Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/59/08. The contractual start date was in November 2014. The final report began editorial review in February 2017 and was accepted for publication in June 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Helen Atherton has received fellowship funding from the National Institute for Health Research (NIHR) School for Primary Care Research (SPCR) during the conduct of the study. Chris Salisbury is a member of the NIHR Health Services and Delivery Research board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Atherton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
Communication technologies are routinely used by the public in everyday life, and there is an expectation that this should extend to health care.
Globally, the use of such technologies in health care is variable. In Denmark, the use of e-mail for consultations in general practice became mandatory in 2009, a measure intended to raise the quality of services delivered to patients, and in 2013 there were four million consultations conducted this way. 1,2 The USA has well-established options, including patient portals for online access to clinicians and routine telephone consultations, which are offered by several of the large health maintenance organisations, under fee for service arrangements. 3
In Finland, e-mails between doctors and patients have been a routine part of care for over a decade. 4 Mobile devices in parts of Africa have vastly increased access to the telephone, as well as to the internet; the potential impact on health care is arguably more transformational than in countries with pre-existing landline networks. 5
In the UK, policy-makers have suggested that alternatives to face-to-face consultations in the general practice setting could have a transformative impact by alleviating staff workload and improving patient access. 6,7 Policy has reflected this, and there has been sustained interest in encouraging general practice to adopt alternatives to the face-to-face consultation. In 2012, the UK Department of Health and Social Care (DHSC) produced a target:
All patients should be able to communicate electronically with their health and care team by 2015.
DHSC. 6
However, this target for implementation was not met. A 2014 policy document from the DHSC and NHS England outlined government proposals8 and suggested that the introduction of alternative methods, such as e-mail or internet video [e.g. Skype™ (Microsoft Corporation, Redmond, WA, USA)], to provide consultations could improve the current provision of primary care in the UK. NHS England has consistently pursued a digital agenda for primary care. Patient Online9 is a NHS England programme, which encourages general practices to:
offer and promote online services to patients, including access to coded information in records, appointment booking and ordering of repeat prescriptions.
NHS England. 9
The scope of Patient Online is set to be extended to the use of online consultation. Most recently, in 2016, General Practice Forward View,7 published by NHS England, outlined an investment of ‘£45 million for a multi-year programme to support the uptake on online consultation systems’7 (contains public sector information licensed under the Open Government Licence v3.0), although the nature of these was unspecified. This agenda has not been limited to England. The NHS in Northern Ireland devised an eHealth and care strategy, which encourages citizens to ‘interact with health care electronically’10 (contains public sector information licensed under the Open Government Licence v3.0), and NHS Scotland has set a target to encourage practices to offer online services to patients, in particular to increase rates of video-consultation use. 11 In Wales, the NHS strategy is for patients to:
use the internet, email and video conferencing to connect with clinicians and care professionals in a way that suits them, potentially reducing delays and costs to the service and service users.
Welsh Assembly. 12
In 2014, GP Access Fund supported 20 pilot projects, to the value of £50M over 1 year, to test new approaches to improve access to general practices. 13,14
An evaluation of the first wave of projects has been published. 15 This evaluation reported that six pilot sites intended to introduce video-consultation tools and six pilot sites trialled e-mail consultations. The conclusion of the report was that non-traditional modes of contact (e.g. video or e-mail consultations) have yet to prove any significant benefits and have had low rates of patient uptake. 15 A second wave of funding under the GP Access Fund has now been released. 14 Several of these pilots also include the use of alternatives to face-to-face consultations, including e-mail consultations, Skype consultations and/or greater use of telephone consultations. Despite the second wave commencing in 2015, the findings from the evaluation have not yet been published by NHS England.
There is pressure on general practice to offer alternative methods of consulting with patients. However, apart from the increased use of telephone consultations, most practices have been slow to adopt alternatives. 16–18 This reflects concerns expressed by GPs about the impact of introducing additional consultation methods and, particularly, concerns about increased workload and achieving safe use. 19,20
Although professional bodies are now making tentative steps towards embracing some of the newer technologies, and supporting practitioners21–23 who wish to use alternatives to the face-to-face consultation, this support has been slow to arrive. This reflects the uncertainty arising from a lack of evidence in the general practice setting, and wider concerns about the general practice workload. This view was supported by the recent report by the Primary Care Workforce Commission,24 which stated that more evidence is required before e-mail or internet video consultations can be recommended as a routine part of primary care.
Given that some general practices have already adopted alternative methods of consulting,17,25 and that there is an increasing expectation that they should be available, this provides an opportunity to provide GPs with guidance for using these new methods, based on best evidence and existing experiences, encouraging those taking them up to do so as safely and effectively as possible, and bringing the maximum benefit for patients and the NHS. 26
Evidence explaining why this research is needed now
The underlying assumptions that drive the policy rhetoric relate to convenience and accessibility for patients and an efficient use of practitioners’ time. 27,28 However, there is little evidence to support such assumptions. The Nuffield Trust,29 among others, have identified the potential for the use of remote consultation in primary care, but also the need for more evidence on the impact of remote consulting.
Evidence to date has assessed the potential impact of some alternatives on clinical outcomes. 30,31 Although trial evidence for some types of alternatives is poor, observational data have pointed towards some clinical benefits, such as improved outcomes from e-mail communication for those with diabetes mellitus and hypertension32 and better monitoring of health concerns with online access to records,33 at least in market-driven health systems. When combined with self-monitoring, telephone and e-mail consultation have been effective in the management of hypertension and diabetes mellitus. 34,35
Studies have sought opinions from patients and health-care professionals on whether or not, and how, they would use alternatives,20,36,37 but these data have been based on hypothetical opinions rather than experience. Other studies have attempted to assess the impact of alternatives to the face-to-face consultation on workload and consultation numbers in primary care settings;38–40 however, these studies have been of low quality,30 or have assessed impact in the context of a patient portal that offers additional functionality,33,41 making it difficult to draw conclusions about the impact of the alternative to the face-to-face consultation alone.
Recent years have seen a plethora of small and local pilot projects and commercial initiatives around specific systems,42,43 which proliferate in an environment of patchy and inconclusive evidence.
What the existing literature does not tell us is under what conditions, with which patients and in which ways alternative methods of consultation actually work. This project addresses this need and builds on previous research by focusing on the experiences of patients and practitioners who have used these alternatives to the face-to-face consultation with different groups of patients for different purposes. 19,44
Where GPs have started to use alternatives to the face-to-face consultation, we can learn from their experiences and from their rationale for introducing them, as well as their reasons for persisting with or discontinuing use. The feasibility of these alternatives to the face-to-face consultation is likely to rely on factors that are identifiable only when they are used in practice (e.g. patient characteristics or the purpose of consultation). Barriers to, and facilitators of, use become apparent as patients and practitioners navigate their way through use. The existing literature on experience can be utilised to develop a picture of how alternatives might be expected to work. 45–47
Existing research has demonstrated a limited understanding of the fact that consultation methods are complex interventions. 30 The lack of good quantitative evidence on technologies such as e-mail and video consultation reflects the difficulties of testing them in trials, as their use has not been clearly defined. 48 Often, distinct elements of the consultation have not been taken into consideration. By developing a theoretical framework, we hope to deconstruct what makes alternatives different from face-to-face consultations, allowing us to assess if and how they should be tested, in relation to the appropriate populations, outcome measures and methodological approach.
This research builds on the previous literature in related fields on how new technologies are adopted and implemented in health care. There has been some research in relation to telehealth interventions to support patients in their own homes. For example, the application of the normalisation process theory to the implementation of telehealth has demonstrated that it is the work involved in adopting new approaches that influences whether or not they normalise in practice; that is, they must fit in with health-care professionals and their roles for successful implementation. 49,50 Other work using the technology acceptance model has highlighted the importance of both usefulness and perceived ease of use in influencing behavioural intentions to use new technology. 51
Work by Greenhalgh et al. 52 on the failed introduction of the HealthSpace communication platform also highlighted the importance of ensuring that the technology used meets people’s perceived needs and fits with their other health-care arrangements. 52 We will take account of these related theoretical perspectives, including insights from the normalisation process theory, the technology adoption model and the diffusion of innovations theory, but we do not propose to base our analysis on any of these specific models.
Health-care needs differ between patient groups. Evidence around how different groups are affected by the introduction of new consultation methods is sparse. Studies have included patient populations in general practice, and this has not tended to include consideration of different patient groups. For telephone consulting, there has been some consideration of the effects on different patient groups, such as patients with brain injuries. 53 However, for other alternatives to the face-to-face consultation, little is known about the impact on different groups of patients. 19,46,54 Existing data from a range of countries and settings indicate that young people, those with tertiary education, the employed and students are more likely to use alternatives to the face-to-face consultation, along with those in poor health. 55,56 It is important to understand more about the use of alternatives to the face-to-face consultation by different patient groups in general practice and whether or not they provide better access to care in relation to need, and, subsequently, their influence on health inequalities.
What is the problem being addressed?
It is important to understand how these alternatives work for patients, and to determine the benefits, advantages and disadvantages for different groups of patients and for a practice as a whole. Some groups are likely to benefit more than others. 55,57 Although attempts have been made to determine the impact of some alternatives on clinical outcomes,30,31,58,59 there has been a lack of focus on appropriate application and implementation, and this is key if we are to inform safe use and to be able to successfully evaluate their use in practice.
Use of alternatives to the face-to-face consultation
The study was designed to explore the use of alternatives to face-to-face consultations, including telephone consultations (but not those used to triage all requests for consultations before offering any face-to-face appointments), e-mail, structured e-consultation systems (e.g. eConsult, Hurley Innovations Ltd, London, UK; askmyGP, GP Access Ltd, Leicester, UK) and internet video [e.g. Skype™ (Microsoft Corporation, Redmond, WA, USA)]. It was expected that in many practices, different combinations of these alternatives to the face-to-face consultation would be offered to varying extents; for example, practices offering internet video consultations are likely also to offer telephone and e-mail consultations.
Furthermore, several methods of communication may be used over the course of one illness. For example, a patient with asthma may have a regular review by completing a structured review form online (which is checked later by the practice nurse), may send an e-mail with a query about their medication, might make a telephone consultation to assess if they need to be seen urgently during an acute attack or may make a face-to-face consultation if their attack does not resolve.
Practices may also offer the same technology for different purposes; for example, most practices allow patients to contact the GP by telephone (most commonly by leaving a message and the doctor telephoning them back), but some practices encourage patients to use telephone consultations as the usual first form of contact. This study explores the use of alternatives to face-to-face consultations for any clinical purpose, including consultations for initial assessment of symptoms or triage, follow-up, chronic disease management and/or discussion of test results. This excludes remote monitoring of health conditions not involving a consultation and also excludes administrative purposes, which do not usually involve direct contact with a clinician (e.g. making an appointment or requesting a repeat prescription).
On the practice side, examples of models of delivery include those that are very simple (e.g. e-mails being routed to the patient’s chosen individual GP for a response) and those that are structurally more complex (e.g. the use of a duty doctor who conducts all telephone and e-mail consultations on any given day).
It is important to note that although we are examining alternatives to the face-to-face consultation, they are not replacements – rather, they are additional methods of consultation. The different type of alternatives to the face-to-face consultation that will be considered are described next.
Types of technology
Telephone consultations
Telephone consultations have been in use for a long time; therefore, the issue for our study is not plausibility but, rather, optimal application. This includes gaining a greater understanding of how practices have addressed potential problems, such as concerns about increased workload or safety.
Several telephone-based initiatives have been introduced in general practice, with a view to reducing GP workload, for example, telephone triage. 60 Some practices offer a system of care in which almost all patients are offered a telephone consultation initially (variously labelled GP Access61 or Doctor First62); however, as the National Institute for Health Research (NIHR) has funded another parallel study that specifically looks at this model of care, we will exclude these approaches from our study.
E-mail consultation
The application and use of e-mail consultation are varied. Some GPs offer e-mail consultations using conventional e-mail programs, whereas others favour asynchronous consultations via a structured online form. 63 There are commercial providers that offer website services to general practices, which can act as a secure host for e-mail consultations (e.g. MySurgeryWebsite). 64 In the case of e-mail communication with patients, NHS Digital has supported NHS policy with the introduction of NHSmail 2. 65 This system allows clinicians to engage in secure e-mail communication with patients, but NHS Digital does not provide guidance on how this might be done.
E-mail consultation includes secure messages sent using webmail. The most commonly described method of applying practice-wide access is via a secure website, whereby patients log in to the practice website and are given the option to send online messages. Responses are received via the patient’s e-mail inbox or an inbox they can access via the website. These sites also tend to offer appointment-booking and repeat prescriptions in the manner of a patient portal, and there is speculation that they could also offer access to medical records. UK policy-makers draw on examples of these sites from the USA, for example, from Kaiser Permanente and the Mayo Clinic, where patient portals are in use. 3,32,66 Thus, UK policy-makers appear to believe that a patient portal system is the most plausible model for the introduction of online consultation,7 despite the fact that this is not backed by robust evidence and has not been tested in a UK setting. Even in the USA, the uptake rate of electronic communication is low and it has not achieved widespread adoption. 67
E-consulting
In this study, e-consulting refers specifically to consultations mediated by software provided by two commercial providers (eConsult, previously known as WebGP,68 and askmyGP69), which claim to manage demand by allowing patients to complete a ‘structured online consultation’. 70 Patients enter information about their symptoms and, in some cases, leave an electronic message for the GP. This provides the GP with a history to enhance the subsequent contact, which is usually made by telephone. eConsult68 software is linked into the practice website and supported by Egerton Medical Information Systems (EMIS; EMIS Web, EMIS Health, Leeds, UK), a main supplier of electronic medical record software in the UK. 71 NHS England has openly supported the roll-out of these software systems in its plans for how general practice will deliver care in the next 5 years, providing:
£45 million [for a] national programme to stimulate uptake of online consultations systems for every practice.
NHS England. 7
Video
There are some examples of the use of internet video to provide consultations in general practice. 42 The use of video consultation is much less well known in UK primary care. There are many reports of practices taking it up (including projects funded by the GP Access Fund, NHS England),14 but little evidence of its feasibility and effectiveness. As described previously, despite six practices piloting video-consultation tools, there was in fact a low level of uptake by practitioners and patients; thus, conclusions could not be drawn about their use. 15 Facilities are emerging to support this type of consultation. For example, EMIS has recently introduced a feature into its systems that provides video consultations, and the feature offers secure communications. 72
Aim
To use a theory-based evaluation approach to understand how, under what conditions, for which patients and in what ways alternatives to face-to-face consultations may offer benefits to patients and practitioners in general practice, and to use this understanding to develop guidance for general practices and a framework for subsequent definitive evaluation.
Objectives
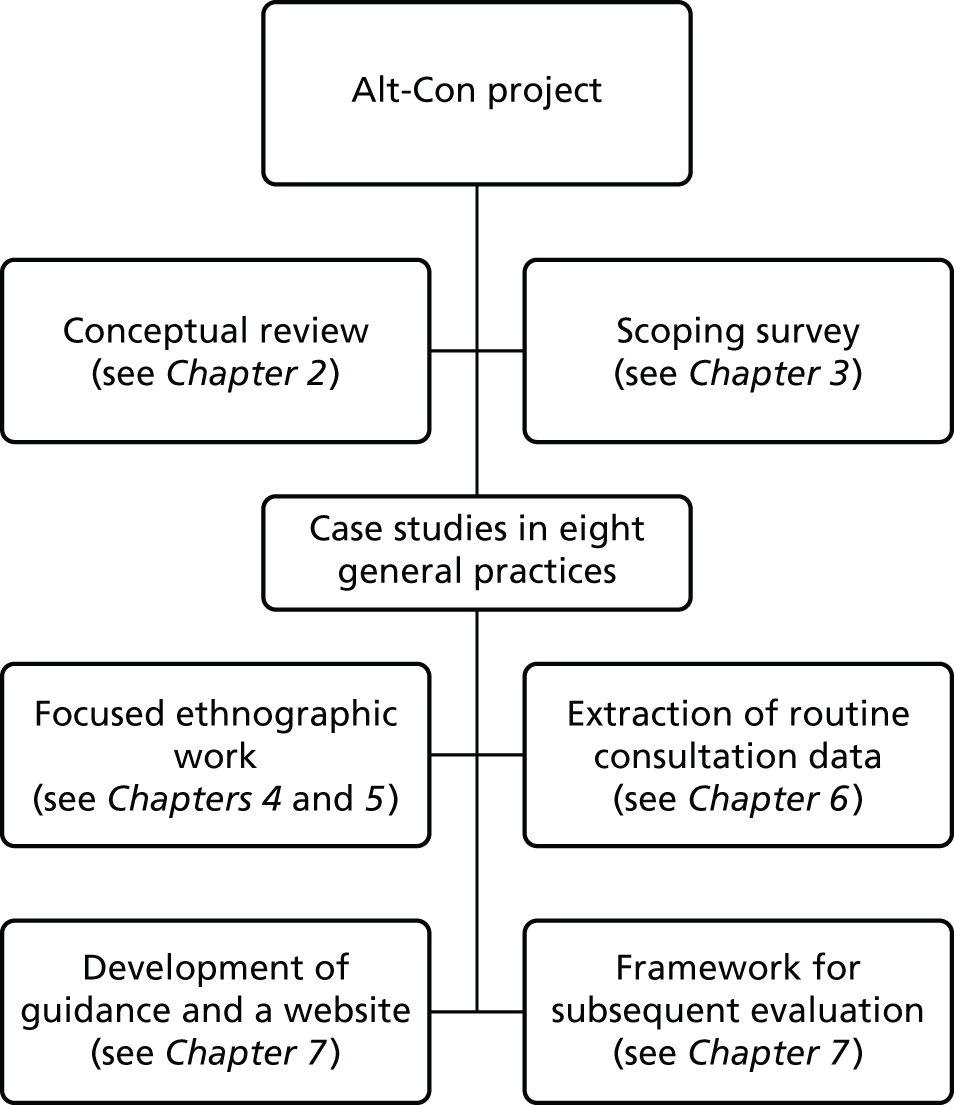
Our study covers the first stages of the MRC’s complex intervention framework, that is, identifying the evidence base, identifying/developing a theory and modelling the process and outcomes. 73 It utilises a mixed-methods case study design. 74 Figure 1 shows a chart outlining the various elements of the project and their relationship.
FIGURE 1.
Different elements of the study and their relationship.
Identifying the evidence base
Objective 1: to conduct a conceptual review, synthesising the literature (qualitative and quantitative) on patients’ and practitioners’ experiences of alternatives to face-to-face consultations, with a particular focus on the views of different groups of patients and factors that promote or hinder the wider implementation and uptake of these alternative forms of consultation.
Developing a theory
Objective 2: to use a scoping exercise to identify the range of ways in which general practices in England and Scotland are currently providing alternatives to face-to-face consultations in order to create a typology of these alternatives.
Objective 3: to identify and recruit approximately eight practices with varied experience of implementing alternatives to face-to-face consultations to act as focused ethnographic case studies.
Objective 4: in the case study practices, to explore how practice context, patient characteristics, the type of technology and the purpose of the consultation appear to interact to determine the feasibility and impact of alternatives to face-to-face consultations, from the perspectives of both patients and staff. This includes the impact on the clinician–patient dynamic. The impact for people living in isolation, people with disabilities, disadvantaged groups and other vulnerable or hard-to-reach groups will be a particular focus.
Objective 5: to identify the factors that act as the main barriers to, and facilitators of, wider use of these alternatives.
Modelling the process and outcomes
Objective 6: to use the findings to develop guidance and a website resource for general practice, detailing the most promising applications of alternatives to face-to-face consultations for different patient groups and different purposes, and in different practice and population contexts.
Objective 7: to treat the provision of alternatives to face-to-face consultations as an intervention, in order to develop a framework for a subsequent evaluation. We will clarify the target population, appropriate outcome measures and best methodological approach for this evaluation.
The research is focused to fill the gaps in the existing evidence base in a way that leads to practical and applicable findings, and provides a framework for future evaluation. It is hoped that the research findings will broaden the scope for research in this area.
Conceptual framework
This study uses a theory-based evaluation approach, which ‘examines the conditions of program implementation and mechanisms which mediate between processes and outcomes as a means to understand when and how programs work’. 75 There are a number of other related approaches to intervention development and evaluation, including logic models,76 realist evaluation,77 intervention mapping78 and causal modelling. 79 Although these approaches have different emphases, they have many ideas in common, including the importance of context in determining outcome and the need to clarify the underlying theory about how an intervention leads to change and clearly specify the intended outcomes. In addition, May et al. 80 have developed the normalisation process theory in order to understand the processes of implementation and integration that lead to innovations becoming embedded in everyday work.
Weiss75 distinguishes between programme theory, which specifies the mechanism of change (the theoretical causal chain for how an intervention leads to intended outcomes), and implementation theory, which describes how the intervention is carried out. This theory-based evaluation approach is helpful in identifying factors that are deemed to be key mediating processes through which an intervention achieves its aims and moderating factors that influence the extent to which process and outcomes are achieved.
In order to develop the programme theory, we drew on a realist approach81 to describe the provision of alternatives to face-to-face consultations in terms of:
-
context [e.g. characteristics of the general practice, the target patient population, the policy framework and the information technology (IT) infrastructure]
-
the theory and assumptions underlying the introduction of an alternative to the face-to-face consultation (how and why different staff members thought that alternatives to face-to-face consultations might lead to benefits)
-
the flow of activities that comprise the intervention (the key processes that occur when patients make use of these alternatives)
-
intended benefits/outcomes (those deemed important to different groups of patients and practitioners).
The implementation theory explored moderating factors that influence the extent to which the process and outcomes are achieved, such as factors acting as barriers to, and facilitators of, practices offering alternatives to face-to-face consultations or to different groups of patients using them.
By focusing on practices that have tried to offer alternatives, including some that deemed their use successful, we aimed to learn lessons about how practices have overcome problems, such as barriers to implementation, and the key factors that made this possible. We will also gain an understanding of the motivations of practitioners who have or have not offered alternatives to the face-to-face consultation, the experience of different groups of patients who have had the opportunity to use these alternatives, the benefits and disadvantages from the perspectives of patients and practitioners, and the problems that remain.
A key focus of interest will be which groups of patients make use of, and have the most to gain from, these alternative forms of access and whether these new approaches are increasing or reducing inequalities of access. This includes consideration of which groups are currently disadvantaged by the limited provision of alternatives to face-to-face care. We will explore the impact of provision of these alternatives on patient satisfaction with access to general practice. We will also explore clinicians’ perceptions of the impact of new forms of consultation on their workload and the appropriateness of the content of patient contacts, as well as factors that would facilitate the wider implementation of these new models of care.
The recently published Wachter report,82 commissioned by the UK DHSC, focused on making IT work in the health service in England, and was largely concerned with implementation at the secondary care level. However, some of the findings were pertinent for the introduction of alternatives to the face-to-face consultation in primary care: ‘digitise for the correct reasons’, and ‘it is better to get digitisation right than to do it quickly’82 (both of these quotations contain public sector information licensed under the Open Government Licence v3.0). This study will explore both the reasons that practices have introduced alternatives to the face-to-face consultation and how they have done it, allowing us to explore perceptions about the ‘right’ way to do this.
Team
The project team was deliberately diverse and was situated across four different universities. Table 1 provides an outline of team member contributions and backgrounds.
| Role in the project | Description of role | Background |
|---|---|---|
| 1. PI (CS) | Led and oversaw the project | GP, background in mixed methods, expert in the field |
| Led and conducted the scoping survey (see Chapter 3) | ||
| Led the analysis of quantitative data from the case study sites (see Chapter 6) | ||
| 2. Co-investigator (BM) | Local PI for two focused ethnographic case study sites | GP, background in mixed methods, expert in the field |
| 3. Co-investigator (JC) | Clinical and methodological input into all elements of the project | GP, background in mixed methods, expert in the field |
| 4. Co-investigator (AG) | Led and conducted the PPI throughout the study (see Chapters 2, 4, 5 and 8) | Patient and public involvement expert |
| 5. Co-investigator (SZ) | Senior lead of focused ethnographic case studies (see Chapters 4, 5, 7). Conducted the conceptual review with HA (see Chapter 2) | Medical sociologist, background in qualitative research |
| 6. Co-investigator (HA) | Day-to-day lead of focused ethnographic case studies and local PI for three focused ethnographic case study sites (see Chapters 4, 5, 7) | Health services researcher, background in mixed methods, expert in the field |
| Conducted conceptual review with SZ (see Chapter 2) | ||
| 7. Project manager and researcher (HB) | Oversaw and managed the entire project | Health psychologist, background in nursing and mixed methods |
| Conducted the scoping survey with CS (see Chapter 3) | ||
| Focused ethnographer for three case study sites | ||
| 8. Researcher (TP) | Focused ethnographer for three case study sites | Medical anthropologist, background in qualitative methods |
| 9. Researcher (AB) | Focused ethnographer for two case study sites | Health services researcher, background in social anthropology and mixed methods |
Structure of the report
Chapter 2 outlines the conceptual review of the literature. Chapter 3 presents the scoping study, which informed identification of the case study sites for recruitment. Chapter 4 details the methods of the focused ethnographic work in our case study sites and Chapter 5 presents the results of this. Chapter 6 describes the routine consultation data obtained from the electronic medical record in each case study site.
Chapter 7 synthesises the different elements of the study, both qualitative and quantitative, and describes how the guidance for the practical application of alternatives to the face-to-face consultation was developed. It includes the framework for future evaluation. The report concludes with the discussion in Chapter 8.
Chapter 2 Conceptual review
This chapter is based on material previously published in Atherton H, Ziebland S. What do we need to consider when planning, implementing and researching the use of alternatives to face-to-face consultations in primary healthcare? Digit Health 2016;2:1–13. 83 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 3.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/3.0/. The text below includes minor additions and formatting changes to the original text.
Background
This conceptual review was informed by realist review, which is a method for synthesising research evidence that is particularly useful in examining complex interventions. 81,84 The methods offer a useful framework for identifying and managing syntheses of existing research and have been applied in such fields as lean thinking in health care,85 internet-based medical education,86 social diffusion in health care,87 social networks and social capital in the self-management of chronic illness88 and the potential health effects of accessing online patient experiences. 89
Policy and practice initiatives need to build on collective wisdom about the successes and failures of previous initiatives; in this review, we sought to identify explanations of why and how various alternatives to face-to-face consultations might work (or not) in primary care.
Aim
To identify and synthesise articles that explore, or test, the effects of alternatives to face-to-face consultations in relation to patient and staff experiences, or describe theories or ideas about the potential effects.
Methods
The review methods drew on Ziebland and Wyke 201289 (Box 1). The review was conducted by HA and SZ.
-
Finalised the review question (see aim).
-
Developed an initial matrix to record the cumulative results from the literature.
-
Drew on considerable existing knowledge of the literature based on our own and colleagues’ bibliographic databases.
-
Conducted a wide-ranging search (with assistance from a librarian) to identify any studies that have explored, or tested, the effects of alternatives to face-to-face consultations in relation to experiences, or described theories or ideas about the potential effects.
-
We examined all resulting titles and abstracts and selected potentially promising papers that could inform thinking.
-
More sources were identified by ‘snowballing’ from reference lists as ideas emerged.
-
A final search for additional studies was made when we had nearly completed the review. Studies were also added when encountered, for example, through discussions and seminars.
-
Each full paper was read by either HA or SZ. No formal quality appraisal tools were used but each paper was considered in relation to its:
-
relevance – does the research address the topic and enable the adding to, adaption or amendment of the initial matrix developed in step 1b?
-
rigour – does the research support the conclusions drawn from it by the authors?
-
-
We identified papers containing important ideas and discussed their relevance during regular meetings throughout the review.
-
This matrix was the main data extraction framework, with new categories incorporated where relevant during the initial reading.
-
The initial ‘map’ or overview identified potential positive and negative effects of alternatives to face-to-face consultations, with particular focus on the impact on inequalities and access, effect on patients and all staff working in primary care, and the potential mechanisms through which each effect might work.
-
A constant comparison approach between reading and the working table was applied. This identified the point at which no new ideas were emerging and ‘saturation’ was reached.
-
We presented the findings at a full project team meeting.
-
We presented and discussed the findings at the Society for Academic Primary Care conference in 2015.
-
At the end of the case study period we presented the findings of the conceptual review and the case studies to the case study practices as part of our stakeholder event.
-
The review was published in a peer-reviewed journal.
Types of studies
The review included material from any study design or article type. Given the changing nature of the field, the review focused on recently published articles (2012 onwards), but included sources from before 2012 where relevant.
Setting
The setting of interest for this review was primary care, but material from related settings (e.g. e-mail consultation between patients and specialists) was included where it provided lessons directly relevant to primary care.
Types of alternatives to the face-to-face consultation
We sought material on the following technologies: telephone consultations (but not those used to triage all requests for consultations before offering any face-to-face appointments), e-mail, e-consultations and internet video (e.g. Skype) technologies, short messaging service (SMS), telehealth and any other ‘care at a distance’ application.
Search for material
Our search was devised in conjunction with an information specialist at the University of Oxford. It was designed to identify articles that have explored, or tested, the effects of alternatives to face-to-face consultations in relation to how patients or staff experience their use, or described theories or ideas about the potential effect.
The search was intended to identify a wide range of study designs and articles. A sensitive search was designed, which yielded a high number of retrieved articles. Databases searched included the Cumulative Index to Nursing and Allied Health Literature, Cochrane Register of Controlled Trials, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, EMBASE, MEDLINE, PsycINFO, Science Citation Index, Social Science Citation Index and Conference Proceedings Citation Index (see Appendix 1 for search strategies). We searched the databases from date of inception to 2015, and then a filter was applied to limit the retrieved articles to those from 2012 onwards.
We used additional sources: (1) key systematic reviews in the field and included studies, (2) papers identified by HA and SZ in the course of our work, (3) papers suggested by experts in the field (including the project team) and (4) papers identified by snowballing from the references lists of interesting and relevant studies.
The news archives of several related news websites and eHealth Insider, Pulse and GP Magazine were all searched for relevant material.
Selecting material
Within the articles identified using the database search, we examined all articles. A two-phase approach was taken; first, titles were examined, before looking at selected abstracts in more depth. Selected articles were then read in full. We checked the reference lists of full studies as we read them. When a ‘key’ paper was identified, we examined the references. The process was iterative, with further material sought as the matrix was populated.
Collation of material and identification of themes
For the purposes of collating material for the review we devised a matrix, which allowed for identification and extraction of key ideas and provided a constant comparison framework.
Either HA or SZ, and sometimes both, read articles. Where useful information was present in a study or article, it was added to the matrix. The matrix template was developed iteratively as material was extracted. For an example of the matrix template see Appendix 2.
Using a matrix allowed us to extract material according to the participants we were interested in, in line with the aims of the wider study: reception staff, nurses, GPs, practice managers, patients (particularly disadvantaged groups) and carers. Additional detail was added as extraction commenced; this meant including other groups (secondary care clinicians, policy-makers, professional bodies) and also acknowledging roles that apply outside a UK setting (e.g. service manager and primary care physician).
We extracted information from the studies by technology type, and initially split it into two categories: positive effects and negative effects. We added a further two categories once the extraction process commenced. These were ‘positive speculation on effects’ and ‘negative speculation on effects.’ This reflected the studies and articles that provided opinion on the technology, and also the studies and articles that included both empirical data and speculation.
Collating material in this way allowed us to identify the potential mechanisms through which each effect might work. Early in the process we (SZ and HA) met to compare the extraction into the matrix and to discuss key themes arising. We continued extraction of material until saturation was reached for the emerging themes.
Appraisal of articles
We did not apply formal quality appraisal tools in this conceptual review; however, each article was considered in relation to:
-
relevance – does the research address the topic and enable us to add to, adapt or amend the initial matrix?
-
rigour – does the research support the conclusions drawn from it by the authors?
When articles were not relevant, we excluded them from those used to develop the matrix. When rigour was in question, we did not exclude the article, but, instead, this was noted for the purposes of interpreting the data.
Synthesis of findings
We identified the main themes from the matrix and put these into an initial ‘map’, using the OSOP90 (one sheet of paper) method for grouping the material. From this point, we used a constant comparison approach: reading the articles and expanding the themes. We met regularly to discuss the data, and this often involved going back to key articles and revisiting themes that were identified earlier in the extraction process.
At this stage, the contents of the matrix and the initial map were shared at a team meeting to obtain input as the analysis progressed. The main themes were also discussed at a patient and public involvement (PPI) workshop (described below).
Theoretical framework
We based our development of the eventual conceptual map on input gained from the wider team and further meetings between the review team (HA and SZ). In organising and structuring the conceptual map, we used the Halford91 sociological framework of health-care work and organisation for information and communications technology (ICT) initiatives.
Halford’s framework91 views that the introduction of new ICT applications threatens to disrupt health-care work and organisation by disrupting social orders mediated by inter-relations of power, knowledge and identity. The analytical framework positions ICT initiatives within orderings of health-care work and organisation, with ICT applications posing three potential disruptions to the organisational, professional and spatial dimensions of health-care work and organisation.
This framework was chosen because it helps to understand, at a general level, how ICT initiatives disrupt the prevailing order of health care. The dimensions of the framework were used to structure the conceptual map, with the acknowledgement that the processes presented are inter-related, shaped by health-care work and organisation, but do not occur independently.
Development of the conceptual map
Once the material had been mapped, we developed it into a series of key questions to be asked when ‘planning, implementing and researching’ alternatives to face-to-face consultations, guided by Halford’s framework. 91 The conceptual map was also used, along with the protocol for the study, to devise a case study guide for the ethnographers to use while conducting the fieldwork. The guide was designed to align the information in the protocol with the information emerging from the review, to ensure that the data collected were in line with the aims of the study and built on existing research. The ethnographic team used it as a supporting guide when conducting the fieldwork.
Patient and public involvement workshop
In order to refine the emerging findings of the review, we held a workshop with patient and public participants. The workshop was facilitated by Andy Gibson. It lasted approximately 3 hours and was attended by five members of the public. We shared the themes from the review, and then members of the research team worked in small groups with the workshop participants to discuss the themes, followed by a whole-group discussion.
Results
Material from 149 separate articles was used in this review, obtained from database searches or snowballing, or via recommendations from team members. They included articles on telephone consulting (29 articles), e-mail/online consulting (34 articles), video consulting (21 articles) and SMS (one article) and articles describing themselves as being about ‘telehealth,’ ‘telecare’ or ‘teleconsultation’ (38 articles). The remainder discussed a combination of communication methods. We found 36 articles that explicitly stated that they were set in primary care, although some were set in multiple health settings. There was a mixture of study and article types, from systematic reviews to commentaries. In total, 56 of the 149 articles were relevant and used when identifying the key themes and devising the conceptual map, and these are each cited at the relevant places in the conceptual map. See Appendix 3 for a full list of the 149 articles identified.
Initial themes
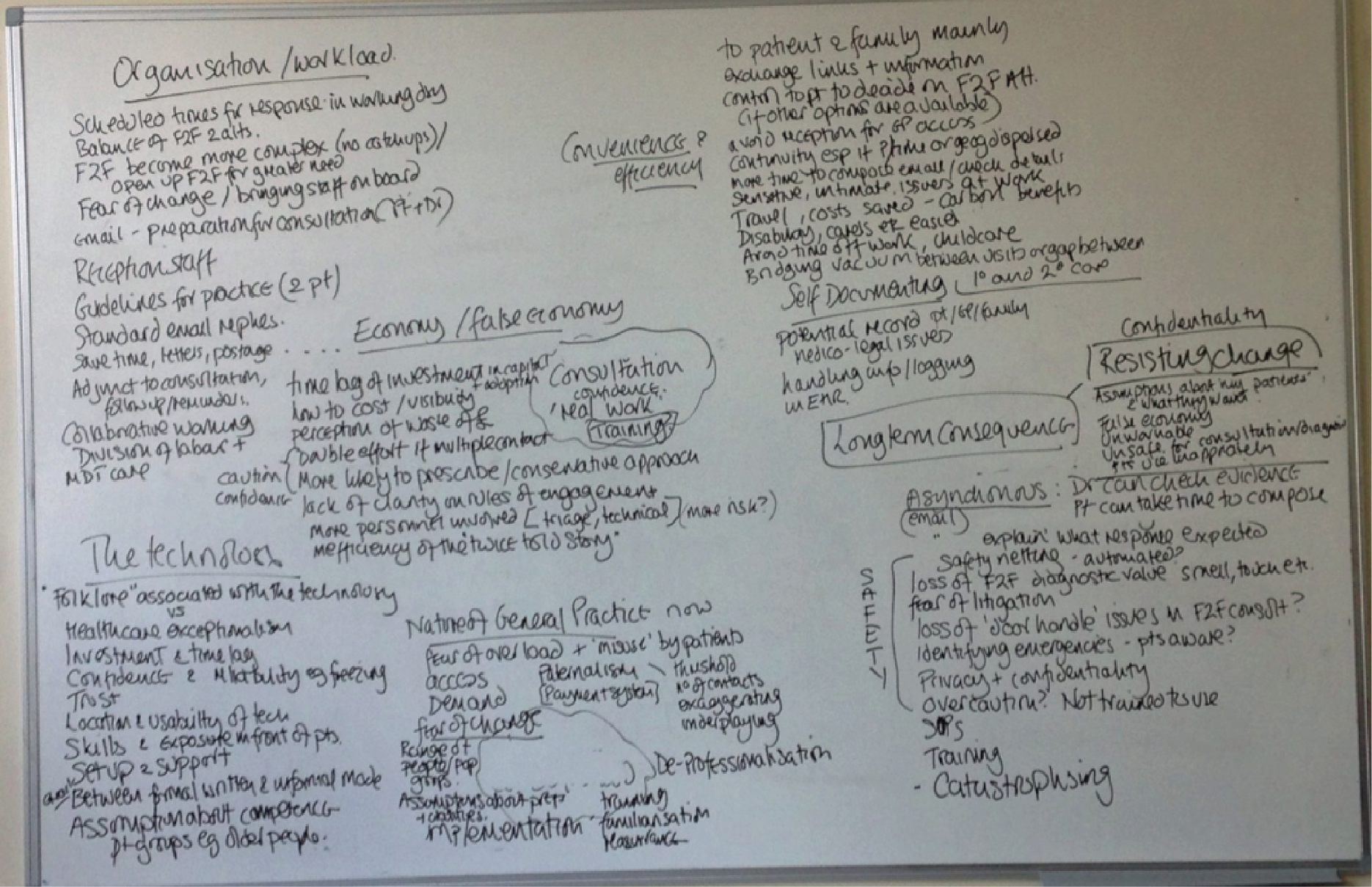
In the initial map, we identified the positive and negative effects of alternatives to face-to-face consultations, the effect on patients and staff working in primary care and other health-care settings and the potential mechanisms through which each effect might work. We identified nine main themes: organisation/workload, convenience and efficiency, the self-documenting nature of alternatives, economy/false economy, the technology itself, the nature of general practice, fear of change, asynchronicity and safety (Figure 2). This map provided the basis for the analysis.
FIGURE 2.
Map of initial themes.
Patient and public involvement workshop
Throughout the discussions, the themes from the review were compared with the perspectives of those attending the workshop. We further explored any differences or possible new ideas within the review material to see if they could add to the conceptual map.
Conceptual map
The final conceptual map covered 10 themes under three headings: organisational disruptions and dynamics, professional disruptions and dynamics and spatial disruptions and dynamics.
Organisational disruptions and dynamics
Uptake and awareness
In settings in which the availability of alternative forms of consultation is a matter for individual practices, rather than being required by policy directives (as in Denmark), then the question is raised as to how patients find out what is available to them at their practice. In a survey of patients’ reasons for not consulting their doctor by e-mail,92 the lack of awareness of the possibility of an e-mail consultation was one of the main reasons for non-use. Primary care professionals have described selectively offering alternatives to patients who they feel are able to use them appropriately. 19,93 Awareness will clearly affect uptake, as will the attitudes of members of the primary care team towards offering these alternatives. There was a lack of material relating to the perspectives of reception staff and their contribution to the uptake and awareness of alternatives, despite their patient-facing role.
Organisation of alternatives to the face-to-face consultation in the health-care setting
Several of the misgivings that have been raised about alternative consultations relate to the organisation and administration of the practice rather than to the consultation itself. Common concerns include what will happen if a part-time member of staff does not pick up an urgent e-mail and if alternatives to the face-to-face consultation will introduce inefficiencies for the practice. 67 Staff sometimes express concerns about whether or not patients will exercise their options responsibly, fearing that the relative ease of sending an e-mail (or a stream of e-mails) may mean that some patients will overconsult or misrepresent their symptoms. 94,95 Although the evidence is limited, in settings in which e-mail consultations have been introduced, they have not, as yet, opened the floodgates for patient demand. 96 Even in practices and health systems in which patients have had the right to e-mail their family doctors for some time, these alternatives are not widely used. 55,97 In Denmark, where e-mail consultations are a standard part of primary care, some doctors admit to managing their patients’ expectations by deliberately delaying their responses to non-urgent e-mails. 44
Primary care is set up to deliver the face-to-face consultation. As yet, there is little evidence about how best to time, conduct and record other forms of consultation. 94,98,99 These uncertainties make changes to service delivery difficult. 30,48 Potential inefficiencies include duplicated consultations if patients consult remotely and then attend the practice or need a home visit. 60,100,101 A study of telephone triage in general practice found that, where telephone triage led to a face-to-face consultation, the duration of this subsequent face-to-face consultation was no shorter, despite a clinician speaking with the patient during the telephone encounter. 102
Making arrangements for recognising and reimbursing some of these alternatives to the face-to-face consultation is an ongoing process. 103,104 In the USA, problems have arisen where reimbursement for Medicare patients is at the discretion of individual insurers, with many patients not being reimbursed for alternative types of communication with their health-care provider. 105
Different alternatives to the face-to-face consultation also differ in their impact on practice organisation. The face-to-face consultation is usually booked via reception staff. This is also the case for most telephone consultations. E-mail can allow patients to bypass the gatekeeping role of the reception staff and obtain direct contact with the primary care professional, or whoever is allocated the task of replying to the e-mail. 19,106 This prospect is sometimes viewed as unacceptably disruptive by clinicians. 107 There is a lack of evidence relating to the roles of team members, such as reception staff, in delivering alternatives to the face-to-face consultation.
Safety
Patient safety is crucial in any form of consultation, but alternatives to the face-to-face consultation present an unknown in terms of what these issues might be. Despite patient safety being cited as a reason to be wary of introducing alternatives to the face-to-face consultation,108 there is very little documentation of what these concerns are. Patient privacy and confidentiality are described as being important, but reports of privacy and confidentiality breaches are few, and collection of these data is uncommon. The Cochrane review of trials relating to e-mail for consultation found that the trials did not report any harms, but this is not the same as stating with confidence that no harms occurred. 30 There is much work to be done in identifying potential patient safety issues and mitigating the risk associated with these.
Organisation of space
As a visual method of consultation, there are considerations to be made when using video conferencing. To benefit from video conferencing, practices may need to allocate a well-lit, private area for the staff to use, as well as reliable connections, so that screens do not freeze mid-consultation. 107,109 This also applies to the systems that the patients are using. 110 A reliable contingency arrangement may be needed in case of technological failure. The potential for ‘freezing’ or image breakdown during a video consultation may have clinical consequences – for example, it can be particularly disturbing for people with mental illness. 109
Professional disruptions and dynamics
Proximity in the consultation
The common feature of all alternatives to the face-to-face consultation is that they are not face to face. A different medium inevitably changes some aspects of the performance of the consultation; these elements may be lost, or may need to be expressed in a different way or performed at a different time, for core elements of the doctor–patient relationship to be maintained. 111,112 There is particular uncertainty around the ‘rules of engagement’ for e-mail and video consultations. 19,44,113 The proximity with the patient that is afforded in the traditional face-to-face consultation permits diagnostic cues, such as smelling the patient’s skin and breath, noting how the patient walks into the room and using casual contact, such as shaking hands, to assess skin temperature and tone. 114,115 The health-care professional may lose some of their ability to check the patient’s understanding, which is often conveyed via non-verbal communication. 116,117 As yet, there is little research indicating whether misunderstandings are increased or diminished with alternatives to the face-to-face consultation.
Professional indemnity
Related to the lack of guidance or consensus on best practice, patient safety and the risk of litigation are often raised when alternatives to the face-to-face consultation are proposed. 93,118 This could be understood as a proxy reason, given that highlighting safety concerns is undoubtedly a more ‘acceptable’ form of resistance than voicing concerns about threats to professional identity and power. However, there is also some evidence that clinicians’ safety concerns are leading to safety-netting, demonstrated by prescribing behaviour; for example, primary care doctors are more likely to prescribe antibiotics during an e-visit than when they consult face to face. 119 This may reflect uncertainty around the medicolegal consequences of this type of prescribing. In trying to understand how alternatives are working, it is necessary to be alert to how safety-netting procedures are enacted.
Health-care professional attitudes
When health-care professionals are asked about their views on using alternatives to the face-to-face consultation, concerns tend to focus on whether or not their clinical duty to provide safe and effective care might be compromised. 37,45 Much of this concern relates to the potential impact of these additional consultation methods on their workload. Fears expressed include increases in consultation volume24,120 and increased administrative load. 20
Those with experience of successfully using alternatives to the face-to-face consultation in their own practice raise similar issues: still feeling uncertain about the long-term effects on their workload and, consequently, their patients. 19 Research suggests that any new technology needs to be seen to enhance what the professional sees as their core role,121 otherwise it is unlikely to be accepted into practice. 122,123
There have been far fewer studies collecting the views and experience of practice nurses on alternatives to the face-to-face consultation, but there is evidence that nurses feel that their role requires proximity to the patient. 111,124–126 In a study of a telehealth self-care support system for people with chronic health problems, the nurses who were providing the service positioned their work as ‘proper nursing’, whereas nurses who were using the telecare system suggested that the calls with patients were ‘just chat’ and doubted that real nursing could be delivered via the telephone. 127 A Norwegian study of nurses working in emergency medicine found that the approach of nurses changed when they consulted remotely: they were more assertive and gave more advice.
Health-care professional skills
An important consideration is whether the technology is familiar and easy for both parties to use or whether it requires new skills. Some health-care professionals worry that their lack of confidence with technology may be exposed, and that such exposure might undermine their authority. 128,129 In a study of breastfeeding support via video consultation, lactation consultants were concerned about technical issues, such as the quality of images, but patients were very satisfied with the remote consultation. The lactation consultants were not confident about undertaking clinical assessments via video – a concern that the authors concluded could be addressed by specific training in using the medium. 110 Although the balance of power within the consultation may change if the primary care professional’s skills come under patient scrutiny,130 this is not necessarily damaging and could even be a helpful shift in longer-term relationship dynamics.
Spatial disruption and dynamics
The nature of the communication medium
There are already many different technologies that patients could use to consult their doctor without meeting face to face, for example telephone, e-mail, SMS and video communication. Although specific platforms are likely to be superseded in a fast-changing field, it is possible to differentiate according to whether the method provides (moving) images, audio or written content, and whether the exchange is in real time or asynchronous. Asynchronicity allows both patients and health-care professionals to send and act on contacts at a time that suits them. For the health-care professional, they can draw upon external resources or check evidence, perhaps providing sources of information for the patient. 67,131 For patients, it allows them time to construct an enquiry, perhaps with help from family or friends, and to send follow-up questions that occur after a consultation. E-mail allows patients to upload images. Methods that allow video connection give health-care professionals the opportunity to view the patient, including visual symptoms (such as a rash) and also, potentially, the patient’s home setting. All of these factors allow for the collection of information on the state of the patient, beyond that communicated verbally.
Patient interface with alternatives to the face-to-face consultation
Where patients have been offered an alternative to the face-to-face consultation, they usually report liking them. 132,133 E-mail and telephone consultations remove the need to attend the GP or nurse’s professional space, which tends to be viewed as a benefit by patients. 67,106,119 Other reported benefits include the convenience of being able to consult while at work,134 to choose when and how to consult and the perceived advantage of avoiding the practice receptionist. 44,124 The ability to communicate with a doctor via e-mail means that the patient can compose a message when something is bothering them, which may be outside office hours. The patient (and their family) may like to exchange information relevant to health and care decisions within their personal contacts. Parents can photograph, record and attach digital files with images of a child’s rash, or recordings of an infrequent cough or breathing difficulty. 44,128 For patients preparing for a visit to hospital, or recovering at home afterwards, these methods can provide a way to keep in touch without necessitating a visit. 111
E-mail exchanges can provide a consultation record, and possibly clearer explanations and subsequent understandings than information obtained during face-to-face contact. 111 This may be particularly advantageous to those who are less articulate or confident in person, those who wish to discuss their consultation with others and those who need help with translation. 94 Some patients may be more willing to disclose intimate or sensitive information via an e-mail than in person or over the telephone – especially if they are at work or in a public place. 44 For others, the reverse will be true, not least because of concerns about confidentiality in e-mails.
Health professionals raise concerns that older patients, disabled patients, people without literacy skills and patients who are less educated3,55 may be disadvantaged through alternatives to the face-to-face consultation. 45 There is some evidence that, for those who have internet access, patients who are disabled, elderly, less confident or living at some distance from the practice are often among those who are particularly keen to use e-mail consultations. 56 Patient skills in using these technologies should be considered. Providing information or training may not be enough on its own. Varsi et al. 131 recommend that patients should be shown how to use a system at a point when it is relevant to them, rather than as part of a general induction to their health-care organisation. If the information does not come at the right time, the patient may not remember the system, or (as is likely in a fast-moving field) the system may have changed by the time they come to use it.
Although there is a lot of speculation about the potential benefits and disadvantages for patients, and particular subgroups of patients, much of it has been written from the health-care professional perspective, and credible empirical evidence from patients is very limited. The perspectives and experiences of patients (and especially those from groups who are assumed to be disadvantaged by the introduction of alternatives to the face-to-face consultation) clearly need further attention when designing, implementing and evaluating systems.
Unintended consequences
It is important when studying alternatives to the face-to-face consultation to consider the potential for unintended consequences. There are numerous examples of technologies that have been tinkered with and adapted in the field,121 some to the extent that their initial purpose is barely recognisable. Changes in one element of care provision can have an impact on other elements of care and the role of other staff. An example is Winthereik and Langstrup’s study,135 in Denmark, of patient and professional behaviours in response to a new portal for pregnant women. The portal was introduced to help women with uncomplicated pregnancies to self-manage, with aims to free up resources for patients with more complicated conditions. They found that, although only a minority of participants engaged in the portal, those who did enacted their active and responsible involvement at the clinic rather than at home. The use of the portal, therefore, provided both more and less than was anticipated: it reconfigured relations in a way that is likely to alter the meaning of care, but not in a manner that was likely to free up resources. In addition, the health-care practitioners, who were supposed to be using the portal to maintain a complete and shared electronic record, were instead printing a paper record and adding their own hand-written notes. The health-care professionals ended up doing more work than before.
Key questions
As the conceptual map was developed, a series of key questions was created (Box 2). These questions were used to form the basis of an essay: ‘What do we need to consider when planning, implementing and researching the use of alternatives to face-to-face consultations in primary healthcare?’. The essay was submitted to and accepted by the Journal of Digital Health and published in September 2016. 83 The content of the essay overlaps with the material presented in this chapter, although the essay was designed for broader application beyond the study.
-
How could patients find out what methods of consultation are offered by their doctor?
-
How will alternatives to the face-to-face consultation be scheduled into existing practice?
-
What impact will alternatives to the face-to-face consultation have on reception and administrative staff work patterns?
-
What are the agreed rules of engagement for the use of alternatives to the face-to-face consultation?
-
What contingency is in place to ensure that communication by asynchronous methods is responded to, and in a timely fashion?
-
How will the expectations of all parties be managed?
-
How can consultations be appropriately administered to avoid duplication of effort?
-
How will alternatives to the face-to-face consultation be documented in the medical record, especially when consulting remotely from the practice?
-
Is reimbursement for alternatives to the face-to-face consultation appropriate? What are the arrangements for reimbursement?
-
What are the potential patient safety issues?
-
How are these (or might these be) mitigated?
-
Are there risks to patient privacy and confidentiality?
-
What are the contingency arrangements for technology failure?
-
What did the designers intend it to do – and (more importantly) how is it used in practice?
-
Does it allow eye-to-eye contact? Is it in real time or is it asynchronous?
-
What is lost in comparison with the copresent consultation?
-
What is the effect on valued aspects of primary care, such as the relationship and continuity of care?
-
What is the alternative to the face-to-face consultation appropriate for? Is it offering a replacement for the face-to-face consultation or is it complementary?
-
Is there a risk of misunderstanding as a result of the change in medium, and can this be accounted for?
-
Will alternatives to the face-to-face consultation change how patients communicate?
-
How are the roles of different team members affected by their use?
-
Are there implications for staffing in the practice?
-
How is medicolegal protection in relation to alternatives to the face-to-face consultation organised and understood in the practice setting?
-
What are the views and concerns of different members of the team about alternatives to the face-to-face consultation?
-
What skills are needed? Is training and support available?
-
Will patients require training or guidance in using alternatives to the face-to-face consultation?
-
Will the introduction of alternatives to the face-to-face consultation allow for flexible working?
-
If so, might this have an impact on primary care staffing recruitment and retention?
-
Are there cost implications?
-
Who was involved in setting up the system and whose work was considered?
-
Is the rationale for introducing an alternative to the face-to-face consultation clear and understandable to all staff members?
-
What impact does it have on all of the different members of the team?
-
Whose core values and interests are served?
-
How is resistance enacted, and by whom?
-
How will patient experiences be collected and recorded?
-
Are there types of consultation that are preferred face to face?
-
What about patients from groups who are often assumed to be disadvantaged in relation to alternatives to the face-to-face consultation (older, disabled, less educated, those with language difficulties)?
-
How might patients use the opportunity to share digital files with their doctors?
-
Are there consequences (either positive or negative) for other elements of the practice, or other aspects of care provision?
-
Are there consequences for other parts of the health system (use of emergency helplines, hospital emergency departments, etc.)?
-
Do (and how do) staff and patients modify new forms of consultation to better meet their needs?
-
How else might the planner, implementer or researcher identify unintended consequences?
Case study guide
The findings of the review fed directly into the case study guide. The case study guide was produced to guide the focused ethnographers in their understanding of the required scope of data collection across the three case study sites. Each ethnographer came from a different background, and two had not conducted research in general practice settings before. The guide was used to ensure that they understood the scope of the focused ethnography and felt confident going into the field.
The guide outlined specific areas of interest, including the staff members they should consider observing (e.g. focusing on reception staff as well as clinical staff), things they might want to look out for (e.g. dynamics within the clinic between staff members) and where they might look (e.g. areas where team members interact beyond the consultation areas) in this particular setting.
The 13-page guide was written systematically, and began by reiterating the objective of the case studies and outlining the participants of interest. Then, for each group of interest, such as reception staff, the tasks required (observation, interview) and the per-protocol approach to conducting the tasks were outlined, and the factors to explore were detailed. These factors were derived from both the protocol and the review findings. The guide finished with a summary of each technology type and the specific factors to explore in relation to these. This was helpful for the ethnographers at the beginning of the study when they were unfamiliar with the research questions. They were told that it was a guide and not a checklist and that it was for their personal reference only. For the case study guide, see Appendix 4.
Conclusion
This conceptual review has identified and synthesised material relating to patient and staff experiences of alternatives to the face-to face-consultation, along with theories and ideas about the potential effects. Key questions to be asked when researching alternatives to the face-to-face consultation have been applied in devising a case study guide, which was used by the focused ethnographers in guiding data collection at case study sites.
The conceptual map and key questions devised here are applied to the interpretation and synthesis of all data collected in this study; this included the focused ethnography and the routine consultation data. The use of the conceptual map and the key questions is demonstrated in the case study results chapter (see Chapter 5) and the synthesis chapter (see Chapter 7), respectively.
Chapter 3 Scoping study
The material in this chapter is republished with permission from the British Journal of General Practice. 136
Introduction
The main aim of this project was to recruit case study practices across three study sites: in and around Bristol; in and around Oxford; and in Lothian and the Highlands and Islands of Scotland. Case study practices had to be using or considering introducing, or to have recently ceased using, alternatives to face-to-face consultations, such as telephone consultations, e-mail consultations, video consultations or e-consultations. We employed a scoping study to identify practices fitting these criteria which could be invited to participate in the main study.
Our secondary aim was to understand the extent of the use of these alternatives to the face-to-face consultation in contemporary general practice.
Methods
The scoping study utilised a number of methods to identify the practices. The main approach was to send a postal survey to all of the practice managers, GP partners and salaried GPs (n = 2719) at all the practices in and around Bristol, Oxford, Lothian and the Highlands and Islands of Scotland (n = 421). This was supplemented by four further approaches: (1) exploring the practices’ websites, (2) contacting companies that offer support in providing alternatives to face-to-face consultations, (3) utilising local and national links with those working in primary care and (4) utilising existing knowledge within the team.
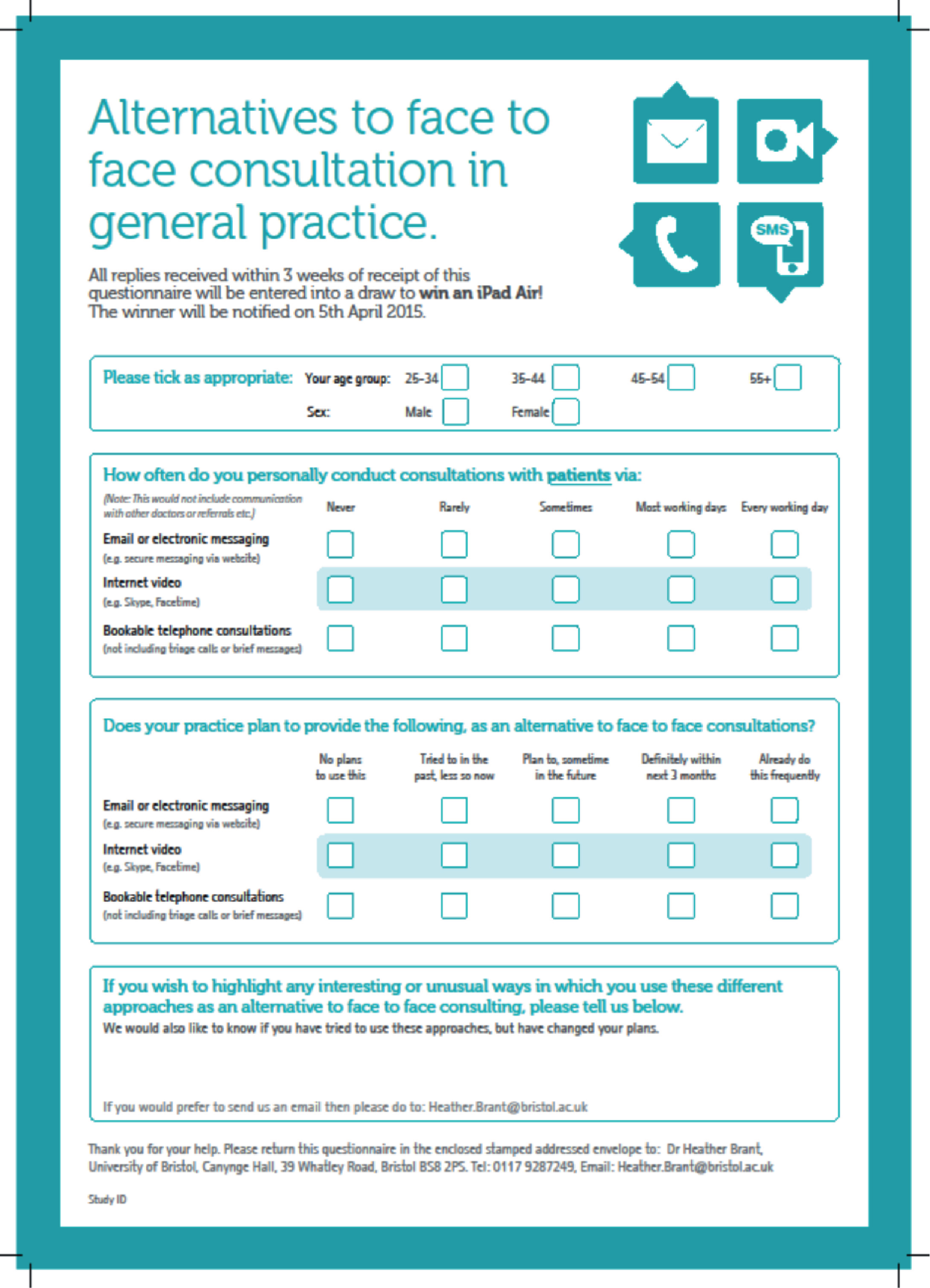
The postal survey
The single-page survey opened with questions about the age and sex of the respondent, followed by two groups of questions. In one group, participants were asked whether their practice currently provided or planned to provide consultations with patients via e-mail or electronic messaging, internet video or telephone. We excluded telephone triage, as this constitutes a contact rather than a consultation and telephone triage is being assessed in an ongoing project funded under the same call. 137 In the other group of questions, participants were asked how often they personally conducted consultations using each of these approaches. Each question in both groups was scored on a 5-point Likert scale. The questionnaire closed with the opportunity for respondents to add information ‘about any interesting or unusual ways in which you use these different approaches’ in a free-text box (Figure 3).
FIGURE 3.
Questionnaire.
Practices within the English study sites were identified through the relevant Clinical Commissioning Group (CCG) websites. For the practices in Scotland, we retrieved details from the Information Services Division Scotland website. Information about the practice managers, GP partners and salaried GPs were accessed via the practice website if one existed. For those practices without a website [53/421 (13%)], we gained the information through a telephone call to the practice.
We posted questionnaires to each of the practice managers, GP partners and salaried GPs. As the focus of this study was on provision of care at a practice level rather than individual GP attitudes, our aim was to receive at least one response from each practice. If no response had been received following a period of 2 weeks, a postal reminder was sent to all of the GPs and the practice manager within the practice, and 2 weeks after this a telephone reminder was made, if appropriate, to the practice manager. We also offered an incentive, with all those who returned a completed questionnaire within a specified time being entered into a raffle for a tablet computer.
Ethics and research governance permissions
The Health Research Authority and the University of Bristol Faculty of Medicine and Dentistry Research Ethics Committee deemed that no ethics permission was needed.
Analysis
We conducted the primary analysis at the practice level, and then subsequently analysed GPs’ personal use of alternative forms of consultation at an individual level. Numerical data were analysed using simple statistical methods supported by Microsoft Excel® 2013 (Microsoft Corporation, Redmond, WA, USA) and Stata® 13 (StataCorp LP, College Station, TX, USA). Where different responses were given by respondents within the same practice, we used the mean result at practice level, rounding to the nearest whole number (since each response was scored from 1 to 5 on a Likert scale). We explored the extent of variation in response by different individuals within the same practice, using the within-practice standard deviation (SD) and the intraclass correlation (ICC) coefficient. Responses regarding GPs’ own use of alternatives to face-to-face consultations were analysed at the individual respondent level. Responses from practice managers were excluded from the individual-level analyses, as they do not consult with patients.
We analysed the results from the free-text box thematically, using NVivo 10 (QSR International, Warrington, UK), and visual mind-mapping was carried out to examine themes and patterns in the data. 90
Exploring practice websites
An attempt was made to access each of the 421 practice websites in our three study areas (186 English and 235 Scottish practices) to see if there was any reference to the use of alternatives to face-to-face consultations. However, websites were not identified for 53 out of 421 practices (13%) at the time of searching (51 of the 53 were in Scotland).
Contacting commercial organisations
A number of companies market software systems to general practices to support them in providing alternatives to face-to-face consultations. We drew up a list of these companies through existing knowledge of the team and extensive searches of the internet. Eight companies were approached to enquire whether or not there were any practices using their technology within our study sites. Although four companies responded, no practices were identified because either the technology was outside our remit, they were reluctant to provide details of the practices that were using their technology, or there were no practices in our study areas.
Utilising local and national links with those working in primary care
In addition to the above methods, we also approached the local CCGs, Health Boards and Primary Care Research Networks in our study areas to ask if there was any awareness of practices adopting any form of alternatives to face-to-face consultations. We were also able to identify any practices or local consortiums that may have been funded by the GP Access Fund. 14 Unfortunately, this approach did not yield any further information, as either we had already identified the sites or there was little knowledge of the local use of alternatives to face-to-face consultations. Our enquiries also demonstrated that, although many sites receiving funding from the GP Access Fund14 had said that they would implement alternatives to face-to-face consultations, such as video-consultation, we were not able to identify any that had actually done so at that point in time.
Results
Postal survey
Of the practices approached, 163 out of 186 practices (88%) in England and 156 out of 235 practices (66%) in Scotland responded, giving an overall practice response rate of 76% (n = 319/421). In addition, 40% of English and 25% of Scottish surveys were returned with an overall individual response rate of 33% (n = 889/2719). The number of responses per practice ranged from 1 to 11.
Profile of respondents
Participating practices were significantly larger (in terms of numbers of registered patients and doctors per practice) than those that did not participate. There were no significant differences between responding and non-responding practices in terms of their deprivation score (Table 2). Of the 696 respondents who reported their sex, 59% (413/696) were female. Respondents categorised their ages as 25–34 years (n = 90/889; 10%), 35–44 years (n = 239/889; 27%), 45–54 years (n = 362/889; 41%) or ≥ 55 years (n = 189/889; 21%). Of all the responses, 12% (105/889) came from practice managers and 88% (784/889) from doctors.
| Characteristic | Responses, n (95% CI) | p-value | |
|---|---|---|---|
| Responders | Non-responders | ||
| Number of doctors working in the practice | 6.05 (5.72 to 6.37) | 3.71 (3.22 to 4.20) | p < 0.001 |
| Number of patients registered with the practice | 7732 (7265.90 to 8197.58) | 6971 (3780.98 to 5322.68) | p < 0.001 |
| Deprivation associated with the practice – England (n = 186)a | 16.62 (15.01 to 18.23) | 19.74 (14.65 to 24.84) | p = 0.20 |
| Deprivation associated with the practice – Scotland (n = 235)b | 7.33 (5.13 to 9.52) | 5.76 (3.23 to 8.29) | p = 0.38 |
The current and planned use of alternatives to face-to-face consultations at the practice level
Although the majority of practices reported routinely offering telephone consultations, few (6%) reported facilitating e-mail consultations (Table 3). One-fifth of practices intended to offer e-mail consultations in the future, but half of the practices had no such plan. None of the respondent practices reported offering internet video consultations, and very few reported any plans to do so in the future. There was also evidence that 21% of practices had previously offered e-mail, and that 10% had previously offered internet video, but that they had subsequently withdrawn these services.
| Does your practice plan to provide the following as an alternative to face-to-face consultations? | Practice-level plans, n (%) | Total, n | ||||
|---|---|---|---|---|---|---|
| No plans to use this | Tried to in the past, less so now | Plan to sometime in the future | Definitely within the next 3 months | Already do this frequently | ||
| E-mail or electronic messaging (e.g. secure messaging via a website) | 169 (53%) | 66 (21%) | 51 (16%) | 14 (4%) | 18 (6%) | 318 |
| Internet video [e.g. Skype, FaceTime (Apple Inc., Cupertino, CA, USA)] | 273 (86%) | 31 (10%) | 13 (4%) | 1 (0%) | 0 | 318 |
| Bookable telephone consultations (not including triage calls or brief messages) | 30 (10%) | 16 (5%) | 30 (9%) | 31 (10%) | 211 (66%) | 318 |
There were some inconsistencies between respondents within the same practice about their practice’s use of telephone (within-practice SD 0.91, ICC 0.53) and e-mail consultations (SD 1.1, ICC 0.39). There was less variation between respondents about their practice’s use of video consultation (SD 0.52, ICC 0.20), related to the limited use of this consultation method in general.
The current provision of alternatives to face-to-face consultations at an individual general practitioner level
The majority of GPs reported personally providing telephone consultations on most working days or every working day (79%). Only 8% of GPs reported providing e-mail consultations on most working days or every working day, whereas 45% did so rarely or sometimes and just under half (47%) never provided e-mail consultations. Furthermore, 99% stated that they never conduct consultations via internet video (Table 4). Provision of telephone, e-mail or video consultations did not vary by GP age or sex, or by study site (data not shown).
| How often do you personally conduct consultations with patients via: | Frequency, n (%) | Total, n | ||||
|---|---|---|---|---|---|---|
| Never | Rarely | Sometimes | Most working days | Every working day | ||
| E-mail or electronic messaging (e.g. secure messaging via website) | 364 (47%) | 248 (32%) | 102 (13%) | 44 (6%) | 17 (2%) | 775 |
| Internet video (e.g. Skype, FaceTime) | 752 (99%) | 10 (1%) | 1 (0%) | 0 | 0 | 763 |
| Bookable telephone consultations (not including triage calls or brief messages) | 68 (9%) | 30 (4%) | 69 (9%) | 147 (19%) | 465 (60%) | 779 |
Thematic analysis of free text
All respondents were invited to complete a free-text box to ‘highlight any interesting or unusual ways in which you use these different approaches as an alternative to face-to-face consulting’ and 249 out of 889 responses (28%) included some form of free text.
Rather than answering the question posed, the majority of the respondents described their views on the idea of introducing e-mail or video consultations. Most of these comments expressed resistance to the idea of e-mail or video consultations. Only a few opinions were related to actual experience, and many respondents expressed strong views, despite reporting no actual experience of using such methods (e.g. ‘only politicians and the naive would think this a good idea’).
A number of GPs expressed concerns that adopting e-mail or video consultation would add to their already demanding workload:
Increasing access options, increases GP stress . . .
E-mail is a nightmare – access all the time and hundreds of e-mails.
Currently overwhelmed and under resourced.
or that it would have a negative impact on the practice:
If we take on e-mail consultations we will have possibly hundreds of emails. Who will deal with them? Medicolegal consequences of delay we have no capacity, this will possibly increase workload.
We already get > 100 e-mails EACH daily. This would open the floodgates and we would drown. It is unmanageable.
We are all too busy to synchronise this.
The practicalities of managing alternatives to face-to-face consultations were also voiced as a concern:
We have talked about these being future possibilities but I have concerns about managing the amounts via e-mail - difficult to cap them.
At the moment there is no way of providing protected time for e-mail consulting and would therefore be reticent to encourage this.
E-mail’s a problem as difficult to store but can copy the essentials into system. It doesn’t save much time. Text is worse as have to make separate note so not used routinely.
The respondents also expressed a fear that offering alternatives to face-to-face consultations would be a challenge in terms of privacy and confidentiality, and would increase clinical risk with medicolegal consequences:
It’s a personal preference but I find the increased access too intrusive and increases risk of information getting lost/filed with other documents.
We have discussed use of e-mail communication but find there is a risk of e-mails not being acted upon when certain GPs are on leave leading to unnecessary risk and delay.
I feel the level of risk with these are higher than a face-to-face or phone.
Issue with confidentiality using e-mail.
Query issues with medicolegal problems + confidentiality.
Practical issues, such as the reliance on appropriate internet provision and broadband reliability, and local concerns about information governance were mentioned as further barriers to implementation:
Internet connection currently barely up to current software requirements for e-referrals etc. Don’t have software & hardware capacity for more modern techniques.
I have tried to discuss use of internet video consults. Health Board have concerns re security - additionally agreeing role out of suitable user friendly secure system may be an issue.
We are not allowed to use the internet due to confidentiality.
alongside a concern that there could be an additional cost to the practice:
Need additional funding/additional admin time (reduced clinical time) to accommodate.
Funds are the only barrier currently.
Skype/facetime would involve investment in IT. This is not funded by our CCG.
A few GPs had experience of some vulnerable and elderly people who preferred alternative consultation methods, whereas others thought that these same groups would be disadvantaged:
Concern that most vulnerable (deaf/blind/elderly/demented/mentally ill) least able to access and so unintentionally disadvantaged.
Very elderly population – technology difficult.
Most of my patients with real health needs are > 85 yo [years old] and not skyping. Most of the patients with electronic ‘wants’ are < 45.
A few GPs mentioned experience of benefits of using an alternative to a face-to-face consultation, such as patients being able to send pictures of a transient rash or an audio file of a child’s cough:
I think patients using media, e.g. bringing in photos of their transient rashes, or recordings of their baby’s cough are great.
In combination with phone consult (and with consent) I have got patients to text me photos of problem e.g. rash, eye inflammation to help confirm diagnosis or whether need to be seen etc.
or their use as part of ongoing medical care and a way of providing patient support or for sharing information:
In my experience telephone consultations useful for F/U [follow up] of problems.
I kept in weekly contact with a T1 DM pt [type 1 diabetes mellitus patient] by text.
E-mail and telephone are usually simple issues such as drug queries or results. Patients report blood pressure I e-mail advice leaflets/links.
The use of alternatives to face-to-face consultations was also seen as a way of managing the practice workload:
We encourage patients to use email to send info to us (stops clogging up the phone lines).
Telephone very effective use of time and resources esp. follow ups.
Some respondents also reported benefits for their patients who preferred to use e-mail because of communication difficulties or disabilities that made it difficult to get to the surgery:
I use e-mail for one patient who has MND [motor neurone disease] and so cannot speak on phone.
E-mail really helpful for deaf patients (who sometimes send me an e-mail before attending a consultation to save time) and for tracheostomy patients.
Some also mentioned using e-mail with particular ‘selected’ patients, and being in e-mail contact with their own GPs:
For what it is worth, my GP has e-mailed me but only as a ‘special patient’!
Exploring practice websites
Within the practice website search, 128 out of 184 English and 125 out of 184 Scottish practices stated that they offered telephone consultations (not including those used for triage). These ranged from same-day call-back to booking a telephone consultation in advance. Five English practices and one Scottish practice offered an electronic messaging service (e-consultations), and four English practices and one Scottish practice invited patients to e-mail their doctor; however, for one there did not appear to be an e-mail address provided, and one English practice had a ‘webform’ box on their site for non-urgent messages. None mentioned offering video consultations. Although some of this information was clearly displayed, for some of the alternatives to the face-to-face consultation offered, particularly e-mail, it was difficult to find the information on practice websites. It was useful to cross-reference the findings from the website search with those from the survey, as sometimes websites were out of date. It was also useful to acknowledge the website information that applied to the case study practices selected for the ethnographic phase of the study, as this gave us more background on the practices we were going to approach for recruitment to the case studies.
Video consultations
As anticipated, the results of the scoping study confirmed that few practices used video consultations. Therefore, we approached practices external to the study sites, in order to invite those using video consultations to participate in interviews.
In order to target recruitment, we approached practices that had spoken publicly about their use of video consultations or responded to a Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) plea, or that had been funded by the GP Access Fund14 to employ video consultations. Further detail on the recruitment of users of video consultations can be seen in Chapter 4.
These additional interviews were used to expand our insights about the use of video consultations, given that we were able to identify only one practice in our study area that used video consultations, and this usage was very sporadic. These interviews are reported alongside the findings from case study practices.
Conclusion
Despite the policy pressure to introduce consultations by e-mail and internet video, this study not only demonstrated that use is limited, but also identified a general reluctance among GPs to implement alternatives to face-to-face consultations other than the telephone. However, it is worth acknowledging that shortly after conducting the survey, many practices introduced e-consult methods, precipitated by the GP Access Fund. 14 These developments would not be reflected in our survey results. Findings from the survey underline that both the reluctance and enthusiasm for these alternatives to face-to-face consultations are mainly speculative and reflect the fears of the profession around the burgeoning workload and concerns relating to professional identity. The free-text responses are indicative of wider concerns and match what is reported in the existing literature.
Regardless of the dearth of practices utilising alternatives to face-to-face consultations, it was possible to identify a number of practices suitable to act as case study sites within our study area. Although some practices declined an invitation to participate, we were able to recruit eight practices across the three sites. The process of case study practice selection is described in Chapter 4.
Chapter 4 Focused ethnographic case studies, methodology and description of sites
Rationale for the methodological approach
Focused ethnography approach
This study used team-focused ethnographic methods. In a focused ethnography, rather than embedding a single researcher in a social setting for a lengthy period, more targeted data collection is used to explore the study topics. Using existing information from the literature and from what is known in clinical practice helps to determine the research question and, subsequently, to generate findings that are relevant and useful. 139
This project is a team-based ethnography as it involved three ethnographers working across a total of eight general practice sites in three regions (Scotland, Oxford and Bristol). Team-based ethnographies have become increasingly popular across disciplines. 140–142 This trend has been linked to funding bodies that encourage multidisciplinary team-based research, because of the wider range of expertise that will be brought to a project. 140,142 The use of a team-focused ethnography for this study has been explored further by Bikker et al. 143
Although ethnographic methods have been used in primary care for several notable studies,144–146 they have usually required an intensive period of immersion (often by a sole researcher) in the study setting. The focused ethnographic approach lends itself well to health services research, because it is an efficient way to obtain an insightful understanding of concepts and processes within the fast-moving context of health-care policy development. This method was particularly suited to this study’s research questions as it allowed data to be collected on a predefined topic guided by the conceptual review work, while emphasising the importance of the context and the cultural landscape of the practices within a limited time frame.
Focused ethnographic team
Composition
The case study team consisted of three researchers with experience of ethnographic research who were employed to conduct the focused ethnographic fieldwork. Although having three researchers collecting data was time efficient, to minimise the costs, two of the researchers were employed solely for the duration of the data collection (12 months). The third researcher was employed for the duration of the project (27 months) and also took on the role of project manager. The ethnographic researchers were based in two universities in England and one in Scotland. They had different backgrounds, which included medical and social anthropology, nursing and mixed-methods research methodologies. The three ethnographers were managed by two co-applicants: Helen Atherton on a day-to-day basis with input from Sue Ziebland (see Table 1, Chapter 1). This subteam of five researchers made up the ‘focused ethnographic team’. The wider study team was also involved in providing a ‘check’ on the data the ethnographic team were collecting.
Communication
Steps were taken to ensure that the focused ethnographic team worked cohesively on the data collection and analysis. Over the period of the fieldwork and analysis, this involved:
-
the focused ethnographic team setting out a strategy for teamworking during their initial meeting
-
the three ethnographers having a weekly telephone meeting
-
the three ethnographers and the day-to-day focused ethnographic team lead (HA) having a fortnightly telephone meeting
-
the three ethnographers contacting the day-to-day lead (HA) via e-mail or telephone, when necessary
-
the day-to-day lead meeting regularly with the senior focused ethnographic team lead (SZ)
-
the entire focused ethnographic team attending three data collection and analysis workshops over the course of the project: two in Oxford and one in Edinburgh
-
the ethnographers attending the project meetings (both face-to-face and telephone meetings) during the 12 months of fieldwork, allowing for updates to be made to the wider study team, and for the ethnographers to hear about the progress of all elements of the project.
Patient and public involvement
We recruited three PPI representatives who reviewed the information sheet and consent forms, leading us to make to a number of improvements. These included:
-
rewording the titles
-
removing all abbreviations
-
an expansion of the information provided about observing consultations between the doctor and the patient/carer
-
simplification of the information provided to patients and carers invited to participate in an interview.
The three PPI representatives were recruited through a request for involvement circulated via the newsletter of ‘People in Health West of England’. Support was provided by the PPI lead, Andy Gibson. Andy Gibson explained the aims of the project and the purpose of involvement activities to potential participants. Feedback was given to participants on the amendments made to the ethics application as a result of their contribution.
Case study recruitment
Selection of sites
We recruited eight practices as planned. Two were in Scotland, three were in Oxfordshire and three were in Bristol. The scoping survey (see Chapter 3) was used to identify potential practices. Based on our survey data, we constructed a matrix of practices detailing various practice characteristics. Characteristics included experience of implementing different types of alternatives to face-to-face consultations; the size of population the practices serve; and location, in terms of whether it is urban or rural and deprived or affluent (based on deprivation scores). We then selected practices to approach, ensuring that we covered a range of demographic characteristics and applications of alternatives to the face-to-face consultation, for example ‘currently using’, ‘tried and rejected’ or ‘substantially modified their plans to use’ alternatives.
We sent invitation letters to practices, followed by telephone calls to the practice manager and/or GP to ensure that the invitation had been received. When practices were interested, a researcher visited to provide more information and discuss the implications of participation. Practices that declined to participate stated excessive workload and/or staff shortages as the reason.
Data collection and management
The remit of the focused ethnography was guided by the findings from the conceptual review, which helped to shape the case study guide and the staff and patient topic guides (see Chapter 2 for a fuller explanation and see Appendix 4 for the case study guide).
One ethnographer was based at each practice. Data were gathered through non-participant observation, informal conversations and semistructured interviews with practice administration staff, GPs and patients. Practice documents and protocols on alternatives to the face-to-face consultations were reviewed. Anonymised data about consultations were collected and these contributed to a quantitative analysis (see Chapter 6).
Consent and observational work
The ethnographers observed practice staff in all areas of the practice, such as clinical areas, reception desks and administrative offices. Observations included consultations, both face to face and alternatives to face-to-face consultations.
In the first instance, the practice manager agreed to the practice participating in the research and informed all staff that the ethnographers would be situated in the practice for a number of weeks.
On commencing the research within the practice, informed consent for observation was sought by the ethnographer from all members of the practice. This involved providing all staff members with an information sheet about the study and providing a consent form. The information sheet outlined that the ethnographers may observe them at work, engage in informal conversation and take notes. They were given up to 1 week to read the sheet and complete the consent form before a further enquiry was made. Some staff members were not based in the practice and declined to consent, on the basis that we would not be observing them. A small number of staff members declined to consent. We ensured not to engage them in informal conversation or directly observe their work. We did not take notes on any work they were engaged in. In addition, those consenting were informed that, at any point during the research period, they could decline observation or conversation. Staff members engaging in interviews were given an additional information sheet and completed an additional consent form for participation in the interview.
Observations of consultations were at the discretion of the GP. Patients were invited to consent to their face-to-face consultation being observed, given an information sheet and asked to consent to the observation. For observation of telephone and e-mail consultations, the ethnographers were not party to patient-identifiable data and so consent was not required; however, the clinician was able to decline the observation if they felt that it was not appropriate. If the ethnographer observed the GP within their consulting room but outside a consultation, they took notes but did not make notes relating to a patient or their condition, being focused only on how the GP worked (e.g. when they responded to e-mail consultations or when they scheduled their telephone consultations). Data were collected using field notes in all cases, and these did not include patient-identifiable data.
Summary profile
In each practice, the ethnographers completed a summary profile for that practice. This was designed to capture the detail obtained by the ethnographers in the field in their own words. It included, among other details, the types of alternative consultations that are (or were) provided, how these are/were provided (e.g. timing, volume, staffing) and any parameters for the types of patients who are/were allowed or encouraged to use alternatives to face-to-face consultations, including variations between practitioners. Over the course of the data collection, the ethnographers added any new observations about the practice to the summary profile template for each of the eight sites. This allowed individual field notes to be transformed into a common format. As a result, comparing the observations between practices became more straightforward, even though the personal styles of completing field notes differed between the ethnographers. At the start of the data collection, the discussion about the research topics among the focused ethnographic team was more general, reflecting the exploratory nature of the study and the process of familiarisation with the field. However, as the data collection progressed, the format of the summary profile template evolved and became more focused on alternatives to the face-to-face consultation.
The ethnographers recorded their own field notes during observations. In more formal settings, such as practice meetings, minimal notes were made by ethnographers in real time, followed by more detailed field notes retrospectively.
Document collection
In each of the case study practices, we sought to review notes and minutes from practice meetings over the preceding 6-month period. Some practices were reluctant to give our researchers full access to these notes and minutes, and so the practice managers in each practice reviewed the minutes, identifying and extracting any relevant information.
In each practice, researchers requested that they be invited to observe practice meetings during which alternatives to the face-to-face consultation would be discussed. In the end, this was the case for only one meeting in one practice, where the researcher attended the meeting and kept notes.
Semistructured interviews
Each interview participant provided informed consent. Interviews were digitally recorded, using an encrypted recorder. The files were transcribed verbatim by a professional transcription service.
Staff interviews were usually conducted in the general practice (one GP was interviewed at home). Additional interviews relating to video consultation at non-case study sites were conducted over the telephone. Information was collected on sex, age, ethnicity, role in the practice, length of time in the role, length of time since qualifying and the type of alternative to the face-to-face consultation used.
Patient and carer interviews were conducted at a location of their choosing, usually their home (or the general practice). Information was collected on sex, age, ethnicity, whether or not they were a carer, whether or not they had a long-term condition or disability, level of education and occupation.
The initial design of the topic guides was based on the findings of the conceptual review and templates used by focused ethnographic team members in previous studies. The topic guides were then revised iteratively among the ethnographic team once the ethnographers were working in the field, and a final topic guide was agreed on for both staff and patient interviews. The staff topic guide differed slightly according to the staff member being interviewed; for example, GPs were asked specifically about how the alternative to the face-to-face consultation affected their relationship with patients (see Appendix 5 for the topic guide).
Interview participant recruitment
Case study site staff
Once they had been conducting observations in the practice for a few weeks, the ethnographers identified relevant staff members to participate in the interviews. The ethnographers had made contact with potential interviewees during non-participant observation, and provided them with the information sheet relating to the interview. If they were willing to participate, an interview was arranged at a time that was convenient for the staff member.
In each practice, administrative staff (including receptionists), GPs and nurses were recruited to be interviewed. When relevant, other members of the practice team were also interviewed, for example, a rural health worker in one practice, a patient manager and an IT manager in another. The team of ethnographers remained in close contact throughout the process, to ensure that the range of staff members being interviewed was suitably varied in regard to factors such as role in the practice, knowledge or involvement in alternatives to the face-to-face consultation.
At the protocol stage, we intended to interview allied health professionals working in general practice, such as phlebotomists and community-based pharmacists. However, it became apparent during observations that, where allied health professionals were working in the practices, they had little to no involvement in the introduction or use of alternatives to face-to-face consultations. Recognising the importance of the wider study team members within general practice, each ethnographer engaged in informal conversations with these staff members to ensure that their perspectives were covered. These conversations were recorded in the researcher’s field notes and subsequently referred to in the structured summary profile.
Users of video consultation
As described in Chapter 3, we recruited an additional four participants from outside the case study sites. These were general practice staff members who were using, were about to use or employed a system that used video consultations.
-
We approached practices that had been funded by the GP Access Fund14 to employ video consultations.
-
We approached practices that had publicised their use of video consultation in news articles or reports.
-
We posted a message on Twitter:
Has your practice offered patients video/skype consults? We are looking for GPs to do a 30m phone interview for AltCon study.
Helen Atherton has 865 Twitter followers and tweets about digital health in primary care.
-
We used personal contacts (HA and CS) obtained via related research studies.
Two participants were recruited via Twitter, and a further two were recruited via personal contacts (HA). We were unable to contact all of the GP Access Fund14 practices and, in the case of those we did contact, we could not identify individuals who were using video consultation. We received no reply from the practices that had publicised their use of video consultation via news articles or reports.
Patients/carers
The aim was to interview patients with different characteristics in relation to age, sex, ethnicity, disability, frequency of attendance and whether or not they had long-term health conditions. All patients invited to participate in interviews had experience of using an alternative to the face-to-face consultation within the practice.
Initially, patients were identified opportunistically, based on those who had engaged in contact with the practice via an alternative to the face-to-face consultation. In subsequent interviews, patients were purposively sampled to ensure that participants with the range of characteristics listed above were included. Practice staff and GPs helped to identify patients and carers and provided potential participants with a study information pack, either via post or in person when attending the practice. This pack included information about the study, an invitation to take part and a reply slip, which they could return via prepaid post. The researcher then called to arrange a convenient time for the interview.
Hard-to-reach and disadvantaged groups
In using a purposive sampling technique, we specifically included people who were identified in the protocol as being in hard-to-reach groups with regard to accessing general practice. Examples included parents/carers of people with complex needs, young men, the vulnerably housed and minority ethnic groups.
The other groups of interest were those that might be disadvantaged by limited provision of alternatives to the face-to-face consultation. These groups were described in the protocol, and further relevant groups were identified in the conceptual review (see Chapter 2). These included patients with mental health conditions, patients living in rural areas, patients with restricted mobility, patients with hearing loss, patients at a great distance from the practice (e.g. working away) and patients with low health literacy and/or low computer literacy.
The aim was to look at the range of problems and issues for these groups, rather than making statements about specific population subgroups. To make it easier for people in these groups to participate, there was flexibility about timings and locations for interviews, with telephone interviews offered when appropriate. Participants in hard-to-reach and disadvantaged groups were identified by the practices so that they could be invited to interview.
Quantitative data
Quantitative data on the numbers and types of consultations recorded were collected from the six English practices, as they all used the same electronic medical record system (the Scottish practices used another system). The ethnographer in each of the practices enquired as to how consultation types were recorded and then conducted an audit of the reliability of this record-keeping by observing practitioners at work and asking a GP to review the last 20 consultations in which each of the alternatives to face-to-face consultations was used in the practice and note whether or not the type had been accurately recorded. Any use of protocols was also noted. Further details of the method and analysis of the quantitative data can be found in Chapter 6.
Data analysis
Coding
The coding frame for analysis of the ethnographic data was devised by the focused ethnographic team at a face-to-face meeting early in the data collection period. Each ethnographic team member had read a series of field notes and transcripts, and contributed to devising a coding structure for the staff data and another different coding structure for the patient data, which comprised interview data only. The three ethnographers read and coded interview transcripts and field notes [using the comment facility in Microsoft Word 2013 (Microsoft Corporation, Redmond, WA, USA)]. Once the coding frame was in place, the field notes were coded and each ethnographer condensed their findings into a summary profile. The day-to-day lead (HA) read the coding of the field notes into the summary profile and read every transcript, checking the coding to ensure reliability and comparability, and adding or making adjustments where relevant. The transcripts and summary profiles were then entered into NVivo software, which allowed thematic reports to be generated.
Analysis
A series of NVivo reports were generated to gather related sections of the data together. At this point, two of the ethnographers had completed their contracts. The day-to-day lead of the focused ethnographic team (HA), senior team lead (SZ) and remaining ethnographer (HB) read all of the reports. They applied the OSOP method90 to identify the line of argument in each thematic report and identify outliers or negative cases. The data from the staff and patient interviews and the field notes were integrated, and a condensed summary was produced for each thematic code.
At this point, the wider study team became involved and were paired with the remaining members of the ethnographic team to discuss the interpretation of the data (HA and BM, HB and CS, SZ and JC). The core messages were presented at a wider team meeting and the analysis refined through discussion among all the team members.
In addition, we held a stakeholder workshop to present and discuss the initial findings and their application. Attendees included academics, policy-makers and health-care professionals. The responses from the workshop delegates were considered during the final stages of the data synthesis. See Chapter 7 for further information on the stakeholder workshop.
Ethics and research governance permissions
Ethics approval was obtained from NHS Yorkshire and the Humber-South Yorkshire Research and Ethics Committee on 23 March 2015 (15/YH/0135). NHS research and development approvals were obtained for the health boards (Scotland) and the CCGs (England) for the participating practices. Approval, via a substantial amendment, was obtained to recruit and interview four general practice staff from practices outside the case study sites. Consent was obtained from primary care staff and patients participating in the focused ethnography. Participation was voluntary and the optional nature of the study was explained in the information sheet.
Description of the case study sites
We approached 20 practices and invited them to participate. Of these, one practice had closed and we received no response from two others. Nine practices declined to participate, stating excessive workload and/or staff shortages as the reason. Eight case study sites were recruited in total, and details of these practices and the period of time spent in each practice can be seen in Table 5. A more detailed summary of each practice can be found in Appendix 6, which includes contextual information about the practices collected by the ethnographers during the course of their observations.
| Practice reference | Size of practice | Location of practice | Deprivation scorea,b | Alternative to the face-to-face consultation used | Number of days spent in observation |
|---|---|---|---|---|---|
| A | 18,353 registered patients | Inner city | Deprived (3) | Telephone consultations, e-consultationsc and isolated use of e-mail | 25 |
| B | 8954 registered patients | Inner city | Deprived (3) | Telephone consultations, isolated use of e-mail | 19 |
| C | 15,000 registered patients | Inner city | Mixed (4) | Telephone consultations, e-consultationsc and isolated use of e-mail | 18 |
| D | 1938 registered patients | Rural | Mixed (5) | Telephone, video (and e-mail?) | 8 |
| E | 7196 registered patients | Inner city | Deprived (1) | Telephone, e-consultationsc and isolated use of e-mail | 17 |
| F | 13,778 registered patients | Semirural | Affluent (10) | Telephone, e-mail | 25 |
| G | 13,511 registered patients | Semirural | Mixed (6) | Telephone, e-mail | 16 |
| H | 6597 registered patients | Inner city | Affluent (10) | Telephone, e-mail | 11 |
Description of interview participants
Staff interview participants
We interviewed 45 members of staff from the case study sites, and a further four from other practices. In the case study sites, we interviewed 19 GPs, eight practice managers, two deputy practice managers, one practice co-ordinator, two senior practice nurses, three practice nurses and one nurse practitioner, one rural health worker, four senior receptionists, one receptionist, one patient service manager, one practice administrator and an IT manager. The four participants from practices outside the case study sites were three GPs and one practice manager. Various different types of alternatives to the face-to-face consultation were used by staff in the case study sites. All GPs and nurses were using telephone consultations.
The participants from outside the case study sites were interviewed about video consultation; one had used video consultation with patients, two had limited experience of using video consultation with patients and one practice manager was in the process of setting up a video-consultation service.
Of the 48 staff interviewed, 33 were female. The age of participants ranged from 31 to 68 years. The majority of participants were white British. For clinical staff, the length of time since qualifying varied from 7 years to 40 years. Staff had been in their current role for varying amounts of time, from 10 months to 31 years. Of the GPs, 16 were partners and six were salaried.
Full details about staff interview participant characteristics can be found in Appendix 7.
Patient and carer interview participants
We interviewed 39 patient and carer participants. All participants were using or had used an alternative to the face-to-face consultation with a health-care professional at their practice. We collected information on their ethnicity, age, sex, current health conditions and whether or not they were carers, alongside information about their level of education and current employment status. Full details about patient interview participant characteristics can be found in Appendix 8.
Hard-to-reach and disadvantaged groups
The sample included a wide range of participants who may find it difficult to engage with general practice settings for varying reasons. These included a parent looking after a disabled child, an asylum seeker who was vulnerably housed, two men aged < 30 years (who typically do not engage in health care) and three participants in minority ethnic groups with English as a second language.
The sample also included patients who may find themselves disadvantaged by the current limited provision of alternatives to the face-to-face consultation, namely six patients with mental health conditions, four patients living in a very rural area, nine patients with restricted mobility and two patients with hearing loss.
Patient and public involvement and young people
The age range of our patient/carer participant sample was wide, but it did not include any participants younger than 24 years (range 24–91 years). Young persons below the age of 18 years were not eligible for inclusion in the study. Being mindful of the potential importance of alternatives to the face-to-face consultation in young people, we sought to obtain the views of young adults to supplement the study. We did this by organising a PPI event for young people. We were able to do this via ‘Bristol Young Health Watch’, a group of young people aged between 16 and 19 years who work alongside the Bristol CCG. The study PPI lead (AG) met with the group during one of their regular existing meetings. Group members were asked to comment on a number of issues related to alternatives to face-to-face consultations in primary care. These comments were recorded on flip charts during the meeting.
Although the people attending the workshop felt comfortable with potentially using new technology to access GP services, they reported similar concerns to other patient groups about issues of confidentiality, being able to exert choice over when to use alternatives and seeing these as a supplement rather than an alternative to face-to-face consultations. The content of the discussion was used to provide context for the findings obtained via interviews and observation.
Chapter 5 Case study results
Introduction
We have framed the findings in this report in terms of the key objectives and research questions set out in our protocol.
In Chapter 2, we presented our conceptual map, which covered 10 themes under three headings. The three headings were derived from Halford’s sociological framework of health-care work and organisation for ICT initiatives. These were organisational disruptions and dynamics, professional disruptions and dynamics, and spatial disruptions and dynamics. We added an additional heading for unintended consequences. The conceptual map informed the field work. At the end of this chapter, we will show how our interpretation of the findings relates to these headings used in the conceptual map.
Results are presented using the following groupings:
-
Understand how and in what ways alternatives to face-to-face consultations may offer benefits to patients and practitioners in general practice.
-
Understand for which patients alternatives to face-to-face consultations may offer benefits.
-
Understand under what conditions alternatives to face-to-face consultations may offer benefits to patients and practitioners in general practice.
Understand how and in what ways alternatives to face-to-face consultations may offer benefits to patients and practitioners in general practice
Rationale for introducing an alternative to the face-to-face consultation
We observed a range of rationales for introducing an alternative to the face-to-face consultation, and these were not mutually exclusive. Different rationales were expressed by different members of staff within the same practice. For instance, in practice F, one GP said that telephone consultations could be a useful way to manage their work more efficiently:
Obviously it’s, it’s easier for us, it’s much more time efficient to phone a patient and often more convenient for them as well.
GP1, practice F
However, the patient manager suggested that the rationale was to give GPs more time to consult with patients who had complex needs. The practice nurse suggested that it was to provide a better and more convenient service for their patients.
At another practice (practice A), the practice manager explained the rationale of adopting an e-consult service as ‘making the GPs’ lives easier’ and ‘to keep people away’; this was a perspective with which one of the GPs concurred, saying that it was ‘to try to manage demand’. In contrast, their colleague, a GP, was ‘looking at how to make ourselves more accessible’, which ‘coincided with the time that the Prime Minister’s Challenge Fund money was going around’.
Such variation suggests several possibilities, including:
-
The decision to implement an alternative to the face-to-face consultation was not fully shared within the practice.
-
The introduction of an alternative to the face-to-face consultation may not have been based on a single rationale.
-
There were differing experiences of the alternative to the face-to-face consultation between members of staff.
-
Staff members may have retrofitted the rationale for the introduction.
Rationales observed and described by staff included:
-
the desire to be a modern practice and respond to the expectations of busy, time-poor patients –
There’s quite a drive, patients very often expect to be able to e-mail us, they want to e-mail us and you know, we like to try and go with the times and you know, reflect what our patients want, so that’s part of a driver for it.
GP2, practice F
-
an alternative being the only way of providing health care for patients in remote locations, or with other barriers to attending the practice –
The only reason for having it on the [name of area] is because physically we’re separated by the water and we don’t go out there every day.
Practice manager, practice D
-
the acknowledgement that the previous system was broken and unethical in providing a first come, first served system that left patients without appointments that they needed –
We were working exceptionally hard, but we were aware that there was a good proportion of our patients who weren’t getting into the system at all and that is very concerning to me. I think if you have a limited resource the only ethical way to distribute that resource is to find out what’s out there and then prioritise, you know . . . And there’s no question that the system we previously ran caused real harm.
GP1, practice E
-
the recognition that reception staff and telephone lines were overwhelmed –
We are aware that we have a very old-fashioned telephone system which doesn’t really have enough lines, but we haven’t been able to do anything about that. So it is quite difficult, embarrassingly difficult for patients to ring in at many times of the day.
GP2, practice A
-
to manage demand and improve efficiency –
It [the introduction of telephone consultations] was done to try and reduce pressure of face-to-face appointments.
GP2, practice C
Alternatives to the face-to-face consultation came into being in different ways. Some practices demonstrated resourcefulness, drawing upon existing structures (e-mail and telephone), whereas practice D developed internet video-consultations from an existing facility for communication between health-care professionals.
In some cases, funding for free pilots and specific project support, such as the GP Access Fund,14 provided a stimulus for trying e-consultation software:
Our pilot of [e-consultation system] is about to come to an end. We were given this on free trial basis to see what we, and our patients would make of it . . . Patient satisfaction has been good and we’re pretty sold on the concept.
GP1, practice E
Marketing strategies employed by these e-consultation companies claimed that the software would increase access while reducing workload:
So I think one of the things that they said at the initial presentation was that it would be, you would perhaps deal with two or three interventions in the space of seeing a patient.
GP2, practice A
The locality of the practice and a consideration of the population it served were often key in the decision about which alternative to the face-to-face consultation to implement, although assumptions (e.g. about the likely uptake) were sometimes ill founded, with uptake being subsequently low (see Chapter 6 for an analysis of the routine consultation data in the case study practices). Although representatives of one of the practices told us that they had discussed the introduction of the alternative to the face-to-face consultation with their patient advisory group, there was little indication that practices had reviewed a range of options with either patients or the whole practice team. Instead, it was deemed adequate for practices or GPs to have considered what they personally understood to be the patient perspective.
Uptake was influenced by patient awareness; for example, where alternatives to the face-to-face consultation were adopted across the practice there was widespread advertising (Box 3), although this had initially been a challenge.
She told me that getting the message out to their patients about [e-consult software] was challenging and that they had put a message on their answer-phone, there is a large poster in the waiting room as you arrive into the practice and there was a message on the electronic screen in the waiting room. She also told me that the practice manager had been tweeting about the change.
The offer of an alternative to the face-to-face consultation was observed to be dependent upon practice staff members’ perceptions of it, in terms of its purpose, when it should be used and their own beliefs and attitudes towards it. Inconsistencies in promotion were linked to attitudes about the alternative to the face-to-face consultation. This led patients to ‘stumble’ across the alternative to the face-to-face consultation:
I went online and it [eConsult] cropped up online. I wasn’t actually looking for it at the time, I just came over it by accident online. I think it’s a very good system, actually. I think it is.
59-year-old female patient with multiple comorbidities, practice E
Not all staff members embraced the use of alternatives to the face-to-face consultation. Individual use by staff was predominantly attributable to personal characteristics [e.g. confidence, experience, familiarity with/tolerance of the system, own skill set (both clinical and technological), own sense of professional identity and their ability/willingness to adapt]:
I have had a lifelong problem with using the phone – I am very visual, and am unusually good at reading faces and body language, and find the phone takes away a huge amount of information, so get very stressed. They tell me I’m actually not bad on the phone, but it always feels difficult to do.
GP2, practice E
This did not apply only to clinical staff; reception staff held opinions about the merits of alternatives to the face-to-face consultation, and they were often responsible for its promotion:
It [telephone consulting] is not the best way I don’t think, not really. Face to face is always better.
Receptionist, practice B
There was a complexity observed whereby no one key reason emerged to explain any reluctance to promote alternatives.
Organisation of workload
Workload was a key issue for practices, and alternatives to the face-to-face consultation offered a way to organise this. Depending on how practices organised the working day, alternatives to the face-to-face consultation could offer flexibility to both staff and patients. GPs and nurses could prioritise their work by choosing when, and in what order, to reply to messages or make telephone calls, rather than taking them as they are scheduled:
If I’ve got a quick injection it’ll take me a couple of minutes, I would maybe tag on a quick one [telephone consultation] of my tasks in between, outside the dedicated slots. I can be doing two or three in between patients, some days I might not get any as well as the two I get, and then of course we’ve got the e-mail stuff.
Nurse, practice F
This allowed them to work more flexibly, fitting around traditional consulting times:
I think it [telephone consulting] has improved my satisfaction and possibly my stress levels as well . . . I’m able to manage my time a bit better.
GP2, practice H
However, they also raised the possibility that the working day could be stretched and include considerable ‘hidden work.’ For example, there was an observation that alternatives to the face-to-face consultation tended to be undertaken by GPs or nurses before the beginning, or after the end, of face-to-face consulting sessions:
All of the telephone consultations aren’t appointmented [sic] in a given slot, they’re just an addition to the workload already.
Practice nurse, practice B
A key example was the assumption that telephone consultations could be shorter than face-to-face consultations. Those practices that scheduled them allocated less time to telephone consultations than face-to-face consultations. Their length, however, appeared to be similar to that of a face-to-face consultation:
But we’d thought that we might be able to do two things, two, do two telephone consultations in the time it took to do a face to face . . . and that hasn’t proved to be the case.
Practice manager, practice F
Although the working day could be organised to include booked e-consultations and telephone appointments, there seemed to be some acceptance of a trade-off between flexibility and additional work. This was illustrated by an informal conversation with a nurse in practice B (Box 4).
Their telephone consultations are not pre-allocated but are slotted in therefore in addition to existing work and often done in their admin time. She would like to see some of these telephone consultations pre-booked so that they aren’t shouldering additional work however this would be at the cost of the flexibility they currently have.
Flexibility was a relative term in relation to workload. E-consultation provided patients with a flexible approach, available 24 hours a day. However, four of our practices using these systems were engaged in a complicated system requiring the administrative staff to monitor new e-consultations. They had to first inform the GP, and then the GP had a large amount of information to read before deciding on a course of action:
The process as it’s set up at the moment, it is laborious . . . the patient submits something on the web form, that comes to the administration by an e-mail, the administration forwards it to our personal e-mail accounts and also puts a message on the virtual surgery list to say it’s there so we don’t overlook it. I don’t think personally I would overlook it, but maybe other people would. Then sometimes I’ll pick up the phone, but otherwise I will reply to the administration copying in my secretary with a bit of bumf I put at the top to the administrator saying, ‘Please forward this back to the patient cutting out this bit of bumf’.
GP2, practice C
With telephone consultation, the flexibility that alternatives to the face-to-face consultation offered the GPs and nurses meant that patients did not know when to expect a call. In some practices, the patient was given a time period within which to expect a telephone call, but this could be lengthy and not necessarily held to:
Oh yeah, well no they turn round and say if it’s in the morning, [GP] will ring you between 11.10 and 11, so in my mind I usually say right that means half past 11. It’s never usually when they say because obviously he has to wait until he finishes his morning surgery, so I totally understand that, but I know he’s going to ring me in the morning. Or again, it will be – if it’s in the afternoon, it will be between 4 and 5 or something. I try and tie them down, but I’m wasting my breath.
50-year-old male patient with multiple comorbidities, practice C
If the patient missed the call, for whatever reason, this might lead to a delay in receiving care or a different course of action (Box 5). What was a convenient way to consult became inconvenient for the patient, despite it offering flexibility for the clinicians.
I observed a call with a patient who called previously requesting a sick-note, the GP had rung them but they had missed the call so they [the patient] were ringing again. He was told that the GP had requested to see the patient before issuing the sick note but the patient said that he couldn’t come in to see the GP so a telephone consultation was booked for him.
Conversion to a different consultation type
Workload was affected if an alternative to the face-to-face consultation converted to a face-to-face consultation. Apart from consultations with young children, there was a lack of consensus among clinicians about the kinds of patients or problems that were more likely to be converted to a face-to-face appointment (Box 6).
They then began to ask each other about how many telephone consultations were converted to face-to-face consultations and realised they varied between the clinicians. GP1 then proceeded to consider how telephone consultations outcomes were dependant on a number of factors, e.g. time of day, day of the week etc.
During consultations, clinicians had to elicit the nature of the patient’s problem, which might be more difficult to assess remotely. Observed discussions between practitioners suggested that their approaches varied, with one GP feeling that being face to face did not add anything when patients were consulting on particular conditions:
Diagnosis of a UTI [urinary tract infection], for instance, is primarily on the history . . . So, a thing like that, by the time you’ve asked them the right questions and made a diagnosis and treated them you might as well do that on the phone as actually seeing them in person, because it adds nothing to the consultation.
GP1, practice D
The lack of physical cues on the telephone or via e-mail/e-consultation meant that some clinicians were cautious and converted an alternative to the face-to-face consultation to a face-to-face consultation. A clinician was observed converting a telephone consultation to a face-to-face consultation, despite deeming it unnecessary, as illustrated in the following field note extract (Box 7).
Some of the calls were regarding fairly minor complaints and although she gave me [and the caller] the impression that it was not necessary for them to be seen [by her use of language, tone of voice and facial expressions to me] they often were still offered an appointment which appeared paradoxical. She told me that this was either because it was clearly what the caller wanted or that she couldn’t be sure over the phone how to proceed.
We also saw conversions between different types of alternative to the face-to-face consultation (e.g. from e-consult to telephone consultation) when the patient had not provided enough information via the online form, or when the content was contentious (e.g. requesting a referral). This led to repetition of content during subsequent consultations.
Adaptation
The alternatives to the face-to-face consultation underwent adaptation once they had been introduced. Adaptation did not occur in the same way for all practices, involving decisions to continue, revise or discontinue offering alternatives. Sometimes practices were surprised by patient uptake – whether this was higher or lower than anticipated:
We created more telephone slots because there was a demand for it.
Practice administrator, practice D
Continuous improvement and refinement of the service was observed, reflecting population needs (e.g. during an informal conversation, a practice administrator in practice D explained that they offered telephone consultation slots during after-school hours for school-aged children). When practices introduced an alternative to the face-to-face consultation, this was often with an expectation that patients and staff would use them in the same way as they had been designed to work; however, both staff and patients applied adaptations. Some patients found ways to access what they required despite the inflexibility of formats:
All I want is a blood test, which takes me like 3 seconds to say, but filling on the online it was remarkably detailed. So I had to make up something. I made up heavy periods, it’s not made up, it’s kind of true, but because they didn’t have, ‘I want a blood test.’ Then that’s why it took half an hour and then it was like, ‘Tell me this, what size clots? How often? What like…’ It was like, ‘Blimey that took a lot of time.’ But it took my time and not their time, which is efficient in terms of the NHS.
48-year-old female with mental health problems, practice A
This patient adapted the e-consult system to try and ensure that they received the treatment they were seeking.
Understand for which patients alternatives to the face-to-face consultation may offer benefits
Patient–clinician relationship
Clinicians reflected on the types of patients with whom they consulted using alternatives to the face-to-face consultation. Some clinicians thought that the use of alternatives to face-to-face consultations enhanced their relationships with patients and, therefore, they would promote and encourage their use, whereas others felt that it inhibited the relationship and the dynamic of the consultation:
‘think it [a telephone consultation] is good at sort of maintaining your doctor/patient relationship, because I think that they feel that you’re listening to them and following up and that rapport is maintained, so I think that’s a positive thing.
GP3, practice A
There was some disagreement among patient respondents on whether having an existing relationship was important before using an alternative to the face-to-face consultation, such as a telephone consultation – some patients felt that it was essential, whereas others were more ambivalent. For the former, they felt that it resulted in the consultations being quicker, as a result of the GP knowing the history of the patient:
I mean, I know my GP very well and she knows me . . . I’m less confident with another GP because they don’t really know me.
59-year-old female patient with comorbidities, practice E
Types of patients and conditions
Clinicians held assumptions about which patients were most likely to be suitable for the use of alternatives to face-to-face consultations.
In some cases, these were based on age group, ethnic group or socioeconomic status:
It’s just by knowing them, really. I mean, yeah, just by knowing them and what they’re like I suppose. You can usually tell from their address to be honest whether they’re going to be appropriate for an e-mail, of whether they’d be sensible enough to use e-mail.
GP1, practice G
One GP commented that telephone consultations were best used with patients who had been born in the UK, and thus had shared knowledge and assumptions about how the system works:
I do notice that generally the patients that are born and raised in the UK, you can process their problems quicker, and that’s just simply because, like I say, communication, shared cultural links that you have, and that’s amazing how much that makes a difference and the more you do it you just think, gosh, it’s turns of phrase or just general understanding about conditions and what happens.
GP1, practice B
Clinicians also talked about the category of the ‘sensible patient’ or the ‘known patient’ who could be relied upon to give a fluent account without being seen, an example being ‘special patients’ such as friends and other professionals (Box 8):
I think some of that gives you a feel of how sensible do I think the patient is? How confident am I that they’ll give me good information?
GP1, practice B
He has 10 patients to whom he has given his personal number to but some are also friends. Or patients who then become friends. Some patients are academics and they become social friends then you meet some during leisure activities and while this goes against the general guidelines but who is a friend and who is not and who is a patient? It is a very grey area, especially when you have been doing this for 15 years.
Asynchronous and textual methods were recognised as useful for people who were very anxious or found face-to-face contact difficult, who had hearing or communication difficulties and those who ‘struggle to express themselves’:
I have a patient who is so anxious she can’t speak, but she can write, so she can send a text and I’ve had lots of concerns about her safety. So that was one reason, and the receptionists couldn’t understand her, nobody could understand her.
GP2, practice A
This was reflected by some patients who reported the benefits of being able to express themselves better through the use of alternatives to face-to-face consultations, such as e-mail:
Well, I feel that you can express yourself better, I think, for me, message, writing it down, you know, typing it. I just feel sometimes if you are, like, if I’m really not feeling good I can’t really express it.
44-year-old female patient who is a carer with mental health problems, practice E
Alternatives to the face-to-face consultation were considered potentially unsuitable if a new health problem was being presented, if the patient was elderly and confused or isolated, or if the patient was using a complex array of medicines. GPs also preferred to see a patient face to face if a translator was needed, if people had strong accents or when the health-care needs were complex. Some GPs said that they would always squeeze in an extra appointment for a child to be seen face to face:
. . . because the stakes are too high with children.
GP, practice D
E-mail was seen as useful for GPs to share and gather information when co-ordinating complex health-care packages with patients accessing multiple treatment centres:
She had seen the consultant in [hospital 1] who said it was entirely appropriate that she would have this surgery done and the exceptional funding. It got quite complicated because of dealing with [hospital 1] and dealing with [hospital 2], and so [hospital 1] were e-mailing me and [hospital 2], I was getting paper letters through, but I also wanted to keep her in the loop as well because she was not a person who would abuse the service basically, so I would say ‘When you’ve heard from [hospital 1] can you let me know so then I can chase up [hospital 2].
GP2, practice B
Some GPs told us that they gave their personal e-mail or mobile phone number to patients who were terminally ill, or to their family carers for use in emergencies.
Telephone consultations and e-consultations were considered most appropriate for factual, practical, single-issue, straightforward and follow-up appointments, according to both staff and patients. Some GPs suggested that they were particularly valuable for ‘the easy stuff’, for example recurrent issues for which the patient was already aware of what they needed (e.g. this included chest infections, antibiotics for recurrent urinary infections and anti-anxiety medication for a long-haul flight):
You know, why would you be doing something complicated on the phone? That’s the whole, that is the take-home message. You shouldn’t be. Do the easy stuff on the phone.
GP1, practice E
Nurses in particular found alternatives to the face-to-face consultation, such as the telephone, useful for managing patients with diabetes mellitus:
So I sorted her on the insulin a few, probably 2 months ago now, and I’m trying to get her, I’m putting her dose up, she’s very reluctant, so I ring her about every 2 weeks at the moment just trying to get her to take more insulin . . . But I wouldn’t normally follow anybody else up like that . . . So, yes, so I’m trying to really keep her on track, I suppose to keep her motivated and trying to keep her going.
Nurse, practice C
Nurses often used the telephone, but also e-mail, for specific tasks such as ‘discharge checks’ and ‘medication reviews’. Nurses reported that not only was this for patients’ convenience, but also to allow flexible working and to monitor patients who were non-attenders.
Alternatives to the face-to-face consultation were also useful for people seeking advice about the side effects of medicines, and telephone calls were used by GPs for checking that symptoms had improved and did not require further investigation (‘safety-netting’):
I guess just following up medications that you might have started just to make sure you know they’re not getting side effects or, I’d say sick certificates is another one, just sort of checking on how somebody is before issuing another certificate.
GP1, practice F
The use of alternatives to the face-to-face consultation was reliant on the judgement of the clinicians with regard to whom it might work for and for which problems. As demonstrated here, the judgement varied, and as described previously, we also observed these judgements being made about whether or not to convert to a face-to-face consultation. In both cases, this influences the patterns of use.
Patients’ perspectives of alternatives to the face-to-face consultation
Although patients were not involved in choosing what types of alternative to the face-to-face consultation their practice offered, they could exercise agency by waiting for a face-to-face appointment instead. Patients who had recently used an alternative to the face-to-face consultation told us that benefits included that they did not need to travel, or sit in a waiting room full of ‘bugs and germs’:
A doctor’s surgery is full of bugs and germs and I didn’t want to be sitting next to people who might pass something onto you . . . Yeah, it’s one of the worst places to be, really, isn’t it, if you’re not well?
40-year-old woman with cancer, practice D
The participant quoted above also said that she considered visiting the practice a waste of her time.
Patients expressed the view that alternatives to face-to-face consultations were more efficient for themselves and the practice. An e-mail or e-consult allowed the patient to keep a record of the consultation; they could take time to prepare what they wrote and make sure that they had covered everything. This was particularly important for those who found the practice intimidating or had trouble remembering what they wanted to discuss with the GP.
Another benefit that patients ascribed to using e-mail or e-consultations was that they could send a direct message and not have to trouble the receptionist. This was more efficient, quicker than trying to get through on the telephone and preferred by those who found the receptionists intimidating. Some liked the idea that the GP could make the decision about whether or not the problem was sufficiently urgent for an appointment, rather than the onus falling on either the patient or the receptionist:
Then the decision whether I need to be seen is his [the GP’s] . . . if you phoned the receptionist, you haven’t got a hope in hell.
76-year-old male patient with comorbidities, practice F
Patients saw alternatives to face-to-face consultations as suitable for ‘basic’ consultations:
If it was e-mail sort of basic stuff, but like if there was more sort of like in-depth stuff, I would probably use the phone, or go down there or you know, I wouldn’t e-mail anything like how I was feeling or anything like that, I’d rather talk to somebody or have a phone appointment.
41-year-old female patient with mental health problems and diabetes mellitus, practice C
Another woman with mental health problems explained that, as she was comfortable with the technology, she liked being able to decide how she wanted to consult:
I think part of the thing with me is I generally feel – is the term empowered? I feel pretty empowered to pick and choose methods of communication that suit me.
34-year-old female patient with mental health problems, practice C
When asked about the quality of care they received in a telephone consultation, a patient from practice D said that it was comparable to face-to-face consultations:
‘The exact same’ as the face-to-face consultation. I’d say it’s the exact same, I don’t see any problems with the call at all . . . I think you still get good care.
54-year-old male patient with diabetes mellitus, practice E
Patients were aware that a face-to-face consultation, with time and physical contact, as well as the opportunity for non-verbal communication, was needed to discuss more complex health problems:
Yes, I mean even when – even though I’m talking to [name of GP] on the end of the phone, there – it’s still more impersonal than face to face, obviously. Because what you’re lacking is that sort of physical interaction, you know, when the subliminal reading body languages and all that sort of thing. But it serves a purpose.
50-year-old male patient with multiple comorbidities, practice C
For patients using e-consultations, there were positive experiences, including that ‘it was straightforward to use’, ‘it made life easier’ and they appreciated the quick turnaround.
However, some patients worried about whether or not their GP’s system worked properly, wondering how long they would have to wait for a response, or felt frustrated by a long list of seemingly irrelevant questions on the standardised form. One patient voiced a concern that no-one seemed to be taking ownership or responsibility for her GP’s e-consult system:
I just found out there is nobody owning the system or responsible for looking after it. If it is a serious project, I would expect someone to be taking control of it, making sure everyone has a reply or something.
34-year-old female patient with young children, practice A
When the patient felt that they needed to see a doctor but there were no appointments available, the opportunity to talk on the telephone or send a message was sometimes perceived as ‘better than nothing’:
There’s a set amount of things that they can ascertain without looking at it. It’s better than nothing, but not 100 per cent.
50-year-old female patient, practice D
As observed among clinicians, patients were applying their own judgement about the suitability of an alternative to the face-to-face consultation for different conditions and situations.
Understand under what conditions alternatives to the face-to-face consultation may offer benefits to patients and practitioners in general practice
Lack of shared understanding within the practice
There was not always a shared understanding of what was happening, or who was doing what or why in relation to alternatives to the face-to-face consultation. A GP from practice C stated, during an informal conversation, that ‘I do the same as every-one else in the practice,’ but was not able to confirm what this was. This was especially true for the practice managers, who would give a different account of the roles of the reception and clinical staff compared with those described by the staff in question during our observations:
They don’t know that I know this, but I know that they will have patients . . . who e-mail them and that is patients probably that they have had a longstanding relationship with . . . The thing with – e-mail is, it is very difficult to close the conversation off, as you know. So it goes backwards, forwards, backwards, forwards.
Practice manager, practice A
Another practice revealed that their use or acceptance of alternatives to face-to-face consultations differed from their colleagues, as a ‘practice-wide’ versus a ‘lone wolf’ approach:
I know that [name of lead GP] has given his e-mail out on a couple of occasions and, generally speaking, it’s not abused . . . I think if I took a poll round, it would be a small percentage of GPs that have given patients their work e-mail address.
Practice manager, practice E
A key example of the lack of shared understanding was the use of e-mail. Many of the GPs in the case studies used e-mail, unbeknown to their colleagues. Furthermore, although some of the practices offered a webform e-mail system, many of their staff were unaware of this. In one practice (B), there was confusion regarding the status of both e-mail and e-consult software. The GPs thought that the e-mail system would and should continue, the practice manager felt that they would continue only with one or the other, depending on whether the e-consult software was a success, and the reception staff thought that the e-mail system was being phased out:
If we continue with e-consult through the [e-consultations] package which we haven’t made a decision on yet, if we did, we may look at whether we somehow switch off our own, or feed into that, so there’s one system.
Practice manager, practice B
Both patients and staff demonstrated difficulty in defining a consultation, leading to uncertainty about what distinguished telephone ‘triage’ from a telephone ‘consultation’. A patient from practice A described the e-consult as ‘it’s a triage system, an electronic triage.’ Communications via telephone and e-mail were often not seen as consultations, but as background information, a perspective that was reinforced if the patient was then asked to come in for a face-to-face consultation. This confusion also led to problems with recording encounters involving alternatives to the face-to-face consultation. For example, we observed administrative enquiries by telephone being recorded as telephone consultations. Other reports suggested that some communications with patients were seen as unofficial, and, therefore, had not been recorded (e.g. some e-mails and personal telephone calls). There was evidently a lack of discussion among practice staff and with patients about exactly what was happening and why.
Where there were policies, we observed interesting contradictions between practice policies and what GPs actually do. For example, a GP who was routinely using e-mail with selected patients described during interview how, as a practice, they were trying to discourage patients from sending e-mails to the practice:
What we’re envisaging is . . . saying, ‘No reply @ X Medical Practice,’ to make it a bit more obvious that you’re not meant to reply as well as putting the other bits in the letter saying this is a non-reply, if you do need to contact the practice then do it through traditional means, and these are what they are.
GP3, practice F
In practice B, there was an example of a patient who had been using e-mail with two previous GPs. Her most recent GP had left, and her new GP would not engage in e-mail communication with her (by not responding at all). This was a big change for the patient, who had used e-mail consultation for a long time. It demonstrated that alternatives could be taken away, as well as offered, where their use was not a practice-wide decision.
Role of reception staff
Practices differed in where the workload was shifted and who appeared to have control over allocating the tasks. Reception staff were often involved in the administration of alternatives to the face-to-face consultation. One form of e-consult involved a manual step, whereby the reception staff allocated the patient to an appointment/contact using a protocol. The onus was on the reception staff to make the right decision:
Not all reception staff are good at that. So, you know, [e-consult software], flu symptoms, you know what’s in it. [e-consult software] full stop could be anything, you know, so you don’t know until you’ve click, click, clicked into it and opened up the letter to find out that it was urgent or not urgent. So there’s a wee bit of training still there.
GP1, practice E
Both the observations of the reception staff and the interview data suggest that alternatives to face-to-face consultations were not routinely offered to patients who asked for an appointment, unless there were no face-to-face appointments available. Telephone consultation, in particular, was used as a tool for managing demand:
They’re often offered, personally I offer them if there isn’t a telephone, a routine face-to-face appointment, so it’s always offered as a kind of secondary option.
Receptionist, practice G
The GPs and management did not mention potential difficulties for their reception staff. They deemed dealing with alternatives to face-to-face consultations an acceptable part of their role in managing patient demand. However, this did create extra work for reception staff, whether explicit or implicit:
And if there’s a red slash, we’re going, ‘Oh, somebody’s missed that telephone call. It’s purple.’ But it relies on somebody to manually pick that up. So if I was not here and [my deputy] was dealing with something in the call room, she might not look for that for half an hour. And by that time usually the patient’s rung in saying, ‘The doctor hasn’t rung me.’ And then we have to react by getting to the doctor and saying, ‘Did you not ring that patient?’ It might be he has tried them and they’ve not been there. But we have to deal with that then. So there, there can be some extra work.
Receptionist, practice F
The role of the receptionist in administering alternatives to the face-to-face consultation was key, but not always adequately considered when organising these consultation types in the practice.
Practice investment and training
On a practical level, investment and training at the practice level were key. E-consult systems, or provision of more telephone lines, required substantial investment:
So you’ve patients ringing in, doctors can’t get lines out because we’ve got limited amount of time, so with the new system it’s cloud based, we can limit the calls in so that people aren’t hanging for ever, they’ll either get the engaged tone or they’ll be sort of like 4th or 5th in the line, but the lines out will be I think unlimited, but certainly enough for the doctors to call out while patients are still ringing in.
Deputy practice manager, practice F
The availability of pilots and the GP Access Fund14 money had helped some practices that had been considering investing in e-consult systems:
We were probably going to buy it anyway, it’s always great when you don’t have to in the end. I think it’s if we were paying for it, we would have to look at the business case for it more closely. If we didn’t have significant uptake of it, if it didn’t give us value for money we would have to stop doing it. So I suppose that’s the bottom line isn’t it? It’s that it would be a significant number of thousands of pounds to buy it, so we’d have to be saving that amount of doctor/nurse time.
GP2, practice A
One manager hesitantly mentioned that the cost could be offset by reducing staffing levels, although cost–benefit considerations were not fundamental to all decisions:
We don’t do anything on a financial basis, otherwise we wouldn’t operate at all.
Practice manager, practice C
A GP reasoned that the cost of the £1000 per month system would require the practice to lose one of the reception staff. There were unintended consequences, such as the cost of additional patient call-backs related to electronic forms of alternatives (e.g. e-mail or e-consultations):
Well I suppose initially, is there a cost? Well you’d say technically you’ve got to phone patients back, so there’s a phone call cost.
Practice manager, practice C
Financial investment included the outlay involved in training staff, which practices were reluctant to invest in. New systems require changes in workflow, roles and responsibilities, and staff having to learn how to use new processes. The majority of practices chose to deliver in-house or ad hoc training, with the main cost being related to covering staff time away from their normal duties:
Some of the doctors have done, in their own sort of like study time that they’re allocated, have done telephone consultation courses, but that’s been, we haven’t organised anything as a practice for them.
Deputy practice manager, practice G
Many staff reported having no training at all, with training focused on the GPs who would be using the consultation method, despite other team members being involved in its administration:
I never had any training in using the telephone as a consultation method, so I just picked it up, did what I thought was appropriate, yes.
Nurse, practice A
One staff member (practice F) described training as ‘being the poor partner, the poor relation’.
Investment and training featured far less in our observations and accounts than the aforementioned workload, which was clearly a priority.
Logistics
There were many practical issues associated with introducing alternatives to the face-to-face consultation, which were not always adequately considered beforehand. In the one site where video consultation was used, the technology fell short of what was needed because of a lack of facilities, slow computers and insufficient bandwidth. Video-consultations could be time-consuming to set up, especially if used infrequently, and the video images were not always good enough. There was also the challenge of keeping a child still in front of the video camera. Because of this, there was an expectation that video consultations might not work and consultations defaulted to the telephone:
And when we do use video it’s actually quite uncommon because most of the time, as I said, you can deal with it on the phone and the problems with the quality of video are such that you don’t get anything extra from doing it.
GP1, practice D
Similarly, the use of e-mail and e-consultations relied on adequate technology and staff surveillance. There were concerns around e-mails arriving at the correct destination, systems being unstaffed and the lack of clarity about when the patient should expect a response. Some practices chose to use automated responses to inform patients when they could expect a reply from the doctor. We saw examples of missed e-consultations being either not noticed by the practice or not acted on. In one case, the patient had to follow this up by contacting the practice online for a second time. As described, these consultations often reverted to face-to-face consultations.
There was a concern around patients using e-mail in ways that might compromise their safety. This required ensuring that patients were informed that their messages may be read by other practice staff, and what would happen if the e-mail was missed or not read. One patient described the use of an out-of-office message by her GP to let her know he was not available:
If you e-mail a doctor you, it’s useful to know that they’ve got that e-mail . . . because I got that bounced straight back it was like okay, plan B . . . because the bounce back, you know because the out of hours bounced back at me it meant I could rethink what I was going to do.
39-year-old female patient, practice G
One of the greatest challenges with telephone consultations, for both patients and practitioners, was the difficulty in getting through on the telephone, whether that was a result of not having enough lines, having poor telephone reception or patients not being available to answer (which often required the clinician to leave a message raising security concerns). There was a limit to how many call-backs were practical, which was determined by the clinician’s judgement. Even if more telephone lines were provided, the number of calls that could be answered was limited by the number of receptionists. Some of these logistical challenges became apparent only once the alternative to the face-to-face consultation was in place, rather than being considered or identified beforehand. This led to the kind of adaptation we described earlier in this chapter.
Recording the consultation and storing data
Record-keeping is important for patient safety, the measurement of workload and medicolegal purposes. None of the systems for alternatives to face-to-face consultations was well integrated with the GP-computerised records systems; therefore, practices tried to adapt what they would do for face-to-face consultations.
Not only did different practices use different methods for recording the content of alternatives to face-to-face consultations, but staff within practices also varied in terms of their attitudes towards this (see Chapter 6), leading to a lack of internal consistency. For example, some practitioners deleted their e-mails, whereas others saved them to a document store. One practice printed and then scanned their e-mails to include them into the patients’ records, whereas another practice recorded all their scheduled telephone consultations in a big red book in reception before putting them into the electronic health record, regarding the book as a back-up:
So the book is basically as a second back-up, so if the system broke down or we didn’t have any electricity or we didn’t have, so the computer just crashed we are still going to be able to phone this patient and we know exactly who has requested a call. But we also print out all the lists every night so the lists of who is coming in for an appointment is there, so we always have a safety net. So, yeah so the book is the magic book [laughter].
Practice manager, practice H
The lack of integration between the systems used for consultation, such as e-mail, with the patient record system resulted in ‘fiddly/clunky work’, especially for the administrative staff who were tasked with routing the e-mail to the GP, where it came into a central account, and sending out the responses. This all created work that could be reduced with better technology, such as integration with EMIS (the practice’s GP computer records system):
Ultimately, it will be tailored so that it goes straight into our EMIS system. So the patient enters the system, they send that e-mail, that e-mail then goes straight into EMIS and it is coded and it is dealt with there . . . At the moment, it is a bit clunky insomuch as the consultation then has to be put into EMIS, but that will change.
Practice manager, practice A
Technology was perceived as acting as a hindrance, and, as demonstrated by the example above from Practice H, was not always to be trusted.
Information governance and clinical governance
Attempts had been made to ensure confidentiality and consent in conducting the consultation, but this was led by individual clinicians applying their own standards (e.g. leaving ambiguous answerphone messages, or avoiding the assumption that the person answering the telephone is the right person):
The first thing you do is you ascertain that you’re talking to the right patient. That’s why, when I leave messages on the answer machine, it’s very basic. ‘Hello, I want to talk to Mr John Smith. This is [own name] from the doctor’s surgery, could you please give me a call back?’ Or I might actually add, ‘don’t worry, it’s nothing serious’.
Nurse, practice D
Decisions were sometimes made in conjunction with the patient. Consent was sometimes taken as implied when using online methods:
By them e-mailing me I’m assuming they’ve got, they’ve given me consent to reply back to them with their information. But yeah I’m, yeah you’re right, it is a risk there but it’s a risk I’m willing to take because I think the patients have, would prefer, the patients are happy to turn a risk on, you know take a risk that sending e-mails to non-secure addresses.
GP1, practice G
Practices were knowledgeable about the appropriate processes required to ensure privacy and confidentiality, but this did not necessarily translate into application when dealing with patients. Instead we heard about ‘instinct’ and ‘listening skills.’ Reception staff were tasked with confirming numbers and providing information on protocols (numbers of times the GP will try to call, times to call) as described by a receptionist from practice G:
I mean obviously you don’t give any information away . . . it might be to their relatives, but you do have to keep confidential things . . . you might be phoning a home number to speak to the wife, and then the husband answers the phone . . . ’Oh hallo, it’s the doctor’s surgery isn’t it?’ And you can’t even say, ’No’. So you have to be tactful and not give any, you know, disclose anything.
Receptionist, practice G
Tying in with the previous sections Recording the consultation and storing data and Adaptation, changes and solutions were arising in an ad hoc fashion, rather than through using a formal framework.
This extended to the view that clinicians had to trust their patients, and patients needed to take some responsibility with regard to confidentiality:
I don’t see there’s much difference in speaking to a patient on the phone as compared to speaking to them in the room . . . I suppose I can’t be entirely sure if somebody comes in and tells me their name that they are that person . . . You can just have to trust them. So I, I don’t really have views on confidentiality in terms of phone calls.
GP2, practice H
This was appreciated by some of the patients, who generally felt a degree of trust in their practice approach to confidentiality:
I’m assuming correct sort of checks and balances have been put in place anyway and the people that work behind the reception have to obviously sign for confidentiality, so yeah. Be a bit wary if the cleaner come in with access to my account.
50-year-old male patient with multiple comorbidities, practice C
Conversely, e-mail seemed to be a special case. As it was often used by individual GPs, rather than as a practice policy, it was the least standardised form in use. GPs used their own initiative with regard to storing e-mail communication, deletion of e-mails, recording e-mail consultations in patients’ records and what to do with any attachments, such as pictures. There was a sense that, for small numbers of patients, the clinician knew well that this could be managed and that it required higher levels of trust and discretion:
So I think I’m equitable in giving out my e-mail, but actually that’s why I manage to edit it down to about 20 active e-mail relationships at any one time.
GP1, practice H
General practitioners described using e-mail sparingly and being aware that it is not openly available.
Protocols existed for the use of alternatives to the face-to-face consultation in some practices. For example, software packages, such as those for e-consultation, were associated with a strict protocol for recording in some practices, but less so in others. However, staff members’ knowledge and use of such protocols varied greatly in line with the variation we observed in how alternatives to the face-to-face consultation were in use.
Understanding how the findings relate to the conceptual review
In this final section, we briefly demonstrate how our interpretation of the findings relate to the conceptual map that we devised in Chapter 2.
Where we present our understanding of how and in what ways alternatives to face-to-face consultations may offer benefits to patients and practitioners in general practice, we see a range of rationales, which were not always agreed or shared throughout the practice team. The organisation of workload and adaptation of alternatives to the face-to-face consultation are related to organisational disruptions and dynamics, and also to the roles and relationships between members of the practice team. Decisions about whether or not an alternative to the face-to-face consultation was included as a scheduled part of the working day, or picked up as an extra task between appointments, were made at the organisational level. Such decisions could support or disrupt the dynamics of the patient–practitioner relationship, including continuity of care and speed of access.
Where we present our understanding for which patients alternatives to face-to-face consultations may offer benefits, we saw that different professional and support staff (including receptionists) determined the type of patients, conditions and circumstances that were considered appropriate for alternatives to face-to-face consultations, or conversion to a face-to-face appointment. We observed that practice staff often did not know how members of the team were making these decisions, or even which consultation methods their colleagues were using routinely.
In understanding under what conditions alternatives to face-to-face consultations may offer benefits to patients and practitioners in general practice, we observed all three factors: spatial dynamics in the lack of understanding about what was happening, organisational and professional dynamics in the role of reception staff and the application of a form of information governance. Organisational dynamics were heavily at play: practice investment, training, logistics and recording the consultation and storing data.
Unintended consequences were evident throughout our findings, cross-cutting every section of this chapter and often influenced by assumptions held before implementation. For example, GPs and other practice staff had been surprised to find that demand for the non-face-to-face consultation was considerably lower than anticipated. Staff suggested that patients might need educating to get used to a new service, to accept the change, to become IT savvy or to be more adaptable. As we have noted, practice staff sometimes seemed reluctant to tell patients that an alternative to the face-to-face consultation was available.
Assumptions about uptake included the view that young, digitally aware people would want to use technology rather than consult face to face. We interviewed a GP who had offered Skype consultations but found that uptake was considerably lower than expected; they explained that this was a surprise:
So we all thought that actually there would – there would be demand out there. So [name of city] is a very young city and . . . has the highest smart phone penetration of any other city, of any city in the UK. So fairly digitally switched on.
GP, large practice in the West Midlands (outside case study sites)
When new systems are introduced, there are no guarantees that patients and staff will use them as designers intended; indeed, adaptation and bricolage are normal, as people find new ways to incorporate the technology into their working lives. Practices reviewed changes and made decisions to continue, revise or discontinue new systems.
Another assumption that was not always borne out was that telephone consultations would be quicker than face-to-face consultations. Some practices allocated less time in the appointment book for telephone consultations. The flexibility of alternatives to the face-to-face consultation had implications for workload, allowing for consultations to be slotted in, but (depending on how the practice decided to organise the doctors’ working day) could also lead to ‘hidden work’ that was not acknowledged. The lack of physical cues in a telephone call or e-mail meant that the GP sometimes decided that a face-to-face consultation was necessary, thereby increasing the number of consultations. These unexpected consequences have implications for the implementation of alternatives to the face-to-face consultation. They are considered alongside the other findings in Chapter 7, in which we synthesise our findings.
Chapter 6 Collection and analysis of routine consultation data
Introduction
Alongside the collection of qualitative data in case study practices, we collected quantitative data. We sought to understand the numbers and characteristics of patients using different types of alternatives to face-to-face consultations. In particular, we aimed to consider the feasibility of using routine records for this purpose, as this is important for planning future research.
Detailed data about consultations are, in theory, available in most general practice computer systems. Almost all general practices in the UK use electronic appointment systems, which log the date and time of the appointment, the clinician with whom the appointment was made and the type of appointment booked (e.g. regular pre-booked face-to-face consultation, booked telephone consultation, home visit request). Once the patient consults, the clinician enters details of the consultation in the electronic medical records, including the date and type of consultation, the clinician’s name (which can be linked to their role, e.g. GP or nurse) and codes and text about the content of the consultation. The appointment system and the electronic medical records system may be integrated (e.g. EMIS147), or the appointment system may stand alone [e.g. FrontDesk148 (EMIS Health, Leeds, UK)].
However, there are concerns about the reliability of these routine data when used for research purposes. Examples of the potential inaccuracies include telephone consultations being recorded as the default (face to face), rather than being manually changed to the correct type, not all consultations starting with an appointment booking (e.g. an unscheduled telephone call from a patient) and inconsistencies within and between practices in how appointments and consultations are recorded. The issues related to the recording of consultations in routine general practice is explained in more detail in Appendix 9. Furthermore, there are potential practical problems with data extraction that need to be resolved, in order to use the data in any future evaluation.
Aim
The aim of this phase of the research was to examine the feasibility of using routinely collected data to assess the number of consultations of different types in UK general practice.
Objectives
-
Within the case study practices, to explore their approach and any policies towards the recording of different consultation types.
-
To assess the reliability with which different types of consultation were recorded.
-
To explore the feasibility of analysing pseudo-anonymised data about consultation content from practice record systems.
-
To quantify (subject to identified constraints of feasibility and reliability) the extent to which alternatives to the face-to-face consultation are used, including the number of patients using each type of alternative and use by patients from different groups defined in terms of age, sex, deprivation and multimorbidity.
Methods
Practice policies
In each case study practice, the local researcher asked GPs how they recorded consultation type in the patient record. Different consultation types included telephone, e-mail, e-consultations, Skype and any other alternatives, as applicable. The researchers asked how consultations should be recorded, how reliably the GPs thought they recorded different types of consultations themselves and if they believed that other doctors in the practice used the same processes. If the practice had any formal policy for recording different types of consultation, the researchers collected examples of these. The researchers observed how different types of consultation were recorded in patients’ records at the time of consultation, and reflected on how this compared with stated practice policy. The researchers were asked to be alert to any systematic biases in recording; for example, pre-booked telephone consultations might be reliably recorded as telephone calls, but incoming calls from patients might not be.
Assessing the reliability of data recording
Where possible, the researchers audited the reliability of data recording by identifying individual consultations of different types, using sources other than the computerised consultation records, and comparing how these were recorded in patients’ records. In some cases, it was possible to cross-reference by identifying different types of appointment in the appointment system and then to open the patient’s consultation record to see whether and how the consultation was recorded. For e-mail consultations, it was possible for the GP to use the e-mail system to identify consultations. GPs were also asked to remember any recent examples of consultations of a particular type that could be compared with the practice record. Researchers were asked to identify a minimum of 20 consultations of each type in each practice, and to record their findings on a structured summary (see Appendix 10).
Extracting pseudo-anonymised data
All six of the case study practices in England used the EMIS computer system, whereas the two practices in Scotland both used Vision149 software (In Practice Software Ltd, London, UK), which serves the same purpose. Similar data appeared to be available for extraction in both systems, but, because of the difficulties of combining data from the different systems, we focused on establishing the feasibility of extracting and analysing pseudo-anonymised data from the EMIS system. 150 This is the most widely used GP computer system in the UK. One of the English practices used EMIS for their clinical records, and a separate but linked system for appointments (FrontDesk148). In this practice, it was necessary to collect data from EMIS and FrontDesk separately and merge them.
Because key variables needed for the analysis were contained in different parts of the computer system (patient register, appointments system and consultation records), it was necessary to develop three electronic searches of the medical records and then to merge the outputs, using a linked pseudo-anonymised identifier.
Searches were based on all patients registered on the date the search was done. Searches were carried out between 11 November 2015 and 7 March 2016 in different practices. We estimated that this would lead to a slight underestimation of annual consultation rate (because some patients leaving or joining the practice would not contribute a full year’s data), but to adjust for this by collecting dates of registration would have added a further complication to data extraction and analysis, and was not considered to be essential for this feasibility study.
Patient details
The first search provided details of each registered patient in the practice and their demographic characteristics, including age, sex, ethnicity and deprivation based on the Index of Multiple Deprivation (IMD) derived from the patient’s postcode. Deprivation is associated with a high IMD score and a low IMD rank – in our data set, quintile 1 was the most deprived.
The search included variables for a range of chronic conditions to create an index of multimorbidity at the individual patient level. Patients with specific chronic conditions can be identified based on clusters of Read codes for each condition defined by the Quality and Outcomes Framework business rules. 151 We developed a search within EMIS, which extracted information about whether or not each patient’s record had any of these disease codes, in a form that could be exported to Excel for analysis. Details of the disease clusters are provided in Appendix 11. We calculated a multimorbidity score for each patient by summating the number of chronic conditions, and created a binary multimorbidity variable for patients with a score of two or more. As with all such multimorbidity indices,152 the prevalence of multimorbidity will depend on the diseases included and how they are coded, so the multimorbidity indicator developed for this study cannot necessarily be directly compared with other indicators. The multimorbidity search routine and Excel score sheet will be made freely available as a resource to practices. 153
Details of appointments
We extracted data on all appointments between 12 November 2014 and 11 November 2015. This included details of patient identifier, date of appointment, type of appointment, whether or not the patient attended, appointment time and consultation duration.
Details of consultations
We extracted data for all clinical consultations within the same 12-month period. This provided details of the patient identifier, date of consultation, type of consultation and professional type. We excluded all entries that had a ‘consultation type’ of an administrative nature (e.g. hospital letters, test results, requests for a repeat prescription).
Analysis
Pseudo-anonymised results for each practice were exported, merged, cleaned and analysed. It was not possible to identify any patient using the data extracted from practices.
In an initial stage of data processing, we listed the full range of consultation types and professional types used in each practice. Different practices used different consultation types with similar labels to mean the same thing. For example, ‘GP surgery’, ‘routine surgery’ and ‘urgent appointment’ all refer to face-to-face consultations in surgery. We recategorised all consultation types into a smaller number of types, based on analysis of the number of consultations of each type, and taking account of observations from the focused ethnographic case studies and audit of reliability of coding. We sought to be consistent with the approach used by Chris Salisbury in a previous large national study of general practice consultation rates based on the Clinical Practice Research Database. 18 The recoding matrix for consultation types is shown in Appendix 12.
We recoded all entries into a small number of common categories for:
-
surgery (face-to-face consultation)
-
telephone consultation
-
e-consult
-
home visit
-
e-mail received from patient
-
e-mail sent to patient
-
e-consult alert (an incoming message from e-consult software)
-
Other (letter received from patient or sent to patient)
-
not a consultation.
We defined a consultation as a two-way communication between a clinician and a patient for clinical purposes, excluding administrative purposes. We categorised ‘surgery’, ‘telephone’, ‘e-consult’, ‘home visit’ and ‘e-mail sent’ as ‘consultations’.
Similarly, we recoded professional types as:
-
GP
-
nurse or health-care assistant (HCA)
-
other clinician
-
administrative/managerial.
The recoding matrix for professional types is shown in Appendix 13.
We included consultations by GPs, nurses and HCAs in the analysis, and excluded entries categorised as ‘other clinician’ or ‘administrative/managerial staff’.
We used simple descriptive statistics to describe the variables in the data, including the proportion of patients with different characteristics.
It became clear that not all of the practices had offered alternatives for the whole period over which we had collected data, with the last practice fully implementing the alternative to the face-to-face consultation for which they had been included in this study (e-consultations) in May 2015. We therefore restricted analysis to the 6-month period from 11 May 2015 to 11 November 2016, and calculated mean annual consultation rates by multiplying the observed number of consultations by 1.973 (365/185). We calculated the annual consultation rate by type of professional and type of consultation, using the categories described above. We calculated the annual rate of consultations of each type according to patient age, sex, ethnicity, deprivation and whether or not they had multimorbidity.
We used regression models to explore the independent effect of each of these factors on the rates of each type of consultation. As a preliminary step, we undertook an exploratory analysis to determine the most appropriate form of analysis, given the highly skewed nature of the data (counts of consultations). All analyses were conducted using negative binomial models, which provided a better fit than using Poisson regression.
We attempted to analyse the mean duration of different types of consultations; however, this proved to be impossible for reasons described in more detail in the results section.
One question of interest is whether alternatives to the face-to-face consultation are used as a form of triage and are then followed by a face-to-face consultation within the next few days or if they act as a definitive consultation. We created a matrix in which each consultation acts as an index, and then we analysed how many other consultations of each type occurred in the 14-day period beginning on the same date.
Results
Practice policies
Practices were selected for our case studies because they used different forms of alternative to a face-to-face consultation; therefore, we did not observe or audit consultations of all types in all practices.
Within the computer system, there are some standard consultation types, such as ‘telephone consultation’ or ‘administration’, but practices can create their own consultation types. Some practices did this, for example, to define appointment types for urgent appointments, same-day appointments or routine pre-bookable appointments. Even when practices used standard types provided by EMIS, practices used different types to mean the same thing, or the same type to mean different things. In some practices, although the type of consultation was usually recorded in some way, how this was done varied from doctor to doctor, and there was no clear policy or norm. The reliability of coding also appeared to vary by consultation type, so face-to-face surgery consultations (the default) were nearly always coded reliably. As a new technology implemented in a fairly structured way, e-consult entries appeared to be coded reliably where there was a protocol for their use. By contrast, the use of telephone consultation appeared to have grown in a more informal and organic way, and no practices had protocols to determine how these should be recorded.
E-mail consultations were recorded in varied and irregular ways, reflecting that these consultations involved the use of e-mail software not integrated with the main EMIS patient record system. Therefore, recording these consultations required an extra step to copy and paste the e-mail into the notes. Some practices had a policy of doing this, and estimated that it happened most of the time. One GP stored his practice-related e-mails in a private folder, but did not upload these to the patient records (although he did note that an e-mail had occurred). He explained that copying them to the patient records would create extra work, but accepted that it meant that his work involved in considering and responding to e-mails was therefore hidden. Unrecorded e-mail consultations also meant that the patient record was incomplete.
Assessing the reliability of data entry of consultation types
We conducted audits in the practices to assess whether or not consultations were recorded systematically and accurately, based on up to 20 consultations of each type in each practice. The use of some alternatives was infrequent, making it difficult to find 20 consultations to audit. In some practices, the recording of consultations was too varied and idiosyncratic to audit against a standard. In the two practices that used Vision (rather than EMIS) to keep records, staff could not audit the number of consultations of different types, or extract data for more detailed analysis; therefore, the comments below are based on their understanding of the situation, rather than data from records. In Table 6, the numbers represent the number of consultations of each type included in the audit (the denominator) and the number recorded using the appropriate consultation type (the numerator).
| Practice | Computer system | Type of alternative consultationa | |||
|---|---|---|---|---|---|
| Telephone | Video | E-consult | |||
| A | EMIS | 18/20 | 2/6 | 10/10 | |
| B | EMIS | 32/35 | |||
| C | EMIS | 20/20 | 2/8 | 7/8 | |
| F | EMIS | 26/30 | No datab | ||
| G | EMIS | 16/20 | 20/20 | ||
| H | EMIS | 20/20 | 8/17 | ||
| D | Vision | Idiosyncraticc | Noted in free text only | ||
| E | Vision | Idiosyncraticc | No auditd | ||
| Total (among EMIS practices included in the data analysis) | 132/145 (91%) | 32/51 (63%) | 17/18 (94%) | ||
The results shown in Table 6 suggest that telephone consultations were recorded reasonably reliably across practices, but e-mail consultations were not. Although, overall, 63% of e-mail consultations were coded, this was largely due to the reliability of coding in just one practice. Coding of consultations resulting from the use of e-consultations appeared to be reasonably reliable, in accordance with protocols which were used in all three case study practices. These protocols had all been devised by the individual practices.
Feasibility of assessing the use of alternatives to the face-to-face consultation
We set out to assess the feasibility of analysing consultation data from routine records, rather than seeking definitive data on the frequency of consultation types. Because of this focus on feasibility, we report below as ‘results’ some issues we identified in conducting the analyses, as well as the results of the analyses themselves.
Issues with data cleaning
Initial data cleaning identified a number of issues that make this type of analysis difficult:
-
Some patients are excluded from extracts of patient data in some practices, for example patients who have died. Whether these patients are included or excluded appears to depend on the data access permissions of the individual who is logged in when the search is run.
-
Some items held as separate variables within EMIS were merged into one column when the data were exported to Excel, but had to be split again for analysis.
-
There were difficulties in handling dates, which were stored in different ways in EMIS (the source), Excel (how the data are exported) and Stata (the statistics package into which the data were imported for analysis).
-
Some professional or consultation types created by practices contained typographical errors or different terms (e.g. dietician vs. dietitian; health-care assistant vs. HCA), so the data had to be visually inspected for each practice to resolve this.
Because of the above problems, a considerable amount of cleaning and reformatting of the data from each individual practice was necessary before the data sets could be merged for analysis.
Patient demographics
Appendix 14 shows the characteristics of the patient population in each practice. These data highlight some aspects of the variation between the practices, which were selected to include different locations, sociodemographic profiles of the patients and size. Several have a high proportion of younger patients; in three practices about three-quarters of the patient population are aged < 45 years, and there are few elderly patients (Figure 4). Two are in deprived areas, with a high proportion of patients from ethnic minority groups, whereas practice H serves many students. In three practices, around half of the patients live in areas within the highest quintile for deprivation, whereas (at the other extreme) 79% of patients in one practice live in areas within the lowest deprivation quintile. The recording of ethnicity was variable, covering around two-thirds of all patients.
FIGURE 4.
Distribution of patients’ age by practice.
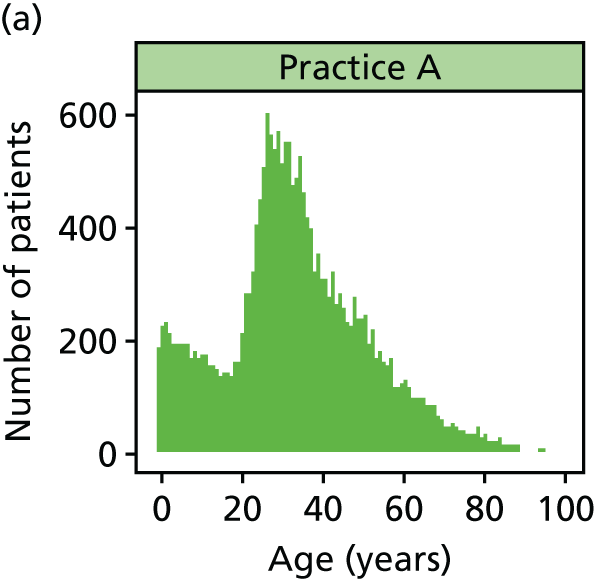
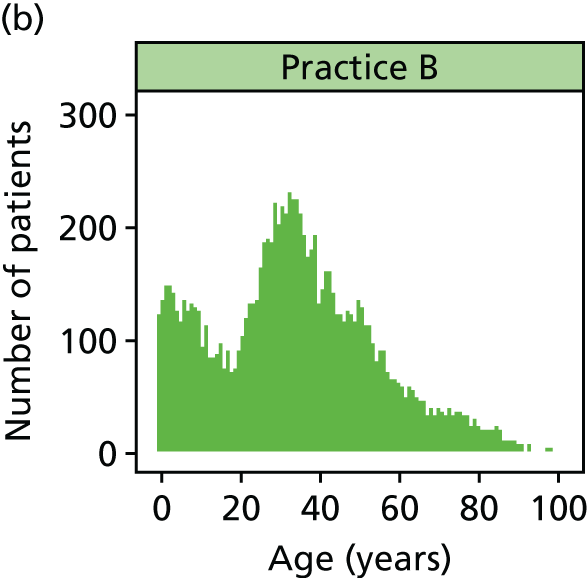
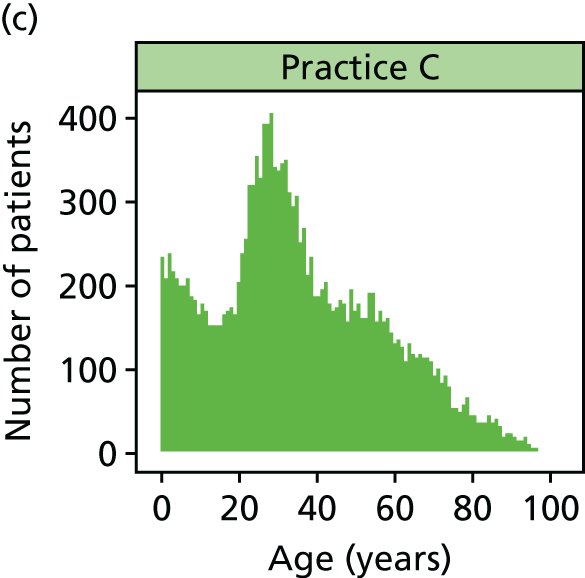
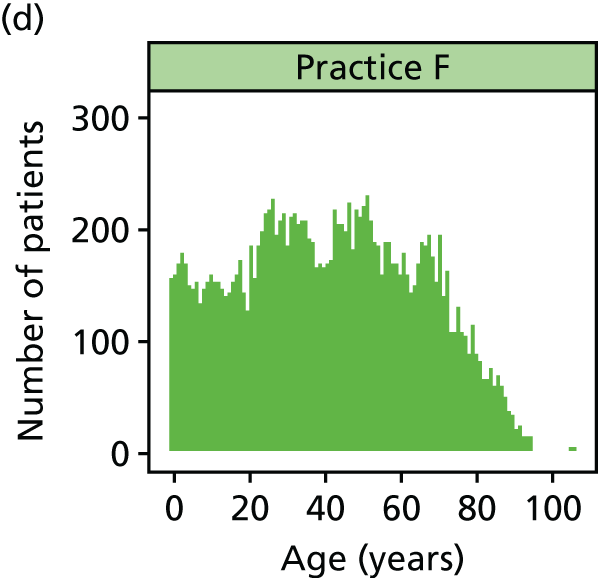
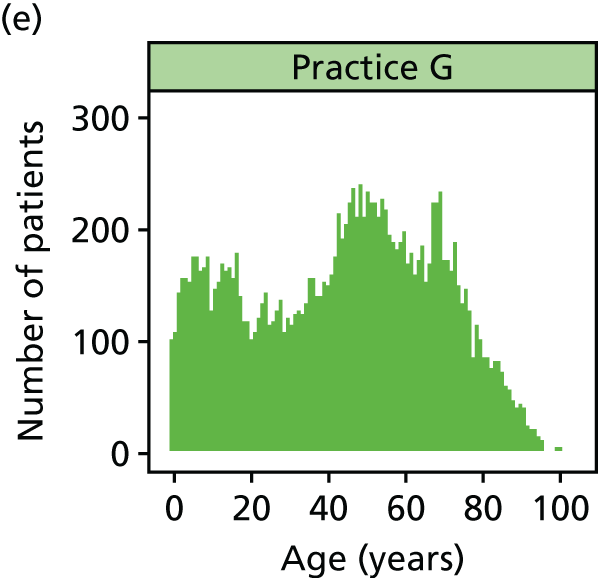
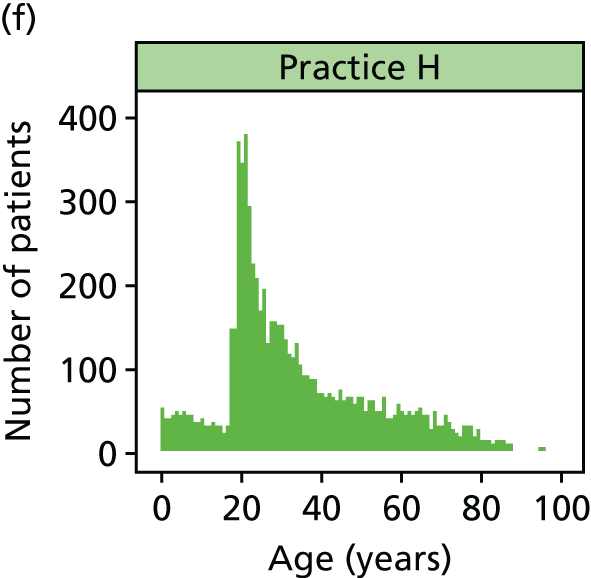
Multimorbidity
Using the set of 15 conditions defined earlier in this chapter, 34% of all patients (n = 26,362) and 39% (n = 24,257) of adult patients aged ≥ 18 years had one or more of these long-term conditions. If multimorbidity is defined as two or more of these conditions, 11% of all patients (n = 8314) and 13% of adult patients (n = 8264) had multimorbidity. These figures are compared with the population of England in Appendix 15. The prevalence of chronic conditions and multimorbidity in each case study practice is shown in Appendix 16.
The prevalence of chronic conditions identified in our case study practices was similar to that reported nationally, except for respiratory conditions. The code set used to define asthma included patients who had either a diagnostic code or a relevant prescription, and this may have led to an overestimation of prevalence. Appendix 17 shows how multimorbidity was associated with age. As expected, there was a clear positive relationship between the prevalence of multimorbidity and increasing age. These data, along with the details of prevalence of individual conditions reported above, accord with expected patterns18 and support the reliability of the approach we used to capture multimorbidity.
Annual consultation rates
The full data set included data on 274,517 entries relating to 77,513 patients contributing to the data set. There were entries related to 209,677 valid consultations in the relevant 6-month period with 46,817 patients. Of these, 79.8% (n = 167,363) were face-to-face consultations in surgery, 61.6% (n = 129,197) were consultations with a GP and 43.0% (n = 90,113) were face-to-face consultations in surgery with a GP.
The overall consultation rate (with GPs or nurses in general practice) varied from 3.85 to 7.47 consultations per patient per year in participating practices, with an overall mean of 5.34 consultations. This is similar to the national average consultation rate of 5.16 consultations, based on data on 398 English general practices in 2013–14, using similar definitions and methods. 18 Nevertheless, four of the practices in this study had low consultation rates. These were the practices serving younger populations, with a consultation rate of only 3.85 consultations per patient per annum in the practice serving a predominantly student population.
The annual consultation rates in this study are only estimates, because the inflation from a 6-month period to calculate an annual rate does not take account of the busier winter months from mid-November to mid-May. Furthermore, as previously mentioned, the denominators consider all patients registered at the practice on a specific date, some of whom may have already left or not yet joined the practice during the 6-month period analysed.
The mean rates of consultation of each type and by each type of professional are shown in Appendix 18.
However, it is more informative to consider the rate of consultations of each type in each practice individually, because not all consultation types were offered in all practices. These data are shown in Table 7.
| Consultation type | Type of professional | Number of consultations | ||
|---|---|---|---|---|
| GP, ratea (%)b | Nurse or HCA, ratea (%)b | Total, ratea (%)b | ||
| Practice A | ||||
| Surgery | 1.8216 (39.06) | 1.3715 (29.41) | 3.1931 (68.48) | 29,761 |
| Telephone | 1.3507 (28.97) | 0.0798 (1.71) | 1.4305 (30.68) | 13,333 |
| E-consult | 0.0108 (0.23) | 0.0108 (0.23) | 101 | |
| Home visit | 0.0209 (0.45) | 0.0069 (0.15) | 0.0278 (0.60) | 259 |
| E-mail sent | 0.0009 (0.02) | 0.0009 (0.02) | 8 | |
| Total | 3.2049 (68.73) | 1.4582 (31.27) | 4.6631 (100) | |
| Number of consultations | 29,871 | 13,591 | 43,462 | 43,462 |
| Practice B | ||||
| Surgery | 2.2471 (49.03) | 1.8300 (39.93) | 4.0771 (88.95) | 18,559 |
| Telephone | 0.3533 (7.71) | 0.1079 (2.35) | 0.4611 (10.06) | 2099 |
| E-consult | 0 | |||
| Home visit | 0.0299 (0.65) | 0.0154 (0.34) | 0.0453 (0.99) | 206 |
| E-mail sent | 0 | |||
| Total | 2.6303 (57.39) | 1.9532 (42.61) | 4.5835 (100) | |
| Number of consultations | 11,973 | 8891 | 20,864 | 20,864 |
| Practice C | ||||
| Surgery | 2.4929 (48.70) | 1.6158 (31.56) | 4.1087 (80.26) | 31,979 |
| Telephone | 0.8327 (16.27) | 0.0560 (1.09) | 0.8887 (17.36) | 6917 |
| E-consult | 0.0114 (0.22) | 0.0114 (0.22) | 89 | |
| Home visit | 0.1006 (1.97) | 0.0098 (0.19) | 0.1104 (2.16) | 859 |
| E-mail sent | 0 | |||
| Total | 3.4377 (67.15) | 1.6816 (32.85) | 5.1192 (100) | |
| Number of consultations | 26,756 | 13,088 | 39,844 | 39,844 |
| Practice F | ||||
| Surgery | 2.6488 (47.75) | 2.3711 (42.74) | 5.0200 (90.49) | 37,018 |
| Telephone | 0.3481 (6.28) | 0.0734 (1.32) | 0.4215 (7.60) | 3108 |
| E-consult | 0 | |||
| Home visit | 0.0311 (0.56) | 0.0427 (0.77) | 0.0738 (1.33) | 544 |
| E-mail sent | 0.0107 (0.19) | 0.0216 (0.39) | 0.0323 (0.58) | 238 |
| Total | 3.0387 (54.78) | 2.5088 (45.22) | 5.5475 (100) | |
| Number of consultations | 22,408 | 18,500 | 40,908 | 40,908 |
| Practice G | ||||
| Surgery | 2.4940 (33.39) | 3.1839 (42.63) | 5.6778 (76.02) | 39,397 |
| Telephone | 1.6007 (21.43) | 0.0259 (0.35) | 1.6267 (21.78) | 11,287 |
| E-consult | 0 | |||
| Home visit | 0.1401 (1.88) | 0.0127 (0.17) | 0.1528 (2.05) | 1060 |
| E-mail sent | 0.0115 (0.15) | 0.0115 (0.15) | 80 | |
| Total | 4.2463 (56.85) | 3.2225 (43.15) | 7.4688 (100) | |
| Number of consultations | 29,464 | 22,360 | 51,824 | 51,824 |
| Practice H | ||||
| Surgery | 2.0082 (52.17) | 1.2095 (31.42) | 3.2177 (83.59) | 10,679 |
| Telephone | 0.5833 (15.15) | 0.0102 (0.27) | 0.5936 (15.42) | 1970 |
| E-consult | 0 | |||
| Home visit | 0.0283 (0.74) | 0.0006 (0.02) | 0.0289 (0.75) | 96 |
| E-mail sent | 0.0090 (0.23) | 0.0090 (0.23) | 30 | |
| Total | 2.6289 (68.30) | 1.2203 (31.70) | 3.8492 (100) | |
| Number of consultations | 8725 | 4050 | 12,775 | 12,775 |
As well as highlighting the variation in overall consultation rate between the participating practices, these data also show considerable variation between practices in both the rate and proportion of alternative types of consultations (noting that not all practices offer all of the alternatives). For example, the proportion of all consultations conducted by telephone varies from 8% to 31%. Among practices offering e-mail consultations, the highest proportion of consultations conducted in this way is 0.58% in one practice, with other practices conducting only 0.02% of consultations in this way. E-consultations also appear to be very rarely used, accounting for 0.22% and 0.23% of consultations in those practices that offer them. It is important to note that, across all practices, face-to-face consultations in surgery still account for the vast majority (79.8%) of all consultations, with home visits accounting for another 1.4% of consultations. As anticipated, the use of alternatives to face-to-face consultations in our case study practices was higher than the national average (86% of consultations in a study of 398 English practices were conducted face to face in surgery). 18 However, among the case study practices chosen because of their interest in the use of alternatives, such approaches account for only a small proportion (18.7%) of all consultations, and 98.6% of these were telephone consultations.
We then explored the extent to which different consultation types were used by patients of different ages, sex, deprivation and multimorbidity. These results are shown in Appendix 19. All of these analyses should be considered as being exploratory, given the small numbers of consultations within some cells, the issues about the reliability of coding previously highlighted and the fact that not all types of alternative were offered in all practices. However, they do demonstrate some general trends and also demonstrate the feasibility of this type of analysis subject to these limitations.
Patterns in consultation rate by age are illustrated in Figure 5, which shows rates of consultations in natural units and also on a logarithmic scale (base 10). This better demonstrates the pattern of rates of each type of consultation in different age groups, given the much lower rates for alternatives to face-to-face consultations.
FIGURE 5.
Rates of different types of consultation by age group. (a) Natural units and (b) logarithmic scale.
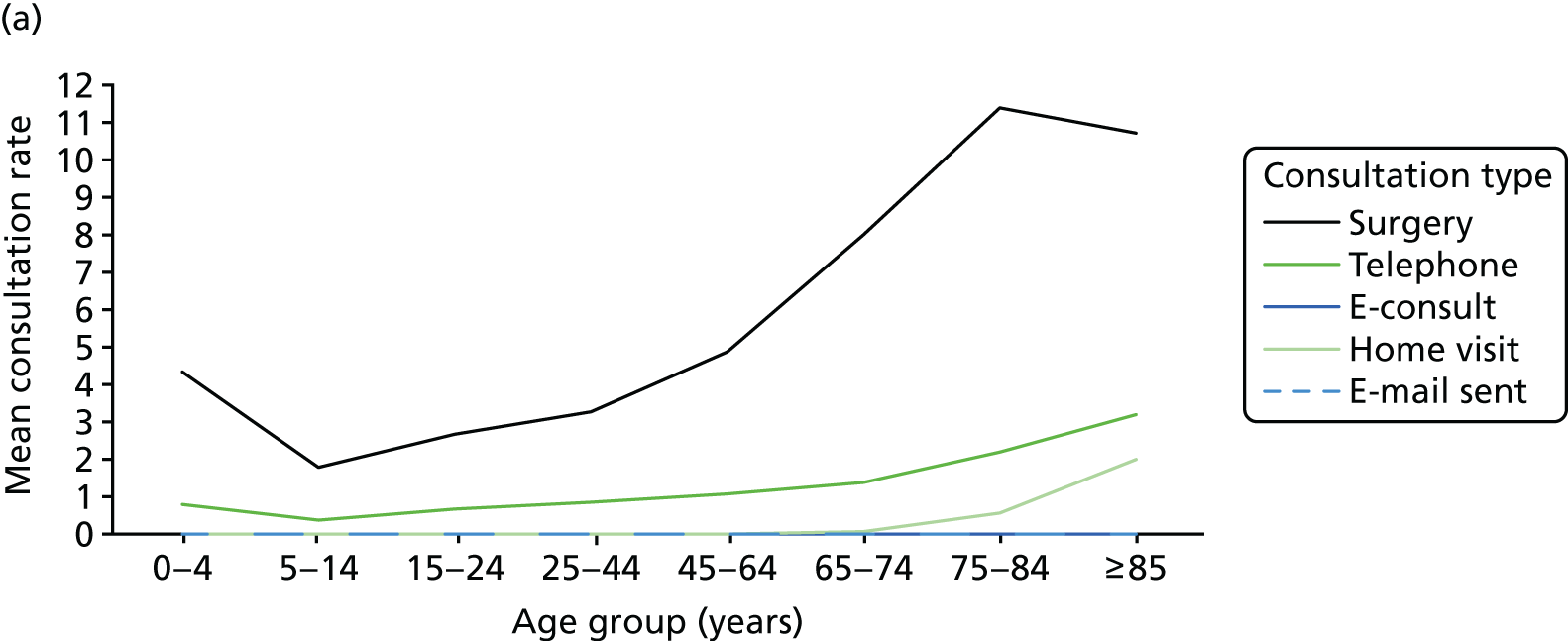
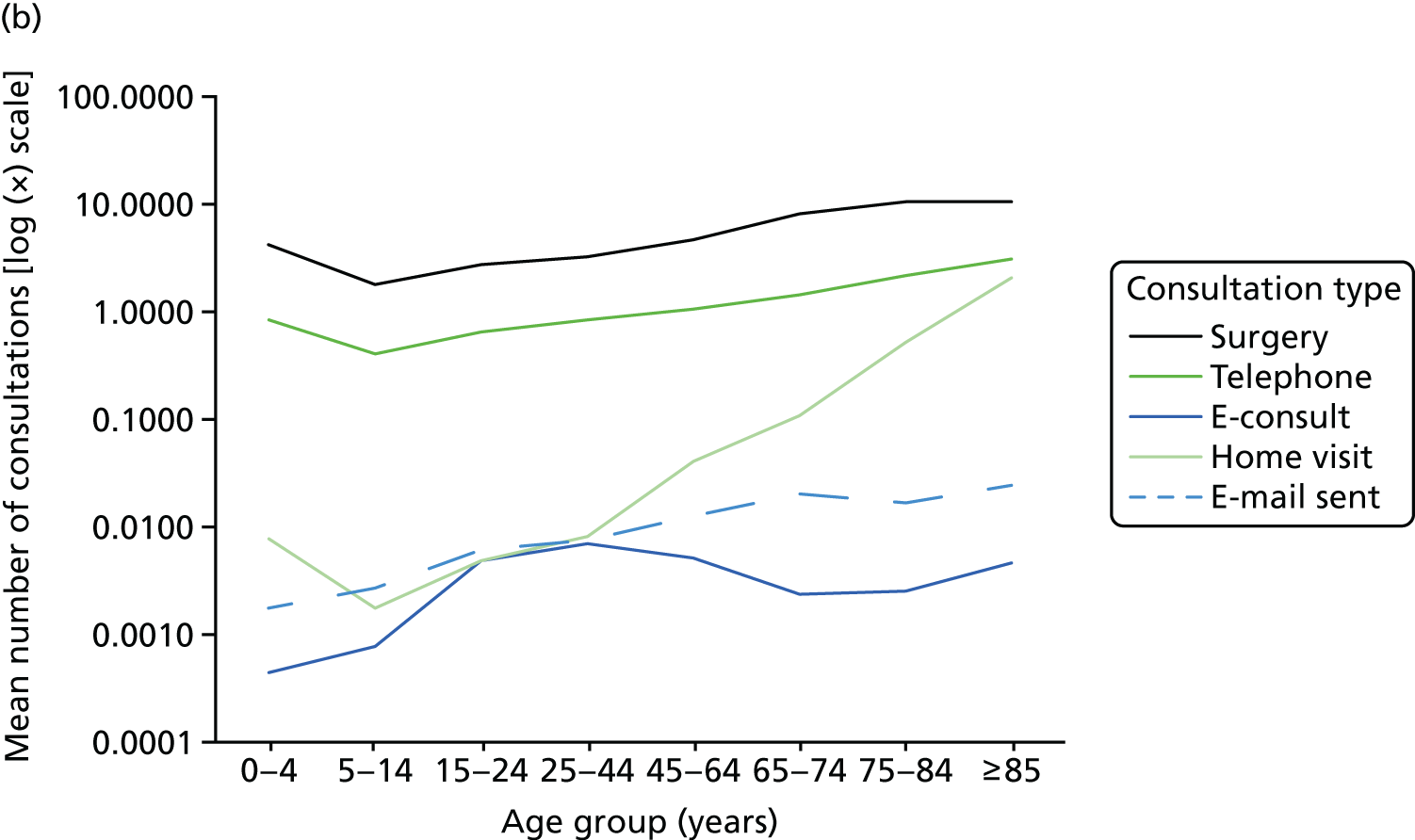
Rates of telephone and surgery consultations follow a similar pattern, with higher rates in babies and older people. Unsurprisingly, there is a strong association between older age and home visit rates. There is a trend towards greater use of e-consultations (but not e-mails) among young adults, although this should be interpreted with caution, as numbers of consultations of these types are small.
Appendix 19 shows that females had higher rates of most types of consultation than males. The numbers of e-mails sent were similar in both sexes, but the total number of e-mails was very small. Appendix 19 also suggests that patients from non-white ethnic groups had a higher rate of telephone consultations and a lower rate of home visits and electronic consultations than white patients.
In this univariate analysis, rates of surgery consultations and e-mails appeared to be highest in the least deprived quintile, but this analysis does not take account of confounding factors, such as age (see Appendix 19).
Unsurprisingly, there is a strongly positive relationship between multimorbidity and consultation rate (see Appendix 19), and patients with more chronic diseases have more consultations of all types (see Appendix 20).
It is important to note that the above findings relate to crude rates, and there are obvious associations between variables (e.g. multimorbidity is more common in older people, and practices in less deprived areas tend to have more elderly patients). In order to explore the independent association between these variables and the use of alternatives to face-to-face consultations, we conducted a multivariate analysis using negative binomial regression models to provide adjusted estimates.
Multivariate analysis
The rate of face-to-face consultations in surgery was higher in older patients, women, those from non-white ethnic groups and those with multimorbidity (Table 8). Patients living in the least deprived quintile had slightly higher face-to-face consultation rates than those in the most deprived quintile. The rate of telephone consultations showed similar relationships with patient characteristics, except that there were no strong relationships with ethnicity or deprivation (Table 9).
| Characteristic | IRR | Robust standard error | 95% CI | p-value |
|---|---|---|---|---|
| Age group (years) | ||||
| 0–4 | 1.6842910 | 0.0818203 | 1.5313240 to 1.8525380 | < 0.001 |
| 5–14 | 0.6349070 | 0.0420091 | 0.5576860 to 0.7228206 | < 0.001 |
| 15–24 | 0.8456574 | 0.0628591 | 0.7310099 to 0.9782855 | 0.024 |
| 25–44 | ||||
| 45–64 | 1.2563120 | 0.0401321 | 1.1800660 to 1.3374840 | < 0.001 |
| 65–74 | 1.7430290 | 0.0861334 | 1.5821280 to 1.9202930 | < 0.001 |
| 75–84 | 2.0259240 | 0.1113851 | 1.8189640 to 2.2564320 | < 0.001 |
| ≥ 85 | 1.6631920 | 0.1746465 | 1.3538180 to 2.0432630 | < 0.001 |
| Sex | ||||
| Female | ||||
| Male | 0.6322535 | 0.0190713 | 0.5959579 to 0.6707596 | < 0.001 |
| Ethnicity | ||||
| White | ||||
| Other | 1.1821780 | 0.0636151 | 1.0638440 to 1.3136730 | 0.002 |
| IMD quintilea | ||||
| 1 | ||||
| 2 | 0.9888322 | 0.0569208 | 0.8833327 to 1.1069320 | 0.845 |
| 3 | 0.9941373 | 0.0821511 | 0.8454868 to 1.1689230 | 0.943 |
| 4 | 0.9450728 | 0.0617305 | 0.8315076 to 1.0741480 | 0.387 |
| 5 | 1.1697980 | 0.0932437 | 1.0006040 to 1.3676020 | 0.049 |
| Morbidity | ||||
| None | ||||
| One morbidity | 1.9252370 | 0.0835421 | 1.7682670 to 2.0961410 | < 0.001 |
| Multimorbidity | 3.1680350 | 0.1325233 | 2.9186570 to 3.4387210 | < 0.001 |
| Constant | 1.4510300 | 0.1495145 | 1.1856830 to 1.7757610 | < 0.001 |
| /lnalpha | 0.1752019 | 0.0456236 | 0.0857813 to 0.2646226 | |
| Alpha | 1.1914870 | 0.0543599 | 1.0895680 to 1.3029390 | |
| Characteristic | IRR | Robust standard error | 95% CI | p-value |
|---|---|---|---|---|
| Age group (years) | ||||
| 0–4 | 1.2321440 | 0.2213758 | 0.8664201 to 1.7522430 | 0.245 |
| 5–14 | 0.5864140 | 0.1060724 | 0.4113735 to 0.8359346 | 0.003 |
| 15–24 | 0.7625089 | 0.0848378 | 0.6131109 to 0.9483111 | 0.015 |
| 25–44 | ||||
| 45–64 | 1.0322340 | 0.0812444 | 0.8846718 to 1.2044090 | 0.687 |
| 65–74 | 1.1082510 | 0.1132202 | 0.9071483 to 1.3539350 | 0.314 |
| 75–84 | 1.3608050 | 0.1570561 | 1.0853130 to 1.7062260 | 0.008 |
| ≥ 85 | 1.6107170 | 0.2832200 | 1.1411650 to 2.2734750 | 0.007 |
| Sex | ||||
| Female | ||||
| Male | 0.5901140 | 0.0200467 | 0.5521027 to 0.6307423 | < 0.001 |
| Ethnicity | ||||
| White | ||||
| Other | 1.2748790 | 0.1685703 | 0.9838278 to 1.6520320 | 0.066 |
| IMD quintilea | ||||
| 1 | ||||
| 2 | 0.8243994 | 0.0645600 | 0.7070965 to 0.9611620 | 0.014 |
| 3 | 0.7046140 | 0.2207291 | 0.3813307 to 1.3019690 | 0.264 |
| 4 | 0.8387277 | 0.2060208 | 0.5182462 to 1.3573940 | 0.474 |
| 5 | 0.9238392 | 0.4086180 | 0.3882454 to 2.1982970 | 0.858 |
| Morbidity | ||||
| None | ||||
| One morbidity | 2.0175740 | 0.1439363 | 1.7542990 to 2.3203600 | < 0.001 |
| Multimorbidity | 3.7713810 | 0.3151042 | 3.2017050 to 4.4424190 | < 0.001 |
| Constant | 0.4417634 | 0.1094456 | 0.2718361 to 0.7179140 | 0.001 |
| /lnalpha | 1.2265010 | 0.1808968 | 0.8719502 to 1.5810530 | |
| Alpha | 3.4092810 | 0.6167280 | 2.3915700 to 4.8600690 | |
For electronic consultations (e-consultations or e-mail consultations, combined), some of these relationships were quite different. Electronic consultations were less common in children and more common in patients who were white and those who lived in more affluent areas (Table 10).
| Characteristic | IRR | Robust standard error | 95% CI | p-value |
|---|---|---|---|---|
| Age group (years) | ||||
| 0–4 | 0.1758768 | 0.1056677 | 0.0541754 to 0.5709719 | 0.004 |
| 5–14 | 0.2650287 | 0.1900929 | 0.0649778 to 1.0809880 | 0.064 |
| 15–24 | 0.7166553 | 0.0788415 | 0.5776529 to 0.8891062 | 0.002 |
| 25–44 | ||||
| 45–64 | 0.8859132 | 0.1073822 | 0.6985804 to 1.1234810 | 0.318 |
| 65–74 | 0.8148025 | 0.2220978 | 0.4775656 to 1.3901820 | 0.452 |
| 75–84 | 0.6133808 | 0.3085860 | 0.2288226 to 1.6442260 | 0.331 |
| ≥ 85 | 0.6608525 | 0.1424938 | 0.4330793 to 1.0084200 | 0.055 |
| Sex | ||||
| Female | ||||
| Male | 0.8209210 | 0.1636159 | 0.5554569 to 1.2132560 | 0.322 |
| Ethnicity | ||||
| White | ||||
| Other | 0.5982574 | 0.1352804 | 0.3840705 to 0.9318911 | 0.023 |
| IMD quintilea | ||||
| 1 | ||||
| 2 | 1.3293110 | 0.3677209 | 0.7729707 to 2.2860750 | 0.303 |
| 3 | 2.4601750 | 0.7504218 | 1.3530870 to 4.4730740 | 0.003 |
| 4 | 2.5731730 | 0.7675142 | 1.4340900 to 4.6170170 | 0.002 |
| 5 | 2.4858550 | 1.1177120 | 1.0297950 to 6.0006800 | 0.043 |
| Morbidity | ||||
| None | ||||
| One morbidity | 1.8807280 | 0.1852671 | 1.5505130 to 2.2812670 | < 0.001 |
| Multimorbidity | 3.4406950 | 0.3964617 | 2.7451410 to 4.3124870 | < 0.001 |
| Constant | 0.0037364 | 0.0011881 | 0.0020035 to 0.0069683 | < 0.001 |
| /lnalpha | 3.9855640 | 0.1663819 | 3.6594620 to 4.3116670 | |
| Alpha | 53.8156500 | 8.9539500 | 38.8404300 to 74.5646700 | |
Feasibility of assessing duration of consultations
We explored the feasibility of determining the duration of different types of consultations using routine data recorded in the EMIS system. It proved impossible to reliably attribute durations to different types of consultation for a variety of reasons, including an inability to link consultations to duration (which is held in the appointments file) when there was more than one consultation on one day, problems with unfeasibly long consultations and missing data. These problems were particularly relevant to telephone consultations, which were often followed by a surgery consultation on the same day.
Patients reconsulting within 14 days
Table 11 shows the proportion of consultations of each type that were followed by another consultation within the subsequent 14 days, including the index day and the types of reconsultation. In interpreting these data, it is important to note that the same consultation may be included as a reconsultation, but could also form an index consultation for another subsequent reconsultation.
| Type of consultation | Number of patients | Number of patients (%) who reconsulted within 14 days by type of reconsultation | |||||
|---|---|---|---|---|---|---|---|
| Surgery | Telephone | E-consult | Home visit | E-mail sent | No reconsultation | ||
| Surgery | 167,393 | 70,975 (42.40) | 23,625 (14.11) | 60 (0.04) | 1565 (0.93) | 229 (0.14) | 87,760 (52.43) |
| Telephone | 38,714 | 19,499 (50.37) | 11,405 (29.46) | 30 (0.08) | 1424 (3.68) | 42 (0.11) | 14,596 (37.70) |
| E-consult | 190 | 75 (39.47) | 58 (30.53) | 14 (7.37) | 2 (1.05) | 0 (0.00) | 73 (38.42) |
| Home visit | 3024 | 1039 (34.36) | 934 (30.89) | 0 (0.00) | 898 (29.70) | 3 (0.10) | 1187 (39.25) |
| E-mail sent | 356 | 138 (38.76) | 26 (7.30) | 0 (0.00) | 2 (0.56) | 46 (12.92) | 187 (52.53) |
| Total | 209,677 | 91,726 (43.75) | 36,048 (17.19) | 104 (0.05) | 3891 (1.86) | 320 (0.15) | 103,803 (49.51) |
Table 11 shows that 50% of patients having a telephone consultation had a subsequent surgery consultation within 14 days, and 29% had another telephone consultation. Some patients will have had both, so 62% of patients had another consultation (compared with 48% of patients who had a surgery consultation then having another consultation within 14 days). For patients having an e-consult, 39% also had a surgery consultation and 31% also had a telephone consultation (62% had at least one additional consultation) within 14 days.
A similar analysis restricted to GP consultations only is shown in Appendix 21.
Table 12 shows that 29% of patients having a GP surgery consultation also had another consultation within 14 days (including 23% having another face-to-face consultation at surgery or at home), whereas 54% of patients having a telephone consultation also had another form of consultation (including 41% also have a face-to-face consultation).
| All practices | Percentage of patients who reconsulted within 14 days | |
|---|---|---|
| Type of consultation | If the initial consultation was with a GP | If the initial consultation was with a GP or nurse |
| Surgery | 29.4 | 47.6 |
| Telephone | 54.0 | 62.3 |
| E-consult | 55.3 | 61.6 |
| Home visit | 55.5 | 60.7 |
| E-mail sent | 39.6 | 47.5 |
| Total | 36.8 | 50.5 |
Conclusions
This feasibility study has enabled us to reach the following conclusions of relevance to future research and evaluation of the use of alternatives to face-to-face consultations:
-
It is technically feasible and relatively straightforward to extract data from routine general practice computer systems for analysis of the rates of different types of consultation.
-
This process is, however, much more difficult than it need be, because of the idiosyncratic way in which practices record types of consultation, which varies both within and between practices. Software systems need to be designed to encourage practice staff to enter details of consultations in a consistent and reliable way.
-
Based on our limited audit in six case study practices, it appears that the recording of telephone consultations and e-consult consultations was not fully reliable, but, given that > 90% of consultations of these types were entered correctly in the notes, this is sufficiently reliable for analysis. However, e-mail consultations were not reliably entered in the notes, so analysis of e-mail consultation rates would underestimate the true rate by about 50%.
-
At present, it is not possible to reliably extract data about the duration of consultations for analysis in EMIS practices. These data are held within the system, but, as far as we can ascertain, it is not possible to extract these using routine searches.
-
We have developed a new and relatively simple method to generate a multimorbidity score for patients in practices using EMIS software. Previously, there has been no easy way to generate a multimorbidity score in routine practice. The search routine and report will be made available on the project website for use by practices and researchers.
-
Notwithstanding the limitations of the reliability of data recording, it is clear that the use of alternatives to the face-to-face consultation, other than telephone consultations, is extremely low. Electronic consultations as a whole (e-consultations or e-mail) represented much less than 1% of all consultations in all practices, with the highest rate being 0.23% in one practice. As such, discussions about whether these consultations increase or decrease demand on practices are moot, given the current levels of use.
-
Telephone consultations are much more established and have been used for many years, but, even so, account for only 18% of all consultations, with a maximum of 31% in the practice that used the telephone to the greatest extent. The key finding is that the vast majority (80%) of consultations are still conducted face to face in surgery, even in case study practices selected because they were attempting to make more use of alternatives to face-to-face consultations.
-
The pattern of consultation rates in relation to patient characteristics was broadly as expected, with higher rates in children and the elderly, women, patients from ethnic minority groups and patients with multimorbidity. Face-to-face consultation rates were slightly higher in the least deprived areas, and telephone consultations slightly higher in the most deprived areas, but otherwise there was no strong relationship with deprivation for these consultation types.
-
However, for electronic consultations, some of these patterns were reversed, with the highest rates in young adults and white patients. There was also a clear trend towards higher rates of e-mail consultations in the less deprived areas. These findings could be interpreted as indicating that provision of electronic consultations increases inequalities of access, or, alternatively, that offering different forms of communication provides a range of routes to care that suit the needs of different sectors of the population. However, low usage levels mean that it is not currently possible to say.
-
Most consultations by telephone, e-mail or e-consult are followed by another consultation (often face to face) within 14 days, and this is more common than after an initial face-to-face consultation. Therefore, any analysis of the use of alternatives to face-to-face consultations needs to take account of knock-on effects in the next 2 weeks.
Chapter 7 Synthesis and framework for future evaluation
Introduction
Throughout this study, both qualitative and quantitative data were collected, guided by a literature review, with the aim of developing a theoretical framework to inform future implementation and evaluation of alternatives to face-to-face consultations in general practice. This chapter describes the process of synthesising the findings from the various sources of data. This includes implications for future research, as well as the development of a web resource, based on our findings, to support practitioners and policy-makers who are thinking about the introduction of alternatives.
Methods for synthesis
A conceptual literature review informed our approach to conducting the focused ethnography in the case study sites. The analysis of the qualitative data followed a stepwise process, whereby the ethnographic team developed the coding frame that was applied to all of the data. As the data collection became complete, a summary document was produced by the ethnographic team for each of the codes, which was then shared and discussed with the wider team. Similarly, the analysis of the quantitative data (as described in Chapter 6) was also discussed within the team. As a team, we reached a consensus on the findings. It was then necessary to validate and optimise these further with a range of professionals, from a range of perspectives, at a stakeholder workshop, to ensure that any theory and resource development would be applicable to those for whom it was intended.
Stakeholder workshop
A range of stakeholders were invited to a workshop event on 18 October 2016 at a central location in London. The 25 attendees included GPs from participating case study practices (n = 5), policy-makers from NHS England with a particular interest in the introduction of digital technologies (n = 4), academics with relevant interests (n = 5), patient and public representatives (n = 4), one person from a primary care consortium and one individual from each of the following: the British Medical Association, the Royal College of General Practitioners, NHS Digital, NIHR and the Hurley Group (which promotes eConsult, an e-consultation software).
Following an introduction to the overall study and its aims and methods, the findings were presented through a series of brief presentations on key questions that we intended to use as the basis for the eventual web resource:
-
What were practices trying to do and why?
-
Whom is the alternative to the face-to-face consultation for and why?
-
How do we get implementation of alternatives to the face-to-face consultation right?
-
How will we know if implementation has worked?
Following each of the presentations, the stakeholders were invited to consider three questions within their table groups, which they then fed back to the room:
-
Do you think we have identified the right issues?
-
Is there anything we have missed?
-
What advice would you expect from our web resource?
The findings from these discussions were recorded on flip-charts and used to refine the structure and content of the web resource (described in Implications for practice and service delivery).
Patient and public involvement input to the synthesis
Patients, carers and members of the public inputted to the stakeholder workshop in two ways. First, four members of the public attended the workshop. These included people with experience of caring for an elderly parent, people with diabetes mellitus and people with depression. In order to ensure that young people’s perspectives were also included, we also invited members of Bristol Young Healthwatch, but none was able to attend. However, we had already elicited their opinions on alternatives to face-to-face consultations in a workshop specifically for young people, and were therefore still able to incorporate their views.
The public contributors who attended the stakeholder workshop actively contributed to the discussions, indicating where there may be areas of consensus and potential disagreement in the adoption and use of alternatives to face-to-face consultations between patients and health-care professionals. Specifically, they suggested that an aim to deliver consultations in an efficient manner, making best use of everyone’s time, would be something that would be shared by both patients and health-care professionals. They also felt that patients should be involved in any decisions about the method of consultation to be used, rather than this being a decision made solely by health-care professionals.
They thought that it was important that the web resource should include material that was aimed at patients and carers, to better inform them about the pros and cons of alternatives to face-to-face consultations. The PPI representatives also thought that the resource should include information on how practices can inform patients and carers on the introduction of alternatives to face-to-face consultations, recognising that one of our findings was that this was not always done well. They discussed issues such as whether to inform specific patient groups or to inform patients more generally.
The views of the PPI representatives concurred with our focus in this project. This included ensuring that the views of carers were considered, and that the use of alternatives to the face-to-face consultation was not limited to communication with GPs, but could include other members of the practice (e.g. nurses or nurse practitioners).
Programme theory
The underlying basis for this research programme was to gain a greater understanding of the use of alternatives by developing a programme theory which would set out how, under what conditions, for which patients and in what ways these alternatives may offer benefits to patients and practitioners in general practice. This would be based on a realist perspective to describe the provision of alternatives to face-to-face consultations in terms of:
-
context
-
mechanism – the theory and assumptions underlying the intervention and the flow of activities that comprise the intervention
-
intended benefits/outcomes.
In addition, we wanted to explore implementation in terms of moderating factors that influence the extent to which the process and outcomes are achieved, such as factors acting as barriers to, and facilitators of, practices offering alternatives to face-to-face consultations or to different groups of patients using them.
Context
The introduction of alternatives to the face-to-face consultation needs to be understood within the current policy context, which has consistently promoted the use of new technology to modernise health care. 7,14 Over the last decade, the idea of online systems to improve access to health care has been repeatedly highlighted as an example of how the NHS will better respond to patients’ needs in the future.
However, our survey of practices demonstrated that, despite a great deal of enthusiastic policy-making and government incentives aimed at increasing the use of alternatives to the face-to-face consultation, with the exception of telephone consulting, these are not at all widespread. Even in the case study practices, where service providers have attempted to introduce innovation, our analysis of routine consultation data showed that use levels for alternatives to the face-to-face consultation were low.
The responses to our survey, and to our interviews, suggest considerable unease at the prospect of introducing new means of accessing a service that is already failing to cope with patient demand. Even though clinicians acknowledged that one motivation for introducing new technologies might be to control the perceived unmanageable workload, many felt that these technologies would increase, rather than reduce, demands on their time, or felt that they did not have the energy or time to put the required changes into place.
These reactions need to be understood within a local context in which general practice is under severe strain. There were many examples in our interview data of practice staff feeling unable to provide a functional service that met patients’ needs or policy-makers’ expectations, leading them to explore options for managing this demand, options that included alternatives to the face-to-face consultation. Interviewees, both patients and staff, described a system that they felt was falling short of providing reasonable access to primary care and this was a source of stress for both service users and providers.
In this context, for some practices, the rationale for introducing a face-to-face consultation was the need to ‘do something’ to change their practice organisation with respect to access to care for patients, even if they were not sure whether or not the change would lead to improvements. However, introducing a change to practice organisation where there is not the capacity to implement it effectively has the potential to lead to problems of implementation, and these were observed in our case study sites.
From our practice observations, a key factor in the introduction of alternatives in the case study practices in England was the financial support provided by the GP Access Fund. 14 Many of the consortia of practices that were successful in bidding for funds included plans to introduce online or Skype consultations. This meant that practices within successful consortia were often given free access to e-consult systems (which would otherwise incur a cost), along with training and project management support. Two of our case study sites were trialling e-consultations funded this way, and one practice was using e-mail as part of a GP Access Fund14 project. One of the practices in Scotland was using an e-consult system as part of a free pilot offered by the e-consult company. The practice liked the system, but felt that it could not justify the cost and decided instead to incorporate features of the e-consult system into its own website, which would cost far less.
Mechanism and intended outcomes
In our focused ethnographic fieldwork, it was not always apparent that the reasons behind a decision to adopt alternative consulting methods had been clearly thought through and discussed within the practice. Members of the wider primary care team were not necessarily involved in the decision to implement, and, in the case of e-mail, were sometimes unaware of the fact that an alternative had been implemented. Decisions to implement were often led by one or two enthusiasts in the practice, with others going along with the decision and, on occasion, others openly disapproving.
Rationales for introducing new forms of consulting included more efficient management of demand, improving access to patients and to be seen as a modern practice. It was not always clear, however, that even when an expressed aim was vocalised, that there was a theoretical basis as to how the proposed innovation was likely to deliver that aim, particularly in respect of improved efficiency. There were a few exceptions to this; for example, in the remote and rural practice, video consulting was intended to overcome difficult, and sometimes impossible, journeys to the practice.
Interviews with patients suggested that they were interested in using these technologies (particularly telephone and e-mail), which they saw as a means of reducing the time they had to expend arranging to see and consult clinicians (particularly for what they termed ‘simple’ problems). The use of alternatives to the face-to-face consultation could also be much more convenient, as well as time-saving, particularly for people who have difficulty physically getting to a surgery, either for geographical reasons or because of illness. The asynchronous nature of some alternatives, such as e-mail, meant that patients could send a message at a time that suited them and then read the response later, rather than having their diary dictated by appointment availability. The use of e-consulting and telephone consulting was seen as a quicker form of access without needing to wait for an appointment, although this was not always the reality.
In summary, patients’ hopes were based around improved access, and there were practice staff who expressed similar views. However, in contrast, a clear motivation for practice staff was to manage demand, even if the potential impact on patient access to care was as yet unknown. There were examples in the interviews of staff hoping that alternatives to the face-to-face consultation would ‘keep patients away’ or act as a triage mechanism, in order to reserve face-to-face consultations for those patients who were felt to need them, but conversely, there were staff who hoped that patients would receive better access and more convenient care. Clinicians hoped that e-consulting systems would provide more structured information exchange, which would be more efficient. Both practice staff and patients believed that it might be possible to deal with simple problems more quickly and easily, so that longer face-to-face consultations could be used for problems that required proximity.
There was, therefore, a tension between two contrasting perspectives. One perspective was the aim to increase access, even at the price of increased workload (because, if there is currently a problem of poor access because of unmet demand, improved access would potentially lead to more patients consulting). The contrasting perspective was the aim to reduce practice workload, even at the price of placing restrictions on patient access. In this scenario, alternatives to face-to-face consultations were seen as a way of channelling patient demand in ways that would be quicker for the clinicians to deal with, even if this was not necessarily the patient’s preferred option. These contrasting perspectives highlight a number of important considerations and assumptions about how the introduction of alternatives to the face-to-face consultation might achieve the desired benefits.
First, one way in which these perspectives might be reconciled is if the use of alternatives to the face-to-face consultation leads to more efficient working, so that access could be increased, while also decreasing practice workload. Both clinicians and patients tended to assume that the use of alternatives would be time-saving overall, even if this was attributable to the redistribution of consultation time across, for example, different patient groups. However, there was a tendency for staff to ignore the workload occurring at the practice level. Doctors and nurses sometimes observed that they were expected to deal with alternatives to the face-to-face consultation in addition to, rather than instead of, their usual number of consultations, by slotting them in between face-to-face consultations or tagging them on at the end of the day. Staff in our practices expressed views suggesting that other members of the team did not fully recognise the impact on them. Reception staff were expected to add to their workload without any planning or allowance for this. There were few instances of practices taking steps to evaluate the overall workload associated with their use. This is an important point because, although previous studies have shown that telephone consultations are indeed shorter than face-to-face consultations (mean of 5.4 minutes vs. 9.2 minutes, respectively18), telephone consultations are also associated with a higher proportion of reconsultations. Thus, after taking account of the proportion of reconsultations telephone consultations do not appear to be time-saving overall. 60 The fact that many practices implemented e-consultations only after they were given financial incentives to do so suggests that they were uncertain about the potential impact on workload, otherwise there would be a good business case to implement them without the need for any subsidy (unless the financial support was just to cover set-up costs).
Second, the ‘mechanism of action’ largely relates to implementation. Alternatives to the face-to-face consultation may improve access for patients if they are able to choose what form of consultation is most appropriate for them in a given situation. However, in some cases (related to the practice motivation to control workload rather than to improve access), practices used alternatives to the face-to-face consultation to control how patients gain access to care. For example, in some practices, receptionists suggested telephone consultations only once all face-to-face consultations were fully booked, or required patients to have a telephone consultation first. In some situations, this could be convenient for patients, but in other situations it was much less convenient for a patient if they had to ensure that they were available on the phone and to keep the whole day free because they did not know when they would be called.
On a related note, several practice interviewees described the need to ‘educate’ patients in using alternatives to the face-to-face consultation. This may simply refer to raising awareness of their availability, and we observed that some practices needed to put more effort into informing patients about the options that were available. However, it could also imply that staff felt that patients may use them in ways that the staff deemed inappropriate. This suggests that part of the mechanism of action was managing patients’ expectations of access to general practice.
Third, the argument that alternatives were useful for ‘simple’ problems assumed that both patients and clinicians can reliably tell in advance which problems are straightforward, and that both parties have a shared view about which problems can be managed remotely. Some of the interviews suggested that some staff do not have confidence that patients can always tell which type of consultation medium is appropriate. This relates to the comments about the need to educate patients, as described above, and the inconsistent way in which some practices asked patients to tell receptionists the reasons for some types of consultation request, but not others. This point is also supported by the finding that many clinicians applied alternatives to the face-to-face consultation selectively with patients that they deemed ‘sensible’, stating that they feared that these alternatives might be used inappropriately by other patients. This finding has also been observed in a previous study. 19
Finally, there was an assumption evident across interviews with patients, doctors and receptionists that face-to-face consultations were viewed as the ‘ideal’ and that an alternative was second best, but better than no access at all. Some patients described not wanting to be ‘fobbed off’ with a telephone consultation, although clinicians sometimes expressed the view that alternatives to the face-to-face consultation were necessary because they could not meet demand for face-to-face consultations. Therefore, use was not necessarily a preferred option for either patient or doctor, but sometimes applied as a response to a problem of undercapacity; this was especially the case for telephone consultation. However, it was acknowledged that alternatives to the face-to-face consultation brought benefits that somewhat offset what was being lost in not having a face-to-face consultation, and for some patients the use of an alternative to the face-to-face consultation was clearly preferable.
Unintended consequences
Although patients (and some practice staff) saw improvements in access to care as a benefit, this did not take away from their worries about demand. Even if the use of alternatives to the face-to-face consultation does mean that consultations can be conducted more quickly and efficiently, there was a concern that increased access will increase demand, outstripping any efficiency gains. Concerns about supply-induced demand caused by offering access to alternatives to the face-to-face consultation were demonstrated by GPs; however, we did not find evidence about whether or not the provision of alternatives does indeed lead to supply-induced demand. Our case study practices experienced the opposite problem, in that use was so infrequent as to question the investment in these new approaches. It is unclear if low uptake results from GPs applying the use of alternatives selectively, patients not being aware of their availability or not wishing to use them, or problems with implementation.
A further unintended consequence expressed was the possibility that the provision of alternatives to the face-to-face consultation might lead to increased consultation rates among groups of patients who are confident with technology. These people may have fewer health needs, and self-care because access to primary care is currently difficult. Lowering the threshold to access would not only increase practice workload, but could also increase health inequalities. This point is considered further under the discussion about the impact on different patient groups.
Implementation
Contextual factors affecting implementation
A range of contextual factors affected which alternatives were implemented and how they were implemented, often in relation to practice population and geography. Our case studies illustrated extreme examples of this. The introduction of video consulting at the rural practice in Scotland was motivated by the difficulty of reaching a doctor by boat, whereas the use of e-mail consultations at another was partly related to the large student population. However, practice culture was also very important, with some of the case study practices introducing alternatives to the face-to-face consultation because they had a long history of being innovative, and they wanted to be forward-looking. As previously noted, in England, the support provided by the GP Access Fund14 was another contextual factor affecting implementation. Some practices had introduced e-consulting systems chosen by their local consortium, without necessarily having thought through how these systems would be used in their practice.
Moderating factors affecting implementation, barriers and facilitators
The GP Access Fund14 also acted as an important facilitator of implementation, providing an impetus to change, financial support and, in some cases, training and support with protocols for provision of a new service. Innovations introduced in this way were more likely to be accompanied by campaigns to raise patient awareness, including messages in the waiting room and in practice websites, although this did not necessarily relate to increased uptake levels.
It was clear that in several practices, introduction was driven by one or two ‘innovators’ in the practice. This could act as a facilitator of implementation, but could also lead to inconsistency. In some practices, it was evident that practice staff were working in different ways, not necessarily knowing how others were working, and with no formal practice policy on how to apply or use an alternative to the face-to-face consultation.
There were several barriers to implementation. These included a lack of training for practice staff, particularly receptionists. In some practices, receptionists felt that there was a lack of awareness from both patients and doctors of the complexity of their role. Furthermore, the use of alternatives to the face-to-face consultation had grown organically in most practices without a plan, and new ways of working had not necessarily been implemented in an efficient or organised way.
Structural factors also had a major influence on implementation. The use of video consulting in one practice was constrained by the inconvenience of using the equipment. Many practices experienced problems because of the limitations of their GP computer records systems, which made it difficult to include records of e-mails or e-consultations. Changes in the use of the telephone for consulting sometimes required more telephone lines than were available.
There were also more subtle factors that acted to impede or modify use, and these were related to the impact on professional identity. New ways of working could be perceived as a threat to aspects of work that were seen as fundamental to professional values. For example, a core tenet of general practice is the importance of the doctor–patient relationship, and forms of consulting that are not based on face-to-face contact may have an impact on that relationship. Alternatives to the face-to-face consultation have often been promoted on the basis of quick and convenient access to care, but clinicians in the case studies speculated that this may be seen as being to the detriment of continuity of care (associated with relationships), as well as potentially to the quality and safety of care.
Some forms of alternatives to the face-to-face consultation were associated with changes in professional roles, for example the greater use of nurses to conduct telephone consultations. This was seen positively by some staff, and has the potential to increase staffing capacity, but in other cases was perceived negatively, with some staff (both nurses and doctors) feeling that the nurse’s time might not be used appropriately. One example of how alternatives to the face-to-face consultation were associated with changes to professional roles is a system (not observed in our case studies, but widely reported during our research) in which practices contract with another organisation so that patients have the opportunity to have a telephone or video consultation with a doctor unconnected with the practice, and who does not have access to the patients’ records. 18,154,155 Such developments challenge some of the key principles on which general practice is based, such as the provision of comprehensive, co-ordinated care provided through a single point of contact. However, this approach can improve access and expand the GP workforce by employing doctors working from home who cannot or do not wish to work in routine general practice. Given the scale of these changes, it is not surprising that the implementation of alternatives to the face-to-face consultation is met with resistance from some professional staff, which may have more to do with the implications for their professional values than it is related to the technology itself, and this was highlighted in the conceptual review (see Chapter 2).
Effects on different patient groups
One of the questions of interest for this research was the impact on different groups, including which groups might be most suitable for different forms and the possibility of increasing health inequalities if other groups are unsuitable. The key finding from our study is that, although individual patients’ perspectives varied, these could not be predicted based on factors such as age, sex or health status. In addition, there was a recognition that an individual patient’s reasons and ability to use a particular form of consultation may change over time and with experience.
Those who contributed to the stakeholder workshop felt that many of the assumptions about which patients benefit most were challenged by the evidence and, therefore, it would be more appropriate to consider how and when to use alternatives to the face-to-face consultation, rather than with which groups. Some forms have primarily been viewed as a way to respond to requests for quick access to care, but stakeholders felt that the same technologies might be more useful for follow-up and monitoring, rather than for initial assessment.
Although differences between patient groups were fewer than might have been anticipated, some concerns were expressed about the potential to increase health inequalities. This is supported to some extent by the findings reported in Chapter 6, that the characteristics of patients using e-consultation (more common in white, affluent, young adults) were in marked contrast to those of patients using telephone or face-to-face consultation. This could be interpreted as providing choice and improving access for people who find conventional forms of access to be inconvenient. However, it could represent inequity, by diverting resources and consultation time to the groups of patients with the fewest health needs. Given the very low number of patients using e-mail or e-consultations, it is important not to overinterpret these findings.
Implications for evaluation
Our aim was to understand how, under what conditions, for which patients, and in what ways, alternatives to face-to-face consultations may offer benefits to patients and practitioners in general practice and to determine which research methods were likely to be feasible to answer these questions.
The results of our research have provided useful data to inform the design of studies to undertake a formal evaluation of alternatives to face-to-face consultations. These include:
-
the number of practices currently using different types
-
the likelihood that practices and their patients will try these out
-
what outcomes are important to practices and their patients and what they expect to be achieved from introducing alternatives
-
to what extent alternatives are implemented differently in different settings and for which purposes
-
the feasibility of measuring the impact of alternatives on consultation rate and length, wider consulting behaviour and secondary care use
-
the groups of patients who are likely to be advantaged or disadvantaged by the introduction of alternatives
-
the types of methodology that are likely to be suitable to answer different research questions for different types.
The feasibility of answering these research questions depends on the level of development and current implementation of the technology under investigation.
One important consideration is the appropriate time at which to conduct an evaluation. Ideally, this would not be done too soon after implementation before the change has bedded down. However, neither should evaluation be conducted when it is too late to have an impact.
Potential research questions
In respect of alternatives to face-to-face consultations, our research has been partly about generating hypotheses, in order to create a logical framework for future definitive studies. Our work has indicated a need for further research on a range of questions:
-
Is it possible to improve the uptake of alternatives to face-to-face consultations and, if so, does this lead to benefits for patients and general practices?
-
What is the impact on access to care as perceived by patients (speed of access, convenience, timely access to care that meets their perceived needs)?
-
What is the impact on NHS workload and, in particular, on different sectors of the NHS (primary and secondary care) and different professional groups (doctors, nurses, receptionists and administrative staff)?
-
What is the impact on the quality and safety of patient management?
-
For which patients and for which conditions are different forms of alternatives most efficient and effective?
-
How do different forms of consultation change the content of the consultation?
-
How satisfied are clinicians and patients with different forms of alternative to the face-to-face consultation?
Our research has shown that telephone consultations are well established, whereas other forms of alternatives to the face-to-face consultation are very little used. Therefore, future research would need to apply different methods and explore different questions for these different technologies, and these are described below.
Telephone consulting
Telephone consulting is the only widespread alternative to the face-to-face consultation in common use. Although a large body of literature exists on telephone consulting [both qualitative and quantitative, including randomised controlled trials (RCTs)],60,156,157 most of this addresses the use of telephone triage of requests for same-day appointments and for out-of-hours work. There is some qualitative research on the use of telephone consultations for follow-up conditions and in long-term condition management, but little in the way of quantitative research, with a few exceptions for specific diseases. 108,158–160 There is a need, therefore, to consider the impact on the quality and safety of patient management and NHS and patient resource use of the introduction of structured telephone follow-up of acute and long-term conditions.
The best way to determine quantitative outcomes (see Table 13) would be to conduct a RCT. This could be randomised at the patient level, but would rely on GPs to recruit and randomise the patients, which is unlikely to be successful. Instead, a cluster randomised trial along the lines of the ESTEEM trial60 is likely to be more successful. An alternative might be a controlled before-and-after study. A qualitative process evaluation could be readily embedded in such a study, possibly within a realist evaluation framework. An economic evaluation with a wide scope would also be essential, because the impacts of this change in practice might be felt in several sectors of the NHS (e.g. role substitution in primary care, changes in the numbers of investigations or use of outpatient or emergency departments).
In recent years, the use of telephone consultations as the main first point of contact for all consultations has been promoted and widely taken up by practices. We did not include such practices within our case studies, because these schemes are well established and now need to be evaluated using different research methods to assess outcomes.
E-consulting
We have identified very low uptake of e-consultations in this research. These systems incur a subscription charge, and, to be cost-effective, would have to be both widely used and reduce practice workload considerably. Research into these systems should begin with further investigation to determine why, as we observed, there is low uptake and how much time it takes a patient to complete the online forms and for clinicians to read them. If it appears that these systems can be made more attractive to patients, there is potential to see how their usage may affect the workload of the practice. Depending on the likely uptake of the intervention, this could be as an individually randomised trial (e.g. patients willing to use the system are randomised to those given immediate and delayed access after 1 year) or, if taken up by large numbers, as a cluster RCT. The study would explore the impact of the intervention on the outcomes described in Table 13. Such a trial should have an inbuilt qualitative process and economic evaluation.
E-mail consulting and webmail
In contrast to structured e-consultation methods, the use of e-mail for patients to enter into a two-way dialogue with the clinician is less well developed in the UK. It is a technology with which many are familiar and it is potentially inexpensive to introduce. However, as is clear from our case study practices, robust systems for handling e-mail have not been established in practices, and this would be difficult to achieve using standard e-mail (e.g. establishing with confidence the identity of patients using the system). Webmail has the potential to be more secure, requiring a logon from the patient. Such systems can be provided through practice websites. They would involve simple triage questions with respect to the nature of the problem to determine the suitability of the medium (e.g. speed of response, considered need for examination). Our work highlights serious concerns from clinicians about being overloaded, by lowering the bar to consultation and inappropriate use of e-mail as a means of fast-tracking to a face-to-face appointment. Unfortunately, there appears to be little in the way of quantitative research on the impact of the use of e-mail on workload, and on the analysis of the content of e-mails in comparison with face-to-face and telephone consulting for similar problems.
Clinicians would have to be reassured that the interventions will be introduced in a controlled manner. As with e-consulting, research should include Phase II research to develop and test the feasibility of robust webmail systems. Once such systems have been devised, then it is possible to consider introduction of webmail for a restricted number of interested patients who could be randomised to having immediate and delayed access. Embedded studies would explore how the content of e-mails compares with face-to-face and telephone consultations and patients’ and clinicians’ perceptions of the use of the medium. A reasonable intervention period (at least 1 year) would be required, as it takes time for people to become used to using new systems.
Video consulting
Although there is a relatively large body of literature exploring the potential for video consulting, many studies are small and descriptive. 59,124 This is particularly true of primary care consultations, mainly demonstrating the potential for the medium, rather than exploring its impact on the content of the consultation or on GP workload or patient satisfaction. There have been no RCTs in general practice, and those studies in the UK have been confined to patient attitudes to video-consultation.
The major hurdle in undertaking research into video-consultation in the UK will be to encourage GPs and practice nurses to use it initially. Before undertaking any trials in the UK, it will be important to address the barriers to these consultations that we have identified. These include the attitudinal and logistical barriers identified by clinicians and the technical difficulties that may be encountered working within the heavily firewalled, low bandwidth systems of the NHS. Thereafter, it will be necessary to explore those types of patients for whom video-consultation is most appropriate, how video-consultations differ in length, content and quality from face-to-face and telephone consultations and patients’ and clinicians’ experience of these different media. At present, the use of video-consultation is so minimal that we are unable to answer these questions. Given the mismatch between the rhetoric and financial support being given to video-consultation compared with the almost non-existent use of it, the priority should be a cautious stepwise introduction, beginning with overcoming technical difficulties and establishing feasibility and potential impact, before widespread implementation of this approach. Once the use of video-consultation is more established, it may be possible to consider RCTs of the use of the medium versus face-to-face and telephone consultations.
Which patients
With the exception of telephone consulting, all new forms of consulting require an internet connection. Almost 8 in 10 households now have fixed broadband access at home and 61% of people regularly access the internet by phone or tablet. 161 According to Ofcom in 2015, 68% of people aged > 55 years owned a smartphone, rising to 90% in younger age groups. At least until 2015, around 25% of non-smartphone users were converting to smartphone use each year. 162 However, not all people who own a smartphone have large data allowances and this could be a problem for people with modest incomes who have no Wi-Fi connection. In contrast, home broadband usage appears to have peaked. 161 People in the poorest households rely more on mobile phones than fixed broadband for internet access. 162 It is clear that, for those consultation formats requiring internet connectivity, there may be a significant number of people excluded from their use, largely older and poorer people.
Analysis of our own data supported this finding and indicated that, although the demography of patients using telephone consulting was largely similar to the demography of patients attending the surgery, e-consultations tended to be carried out with younger and more affluent patients. There were insufficient instances of use of video consulting to determine the demography of users with confidence.
Interviews and observations with clinicians and patients also indicated that telephone consultations were more challenging for people who have communication difficulties (primarily those who did not use English as a first language or who had hearing problems), learning difficulties or cognitive impairment. However, for some of these groups, written communication such as webmail/e-mail and e-consulting systems might be helpful. Future developments would have to be carefully planned to ensure that the introduction of these technologies was not at the expense of those who may not have access to or be able to use them.
The choice of patient group relates closely to the question of how alternatives to the face-to-face consultation are implemented and for which purposes. If patients can choose from a range of consultation options that are equally available, then the patient group using each type of consultation will be determined by patients themselves. If use of alternatives to the face-to-face consultation is mandated by the practice as the default way to gain access to care, it will be important to facilitate other routes to care for these groups with particular needs, as described above.
Which technology
In summary, our research suggests that there are three types of technology that are priorities for robust evaluation, because they are being widely implemented in the absence of evidence. In each case, the research needed is less to do with the technology and more to do with the impact of the system redesign. The three priorities currently for evaluation of alternatives are as follows:
-
The use of the telephone for follow-up consultations; as previously noted, most attention has been given to the use of the telephone for initial consultations or triage, but there is great scope for use of the telephone for follow-up and monitoring of previously diagnosed problems, review of chronic conditions, support for self-management and simple queries. As we observed in the case studies, many practices use the telephone in a variety of ways that are often ad hoc. There have been several studies of telephone support for a range of specific chronic conditions,158 but few studies of a whole-system redesign that maximises the use of telephone consulting for follow-up in an organised way. 159,160
-
E-consulting systems are being heavily promoted, and their implementation has accelerated greatly as a result of the GP Access Fund. 14 These systems often come with support and standardised protocols, and have often been acquired as a result of the decision of all the doctors in the practice. The use of these systems is quite formalised, which may facilitate research. Despite the attention given to these systems, there is very little evidence about their impact, and this is therefore a priority for research. However, in our case studies, we observed very poor uptake of these interventions, despite their being heavily promoted by practices. It would be important to explore the reasons for this, before embarking on a large-scale evaluation.
-
The use of ‘telephone-first’ models of access to care. This is currently being studied by another research team using mixed methods, including a before-and-after study of patient experience and hospital utilisation, qualitative interviews with patients and analysis of routine data about consultation rates, waiting times and continuity of care in a sample of practices. These studies will provide much-needed evidence, but will inevitably share the limitations of all such quasi-experimental studies, particularly the potential for confounding and selection bias. It is likely that practices that take up telephone-first models differ from other practices in important ways (particularly relating to local context and practice culture) that are hard to measure. Nevertheless, this is likely to be the best evidence available, as a true experimental study, such as a RCT, would probably be impossible to conduct.
Clearly, many of the issues above will pose a challenge to future research in the area. Particularly for those interventions that are little used currently (e.g. webmail/e-mail and video consulting), many clinicians will need to be persuaded of the possible long-term benefits, and will probably require some form of support/incentive to identify and agree the need for the change in their current practice.
Is there a need for a standard implementation of alternatives to the face-to-face consultation in undertaking research?
Our research shows that similar technologies are implemented differently in different practices. Some of these had been planned carefully and others had evolved, possibly not always with a great deal of thought. Implementations were sometimes somewhat piecemeal, with not all clinicians involved in their use and with no written or accepted protocols for handling them. It seems very likely that, regardless of the final implementation, one that has been planned and agreed with members of the practice team is more likely to be successful than one that has not. For the purposes of researching the impact of alternatives to face-to-face consultations, it makes sense to ensure that practices agreeing to take part in research should be supported to develop protocols for handling novel consultations in a way that suits their practice demography and existing management style to increase the chances of a successful implementation. However, it is likely, for example, that a solution that suits a remote and rural island practice will not necessarily suit an inner-city practice with a large non-English-speaking population. It is also possible that the implementation will evolve with time as practices gain experience. Alternatives to the face-to-face consultation are a good example of a complex intervention, and a range of research designs may be more or less applicable. A rigid, unalterable intervention, such as is normal for a traditional RCT, is unlikely to be appropriate. Regardless of approach, it will be important to specify the key features of the alternative to the face-to-face consultation (which, depending on study design, may be an intervention) that are fundamental to its intended purpose, and, therefore, must be implemented as planned, and those features that are flexible and appropriate for local modification.
Although there are many other potential uses of alternatives apart from the three listed above, these are less established, and attention should be given to further development and feasibility testing before definitive evaluation. In the case of some technologies, such as video consulting, for which there is little experience of use in primary care and different technological options are available, it will be important, prior to attempting to assess impact, to determine which are most accepted and used by clinicians and patients.
Measures of the process of care
This research has highlighted the range of factors that may act as mediators or moderators to the successful implementation of alternatives to the face-to-face consultation. Some of these factors are related to the presumed mechanisms and assumptions about how they might improve general practice (e.g. that managing an e-consultation will be quicker than a face-to-face consultation, leading to lower practice workload and shorter waits for a face-to-face appointment). In future research, it will therefore be important to assess these factors as measures of the process of care. This will help to illuminate how and why the intervention was effective, or if it was not effective, whether this was because of a failure to deliver the intervention as intended or a failure of the intervention to have the desired effect. Some factors, such as the number of consultations of different types, could be considered as measures of the process of care or as the outcome of the implementation. We have therefore considered both process and outcome measures together in Table 13.
Measures of outcome
The parameters best used to capture the outcomes of most importance will depend on the chosen methodology and the type of alternative to the face-to-face consultation under investigation. However, the key outcomes that matter to patients, practice staff and the NHS are listed in Table 13. Some of these outcomes are a direct result of the use of alternatives to the face-to-face consultation, whereas others may well be related and are important to patients (e.g. health-related quality of life), practices (e.g. staff morale) and the NHS (e.g. possible knock-on effects on emergency department attendance rates).
| Parameter | Potential source | Feasibility |
|---|---|---|
| Patients: measures of access to care | ||
| Awareness of availability | Questionnaire: PROM | Suitable questions may need to be developed |
| Time taken to contact the practice | PROM | Suitable questions exist (e.g. in the GP Patient Survey163) |
| Ability to get consultation type of choice (or one at all) | PROM and/or audit | Suitable questions exist (e.g. in the GP Patient Survey163) |
| Ability to get consultation with clinician of choice | PROM | Suitable questions exist (e.g. in the GP Patient Survey163) |
| Ability to get appointment/consultation as soon as patient would like | PROM | Suitable questions exist (e.g. in the GP Patient Survey163) |
| Time taken up by consultation (including getting to the surgery and waiting, time completing online questionnaire or time waiting for a telephone call, as relevant) | PROM | Questions can be adapted from existing questionnaires, including the GP Patient Survey163 |
| Satisfaction with convenience of appointment | PROM | Suitable questions exist (e.g. in the GP Patient Survey163) |
| Satisfaction with interpersonal nature of the consultation | PROM | Suitable questions exist (e.g. in the GP Patient Survey163) |
| Perceptions of support for self-care | PROM | Validated questions exist |
| Health-related quality of life | PROM | Validated measures exist (e.g. the EQ-5D or the SF-36), but lack sensitivity for primary care consultations |
| Satisfaction with the outcome of the consultation | PROM | There is a lack of generic measures of the outcome of primary care consultations, but a suitable measure has recently been developed164 |
| Quality of the consultation | Observed or recorded consultations | There are approaches to the assessment of consultation quality, although they are very labour intensive |
| Practices: measures of workload, cost and staff satisfaction | ||
| Number of patient requests for different types of appointment | Audit | Audit may require bespoke data collection at reception or via portals for e-consultation |
| Length of consultations | Routine data from GP system | Difficult to extract for analysis at present (see Chapter 6). Prone to errors if clinicians do not open and close patients records at the beginning and end of consultations – this is likely to be a particular problem with some forms of alternatives to the face-to-face consultation |
| Total number of consultations of different types in the practice over 12 months | Routine data from GP system | Feasible, as demonstrated in Chapter 6. Dependent on all forms of consultation being reliably entered in patient records |
| Total number of consultations with different types of staff over 12 months | Routine data from GP system | Dependent on reliability of recording of all consultations and staff type |
| Number of consultations completed with advice or prescription only | Routine data from GP system | May have to be derived indirectly from lack of subsequent consultations |
| Number of problems dealt with in each consultation | Audit of sample | In theory, this should be available from routine data, but because many problems are entered as free text rather than coded, this would require manual analysis of individual consultations |
| Content of consultations | Established consultation analysis tools following direct observation or recordings; analysis of computer records | Observation or recording of a sufficient number of consultations is laborious. Analysis of GP records may not fully represent consultation content |
| Number of patients directed to other sources of care | Audit of sample or routine data | Could be collected from routine data if practices use structured data entry for each consultation |
| Number of follow-up consultations within 14 days | Routine data from GP system | We have demonstrated the feasibility of doing this and associated difficulties in Chapter 6 |
| Number of patients who do not attend | Routine data from GP system | Feasible from routine appointment systems |
| Total consultation time per annum, taking account of number and duration of all consultations | Routine data from GP system | Limitations relating to data about duration apply |
| Cost of primary care at the practice level | Routine data from GP system | Based on data about consultation numbers and duration and staff type. Limitations relating to data about duration apply |
| Staff perceptions of training and competence to use alternatives | Staff survey | Suitable questions may need to be developed |
| Staff satisfaction and morale | Staff survey | Validated questions can be used or adapted from existing questionnaires |
| The NHS | ||
| Rates of use of out-of-hours services, emergency departments, outpatient consultations, emergency admissions | Routine data | All available from Hospital Episode Statistics,165 except out-of-hours services. Data may be available in GP records, but not standardised and difficult to extract |
| Quality and safety of care | Audit of sample | Will require expert review, sometimes difficult to achieve agreement |
| Number and cost of investigations | GP records | Can be difficult to extract and cost reliably |
| Number and cost of prescriptions | GP records or NHS Prescription Services | Feasible |
| Cost of care from all NHS sources | Combining data sources described above | Dependent on reliability and completeness of all data |
The parameters listed in Table 13 reflect the priorities of patients and practitioners identified in this research and we have proposed suitable measures and made comments about their feasibility based on the experience of the research team.
Feasibility of practice recruitment
In order to evaluate alternatives to the face-to-face consultation in a rigorous research design, it will be necessary to recruit a sufficient number of practices in a range of settings. However, our survey of practices reported in Chapter 3 demonstrated a low level of willingness to implement. Therefore, a prospective study may be impossible to conduct, unless alternatives to the face-to-face consultation are developed that appear to offer advantages to general practices and are implemented for the purpose of evaluation. The only evaluative research that would appear to be possible at present would be studies of approaches that are being widely implemented, such as new forms of telephone consulting or the introduction of e-consultation.
Feasibility of patient recruitment
We did not seek to recruit patients on a large scale in this study, but previous experience suggests that it is possible to recruit at least 39% of people attending general practice to complete a questionnaire166 and 78% to allow access to their records for analysis of consultation rates. 60 However, the feasibility of patient recruitment to research on some forms of alternatives to the face-to-face consultation will be constrained by the small number of patients using them.
Sample size
In the study reported in Chapter 6, up to 30% of consultations were conducted by telephone. With a telephone consulting rate of between 0.4 and 1.4 consultations per patient per year at different practices, it would be feasible to recruit a large number of patients within a short period. In contrast, e-consultations accounted for < 1% of all consultations in the three case study practices that provided them. Therefore, it would not currently be feasible to evaluate the impact of e-consultations unless uptake increases.
Feasibility of data collection for process measures and outcomes
Table 13 above shows that most measures can be collected from patient-reported outcome measures or routine GP computerised records. Suitable questions are available from validated patient questionnaires for most of the relevant variables. Our research has demonstrated that routinely acquired data from GP computer systems can be interrogated to determine the number and types of consultations, including the number of subsequent consultations within 14 days. It was also possible to describe characteristics of the demography and medical history of patients using these consultations, as well as the professional characteristics of the clinicians consulted. Although not carried out in this study, it would also be feasible to collect data from GP computerised records of prescriptions and investigations.
However, the quality of recording of data in general practice is variable, particularly in respect of accurately recording consultation type. We found that telephone consulting was systematically under-recorded and that e-mail consultations were particularly poorly recorded. It was difficult to detect if a telephone consultation was for triage or a complete consultation (although the former may be inferred through searching for follow-up consultations within a defined period after the index consultation). Some forms of e-consulting systems (e-consult) were designed to remind GPs to record them, and as a result, were better recorded.
Although consultation type may not have been well coded, there were instances when this could be deduced from free text within the consultation record. Research utilising machine-learning techniques is promising in terms of identifying consultation type from free-text entry. 167 Although we did not use these in our research, we are aware that algorithms have also been devised that can infer the likely consultation type from arrival time, start time and consultation length. 168
The use of routinely recorded data in primary care therefore poses problems of accuracy and completeness. It seems unlikely that clinicians will improve the accuracy of their recording in the absence of changes to the design of current GP consulting software. Potentially, incentives may improve this. If this is not possible, it has implications for the size of studies that may be needed to demonstrate changes in outcomes.
The website resource
The stakeholder workshop was helpful in terms of crystallising some of the key messages from this study. Feedback from stakeholders was used to identify actionable messages for practices and policy-makers. We used these as the basis for a website resource, under the following headings:
-
Why do you want to introduce an alternative to face-to-face consultations?
-
Which alternative are you interested in?
-
Who is it for and why?
-
How do we get it right?
-
How will we know if it has worked?
The web resource was developed with the help of the website team at the University of Bristol (Figure 6). It was agreed that the resource should be simple, accessible and intuitive, and designed to address the issues that the user would find most helpful. Given the variability in the rationale for, and implementation of, alternatives to the face-to-face consultation, the principle of the resource was to provide a self-appraisal and guidance tool, rather than providing standardised recommendations. The user would be guided to consider a series of key questions relating to the introduction of alternatives to the face-to-face consultation, and the responses to these questions would suggest things to consider and links to sources of guidance. In broad terms, the web resource was structured to follow the topics covered at the stakeholder workshop, that is, the need to consider the rationale for the introduction of an alternative, who the practice was expecting to use it and for what purposes, suggestions about pitfalls to avoid in implementation and ideas about how to monitor and assess the success of the initiative. Because we were aware that users might not access the website in a linear fashion, a side bar was present throughout the resource to allow the user to go back or progress onto another section. We were also aware that some users may not access the resource at the beginning if they had searched using specific terms, so the sidebar helped the user to navigate the site.
FIGURE 6.
Screenshot of website resource. Reproduced with permission from the University of Bristol.
Once complete, the website resource was viewed and commented on further by the PPI representatives. The final website can be reached at www.bristol.ac.uk/primaryhealthcare/researchthemes/alt-con/resources/.
An outline of the structure of the resource is provided in Appendix 22.
The development of the website resource has been through a rigorous process, beginning with the ethnographic researchers and extended to the wider study team through to stakeholders and PPI representatives. The synthesis of the feedback from the stakeholder workshop with the study findings has been crucial. The study team feels confident that the website provides an informed and evidence-based resource to guide potential users of alternatives to face-to-face consultations.
Chapter 8 Discussion
Summary of the main findings
We set out to understand how, under what conditions, for which patients and in what ways alternatives to face-to-face consultations may offer benefits to patients and practitioners in general practice, and to use this understanding to develop guidance for general practices and a framework for subsequent definitive evaluation.
The first stage of our research was a conceptual review, which culminated in ‘key questions to consider when planning, implementing and researching alternatives to face-to-face consultations’. 83 This review helped to provide a focus for some of the subsequent stages of research, but was also designed for broader use beyond our study and to act as a guide for practitioners, policy-makers and researchers.
We found that alternatives to the face-to-face consultation are not in widespread use in general practice in the UK, with the exception of telephone consulting. In the scoping survey, conducted in three areas of the UK, we found barely any use of video consulting and very little use of e-mail or electronic consultation. Bookable telephone calls were used by most, but not all, of the GPs surveyed. When asked about intentions to introduce alternatives to the face-to-face consultation, the majority of practices had no plans to use video or electronic messaging, and 10% of respondents did not plan to introduce bookable telephone consultations. Free-text comments mostly expressed resistance to the idea of e-mail or video-consultations, although only a few opinions were related to experience of an alternative to the face-to-face consultation. Thus, despite the policy pressure to introduce consultations by e-mail and internet video, as described in Chapter 1, there is little actual use and a general reluctance among GPs to implement alternatives, other than the telephone, to face-to-face consultations.
The scoping study guided recruitment of the case study sites. Even in the eight case study sites, selected because alternatives to the face-to-face consultation were in use or had been in use, actual levels of use were low. Our analysis of routine consultation data in these eight practices showed that telephone consultations accounted for only 18% of all consultations. Among practices offering e-mail consultations, the highest proportion of consultations conducted in this way was 0.58% in one practice, with other practices conducting only 0.02% of consultations in this way. E-consultations were also very rarely used, accounting for 0.22% and 0.23% of consultations in those practices that offer them. In the one case study practice that used video, levels of use were so low that it was not possible to include them in this analysis. Across all eight of the case study practices (chosen because of their interest in using alternatives) the vast majority of consultations (80%) are still conducted face to face in surgery. These low levels of usage of alternatives to the face-to-face consultation challenge assumptions by policy-makers that alternatives will necessarily lead to replacement of, or reduction in, face-to-face consultations, and raise questions about whether or not it is appropriate to actively fund alternatives to the face-to-face consultation.
The lack of practices offering video consultation, and low levels of use in our case study site, led us to conduct four additional interviews outside the case study sites. These interviews were with people setting up or using video-consultation services in primary care. Two of these had very limited experience of using video consultation with patients as a result of low uptake. We had originally hoped to recruit additional participants from those practices that had been awarded funding under the GP Access Fund14 and had stated that they would use video consultation. Of the practices that were contactable, it was not possible to identify any practice that had gone ahead and routinely offered video consultation in this way. For several of the awarded projects, it was not possible to contact anyone involved, and there were no published results of the projects available. Therefore, it was not possible to collect much information on the application of video consultation in general practice.
In our case study practices, the uptake of e-mail consultation was closely related to whether, how and to whom individual GPs offered this type of consultation. GPs tended to do this selectively, basing the decision on familiarity with the patient, or other characteristics of the patient or their health condition. For other alternatives to the face-to-face consultation, the role of reception staff was crucial in offering these consultation types. The conceptual review found almost no evidence about how the wider practice staff members influence uptake; by observing these staff members in our focused ethnography, we found that receptionists and administrators had a crucial role in whether or not new consultation methods were offered to patients.
Despite low use and uptake levels, our case study practices were all using alternatives to the face-to-face consultation in varying formats. We were thus able to explore their rationales for introducing these alternatives. The rationales included:
-
the desire to be a modern practice and to respond to the expectations of busy, time-poor patients
-
alternatives being the only way of providing health care for patients in remote locations, or with other barriers to attending the practice
-
the acknowledgement that the previous system was broken and unethical in providing a first come, first served system that left patients without appointments that they needed
-
the recognition that reception staff and telephone lines were overwhelmed
-
the desire to manage demand and improve efficiency.
The rationales were not mutually exclusive; different team members described different understandings of the rationale in their own practice.
During this study, we set out to understand which patients may benefit, or not, from alternatives to the face-to-face consultation. The conceptual review showed that health-care professionals worry about certain groups being disadvantaged by alternatives to the face-to-face consultation, but these concerns were largely speculative. The patients interviewed in our case study sites included many from disadvantaged groups. For the patients, the benefits of alternatives to the face-to-face consultation reflected the characteristics of the medium (e.g. remote, asynchronous or text based). Regardless of socioeconomic circumstances, patients said that they liked the efficiency and convenience offered by alternatives to the face-to-face consultation. Both health-care professionals and patients agreed that there were certain conditions or issues that would require a face-to-face consultation. Health-care professionals made assumptions about the types of patients who were suitable for engagement in alternatives to the face-to-face consultation, referring to the ‘sensible patient.’ For both patients and staff, there were times when alternatives to the face-to-face consultation represented a second-best option. This was particularly the case with telephone consultation, which was also the approach used most frequently, and was well integrated within the practices.
Our examination of routine consultation data meant that we could explore the characteristics of patients engaging in alternatives to the face-to-face consultation. Within the case study practices, the pattern of consultation rates was broadly in line with what we would expect, with higher rates in children and the elderly, women, patients from ethnic minority groups and patients with multimorbidity. Surgery consultation rates were slightly higher in the least deprived areas, and telephone consultations were slightly higher in the most deprived areas, but otherwise there was no strong relationship with deprivation for these consultation types. For electronic consultations, some of these patterns were reversed, with the highest rates in young adults and white patients. There was also a clear trend towards higher rates of e-mail consultations in the less deprived areas. Low usage levels for e-mail consultations and the limited quality of the data available mean that it is not currently possible to say why this might be, although our observation about GPs’ (and perhaps receptionists’) selectivity about ‘suitable’ patients may be a factor. There may be other reasons why the provision of e-mail consultations increases inequalities of access. If a range of routes to care are offered, they may suit the needs of different sectors of the population.
In Chapter 7, we showed how we synthesised our findings from all of the different components of our research to develop a programme theory to articulate the mechanisms through which alternatives to the face-to-face consultation might offer advantages, and the potential benefits to patients and practices. This chapter also highlights the importance of local practice and population context in respect of how alternatives might be implemented, and how these alternatives might have different consequences in different types of setting. Chapter 7 then makes use of the programme theory to develop a framework for subsequent evaluation of the use of alternatives to the face-to-face consultation.
In analysing and synthesising our data, we took account of related theoretical perspectives, including insights from the normalisation process theory, the technology adoption model and the diffusion of innovations theory. 51,52,80 We did not base our analysis on any of these specific models, but were able to draw on their key tenets in interpreting our findings and devising our recommendations. In considering the contextual and moderating factors relating to implementation, we aligned with the normalisation process theory in focusing on the different kinds of work that people do in enacting a new practice. We also drew on the diffusion of innovation theory when understanding how one or two key actors within the practice could influence implementation, although, unlike the pattern described in the theory, we did not necessarily see the spread of the innovation throughout the practice. The perceived usefulness and ease of use of a new technology, as described in the technology acceptance model, were aligned with observations about a perceived threat to professional identity and a perceived challenge to the core elements of general practice being key to the ‘usefulness’, or lack thereof.
Strengths and limitations of the study
Conceptual review
The review provided a comprehensive assessment of the recent literature in relation to alternatives to the face-to-face consultation. We included opinion pieces, as well as studies including qualitative or quantitative data. The review provided a conceptual framework for the data collection and analysis, highlighting under-researched groups and topics for the case studies and suggestions for future evaluation. The conceptual analysis focused on the ideas present in the articles that we reviewed and did not attempt to synthesise numerical or thematic analyses from empirical papers. There were limitations to the approach taken in conducting the review. In restricting the database search to the previous 3 years, some relevant studies may have been missed. We aimed to include all relevant ideas, but some fledgling ideas, for example, from discussion sections of apparently tangential studies, may have been missed among the large amounts of material within the review. To help mitigate this, we asked three leading research and policy experts in the field to comment on the draft review and highlight any ideas we had missed. The applied focus of the conceptual review is a strength in a fast-moving field that lacks a substantial empirical evidence base.
Scoping study
The practice survey is the first in the UK designed to assess the use, and planned use, of alternatives to the face-to-face consultation in primary care from the perspective of GPs and practice managers. The large number of practices represented in this survey is a strength of this study. In this postal survey of general practice in three areas of England and Scotland, at least one response was obtained from a high proportion of practices (76%), which could be a reflection on the strength of feeling for this subject, but could also be related to the brief structure of the questionnaire and the incentive offered (a tablet computer in a prize draw). These practices were representative of all practices approached in terms of size, region and deprivation. The use of free-text comments, as well as the closed questions of the survey, added to the understanding of GPs’ concerns.
The survey included practices from areas with a range of characteristics: urban to rural, inner city to remote, and affluent to deprived locations. Such practices have differing local contexts, policies and incentives to implement alternatives to face-to-face consultations. The study covered only three broad geographical areas; practices in other areas of the UK could be using alternatives to face-to-face consultations differently.
We found in the case study work that there was different awareness of alternative methods among different members of the team; therefore, depending on which member(s) of staff replied to the survey, a different picture might emerge. The very idea of offering consultations using an alternative medium was controversial in some practices, especially where this was not an official practice policy. Therefore, it is also possible that there was some response bias169 whereby responders might have been reluctant to admit to using e-mail or internet video. With free-text comments, those who responded may have particularly strong views about the topic. Although the practice-level response rate was high, the response rate from individuals was lower. As such, the findings from this survey offer a previously unknown insight into the current use of alternatives to face-to-face consultations, but may not be generalisable.
The results of the survey were accompanied by further scoping methods, a strength of the study. Access to the practice websites was used both to check information given via the survey (and to add information from practices that had not responded). We had not anticipated the number of practices without active websites at the time of the scoping exercise. Supplementing this further by utilising contacts with local or national knowledge of the use of alternatives to the face-to-face consultation within primary care and approaching companies supporting practices in providing alternatives was another strength to the scoping exercise.
Focused ethnographic case studies
There are several advantages to using a team-based focused ethnography in multiple sites. It is a quick approach, and data can be collected at different sites concurrently. This speed is advantageous in research areas where the policy context is constantly changing. Similar fieldwork completed by one ethnographer would take much longer. Using multiple sites over a wide geographical area allowed for the capture of diversity in the use of communication technologies across several different locations.
Team working has benefits; in this study, it offered the opportunity for reflection and sense-checking, made the work less lonely and isolated and allowed for the sharing of ways of working, with the ethnographers building research skills. The regular meetings among the focused ethnographic team members allowed for constant comparison of the data and appraisal of the emerging areas of interest to explore further.
There were also some challenges presented by this approach. The nature of the posts required the appointment of ethnographers who had similar skills and were likely to get on with each other, something that was challenging when looking for specialist skills across three employing universities (University of Bristol, University of Edinburgh and University of Oxford). Data management was a huge task for the day-to-day lead (HA); for example, there was a lot of time taken to check coding across all transcripts and to ensure that data were safely and appropriately saved and stored. Research assistants employed in the senior ethnographer’s wider team (SZ) were drafted in to assist with entering coded transcripts onto NVivo (this requirement had not been anticipated) to free up time for the ethnographers to contribute to the analysis.
Another challenge was to ensure appropriate comparisons between case study sites that had been selected because they were using different approaches in different contexts, and were also located in very different geographical areas and managed separately by our ethnographers. Feedback from our ethnographers led to an initial period of adjusting the study documents (i.e. interview questions and coding framework), to balance the focus on the anticipated themes from the research questions and the emergent issues that were captured within the context of the different practices.
Ideally, each of our ethnographers would have visited the case study sites other than their own, to obtain a better grasp of the field and to compare perspectives between team members. Furthermore, longer contracts for our ethnographers would have allowed for more in-depth sharing of field notes and more face-to-face meetings, as well as for all three of the field ethnographers to be involved throughout the data analysis and writing up. The wider study team were engaged at the data analysis stage, and having input from experienced researchers with different disciplinary backgrounds, including general practice, was invaluable to the interpretation and final stages of the project. These fruitful discussions led to an understanding of:
-
how varied the case study practice cultures were in the experience of the GP members of the wider study team
-
potential audiences for the study findings and how to translate the information to practice teams
-
different practices about what gets recorded and timed as a ‘consultation’.
The case study sites were selected on the basis of their varied use of alternatives to the face-to-face consultation. We included a range of urban and rural practices, covering a broad geographical area, and having a wide range of deprivation scores. Some of the practices served communities with low levels of patients from ethnic minority backgrounds. Some practices had a high proportion of younger patients, which may have been connected to their willingness to offer alternatives to the face-to-face consultation. We interviewed patients from a wide range of ages, health conditions and socioeconomic groups.
Routine consultation data
The study set out to assess the feasibility of analysing consultation data from routine records, rather than necessarily providing definitive results about the frequency of consultations of each type. Because of this focus on feasibility, issues in conducting the analysis have been described. As described in Chapter 6, a series of problems associated with the data collected were identified, only some of which were foreseen. The data required a considerable amount of cleaning and reformatting from each individual practice before the data sets could be merged for analysis. For all types of alternative to the face-to-face consultation, the recorded number of consultations is likely to be an underestimate of the true number of consultations because of the recording limitations discussed in the chapter. Finally, not all practices offered the relevant forms of alternatives to the face-to-face consultation during the whole year covered by the data collection period. For this reason, data were analysed from the second 6-month period (mid-May to mid-November). This may also lead to an underestimation of consultation rates, because it omits the winter months, which are the periods of greatest demand. Despite these limitations, there would have to be an enormous element of under-recording to change the key conclusion, which is that the use of alternatives to face-to-face consultations, other than telephone consultations, is extremely limited.
Impact of patient and public involvement
Patient and public involvement had a positive impact on the study in a number of ways, and these are briefly outlined here.
Advisory group
Throughout the study, there were two PPI representatives in the advisory group. They were not connected with the PPI in the main part of the study, and provided an independent view on the PPI work and critical feedback on the PPI work that was undertaken. Importantly, they helped to ensure that the patient and carer perspective was a central concern in carrying out this work.
Workshop on the conceptual review
The issues raised in the PPI workshop were compared with the findings of the review. Doing this helped to confirm the relevance of issues raised in the literature. The feedback was also used to direct analysis and search for additional literature.
Focused ethnographic case studies
Patient and public involvement input helped to modify the patient-facing documents used in the study. The title of the study on the information sheets and consent forms was modified in response to PPI advice, and all abbreviations were removed from the documents. The information on observing the consultation between the doctor and the patient/carer and that provided to patients and carers invited for interviews was expanded to include more information.
Involving young people in our work helped us to broaden the range of patient and public perspectives in our project. This work confirmed that young people felt comfortable with the use of new technology to facilitate alternatives to face-to-face consultations. However, crucially, it also confirmed that they share the concerns expressed by other patient groups about the use of alternatives to face-to-face consultations. Without this element, the viewpoint of younger people would have been missing from our study.
Stakeholder workshop
Public contributors actively contributed to the discussions, pointing out where there may be areas of consensus and potential disagreement in the adoption and use of alternatives to face-to-face consultations between patients and health-care professionals. The impact of PPI on the synthesis of the study findings is described in Chapter 7.
Comparison with other studies
Although previous surveys have been conducted, the levels of use recorded in our scoping survey are lower than previous estimates reported from surveys conducted in Europe. 97,170 Fewer practices offer e-mail or video consultations than often envisaged. 171
We observed in our routine consultation data that there was a strongly positive relationship between multimorbidity and consultation rates; patients with more chronic diseases have more consultations of all types. This concurs with findings from a secondary analysis of European survey data, which found that patients’ use of e-mail to communicate with their health-care provider was positively correlated with multimorbidity, with use increasing for every additional condition. 55
Our conceptual review (see Chapter 2) highlighted a lack of evidence about the use of video consultation in primary care settings. There are examples of use in mental health conditions and palliative care, for which pilot studies have explored the feasibility of using video. 172–174 This reflects our observation that the use of video consultation is in its infancy. The first evaluation of the GP Access Fund14 found that video consultations had a low rate of patient uptake and were yet to show benefits. 15 The results of the second evaluation are pending; 14 out of the 37 sites anticipated that they would implement some form of video consultation. 175
At the time of writing, there are no published studies relating to e-consultations; however, we know of local evaluations of e-consult use in CCGs under way across England, and these are set to publish in the next few months. These studies may add to what we have found and inform future evaluations of e-consultations. Despite the lack of evidence, NHS England have committed to funding e-consultation systems in general practice from December 2017. 7
NHS England have also committed to funding ‘telephone tools’ in general practice, referring to ‘telephone consultation’. 7 We noted that the distinction between telephone consultation and telephone triage was often blurred by practice staff (and sometimes by patients too) and this was reflected in the recording of the consultation. It is not clear whether or not those making policy have made this distinction. A recent trial of telephone triage in general practice60 found that introducing telephone triage delivered by a GP or nurse was associated with an increased number of primary care contacts in the 28 days after a patient’s request for a same-day GP consultation, although costs were similar to usual care. In keeping with our findings, this study concluded that whole-system implications should be assessed when considering the introduction of a new system. We have highlighted the risk of unintended consequences when introducing new forms of consultation, and the need to involve the entire practice team.
US-based studies of e-mail consultation have explored associations between the use of patient–clinician e-mail and a range of outcomes. In one study, patient use of secure e-mail with clinicians was not found to be associated with an increase in the use of clinical services 7–18 months after first use. Although it was associated with an initial increase in activity by e-mail users, this did not persist beyond 6 months. 41 Another study found that use of e-mail was associated with an improvement in clinical markers for diabetes mellitus among their patients. 32
These US studies are possible because of the widespread use of patient portals by individual health maintenance organisations. These portals are used for optional electronic messaging, appointment booking and providing test results, as well as operating as an electronic health record. They ensure that data on consultation number and type are recorded in a standardised way. It allows for the analysis of data on patient health status and utilisation of health services from large numbers of patients. As we have demonstrated in our analysis of routine consultation data (see Chapter 6), this type of analysis is more difficult in the UK, where infrastructure to facilitate accurate records about the numbers and types of consultations is less readily available, and protocols for recording newer consultation types are not in place.
However, although these studies allow for associations between e-mail and outcomes to be explored, there is limited evidence about the organisational and relational dynamics that contribute to change. 66 This is something we were able to explore in our study, allowing us some understanding of the possible mechanisms of action for alternatives to the face-to-face consultation.
Our study suggests that the desire to use alternatives to the face-to-face consultation to improve patient access to care is often combined with a perceived need to reduce, or better manage, general practice workload. A concern about whether improving access through use of alternatives to the face-to-face consultation will increase rather than decrease workload pressure is also evident in much previous research on the use of alternatives, such as telephone60 or e-mail consultations. 19 This can be understood in terms of the phenomenon of supply-induced demand, which has recently been considered in a briefing paper from the Nuffield Trust. 176 Although not specifically relating to alternatives to the face-to-face consultation, this paper identified different ways in which new and more accessible forms of service can lead to a new and increased demand for care for problems that patients would otherwise have managed themselves. Clear evidence to support or refute this idea is limited, but it was a concern of some of the staff in practices considering implementation of alternatives to face-to-face consultations. Those staff who were enthusiastic about the potential of using an alternative to a face-to-face consultation were sometimes surprised that there was little evidence of an efficiency gain within their own practice. Future implementation of alternatives should carefully monitor the impact on overall health service utilisation, both within and beyond general practice.
Some of our findings support the existing qualitative literature. In earlier studies of e-mail consultation, GPs described selectively choosing with which patients to engage in an e-mail consultation,19 in much the same way that our participants referred to choosing ‘sensible’ patients. The suitability of e-mail for straightforward and uncomplicated questions or conditions was reported in a Danish study. 44 A conversation analysis of telephone consultation found that patients were less likely to raise additional problems with the GP during a telephone consultation than during a face-to-face consultation. 177 This fitted with our finding that patients and doctors were in accord that the telephone was good for ‘basic’ problems, and that a face-to-face consultation was needed for multiple issues, or new or complex problems.
In the time that this study has been under way, there have been several policy documents published that make reference to alternatives to the face-to-face consultation in general practice settings. The General Practice Forward View,7 published by NHS England, has outlined a commitment to funding telephone and e-consultation tools. The Nuffield Trust issued a report on the ‘Digital Patient’ in primary care,29 which summarised the evidence to date for remote consultation (including the publication of our scoping survey). This report also drew on a case study example for video consultations, reiterating our finding that video consultation is not currently widely offered. The recommendations in the report were to ensure that the technology meets the needs of users, to focus on people likely to benefit in the short term and to provide reassurance to patients and professionals regarding information governance. 29
The Primary Care Workforce Commission report, commissioned by the incumbent Health Secretary and published in 2015, concluded that more evidence is required before alternatives to the face-to-face consultation can be recommended as a routine part of care. 24 Our findings are in agreement with this. We have outlined how this evidence might feasibly be obtained, as well as the key questions that should be answered.
Implications for practice and service delivery
We have devised a web resource for GPs, practice staff and commissioners. Given the variability in the rationale for and implementation of alternatives to the face-to-face consultation, the principle of the resource was to provide a self-appraisal and guidance tool. It is envisaged that potential users will dip in and out of the resource depending on their needs and interest. Our study findings informed five key headings that were felt to be useful for practices.
-
Why do you want to introduce an alternative to face-to-face consultations?
In signposting users to the appropriate information and resources, it is important to understand their reason for considering the introduction in the first place, as this allows us to identify what are likely to be the biggest issues for them.
-
Which alternative are you interested in?
The differences between the different types of alternatives to the face-to-face consultation have an impact on implementation. The information provided in this section is tailored to each type.
-
Who is it for and why?
This section asks users to consider those patients to whom they hope to offer alternatives to the face-to-face consultation, and for what purpose.
-
How do we get it right?
This section tackles how users might get it ‘right’ on a patient level, on a professional and personal level, and on an organisation and systems level. It notes possible unintended consequences.
-
How will we know if it has worked?
This section asks the users what they want to measure and suggests how they might do it. It encourages a process of ongoing reflection.
The website is particularly relevant for commissioners. The recent introduction of sustainability and transformation plans are likely to affect how general practice delivers services, and, consequently, whether and how commissioners and practices introduce and develop their use of alternatives to the face-to-face consultation, if they have not already. The 5-year sustainability and transformation programmes are focused on local planning and could have implications for diversification of service delivery between areas. The programmes focus on three headline areas: ‘improving quality and developing new models of care,’ ’improving health and wellbeing’ and ‘improving efficiency of services’. 178
Uptake was low across all types of alternatives to the face-to-face consultation. This was especially the case for video. Despite this low level of uptake, video consultation is still regarded as potentially transformative in general practice,7 and accounts of successful use are documented in news articles42 and reports. 29 However, our efforts to find practices that were using video were to little avail. We can provide little information about the use of video for GP consultations, beyond the snapshot available in these publications. Our findings suggest that the reality of trying to implement video consultations is very different from the theory of what it might offer, and this has implications for practice and service delivery. Despite this, novel methods of offering patients an alternative to the face-to-face consultation, such as video, have arisen since the inception of this study. Commercial organisations offering services such as an ‘app’ that allows you to have a video or telephone consultation with a GP are being commissioned by NHS general practices in some parts of the UK, although this has not been evaluated and use is not yet widespread. 154
Research recommendations
Our research has largely been hypothesis-generating, to create a logical framework for future evaluations. Our work has indicated a need for further research on a range of questions, as previously listed in Chapter 7.
-
Is it possible to improve uptake of alternatives to face-to-face consultations and, if so, does this lead to benefits for patients and general practices?
-
What is the impact on access to care as perceived by patients (speed of access, convenience, timely access to care that meets their perceived needs)?
-
What is the impact on NHS workload and, in particular, the impact on different sectors of the NHS (primary and secondary care) and different professional groups (doctors, nurses, receptionists and administrative staff)?
-
What is the impact on the quality and safety of patient management?
-
For which patients and for which conditions are different forms of alternatives most efficient and effective?
-
How do different forms of consultation change the content of the consultation?
-
How satisfied are clinicians and patients with different forms of alternative to the face-to-face consultation?
-
We have used a mixture of qualitative and quantitative methods to explore some of these questions and to identify key questions for further evaluation and observational research. Future research may need to explore different questions for each of the different technologies. However, unless or until uptake of e-consultations or video consultations increases, it will be impossible to measure impacts.
In Chapter 7, we have discussed in some detail the most relevant questions in relation to each of the different forms of alternative to the face-to-face consultation, along with discussion about the most appropriate research designs, the target population, relevant outcomes and issues of feasibility such as recruitment, sample size and data collection. In brief, we concluded that telephone consultation is already in widespread use, but evidence is lacking on the use for patient management and follow-up, by which means the quality and safety of these approaches could be assessed. Conversely, e-consultations are a very new approach to the consultation and so research into these systems should begin with an investigation into the low patient uptake, followed by an assessment of their impact on workload in the practice. For e-mail consultation, research should begin by devising systems through which to deliver e-mail consultation. Once a system is devised, it could be tested to assess the impact on workload, with embedded studies that assess the content of e-mails, and the views of patients and professionals on its use. Video consulting presents a challenge, given the current low levels of use. First steps would be to identify barriers to use. From there, it would be necessary to explore those patients for whom it is most appropriate, how video consultations compare with other types of consultation with respect to content and quality, and patient and clinician experience.
Finally, we suggest that there are three types of alternatives to the face-to-face consultation that are priorities for robust evaluation because they are being widely implemented in the absence of evidence; these are:
-
the use of telephone for follow-up consultations
-
e-consulting systems
-
the use of telephone-first models of access to care.
Although there are different research questions associated with the above three types, we would stress that the research design should focus more on how the service, including relationships, expectations and patterns of work, is redesigned, than on the nature of the technology itself.
As part of this study, we have outlined the key outcomes that matter to patients, practice staff and the NHS (outlined in detail in Chapter 7). These include measures of access to care, measures of workload, cost and staff satisfaction, and measures directly related to use of the NHS. Given the low levels of uptake and use observed at present, evaluative research would be most feasible for approaches that are being widely implemented, such as telephone consulting and e-consult systems. There are issues to overcome in conducting future research. These concern the recruitment of patients and the feasibility of data collection for outcomes; we have demonstrated that routinely acquired data from GP computer systems can be used, although the quality is variable. The size of studies may have to be adjusted to reflect the accuracy and completeness of data collected this way.
Conclusions
Alternatives to the face-to-face consultation are not currently in mainstream use in general practice, and we observed a low level of uptake in our case study practices. We have identified the underlying assumptions and logic that patients and staff report in relation to the use of these alternatives, and have shown that different stakeholders have different perspectives on what they hope to achieve through the use of alternatives to the face-to-face consultation. Through observation of real-life use of different forms of alternative, we have gained an understanding of how, under what circumstances and for which patients such alternatives might result in benefits or in potential unintended adverse consequences. We have used this understanding to develop a framework and recommendations for future evaluation of the use of alternatives to face-to-face consultations. The current very low level of uptake of alternatives and the lack of clear evidence of benefit may influence their uptake on a wider scale, something which is favoured by policy-makers. We have highlighted key issues for practices and policy-makers to consider and have made recommendations about priorities for further research to be conducted before or alongside future roll-out of alternatives to face-to-face consultations.
Acknowledgements
We would like to thank all of the staff and patients at the eight case study practices, the participants in the video-consultation interviews, the respondents to our scoping survey and the various stakeholders who participated in this research. Without them, it would not have been possible to conduct this study.
We would like to thank our PPI contributors for their invaluable input throughout this project.
We would like to thank the steering committee members, who were generous in giving their time and advice throughout the project. In addition, Dr Becca Robinson provided input from the perspective of the Bristol CCG; we are grateful for her contributions.
We are grateful to Mrs Caroline Jordan, Dr Angela Martin and Dr Lucy McCloughan for their ongoing administrative and management support throughout the project.
Steering group members
Professor Richard Baker (Professor Emeritus, DH Studies, University of Leicester).
Professor Frances Griffiths (Professor, Division of Health Sciences, University of Warwick).
Linda Prosser (Director of Assurance and Delivery, NHS England Southwest).
Elly Bernard (Project Management Office Manager, One Care Consortium, Bristol).
Lynn Tatnell (PPI representative 2014–15).
Faith Harris-Golesworthy (PPI representative 2014–15).
Gail Thornton (PPI representative 2016).
Adele Webb (PPI representative 2016).
Other contributors
Nia Roberts (Librarian, University of Oxford) devised and ran the searches in the conceptual review.
Mei Lau (Research Assistant, University of Oxford) assisted in organising the databases for the conceptual review.
Dr Kerry Walker (Research Assistant, University of Bristol) provided administrative support in conducting the scoping survey.
Dr Ludivine Garside (Senior Research Associate, University of Bristol) analysed the routine consultation data.
Keira Pratt-Boyden (Research Assistant, University of Oxford) organised the coded qualitative data into NVivo software.
Thuy Phan (Research Assistant, University of Oxford) organised the coded qualitative data into NVivo software.
Dr Abi Eccles (Research Fellow, University of Warwick) assisted in putting the report together.
Helen McGowan (Research Projects Administrator, University of Warwick) assisted in putting the report together.
Patient and public involvement contributors
Valerie Keston-Hole (PPI workshop participant 2015).
Dirk Day (PPI workshop participant 2015).
Bala Balenthiran (PPI workshop participant 2015).
Bernard Gudgin (PPI workshop participant 2015).
Derek Shaw (PPI workshop participant 2015).
Lynn Tatnell (PPI representative 2014–15).
Faith Harris-Golesworthy (PPI representative 2014–15).
Gail Thornton (PPI representative 2016).
Adele Webb (PPI representative 2016).
Anne-Laure Donskoy (PPI representative 2016).
Sandra Tweddell (PPI Representative 2016).
Members of Young Healthwatch Bristol (2016).
Contributions of authors
Dr Helen Atherton (Assistant Professor, Primary Care) contributed to the conception and design of the overall study, was the principal investigator in Oxford and was the day-to-day lead of the ethnographic team. She co-wrote the conceptual review and analysed the qualitative data. She led on the report, drafting Chapters 1, 2, 4, 5 and 8, and contributing to all other chapters and elements of the report.
Dr Heather Brant (Senior Research Associate, Ethnography) was the project manager responsible for the day-to-day running of the project, and was the researcher at the Bristol site. She led on the scoping study, drafted Chapters 3 and 5 and contributed to Chapter 4. She undertook the ethnographic research at the case study sites near Bristol and analysed the qualitative data.
Professor Sue Ziebland (Professor, Medical Sociology) contributed to the conception and design of the study, co-wrote the conceptual review, provided guidance and support for the focused ethnography, analysed the qualitative data and contributed to the report.
Ms Annemieke Bikker (Research Fellow, Ethnography) was the researcher at the Edinburgh site. She conducted the ethnographic research at the case study sites in Scotland.
Professor John Campbell (Professor, General Practice and Primary Care) contributed to the conception, design and ongoing review of study delivery and write-up.
Dr Andy Gibson (Associate Professor, Patient and Public Involvement) led the PPI in the project and contributed to writing the report.
Professor Brian McKinstry (Professor, Primary Care e-Health) contributed to the conception and design of the study, was the principal investigator in Scotland, recruited the Scottish practices and substantially contributed to Chapter 7.
Dr Tania Porqueddu (Research Fellow, Ethnography) was the researcher at the Oxford site. She undertook the ethnographic research at the case study site in Oxfordshire.
Professor Chris Salisbury (Professor, Primary Health Care) was the chief investigator and had overall responsibility for the conduct of the study. He contributed to the conception and overall design of the study, led the quantitative analysis, drafted Chapters 6 and 7 and contributed to all other chapters of the report.
All authors were involved in critically revising the final report for important intellectual content.
Publications
Atherton H, Ziebland S. What do we need to consider when planning, implementing and researching the use of alternatives to face-to-face consultations in primary healthcare? Digit Health 2016;2.
Brant H, Atherton H, Ziebland S, McKinstry B, Campbell JL, Salisbury C. Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice. Br J Gen Pract 2016;66:e460–6.
Bikker AP, Atherton H, Brant H, Porqueddu T, Campbell JL, Gibson A, et al. Conducting a team-based multi-sited focused ethnography in primary care. BMC Med Res Methodol 2017;17:139.
Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, et al. Alternatives to the face-to-face consultation in general practice: focused ethnographic case study. Br J Gen Pract 2018;68:293–300.
Brant H. Atherton H. Bikker A. Porqueddu T. Salisbury C. McKinstry B. et al. Receptionists’ role in new approaches to consultations in primary care: focused ethnographic study. Br J Gen Pract 2018; in press.
Data sharing statement
Anonymised data from the scoping study and the qualitative elements of the focused ethnography can be obtained from the chief investigator, Professor Chris Salisbury, on request.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Danish Government . Den Digitale Vej Til Fremtidens Velfærd 2011. https://horsensbibliotek.dk/om-bibliotekerne/projekter/den-digitale-vej-til-fremtidens-velfaerd (accessed 8 February 2017).
- Danish Medical Association . Aktivitet Og Økonomi I Almen Praksis I Dagtid Og Vagttid 2003 Til 2013 2014. www.laeger.dk/portal/pls/portal/!PORTAL.wwpob_page.show?_docname=10539072.PDF (accessed 8 February 2017).
- Pearl R. Kaiser Permanente Northern California: current experiences with internet, mobile, and video technologies. Health Aff (Milwood) 2014;33:251-7. https://doi.org/10.1377/hlthaff.2013.1005.
- Castrén J, Niemi M, Virjo I. Use of email for patient communication in student health care: a cross-sectional study. BMC Med Inform Decis Mak 2005;5. https://doi.org/10.1186/1472-6947-5-2.
- Aker JC, Mbiti IM. Mobile phones and economic development in Africa. J Econ Perspect 2010;24:207-32. https://doi.org/10.1257/jep.24.3.207.
- Department of Health and Social Care . The Power of Information: Putting All of Us in Control of the Health and Care Information We Need 2012. www.gov.uk/government/uploads/system/uploads/attachment_data/file/213689/dh_134205.pdf (accessed 9 February 2017).
- NHS England . General Practice Forward View 2016. www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf (accessed 8 February 2017).
- Transforming Primary Care. Safe, Proactive, Personalised Care for Those Who Need It Most. London: DHSC and NHS England; 2014.
- NHS England . Patient Online 2016. www.england.nhs.uk/ourwork/pe/patient-online/ (accessed 8 February 2017).
- Health and Social Care Board . EHealth and Care Strategy for Northern Ireland 2016. www.health-ni.gov.uk/sites/default/files/publications/dhssps/interactive-ehealth-strategy.pdf (accessed 8 February 2017).
- NHS Scotland . EHealth Strategy 2014–2017 2015. www.gov.scot/Resource/0047/00472754.pdf (accessed 7 February 2017).
- Welsh Government . Informed Health and Care. A Digital Health and Social Care Strategy for Wales 2015. http://gov.wales/docs/dhss/publications/151215reporten.pdf (accessed 8 February 2017).
- Todd R. £50m GP Fund for Expanded Access 2013. www.ehi.co.uk/news/EHI/8931/%C2%A350m-gp-fund-for-expanded-access (accessed 8 February 2017).
- GP Access Fund. London: NHS England; 2015.
- NHS England . Prime Minister’s Challenge Fund: Improving Access to General Practice. First Evaluation Report: October 2015 2015. www.england.nhs.uk/wp-content/uploads/2015/10/pmcf-wv-one-eval-report.pdf (accessed 8 February 2017).
- Whitfield L. Netscape Navigators 2013. www.digitalhealth.net/2013/02/netscape-navigators/ (accessed 8 February 2017).
- British Medical Association . The Future of General Practice – Survey Results 2015. http://bma.org.uk/working-for-change/negotiating-for-the-profession/bma-general-practitioners-committee/surveys/future-of-general-practice (accessed 8 February 2017).
- Hobbs FD, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet 2016;387:2323-30. https://doi.org/10.1016/S0140-6736(16)00620-6.
- Atherton H, Pappas Y, Heneghan C, Murray E. Experiences of using email for general practice consultations: a qualitative study. Br J Gen Pract 2013;63:e760-7. https://doi.org/10.3399/bjgp13X674440.
- Hanna L, May C, Fairhurst K. The place of information and communication technology-mediated consultations in primary care: GPs’ perspectives. Fam Pract 2012;29:361-6. https://doi.org/10.1093/fampra/cmr087.
- British Medical Association . Developing General Practice Today: Providing Healthcare Solutions for the Future 2013. www.bma.org.uk/-/media/files/pdfs/news%20views%20analysis/bma%20developing%20general%20practice%20report%20v2.pdf (accessed 13 February 2017).
- Royal College of General Practitioners . An Inquiry into Patient Centred Care in the 21st Century: Implications for General Practice and Primary Care 2015. www.rcgp.org.uk/policy/rcgp-policy-areas/inquiry-into-patient-centred-care-in-the-21st-century.aspx (accessed 8 February 2017).
- Ware J, Mawby R. Patient Access to General Practice: Ideas and Challenges from the Front Line. London: Royal College of General Practitioners; 2015.
- Roland M, Barber N, Imison C, Howe A, Rubin G, Storey K. The Future of Primary Care: Creating Teams for Tomorrow. London: Health Education England; 2015.
- Digital Health . You Don’t Have Mail Consultations 2013. www.digitalhealth.net/2013/02/you-dont-have-mail-consultations/ (accessed 9 February 2017).
- Atherton H. Use of email for consulting with patients in general practice. Br J Gen Pract 2013;63:118-19. https://doi.org/10.3399/bjgp13X664072.
- Whitfield L. Lib Dem Manifesto Promises GPs by Skype 2015. www.digitalhealth.net/2015/04/lib-dem-manifesto-promises-gps-by-skype/ (accessed 8 February 2017).
- Wheeler B. David Cameron Promises Seven-Day GP Access by 2020. London: British Broadcasting Corporation; 2014.
- Castle-Clarke S, Imison C. The Digital Patient: Transforming Primary Care?. London: Nuffield Trust; 2016.
- Atherton H, Sawmynaden P, Sheikh A, Majeed A, Car J. Email for clinical communication between patients/caregivers and healthcare professionals. Cochrane Database Syst Rev 2012;11. https://doi.org/10.1002/14651858.CD007978.pub2.
- Bunn F, Byrne G, Kendall S. Telephone consultation and triage: effects on health care use and patient satisfaction. Cochrane Database Syst Rev 2004;4. https://doi.org/10.1002/14651858.CD004180.pub2.
- Zhou YY, Kanter MH, Wang JJ, Garrido T. Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Aff 2010;29:1370-5. https://doi.org/10.1377/hlthaff.2010.0048.
- Palen TE, Ross C, Powers JD, Xu S. Association of online patient access to clinicians and medical records with use of clinical services. JAMA 2012;308:2012-19. https://doi.org/10.1001/jama.2012.14126.
- McKinstry B, Hanley J, Wild S, Pagliari C, Paterson M, Lewis S, et al. Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.f3030.
- Wild SH, Hanley J, Lewis SC, McKnight JA, McCloughan LB, Padfield PL, et al. Supported telemonitoring and glycemic control in people with type 2 diabetes: the telescot diabetes pragmatic multicenter randomized controlled trial. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1002098.
- Dudas RA, Crocetti M. Pediatric caregiver attitudes toward email communication: survey in an urban primary care setting. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2738.
- Neville RG, Marsden W, McCowan C, Pagliari C, Mullen H, Fannin A. A survey of GP attitudes to and experiences of email consultations. Inform Prim Care 2004;12:201-6. https://doi.org/10.14236/jhi.v12i4.127.
- Kummervold PE, Trondsen M, Andreassen H, Gammon D, Hjortdahl P. Patient-physician interaction over the internet. Tidsskr Nor Laegeforen 2004;124:2633-6.
- Katz SJ, Moyer CA, Cox DT, Stern DT. Effect of a triage-based e-mail system on clinic resource use and patient and physician satisfaction in primary care: a randomized controlled trial. J Gen Intern Med 2003;18:736-44. https://doi.org/10.1046/j.1525-1497.2003.20756.x.
- Katz SJ, Nissan N, Moyer CA. Crossing the digital divide: evaluating online communication between patients and their providers. Am J Manag Care 2004;10:593-8.
- Meng D, Palen TE, Tsai J, McLeod M, Garrido T, Qian H. Association between secure patient–clinician email and clinical services utilisation in a US integrated health system: a retrospective cohort study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009557.
- Price C. Patients Give Thumbs Up to GP Skype Pilot 2015. www.pulsetoday.co.uk/home/finance-and-practice-life-news/patients-give-thumbs-up-to-gp-skype-pilot/20009161.article#.VcoIIPlVhBd (accessed 9 February 2015).
- Andreassen HK, Kjekshus LE, Tjora A. Survival of the project: a case study of ICT innovation in health care. Soc Sci Med 2015;132:62-9. https://doi.org/10.1016/j.socscimed.2015.03.016.
- Hansen CS, Christensen KL, Ertmann R. Patients and general practitioners have different approaches to e-mail consultations. Dan Med J 2014;61.
- Goodyear-Smith F, Wearn A, Everts H, Huggard P, Halliwell J. Pandora’s electronic box: GPs reflect upon email communication with their patients. Inform Prim Care 2005;13:195-202. https://doi.org/10.14236/jhi.v13i3.597.
- Neville RG, Marsden W, McCowan C, Pagliari C, Mullen H, Fannin A. Email consultations in general practice. Inform Prim Care 2004;12:207-14. https://doi.org/10.14236/jhi.v12i4.128.
- Edirippulige S, Levandovskaya M, Prishutova A. A qualitative study of the use of Skype for psychotherapy consultations in the Ukraine. J Telemed Telecare 2013;19:376-8. https://doi.org/10.1177/1357633X13506523.
- Armfield NR, Gray LC, Smith AC. Clinical use of Skype: a review of the evidence base. J Telemed Telecare 2012;18:125-7. https://doi.org/10.1258/jtt.2012.SFT101.
- Mair FS, Hiscock J, Beaton SC. Understanding factors that inhibit or promote the utilization of telecare in chronic lung disease. Chronic Illn 2008;4:110-17. https://doi.org/10.1177/1742395308092482.
- Mair F, May C, Murray E, Finch T, Anderson G, O’Donnell C, et al. Understanding the Implementation and Integration of e-Health Services. Southampton: NIHR, Service Delivery and Organisation programme; 2009.
- Davis FD, Bagozzi R, Warshaw P. User acceptance of computer technology: a comparison of two theoretical models. Manag Sci 1989;35:982-1003. https://doi.org/10.1287/mnsc.35.8.982.
- Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. BMJ 2010;341. https://doi.org/10.1136/bmj.c5814.
- McKinstry B, Watson P, Elton RA, Pinnock H, Kidd G, Meyer B, et al. Comparison of the accuracy of patients’ recall of the content of telephone and face-to-face consultations: an exploratory study. Postgrad Med J 2011;87:394-9. https://doi.org/10.1136/pgmj.2010.101287.
- McKinstry B, Walker J, Campbell C, Heaney D, Wyke S. Telephone consultations to manage requests for same-day appointments: a randomised controlled trial in two practices. Br J Gen Pract 2002;52:306-10.
- Newhouse N, Lupiáñez-Villanueva F, Codagnone C, Atherton H. Patient use of email for health care communication purposes across 14 European countries: an analysis of users according to demographic and health-related factors. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.3700.
- Lupiañez-Villanueva F, Maghiros I, Abadie F. Strategic Intelligence Monitor on Personal Health Systems phase 2 (SIMPHS 2) Citizens and ICT for Health in 14 EU Countries: Results from an Online Panel. Seville: European Commission Joint Research Centre, Institute for Prospective Technological Studies; 2013.
- Kruse RL, Koopman RJ, Wakefield BJ, Wakefield DS, Keplinger LE, Canfield SM, et al. Internet use by primary care patients: where is the digital divide?. Fam Med 2012;44:342-7.
- Goldzweig CL, Orshansky G, Paige NM, Towfigh AA, Haggstrom DA, Miake-Lye I, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med 2013;159:677-87. https://doi.org/10.7326/0003-4819-159-10-201311190-00006.
- Fatehi F, Armfield NR, Dimitrijevic M, Gray LC. Clinical applications of videoconferencing: a scoping review of the literature for the period 2002–2012. J Telemed Telecare 2014;20:377-83. https://doi.org/10.1177/1357633X14552385.
- Campbell JL, Fletcher E, Britten N, Green C, Holt TA, Lattimer V, et al. Telephone triage for management of same-day consultation requests in general practice (the ESTEEM trial): a cluster-randomised controlled trial and cost-consequence analysis. Lancet 2014;384:1859-68. https://doi.org/10.1016/S0140-6736(14)61058-8.
- GP Access Ltd . GP Access 2016. gpaccess.uk/ (accessed 8 February 2017).
- Productive Primary Care . Productive Primary Care 2016. www.productiveprimarycare.co.uk (accessed 8 February 2017).
- Al-Ubaydli M. Online consultations can save valuable time for both patients and doctors. Guardian 2013. www.theguardian.com/healthcare-network/2013/sep/17/online-consultation-save-doctors-time (accessed 9 February 2017).
- My Surgery . My Surgery Website 2016. www.mysurgerywebsite.co.uk/live/websites/website-features (accessed 8 February 2017).
- NHS Digital . NHSmail 2015. http://systems.hscic.gov.uk/nhsmail/future (accessed 8 February 2017).
- Otte-Trojel T, Rundall TG, de Bont A, van de Klundert J, Reed ME. The organizational dynamics enabling patient portal impacts upon organizational performance and patient health: a qualitative study of Kaiser Permanente. BMC Health Serv Res 2015;15:1-12. https://doi.org/10.1186/s12913-015-1208-2.
- Bishop TF, Press MJ, Mendelsohn JL, Casalino LP. Electronic communication improves access, but barriers to its widespread adoption remain. Health Aff (Milwood) 2013;32:1361-7. https://doi.org/10.1377/hlthaff.2012.1151.
- WebGP e . EConsult WebGP 2016. https://econsult.net/ (accessed 8 February 2017).
- GP Access Ltd . AskmyGP 2016. http://askmygp.uk/ (accessed 8 February 2017).
- Adamson SC, Bachman JW. Pilot study of providing online care in a primary care setting. Mayo Clin Proc 2010;85:704-10. https://doi.org/10.4065/mcp.2010.0145.
- EMIS Health . EConsult 2016. www.emishealth.com/products/econsult/ (accessed 8 February 2017).
- EMIS Health . Video Consult 2016. www.emishealth.com/products/video-consult/ (accessed 8 February 2017).
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Yin RK. Case Study Research: Design and Methods. London: Sage; 2003.
- Weiss CH. Theory-based evaluation: past, present, and future. New Dir Eval 1997;76:41-55. https://doi.org/10.1002/ev.1086.
- WK Kellogg Foundation . Logic Model Development Guide 2006. www.wkkf.org/resource-directory/resource/2006/02/wk-kellogg-foundation-logic-model-development-guide (accessed 8 February 2017).
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Bartholomew LK, Parcel GS, Kok G. Intervention mapping: a process for developing theory- and evidence-based health education programs. Health Educ Behav 1998;25:545-63. https://doi.org/10.1177/109019819802500502.
- Hardeman W, Sutton S, Griffin S, Johnston M, White A, Wareham NJ, et al. A causal modelling approach to the development of theory-based behaviour change programmes for trial evaluation. Health Educ Res 2005;20:676-87. https://doi.org/10.1093/her/cyh022.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: Sage; 2006.
- Wachter RM. Making IT Work: Harnessing the Power of Health Information Technology to Improve Care in England Report of the National Advisory Group on Health Information Technology in England 2016. www.gov.uk/government/uploads/system/uploads/attachment_data/file/550866/Wachter_Review_Accessible.pdf (accessed 8 February 2017).
- Atherton H, Ziebland S. What do we need to consider when planning, implementing and researching the use of alternatives to face-to-face consultations in primary healthcare?. Digit Health 2016;2:1-13. https://doi.org/10.1177/2055207616675559.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Mazzocato P, Savage C, Brommels M, Aronsson H, Thor J. Lean thinking in healthcare: a realist review of the literature. Qual Saf Health Care 2010;19:376-82. https://doi.org/10.1136/qshc.2009.037986.
- Wong G, Greenhalgh T, Pawson R. Internet-based medical education: a realist review of what works, for whom and in what circumstances. BMC Med Educ 2010;10. https://doi.org/10.1186/1472-6920-10-12.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Vassilev I, Rogers A, Sanders C, Kennedy A, Blickem C, Protheroe J, et al. Social networks, social capital and chronic illness self-management: a realist review. Chronic Illn 2011;7:60-86. https://doi.org/10.1177/1742395310383338.
- Ziebland S, Wyke S. Health and illness in a connected world: how might sharing experiences on the internet affect people’s health?. Milbank Q 2012;90:219-49. https://doi.org/10.1111/j.1468-0009.2012.00662.x.
- Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ 2006;40:405-14. https://doi.org/10.1111/j.1365-2929.2006.02467.x.
- Halford S, Lotherington AT, Obstfelder A, Dyb K. Getting the whole picture?. Inform Comm Soc 2010;13:442-65. https://doi.org/10.1080/13691180903095856.
- Nijland N, van Gemert-Pijnen JE, Boer H, Steehouder MF, Seydel ER. Increasing the use of e-consultation in primary care: results of an online survey among non-users of e-consultation. Int J Med Inform 2009;78:688-703. https://doi.org/10.1016/j.ijmedinf.2009.06.002.
- Hanna L, Fairhurst K. Using information and communication technologies to consult with patients in Victorian primary care: the views of general practitioners. Aust J Prim Health 2013;19:166-70. https://doi.org/10.1071/PY11153.
- Cohn A. The benefits of encouraging patients to email their doctor: a review of individual practice. Arch Dis Child Educ Pract Ed 2014;99:152-6. https://doi.org/10.1136/archdischild-2013-305856.
- van Gurp J, van Selm M, van Leeuwen E, Hasselaar J. Transmural palliative care by means of teleconsultation: a window of opportunities and new restrictions. BMC Med Ethics 2013;14. https://doi.org/10.1186/1472-6939-14-12.
- Najera C, Ivorra J, Chalmeta I, Grau E, Valero JL, Garcia-Armario MD, et al. Activity of telephone consultation to nursing by request in rheumatology. Ann Rheum Dis 2013;72.
- Ortega Egea JM, González MV, Menéndez MR. eHealth usage patterns of European general practitioners: a five-year (2002–2007) comparative study. Int J Med Inform 2010;79:539-53. https://doi.org/10.1016/j.ijmedinf.2010.05.003.
- Travers CP, Murphy JF. Neonatal telephone consultations in the National Maternity Hospital. Ir Med J 2014;107:251-2.
- Majeed A. Data from one GP to inform the debate whether patients should be able to email their general practitioner. BMJ 2014;349. https://doi.org/10.1136/bmj.g5766.
- Huibers L, Koetsenruijter J, Grol R, Giesen P, Wensing M. Follow-up after telephone consultations at out-of-hours primary care. J Am Board Fam Med 2013;26:373-9. https://doi.org/10.3122/jabfm.2013.04.120185.
- Raven M, Butler C, Bywood P. Video-based telehealth in Australian primary health care: current use and future potential. Aust J Prim Health 2013;19:283-6. https://doi.org/10.1071/PY13032.
- Holt T, Fletcher E, Warren F, Richards S, Salisbury C, Calitri R, et al. Telephone triage systems in UK general practice: analysis of consultation duration during the index day in a pragmatic randomised controlled trial. Br J Gen Pract 2016;66. https://doi.org/10.3399/bjgp16X684001.
- Crotty BH, Tamrat Y, Mostaghimi A, Safran C, Landon BE. Patient-to-physician messaging: volume nearly tripled as more patients joined system, but per capita rate plateaued. Health Aff 2014;33:1817-22. https://doi.org/10.1377/hlthaff.2013.1145.
- Pedersen KM, Andersen JS, Søndergaard J. General practice and primary health care in Denmark. J Am Board Fam Med 2012;25:34-8. https://doi.org/10.3122/jabfm.2012.02.110216.
- Facchiano L, Snyder CH. Challenges surrounding provider/client electronic-mail communication. J Nurse Pract 2011;7:309-15. https://doi.org/10.1016/j.nurpra.2011.01.016.
- Ruiz IS, García GP, Riquelme I. E-mail communication in pain practice: the importance of being earnest. Saudi J Anaesth 2014;8:364-7. https://doi.org/10.4103/1658-354X.136434.
- Van Gurp J, Hasselaar J, van Leeuwen E, Hoek P, Vissers K, van Selm M. Connecting with patients and instilling realism in an era of emerging communication possibilities: a review on palliative care communication heading to telecare practice. Patient Educ Couns 2013;93:504-14. https://doi.org/10.1016/j.pec.2013.07.002.
- McKinstry B, Hammersley V, Burton C, Pinnock H, Elton R, Dowell J, et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010;19:298-303. https://doi.org/10.1136/qshc.2008.027763s.
- DE Weger E, Macinnes D, Enser J, Francis SJ, Jones FW. Implementing video conferencing in mental health practice. J Psychiatr Ment Health Nurs 2013;20:448-54. https://doi.org/10.1111/j.1365-2850.2012.01947.x.
- Rojjanasrirat W, Nelson EL, Wambach KA. A pilot study of home-based videoconferencing for breastfeeding support. J Hum Lact 2012;28:464-7. https://doi.org/10.1177/0890334412449071.
- Wibe T, Helleso R, Varsi C, Ruland C, Ekstedt M. How does an online patient-nurse communication service meet the information needs of men with recently diagnosed testicular cancer?. ISRN Nurs 2012;2012.
- Wynn R, Bergvik S, Pettersen G, Fossum S. Clinicians’ experiences with videoconferencing in psychiatry. Stud Health Technol Inform 2012;180:1218-20.
- Jiwa M, Meng X. Video consultation use by Australian general practitioners: video vignette study. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2638.
- Foster J, Jessopp L, Dale J. Concerns and confidence of general practitioners in providing telephone consultations. Br J Gen Pract 1999;49:111-13.
- Scharff JS. Clinical issues in analyses over the telephone and the internet. Int J Psychoanal 2012;93:81-95. https://doi.org/10.1111/j.1745-8315.2011.00548.x.
- Little P, White P, Kelly J, Everitt H, Mercer S. Randomised controlled trial of a brief intervention targeting predominantly non-verbal communication in general practice consultations. Br J Gen Pract 2015;65:e351-e6. https://doi.org/10.3399/bjgp15X685237.
- Little P, White P, Kelly J, Everitt H, Gashi S, Bikker A, et al. Verbal and non-verbal behaviour and patient perception of communication in primary care: an observational study. Br J Gen Pract 2015;65:e357-65. https://doi.org/10.3399/bjgp15X685249.
- Van Gurp JLP, Hasselaar J, Vissers K, Van Leeuwen E, Van Selm M. How technologized care can lead to compassionate professional involvement: a longitudinal, qualitative multiple case study about teleconsultation in palliative home care. Palliat Med 2014;28.
- Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med 2013;173:72-4. https://doi.org/10.1001/2013.jamainternmed.305.
- MacNeill V, Sanders C, Fitzpatrick R, Hendy J, Barlow J, Knapp M, et al. Experiences of front-line health professionals in the delivery of telehealth: a qualitative study. Br J Gen Pract 2014;64:e401-7. https://doi.org/10.3399/bjgp14X680485.
- Greenhalgh T, Swinglehurst D, Stones R. Rethinking resistance to big IT: a sociological study of why and when healthcare staff do not use nationally mandated information and communication technologies. Health Serv Deliv Res 2014;2.
- Hendy J, Fulop N, Reeves BC, Hutchings A, Collin S. Implementing the NHS information technology programme: qualitative study of progress in acute trusts. BMJ 2007;334. https://doi.org/10.1136/bmj.39195.598461.551.
- Hendy J, Reeves BC, Fulop N, Hutchings A, Masseria C. Challenges to implementing the national programme for information technology (NPfIT): a qualitative study. BMJ 2005;331:331-6. https://doi.org/10.1136/bmj.331.7512.331.
- Johansson AM, Lindberg I, Söderberg S. The views of health-care personnel about video consultation prior to implementation in primary health care in rural areas. Prim Health Care Res Dev 2014;15:170-9. https://doi.org/10.1017/S1463423613000030.
- Tjora A. The technological mediation of the nursing-medical boundary. Sociol Health Illn 2000;22:721-41. https://doi.org/10.1111/1467-9566.00228.
- Hakimnia R, Holmstrom IK, Carlsson M, Hoglund AT. Exploring the communication between telenurse and caller-a critical discourse analysis. Int J Qual Stud Health Well-Being 2014;9. https://doi.org/10.3402/qhw.v9.24255.
- Segar J, Rogers A, Salisbury C, Thomas C. Roles and identities in transition: boundaries of work and inter-professional relationships at the interface between telehealth and primary care. Health Soc Care Community 2013;21:606-13. https://doi.org/10.1111/hsc.12047.
- Gupta SG. Tips for telephone and electronic medical consultation. Indian J Pediatr 2013;80:944-8. https://doi.org/10.1007/s12098-013-1191-8.
- Brewster L, Mountain G, Wessels B, Kelly C, Hawley M. Factors affecting front line staff acceptance of telehealth technologies: a mixed-method systematic review. J Adv Nurs 2014;70:21-33. https://doi.org/10.1111/jan.12196.
- Avey JP, Hobbs RL. Dial in: fostering the use of telebehavioral health services in frontier Alaska. Psychol Serv 2013;10:289-97. https://doi.org/10.1037/a0028231.
- Varsi C, Gammon D, Wibe T, Ruland MC. Patients’ reported reasons for non-use of an internet-based patient-provider communication service: qualitative interview study. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2683.
- Haun JN, Lind JD, Shimada SL, Martin TL, Gosline RM, Antinori N, et al. Evaluating user experiences of the secure messaging tool on the Veterans Affairs’ patient portal system. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.2976.
- Houston TK, Sands DZ, Jenckes MW, Ford DE. Experiences of patients who were early adopters of electronic communication with their physician: satisfaction, benefits, and concerns. Am J Manag Care 2004;10:601-8.
- Andreassen HK. What does an e-mail address add? – Doing health and technology at home. Soc Sci Med 2011;72:521-8. https://doi.org/10.1016/j.socscimed.2010.11.026.
- Winthereik BR, Langstrup H, Mol AM, Moser I, Pols J. Care in Practice: On Tinkering in Clinics, Homes and Farms. Bielefield: Transcript Verlag; 2010.
- Brant H, Atherton H, Ziebland S, McKinstry B, Campbell JL, Salisbury C. Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice. Br J Gen Pract 2016;66:e460-6. https://doi.org/10.3399/bjgp16X685597.
- NIHR Journals Library . HS&Amp;DR – 13 59 40: Tele-First: Telephone Triage As an Alternative to Face to Face Contact in General Practice 2015. www.nets.nihr.ac.uk/projects/hsdr/135940 (accessed 8 February 2017).
- Office for National Statistics . English Indices of Deprivation 2015 2015. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 14 March 2018).
- Higginbottom GM, Pillay JJ, Boadu NY. Guidance on performing focused ethnographies with an emphasis on healthcare research. Qual Rep 2013;18:1-6.
- Jarzabkowski P, Bednarek R, Cabantous L. Conducting global team-based ethnography: methodological challenges and practical methods. Hum Relat 2015;68:3-33. https://doi.org/10.1177/0018726714535449.
- Schlesinger P, Selfe M, Munro E. Inside a cultural agency: team ethnography and knowledge exchange. J Art Manag Law Soc 2015;45:66-83. https://doi.org/10.1080/10632921.2015.1039741.
- Scales K, Bailey S, Lloyd J. Separately and together; reflections on conducting a collaborative team ethnography in dementia care. Enquire 2008;6:24-49.
- Bikker AP, Atherton H, Brant H, Porqueddu T, Campbell JL, Gibson A, et al. Conducting a team-based multi-sited focused ethnography in primary care. BMC Med Res Methodol 2017;17. https://doi.org/10.1186/s12874-017-0422-5.
- Alderson SL, Russell AM, McLintock K, Potrata B, House A, Foy R. Incentivised case finding for depression in patients with chronic heart disease and diabetes in primary care: an ethnographic study. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005146.
- Gabbay J, May Al. Evidence based guidelines or collectively constructed ‘mindlines?’ Ethnographic study of knowledge management in primary care. BMJ 2004;329. https://doi.org/10.1136/bmj.329.7473.1013.
- McDonald R, Harrison S, Checkland K, Campbell SM, Roland M. Impact of financial incentives on clinical autonomy and internal motivation in primary care: ethnographic study. BMJ 2007;334. https://doi.org/10.1136/bmj.39238.890810.BE.
- EMIS Health . EMIS Health: Primary Care 2016. www.emishealth.com/products/primary-care/ (accessed 8 February 2017).
- Front Desk Incorporated . Front Desk 2016. www.frontdeskhq.com/ (accessed 9 February).
- In Practice Systems Ltd . Vision for GP Practices 2017. www.inps.co.uk/vision/gp-practices (accessed 9 Feb 2017).
- EMIS Health . EMIS Web Most Widely Used GP System 2013. www.emishealth.com/news-events/news/emis-web-most-widely-used-gp-system/ (accessed 8 February 2017).
- NHS Digital . QOF Business Rules v34.0 2016. http://content.digital.nhs.uk/qofbrv34 (accessed 8 February 2017).
- Violan C, Foguet-Boreu Q, Flores-Mateo G, Salisbury C, Blom J, Freitag M, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0102149.
- Salisbury C. Multimorbidity Search Tool for EMIS Practices 2017. www.bristol.ac.uk/primaryhealthcare/resources/multimorbidity-tool/ (accessed 9 February 2017).
- Babylon . Babylon 2017. www.babylonhealth.com/ (accessed 10 February 2017).
- Push Dr Ltd . Push Doctor 2017. www.pushdoctor.co.uk/ (accessed 10 February 2017).
- Richards DA, Meakins J, Tawfik J, Godfrey L, Dutton E, Richardson G, et al. Nurse telephone triage for same day appointments in general practice: multiple interrupted time series trial of effect on workload and costs. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7374.1214.
- Lattimer V, George S, Thompson F, Thomas E, Mullee M, Turnbull J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. The South Wiltshire Out of Hours Project (SWOOP) Group. BMJ 1998;317:1054-9. https://doi.org/10.1136/bmj.317.7165.1054.
- Pinnock H, Adlem L, Gaskin S, Harris J, Snellgrove C, Sheikh A. Accessibility, clinical effectiveness, and practice costs of providing a telephone option for routine asthma reviews: Phase IV controlled implementation study. Br J Gen Pract 2007;57:714-22.
- Salisbury C, O’Cathain A, Thomas C, Edwards L, Gaunt D, Dixon P, et al. Telehealth for patients at high risk of cardiovascular disease: pragmatic randomised controlled trial. BMJ 2016;353. https://doi.org/10.1136/bmj.i2647.
- Salisbury C, O’Cathain A, Edwards L, Thomas C, Gaunt D, Hollinghurst S, et al. Effectiveness of an integrated telehealth service for patients with depression: a pragmatic randomised controlled trial of a complex intervention. Lancet Psychiatry 2016;3:515-25. https://doi.org/10.1016/S2215-0366(16)00083-3.
- Ofcom . Internet and Online Content 2015. www.ofcom.org.uk/__data/assets/pdf_file/0017/13445/uk_5.pdf (accessed 8 February 2017).
- Ofcom . Telecoms and Networks 2015. www.ofcom.org.uk/__data/assets/pdf_file/0013/14116/uk_4.pdf (accessed 8 February 2017).
- NHS England . GP Patient Survey 2016. https://gp-patient.co.uk/surveys-and-reports (accessed 8 February 2017).
- Murphy M, Hollinghurst S, Salisbury C. Agreeing the content of a patient-reported outcome measure for primary care: a Delphi consensus study. Health Expect 2017;20:335-48. https://doi.org/10.1111/hex.12462.
- NHS Digital . Hospital Episode Statistics 2016. http://content.digital.nhs.uk/hes (accessed 8 February 2017).
- Ipsos MORI. GP Patient Survey – National Summary Report. London: NHS England; 2016.
- Velupillai S, Mowery D, South BR, Kvist M, Dalianis H. Recent advances in clinical natural language processing in support of semantic analysis. Yearb Med Inform 2015;10:183-93. https://doi.org/10.15265/IY-2015-009.
- MacRury S, Finlayson J, Hussey-Wilson S, Holden S. Development of a pseudo/anonymised primary care research database: proof-of-concept study. Health Informatics J 2016;22:113-9. https://doi.org/10.1177/1460458214535118.
- Cockburn J, Campbell E, Gordon JJ, Sanson-Fisher RW. Response bias in a study of general practice. Fam Pract 1988;5:18-23. https://doi.org/10.1093/fampra/5.1.18.
- Bertelsen P, Stub Petersen L. Danish citizens and general practitioners’ use of ICT for their mutual communication. Stud Health Technol Inform 2015;216:376-9.
- Armstrong S. Finally, the NHS goes digital. Or does it?. BMJ 2015;351. https://doi.org/10.1136/bmj.h3726.
- Stain HJ, Payne K, Thienel R, Michie P, Carr V, Kelly B. The feasibility of videoconferencing for neuropsychological assessments of rural youth experiencing early psychosis. J Telemed Telecare 2011;17:328-31. https://doi.org/10.1258/jtt.2011.101015.
- Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry 2013;170:256-62. https://doi.org/10.1176/appi.ajp.2012.12081064.
- Taylor A, Morris G, Pech J, Rechter S, Carati C, Kidd MR. Home Telehealth Video Conferencing: Perceptions and Performance. JMIR Mhealth Uhealth 2015;3. https://doi.org/10.2196/mhealth.4666.
- NHS England . Wave Two 2016. www.england.nhs.uk/gp/gpfv/redesign/improving-access/gp-access-fund/wave-two/ (accessed 8 February 2017).
- Rosen R. Meeting Need or Fuelling Unnecessary Demand? Understanding the Impact of Improved Access to Primary Care. London: Nuffield Trust; 2014.
- Hewitt H, Gafaranga J, McKinstry B. Comparison of face-to-face and telephone consultations in primary care: qualitative analysis. Br J Gen Pract 2010;60:e201-12. https://doi.org/10.3399/bjgp10X501831.
- Sustainability and Transformation Plans (STPs) Explained. London: The King’s Fund; 2016.
- NHS Digital . Quality and Outcomes Framework (QOF) – 2014–15 n.d. https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/quality-and-outcomes-framework-qof-2014-15 (accessed 7 May 2018).
Appendix 1 Search strategies used in the conceptual review
MEDLINE
Date searched: 13 January 2015.
Search strategy
| # | MEDLINE search strategy | Results |
|---|---|---|
| 1 | Remote Consultation/ | 3643 |
| 2 | (e-consult* or econsult* or teleconsult*).ti,ab. | 851 |
| 3 | (tele* adj5 consult*).ti,ab. | 1718 |
| 4 | ((email* or e-mail*) adj5 (consult? or consultation?)).ti,ab. | 99 |
| 5 | ((online or electronic or web or web-based or internet* or virtual* or digital or portal?) adj5 (consult? or consultation?)).ti,ab. | 664 |
| 6 | ((video* or skyp*) adj5 (consult? or consultation?)).ti,ab. | 631 |
| 7 | ((multimedia or multi media) adj5 (consult? or consultation?)).ti,ab. | 20 |
| 8 | (remote adj5 (consult? or consultation?)).ti,ab. | 307 |
| 9 | ((email* or e-mail*) and (consult? or consultation?)).ti. | 30 |
| 10 | ((online or electronic or web or web-based or internet* or virtual* or digital or portal?) and (consult? or consultation?)).ti. | 192 |
| 11 | ((video* or skyp*) and (consult? or consultation?)).ti. | 134 |
| 12 | ((multimedia or multi media) and (consult? or consultation?)).ti. | 9 |
| 13 | (remote and (consult? or consultation?)).ti. | 69 |
| 14 | ((telehealth or telemedicine or telemonitor*) and (consult? or consultation?)).ti,ab. | 1129 |
| 15 | ((tele-health or tele-medicine or tele-monitor*) and (consult? or consultation?)).ti,ab. | 15 |
| 16 | ((cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?) and (consult? or consultation?)).ti,ab. | 170 |
| 17 | (((text or mobile or short or brief) adj messag*) and (consult? or consultation?)).ti,ab. | 35 |
| 18 | ‘Referral and Consultation’/ or exp Professional-Patient Relations/ | 168,421 |
| 19 | telecommunications/ or electronic mail/ or exp telemedicine/ or telephone/ or exp cellular phone/ or videoconferencing/ or Hotlines/ or Text Messaging/ or exp internet/ | 84,227 |
| 20 | 18 and 19 | 4547 |
| 21 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media)).ti. | 144 |
| 22 | (((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) adj5 (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media)).ti,ab. | 941 |
| 23 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?)).ti. | 1 |
| 24 | (((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) adj5 (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?)).ti,ab. | 40 |
| 25 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and ((text or mobile or short or brief) adj messag*)).ti. | 0 |
| 26 | ((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and ((communicat* or relation*) adj5 (text messag* or short messag* or brief messag* or mobile messag*))).ti,ab. | 8 |
| 27 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 20 or 21 or 22 or 23 or 24 or 25 or 26 | 11,036 |
| 28 | systematic review.ti,ab. | 52,561 |
| 29 | meta analysis.pt. | 51,754 |
| 30 | MEDLINE.tw. | 61,188 |
| 31 | (Qualitative and synthesis).ti,ab. | 3439 |
| 32 | (meta-synthesis* or meta synthesis* or metasynthesis).ti,ab. | 385 |
| 33 | (meta-ethnograph* or metaethnograph* or meta ethnograph*).ti,ab. | 186 |
| 34 | (meta-study or metastudy or meta study).ti,ab. | 50 |
| 35 | systematic review*.ti,ab. and qualitative research/ | 289 |
| 36 | (realist review? or mixed review? or mixed method? review?).ti,ab. | 180 |
| 37 | 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 | 127,413 |
| 38 | 27 and 37 | 226 |
| 39 | limit 38 to english language | 217 |
| 40 | exp Attitude/ | 269,059 |
| 41 | exp Professional-Patient Relations/ | 120,163 |
| 42 | personal satisfaction/ | 11,509 |
| 43 | consumer satisfaction/ or patient satisfaction/ or patient preference/ | 80,300 |
| 44 | nurse’s practice patterns/ or physician’s practice patterns/ | 43,097 |
| 45 | (experience? or experiential or attitud* or opinion? or view* or satisf* or dissatis* or perception? or perspective? or perceive? or prefer* or enthus*).ti,ab. | 1,909,121 |
| 46 | 40 or 41 or 42 or 43 or 44 or 45 | 2,171,500 |
| 47 | 27 and 46 | 6391 |
| 48 | Program Evaluation/ | 46,858 |
| 49 | ((program* or process*) adj5 (evaluat* or analy*)).ti,ab. | 93,067 |
| 50 | (barrier? or obstacle? or objection? or challeng* or difficult*).ti,ab. | 1,021,768 |
| 51 | (facilitat* or encourag* or empower* or embed* or engag* or benefit* or attract* or integrat*).ti,ab. | 1,328,578 |
| 52 | (implement* or adopt* or utiliz* or utilis* or access*).ti,ab. | 1,035,525 |
| 53 | 48 or 49 or 50 or 51 or 52 | 3,038,396 |
| 54 | 27 and 53 | 5144 |
| 55 | qualitative research/ | 21,409 |
| 56 | *interviews as topic/ or focus groups/ or narration/ | 25,742 |
| 57 | exp Questionnaires/ | 317,408 |
| 58 | observation.ti. | 25,933 |
| 59 | interview?.ti. | 26,741 |
| 60 | (qualitative adj2 (interview* or study)).ti,ab. | 24,246 |
| 61 | (qualitative or focus group? or story or stories or narration or narrative* or discourse or discursive or grounded theory or ethnogra* or phenomenolog*).ti,ab. | 200,298 |
| 62 | (questionnaire? or survey? or feedback).ti,ab. | 710,635 |
| 63 | 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 | 1,061,701 |
| 64 | 27 and 63 | 2872 |
| 65 | 47 or 54 or 64 | 8639 |
| 66 | limit 65 to english language | 8043 |
EMBASE
Date searched: 13 January 2015.
Search strategy
| # | EMBASE | Results |
|---|---|---|
| 1 | teleconsultation/ | 6342 |
| 2 | (e-consult* or econsult* or teleconsult*).ti,ab. | 1027 |
| 3 | (tele* adj5 consult*).ti,ab. | 2379 |
| 4 | ((email* or e-mail*) adj5 (consult? or consultation?)).ti,ab. | 153 |
| 5 | ((online or electronic or web or web-based or internet* or virtual* or digital or portal?) adj5 (consult? or consultation?)).ti,ab. | 949 |
| 6 | ((video* or skyp*) adj5 (consult? or consultation?)).ti,ab. | 729 |
| 7 | ((multimedia or multi media) adj5 (consult? or consultation?)).ti,ab. | 23 |
| 8 | (remote adj5 (consult? or consultation?)).ti,ab. | 385 |
| 9 | ((email* or e-mail*) and (consult? or consultation?)).ti. | 39 |
| 10 | ((online or electronic or web or web-based or internet* or virtual* or digital or portal?) and (consult? or consultation?)).ti. | 248 |
| 11 | ((video* or skyp*) and (consult? or consultation?)).ti. | 148 |
| 12 | ((multimedia or multi media) and (consult? or consultation?)).ti. | 8 |
| 13 | (remote and (consult? or consultation?)).ti. | 84 |
| 14 | ((telehealth or telemedicine or telemonitor*) and (consult? or consultation?)).ti,ab. | 1457 |
| 15 | ((tele-health or tele-medicine or tele-monitor*) and (consult? or consultation?)).ti,ab. | 29 |
| 16 | ((cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?) and (consult? or consultation?)).ti,ab. | 300 |
| 17 | (((text or mobile or short or brief) adj messag*) and (consult? or consultation?)).ti,ab. | 56 |
| 18 | consultation/ or doctor patient relation/ or nurse patient relationship/ | 170,188 |
| 19 | *e-mail/ or *internet/ or *mobile phone/ or *telecommunication/ or *telephone/ or *text messaging/ or *videoconferencing/ or exp *telehealth/ | 54,585 |
| 20 | 18 and 19 | 3164 |
| 21 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media)).ti. | 158 |
| 22 | (((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) adj5 (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media)).ti,ab. | 1359 |
| 23 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?)).ti. | 2 |
| 24 | (((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) adj5 (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?)).ti,ab. | 60 |
| 25 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and ((text or mobile or short or brief) adj messag*)).ti. | 1 |
| 26 | ((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and ((communicat* or relation*) adj5 (text messag* or short messag* or brief messag* or mobile messag*))).ti,ab. | 10 |
| 27 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 20 or 21 or 22 or 23 or 24 or 25 or 26 | 13,678 |
| 28 | systematic review.ti,ab. | 64,358 |
| 29 | meta analysis/ or ‘meta analysis (topic)’/ or ‘systematic review’/ or ‘systematic review (topic)’/ | 154,027 |
| 30 | MEDLINE.tw. | 72,060 |
| 31 | (Qualitative and synthesis).ti,ab. | 3785 |
| 32 | (meta-synthesis* or meta synthesis* or metasynthesis).ti,ab. | 377 |
| 33 | (meta-ethnograph* or metaethnograph* or meta ethnograph*).ti,ab. | 181 |
| 34 | (meta-study or metastudy or meta study).ti,ab. | 59 |
| 35 | systematic review*.ti,ab. and exp qualitative research/ | 777 |
| 36 | (realist review? or mixed review? or mixed method? review?).ti,ab. | 192 |
| 37 | 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 | 208,719 |
| 38 | 27 and 37 | 354 |
| 39 | limit 38 to english language | 340 |
| 40 | exp *attitude/ | 189,912 |
| 41 | doctor patient relation/ or nurse patient relationship/ | 110,766 |
| 42 | satisfaction/ | 30,068 |
| 43 | patient satisfaction/ or patient preference/ | 95,228 |
| 44 | (experience? or experiential or attitud* or opinion? or view* or satisf* or dissatis* or perception? or perspective? or perceive? or prefer* or enthus*).ti,ab. | 2,406,027 |
| 45 | 40 or 41 or 42 or 43 or 44 | 2,601,000 |
| 46 | 27 and 45 | 6966 |
| 47 | exp program evaluation/ | 3463 |
| 48 | ((program* or process*) adj5 (evaluat* or analy*)).ti,ab. | 120,143 |
| 49 | (barrier? or obstacle? or objection? or challeng* or difficult*).ti,ab. | 1,278,412 |
| 50 | (facilitat* or encourag* or empower* or embed* or engag* or benefit* or attract* or integrat*).ti,ab. | 1,631,843 |
| 51 | (implement* or adopt* or utiliz* or utilis* or access*).ti,ab. | 1,286,296 |
| 52 | 47 or 48 or 49 or 50 or 51 | 3,724,026 |
| 53 | 27 and 52 | 6557 |
| 54 | grounded theory/ or naturalistic inquiry/ or qualitative research/ | 29,676 |
| 55 | exp *interview/ | 7584 |
| 56 | exp Questionnaire/ | 422,043 |
| 57 | observation.ti. | 29,376 |
| 58 | interview?.ti. | 27,429 |
| 59 | (qualitative adj2 (interview* or study)).ti,ab. | 28,300 |
| 60 | (qualitative or focus group? or story or stories or narration or narrative* or discourse or discursive or grounded theory or ethnogra* or phenomenolog*).ti,ab. | 238,686 |
| 61 | (questionnaire? or survey? or feedback).ti,ab. | 904,101 |
| 62 | 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 | 1,264,073 |
| 63 | 27 and 62 | 5679 |
| 64 | 46 or 53 or 63 | 11,230 |
| 65 | limit 64 to english language | 10,471 |
PsycINFO
Date searched: 13 January 2015.
Search strategy
| # | PsycINFO | Results |
|---|---|---|
| 1 | (e-consult* or econsult* or teleconsult*).ti,ab. | 115 |
| 2 | (tele* adj5 consult*).ti,ab. | 380 |
| 3 | ((email* or e-mail*) adj5 (consult? or consultation?)).ti,ab. | 26 |
| 4 | ((online or electronic or web or web-based or internet* or virtual* or digital or portal?) adj5 (consult? or consultation?)).ti,ab. | 196 |
| 5 | ((video* or skyp*) adj5 (consult? or consultation?)).ti,ab. | 328 |
| 6 | ((multimedia or multi media) adj5 (consult? or consultation?)).ti,ab. | 2 |
| 7 | (remote adj5 (consult? or consultation?)).ti,ab. | 32 |
| 8 | ((email* or e-mail*) and (consult? or consultation?)).ti. | 10 |
| 9 | ((online or electronic or web or web-based or internet* or virtual* or digital or portal?) and (consult? or consultation?)).ti. | 34 |
| 10 | ((video* or skyp*) and (consult? or consultation?)).ti. | 54 |
| 11 | ((multimedia or multi media) and (consult? or consultation?)).ti. | 0 |
| 12 | (remote and (consult? or consultation?)).ti. | 6 |
| 13 | ((telehealth or telemedicine or telemonitor*) and (consult? or consultation?)).ti,ab. | 216 |
| 14 | ((tele-health or tele-medicine or tele-monitor*) and (consult? or consultation?)).ti,ab. | 3 |
| 15 | ((cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?) and (consult? or consultation?)).ti,ab. | 36 |
| 16 | (((text or mobile or short or brief) adj messag*) and (consult? or consultation?)).ti,ab. | 13 |
| 17 | exp Professional Consultation/ or therapeutic processes/ | 27,730 |
| 18 | internet/ or exp electronic communication/ or telemedicine/ or telephone systems/ or telecommunications media/ or cellular phones/ or teleconferencing/ | 36,334 |
| 19 | 17 and 18 | 439 |
| 20 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media)).ti. | 45 |
| 21 | (((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) adj5 (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media)).ti,ab. | 350 |
| 22 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?)).ti. | 0 |
| 23 | (((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) adj5 (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?)).ti,ab. | 9 |
| 24 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and ((text or mobile or short or brief) adj messag*)).ti. | 0 |
| 25 | ((patient? adj3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and ((communicat* or relation*) adj5 (text messag* or short messag* or brief messag* or mobile messag*))).ti,ab. | 3 |
| 26 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 19 or 20 or 21 or 22 or 23 or 24 or 25 | 1670 |
| 27 | systematic review.ti,ab. | 10,570 |
| 28 | meta analysis/ or ‘systematic review’.md. | 13,931 |
| 29 | MEDLINE.tw. | 7576 |
| 30 | (Qualitative and synthesis).ti,ab. | 1107 |
| 31 | (meta-synthesis* or meta synthesis* or metasynthesis).ti,ab. | 293 |
| 32 | (meta-ethnograph* or metaethnograph* or meta ethnograph*).ti,ab. | 120 |
| 33 | (meta-study or metastudy or meta study).ti,ab. | 46 |
| 34 | systematic review*.ti,ab. and qualitative research/ | 66 |
| 35 | (realist review? or mixed review? or mixed method? review?).ti,ab. | 84 |
| 36 | 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 | 22,514 |
| 37 | 26 and 36 | 48 |
| 38 | limit 37 to english language | 47 |
| 39 | exp attitudes/ | 270,510 |
| 40 | therapeutic processes/ | 19,101 |
| 41 | satisfaction/ or client satisfaction/ or consumer satisfaction/ or dissatisfaction/ | 17,949 |
| 42 | (experience? or experiential or attitud* or opinion? or view* or satisf* or dissatis* or perception? or perspective? or perceive? or prefer* or enthus*).ti,ab. | 1,165,793 |
| 43 | 39 or 40 or 41 or 42 | 1,248,546 |
| 44 | 26 and 43 | 1070 |
| 45 | exp Program Evaluation/ | 16,799 |
| 46 | ((program* or process*) adj5 (evaluat* or analy*)).ti,ab. | 52,284 |
| 47 | (barrier? or obstacle? or objection? or challeng* or difficult*).ti,ab. | 349,871 |
| 48 | (facilitat* or encourag* or empower* or embed* or engag* or benefit* or attract* or integrat*).ti,ab. | 548,566 |
| 49 | (implement* or adopt* or utiliz* or utilis* or access*).ti,ab. | 322,900 |
| 50 | 45 or 46 or 47 or 48 or 49 | 1,037,734 |
| 51 | 26 and 50 | 938 |
| 52 | qualitative research/ or grounded theory/ or observation methods/ | 11,560 |
| 53 | (focus group or interview or qualitative study).md. | 219,298 |
| 54 | exp *interviews/ | 7834 |
| 55 | questionnaires/ or exp surveys/ | 20,924 |
| 56 | observation.ti. | 3541 |
| 57 | interview?.ti. | 9280 |
| 58 | (qualitative adj2 (interview* or study)).ti,ab. | 30,171 |
| 59 | (qualitative or focus group? or story or stories or narration or narrative* or discourse or discursive or grounded theory or ethnogra* or phenomenolog*).ti,ab. | 238,150 |
| 60 | (questionnaire? or survey? or feedback).ti,ab. | 388,131 |
| 61 | 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 | 712,416 |
| 62 | 26 and 61 | 733 |
| 63 | 44 or 51 or 62 | 1476 |
| 64 | limit 63 to english language | 1409 |
Cumulative Index to Nursing and Allied Health Literature
Date searched: 13 January 2015.
Search strategy
| # | Cumulative Index to Nursing and Allied Health Literature | Results |
|---|---|---|
| 1 | (MH ‘Remote Consultation’) | 597 |
| 2 | TI ( e-consult* or econsult* or teleconsult* ) OR AB ( e-consult* or econsult* or teleconsult* ) | 121 |
| 3 | TI tele* N5 consult* OR AB tele* N5 consult* | 406 |
| 4 | TI ( ((email* or e-mail*) N5 (consult? or consultation?)) ) OR AB ( ((email* or e-mail*) N5 (consult? or consultation?)) ) | 22 |
| 5 | TI (((online or electronic or web or web-based or internet* or virtual* or digital or portal?) N5 (consult? or consultation?))) OR AB (((online or electronic or web or web-based or internet* or virtual* or digital or portal?) N5 (consult? or consultation?))) | 75 |
| 6 | TI (((video* or skyp*) N5 (consult? or consultation?))) OR AB (((video* or skyp*) N5 (consult? or consultation?))) | 142 |
| 7 | TI (((multimedia or multi media) N5 (consult? or consultation?))) OR AB (((multimedia or multi media) N5 (consult? or consultation?))) | 2 |
| 8 | TI ((remote N5 (consult? or consultation?))) OR AB ((remote N5 (consult? or consultation?))) | 20 |
| 9 | TI (((e-mail* or e-mail*) and (consult? or consultation?))) OR TI (((online or electronic or web or web-based or internet* or virtual* or digital or portal?) and (consult? or consultation?))) OR TI (((video* or skyp*) and (consult? or consultation?))) OR TI (((multimedia or multi media) and (consult? or consultation?))) OR TI ((remote and (consult? or consultation?))) | 74 |
| 10 | TI (((telehealth or telemedicine or telemonitor*) and (consult? or consultation?))) OR AB (((telehealth or telemedicine or telemonitor*) and (consult? or consultation?))) | 95 |
| 11 | TI (((tele-health or tele-medicine or tele-monitor*) and (consult? or consultation?))) OR AB (((tele-health or tele-medicine or tele-monitor*) and (consult? or consultation?))) | 1 |
| 12 | TI (((cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?) and (consult? or consultation?))) OR AB (((cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?) and (consult? or consultation?))) | 0 |
| 13 | TI ((text messag* or short messag* or brief messag* or mobile messag*) AND (consult? or consultation?)) OR AB ((text messag* or short messag* or brief messag* or mobile messag*) AND (consult? or consultation?)) | 4 |
| 14 | ((MH ‘Referral and Consultation’) OR (MH ‘Professional-Patient Relations+’)) AND ((MH ‘Telecommunications’) OR (MH ‘Instant Messaging’) OR (MH ‘Internet+’) OR (MH ‘Telehealth’) OR (MH ‘Telemedicine’) OR (MH ‘Telenursing’) OR (MH ‘Telepsychiatry’) OR (MH ‘Telephone’) OR (MH ‘Text Messaging’) OR (MH ‘Videoconferencing’)) | 2958 |
| 15 | TI ((patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (e-mail or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media))) OR AB ((((patient? N3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) N5 (e-mail or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media))) | 118 |
| 16 | TI ((patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?))) OR AB ((((patient? N3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) N5 (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?))) | 1 |
| 17 | TI ((patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (text messag* or short messag* or brief messag* or mobile messag*))) OR AB (((patient? N3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and ((communicat* or relation*) N5 (text messag* or short messag* or brief messag* or mobile messag*)))) | 2 |
| 18 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 13 OR 14 OR 15 OR 16 OR 17 | 4145 |
| 19 | (MH ‘Systematic Review’) | 20,084 |
| 20 | (MH ‘Meta Analysis’) | 15,132 |
| 21 | TI ‘systematic review’ OR AB ‘systematic review’ | 16,924 |
| 22 | TI medline OR AB medline | 16,304 |
| 23 | TI (Qualitative and synthesis) OR AB (Qualitative and synthesis) | 765 |
| 24 | TI ((meta-synthesis* or meta synthesis* or metasynthesis)) OR AB ((meta-synthesis* or meta synthesis* or metasynthesis)) | 513 |
| 25 | TI ((meta-ethnograph* or metaethnograph* or meta ethnograph*)) OR AB ((meta-ethnograph* or metaethnograph* or meta ethnograph*)) | 110 |
| 26 | TI ((meta-study or metastudy or meta study)) OR AB ((meta-study or metastudy or meta study)) | 950 |
| 27 | TI (realist review? or mixed review? or mixed method? review?) OR AB (realist review? or mixed review? or mixed method? review?) | 88 |
| 28 | 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 | 46,663 |
| 29 | 18 AND 28 | 48 |
| 30 | 18 AND 28 – Limited to English | 47 |
| 31 | (MH ‘Attitude+’) | 211,148 |
| 32 | (MH ‘Professional-Patient Relations+’) | 52,385 |
| 33 | (MH ‘Consumer Satisfaction’) OR (MH ‘Patient Satisfaction’) | 31,099 |
| 34 | (MH ‘Practice Patterns’) | 4882 |
| 35 | TI (experience? or experiential or attitud* or opinion? or view* or satisf* or dissatis* or perception? or perspective? or perceive? or prefer* or enthus*) OR AB (experience? or experiential or attitud* or opinion? or view* or satisf* or dissatis* or perception? or perspective? or perceive? or prefer* or enthus*) | 271,933 |
| 36 | 31 OR 32 OR 33 OR 34 OR 35 | 431,877 |
| 37 | (MH ‘Program Evaluation’) | 19,035 |
| 38 | TI (((program* or process*) N5 (evaluat* or analy*))) OR AB (((program* or process*) N5 (evaluat* or analy*))) | 21,128 |
| 39 | TI ((barrier? or obstacle? or objection? or challeng* or difficult*)) OR AB ((barrier? or obstacle? or objection? or challeng* or difficult*)) | 157,274 |
| 40 | TI ((facilitat* or encourag* or empower* or embed* or engag* or benefit* or attract* or integrat*)) OR AB ((facilitat* or encourag* or empower* or embed* or engag* or benefit* or attract* or integrat*)) | 211,725 |
| 41 | TI ((implement* or adopt* or utiliz* or utilis* or access*)) OR AB ((implement* or adopt* or utiliz* or utilis* or access*)) | 166,978 |
| 42 | 37 OR 38 OR 39 OR 40 OR 41 | 460,045 |
| 43 | (MH ‘Qualitative Studies+’) | 71,654 |
| 44 | (MH ‘Interviews+’) OR (MH ‘Focus Groups’) | 134,811 |
| 45 | (MH ‘Questionnaires+’) | 184,448 |
| 46 | TI (observation or interview) OR AB (qualitative or focus group? or story or stories or narration or narrative* or discourse or discursive or grounded theory or ethnogra* or phenomenolog*)) OR TI (qualitative or focus group? or story or stories or narration or narrative* or discourse or discursive or grounded theory or ethnogra* or phenomenolog*)) OR AB (questionnaire? or survey? or feedback) OR TI (questionnaire? or survey? or feedback) | 134,736 |
| 47 | 43 OR 44 OR 45 OR 46 | 354,135 |
| 48 | 36 OR 42 OR 47 | 884,801 |
| 49 | 18 AND 48 | 3288 |
| 50 | 18 AND 48 – limited to English | 3261 |
Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects
Date searched: 13 January 2015.
Search strategy
| ID | Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects |
|---|---|
| #1 | MeSH descriptor: [Remote Consultation] explode all trees |
| #2 | (e-consult* or econsult* or teleconsult*):ti,ab,kw (Word variations have been searched) |
| #3 | (tele* near consult*):ti,ab,kw (Word variations have been searched) |
| #4 | ((email* or e-mail*) near (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #5 | ((online or electronic or web or web-based or internet* or virtual* or digital or portal?) near (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #6 | ((video* or skyp*) near (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #7 | ((multimedia or multi media) near (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #8 | (remote near (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #9 | (email* or e-mail*) and (consult? or consultation?):ti (Word variations have been searched) |
| #10 | ((online or electronic or web or web-based or internet* or virtual* or digital or portal?) and (consult? or consultation?)):ti (Word variations have been searched) |
| #11 | ((video* or skyp*) and (consult? or consultation?)):ti (Word variations have been searched) |
| #12 | ((multimedia or multi media) and (consult? or consultation?)):ti (Word variations have been searched) |
| #13 | (remote and (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #14 | ((telehealth or telemedicine or telemonitor*) and (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #15 | ((tele-health or tele-medicine or tele-monitor*) and (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #16 | ((cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?) and (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #17 | (((text or mobile or short or brief) next messag*) and (consult? or consultation?)):ti,ab,kw (Word variations have been searched) |
| #18 | MeSH descriptor: [Referral and Consultation] this term only |
| #19 | MeSH descriptor: [Professional-Patient Relations] explode all trees |
| #20 | #18 or #19 |
| #21 | MeSH descriptor: [Internet] explode all trees |
| #22 | MeSH descriptor: [Telecommunications] this term only |
| #23 | MeSH descriptor: [Telephone] explode all trees |
| #24 | MeSH descriptor: [Electronic Mail] explode all trees |
| #25 | MeSH descriptor: [Videoconferencing] this term only |
| #26 | MeSH descriptor: [Telemedicine] explode all trees |
| #27 | #21 or #22 or #23 or #24 or #25 or #26 |
| #28 | #20 and #27 |
| #29 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media)):ti (Word variations have been searched) |
| #30 | (((patient? near/3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) near (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media)):ti,ab,kw (Word variations have been searched) |
| #31 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?)):ti (Word variations have been searched) |
| #32 | (((patient? near/3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and (communicat* or relation*)) near (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?)):ti,ab,kw (Word variations have been searched) |
| #33 | (patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and ((text or mobile or short or brief) adj messag*)):ti (Word variations have been searched) |
| #34 | ((patient? near/3 (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps)) and ((communicat* or relation*) near (text messag* or short messag* or brief messag* or mobile messag*))):ti,ab,kw (Word variations have been searched) |
| #35 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #28 or #29 or #30 or #31 or #32 or #33 or #34 |
Science Citation Index, Social Science Citation Index and Conference Proceedings Citation Index – Science
Date searched: 13 January 2015.
Search strategy
| Set | Results | Science Citation Index, Social Science Citation Index and Conference Proceedings Citation Index – Science |
|---|---|---|
| 1 | 3542 | TOPIC: (e-consult* or econsult* or teleconsult*) OR TOPIC: (tele* NEAR/5 consult*) OR TOPIC: (((email* or e-mail*) NEAR/5 (consult? or consultation?))) OR TOPIC: (((online or electronic or web or ‘web-based’ or internet* or virtual* or digital or portal?) NEAR/5 (consult? or consultation?))) OR TOPIC: (((video* or skyp*) NEAR/5 (consult? or consultation?))) OR TOPIC: (((multimedia or ‘multi media’) NEAR/5 (consult? or consultation?))) OR TOPIC: ((remote NEAR/5 (consult? or consultation?))) |
| 2 | 763 | TITLE: (tele* AND consult*) OR TITLE: (((email* or e-mail*) AND (consult? or consultation?))) OR TITLE: (((online or electronic or web or ‘web-based’ or internet* or virtual* or digital or portal?) AND (consult? or consultation?))) OR TITLE: (((video* or skyp*) AND (consult? or consultation?))) OR TITLE: (((multimedia or ‘multi media’) AND (consult? or consultation?))) OR TITLE: ((remote AND (consult? or consultation?))) |
| 3 | 826 | TOPIC: (((telehealth or telemedicine or telemonitor*) and (consult? or consultation?))) OR TOPIC: (((tele-health or tele-medicine or tele-monitor*) and (consult? or consultation?))) OR TOPIC: (((‘cell phone?’ or ‘cellular phone?’ or ‘cellular telephone?’ or ‘mobile phone?’ or ‘mobile telephone?’ or ‘smart phone?’ or smartphone? or iphone? or ‘android phone?’ or ipad? or ‘tablet computer?’ or ‘mobile computer?’ or ‘mobile device?’) and (consult? or consultation?))) OR TOPIC: ((((text or mobile or short or brief) NEXT messag*) and (consult? or consultation?))) |
| 4 | 26 | TITLE: ((patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media))) OR TITLE: ((patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and (cell phone? or cellular phone? or cellular telephone? or mobile phone? or mobile telephone? or smart phone? or smartphone? or iphone? or android phone? or ipad? or tablet computer? or mobile computer? or mobile device?))) OR TITLE: ((patient? and (doctor? or physician? or clinician? or nurse? or general practitioner? or gp or gps) and (communicat* or relation*) and ((text or mobile or short or brief) NEXT messag*))) |
| 5 | 290 | TOPIC: ((patient? NEAR/3 (doctor? or physician? or clinician? or nurse? or ‘general practitioner?’ or gp or gps))) AND TOPIC: (((communicat* or relation*) NEAR/5 (email or e-mail or online or electronic or web or web-based or internet* or virtual* or digital or portal? or video* or skype or multimedia or multi-media))) |
| 6 | 5 | TOPIC: ((patient? NEAR/3 (doctor? or physician? or clinician? or nurse? or ‘general practitioner?’ or gp or gps))) AND TOPIC: (((communicat* or relation*) NEAR/5 (‘cell phone?’ or ‘cellular phone?’ or ‘cellular telephone?’ or ‘mobile phone?’ or ‘mobile telephone?’ or ‘smart phone?’ or smartphone? or iphone? or ‘android phone?’ or ipad? or ‘tablet computer?’ or ‘mobile computer?’ or ‘mobile device?’))) |
| 7 | 4 | TOPIC: ((patient? NEAR/3 (doctor? or physician? or clinician? or nurse? or ‘general practitioner?’ or gp or gps))) AND TOPIC: (((communicat* or relation*) NEAR/5 (‘text messag*’ or ‘short messag*’ or ‘brief messag’ or ‘mobile messag*’))) |
| 8 | 4045 | 7 OR 6 OR 5 OR 4 OR 3 OR 2 OR 1 |
| 9 | 227,199 | TOPIC: (‘systematic review*’ or metaanalys* or ‘meta-analys*’) OR TOPIC: (medline) OR TOPIC: ((Qualitative and synthesis)) OR TOPIC: ((meta-synthesis* or ‘meta synthesis*’ or metasynthesis)) OR TOPIC: (meta-ethnograph* or metaethnograph* or ‘meta ethnograph*’) OR TOPIC: (meta-study or metastudy or ‘meta study’) OR TOPIC: (‘realist review?’ or ‘mixed review?’ or ‘mixed method review?’ or ‘mixed methods review?’) |
| 10 | 152 | 9 AND 8 |
| 11 | 2,506,676 | TOPIC: (experience? or experiential or attitud* or opinion? or view* or satisf* or dissatis* or perception? or perspective? or perceive? or prefer* or enthus*) |
| 12 | 1375 | 11 AND 8 |
| 13 | 5,990,498 | TOPIC: (((program* or process*) NEAR/5 (evaluat* or analy*))) OR TOPIC: (barrier? or obstacle? or objection? or challeng* or difficult*) OR TOPIC: (facilitat* or encourag* or empower* or embed* or engag* or benefit* or attract* or integrat*) OR TOPIC: (implement* or adopt* or utiliz* or utilis* or access*) |
| 14 | 2156 | 13 AND 8 |
| 15 | 1,221,445 | TITLE: (observation* or interview*) OR TOPIC: (qualitative or ‘focus group?’ or story or stories or narration or narrative* or discourse or discursive or ‘grounded theory’ or ethnogra* or phenomenolog*) OR TOPIC: (questionnaire? or survey? or feedback) |
| 16 | 638 | 15 AND 8 |
| 17 | 2806 | 16 OR 14 OR 12 |
| 18 | 2702 | 16 OR 14 OR 12 – limited to English |
| 19 | 149 | 9 AND 8 – limited to English |
Appendix 2 Matrix template for the conceptual review
| Reception staff | Nurses | GPs/primary care physicians | Practice managers/service managers | Others (secondary care clinicians, policy-makers, professional bodies) | Patients (about them and by them) | ‘Disadvantaged’ patients/groups of patients | Carers (including parents) | |
|---|---|---|---|---|---|---|---|---|
| Telephone | ||||||||
| Positive | ||||||||
| Negative | ||||||||
| Positive speculation | ||||||||
| Negative speculation | ||||||||
| Positive | ||||||||
| Negative | ||||||||
| Positive speculation | ||||||||
| Negative speculation |
Appendix 3 Conceptual review: list of relevant articles identified in the search
Abi Tayeh R, Joseph J. Telephone contact between patients and rheumatology department in a private healthcare system. Ann Rheum Dis 2014;73:1151–2.
Andreassen HK. What does an e-mail address add? – Doing health and technology at home. Soc Sci Med 2011;72:521–8. https://doi.org/10.1016/j.socscimed.2010.11.026
Armfield NR, Edirippulige SK, Bradford N, Smith AC. Telemedicine – is the cart being put before the horse? Med J Aust 2014;200:530–3.
Atherton H. Use of email for consulting with patients in general practice. Br J Gen Pract 2013;63:118–19. https://doi.org/10.3399/bjgp13X664072
Atherton H, Pappas Y, Heneghan C, Murray E. Experiences of using email for general practice consultations: a qualitative study. Br J Gen Pract 2013;63:e760–7. https://doi.org/10.3399/bjgp13X674440
Atherton H, Sawmynaden P, Sheikh A, Majeed A, Car J. Email for clinical communication between patients/caregivers and healthcare professionals. Cochrane Database Syst Rev 2012;11:CD007978.
Avey JP, Hobbs RL. Dial in: fostering the use of telebehavioral health services in frontier Alaska. Psychol Serv 2013;10:289–97. https://doi.org/10.1037/a0028231
Banbury A, Roots A, Nancarrow S. Rapid review of applications of e-health and remote monitoring for rural residents. Aust J Rural Health 2014;22:211–22. https://doi.org/10.1111/ajr.12127
Bishop TF, Press MJ, Mendelsohn JL, Casalino LP. Electronic communication improves access, but barriers to its widespread adoption remain. Health Aff (Milwood) 2013;32:1361–7.
Boman K, Olofsson M, Berggren P, Sengupta PP, Narula J. Robot-assisted remote echocardiographic examination and teleconsultation: a randomized comparison of time to diagnosis with standard of care referral approach. JACC Cardiovasc Imaging 2014;7:799-803.
Breen LA, Kariyawasam D, McGowan BM, Powrie JK, Carroll PV. Nurse-led Telephone Consultation Offers Patients With Graves Disease a Satisfying Means of Follow-Up Care. Endocrine Society, 94th Annual Meeting and Exposition, abstract no. 26459, Houston, TX, 23–26 June 2012.
Brewster L, Mountain G, Wessels B, Kelly C, Hawley M. Factors affecting front line staff acceptance of telehealth technologies: a mixed-method systematic review. J Adv Nurs 2014;70:21–33. https://doi.org/10.1111/jan.12196
Brockes C, Frei A, Schmidt-Weitmann S, Zimmerli L, Battegay E, Lennart Neumann C, et al. Medical online consultation regarding hypertension. J Hypertonie 2013;17:7–10.
Burgess M, Andiappan M, Chalder T. Cognitive behaviour therapy for chronic fatigue syndrome in adults: face-to-face versus telephone treatment: a randomized controlled trial. Behav Cogn Psychother 2012;40:175–91.
Burke P, O’Brien T, Korn S. Attitudes and experiences of telehealth video consultations among dermatologists in Victoria. Australas J Dermatol 2013;54:6–7.
Burns CL, Ward EC, Hill AJ, Malcolm K, Bassett L, Kenny LM, Greenup P. A pilot trial of a speech pathology telehealth service for head and neck cancer patients. J Telemed Telecare 2012;18:443–6. https://doi.org/10.1258/jtt.2012.GTH104
Campbell JL, Fletcher E, Britten N, Green C, Holt TA, Lattimer V, et al. Telephone triage for management of same-day consultation requests in general practice (the ESTEEM trial): a cluster-randomised controlled trial and cost-consequence analysis. Lancet 2014;384:1859–68.
Campbell-Richards D, Morris J, Sudra R, Vijayaraghavan S, O’Shea T, Greenhalgh T, et al. Online outpatient consultations: the patient perspective. Diabet Med 2014;31:165.
Castro LA, Favela J, Garcia-Pena C. Effects of communication media choice on the quality and efficacy of emergency calls assisted by a mobile nursing protocol tool. Comput Inform Nurs 2014;32:550–8.
Chen CH, Young TH, Huang CH, Chang HH, Chen CL, Chien HF, et al. Patient-centered wound teleconsultation for cutaneous wounds: a feasibility study. Ann Plast Surg 2014;72:220–4. https://doi.org/10.1097/SAP.0000000000000031
Chi NC, Demiris G. A systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare 2015;21:37–44. https://doi.org/10.1177/1357633X14562734
Choi H, Kim J. Effectiveness of telemedicine: videoconferencing for low-income elderly with hypertension. Telemed J E Health 2014;20:1156–64. https://doi.org/10.1089/tmj.2014.0031
Chu VH, Sexton DJ. Editorial commentary: telephone consultation for Staphylococcus aureus bacteremia: opening Pandora’s box. Clin Infect Dis 2013;56:536–8.
Churcher J. On: skype and privacy. Int J Psychoanal 2012;93:1035–7. https://doi.org/10.1111/j.1745-8315.2012.00610.x
Cohn A. The benefits of encouraging patients to email their doctor: a review of individual practice. Arch Dis Child Educ Pract Ed 2014;99:152–6. https://doi.org/10.1136/archdischild-2013-305856
Consumer Reports. The Doctor Will E-Mail You Now: Five Reasons Patient Portals Can Lead to Better Health. 2014. URL: www.consumerreports.org/cro/magazine/2014/01/the-doctor-will-email-you-now/index.htm (accessed 8 February 2017).
Crotty BH, Tamrat Y, Mostaghimi A, Safran C, Landon BE. Patient-to-physician messaging: volume nearly tripled as more patients joined system, but per capita rate plateaued. Health Aff (Milwood) 2014;33:1817–22. https://doi.org/10.1377/hlthaff.2013.1145
Crotty BH, Mostaghimi A, Landon BE. Teaching electronic patient-doctor communication using a patient web portal. J Gen Intern Med 2013;28:S480.
Daniel SJ, Wu L, Kumar S. Teledentistry: a systematic review of clinical outcomes, utilization and costs. J Dent Hyg 2013;87:345–52.
de Jong CC, Ros WJ, Schrijvers G. The effects on health behavior and health outcomes of Internet-based asynchronous communication between health providers and patients with a chronic condition: a systematic review. J Med Internet Res 2014;16:e19.
DE Weger E, Macinnes D, Enser J, Francis SJ, Jones FW. Implementing video conferencing in mental health practice. J Psychiatr Ment Health Nurs 2013;20:448–54. https://doi.org/10.1111/j.1365-2850.2012.01947.x
Dickinson R, Hall S, Sinclair JE, Bond C, Murchie P. Using technology to deliver cancer follow-up: a systematic review. BMC Cancer 2014;14:311. https://doi.org/10.1186/1471-2407-14-311
Do Campo J, Hannan T, Pava C. ‘Skype me doc’ (telehealth consultations). Intern Med J 2013;43:40.
dos Santos MT, Moura SC, Gomes LM, Lima AH, Moreira RS, Silva CD, Guimarães EM. Telehealth application on the rehabilitation of children and adolescents. Rev Paul Pediatr 2014;32:136–43.
Dudas RA, Crocetti M. Pediatric caregiver attitudes toward email communication: survey in an urban primary care setting. J Med Internet Res 2013;15:e228. https://doi.org/10.2196/jmir.2738
Engle X, Aird J, Tho L, Bintcliffe F, Monsell F, Gollogly J, Noor S. Combining continuing education with expert consultation via telemedicine in Cambodia. Trop Doct 2014;44:62–8. https://doi.org/10.1177/0049475513515654
Facchiano L, Snyder CH. Challenges surrounding provider/client electronic-mail communication. J Nurse Pract 2011;7:309–15.
Fatehi F, Martin-Khan M, Smith AC, Russell AW, Gray LC. Patient satisfaction with video teleconsultation in a virtual diabetes outreach clinic. Diabetes Technol Ther 2015;17:43–8.
Foster J, Jessopp L, Dale J. Concerns and confidence of general practitioners in providing telephone consultations. Br J Gen Pract 1999;49:111–13.
Frade S, Rodrigues H. Benefits, challenges and impact of teleconsultation – a literature review. Stud Health Technol Inform 2013;192:1157.
Freeman KA, Duke DC, Harris MA. Behavioral health care for adolescents with poorly controlled diabetes via Skype: does working alliance remain intact? J Diabetes Sci Technol 2013;7:727–35.
Garrett CC, Hocking J, Chen MY, Fairley CK, Kirkman M. Online sexual health consultations: examining young people’s privacy and security concerns. Eur J Contracept Reprod Health Care 2013;18:S111.
Goodyear-Smith F, Wearn A, Everts H, Huggard P, Halliwell J. Pandora’s electronic box: GPs reflect upon email communication with their patients. Inform Prim Care 2005;13:195–202.
Greenhalgh T, Swinglehurst D, Stones R. Rethinking resistance to big IT: a sociological study of why and when healthcare staff do not use nationally mandated information and communication technologies. Health Serv Deliv Res 2014;2(39).
Grustam AS, Severens JL, Van Nijnatten J, Koymans R, Vrijhoef HJM. Cost-effectiveness of telehealth interventions for chronic heart failure patients: a literature review. Int J Technol Assess Health Care 2014;30:59–68.
Gupta SG. Tips for telephone and electronic medical consultation. Indian J Pediatr 2013;80:944–8. https://doi.org/10.1007/s12098-013-1191-8
Hakimnia R, Holmstrom IK, Carlsson M, Hoglund AT. Exploring the communication between telenurse and caller-a critical discourse analysis. Int J Qual Stud Health Well-being 2014;9:24255.
Haluza D, Jungwirth D. ICT and the future of health care: aspects of doctor-patient communication. Int J Technol Assess Health Care 2014;30:298–305. https://doi.org/10.1017/S0266462314000294
Hanna L, Fairhurst K. Using information and communication technologies to consult with patients in Victorian primary care: the views of general practitioners. Aust J Prim Health 2013;19:166–70. https://doi.org/10.1071/PY11153
Hanna L, May C, Fairhurst K. The place of information and communication technology-mediated consultations in primary care: GPs’ perspectives. Fam Pract 2012;29:361–6. https://doi.org/10.1093/fampra/cmr087
Hansen CS, Christensen KL, Ertmann R. Patients and general practitioners have different approaches to e-mail consultations. Dan Med J 2014;61:A4863.
Harris MA, Hood KK, Mulvaney SA. Pumpers, skypers, surfers and texters: technology to improve the management of diabetes in teenagers. Diabetes Obes Metab 2012;14:967–72. https://doi.org/10.1111/j.1463-1326.2012.01599.x
Harrison S, Stadler M, Ismail K, Amiel S, Herrmann-Werner A. Are patients with diabetes mellitus satisfied with technologies used to assist with diabetes management and coping?: a structured review. Diabetes Technol Ther 2014;16:771–83.
Hasselberg M, Beer N, Blom L, Wallis LA, Laflamme L. Image-based medical expert teleconsultation in acute care of injuries. A systematic review of effects on information accuracy, diagnostic validity, clinical outcome, and user satisfaction. PLOS ONE 2014;9:e98539.
Haun JN, Lind JD, Shimada SL, Martin TL, Gosline RM, Antinori N, et al. Evaluating user experiences of the secure messaging tool on the Veterans Affairs’ patient portal system. J Med Internet Res 2014;16:e75. https://doi.org/10.2196/jmir.2976
Hendy J, Fulop N, Reeves BC, Hutchings A, Collin S. Implementing the NHS information technology programme: qualitative study of progress in acute trusts. BMJ 2007;334:1360.
Hendy J, Reeves BC, Fulop N, Hutchings A, Masseria C. Challenges to implementing the national programme for information technology (NPfIT): a qualitative study. BMJ 2005;331:331–6.
Himle MB, Freitag M, Walther M, Franklin SA, Ely L, Woods DW. A randomized pilot trial comparing videoconference versus face-to-face delivery of behavior therapy for childhood tic disorders. Behav Res Ther 2012;50:565–70.
Hofstede J, de Bie J, van Wijngaarden B, Heijmans M. Knowledge, use and attitude toward eHealth among patients with chronic lung diseases. Int J Med Inform 2014;83:967–74. https://doi.org/10.1016/j.ijmedinf.2014.08.011
Holt T, Fletcher E, Warren F, Richards S, Salisbury C, Calitri R, et al. Telephone triage systems in UK general practice: analysis of consultation duration during the index day in a pragmatic randomised controlled trial. Br J Gen Pract 2016;66:e214–8.
Houston TK, Sands DZ, Jenckes MW, Ford DE. Experiences of patients who were early adopters of electronic communication with their physician: satisfaction, benefits, and concerns. Am J Manag Care 2004;10:601–8.
Huibers L, Koetsenruijter J, Grol R, Giesen P, Wensing M. Follow-up after telephone consultations at out-of-hours primary care. J Am Board Fam Med 2013;26:373–9. https://doi.org/10.3122/jabfm.2013.04.120185
Ireland S, Kent B. Telephone pre-operative assessment for adults: a comprehensive systematic review. JBI Libr Syst Rev 2012;10:1452–503.
Jiwa M, Meng X. Video consultation use by Australian general practitioners: video vignette study. J Med Internet Res 2013;15:e117. https://doi.org/10.2196/jmir.2638
Joffe E, Turley JP, Hwang KO, Johnson TR, Johnson CW, Bernstam EV. Errors in after-hours phone consultations: a simulation study. BMJ Qual Saf 2014;23:398–405. https://doi.org/10.1136/bmjqs-2013-002243
Johansson AM, Lindberg I, Söderberg S. The views of health-care personnel about video consultation prior to implementation in primary health care in rural areas. Prim Health Care Res Dev 2014;15:170–9. https://doi.org/10.1017/S1463423613000030
Johansson AM, Lindberg I, Söderberg S. Patients’ experiences with specialist care via video consultation in primary healthcare in rural areas. Int J Telemed Appl 2014;2014:143824. https://doi.org/10.1155/2014/143824
Joseph P, Leong K, Banerjee M, Leong KS. The effectiveness of telephone consultation in patients with diabetes. Diabet Med 2014;31:173.
Keely E, Liddy C, Afkham A. Utilization, benefits, and impact of an e-consultation service across diverse specialties and primary care providers. Telemed J E Health 2013;19:733–8. https://doi.org/10.1089/tmj.2013.0007
Knapp M. Tele-video consultations: a useful adjunct for regional nephrology? Nephrology 2013;18:62.
Koivunen M, Saranto K. Nursing professionals’ experiences of the facilitators and barriers to the use of telehealth applications: – a systematic review of qualitative evidence. JBI Libr Syst Rev 2012;10:3894–906.
Labacher L, Mitchell C. Talk or text to tell? How young adults in Canada and South Africa prefer to receive STI results, counseling, and treatment updates in a wireless world. J Health Commun 2013;18:1465–76. https://doi.org/10.1080/10810730.2013.798379
Labrie N, Schulz PJ. Does argumentation matter? A systematic literature review on the role of argumentation in doctor-patient communication. Health Commun 2014;29:996–1008.
Lam R, Lin VS, Senelick WS, Tran HP, Moore AA, Koretz B. Older adult consumers’ attitudes and preferences on electronic patient-physician messaging. Am J Manag Care 2013;19:eSP7–11.
Lee SAS, McElroy S. Telepractice is a new method for providing services to children with Autism Spectrum Disorder (ASD): this scoping review summarizes existing research and identifies research gaps. Evid Based Commun Assess Interv 2012;6:177–80.
Lemieux J, Tran A, Brienza V, Jurencak R. Telephone consultation usage in a pediatric rheumatology clinic: considerations in optimizing nursing resources. Arthritis Rheum 2013;65:S1194.
Liddy C, Maranger J, Afkham A, Keely E. Ten steps to establishing an e-consultation service to improve access to specialist care. Telemed J E Health 2013;19:982–90. https://doi.org/10.1089/tmj.2013.0056
Little P, White P, Kelly J, Everitt H, Gashi S, Bikker A, Mercer S. Verbal and non-verbal behaviour and patient perception of communication in primary care: an observational study. Br J Gen Pract 2015;65:e357–65. https://doi.org/10.3399/bjgp15X685249
Little P, White P, Kelly J, Everitt H, Mercer S. Randomised controlled trial of a brief intervention targeting predominantly non-verbal communication in general practice consultations. Br J Gen Pract 2015;65:e351–e6. http://dx.doi.org/10.3399/bjgp15X685237
Lundvoll Nilsen L, Andreassen HK. Videoconferencing in acute and non-acute medical work. Stud Health Technol Inform 2013;190:36–8.
Lupiañez-Villanueva F, Maghiros I, Abadie F. Strategic Intelligence Monitor on Personal Health Systems phase 2 (SIMPHS2) Citizens and ICT for Health in 14 EU Countries: Results from an Online Panel. Seville: European Commission Joint Research Centre, Institute for Prospective Technological Studies; 2012.
MacNeill V, Sanders C, Fitzpatrick R, Hendy J, Barlow J, Knapp M, et al. Experiences of front-line health professionals in the delivery of telehealth: a qualitative study. Br J Gen Pract 2014;64:e401–7. https://doi.org/10.3399/bjgp14X680485
Majeed A. Data from one GP to inform the debate whether patients should be able to email their general practitioner. BMJ 2014;349:g5766. https://doi.org/10.1136/bmj.g5766
Marconi GP, Chang T, Pham PK, Grajower DN, Nager AL. Traditional nurse triage vs physician telepresence in a pediatric ED. Am J Emerg Med 2014;32:325–9. https://doi.org/10.1016/j.ajem.2013.12.032
Markus PA, Leatherwood SM. How to safely communicate by e-mail with patients. J Med Assoc Ga 2012;101:38.
McKinstry B, Hammersley V, Burton C, Pinnock H, Elton R, Dowell J, et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010;19:298–303. https://doi.org/10.1136/qshc.2008.027763
Meher SK, Biswas A, Ratha BK. Legal issues among doctors in the implementation of teleconsultation: a study at AIIMS, New Delhi, India. Stud Health Technol Inform 2013;192:1107.
Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med 2013;173:72–4. https://doi.org/10.1001/2013.jamainternmed.305
Mignerat M, Lapointe L, Vedel I. Using telecare for diabetic patients: a mixed systematic review. Health Policy Technol 2014;3:90-112.
Mohammad M, Freeman M. Integrated diabetes care: the benefit of e-consultations. Diabet Med 2014;31(Suppl. 1):161.
Moravej H. Are general physicians prepared to respond to telephone consultations? Iran J Pediatr 2012;22:575–6.
Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol 2013;8:472–81.
Moth G, Huibers L, Christensen MB, Vedsted P. Drug prescription by telephone consultation in Danish out-of-hours primary care: a population-based study of frequency and associations with clinical severity and diagnosis. BMC Fam Pract 2014;15:142. https://doi.org/10.1186/1471-2296-15-142
Muscarella M, Kranenburg-van Koppen L, Grijpink-van den Biggelaar K, Drop SL. Global application of disorders of sex development-related electronic resources: e-learning, e-consultation and e-information sharing. Endocr Dev 2014;27:268–83.
Muskens EM, Lucassen P, Groenleer W, van Weel C, Oude Voshaar R, Speckens A. Psychiatric diagnosis by telephone: is it an opportunity? Soc Psychiatry Psychiatr Epidemiol 2014;49:1677–89. https://doi.org/10.1007/s00127-014-0861-9
Najera C, Ivorra J, Chalmeta I, Grau E, Valero JL, Garcia-Armario MD, et al. Activity of telephone consultation to nursing by request in rheumatology. Ann Rheum Dis 2013;72(Suppl. 3):1090.
Neergaard MA, Warfvinge JE, Jespersen TW, Olesen F, Ejskjaer N, Jensen AB. The impact of ‘modern telecommunication’ in palliative care – the views of the professionals. Telemed J E Health 2014;20:24–31. https://doi.org/10.1089/tmj.2013.0047
Neville RG, Marsden W, McCowan C, Pagliari C, Mullen H, Fannin A. A survey of GP attitudes to and experiences of email consultations. Inform Prim Care 2004;12:201–6.
Newhouse N, Lupiáñez-Villanueva F, Codagnone C, Atherton H. Patient use of email for health care communication purposes across 14 European countries: an analysis of users according to demographic and health-related factors. J Med Internet Res 2015;17:e58. http://dx.doi.org/10.2196/jmir.3700
O’Cathain A, Knowles E, Turner J, Nicholl J. Acceptability of NHS 111 the telephone service for urgent health care: cross sectional postal survey of users’ views. Fam Pract 2014;31:193–200.
Oliveira TC, Barlow J, Gonçalves L, Bayer S. Teleconsultations reduce greenhouse gas emissions. J Health Serv Res Policy 2013;18:209–14. https://doi.org/10.1177/1355819613492717
Ortega Egea JM, González MV, Menéndez MR. eHealth usage patterns of European general practitioners: a five-year (2002-2007) comparative study. Int J Med Inform 2010;79:539–53. https://doi.org/10.1016/j.ijmedinf.2010.05.003
Patel PB, Vinson DR. Physician email and telephone follow-up after emergency department visit improves patient satisfaction: a cross-over trial. Ann Emerg Med 2011;1:S252.
Pearl R. Kaiser permanente Northern California: current experiences with internet, mobile, and video technologies. Health Aff (Milwood) 2014;33:251–7.
Pedersen KM, Andersen JS, Søndergaard J. General practice and primary health care in Denmark. J Am Board Fam Med 2012;25(Suppl. 1):34–8. https://doi.org/10.3122/jabfm.2012.02.110216
Peleg R, Nazarenko E. Providing cell phone numbers and e-mail addresses to patients: the patient’s perspective, a cross sectional study. Isr J Health Policy Res 2012;1:32. https://doi.org/10.1186/2045-4015-1-32
Philip S, Milne N, Page C, McCallum C, Kelday A, Gilmour T, et al. Teleconsultation is an effective method of supporting diabetes care in a remote and rural setting. Diabet Med 2014;31:175.
Plener I, Hayward A, Saibil F. E-mail communication in the management of gastroenterology patients: a review. Can J Gastroenterol Hepatol 2014;28:161–5.
Purc-Stephenson RJ, Thrasher C. Patient compliance with telephone triage recommendations: a meta-analytic review. Patient Educ Couns 2012;87:135–42. https://doi.org/10.1016/j.pec.2011.08.019
Pygall S-A. Improving patient care with the use of telephone consultations. Prim Health Care 2012;22:28–30.
Raven M, Butler C, Bywood P. Video-based telehealth in Australian primary health care: current use and future potential. Aust J Prim Health 2013;19:283–6. https://doi.org/10.1071/PY13032
Rezende EJ, Tavares EC, Alves HJ, dos Santos Ade F, de Melo Mdo C. Teleconsultations in public primary care units of the city of belo horizonte, Brazil: profile of patients and physicians. Telemed J E Health 2013;19:613–18. https://doi.org/10.1089/tmj.2012.0179
Rojjanasrirat W, Nelson EL, Wambach KA. A pilot study of home-based videoconferencing for breastfeeding support. J Hum Lact 2012;28:464–7. https://doi.org/10.1177/0890334412449071
Roland M, Barber N, Imison C, Howe A, Rubin G, Storey K. The Future of Primary Care: Creating Teams for Tomorrow. London: Health Education England; 2015. URL: http://hee.nhs.uk/wp-content/blogs.dir/321/files/2015/07/The-future-of-primary-care.pdf (accessed 8 February 2017).
Rubin MN, Wellik KE, Channer DD, Demaerschalk BM. A systematic review of telestroke. Postgrad Med 2013;125:45–50. https://doi.org/10.3810/pgm.2013.01.2623
Ruiz IS, García GP, Riquelme I. E-mail communication in pain practice: the importance of being earnest. Saudi J Anaesth 2014;8:364–7. https://doi.org/10.4103/1658-354X.136434
Sabesan S, Kelly J, Evans R, Larkins S. A tele-oncology model replacing face-to-face specialist cancer care: perspectives of patients in North Queensland. J Telemed Telecare 2014;20:207–11.
Saied A, Sherry SJ, Castricone DJ, Perry KM, Katz SC, Somasundar P. Age-related trends in utilization of the internet and electronic communication devices for coordination of cancer care in elderly patients. J Geriatr Oncol 2014;5:185–9.
Salles N, Baudon MP, Caubet C, Dallay F, Chaleuil M, Magne S, et al. Telemedicine consultations for the elderly with chronic wounds, especially pressure sores. Eur Res Telemed 2013;2:93–100.
Scharff JS. Clinical issues in analyses over the telephone and the internet. Int J Psychoanal 2012;93:81–95. https://doi.org/10.1111/j.1745-8315.2011.00548.x
Schickedanz A, Huang D, Lopez A, Cheung E, Lyles CR, Bodenheimer T, Sarkar U. Access, interest, and attitudes toward electronic communication for health care among patients in the medical safety net. J Gen Intern Med 2013;28:914–20. https://doi.org/10.1007/s11606-012-2329-5
Schulz TR, Richards M, Gasko H, Lohrey J, Hibbert ME, Biggs BA. Telehealth: experience of the first 120 consultations delivered from a new refugee telehealth clinic. Intern Med J 2014;44:981–5. https://doi.org/10.1111/imj.12537
Scrivo R, Priori R, Coppola M, Minniti A, Brandt J, Picarelli G, et al. Use of a contact center telephone helpline in rheumatology outpatient management: A five-year experience analysis and patients’ perception. Mod Rheumatol 2014;24:585–9.
Segar J, Rogers A, Salisbury C, Thomas C. Roles and identities in transition: boundaries of work and inter-professional relationships at the interface between telehealth and primary care. Health Soc Care Community 2013;21:606–13. https://doi.org/10.1111/hsc.12047
Seguranyes G, Costa D, Fuentelsaz-Gallego C, Beneit JV, Carabantes D, Gomez-Moreno C, et al. Efficacy of a videoconferencing intervention compared with standard postnatal care at primary care health centres in Catalonia. Midwifery 2014;30:764–71.
Sharwardy SN, Parveen S, Sarwar H, Rahman Z. An analysis of a videoconference-based teleconsultation system in Bangladesh. J Telemed Telecare 2012;18:303–4. https://doi.org/10.1258/jtt.2011.110004
Shepherd E. Use Skype to Boost Access to GP Services ‘Can Patients be Accurately Assessed Using Skype and Email?’. 2014. URL: www.nursingtimes.net/can-patients-be-accurately-assessed-using-skype-and-email/5070058.blog (accessed 8 February 2017).
Sifferlin A. The doctor will Skype you now. Telemedicine apps aim to replace nonemergency visits. Time 2014;183:12.
Stoop EM, de Wijkerslooth TR, Bossuyt PM, Stoker J, Fockens P, Kuipers EJ, et al. Face-to-face vs telephone pre-colonoscopy consultation in colorectal cancer screening; a randomised trial. Br J Cancer 2012;107:1051–8. https://doi.org/10.1038/bjc.2012.358
Tan K, Lai NM. Telemedicine for the support of parents of high-risk newborn infants. Cochrane Database Syst Rev 2012;6:CD006818. https://doi.org/10.1002/14651858.CD006818.pub2
Tan L, Hu W, Brooker R. Patient-initiated camera phone images in general practice: a qualitative study of illustrated narratives. Br J Gen Pract 2014;64:e290–4. https://doi.org/10.3399/bjgp14X679723
Thompson-Coon J, Abdul-Rahman AK, Whear R, Bethel A, Vaidya B, Gericke CA, et al. Telephone consultations in place of face-to-face out-patient consultations for patients discharged from hospital following surgery: a systematic review. BMC Health Serv Res 2013;13:128.
Tjora A, Tran T, Faxvaag A. Privacy vs usability: a qualitative exploration of patients’ experiences with secure Internet communication with their general practitioner. J Med Internet Res 2005;7:e15.
Travers CP, Murphy JF. Neonatal telephone consultations in the National Maternity Hospital. Ir Med J 2014;107:251–2.
van der Kop ML, Karanja S, Thabane L, Marra C, Chung MH, Gelmon L, et al. In-depth analysis of patient–clinician cell phone communication during the WelTel Kenya1 antiretroviral adherence trial. PLOS ONE 2012;7:e46033.
van Gurp J, Hasselaar J, van Leeuwen E, Hoek P, Vissers K, van Selm M. Connecting with patients and instilling realism in an era of emerging communication possibilities: a review on palliative care communication heading to telecare practice. Patient Educ Couns 2013;93:504–14.
van Gurp J, van Selm M, van Leeuwen E, Hasselaar J. Transmural palliative care by means of teleconsultation: a window of opportunities and new restrictions. BMC Med Ethics 2013;14:12. https://doi.org/10.1186/1472-6939-14-12
Van Gurp JLP, Hasselaar J, Vissers K, Van Leeuwen E, Van Selm M. How technologized care can lead to compassionate professional involvement: a longitudinal, qualitative multiple case study about teleconsultation in palliative home care. Palliat Med 2014;28:587.
van Velthoven MH, Tudor Car L, Car J, Atun R. Telephone consultation for improving health of people living with or at risk of HIV: a systematic review. PLOS ONE 2012;7:e36105. https://doi.org/10.1371/journal.pone.0036105
Varsi C, Gammon D, Wibe T, Ruland CM. Patients’ reported reasons for non-use of an internet-based patient-provider communication service: qualitative interview study. J Med Internet Res 2013;15:e246.
Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev 2012;12:CD007457. https://doi.org/10.1002/14651858.CD007457.pub2
Waterman BR, Laughlin MD, Belmont PJ, Schoenfeld AJ, Pallis MP. Enhanced casualty care from a Global Military Orthopaedic Teleconsultation Program. Injury 2014;45:1736–40.
Weiner JP. Doctor–patient communication in the e-health era. Isr J Health Policy Res 2012;1:33. https://doi.org/10.1186/2045-4015-1-33
Wibe T, Helleso R, Varsi C, Ruland C, Ekstedt M. How does an online patient-nurse communication service meet the information needs of men with recently diagnosed testicular cancer? ISRN Nurs 2012;2012:260975.
Winthereik BR, Langstrup H. When Patients Care (Too Much) for Information. In Mol AM, Moser I, Pols J, editors. Care in Practice: On Tinkering in Clinics, Homes and Farms. Bielefield: Transcript Verlag; 2010. pp. 195–213.
Woolford SJ, Blake N, Clark SJ. Texting, tweeting, and talking: e-communicating with adolescents in primary care. Contemp Pediatr 2013;30:12–18.
Wynn R, Bergvik S, Pettersen G, Fossum S. Clinicians’ experiences with videoconferencing in psychiatry. Stud Health Technol Inform 2012;180:1218–20.
You A, Kawamoto J, Smith JP. A pharmacist-managed telemedicine clinic for hepatitis C care: a descriptive analysis. J Telemed Telecare 2014;20:99–101. https://doi.org/10.1177/1357633X13519043
Zanaboni P, Knarvik U, Wootton R. Adoption of routine telemedicine in Norway: the current picture. Glob Health Action 2014;7:22801. https://doi.org/10.3402/gha.v7.22801
Appendix 4 Case study guide
Objective of the case studies
-
In the case study practices, to explore how practice context, patient characteristics, type of technology and the purpose of the consultation appear to interact to determine the feasibility and the impact of alternatives to face-to-face consultations, from the perspectives of both patients and staff. This includes the impact on the clinician–patient dynamic.
-
The impact for isolated, disabled, disadvantaged and other vulnerable or hard-to-reach groups will be a particular focus.
We are interested in the following groups:
Staff: GPs, nurses, reception staff, practice management, administrative staff, other staff (practice-based and community-based nurses, pharmacists and allied health professionals, such as phlebotomists or community-based physiotherapists).
Patients: all patients, with particular interest in carers, family members and disadvantaged groups.
We are interested in the following consultation technologies:
-
e-mail, including patient portals, web portal and standard e-mail
-
telephone
-
video consultations
-
SMS.
We are hoping to build on themes that have been well reported in the literature with regard to GPs and patient perspectives on the advantages and disadvantages of using alternatives to the face-to-face consultation. Please see the full protocol for the background to the project and a summary of these factors.
The factors within alternatives to the face-to-face consultation that we aim to explore have come from the findings of our realist review and from the patient–public involvement workshop that we held in April 2015. The workshop was attended by five members of the public. We briefly described the study and asked the group to consider three key issues:
-
If GPs offer consultations without the need for the patient to visit the practice (e.g. by telephone, e-mail or video conferencing), what do you see as the benefits and disadvantages to patients?
-
What about practice staff, what might be the benefits and disadvantages to them?
-
What do you think might encourage or discourage both practices and patients to adopt this approach to consultations?
You should consider the factors listed here when conducting observations and interviews, but it is not an exhaustive or a prescriptive list.
Reception staff
| Tasks | Per-protocol approach | Factors to explore |
|---|---|---|
|
|
|
|
|
|
Practice managers
| Tasks | Per-protocol approach | Factors to explore |
|---|---|---|
|
|
|
|
|
|
|
|
General practitioners
| Tasks | Per-protocol approach | Factors to explore |
|---|---|---|
|
|
|
|
|
Nurses
| Tasks | Per-protocol approach | Factors to explore |
|---|---|---|
|
|
|
Wider team
| Tasks | Per-protocol approach | Factors to explore |
|---|---|---|
|
|
|
Patients
| Tasks | Per-protocol approach | Factors to explore |
|---|---|---|
|
|
|
Isolated, disabled, disadvantaged or vulnerable or hard-to-reach groups and carers
| Tasks | Per-protocol approach | Factors to explore |
|---|---|---|
|
|
|
The following table includes factors that you should be aware of that relate to the specific type of alternatives to the face-to-face consultation.
| Technology | Factors to be aware of |
|---|---|
E-mail
|
|
| Portals |
|
| WebGP |
|
| Video |
|
Telephone
|
|
The following table includes specific issues you should consider before commencing the ethnography.
| Specific issues | Factors |
|---|---|
| Level of engagement with patient | How to read an alternative to the face-to-face consultation? |
| Software/hardware | Efficient support system for fixing and maintaining equipment? |
| Set-up | When this change was introduced, was there any co-design? |
| ‘Early adopters’ | Those using alternatives to the face-to-face consultation in the UK may be unusual, and this should be considered |
| Characteristics of the general practice | The target patient population, the policy framework and the IT infrastructure |
Appendix 5 Topic guides for semistructured interviews
-
Interviews will last up to 1 hour.
-
Begin by collecting demographic information using the facesheet.
-
Where practices are no longer using alternatives, please apply the prompts in the past tense.
-
Please substitute ‘alternatives to the face-to-face consultation’ for the relevant technology.
Topic guide for reception and administrative staff
1. What is it like to work in this practice?
-
What is your role?
-
Collaborative working, i.e. involvement in decision-making?
-
Pros and cons.
2. Your role in alternatives to the face-to-face consultation
-
Clarify scope of involvement and role.
-
Role in administering alternatives to the face-to-face consultation (how role may have changed over time).
3. Introduction of alternatives to the face-to-face consultation
-
What is your understanding of why was it introduced?
-
How long did it take you to get used to?
-
How has it had an impact on how you do your job, e.g. appointment systems?
-
Did you have to have training? What form did this take? If not why not?
-
How are security and confidentiality addressed? Are you happy with the systems in use?
4. Delivery of alternatives to the face-to-face consultation
-
Type of alternatives to the face-to-face consultation they can offer to patients?
-
Types of patients allowed/encouraged to use alternatives?
-
Which patients take it up?
-
Benefits to the patient?
5. Impact of alternatives to the face-to-face consultation on role
-
Has it had any impact on your job role, satisfaction, stress?
-
Have you encountered any difficulties? How have these been addressed?
-
Has it changed your perspective of the practice as a place to work?
6. View of alternatives to the face-to-face consultation used in the practice
-
What has the impact been in the practice?
-
Where use has ceased, what has changed?
-
Benefits to the practice?
7. Personal views of alternatives to the face-to-face consultation
-
What are your thoughts on the future of alternatives to the face-to-face consultation in general practice?
-
Where do you think it will go? Does it excite/worry you?
Topic guide for nurses
1. What is it like to work in this practice? (just before I start this interview)
-
What is your role?
-
Collaborative working, i.e. involvement in decision-making?
-
Pros and cons.
2. Your role in alternatives to the face-to-face consultation
-
Clarify scope of involvement and role (GP involvement? Individual vs team use?)
-
Role in administering alternatives to the face-to-face consultation (how role may have changed over time).
3. Introduction of alternatives to the face-to-face consultation
-
How did use come about? Were you involved?
-
If not, how did you end up using alternatives to the face-to-face consultation?
-
Did you have to have training? What form did this take? If not why not?
-
How are security and confidentiality addressed? Are you happy with the systems in use?
4. Delivery of alternatives to the face-to-face consultation
-
Type of alternatives to the face-to-face consultation you engage in? Why this type?
-
How long did it take you to get used to?
-
Who uses it, why and what happens as a result? E.g. type of patients encouraged to use it, others discouraged?
-
What are the benefits to your patients?
-
Impact on dynamic/relationship with patient.
-
Experienced any critical incidents/significant events?
5. Impact of alternatives to the face-to-face consultation on role
-
Has it had any impact on your job role, satisfaction, stress?
-
Have you encountered any difficulties? How have these been addressed?
-
What are your feelings about level of responsibility in your role when using alternatives to the face-to-face consultation?
-
Has it changed your perspective of the practice as a place to work?
6. View of alternatives to the face-to-face consultation use in the practice
-
Have views about technology in the practice changed since introducing alternatives to the face-to-face consultation?
-
Where use has ceased, what has changed?
-
Benefits to the practice?
7. Personal views of alternatives to the face-to-face consultation
-
What are your thoughts on the future of alternatives to the face-to-face consultation in general practice?
-
Where do you think it will go? Does it excite/worry you?
Topic guide for GPs
1. What is it like to work in this practice? (Just before I start this interview)
-
What is your role?
-
Collaborative working, i.e. involvement in decision-making?
-
Pros and cons.
2. Your role in alternatives to the face-to-face consultation
-
Clarify scope of involvement and role (GP involvement? Individual vs team use?)
-
Role in administering alternatives to the face-to-face consultation (how role may have changed over time).
3. Introduction of alternatives to the face-to-face consultation
-
How did use come about? Were you involved?
-
If not how did you end up using alternatives to the face-to-face consultation?
-
Did you have to have training? What form did this take? If not why not?
-
How are security and confidentiality addressed? Are you happy with the systems in use?
-
Any steps taken to ensure medicolegal protection?
4. Delivery of alternatives to the face-to-face consultation
-
Type of alternatives to the face-to-face consultation you engage in? Why this type?
-
How long did it take you to get used to?
-
Who uses it, why and what happens as a result? E.g. type of patients encouraged to use it, others discouraged?
-
What are the benefits to your patients?
-
Impact on dynamic/relationship with patient.
-
Experienced any critical incidents/significant events?
-
How do you record these consultations?
5. Impact of alternatives to the face-to-face consultation on role
-
Has it had any impact on your job role, satisfaction, stress?
-
Have you encountered any difficulties? How have these been addressed?
-
What are your feelings about level of responsibility in your role when using alternatives to the face-to-face consultation?
-
Has it changed your perspective of the practice as a place to work?
6. View of alternatives to the face-to-face consultation use in the practice
-
Have views about technology in the practice changed since introducing alternatives to the face-to-face consultation?
-
Where use has ceased, what has changed?
-
Benefits to the practice?
7. Personal views of alternatives to the face-to-face consultation
-
What are your thoughts on the future of alternatives to the face-to-face consultation in general practice?
-
Where do you think it will go? Does it excite/worry you?
Topic guide for wider members of the team (health-care professionals)
1. What is it like to work in this practice (just before I start this interview)
-
What is your role?
-
Collaborative working, i.e. involvement in decision-making?
-
Pros and cons.
2. Your role in alternatives to the face-to-face consultation
-
Clarify scope of involvement and role (Individual vs team use?)
-
Role in administering alternatives to the face-to-face consultation (how role may have changed over time).
3. Introduction of alternatives to the face-to-face consultation
-
How did use come about? Were you involved?
-
If not how did you end up using alternatives to the face-to-face consultation?
-
Did you have to have training? What form did this take? If not why not?
-
How are security and confidentiality addressed? Are you happy with the systems in use?
4. Delivery of alternatives to the face-to-face consultation
-
Type of alternatives to the face-to-face consultation you engage in? Why this type?
-
How long did it take you to get used to?
-
Who uses it, why and what happens as a result? E.g. type of patients encouraged to use it, others discouraged?
-
What are the benefits to your patients?
-
Impact on dynamic/relationship with patient.
-
Experienced any critical incidents/significant events?
-
How do you record these consultations?
5. Impact of alternatives to the face-to-face consultation on role
-
Has it had any impact on your job role, satisfaction, stress?
-
Have you encountered any difficulties? How have these been addressed?
-
What are your feelings about level of responsibility in your role when using alternatives to the face-to-face consultation?
-
Has it changed your perspective of the practice as a place to work?
6. View of alternatives to the face-to-face consultation use in the practice
-
Have views about technology in the practice changed since introducing alternatives to the face-to-face consultation?
-
Where use has ceased, what has changed?
-
Benefits to the practice?
7. Personal views of alternatives to the face-to-face consultation
-
What are your thoughts on the future of alternatives to the face-to-face consultation in general practice?
-
Where do you think it will go? Does it excite/worry you?
Topic guide for practice manager
1. What is it like to work in this practice (just before I start this interview)
-
What is your role?
-
Collaborative working, i.e. involvement in decision-making?
-
Pros and cons.
2. Your role in alternatives to the face-to-face consultation
-
Clarify scope of involvement and role.
-
Role in development and introduction of alternatives to the face-to-face consultation in the practice.
3. Introduction of alternatives to the face-to-face consultation
-
Reasons for introduction, perceived benefits? Who was involved in establishing alternatives to the face-to-face consultation?
-
Alternatives to the face-to-face consultation occurring throughout or just by certain staff?
-
Investment by the practice in alternatives to the face-to-face consultation.
-
Are there protocols in place for use? How did these come about?
-
How were systems for information handling developed?
-
How are security and confidentiality addressed?
-
How long did it take to embed into the practice?
4. Delivery of alternatives to the face-to-face consultation
-
Types of alternatives to the face-to-face consultation on offer in practice?
-
Which members of practice staff involved and why?
-
Which patients use it and why?
-
Parameters around who can use alternatives to the face-to-face consultation and what for?
5. Alternatives to the face-to-face consultation and information handling
-
Experienced any data breaches?
-
How have medicolegal concerns been addressed?
-
Have any issues arisen with the computer systems, appointment systems or telephone systems?
-
Have there been any critical incidents/significant events?
-
Training of staff in using alternatives to the face-to-face consultation
-
How have patients been informed about alternatives to the face-to-face consultation?
-
Impact on workload, workforce planning, utilisation of resources.
-
Difficulties encountered and how these have been addressed?
6. Impact of alternatives to the face-to-face consultation on role
-
Has it had any impact on your job role, satisfaction, stress?
-
Has it had any impact on the roles of the staff you manage?
7. View of alternatives to the face-to-face consultation use in the practice
-
Have views about technology in the practice changed since introducing alternatives to the face-to-face consultation?
-
What have been the benefits of the different types of alternatives to the face-to-face consultation to the practice?
-
What barriers have been encountered in using alternatives to the face-to-face consultation?
-
Where use has ceased, what has changed?
8. Personal views of alternatives to the face-to-face consultation
-
What are your thoughts on the future of alternatives to the face-to-face consultation in general practice?
-
Where do you think it will go? Does it excite/worry you?
Appendix 6 Description of the case study practices
Each account was written by the ethnographer working in the practice.
Practice A
Practice A was a large practice with > 18,000 registered patients served by four GP partners, seven salaried GPs, one GP trainee and one clinical pharmacist independent prescriber. There are six practice nurses, three of which hold minor illness clinics, three treatment room nurses supported by two HCAs and one phlebotomist. There was a practice manager and an operations manager supported by a large team of admin and reception staff. There are 12 members of reception staff (plus a further two in a sister practice located nearby that are included within the practice), three of which are full time. They start on a probation period and are expected to complete a list of competencies within 6 months of starting. The receptionists work a shift pattern to accommodate the extended hours that the practice operates – many work 1 week of earlies followed by a week of lates with some starting midday. It manages two sister practices, one that was next door and one that was in the neighbouring county.
It was an inner-city practice that was in a deprived area with an IMD score of three, but with pockets of affluence. It serves an incredibly diverse population. It was located within a multicultural area with a high percentage of their patients being non-English speakers. The practice also hosts a local drugs project and a service for new immigrants. It had access to translation services (either face-to-face or via telephone), a high prevalence of drug and alcohol problems with a number of probation hostels within their boundary while including areas with high levels of students and professionals. The practice struggles to recruit and retain staff (in line with national challenges). It had an active patient participation group.
The practice had recently (since March 2015) been piloting e-consult software hosted by a local consortium, so it was provided at no cost to the practice; however, one of their GPs had been to a presentation by the group that devised the software and was considering introducing it before it was offered for free as a pilot. However, the uptake by patients of e-consult software was low. The practice also offers telephone consultations, as advertised on their website, but this was in an ad hoc way. This information was supported by the results from the GP survey. Consultations by e-mail or internet video are not officially offered, however, I learnt that some of the GPs do use e-mail with selected patients. They also operate a telephone triage system where there can be a blurring between triage and consult.
The practice manager was very keen on the use of technology and since I completed data collection had introduced Wi-Fi in the waiting room to encourage patients to use online services. Many of the staff, in particular the GPs, have smart phones with them and regularly respond to texts, etc. In addition, the practice offers patients the ability to book appointments or order prescriptions online but they need to register first and patients are encouraged to log their arrival on a screen in the waiting room. Information was provided to the waiting room via an electronic screen. The practice relies heavily on technology for all its internal correspondence using EMIS to communicate about clinical matters and e-mail for non-clinical. They rarely speak to each other by phone or even face to face. The different staff groups seem to share separate social areas and do not interact with each other very often. The doctors rarely leave their consulting rooms. The different staff groups seem to share separate social areas and do not interact with each other very often. The practice participates regularly in research and was very familiar with the whole process.
Alternatives offered:
-
Telephone – telephone consultation was open to all patients with an ad hoc approach to scheduling.
-
E-mail – only a couple of GPs used e-mail consultations with selected patients.
-
E-consult – the practice had been recently piloting e-consult software with an ad hoc approach to scheduling.
Practice B
Practice B was a moderately sized practice with c. 9000 registered patients served by three GP partners, seven salaried GPs, one GP trainee and one clinical pharmacist independent prescriber. This was supplemented by the regular use of locum doctors. There are three practice nurses, one treatment room nurse supported by one health care assistant. The practice manager was supported by a team of seven admin and eight reception staff. There was little staff turnover and many of the staff have worked in the practice for a number of years. New employees are the result of either expansion or to replace those who have retired. There was no formal training for the receptionists but they begin with two weeks where they observe the existing reception staff and then they will be supervised for a further two weeks depending on their progress.
The practice operates from 8.30 a.m.–6.30 p.m. each day with an extended opening on Monday (until 7.30 p.m.) and run a morning clinic one Saturday a month. The receptionists work a shift pattern to accommodate the hours that the practice operates. It did not operate a triage system so patients who request a same day appointment will be given one if one is available. These are not seen as for emergency reasons only but a method of offering routine appointments. Similarly, if someone requests a home visit this was accepted and added to a central list of requested home visits that the GPs share among themselves and do after morning surgery was complete. There was some interaction between the differing staff groups and the doctors regularly meet each day, this often includes the clinical pharmacist and the practice manager. While I have been in the practice I have noticed that the practitioners leave their consulting room doors open when they are not seeing patients. By doing this it makes for a more accessible environment and invites interactions between the staff.
The practice resides in a brand new building, opened late September 2015, which it shares with another smaller practice and also hosts a Citywide Community Health service. In addition, there was a strong corporate image with all the staff (with the exception of the GPs and practice manager) wearing uniforms. It was an inner-city practice that was in a deprived area with an IMD score of three. It serves a diverse population. It was located within a multicultural area with a high percentage of their patients being non-English speakers, with patients coming from India, Somalia and Eastern Europe in the main.
The practice offers telephone consultations and this was advertised on their website. This was managed in a semistructured way, with some appointments ring-fenced for telephone consultations. Consultations by e-mail are not officially offered currently, however, I learnt that some of the GPs do use e-mail with selected patients. In addition, although they do not offer internet video currently, the Practice Manager was very keen to introduce Skype consultations after attending a presentation from a GP currently using Skype. This was supported by the results from the GP survey. The practice relies heavily on technology for all its correspondence using the practice software to communicate about clinical matters and e-mail for non-clinical. They rarely speak to each other by phone but often speak face-to-face. Since the move to the new building many of the practices have changed and one of these was less access to each other. Many of the staff, in particular the GPs, have smart phones on them and are regular responding to texts etc. In addition, the practice offers patients the ability to book appointments or order prescriptions online but they need to register first. The practice participates infrequently in research and despite being unfamiliar with the whole process they were very interested and welcoming.
Alternatives offered:
-
Telephone – telephone consultation was open with all patients.
-
E-mail – only a couple of GPs used e-mail consultations with selected patients.
Practice C
Practice C was a large practice with c.15000 patients served by eight GP partners and five salaried GPs. There are six practice nurses and three HCAs, and the practice was managed by one business partner/practice manager supported by seven admin staff and fourteen receptionists (two of which are dedicated to the treatment room). The turnover of staff was marginal with staff being in post from within the last few months to decades. There was little evidence of the use of locum staff. The receptionists do not wear a uniform and their training was fairly informal – they observe an experienced receptionist for 2–4 weeks and then are supervised for a further 2–4 weeks until they feel and appear competent.
The practice operates from 08.00 a.m.–6.30 p.m. Monday to Friday and 8.30 a.m.–12.15 p.m. on a Saturday (pre-booked appointments only). The GPs meet for lunch each day between 12.15–12.45 p.m. in the communal coffee area and sometimes they are joined by the Practice Manager but it was made clear to the rest of the practice staff that this was protected time and they do not expect to be disturbed. The nurses then have their lunch, 12.45–13.15 p.m. and then the rest of the staff have theirs – sometimes they share the space with the nursing staff.
This practice serves a diverse area including patients for whom English was a second language from eastern European countries, Somalian and Asian populations, a large travellers’ community and a large student population. Many of their patients are transient, but some such as the travellers remain on their books despite moving around. They also cover a large nursing home.
It was an innovative practice offering telephone consultations, e-consults and e-mail in the form of a web form all which was promoted on the website. Consultations using internet video was not offered. Although e-consult software was currently being piloted, the practice manager told me she had attended a presentation from the NHS GP partnership responsible for devising the e-consult software and was considering introducing it to the practice until they had been approached top pilot the system, however, the uptake by patients of e-consults or the use of the Web Form was low. The practice had a structured approach to scheduling e-consults and telephone consultations.
The practice offers patients the ability to book appointments or order prescriptions online but they need to register first. They are very keen to improve access for their patients and alongside the alternative to the face-to-face consultation and online booking they offer a patient partner service whereby patients ring a number and can then select an appointment from a range of options for three days ahead. Access to same day appointments was incredibly good with the practice offering duty doctor appointments, uncapped ‘sit & wait clinics’ (one in the morning and one in the evening) and an ‘open surgery’ in the afternoon.
The practice relies heavily on technology for all its correspondence using the practice software to communicate about clinical matters and e-mail for non-clinical and they rarely speak to each other by phone. Many of the staff, in particular the GPs, have smart phones on them and are regular responding to texts etc. The practice participates in a number of research projects so the process was familiar to most of the staff.
Alternatives offered:
-
Telephone – telephone consultation was open with all patients with an ad hoc approach to scheduling.
-
E-mail – a couple of GPs used informal e-mail consultations with selected patients but there was a more formal Webform approach with structured scheduling.
-
E-consult – the practice had been recently piloting e-consulting software with a structured approach to scheduling.
Practice D
Practice D was a salaried practice with c. 2000 registered patients. There were two full-time male GPs (who run the video-consultation link between the practice and another remote surgery), one part time female GP, one GP who was on maternity leave and was due to return in May, one part time female practice nurse, one part time female health care assistant, one female practice manager who manages one practice in total, and three female reception and admin staff of which two also work in other salaried practices. The practice was closely related with another more remote practice. Two full time GPs work in both practices. A pharmacy was at the bottom of the road, and the hospital at the top. The medical centre was in the middle. About three years ago the practice moved into a new large, spacious building with views over the bay. The nurses also had a common room in the building (filled with laughter, chat and biscuits) and see patients there as well. They work with, but are separate from, the practice team.
There was a fortnightly rota system for the remote practice for the two GPs. The GP on the rota took all the calls for 14 days to cover the remote practice. Video consulting was used with patients from this remote practice only. The video-consulting room in the practice was quite small and had a chair, desk and the video call machine. It’s like a phone with a small screen, phone and computer in it. It was also used by other staff, but the room needs to be booked and vacated if the GP needs to make a video-consultation. The video-consultation used in the remote surgery was on a desk in the (small) waiting room. The video-consultation link was part of a project (since November 2014), which initially runs for two years. According to GP1 there are about 160 people living in the remote region.
What stood out for me was the friendly and serious atmosphere in reception. However, I observed little interaction between the admin/reception staff and the GPs and there was not much chat in the reception. GP1 walked frequently into the reception and his mannerisms seemed to cheer up the staff. Also the video consulting was perceived as part of the project, which was part of the work of two GPs only. The practice did not have a website other than the standard one created by the Health Board. The computer system used was Vision. A face-to-face consultation was 15 minutes and a telephone consultation was 5 minutes.
Alternatives offered:
-
Telephone –the GP had telephone slots (about six a day) and the receptionist will add more at the end of the day if needed. In Vision appointments, headings are Beige for telephone consultation and written as, for example, ‘Mon AM Tel.’.
-
Video-consultation – was used as part of the communication with the people living remotely. It was not much used (technical issues, low uptake).
-
E-mail – was used occasionally by GP2 and the practice nurse to organise the practical aspects of care. Admin e-mail was on the patient leaflet.
Practice E
Practice E had c. 7000 registered patients. It was a salaried practice and located in a deprived area. There are nine GPs (seven female and two male; the male lead GP and one female GP are full time and the rest work part time); four female nurses (a lead practice and triage nurse, a primary care nurse, two treatment room nurses of which one left. The practice was in the recruitment process for several nurse positions); one practice manager and one assistant practice manager (both female); nine reception and office staff (of which eight female). At the end of the fieldwork two new reception staff had been recruited. The receptionists work in shifts between the front reception and the back office where all the phone calls from the patients seeking appointments are answered.
The practice had moved into a new large, modern, spacious the building over two years ago. Besides the practice, the building also houses a café and a range of health social care and family support services. The practice staff were positive about the building. The practice was based over two floors, with all the treatments rooms and reception at the ground floor. The corridor to the treatment rooms and the door to the reception are locked and staff use their pass to enter. There was a self-check-in next to the reception. I observed the machine out of order on several occasions.
I observed a lot of interaction between the (clinical, office, practice manager, assistant practice manager and most of the reception) staff, both formally and informally. There was a social/meeting area, which seemed well attended during break times. Practice and staff meetings were held every Tuesday. On the corridor was a monthly staff reward system called ‘Pat on the back’. Every month each staff member of practice nominate one other staff member for an achievement or for support.
The practice had a website and a Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) page (managed by the lead GP).
My experience during the fieldwork was that the staff were very welcoming and open to the research. They were very supportive of each other and committed to their practice population and it was a real pleasure to work in this practice.
Alternatives offered:
-
Telephone – the practice uses a patient call-back system, since 2012. There are 18 potential telephone slots per clinic (morning/afternoon). The (5-minute) slots get populated on the day by the reception staff and then it was up to the GP who they bring into the practice during that same clinic (face-to-face was 10 minutes).
-
E-consult – the practice was at the time of the fieldwork piloting for free e-consult software. This was an internet call back request system. The software was from the same company that provides the Patient Call-back system. The e-consult software was reported as costing £12,000 a year and was used by about 10% of the patients. Although they like the system, the practice cannot justify the cost and are in the process of incorporating features of the e-consult software into their own website.
-
E-mail through the practice website – was option on website, called ‘Request call back’, to send a question to the practice. Like the queries sent by e-consult software, the patients’ questions/issues arrive in the practice e-mail inbox and are dealt with in the same manner as e-consult software. At the moment it was like a speedy version of e-consults. It had a disclaimer.
-
E-mail was used informally by the lead GP with some patients. When one of the receptionists explained the registration process to me in detail, she points out that there was a box for e-mail.
Practice F
Practice F had c.14,000 registered patients. It was located in a rural location with high levels of affluence (IMD 10) and low levels of diversity. There are seven GP partners, three salaried GPs, two registrar GPs, three regular GP locums, seven practice nurses, five health care assistants, seven managers, 14 receptionists and 11 admin staff.
The 25 reception and admin staff were co-located. Everyone had somebody who can substitute them. The reception team deals with patients while secretary and scanning persons do not. All staff in the team were female. Reception opens at 8.00 a.m. since it’s also a health centre, and thus comprises other NHS services and also non-NHS services. The door opens at 8.20 a.m. to let people in who often queue although appointments start at 8.30 a.m. Scattered around the office, especially around the admin part, there are cards hanging with messages like ‘Laugh’ or ‘Remember it’s nice to be nice’ or ‘Be the person others can count on to get things done’ and ‘you may not find the job you love but you can love the job you found’.
This was a rural modern practice housed in a fairly new building (four years old). The building was on two floors, the practice only uses first floor and part of the second floor and lends the ground floor and some rooms on the second floor. The first floor had: the front desk reception, nurses’ clinics, GPs’ clinics, admin and call centre area, and dispensary area. The second floor had the staff common room, meeting rooms, facility offices and rooms to rent out. The first floor had an internal corridor for GPs to use when they do not want patients to see them when they are in and want to go from one side to the other side of the building.
The practice operates: Monday to Thursday 8.30 a.m.–12 p.m./2.30–5.30 p.m.; Friday 7.30 a.m.–12 p.m./2.30–6.30 p.m. Nurses have slightly different hours and blood clinics work during lunch breaks. It offers a range of online facilities to its patients (i.e. appointment booking, order or repeat prescriptions online, online access to view test results).
Practice meetings were held on Fridays: meetings rotated between clinical team, district nurses, patient information meetings and education meetings. Staff met once a quarter. Wednesday lunch times were when reception and administrators held their meetings.
Alternatives offered:
-
Telephone – telephone consultation was open with all patients.
-
E-mail – e-mail consultations only with selected patients.
Practice G
Practice G had c. 13,500 registered patients. It was located in a semi-rural location with high levels of affluence (IMD score of 10) and low levels of diversity. There were 11 GPs, five nurses, four health care assistants, five practice managers, 11 receptionists and seven dispensary staff. The main site building normally had two receptionists working at the surgery at the same time, whereas site two only had one. In site one, receptionists work one next to the other with the screen in the middle of the two desks. They answer phone calls and turn to go at the front and speak to patients when they ring the bell. This can often create an atmosphere of tension within the call centre, as receptionists constantly have to juggle between the front reception, the phone ringing at the back and administrative tasks. At this site, receptionists only work part time and they all live locally.
The practice was large with two associated practices situated in two small rural towns. The practice was based within two different buildings. The main building was situated at the centre of a rural town 7.7 miles from the main city in the county. It was a one-floor building comprising of two waiting rooms, a small reception, a call centre room and administrative office, the practice manager and secretary offices, a kitchen, a common room, eight clinic rooms and a dispensary. Differently from practice 1, the lack of common spaces, and also the more confined structure of the practice, did not allow much interaction among different members of staff. The common room was also less utilised and mainly used for meetings. An interesting feature about this practice was that there was not a receptionist within the reception space but there was a bell that patients can ring whenever they arrive at the practice reception. Next to the reception there was a screen where patients can sign in as they arrive. The call centre at the back, where the two receptionists spend their time, had a TV screen where images from the various CCTV cameras around the practice are streamed: one camera was found in the reception where receptionists can see patients who have just rang the bell asking for their attention, one in each waiting room and one in the car park pointed at the GP’s parking space to monitor their movements. The second building site was situated 4.3 miles from the main surgery. It’s a one-floor building with a small reception with one receptionist and a waiting room, and two clinic rooms. There are about six GPs who mainly work in this practice although they do also work in the main practice site when needed.
The clinic operated Monday to Friday 8.30 a.m.–6.30 p.m.; extended hours Monday, Tuesday and Wednesday 6.30–7.30 p.m. and they offer a range of online facilities to arrange appointments, order repeat medication, check online test results, access online medical records, access travel risk assessments, change personal details and complete online monitoring forms for blood pressure.
Alternatives offered:
-
Telephone – telephone consultation was officially used with patients and also booked as an alternative to face-to-face consultation.
-
E-mail – informal e-mailing with selected patients.
Practice H
Practice H had c. 6500 registered patients. It was an inner city practice was moderate levels of deprivation (Index of Multiple Deprivation 6) and diversity. There were five GPs, two nurses, one practice manager, two admin staff, five reception staff, one secretary and one IT manager. The reception team was composed of a senior receptionist and four receptionists, although during the observation there were only three receptionists working there as one had left and it took them a few months to hire a new receptionist. The reception room was an open space where the staff pigeon hole is also found. Thus, other staff members regularly go there to check their mail and occasionally stop to chat with the receptionists, especially the senior receptionist who had been there the longest.
The practice was situated in the town centre and was within walking distance from the train station. The practice building was a four-floor listed Victorian house and had been the base of the practice since it was first established. The reception, the waiting room and one of the nursing treatment rooms are situated on the first floor. The ground floor had a waiting room and two GPs treatment rooms. On the second floor there are more two more GPs treatment rooms, while the third floor was where the admin and the manager have their offices and where the kitchen and common rooms are located. When compared with the other two practices, this practice was relatively small in size.
The practice opened from 8.00 a.m. until 6.00 p.m. Monday to Friday. Extended surgery times are: Tuesdays 6.30–8.00 p.m., every other Thursday 6.30–8.00 p.m. and Fridays 7.00–8.00 a.m.
Alternatives offered:
-
Telephone – telephone consultation was officially used with patients and also booked as an alternative to face-to-face consultation.
-
E-mail – informal e-mailing with selected patients.
Appendix 7 Staff interview participant characteristics
| Sex | Age (years) | Role description | Length of time within role | Use of alternatives to the face-to-face consultation |
|---|---|---|---|---|
| F | 46 | GP partner | 19 years | E-consultations, telephone, e-mail and text messaging |
| F | 58 | GP partner | 30 years | E-consultations, telephone, e-mail and text messaging |
| M | 31 | GP partner | GP partner for 5 months, GP for 2 years | Telephone |
| M | 38 | GP partner | 6 years | Telephone and text messaging (to send results) |
| F | 50 | GP partner | 6 years | Telephone, e-mail and texting messaging (to send results) |
| F | 43 | GP partner | 11 years | E-consultations, telephone and e-mail |
| M | 55 | GP partner | 18 years | E-consultations, telephone and e-mail |
| M | 31 | GP partner | 10 months | Telephone and e-mail |
| M | 49 | GP partner | 12 years | Telephone and e-mail |
| F | 54 | GP partner | 14 years | Telephone and e-mail |
| M | 38 | GP partner | 8 years | Telephone and e-mail |
| F | 49 | GP partner | 9 years | Telephone and e-mail |
| M | 47 | GP partner | 3–4 years | Telephone and e-mail |
| M | 52 | GP partner | 15 years | Telephone and e-mail |
| M | 55 | Principal GP partner | 26 years | Telephone and e-mail |
| M | 42 | Medical director and GP partner | 5 months | Telephone and video |
| F | 50 | Salaried GP | 6 months (but was also partner in previous practice) | E-consultations, telephone and e-mail |
| M | 55 | Salaried GP | 16 years (at current practice) | Telephone, e-mail and video |
| M | 59 | Salaried GP | 6 months | Telephone, e-mail and video |
| M | 41 | Salaried GP | 4 years | Telephone, e-consultations and e-mail |
| M | 48 | Salaried GP | 18 years | Telephone and e-mail |
| F | 50 | Salaried part time GP | 19 years | Telephone and e-consultations |
| F | 50 | Partner practice manager | 8 years | N/A |
| F | 56 | Practice manager | 8 years | N/A |
| M | 50 | Practice manager | 4 years | N/A |
| F | Not answered | Practice manager | 10 years | N/A |
| F | 60 | Practice manager | 1–2 years | N/A |
| F | 57 | Practice manager | 13 years | N/A |
| F | 56 | Practice manager | 4 years | N/A |
| F | 38 | Practice manager | 3 years | N/A |
| F | 51 | Practice manager | 5 years | About to start using video |
| F | 36 | Assistant practice manager | 18 years | N/A |
| F | 52 | Deputy practice manager | 13 years | N/A |
| F | 55 | Patient service manager | 2 years | Telephone |
| F | 59 | Practice nurse | 10 years | Telephone and e-mail |
| F | 54 | Practice nurse | 15 years | Telephone |
| F | 50 | Practice nurse | 4 years | Telephone |
| F | 59 | Practice nurse | 33 years | Telephone |
| F | 56 | Practice nurse | 20 years | Telephone |
| F | 61 | Senior practice nurse | 20 years | Telephone and e-mail |
| F | 53 | Senior receptionist | 14 years | Telephone and e-mail |
| F | 53 | Senior receptionist | 1 year | Telephone |
| F | 51 | Receptionist | 3.5 years | Telephone and e-mail |
| F | 48 | Receptionist | 13 years | N/A |
| F | 46 | Receptionist | 7 years | N/A |
| F | 51 | Practice coordinator | 9 years | N/A |
| F | 45 | Practice administrator | 11 years | Telephone and e-mail |
| F | 51 | Support worker | Not answered | Video |
| M | 68 | IT manager | 13 years | N/A |
Appendix 8 Patient interview participant characteristics
| Sex | Age (years) | Carer | Long-term condition/disabilities | Education level |
|---|---|---|---|---|
| F | 48 | No | Mental health condition | Degree |
| F | 59 | No | Mental health condition | Degree |
| Transgender | 53 | No | Mobility issues | Vocational award |
| M | 23 | No | Not answered | A level |
| F | 34 | Yes | None | Postgraduate award |
| M | 39 | No | Restricted mobility and impaired eyesight | Not answered |
| F | 36 | No | None | Degree |
| F | 26 | No | Hyperthyroidism, labyrinthitis and seizures | GCSE/O level |
| F | 34 | No | Mental health condition | Postgraduate award |
| F | 56 | Yes | Two long-term conditions and restricted mobility | Not answered |
| M | 31 | No | Has a pacemaker that requires regular checks | Degree |
| M | 26 | No | None | Degree |
| F | 73 | No | COPD, impaired hearing and restricted mobility | Not answered |
| M | 50 | No | Multimorbidities | Not answered |
| F | 41 | No | Mental health condition and other multimorbidities | Not answered |
| F | 40 | Yes | Cancer | Higher/A Level |
| F | 52 | No | Diabetes mellitus | GCSE/O level |
| F | 50 | Yes | None | Degree |
| F | 37 | Yes | None | Postgraduate award |
| F | 32 | Yes | Has a long-term condition, but not stated | Secondary school educated |
| F | 59 | No | Multimorbidities | Secondary school educated |
| M | 54 | Not answered | None | Secondary school educated |
| F | 54 | No | Diabetes mellitus | Secondary school educated |
| F | 44 | Yes | Mental health condition | Attending college at moment |
| M | 76 | No | Multimorbidities | A level |
| F | 48 | Yes | None | Vocational award |
| F | 91 | No | Multimorbidities and hearing impairment | Vocational award |
| F | 84 | No | Heart condition | A level |
| M | 56 | No | Multimorbidities and restricted mobility | Degree |
| M | 53 | No | Type 2 diabetes mellitus | Degree |
| M | 75 | No | Asthma and diabetes mellitus | Secondary school educated |
| F | 39 | Yes | Asthma | Degree |
| M | 31 | No | Recurrent mouth sores | Degree |
| M | 58 | No | Diabetes mellitus and restricted mobility | Degree and vocational training |
| M | 65 | No | Heart condition | Postgraduate award |
| F | 79 | Yes | Multimorbidities and restricted mobility | Vocational award |
| F | 57 | No | Vascular varicose veins, high blood pressure and depression | A level |
| F | 73 | No | Osteoporosis, cancer and thyroid problems | Postgraduate award |
| F | 24 | No | Bipolar disorder | A level |
Appendix 9 Issues related to the recording of consultations in routine general practice computer systems
At the beginning of a consultation, a clinician will usually select the patient’s name in the appointment system. The computer records the identity of the person conducting the appointment from their log-in details and opens a consultation record entry. Each consultation entry has a designated consultation type (e.g. face-to-face surgery consultation or telephone consultation), which may be determined by the type of appointment booked or by a system default (which can be changed for each consultation). The type of consultation is not necessarily the same as the type of appointment and may be recorded in different parts of the computer record.
Most practice computerised appointment systems record the times at which the patient checks in, and the time at which the consultation started and ended. If a patient does not attend, this may be recorded in the appointment system and in the individual patient’s medical record. This might happen automatically, or be done manually, depending on the computer system and the practice policy. Therefore, it should be possible to collect substantial amounts of useful data from routine records to allow analysis of numbers of appointments and consultations of different types, by different types of patients, with different types of clinicians, and including details of waiting times, consultation duration, and attendance and non-attendance rates.
However, there are a number of issues that make this more complicated:
-
The clinician conducting the consultation may not be the same as the clinician with whom the appointment was booked.
-
The clinician conducting the consultation is identifiable from their log-in details, which also identifies their professional status (e.g. GP, practice nurse), but some practices attribute a variety of professional types to individual log-in records (e.g. ‘assistant’), which may not clearly indicate their profession.
-
The type of appointment booked may not be the same as the type of consultation conducted. For example, a receptionist may add a patient’s name to a slot intended for a booked face-to-face appointment with a free-text comment saying that the patient has requested a telephone call. When the GP selects this appointment, the consultation record may default to a face-to-face surgery consultation. The GP should edit the appointment type to ‘telephone consultation’, but this may not always happen.
-
Not all consultations start with an entry in the appointments system, and not all appear in the consultation record. For example, incoming telephone calls from patients that have not been pre-booked should be recorded in the patient’s clinical record, but will not appear in the appointments system, and are recorded only as telephone consultations, rather than the default of ‘face-to-face surgery’ (only if the GP remembers to edit the consultation type). Communications via e-mail may be recorded in a variety of ways. Depending on local policy, practice e-mails may not appear in the clinical records as consultations. The practice may file an e-mail in a section of the patient’s record for documents (like letters). An e-mail or e-consult communication will be recorded as a consultation only if it is entered as such in the consultation records part of the system. There is a range of standard consultation types that users can choose from, or they may create their own consultation types.
-
Although many variables about appointments and consultations are recorded in practice computer systems, they are not necessarily all available to be searched or extracted. For example, in EMIS (the most widely used GP computer system), details of consultation duration are recorded in the appointments system, but not in the consultation record; therefore, consultations that did not result from a pre-booked appointment will not have a recorded duration.
-
The ways in which data are recorded vary by type of GP computer system, between practices (in accordance with local practice policies) and even within practices, as a result of variations between different members of staff.
Appendix 10 Data collection sheet to assess the reliability of recording of alternative consultation types
Practice name: ________________________________________________________________
Structured summary date of completion: ______________________
Computer system e.g. EMIS web, EMIS PCS, system one etc.: _____________________________
Please complete the table below, completing the columns as applicable for each type of alternative offered in the practice.
| Telephone | E-consult or other internet messaging system | Skype or other internet video | ||
|---|---|---|---|---|
| 1. Is this alternative used in this practice? | Yes [ ] No [ ] | Yes [ ] No [ ] |
Yes [ ] No [ ] Specify which system below: |
Yes [ ] No [ ] Specify which system below: |
| 2. How are these recorded in the consultation screen (i.e. consultation type; read coded entry?) | ||||
| 3. Comments on how reliably these are entered and major sources of variation e.g. between different doctors or consultations under different circumstances | ||||
| 4. Audit of more than 20 consultations in a regular session e.g. a specific telephone consulting session or e-mail consulting session. |
How did you find consultations? How many consultations did you look at? [ ] Of these How many were recorded in the way stated in Q2? [ ] |
How did you find consultations? How many consultations did you look at? [ ] Of these How many were recorded in the way stated in Q2? [ ] |
How did you find consultations? How many consultations did you look at? [ ] Of these How many were recorded in the way stated in Q2? [ ] |
How did you find consultations? How many consultations did you look at? [ ] Of these How many were recorded in the way stated in Q2? [ ] |
| 5. Audit of more than 20 consultations not in a regular session e.g. taken during or at the end of a routine surgery. How many consultations did you look at? Of these How many were recorded in the way stated in Q2? |
How did you find consultations? How many consultations did you look at? [ ] Of these How many were recorded in the way stated in Q2? [ ] |
How did you find consultations? How many consultations did you look at? [ ] Of these How many were recorded in the way stated in Q2? [ ] |
How did you find consultations? How many consultations did you look at? [ ] Of these How many were recorded in the way stated in Q2? [ ] |
How did you find consultations? How many consultations did you look at? [ ] Of these How many were recorded in the way stated in Q2? [ ] |
| 5. Does the practice do any regular reports of their use of this alternative e.g. number of telephone calls in a month? If so, please describe and bring copies of reports as long as they do not have any patient identifiers |
Yes [ ] No [ ] Specify type of reports below: |
Yes [ ] No [ ] Specify type of reports below: |
Yes [ ] No [ ] Specify type of reports below: |
Yes [ ] No [ ] Specify type of reports below: |
| 6. Other comments? |
Appendix 11 Clusters of diseases used to create a multimorbidity score
The conditions with available code clusters were:
-
chronic kidney disease
-
heart failure
-
hypertension
-
coronary heart disease
-
peripheral arterial disease
-
stroke
-
diabetes mellitus
-
asthma
-
chronic obstructive pulmonary disease
-
epilepsy
-
atrial fibrillation
-
severe mental health problem (e.g. schizophrenia, psychotic illness)
-
depression
-
dementia
-
learning disability
-
rheumatoid arthritis.
We extracted information about whether or not each patient had any of these disease clusters. If a patient was recorded as having both asthma and chronic obstructive airways disease (COPD), this was coded just once as a ‘respiratory condition’ to avoid the risk of double-counting. If a patient was coded as having epilepsy and also had a code for ‘epilepsy resolved’, they were not included as having epilepsy. Patients were included as having depression only if they were included in the depression code cluster and had also had a prescription for an antidepressant in the last 3 months.
It was necessary to run separate searches for each of the above conditions. We created a report in EMIS that ran each of the searches sequentially and amalgamated the findings into a report with one row per patient and one column per disease, for export to Microsoft Excel.
We calculated a multimorbidity score for each patient by summating the number of chronic conditions, and created a binary multimorbidity variable for patients with a score of two or more.
Appendix 12 Recoding the consultation type in each case study practice
| Consultation types as recorded | Coding for analysis | Practice | |||||
|---|---|---|---|---|---|---|---|
| A | H | G | C | F | B | ||
| Awaiting clinical code migration to EMIS Web | Not consultation | Awaiting clinical code migration to EMIS Web | Awaiting clinical code migration to EMIS Web | Awaiting clinical code migration to EMIS Web | Awaiting clinical code migration to EMIS Web | Awaiting clinical code migration to EMIS Web | Awaiting clinical code migration |
| Clinic note | Surgery | Clinic note | Clinic note | Clinic note | Clinic note | Clinic note | |
| Discussion with colleague | Not consultation | Discussion with colleague | Discussion with colleague | Discussion with colleague | Discussion with colleague | Discussion with colleague | Discussion with colleague |
| E-consult | E-consult | E-consult | |||||
| E-mail consultation | E-consult | E-mail consultation | E-mail consultation | ||||
| E-mail received from carer | E-mail received | E-mail received from carer | |||||
| E-mail received from patient | E-mail received | E-mail received from patient | E-mail received from patient | E-mail received from patient | E-mail received from patient | ||
| E-mail received from third party | E-mail received | E-mail received from third party | |||||
| E-mail sent to carer | E-mail sent | E-mail sent to carer | |||||
| E-mail sent to patient | E-mail sent | E-mail sent to patient | E-mail sent to patient | E-mail sent to patient | E-mail sent to patient | ||
| Emergency appointment | Surgery | Emergency appointment | |||||
| Emergency consultation | Surgery | Emergency consultation | |||||
| Face-to-face consultation | Surgery | Face-to-face consultation | Face-to-face consultation | Face-to-face consultation | Face-to-face consultation | Face-to-face consultation | |
| Face-to-face consultation with relative/carer | Surgery | Face-to-face consultation with relative/carer | Face-to-face consultation with relative/carer | ||||
| GP surgery | Surgery | GP surgery | GP surgery | GP surgery | GP surgery | GP surgery | GP surgery |
| Group consultation | Other | Group consultation | |||||
| Home visit note | Home visit | Home visit note | Home visit note | Home visit note | Home visit note | Home visit note | Home visit note |
| Inbound document | Not consultation | Inbound document | Inbound document | Inbound document | Inbound document | ||
| Joint consultation | Surgery | Joint consultation | |||||
| Mail from patient | Other | Mail from patient | Mail from patient | Mail from patient | |||
| Mail to patient | Other | Mail to patient | Mail to patient | Mail to patient | |||
| Night visit note | Home visit | Night visit note | |||||
| Nursing home visit note | Home visit | Nursing home visit note | Nursing home visit note | ||||
| Nurse telephone triage | Telephone | Nurse telephone triage | |||||
| Outbound referral | Not consultation | Outbound referral | Outbound referral | Outbound referral | Outbound referral | Outbound referral | Outbound referral |
| Residential home visit note | Home visit | Residential home visit note | |||||
| Routine consultation | Surgery | Routine consultation | |||||
| Telephone call from a patient | Telephone | Telephone call from a patient | Telephone call from a patient | Telephone call from a patient | Telephone call from a patient | ||
| Telephone call from relative/carer | Telephone | Telephone call from relative/carer | Telephone call from relative/carer | Telephone call from relative/carer | Telephone call from relative/carer | ||
| Telephone call to a patient | Telephone | Telephone call to a patient | Telephone call to a patient | Telephone call to a patient | Telephone call to a patient | Telephone call to a patient | |
| Telephone call to relative/carer | Telephone | Telephone call to relative/carer | Telephone call to relative/carer | Telephone call to relative/carer | Telephone call to relative/carer | ||
| Telephone consultation | Telephone | Telephone consultation | Telephone consultation | Telephone consultation | Telephone consultation | Telephone consultation | Telephone consultation |
| Telephone triage encounter | Telephone | Telephone triage encounter | Telephone triage encounter | ||||
| Third-party consultation | Other | Third-party consultation | Third-party consultation | Third-party consultation | Third-party consultation | Third-party consultation | Third-party consultation |
| Urgent consultation | Surgery | Urgent consultation | |||||
| WebGP alert | WebGP alert | WebGP alert | |||||
Appendix 13 Recoding professional type in each case study practice
| Professional user types as recorded | Recoded category | Practice | |||||
|---|---|---|---|---|---|---|---|
| A | H | G | C | F | B | ||
| Analyst | Admin | Analyst | Analyst | Analyst | Analyst | Analyst | Analyst |
| Appointments clerk | Admin | Appointments clerk | Appointments clerk | Appointments clerk | Appointments clerk | Appointments clerk | Appointments clerk |
| Associate practitioner – GP | GP | Associate practitioner – GP | Associate practitioner – GP | Associate practitioner – GP | Associate practitioner – GP | Associate practitioner – GP | |
| Associate practitioner – nurse | Nurse or HCA | Associate practitioner – nurse | Associate practitioner – nurse | Associate practitioner – nurse | |||
| Chiropodist/podiatrist | Other clinician | Chiropodist/podiatrist | Chiropodist/podiatrist | Chiropodist/podiatrist | Chiropodist/podiatrist | ||
| Clerical worker | Admin | Clerical worker | Clerical worker | Clerical worker | Clerical worker | Clerical worker | Clerical worker |
| Clinical assistant | GP | Clinical assistant | Clinical assistant | Clinical assistant | Clinical assistant | ||
| Clinical coder | Admin | Clinical coder | Clinical coder | Clinical coder | |||
| Community administrator | Admin | Community administrator | Community administrator | Community administrator | Community administrator | Community administrator | Community administrator |
| Community mental health nurse | Other clinician | Community mental health nurse | |||||
| Community nurse | Nurse or HCA | Community nurse | Community nurse | Community nurse | Community nurse | Community nurse | Community nurse |
| Community practitioner | Nurse or HCA | Community practitioner | Community practitioner | Community practitioner | Community practitioner | Community practitioner | Community practitioner |
| Consultant | Other clinician | Consultant | Consultant | Consultant | Consultant | Consultant | Consultant |
| Counsellor | Other clinician | Counsellor | Counsellor | Counsellor | Counsellor | Counsellor | |
| Desktop support administrator | Admin | Desktop support administrator | Desktop support administrator | Desktop support administrator | Desktop support administrator | Desktop support administrator | Desktop support administrator |
| Dietitian | Other clinician | Dietitian | Dietitian | ||||
| Dispenser | Other clinician | Dispenser | Dispenser | Dispenser | Dispenser | Dispenser | Dispenser |
| Enrolled nurse | Nurse or HCA | Enrolled nurse | Enrolled nurse | Enrolled nurse | Enrolled nurse | ||
| GP registrar | GP | GP registrar | GP registrar | GP registrar | GP registrar | GP registrar | GP registrar |
| General medical practitioner | GP | General medical practitioner | General medical practitioner | General medical practitioner | General medical practitioner | General medical practitioner | General medical practitioner |
| Health-care support worker | Nurse or HCA | Health-care support worker | Health-care support worker | Health care support worker | Health-care support worker | Health-care support worker | Health-care support worker |
| Health records administrator | Admin | Health records administrator | |||||
| Health records clerk | Admin | Health records clerk | |||||
| HCA | Nurse or HCA | HCA | HCA | HCA | HCA | HCA | HCA |
| Helper/assistant | Nurse or HCA | Helper/assistant | |||||
| House officer – post registration | GP | House officer – post registration | House officer – post registration | ||||
| Manager | Admin | Manager | Manager | Manager | Manager | Manager | Manager |
| Medical records clerk | Admin | Medical records clerk | Medical records clerk | ||||
| Medical secretary | Admin | Medical secretary | Medical secretary | Medical secretary | Medical secretary | Medical secretary | |
| Medical student | Other clinician | Medical student | Medical student | Medical student | |||
| Midwife | Other clinician | Midwife | Midwife | Midwife | Midwife | Midwife | Midwife |
| Modern matron | Nurse or HCA | Modern matron | |||||
| Nurse consultant | Nurse or HCA | Nurse consultant | Nurse consultant | Nurse consultant | |||
| Nurse manager | Nurse or HCA | Nurse manager | Nurse manager | Nurse manager | |||
| Occupational therapist | Other clinician | Occupational therapist | Occupational therapist | ||||
| Paramedic specialist practitioner | Other clinician | Paramedic specialist practitioner | |||||
| Pharmacist | Other clinician | Pharmacist | Pharmacist | Pharmacist | Pharmacist | Pharmacist | |
| Phlebotomist | Nurse or HCA | Phlebotomist | Phlebotomist | Phlebotomist | Phlebotomist | Phlebotomist | Phlebotomist |
| Practitioner | Other clinician | Practitioner | Practitioner | ||||
| Receptionist | Admin | Receptionist | Receptionist | Receptionist | Receptionist | Receptionist | Receptionist |
| Salaried GP | GP | Salaried GP | Salaried GP | Salaried GP | Salaried GP | Salaried GP | Salaried GP |
| Secretary | Admin | Secretary | Secretary | Secretary | Secretary | Secretary | |
| Senior administrator | Admin | Senior administrator | |||||
| Senior clinical medical officer | GP | Senior clinical medical officer | |||||
| Sessional GP | GP | Sessional GP | Sessional GP | Sessional GP | Sessional GP | Sessional GP | Sessional GP |
| Sister/charge nurse | Nurse or HCA | Sister/charge nurse | Sister/charge nurse | ||||
| Specialist nurse practitioner | Nurse or HCA | Specialist nurse practitioner | Specialist nurse practitioner | Specialist nurse practitioner | Specialist nurse practitioner | Specialist nurse practitioner | Specialist nurse practitioner |
| Staff nurse | Nurse or HCA | Staff nurse | Staff nurse | Staff nurse | |||
| Student practice nurse | Nurse or HCA | Student practice nurse | Student practice nurse | ||||
| System administrator | Admin | System administrator | System administrator | System administrator | System administrator | ||
| System worker | Admin | System worker | System worker | ||||
Appendix 14 Demographic details of patients by practice
| Characteristic | Practice, n (%) | Total (A, B, C, F, G and H) | ||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | F | G | H | n (%) | Cumulative % | |
| Age (years) | ||||||||
| 0–4 | 1042 (5.7) | 663 (7.4) | 1083 (7.1) | 823 (5.7) | 652 (4.8) | 221 (3.4) | 4484 (5.8) | 5.8 |
| 5–14 | 1729 (9.4) | 1129 (12.6) | 1758 (11.4) | 1466 (10.1) | 1597 (11.7) | 377 (5.8) | 8056 (10.4) | 16.2 |
| 15–24 | 2064 (11.2) | 974 (10.8) | 2123 (13.8) | 1609 (11.1) | 1349 (9.9) | 2034 (31.1) | 10,153 (13.1) | 29.3 |
| 25–44 | 8894 (48.4) | 3698 (41.2) | 5604 (36.5) | 3909 (26.9) | 2795 (20.4) | 2209 (33.7) | 27,109 (35) | 64.2 |
| 45–64 | 3639 (19.8) | 1810 (20.2) | 3108 (20.2) | 3733 (25.7) | 4040 (29.5) | 1089 (16.6) | 17,419 (22.5) | 86.7 |
| 65–74 | 653 (3.6) | 360 (4) | 986 (6.4) | 1654 (11.4) | 1784 (13) | 367 (5.6) | 5804 (7.5) | 94.2 |
| 75–84 | 284 (1.5) | 247 (2.8) | 457 (3) | 955 (6.6) | 1026 (7.5) | 188 (2.9) | 3157 (4.1) | 98.3 |
| ≥ 85 | 84 (0.5) | 100 (1.1) | 237 (1.5) | 400 (2.7) | 447 (3.3) | 63 (1) | 1331 (1.7) | 100 |
| Total | 18,389 (100) | 8981 (100) | 15,356 (100) | 14,549 (100) | 13,690 (100) | 6548 (100) | 77,513 (100) | |
| Sex | ||||||||
| Female | 8566 (46.6) | 4271 (47.6) | 7579 (49.4) | 7295 (50.1) | 6958 (50.8) | 3093 (47.2) | 37,762 (48.7) | 48.7 |
| Male | 9823 (53.4) | 4710 (52.4) | 7777 (50.6) | 7254 (49.9) | 6732 (49.2) | 3455 (52.8) | 39,751 (51.3) | 100 |
| Total | 18,389 (100) | 8981 (100) | 15,356 (100) | 14,549 (100) | 13,690 (100) | 6548 (100) | 77,513 (100) | |
| Ethnicity | ||||||||
| White | 10,820 (58.8) | 3868 (43.1) | 8432 (54.9) | 9635 (66.2) | 7752 (56.6) | 4968 (75.9) | 45,475 (58.7) | 58.7 |
| Other | 4999 (27.2) | 2860 (31.8) | 2027 (13.2) | 338 (2.3) | 325 (2.4) | 965 (14.7) | 11,514 (14.9) | 73.5 |
| Unknown | 306 (1.7) | 84 (0.9) | 98 (0.6) | 603 (4.1) | 2584 (18.9) | 66 (1) | 3741 (4.8) | 78.3 |
| Missing | 2264 (12.3) | 2169 (24.2) | 4799 (31.3) | 3973 (27.3) | 3029 (22.1) | 549 (8.4) | 16,783 (21.7) | 100 |
| Total | 18,389 (100) | 8981 (100) | 15,356 (100) | 14,549 (100) | 13,690 (100) | 6548 (100) | 77,513 (100) | |
| IMD quintilea | ||||||||
| 1 | 9949 (54.1) | 4363 (48.6) | 7406 (48.2) | 0 (0) | 1 (0) | 917 (14) | 22,636 (29.2) | 29.2 |
| 2 | 3997 (21.7) | 4031 (44.9) | 3110 (20.3) | 927 (6.4) | 2 (0) | 685 (10.5) | 12,752 (16.5) | 45.7 |
| 3 | 1104 (6) | 363 (4) | 828 (5.4) | 2668 (18.3) | 1122 (8.2) | 3302 (50.4) | 9387 (12.1) | 57.8 |
| 4 | 3034 (16.5) | 166 (1.8) | 3454 (22.5) | 3332 (22.9) | 1762 (12.9) | 1003 (15.3) | 12,751 (16.5) | 74.3 |
| 5 | 270 (1.5) | 52 (0.6) | 555 (3.6) | 7616 (52.3) | 10,802 (78.9) | 639 (9.8) | 19,934 (25.7) | 100 |
| Missing | 35 (0.2) | 6 (0.1) | 3 (0) | 6 (0) | 1 (0) | 2 (0) | 53 (0.1) | 100 |
| Total | 18,389 (100) | 8981 (100) | 15,356 (100) | 14,549 (100) | 13,690 (100) | 6548 (100) | 77,513 (100) | |
Appendix 15 Prevalence of conditions in study practices and nationally
| Conditions | Patients, n (%) | Prevalence rate in England,b % | |
|---|---|---|---|
| Alla | Aged ≥ 18 yearsa | ||
| Chronic kidney disease | 2214 (2.9) | 2213 (3.5) | 4.1 (≥ 18 years) |
| Heart failure | 452 (0.6) | 452 (0.7) | 0.7 |
| Hypertension | 8336 (10.8) | 8331 (13.3) | 13.8 |
| Coronary heart disease | 1661 (2.1) | 1661 (2.6) | 3.2 |
| Peripheral arterial disease | 400 (0.5) | 400 (0.6) | 0.6 |
| Stroke | 1069 (1.4) | 1062 (1.7) | 1.7 |
| Diabetes mellitus | 3141 (4.1) | 3116 (5.0) | 6.4 (≥ 17 years) |
| Respiratoryc | 13,152 (17.0) | 11,186 (17.8) | 7.8 (6.0 asthma; 1.8 COPD) |
| Current epilepsyd | 876 (1.1) | 825 (1.3) | 0.8 (≥ 18 years) |
| Atrial fibrillation | 1090 (1.4) | 1090 (1.7) | 1.6 |
| Severe mental health | 831 (1.1) | 827 (1.3) | 0.9 |
| Current depression | 5504 (7.1) | 5454 (8.7) | 7.3 (≥ 18 years) |
| Dementia | 416 (0.5) | 416 (0.7) | 0.7 |
| Learning disabilities | 360 (0.5) | 323 (0.5) | 0.4 |
| Rheumatoid arthritis | 518 (0.7) | 505 (0.8) | 0.7 (≥ 16 years) |
| Any of the above | 26,362 (34.0) | 24,257 (38.6) | |
| ≥ 2 of the above | 8314 (10.7) | 8264 (13.2) | |
| Total | 77,513 (100) | 62,809 (100) | |
Appendix 16 Prevalence of conditions by practice: patients aged ≥ 18 years
| Condition | Practice, n (col%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | H | G | C | F | B | |||||||
| Chronic kidney disease | 293 | 1.9 | 71 | 1.2 | 766 | 7 | 459 | 3.8 | 399 | 3.4 | 225 | 3.2 |
| Heart failure | 59 | 0.4 | 13 | 0.2 | 156 | 1.4 | 91 | 0.8 | 89 | 0.8 | 44 | 0.6 |
| Hypertension | 1151 | 7.6 | 334 | 5.7 | 2431 | 22.2 | 1552 | 12.9 | 2072 | 17.5 | 791 | 11.4 |
| Coronary heart disease | 197 | 1.3 | 81 | 1.4 | 420 | 3.8 | 388 | 3.2 | 438 | 3.7 | 137 | 2 |
| Peripheral arterial disease | 66 | 0.4 | 11 | 0.2 | 115 | 1.1 | 99 | 0.8 | 81 | 0.7 | 28 | 0.4 |
| Stroke | 129 | 0.8 | 48 | 0.8 | 320 | 2.9 | 209 | 1.7 | 261 | 2.2 | 95 | 1.4 |
| Diabetes mellitus | 533 | 3.5 | 153 | 2.6 | 648 | 5.9 | 727 | 6 | 606 | 5.1 | 449 | 6.5 |
| Respiratory condition | 2535 | 16.7 | 812 | 13.8 | 2089 | 19.1 | 2444 | 20.3 | 2265 | 19.2 | 1041 | 15 |
| Current epilepsy | 175 | 1.2 | 47 | 0.8 | 140 | 1.3 | 193 | 1.6 | 175 | 1.5 | 95 | 1.4 |
| Atrial fibrillation | 107 | 0.7 | 63 | 1.1 | 375 | 3.4 | 184 | 1.5 | 284 | 2.4 | 77 | 1.1 |
| Severe mental health condition | 288 | 1.9 | 65 | 1.1 | 90 | 0.8 | 180 | 1.5 | 108 | 0.9 | 96 | 1.4 |
| Current depression | 1180 | 7.8 | 385 | 6.6 | 925 | 8.5 | 1312 | 10.9 | 1063 | 9 | 589 | 8.5 |
| Dementia | 28 | 0.2 | 21 | 0.4 | 156 | 1.4 | 90 | 0.7 | 101 | 0.9 | 20 | 0.3 |
| Learning disabilities | 64 | 0.4 | 6 | 0.1 | 29 | 0.3 | 111 | 0.9 | 71 | 0.6 | 42 | 0.6 |
| Rheumatoid arthritis | 81 | 0.5 | 25 | 0.4 | 171 | 1.6 | 87 | 0.7 | 109 | 0.9 | 32 | 0.5 |
| Any of the above | 4863 | 32 | 1582 | 27 | 5205 | 47.6 | 5047 | 41.9 | 5148 | 43.6 | 2412 | 34.8 |
| Two or more of any of the above | 1317 | 8.7 | 385 | 6.6 | 2064 | 18.9 | 1836 | 15.2 | 1829 | 15.5 | 833 | 12 |
| Total | 15211 | 100 | 5870 | 100 | 10,945 | 100 | 12,040 | 100 | 11,810 | 100 | 6933 | 100 |
Appendix 17 Proportion of patients with multimorbidities in different age groups (aged ≥ 18 years)
| Age group (years) | Multimorbidities (all practices) | |||||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | Total | ||||||
| n | row% | col% | n | row% | col% | n | col% | |
| 18–24 | 7762 | 97.2 | 14.2 | 227 | 2.8 | 2.7 | 7989 | 12.7 |
| 25–44 | 26,013 | 96.0 | 47.7 | 1096 | 4.0 | 13.3 | 27,109 | 43.2 |
| 45–64 | 14,902 | 85.6 | 27.3 | 2517 | 14.4 | 30.5 | 17,419 | 27.7 |
| 65–74 | 3964 | 68.3 | 7.3 | 1840 | 31.7 | 22.3 | 5804 | 9.2 |
| 75–84 | 1501 | 47.5 | 2.8 | 1656 | 52.5 | 20.0 | 3157 | 5.0 |
| ≥ 85 | 403 | 30.3 | 0.7 | 928 | 69.7 | 11.2 | 1331 | 2.1 |
| Total ≥ 65 | 5868 | 57.0 | 10.8 | 4424 | 43.0 | 53.5 | 10,292 | 16.3 |
| Total | 54,545 | 86.8 | 100 | 8264 | 13.2 | 100 | 62,809 | 100 |
Appendix 18 Consultation rates (all practices) by type of consultation and type of professional
| Consultation type | Number of consultations | Type of professional, ratea (%)b | ||
|---|---|---|---|---|
| GP (n = 129,197) | Nurse or HCA (n = 80,480) | Total (n = 209,677) | ||
| Surgery | 167,393 | 2.2937 (42.98) | 1.9670 (36.86) | 4.2607 (79.83) |
| Telephone | 38,714 | 0.9237 (17.31) | 0.0618 (1.16) | 0.9854 (18.46) |
| E-consult | 190 | 0.0048 (0.09) | 0.0048 (0.09) | |
| Home visit | 3024 | 0.0613 (1.15) | 0.0157 (0.29) | 0.0770 (1.44) |
| E-mail sent | 356 | 0.0050 (0.09) | 0.0040 (0.08) | 0.0091 (0.17) |
| Total | 209,677 | 3.2885 (61.62) | 2.0485 (38.38) | 5.3370 (100) |
Appendix 19 Rates of different types of consultation by age group, sex, deprivation, ethnicity and multimorbidity
Rates of different types of consultation by age group (all practices)
| Age group (years) | Consultation type | Number of consultations | |||||
|---|---|---|---|---|---|---|---|
| Surgery (n = 167,393) | Telephone (n = 38,714) | E-consult (n = 190) | Home visit (n = 3024) | E-mail sent (n = 356) | Total (n = 209,677) | ||
| 0–4 | 4.2869 | 0.8408 | 0.0004 | 0.0079 | 0.0018 | 5.1379 | 11,677 |
| 5–14 | 1.7905 | 0.4330 | 0.0007 | 0.0017 | 0.0027 | 2.2287 | 9100 |
| 15–24 | 2.6920 | 0.6617 | 0.0049 | 0.0049 | 0.0060 | 3.3694 | 17,339 |
| 25–44 | 3.2564 | 0.8913 | 0.0075 | 0.0081 | 0.0071 | 4.1704 | 57,302 |
| 45–64 | 4.8703 | 1.0862 | 0.0050 | 0.0385 | 0.0125 | 6.0125 | 53,083 |
| 65–74 | 7.9490 | 1.3930 | 0.0024 | 0.1074 | 0.0201 | 9.4719 | 27,864 |
| 75–84 | 11.3248 | 2.2192 | 0.0025 | 0.5293 | 0.0169 | 14.0927 | 22,550 |
| ≥ 85 | 10.7291 | 3.1796 | 0.0044 | 2.0160 | 0.0237 | 15.9528 | 10,762 |
| Total | 4.2607 | 0.9854 | 0.0048 | 0.0770 | 0.0091 | 5.3370 | 209,677 |
Rates of different types of consultation by sex (all practices)
| Sex | Consultation type | Number of consultations | |||||
|---|---|---|---|---|---|---|---|
| Surgery (n = 167,393) | Telephone (n = 38,714) | E-consult (n = 190) | Home visit (n = 3024) | E-mail sent (n = 356) | Total (n = 209,677) | ||
| Female | 5.0794 | 1.2370 | 0.0065 | 0.1007 | 0.0086 | 6.4321 | 123,108 |
| Male | 3.4831 | 0.7464 | 0.0033 | 0.0544 | 0.0095 | 4.2967 | 86,569 |
| Total | 4.2607 | 0.9854 | 0.0048 | 0.0770 | 0.0091 | 5.3370 | 209,677 |
Rates of different types of consultation by deprivation quintile (all practices)
| IMD quintilea | Consultation type | Number of consultations | |||||
|---|---|---|---|---|---|---|---|
| Surgery (n = 167,343) | Telephone (n = 38,696) | E-consult (n = 190) | Home visit (n = 3024) | E-mail sent (n = 355) | Total (n = 209,608) | ||
| 1 | 3.8195 | 1.0713 | 0.0064 | 0.0613 | 0.0004 | 4.9589 | 56,894 |
| 2 | 3.9908 | 0.9274 | 0.0065 | 0.0775 | 0.0029 | 5.0052 | 32,350 |
| 3 | 3.8959 | 0.7730 | 0.0025 | 0.0496 | 0.0143 | 4.7354 | 22,530 |
| 4 | 3.9292 | 0.9239 | 0.0082 | 0.0935 | 0.0104 | 4.9652 | 32,089 |
| 5 | 5.3247 | 1.0652 | 0.0009 | 0.0970 | 0.0194 | 5.3389 | 65,745 |
| Total | 4.2624 | 0.9856 | 0.0048 | 0.0770 | 0.0090 | 6.5071 | 209,608 |
Rates of different types of consultation by Index of Multiple Deprivation quintile: logarithmic scale (all practices)
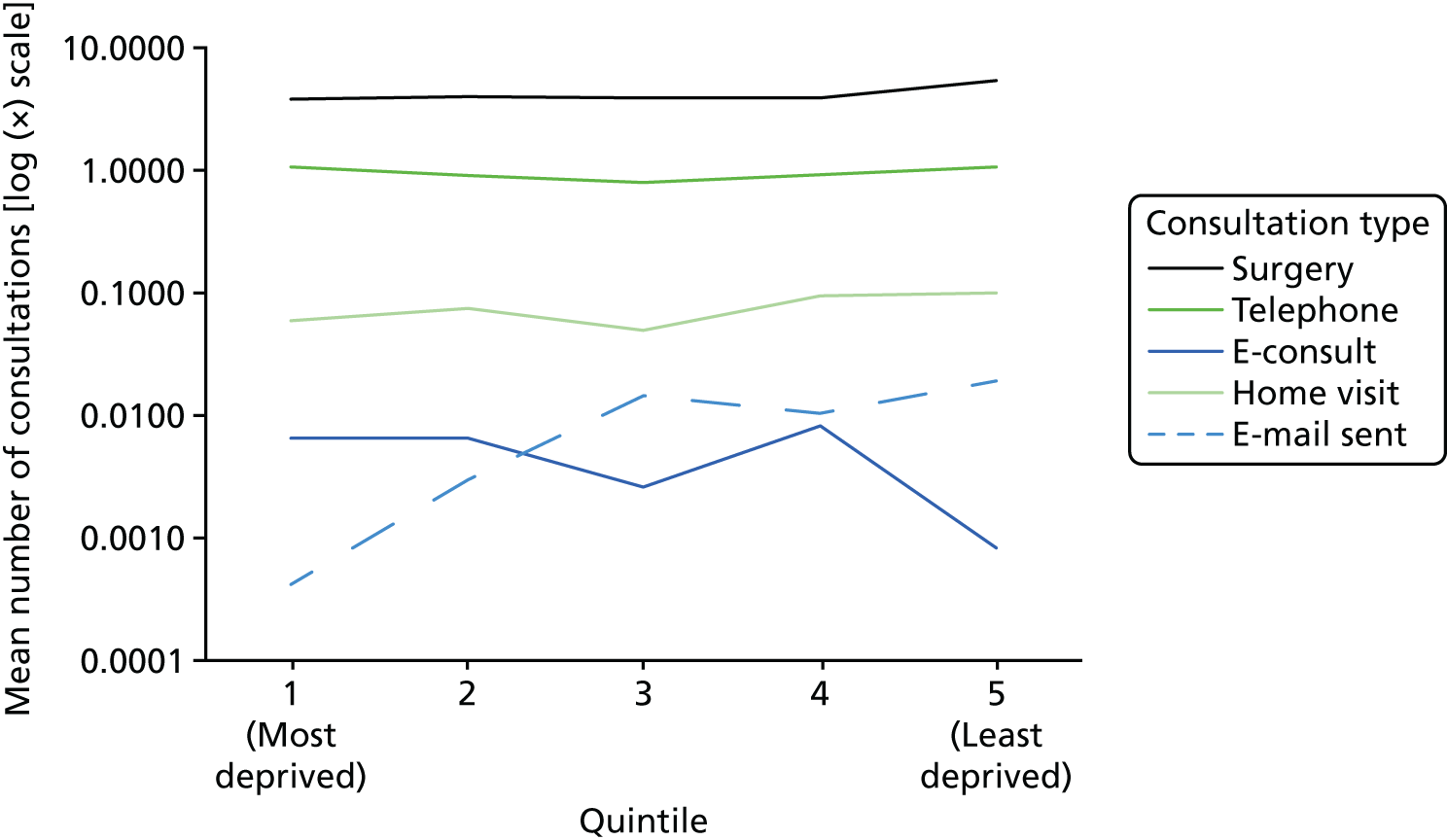
Rates of different types of consultation by ethnicity (all practices)
| Ethnicity | Consultation type | Number of consultations | |||||
|---|---|---|---|---|---|---|---|
| Surgery (n = 167,393) | Telephone (n = 38,714) | E-consult (n = 190) | Home visit (n = 3024) | E-mail sent (n = 356) | Total (n = 209,677) | ||
| White | 4.4687 | 1.0098 | 0.0063 | 0.0762 | 0.0125 | 5.5734 | 128,462 |
| Other | 4.1122 | 1.1141 | 0.0048 | 0.0332 | 0.0014 | 5.2657 | 30,730 |
| Unknown | 6.2971 | 1.6808 | 0.2347 | 0.0121 | 8.2247 | 15,595 | |
| Missing | 3.3453 | 0.6760 | 0.0020 | 0.0738 | 0.0045 | 4.1016 | 34,890 |
| Total | 4.2607 | 0.9854 | 0.0048 | 0.0770 | 0.0091 | 5.3370 | 209,677 |
Rates of different types of consultation by morbidity and multimorbidity (all practices)
| Morbidity | Consultation type | Number of consultations | |||||
|---|---|---|---|---|---|---|---|
| Surgery (n = 167,393) | Telephone (n = 38,714) | E-consult (n = 190) | Home visit (n = 3024) | E-mail sent (n = 356) | Total (n = 209,677) | ||
| None | 2.6783 | 0.6070 | 0.0034 | 0.0091 | 0.0057 | 3.3035 | 85,645 |
| One morbidity | 5.5053 | 1.2636 | 0.0067 | 0.0513 | 0.0121 | 6.8389 | 62,560 |
| Multimorbidity | 11.2946 | 2.7098 | 0.0100 | 0.5501 | 0.0233 | 14.5878 | 61,472 |
| Total | 4.2607 | 0.9854 | 0.0048 | 0.0770 | 0.0091 | 5.3370 | 209,677 |
Appendix 20 Rates of different types of consultation by number of morbidities: natural units and logarithmic scale
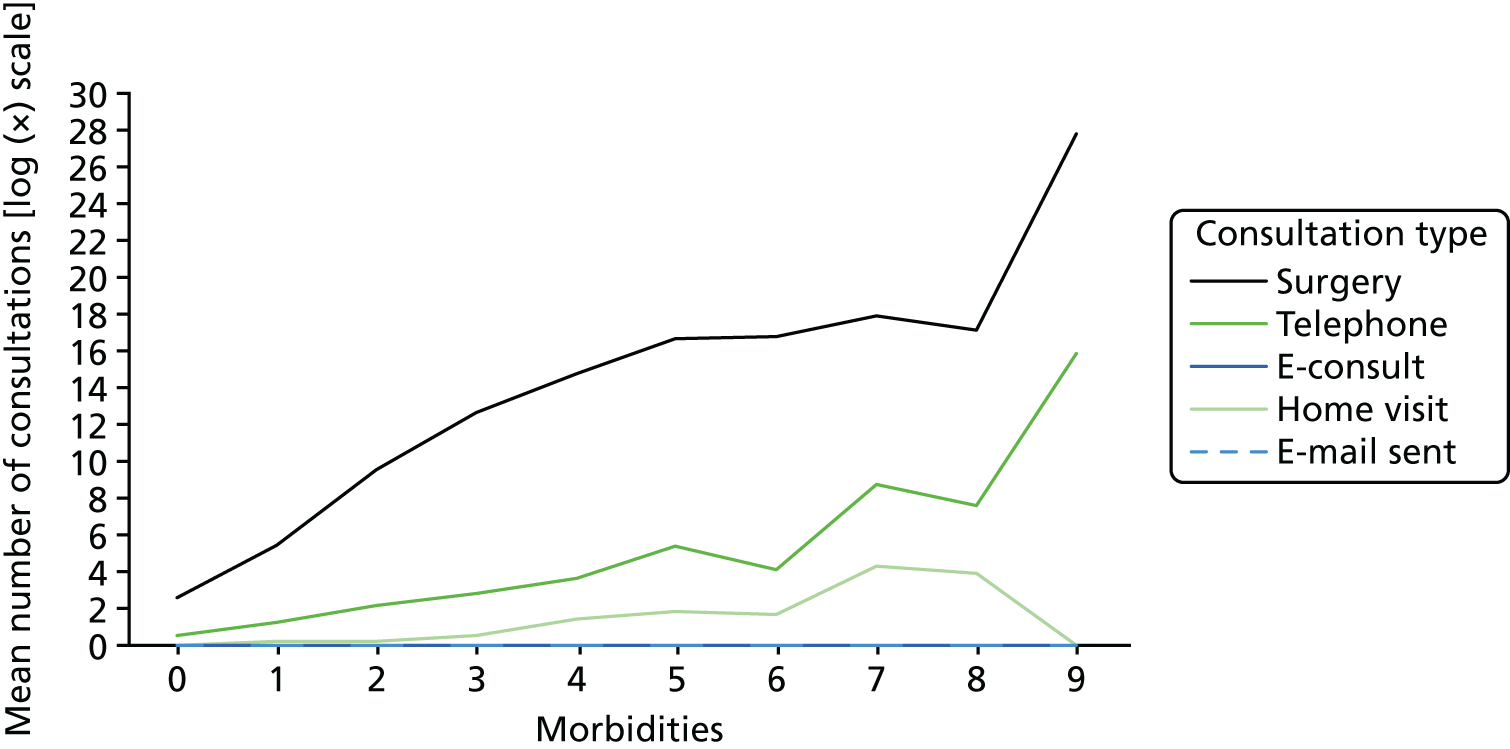
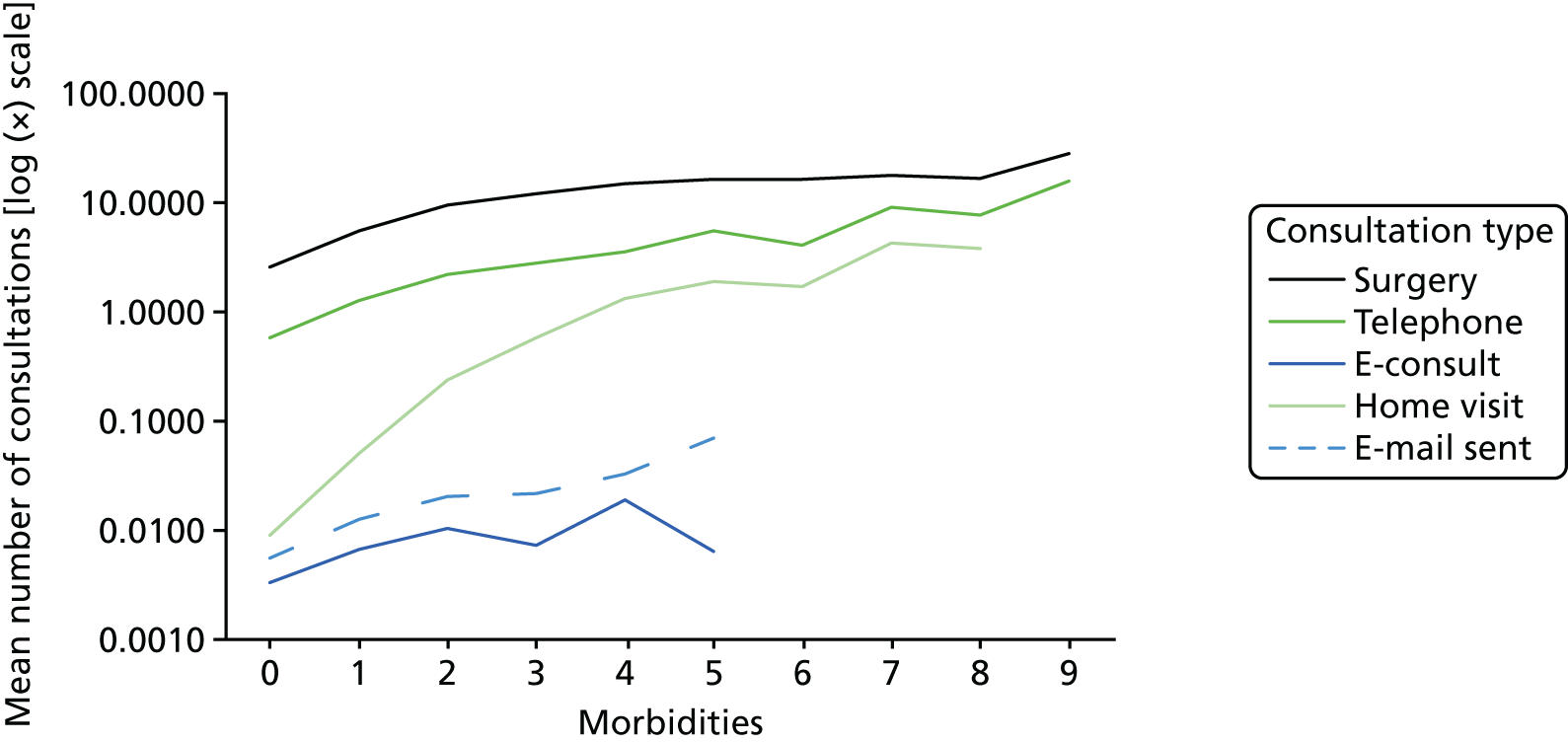
Appendix 21 Consultations and reconsultations with general practitioner only
| Type of consultation | Number of patients consulting | Number (%) of patients who reconsulted within 14 days by consultation type | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgery | Telephone | E-consult | Home visit | E-mail sent | No reconsultation | ||||||||
| Surgery | 90,113 | 20,398 | 22.64 | 10,224 | 11.35 | 38 | 0.04 | 737 | 0.82 | 108 | 0.12 | 63,639 | 70.62 |
| Telephone | 36,288 | 13,751 | 37.89 | 10,555 | 29.09 | 27 | 0.07 | 1241 | 3.42 | 36 | 0.10 | 16,688 | 45.99 |
| E-consult | 190 | 58 | 30.53 | 58 | 30.53 | 14 | 7.37 | 2 | 1.05 | 0 | 0.00 | 85 | 44.74 |
| Home visit | 2409 | 625 | 25.94 | 723 | 30.01 | 0 | 0.00 | 622 | 25.82 | 3 | 0.12 | 1073 | 44.54 |
| E-mail sent | 197 | 52 | 26.40 | 15 | 7.61 | 0 | 0.00 | 1 | 0.51 | 28 | 14.21 | 119 | 60.41 |
| Total | 129,197 | 34,884 | 27.00 | 21,575 | 16.70 | 79 | 0.06 | 2603 | 2.01 | 175 | 0.14 | 81,604 | 63.16 |
Appendix 22 An outline of the structure of the web resource
Figure 6, Chapter 7 is a screenshot of the homepage for the website.
The structure of the website follows a three-level hierarchy.
On the front page, there is a small amount of text to introduce the site and its aims and objectives, and a side bar that provides a link back to the main Alt-Con front page, links to each of the five main headings (as listed below) and one link to the different Alt-Con choices. The user can go either to the top level or directly to the page of interest.
The same side bar remains on each page, allowing the user to navigate between pages. In addition, the pages include hyperlinks to take the user to specific pages of interest.
-
Level 1: front page.
-
Level 2: why do you want to introduce an alternative to a face-to-face consultation? With three options, each leading to a separate page:
-
Level 3: convenience for patients.
-
Level 3: increasing access.
-
Level 3: to manage demand.
-
-
Level 2: who is it for and why? With two options, each leading to a separate page:
-
Level 3: who is it for?
-
Level 3: for what purpose?
-
-
Level 2: how can you get it right? With three options, each leading to a separate page:
-
Level 3: on a patient level.
-
Level 3: on a professional and personal level.
-
Level 3: on an organisational and systems level.
-
-
Level 2: how will we know if it has worked? With two options, each leading to a separate page:
-
Level 3: what do you want/should you measure?
-
Level 3: how can I/should I measure it?
-
-
Level 2: which alternative are you interested in? And then four buttons:
-
Level 3: telephone.
-
Level 3: e-mail.
-
Level 3: e-consult.
-
Level 3: video.
-
List of abbreviations
- CCG
- Clinical Commissioning Group
- DHSC
- Department of Health and Social Care
- EMIS
- Egerton Medical Information Systems
- GP
- general practitioner
- HCA
- health-care assistant
- ICC
- intraclass correlation
- ICT
- information and communications technology
- IMD
- Index of Multiple Deprivation
- IT
- information technology
- MRC
- Medical Research Council
- NIHR
- National Institute for Health Research
- OSOP
- one sheet of paper
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- SD
- standard deviation
- SMS
- short messaging service
