Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1017/18. The contractual start date was in February 2013. The final report began editorial review in March 2017 and was accepted for publication in July 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Godfrey et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
In this chapter, we set out the background to and rationale for the study. We review evidence on the meaning of person-centred care, considered a benchmark of care quality, with reference to the care of people with dementia on acute hospital wards. We then describe the development of an intervention to improve the care of hospitalised older people with dementia, the theory of change underpinning it and the objectives of the research to evaluate it.
Improving care of people with dementia in hospital: a policy priority
Improving the care of people with dementia has been identified as a policy priority in the UK and internationally over the last decade. This has resulted in the development of national dementia strategies in England1, Wales2 and Scotland. 3,4 Similar initiatives have been introduced in other European countries5 and in Australia6,7 and New Zealand. 8 In the UK, the policy and strategic objectives include improving care quality for people with dementia in acute hospitals (objective 8 of the English strategy1 and target 2 of the 1000 Lives Plus campaign for Wales2); and making hospitals more ‘dementia friendly’. 3 Both objectives are prioritised in the Prime Minister’s Dementia Challenge. 9,10
Older people are the main users of acute hospital beds, and around half of patients who are aged ≥ 70 years have a cognitive impairment, including dementia, delirium and delirium on dementia. 11–13
The needs of people with dementia in hospital are multiple and complex. They include care needs relating to functional impairments, a consequence of physical comorbidities common among those in advanced older age; expressive, emotional and communication needs, which vary depending on the nature, severity and impact of their cognitive impairment; and medical needs resulting from the type of acute event precipitating hospital admission, which may also exacerbate the dementia (e.g. pain and infection).
People on hospital wards living with dementia are at heightened risk of unintended adverse events. These events include delirium and falls that contribute to increased mortality, longer length of hospital stay and poor health outcomes such as loss of independence and new care home admissions,11,12,14,15 with the attendant resource implications. 16,17 Being in hospital may be experienced as frightening and engender feelings of anxiety, distress and agitation18–22 as a consequence of the busy and unfamiliar environment. Features of physical design, organisational structure, care climate and care processes that do not take account of individuals’ vulnerability and reduced resilience may exacerbate distress and contribute to poor outcomes. 21,22
The dominance of older people on acute wards and the prevalence of dementia among those hospitalised means that care delivery to people with a cognitive impairment is a litmus test of the quality of hospital care. Yet, despite the frequency with which people with dementia utilise acute care, evidence from systematic reviews,21,22 recent in-depth studies18,23,24 and national audits25,26 suggests that the needs of people in this group are often under-recognised and inadequately addressed.
Care of hospitalised older people with dementia
Studies have identified the organisational and cultural features of acute care delivery that have a negative impact on the care of patients with dementia. These include inflexible care routines that privilege the performance of medical and physical care tasks over time spent with patients,27,28 and physical environments that are difficult to navigate. 21,22,25 The nature and quality of staff interactions with patients has been regarded as problematic, with staff encounters that are primarily task focused and involve limited engagement of the person at a personal level;17–19,21,22,24,25,29–33 and communication practices that are poorly responsive to the emotional needs of patients17,21–25,27,30–32 and/or lead to a failure to ‘see’ and act on behavioural cues that might indicate distress or pain. 34,35 Studies have reported stigmatising and negative attitudes towards people with dementia among some staff and that such patients should not be admitted to acute wards. 27,29–32 Often conveyed as ensuring their safety and that of other patients, the consequence is to see people with dementia as ‘other’. Conversely, staff with knowledge of dementia express lower perceived strain in caring for a person with dementia and less negative attitudes. 32 Research with caregivers has reported inadequate support for their relative with nutrition and hydration,17 both risk factors for delirium;36 the person with dementia not being treated with dignity and respect;17,22,24,27,37,38 and limited engagement in decision-making, for both the person with dementia and the caregiver. 17,22,37 A key factor, contributing to poor care delivery from UK studies, is lack of knowledge and skill in dementia care. 20,22,25,38
Person-centred care: a marker of care quality
What is person-centred care?
‘Person-centred’ care has become ubiquitous in UK health and social care policy discourse as synonymous with care quality. Prioritised in the National Service Framework for Older People,39 it is viewed as key to upholding dignity in care40 and forms one of the key Principles of Nursing Practice developed by the Royal College of Nursing (RCN). 41 However, either its meaning in policy is implicit or there is varying emphasis on different domains. It is commonly conveyed as individualised care, holistic care, choice, autonomy and dignity; and the use of the term, and the particular emphasis attached to it, has varied over time and in relation to wider policy interests (see Appendix 1 for a document review).
From research, there is a similar lack of clarity on what is person-centred care. Two systematic reviews examined its meaning in health,42,43 although they adopted different perspectives. Kogan et al. 42 explored research relating to older people, and Sharma et al. ’s43 review of reviews addressed understanding of person-centeredness in nursing and medicine. Both concluded that there was no consensus on meaning, posing difficulties in operationalising the concept. Neither included studies in acute care, and only 3 out of 132 papers in Kogan’s review related to people with dementia, all of which were conducted in long-term care. To explore this further, we consider theoretical conceptions of personhood and person-centred care in dementia and draw on research evidence to explore what quality care might look like for people with dementia on acute wards.
Theoretical conceptions of person-centred care in dementia
Personhood in dementia
Kitwood’s44 theoretical model of ‘personhood’ has been enormously influential as the basis for ‘person-centred’ care in dementia. He drew attention to the way in which people’s experience, behaviours and actions do not simply arise as a consequence of neurological deficits. They are also shaped by interactional processes that result in the erosion of personhood and the consequent invisibility and diminishing of the person; in essence, loss of cognition is equated with being a non-person, with a deleterious impact on the individual. Similarly, Sabat45 has explored how the social positioning of people with dementia affects how they are related to, considered and conceptualised, and which in turn affects their personhood, their behaviour and their interactions with others. This theory projects the malign impact of ‘others’ (whether at institutional, organisational, social or interpersonal levels) on the person’s sense of self.
Based on humanistic values and person-centred psychotherapy,46 Kitwood suggests that a person with dementia can sustain relative well-being if personhood is maintained. Drawing on empirical research in long-term care, he defines five psychological needs (not unique to people with dementia) to establish the main foci of interventions for sustaining personhood: comfort, attachment, inclusion, occupation and identity. Although the concept of ‘person-centred’ has been criticised for its ‘individual’ emphasis,47 ‘personhood’ as articulated by Kitwood and Sabat is relational, the underpinning assumption being that the person is embedded in relationships in a social world. Person-centred care, therefore, is care that meets the person’s psychological and social needs, informed by values of respect and concern for others, and that has been summarised in the VIPS model. 48 Here, person-centred care comprises four elements: valuing people with dementia and those who care for them (V); treating people as individuals (I); looking at the world from the perspective of the person with dementia (P); and positive social environment such that the person can experience well-being (S). The significance of the quality of the relationship with persons with dementia is uncontested. Less evident is how to operationalise an appropriate response to the psychological and social needs identified by Kitwood44 into settings that are temporary, geared to specific purposes and where relationships are short-lived and transient, as are acute wards. Indeed, it is argued that operationalising person-centred care will vary with the nature of the setting in which it is delivered. 49
Embodiment and dementia
Recent developments in understanding dementia have drawn on theories of embodiment. 50–53 Kontos50 directs attention at the way in which people with dementia express selfhood through their embodied way of ‘being in the world’ (i.e. through activity and engagement rather than reflection or contemplation). She contends that selfhood that resides in the pre-reflective body has two origins. The first is primordial, whereby ‘selfhood emanates from the body’s power of natural expression, and manifests in the body’s inherent ability to apprehend and convey meaning’. 50 This is seen, for instance, in how people, including those with severe dementia, communicate with gestures, body movements and facial expressions, which carry meaning in interpersonal communication; they are reflective of agency or intentionality. The second origin of selfhood is the sociocultural dimension of the pre-reflective body: people’s actions and interactions convey deeply internalised, socioculturally specific ways of being in the world. For example, people with severe dementia may converse with each other following normative rules of engagement (e.g. turn-taking), although the content may seem unintelligible to the listener. She argues that the notion of embodied selfhood refers to the complex inter-relationship between primordial and social characteristics of the body, which reside below the threshold of cognition, are grounded in the pre-reflective level of experience and are manifest primarily in corporeal ways. Understanding the ways in which people are embodied is to challenge the assumption that there is loss of agency with cognitive impairment. The conception of embodied communication as meaningful has implications for engaging with people with dementia in acute care. Hughes53 considers that if one is to share, if not fully understand, the world of a person with dementia, one must draw on myriad non-verbal and expressive cues, and to make sense of them requires knowledge of the person.
Practice of person-centred care on acute wards
Research relating to older people with dementia on acute wards primarily highlights difficulties in care practice, and evidence reviews conclude that a chasm exists between the rhetoric of ‘person-centred care’ and actual delivery. 21,22 Apart from a recent study,24 this research does not draw on a theoretical conception of ‘person-centred’ care in dementia, although several studies offer insight into what person-focused practice might look like.
Studies on the quality of care delivery on acute wards have been mainly small scale, employing ethnographic18–20,30,33 or mixed methods, including interviews with caregivers. 23,24,29,31,32,54 Two20,54 drew out components of good practice from observation, interviews and conversations with patients. Tolson et al. ,54 employing critical incident interviewing with patients (possible with only a small number) and caregivers, identified four themes within a temporal frame around which components of quality practice could be delineated. ‘Settling in’ referred to the process of adjustment involving responsiveness to emotional signifiers and acknowledgement of the person as valued and part of a family/social network. Its significance stemmed from the person’s need for reassurance, given the disorientation and distress resulting from being in an unfamiliar environment. ‘Visible love’ by engaging with the affective dimension of caring, including the connections between the patient and family, generated a sense of the person’s worth. ‘Reaching me, reaching you’ related to the interactional quality of encounters in which sharing and knowing assumed central importance. ‘My condition’ embraced the acute illness, existing health problems and the cognitive impairment. Quality practice meant achieving a ‘balance of care’ based on understanding the inter-relationship between these three. ‘Best’ practice in acute care required attention to the particular needs of people consequent on the cognitive impairment; strategies that promoted ‘settling in’, thereby enabling people to feel valued; and proactive communication that facilitated connections with the person’s biography and significant relationships in providing care.
Norman20 identified two further components pertinent to ‘good’ practice. First, patients were viewed not just as passive ‘recipients’ of care but as active agents, conveying a sense of ‘self’ in their actions and interactions. When staff viewed what patients did as meaningless or problematic, it resulted in a construction of patients as reduced and dependent. Conversely, seeing patients’ actions and interactions as meaningful drew forth a staff response that reinforced the person’s individuality and sense of self. Second, a distinction was drawn between two types of nursing work, ‘practical’ and ‘emotional’, similar to that in recent literature between ‘task-centred’ and ‘person-centred’. ‘Practical’ work was defined by minimal collaboration in which a provider/recipient relationship prevailed; ‘emotional’ work involved higher levels of collaboration, including prioritising patients’ needs. However, this binary conception of forms of work in the context of people with dementia on acute wards appears limited. Instead, employing the conception of Tolson et al. 54 of the ‘balance of care’, it would seem more useful to consider ‘practical’ and ‘emotional’ work not as polar opposites, but as infused, one with the other.
Nilsson et al. ’s32 ethnographic study on a cardiology unit offers negative evidence in support of Tolson’s ‘balance of care’ conception. The overarching category, ‘falling behind’, refers to the way in which patients’ needs associated with dementia went largely unnoticed until they escalated and emerged as problems that disrupted the usual flow or threatened safety issues in the unit. The response generated was reactive and not proactive, with negative consequences for patients, relatives and staff. Clissett et al. 24 employed Kitwood’s44 conception of the basic needs necessary to sustain personhood as an a priori framework to determine what was person-centred care, namely care that offered comfort, attachment, inclusion, occupation and identity. They concluded that although staff promoted attachment and inclusion, there was little evidence that they supported patients’ sense of identity, occupation and comfort; and that practice was poor in these areas. Their conclusions and interpretations do not flow unambiguously from the empirical data presented. First, the content of what was contained within these domains appeared somewhat arbitrary. Second, the way findings were presented (conveying accounts of how these needs were met followed by missed opportunities) meant that the weight given to positive aspects of practice, in relation to lost opportunities, is unclear from the illustrative data. Third, what shaped these positive and negative features of practice were not elucidated, as the focus was on the interpersonal level of staff–patient engagement. Fourth, there is an assumption that needs conceived of as necessary to secure well-being developed in a care homes context are equally relevant to acute care.
Another recent qualitative comparative study of care delivery to people with a cognitive impairment on a specialist medical and mental health unit and standard care wards within a randomised controlled trial33 provides further clarity on what person-centred practice might look like on acute wards. This involved a subsample of 60 (30 in each group) out of 90 trial participants observed using dementia care mapping and unstructured observation captured in fieldnotes. Many aspects of practice were similar across specialist and standard care wards: crowded, noisy physical environments; delivery of care in a routine and task-oriented fashion; communication that was usually brief or absent when meeting physical care needs; and the prioritisation of physical over emotional needs. Some features of person-centred care were observed, described as care that included personal communication during routine care tasks, validating patient concerns, facilitating independence and delivering care at a relaxed pace. The main difference between standard care and the specialist unit related to the work carried out within the activities room, with designated activities co-ordinators in the specialist dementia unit. The authors concluded that the profile of patients on both ward types was similar (high dependency resulting from acute illness, functional dependency, behavioural and psychological problems with increased cognitive impairment). Although the activities programme was very successful for some people, severity of illness and impairment meant that others could not participate. The trial,55 of which this qualitative study was a component, is the only published research to date that has examined the outcomes of care practice on specialist medical and mental health units compared with standard care. The findings reported increased satisfaction among caregivers on the specialist unit but no significant differences in organisational or clinical outcomes.
In summary, although person-centred care is presented as a marker of care quality in health research, there is no consensus on its meaning. Although the humanistic values underpinning person-centeredness offer a guide for practice, further work is needed to concretise what this person-centred practice might look like in an acute ward environment, and what methods and tools might be effective in improving practice.
Developing the observation tool
The Person, Interactions and Environment (PIE) observation tool was developed for use in the first national audit of dementia on NHS hospital wards25 during a 3-year research study (2008–10). The aim was to develop and feasibility test an easy-to-use tool to:
-
enable local observers (staff or volunteers) to view care from the perspective of the person with dementia
-
provide observers with a means (and vocabulary) to report on care quality based on the findings
-
enable the care provided to be compared with that of other hospitals nationally
-
produce data for use by ward staff to develop action plans to improve practice.
The study was overseen by a steering group for the National Audit of Dementia (NAD), comprising professional and ‘experiential’ dementia experts (including individuals with dementia, and caregivers).
Process of Person, Interactions and Environment tool development
The first phase involved iterative scoping reviews to examine the concept of person-centeredness, and the observation tools used to measure it in an acute setting that could potentially be adapted for the audit. The literature review identified several potential candidate tools. However, these were based on nursing models and not dementia specific;56,57 or they were dementia specific but not tailored for use in an acute setting;58–60 or the complexity, level of expertise required and cost involved in using the tool made it impractical. 59,60 It was agreed to develop a new observation tool for the audit.
A subsequent systematic search of the literature was undertaken to explore the dimensions of care valued by hospitalised older people generally and by those with dementia specifically. The findings from this review were discussed through a process of stakeholder consultation via focus groups with staff and patient representatives from different specialties in four hospitals, and a patient and public involvement group. The purpose was to inform the content and structure of the proposed tool and how it might be used in hospital.
The PIE tool has three dimensions: person, interactions and environment. These represent the elements of knowing and using information about the patient as a person in care delivery, the quality of staff–patient interaction, and the effect of the immediate organisational and physical environment. They reflect inter alia the personhood of the individual, including their subjective experience (incorporating biography, values, life preferences and significant relationships); the interactional or relational character of the social world in which the person is embedded and that shapes sense of self and identity; and the nature of the surrounding physical, social and care environment that provides the context in which care is delivered. Drawing on interactionist44 and social positioning45 theories of dementia, it was understood that the type and severity of the cognitive impairment both have an impact on the individual’s experience of the interpersonal, social and physical world, which in turn affects the person with the condition. This dynamic has implications for the care delivery of people living with dementia on acute wards.
The feasibility of the draft tool and guidance was tested in seven hospitals (18 wards) and through further consultation with the advisory group. Key criteria were that it should be acceptable to staff and feasible for use with minimal resources.
Following modifications and refinements, the PIE tool and guidance were presented in the form of a workbook manual and a one-day workshop to train hospital staff in its use. For audit purposes, PIE involved gaining informed consent to observe the care of up to six patients with dementia or problems in a ward area in real time. Observations were conducted by two staff (one external to the ward), who paired up to observe different patients for at least two periods of 2 hours (one in the morning and one over lunchtime). Following reflection and feedback with the ward team, each ward identified one aspect of good practice and one requiring improvement, with achievable short-term and longer-term actions to be undertaken at ward, directorate and trust/health board levels.
Use of Person, Interactions and Environment in the National Audit of Dementia
An enhanced audit component of the NAD was conducted in a subsample of 55 hospitals (145 wards), and included PIE. The findings from PIE observations, conveyed in the published report,25 were that care and communication were generally reactive and based on an organisationally set, task-driven routine rather than being person-focused, flexible and proactive. Although there were ‘pockets’ of positive, individualised care in the practice of individual staff, or as elements of ward practice, only a handful of wards (5/105) reported practices that were consistently focused on the person. There were periods of care-based activity interspersed with inactivity, leading to lack of attention and stimulation. The environment was often impersonal and dementia unfriendly, with a lack of orienting cues, dementia aids or areas for socialising.
Although the findings were not novel, the breadth of coverage underscored the nature and extent of the problem of care delivery to patients with dementia. Furthermore, a comparison between wards offered preliminary evidence of ‘propellers’ or features of staff–patient interaction that supported person-focused communication, suggesting scope to enhance care.
As the primary purpose of the audit was to document current practice, the process of translating action-planning at ward level to effect organisational change, and the systems and mechanisms required to support and sustain it, was not developed. Nor was there an attempt to examine whether action plans derived from observation affected staff practice, patients’ care experience or health outcomes. These conclusions prompted the current study: the development of PIE as a generalisable practice development process in conjunction with the PIE observation tool (PIE Programme), and an evaluation of its effectiveness in improving care for people with dementia on acute wards.
From the Person, Interactions and Environment observation tool to the Person, Interactions and Environment programme
The PIE Programme (referred to henceforth as PIE), tools, guidance, implementation process, manual and ‘theory of change’ were elaborated on as part of this current study.
This further development involved an iterative review of the literature on implementing change, a workshop with staff across the Yorkshire and the Humber region who had used PIE in the NAD, and participation in workshops with NHS hospital staff (RW, JC and MG). These workshops were conducted as part of a Quality Mark for Elder-Friendly Hospital Wards, launched by the Royal College of Psychiatrists in partnership with the Royal College of Physicians, the British Geriatrics Society, the RCN and Age UK. Within these fora, we tested out the further acceptability and use of PIE as a strategy and process to support cultural and practice change on acute wards to meet the needs of patients with dementia.
The Person, Interactions and Environment intervention and implementation process
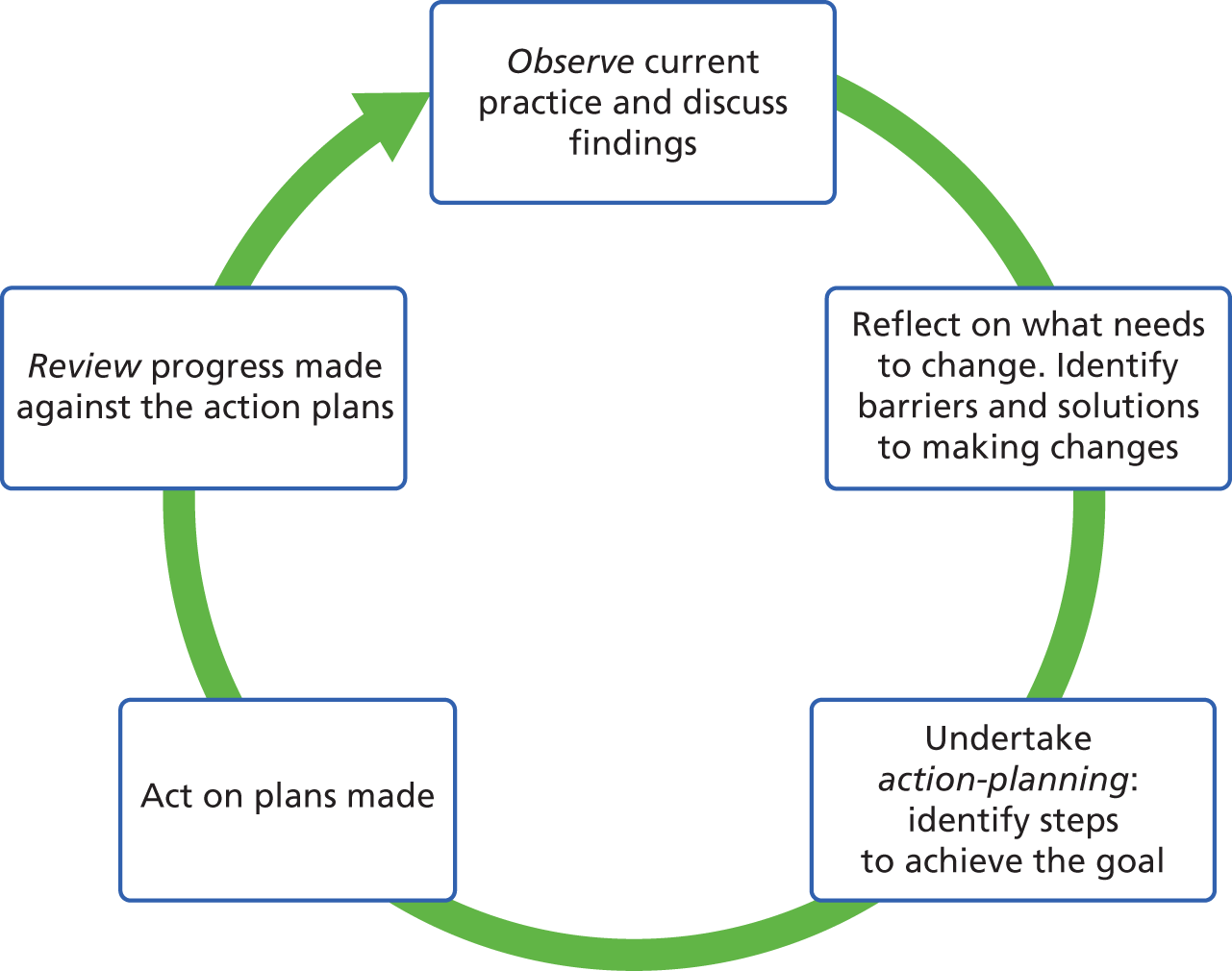
PIE adopts a systematic approach, using a set of steps to implement and embed change in routine care on hospital wards, each step being supported by tools and guidance. Implementation is a cyclical process comprising observation of current practice (observation tool and guidance). Observation is a means to, first, document care as delivered and, second, consider the impact of the care on patients with dementia to promote fresh insights and potentially challenge existing practice. Reflection on observations is the basis for identifying goals and action plans to improve practice (action-planning tool and guidance). Goals for change are prioritised and action plans are formulated. Action plans specify steps to move from current practice towards achieving goals; how these will be taken forward and by whom; and how they will be communicated to the wider staff group to extend the programmes’ reach and engage them in action. A review of progress against planned action, including an appraisal of barriers to and facilitators of change (review tool and guidance), enables an adjustment of action and/or a review of goals. The process is illustrated in Figure 1.
FIGURE 1.
The PIE service improvement process.
Implementation team
An additional mechanism to effect change is the establishment of an implementation team to lead it. Its core membership comprises a ward manager or senior nurse with the authority and legitimacy to drive the programme; a matron or practice development lead outside the ward to provide organisational and facilitative support, and act as a conduit between ward-based initiatives and dementia strategies at the departmental and hospital levels; and ward staff involved in directly providing care to patients, such as nurses, therapists and health-care assistants (HCAs). Within these parameters, the size and make-up of the team is flexible.
This conception synthesises a top-down and bottom-up approach to change:61 the active involvement of senior staff to secure organisational commitment to introducing and embedding the programme; and the engagement of those directly in delivering it, to ensure that their views and experiences inform the pace and direction of change. 62–64 The responsibilities of the team include:
-
raising awareness of PIE among the whole staff group
-
organising observations, action-planning and review of progress
-
engaging ward staff in change through discussion of priorities and action plans
-
reviewing what systems and mechanisms need to be put in place to support sustainability.
Strategies to support implementation
Several strategies are in place to support implementation: a PIE manual, and an interactive training workshop to introduce participants to PIE.
Person, Interactions and Environment manual
The manual is organised as a workbook and comprises three sections. Section 1 describes the PIE purpose and rationale, specifically why people with acute illness living with dementia require a tailored and dementia-sensitive approach to meet their care needs and facilitate recovery. Section 2 provides an overview of the cyclical process of change involving observation, reflection, action-planning, action and review. Section 3 details each step in the implementation process (observation, action-planning and review), the tools for each step, guidance on using the tools and a flow chart to indicate what should happen and when. Worked-out exemplars of observations, action plans and reviews are provided.
Person, Interactions and Environment introductory workshop
PIE is introduced in a one-day workshop to familiarise participants with the programme. The first part of the workshop conveys, through various media (role play, drama, video clips), how the social and spatial environment of an acute ward may be perceived by persons with a cognitive impairment. This is aimed at sensitising staff to how people with dementia may experience the world around them. Observation of encounters between professionals and people with dementia are presented via drama and video clips, for example the ‘Come feel with me’ DVD (digital versatile disc). 65 The purpose is to elicit critical refection on how people with dementia may express agency through embodied action, thereby directing attention on ‘knowing the person’ to interpret behaviour and action. The second part of the workshop takes participants through each step in the observation, action-planning, action and review cycle, preparatory to introducing PIE on their ward.
Theory of change
In designing the PIE implementation process, we drew on normalisation process theory (NPT)66 as a sensitising framework. From the range of theories available on implementation,67,68 our use of NPT stems from its sociological focus and the utility of the broad constructs that constitute it. In contrast to psychological theories of change that address individual behaviour, NPT focuses on microsocial processes that affect the implementation of a practice (or technique) in an organisation or clinical setting to account for how individuals and organisations understand and make sense of the new practice, engage with it, participate in the work relating to it, and reflect or appraise its effects in relation to valued goals. NPT appeared most apt for PIE implementation. PIE is a whole-ward intervention; it does not simply involve change in individual behaviour, but also requires organisational, cultural and team-level change. Furthermore, the PIE intervention uses and alters roles and patterns of communication among staff and between staff and patients. Changed meanings, practices, roles and relationships are intended to become part of ‘the way we do things here’ (ward culture).
Within NPT, ‘normalisation’ refers to the work of individuals as they engage in activities that become routinely embedded in knowledge and practice. NPT postulates four generative mechanisms that operate individually and collectively to explicate how practices become ‘normalised’ within routine care: coherence, cognitive participation, collective action and reflexive monitoring. New practices, the theory contends, become routinised when:
-
the work that defines and organises a practice or intervention is understood as meaningful and invested in, in respect of the knowledge, skills, behaviours and actions required to implement it at an individual and collective level (coherence)
-
the work is perceived as worthwhile and appropriate for the commitment of individual time and effort in order to bring about the intended outcome (cognitive participation)
-
work practices, and the division of labour through which these are carried out, are modified or adapted to incorporate the change or intervention into the social system of the host organisation (collective action)
-
those engaged appraise the effects as attributable to the intervention and congruent with valued goals (reflexive monitoring).
In PIE, the work of generating coherence begins with the introductory workshop, with its content and participatory nature focused on a range of ways for participants to ‘see the world’ from the perspective of the person with dementia. This continues with the first step in the improvement cycle, namely staff’s real-time observation of patients with dementia. Taking a ‘step back’ from work roles to observe ‘persons, practice and context’ for a short time, as an ‘outsider’ looking in, will, it is assumed, help staff to ‘see’ things in a different way (coherence). This is the prerequisite to reflect on, and examine, what may have been taken-for-granted assumptions, activities and practices. In contrast to the use of the PIE observation tool in the NAD, the number of observations, by whom and when, are flexible, to facilitate local buy-in. Collective discussion of observations within the PIE team further reinforces coherence, and by establishing the need for, and possibility of, change, will secure cognitive participation. These reflections form the starting point for identifying goals for change and the necessary steps or action plans to achieve the goals. Action-planning, including who does what and how it will be communicated and discussed within the wider team, is intended to pursue the work of collective action. A review of progress and reappraisal of goals and actions in the light of what works will, it is assumed, act as leverage to continue the process (reflexive monitoring).
The PIE implementation process is systematic and tools are provided for each step (observation, action plans and reviews). However, the content – how observations are conducted (the number conducted, and for how long, by whom and when they are conducted), the goals identified and the action plans pursued – is flexible and tailored to individual wards. Implementation is conceived of as a process and not a one-off event. 69 A significant dimension of PIE implementation is temporality. Change through successive observation, action-planning, action and review cycles mean that the process is likely to be non-linear and multidirectional,70,71 the success (or failure) of action plans creating the conditions for subsequent review and new/reworked action plans. The commitment and skill of those leading the change and in working through each phase of the improvement cycle will affect implementation and outcomes, so that there is a degree of unpredictability of the process (and the outcomes).
PIE is an exemplar of a complex intervention. 72 It contains multiple interacting components; the levels at which change is directed are several (individual, collective and organisational); and there is flexibility in delivering it. The change process is emergent and non-standardised. 73 The ward setting within which the intervention is being introduced, and with which it interacts, is also dynamic, adding another level of complexity. 74
The research study
The overall research purpose was to examine whether or not PIE enhanced the care of older people on acute wards living with dementia, how this was achieved, and whether or not, and in what ways, this had an impact on ward practice, patient and caregiver experiences and selected clinical outcomes.
The objectives of the process and outcomes evaluation of PIE were to:
-
provide a descriptive and explanatory account of how staff engaged with PIE in the real-life context of acute ward delivery
-
test out and refine the causal assumptions underpinning PIE (the theory of change)
-
explore the impact of PIE on practice, patient and caregiver experiences and clinical outcomes.
The research questions posed address the PIE process and outcomes at several levels. The specific questions were as follows.
Process of change
-
How is delivery of PIE achieved, and what is actually delivered?
-
How does PIE produce change, or, conversely, if the intended changes do not occur, is this because of poor/inadequate theory or poor implementation?
-
How and in what ways is PIE implementation (and outcomes) affected by the organisational and resource context of acute care delivery?
Outcomes
-
Does PIE change ward staff practice in ways that are consistent with person-focused care?
-
Is PIE effective in improving care for people with a coincidental dementia on acute wards, as experienced by those patients and/or observed by their relatives/caregivers?
-
Is there preliminary evidence of effectiveness of PIE in improving selected clinical outcomes (days in delirium and falls rate)?
Chapter 2 Evaluating Person, Interactions and Environment: methodology and methods
Introduction
This chapter elucidates the methodology and methods employed in performing a process and outcomes evaluation of PIE. It includes the rationale for the design, sampling strategy, data collection methods and analysis; the ethical issues posed; and how public and patient participation was pursued.
Methodology
We performed a comparative, longitudinal, mixed-methods case study. Case-based research75–79 is characterised by the depth and detail of information collected within naturally occurring, bounded settings, in which the boundary between the setting and focus of interest is permeable. 78 In this study, the analytic lens was care delivery to older people with dementia hospitalised on NHS acute wards. This is one facet of ward work, which is also affected by contextual factors outside the ward.
The distinctiveness of the approach is its systemic and holistic perspective. Ragin and Becker75 argue that:
The . . . case oriented approach places cases, not variables centre stage. But what is a case? Comparative social science [answers this question] . . . Boundaries around places and time periods define cases.
Ragin and Becker, p. 575
Embedded in this conception is that cases are complex systems in which:
[T]rajectories and transformations depend on all of the whole, the parts, the interactions among parts and whole, and the interactions of any system with other complex systems among which it is nested and with which it intersects.
Ragin and Becker, p. 275
The rationale for adopting a case study design flowed from the nature of PIE and the setting in which change was introduced. PIE exhibits several features of complex interventions:72 the number and difficulty of behaviours and practices required to implement and deliver it; the levels at which change is required (individual, collective and organisational); the degree of flexibility permitted in delivering it; and the dynamic environment in which it is being implemented. The setting for initiating and implementing PIE is the acute ward; the evaluation of effectiveness requires an understanding of ‘how’ and ‘why’ change occurs within this organisational context. The comparative focus enables the exploration of commonalities and differences between cases to develop an explanatory account that extends beyond the specificity of each case.
We sought to provide a rich description of care delivery to patients with dementia in the spatial, temporal and organisational setting of the hospital ward; to understand how, and the conditions in which, PIE effects change over 18 months; and, conversely, why change occurs in some circumstances and not in others. An embedded process evaluation examined how PIE was understood and enacted by staff in real time.
Methods
Sampling strategy
Our intention was to recruit eight wards in four acute NHS trusts. Cases were sampled purposively. Wards with a substantial proportion of older people with dementia among their patient intake were identified in trusts (care of older people wards, dementia wards and trauma orthopaedic wards), varying in size and type of catchment locality in three English regions. We employed criteria of ‘readiness’ to implement PIE,80 informed by previous research on delirium prevention:81
-
interest expressed among senior acute hospital staff in taking part in research to improve person-centred care for people with dementia
-
agreement of senior ward staff to engage in a practice improvement programme over 18 months
-
commitment from a clinical lead at directorate level or an individual with responsibility for practice development to assume a leadership role in initiating and facilitating PIE.
Site recruitment
Using networks developed through the NAD, letters of invitation were sent to named individuals (directorate leads, practice development leads and ward managers) in 13 NHS hospital trusts in different English regions, and followed up with telephone conversations. Those indicating interest in taking part were sent an ‘expression of interest’ pro forma, which encapsulated the ‘readiness’ criteria. This was a signed commitment by a ward manager, directorate matron and practice development lead to take part and to assume responsibility for initiating and facilitating PIE.
Meetings with staff at ward and directorate level were organised in each of five acute trusts that expressed interest. These offered diversity in their size (small, medium or large), type of catchment locality (small towns with rural hinterland, large city, metropolitan area, and a geographically dispersed locality of large towns and villages) and geographical location (north, central and south English regions). They spanned 11 wards: three medical, care of older people wards; two dementia wards; four acute trauma wards; one acute stroke ward; and one older people’s rehabilitation ward. All trusts and wards agreed to participate in the research, returning their signed forms. Based on initial meetings with directorate and ward staff during recruitment, wards varied in their degree of ‘dementia awareness’ (reinforced in data collection).
We agreed to oversample and include these trusts and linked wards; prior experience of research in acute hospitals suggested that organisational turbulence was common (e.g. changes to ward models, ward reorganisation and bed closures). This proved prescient. Before fieldwork began, one of the sites (an orthopaedic trauma ward) dropped out because of staffing difficulties. Appendix 2 provides a summary of the structure of participating sites.
Data collection methods
A common set of data was collected for each ward over a 7- to 8-week period at baseline, and at 9 and 18 months following PIE implementation for those wards that pursued PIE.
We collected qualitative data via interviews with staff to examine their views on care delivery and the meaning of person-centred care; explored how routine care was accomplished in time and space using ethnographic observations and informant interviews with staff; conducted in-depth case studies with patients and their relatives or caregivers to understand how people with dementia experienced care through observation of patients over their acute episode and conversations ‘in the moment’ with them, and interviews and conversations with relatives/caregivers; and built up a picture of how their journey into and through the ward unfolded in time, via case notes and observations of handover and multidisciplinary team (MDT) meetings.
Quantitative data relating to ward structure (trust policy, resources and priorities) and physical environment; organisation (staff and patient profiles) and care culture (staff questionnaire), which shape care delivery and patient experience, were collected. Outcome data to examine the impact of PIE were collected at baseline and at 9 and 18 months for selected clinical outcomes (days in delirium and falls), although the systematic collection of these data across all implementation sites proved problematic (see below).
Ward structure and organisation
Physical environment
A description of the physical environment of each ward was constructed from observation.
Patient profile
A patient profile was created using a common pro forma for all wards in a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet. All patients on the ward and all new admissions during each data collection period were included. For each patient, we collected demographic (age, gender, and residence prior to admission), clinical (reason for admission, dementia diagnosis, probable dementia/memory problems and delirium) and service variables (date of admission and discharge, length of inpatient stay, discharge destination and readmission within 30 days). We adopted a pragmatic approach to the problem of poorly diagnosed dementia25 by classifying patients with a formal diagnosis and those assessed during their admission with probable dementia. In the report, we use ‘dementia’ to include both.
The collection of patient profile data required negotiation with trusts and wards to facilitate completion, as the data had to be provided in anonymised format and input by trust staff. Researchers made strenuous efforts to ensure that the pro forma was completed as fully and accurately as possible – a not inconsiderable task – and some funding was provided to wards to support this. The resulting data set provides a picture of variation in the patient journey between ward types and across trusts from admission to discharge.
Staffing profile
As well as collecting information on staff mix and staffing complement, researchers noted actual staff numbers during observed shifts and whether these staff were permanent, temporary, Bank or agency. This provided a more accurate picture of the meaning of staff shortages and difficulties than simple reference to the designated staffing levels that should occur.
Care culture, staff knowledge and understanding of person-centred care
The Climate for Care Questionnaire28 comprised 38 items relating to staff views on the shared philosophy of ward care, adequacy of resources, mutual support, feeling safe, improving practice, involvement, developing skills, time pressures and team working. It was slightly modified to include core MDT members such as therapists and medical staff (see Appendix 3).
All staff were asked to complete the questionnaire anonymously; responses were voluntary and were returned by being placed in a sealed envelope in a box file kept in a shared area where the researcher could collect them. Most returns were from nurses and HCAs. Completion rates varied between wards, with an overall response rate of just under 50% among nursing and care staff. It is difficult to be precise in that the calculation was based on staff complement, but the level of vacancies carried by wards varied between wards and over time. We sought to maximise response using different methods: ward managers were asked to remind staff during handovers; ward clerks were approached to keep the box for completed questionnaires in a prominent place (staff room or nurses’ station); and researchers gave out questionnaires to individual staff present during observation. It was notable that wards in which fieldwork revealed poor staff morale had a low response rate. In total, there were 104 respondents.
We conducted qualitative interviews, using a topic guide, with a purposive sample of ward staff at different levels of seniority and discipline (e.g. medical, nursing, therapy and care staff) and different roles (ward clerk, housekeeping and domestic staff). The topic guide was employed as an aide-memoire and interviewees were invited to discuss issues of importance to them. Conducted prior to PIE implementation, the purpose of the interviews was to explore how staff understood the meaning of person-centred care for people with dementia and the factors from their perspective that affected care delivery. The interview times varied between 30 minutes and 1 hour; they were subject to interruptions, and were often rescheduled and resumed opportunistically in gaps between frenetic activity. Interviews were audio-recorded (with a few exceptions when staff declined) and fully transcribed. In total, 56 interviews were conducted.
These included trust strategies and performance, ward-based assessment and care protocols for patients with cognitive impairment (dementia and delirium), treatment and care planning documentation, care pathways for dementia and delirium, and policies and procedures.
Organisation of care, ward routines and practices
Ethnographic observation was employed to develop an understanding of the pattern of ward activity and routines and how care for people with dementia was accomplished. This incorporated informant conversations with staff to clarify issues raised in the observation and to seek their perspective (albeit sensitive to staff’s work demands). 82 It provided a richer account of what was happening, including what people took for granted or were unable to articulate.
Each ward was visited by a researcher before fieldwork began to acquire familiarity with the spatial environment and to develop an initial observational strategy: where to observe, when to observe and the key actors involved. This provided an opportunity for the researchers to acquaint staff with the study and to respond to any questions about it.
Observation occurred over approximately 8 weeks in each of 10 wards at baseline. Researchers covered a variety of shifts: early morning, afternoon and night, weekdays and weekends. They observed the daily pattern of work, regular routines (ward rounds, multidisciplinary meetings and handovers) and special events (staff away-days). Field notes captured descriptions of settings, events, interactions and activities. Contemporaneous jottings in the field were written up as expanded accounts as soon as possible after observation (observation sessions usually occurred over a 3-hour period to facilitate this). 83–85 A field note journal was maintained in chronological order. It included initiatives introduced at hospital or ward level relating to care of people with dementia or pertinent to the ward case study (e.g. discussion and proposals around ward moves, staffing and hospital/trust performance). The researchers’ impressions and reactions to interactions, activities and episodes were recorded separately, as adopting such methods of reflexivity is an important quality check when undertaking such research. 85
For general observation, the focus was on routine practice. Observational notes did not record the names of individuals, only whether they had a professional role or if they were a patient or visitor. Neither did the researcher engage in observations of one-to-one clinical encounters between staff and patients; in cubicles where clinical examinations were being carried out; in spaces deemed private, such as behind curtains, in toilets or bathrooms; or in other spaces considered inappropriate by senior staff.
During observation, researchers were often asked for assistance by patients. Our approach was to respond to such requests by explaining the researcher’s role and by alerting a staff member, except when the request involved normal courtesies (e.g. opening a carton of juice left on a tray, moving a drink closer to the patient or providing directions) and did not require medical or functional knowledge (as in providing assistance with standing or walking). This generally worked well.
Approximately 30 hours’ general observation occurred on each of 10 wards at baseline (this varied somewhat with the size of the ward). A total of 295 hours’ observation was carried out.
Further observation for the same duration and over the same time periods occurred at interim (four wards) and at follow-up (two wards), reflecting the stage to which PIE implementation was pursued. A total of 175 hours of further observation was carried out.
Patient case studies
We intended to recruit up to six patients with a cognitive impairment on each ward, at each data point, for in-depth study. The purpose was to explore patients’ experience of care and their relatives’ or caregivers’ views about the care and their involvement in decision-making. Through conversations ‘in the moment’ with the patient during observation, we sought to include people with moderate to severe impairment in ways that were meaningful and ethical, as the method does not require verbal facility or the ability to recall. This would also enable us to locate individuals’ care experiences in the context of staff communication practices with them and the organisational, social and spatial environment of their ward. Additionally, we intended to conduct qualitative interviews with the patient’s relative or caregiver, review medical and care notes, and observe multidisciplinary meetings at which the person’s care and discharge plan was discussed.
Early on, it was evident that triangulation of data for patient case studies was very time-consuming. Because of the length of time these patients spent on the ward, and the depth and quality of data as a result of following patients to discharge, the research team proposed (supported by the Health Services and Delivery Research programme) to reduce the number of patient case studies, so as not to sacrifice depth for breadth of coverage. Purposive sampling was pursued to identify two patients at each site at each data point, selected as critical exemplars of those with dementia in acute wards. They included people unable to communicate verbally or perceived as challenging for staff to manage. The observation of selected patients enabled us to expand understanding of care routines that were not easily accessible through general observation but could be explored through the prism of individual patient journeys, for example the often convoluted process of discharge planning. Each patient/case study involved 5 or 6 hours’ additional focused observation. Appendix 4 provides pen-pictures of two of them. A total of 31 patient case studies were completed: 156 hours’ observation and conversations ‘in the moment’, and 28 interviews with relatives.
A summary of qualitative data by ward for different phases of data collection is presented in Appendix 5.
Person, Interactions and Environment process evaluation methods
An embedded process evaluation86 addressed the following research questions derived from NPT concepts, using a similar approach to that we employed in two recent studies. 87,88
-
Were the strategies employed to engage staff (interactive workshops and manual) sufficient to engender a sense of purpose around the beliefs and values that inform person-focused care for people with dementia (coherence)?
-
Was the process for leading and implementing PIE (team and service improvement cycle) perceived as worthwhile and feasible to invest in to effect change in ward culture and practice (cognitive participation)?
-
Was the work involved in pursuing PIE implementation (observation, action-planning and review) conceived of as necessary and effective in engaging staff in implementing and sustaining change (collective action)?
-
Did staff individually and collectively appraise PIE as worthwhile for themselves and their patients in benefits or outcomes achieved (appraisal)?
We utilised mixed methods to examine how delivery was achieved, what was actually delivered, the mechanisms of change and the effect of contextual factors on delivery. 89,90
-
Observation of PIE action-planning and review meetings to provide a contemporaneous account of the intervention: how it was activated, who was involved, problems encountered and solutions developed. Given the locally determined nature of the content (flexibility) within a systematic process, the question relating to fidelity is couched in terms of how precisely each step in implementation was pursued and proceeded to the next phase. 91
-
Conversations/informant interviews with implementation team members to explore how the programme was understood and communicated to the wider ward team; how different programme components were implemented (tools and guidance); and whether they were perceived as necessary, sufficient and of value in facilitating change. These took place at intervals of around 3 weeks within full and partial implementation wards.
-
Collection and analysis of PIE documentation: observation, action-planning and review tools to examine the content of the programme as enacted.
-
Staff narrative accounts of the process: interviews with a sample of PIE team members at the conclusion of implementation provided retrospective reflection on the process and impact of change. Additionally, we conducted interviews with individuals in sites that had not implemented PIE to explore implementation barriers (29 interviews with 37 staff).
-
Events ‘log’: a contemporaneous ‘events’ log was maintained by researchers to capture change in policies, systems and procedures outside PIE implementation that might affect the change process and outcomes. This included initiatives undertaken by the trust aimed at improving the care of people with dementia.
We had intended to organise two cross-site workshops at interim and conclusion of implementation to compare experiences and the contextual factors influencing these. Because of the unevenness of PIE implementation and the wide geographical location of sites, this did not prove feasible. One cross-site meeting occurred of staff in wards in two geographically distant hospitals within Seaford Trust (see Chapter 5).
Impact of Person, Interactions and Environment
Ward staff practices
Ethnographic observations and interviews with staff (as above) were conducted at 9 and 18 months where PIE implementation occurred.
Patient and relative/caregiver experiences of care
The sources of data were ethnographic observations and patient case studies.
Clinical outcomes
We sought to collect quantitative data on delirium incidence, days in delirium and falls at baseline and at 9 and 18 months. Delirium and falls are the most common unintended adverse events affecting older people admitted to hospital. We hypothesised that the rate of falls and days in delirium would be affected by improvements in care practice.
Delirium is a common, serious and unrecognised condition on acute wards;13,36,92,93 dementia is a risk factor for delirium36,94,95 and delirium accelerates cognitive decline. 96 Delirium incidence is associated with environmental (e.g. setting, lighting, and sensory overload) and care-related factors (e.g. fluid and nutritional intake, mobilisation and cognitive stimulation) that interact with patient vulnerability,36,97 and is regarded as a critical marker of care quality. 36,97 Data on delirium incidence and occurrence are not routinely collected in hospital, in part reflecting poor knowledge of the condition. 93,97,98 In this study, we employed the validated Delirium Observation Screening (DOS) scale,99 a 13-item scale developed to facilitate the early recognition of delirium, which is based on the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition100 criteria. It comprises a single sheet completed at least once daily by nurses as they attend to patients, with a score of > 3 indicating delirium (see Appendix 6).
We negotiated for the DOS scale to be incorporated into ward practice so as to prospectively collect information to monitor delirium rates and days spent with incident delirium. Although the completion of the DOS was reported to take < 1 minute, and therefore was not resource-intensive, staff found that it took considerably longer. The DOS scale was not consistently completed, with wards citing staffing difficulties as a reason for lack of completion. Several wards on which staff were already sensitive to the observational cues of ‘acute confusion’ and valued the information to inform practice (including both dementia wards) completed DOS. A high incidence of delirium and of days in delirium on these wards did not (from observation) reflect poor care quality.
Regarding falls, systematic reviews101,102 suggest a modest reduction in the falls rate with multifactorial interventions in hospital settings. The National Patient Safety Agency103 concluded that the most useful measure of falls is the number of falls per 1000 occupied bed-days. Reported falls for patients admitted during each phase of data collection were recorded as one of the patient profile variables on the Microsoft Excel datasheet, and a calculation was made of the rate of falls per 1000 occupied bed-days. Unfortunately, there was a considerable number of missing patient profile data, including those on falls for the two wards that successfully implemented PIE. When such data were available, we have reported them. However, the interpretation of the data is not straightforward. Not only do risk factors for falls relate to the actions of ward staff, but there are also patient-specific factors that give rise to variability in rates. Thus, risk increases with advanced age, presence of dementia, delirium and frailty, so that ward patient profile will affect the falls rate. 104 Similarly, as hospital-related falls occur as a consequence of mobilising and recovering from illness, practices regarding the balance of risk, promoting rehabilitation and respecting autonomy will also affect the falls rate. 104 Overall, the data obtained on falls were patchy across sites. On both clinical outcome measures, then, we were unsuccessful in securing reliable and consistent data for all wards. The attempt to do so has raised useful questions regarding feasibility, which we consider in Chapter 6.
Service outcomes (length of stay, readmissions within 30 days and discharge destination) were collected as part of the patient profile data set.
Analysis
Qualitative data (interview transcripts and ethnographic field notes) were analysed using grounded theory methods,105 including simultaneous data collection and analysis, constant comparison, searching for negative cases and memo writing. Descriptive and analytic codes were developed into higher-order categories through processes of data reduction and reassembly. First, an analysis was pursued for each data set (interviews, observations, patient case studies) within individual wards (the case study). We then compared analytic themes across these data sets, drawing out, for example, similarities and differences between staff interviews and observations on the understanding and practice of person-centred care. Through regular research team meetings, the emerging data from individual case studies, and reflections on them, were discussed. The similarities and differences between wards were drawn out, and we identified topics for more focused observation and ideas of analytic interest to pursue. Hypotheses were generated to explore and account for variation between cases; these were tested out through a cross-case comparison and search for alternative explanations.
Regarding ward practices with respect to patients with dementia, we proceeded as follows. From initial observations, we focused on aspects of practice relating to the work of communication, routine care tasks, responses to different types of distress, the strategies adopted and the attitudes and knowledge that informed them. For each case study, all incidents and episodes relating to this work were mapped, alongside the environmental, organisational and interactional contexts in which they occurred and the physical and emotional responses of patients. Through a comparison between the incidents and episodes captured in memos, we identified patterns of action and interaction. These patterns and what shaped them were refined through cross-case comparison. For example, the open code ‘distress’ was explored through a perusal of all incidents and episodes pertaining to it. Through constant comparison, different forms of distress were identified, which varied by how the distress was manifested, the perceived need giving rise to it and the persistence of its expression. Staff responses were similarly coded and categorised based on the type of response and the context in which it occurred. The relationship between the varied forms of distress and the responses to them were interrogated to identify patterns, which were further refined through a comparison between cases.
A similar analytic process was pursued in relation to PIE implementation. Qualitative data from interviews, workshop notes, observation of action-planning and review meetings, and examination of completed documentation were drawn together for each ward in chronological order. This provided a within-case descriptive account of implementation over time, the nature of the engagement of staff with each step in the cycle and the barriers encountered, using NPT as a sensitising framework. The emphasis was on delineating the sequence of implementation steps over time and in the context of events within the hospital and trust; the conditions that had an impact on the temporal flow of action, and their consequences, whether persisting with or abandoning PIE. We then examined implementation processes, through a cross-case comparison, to discern generalisable features that might account for variation. An analysis of the qualitative data was conducted manually, moving iteratively between the empirical data, sense-making in relation to the data and reflection on the literature.
Quantitative data were analysed using descriptive statistics.
Research team
Three investigators conducted the case studies with the academic support of the lead author (an experienced qualitative researcher and teacher in qualitative methods). The three attended a 5-day module on the theory and practice of qualitative research at the University of Leeds, which included ethnographic methods and analytic strategies. All four met regularly (at least monthly) to consider emerging findings and problems encountered. Between meetings, telephone conversations and e-mail discussions facilitated dialogue and mutual support, as the observations made heavy demands on researchers both practically and emotionally. The wider research team, including the chief investigator, met every 2 months to discuss progress. This was in addition to receiving support and advice from the Programme Management Group.
Ethics
Ethics approval for the study was obtained from the National Research Ethics Committee Yorkshire & The Humber Bradford (reference 12/YH/0442). The main ethical issues were securing the consent of patients to take part in specific ward observations, conversations and interviews, especially those who might have dementia or delirium, and not seeking formal consent for the general observations of ward routines.
Patient consent
The consent procedures adhered to the Mental Capacity Act 2005106 and accompanying Code of Practice. 107 First, when an individual was identified by staff as having a cognitive impairment, we considered how best to approach that person, with advice from ward staff (e.g. times when the person might be more alert, or when their relative was present). Second, the researcher explained the study in clear terms and ascertained whether or not the person understood the information. Third, if the person was deemed unable to make a decision about participating in the research, we sought information regarding a suitable personal consultee (close relative or friend), either from the patient or from a staff member. Every effort was made to secure a suitable personal consultee, or, in their absence, a nominated consultee to give patients without next of kin the opportunity to participate. If the consultee advised that a patient who lacked capacity would be willing to take part in the study, then that person was included, providing that they showed no signs of unwillingness (e.g. becoming distressed, upset or anxious in the presence of the researcher or when discussing the study). Consent was ongoing. The researchers checked that people were willing to continue, and were sensitive to signs of distress, including verbal and non-verbal cues.
General ward observations
The decision not to seek research consent for the general observations of ward routines was carefully considered. As observations were unobtrusive, carried out in public or semipublic spaces, and did not identify individual staff, patients or visitors by name, we considered that it would be impractical, and probably more intrusive, to seek formal written consent from all those present. Instead, we sought informal, verbal consent. Before each observation, the researcher reported to a senior staff member and introduced themselves to any staff they had not previously met, doing this at an opportune moment that did not interfere with the workflow. At the end of each observation period, the researcher ‘signed out’ with the senior staff. It should be emphasised that, throughout the study, observations were conducted with the full knowledge, support and co-operation of ward staff. If anyone appeared unhappy, distressed or uncomfortable by our presence on a particular occasion, we did not include them in the observation. This happened rarely. There were several instances when a patient became annoyed with the researcher when she indicated that she was unable to help the patient leave the ward and return home (call a taxi or get their coat). More often, when a patient was distressed and no staff member was available, the researcher sat with the person and sought to provide reassurance.
In the report, we have used pseudonyms throughout – for trusts, wards, staff, patients and caregivers – and have altered some biographical details to protect anonymity, privacy and confidentiality.
Patient and public involvement
There were several strands to our patient and public involvement strategy.
We involved our well-informed local older person’s group (approximately 15 people), with whom we have a longstanding relationship. This is a subgroup of a forum, established by the local authority, that comprises approximately 300 retired local people who are consulted on health and social policy issues. The subgroup has been acting as an advisory body in all aspects of our delirium and dementia research since July 2007. Three meetings of the group took place: at the beginning to inform data collection methods and contribute to the ethics application; following the conclusion of baseline data collection in the first two sites to reflect on the emerging findings and their implications for further data collection; and at the end of the study to discuss issues around PIE implementation.
Two meetings were held with people with dementia, one of which also involved caregivers. One meeting occurred with people with dementia and/or memory problems (n = 5). This ‘memoires’ group is a longstanding group of people who meet weekly for social, leisure and arts-based activities, and is organised by one of the locality-based neighbourhood networks for older people in inner-city Leeds. We held another meeting with people with dementia and their caregivers, hosted by another neighbourhood network in an outer suburb (n = 34). In both meetings, we discussed our emerging findings in relation to people’s experiences of acute care (i.e. people with dementia and their relatives). These meetings were organised to include the voices of people with dementia in the study, especially given that the cross-site workshops did not happen.
Two caregivers of relatives with dementia, recruited through the Alzheimer’s Society Research Network, were engaged as co-applicants and played a key role at all stages of the research. Our steering group also included a person with dementia and his caregiver, both of whom participated in discussions about direction and progress.
Chapter 3 Case study profiles
Introduction
This chapter describes the structural, organisational and cultural context of the study wards prior to PIE implementation. It also situates each ward within the wider hospital and trust environment, with specific focus on the policies in place, and the priority attached to, and investment in, services for older people with dementia. At the same time, direction and resource deployment at trust (and hospital) level is shaped by national policy priorities, regulatory requirements and resource constraints. The interactions between these levels create a fluid and dynamic environment for service delivery in wards and to patients.
National policy context: dementia
When the study began, in early 2013, the timing seemed propitious. National policy on improving the care of people with dementia had been given impetus with publication of the Prime Minister’s Challenge on Dementia 2015. 9 This coalesced with other policy drivers: the report of the Francis inquiry, published in March 2013,108 on the failings in Mid Staffordshire NHS Foundation Trust, particularly around the care of frail, older patients; and the findings of the first National Audit of Dementia Care on acute wards. 25
Interest in improving hospital care for patients with dementia was reflected across the five trusts. All had in place, or were in the process of developing, dementia strategies, although the content of these varied.
City NHS Trust
Organisation
City Trust is a long-established foundation trust, being among the first wave to achieve foundation status. It provides services to a core population of around 500,000, and employs > 5000 staff. Acute services are mainly located within a 900-bed hospital, with an 80-bed facility providing rehabilitation and outpatient provision from a separate site. It is a large, busy trust, with > 120,000 accident and emergency (A&E) department attendances annually. Situated in a region with a post-industrial heritage and a diverse culture, its diversity has contributed to an increased demand on health and social care provision at both ends of the age spectrum.
Since attaining foundation status, City Trust had generated an annual surplus. However, annual reports noted the challenge of securing improvements in quality and performance, managing reduced income growth, identifying efficiency savings and responding to the demands of a multiethnic population within one of the most deprived English local authorities.
Up until 2011, the trust was assessed as meeting the performance targets set by the national regulator, Monitor. During 2012 and 2013, performance targets on waiting times for treatment were breached, resulting in a review by the NHS Support Team, the launch of a comprehensive turnaround programme, and a return to compliance in April 2013. In January 2014, the Care Quality Commission (CQC) issued a report on an unannounced inspection the previous October on the main hospital site and assessed that action was needed in several areas, including respecting and involving people who use services and assessing and monitoring the quality of provision. A warning notice was issued on staffing because of staff vacancies carried. Strategic action centred on making improvements in problem areas, including the recruitment of staff, for implementation during 2014. A CQC inspection in October 2014 assessed the trust as ‘requiring improvement’; medical care was ‘good’ at both hospital sites. A change in leadership at board and senior management level at this time created some organisational instability. This was the context in which the strategic priorities around the care of people with dementia were established.
Care of people with dementia
A strategic trust priority from 2011 to 2012 was improving the physical environment for patients with dementia. City Trust was successful in securing external funding for this purpose, augmented by investment through its capital improvement programme. The design and execution of the changes on several older people’s wards was described as ‘exemplary’ in the CQC’s 2014 inspection report. The 2013/14 annual report announced the extension of the improvement programme to the second hospital.
Since 2012, a rolling programme of ‘dementia awareness’ training tailored to different staff groups had been delivered jointly by the dementia lead within the elderly services directorate and the trust’s practice development lead. Both subsequently launched an initiative to recruit ‘dementia champions’. The appointment of a lead nurse for dementia in 2014 instigated a dementia strategy through the formation of a multidisciplinary dementia steering group.
City Trust Person, Interactions and Environment wards
Two wards took part in the study: a rehabilitation ward for older people located in the 80-bed hospital a distance from the main hospital site (Rivermead), and a trauma orthopaedic ward in the main hospital (Cedar).
Rivermead: structure and organisation of care delivery
Rivermead is a ‘step-down’ ward for rehabilitation. The hospital in which it is located previously had more inpatient wards but now mainly comprises outpatient services and rehabilitation beds, acute services being centralised in the main hospital. Bed numbers fluctuate according to bed management demands: usually 27 during ‘winter pressures’ and 23 at other times.
Physical environment
At baseline and during interim data collection, Rivermead comprised 27 beds (three side rooms and four six-bedded bays). Three bays contained a round table, large enough for four chairs. The fourth bay was less spacious, with a coffee table and two chairs. Outside the time of ‘winter pressures’, a bed was removed from each bay, allowing more space around the table. It was common to see staff seated here, note-writing; patients were seen here rarely.
The physical environment was cramped. There was one very small office and one similar-sized staff room. There was no designated space for activities with patients; corridors and bays constituted the only communal spaces.
Each bay was painted a different colour. There were pictures dotted around (local images of the city). The patient toilets had clear visual signage and Braille. The toilet door frames were painted red as a visual cue. Staff were heard directing patients by telling them to head for the door with the red frame.
Patient profile
There were 123 admissions over 7 weeks at baseline, eight of which were readmissions (approximately 18 admissions per week). All of those admitted had come from the main hospital following an acute episode. The median length of stay was 14 days (range 1–48 days). Table 1 provides a summary of the patients’ sociodemographic characteristics.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| 65–69 | 1 (1) |
| 70–74 | 0 |
| 75–79 | 17 (14) |
| 80–84 | 32 (26) |
| 85–89 | 38 (31) |
| 90–94 | 30 (24) |
| ≥ 95 | 5 (4) |
| Gender | |
| Men | 28 (22) |
| Women | 95 (77) |
| Residence prior to acute admission | |
| Own home | 108 (88) |
| Extra-care housing | 2 (2) |
| Intermediate care | 1 (1) |
| Residential care home | 2 (2) |
| Nursing home | 2 (2) |
| No information | 8 (6) |
More than half of the patients were in advanced older age (i.e. aged ≥ 85 years), and women dominated. Most patients had been living in their own home before the event that had precipitated their acute admission.
Over one-third (n = 44) of patients had an ongoing cognitive impairment: 36 had a diagnosed dementia and eight had been assessed as having probable dementia. Almost one-fifth had delirium (n = 24), of whom 12 had both delirium and dementia. Thus, just under half of patients (n = 56) on this ward had a cognitive impairment on admission. Just over half of patients had delirium during their stay (n = 64), although for most of them the mean number of days in delirium was 3 (range 1–27 days). Only one-quarter (n = 32) of patients were identified as having no cognitive impairment either on or during admission.
The reasons for admission are shown in Figure 2, although for most patients multiple factors (medical, functional and cognitive) were implicated.
FIGURE 2.
Rivermead: reasons for admission. COPD, chronic obstructive pulmonary disease; SOB, shortness of breath.
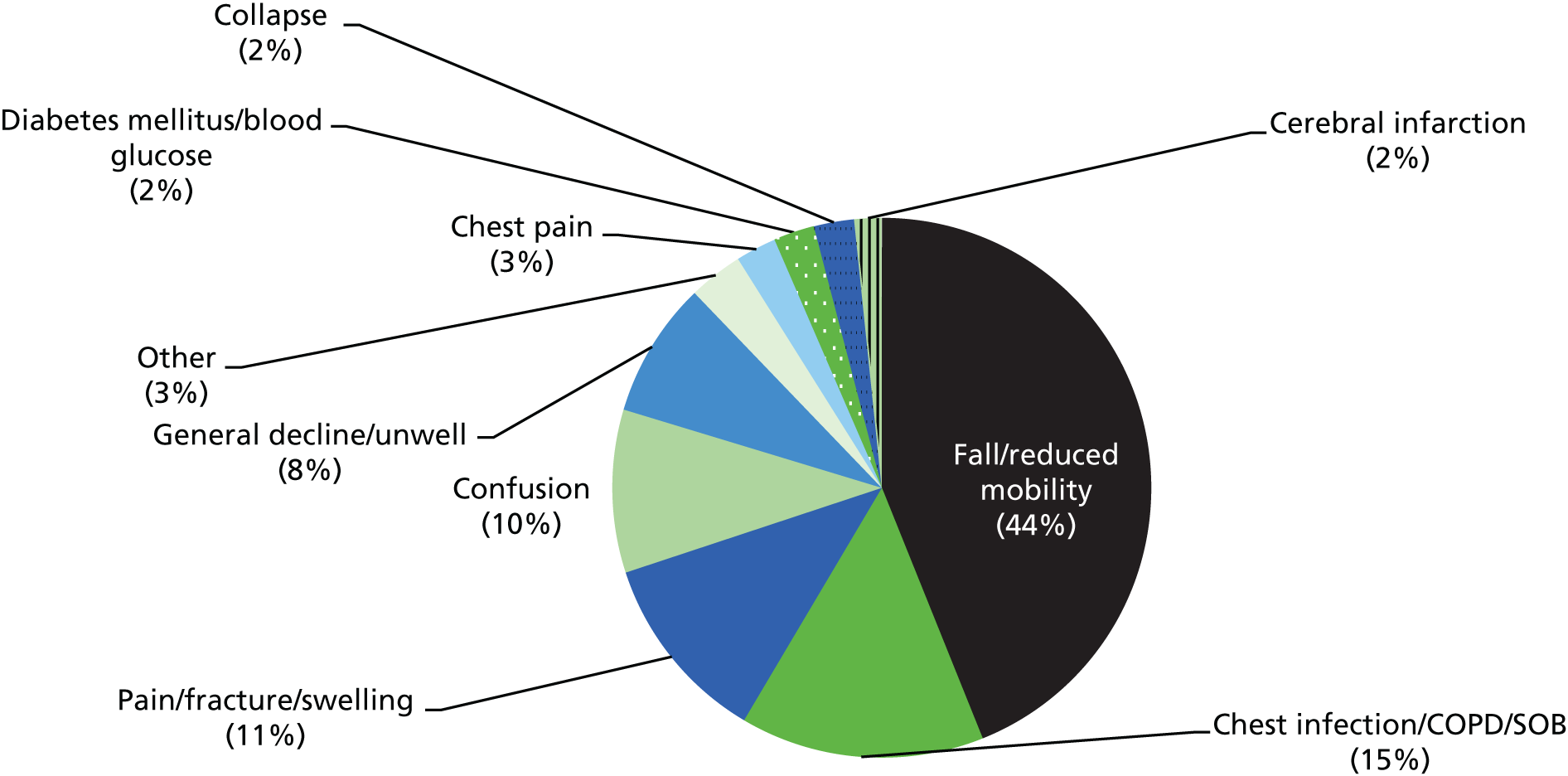
A further indication of a patient’s degree of frailty is their discharge destination (Figure 3). Ten per cent of patient discharges involved a new long-term care admission; a further 10% of patients were discharged to intermediate care for additional rehabilitation; and 2% died in hospital.
FIGURE 3.
Rivermead: discharge destination.
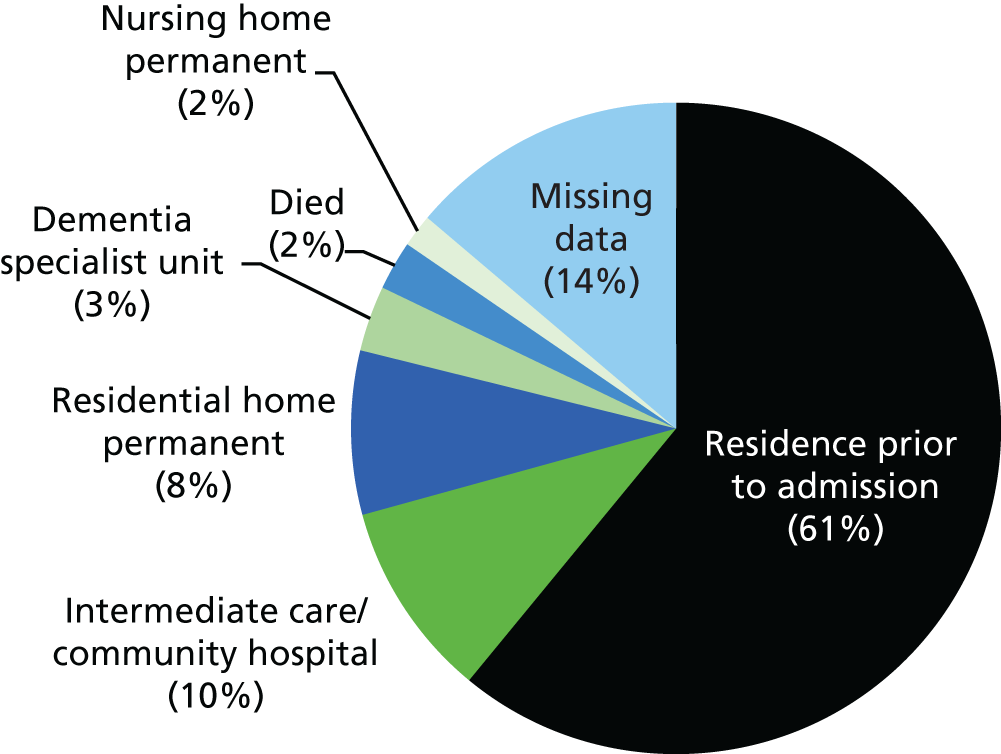
Staff profile
The nursing/care staff complement was 30 full-time equivalent (FTE) staff (25 in post). On the early shift (from 07.00), there were three qualified nurses and four HCAs (a ratio of registered staff to patients of 1 : 9); on the late shift (from 13.00), there were three nurses and three HCAs; and on the night shift, there were two nurses and two HCAs. On each shift observed, overall staffing levels were met over the course of observation. However, when a staff shortage occurred, a HCA replaced a qualified member of staff for that shift and the ratio of qualified to unqualified staff was reduced. It was not uncommon for Bank or agency staff to provide shift cover or to ‘special’ a patient on a one-to-one basis (typically a person who was agitated or distressed). The ward manager regularly provided direct patient care as and when needed.
Rivermead: care culture
At the start of fieldwork (February 2014), Rivermead had a stable ward leadership and purpose. The staff group had worked together for a long time (median 4 years and 3 months, and up to 25 years among those completing the Climate of Care questionnaire; n = 15), reflecting the broader profile of a stable team.
The responses to the Climate of Care questionnaire indicated that staff shared an explicit philosophy of care and culture of caring, were respectful of each other’s skills and knowledge, and valued patient involvement in decision-making. The ward manager was viewed as someone who inspired confidence, consulted the team about daily problems, acted in a caring manner towards the team, was explicit about the care standards expected and set an example in hands-on care, actively coaching individuals. At ward level, staff felt supported and engaged, a picture reinforced from observation and interviews. The ward manager was a key driver in shaping the care culture: an experienced nurse and manager, she perceived her role in priority order as ‘looking after my patients’; ‘looking after my staff’ (emotionally, developing knowledge and skills, and encouraging them to participate and further their careers); and ‘as a manager’, ensuring compliance with trust policies and procedures. She had undertaken advanced training in dementia, and conveyed, in values and practice, a commitment to providing individualised care to patients.
There were mixed views regarding staff relationship vis-à-vis the trust. The downside of being located at a distance from the main hospital site was poor communication and links with senior or specialist colleagues. There was a sense that colleagues in the main hospital lacked understanding of the ward’s purpose (rehabilitation), and had little appreciation of their particular skills and the complexity of the patients with whom they worked. Positively, they valued the sense of camaraderie engendered among staff in the smaller site and the greater autonomy and predictability of the work. External pressures on day-to-day-work were viewed as constraining their ability to deliver the quality of care they aspired to provide. Among some staff, a source of stress was the lack of time to reflect on ways to improve care delivery. As the bridge between the hospital and ward, senior staff, particularly the manager, sought to contain the tension between the priorities and requirements of the trust and their espoused values on providing individualised care and supporting staff. This, along with their physical separation from the main hospital, meant that the ‘troubles’ of the trust around meeting performance targets, and the changes at trust and senior management team level, were less salient for the ward team. Furthermore, the stability of the staff team meant that although there was recourse to Bank and agency staff to cover some shifts, hospital staff vacancy levels had less of an impact on Rivermead than on other wards with an unstable staff group.
Cedar: structure and organisation of care delivery
This orthopaedic trauma ward had moved to a temporary location at the end of 2013 and there was uncertainty surrounding its future purpose. Subsequently, following bed closures and ward remodelling, a new ward was created, involving half of the beds on a former older people’s ward and half for older trauma patients. This ward came into existence in August 2014 and agreed to participate in the study, with fieldwork commencing in September 2014. Given the late entry of this ward into the research, it was agreed that PIE implementation would occur over 9 months rather than the 18 months originally envisaged.
Of the 28 beds on this ward, 14 were for patients aged ≥ 60 years with fractured neck of femur; the remainder were for older, medical patients.
Physical environment
Physically, the ward was vast and modern in design, comprising one long corridor, 12 side rooms and four four-bedded bays (three female and one male). Each bay had a television, two large windows and a notes trolley. All patients had a whiteboard above their bed, on which their name was written. It was not possible to see into the bays without physically entering them. There was a room for relatives, two meeting rooms and a sisters’ office, but no day room.
The ward had been renovated using similar design principles as the ‘healing environment’ wards elsewhere in the hospital. The corridor was decorated in pleasant colours, including images of generic scenery, and included two three-seater chairs opposite a television. It was usual to see staff and patients seated here (staff writing; patients watching television or undertaking a ward activity). Toilets had clear signage (male/female cartoon/silhouette) and the surrounding walls were painted red as a visual cue. Information boards were placed around the ward, including boards about delirium and dementia.
Patient profile
During baseline, there were 190 admissions to Cedar over 7 weeks, four of which were readmissions (approximately 27 per week). The median length of stay was 7 days (range 1–47 days), facilitated by access to ‘step-down’ beds (Rivermead or similar). Table 2 provides a summary of the patients’ sociodemographic characteristics.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| 29–64 | 14 (7) |
| 65–69 | 5 (3) |
| 70–74 | 15 (8) |
| 75–79 | 25 (13) |
| 80–84 | 47 (25) |
| 85–89 | 49 (26) |
| 90–94 | 27 (14) |
| ≥ 95 | 8 (4) |
| Gender | |
| Men | 77 (41) |
| Women | 113 (59) |
| Residence prior to acute admission | |
| Own home | 58 (31) |
| Residential care home | 4 (2) |
| Nursing home | 10 (5) |
| No information | 118 (62) |
Just under half of patients were in advanced older age (44% were aged ≥ 85 years). The majority for whom data were available had lived in their own homes before being admitted to hospital.
On admission, at least one-third (n = 62; missing data, n = 96) of patients had an ongoing cognitive impairment: 41 with a diagnosed dementia and 21 assessed with probable dementia. Eight patients were identified with delirium, of whom seven also had dementia (missing data, n = 120). For those patients for whom data were available (approximately half, n = 94), just over half (n = 50) had a cognitive impairment on admission. Of the data collected on delirium during admission (missing data, n = 157), 18 patients had delirium (median of 3 days in delirium; range 1–12 days).
The reasons for admission to Cedar are shown in Figure 4. The pattern reveals a more acute profile than in Rivermead, suggested also by the relatively high proportion of patients who died during their admission (15%).
FIGURE 4.
Cedar: reasons for admission. COPD, chronic obstructive pulmonary disease; SOB, shortness of breath; UTI, urinary tract infection.
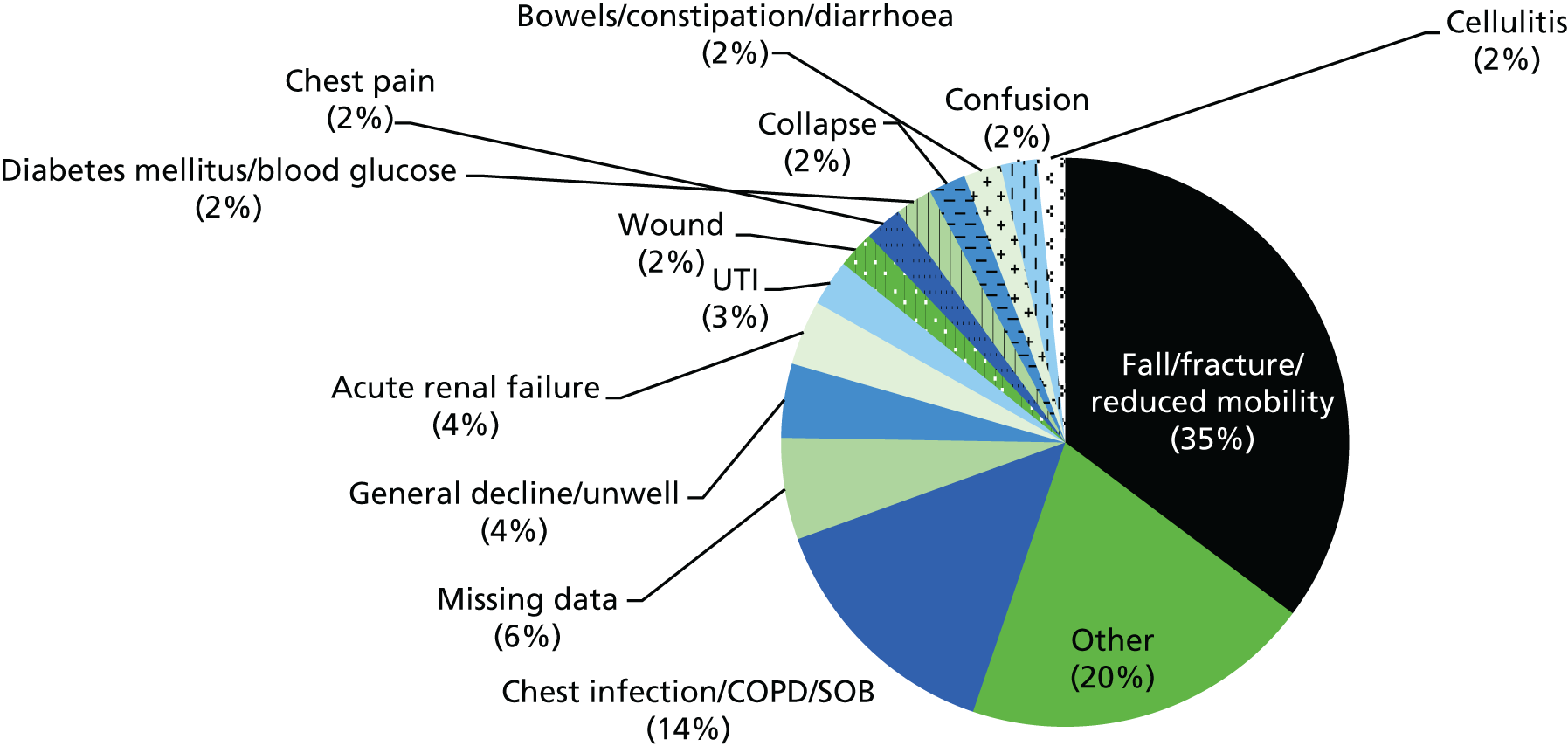
The data on discharge destination (Figure 5) reflected the fact that a significant minority of patients on this ward were discharged to the ‘step-down’ ward when they were medically stable but still insufficiently recovered to return to their usual residence. The symbiotic relationship between the acute older people’s wards and rehabilitation wards such as Rivermead contributed to the very short length of stay on Cedar, the ‘step-down’ wards providing additional therapy for patients deemed not safe to be discharged.
FIGURE 5.
Cedar: discharge destination.
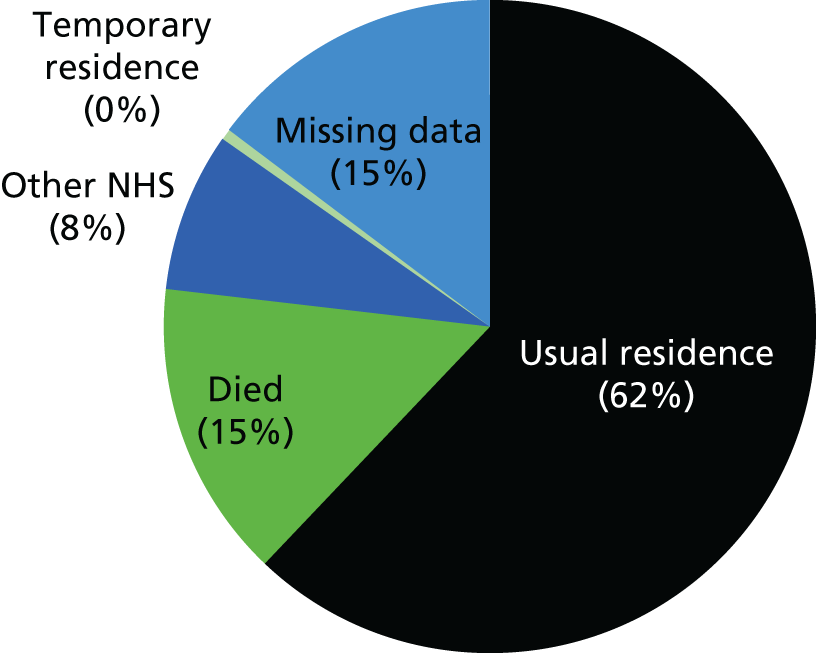
Staff profile
The ward team comprised 35 FTE staff. Staff complement on the early shift (from 07.00) was five qualified nurses and three HCAs (a ratio of registered staff to patients of 1 : 5.6); on the late shift (from 13.00), it was four nurses and three HCAs; and at night, it was two nurses and three HCAs. In three-quarters of shifts observed, the actual numbers of staff were consistent with intended staffing. This was achieved by having one fewer qualified and one additional HCA, or by using Bank or agency staff; one-quarter of observed shifts were down by one staff member.
Cedar: care culture
The ward manager had spent most of her working life nursing older people and, like her colleague on Rivermead, was an experienced ward manager. Although a number of team members had come with her from a care of older people’s ward, melding a staff group into a team with a dual focus on complex medical conditions and orthopaedic trauma was still a work in progress when fieldwork commenced. The level of patient dependency was regarded as high, and the physical demands of providing care weighed heavily on staff, as many patients required two people to assist them with personal care.
In interviews, the ward manager conveyed a strong ethos of individualised care, tempered with an acknowledgement of the reality of the multiple and simultaneous demands on staff. The work of a ward manager was presented as balancing different and competing interests: meeting hospital targets regarding flow and spending time with patients, reducing falls risk and undertaking rehabilitation work towards functional improvement.
From their responses to the Culture of Care questionnaire (n = 14), staff echoed the priority that their manager attached to individualised care, treating patients with dignity, putting effort into providing good-quality care, meeting patients’ care needs, and involving patients and caregivers in decision-making. They valued the skills, competence and support of colleagues; had trust and confidence in each other; communicated and worked well as part of the MDT; and felt able to bring up issues and challenge practice. The manager was perceived as inspiring confidence, consulting with the team about daily problems, acting in a caring manner towards staff, being explicit about the care standards expected and setting an example in hands-on care.
Similar to colleagues on Rivermead, staff on Cedar perceived a gap between their aspiration to provide individualised care and the inadequate support and resources for spending time with patients and developing new skills. In comparison with Rivermead staff, they were less critical of the resources available to them at the hospital level, particularly valuing the access they had to expertise on aspects of care. This probably reflected their physical proximity on the main hospital site, being closer to decision-making structures. For senior ward staff, particularly the manager, hospital priorities on patient flow, reducing length of stay and cutting beds imposed a heavy burden, as they were closer to the everyday impact of these pressures.
Valley NHS Trust
Organisation
Valley NHS Foundation Trust provides acute, rehabilitation and community services in hospital and community settings for a geographically dispersed rural and urban population of > 200,000. It covers an area of > 700 square miles in north-west England and acquired foundation status in 2010.
When the study began, the main hospital had 395 beds for acute, elective and specialist care, and some 55,000 A&E department attendances annually. It had a strong local presence and community connection, reflected in its large volunteer base, with around 400 volunteers carrying out over 30 different roles across wards and departments. The trust also managed three community hospitals in different locations across its wide area.
Annual reports between 2010/11 and 2013/14 revealed an organisation consistently meeting national targets on finance and governance, clinical safety and effectiveness and which had been operating with a relatively stable trust leadership. Similar to City Trust, Valley had invested heavily in the modernisation of its built environment, including improving the ward’s physical environment.
As in other study trusts, NHS reorganisation posed considerable uncertainty for forward planning. Simultaneously with organisational upheaval, the following challenges were noted: delivering safe and quality care, and managing a 3–5% year-on-year increase in volume demand on services alongside the requirement on providers to find efficiencies of 4–5% per annum to absorb the growth within a fixed overall real-term budget. The dual strategy pursued in meeting these competing demands was to cut costs and develop new services to grow income.
Care of people with dementia
Local strategic priorities included reducing ‘slips, trips and falls’, which were viewed as a particular risk for people with dementia. Initiatives included the development of a system to more accurately monitor falls; the introduction of screening, assessment and evaluation tools to improve risk management processes; the purchase of monitoring equipment to reduce falls incidence; the provision of floor-level beds for patients at high risk of falling out of bed; and the inclusion of falls prevention and bed rail use in mandatory training.
For people with dementia, priorities were improving nutritional care and implementing the ‘Butterfly Scheme’. The former involved the expansion of an established ‘feeding buddy’ system with trained volunteers to assist vulnerable patients to eat and drink. The ‘Butterfly Scheme’, introduced in 2011, used a butterfly symbol to highlight the needs of patients with a dementia diagnosis; provided staff with practical guidance to meet the needs of these patients; and alerted staff to the collection and use of information from relatives to better engage with these patients and to inform care planning. The scheme was supported through mandatory training for the clinical and support staff who directly provided care.
Increasing staff awareness of dementia was prioritised through a programme of ‘dementia champions’, and the creation of more ‘dementia-friendly’ environments was pursued through ward refurbishment in 2013/14, supported by external funding.
Valley Trust Person, Interactions and Environment wards
Two hospital wards participated in the study: an acute trauma ward (Oak) and a care of older people ward (Ambridge). Both had benefited from funding to improve the ward environment, which had been completed on Oak before fieldwork commenced. During most of baseline, Ambridge was in a temporary location because of refurbishment, moving into its permanent space in the final weeks. The moves created environmental disruption and upheaval for staff and patients.
Oak: structure and organisation of care delivery
Oak ward was a 28-bed, acute orthopaedic trauma ward. Around 30 months before the study, there had been a change in medical leadership: orthogeriatric consultants had been introduced alongside orthopaedic surgeons to provide comprehensive geriatric assessment and care planning for older patients. This involved separate MDT meetings on a twice-weekly basis.
Physical environment
Oak ward was organised as six four-bed bays (12 male and 12 female) and four single rooms (two male and two female). The male and female bays were located along corridors at right angles to each other, with a small workstation in the space between. The waist-high walls bordering the workstation desk created a sense of an open space around this working area. There was a separate day room and relatives’ room, a staff room, and an office for the ward manager and senior orthopaedic nurse. The decor was bright, with good natural light; feature walls in each bay were painted in different colours and there were clocks in each bay displaying the time and date.
Patient profile
There were 174 people admitted during baseline, of whom one was a readmission. This was a mixed-age profile (range 16–101 years). There were two distinct admission patterns: younger people with limb fractures typically sustained in motoring accidents, and people in advanced older age with fractured neck of femur and comorbid chronic health problems. The median length of stay was 9 days (range 1–78 days). Table 3 provides a summary of patients’ sociodemographic characteristics.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| < 40 | 23 (13) |
| 40–49 | 16 (9) |
| 50–64 | 21 (12) |
| 65–69 | 5 (3) |
| 70–74 | 5 (3) |
| 75–79 | 24 (13) |
| 80–84 | 23 (13) |
| 85–89 | 35 (20) |
| 90–94 | 19 (11) |
| ≥ 95 | 3 (2) |
| Gender | |
| Men | 77 (44) |
| Women | 97 (56) |
| Residence prior to acute admission | |
| Own home | 148 (85) |
| Residential care home | 4 (2) |
| Nursing home | 19 (11) |
| Dementia unit | 1 (0.5) |
| No information | 2 (1) |
Whereas around one-quarter of patients overall had a diagnosis of dementia or were assessed as having probable dementia on admission, this applied to 40% of those ≥ 80 years. Furthermore, 9% had a delirium on admission, the majority of whom (11/15) had delirium on dementia. Most people had been admitted from their own home; 13% were residents in a nursing or residential care home. Just over one-third of older people (aged ≥ 65 years) had delirium during their inpatient stay (36%), and the median number of days in delirium was 4 (range 1–28 days).
The reasons for admission to Oak ward are shown in Figure 6. Given the nature of the ward, admissions were dominated by orthopaedic trauma; among older people, the largest single reason was a fractured hip.
FIGURE 6.
Oak: reasons for admission.
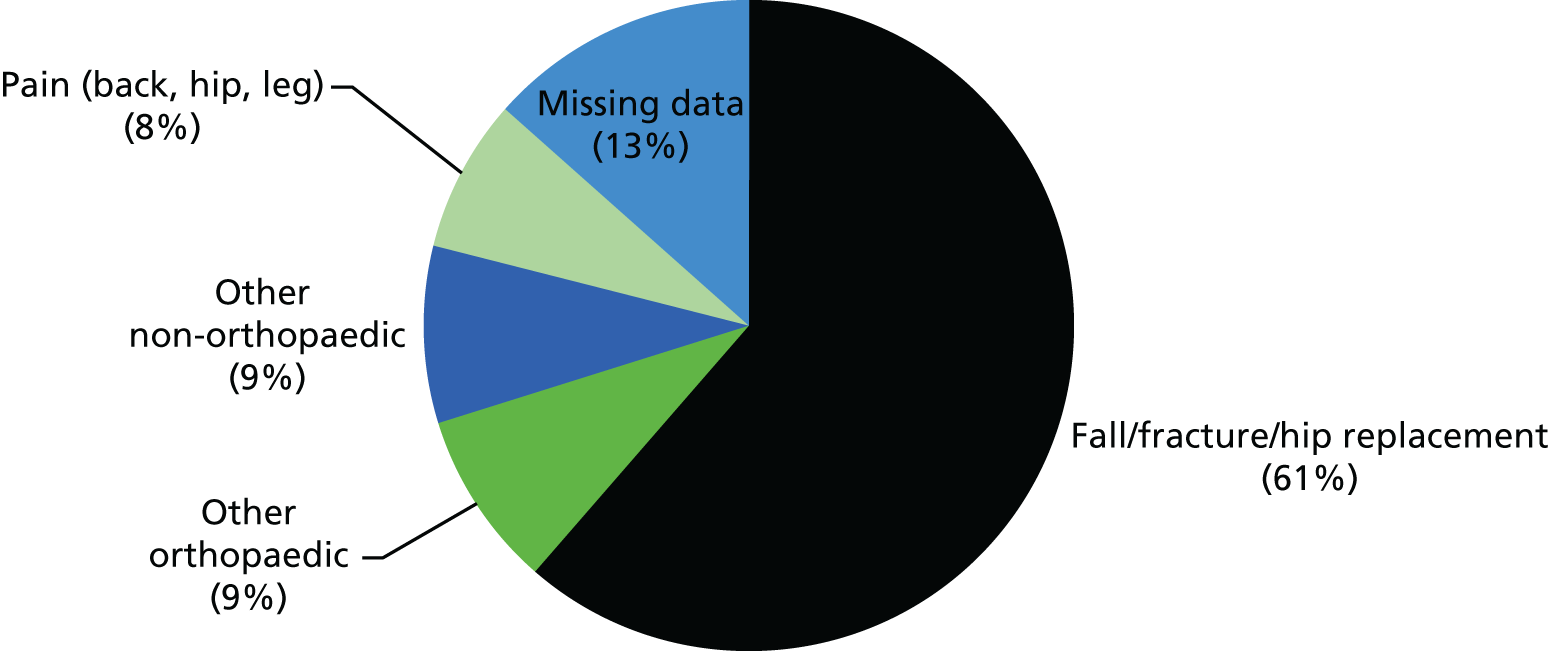
Patient destinations on discharge are shown in Figure 7; 5% died in hospital and, of the rest, 9% went to a new permanent nursing or residential care home (although this applied to just under one-fifth of older patients).
FIGURE 7.
Oak: discharge destination.
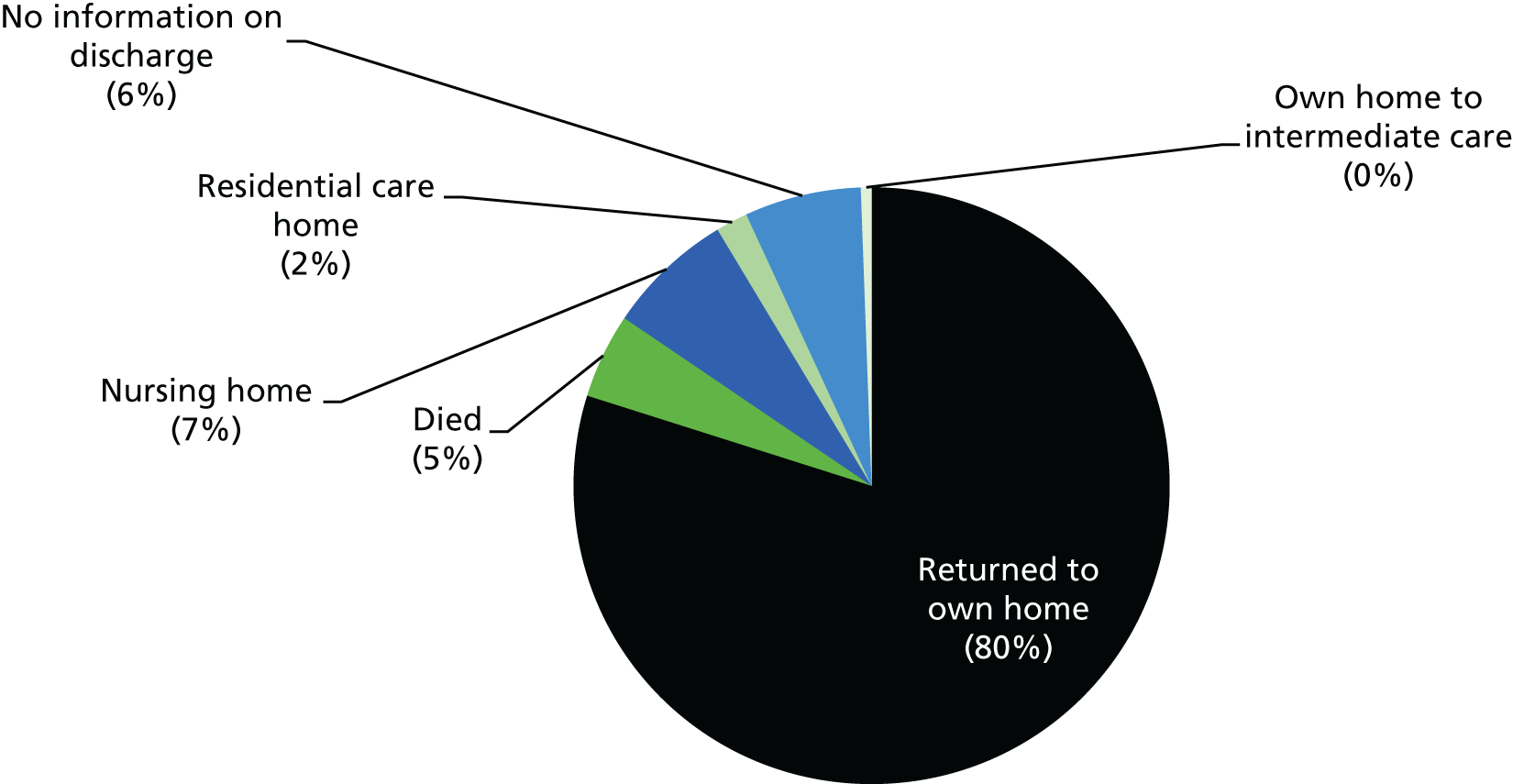
Staff profile
The ward complement was 33 FTE staff. Typically, this was organised as three qualified nurses and four HCAs on the early shift (ratio 1 : 9.3 registered staff to patients); three qualified nurses and four HCAs on the late shift: and, at night, two qualified nurses and three HCAs. Additionally, a specialist orthopaedic nurse practitioner working across A&E and the ward provided expertise and support during the day from Monday to Friday; and the ward manager was a visible presence, providing hands-on care when required. Even so, during most of baseline fieldwork, the ward was considerably short-staffed as a consequence of sickness, vacancies and secondments. This resulted in considerable daily work for the manager/senior sister to secure cover either by cajoling existing staff to work additional shifts or by using Bank staff (Bank staff constituted nearly one-third of staff during most of the observed shifts).
Oak: care culture
During baseline (end of November 2013 to early February 2014), the ward team was undergoing change. Until then, it had been relatively stable, with a strong, supportive team ethos. The manager had been in post for 6 years, first as a junior sister and then as manager, and many of the nursing and care staff had worked together for ≥ 5 years. However, several nurses had left or were in the process of leaving when fieldwork commenced; difficulties and delays in recruiting new staff resulted in the use of temporary staff, which had an impact on workload and ward morale.
The manager placed high value on supporting her staff, considering that a ‘stressed’ staff member affected everyone, both colleagues and patients. Observation revealed a leader who was a visible and cheerful presence on the ward and who conveyed to staff that their work was appreciated. Delivering ‘quality care’ was seen to require attention to patients’ emotional as well as physical and care needs; furthermore, spending time with patients was conveyed as a necessary and valued part of nursing and care work. The current staffing difficulties were regarded as compromising the realisation of this vision. In her interview, the manager envisaged that an aspect of her role was to absorb pressures from senior management so as to sustain a calm and ‘happy’ care environment. This conception of the ward leader as ‘buffer’ between the demands of senior management and the day-to-day work of providing direct patient care was felt as isolating and stressful.
The change in the staff team was evident among those completing the Climate for Care questionnaire (n = 14). Respondents were equally divided between those who had worked on the ward for between 1 and 6 months and those who had been there for ≥ 5 years. Staff reported that they shared an explicit philosophy of care, that there existed a culture of caring for patients and that the psychological aspects of care were highly valued, as was the involvement of patients and their caregivers. Staff were generally negative about the adequacy of support services to enable them to spend time with patients and also considered that there were insufficient numbers of staff who had the knowledge and skills to provide quality patient care. This was felt across the board: among both long-standing staff members and those who had been in post for ≤ 6 months.
Respondents considered that the quality of care provided by the MDT met patients’ individualised needs and was responsive to the needs of caregivers; staff were viewed as treating patients with dignity and respect; there was good communication between team members; and people worked well together and were supportive of each other. The general view was that there was insufficient time to reflect on performance and ways of improving care delivery. This view was supported by observation: staff members were in continuous motion, a combination of the physical demands of patients who were immobile and staff shortages. External pressures acted as a constraint on delivering the quality of care that they aspired to provide. The team viewed the ward manager as supportive, a visible presence and a role model in delivering hands-on care. In contrast, their perception of the hospital management was negative: they considered that staff views were not listened or responded to, and that support for staff at ward level, when needed, was not forthcoming.
Ambridge: structure and organisation of care delivery
Ambridge was a 30-bed care of older people ward, although bed numbers were reduced to 29 during baseline because of staffing shortages. The ward was designated for patients with ‘acute and complex needs’.
Physical environment
The layout of Ambridge was similar to that of Oak ward, with male and female bays located on corridors at right angles to each other. Along each corridor, there were three four-bedded bays and three single rooms with separate patient toilets and a bathroom. One side room on each corridor was en suite. There were some concessions to the creation of a ‘dementia-friendly’ physical environment, such as the toilet signage. However, the flooring was shiny in places, there was little natural light and the decor was worn and tired. There was a large nurses’ station in a box shape between the corridors, such that the bays were not observable from this location.
There was a designated day room (labelled ‘patient lounge’ on a small notice on the door). The space had multifunctional uses: a place for MDT meetings; for staff to do paperwork; for visitors to wait while the patient they had come to see was receiving medical or personal care; and occasionally where a patient might sit alone, watch television or converse with a visitor. A monochrome, functional space with unforgiving florescent lighting, its size offered the potential for patients to sit around one of three tables near the window or in the lounge area, which had seating for nine and was where the television was located. However, the room had the appearance of a storage area. It was generally full of stacked chairs; and walking frames, two hoists and physiotherapy equipment blocked access to the small bookshelf and its stack of books. This was the environment in which care delivery as observed occurred, and was typical of old-style wards in hospitals dating from the 1960s.
Patient profile
There were 171 people admitted to Ambridge over 9 weeks (around 17 per week), of whom two were readmissions. (Baseline fieldwork extended a further 2 weeks here, compared with other sites, to take account of the disruption caused by the move to the new space.) The median length of stay was 11 days (range 1–89 days). Table 4 shows the patient profile.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| 65–69 | 1 (1) |
| 70–74 | 6 (3) |
| 75–79 | 18 (10) |
| 80–84 | 51 (30) |
| 85–89 | 50 (29) |
| 90–94 | 37 (22) |
| ≥ 95 | 8 (5) |
| Gender | |
| Men | 80 (47) |
| Women | 90 (53) |
| No information | 1 (–) |
| Residence prior to acute admission | |
| Own home | 144 (84) |
| Residential care home | 19 (11) |
| Nursing home | 7 (4) |
| Intermediate care | 1 (–) |
Over half of the patients were in advanced older age (56% were aged ≥ 85 years). One-quarter had a diagnosis of, or probable, dementia. From fieldwork (handover, MDT meetings and observation), this appeared an underestimate and inconsistent with findings from other care of older people study wards. Just under one-fifth of patients (n = 30) had delirium on admission, of whom most (21/30) had a delirium on dementia. Data on delirium incidence were not collected.
The reasons for admission to Ambridge ward are shown in Figure 8.
FIGURE 8.
Ambridge: reasons for admission. AF, atrial fibrillation; COPD, chronic obstructive pulmonary disease; SOB, shortness of breath; TIA, transient ischaemic attack; UTI, urinary tract infection.
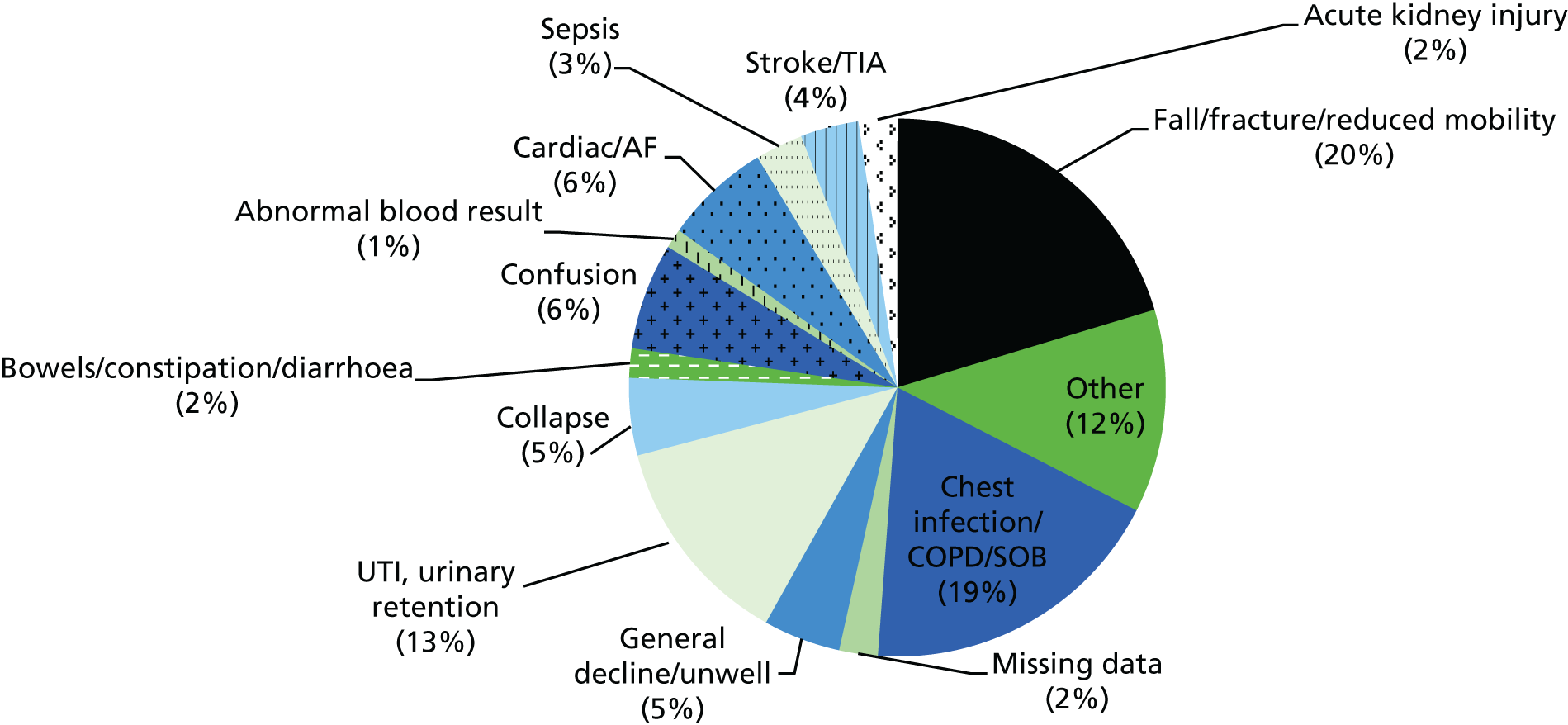
Discharge destinations are shown in Figure 9. Two-thirds of patients returned to their own homes on discharge, a smaller proportion than in Oak, reflecting a higher number who died during admission (9%) and a higher proportion of new admissions to long-term care (13%) or to hospice/palliative care (2%).
FIGURE 9.
Ambridge: discharge destination.
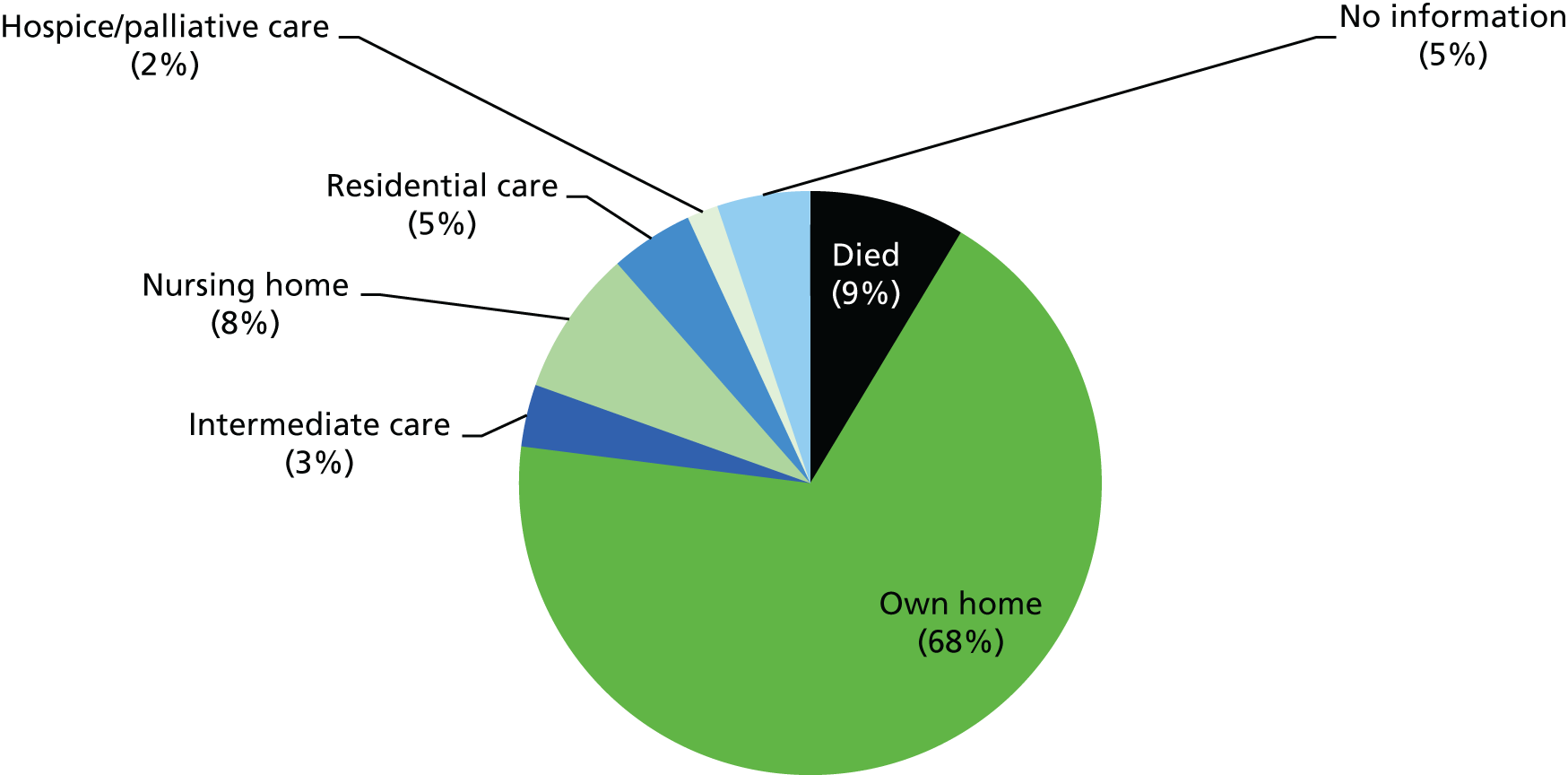
Staff profile
The staffing complement was 33. Four qualified nurses and four HCAs were on the early shift (a ratio of registered staff to patients of 1 : 7.2); three nurses and four HCAs were on the late shift; and two nurses and three HCAs were on at night. Thus, for a slightly larger bed base than Cedar ward in City Trust, the ward had a smaller staff complement and the proportion of registered to care staff was also lower. Although most shifts had the requisite numbers of staff, observed shifts indicated at least one and often two or more Bank or agency staff. Shortly before fieldwork began, one of two senior sisters had left to manage the newly opened ‘winter pressures’ ward and a staff nurse had been promoted to junior sister. During a substantial period of fieldwork, both the remaining senior sister and the ward manager were on sick leave and the ward was managed by the junior sister, without additional senior staff support.
Ambridge: care culture
Similar to Oak, Ambridge was a ward in transition. This had a spatial dimension (being parked in a temporary location while awaiting the move to its permanent, refurbished home) and a staff dimension (change in ward leadership and departure of experienced staff). Both contributed to disruption.
During most of baseline, the junior sister managed the ward. An experienced nurse, this was her first management post. She expressed strong commitment to providing care that treated ‘people as individuals’ and therefore placed store on finding out their concerns and wishes, including people unable to communicate through language. The combination of few experienced staff on the team, others in post only a short time, and reliance on temporary staff to cover shortages, exacerbated the difficulty in creating and sustaining a coherent ward culture. Whereas some on the ward had chosen to work with older people, and had knowledge and understanding of dementia, others had not.
There were only four respondents to the Culture of Care questionnaire: two had worked on the ward for 12 and 10 years, and the others had done so for 5 and 6 months. Their responses echoed the views of staff from informant conversations during observations and formal interviews. They conveyed common values: placing emphasis on caring for and supporting patients, and seeing the involvement of patients and caregivers as important. Yet they considered that there was an absence of resources and support to allow them to spend time with patients, and insufficient staff to provide quality care; and as a team, they did not review how to improve care delivery. Although supportive of each other, they reported an inability to challenge poor practice or to raise difficult issues with colleagues. They were most negative about the hospital, perceiving that their concerns and opinions were neither listened to nor responded to, and that assistance was not available when needed.
Ironbridge NHS Trust
Organisation
Ironbridge Trust, similar to City, is a long-established foundation trust. It provides acute, elective, specialist and some community services to a core population of around 650,000. The location of a major trauma centre, it has > 150,000 A&E attendances annually. With around 2000 inpatient beds and employing some 16,000 staff, it is one of the largest trusts in the country and one of the biggest local employers.
Annual trust reports between 2010/11 and 2013/14 presented an organisation that, in leadership, efficiency, safety and caring, was successful and consistently meeting national and local targets. Similar to other study trusts, it presented as being challenged by the multiple and competing political, organisational, performance, financial and regulatory demands.
A major transformation in service delivery was initiated by the integration of adult community and acute services from spring 2011. A further integrative step from autumn 2014 involved combining the Directorate of Geriatric and Stroke Medicine and the Primary and Community Services Care Group, a union with a direct impact on our study ward.
Care of people with dementia
From 2011/12, the trust’s strategic priorities included improving the care of people with dementia and creating ‘dementia-friendly’ physical environments on care of older people wards.
In 2011, a new ward was established that was dedicated for older patients with dementia undergoing hip fracture surgery; and, in 2012, an integrated multiprofessional care pathway for patients with both dementia and delirium was implemented, supported by training. A discreet symbol was developed (as in Valley wards) to enable staff to recognise people with dementia; this was aligned with a personal information booklet, ‘All About Me’, launched in spring 2014, for use by patients with confusion/dementia and their caregivers.
Ironbridge Person, Interactions and Environment wards
Two Ironbridge wards initially expressed interest in participating in PIE: a trauma orthopaedic ward and an acute dementia ward. Both met our ‘readiness’ criteria. Before fieldwork commenced in January 2014, the trauma ward withdrew, citing staffing difficulties. Efforts to engage another ward were unsuccessful.
Netherton: structure and organisation of care delivery
Netherton was an acute medical ward for those aged ≥ 70 years with comorbid dementia or delirium/acute confusion. It was not a specialist dementia ward:59 it did not employ specialist mental health staff, therapy input was similar to that in other care of older people wards, and it had no additional staff providing activities. During baseline, Netherton comprised 28 beds (including one bed for ‘winter pressures’, which was consistently in use during fieldwork).
Physical environment
Netherton was organised in four six-bedded bays and four single rooms: one male and three female bays. The bays were colour-coded (purple, yellow, blue or green). Each had a small table near a window at which staff sometimes sat to write. The single rooms were relatively spacious and pleasant with natural daylight.
The ward presented as a bright, airy, clean and open environment. Each bay was separated by a low divider (work surface, no doors), opening on to a wide corridor with a large skylight, exuding a sense of spaciousness and allowing ample daylight. There was a very small workstation down the entrance corridor with space for a single computer. There was a table in the corridor around which there was space for 4–6 people to sit (which patients and staff did, interchangeably).
Off the bays (opposite the work station) was a large L-shaped day room with a separate door and half-height windows overlooking the hospital grounds. Painted in neutral colours, it had three tables with ample seating for dining and socialising. At the far end was a lounge space with chairs and a television (there were no televisions in the bays). Various reminiscence/household objects were laid on side tables (an old-style radio, an alarm clock and games); on the walls were old brand adverts and pictures of the locality. A small, enclosed room off this served as a private space, and had a settee, chair, lamp and bookshelf. It was slightly shabby, but homely, in appearance.
Off the corridors to the left and right of the central ward space, and opposite the bays, were the patient toilets, shower room and single rooms. The toilets had visible signage, and toilet seats and rails that were dark blue, contrasting with the otherwise white suites. The location of the toilets allowed patients who were mobile the opportunity to walk between their bed in the bay and the toilet. Further along from these rooms was a designated staff space (a toilet with key access and a small room). There was an atmosphere of calmness and quiet efficiency, with staff and patients sharing communal spaces.
Patient profile
There were 75 people admitted during baseline (an average of eight per week), and no readmissions. Most patients came directly from A&E or the assessment unit (70%; 52/75); just under one-third had been admitted from other hospital wards. The median length of stay was 41 days (range 1–126 days); extended lengths of stay were attributed to changes in the system for financially assessing patients, resulting in delays to some patients being discharged. Table 5 summarises the patients’ sociodemographic profile.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| 60–64 | 1 (1) |
| 65–69 | 0 (0) |
| 70–74 | 3 (4) |
| 75–79 | 9 (12) |
| 80–84 | 14 (19) |
| 85–89 | 30 (40) |
| 90–94 | 16 (21) |
| ≥ 95 | 2 (2) |
| Gender | |
| Men | 18 (23) |
| Women | 57 (76) |
| Residence prior to acute admission | |
| Own home (including sheltered housing) | 66 (88) |
| Residential care home | 3 (4) |
| Nursing home | 5 (6) |
| Assisted living | 1 (1) |
Just under two-thirds of patients were in advanced older age, a slightly older profile than in other participating wards, and women dominated. Most had been admitted from their own home.
Most patients (n = 70, 93%) had dementia (the remaining patients had delirium but not dementia). Nearly two-thirds (60%; 31/52) of new acute admissions had delirium. Overall, 70% (54/75) had delirium during their stay, of whom nine (13%) were in delirium for ≥ 30 days. The median number of days in delirium was 16 (range 1–57 days). The reasons for admission are shown in Figure 10.
FIGURE 10.
Netherton: reasons for admission. UTI, urinary tract infection.
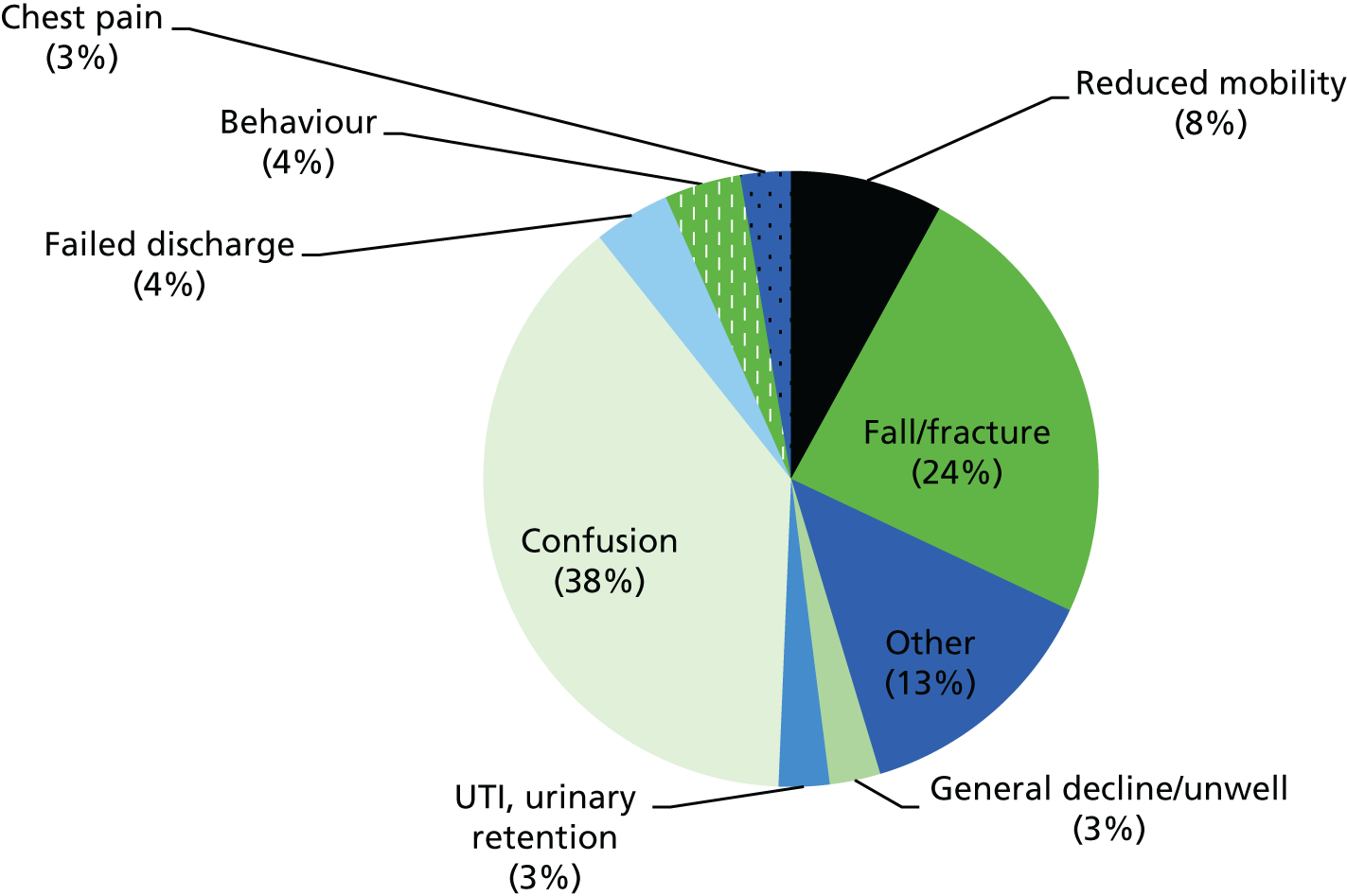
Discharge destination data were available for 44 patients (the remaining 25 still being in the ward at the end of data collection). These are presented in Figure 11.
FIGURE 11.
Netherton: discharge destination.
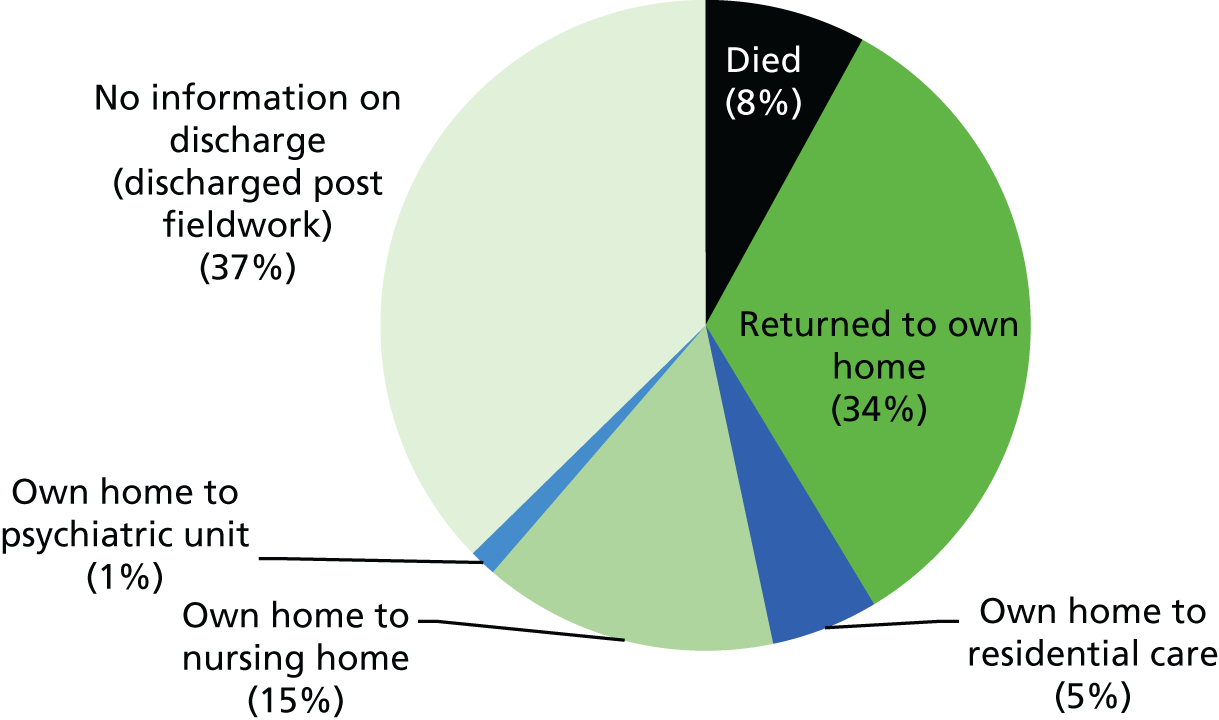
Of those for whom information was available, 25 (57%) were discharged to their own home; one-fifth involved new admissions to long-term, mainly nursing home, care.
Staff profile
The ward team comprised 35 staff. The typical staffing complement was five nurses and three HCAs (early shift); four nurses and three HCAs (late shift); and two nurses and two HCAs (night shift). The ratio of registered nurses to patients on the day shift was 1 : 5.6. The staffing complement was generally maintained during baseline, although, as elsewhere, staff shortages on a shift involved the substitution of a HCA for a nurse.
Netherton: care culture
An established, stable team, half of them had worked together for at least the 8 years in which the current ward model had operated (acute, dementia care). This included senior staff (ward manager, senior sister and charge nurse) who had a wealth of knowledge and skill in caring for people with dementia, acquired through formal self-directed learning, personal and professional experience. They conveyed, through formal and informal mechanisms, a consistent and coherent team ethos and a commitment to the ongoing appraisal of work practices. Twice-yearly away days were held for staff to examine practice and identify problem areas to work on. Everyone was expected to attend (the away days were organised as two separate days to facilitate participation). Through these various mechanisms, new staff were enculturated into a style of team working that emphasised continuous improvement as ‘how we do things on this ward’. The ethos of person-focused care was reflected in the responses to the Culture of Care questionnaire, completed by just over half of the team (n = 18).
Consensus existed among respondents that the team shared an explicit philosophy of care; the psychological needs of patients were considered; involving patients and their carers was an important part of the work; and these values and expectations were communicated to new staff. There was agreement that patients were treated with dignity and respect; they experienced individualised care, and patients’ and families’ care needs were met (reflected in research observations).
Most respondents agreed that there were sufficient ward resources to deliver good care, including staff with the requisite knowledge and skills to provide it. Just under half regarded staffing levels as insufficient to allow them to spend enough time with patients.
They felt supported as a team, could rely on each other, were relatively comfortable about bringing up problems with colleagues and felt that they could influence ward decision-making. In agreement with staff on other study wards, there was too much work to do in too little time, but they particularly valued the learning and development opportunities available.
Strong, positive feedback was received about the ward’s leadership and management style, especially the support provided and clarity of expectations around achieving care excellence. Perceptions of the wider hospital were mixed, although views were more neutral to positive about the availability of training opportunities and access to resources.
Central NHS Trust
Organisation
This foundation trust is one of the largest in England, employing around 11,000 staff (one of the top five employers in the region). It treats more than 1.2 million people and has 250,000 A&E attendances annually. Acute services are primarily located in one main hospital, with additional beds in two smaller hospitals. The study wards were located in one of these, comprising around 229 beds and providing a range of community, outpatient, inpatient and emergency care services. This hospital was situated approximately 6 miles from the main hospital, within a self-defined, organisational community (it has its own local authority) of 250,000 people.
Trust board annual reports from 2011/12 reveal an organisation in which balancing finances was a persistent and significant challenge. In 2013, the trust’s contingency fund was under pressure; the research site hospital was in overspend by 15% and had not delivered on its cost improvement programme. A plan to reduce costs by closing flexi beds was set in train; and the financial position of the hospital was in focus, including weekly rectification update meetings. The trust was also reviewing staffing models as a cost-saving measure.
By November 2013, the A&E waiting time performance target had been missed for five consecutive quarters, creating concern that Monitor would intervene and prompting micro-management to regain control. All elective inpatient surgery was temporarily suspended, which resulted in failure to meet the 18-week referral-to-treatment target and the creation of a backlog in excess of 1000. The research site hospital met A&E waiting time targets, but, with significant pressure on the trust affecting all sites, work was conducted to review capacity and demand.
A CQC inspection in autumn 2013, the results of which were published in January 2014, deemed the trust as requiring improvement on all criteria apart from ‘effective’. The trust board and senior management were under considerable pressure to balance development and redesign against significant challenges, including winter pressures, increased activity and securing financial recovery.
Care of people with dementia
Local strategic priorities during 2011–14 included a programme to deliver improvements to the care of people with dementia and delirium, including policy, ward environment and drug treatment. The dementia strategy and steering group selected key areas to monitor, including education, improved pathways, metrics, and the embedding of personalised ‘all about me’ documentation into practice. A supported integrated discharge team was established to facilitate the timely discharge of frail elders, and joint old-age medical and old-age psychiatry were to be available on every site. The trust dementia steering group placed emphasis on improving dementia screening rates, which were well below target. Of the trust hospitals, the research site had best compliance with screening: from 3% in September 2013 to 33% in December 2013 (the target was 90%).
A trust-wide ongoing programme of ‘dementia awareness’ training had been delivered before the start of the research, tailored to different staff groups, with the intention of utilising a group of ‘dementia champions.’ In recognition of the increasing number of patients with dementia, 30 mental health nurses were recruited to Bank staff, and some volunteers received specialist training in dementia in the main hospital, with a rollout plan to other sites.
Central Trust Person, Interactions and Environment wards
Three wards took part in the study; collectively, they formed the elderly care directorate in this hospital. Denton is a rehabilitation ward for people with dementia who are medically stable; similar to Netherton, it is not a specialist dementia ward. Beech is a mixed trauma and care of older people ward, and Rose is a stroke ward. On all three, baseline data collection began as planned in July 2013.
Denton: structure and organisation of care delivery
Denton comprised 13 beds. A designated ‘enhanced recovery ward’, it was intended to provide dedicated support to people with dementia who were medically fit and mobile and would benefit from the expertise and calmer environment offered there. It was also part of the trust’s winter initiatives to manage patient flow. When fieldwork began, the ward was relatively new, having opened in January 2013. Early in the data collection phase, it emerged that long-term funding to the ward was insecure and that bed numbers were not included in the hospital total. The ward underwent waves of imminent closure threats. The impetus for keeping the ward open came from clinicians who were passionate about having access to a resource for people with dementia and from positive feedback from patients and relatives.
Physical environment
The physical environment was spacious. There were two six-bedded bays (male and female) and one side room. The impression was of a less medicalised environment than other wards on the site. Décor was neutral and there was some signage for the bathroom. The staff office had clear visibility into the open, spacious day area, where patients and staff spent most time. In this area there were four round tables each with four chairs, at which patients, visitors and staff sat. In addition, there were some high chairs in a row, and more stacked chairs for visitors. There was access to a small garden with a bench.
Patient profile
During baseline, there were 39 people admitted over 9 weeks (approximately four per week), of whom one was a readmission. Patients were admitted from other wards in this hospital, following an acute stay. The median length of stay was 25 days (range 4–79 days). Table 6 summarises the patients’ sociodemographic characteristics.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| 65–69 | 2 (5) |
| 70–74 | 1 (3) |
| 75–79 | 5 (13) |
| 80–84 | 6 (15) |
| 85–89 | 12 (31) |
| 90–94 | 9 (23) |
| ≥ 95 | 3 (8) |
| Gender | |
| Men | 15 (38) |
| Women | 24 (62) |
| Residence prior to acute admission | |
| Own home | 34 (87) |
| Residential care home | 4 (10) |
| Nursing home | 1 (3) |
More than half of patients were in advanced older age (median 88 years), and the majority were women. Most had lived at home before their acute admission. All (n = 39) had dementia; one-quarter (n = 10) had delirium (of whom seven had delirium on dementia). During their admission, most patients had delirium (n = 33); the median number of days in delirium was 11 (range 1–36 days). The reasons for admission are shown in Figure 12.
FIGURE 12.
Denton: reasons for admission. UTI, urinary tract infection.
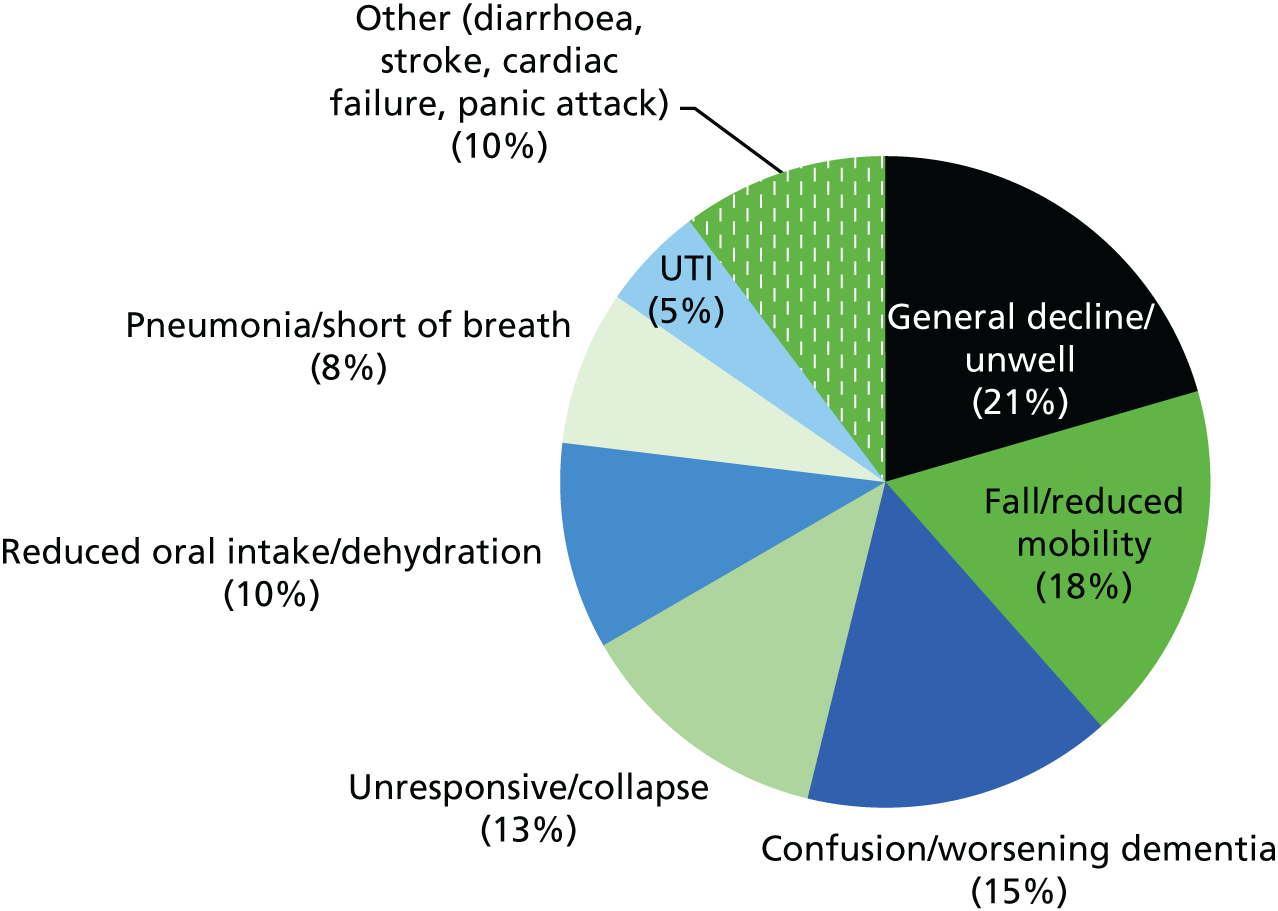
A further indicator of the frailty of the patient profile is the discharge destination pattern (Figure 13), which shows that 16% of patients died and 38% went to long-term care.
FIGURE 13.
Denton: discharge destination.
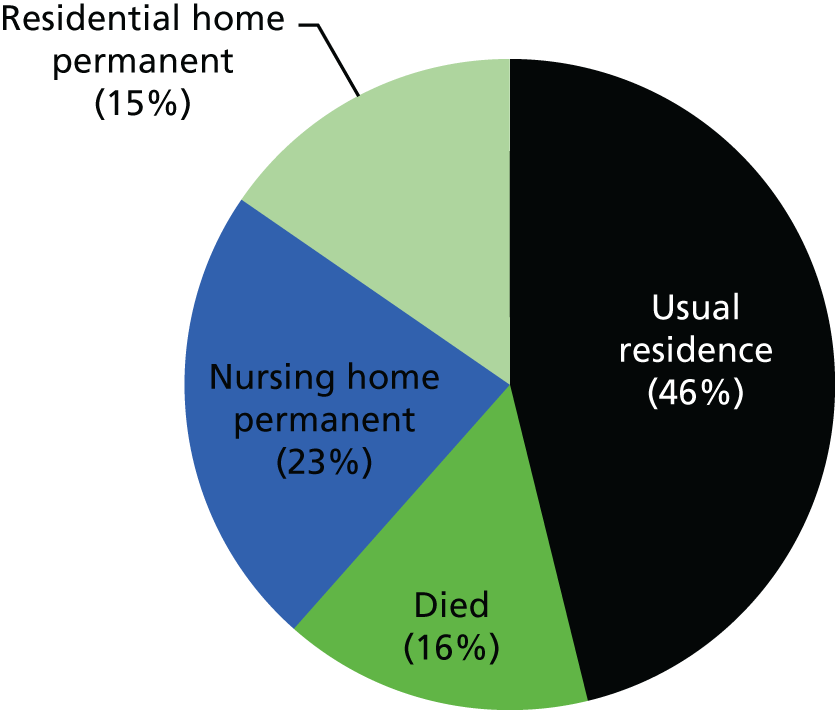
Staff profile
The ward team comprised 12 staff. The staffing complement was two qualified nurses and two HCAs during the day, and two qualified nurses and one HCA at night (a patient-to-registered-staff ratio of 1 : 6). A geriatrician provided a weekly patient review meeting, and a junior doctor was primarily based on the ward; this post was not permanent. Therapy cover was provided by the senior occupational therapist with an interest in dementia and by therapists who might follow patients from their previous ward.
Denton: care culture
Most staff had worked together since the ward opened, some 7 months prior to baseline. All had chosen to work there because they had an interest in dementia. Many of the resources on the ward – for example games and reminiscence materials – had been purchased through fundraising initiatives by ward staff. There was heightened goodwill among staff, patients and relatives in joint working towards such initiatives.
Ten Culture of Care questionnaires were completed: eight by nursing and care staff, and one each by a doctor and a housekeeper.
There was consensus that the team had a caring approach, shared an explicit philosophy of care, placed high value on the psychological care of patients and the provision of enabling support, and regarded the involvement of patients and caregivers as very important. There was agreement that the team had access to adequate resources and that they routinely engaged in reflection and discussion aimed at improving care delivery.
The perceptions of the MDT were almost unanimously positive, with good working relationships. There was a consensus that patients were treated with dignity and respect, that they experienced good individualised care and that patients’ and families’ care needs were usually met. Observation supported this picture, attesting to a style of collaborative work with families that embraced sensitivity and responsiveness to their anxieties and concerns. There was very positive feedback about the emotional and practical support offered within the team, with respondents unanimous about the trust, competence and confidence they shared, and that they felt comfortable about discussing difficult issues together.
There was a slightly mixed response with regard to balancing resources and demands. Although some considered that there was too much work to do in too little time, most agreed that they could follow best practice within existing resources. They were generally very positive about ward learning and development opportunities.
Universal, strong, positive support about all aspects of ward leadership and management was conveyed: the ward manager was reported to consult daily with the team and to be an ongoing presence who was involved in hands-on patient care.
The most variable responses were provided to questions about the hospital, indicating mixed views about hospital resources, access to expert assistance and the responsiveness of hospital management to staff concerns. It was largely agreed that the hospital provided adequate training opportunities and treated staff with dignity, and that staff had the authority to make decisions.
Comparing all wards in the study, Denton respondents were most universally positive, summed up in the comment of a HCA:
I have worked on [Denton] since it opened . . . I have never been as happy since I started working for the trust. It is a lovely well-run ward . . . patients get great care here.
Beech: structure and organisation of care delivery
This ward provides care to a mix of older people with complex medical needs and those who suffered orthopaedic trauma, primarily fractured neck of femur. During baseline, the ward usually had 24 beds: 12 trauma and 12 medical. There was an additional bay, open as part of the hospital’s capacity-management strategy, making a total of 31 beds (over five bays and three side rooms). Historically, the ward had undergone many changes over the years (of purpose, size, patient group and physical location).
Physical environment
The ward appeared a ‘busy’, cluttered physical space, with people, artefacts and equipment. There were no meeting rooms and no day room: team and MDT meetings were held in the ward manager’s office or the staff room. The environment was not ‘dementia friendly’; the bays all looked the same and had no orienting features. Each bed had a pay-per-use television and radio screen.
Patient profile
During baseline, admission data were recorded for approximately 5 weeks, during which there were 60 admissions (12 per week). The median length of stay was 20 days (range 4–153 days). The physical and cognitive abilities of patients varied. For example, ability to mobilise spanned those who walked around the ward independently to people who were mostly in bed. Many patients were physically frail, requiring assistance to transfer or to mobilise. Table 7 summarises the patients’ sociodemographic characteristics.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| 65–69 | 1 (2) |
| 70–74 | 6 (10) |
| 75–79 | 7 (12) |
| 80–84 | 11 (18) |
| 85–89 | 10 (17) |
| 90–94 | 17 (28) |
| ≥ 95 | 8 (13) |
| Gender | |
| Men | 13 (22) |
| Women | 47 (78) |
| Residence prior to acute admission | |
| Private residence | 50 (83) |
| Residential care home | 4 (7) |
| Nursing home | 1 (2) |
| Respite care | 1 (2) |
More than half of patients were in advanced older age (median 87 years; range 67–99 years). The majority had lived at home (including many who had caregivers) prior to the event that had brought them into hospital. Just over one-third had dementia (n = 21). Given the age profile of these patients, and based on observation, this probably underestimated the dementia prevalence (data were incomplete; data were missing for 27 patients. On admission, at least one-fifth had delirium (n = 12; missing data, n = 27). Of those who were assessed for delirium during their admission (n = 18; missing data, n = 42), almost half were identified as having a delirium (n = 8) for a median of 3 days (range 1–15 days). The reasons for admission are shown in Figure 14.
FIGURE 14.
Beech: reasons for admission. AF, atrial fibrillation; TIA, transient ischaemic attack; UTI, urinary tract infection.
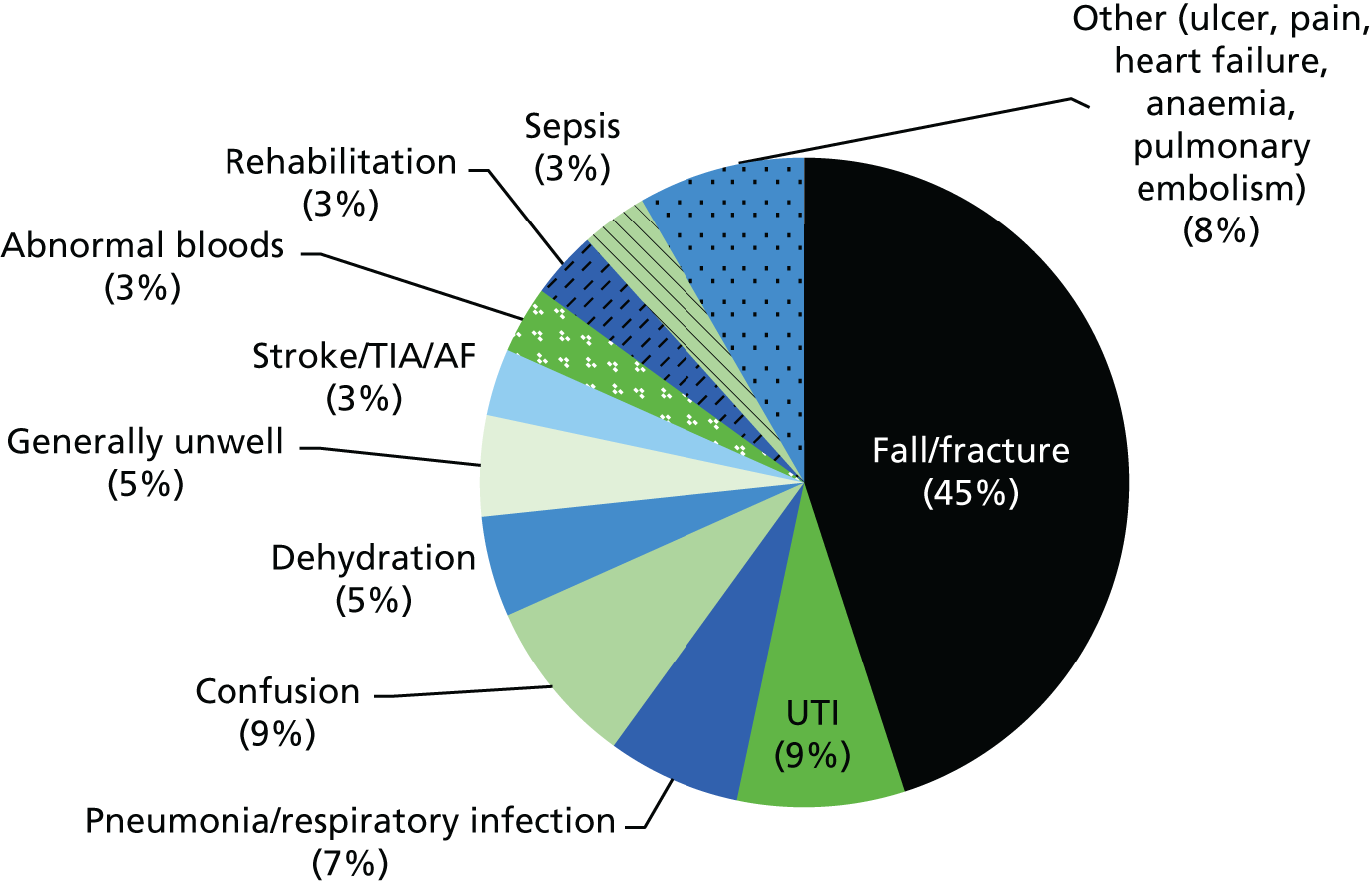
Data on discharge destination are presented in Figure 15. Just under three-quarters of patients returned to their usual residence on discharge; a further quarter were equally divided between those who died and those who were newly admitted to long-term care.
FIGURE 15.
Beech: discharge destination.
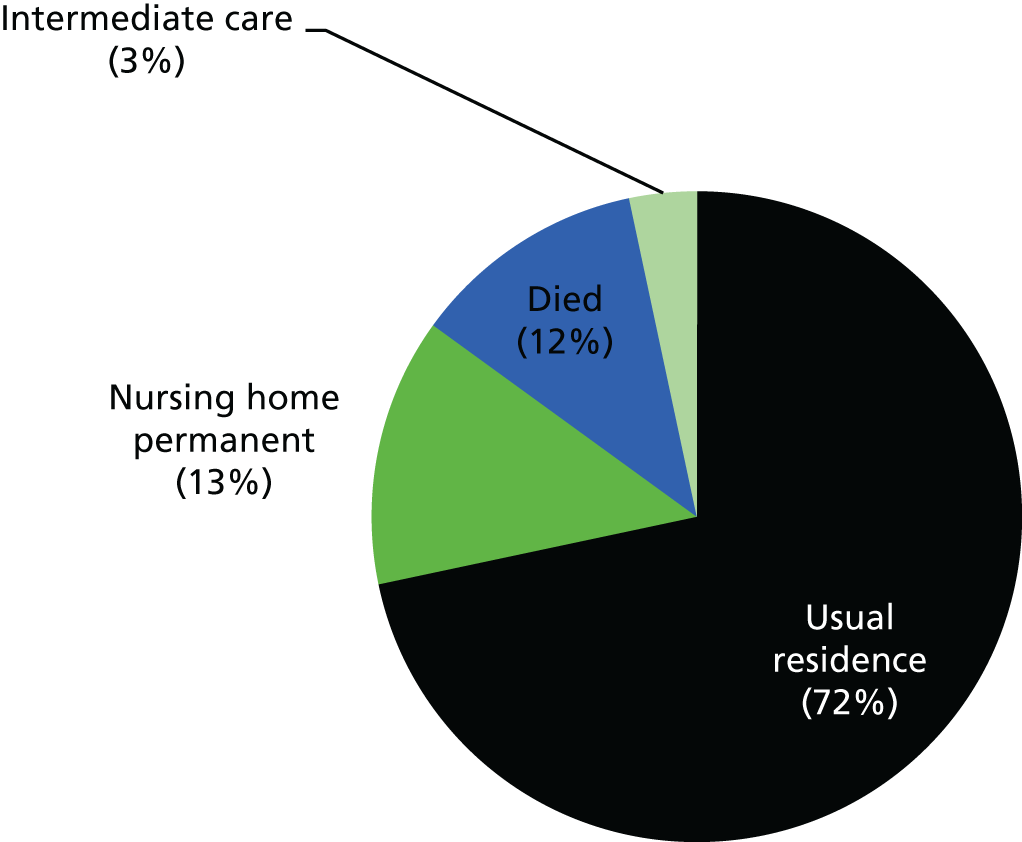
Staff profile
Detailed information on staffing complement was unavailable (accounted for in part from variability of available beds). Shifts were commonly staffed using Bank or agency workers, and it was not uncommon for such staff to ‘special’ a patient on a one-to-one basis (typically someone who was agitated or distressed). The ward manager was primarily engaged in management tasks and was rarely involved in direct patient care.
Beech: care culture
The ward model was relatively new, and there was considerable ongoing work necessary, from the ward manager’s perspective, to construct a team and forge a common care ethos; this was made more difficult by a shortage of permanent staff and a reliance on temporary workers. This was reflected in the responses to the Culture of Care questionnaire, completed by five staff only (two nurses, one HCA, one geriatrician and one who did not provide his or her job role). Interpretations of the questionnaire data are limited, given the paucity of data; however, there are clear patterns in the responses that echo those derived from observation and interviews. Of all of the wards, the respondents here were most negative.
Generally, the respondents conveyed that among the team there was low value placed on involving patients and caregivers, insufficient basic ward equipment, inadequate support to allow time to be spent with patients, and no routine mechanism for improving care delivery. Regarding multidisciplinary working, there were mixed views: although communication was perceived as good, it was felt that patients did not experience individualised care (a view shared by the ward manager during an informant interview). With regard to decision-making, respondents considered that they had little influence in how the work was managed, and that there was too much pressure on resources and demands, such that there was insufficient time to deliver best care and pursue appropriate training. Although the manager was perceived as available and supportive, she was not visible in direct care provision. Respondents indicated that they did not feel well supported by the hospital, were not fairly rewarded for their work and were not treated with respect, and that management did not listen to their concerns.
Rose: structure and organisation of care delivery
Rose ward was for patients recovering from stroke who required medical care and rehabilitation. Non-stroke patients with medical needs were also admitted, including those with palliative care needs, particularly into the four single rooms, of which there was a shortage in this hospital. The ward had 23 beds (sometimes 24, with an additional bed in the male bay). It seemed, from the patient profile, that the ward was evolving from a specialist unit into a mixed medical ward.
Physical environment
Similar to Beech, the physical environment was ‘busy’, clinical and not ‘dementia friendly’. There were three bays, two female (one eight-bedded and one five-bedded) and one male (with six beds), as well as four single rooms. Some bays only were within view of the nursing station. A staff member was based in one bay opposite the nursing station (a stroke data co-ordinator who had been a HCA).
There was an office used by staff and for relatives’ meetings, and a small, cluttered staff room. Both were planned to be refurbished to better fit their purpose. There was no day room. A large therapy room at the end of the ward contained a small therapy office, lots of equipment and open space. The ward had a stroke-friendly garden, built with money raised by ward staff.
Patient profile
During baseline there were 167 people admitted over 8 weeks (approximately 21 per week). The median length of stay was 5 days (range 1–91 days). Table 8 provides a summary of the patients’ sociodemographic characteristics.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| 18–64 | 48 (29) |
| 65–69 | 12 (7) |
| 70–74 | 19 (11) |
| 75–79 | 14 (8) |
| 80–84 | 36 (22) |
| 85–89 | 21 (13) |
| 90–94 | 11 (7) |
| ≥ 95 | 6 (4) |
| Gender | |
| Men | 81 (49) |
| Women | 86 (51) |
| Residence prior to acute admission | |
| Own home | 157 (94) |
| Residential care home | 4 (2) |
| Nursing home | 4 (2) |
| Care home other | 1 (1) |
The age (median 77 years, range 18–99 years) and physical and cognitive abilities of patients varied considerably. Given the age range and variability of recovery, there was potential for added complexity. Some patients had life-changing, newly acquired disabilities and others aimed to resume paid work following their recovery. Many of those currently on the ward required staff assistance to transfer or to mobilise.
The majority had lived at home before their acute admission. On admission, 13 patients (8%) had dementia and three had delirium. Among those assessed for delirium during their admission (n = 19; missing data, n = 148), over half were identified as having delirium (n = 11), for a median of 4 days (range 1–7 days). The reasons for admission are shown in Figure 16. Just under half of patients had suffered a stroke; the remainder had been admitted for various acute medical conditions.
FIGURE 16.
Rose: reasons for admission. CVA, cerebrovascular accident; FAST, Facial drooping, Arm weakness, Speech difficulties, Time to call emergency services; SOB, shortness of breath; TIA, transient ischaemic attack; UTI, urinary tract infection.
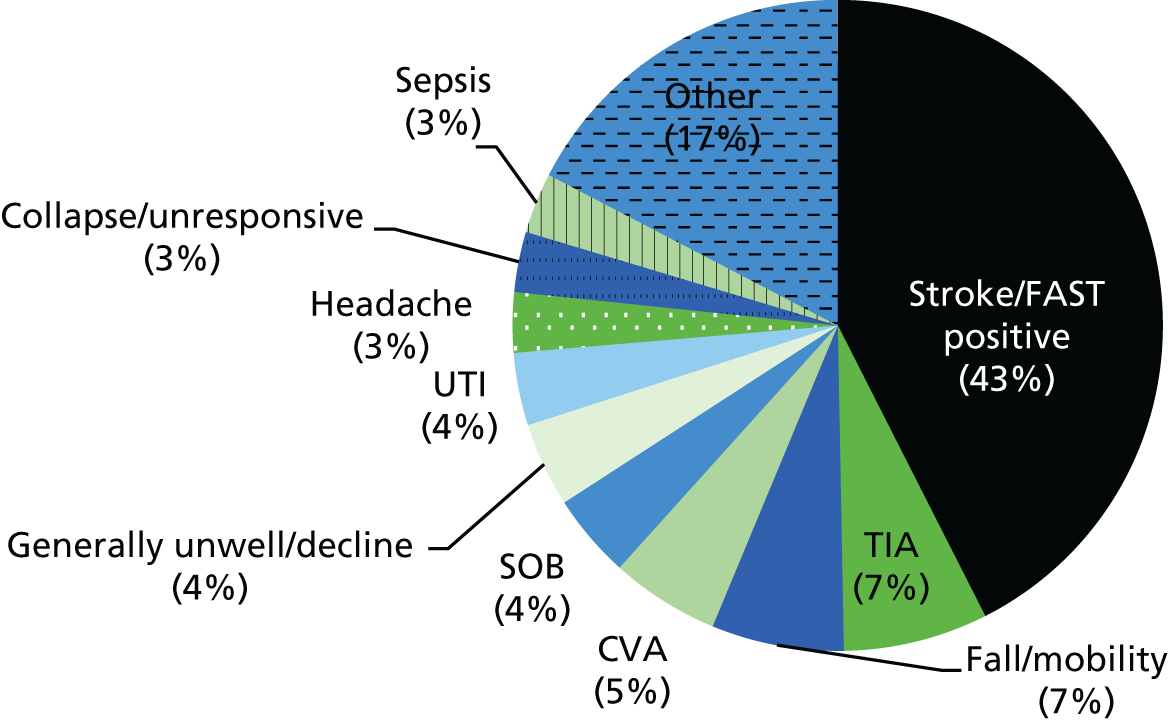
Data on discharge destination are shown in Figure 17.
FIGURE 17.
Rose: discharge destination.
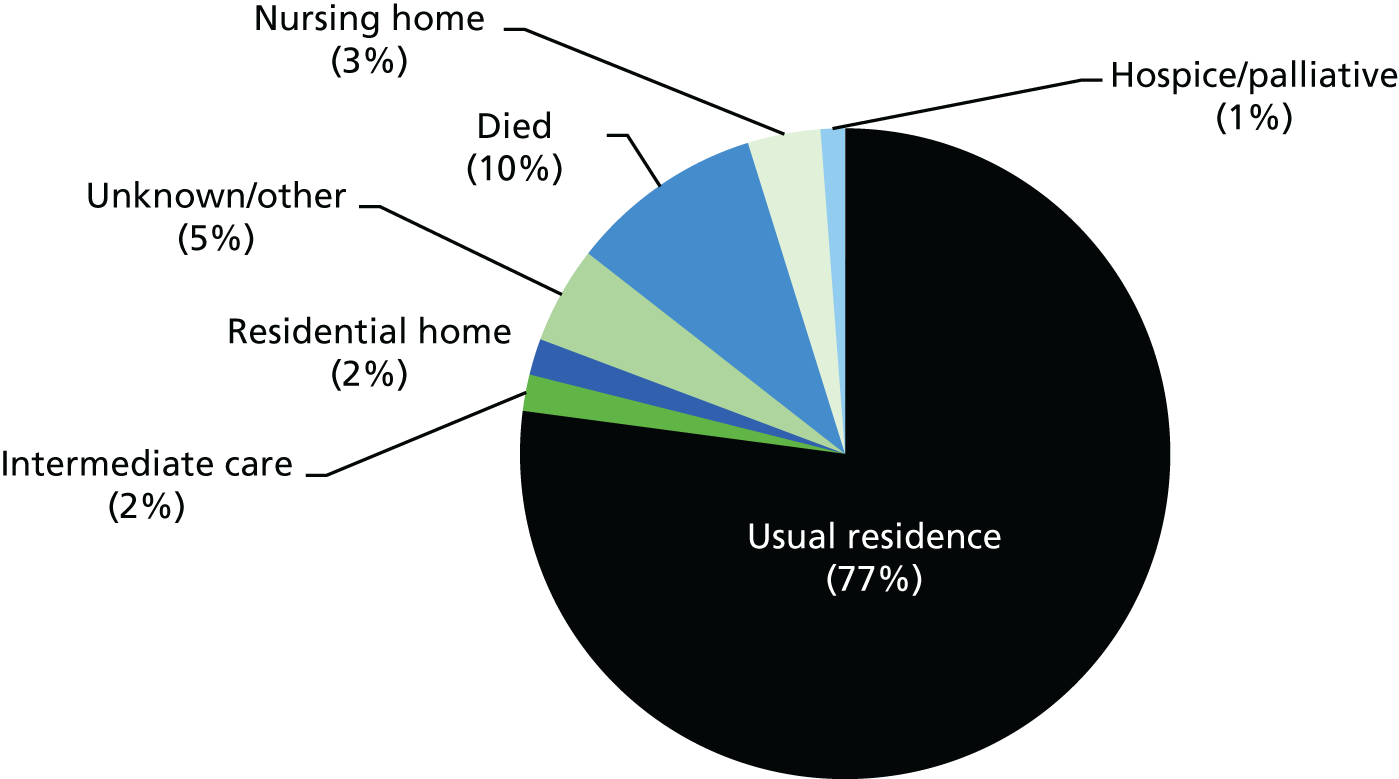
The proportion of patients discharged to their usual residence was reflective of a population who, before admission, was slightly younger and healthier than that of other wards in this study. Additionally, patients here benefited from access to the Early Supported Discharge and Hospital at Home services, both of which facilitated the continuation of monitoring, nursing support and rehabilitation on acute discharge.
Staff profile
The senior ward management team included a manager, a sister, a charge nurse and a senior stroke co-ordinator (the role of the last of these was to identify and co-ordinate stroke patients admitted to any part of the hospital). There was also a co-ordinator from the Stroke Association, who performed the function of patient and family liaison and was a link to facilitate the patients’ transition between the ward and their own home on discharge. The staffing complement was four nurses and three HCAs on the early shift; three nurses and two HCAs on the late shift; and three nurses and two HCAs at night (a registered staff-to-patient ratio of 1 : 6).
Rose: care culture
Based on observation and staff interviews, the manager had ward presence but limited patient contact. She was newly promoted and appeared stretched. She was supported by the sister and the charge nurse, both of whom were visible and active in providing direct patient care and had long experience of working on the ward. Several HCAs had been based on the ward for many years. The existence of a stable group of staff at different levels over time provided continuity and a strong sense of collegiate working. Morale was affected by staffing difficulties, as was working in a physical environment regarded as ‘tired’, cluttered and dark. The manager considered that her staff team were overburdened and was protective of them, for example being careful to ensure that feedback on performance and critical incidents was conveyed and reflected on constructively.
The responses to the Culture of Care questionnaire (12/30 questionnaires returned from nursing, medical and therapy staff) indicated mixed views about the care and ward working environment. Positively, it was reported that the team shared an explicit philosophy of care and that the involvement of patients and caregivers was valued. However, staff considered that there was inadequate support to allow them to spend time with patients. They conveyed a positive sense of providing good care and working as a team, for example indicating that staff worked well within the MDT, provided individualised care and treated patients with dignity and respect. Respondents were largely neutral about team support, raising difficult issues and being able to participate in ward decision-making. There was much disagreement about the extent to which resources and demands negatively affected work and care, although there was agreement on the availability of, and access to, training. Ward leadership was perceived as positive, although, in comparison with City, Ironbridge and Seaford wards, this was expressed in less enthusiastic terms. The perception of support from the hospital was mixed; respondents were generally positive about being able to obtain expert assistance when needed and being treated with dignity and respect.
Seaford NHS Trust
Organisation
Seaford Trust is one of the largest in England, with five hospitals, spread over a wide geographical, socioeconomically diverse area and serving a population of approximately 759,000. The three acute hospitals (two of which were involved in PIE) employ > 7500 staff and serve a bed base of 1107. It was awarded foundation trust status in 2009.
Trust annual reports from 2010–11 to 2013–14 present a picture of high performance and future uncertainty that was similar to that in other participating trusts. In the recent past, it had received the accolade of Trust of the Year, was the top performing hospital in the Healthcare, Excellence and Leadership Awards and met all of Monitor’s governance and financial targets. In the 2 years from 2012 to 2013, the pattern of high performance was seen to persist, although the foreshadowed difficulties included an increasing demand on services, particularly as a result of ‘winter pressures’.
A major strategic initiative pursued was the development of a Shared Purpose Framework and set of values that would guide practice, which was launched in 2013, when the study began. This was intended as the starting point for a programme of cultural change and was aimed at engaging staff at all levels around four key purposes: person-centred care, safe care, effective care, and creating an effective workplace culture to sustain and enable quality improvement.
Care of people with dementia
Dementia per se was not identified as a key priority in trust annual reports until the 2012/13 report. This announced two key initiatives: the establishment of a dementia team and a new Enhancing Quality Programme pathway for dementia, both launched in early 2013. The dementia team comprised a matron, two experienced nurses and a consultant working closely with them to lead improvements and support the implementation of the dementia strategy. The matron and specialist nurses were attached to each of three district general hospitals in the trust, including the two study wards.
The dementia team was in post for < 1 year when the research began but had already instigated several initiatives that were quickly and widely acknowledged. In 2013, they won the trust’s Caring Award for their work, which included a trust pathway for dementia care, staff dementia training, a ‘confusion pathway’ and a pocket guide to preventing falls and managing confusion, in collaboration with the falls matron.
Seaford Trust Person, Interactions and Environment wards
These were the last wards recruited, partly owing to the arm’s-length negotiations required for set-up. Even so, data collection and other research activity ran largely according to the planned timetable owing to a relatively (compared with the other sites) stable situation, in that both wards retained their specialisms (one orthopaedic and one frailty/rehabilitation) over the research time frame.
Poplar: structure and organisation of care delivery
The easternmost site, where Poplar ward is located, is an acute hospital with 388 beds providing a range of emergency and elective services and comprehensive trauma, orthopaedic, obstetrics, general surgery and paediatric services. The hospital dates back to the 1930s, when the original building was constructed. Between 1996 and 1998, most services were relocated and expanded into a new hospital building linked to the original facilities.
The hospital has several specialist units and new staff accommodation. Co-located on the site are mental health facilities for working-age adults and older people run by the local NHS and Social Care Partnership (mental health) trust.
Poplar is a 22-bed orthopaedic ward for older people. Most patients are admitted as emergencies following a fall and the sustaining of a fractured neck of femur.
As baseline data collection started, the ward clerk, who had agreed to assist with accessing the ward profile data, sustained a fall and was hospitalised with bilateral ankle fractures. She was off sick for the whole period, which made data collection a challenge, as the researcher did not have access to the electronic patient data.
Physical environment
Poplar comprises three six-bedded bays, two single rooms and one double room and is situated in the new (1990s) building. There are usually one male and two female bays, all of which are colour-coded. The rooms are fairly spacious, and there are small tables and chairs at the far end of each bay, near the windows. Other chairs, for visitors, are at the entry to the bays. All of the bays and rooms have clocks and date calendars. The ward had relocated twice just before the study began, and its current ‘home’ meant the loss of a day room: a source of regret among staff.
Patient profile
At baseline there were some 90 admissions, all emergencies, having a median length of stay of 15 days (range 1–36 days). For the reasons above, there are many missing data. Table 9 presents the Poplar patient profile.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| 65–69 | 3 (3) |
| 70–74 | 5 (6) |
| 75–79 | 12 (13) |
| 80–84 | 21 (23) |
| 85–89 | 21 (23) |
| 90–94 | 20 (22) |
| ≥ 95 | 6 (7) |
| No information | 2 (2) |
| Gender | |
| Men | 27 (30) |
| Women | 61 (68) |
| No information | 2 (2) |
| Residence prior to acute admission | |
| Own home | 46 (51) |
| Extra-care housing | 1 (1) |
| Intermediate care | 0 (0) |
| Residential care home | 10 (11) |
| Nursing home | 0 (0) |
| No information | 33 (37) |
Patients were mostly aged ≥ 80 years and female. The majority were admitted from home following a fall. According to documentation, approximately 50% of patients had a degree of cognitive impairment at any one time. This is supported by staff interview data, although the numbers appeared to fluctuate upwards. Data on delirium were not collected. Figure 18 reports the reasons for admission.
FIGURE 18.
Poplar: reasons for admission. ‘Other’ includes dislocated hip, hip fracture, wrist fracture, displaced neck of femur, cellulitis.
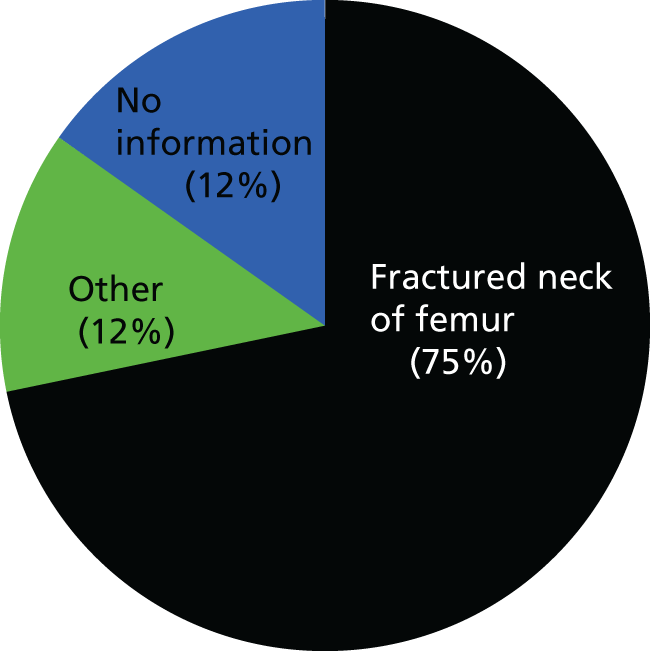
Data on discharge destination are presented in Figure 19.
FIGURE 19.
Poplar: discharge destination.
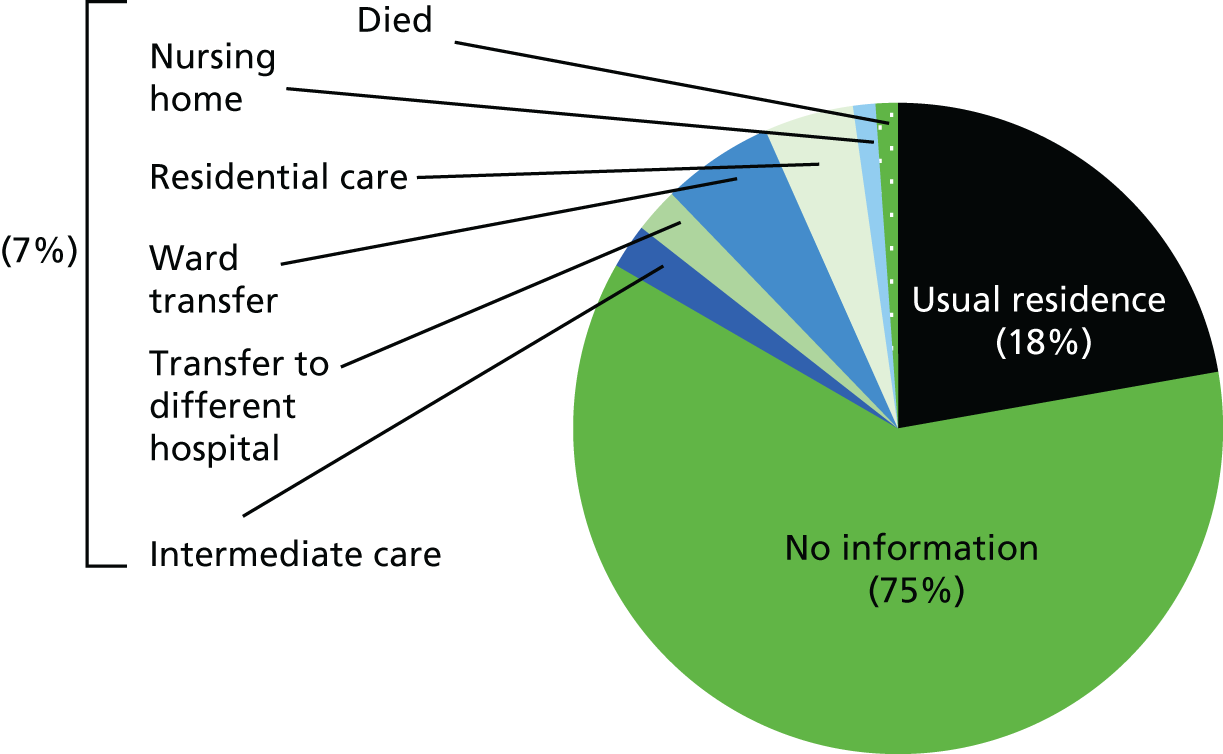
For more than half of patients discharged at baseline, their destination was not recorded, reflecting difficulties with data collection. Nor is there any information on discharge for those patients remaining on the ward at baseline. Of those for whom information is available, some three-quarters were discharged to their usual residence, and the rest were divided between intermediate care placements, transfers to another hospital and long-term care.
Staff profile
The staff complement was 33 [15 nurses, two associate practitioners (APs) and 16 HCAs] meaning that it was comparatively well resourced. This was mainly the result of a determined ward manager who felt very protective towards her ward and staff. Cover was at least four registered staff and four HCAs per day shift and two registered staff and two HCAs per night shift (a ratio of registered staff to patients of 1 : 5.6. Some staff worked long shifts (07.30 to 20.30); others worked conventional early or late shifts. There was much flexibility, including part-time and internal rotation and permanent nights. There were nine orthopaedic consultants attached to the ward.
Poplar: care culture
Twelve questionnaire responses were received from the 20 distributed (mainly nurses and HCAs, with one volunteer and one student nurse). Although most had not worked for long on the ward (seven had done so for < 2 years), most had worked in the hospital for between 5 and 21 years and were experienced in the care of older people.
Responses showed strong agreement on the existence of a shared philosophy of care that valued psychological support and involving patients and caregivers. It was considered that the ward had sufficient equipment and skills among the team. The interviews further suggested a strong team who could rely on each other, as well as shared information and skills. Team members considered that they had influence on decision-making and that there was time to share task-related information. There was strong support for the leadership and management style of the ward manager in all areas. In particular, she was seen as an ongoing ward ‘presence’, supportive and protective of her staff and keen to ensure that everyone received appropriate training. She was also viewed as keen to appoint staff with a particular interest in dementia care. The dementia nurse linked to the ward was highly respected and much appreciated. She had worked on Poplar prior to her role change and was well known.
Most staff agreed that there was too much work to do in too little time and without adequate resources. They generally felt that they were not listened to by senior managers, and nor were they rewarded for their work. This is largely supported by comments from the 2014 CQC inspection regarding leadership (which included evidence of bullying and harassment). Moreover, there was some resentment about a recent ward move from an environment that staff perceived as more conducive to the well-being of patients, and a sense that other wards, less skilled in dementia care, tended to send people with dementia to their ward.
Crane: structure and organisation of care delivery
Crane is a 26-bed ward based in the westernmost hospital. Opened in 1979, the hospital was part of a plan to expand the town and surrounding area in the late 1960s by relocating people from London. It employs about 2500 people and has 476 beds. It offers a wide range of specialist facilities and services, including a shop run by Friends of the Hospital, a volunteer-run society, providing basic goods and services to patients and visitors, which raised £2.5M in donations.
Physical environment
The ward comprised four bays, three with six beds and one with five, each of which had a shower room: two bays were designated for women and two for men. The smaller bay had previously been a dayroom. Each bay had a sink at the far end; there was no space for tables and chairs. Clocks showing the time and date had recently been hung above the entrance to each bay.
Beyond the end door there was a linking corridor leading to another ward. This also housed three side rooms that appeared very separate from the main ward, although they were part of it. Further on, and linking with the next ward, was an annexe of half a dozen ‘winter beds’ (that were often open well into late spring/early summer and that, when open, usually took one or two staff from Crane). On the right side of the corridor were storerooms, the nurses’ station, the ward manager’s office, a meeting room which also housed the medication trolleys, and the patient toilets. The nurses’ station was located opposite the first two bays and next to the ward manager’s office. The medical notes were stored there, and the space became overcrowded when medical and nursing staff were reviewing patient notes. The ward clerk’s desk was also sited there.
Patient profile
There are a large number of days towards the end of the baseline for which there is no documentation, as the acting ward manager, who had been maintaining records, left around this time.
During baseline there were 121 admissions. The median length of stay was 8.5 days (range 1–64 days). The sociodemographic patient profile is presented in Table 10.
| Characteristic | n (%) |
|---|---|
| Age range (years) | |
| < 65 | 1 (< 1) |
| 65–69 | 1 (< 1) |
| 70–74 | 4 (3) |
| 75–79 | 23 (19 ) |
| 80–84 | 27 (22) |
| 85–89 | 37 (30) |
| 90–94 | 20 (16) |
| ≥ 95 | 8 (7) |
| Gender | |
| Men | 69 (57) |
| Women | 52 (43) |
| Residence prior to acute admission | |
| Own home | 92 (75) |
| Intermediate care | 1 (< 1) |
| Residential care home | 15 (12) |
| Nursing home | 7 (6) |
| No information | 6 (5) |
The majority of patients were in their eighties, and there were slightly more men than women. Three-quarters had been admitted from their own homes. From documentation and staff interviews, at least half of the patients had dementia, but this fluctuated upwards to over three-quarters at times.
The reasons for admission are shown in Figure 20. Many included multiple pathologies, and those categorised as ‘other’ included undifferentiated diagnoses, various cancers, and heart and autoimmune diseases, plus long-term conditions or infections.
FIGURE 20.
Crane: reasons for admission. ‘Other’ includes cellulitis, heart failure, shortness of breath, cancer and urinary tract infection.
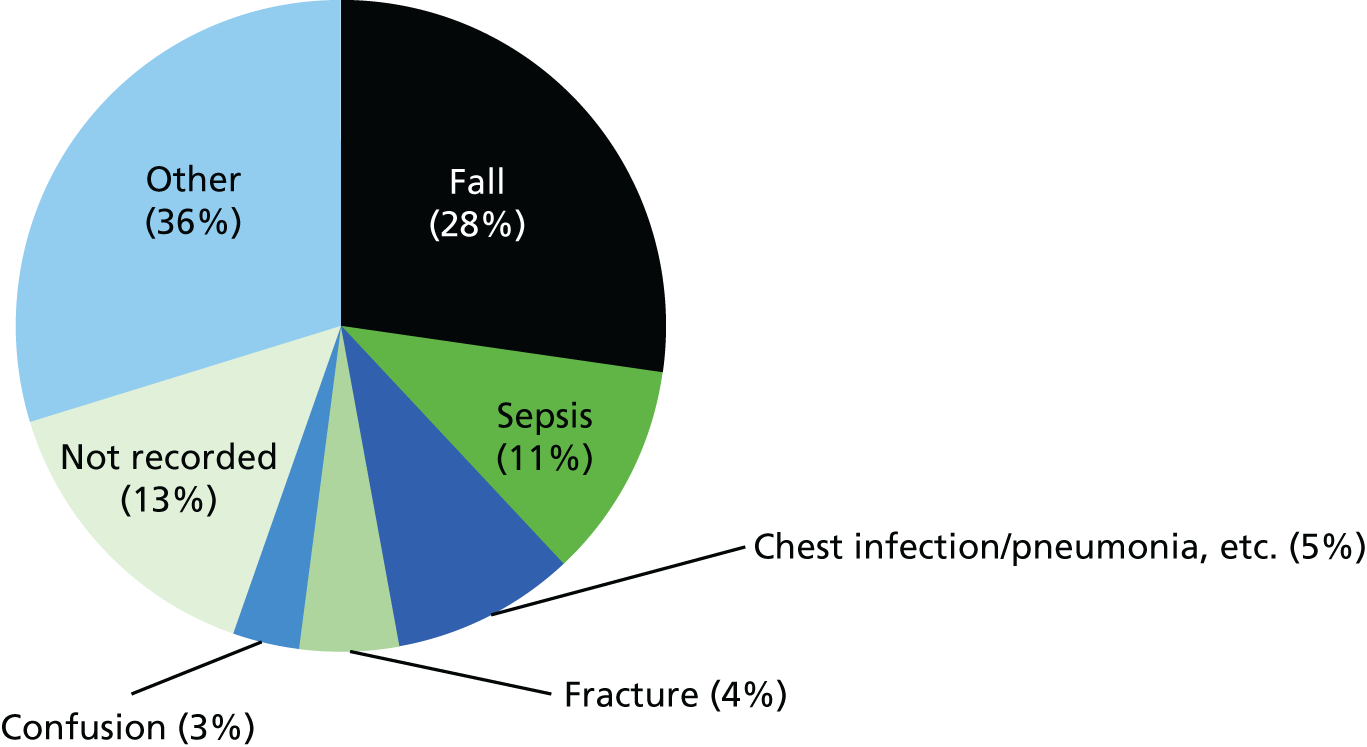
The data on destination at discharge (Figure 21) indicate that most patients returned to their usual residence, although there is considerable missing information, including in respect of those who remained on the ward at the end of baseline data collection. There were also a number of deaths on the ward during this time.
FIGURE 21.
Crane: discharge destination. IC, intermediate care.
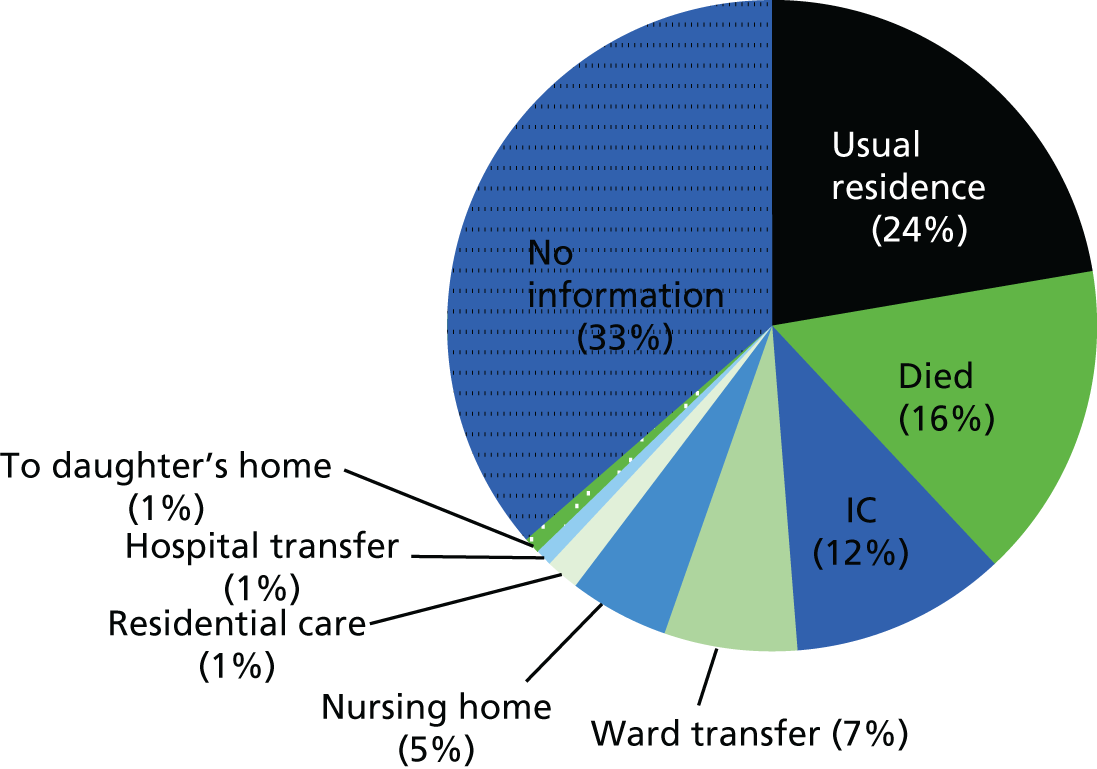
Staff profile
There were 40 staff on the rota at baseline, but many were part-time. The staffing complement was five nurses (including a sister) and four HCAs during the day, and two nurses and two HCAs at night. Most worked long shifts, from 07.30 to 20.30, and many rotated to nights. Two staff were reallocated to ‘winter pressures’ beds, when open, on a rotational basis. The ratio of registered staff to patients was 1 : 4.4.
Crane: care culture
Five responses were received from the 13 Climate for Care questionnaires distributed. This is a small and unrepresentative sample, limiting interpretation of the findings. Two of the respondents were experienced, one having spent 12 years on the ward; the others had been there for < 1 year.
The questionnaire responses and interviews suggested that there was support for a shared philosophy of care; psychological aspects were highly valued, expectations were communicated and staff were knowledgeable. There was support for the effectiveness of the MDT, with occupational therapists being particularly valued as a fount of information. Staff reported trying to shift from a task-orientated approach towards supporting patients’ families. Their approach to dementia care was shaped by the lead dementia specialist nurse based at the site and considered an enormous support through the provision of education and advice. She saw her role as offering a resource for practice-based learning and modelling care. Her work was acknowledged at senior management level, including by the deputy nurse for quality and the senior consultant. As with Poplar, there was support for the leadership style of the ward manager, which, at baseline, was an ‘acting’ one. Overall, the picture depicted was of an enthusiastic, motivated and optimistic workforce.
Less positively, there was ambivalence about the availability of wider trust support. Respondents considered there to be too much work for the time available and that resources were inadequate. In particular, there was insufficient time to sit with individual patients, it was difficult to take staff from the wards for them to undergo training, and the physical environment was regarded as noisy and cramped. Similar to Poplar, ward staff complained of a lack of social space and the loss of a bathroom. They also expressed frustration at the paucity of step-down facilities, which meant that patients remained on the ward longer than was ideal for their well-being.
Summary
Improving the care of people living with dementia was becoming a priority in all participating trusts. On most study wards, changes to the physical environment to make it more dementia friendly had recently occurred or were under way during fieldwork. Although the changes had created more attractive and easier-to-navigate environments, communal or patient spaces were very limited, except on Netherton and Denton. All trusts had introduced dementia-awareness training programmes and had initiated, or were in the process of establishing, a network of ‘dementia champions’.
Wards varied in their organisation and care culture. On several, staff shortages contributed to low morale. A common theme in the responses to the Culture of Care questionnaire was the problem of delivering high-quality care, being seen to embrace spending time with patients and ‘having too much to do in too little time’.
The number of people in advanced older age (aged ≥ 85 years) was highest in the dementia wards, followed by rehabilitation, care of older people and orthogeriatric wards. It was lowest on stroke and orthopaedic trauma, reflecting their wider age profile. The prevalence of dementia followed this pattern. This interpenetration of advanced older age and physical, cognitive, practical, emotional and medical needs poses major challenges for staff in the delivery of appropriate care.
Chapter 4 Person-centred care: meaning and practice
Introduction
On all study wards, the daily work of care was largely delivered to patients with complex needs. In this chapter, we explore staff perceptions of the meaning of person-centred care, and how care was accomplished prior to PIE implementation. Establishing staff understanding of person-centred care and the pattern of ‘usual care’ for people with dementia provided the baseline against which to explore what quality care might look like in practice and how it could be improved.
Person-centred care: staff perspective
‘Individualised care’
On all wards, staff typically conveyed person-centred as ‘individualised care’, ‘seeing the person and not the medical condition’ and ‘tailoring care around the person’. The term was often presented as a short-hand descriptor of ‘good practice’ or ‘quality care’ that staff aspired to deliver:
All my patients are elderly and very, very vulnerable, and they might not have dementia as their diagnosis; a little bit forgetful . . . scared . . . muddled; they’re out of their own environment . . . I firmly believe you give [person-centred care] to everybody that you nurse.
Manager, Rivermead Ward, City Trust
Multiple meanings were ascribed to the term ‘person-centred’ that have been variously referred to as according respect, acknowledging people’s essential human dignity, treating people as individuals and finding out what is important to them relevant to their treatment and care. Staff who had been in practice or had undertaken professional training prior to the policy use of the term ‘person-centred’ tended to refer instead to ‘individualised patient care’. Yet the meaning they attached to ‘patient-centred’ was no different to what others referred to as ‘person-centred’.
‘Person-centred’ care on acute wards
Pressed to elaborate on the meaning of ‘person-centred’, interviewees offered examples that varied from addressing patients by their preferred name, being flexible about such care routines as washing and serving breakfast, providing a choice of meals, respecting privacy, personalising bed space (family photographs) and involving patients in decision-making on treatment and care. Thus, the content varied from the courteous and respectful to meaningful engagement based on knowledge of the person. Different professionals on different wards placed more or less emphases on these various dimensions of ‘person-centeredness’.
Generally, HCAs and less experienced staff appeared unfamiliar with the term:
Person-centred care – do you mean looking after a certain person?
HCA, Ambridge Ward, Valley Trust
And:
Is that where you . . . set out a care plan for that person . . . I think that’s what it means, setting out a care plan for that person that has that condition.
HCA, Poplar Ward, Seaford Trust
Unfamiliarity with the term or an inability to articulate what it meant did not imply a lack of attention to the person or denote depersonalising care practices. On all wards, individual care staff accorded value to spending time with patients, building trust and engendering a sense of safety. Despite a lack of formal dementia training, these workers explained how they drew on personal knowledge to make a connection with how the patient might be feeling. From her own experience of being an inpatient, one HCA emphasised the emotional and practical work necessary to assuage patients’ anxieties:
When I’ve been to patients here, and you said you’d be back in a minute and you weren’t, I didn’t understand how frustrating that was until I experienced that myself. For somebody to say to you: ‘I’ll be back in a minute’ and then you never see them again and then all of a sudden this person’s gone off shift. [And] not being told your diagnosis, what’s going on . . . well they don’t get angry. But I was angry that I was just left there . . . So now I say with their permission, ‘do you want me to go and see what’s going on for you’? I will then come and read the Kardex (the patient’s case notes) and if I can give them any information . . . because a lot of them think that they’re being shoved into homes . . . Just to know that they’re still in control because to lose control must be awful.
HCA, Rivermead Ward, City Trust
An empathic connection with the patient’s experience informed an approach to action aimed at reducing uncertainty and perceived loss of control.
‘Seeing the person, not the dementia’
Most participants did not distinguish between ‘person-centeredness’ for patients generally and for people with dementia, for whom ‘person-centred’ translated into ‘seeing the person, not the dementia’:
. . . it’s about . . . the individual as a human being before they are a condition or a set of circumstances, and before you attach the labels and treatments you acknowledge that they are a person . . . I’m not sure that I would particularly say that the person with dementia is different . . . although it might be more challenging to identify how you respond . . . you might have to . . . get information from a wider range of sources.
Practice development co-ordinator, Ironbridge Trust
The way staff translated the espoused values of ‘individualised care’ into practice for patients with dementia revealed important differences between those who were knowledgeable about the condition, whether derived from experience or from training, and those with poor understanding of it. First, we describe staff views on what was necessary to provide individualised care and the conditions that shaped practice; and, second, we draw out the specific knowledge and skill required, and challenges posed, in delivering individualised care to people with dementia.
‘Knowing the person’
There was consensus that ‘knowing the person’ was crucial to delivering ‘individualised care’. Relevant knowledge, as a minimum, included aspects of the person’s life history, significant relationships, and likes and dislikes pertinent to care delivery (e.g. food preferences and their preferred name).
Systems and processes to ‘know the person’
Most wards had mechanisms in place (or were introducing them) to gather biographical knowledge, using such tools as ‘this is me’ or ‘see who I am’ booklets. These were frequently alluded to by staff as a resource to begin a conversation. As a means of engaging close relatives in dialogue about the person at admission, the tools performed a useful function. The collection of biographical information to inform practice required that staff place value on eliciting such knowledge; that when information was sought from family members, staff efforts were reciprocated; and that the knowledge acquired was used in day-to-day staff–patient interactions:
This can be really helpful . . . because you have something to talk about to the patient . . . if you take time to read it . . . then when they’re agitated or upset you can sit down and talk to them about things they used to do and just try and interest them and get them settled again.
Nurse, Crane Ward, Seaford Trust
On all wards, the completion of formal biographical tools was very patchy, and, when recorded, their use was inconsistent. Moreover, unless these tools were employed as ‘living’ documents, and built on through subsequent interactions with the patient and family, they were of limited value.
Several wards had a strong culture of eliciting and sharing personally meaningful information about patients, whether informally or via such routine mechanisms as daily handovers and MDT meetings. This was a ‘live’ process, whether additional to, or in the absence of, the formal recording of biographical knowledge.
Dialogue with patients’ ‘significant others’ was an important source of personally meaningful knowledge. Its collection and use was predicated on the value attached to engaging with relatives/friends routinely, particularly during visiting times.
At one end of the spectrum, there were wards, particularly but not exclusively dementia wards, where senior staff placed high value on nursing and care staff ‘knowing the person’ through ongoing conversations with family members. It was also acknowledged that organisational factors could act as impediments:
We like to build up close relationships with the family where we can . . . just talking to them and seeing that staff talk to them . . . We try to encourage staff to walk around at visiting time and ask relatives: ‘is there anything you want to know’. . . And [charge nurse] is very good at that . . . But it can be hard . . . because visiting times tend to coincide with shift end times.
Manager, Netherton Ward, Ironbridge Trust
On some of these wards, a division of labour existed such that senior staff assumed primary responsibility for engaging with families. Observation during visiting times showed that these staff spent much of the time in conversations with relatives, both proactively seeking out particular family members and conveying an openness to talk when approached.
At the other end of the spectrum, there were wards on which staff appeared more ambivalent about collaborative work with relatives. While acknowledging the importance of relatives in the patient’s life, staff emphasised in their talk how family members’ interests did not necessarily coincide with the patient’s interests. Stories of patients and families staff had dealt with were recounted to illustrate the problem of interfamilial conflicts and divergent preferences of patients and caregivers regarding future care, including discharge destination. ‘Close others’ were often perceived as having ‘unreal’ expectations of what was possible in terms of recovery or what was feasible for services to provide. Their stance could be termed ‘hesitant’ collaboration: acknowledging the need to work with families to facilitate the person’s recovery and onward movement, but viewing this as a source of stress.
Staff on most wards adopted a ‘negotiated’ collaborative stance: families were viewed as a resource and source of support, but their interests and those of the patient might diverge, and family members might not agree with each other about what was best for the patient. Nevertheless, the emphasis was on negotiating between different interests and views. These varied stances and their consequences are conveyed in the following quotation:
It’s very rare to have a ‘difficult family’ on this ward and I think that’s because of all the good work that the nurses do, especially when there’s terminal issues and . . . it’s quite difficult for the family . . . The approach that the nurses take here because they have this interest and it’s seen as the thing to do to talk to the family [means] it’s noticeable how it’s very rare I’ll have a family that have got to the point of distress and aggravation . . . It happens a lot on other wards: you know, ‘what’s happening to my dad, no-one’s telling me anything?’ . . . Rarely happens here. ‘No one’s listening to my dad, no-one’s feeding him’, never happens here . . .
Senior consultant, Ironbridge Trust
Valuing time with patients
Most staff emphasised that ‘knowing the person’, a precondition for delivering ‘individualised care’, meant spending time with people. Expenditure of time required that value was placed on talking to patients and having sufficient staff to do it. As noted elsewhere, this was dependent on the legitimacy accorded to such work by senior staff, conveyed through formal supervision, team meetings and the mirroring of ‘good practice’.
Time: a scarce resource
The ward care environment was a key factor in the legitimacy attached to spending time with patients; also significant was the support proffered by middle managers in proximate seniority to the ward. At this level, and reflecting wider demand and supply pressures, mixed messages were conveyed. In Seaford Trust, both study wards had secured a generous staffing complement in recognition of the complexity of their patient profile in comparison with wards elsewhere. However, the ward risked having staff taken off shift to support a neighbouring ward. The message staff ‘heard’ was that if they had the time to talk to patients, they had too little work to do.
Ward pressures created conflict between the aspiration to spend time with patients and the limits imposed by organisational constraints. The espoused value among senior ward staff that nurses and HCAs should sit with and talk to patients was compromised by staff sickness, vacancies and recruitment difficulties. As a consequence, staff often spent most of their shift ‘on the move’. Time spent with patients was short and limited to encounters relating to the ‘bodywork of care’109 (washing, dressing, toileting and assisting with mealtimes) or delivering clinical and therapeutic care (observations, dispensing medication and mobilising). Similarly, periods of heavy demand, for example during ‘winter pressures’, constrained the time spent with individual patients.
‘Knowing the person with dementia’
‘Knowing the person with dementia’ posed challenges at several levels: in the time and skill required to communicate with the person, especially with loss of language, and in the nature and depth of knowledge required to understand the person ‘in their world’.
There were staff on some wards whose contact with patients with dementia was primarily limited to carrying out routine tasks. There were others for whom engaging with these patients was highly valued: spending time with them was a means through which a relationship of trust could develop. Furthermore, knowing something of the person could provide an opening to pursue a conversation, which, in turn, reinforced their ‘personhood’:
Personally, I’d get to know them . . . sit and just ask questions about the past, what they used to do . . . communication is everything because if you can get something back from them . . . you can work on that and . . . build up a friendship . . . earning their trust.
HCA, Rivermead Ward, City Trust
A different level of knowledge: understanding the person ‘in their world’
For staff with an understanding of dementia, ‘knowing the person’ involved more than biographical knowledge. It encompassed a deeper knowledge of the person, including what was personally meaningful to them and what evoked emotion (whether positive, such as joy, or negative, such as anger, irritation and distress). A prerequisite to acquiring such knowledge was an ‘imaginative connection with the person’, whether professionally or experientially derived.
Many staff had experience of working with people with dementia and they understood that being in hospital could be disorienting and frightening. Some connected in their imagination with the emotional impact of being in a strange place where patients were metaphorically ‘pushed and prodded’:
A lot of people don’t sit down and think, ‘oh what would it actually be like if I had dementia’, and you think what it must be like: all them strange faces; we’re coming at them; we’re moving them; we’re hands on them . . . what must that actually feel like if you don’t understand what are going on.
Occupational therapist, Cedar Ward, City Trust
The process whereby care staff drew on their imagination to make a connection with the person with dementia was underscored by recognition, even if implicit, of their common essential ‘personhood’. Seeing the person as ‘someone like us’ appeared central to valuing and engaging with them.
Communicating with patients, particularly those unable to express themselves verbally, required considerable time and a complex skill set. Being attuned to observational cues did not mean that one could easily interpret people’s needs. Spending time with the person to seek out and make sense of observable action and reactions was also necessary:
. . . sometimes they’ll be trying to get up and you think they’re just trying to get up but really they need to go to the toilet but they can’t voice that. So you have to be able to judge . . . And it . . . does get quite difficult to understand what their needs are, what they’re trying to communicate with you if you don’t spend a lot of time with them . . .
Staff nurse, Crane Ward, Seaford Trust
For staff on dementia wards, overlaying the salience and value attached to ‘individualised’ care was how to make it work in a meaningful way, taking account of the complexity of delivering such care in practice. This required a particular form of ‘knowing’: seeking to understand and respond, cognitively and emotionally, to where the person was at ‘in their world’ (i.e. how they experienced reality).
In the following quotation, the nurse explains why it is necessary to understand the perspective of the patient, ‘Daniel’. Daniel did not communicate verbally and often hit out at staff when receiving personal care. In describing working with him, the nurse highlights the significance of physical contact and of trying different things to find out what works with each person. She notes how important it is to understand that Daniel’s dignity has been compromised by his condition and that staff have a role in sustaining it, even if Daniel is not aware of what he is doing:
Daniel can’t take instructions, he doesn’t understand instructions. So really you can understand why he gets so frustrated, because if we didn’t understand something, if someone spoke to us in a different language and tried taking our clothes off or something like that we’d start hitting out. So . . . we have to understand where he’s coming from, we have to get in the mindset of him. Do you know where I’m coming from? How do you do that? Holding his hand, he likes to hold people’s hands, he shakes people’s hands, he smiles, laughing, if you say something. So you laugh with him and say, ‘Oh come on then Daniel’. He does like that, that’s the thing. But we’ve also got to remember if he knew what he was doing he’d be absolutely mortified. It’s not that man, the man that we, that his family know . . . that’s sitting down and likes to eat, and likes to laugh and joke about with you. It’s not the man in the bathroom. The man in the bathroom is completely different and he’s scared more than anything; you can see that he’s scared . . . What we’ve found is . . . hold his hands and talk to him face to face, get eye contact and then someone changes him from behind. Then it works out better.
Staff nurse, Denton Ward, Central Trust
This account exemplifies several distinct features of the work of ‘knowing’ and engaging with the person with dementia in a positive way. It demonstrates how personally meaningful knowledge derived from multiple sources can assist with interpreting embodied communication. It underscores the importance of interpersonal skills, including the sensitive use of touch and eye contact, to convey empathy. It illustrates the need for specific knowledge about dementia and how it affects the person. Alongside openness to embodied communication, it is understood that communication is imbued with meaning, although this might not be immediately ‘knowable’. It recognises that there is an element of uncertainty and unpredictability about how the person will respond in a given situation such that strategies to engage him/her are emergent, built up through trial and error and will likely involve creative, tailor-made solutions. It was often this distinctive knowledge and skill that staff, particularly those providing direct care, reported that they lacked.
People with dementia as ‘other’
There were wards on which some staff expressed in their talk embedded assumptions that people with advanced dementia, particularly, had lost their ‘personhood’. The language they employed in informant interviews conveyed the sense of the person with dementia as ‘other’. People with dementia were a collective or group (‘the dementia patients’) characterised by their ‘problematic behaviours’, typically ‘aggressive’ and ‘wanderers’. The ‘dementia patients’ were viewed as posing difficulties for staff, who derived little personal or professional satisfaction from working with them: ‘we duck and dive to avoid being hit’ and ‘we spend our days trying to keep them in the ward safe and not fall’.
This conception of ‘the demented patients’ as ‘other’ was associated with the view that such people had no place on general wards but should be in specialist units. Although this view was atypical among staff in this study, unlike in other research,27,29–32 it was found among those without personal or work experience or knowledge of dementia. Referring to the challenges of working with colleagues who lacked such knowledge, one interviewee commented:
Some of them say ‘we don’t want to work in here because of the dementia people, how they behave’. I do feel for them to be honest because if they had the knowledge and the skill, I don’t think anyone could say that . . .
Staff nurse, Ambridge Ward, Valley Trust
Although poor dementia knowledge was commonly attributed to temporary staff, including Bank and agency workers, the picture was more complicated. Routine reliance on temporary staff tended to reflect organisational instability, including staff shortages, poor team morale, and changes to the ward profile and model as a consequence of bed closures and reorganisation. Organisational instability, in turn, exacerbated the problem of creating and sustaining a care environment that supported ‘personhood’, thereby ensuring that the ward team mirrored respectful practice. Thus:
No I wouldn’t say that was shared . . . [conception of ‘individualised care]. We don’t normally talk . . . We just come to work . . . and do what we’re supposed to do, then we go home. It would be nice if one day we sat down as members of the team in this ward to talk about things; the challenges that we have and what it is that we can do with that.
Staff nurse, Ambridge Ward, Valley Trust
Now, drawing on ethnographic observation and patient case studies, we consider how care was accomplished in practice for people with dementia, how this varied between wards, and the implications for what ‘quality’ care might look like in this setting. We set the scene by conveying in broad outline the rhythm of ward life.
Accomplishing care: ward routines and practices
Routines
The daily routine and the tasks that constituted it had a similar shape and content on all acute wards, although the timing and degree of flexibility varied.
On some wards, the day for patients started early, at around 06.30, as night staff began washing and dressing the few patients who were awake. Activity in corridors and by the nurses’ station began with the arrival of the early morning shift at 07.00, although bays and rooms remained in semidarkness. Nursing handover from the night shift signalled the start of the new day. Each patient was briefly discussed: whether or not they were settled during the night, adverse events that transpired, action to be taken during the day. Snippets of information gleaned from patients during the shift were shared (e.g. ‘whenever we talk about home, she becomes teary and doesn’t want a care home’).
Staff were allocated a working area, with often one HCA for each bay and one nurse for two bays. After handover, the dispersal of staff to their work locations signalled the washing and dressing of patients and the preparation of breakfast. Most wards allowed a degree of flexibility in the order of these activities, but for all wards this was a pressured, busy time, the aim being to get patients ready before the arrival of the rest of the MDT. On some wards, the lights were turned on in the bays straight away; on others, the ‘lighting up’ of patient areas was pursued at a more leisurely pace. Staff moved from patient to patient, seeing who was awake and who needed help with toileting and washing. Domestic or cleaning staff were often present from this time.
Breakfast was typically served from 08.00 onwards: the clatter of trolleys added to the chatter of staff as they greeted patients, moving quickly in and out of bays and rooms with trays. On all wards, there were those who required either direct help or coaxing and encouragement to eat, tasks that could occupy a HCA with a single individual for 30 minutes. With one or, at most, two staff in a bay of five or six patients, several of whom required assistance, patients who just needed encouragement might be overlooked or left waiting. Although personal care tasks were the primary domain of HCAs, a strict division of labour between nurses and HCAs was atypical. On most wards, once it seemed that sufficient progress had been made with getting patients up, and breakfast was under way, at around 08.30 or 09.00, nurses would begin medication rounds. This was another pressured task, as different patients might need medication before or after eating, or pain relief in advance of seeing the therapist.
From 09.00, the pace of work shifted up a gear with the arrival of other members of the MDT – therapists and doctors, phlebotomists, pharmacists, porters, the ward clerk – adding to the cacophony of sounds: telephones ringing, buzzers buzzing, trolleys squeaking and patients calling out. To the external observer, the picture conveyed was of ordered chaos as each professional went about their specific tasks, working through with patients: doctors doctoring, therapists mobilising, nurses medicating and care staff moving quickly in and out of bays assisting with care tasks. The multiple and competing demands on staff during this period meant that calls for assistance were not always responded to speedily, particularly when a patient required the help of more than one staff member with personal care. Shouts of ‘too late; I’ve done it . . . the bed’s a mess’ were not uncommon, as assistance with toileting was not responded to quickly enough, adding to the pressure on staff and the distress of patients.
By late morning, patients were dozing or propped up with pillows, and those well enough to get up were dressed and sitting on a chair by the bed; the ward round was under way and therapists were occupied in one-to-one work with individuals. On several wards, the placement of tables and chairs in spaces in or between bays facilitated conversations between people; however, with the exception of Netherton and Denton (dementia wards), on most wards there was limited or no collective space for activities or interaction. Where communal rooms existed, they were rarely used by patients; more often they were used by staff. Wards varied in the extent to which patients used the ward space beyond their immediate location around the bed and in the bay. On some wards, it was unusual to see patients moving about the bays and in the corridors. Although partly due to lack of space and people being unable to move because of frailty, pain or hip replacement, it also reflected the care environment. On some wards, unsupervised movement was discouraged as it was seen to be symptomatic of ‘wandersome’ behaviour and, therefore, placing patients at risk of falling. On others, staff were accepting of patients walking about and they kept an eye out for, and were ready to provide supportive assistance to, individuals whose mobility was poor.
At midday, the round of mealtimes, toileting and dispensing of medication resumed. It was common for staff to have spent most of the morning into early afternoon (from 07.00 to 14.00) on their feet, apart from a short break mid-morning.
On several wards, open visiting from late morning saw a trickle of visitors, who were often encouraged to assist their relative/friend with eating. On most wards, visiting times were scheduled for up to 2 hours from 14.00, and up to 2 hours from 18.00. In practice, there was considerable flexibility: when patients were very ill, or when visitors had come a distance or had simply arrived early. The steady stream of visitors in the afternoon altered the ward rhythm as movement and noise emanated from patients and visitors. Their departure heralded the repetition of routine tasks: meals, clinical observations, toileting and then visiting again. The exiting of visitors in the evening was the signal for commencing night work. Formal handover from day to night staff reversed the sequence of the early morning, and another busy period began of putting patients to bed, toileting and administering medications. For patients, the dimming of the central lights in the bays signalled the day’s end, although movement within bays and between beds, bays and toilets continued into the night.
The apparent orderliness of the routine was deceptive; it was punctured by the moaning and shouting out of people in distress, a flurry of activity with the arrival of a new patient on a trolley, the pacing of a patient by the entrance to the ward anxious to leave and being remonstrated with by staff, or a sudden crisis event such as a patient collapsing or falling. For several people with a cognitive impairment on each ward, the period of late afternoon/early evening often presaged extreme agitation and distress. This manifested in shouting out or pacing up and down the bay and corridor. Such behaviour was disruptive to other patients. It was also difficult for staff to manage as many of them were near the end of a 12-hour shift. For staff, too, the semblance of orderly transfer from the day to the night shift could be disrupted and protracted: crises or staff shortages during the day meant that the ‘day’ jobs were not completed to time. Although the ‘burden’ of organising and managing completion of the shift ‘work’ fell heavily on senior ward staff, the unfinished tasks were also assumed by nurses overextending the day shift and adding to the ‘night’ work.
Practices
From a comparative analysis of fieldnotes within and across sites, we could discern a continuum of practices supportive of, or barriers to, sustaining personhood, and the organisational, spatial and care environmental factors that shaped them. We report on three inter-related illustrative features of practice: communication, toileting and continence (exemplar of personal care), and responding to distress. How staff communicate with patients may either contribute to patient distress or ameliorate it; and staff responsiveness to requests for assistance with toileting will be shaped by the ability of patients to convey their needs and by ward organisational and environmental factors. Our intention here is to draw out what might be the dimensions of ‘person-centeredness’ in practice in the specific context of the acute ward.
Communication
A common critique of nursing practice generally,110,111 and of the care of people with dementia specifically, from research17–19,21,22,24,25,29–33 is the dominance of task-focused communication over ‘person-centred’ communication. Practice in our study, even at baseline, was considerably more differentiated and nuanced than this binary conception implies.
A continuum of communication practices was discerned. At one end of the spectrum were wards on which interactions between staff and patients were viewed as opportunities to communicate with the person with dementia at a social and emotional level. At the opposite end were wards on which staff–patient communication concerned tasks relating to care, clinical or therapy work. These encounters could be suffused with warmth and concern; they could also entail a lack of responsiveness to expressed emotion that was painful for researchers to observe. Among most wards at baseline, the communication style was mixed, and was located along a continuum between these extremes: varying levels of personally meaningful communication and/or inconsistency within teams.
Personally meaningful and engaging communication
On both dementia wards, there existed a consistent and coherent care ethos among senior staff that ‘knowing the person with dementia’ was fundamental to care that recognised the individual’s ‘personhood’. Spending time with patients and relatives was legitimised by senior staff and mirrored in how they went about their daily work. It was reinforced in individual supervision and mechanisms for team reflection and practice review (ward-based training and regular events, such as twice-yearly away days).
The field note quoted below illustrates how these staff employed a personally engaging communication style with patients while carrying out routine tasks. This form of communication was an expectation on all staff, irrespective of role, as an essential feature of care delivery. The time of the encounter is pertinent in that the ward rhythm from early through to late morning was observed as ‘hectic’, with staff continuously on the move:
Field note: 10.30 Friday
In one of the male bays there are five men each sat next to their bed . . . Two care staff come into the bay and begin to make up the beds, changing the sheets. They chat with Max as they do his bed, initiating conversation with him about his travels in South Africa: ‘why did you like to travel?’ Although Max has been on the ward only a couple of days, staff demonstrate knowledge of his personal history. A conversation ensues, moving on to his proficiency in different languages.
Netherton Ward, Ironbridge Trust
In their conversations, staff drew on their knowledge of the person and built on it to communicate at a personally meaningful level. The process both reinforced the person’s sense of self and offered reassurance and a sense of security when the person was confused, disoriented or distressed.
In the following episode, a staff nurse sat at the bedside of a patient, Annie. With poor ability to communicate verbally, Annie had periodically conveyed observable signs of distress and agitation (moaning and pulling at her jumper). As well as reinforcing the significance of personally meaningful knowledge to facilitate engagement, there were features of this encounter that typified a style of communication that sought to connect with the person: the use of touch and of positive emotional memory to alleviate distress:
Field note: Saturday 14.45
Staff nurse Ellie comes into the bay and goes over to Annie. She sits down by the bedside and takes Annie’s hand in hers, looking directly at her: ‘Where’s your lovely smile, Annie?’ Annie responds with a wide smile looking at Ellie. ‘Annie, would you like to sing with me, that song you’ve said you really like?’ Ellie begins to sing: Lady in red. Annie joins in, hesitantly at first; then more confidently; she knows most of the words. Ellie remains with her singing and talking for about 15 minutes until called away.
Netherton Ward, Ironbridge Trust
Over the afternoon, several staff came to sit with Annie, using touch and voice to connect with her, illustrating a collective team response (and also highlighting how such encounters could be cut short as a result of the myriad, competing demands made on staff).
Although not every interaction on these wards was conducted utilising this personally engaging style, and not every staff member had the level of interpersonal skill shown in the above quotations, this was the dominant mode of communication with people with dementia and was regarded as an expectation of ‘the way we do things around here’.
Task-focused communication
Varied forms of task-focused communication could be distinguished on all wards: respectful, warm and task-focused; minimal verbal exchange; and unresponsive to patients’ expressed emotion. These different forms could be construed as more or less problematic depending on the context.
Here, the content of the exchange was related to the task, although the form was warm and respectful. The episode below unfolded over 20 minutes after lunch, a lull following the ‘busyness’ of mealtime:
Field note: 13.10–13.30
From one of the bays, I hear Edie talking in an agitated fashion. I look in, she’s sitting on the chair by the bed and is pulling at the blanket covering her legs . . .’You’re c. . .’, Edie says to no one in particular. Different staff members pop their heads into the bay briefly, acknowledge Edie but don’t go in.
Edie speaks out at intervals over the next ten minutes . . . Now she is slumped over a bit, her eyes closed . . . no one has been in the bay for the past half hour.
Two staff go into the bay: ‘Edie, Edie’. . . they call her in a cheerful and friendly tone of voice. Drawing the curtains around her, they again say her name to waken her/get her attention. ‘We’ll just get you into bed’. She laughs . . . they chat together – how is she feeling, does she need anything – as they help her into bed. She responds as if she enjoys the company and attention.
Ambridge Ward, Valley Trust
These were interactions in which there was limited verbal communication with patients as staff concentrated on their task. In the account quoted below, following a brief salutation, care tasks were performed in relative silence, and without explanation, with an unwell patient, who had severe dementia and limited verbal facility:
Field note: 12.40
I sit in the bay. The patient (Alice) is sitting in her chair; the food arrives. The nurse puts it on the table in front of her and says ‘that’s yours’; without making eye contact, she walks away. Alice sits up and moves forward to the edge of the chair. She slowly picks up the napkin and unfolds it; ignoring the food, she plays with the napkin: folding and unfolding it. After 5 minutes another nurse arrives, gets a chair and sits beside Alice. She physically assists Alice to eat, cutting up her food and taking the spoon with food to her mouth for the next 10 minutes. There is no talk between them. With food still on the plate, the nurse writes in what appears to be a food chart and leaves. Alice seems aware of food on her plate but doesn’t eat any more.
Beech Ward, Central Trust
What elevated these encounters with people with dementia as diminishing their ‘personhood’ was the dissonance between the personal nature of the task (physically assisting the person to eat) and the way in which it was done.
This form of communication ignored, or at least was unresponsive to, the patient’s embodied and emotional cues. In the first example below, the patient appears disoriented to place, although she expresses this quietly, more as a question than as evident distress, and addressing no one in particular until a nurse enters the bay:
Field note: 16.55
The lady in bed 5 talks quietly but audibly; she is not addressing or looking at anyone in particular. I don’t know if she is aware we are here. She says ‘where am I’ repeatedly and ‘put my head up’ and at one point when a nurse comes into the bay exclaims: ‘please!’. The nurse says ‘I wish I could, I wish I was an octopus’ and asks down the corridor ‘is Joan about? To sit somebody up’. A HCA comes in and she and the nurse then pull the curtain around bed 5. They adjust the patient’s position and give her instructions: ‘hold on to that . . . we need you to hold on to that so we can help you’; ‘put your head up.’ The lady makes a noise. One staff says to another: ‘It’s no wonder our backs are absolutely knackered’. The curtains are drawn back and the patient is sitting upright on the bed with her head on the pillow. The food on her tray has so far been untouched. The table is drawn up within the patient’s reach and one staff member stays to assist her with eating, spooning food into her mouth and talking to her a little, ‘you need to eat something’.
Oak Ward, Valley Trust
Although staff respond to the request, ‘put my head up’, they ignore the question about where she is. Over the next hour she continues periodically, in a low voice, to say ‘where am I’, until she falls asleep.
In the following further example, the patient exhibited distress (moaning and crying out), repeatedly asked for her mother, and at one point reached out her hand as if seeking comfort. Although the two staff assisting her focused on making her physically comfortable, they did not respond to her at an emotional level:
Field note: 11.40
All the patients in the bay are in bed, in their nightclothes. A nurse and HCA have been with Peggy; the curtains are pulled around her bed. I hear both staff giving Peggy instructions, asking her to move. She calls out ‘ah!’ (sounding like in pain) repeatedly for most of the time they are with her; then she quietens down. She says she’s cold, and ‘I love me mother’. Neither staff makes a response to this. When the curtain is drawn back, Peggy now faces forward a little more, still lying down and largely facing upwards. She continues talking ‘where’s me mother? She’s looking after me?’ She moans as though in pain from being moved, ‘my legs, my legs’; talks about her mother, and ‘please, help’. The HCA and nurse don’t engage with her talk. At one point, Peggy reaches her hand toward one of the staff whose hand is nearby; the staff member moves her hand away, intent on what she is doing [very sad to watch]. Having completed their task, they both leave the bay.
Cedar Ward, City Trust
Engaging with people with dementia at an emotional level, particularly when the person seemed in a world unrelated to the reality of the here and now, was viewed as difficult for some staff. Even so, an inability to ‘see’ and respond to embodied communication and to empathically connect with the patient’s distress could exacerbate such distress.
There were several wards on which little personally meaningful communication was initiated by staff generally with people with dementia, although some individuals responded to patients’ expressed emotion, offering reassurance and empathy. On most wards, and for most staff, task-focused communication occurred in some contexts, most commonly in a warm and respectful manner. Even so, there was considerable variation in the extent to which the style of communication staff adopted was responsive to expressed or embodied emotion, particularly with patients who had little or no verbal facility or were perceived as being challenging to manage.
Mixed communication styles
Even within the same wards, staff adopted neither a consistently personally meaningful nor a consistently task-focused communication style. Variability is vividly illustrated in the following quotation:
Field note: 10.25 am–11.45 am
10.25: In the bay, I see Pat fiddling with her cover as she murmurs: ‘oh dear’ . . . then: ‘Joyce, Emma, I’ll come over to you’ . . . ‘don’t let me fall’. A nurse calls from behind another patient’s curtain to ask ‘what’s the matter’. Getting no reply, she continues with what she’s doing. Pat continues to murmur.
10.45: Two doctors on ward round approach Pat. As the other patients in the bay watch with apparent curiosity, one doctor introduces himself: ‘Good morning, how are you? Do you feel OK?’ Pat responds: ‘yes’. Each subsequent question from the doctor is responded to with ‘yes’: (‘have you stood up and walked yet? Have the physios been? Can you show me your tongue? Are you drinking enough water?’ He asks if she knows where she is and she responds ‘in hospital’. The second doctor comments to the first that she was in retention, and they proceed to discuss symptoms and diagnosis as she’s asked to breathe in and out. They agree to put her on antibiotics. They thank the patient; tell her to drink water and move on to the next patient.
11.45: Pat starts murmuring again. Her neighbour in the next bed asks what is wrong but she doesn’t respond. The [AP associate practitioner] who is in the bay goes over to Pat; crouches down to Pat’s level and takes her hand: ‘Are you comfortable?’ Pat asks when she can go home. ‘You can go home when you’re eating and drinking better – that’s why I’m nagging you’. Pat responds: says ‘you’re not nagging, you’re very nice people’. She tells the AP she’s not a big eater, who responds in a reassuring tone of voice: ‘I know’ and asks if she puts a small portion on a smaller plate could Pat manage to eat a bit. Pat responds with ‘yes’ but she cannot remember what she’s ordered.
Poplar Ward, Seaford Trust
Although the patient appears disorientated to place (thinks she is falling) and person (calling for Joyce and Emma) and is distressed, she answers the doctor’s questions appropriately. The doctors focus on physical problems (hydration, mobilisation, elimination, cardiac and breathing difficulties) and perform a cognitive test in conversational style, although they also talk over the patient about her symptoms. The AP, using body language (touch, bending down to Pat’s eye level), tries to elicit what is wrong – comfort, hydration, nutrition – and suggests a solution to Pat’s verbalisation of the problem (anxiety about going home) and immediate issue (smaller portions of food). With time and patience, Pat is enabled to express anxiety and her immediate need.
Communicating with patients with limited verbal facility was challenging for staff. It demanded time and work to interpret the meaning of their expressive gestures and emotion. It also required understanding that these had meaning as intelligible manifestations of a social, relational and embodied self.
Toileting and continence
Of considerable significance in ward routines was the ‘bodywork of care’109 relating to toileting and continence. Ordinarily a private act, on the hospital ward it had the character of a ‘public’, medical event. Bowel and bladder functioning was an ongoing topic of talk of staff with patients during clinical observations and in medical encounters, for example on ward rounds. In daily handovers, issues relating to urine output and bowel movements were a focus of discussion as observable indicators of infection and explanation for increased confusion. In MDT meetings, incontinence, particularly of faeces, was regarded as a key risk factor requiring 24-hour care, particularly if the person lived alone or could be at risk of falling during the night. Thus, assistance with toileting was more than a care task; it assumed clinical significance.
For patients, toileting was an essentially private act. In the context of dependence (immobility or loss/reduced control of bowel and bladder), the management of, and staff responsiveness to, needs relating to toileting was a major source of anxiety. Among those who were incontinent and wearing pads, the physical sensation of passing urine or faeces, and consequently feeling wet and dirty, contributed to their distress. There were many occasions during observation and conversations with her when Brenda, a 90-year-old patient with dementia on Oak ward, indicated that she needed the toilet, and pressed the buzzer. Although Brenda had been provided with incontinence pads during her stay, these did not alleviate her fear of ‘accidents’. The urgency of her need meant that the response was often not quick enough and she felt unclean and embarrassed that staff had to deal with the dirty pad and ‘wipe my bottom’. She tried to get out of bed several times during the night. While this was interpreted as ‘wandering’ by some ward staff (her case notes indicated that she had had delirium earlier in her admission and had tried to climb out of bed), for Brenda’s family it replicated her practice of getting up during the night in her own home to go to the toilet. On the ward, it served to reinforce the professional assessment of her as a ‘falls risk’.
With regard to illustrative tasks of care, we distinguished between types of staff response, namely anticipatory, enabling, sensitivity to the emotional significance of practical needs, and the task as object of the work. These were shaped inter alia by the care environment and ward context, specifically place (physical environment) and time (what happened and when).
Anticipatory
This pattern was exemplified in practice on Netherton ward. The ward physical environment facilitated staff ‘seeing’ observational cues and anticipating needs. The four six-bed bays, while separated from each other by ceiling-height walls, opened directly on to the main corridor, with a waist-high wall between bay and corridor. The two main patient toilets (separate male and female with visible signage) were located in the corridor near the centre of the ward. This area was used as a shared patient and staff space: both groups were observed seated around the table placed here. The ward clerk was usually based in the nearby small nurses’ station with space only for a computer and trolley on the desk and a trolley with patients’ notes alongside. From the corridor and shared space, patients in the bays were in the sight of staff; staff were also allocated to work in a particular bay (or single rooms), although they helped each other when needed. With the exception of the three single rooms, staff and patients were visible to each other.
As noted above, there was an expectation on staff here that they should spend time with patients. They were also sensitive to observational cues to expressed need by people who had limited ability to use language. This is illustrated in the scenarios below, which occurred at different times of the day and evening, indicating that the response was not time dependent:
Field note: 11.20
Gabbi moves out of the bay using her frame. She stops, looks around at the entrance with a puzzled look on her face. A HCA sees her: ‘Do you want the toilet, Gabbi?’ Her face lights up and she nods. The HCA suggests that they walk together and at the toilet door, she opens the door for Gabbi and waits outside. The HCA says to a staff member nearby: ‘That’s normal’ (Gabbi frequently needs the toilet, but needs orienting to get there).
Field note: 16.00
Tom, who is very frail and wobbly on his feet, makes his way out of the bay toward the toilet. The discharge co-ordinator notices him: ‘Is he alright?’ A HCA goes over to help him as he’s getting agitated – maybe he’s disoriented. He walks with Tom to the toilet, waits for him, then he guides him back to his bed when he’s finished.
Field note: 20.55
Paul is walking again. A nurse chats to him, notices he is pulling his trousers a bit. She discreetly asks him: ‘Are you wanting the toilet?’ ‘Pardon?’ She repeats the question. ‘Yes’, he says. ‘Come with me, we’ll go together.’
Netherton Ward, Ironbridge Trust
For people with dementia, orientation to and from the toilet posed a difficulty and, even if mobile, they required assistance in finding their way.
Enabling
These scenarios illustrate another aspect of practice, namely the enabling approach adopted. Staff provided an unobtrusive steer while supporting patients’ own initiative, guiding them to the toilet and back to their bed. They provided support only if necessary, checking this with the person. This attention and effort of the team in assisting with toileting flowed from the value that they attached to being responsive and to the enabling of independent action. Encouraging and assisting patients to walk to the toilet contributed to the goal of optimising mobility. This work was transformed from a chore to an opportunity to support mobility, part of the broader objective of sustaining residual competence and skills.
The anticipatory, enabling approach to this task was observed across the team, including the ward clerk. All staff (in various roles and at different levels of seniority) were observed to be responsive to individuals’ needs for assistance. Although HCAs most often followed through with help, others were vigilant in picking up on patient cues. Staff ability to anticipate need necessitated shared knowledge of the person; knowledge also communicated informally to team members who might be new and therefore not ‘in the know’.
Sensitivity to the emotional significance of expressed need
‘Sensitivity to the emotional significance of expressed need’ is illustrated in the scenario below. Once the practical need was identified, the senior nurse responded to it immediately. She ‘listened’ to the patient’s distress to ascertain the nature of the problem and to provide reassurance at an emotional and a practical level. This episode occurred during the morning rush:
Field note: 07.50
A lady in side room 3 comes into the corridor. I talk to her a little. She looks upset, and tells me that she needs the toilet. I see the manager in the corridor helping another patient . . . I tell her about the patient in room 3 and she makes her way toward the room. A nearby HCA notices and says that she checked with this lady and that she didn’t seem to have had a bowel movement. The patient clearly feels unwell. The ward manager asks her if she is constipated. She starts to cry. The manager gets her to sit down, kneels in front of her and talks to her . . . The patient weeps a little . . . she says she wants her husband. The ward manager reassures her that her husband will be coming later and she will give her medication to deal with the constipation.
Rivermead Ward, City Trust
Constraints on responsiveness
Awareness of need was shaped by the physical environment and staff availability during periods of intense activity. The physical layout of some wards and the siting of single rooms did not allow for easy visibility of patients, such that staff members could not anticipate patients’ needs unless in the vicinity. This included, for example, single rooms located a distance from the nursing station and/or separate bays organised as rooms with full-height walls and doors that, when closed, meant that patients were not visible to staff. To ‘see’ what was happening in the bays (and single rooms), staff had to physically enter them. Although a HCA was usually allocated to each bay, during ‘busy’ periods there were times when there were no staff in a bay, as they had been called away to provide assistance elsewhere.
There were also specific times during which constraints operated to affect responsiveness: during the handover from day to night staff, during busy periods, and at night when staffing was much reduced. Although individual staff might have experiential and skill-based knowledge of people with dementia and/or the capacity to make empathic connection with patients’ experiences, their ability to anticipate need and respond proactively was limited by the physical and organisational context.
The following scenario occurred during the busy morning period. Responsiveness to the patient’s request was affected by the multiple, simultaneous tasks required of staff and the priority attached to some, such as medication administration. It was not permitted for dispensing nurses to leave the medication trolley unattended, which meant that, during the dispensing of medication, their physical presence in the bay did not denote that they were available to respond:
Field note: 09.00
A patient in the bay tells me she would like to go to the toilet. I go to the nurse who is giving out medication. The nurse presses the patient’s buzzer; the HCA comes back into the bay, sees the buzzer and the nurse says that the patient wants the toilet. The HCA says to the nurse that the patient has just been and that she is behind with the breakfasts. She then goes over to the patient and asks her ‘can you wait a minute or are you desperate for the toilet?’ The patient replies she can wait. Five minutes later she buzzes again; this time a nurse comes and takes her.
Rivermead Ward, City Trust
On most wards, as here, nurses and HCAs helped each other with requests for help with practical tasks; similarly, senior staff were actively involved in care, conveying in their practice the value attached to this work, and mirroring collaboration between staff who had different roles and responsibilities.
The task as object of the work
This is where the task is pursued simply as a job to be done. The staff member responds to the request but there is no interpersonal exchange. For example, the person may be supported to go to the toilet, but this is done in silence.
Experience of distress and the response
Patients on acute wards are at high risk of experiencing distress: pain and discomfort as a consequence of being ill and the medical procedures carried out on them; anxiety about the potential for recovery; and fear about their ability to resume valued aspects of life that give pleasure. There is also the sense of loss of control, which is particularly acute for people with dementia. For these patients, as well, their distress is compounded by the effects of a condition that has a negative impact on their capacity to make sense of and negotiate an ‘alien’ environment. Additionally, the temporary absence of familiar artefacts and people who provide a ‘handhold’ to a concretely present reality or to past memories,112 and the loss of ‘competence’ that ensues as a consequence of the unfamiliarity of faces, places and routines, further aggravates their distress. These factors affect how people feel and act. Another source of distress is disorientation and heightened fear from hallucinations that accompany forms of delirium or acute confusion,113–115 of which patients with dementia are at particular risk.
Disorientation and feeling ‘muddled’ were common sources of distress among patients with dementia. Bridie, unlike many others with dementia on our study wards, was able to articulate her disorientation. In a conversation ‘in the moment’, she described the myriad ways in which she felt ‘muddled’: being in a strange place where ‘you don’t know what to do or what’s expected of you’; where ‘it was tiring’ trying to figure it out, to work out ‘what the rules were’ and ‘to be doing things you’re not used to’; where other patients too ‘don’t know if they’re on their head or their hands’; where it can ‘be different every day’ and you’re ‘not used to chaos in your life, are you?’. It was not nice, she added, ‘to be muddled up all the time’, not just yourself but others as well: ‘you can’t just put all these people muddled up together and expect them to be happy’.
Many patients with dementia were unable to verbalise their needs and conveyed their distress through behaviour and action. We can delineate different forms of distress and staff response to them: episodic distress, in respect of an immediate unmet need; persistent distress, the source of which was unclear and which appeared impervious to action by staff, or at least only temporarily; and distress manifested as agitation, verbal aggression or hitting out. Whereas some forms of distress called forth an empathic response, others elicited fear, anger and restraining action that addressed the behaviour and not the person.
Episodic distress
This is distress in the context of an unmet need, the nature of which might not be immediately evident and/or requires interpretation on the part of those responding. In the example below, staff initially drew on their knowledge of the person to engage with Peter. When this did not alleviate his distress, an alternative source and approach was suggested during a discussion between the HCAs, who observed that he was fiddling with his hearing aid:
Field note: 11.30
Peter appears very agitated. He is fiddling with hearing equipment, calling for his wife, then ‘help me. I want to go home’. The HCA in the bay knows him from a previous admission, know he likes singing and tries to encourage him to sing, without success. She speaks to her colleague and they consider that his hearing aid might need new batteries. They agree to ask his wife about it when she visits. Later, Peter is observed as more settled; his hearing aid is working and he’s singing: ‘Singing in the rain’.
Poplar Ward, Seaford trust
Recognising that distress was an appropriate response and did not necessarily need to be ‘fixed’ required particular sensitivity on the part of staff whose role emphasised ‘doing’:
Field note:
A HCA stands at the table writing, the lady in bed 4 starts to cry. The HCA notices and goes straight to her, asking; ‘what’s the matter? Are you in pain?’ The patient shakes her head and says ‘remembering’ (a new song just started playing); the HCA appears to realise that this is what might be triggering the emotion. She asks if she would like another song on. The patient says ‘no’ and shakes her head. The HCA offers a sympathetic tone, strokes her head, holds her hand, and says ‘are they good memories?’ The patient nods. ‘Are you remembering all those dances you went to?’ The patient says something I can’t hear. The HCA stays with her a little. The HCA leaves her; the patient continues crying gently, looking straight ahead.
Rivermead Ward, City Trust
The HCA simply and calmly asked the patient why she was crying, and understood that it was all right for her to cry, and to relive her memories, stimulated by the music. She offered her physical (stroking her head, touching her hand) and verbal comfort and left her alone, and seemed aware of her (checking back) after the song finished.
Persistent distress
There were always a number of patients on all wards who expressed persistent and observable distress – moaning, crying out, shouting – that was not easily assuaged. At most, an empathic staff response secured temporary respite, as, for example, with Annie on Netherton, described earlier. Practical solutions, such as continually checking on the patient, asking if he or she wanted to go to the toilet, or offering food, had no effect. The inability of staff to identify, from their repertoire of solutions to practical problems, how to temper distress gave rise to their frustration and helplessness. Additionally, staff awareness of the impact on other patients added to the difficulties in responding. The following account summarises an incident from Rivermead, but such episodes were observed on all wards, evoking a similar response in most of them:
For several days, the researcher had heard Rosa crying from out in the bay. She called out for help and cried; appearing in deep distress. Staff went over to her periodically, asked her if she wanted to go to the toilet, if she was in pain, if she needed anything. Rosa didn’t respond but continued to cry out. One particular staff member would sit for a little while with Rosa, holding her hand; when she left, Rosa resumed crying. Other patients on the ward were affected by Rosa’s cries: ‘It’s hell here’, the researcher overheard one patient saying to another.
When the researcher returned to the ward several days later, she noted that Rosa had been moved from the bay to a side room which was some distance from the bays and the nurses’ station. She continued to call out as before. The researcher noticed that as a staff member passed by the door to her room, she would pop her head in: ‘are you all right Rosa’. Apart from engaging in routine tasks, staff didn’t tend to stay with her. They told the researcher that Rosa also cried out when her relatives visited.
Rivermead Ward, City Trust
One solution to the constancy of the expression of distress was to establish physical distance by moving the patient from a bay into a single room (Cecil’s experience; see Appendix 4). Although ameliorating the distress of other patients, this created dissonance among staff who aspired to being responsive to patient need.
Distress manifested as agitation
When the person’s expression of persistent distress included forms of action and interaction regarded as ‘difficult’ or ‘unacceptable’, such as shouting, swearing or hitting out, the response of staff was more mixed, evoking both empathic connection and ‘telling off’:
Field note 11.00–12.30; 19.30–21.00
Of the four beds in this bay, three of them (Beds 1, 3 & 4) have a flower above the bed, indicating that the patient in each of these beds has dementia. All of the patients in the bay are in bed and wearing their night clothes. During this observation, there are multiple streams of activity. The woman in bed 3 is distressed or unsettled to some degree almost constantly: pulling her bedsheets off, fiddling with the sheets or her nightie, talking to herself, seemingly random and very loud shouts (often swearing, occasionally for help). Her distress sometimes fleetingly disappears and she smiles at staff. The woman opposite her in bed 1 is rattled by the noise and occasionally shouts over to her to be quiet; that she shouldn’t be allowed to make that noise, it’s not fair on others ‘it’s time she left’.
Over the next hour, different members of staff approach the woman in Bed 3 and attempt various tasks with her: taking bloods and doing clinical observations. She refuses verbally and physically, pushing them away and appears unable to understand what they want. At different times, several staff come into the bay, talk to her politely, addressing her by name and make eye contact, but the patient’s gestures and language are aggressive. No one stays with her.
At one point, the patient in bed 1 adopts a more sympathetic tone toward the person in bed 3: ‘what are you saying love? Are you alright? You don’t look alright but then I suppose that’s not up to me . . .’ On each occasion, a staff member comes into the bay, they brightly say ‘hello’ to the patient in bed 1 – she generally presents as pleasant and chatty and appears easy to engage with.
The patient in bed 3 continues to talk to herself, fiddles with her blanket, swears frequently when shouting/talking. No one responds; she is isolated in her own world with these conversations. Then she looks up and says ‘hello’ and talks to me. For a few minutes she looks happy and relaxed. When she relaxes, her whole demeanour softens and she talks more calmly, and laughs often. She talks about where she lives and about her mother.
Observation mid-to-late evening reveals a similar pattern: the patient in bed 3 periodically talks to herself, lists names, counts them on her fingers and cries a little. During one of these episodes a HCA goes to her, takes her arm and rubs it gently, speaking softly, offering comfort. When she leaves, the patient resumes talking to herself and cries again.
Cedar Ward, City Trust
Critical in supporting people with dementia on acute wards was understanding that there was an underlying meaning to their actions and interactions and that making a connection with the person in ‘their world’ was necessary in appropriately responding to them. The following example is illustrative:
Field note: 21.45–23.40
Daniel, has been walking continuously up and down the corridor and in the bay since about 22.00. Now and again he stops, picks something up, puts it down, moves things about, straightens things or pushes them away (chair, bin). Other patients are either in bed or getting ready for bed; the lights are dimmed in one of the bays where everyone is in bed.
22.40: The nurse and HCA talk about how best to get Daniel to settle. They conclude that as long as he doesn’t disturb other patients, they will leave him for a while.
23.15: Daniel is still walking in the corridor. I notice that he sometimes places his hand on his tummy/groin area or undoes or redoes his trouser fly. The student nurse, Maeve, notices this. She puts her arm around Daniel’s shoulders, speaks to him using his name, holds his hand, asks if he wants the toilet and suggests they walk there together. He refuses; becomes more agitated. Maeve tries again five minutes later with assistance from the HCA – saying she can’t leave him wet. This time he goes with her.
23.20: I can hear Maeve talking to Daniel in the toilet. He comes out, changed nightclothes on and pad changed. Maeve and the HCA help him to bed.
I hear Maeve and the HCA talking to each other about how Maeve managed to get him to the toilet and to bed. Maeve indicated it wasn’t a problem in that once in the toilet, Daniel just wanted to hold her hand and with this he was okay. They continued to share different ideas and solutions about what worked for different patients.
Denton Ward, Central Trust
This episode occurred during the night shift, when four staff were on duty. Even so, staff responded with patience and effort, attempting to engage with Daniel and work collaboratively with him.
For staff without knowledge of dementia or skill in responding to it, a focus on the behaviour as lacking purpose or meaning could elicit ‘controlling’ action:
Field note: 12.00–13.00
12.00: The male patient . . . walks around, sometimes standing still by the nursing station, he appears to be waiting to leave and occasionally voices that he wants to go or that he wants his money. Staff acknowledge him as they walk past, asking him to go to his chair and eat otherwise his food will get cold. He says he doesn’t want food . . . But they don’t stop; they are in continuous motion as they move into and through the bays.
12.15: The man is now waiting by the Nurses station and appears agitated. A member of staff walks past him asking ‘do you want some pudding Mr X?’ He doesn’t respond and is clearly preoccupied with something else. He sees someone walk toward the ward entrance/exit and begins to follow. I hear him say ‘bloody hell’ (it sounds like the door has closed). A member of staff down the corridor calls to him ‘come back down here for us, I can’t run’. He mutters ‘stuck here all day’. He walks with a stick, wearing jeans, a nursing gown, and a jacket. He says; ‘I need my money, I keep telling her, I should be home now’. He starts to walk slowly toward the female end of the bay, the ward clerk is near and asks him: ‘what’s the matter’, using his name, and saying he doesn’t want to go down that side, suggesting he go back to his bed. He replies ‘oh I’m not stopping’. He becomes more agitated, saying he’s been waiting two hours and wants his money. Someone suggests he sit down (meaning in the bay; he goes to the nurses’ station and sits down . . . He mentions money again . . . Staff nearby discuss this patient, I hear ‘he’s suddenly just gone hasn’t he . . . he was alright this morning.
Ambridge Ward, Valley Trust
Despite awareness among several staff involved in the episode that the patient had become more confused, his agitation was attributed to the confusion and not perceived as having meaning. Staff were also focused on the fact that it was lunchtime, mealtimes being one of the prioritised events of the day that, for a short period, consume most ward resources. However, repeated instructions to ‘sit down’ and to go back to his ‘bed’ increased the patient’s agitation. Episodes that similarly elicited an ‘instructional’ response included female patients standing near the ward entrance in the early afternoon who, from their demeanour and talk, were waiting for their children: ‘where are the babies’.
This form of ‘controlling’ action was also an organisational strategy on some wards, reflective of how patients deemed ‘difficult’ and as requiring one-to-one support were ‘managed’. This involved one-to-one assistance provided by ‘specials’ or ‘sitters’. These included Bank or agency HCAs in Valley, mental health trained nurses in Central, and security staff in Seaford. Typically, these ‘specials’ engaged in surveillance and control: sitting or walking with the patient either in silence or with short, sharp injunctions to ‘sit down’ or ‘don’t do that’. The determining factor in the response was how the work was defined, namely as control and management, and not the experience or profession of the staff member. On other wards, ‘specials’ were employed as an extra pair of hands to aid a group of patients or in a bay, which could be a positive experience for patients.
Summary
The conception of ‘person-centred’ care held by staff mirrors that in policy and practice. Meanings were multiple and varied, although the concept was most commonly understood as ‘individualised care’. Drawing out what this might mean for patients with dementia led to a nuanced and particular account.
Our findings reinforce and extend, from previous research,20,54 what good practice might look like on acute wards and concretise the significance of embodied communication in engaging meaningfully with patients living with dementia.
Chapter 5 Process of Person, Interactions and Environment implementation
Introduction
This chapter examines PIE implementation over 18 months. This focus on process over time conceptualises improvement interventions not as single, discrete changes but as ‘facilitated evolution’. 116
Not all wards proceeded to PIE adoption. We distinguished between ‘full implementers’, ‘partial implementers’ and ‘non-implementers’. ‘Full implementer’ wards pursued change over 18 months broadly as intended (two wards within a single trust). ‘Partial implementers’ were located on a continuum between those that made some progress but did not persist to full adoption (two wards in two different trusts) and those that were lost early during installation (two wards in the same trust). ‘Non-implementers’ did not even begin PIE installation (four wards in three trusts) (Table 11).
| Trust and ward | Implementers | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Full | Partial | Non | ||||||||
| Trust | Seaford | City | Ironbridge | Central | City | Valley | Central | |||
| Ward | Poplar | Crane | Rivermead | Netherton | Beech | Rose | Cedar | Ambridge | Oak | Denton |
Stages of implementation
Initially, we examined these implementation patterns as they unfolded over time. First, we compared the constellation of factors that shaped PIE implementation on wards that varied in the extent to which the process was pursued. Second, we compared implementation processes between wards to discern generalisable features that might account for variation.
We found it useful to draw on a stages-of-implementation framework from a review69 of implementation research to explore, in more depth, the factors that contributed to progress (or were barriers to it) at each stage. The framework comprises six stages (Box 1).
Exploration and adoption: making a decision about whether or not to proceed based on the match between the needs of the organisation, assessment of the intervention as relevant and the resources required to carry it through.
Programme installation: active preparation to begin implementation, for example introducing the programme to staff, recruiting people to lead the work and organising training.
Initial implementation: first steps in making change happen. Typically a challenging period during which confidence in the decision to adopt is being tested and the implications of the resource investment are becoming evident.
Full adoption: programme becomes fully operational.
Innovation: period during which the programme is being refined and expanded; desirable changes are being considered for inclusion as part of routine practices.
Sustainability: the goal at this stage is long-term survival of the practices introduced.
In this study, exploration and adoption occurred through informal discussion and meetings with senior ward staff and middle managers at directorate level about participation in the research and what it would involve, and securing their signed agreement to invest in the necessary support and resources, thereby meeting our ‘readiness’ criteria. Programme installation took planning for change a step further through the preparatory work of implementation: facilitating PIE workshops and identifying staff to take part with a view to making up the PIE team. The phase of initial implementation started with observation, the first step in the improvement cycle. Full adoption involved completing a full action-planning and review cycle. Stages of innovation and sustainability entailed embedding change in routine practice.
All wards had gone through exploration and adoption; nevertheless, further preparatory work by the research team was necessary to support first steps in PIE installation. Less than 6 months after agreement to implement PIE, organisational changes having an impact on wards (e.g. temporary and permanent moves to new locations) and personnel moves, involving key staff at ward and middle manager level, meant that relationships had to be developed anew with incumbent staff in leadership roles. Additionally, negotiation of the organisation of the preparatory workshops and securing attendance of staff who would constitute the PIE team was pursued ward by ward, drawing on our evolving knowledge through fieldwork of staff with an interest in dementia care and respect of their peers. The fluid and dynamic nature of large organisations means that this first stage is unlikely to occur as a once-and-for-all agreement.
Full implementers
Engagement with Person, Interactions and Environment to programme installation
Both Seaford wards implemented PIE to timescale over 20 months (February 2014–October 2015, Poplar) and 19 months (May 2014–December 2015, Crane). Each was located around the middle of the continuum in their responsiveness to patients with dementia and being person-focused in their practice (see Chapter 4). The first step in programme installation occurred with the introductory workshops. The recent establishment of a specialist dementia team in the trust opened up the possibility of developing reciprocal linkages of mutual benefit to improve practice. Over several meetings with the PIE researcher, the dementia team lead expressed interest in the team becoming actively involved in PIE.
Workshops
Separate workshops were organised for each ward because of the geographical distance between the two hospitals. These workshops occurred shortly after baseline and were intended for staff who had expressed an interest in assuming leadership of the programme. They comprised informally emergent dementia ‘champions’: nurses, HCAs and therapists involved in direct patient care; and both senior staff from the ward and those with a remit for service improvement (practice development lead, specialist dementia nurses). Participants expressed enthusiasm at taking part, and at the conclusion of the workshop they made plans to get together and organise observations.
Person, Interactions and Environment teams
The wards differed in the composition of their PIE teams. The Poplar team comprised nursing and care staff at different levels of seniority (practice development facilitator, dementia nurse specialist, ward sister, staff nurses, HCAs and therapy assistant). Joint leadership was assumed by the practice development facilitator and the dementia nurse. Both were external to routine ward work and had a developmental role in relation to staff on the ward. The dementia nurse had previously worked on Poplar and attracted considerable respect from staff. The ward manager was not a formal team member but provided active support, facilitation and encouragement.
On Crane, the PIE team comprised the lead dementia nurse specialist, a senior occupational therapist (OT), OT, two therapy assistants and a ward sister. At the outset, there was no direct involvement of front-line nursing and care staff.
From installation to initial implementation: a critical stage
The first PIE cycle on Poplar began after the introductory workshop. Five team members, working in pairs, conducted 5 hours’ observation over different times of the day, including a weekend, in time spans of around 1 hour. For both the observers and the observed, it was perceived as ‘out of their comfort zone’ at the beginning. ‘Observers’ found it difficult to look without acting, and the objects of observation, the ‘observed’, were wary:
’Why are you doing that?’ . . . Now no-one takes any notice of us [observing] do they? . . . they see it as supporting them . . . and it’s made everyone aware of dementia.
Senior nurse, Poplar Ward
In this cycle, there was a gap of around 6 weeks between the observations and the development of action plans during which very little PIE work occurred. Local contextual and situational factors were implicated. The ward was temporarily re-sited because of refurbishment creating disruption for staff; this was the second move, and it came not long after the ward had moved to what had been intended to be its permanent home. An imminent CQC site visit also absorbed the energies of senior staff. Both contributed to difficulties for the team in identifying a mutually convenient time to meet, reflecting on their observations and developing action plans.
Informal discussions between individual team members helped to sustain momentum, as the practice development facilitator, supported by the dementia nurse, acted as a PIE ‘driver’. Together they reviewed the observations, and agreed a process for communicating findings and for extending discussion to the wider staff group. All observations were organised as claims (positive or favourable), concerns (negative or unfavourable) and issues (areas of potential disagreement). This method, from Fourth Generation Evaluation,117 was being employed with staff across the trust to engage different stakeholders on a common vision to improve care culture. Observations under each heading were captured on paper and displayed in the staff room, inviting comment.
The journey to initial implementation on Crane was considerably slower than on Poplar. Only one set of observations had taken place by the end of May, and no work on action-planning had occurred. Partly, this reflected situational factors at ward level: the acting ward manager, who had been supportive of the research, retired as implementation started. Ward leadership, for a period, was held by two acting-up sisters, one of whom was on leave when the initial implementation began.
A new ward manager with a practice development background was appointed in June 2014. The research team proposed a second workshop to focus on action-planning and to re-energise the PIE process. This was well attended, including by the incoming manager. It generated renewed enthusiasm and resulted in a planned meeting to organise further observations. Implementation resumed in August 2014, some 5 months after the first workshop, and the lead specialist dementia nurse assumed responsibility for steering PIE. Team members included a ward sister, a senior OT who attended the workshop, and several of her staff (an OT and a therapy assistant).
Although both wards experienced some disruption (physical relocation and transition to a new ward manager), which extended the timeline from installation to initial implementation, such changes were temporary. Critical at this juncture in moving PIE forward was the proactive role assumed by external ‘drivers’, and the role enacted first by the Poplar ward manager and then by the new ward manager on Crane, as a facilitator, supporting and encouraging staff to get involved.
From initial implementation to full adoption
The first action plan developed on Poplar established several broad areas to work on, with short- and medium- to longer-term action around communication, nutrition and activities. An important feature of action-planning was the way in which observations generated creative solutions to address multiple issues simultaneously. Box 2 presents an action plan around mealtimes as a social event, starting in a single bay. Addressing several goals, it was initially directed at communication. It set in train a stream of work beginning with small steps, and subsequently was expanded to all bays through the process of appraisal and review (including new observations). An additional goal to which the initiative contributed was patient mobilisation; getting people up and moving between bed and tables.
This action plan was developed through reflection and discussion of observation of a joint activity (creating a mural for the ward) involving patients on the ward and young people, part of a time-limited, intergenerational project. Patients, including those with dementia and limited language, demonstrated enthusiasm and enjoyment, and talked about aspects of their lives that had been unknown to staff, as they took part in the activity. Reflecting on their observation, staff were surprised at what could be gleaned about people’s lives through patients talking to each other in a convivial setting.
This prompted the plan to get patients to eat lunch communally (e.g. using tablecloths and flowers) with music played after, making it a social event. As noted in Chapter 3, this ward had space for tables and chairs in the bays but these were primarily used by staff to do paperwork. It was agreed that the plan would start in one bay and extend to others, depending on progress. It required negotiation with staff beyond the ward to pursue (e.g. infection control and catering), as well as the agreement of the ward manager and wider team. With catering, for example, one of the issues raised was the size of meal portions: patients found that the standard portions were too large and therefore unappetising, and, with support from the housekeeper, the contracted agency that supplied the meals agreed. Sitting with patients during the meal allowed staff to observe patients’ dietary intake but unobtrusively. This was seen to work as a social event and as a means to encourage eating (the dietitian who worked on the ward also became interested and involved in the work).
On Crane, implementation began in earnest following the second workshop and continued thereafter. For the first cycle there were four sets of observations, typically conducted in pairs, each 1 hour long, undertaken at different times and in different spaces. Plans arising from these included immediate action on nutrition: eliciting patients’ food preferences and ensuring the consistent use of food charts, initiating work to increase activities with patients, and including the engagement of ‘dementia visitors’ in the work (a recent initiative via the dementia team, these were volunteers who came to the ward once weekly) (Box 3).
One of the first sets of observations concerned the level of noise on the ward, in particular the constant music from the radios, which was felt to be mainly for the benefit of staff. Reflection on its potential adverse impact on patients with dementia (overstimulation and an increase in stress) and discussion among the implementation team about the therapeutic effect of music resulted in an initial short-term action plan including monitoring the use of music for 1 week; discussing with patients the music they enjoyed; eliciting ideas from staff about the appropriate use of music, including how to manage varied preferences (use of headphones, etc.); and using observations within the wider staff group to engage them in reflection about how they might feel if they were hospitalised.
A review of the action plans led to the introduction of music during lunchtime. As several patients enjoyed singing along to the CDs, a further action plan was identified: to establish whether or not there was interest in having a regular singing session a couple of days every week, and to organise a trial session involving Christmas carols (meeting in December).
This example is illustrative of the emergent nature of implementation and change. Action plans evolved through the dynamic of action and appraisal of progress; this in turn opened up further possibilities that had not been anticipated at the outset. Observation about noise from the radio resulted in a plan to elicit patient preferences about the music played on the ward; moved on to establishing music as a collective and purposeful activity at lunchtime; and then extended to plans for a regular monthly singing session, as patients appeared to derive pleasure from joining in. Similar to Poplar, a small step at one level could lead to a significant change in how things were usually done, with space and momentum created through the action-planning and review process.
Full adoption towards sustainability
On Poplar, by the conclusion of the study, ‘mealtime as a social event’ had not only been extended to all bays but had been incorporated into the ward routine. There were aspects of the initiative that required ongoing work based on experience: men appeared more reluctant to engage than women, and staff needed to consider which patients would get on with each other.
PIE observations continued periodically throughout the research. New issues that were identified and that resulted in immediate action plans to pursue included ensuring that patients did not feel isolated, ignored or disconnected (e.g. leaving curtains closed around patients post care delivery, being mindful not to exclude patients from discussions when within earshot, and regularly checking that the clocks in the bays were accurate in time and date).
A persistent focus of action-planning was the provision of stimulating activities for patients who were well enough to take part but insufficiently recovered to be discharged, including puzzles, newspapers, games and reminiscence resources (RemPod, Stroud, UK). Plans required identifying staff time and sources of funding to purchase materials. By the end of the third improvement cycle, reviews indicated some positive change: staff sitting with, and encouraging, patients to read and using pictures as prompts for conversation. Overall, these action plans were evaluated as ‘partially met’. Engagement was constrained by staff availability, which waxed and waned depending on demand, patient flow and level of patient acuity, which was unpredictable.
Over time, the composition of the PIE team changed as some members moved on and were replaced by new staff. Although never a formal member of the team, the ward manager continued to play a crucial enabling role in supporting and encouraging staff to get involved in PIE and in facilitating the communication of action plans to the wider staff group. Her commitment to PIE, the authority and legitimacy this gave to implementation work, and the support provided to enable staff to take time out to do observations were critical to the process. Her inclusive management style was a factor in involving HCAs directly in the PIE team. One HCA, when asked by the researcher why she felt able to take the initiative with PIE, commented, ‘the ward manager treats all her staff as equals’ and ‘there is no hierarchy here’. Another HCA, who took special interest in nutrition (which dovetailed with PIE action plans), also reported that her enthusiasm was a result of the ward manager’s encouragement. Apart from a period of absence (as a result of injury), the ward manager was present throughout the research but retired just as it came to a close.
On Crane, alongside ‘music as stimulating activity’, which expanded in form and content over time, new action plans identified and pursued included encouraging patients who were well enough and near to discharge to dress in their own clothes during the day, something that was not usual on this ward. This was viewed as supporting the normalisation of the transition from hospital to home and encouraging independence. It was also aimed at nursing, care and therapy staff to increase person-focused interaction while they helped the person choose their clothes and assisted them to get dressed. Making this happen involved negotiating with relatives to bring in clothing and ensuring that staff went about the work with individual patients.
Four PIE cycles were completed on Crane by the end of the study. Subsequent observations were shorter – around 30 minutes’ duration – to make the process manageable given the demands on staff time. Ward staff who were not part of the PIE team conducted some observations, extending the programme’s reach. An explicit objective of the manager, integrated into action plans, was to engage the wider staff team in discussion about change and provide opportunities for them to put forward ideas through team meetings and handovers. Inclusivity was valued as a principle of teamworking and a strategy to ensure that staff ‘buy-in’ to change. For example, the use of food charts was systematised through flagging up, on handover sheets, which patients needed them.
Trying out different ideas around activities to increase stimulation for patients was an ongoing topic of action plans; this included encouraging the use of reminiscence materials secured for the ward via the dementia team and creating themed ‘memory boxes’ to add to them. This work tended to proceed in fits and starts. Initially, it was very successful and had the support of the ‘dementia visitor’, a volunteer who came to the ward once-weekly, and two nurses who were keen to take part. As on Poplar, success depended on demands, and the investment of time and staff was an ongoing issue, particularly during winter pressures, when the team helped to cover an additional six beds. The cramped nature of the environment and lack of separate space for patients outside the bays was an additional constraint. In addition, on this ward, engagement in activities was assessed as being ‘partially’ implemented. The long-term plan, advocated by the specialist dementia team through the dementia strategy, was the recruitment of an activities organiser to work with a number of wards, including Crane, to enhance activities for patients.
The composition of the PIE team for a long time did not extend beyond senior nurses, OTs and therapy assistants. As therapists rotated between wards, this meant that individuals changed, although ongoing therapy involvement was maintained. More than 12 months into implementation, a staff nurse was ‘recruited’ to the PIE team. Even so, success in accomplishing specific action plans required the active engagement of front-line staff, including nurses and HCAs (e.g. music at lunchtimes, observational monitoring of nutrition intake and encouraging patients to dress in their own clothes). Strategies to enable ‘buy-in’ of the changes were both essential and contributed to translating plans into action on the ward.
Joint action between Person, Interactions and Environment teams
A cross-site workshop, a significant event for members of both PIE teams, was held in spring 2015, just under 1 year following PIE introduction. This was instigated by the Poplar team. Ten staff from both wards took part, including the dementia specialist nurse from a third trust hospital; the researcher was also invited. Networking between wards initiated through the meeting was important in facilitating a shift from PIE adoption to programme innovation.
The meeting provided opportunity for reflection on what needed to be done, using the claims, concerns and issues framework. There was considerable enthusiasm about being part of a process that actively involved staff on the front line in collaborative action to effect change, which in turn encouraged them to use their initiative to try out new ideas. They perceived a change in practice: increased use of the ‘This is Me’ booklet; greater involvement with patients’ families; and a heightened awareness of patient experience as being at the centre of what they did. Concerns centred on time constraints, how to sustain PIE after the research ended and how to embed changes in routine practice. Ideas on joint action to pursue included incorporating information on PIE into a general induction pack for staff and involving all new staff in undertaking a short PIE observation with a link PIE team member.
Throughout the day, there were explicit links made between the PIE objective of enhancing person-centred care and the trust’s shared purpose framework; the critical role played by the specialist dementia team in championing PIE and the dementia team’s conception of PIE as a vehicle through which aspects of the dementia strategy could be pursued. Both were viewed as operating in synergy one with the other.
Did implementation work as intended?
Drivers, facilitators, teams and networks
We had conceptualised the process of PIE implementation as requiring simultaneous top-down and bottom-up leadership. This was encapsulated in a team involving senior ward staff, those at the ‘sharp end’ of care delivery, and practice development expertise to provide external support and a voice for PIE between the ward and middle managers. Even so, we considered that senior ward staff would assume a leadership role for PIE.
On both Seaford wards, the ‘external facilitators’ were the key ‘drivers’ of change. They were committed and motivated to improve care delivery, either as part of their broader role in enabling cultural and practice change in the trust or because of their interest and remit to improve care of people with dementia. Ward managers also acted as ‘drivers’ of change, although not as we had envisaged. Instead, they were change ‘facilitators’: on the one hand legitimating staff time and investment in PIE, and on the other hand extending its reach to the whole staff group. it was neither feasible nor practicable for managers to lead PIE; their day was dominated by work to ensure that the ward operated in a smooth, safe and effective fashion. But the teams were also essential. Team members pursued action on the ward and also contributed to generating interest and enthusiasm among their colleagues. On both wards, albeit in different ways, the interface between members of the PIE team and wider staff group was an additional factor in extending the reach of PIE across the ward.
The role played by the specialist dementia team extended beyond driving PIE at ward level. The establishment of the team was consequent on a trust board initiative; it had strong high-level support and both formal and informal links with senior managers and the board. For the dementia lead nurse, PIE was conceived of as a vehicle through which the dementia strategy was pursued, and one method for achieving practice change for hospitalised patients living with dementia. This encapsulated her vision of improvement through simultaneous high-level strategic initiatives and ground-level practice change. Nevertheless, maintaining this duality was perceived as an ongoing challenge for the team within a large, geographically dispersed organisation and several large hospitals serving very different catchment populations. Such a vision was not evident in any of the other study trusts. Although high-level support for PIE occurred through the dementia team’s vertical and horizontal networks, staff on Crane and Poplar were actively involved in supporting the work of the dementia specialists in their respective hospitals, as, for example, the dementia cafés. Patients from both wards were observed being taken to events by staff.
On Poplar, the practice development facilitator also played an important role in making PIE visible in the hospital and trust, through presentations to middle and senior managers, as an exemplar of a process of cultural change. The existence of a clearly articulated, unifying vision by the trust with explicit goals for quality improvement was aligned with the change model pursued in PIE. PIE was conceived of as synergistic with key strategic trust priorities and, therefore, as a legitimate target for the investment of time and resources.
Person, Interactions and Environment change process
The full adoption and routinisation of PIE in Poplar and Crane enables us to draw out how and in what ways the change process as envisaged was carried through in practice, and, conversely, what was different from partial and non-implementer wards.
Implementation spiral
We envisaged implementation proceeding in cyclical and sequential fashion: through observation, reflection, action-planning, action and review. Interest was in whether or not the functions reflected in each step were necessary. In practice, the process took the form of a spiral, with simultaneous reviewing, amending action plans and actions in pursuit of them, alongside identifying new action plans, all at the same meeting. As actions were reviewed, some were abandoned as unworkable or an unnecessary addition; others became fully embedded in ward routines, becoming part of ward culture; still others were extended beyond the areas in which they were tried out. This was most pronounced on Crane ward (Figures 22 and 23). Thus, although each step was a necessary component of implementation, change occurred as an interactive spiral movement.
FIGURE 22.
Person, Interactions and Environment implementation on Crane, Seaford Trust. Dark green, researcher- and/or PIE leader-led actions and documentation; blue, PIE team members’ documentation; light green, PIE team leaders’ documentation.
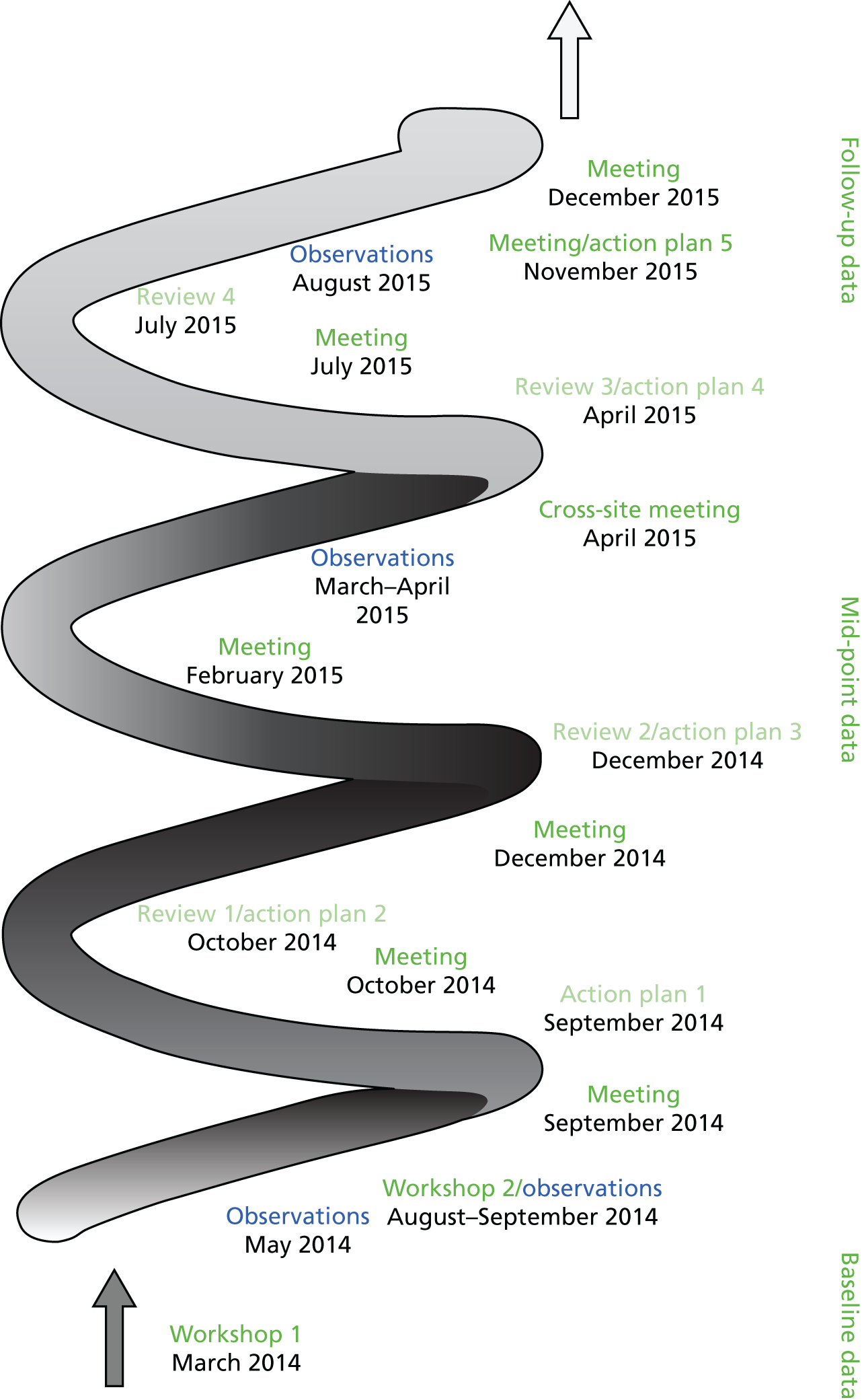
FIGURE 23.
Person, Interactions and Environment implementation on Poplar, Seaford Trust. Dark green, researcher- and/or PIE leader-led actions and documentation; blue, PIE team members’ documentation; light green, PIE team leaders’ documentation.
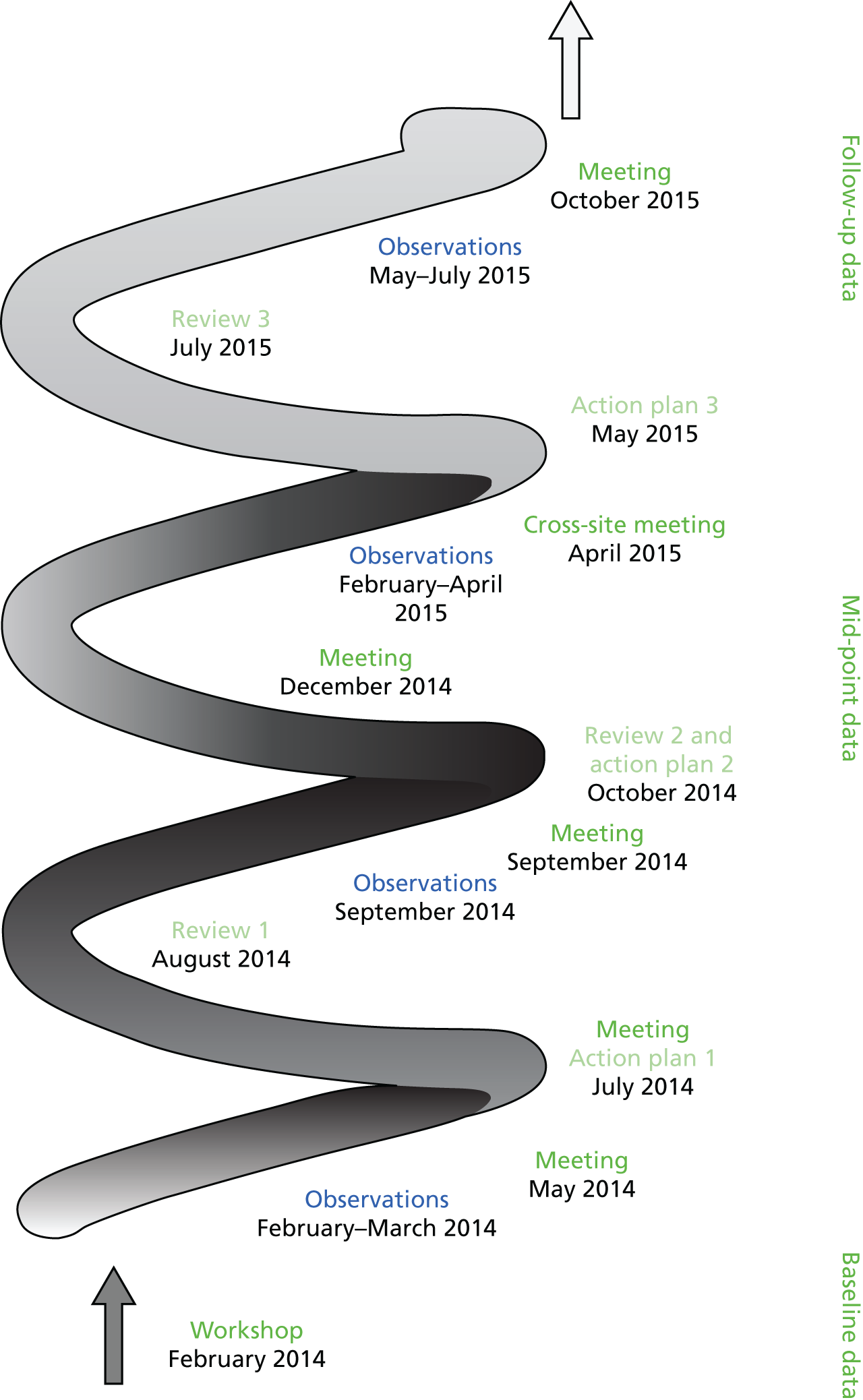
Conduct of observation
The manual and guidance on observation suggested that observations could be conducted in pairs over about 1 hour, with each observer focusing on several patients (focus on individual patients was the approach adopted in the NAD, influenced by dementia care mapping). Whereas initial observations on both wards proceeded in this way, subsequent observations were much shorter. In part, the involvement of several pairs of staff at different times and in different locations built up a composite picture of patterns of action and interaction that fewer observations over a longer time could not achieve. In part, it made the conduct of observation feasible in the context of a busy ward and distributed the experience of carrying out observations among a larger number of people. Similarly, the focus of observation broadened to include not only patients but ward routines and the impact that these had on patients. These changes were incorporated into the manual.
A feature of the conduct of observation, emphasised in guidance and reinforced in the workshop, was that, in their recording and feedback to staff, observers should convey what was positive about practice as well as what needed to change. Thus, observations were aimed at simultaneously establishing objectives for change and ensuring that staff continued to feel valued, motivated and engaged in the improvement process.
On both Seaford wards, in presenting feedback, the PIE teams refrained from directly criticising individual colleagues’ communication practices. Nevertheless, it was evident from action plans that staff communicative practices featured in one way or another in most of them: in the emphasis placed on expanding opportunities for socialisation and interaction between patients and staff and between patients themselves; and in making the quality of the encounter with patients central to routine work (e.g. action on encouraging patients to dress in their own clothes had the dual objectives of staff spending time with patients while they helped them to dress).
Documentation
Completing PIE documentation on both wards often followed on from the action-planning meetings, as it required both time and access to writing space. This had implications for the timing and flow of action. As it was team members with designated office space, namely the practice development lead on Poplar and the lead dementia nurse on Crane, who undertook this task, it was completed post hoc when time permitted and often relied on the researcher’s contemporaneous record of the discussion (the researcher attended, on invitation, nearly all of the PIE meetings).
Although the content of PIE documentation was seen as useful, providing a broad framework to consider goals and steps to achieve them, it was felt to involve unnecessary duplication. The need for simplification was discussed with the research team, and revised documentation was developed, tried out and shared with other sites. Over time, as the action-planning and review process became embedded, meeting notes that conveyed the rationale for action and review provided a steer for framing and appraising goals and progress, and the action and review forms simply summarised action points. In this respect, the systematic format for structuring action plans and reviews appeared necessary at the outset to implement a different way of working. As the process became embedded, there was less reliance on the format to make change happen (i.e. local adaptation occurred without compromising the function).
Person, Interactions and Environment and normalisation process theory
On both wards, although implementation was neither smooth nor linear, each of the change steps was necessary and facilitated movement forward. Observation and reflection sensitised staff to aspects of routines and practices that they had previously taken for granted; once observers resolved their initial wariness about whether or not they were doing it ‘right’, observation was viewed as feasible and enjoyable and offered new insight. Thus, the process generated coherence among PIE team members and increased interest and motivation to move to the next step, namely action-planning (cognitive participation). Collective reflection and discussion on observations gave rise to creative action to effect change that was perceived as meaningful and worthwhile (collective action). The work of negotiating step changes, with different team members taking responsibility, reinforced coherence, participation and action. Actions involved different PIE members in ways that provided opportunities to reach beyond their existing roles (e.g. HCAs on Poplar). Simultaneous review of progress (appraisal), modifying goals and action plans, and extending existing work into new areas generated by experience of plans in action further enhanced coherence and cognitive participation. PIE was seen as a useful and effective means of making change happen.
Several aspects of PIE implementation on both wards add further insight into the mechanisms of change and, therefore, how the NPT framework could be further elaborated on in particularly complex and dynamic environments, such as acute wards.
First, to achieve ‘normalisation’ of new ways of doing things, strategies to generate mechanisms of change (coherence, cognitive participation, collective action and appraisal) needed to occur at multiple levels. It was not sufficient for the PIE team to make sense of the intervention to distinguish it from their current ways of working, and to buy into the work as a worthwhile investment; front-line staff also had to be engaged. Without their active participation, the depth and reach of action plans to achieve coverage across the ward would not happen. In this, the ward manager as ‘facilitator’ assumed a key role in enabling this to occur. On both wards, strategies to secure engagement in the change process beyond PIE teams were actively pursued through established, routine fora, for example handovers and board rounds as well as staff meetings and supervision.
Second, there was the dynamic environment of acute wards. Staff turnover was one aspect of this; another was the unpredictability of the pattern of ward work. Staff turnover affected both PIE teams: a HCA on the Poplar team moved on from the ward within a couple of months of the first cycle; and the rotation of therapists on Crane meant that individual team members changed regularly. There were no difficulties in recruiting new people to replace those who left, itself an indication that PIE was valued and worthwhile.
Unpredictability in the work pattern derived from the particular conjunction of patient need and profile at any one point in time, and the variable weight of demand on routines and practices. ‘Winter pressures’ were often cited as contributing to high demand, but in actuality duration was elongated as the additional beds extended from November to June. Sustaining understanding and ‘buy-in’ to PIE (coherence and cognitive participation) required processes for renewal. For example, involving an interested individual to carry out observation, paired with a more experienced team member, proved useful. Time and situational factors pertaining to work patterns and flow meant that coherence and cognitive participation might require reinvigorating prior to securing collective action. Maintaining morale and belief in the possibility of change during periods when demand on staff surged required flexibility in devising and implementing action plans.
Evaluating progress through appraising action, and delegating aspects of the work to different team members with appropriate support, had the potential to reinforce coherence, participation and collective action, and to extend and deepen reach of the action. Critical appraisal and reflection on why actions were not pursued as intended (i.e. whether alternative strategies to reach the same goal needed to be considered, or whether the goal should be changed) also improved action-planning. The generative mechanisms then operated interactively, between levels and over time, and not in a linear fashion. Sustaining momentum in a dynamic environment meant that the generative mechanisms theorised as necessary to ‘normalise’ new innovations in practice were not one-off achievements but had to be reworked until they were no longer recognised as new but were simply part of ‘the way we do things’.
Organisational context
At the trust level, PIE implementation was bookended by a negative CQC inspection report and an outcome that resulted in the trust being placed in ‘special measures’, although care on medical wards, including on older people’s wards, was judged to be good. Implementation took place between the first visit by the regulator in March 2014 and ended (for research purposes) with the results of the second visit in November 2015.
Although work relating to the CQC inspection, subsequent outcome and responsive action dominated the business of the trust board and senior managers, it did not appear to have a direct impact on PIE progress or the day-to-day work of the wards. Related issues, including changes in personnel at board and senior management, were similarly not seen as directly affecting ward organisation and practices. What appeared decisive was that, despite these events, trust strategic priorities remained unchanged. Action taken by the board in response to the findings of the inspection included intensifying the drive to engage staff at all levels in joint work to translate shared values into improving services. For ward staff, the factors that had most resonance for organisation and care delivery were demand on beds and the availability of resources to facilitate the timely flow of patients in and through the ward and transitioning beyond it. The systemic pressures staff on Poplar and Crane experienced in relation to demand and flow were a constant. They occurred before and after the trust was placed in special measures and were not affected by the remedial action taken by the board in addressing the CQC recommendations. We return to this in comparing the experience here with that of City Trust, which also received a poor CQC rating at about the same time as Seaford, with very different consequences for PIE.
In addition to the general problem of demand and flow, there were specific contextual features of Crane that influenced PIE implementation in practice: ward design and layout, and the cramped nature of the space. The latter in particular made PIE observations by staff difficult, as there was no obvious place from which to discreetly observe patients and staff. The lack of a day room, much wanted by staff, meant that, as with Poplar, finding a meeting venue was problematic. In the later stages, the OTs offered one of their rooms off-ward, when it was not in use. After the creation of hubs at each site (resource rooms where events were held and material on continuing professional development was freely available), meetings were held here. Ward factors also included the recurrence of norovirus, which twice meant ward closure and a halt to PIE activity (and delayed fieldwork).
Partial implementers
There were two ‘true’ partial implementer wards and two others that took faltering steps towards PIE installation. Located betwixt and between partial and non-implementation, these are discussed under non-implementers as, although they intended to proceed, in actuality movement was cut short very early.
Over a period of 12–18 months, Netherton and Rivermead moved through the phase of initial implementation but did not proceed to full PIE adoption. Interest and enthusiasm carried senior staff on Beech and Rose wards (Central Trust) to PIE installation, but both just crossed the threshold into initial implementation and did not go further. They are discussed along with Denton ward, the third ward in this trust, which, although characterised as a non-implementer, is not qualitatively different in the implementation stage reached from Beech and Rose, having stalled at the boundary of initial implementation.
Engagement with Person, Interactions and Environment
Rivermead and Netherton were initially ‘slow’ to get going (not dissimilar to Seaford wards) and then moved forward with initial implementation, albeit in fits and starts. Neither, for various reasons, proceeded to full PIE adoption.
In terms of practice with patients living with dementia (see Chapter 4), staff on Netherton were observed as being at the high end of the quality continuum; those on Rivermead were in the middle, similar to Seaford wards.
More so than in other PIE wards, Netherton in Ironbridge Trust had in place multiple facilitating factors that augured positive engagement with PIE. The introductory meeting with staff revealed a passionate commitment to continuous improvement in care delivery for their patients, directorate-level support to facilitate the research, and interest among the training and practice development team to assist with PIE. Senior ward staff had worked together over a long period and had created a cohesive team.
The ward team in Rivermead was similarly long-established and cohesive. The manager was very supportive of improving the care of people with dementia and had worked closely with the practice development lead (who was identified as the external ‘driver’); both had a particular interest in dementia care.
Senior staff on both wards had an interest in delirium, understood the value of delirium screening and worked to facilitate the collection of DOS data as part of routine nursing observations.
Workshops and Person, Interactions and Environment teams
The Netherton introductory workshop in early November 2013 was attended by a nucleus of seven staff of different levels of seniority and roles (a manager, a charge nurse, staff nurses, HCAs and an occupational therapist attached to the ward) who would form the PIE team. Training and practice development staff also took part, the intention being that they would support Netherton in implementing PIE. Feedback on the workshop was very positive, and ward staff indicated a willingness and enthusiasm to get going.
From Rivermead, nine staff attended the PIE workshop in February 2014 (two sisters, two staff nurses, three HCAs, a housekeeper and a therapy assistant). Their composition reflected engagement and interest among the staff group in a diversity of roles. Although they did not formally constitute a PIE team, there was tacit understanding that they would take responsibility for leading on PIE with the support of the trust’s practice development lead, who would steer implementation on the ward.
At the conclusion of the workshops, both wards had plans under way for PIE installation: actual and virtual PIE teams and identified support outside the wards. Some aspects were tentative: how a loosely organised team would work (Rivermead) and how practice development support would contribute to PIE (Netherton).
Initial implementation: a sticking point?
Following the workshop, at the instigation of the Netherton PIE team, the site researcher met with them to discuss the process and tasks. The ward manager suggested that she would lead PIE and that they would carry out practice observations to build their confidence during December. The first PIE cycle began in earnest with observations from mid-January 2014. These were conducted over a 2-hour period in pairs on two occasions, at different times of the day (mid-morning and afternoon). Staff initially felt inhibited and anxious, concerned that colleagues might act differently knowing that they were being observed, similar to Seaford. Afterwards, they met to share reflections.
Observations indicated positive features of practice (staff being responsive to and reassuring anxious patients; encouraging interaction between patients; offering choice of food and drink and going about it straight away; ward being clean; patients in beds appearing content; other patients being up and about in the day room and corridor). Feedback was provided to staff on shift and welcomed as acknowledging the strength of teamworking. Immediate action was initiated from these observations: the introduction of short, staggered staff breaks in the morning to ensure responsiveness during a period when staff were relatively invisible in the bays (observed through buzzers going unanswered, and patients being left waiting longer than usual for assistance), and attention to the temperature of the ward for patients who were inactive by offering blankets (staff who were constantly in motion did not notice this).
Over the following 2 months (February–March 2014), further observations occurred involving all seven PIE team members and practice development co-ordinator. The additional support that had been anticipated from staff at directorate level did not materialise. Apart from individual examples of a particular patient being ignored or a dozing patient not being offered a drink, observation elicited a picture of responsive practice, an image with which the ward ‘outsider’ – the practice development co-ordinator – concurred. A facilitation meeting between members of the research team, the PIE team lead and the senior charge nurse was held in early April 2014 to support the translation of observations into action plans. It was reported that plans on reducing noise in the morning and increasing activities were being developed from the second set of observations.
By summer 2014, 6 months after initial implementation began, progress had stalled. An examination of action plans from previous observations by the research team revealed difficulties in moving beyond a general ‘wish’ list to identifying specific steps and the devolution of responsibilities to achieve them. For example, although the use of volunteers to support activities such as reminiscence, exercise groups and games was identified as an action, as was increasing activities provided by staff to patients, concrete steps to take these forward were vague (‘manager to pursue’). Indeed, from informant conversations with PIE team members, although they concurred with the objective of doing more stimulating activities with patients, they felt that this could not be done with their existing staff complement. Similarly, engaging volunteers was viewed as a good idea, but the steps to make it happen had not been worked through.
The research team offered a further half-day workshop to consider action-planning and review, held in August 2014, when interim data collection was to start. Five PIE team members attended, including two senior staff. Anonymous ethnographic observations were used to explore practice in its organisational context. These were intended to provoke a discussion of factors shaping practice that might be a focus for change without ‘blaming’ individuals and to work through action-planning around concrete examples. Evident from discussion was the openness of the team to debate aspects of practice that were regarded as contentious (use of language and terms of endearment with patients). The workshop appeared to generate renewed enthusiasm as had previously occurred with Crane. It was agreed that they would develop an action plan for discussion with ward staff at the forthcoming 6-monthly staff away day in November (to which the researcher was invited). Thus, as the PIE implementation phase approached 9-month interim data collection, there was the prospect of resumption.
In Rivermead, similar to Seaford wards, nearly 3 months elapsed between the introductory workshop and the first set of observations. In May 2014, three pairs of staff (three HCAs, a housekeeper, a nurse and a ward manager) conducted observations at different times of the day: early afternoon, teatime and late evening, over 2 hours on each occasion. Reflections on observations occurred informally afterwards. Despite the number, range and length of observations, documentation revealed a relatively superficial portrayal of practice and goals for improvement, largely related to professional ‘visitors’ to the ward (pharmacists, phlebotomists, porters and medical staff). For example, a positive feature of practice was greeting every patient on entering the bay; this contrasted with what was regarded as poor practice, that ‘visiting’ professionals did not do likewise. Observers here were mainly care staff, posing the question whether or not their social location made it more difficult to raise issues of practice; in other sites, observations were undertaken by a more hierarchically diverse group. Yet feedback with the researcher revealed that observers had ‘seen’ and noted little interaction between staff and patients for long periods in the evening, but as it was interpreted as requiring additional staff to resolve it did not feature as a goal for change. ‘Knowledge’ of the problem was uncontested; their judgement that they were powerless to act on it had an impact on its utility as a focus of action-planning.
Informal conversations between virtual PIE members occurred to discuss observations, but no formal meeting to pursue action-planning took place. The practice development co-ordinator, who was to provide a steer for PIE implementation, had taken up the post of matron shortly after the PIE workshop. Although she had negotiated time for PIE, her working life was absorbed by organisational demands: staffing shortages and a wide-ranging reorganisation of ward models and bed closures following a poor CQC inspection (inadequate staffing being a particular focus of concern). The ward manager was also on sickness leave in the month following observations. Similar to Netherton, the PIE implementation record had stuck on observation.
Starting again
In Netherton, the away day in November 2014 was attended by half of the ward team (a second day was to involve remaining staff). The site researcher and PIE team facilitated discussion about PIE. Ward observations were considered in groups charged with identifying priorities and action plans arising from them. Deliberations (recorded for the PIE team to work on afterwards) were wide-ranging, generating lots of ideas, varying from staff training in working with patients deemed ‘challenging’ to reducing bed numbers to allow for more time with individuals. From subsequent discussions on the day, senior staff appeared preoccupied with changes occurring at ward level: what they perceived as increased medical acuity and dependency of their patient profile, a push from managers to speed patient flow (a recent managerial directive to all wards required reduction in length of inpatient stay), and concerns around staffing, particularly the loss of a qualified member of staff ‘taken away’ to cover neighbouring wards as the hospital entered ‘winter pressures’.
Following the away day, action-planning stalled again; the length of time since observations had taken place and the changes in the ward patient profile since then were arguments proffered by senior staff for carrying out a further set of observations. These were organised with external support from practice development/clinical education colleagues. This would be a new start.
A second PIE cycle was begun in February 2015 with ‘external’ ward observers. Observations were conducted over 1 week at different times and locations. As before, feedback was very positive, reinforcing the picture of person-focused practice. As a means of reinforcing and celebrating the quality of care delivered on the ward, and to their professional peers beyond, PIE observation was successful. The OT who had conducted some observations with colleagues took the initiative in writing up action plans from them but was reluctant to assume a leadership role in PIE, viewing her position as a ‘part-time’ member of the ward team (with nurses and HCAs perceived as the ‘core’).
In the months that followed, prompts by the site researcher revealed little further progress: the PIE team had not met. This remained the position at the end of December 2015. Their difficulty in developing action plans (recognised by senior ward staff) suggested that a contributory factor was a ceiling effect around identifying areas for improvement at least in the context of existing resources. The staff group (and senior staff) had many ideas for desired changes, but they were seen to require additional staffing.
Final data collection was delayed, as the timing coincided with a CQC inspection; interim collection had also been delayed because of infection and ward closure. The timescale for study completion meant that a further round of data collection was not feasible.
In Rivermead, informant conversations between the researcher and PIE team members between July and September 2014 revealed that ward staff were working day to day; there was neither the time nor the ‘headroom’ to do more than get through the daily routine. ‘Winter pressures’ beds (an additional five) were still open on the ward: they closed and reopened during the same week in September. The matron (external PIE lead) continued to be enmeshed in work around staffing, bed closures and ward remodelling. The research team offered a workshop to help with moving PIE on; this was not taken up.
With autumn behind and winter approaching, the anticipation of increased demand made the prospect of resuming PIE remote. Senior staff indicated that although the team had made positive changes over the years ‘in the small things’ (respectful of patients’ dignity and privacy), moving to the next step required a more fundamental examination of their practice and review of resources. Yet the daily pressures on staff made this ‘out of time’.
Late December 2014, the matron held an action-planning meeting with the PIE team. Action plans were discussed and the team was to develop and consider them with the wider staff group. The confluence of elapsed time since the observations, demand pressures on the ward and long-term sickness among established staff resulted in no further work on PIE.
Interim data collection began in January 2015, a heightened period of ‘winter pressures’. Observation indicated no discernible improvement in practice that might be attributable to PIE, unsurprising given that implementation had not been pursued.
Partial implementers: barriers and facilitators
Drivers and teams
On both ‘partial implementer’ wards, leadership (or rather its absence) was a barrier to pursuing PIE. Nevertheless, the form it took and its relative weight in interaction with organisational and ward level contextual factors differed between them.
On Netherton, the ward manager assumed the PIE leadership role but only partially enacted it, and the ‘external’ facilitator, who had helped with observations, was not called on to assist in driving PIE. The OT took on some of these tasks, going through observations and completing documentation on action plans. In the light of her perceived peripheral position in the team, her role was viewed as supportive only. This suggests that external facilitation is critical to successful implementation, albeit aligned with the active support and encouragement of the manager, as on Seaford wards. The work of ward management, being the bridge between patients and staff on the one hand and the organisation on the other, in an ever-changing, dynamic context, made it difficult, if not impossible, to assume leadership of PIE as well. The strength and cohesiveness of the senior management team suggested that it might be different on Netherton: it was not.
However, the ward had invested considerable resources in observation, including involvement in additional workshops and meetings aimed at energising the PIE process. Staff were enthusiastic, and senior staff actively facilitated time to conduct them. This included people who were not members of the PIE team, such as, for example, the ward clerk, who played a pivotal role in the smooth running of the ward. Their principal difficulty was in translating observations into meaningful action to take practice forward.
We hypothesise that two linked features of the care environment are implicated, providing a plausible, explanatory account of the inability of Netherton to proceed to full adoption: the high quality of practice on the ward and the existence of well-established mechanisms and processes to pursue continuous practice improvement. The positive picture of practice conveyed through the use of the tool was consistent with baseline and interim data collection (observation and interviews with stakeholders external to the ward). Analysis revealed a strong, shared ethos of person-focused care and high value placed on all staff in spending direct time with patients (and relatives) as an essential component of their day-to-day routine. From data presented in Chapter 4, Netherton was one of two wards in which understanding and practice of person-centred care for people living with dementia was most highly developed (Denton being the other). This was enabled and reinforced through team reflection, discussion and review via away days, and built on routinely through handovers, supervision, mirroring and applauding good practice. Although the problem was not ‘solved’, and would always be a work in progress, as evidenced in the new challenges posed with a potentially altered patient profile, the mechanisms they had developed to effect change were not obviously wanting. In this context, the PIE observation tool offered a systematic and novel approach to enhance their systems, but the rest did not offer benefits over and above what already existed. Ward staff had not abandoned goals for change; often expressed were organisational goals to which they aspired, namely a reduction in the size of the ward to allow them to provide more one-to-one support, and staffing levels that would enable them to deliver therapeutic care and stimulating activities.
The PIE team in Rivermead was more of an informal group of staff who had worked together with the ward manager over a long period and who had particular interest in improving the care of people with dementia on their ward. Apart from the manager, they comprised mainly unqualified and support staff (HCAs, a housekeeper and a therapy assistant). Similar to Netherton, although they conducted multiple observations, they experienced barriers in translating their observations into meaningful action plans that could take practice forward. Their difficulties could be viewed as reinforcing the necessity for, and the form of, the PIE ‘driver/team’ model: the inclusion of a staff mix to ensure the authority and legitimacy of the change process, vertically beyond the ward and horizontally among their peers. The ward manager, although supportive and encouraging, assumed a mainly facilitative role, necessary, as observed in Seaford, but insufficient to provide effective leadership of PIE on account of ward demands. If the matron had been able to ‘drive’ PIE as intended, this would have enhanced the legitimacy of the action-planning process and provided staff with the confidence to challenge practice. Her inability to do this was an expression of the wider organisational context. Even so, there were also indications that one of the difficulties in pursuing action plans that would make a difference was staff belief that they were impossible to pursue with their existing staffing. Evident, then, were multiple and interacting contextual features that elucidate the interaction between an innovation and its context, and expressed in such comments as ‘we’re as good as we could be with the resources we’ve got’. In both partial implementer wards, although for different reasons, coherence and cognitive participation of PIE as a vehicle for change initially secured was lost.
Vertical and horizontal networks
Absent on both Netherton and Rivermead were what we termed vertical and horizontal networks linking the action on PIE beyond the immediate environment of the ward to wider networks of support on dementia, as in Seaford. In part, this reflected the absence of an external driver who could provide such a link; it was also affected by the perceived lack of congruence between the direction pursued within the trusts on the immediate priorities for action on dementia and focus of PIE on ward-level practice change.
There were other dementia improvement initiatives being carried out in City and Ironbridge Trusts. Unlike in Seaford, these operated in parallel with PIE and there was no interchange between them. In both trusts, the recruitment of ‘dementia champions’ was a key element of the dementia strategy, and the champion model broadly operated in a similar fashion in both.
In Ironbridge, focus was on developing a dementia champions network with two champions in each area (clinical and non-clinical). The requirement on them was to attend a minimum number of meetings per year and to raise awareness of dementia within their work spheres. The aim was to generate interest among staff at all levels, thereby building awareness of dementia in small steps from what was considered to be a low base of understanding. Staff on Netherton expressed impatience at the evolutionary nature of the approach: improving ward practice needed to be addressed, and a focus on enhancing general awareness would not achieve this. As the Seaford Trust experience indicated, there is no necessary conflict between adopting parallel approaches (practice change alongside enhancing general awareness). For Netherton staff, the lines of difference were an expression of what they viewed as the low priority attached to patients with dementia with high-level needs. In City, the vision conveyed by the matron who played an important enabling role in the dementia champions initiative was that, once the ‘champions’ were in place on each ward, they could use PIE to improve practice. This initiative too was affected by organisational upheaval and there was little indication over the course of fieldwork of diffusion of the dementia champions network and its reach into wards to improve practice.
Organisational context
In comparison with the other ‘partial implementers’, the organisational context on Netherton, and within which PIE was being introduced, was relatively stable and benign. A process of integration of the Elderly Care Directorate and Community Services was under way during interim data collection, and, although it involved senior ward staff in additional work, it was perceived as a welcome development.
Micro-system change at ward level was a perceived shift in the patient profile from baseline. During interim data collection, a persistent topic of staff informant conversations and interviews was that the patient profile had become more medically acute and physically dependent. As an ongoing presence on the ward, the researcher was conscious of the level of emotional and physical work undertaken by staff to maintain a proactive and responsive approach, to relieve and manage distress and agitation among people with delirium and dementia, and to sustain a relatively calm environment.
Patient data collected at interim supported staff perception of a change in the patient profile. The age and gender profile was similar for the two time periods, as was the prevalence of dementia (93% and 98%, respectively) and delirium on admission (80%). At interim, however, one-fifth of patients were admitted from long-term care, double that at baseline. The mean length of stay had also reduced, from 42 to 31 days. These indicators would tend to suggest a more dependent patient profile, a picture that was supported by research observation. Thus, fewer patients were seen routinely walking about on the ward than previously. Staff perceived that more of their patients were presenting challenging behaviour (acting out in anger at staff, shouting, and being unpredictable in their actions and interactions). Such a change was not discernible from fieldwork: at baseline also, staff were working with many patients with delirium and dementia whose agitation and distress escalated during late afternoon and at night. Furthermore, although the staffing complement was unchanged between baseline and interim, fieldwork indicated that during the morning and afternoon shifts, actual staffing was frequently down by one nurse, who typically had been moved to support a neighbouring ward. Qualitatively, many staff projected weariness in their body stance, which had been unnoticed during baseline. This might have reflected the timing of data collection phases: baseline occurred between mid-August and early November, whereas interim fieldwork was from the end of November to the beginning of February, a period of heightened demand on beds.
As indicated above, the problem of leadership as it had an impact on PIE implementation in Rivermead was shaped by turbulence in the trust. By summer 2014, organisational changes resulted in high work pressure on the ward as the effects of ward closures (30 beds across care of older people wards) percolated to ward level. Across the trust, the level of admissions was regarded as unprecedented. For ward staff and middle managers it meant an absence of ‘headroom’ for reflection and planning as ‘firefighting’ consumed the working day: ‘we’re so focused on the basics today that we have no time to look at tomorrow’. Work pressures contributed to reduced morale. It was also observed that sickness and staff vacancies had resulted in more extended use of Bank staff. In informant interviews, staff expressed hope that PIE would be picked up again when timing was more favourable. Work pressures persisted on Rivermead through interim data collection between January and March 2015, and several staff left, exacerbating staffing difficulties.
A further full CQC inspection in October 2014, reporting in April 2015, resulted in an overall assessment of ‘requiring improvement’. Governance and staffing levels were identified as issues to address. A reorganisation of middle and senior manager tiers was aimed at addressing the former; the persistence of recruitment difficulties contributed to further bed closures and ward reorganisation. In summer 2015, a decision was taken by senior managers to close Rivermead with immediate effect; the manager being informed the week before it was to take place. Over several weeks, concerted opposition from clinicians resulted in revision of the plans: the merger of two wards. As a strategy to retain staff with perceived expertise in care of older people and a resource built up over several years, it was unsuccessful. Many staff had already moved to other posts, and what had been a stable ward team dispersed. The end of Rivermead ward brought the research here to a conclusion.
Non-implementers
Creating local engagement with Person, Interactions and Environment
Based on their response to PIE, we characterised non-implementers as ‘tentative’: wards that expressed continued interest in PIE but timing for change was wrong; and ‘disengaged’, wards that did not engage with PIE after reassessment of the decision to proceed (i.e. ‘true’ non-implementers).
Tentative implementers
The three wards in Central Trust were ‘tentative’ implementers. Although two of them – Rose and Beech – took faltering steps to PIE installation, and the third – Denton – made no progress beyond the exploration and adoption stage, the factors that shaped their varied responses were the same.
Denton, a dementia ward, was established in early 2013 to provide support to people with dementia who were ‘medically fit’ but would benefit from ‘enhanced recovery’ (see Chapter 3). From a performance perspective, an additional objective was to facilitate the timely flow of patients from the acute wards of those deemed ‘challenging’ and either ‘unsafe’ to return home or likely to need long-term care placement. The staff team had been recruited for their knowledge and interest in working with people living with dementia, and care delivery, similar to that on Netherton, was person centred. From the outset, staff were enthused by the potential of PIE to enhance the care of people admitted to the ward. Shortly after fieldwork began, it became evident to the research team that its continued existence was uncertain. From one week to another, the site researcher was apprised of varied accounts of the future of the ward oscillating between closure, expansion and permanence. By the autumn of 2013, the dominant narrative was closure, ostensibly because of the lengthy stay of the patients admitted. Although work practices were directed at supporting individual patients, and staff in their own time pursued fundraising initiatives to enhance what they could offer, a consequence of the lack of a clear strategic vision for the ward at hospital and trust level was that goals for improvement were immediate to short term. Even so, the ward manager assumed the role of PIE ‘champion’, advocating with peers on Beech and Rose wards to engage with PIE, and took the lead in organising and facilitating PIE workshops.
Both Beech and Rose ward managers were open that knowledge of dementia among staff, and care of people with dementia on their corresponding wards, required improvement. Additionally, both wards were in transition. The Rose manager was new in post and was building relationships with the team; her Beech ward colleague, although very experienced, had assumed leadership of a new ward model and staff group. For her, forging a team ethos and ward culture was regarded as a work in progress. Both expressed interest in being actively involved in PIE.
These three, along with three staff from Rose, Beech and Denton wards, respectively, took part in a joint PIE workshop in early November 2013. The event sparked interest in using PIE. At its conclusion, all three ward managers arranged to meet and discuss how to work jointly to take PIE forward. They anticipated working collaboratively to support each other. There were potential difficulties: Beech had moved physical location and the manager had been informed that the ward purpose was changing from an acute medical facility to a step-down assessment unit. The perception of managers on these wards, and conveyed in informant accounts, was of decisions being discussed and pursued at trust and senior management levels, and the involvement of them at the point at which decisions had been arrived. Furthermore, changes could not be communicated to their staff until the decision had been actioned. Although the research remit did not extend to decision-making beyond the ward, staff on all three conveyed, in interviews and informant conversations, their sense of being continuously ‘acted on’ with regard to changes in their work roles and environments in which they had little input to shape. For the Beech ward manager, the proposed change in ward model was the third in as many years.
In some respects, Beech and Rose wards were unlikely implementers in that the scale of change required to improve practice was considerable. Even so, PIE was regarded as a lever to effect improvement. Following the workshop, Denton, Beech and Rose managers, working in pairs, undertook several practice observations on Beech and Rose, respectively. The research team offered a further workshop on action-planning, which was difficult to organise: Beech was in transition between an acute ward and step-down unit, maintaining both functions with a lower staff complement, and Denton’s future was uncertain. In spring 2014, the Denton ward manager confirmed that the decision to close the unit had been definitively made; Rose ward was also planned for future closure, and further changes to the Beech ward model were being planned. Staff on all three wards were reported to be demoralised and looking to move on: they were unable to continue with PIE.
Non-implementers: revisiting the exploration and adoption stage
In Valley Trust, the senior nurse for older people, and the intended ‘driver’ of PIE on both Ambridge and Oak wards, moved to a new post during baseline fieldwork. Although the research team sought to involve a staff member at a similar level, no one was identified. Facilitation support at ward level was not forthcoming either, in part reflecting staffing shortages on both wards. Two out of three introductory workshops organised for staff on both wards during January and February 2014 were poorly attended; a third was offered but cancelled on the day as staff could not be released. No senior ward staff were able to attend any of the workshops.
Feedback from the workshops posed the question as to how those attending perceived PIE: as an approach to engaging them in a process of change, or as training in dementia care. The first part, on the dementia experience, was perceived as valuable; the second, on implementing PIE, was not viewed as salient to their current concerns, namely getting through daily tasks with patients. For some participants, the gap between current practice and ‘person-centred’ care was so wide that improving care required basic knowledge and skills in dementia care to move forward; for others, the care they provided was as person-centred as it could be with the resources at their disposal.
Further attempts to organise workshops were unsuccessful, including pursuing negotiation at directorate level for support. Both ward managers indicated that PIE implementation was not possible; it was ‘out of time’. The current constellation of factors, staffing difficulties on both wards and senior staff moves on one, indicated that if circumstances changed, pursuing PIE might be possible. The research team agreed to contact ward managers later in the year. Over the following 6 months, the research team made several attempts to re-engage senior ward staff on both Oak and Ambridge: some had moved on, staffing difficulties persisted and the trust’s priority was dementia training with staff.
Similar to all recruited wards, ‘buy-in’ to PIE had been negotiated and ‘readiness’ criteria had been met. The departure of the senior nurse who was to drive PIE curtailed further engagement. Attempts to pursue PIE occurred, first through discussion at directorate level on how to identify a replacement ‘driver’, and then by returning to the stage of ‘exploration and adoption’ with ward managers. Neither was successful. Although the senior nurse had acted as a ‘change champion’ through the initial exploration and adoption stage, there was no one willing to assume this role on her departure. Whereas change ‘champions’ can play a pivotal role in facilitating innovation, their effectiveness also depends on whether or not they can harness networks of support to carry it through. 80,118 Regarding PIE, those networks did not survive the ‘champion’s departure, although here too there appeared a lack of resources at ward level to pursue a service improvement process requiring ‘headroom’ to action.
Cedar ward in City Trust, the companion ward to Rivermead, was the outcome of ward reorganisation, an amalgamation of medical and orthopaedic beds resulting from a reduction in beds within the hospital. A late entrant to the study within weeks of its creation, the task for senior ward staff was to construct a team and develop systems and mechanisms to deliver care to a new patient group.
Although a number of staff from the original older people’s ward had attended the PIE workshop, there was no further engagement at any level in PIE. As with Rivermead, the PIE driver had no capacity to lead the work, and the same demand pressures and organisational change at City Trust that had an impact on Rivermead also affected Cedar ward directly. Reflecting, the ward manager considered that the decision to take part in the research had involved an underestimation of the level of work involved in forging a new team, which, coupled with demand pressures, meant that ‘timing’ was not right. Although the ‘timeliness’ of an intervention is a feature of context receptivity in adoption, it has not been an explicit focus of research interest. 80 We suggest that although ‘timing’ is a relevant ‘readiness’ criterion in site selection, it does not determine successful implementation in the absence of a facilitative organisational context.
Summary
Only the Seaford trust wards had all of the conditions in place to effect PIE implementation. In essence, interaction between micro-level features at ward level and a facilitative organisational environment created the conditions for a receptive context for change on these wards. Elsewhere, organisational turbulence having multiple impacts at ward level resulted in an organisational environment that was unreceptive to change.
Chapter 6 Outcomes of Person, Interactions and Environment
Introduction
This chapter examines outcomes of PIE: in improving ward practice; in enabling a positive experience of care for people with dementia and their relatives/caregivers; and in providing preliminary evidence of effectiveness with regard to clinical outcomes (delirium and falls).
Person, Interactions and Environment implementation and practice change
On both Poplar and Crane wards, where full PIE adoption occurred, there were discernible changes to ward practice, directly attributable to the intervention. The experience of doing observation reinforced its value as a means to ‘see’ action and interaction in a different way:
It’s allowed us to step back and look at what we’re doing. ‘Cause when we’re right in the middle of it it’s all quite difficult, seeing what’s going on and what you should be doing.
Staff nurse, Poplar Ward
Senior staff also saw new ways of ‘seeing’, as indicated in the discussion with the dementia specialist team:
And it’s the good stuff that you don’t pick up unless you’re doing the observations and you realise – because you don’t have the time to see it.
Because you’re in the middle of it.
And you do see much more when you just step back and watch.
Dementia specialist nurses, PIE meeting December 2015
The observations heightened staff’s perceptions of what it was like to be a patient: ‘I didn’t realise the levels of noise and stuff around patients . . . or what an effect that has . . .’. At the heart of work initiated through PIE was an increasing awareness that patient experience should be at the centre of how staff worked. It reinforced the necessity for additional work by staff to facilitate a ‘connection’ with the person so as to pursue the work of ‘recovery’. Creating opportunities for communication between staff and patients in a ‘normal’ setting contributed to the collection of meaningful knowledge about the person. For example, on Poplar the practice of patients sitting around tables for lunch was a significant change resulting from PIE action plans. Observation and staff reports indicated that the broader objectives of the activity – to improve nutrition and to enhance social interaction and communication – were achieved. Staff reported that patients had better appetites and were socialising with others at the table, as well as benefiting from being mobilised more often by way of walking to the table. Social interchange in an informal environment enabled staff to discover new things about the person and pick up more information about individuals’ dietary likes and dislikes.
On Crane, similarly, the focus on nutrition led to regular ‘lunch-club-style’ events in the middle of bays, against the odds, given the restricted space. This resulted in improved communication between staff and patients; and more interaction between patients, albeit their exchanges were often largely incomprehensible to outsiders. Events such as the dementia cafés, held off-ward, provided opportunities for patients who were well enough to socialise in a convivial environment. Although not initiated through PIE, the provision of support to attend was integrated into PIE action plans.
The PIE process, observation and space to reflect collectively on practice, along with the observable changes that were set in train, gave staff confidence that they could make a difference, including those who were not directly involved in PIE teams.
I think it’s just made us more aware of what we can achieve . . . as the word has spread, there’s been more of an understanding.
HCA, follow-up, Poplar Ward
On both wards, staff felt able to challenge aspects of established practice, including those that involved other services, for example negotiating with external caterers to serve smaller portions and a wider selection of finger-food to support the nutritional intake of frail patients.
These practice changes represented steps forward, contributing to an enhanced patient experience. They had a positive impact on ward care culture in myriad ways even if not fully transformative of the care culture. Respectful, warm, task-focused communication practices still dominated in routine staff–patient encounters, particularly during busy periods, although staff’s responsiveness to patients’ emotional needs during tasks was also observed:
HCA returns to patient in bed 1 and pulls the curtains round. ‘Can you wash your face?’ she asks. Then ‘you’re a bit down in the dumps today, Ron. What are you thinking about?’ He says his wife. The HCA provides reassurance, reminds him his wife phoned yesterday and said she is coming in today . . . that she wanted a rest yesterday so couldn’t come. She asks the patient to stand up as she continues to help him wash. She encourages him to walk a few steps – ‘it will do you good’.
Field note, Crane Ward, interim, February 2015
Staff perceptions of Person, Interactions and Environment
Interviews with staff at the conclusion of the study showed that PIE had harnessed enthusiasm and engendered confidence, collaboration, a sense of empowerment and agency, including among unqualified staff, in trying out new ways of working. They also talked about the time pressures on them from increased throughput and higher patient dependency, both of which affected the time that they were able to spend with individual patients, thereby reinforcing the criticality of staff outside the ward in driving change. Given the timing (winter 2015), this probably reflected seasonal variation in demand, although the lengthening period during which ‘winter pressures’ beds remained open on most sites suggested ongoing high demand:
Because we’ve been really busy, we’ve had a lot more patients with higher needs and I think we’ve struggled . . . to achieve what we had been achieving . . . We come up with the ideas, but it needs someone [to say] ‘yes that’s OK let’s do that’ . . . Whereas if you’ve not got that support I think some of it might flounder.
HCA, Poplar Ward
Some staff were impatient at what they regarded as the slow speed of change. The lack of involvement of front-line staff in the Crane PIE team was a disappointment to some senior staff. Yet without the engagement of nurses and HCAs in pursuing action plans, PIE adoption would not have occurred and nor would its reach have gone beyond the PIE team. The Crane manager considered that PIE had stimulated reflection and action across the team as a whole, but that sustaining the process would necessitate renewal through the involvement of new staff in PIE. One proposal being considered at the conclusion of the study was to initiate new staff through the use of the observation tool alongside an experienced ‘observer’.
On both wards, plans were in train to continue PIE beyond the study conclusion. A further year on, PIE had been sustained in Crane, with the increased participation of front-line staff. The merger of Poplar with another ward encompassed plans to extend PIE to the joint ward.
Impact on patient and caregiver experience
From observation at baseline, we characterised care delivery on both wards as competent, caring and broadly responsive to people’s expressed needs, although time to respond was slower during busy periods (early to mid-morning and during mealtimes). There were staff who were particularly sensitive to the emotional needs of people with dementia, and used their knowledge of the person to anticipate and respond to those who were unable to communicate verbally. Openness to, and engagement with, families was distributed among all staff, from HCAs to ward managers, a collaborative, negotiated response to relatives and caregivers being an expectation of everyone. These features of care delivery contributed to a positive experience of care from patient case studies on both wards (six at baseline and five over the course of PIE implementation).
Experience of care
Without exception, patients and relatives at baseline described their experience of care in positive terms: staff were kind and responsive when patients needed assistance; and relatives indicated that staff made themselves available to discuss their concerns, kept them informed about what was happening and involved them in decisions about the future. In the detail, we get a more nuanced picture of both experiences in context of what was viewed as ‘good’ and variability in responding to preferences and needs.
Warmth and responsiveness
The characterisation of care delivery on both Seaford wards as ‘warm, sensitive and task focused’ was mirrored in the case studies. From observations and ‘conversations in the moment’, patients conveyed that staff were responsive to their requests for assistance but that they had also learned how to get a response, for example by ‘seizing the right moment’:
Well, I wait till I think they’re not busy. If they’re rushing, rushing backward and forward, I keep quiet. But if they’re just wandering, I’ll say, ‘nurse’, like that and they come over. But if I see them running then I wouldn’t because I think, well they’re off to do something important.
Rose, Poplar Ward
Lily, moved from a bay to one of the single rooms, similarly expressed the sense of being patient and seeking acknowledgement that she looked for help only when it was ‘important’:
I press my buzzer and if they don’t come there and then, I wait a bit longer and I have another press. Because I must realise they’ve got work elsewhere. So you just sit and wait until they can get to you. But it’s really . . . important you keep your finger on the buzzer; but I wouldn’t do that if it wasn’t important.
Lily, Poplar Ward
Iris had also moved from a bay to a single room – not of her choosing – and she had developed a meticillin-resistant Staphylococcus aureus (MRSA) type infection. Her daughter said that Iris had been very upset and agitated about the move but had settled after a while. Now she considered her mother to be content on the ward:
She was very frightened about coming in to hospital. It’s her one dread – being in hospital. I know it’s a terrible thing to say but this has actually done her good because it’s taken away her fear of hospitals now.
Iris’s daughter, Poplar Ward
John’s daughter-in-law talked about the lack of staff time spent directly sitting with patients. As a HCA in a residential care home, she acknowledged the importance of spending time with people but viewed this as requiring more staff on the ward as the nurses were so busy: ‘they’re always darting about quite a bit’, although they ‘always they do go out of their way to make sure that the patients are comfortable’ and ‘they come and make sure that we’re OK [relatives]’.
Other patients: source of disturbance, friendliness and reciprocal help
Being on a ward meant that proximity to other patients was a source of conviviality and disturbance. Women interviewed considered that ‘friendliness’ was important. They distinguished between liking to sit and talk with people, ‘being sociable’ and being ‘best friends’: ‘you get friendly . . . it’s not a good thing to try to make friends because it doesn’t last’. Daisy described her relationship with other patients as ‘vaguely to talk to’, but she had become good friends with Bessie. Conveyed in her account is a level of understanding and acceptance of others’ disorientation:
Bessie and I are quite good friends now . . . but I still haven’t found her husband though [Daisy laughs] . . . She does get in a muddle sometimes looking for Fred. She says: ‘where’s Fred?’
Daisy, Crane Ward
The conversation with Daisy was punctuated with her interjections to Bessie: ‘are you all right, Bessie’; ‘Careful Bessie . . . she doesn’t look safe’ [to the researcher].
Rose liked to sit with people and talk, ‘getting on’ but not being ‘close friends’. She was sanguine about other patients calling out:
You can look around at everything and think, ‘oh I wish they wouldn’t do that’. I don’t like the way they do that . . . but that’s only your personal opinion. I can’t judge what all these people think . . . There’s a lady, she does a lot of shouting . . . I think she’s a very disturbed person . . . but if you pull the clothes over your head and don’t listen, it’s OK . . . when they moan and groan there’s a reason for it . . . they’re unhappy . . . with myself I’m perfectly happy as things are [Rose laughs good-humouredly].
Rose, Poplar Ward
Lily had been moved to a single room from a bay because of disturbance from other patients, who she described as ‘rowdy and grumbly’. She felt better on her own: ‘it’s a rest’ [being in bed].
Men interviewed appeared less interested in the potential for conviviality and social interchange. John was moved to a single room: he was unable to sleep because another patient was shouting out during the night. His daughter-in-law would have preferred that he stayed in the bay for the company but understood that he preferred to be on his own. He found enjoyment in looking at the birds through the window; enjoyment in nature replicated how he spent time at home. Robert was happy to sit with people in the bay and found comfort in the routine: ‘I was in the medical corps in the war . . . it’s got to be run as a routine’.
Going home
Everyone wanted to resume life as before. Apart from Rose, who was to return to her care home, patients’ destinations were uncertain. It was not always clear from patients how much involvement they had with the decision about planning for discharge. In part this reflected memory difficulties. Rose hoped to return to her care home but indicated that she did not know when this would happen; her daughter reminded her that she was being discharged within a couple of days. There was a sense from patients’ talk that there had been discussion but that, ultimately, the decision was not in their hands; it rested elsewhere, not only with professionals but with close relatives. Thus, although Robert hoped to go back home, his relatives had talked to him of going into care:
I know they’ve been thinking of me going into another place where I could talk to other people and that . . . but . . . in some ways I would and others I wouldn’t.
Robert, Crane Ward
Lily was not sure how much longer she would be in hospital except that the doctor had said that she would be ready when she could walk a little way, adding, ‘they know better than me’.
Relatives, on the other hand, described how they were very much involved in the decision about discharge, a process perceived as emotional and conflicting in reconciling their relative’s wish to resume life as before with their deteriorating health.
Did Person, Interactions and Environment make a difference to patient experience?
The five patient case studies following PIE implementation were purposively selected to include those who were frailer as critical exemplars of patients perceived to be more challenging and therefore particularly testing of progress made. All had limited ability to communicate verbally, although this varied depending on the time of day, and they deteriorated over time.
Experience of care
Similar to baseline, relatives assessed care as very good: staff were described as kind and responsive, and available to discuss the carer’s problems and concerns. Emily’s daughter visited her mother daily: ‘If I only mention something to the nurses, it’s dealt with’. Acknowledged, too, was the significance of staff caring for her mother: ‘she doesn’t take much in. I don’t think they could do much more for her’.
Observation and conversation with patients revealed a deteriorating trajectory of inter-related physical and cognitive impairment. Frail when first encountered, these people alternately conveyed frustration at others not responding to them in relation to their conception of reality, and derived pleasure in the moment from encounters with others, including the researcher.
It was in respect of these patients that understanding of, and emotional engagement with, them ‘in their world’ was not consistent across staff on either ward, even though they generally acted with warmth and kindness in carrying out day-to-day tasks.
Dorette was French in origin but had lived in England for decades; she was often distressed, wanting to get to the train station, and had reverted to her first language. She called out frequently to be taken to ‘Gare St Lazare’, expressing anger and frustration in the absence of a response. Although some staff would talk with her about her life, others would ignore her. She evinced pleasure when staff spoke to her in French, smiling, apparently at their faltering efforts (including the site researcher’s) with the language. At other times she became angry when asked to do a task (e.g. changing her clothes when wet) as it would make her late for the train. Annie often shouted out in protest during routine observations or personal care work but was comforted by touch – holding her hand and stroking her hair – when distressed. Connie often expressed her desire to go home, get off the ward and catch a bus back home. When a staff member sat with her, she talked animatedly about the place where she grew up and had spent all her life and to where she talked of returning; she never spoke of the care home she had lived in for some time.
From observation, staff at follow-up appeared more responsive to patients’ embodied action as meaningful, and sought to address care needs. Thus, Emily, exemplifying the ‘unco-operative’ patient, repeatedly tried to pull out the intravenous line (for hydration), scratched staff when angry and was reluctant to eat and drink when assisted. Staff would sit with her, and discovered that fortified drinks and dessert were the only things that she would touch. As she transitioned to being unresponsive and sleeping most of the time, the work of ‘care’, including that relating to nutrition, hydration and elimination, became increasingly challenging to carry out; comfort through touch seemed all-important. For these patients, responding cognitively and emotionally to them ‘in their world’ also enabled care tasks to be completed.
These patients, with the exception of Connie, did not take part in mealtimes as ‘social events’; either they were too ill and in bed (Emily) or they did not want to do so. Connie was the exception, and she also enjoyed being taken to the dementia café. She was joyous at the music, joined in the singing and conveyed how much she loved being around the children who had come along from the local primary school. Returning to the ward, she became preoccupied again with getting the bus home and being taken to the bus stop.
These illustrative accounts attest to the challenge of working with patients whose hold on a ‘shared reality’ diminished,112 even while moments of pleasure and joy were experienced, facilitated through sensory and emotional engagement with others.
Declining trajectory: physical and cognitive
Cognitive deterioration among these patients was interlinked with physical decline. Within a week of her operation, Dorette was being assisted to walk with a walking frame and described as ‘medically fit’ for discharge on the ward round. Ten days subsequently, she was ‘poorly’, receiving blood transfusions, indicated that she was very tired and wanted to sleep all the time. In conversation with the researcher, she expressed a wish that she ‘had wings’ to take her home. Unable to stand, even with assistance, she lay in bed or was helped to sit on the chair by the bed. Repeated attempts by therapists to get her up and moving failed, further contributing to physical deterioration. This pattern in different forms applied to other patient case studies. Activities initiated through PIE, such as communal mealtimes, and opportunities for patient–patient and staff–patient interaction, occurred around them and they were too ill to take part. Emily and Annie died in hospital; Dorette and Beatrice were newly admitted to long-term care following 50 and 73 days’ hospital stay, respectively. Connie and Beatrice were still on the ward at the conclusion of fieldwork. It was planned that Beatrice would go to a nursing home when a suitable place was found; a different care home placement was being sought for Connie, as she was perceived as too dependent to return to her previous care home.
In summary, at each time point, patients (and close relatives) perceived staff as warm, caring and responsive. Patients were ‘forgiving’ of staff not always being available when needed, and spoke of choosing an opportune moment to ask for assistance. Ethnographic observation suggested that, apart from busy periods, patients were responded to quickly on both wards when they expressed a need, unlike on some other study wards. For relatives, that staff made themselves available, heard their concerns and addressed them inculcated trust in the care provided to their relative.
Observation indicated two aspects of practice that changed as a result of PIE with a positive impact on patient experience: enhanced sociability and sense of well-being from communal mealtimes; and pleasure and shared memories evoked by listening together at music sessions. For staff, these activities provided opportunities to acquire personally meaningful knowledge of the person to make sense of their behaviour and action and provide appropriate emotional support, realising the meaning of a ‘person-centred’ approach in their practice. For people with severe dementia, this ‘person-focused’ practice was more inconsistent within staff teams. Although all staff engaged with such patients with warmth and care, responding to the emotional needs of those whose sense of a shared reality had diminished required a level of knowledge and skill not shared by everyone – as well as time.
Clinical outcomes
Days in delirium
Before the research, none of the wards had routinely used a screening tool for delirium; although City Trust was considering introducing the SQiD,119 a single question asked of relatives to assess onset of increased confusion. The collection of DOS data was inconsistent. Unfortunately, although there were some data on days in delirium for both Seaford wards at baseline, none was collected at subsequent time points. Thus, on both Seaford wards at baseline, one-fifth of patients for whom DOS data were collected screened positive for delirium, although, for most of them, the number of days in delirium was small (median = 4 days). Mid-way during baseline, both wards stopped collecting DOS data, deeming this too onerous to pursue. On Crane (care of older people ward), most patients who had screened positive for delirium at baseline had dementia (75%); the proportion was small (30%) on Poplar (orthopaedic trauma ward).
Both partial implementer wards – Netherton and Rivermead – collected consistent DOS data at baseline and interim data collection points. Although neither proceeded far with PIE implementation, it is of interest to examine delirium rates on both wards in order to highlight some challenges in collecting and interpreting results. Table 12 reports delirium rates at both time points.
| Outcome | Time point | |||
|---|---|---|---|---|
| Netherton ward | Rivermead ward | |||
| Baseline | Interim | Baseline | Interim | |
| Patients with delirium on admission to ward, n/N (%) | 31/52 (60) | 66/87 (76) | 24/123 (20) | 33/110 (30) |
| Patients with delirium during their stay on the ward, n/N (%) | 54/75 (70) | 75/87 (86) | 64/110 (59) | 72/110 (66) |
| Days in delirium, median (range) | 16 (1–57) | 20 (1–44) | 10 (1–27) | 9 (1–27) |
| Patients ≥ 30 days in delirium (n) | 7 | 6 | – | – |
Delirium occurrence (on admission and during inpatient stay) was considerably higher on Netherton than on Rivermead, which was unsurprising as most patients admitted had dementia (the few who did not had been assessed as having delirium). The co-occurrence of delirium and dementia was evident from patient profiles for all participating wards (see Chapter 3). Further people with dementia are at particular risk of developing delirium. 36,94,95 However, from multiple sources of data (observation, patient case studies), we found that care quality for people with dementia on Netherton was consistently high. Most people during their admission experienced delirium at some point, including the small number who were not admitted with it. The number of patients experiencing extended delirium (≥ 30 days) was very small and was similar across time points.
Although the overall number of patients with incident delirium across time points is too small to draw inferences about the relationship with care quality, the results highlight the scale of the problem of delirium among this ‘at-risk’ group, given the level of distress caused to patients120–122 and the challenges in providing appropriate care as a consequence. To make meaningful inferences about the relationship between delirium and care delivery would require the collection of delirium data over a longer period of time pre and post intervention with a sufficient sample size to make the necessary adjustments to reflect varying levels of risk.
Falls
Similar to delirium, falls data were not collected consistently in Seaford wards. Table 13 provides the number and rate of reported falls per 1000 occupied bed-days for Netherton and Rivermead wards at baseline and interim.
| Outcome | Time point | |||
|---|---|---|---|---|
| Netherton Ward | Rivermead Ward | |||
| Baseline | Interim | Baseline | Interim | |
| Falls per 1000 occupied bed-days (n) | 9 | 27 | 25 | 18 |
As discussed (see Chapter 2), risk factors for falls not only relate to the actions of staff, but patient-specific factors are also implicated, including advanced older age, dementia, delirium and frailty, as are practices regarding rehabilitation. 101 Furthermore, the pattern of falls fluctuates, and it is argued that pre- and post-intervention data need to be collected over ≥ 9 months to deal with potential confounders resulting from changes in staffing, case mix, activity or recording practices. 101 The threefold increase in the falls rate in Netherton, for example, between baseline and interim is likely to reflect the more dependent patient profile than at baseline. Field notes during interim did not indicate that the quality of care delivered had deteriorated. Similarly, the reported reduction in the rate of falls on Rivermead at interim does not, from observational data, imply that the quality of care had improved; rather, staffing difficulties that placed increased pressures on ward staff suggested that staff were able to spend less time with patients with dementia at interim. The multiple and interacting risk factors for falls (as for delirium) present considerable challenges in drawing inferences about the impact of an intervention to improve care delivery on falls rate. Here, also, larger samples to deal with confounders, and a longer timespan for data collection to take account of seasonal and case-mix variation, would be necessary to detect meaningful change.
Summary
On both wards in which PIE was fully adopted, real, observable practice changes occurred, and these were sustained over time. There was evidence that the care experience of some patients who benefited from the practice changes improved, although the most visible changes did not have an impact on those who were too ill to take part. We cannot draw any conclusions about the impact on clinical outcomes as neither of the full implementer wards collected consistent data on delirium or falls. From the literature, and from the examination of falls and delirium in the partial implementer wards, we can conclude that although these outcomes are relevant to explore as indicators of care quality, meaningful interpretation of their impact would require considerably larger patient samples, collected over a more extended before-and-after period to take account of confounders.
Chapter 7 Discussion and conclusions
Introduction
The research aim was to evaluate PIE as an intervention to improve the care of people living with dementia on acute hospital wards, effecting care that was more person-centred. The objectives were to understand how PIE worked in acute care (process of change) and what contributed to its success (or not); to examine its effectiveness in changing staff practices, thereby improving the patient and caregiver experience; and to seek preliminary evidence of its impact on selected clinical outcomes (delirium and falls). An additional objective was to develop insight into what person-centred care might look like in practice in an acute hospital setting.
When our research began in 2013, the timing seemed propitious. There was renewed UK policy impetus on improving care quality for people with dementia, including on acute hospital wards, resulting in national performance targets on identifying people with dementia and improving staff knowledge and skills of staff through training. 1–4,9 The findings of the first national audit of dementia in general hospitals provided a spur to trusts to make improving care of people with dementia a strategic priority. At the same time, there was uncertainty about the impact of major structural and organisational change in the NHS alongside ongoing challenges: achieving continuous improvements in performance, quality of care and the hospital environment; identifying efficiency savings; managing the impact of reductions in social care provision on patient flow; and responding to year-on-year increased demand with reduced income growth. Both sets of challenges found expression within participating trusts and wards in the context of local history, health and social care economy and relationships, and economic situation.
Discussion
Patients with dementia on acute wards: the challenge for care providers
The patient profile on wards dominated by older people (dementia, care of older people and orthogeriatric wards) revealed the scale of the challenge in acute hospitals to improve the care of people with dementia. People with a cognitive impairment, including delirium, constituted at least half of the patient profile. Many had moderate to severe impairment; they lacked the ability to communicate verbally, and required assistance with personal care and active support with eating and drinking. On every ward there were patients who called out repeatedly, seemingly in deep distress. Acute care for people living with dementia, therefore, cannot be conceived of as peripheral to, or disruptive of, the routine work of ward staff, but is a central feature of it. 23,24,29,30 As well as the health event that precipitated acute admission, these patients were in advanced older age and had multiple health problems; they were physically frail and had care networks that were often fragile. Achieving a ‘balance of care’54 in an acute setting required the delivery of clinical, therapeutic and personal care based on an understanding of the interaction between these multiple and complex needs, including cognitive impairment, and how they mediated the process of recovery. Although all participating wards had introduced training in caring for people with dementia, the level of skill required to respond to the complexity of need of their patient profile was not generally addressed on these programmes.
On all wards, medical, nursing and care work was generally perceived by staff as rewarding, physically hard, emotionally taxing and demanding of specific skills, expertise and knowledge of dementia and delirium. Some staff on most general wards (i.e. not the dementia wards) felt ill-equipped in terms of training and resources to provide appropriate support. They conveyed a gap between a broadly supportive and engaging staff culture at ward level and ambiguity and tensions between competing priorities at the level of the hospital that affected their day-to-day working practices. The width of the gap varied considerably between trusts.
Three out of 10 wards did not attain the RCN staff-to-patient ratio for safe working on older people’s wards,123 namely eight staff for 28 beds, a ratio of 1 : 3.5. Most did not meet the recommended ratio of registered nurse to HCA of 65 : 35. The picture was bleaker than this suggests in that, on several wards, the staff complement was maintained only through the extensive use of Bank and agency staff, with consequences for staff morale, the sustainability of a coherent care culture and the availability of ‘headroom’ to engage in service improvement. Of the two wards that successfully implemented PIE, both had a relatively generous staff complement, a ratio of registered staff to patients of 1 : 5.6 (Poplar) and 1 : 4.4 (Crane), although here, too, staff were often moved to support other wards when numbers were depleted.
Across most wards, environmental changes to create more ‘dementia-friendly’ spaces had occurred, making for more attractive environments that were easier to navigate. However, communal or patient space was extremely limited, and the layout of some wards meant that the scope for movement of patients to recover or sustain mobility was restricted.
‘Person-centred’ care: meaning, content and practice
Meaning and content
’Person-centred’ care in UK health policy has, over nearly two decades, set the standard for care quality. In health policy discourse, the concept has become a portmanteau term with multiple meanings, for example ‘individualised care’, ‘seeing the person and not the medical condition’, ‘tailoring care around the person’ and care that accords dignity and respect (see Appendix 1). Furthermore, there has been varied policy emphasis at different times on particular aspects or dimensions of ‘person-centred’ care, currently ‘compassionate care’. 113,114,124
There is a similar lack of consensus on the meaning of person-centred care from research. Although theoretical conceptions of personhood and person-centred care in dementia provide a powerful value base to inform practice,44–48 there is a dearth of research on what practice might actually look like for people living with dementia in acute care,49,115 as most such research has been undertaken in long-term care. Yet care delivery in acute hospitals has specific purposes (treatment and recovery); the physical environment is intended as a temporary and ordered space geared to these purposes; and relationships within the setting, although of major significance, are short term and transient. An important aspect of this study is the insight provided on the dimensions of care practice on acute wards that has the person with dementia at its centre, the knowledge and skills that underpin them, and the organisational and cultural factors that are necessary to support them.
Practice
Staff understanding of person-centred care was consistent with the multiple descriptions and explanations of ‘person-centeredness’ in the policy and research literature. It was variously referred to as ‘individualised care’, ‘seeing the person and not the medical condition’ and ‘tailoring care around the person’. For most staff, it denoted ‘good practice’ or ‘quality care’, which staff aspired to deliver to all patients and not only to those with a cognitive impairment. The extent to which the aspiration could be translated into ward work was viewed as constrained by the pressures of demand, resources of time and staffing and operational priorities, mostly external to the ward and outside their immediate control. Organisational constraints on spending time with patients were real and included the legitimacy attached to such work by middle managers negotiating between competing national, local and organisational priorities.
Comparing how care was actually accomplished, we discerned a continuum of practices supportive of, or barriers to, sustaining personhood, and the organisational, spatial and care environment factors that shaped them.
Although the literature adopts a binary conception of person-centred versus task-focused communication, we delineated between more differentiated styles of communication that we termed as follows: personally meaningful and engaging with the person; respectful, warm, task focused; minimal verbal exchange; and communication unresponsive to patients’ expressed emotion. These reflected more of a continuum than fixed points. On most wards, the style was mixed, albeit dominated by warm, respectful and task-focused communication.
A ‘personally meaningful’ communication style required the ability to make an imaginative connection cognitively and emotionally with how the person might be experiencing the ‘social world’. This has been variously referred to as ‘caring imagination’125 and ‘embodied selfhood’. 50,51 For some staff, this was developed through personal knowledge of dementia; for others this was through advanced learning and professional experience. ‘Imaginative connection’ with the person was seen to involve time and effort to ‘see’ and make sense of non-verbal communication and emotion126 and to understand such embodied communication as meaningful, a source of agency20,54 and reflective of personhood even where linguistic ability was lost. At the other end of the spectrum, minimal engagement and communication that was unresponsive to expressed emotion typified an approach that viewed the person with dementia as ‘other’, and without agency. A critical point was that these observed methods of communication were preformed and were not influenced or shaped by PIE.
The multiple needs of this patient profile on hospital wards required nursing, therapy and care work that embraced such tasks as administering medication, assisting with toileting, nutrition and hydration and supporting mobilisation. In the conduct of such tasks, we delineated approaches to practice that were responsive and supportive of recovery in respect of people with dementia. These are termed anticipatory; enabling; and sensitivity to the emotional significance of practical needs. Knowledge of the person, including routines, preferences, anxieties and ways of communicating need, facilitated an anticipatory response to a practical need, particularly when the person was unable to communicate verbally. Providing assistance in a way that built on the person’s level of competence increased their confidence and was supportive of independent action. A further feature of a responsive approach was sensitivity to the emotional significance of expressed need. For example, need for assistance with personal care tasks such as toileting is not comparable with help with picking up a paper from the floor: it has symbolic and emotional meaning in terms of control over basic personal care tasks, as well as ‘being’ and feeling ‘clean’. In contrast to anticipatory, enabling and emotionally responsive approaches to tasks were approaches in which completion of the task was the sole object of the work such that the person was treated as ‘object’.
Responsiveness to the needs of people with dementia also required particular knowledge and skills relating to dementia and how it affected the person. This recognised that there was an element of uncertainty and unpredictability about how the person would respond in a given situation such that strategies to engage him or her were emergent, built up through trial and error and likely to involve creative, tailor-made solutions. This practice knowledge and skill was often what ward staff, particularly those providing direct care, reported that they lacked. The application of general values to sustaining personhood, we would argue, does not provide a sufficient guide to practice in acute care settings in the absence of a ‘caring imagination’ and dementia-specific knowledge and skills. Although these dimensions of practice are not necessarily exhaustive, they were sufficiently sensitive to differentiate study wards, suggesting a continuum of supportive practices and the factors that contributed to them.
Implementing Person, Interactions and Environment: interaction of micro-, meso- and macro-level factors
Despite the gap between the quality of health care that patients should receive and what actually happens, programmes to secure improvements in care quality have demonstrated inconsistent, variable and patchy results. 116,127,128 This in part reflects the fact that such interventions are more appropriately construed as events in multilayered and interacting systems, meaning that the organisational, political and social contexts in which the intervention is located are not simply background noise; they are part of the programme of change74,89,90,116,129–131 and interact with it. Other features of complexity include the multiplicity of programme components and their dynamic and emergent nature such that different groups interact with programmes in different ways.
PIE was fully adopted in only two out of 10 study wards, and had proceeded to innovation and sustainability in those two. To explore why some wards adopted PIE and others did so only partially or not at all, we examined the relationship between what was intended to happen and what actually happened, and the interface with the organisational context over time, using a stages-of-implementation framework. 69
Micro-level facilitators of and barriers to change
The factors contributing to the failure to proceed with PIE adoption were multiple and interactive. At a micro ward level they included leadership and stakeholder engagement, ‘fit’ with strategic priorities and the perceived salience of PIE to achieve valued goals.
Drivers, facilitators, teams and networks
Engagement in PIE from initial implementation through innovation to sustainability required active leadership outside the day-to-day demands of managing a ward; facilitative support and encouragement from senior ward staff; and collective team involvement to make change happen. These dimensions of PIE leadership and stakeholder engagement provided the necessary levers of change: key individuals beyond the ward whose professional authority and vertical networks legitimated the priority attached to the work of improvement in the face of competing priorities; senior ward staff facilitating and encouraging direct involvement in the change process and in ensuring that planned changes were communicated to the wider staff team; and implementation team members with respect of their peers to extend the reach of the intervention to the ward. Only in Poplar and Crane were all of these elements in place; the absence of one or more of them contributed to the failure to proceed to full adoption.
The conception of ‘facilitation’ in our study differs from that projected in some frameworks for implementing change, for example PARiHS (Promoting Action on Research Implementation in Health Services)132–134 and practice development,135–137 both of which place emphasis on skilled facilitation in effecting change. Here, the ward manager as facilitator did not ‘drive’ implementation but played a critical role in extending its reach to the whole ward, which was necessary to effect practice change.
‘Fit’ with strategic priorities
PIE was not the only initiative aimed at improving the care of people with dementia under way in participating trusts. In Seaford, there was heavy investment at strategic trust level with the establishment of a team of three specialist dementia matrons in early 2013, attached to each of three district general hospitals in the trust, including the two wards in our study. They worked directly with ward staff to mirror good practice in dementia care, provided support and in-depth training around communication and in anticipating and responding to challenging behaviour, and engaged in high-level organisational changes at trust level (e.g. developing dementia pathways). From the outset, the dementia specialists embraced PIE as one vehicle through which to pursue practice change; the team lead acted as ‘driver’ of PIE in one ward and one of the dementia nurses actively supported PIE in the other. The lead specialist matron had both seniority and a direct line to the senior management team, and provided a conduit between senior managers and the ward in both directions, securing high-level commitment and resource for local PIE initiatives; these in turn were celebrated as exemplars of the wider strategy in action. In this respect, PIE and the trust dementia strategy were synergistic.
In other trusts (City and Ironbridge), a high-level priority, and one centrally driven, was the creation of dementia champions and the initiation of awareness training for staff at all levels around dementia. The role appears to have been variously interpreted: from increasing awareness of dementia within a work arena; as a mirror of good practice vis-à-vis colleagues; and as a change mechanism within a workplace. How the recruitment of ‘champions’ would translate into a means of changing practice at ward level was not clear; however, the conception underpinning the approach was that the creation of a wide network of ‘champions’, who would meet together at intervals, would lead to change at workplace level. In City, the matron who had championed PIE envisaged that the initiative would feed into the use of PIE at ward level, a vision that was not necessarily shared among those involved in developing the dementia strategy. For staff on Netherton, the champions initiative appeared diffuse and lacking in depth and impact. Furthermore, as the initial focus of the initiative was on raising general awareness of dementia, this was not seen to address staff perception of the problem, namely how ward staff were to be provided with the skills necessary to work with challenging patients.
Salience of Person, Interactions and Environment to achieve valued goals
Focus of PIE in addressing practice change generated interest and enthusiasm among staff on wards that varied in the quality of care and, therefore, scope for practice change. In both wards in Seaford, the process of PIE implementation engendered confidence, collaboration, a sense of empowerment and agency among the staff group, including among HCAs in trying out new ways of working. Positive change was visible and in turn acted as a spur to keep going.
Among ‘partial’ implementers, PIE was embraced enthusiastically at the outset. In Netherton, observation reinforced pride among the staff team of the general quality of care provided. Herein lay the difficulty. Translating observations into action plans that addressed valued goals proved more difficult. What was not articulated in the beginning was that the prime goal of senior staff was a reduction in the size of the ward and an increase in staff time to provide stimulating activities. Neither of these goals were, seen as actions that could be pursued through PIE. This poses the question of whether or not there exists a quality ‘ceiling’ effect in terms of a ‘person-focused’ approach within the constraints of acute care delivery. Additionally, within this ward, there existed a team culture and routine systems and mechanisms to engage in deliberative practice reflection to secure quality improvement; apart from observation, the additional work of PIE seemed superfluous.
Enthusiasm and interest in improving practice also required supportive environments to sustain belief in staff agency to affect change so that investment of time and resources was seen as worthwhile. Demand pressures and organisational uncertainty dampened both, evident not only in Rivermead but in all three Central Trust wards.
Meso- and macro-level facilitators/barriers to change
Organisational turbulence
Features of leadership and fit with strategic priorities were local expressions of forces operating at meso and macro levels. Although our starting point was understanding that organisations in which interventions are inserted are dynamic, what was surprising was the degree of organisational instability and turbulence encountered in the study and the impact of decision-making and action at senior and middle management on the capacity of staff at ward level to engage in change.
Although all participating wards experienced staff shortages and demand pressures, two wards experienced a level of staff shortages and service delivery pressures that affected the resources available to provide the headroom to pursue service improvement. For example, on the non-implementer Valley Trust wards, there was an absence of all aspects of leadership when the research commenced. Although ‘buy-in’ at ward and directorate levels to engage with PIE had been negotiated at the outset, the departure of the senior nurse during fieldwork, who had championed PIE participation during baseline fieldwork, stalled and then curtailed further engagement, resulting in the withdrawal of both wards prior to PIE installation. This was one facet of a deeper organisational problem. Although change ‘champions’ who are in a position to harness support within an organisation can play a pivotal role in leading change,80,118 personal influence may not outlast individuals in the absence of organisational support. PIE found no resonance at either ward or middle management levels: ward staff had neither the headroom to pursue service improvement nor the support from middle managers, whose priority was on managing performance, demand and patient flow. 138,139
Four out of the 10 wards closed during the research, either suddenly or over a protracted period. In Rivermead, closure was sudden, within 1 week of being announced, part of a major reorganisation of ward models and bed reductions in response to a staffing shortage and financial restructuring. The same factors had contributed to the absence of a PIE ‘driver’ on this ward to support implementation. With Denton, Beech and Rose wards, remodelling and closure occurred over a protracted period, during which proposals shifted and changed, demonstrating a lack of clarity and transparency in decision-making at executive and senior management level, and sapping the morale and motivation of staff to future plan, critical to the pursuance of a care improvement initiative.
Cedar Ward in City Trust differed from these others in one respect. It was formed as result of ward remodelling, an amalgamation of medical and orthopaedic beds resulting from a reduction in the hospital bed base. Cedar was a late entrant to the study within weeks of its creation, and the ward manager considered, in retrospect, that their priority had been to construct a team and to develop systems and mechanisms to deliver care to a new patient group, and that PIE implementation was ‘out of time’. Although the ‘timeliness’ of an intervention is a feature of context receptivity in adoption, it has not been an explicit focus of research interest. 80 We suggest that, although ‘timing’ is a relevant ‘readiness’ criterion for site selection, it does not determine successful implementation in the absence of a facilitative organisational context, as the experience of Rivermead, the second ward in this trust, attests.
In a programme of research on quality and safety in the NHS,139 the authors concluded that success in implementing quality improvement initiatives required that the process was adequately resourced. This included time for staff involvement in changing practices and acknowledgement of the effort, expertise and investment necessary to make such approaches work. We would further argue that time and investment of energy, enthusiasm and commitment requires cognitive and emotional space to plan and work towards an aspired future, difficult if not impossible to mobilise in context of organisational uncertainty and staff disengagement and disempowerment. These findings also reinforce the conception of interventions as ‘events in systems that either leave a lasting footprint or wash out depending on how well the dynamic properties of the system are harnessed’50 or equally, as here, where factors at organisational level act as barriers to engagement in a change process at the front line. The corollary is that ‘readiness’ to engage in service improvement initiatives requires a better understanding of ‘receptive contexts’. 140
Normalisation process theory
Normalisation process theory offered a useful framework to consider what might be the components of the PIE change process. However, even on successful implementer wards, strategies to generate mechanisms of change (coherence, cognitive participation, collective action and reflexive monitoring) needed to occur at multiple levels. Here, ward managers as change facilitators played a crucial role in engaging staff beyond the implementation teams in PIE, using routine communication mechanisms (handover and team meetings) to ensure their ‘buy-in’. Furthermore, ‘buy-in’ at all levels was not achieved once and for all. The dynamic nature of ward environments meant that, for PIE adoption to proceed, PIE teams were confronted with the task of developing systems for the renewal of staff engagement in sustaining the programme. The experience of ‘partial’ implementers also attests to the fact that the generative mechanisms hypothesised in NPT require ‘receptive’ organisational contexts to effect routinisation (i.e. they do not work in isolation).
Impact and outcomes of Person, Interactions and Environment
Evidence from observation and staff interviews on both full adoption wards suggests that the PIE Programme had a significant impact on practice. Specific changes, as for example, communal meals, increased staff knowledge of patients, staff–patient interaction, patient–patient interaction and nutrition intake, were introduced. Observation and interviews indicated that providing opportunities for patients to socialise facilitated patients conversing with each other as well as with staff. Although the content of patient–patient conversation was not always meaningful to the observer, it conveyed a sense of warmth, conviviality and sociability that was absent on other wards, and similar to what occurred on the dementia wards through communal dining. It reinforced the ‘friendliness’ and ‘looking out’ for each other expressed by some patients with their fellows, and was of demonstrable benefit. 141,142
There was also evidence that practice change had a positive impact on the experience of patients and caregivers, although the heterogeneity of need and severity of impairment meant that some of the more visible changes did not affect everyone equally. Indeed, findings throw into relief the varied needs of patients on acute wards living with dementia: opportunities for social interaction and activities may be valued by some but not all; for others, the use of touch and emotional connection with the person in ‘their world’ involving time spent in one-to-one contact may be more appropriate.
We are unable to draw any conclusions about the effect of PIE on clinical outcomes, as data on delirium and falls were not collected on these wards.
Learning from Person, Interactions and Environment implementation
Within the full adoption wards, PIE was effective in identifying a need for change and providing a systematic method to pursue action-planning and appraisal where organisational supports were in place. Observations generated creative solutions to address multiple issues simultaneously; action plans established a stream of work from small steps through the appraisal process; and the bottom-up/top-down approach enhanced sustainability and reach. 138
There are aspects of learning from the research and experience of PIE implementation to incorporate into refinements of the guidance and tools. First, the dimensions of person-focused practice from the research relating to communication, tasks and managing distress may provide an explicit focus for service improvement, albeit without constraining the flexibility and creativity of implementers. Second, the content of some of the PIE documentation may be simplified without undermining its function in the process. Thus, the distinction made in the action-planning documentation between short-, medium- and long-term action plans appeared unnecessarily complicated and unhelpful. A key factor in teams getting going and keeping going was identifying goals and priorities around which staff could be mobilised to act. Indeed, the difference between short-, medium- and long-term action plans is likely to be in the number of steps required to achieve longer-term goals. At the same time, progress in working through the steps to achieve a longer-term goal may involve a reassessment/review of the goal and/or how to pursue it. Third, while some simplification of the documentation is suggested, we consider that completion of observation, action-planning and review tools through initial and full implementation is helpful in systematising engagement with the process, as others have argued. 74 Fourth, it became evident early on that additional support and guidance to translate observations and reflections into action plans was required and provided, requiring the expansion of this part of the manual.
Generalisability of Person, Interactions and Environment
Is the PIE method too difficult for widespread use on acute wards? Would an alternative approach to service improvement be more effective? It is difficult to draw clear conclusions here. On the one hand, there is little research on what strategies for implementing innovations work in health settings or which work better for which kind of intervention. A compilation of implementation strategies143 identified nearly 70, of which most complex interventions involve several in combination (as in PIE).
One strategy for improving care delivery, and a key element of the national dementia strategy, is the provision of staff training. There has been considerable investment in training staff in the care of people with dementia in hospital. Between the first and second national audits of dementia in general hospitals in England and Wales,25,26 there had been a threefold improvement in the proportion of hospitals with a training and knowledge framework in place to identify the skills required of staff to work with and care for people with dementia (from one-quarter to just over three-quarters of hospitals). However, a recently published review144 of training for hospital staff concluded that of the 14 studies identified relating to 10 training programmes (four were a repeat of the original interventions with amendments), all except four evaluated learning, staff attitudes and confidence. The four that examined changes in practice relied only on staff self-reported data. Similarly, there were no studies that assessed patient and family members’ experience of care following training. Most studies employed pre- and post-research designs, and the methodological quality was rated as mixed. The authors concluded that the evidence of effectiveness of training on changing care practice and influencing patient outcomes was very limited. Another strategy highlighted in the national audits25,26 is the introduction of dementia champions. The second audit26 concluded that although the vast majority of hospitals (82%) had a champion for dementia at directorate level, and around three-quarters of hospitals had a champion at ward level, there was a dearth of evidence as to the impact of such roles on day-to-day practice. The report concluded that focus of attention in future audits should be on practice and not only systems and strategies.
Conclusions and limitations
PIE has the potential to improve the care of older people living with dementia on acute wards when implemented. However, findings are indicative for two reasons. First, as data on delirium and falls were not systematically collected on wards where PIE was implemented, there is no evidence of whether or not the programme is effective in improving clinical outcomes. Second, although PIE worked as intended on two wards to effect change in practice, it was not adopted in most study wards.
Research implications
Several broad areas for further research are indicated.
The combined and interactive effect of advanced older age, dementia exacerbated by delirium, chronic health problems and acute events presents enormous challenges for staff in providing quality care. There is pressing need for further research to identify more precisely the skill mix and resources necessary to provide person-focused care to this frail patient group across the spectrum of acute medical, functional, therapeutic and supportive needs. At the same time, more insight is required about the recovery trajectories of patients with such complex and multidimensional needs, and the contingencies that affect and shape them, in order to provide the most appropriate place and type of care to facilitate recovery.
Implementing innovations to change practices in complex organisations, such as acute wards, requires more in-depth understanding of contextual factors that affect the capacity of organisations to absorb and embed new practices. Longitudinal research that examines the dynamic between interventions and the environments in which they are inserted is needed. In particular, we require understanding of what are ‘receptive change’ contexts, suggesting a parallel line of investigation to that focusing on application of theories to the development and implementation of interventions to secure service improvement.
Acknowledgements
We are extremely grateful to the NHS organisations that took part in the study. The requirements of anonymity mean that we cannot name them; only they know who they are. They include the managers, research and development staff and local collaborators who opened the door to the research, negotiated with wards to participate and in different ways facilitated the research. Without their invaluable support, the study would not have been possible.
To the ward managers and staff and patients in our participating wards, we owe an enormous debt of gratitude. Invariably, they made us welcome, tolerated and facilitated our ongoing presence even though being observed must have felt difficult and intrusive at times, plied us with cups of tea to keep us going and answered our questions on the hoof with patience, interest and good humour, despite being often inordinately stretched and busy. We are also very appreciative of those staff who gave their time to take part in interviews and complete questionnaires, thereby sharing their views and experiences with us.
We felt privileged to share the experiences of patients and their relatives; we learned an enormous amount from our observations and conversations ‘in the moment’ and hope that we can convey some of that through this report.
Our final group of research participants were those who took part in the PIE Programme; we are so grateful to those who put effort, vision and creative energy into the process of implementation.
Finally, the research team want to thank those members of our Programme Management Group who contributed enormously to the development and conduct of the research at different time points:
Jill Clayton is a senior nurse with older people who has considerable practice and professional development expertise in respect of the care of people with dementia. She was closely involved in the development of the PIE observation tool for the National Audit of Dementia, was joint lead on the workshops provided for stakeholders across all sites in this research study, and shared her knowledge with the research team both within Programme Management Group meetings and on the many train journeys we took together to run the PIE workshops.
Chloe Hood is the programme manager for the National Dementia Audits and for the Quality Mark in Elder Friendly Hospital Wards under the auspices of the Royal College of Psychiatrists. She was involved in the conception of the study and in the early work to develop the PIE Programme, particularly the action-planning element. She contributed to Programme Management Group meetings, including sharing her experience of the Quality Mark initiative.
Anabella Padilla-Lamb from the Alzheimer’s Society Research Network provided valuable advice and input to our Programme Management Group, ensuring that the voice of caregivers and of people living with dementia remained at the heart of the research.
Finally, thanks go to our study advisory group members [Professor Gillian Parker (University of York); Professor Francine Cheater (University of East Anglia); Trevor Jarvis, Dementia Ambassador; and Anne Jarvis] for their invaluable contribution and support during the research.
Contributions of authors
Ms Mary Godfrey has expertise in qualitative research and experience in mixed-methods studies involving the development and evaluation of complex interventions. She was involved in all aspects of the study from inception to completion, including drafting and editing all sections of the final report.
Professor John Young is an academic geriatrician with expertise in multimethod research designs including randomised controlled trials, systematic reviews, and qualitative and health economic studies relating to older people. He is on the steering group for the National Dementia Audits. Professor Young was chief investigator and involved in all aspects of the study from inception to completion, including editing all sections of the report.
Ms Rosemary Shannon is a health services researcher with experience of conducting mixed-methods studies and expertise in qualitative research methods. She was involved in data collection and analysis in three trusts, drafting sections of the report and editing all sections.
Dr Ann Skingley is a health services researcher with expertise in qualitative research and a disciplinary nursing background. She was involved in data collection and analysis in one trust, drafting sections of the report and editing all sections.
Ms Rosemary Woolley was a senior research fellow in the Academic Unit of Elderly Care and Rehabilitation and project manager of the research until November 2015. She had been involved in the development of the PIE observation tool for use in the National Dementia Audit. She was involved in the conception of the study and in data collection and analysis in two hospitals until leaving on account of illness.
Mr Frank Arrojo is a research network volunteer for the Alzheimer’s Society with experience of a close relative living with dementia. He contributed to the study conception and to Programme Management Group meetings and commented on the final report.
Professor Dawn Brooker has an international reputation in the field of person-centred care service development for people with dementia. She was involved in protocol development and contributed to Programme Management Group meetings and to the final report.
Professor Kim Manley has an international reputation for the development of effective workplace cultures in health care linked to the provision of quality services that are person centred. She has extensive experience in participatory action research and the use of observation tools to change practice. She has been a Steering Group Member for the National Audit of Dementia. She contributed to all aspects of the research including edits of the final report.
Professor Claire Surr is an expert in dementia care mapping and was instrumental in the development of Dementia Care Mapping (DCM) 8. She was involved in protocol development, and contributed to Programme Management Group meetings and to edits of the final report.
Data sharing statement
This is a qualitative study and therefore the data generated are not suitable for sharing beyond those contained within the report. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Living Well With Dementia: A National Dementia Strategy. London: Department of Health; 2009.
- 1000 Lives+: Improving Dementia Care. Cardiff: NHS Wales; 2010.
- Healthcare Quality Strategy for NHS Scotland. Edinburgh: Scottish Government; 2010.
- Scotland’s National Dementia Strategy 2013–2016. Edinburgh: Scottish Government; 2013.
- Alzheimer Europe . National Dementia Plans n.d. www.alzheimer-europe.org/Policy-in-Practice2/National-Dementia-Plans/ (accessed 13 December 2016).
- National Framework for Action on Dementia 2006–2010. Sydney, NSW: NSW Department of Health on behalf of AHMC; 2006.
- National Framework for Action on Dementia 2015–2019. Sydney, NSW: NSW Department of Health on behalf of AHMC; 2015.
- New Zealand Framework for Dementia Care. Wellington: Ministry of Health; 2013.
- Prime Minister’s Challenge on Dementia 2015: Delivering Major Improvements in Dementia Care and Research by 2015. London: Department of Health; 2012.
- Prime Minister’s Challenge on Dementia 2020. London: Department of Health; 2015.
- Who Cares Wins. London: Royal College of Psychiatrists; 2005.
- Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009;195:61-6. https://doi.org/10.1192/bjp.bp.108.055335.
- Goldberg SE, Whittamore KH, Harwood RH, Bradshaw LE, Gladman JRF, Jones RG. on behalf of the Medical Crises in Older People Study Group . The prevalence of mental health problems among older adults admitted as an emergency to a general hospital. Age Ageing 2012;41:80-6. https://doi.org/10.1093/ageing/afr106.
- Mukadam N, Sampson EL. A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. Int Psychogeriatr 2011;23:344-55. https://doi.org/10.1017/S1041610210001717.
- George J, Long S, Vincent C. How can we keep patients with dementia safe in our acute hospitals? A review of challenges and solutions. J R Soc Med 2013;106:355-61. https://doi.org/10.1177/0141076813476497.
- Caspe Healthcare Knowledge Systems . An Economic Analysis of the Excess Costs for Acute Care for Patients With Dementia n.d. www.chks.co.uk/userfiles/files/Dementia_an_economic_analysis.pdf (accessed 5 October 2016).
- Counting the Cost: Caring for People with Dementia on Hospital Wards. London: Alzheimer’s Society; 2009.
- Porock D, Clissett P, Harwood RH, Gladman JR. Disruption, control and coping: responses of and to the person with dementia in hospital. Ageing Soc 2015;35:37-63. https://doi.org/10.1017/S0144686X13000561.
- Cowdell F. The care of older people with dementia in acute hospitals. Int J Older People Nurs 2010;5:83-92. https://doi.org/10.1111/j.1748-3743.2010.00208.x.
- Norman R. Observations of the experiences of people with dementia on general hospital. J Res Nursing 2006;11:453-65. https://doi.org/10.1177/1744987106065684.
- Moyle W, Olorenshaw R, Wallis M, Borbasi S. Best practice for the management of older people with dementia in the acute care setting: a review of the literature. Int J Older People Nurs 2008;3:121-30. https://doi.org/10.1111/j.1748-3743.2008.00114.x.
- Dewing J, Dijk S. What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia 2016;15:106-24. https://doi.org/10.1177/1471301213520172.
- Innes A, Kelly F, Scerri C, Abela S. Living with dementia in hospital wards: a comparative study of staff perceptions of practice and observed patient experience. Int J Older People Nurs 2016;11:94-106. https://doi.org/10.1111/opn.12102.
- Clissett P, Porock D, Harwood RH, Gladman JR. The challenges of achieving person-centred care in acute hospitals: a qualitative study of people with dementia and their families. Int J Nurs Stud 2013;50:1495-503. https://doi.org/10.1016/j.ijnurstu.2013.03.001.
- Report of the National Audit of Dementia Care in General Hospitals. London: Royal College of Psychiatrists; 2011.
- Young J, Hood C, Gandesha A, Souza R. National Audit of Dementia Care in General Hospitals 2012–13: Second Round Audit Report and Update. London: Healthcare Quality Improvement Partnership (HQIP); 2013.
- Calnan M, Tadd W, Calnan S, Hillman A, Read S, Bayer A. ‘I often worry about the older person being in that system’: exploring the key influences on the provision of dignified care for older people in acute hospitals. Ageing Soc 2013;33:465-85. https://doi.org/10.1017/S0144686X12000025.
- Patterson M, Nolan M, Musson G. From Metrics to Meaning: Culture Change and Quality of Acute Hospital Care for Older People. London: Her Majesty’s Stationery Office; 2011.
- Borbasi S, Jones J, Lockwood C, Emden C. Health professionals’ perspectives of providing care to people with dementia in the acute setting: toward better practice. Geriatr Nursing 2006;27:300-8. https://doi.org/10.1016/j.gerinurse.2006.08.013.
- Moyle W, Borbasi S, Wallis M, Olorenshaw R, Gracia N. Acute care management of older people with dementia: a qualitative perspective. J Clin Nurs 2011;20:420-8. https://doi.org/10.1111/j.1365-2702.2010.03521.x.
- Clissett P, Porock D, Harwood RH, Gladman JR. The responses of healthcare professionals to the admission of people with cognitive impairment to acute hospital settings: an observational and interview study. J Clin Nurs 2014;23:1820-9. https://doi.org/10.1111/jocn.12342.
- Nilsson A, Rasmussen BH, Edvardsson D. Falling behind: a substantive theory of care for older people with cognitive impairment in acute settings. J Clin Nurs 2013;22:1682-91. https://doi.org/10.1111/jocn.12177.
- Goldberg SE, Whittamore KH, Pollock K, Harwood RH, Gladman JRF. Caring for cognitively impaired older patients in the general hospital: a qualitative analysis of similarities and differences between a specialist Medical and Mental Health Unit and standard care wards. Int J Nurs Stud 2014;51:1332-43. https://doi.org/10.1016/j.ijnurstu.2014.02.002.
- Morrison RS, Siu AL. A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. J Pain Symptom Manage 2000;19:240-8. https://doi.org/10.1016/S0885-3924(00)00113-5.
- Sampson EL, White N, Lord K, Leurent B, Vickerstaff V, Scott S, et al. Pain, agitation, and behavioural problems in people with dementia admitted to general hospital wards: a longitudinal cohort study. Pain 2015;156:675-83. https://doi.org/10.1097/j.pain.0000000000000095.
- Delirium Prevention, Diagnosis and Management. Manchester: National Institute for Health and Care Excellence; 2010.
- Jurgens FJ, Clissett P, Gladman JR, Harwood RH. Why are family carers of people with dementia dissatisfied with general hospital care? A qualitative study. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-57.
- Thompson R, Heath H. Dignity in Dementia: Transforming General Hospital Care. Summary of Findings from a Survey of Carers and People Living with Dementia. London: Royal College of Nursing; 2011.
- National Service Framework for Older People. London: Department of Health; 2001.
- Dementia: Supporting People with Dementia and Their Carers in Health and Social Care. London: National Institute for Health and Care Excellence; 2006.
- Principles of Nursing Practice: Principles and Measures Consultation. Summary Report for Nurse Leaders. London: RCN; 2010.
- Kogan AC, Wilber K, Mosqueda L. Person-centered care for older adults with chronic conditions and functional impairment: a systematic literature review. J Am Geriatr Soc 2016;64:e1-7. https://doi.org/10.1111/jgs.13873.
- Sharma T, Bamford M, Dodman D. Person-centred care: an overview of reviews. Contemp Nurse 2015;51:107-20. https://doi.org/10.1080/10376178.2016.1150192.
- Kitwood T. Dementia Reconsidered: The Person Comes First. Buckingham: Open University Press; 1997.
- Sabat SR. The Experience of Alzheimer’s Disease: Life Through a Tangled Veil. Oxford: Blackwell Publishers Ltd; 2001.
- Rogers C. On Becoming a Person: A Therapist’s View of Psychotherapy. Boston, MA: Houghton Mifflin Company; 1961.
- Nolan M, Ryan T, Enderby P, Reid D. Towards a more inclusive vision of dementia care practice and research. Dementia: Int J Soc Res Pract 2002;1:193-211. https://doi.org/10.1177/147130120200100206.
- Brooker D. What is person-centered care in dementia?. Revi Clin Gerontol 2004;13:215-22. https://doi.org/10.1017/S095925980400108X.
- Edvardsson D, Winblad B, Sandman PO. Person-centred care of people with severe Alzheimer’s disease: current status and ways forward. Lancet Neurol 2008;7:362-7. https://doi.org/10.1016/S1474-4422(08)70063-2.
- Kontos P. Ethnographic reflections on selfhood, embodiment and Alzheimer’s disease. Ageing Soc 2004;24:829-49. https://doi.org/10.1017/S0144686X04002375.
- Kontos P. Embodied selfhood in Alzheimer’s disease: rethinking person-centred care. Dementia: Int J Soc Res Pract 2005;4:553-70. https://doi.org/10.1177/1471301205058311.
- Phinney A, Chesla CA. The lived body in dementia. J Aging Stud 2003;17:283-99. https://doi.org/10.1016/S0890-4065(03)00029-X.
- Hughes JC. ‘Y’ feel me?’ How do we understand the person with dementia?. Dementia 2013;12:348-58. https://doi.org/10.1177/1471301213479597.
- Tolson D, Smith M, Knight P. An investigation of the components of best nursing practice in the care of acutely ill hospitalized older patients with coincidental dementia: a multi-method design. J Adv Nurs 1999;30:1127-36. https://doi.org/10.1046/j.1365-2648.1999.01194.x.
- Goldberg SE, Bradshaw LE, Kearney FC, Russell C, Whittamore KH, Foster P, et al. Care in specialist medical and mental health unit compared with standard care for older people with cognitive impairment admitted to general hospital: randomised controlled trial (NIHR Team Trial). BMJ 2013;347. https://doi.org/10.1136/bmj.f4132.
- Dewing J. RCN Workplace Resources for Practice Development. London: Royal College of Nursing; 2006.
- McCormack B, Henderson E, Wilson V, Wright J. Making practice visible: the Workplace Culture Critical Analysis Tool (WCCAT). Practice Dev Healthcare 2009;8:28-43. https://doi.org/10.1002/pdh.273.
- Dean R, Proudfoot R, Lindesay J. The quality of interactions schedule (QUIS): development, reliability and use in the evaluation of two Domus units. Int J Geriat Psychiat 1993;8:819-26. https://doi.org/10.1002/gps.930081004.
- Brooker D, Surr CA. Dementia Care Mapping: Principles and Practice. Bradford: University of Bradford; 2005.
- Dementia Care Mapping: Principles and Practice, Third edition. Bradford: University of Bradford; 2010.
- Sabatier PA. Top down and bottom up approaches to implementation research: a critical analysis and suggested synthesis. J Pub Pol 1986;6:21-48. https://doi.org/10.1017/S0143814X00003846.
- Lukas CV, Holmes SK, Cohen AB, Restuccia J, Cramer IE, Shwartz M, et al. Transformational change in health care systems: an organizational model. Health Care Manage Rev 2007;32:309-20. https://doi.org/10.1097/01.HMR.0000296785.29718.5d.
- Bate P, Mendel P, Robert G. Organising for Quality: The Improvement Journeys of Leading Hospitals in Europe and the United States. Oxford: Radcliffe Publishing; 2008.
- Powell AE, Rushmer RK, Davies HTO. A Systematic Narrative Review of Quality Improvement Models in Health Care. Edinburgh: Quality Improvement Scotland; 2009.
- De Bellis A, Bradley SL, Wotherspoon A, Walter B, Guerin P, Cecchin M, et al. Come into my World – How to Interact with a Person who has Dementia: An Educational Resource for Undergraduate Healthcare Students on Person-centred Care. Adelaide, SA: Flinders University, Hyde Park Press; 2009.
- May C, Finch T. Implementing, embedding and integrating practices: an outline of normalization process theory. Sociol 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003;362:1225-30. https://doi.org/10.1016/S0140-6736(03)14546-1.
- Grol RP, Bosch MC, Hulscher ME, Eccles MP, Wensing M. Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q 2007;85:93-138. https://doi.org/10.1111/j.1468-0009.2007.00478.x.
- Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, National Implementation Research Network (FMHI Publication #231); 2005.
- Rogers PJ. Using programme theory to evaluate complicated and complex aspects of interventions. Evaluation 2008;14:29-48. https://doi.org/10.1177/1356389007084674.
- Stame N. Theory-based evaluation and types of complexity. Evaluation 2006;10:58-76. https://doi.org/10.1177/1356389004043135.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Hawe P, Shiell A, Riley T. Complex interventions: how ‘out of control’ can a randomised controlled trial be?. BMJ 2004;328:1561-3. https://doi.org/10.1136/bmj.328.7455.1561.
- Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Community Psychol 2009;43:267-76. https://doi.org/10.1007/s10464-009-9229-9.
- Ragin C, Becker H, Ragin C, Becker H. What is a Case? Exploring the Foundations of Social Inquiry. Cambridge: Cambridge University Press; 1992.
- Ragin C, Byrne D, Ragin C. The Sage Handbook of Case-based Methods. London: Sage; 1992.
- Stake R. The Art of Case Study Research. London: Sage; 1995.
- Yin R. Case Study Research: Design and Methods. London: Sage; 2009.
- Byrne D, Byrne D, Ragin C. The Sage Handbook of Case-based Methods. London: Sage; 2013.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Young J, Cheater F, Collinson M, Fletcher M, Forster A, Godfrey M, et al. Prevention of delirium (POD) for older people in hospital: study protocol for a randomised controlled feasibility trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0847-2.
- Atkinson P. For Ethnography. London: Sage; 2015.
- Spradley JP. Participant Observation. Belmont, CA: Wadsworth; 1980.
- Lofland J, Snow D, Anderson L, Lofland LH. Analysing Social Settings: A Guide to Qualitative Observations and Analysis. Belmont, CA: Wadsworth; 2006.
- Emerson RM, Fretz RI, Shaw LL. Writing Ethnographic Fieldnotes. Chicago, IL: University of Chicago Press; 1995.
- Moore G, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process Evaluations of Complex Interventions: UK Medical Research Council (MRC) Guidance. London: Medical Research Council; 2011.
- Godfrey M, Smith J, Green J, Cheater F, Inouye SK, Young JB. Developing and implementing an integrated delirium prevention system of care: a theory driven, participatory research study. BMC Health Serv Res 2013;13:1-15. https://doi.org/10.1186/1472-6963-13-341.
- Clarke D, Godfrey M, Hawkins R, Sadler E, Harding G, Forster A, et al. Implementing a training intervention to support caregivers after stroke: a process evaluation examining the initiation and embedding of programme change. Implement Sci 2013;8:1-15. https://doi.org/10.1186/1748-5908-8-96.
- Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q 2001;79:281-315. https://doi.org/10.1111/1468-0009.00206.
- Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q 2010;88:500-59. https://doi.org/10.1111/j.1468-0009.2010.00611.x.
- Century J, Cassata A, Rudnick M, Freeman C. Measuring enactment of innovations and the factors that affect implementation and sustainability: moving toward common language and shared conceptual understanding. J Behav Health Serv Res 2012;39:343-61. https://doi.org/10.1007/s11414-012-9287-x.
- Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing 2006;35:350-64. https://doi.org/10.1093/ageing/afl005.
- Collins N, Blanchard MR, Tookman A, Sampson EL. Detection of delirium in the acute hospital. Age Ageing 2010;39:131-5. https://doi.org/10.1093/ageing/afp201.
- Davis DH, Muniz Terrera G, Keage H, . Delirium is a strong risk factor for dementia in the oldest-old: a population-based cohort study. Brain 2012;135:2809-16. https://doi.org/10.1093/brain/aws190.
- MacLullich AM, Beaglehole A, Hall RJ, Meagher DJ. Delirium and long-term cognitive impairment. Int Rev Psychiatry 2009;21:30-42. https://doi.org/10.1080/09540260802675031.
- Fong TG, Jones RN, Shi P, Marcantonio ER, Yap L, Rudolph JL, et al. Delirium accelerates cognitive decline in Alzheimer disease. Neurology 2009;72:1570-5. https://doi.org/10.1212/WNL.0b013e3181a4129a.
- Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet 2014;383:911-22. https://doi.org/10.1016/S0140-6736(13)60688-1.
- Davis D, MacLullich A. Understanding barriers to delirium care: a multicentre survey of knowledge and attitudes amongst UK junior doctors. Age Ageing 2009;38:559-63. https://doi.org/10.1093/ageing/afp099.
- Schuurmans MJ, Shortridge-Baggett LM, Duursma SA. The Delirium Observation Screening Scale: a screening instrument for delirium. Res Theory Nurs Pract 2003;17:31-50. https://doi.org/10.1891/rtnp.17.1.31.53169.
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. American Psychiatric Association; 2000.
- Oliver D, Connelly JB, Victor CR, Shaw FE, Whitehead A, Genc Y, et al. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ 2007;334. https://doi.org/10.1136/bmj.39049.706493.55.
- Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in nursing facilities and hospitals. Cochrane Database Syst Rev 2010;1. https://doi.org/10.1002/14651858.CD005465.pub2.
- Healey F, Scobie S. Slips, Trips and Falls in Hospital. London: National Patient Safety Agency; 2007.
- Oliver D, Healey F, Haines TP. Preventing falls and fall-related injuries in hospitals. Clin Geriatr Med 2010;26:645-92. https://doi.org/10.1016/j.cger.2010.06.005.
- Charmaz K. Constructing Grounded Theory. Thousand Oaks, CA: Sage; 2014.
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Mental Capacity Act 2005 Code of Practice. Norwich: The Stationery Office; 2007.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationary Office; 2013.
- Twigg J. Carework as a form of bodywork. Ageing Soc 2000;20:389-411. https://doi.org/10.1017/S0144686X99007801.
- Bolster D, Manias E. Person-centred interactions between nurses and patients during medication activities in an acute hospital setting: qualitative observation and interview study. Int J Nurs Stud 2010;47:154-65. https://doi.org/10.1016/j.ijnurstu.2009.05.021.
- Corbin J. Is caring a lost art in nursing?. Int J Nurs Stud 2008;45:163-5. https://doi.org/10.1016/j.ijnurstu.2007.09.003.
- Miesen B. Care-giving in dementia: contours of a curriculum. Dementia 2010;9:473-89. https://doi.org/10.1177/1471301210381680.
- Dementia Nursing: Vision and Strategy. London: Department of Health; 2016.
- Dewar B, Nolan M. Caring about caring: developing a model to implement compassionate relationship centred care in an older people care setting. Int J Nurs Stud 2013;50:1247-58. https://doi.org/10.1016/j.ijnurstu.2013.01.008.
- McCormack B. Person-centredness in gerontological nursing: an overview of the literature. J Clin Nurs 2004;13:31-8. https://doi.org/10.1111/j.1365-2702.2004.00924.x.
- Øvretveit J. Understanding the conditions for improvement: research to discover which context influences affect improvement success. BMJ Qual Saf 2011;20:i18-23. https://doi.org/10.1136/bmjqs.2010.045955.
- Guba E, Lincoln Y. Fourth Generation Evaluation. Newbury Park, CA: Sage; 1989.
- Damschroder LJ, Banaszak-Holl J, Kowalski CP, Forman J, Saint S, Krein SL. The role of the champion in infection prevention: results from a multisite qualitative study. Qual Saf Health Care 2009;18:434-40. https://doi.org/10.1136/qshc.2009.034199.
- Sands MB, Dantoc BP, Hartshorn A, Ryan CJ, Lujic S. Single Question in Delirium (SQiD): testing its efficacy against psychiatrist interview, the Confusion Assessment Method and the Memorial Delirium Assessment Scale. Palliat Med 2010;24:561-5. https://doi.org/10.1177/0269216310371556.
- Duppils GS, Wikblad K. Patients’ experiences of being delirious. J Clin Nurs 2007;16:810-18. https://doi.org/10.1111/j.1365-2702.2006.01806.x.
- O’Malley G, Leonard M, Meagher D, O’Keeffe ST. The delirium experience: a review. J Psychosom Res 2008;65:223-8. https://doi.org/10.1016/j.jpsychores.2008.05.017.
- Bélanger L, Ducharme F. Patients’ and nurses’ experiences of delirium: a review of qualitative studies. Nurs Crit Care 2011;16:303-15. https://doi.org/10.1111/j.1478-5153.2011.00454.x.
- Safe Staffing for Older People’s Wards: RCN Summary Guidance and Recommendations. London: Royal College of Nursing; 2012.
- Compassion in Practice, Nursing, Midwifery and Care Staff: Our Vision and Strategy. Leeds: Department of Health; 2012.
- Hamington M. Embodied Care: Jane Addams, Maurice Merleau-Ponty, and Feminist Ethics. Urbana, IL: University of Illinois Press; 2004.
- Mills M. Narrative identity and dementia: a study of emotion and narrative in older people with dementia. Ageing Soc 1997;17:673-98. https://doi.org/10.1017/S0144686X97006673.
- Auerbach AD, Landefeld CS, Shojania KG. The tension between needing to improve care and knowing how to do it. N Engl J Med 2007;357:608-13. https://doi.org/10.1056/NEJMsb070738.
- Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf 2012;21:876-84. https://doi.org/10.1136/bmjqs-2011-000760.
- Davidoff F. Heterogeneity is not always noise: lessons from improvement. JAMA 2009;302:2580-6. https://doi.org/10.1001/jama.2009.1845.
- Fitzgerald L, Ferlie E, Wood M, Hawkins C. Interlocking interactions, the diffusion of innovations in health care. Human Rel 2002;55:1429-49. https://doi.org/10.1177/001872602128782213.
- Dopson S, Fitzgerald L, Ferlie E. Understanding change and innovation in healthcare settings: reconceptualising the active role of context. J Change Manage 2008;8:213-31. https://doi.org/10.1080/14697010802133577.
- Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care 1998;7:149-58. https://doi.org/10.1136/qshc.7.3.149.
- Rycroft-Malone J, Kitson A, Harvey G, McCormack B, Seers K, Titchen A, et al. Ingredients for change: revisiting a conceptual framework. Qual Saf Health Care 2002;11:174-80. https://doi.org/10.1136/qhc.11.2.174.
- Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implement Sci 2008;3. https://doi.org/10.1186/1748-5908-3-1.
- McCance T, Gribben B, McCormack B, Laird EA. Promoting person-centred practice within acute care: the impact of culture and context on a facilitated practice development programme. Intl Pract Dev J 2013;3.
- McCormack B, Dewing J, McCance T. Developing person-centred care: addressing contextual challenges through practice development. Online J Issues Nurs 2011;16.
- Manley K, McCormack B, Wilson V, Manley K, McCormack B, Wilson V. Practice Development in Nursing: International Perspectives. Oxford: Blackwell; 2008.
- West M, Baker R, Dawson J, Dixon Woods M, Lilford R, Martin G, et al. Quality and Safety in the NHS: Evaluating Progress, Problems and Promise. Lancaster: Lancaster University; 2010.
- Dixon-Woods M, Baker R, Charles K, Dawson J, Jerzembek G, Martin G, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106-15. https://doi.org/10.1136/bmjqs-2013-001947.
- Pettigrew AM, Ferlie E, McKee L. Shaping Strategic Change. London: Sage; 1992.
- The Psychological and Social Needs of Patients. London: BMA; 2011.
- Fredman L, Hawkes WG, Black S, Bertrand RM, Magaziner J. Elderly patients with hip fracture with positive affect have better functional recovery over 2 years. J Am Geriatr Soc 2006;54:1074-81. https://doi.org/10.1111/j.1532-5415.2006.00786.x.
- Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev 2012;69:123-57. https://doi.org/10.1177/1077558711430690.
- Scerri A, Innes A, Scerri C. Dementia training programmes for staff working in general hospital settings – a systematic review of the literature. Aging Ment Health 2017;21:783-96. https://doi.org/10.1080/13607863.2016.1231170.
- A New Ambition for Old Age: Next Steps in Implementing the National Service Framework for Older People. London: The Stationery Office; 2006.
- Dignity . The Dignity in Care Campaign n.d. www.dignityincare.org.uk/About/Dignity_in_Care_campaign/ (accessed 15 June 2018).
- Tadd W, Hillman A, Calnan S, Calnan M, Bayer T, Read S. Dignity in Practice: An Exploration of the Care of Older Adults in Acute NHS Trusts. London: Her Majesty’s Stationery Office; 2011.
- High Quality Care For All: NHS Next Stage Review Final Report. London: Department of Health; 2008.
- Balint E. The possibilities of patient-centred medicine. J R Coll Gen Pract 1969;17:269-76.
- McWhinney I, Stewart M, Roter D. Communicating with Medical Patients. London: Sage; 1989.
- Byrne P, Long B. Doctors Talking to Patients. London: HMSO; 1976.
- Stewart MA, Brown J, Weston W, McWhinney I, McWilliam C, Freeman T. Patient-centred Medicine: Transforming the Clinical Method. London: Sage; 1995.
- Laine C, Davidoff F. Patient-centered medicine: a professional evolution. JAMA 1996;275:152-56. https://doi.org/10.1001/jama.1996.03530260066035.
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med 2000;51:1087-100. https://doi.org/10.1016/S0277-9536(00)00098-8.
- Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- Gerteis M, Edgman-Levitan S, Daley J, Delbanco T. Through the Patient’s Eyes: Understanding and Promoting Patient-centred Care. San Francisco, CA: Jossey-Bass; 1993.
- Goodrich J, Cornwell J. Seeing the Person in the Patient: The Point of Care Review Paper. London: The King’s Fund; 2008.
- Shaller D. Patient-centered Care: What Does It Take?. Oxford: Picker Institute and The Commonwealth Fund; 2007.
- Person-centred Care Made Simple. London: The Health Foundation; 2014.
- Person-centred Care in Europe: A Cross-country Comparison of Health System Performance, Strategies and Structures. Oxford: Picker Institute Europe; 2016.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Strategic Narrative: Achieving Sustainable Quality in Scottish Healthcare, A 2020 Vision. Scottish Government/NHS Scotland; 2012.
- Dignity in Dementia: Transforming General Hospital Care, Summary of Findings from Survey of Carers and People Living with Dementia. London: RCN; 2011.
- Dignity in Dementia: Transforming General Hospital Care, Summary of Findings from Survey of Professionals. London: RCN; 2011.
- Firth-Cozens F, Cornwell J. The Point of Care: Enabling Compassionate Care in Acute Hospital Settings. London: The King’s Fund; 2009.
Appendix 1 Person-centred care in policy
What is ‘person-centred’ care in policy?
‘Person-centred’ care has become ubiquitous in UK health and social care policy discourse as synonymous with care quality. Its meaning in policy, however, either is implicit or involves varying emphasis on different domains. It is commonly conveyed as individualised care, holistic care, choice, autonomy and dignity. Moreover, the use of the term, and the particular emphasis attached to it, has varied over time and in relation to wider policy interests.
One of the first UK policy documents to use the term ‘person-centred’ care was the National Service Framework for Older People (NSFOP). 39 In Standard 2, it refers to the requirement on health and social care services to ensure that this group of people receive appropriate and timely packages of care that meet their individual needs, regardless of health and social services boundaries. This treatment of older people as individuals was conceived as listening to them, involving them in all decisions about their care and needs, enabling them to make choices about their care and providing a co-ordinated and integrated service response. This was to be achieved through the single assessment process, integrated commissioning arrangements and integrated service provision between health and social care. It was incumbent on staff that services should be delivered in a manner that accorded respect and dignity. In Standard 7 relating to older people with mental health problems, including dementia, the hallmark of a quality system of care was that it be:
comprehensive, multidisciplinary, accessible, responsive, individualised, accountable and systematic.
Person-centred’ care, then, was a multidimensional construct with interactional, relational and systemic components.
There was no explicit reference to ‘person-centred’ or ‘person-centeredness’ in respect of care in general hospitals in the NSFOP, the emphasis was on promoting dignity and privacy (Standard 4). It was asserted that care in hospital should be underpinned by ‘fundamental principles for the promotion of dignity’ (p. 5239 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). This was translated into the creation of physical and care environments that were clean, offered privacy, promoted independence, provided for personal care needs, access to specialist care and advice from staff trained in caring for older people.
Subsequently, the term ‘dignity’ became the standard bearer to carry care quality in policy, being the focus of a campaign with particular emphasis on older people and care on hospital wards. A New Ambition for Old Age,145 which set out further steps in implementing the NSFOP, had dignity in care at its center (Programme 1, p. 4). This was followed by the launch of a campaign for dignity in care by the Department of Health in November 2006, the aim of which was 'to put dignity at the heart of care' and to create dignity champions in every health-care organisation to promote it. 146 The primary emphasis in this campaign on the behaviour and attitudes of individual staff was criticised on the grounds that these exist within a complex set of organisational cultures and competing priorities that have an impact on individual and team approaches to the care and treatment of older people. 28,147
In its vision for modernising the NHS, High Quality Care for All,148 the government emphasised the values of respect, dignity and compassion. It was noted in the preface of the paper that:
[T]he NHS touches our lives at times of most basic human need, when care and compassion are what matter most.
In this paper, the term ‘person-centred’ was not used. The vision for change was of a locally led, patient-centred and clinically driven NHS; providing quality care, namely care that was personalised, safe and clinically effective:
safe, personalised, clinically effective care [and] locally led patient-centred and clinically driven change.
Whereas ‘person-centred’ had been applied in a generic sense across sectors and services within the NSFOP, the term ‘patient-centred’ was more commonly utilised in a health context. Nevertheless, both terms were used interchangeably to encompass similar content. The policy shift towards dignity, respect and compassionate care did, however, direct attention to the relational aspects of care delivery and, therefore, to how care was experienced by those receiving it.
Person-centred care: people with dementia
Regarding the care of people with dementia, National Institute for Health and Care Excellence guidelines40 made specific reference to Kitwood’s theoretical model of ‘personhood’,44 the only policy document up to this point to locate person-centeredness in a theoretical framework. Many of the recommendations reflected values deemed supportive of ‘personhood’:
-
the human value of people with dementia, regardless of age or cognitive impairment, and of those who care for them
-
the individuality of people with dementia, with their unique personality and life experiences among the influences on their response to the dementia
-
the importance of the perspective of the person with dementia
-
the significance of relationships and interactions with others to the person with dementia, and their potential for promoting well-being.
The fourth principle places explicit emphasis on ‘relationship-centred care’ as a component of ‘person-centeredness’ in the emphasis placed on social networks and social interaction. Recommendations on hospital care included provision of services that addressed personal and social care needs and the mental and physical health of people with dementia, through specialist assessment involving medical and liaison teams and a co-ordinated and integrated approach to delivery.
The first national dementia strategy1 did not use the term ‘person-centred’, although its focus on the social inclusion of people with dementia by reducing stigma and empowering people to make choices has also been subsumed under the term. The vision underpinning the strategy was that everyone with dementia would have access to needed care and support wherever they lived, and that:
. . . public and professionals . . . are well informed . . . fear and stigma associated with dementia have been allayed . . . false beliefs that dementia is a normal part of ageing . . . have been corrected . . . families affected by dementia know where to go for help, what services to expect . . . quality of care is high . . .
Department of Health, p. 15. 1
This emphasis on equitable, antidiscriminatory, accessible and quality services reflected the chasm between the vision and the contemporary reality of provision. The priority was the creation of a service infrastructure to establish the conditions in which relational dimensions of quality care could flourish. Although improving general hospital care for people with dementia was a policy objective, the primary emphasis was on strategic initiatives (identifying leadership for dementia, establishing a care pathway and commissioning specialist liaison older people’s mental health teams).
Experience of care: patient or person centred?
Although the term ‘person-centred’ was introduced into policy around 2000, by the end of the decade it was still not embedded in the policy lexicon. Neither had it supplanted ‘patient-centred’, as both terms co-existed in different policy contexts.
The concept of ’patient-centred’ care is rooted in a shift from the traditional biomedical model in favour of embracing personal choice and autonomy for people receiving health services. ‘Patient-centred‘ care was defined by Balint149 as care that understands the patient as a unique human being, and a patient-centred approach was one in which ‘the physician tries to enter the patient’s world to see the illness through the patient’s eyes’. 150 It was viewed as representing a style of consulting in which the doctor used the patient’s knowledge and experience to guide the interaction,151 forging a therapeutic alliance in which power and responsibility was shared152 to deliver care that was ‘closely congruent with, and responsive to patients’ wants, needs and preferences’. 153 Even so, debate has continued as to its precise meaning, although Mead and Bower154 argue that the term ‘has been used to refer to so many different concepts that its scientific utility may have been compromised’.
An internationally recognised and widely used definition of patient-centred care that has been influential in North American health policy is that from the US Institute of Medicine. This comprises several components: a partnership model of health involving practitioners, patients and families, decision-making that respects patients needs and preferences, and knowledge and support to make decisions and engage in self-care. 155
Importantly, the Institute of Medicine conception goes beyond the relational dimension. Informed by the work of Gerteis et al. ,156 seven dimensions of patient-centred care were identified: respect for patients; co-ordination and integration of care; information, communication and education; physical comfort, emotional comfort/alleviation of fear and anxiety; involvement of family/friends; transition; and continuity. Further layers of responsibility on health systems at service, sector and programme level were added to ensure that organisational processes and regulatory and governance frameworks were underpinned by these principles.
Until the mid-2000s, this conception of patient-centred care was also reflected in influential UK-based policy organisations. The King’s Fund Point of Care Programme157 was intended to work alongside front-line staff and their managers and focus attention on patients’ experience of care in the NHS. The authors argued that the quality of a patient’s experience was seeing the person and not just the patient and being related to with compassion and kindness. They emphasised that the paradigm shift toward ‘patient experience’ was not simply about the relational dimension of care. Rather, different aspects of the experience – the process of care and treatment, the environment in which it occurs, the physical sense of the place – come together with the manner in which it is delivered to inform the subjective experience.
In projecting a definition of quality to capture the experience of ‘the person in the patient’, Goodrich and Cornwell157 drew on the Institute of Medicine’s155 definition of patient-centred care and the dimensions that constitute it. These were similar to those adumbrated in the NSFOP under the term ‘person-centred’.
A consultative exercise commissioned by the Picker Institute around the same time concluded that the factors contributing to patient-centred care based on the Institute of Medicine’s definition were158 leadership; strategic vision clearly and constantly communicated to every member of the organisation; involvement of patients and families at multiple levels; care for the caregivers through a supportive work environment; systematic measurement and feedback; quality of the built or physical environment; and supportive technology. The delivery of patient-centred care was seen to require action at multiple and interacting levels: organisational, cultural, environmental, individual and relational, as well as the qualitative dimensions of the work environment of those delivering care.
Although describing similar ideas, the term ‘patient centred’ has been the subject of critique on the basis that it still addresses the person as ‘patient’ (i.e. in context of their illness or condition). Person-centred is seen to cover a wider range of settings other than health. It also implies a person as both a social and relational being, and part of a wider social network that shapes the pattern of daily life and sense of well-being.
Ascendancy of person-centred care in UK health and social care policy
Over the last decade, the concept of person-centred care has become the term most widely used in UK policy discourse, yet its meaning and how it should be enacted in practice is ambiguous and fluid. In different areas of health policy, there are varied nuances of meaning. Considerable work has been undertaken by organisations aiming to influence policy in order to achieve consensus on meaning and content.
The Health Foundation159 identified a framework of four basic principles to guide the ‘new’ relationship between providers and users of health services to secure care tailored to individual needs: dignity, compassion and respect at the centre of care delivery; care that is co-ordinated; care that is personalised; and developing and supporting people’s own strengths to live a good life. 159
This summarises person-centred care as individualised, caring and enabling; involving collaboration between professionals and those using services; providing people with the knowledge, skills and confidence to manage and make informed decisions about their health and health care; and co-ordinated and delivered in a manner that accords dignity, compassion and respect to the person.
This embraces principles relating to care systems to enable people live a ‘good life’ and those geared to the care delivery process and the relational encounter. It is similar to the Institute of Medicine’s definition of patient-centred, with the important exception that understanding of personalised care and the focus of co-ordination goes beyond health.
The similarities and differences between the concepts of ‘patient-centred’ and ‘person-centred’ are noted in a policy briefing by the Picker Institute. 160 Recognising that both terms described similar ideas, ‘person-centred’ was preferred: it embraced a wider range of care settings, recognised people as individuals rather than as ‘patients’, and was better able to reflect the important role of people’s families, friends and caregivers in their health and well-being. Furthermore, it opened up a more inclusive model for building a quality health system by encompassing people who lacked health literacy or capacity. Whereas in dementia the concept of ‘personhood’44 and the persistence of self45 had countered the dominant biomedical model, an inclusive conception of ‘person-centred’ care also posed a challenge in actualising principles of enablement and collaboration for and with people with dementia, particularly those with moderate or severe impairment.
Translating person–centred care into service development and delivery for people with dementia
The major challenges in the NHS, which include increased demand, fundamental structural and cultural change and the context of economic austerity, have prioritised achievement of health efficiencies. As a result, ‘person-centeredness’ in policy discourse has assumed a double-edged meaning. For example, involvement in decision-making and effecting choice, both of which are regarded as dimensions of person-centred care, have found expression in such initiatives as personalised budgets aimed simultaneously at meeting productivity and ‘patient as person’ objectives, and pose considerable challenges in respect of people with dementia. The Health and Social Care Act 2012161 places a legal duty on NHS England and Clinical Commissioning Groups to involve patients in their care. However, increasingly decision-making on local health priorities are driven by budgetary constraints, posing the question as to what level of involvement and by whom, defines a service as ‘person-centred’. The Scottish Government’s 2020 Vision162 states that:
care will be provided to the highest standards of quality and safety, with the person at the centre of all decisions.
Less evident is what ‘being at the centre of decisions’ looks like, especially for people with dementia.
Some aspects of the direction of travel may be seen in more recent policy documents. There is emphasis on singular dimensions of person-centred care, particularly at the interpersonal level of the professional–person interaction.
The first Prime Minister’s Challenge on Dementia10 set out three broad objectives: driving improvements in health and care; creating dementia friendly communities; and committing to increased research, which also includes engagement of people with dementia. Under the rubric of these objectives were infrastructural and service development initiatives: increasing diagnostic rates through improvements in awareness, including in acute hospitals, education and training of the health workforce, geared to role and purpose; a NHS guarantee of a written integrated personalised care plan; and better assessment and support for caregivers. Although the term ‘person-centred’ care was not explicitly used in the document, components of it featured heavily, namely a ‘personalised care plan’, relationship-focused care, and ‘seeing the person’, not the dementia, through strategies designed to enhance social inclusion.
The Foreword in the recent Prime Minister’s Challenge10 refers to compassionate care, and:
that kindness, care and dignity take precedence over structures and systems.
Although the broad objectives remained the same as those set out in the first Challenge, they were now couched in terms of outcomes articulated through engagement of people with dementia, including staff/professional encounters based on compassion, dignity and caring; a partnership approach involving listening, offering and supporting people to make choices about their health and care; and ensuring more consistency of access, care and standards of provision. However, the notion of ‘compassionate care’, delivered through encounters that accord dignity and respect for the person, dominates.
The focus on the relational dimensions of health care in professional and policy discourse is not surprising, following on from the Mid Staffordshire hospital scandal. Interpersonal aspects of the nursing role, namely care, dignity and respect, were conveyed by the RCN as critical in transforming acute hospital care for people with dementia. 163,164 Moreover, the language of ‘compassion’ and ‘compassionate care’ has increasingly dominated policy. The nursing vision for care, as explicated in the ‘6 Cs’ of care, compassion, competence, communication, courage and commitment,124 presents the nursing role primarily in interpersonal and social terms and applies the same model to the care of people with dementia. 113 This is not to suggest that the relational dimension of ‘person-centeredness’ is unimportant; it is the extent to which it directs attention from the organisational, environmental and systemic dimensions that facilitate person-centred care at the relational level that is problematic. As elucidated in a King’s Fund paper,165 enabling compassion that involves staff openness to distress and suffering also requires the existence of teams that are supportive of staff and of organisational cultures that create and sustain healing environments.
Appendix 2 Summary trust and ward profiles
| Characteristic | Trusts and wards | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Seaford | City | Ironbridge | Central | Valley | ||||||
| Population |
759,000 Wide geographical spread (small city, towns and rural hinterland) |
500,000 City with diverse cultural and ethnic mix |
650,000 City with diverse ethnic and cultural mix |
1,200,000 Wide geographical spread: ethnically diverse city and suburban town |
200,000 Geographically dispersed rural area |
|||||
| Type of hospital | Large teaching | Large teaching | Large teaching | Large teaching | Small district | |||||
| Number of staff | 7500 | 5200 | 16,000 | 11,000 | 2400 | |||||
| Number of beds | 1100 (over a number of hospitals) | 900 (large hospital and small hospital on separate site) | 2000 (across a number of hospitals) | Wards within suburban hospital (229 beds) | 395 | |||||
| Poplar | Crane | Rivermead | Cedar | Netherton | Beech | Rose | Denton | Ambridge | Oak | |
| Type of ward | Trauma orthopaedic (older people) | Medical: care of older people | Rehab: older people | Older people medical/acute trauma | Dementia | Older people medical/ trauma/orthopaedic | Stroke/medical/palliative |
Dementia Rehab |
Older people/medical | Mixed age: trauma/orthopaedic |
| Number of beds | 22 | 26 | 27 | 28 | 27/28 | 24 | 23 | 13 | 30 | 28 |
| Staffing ratio |
E 4 : 4 L 4 : 4 N 2 : 2 |
E 5 : 4 L 5 : 4 N 2 : 2 |
E 3 : 4 L 3 : 3 N 2 : 2 |
E 5 : 3 L 4 : 3 N 2 : 3 |
E 5 : 3 L 4 : 3 N 2 : 2 |
NA |
E 4 : 3 L 3 : 2 N 3 : 2 |
E 2 : 2 L 2 : 2 N 2 : 1 |
E 4 : 4 L 3 : 4 N 2 : 1 |
E 3 : 4 L 3 : 4 N 2 : 3 |
Appendix 3 Questionnaire for ward staff
Appendix 4 Patient case studies
Appendix 5 Summary data collection
| Time point | Name and type of ward | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Central Trust | Ironbridge Trust | Valley Trust | City Trust | Seaford Trust | ||||||
| Rose: stroke | Denton: older people (dementia) | Beech: older people + #NOF | Netherton: older people (dementia) | Oak: trauma orthopaedic | Ambridge: older people | Rivermead: older people | Cedar: older people + #NOF | Poplar: trauma and orthogeriatrics | Crane: older people | |
| Baseline | ||||||||||
| Dates of data collection | July–November 2013 | July–November 2013 | July–November 2013 | August–November 2013 | November 2013–January 2014 | November 2013–March 2014 | February–April 2014 | September–November 2014 | December 2013–February 2014 | February–March 2014 |
| General ward observation, hours (n) | 22 | 26 | 19 | 39 | 33 | 38 | 34 | 33 | 24 | 27 |
| Patient case studies (n of patients) | 0 | 3 | 3 | 2 | 2 | 2 | 2 | 2 | 3 | 3 |
| Patient observation, hours (n) | 5 | 4 | 5 | 6 | 6 | 5.5 | 6 | 5 | 5 | |
|
Staff interviews (n) Conception of person-centred care |
2 | 5 | 2 | 10 | 6 | 8 | 6 | 7 | 5 | 5 |
| Interim | ||||||||||
| Dates of data collection | November 2014–May 2015 | January–March 2015 | November 2014–February 2015 | January–March 2015 | ||||||
| General ward observation, hours (n) | 31 | 34 | 29 | 26 | ||||||
| Patient case studies (n of patients) | 2 | 2 | 1 | 2 | ||||||
| Patient observation, hours (n) | 6 | 6 | 3 | 4.5 | ||||||
|
Staff interviews (n) Process of implementation of PIE |
7 | 4 | 4 (5 staff) | 3 (4 staff) | ||||||
| Outcome | ||||||||||
| Dates of data collection | August–October 2015 | October–December 2015 | ||||||||
| General ward observation, hours (n) | 29 | 26 | ||||||||
| Patient case studies (n of patients) | 1 | 1 | ||||||||
| Patient observation, hours (n) | 4 | 4 | ||||||||
|
Staff interviews (n) PIE: barriers and experience |
1 | 1 | 1 | 3 | 3 (5 staff) | 3 (7 staff) | ||||
Appendix 6 Delirium Observation Screening Tool
List of abbreviations
- A&E
- accident and emergency
- AP
- associate practitioner
- CQC
- Care Quality Commission
- DOS
- Delirium Observation Screening
- FTE
- full-time equivalent
- HCA
- health-care assistant
- MDT
- multidisciplinary team
- NAD
- National Audit of Dementia
- NPT
- normalisation process theory
- NSFOP
- National Service Framework for Older People
- OT
- occupational therapist
- PIE
- Person, Interactions and Environment
- RCN
- Royal College of Nursing
