Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/198/07. The contractual start date was in July 2015. The final report began editorial review in May 2017 and was accepted for publication in August 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Fran Toye, Kate Seers and Karen Barker authored two studies that are included in this qualitative evidence synthesis. Kate Seers is a Health Services and Delivery Research board member and a Health Services Research Commissioning board member.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Toye et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
A recent systematic review1 of population studies indicates that as many as 28 million adults in the UK are affected by chronic pain. Population estimates suggest that around 25% of adults around the world suffer with moderate or severe pain,2–6 and for between 6% and 14% of these adults this pain is disabling. 6,7 We know that living with chronic pain can be challenging and that patients do not always feel valued or believed by health-care professionals (HCPs). 8 To improve these patients’ experiences of health care, we need to understand what is going on from the perspective of the HCP. In particular, we need to understand why it is that working with people with chronic non-malignant pain can result in patients experiencing this as an adversarial relationship. If we can understand what it is like to be a HCP providing health care to people with chronic non-malignant pain, and in particular its challenges and rewards, this understanding can facilitate improvements in the experience and quality of health care for this large group of people.
Chronic pain can be particularly challenging for HCPs to treat because it persists beyond the expected healing time and is not amenable to routine methods of pain control. 9 This is complicated by the finding that pain is not always explained by a specific pathology. 6 HCPs find working with patients with chronic pain very complex. For example, HCPs describe feeling ‘bombarded by despair’ under the pressure of not being able to fix the person in pain. 10 They can also find it a challenge to balance empathy with ‘not getting too involved’. 10 Allegretti and colleagues11 describe the challenges for general practitioners (GPs) and highlight mismatches in patients’ and clinicians experiences of health care. Others report feelings of frustration and discord in the patient–clinician relationship. 12 It is not uncommon for patients to report dissatisfaction with their HCP interaction and this is likely to influence their decisions and actions. 13 The rationale for this study is underpinned by the need to facilitate ‘patient-centred medicine’. 14 Mead and Bower15 identified five key dimensions of patient-centred medicine: (1) taking a biopsychosocial perspective; (2) framing the ‘patient-as-person’; (3) sharing power and responsibility; (4) therapeutic alliance, which hinges on an effective personal relationship; and (5) ‘doctor-as-person’, which recognises the influence that HCPs’ personal characteristics and responses can have on care. Mead and Bower15 indicate that patient-centred care requires HCPs to be self-aware of their emotional responses and reactions: ‘sensitivity and insight into the reactions of both parties can be used for therapeutic purposes’. Thus, understanding the experience of providing health care to people with chronic non-malignant pain from the perspective of the HCP can have important implications for delivery of health care, decision-making and health-care quality. The findings will allow HCPs and their managers to understand, in detail, the challenges of providing health care to this complex group of patients and, thus, facilitate improvements to the quality of health care. In addition, a mutual understanding of what it is like to provide and receive health care for chronic non-malignant pain can facilitate a therapeutic partnership from the perspective of both patients and their HCPs.
The aim of qualitative evidence synthesis (QES) in health care is to systematically review and integrate findings in order to increase our understanding of the complex processes of health care and, thus, improve the experience and quality of that care. The proliferation of qualitative studies can make it difficult to access and utilise qualitative knowledge to inform practice and policy. 16 The Cochrane Qualitative Research Methods Group acknowledges the importance of including qualitative findings within evidence-based health care,17 and insights from several meta-ethnographies have contributed to a greater understanding of complex processes in health care, for example medicine-taking,18 diabetes,19 antidepressants,20 chronic musculoskeletal pain8 and chronic pelvic pain. 21 There are various methods for synthesising qualitative research. 16,22–25 An important distinction made in synthesis approaches is between (1) those that aim to describe or ‘aggregate’ findings and (2) those that aim to interpret these findings and develop conceptual understandings or ‘theory’. 26 Our aim is to develop conceptual understanding. We will use the methods of meta-ethnography developed, refined and reported by Toye and colleagues8 in a previous meta-ethnography of patients’ experience of chronic musculoskeletal pain.
Objectives
-
To undertake a QES (meta-ethnography)26–28 that will increase our understanding of what it is like for HCPs to provide health care to people with chronic non-malignant pain and, thus, to inform improvements in the experience and quality of health care.
-
To make our findings easily available and accessible through a short film.
-
To contribute to the development of methods for QES that aim to bring together qualitative research findings so that health care can be improved.
Chapter 2 Methods
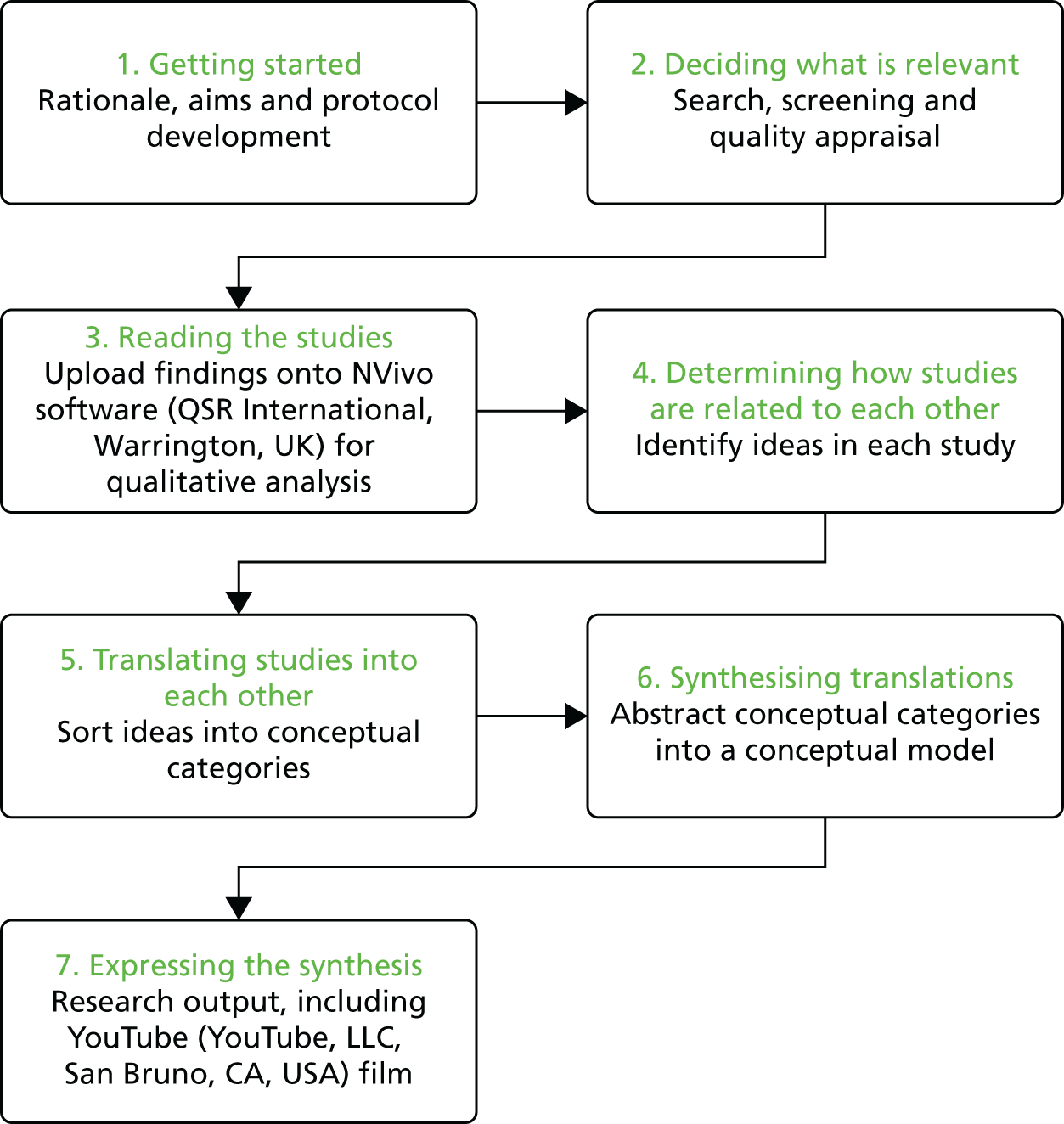
There are seven stages to meta-ethnography (outlined in Figure 1). Stage 1 incorporates the rationale, aims and protocol development. Stage 2 involves deciding what is relevant to the synthesis through a systematic search, screening and appraisal. The analytical stages in meta-ethnography involve overlapping research activities: reading the studies (stage 3), determining how the studies are related (stage 4), translating the studies into each other (stage 5) and synthesising the translations (stage 6). The final stage (stage 7) involves the output and dissemination of findings.
FIGURE 1.
The stages of meta-ethnography.
Stage 1: getting started
This stage incorporates the background, rationale, aims and protocol development.
Stage 2: deciding what is relevant
In their original text on meta-ethnography, Noblit and Hare26 do not advocate an exhaustive literature search, and the number of studies included in meta-ethnographies ranges widely. 22,24,27 The aim of meta-ethnography is not to perform statistical analyses but to draw on knowledge for conceptual development. Some argue that including too many studies makes the analysis ‘unwieldy’. 27,29 However, we aimed to produce a conceptual analysis with a weight of evidence that has resonance with the health research community and thus undertook a systematic search of the published literature. Our previous meta-ethnography has demonstrated the value of undertaking a systematic search and including a larger number of studies into a QES. 28
Searching and screening
Inclusions
We included studies that explored HCPs’ experiences of providing health care to adults with chronic non-malignant pain.
Exclusions
We excluded studies of acute pain, head pain, arthritis (including osteoarthritis and rheumatoid arthritis) or patient experience, and studies in which HCPs’ experiences could not be disentangled from the experiences of others (e.g. patients, carers or family members).
We searched five electronic bibliographic databases [MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO and Allied and Complementary Medicine Database (AMED)] using terms adapted from the InterTASC Information Specialists’ Sub-Group search filter resource. 30–33 The InterTASC Information Specialists’ Sub-Group is a group of information professionals supporting research groups producing technology assessments for the National Institute for Health and Care Excellence (URL: www.york.ac.uk/inst/crd/intertasc/; accessed 24 July 2017).
We developed the search strategy with an information specialist and used a combination of specific subject heading terms and free-text terms (Table 1). We did not use the ‘clinical query limits’ option for qualitative research in our searches, as we had found that this can filter out relevant qualitative studies. To ensure value for money, we did not include citation checks, hand-searching, grey literature or Doctor of Philosophy (PhD) searches. Previous experience has shown us that these strategies do not necessarily add significant conceptual value to large meta-ethnographies. 28 Two reviewers screened the titles, abstracts and full texts of potential studies for relevance.
| Database | Terms | |||
|---|---|---|---|---|
| Qualitative research | Pain | |||
| Subject heading | Free text | Subject heading | Free text | |
| MEDLINE | ATTITUDE TO HEALTHCARE/INTERVIEWS AS TOPIC/FOCUS GROUPS/NURSING METHODOLOGY RESEARCH/ATTITUDE TO HEALTH |
Qualitative ADJ5 (theor* OR study OR studies OR research OR analysis)/ethno*/emic OR etic/phenomenolog*/ hermeneutic*/heidegger* OR husserl* OR colaizzi* OR giorgi* OR glaser OR strauss OR (van AND kaam*) OR (van AND manen) OR ricoeur OR spiegelberg* OR merleau/constant ADJ3 compar*/focus ADJ3 group*/grounded ADJ3 (theor* OR study OR studies OR research OR analysis)/narrative ADJ3 analysis/discourse ADJ3 analysis/(lived OR life) ADJ3 experience*/ (theoretical OR purposive) ADJ3 sampl*/(field ADJ note* ) OR (field ADJ record* ) OR fieldnote*/ participant* ADJ3 observ*/action ADJ research (digital ADJ record) OR audiorecord* OR co AND operative AND inquir* /co-operative AND inquir* (semi-structured OR semistructured OR unstructured OR structured) ADJ3 interview*/(informal OR in-depth OR indepth OR ‘in depth’) ADJ3 interview*/(‘face-to-face’ OR ‘face to face’) ADJ3 interview*/’IPA’ OR ‘interpretative phenomenological analysis’/’appreciative inquiry’ social AND construct*/poststructural* OR (post structural*) OR post-structural* /postmodern* OR (post modern*) OR post-modern*/ feminis*/humanistic OR existential OR experiential |
BACK PAIN/CHRONIC PAIN/PAIN/PAIN MANAGEMENT/FIBROMYALGIA/ |
(chronic* OR persistent* OR long-stand* OR longstand* OR unexplain* OR un-explain*) ADJ5 pain Fibromyalgia ‘back ache’ OR back-ache OR backache ‘pain clinic’ OR pain-clinic* pain adj5 syndrome* |
| PsycINFO | QUALITATIVE RESEARCH/INTERVIEWS/GROUP DISCUSSION/GROUNDED THEORY/CONTENT ANALYSIS/LIFE EXPERIENCES/PHENOMENOLOGY/ETHNOGRAPHY/ | CHRONIC PAIN/LOW BACK PAIN/MUSCULOSKELETAL PAIN/PAIN/PAIN CLINIC/BACKACHE/FIBROMYALGIA/ | ||
| EMBASE | QUALITATIVE RESEARCH/QUALITATIVE RESEARCH/PHENOMENOLOGY/PERSONAL EXPERIENCE/ATTITUDE | BACK PAIN/CHRONIC PAIN/LOW BACK PAIN/MUSCULOSKELETAL PAIN/PAIN/PAIN CLINICS/FIBROMYALGIA/PAIN MANAGEMENT/ | ||
| CINAHL | QUALITATIVE STUDIES/QUALITATIVE VALIDITY/PHENOMENOLOGY/PHENOMENOLOGICAL RESEARCH/ETHNOGRAPHIC RESEARCH/ANTHROPOLOGY, CULTURAL/OBSERVATIONAL METHODS/PARTICIPANT OBSERVATION/LIFE EXPERIENCES/LIFE HISTORIES/ATTITUDE TO LIFE/ETHNOLOGICAL RESEARCH/ETHNONURSING RESEARCH/NATURALISTIC INQUIRY/FOCUS GROUPS/GROUNDED THEORY/PURPOSIVE SAMPLE/THEORETICAL SAMPLE/SNOWBALL SAMPLE/FIELD STUDIES/FIELD NOTES/CONSTANT COMPARATIVE METHOD/CONTENT ANALYSIS/DISCOURSE ANALYSIS/THEMATIC ANALYSIS/ | PAIN/PAIN CLINICS/CHRONIC PAIN/FIBROMYALGIA/PAIN CLINICS/ | ||
| AMED | ATTITUDE/INTERVIEWS/ | PAIN/FIBROMYALGIA/BACKACHE/ | ||
Quality appraisal
Although there are many frameworks suggested for appraising the quality of qualitative research, there is no consensus on what makes a study ‘good’. 27,34 However, a growing number of researchers are appraising studies for the purpose of QES. 24
Although we did not intend to use rigid guidelines for determining inclusion, we used three methods of quality appraisal to frame our discussions:
-
The questions developed by the Critical Appraisal Skills Programme (CASP) for appraising qualitative research (Box 1). 35 We assigned a numerical score to each question to indicate whether we felt that the CASP question (1) had not been addressed, (2) had been addressed partially or (3) had been extensively addressed, thus giving a possible score range of 10–30. 8 We used the CASP in this way in a previous meta-ethnography of patients’ experience of living with chronic non-malignant pain, in which we found that satisfactory papers scored at least 19. 8
-
A list of seven themes (Table 2) developed from a qualitative study embedded in a previous meta-ethnography funded by the Health Services and Delivery Research (HSDR) programme. 36 Unlike CASP, these themes were developed specifically for meta-ethnography. For example, CASP does not focus specifically on conceptual clarity as a facet of quality, which is a distinguishing feature of meta-ethnography.
-
We categorised, as suggested by Dixon-Woods and colleagues,34 a ‘key paper’ that was ‘conceptually rich and could potentially make an important contribution to the synthesis’; a ‘satisfactory paper’; a paper that is irrelevant to the synthesis; and a paper that is methodologically fatally flawed.
-
Was there a clear statement of the aims of the research?
-
Is a qualitative methodology appropriate?
-
Was the research design appropriate to address the aims of the research?
-
Was the recruitment strategy appropriate to the aims of the research?
-
Were the data collected in a way that addressed the research issue?
-
Has the relationship between researcher and participants been adequately considered?
-
Have ethical issues been taken into consideration?
-
Was the data analysis sufficiently rigorous?
-
Is there a clear statement of findings?
-
How valuable is the research?
Reproduced from CASP. 35 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC-SA 3.0) license, which permits others to distribute, remix, adapt and build upon this work, for non-commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc-sa/3.0/.
| Question | Response |
|---|---|
| 1. Is the background/rationale/aim described? | Yes/no/not clear |
| 2. Is the sample described? | Yes/no/not clear |
| 3. Is the researcher’s perspective clear | Yes/no |
| 4. Has the researcher challenged their own interpretation? | Yes/no/not clear |
| 5. Does the researcher’s interpretation come from the original data? | Yes/not clear |
| 6. Can you identify the ideas in this study (or do you find yourself recoding)? | Yes/no/not always |
| 7. Has this changed your thinking/made you think? (Describe in what way) | Yes/no |
Two reviewers appraised each paper, and if they were unable to reach an agreement the study was sent to a third reviewer for the final decision.
GRADE-CERQual
We also utilised the Grading of Recommendations Assessment, Development and Evaluation Confidence in the Evidence from Reviews of Qualitative research (GRADE-CERQual) framework37 (URL: www.cerqual.org/; accessed 24 July 2017), which aims to help reviewers to assess and describe how much confidence readers can place in review findings, in other words ‘the extent to which the review finding is a reasonable representation of the phenomenon of interest’. 37 GRADE-CERQual proposes four distinct areas to rate for each review finding before assessing overall confidence. We aimed to explore how these domains were useful in assessing the confidence in a conceptual QES.
Methodological limitations
In GRADE-CERQual, methodological limitations are the ‘extent to which there are problems in the design or conduct of the primary studies that contributed evidence to a review’. 37 Reviewers are required to provide an evaluation of the methodological quality of the studies supporting each of the review findings.
Relevance
In GRADE-CERQual, relevance is the ‘extent to which the body of evidence from the primary studies supporting a review finding is applicable to the context specified in the review question’. 37 Reviewers are required to provide an evaluation of the relevance of the studies supporting each of the review findings.
Adequacy of data
In GRADE-CERQual, adequacy of data is an ‘overall determination of the degree of richness and quantity of data supporting a review finding’. 37 Rich data provide ‘sufficient detail to gain an understanding of the phenomenon we are studying’. 37 Reviewers should describe the adequacy of data for each finding.
Coherence
In GRADE-CERQual, coherence considers whether or not the finding is well grounded in the primary studies. Reviewers should demonstrate that there has been no ‘attempt to create findings that appear more coherent through ignoring or minimising important disconfirming cases’,37 in other words demonstrate that they are not cherry-picking evidence to support an a priori concept. They should describe consistency and inconsistency along with possible explanations for any variations found across studies or cases.
Overall confidence
Finally, GRADE-CERQual reviewers give an overall rating of confidence for each individual review finding. The suggested ratings are high, moderate, low or very low. Lewin and colleagues37 indicate that ‘it may be difficult to achieve “high confidence” for review findings in many areas, as the underlying studies often reveal methodological limitations or there are concerns regarding the adequacy of the data’.
Stage 3: reading the studies
This stage of meta-ethnography involves thoroughly reading and re-reading the studies to identify and describe the ideas or concepts. 26 The raw data of meta-ethnography are ideas or concepts in the primary studies. To allow us to refer to the original studies, we uploaded the study findings onto NVivo 11 software (QSR International, Warrington, UK) for qualitative analysis. NVivo is particularly useful for collaborative analysis as it allows the team to keep a record and compare the reviewers’ unique interpretations. NVivo 11 also allows the researchers to write memos and link them to data in order to keep track of developing analysis. We maintained a Microsoft Excel® database (Microsoft Corporation, Redmond, WA, USA) of study demographics, appraisal and decisions on inclusion or exclusion. We read the studies in batches related to the topic/professional group and in the order in which they were retrieved, and did not use an index paper. In other meta-ethnographies, for example those of Campbell and colleagues,27 researchers have used an index paper as a way of ‘orienting the synthesis’. 38 In these examples, concepts from an early or index paper are used for comparison with concepts from subsequent studies. However, we felt that there were methodological issues with using an index paper:
-
How do we decide which paper to use as an index paper?
-
How do we define a ‘classic’ paper with no consensus about what makes a study good?
-
An index paper can have a dramatic effect on the resulting interpretation.
-
Using an index paper can mean that we become constrained by a priori concepts. This is important because we will not necessarily find the conceptually rich papers first. The process of searching and analysing is iterative and analysis does not start when the full body of data is collected but continues alongside data collection.
-
When synthesising a large number of studies, comparing concepts across these studies from an index paper can become unwieldy.
Stage 4: determining how studies are related to each other
Determining how studies are related to each other involves creating ‘a list of key metaphors, phrases, ideas and/or concepts’ (p. 28). 26 The purpose of careful reading in meta-ethnography is to identify and describe the ‘metaphors’/ideas/concepts in each study and ‘translate’ or compare them to those found in other studies. This is fundamental to meta-ethnography because concepts are the raw data of the synthesis. However, at times it can be a challenge to decipher the concepts from primary studies. 36 Two reviewers read each paper to identify and describe the concepts and compiled a list of concepts from the original papers. Our analysis was based on clearly articulated concepts from the originating papers. Schütz39 distinguishes between (1) first-order constructs (the participants’ ‘common sense’ interpretations in their own words) and (2) second-order constructs (the researchers’ interpretations of first-order constructs). In meta-ethnography, the ‘data’ are second-order constructs that are further abstracted to develop third-order constructs (reviewer’s interpretations of second-order constructs). However, the distinction between first- and second-order constructs is not clear-cut:40 primary authors choose narrative exemplars to illustrate a second-order construct. Meta-ethnography attempts to identify themes not from original narrative data but from the reported concepts. We did not recode narrative data as any attempt to recode is not embedded in the primary research process. Rather, we excluded data from analysis if both reviewers could not decipher a clear concept.
Owing to the scale of the study and the potential number of second-order constructs, our interpretation of each concept needed to combine clarity, precision and brevity. We therefore used a combination of the author’s description of the second-order construct (which briefly and clearly described the construct), and our interpretation of the construct (if the original was unclear or lengthy). In some cases, we found that there was a section of narrative exemplar provided by the original authors that was enough to give the essence of the concept. Our aim was to compile a list of concise interpretations of second-order constructs that were grounded in the primary studies.
Stage 5: translating studies into each other
The next stage in meta-ethnography involves exploring how the concepts are related to each other and, thus, sorting concepts into conceptual categories. 26 All three reviewers organised, discussed and then reorganised the concepts into categories. ‘Translation’ is achieved through the constant comparative method41 through which the reviewers begin to see similarities and differences and organise concepts into further abstracted conceptual categories.
Stage 6: synthesising translations
The next stage of meta-ethnography is to synthesise, or make sense of, the conceptual categories by developing overarching themes and integrating these themes into a conceptual model. This is part of an ongoing process in which findings are further abstracted to form a conceptual framework. We planned to develop a line-of-argument synthesis, which involves ‘making a whole into something more than the parts alone imply’ (p. 28). 26 In our experience of performing large meta-ethnographies, a line of argument can incorporate reciprocity and refutation into a useful conceptual model. This is achieved by constantly comparing concepts and developing ‘a grounded theory that puts the similarities and differences between studies into interpretive order’ (p. 64). 26 We described and printed conceptual categories on postcards and sent these to our advisory group members to read and sort into thematic groups. Then, during the next advisory group workshop, members formed small groups to discuss and reorganise the postcards together. Each of the groups then chose a spokesperson to describe its themes. The complete advisory group then discussed and agreed on the final overarching themes. The aim of the workshop was to develop thematic groups that would underpin a conceptual model. Once the thematic groups had been finalised at the advisory group meeting, all three reviewers discussed and agreed on a conceptual model that they felt was greater than the sum of the individual themes.
Stage 7: expressing the synthesis
The final stage of meta-ethnography involves output and dissemination of findings. Our outputs included a short YouTube film (YouTube, LLC, San Bruno, CA, USA) (see Report Supplementary Material 1; URL: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1419807/#/documentation). The script for the film was woven together from narrative exemplars from the primary studies to illustrate each overarching theme. The reviewers worked closely alongside a media company, RedBalloon (URL: www.redballoon.co.uk/; accessed 24 July 2017), which specialises in outputs from qualitative research. The team had worked successfully together to produce a film from a previous HSDR-funded meta-ethnography that explores patients’ experiences of living with chronic musculoskeletal pain (www.youtube.com/watch?v=FPpu7dXJFRI; accessed 24 July 2017).
Chapter 3 Findings
This is a full report of findings reported in Toye and colleagues42 (Reproduced from Toye et al. 42 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/) and Toye and colleagues43 (Reproduced from Toye et al. 43 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/).
Search results
The results of the systematic search are shown in Figure 2. We screened 954 potentially relevant studies and excluded 770 after screening the abstracts. We retrieved 184 full-text articles and excluded 101 for the following reasons:
FIGURE 2.
Systematic search results.
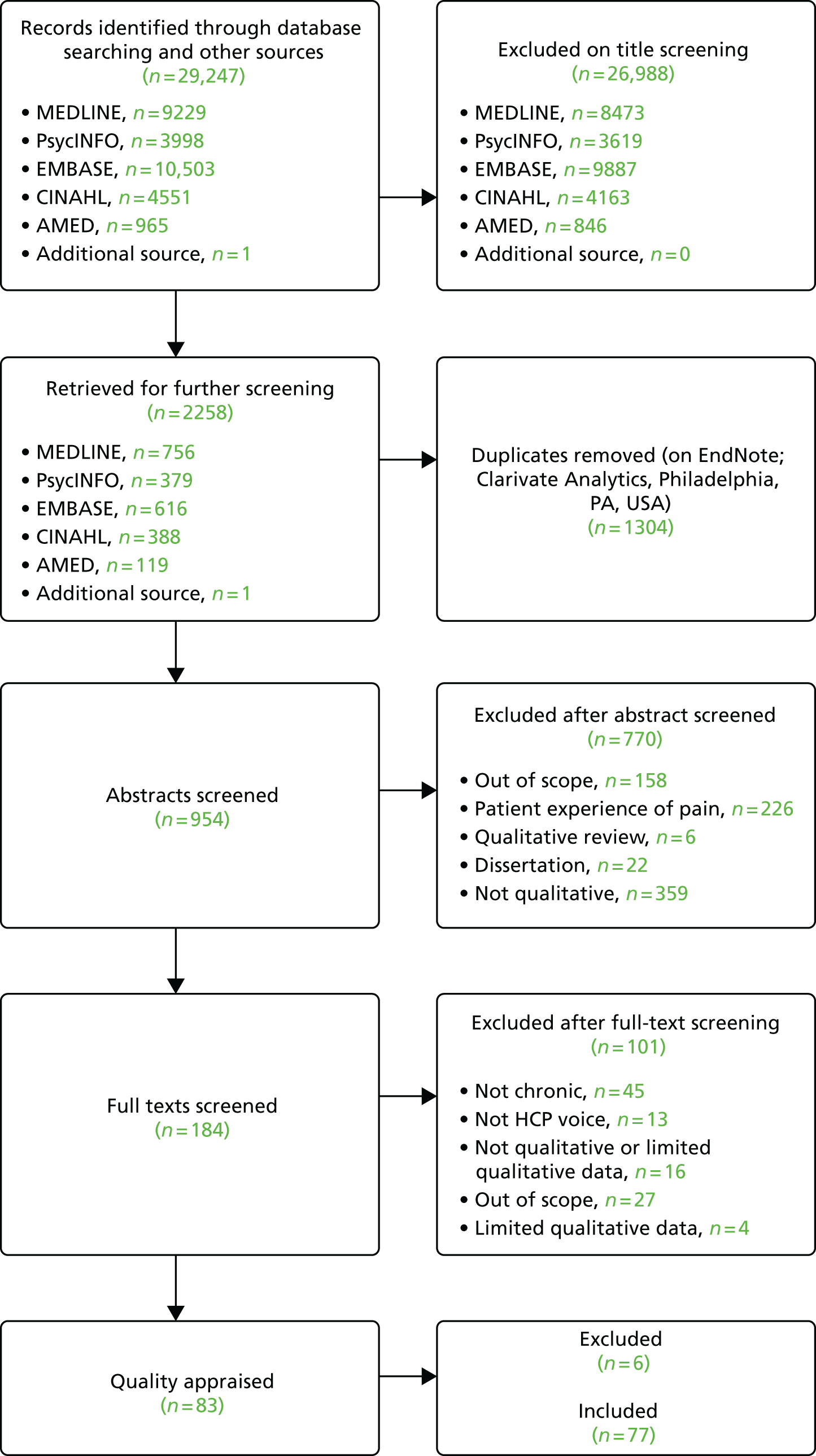
Of the 83 potential studies, we unanimously excluded six on the grounds of methodological report. 144–149 We included 77 published studies reporting the experiences of > 1551 HCPs. 11,150–225 Table 3 provides the author, year of publication, professional/topic group, geographical context, number of participants, data collection and analytical methods for each study. HCPs included a diversity of doctors, nurses and allied health professionals in various contexts and geographical locations. Not all of the studies reported the number of participants from specific professional groups, which meant that it was not possible to give the exact sample number from each profession. The majority of studies were from the USA, the UK, Canada and Sweden. The sample size from the studies ranged from 6 to 103 (average 22). One focus group study165 and three ethnographic studies156,200,223 did not report their sample size.
| First author and year | Location | n | Data collection | Analytical approach | Professional group/topic |
|---|---|---|---|---|---|
| Afrell 2010151 | Norway | 6 | Focus groups | Phenomenology | Specialist physiotherapists |
| Allegretti 201011 | USA | 13 | Semistructured interview | Immersion–crystallisation | Primary care physicians/GPs |
| Åsbring 2003152 | Sweden | 26 | Semistructured interview | Grounded theory | Fibromyalgia |
| aBaldacchino 2010153 | UK | 29 | Focus groups and interviews | Framework analysis | Opioid prescription |
| Barker 2015154 | UK | 7 | Semistructured interviews | Action research | Specialist physiotherapists |
| aBarry 2010155 | USA | 23 | Semistructured interview | Grounded theory | Opioid prescription |
| Baszanger 1992156 | France | NK | Ethnography | Grounded theory | Chronic pain services |
| aBerg 2009157 | USA | 16 | Semistructured interview | Thematic analysis | Opioid prescription |
| Bergman 2013158 | USA | 14 | Interviews | Thematic analysis | Primary care physicians/GPs |
| Blomberg 2008159 | Sweden | 20 | Focus groups | Grounded theory | Nursing |
| Blomqvist 2003160 | Sweden | 52 | Interviews | Content analysis | Older adults |
| aBriones-Vozmediano 2013161 | Spain | 9 | Semistructured interview | Discourse analysis | Fibromyalgia |
| Cameron 2015162 | UK | 13 | Semistructured telephone interviews | Thematic analysis | Older adults |
| Cartmill 2011163 | Canada | 10 | Semistructured interview | Grounded theory | Chronic pain services |
| Chew-Graham 1999164 | UK | 20 | Semistructured interview | Grounded theory | Primary care physicians/GPs |
| Clark 2004165 | USA | NK | Focus groups | Ethnography | Pain in aged care facilities |
| Clark 2006166 | USA | 103 | Semistructured interviews | Content analysis | Pain in aged care facilities |
| Côté 2001167 | Canada | 30 | Focus groups | Thematic analysis | Pain-related work disability |
| Coutu 2013168 | Canada | 5 | Semistructured interviews | Thematic analysis | Pain-related work disability |
| Dahan 2007169 | Israel | 38 | Focus groups | Immersion–crystallisation | Guidelines |
| Daykin 2004170 | UK | 6 | Semistructured interviews | Grounded theory | Physiotherapists |
| Dobbs 2014171 | USA | 28 | Focus groups | Content analysis | Pain in aged care facilities |
| Eccleston 1997172 | UK | 11 | Q-analysis | Q-analysis | Mixed professionals |
| Espeland 2003173 | Norway | 13 | Focus groups | Phenomenology | Guidelines |
| aEsquibel 2014174 | USA | 21 | Interviews | Immersion–crystallisation | Opioid prescription |
| aFontana 2008175 | USA | 9 | Semistructured interview | Emancipatory research | Opioid prescription |
| Fox 2004176 | Canada | 54 | Focus groups | Thematic analysis | Pain in aged care facilities |
| aGooberman-Hill 2011177 | UK | 27 | Semistructured interview | Thematic analysis | Opioid prescription |
| Gropelli 2013178 | USA | 16 | Semistructured interviews | Content analysis | Pain in aged care facilities |
| Hansson 2001179 | Sweden | 4 | Interviews | Grounded theory | Pain-related work disability |
| Harting 2009180 | The Netherlands | 30 | Focus groups | Content analysis | Guidelines |
| Hayes 2010181 | Canada | 32 | Focus groups and interviews | Grounded theory | Fibromyalgia |
| Hellman 2015182 | Sweden | 15 | Semistructured interviews | Thematic analysis | Pain-related work disability |
| Hellström 1998183 | Sweden | 20 | Interviews | Phenomenology | Fibromyalgia |
| Holloway 2009184 | Australia | 6 | Semistructured interviews | Constant comparison | Pain in aged care facilities |
| aHolloway 2009185 | Australia | 6 | Semistructured interviews | Constant comparison | Pain in aged care facilities |
| Howarth 2012186 | UK | 9 | Interviews and focus groups | Grounded theory | Chronic pain services |
| aKaasalainen 2007187 | Canada | 66 | Interviews and focus groups | Grounded theory | Pain in aged care facilities |
| Kaasalainen 2010188 | Canada | NK | Interviews and focus groups | Thematic analysis | Pain in aged care facilities |
| aKaasalainen 2010189 | Canada | 53 | Interviews and focus groups | Case study analysis | Pain in aged care facilities |
| aKilaru 2014190 | USA | 61 | Semistructured interview | Grounded theory | Opioid prescription |
| aKrebs 2014191 | USA | 14 | Semistructured interview | Immersion–crystallisation | Opioid prescription |
| Kristiansson 2011192 | Sweden | 5 | Interviews | Narrative analysis | Primary care physicians/GPs |
| Liu 2014193 | Hong Kong | 49 | Interviews and focus groups | Content analysis | Pain in aged care facilities |
| Löckenhoff 2013194 | USA | 44 | Focus groups | Content analysis | Mixed HCPs |
| Lundh 2004195 | Sweden | 14 | Focus groups | Constant comparison | Primary care physicians/GPs |
| MacNeela 2010196 | Ireland | 12 | Critical incident interview | Thematic analysis | Primary care physicians/GPs |
| McConigley 2008197 | Australia | 34 | Interviews and focus groups | Thematic analysis | Pain in aged care facilities |
| aMcCrorie 2015198 | UK | 15 | Focus groups | Grounded theory | Opioid prescription |
| Mentes 2004199 | USA | 11 | Semistructured interviews | Thematic analysis | Pain in aged care facilities |
| O’Connor 2015200 | USA | NK | Ethnography | Constant comparison | Chronic pain services |
| Øien 2011201 | Norway | 6 | Interviews, focus groups, observation | Case study | Physiotherapists |
| Oosterhof 2014202 | The Netherlands | 10 | Interviews and observation | Thematic analysis | Chronic pain services |
| Parsons 2012203 | UK | 19 | Semistructured interviews | Framework analysis | Mixed professionals |
| Patel 2008204 | UK | 18 | Semistructured interview | Thematic analysis | Primary care physicians/GPs |
| aPatel 2009205 | UK | 18 | Semistructured interview | Thematic analysis | Primary care physicians/GPs |
| Paulson 1999206 | Sweden | 21 | Interviews | Phenomenology | Fibromyalgia |
| Poitras 2011207 | Canada | 9 | Semistructured interviews | Thematic analysis | Guidelines |
| aRuiz 2010208 | USA | 21 | Focus groups and interviews | Grounded theory | Older adults |
| Schulte 2010209 | Germany | 10 | Semistructured interview | Thematic analysis | Primary care physicians/GPs |
| Scott-Dempster 2014210 | UK | 6 | Semistructured interviews | Interpretative phenomenological analysis | Specialist physiotherapists |
| aSeamark 2013211 | UK | 22 | Interviews and focus groups | Thematic analysis | Opioid prescription |
| Shye 1998212 | USA | 22 | Focus groups | Immersion–crystallisation | Guidelines |
| aSiedlecki 2014213 | USA | 48 | Interviews | Grounded theory | Nursing |
| Slade 2012214 | Australia | 23 | Focus groups | Grounded theory | Physiotherapists |
| Sloots 2009215 | The Netherlands | 4 | Semistructured interviews | Thematic analysis | Chronic pain services |
| Sloots 2010216 | The Netherlands | 10 | Semistructured interviews | Thematic analysis | Chronic pain services |
| aSpitz 2011217 | USA | 26 | Focus groups | Thematic analysis | Opioid prescription |
| aStarrels 2014218 | USA | 28 | Telephone interview | Grounded theory | Opioid prescription |
| Stinson 2013219 | Canada | 17 | Focus groups | Thematic analysis | Chronic pain services |
| Thunberg 2001150 | Sweden | 22 | Interviews | Grounded theory | Chronic pain services |
| Toye 2015220 | UK | 19 | Focus groups | Grounded theory | Mixed professionals |
| Tveiten 2009221 | Norway | 5 | Focus groups | Content analysis | Chronic pain services |
| Wainwright 2006222 | UK | 14 | Interviews | Thematic analysis | Primary care physicians/GPs |
| Wilson 2014223 | UK | NK | Interviews, documents | Ethnography | Guidelines |
| Wynne-Jones 2014224 | UK | 17 | Semistructured interviews | Constant comparison | Pain-related work disability |
| Zanini 2014225 | Italy | 17 | Semistructured interviews | Thematic analysis | Chronic pain services |
Quality assessment and inclusion
Table 4 provides the outcome of appraisal: the CASP score from each reviewer [from 10 (low) to 30 (high)]; the difference in CASP score between reviewers; the seven themes developed from a previous meta-ethnography;8 the global quality score (key, satisfactory, uncertain, irrelevant or fatal flaw); and reviewers’ assessment of potential value based on CASP question 10 (‘how valuable is the research?’). The difference in CASP score between two reviewers ranged from –4 to 2 (a possible score of 10–30). They did not agree about the inclusion of four studies,172,178,196,201 which were subsequently included by a third reviewer. Two reviewers agreed that 89% of primary authors had reported their study aim and 84% had described their sample. They agreed that 89% of the authors had not reported their perspective and its potential influence on findings and 69% had not reported methods for challenging their interpretation. Reviewers also agreed that only 65% of authors had provided clear examples to demonstrate that their findings were drawn from the data and only 55% of authors had clearly described all their findings. Twenty-eight studies11,150,151,153,154,156,157,159,165–167,174,176,179,187,190,195,204,207–209,211–214,221–223 were reported as having ‘changed the thinking’ of at least one reviewer. However, reviewers’ appraisal comments (see Appendix 1) suggested that, even if they did not change their thinking, the primary studies encouraged reviewers to think. Two reviewers unanimously appraised five studies150,151,214,222,223 as ‘key papers’ and 72 as ‘satisfactory’ (see Table 3). At least one reviewer appraised 26 studies11,150,151,154,156,157,160,170,171,176,187,190,191,195,198,204,205,210,211,214,219–223,225 as potentially making a ‘valuable’ contribution to the analysis. They agreed on 21 of 26 of the valuable studies. To allow readers to evaluate the transferability of findings, Table 5 shows the reviewers’ assessment of relevance (direct, indirect, partial or uncertain) and aim of each study. We rated 60 studies11,150,152–164,168–171,173–178,180,181,183–188,190–193,195,196,198,200–211,214,215,217,218,221,222,224,225 as directly relevant, seven151,165,166,197,219,220,223 as indirectly relevant, nine172,179,182,189,194,199,212,213,216 as partially relevant and one167 as uncertain.
| In/out | First author and year | Reviewer 1 CASP score | Reviewer 2 CASP score | Difference between CASP scores | Theme | Global quality and value score (CASP question 10) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Rationale/aim described? | 2. Sample described? | 3. Researcher’s perspective clear? | 4. Challenged interpretation? | 5. Does interpretation come from the data? | 6. Can you identify the ideas? | 7. Has this changed your thinking? | ||||||
| In | Thunberg 2001150 | 27 | 27 | 0 | Y | Y | N | Y | Y | N (Y) | Y (N) | KP and V2 |
| In | Slade 2012214 | 28 | 29 | –1 | Y | Y | N | Y | Y | Y | Y | KP and V2 |
| In | Wainwright 2006222 | 28 | 28 | 0 | Y | Y | N | Y | Y | Y | Y (N) | KP and V2 |
| In | Afrell 2010151 | 29 | 29 | 0 | Y | Y | N | Y | Y | Y (N) | Y | KP and V2 |
| In | Wilson 2014223 | 29 | 30 | –1 | Y | Y | N (Y) | Y | Y | Y | Y | KP and V2 |
| In | Tveiten 2009221 | 26 | 28 | –2 | Y | N | N | N | Y | Y | Y (N) | SAT and V2 |
| In | Kaasalainen 2007187 | 27 | 27 | 0 | Y | Y | N | Y | Y | Y | Y (N) | SAT and V2 |
| In | Kilaru 2014190 | 27 | 27 | 0 | Y | N | N | N | Y | Y | Y (N) | SAT and V2 |
| In | Krebs 2014191 | 27 | 28 | –1 | Y | Y | N | Y | Y | Y | N | SAT and V2 |
| In | Lundh 2004195 | 27 | 29 | –2 | Y | Y | N | N | Y | Y | N (Y) | SAT and V2 |
| In | Fox 2004176 | 27 | 27 | 0 | Y | Y | N | Y | Y | Y | Y | SAT and V2 |
| In | Allegretti 201011 | 28 | 29 | –1 | Y | Y | N | Y | Y | Y | Y | SAT and V2 |
| In | Baszanger 1992156 | 28 | 27 | 1 | Y | Y | N | N | N | N | Y (N) | SAT and V2 |
| In | Daykin 2004170 | 28 | 28 | 0 | Y | Y | N | Y | Y | Y (N) | N | SAT and V2 |
| In | McCrorie 2015198 | 28 | 29 | –1 | Y | Y | N | Y | Y | Y (N) | N | SAT and V2 |
| In | aPatel 2008204 | 28 | 29 | –1 | Y | Y | N | Y | Y | Y | Y | SAT and V2 |
| In | Zanini 2014225 | 28 | 28 | 0 | Y | Y | N | Y | Y | Y | N | SAT and V2 |
| In | Barker 2015154 | 29 | 29 | 0 | Y | Y | Y | Y | Y | Y | N (Y) | SAT and V2 |
| In | Berg 2009157 | 29 | 29 | 0 | Y | Y | N | Y | Y | Y | Y (N) | SAT and V2 |
| In | Scott-Dempster 2014210 | 29 | 29 | 0 | Y | Y | N | Y | Y | Y | N | SAT and V2 |
| In | Toye 2015220 | 29 | 29 | 0 | Y | Y | N | Y | Y | Y | N | SAT and V2 |
| In | Blomqvist 2003160 | 26 | 28 | –2 | Y | Y | N | Y | N | Y | N | SAT and V1 |
| In | Dobbs 2014171 | 27 | 28 | –1 | Y | Y | N | Y | Y | Y | N | SAT and V1 |
| In | Seamark 2013211 | 27 | 26 | 1 | Y | Y | N | Y | Y | Y | Y (N) | SAT and V1 |
| In | Stinson 2013219 | 27 | 25 | 2 | Y | Y | N | Y | Y | Y | N | SAT and V1 |
| In | aPatel 2009205 | 28 | 28 | 0 | Y | Y | N | Y | Y | N | N | SAT and V1 |
| In | Cameron 2015162 | 22 | 22 | 0 | Y | N | N | N | N | N | N | SAT |
| In | Chew-Graham 1999164 | 22 | 23 | –1 | Y | Y | N | N | N | Y | N | SAT |
| In | Coutu 2013168 | 22 | 21 | 1 | Y | N | N | Y | Y | N | N | SAT |
| In | Löckenhoff 2013194 | 22 | 22 | 0 | N (Y) | Y | N | N | N | N | N | SAT |
| In | Åsbring 2003152 | 23 | 24 | –1 | Y | N | N | N | N | Y | N | SAT |
| In | Shye 1998212 | 23 | 24 | –1 | Y | Y | N | N | Y | Y (N) | Y (N) | SAT |
| In | Siedlecki 2014213 | 23 | 24 | –1 | Y | Y | N | N | N | N | Y (N) | SAT |
| In | Baldacchino 2010153 | 24 | 23 | 1 | Y | N | N | N | Y | Y (N) | Y | SAT |
| In | Côté 2001167 | 24 | 25 | –1 | Y | Y | N | Y | Y | Y | Y (N) | SAT |
| In | Hellström 1998183 | 24 | 25 | –1 | Y | Y | N | N | Y (N) | Y | N | SAT |
| In | Kristiansson 2011192 | 24 | 24 | 0 | Y | Y | N (Y) | N | N | N | N | SAT |
| In | Parsons 2012203 | 24 | 25 | –1 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Fontana 2008175 | 25 | 24 | 1 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Clark 2004165 | 25 | 26 | –1 | Y | Y | N | Y | N | Y | Y | SAT |
| In | Harting 2009180 | 25 | 25 | 0 | Y | Y | N | Y | N | N | N | SAT |
| In | Hayes 2010181 | 25 | 26 | –1 | Y | Y | N | Y | Y | N | N | SAT |
| In | McConigley 2008197 | 25 | 26 | –1 | Y | Y | N | Y | N | Y (N) | N | SAT |
| In | Poitras 2011207 | 25 | 26 | –1 | Y | Y | N | Y | N | Y | Y (N) | SAT |
| In | Ruiz 2010208 | 25 | 25 | 0 | Y | Y | N (Y) | Y | Y | Y | N (Y) | SAT |
| In | Sloots 2010216 | 25 | 25 | 0 | Y | Y | N | Y | Y | N | N | SAT |
| In | Wynne-Jones 2014224 | 25 | 25 | 0 | Y | Y | N | Y | Y | N | N | SAT |
| In | Bergman 2013158 | 26 | 25 | 1 | Y | Y | N (Y) | Y | Y | Y (N) | N | SAT |
| In | Cartmill 2011163 | 26 | 26 | 0 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Clark 2006166 | 26 | 27 | –1 | Y | Y | N | Y | Y | Y | Y | SAT |
| In | Dahan 2007169 | 26 | 27 | –1 | Y | Y | N | Y | Y | N | N | SAT |
| In | Gooberman-Hill 2011177 | 26 | 28 | –2 | Y | Y | N | Y | Y | N (Y) | N | SAT |
| In | Hansson 2001179 | 26 | 27 | –1 | Y | Y | N | Y | N (Y) | Y | Y (N) | SAT |
| In | Holloway 2009184 | 26 | 26 | 0 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Holloway 2009185 | 26 | 26 | 0 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Kaasalainen 2010189 | 26 | 27 | –1 | Y | Y | N | Y | Y | N | N | SAT |
| In | O’Connor 2015200 | 26 | 27 | –1 | Y | Y | N | N | N | Y | N | SAT |
| In | Schulte 2010209 | 26 | 27 | –1 | Y | Y | N (Y) | Y | N | Y | Y (N) | SAT |
| In | Sloots 2009215 | 26 | 27 | –1 | Y | Y | N | N (N) | Y | Y | N | SAT |
| In | Starrels 2014218 | 26 | 27 | –1 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Barry 2010155 | 27 | 26 | 1 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Blomberg 2008159 | 27 | 28 | –1 | Y | Y | N | Y | Y | Y | Y (N) | SAT |
| In | Briones-Vozmediano 2013161 | 27 | 28 | –1 | Y | Y | N | Y | Y (N) | Y | N | SAT |
| In | Espeland 2003173 | 27 | 27 | 0 | Y | Y | Y (N) | Y | Y | N | N | SAT |
| In | Esquibel 2014174 | 27 | 28 | –1 | Y | Y | N | Y | Y | Y | Y (N) | SAT |
| In | Hellman 2015182 | 27 | 28 | –1 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Howarth 2012186 | 27 | 27 | 0 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Kaasalainen 2010188 | 27 | 27 | 0 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Liu 2014193 | 27 | 28 | –1 | Y | Y | N | Y | Y | Y (N) | N | SAT |
| In | Mentes 2004199 | 27 | 27 | 0 | Y | Y | N | Y | N | Y | N | SAT |
| In | Oosterhof 2014202 | 27 | 26 | 1 | Y | Y | N (Y) | Y | Y | N | N | SAT |
| In | Paulson 1999206 | 27 | 27 | 0 | Y | Y | N | Y | N (Y) | N | N | SAT |
| In | Spitz 2011217 | 27 | 27 | 0 | Y | Y | N | Y | Y | Y | N | SAT |
| In | Eccleston 1997172 | 20 | 25 | –5 | Y (N) | Y | N (Y) | Y (N) | Y | N | N | SAT/FF |
| In | MacNeela 2010196 | 21 | 22 | –1 | N | N | N | N | N | N | N | SAT/FF |
| In | Øien 2011201 | 23 | 24 | –1 | Y | Y | N | Y (N) | N (N) | N (N) | N | SAT/FF |
| In | Gropelli 2013178 | 21 | 21 | 0 | Y | Y | N | N | N | N (N) | N | SAT/FF |
| Out | Kotarba 1984149 | 14 | 13 | 1 | N | N (N) | N | N | N | N (N) | N | FF |
| Out | Dysvik 2010148 | 18 | 17 | 1 | N | N (Y) | N | N (N) | N | N | N | FF |
| Out | Hadker 2011147 | 19 | 19 | 0 | N (Y) | N (Y) | N | N (N) | N | N | N | FF |
| Out | Schofield 2006144 | 19 | 19 | 0 | Y | N | N | N | N | N | N | FF |
| Out | Crowe 2010146 | 21 | 25 | –4 | N | N | N | N | N | N | N | FF |
| Out | Corbett 2009145 | 23 | 23 | 0 | Y | Y | N | Y | N (Y) | N (N) | N | FF |
| Out | Corrigan 2011116 | 21 | 21 | 0 | N (Y) | N (Y) | N | N | N | N (N) | N | Irrelevant |
| Out | Coutu 2013168 | 24 | 25 | –1 | N (Y) | N | N | N | N (Y) | N | N (N) | Irrelevant |
| First author and year | Relevance | Study aim |
|---|---|---|
| Afrell 2010151 | Indirect | To find out how physiotherapists experienced the influence of systematically prepared key questioning on their relation to, and understanding of, patients with long-standing pain |
| Allegretti 201011 | Direct | To explore shared experiences among chronic low back pain patients and their physicians |
| Åsbring 2003152 | Direct | To investigate:
|
| Baldacchino 2010153 | Direct | To describe physicians’ attitudes and experience of prescribing opioids to people with chronic non-cancer pain and a history of substance abuse |
| Barker 2015154 | Direct | To evaluate the implementation of acceptance and commitment therapy to physiotherapy-led pain rehabilitation programme |
| Barry 2010155 | Direct | To examine physicians’ attitudes to and experiences of treating chronic non-cancer pain |
| Baszanger 1992156 | Direct | To examine how physicians, specialising in pain medicine, work at deciphering chronic pain |
| Berg 2009157 | Direct | To explore providers’ perceptions of ambiguity and then to examine their strategies for making diagnostic and treatment decisions to manage chronic pain among patients on methadone maintenance therapy |
| Bergman 2013158 | Direct | To understand the respective experiences of patients with chronic pain and primary care practitioners communicating with each other about pain management in the primary care setting |
| Blomberg 2008159 | Direct | To explore district nurses’ care of chronic pain sufferers and to create a theoretical model that can explain the variation in district nurses’ experiences of caring for these patients |
| Blomqvist 2003160 | Direct | To explore nursing and paramedical staff perceptions of older people in persistent pain and their day-to-day management of pain |
| Briones-Vozmediano 2013161 | Direct | To explore experiences of fibromyalgia management, namely diagnostic approach, therapeutic management and the health professional–patient relationship |
| Cameron 2015162 | Direct | To explore current attitudes and approaches to pain management of older adults from the perspectives of HCPs representing multidisciplinary teams |
| Cartmill 2011163 | Direct | To explore the experience of clinicians during the transition from working as an interdisciplinary team to providing a transdisciplinary model of care in a programme for chronic disabling musculoskeletal pain |
| Chew-Graham 1999164 | Direct | To understand how GPs understood chronic low-back pain, how they approached the consultation and how they conceptualised the management of this problem |
| Clark 2004165 | Indirect | To describe the kinds of pain assessments nursing home staff use with nursing home residents and the characteristics and behaviours of residents that staff consider as they assess pain |
| Clark 2006166 | Indirect | To explore the perceptions of a nursing home staff who participated in a study to develop and evaluate a multifaceted pain management intervention |
| Côté 2001167 | Uncertain | To explore the views of chiropractors about timely return to work, to identify the approaches used and to learn about perspectives on the barriers to, and facilitators of, successful return to work with musculoskeletal disorders |
| Coutu 2013168 | Direct | To define and describe scenarios depicting the differences between clinical judgement, workers’ representations of their disability and clinicians’ interpretations of these representations |
| Dahan 2007169 | Direct | To identify the barriers to, and facilitators of, the implementation of low-back pain guidelines from family practitioners’ perspective |
| Daykin 2004170 | Direct | To explore physiotherapists’ pain beliefs with the purpose of highlighting the nature of their beliefs and the role they played within their management of chronic low-back pain |
| Dobbs 2014171 | Direct | To explore:
|
| Eccleston 1997172 | Partial | To explore how sense is made of the causes of chronic pain |
| Espeland 2003173 | Direct | To identify and describe:
|
| Esquibel 2014174 | Direct | To explore the experiences of adults receiving opioid therapy for relief of chronic non-cancer pain and those of their physicians |
| Fontana 2008175 | Direct | To critically examine subjective factors that influence the prescribing practices of registered nurses for patients with chronic non-malignant pain |
| Fox 2004176 | Direct | To identify barriers to the management of pain in long-term care institutions |
| Gooberman-Hill 2011177 | Direct | To explore GPs’ opinions about opioids and decision-making processes when prescribing ‘strong’ opioids for chronic joint pain |
| Gropelli 2013178 | Direct | To determine nurses’ perceptions of pain management in older adults in long-term care |
| Hansson 2001179 | Partial | To elucidate life lived with recurrent, spine-related pain and to explore the development from work to disability pension |
| Harting 2009180 | Direct | To gain an in-depth understanding of the determinants of guideline adherence among physical therapists |
| Hayes 2010181 | Direct | To explore knowledge and attitudinal challenges affecting optimal care in fibromyalgia |
| Hellman 2015182 | Partial | To explore and describe health professionals’ experience of working with return to work in multimodal rehabilitation for people with non-specific back pain |
| Hellström 2015183 | Direct | To explore the clinical experiences of doctors when meeting patients with fibromyalgia |
| aHolloway 2009184 | Direct | To explore the experiences of nursing assistants who work with older people in residential aged care facilities (chronic pain example) |
| aHolloway 2009185 | Direct | To explore the experiences of nursing assistants who have worked with older people in residential aged care facilities who are in pain |
| Howarth 2012186 | Direct | To explore person-centred care from the perspectives of people with chronic back pain and the interprofessional teams that cared for them |
| Kaasalainen 2007187 | Direct | To explore the decision-making process of pain management of physicians and nurses and how their attitudes affect decisions about prescribing and administering pain medications among older adults in long-term care |
| Kaasalainen 2010188 | Direct | To explore the perceptions of health-care team members (regulated and non-regulated staff) and nurse managers (management staff) regarding the nurse practitioner role in pain management in long-term care |
| Kaasalainen 2010189 | Partial | To:
|
| Kilaru 2014190 | Direct | To identify key themes regarding emergency physicians’ definition, awareness, use and opinions of opioid prescribing guidelines |
| Krebs 2014191 | Direct | To understand physicians’ and patients’ perspectives on recommended opioid management practices and to identify potential barriers to, and facilitators of, guideline-concordant opioid management in primary care |
| Kristiansson 2011192 | Direct | To understand and illustrate what GPs experience in contact with chronic pain patients and what works and does not work in these consultations |
| Liu 2014193 | Direct | To explore nursing assistants’ roles during the process of pain management for residents |
| Löckenhoff 2013194 | Partial | To examine how perceptions of chronological time influence the management of chronic non-cancer pain in middle-aged and older patients |
| Lundh 2004195 | Direct | To explore and describe what it means to be a GP meeting patients with non-specific muscular pain |
| MacNeela 2010196 | Direct | To examine how GPs represent chronic low-back pain in an applied context, especially in relation to psychosocial care |
| McConigley 2008197 | Indirect | To develop recommendations and a related implementation resource ‘toolkit’ to facilitate implementation of pain management strategies in Australian residential aged care facilities |
| McCrorie 2015198 | Direct | To understand the processes that bring about and perpetuate the long-term prescribing of opioids for chronic non-cancer pain |
| Mentes 2004199 | Partial | To evaluate whether or not information from family members/friends about patients’ lifelong pain behaviour improves pain detection in cognitively impaired residents and to evaluate pain information from caregivers |
| O’Connor 2015200 | Direct | To explore patterns of communication and decision-making among clinicians collaborating in the care of challenging patients with chronic low-back pain |
| Øien 2011201 | Direct | To describe communicative patterns about change in demanding physiotherapy treatment situations |
| Oosterhof 2014202 | Direct | To explore which factors are associated with a successful treatment outcome in chronic pain patients and professionals participating in a multidisciplinary rehabilitation programme |
| Parsons 2012203 | Direct | To explore beliefs about chronic muscular pain and its treatment and how these beliefs influenced care seeking and ultimately the process of care |
| aPatel 2008204 | Direct | To explore GPs’ experiences of managing patients with chronic pain from a South Asian community |
| aPatel 2009205 | Direct | To explore the experiences of and needs for management of people from a South Asian community who have chronic pain |
| Paulson 1999206 | Direct | To explore the experiences of nurses and physicians in their encounter with men with fibromyalgia |
| Poitras 2011207 | Direct | To identify barriers and facilitators related to the use of low-back pain guidelines as perceived by occupational therapists |
| Ruiz 2010208 | Direct | To explore the attitudes of primary care practitioners towards chronic non-malignant pain management in older people |
| Schulte 2010209 | Direct | To understand the factors that influence whether or not referrals from GPs are made, and at what stage, to specialised pain centres |
| Scott-Dempster 2014210 | Direct | To explore physiotherapists’ experiences of using activity pacing with people with chronic musculoskeletal pain |
| Seamark 2013211 | Direct | To describe the factors influencing GPs’ prescribing of strong opioid drugs for chronic non-cancer pain |
| Shye 1998212 | Partial | To gain understanding about why a controlled intervention to reduce variability in lumbar spine imaging test rates for low-back pain patients was ineffective |
| Siedlecki 2014213 | Partial | To explore and understand nurses’ assessment and decision-making behaviours related to the care of patients with chronic pain in the acute care setting |
| Slade 2012214 | Direct | To investigate how physiotherapists prescribe exercise for people with non-specific chronic low-back pain in the absence of definitive or differential diagnoses |
| aSloots 2009215 | Direct | To explore which factors lead to tension in the patient–physician interaction in the first consultation by rehabilitation physicians of patients with chronic non-specific low-back pain who are of Turkish and Moroccan origin |
| aSloots 2010216 | Partial | To explore which factors led to dropout in patients of Turkish and Moroccan origin with chronic non-specific low-back pain who participated in a rehabilitation programme |
| Spitz 2011217 | Direct | To describe primary care providers’ experiences of and attitudes towards, as well as perceived barriers to, and facilitators of, prescribing opioids as a treatment for chronic pain among older adults |
| Starrels 2014218 | Direct | To understand primary care providers’ experiences, beliefs and attitudes about using opioid treatment agreements for patients with chronic pain |
| Stinson 2013219 | Indirect | To explore the information and service needs of young adults with chronic pain to inform the development of a web-based chronic pain self-management programme |
| Thunberg 2001150 | Direct | To explore the way HCPs perceive chronic pain |
| Toye 2015220 | Indirect | To understand the impact on HCPs of watching and discussing a short research-based film about patients’ experience of chronic musculoskeletal pain |
| Tveiten 2009221 | Direct | To develop knowledge of the dialogue between the health professionals and the patient in the empowerment process at a pain clinic |
| Wainwright 2006222 | Direct | To explore the dilemma of treating medically explained upper-limb disorders |
| Wilson 2014223 | Indirect | To understand both the meaning of a clinical practice guideline for the management of non-specific low-back pain and the sociopolitical events associated with it |
| Wynne-Jones 2014224 | Direct | To explore GPs’ and physiotherapists’ perceptions of sickness certification in patients with musculoskeletal problems |
| Zanini 2014225 | Direct | To identify aspects important to address during a consultation to build a partnership with patients with chronic pain |
Coding and conceptual categories
We coded batches of studies in the following order according to topic/professional grouping:
-
Ten studies reported the experiences of primary care physicians/GPs. 11,158,164,192,195,196,204,205,209,222
-
Four studies explored the experiences of a mixed group of HCPs. 172,194,203,220
-
Three studies explored the experiences of physiotherapists. 170,201,214
-
Three studies explored the experiences of physiotherapists specialising in chronic pain management. 151,154,210
-
Five studies explored the experiences of a mixed group of HCPs providing health care to people with fibromyalgia. 152,161,181,183,206
-
Eleven studies explored the experiences of a mixed group of HCPs working in specialist chronic pain services. 150,156,163,186,200,202,215,216,219,221,225
-
Five studies explored the experiences of a mixed group of HCPs working in pain management related to employment. 167,168,179,182,224
-
Twelve studies explored the experiences of a mixed group of HCPs prescribing opioids to patients with chronic pain. 153,155,157,174,175,177,190,191,198,211,217,218
-
Six studies explored the experiences of a mixed group of HCPs utilising guidelines for chronic pain. 169,173,180,207,212,223
-
Three studies explored the experiences of a mixed group of HCPs working with older adults. 160,162,208
-
Thirteen studies explored the experiences of a mixed group of HCPs working with older adults in long-term care facilities. 165,166,171,176,178,184,185,187–189,193,197,199
-
Two studies explored nurses’ experiences of providing health care to people with chronic non-malignant pain. 159,213
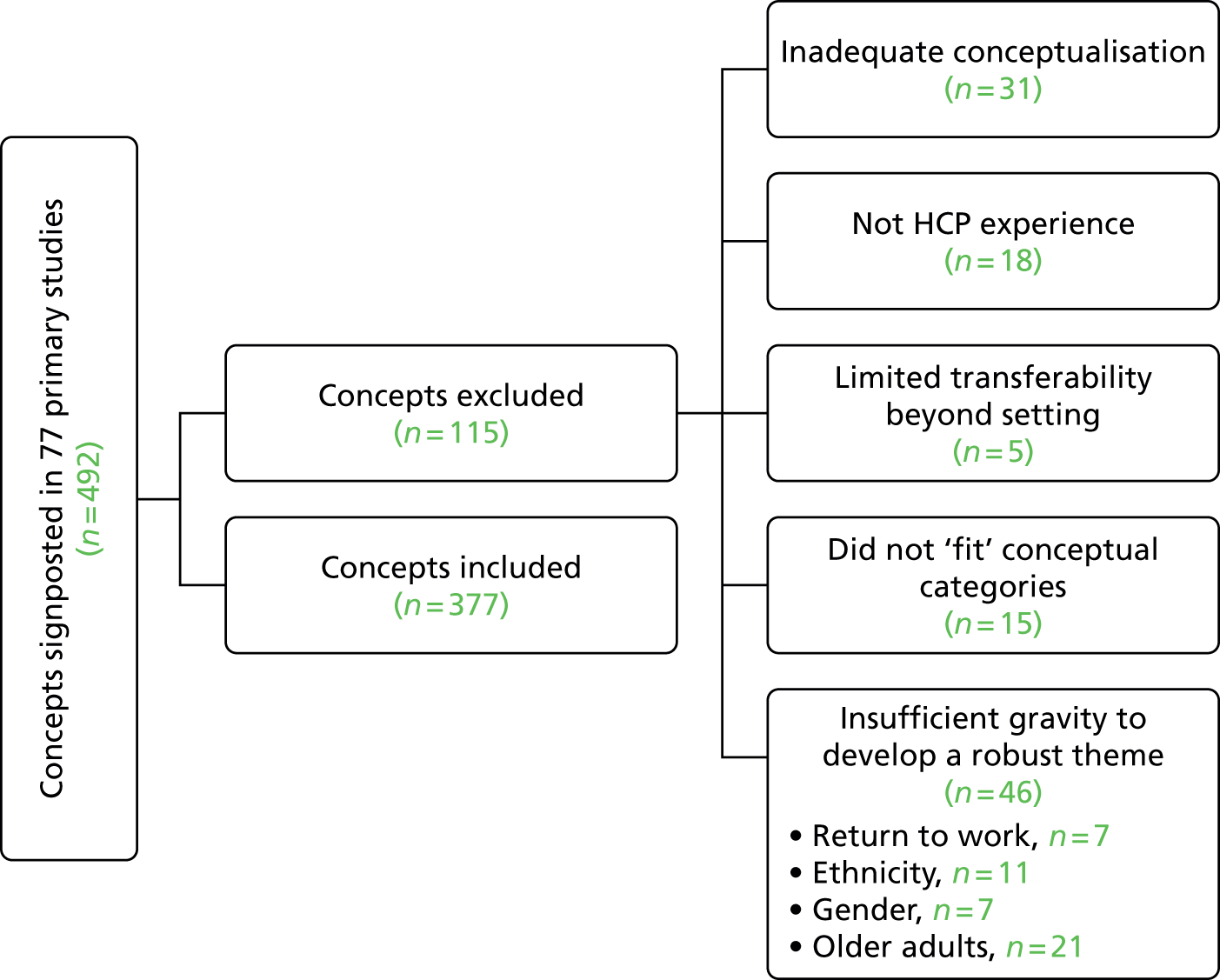
Appendix 2 provides a coding report of included and excluded concepts. Two reviewers identified 492 potential concepts in 77 primary studies (Figure 3). They excluded 115 potential concepts for the following reasons: inadequate conceptualisation (31 concepts in 17 studies11,150,155,160,162,169,173,178,181,188,192,196,197,206,208,219); did not explore HCP experience (18 concepts in seven studies168,174,198,202,203,215,223); and explored a topic with limited transferability beyond a specific context (five concepts in five studies166,167,197,208,223). We agreed that for some topics there were insufficient concepts to allow us to develop robust conceptual categories: return to work (seven concepts in two studies167,182), ethnicity (11 concepts in five studies171,204,205,215,216), gender (seven concepts in one study206) and older people (21 concepts in nine studies159,160,162,165,176,187,194,199,208). Fifteen potential concepts did not fit our developing conceptual analysis (Table 6).
FIGURE 3.
Concepts that were included and excluded.
| First author and year: qualitative finding | Description of finding |
|---|---|
| Barry 2010:155 logistical factors – ancillary staff | Physicians expressed concern that they had an insufficient number of qualified staff to implement pain management |
| Barry 2010:155 logistical factors – insurance coverage | Concerns about the logistics of insurance coverage for pain management services and the difficulty in characterising patients’ pain status because of restrictions from insurance companies |
| Fontana 2008:175 critical analysis | Conflicts of interest in which the patients’ best interests are given a low priority. Nurses did not see prescribing decisions as ethical ones and, as a result, did not recognise the conflicts that were at work when they made these decisions |
| Holloway 2009:184 initiating clinical care | The ability to provide pain management for residents when needed varied considerably between facilities; for some it involved basic care such as emotional support, positioning and using hot-packs, whereas in other facilities they administered pain medication and had responsibility for monitoring the effectiveness of the pain management interventions and documentation |
| Holloway 2009:185 perfect positioning (rewards of getting it right) | Assistants felt sustained and fulfilled by the rewarding aspects of caring. All spoke of their passion for, enjoyment of and love for their work (and this is why they stayed in it). Despite the emotional distress associated with observing people in pain, assistants gained satisfaction from seeing residents relieved of pain. Discussed poor financial remuneration |
| Kaasalainen 2010:188 interactions with long-term care staff and managers | Nurse practitioner was viewed as a nurse with added skills who assisted other health-care team members with managing uncontrolled pain and was often used as an additional resource for nurses |
| Liu 2014:193 instigator implementing non-pharmacological interventions | Skills in distraction, reassurance and being gentle. Nursing assistants explained how they distracted or reassured residents who were in pain |
| Löckenhoff 2013:194 age differences in time horizons (treatment planning) | Consistently reported that they planned and administered pain management regimens for the long term |
| Lundh 2004:195 variation 1 | I can feel very curious! What do these symptoms stand for? |
| Oosterhof 2014:202 experiences concerning the treatment outcome (learning new behaviour) | HCPs recognised that change takes effort and a combination of explanation and practice. Some managed to learn and implement new behaviour because they have always been active or because of good body awareness or physical preference. Others find it difficult to keep up effort because of personal problems and poor social support |
| Scott-Dempster 2014:210 ‘It’s not a One Trick Pony’ | Physiotherapists regarded activity pacing as part of the pain management tool box. Activity pacing was not described as something that was clearly definable or had fixed parameters. Achieving this flexibility could be challenging, as it meant that the physiotherapist had to adapt activity pacing for each individual |
| Seamark 2013:211 cost | Some did not consider cost and prescribed what was needed. Others felt that it was important to bear in mind |
| Siedlecki 2014:213 core concepts/taking ownership | Some did not take ownership of the problem and saw it as someone else’s problem |
| Stinson 2013:219 barriers to care (patient-specific barriers) | Difficult to maintain a consistent pain management regimen because of time commitments and reluctance of younger people |
| Stinson 2013:219 pain management strategies (support systems) | HCPs recognised the importance of peer support for patients |
All reviewers organised the remaining 377 concepts into 42 conceptual categories. Table 7 gives an example of one of the conceptual categories (‘is the pain real?’) and its included concepts. Our description of the concepts that formed the raw data of analysis were a combination of the primary author’s description of the second-order construct (in which they briefly and clearly described the construct), and our interpretation of the construct (if the original was unclear or lengthy). In some cases we found that there was a section of narrative exemplar provided by the original authors that adequately described the essence of the concept.
| First author/year and qualitative finding | Description of finding |
|---|---|
| Åsbring 2003:152 illness vs. disease | HCP scepticism for conditions characterised by a lack of objective measurable values that would make it possible to establish cause. Fibromyalgia and chronic fatigue described as illness not disease. There was some doubt regarding this scientific ideal |
| Åsbring 2003:152 moral judgement of illness | Biomedical disease was regarded as more threatening to self than ‘illness’. Suggestion that patients think they cannot live with it because they have not experienced something ‘really threatening’. An individual who claims to be sick must also look sick to be accepted as such. Sometimes doubted legitimacy of person |
| Bergman 2013:158 acknowledgement of the reality of pain and the search for objective evidence (primary care practitioners) | Search for objective evidence of pain is a crucial part of evaluation (particularly with opioids). Struggled with the dilemma of how to respond in the absence of physical findings. Looked for behavioural and non-verbal cues to indicate presence/absence of pain. Doubted legitimacy in the absence of evidence. Others acknowledged the subjective nature of pain and importance of believing patients |
| Esquibel 2014:174 effect of chronic opioid therapy on doctor–patient relationship – examples of chronic opioid therapy embittering the doctor–patient relationship | Opioid therapy can become the source of conflict and mistrust. Clinical encounters can become largely overshadowed by opioid medication discussion or controversy. Physicians tend to question the validity of their patient’s pain and do not approve of opiate pain medication as treatment |
| Hayes 2010:181 definition and diagnosis | Questioned the validity of fibromyalgia itself and recognised the impact of this doubt. Doctors did not like clinical situations in which they did not feel in control: The patients tell me with a smile on their lips that they are suffering immensely from all kinds of bodily disorders. How on earth can they look so terribly healthy? |
| Holloway 2009:184 clinical decision-making | Assistants relied on their knowledge of the resident. They spent time with residents and knew their behaviours and moods, so were able to detect changes. They made personal judgements that influenced clinical decisions about pain. Some felt that residents exaggerated pain and changed pain report to ‘more appropriate’ level |
| Kaasalainen 2010:189 health-care providers | Staff did not always believe residents’ reports of pain, or felt that they were overstating their pain. At times, staff felt they needed to ‘second guess’ the residents’ reports |
| Lundh 2004:195 an inconsistent patient | She had ten different symptoms and looked totally healthy! Then you are surprised! |
| MacNeela 2010:196 representing the person’s experience (work and legal issues) | Return to work was synonymous with recovery and successful adjustment, but work avoidance and ulterior motives were part of the script for chronic low-back pain. Could highlight doubt and risk rather than person’s ‘plight’: I mean that could be genuine . . . You’d have to be on guard this man isn’t laying it on |
| Siedlecki 2014:213 nurse characteristics – discernment | Nurses described the importance of knowing their patients to discern appropriate pain management:You can look at that patient and many times what they tell you verbally may not be consistent with what we see . . . they may be very calmly in bed or fall asleep as they’re talking to you but they tell you their pain is a 10/12 |
| Stinson 2013:219 barriers to care (societal barriers) | HCPs described the societal tendency to cast doubt on the veracity of chronic pain: This isn’t something that people can see and so a lot of people, I think, feel like they’re not believed either by their friends or by their family or their health care practitioners um and that is also I guess a big issue |
Once the reviewers had agreed on a description of each conceptual category, Fran Toye wrote a statement of this finding in the first person.
For example:
This conceptual category described how endless paperwork eats into HCPs’ limited patient time
became:
This endless paperwork eats into my limited patient time.
We have found that writing concepts in the first person is a powerful way for reviewers and their advisory group members to fully engage in the meaning and sentiment of each concept. It also facilitates the use of accessible language for a diverse audience in both analysis and dissemination.
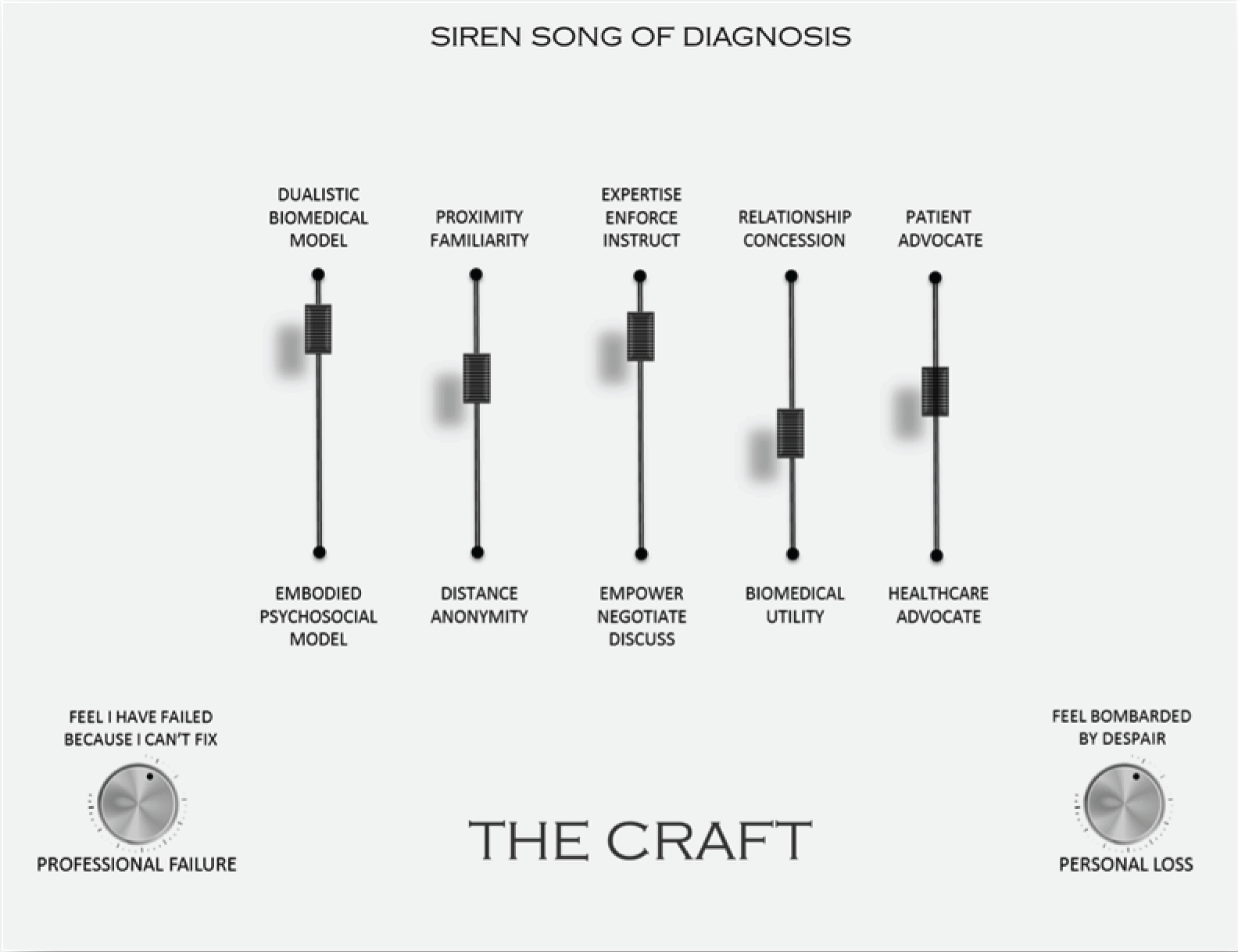
Table 8 provides a description of each of the 42 conceptual categories written in the first person. The reviewers worked with a research fellow and a project advisory group that included patients and HCP members to further abstract these 42 conceptual categories, printed on postcards, into six overarching themes that underpin HCPs’ experience of providing health care to people with chronic non-malignant pain (Figure 4). Table 9 provides a list of the conceptual categories underpinning each of the six final themes. Table 10 shows the number of studies and concepts for each theme organised by topic/professional group. It also indicates the global appraisal score given for individual studies supporting the theme.
| Conceptual category title | Description of conceptual categorya |
|---|---|
| My professional duty | It is my professional duty to provide the care that I see fit and my patient’s duty to follow my professional advice. Professional competence is paramount. Do not let your patient dictate what to do |
| This endless paperwork takes time | This endless paperwork eats into my limited patient time |
| It takes time to get to know someone | I need to get to know my patient if I am going to help them, but this takes time. Because my time is restricted I tend to focus on the person’s physical body rather than on the person sitting in front of me. Sometimes I even avoid seeing patients with chronic pain |
| I am my patient’s advocate | I am an advocate for my patient and it is my job to mediate between them and other staff and organisations. This advocacy makes our relationship strong but it can come with personal risks of loss or failure |
| Seeing a fellow human | It is important to get to know my patients, recognise their losses and regard them with dignity. However, I also need to balance the emotional burden that comes with engaging with a fellow human being |
| The conflicting role of gatekeeper | Being a gatekeeper to other services conflicts with my role as caregiver (GP) |
| Learning the craft of pain management | You learn to treat chronic pain through experience. My personal experience of pain, my life experience and my professional experience are what make me a good clinician |
| We did not learn this in class | I didn't learn how to treat chronic pain in my clinical education. I am underskilled in chronic pain management, particularly psychological strategies and medication |
| Guidelines: take them or leave them | The guidelines for back pain just give me more paperwork to read. I can take them or leave them |
| Guidelines: support psychosocial model | The guidelines for back pain are useful because they give weight to a psychosocial explanations rather than overemphasising biomedical explanation |
| Guidelines: to convince others about my decisions | Sometimes I use the guidelines for back pain to convince patients and other clinicians that I am making the right decision; ‘look I am following this to the letter!’ |
| Guidelines: constrain expert knowledge | The guidelines for back pain challenge or even constrain my expert knowledge |
| Guidelines: prevent individualised care | The guidelines for back pain do not allow me to provide individualised treatment for my patient |
| Exhausted by the sense of loss | I am a ‘helpless helpoholic’. I have a strong yearning to help but am constantly frustrated and disappointed. I am on a hiding to nothing and whatever I do is not enough. I am overwhelmed and exhausted by the sense of loss |
| A sense of failure | I find it a challenge to alter my professional mandate, which is to diagnose what the problem is and fix it. If I do not fix something I feel that I have failed. ‘Difficult patients’ are those you cannot fix |
| I am not a psychologist | I feel a bit uncomfortable treating the ‘psychological’ aspects of pain (e.g. depression) – is this really my job? |
| The challenge of biomedical ambiguity | At times I feel a bit anxious because I cannot locate the pain or give it a medical diagnosis. Pain remains ambiguous and hard to explain |
| It is difficult to access specialist services | It is really difficult to access specialist pain (and addiction) services |
| What is the point of referring to other services? | My patient did not get what I expected from pain management services. Are they really the experts? They tend to overemphasise medication. What are they offering that I cannot provide? |
| Finding common ground | It is important to work together with my patient for mutual understanding and co-operation. Finding common ground can be a challenging process of negotiation |
| Conflicting agendas | If you and your patient do not have a shared agenda this can cause tension. Patients often expect a cure, a specific test or a referral when this is not on my agenda |
| Show them you believe them | I need to show patients that I believe them |
| It’s a matter of give and take | I sometimes provide things that my patients ask for in order to maintain our relationship, even when I know there is little point. My decisions are not always taken on clinical grounds. At times you need to balance long- and short-term gains |
| Patient empowerment is easier said than done | It is difficult to navigate between professional and patient expertise. When do I let my patient make the decision (especially when I think they are making a mistake)? Although I should let them be in control, it can be easier to take charge |
| Feigning diagnostic certainty | My patients cling ‘tenaciously’ to the biomedical model and sometimes I ‘feign diagnostic certainty’ so that they continue to trust me. However, I sometimes worry that this is dishonest |
| Healing supersedes fixing | Healing is a journey that I take in partnership with my patient. Sitting alongside rather than constantly trying to diagnose and fix can take away the sense of failure for both of us |
| Betwixt biomedical and psychological explanations | Patients do not want to shift from a biomedical explanation to a psychosocial one. The biomedical model is more socially acceptable in our culture. Trying to shift my explanation can make it very difficult for me to maintain a good relationship with my patient |
| Bridging biomedical and psychosocial | When I shift from biomedical explanation to a psychosocial explanation I use strategies to avoid alienating my patient. This does not resolve the uncertainty but circumvents the problem by using other labels or treatments that can be ambiguous |
| I am in the best position to know the patient but no one listens to me | Even though, on the front line, I am in a ‘the perfect position’ to get to know the patient and help manage their pain, I am ignored or undermined by my colleagues who do not listen to what I have to say |
| Mutual professional respect facilitates care | A mutual and respectful relationship with my colleagues can facilitate the kind of communication that underpins effective pain management |
| Proximity and continuity facilitate team work | Working in the same place as my colleagues facilitates the collaboration necessary for effective pain management |
| Breaking down professional boundaries | We should break down professional boundaries and hierarchies and work together as a team. This involves knowing and valuing what each professional can offer, helping out and sharing knowledge |
| Picking up the pieces | I sometimes have to spend time undoing what another health professional has done or said. I have to pick up the pieces |
| The siren song of diagnosis | I focus on the biomedical disease not the person. Biomedical disease takes precedence; it is something. However, I know that this model did not fit chronic pain |
| Pain is embodied, not dualistic | I focus on the person, rather than the part of the body in pain. I focus on my patient’s suffering beyond their bodily pain. Pain is multidimensional and my ‘gaze’ therefore needs to be multifocal |
| The test results can come back to you like a boomerang | Getting an X-ray might reveal something that is not the cause of the pain and create an additional problem to deal with. A red herring |
| You need to cover your back | I will get an X-ray done just in case there are any legal repercussions. I want to be certain I have not missed anything |
| The X-ray will rule out anything serious | I will get an X-ray to rule out serious pathology. There have been examples of missed cases. I want to reassure my patient that there is nothing serious, even though I am certain that there is nothing there |
| I will let you have an X-ray | This describes the strategic use of X-rays in maintaining patient relations and trust (i.e. I am prepared to bend the rules for you). Some ordered X-rays because the patient asked for one, or as a compromise for a preferred or less accessible service |
| X-ray will buy me time | This describes X-ray referral as a means of biding time or buying time. It is sometimes quicker just to order an X-ray. It might also save time en route to a different service |
| Is the pain real? | I sometimes feel sceptical about my patient’s pain. What I see and what they tell me does not always fit. I find myself ‘second guessing’. However, I am aware of the social doubt about chronic pain and know that it is not wise to ‘judge a book by its cover’ |
| The moral dimension of pain management: I hate to say it but . . . | There are always those who complain more than others; who are just seeking attention or who demand things; who are non-compliant or unmotivated. However, we should not judge a book by its cover |
FIGURE 4.
Illustration of conceptual analysis with advisory group.
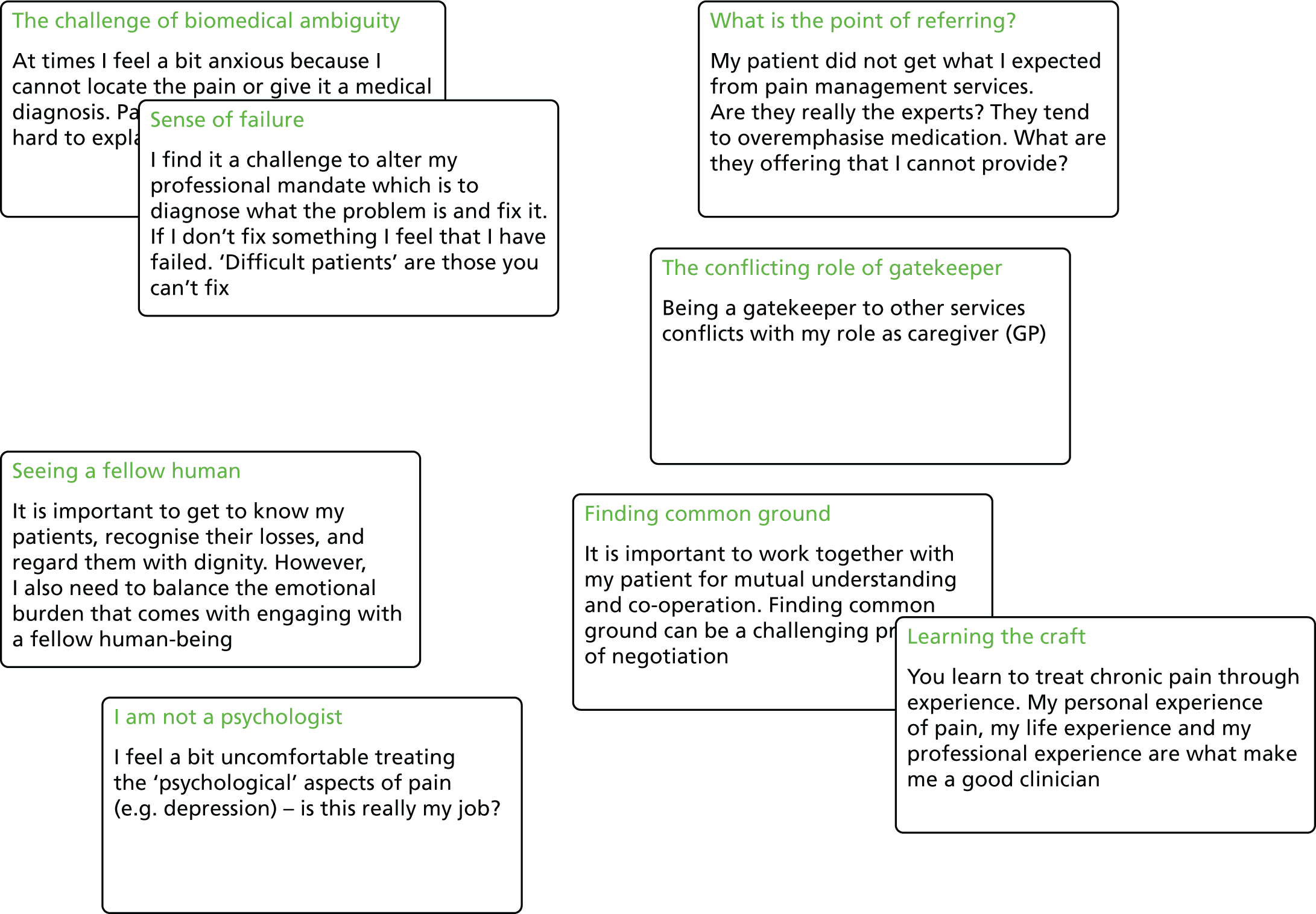
| Final theme | Conceptual category underpinning theme |
|---|---|
| Sceptical cultural lens and siren song of diagnosis | Is the pain real? |
| The moral dimension of pain management: ‘I hate to say it but . . .’ | |
| Navigating juxtaposed models of medicine | ‘The siren song of diagnosis’ |
| Betwixt biomedical and psychological explanations | |
| Pain is embodied, not dualistic | |
| Healing supersedes fixing | |
| This endless paperwork takes time | |
| It takes time to get to know someone | |
| Navigating the patient–clinician borderland | My professional duty |
| Finding common ground | |
| Conflicting agendas | |
| Show them you believe them | |
| It’s a matter of give and take | |
| ‘Patient empowerment is easier said than done’ | |
| Feigning diagnostic certainty | |
| Bridging biomedical and psychosocial | |
| The challenge of dual advocacy | Picking up the pieces |
| I am my patient’s advocate | |
| The conflicting role of gatekeeper | |
| It is difficult to access specialist services | |
| What is the point of referring to other services? | |
| Mutual professional respect facilitates care | |
| Proximity and continuity facilitate team work | |
| Breaking down professional boundaries | |
| I am in the best position to know the patient but no one listens to me | |
| Personal costs | The challenge of biomedical ambiguity |
| A sense of failure | |
| Seeing a fellow human | |
| Exhausted by the sense of loss | |
| The craft of pain management | Learning the craft of pain management |
| We did not learn this in class | |
| I am not a psychologist | |
| Guidelines: take them or leave them | |
| Guidelines: constrain expert knowledge | |
| Guidelines: prevent individualised care | |
| Guidelines: to convince others about my decisions | |
| Guidelines: support psychosocial model | |
| The test results can come back to you like a boomerang | |
| You need to cover your back | |
| The X-ray will rule out anything serious | |
| I will let you have an X-ray | |
| X-ray will buy me time |
| Global appraisal score | First author/year | Theme (number of concepts) | Topic professional group | |||||
|---|---|---|---|---|---|---|---|---|
| Sceptical cultural lens and siren song of diagnosis | Navigating juxtaposed models | Navigating the patient–clinician borderland | Challenge of dual advocacy | Personal cost | The craft of pain management | |||
| Valuable | Allegretti 201011 | 2 | 1 | 2 | Primary care physicians/GPs | |||
| SAT | Bergman 2013158 | 2 | 2 | 1 | 2 | 1 | ||
| SAT | Chew-Graham 1999164 | 1 | 2 | |||||
| SAT | Kristiansson 2011192 | 1 | 9 | 2 | 5 | |||
| Valuable | Lundh 2004195 | 1 | 2 | 1 | 4 | 1 | ||
| Uncertain | MacNeela 2010196 | 3 | 1 | 2 | 1 | 1 | ||
| Valuable | Patel 2008204 | 1 | 1 | |||||
| Valuable | Patel 2009205 | 2 | ||||||
| SAT | Schulte 2010209 | 1 | 3 | |||||
| KP | Wainwright 2006222 | 3 | 6 | |||||
| Uncertain | Eccleston 1997172 | 1 | 1 | Mixed | ||||
| SAT | Löckenhoff 2013194 | 1 | ||||||
| SAT | Parsons 2012203 | 2 | 1 | 2 | ||||
| Valuable | Toye 2015220 | 1 | 4 | 1 | 4 | |||
| Valuable | Daykin 2004170 | 1 | 1 | 2 | 4 | Physiotherapy | ||
| Uncertain | Øien 2011201 | 3 | 1 | |||||
| KP | Slade 2012214 | 2 | 3 | 1 | 4 | |||
| KP | Afrell 2010151 | 6 | 1 | 2 | Special physiotherapy | |||
| Valuable | Barker 2015154 | 2 | 2 | 3 | 1 | |||
| Valuable | Scott-Dempster 2014210 | 2 | 6 | 1 | ||||
| SAT | Åsbring 2003152 | 3 | 2 | 3 | 2 | 1 | Fibromyalgia | |
| SAT | Briones-Vozmediano 2013161 | 1 | 2 | 1 | 2 | |||
| SAT | Hayes 2010181 | 1 | ||||||
| SAT | Hellström 2015183 | 1 | 3 | 2 | 3 | |||
| SAT | Paulson 1999206 | 1 | ||||||
| Valuable | Baszanger 1992156 | 5 | 4 | Specialist chronic pain services | ||||
| SAT | Cartmill 2011163 | 1 | 3 | |||||
| SAT | Howarth 2012186 | 3 | 1 | |||||
| SAT | O’Connor 2015200 | 2 | 3 | |||||
| SAT | Oosterhof 2014202 | 3 | 1 | |||||
| SAT | Sloots 2009215 | 1 | ||||||
| SAT | Sloots 2010216 | 3 | ||||||
| Valuable | Stinson 2013219 | 1 | 1 | 2 | 1 | 4 | ||
| KP | Thunberg 2001150 | 1 | 4 | 3 | 1 | |||
| Valuable | Tveiten 2009221 | 3 | 1 | |||||
| Valuable | Zanini 2014225 | 2 | 1 | |||||
| SAT | Côté 2001167 | 1 | 1 | 2 | 2 | 1 | Work disability | |
| SAT | Coutu 2013168 | 1 | 2 | |||||
| SAT | Hansson 2001179 | 1 | ||||||
| SAT | Hellman 2015182 | 2 | ||||||
| SAT | Wynne-Jones 2014224 | 1 | 2 | 1 | 1 | |||
| SAT | Baldacchino 2010153 | 1 | Prescription of opioids | |||||
| SAT | Barry 2010155 | 2 | 2 | 1 | 4 | 1 | 3 | |
| Valuable | Berg 2009157 | 1 | 1 | 1 | 1 | |||
| SAT | Esquibel 2014174 | 3 | 2 | 1 | ||||
| SAT | Fontana 2008175 | 2 | 1 | |||||
| SAT | Gooberman-Hill 2011177 | 1 | ||||||
| Valuable | Kilaru 2014190 | 1 | ||||||
| Valuable | Krebs 2014191 | 1 | 2 | |||||
| Valuable | McCrorie 2015198 | 2 | 1 | 1 | 2 | 1 | ||
| Valuable | Seamark 2013211 | 1 | 1 | |||||
| SAT | Spitz 2011217 | 2 | 1 | 2 | ||||
| SAT | Starrels 2014218 | 1 | ||||||
| SAT | Dahan 2007169 | 1 | 3 | 1 | 2 | 2 | Guidelines | |
| SAT | Espeland 2003173 | 1 | 6 | 1 | ||||
| SAT | Harting 2009180 | 1 | 6 | |||||
| SAT | Poitras 2011207 | 2 | 1 | 2 | 6 | |||
| SAT | Shye 1998212 | 6 | 1 | |||||
| KP | Wilson 2014223 | 4 | ||||||
| Valuable | Blomqvist 2003160 | 3 | 1 | 2 | Older adults | |||
| SAT | Cameron 2015162 | 1 | 1 | |||||
| SAT | Ruiz 2010208 | 1 | 3 | |||||
| SAT | Clark 2004165 | 1 | 1 | 1 | 2 | Pain in aged care facilities | ||
| SAT | Clark 2006166 | 1 | 2 | |||||
| Valuable | Dobbs 2014171 | 1 | 1 | 1 | ||||
| Valuable | Fox 2004176 | 2 | 4 | 2 | 1 | |||
| Uncertain | Gropelli 2013178 | 1 | 1 | |||||
| SAT | Holloway 2009184 | 1 | 2 | 1 | ||||
| SAT | Holloway 2009185 | 2 | 5 | |||||
| Valuable | Kaasalainen 2007187 | 1 | 2 | |||||
| SAT | Kaasalainen 2010188 | |||||||
| SAT | Kaasalainen 2010189 | 1 | 1 | 2 | 2 | |||
| SAT | Liu 2014193 | 3 | 3 | |||||
| SAT | McConigley 2008197 | 1 | 3 | |||||
| SAT | Mentes 2004199 | 2 | 2 | |||||
| SAT | Blomberg 2008159 | 1 | 4 | Nursing | ||||
| SAT | Siedlecki 2014213 | 2 | 1 | 2 | 4 | 3 | 1 | |
Assessment of confidence in findings (GRADE-CERQual)
Indicators of confidence in each review finding are shown in Table 11 [including the number of studies rated as key/valuable or satisfactory (methodological limitations); the number of concepts (adequacy); the number of studies out of 77 (coherence); an assessment of study relevance; and our overall assessment of confidence]. We rated our confidence in the review finding as high when it was supported by more than half of the studies. However, there is currently no agreed way of assessing confidence.
| Review finding | Methodological limitations: satisfactory (key) | Relevance | Adequacy (number of concepts) | Coherencea (number of studies out of 77) | Assessment of confidence |
|---|---|---|---|---|---|
| Sceptical cultural lens and siren song of diagnosis | 29 (0) | 22 direct, 4 indirect, 2 partial, 1 uncertain | 43 | 29150,152,155,158,160,165–167,169–174,181,183,184,189,191,192,195,196,198,203,213,217–220 | Moderate |
| Navigating juxtaposed models of medicine | 42 (2) | 37 direct, 4 indirect, 2 partial, 1 uncertain | 77 | 4411,150–152,154–163,165,167,168,170,172,174–176,180,183,189–191,195,196,198,200,203,204,206,207,210,211,213–215,217,219,220,222 | High |
| Navigating the patient–clinician borderland | 34 (2) | 29 direct, 3 indirect, 3 partial, 1 uncertain | 92 | 3611,150–152,154–157,161,164,167–169,173,174,183,192,194–196,198,201,202,207,209,210,212–214,216,219–222,224,225 | Moderate |
| The craft of pain management | 29 (2) | 27 direct, 2 indirect, 1 partial, 1 uncertain | 60 | 31152–155,157,158,167,169–171,173,175–178,180,186,189,195–197,202,203,207,208,211,213,214,217,223,224 | Moderate |
| Challenge of dual advocacy | 35 (1) | 26 direct, 4 indirect, 5 partial, 1 uncertain | 70 | 36150,155,158,159,161–163,165–167,169,176,178,179,182,184–187,189,192,193,196–200,205,207–209,212–214,219,224 | Moderate |
| Personal cost | 32 (1) | 28 direct, 4 indirect, 1 partial, 0 uncertain | 71 | 3311,151,152,154,155,157,158,160,161,164,165,169–171,176,183–185,187,192,193,195,198,199,201,204,210,213,219–221,224,225 | Moderate |
Conceptual themes
We illustrate the six themes with narrative exemplars. The film output ‘Struggling to support people to live a valued life with chronic pain’ can be watched on YouTube (see Report Supplementary Material 1; URL: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1419807/#/documentation).
A sceptical cultural lens and siren song of diagnosis
This theme describes a cultural lens that provides a sceptical view of chronic pain. With this view, clinical work focuses on determining whether pain is ‘something’ (biomedical) or ‘nothing’. Although some acknowledged the dangers of ‘judging a book by its cover’, HCPs viewed the world through this sceptical lens and at times found themselves making non-clinical judgements about whether a patient’s pain was real or imagined. HCPs described how they could experience a dissonance between what they saw and what the patient said:
Sometimes I could have a patient sitting there and saying that they are hurting, 10 out of 10, and they are sitting like you and I.
Bergman 2013158
Some people say ‘This is the worst pain I’ve had in my whole life’ without any real sort of physical signs of pain so it’s really tough; we have a complex job in assessing that.
Kaasalainen 2010189
The patients tell me with a smile on their lips that they are suffering immensely from all kinds of bodily disorders. How on earth can they look so terribly healthy?
Hellström 2015183
However, HCPs recognised the dangers of their scepticism and acknowledged a need to not make hasty judgements. Although they knew that patients did not always look like they were in pain, HCPs remained ‘on guard’ against being exploited by fraudulent claims of pain:
You’d have to be on guard this man isn’t laying it on.
MacNeela 2010196
It is not clear to me why he is the way he is . . . this catastrophic pain and what he is telling himself about it . . . but there is always a little bit . . . of concern; am I being manipulated, is this really real?
Esquibel 2014174
Such people . . . ones whose wishes you cannot fathom – provoke anger and frustration because at some point, you don’t always know how to verify their complaints. You feel somewhat exploited. It is a very unpleasant feeling.
Dahan 2007169
Health-care professionals thus engaged in moral ‘boundary work’ in order to second-guess patients’ claims and determine credibility. The process of boundary work hinged on a multiplicity of dualities superposed on a polarity of ‘good’ and ‘bad’ (Figure 5).
FIGURE 5.
Dualities of moral boundary work.
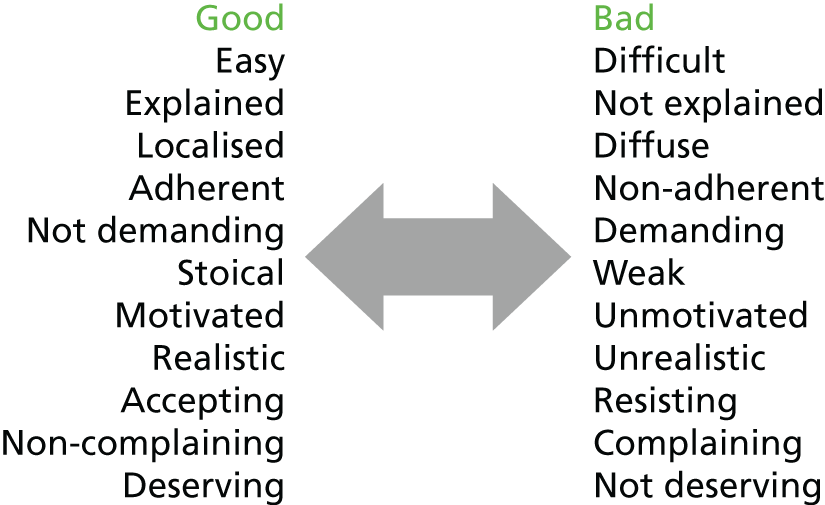
In contrast, some HCPs recognised that moral boundary work was flawed and advocated trust as the basis of a therapeutic relationship:
Sometimes we say ‘oh she came in with back pain but I don’t think she’s really in pain’ . . . but really even if somebody is in pain and distress, [it] doesn’t always have to be in how they present themselves . . . that doesn’t mean she is not in pain.
Toye 2015220
I hate to say it . . . but I used to be one of the people that used to say, ‘Oh, well, they are probably just wanting attention’. But I’ve changed in that matter. People are in pain, and it’s not just to get attention.
Clark 2006166
Pain is so subjective and so that’s where the difficulty lies . . . I find it hard to say how someone’s pain can be judged by someone else . . . You have to show a patient you’re empathetic to him. There is a pain. Pain is real.
Bergman 2013158
Navigating juxtaposed models of medicine
This described HCPs’ challenge of navigating juxtaposed models of medicine: the biomedical and the biopsychosocial. HCPs described a culturally entrenched pull towards the biomedical ‘siren song of diagnosis’. 214 Clinical work, therefore, hinged on proving (or disproving) the presence (or absence) of something ‘real’:
Being able to track something gives me more comfort than going by what you’re telling me . . . because I like to see proof . . . You [want to] . . . be convinced that you’re treating something and that what you’re treating is real.
Berg 2009157
I will listen to their story, I will examine them and I always say you have got to exclude the physical first that is your job . . . I think as doctors we have an obligation to exclude the physical first and not jump into [psychosocial explanations] because it reduces the patient to being an un-necessary complainer and I don’t believe that they really are.
Wainwright 2006222
Unexplained symptoms such as chronic pain were felt to obscure ‘real’ health problems such as diabetes or heart conditions:
They don’t seem to worry about issues that might be real . . . his cholesterol is high, he’s not worried . . . There are some other issues that he needs to attend to, and he’s not worried. His father died when he was 52. He’s not worried. He was 53.
Bergman 2013158
Even those HCPs who advocated a biopsychosocial model could make an abrupt shift towards psychosocial explanations only after they had excluded something biomedical. After this shift, clinical work moved away from diagnosis towards persuading patients that psychosocial factors influenced pain. This abrupt shift, indicating a dualistic biopsychosocial model, could threaten the therapeutic relationship:
The terminology . . . psychiatric and psychological . . . have a stigma attached to them that is not intended . . . we accept that patients with long term pain will have a psychological component to it but actually labelling it as that.
Toye 2015220
Health-care professionals recognised the potential tension and, therefore, would default to biomedical explanations or use ‘bridging’ strategies to smooth, or even conceal, the shift from biomedical to psychosocial explanations. These explanations still tended to focus on the physicality of the body:
If you present [the pain explanation] as a completely airy fairy psychological . . . then they are going to go away dissatisfied . . . you have got to lead them in gently . . . there is an element of mind and body that contribute.
Wainwright 2006222
If you start from the body and if you ask a little carefully how things work when you are physically like that, then it is not threatening, and you can approach things, like, through the body.
Afrell 2010151
Some HCPs felt that offering a diagnosis helped patients to move forward, or gave a sense of relief. Some might even ‘feign diagnostic certainty’222 to achieve this goal:
The fact that they tell you that you have a problem that’s not just to do with your nerves and that there’s something wrong physically . . . Just that gives you a certain sense of relief.
Briones-Vozmediano 2013161
Once I give [a diagnosis] . . . I am ready to say . . . let’s stop doing tests. Let’s stop sending you to lots of different doctors looking for a cure . . . let’s try and make you better . . . [they] have more tests than is good for them.
Wainwright 2006222
Well, if she seems to have use for a diagnosis to achieve her goal, I’ll gladly help her.
Hellström 2015183
Others voiced ethical concerns about the deception of feigning diagnostic certainty:
I am very happy for a person to treat the whole person and we do it all the time . . . But I think giving it a label that actually has no justification I think is misleading to the patient and I actually feel quite strongly about that.
Wainwright 2006222
Not all HCPs utilised a dualistic biopsychosocial model. Some did not make an abrupt shift towards psychosocial explanations but, rather, utilised an embodied biopsychosocial approach with ‘no breaking point where the physical becomes psychological’. 156 In these cases, there was a sense that pain is multidimensional and that the ‘physician gaze’226 is multifocal. Clinical work involved understanding a person’s suffering from the outset of health care, alongside attempts to define pain in biomedical diagnostic terms. These HCPs described an embodied approach to health care underpinned by the aim of understanding that a person is suffering from ‘something’:
If there isn’t a physiological problem, it doesn’t mean that there isn’t an illness, and if the patient is suffering then we should look at the problem and how we can help.
Wainwright 2006222
While we talked . . . many losses came up and I began myself to think about what all this was about in fact, what is this pain? Where it came out that there was a lot of disappointment, where there was divorce and . . . yes, it can’t be purely physiological.
Afrell 2010151
Once a person’s life has fallen apart it’s not so much about the pain and the injury anymore. It’s about all these other things in their life and it’s all these other things that need to be addressed in order to get them better and get them back on track.
Cartmill 2011163
Those who utilised an embodied psychosocial model recognised that sitting alongside and supporting patients, rather than trying to ‘fix’ them, could be rewarding for both the patient and their HCP. There was also a sense that sitting alongside a person on a healing journey, rather than holding on to the professional desire to ‘fix’, could take away the sense of professional failure and be rewarding for both the patient and the professional:
[It is] a journey rather than ‘this is my one chance . . . and I have to get it all done in one go’ . . . It's about moving away from that place of stuckness and creating a little bit of momentum . . . you know when you're pushing a car.
Toye 2015220
[The] traditional model . . . doesn’t allow people to express how pain has affected their whole life, it is very homed in to the particular area of the body and trying to fix it . . . [I] find it more satisfying to work in a way that acknowledges and discusses the impact.
Scott-Dempster 2014210
Some described how time restrictions and demands in the health-care system could encourage HCPs to focus on the physical body:
The biggest problem in the whole thing is lack of time. Typically these are complex people with multiple problems, and you really could spend the whole appointment, more than one whole appointment, just talking about this.
Krebs 2014191
We are limited by the amount of time with the patient. I know this sounds bad, but [talking about pain] opens a can of worms.
Siedlecki 2014213
I think as a clinician [you] focus straightaway on . . . a biological type approach to it. I think some of the psychological feelings get more brushed over perhaps . . . very often there is not the space in the consultation.
Toye 2015220
Navigating the patient–clinician borderland
This theme describes the complexity of navigating the borderland between patient and HCP. First, there is a need for give and take in order to maintain a therapeutic relationship. Second, there is a need to negotiate effective control of the therapeutic decisions. Integral to a negotiated relationship is the need to find common ground. Tension could arise when the patient and the HCP did not share an agenda, in particular when the patient’s expectations of diagnosis, treatment and cure were not met. The challenge for HCPs became to find this common ground or lose the patient’s trust:
People feel let down by their doctors . . . The degree of satisfaction is very low . . . basically because we don’t solve their problem . . . They go from one to the other, they find a doctor who gives them hope and they go to him.
Briones-Vozmediano 2013161
We kept having a difference of opinion: we think that your back isn’t damaged; we think the pain is caused by a false danger message from your brain while there is no tissue damage in your body. He said: I can’t understand that . . .
Oosterhof 2014202
To effectively maintain an effective therapeutic relationship, HCPs sometimes made clinical choices that they might regard to be of doubtful medical utility because this was what the patient wanted (e.g. referring for an X-ray, prescribing painkillers or referring to secondary health care). Maintaining a therapeutic relationship was described as a matter of give and take and attempts to balance long- and short-term gains were therefore described as integral to clinical work. Concessions were sometimes necessary:
Sometimes patients refuse to believe that their condition cannot be treated . . . and insistently ask for a series of medical investigations that you, as a doctor, would not perform. In such cases, a medical investigation can work as a therapy because it . . . shows that you listened to them.
Zanini 2014225
There definitely have been times when I’ve issued a [sick] note just purely because it’s became so antagonistic in a consultation that’s what I’ve done.
Wynne-Jones 2014224
Health-care professionals described the challenge of negotiating control of therapeutic decision-making and of deciphering the borderline between professional expertise and patient empowerment. HCPs were on guard against being ‘bullied’ into clinical decisions, but at the same time they wanted the patient to be involved in clinical decisions. HCPs described times that they found it difficult to stand back and let patients make a decision that they considered to be the wrong one:
I recognise that . . . we are trying to promote learning by giving choice and allowing people to get it wrong . . . get that, although it is still hard . . . not to give advice when I see . . . that the advice can be really helpful.
Barker 2015154
Trying to allow myself to listen objectively and to . . . sit with the fact that actually [the patient] might want to do something which is wholly unsensible, but allowing that to happen if that truly is what they want.
Scott-Dempster 2014210
When opinions conflicted, the HCP ‘short-circuit’ tended to take control. 221 This navigational strategy utilised a model of un-negotiated HCP ownership over clinical decision-making. 214 Here, professional knowledge is paramount and part of clinical work is to persuade patients to follow their recommendation. Patients were allowed to participate in decisions, but only up to a point. Clinical work was to tell the patient what to do and hope that they did what you wanted:
How do you get them to do what you want?
Slade 2012214
[Some say] ‘I know so much more about my illness than you do and I’m going to tell you what to do.’ . . . You want to have a team effort . . . but you also don’t want to be bullied . . . they can be the toughest patients to deal with.
MacNeela 2010196
However, there was a sense that trying to enforce control or ‘adherence’ was not effective. An alternative strategy involved enquiry and negotiation, rather than persuasion or enforcement and, here, clinical work incorporated ‘wondering together with the patient’:221
If you share your knowledge, not by telling that you are right, but really share what you know about the drugs and the effect . . . then you offer the patient an opportunity to think and decide by himself.
Tveiten 2009221
There’s something magical in this. If I’ve understood what the patient wants from me, and he understands what I’m going to do with him, then I have a good chance of succeeding.
Côté 2001167
Patients have to embrace our suggestion because they are convinced that it is the right one and not because we want them to choose a particular option. If you propose something that is inconsistent with their experience or knowledge, there is a risk that they will not listen to you.
Zanini 2014225
This theme was not supported by studies that explored the experience of HCPs in care facilities for older adults and this might indicate a difference in experience in these situations.
The challenge of dual advocacy
This theme describes the HCP as simultaneously an advocate of the patient and the health-care system. Although representing the patients’ interests, they are also a cog in a larger health-care system. At times it could feel like cogs in the machine were working against the patient and each other. HCPs could find themselves in a position of mediation or gatekeeping within the health and social care system. At times, this might involve undoing the work of other HCPs, and some HCPs felt like a linchpin keeping the ‘wheels’ of the system in place:
I mean it’s a dual role for us obviously we’re responsible for someone’s physical health and this is the second role that we have as a sort of gatekeeper to, you know getting incapacity benefits and the two sometimes don’t sit very comfortably.
Wynne-Jones 2014224
It all ends up on our doorstep. It is not only we who face the system – we are mediators of sorts between the patient and the system. Not only must we work with the patient against the system, but with the system as well.
Dahan 2007169
I think it’s good to take ownership . . . as soon as someone gets sort of uncomfortable they will shift to a different prescriber . . . And I honestly think it’s like a ship without a rudder and it’s just going round and round in circles.
McCrorie 2015198
At times it felt difficult to access effective specialist services:
There is a really big access issue with the pain clinics right now . . . while I can refer them, their likelihood of getting an appointment, even with strong advocacy from me, is very low.
Barry 2010155
Many cases are being referred to rheumatology and rehabilitation, to specialist doctors in rehabilitation and some are sent to psychiatry . . . but not all patients are given this opportunity, it’s not open to everyone because there just aren’t the resources to offer these services to everyone.
Briones-Vozmediano 2013161
There was a sense of mismatch between what primary care practitioners expected from secondary care and what they received:
Every time I send somebody to chronic pain [clinic] they come out with more medication, or injections.
McCrorie 2015198
Often I find that they are not accomplishing any more than I was and [patients] are often sent back to me with them [pain specialists] essentially saying, ‘we did our best’. It’s very frustrating, because if they were easy patients they wouldn’t have been seeing them.
Barry 2010155
Others described a working health-care system in which the cogs work smoothly together. This system incorporated the benefits of reciprocity, mutuality and collaboration between HCPs and the benefits of being able to break down or cross professional boundaries and hierarchies. Being confident in other professionals’ capabilities, reciprocal respect, team intelligence and shared knowledge could underpin an effective chronic pain service. Geographical proximity and continuity of staff were described as facilitating teamwork, whereas hierarchical relations could impede effective communication and pain management:
We get a lot of mileage about slapping each other on the back a little bit. And increasing other members of the team’s confidence by respecting other members of the team, their profile is improved, I think.
Howarth 2012186
There’s no sort of hierarchy. There’s the team, then there’s the clinical practice lead and then there’s management. But amongst the team there’s no real hierarchy.
Cartmill 2011163
If the team sort of echoes the same message and provides richness in terms of their different perspective on it but it all sort of amounts to the same message, then I think there’s less confusion for the poor clients.
Cartmill 2011163
Contrary to this, in residential care facilities, unqualified front-line staff described how they could feel disempowered by qualified professionals:
We’re at the bottom of the ladder, but we do the most important job . . . I mean we’re the ones in the wards and spend the bulk of the time with the residents.
Holloway 2009185
They act like the only thing we’re good for is to go clean butts . . . they really need to realise that we spent all this time with these residents . . . and we do know a little bit about what’s going on . . . they need to give us a little bit more respect.
Clark 2006166
I’ve charted many times . . . the patient screaming, yelling, pulling hair, blah, blah, blah, and right underneath my charting the doctor writes, ‘Stable’.
Fox 2004176
Personal costs
This theme described the emotional costs of providing health care to people with chronic non-malignant pain. On the one hand, the biomedical model could create a sense of professional failure for not being able to fix the problem. On the other hand, an embodied approach to pain management could incur a personal cost. As chronic pain did not comfortably fit the biomedical model, some HCPs felt challenged because they could not locate or define pain biomedically:
I’m a scientist, at least I like to have objective things, numbers, data, pictures, lab results. I actually don’t like the challenge of trying to read a person’s mind.
Berg 2009157
Unpleasant emotions, they explained, can cause as much suffering as physical pain. What, then, is pain? And can it be quantified or even identified as a pure sensation?
Clark 2004165
The problem is that there is no objective test to diagnose these patients. I don’t have a test that enables me to say: ‘this patient has fibromyalgia or doesn’t have fibromyalgia’.
Briones-Vozmediano 2013161
Being unable to diagnose a problem and offer a cure instilled a strong feeling of professional failure. HCPs found it professionally challenging to be unable to ‘fix’ people despite a strong desire to fix things. HCPs became frustrated and demoralised, and at times they could feel ‘on a hiding to nothing’; ‘how did we fail them?’:213
It’s awful, and I think it’s demoralizing when you leave people in pain. That’s just so disrespectful. I mean you’re supposed to be a doctor, you’re supposed to relieve pain and suffering, and you ignore the pain.
Barry 2010155
You become a doctor not to tell people I can’t do anything, I can’t find anything, you have this perception of yourself as well that you’re going to sort it out and if you can’t sort it out, it’s frustrating. What’s the point of you being there?
Patel 2008204
No matter what I do, I can use prescription pad and pen and do sleight-of-hand feats and stand on my knees and perform conjuring tricks! Nothing helps!
Lundh 2004195
An embodied approach to pain management involved recognising the overwhelming loss of a fellow human being and this could come with a personal cost:
We forget how much chronic pain affects the patient. They lose their jobs, they have emotional stress and depression and the depression itself is a big loss of productivity to the patient but also to the entire family and to the community.
Siedlecki 2014213
What they need is somebody to sit and talk with them and rub their back or they need company and they need understanding and compassion and you can’t give them that in a pill.
Fox 2004176
Health-care professionals recognised a need to balance the emotional burden of familiarity:
Trying to listen to the person . . . sort of empathise . . . [but] almost protected professionally . . . trying to see where that person was coming from but not letting it become too personal . . . I’ve used the phrase detached empathy.
Toye 2015220
The craft of pain management
The final theme described clinical work as an experience-based competence or ‘craft’. 170 This craft was gained from experience and patient mileage rather than through didactic education or research. At times HCPs felt underskilled in chronic pain management, particularly in relation to psychological therapies:
The problem is, we don’t know how to treat pain. And so everybody is telling me I’m not treating pain well, but nobody is helping me figure out how to treat the pain.
Spitz 2011217
I am not a psychologist . . . Someone bringing out a lot about their past . . . we don’t want to say the wrong thing and it be to someone’s detriment . . . you don’t want to open this can of worms.
Barker 2015154
It’s fine saying [to a patient] yes well you know that is part of the pain . . . you feel depressed with it . . . I don’t really feel I’m at all competent in knowing what to say to try and help them round that.
Parsons 2012203
Personal experience and maturity, patient mileage and learning from more-skilled professionals (apprenticeship) were described as integral to craft knowledge:
One becomes more stable as a person [with age], and does not really have the same demands and does not believe that one can do everything, that one is able to solve everything . . . Young doctors can have in them, that they believe that they will solve everything.
Åsbring 2003152
New grads can’t learn all of this, they need a certain number of years, you can’t teach them all of this, there’s so much they’ve got to learn.
Slade 2012214
If you have a patient who’s not responding the way that you expect, it’s nice to have someone there who can have a look and see . . . you can see and hear what everybody else is doing and that is how you learn . . . it’s like osmotic learning.
Slade 2012214
Pragmatic use of guidelines
There was a sense that evidence-based guidelines could challenge or constrain craft knowledge. Although some HCPs felt that evidence guidelines supported a holistic approach,180,207 there was a stronger feeling that guidelines did not facilitate individualised care:
Treatment has to be tailored to patients’ needs and prescriptive guidelines promoting ‘one size fits all’ is not acceptable.
Wilson 2014223
If you work according to the guidelines, you are constrained in your performance . . . what would be left of your independence, your own competence, your own practical experience . . . Am I to conclude then that my training was useless?
Harting 2009180
Most pain specialists spend most of their time treating people with low back pain that’s what we do. And a guideline comes out that says, you’re not needed. Full stop. It can be managed without any reference to you whatsoever . . . no need for doctors and nurses.
Wilson 2014223
Health-care professionals showed limited attention to guidelines in clinical decision-making. Clinical work was about the craft of learning from doing things:
My experience is that therapists say they adhere to the guidelines, although they still all work in different ways.
Harting 2009180
Such a huge heap, such a bundle of paper, such a bundle of characters . . . we have been educated to do things. So if you give this group a pile of papers, who will read them? I think nobody will.
Harting 2009180
Health-care professionals framed guidelines within the remit of their own professional knowledge and used them pragmatically and flexibly:
But of course, I’m free to take or leave these things, to look at whether they suit my own ideas of how to approach my patients.
Harting 2009180
Of course, it is not necessary to follow the guidelines exactly; it is more like: this is roughly the approach, regardless of the background you have.
Harting 2009180
For example, some used the evidence guidelines as a tool to convince patients or colleagues that their professional decision was the right one:
In the case of disagreement . . . about the treatment policy, you can always turn to the guidelines, and you can argue while showing them these national guidelines.
Harting 2009180
Health-care professionals described the decision to refer a patient for clinical testing as a craft. This highlights the multiplicities of clinical decision-making whereby HCPs face the challenge of balancing varied competing interests in order to achieve an optimum outcome (Figure 6).
FIGURE 6.
Multiplicity of clinical decision-making: do I refer for a test?
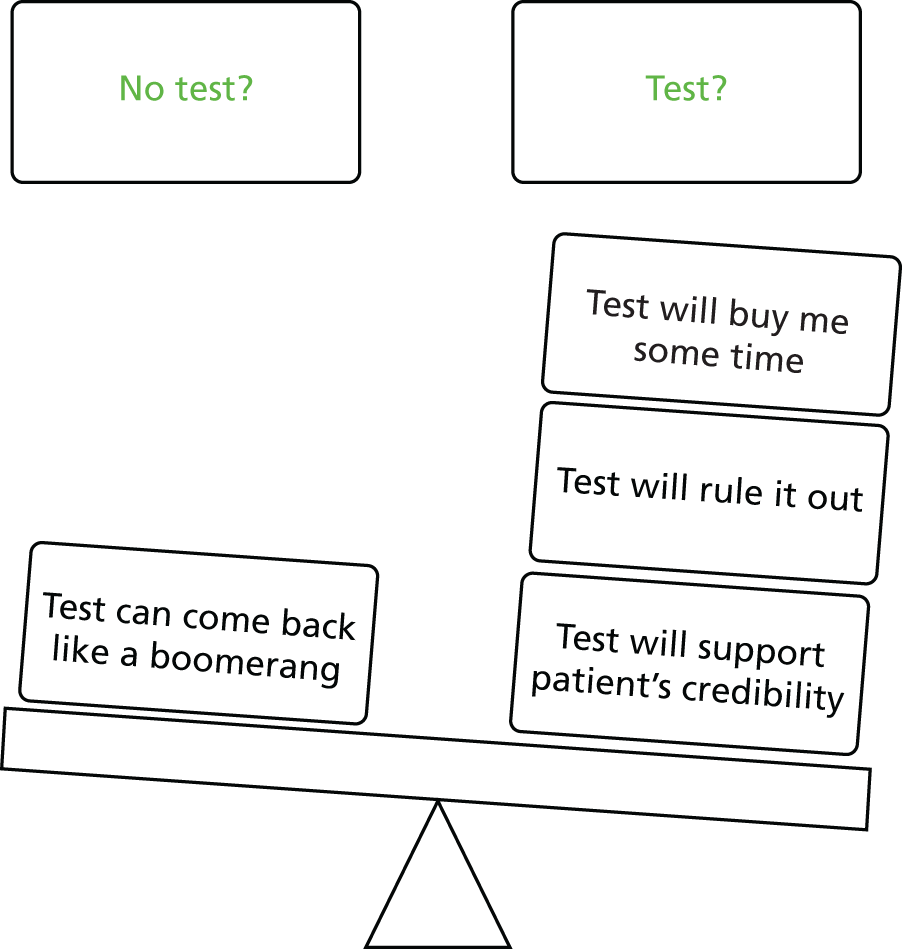
First, a test or investigation might be used to confirm or to rule out serious pathology. This might be to reassure patients or HCPs, or alternatively to convince a patient or HCP that there was no pathology:
‘Wear and tear’ is, in a way, quite nice to have. Most are satisfied with that . . . nothing dangerous, and nothing that needs surgery. It’s a short version of an explanation.
Espeland 2003173
At times, there might be a need to rule out pathology as a defence against complaints of malpractice. 173 However, there was a sense of ambivalence regarding the usefulness of tests in clinical decision-making:
What are we afraid of? After all, it occurs to every doctor sitting here that he may just miss something. That is how we were taught, we were told watch out, you may miss something. How much did we miss? Almost nothing.
Dahan 2007169
X-rays could also be used strategically to support patients’ credibility and to maintain trust. Referring a for an investigation was felt to be a strong statement that patient I hear you, believe you and I am even prepared to bend the rules for you. Some ordered X-rays because the patient asked for one, or as a compromise for a preferred or less accessible service:
[An X-ray referral] is interpreted as a definite signal that the physician thinks it is something physical. It means . . . [the patient] can come home and say, ‘I had an X-ray’, and then everybody will realise I have pain in my back.
Espeland 2003173
Investigations could also be used as a means of biding time or buying time. It was sometimes quicker just to order an X-ray. It might also save time en route to a different service:
I buy time by ordering an imaging test, even though I know it will not be helpful . . . It buys time . . . It’s a kind of therapy. It reassures the patient that they’re being cared for.
Shye 1998212
Sometimes I found myself referring a person for an X-ray in order to clear the waiting room and allow myself 2 minutes of breathing time . . . the patient keeps quiet while I write out his referral. Sometimes you find yourself doing this and it goes against any reasoning or logic.
Dahan 2007169
Some erred on the side of caution in ordering investigations and considered the potential repercussions of securing a false positive:
He’s got a scan of his disc, it’s there [a disc bulge], but I think he’s had it for years . . . but he’s now fixated on a disc.
Slade 2012214
It come back at me like a boomerang: ‘now I’m worn out, I can’t work any more, I’ll go over to social security benefit’.
Espeland 2003173
A word of caution given was to think very carefully about the person for whom the test was being done:
[Be] very self-aware when you're thinking about doing tests . . . sometimes in chronic pain doctors are doing the tests for themselves not for the patient . . . that uncomfortableness with not being able to fix or do something . . .
Toye 2015220
Conceptual model
The final phase of meta-ethnographic analysis is to develop a conceptual model that is abstracted from, but more than, the sum of its themes. The reviewers developed a model that helps us to understand the experience of providing health care to people with chronic non-malignant pain (Figure 7). The model is underpinned by a series of tensions: (1) between a dualistic biomedical model and an embodied psychosocial model; (2) between professional distance and proximity; (3) between professional expertise and patient empowerment; (4) between a need to make concessions in order to maintain relationships and known biomedical utility; and (5) between patient advocacy and health-care system advocacy.
FIGURE 7.
Conceptual model: complexity of providing health care to people with chronic non-malignant pain.
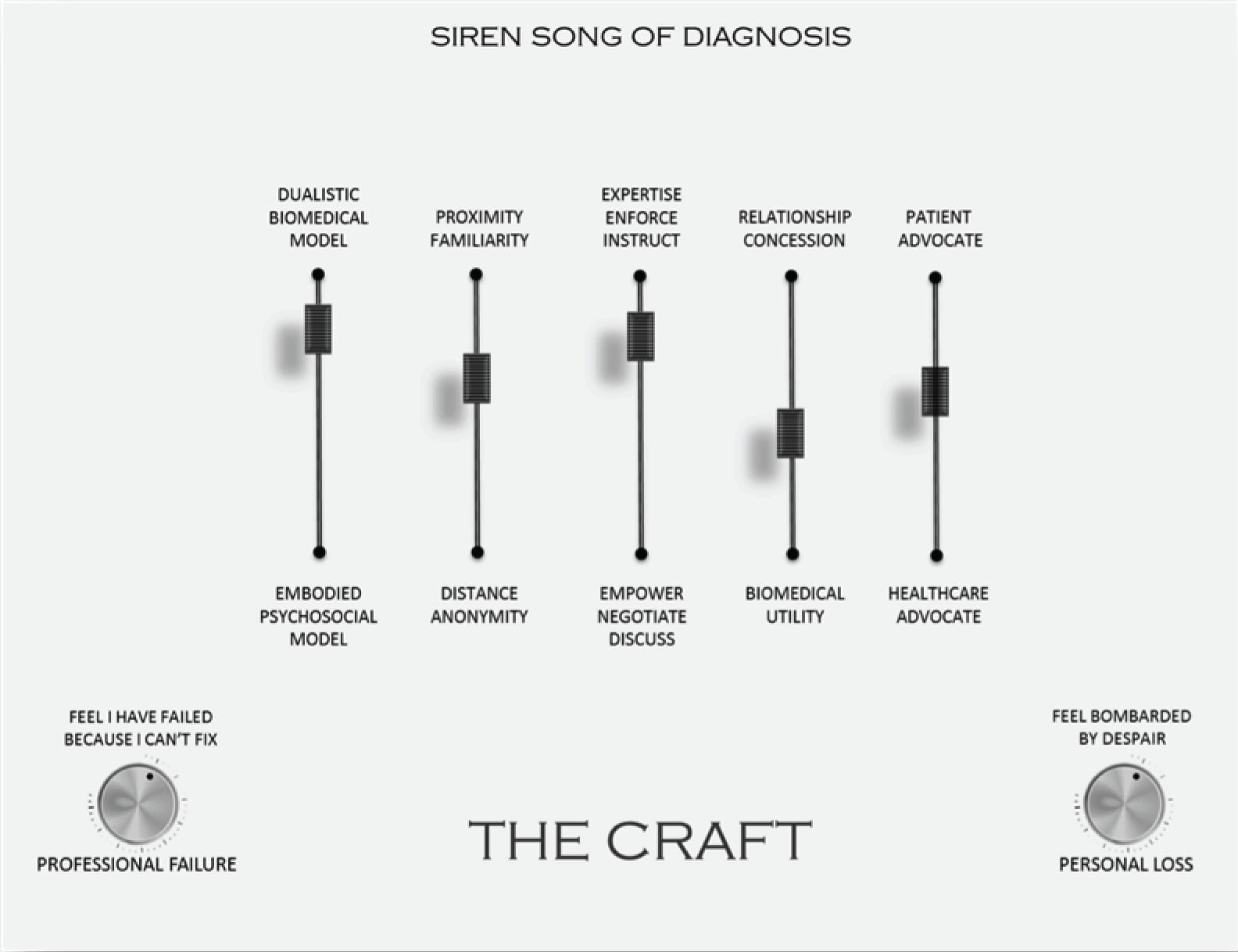
We conceptualised these tensions, on a mixing console, as underpinning the craft of chronic non-malignant pain management. The poles are neither inherently good nor bad; just as bass and treble are neither inherently good nor bad. It is the correct mix within a context that contributes to the quality of music. Our console also incorporates the pitch or level of loss, both professional and personal, that can contribute to the harmony or dissonance of a therapeutic encounter.
Opioid prescription
The reviewers also identified 76 concepts in 17153,155,157,161,174,175,177,187,189–191,198,208,211,213,217,218 of the 77 studies that uniquely explored the experience of prescribing opioids to patients with chronic non-malignant pain. The reviewers discussed and organised the 76 concepts (see Appendix 3) into 19 conceptual categories (Table 12), and then into six themes that underpin HCPs’ experience of prescribing opioids to patients with chronic non-malignant pain:
-
should I, shouldn’t I?
-
pain is pain
-
walking a fine line
-
social guardianship
-
moral boundary work
-
regulations and guidelines.
| Conceptual category title | Description of conceptual category |
|---|---|
| A battleground | This describes how the clinical arena for prescribing opioids can become a battleground in which mistrust pervades and the HCP sometimes has to make some concessions to move forward |
| It’s quite a taboo | This describes the stigma of opioids, a culture hostile to long-term opioid use and the taboo of prescribing. HCPs compared their own prescribing practice with that of their colleagues and were concerned over being judged by their peers. Some felt that they had a personal responsibility to protect society from the consequences of drug misuse. There is sense of policing drug use |
| Concerns over misuse | This describes concerns over misuse of opioid prescriptions |
| I don’t want to feed a habit | This describes the concern about causing addiction or feeding a habit if there was already a history of abuse |
| Only as a last resort | This describes opioid treatment as a last resort. There needs to be a pretty good reason to prescribe opioids |
| It’s not gonna be my little old lady | This describes the moral boundary work to determine which patients are likely to misuse prescriptions. You have to go with your gut. This boundary work is complex and incorporates non-clinical judgements. However, some sensed the dangers of judging a book by its cover |
| No diagnosis is a trigger for suspicion | This describes an unwillingness to prescribe opioids to those who have chronic conditions with no biomedical cause, or in whom symptoms are vague. Suspicion arose when observed symptoms did not match the patients report (dissonance) |
| It’s my name on the bottle | This describes concerns about possible legal or regulatory sanctions as a consequence of prescribing opioids as treatment for chronic pain |
| Addiction not a barrier | This describes a view that drug addiction should not be a barrier to opioid prescription for pain. You can have pain and also addiction and you need to balance the benefits of adequate pain control |
| Pain is pain (non-malignant or malignant) | This describes how in theory pain is pain, whether malignant or not, and that this should not have an impact on the decision to prescribe. However, in practice it is different. The decision is complicated by the length of time that opioids would be prescribed for non-malignant pain and the fear of causing addiction. There is a sense that experience working in palliative care facilitates prescribing for non-malignant pain |
| Walking a fine line between gains and losses | This describes the need to carefully balance the benefits and adverse effects of opioids. An emphasis on adverse effects might lead to unnecessary suffering, or to a patient seeking out more harmful methods of pain control. Some HCPs erred on side of benefits and others on the side of harm. There was a sense that patients also have to walk this fine line and make difficult decision |
| Balancing adverse effects in older adults | This describes concerns over prescribing opioids to older adults because of the potential severity and impact of adverse effects (e.g. polypharmacy, cognitive function and falls). In principle, age should not make a difference, but in practice it does. Sense that you needed specialised knowledge to prescribe in this area |
| I learnt the hard way | This describes how a HCP had prescribed opioids in the past and got their fingers burnt. At times there was a feeling of being ‘deceived’ by patients. However, there was also an understanding that part of clinical work was to learn from your mistakes |
| Should I, Shouldn’t I? | This describes a sense of uncertainty about when to prescribe opioids and a feeling of ambiguity about the effects of medication. At times HCPs referred to other HCPs or prescribed medication in order to buy some time. This uncertaintly was compounded by not having the time to get to know the patient. A ‘let’s just wait and see what happens’ perspective |
| Lack of expertise in addiction | This describes a perceived lack of expertise in chronic pain and addiction |
| Prescribing guidelines: positive | This describes a positive attitude to guidelines that can be used to justify clinical decisions and help to deal with ‘challenging’ patients. Some also felt that guidelines could help to prevent potential social harm from abuse or misuse |
| Prescribing guidelines: negative | This describes a negative view of prescribing guidelines (the legislature seen as practising medicine without a licence). Guidelines can be used as a reason not to prescribe to those who need it and can interfere with professional autonomy. Some felt that guidelines would only be used pragmatically to support usual care |
| Opioid agreements: negative view | This describes a negative view of opioid prescribing agreements and drug screening as striking a blow at the heart of the patient–clinician relationship by creating mistrust and hostility. Also a feeling that they are ineffective at stopping misuse of opioids |
| Opioid agreements: positive view | This describes a more positive view of opioid prescribing agreements that struck a blow at drug misuse. They were useful in establishing boundaries and opening up honest discussion |
A core concept overarching all six themes was a sense of ambiguity surrounding opioid prescribing. We illustrate the six themes with narrative exemplars. Indicators of confidence in our review findings as recommended in the GRADE-CERQual framework37 are given in Table 13.
| Review finding | Methodological limitations (satisfactory studies) | Relevance (partial or direct) | Adequacy (number of concepts) | Coherence (number of studies out of 17) | Assessment of confidence |
|---|---|---|---|---|---|
| Should I, shouldn’t I? | All | 9 direct | 19 | 9155,157,161,174,175,177,191,198,217 | High confidence |
| Pain is pain | All | 5 direct, 1 partial | 8 | 6153,177,187,189,211,217 | Moderate confidence |
| Walking a fine line | All | 9 direct, 2 partial | 20 | 11153,157,162,177,187,188,190,194,208,211,217 | High confidence |
| Social guardianship | All | 10 direct, 1 partial | 17 | 11153,155,157,174,175,177,190,191,208,211,217 | High confidence |
| Moral boundary work | All | 12 direct, 2 partial | 27 | 14153,155,157,174,175,177,190,191,198,208,211,213,217,218 | High confidence |
| Regulations and guidelines | All | 8 direct | 18 | 8155,157,175,177,190,191,217,218 | Moderate confidence |
Should I, shouldn’t I?
The theme ‘should I, shouldn’t I?’155,157,161,174,175,177,191,198,217 described uncertainty about when to prescribe opioids, and a feeling of ambiguity about the effects of medication:
Depending on who I run into, I may get into all kinds of problems . . . ‘You’re just being unfair because he’s a drug addict . . .’. But if I run into somebody else, they might say ‘No . . . that was a good clinical decision‘.
Berg 2009157
The aetiology of the disease is not really known and you have few means of knowing what you’re doing. You’re treating the pain and you don’t know why there is no response . . . No matter what you give them, the pain doesn’t go away.
Briones-Vozmediano 2013161
Some felt that clinical education did not prepare them to make these decisions:
We took an advanced pharm[acology] class, and we discussed it in one lecture, but that was it. Isn’t that ridiculous considering how many people we see in pain?
Fontana 2008175
Nobody here knows how to treat pain in anybody who has a history [of addiction] and already on something like methadone. Nobody knows how to treat them . . . Most of us in primary care end up [doing it] by default. But that’s not good.
Barry 2010155
Uncertainty was compounded by the sense that specialist referrals were either restricted or unproductive:
Often I find that they are not accomplishing any more than I was and [patients] are often sent back to me with them [pain specialists] essentially saying, ‘we did our best.’ It’s very frustrating, because if they were easy patients they wouldn’t have been seeing them.
Barry 2010155
Pain is pain
The theme ‘pain is pain’153,177,187,189,211,217 was underpinned by the concept that if a person is in pain then the primary aim of the HCP should be to try to relieve their pain. If a person is in pain, even drug addiction should not be a barrier to opioid prescription:
At the end of the day, if someone’s got chronic pain it doesn’t matter if they’re addicted to painkillers if it sorts out their quality of life.
Gooberman-Hill 2011177
I had a guy last week who’d been stabbed . . . and he had to discharge himself because they wouldn’t give him any pain control . . . he wasn’t even getting his prescribed dose of methadone . . . there’s a protocol . . . they choose not to know about it and it’s just pure stigma.
Baldacchino 2010153
However, HCPs felt that the decision to prescribe opioids was complex and that, although in theory pain is pain, in practice it is different. HCPs described differences in practice that would make them less likely to prescribe opioids. For example, in the case of chronic non-malignant pain, they would need to carefully balance the risks and benefits of long-term opioid prescription:
With [malignant pain] . . . your aim always is to get complete relief of pain . . . For chronic pain . . . you’ve got to weigh up . . . the potential side effects . . . you are not necessarily going to get them pain free because they’ve got the rest of their lives to live.
Seamark 2013211
Health-care professionals explicitly compared prescribing practices for palliative care and chronic non-malignant pain:
We tend to focus too much on pain control for palliation as opposed to just everyday clients. Certainly nobody wants to die in pain, but nobody wants to live in pain either.
Kaasalainen 2007187
It might be that you are . . . just getting them through the last few weeks . . . so maybe we feel more comfortable, whereas the patient with chronic back pain you don’t how long you’re going to be treating . . . I think it’s a risk–benefit issue.
Spitz 2011217
Walking a fine line
The theme ‘walking a fine line’153,157,162,177,187,188,190,194,208,211,217 described the need for HCPs to carefully balance the benefits and adverse effects of opioids. On the one hand, emphasising adverse effects might lead to unnecessary pain, but, on the other hand, emphasis on pain control might lead to harm or abuse:
There are two mistakes you make . . . the mistake of undertreating or of giving medicines that end up being sold or used for unintended purposes. You’re going to make errors both ways, and I think it’s generally better to risk opiates being misused versus not treating someone’s pain.
Berg 2009157
This sense of walking a fine line was heightened when prescribing opioids for older adults, and HCPs felt that specialised knowledge was necessary to effectively prescribe opioids to older people with chronic pain. Although in theory age should not affect decisions, there was a sense that in practice it did:
But there are safety issues, and at the end of the day if they came to grief . . . you’d feel . . . excessive side effects . . . that contributed to some major event . . . So we walk a fine line sometimes between giving adequate pain relief and giving safe treatment.
Gooberman-Hill 2011177
Older people metabolise medication differently . . . so you don’t want to give them medication that’s going to impair their ability to function . . . You don’t want to interfere with their ability to make judgements and so on, so I don’t like using opioids in elderly people at all.
Ruiz 2010208
I just have a hard time prescribing opioids in my older patients. I get frightened with 80+ year olds; how are they going to respond? Am I going to absolutely drop them to the floor even with a small dose?
Spitz 2011217
Social guardianship
The theme ‘social guardianship’153,155,157,174,175,177,190,191,208,211,217 described a culture hostile to opioid use and the professional taboo of prescribing opioids for chronic non-malignant pain. HCPs compared their own practise with that of their colleagues and were worried that they would be harshly judged by their peers for prescribing opioids. Some felt a personal responsibility to protect society from the consequences of opioid misuse and viewed certain patients with suspicion, particularly those who requested opioids. To protect society, some implemented strategies to control patients’ behaviour (e.g. bottle checks, opioid contracts and background checks). HCPs were also concerned that opioid prescriptions might be diverted to others:
I am a naysayer on opiates . . . too much of my day is spent policing how many [opioids] have been prescribed and how many times a patient is a return patient and how often they visited requesting opiate prescriptions.
Kilaru 2014190
If you prescribe to a population where you think diversion is going on, you definitely have a responsibility. I also worry about who is getting the drug, is it my son? I mean, we are members of society after all.
Fontana 2008175
Some HCPs discussed indicators of potential abuse (e.g. lost prescriptions, early requests for medication and frequent attendance), whereas others acknowledged that these might actually indicate poorly managed pain and, therefore, a greater need for pain relief:
If people are taking it genuinely for pain they tend to stick to the prescribed dosage . . . addicts tend to be the ones who are always ordering early . . . you don’t lose your tablets if you are . . . getting great benefit from them for pain.
Baldacchino 2010153
The concern would be is this pain real, or is it just put on to obtain opioid? . . . I mean, an assessment of the pain and whether I think it’s genuine or not. I think it’s very difficult; it’s something I’m currently dealing with at the moment, and not very successfully.
Seamark 2013211
Moral boundary work
The theme ‘moral boundary work’153,155,157,174,175,177,190,191,198,208,211,213,217,218 was underpinned by the clinical work of deciding whose pain is ‘real’ and thus who should be prescribed opioids. There was a sense of an underlying unwillingness to prescribe opioids for pain with no clear biomedical cause, or if symptoms were vague. Suspicion arose when there seemed to be dissonance between the patient’s report of pain and the symptoms observed by the professional:
A lot of patients . . . they really need it . . . based on their underlying pathology . . . a patient who has a cancer or a real anatomic foundation . . . you have to count on more observation, combined with other clinical data . . . you pretty much know who is abusing and who is not.
Krebs 2014191
I think for patients who have chronic pain it’s more challenging and I think that’s the place where I’m constantly rethinking my practice . . . You’re always on the fence: am I doing the right thing for my patient?
Kilaru 2014190
Health-care professionals described good patients (e.g. those who made appropriate demands, took advice and did not cause trouble) and ‘difficult’ patients (the demanding, non-adherent and trouble-making):
For those patients that have a legitimate reason for wanting to take it and if I can trust them . . . most of these are older patients of mine. They never request early refills, they don’t go to the [emergency room] in between visits to get them . . .
Krebs 2014191
Non-clinical moral judgements or gut feelings contributed to prescribing decisions. HCPs recalled episodes when they had made a mistake by trusting ‘the wrong’ patient. Over time they felt that they had become better at making the right decision. Examples were given of HCPs getting their fingers burned when prescribing opioids, along with an understanding that lessons had to be learnt from mistakes:
At times there was a feeling of being ‘deceived’ by patients so that you prescribed opioids:
I’ve had trust in people, and it’s been betrayed – sometimes the trust is betrayed multiple times. I find I’m not always that great a judge of who to trust and who not to trust, so, I don’t trust my own judgement on trust all the time . . . I think people feel like they’ve been violated, you know, cheated, like they’ve been taken advantage of. I feel some of that, too. Ultimately you feel you’ve made a poor judgement, and you get mad at yourself . . . My impression was that he had a true ankle problem. Then you find out it was all lies, but you know, at that time and at that moment, that was my assessment, and I did it. You’re allowed to make mistakes.
Berg 2009157
Prescribing . . . is a sort of rather woolly, nebulous product . . . I’ve been moulded by the successes and the failures . . . we all learn on the hoof, don’t we? . . . I think everybody’s fingers get burnt with people who you give the opioids to with a more trusting attitude.
Seamark 2013211
However, some sensed the dangers of judging a book by its cover and acknowledged that basing clinical decisions on their gut feeling might not be fair or accurate:
There’s a disconnect . . . even if it’s the sweetest little 85-year-old woman who looks like your grandmother, versus, you know, some guy from the ghetto wearing his pants down at his knees . . . it shouldn’t really matter.
Starrels 2014218
Regulations and guidelines
The theme ‘regulations and guidelines’155,157,175,177,190,191,217,218 described HCPs’ views about external regulation of opioid prescription (specifically guidelines, opioid agreements and drug screening). Some described a negative view of prescribing guidelines and felt that they interfered with professional autonomy, an example of the ‘legislature practising medicine without a licence’:190
You’re there to help them and they can tell you their deepest, darkest secrets, but yet you’re policing them . . . I like to see the person as a person . . . You can’t do your job when you are thinking about these things.
Krebs 2014191
There could be negative implications to that if patients are actually leaving the emergency department because of the way they interpret that [regulations] poster . . . there’s potential that sick patients could actually leave your emergency department when they need help.
Kilaru 2014190
Health-care professionals feared legislative reprimand if they prescribed outside guidelines:
My name is on that bottle . . . I had a patient die. He took the entire bottle, and the police came to see me because they found him dead with the empty bottle with my name on it . . . I won’t accept that burden.
Fontana 2008175
[GPs] are scared of being in front of the coroner . . . with a load of angry family and relatives wagging a finger at us, when all we’re trying to do is really help . . . if it works, brilliant. If it doesn’t work . . . people are very quick to criticise.
Gooberman-Hill 2011177
Others described a negative view of opioid prescribing agreements and drug screening as striking a blow at the heart of a patient–clinician relationship by creating mistrust and hostility:
It can really strike a major blow to trust in the doctor patient relationship when you ask someone to sign a piece of paper . . . if there is already mistrust between the patient and the doctor, it could heighten that mistrust . . .
Starrels 2014218
Some used guidelines pragmatically as leverage or to justify decisions and thus help them to deal with ‘challenging’ patients:
I tell them this is standard protocol. I’m not singling you out. I’m not picking on you. I’m not treating you like an addict. This would happen to anybody. If you take our chronic pain meds long enough, anybody will become physically dependent on them.
Krebs 2014191
[An agreement] gives me leverage or comfort in discontinuing the medication . . . because we’ve kind of laid it out from the beginning that those behaviours were not okay . . . it made my life a little easier, but I’m not sure it did the patients a giant service.
Starrels 2014218
Others described a more positive attitude to regulation. For example, opioid agreements could be useful in establishing boundaries and opening up honest discussion:
I think it improves the care, because you are able to then have more open and frank discussions around their pain . . . and [about] other things going on in their life . . . In the best of circumstances it actually will make for a deeper more trusting relationship.
Starrels 2014218
Conceptual framework: prescribing opioids
Our conceptual model (Figure 8) hinges on the HCP’s need to decipher the ambiguity surrounding opioid prescription for chronic non-malignant pain (should I, shouldn’t I?). Social suspicion and hostility towards opioids (social guardianship) will tip the balance for prescribing towards the negative, whereas the pre-eminence of pain (pain is pain) might tip the balance towards prescribing. The decision is not clear-cut. First, HCPs might make non-clinical judgements about the person (moral boundary work). Second, they must determine the balance of positive and adverse effects for each individual (walking a fine line). Last, there is a sense of professional ambivalence towards prescribing guidelines (regulations and guidelines). This conceptual model demonstrates the complexity of making a decision to prescribe opioids to someone with non-malignant pain. It also demonstrates that the decision is influenced by intra- and interpersonal factors and broader external concerns.
FIGURE 8.
Conceptual model: the ambiguity of prescribing opioids to patients with chronic non-malignant pain.
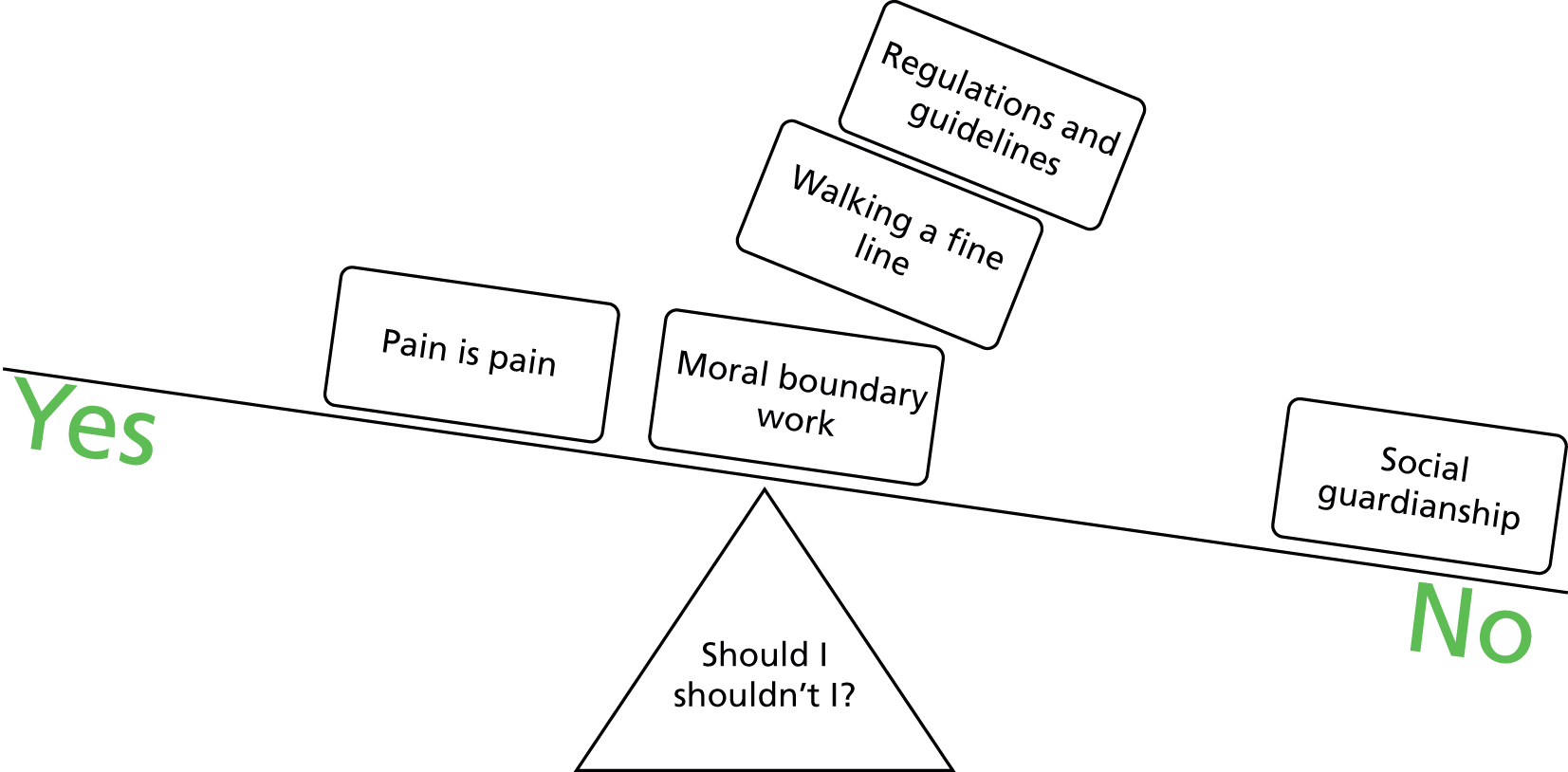
Discussion
We aimed to undertake a QES using the methods of meta-ethnography reported by Toye and colleagues8 to increase our understanding of what it is like for HCPs to provide health care to people with chronic non-malignant pain and thus to inform improvements in the experience and quality of health care. At the outset of this study, we had intended to include HCPs’ experience of treating chronic non-malignant musculoskeletal pain in order to mirror a previous QES of patients’ experience of chronic non-malignant musculoskeletal pain. However, our preliminary reading indicated that HCPs’ experiences of treating chronic non-malignant pain were not boundaried to a particular body system, but were a summative experience that cut across conditions. After consultation and agreement with our advisory group, we therefore sought and attained permission from the funders to remove ‘musculoskeletal’ from our study title. Our search strategy then focused generically on chronic non-malignant pain. Further research might focus on specific diagnoses (such as neuropathic, visceral, pelvic or phantom pain or arthritis) to explore potential similarities and differences in HCPs’ experiences of treating these conditions.
This is the first time that such a synthesis has been undertaken on this topic. Already we know that, from the patient perspective, the experience of health care can be adversarial. 8 Patients with chronic pain struggle to affirm their sense of self; their present and future appears unpredictable; they search for a credible explanation for their pain; they do not always feel heard, believed or valued by HCPs; and they struggle to prove themselves in the face of scepticism. 8 Our findings can help us to consider this experience of health care from the perspective of HCPs. We identified six themes from 77 studies that help to explain the HCP experience of providing health care to people with chronic non-malignant pain and six themes specific to the experience of prescribing opioids to this group of patients. The innovation of our conceptual model is to propose a series of tensions that are integral to the experience of providing health care to people with chronic non-malignant pain. These tensions were between a dualistic biomedical model and an embodied psychosocial model; professional distance and proximity; professional expertise and patient empowerment; the need to make concessions to maintain therapeutic relationships and the need for evidence-based utility; and patient and health-care system advocacy. This model may be transferable to other chronic conditions.
A sceptical cultural lens and siren song of diagnosis
From the HCP perspective, the findings highlight a deep-seated cultural scepticism towards people with chronic non-malignant pain. This scepticism influences a powerful gravitational pull towards the biomedical model and siren song of medical diagnosis. The biomedical model takes disease to be an objective biomedical category not influenced by psychosocial factors or judgements about moral worthiness. 227 Alternatively, the biopsychosocial model focuses on the embodied experience of illness. 227 HCPs describe the challenge of navigating juxtaposed biomedical and biopsychosocial models. Although many HCPs may feel that they adhere to a biopsychosocial model, our findings indicate a dualistic approach whereby HCPs make a sudden shift to biopsychosocial explanations after exhausting attempts to decipher a diagnosis. In essence, psychosocial aspects are ‘grafted onto the somatic’ core (p. 44). 228 Our interpretation supports the need for a more embodied biopsychosocial model that focuses on the personal meaning of pain. Embodiment theory has its roots in the writings of Merleau-Ponty,229 who breaks down the dualism of mind and body and focuses on the personal meaning of suffering. Personal meaning always accompanies the experience of pain. 228,230 From a patient perspective, both covert and overt scepticism from HCPs, along with a cultural pull towards biomedical explanations, may help to explain why patients with chronic pain can experience a strong sense of not being believed. 8 An abrupt shift in explanation towards the psychosocial by HCPs may exacerbate this loss of credibility, particularly in the context of persisting cultural dualisms (real/unreal, physical/mental, medical/psychological and body/mind). We know that people in chronic pain can feel a profound sense of shame and stigma because they do not fit the dominant medical discourse and that they struggle to prove to others that they are a credible and ‘good’ person. 8 A more embodied non-dualistic biopsychosocial approach at the outset might help HCPs to support patients with chronic pain. These findings highlight that both HCPs and their patients share a struggle to negotiate dual explanatory models for pain. However, although the patient might persevere in efforts to find a medical diagnosis in order to gain credibility, the HCP might make an abrupt shift towards the biopsychosocial, and this is a potential source of tension.
Navigating the patient–clinician health-care interface
From the HCP perspective, our findings demonstrate the complexity of navigating the interface between themselves, patients and the health-care system. Navigating the patient–clinician borderland, the challenge of dual advocacy and the craft of pain management all indicate the challenges of managing this interface. The finding that HCPs sometimes make concessions that are not evidence based in order to maintain effective relationships may have implications for policy and practice. For example, it might help to explain why an increasing number of HCPs are prescribing opioids despite very limited evidence for long-term opioid therapy for chronic pain before the end of life,231–233 or why a doctor may refer a patient for an investigation when its efficacy is not well supported. The findings demonstrate that HCPs can struggle to find a balance between providing professional expertise and empowering their patients. At times, this can mean that they feel pressed into making decisions of limited clinical utility. The short circuit can be to take control of the clinical encounter, thus alienating the patient from any sense of control.
Our findings indicate that HCPs can find it a challenge to simultaneously represent the patient and the health-care system. They also demonstrate the benefits of mutual respect and shared knowledge for an effective chronic pain service, and suggest that recognising mutual skills and combined knowledge of colleagues rather than focusing on differences might benefit health care. From the patient perspective, we know that the person with chronic pain experiences an ambivalent relationship with the health-care system and can feel trapped in a system that is not meeting their needs. 8 The craft of pain management describes clinical work as an experience-based competence that at times could feel constrained by external guidelines. At times HCPs felt underskilled in chronic pain management, particularly in relation to psychological therapies.
Personal costs
The findings demonstrate that from a HCP perspective there are emotional costs involved in providing health care to people with chronic non-malignant pain. HCPs can feel that they have failed in their professional duty to find and fix a medical problem. On the other hand, those who take time to understand their patients’ personal losses can feel ‘bombarded by despair’. 220 We know that from a patient perspective there are also profound personal losses. The person is struggling with an overwhelming loss of present and future self and does not always feel valued as a person in health care. They look back nostalgically to the past self and feel a sense of great loss. They describe a fundamental need for their HCP to believe and bear witness to their suffering. 8 Our findings have clinical implications: how do we support HCPs to sit alongside patients and yet not be able to fix them, without experiencing the losses of failure? It might be useful for clinical educators to consider overlaps in training need between palliative care, which by definition does not aim at cure, and chronic pain management. HCPs included in this review did not discuss their own personal life context, which may, at times, contribute to and make HCPs less resilient to personal or professional losses. Our findings suggest that it may be useful to frame a more embodied approach as one that has advantages for both patients and HCPs. Although seeing the patient as a fellow human can impose a personal burden, it can also provide a mutual and positive human experience. 234 Sitting alongside a patient frames the clinician as an advocate, rather than adversary. Charon235 demonstrates that sitting alongside a patient, although emotional, can have a positive impact on work satisfaction by allowing clinicians to interact on a human level. This may take the pressure off clinicians to fix their patients.
Using the conceptual model in clinical education
We present our conceptual model as a mixing console that can help us to understand, think about and modify our experience of providing health care to people with chronic non-malignant pain. The model is underpinned by a series of tensions:
-
biomedical model versus an embodied psychosocial model
-
professional distance versus professional proximity
-
professional expertise versus patient empowerment
-
making concessions to maintain an effective relationship versus biomedical utility
-
patient advocate and health-care system advocate.
Health-care professionals can use this mixing console to help them to think about their encounters with patients with chronic pain, for example:
-
Am I making a sudden shift to psychosocial explanations?
-
Am I considering psychosocial factors at the outset?
-
Do I understand this patient’s experience or am I too distant?
-
Am I trying to enforce my decisions?
-
Am I making a concession and for whose benefit?
-
How is my patient experiencing this dual advocacy?
-
What personal impact is this having on me?
-
Am I feeling like I have failed?
Our console will allow HCPs to consider their individual mix and contemplate a re-mix if necessary in order to successfully support people with chronic pain, or to individualise their approach for different patients. Using the mixing console could potentially be used to help appreciate and alter the tensions during a consultation with a patient. This fits in with Mead and Bower’s15 framework for patient-centred care, which recognises both the importance of the therapeutic alliance and the influence that HCPs’ personal characteristics and responses can have on care. Further research to explore the usefulness of this console within a therapeutic encounter would add benefit to this QES.
Opioid prescription
Despite recent guidelines suggesting that patients might not benefit, there has been a significant rise in opioid prescription for chronic non-malignant pain. 231,232 The findings do not indicate that the limited efficacy of opioids for chronic non-malignant pain is the primary barrier to prescribing. Our findings indicate ambiguity surrounding the prescription of opioids to patients with chronic pain. Although some were aware of the adverse effects of opioids, they were concerned that choosing not to prescribe would lead to unnecessary suffering. Although HCPs discussed the potential harm from opioids, there was also a feeling of personal responsibility to police and protect society from opioid misuse. A more positive and collaborative frame for making the decision to prescribe, or not, might be useful, for example emphasising the limited efficacy and serious adverse effects of opioids. 231,232 The findings demonstrate ambivalence towards the external regulation of opioid prescription. There was a sense that regulation limited professional autonomy and that there should be freedom to prescribe. Some felt that regulation could lead to mistrust and hostility. Others felt that opioid agreements could help to open up honest discussion. Others used them to justify difficult or unpopular decisions. In view of the rise of opioid prescription and recent guidance, further research to explore HCPs’ experience and view of guidelines would be useful. Although we did not set out to explore the experience of prescribing opioids for chronic non-malignant pain, the findings indicate that opioid prescription is an important facet of the HCP experience. In qualitative research methodologies, unexpected findings can demonstrate that the reviewers have not been constrained by a priori concepts. Research to explore patients’ experience of deciding to take opioids for chronic pain is also timely. This would help us to understand the motivations and experiences of those with chronic pain and the HCPs trying to manage that pain.
Film outputs from qualitative research
We produced a film output to present themes from this QES. Findings from a previous meta-ethnography of patients’ experience of living with chronic pain have received > 29,000 views. YouTube comments suggest that it resonates with experience and that watching the film can make people think. The film has also been utilised in pain management education. 220 Qualitative research aims to understand a variety of perspectives and it can be challenging to demonstrate specific impacts on health care. Its value includes encouraging us to think outside our own experience and challenge our values and practices. 10 Parsons and colleagues236 argue that the impact of visual representations of qualitative research might be a ‘subtle shift in viewers’ perspectives’. Visual media lend themselves to an interactive, or dialectic, style of learning,237–245 which can evoke, provoke and stimulate ideas. 239 They can be powerful because they facilitate emotional engagement beyond that from reading reports. 236,246 Performative methods have been used in clinical education to facilitate learning through dialogue246–249 and to develop empathetic understanding. 241,242,250,251 Through film, viewers can access different perspectives in a safe environment and explore their own clinical practice. Although there are diverse ways of knowing,252 evidence-based medicine has a strong strand of objective modes of knowledge, or episteme. Greenhalgh253 invites us to challenge accepted ways of knowing and incorporate other forms of knowledge, knowledge that can be conceptualised as a dynamic process occurring at the interface between ideas and audience. Future research to explore the impact of this film on relevant stakeholders would help us to understand the impact of qualitative research films on health-care experience.
Methodological issues
Are we constrained by a priori concepts?
The findings of qualitative research will inevitably be the authors’ interpretation. It is impossible to conceptualise, or think, without existing categories in mind, and researchers will always bring existing ideas and points of view into their thinking and analysis. This should not be seen as a weakness in qualitative methodologies; on the contrary, useful qualitative analysis hinges on utilising existing concepts. This resonates with Blumer’s sensitising rather than definitive concepts: ‘definitive concepts provide prescriptions of what to see, sensitising concepts merely suggest directions along which to look’ (p. 7). 254 It is more useful to consider qualitative analysis not as a linear, but as a dialectic process in which tension between existing and new concepts can create innovative ways of thinking. 255 Researchers contemplate their data with an open mind but not an empty head. 256 Existing concepts become a limitation only if you are reluctant to change them. This is why it is necessary to collaboratively challenge developing concepts in a team environment in which reviewers feel safe to challenge each other. The strength of our team was that members felt free to agree, disagree or change their mind within the safety of the group.
How much should we search for?
Campbell and colleagues,27 in their meta-ethnographies of 25 and 37 studies, suggest that ‘40 papers is realistic [in order] . . . to maintain sufficient familiarity’. Toye and colleagues28 suggest that it is possible to include a larger number of studies in reviews. The size of a QES will ultimately depend on the aims and resources available (both financial and published). Researchers and funders should consider whether or not an exhaustive search of the literature will add value. A growing volume of published qualitative research means that there will inevitably be an increase in the potential number of studies for qualitative syntheses. Reviewers therefore need to consider what they include. However, there are issues to consider when deciding what not to include. Fundamentally, how do we determine which are the most valuable studies?
We made the decision to systematically search for, and include, all papers that we felt were ‘good enough’. Some qualitative researchers suggest a more targeted approach to sampling data. For example, you could stop searching for new data when ‘theoretical saturation’ is reached (i.e. when collecting additional data seems to add no more insight). 41 This is more comparable with the sampling strategies commonly used in qualitative research. One option might be to start your search with a single database and expand as analysis proceeds. 23 However, there are some important issues to consider when deciding what to include or exclude from QES. Importantly, reviewers do not necessarily find the conceptually rich papers first. This means that reviewers may need to read and consider several ‘thin’ studies before finding rich and key concepts. Sometimes gravitational concepts develop from a small number of studies; yet at other times it may take a larger number. We also need to consider recent development that aims to evaluate confidence in QES, specifically GRADE-CERQual for determining confidence in reviews. GRADE-CERQual considers adequacy of data (overall determination of the degree of richness and quantity of data supporting a review finding) and coherence (whether or not the finding is well grounded in the primary studies and whether or not reviewers have considered variations across studies), as important determinants of confidence. We feel that a systematic exploration of the available research can contribute to confidence in findings. It is also important to consider that if review findings are to be used to influence policy and practice we may be more confident in the adequacy of data if the finding is drawn from a large pool. Although it can be time-consuming, it can add confidence if we systematically search for all relevant studies.
How can we determine confidence in review findings?
There have been calls to standardise reporting of qualitative syntheses,29,257,258 but there is currently no agreed way of making an assessment of confidence for QES. As qualitative analysis is underpinned by an interpretive framework, efforts to regulate it will always be complicated by varying opinions vis-à-vis quality. 34,36 Establishing confidence in the output of qualitative research synthesis (ConQual)259 and GRADE-CERQual37 offer overlapping but distinct approaches for determining confidence in QES.
‘Methodological limitations’ (‘dependability’)
Both ConQual259 and GRADE-CERQual37 consider the quality of included primary studies to be an important determinant of confidence in a particular review finding. GRADE-CERQual refers to this as methodological limitations and ConQual refers to this as dependability. However, determining quality in qualitative research is complex and unresolved. Although there are a growing number of frameworks for appraising the quality of qualitative research,27,34 and a growing number of reviewers appraising primary studies,24 a significant number of qualitative reviewers take a legitimate choice not to appraise for the purpose of QES. 27 This choice does not imply low quality. Indeed, although quality appraisal might help us to recognise methodological flaws, it does not necessarily help us to appraise the value of findings. 36
We found that the CASP was a useful way of framing discussions on quality and papers that we considered to be ‘key’ did gain higher CASP scores. However, this threshold was not clear-cut and it is unlikely to be useful as a threshold score for determining inclusion in and exclusion from qualitative syntheses. There was a much higher level of agreement on CASP score35 than in our previous study. 8 This may be because the reviewers have developed their view on what constitutes quality over the process of working together for several years. ‘Satisfactory’ papers all scored ≥ 20 on CASP, similar to a previous study in which satisfactory papers scored ≥ 19. However, two studies scoring > 20 were still excluded as ‘fatally flawed’. The reviewers found it challenging to decipher the concepts in these studies.
We also aimed to test the usefulness of a list of themes developed from a qualitative study embedded in a previous meta-ethnography funded by the HSDR programme (see Table 2). 36 Unlike CASP, these themes were developed specifically for meta-ethnography. Findings from this appraisal confirmed that qualitative studies are very likely to report their rationale, aim and sample adequately. However, there are areas for improvement, specifically:
-
Qualitative authors do not always give readers adequate insight into the researcher’s perspective.
-
They do not always report how they have challenged their own interpretation.
-
They do not always use appropriate exemplification to show that their interpretation has come from the data.
-
They do not always articulate their concepts with adequate clarity.
Fundamental to conceptual qualitative syntheses is the capacity of included studies to make the reviewers think and develop concepts. Studies reported as having ‘changed the thinking’ of at least one reviewer tended to score higher. Appraisal comments (see Appendix 1) suggest that even if it did not change thinking, the primary studies did encourage reviewers to think.
Finally, although reviewers agreed that if studies were ‘key’, ‘fatally flawed’ or ‘irrelevant’,23 the large majority of studies were judged to be ‘satisfactory’. This confirms findings from our previous study. 8 It would be useful to find ways in which we can be more discerning about what to include. We felt that the CASP question 10 (how valuable is this study?) had face value in providing a particular reviewer’s appraisal of value. Further research to explore ways of deciphering the potential value of particular qualitative findings would be useful, particularly in the context of research proliferation.
Reviewers and funders need to consider why we are spending a lot of time appraising studies and whether or not this has any impact on review findings. Does it make any significant difference if we include studies with a poor methodological report27,260 (particularly if our unit of analysis is a concept)? Fundamentally, some concepts will exert a strong influence on concept development and other concepts will not. The reasons for this are complex and will depend on factors that include a priori knowledge of the reviewer and the persuasiveness of the written primary findings. We think that, for the purposes of determining confidence of review findings for GRADE-CERQual, an appraisal of either ‘satisfactory’ or ‘not satisfactory’ would therefore be fit for purpose. QES is a time-consuming process and time might be better spent abstracting concepts rather than pettifogging over fine details of appraisal, particularly when there is no agreed method for determining what good quality is.
What is a satisfactory study for qualitative evidence synthesis? Suggested themes for future research
For future QES, the questions shown in Table 14 might help reviewers to consider whether or not a study is satisfactory for inclusion into meta-ethnographies. This list of questions is intended as food for thought, rather than as an appraisal checklist. Future research could explore the utility of these questions for conceptual QES. Importantly, reviewers need to consider whether or not their chosen appraisal criteria have any real impact on their decision to include studies. Although we agree that it is vital to exclude studies that are methodologically fatally flawed as this will have a direct impact on the truth claims (e.g. if the study is unethical), we would argue that as long as studies are satisfactory, then appraisal for conceptual reviews hinges on being able to extract clear concepts. Studies that lack conceptual insight will not influence analytical decisions and, therefore, are unlikely to have an impact on conceptual development; they will therefore do no harm.
| CASP question | Answer |
|---|---|
| Was there a clear statement of the rationale and aims?a | Yes/no |
| Was the research design appropriate to address the aims of the research?a | Yes/no |
| Was the recruitment strategy appropriate to the aims of the research?a | Yes/no |
| Has the relationship between researcher and participants been adequately considered?a | Yes/no |
| Has the researcher adequately challenged their own interpretation? | Yes/no |
| Does the researcher’s interpretation come from the original data? | Yes/no |
| Can you identify the concepts in this study (or do you find yourself recoding)? | Yes/no |
| Have the findings made you think? | Yes/no |
| Is the research potentially valuable?a | Yes/no |
Relevance
We agree that studies included in a review should be relevant to the topic under review. However, studies that we rated as ’partially’, ’indirectly’ or ’uncertainly’ relevant also contained useful concepts (i.e. although a study may be partially relevant, it may contain some concepts relevant to the topic under exploration). We think that for the purposes of determining confidence of review findings for GRADE-CERQual reviewers should include only concepts that are relevant to the topic, but these concepts may be present in studies that are partially or indirectly relevant.
Adequacy
Adequacy regards the depth of data supporting each finding. Lewin and colleagues37 define it as ‘the ‘overall determination of the degree of richness and quantity of data supporting a review finding’. However, how can reviewers/readers determine the degree of richness or quantity of data that is adequate to support a finding? It may be useful to conceptualise adequacy in terms of gravity and gravitational pull. One could argue that as data contribute to the development of a concept, they begin to create their own gravitational pull that moulds them into shape. At this point the number of data is adequate. Concepts develop as part of a dialectic process and it would therefore be impossible to define the point at which the concept is pulled into a coherent shape. Thus, determination of adequacy is complex and subjective. Qualitative researchers should demonstrate that their interpretations have gravitational pull. This can be challenging as an appraisal of gravitational pull is qualitative. However, it can help the reader if reviewers provide clear information about the source of their concepts, along with clear and appropriate exemplification of this concept. If the reader feels that the narrative exemplar does not illuminate the reviewers’ concept then this will decrease the gravity of that concept. This resonates with Munn and colleagues’259 concept of ‘credibility’ as the ‘the congruency between the author’s interpretation and the supporting data’ (p. 4259).
It also important to consider that a single concept can exert a strong gravitational pull and that gravity has a qualitative component. We advocate caution regarding making truth claims purely on sheer weight of data; the tale of the Emperor’s New Clothes has taught us the validity of a small voice. Single concepts can stimulate a new way of thinking or highlight possible areas in which research is timely. We need to consider our own views about the purpose of qualitative research:
-
Do we aim to stimulate thinking and understanding through qualitative research?
-
Do we aim to increase our understanding of different experiences of living in the world?
-
Do we aim to develop theories that underpin complex processes?
In all these cases, size may not matter. Indeed, we would want our syntheses to include some unique concepts that challenge our thinking. However, qualitative reviewers cannot ignore the issue of size; they face the same questions as primary researchers grappling with the questions – how many qualitative interviews is enough?261 A large review can appear, and may arguably be, more ‘adequate’ than a small review. If 40 studies support a concept, then this is in some way different from only five studies supporting it. If the aim is to stimulate ideas and contribute to a particular field of enquiry, then ‘adequacy’ may not be our only concern. If our aim is to develop robust gravitational concepts, we should consider both the economy and diseconomy of scale. For our purposes, we have gained confidence from including a large body of qualitative studies. We cannot know whether or not these findings would be qualitatively different had we included fewer studies. For the purposes of determining confidence of review findings for GRADE-CERQual reviewers, it is useful to provide a tally of the concepts that support each finding so that the reader can make their own assessment about adequacy for purpose. The power of concepts to make us think, however, is not based on quantity of data included. However, qualitative health researchers live in a research culture that values numbers and economies of scale and there is a real danger that potential stakeholders continue to undervalue the contribution that qualitative research can make towards improving people’s experiences of health care.
Coherence
Coherence considers the consistency (and difference) across studies. We agree that it is important to demonstrate to readers that concepts have not been cherry-picked and that it is therefore important to present concepts that do not fit the analysis. However, we do not feel that inconsistency necessarily negates confidence in a particular finding. An insightful concept might appear in a single study or it may represent a point of view that is untapped in other studies. We agree that it is useful to provide information about consistency for the same reasons that it is important to provide information about adequacy; readers should know where the concepts come from. We think that for the purposes of determining confidence of review findings for GRADE-CERQual it may be useful to provide a tally of individual studies supporting the finding and, importantly, to present concepts that do not fit the conceptual analysis. However, as we have said:
-
Qualitative research does not aim to be representative or true in a positivist sense, but aims to generate useful ideas.
-
The tale of the Emperor’s New Clothes has taught us the validity of a small voice.
It is important to consider these issues when utilising tools such as ConQual259 and GRADE-CERQual37 as well as reporting guidelines, such as the imminent meta-ethnography reporting guidelines (eMERGe; www.stir.ac.uk/health-sciences-sport/research/groups/emerge/; accessed 22 January 2018). Although these tools can definitely encourage reviewers and readers to think, the issue of quality in qualitative research is complex and these tools cannot guarantee confidence in findings. Thus, access to a GRADE-CERQual chart in an appendix does not remove the need for intellectual scrutiny on the part of reviewer or reader. Indeed, the tools were not intended to encourage a tick-box exercise, but to allow the reviewers and readers to consider issues of quality and utility. We need to consider that readers working outside an interpretive methodological tradition might not be familiar with the complexity of quality in qualitative research. For example, although both ConQual259 and GRADE-CERQual37 advocate quality appraisal, we cannot ignore the fact that a significant number of reputable qualitative reviewers have pro-actively chosen not to appraise. 27 This is not surprising in the light of the fact that there is no agreed means of determining quality. We need to consider the dangers of yielding to methodological monopolies and continue to challenge our ideas about what is good.
Credibility
Munn and colleagues259 propose an additional criterion, credibility, for establishing confidence in the findings of qualitative research syntheses. Credibility is a global evaluation of ‘fit’ (‘equivocal’, ‘unequivocal’ or ‘unsupported’) between the primary data and the reviewers’ interpretations as demonstrated by adequate exemplars. This resonates with concept–indicator fit. 262 We feel that concept–indicator fit underpins good-quality qualitative research and would therefore consider it fundamental to a quality assessment. 36 However, deciding whether or not the author has provided ‘an illustration that is beyond reasonable doubt’36 is the reader’s personal judgement.
Conceptual insight
Conceptual insight is fundamental to meta-ethnographic aims and, therefore, primary authors need to provide an adequate and clear description of their concept. In addition to clarity, a concept should allow reviewers to think with it. Neither conceptual clarity nor strength is considered in either GRADE-CERQual or ConQual. There were 18 studies11,150,155,160,162,169,173,178,181,187,188,192,196,197,202,206,208,219 that provided inadequate conceptualisation in at least one finding (see Appendix 2) and one study188 from which we felt unable to include a single concept into our analysis.
Overall confidence in review
This was a large QES and we rated our confidence as high when more than half of the reviews (n ≥ 39) supported the finding. However, there is no agreed way to determine how many data provide sufficient gravity to support the validity of a concept. One concept may be weightier than 10 other concepts. Attempts to rate overall confidence raise important issues for reviewers. Importantly, are we in danger of slipping into a positivist fallacy that qualitative research can help us to find ‘the’ right answer. Qualitative research encourages us to think outside our own box and develop a questioning approach that can be utilised in policy and practice decision-making. It cannot provide the answer, but can provide concepts to think with and encourage us to see things from a different vantage point and to challenge our thinking and practice.
Chapter 4 Implications for education, policy and practice
We aimed to undertake a QES using the methods of meta-ethnography reported by Toye and colleagues8 to increase our understanding of what it is like for HCPs to provide health care to people with chronic non-malignant pain and thus to inform improvements in the experience and quality of health care. Patients report dissatisfaction with their HCP interaction13 and the relationship between patients and HCPs can have a significant effect on health outcomes. Already we know that, from the patient perspective, the experience of health care can be adversarial. 8 It seems likely that HCPs’ responses can have an impact on quality of care. Thus, understanding the experience of providing health care to people with chronic non-malignant pain from the perspective of the HCP can have important implications for delivery of health care, decision-making and health-care quality.
Our findings can help us to consider the experience of health care from both perspectives and understand tensions that may contribute to this adversarial experience. Specifically:
-
The findings indicate an underlying scepticism that might contribute to an adversarial relationship between HCP and patient. Believing patients’ experiences may provide a more secure foundation for an effective therapeutic relationship.
-
The findings indicate a dualistic approach whereby HCPs make a sudden shift from biomedical to biopsychosocial explanations for pain after exhausting attempts to decipher a diagnosis. This abrupt shift may exacerbate a sense of loss of credibility for patients.
-
The findings indicate that some HCPs engage in judgements about what is real or not real, which are underpinned by a cultural duality of real (biomedical) and not real (psychosocial).
-
The findings suggest that an embodied, rather than dualistic, biopsychosocial model that focuses on the personal meaning of pain from the outset might help to lessen the adversarial experience and also reduce the HCP’s sense of failure.
-
The findings have clinical and educational implications. How can we enable HCPs to manage the tensions that underpin the experience of providing health care to people with chronic non-malignant pain? How do we recognise and support the complexity of skills and emotional cost of providing health care to people with chronic non-malignant pain?
-
The findings highlight the benefits of reciprocity, mutuality and collaboration between HCPs and the benefits of being able to break down or cross professional boundaries and hierarchies.
-
The findings highlight a need to consider the emotional costs to HCPs of treating patients with chronic pain.
We invite HCPs to use our ‘mixing console’ to help them to think about their encounters with patients. This console may be transferable to other chronic conditions.
Chapter 5 Recommendations for research
-
Future research to explore HCPs’ experiences with chronic non-malignant pain in diverse ethnic groups, gender-specific contexts and in older people living in the community would make a valuable contribution to the evidence base on people’s experiences of living with chronic pain.
-
Future research to explore the application and usefulness of our conceptual model in education and practice would add value to this research.
-
Future research to explore the application and usefulness of our film output in education and practice would add value to this research.
-
Future research to explore the value added to QES by quality appraisal and the relevance of GRADE-CERQual for evaluating confidence in meta-ethnography findings would make a useful contribution to QES methodology.
-
Further research on how QES can be used to inform commissioning, policy and practice would contribute to knowledge on effective dissemination of qualitative research.
Acknowledgements
We would like to thank:
-
the National Institute for Health Research HSDR programme for funding this study
-
the authors of the included qualitative studies
-
the HCPs who shared their stories for the included studies
-
Cathy Jenkins for her contribution to the visualisation of our conceptual model
-
our study advisory group and Meredith Newman for chairing this group of patients and HCPs
-
our anonymous reviewers whose feedback strengthened the final report.
Contributions of authors
Fran Toye (Dr, Qualitative Researcher) made a substantial contribution to the design, acquisition, analysis and interpretation of data, drafted the first, subsequent and final versions of the report and designed the visual outputs.
Kate Seers (Professor, Qualitative Researcher) made a substantial contribution to the design, acquisition, analysis and interpretation of data, revised all versions of the report for important intellectual content and approved the final version.
Karen Barker (Associate Professor, Qualitative Researcher) made a substantial contribution to the design, acquisition, analysis and interpretation of data, revised all versions of the report for important intellectual content and approved the final version.
Publications
Toye F, Seers K, Barker KL. Meta-ethnography to understand healthcare professionals’ experience of treating adults with chronic non-malignant pain. BMJ Open 2017;7:e018411.
Toye F, Seers K, Tierney S, Barker K. A qualitative evidence synthesis to explore healthcare professionals’ experience of prescribing opioids to adults with chronic non-malignant pain. BMC Fam Pract 2017;18:94.
Data sharing statement
Requests for access to data should be addressed to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Fayaz A, Croft P, Langford RM, Donaldson LJ, Jones GT. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010364.
- Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287-333. https://doi.org/10.1016/j.ejpain.2005.06.009.
- Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet 1999;354:1248-52. https://doi.org/10.1016/S0140-6736(99)03057-3.
- König HH, Bernert S, Angermeyer MC, Matschinger H, Martinez M, Vilagut G, et al. Comparison of population health status in six European countries: results of a representative survey using the EQ-5D questionnaire. Med Care 2009;47:255-61. https://doi.org/10.1097/MLR.0b013e318184759e.
- Covinsky KE, Lindquist K, Dunlop DD, Yelin E. Pain, functional limitations, and aging. J Am Geriatr Soc 2009;57:1556-61. https://doi.org/10.1111/j.1532-5415.2009.02388.x.
- Croft P, Peat G, Van-der-Windt D. Primary care research and musculoskeletal medicine. Prim Health Care Res Dev 2010;11:4-16. https://doi.org/10.1017/S1463423609990272.
- Smith BH, Elliott AM, Chambers WA, Smith WC, Hannaford PC, Penny K. The impact of chronic pain in the community. Fam Pract 2001;18:292-9. https://doi.org/10.1093/fampra/18.3.292.
- Toye F, Seers K, Allcock N, Briggs M, Carr E, Andrews J, et al. A meta-ethnography of patients’ experiences of chronic non-malignant musculoskeletal pain. Health Serv Deliv Res 2013;1.
- Merskey H, Bogduk N. Classification of Chronic Pain. Definitions of Chronic Pain Syndromes and Definition of Pain Terms. Seattle, WA: International Association for the Study of Pain; 1994.
- Toye F, Jenkins S. ‘It makes you think’ – exploring the impact of qualitative films on pain clinicians. Br J Pain 2015;9:65-9. https://doi.org/10.1177/2049463714549776.
- Allegretti A, Borkan J, Reis S, Griffiths F. Paired interviews of shared experiences around chronic low back pain: classic mismatch between patients and their doctors. Fam Pract 2010;27:676-83. https://doi.org/10.1093/fampra/cmq063.
- Breen A, Austin H, Campion-Smith C, Carr E, Mann E. ‘You feel so hopeless’: a qualitative study of GP management of acute back pain. Eur J Pain 2007;11:21-9. https://doi.org/10.1016/j.ejpain.2005.12.006.
- Dwamena F, Holmes-Rovner M, Gaulden C, Jorgenson S, Sadigh G, Sikorskii A, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012;12. https://doi.org/10.1002/14651858.CD003267.pub2.
- Balint M. The doctor, his patient, and the illness. Lancet 1955;268:683-8. https://doi.org/10.1016/S0140-6736(55)91061-8.
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med 2002;51:1087-110. https://doi.org/10.1016/S0277-9536(00)00098-8.
- Sandelowski M, Barrosso J. Handbook for Synthesising Qualitative Research. New York, NY: Springer Publishing; 2007.
- Noyes J, Popay J, Pearson A, Hannes K, Booth A, Higgins J, et al. Cochrane Handbook for Systematic Reviews. Chichester: John Wiley & Sons; 2008.
- Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy 2002;7:209-15. https://doi.org/10.1258/135581902320432732.
- Campbell R, Pound P, Pope C, Britten N, Pill R, Morgan M, et al. Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Soc Sci Med 2003;56:671-84. https://doi.org/10.1016/S0277-9536(02)00064-3.
- Malpass A, Shaw A, Sharp D, Walter F, Feder G, Ridd M, et al. ‘Medication career’ or ‘moral career’? The two sides of managing anti-depressants: a meta-ethnography of patients experience of antidepressants. Soc Sci Med 2009;68:154-68. https://doi.org/10.1016/j.socscimed.2008.09.068.
- Toye F, Seers K, Barker K. A meta-ethnography of patients’ experiences of chronic pelvic pain: struggling to construct chronic pelvic pain as ‘real’. J Adv Nurs 2014;70:2713-27. https://doi.org/10.1111/jan.12485.
- Dixon-Woods M, Booth A, Sutton A. Synthesizing qualitative research: a review of published reports. Qual Res 2007;7:375-422. https://doi.org/10.1177/1468794107078517.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative research evidence: a review of possible methods. J Health Serv Res Policy 2005;10:45-53. https://doi.org/10.1177/135581960501000110.
- Hannes K, Macaitis K. A move to more systematic and transparent approaches in qualitative evidence synthesis: update on a review of published papers. Qual Res 2012;12:402-42. https://doi.org/10.1177/1468794111432992.
- Barnett-Page E, Thomas J. Methods for Synthesis of Qualitative Research: A Critical Review. Economic and Social Research Council Research Methods 2009 n.d. http://eprints.ncrm.ac.uk/690/1/0109%2520Qualitative%2520synthesis%2520methods%2520paper%2520NCRM.pdf (accessed 10 August 2017).
- Noblit G, Hare R. Meta-Ethnography: Synthesising Qualitative Studies. Newbury Park, CA: Sage Publications; 1988.
- Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess 2011;15. https://doi.org/10.3310/hta15430.
- Toye F, Seers K, Allcock N, Briggs M, Carr E, Barker K. Meta-ethnography 25 years on: challenges and insights for synthesising a large number of qualitative studies. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-80.
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12. https://doi.org/10.1186/1471-2288-12-181.
- Wong SS, Wilczynski NL, Haynes RB. on behalf of Hedges Team . Developing optimal search strategies for detecting clinically relevant qualitative studies in MEDLINE. Stud Health Technol Inform 2004;11:311-16.
- Wilczynski NL, Marks S, Haynes RB. Search strategies for identifying qualitative studies in CINAHL. Qual Health Res 2007;17:705-10. https://doi.org/10.1177/1049732306294515.
- McKibbon KA, Wilczynski NL, Haynes RB. Developing optimal search strategies for retrieving qualitative studies in PsycINFO. Eval Health Prof 2006;29:440-54. https://doi.org/10.1177/0163278706293400.
- Walters LA, Wilczynski NL, Haynes RB. on behalf of Hedges Team . Developing optimal search strategies for retrieving clinically relevant qualitative studies in EMBASE. Qual Health Res 2006;16:162-8. https://doi.org/10.1177/1049732305284027.
- Dixon-Woods M, Sutton A, Shaw R, Miller T, Smith J, Young B, et al. Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. J Health Serv Res Policy 2007;12:42-7. https://doi.org/10.1258/135581907779497486.
- Critical Appraisal Skills Programme . Critical Appraisal Skills Programme: Making Sense of Evidence About Clinical Effectiveness: 10 Questions to Help You Make Sense of Qualitative Research n.d. http://docs.wixstatic.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf (accessed 10 August 2017).
- Toye F, Seers K, Allcock N, Briggs M, Carr E, Andrews J, et al. ‘Trying to pin down jelly’ – exploring intuitive processes in quality assessment for meta-ethnography. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-46.
- Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLOS Med 2016;12. https://doi.org/10.1371/journal.pmed.
- Pope C, Mays N, Popay J. Synthesizing Qualitative and Quantitative Health Research: A Guide to Methods. Berkshire: Open University Press; 2007.
- Schütz A. Collected Papers 1. The Hague: Martinus Nijhoff; 1962.
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-21.
- Charmaz K. Constructing Grounded Theory. Thousand Oaks, CA: Sage Publications; 2006.
- Toye F, Seers K, Barker KL. Meta-ethnography to understand healthcare professionals’ experience of treating adults with chronic non-malignant pain. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-018411.
- Toye F, Seers K, Tierney S, Barker KL. A qualitative evidence synthesis to explore healthcare professionals’ experience of prescribing opioids to adults with chronic non-malignant pain. BMC Fam Pract 2017;18. https://doi.org/10.1186/s12875-017-0663-8.
- Jeffrey E, Foster E. A qualitative investigation of physical therapists’ experiences and feelings of managing patients with nonspecific low back pain. Phys Ther 2012;92. https://doi.org/10.2522/ptj.20100416.
- Skelton AM, Murphy EA, Murphy RJ, O’Dowd TC. Patient education for low back pain in general practice. Patient Educ Couns 1995;25. https://doi.org/10.1016/0738-3991(95)00807-C.
- Skelton AM, Murphy EA, Murphy RJ, O’Dowd TC. General practitioner perceptions of low back pain patients. Family Pract 1995;12. https://doi.org/10.1093/fampra/12.1.44.
- Elder N, Ricer R, Tobias B. How respected family physicians manage difficult patient encounters. J Am Board Fam Med 2006;19. https://doi.org/10.3122/jabfm.19.6.533.
- Carr EC, Worswick L, Wilcock PM, Campion-Smith C, Hettinga D. Improving services for back pain: putting the patient at the centre of interprofessional education. Qual Prim Care 2012;20:345-53.
- Karstens S, Joos S, Hill JC, Krug K, Szecsenyi J, Steinhäuser J. General Practitioners views of implementing a stratified treatment approach for low back pain in Germany: a qualitative study. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0136119.
- Roberts C, Adebajo AO, Long S. Improving the quality of care of musculoskeletal conditions in primary care. Rheumatology 2002;41:503-8. https://doi.org/10.1093/rheumatology/41.5.503.
- May C, Allison G, Chapple A, Chew-Graham C, Dixon C, Gask L, et al. Framing the doctor–patient relationship in chronic illness: a comparative study of general practitioners’ accounts. Sociol Health Illn 2004;26. https://doi.org/10.1111/j.1467-9566.2004.00384.x.
- McIntosh A, Shaw FM. Barriers to patient information provision in primary care: patients’ and general practitioners’ experiences and expectations of information for low back pain. Health Expect 2003;6. https://doi.org/10.1046/j.1369-6513.2003.00197.x.
- Miller S, Pinnington A. Straightforward consultation or complicated condition? General practitioners’ perceptions of low back pain. Eur J Gen Pract 2003;9. https://doi.org/10.3109/13814780309160385.
- Rogers WA. Whose autonomy? Which choice? A study of GPs’ attitudes towards patient autonomy in the management of low back pain. Fam Pract 2002;19:140-5. https://doi.org/10.1093/fampra/19.2.140.
- Sanders T, Foster NE, Ong BN. Perceptions of general practitioners towards the use of a new system for treating back pain: a qualitative interview study. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-49.
- Barker KL, Reid M, Lowe CJM. Divided by a lack of common language? A qualitative study exploring the use of language by health professionals treating back pain. BMC Musculoskelet Disord 2009;10. https://doi.org/10.1186/1471-2474-10-123.
- Billis V, McCarthy J, Stathopoulos I, Kapreli E, Pantzou P, Oldham A. The clinical and cultural factors in classifying low back pain patients within Greece: a qualitative exploration of Greek health professionals. J Eval Clin Pract 2007;13. https://doi.org/10.1111/j.1365-2753.2006.00698.x.
- Magnusson JE, Fennell JA. Understanding the role of culture in pain: Māori practitioner perspectives relating to the experience of pain. N Z Med J 2011;124:41-5.
- May S, Greasley A, Reeve S, Withers S. Expert therapists use specific clinical reasoning processes in the assessment and management of patients with shoulder pain: a qualitative study. Aust J Physiother 2008;54:261-6. https://doi.org/10.1016/S0004-9514(08)70005-9.
- McDonald DD. Trialing to pain control: a grounded theory. Res Nurs Health 2014;37:107-16. https://doi.org/10.1002/nur.21584.
- Montali L, Monica C, Riva P, Cipriani R. Conflicting representations of pain: a qualitative analysis of health care professionals’ discourse. Pain Med 2011;12:1585-93. https://doi.org/10.1111/j.1526-4637.2011.01252.x.
- Ong BN, Hooper H. Comparing clinical and lay accounts of the diagnosis and treatment of back pain. Sociol Health Illn 2006;28:203-22. https://doi.org/10.1111/j.1467-9566.2006.00488.x.
- Ong BN, Hooper H. Involving users in low back pain research. Health Expect 2003;6:332-41. https://doi.org/10.1046/j.1369-7625.2003.00230.x.
- Pincus T, Vogel S, Breen A, Foster N, Underwood M. Persistent back pain – why do physical therapy clinicians continue treatment? A mixed methods study of chiropractors, osteopaths and physiotherapists. Eur J Pain 2006;10:67-76. https://doi.org/10.1016/j.ejpain.2005.01.008.
- Vegni E, Mauri E, Moja EA. Stories from doctors of patients with pain. A qualitative research on the physicians’ perspective. Support Care Cancer 2005;13:18-25. https://doi.org/10.1007/s00520-004-0714-2.
- Askew R, Kibelstis C, Overbaugh S, Walker S, Nixon-Cave K, Shepard KF. Physical therapists’ perception of patients’ pain and its effect on management. Physiother Res Int 1998;3:37-58. https://doi.org/10.1002/pri.121.
- Cruz EB, Moore A, Cross V. Clinical reasoning and patient-centred care in musculoskeletal physiotherapy in Portugal – a qualitative study. Man Ther 2012;17:246-50. https://doi.org/10.1016/j.math.2012.02.007.
- Dean G, Smith A, Payne S, Weinman J. Managing time: an interpretative phenomenological analysis of patients’ and physiotherapists’ perceptions of adherence to therapeutic exercise for low back pain. Disabil Rehabil 2005;27. https://doi.org/10.1080/0963820500030449.
- Perreault K, Dionne CE, Rossignol M, Morin D. Interprofessional practices of physiotherapists working with adults with low back pain in Quebec’s private sector: results of a qualitative study. BMC Musculoskelet Disord 2014;15. https://doi.org/10.1186/1471-2474-15-160.
- Sanders T, Foster E, Bishop A, Ong BN. Biopsychosocial care and the physiotherapy encounter: physiotherapists’ accounts of back pain consultations. BMC Musculoskelet Disord 2013;14. https://doi.org/10.1186/1471-2474-14-65.
- Smart K, Doody C. The clinical reasoning of pain by experienced musculoskeletal physiotherapists. Man Ther 2007;12. https://doi.org/10.1016/j.math.2006.02.006.
- Francke AL, Lemmens AB, Abu-Saad HH, Grypdonck M. Nurses’ perceptions of factors influencing the use of a pain program. J Pain Symptom Manage 1997;14:300-10. https://doi.org/10.1016/S0885-3924(97)00240-6.
- Larsson H, Blomqvist K. From a diagnostic and particular approach to a person-centred approach: a development project. J Clin Nurs 2015;24:465-74. https://doi.org/10.1111/jocn.12628.
- Parke B. Gerontological nurses’ ways of knowing. Realizing the presence of pain in cognitively impaired older adults. J Gerontol Nurs 1998;24:21-8. https://doi.org/10.3928/0098-9134-19980601-08.
- Droes NS. Role of the nurse practitioner in managing patients with pain. Internet J Adv Nurs Pract 2004;6.
- Schers H, Wensing M, Huijsmans Z, van Tulder M, Grol R. Implementation barriers for general practice guidelines on low back pain a qualitative study. Spine 2001;26:E348-53. https://doi.org/10.1097/00007632-200108010-00013.
- Bussieres AE, Patey AM, Francis JJ, Sales AE, Grimshaw JM, Canada PT, et al. Identifying factors likely to influence compliance with diagnostic imaging guideline recommendations for spine disorders among chiropractors in North America: a focus group study using the Theoretical Domains Framework. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-82.
- Ottenheijm RP, Hesselmans NJ, Kemper A, Moser A, de Bie RA, Dinant GJ, et al. GPs’ perspectives on the diagnostic work-up in patients with shoulder pain: a qualitative study. J Eval Clin Pract 2014;20:239-45. https://doi.org/10.1111/jep.12114.
- Peiris D, Williams C, Holbrook R, Lindner R, Reeve J, Das A, et al. A Web-based clinical decision support tool for primary health care management of back pain: development and mixed methods evaluation. J Med Internet Res 2014;16. https://doi.org/10.2196/resprot.3071.
- Stenner K, Courtenay M. The role of inter-professional relationships and support for nurse prescribing in acute and chronic pain. J Adv Nurs 2008;63:276-83. https://doi.org/10.1111/j.1365-2648.2008.04707.x.
- Stenner K, Courtenay M. Benefits of nurse prescribing for patients in pain: nurses’ views. J Adv Nurs 2008;63:27-35. https://doi.org/10.1111/j.1365-2648.2008.04644.x.
- Bjorner T, Kjolsrod L. How GPs understand patients’ stories: a qualitative study of benzodiazepine and minor opiate prescribing in Norway. Eur J Gen Pract 2002;8:25-30. https://doi.org/10.3109/13814780209160825.
- Strand LI, Kvale A, Raheim M, Ljunggren AE. Do Norwegian manual therapists provide management for patients with acute low back pain in accordance with clinical guidelines?. Man Ther 2005;10:38-43. https://doi.org/10.1016/j.math.2004.07.003.
- Haskins R, Osmotherly G, Southgate E, Rivett A. Physiotherapists’ knowledge, attitudes and practices regarding clinical prediction rules for low back pain. Man Ther 2014;19. https://doi.org/10.1016/j.math.2013.09.005.
- Josephson I, Bulow P, Hedberg B. Physiotherapists’ clinical reasoning about patients with non-specific low back pain, as described by the International Classification of Functioning, Disability and Health. Disabil Rehabil 2011;33:2217-28. https://doi.org/10.3109/09638288.2011.563819.
- Josephson I, Hedberg B, Bülow P. Problem-solving in physiotherapy – physiotherapists’ talk about encounters with patients with non-specific low back pain. Disabil Rehabil 2013;35:668-77. https://doi.org/10.3109/09638288.2012.705221.
- Miller WL, Yanoshik MK, Crabtree BF, Reymond WK. Patients, family physicians, and pain: visions from interview narratives. Fam Med 1994;26:179-84.
- McGee SJ, Kaylor BD, Emmott H, Christopher MJ. Defining chronic pain ethics. Pain Med 2011;12:1376-84. https://doi.org/10.1111/j.1526-4637.2011.01192.x.
- Lærum E, Indahl A, Skouen JS. What is ‘the good back-consultation’? A combined qualitative and quantitative study of chronic low back pain patients’ interaction with and perceptions of consultations with specialists. J Rehabil Med 2006;38:255-63. https://doi.org/10.1080/16501970600613461.
- Rutledge N, Cantero P, Ruiz J. Managing chronic pain in low income overweight Latinos: provider perceptions. Commun Nurs Res 2013;46:639-40.
- Øien AM, Iversen S, Stensland P. Narratives of embodied experiences – therapy processes in Norwegian psychomotor physiotherapy. Adv Physiother 2007;9:31-9. https://doi.org/10.1080/14038190601152115.
- Øien AM, Råheim M, Iversen S, Steihaug S. Self-perception as embodied knowledge – changing processes for patients with chronic pain. Adv Physiother 2009;11:121-30. https://doi.org/10.1080/14038190802315073.
- Wootton IM, Wood V, Cook F. Who wants expert patient programmes for chronic mechanical spinal pain? An investigation into the value of, and recruitment to, an expert patient programme as part of the physiotherapy management of chronic spinal pain. Physiotherapy 2008;94:78-84. https://doi.org/10.1016/j.physio.2006.12.012.
- Thomson D. An ethnographic study of physiotherapists’ perceptions of their interactions with patients on a chronic pain unit. Physiother Theory Pract 2008;24:408-22. https://doi.org/10.1080/09593980802511805.
- Bullington J, Nordemar R, Nordemar K, Sjöström-Flanagan C. Meaning out of chaos: a way to understand chronic pain. Scand J Caring Sci 2003;17:325-31. https://doi.org/10.1046/j.0283-9318.2003.00244.x.
- Doran J. Experiencing wellness within illness: exploring a mindfulness-based approach to chronic back pain. Qual Health Res 2014;24:749-61. https://doi.org/10.1177/1049732314529662.
- Howarth M, Warne T, Haigh C. Pain from the inside: understanding the theoretical underpinning of person-centered care delivered by pain teams. Pain Manag Nurs 2014;15:340-8. https://doi.org/10.1016/j.pmn.2012.12.008.
- Buchbinder M, Wilbur R, McLean S, Sleath B. ‘Is there any way I can get something for my pain?’ Patient strategies for requesting analgesics. Patient Educ Couns 2015;98:137-43. https://doi.org/10.1016/j.pec.2014.10.021.
- Buijs PC, Lambeek LC, Koppenrade V, Hooftman WE, Anema JR. Can workers with chronic back pain shift from pain elimination to function restore at work? Qualitative evaluation of an innovative work related multidisciplinary programme. J Back Musculoskelet Rehabil 2009;22:65-73. https://doi.org/10.3233/BMR-2009-0215.
- Thunberg KA, Hallberg LR. The need for organizational development in pain clinics: a case study. Disabil Rehabil 2002;24:755-62. https://doi.org/10.1080/09638280210124356.
- Valjakka AL, Salantera S, Laitila A, Julkunen J, Hagelberg NM. The association between physicians’ attitudes to psychosocial aspects of low back pain and reported clinical behaviour: a complex issue. Scand J Pain 2013;4:25-30. https://doi.org/10.1016/j.sjpain.2012.08.003.
- Kotarba JA. Perceptions of death, belief systems and the process of coping with chronic pain. Soc Sci Med 1983;17:681-9. https://doi.org/10.1016/0277-9536(83)90374-X.
- Cedraschi C, Robert J, Goerg D, Perrin E, Fischer W, Vischer TL. Is chronic non-specific low back pain chronic? Definitions of a problem and problems of a definition. Br J Gen Pract 1999;49:358-62.
- Cedraschi C, Robert J, Perrin E, Fischer W, Goerg D, Vischer TL. The role of congruence between patient and therapist in chronic low back pain patients. J Manipulative Physiol Ther 1996;19:244-9.
- Sloan TJ, Walsh DA. Explanatory and diagnostic labels and perceived prognosis in chronic low back pain. Spine 2010;35:E1120-5. https://doi.org/10.1097/BRS.0b013e3181e089a9.
- Al-Shaer D, Hill PD, Anderson MA. Nurses’ knowledge and attitudes regarding pain assessment and intervention. Medsurg Nurs 2011;20:7-11.
- Ferrell B. Ethical perspectives on pain and suffering. Pain Manag Nurs 2005;6:83-90. https://doi.org/10.1016/j.pmn.2005.06.001.
- Walker JM, Akinsanya JA, Davis BD, Marcer D. The nursing management of elderly patients with pain in the community: study and recommendations. J Adv Nurs 1990;15:1154-61. https://doi.org/10.1111/j.1365-2648.1990.tb01707.x.
- Gillmore R, Hill T. Reactions to patients who complain of pain: effects of ambiguous diagnosis. J Appl Soc Psychol 1981;11. https://doi.org/10.1111/j.1559-1816.1981.tb00819.x.
- Haq I, Fuller J, Dacre J. The use of patient partners with back pain to teach undergraduate medical students. Rheumatology 2006;45:430-4. https://doi.org/10.1093/rheumatology/kei167.
- Chancellor J, Martin M, Liedgens H, Baker G, Müller-Schwefe HH. Stated preferences of physicians and chronic pain sufferers in the use of classic strong opioids. Value Health 2012;15. https://doi.org/10.1016/j.jval.2011.07.002.
- Walker JM. Caring for elderly people with persistent pain in the community: a qualitative perspective on the attitudes of patients and nurses. Health Soc Care Community 1994;2:221-9. https://doi.org/10.1111/j.1365-2524.1994.tb00168.x.
- Parsons A, Mamdani M, Bhattacharyya O, Fortin CM, Melo M, Salmon C, et al. Narcotic analgesic utilization amongst injured workers: using concept mapping to understand current issues from the perspectives of physicians and pharmacists. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-280.
- Kaasalainen S, Brazil K, Akhtar-Danesh N, Coker E, Ploeg J, Donald F, et al. The evaluation of an interdisciplinary pain protocol in long term care. J Am Med Dir Assoc 2012;13:664.e1-8. https://doi.org/10.1016/j.jamda.2012.05.013.
- Tousignant-Laflamme Y, Tousignant M, Lussier D, Lebel P, Savoie M, Lalonde L, et al. Educational needs of health care providers working in long-term care facilities with regard to pain management. Pain Res Manag 2012;17:341-6. https://doi.org/10.1155/2012/506352.
- Corrigan C, Desnick L, Marshall S, Bentov N, Rosenblatt RA. What can we learn from first-year medical students’ perceptions of pain in the primary care setting?. Pain Med 2011;12:1216-22. https://doi.org/10.1111/j.1526-4637.2011.01150.x.
- Costa-Black KM, Durand MJ, Imbeau D, Baril R, Loisel P. Interdisciplinary team discussion on work environment issues related to low back disability: a multiple case study. Work 2007;28:249-65.
- Gunby SS. The lived experience of nursing students in caring for suffering individuals. Holist Nurs Pract 1996;10:63-7. https://doi.org/10.1097/00004650-199604000-00010.
- Eifried S. Bearing witness to suffering: the lived experience of nursing students. J Nurs Educ 2003;42:59-67.
- Noll E, Key A, Jensen G. Clinical reasoning of an experienced physiotherapist: insight into clinician decision-making regarding low back pain. Physiother Res Int 2001;6:40-52. https://doi.org/10.1002/pri.212.
- Undeland M, Malterud K. Diagnostic interaction: the patient as a source of knowledge?. Scand J Prim Health Care 2008;26:222-7. https://doi.org/10.1080/02813430802325086.
- Espeland A, Baerheim A. General practitioners’ views on radiology reports of plain radiography for back pain. Scand J Prim Health Care 2007;25:15-9. https://doi.org/10.1080/02813430600973459.
- van WP, Beetsma A, Neels H, Roussel N, Nijs J. Physical therapists should integrate illness perceptions in their assessment in patients with chronic musculoskeletal pain; a qualitative analysis. Man Ther 2014;19. https://doi.org/10.1016/j.math.2013.11.006.
- Steihaug S, Malterud K. Part process analysis: a qualitative method for studying provider–patient interaction. Scan J Public Health 2003;31:107-13. https://doi.org/10.1080/14034940210134031.
- Dysvik E, Furnes B. Nursing leadership in a chronic pain management group approach. J Nurs Manag 2012;20:187-95. https://doi.org/10.1111/j.1365-2834.2011.01377.x.
- Baker C, Gallois C, Driedger SM, Santesso N. Communication accommodation and managing musculoskeletal disorders: doctors’ and patients’ perspectives. Health Commun 2011;26. https://doi.org/10.1080/10410236.2010.551583.
- Wermeling M, Scherer M, Himmel W. GPs’ experiences of managing non-specific neck pain – a qualitative study. Fam Pract 2011;28:300-6. https://doi.org/10.1093/fampra/cmq109.
- Nielsen M, Keefe J, Bennell K, Jull A. Physical therapist-delivered cognitive-behavioral therapy: a qualitative study of physical therapists’ perceptions and experiences. Phys Ther 2014;94:197-210. https://doi.org/10.2522/ptj.20130047.
- Kee CC, Epps CD. Pain management practices of nurses caring for older patients with osteoarthritis. West J Nurs Res 2001;23:195-210. https://doi.org/10.1177/019394590102300207.
- Manias E. Complexities of pain assessment and management in hospitalised older people: a qualitative observation and interview study. Int J Nurs Stud 2012;49:1243-55. https://doi.org/10.1016/j.ijnurstu.2012.05.002.
- Blondal K, Halldorsdottir S. The challenge of caring for patients in pain: from the nurse’s perspective. J Clin Nurs 2009;18:2897-906. https://doi.org/10.1111/j.1365-2702.2009.02794.x.
- Hildebran C, Cohen DJ, Irvine JM, Foley C, O’Kane N, Beran T, et al. How clinicians use prescription drug monitoring programs: a qualitative inquiry. Pain Med 2014;15:1179-86. https://doi.org/10.1111/pme.12469.
- Donovan J. Learning disability nurses’ experiences of being with clients who may be in pain. J Adv Nurs 2002;38:458-66. https://doi.org/10.1046/j.1365-2648.2002.02207.x.
- Ladak SS, McPhee C, Muscat M, Robinson S, Kastanias P, Snaith K, et al. The journey of the pain resource nurse in improving pain management practices: understanding role implementation. Pain Manag Nurs 2013;14:68-73. https://doi.org/10.1016/j.pmn.2011.02.002.
- Skjutar A, Schult M-L, Christensson K, Müllersdorf M. Indicators of need for occupational therapy in patients with chronic pain: occupational therapists’ focus groups. Occup Ther Int 2010;17.
- Wainwright D, Boichat C, McCracken LM. Competing patient and professional agendas in service development. J Health Organ Manag 2014;28:777-94. https://doi.org/10.1108/JHOM-08-2013-0157.
- Hooten WM, Vickers KS, Shi Y, Ebnet KL, Townsend CO, Patten CA, et al. Smoking cessation and chronic pain: patient and pain medicine physician attitudes. Pain Pract 2011;11:552-63. https://doi.org/10.1111/j.1533-2500.2011.00462.x.
- Beattie A, Shaw A, Yardley L, Little P, Sharp D. Participating in and delivering the ATEAM trial (Alexander technique lessons, exercise, and massage) interventions for chronic back pain: a qualitative study of professional perspectives. Complement Ther Med 2010;18:119-27. https://doi.org/10.1016/j.ctim.2010.05.037.
- Spiers J. Expressing and responding to pain and stoicism in home-care nurse–patient interactions. Scand J Caring Sci 2006;20:293-301. https://doi.org/10.1111/j.1471-6712.2006.00407.x.
- Tellier PP, Belanger E, Rodriguez C, Ware MA, Nancy PN. Improving undergraduate medical education about pain assessment and management: a qualitative descriptive study of stakeholders’ perceptions. Pain Res Manag 2013;18:259-65. https://doi.org/10.1155/2013/920961.
- Mackintosh-Franklin C. The impact of experience on undergraduate preregistration student nurses’ responses to patients in pain: a 2-year qualitative longitudinal study. Pain Manag Nurs 2014;15. https://doi.org/10.1016/j.pmn.2012.08.009.
- Samuels JG, Leveille DM. Senior nursing students’ clinical judgments in pain management. Nurse Educ 2010;35:220-4. https://doi.org/10.1097/NNE.0b013e3181ed83da.
- Coutu MF, Legare F, Stacey D, Durand MJ, Corbiere M, Bainbridge L, et al. Occupational therapists’ shared decision-making behaviors with patients having persistent pain in a work rehabilitation context: a cross-sectional study. Patient Educ Couns 2015;98:864-70. https://doi.org/10.1016/j.pec.2015.03.015.
- Schofield P. Talking to older people in care homes: perceptions of their pain and their preferred management strategies. Results of a pilot study. Int J Disability Hum Dev 2006;5. https://doi.org/10.1515/IJDHD.2006.5.1.53.
- Corbett M, Foster N, Ong BN. GP attitudes and self-reported behaviour in primary care consultations for low back pain. Fam Pract 2009;26:359-64. https://doi.org/10.1093/fampra/cmp042.
- Crowe M, Whitehead L, Jo Gagan M, Baxter D, Panckhurst A. Self-management and chronic low back pain: a qualitative study. J Adv Nurs 2010;66:1478-86. https://doi.org/10.1111/j.1365-2648.2010.05316.x.
- Hadker N, Garg S, Chandran B, Crean M, McNett M, Silverman L. Efficient practices associated with diagnosis, treatment and management of fibromyalgia among primary care physicians. Pain Res Manage 2011;16. https://doi.org/10.1155/2011/367059.
- Dysvik E, Stephens P. Conducting rehabilitation groups for people suffering from chronic pain. Int J Nurs Pract 2010;16. https://doi.org/10.1111/j.1440-172X.2010.01825.x.
- Kotarba A, Seidel V. Managing the problem pain patient: compliance or social control?. Soc Sci Med 1984;19. https://doi.org/10.1016/0277-9536(84)90029-7.
- Thunberg KA, Carlsson SG, Hallberg LRM. Health care professionals’ understanding of chronic pain: a grounded theory study. Scan J Caring Sci 2001;15. https://doi.org/10.1046/j.1471-6712.2001.1510099.x.
- Afrell M, Rudebeck CE. ‘We got the whole story all at once’: physiotherapists’ use of key questions when meeting patients with long-standing pain. Scand J Caring Sci 2010;24:281-9. https://doi.org/10.1111/j.1471-6712.2009.00718.x.
- Åsbring P, Närvänen A. Ideal versus reality: physicians perspectives on patients with chronic fatigue syndrome (CFS) and fibromyalgia. Soc Sci Med 2003;57:711-21. https://doi.org/10.1016/S0277-9536(02)00420-3.
- Baldacchino A, Gilchrist G, Fleming R, Bannister J. Guilty until proven innocent: a qualitative study of the management of chronic non-cancer pain among patients with a history of substance abuse. Addict Behav 2010;35:270-2. https://doi.org/10.1016/j.addbeh.2009.10.008.
- Barker KL, Heelas L, Toye F. Introducing acceptance and commitment therapy to a physiotherapy led pain rehabilitation programme: an action research study. Br J Pain 2015;10:22-8. https://doi.org/10.1177/2049463715587117.
- Barry DT, Irwin KS, Jones ES, Becker WC, Tetrault JM, Sullivan LE, et al. Opioids, chronic pain, and addiction in primary care. J Pain 2010;11:1442-50. https://doi.org/10.1016/j.jpain.2010.04.002.
- Baszanger I. Deciphering chronic pain. Sociol Health Illn 1992;14:181-215. https://doi.org/10.1111/1467-9566.ep11343694.
- Berg M, Arnsten H, Sacajiu G, Karasz A. Providers’ experiences treating chronic pain among opioid-dependent drug users. J Gen Intern Med 2009;24. https://doi.org/10.1007/s11606-009-0908-x.
- Bergman AA, Matthias MS, Coffing JM, Krebs EE. Contrasting tensions between patients and PCPs in chronic pain management: a qualitative study. Pain Med 2013;14:1689-97. https://doi.org/10.1111/pme.12172.
- Blomberg AM, Hylander I, Törnkvist L. District nurses’ involvement in pain care: a theoretical model. J Clin Nurs 2008;17:2022-31. https://doi.org/10.1111/j.1365-2702.2007.02222.x.
- Blomqvist K. Older people in persistent pain: nursing and paramedical staff perceptions and pain management. J Adv Nurs 2003;41:575-84. https://doi.org/10.1046/j.1365-2648.2003.02569.x.
- Briones-Vozmediano E, Vives-Cases C, Ronda-Pérez E, Gil-González D. Patients’ and professionals’ views on managing fibromyalgia. Pain Res Manag 2013;18:19-24. https://doi.org/10.1155/2013/742510.
- Cameron PA, Smith, Blair H, Schofield Patricia A. Pain and rehabilitation. J Physiother Pain Assoc 2015;38:17-28.
- Cartmill C, Soklaridis S, Cassidy J. Transdisciplinary teamwork: the experience of clinicians at a functional restoration program. J Occup Rehabil 2011;21. https://doi.org/10.1007/s10926-010-9247-3.
- Chew-Graham C, May C. Chronic low back pain in general practice: the challenge of the consultation. Fam Pract 1999;16:46-9. https://doi.org/10.1093/fampra/16.1.46.
- Clark L, Jones K, Pennington K. Pain assessment practices with nursing home residents. West J Nurs Res 2004;26:733-50. https://doi.org/10.1177/0193945904267734.
- Clark L, Fink R, Pennington K, Jones K. Nurses’ reflections on pain management in a nursing home setting. Pain Manag Nurs 2006;7:71-7. https://doi.org/10.1016/j.pmn.2006.02.004.
- Côté P, Clarke J, Deguire S, Frank JW, Yassi A. Chiropractors and return-to-work: the experiences of three Canadian focus groups. J Manipulative Physiol Ther 2001;24. https://doi.org/10.1067/mmt.2001.115267.
- Coutu MF, Baril R, Durand MJ, Cote D, Cadieux G. Clinician–patient agreement about the work disability problem of patients having persistent pain: why it matters. J Occup Rehabil 2013;23:82-9. https://doi.org/10.1007/s10926-012-9387-8.
- Dahan R, Borkan J, Brown JB, Reis S, Hermoni D, Harris S. The challenge of using the low back pain guidelines: a qualitative research. J Eval Clin Pract 2007;13:616-20. https://doi.org/10.1111/j.1365-2753.2007.00855.x.
- Daykin AR, Richardson B. Physiotherapists’ pain beliefs and their influence on the management of patients with chronic low back pain. Spine 2004;29:783-95. https://doi.org/10.1097/01.BRS.0000115135.19082.97.
- Dobbs D, Baker T, Carrion IV, Vongxaiburana E, Hyer K. Certified nursing assistants’ perspectives of nursing home residents’ pain experience: communication patterns, cultural context, and the role of empathy. Pain Manag Nurs 2014;15:87-96. https://doi.org/10.1016/j.pmn.2012.06.008.
- Eccleston C, De CACA, Rogers WS. Patients’ and professionals’ understandings of the causes of chronic pain: blame, responsibility and identity protection. Soc Sci Med 1997;45:699-710. https://doi.org/10.1016/S0277-9536(96)00404-2.
- Espeland A, Baerheim A. Factors affecting general practitioners’ decisions about plain radiography for back pain: implications for classification of guideline barriers – a qualitative study. BMC Health Serv Res 2003;3. https://doi.org/10.1186/1472-6963-3-8.
- Esquibel AY, Borkan J. Doctors and patients in pain: conflict and collaboration in opioid prescription in primary care. Pain 2014;155:2575-82. https://doi.org/10.1016/j.pain.2014.09.018.
- Fontana JS. The social and political forces affecting prescribing practices for chronic pain. J Prof Nurs 2008;24:30-5. https://doi.org/10.1016/j.profnurs.2007.06.002.
- Fox P, Solomon P, Raina P, Jadad A. Barriers and facilitators in pain management in long-term care institutions: a qualitative study. Can J Aging 2004;23:269-80. https://doi.org/10.1353/cja.2004.0032.
- Gooberman-Hill R, Heathcote C, Reid CM, Horwood J, Beswick AD, Williams S, et al. Professional experience guides opioid prescribing for chronic joint pain in primary care. Fam Pract 2011;28:102-9. https://doi.org/10.1093/fampra/cmq083.
- Gropelli T, Sharer J. Nurses’ perceptions of pain management in older adults. Medsurg Nurs 2013;22:375-82.
- Hansson M, Boström C, Harms-Ringdahl K. Living with spine-related pain in a changing society – a qualitative study. Disabil Rehabil 2001;23:286-95. https://doi.org/10.1080/096382801750143625.
- Harting J, Rutten GM, Rutten ST, Kremers P. A qualitative application of the diffusion of innovations theory to examine determinants of guideline adherence among physical therapists. Phys Ther 2009;89. https://doi.org/10.2522/ptj.20080185.
- Hayes M, Myhal C, Thornton F, Camerlain M, Jamison C, Cytryn N, et al. Fibromyalgia and the therapeutic relationship: where uncertainty meets attitude. Pain Res Manag 2010;15. https://doi.org/10.1155/2010/354868.
- Hellman T, Jensen I, Bergström G, Busch H. Returning to work – a long-term process reaching beyond the time frames of multimodal non-specific back pain rehabilitation. Disabil Rehabil 2015;37:499-505. https://doi.org/10.3109/09638288.2014.923531.
- Hellström O, Bullington J, Karlsson G, Lindqvist P, Mattsson B. Doctors’ attitudes to fibromyalgia: a phenomenological study. Scand J Soc Med 1998;26:232-7. https://doi.org/10.1177/14034948980260030201.
- Holloway K, McConigley R. Descriptive, exploratory study of the role of nursing assistants in Australian residential aged care facilities: the example of pain management. Australas J Ageing 2009;28:70-4. https://doi.org/10.1111/j.1741-6612.2009.00360.x.
- Holloway K, McConigley R. Understanding nursing assistants’ experiences of caring for older people in pain: the Australian experience (corrected). Pain Manag Nurs 2009;10:99-107. https://doi.org/10.1016/j.pmn.2008.10.001.
- Howarth M, Warne T, Haigh C. ‘Let’s stick together’ – a grounded theory exploration of interprofessional working used to provide person centered chronic back pain services. J Interprof Care 2012;26. https://doi.org/10.3109/13561820.2012.711385.
- Kaasalainen S, Coker E, Dolovich L, Papaioannou A, Hadjistavropoulos T, Emili A, et al. Pain management decision making among long-term care physicians and nurses. West J Nurs Res 2007;29:561-80. https://doi.org/10.1177/0193945906295522.
- Kaasalainen S, Martin-Misener R, Carter N, Dicenso A, Donald F, Baxter P. The nurse practitioner role in pain management in long-term care. J Adv Nurs 2010;66:542-51. https://doi.org/10.1111/j.1365-2648.2009.05206.x.
- Kaasalainen S, Brazil K, Coker E, Ploeg J, Martin-Misener R, Donald F, et al. An action-based approach to improving pain management in long-term care. Can J Aging 2010;29:503-17. https://doi.org/10.1017/S0714980810000528.
- Kilaru S, Gadsden M, Perrone J, Paciotti B, Barg K, Meisel F. How do physicians adopt and apply opioid prescription guidelines in the emergency department? A qualitative study. Ann Emerg Med 2014;64. https://doi.org/10.1016/j.annemergmed.2014.03.015.
- Krebs EE, Bergman AA, Coffing JM, Campbell SR, Frankel RM, Matthias MS. Barriers to guideline-concordant opioid management in primary care – a qualitative study. J Pain 2014;15:1148-55. https://doi.org/10.1016/j.jpain.2014.08.006.
- Kristiansson MH, Brorsson A, Wachtler C, Troein M. Pain, power and patience – a narrative study of general practitioners’ relations with chronic pain patients. BMC Fam Pract 2011;12. https://doi.org/10.1186/1471-2296-12-31.
- Liu YW. Exploring nursing assistants’ roles in the process of pain management for cognitively impaired nursing home residents: a qualitative study. J Adv Nurs 2014;70:1065-78. https://doi.org/10.1111/jan.12259.
- Löckenhoff E, Laucks S, Port D, Tung J, Wethington E, Reid MC. Temporal horizons in pain management: understanding the perspectives of physicians, physical therapists, and their middle-aged and older adult patients. Gerontologist 2013;53. https://doi.org/10.1093/geront/gns136.
- Lundh C, Segesten K, Björkelund C. To be a helpless helpoholic – GPs’ experiences of women patients with non-specific muscular pain. Scand J Prim Health Care 2004;22:244-7. https://doi.org/10.1080/02813430410006756.
- MacNeela P, Gibbons A, McGuire B, Murphy A. ‘We need to get you focused’: general practitioners’ representations of chronic low back pain patients. Qual Health Res 2010;20:977-86. https://doi.org/10.1177/1049732310364219.
- McConigley R, Toye C, Goucke R, Kristjanson LJ. Developing recommendations for implementing the Australian Pain Society’s pain management strategies in residential aged care. Australas J Ageing 2008;27:45-9. https://doi.org/10.1111/j.1741–6612.2007.00266.x.
- McCrorie C, Closs SJ, House A, Petty D, Ziegler L, Glidewell L, et al. Understanding long-term opioid prescribing for non-cancer pain in primary care: a qualitative study. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0335-5.
- Mentes C, Teer J, Cadogan P. The pain experience of cognitively impaired nursing home residents: perceptions of family members and certified nursing assistants. Pain Manag Nurs 2004;5. https://doi.org/10.1016/j.pmn.2004.01.001.
- O’Connor BB, Eisenberg DM, Buring JE, Liang CL, Osypiuk K, Levy DB, et al. Within-team patterns of communication and referral in multimodal treatment of chronic low back pain patients by an integrative care team. Glob Adv Health Med 2015;4:36-45. https://doi.org/10.7453/gahmj.2014.076.
- Øien AM, Steihaug S, Iversen S, Råheim M. Communication as negotiation processes in long-term physiotherapy: a qualitative study. Scand J Caring Sci 2011;25:53-61. https://doi.org/10.1111/j.1471-6712.2010.00790.x.
- Oosterhof B, Dekker JH, Sloots M, Bartels EA, Dekker J. Success or failure of chronic pain rehabilitation: the importance of good interaction – a qualitative study under patients and professionals. Disabil Rehabil 2014;36:1903-10. https://doi.org/10.3109/09638288.2014.881566.
- Parsons S, Harding G, Breen A, Foster N, Pincus T, Vogel S, et al. Will shared decision making between patients with chronic musculoskeletal pain and physiotherapists, osteopaths and chiropractors improve patient care?. Fam Pract 2012;29:203-12. https://doi.org/10.1093/fampra/cmr083.
- Patel S, Peacock S, McKinley R, Carter DC, Watson PJ. GPs’ experience of managing chronic pain in a South Asian community – a qualitative study of the consultation process. Fam Pract 2008;25:71-7. https://doi.org/10.1093/fampra/cmn012.
- Patel S, Peacock SM, McKinley RK, Clark-Carter D, Watson PJ. GPs’ perceptions of the service needs of South Asian people with chronic pain: a qualitative enquiry. J Health Psychol 2009;14:909-18. https://doi.org/10.1177/1359105309341003.
- Paulson M, Danielson E, Norberg A. Nurses’ and physicians’ narratives about long-term non-malignant pain among men. J Adv Nurs 1999;30:1097-105. https://doi.org/10.1046/j.1365-2648.1999.01162.x.
- Poitras S, Durand MJ, Côté AM, Tousignant M. Use of low-back pain guidelines by occupational therapists: a qualitative study of barriers and facilitators. Work 2011;39:465-75. https://doi.org/10.3233/WOR-2011-1196.
- Ruiz JG, Qadri SS, Nader S, Wang J, Lawler T, Hagenlocker B, et al. Primary care management of chronic nonmalignant pain in veterans: a qualitative study. Educ Gerontol 2010;36:372-94. https://doi.org/10.1080/03601270903212450.
- Schulte E, Heift A, Welke J, Hermann K, Schäfer M, Boemke W. Specialised pain therapy from the general practitioners’ perspective: a qualitative assessment. J Pain Manag 2010;3.
- Scott-Dempster C, Toye F, Truman J, Barker K. Physiotherapists’ experiences of activity pacing with people with chronic musculoskeletal pain. An interpretative phenomenological analysis. Physiother Theory Pract 2014;30:319-28. https://doi.org/10.3109/09593985.2013.869774.
- Seamark D, Seamark C, Greaves C, Blake S. GPs prescribing of strong opioid drugs for patients with chronic non-cancer pain: a qualitative study. Br J Gen Pract 2013;63:e821-8. https://doi.org/10.3399/bjgp13X675403.
- Shye D, Freeborn DK, Romeo J, Eraker S. Understanding physicians’ imaging test use in low back pain care: the role of focus groups. Int J Qual Health Care 1998;10. https://doi.org/10.1093/intqhc/10.2.83.
- Siedlecki L, Modic MB, Bernhofer E, Sorrell J, Strumble P, Kato I. Exploring how bedside nurses care for patients with chronic pain: a grounded theory study. Pain Manag Nurs 2014;15. https://doi.org/10.1016/j.pmn.2012.12.007.
- Slade SC, Molloy E, Keating JL. The dilemma of diagnostic uncertainty when treating people with chronic low back pain: a qualitative study. Clin Rehabil 2012;26:558-69. https://doi.org/10.1177/0269215511420179.
- Sloots M, Scheppers EF, Bartels EAC, Dekker JHM, Geertzen JHB, Dekker J. First rehabilitation consultation in patients of non-native origin: factors that lead to tension in the patient–physician interaction. Disabil Rehabil 2009;31:1853-62. https://doi.org/10.1080/09638280902847085.
- Sloots M, Dekker JH, Pont M, Bartels EA, Geertzen JH, Dekker J. Reasons of drop-out from rehabilitation in patients of Turkish and Moroccan origin with chronic low back pain in the Netherlands: a qualitative study. J Rehabil Med 2010;42:566-73. https://doi.org/10.2340/16501977-0536.
- Spitz A, Moore AA, Papaleontiou M, Granieri E, Turner BJ, Reid MC. Primary care providers’ perspective on prescribing opioids to older adults with chronic non-cancer pain: a qualitative study. BMC Geriatr 2011;11. https://doi.org/10.1186/1471-2318-11-35.
- Starrels L, Wu B, Peyser D, Fox D, Batchelder A, Barg K, et al. It made my life a little easier: primary care providers’ beliefs and attitudes about using opioid treatment agreements. J Opioid Manag 2014;10. https://doi.org/10.5055/jom.2014.0198.
- Stinson J, White M, Isaac L, Campbell F, Brown S, Ruskin D, et al. Understanding the information and service needs of young adults with chronic pain: perspectives of young adults and their providers. Clin J Pain 2013;29:600-12. https://doi.org/10.1097/AJP.0b013e31826dce65.
- Toye F, Jenkins S, Seers K, Barker K. Exploring the value of qualitative research films in clinical education. BMC Med Res 2015;15.
- Tveiten S, Meyer I. ‘Easier said than done’: empowering dialogues with patients at the pain clinic – the health professionals’ perspective. J Nurs Manag 2009;17:804-12. https://doi.org/10.1111/j.1365-2834.2008.00921.x.
- Wainwright D, Calnan M, O’Neil C, Winterbottom A, Watkins C. When pain in the arm is ‘all in the head’: the management of medically unexplained suffering in primary care. Health Risk Soc 2006;8:71-89. https://doi.org/10.1080/13698570500532512.
- Wilson N, Pope C, Roberts L, Crouch R. Governing healthcare: finding meaning in a clinical practice guideline for the management of non-specific low back pain. Soc Sci Med 2014;102. https://doi.org/10.1016/j.socscimed.2013.11.055.
- Wynne-Jones G, van DD, Ong BN, Bishop A, Cowen J, Artus M, et al. Perceptions of health professionals towards the management of back pain in the context of work: a qualitative study. BMC Musculoskelet Disord 2014;15. https://doi.org/10.1186/1471-2474-15-210.
- Zanini C, Sarzi-Puttini P, Atzeni F, Di FM, Rubinelli S. Doctors’ insights into the patient perspective: a qualitative study in the field of chronic pain. Biomed Res Int 2014:514230-1. https://doi.org/10.1155/2014/514230.
- Foucault M. The Birth of the Clinic. Abingdon: Routledge Classics; 2003.
- Engel G. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129-36. https://doi.org/10.1126/science.847460.
- Grace V. Embodiment and meaning. J Conscious Stud 2003;10:41-60.
- Merleau-Ponty M. Phenomenology of Perception. London: Routledge; 1962.
- Wall P. Pain: The Science of Suffering. London: Phoenix; 1999.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Recomm Rep 2016;65:1-49. https://doi.org/10.15585/mmwr.rr6501e1.
- Royal College of Anaesthetists . Opioids Aware: A Resource for Patients and Healthcare Professionals to Support Prescribing of Opioid Medicines for Pain. A Public Health England Funded Project 2016. www.rcoa.ac.uk/faculty-of-pain-medicine/opioids-aware (accessed 10 August 2017).
- Chou R, Deyo R, Devine B, Hansen R, Sullivan S, Jarvik JG, et al. The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain. The Evidence Report Technology Assessment n.d. www.effectivehealthcare.ahrq.gov/ehc/products/557/1971/chronic-pain-opioid-treatment-report-141205.pdf (accessed 10 August 2017).
- Levinas E. Totality and Infinity: An Essay on Exteriority. Pittsburgh, PA: Duquesne University Press; 1969.
- Charon R. Narrative Medicine – Honoring the Stories of Illness. Oxford: Oxford University Press; 2006.
- Parsons J, Heus L, Moravac C. Seeing voices of health disparity: evaluating arts projects as influence processes. Eval Program Plann 2013;36:165-71. https://doi.org/10.1016/j.evalprogplan.2012.03.003.
- Yallop JJG, deVallejo IL, Wright P. Editorial: Overview of the Performative Social Science Special Issue n.d. www.qualitative-research.net/index.php/fqs/article/view/375/817 (accessed 10 August 2017).
- Denzin N. The reflexive interview and a performative social science. Qual Res 2001;1:33-46. https://doi.org/10.1177/146879410100100102.
- Gergen M, Jones K. Editorial: a conversation about performative social science. Forum Qual Soc Res 2008;9.
- Colantonio A, Kontos PC, Gilbert JE, Rossiter K, Gray J, Keightley ML. After the crash: research-based theater for knowledge transfer. J Contin Educ Health Prof 2008;28:180-5. https://doi.org/10.1002/chp.177.
- McCullough M. Bringing drama into medical education. Lancet 2012;379:512-13. https://doi.org/10.1016/S0140-6736(12)60221-9.
- Rosenbaum ME, Ferguson KJ, Herwaldt LA. In their own words: presenting the patient’s perspective using research-based theatre. Med Educ 2005;39:622-31. https://doi.org/10.1111/j.1365-2929.2005.02181.x.
- Saldana J. Dramatizing data: a primer. Qual Inq 2003;9:218-36. https://doi.org/10.1177/1077800402250932.
- Lafreniere D, Cox SM. Performing the human subject: arts-based knowledge dissemination in health research. J Appl Arts Health 2012;3:243-57. https://doi.org/10.1386/jaah.3.3.243_1.
- Rossiter K, Kontos P, Colantonio A, Gilbert J, Gray J, Keightley M. Staging data: theatre as a tool for analysis and knowledge transfer in health research. Soc Sci Med 2008;66:130-46. https://doi.org/10.1016/j.socscimed.2007.07.021.
- Parsons JA, Boydell KM. Arts-based research and knowledge translation: some key concerns for health-care professionals. J Interprof Care 2012;26:170-2. https://doi.org/10.3109/13561820.2011.647128.
- Kontos PC, Poland BD. Mapping new theoretical and methodological terrain for knowledge translation: contributions from critical realism and the arts. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-1.
- de la Croix A, Rose C, Wildig E, Willson S. Arts-based learning in medical education: the students’ perspective. Med Educ 2011;45:1090-100. https://doi.org/10.1111/j.1365-2923.2011.04060.x.
- Jonas-Simpson C, Mitchell GJ, Carson J, Whyte C, Dupuis S, Gillies J. Phenomenological shifts for healthcare professionals after experiencing a research-based drama on living with dementia. J Adv Nurs 2012;68:1944-55. https://doi.org/10.1111/j.1365-2648.2011.05877.x.
- Walsh M. Narrative pedagogy and simulation: future directions for nursing education. Nurse Educ Pract 2011;11:216-19. https://doi.org/10.1016/j.nepr.2010.10.006.
- Todres L. Being with that: the relevance of embodied understanding for practice. Qual Health Res 2008;18:1566-73. https://doi.org/10.1177/1049732308324249.
- Greenhalgh T, Howick J, Maskrey N. Evidence based medicine: a movement in crisis?. BMJ 2014;348. https://doi.org/10.1136/bmj.g3725 (accessed 10 August 2017).
- Greenhalgh T. What is this knowledge that we seek to ‘exchange’?. Milbank Q 2010;88:492-9. https://doi.org/10.1111/j.1468-0009.2010.00610.x.
- Blumer H. What is wrong with social theory. Am Sociol Rev 1954;18:3-10. https://doi.org/10.2307/2088165.
- Forster M, Beiser FC. Cambridge Companion to Hegel. Cambridge: Cambridge University Press; 1993.
- Richardson R, Hans Kramer E. Abduction as the type of inference that characterizes the development of a grounded theory. Qual Res 2006;6:497-513. https://doi.org/10.1177/1468794106068019.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2012;11. https://doi.org/10.1186/1741-7015-11-21.
- France EF, Ring N, Noyes J, Maxwell M, Jepson R, Duncan E, et al. Protocol-developing meta-ethnography reporting guidelines (eMERGe). BMC Med Res Methodol 2015;15. https://doi.org/10.1186/s12874-015-0068-0.
- Munn Z, Porritt K, Lockwood C, Aromataris E, Pearson A. Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-108.
- Elmir R, Schmied V, Wilkes L, Jackson D. Women’s perceptions and experiences of a traumatic birth: a meta-ethnography. J Adv Nurs 2010;66:2142-53. https://doi.org/10.1111/j.1365-2648.2010.05391.x.
- Baker SE, Edwards R. How Many Qualitative Interviews is Enough?. National Centre for Research Methods Review Paper: Expert Voices and Early Career Reflections on Sampling and Cases in Qualitative Research 2012 n.d. http://eprints.ncrm.ac.uk/2273/ (accessed 10 August 2017).
- Seale C. The Quality of Qualitative Research. London: Sage Publications; 1999.
Appendix 1 Log of appraisal comments
| First author/year | Appraisal comments |
|---|---|
| Afrell 2010151 | This was a very thought provoking account. Made me think directly about applicability of qualitative findings to clinical practise. Resonated with my own work. Highly relevant practical application of qualitative work. Key themes about ambivalence, resonates with Victor Turner again (fructile chaos) |
| Allegretti 201011 | Exemplars well chosen. Surprised by idea that HCPs used biopsychosocial model (but in teaching hospital). Reinforces Helman’s ideas that it is a challenge to impose cultural models that do not fit onto someone (here patients). Interesting but not key |
| Åsbring 2003152 | Fibromyalgia and chronic fatigue not entirely sure which diagnosis for clinicians, mixed diagnosis makes it a bit muddy but agree about overlap so adds insight. Does not describe methods of rigour, just ‘Strauss and Corbin’. Not clear always if interpretation from data. Not all key ideas have exemplars. Sometimes drift into discussion not grounded in the data. Very negative view of HCP. However, resonates with notion of moral narrative |
| Baldacchino 2010153 | Findings brief. Changes thinking – I had not considered this subgroup. This is the first study on barriers to opioid prescription. Very minimal report of method but ‘no harm’. Maybe limited applicability as about those with history of substance abuse |
| Barker 2015154 | Co-authored |
| Barry 2010155 | Minimal abstraction of ideas (19 themes). Can identify ideas as limited abstraction. Not great. Little analytical work. Might add to a theme but no key ideas. Hard to read |
| Baszanger 1992156 | Ethnographic style and findings not always clear. Not always clear if interpretation from data. Ethnographic style. Not lengthy quotes. High on interpretation of observations. Interesting but very long winded and needed deciphering. Hard read |
| Berg 2009157 | Like idea of ambiguity – focus on problem of opioids or focus on problem of pain control. Insight into ambiguities of medical practise. It is not clear cut (diagnostic ambiguity) |
| Bergman 2013158 | Did not change thinking, but introduction to difficulties of opioids prescription. Resonant account |
| Blomberg 2008159 | Not great rationale for focus groups but OK. Insight into district nurse. I liked idea introduced that nurse can become passive if collaboration and organisational support are not available. Provides a clear model. A bit so-what-ish |
| Blomqvist 2003160 | Thin on exemplar |
| Briones-Vozmediano 2013161 | No change of ideas but resonant. Insightful comment:no matter what you give them the pain does not go away |
| Cameron 2015162 | Not entirely sure how study recruited ‘convenience sample’. Thinking not changed but made me think about phenomenology of age and pain. Heterogeneous sample makes it more difficult to transfer findings. However, may help to contribute to a theme on ageing and pain |
| Cartmill 2011163 | Not change thinking but made me think about organisation focus in chronic pain management. Areas to learn from. Focus of aim = effective teamwork in functional restoration programme |
| Chew-Graham 1999164 | Method not described (just ‘grounded theory’). Not always clear if interpretation comes from data. Draws heavily on knowledge from a previous study and sociological frameworks. Presents bleak view of HCPs. Raises some resonant points |
| Clark 2004165 | Thinking more about persistent pain management in residential care. I had discarded it but seem to be shared characteristics exacerbated by the issue of age. Not always clear if it comes from the data. Narrative exemplars a bit thin |
| Clark 2006166 | Thinking more about pain in nursing homes. Importance of auxiliary nurse and collaborative with physicians. Query transferability as relates to interviews after a global pain intervention study in nursing homes. Interviewed those in treatment arm and control arm. However, some resonant accounts |
| Corbett 2009145 | Thin description. Out |
| Corrigan 2011116 | No comment. Out |
| Côté 2001167 | New insight from chiropractors – did not anticipate sense of professional isolation |
| Coutu 2013168 | Difficult to get clear sense of HCP as findings from HCP–patient dyads. Dyads make it difficult as observing space between two parties so difficult to decipher experience from a particular stance. A bit thin |
| Crowe 2010146 | Sample not described. No gravitational ideas. No evidence of analysis/idea abstraction |
| Dahan 2007169 | Themes not pulled together very clearly but second-order concepts OK. Nothing new but resonant. Makes interesting parallel to dealing with terminal illness. Also difficulties that arise from being ‘in the middle’ in primary care |
| Daykin 2004170 | Not changed thinking but thoughtful account. Shows complexity of ‘good/bad’ (i.e. not just about chronicity/complexity but also patient locus of control). Daykin feels that HCPs do not judge challenging patient on personal characteristics (this may be naive). Enjoyed and know author well. A very generous interpretation of HCPs |
| Dobbs 2014171 | Several ideas in one heading. No change but have become more inclined to include nursing assistant and residential papers. Need to include persistent pain in residential care (ethical decision) |
| Dysvik 2010148 | No comment |
| Eccleston 1997172 | Really nice intro set in social science literature. Q-analysis – quantitative treatment of narrative data. Only one account relevant to this study. I would not include as no clear thematic ideas but maybe decision grounded in dislike of quantifying qualitative data. I think it sits outside phenomenological tradition. (Other reviewers ‘in’) |
| Espeland 2003173 | Resonant. Bit thin but adds to a theme |
| Esquibel 2014174 | Do not think concepts in tables match narrative analysis. Conceptualised a bit too far and making assumptions. Changed thinking – insight into construction of good and bad patients. Very nice introduction and description of benefits of narrative. Some nice data |
| Fontana 2008175 | No change but reinforcing need to include this cohort. Themes beginning to resonate in this group (e.g. time/communication empathy) |
| Fox 2004176 | Researchers perspective not available and this is important in a ‘critical analysis’ which is grounded in a perspective. Seems to come from data, but suspicious because highlights power structures. Not considered nursing perspective before. Makes me think about different organisational/cultural perspective. Interesting analysis. Quite negative view of HCPs |
| Gooberman-Hill 2011177 | Not always clear gravity. Not changed thinking. Different prescribing opinions for type of pain (e.g. elderly and comorbidity). Chronic joint pain. A little uncertainty on inclusion? Arthritic (only because know the team) |
| Gropelli 2013178 | Thin. Appears to have an axe to grind. Exemplars not well chosen to support themes. Untranslatable. Third reviewer ‘in’ |
| Hadker 2011147 | No comment. Out |
| Hansson 2001179 | A bit thin as this is a small section on a wider study on patient experience. Verging on uncertain but potential useful bolstering to theme. A bit thin and difficult to transfer outside specific context. Might contribute to a thematic category |
| Harting 2009180 | A priori ideas make it difficult and felt ‘shoe horned’ a bit. A bit deductive. Uses a framework. A priori themes interfere with findings and not clear if interpretation entirely from data. Titles reduce clarity. A priori themes reduce clarity |
| Hayes 2010181 | Not always a strong gravitational pull to a clear idea. A bit generic. Thin but resonant. Like term ‘it’s a fuzzy concept’ – reminds me of difficulties of anomaly |
| Hellman 2015182 | Bit repetitive, but adds gravity |
| Hellström 2015183 | No new thinking. But like the ideas of anomaly. GPs avoid biomedical anomaly by referring on (shift buck). This is like liminality (fructile chaos, anomaly, liminality – positive spin could be phoenix idea). Problem = very harsh representation of HCP (e.g. talk about ‘deviant personality’) Otherwise ideas nice. In science an anomaly is used for a situation where one is faced with something that challenges the paradigm induced expectations that govern normal science |
| Holloway 2009184 | No change but more insight into nursing assistant role in front line. Nursing assistant an important part of the team. Very similar to Holloway 2009185 |
| Holloway 2009185 | No new ideas but brings in nursing assistant views. Importance of HCP team |
| Howarth 2012186 | Thinking about collaborative working and space/physical environment. Team work. Clear and concise gravitational themes |
| Kaasalainen 2007187 | Some lovely data that gives insight into experience and suggests a way forward: nobody wants to die in pain but no one wants to live in pain either people think she is in bed resting . . . well guess what, she’s in bed looking at the ceiling and thinking about her painMum |
| Kaasalainen 2010188 | Not always abstracted ideas fully. Titles a bit generic and ideas hidden a bit |
| Kaasalainen 2010189 | Resonant ideas |
| Kilaru 2014190 | Developing ideas on opioids |
| Kotarba 1984149 | No comment |
| Krebs 2014191 | No change but thinking about concept of ‘gut feeling’ used to judge patients. Like the sampling ‘who may think differently on this topic to you’ |
| Kristiansson 2011192 | Difficult to extract ideas from narrative. Use ‘stanzas’. Found narrative style difficult to extract second-order concepts |
| Liu 2014193 | Resonant but on thin side |
| Löckenhoff 2013194 | Verging on uncertain. Thin study. Towards deductive/framework approach. Focus on timelines rather than allowing data to speak. Also older age is 60+ years so not that old |
| Lundh 2004195 | Positive view of HCPs. I liked it. A positive non-judgemental view |
| MacNeela 2010196 | Uncertain whether or not to include. I did not follow methods. A bit scrappy. Poor organisation of findings section made extraction of ideas cumbersome. Some interesting findings. Titles not consistent. Mixed-method qualitative design |
| McConigley 2008197 | Not given examples to support analysis. Highlight issues for careworkers and non-professional staff. Satisfactory but uncertain transferability – about implementation of guidelines for pain in residential care (Australia) could be in this section or in guidelines section. Thin on exemplar |
| McCrorie 2015198 | Not different but resonant. ‘Unfolding’ of treatment with no plan. Responsibility shift again. Ideas coming through |
| Mentes 2004199 | Thin |
| O’Connor 2015200 | Not changed thinking, but thinking about team dynamic and context of care. Theme emerging = team/integrative context of care |
| Øien 2011201 | Very thin account of 11 cases. Norwegian specialty so query transferability. However, interesting theme of seeking common ground. Some resonance |
| Oosterhof 2014202 | A bit thin on HCP ideas. Based on one example – analysis does not come through. A bit thin but resonant and may contribute |
| Parsons 2012203 | Mixed private NHS and complementary therapy – some difficulty deciphering patient HCP data. May contribute to wider theme. Some interesting idea development. Deductive pole of analysis |
| Patel 2008204 | Made me think about overlap between experience of different cultural groups that could help us to understand and articular challenges. I enjoyed reading this. Concise and clear. Raised questions and food for thought, particularly in an anthropological context |
| Patel 2009205 | Does not offer much more than Patel 2008,204 but different themes on service provision that might contribute to a theme |
| Paulson 1999206 | Not always clear if interpretation from HCP or patient. Data not always used to support theme. Not changed thinking but made me think about gender expectations in HCP/patient discussions/attitudes. Demonstrates need for a gender study. Some important ideas but not very good illustrative data at times |
| Poitras 2011207 | Deductive? First insight into relationship between professional groups and its impact on effectiveness of care. I do not like the way that authors ‘dump’ codes that are not consistent in accounts this does not fit qualitative philosophy. Negative case can illuminate constant comparison |
| Ruiz 2010208 | Unable to decipher nurses from medical opinions in this |
| Schofield 2006144 | No comment |
| Schulte 2010209 | Data a bit thin. No in-depth exemplars. Removed sections about interviews with patients. This is about relationship with second and third care specialists. Limited scope. Does not probe GPs expectations of pain clinics and that is a shame, in view of title. Overall a bit thin but may contribute to a category |
| Scott-Dempster 2014210 | Co-authored |
| Seamark 2013211 | Changed thinking – consider that there is a perceived difference to cancer pain. Resonated and helps build concepts |
| Shye 1998212 | Hard to tell how ‘valuable research is’ at outset. Change thinking – yes; thought about the game-playing of tests that occurs (context demands/patient demand). Scope uncertainty – not specifically about use of guidelines for patients with chronic pain, but included to scan results for relevance. Nice description of relevant themes. Made me think of complexity of ‘playing the game’ that GPs have to do |
| Siedlecki 2014213 | Sometimes quotes do not match interpretation. Made me think about those with chronic pain on wards. An important insight into experiences of patient with chronic pain in an acute setting (e.g. do not cut home medications when in hospital if person has chronic pain). Some methodological flaws but still something positive about it. Not sure what the grounded theory is |
| Slade 2012214 | Clear and interesting themes with well supported and thoughtful discussion. Presents a key idea related to paradox of acute vs. chronic pain: (1) acute model (gain trust, quick gains, medication expectations); (2) chronic model. Makes me think – why do we need two models at all? Not helpful to use two models for gaining improvements. Possible negative impact on gaining trust |
| Sloots 2009215 | No comment |
| Sloots 2010216 | A few ideas not transparent and, therefore, not included – low gravity. Not changes thinking about culture differences as barrier. The barriers appear same if we frame any patient as if they were from a different culture. Some interesting thoughts. A bit on the thin side. Different cultural perspective sparks ideas |
| Spitz 2011217 | Used mixed methods so focuses on numbers a bit. A bit thin but insight into different influences in older patients |
| Starrels 2014218 | This paper gets a high score and raises issue of score not telling all. It is a bit thin but resonant and adds to gravity of themes |
| Stinson 2013219 | Not full gravitational pull but different perspective from younger people with pain. May contribute |
| Thunberg 2001150 | Thoughtful overarching core category of ambiguity which might lead to an important theme in analysis. Introduces concept of ambiguity: (a) ideal (holistic); (b) practice – practices of medicine based on clear professional boundaries, biomedicine, tests. Idea – ambiguity akin to liminality (fructile chaos) – Victor Turner |
| Toye 2015220 | Co-authored |
| Tveiten 2009221 | Bit vague on sample/nice ideas/metaphors. I am thinking more and more about tension – what should do and path of least resistance. Nice metaphor ‘wondering together’; ‘short circuit’ it is easier to let our own competence be paramount and not always allow participation. Highlight tension between empowerment and professional role ‘easier said than done’ |
| Wainwright 2006222 | Like it. Arm pain – not specific origin. May be key but difficult to tell early on. Made me think about problems of bio–psych–social as linear rather than venn-diagrammatically (see Victoria Grace) |
| Wilson 2014223 | Made me consider discourse of medicine and boundary management in health care. This explores boundary work of medicine language and process. Not all relevant but what is relevant is key to debate (potentially) |
| Wynne-Jones 2014224 | Lacks structure and some areas of themes repeated in sections. However, resonant and in scope |
| Zanini 2014225 | Supports well what I know and includes key ideas. A useful account of themes that is likely to be included in review findings |
Appendix 2 Concepts included in and excluded from the analysis
Findings with inadequate conceptualisation
-
Allegretti 2010:11 convergence – many barriers exist to care.
-
Barry 2010:155 physician factors – continuity of care.
-
Blomqvist 2003:160 activities to manage pain.
-
Blomqvist 2003:160 activities to manage pain – no activity.
-
Cameron 2015:162 psychology, negative thoughts, coping and reinforcement.
-
Dahan 2007:169 the guideline – practical issues in relation to low-back pain guideline implementation.
-
Espeland 2003:173 the GP’s professional dignity.
-
Gropelli 2013:178 inability to recognise an individualised plan of care.
-
Gropelli 2013:178 nurses’ perceptions about older adults and families.
-
Gropelli 2013:178 nurses’ perceptions and the possible lack of self-awareness cause barriers.
-
Hayes 2010:181 treatment and management.
-
Kaasalainen 2007:187 barriers and facilitators – barriers.
-
Kaasalainen 2007:187 barriers and facilitators – facilitators.
-
Kaasalainen 2010:188 influential factors.
-
Kaasalainen 2010:188 nurse practitioner role in pain management in long-term care.
-
Kaasalainen 2010:188 perceived outcomes.
-
Kristiansson 2011:192 helped her.
-
Kristiansson 2011:192 life hurts.
-
Kristiansson 2011:192 sad and still.
-
MacNeela 2010:196 professional knowledge – a schema for back pain.
-
McConigley 2008:197 strengths to assist in the implementation process.
-
Oosterhof 2014:202 experiences concerning the treatment outcome (maintaining new behaviour).
-
Paulson 1999:206 needing human support (feeling alone and forlorn).
-
Paulson 1999:206 needing human support (searching for sympathy).
-
Paulson 1999:206 struggling for relief from pain (not being taken seriously).
-
Paulson 1999:206 struggling for relief from pain (seeking explanation and wanting to be cured).
-
Ruiz 2010:208 value of ancillary services.
-
Stinson 2013:219 pain management strategies (physical strategies).
-
Stinson 2013:219 service delivery recommendations.
-
Thunberg 2001:150 professionals’ caring reality: hierarchy.
-
Thunberg 2001:150 professionals’ caring reality: medical–physical treatment.
Concepts that did not explore health-care professionals’ experiences
-
Coutu 2013:168 harmony scenario.
-
Esquibel 2014:174 utility and proper usage.
-
Esquibel 2014:174 addiction.
-
McCrorie 2015:198 patient drivers to seek help.
-
Oosterhof 2014:202 experiences concerning the interaction – being involved.
-
Oosterhof 2014:202 experiences concerning the interaction – being taken seriously.
-
Oosterhof 2014:202 experiences concerning the treatment outcome (organisational problems).
-
Parsons 2012:203 legitimating suffering (patients’ beliefs about receiving a diagnosis label for their pain).
-
Parsons 2012:203 legitimating suffering (the interaction between patients and health professionals’ beliefs about pain causation).
-
Parsons 2012:203 the evolving nature of patients’ and health professionals’ models of understanding chronic musculoskeletal pain (patients’ and health professionals’ beliefs about pain causation).
-
Parsons 2012:203 the evolving nature of patients’ and health professionals’ models of understanding chronic musculoskeletal pain (patients’ adaptation of causation belief).
-
Parsons 2012:203 development and tailoring of consultation and treatment approaches throughout patients’ illness careers (patients’ beliefs about consulting for and treatment of chronic musculoskeletal pain).
-
Sloots 2009:215 credibility with regard to foreign diagnosis.
-
Sloots 2009:215 trust in the rehabilitation physician.
-
Wilson 2014:223 articles of association.
-
Wilson 2014:223 calling for withdrawal of the guidance.
-
Wilson 2014:223 extraordinary general meeting.
-
Wilson 2014:223 the blog.
Concepts with limited transferability beyond specific context
-
Clark 2006:166 changes in pain knowledge, attitudes and practice – knowledge.
-
Côté 2001:167 approaches to manage occupational injuries – contact with the workplace.
-
McConigley 2008:197 toolkit development.
-
Ruiz 2010:208 value of computerised patient record system as a support tool.
-
Wilson 2014:223 guideline development group membership list.
Concepts with insufficient primary data to develop robust themes
Return to work
-
Côté 2001:167 barriers and facilitators of return to work – related to workplace.
-
Côté 2001:167 timely return to work.
-
Hellman 2015:182 multimodal rehabilitation created a foundation for a continuous return to work process – improving conditions for returning to work.
-
Hellman 2015:182 multimodal rehabilitation created a foundation for a continuous return to work process – creating a sustainable action plan.
-
Hellman 2015:182 return to work – a long-term process reaching beyond the time frames of multimodal rehabilitation.
-
Hellman 2015:182 the patients’ needs and conditions directed features within rehabilitation.
-
Hellman 2015:182 the professionals’ attitudes directed features within rehabilitation – promoting health and well-being rehabilitation warranty.
Ethnicity
-
Dobbs 2014:171 cultural, religious, and gender influences of resident pain care by certified nursing assistants.
-
Patel 2008:204 communication.
-
Patel 2008:204 consulting behaviour.
-
Patel 2008:204 presentation of pain.
-
Patel 2009:205 addressing patients psychosocial needs via counselling and cognitive–behavioural therapy.
-
Patel 2009:205 opportunities for increasing practitioners’ understanding of pain in a multicultural community.
-
Patel 2009:205 provisions required for community support.
-
Sloots 2009:215 communication.
-
Sloots 2009:215 responsibility for illness and treatment.
-
Sloots 2009:215 symptom presentation.
-
Sloots 2010:216 reasons for dropout in rehabilitation patients (communication and use of interpreters).
Gender
-
Paulson 1999:206 needing human support (being weary of life).
-
Paulson 1999:206 needing to be manly – being ashamed.
-
Paulson 1999:206 struggling for relief from pain (suffering from variable pain that is difficult to express and explain).
-
Paulson 1999:206 needing human support (withholding one’s innermost feelings).
-
Paulson 1999:206 needing to be manly – being strong and effective.
-
Paulson 1999:206 needing human support (suffering reduced self-confidence).
-
Paulson 1999:206 naive reading.
Older people
-
Blomberg 2008:159 detecting pain problems.
-
Blomberg 2008:159 detecting pain problems – patients’ abilities to communicate pain to district nurses.
-
Blomqvist 2003:160 care-related pain.
-
Blomqvist 2003:160 concealed pain.
-
Blomqvist 2003:160 endured pain.
-
Blomqvist 2003:160 inarticulate pain.
-
Cameron 2015:162 communication, confusion and questioning.
-
Cameron 2015:162 consultation time and historical events (time of life).
-
Cameron 2015:162 information retrieval.
-
Cameron 2015:162 mobility in older adults.
-
Cameron 2015:162 physiology, comorbidities and signs of ageing.
-
Clark 2004:165 behavioural and visual cues to pain.
-
Fox 2004:176 barriers to the assessment and treatment of pain – patient-related barriers (difficulty administering medications to patients).
-
Fox 2004:176 barriers to the assessment and treatment of pain – patient-related barriers (cognitive impairment).
-
Fox 2004:176 barriers to the assessment and treatment of pain – patient-related barriers (patients’ reluctance to report pain).
-
Fox 2004:176 facilitation of the assessment and treatment of pain – family support.
-
Kaasalainen 2007:187 lack of awareness of residents’ pain.
-
Löckenhoff 2013:194 age differences in time horizons (long-term prognosis).
-
Löckenhoff 2013:194 self-management of chronic pain.
-
Mentes 2004:199 pain on movement.
-
Ruiz 2010:208 pain as part of growing old.
Concepts that did not fit the conceptual analysis
-
Barry 2010:155 logistical factors – ancillary staff.
-
Barry 2010:155 logistical factors – insurance coverage.
-
Fontana 2008:175 critical analysis.
-
Holloway 2009:184 initiating clinical care.
-
Holloway 2009:185 perfect positioning (rewards of getting it right).
-
Kaasalainen 2010:188 interactions with long-term care staff and managers.
-
Liu 2014:193 instigator implementing non-pharmacological interventions.
-
Löckenhoff 2013:194 age differences in time horizons (treatment planning).
-
Lundh 2004:195 variation 1.
-
Oosterhof 2014:202 experiences concerning the treatment outcome (learning new behaviour).
-
Scott-Dempster 2014:210 ‘it’s not a one trick pony’.
-
Seamark 2013:211 cost.
-
Siedlecki 2014:213 core concepts/taking ownership.
-
Stinson 2013:219 barriers to care (patient-specific barriers).
-
Stinson 2013:219 pain management strategies (support systems), HCPs recognised the importance of peer support for patients.
Concepts included in analysis
-
Afrell 2010:151 a change of the relation to the patient – facing the negative.
-
Afrell 2010:151 a change of the relation to the patient – reconsidering the professional mandate.
-
Afrell 2010:151 a change in the patient – starts the processing.
-
Afrell 2010:151 the physiotherapists’ insights into the patient as a person – the patient’s view of the connection between body and life comes out.
-
Afrell 2010:151 the physiotherapists’ insights into the patient as a person – the pain is near to feelings.
-
Afrell 2010:151 the physiotherapists’ insights into the patient as a person – the pain mirrors life experience.
-
Afrell 2010:151 the physiotherapists’ insights into the patient as a person – the patient has the words.
-
Allegretti 2010:11 convergence – current treatments are ineffective.
-
Allegretti 2010:11 convergence – patients suffered from severe or serious chronic low-back pain.
-
Allegretti 2010:11 divergence – treatment goal of reducing pain versus improving function.
-
Allegretti 2010:11 divergence – biomedical versus biopsychosocial model.
-
Allegretti 2010:11 divergence – the importance of a definitive diagnosis.
-
Åsbring 2003:152 illness and the professional role.
-
Åsbring 2003:152 illness versus disease.
-
Åsbring 2003:152 moral judgement of illness.
-
Åsbring 2003:152 moral judgement of patient.
-
Åsbring 2003:152 strategies to manage patients with illness – adjusting the ideal to reality.
-
Åsbring 2003:152 strategies to manage patients with illness – doing something concrete.
-
Åsbring 2003:152 strategies to manage patients with illness – giving the patient responsibility.
-
Åsbring 2003:152 strategies to manage patients with illness – keeping a distance or getting closer.
-
Åsbring 2003:152 strategies to manage patients with illness – trying to find causes other than biomedical ones.
-
Åsbring 2003:152 strategies to manage patients with illness – trying to get the patient to accept the situation.
-
Baldacchino 2010:153 factors associated with abuse, misuse or diversion of prescription opioids.
-
Baldacchino 2010:153 judgements about whether or not patient is substance user affects chronic non-cancer pain management.
-
Baldacchino 2010:153 management of chronic non-cancer pain among people with a history of substance abuse.
-
Baldacchino 2010:153 physicians’ attitudes to prescribing opioids for chronic non-cancer pain management.
-
Barker 2015:154 it’s quite a long way from physiotherapy.
-
Barker 2015:154 reconstructing ‘acceptance’.
-
Barker 2015:154 understanding pain as an embodied experience.
-
Barker 2015:154 it’s quite a long way from physiotherapy.
-
Barker 2015:154 value-based goals a profound motivation for positive change.
-
Barry 2010:155 physician factors – opioid agreements.
-
Barry 2010:155 logistical factors – addiction referrals.
-
Barry 2010:155 logistical factors – diagnostic workup.
-
Barry 2010:155 logistical factors – pain management referrals.
-
Barry 2010:155 logistical factors – time.
-
Barry 2010:155 patient factors – attitudes towards opioid analgesics.
-
Barry 2010:155 patient factors – cost of specialty pain management.
-
Barry 2010:155 patient factors – motivation.
-
Barry 2010:155 patient factors – physician responsiveness to patients’ pain.
-
Barry 2010:155 physician factors – aberrant behaviours.
-
Barry 2010:155 physician factors – coexisting disorders.
-
Barry 2010:155 physician factors – expertise in pain management.
-
Barry 2010:155 physician factors – expertise in treating co-occurring chronic pain and opioid addiction.
-
Barry 2010:155 physician factors – interest in pain management.
-
Barry 2010:155 physician factors – pain assessment.
-
Baszanger 1992:156 centre 1 – establishing the patients pain situation.
-
Baszanger 1992:156 centre 1 – formulating advice to patients (a logic of description and demonstration).
-
Baszanger 1992:156 centre 1 – formulating advice to patients (face-to-face relations and the work of justification).
-
Baszanger 1992:156 centre 2 – establishing the patient’s pain situation.
-
Baszanger 1992:156 centre 2 – formulating advice to patients a logic of explanation and conviction.
-
Baszanger 1992:156 centre 2 – mutual involvement and the work of agreeing.
-
Berg 2009:157 practising in a context of ambiguity – decision-making frameworks.
-
Berg 2009:157 practising in a context of ambiguity – response to ambiguity.
-
Berg 2009:157 practising in a context of ambiguity – the ambiguity of pain.
-
Berg 2009:157 practising in a context of ambiguity; decision-making frameworks – pain management strategies.
-
Berg 2009:157 practising in a context of ambiguity; decision-making frameworks – perception and management of treatment risks (risk of deception).
-
Berg 2009:157 practising in a context of ambiguity; decision-making frameworks – perception and management of treatment risks.
-
Berg 2009:157 practising in a context of ambiguity; decision-making frameworks – perception and management of treatment risks (risk of disciplinary consequences).
-
Berg 2009:157 practising in a context of ambiguity; decision-making frameworks – perception and management of treatment risks (risk of abuse).
-
Berg 2009:157 treatment goals.
-
Berg 2009:157 acknowledgment of the reality of pain and the search for objective evidence (primary care practitioners).
-
Bergman 2013:158 recognition of patient individuality and consideration of relationship history.
-
Bergman 2013:158 role of discussing pain versus other primary care concerns.
-
Blomberg 2008:159 detecting pain problems – other professionals’ pain care collaborations with district nurses.
-
Blomberg 2008:159 detecting pain problems – the organisation’s pain care support regarding district nurses.
-
Blomberg 2008:159 district nurses involvement in pain care.
-
Blomberg 2008:159 responding to pain problems.
-
Blomqvist 2003:160 exaggerated pain.
-
Blomqvist 2003:160 real pain.
-
Blomqvist 2003:160 self-inflicted pain.
-
Blomqvist 2003:160 trivial pain.
-
Briones-Vozmediano 2013:161 diagnostic approach (health professionals).
-
Briones-Vozmediano 2013:161 evaluation of the health professional–patient relationship.
-
Briones-Vozmediano 2013:161 therapeutic management (health professionals).
-
Cameron 2015:162 consultation time and historical events (consultation time).
-
Cameron 2015:162 information retrieval.
-
Cameron 2015:162 physiology, comorbidities and signs of ageing.
-
Cameron 2015:162 resources.
-
Cartmill 2011:163 communication and collaboration among colleagues.
-
Cartmill 2011:163 organisational structure.
-
Cartmill 2011:163 the client population.
-
Chew-Graham 1999:164 making and negotiating a diagnosis.
-
Chew-Graham 1999:164 the doctor–patient relationship – negotiation or conclusion.
-
Clark 2004:165 relationship-centred cues to residents’ pain.
-
Clark 2004:165 resident characteristics and attitudes – resident attitudes.
-
Clark 2004:165 resident characteristics and attitudes – resident behaviours.
-
Clark 2004:165 uncertainty in pain assessment.
-
Clark 2006:166 changes in pain knowledge, attitudes and practice – attitudes.
-
Clark 2006:166 changes in pain knowledge, attitudes and practice – practice.
-
Clark 2006:166 progressive solutions and suggestions for changing practice.
-
Côté 2001:167 approaches to manage occupational injuries – chiropractic’s strength in diagnosis and treatment.
-
Côté 2001:167 approaches to manage occupational injuries – patient-centred care.
-
Côté 2001:167 barriers and facilitators of return to work – related to the worker.
-
Côté 2001:167 barriers and facilitators of return to work – related to rehabilitation.
-
Côté 2001:167 barriers and facilitators of return to work – related to payer.
-
Coutu 2013:168 little known about worker’s representations, modifiable problem targeted.
-
Coutu 2013:168 little known about worker’s representations, non-modifiable problem targeted.
-
Coutu 2013:168 scenario of differences between clinical judgement and worker’s representations.
-
Dahan 2007:169 patient–doctor interaction and relationship.
-
Dahan 2007:169 the guideline – practical issues in relation to low-back pain guideline implementation.
-
Dahan 2007:169 the physician’s low-back pain treatment agenda.
-
Daykin 2004:170 ‘good’ patients and the challenge of ‘difficult’ patients.
-
Daykin 2004:170 ‘good’ patients and the challenge of ‘difficult’ patients – impact of treating difficult patients.
-
Daykin 2004:170 developing craft knowledge.
-
Daykin 2004:170 developing craft knowledge – enlarging one’s tool bag.
-
Daykin 2004:170 developing craft knowledge – gaining patient mileage.
-
Daykin 2004:170 developing craft knowledge – personal pain experience.
-
Daykin 2004:170 pain beliefs within the therapeutic encounter.
-
Daykin 2004:170 the role of empathy in certified nursing assistant’s care of residents with pain.
-
Dobbs 2014:171 attitudes as barriers to communication about resident pain care.
-
Dobbs 2014:171 worker strategies to detect pain.
-
Eccleston 1997:172 Q-analysis (professional accounts).
-
Espeland 2003:173 access to radiology services.
-
Espeland 2003:173 pressure from other health-care providers or social security.
-
Espeland 2003:173 the GP’s expectations about the consequences of ordering radiography.
-
Espeland 2003:173 the GP’s perception of patients’ wishes for radiography.
-
Espeland 2003:173 the GP’s perception of whether or not the patient really is ill.
-
Espeland 2003:173 the GP’s response of keeping control and trying to help.
-
Espeland 2003:173 the GP’s uncertainty – radiography just to be sure.
-
Espeland 2003:173 effect of chronic opioid therapy on doctor–patient relationship – examples of chronic opioid therapy embittering the doctor–patient relationship.
-
Esquibel 2014:174 effect of chronic opioid therapy on doctor–patient relationship – perspectives on ideal and difficult patients.
-
Esquibel 2014:174 effect of chronic opioid therapy on doctor–patient relationship – prescribing opioids (an unwanted burden, an ineffective solution).
-
Esquibel 2014:174 right to pain medications.
-
Esquibel 2014:174 understanding pain.
-
Fontana 2008:175 critical analysis – in the best interest of society.
-
Fontana 2008:175 critical analysis – in the best interest of the patient.
-
Fox 2004:176 barriers to the assessment and treatment of pain – caregiver-related barriers (beliefs and knowledge).
-
Fox 2004:176 barriers to the assessment and treatment of pain – caregiver-related barriers (insensitivity to patients’ pain).
-
Fox 2004:176 barriers to the assessment and treatment of pain – system-related barriers (documentation).
-
Fox 2004:176 barriers to the assessment and treatment of pain – system-related barriers (insufficient time for nursing staff).
-
Fox 2004:176 barriers to the assessment and treatment of pain – system-related barriers (lack of communication).
-
Fox 2004:176 barriers to the assessment and treatment of pain – system-related barriers (frustration).
-
Fox 2004:176 facilitation of the assessment and treatment of pain.
-
Fox 2004:176 facilitation of the assessment and treatment of pain – demonstrating understanding and compassion.
-
Fox 2004:176 facilitation of the assessment and treatment of pain – teamwork.
-
Gooberman-Hill 2011:177 are opioids the best option – managing adverse effects and assessing vulnerable patients.
-
Gooberman-Hill 2011:177 are opioids the best option – the importance of previous experience.
-
Gooberman-Hill 2011:177 are opioids the best option – views about opioid addiction, withdrawal and misuse.
-
Gooberman-Hill 2011:177 are opioids the best option.
-
Gropelli 2013:178 failure to communicate.
-
Gropelli 2013:178 lack of education.
-
Hansson 2001:179 working guided by medical ethics.
-
Harting 2009:180 confirmation stage.
-
Harting 2009:180 decision stage.
-
Harting 2009:180 implementation stage.
-
Harting 2009:180 knowledge stage – acquainted with innovation.
-
Harting 2009:180 knowledge stage – understanding of innovation.
-
Harting 2009:180 persuasion stage.
-
Hayes 2010:181 definition and diagnosis.
-
Hellman 2015:182 a coherent link with external actors facilitated the return to work process – enabling collaboration.
-
Hellman 2015:182 conflicting interests between implicit attitudes and explicit guidelines.
-
Hellström 2015:183 adhering to the biomedical paradigm.
-
Hellström 2015:183 avoiding recognising fibromyalgia as a possible biomedical anomaly.
-
Hellström 2015:183 establishing an instrumental relationship.
-
Hellström 2015:183 managing clinical uncertainty.
-
Hellström 2015:183 prioritising diagnostics.
-
Holloway 2009:184 advocating for residents.
-
Holloway 2009:184 clinical decision-making.
-
Holloway 2009:185 extended roles – clinical judgements.
-
Holloway 2009:185 extended roles – nagging.
-
Holloway 2009:185 perfect positioning.
-
Holloway 2009:185 perfect positioning (emotional attachment).
-
Holloway 2009:185 perfect positioning (frontline).
-
Holloway 2009:185 perfect positioning (knowing the resident).
-
Holloway 2009:185 perfect positioning (teamwork).
-
Howarth 2012:186 collective efficacy.
-
Howarth 2012:186 interprofessional development through negotiated space.
-
Howarth 2012:186 team maturity.
-
Kaasalainen 2007:187 reluctance of health-care providers to use opioids.
-
Kaasalainen 2007:187 uncertainty about the accuracy of pain assessment and diagnosis.
-
Kaasalainen 2007:187 working to individualise pain treatments.
-
Kaasalainen 2007:187 influence of physician trust of the nurse on prescribing patterns.
-
Kaasalainen 2010:189 health-care providers.
-
Kaasalainen 2010:189 residents/family.
-
Kaasalainen 2010:189 system.
-
Kilaru 2014:190 associations with underlying attitudes towards opioid prescribing.
-
Kilaru 2014:190 attitudes towards guidelines – liability.
-
Kilaru 2014:190 attitudes towards guidelines – patient diversion.
-
Kilaru 2014:190 attitudes towards guidelines – physician autonomy.
-
Kilaru 2014:190 attitudes towards guidelines – public health.
-
Kilaru 2014:190 definition and awareness of guidelines – hospital-based guidelines.
-
Kilaru 2014:190 definition and awareness of guidelines – state and national guidelines.
-
Kilaru 2014:190 how physicians use guidelines – communication.
-
Krebs 2014:191 need to protect patients from harm.
-
Krebs 2014:191 inadequate time and resources.
-
Krebs 2014:191 opioid monitoring as a ‘law enforcement’ activity.
-
Krebs 2014:191 relying on general impressions of risk.
-
Kristiansson 2011:192 distressed, offended and disappointed.
-
Kristiansson 2011:192 prepare for a race.
-
Kristiansson 2011:192 build a safe relationship.
-
Kristiansson 2011:192 no help.
-
Kristiansson 2011:192 see how it goes.
-
Kristiansson 2011:192 she disappointed.
-
Kristiansson 2011:192 she was really sad.
-
Kristiansson 2011:192 very high risk.
-
Kristiansson 2011:192 wants to try.
-
Kristiansson 2011:192 her whole tiredness over me.
-
Kristiansson 2011:192 scolded.
-
Kristiansson 2011:192 while away one’s days.
-
Kristiansson 2011:192 will be challenged.
-
Kristiansson 2011:192 not obvious without own assessment.
-
Kristiansson 2011:192 receive a dressing-down.
-
Kristiansson 2011:192 want to examine before a doctor’s letter.
-
Liu 2014:193 level of familiarity.
-
Liu 2014:193 pain assessor.
-
Liu 2014:193 reporter – appreciation of the importance of their role as proxy report.
-
Liu 2014:193 reporter – submissive attitudes.
-
Liu 2014:193 subordinate implementing prescribed medications.
-
Liu 2014:193 subordinate implementing prescribed medications – underused reassessor.
-
Löckenhoff 2013:194 age differences in time horizons (concerns about future side effects).
-
Löckenhoff 2013:194 patient–provider relationship.
-
Lundh 2004:195 an inconsistent patient.
-
Lundh 2004:195 devotion to help.
-
Lundh 2004:195 being a helpless helpoholic.
-
Lundh 2004:195 frustration.
-
Lundh 2004:195 helplessness.
-
Lundh 2004:195 ineffective tools.
-
Lundh 2004:195 variation 2.
-
Lundh 2004:195 variation 3.
-
MacNeela 2010:196 representing the person’s experience (depression).
-
MacNeela 2010:196 representing the person’s experience (social categories).
-
MacNeela 2010:196 representing the person’s experience (work and legal issues).
-
MacNeela 2010:196 the therapeutic relationship.
-
MacNeela 2010:196 the therapeutic relationship (gatekeeper).
-
MacNeela 2010:196 the therapeutic relationship (moral guardian).
-
MacNeela 2010:196 the therapeutic relationship (patient guide).
-
McConigley 2008:197 barriers to implementation – resource issues.
-
McConigley 2008:197 barriers to implementation – work role issues.
-
McConigley 2008:197 needs associated with implementation.
-
McConigley 2008:197 strengths to assist in the implementation process.
-
McCrorie 2015:198 features of transactions between patients and GPs – continuity of care.
-
McCrorie 2015:198 features of transactions between patients and GPs – mutuality and trust in the relationship.
-
McCrorie 2015:198 features of transactions between patients and GPs – locating control and responsibility for change.
-
McCrorie 2015:198 features of transactions between patients and GPs – absence of a shared management plan.
-
Mentes 2004:199 distraction, inspection and telling the charge nurse.
-
Mentes 2004:199 knowing the resident.
-
Mentes 2004:199 pain assessment face and eyes.
-
O’Connor 2015:200 being under one roof.
-
O’Connor 2015:200 case conferences or team meetings.
-
O’Connor 2015:200 patients as whole persons.
-
O’Connor 2015:200 patients help themselves.
-
O’Connor 2015:200 training.
-
Øien 2011:201 ambivalence and uncertainty.
-
Øien 2011:201 impatience and disagreement.
-
Øien 2011:201 seeking for common ground – a demanding negotiating process.
-
Oosterhof 2014:202 experiences concerning the interaction (being open).
-
Oosterhof 2014:202 experiences concerning the interaction (giving a clear explanation).
-
Oosterhof 2014:202 experiences concerning the treatment outcome – acknowledgement for the physical part or the pain.
-
Oosterhof 2014:202 experiences concerning the treatment outcome (shared understanding of the pain).
-
Parsons 2012:203 legitimating suffering (health professionals’ beliefs about being able to diagnose chronic musculoskeletal pain).
-
Parsons 2012:203 the evolving nature of patients’ and health professionals’ models of understanding chronic musculoskeletal pain (patients’ and health professionals’ beliefs about pain causation).
-
Parsons 2012:203 the evolving nature of patients’ and health professionals’ models of understanding chronic musculoskeletal pain (health professionals’ adaptation of causation beliefs).
-
Parsons 2012:203 development and tailoring of consultation and treatment approaches throughout patients’ illness careers (HCPs’ beliefs about consulting for and treatment of chronic musculoskeletal pain).
-
Patel 2008:204 GPs’ personal challenges.
-
Patel 2008:204 psychosomatic interpretations.
-
Patel 2009:205 expectation mismatch.
-
Patel 2009:205 the challenges of secondary care services.
-
Paulson 1999:206 needing human support (disturbing feelings).
-
Poitras 2011:207 clinical relevance.
-
Poitras 2011:207 environment – work organisation.
-
Poitras 2011:207 environment – work organisation.
-
Poitras 2011:207 peers and stakeholders.
-
Poitras 2011:207 therapists – agreement with the guidelines.
-
Poitras 2011:207 therapists – compatibility with current practice.
-
Poitras 2011:207 therapists – impact on low-back pain disability.
-
Poitras 2011:207 therapists – understandability of the guidelines.
-
Ruiz 2010:208 waiting times for pain clinic.
-
Ruiz 2010:208 concerns about using pain medications (addiction dependency).
-
Ruiz 2010:208 concerns about using pain medications (medication diversion).
-
Ruiz 2010:208 concerns about using pain medications (side effects).
-
Ruiz 2010:208 poor training in pain management (on-the-job training).
-
Ruiz 2010:208 poor training in pain management (self-directed learning).
-
Ruiz 2010:208 poor training in pain management (training as a student resident).
-
Schulte 2010:209 communication between GPs and pain specialists.
-
Schulte 2010:209 GPs’ attitude towards pain specialists.
-
Schulte 2010:209 referral from GPs to specialised pain centres.
-
Schulte 2010:209 experiences of GPs after referral to specialist pain clinics.
-
Scott-Dempster 2014:210 changing practice from ‘fix it’ to ‘sit with’.
-
Scott-Dempster 2014:210 process of realisation that life can be different – encourage self-reflection.
-
Scott-Dempster 2014:210 process of realisation that life can be different – realise I can do something.
-
Scott-Dempster 2014:210 process of realisation that life can be different.
-
Scott-Dempster 2014:210 process of realisation that life can be different – encourage self-reflection.
-
Scott-Dempster 2014:210 process of realisation that life can be different – discover through trying.
-
Scott-Dempster 2014:210 process of realisation that life can be different – patients can’t see.
-
Seamark 2013:211 chronic non-cancer pain is seen as different from cancer pain.
-
Seamark 2013:211 concerns around tolerance and addiction.
-
Seamark 2013:211 difficulties in assessing pain.
-
Seamark 2013:211 effect of experience and events.
-
Shye 1998:212 access to referral services.
-
Shye 1998:212 management expectations a double bind.
-
Shye 1998:212 patient characteristics.
-
Shye 1998:212 patient expectations – building and maintaining trust.
-
Shye 1998:212 time the scarcest resource.
-
Shye 1998:212 ambiguity of internal referral processes.
-
Siedlecki 2014:213 core concepts – frustration.
-
Siedlecki 2014:213 core concepts – moral distress.
-
Siedlecki 2014:213 core concepts – taking ownership.
-
Siedlecki 2014:213 core concepts – tenacity.
-
Siedlecki 2014:213 nurse characteristics – attitude.
-
Siedlecki 2014:213 nurse characteristics – discernment.
-
Siedlecki 2014:213 nurse characteristics – knowledge.
-
Siedlecki 2014:213 system barriers.
-
Slade 2012:214 blame game – physiotherapists are critical when care-seekers fail to improve.
-
Slade 2012:214 physiotherapists are challenged by diagnostic uncertainty (physiotherapists use surrogates for pathoanatomical diagnoses to provide solutions).
-
Slade 2012:214 physiotherapists are challenged by diagnostic uncertainty (communicating the truth is difficult – physiotherapists feel pressured to diagnose).
-
Slade 2012:214 physiotherapists perceive that care-seekers want a clear diagnosis.
-
Slade 2012:214 physiotherapists seek ‘certainty’ from experienced colleagues (professional ‘experts’ are attractive models).
-
Slade 2012:214 physiotherapists seek ‘certainty’ from experienced colleagues (workplace culture and mentors are important).
-
Slade 2012:214 practitioners feel underprepared by traditional education models (physiotherapists believe they are underprepared by their education).
-
Slade 2012:214 practitioners feel underprepared by traditional education models (experience is the real teacher).
-
Slade 2012:214 practitioners feel underprepared by traditional education models (physiotherapists believe they are underprepared by their education).
-
Sloots 2009:215 expectations regarding the aim of treatment.
-
Sloots 2010:216 reasons for dropout in rehabilitation patients (acknowledgement or legitimisation of the pain complaints).
-
Sloots 2010:216 reasons for dropout in rehabilitation patients (credibility with regard to foreign diagnosis).
-
Sloots 2010:216 reasons for dropout in rehabilitation patients (trust in the rehabilitation physician).
-
Spitz 2011:217 facilitators of opioid use – perceived patient-level barriers to opioid use.
-
Spitz 2011:217 frustration treating pain in primary care.
-
Spitz 2011:217 greater comfort using opioids in patients receiving palliative care.
-
Spitz 2011:217 provider barriers to opioid use – concerns about opioid abuse, misuse or addiction.
-
Spitz 2011:217 provider barriers to opioid use – concerns about regulatory and or legal sanctions.
-
Spitz 2011:217 provider barriers to opioid use – fear of causing harm.
-
Spitz 2011:217 provider barriers to opioid use – pain subjectivity.
-
Spitz 2011:217 providers’ opioid prescribing practices and attitudes.
-
Starrels 2014:218 beliefs about the utility of opioid treatment agreements – prevention of opioid misuse.
-
Starrels 2014:218 beliefs about the utility of opioid treatment agreements – diagnosis of opioid misuse.
-
Starrels 2014:218 beliefs about the utility of opioid treatment agreements – physician self-protection.
-
Starrels 2014:218 perceived effect of opioid treatment agreement use on the therapeutic alliance.
-
Starrels 2014:218 perception of patients’ risk of misuse.
-
Stinson 2013:219 barriers to care (health-care systems barriers).
-
Stinson 2013:219 barriers to care (societal barriers).
-
Stinson 2013:219 pain impact (future).
-
Stinson 2013:219 pain impact (physical impact).
-
Stinson 2013:219 pain impact (role functioning).
-
Stinson 2013:219 pain impact (social and emotional impact).
-
Stinson 2013:219 pain management strategies (pharmacological strategies).
-
Stinson 2013:219 pain management strategies (psychological strategies).
-
Thunberg 2001:150 professional ambiguity.
-
Thunberg 2001:150 professionals’ thoughts on ideal care.
-
Thunberg 2001:150 professionals’ thoughts on ideal care (holistic approach).
-
Thunberg 2001:150 professionals’ thoughts on ideal care (the patient in his or her context).
-
Thunberg 2001:150 professionals’ thoughts on ideal care (validating).
-
Thunberg 2001:150 professionals’ caring reality.
-
Thunberg 2001:150 professionals’ caring reality illness carried by the patient.
-
Thunberg 2001:150 professionals’ caring reality monofactorial aetiology.
-
Thunberg 2001:150 professionals’ caring reality objective analysis.
-
Toye 2015:220 a glimpse beneath the surface.
-
Toye 2015:220 a glimpse beneath the surface (the challenge of clinical time constraints).
-
Toye 2015:220 bombarded by despair – I’ve used the phrase detached empathy.
-
Toye 2015:220 bombarded by despair – it was a bit uncomfortable listening to the things she said.
-
Toye 2015:220 a glimpse beneath the surface (I can now see her struggle to perform pain).
-
Toye 2015:220 reconstructing the clinical encounter as a shared journey – we are going to chip away at this in bite-sized chunks.
-
Toye 2015:220 reconstructing the clinical encounter as a shared journey – this is a journey to healing not fixing.
-
Toye 2015:220 pitfalls of the medical model – the challenge of ‘sitting with’ (not fixing).
-
Toye 2015:220 pitfalls of the medical model – the challenge of breaking down the dichotomy of mind and body.
-
Tveiten 2009:221 challenges of conducting a dialogue.
-
Tveiten 2009:221 different dialogues and varying purposes.
-
Tveiten 2009:221 patient participation and the patient as an expert – easier said than done.
-
Tveiten 2009:221 the importance and characteristics of the good dialogue.
-
Wainwright 2006:222 clinical uncertainty.
-
Wainwright 2006:222 psychosocial problems and the doctor–patient relationship.
-
Wainwright 2006:222 psychosocial problems and the doctor–patient relationship (negotiated diagnosis).
-
Wainwright 2006:222 psychosocial problems and the doctor–patient relationship (covert shift to the psychosocial paradigm).
-
Wainwright 2006:222 psychosocial problems and the doctor–patient relationship (negotiated diagnosis).
-
Wainwright 2006:222 psychosocial problems and the doctor–patient relationship (overt shift to the psychosocial paradigm).
-
Wainwright 2006:222 psychosocial problems and the doctor–patient relationship – covert shift to the psychosocial paradigm (bridging technologies: fibromyalgia).
-
Wainwright 2006:222 psychosocial problems and the doctor–patient relationship – covert shift to the psychosocial paradigm (bridging technologies: amitriptyline).
-
Wilson 2014:223 symbolic languages – legitimisation of practice.
-
Wilson 2014:223 symbolic languages – diagnostic expertise.
-
Wilson 2014:223 symbolic languages – the evidence base.
-
Wilson 2014:223 symbolic languages – the individual patient.
-
Wynne-Jones 2014:224 approaches to evaluating patients’ work problems.
-
Wynne-Jones 2014:224 issuing of fit notes – GP as ‘patient advocate’.
-
Wynne-Jones 2014:224 perceived ability to manage ‘work and pain’.
-
Wynne-Jones 2014:224 policies and penalties in the workplace.
-
Zanini 2014:225 patients’ perspectives of their health condition.
-
Zanini 2014:225 patients’ perspectives of treatments.
Appendix 3 Concepts included in the opioid concept analysis
Baldacchino 2010153
-
Factors associated with abuse, misuse or diversion of prescription opioids.
-
Judgements about if patient is substance user affect chronic non-cancer pain management.
-
Management of chronic non-cancer pain among people with a history of substance abuse.
-
Physicians’ attitudes to prescribing opioids for chronic non-cancer pain management.
Barry 2010155
-
Physician factors: opioid agreements.
-
Patient factors: attitudes towards opioid analgesics.
-
Patient factors: motivation.
-
Patient factors: physician responsiveness to patients’ pain.
-
Physician factors: aberrant behaviours.
-
Physician factors: coexisting disorders.
-
Physician factors: expertise in pain management.
-
Physician factors: expertise in treating co-occurring chronic pain and opioid addiction.
-
Physician factors: interest in pain management.
-
Physician factors: pain assessment.
Berg 2009157
-
Practising in a context of ambiguity: decision-making frameworks.
-
Practising in a context of ambiguity: the ambiguity of pain.
-
Practising in a context of ambiguity: decision-making frameworks – pain management strategies.
-
Practising in a context of ambiguity: decision-making frameworks – perception and management of treatment risks.
-
Practising in a context of ambiguity: decision-making frameworks – perception and management of treatment risks (risk of disciplinary consequences).
-
Practising in a context of ambiguity: decision-making frameworks – perception and management of treatment risks (risk of deception).
-
Practising in a context of ambiguity: decision-making frameworks – perception and management of treatment risks (risk of abuse).
-
Treatment goals.
Briones-Vozmediano 2013161
-
Therapeutic management (health professionals).
Cameron 2015162
-
Information retrieval.
-
Physiology, comorbidities and signs of ageing.
Esquibel 2014174
-
Effect of chronic opioid therapy on doctor–patient relationship: examples of chronic opioid therapy embittering the doctor–patient relationship.
-
Effect of chronic opioid therapy on doctor–patient relationship: prescribing opioids – an unwanted burden, an ineffective solution.
-
Effect of chronic opioid therapy on doctor–patient relationship: perspectives on ideal and difficult patients’ right to pain medications.
Fontana 2008175
-
Critical analysis: in the best interest of society.
-
Critical analysis: in the best interest of the nurse.
-
Critical analysis: in the best interest of the patient.
Gooberman-Hill 2011177
-
Are opioids the best option?
-
Are opioids the best option? Managing adverse effects and assessing vulnerable patients.
-
Are opioids the best option? The importance of previous experience.
-
Are opioids the best option? Views about opioid addiction, withdrawal and misuse.
Kaasalainen 2007187
-
Reluctance of health-care providers to use opioids.
-
Working to individualise pain treatments.
Kaasalainen 2010189
-
Residents/family.
Kilaru 2014190
-
Associations with underlying attitudes towards opioid prescribing.
-
Attitudes towards guidelines: liability.
-
Attitudes towards guidelines: patient diversion.
-
Attitudes towards guidelines: physician autonomy.
-
Attitudes towards guidelines: public health.
-
Definition and awareness of guidelines: hospital-based guidelines.
-
Definition and awareness of guidelines: state and national guidelines.
-
How physicians use guidelines: communication.
Krebs 2014191
-
Need to protect patients from harm.
-
Inadequate time and resources.
-
Opioid monitoring as a ‘law enforcement’ activity.
-
Relying on general impressions of risk.
Löckenhoff 2013194
-
Age differences in time horizons (concerns about future side effects).
-
Patient–provider relationship.
McCrorie 2015198
-
Features of transactions between patients and GPs: mutuality and trust in the relationship.
-
Features of transactions between patients and GPs: locating control and responsibility for change.
-
Features of transactions between patients and GPs: absence of a shared management plan.
Ruiz 2010208
-
Concerns about using pain medications (addiction dependency).
-
Concerns about using pain medications (medication diversion).
-
Concerns about using pain medications (side effects).
Seamark 2013211
-
Chronic non-cancer pain is seen as different from cancer pain.
-
Concerns around tolerance and addiction.
-
Difficulties in assessing pain.
-
Effect of experience and events.
Siedlecki 2014213
-
Nurse characteristics: attitude.
Spitz 2011217
-
Facilitators of opioid use: perceived patient-level barriers to opioid use.
-
Greater comfort using opioids in patients receiving palliative care.
-
Provider barriers to opioid use: concerns about opioid abuse, misuse or addiction.
-
Provider barriers to opioid use: concerns about regulatory and/or legal sanctions.
-
Provider barriers to opioid use: fear of causing harm.
-
Provider barriers to opioid use: pain subjectivity.
-
Providers’ opioid prescribing practices and attitudes.
Starrels 2014218
-
Beliefs about the utility of opioid treatment agreements: prevention of opioid misuse.
-
Beliefs about the utility of opioid treatment agreements: diagnosis of opioid misuse.
-
Beliefs about the utility of opioid treatment agreements: physician self-protection.
-
Perceived effect of opioid treatment agreement use on the therapeutic alliance.
-
Perception of patients’ risk of misuse.
List of abbreviations
- AMED
- Allied and Complementary Medicine Database
- CASP
- Critical Appraisal Skills Programme
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- ConQual
- establishing confidence in the output of qualitative research synthesis
- GP
- general practitioner
- GRADE-CERQual
- Grading of Recommendations Assessment, Development and Evaluation Confidence in the Evidence from Reviews of Qualitative research
- HCP
- health-care professional
- HSDR
- Health Services and Delivery Research
- QES
- qualitative evidence synthesis