Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/209/02. The contractual start date was in April 2014. The final report began editorial review in January 2017 and was accepted for publication in June 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Lizanne Harland reports personal fees from Bristol Clinical Commissioning Group (CCG) and Gloucestershire CCG outside the submitted work. Lesley Wye is a member of the Health Services and Delivery Research (HSDR) Prioritisation Commissioning Panel. Chris Salisbury is a board member of the National Institute for Health Research (NIHR) HSDR programme, which funded this project. He is also a board member of the NIHR School for Primary Care Research.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Horrocks et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction, background and aim of the study
This chapter provides the rationale for the study, outlines the policy context for community nursing service provision and describes some of the challenges in measurement of service quality within community nursing.
Introduction
Public perceptions and trust in the medical and nursing profession were shaken by the Bristol Royal Infirmary inquiry in 20011 and the failings in care at the Mid Staffordshire NHS Foundation Trust,2 both of which related to care quality in hospitals. NHS England (NHSE)3 responded with The 6Cs and Compassion in Practice, a paper characterising provision of high-quality nursing under the categories of the six ‘Cs’ – ‘care’, ‘compassion’, ‘courage’, ‘communication’, ‘commitment’ and ‘competence’– that could be applied to nursing in any health-care setting, and that has since been rolled out to include all practitioners in the NHS. The importance of having well-educated, graduate practitioners providing leadership at the front line in the nursing workforce to ensure the care and safety of patients has also been confirmed. 4 Since 2016, Nursing and Midwifery Council (NMC) revalidation has been introduced for registered practitioners to ensure that adherence to the code of professional standards for nurses in care delivery is being upheld. 5 However, the setting and monitoring of care standards is somewhat easier in the acute sector than in the community, and it is notable that the majority of work in relation to assessing nursing care quality has been undertaken in a hospital setting. Given the comparative invisibility of care delivery in patients’ homes, it is crucial that care quality can be monitored to protect patients.
Nurses constitute the largest service group within community-based health provision and work in a range of roles supporting patients in their homes to prevent unnecessary hospital admission and facilitate timely discharge. They may work in specialist roles, such as palliative care or heart failure, or as part of nursing teams (e.g. district nurses and community matrons), providing a full range of nursing care to people who are housebound, therefore serving the most vulnerable and frail NHS users. 6 Care provided in the home is largely invisible to planners and managers and, therefore, it is crucial to understand how quality measures for community nursing are identified and their usefulness for assuring service quality. 7,8 Although an understanding of how to measure the quality of services is growing in the hospital and primary care sectors, comparatively little is known about how best to measure service quality in the community nursing sector,9 or how patients perceive the value of current quality indicators.
The setting and measurement of quality standards have been formally incorporated into community health service commissioning decisions since 2009 and a database of quality indicators (QIs) has been published for use in community services. 10 The use of standardised QIs across community services should, in theory, enable similar services to be compared. Despite substantial investment in QI schemes, however, little is known about how quality measures are used in practice and their usefulness in improving and monitoring quality in nursing. A recent report by The King’s Fund found that community care providers still lacked ‘robust, comparable national indicators that would enable them to benchmark their performance’ and that information technology (IT) and infrastructure were underdeveloped to support quality measurement. 11 The report covered the full range of community services; however, many community services actually take place in clinic and health centre settings and provide time-limited episodes of care for which outcome measures may be readily identified. In contrast, quality measurement in community nursing is complicated by the fact that the majority of service users are cared for in the home and have complex and long-term health problems or deteriorating conditions, making suitable outcome measures difficult to design. 12,13
Quality indicators are measures that aim to numerically describe a service to enable comparison or to assess improvement. 10,14,15 They can come from multiple sources, including Transforming Community Services,10 Community Information Data Set16 and National Institute for Health and Care Excellence (NICE) quality standards,17 in addition to local derivation. 18 The concept of quality measurement in health care incorporates a range of different dimensions,19–21 and perspectives on quality measurement can vary between commissioners, providers and service users. 18 Donabedian’s health-care quality framework19 comprises three domains, namely structure (the organisational system or environment under which care is provided, e.g. training of staff, staffing levels), process (e.g. components of service provision) and outcome measurement (the consequences for health of the care delivered). There has been debate about the relative importance of process and outcome measures in quality assurance. 21 Although outcomes represent the ultimate goals of health care and are more easily measured and understood by service users, they can be affected by extraneous factors outside the control of the health service and may not be apparent at the time of care delivery, so are more difficult to attribute. For this reason they may be mistrusted by service providers. 7,18,22 Process indicators, in contrast, are likely to be within the scope of the health-care provider and less likely to be influenced by external factors, but are less easily measured or understood by those outside the service. 22
More recently, NHS quality of care assessment has reflected an emphasis on efficient use of resources and effectiveness, the latter reflecting both clinical outcomes and user experience. 21 This approach was incorporated and further developed within the current NHS quality domains, namely patient experience and clinical effectiveness, with the addition of patient safety. 23 At the time of the current study, these quality domains were incorporated into an annual, nationally mandated quality scheme called Commissioning for Quality and Innovation (CQUIN). The CQUIN scheme, included within the NHS standard contract, offers community services providers additional income to meet quality goals (e.g. improvements in end-of-life care planning) by measuring quality outcome indicators (such as the number of people with a record of death in a preferred place). 24 The intention was to allow commissioners to negotiate with health-care providers on developing services to meet local priorities, while operating within a broader national framework based on national and international best practice. The scheme has the potential to provide information for comparison purposes and incentivise innovative practice and higher-quality aspirations locally. However, a national evaluation of the scheme (which included both acute and community providers) found that few of its interviewees consulted national indicators when developing their CQUIN schemes and that the variety of local indicators that emerged were often unclear or lacking in precision, making it difficult to follow up performance or benchmark services. 25 Several recommendations were made, including reducing the number of local CQUINs schemes and the provision of a small number of benchmarking QIs with a menu of appropriate indicators for use in acute and community settings. Since the changes following the implementation of the Health and Social Care Act 2012,26 it is unclear how, if at all, use of the CQUIN scheme has changed under Clinical Commissioning Groups (CCGs) led by general practitioners (GPs) and how useful it is in the context of measuring quality in community nursing.
The delivery of NHS community nursing services is also subject to a number of quality requirements or key performance indicators (KPIs) incorporated within the standard NHS contract for monitoring and accountability purposes. 27,28 National quality requirements applicable for community nursing include ‘duty of candour’ and ‘never events’, that is, the need for staff to speak up if they are aware of ‘near miss’ incidents of potential harm to patients in order that learning can be gained to prevent similar harms from happening in future. A medication error involving insulin (much of which is administered by community nurses in patients’ homes) would be designated a ‘never event’, as its impact on the patient could be catastrophic. 29 The duty of candour states that staff should be honest and transparent in their communications with patients and their relatives when things go wrong. 30 The contract also includes locally agreed incentive schemes and requires reporting on service quality issues, such as complaints, serious incidents, staff numbers and skill mix, all of which can provide a regular snapshot of real-time feedback on service quality. In addition, providers are required to provide feedback from patients and staff on a regular basis.
Regular approval from the Care Quality Commission (CQC)31 is another requirement of community nursing service providers. CQC inspection overlaps with several areas incorporated in the NHS standard contract, but also includes quality standards related to ‘caring’. Caring is defined as the degree of dignity, respect and compassion while receiving care, people being involved as partners in their care and people who use the services receiving support to cope emotionally with their condition, none of which is directly monitored by the NHS contract. Another key difference relates to the approach to monitoring quality, which always involves an observation of practice and assessment of leadership, as well as an inspection of relevant documentation and talking directly to front-line staff and patients. Taken together, there appears to be a battery of quality assurance requirements on which community service providers report, suggesting a large workload to set, monitor and report on indicators of service quality, without evidence of their perceived usefulness for community nursing from the perspectives of commissioners or service providers and those in receipt of nursing care.
Quality indicator schemes have the potential to improve care quality by provision of feedback to clinicians to improve performance and reduce variation between services, yet there is a body of evidence that suggests that there can be unintended consequences of their use. 32 Unintended consequences documented in the literature included data collection using IT interfering with patient interactions and demotivation of clinicians when they felt their professional judgement being over-ruled. A study exploring primary care professionals’ experiences of the GP Quality and Outcomes Framework, a pay-for-performance quality scheme, suggested that the nature of professional and patient consultations had changed since its introduction, with patient centredness and continuity negatively affected. 33,34 Rambur et al. ,35 reporting on UK studies that included nurses, found evidence of ‘measure fixation’, that is, inappropriate attention on isolated aspects of care conflicting with patient-centred care. 36,37 Although the nurses referred to above tended to work in general practice or acute settings, little is known about the impact of incentivised QIs such as CQUINs on care delivered by community nurses. Furthermore, incentivised QIs for nursing that have been applied in acute care have been rolled out into the community, taking little account of the differing care context for nurses,38 and it is not clear how useful these are for assessing quality from the perspectives of commissioners, providers, patients or front-line community nursing staff.
In this report, findings are presented from a study comprising a collaboration between four universities (University of the West of England, Bristol; University of Bristol; London School of Hygiene and Tropical Medicine; and University of Manchester) and a NHS partner (the NHS Bristol CCG). Patient and public involvement in the study was integrated firmly at the outset by the inclusion of a lay co-applicant, who instigated the initial research question of how the use of performance indicators might affect nurses’ delivery of personalised care. The study aimed to understand how QIs were being selected and applied in the community nursing context, whether or not these were considered useful by patients, commissioners and providers, and how they could best be used to confer benefit to patients being cared for by community nurses.
Background
The recent background for community nursing provision has been one of continuing organisational change and financial pressure. The NHS is expected to make £22B in efficiency savings by 2020. 39 A key factor in meeting this target is to shift care from acute service provision to the community, placing increased pressure on community services to reduce avoidable hospital admissions and enable the timely discharge of patients. The following section presents the key themes from our review of the literature, which drew on both a structured search of research relating to quality and community nursing and the knowledge of relevant literature within the research management group (see Appendix 1 for the search strategy). It outlines recent policy in the arena of commissioning and community service provision, including the drive to integrate health and social care services, workforce issues and the care context for community nursing, against which the measurement of service quality takes place.
Policy context for community nursing services
The study commenced in 2014, soon after the implementation of the Health and Social Care Act 2012,26,40 with the newly formed CCGs having been in place just over 1 year. Alongside the new commissioning organisations, Transforming Community Services had required NHS organisations in England to be either commissioner or provider. 40 New models of community services providers, for example social enterprises and community foundation trusts, were announced in the Next Stage Review as well as a flexible standard contract to enable commissioners to:
hold community health services to account for quality and health improvement.
p. 4441
Many of these organisations were only created in 2010/11 with 3- to 5-year contracts. A quality framework for community services was also published, which identified 76 QIs reflecting the six areas contained in Transforming Community Services. 10 Community teams were expected to choose and implement a few of these indicators, adapting them to their local circumstances, but at least one commentator expressed doubts that nurses would be given full budgetary control to implement them. 42
The increased integration of health and care services and funding to improve the quality of services for older and disabled people was announced in the Better Care Fund (BCF) spending review (£3.8B worth of funding in 2015/16). 43 In theory, the programme would directly affect the delivery of community nursing, as community nurses play a key role in looking after older and disabled people in their homes. The establishment of new models of care, such as multispecialty community providers, which are vehicles for integrating health and social care, was encouraged in the Five Year Forward View;39 these models are likely to impact on the way that community nursing provision is delivered in future. The main challenges facing commissioners have been identified as the need to consult and engage with patients, and the use of competitive tendering and outcomes-based contracts as organisations move to the new models of care. 44 Furthermore, a major problem hampering community services commissioning was said to be a lack of reliable data and suitable outcome measures, both essential components of outcomes-based commissioning. 44 These components must be in place to allow the benchmarking and evaluation of value-for-money services.
Community nursing services are central to effective integrated care provision, but appropriate outcome measures to assess the impact of integrated care require co-production across organisations and tailoring to those organisations’ priorities for service delivery. 45 The development of meaningful outcomes can be a lengthy process, and this is currently at an early stage. A survey of health and social care managers found that interprofessional working (IPW) for older people, an aspect of integrated care, tended to focus on time-limited, problem-specific interventions, with intermediate care services the most frequently identified model of provision. 46 Intermediate care services are short-term, high-input nursing and therapy care provided to patients at risk of hospital admission or post discharge from hospital, with a focus on support and rehabilitation. The avoidance of hospital admission and recovery from acute episodes of ill health are valid health-care outcomes for intermediate care service input, but they do not reflect continuity of care, which is arguably a better indicator of high-quality integrated care, particularly from the perspective of patients with long-term conditions and their carers. 18 Time, resources and good communication between front-line clinicians and managers are all required to facilitate effective integrated care, but disparities have been reported between, on the one hand, the expectations of leaders in terms of the speed of change required and, on the other hand, the expectations of front-line staff in terms of the feasibility of such change in practice. 47 It is not known how the impact of individual services, such as community nursing, will be attributed for quality monitoring purposes in the developing integrated care context.
Workforce issues
A responsive and high-quality community nursing service is vital for meeting the policy aims of reducing pressure on acute services and, therefore, reducing NHS costs. Historically, decisions about the structure and deployment of nursing teams have been based on tradition and so can be inconsistent and non-systematic. 48 Longstanding issues include a large number of vacancies and a lack of consensus on the most appropriate way to use staff to meet patient need (i.e. whether the service should be generalist or specialist led, or the level of skill mix required in teams). Shortages in community nurse staffing levels have been claimed to lead to patients being readmitted to hospital. 49 The Royal College of Nursing (RCN) has repeatedly stressed that, despite the policy drive to move care into the community and closer to people’s homes, community nursing numbers have declined. There was a 42% fall in district nurse-trained nurses between 2004 and 2014,50,51 and the overall proportion of nursing staff employed to provide general nursing care to people in their own homes has changed little. 52
Patient safety is a fundamental NHS quality measure. A new commissioning framework for community nursing,53 produced following the recommendations of the Francis report,2 takes into account safe staffing. The quality measures incorporated in the framework include access to professional development, use of evidence-based metrics for patient outcomes and experience, and KPIs to demonstrate evidence of workforce planning. District nursing providers, however, still require evidence-based operational scheduling tools to determine the requisite numbers and skill mix of staff needed to deliver care to patients at home. These, in turn, need to be compatible with a population needs-informed community nursing workforce forecasting tool before outcomes and performance can be compared across organisations. 48 Without such tools, it is difficult to know how to benchmark organisational performance and measure quality improvement in community nursing.
The staffing of community nursing teams has been bolstered by the introduction of skill mix, that is, the inclusion of nursing assistants to undertake specific roles in patient care. A National Institute for Health Research-funded study found that nursing assistants made up one-quarter of the community nursing workforce. The study found that senior managers appreciated the breadth of skills offered by skill mix and the consequent freeing up of registered nurse time for more complex nursing care. 54 When nursing assistants have been used effectively in relation to medication visits, they have been shown to improve access, reduce the pressure on qualified staff and have the potential to reduce costs. 29–40,42–55 Despite the positive evidence for skill mix, a survey conducted by the RCN Eastern suggested that nearly half of the 139 respondents found that skill mix in their teams was insufficient to meet patient need. 49 However, the use of skill mix with nursing assistants working within tightly defined roles in the community could result in increased delivery of task-focused nursing care as, from a patient perspective, those with complex morbidities might experience more than one nurse from the same team calling to provide different aspects of care, with a detrimental impact on continuity of care and, therefore, on perceived quality.
Measuring quality in community nursing
The policy drive for clinical effectiveness quality outcomes and increased provider competition has required community nursing services to adopt some of the commercial approaches associated with private sector organisations to demonstrate that the commissioners’ requirements are being met, for example production of evidence about patient and GP satisfaction with the service, regular updating of practice to demonstrate adherence to international best practice and demonstration of value for money. 56 Measuring clinical effectiveness in community nursing, however, is challenging; patients are generally older and frail, with deteriorating conditions and comorbidities that make it difficult to establish meaningful indicators (e.g. wound care outcomes depend on a number of factors such as the physical, social and environmental context of the patient). 57 A further challenge is attributing a change in health status to a particular intervention delivered by nurses, as community nurses tend to work alongside other services, agency staff and informal carers. Unlike in a hospital or a nursing home setting, community nurses are not able to oversee patients continuously to ensure compliance with best practice. 57
Measures of productivity, such as nurse–patient contacts and fulfilment of visits within designated time limits, have been used as a measure in district nursing as a proxy for clinical effectiveness. Such measures are comparatively easy to draw down from clinical databases. With the adoption of assessment and monitoring tools that measure clinical effectiveness for outcomes such as end-of-life care, patient safety and patient satisfaction, the need for accurate documentation has become an even greater necessity. Such tools are completed in the home by community nurses themselves in the context of clinical care and now serve the dual purpose of populating service quality databases. The new commissioning framework for community nursing recommends investment in new technology to both increase patient independence and enable community staff to record care activity more efficiently. 53 The importance of having an appropriate IT infrastructure in place in the community to deliver the intended aims of the quality schemes has been emphasised and is driving forward the implementation of mobile technology in the community. 58,59 However, there is a risk that the use of technology will facilitate the collection of outcomes that are not necessarily meaningful in relation to community nursing service quality, simply because it is possible to capture the data.
Summary
Despite recent progress in developing a framework for commissioning community nursing, there remain a number of practical challenges in measuring community nursing service quality. The impact of workforce issues and organisational changes such as IT implementation may not be fully understood in relation to community nursing. The nature of the work community nurses do, frequently over a lengthy time scale, makes finding suitable quality measures difficult. Moreover, it is not known how suitable or valid it is to use measures developed in acute settings for the purposes of assessing service quality in the community. There is a gap in the literature about the type of quality measures in use by commissioners and their effectiveness in really monitoring and improving the quality of community nursing care. Recent drives to encourage new forms of integrated organisations are likely to involve community nursing, and hence appropriate measures of quality will need to be determined.
In this study, we aimed to investigate how quality metrics are selected and agreed between commissioners and providers of community nursing services, as well as how these metrics are subsequently used in practice with the purpose of understanding how to improve them for the benefit of patients. We also focused on the perceived usefulness of current measures in improving quality of care provision, including patient and carer perspectives, and explored the challenges facing service providers in collecting information relating to quality of care.
Chapter 2 sets out the methodology of this three-phase, mixed-methods study. For clarity, this is immediately followed in Chapter 3 by the findings of the first phase, the national CQUIN survey. The following five chapters (see Chapters 4–8) report the case study findings. Chapter 9 draws together the findings from all of the data streams, which are then discussed in the final chapter (see Chapter 10) of the report.
Chapter 2 Study objectives, design and methodology
This chapter details the design and methodology of this mixed-methods study. The overall aims and objectives of the study are introduced below, followed by information about components of the study design and conduct. The chapter also includes information on how patient and public involvement contributed to and informed many aspects of both design and methodology; the process for gaining NHS ethics and research and development (R&D) approvals for the study; and a summary of deviations from the original protocol.
Aims and objectives
The study aimed to investigate the selection, application and usefulness of quality measures in use for community nursing from April 2014 to June 2016 in order to identify how they are used and the factors that influence their usefulness in achieving their intended goals of ensuring high-quality care for patients.
The research questions developed for the study were:
-
Which QIs are selected locally, regionally and nationally for community nursing?
-
How are they selected and applied?
-
What is their usefulness to patients, commissioners and community provider staff?
The associated study objectives were to:
-
map QIs in use for community nursing
-
identify the processes for the selection of QIs for community nursing at local, regional and national level
-
clarify the processes for introducing and applying QIs into community nursing services and to explore how data are collected, analysed and quality assured
-
explore the usefulness of indicators in terms of meeting priorities, assessing the quality of services, influencing commissioning decisions and bringing about changes in service delivery from the perspectives of patients, front-line teams and commissioners (Figure 1).
FIGURE 1.
Flow diagram of study methodology. a, Interviews will also explore selection; b, interviews will also explore selection and application.
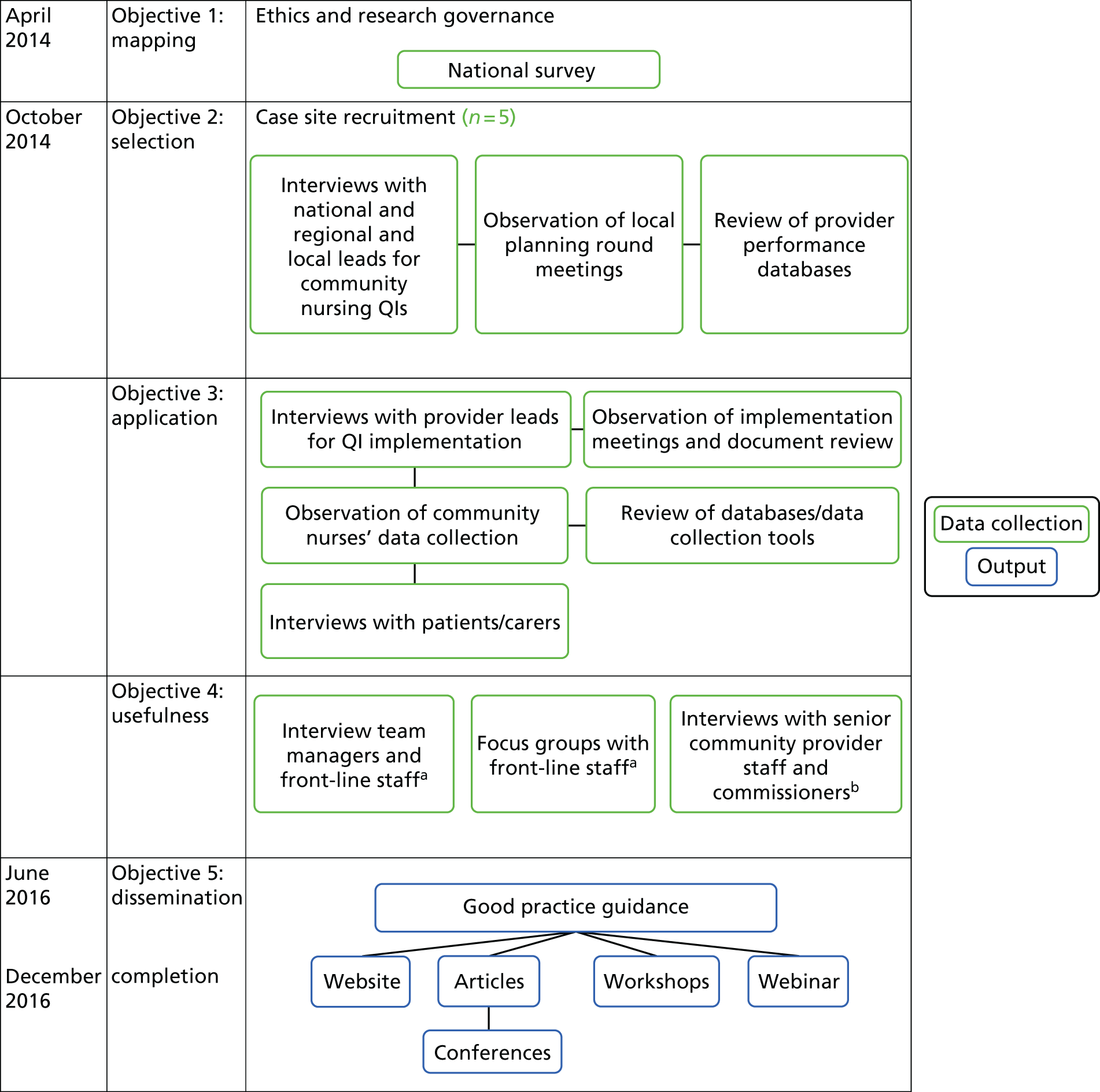
A mixed-methods design in three phases was utilised, which comprised:
-
phase 1 – a national cross-sectional survey of QI schemes
-
phase 2 – an in-depth qualitative case study of the selection, application and usefulness of quality measures in use for community nursing in five study sites
-
phase 3 – a series of stakeholder engagement workshops to validate and check the transferability of our findings.
Mixed-methods design and conceptual framework
The study used a pragmatic mixed-methods design involving an integrative approach of ‘connecting’ quantitative and qualitative data rather than ‘merging’ or ‘embedding’. 60 Mixed methods were employed sequentially to provide both breadth (phase 1) and depth of description of QI use in community nursing (phase 2). Quantitative data were collected first to describe the range of QI and incentive schemes in use nationally in community nursing during 2014/15, and then to give a sample of providers from which to purposively select five sites for the case study. Case study research enables an in-depth exploration of contemporary events using a combination of qualitative data collection methods. Such methods include interviews, non-participant observation and documentary analysis. 61,62 One of the strengths of the case study approach is that it enables the triangulation of data, thus supporting the validity of the overall analysis. Our case study in multiple sites built on the survey findings by exploring in depth the relationship between policy directives on quality measurement and influences on local implementation. It enabled the identification and probing of the processes of selection and application of QI schemes and other quality measures currently used by community nurses, as well as an insight into the perceived effectiveness of such measures for the purpose of assessing service quality.
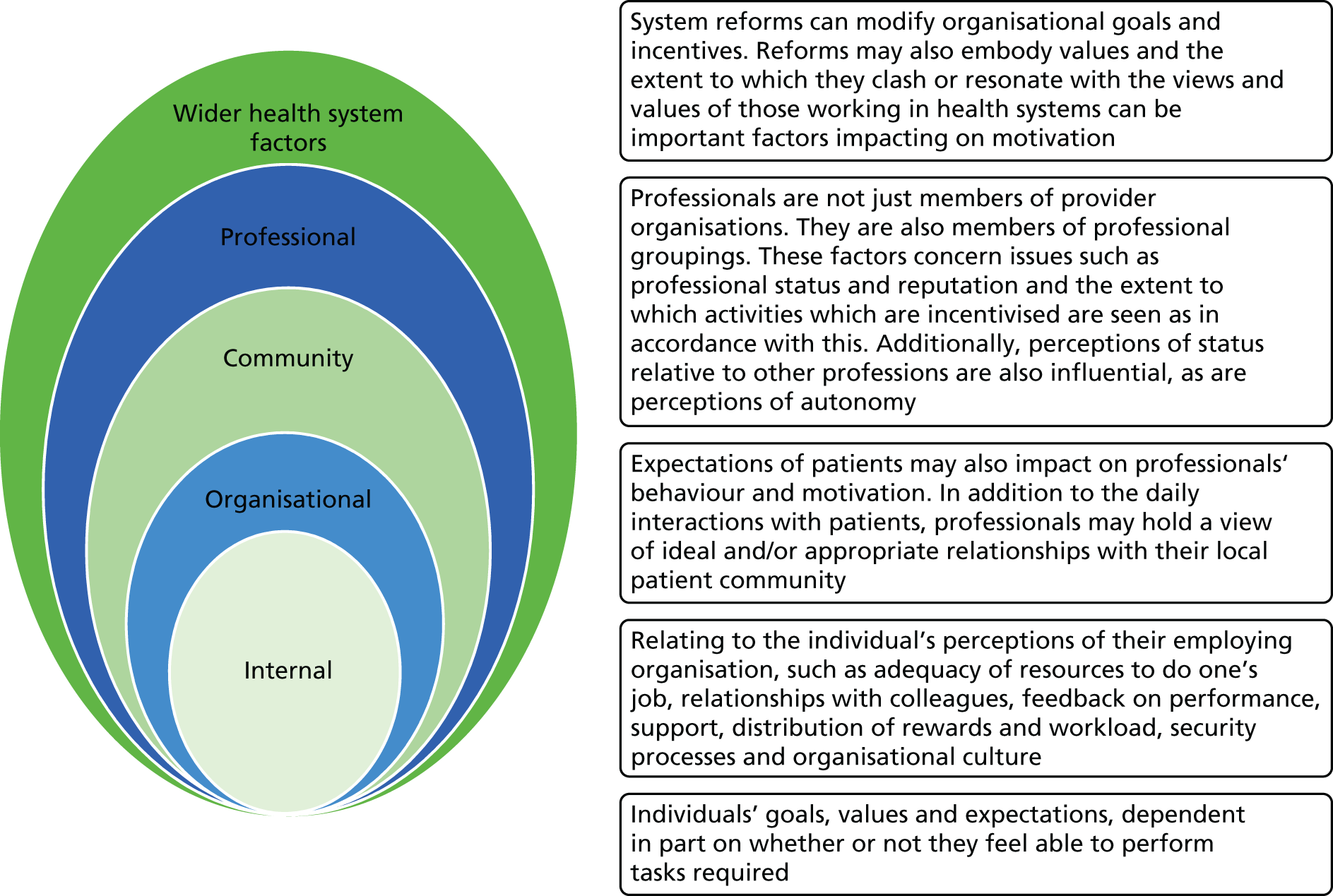
Individual and local factors can affect the success of national policy implementation, so an understanding of the interplay between these is fundamental in ensuring that any benefits from national initiatives, such as QI schemes, are obtained. To conceptualise our study, we used a framework originally developed by Franco et al. ,63 which had been utilised successfully in our earlier work. 32 This multilevel framework includes factors that influence individual behaviour and attitude, and incorporates organisational and wider health system contexts and relationships, helping explain the interplay between them. These contexts are all likely to have a bearing on which QIs get selected, as well as how they are applied in practice.
We ‘co-produced’ this project by working in partnership throughout the research process with patient and carer representatives, commissioners and community nurses, who were part of the larger study team. This included drawing on their expertise and knowledge when formulating the research question(s), scoping the literature, collecting and analysing data, and identifying the key messages, mediums and target audiences for dissemination. In a subsequent phase (phase 3), we held engagement events with commissioners, health-care practitioners, patients and carers in 10 locations nationally to check our analyses and interpretation of evidence to improve the dependability and transferability of our findings and also to support the development of good practice guidance (see Appendices 2–4).
Setting
The study provided a national snapshot of QI schemes applying to community nursing, followed by an investigation of the selection, application and implementation of QI schemes in five sites across England. Each case site comprised a dyad of a community nursing service provider contracted to provide NHS services and their associated CCG. At least one case study site was an independent provider. The included community nurses were registered nurses providing home-based nursing care to adults. A geographical spread of case sites and different types of community nursing provider enhanced the reach of the project and transferability of findings.
For clarity, the methodology of the national survey will be reported first, followed by the case study.
Phase 1: national survey
Design and sampling
The original intention was to conduct an electronic cross-sectional survey of all 211 CCGs across England in order to identify their community nursing service providers and associated QI schemes. The first step was to identify potential respondents by using the CCG information and contact details available online from NHSE to identify departments and/or commissioners responsible for quality or commissioning community nursing services. It became clear quickly that the requisite information was generally not available online. Although using the telephone number given occasionally resulted in correctly identifying a potential respondent, this was a laborious and time-consuming approach. In April 2014, at the time of the survey, the CCGs were comparatively new organisations, having only recently been established after the implementation of the Health and Social Care Act 2012. 26 Often it was not easy for the local administrators answering the telephone to identify the correct personnel responsible for commissioning community nursing, and they frequently suggested that the researcher submit the questions through a Freedom of Information (FOI) request; this was therefore adopted as the main method of data collection.
Data collection
Once the appropriate avenue for submitting a FOI request to a CCG was identified, the following three questions were asked.
-
Who commissions community nursing services for your CCG and what are their contact details?
-
What QI scheme(s) covering community nursing services are being used for 2014/15?
-
Which organisation provides your community nursing services and what is the nature of this provision, for example NHS, social enterprise, voluntary organisation or private?
Data comprising a mix of CQUINs, local QIs and KPIs were received in a variety of formats – electronic spreadsheets, word documents and copies of contracts – all with varying degrees of completeness. As the second phase of the project aimed to examine, in detail, the processes around quality measurement in community nursing, and as the aim of the current phase was to gain a broad national quality snapshot, it was decided to focus on CQUINs only for the analysis. CQUINs were also submitted in a format sufficiently consistent to allow a cross-organisation comparison, and allowed variation and local priorities to be identified nationally. All of the organisational details and CQUINs data were entered onto a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet, and were cleaned by checking for anomalies or inconsistencies across fields.
Analysis
For each CQUIN, we recorded the NHS region and CCG area and, when supplied, the indicator name, its descriptor and the rationale for its use. The CQUINs were then categorised as ‘national’ (pertaining to the national indicator scheme) or ‘local’ (reflecting local needs and conditions), as defined by the NHSE CQUIN guidance. As the CQUINs documentation we received only rarely specified community nursing services in the title, it was necessary to identify which CQUINs applied to nursing. To identify and code community nursing CQUINs, three researchers with professional experience of either community nursing or commissioning, working in pairs, scrutinised the associated description and rationale to determine whether or not the CQUIN applied to nursing. At least one of the following criteria had to be met for this purpose:
-
Community nurses are directly involved in gathering data about quality.
-
Community nurses’ activities constitute an essential contribution to the achievement of the CQUIN.
There is significant variation in the configuration of community services,11 which could affect the above coding. To be inclusive, when it was not possible to be certain whether or not the CQUIN applied to community nursing, the CQUINs were coded as ‘possible’ (e.g. if a CQUIN applied to a reablement service and it was not clear if the local service included a community nurse) or ‘definite’ (e.g. if it clearly related to community nursing service provision, or if such nurses collected data for the purposes of quality measurement).
Next, community nursing CQUINs were further coded by applying the following quality dimensions to each:
-
patient safety, clinical effectiveness and patient experience, or a combination of these dimensions23
-
structure, that is, contributing to the underpinning service requirements (e.g. staff numbers, appropriate training, infrastructure, building and equipment); process, that is, activities carried out by staff in relation to service delivery; or outcome, that is, the assessment of the impact of health activities on patients. 19
Initial coding was conducted by one researcher, with a 10% sample recoded by a second researcher; any differences were resolved by discussion prior to completion of coding.
Since the national evaluation of CQUINs25 had recommended the promotion of the use of a Pick List and evidence-based indicators, a final exercise investigated whether or not the community nursing CQUIN indicators had identifiable sources: indicator names, descriptors and rationales were searched for mention of particular documents (e.g. NHS Outcomes Framework)27 and for particular organisations (e.g. NICE). Exact wording drawn from community indicators in the CQUINs Pick List (a database of evidence-based QIs for users of the CQUIN scheme),24 was also used as a search term to identify any local CQUINs which had incorporated indicators from the Pick List. When a source was identifiable, the CQUIN was coded accordingly. Three researchers, two of whom had professional health-care backgrounds, collaborated to produce these coding schemes.
The resulting data were descriptively analysed using IBM SPSS Statistics 20.0 (IBM Corporation, Armonk, NY, USA). The methods and emerging findings of the survey were made available on the project website.
The next section describes the design and methodology of the case study.
Phase 2: case study
A case study is a preferred method for examining, in detail, contemporary events over which it is not possible or desirable to exert control. 61,62 It constitutes an in-depth exploration of a ‘bounded system’ (p. 61),62 or ‘case’, over time, through the use of multiple data sources, rich in context and detail. The proposed case study was to explore in depth the processes in use for measuring quality in community nursing services in England. The aim was to collect data over the duration of the annual commissioning cycle, focusing on agreeing contracts and quality monitoring and evaluation in order to understand the processes involved. We also aimed to investigate the impact on front-line staff and patients and their carers of the application of quality measures in practice, and the perceptions of all participants of the usefulness of such measures for determining the quality of nursing. Following the Health and Social Care Act 201226 and the implementation of clinical commissioning organisations, and in discussion with the research management group, it was decided to explore whether or not the new organisational context might determine or help to explain any variations found across different sites. A multisite case study approach was therefore deemed appropriate and we recruited five case sites across the country.
Sampling
Purposive sampling enables researchers to select sites on the basis of their potential to provide data on the contextual factors considered to be significant for the investigation. 64 In discussion with the research management group, a shortlist of 10 potential case sites was identified, from which seven were approached and five were recruited. Once identified as potential sites, both the commissioning and the provider organisation were approached separately, but concurrently, via the people named as responsible for commissioning and managing community nursing in the organisations. Each organisation was advised that it could not be used as a case site if the other organisation chose not to participate. The case sites were identified on the basis of the findings of the survey, selected using the following inclusion criteria:
-
variation in geographical location across England
-
range and number of QI schemes in operation across community nursing services
-
range of provider organisation type (NHS and independent).
Although there is no consensus on the number of case sites to include in a multisite case study, five sites enabled depth of study, while also enabling sufficient cross-comparison to check for consistency. 65 One of three researchers was allocated to be the main contact for data collection within each site to enable trust to be established and an in-depth knowledge of the site to be developed. The nurse researcher visited all the sites in which front-line observations took place. This arrangement enabled sufficient depth of knowledge in relation to commissioning at each site and cross-case understanding of evidence relating to front-line staff, patients and informal carers.
Participant inclusion criteria
-
National and regional quality leads from NHSE in a position to provide understanding about the influence of national and regional quality directives on local implementation of quality schemes.
-
Commissioners and community service provider managers directly responsible for community nursing services and, in particular, agreeing and implementing QI schemes.
-
Registered community nurses delivering nursing care to people aged ≥ 18 years in their own homes. This criterion included district nursing teams, integrated care teams, integrated community nursing teams, community matrons and community nurses for older people, who provide home-based care for adults with multiple and advanced long-term conditions requiring nursing and palliative care services. The service aims for these community nurses are to enable people with long-term or deteriorating conditions to live independently for as long as possible, reduce avoidable hospital admissions by timely nursing interventions and facilitate the discharge of patients not requiring hospital care.
-
Patients (adults aged ≥ 18 years) or their carers receiving care from community nurses in their own homes were also recruited to the study for interview. Interpreters were available if required.
Participant exclusion criteria
-
Community nurses providing children’s, mental health and learning disabilities nursing were excluded as joint commissioning arrangements often apply in relation to these services and these would have broadened the scope of the project significantly, causing a loss of focus.
-
Patients were excluded from this study if they were aged < 18 years, in the final stages of terminal illness, or could not give informed consent (or, in the case of reduced mental capacity, consent could not be gained from their legal representative).
Case study sites
Each site comprised a CCG and a service provider. Community nursing services were provided by four NHS organisational types (community trusts, combined acute and community trusts or community foundation trusts) and one social enterprise. In all of the case sites, community nurses were located in geographically based teams of various configurations serving a number of general practices. They are accessed by a single point of entry system, whereby there is one centralised telephone number for referrers and other patients.
Pseudonyms have been used and any similarity with existing place names is unintentional. A summary of the characteristics of each case site is provided in Table 1.
| Characteristic | Site | ||||
|---|---|---|---|---|---|
| Alderton West | Beechbury | Cedarham | Dogwoodheath | Elmhampton | |
| Type of area | Urban | Urban | Urban | Urban | Rural |
| Deprivation relative to the national average | Higher than average | Higher than average | Higher than average | Higher than average | Lower than average |
| Approximate number of general practices covered by case site CCG | 50 | 40 | 50 | 60 | 80 |
| Approximate size of population served by case site CCG | 1,000,000 | 300,000 | 300,000 | 300,000 | 500,000 |
| Total number of CCGs in the area | 4 (3 commission jointly) | 3 (all commission jointly) | 2 (both commission jointly) | 3 (all commission independently) | 1 |
| Approximate size of population served by provider | > 1,000,000 | 800,000 | 600,000 | 300,000 | 500,000 |
| Type of provider | NHS community foundation trust | NHS community trust | NHS acute and community foundation trust | Social enterprise | NHS foundation trust |
Once permission was granted for the case study to be carried out, local senior managers (commissioners and providers) identified suitable meetings for the researchers to observe, as well as members of their organisation who could assist us in recruiting individuals from the requisite staff groups. With the assistance of administrative staff in the case study sites, potential participants were sent study information sheets so that they could decide whether or not to participate. The methods for recruiting service users to the study are explained below.
Data collection
Observations, interviews and focus groups were the main methods of data collection. Semistructured interviews were used as they enable sufficient focus on the topic under investigation while allowing flexibility for the participants to introduce new ideas and experiences for study. These were audio-recorded and undertaken using purpose-designed interview schedules guided by the research questions and advice from members of the research management group. In particular, the patient reference group provided advice on the interview schedule designed for patients and carers. Four experienced researchers with varying backgrounds, including two with experience of professional practice in the NHS, collected data. The data collection methods used in each site are shown in Table 2.
| Research question | Objective | Data collection method |
|---|---|---|
| How are QIs selected and applied? | Selection: to identify the processes for the selection of QIs for community nursing at local, regional and national level |
Semistructured interviews with national, regional and local community QI leads in each case study site Non-participant observation of local commissioning/contract meetings where QIs were discussed, selected, developed and/or monitored. Documentary review |
| Application: to clarify the processes for introducing and applying QIs into community nursing services and to explore how data are collected, analysed and quality assured |
Semistructured interviews with provider leads responsible for QI implementation Observation of meetings between provider leads responsible for implementation and front-line provider staff Shadowing of community nursing staff to observe QI data collection. Documentary review |
|
| What is their usefulness to patients, carers, commissioners and community provider staff? | Usefulness: to explore the usefulness of indicators in terms of meeting priorities, assessing the quality of services, influencing commissioning decisions and bringing about changes in service delivery from the perspective of patients, front-line teams and commissioners |
Semistructured interviews with patients and carers Focus groups and semistructured interviews with clinical team managers and front-line clinicians Semistructured interviews with senior community provider and commissioners |
One-to-one semistructured interviews were conducted with commissioners and provider managers. Observations of internal meetings or combined CCG/provider meetings (where QIs for community nursing were on the agenda) were also undertaken. Joint meetings between the commissioners and their service provider managers and internal quality meetings within the local service provider organisations were observed. The aim of the observations was to learn about the local priorities and contextual quality issues for commissioners and provider managers, and to understand the professional roles and relationship between staff in the different organisations. Interviews for commissioners and service providers covered the processes used for identifying suitable QIs and the policy-drivers underpinning their choices; perceived usefulness of QIs for service quality improvement; characteristics of effective schemes and perceptions of how well CQUIN schemes have worked for community nursing.
One-to-one semistructured interviews were conducted with nurse team leaders and an observation of team meetings was undertaken when the monitoring or application of QIs was on the agenda. Interview topics included perceptions of how front-line staff feed into the process of selection and implementation of QIs; systems for recording data; the extent to which selected indicators are under the control of the clinician; barriers to implementation; and benefits or service improvements deriving from indicator use.
Focus groups were conducted with front-line staff to explore their views and experiences of QIs being used for community nursing. In addition, front-line observations were undertaken by a community nurse-trained researcher to observe processes of QI data collection and recording during patient visits. Indicative topics for focus groups with front-line staff included awareness of current indicators; the extent to which staff feel able to influence or participate in selection of QIs; confidence in QIs as a reflection of service quality; extent to which staff are in control of factors that could influence achievement of particular QIs; how quality data are recorded; challenges for front-line teams in implementing indicators; and perceptions of impact on patient care. Front-line staff were recruited via their managers, or through newsletters to the organisation.
Table 3 details the number of participants contributing data in interviews and focus groups, and meetings observed in each case site.
| Data collection | Number of events (number of participants) | ||||
|---|---|---|---|---|---|
| Alderton West | Beechbury | Cedarham | Dogwoodheath | Elmhampton | |
| Interview | |||||
| Commissioners | 3 (3) | 4 (4) | 4 (4) | 4 (5) | 4 (5) |
| Provider managers | 3 (3) | 7 (7) | 2 (2) | 5 (5) | 5 (5) |
| Community nursing team leaders | 2 (2) | 2 (2) | 1 (1) | 1 (2) | 3 (3) |
| Patients (patients, carers) | 3 (1, 2) | 1 (0, 1) | 4 (4, 0) | 2 (2, 0) | 3 (2, 1) |
| Total | 10 (11) | 14 (14) | 11 (11) | 12 (14) | 15 (16) |
| FG | |||||
| Front-line staff | 1 FG (6) | 2 FGs (5) | 3 FGs (11) | 1 FG (15) | 2 FGs (8) |
| Meetings observed | |||||
| Commissioners and provider managers | 4 (35) | 3 (34) | 2 (38) | 2 (14) | 3 (34) |
| Commissioners only | 2 (9) | ||||
| Provider managers only | 2 (9) | 1 (8) | 2 (37) | 1 (11) | 1 (11) |
| Community nursing managers/team leaders | 2 (33) | 1 (9) | 1 (11) | ||
| Total | 8 (77) | 4 (42) | 4 (75) | 6 (43) | 5 (56) |
Many of the data that inform quality measurement in community nursing are collected by front-line nurses themselves. Observation and shadowing of front-line staff was therefore undertaken to observe how data for QIs were documented during the course of delivering and recording patient care in the home. A researcher with a professional community nursing, albeit not district nursing, background (SH), undertook all the shadowing. The choice of using a registered nurse who was not a district nurse but had a community background was made to preserve the balance between ‘insider’ and ‘outsider’ status of the researcher to understand and identify with the front-line teams and preserve patient dignity, but also to maintain the professional distance that permits adequate observation and data collection. 66 Participating case sites identified members of nursing teams who were prepared to be shadowed and visits were arranged at times to suit the nurses, avoiding the winter pressures period. Handover meetings or safety briefings were also attended and the use of computer software for documenting activity and outcomes of care was observed. A contemporaneous diary was written and evidence from shadowing nursing staff in the home was recorded separately on purpose-designed observation schedules. In each case site, any key documents detailing the selection, monitoring and evaluation of quality measures in use for community nursing, such as CQUINs, NHS contract sections 4 and 6, and community dashboards, were requested. Table 4 shows the number of front-line nurses shadowed and the number of home visits made in each case site.
| Front-line observation | Site | ||||
|---|---|---|---|---|---|
| Alderton West | Beechbury | Cedarham | Dogwoodheath | Elmhampton | |
| Number of shadowing sessions (community nurses shadowed) | 3 (3) | 2 (2) | 4 (4) | 0 | 4 (3) |
| Total number of home visits undertaken | 12 | 11 | 21 | 0 | 22 |
| Assessment | 1 | 0 | 2 | 0 | 1 |
| Assessment and follow-up | 0 | 0 | 0 | 0 | 1 |
| Follow-up visits | 11 | 11 | 18 | 0 | 19 |
| Assessment and discharge | 0 | 0 | 0 | 0 | 1 |
| Discharge visits | 0 | 0 | 1 | 0 | 0 |
See Appendix 5 for interview, focus group and observation schedules used to collect data from commissioners, provider managers and front-line staff.
A combination of approaches was used to identify patient (patient and/or carers) participants. We aimed to conduct one-to-one semistructured interviews with people initially identified from the shadowing of front-line staff. This strategy had limited success owing to the age and infirmity of such patients and their carers. To ensure sufficient representation from patients and carers in the study, we supplemented one-to-one interviews with a locally derived focus group. Patient and carer interviews included questions about their perceptions and understanding of high-quality nursing care. The current QIs applying to community nursing were then explained and patients and carers were asked their views on these for assessing community nursing service quality. Any further areas that patients and carers felt were important indicators of nursing quality were noted.
See Appendix 6 for interview and focus group schedules used to collect data from patients and carers.
Data analysis
The case study generated multiple sources of qualitative data from the sites, including interviews with patients, local senior managers (commissioner and providers) with a role in quality implementation, community nursing team leaders, focus groups with front-line nurses, observations of front-line nursing staff and quality meetings, and documentation relating to the selection, application or monitoring of quality. Interview data were audio-recorded and transcribed verbatim, and contemporaneous notes were made during the observation of meetings and the shadowing of front-line staff. Data were anonymised and entered into NVivo 10 software (QSR International, Warrington, UK), or, in the case of front-line observations, into a Microsoft Excel® spreadsheet to aid comparison.
Qualitative data analysis drew on constant comparison techniques by which analysis proceeded with and informed data collection,67 with members of the research team liaising regularly to share their interpretations of findings from the case sites. Data were open coded initially to generate concepts that were then validated by comparison and discussion with members of the research team, whose composition reflected key audiences. Once the codes were agreed, these were used to construct a coding framework within NVivo and a team approach to coding proceeded, with each member of the team taking responsibility for coding a particular set of data across the sites [e.g. one member of the team coded all of the provider manager interviews (KP) and another coded all of the commissioner manager interviews (CP)]. All members of the team coded the meetings that they themselves had observed. Front-line team focus group data were analysed by one researcher (LD) and the service user interview, shadowing and observation data were analysed by the nurse researcher (SH). In this way, the research team gained a cross-site perspective. The individual coding databases were merged regularly into an NVivo master database to check progress and assess whether or not there were any differences in the way codes were being applied. The resulting codes were then further analysed to determine their attributes and dimensions, resulting in themes relating to selection, application and usefulness of QIs in the case study sites.
An adapted version of the five-level analysis theoretical framework developed by Franco et al. 63 was used to aid our interpretation of the interview and focus group data (Figure 2). This framework was developed in previous work that examined the relationship between financial incentives and behaviour in a range of primary care and community settings in health care. 32 It is applicable to the selection and implementation of all types of QI schemes, not only those that include financial incentives. The framework assisted in enabling the matching of codes and emerging themes with potential contextual facilitators and barriers to use of quality measures in terms of meeting priorities, assessing service quality, influencing commissioning and bringing about changes in service delivery. To increase the rigour of the analysis, use of multiple sources of data provided opportunities for comparison and contrast across accounts. For example, patients’ views, expectations and experiences demonstrated an alternative perspective on the values driving selection and application of QIs by commissioners and health-care providers.
Documentary analysis was limited due to the relative paucity and incompleteness of documents supplied to the research team across the case sites. The standard NHS contract was analysed to assess the degree of content relating to quality of community nursing services. When it was possible to obtain documents containing information about QIs, these were analysed to identify which QIs were being used for contracting community nursing in 2015/16. Documents included quality reports, ‘dashboards’ and schedules 4 and 6 of the NHS contract from the case sites (see Chapter 4). The analysis compared how, or if, quality measures related to the professional standards set out in Vision and Strategy for Nursing, Midwives and Care Staff 3 and CQC quality criteria now being applied to community services. The documentary analysis was undertaken by a member of the research team who was actively working as a community nurse at the time of the study.
The next section describes the organisation of the stakeholder engagement events.
Phase 3: stakeholder engagement
Evidence suggests that research is most effectively disseminated using multiple vehicles, ideally with face-to-face interaction. 68 Dissemination events were an integral part of the study design and were planned to start towards the final few months of the project. We planned to hold workshops across the country, both putting on special events ourselves and contributing to other organisations’ meetings and conferences in order to check the study’s emerging findings and develop our good practice guidance with a wider audience. These events were intended to include a mixed group of commissioners, service managers, front-line staff, patients and carers. Owing to the time constraints on NHS staff, these were timetabled to last either a morning or an afternoon, when possible, and attendees were able to hear about emerging findings from the study and discuss the good practice guidance.
Researchers contacted participating case sites and used personal and professional contacts and networks in different parts of the country to identify other organisations that might be interested and willing to assist in holding a workshop locally. Once a workshop was agreed in principle, a key local lead for community nursing was identified and asked to give an introduction to the day. An experienced facilitator with a commissioning background, a member of the core research team and one other member of the wider team involved in the project facilitated the workshops. To gain stakeholder feedback about some of the study findings as well as statements from the draft good practice guidance, a key activity during the workshop was to engage small delegate groups in a deliberative dialogue exercise. 69 These small group discussions were distinct from focus groups in so much as data were not collected with which to inform the study; rather they were designed to discuss our findings in relation to delegates’ own experiences. Each workshop produced feedback on emerging findings and draft good practice guidance. Nursing participants received certificates of attendances for professional revalidation purposes. Participants completed evaluation forms and facilitators reflected on each workshop, making adjustments to timing and materials in response to feedback (see Appendix 2).
Projected outputs
-
Development of a project website on which outputs based on emerging findings of the study have been published (www.QuICN.uk). As our NHS co-applicants stressed the importance of getting findings out early, we began to disseminate emerging findings via our website within 6 months of starting the project, with the analysis of the national QI database and publication of discussion papers (www.quicn.uk).
-
Publications, including the full report, evidence summaries for participants and other stakeholders, peer-review journals, local NHS newsletters and A5 laminates, are in progress.
-
Using the findings of our project we have developed good practice guidance (see Appendix 4) on how best commissioners and managers can approach the selection and application of appropriate quality measures for community nursing and their perceived usefulness from the patient and carer perspectives.
Patient and public involvement
There has been substantial input from service users (patients, carers and/or members of the public) throughout the study. In earlier work to develop local QIs for community services in Bristol, a service user expressed concern that the administration and collection of data for QIs would distract community nurses from delivering patient-centred care. This individual was a co-applicant on the successful proposal and has been the co-lead on the user aspect of this study. As a former performance manager and member of the local community health forum, he contributed to designing the study and recruiting other lay people to become involved by sitting on the research management group and/or being part of a service user reference group (SURG) for the study. The SURG has contributed to the design of data collection tools for patients and carers, including an aide-memoire to assist researchers in covering topics thought by members to be important (see Appendix 6), the interpretation of findings and the content of the final report. SURG members have also been involved in the development and delivery of the stakeholder engagement workshops. In addition, a member of SURG was involved in interviewing and selecting research staff.
Patients and carers have attended workshops where emerging findings have been discussed and contributed to the interpretations of evidence and development of good practice guidance.
Ethics and NHS permissions
We considered our project to be low risk (as it is not an intervention study and we were not recruiting patients unable to give informed consent for interviews). Therefore, on advice received from NHS ethics, we initially submitted via the proportionate review process. On their closer scrutiny, the project was deemed to involve risk as it involved the shadowing of front-line staff during patient visits, and the submission was, therefore, forwarded to the next full NHS ethics meeting. At this meeting, the proposal to include the shadowing of front-line staff was considered to be intrusive to patients. Moreover, the frailty of community nurse patients, some with fluctuating mental capacity to give informed consent for an observer to be present, led to the project then being referred to a specialist NHS Ethics Committee. Approval for the study was finally obtained in July 2014 (National Research Ethics Service Committee Yorkshire & The Humber – Leeds West 14/YH/1059). The process for shadowing front-line staff to observe documentation of quality data in the field (i.e. patients’ homes) required that nurses visiting patients a few days before the day of the observation visit took a study information sheet to patients in order to allow them to consider the nurses’ involvement in this aspect of the study. On the day of shadowing, the visiting nurse was consented to the study and went into the home alone to see the patient to ask if they would agree to a nurse researcher being present to observe their nurse for that visit. If they answered positively, the researcher was admitted. The researcher then obtained verbal permission from the patient to observe the nurse. Formal written consent to take part in the study was not required from patients themselves, as they were not study participants and no identifiable data were collected from or about them. We subsequently sought and received additional ethics permission to recruit patients to a focus group when we found that we were unable to recruit enough patients via front-line observation visits. These participants were recruited through the SURG.
We were unable to start NHS R&D permissions until we had identified potential case sites from the survey findings. Recruitment entailed initial contacts to both a community services provider and a commissioner from the local CCG, and approval to participate from both partners was required before an application for NHS permissions could be sought (this was sometimes a time-consuming process). Commissioning organisations were comparatively new and there were difficulties identifying the appropriate person within the organisation to give approval. Moreover, community nursing services provider organisations have a range of types (e.g. NHS community trust, combined acute and community organisations, independent or private), meaning that it was sometimes difficult to find the person who could take responsibility for signing up to the project. The NHS permissions process was lengthy and involved duplication and slight variation of requirements across the sites, where each application was considered separately. Owing to the multiplicity of data collection methods and range of participants in a mixed-methods study, there was a large amount of related paperwork for R&D departments to review. This created a lot of extra work for both the R&D departments and the research team. Overall, the administration involved in the permissions process was time-consuming for each organisation, and, on one occasion, having just achieved successful sign-off from R&D in one site, permission was suddenly withdrawn by the provider without explanation. One other case site took several months to obtain internal agreements, having initially expressed interest to the researcher, so we eventually withdrew and selected another site from the list in a similar area. We were eventually able to recruit and obtain permission for all 10 organisations constituting the five case sites, although we were late starting data collection in two sites.
Deviation from the original protocol
Given the degree of organisational change and workforce pressures present during the course of this study, we were fortunate to have established good links with our case sites and to be allowed access to undertake data collection. However, the following small changes to the protocol had to be accepted.
The number of national and regional NHSE quality leads we interviewed was comparatively small. The interviews we conducted suggested that their strategic role with CCGs and current priorities tended towards the acute rather than the community sector and, although they were knowledgeable, their actual role in relation to quality process implementation in community settings appeared to be more limited. These interviews were, however, very useful for informing subsequent data collection in the case sites.
As explained earlier in this chapter, we took a pragmatic decision to alter our means of data collection for the national survey in response to the incompleteness of the CCG data available online at the time of the survey. We had planned to undertake an electronic survey, but the requisite e-mail addresses were not provided online owing to data protection, and the telephone numbers supplied usually went to a local administrative assistant who did not know to whom our enquiry should be directed. We were frequently asked to go through FOI channels to access the information we required, as these departments were set up to provide advice on a range of topics, so we used this as our main method of data collection. We also decided to focus our analysis on CQUIN data only for this part of the study, as only these data were provided in a form that was sufficiently comparable across organisations.
One case site did not allow us to shadow their front-line staff. As it had been hoped to recruit patients for interview from the shadowing exercise, this led to the provider organisation helping us with the identification of patients by offering us access to their local patient group, with limited success. There was considerable similarity in the findings from the four sites where front-line shadowing did take place, and evidence from the focus group of front-line staff that was held there confirmed that the same contextual pressures and views on quality measurement found in other sites pertained.
The supporting documentary analysis we had planned was constrained by the variation in the documents supplied to us by the case sites. We were able to compare CQUINs across the sites again, but, owing to the changes in the CQUIN schemes over time and current policy-drivers, the variation in what sites were doing nationally and locally had reduced. There may also have been some concerns in case sites at the potential sensitivity of documents being used.
Chapter 3 National survey findings
In this and the next five chapters (see Chapters 4–8) we present our findings. In this chapter, we present the findings from the national survey of CCGs that aimed to identify the number and variety of CQUIN QIs in use for community nursing in 2014–15, conducted across all of the CCGs in England. The first section of the chapter presents the findings from the descriptive statistical analysis; the second section details the findings arising from the content analysis of the data.
Descriptive statistical analysis of data
Response rate
All the CCGs contacted (n = 211) acknowledged our initial approach.
Of these, 25 CCGs either had no information ready to send us, or replied that they were unwilling to send us any. A further 27 CCGs sent us only information about KPIs or other QIs. A total of 159 (75%) CCGs sent us CQUIN data. The response rate by region was North, n = 56 (82.3%); Midlands and East, n = 49 (81.7%); South n = 36 (69.2%); and London, n = 18 (58.1%).
The CQUIN scheme entails organisations meeting both national and local QIs. At the time of data collection, national CQUINs comprised the Friends and Family Test (FFT), National Safety Thermometer (NST) and, in acute settings, The National Dementia and Delirium CQUIN. As all providers were obliged to meet the criteria set within the national CQUINs, the findings presented here relate to only local CQUINs that definitely involved community nursing services (community nursing CQUIN). These included CQUINs focused on the prevention and treatment of pressure ulcers (PUs), which extended the requirements of the NST, and dementia (not nationally mandated for community settings). Of the 159 respondents who sent us CQUIN data, 145 (68.7% of all those contacted) sent information about at least one local CQUIN definitely related to community nursing. The findings concerning those local CQUINs that possibly applied to community nursing can be found on the project website (www.quicn.uk). The following sections of this chapter focus only on the 145 CCGs that sent us definite community nursing CQUINs.
Organisation of care information
The 145 CCGs that provided information on local community nursing CQUINs commissioned community nursing services from 78 provider organisations. Of these, NHS trusts providing both community and acute services were the predominant form of organisation (n = 36, 46.1%), with NHS community health-care trusts the second most dominant type of organisational structure (n = 27, 34.6%). Social enterprises (n = 13, 16.7%) and private providers (n = 2, 2.6%), both comparatively new entities in community provision, together constituted < 20% of community nursing service provision. Table 5 shows the regional variation in the number of CCGs associated with each of these 78 community nursing service providers.
| Number of CCGs served by each provider | Region, n (%) | |||
|---|---|---|---|---|
| London | Midlands and East | North | South | |
| 1 | 5 (50.0) | 6 (30.0) | 17 (51.5) | 7 (46.7) |
| 2 | 3 (30.0) | 7 (35.0) | 9 (27.3) | 2 (13.3) |
| 3 | 1 (10.0) | 2 (10.0) | 5 (15.2) | 3 (20.0) |
| 4 | 0 | 4 (20.0) | 2 (6.1) | 2 (13.3) |
| 5 | 0 | 0 | 0 | 1 (6.7) |
| 6 | 1 (10.0) | 1 (0.5) | 0 | 0 |
| Total number of providers | 10 (100) | 20 (100) | 33 (100) | 15 (100) |
Commissioning support units or other suppliers such as private consultants provided commissioning advice and support to CCGs as they assumed their new role. One hundred and thirteen (78%) CCGs provided information linking them with a commissioning support unit. It was not possible to discern details of any commissioning support unit support for 32 CCGs.
Number of local community nursing CQUINs set
From the 145 CCGs in our data set, we received details of 484 local community nursing CQUINs. The average number of local community nursing CQUINs set by CCGs was three, with a minimum of one and a maximum of 12.
The picture looked different for community nursing service providers as, in many of these cases, they were providing services for more than one CCG. On average, providers were implementing four to six local CQUINs. Twelve providers were each associated with only one local community nursing CQUIN. Fifteen of the 82 providers in the data set had to deliver on relatively high community nursing CQUIN numbers (> 10).
Analysis of local community nursing CQUINs
As the focus of the wider study is on process, including an exploration of the way in which CCGs and providers collaborate to select and implement CQUINs, findings are presented for the total number of local community nurse CQUINs (n = 484). The majority of local community nurse CQUINs (n = 309) were uniquely worded, suggesting that they were tailored to local circumstances. First, the local community nurse CQUINs were analysed for their fit with the main quality domains used by CQUIN schemes.
Quality dimensions
The local community nurse CQUINs were analysed for their fit with the main quality domains used by CQUIN schemes, namely patient safety, patient experience and effectiveness of care (quality dimension 1),23 and Donabedian’s domains for measuring health-care quality, namely structure, process and outcome (quality dimension 2). 19 The complexity of community nurse CQUINs in use was made evident by the fact that 143 (29.6%) community nurse CQUINs addressed a combination of two or three aspects of quality dimension 1. Similarly, 122 (25.2%) community nurse CQUINs focused on more than one aspect of quality dimension 2. Owing to a lack of information, six (1.2%) community nurse CQUINs were undetermined with respect to quality dimension 1, and eight (1.7%) could not be related to a specific aspect of quality dimension 2. The aspect of quality dimension 1 most frequently addressed was effectiveness of care (417 community nurse CQUINs, 86.2%). The aspect of quality dimension 2 most frequently addressed was process (336 community nurse CQUINs, 69.4%) (Table 6).
| Quality dimension aspect | Number of community nursing CQUINs (%)a (N = 484) |
|---|---|
| Effectiveness of care | 417 (86.2) |
| Patient safety | 116 (24.0) |
| Patient experience | 93 (19.2) |
| Process | 336 (69.4) |
| Structure | 163 (33.7) |
| Outcome | 116 (24.0) |
It was notable that, of the 417 CQUINs addressing effectiveness of care, only 81 (19.4%) focused on outcome. Of these, only 27 (6.5%) focused on outcome alone (i.e. not in combination with either structure or process). Examples include:
Onward referral to ensure diagnosis [of dementia].
Quality dimension 1 – effectiveness; quality dimension 2 – process and outcome
Reduction in the prevalence of all pressure ulcers.
Quality dimension 1 – patient safety and effectiveness of care; quality dimension 2 – outcome
Of the 209 CQUINs aiming to address patient safety and patient experience, only five (2.4%) focused on both these aspects of quality dimension 1.
Distribution of local community nurse CQUINs across care themes
The intended aim or goal of each local community nurse CQUIN as stated by the organisation was coded into 13 care themes (Figure 3). A specific clinical focus accounted for 202 (41.7%) of the total number of community nurse CQUINs, namely long-term conditions and care planning (58, 11.8%), end-of-life care (36, 7.4%), dementia (34, 7.0%), PUs (34, 7.0%), falls (24, 5.2%), addiction (9, 1.9%) and care of older people (7, 1.4%). A further 191 CQUINs (39.5%) related to organisation of care (83, 17.1%), organisational issues (80, 16.5%) or admission and discharge (28, 5.8%). Fifty-three (10.9%) CQUINs addressed patient safety (28, 5.8%) or patient experience (25, 5.2%). In addition, 38 (7.9%) had a non-specific focus on clinical effectiveness. The preponderance of CQUINs addressing organisational aspects of care and/or service provision suggests that commissioners and providers alike were focused on adapting the service to the demands of the changing health-care landscape in England.
FIGURE 3.
Distribution of community nursing CQUINs across care themes (n = 484).
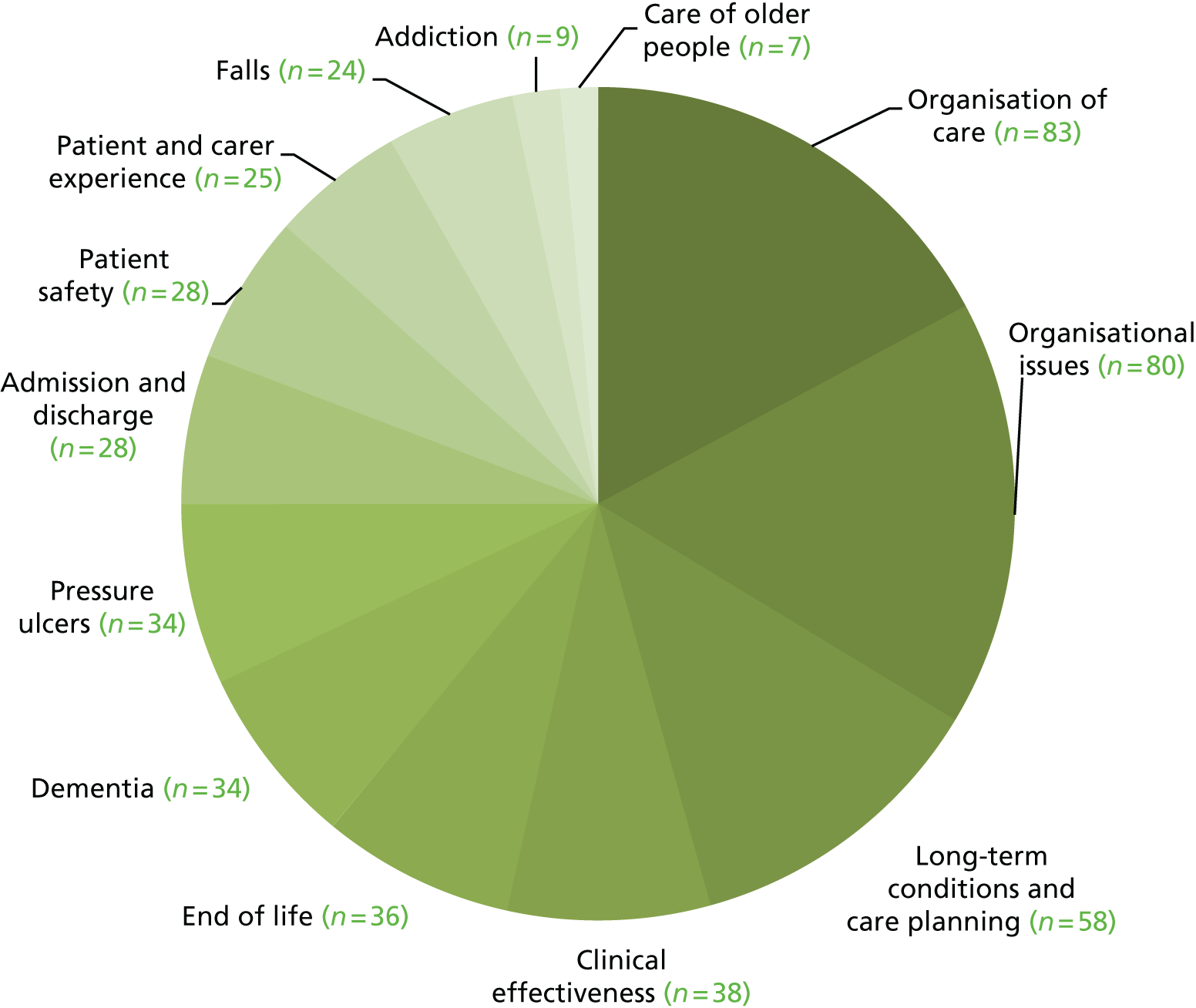
Care themes and quality dimensions
Provider organisation type did not seem to be associated with any particular differences in the analysis of quality dimensions of CQUINs in use. When examining the relationship between care themes and quality dimensions, it appeared that, of the 191 CQUINs relating either to organisation of care, organisational issues or admission and discharge, all focused on structure [e.g. ‘Review and development of community staff workload and dependency tool’ (organisational issues)] and/or process {e.g. ‘To embed the use of the risk stratification tool to ensure that high risk patients are identified for review by proactive care multidisciplinary teams’ [MDTs] (organisation of care)}. Nearly all these CQUINs addressed effectiveness of care (n = 183, 95.8%); only 14 (7.3%) focused on outcomes, with only 18 (9.4%) addressing patient experience and only 15 addressing (7.8%) patient safety.
Many of the CQUINs addressing an identified clinical condition related to effectiveness of care, ranging from nine (100%) concerning addiction to 19 (79.2%) for falls. CQUINs addressing patient safety and patient experience were almost entirely mutually exclusive. Nearly all of the CQUINs which focused on falls (n = 22, 91.7%) and PUs (n = 32, 94.1%) related to patient safety; however, none addressing these areas of care was associated with patient experience. There were no CQUINs addressing patient experience and end-of-life care or dementia. More than 75% of CQUINs that focused on an identified clinical condition were associated with process, with the exception of dementia (n = 21, 6.8%) and PUs (n = 14, 41.2%). The proportion of CQUINs linked to structure ranged from four (16.7%) for falls to 13 (36.1%) for end-of-life care. No ‘structure’ CQUINs were directed at care of older people. The proportion of CQUINs focused on outcome varied considerably across the identified conditions, ranging from 0% for addiction to 24 (70.6%) for PUs. Table 7 shows the relationship between identified clinical conditions and aspects of both quality dimensions.
| Care theme | Quality dimension, n (%) | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | |||||
| Patient safety | Patient experience | Effectiveness of care | Structure | Process | Outcome | |
| Long-term conditions and care planning (58) | 2 (3.4) | 22 (37.9) | 53 (91.4) | 19 (32.8) | 47 (81.0) | 22 (37.9) |
| End-of-life care (36) | 0 (0) | 21 (58.3) | 31 (86.1) | 13 (36.1) | 29 (80.6) | 18 (50.0) |
| Dementia (34) | 0 (0) | 1 (2.9) | 33 (97.1) | 12 (35.3) | 21 (61.8) | 1 (2.9) |
| PUs (34) | 32 (94.1) | 0 (0) | 33 (97.1) | 7 (20.66) | 14 (41.2) | 24 (70.6) |
| Falls (24) | 22 (91.7) | 0 (0) | 19 (79.2) | 4 (16.7) | 23 (95.8) | 2 (8.3) |
| Addiction (9) | 0 (0) | 0 (0) | 9 (100) | 2 (22.2) | 7 (77.8) | 0 (0) |
| Care of older people (7) | 7 (100) | 3 (42.9) | 7 (100) | 0 (0) | 7 (100) | 1 (14.3) |
The findings concerning the CQUINs’ relationship to the aspects of both quality dimensions suggest an assumption on the part of commissioners that focusing on process implies effectiveness of care. It was also notable that to fit with safety, experience and care effectiveness quality measures, CQUINs should arguably be construed as outcomes. However, the application of Donabedian’s domains in our analysis showed that the majority of measures in use for local CQUINs were actually measures concerning process. 19
Local community nurse CQUIN source
An identifiable source was found for 189 (39.0%) local community nurse CQUINs (Table 8). In some cases, CQUINs were associated with more than one source. The most frequently occurring source was the ‘national CQUIN scheme’, including five community nurse CQUINs taken from the Pick List (n = 39); community nurse CQUINs concerning end-of-life care (n = 10, 26.3%) and dementia (n = 9, 23.7%) accounted for 50% of these CQUINs. There was no other discernible association between this source and any other goals or themes covering an area of care.
| Source of CQUIN | Number of CQUINs |
|---|---|
| National CQUIN Scheme (including Pick List) | 39 |
| Research evidence (without details) | 26 |
| NICE | 22 |
| Local evidence | 21 |
| NHS Outcomes Framework | 17 |
| Francis Report | 14 |
| Research evidence (with details) | 12 |
| Other national reports | 9 |
| National agenda or priority | 6 |
| National guidance or policy | 5 |
| Other national frameworks | 5 |
| NHS BCF | 4 |
| NHS End of Life Care Strategy 2008 | 3 |
| Caldicott2 | 2 |
| National Dementia Strategy | 2 |
| Serious Case and Domestic Homicide Review | 2 |
| 2011 census | 1 |
| High Impact Action for Nursing and Midwifery | 1 |
| NHSE ‘Everyone Counts’ | 1 |
| NHSE National Quality Board | 1 |
| NHS Next Stage Review Final Report | 1 |
| Total | 194a |
Content analysis of key care themes
Given NHSE policy priorities in relation to the reduction of avoidable hospital admissions and timely patient discharge,24 it was surprising to find that this was not apparently an explicit key goal in relation to choice of CQUINs for community nursing. Although the categorisation of care themes in the survey gives a broad indication of CCG priorities in relation to community nursing, we investigated four areas of particular importance in community nursing day-to-day work to see if a link with admissions avoidance or timely discharge was evident therein: organisation of care and organisational issues, long-term conditions, care planning and end-of-life care.
Organisation of care and organisational issues
Closer examination of the content of CQUINs within the dominant care themes of organisational issues and organisation of care revealed a focus on four categories: the care model, integration, ‘Francis’ CQUIN and 7-day working.
The care model
The care model refers to the configuration of community nursing services with its multidisciplinary partners in order to deliver care. 6,70 Traditionally, in England, district nursing services were attached to general practices and generally based near or in their premises. The survey findings suggest that commissioners and providers were in various stages of moving more closely towards a distinctive new care model of expanded relationships: placing larger teams of community nurses around clusters of general practices primarily, but also into ‘neighbourhood teams’ or ‘integrated teams’, ‘virtual ward’ or ‘community wards’ in order to provide capacity and expertise to respond to patients with deteriorating conditions who might otherwise be admitted to hospital.
Within these care model indicators, there was a focus on care planning, particularly increasing the number of patient care plans and the time frames in which they were completed and MDT meetings. There were CQUIN indicators related to increasing the frequency of these meetings, assuring full multidisciplinary attendance and the importance of building relationships with GPs and primary care to secure long-term teamwork and commitment.
Integration
Closely linked to the care model, integration CQUINs related largely to structural outcomes such as linking IT systems across organisational boundaries in order to improve communication and relationships. Integration of IT systems concentrated on shared communication across acute and primary care, with few direct references to social care IT systems. A handful of local indicators related to patients holding their own health records; these centred on patient discharge passports detailing ongoing care and therapy needs. More emphasis was placed on relationships with primary care rather than acute trusts and there were few references to working partnerships with the voluntary sector, mental health services or engaging with local community initiatives.
‘Francis’ indicators
A number of organisational CQUIN indicators were influenced by recommendations from the Francis report. 2 These focused on putting systems in place to ensure that organisations were responding effectively to incidents and complaints; some required independent panels to review complaints procedures and to share the learning across organisations. Other ‘Francis’ indicators examined staffing levels with a view to greater transparency around safety, which is especially important as there is no ‘cut off’ to the numbers on a district nursing caseload. Despite this, there were notably few indicators linking safe staff levels to a caseload weighting classification system, which would link staffing levels and skill mix to patient need and mix within each caseload.
There was some emphasis on community nursing workforce development, which aimed to expand nursing competencies, embed the 6Cs3 and promote regular staff supervision. Staff experience is considered to be an important measurement of the quality of health-care provision. 71 The administration of surveys, particularly the ‘Cultural Barometer’,72 was also incentivised in order to access staff views about the care they provided and attitudes to their working environment.
Seven-day working
Some organisational CQUINs incentivised a 7-day approach to community provision with a view to promoting patient discharge from hospital. A minority of indicators aspired to enable weekend provision equal to a normal week day; the majority aimed to enhance a particular aspect of care, such as setting targets for services for 7-day working specifically for patients known to the MDT with a care plan in place. Few of these indicators included detail of the necessary steps to scope current provision and plan the development and extension of services. As CQUIN schemes are time limited and the regulations require the service innovation funded to be incorporated into normal provision, going forward this would be an important consideration.
Long-term conditions and care planning
The management of patients with long-term conditions is a core role for community nurses,52 representing the second major care theme within local CQUIN indicators (after organisational issues). Many of the organisational indicators were to instigate changes to support better management of people with long-term conditions and there are some overlaps within subthemes, particularly around a more integrated multidisciplinary care-planning way of working. Other dominant subthemes within this category included embedding patient self-care approaches and psychological assessments into long-term condition management in the community, utilising telephone self-care hubs and ‘rescue’ care plans, where patients can be taught to recognise signs of exacerbation and take steps to self-manage their condition or seek help. Secondary subthemes included training, telehealth and better-supported discharge.
Scrutiny of long-term condition indicators highlighted divergent approaches to management and care. One-third of the local CQUINs for long-term conditions were generalist in their focus; that is, they proposed macro strategies to improve care across a range of conditions, like better integration, self-management methods and supported discharge. Two-thirds of indicators were specialist in their make-up; that is, they focused on improvements in one specific condition. The long-term conditions specified most commonly were chronic obstructive pulmonary disease and other respiratory diseases, diabetes, stroke and heart failure, with one CQUIN specifying dementia. Within the ‘specialist’ indicators, there was an emphasis on upskilling community matrons through training and by creating closer links between the matrons and specialist nurses. There was also an emphasis on early identification of patients and on development of care pathways relating to a specific condition.
Many of the indicators relating to long-term conditions were directed at the community matrons, as case managers, to support ‘in-reach’ discharge planning, as the main recipients of training in specific specialisms and to support joint working with specialist nurses. Community matrons or case managers, however, represent only a small proportion of the community nursing workforce, with much of the front-line nursing care being undertaken by lower-banded community nurses. 73
Supporting the carers of people with a long-term condition was an important strand of local CQUINs; however, it was one of the least dominant subthemes. Indicators involved more formal identification of carers alongside people with a long-term condition to ensure that they were ‘signposted’ to appropriate support for financial advice, local groups and respite care.
End-of-life care
Care provision for people choosing to die at home is another core area of care for community nursing services,52 though it was not prioritised in relation to CQUIN indicators in comparison with organisational issues and long-term conditions. Dominant subthemes related to the identification of patients nearing the end of their lives and recording them on a palliative register, particularly those who had a diagnosis other than cancer, to offer them (and their family) opportunities to plan their care. Other dominant subthemes focused on effective care planning: in increasing the numbers of plans; in ensuring the completeness of the documentation to include a preferred place of care and resuscitation decisions; and in communicating these plans across services and organisations to support patients’ choices and preferences.
Effective multidisciplinary working was also incentivised in end-of-life care CQUIN indicators. Indicators sought to embed attendance at multidisciplinary meetings involving specialist hospice nurses at practice level, but also cross-organisational meetings at a strategic level to standardise provision, and multidisciplinary, multiorganisational post-death reviews to explore cases in which patients did not achieve their preferences.
To a lesser extent, some indicators concerned enhancing nursing competencies by the provision of tailored end-of-life training. The types of training ranged from broad mandatory sessions to focusing on the specifics of advanced care planning and embedding the lessons of recent findings from the withdrawal of the Liverpool Care Pathway. Bereavement care also featured as a lesser subtheme, with an emphasis on follow-up care with relatives and, in some cases, the development of a bereavement care plan for people who had spent many years caring for a sick relative.
Reducing admissions and timely discharge
Overall, closer scrutiny of the organisational CQUINs suggested commissioners putting in place some of the structural requirements, such as IT and training, to develop a responsive community nursing service and facilitate integrated working within MDTs, both of which are essential as an alternative to hospital provision. An implicit focus on reducing both patient admissions to, and time spent in, the acute sector, was discernible in CQUINs concerning long-term conditions, particularly where they addressed macro strategies for improving care, patient self-care and staff training. Similarly, the end-of-life care CQUINs included a focus on staff skills to enable community nurses to support patients who choose to die at home. Scrutiny of the four care themes from the survey (organisation of care and organisational issues, long-term conditions, care planning and end-of-life care), which together accounted for 75.8% of the CQUINs recorded, revealed an implicit drive to increase community-based care provision. If the 28 (5.8%) CQUINs directly focused on admission avoidance or reduction are also included, the proportion of these CQUINs rises to > 80%. This suggests that reducing hospital admissions and facilitating timely discharge were key targets for the measurement of quality in community nursing for the CCGs participating in the survey.
Summary
The survey analysis provided a snapshot of the range and variation of CQUIN schemes applying to community nursing nationally and the types of organisations involved in commissioning and providing nursing services since implementation of the Health and Social Care Act 2012. 26 Although CCGs tend to commission services from a single provider, it is evident that nearly half of the provider organisations deliver services for more than one CCG, suggesting a considerable workload in relation to CQUIN negotiation for providers. The number of CQUINs varied in each organisation but averaged < 10 (as suggested by the guidance for CQUIN 14/15), and this did not appear to be associated with the numbers of organisations involved.
Scrutinising the survey data in relation to aspects of the two quality dimensions, namely patient safety, patient experience and effectiveness of care, and structure, process and outcome, revealed the complexity of community nursing CQUINs in use. It was clear that a sizeable proportion of CQUINs addressed more than one of these aspects. It was also notable that, although the aspect of quality dimension 1 most frequently addressed was effectiveness of care, only a relatively small percentage of CQUINs focused on outcome, either alone or in combination with at least one other aspect of quality dimension 2. Process was the aspect of quality dimension 2 most often addressed, despite the presumption that CQUINs are designed to address safety, experience and care effectiveness, all of which should arguably be construed as outcomes. These findings suggest an assumption that focusing on process implies effectiveness of care. As nearly 60% of the CQUINs examined explicitly addressed organisation concerns, with many of the remainder implicitly focusing on the structure or processes within organisations, these findings together suggest that all of the CCGs recruited to the survey, along with their community nursing providers, were focused almost exclusively on adapting to the demands of the changing landscape of health-care provision in England. This perception was reinforced by the content analysis of the four care themes, namely (1) organisation of care and organisational issues, (2) long-term conditions, (3) care planning and (4) end-of-life care, where an implicit drive towards reducing patient admission to, and time spent in, hospital was evident.
The findings from the survey highlighted particular issues in relation to the case study phase of our research, namely the way in which the quality of outcomes was being assessed and the focus on developing structures and processes to meet the rising demand for community-based care. In the next chapter we present a description of our case studies and our findings concerning the local context for community nursing quality measurement within them.
Chapter 4 Findings 1: the case study sites and the current context of measuring community nursing quality
This chapter outlines the structures of the organisations commissioning and providing community nursing services in the five case study sites. Information about CQUINs and other quality measures which provider organisations were expected to meet in 2014/15 and 2015/16 is presented after the case site description.
Case study sites
Each site comprised a CCG and a service provider. Community nursing services were provided by four NHS organisations (community trusts, combined acute and community trusts or community foundation trusts) and one social enterprise. In all of the case sites, community nurses were located in geographically based teams serving a number of general practices. Teams were accessed by a single point of entry system, whereby there was one centralised telephone number for referrers and other patient enquiries. For tables summarising the characteristics of the case sites and the numbers and types of participants, see Chapter 2.
The following text provides more details of the commissioning and provider organisations. Pseudonyms have been used and any similarity with existing place names is unintentional.
Alderton West
(Data collection 25 May 2015–10 May 2016.)
Alderton West is a large urban area. Deprivation in the area is higher than average and life expectancy for both men and women is lower than the England average. Smoking-related deaths are higher than the England average. Mortality rates for those aged < 75 years from cancer and cardiovascular disease are significantly higher than the average for England. One NHS commissioning organisation, the NHS Alderton West CCG, is responsible for managing the contract with the community care provider, Alderton Community NHS Foundation Trust (ACFT), on behalf of two other CCGs, which also commission services from this provider. Alderton West CCG is associated with approximately 50 general practices covering a population of approximately 300,000. ACFT provides > 30 different community services for adults, including some inpatient beds. The district nursing teams are organised in multidisciplinary integrated teams of varying sizes and cover the whole city. ACFT provides community services for a total of four CCGs, covering a population of > 1,000,000.
Beechbury
(Data collection 14 April 2015–25 April 2016.)
The second case site, Beechbury, is a large urban area. There is a high level of deprivation compared with the average for England and a higher than average proportion of people smoking and dying from smoking-related diseases. Premature deaths in those under the age of 75 years from cardiopulmonary diseases and cancer are also higher than the England average. The NHS Beechbury CCG is one of three CCGs that cover the city. Beechbury CCG’s area of responsibility comprises > 40 general practices covering a population of approximately 300,000. Community nursing services are commissioned from Beechbury Community NHS Healthcare Trust (BCHT), which provides a range of health services across the area. BCHT also delivers care commissioned by the two other CCGs for a total population of approximately 800,000.
Despite the existence of separate CCGs, many aspects of commissioning and quality and performance oversight are conducted jointly across the CCG group in collaboration with BCHT. Beechbury CCG and BCHT also work to deliver community-based care in partnership with local authority and voluntary sector organisations, as well as other NHS trusts. The health and social care structures for delivering care in the Beechbury site have undergone significant redesign over the last few years and community nurses work in a number of MDTs. Team management posts are held by staff from different professions and support from a range of senior clinical staff is built in to the management structure, including a named individual whose remit is overseeing quality issues.
Cedarham
(Data collection 6 July 2015–29 May 2016.)
Cedarham is a large urban area. Community services are commissioned by NHS Cedarham CCG which covers nearly 50 general practices serving approximately 300,000 people. Community nursing services are provided by a combined acute and community care organisation, Cedarham NHS Foundation Trust (CFT). One other neighbouring CCG also commissions services from CFT, which provides services for an ethnically diverse population of approximately 600,000 people. Deprivation in the area is higher than average. Life expectancy for men is lower than the England average, but for women it is higher than average. Smoking-related deaths and mortality rates among those under 75 years for cancer and cardiovascular disease are higher than the England average. The supervision and oversight of quality issues in CFT community nursing services is the remit of a senior manager with a community nursing background, who has direct contact with locality managers. The development of integrated care is an organisational priority for the trust.
Dogwoodheath
(Data collection 18 February 2015–11 February 2016.)
NHS Dogwoodheath CCG is one of three CCGs with responsibility for commissioning community-based care for people living in a large urban environment, with a population of approximately 300,000. Commissioning is conducted independently by each CCG in the area. The health of people living here is generally worse than the England average, with the rate of smoking-related deaths and the number of people dying prematurely from cardiovascular disease and cancer being considerably higher than average. Community nursing services are delivered by Dogwoodheath Respond (DHR), a social enterprise. Community nurses work in MDTs, usually managed by a team leader with either a nursing or a therapy background.
As well as working with approximately 60 local general practices, both the CCG and DHR collaborate with a range of other organisations involved in delivering care, including acute and community-based NHS trusts, local authority organisations, the private sector and the voluntary sector. Both Dogwoodheath CCG and DHR work closely together to monitor quality issues. Communication and collaboration between them are facilitated by their occupying premises near one another.
Elmhampton
(Data collection 11 February 2015–30 November 2015.)
Elmhampton is a large, predominantly rural area also containing several large towns. The population of around 500,000 people is slightly older than the national average and has a higher than average life expectancy. Levels of deprivation are below the national average, although pockets of deprivation do exist. The prevalence of smoking and obesity in adults here lies within the national average range, and smoking-related deaths, as well as cardiovascular disease or cancer mortality in those aged < 75 years, are lower than national rates. NHS Elmhampton CCG operates in several localities with approximately 80 general practices. It is the sole CCG for the area and commissions community nursing and some other services from Elmhampton NHS Foundation Trust (EFT), also covering the same geographical area. EFT has been delivering community services for 5 years and working with the CCG since its inception. At the time of the study, EFT was in the process of service redesign, working towards integration. A particular priority for the service is to develop specific integrated pathways to assist particularly vulnerable patient groups.
Participants in the case study sites
A total of 111 individuals (commissioners, provider managers, community nursing team leaders, front-line community nurses, patients and carers) took part in 62 interviews and nine focus groups across the five sites. A further focus group of eight patients and carers took place locally. Members of the research team observed 27 meetings attended by commissioners, provider managers and/or community nursing team leaders.
Four of the five sites consented to a nurse researcher shadowing community nurses during their day-to-day work to observe processes in place for recording QI data both in patients’ homes and in the nurses’ community bases. Twelve community nurses were shadowed in 13 sessions and visited 66 patients in their homes. Three patients refused for their nurse to be observed on the day of visit. On average, home visits lasted just under 30 minutes, but the range was from 10 to 95 minutes. In addition to visits, front-line nursing staff were observed completing their records on computers at their base and other administrative tasks such as referrals and ordering equipment. Handover meetings were observed at each participating case site.
CQUINs in use in 2014/15
Documentary data collected for phase 1 of the study identified that all of the case sites implemented two national CQUINs in 2014/15, namely the FFT and the NST, involving the measurement of catheter-acquired urinary tract infections (CAUTIs), new PUs and falls. The fourth domain of the NST was not reported on in the community. Some sites also included local CQUINs for community nursing that complemented/added to the national requirements concerning PU and falls measurement and reporting. In addition, some implemented local CQUINs focusing on dementia. Phase 1 analysis revealed that number of local CQUINs implemented for community nursing across the case sites in 2014/15 ranged from 1 to 12, with Dogwoodheath (the social enterprise) adopting the largest number. There was some commonality in the areas of care addressed, namely dementia care, discharge planning/review, multidisciplinary working, patient education and patient experience (Table 9). However, there was also variation across the sites in areas of care prioritised through the adoption of CQUIN ‘stretch’ targets, as shown in Table 9.
| CQUIN detail | Site | ||||
|---|---|---|---|---|---|
| Alderton West | Beechbury | Cedarham | Dogwoodheath | Elmhampton | |
| Number | 1 | 5 | 3 | 12 | 3 |
| Care plan development | 1 | ||||
| Catheter care | 1 | ||||
| Dementia care | 3 | 2 | 1 | ||
| Discharge planning/review | 1 | 1 | |||
| Falls | 2 | ||||
| Multidisciplinary working | 1 | 1 | 2 | ||
| Patient education | 2 | 2 | |||
| Patient experience | 1 | 1 | |||
| Organisational communication | 1 | ||||
| PUs | 1 | ||||
Table 9 shows only those CQUINs that were definitely applicable to community nursing in 2014/15 in each site. There were other CQUINs included in the provider organisation contracts that may have applied to community nursing. Areas of care addressed by these CQUINs included many of those listed in Table 9, as well as training for non-registered nursing staff and learning from safeguarding.
Quality measures used in the case sites in 2015/16
In response to our request for documentary data, the case study sites submitted a mixture of details from schedule 4 and/or schedule 6 of the NHS standard contract, as well as dashboards or scorecards through which quality requirements were measured and reported. There was no set format for these; some looked at specific aspects of monitoring, for example a dashboard concerning only workforce compared with others incorporating all the national and local contractual quality requirements. One case study site submitted the local quality requirements (schedule 4), an example of the dashboard and a scorecard with considerable overlap in what was being reported on in each. No case site submitted a complete data set in this regard (Table 10).
| Study site | Type of documentation | |||
|---|---|---|---|---|
| Schedule 4 | Schedule 6 | Dashboard | Scorecard | |
| Alderton West | Proposed local quality requirements 2016/17 | ? | Provider dashboard 2015/16 reporting on operational national and local quality requirements | Scorecard (November 2015) reporting on safety, patient experience, workforce and efficiency, training, human resources, governance, activity and essential care standards |
| Beechbury | ? | ? | ? | Scorecard of KPIs (October 2015) contained in an Integrated performance report reporting on CQC key domains: safe, effective, caring, responsive, well led with an extra category of finance |
| Cedarham | ? | ? | District nurse quality dashboard (2015); workforce update and dashboard (August 2015) | |
| Dogwoodheath | Local quality requirements 2015/16 | Local reporting requirements 2015/16 | ? | ? |
| Elmhampton | Local quality requirements 2015/16 | Service development and improvement plan 2015/16 | ||
| Data quality improvement plan 2015/16 | ||||
Alderton West commissioners were particularly focused on partnership working, patient consultation and education. It was also their intention to work towards achieving NHSE outcomes such as improved life expectancy, improved patient experience and moving care outside hospitals and closer to people’s homes where possible. Documentary analysis revealed that the service’s quality dashboard for 2015/16 contained 44 local quality requirements applicable to community nursing. Indicators included measures for access to services, delayed transfers of care and completed assessments, response times for patient complaints, the number of serious incidents, never events, staff appraisals and training, vacancy rates and reporting on the NST as reported below.
Beechbury Community Health Trust’s quality reporting for care is aligned with the five CQC quality domains and the fundamental standards of care. The trust was obliged to meet > 40 QIs for community nursing services, although some of these applied only to caring for patients in residential settings. Particular attention appeared to be focused on patient safety, the responsiveness of the organisation and on staff experience and capacity.
The Cedarham commissioners agreed with the trust not to have any CQUINs for the contractual year 2015/16. Nevertheless, a district nursing quality dashboard for that period indicated that they were collecting data on a number of local quality requirements: sickness and vacancy rates; governance issues around the numbers of incidents and complaints; caseload size; the percentage of face-to-face contact time and the number of grade 3–4 PUs and falls. Also captured were the number of contacts for palliative care and with general practices. Other highlighted areas were medicines management, serious incident reporting, training of staff for safeguarding adults, patient experience and patient safety. Copies of the dashboards were placed on staff noticeboards in the bases (front-line observation notes).
Dogwoodheath Respond was expected to meet approximately 20 local quality requirements regarding community-based care in Dogwoodheath in 2015/16, including some relating to waiting times and end-of-life care. There was a particular focus on community nursing issues rather than broader governance compared with other case site studies, and on capturing patient experience through a range of surveys, which formed many of the requirements. Local reporting requirements included information about referrals and case management.
In Elmhampton, the EFT was required to meet 10 QIs for community nursing services. Over half of these related to patient safety, the remainder being involved with the responsiveness of the organisation. There were additional indicators relating to transfers of care that could also involve this service. Again, in at least one of the main bases there was a noticeboard with quality data posted so that staff could see how the well the organisation was doing (front-line observation notes).
All of the participating sites had CQC inspections at one point during data collection for this study.
CQUINs
The four case sites with CQUINs in 2015/16 implemented two national CQUINs for that period focusing on dementia and urgent and emergency care; the CQUIN regarding the latter mainly concerned admission avoidance and discharge planning.
Local CQUINs definitely applying to community nursing services in 2015/16 in Alderton West, Beechbury, Dogwoodheath and Elmhampton are presented in Table 11. The range of the number of CQUINs adopted in different sites was slightly smaller than in 2015/16, varying from two to six. Dogwoodheath implemented the most CQUINs, as was the case in 2014/15.
| CQUIN detail | Site | |||
|---|---|---|---|---|
| Alderton West | Beechbury | Dogwoodheath | Elmhampton | |
| Number | 3 | 2 | 6 | 2 |
| Catheter care | Yes | |||
| Discharge planning/review | Yes | Yes | ||
| Multidisciplinary working | Yes | Yes | Yes | |
| Patient activation/well-being | Yes | Yes | ||
| Patient education | Yes | |||
| Patient experience | Yes | |||
| PUs | Yes | Yes | ||
| Safeguarding | Yes | |||
Across these four sites, only one further CQUIN was identified that could possibly apply to community nursing. This indicator focused on the processes in place in Elmhampton with respect to the transition of care for individuals with ongoing continence problems from the children’s services to those for adults.
The context of care
National policy directs and influences the way that health service quality is measured and applied in the context of community nursing. Throughout the study, we found that front-line staff, patients and carers were keen to offer their thoughts about local issues affecting the quality of care provided and its measurement. In the following section, we present findings related to the context of quality measurement in community nursing in relation to the national picture and across the five study sites locally. In discussion within the research team it was evident from the within-case analyses that there was a great deal of similarity in findings with respect to all our emergent themes. We have therefore presented findings from a cross-case analysis in this chapter and in the following chapters using data drawn from all of the sources across the five case study sites, as well as the data from the NHSE interviewees.
Identifiers for quoted excerpts from interviews and focus groups in this chapter are shown in Table 12. Excerpts from field notes recorded during the observation of meetings and of front-line staff at work are labelled accordingly.
| Participant | Identifier |
|---|---|
| Carer | C |
| Commissioner | CM |
| Community nurse (focus group) | CNFG |
| Community nursing team leader (provider) | NTL |
| Focus group carer (non-case study site) | FGC |
| Focus group patient (non-case study site) | FGP |
| NHSE: national officer | N |
| NHSE: regional officer | R |
| Patient | P |
| Provider business/performance manager | BM |
| Provider manager: director/manager of nursing services or of quality | PM |
In each case, an individual participant is identified by a unique number preceded by the name of the case site (e.g. Beechbury CNFG1), except for the local patient and carer focus group FGP1/FGC1.
Cross-cutting themes emerging from the data in relation to the current context of community nursing quality measurement included national–local interface, reorganisation of care, IT implementation and community nursing caseloads.
National–local interface
We investigated the way in which national policy about quality in community nursing is transmitted to local commissioners and providers, focusing on the role played by NHSE and the regional area teams. One of the main roles played by the national and regional bodies is to facilitate communication between the different actors in order to achieve a better understanding of the practical implications of national policy. For example, NHSE have organised a series of workshops across the country to collect views on what works in community service provision. These workshops heavily influenced the publication of the Framework for Commissioning Community Nursing. 53
Within the regions, area teams monitor CCG performance via standardised quality assurance processes. These involve having regular meetings with CCGs and receiving regular submission (monthly, bi-monthly, quarterly) of specific information requirements:
So we routinely have safety thermometer reports. So our analytical teams will always provide those. So we have dashboards that are looking at community, and acute providers. And they’ll bring a number of different indicators, so whereas that’s from safety thermometer, from the national SI [serious incident] reporting system, it’s from activity information around delayed transfers for care. There’s a vast amount of indicators that we’d routinely get, and we get that on the monthly basis. We tend to pull that together in a dashboard. The providers have their own, but we have that overview of all services.
R2
However, one regional participant stated that the area teams do not pursue the monitoring of QIs in great detail:
We probably don’t input hugely into any contractual quality indicators but we will be looking at quality sort of generally across contracts that we have responsibility for.
R1
Similarly, another regional participant explained that during their performance meetings with CCGs, QIs are discussed, but not every single one of them:
We do discuss [indicators] . . . and we tend to have an update on that. But I think if we discussed every CQUIN that every provider [had] . . . I just don’t think you could accommodate it.
R2
The main reasons are lack of resources in the area teams and the need to preserve the autonomy of local commissioners. Prior to being authorised, CCGs went through a rigorous authorisation process in which they had to meet a number of centrally defined criteria, including their ability to commission for quality. One regional interviewee stated that, although the regional teams needed perhaps to do more, detailed monitoring of CCGs would require a lot of resources that are currently lacking. The interviewee stressed, however, that it is, on the whole, better that the regional or national bodies give commissioners the flexibility they need, as long as they are assured by concrete evidence that standards of quality are improving:
Maybe, do we need to look at those things specifically . . . I’m really not sure we’ve got the resources to do that. My view is that we should trust the system to do what it does, so not getting involved is probably the right thing to do, as long as we can see the evidence that it is happening.
R1
Another regional participant agreed that one of the main roles of the area teams was to facilitate implementation of national policy by CCGs. During their regular meetings with commissioners, for example, the area team performs this facilitating role:
So it’s usually a two-way meeting. So we provide updates. So what’s coming from the central team, what’s going on in NHS England, and then anything else, you know, whether it be finance from FFT reports or anything like that. So we try to get information to them as quickly as possible. And then we tend to talk around some of the good practice or challenges that they’re having locally. And it’s just about a shared understanding, see if we can help or support or direct.
R2
One regional team participant emphasised that a lack of robust data on community nursing made monitoring of the service difficult:
And if we’re talking about district nursing, community nursing, there is not a data set, a nationally agreed data set. So it’s hard and you find that you concentrate on talking about the services where there is information. And that means that we spend less time talking about community services and less time talking about mental health services because there is not such a great wealth of data and we spend an awful lot of time talking about acute trusts.
R1 (bold has been used for emphasis)
Another participant stated that although the area team examines data from CCGs as part of the assurance process, data sets are used more to generate discussions about the real state of services than being accepted in the absence of further triangulation:
Data can start a conversation. And it’s about working with the CCG to validate some of that data. So we don’t always take it at face value, but it would always start the conversation. And most of the time, the information that the CCGs have, and providers have, it matches up, but not always. And that’s about having those conversations.
R2
Reorganisation of care
The widespread reorganisation of structures for providing care was seen to be a factor having a direct impact on the quality of care provision and, therefore, on issues affecting measurement of care quality. Changes to community nursing working conditions were common across all five case sites as organisations were moving to the provision of extended nursing hours intended to reduce avoidable hospital admissions, improve timely discharge and improve efficiency. These included altered working hours for front-line staff and changed modes of working such as moving to integrated health-care services or hub-and-spoke systems, in which community nurses work in teams from a central base covering a number of GP surgeries, rather than being based with individual general practices. It was also apparent that there was an expectation that such changes were likely to continue in the longer term:
There have been some changes following the merger of mental health and community and larger integrated teams providing service, some shifts 2–10 p.m. plus the overnight service. The next development is ‘agile’ working – the trust wants to get rid of the current base and have nurses working from home.
Elmhampton (front-line observation notes)
The integration of health-care services was generally viewed positively by front-line staff, although the process of change caused some challenges for day-to-day working. Case sites were at varying stages in this process, but the issues relating to the establishment of new organisational structures were common. Confusion was expressed about line management relationships (in part the result of some management posts being unfilled at the time of the study). Some team leaders were either temporarily without direct line management, or in the process of changing roles themselves:
. . . my manager doesn’t actually know how that’s going to impact, how we’re going to be integrated, you know. So I mean all that is up in the air at the moment.
Elmhampton CNFG1
And there’s been this massive, massive consultation . . . and it’s now putting staff into the posts in different areas, in these different roles with different titles.
Elmhampton CNFG2
Nevertheless, the benefits of changing modes of working were noted by many and seen as necessary to enable nurses to continue to give the best quality of care in the context of increasing caseloads. One gave a clear description of the benefits of the workforce planning made possible through the hub-and-spoke model:
Things have improved . . . It’s not like my staff. It’s our staff. It’s our team, it’s our patient . . . And say for instance . . . I haven’t got staff in my team . . . by the time we do the team planning, the other team would have identified okay . . . So with that, if I’m short, I can always fill the gap . . . which has actually helped a lot.
Cedarham CNFG2
However, not all aspects of restructuring were welcomed by the front-line staff. There was some disquiet expressed at proposed role changes in one site that was moving to a more generalised service model, where a district nurse said that district nurses did not want to be specialists and community matrons did not want to be district nurses:
Still in the process of moving to an integrated team and this has involved moving offices in order to be in close proximity with one another. Some people are not keen on being integrated as community matrons do not want to go back to management duties [they will be leading the district nursing team] and district nurses do not necessarily want to learn the skills of the community matron.
Beechbury (front-line observation notes)
Changes to working hours, such as incorporation of the twilight shift (6–10 p.m.) into the day shift, had resulted in nurses leaving because the new hours were incompatible with their home lives and child care provision:
A lot of people did the twilight shift because it suited them. 6 o’clock till 10; they didn’t have to sort out any child care, they could pick their children up and take their children to school . . .
Beechbury CNFG1
There was some evidence that shift changes had also had a negative impact on patients due to the same number of staff being spread more thinly. Patients requiring insulin are prioritised for early visits in a community nursing caseload. A patient whose care had changed since the adjusted hours reported that her daily visit had been delayed, which had an impact on when her carers were able to get her up and resulted in her having to stay in bed later in the morning:
There used to be two [nurses] say start at 8.30 not just one at 8.30 till 10 and they find it a struggle to get round all the diabetics and maybe the two bowel ones that they do before 10 o’clock, and we need it before 10 because our carers come, we can’t get up until the nurse has been, but it is a struggle for them because of the new times that they are working.
Elmhampton P1
Recruitment and retention of staff were reported to be a problem in every case site, as evidenced at one organisational meeting:
There is an ongoing increase in vacancies. The HR [human resources] manager reported that a lot of staff are leaving. Recruitment is in progress, but it is not proceeding fast enough to replace staff. Exit interviews are ongoing.
Alderton West meeting (field notes)
In one focus group in Cedarham, a nurse spoke of an area within her case site having around 50% agency staff. In this case site one period of nurse shadowing was conducted with an agency staff member of the team. In discussion, it transpired that the nurse had been a temporary member of the team for nearly a year and preferred the flexibility it afforded. Evidence from focus groups suggested that the overall quality of care received by patients was felt to be affected by vacancies:
If your team’s well staffed you’re going to provide better care. If you’re struggling with five staff on 70 visits, you’re just not, the standard of the level of care is not going to be the same as if you’ve got a fully staffed team.
Dogwoodheath CNFG1
A regional participant focused on the challenge of staff shortages and the need to move more resources into community nursing:
I think it’s very challenged. I think recruitment and retention . . . There is a need to involve the nurses much more, and devise care and long-term conditions, and how that’s being managed locally without them needing to go into the acute setting . . . I think community nursing, I think needs quite a significant amount of investment. If we want to achieve . . . reduce the number of admissions to hospital, then we need to invest in our community services, and the district nursing being quite key to that.
R2
It appeared that, in at least one case site, considerable effort and expense were being successfully invested in improving recruitment:
The trust reported enormous success in district nurse [DN] recruitment. 42% of their vacancies have gone to community nurses. Some of the things they did to attract staff was to re-brand themselves and increased their reputation and started a massive advertising campaign. This year they recruited 24 new DNs, last year they recruited only six.
Cedarham meeting (field notes)
However, it was evident that this development had still to be felt on the ground. During one observation session with front-line staff in Cedarham, the nurse whom the researcher accompanied said that she had worked until 10 p.m. the previous evening, although her shift had officially finished at 4 p.m. On the following day when observation commenced, she had started work again at 8 a.m.
A strategy to combat the problem of recruitment and retention, common to all the case sites, involved the introduction of more, but less well-qualified staff, into the team. A national participant offered this view of the matter:
There’s also the issue of skill mix in some of the teams, so how are they using skill mix? Does it always take a community nurse to do that, or could they be using community volunteers or health-care assistants in a different way, so it’s about just stopping for a moment and thinking, do we need to do things the way we’ve always done them?
N1
However, greater skill mix was not necessarily leading to perceived improvement in care quality:
At the moment we seem to be getting a lot of [band] fours, a lot of [band] threes. And what we need is staff with the knowledge and the skill to do the work . . . You can look at someone’s team and think, oh, they’re fully staffed. Well they might be fully staffed, but not with the skill you need to do the work appropriately.
Alderton West CNFG1
Concern was also voiced that larger teams could result in lack of continuity for patients and carers:
The CCG quality manager added that too many people see the same patient so there is no continuity of care . . . consistency has an impact on the deterioration of the patient. Getting the structure right is key.
Beechbury meeting (field notes)
Asked about some of the key challenges facing the work of district nurses, and therefore the quality of care provision, one NHSE national lead interviewee summarised them as having access to good IT systems, working in geographically organised teams and having the right skill mix in each team:
I think a big issue, a massive issue, for community nurses is technology, and where they have access to good IT and they can use it, it makes a hell of a lot of difference to the work. I think the way teams organise themselves, so, you know, are they working together, are they working around a GP practice, are they working as a geographical team, because again, that’s been shown that they can waste a lot of time travelling around, so there’s that issue as well.
N1
Information technology implementation
In all the sites, new IT systems were being developed. However, investment in IT services to support front-line care received mixed reactions from staff. Although its potential was recognised and welcomed, IT implementation issues were a challenge everywhere. Problems included staff having to learn the different IT systems, sometimes more than one at the same time, while sometimes also coping with outdated hardware. This became apparent during sessions shadowing community nurses. In Alderton West, staff were using a new system for recording care and activity, a different system for recording their mileage and, at the same time, implementing a new work allocation system:
Currently nurses are getting used to a new electronic mileage calculator – this is not linked to RiO [an electronic care record system for health and social care organisations] and is leading to too much time being ‘wasted’ on completing returns, and hence delays in recouping outlay for petrol . . . The team leader was complaining about the imposition of a new allocation tool for staff and asked who had been involved in its piloting as she thought it was not fit for purpose in her large team – several shortcomings had been identified . . . The team are supposed to use laptops but these are heavy and unwieldy . . . no-one in this team was using them routinely.
Alderton West (front-line observation notes)
In Cedarham, a new electronic care record (successfully used in the acute side of the organisation) had been introduced at the same time as staff were piloting a device to record nursing notes electronically for use in patients’ homes. On one day of the front-line observations both new technologies were causing problems for staff in writing up their work and planning workload allocation for the team. In some instances, a lack of availability of assistance when ‘teething problems’ occurred compounded any IT problems:
Some of the good things are definitely, I mean I wanted EPR [electronic patient records] for so long because it drove me mad doing notes onto electronic records so it’s just some of it getting used to it because you’ve not just got your [IT package], and you’ve got your [mobile IT package] so again they work differently as well so it’s a lot of new learning to do . . . It’s not till you start doing something that you come up with all the questions . . . the people that were [teaching] moved on so there is nobody there to ask, so a lot of things have been done incorrectly.
Beechbury CNFG3
In some of the sites, it appeared that staff actively resisted using new systems:
The senior quality and safety manager asked whether the safer staffing electronic tool had helped with regards to data collection and ensuring safer staffing requirements are met. The associate director explained that there had been issues when implementing the tool, most notably getting staff to access and use the system.
Alderton West meeting (field notes)
There were particular problems noted with some less recently qualified community nurses, more used to paper documentation held in the home and at the office, who were not used to having to input all relevant information on to computer. This staff group were reported to lack confidence and to need a great deal of support in order to adapt to new IT systems:
We had people in tears. I can just remember the person in the corridor out there in tears saying ‘I need to leave’. They will come to the computer and they’ll be shaking. And it’s like, ‘It’s fine. You’re not going to do anything wrong. You’re not going to delete someone’s clinical record. The computer won’t let you do that anyway’.
Elmhampton PM4
Some front-line staff argued that new technology interfered with good communication:
The people whose houses we go into, to be honest, you can’t sit down and type in front- and I find that rude anyway.
It’s unprofessional.
Like we’re more interested in documenting than actually seeing the patient.
You find a lot more out with the patient if you’re sitting with them and talking face to face.
As front-line observations demonstrated that nurses were documenting sometimes quite lengthy care notes on paper records in front of patients in the home, it may be that it is unfamiliarity and the attendant difficulties of using new technology that influence this perception. At one shadowing session, during a conversation with a patient, a nurse commented that computers can present barriers to the patients; however, the patient, a nonagenarian, unexpectedly disagreed, saying that people need to move with the times.
Front-line observations confirmed the challenges for staff navigating new software: having increased equipment to carry or keep in the back of the car and time required to input care data in all the sites. Other issues arise with technology in the community due to connectivity problems.
Although all of the sites had made an attempt to implement mobile working in community nursing services, this process had been hampered by unreliable connectivity in a number of areas, both urban and rural. Some nurses were reported to be uncomfortable about using tablets or other small hand-held devices in patients’ homes. One manager was concerned about nurses’ safety in this regard. There were reports of nurses waiting until after a visit to enter their data electronically, doing so while sitting in their cars. This raised issues concerning their own health and also about their physical safety in some circumstances.
Community nursing caseloads
A factor reported as adding to pressures on front-line staff was the increasingly complex nature of patients on the community nursing caseload, whose care can entail a considerable amount of community nursing time. The situation was often compounded by staff shortages and high sickness rates, in some cases associated with individuals struggling to cope with extensive changes to their traditional ways of working. The extent of staff sickness was an item discussed at many of the meetings observed, in terms of both concern for staff well-being and its logistical impact on the service:
The CCG quality manager asked if it will be possible to find out the themes involved in long-terms sickness rates and stress.
Beechbury meeting (field notes)
Staff sickness and vacancies were also quality measures to be monitored regularly and reported to the CCG.
In the Dogwoodheath focus group, one nurse estimated that 80% of her caseload was made up of patients with complex needs. Complex care is in itself generally viewed positively and as an opportunity to enhance and practise a range of nursing skills, but the consequent increased support for the patient can create difficulties, as reported in another focus group:
We are doing more acute things now in the patients’ home. We do IVs [intravenous (injections or infusions)], PICC [peripherally inserted central catheter] line care. We are now even starting blood transfusions . . . which then takes a district nurse or a community nurse off the radar for at least between 2 and 4 hours . . . And this is adding stress . . . we love doing these things . . . you get your teeth into it. It’s brilliant. But you need the extra people on the ground – simple.
Elmhampton CNFG3
It was evident that there was ever-increasing demand on community nursing time:
The head of nursing for adult community services said that last month referrals have jumped to 30,000. There usually are 26,500 visits a month for 130 staff.
Cedarham meeting (field notes)
Moreover, the unique nature of the community nursing caseload is that it cannot be ‘full’ or ‘closed’, so that if a patient is deemed fit enough to leave hospital and able to go home, they will be discharged and become part of the caseload regardless of any staffing issues the community nurses may be experiencing:
You’ve got no full case load. You know, in hospital when your 30 beds are filled, that’s it, you can’t have any more patients on the ward. In the community, you just have referral, referral, referral and they’re home. You can’t say, oh, I can’t take this patient because we haven’t got enough staff.
Alderton West CNFG2
A team leader in Cedarham talked about how busy the service is, commenting that ‘his hands were tied’, as there was an organisational cap on the use of bank or agency staff in the service:
. . . has 18 members of staff but would like 12 on each shift. They like to allocate about 20 [units of time] per nurse – unless staff hold positions of responsibility which means they cannot be patient facing. Emphasised that district nurses do not have a waiting list – ‘if a patient needs DN [district nurse] care they need it today’. Patient expectations are high – think everything should be available to them on NHS and they should not have to contribute to care costs.
Cedarham (front-line observation notes)
Both provider managers and nursing team leaders felt that increasing demands from patients could be due to staff in acute services and GPs sometimes raising patients’ expectations about the care they will receive in the community, with one participant stating that the service is referred to nationally as the ‘sponge’ service because it is meant to absorb everything. In particular, there were issues noted with nurses having to visit people possessing both cognitive ability and dexterity in order to administer injections, when these patients could be taught how to administer them safely and effectively themselves.
Another common cause of complaint was mobile patients expecting nurses to visit them at home, rather than attending a clinic or general practice. This situation can lead to problems when patients are informed that the nurses will no longer be coming to their home:
And then when you’ve been walking for a little bit, you have to stop anyway most of the time, your hip plays up. And you just can’t move and then you can’t breathe . . . but some nurses don’t seem to understand that, it happened a few months ago. And I was quite angry about it and I was really upset . . . I’d only seen her once before, and she was doing my legs and . . . when she’d finished she said ‘I have to inform you that you’ve been seen out twice, so I have to say, we won’t be coming any more.’ I said ‘What do you mean?’ She said ‘Well, you’ll have to go up to the clinic’.
FGP1
These data showed that there can be a mismatch between patient and community nurse expectations of what obligations the service has in terms of providing their care. There appears to be a need for clearer communication to patients about this issue. In one case site the community nursing service decided that firm action needed to be taken; strategies included raising this issue at meetings between the head of nursing and commissioners, and between front-line nurses and general practices, as well as being prepared to deal with patient complaints in this regard:
The chair stressed that it is time that the nursing service put their foot down. A lot of complaints from patients are from patients that the service should not have taken on anyway. So ‘we need to put in place processes to stop inappropriate use of the service’ . . . The chair stressed that when nurses get an inappropriate referral they should not take it on but they should make sure that they give detailed feedback why the referral was not appropriate . . . The chair said that she hears from nurses that they accept most referrals in order to avoid complaints from patients. This should not be happening because ‘we are prepared to deal with complaints about inappropriate referrals’.
Cedarham Meeting (field notes)
It is hard to plan for the resultant, largely unpredictable nature of additions to the district nursing caseload. Once a patient is on the caseload, owing to the complexity of their health needs, they are less likely to be discharged than they would be from other services:
District nursing is very generic from continence to palliative . . . once they’re on your caseload you’re looking at prevention, management, whether it’s acute or long-term condition, and then it’s sustaining that to prevent the illness and prevent them going into hospital. So you can’t discharge many patients either, very quickly, like you can with other specialist services.
Alderton West CNFG3
In this context it is worth noting that community nursing services are commissioned through a block contract, with no reference to the number of patients on the caseload and, therefore, with no contractual flexibility regarding the feasibility of service provision in terms of the ratio of patients to staff.
Summary
The five case sites comprised four urban localities and one rural locality; all of the former were areas of high deprivation compared with the national average. Population sizes were comparable across the sites. Organisation of the community nursing services differed little between the sites, being mainly geographically based. One site (Alderton West) had a mixed provision, with some nurses located in teams attached to particular general practices and other larger teams being geographically based. Community nurses operated in integrated or multidisciplinary community teams in three of the sites. Community nursing services were provided by two NHS foundation community trusts, one NHS foundation trust offering both acute and community services, one NHS community trust and one social enterprise.
There was a notable range in the number of local CQUINs implemented across the case study sites in both 2014/15 and 2015/16. Nevertheless, most of the four sites using CQUINS in 2015/16 had reduced the number of those adopted compared with the previous year, although Dogwoodheath continued to have the greatest number. Variations in local priorities were evident in the focus of local CQUINs adopted in the different sites in both years. Other quality requirements for community nursing in 2015/16 reflected a common concern across the five case study sites for issues relating to patient experience and safety, as well as for staff development and well-being.
The national and regional NHSE representatives interviewed made it clear that they cannot undertake the monitoring of organisation performance in terms of quality comprehensively, due to a lack of resources and of robust quality data concerning community nursing services. Moreover, there is an explicit agenda to promote CCG flexibility and autonomy. The combination of these factors has implications for the consistency of quality standards achievable across different CCGs and providers. However, it may be impractical to assume such consistency is achievable in any circumstances, given the impact that local conditions can have on a service. The variety in the number and focus of indicators in use across the five case sites during the period of data collection evidence the differences in organisational priorities; these priorities could not be accommodated if CCGs were not able to decide how to respond to local conditions.
It appeared that reorganisation in response to the new care landscape in the UK involved a degree of restructuring in all the case sites. Although many aspects of these changes were welcomed by staff, a sizeable minority were reported to be struggling with altered shift patterns, new geographical configurations of teams and updated or problematic IT systems. Moreover, recruitment, retention and sickness rates among community nurses were an issue in all the case study sites.
All these factors appeared to have an impact on the ability of staff to deliver a high-quality service, which was further compounded by the increasing complexity of caseload management. Although increasing the numbers of staff through increasing skill mix was a favoured solution for this problem, the data showed that it did not necessarily alleviate the situation, as numbers of nurses with the requisite high-level skills were not always available.
The overall picture of the community nursing services in all the case sites was, therefore, of a service under pressure, struggling to deliver care to the required standard. This situation calls into question the feasibility of improving the quality of care for patients without the investment of additional resources into the service.
Chapter 5 Findings 2: selection
The process of using indicators to assess quality in community nursing starts with the selection of appropriate measures. Indicators can be nationally mandated, or may be chosen to address local concerns. The first main objective of our study was to explore how QIs were selected in the case sites.
Identifiers for quoted excerpts from interviews and focus groups in this chapter are shown in Table 13. Excerpts from field notes recorded during observation of meetings and of front-line staff at work are labelled accordingly.
| Participant | Identifier |
|---|---|
| Carer | C |
| Commissioner | CM |
| Community nurse (focus group) | CNFG |
| Community nursing team leader (provider) | NTL |
| Focus group carer (non-case study site) | FGC |
| Focus group patient (non-case study site) | FGP |
| NHSE: member of central national nursing team | N |
| NHSE: regional officer | R |
| Patient | P |
| Provider business/performance manager | BM |
| Provider manager: director/manager of nursing services or of quality | PM |
In each case, an individual participant will be identified by a unique number preceded by the name of the case site (where applicable) (e.g. Beechbury CNFG1; FGP2).
Themes identified for ‘selection’ included processes used to select indicators, indicator appropriateness and inclusion of all relevant stakeholders.
Processes used to select indicators
Typically, providers and commissioners enter into negotiation, with both sides clarifying their priorities. Commissioners reported that, every contractual year, they present to their providers an initial list with QIs and suggestions for local CQUINs. They then spend a period of a few months discussing the feasibility of these indicators with the providers. The process of selecting the initial list of indicators usually takes into consideration national guidance, their local priorities and commissioning intentions, and any gaps in quality identified locally throughout the year. Sources for the selection of indicators, according to commissioners, derived from:
-
compliance with national policy guidance and national indicators, for example time scales for conducting root cause analyses for serious incidents, Five Year Forward View,28 NHSE commissioning priorities
-
national quality requirements that may need to be supported by additional local requirements
-
local commissioning priorities resulting from CCG membership consultation
-
the KPIs included in the service specifications for particular clinical conditions
-
CQUINs (national and local); previous CQUINs tend to become KPIs
-
any gaps in service provision identified via the monitoring of services throughout the year (including quality visits by commissioners to the providers)
-
suggestions from the providers.
At the time the project was conducted the annual process of commissioning for selection for quality measures had been starting between September and November each year and ending with the signing of the contract in April. Although the agreement of the local QIs and CQUINs is meant to be a collaborative exercise, it was acknowledged by both commissioners and provider managers that the selection process is usually driven by the former:
The CQUINs were really very much designed by the commissioners and then fairly late on they had a conversation with our contracting team. I think it was really almost towards the very end when they were almost signed and sealed that it became a ‘do you want to comment?’ . . . I think we found out a couple of weeks before the end of the contracting time.
Beechbury PM1
Provider managers certainly felt that they should have the opportunity to work jointly with commissioners to develop indicators. For some of them, their reason for this was previous experience of commissioners not always being aware of relevant issues concerning systems in place:
I think one of the biggest issues is commissioners setting up indicators that they don’t actually understand and they have read somewhere or pulled out somewhere, and actually defining what it is that you’re counting in the first place.
Dogwoodheath BM1
It appeared that a lot of discussion can take place between commissioners and providers about the level of detail and the amount or type of information that commissioners need. This impression was reinforced at meetings where details of prospective indicators were on the agenda:
The CCG finance and performance manager said that they could start by tracking down what they need to reduce, e.g. length of stay, etc., and then have a measurable target . . . There has to be some learning. The provider head of performance said that they first have to come up with a sensible suggestion which they could then discuss with the finance director and the trust board. He said the question is whether the trust can agree to any reduction given how little understanding there is around the issue and how many parties are involved.
Alderton West meeting (field notes)
Given the complicated nature of discussions and the complexity of service activities, it is unsurprising that participants reported that this process can be fairly lengthy and time-consuming before agreement is reached between the parties:
It took us 25 iterations before we got the first spec signed off. Twenty-five drafts.
Dogwoodheath PM1
Some commissioners felt that this can be because the process involves consultation of staff at all stages of the process. It was also noted that GPs can influence both the operationalisation and the adoption of indicators and a few provider managers stated some difficulties in this respect. To avoid such problems, in Elmhampton a community nursing best practice group discussed potential challenges with GPs to help define and/or refine the indicators under consideration:
All the GPs are advocating using the [personalised care planning tool] plan. It’s 45 pages long . . . There are elements of it that are really good and what we’re going back to the CCG and saying is, there are some bits that we absolutely want to use but it’s too short a time frame to get everybody using the same tool . . . we’re all using different paperwork . . . It’s at times like that that I will take that to the senior district nursing group and go, I don’t know, what do I do? How can we manage this? They normally come up with some really good and positive suggestions and so it works.
Elmhampton PM2
The processes of selection appeared often to be based in what had happened in the past or in what data are available. One business manager thought that this could result in the selection of indicators that are not really fit for purpose:
That’s one of the key concepts we’re really trying to push – it’s to start with ‘What is it we want to know?’ . . . Often my experience is we’ve started [with] ‘What data have we got?’ That’s what we use and therefore it doesn’t generate that improvement that perhaps all the effort put into collecting and measuring that data should result in . . .
Beechbury BM2
It was generally agreed that indicators should be meaningful, specific, patient related, achievable and SMART (specific, measurable, appropriate, realistic and time bound). 74 Consistent terminology should be used and data collection processes should be simple and systematic and make use of mechanisms already in place. It was also thought essential that resources are provided for collection of quality data to avoid any detrimental effect on front-line clinical services and that the stability of core services must be ensured with staff overload avoided. Participants noted the importance of, and the challenges involved in, ‘keeping the day-to-day work safe’, although there could be differences of opinion about what this actually entailed:
The head of quality [CCG] said that it had been agreed that the CQUIN would be implemented in two neighbourhood teams [NTs]. He felt that it is too restricted to implement only in specialist teams, as this is too small a beginning to the CQUIN implementation. He is happy for it to be rolled out to two NTs, in line with the requirements of the national CQUIN. The director of nursing [provider] responded that the trust wanted to work with the spirit of the CQUIN, but that it is very late in the year to do so, and front-line teams are experiencing winter pressures on their workload. She said that, given the time frame, she felt that it was reasonable to restrict the CQUIN implementation to specialist teams, as it would be far too onerous to roll out to NTs. The CCG contract manager said that a contract variation has been put forward to change the CQUIN, and a decision is awaited from the management board.
Beechbury meeting (field notes)
Indicator appropriateness
During the discussions between commissioners and providers, one key factor determining which QIs to include appeared to be deciding how feasible or achievable indicators are. Commissioners indicated that, because of the financial element, the negotiation of CQUINs focuses particularly on the issue of indicator achievability, with the caveat that they should not be too easy to achieve, in order to provide value for money. It was felt that a lot of debate and frustration during the application of CQUINs can be avoided if the indicators are clearly stated in the contract and are also measurable:
[Providers] want something that they can deliver basically. So if it’s having something that’s either too difficult to measure or can’t be measured or too woolly . . . we know that we’re not going to get anywhere with that.
Cedarham CM1
However, despite reported attempts to develop feasible and achievable indicators, some participants more closely involved with the practical delivery of care stated that some indicators in use were not fit for purpose. Problems stated included indicator requirements conflicting with those of good nursing practice and adoption of indicators designed for inpatient settings without adjustment for use in the community:
The commissioners decide what we’re going to do and then that’s passed on . . . a couple of times we’ve had CQUINs that have just been so poorly thought out that we’ve been set up to fail.
Alderton West NTL1
Nurses expressed unease when they felt that care delivery was being driven by a QI protocol as opposed to professional judgement. There was concern expressed at a team leaders’ meeting during discussion of an indicator for which data collection processes were not aligned with recommended clinical practice:
One of the nurse team leaders asked about the need to continue doing urinalysis on patients. She said that this is not good practice, but as it is included in a quality indicator, nurses are having to do it more often than clinically indicated.
Alderton West meeting (field notes)
A similar opinion was expressed by a front-line nurse in Beechbury:
Purpose T [a pressure ulcer risk assessment tool] carried out on every patient – although the nurse commented that in her view, clinical judgement should take precedence over whether this is an essential standard to meet.
Beechbury (front-line observation notes)
Some indicators were reported to have caused offence, such as requirements to ask all patients about alcohol consumption or continence.
Another issue arose through national requirements for community providers to achieve nationally mandated CQUINs originally designed for application in acute settings:
What you immediately run into actually, is that they are the set ones nationally. Everybody has got to do them but it doesn’t quite match what community services provide.
R3
Provider organisations stand to lose income in relation to non-achievement of QI targets for PU prevention (an accepted marker for good-quality nursing care in the acute care sector), and new approaches to risk manage responsibility for PUs had been instigated in all the case sites, including the introduction of purpose-designed patient information leaflets about PU prevention.
This indicator (based on best practice) was criticised by community nurses as sometimes conflicting with patient-centred care:
. . . a 15-year-old who’d been in a road accident and had two toes amputated.
Beechbury CNFG4
At the other end of the spectrum, patients in the terminal phase of their illness may have to be disturbed to be repositioned in bed in order to comply with the PU prevention protocol. If PUs did occur in these circumstances, a serious incident investigation would be triggered:
If they’re comfortable, do they [managers] really want us moving them around just to check their bottom . . . when we know that they’ve got 7 days or less to live? Patient centred, you could argue, is whether it’s appropriate to do these things to the patient at the time. So to roll the patient who actually is nice and settled . . .
It’s distressing actually for a lot of them. They really don’t want it. A lot just want to be left.
We spend all this time trying to keep them in a state where they’re not agitated and then agitate them.
And I just think how can they [managers] justify that [serious incident investigation] because the body’s breaking down. The oxygen levels have dropped.
Another factor impacting on the lack of suitability of the PU prevention indicator in community settings was that, unlike in the acute sector, this indicator was not entirely within nurses’ sphere of influence:
I mean, even if you went into a patient every day, I mean it’s only, what?
Maximum of an hour a day. So you’ve got 23 hours of not [being able to oversee them], legs going back down again, cushion going . . .
Yes. You know? It is – more the patient’s responsibility – isn’t it? – to take on our advice that we’ve given and, you know, help us in helping them, whereas in the hospital . . . you’re there more so you can encourage them more. Oh, you know, come on, you know, can you lay on your side for a bit? You know?
Inclusion of all relevant stakeholders
A common opinion among participants was that indicators should incorporate both clinician and patient perspectives. Commissioners reported valuing indicators agreed after discussion and input from the providers. They felt that ownership from the provider was essential for the success of a CQUIN and that community nursing staff will be more committed and willing to implement indicators that they have helped shape. One provider business manager thought that, to promote engagement and/or ownership from the service, it could be useful to move towards standardising questions rather than answers, so that staff would be able to self-select measures appropriate for their practice.
Provider managers agreed that having informed professional input enhances the quality of any measures developed and helps to establish ownership among nursing staff. The data revealed that, in a number of the case sites, initiatives were being put in place to ensure that staff views could contribute to indicator development, and most provider managers said that staff had some input into indicator identification and selection. Nevertheless, community nurses across all five case sites refuted this view, describing the process as ‘a top-down’ approach; the general feeling expressed by the nurses was that indicators were imposed when and if there were signs of possible problems. Many nurses were unsure who was involved in the selection process and were suspicious of QIs, feeling that they could be used punitively with staff:
I think it’s the people that put the numbers in the computers and think, ooh, this looks a bit dodgy there, and we’ll send it down I honestly do.
Yes.
They haven’t got a clue what’s going on.
It’s probably risk assessed, isn’t it?
I think, you know, if you’ve put lots of Datix [serious incident forms; Datix Ltd, London, UK] in for pressure sores, then they’re obviously going to audit that.
In one site, a nurse commented on the language of ‘harm-free’ care and the implication that they were otherwise treating patients in a way that was detrimental to their health:
So it’s meant to be a useful tool to improve care [NST], now it seems to be to find out why we’re getting . . .
Measuring to see how bad we are, yes.
I think that’s why it’s worded wrong, because it’s all about harm. So you feel it’s negative from the start, because they’re trying to find out how much harm you’ve created.
A provider quality analyst from Beechbury who worked closely with front-line staff on quality data reiterated the importance of the vocabulary used when talking about quality, preferring the phrase ‘see how you are doing’ to more punitive and management language about missed targets and performance.
Community nurses said their role was poorly understood by commissioners and many examples showed how their work differs from that of nurses working in hospitals. Differences include the need to factor in time spent travelling to patients’ homes, tabling visits to fit around medication timings, connectivity problems with mobile technology, unrecorded work necessitated by other ‘missing’ services, isolation of patients, lone working and the practicalities of working in people’s homes. These differences underpin nurses’ views that QIs for community nursing could be made more useful and better reflect the quality of care given if the nurses themselves played an active role in their design and analysis, rather than simply collecting the data. Nurses indicated that they would appreciate being involved in the whole process of quality assessment. When asked how quality measures could be made more meaningful for them, nurses in one site responded:
Maybe involving us in, you know designing the indicators, you know . . .
And that you saw some good come out of doing it . . .
And being involved in action planning to improve it when you get the results.
Patients are not involved in identifying or selecting indicators generally. There was only one instance of patient involvement in the development of an indicator in the data, concerning wound care:
We surveyed about 21 patients to ask them what they want from wound healing. What’s the thing that upsets them most about their wounds? And it talked about things like pain and healing rates, so that was a quite useful exercise.
Cedarham PM2
Some participants showed an awareness that perceptions of what makes care ‘good’ may differ between patients and professionals. Nevertheless, there was evidence of intention to tackle the issues of involving patients appropriately in indicator selection processes.
A number of commissioners thought that the future direction of travel for measuring quality will be towards outcomes-based measuring, dependent on patient input:
It might be more on the patient outcomes and I think that’s the direction that we’re going in . . . waiting times are important because you can monitor the access but we are working more and more on patient outcomes. So when we’re redesigning or designing from scratch a service, part of the public engagement would be what outcome would you expect from this service and then we use them as our core qualitative measures.
Dogwoodheath CM1
Summary
The data showed that, despite stated aspirations to involve other stakeholders, particularly front-line nurses and service users, current processes of selection largely involve a ‘top-down’ process involving commissioners and senior provider managers. The fact that the process is already very time-consuming must mitigate wider stakeholder involvement without radical restructuring and reordering of QI selection.
Nevertheless, the disadvantage of excluding community nurses from the selection process appeared to have sometimes given rise to measures which could clash with provision of patient-centred care. This situation inevitably placed nurses in an invidious position, as they were duty bound to apply the indicators while simultaneously bearing a professional obligation to deliver care in line with best clinical practice.
Despite participants’ stated concerns to select feasible indicators, the decision to extend quality measures suitable for acute settings into the community without appropriate modification appeared to render some quality measures as problematic from the nurses’ viewpoint. It was apparent that, where nationally mandated indicators are concerned, this matter was out of commissioners’ hands.
The combination of all these factors implied that nurses were being placed in unnecessarily stressful situations with respect to care quality measurement. This appeared to exacerbate further the current difficulties experienced with the delivery of community nursing services, as detailed in Chapter 4.
Chapter 6 Findings 3: application
Application refers to the processes around implementation of QIs in practice; that is, how selected indicators for community nursing were introduced to the nurses, whether or not any further training was offered, how data were collected and quality assured and any resulting feedback for staff.
Identifiers for quoted excerpts from interviews and focus groups in this chapter are shown in Table 14. Excerpts from field notes recorded during observation of meetings and of front-line staff at work are labelled accordingly.
| Participant | Identifier |
|---|---|
| Carer | C |
| Commissioner | CM |
| Community nurse (focus group) | CNFG |
| Community nursing team leader (provider) | NTL |
| Focus group carer (non-case study site) | FGC |
| Focus group patient (non-case study site) | FGP |
| NHSE: member of central national nursing team | N |
| NHSE: regional officer | R |
| Patient | P |
| Provider business/performance manager | BM |
| Provider manager: director/manager of nursing services or of quality | PM |
In each case, an individual participant is identified by a unique number preceded by the name of the case site (where applicable) (e.g. Beechbury CNFG1; FGP2).
Themes identified for ‘application’ included QI monitoring, communication about indicators within provider organisations, data collection processes and data quality.
Quality indicator monitoring
Quality measurement in a service is a component of quality monitoring. Routine monitoring of QIs happened in all of the case sites by means of ‘dashboards’ and scorecards, usually reviewed at regular quality meetings, which were either limited to individual organisations or attended by representatives of both the CCGs and the providers. All of the quality review meetings observed included these items on the agenda:
They discussed the following indicators from the dashboard: a. Mandatory training: the CCG quality manager observed that a number of indicators relating to mandatory training had not met the required contractual threshold. The provider head of performance explained the process that the trust have in place in order to monitor non-compliance and improve staff completing the relevant training requirements.
Alderton West meeting (field notes)
One participant described these joint meetings as an important part of monitoring because they allowed commissioners to be both reactive and proactive when it comes to quality issues:
[The meeting membership] can set its own agenda and it can hold the trust to account . . . it can react to quality issues that it sees in community services.
Cedarham CM2
In relation to the monitoring of indicators, it appeared that commissioners relied mainly on the written evidence presented to them by the providers. This was often categorised according to ‘risk ratings’ – green, amber and red – reported through the performance dashboards:
The chair asked what the risk rating for quality in relation to staff numbers was. The trust said it is red for recruitment and amber for quality.
Cedarham meeting (field notes)
However, one commissioner implied that an element of trust was essential when considering the credibility of reports. A number of commissioners relied only on provider self-reported data, but others supplemented the data from providers with visits to various practice settings, both announced and unannounced. One commissioner stressed that it was important that such visits were led by members of staff with a detailed understanding of the service under inspection.
Another commissioner explained that the purpose of the scheduled visits (which included shadowing of district nurses at work) was not so much a formal inspection of the provider’s performance as an effort to understand the challenges the service might be facing. A commissioner working with a rurally based provider emphasised the value of visits by commissioners in understanding the work district nurses are doing. The following quotation indicates that the quality of a lot of care that district nurses are offering is not easy to capture:
I went to this one very isolated farm in the middle of nowhere – this little old lady, 85, on her own; and it was the only contact she had and actually, the district nurses do have to do a bit of the social thing, and just checking they’re all right. So it’s all through the conversation and you can see there are key points coming out . . . actually seeing it in reality . . . it really brought it down to that patient level.
Elmhampton CM2
In some sites, instead of monitoring on the basis of referrals and activity, commissioners and providers were moving into monitoring community nursing services in terms of caseload and patient pathways through integrated teams. This development was not without its problems in terms of measuring quality, mainly due to the reported initial uncertainty and lack of knowledge about the numbers of patients being supported by the teams, and about the length of time a patient may spend on the team caseload. Gaining this information was seen as a priority for the quality of the service to be monitored effectively.
Some commissioners complained that the guidance for the national CQUINs is not always clear. For example, commissioners were confused about how to apply the CQUIN on reducing avoidable emergency admissions (2015/16 contracting year):
It’s a new CQUIN for this year on reducing the proportion of avoidable emergency admissions. It looks a bit too complicated and they’ve not put any metrics in and they’ve not put any targets.
Elmhampton CM1
Some indicators are reported to be more difficult to apply than others and require a developmental approach. In these cases participants agreed that 2 or 3 years might be needed for criteria to be met, with commissioners and providers agreeing the stages and milestones for each year.
In addition to the use of ‘dashboards’ and scorecards, provider managers stated a range of different strategies in use in their organisations to monitor the quality of the service, which were used on an ongoing basis. These included assigning practice teachers to inspect a sample of community nurses’ case notes on a monthly basis, to ensure that care delivered was appropriate for each patient:
We have community practice teachers who go into every single [community nursing] team once a month. They select five case files and they go through those, using a standard template to check things off, then they submit that data. Everybody is aware of that, the teams are aware, the team manager’s aware, everybody knows [when] they have to be done by . . . that’s very much embedded.
Alderton West PM4
Other initiatives involved undertaking regular audits in different areas (e.g. wound care and hand hygiene), and appointing leaders and champions for particular indicators to liaise with and encourage front-line staff to meet required criteria. However, in some case sites a lack of time was reported as a significant barrier to monitoring quality:
I think the difficulties for us are around manpower to do that in time . . . my ideal would be that somebody works with every nurse at least once a month to take a view of their practice, conduct with patients, what they’re writing down. We don’t have the staff to do that, it just goes by the by.
Cedarham PM2
It was noted that improving quality requires close collaboration between commissioners and providers, and many participants stated the importance of maintaining good relationships in this respect. This perspective was noted at an internal CCG meeting held prior to a joint quality review meeting with the provider:
Points were raised from the minutes of the previous meeting, some discussion about how to take things forward with respect to a CQUIN that had not been achieved. The focus appeared to be on gaining clarity about issues and challenging the provider where necessary, while still maintaining cordial relations.
Dogwoodheath meeting (field notes)
Communication about indicators within the provider organisation
The data revealed that most information about indicators is relayed to front-line staff and reported back through existing management structures and team meetings, as well as through internal bulletins or newsletters. Some managers make a point of visiting community bases regularly, whereas others rely on e-mails and other electronic communication:
The head of planning and performance explained that a link to the Friends and Family Test is circulated on e-mail now and is advertised in the staff newsletter.
Elmhampton meeting (field notes)
It was noted that effective face-to-face communication can be hampered by geography or the size of community teams:
So getting the message to them, when geographically they’re spread over Cedarham, that’s always really difficult. They’re always out and about, so you’re trying to meet up and get the message to them on a regular basis.
Cedarham PM1
A theme which came through strongly across the case sites from community nurses was the lack of communication with them prior to the implementation of a new QI. Nurses could be told of an indicator only days before it was due to be used, potentially creating problems from the outset. Several examples were given, including the following from a focus group which included some senior nursing staff:
You may even want to ask my colleagues now, did they know there was a [named] CQUIN coming in the next couple of months?
No.
Right, so . . . our managers know about it, but they haven’t told anyone else. And we’re looking at the training for it . . . and so on. But all that’s happening behind closed doors.
. . So it’s something else they’ll be doing they know nothing about . . .
How good would that be just to let us know so we can start preparing . . . our own learning from learning and development, a course you’ve got to attend.
Although there was acknowledgement that community nurses generally provide very good care and work extremely hard, a common theme found in the managers’ data was that they often do not fully appreciate the importance of collecting indicator data, or do not understand why they are being asked to do so. It was noted that it was often challenging to engage staff in this respect, particularly as most nurses, if short of time, always prioritise direct patient care above QI data collection. One manager felt that there was a vicious circle in operation, in that a lack of attention to data collection inevitably led to poor-quality data; she felt that this only reinforced nurses’ views that data are not worth collecting in the first place. There were also problems acknowledged with the clarity of communication between different levels in the organisation, so that by the time relevant information reached front-line staff, instructions regarding data collection could be quite confusing and lack sufficient detail.
Managers were generally aware of the need to help staff understand the importance of collecting the required quality data, although some interviewees also acknowledged that the organisations have more to do to in this regard. It was also recognised that staff are more likely to embrace an indicator if they can see how it brings clear benefits either to patients or themselves. A national participant noted that a problem with achieving CQUINs is that often the teams that have worked for them do not know what resulting benefits may have accrued, because the funding gained goes to the organisation rather than directly to the teams that implemented them:
They do it to get the money and then . . . either it doesn’t make that much difference or they get the money, but that particular team doesn’t get the money, it goes into the organisation.
N1
In one organisation, a business manager visited the front-line nursing teams to explain the CQUINs in detail and to highlight their importance and how, if good-quality data were collected, the service could be improved:
I gave a presentation to a district nursing team event recently . . . I ran them through all the CQUINs and say this is why we do the CQUINs, this is what the aim of the CQUINs was . . . the feedback was that it was helpful because they could actually see what it was all about . . . I showed them the activity graphs and how activity had increased and I said ‘because you collect your activity data, because you actually log it on RiO [an electronic care record system for health and social care organisations] we are able to show them that it’s gone up by 7.2%, we can show them how run off your feet you are’.
Elmhampton BM1
He reported that the quality and consistency of data collected improved significantly after this visit. However, front-line staff are not always informed about how the data they collect are used. Community nurses commonly reported that they received only limited feedback on their QI outcomes and some of the provider managers interviewed noted this to be a failing of the system and an issue that needed to be addressed:
That’s really important, about giving feedback back into the nurses . . . it’s all around morale and how you look after your staff.
Cedarham PM2
In one case site, however, regular feedback from management was identified:
They sort of bring everything together and collate the figures. And in most cases will get back to us . . . And they do a graph for each [area] for each month. And our managers will normally come back. If we are doing well, we’ve been commended. If we are not, she feels disappointed.
Cedarham CNFG2
In a different focus group from this same case site, a senior nurse spoke of their collaborative approach to feedback and analysis:
What we tend to do with our team when we achieve something better, we might buy just a cake and celebrate . . . And we look at it and say what went wrong and again like the patients’ survey. When somebody brings, I said . . . Please open and let me know what your patients say. So that way we look at what the key themes within the area, whatever they say, oh, nurses are normally late. They don’t call me or whatever. Then we work around that . . . Because when we fall, we fall together. When we rise, we rise together.
Cedarham CNFG9
In a different site, during an internal provider meeting to discuss CQUIN achievement, the senior manager chairing the meeting made a point of asking that front-line staff be congratulated on their work and asked for input about how to use the money accruing:
The chair reiterated that the community staff have done ‘a fantastic job’ and asked that they should be told this. Money that has been earned through meeting the CQUIN targets is now available, and she asked that staff should be consulted about possible ways of spending it.
Dogwoodheath Meeting (field notes)
Data collection processes
Some participants stated that combining a number of apparently simple processes can result in a very complex system and that frequent ongoing monitoring is required to get an accurate picture of quality in the service, which is not always possible due to capacity issues. Data collection was generally acknowledged to be time-consuming, particularly where duplication of data entry is unavoidable. All data need to be recorded electronically, but some are still collected initially by hand on paper. Although there was a focus in most sites of reducing this activity as soon as possible, it was also acknowledged that it would probably not be possible to remove paper notes completely:
We have to have notes in the patient’s home . . . it’s not just us that are involved with those patients; we’ve got adult social care; we’ve got GPs. We’ve got a lot of family that would like to be more involved in the care . . . so our home notes are integral to good, personalised care. But at the same time we need to put things [on computer].
Elmhampton PM4
The increasing emphasis on documenting information for quality purposes was perceived as having been accompanied by a decrease in the time available to spend with patients, so that nurses felt that their workload was being driven by indicator reporting requirements:
It’s totally taken over. Patients don’t come anywhere near priority now, they’re right down at the bottom. It’s all these targets, audits, data this that and the other.
But the hardware isn’t up to speed yet, that’s the problem.
And I think over the years, face to face contact with patients has gone down, because you’re spending more of the afternoons on a computer.
From a patient point of view, although recognising the time taken to complete notes, the nursing records held in the home were a valuable resource and found to facilitate involvement in their own care, enabling them to monitor progress and also accurately to inform other visiting professionals of current nurse input:
Yes. I mean, I think the nurses have a heck of a lot of paperwork to do. I mean, B is writing for ages when she’s here but every single thing is focused on; everything is jotted down. The notes are left here so she’s not writing down anything that we can’t know about. So we know what the blood pressure was that day. We know the blood test results, and it’s wonderful . . . If the doctor rang and wanted to know what his blood pressure was, I’d know instantly because it’s there in the notes.
Alderton West C1
One unintended consequence of increasing electronic data recording, which has the potential to reduce nurse time spent documenting quality information, is that patients could be potentially excluded from the benefits of having access to paper care records in the home. However, it appeared that the amount of documentation required can impact heavily on nurse workload, in particular the need for data to be recorded in a variety of formats:
It’s all in the patient’s notes, documentation I think, some people have the [electronic] notebooks . . . And online as well, put it on the system.
Yes . . . We still have paper notes and [IT package 1] . . . and some practices have [IT package 2] as well so we have to fax or e-mail consultations for them to get on to their systems. So it’s all, it’s quite difficult at times because some of them are triple entry.
There is a national drive to encourage patients to take some responsibility for their own care and prevention of further health problems. This has been interpreted in at least one site as requiring a signature from the patient to say they understand their responsibilities to avoid PUs occurring. However, in the context of financial penalties for not achieving quality outcomes it could suggest an element of defensive record keeping as such a record could constitute evidence that the nurses had done all in their power to prevent the PU and would be helpful, perhaps, in reporting back to the commissioners. Additionally, for safeguarding reasons, the nurses recorded in the notes the fact that all options regarding prevention and equipment had been discussed with the patient or carer. During a shadowing session, a staff nurse at a handover meeting reported a problem with a patient who had been discharged from hospital that day, provoking an immediate response from the team leader:
Another nurse brought up a newly discharged patient from hospital who has come onto caseload with a black heel (PU) – ‘to be Datixed immediately’. PUs are a quality standard – ‘need to demonstrate it did not start in our service’, ‘to be done ASAP’.
Cedarham (front-line observation notes)
Datix (Datix Ltd, London, UK) is the electronic serious incident reporting proforma used in provider organisations. If a patient on the caseload was identified as having a grade 3 or 4 PU (classed as moderate/severe), a serious incident investigation would be triggered. These investigations include interviews with the staff involved and scrutiny of care records leading up to the date the PU was identified. Such investigations are badged as learning opportunities for staff but can be construed as punitive and take a long time to complete:
I think there’s a fear as well, isn’t there, that the finger’s going to be pointed. People do feel scapegoated. I did. I felt terrible. I wasn’t even here when the woman developed it, I was off.
Beechbury CNFG3
During a shadowing session in Elmhampton, one clinical leader said that she thought she spent about 30% of her time on investigations prompted by the Datix system.
Collecting QI data appeared both to have an impact on, and be affected by, difficulties for the workforce arising from issues associated with the complexity of the caseload, adapting to new IT systems, high levels of sickness and staff shortages, as outlined in Chapter 4. Many of the participants mentioned the degree of support community nurses have required to enter quality data onto the computer systems:
A lot of this stuff depends on the inputters. And many of the inputters are the clinicians and the people at the front line. So they have to have access to good IT systems to input the data as well. And sometimes, you know, the systems are slow and clunky.
Alderton West PM2
Recording ‘outcomes of care’ is a key community nursing performance QI. Nurses are required to record the outcomes of their visits on a daily basis. As outlined previously, electronic care records often cannot be updated when nurses are out on visits due to connectivity problems, so ‘outcoming’ (the updating of visit outcomes in order to enable ongoing planning for allocation of workload) must therefore be undertaken when nurses access the live records back at base. Several nurses spoke of working out of hours to meet the requirement:
You stay over your time. On your day off, you come in. Because you don’t want your name to be called as someone who has not done their outcome.
Cedarham CNFG4
It was also noted to be difficult to collect data from some patients on the community caseload, as many of them are frail or lack capacity. In some instances there may also be language problems adding to the challenges. Patient satisfaction surveys are either posted or taken into patients’ homes and left there for completion. Nursing team leaders did not think it ethical for nurses to sit with patients while they complete a survey.
A suggestion was made that it might be better if such forms were administered by an independent body. This would have an additional advantage of circumventing another factor which may contribute to the apparently low completion rates – that the nurses do not like to give the forms out – expressed by one nurse in Elmhampton as feeling ‘like touting for compliments’. At one nurse team leader meeting, it was clear that some nurses did not think that they should be responsible for collecting these data from patients at all:
Manager 2 said that an envelope should be given out with the forms so that staff can collect them. Team leader 7 said that it should not be the nurses’ responsibility to collect responses.
Alderton West meeting (field notes)
Data quality
The quality of data collected by the front-line teams was sometimes considered to be poor or incomplete and it was reported that in some cases clinicians complete instruments incorrectly or do not record activity (e.g. providing a patient with an educational trigger tool, or emotional support and reassurance provided). This obviously has an effect on the robustness of information available about relevant quality issues in the organisation. A data analyst manager in Dogwoodheath noted that the community nursing service was ‘probably not one of our top performers in terms of data quality’. A nurse in the same site suggested that one of the reasons for the hasty or incorrect completion of indicator data was the result of staffing shortages causing staff to feel under pressure:
We are so short-staffed . . . time’s being taken away from patients, filling these audits and quality measures in, we’re rushing them, so they’re probably not being filled in correctly. And then all our results probably aren’t accurate, which is then making us look worse than we are.
Dogwoodheath CNFG5
Another reason given for incomplete data being recorded during front-line observations was that computer systems required a time allocation for each task entered; a lengthy process. Nurses could either estimate the time spent or omit recording some care tasks they had carried out on the computer. This suggests that the full extent of nursing care given is not routinely electronically recorded. Managers, therefore, may not be aware of all the components of care given, so this is not taken into account with regard to quality assessment or measurement.
The possibility of erroneous data collection was compounded by the ambiguous wording of some indicators. An example that caused confusion for some nurses was the categorisation of PUs as ‘new’ or ‘old’ with a timing specified ‘within the last 72 hours’:
So are you supposed to record if someone has had a PU that is older than 72 hours or is it anything that just occurred in 72 hours or do you put that as an old one or is old technically if it’s happened in a different trust and it’s always a new one if it’s happened in our trust?
Beechbury CNFG1
Targeted efforts to improve data quality include offering relevant training. However, it appeared that staff do not always have time to attend training offered prior to implementing a new QI, due to competing workload pressures. It can therefore be impossible to release staff from front-line care for this purpose:
You plan for everyone to go but then circumstances arrive in each and every team that means you have to keep staff at base, doing the work, rather than sending them on training.
Dogwoodheath CNFG4
In a number of provider organisations, this situation had led to contractual breaches. In one case, the provider failed to meet a CQUIN target for training due to staff shortages and sickness and was subsequently financially penalised.
External factors, such as the patient environment, can have an impact on the successful implementation and achievement of QIs in the community. It was noted that, even where staff can attend relevant training, it usually occurs in the context of a training environment rather than in the patient’s home. The different conditions operating in these environments can make it difficult to apply apparently straightforward indicators during an actual episode of care:
You will get training on them [indicators] but it’s very different in a training environment, they will show you, well you do it like this, this and this, but when you actually get into the patient’s home . . . it’s never straightforward, and it’s really hard to determine actually, what I am writing where and what I am supposed to be writing, and how to classify and define things they are asking for.
Beechbury CNFG1
In all the sites, data were collected on a set day of the month for the audit of nationally mandated indicators, including those recording CAUTIs, falls and PUs. Observations conducted in Elmhampton on ‘NST day’ bore out evidence from focus group data across the sites suggesting this was a paper exercise where visits were conducted as usual and then, once back at the office, the paperwork was completed and passed to the administrative team to upload onto the national database. Only patients actually seen on the day of the audit were included in data collection, so that patients with ulcers or urinary tract infections seen on other days of the week were excluded, regardless of their clinical condition:
A patient had called to say his leg catheter bag had bloody urine in it so we visited to assess – the nurse wanted to prescribe antibiotics as he had previously nearly died with sepsis. GP said to wait, as no sign and symptoms of systemic infection. Therefore the safety thermometer returns did not show any patients with catheters with infection either. The nurse said virtually every person with a catheter would have a UTI [urinary tract infection].
Elmhampton (front-line observation notes)
If the audit was conducted on the same day of the month each time, owing to length of stay on the caseload, the same people might be included a number of times.
In relation to the FFT, another national mandatory QI, staff reported problems in obtaining feedback from patients. In the acute sector, once care is completed, patients are asked to complete the survey when they are discharged. The low level of discharges from the community nurse caseload where a patient is well enough to complete a survey means that, in order to meet a desired response rate, nursing staff might have to ask the same person more than once:
Yes, but we have to get a certain number done each month. So say like 30 per team. So we’ve actually exhausted all of the patients now because we have 113 patients in my team and we’ve, you know, questioned them, questioned them, questioned them with the same survey.
Cedarham CNFG4
During shadowing sessions in one case site, it became apparent that collecting data for this indicator was not a priority for the nurses:
FFT – done on paper questionnaire [in patients’ notes], meant to be done regularly but done ‘when remembered’.
Elmhampton (front-line observation notes)
Various methods were observed to be in use to ensure response rates. Front-line staff across the sites reported that their managers had tried introducing incentives or prizes to teams to increase distribution rates. Another strategy noted was to include the relevant forms in the patient records to be used at discharge. However, overall, an ad hoc approach seemed to be used, where QI feedback to managers filtered down to staff and a ‘drive’ for improved completion rates would then ensue.
Summary
In all the case sites it was clear that significant resources are invested in collecting and analysing data for quality purposes and monitoring providers’ performance against quality and KPIs. However, it was also clear that the current system can produce only a partial, and sometimes inaccurate, picture of how well the community nursing service is operating in terms of delivering high-quality care. Although participants reported occasional initiatives to assess quality in the service through methods complementing the use of the ubiquitous scorecards and dashboards, both CCGs and provider organisations lacked resources to undertake regular, comprehensive monitoring by other means.
Organisational systems and work pressures appeared to frequently present obstacles to clear communication with community nurses about the use of QIs, both prior to and after their application. Nevertheless, there were some examples of constructive action that could be taken to improve the situation. An irony of the current system was that, where contractual conditions for staff training were breached due to work pressures, the resulting financial penalties resulted in the organisation incurring further curtailing of resources, potentially exacerbating the situation.
The time required for quality data collection was another area which appeared sometimes to cause conflict between nurses’ responsibilities to the organisation and to their patients, in which case nurses seemed invariably and understandably to prioritise the latter. It was clear that the duplication of data, particularly through the use of both paper and electronic systems of record keeping, was an undesirable use of the nurses’ time, when considered from an organisational perspective. Nevertheless, it was also clear that maintaining paper notes to be kept in patients’ homes is an essential component of good clinical care and was valued by patients and carers.
Data from all the case sites portrayed a picture of a system in which significant effort and resources are spent to monitor service quality with results that, at best, arguably lack effectiveness and, at worst, exacerbate the pressures under which community nurses currently operate.
Chapter 7 Findings 4: usefulness
The main rationale for measuring quality in community nursing through the use of QIs is to improve the care provided to patients and carers. 32 The third main objective of the study was to discover how useful study participants perceived the QIs selected and applied within their organisations to be in this respect.
Identifiers for quoted excerpts from interviews and focus groups in this chapter are shown in Table 15. Excerpts from field notes recorded during observation of meetings and of front-line staff at work are labelled accordingly.
| Participant | Identifier |
|---|---|
| Carer | C |
| Commissioner | CM |
| Community nurse (focus group) | CNFG |
| Community nursing team leader (provider) | NTL |
| Focus group carer (non-case study site) | FGC |
| Focus group patient (non-case study site) | FGP |
| NHSE: member of central national nursing team | N |
| NHSE: regional officer | R |
| Patient | P |
| Provider business/performance manager | BM |
| Provider manager: director/manager of nursing services or of quality | PM |
In each case, an individual participant is identified by a unique number preceded by the name of the case site (where applicable) (e.g. Beechbury CNFG1; FGP2).
Themes identified for ‘usefulness’ included contractual issues and benchmarking; impact of collecting data about quality; limitations of current indicators; and how to measure quality in community nursing.
Contractual issues and benchmarking
A regional representative of NHSE recounted how the introduction of CQUINs for community services had not been well received:
When the first sort of guidance came out, community services were quite angry because it was seen as almost a penalty, that you were pulling money back and then you were reissuing it if they improved quality. So you know it wasn’t received terribly well.
R3
However, commissioners reported seeing the value of CQUINs as providing a focus on specific service improvements. Nevertheless, there was a perception that the application of CQUINs needs to change. Although the premise behind a CQUIN is that targets can be set and measured along a trajectory, it was acknowledged that it is not often that ‘you can ever distil anything down to be that simple’. It was reported that many CQUINs have been adapted to be made more qualitative and with broader scope than originally intended.
There were differing views among commissioners about how a provider’s perception of a CQUIN’s achievability affected their attitude towards it. One commissioner said that CQUINs can act as an incentive if the provider perceives them as achievable; in contrast, another commissioner said that if the CQUINs were too easy to achieve, the provider would tend to direct the CQUIN money to other services in the organisation.
Some commissioners tried to make sure that CQUINs achieved intended outcomes, even after they had been embedded in an organisation. In some cases, providers were asked to conduct a full analysis of associated outcome benefits for patients and the service. Providers complained about the fact that past CQUINs are usually included in the contract without extra funding. This results in the service having to meet an increasing number of targets while being unable to refuse to take on new patients, no matter how the community nursing caseload grows or how complex it becomes. This situation is compounded by the ongoing block nature of the community nursing contract, which is based on volume rather than the nature of the service being provided.
One commissioner felt that it was not at all clear if or how achievement of the national CQUINs was monitored by NHSE or their regional area teams, and cited instances of provider organisations interpreting national CQUINs idiosyncratically or adapting them to suit their own circumstances. In contrast to acute care services, contracts relating to community care services at the time of data collection did not contain national targets which could result in financial sanctions if not met by providers. However, similar to acute care services, in community care services commissioners could withhold payment to providers if certain conditions in the contract, usually related to timely submission of data, were not met. One commissioner doubted the effectiveness of financial penalties in improving quality of care:
You do need to be able to hold the trust to account, but penalties are not necessarily the best way to do that. But, nevertheless, they are formally in the contract and are potentially a contract lever.
Cedarham CM2
In one case site, the non-achievement of CQUINs led to negotiation concerning the resulting financial implications:
Three CQUINs have not been achieved, including attendance at information sharing meetings, as there was no evidence to support this. The provider business manager stated that attendance had happened, but had unfortunately not been minuted. The GP [chair] replied that the CCG would ‘take it on trust’ . . . the provider business manager also raised the issue of dementia training for staff, saying that the target had been set with all good intentions of supporting it. Due to recruitment patterns, targets in the early part of the year had not been met, but she assured the meeting that all staff had been booked on to training for the second half of year. So the provider appeared to have done well in this respect, but according to the letter of the contract, did not achieve the set target. GP suggested over-riding the initial decision to consider the provider in breach of contract in this respect, but the CCG director of quality governance said that she was unwilling to ignore her staff’s recommendation in such an arbitrary fashion. She agreed to review the situation.
Dogwoodheath meeting (field notes)
A number of participants bemoaned the lack of formal benchmarking systems for QIs. It was notable that many commissioners interviewed were not aware of the Pick List (the national database of CQUIN indicators that commissioners can use), or of the QIs database available at NICE. One commissioner specifically stated that it would be helpful to have such a website, so that commissioners could have access to it and adapt relevant CQUINs to their local circumstances:
Wouldn’t it be great if there was a database online, you could go in, you could say I want a CQUIN around pressure ulcers? . . . It’s not about copying them, because I realise that locally there will be different health economies and different situations.
Alderton West CM1
Provider managers also wanted to be able to benchmark their quality and performance against other providers of community nursing services. In order to undertake such comparisons, two case sites belonged to the in-house NHS Benchmarking Network (www.nhsbenchmarking.nhs.uk/). For all the sites, however, informal benchmarking was the norm, with individual managers contacting nursing organisations, for example the Queen’s Nursing Institute (QNI) and the Directors of Nursing networks, or engaging in ad hoc conversations with counterparts in other provider organisations. Although much of the information gleaned in this way was acknowledged to be anecdotal, the advantages cited of this interorganisational contact included the opportunity to learn from other providers:
We’ve borrowed several of the models and the ideas from [provider] that they’ve tried and that have worked. And we’ve talked to them about what the pitfalls were, et cetera, so from the perspective of sharing good practice that has been quite useful.
Elmhampton BM1
Impact of collecting data about quality
Some evidence of direct positive impact on care resulting from the application of QIs was apparent across the case sites. Areas of care reported to have been positively affected by the implementation of QIs included PU prevention, discharge and dementia screening. Positive results of indicator implementation were usually couched by managers in terms of QIs having helped to raise staff awareness of, and improve attitudes towards, relevant issues and changes in practice.
Some participants said that having indicators in place and monitoring them regularly were useful in terms of increasing transparency of services, provider accountability and confidence among both commissioners and provider staff in the quality of service being delivered. One commissioner felt that frequent reporting requirements (usually monthly) provided a mechanism for driving the quality agenda, and had proved to do so. A business manager noted the importance of QIs as being an inherent part of organisational activity, as he felt that without them, it would not be possible to have a clear picture of the service being delivered.
Despite the apparent lack of feedback about service quality in most of the case sites, some nurses were able to identify examples in which they had benefited directly from QIs, particularly in relation to the technology and documentation allied with integration. Teams spoke of being able to access information about their patients which they would previously have only known by word of mouth, a tool that can be seen to be particularly useful for night staff:
It’s [IT package 1] opened up now with [service X] and, you know, speech and language we can see, and a few other bits . . .
Yes, that’s just come in. And also for alerts, you know, for patients that obviously are, could be potentially abusive, or they’ve got a rabid dog, or you know, you’ve got a little alert.
Other benefits reported by the nurses from achievement of QIs were increased funding for district nurse training, new equipment for community nursing teams and extra capacity to assist with administration involved with Datix investigations.
The only time that we’ve really known was the, when the DN [district nurse] students last year got funded through CQUIN money.
Didn’t we get them [independent vascular services] nurses from some kind of target?
Dementia target, yes . . .
We had some equipment bought for our service.
We did yes. And wasn’t the mobile working supposed to have come from that, extra money somewhere . . .
We’re supposed to be getting some of them Doppler machines as well aren’t we?
A nurse in another case site was able to identify a successful outcome of Datixing:
We ended up getting another full-time member of staff because we actually put a Datix in to do with staffing. And our community matron phoned up and said ‘what’s this about staffing? I didn’t know you were short’ . . . You know, because nothing was being written down . . . We started putting in all our extra hours. And then we, luckily, managed to get our staff.
Elmhampton CNFG6
However, QIs were not always associated with obvious benefit and could sometimes cause unintended and undesirable consequences:
We suddenly then had to start visiting patients that were at risk of developing pressure ulcers far more frequently than we ever had done and it actually incurred another 1400 visits per year for the community nursing team, without any additional capacity to do that . . . other visits had to give way, so things that weren’t life threatening perhaps, like a continence reassessment . . . the work to achieve the CQUIN visit would take priority over that sort of continence care.
Dogwoodheath PM1
Reservations noted above about the introduction of new IT systems notwithstanding, it was thought that this had helped to demonstrate the pressures affecting services and had also enabled some community nursing teams to compare their own performance with those of others in the same organisation.
Perhaps owing to the reservations about validity and reliability of QI data and associated workload pressures, front-line staff were guarded in their responses to the usefulness of QIs being used in practice. Patients, on the other hand, were largely positive about the idea of nurses reporting back to managers on quality and the goals of national and local QIs currently in use, but were not always in agreement that they should be used as measures of community nursing service quality.
Nevertheless, nurses, patients and carers all spoke (albeit with some reservations) about benefits arising from QI application with respect to some clinical conditions, namely CAUTIs, PUs and falls. Several patient participants had indirect experience of people who had become acutely ill with a urinary tract infection and were aware of how people can become confused and their health can deteriorate, so considered it an important indicator:
Oh I think it’s a good thing because a kidney infection is a severe complaint. I’ve had them in the past. I have and I tell you something they are no joke.
Cedarham P2
However, some reservations were raised with regard to whether or not these could be prevented by good nursing care. One patient, who was a wheelchair user, commented:
I am not sure that’s nursing care or not to be honest with you. I mean for spinal patients it’s probably not, because a lot of them are in manual chairs which propel and their hands are touching a wheel and then you touch this and then you are bringing your own infection to yourself.
Elmhampton P1
Although agreeing that CAUTIs are an important negative outcome for people with urinary catheters, one carer focused on nursing activities, doubting whether or not the indicator in use provided a sufficient link with important nursing processes, that is, correct and timely catheter care and nursing assessment and monitoring to prevent infection:
I am not sure that highlights the quality of the care of the catheter as it does not indicate the bags have been changed regularly, it doesn’t indicate a record being kept of when the catheter was inserted and whether it was changed every 6 weeks or 12 weeks.
Beechbury C1
There was consensus among patients that preventing PUs is important for their comfort and safety:
Oh obviously yes, it is important for the nurses to know, of course it is, without a doubt.
Alderton West P1
However, some participants called into question the validity of the measure in relation to district nursing quality, due to difficulties in distinguishing some pressure lesions from moisture lesions and the lack of 24-hour nursing supervision of patients:
You can’t really blame the nurse for that, I wouldn’t have thought. They can’t be there 24/7, can they? And, as you say, if the patient is not feeling like moving, this can happen . . . But it’s – I suppose if somebody lives on their own and they’re not getting any help from somebody, other than the nurse coming in, I suppose pressure sores can develop. But, you know, I listen very carefully to the information I’m given and [husband] is asked to move every hour without fail and I try to encourage him to do that.
Alderton West C1
At an operational meeting for front-line nurses in Cedarham, a graphic illustration of this problem was discussed during a review of patients with PUs on the caseload:
The next incident referred to a patient who was chair bound but somehow went to an airport and sat there for hours, after which he developed an ulcer. The nurses felt that the patient needs to be co-operative – he has been given all the relevant information but the problem is how to change his personality and attitude. There is no particular learning from this case, but just to highlight the fact that nurses cannot do a lot if the patient is not co-operative.
Cedarham meeting (field notes)
There remains some debate around correct identification of PUs, with some wounds being attributed to the effects of moisture and, therefore, exempt from being counted as a PU.
Despite misgivings about interpretation of wording, the focus group evidence from nurses suggested recognition that collecting quality data, with respect to falls, can lead on to a full falls assessment for the patient. This was considered to be important, as falls can be a sign of deteriorating health and nurses would not necessarily routinely ask patients if they had fallen in the absence of the indicator. Patients agreed that an indicator relating to falls is important and that nurses would not otherwise be aware if they did not ask the patient:
She slipped out of the chair. They think she slipped out of the chair, we don’t know whether she tried to stand up or what she did but I think she just slipped out of her chair because her blood sugars weren’t very good yesterday. We got her back into the chair but I don’t think the district nurses would be aware that she slipped out of the chair and I haven’t told them . . .
Beechbury C1
To patients, the important part of the falls QI is what is done with the information:
Yes I think it is. It hasn’t happened to me but yes I think that people who are elderly, stumbling, falling – yes it should be noted, recorded and perhaps passed onto the doctor, information.
Elmhampton P1
And I think they should be making a phone call to check. It’s not going to take a lot. I know phone calls do, but you know, it’s caring isn’t it? And it’s ideal for, you think, oh that was nice of them . . . Well it’s following it up, isn’t it? It’s following up. And they, it needs to be followed up.
FGC1
Limitations of current indicators
A common criticism of indicators in use was that they focus on counting activity, rather than recording quality processes and, as such, do not provide an accurate reflection of the quality of community nursing on their own:
What we don’t have is an opportunity to actually record [information] . . . you might be going in to do medication but, actually, a lot of your time might be spent trying to talk the [alcoholic] patient round into having their medication and maybe not having a drink today, and you can’t record that.
Alderton West NTL2
A lot of the indicators in use focused on measuring quality by counting things that could be counted. This is unsurprising, as some participants said that process measures (e.g. number of referrals or number of visits) are easier to measure than measuring quality of care. One provider manager used the example of community nurses being required to have regular meetings with GPs; however, data were only collected about the number of meetings attended, rather than on any outcomes for patients arising from them.
The danger of the ‘counting’ approach was articulated by a national lead who was aware of criticism that some CQUINs seemed to be a box-ticking exercise without any concrete benefits resulting from them:
Some people I go up to talk about, oh, it’s great because it gave them money to do X, Y, or Z, and other teams are quite cynical, that they’ll do all this work and then they don’t see any benefit from it, so I think it’s mixed.
N1
There was a perception that patient experience can be assessed through patient surveys, and managers in most sites reported that the collection of patient experience data was good and showed general satisfaction with care. However, it was also noted how difficult it can be to formulate appropriate wording and questions. Furthermore, when a patient is unable to complete a survey independently, it was also recognised that results can be affected by whoever helps the patient with this task. A further issue relating to this process was the staff perception that patients would be afraid to complain:
A patient can be thinking, ‘OK, do I really be really honest?’ Because they’re still on the caseload. So ’if I was to write something really bad, is that going to impact on my care that I’m going to receive afterwards?’
Elmhampton CNFG7
This observation was borne out of evidence from patient interviews and calls into question the validity of the survey with community patients:
Probably one of the best ways is by questionnaires and questioning the people who are receiving the service and getting anonymous feedback where people can feel that they can write down exactly what is going on without thinking ‘I don’t want to’, as people are always frightened of complaining in case it reflects on the care that they get later on aren’t they?
Beechbury C1
Misunderstandings as to the purpose of such forms can also arise. One patient said that being surveyed to ask if she would recommend the nursing service to friends and family sounded as though the service was marketing itself, when she perceived it not to have sufficient resources to expand:
I can remember having one leaflet, whether it was for the district nurses or not I wouldn’t like to say but I am a bit sceptical on that, because why are they sort of trying to advertise that when they are having a job to keep up with, what they are doing? [Laughs]
Elmhampton P2
The limited use of QIs in some clinical situations was demonstrated during a shadowing session with front-line staff in Alderton West:
Brief discussion about quality indicator for the service – admissions avoidance – difficulty showing effectiveness with this indicator since admissions were not being reduced overall – but thinks this is because profile of caseload increasingly old and ill with complex comorbidities.
Alderton West (front-line observation notes)
How to measure quality in community nursing
It was generally acknowledged that quality in community nursing care is difficult to measure, partly owing to the nature of the service:
It’s difficult to monitor it [community nursing] because it is out and about and delivered in patients’ homes . . . by its nature it is quite hidden and it is difficult to assess how good that’s been without relying on your patients to tell you really.
Elmhampton PM3
This situation appears even more complex when viewed in the context of other national policy requirements. One commissioner explained:
It’s certainly made monitoring [even] things like workforce trajectories, which should be very, very simple to monitor, quite challenging because you’re looking at core workforce plus BCF workforce plus whatever an individual CCG might be commissioning for an area. So if you’ve got a pool of nurses for one bit and a pool of nurses for that bit, do they still count for that bit, and how do you measure things?
Beechbury CM2
Both commissioners and providers thought that moving towards outcomes-based commissioning would enable a more sophisticated assessment of quality. It was generally thought that there is a need to use a mixture of narrative and hard metrics and to focus on collecting more in-depth data about smaller numbers of patients/incidents in order to gain a better assessment of quality in community nursing. Interviewees gave examples of some initiatives implemented to improve quality by focusing in more depth on relevant issues [e.g. the inspection of case files by community practice teachers in Alderton West (see Chapter 6)]. A similar focus on using case files as evidence of the quality of community nursing care was found in Beechbury:
In order to demonstrate effective multidisciplinary working the organisation has to present a case study to the commissioners – the community matron has prepared a case study of a patient with whom she worked who, previous to her involvement, was a frequent 999 caller and GP call out patient . . . Since her input reviewing medication and referrals involving the district nurses and other members of the team to monitor concordance with medication, has had no 999 calls or GP call outs . . . Evidence of monthly MDT meetings attendance is also required for this CQUIN.
Beechbury (front-line observation notes)
Examples cited in other case sites included multidisciplinary mortality reviews in the case of sudden unexpected deaths and learning networks open to all staff (including those in clerical and administrative posts), where key information from the provider’s quality and safety group is presented and discussed.
Some participants suggested that differential targets may be required for measuring quality in areas of socioeconomic deprivation or with differing clinical conditions. Different types of service delivery could also require different outcome measures, for example a rapid response service to avoid acute admission compared with a service supporting patients living with long-term conditions. One commissioner stated that a balance needs to be struck between standardised quality measures and allowing providers to have the flexibility to improve services as long as they can show that overall outcomes are met.
It was felt that community nursing QIs should have a holistic focus (looking at all factors that may affect an individual’s recovery), measuring real health outcomes instead of counting interventions that may not necessarily result in healing. A national lead emphasised the need to make the most of every nurse–patient encounter:
But if you are a community nurse for example, just going in and saying oh yes, here is a leg ulcer, that’s what it measures, that’s the dressing that we put on it. But actually in that space of time with the individual who might be sat there with a glass of beer on the side, with an ashtray full of cigarettes, is clearly overweight and is not doing any exercise; the quote for me is, well what next? So within that space and time that the nurses are providing that clinical intervention for that particular problem, actually where is the intervention in terms of okay, what other things do we need to address in order to help you heal?
N2
Many ideas about increasing the usefulness of QIs were offered by nurses and patients. QI documentation could be useful as an aide-memoire for good-quality patient care and those that incorporated training requirements could enable nurses to access staff development. Retention of QI information on IT databases that would not previously have been stored, such as venepuncture data, was considered to be helpful for other purposes such as providing evidence to build a business case for more staff or efficient streamlining of Datix investigations:
I think if they can pull off what they’re pulling off, it’s great isn’t it? Because that’s a form we’re not filling in.
Elmhampton CNFG2
When indicators were able to indicate effectiveness, these were viewed as especially useful:
When there was the CQUIN . . . You could see they had like safety crosses, didn’t they? You would see when you got a PU in there, and at the end of the month . . . You would see that they’re coming down. So that was a good way of saying that yes, there was one, but we’ve put this in place and they’re now healing. And you could record healing or, in hospital, or static.
Alderton West CNFG4
Quality indicators could also be used with patients to demonstrate effectiveness of care. In the patient focus group, one participant with complex comorbidities talked about setting milestones or goals in relation to measuring progress with care and how difficult it was to say whether or not she was improving owing to the long-standing nature of her illness. The use of small goals such as those used by physiotherapists was thought to be a good use of indicators that could be applied in nursing too:
I think that’s, I think it’s good to have and we can prove it because we’ve had goals and we’ve got there, we’ve done it and you get a good sense.
FGP1
Suggestions made by nurses regarding how indicators might better measure the quality of their work involved the inclusion of ‘softer’ indicators alongside the numeric outcomes that are largely used. Nurses do see the value of quantitative measures assessing effectiveness, but suggest a balance needs to be struck. When asked how they measure the quality of their work themselves, they spoke both of direct feedback from their patients and of healing:
What I find anyway is patient feedback, you know, they will say oh that’s really comfortable if you have done a leg dressing or just an injection and oh I didn’t even feel that go in or you know, something like that, that is where I get the majority of my feedback from on a day-to-day basis anyway . . .
I think the fact that you know, if it is a wound or a leg ulcer, the fact that it’s healing . . .
In addition to their own input into QIs, nurses felt that if others involved in the decision-making were to observe them occasionally in their work, this would inform the selection of appropriate indicators. Instances were given of this happening to an extent and were welcomed:
I think it is difficult, isn’t it, when you’re sat in an office to visualise something, isn’t it, and that’s not your background. We’re really pleased that they’re coming out really . . . Because they’re commissioning the services, aren’t they, and it’s nice for them to see what they’re commissioning. The practicalities.
Elmhampton CNFG2
Patients also suggested that managers should go out on visits with staff to assess service quality and that this would be a valid means of both increasing their understanding of the context for care and reporting back on service quality:
I really can’t think how it could be done, other than spot checks.
Alderton West C1
They would have to go around and check them, because, if the head one went around and checked they would see what happened to the people.
Cedarham P1
From the perspective of both patient and front-line staff, it was clear that having sufficient time to spend with patients was important to both nurses and patients, and thought to be a fundamental characteristic of a high-quality service. The length of visits observed during the shadowing sessions ranged from 5 to 95 minutes. There was a notable difference between the average duration of patient visits by senior nurses and specialist community nurses (35 minutes) compared with band 5 district nurses (23 minutes). It was apparent during shadowing sessions in Beechbury and Alderton West that the former enabled a more holistic approach to care, which patients and carers appeared to value. A patient with a young family with a potentially life-limiting condition commented:
She sits down, she has a chat with us and she is straight with us, she is just so nice. It is hard to explain, it is just nice to see her . . . As I say she does check me, I mean she always checks me for everything, you know.
Alderton West P1
Many people receiving community nursing services live alone or may spend most of the day on their own. District nurses aspired to be less task focused during home visits and patients clearly valued an opportunity to have a conversation during a visit:
So you know, if you can’t speak, spend time to speak to a 95-year-old you shouldn’t be in community nursing is my kind of motto.
Cedarham CNFG3
One patient with partial sight and mobility problems expressed succinctly the loneliness and isolation of many people confined to their homes:
Some people have people that come in, some people don’t have, . . . and they wait for the nurse to come, so they could [have a] little talk or a little something, because they’re not just there to give the injection of the medication, sometimes a little bit of talking helps them to go along, help them along the way.
Cedarham P1
Patients frequently valued the ‘willingness’ and kindness of staff delivering the service, making the difference to their perceptions of care quality. It was the staff who were able to have a friendly conversation and ‘know’ them as a person during the course of care delivery who were most appreciated:
I want somebody who is intelligent and who knows the job so that they have the professional capacity, but they are human and caring and you can talk to them on an everyday level about anything, you know. Because we don’t talk about medical things we talk about the garden or anything and that just makes you feel you have a connection with the nurse.
Elmhampton P1
These quotations highlight the importance not only of nurses having sufficient time and the willingness to develop relationships with their patients, but also of including this aspect of care in quality measurement.
Summary
The study data showed that, in the wider context, an unavoidable consequence of the intention to promote flexibility and autonomy for CCGs in terms of QI selection and application was the lack of benchmarking opportunities. Commissioners and provider managers did not feel that there were any easy ways to compare the quality of the care provided through their services with that of other care organisations. These data painted a picture of individuals responsible for quality in the case study organisations having to operate ‘blind’ to a certain extent. There was also some scepticism expressed about the value of the CQUIN system per se.
It was acknowledged that, owing to the nature of the service, it is difficult to measure quality in community nursing. However, participants agreed that current indicators in use were helpful to promote the transparency of the service for commissioners and provider managers, and also brought some benefits to front-line staff in terms of streamlining work systems, particularly with regard to accessing information about their patients. It was also agreed that areas of care addressed by current indicators are important to monitor (e.g. PUs). Nevertheless, it was also reported that QIs were not always associated with obvious benefits and could sometimes cause unintended and undesirable consequences for both the front-line staff and patients.
A significant issue in this regard appeared to be the fact that many indicators focus on counting activity, rather than on linking outcomes to quality processes, and as such do not provide an accurate reflection of the quality of community nursing on their own. Patients, carers and front-line staff shared similar priorities in relation to quality, emphasising the importance of there being sufficient time to offer person-centred or individualised care. A common view among participants was that effective assessment of care quality should entail the use of both hard metrics and narrative; it was noticeable that in most of the sites, there were ongoing attempts to establish processes through which to collect quality data about the ‘softer’, less easy to measure aspects of the service.
In addition, a drive towards using outcomes-based QIs could be more closely aligned with patient-centred care to demonstrate the effectiveness of the service. A few participants suggested that the use of small goals, tailored to the individual (such as those used by physiotherapists), could be appropriate indicators of care quality in the community nursing service.
The study data suggest that the current system of measuring quality in community nursing, although of some value to all stakeholders, has only limited effectiveness, both in relation to representing service quality to planners and managers and in representing the nursing values incorporated in the 6Cs,3 which are important both to users and those delivering front-line care.
Chapter 8 Findings 5: integrated care
In every study site, there was awareness among commissioners and provider managers of health-care provision moving towards new models of care incorporating varying degrees of interorganisational collaboration. In addition to offering views and experience concerning selection, application and usefulness of QIs, it was notable that many participants were concerned about how quality could be measured in the current context of service integration. At the time of data collection, all the participant service providers were involved in promoting joint working with other organisations and attempting to develop shared indicators across community and other services. One case study site was one of the national vanguard sites charged with implementing new models of integrated care emerging from the Five Year Forward View28 and receiving targeted support to this end. 39 As part of the drive to support quality development in these sites, NHSE had organised four events (one in each region), attended by commissioners, providers, practitioners and educationalists to discuss together the opportunities and challenges for community and primary care nurses in the vanguard sites.
Identifiers for quoted excerpts from interviews and focus groups in this chapter are shown in Table 16. Excerpts from field notes recorded during observation of meetings and of front-line staff at work are labelled accordingly.
| Participant | Identifier |
|---|---|
| Carer | C |
| Commissioner | CM |
| Community nurse (focus group) | CNFG |
| Community nursing team leader (provider) | NTL |
| Focus group carer (non-case study site) | FGC |
| Focus group patient (non-case study site) | FGP |
| NHSE: member of central national nursing team | N |
| NHSE: regional officer | R |
| Patient | P |
| Provider business/performance manager | BM |
| Provider manager: director/manager of nursing services or of quality | PM |
In each case, an individual participant is identified by a unique number preceded by the name of the case site (where applicable) (e.g. Beechbury CNFG1; FGP2).
Associated themes emerging from the data were fragmentation of care, negotiation, accountability and indicator impact.
Fragmentation of care
Given the current lack of integrated or ‘joined-up’ care, being a patient in the community has become increasingly complex with the proliferation of different care providers. There was a perception among both commissioners and provider managers that service restructuring has led to a task-focused service where there is very little continuity of care for patients:
The other thing is that the service has become very task focused, when historically you would have expected it to have undertaken a holistic assessment of everybody’s needs . . . The CCG quality manager said that she thought that having smaller teams with case load responsibility and which are well led is crucial.
Beechbury meeting (field notes)
In contrast to this ideal, models of care in the case sites entailed community services being provided by a number of different agencies: some specialist and time limited and some not; some funded and some having to be paid for by patients; equipment can come from different sources or be provided privately. Patients and carers often spoke of the responsibilities for caring for people with complex, long-term, often deteriorating conditions over many years and the problems navigating health and social care boundaries and, for some, managing and worrying about the financial implications of care choices. In the example below, a patient who used a wheelchair related her problems in this regard:
. . . We have got savings, so we have to pay until the money dwindles, which is hard, because it is expensive . . . I am paying about £800 a month in care and the State are paying me about £280 a month. So that’s about £500 a month extra I have to find . . . to have more care or more help around the house . . . I cut it down to basics because we can’t afford to do everything.
Elmhampton P1
In the course of patient interviews it was apparent that several key aspects of health service care important to, and having an impact on, community patients and carers were not picked up in relation to nursing quality measurement, for example transitions between care, continuity and the quality of collaboration or shared working between nurses and agency carers or district nursing and staff in primary care. The patient quoted above also related her problems to getting someone to syringe her ears as requested by her audiologist. She was unable to access the GP surgery easily owing to her immobility and the practice had refused to send their practice nurse, as district nurses were visiting her. A district nurse had syringed her ears without good effect so the patient had to pay someone privately. Soon afterwards her ears had blocked up again:
I am hoping that one of the nurses will syringe my ears. I have been to the audiologist and he says that they are fully blocked and he can’t adjust the hearing aid until I get the wax removed. We had all this back in May and one of the girls did syringe my ears but it didn’t clear and so I had to go to have it done privately . . . That was only in July, so I don’t really want to have it done every 2 months at the price he costs but there is only one nurse on duty who can do it.
Elmhampton P1
In another example, a patient with a PU on discharge from hospital received care from a number of teams visiting her home, but there was disagreement as to who should be providing what care. A specialist enablement team came for a time-limited period, and then district nurses worked alongside agency care staff to deliver personal care:
It was more like a mini row about who was going to do it [check pressure areas] and I thought ‘if I was sat there and in [patient]’s shoes listening to this I wouldn’t be very happy. I would be thinking I am a burden and arguing over who is going to do something for me’; no I wasn’t very happy but it was sorted out; it was finally agreed that the carers would put it [Intrasite Gel, Smith and Nephew, London, UK] on as long as the district nurses double checked the area at least twice a week. But it does seem to be quite, what’s the word, it’s not set in concrete who’s doing what when.
Beechbury C1
One effect of fragmented care provision is that there is little chance for patients to build a trusting relationship with community nurses; this important aspect of nursing care is not considered in relation to quality outcomes:
You can’t communicate with people that you don’t see often. I could communicate far more . . . the [private] carers understand me; I understand them. They know my standards . . . and there’s a real relationship there and caring. Caring. The care from those two girls is awesome. So, obviously, we have a relationship. With somebody who comes in just once a fortnight [like the community nurse], well, you don’t develop a relationship on those terms.
Elmhampton C1
Negotiation
There was broad agreement that integrated services would be beneficial for patients. In this context, communication and integration of the community nursing service with GPs and other related services (e.g. care homes, out-of-hours services, social care) emerged as a main theme. In one case site a unified contract had been developed for cardiac care, irrespective of where the patient was being treated.
In Beechbury, negotiations were in process to develop joint indicators. However, these were proving difficult to conceptualise and required a lot of time for planning and preparation. Key issues identified included a lack of streamlined processes and conflicting priorities:
The chair [CCG] said that he was still struggling with the concept of the shared CQUIN, and asked if the CQUIN could be to actually develop a CQUIN with shared risk. The CCG head of quality said that the providers would be expected to develop a framework within quarter 1. The trust manager said that providers would need a whole year to develop an effective plan for working together. The CCG director of nursing said that that was not acceptable, they cannot have a year without a product, as they cannot justify this spend of public money.
Beechbury meeting (field notes)
It was also noted that negotiating joint monitoring of quality could be hampered by advantages accruing to different provider groups from current financial systems (e.g. incentives for GPs to develop care plans for patients). Other difficulties concerned variation in different organisations’ ways of measuring quality, which mean that it is not always possible to compare quality measurements directly for the same area of care; an example given was the different systems used to measure PUs in a community nursing service and in the local acute provider:
We don’t always know if we’re comparing like for like, and people measure things differently. We saw this around the pressure ulcers . . . one of our local acutes had an extra category, so we weren’t comparing the same things they’d introduced themselves.
Alderton West PM4
There was widespread recognition of the difficulty in aligning quality monitoring systems across health and social care, given the differences in the way quality is measured in the two services. These differences will need to be smoothed out if service integration is to succeed, a task recognised as requiring a considerable amount of time, effort and thought.
Accountability
Correct attribution of a quality measure is problematic in a situation where more than one service provider or carer is involved. Some patients and carers reported living with the uncertainty, contingent on lack of clarity concerning the allocation of responsibility for care:
I’ve had to keep an eye on the carers here and say to them you need to change the bag, weekly and the night bag weekly and I don’t, the district nurses have told the carers that they must do it and it’s down to the carers not the district nurses. The district nurses can only get involved in catheter care when the catheter becomes blocked or there is a problem with it.
Beechbury C1
Commissioners and provider managers were concerned about the inevitable risk involved when quality measures are dependent to any extent on other organisations’ performance or processes and accepted that monitoring QIs in integrated or collaborative services would be difficult. This was evident at a meeting in Beechbury where the development of their proposed joint indicator was being discussed:
CCG manager 1 said that there is support in principle among all parties [Community Services Provider, City Council, Mental Health Trust] for a shared CQUIN. However, there appears to be some anxiety about who will carry ultimate responsibility for delivery of such a CQUIN.
Beechbury meeting (field notes)
Individual commissioners were also mindful of provider concerns in this regard:
The measures that you put in place have to be measures that have the ownership of the provider that is within their control to measure. So you can’t ask them to do something that relies on somebody else measuring it for them.
Dogwoodheath CM2
In a number of case sites, nursing team leaders (not involved in ongoing negotiations about joint indicators), also raised the problem of responsibility and accountability for meeting data collection targets if they have no control over many aspects of the process:
Many of those at the meeting felt that this CQUIN is quite problematic, as there is a new system of care co-ordination which cuts across organisations and which also involves local authority functions – this means that provider staff do not have control over many aspects of the process.
Dogwoodheath meeting (field notes)
Good communication between all organisations involved was thought to be crucial.
Despite the drive towards joint working, persistent practical problems reported included issues of confidentiality and incompatible computer systems. Currently it is only possible to share very limited data across organisations: patients have to approve sharing of their personal and clinical data in many cases. As noted in Chapter 4, general practices, community nursing services and social care services all have different computer systems, making widespread easy electronic communication impossible.
Impact
The data showed that community nurse interactions with other health-care professionals such as GPs, hospital and care staff can have an impact on implementation and achievement of quality standards. An example was given of patients being transferred to district nursing caseloads from hospitals without the required continence assessments:
Most of the INCO [incontinence] assessments are from the hospital . . . but they expect us to do it . . . It is time-consuming because you have to send in your 3 day fluids chart first . . .
And the wards know they are meant to be doing that . . . because the patient has been in a bed, and they’ve been in there for over 3 days. It is their responsibility as part of their assessment to provide a level of quality care . . . knowing why is the person incontinent.
A similar issue was discussed at a quality monitoring meeting in another trust:
Other issues discussed included the necessity to do targeted work with nurses and physiotherapists involved in patient discharge from acute services, as hospital staff appear to lack understanding about community services/facilities. The GP asked about the role of care co-ordinators. A general discussion ensued, with the provider director of quality highlighting the complexity of the service, and the CCG assistant director of quality saying that the issue was on the table for multidisciplinary action.
Dogwoodheath meeting (field notes)
Nevertheless, the data revealed that nurses were mindful of promoting good relationships with other professionals:
GP request to ensure patient attends outpatient appointment following admission for accident and surgery . . . Nurse discussed importance of responding to GP requests in this sort of case – building and cementing good relationships – GPs appreciate them and are always available when required. The nurses are based in the same building as one of the three GP practices they cover and this facilitates good relationships.
Alderton West (front-line observation notes)
In Beechbury, similar good relationships in some areas of cross-organisational practice had been noted, although other aspects of the organisation of care still needed to be addressed:
QM [quality manager] CCG reported that she had undertaken some scheduled visits to three neighbourhood teams in one area. She had identified really good partnership working, including GPs, psychologists and school nurses. In particular, staff feedback indicated improved relationships with GPs. However, the intermediate care team [ICT] was not well integrated and felt separate from other organisations and teams. Estates need to be reviewed, as ICT members feel separate and isolated.
Beechbury meeting (field notes)
Collaboration across health and social care appeared still to be largely underdeveloped. Joint assessment of patients that depended on arranging meetings with social care staff and completion of requisite documentation to meet reporting targets created particular difficulties for community nurses:
That was a few years ago now, but the, you know the target was 21 days you had to do the assessment, get all the information and all that. But you often couldn’t get, you know it’s got to be a joint piece of work and you couldn’t actually get the social worker and all that, so it would go on and on.
Elmhampton CNFG2
However, joint working between different practitioners was not the only factor noted in this regard. Issues affecting one organisation involved in providing care could also impact on how staff in another organisation function, as evidenced at a meeting in Elmhampton:
The community manager reported that the local authority [LA] are in significant financial difficulty, and are putting in place strict criteria with regard to funding, which will impact on the services in the community. There is ongoing communication between the trust and the LA, and this issue will need to be flagged up to the CCG.
Elmhampton meeting (field notes)
In Cedarham, it was noted that, when short of practice nurses, some GPs assumed that the care for which they were responsible could be provided by district nurses:
Relationships with GPs – also trying not to lose money through not achieving targets – see DN [district nurse] service as a way to ensure this does not happen.
Cedarham (front-line observation notes)
Despite ongoing problems in establishing integrated care systems, participants accepted that QIs for community nursing have to take account of collaborative care provision, recognising that quality in community-based care depends on a number of interrelated services. When asked about the effectiveness of existing QIs for community nursing, national and regional participants from NHSE suggested that the focus on quality in community nursing should move to an integrated care approach:
So I think when we talk about quality indicators for community nursing, I think what we need to think about are quality indicators for people who are cared for in the community and look at it from an individual’s point of view, rather than siloing the nursing service, because . . . some individuals have 20, 30 people coming into contact with them, which is not good, so it’s about the experience for that individual, and I think that’s where we need to focus the quality.
N1
A regional participant from NHSE made a similar point:
I think CQUINs, if we really want to improve patient care, I think it’s very rare you’re going to get CQUINs that are just going to involve one organisation. So I think for CQUINs to really work, but it’s really difficult to do, because that’s actually how do you incentivise that part of the patient journey? But actually I think for something to work, to collectively come together. So, say the ambulance service, community services, and acute, let’s come together to develop some really good, tangible CQUINs, would really improve quality.
R2
The development of joint metrics across services involved in integrated care is still in the very early stages and anticipated outcomes are often system outcomes. However, in two case sites it was reported that a joint indicator had helped drive collaboration between services in different sectors, although with variable results. In one site, an indicator requiring the community nursing service to work with adult social care, primary care and members of the voluntary sector where patients were at risk of hospital admission had resulted in improved joint working across the different organisations. However, in another site, where an indicator focused on sharing care plans with primary care, the community nurses felt that they were being challenged to try and find more patients who fit the criteria than were actually on their caseload, in order to meet the targets set.
Blanket implementation of QIs could also cause unintentional conflict with wider MDT partners if there had not been sufficient communication. One team member spoke of a blood sugar monitoring CQUIN that they had had to implement:
So random capillary glucose monitoring. And if that was abnormal you’d do an HbA1c [glycated haemoglobin], or you’d be liaising and faxing the GP with all kinds of results and the GP would then have to act upon it, and most we found that 80% of the GPs knew nothing about it . . . And when we were faxing GPs with the results, their fax machines were burning out and breaking down because about four million faxes going through every day, because the amount of visits we do and the amount of abnormal blood sugar levels you find, the system would crash . . .
Alderton West CNFG5
Summary
All the case sites were addressing the issue of providing community nursing care in collaboration with other organisations, with widespread recognition and acceptance among the study participants of the need for effective quality measures of integrated care. The problems arising for patients due to the current fragmentation of care services served to emphasise this need.
However, it was also widely recognised that measuring the quality of integrated care brings its own problems. Key issues identified include lack of streamlined processes, including IT, conflicting priorities and agreeing appropriate allocation of responsibility for meeting indicator criteria. Unsurprisingly, joint indicators across organisations seemed difficult to conceptualise and to require a lot of time for planning and preparation.
Of particular interest in this context was that, when compared with the rest of the sample, the one vanguard site in the study appeared to be struggling with very similar problems in this regard. A major factor affecting the development of joint working appeared to be the ongoing resource and staffing difficulties experienced in all the sites, which made transforming existing practice conditions and organisational systems, while continuing to provide effective patient care, challenging.
Chapter 9 Synthesis of findings
The previous six chapters have presented our findings from the national survey and case study to investigate which measures are being used to assess quality for community nursing services and how they are applied in practice. Their usefulness has been explored from the perspectives of commissioners, providers, front-line staff and patients.
In this chapter we draw together the study findings using Franco et al. ’s theoretical framework63 (see Figure 2) to help explain the interplay of national and local factors in determining the organisational, professional and individual factors having an impact on the measurement of quality in community nursing.
Analysis framework
Consideration of the study findings in relation to Franco et al. ’s framework63 has allowed exploration of how different factors influencing quality in community nursing relate to one another. We discuss these issues firstly in relation to factors within the wider health systems, categorised at the outer level of the framework (see Figure 2), moving sequentially inwards to end with consideration of conditions affecting community nurses as individuals.
Wider health systems factors
The main findings from the nationwide survey of CCGs revealed that in 2014/15 there were still few providers of community nursing services outside the NHS fold. Social enterprises and private providers constituted < 20% of community nursing service provision working with CCGs in our sample. Nearly half of community provider organisations were serving more than one CCG, which can arguably be assumed to contribute to a challenging workload for these organisations.
The focus on incentivised QIs in this survey suggested that the main objectives of commissioners in 2014/15 were to use the CQUIN scheme to develop community nursing organisations in order to meet the aims of the BCF, that is to provide care closer to home and outside hospital wherever possible, within a more integrated service provision. No appreciable differences appeared in relation to the numbers of CQUINs or overall goals of these in respect of provider organisational type, though within these categories there were small differences in terms of local priorities. There appeared to be a preponderance of QIs focused on ‘process’, that is, the way services are delivered, as opposed to outcomes, suggesting commissioners and providers accepted that a link to improving the way in which community nursing services are delivered will lead to improved health outcomes.
It is clear from the findings of both the survey and the case study that wider health systems factors affecting community nursing services and those delivering or receiving care arise from reorganisation of structures at both the national and local level following the passage of the Health and Social Care Act 2012. 26 The creation of NHSE, and its role in mandating national QIs for adoption by CCGs, appears to have had some unforeseen consequences (e.g. the rolling out of indicators from hospital to community settings). There seems to have been little consideration of possible variations in methods and context of care delivery in relation to different settings and possible effects on the usefulness or appropriateness of relevant indicators; our study findings show that the value of some of the indicators in use in the community are questionable in this respect. The lack of comprehensive benchmarking opportunities for both CCGs and providers compounds this situation, as there is no national forum for relevant discussion.
The diversity of health service providers resulting from the Health and Social Care Act 2012,26 namely NHS organisations, not-for-profit bodies and private companies, has resulted in increased competition between community providers. Although this was a stated aim of the Act, our findings have shown potential difficulties for NHS community providers. Private providers or larger providers can take advantage of scales of economy and existing infrastructure, which many fairly new entities, such as social enterprises, do not have. Following implementation of the Act in 2013, the financial reins are now held by CCGs, who are responsible for allocation of funds to providers. There is no system for matching funds available to service demand in community nursing; in none of our case sites had the providers been successful in negotiating a different basis for payment for community nursing services, other than the standard block contract. This factor, combined with the drive to offer care in the community to patients with increasingly complex conditions and the obligation of the community nursing service to accept all referrals, has resulted in a situation where the service appears to be struggling to provide care which truly meets patient need and, at times, borders on being unsafe. 75 The situation is further compounded by national problems concerning recruitment and retention of community nurses. 75 In this context, the requirement for providers to meet criteria for QIs appears at best to have only a limited effect and, at worst, may actually impact adversely on the quality of care that community nurses are able to deliver.
Although all parties involved appeared to welcome the move towards establishing integrated care structures for community-based patients, our findings show that difficulties concerning logistics, communication and culture change between and within organisations persist; none of the managers interviewed offered any concrete suggestions about how to effect necessary changes. These problems are not restricted to our case sites. Recent literature highlights similar issues in many health and social care organisations, with the lack of resources and time for the creation of suitable interorganisational infrastructure appearing to be a key issue. 76–78
The assignment of financial control to CCGs has also resulted in their having considerable power to determine priorities for care at a local level. The range of local indicators in use across our case sites illustrates both the commonalities and diversity of need operating in different areas. However, our data show that, despite stated intentions to the contrary, providers are often bound by CCG perspectives, rather than the realities of service demand and logistics, of which commissioners appear to be sometimes unaware. Nevertheless, in our study there appears to be little doubt that providers and commissioners are focused on collaborating constructively for the benefit of patients, despite system shortcomings. Methods in use for monitoring and reporting quality, particularly dashboards providing detailed records of performance against targets, can be useful for creating confidence at a managerial level in both commissioning and provider organisations. However, their effectiveness as catalysts for care improvement seems debatable.
Professional
Despite recognition of the usefulness of some QIs, front-line community nurses in our study expressed dissatisfaction about the effect of the current system on their ability to discharge their professional obligations as they understand them. In particular, commissioners’ ignorance of relevant clinical issues with respect to data collection requirements for QIs was highlighted in a few of the case sites as being problematic. An associated issue was that of unintended consequences arising from indicators for specific areas of care being prioritised above consideration of other areas. Many nurses, including those in our study, value highly the provision of care and compassion,79 which can be classed as the ‘softer’ aspects of their role. However, it is acknowledged that these aspects are very difficult both to define and to measure. 79 Conflicts in definition of the nursing role also appeared to be operating. Although it has been established that providing basic personal or social care is not part of the community nursing role, it can be very difficult for nurses to withhold such care when faced with isolated and/or vulnerable patients. Nurses who value the caring and compassionate elements of their professional role may well define the provision of such care as an essential aspect of their role, not as an unnecessary use of their time. In our study, the tendency for indicators to focus on clinical task measurement appeared sometimes to have resulted in nurses having to choose whether to focus on meeting expected targets, such as expected duration of visits, or on ‘softer’ aspects of care; an associated issue involved their having to practise defensively in order to protect themselves and/or the organisation. In their dual role as both professional caregiver and employee, it appears that nurses often have to manage a range of conflicting expectations in relation to measuring quality.
Community
Our data showed clearly that patients value the opportunity to build relationships with the community nurses who care for them, as has been found elsewhere. 80 By contrast, current care provision appears to entail patients having to negotiate fragmented services and interact frequently with a wide range of service providers. 75 Although there may well be system advantages to be gained from organisational changes (e.g. basing community nurses geographically rather than their being linked to particular general practices), these advantages do not necessarily translate to better experience of care for patients on the ground. Despite apparent positive responses, the issues underlying poor quality of evidence from patient surveys found in this study needs to be considered in this context. All the organisations in the study had processes for the involvement of patients and the wider public, but these did not appear to have any direct impact on the way in which quality measures were selected or implemented in community nursing. Given the relative frailty of patients on the community nursing caseload,75 which may impede their engagement with these processes, there appears to be a fundamental difficulty in representing patient views adequately. Caring responsibilities assumed by informal carers (family members and/or friends) are often extremely onerous,81 precluding this group’s ability to take part in processes that require expenditure of time and/or effort. Moreover, patients cannot be considered to be a homogenous group with a unified perspective on specific issues,82 so it cannot be assumed that those who do engage with formal representation within organisations share views and concerns with patients receiving community nursing care. In our study there was an appreciable concordance in the views of patients and carers and those staff delivering front-line care with regard to the aspects of service delivery likely to improve quality. The most important of these was allowing nurses the time to deliver person-centred care.
Organisational
Key issues with respect to measuring quality in community nursing in our study appear to be the lack of involvement of front-line staff in indicator development and/or selection, and the lack of feedback from managers to front-line staff about indicators or their effects. Certainly, the reporting procedures for safety indicators were viewed as punitive by front-line staff, onerous in respect of investigation time by team managers and, financially, a risk for provider organisations. Although some participants reported that quality dashboards could be useful in some respects, there was a general feeling of disengagement and lack of ownership concerning the current systems for measuring quality of community nursing care provision. Many of the front-line staff in our study seemed unaware of, or unable to use, opportunities to influence quality measurement. This may in part be a legacy of nursing’s traditional role within the hierarchical structures of the NHS,83 where there has been little, if any, expectation that nurses providing front-line care will proactively initiate or influence that care at a strategic level. Many of our study participants appeared relatively passive in this regard, a situation undoubtedly compounded by the combination of managing an increasing workload in the context of staff shortages, organisational changes and problems accompanying the implementation of new IT systems. This situation seems to have created an organisational climate in which front-line nurses do not feel they have adequate resources to deliver care in a way that satisfies the personal or professional criteria which they feel they should be meeting.
Internal
One of the most contentious issues affecting individual nurses in our study appeared to be the difficulty that some experienced in adapting to changed computer systems and mobile working, which reportedly undermined their confidence in their ability to function adequately in their changing role. This is not an isolated or new issue; the problems that some workers have when computers are introduced into the workplace have been well documented. 84 In comparison with acute settings, computers have only been introduced relatively recently in many community nursing settings, to a workforce who traditionally have had little engagement with technology in the course of their duties. However, this may well only be a problem in the short term, as more recently qualified nurses are being increasingly recruited into community teams post registration. Of more pressing concern for individual nurses are the related issues of fatigue and stress. High sickness rates are endemic in the community nursing workforce,75 a situation that only increases pressure on a service already struggling to meet demand. A vicious circle can ensue, as individual nurses choose to leave the profession in order to preserve their own health and well-being, thereby exacerbating the problem. 75
Summary
Provider organisations’ explicit goals have had to change and align with current national and local agendas, as interpreted by commissioners. Although providers have always aimed to provide good care for patients and their families, the service now appears to be significantly focused on meeting targets related to relieving pressures in the NHS acute sector and which are of dubious validity in relation to provision of high-quality nursing care in the community. As such, the values implicit in a culture of setting and meeting targets appear at times to clash with those of front-line nursing staff, who consequently feel little engagement or ownership for QIs currently in use.
As professionals, the front-line community nurses expressed concern about the effect on care of some QI targets. The difficulty of measuring ‘softer’ aspects of care appears to prevent recognition of the true quality of the service provided. Many patients and carers consider these aspects of care to be as essential as nurses’ clinical and technical competence. Their obligations as employees to collect data for QIs can at times compromise nurses’ professional autonomy.
The current climate of staff shortages and ongoing logistical problems, which appears at times to be exacerbated by the need to collect data for quality measurement, has contributed to high levels of sickness among community nursing staff. This situation does not bode well for the capacity of the service to provide consistently high-quality care to patients on the community nursing caseload.
Although it is clear that all of the organisations in our study site are striving to improve and measure aspects of care quality, there is some debate about the degree to which they are succeeding. The Framework for Commissioning Community Nursing53 stipulates that quality entails ‘high-quality care’ delivered by a workforce composed of ‘the right people with the right skills in the right place at the right time’ (p. 16),53 and the development of ‘effective relationships’. Given the climate in which all community nursing service providers are currently operating, it is unclear how these aspects of quality are to be achieved.
To validate our analysis and findings we took some of our main findings to a series of 10 stakeholder workshops across the country, where they were discussed in the light of people’s experiences locally (see Appendix 2 for a full report). These discussions consolidated the development of good practice guidance (see Appendix 4).
Chapter 10 Discussion and conclusion
Discussion
In Chapter 9 we collated the findings from the various data streams collected over the course of this mixed-methods study and considered our data in relation to a framework that identified how wider contextual factors interplay with the processes around quality measurement in community nursing. 63 This chapter picks up some of the significant findings from our study and discusses their implications for the use of such measures in community nursing service quality assessment. It concludes by suggesting how quality measurement may be improved for the benefit of patients and carers.
Quality measures in use for community nursing
The national survey of CCGs conducted in 2014 (response rate 69%) found that only a small inroad of < 20% of independent and voluntary sector community nursing service provision had occurred following implementation of the Health and Social Care Act 2012. 26 The remaining community nursing providers were NHS trusts; the majority providing both acute and community services. This pattern of provision suggests that the competitive procurement element of ‘any qualified provider’ enshrined in the Act had been slow to take hold in the realm of community nursing services. Furthermore, evidence from our survey suggested little change had occurred in relation to the number and sources of indicators for commissioning in relation to the CQUIN scheme since the national evaluation in 2013. 25 Despite recommendations from the national evaluation to limit development of local indicators, only a minority of respondents used a validated database as a source of indicator, thus suggesting that these were developed locally in the main. The number and complexity of CQUINs identified in the survey suggested a significant workload associated with selection, monitoring and evaluation of community nursing service quality within the CQUIN scheme alone. Overall it appeared that commissioners were using the scheme to incentivise community providers to shape their services to ensure fitness to provide ‘more care closer to home’,39 potentially prioritising national policy-drivers to reduce pressures on the acute sector over local community nursing service quality priorities.
Workload associated with quality reporting
The substantial workload associated with negotiating and agreeing indicators, and subsequent monitoring and reporting on targets implied by the survey, were borne out of findings from the case study. It was interesting to note in this context that the comparatively large number of CQUINs used in Dogwoodheath appeared irrelevant; workload was reported to be onerous in all of the case study sites. Community services have long been commissioned using a block contract, which has the advantages of low transaction costs and a predictable income for the provider. 85 The introduction of pay-for-performance schemes such as CQUIN as an adjunct to the community block contract in 2010 (despite limited evidence of its success in health-care settings) potentially afforded some flexibility in responding to local need and incentivising service development. 86 However, evidence from the case sites suggested that the potential advantages of such schemes might be offset by the disadvantages, such as lengthy periods of negotiation and the need for regular reporting on targets for accountability purposes. One of the aims of introducing the scheme was to facilitate communication and discussion between commissioners and providers over local needs and services, but despite the number and duration of such negotiations, it was evident that misunderstandings could still prevail. Providers were critical that finances underpinning the CQUIN scheme had been withheld from their allocated funds, and that commissioners had unrealistic targets and did not fully appreciate the risks for already stretched providers in participating with the scheme. In comparison, some commissioners reported provider naivety for not including business analysts in selection of clinical QIs at the start of the scheme, when there was less appreciation of how missed targets might impact them financially. The revised scheme for 2016/17 introduced a reduced set of national CQUINs to apply in the community, with the emphasis on staff health and well-being and physical health of people with serious mental illness. 87 A prescriptive list of indicators has been provided with guidance on the numbers and types of local indicators that are available to be used. Current guidance appears to confirm the perception that the CQUIN scheme for community services providers continues to be used to drive through national policy priorities that reduce pressure on the acute sector rather than focus on local issues affecting nursing care quality.
Front-line nursing staff were critical of the quality measures selected having been rolled out from acute settings, especially where these appeared not to take account of the community context or conflicted with their professional judgement. For pay-for-performance schemes to be effective, health outcomes chosen to be incentivised must be measurable and directly attributable to the care provider. 85 However, our study found that health-care outcomes favoured by NHSE (e.g. the NST) could be difficult to measure meaningfully and could be capable of being influenced by multiple determinants. Although the NST was piloted extensively,38 90% of participating sites were acute or inpatient settings and may not have adequately represented a community context. Community nurses generally work alongside private or social sector staff delivering personal care to patients, so attribution of some health outcomes (such as PUs) can be problematic. 88 Additionally, informal carers, that is, family members and friends, are frequently involved in providing different aspects of care for patients. These typically include personal care, but may also incorporate more complex emergency care tasks. 81 All such activities might contribute to the overall health outcome being measured, yet are not amenable to monitoring in a formal or systematic way.
Furthermore, procedures for data collection in the community were flawed and could result in a reduction of the validity of quality measures in use. Front-line staff were largely responsible for collecting data to report on service quality, but in this study there was scant evidence of electronic data collection methods in use, making the workload associated with data collection more onerous. Nurses recorded care delivered on paper care plans in the patient’s home and jotted down measurements in their diary or relied on memory for recording these later on the community database at the office, suggesting the potential, at the least, for inaccurate recording of quality data. The workload entailed in collecting data on quality measures which were not felt to be invalid, on top of patient care responsibilities, meant that nurses gave data collection low priority, as has been reported elsewhere. 32,37 Our evidence suggested that front-line nurses were relatively uninformed about contractual KPIs or CQUINs and appeared to have only a vague idea of how incomplete or scant pay-for-performance data might impact on their employing organisation. Where feedback on performance is provided to staff, quality is improved and variation in care is reduced,32 so educating staff about quality measures, involving them in selecting appropriate indicators and providing them with regular feedback might counteract current perceptions and improve data quality.
Both front-line staff and managers in provider organisations found the workload incurred for serious incident investigations (quality procedures in response to threats to patient safety), to be onerous. Although designated as learning opportunities and demonstrating openness and transparency under ‘duty of candour’,30 front-line staff found these processes unduly punitive in relation to PU quality measures and they were reported to be time-consuming for their managers to investigate and report. Patient safety is an essential component of a high-quality service, but the current approach to investigate PU occurrence could take months to conclude. Linked, as they are, with contractual reporting obligations, such investigations can create the impression of fact finding for the purposes of correctly assigning blame, in order to ensure the organisation is not penalised, rather than identifying potential learning from the incident, as recommended by Francis. 2 Importantly, negative perceptions such as these could have the unintended effect of front-line staff underscoring PUs or discourage reporting the discovery of a high-grade PU in a timely way.
Unintended consequences
There is a dearth of evidence on unintended consequences of using quality metrics for nursing. 35 Rambur et al. 35 reported that evidence on quality metrics used for other health professionals suggests these can actually lead to decreases in care. Examples given were a lack of focus on patients’ concerns36 and increases in mortality due to measure fixation (that is undue emphasis on the aspect of quality being monitored to the detriment of other aspects of care), a point also made forcefully by Francis. 2 Our study has confirmed the possibility of unintended negative consequences arising from use of pay-for-performance indicators in community nursing services. The use of indicators designed to increase communication and improve care of diabetics almost brought local GP systems to a standstill and detrimentally affected GP community nurse relations. Repeated requests to patients to complete satisfaction questionnaires led instead to irritation with nurses, and inappropriate skin assessments being conducted caused annoyance to patients. At an organisational level, financial penalties were incurred due to staff being unable to attend training designed to enhance care due to front-line staff shortages. All of these instances emphasise the importance of including all stakeholders in indicator development in order to ensure that the intended benefit of such schemes for patients is achieved and to foresee and prevent negative consequences from occurring.
Competing priorities for quality
There is an underlying tension between the competing priorities of commissioners, managers and clinical staff in relation to choice of appropriate service quality measures. Although policy on quality measurement has focused on patient safety, patient experience and clinical effectiveness since 2008,23 financial pressures on the NHS has made more care delivered at or closer to home24 an important target for commissioners. Our analysis of the CQUINs applying to community nurses found that many of these were founded on processes to facilitate closer working in the community and to improve integrated care for patients with long-term conditions. Although these are laudable aims in themselves, they also enable commissioners to deliver on the need to reduce pressure on the acute sector, rather than reflect the quality of community nursing services felt on the ground. Foremost, quality priorities for front-line staff in this study were the impact of staffing problems and an ever-increasing workload on the ability to deliver person-centred care, a value highly regarded by nurses (and the NMC) as representing good-quality care. 11,89 In this view they were supported fully by patients and carers, who reported frequently on the value they attached to individualised care from skilled and compassionate staff, with time to spend. Moreover, patients and carers identified serious problems with quality of continuity of care and difficulties navigating professional boundaries in the community, neither of which have been picked up adequately in relation to current quality metrics for nursing.
The discordance in priorities of commissioners and front-line staff may point to subversion of the values and experiences of professionals delivering care to patients in favour of more strategic objectives. One approach matches highly trained nurses providing skilled professional health treatment to patients within an efficient time frame with ‘softer’ aspects of care being undertaken by less qualified staff, whereas the other opposing perspective values provision of less easily measured aspects of care as an essential component of holistic, compassionate person-centred care. It is probably inevitable in the current situation of increasing demand, high vacancies90 and stretched community nursing services that skill mix will increase, with more task-focused care being undertaken by registered staff without specialist training or health-care assistants, but arguably such an approach mitigates against the standards and values enshrined in the NMC code of practice5 and the reasons why many nurses enter into the profession.
The QNI have identified the urgent need for a standard workforce tool for community nursing in order to ensure the safety of patients and the quality of care provision in response to increasing skill mix and larger geographical teams. Workforce tools that take account of the varying skill levels available in the community nurse team and caseload complexity have been developed around the UK, but none have been adopted countrywide. 48 Dilution of specialist community nurse expertise could pose a risk to care quality4 if sufficient time is not available for staff training and, importantly, supervision of staff delivering care in patients’ homes. 91,92 Staff vacancies and sickness were reported on regularly as part of contract accountability in our case sites, but it was less clear how report of such measures fed into service change or investment. Ironically, an increasingly ‘task-focused’ approach to care provision, as represented by increasing skill mix, could prove to be a false economy. A recent evaluation of the Netherlands’ Buurtzorg model of community nursing, which enables nurses to spend more time with patients and provide both nursing and support care, seems to result in higher staff and patient satisfaction with care at an average cost. 92
Integrated care
Community nursing services have long worked alongside other health and social care providers and, until the recent reorganisation, were closely linked to general practice teams and delivered care to the same patient population. The Transforming Community Services Programme40 has driven widespread changes with regard to expanded and merged community nursing teams. Although important economies of scale were achieved, some disadvantages were incompatibility across different IT systems, loss of proximity leading to reduced opportunity to meet face to face with the local general practice and, arguably, a more corporate approach to care provision. In particular, the latter, although appearing more efficient, could create the potential that a greater number of nurses could be visiting patients across a larger geographical area, resulting in fragmented and task-orientated care for patients. 93 Furthermore, increasing diversification within the community nursing service itself (e.g. introduction of specialists for long-term conditions, end-of-life care and intermediate care teams, community case managers or community matrons as well as nursing assistants), means the potential is increased for an ever more complex provision of nursing care for patients within community nursing services alone. 93
Current health and social care policy is building on the changes introduced in 2009 to develop closer links with the social, independent and voluntary sector. The introduction of shared planning arrangements, trialled in vanguard sites across England, is now being rolled out more widely in sustainability and transformation plans across the country. 94 This policy, although promising much in relation to the management of patients in the community using the most appropriate service provider, brings its own challenges in relation to the delivery of person-centred care and quality assurance. It was notable that the one vanguard site in the study did not appear to be coping with these challenges any more easily than the other case sites. Care delivered in the home is comparatively invisible, where patients may lack mental capacity and be too frail to speak up for themselves, or isolated and completely dependent on services provided, and it is essential that there should be a quality framework safety net and that professionals from all the different sectors are held accountable for outcomes of care delivered. 45 Our study suggests that where quality schemes are incentivised and organisations stand to be penalised financially if targets are not met, there can be particular problems in designing indicators to ensure accountability and shared risks between the partners providing care.
One of the main threats to quality from the changes envisaged in the sustainability and transformation plans is to maintain continuity and allocation of responsibility for care across fragmented provision of services. The development of quality measures that can capture meaningful care attributes appears to be a difficult and time-consuming process, even when focused on only one service component, suggesting a different approach to service quality assessment in these organisations will be essential. Currently, apart from patient experience surveys, the means of measuring care delivered within an integrated care service is at a rudimentary stage. Quality measures that could demonstrate continuity of care and transition between providers were notable gaps in indicator provision, but are essential to patients for good-quality care. Such indicators are likely to become more important as the integration agenda moves forward and to lead to the need for different and more creative measures being put in place for service quality assessment. However, in order for such measures to be developed and effectively applied, it will be essential first to create the infrastructure and establish streamlined communication processes between organisations. Education and preparation for interprofessional working will also be needed for staff required to extend their professional practice to take into account perspectives and traditions associated with other disciplines in health and social care. 78
Study strengths and limitations
The choice of a mixed-methods design incorporating a survey and case study has enabled the team to investigate contemporaneously and in depth, the processes for selecting and applying QIs in community nursing quality assessment. 95 Despite the initial problems of obtaining data from the new CCGs, our survey succeeded in obtaining a 69% response rate, providing good strength of evidence of the national picture in relation to variation in organisations providing community nursing and the number and range of local QIs in use for community nursing in 2014/15. Inferences made about suspected workload involved in respect of selecting and monitoring quality measures based on the survey findings were able to be explored in the case study. The use of five health settings has facilitated comparison of findings across different types of community services provider organisations. Our within-case analysis suggested very little variation in contextual characteristics impacting on how community nursing service quality is measured within the different organisations. This is possibly due to the strong policy-drivers from NHSE for delivery of care closer to home creating some turbulence by pushing forward organisational change and increasing integration in all the sites, following on from the implementation of CCGs in 2013. Although the generalisability of findings from case studies could be argued to be limited, this study has incorporated triangulation into its data collection methods by conducting front-line and meeting observations, which can both inform and validate our interviews conducted with participants in the field. A dissemination phase enabled us to test and validate our findings with stakeholders from around the country, thus reinforcing confidence in our findings.
We purposively selected case site organisations from scrutiny of the findings of the survey, and consequently there may have been some differences between those sites that agreed and those that did not, which might have influenced the case study findings. Two sites we approached initially seemed to agree to participate, but in one case took so long to provide requisite information for the NHS permissions process it had to be abandoned. In another potential site that included a private provider, despite a great deal of enthusiasm from its nursing lead, we were unable to recruit as, at the final stage, a high-level decision meant that the site suddenly withdrew. It is possible that market sensitivity and concerns about confidentiality were behind the decision to withdraw. This experience highlights a number of issues that need to be considered with the wider involvement of private providers in this area of provision. First, claims of the need for confidentiality of commercially sensitive information may make it increasingly difficult to scrutinise the activities of companies in order to understand lessons from which other organisations can learn. Second, an unwillingness to take part in research (which is essential for NHS improvement) will be problematic unless a requirement to support NHS-funded research is made explicit. NHS organisations are themselves subject to a clear expectation that they will support research as a core activity.
It is recognised that people who volunteered to be interviewed or shadowed in the case sites may have been different from those that did not allow access. However, our study design incorporated a dissemination element that enabled our findings to be shared with a range of stakeholders across the country to test out the extent to which our analysis and interpretations resonated with staff and patients in different locations around England. The research team considered the effort and resources expended for this valuable exercise justified, in that these events validated our findings and produced valuable insights into how they could be translated into actionable good practice guidance, all of which significantly enhanced the strength of our study and its outputs. The use of all the above methods of triangulation and validation considerably strengthens the trustworthiness of the findings.
New CCGs were not quite embedded in 2014 when the national survey was undertaken, and this was the reason for a pragmatic decision to use FOI processes as a data collection method. The use of FOI ensured that the organisation found the correct source of information and advice, as telephone operators rarely knew to whom they should address our enquiry, a problem that has been reported elsewhere. 95 Furthermore, utilising the knowledge of our commissioner co-applicant, and in order to increase our response rate, rather than ask people to complete a long questionnaire, we asked them to send us their documentation relating to quality of community nursing in 2014/15. Requesting documentation designed for work purposes resulted in receipt of a variety of documents at different stages of completeness. The most consistently complete data reported the CQUIN scheme and, as our design incorporated an ensuing case study, affording the chance for in-depth analysis of other quality measures, we focused on CQUINs for the survey. This possibly narrowed our focus too closely on this aspect of service quality measurement; however, negotiating and monitoring the scheme proved to be a key area of work for commissioners and enabled insight into the competing quality priorities between commissioners and service providers. The focus on CQUINs also highlighted the difference in emphasis given to front-line concerns and the national agenda. As the scheme was incentivised it also offered the opportunity to add to the meagre literature on the unintended consequences of incentivised care in relation to community nursing. We were able to scrutinise a range of supporting documentation on other measures from commissioners and providers, including front-line staff, although this was comparatively limited owing to variation and incompleteness in the documentation obtained. Commercial sensitivities following the introduction of competitive commissioning may also have influenced what documents were made available to the team.
Owing to the prevailing wider circumstances relating to staff vacancies and a high degree of change impacting on community nursing services, we were sensitive to ensuring that front-line staff shadowing was timed for the convenience of organisations, missing the winter pressures and only commencing when the research team had built a relationship of trust with nursing team leaders. Nevertheless, one of the sites, the social enterprise, did refuse to allow shadowing of staff without giving any explanation, although front-line staff were able to participate in a focus group. As the findings of that focus group were in accord with focus groups in different sites, it is arguable whether or not there would have been different issues emerging in relation to front-line observations but, again, commercial sensitivities may have been behind the decision to deny access. In the other four sites, community nurse team leaders allocated staff for shadowing and in several cases this was a more senior member of the team. Although this might have influenced the findings of observations to an extent, it did enable a more in-depth discussion of care context and quality than might otherwise have been the case.
Lack of parity in documentation received meant that it was difficult to identify any meaningful differences in our cross-case analysis of this aspect of the data collection. The main difference identified was that one case site (a combined acute and community trust) had chosen not to participate in the 2015/16 CQUIN scheme. It was unclear whether this was due to a pragmatic decision to minimise financial risk or because it did not prioritise community services. Additional documentation, such as retrospective quality accounts, was complete and accessible online. In theory these reports enable patients and carers and other stakeholders to access information about service quality. In reality, although quality accounts do provide evidence of provider services’ achievements against quality targets, accompanied by comments from the local Healthwatch organisation, the reports have the appearance of a public-focused marketing brochure (their structure and appearance differed across the case sites, again making comparison unfeasible). Furthermore, the ‘marketing‘ of quality accounts highlights the problem of linking QIs to financial awards and penalties, as it is bound to lead to organisations seeking to market themselves and present the most positive face possible, rather than openly highlight and learn from problems in order to improve them.
Implications for practice
Commissioners and provider managers alike reported difficulties in finding appropriate health outcome QIs for community nursing and applying meaningful targets and goals. In our study, even where patients and carers agreed on the importance of health outcomes being reported nationally, they did not think that such measures could be used to assess nursing quality, having first-hand knowledge of other factors that could influence these outcomes. There was consensus that QIs would be most useful if front-line staff and patients or carers could be involved more closely in the process of selection. The practicalities of achieving this input are yet to be decided. However, clinical QIs that could be used as an aide-memoire by front-line nurses were found to be useful by staff (e.g. assessment of falls). This measure was also considered important by patients and carers and is known to be an indicator of deterioration in health and injuries that could potentially lead to hospital admission. 96 Although agreeing with the importance of a falls assessment, however, patients cautioned that the fact that an assessment had been undertaken was not, of itself, an indicator of high-quality care, placing the quality emphasis instead on provision of follow-up and ongoing monitoring.
Meaningful care quality outcomes for both patients and nurses could be achieved by adopting an approach that incorporates patient-centred care with outcomes of care measurement. Patients with long-term conditions thought that defining appropriate goals with their community nurse and setting small milestones to measure their improvement over the course of an episode of care would be motivating, both enabling them to take more control of their health themselves and also be amenable to measuring a health outcome of importance to them. A small unpublished pilot study suggested this approach fitted in with personalised care planning and was possible in a community nursing context. The use of such measures can have the effect of uncovering related, albeit previously unknown, health concerns of the patient and open a patient-led discussion (S Horrocks and L Wye, University of Bristol, 2014). Small goals or milestones that can be influenced by nursing can arguably give a better reflection of patient-centred care than a standard satisfaction measure. However, such an approach would require education for staff and perhaps entail more time in assessing and monitoring patient progress by front-line nurses. A discussion paper on outcome-based commissioning in the social care sector has emphasised that although there are some benefits to patient-determined goals, it is resource intensive and requires effective systems to accurately identify client needs and overall service objectives and then to manage the processes of monitoring and audit, a finding that may apply likewise in the health-care sector. 97
Helping staff identify how they themselves could use quality data to support their work might encourage greater interest and investment from the front line. Some staff in our study recognised that accessible quality data could potentially support business cases more efficiently than before. In addition, there was evidence of a team having achieved some success with applications for administrative support using such data. At a more senior management level, team managers found the quality dashboard useful for tracking indicators relating to staff activity, sickness and vacancies on a monthly basis. Where feedback of these figures was made available to front-line staff, they were found to be useful in helping teams compare their own outcomes month on month and with other teams in the area (and act as an incentive to improve their own outcomes). 32
Improving practice in assessing service quality
Commissioners and providers in this study were sensitive to the limitations of relying on patient surveys and staff activity level for quality measurement and sought alternative means to demonstrate quality. In all the sites there were examples of good practice in relation to quality, from peer auditing of clinical case notes, to the use of a patient case study presented to commissioners to demonstrate successful multidisciplinary working. The latter had the benefit of harnessing input from the patient, where this was possible, required to be a fundamental aspect of planning in relation to developing sustainability and transformation plans. 98 Although the example above is unlikely to be sufficient to address the monitoring and accountability needs of commissioners and provider service managers, it could be helpful in demonstrating less easily measured aspects of care quality, such as the establishment of trust between a patient with complex needs and the community nursing service, a prerequisite in designing care around the patient.
Our study found that front-line staff rarely have time to record all the details of their assessment of the patient at each visit, prioritising clinical changes and medical updates on the care plans in patients’ homes. An even more reductive report was uploaded onto the computer in the office. Comfort, reassurance and patient education provided routinely during the course of front-line observations was generally not coded as, in order to do so, nurses had to input the time spent on each aspect of care provided and computer data entry therefore became time-consuming and onerous. Where commissioners accompanied nurses on their visits in order to familiarise themselves with care delivery, they had the opportunity to witness aspects of care which often go unrecorded and are less easy to measure, such as the kindness and flexibility of the nurse and the quality of the interaction between nurse and patient and/or carer. Furthermore, these opportunities were found to be instructive in helping commissioners and managers understand the contextual problems staff face, the circumstances in which their patients live, and their need to be able to react to unexpected situations and provide whatever support is necessary in order to carry out the ‘nursing task’ they had come to deliver. It would be unethical, for example, for a nurse to visit a patient to administer medication and, because they happened to arrive before the carer, leave the patient in soiled bedclothes. Currently, it is unlikely to be feasible for commissioners to undertake regular inspections as part of accountability assessment but, with the development of new care collaborations, it will be essential to understand how different professionals work together in the community and this is likely to be best achieved by front-line observation.
Patients and carers in our study regarded inspection as an essential component of quality assessment that both commissioners and managers should undertake as part of their role. The inspection of front-line care delivery is a key aspect of CQC quality assessment of services. Plans currently under consultation with NHS Improvement99 suggest that the CQC key questions around safety, effectiveness, caring, being well led and responsiveness will be incorporated into quality assessment for all NHS service providers, while the number of contractual QIs will be streamlined and rationalised. There may also be untapped potential in using feedback from community nursing staff in relation to service quality assessment. Nurse feedback has been shown to be a good indicator of service quality and concordant with patient outcomes in acute settings. 71,100 In our study, front-line perceptions of quality accorded strongly with those of patients and carers, suggesting that front-line community staff views may also be used as a proxy for patients who, in the community, were reported to be too frail or unwell to complete quality surveys.
Ensure quality indicators selected are fit for purpose
Measures selected must be both appropriate and feasible, and should not conflict with recommended clinical practice. Our evidence suggests that commissioners and provider managers need to allow front-line staff, patients and carers a more forceful voice both in choosing suitable quality measures and in demonstrating service quality more creatively in order to reduce the likelihood of indicators that are not fit for purpose being selected. Moreover, selected quality measures should include a focus on structural issues of importance to front-line community nurses, such as adequate staffing and access to staff development. These have a clear link with provision of safe and person-centred care, which is a fundamental measure of quality for nurses and patients.
Although it is acknowledged that, for accountability reasons, commissioners and service managers need evidence to demonstrate a safe and effective service is being provided, evidence from this study questions the need for the number of quality measures in current use for community nursing and suggests transaction costs associated with monitoring and reporting have not been fully considered. Commissioners should be aware that even small numbers of comparatively routine quality measures can add up to a major workload for provider managers and staff, detracting from care delivery. Streamlining contractual indicators with CQC measures might alleviate the problem.
Quality indicators that work well in acute settings are not necessarily suitable for the community. Evidence on the NST and the FFT in this study suggested that neither were sufficiently piloted in a community context. An apparently straightforward indicator, such as enhancing the well-being of staff, that might work well in an acute setting is likely to prove problematic in a community setting where staff are dispersed geographically in buildings with limited space for staff canteens or sufficient footfall for healthy meals to be delivered locally. Involving representatives from community sectors of health service provision in high-level selection of national indicators could prevent unsuitable indicators being rolled out into the community. Provider managers need to engage nursing teams consistently in quality discussions by providing feedback on care quality and enabling real consultation on appropriate measures for quality assessment.
There was evidence from this study that front-line staff collecting data did not fully appreciate the need for good-quality data to be submitted or the consequence for the service of not having sufficient data on service quality available. Managers need to provide regular feedback focusing on how staff are doing with regard to quality in order to maintain motivation and identify how any difficult issues can be resolved. Some practical suggestions to improve communication between managers and front-line staff coming from the stakeholder events in the final phase of the study included more effective utilisation of IT; regular fora or meetings where people could discuss service quality; newsletters to staff; and opportunities for front-line staff to shadow managers in their meetings with commissioners to appreciate what is involved in quality measurement for the organisation.
Resolve connectivity problems for information technology and support nurses with adapting their practice to make greater use of information technology
If the need for community nurses to be involved in collecting data for quality purposes is to continue, then two things are required: (1) a stronger link between the measures being used as QIs and their usefulness to the clinical nursing needs of patients on the caseload; and (2) greater support for nurses to utilise IT effectively in the community. Evidence of difficulties with connectivity and compatibility suggests that these challenges need to be resolved before rolling IT packages out into practice in order not to discourage nurses and add to busy workloads. Careful assessment of the impact on patients and carers of increased use of IT records is required to ensure that this is not detrimental to service users who find such records a helpful reference when communicating with GPs and other service providers.
Further research
Our findings suggest that further research is required into the costs of administration of QI pay-for-performance schemes in community health settings and how these schemes can be modified to be of greater benefit to patients in supporting quality improvement and innovation in the new integrated care environment.
Research is needed to identify an agreed way of assessing if and how complex interactions between different aspects of care can be weighted and measured in new integrated care organisations. A related and pressing issue is how to minimise transaction costs in relation to time and workload associated with quality monitoring, without compromising patient safety.
More research is also required to identify the most effective way to provide front-line nurses and patients with a voice when quality measures are selected to ensure validity and to ensure that patient priorities are met.
The effectiveness of new configurations of community nursing service provision and its impact on patients and other stakeholders requires assessment in relation to continuity of care for patients and ease of access to the MDT.
Retrospective analysis of the sustainability of CQUIN-funded schemes should be undertaken to identify their longevity once the CQUIN funding has ceased.
A trial of patient-directed outcome measures could be undertaken to identify their usefulness in the community nursing or integrated care context. A pilot study in this area using a slightly adapted Measure Yourself Medical Outcome Profile questionnaire (freely available), suggested that it might provide a measurable clinical outcome for patient-centred care as a QI for community nursing.
On the basis of research suggesting a link between positive nurse assessment of service quality and positive health outcomes for patients in acute settings, the feasibility of using community nurse assessments of service quality as a proxy for their patients could be trialled.
The validity and reliability of closer alignment with CQC approaches for quality measurement in community nursing, including front-line inspection, should be investigated.
Evaluation of the costs and benefits of different methods of stakeholder and public engagement should be undertaken to review the long-term benefits of these to validating research findings and implications for practice.
Conclusion
This study aimed to investigate the ways in which quality in community nursing is measured, specifically the selection, application and usefulness of QIs being used in commissioning community nursing services. The context for the overall question was an awareness that public confidence in nursing quality has been shaken by hospital and care home scandals in recent years. Yet little was known about the quality of services being provided in the home, or how their quality is measured. Our study findings suggest that the quality measures currently in use appear to fulfil the accountability requirements of commissioners and health service provider managers in relation to investment in organisational change, but do not sufficiently capture the values espoused by front-line staff or service users in relation to the experience of care.
Furthermore, the requirement for service providers to meet existing criteria for nationally mandated and local incentivised QIs appears to be risky at a time of financial constraint, have a limited positive effect and could actually impact adversely on the quality of care that nurses are able to deliver because front-line nurse time needs to be utilised in data collection and follow-up. Poorly conceived indicators may also result in unintended negative consequences for patients and other members of the health-care team.
The validity and reliability of data currently collected by front-line community nursing staff is questionable for quality assessment purposes, and the resource that appears to be required to agree, implement and monitor quality measures in practice suggests pay-for-performance approaches to quality measurement may not be cost-effective. In contrast, CQC inspections incorporate quality domains, such as the nature of caring and responsiveness, that encompass the values of patients and nurses more effectively than current health service quality measures, and front-line inspections conducted by objective observers can more fully contextualise service quality. There is an argument to suggest reducing the number of different indicators on which providers must report and adoption of the five CQC domains as a basis for quality measurement.
The need for managers to monitor service quality will, however, continue, and increasing evidence suggests that for this to be meaningful both to community nurses and patients and carers, measures should specifically reflect their concerns about appropriate staffing and resources, such as appropriate time allocation for visits. There is potential for improving quality measures by involving all stakeholders, including patients and front-line staff more effectively, as required for effective outcome-based commissioning. This can be achieved by using more innovative ways of assessing service quality, such as incorporating real-life patient case studies and by consulting staff at each stage of the commissioning cycle. Extended contract time scales currently being discussed by NHSE should facilitate improved engagement with front-line staff, patients and carers in quality assessment. Personalised care planning may present an opportunity to further develop patient-derived goals that could be used as health-care outcomes for community nursing service quality measurement. Although problems with connectivity continue to impede the use of IT for the purposes of data collection in community nursing, in time, new technologies are likely to promote ease of data collection alongside clinical record keeping and could also be used to bring about collaboration across providers in the community.
Acknowledgements
We wish to acknowledge gratefully the valuable support we received from a range of sources that enabled us to complete this project in a timely manner.
Research facilitation and participation
We are extremely grateful to all the individuals in our case study sites who facilitated our access to the participating organisations and to all our participants for the time they generously gave us and their willingness to share their views.
Stakeholder engagement events
The opportunity to include in our final report stakeholder feedback about our findings and draft good practice guidance considerably enhanced our study. We would therefore like to thank all those delegates who took the time and trouble to attend the stakeholder engagement events in support of the project.
Special thanks to Martin Howard, who brought to bear his invaluable expertise and experience in advising and assisting with the facilitation of the workshops.
Service user reference group
We also wish to thank the members of SURG – Geoff Loydon, Joan Bayliss, Jill Boreham, Christine Donald and Enid Smith – who provided us with pertinent advice throughout the project, which helped to ensure that our study processes and discussion of findings incorporated and reflected service user perspectives.
Colleagues
Our thanks also go to Katalin Bagi and Claire Chappell for their sterling support with the financial management of the project throughout its duration, and to Jo Hartland and Paul Roy from the Avon Primary Care Research Collaborative management who were always available for consultation and advice when we needed it.
Study Steering Committee
Finally, we are indebted to our Study Steering Committee members whose considered and judicious advice helped us to maintain and refine focus at key stages of the project.
Contributions of authors
Sue Horrocks (chief investigator) participated in the conception and initial design of the project, contributed to data collection and analysis of both the quantitative and qualitative data and was lead author for the final report.
Katherine Pollard (project manager) contributed to data collection and analysis of both the quantitative and qualitative data, co-led the facilitation of the stakeholder engagement events and contributed to writing the final report.
Lorna Duncan contributed to data collection and analysis of both the quantitative and qualitative data, helped with the facilitation of the stakeholder engagement events and contributed to writing the final report.
Christina Petsoulas contributed to data collection and analysis of the qualitative data, helped with the facilitation of the stakeholder engagement events and contributed to writing the final report.
Emma Gibbard contributed to the design of the project, analysis of the qualitative data, co-led the facilitation of the stakeholder engagement events and contributed to writing the final report.
Jane Cook contributed to the design of the project, analysis of both the quantitative and qualitative data, helped with the facilitation of the stakeholder engagement events and contributed to writing the final report.
Ruth McDonald participated in the conception and initial design of the project, provided material for the final report and helped to revise it for intellectual content.
Lesley Wye contributed to the design of the project and to analysis of the quantitative data, as well as helping to revise the report for intellectual content.
Pauline Allen participated in the conception and initial design of the project, contributed to higher level data analysis, provided material for the final report and helped to revise it for intellectual content.
Pete Husband (service user) participated in the conception and initial design of the project, chaired the project SURG, provided material for the final report and helped to revise it for intellectual content.
Lizanne Harland participated in the conception and initial design of the project, contributed to the analysis of the quantitative data, helped facilitate the stakeholder engagement events, provided material for the final report and helped to revise it for intellectual content.
Ailsa Cameron contributed to the design of the project, provided input to the conduct of the study and helped to revise the report for intellectual content.
Chris Salisbury contributed to the design of the project and the grant proposal, provided input to the conduct of the study and helped to revise the final report for intellectual content.
Publications
Cook J, Horrocks S, Gibbard E, Harland L, Wye L. How commissioning affects community nursing. Nurs Times 2015;111:18–21.
Cook J, Horrocks S. Community nursing quality indicators for end-of-life care in England: identification, preparation, and coordination. Br J Community Nurs 2016;21:119–23.
Petsoulas C, Allen P, Horrocks S, Pollard P, Duncan L, Gibbard E, et al. Using contractual incentives in district nursing in the English NHS: results from a qualitative study. Public Money Manage 2018;38:223–32.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Kennedy I. Learning From Bristol: The Report of the Public Inquiry Into Children’s Heart Surgery at the Bristol Royal Infirmary 1984–1995. London: HMSO; 2001.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary. London: The Stationery Office; 2013.
- NHS England . The 6Cs and Compassion in Practice 2012. www.england.nhs.uk/6cs/ (accessed 31 October 2016).
- Quality with Compassion: The Future of Nursing Education. London: Royal College of Nursing; 2012.
- Code of Conduct: Professional Standards of Practice and Behaviour for Nurses and Midwives. London: NMC; 2015.
- Imison C. Shaping PCT Provider Services. The Future for Community Health. London: The King’s Fund; 2009.
- Thomas LM, Reynolds T, O’Brien L. Innovation and change: shaping district nursing services to meet the needs of primary health care. J Nurs Manag 2006;14:447-54. https://doi.org/10.1111/j.1365-2934.2006.00686.x.
- Edwards M. A nursing perspective. London J Prim Care 2008;1. https://doi.org/10.1080/17571472.2008.11493192.
- While A. Measuring productivity within community nursing. Br J Community Nurs 2008;13. https://doi.org/10.12968/bjcn.2008.13.4.29029.
- Transforming Community Services . Demonstrating and Measuring Achievement: Community Indicators for Quality Improvement 2011. www.gov.uk/government/uploads/system/uploads/attachment_data/file/215624/dh_126111.pdf (accessed 1 December 2016).
- Foot C, Sonola L, Bennett L, Fitzsimons B, Raleigh V, Gregory S. Managing Quality in Community Health Care Services. London: The King’s Fund; 2014.
- Higginson I. Quality of care and evaluating services. Int Rev Psychiatry 1994;6:5-14. https://doi.org/10.3109/09540269409025239.
- Horrocks S, Cook J, Ashton N, Wye L. Made to measure? Assessing feasibility of quality indicators for district nursing. Br J Community Nurs 2012;17:28-34. https://doi.org/10.12968/bjcn.2012.17.Sup9.S28.
- NHS Institute for Innovation and Improvement . Productive Community Services: Releasing Time to Care 2009. http://webarchive.nationalarchives.gov.uk/20101121150230/https://www.institute.nhs.uk/quality_and_value/productivity_series/productive_community_services.html (accessed 25 January 2018).
- Measuring for Quality in Health and Social Care: An RCN Position Statement. London: RCN; 2009.
- NHS Digital . Community Information Data Set 2012. http://content.digital.nhs.uk/comminfodataset (accessed 5 May 2017).
- National Institute for Health and Care Excellence . Quality Standards and Indicators n.d. www.nice.org.uk/standards-and-indicators (accessed 6 December 2016).
- Davies P, Wye L, Horrocks S, Salisbury C, Sharp D. Developing quality indicators for community services: the case of district nursing. Qual Prim Care 2011;19:155-66.
- Donabedian A. The quality of care. How can it be assessed?. JAMA 1988;260:1743-8. https://doi.org/10.1001/jama.1988.03410120089033.
- Maxwell RJ. Dimensions of quality revisited: from thought to action. Qual Health Care 1992;1:171-7. https://doi.org/10.1136/qshc.1.3.171.
- Campbell SM, Roland MO, Buetow SA. Defining quality of care. Soc Sci Med 2000;51:1611-25. https://doi.org/10.1016/S0277-9536(00)00057-5.
- Mainz J. Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care 2003;15:i5-11. https://doi.org/10.1093/intqhc/mzg084.
- High Quality Care for All. NHS Next Stage Review Final Report. London: Department of Health and Social Care; 2008.
- NHS England . Commissioning for Quality and Innovation (CQUIN): 2014 15 Guidance 2014. www.england.nhs.uk/wp-content/uploads/2014/12/sc-cquin-guid.pdf (accessed 25 January 2018).
- McDonald R, Zaide S, Todd S, Konteh F, Hussain K, Brown S, et al. Evaluation of the Commissioning for Quality and Innovation Framework: Final Report n.d. http://hrep.lshtm.ac.uk/publications/CQUIN_Evaluation_Final_Feb2013-1.pdf (accessed 26 January 2018).
- Health and Social Care Act. London: The Stationery Office; 2012.
- The NHS Outcomes Framework 2015/16. London: Department of Health and Social Care; 2014.
- NHS England . 2014/15/NHS/Standard/Contract 2014. www.england.nhs.uk/nhs-standard-contract/14-15/ (accessed 25 January 2018).
- Livingstone C, Wolper S, Rogers T. Improving efficiency and safety for patients who are unable to self-administer insulin. Br J Community Nurs 2013;18:476-81. https://doi.org/10.12968/bjcn.2013.18.10.476.
- Openness and Honesty When Things Go Wrong: The Professional Duty of Candour. London: NMC; 2015.
- Care Quality Commission . About Us: What We Do and How We Do It 2013. www.cqc.org.uk/sites/default/files/20170504_CQC_About-us.pdf (accessed 4 May 2017).
- McDonald R, Cheraghi-Sohi S, Tickle M, Roland M, Doran T, Campbell S, et al. The Impact of Incentives on the Behaviour and Performance of Primary Care Professionals: Report for the National Institute for Health Research Service Delivery and Organisation Programme. London: National Institute for Health Research Service Delivery and Organisation programme; 2010.
- Campbell SM, Braspenning J, Hutchinson A, Marshall M. Research methods used in developing and applying quality indicators in primary care. Qual Saf Health Care 2002;11:358-64. https://doi.org/10.1136/qhc.11.4.358.
- Gillam SJ, Siriwardena AN, Steel N. Pay-for-performance in the United Kingdom: impact of the quality and outcomes framework: a systematic review. Ann Fam Med 2012;10:461-8. https://doi.org/10.1370/afm.1377.
- Rambur B, Vallett C, Cohen JA, Tarule JM. Metric-driven harm: an exploration of unintended consequences of performance measurement. Appl Nurs Res 2013;26:269-72. https://doi.org/10.1016/j.apnr.2013.09.001.
- Powell AA, White KM, Partin MR, Halek K, Christianson JB, Neil B, et al. Unintended consequences of implementing a national performance measurement system into local practice. J Gen Intern Med 2012;27:405-12. https://doi.org/10.1007/s11606-011-1906-3.
- Lester HE, Hannon KL, Campbell SM. Identifying unintended consequences of quality indicators: a qualitative study. BMJ Qual Saf 2011;20:1057-61. https://doi.org/10.1136/bmjqs.2010.048371.
- Power M, Fogarty M, Madsen J, Fenton K, Stewart K, Brotherton A, et al. Learning from the design and development of the NHS Safety Thermometer. Int J Qual Health Care 2014;26:287-97. https://doi.org/10.1093/intqhc/mzu043.
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/ourwork/futurenhs (accessed 1 December 2016).
- Department of Health and Social Care, Transforming Community Services Programme . Transforming Community Services: Ambition, Action, Achievement 2009. http://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_101425 (accessed 25 January 2018).
- Next Stage Review: Our Vision for Primary and Community Care. London: Department of Health and Social Care; 2008.
- Duffin C. Putting ambition into community services. Primary Health Care 2009;19:7-8. https://doi.org/10.7748/phc.19.7.7.s10.
- HM Treasury . Spending Round 2013 2013. www.gov.uk/government/uploads/system/uploads/attachment_data/file/209036/spending-round-2013-complete.pdf (accessed 25 January 2018).
- Monitor . Commissioning Better Community Services for NHS Patients 2015. www.gov.uk/government/uploads/system/uploads/attachment_data/file/397429/Improving_community_services.pdf (accessed 26 January 2018).
- Better Care Fund . How to . . . Understand and Measure Impact 2015. www.england.nhs.uk/wp-content/uploads/2015/06/bcf-user-guide-04.pdf.pdf (accessed 26 January 2018).
- Goodman C, Drennan V, Scheibl F, Shah D, Manthorpe J, Gage H, et al. Models of inter professional working for older people living at home: a survey and review of the local strategies of English health and social care statutory organisations. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-337.
- Haycock-Stuart E, Kean S. Does nursing leadership affect the quality of care in the community setting?. J Nurs Manag 2012;20:372-81. https://doi.org/10.1111/j.1365-2834.2011.01309.x.
- The Queen’s Nursing Institute . Developing a National District Nursing Workforce Planning Framework 2014. www.qni.org.uk/wp-content/uploads/2016/09/district_nursing_workforce_planning_report.pdf (accessed 26 January 2018).
- Sprinks J. District nurse posts being axed despite push for community care. Nurs Stand 2012;26. https://doi.org/10.7748/ns2012.05.26.36.11.p8273.
- Community Nursing: Transforming Health Care. London: RCN; 2011.
- A Workforce in Crisis? The UK Nursing Labour Market Review. London: RCN; 2015.
- District Nursing – Harnessing the Potential. The RCN’s UK Position on District Nursing. London: RCN; 2013.
- NHS England . Framework for Commissioning Community Nursing 2015. www.england.nhs.uk/wp-content/uploads/2015/10/Framework-for-commissioning-community-nursing.pdf (accessed 26 January 2018).
- Pender S, Pearce F. End of life care community services. J Community Nurs 2012;26:4-6.
- Lee CY, Beanland C, Goeman D, Johnson A, Thorn J, Koch S, et al. Evaluation of a support worker role, within a nurse delegation and supervision model, for provision of medicines support for older people living at home: the Workforce Innovation for Safe and Effective (WISE) Medicines Care study. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1120-9.
- Quinn D, Adams J. Developing a community multiple sclerosis nursing service. Nurs Stand 2014;28:46-50. https://doi.org/10.7748/ns.28.37.46.e8293.
- Nancarrow SA. Barriers to the routine collection of health outcome data in an Australian community care organization. J Multidiscip Healthc 2013;6:1-16. https://doi.org/10.2147/JMDH.S37727.
- Blockley D, Large L, Spencer L, Rashid C. Transforming community leg ulcer services. J Community Nurs 2011;25:20-4.
- Bowers B, Pellett C. Measuring the clinical effectiveness of district nurses. Br J Community Nurs 2013;18:332-7. https://doi.org/10.12968/bjcn.2013.18.7.332.
- Cresswell J. Research Design, Qualitative, Quantitative and Mixed Methods Approaches. Thousand Oaks, CA: Sage Publications; 2003.
- Yin R. Case Study Research Design and Methods. Thousand Oaks, CA: Sage Publications; 2009.
- Cresswell J. Qualitative Inquiry and Research Design: Choosing Among Five Traditions. Thousand Oaks, CA: Sage Publications; 1998.
- Franco LM, Bennett S, Kanfer R. Health sector reform and public sector health worker motivation: a conceptual framework. Soc Sci Med 2002;54:1255-66. https://doi.org/10.1016/S0277-9536(01)00094-6.
- Bowling A. Research Methods in Health: Investigating Methods In Health. Maidenhead: Open University Press; 2014.
- Allen P, Keen J, Wright J, Dempster P, Townsend J, Hutchings A, et al. Investigating the governance of autonomous public hospitals in England: multi-site case study of NHS foundation trusts. J Health Serv Res Policy 2012;17:94-100. https://doi.org/10.1258/jhsrp.2011.011046.
- Brewer JD. Ethnography. Buckingham and Philadelphia, PA: Open University Press; 2000.
- Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage Publications; 2007.
- Prior M, Guerin M, Grimmer-Somers K. The effectiveness of clinical guideline implementation strategies–a synthesis of systematic review findings. J Eval Clin Pract 2008;14:888-97. https://doi.org/10.1111/j.1365-2753.2008.01014.x.
- London S. Thinking Together: The Power of Deliberative Dialogue 2016. www.scottlondon.com/reports/dialogue.html (accessed 26 January 2018).
- Davidson P, Halcomb E, Hickman L, Phillips J, Graham B. Beyond the rhetoric: what do we mean by a ‘model of care’?. Aust J Adv Nurs 2006;23:47-55.
- Hazell W. Analysis: CQC Ratings Align With Staff Satisfaction 2015. www.hsj.co.uk/home/analysis-cqc-ratings-align-with-staff-satisfaction/5085358.article (accessed 26 January 2018).
- Rafferty A, Philippou J, Fitzpatrick J, Ball J. ‘Culture of Care’ Barometer: Report to NHS England on Development and Validation of an Instrument to Measure ‘Culture of Care’ in NHS Trusts. London: King’s College London (National Nursing Research Unit); 2015.
- Ball J, Philippou J, Pike G, Sethi G. Survey of District and Community Nurses in 2013: Report to the Royal College of Nursing. London: King’s College London; 2014.
- Doran GT. There’s a S.M.A.R.T. way to write management’s goals and objectives. AMA Forum 1981;70:35-6.
- Maybin J, Charles A, Honeyman M. Understanding Quality in District Nursing Services: Learning from Patients, Carers and Staff. London: The King’s Fund; 2016.
- Ignatowicz A, Greenfield G, Pappas Y, Car J, Majeed A, Harris M. Achieving provider engagement: providers’ perceptions of implementing and delivering integrated care. Qual Health Res 2014;24:1711-20. https://doi.org/10.1177/1049732314549024.
- Vize R. The Revolution Will Be Improvised: Stories and Insights About Transforming Systems 2014. http://leadershipforchange.org.uk/the-revolution-will-be-improvised/ (accessed 5 May 2017).
- Humphries R. Integrated health and social care in England – progress and prospects. Health Policy 2015;119:856-9. https://doi.org/10.1016/j.healthpol.2015.04.010.
- Richardson C, Percy M, Hughes J. Nursing therapeutics: teaching student nurses care, compassion and empathy. Nurse Educ Today 2015;35:e1-5. https://doi.org/10.1016/j.nedt.2015.01.016.
- Stoddart KM. Social meanings and understandings in patient-nurse interaction in the community practice setting: a grounded theory study. BMC Nurs 2012;11. https://doi.org/10.1186/1472-6955-11-14.
- Moule P, Pollard K, Clarke J, Fear C, Lawson B, Thompson R, et al. An integrated approach for individualised support: carers’ views. J Integr Care 2014;22. https://doi.org/10.1108/JICA-09-2014-0034.
- Donskoy AL, Pollard K, Thomas J, Pollard K, Sellman D. Interprofessional Working in Health and Social Care: Professional Perspectives. Basingstoke: Palgrave Macmillan; 2014.
- Mackintosh N, Sandall J. Overcoming gendered and professional hierarchies in order to facilitate escalation of care in emergency situations: the role of standardised communication protocols. Soc Sci Med 2010;71:1683-6. https://doi.org/10.1016/j.socscimed.2010.07.037.
- Parayitam S, Kiran J, Desai MS, Eason MK. Computer attitude as a moderator in the relationship between computer anxiety, satisfaction, and stress. Comput Human Behav 2010;26:345-52. https://doi.org/10.1016/j.chb.2009.11.005.
- Marshall S, Haywood K, Fitzpatrick R. Impact of patient-reported outcome measures on routine practice: a structured review. J Eval Clin Pract 2006;12:559-68. https://doi.org/10.1111/j.1365-2753.2006.00650.x.
- Lagarde M, Wright M, Nossiter J, Mays N. Challenges of Payment-For-Performance in Healthcare and Other Public Services: Design, Implementation and Evaluation 2013. http://researchonline.lshtm.ac.uk/2478790/1/Challenges%20of%20payment%20for%20performance%20in%20healthcare%20and%20other%20public%20services%20final.pdf (accessed 6 December 2016).
- NHS England . CQUIN 2016 17 Guidance 2015. www.england.nhs.uk/nhs-standard-contract/cquin/cquin-16-17/ (accessed 26 January 2018).
- Griffiths P. Can We Measure the Quality of Nursing? 2012. www.health.org.uk/newsletter/can-we-measure-quality-nursing (accessed 26 January 2018).
- Maben J, Morrow E, Ball J, Robert G, Griffiths P. High Quality Care Metrics for Nursing. London: National Nursing Research Unit, King’s College London; 2012.
- Helm C, Bungeroth L. Safe and Effective Staffing: The Real Picture. UK Policy Report. London: RCN; 2017.
- Safe Staffing Levels – A National Imperative. The UK Nursing Labour Market Review 2013. London: RCN; 2013.
- Gray BH, Sarnak DO, Burgers JS. Home Care by Self-Governing Nursing Teams: The Netherlands’ Buurtzorg Model. New York, NY: The Commonwealth Fund; 2015.
- Edwards N. Community Services: How They Can Transform Care. London: The King’s Fund; 2014.
- NHS England . Delivering the Forward View: NHS Planning Guidance 2016 17–2020 21 n.d. www.england.nhs.uk/wp-content/uploads/2015/12/planning-guid-16-17-20-21.pdf (accessed 29 January 2018).
- Allen P, Hughes D, Vincent-Jones P, Petsoulas C, Doheny S, Roberts JA. Public contracts as accountability mechanisms: assuring quality in public health care in England and Wales. Public Manage Rev 2016;18:20-39. https://doi.org/10.1080/14719037.2014.957341.
- Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med 2002;18:141-58. https://doi.org/10.1016/S0749-0690(02)00002-2.
- Bolton J. Emerging Practice in Outcome-Based Commissioning for Social Care: A Discussion Paper 2015. https://ipc.brookes.ac.uk/publications/John_Bolton_Outcome_Based_Commissioning_Paper_April_2015.pdf (accessed 26 January 2018).
- Alderwick H, Dunn P, McKenna H, Walsh N, Ham C. Sustainability and Transformation Plans in the NHS: How Are They Being Developed in Practice 2016. www.kingsfund.org.uk/sites/default/files/field/field_publication_file/STPs_in_NHS_Kings_Fund_Nov_2016.pdf (accessed 26 January 2018).
- NHS Improvement . How We Work n.d. https://improvement.nhs.uk/about-us/how-we-work/ (accessed 29 January 2018).
- McHugh MD, Stimpfel AW. Nurse reported quality of care: a measure of hospital quality. Res Nurs Health 2012;35:566-75. https://doi.org/10.1002/nur.21503.
- Public Services (Social Value) Act 2012. London: The Stationery Office; 2012.
Appendix 1 Literature review: search strategy
We used a two-strand approach to review the literature. We drew on the expertise of the research management group in their particular fields of community nursing, commissioning, NHS contracts and quality measurement (including incentivised quality schemes), to identify salient research and policy papers related to quality measurement in community nursing. We also drew on the QNI, RCN and The King’s Fund for salient reports and papers.
We then conducted a structured search of the literature referring to community nursing provision in England and in countries with similar health-care systems. We placed emphasis on studies conducted relatively recently (i.e. after 2011), but we did not exclude older publications (going back to 2009). We included studies or publications on measuring quality in community nursing and focused on care provision for adults at home. We excluded studies that focused on institutionalised care, mental health care provision or learning disabilities, as well as on children and young people care provision. Table 17 included the databases searched.
| Source | Year (n) | |
|---|---|---|
| 2015 | 2016 | |
| CINAHL Plus | 74 | 1 |
| HMIC | 1 | 0 |
| MEDLINE | 317 | 0 |
| EMBASE | 166 | 1 |
| Web of Science | 126 | 3 |
| Total | 684 | 5 |
The keywords we used were Measur* and quality and community services; quality and indicators and community services; Measur* and qual* and community nursing; Commission* and quality and community services; quality and indicators and measuring and community nursing; quality in community nursing; Commission* for Quality and Innovation.
After deleting duplicates we were left with 281 entries. After reading the abstracts we selected 23 papers for inclusion. We also searched grey literature and added a further three publications. We did not use an evaluation tool of the references we found, as this was an exploratory exercise to assess the extent of the coverage that the issue of measuring quality in community nursing has received in the literature.
In June 2016, we updated the literature review by searching the same databases with the same keywords for 2015–16. This yielded five articles, two of which were rejected after reading the abstracts and three of which were added to the review. Further searches were conducted to focus on specific quality CQUIN indicators, such as the NST and community nursing, to establish the range of research linked specifically to community nursing.
Appendix 2 Stakeholder engagement
Introduction
In this appendix we present the key discussion points from 10 stakeholder engagement events. Eight workshops and two facilitated conference sessions were held over the space of 4 months, from June to September 2016. The workshops were held in different cities across England: Birmingham, Bridgwater (Somerset), Bristol, Leeds, London, Nottingham, Southampton and York. The two conference sessions were in the programme for the conference ‘Community Nursing: Innovation and Transformation’ held in Leeds in July 2016 and for the QNI conference held in London in September 2016. Three or four different members of the research management group with a range of professional backgrounds, including a member of SURG, together with an independent consultant with expertise in group facilitation and commissioning, facilitated each event. After the first workshop, at least one facilitator at each event had been involved in a previous event.
The purpose of the stakeholder engagement events was to:
-
test the emerging findings from the case study sites to check our analyses and interpretation
-
review and improve draft good practice statements and identify further areas of good practice (see Appendices 3 and 4)
-
engage key stakeholders in our research and its outputs to enhance impact.
The workshops were designed to engage a mixed audience of commissioners, service managers, front-line staff, patients and carers, and involve them in a deliberative dialogue exercise. 69 This was achieved in the majority of the events, although, owing to practical reasons, the composition varied and not all stakeholders were represented at every workshop. The eight workshops were attended by a total of 120 delegates; attendance ranged from 10 to 27 individuals at a single event. All stakeholders were represented at three events; it proved impossible to recruit any patients or carers to three events and commissioners were not present at two other events. However, all of the workshops involved at least two of the three stakeholder groups targeted.
Each workshop lasted for 3 hours and followed the same format. Each started with short presentations to set the scene and context for the research. This typically included a keynote presentation focused on quality and community nursing delivered by a local quality or service lead, followed by a short presentation by a member of the research team on the what, why and how of the research. We emphasised here that the research focus was on the ‘how’, that is ‘how is quality measured?’, rather than the ‘what’, that is, ‘what does a good QI for community nursing look like?’ The next stage involved the use of deliberative dialogue,69 where participants worked in small groups to share, discuss and capture their thoughts, ideas and experiences in relation to four findings and associated good practice statements presented (see Boxes 1–4). Key points from these discussions were then fed back to the wider group for further consideration.
Each workshop was evaluated to seek feedback on format, quality of presentations and facilitation, as well as asking participants to identify an action they could take as a result of attending the workshop. The feedback from the first workshop was used to review and refine the workshop content and format for future events.
The two conferences had a greater focus on reaching community nurses. Twenty-four nurses attended the session at the conference held in Leeds and 122 took part in the session at the QNI conference. The conference sessions used the same presentation as the workshops and lasted for approximately 45 minutes. Owing to these time constraints, the discussions focused on one finding only (see Finding 1: indicators are not always fit for purpose). Owing to the scale of these conferences and the timings of the conference programmes, we were unable to evaluate the individual sessions.
The findings presented and discussed at the stakeholder engagement events were those that emerged from data collected through interviews and focus groups with commissioners, providers, front-line staff, patients and carers, across all five case studies. Owing to time constraints it was obviously not possible to offer the opportunity to delegates to discuss more than a few of the many findings which emerged from the study. The findings presented at the stakeholder engagement events were selected because they were consistent across all five sites and suitable for discussion by all stakeholder groups:
-
Not all indicators selected are fit for purpose as the selection process does not always involve all the right people.
-
Indicators rolled out from hospital settings often do not work well in community nursing settings.
-
Staff do not always receive adequate information about indicators either before or after they collect relevant data.
-
Quality in community nursing is hard to measure and a focus on collecting numbers does not give a true reflection of the service being delivered.
It was interesting to note that these findings were all challenges inherent in current processes. The draft good practice statements developed were based on the evidence collected from the case study sites.
To facilitate discussion in their small groups, participants were asked to consider the following questions:
-
Is this finding a key issue for you?
-
Do the good practice statements address this issue?
-
How could the good practice statements be put into practice?
-
How else could this issue be addressed?
Stakeholder discussions
In the following section, key points brought up during the stakeholder discussions at both the workshops and the conference sessions are presented for each of the four findings and their associated good practice statements (see Boxes 1–4). There were common messages and themes that emerged from these discussions which highlighted a degree of interdependency between the four findings.
Finding 1: indicators are not always fit for purpose (Box 1)
Most delegates agreed with this finding, feeling that it reflected their local context and situation. Those that did not fully identify with it had started to put in place processes to improve the level of involvement. However, it became apparent that some front-line staff were not even aware there was a process in place to identify and select QIs or CQUINs.
Reasons given for the importance of engaging and involving all the right stakeholders in the process of selection included the fact that different stakeholders bring different perceptions, expectations, experience and expertise to the process. Gaps in the involvement of some stakeholders, particularly front-line staff and patients and carers, were identified by delegates, reflecting the finding discussed. In addition, suggestions around who should be involved in the process included those working in interdependent organisations (primary, secondary and domiciliary care providers), researchers and experts in quality measurement. The involvement of community nurses in the selection process was proposed by participants as a mechanism to help improve the practical and clinical appropriateness of indicators selected and increase ownership and understanding among front-line staff of the importance of QIs.
Not all indicators selected are fit for purpose as the selection process does not always involve all the right people.
Good practice statements:
-
Actively engage and involve representatives from your key stakeholder groups, including commissioners, providers, community nurses, patients, carers and their representative organisations in the identification and selection of Qis.
-
Actively seek feedback from patients and their carers about their experience and the quality of care that they receive, to identify best medium/mechanism for reaching patients/carers, particularly those who are more vulnerable through frailty, lack of capacity, etc.
-
Be explicit about the intended goal of the QI.
A number of challenges and barriers were identified that could prevent active engagement with all stakeholders in indicator selection. These included the short time scales allowed for the selection process; the time and resources needed to engage and involve the relevant stakeholders; the availability of staff; the ability to engage patients who are often housebound, frail and/or lacking capacity; and the multiplicity of providers and commissioners. Ideas for improving the process and overcoming some of these challenges were put forward, some of which had already been put into practice locally. These included using tools, such as stakeholder analysis, to identify relevant stakeholders; starting the process earlier in the year to enable more time for involvement; holding specific workshops for stakeholder engagement or building it into existing fora; using existing data to identify areas for improvement and develop indicators; and providing staff with training about the processes involved in selecting QIs. There was a general feeling that a more bottom-up approach was needed and that this should utilise existing information, learning and feedback to identify areas for improvement.
Delegates agreed that it was important to actively seek feedback from patients and carers about the quality of the services they receive; there was a particular emphasis on consulting carers in some workshops. Associated barriers and challenges, in addition to the patient group characteristics identified above, included practicalities such as postage, time and resources to gather feedback; issues of representation and difficulties of engaging those who are seldom heard; and ethical issues and implications of staff collecting feedback from patients, including bias, fear of impact on their own care and the lack of anonymity.
There were a number of ideas and examples of current mechanisms that could be put into practice to help improve the engagement and involvement of patients and their carers. This included involving the voluntary sector, such as Healthwatch, to represent the patient voice and to use volunteers to collect feedback from patients. Utilising existing patient groups, such as patient participation groups in general practices, or establishing new patient reference groups were also suggested together with specific events for carers such as carer roadshows. It was also thought that 360-degree feedback could be built into existing processes (e.g. staff and student appraisals), and also that social media could be an effective tool for engagement. There was a strong message from delegates that patients and their carers should be involved throughout their care, from the co-design of services to the selection of QIs, as well as participating in care planning and goal-setting.
There was agreement that there needs to be greater clarity around the purpose and goal of indicators selected. Concerns were raised around the current focus of QIs with participants questioning whether or not they actually measure quality. There was recognition that indicators tend to be more task focused than outcome focused which has possible unintended consequences on care and makes many of them feel like a tick-box exercise. It was suggested that indicators currently focus more on money, organisational or commissioner issues rather than those important to patients; they are thought to tend to be used to judge the quality of care, not to improve it.
There was a consistent message that indicators need to be more person centred, with a greater focus on individual patients’ goals and also to be outcome focused. In particular, the point was made that one size does not fit all. The level of the organisation at which indicators are set was also raised as an issue, suggesting that this should be more at the micro, patient, clinical or local level. It was felt that this could be achieved through the involvement of patients in their care planning, using patient-reported outcome measures and goal-setting tools as an indicator of quality.
As in our wider study data, some of the workshop attendees highlighted the lack of a national suite of outcome measures to facilitate benchmarking. The facilitators noted that there was a lack of awareness of existing Pick Lists and menus of QIs in some of the workshops, even among commissioner attendees. This desire for benchmarking raises a potential tension between developing a bottom-up, patient-centred approach and the advantages of having a shared national suite of indicators.
In terms of the good practice statements, the issue of definitions was raised with regard to some of the terminology used. It was suggested that there needed to be more clarity around what is meant by ‘involvement and engagement’ and what is meant by ‘fit for purpose’.
Finding 2: quality indicators that work in acute settings are not necessarily suitable for community (Box 2)
Workshop participants were quick to identify QIs that matched this finding, citing the FFT, NST, staff well-being and falls CQUINs as examples. There were discussions around the origins and drivers for these indicators and it was noted that many of them had been set at a national level for acute settings, provoking the question of how to raise the community service profile so as to influence the national level. An example related to the staff well-being CQUIN target set for 2016/17. This CQUIN obliges provider organisations to ensure that healthy eating options are available to staff at all times, an unrealistic target in community settings.
As found in our interview data, the workshop participants felt that contextual differences were an important factor to successful indicator implementation. Examples given of the difference in context included environmental factors (a person’s home vs. hospital), interdependencies with other services (whole systems) and associated differing power bases, nursing caseloads and IT systems.
A lack of consideration of the contextual differences was often perceived to hinder the successful implementation and usefulness of indicators. Suggestions made for overcoming these barriers included providing flexibility and time to adapt indicators to the community setting, with an idea of working in partnership with the acute sector. This would need to take into account the local environment, patient needs, local service provision, IT and data collection methods/systems (utilising existing data and data collection methods). An example was given of where the development of leaders and champions for the PU QI had improved compliance in data collection and outcomes. Other suggestions included improvements in communication and IT/information sharing.
Indicators rolled out from hospital settings often do not work well in community nursing settings.
Good practice statements:
-
Ensure that the indicators selected are appropriate for the context within which they are to be applied.
-
Staff must have ownership of the indicator and feel that it is valid as an indicator of their service quality.
-
Ensure that the indicators selected are SMART.
-
Limit the total number of quality of indicators as appropriate to the setting within which they are being implemented.
Participants agreed with the good practice statement that staff need to feel they have ownership of the indicators and that it reflects the service and quality of care being delivered. Some attendees went further, suggesting that information should also be provided to help understand what is working well, share best practice and identify areas for improvement. Discussion linked back to the importance of involving front-line staff in the selection and design of the QIs to facilitate this and the need for data to be relevant and easy to collect, as well as being more person centred.
There was some difference of opinion about whether or not using the SMART acronym was appropriate or even feasible. Concerns were raised around how certain elements of care and the human experience could be measured. Participants provided alternative suggestions, from a revision of the SMART acronym to refocusing an indicator on patient-centred outcome measures. Many agreed that indicators need to be measurable, that the data need to be easy to collect and should utilise both quantitative and qualitative information, including feedback from patients. These opinions all reflect the wider study findings.
Most delegates agreed that it was a good idea to limit the number of QIs. Those that expressed some uncertainty about this statement raised concerns about possible tensions between setting a limit and comprehensively addressing quality issues appropriately.
Finding 3: front-line staff do not receive adequate information about quality indicators (Box 3)
Front-line staff felt that finding 3 resonated with them, with many stating that they often do not receive information about QIs before they are implemented, nor do they receive feedback about how the data they have collected are used. It was clear from the workshops that the understanding of QIs, the consequences of not meeting indicator targets and the awareness of the processes involved in indicator selection and application varied among front-line staff attending. It was generally felt that the issue identified in this finding needs to be addressed.
It was also agreed that there should be feedback mechanisms in place for staff that are timely, relevant, meaningful, open and transparent. Delegates at one workshop suggested that there should be a cycle of involving staff in indicator selection, preparation for data collection, data collection and general feedback. Issues that emerged during discussion included some of the current challenges of data collection (e.g. the time required to collect data and the impact this can have on front-line nurses’ workload). It was also felt that there was often a lack of clarity around the purpose or importance of the data being requested, as well as issues with data quality and IT solutions. These opinions all agreed with the study’s wider interview and focus group data.
Staff do not always receive adequate information about indicators either before or after they collect relevant data.
Good practice statements:
-
Staff who are going to collect data for an indicator should be fully informed well beforehand about what they have to collect, why they are doing so and what will happen to the information they gather.
-
Make sure that front-line staff receive regular and accessible feedback about how data they collect are used and present them with findings so that they can see the usefulness of an indicator in relation to their patients.
-
Invest in streamlining communication systems between different organisations and sectors.
Improving the ownership of indicators was seen as an important step to improving the implementation and usefulness of indicators. It was agreed that nurses need to recognise them as an important mechanism in enabling the delivery of high-quality care. Participants suggested that ensuring indicators have a clear purpose that links back to the patient, service specification, quality domains, key strategic objectives and the NHS constitution, would improve ownership and make it easier for community nurses to understand why they are important. Greater clarity around the importance of the data to be collected and how it would be used was also needed. Use of protected learning time and ‘softer’ intelligence, where staff are given the opportunity each quarter to ask ‘how are things going?’, as well as more time allowed for implementation, engagement and feedback, was suggested as a good way to improve staff understanding of, and engagement with, indicator processes. An example was given by one of the delegates of using a team meeting to share information about an indicator with staff, with subsequent improvement in the amount and quality of indicator data collected.
Communication and information sharing was a strong theme across all the discussions. Participants reflected that there needs to be improved communication between and within organisations around QIs. There were examples given of where organisations had tried to address information sharing and communication through improving IT. This included open access to team folders and organisational dashboards, building into existing mechanisms such as community nurse fora, team meetings, clinical updates, newsletters and websites. Other examples included introducing new mechanisms such as quality boards in community offices, developing champions, using supervision time and embedding relevant information into induction processes. IT was seen as barrier to and a facilitator of this, with examples such as access to team folders seen as a solution, but lack of information and data sharing, particularly where there were interdependent agencies, acting as a barrier.
There were some concerns around the wording of these good practice statements, in that delegates felt that they represented staff as being slightly ‘done to’ rather than as partners in the process. This links back to the need to ensure staff feel engaged and involved in the whole process rather than just an agent for data collection.
Finding 4: not all aspects of nursing care are easy to measure (Box 4)
Although the majority of attendees agreed with finding 4, in two workshops there was some disagreement around whether or not quality is hard to measure. One argument related to the fact that it is possible to measure the improvement in a patient’s health (e.g. if a PU resolves then this is measurable). However, other delegates raised the difficulty of measuring the emotional or human element of care.
Quality in community nursing is hard to measure and a focus on collecting numbers does not give a true reflection of the service being delivered.
Good practice statements:
-
Consider using a mixture of numbers and narrative including a case study approach that involves patients and carers directly.
-
Ensure that the right information is collected to help measure progress towards achievement of an indicator.
There was general agreement that using a mixture of both quantitative and qualitative data (also referred to as ‘hard’ and ‘soft’ or ‘numbers’ and ‘narrative’), gave a better understanding of quality of care. Some front-line staff attendees offered examples of situations where they felt they had been able to provide really good care to patients; however, as this care depended to a considerable extent on the nurses’ skilful use of empathic perception and/or interpersonal skills, it had not been possible for them to record either the care given or the outcome so that this information could feed into the formal quality monitoring process. Delegates at one workshop raised the difficulty in quantifying quality, with those at another noting that quality has a ‘qual’ in it as in ‘qualitative’. In some workshops this finding led back to previous discussions around the focus of QIs. Participants reiterated the need for a greater focus on person-centred goals and outcomes to support quality improvement, feeling that this in turn would influence the type of data collected.
There were challenges considered and barriers identified to achieving more comprehensive data on the quality of community nursing care. These included the lack of skills, resources and time to support data collection and analysis; issues with IT and current data collection and feedback mechanisms; and also the long-term nature of some goals.
To help implement good practice, a number of ideas were put forward primarily focused on the collection of qualitative data, linking back to ideas proposed for collecting feedback from patients. This ranged from utilising existing data and data collection mechanisms such as case note audits, peer review and ‘deep dives’ to using policy-drivers such as the Social Value Act 2012 as a lever. 101 The involvement of the voluntary sector and volunteers in data collection was again raised as a possibility, alongside holding focus groups and collecting patient stories and case studies. The importance of finding ways to capture staff feedback was also noted and suggestions included utilising reflective practice and revalidation processes. There were examples given where patients had been invited in to share their stories and experiences at team meetings or as part of a focus group and it was thought that these had been valuable processes.
Attendees re-emphasised the need for data collection to be simple and where possible, to utilise existing data and systems. In one workshop, however, there was a suggestion that there needed to be a shift in focus from data collection to good record keeping.
It was suggested that the word ‘consider’ should be removed from the first good practice statement, as it was felt that quality measurement should always involve mixed methods. Although participants agreed in principle with the good practice statement that ‘data collected is of high quality’, discussions raised the issue of the meaning of high-quality data. It was felt that this would need further description or definition within the good practice statement, as ‘quality’ means different things to different people. Some of the descriptions offered by delegates of data that might be seen as ‘high quality’ included their being robust, validated or triangulated.
Cross-cutting themes
A number of cross-cutting themes emerged from discussions that reflected many of the challenges currently affecting community nursing. 75 These included issues around recruitment and retention, changing caseloads and increasing workload; the impact of indicator data collection on staff workload and the time available to care for patients; the interdependency of nursing services on other services and the move towards integration of care; the challenges with time scales, IT and documentation; and the lack of communication, engagement and training around QIs with front-line staff. All of these themes reflect our wider study data.
Interestingly, discussion also highlighted the relationship between the four findings presented, with interdependencies noted between all of them. There was a consistent message that the appropriate involvement of the right people, good communication throughout the process and clarity of purpose would address many of the challenges presented within the findings. Another common message was the need to change the focus of indicators to concentrate more closely on patients and their outcomes, together with a focus on improvement rather than judgement.
Workshop evaluation
Eighty-eight evaluation forms were completed across the eight workshops, on 84 (95.45%) of which the workshop was rated overall as either excellent or good. Sixty participants identified an action they could take forward following the workshop. These included:
Evolve CQUIN differently from now on – with those who will be collecting/involved in the indicator collection.
As a commissioner, ensure that development of outcome measures is carried out collaboratively.
Think about greater use of PROMs [patient-reported outcome measures].
Review the research when available, discuss with colleagues.
The research team felt that holding the workshops was a very valuable exercise, as it enabled testing of some of our study findings with wider stakeholder groups, as well as enhancing the quality of the good practice guidance developed following data analysis. However, it was also noted that this series of stakeholder engagement events was extremely resource intensive. In particular, administrative input into the process was substantial. It is recommended that funding for these valuable engagement activities needs to be properly estimated in grant applications submitted to funders.
Summary
Through these events we have reached and engaged with > 260 people, with 120 participants attending the eight workshops together with 146 people in attendance at the conference presentations.
The discussions at the stakeholder engagement events were very useful. First, they not only revealed that the four study findings presented reflected attendees’ views of their local experiences, but also confirmed some of the wider study findings not presented at these events. This suggests that our analysis and interpretation of our study data are accurate and that our findings transfer to other areas of the country. It was notable that none of the attendees found our findings surprising. In turn, the facilitators of the events reflected that the additional information emerging from the discussions did not reveal anything unexpected.
Second, workshop attendees’ feedback confirmed that the good practice statements were reflective of the findings and addressed the key issues. Useful suggestions for improvements were made and these have been incorporated into the final version of the good practice guidance (see Appendix 4). Focusing discussion on how the good practice statements could be implemented helped to identify some of the challenges and possible solutions, enabling delegates to share good practice within their own organisations, which further informed the good practice statements.
The workshops were very positively evaluated and undoubtedly enhanced the robustness of the study findings as well as the good practice guidance developed as a study output. However, they were extremely resource intensive, particularly in terms of administrative input; the cost of such initiatives needs to be properly estimated in grant applications to funders.
Appendix 3 Development of the good practice guidance
The paper below drew on pertinent recent literature and preliminary analyses of data from providers, commissioners, front-line staff, patients and carers. The formulation of this paper was the initial starting point for the development of the good practice guidance.
Appendix 4 Good practice guidance for selecting and applying quality indicators in community nursing
Selection
-
Start the process early to enable time to identify, engage and involve stakeholders in the identification and selection of QIs. Consider starting with the co-design and co-production of service specifications as this will inform the development of person-centred QIs.
-
Actively engage and involve representatives from key stakeholder groups. This may include commissioners, providers, community nurses and other clinicians across all grades, patients, formal and informal carers and their representative organisations, researchers and academics, as well as experts in measurement such as health economists and data analysts.
-
Involve front-line staff in the selection and design of QIs as this will improve ownership and understanding, and ensure that it is a valid indicator of service quality and can be used to improve it.
-
Use information from existing data and learning from previous QIs and link back to service specifications to help inform indicator identification and selection.
-
Be explicit about the purpose and intended goal of a QI. Ensure that the focus is on improving the quality of services and consider using person-centred outcomes.
-
When selecting indicators consider both the intended and possible unintended consequences.
Application
-
Ensure that the total number of QIs is appropriate for the setting within which they are to be implemented and that they link back to the service specification.
-
Avoid introducing too many simple processes which, when all combined, result in an overcomplicated process for staff on the ground.
-
Ensure that the indicators selected are appropriate for the context within which they are to be applied. Take account of individual patients’ needs, the care environment, the current infrastructure (including IT), resources and existing data, as well as the knowledge and skills available.
-
Consider using indicators that are SMART.
-
Develop clear communication and engagement plans to support the identification and delivery of QIs.
-
Make sure all those involved in collecting data, including front-line community nursing staff, are fully engaged in the process and informed well beforehand about what data they have to collect, why they are doing so and what will happen to the information they gather.
-
Make sure that all stakeholders involved in the process, particularly front-line staff, receive timely, regular and accessible feedback about data collected and resulting findings so that these can inform further quality improvement.
-
Invest in streamlining communication systems between different organisations and sectors.
Usefulness
-
Ensure that the right information (data) is collected to help measure progress towards achievement of an indicator.
-
Capture the true quality of the service by varying how it is measured – consider using a mixture of both numbers (quantitative) and narrative (qualitative) data, including case studies and patient stories that involve patients and carers directly.
-
Ensure that the indicator is fit for purpose (i.e. that the intended benefit is being produced).
-
Ensure that the right measures are selected to reflect the goal and consider use of proxy measures for those with long-term outcomes.
Ensure that the data collected reaches an agreed standard and has been validated and triangulated where possible. Consider providing education and training to staff to support data entry, data collection, the understanding of quality and QIs, quality improvement, clinical audit and evaluation.
Appendix 5 Instruments used to collect data from commissioners, provider managers and front-line staff
Interview schedule for commissioners
The interviewer will typically follow each question with additional supplementary questions in order to obtain a clear, in-depth understanding of the interviewee’s answer. Each interview will start by asking the participant for the title of their current post and the length of time for which the post has been held.
Question 1: you kindly provided details of your local QI scheme for our survey. Can I just check we have the correct details please? (Show scheme.)
Question 2a: please could you walk me through the process you go through to identify and select QIs for community nursing?
Question 2b: what were the drivers influencing this process?
Question 3: how useful have QI schemes been in driving quality improvement in community nursing services?
Question 4: what factors have you identified that makes an effective quality scheme for community nursing?
Question 5: specifically looking at financial incentive and penalty schemes such as CQUIN, could you explain how these work locally for community nursing?
Question 6: is there anything I have not asked you but that you think is important for this study to be aware of?
Interview schedule for provider managers
The interviewer will typically follow each question with additional supplementary questions in order to obtain a clear, in-depth understanding of the interviewee’s answer. Each interview will start by asking the participant for the title of their current post and the length of time for which the post has been held.
Question1: what is your involvement with the selection of QIs for community nursing?
Question 2: how useful have QI schemes been in driving quality improvement in community nursing services?
Question 3: to what extent are staff in control of factors that could influence achievement of particular QIs – any examples of these?
Question 4: how could indicators be improved for the benefit of patients?
Question 5: what is the system of data recording for QI monitoring?
Question 6: what are the local barriers/challenges and facilitators for implementation of quality schemes on the ground with front-line staff?
Question 7: how confident are you that QIs accurately reflect service quality?
Question 8: in what ways (if at all) does the need for data collection impact on nurses’ relationships with patients?
Question 9: how can the idea of capturing quality of service be translated into routine practice?
Question 10: is there anything I have not asked you but that you think is important for this study to be aware of?
Interview schedule for community nursing team leaders
The interviewer will typically follow each question with additional supplementary questions in order to obtain a clear, in-depth understanding of the interviewee’s answer. Each interview will start by asking the participant for the title of their current post, the length of time for which the post has been held and the length of time since professional qualification.
Question 1: can we start by looking at the QIs in use for your services and talking about how front-line staff feed into this process in your area?
Question 2: to what extent are staff in control of factors that could influence achievement of particular QIs – any examples of these?
Question 3: what is the system of data recording for QI monitoring?
Question 4: how confident are you that QIs accurately reflect service quality?
Question 5: how useful have QI schemes been in driving quality improvement in community nursing services?
Question 6: what are the local barriers/challenges and facilitators for implementation of quality schemes on the ground with front-line staff?
Question 7: how can the process of capturing quality of service be translated into routine practice without impacting detrimentally on the quality of care?
Question 8: in what ways (if at all) does the need for data collection impact on nurses’ relationships with patients?
Question 9: how could indicators be improved for the benefit of patients?
Question 10: is there anything I have not asked you but that you think is important for this study to be aware of?
Focus group schedule for front-line nurses
The facilitator will typically follow each question with additional supplementary questions in order to obtain a clear, in-depth understanding of a participant’s answer.
Question 1: just to start, how do community nurses know if they are providing a high-quality service or not?
Question 2: can you tell me anything about the KPIs or QIs being collected for community nursing?
Question 3: to what extent have you been able to influence or participate in selection of indicators? (If ‘yes’) can you give any examples of how this has happened?
Question 4: what are your thoughts about these QIs for measuring the quality of community nursing?
Question 5: looking at these, to what extent do you feel front-line staff are in control of achieving these or not? (Facilitator shares some indicators in use locally.)
Question 6: can you explain how the data for quality monitoring purposes (such as for the NST) is collected in your area?
Question 7: what are the pros and cons of these QIs?
Question 8: what are the challenges in collecting QI data for you as front-line clinicians?
Question 9: how, if at all, does data collection for QIs in the course of your normal working day affect your patients?
Question 10: what happens to the data that you collect?
Question 11: what implications are there for the organisations if QIs are/are not met?
Question 12: what feedback, if any, do you get on community nursing service quality from patients and/or from managers?
Question 13: how could the processes for data collection for QIs be improved for front-line staff?
Question 14: are there any other comments you would like to make in relation to measuring quality in community nursing?
Observation schedule for front-line shadowing sessions
| Date and time start and end | Staff grade | ||
| Case site and location | Length of time as a community nurse | ||
| Observation number/code | Gender of nurse | ||
| Observer ID |
| Background/reason for visit (e.g. wound dressing, medication) |
| Location of visit (sitting room, bedroom): | |
| Type of visit (assessment, follow-up, discharge): | |
| People present at the visit: | |
| Nurse activities (what did the nurse do for the patient?): | |
|
The physical things that are present: Nurse equipment: Types and format of nursing records: |
|
|
What data are recorded? How is QI information used and captured? Description of interaction between patient and nurse: |
|
|
Reflections/analytic notes: What analytic questions/issues arise for the observer? |
|
|
Action points? Implications for data collection/fieldwork? Interview questions/topics? |
Observation schedule for organisational meetings
| Date and start time–end time: | |
| Case site and location: | |
| Observation number/code: | |
| Observer ID: | |
| Background to meeting/context: | |
| Location of meeting and description of physical environment (diagram): | |
|
Type of meeting, planning, implementation, appraisal: Other: |
|
| People present (titles and designation): | |
| Agenda item(s) relating to study: | |
|
The physical things that are present: Notes of last meeting: Papers: Reports: Financial information: |
|
| Observation notes (pre meeting): | |
| Observation notes (meeting): | |
| Feelings (the emotions and feelings felt and expressed during the meeting): | |
|
Reflections/analytic notes: What analytic questions/issues arise for the observer? |
|
|
Action points? Implications for data collection/fieldwork? Interview questions/topics? |
Appendix 6 Instruments used to collect data from patients and carers
Interview schedule for patients and carers
The interviewer will adjust the wording appropriately, depending on whether the interviewee is a patient or a carer.
Question 1: please tell me about the care you receive from the nurse(s) who come to visit you at home.
Check that the patient/carer is talking about care they receive from the community nurse(s), rather than from another community service.
Try and find out what the patient/carer thinks are good things about the care they receive.
Try and find out what the patient/carer thinks are bad things about the care they receive.
Question 2: so you are saying that good nursing care involves . . . mention the issues they have talked about in their answer to the first question.
Reverse the bad things they have talked about and ask about them as well as the good things.
Talk to the patient/carer about the measures that apply to community nursing locally, making sure that you explain what they mean, and what issues are involved. For each measure ask:
Question 3: does this issue matter to you personally? Why (not)?
Question 4: do you think that nursing managers need to know about this issue in order to make sure that people get good care from community nurses? Why (not)?
Question 5: you said that good nursing care involves . . . (mention everything they said in answer to the first question). I just want to check if you think that there is anything else that nursing managers should know about, so that they can make sure that community nurses are delivering good care to patients and carers.
Focus group schedule for patients and carers
The interviewer will give each participant a paper with the examples of QIs below to each participant.
Venous leg ulcers should heal within 24 weeks of diagnosis.
An example of a patient experience quality measure is:Patients were able to contact a district nurse when needed, including outside of normal working hours.
An example of a patient safety measure is:Each patient coming on to a community nursing caseload and, where appropriate, their carers, will be educated about the importance of moving position regularly and offered pressure-relieving equipment as needed and sign a form to confirm they understand the importance of using the advice and equipment provided.
The wording of questions will be adjusted as necessary to include all participants.
Question 1: thinking about your experience of community nursing services, which aspects of the service you received were important to you? (Check participants are talking about care they receive from the community nurse(s), rather than from another community service.)
Question 2: how did you judge whether or not a high-quality service was provided?
Question 3: Talk to the patient/carer about the NST, FFT (and a few other indicators that apply to community nursing). Explain what they mean and why they are collected. For each measure ask:
Does this matter to you personally? Why (not)?
Do you think that nursing managers need to know about this in order to make sure that people get good-quality care from community nurses? Why (not)?
Question 4: what do you think about community nursing providers using patient satisfaction surveys?
Question 5: how best can patients and carers express their personal priorities for care? (Probe: explain patient identified goals.) What do you think would be the advantages and disadvantages of using these?
Question 6: what information would you like to know about the community nursing services you use and how would it best be given?
Question 7: I just want to check if you think that there is anything else that I have not asked about, that would be important for us to know in relation to how best to measure the quality of community nurse care?
Glossary
- Better Care Fund
- A programme spanning both the NHS and local government, aiming to provide integrated health and social care for the most vulnerable people in society.
- Block contract
- The NHS payment system used for community health services and mental health services under which a health-care provider receives a lump-sum payment to provide a service irrespective of the number of patients treated.
- Care Quality Commission
- The regulator for the quality of health-care services/providers in England.
- Clinical Commissioning Group
- A clinically led statutory NHS body responsible for the planning and commissioning of health-care services for their local area. Clinical Commissioning Groups were created following the Health and Social Care Act 2012 (Great Britain. Health and Social Care Act. London: The Stationery Office; 2012) and replaced Primary Care Trusts on 1 April 2013.
- Commissioning for Quality and Innovation
- The performance incentive scheme set out in the national NHS standard contract.
- Commissioning for Quality and Innovation Pick List
- A database of evidence-based quality indicators for users of the Commissioning for Quality and Innovation scheme.
- Commissioning support unit
- A NHS or external provider of commissioning support.
- Community nursing
- A field of nursing that is a blend of primary health care and nursing practice with public health nursing. The community health nurse conducts a continuing and comprehensive practice that is preventative, curative and rehabilitative.
- Dashboards
- Spreadsheets with quality indicators that providers of health-care services are required to update monthly.
- Datix (Datix Ltd, London, UK)
- An online serious incident report form.
- District nurse
- A registered nurse who visits people in their own homes or in residential care homes.
- Focus group
- A group of people assembled to participate in a discussion about a research topic.
- Foundation trust
- A not-for-profit, public benefit corporation. Foundation trusts are part of the NHS and provide hospital, mental health, community and ambulance services. They were created to devolve decision-making from central government to local organisations and communities.
- Francis inquiry report
- Published in February 2013, the Francis inquiry report examined the causes of the failings in care at Mid Staffordshire NHS Foundation Trust between 2005 and 2009.
- Freedom of Information
- The public’s right of access to information held by public authorities.
- Friends and Family Test
- A national Commissioning for Quality and Innovation indicator that applies to community as well as hospital services.
- Glycated haemoglobin
- The glycated haemoglobin blood test is used to assess average blood sugar levels over the last 3 months for people diagnosed with diabetes.
- Healthwatch
- The consumer champion for health and social care in England.
- Interprofessional working (for older people)
- A type of integrated care that tends to focus on time-limited, problem-specific interventions.
- Key performance indicators
- Measurable values that demonstrate how effectively a company is achieving key business objectives. Organisations (including the NHS) use key performance indicators to evaluate their success at reaching targets.
- Liverpool Care Pathway
- A UK care pathway (excluding Wales) covering palliative care options for patients in the final days or hours of life. It was developed to help doctors and nurses provide quality end-of-life care.
- Monitor
- The independent regulator of health-care provision in England.
- National Institute for Health and Care Excellence
- An independent organisation, set up by the government in 1999, responsible for deciding which drugs and treatments are available on the NHS in England and Wales.
- National Institute for Health Research
- A UK government body that receives Department of Health and Social Care funding to direct and co-ordinate research programmes for the benefit of NHS patients in England.
- National Safety Thermometer
- A national Commissioning for Quality and Innovation for community services.
- Never events
- Serious incidents of harm to patients that should never occur.
- NHS Benchmarking Network
- An organisation established in 1996 in response to a need for NHS organisations to work together to improve services rather than to continually ‘reinvent the wheel’. It works with its 340-plus members to understand the wide variation in demand, capacity and outcomes evident within the NHS and to define what ‘good’ looks like.
- NHS England
- An executive, non-departmental public body responsible for directly commissioning primary care and specialist services and overseeing the commissioning arrangements created by the Health and Social Care Act 2012.
- Patient and public involvement
- When duty is placed on NHS health-care providers to involve and consult patients and the public.
- Patient participation group
- Made up of volunteer patients attached to general practices, who meet with practice staff each month to discuss the work of the practice. They aim to feed back to the practice patient views and suggestions for improving, changing and developing patient services.
- Patient reference group
- A group of individuals who meet regularly and engage with one or more members of general practice staff (including general practitioners). Patient reference groups started being established during 2011. Practices which formed patient reference groups received additional funding.
- Patient-reported outcome measure
- A method of assessing the quality of care delivered to NHS patients from the patient perspective. Currently covering four clinical procedures, patient-reported outcome measures calculate the health gains after surgical treatment using pre- and post-operative surveys. The four procedures are hip replacements, knee replacements, groin hernia and varicose veins. Providers of NHS-funded care have collected patient-reported outcome measures since April 2009.
- Pay for performance
- A payment model that offers financial incentives to health-care providers for meeting certain performance measures.
- Pressure ulcer
- Also known as bedsores, an injury to skin and underlying tissue resulting from prolonged pressure on the skin. Pressure ulcers most often develop on skin that covers bony areas of the body.
- Primary Care Trust
- A commissioning body before the creation of Clinical Commissioning Groups under the Health and Social Care Act 2012.
- Quality Account
- A report about the quality of services by NHS health-care providers. Each provider annually publishes a report, including the independent sector, and reports are available to the public.
- Quality and Outcomes Framework
- The annual reward and incentive programme detailing general practice achievement results. It rewards practices for the provision of quality care and helps standardise improvement in the delivery of primary medical services.
- Quality indicator
- A measure of health-care quality.
- Queen’s Nursing Institute
- A registered charity dedicated to improving the nursing care of people in their own homes.
- Regional team
- A regional subdivision of NHS England (four in total).
- RiO
- An electronic care record system for health and social care organisations.
- Root cause analysis
- A method of problem-solving used for identifying the root causes of faults or problems. In health care, root cause analysis investigations identify how and why patient safety incidents happen and are used to identify areas for change and to develop recommendations for delivering safer patient care.
- Royal College of Nursing
- A membership organisation and trade union with > 432,000 members in the UK. It was founded in 1916, receiving its royal charter in 1928. The majority of members are registered nurses, but student nurses and health-care assistants are also members.
- Service user reference group
- A small group of service users (patients, carers and members of the public) who contributed to design of data collection tools, the interpretation of findings and the content of the final report.
- Social Value Act 2012
- Legislation that came into force on 31 January 2013 and requires the commissioners of public services to think about how they can also secure wider social, economic and environmental benefits [Great Britain. Public Services (Social Value) Act 2012. London: The Stationery Office; 2012].
- Vanguard sites
- New models of integrated care that emerged from the Five Year Forward View (NHS England. 2014/15 NHS Standard Contract. Leeds and Wakefield: NHS England; 2014), published in October 2014.
List of abbreviations
- ACFT
- Alderton Community NHS Foundation Trust
- BCF
- Better Care Fund
- BCHT
- Beechbury Community NHS Healthcare Trust
- CAUTI
- catheter-acquired urinary tract infection
- CCG
- Clinical Commissioning Group
- CFT
- Cedarham NHS Foundation Trust
- CQC
- Care Quality Commission
- CQUIN
- Commissioning for Quality and Innovation
- DHR
- Dogwoodheath Respond
- EFT
- Elmhampton NHS Foundation Trust
- FFT
- Friends and Family Test
- FOI
- Freedom of Information
- GP
- general practitioner
- IT
- information technology
- KPI
- key performance indicator
- MDT
- multidisciplinary team
- NHSE
- NHS England
- NICE
- National Institute for Health and Care Excellence
- NMC
- Nursing and Midwifery Council
- NST
- National Safety Thermometer
- PU
- pressure ulcer
- QI
- quality indicator
- QNI
- Queen’s Nursing Institute
- R&D
- research and development
- RCN
- Royal College of Nursing
- SMART
- specific, measurable, appropriate, realistic and time bound
- SURG
- service user reference group