Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/77/15. The contractual start date was in June 2016. The final report began editorial review in June 2017 and was accepted for publication in December 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Alison Turner reports membership of the National Institute for Health Research (NIHR) Dissemination Centre Advisory Group. The Strategy Unit (NHS Midlands and Lancashire Commissioning Support Unit) was commissioned to support the Dudley Multispecialty Community Provider (MCP) vanguard, and Alison Turner has been involved in providing evidence analysis in support of the local evaluation of the vanguard. Abeda Mulla reports membership of the NIHR Health Services and Delivery Research (HSDR) Prioritisation Panel (researcher led); The Strategy Unit was commissioned by the Dudley Clinical Commissioning Group (CCG) to deliver a primary care development programme, and Abeda Mulla is involved in providing general practices with service improvement and change support, and evaluating the programme workstreams. The Strategy Unit was also commissioned by NHS England to conduct a rapid research study in the context of General Practitioner (GP) Access, and Abeda Mulla was the technical lead for the project, overseeing all aspects of the analysis and writing the report. Andrew Booth reports being a principal investigator on a NIHR HSDR Evidence Synthesis Centre contract and membership of the NIHR Complex Reviews Research Support Unit Funding Board. Shiona Aldridge works for The Strategy Unit, which was commissioned by NHS England to conduct a rapid research study in the context of GP Access, and she was involved in undertaking the qualitative analysis; she was also involved in providing evidence analysis in support of the local evaluation of the Dudley MCP vanguard. Sharon Stevens reports being involved in providing evidence analysis in support of the local evaluation of the Dudley MCP vanguard and undertaking the evidence review for the NHS England-funded review of managing access in English general practice. Mahmoda Begum reports that, in relation to The Strategy Unit being commissioned by the Dudley CCG to deliver a primary care development programme, she is involved in providing general practices with service improvement and change support, and evaluating the programme workstreams; she was also involved in undertaking the qualitative interviewing and analysis for the NHS England-funded review of managing access in English general practice. Anam Malik reports that, in relation to The Strategy Unit being commissioned by the Dudley CCG to deliver a primary care development programme, she is involved in providing general practices with service improvement and change support, and evaluating the programme workstreams; she was also involved in undertaking the qualitative interviewing and analysis for the NHS England-funded review of managing access in English general practice.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Turner et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Multispecialty community providers as new care models
The publication of the Five Year Forward View (FYFV)1 formally introduced the NHS England (NHSE) strategy for delivering new integrated models of care: ‘the NHS will take decisive steps to break down the barriers in how care is provided between family doctors and hospitals, between physical and mental health, between health and social care’1 (contains public sector information licensed under the Open Government Licence v3.0). At the time of publication, the NHS was facing significant financial pressures; in 2013–14 there was a £90.6M deficit across acute trusts and Clinical Commissioning Group (CCGs),2 and this increased financial burden was exacerbated with a 6.4% fall in public spending in adult social care between 2009–10 and 2015–16. During this period, the population aged ≥ 65 years grew by 15.6%3 and the health-care costs of managing long-term conditions was forecasted to increase by £5B between 2011 and 2018. 4
These cost pressures served to add urgency to the migration of English health and social care economies towards integrated care delivery. 5 The FYFV outlined five pioneering new models of integrated care, to be delivered through a systematic approach of large-scale transformation, with the ambition of providing better quality and experience of health care. These models differed in their involvement of different health and care agencies, but shared one main aim: to reduce the high level of avoidable hospital admissions (20% in 2013),6 while offering improved health-care quality, outcomes and patient satisfaction, which were all becoming increasingly challenging to deliver. 1,7–10
This evidence synthesis concerns itself with the 14 multispecialty, community-based provider vanguards, that is, the multispecialty community provider (MCP) model of care. The MCP focus was a result of the local health economy context; two MCPs requested support from The Strategy Unit (where all but one of the study authors were based), and MCP programme leads (national and local) expressed interest in participating as advisors for the synthesis to ensure relevance to their needs. We follow NHSE’s definition of MCPs:
It is a new type of integrated provider . . . combines the delivery of primary care and community-based health and care services – not just planning and budgets. It also incorporates a much wider range of services and specialists wherever that is the best thing to do.
NHSE. Contains public sector information licensed under the Open Government Licence v3.011
The model was intended to provide accessible, co-ordinated services for patients through professional integration in community settings: ‘one new option to permit groups of general practitioners (GPs) to combine with nurses, other community health services, hospital specialists and perhaps mental health and social care to create integrated out-of-hospital care’ (contains public sector information licensed under the Open Government Licence v3.0). 1
The distinction between the primary and acute care systems (PACSs) and MCP new models of care can be characterised by the role of the acute sector; inherent within MCPs was the emphasis on primary care focus and leadership, whereas PACSs, by definition, required acute and primary care collaboration. As such, the MCP vanguards chosen had the necessary focus on general practice, with primary care development being the priority for local health economies to drive the shift towards transformation of primary care services. This transformation included extended primary care services; innovative care delivery; application of digital technologies; new skills and roles; greater community involvement and collaboration with the voluntary sector; and greater convenience for patients. Through becoming ‘the focus of a far wider range of care needed by their registered patients’,1 the expectation was that MCPs would eventually become the providers of out-of-hospital care delivering a patient-focused model12 within an integrated system that has aligned commissioning and provider incentives. 13
As the vanguard MCPs started their journey, standard principles for operation were provided with the flexibility to adapt for the local context. 11 The emerging care model and contract framework for MCPs14 described the core features of MCPs and ways of contractually supporting a MCP. This included stipulations to:
-
serve the whole population, not just a specific subset (e.g. those aged > 65 years)
-
operate at four different tiers: (1) whole population, (2) people with self-limiting conditions, (3) people with ongoing care needs and (4) patients deemed to be at risk of unscheduled care or high utilisation
-
deliver the MCP through community ‘care hubs’, with each hub serving a community of around 30,000–50,000 people
-
demonstrate financial integration, potentially through a single, multiyear whole-population budget for all MCP services
-
deploy the MCP budget flexibly to reshape the local care delivery system, including incentives and risk-/gain-share agreements.
As a model of care, the emphasis is on system-wide improvement across multiple dimensions of health care,15 often expressed as the triple aim (improving population health, patient experience and cost-effectiveness) or as the quadruple aim16,17 (which also incorporates staff or provider experience). Reflecting the association between staff experience and quality of care,18 we use the term quadruple aim in this review.
Legacy integrated care models
National policy in England has for some time advocated a stronger role and increased accountability for primary care in delivering integrated care. Most notably, Lord Darzi’s High Quality Care For All. NHS Next Stage Review Final Report19 gave rise to integrated care pilots, community-based polyclinics with a primary care function and a renewed focus on practice-based commissioning. The subsequent integrated care and support pioneers were a result of a national partnership, through which an integration plan set out how local structures, such as health and well-being boards, could facilitate health and care agencies to make further steps towards integration. 20 Within this, primary care was said to have:
. . . a key role to play in supporting the local delivery of integrated care, by providing continuity across primary, community and secondary settings, focusing on preventative care and facilitating access to social care, including for carers, through effective coordination of care planning and management and risk stratification.
National Collaboration for Integrated Care and Support20
In parallel to the selection of the integrated care and support pioneers, the Better Care Fund programme was launched, providing the means by which pooled budgets could be used to deliver agreed NHS and local government integration plans. Over time, the integrated care and support programme was absorbed by NHSE and is now simply known as NHSE Pioneers.
At the time of the introduction of the new care models, the evidence base on health-system integration was variable, characterised by a lack of consensus on what constitutes integrated care,21,22 with no single model or approach to integrated care that was feasible for universal application. 23,24 However, although a universal model may not exist, the evidence base of legacy integrated care models offers the prospect of important lessons for what might be considered the ‘active ingredients’ for MCP models of care. 25–29 The ‘critical ingredients’ for integrated care had already been identified as relationship management, staff development and staff retention. 29 There is also a recognition that understanding integrated care requires a framework of the micro (e.g. clinical integration), meso (e.g. professional and organisational integration) and macro (e.g. system integration). 30
Several of the current MCPs began their integrated care journey as pilots, pioneers or GP Access Funds31 (previously known as the Prime Minister’s Challenge Fund) recipients. Although the integrated care pilots/pioneers specifically followed an integrated care agenda, the GP Access Fund31 schemes took a more indirect route to integration, as the focus was ‘to help improve access to general practice and stimulate innovative ways of providing primary care services’ (contains public sector information licensed under the Open Government Licence v3.0). 32 In parallel, in some localities, a more bottom-up approach to community integration developed, such as ‘Healthy Villages’ in Birmingham,33 where community partnerships were established with the NHS and the local authority, again as a result of the combined pressures of demographic and financial challenges. 34 Lack of formal evaluation, compared with the vanguards, means that the learnings and outcomes are difficult to access.
The evaluation of the UK Integrated Care Pioneers found some convergence of activities towards a similar set of specific interventions, including primary care-centred features of multidisciplinary teams (MDTs) and care navigation. 35 It was also noted that these pioneers became less ambitious and more pragmatic in their efforts to achieve horizontal local integration as delivery progressed. 35
Table 1 provides some examples of what might be considered to be the main legacy models of MCPs, such as integrated care approaches, either in England or internationally. The models we have listed in Table 1, and described below, were identified to be of interest to MCP vanguards. These models were mentioned in the ‘value propositions’ that each vanguard was requested to submit with their programme logic models (to request funding from the NHS Transformation Fund in 2016/17). 42 These legacy or international models were mentioned because they resonated with MCP vanguards in their design or aspirations. The Strategy Unit had access to these materials, as we supported the development of the vanguard logic models, and the new care models team gave permission to further use the materials for the purpose of this synthesis. As such, the international models discussed here are not intended to be an exhaustive assessment by the review authors, but rather a reflection of models that were known to, and thus likely to influence, MCP vanguards.
| Name | Location | Timeline | Evaluation/overview |
|---|---|---|---|
| Predecessors to the MCP | |||
| Integrated Care Pilots | England | 2008–10 | RAND Europe, and Ernst and Young LLP (2012)36 |
| Integrated Care Pioneers | England |
First wave: 2014 Second wave: 2015 |
Erens et al. (2016)35 |
| GP Access Funds | England |
First wave: 2014 Second wave: 2015 |
SQW and Mott MacDonald (2016)32 |
| Other models of care that have influenced MCPs | |||
| ACO | USA |
Pioneers: 2012–16 Next generation: 2018 |
L&M Policy Research (2016)37 |
| Alzira | Spain |
First 15-year contract in 1999 Second 15-year contract in 2003 |
de Rosa Torner (2012)38 |
| Buurtzorg | The Netherlands | Founded in 2006 | Gray et al. (2015)39 |
| Gesundes Kinzigtal | Germany | Founded in 2006 | Hildebrandt et al. (2010)40 |
| Nuka | USA – Alaska | Founded in 1999 | Southcentral Foundation (2016)41 |
Accountable care organisations
Of the international models, arguably the key influencer of the new care models was the US accountable care organisation (ACO) approach. ACOs were introduced in 2012, following new legislature for health-care reform in the USA, which directed the Centers for Medicare and Medicaid Services (CMS) Innovation Centre to develop and test new payment and service delivery models through the Patient Protection and Affordable Care Act. 43 ACOs are described as a group of providers that are contractually responsible to a commissioner to provide all of the care for a given population over a defined period of time, and to uphold pre-agreed quality outcomes within a given ‘capitated’ budget or ‘fee-for-service’ agreements. 44 The programme theory for ACOs is that if providers have an opportunity to share in financial rewards (or face penalties), then ACOs will reduce fragmentation and duplication in medical care. It is suggested that the improved communication and co-ordination across providers, physicians and patients will improve the quality of services and reduce spending. 45 The Pioneer ACO programme started in 2012, with 32 pioneer sites chosen by the CMS to participate, and ended in 2016 with eight organisations. 45 Forty-four next-generation ACOs have been selected by the CMS and will begin the programme in 2018. 45
Gesundes Kinzigtal
Gesundes Kinzigtal (meaning ‘healthy Kinzigtal’ – the town in south-west Germany where the model was introduced) is an accountable network of physicians, partnering with a health-care management company, driven by the needs of multimorbid patients requiring co-ordinated care. 46 Long-term contracts were put into place in 2006 with two German non-profit sickness funds to integrate health and care services for their insured populations. The integrated system covers a population of 60,000, of which Gesundes Kinzigtal is in charge of the health-care budget of 31,000 ‘assureds’. 40 It has a responsibility to deliver regionally integrated health and care services, covering all age groups and care settings, with the explicit triple aims of improving the health of the population, enhancing the patient care experience and reducing the per capita costs of care. To date, improved population health outcomes,40 potential cost-effectiveness,47 more appropriate access (decline in overuse, underuse and misuse of health care) and an increase in health-care quality have been reported. In early 2017, the lessons from Gesundes Kinzigtal were applied to the launch of a new integrated care model in a city in northern Germany, which was designed to improve access to health services in two of Hamburg’s disadvantaged suburbs: Billstedt and Horn. We discuss the underpinning evidence around access in integrated systems in Chapter 4.
Alzira
The Spanish ‘Alzira’ model (named after the town where the model was first implemented) is akin to the financially led model of the US ACOs. However, it has a unique feature of private and public contracting, such that the private sector finances the construction and operation of the health-care infrastructure and delivers clinical services through a capitation fee. This reduces the public sector partner role to that of commissioner of health care. 48 The regional government entered into a long-term contract in 1999 for 15 years, and cost-effectiveness benefits were widely reported. 38 Acerete et al. ,49 however, dispute some of the claims, stating that ‘the precise level of cost savings achieved has never been subject to public scrutiny and remains controversial, with a true like-for-like comparison impossible’. 49 The financial innovations of both the ACO and the Alzira models have influenced the vanguards’ contracting and budgeting mechanisms, and we explore this further in Chapter 5.
Nuka
The Nuka System of Care50 is built on the premise that the relationship between the primary care team and the patient/customer-owner is the single most important tool in managing chronic disease, controlling health-care costs and improving the overall wellness of a population. It was developed in the late 1990s by the Southcentral Foundation, a non-profit health-care organisation serving a population of around 60,000 Alaska Native and American Indian people in Southcentral Alaska. 41 The accountability for improved health outcomes in Nuka lies with the partnership of providers and people in the Native Alaskan community, who changed from being the ‘recipients of services’ to the ‘owners’ of their health system, so that they could co-design services and oversee implementation. The Southcentral Foundation’s annual progress report documents outcomes that include increased patient satisfaction and significant reductions in the use of specialist and hospital-based treatment. 51 The key to the success of this model of integrated care is suggested to be the transfer of the partnership ‘power’ to the recipients of services. 51 We explore partnerships for integrated care further in Chapter 6.
Buurtzorg
The Dutch Buurtzorg (neighbourhood care) not-for-profit model was born out of a desire to improve the staff experience of community nurses delivering integrated home care. It aimed to provide an accountable partnership with social innovation, ‘humanity over bureaucracy’, at its core,52 by attempting to shift the care delivery mindset from managerial protocols and administration to clinical autonomy and accountability. 53 Buurtzorg Nederland was founded in 2006, with a small team of professional nurses, and following 10 years of operation, the model has extended to encompass 10,000 nurses in 850 teams in towns and villages all over the Netherlands, and has spread to a further 24 countries. 54,55 In response to criticisms of ‘cherry-picking’ of patients in its reporting of cost-effectiveness, the Dutch Ministry of Health, Welfare and Sport commissioned the consulting firm Klynveld Peat Marwick Goerdeler (KPMG; Amstelveen, the Netherlands) to compare Buurtzorg with other home-care providers. This evaluation showed that, even after controlling for differences in patient characteristics, Buurtzorg remained a low-cost provider of home-care services; the addition of patients’ total costs (nursing home, physician and hospital costs) resulted in Buurtzorg’s total per-patient costs being around average for the Netherlands. 39 Moreover, the quality of care was deemed efficient, as demonstrated by patient satisfaction56 and a high level of staff experience, as shown by Buurtzorg being named the best national employer in 2010–12. 39 Chapters 4–6 provide further support for the inclusion of staff experience as a health-care aim.
Multispecialty community provider progress
As a result of reductions in agency/locum staffing at trusts and commissioner underspends, the Next Steps on the NHS Five Year Forward View57 reported a context of ‘improved financial grip’ in 2017 compared with 2014. A further contributor was the deployment of funding to manage local emergency activity pressures. Here, the MCP and PACS were highlighted as having lower growth in emergency hospital admissions and emergency inpatient bed-days than the rest of England, in the period of January–December 2016, compared with the October 2014–September 2015 vanguard baseline. Of the MCP vanguards, Principia Partners in Health reported absolute reductions in emergency admissions per capita. 57
The Next Steps on the NHS Five Year Forward View57 notes that sample sizes and the duration of implementation may limit the applicability of the results. The same document suggests that vanguards, in particular, are expected to ‘earn their passage’ and take clearer financial accountability for reducing emergency hospitalisation growth in their area, in order to be deemed a success and earn accountable care system (ACS) status. 57 Thus, the definition of vanguard ‘success’, and a more general pressure to report a positive impact, through the measurement of emergency hospital admission growth in the short term, was noted by some commentators to signal a change from a model that is ‘coherent, patient-centric and focused on prevention’, which takes time towards delivering a more tangible measure of success, to one which has to justify central investment. 58 The scaling-down of ambition – ‘the original Forward View vision of PACS and MCPs, as embodied by the vanguards, is still relevant but its collision with reality has produced a more modest set of ambitions and a less all-encompassing definition of success’58 – resonates with the previous assessments of integrated care pioneers. 35
However, this might not be the case for all vanguards; those that are more established and moving from being experimental to business as usual – ‘A few areas (particularly some of the MCP and PACS vanguards) in England are on the road to establishing an ACO, but this takes several years’57 (contains public sector information licensed under the Open Government Licence v3.0) – may become more ambitious, with the formation of ACSs initiating ‘the biggest national move to integrated care of any major western country’. 57 The first eight candidates for ACSs were announced in June 2017,59 with the remit to retain existing health and social care structures (this is different from ACOs), to deliver integrated care with increased financial accountability, negating the need for burdensome annual transactional negotiations. 57,60
Aim and objectives
The aim of this synthesis was to provide decision-makers in health and social care with an ‘actionable’ evidence base for the MCP model of care. We believe that this synthesis, based on realist principles, can serve as a ‘blueprint’ with ‘active ingredients’ to inform the design and delivery of current and future iterations of the MCP model. 61
Specifically, the objectives of the synthesis were to:61
-
articulate the underlying programme theories of the MCP model of care, by mapping the logic models of the 14 MCP vanguards, selecting and prioritising significant theories for investigation
-
identify sources of theoretical, empirical and practice evidence to test selected programme theories
-
appraise, extract and analyse evidence, reconciling confirmatory and contradictory evidence
-
develop the synthesis, explaining how the mechanisms used in different contexts contribute to outcomes and process variables
-
consult with key stakeholders to validate the findings and to test their applicability to different contexts
-
finalise the synthesis, incorporating stakeholder feedback
-
disseminate the findings, preparing a series of practical tools to support knowledge.
Chapter 2 Review methodology: stakeholder engagement, programme theory elicitation and analysis of the literature
On initiation, the review team registered a review protocol with the PROSPERO database and published an expanded version within a peer-reviewed journal. 61 This chapter first describes how we analysed existing logic models to identify programme theories and then engaged with stakeholders in order to verify and elucidate these potential programme theories. Subsequently, we conducted a systematic search of the relevant literature, supplemented by further purposive explorations for evidence, underpinning each programme theory component. Key to the review strategy was our realisation that we needed to prioritise programme theory that could most inform the current development of MCPs. A two-level approach was used to populate, first, full programme theory reviews (R1–3), and then, second, a larger range of programme theory maps (M4–7), which seek to identify the key evidence underpinning additional important programme theory components prioritised by the stakeholders. Just as an intervention may have multiple intervention components, each triggering one or more mechanisms, so too a programme theory can be seen to have multiple theory components, each engaging with one or more mid-range theories. In actuality, when a programme is delivering against the intended outcomes, all of the programme theory components operate synergistically and interactively. However, for evaluation purposes, theory components are best dissected as separate entities and explored, in this report, via either programme theory reviews or programme theory maps. By programme theory component, we therefore refer to the most meaningful level of granularity for the overarching programme theory to be examined, by mapping and assembling the literature.
This chapter seeks to follow the reporting standards advocated by the National Institute for Health Research (NIHR)-funded Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) project. 62 We describe how we carried out our review, following the steps outlined in comparable projects. 63 We have found it helpful to follow Pawson’s64 time and task template for a realist synthesis. Specifically, with regard to searching for evidence, we have broadly followed the six principal elements identified in a forthcoming chapter on the ‘realist search’. 65
As stated in the previous chapter, the aim of our realist synthesis was to provide decision-makers in health and social care with a practical evidence base relating to the MCP model of care.
Justification for the choice of a realist/best-fit framework synthesis
Best-fit framework synthesis
We took the innovative approach of using a best-fit framework synthesis as a means of organising and mapping data, as a prequel to a formal realist synthesis. A best-fit framework synthesis offers a rapid tool by which to facilitate data extraction and analysis, and thus maximise the value of the interpretive synthesis in a way that is amenable to the production of practical recommendations. 66 Framework synthesis is considered ‘especially suitable in addressing urgent policy questions where the need for a more fully developed synthesis is balanced by the need for a quick answer’. 67 A best-fit framework synthesis offers a pragmatic variant of framework synthesis. Instead of spending a disproportionate amount of time in developing a definitive conceptual framework with stakeholders, a best-fit framework synthesis uses the best-available conceptual or instrumental frameworks as a starting point for extracting and analysing the data. In doing so, it harnesses ‘the recognised strengths of both framework and thematic synthesis’. 68 Furthermore, in this project, we specifically sought frameworks with ‘practitioner credibility’ with those working within a rapidly developing area of models of care. Framework synthesis was thus selected as a vehicle for the future dissemination of findings. A best-fit framework synthesis was subsequently combined with a synthesis following realist principles, which is particularly suited to exploring what works, when, for whom and in what circumstances.
The realist principles used in this project derive from the need to use methods that acknowledge the inherent complexity within programmes of change and their evaluation. 69 Although the initial development of the realist methodology focused on realist evaluation, using purposely collected and readily available primary data, Pawson64 subsequently identified the need for, and documented, a corresponding process within the emerging science of reviews. The realist synthesis approach has been consolidated and explored more fully, as demonstrated by Rycroft-Malone et al. 70 in 2012. Particularly influential is the trend to combine elements of realist evaluation and synthesis in order to optimise relevance and transferability. The realist approach acknowledges that interventions do not necessarily transfer easily from one setting to another, and offers deeper insights into the contextual factors involved in change. Realist approaches have been demonstrated as having particular utility within the NIHR’s Health Services and Delivery Research (HSDR) programme-funded projects. 63,71,72
Programme theory development and refinement requires undertaking a series of activities. These activities do not necessarily take place sequentially, and are typically iterative. However, we present them serially for transparency and ease of understanding. We undertook the following activities, reinterpreted from Pawson64 and others in a forthcoming book chapter (due for publication in June 2018):65
-
formulating specific questions as lines of inquiry73
-
exploring a proposed area of research to identify previously published research and, if necessary, refining the research question (the background search)64
-
identifying theories as hypothetical explanatory accounts (initial programme theories) of how an intervention works (the search for programme theories)64
-
identifying empirical evidence to test and refine the initial programme theory (the search for empirical evidence)64
-
responding to new information needs that emerge during testing and refining the initial programme theory (the final search to refine programme theories)64
-
documenting the search process in an explicit and transparent manner. 62,74
A realist synthesis is theory driven and seeks to unearth ‘the unseen elements of a programme (the mechanisms) that lead to its success or failure’. 72 Configurations of contexts, mechanisms and outcomes are mapped to show how particular contexts or conditions trigger mechanisms to generate outcomes. Multiple mechanisms may be activated within each intervention, each representing a ‘pathway from resource to reasoning and response’. 75 The reasoning and response may derive from the perspectives of the receivers, the organisers or those delivering the programmes. 76
Programme theory ‘describes the theory built into every programme’,62 being expressed as ‘if we provide these people with these resources it may change their behaviour’. 77 A strength of realist synthesis is its facility to accommodate diverse sources of evidence when ‘reconstructing’ programme theories. It draws from a systematic process that includes stakeholder engagement, an overview of relevant extant theory62 and close examination of primary research. 64 Such an approach faces three challenges: (1) many commentaries may not articulate a programme theory, or at least may not make a particular programme theory explicit; (2) programme theories may be expressed in a variety of forms and formats, making translation and comparison problematic; and (3) the non-standardisation of format makes it difficult to prioritise theories for further exploration.
However, important adaptations from the classic realist approach acknowledge our ready access to an explicit source of programme theory (i.e. the logic models produced by the local MCP teams). Although programmes of change (i.e. New Care Models programmes) may be considered to be ‘theories incarnate’;69 these theories truly ‘take on flesh’ when realised within the structure of logic models. In this review, we developed a theory by analysing the definitive published logic models, along with their associated narratives, as a source of articulated theories about ‘what works’ in MCP models and the conditions that might result in the achievement of programme success.
For the purposes of this review, a MCP was considered to be ‘a new type of integrated provider’ that ‘combines the delivery of primary care and community-based health and care services’ with the result that ‘services previously based in hospitals’ (e.g. outpatient clinics, diagnostic, day surgery, etc.) may be delivered in the community. It may also involve the integration of ‘mental and physical health services and, potentially, social care provision, together with NHS provision’ [adapted from NHSE (2016);11 contains public sector information licensed under the Open Government Licence v3.0].
As this definition implies, successful implementation and transformational change are contingent on diverse factors that must be acknowledged within a review approach that accommodates complexity and contingency. As a consequence, we selected a theory-driven approach to evidence synthesis, underpinned by the realist philosophy of science and causality. 78
Review questions
Our original review questions were as follows:61
-
What are the foremost theories of change inherent within the MCP model of care?
-
What seem to be the ‘active ingredients’ that should inform the design of MCP models of care?
-
What are the social and cultural conditions that influence (enabling and blocking) change within MCP models of care, and how do these mechanisms operate in different contexts?
-
What are the key knowledge gaps and uncertainties in relation to the design, implementation and evaluation of MCP models of care?
Changes to the review process
No major changes to the review process were made subsequent to the publication of the review protocol. 61 However, to maximise the utility of the realist synthesis for project stakeholders, and to enhance its value for NIHR, we decided to complement our approach to full realist reviews of key programme theory components with a broadly analogous process of ‘mapping’ for other components identified during the identification of a programme theory.
This mapping approach combines elements of the realist review process,64 rapid realist review approaches79 and features utilised in systematic mapping. 80 Specifically, rapid realist methodology seeks to incorporate the theory specification of a realist review,64 with the boundary clarification aim of a scoping review. 81 In contrast to a systematic review, systematic mapping does not aim to answer a specific question. Instead, it ‘collates, describes and catalogues available evidence (e.g. primary, secondary, quantitative or qualitative) relating to a topic of interest’. 80,82 Included studies are used to develop a greater understanding of concepts and to identify knowledge gaps and knowledge clusters. Systematic mapping aims to share the same characteristics of being systematic, explicit and reproducible that are possessed by systematic reviews, but can be used to address open-framed questions on broad topics. Systematic mapping is particularly valuable for broad, multifaceted questions, as revealed by our identification of programme theory components, whereby a topic of interest is not considered suitable for systematic review.
Identification of programme theories
A ‘classic’ realist synthesis begins with the identification of opinions and commentaries as a source of programme theories for which evidence is later sought.
Multispecialty community providers as new care models represent complex social programmes, involving multiple stakeholders or actors, structures and organisations. We were able to harness a ready source of programme theory, in the form of logic models developed by 12 of the 14 MCPs. These logic models were submitted to NHSE as part of its programme documentation in the first year of new care model funding. Although falling short of a standardised format, all were informed by the conventions of logic model presentation. 83 Logic models ‘outline the inputs, processes, outputs and outcomes of a programme’84 in an accessible diagrammatic form, typically with accompanying notation and/or explanatory text. The logic models developed by the vanguards typically follow the model recommended in The Magenta Book: Guidance for Evaluation,85 which lends itself to the CIMO (context, intervention, mechanisms, outcomes)73 framework within which we planned the search strategy.
An initial rapid desk-based analysis of the MCP vanguard applications identified that multiple interventions and mechanisms are being developed at the micro, meso and macro levels [e.g. extensivist primary care, multidisciplinary community teams, social prescribing (interventions), community assets and social capital (mechanisms)]. Resources can be ‘material, cognitive, social or emotional’. 77 Resources identified within NHSE’s MCP Framework: Working Document86 include design, evaluation, integrated commissioning, patient and community empowerment, technology, workforce, leadership and engagement.
Formulating specific lines of inquiry
In many realist reviews, the research team needs to ‘surface’ programme theories from interviews with stakeholders, and from the published literature and more ephemeral contributions, such as blogs and newspapers. Our access to the formal logic model submissions submitted by vanguards as a requirement for applications for funding allowed us to explore a full spread of interventions, as identified by the vanguards, against a backdrop of different contextual characteristics. The selection of vanguard sites holds an inherent advantage in offering a form of ‘intensity sampling’. However, from a methodological point of view, the concept of a ‘vanguard’ holds an inherent risk of selection bias (i.e. the likelihood that sites have been selected according to their readiness for new care models). So, although we sought to explore the implementation of new care models across a diverse sample of care providers, the total sample itself had been preselected. Such caution is particularly important when looking to apply review findings to roll out and sustainability for ‘failed’ vanguard applications and for those sites that could not aspire to a vanguard application. Nevertheless, existing MCP vanguards represent significant diversity of both contexts and target populations, as acknowledged in our choice of an approach that emphasises ‘what works for whom under what circumstances’,69 and offer the potential to identify context-specific issues and constraints at a particular level, even where a general pattern of successful implementation appears to prevail. Under these conditions, it becomes particularly important to implement a series of validation checks and balances within the strategy for data synthesis.
Strategy for programme theory identification
The extraction and articulation of programme theories offers a foundation for the entire realist synthesis project. We analysed all available MCP logic models (12 of the 14 sites), supplemented by related documentation available in the public domain (via vanguard websites and the NHSE website). We worked systematically through all of the available logic models, extracting causal links in the form of ‘if–then’ statements. 87 We then grouped these if–then statements thematically within a spreadsheet (Table 2) and sought to reconstruct the causal pathways into an aggregated logic model that represented the integrated programme theory from across multiple sites (see Chapter 3).
| Statements | |
|---|---|
| If . . . | Then . . . |
| Commissioners fund new community facilities | Community services will increase capacity |
| Commissioners fund new community facilities | Acute services will discharge patients to community facilities (step-down) |
| Commissioners fund new community facilities | Health-care professionals will treat more patients closer to or at home |
| Commissioners fund new community facilities | Practitioners can support the patients most likely to need acute care |
| Commissioners fund paramedic practitioner roles to support home visiting | Fewer patients will attend A&E departments |
| Commissioners fund paramedic practitioner roles to support home visiting | GPs will refer fewer patients for emergency admissions |
| Commissioners fund paramedic practitioner roles to support home visiting | Commissioners will negotiate disinvestment in acute beds |
When causal links were incomplete, an attempt was made to verify these links from the logic model of an alternative source. When this was not possible, these orphan links were ‘parked’ for later review and rationalisation. Logic models are sometimes criticised for being ‘rigid’ and for not making explicit the causal pathways through which change occurs. 84 Closer examination of our data source confirmed these complexities – sometimes nodes or links between logic model components were imperfectly articulated; in other instances, intermittent links were omitted, resulting in incomplete causal pathways.
An investigation of the full set of available logic models was intended to reveal the diversity of the different programme theories underlying MCPs, while also uncovering fundamental local differences in approach or emphasis. The resultant set of programme theories was compiled for discussion with the advisory group.
At the same time, team members were sensitising themselves to different interpretations of the new care models initiatives through official documents, local guidance, independent commentaries and blogs and current awareness services, such as the Health Service Journal, The Commissioner Newsletter and NHSE’s New Care Models Bulletin. Broader exploration of the wider historical and political context also took place; for example, via the literature on large-scale transformation. 42,88
As a model of care comprising a broad range of interventions, the MCP model generated multiple programme theory components. The richness of the data is significant – we extracted, in total, 1394 if–then statements. All statements were coded using the agreed best-fit framework and then grouped into themes that emerged from the data. This allowed us to compare the MCP programmes in terms of context, mechanism and outcome configurations efficiently and rapidly within the subsequent realist synthesis. 79
We developed twelve draft theories:
-
innovative services deliver sustainable care
-
community-based, co-ordinated care is more accessible
-
collective responsibility improves quality and safety outcomes
-
multidisciplinary teams provide continuity of care
-
local MCP contracting delivers ACOs
-
pooled budgets incentivise integrated care providers
-
fostering relational behaviours builds resilient communities
-
integrated care navigators increase workforce capacity
-
engaged and trained staff lead cultural change
-
new ways of working enable staff resilience
-
evaluation activities sustain transformational change
-
information-sharing enables effective collaboration.
By cataloguing the different programme theories underlying MCPs, as identified from the logic models (reported in Chapter 3 of this report), we were able to identify underpinning mechanisms by which different programme components achieve their effect, as perceived by those actively involved in designing and implementing the New Care Models programmes across the vanguard sites.
Agreeing the focus of the review
To agree the focus of the review, we presented our initial programme theory components and a basic overview of constituent if–then statements at a 1-day stakeholder meeting. Our stakeholder event included the following people:
-
an academic, who was the chief investigator of another HSDR programme-funded New Care Models project (reference number 15/77/10)
-
the accountable officer/chief clinical officer of a CCG, which was a MCP vanguard site
-
the chief officer of a CCG, which was a MCP vanguard site
-
a communications consultant and fellow
-
the Director of Primary Care in a CCG
-
an evaluation lead in NHSE
-
an executive director of a MCP vanguard site
-
a regional manager of the New Care Models programme in NHSE
-
two patient and public representatives
-
the Director of Strategy of a community health-care foundation trust.
We presented our initial programme theorising as ‘propositions about how new care models are intended to work’, and invited participants to comment on these ideas and refine, extend and prioritise them.
Contribution of the project advisory group
A detailed assessment of the area under study identified a lack of a single appropriate framework. In June 2016, the project advisory group was briefed on the aims, objectives, scope and approach of the study, with a specific focus on the best-fit framework synthesis approach, sharing with them a tentative framework with which the review team intended to support the realist synthesis. The discussion proved to be extremely fruitful, as the review team were made aware of a forthcoming framework from NHSE.
Working with the advisory group allowed us to test the proposed approach and programme theories with key stakeholder groups. It also made us aware of relevant work within the New Care Models programme and the vanguard sites. For example, the review team secured early sight of an implementation matrix being developed by NHSE, which sets out the key characteristics and expectations of new care models.
Creation of a metaframework
Subsequently, we identified five existing frameworks to cover the various aspects relevant to the MCP model of care. These were derived from three relevant guidance documents for MCPs (a, b and e) and two integrated care frameworks (c and d):
-
the eight enablers of transformation in The Forward View into Action: New Care Models: Update and Initial Support89
-
MCP Framework: Working Document 86
-
Framework on Integrated, People-Centred Health Services 90
-
System Leadership: Lessons and Learning from AQuA’s Integrated Care Discovery Communities 91
-
The Multispecialty Community Provider (MCP) Emerging Care Model and Contract Framework. 11
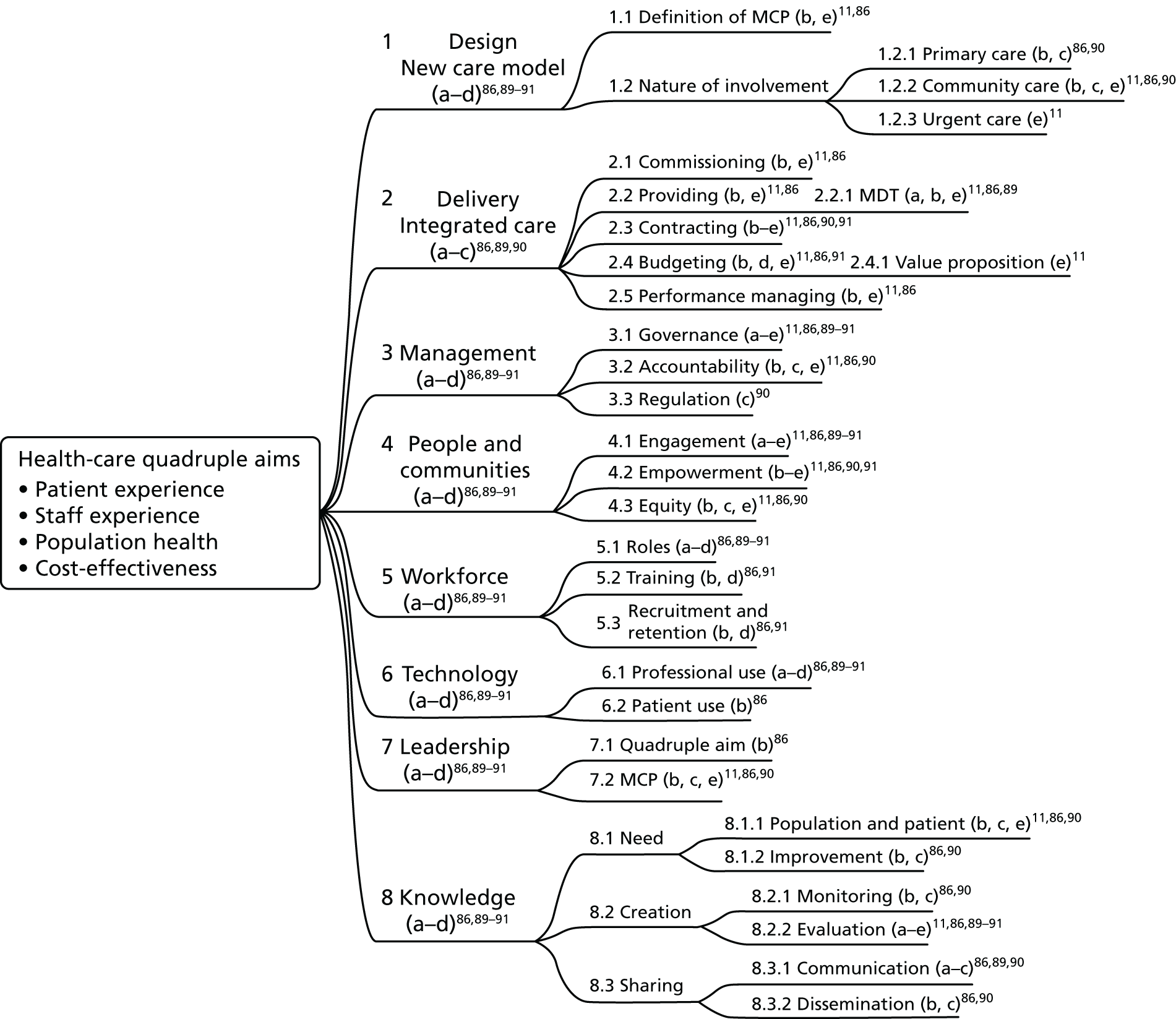
Finally, a sixth quadruple aim framework was identified to capture the intended outcomes, namely, patient experience; the health of the population; health-care costs; and staff experience. 17 The chosen frameworks each contributed unique elements, and so we followed the approach, previously reported by Carroll et al. ,68 of merging the six frameworks into a single metaframework. Essentially, the best-fit framework provided an additional analytical lens for the data, separate from the realist terminology and principles, and offered resonance with the world view of the stakeholders. By combining the six frameworks within a single metaframework, we constructed both a conceptual map and a vehicle for the organisation and extraction of data (Figure 1).
FIGURE 1.
Best-fit framework.
Strategy for prioritisation and finalisation of the candidate programme theories
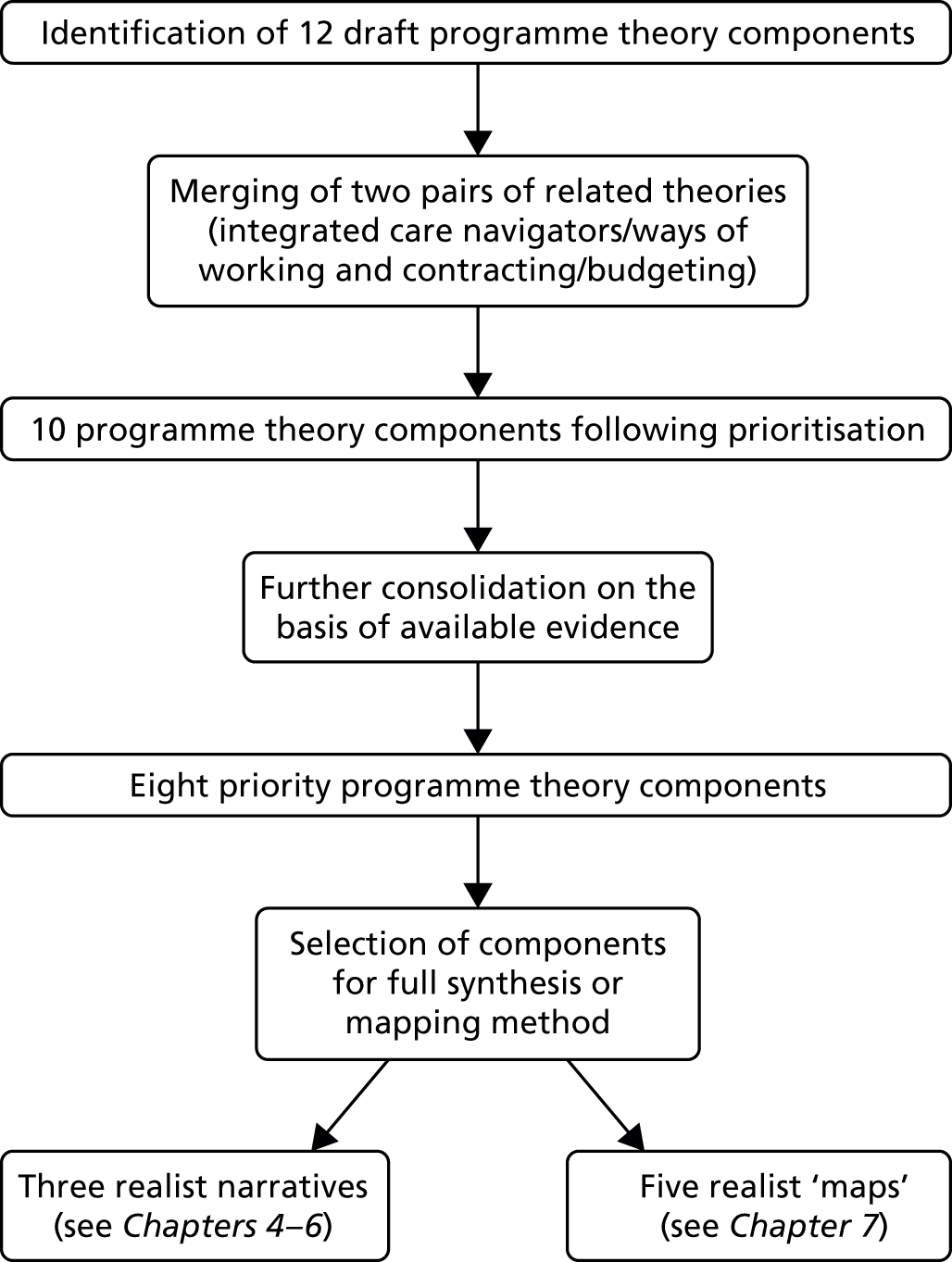
Following the stakeholder workshops, we held a review team meeting to reflect on the issues raised and to agree the focus of the review. We chose not to utilise a formal method of prioritisation, recognising that our stakeholder event had not been organised on representation principles; instead, stakeholders offered valuable perspectives on the 12 individual programme theory components and the composite programme theory (Figure 2). It was interesting to observe a strong consensus on priorities across professional and lay representation, even when more overtly public- or patient-focused programme theory components featured in the candidate list.
FIGURE 2.
Identification and prioritisation of programme theories.
As a result of the stakeholder event, the review team:
-
merged several related programme theory components in which synergies were identified
-
refined the wording of several programme theory components to make them more accurate or salient
-
prioritised several theory components for full realist review, while allocating the remaining theories to a broad focused mapping approach (see Box 1).
The stakeholder group had also initiated an informative discussion on the possible unintended consequences of specific elements of the MCP model; for example, how moving diagnostic services into the community might stimulate increased locality demand with a consequent effect on false positives, referrals and admissions.
A flow diagram and narrative was developed for each draft theory (see Chapters 4–7), which were reviewed with the project advisory group in October 2016. The group was asked to validate theories and to prioritise those appropriate for realist review. This conversation was supplemented with telephone interviews with each of the three MCP leads on the advisory group. From working with the group, we were able to merge two of the theory components (integrated care navigators and ways of working) into one and prioritise three theory components for realist review (see Chapters 4–6 and Figure 2). The group opted to prioritise theory components that represent the more innovative aspects of the MCP model, typically those for which coverage by existing reviews is more limited. We proposed to conduct mapping reviews for the remaining theory components (see Chapter 7) to provide realist-oriented overviews of the key review literature.
We subsequently merged the two theories relating to contracting and budgeting, resulting in 10 theories (four prioritised for realist review, with the remaining six subject to mapping review; see Figure 2). Finally, a detailed examination of the respective evidence bases underpinning the programme theories indicated further commonalities in arriving at the following programme theories (Box 1) for exploration through the theoretical literature and the empirical evidence (three for review and five for maps).
If primary care providers grow (new/expanded roles, additional services, hubs, extended hours) to deliver place-based services, then patients will access more specialist care within community settings.
R2: place-based contracting and payment systems incentivise shared accountabilityIf commissioners award place-based contracts (incorporating new accountability and governance models, capitated budgets and risk-sharing), then providers will adopt integrated working.
R3: fostering relational behaviours builds resilience within communitiesIf commissioners and providers develop mutually beneficial relationships and co-produce services (with patients, the public, the voluntary sector, community groups, local businesses and other public services) within local communities, then health and care services will support local communities to build resilience.
Programme theory component maps M1: collective responsibility improves quality and safety outcomesIf providers share a collective responsibility for outcomes through standard integrated pathways, then providers will improve the quality and safety of care.
M2: multidisciplinary teams provide continuity for patients with long-term conditions/complex needsIf primary care providers deliver care via MDTs (organised around natural communities), then patients with long-term conditions/complex needs will experience better continuity of care.
M3: engaged and trained staff expedite cultural changeIf commissioners and providers train and fully engage staff in service transformation, then staff will drive the cultural change that underpins new ways of working.
M4: system learning embeds and sustains transformational changeIf MCPs learn and adapt quickly using evaluation/monitoring loops and knowledge-sharing, then MCPs will sustain transformational change.
M5: proactive population health is dependent on shared and linked dataIf MCP staff are not able to access shared/linked data, then patients will continue to experience fragmented care.
The draft conceptual model was verified with key stakeholders from within the MCP vanguards and NHSE via individual follow-up telephone interviews (February to March 2017). Advisory group members and wider contacts were thus used to ensure that the model was fit for purpose and meaningful to decision-makers and practitioners.
The methodology we employed offered a systematic vehicle for harnessing the exploratory potential of the realist lens within an accelerated time scale for practitioner benefit. Thematic coding against the best-fit framework allowed us to synthesise the underlying programme theories behind the MCP model by building up causal chains. This was followed by the identification of theoretical, empirical and practice evidence with which to test the programme theories, and appraisal, extraction and analysis of evidence, to include reconciling confirmatory and contradictory evidence.
Identifying and searching for abstract theories
Once the candidate programme theories were finalised, the next step was to seek to make connections between these lower-level service-based theories and higher-level, more abstract theories. This allowed us to develop a series of hypotheses that would be testable against empirical studies identified from systematic searching. More importantly, the level at which such theories operate would make it possible to produce transferable lessons about how, and in what circumstances, new care models produce their intended outcomes.
To identify the abstract theories, we pursued references from within the relevant literature, in particular analyses, commentaries and opinion pieces. This required looking beyond the actual programme theory to identify more specific mechanisms that might be activated by a MCP component (e.g. governance and control, local identity and place, collective ownership). In doing this, we sought to answer such questions as ‘how might we typify this intervention?’, ‘what core underlying idea is at work here?’ and ‘what other interventions are underpinned by similar ideas?’. Several key ideas underpinned more than one of the prioritised programme theories:
-
demand management
-
shared accountability
-
community ownership and resilience.
Abstract theories also emerged from the search for empirical evidence, as described below (see Table 3). Programme theory-related searches do not distinguish between empirical and theoretical literature, so it is efficient to look for examples of each when reviewing identified items. Our systematic approach, utilising Publish and Perish 5.23.9 software [(Harzing.com, Hendon, UK) see Data extraction, quality assessment and synthesis for the realist reviews] represents an improved and more auditable strategy than that used in comparable projects, such as screening the first five pages of Google Scholar (Google Inc., Mountain View, CA, USA) results. 63
Searching for empirical evidence and selection of studies
The next stage of our realist synthesis involved searching for empirical evidence in order to test and refine our programme theories. Following initial validation and prioritisation of the programme theories, we translated key concepts into a search strategy for four core bibliographic databases: MEDLINE, Health Management Information Consortium (HMIC), Cumulative Index to Nursing and Allied Health Literature (CINAHL) and EMBASE (for a sample MEDLINE search strategy, see Appendix 2). A systematic search was conducted to identify research- and practice-derived evidence produced between January 2000 and December 2016. Given that we were unable to identify a specific date from which the forerunners of the MCP model became apparent, any date cut-off point should be considered arbitrary. We therefore sought to achieve a balance that captures the historical legacy of a variety of MCP models, but which focuses on contemporary evidence. We considered that the team would be able to implement a cut-off date of 2000 in a more consistent manner than by calculating a 15-year cut-off date. The bibliographic databases searched included MEDLINE, PreMEDLINE, CINAHL, EMBASE, HMIC and The Cochrane Library, together with grey literature sources, such as The King’s Fund and the Nuffield Trust.
A search strategy was developed by qualified information specialists within the review team to identify published studies against which to test our theories (see Appendix 2). Candidate search terms were identified by analysing documentation, including logic models, from the MCP demonstrator sites. Terms were reviewed by the review team, with particular support from The Strategy Unit colleagues involved in supporting new care models. Further input came from the advisory group set up to support the synthesis.
The strategy covered all four prioritised theories, to avoid potential duplication from running separate searches. Results were screened and supplemented with searches of grey literature sources (see Appendix 3).
Test screening of a single set was initially performed independently by both screeners for 25% of the included records (Table 3). Regular debriefing sessions were held after each batch of records (e.g. after the first 100) to ensure ongoing consistency and identify any systemic reasons for disagreement. As the review team became more sensitised to the types of evidence available, this figure was downgraded to 20% for the remaining batches. Once acceptable agreement was reached, screening proceeded on an individual basis. Test screening was undertaken in batches to check consistency first. Disagreements were referred to one of the principal investigators.
| Broad themes | Number of records screened | Test screening percentage | Screeners |
|---|---|---|---|
| Access | 7965 | 25% (n = 1992) | Three pairs/six screeners |
| MCP | 2230 (2160 from searches, plus 70 additional records) | 25% (n = 558) | One pair/two screeners |
| Community | 8772 | 20% (n = 1755) | Two pairs/three screeners |
| Contracting | 2695 [original total of 2741, but identified 46 duplicates in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA)] | 20% (n = 540) | Three pairs/three screeners |
| Ways of working | 8843 | 20% (n = 1770) | Three pairs/three screeners |
Data extraction, quality assessment and synthesis for the realist reviews
To address the study questions, we sought a recognisably vast and diffuse evidence base with literature comprising four main types:
-
before-and-after studies or interrupted time series from previous or current initiatives [i.e. MCPs or forerunners, such as ACOs (in the USA)]
-
descriptive reports/case studies of current MCP initiatives, offering contextual detail and programme theory
-
commentaries, editorial and opinion pieces on the characteristics and rationale of MCPs and their forerunners
-
policy documents (e.g. from NHSE). 61
For all types of evidence, we focused on their theoretical or contextual contribution, recognising that formal quality assessment of such heterogeneous items would be of little value. For conceptual and contextual types of evidence, we employed a reflexive approach to locate the contribution of each item within the overall body of evidence and to assess its specific contribution.
Our quality procedures were strengthened by an iterative, purposive search for additional confirmatory or disconfirming evidence. Our overall method for quality assessment therefore acknowledged the trade-off between relevance and rigour. 71 In doing this, we sought to clearly identify whether materials had been selected for rigour, for context or for conceptual contribution. In addition, the quality and relevance of the evidence was assessed during the synthesis process, as each lead author weighed up how each individual item contributed to the development of the overall narrative account and to the review question and aims. This approach, which contrasts with the processes of formal quantitative study appraisal, is common within more interpretive synthesis methodologies. 92
Literature of interest could pertain more widely to large-scale transformation as effected by, for example, ACOs (see Chapter 1), or broadly to the different new care model initiatives launched under the FYFV,1 or it could relate specifically to the MCPs. We anticipated generic difficulties with searching for complex social phenomena,93 together with specific difficulties in searching for terms associated with integrated care,94 and thus placed particular emphasis on following up reference lists and conducting forward citation-searching to identify additional evidence. We also anticipated a limited literature examining UK-based MCPs and, therefore, sought to broaden the usefulness of the review by exploring the ‘intellectual heritage’ of the MCP model61 as identified in Chapter 1. In interpreting ‘evidence’, we adopted Williams and Glasby’s95 definition from the management domain, comprising empirical evidence from research; practice-based and experiential evidence from service delivery; and theoretical evidence. Consequently, our search strategy sought to include research studies (trials and reviews), service evaluations and case studies, in addition to thought-leading papers.
For the full realist reviews, we grouped studies together by programme theory. Each item of evidence was used to test the individual programme theory component and the degree to which studies supported, nuanced or challenged that theory. Each review was written up as a narrative account, following the example offered in previous commissioned realist syntheses. 63 As described in Strategy for prioritisation and finalisation of the candidate programme theories, this provides a transparent and auditable account of how each study contributed to theory testing, while allowing the reader to engage with the study findings and our interpretations of them. This process also allowed us to assess the quality of studies supporting, or contradicting, each programme theory component. We offer a summary of the theories in the next chapter before proceeding through each of the realist reviews and realist mapping reviews in turn, in the subsequent sections of the report.
We were aware that relatively few papers within our wider systematic search of related literature looked specifically at the characteristics of MCPs.
The development of the search strategy was iterative; as further keywords were identified within the accompanying narrative, each programme theory component lead ran supplementary search strategies to identify further relevant material. Materials were sifted by each reviewer, and references were privileged, first by relevance (e.g. UK based and contemporary), and then by their reach and significance (i.e. systematic reviews, multiple case studies to increase generalisability). As this was an interpretative and theory-testing review, the emphasis was on indicative evidence that could offer insights, rather than a comprehensive and exhaustive identification of the literature.
Our preferred pragmatic approach to data extraction was to use Google Forms (Google Inc., Mountain View, CA, USA), rather than NVivo (QSR International, Warrington, UK), which has been used by comparable teams. 63 This enabled us to collate, categorise and code information more rapidly, using drop-down categories in recognition of the specific mapping role of these reviews. This approach allows for a formative assessment of review categories and the contributions of literature extracted to date, and identifies gaps for further purposive searching. This approach also enabled us to itemise mechanisms and outcomes, and to map the papers that address these mechanisms and outcomes. A prototype form was developed and tested, incorporating the data extraction logic of ‘confirming/negating/modifying evidence’ from a previous comparable review. 70 One form was completed for each paper.
Data extraction, quality assessment and synthesis for the mapping reviews
For each of the four mapping reviews, we started with a core set of documents (step 1). We then used accepted ‘pearl-growing’ and ‘citation-chasing’ strategies96 to follow up citations and references (step 2). As the intention was to describe and engage with relevant bodies of literature, illustrated by substantive contributions, rather than analysing and interpreting the findings, we did not seek to be comprehensive. We accept that other relevant items could be identified, but we believe that our focus on reviews, overviews and key empirical studies offers a structured foray into these contiguous fields. This interpretive process was selected to correspond to the underlying intent of the overall review methodology and, therefore, contrasts with the more familiar aggregative search procedures utilised by a systematic review. Nevertheless, the search procedures were designed to be auditable, reproducible and ‘systematic’, utilising structured search software (the use of Publish and Perish is described later in this section).
Finally, as particular themes or intervention components were identified, we sought to purposively identify reviews from the broader literature (step 3). Given that the separation of the overarching programme theory into component programme theories and the relative emphasis of review and mapping approaches was decided on primarily pragmatic and logistic grounds, we sought to be as parsimonious and efficient as possible (e.g. when a paper contributed to multiple component theories, one person read it and extracted data for the benefit of the other analytical subteams).
We used a formalised process for searching Google Scholar using the freely available Publish or Perish software to identify, capture and document citation patterns. This process augmented the necessarily limited searches of title and abstract that characterise systematic reviews. We had already identified in our protocol the need for broad full-text searching to identify concepts otherwise buried within journal articles, books or reports. An exemplar for M7 is shown in Table 4.
| M7 system learning embeds and sustains transformational change | |||
|---|---|---|---|
| If MCPs learn and adapt quickly using evaluation/monitoring loops and knowledge-sharing, then MCPs will sustain transformational change | |||
| Concepts | Concept 1 | Concept 2 | Number of references |
| MCPs | Training | 31 | |
| MCP | Training | 59 | |
| MCPs | Transformational change | 59 | |
| MCP | Transformational change | 33 | |
| MCPs | Organisational learning | 22 | |
| MCP | Organisational learning | 61 | |
| Total before removal of duplicates | 264 | ||
| Final total | 99 | ||
Papers identified from the new care models systematic searches (see Table 3), together with the results of individual forays into the literature (pursuing references, citation searches and full-text Google Scholar searching), were initially mapped to any of the component theories identified by the review team. For data extraction, in contrast with the extraction approach used for the reviews, our realist mapping methodology looked for the presence of key contributions to the programme theory, either in supporting or contributing additional insights or nuances (e.g. around the influence of context), or by negating or challenging the theory. A sample data extraction form can be found in Appendix 4.
Follow-up to realist reviews and realist maps
Once a preliminary analysis had been undertaken for a substantive proportion of the realist reviews and maps, the team convened a stakeholder event in Birmingham in May 2017. This small group event targeted MCP vanguard sites, together with the project advisory group members.
In accordance with the NHS Health Research Authority’s statement on public involvement, members of the public/NHS staff were involved in the research process as part of the planning and design of this review. They helped to co-produce the findings, rather than the event being to/for/about them. Our focus group was conducted with members as ‘part of an advisory group, providing valuable knowledge and expertise based on their experience’97 and thus, their involvement did not require ethics approval. This was confirmed by the Health Research Authority’s decision tool assessment. 98
We invited advisory group members, MCP vanguard teams and other stakeholders who had been in contact with the project via related communication activities. On the day, 11 attendees participated, in addition to seven members of the core project team. Of these, two individuals were patient and public involvement (PPI) representatives; three represented commissioners; three came from MCP sites; two were communications specialists; and one was a NHSE lead. We chose a central Birmingham venue because of its accessibility and convenience for many of the 14 MCP vanguards.
The purpose of this event, using focus group methodology, was to explore three key questions:
-
Can community-based, co-ordinated care manage demand?
-
Can place-based contracting and payment systems incentivise shared accountability?
-
Can partnerships with community groups, local small and medium-sized enterprises and other public services build community resilience?
Designed in the format of a focus group and influenced by the realist interviewing technique,99 this stakeholder event offered an opportunity to test and validate the finalised programme theory components and emerging findings with key stakeholder groups. On the day, the project lead and other core team members delivered an introduction to the project (aims/objectives/progress to date) and then walked attendees through the emerging findings for each of the three theory components (R1–R3). Participants were then invited to join a discussion on a relevant theory component. Permission was obtained to record the three discussions, subject to good data management procedures and the lead for each theory component then summarised the group’s responses to the articulated theory and emerging findings (i.e. whether or not these were complete and accurate and whether or not findings resonated with their experience in their various contexts).
As a result, the team was able to collect and analyse a broad range of insights from participants, including decision-makers and operational staff from current and planned MCPs; research and support services staff; and PPI representatives.
Chapter summary
In this chapter, we have described the iterative process through which we integrated data from the preliminary logic models with insights from stakeholders and broader findings from the literature. In following the RAMESES guidelines,62 we have sought to make the process as transparent as possible. We have explained our reasons for selecting a realist review methodology, and described how we searched for programme theories, how we selected our programme theories, how we identified and selected papers and how we synthesised the papers.
Chapter 3 Programme theory
In Chapter 2, we set out the methodology for deriving the eight programme theory components (Box 2). In this chapter, we describe our understanding of these final refined programme theory components (see Box 2), illustrated by selected quotations from MCP vanguard logic models. These components have been gleaned from the analysis of individual logic models to capture causal links, through if–then statement extraction, followed by reconstruction of causal pathways, according to common themes. The logic models prepared by the MCP vanguards varied greatly in terms of the granularity and depth of detail, perhaps reflective of the maturity of the transformation programmes; those which were building on a legacy of earlier initiatives, such as GP Access Funds31 (previously known as the Prime Minister’s Challenge Fund), typically comprised multiple models to represent key activities.
R1: community-based, co-ordinated care is more accessible.
R2: place-based contracting and payment systems incentivise shared accountability.
R3: fostering relational behaviours builds resilience within communities.
M1: collective responsibility improves quality and safety outcomes.
M2: MDTs provide continuity for patients with long-term conditions/complex needs.
M3: engaged and trained staff expedite cultural change.
M4: system learning embeds and sustains transformational change.
M5: proactive population health is dependent on shared and linked data.
The MCP programme theory components encompass an intricate set of overlapping activities and assumptions, highlighting the inherent interdependencies within such a complex service transformation. It is important to note that this complexity is evident in the design of the MCP vanguards and is described in the logic model narratives. For example, the Principia MCP describes the engagement of patients in self-care as a strategy for reducing demand on community-based services, with the aim of releasing capacity within community services, to accommodate a shift from hospital-based to community-based care, and within hospitals to build excellence within core services. 100
Dudley CCG’s approach reflects the different needs of different groups, but with a common focus on access, co-ordination and continuity of care, advocating a central role for primary care in driving integration of care across services. 101
The programme theory components are notable in their coverage of both interventions (what MCPs will do) and ways of working (how MCPs will design and deliver services). The components relate to interventions, such as new contracts, as well as behaviours, such as community involvement. The permutation of activities is shaped by contextual factors, which differ across the 14 MCP vanguards. The documentation associated with MCP logic models recognises enablers of, and barriers to, change but makes little explicit reference, with limited exceptions, to what might be referred to, in realist methodology, as mechanisms.
As described in Chapter 1, the new care models formed an integral part of the FYFV vision,1 signalling a more explicit shift towards system-wide and place-based transformation. As implementation progresses, commentators have advocated a focus beyond integration to a more cohesive approach to population health. 102,103
In this chapter, the underlying logic of each theory component is described further and depicted in a logic model representation, with an accompanying narrative. These were originally developed for stakeholder engagement activities during the study. From MCP vanguard documentation, it is clear that thinking has been influenced, to an extent, by legacy models within the NHS and international models of care; we have indicated models we believe to be pertinent to the various programme theory components.
R1: community-based, co-ordinated care is more accessible
If primary care provision is enhanced (new/expanded roles, additional services, hubs, extended hours) to deliver place-based services then patients will access more specialist care within community settings, rather than the hospital.
Programme theory component ‘R1’ articulates the hypothesis that co-ordinated care is more accessible if it is located closer to home, and will lead to improved health and service outcomes. This theory component describes primary care-led delivery, with accountability/duty of care for patients organised around registered lists. Co-ordinated care is organised around ‘natural communities’ or ‘hubs’ and delivered by MDTs comprising generalists and specialists from the NHS, independent practice, social care, community services and third-sector services. The intention is that a stronger community focus will encourage people to access more services closer to home; the expectation is that accessible co-ordinated care delivered closer to home will help to manage demand, improve patient and staff experience, and improve the efficiency of services. Improved access with features of timeliness, virtual interactions, self-management and joined-up care will contribute to achieving quadruple aim outcomes. Figure 3 shows the logic model and Figure 4 the narrative developed by the project team for the focus group.
FIGURE 3.
Programme theory component R1: logic model.
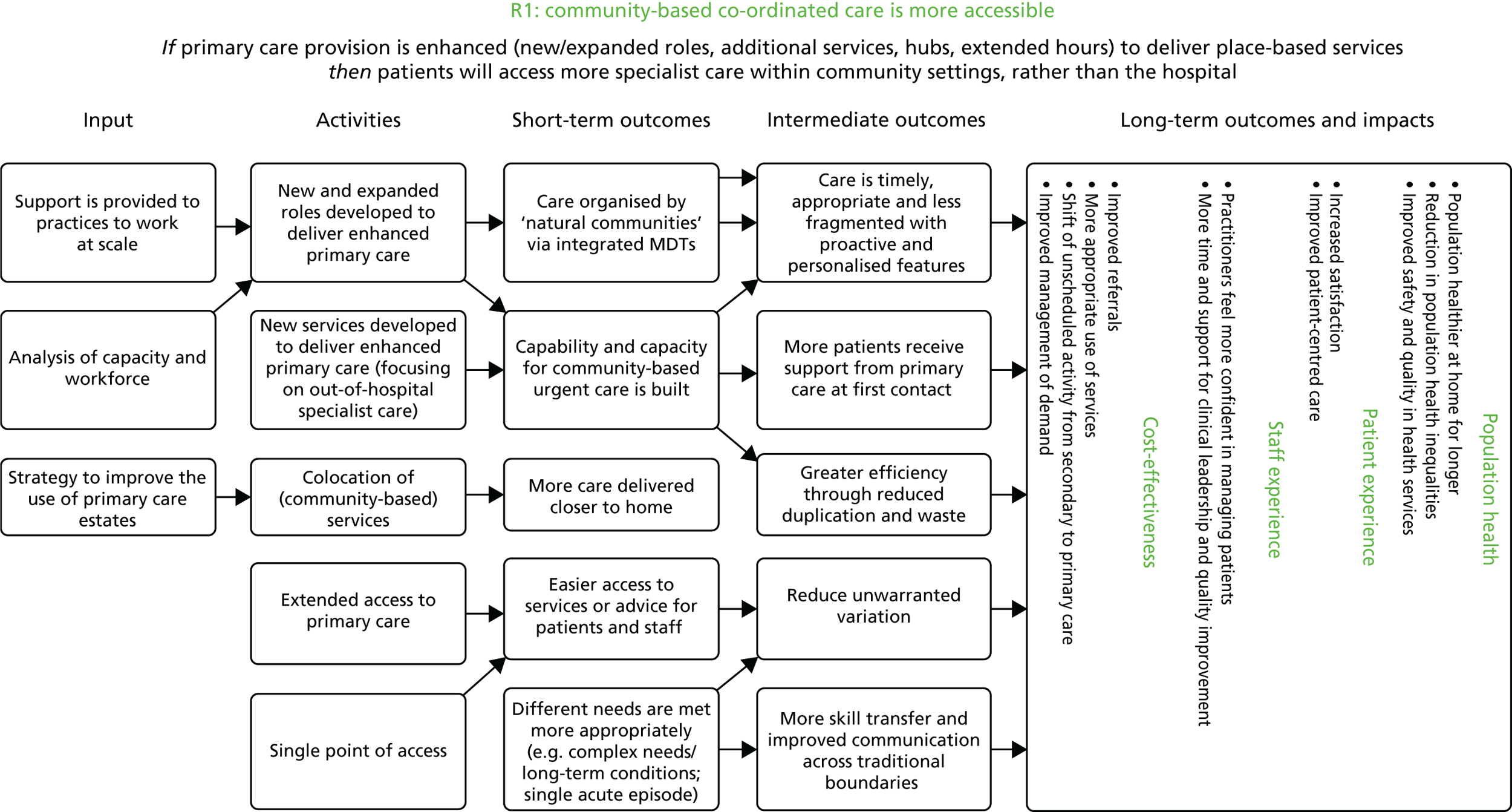
FIGURE 4.
Programme theory component R1: narrative. A&E, accident and emergency; ANP, advanced nurse practitioner; GPwSI, general practitioner with specialist interests; HCA, health-care assistant.
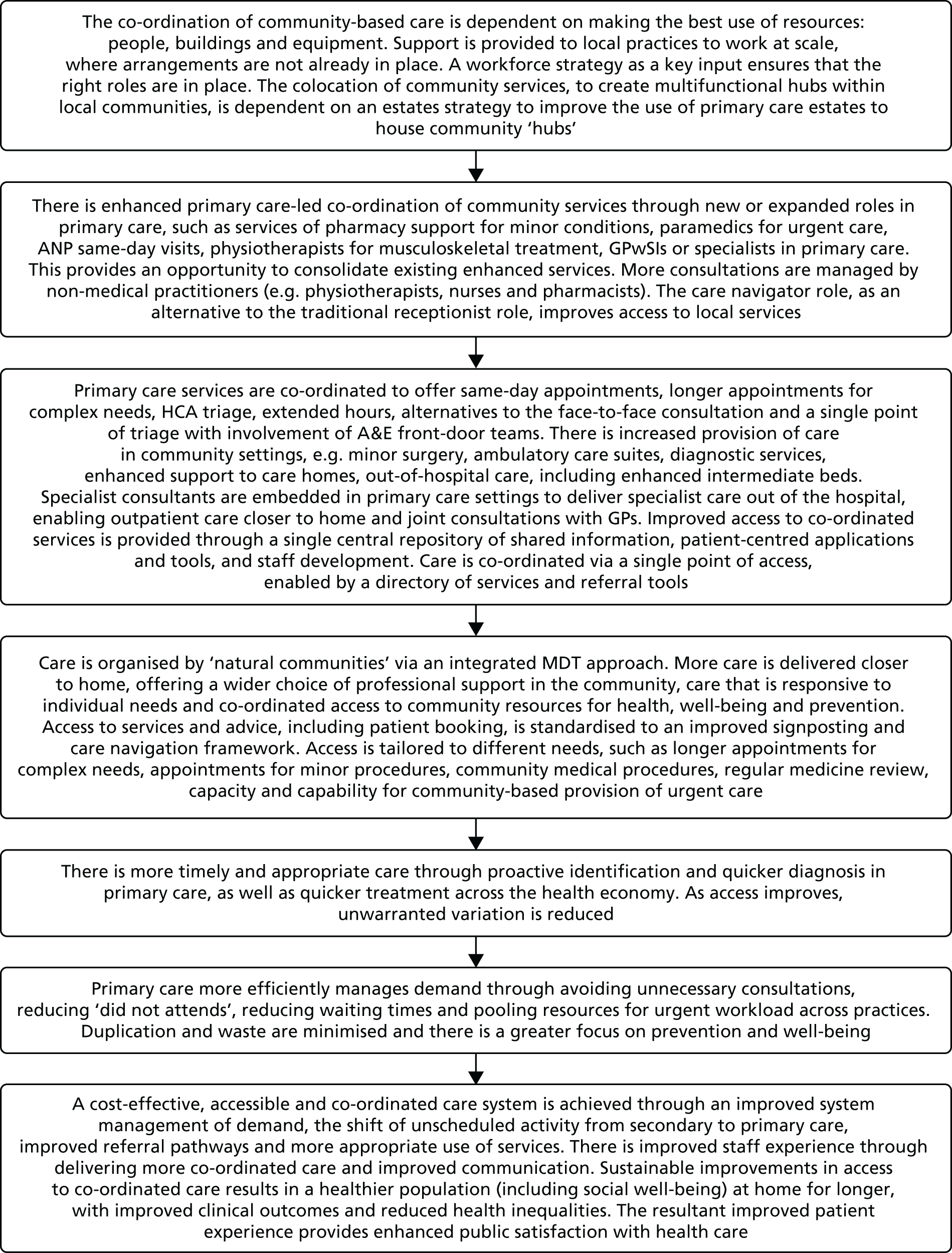
An enhanced capacity to deliver primary care services, through the creation of new roles (such as practice-based pharmacists) and the expansion of existing roles [such as advanced nurse practitioners (ANPs)], is a key element of the MCP model. This is demonstrated by Principia MCP’s vision for better deployment of clinicians to enable more prompt management of acute conditions and improved quality of care for long-term conditions. 100
The Stockport Together MCP aims to improve the interface between primary and secondary care, via the ‘Consultant Connect’ service, which enables GPs to consult secondary care clinicians for specialist advice by telephone. 104
Several vanguards anticipate a significant impact of the expanded primary care model on reducing the GP workload, for example: ‘50% of work done by GPs could be carried out by more cost-effective resource’. 105 Implicit assumptions to the creation of such a team include that these additional roles can be filled, and demand for GP consultations can be shifted to other clinicians, with an associated potential unintended consequence whereby more desirable roles or areas create a market effect.
The MCPs differentiate within their models between the approaches to delivery of acute episodic care and care for complex and long-term conditions; for example, the Connected Care MCP describes an approach to improve access and capacity within primary care, through interventions such as electronic triage and proactive care. 106,107
Although the models share a common ambition to improve accessibility through care closer to home, with many sharing features of extended general practice opening hours or a single point of access to MCP services, local innovations include the concept of the ‘Apple Store-style kiosks’ within practices108 to improve care navigation and reduce the need for receptionists. The Encompass MCP describes a model of working with paramedics to provide urgent home visits with the aim of preventing hospital admissions, now being replicated elsewhere. 109,110 However, such a model is vulnerable to pressures on the 999 service to answer calls in time, which can lead to subsequent withdrawal of the service and increased demands on local GP home-visiting services. 111
The vision of enhanced primary care is not new to the New Care Models programme, and several of the MCP vanguards are building on earlier experience, as participants in earlier initiatives (see Chapter 1), including Darzi centres,112 the GP Access Fund31 (formerly the Prime Minister’s Challenge Fund) and the Integrated Care Pioneers. 113 Influences from international models of care (see Chapter 1) are also evident in the documentation relating to the MCP model; examples include New Zealand’s experiences of transforming primary care;114 Buurtzorg’s model of neighbourhood care115 and the Esther model of co-ordinated care from Sweden. 116
R2: place-based contracting and payment systems incentivise shared accountability
If commissioners award place-based contracts (incorporating capitated budgets and risk-/gain-sharing) then providers will share accountability for population health, cost-effectiveness, patient experience and staff experience.
This programme theory component is predicated on the development and deployment of ‘hard’ levers for change. 117 The need for these hard levers to facilitate integrated care was recognised early on in the New Care Models programme. 11 Earlier attempts to integrate services118 had identified barriers; learning suggested that levers were needed to improve outcomes and encourage place-based accountability. These were capitation, risk- and gain-sharing, differential outcome-based payments and payments for performance incentives. 119,120 Such levers are reflected in early thinking encapsulated in the MCP vanguard logic models, demonstrated by Principia’s intention to develop a single system-wide budget to enable system-wide transformation and delegated decision-making. 100
NHS England has subsequently worked with a subset of six MCP vanguards to develop a contracting framework11 and draft contract documents. 14 Dudley121 was the first of these MCP vanguards to commence formal procurement, in June 2017.
Figure 5 shows the logic model and Figure 6 shows the narrative developed by the project team for the focus group.
FIGURE 5.
Programme theory component R2: logic model.
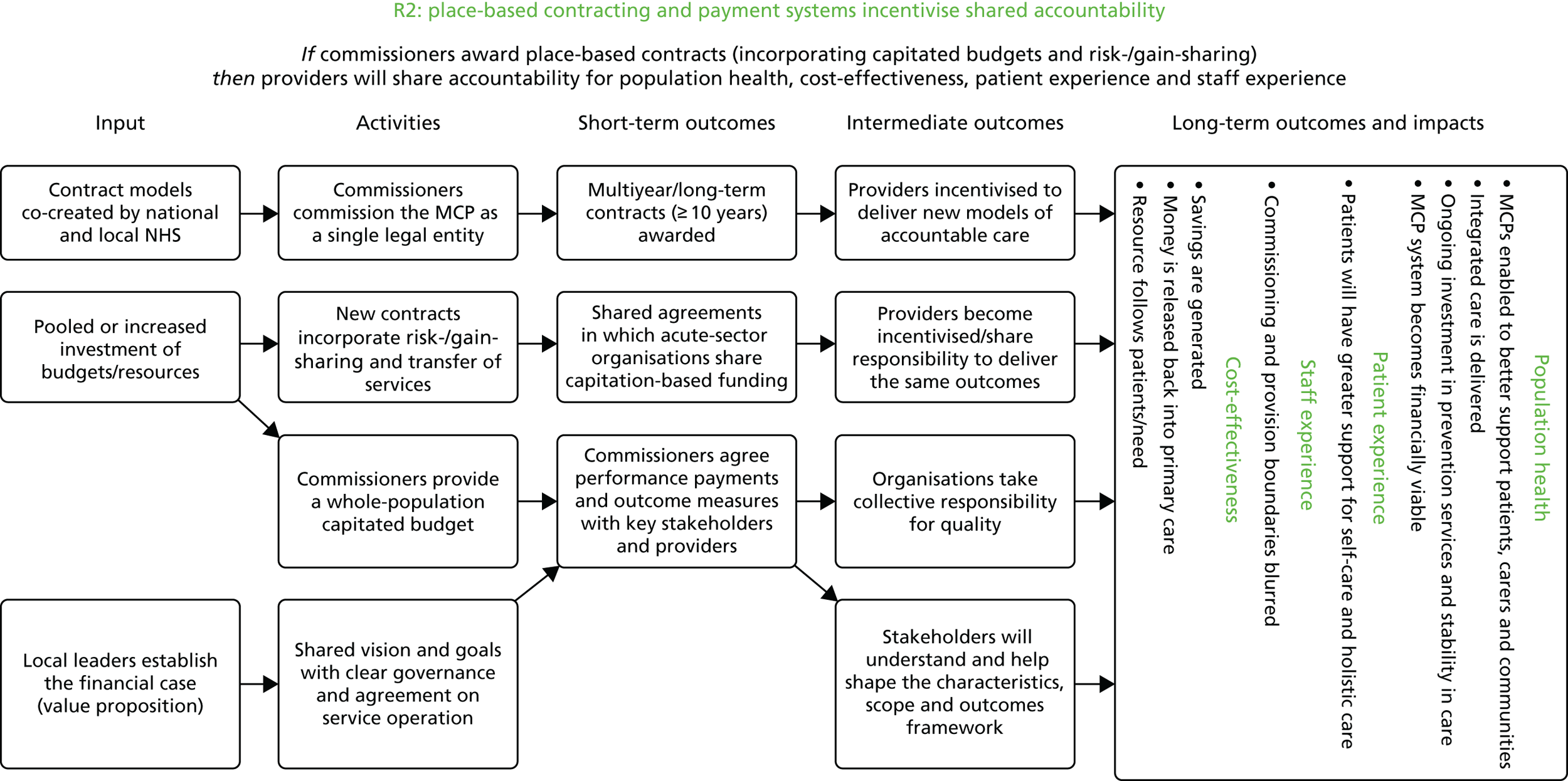
FIGURE 6.
Programme theory component R2: narrative.

NHS England’s framework outlines three different contract options for establishing a MCP model of care:11
-
a virtual MCP contract
-
a partially integrated MCP contract
-
a fully integrated MCP contract.
The different contract options available present a different mix of risks and benefits. For example, the fully integrated contract results in primary care services being reprocured. NHSE acknowledges that these contracts may mean more disruption and potential additional complications for local leaders in return for more freedom to redesign care. The partially integrated contract offers GPs the flexibility to enter alliance agreements with the option to return to General Medical Services/Personal Medical Services contracts. The virtual contract offers the benefit of minimum disruption balanced against the risk of limited freedom to change structures.
A key feature of the MCP contract framework is the population-based budget:
Merging separate existing funding streams into a single payment made to the MCP should allow for more flexible allocation of resource, directed towards the areas in which the funds will have the greatest impact on population health care.
NHSE. 11
In recognition of the risks involved in capitation, the contract also incorporates risk- and gain-sharing agreements ‘to ensure that the payment system does not inhibit the path to transformational, system-wide change’ (contains public sector information licensed under the Open Government Licence v3.0). 11 The framework has been developed to enable commissioners and primary care providers to determine the scale and pace of change, and, depending on local contextual factors, to develop a contracting solution that works for them. 11
The built-in flexibility enables GP practices to determine their relationship with the MCP – either as an alliance partner or as an employee. 122
The contract frameworks not only build on the lessons from legacy models (see Chapter 1) within the NHS, such as the Better Care Fund123 and the Integrated Care Pioneers124 models, but also the experiences of delivering the Quality and Outcomes Framework (QOF)125 and joint commissioning. Looking beyond the NHS, lessons may be harvested from relevant international models (see Chapter 1), such as the ACO model126 in the USA, Gesundes Kinzigtal127 in Germany and the Alzira model128 in Spain.
R3: fostering relational behaviours builds resilience within communities
If commissioners and providers develop mutually beneficial relationships and co-produce services (with patients, the public, the voluntary sector, community groups, local businesses and other public services) within local communities, then health and care services will support local communities to build resilience.
This programme theory component reflects a shift towards a system-based approach to transformation, based on collaboration, to develop a more holistic approach to health and well-being. Figure 7 shows the logic model and Figure 8 shows the narrative, developed by the project team for the focus group. This longer-term view, encouraged by the New Care Models programme11 is reflected in the design of MCPs, many of which set out an early ambition to work with local communities to tackle issues, such as social isolation and public health issues. A key characteristic of these relational behaviours is the emphasis on partnership working – with other public services, third-sector organisations, community groups and local businesses. One example is the Schools App Challenge,129 which is part of a range of prevention interventions targeted at different groups intended to encourage lifestyle changes, with the aim of improving health outcomes and reducing harmful behaviours in the long term. 105 As part of the same programme, HealthPods (pop-up facilities that offer health checks, well-being advice and assessments, which are aimed at reaching groups that may be missed by current services)105 are being used to target higher-risk and hard-to-reach groups.
FIGURE 7.
Programme theory component R3: logic model. JSNA, Joint Strategic Needs Assessment.
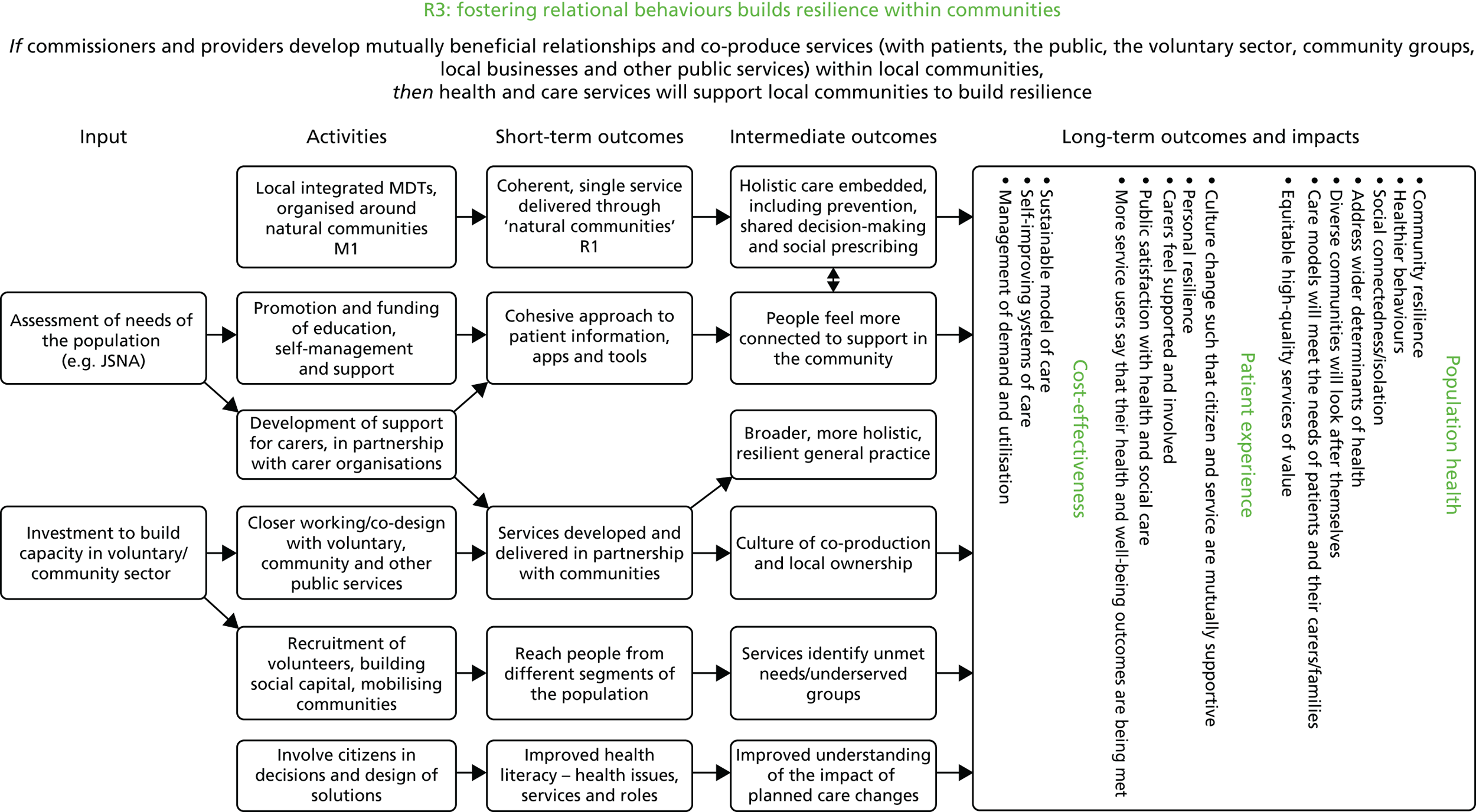
FIGURE 8.
Programme theory component R3: narrative.
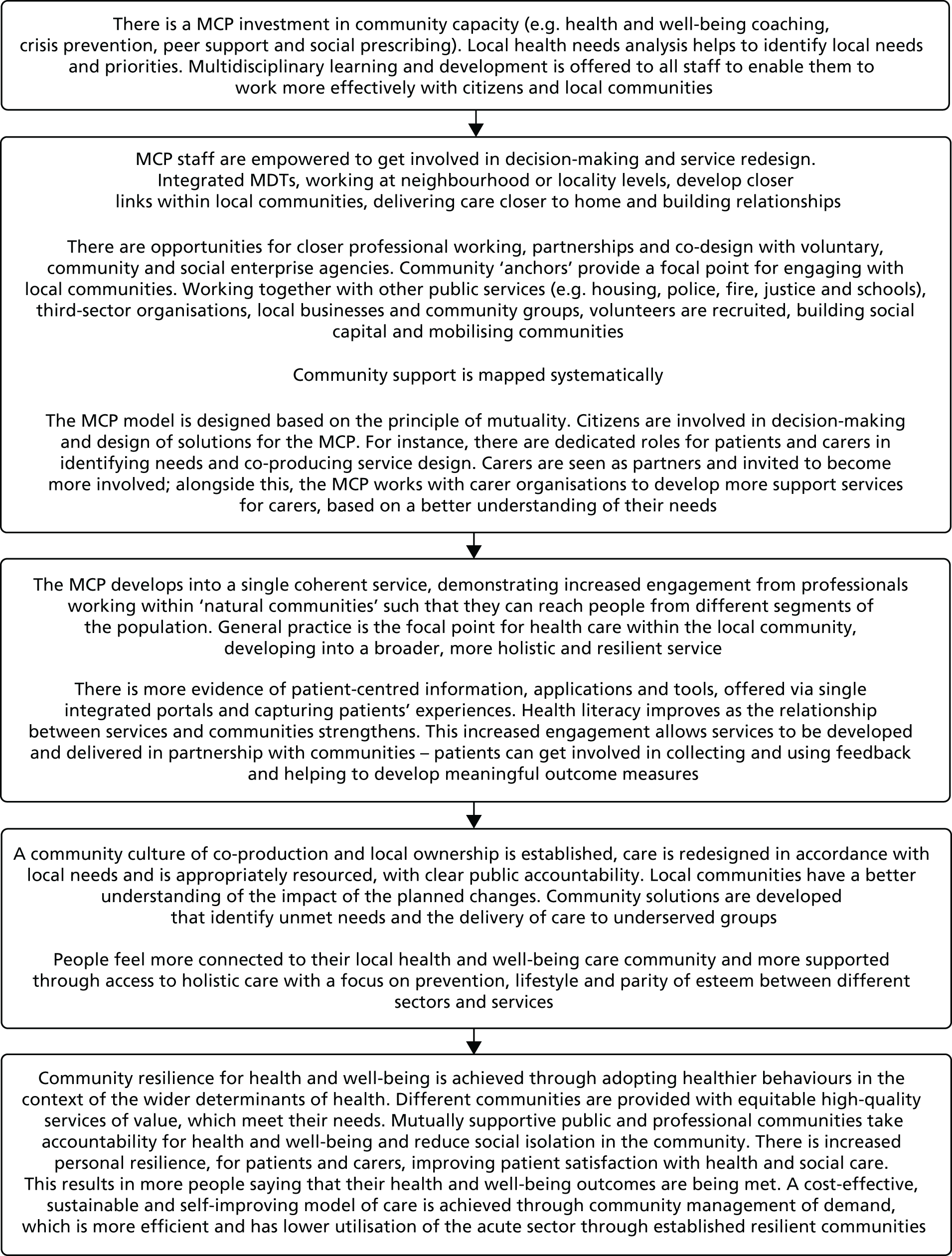
The emphasis on prevention signals a shift in the relationship between health services, patients and communities, reflected in Dudley CCG’s emphasis on collective ownership and responsibility. 130 Many MCP logic models refer to building social capital, leveraging community-based assets and recruiting volunteers and peer-support workers to take on both patient-facing and non-patient-facing roles. The Erewash MCP explains how social capital contributes to the theory of change by reducing social isolation and increasing participation in health choices, leading to lower use of secondary care services. 131 Recognising that some patients have increased access to information through mobile technologies, the MCPs describe the expectations around patients’ personal responsibilities, outlining a more active role in decisions about their health care and about local health services.
This ambition for a new relationship with local communities reflects a gradual direction of travel within public services and earlier initiatives, such as the Integrated Care Pioneers124 and Expert Patient programmes, may offer valuable learning. 4 Vanguards have also referenced experiments, such as the social prescribing programme in Rotherham132 and Nesta’s People Powered Health133 programme, reflecting the uptake of learning from experiments around the UK within the New Care Models programme.
M1: collective responsibility improves quality and safety outcomes
If providers share collective responsibility for outcomes through standard integrated pathways, then providers will improve the quality and safety of care.
Responding to the complexity of health service transformation, the MCP vanguards acknowledge that shared responsibility will improve outcomes and tackle perverse incentives. The suggestion is that a collective approach by providers of MCP care will help to tackle issues of quality, for example, unwarranted variation. Figure 9 shows the logic model and Figure 10 shows the narrative, developed by the project team for the focus group.
FIGURE 9.
Programme theory component M1: logic model. JSNA, Joint Strategic Needs Assessment.
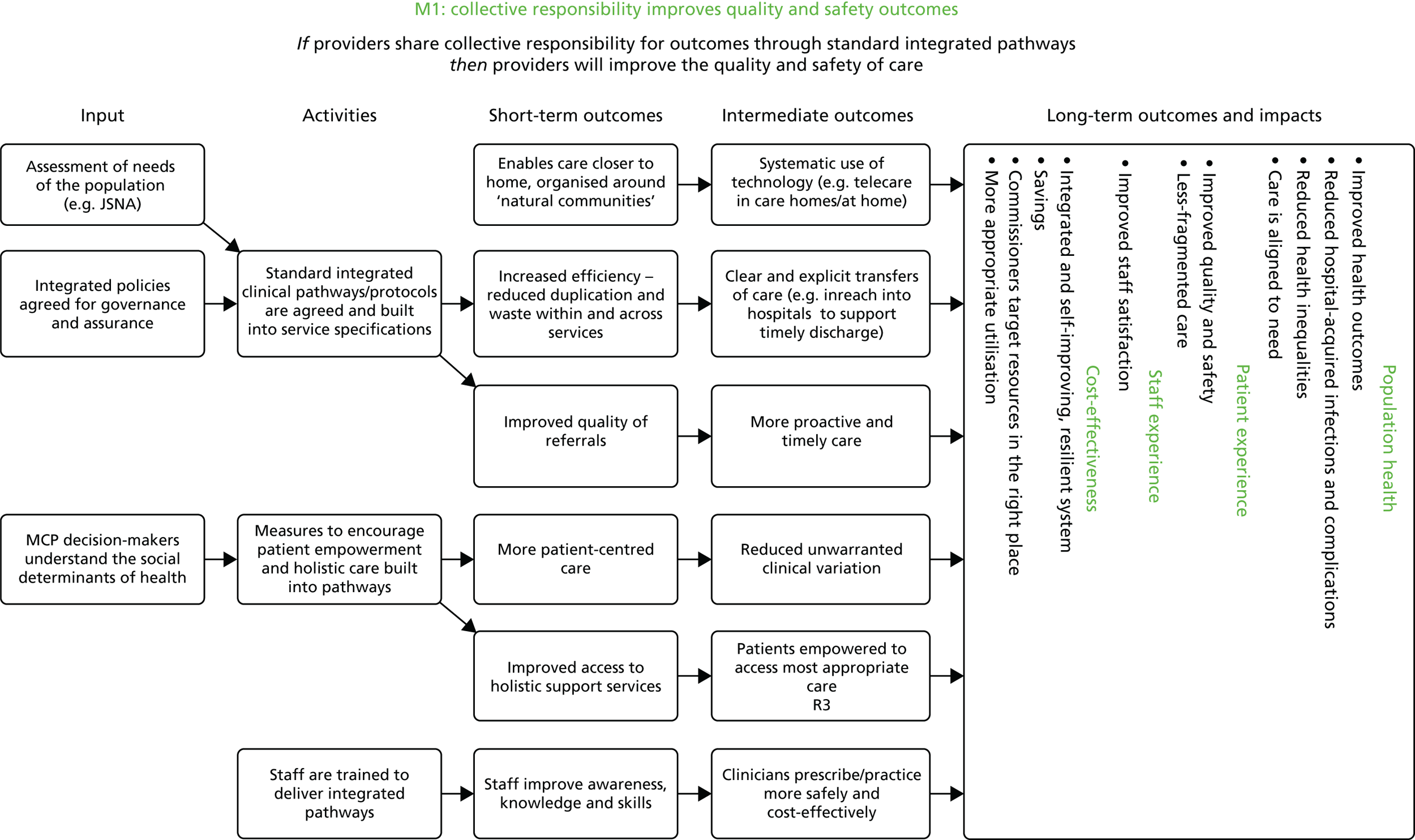
FIGURE 10.
Programme theory component M1: narrative.
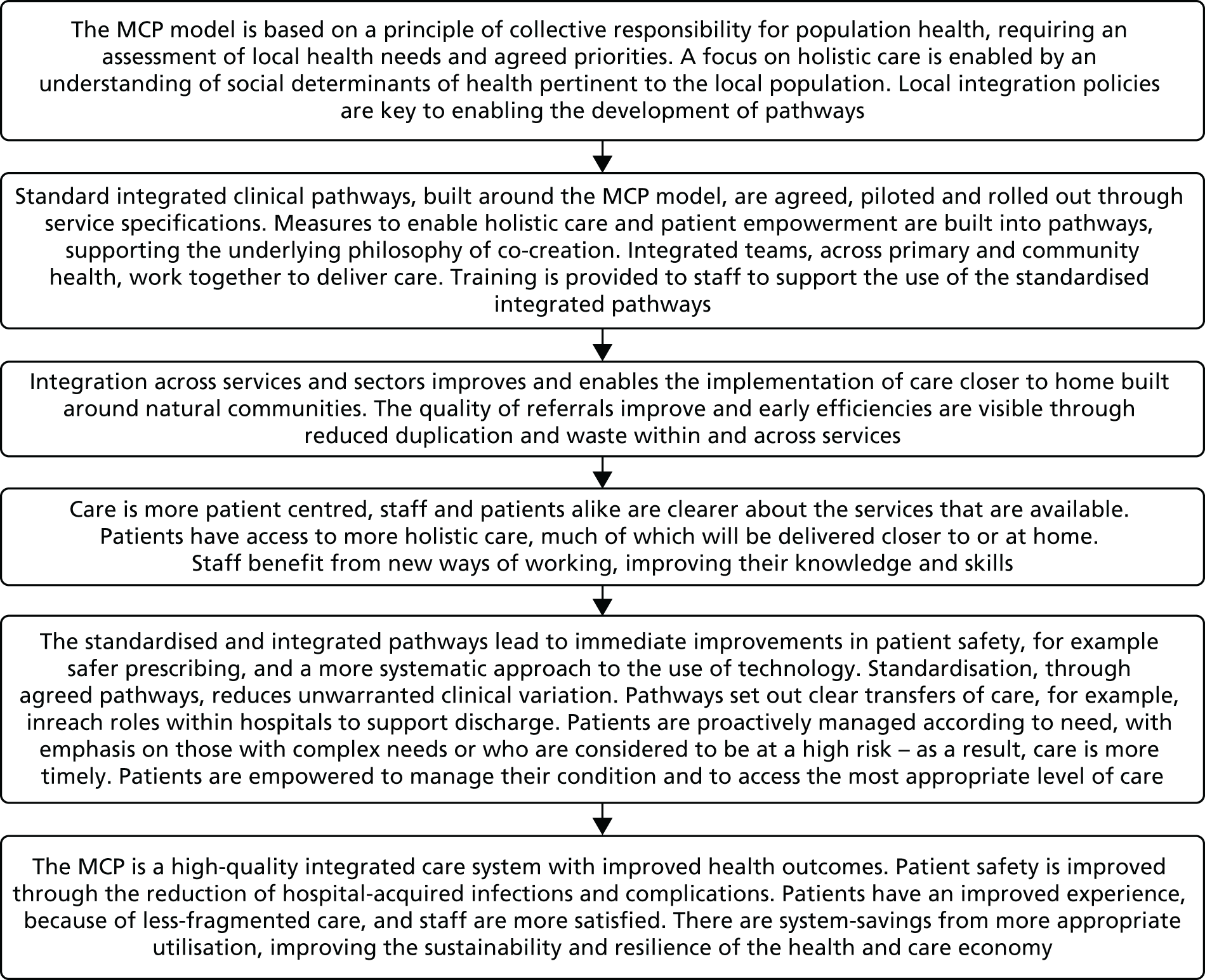
The need for a co-ordinated and collective provider responsibility is being formalised by new contracting forms. 11,122 Key to the shift towards collective responsibility is the development of shared outcomes, with several vanguards committing to co-produced outcomes to ensure that what matters to patients is measured. The prior information notice to procure a MCP for Dudley references a new outcomes framework,122 replacing the QOF,125 to be supported by systems and processes to ensure standardisation in care delivery and data collection. This particular aspect of the MCP model depends on new contracting arrangements and cultural change to adopt a system-oriented, rather than an organisation-oriented, approach:
A multi-disciplinary approach to developing shared care will ensure that specialists and generalists are working together in the shared interests of their patient; and patients will be clear how the different clinicians are working together with them, providing clear continuity of care, to contribute to the management of their condition.
Dudley CCG134
This highlights the interdependencies inherent within the MCP model and the acknowledgement that change is dependent on a variety of mechanisms. Integrated pathways provide a focal point for bringing together processes, people and technology, and MCPs are learning from the experience of earlier NHS policy initiatives from the 2000s,24 and international models, such as Alzira128 in Spain and Esther116 in Sweden (see Chapter 1).
M2: multidisciplinary teams provide continuity for patients with long-term conditions/complex needs
If primary care providers deliver care via MDTs (organised around natural communities), then patients with long-term conditions/complex needs will experience better continuity of care.
The MDT is a core element of many of the vanguard MCP models, with teams taking on responsibility for planning care within agreed neighbourhoods. The MDT – which comprises different combinations of GPs, nurses, social workers, link workers, pharmacists, physiotherapists and others – is tasked with identifying high-risk populations and developing care plans with patients. A primary care-led model is thought to increase the continuity of care. 135 Figure 11 shows the logic model and Figure 12 shows the narrative developed by the project team for the focus group.
FIGURE 11.
Programme theory component M2: logic model. JSNA, Joint Strategic Needs Assessment; LTC, long-term condition.
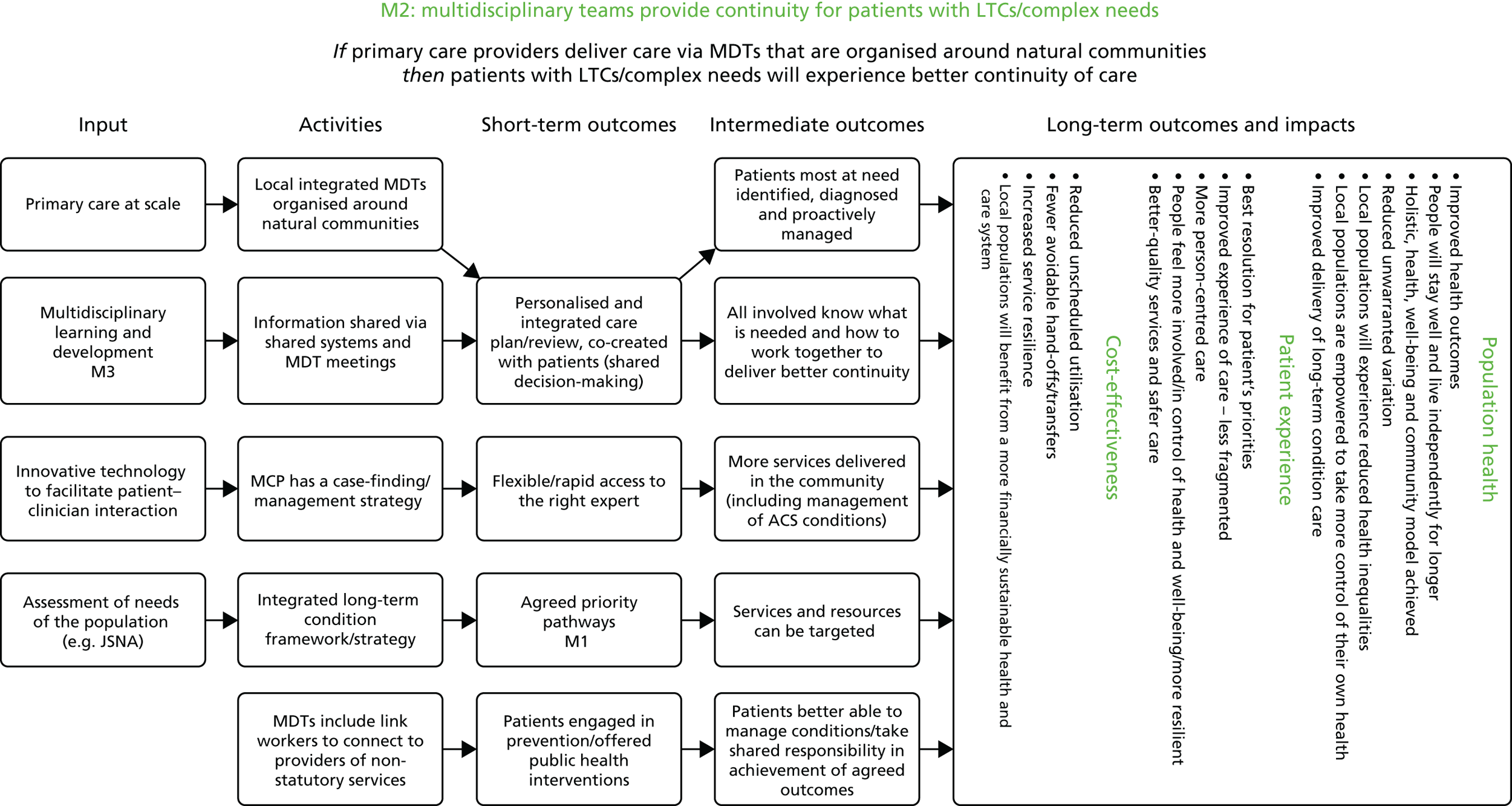
FIGURE 12.
Programme theory component M2: narrative.
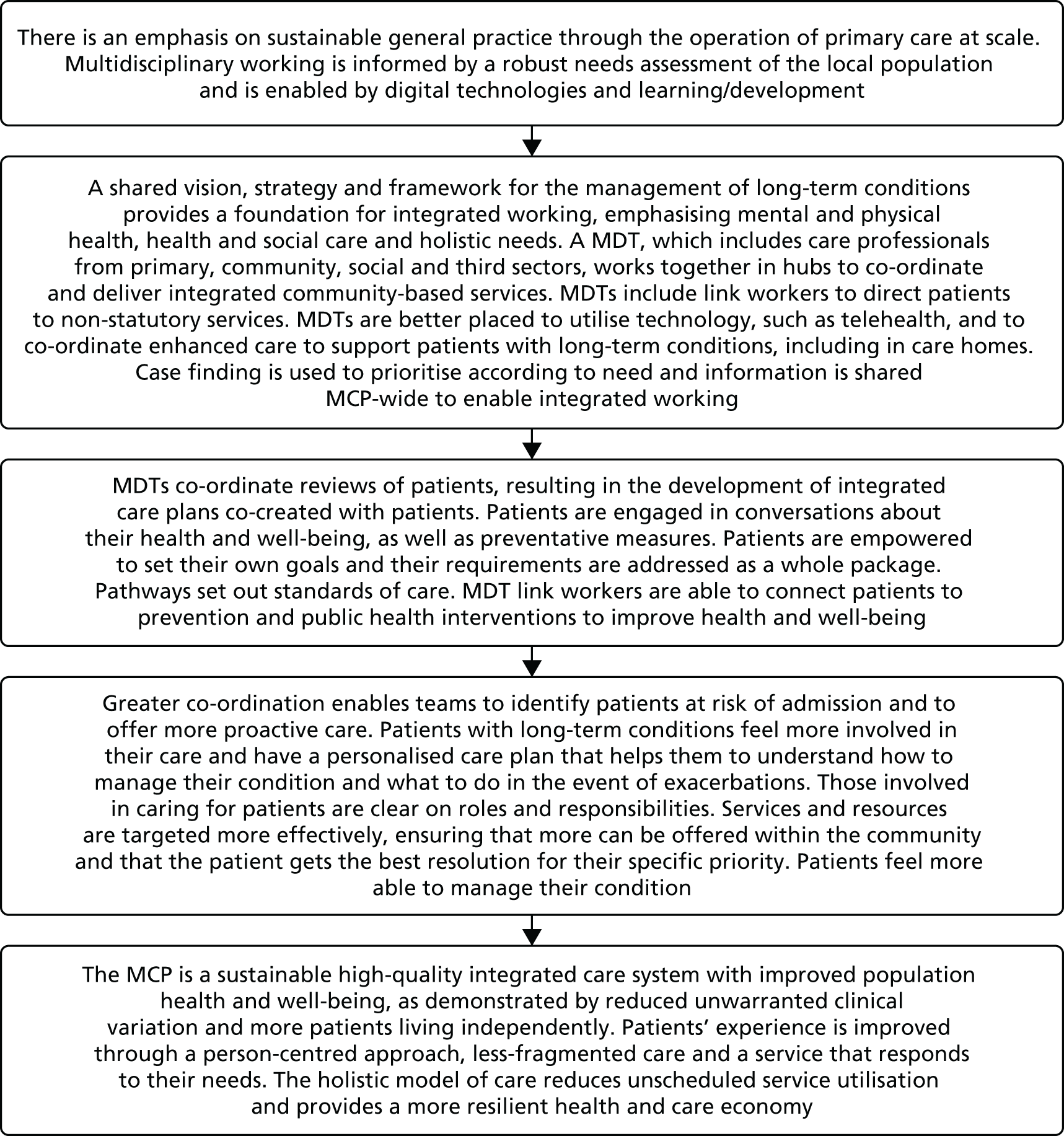
Many of the MCP vanguards describe a more holistic role for MDTs, through prevention and working with public health and community groups to address wider determinants of health, social isolation and general well-being issues, through interventions such as social prescribing. A social prescribing programme has also commenced in Encompass MCP, enabling the voluntary-sector umbrella organisation Red Zebra136 to start to build a MCP-wide database of voluntary and community services that service users and practitioners will be able to access via the social-prescribing service team. 109
Described as ‘teams without walls’,130 MDTs are empowered to deliver more proactive care, thus contributing to the overall goal of managing demand and service utilisation. It is expected that the multidisciplinary approach will be key to achieving the quadruple aim, as exemplified by the extended primary care teams in the Southern Hampshire MCP, set up to support patients with complex needs. 137
Multidisciplinary working carries an implied interdependency with broader community relationships (see Chapter 3, R3: fostering relational behaviours builds resilience within communities), for example, additional capacity through the use of volunteers. Voluntary link workers are often perceived as unrestricted by specialism, which enables a more holistic view of an individual’s needs beyond medical conditions. 122
Multidisciplinary teams feature as a key element of the Integrated Care Pioneers35 and in many other models internationally (see Chapter 1), including ChenMed138 and the Nuka model in Alaska,139 suggesting a broad and varied evidence base to inform the MCP model.
M3: engaged and trained staff expedite cultural change
If commissioners and providers train and fully engage staff in service transformation, then staff will drive the cultural change that underpins new ways of working.
This programme theory component reflects a common thread running through the planned interventions and innovations of MCPs; that is, the pervasive recognition that service transformation is dependent on empowered and engaged staff to initiate and maintain service change:
The success of an MCP depends on how it grows and deploys its assets. [. . .] And it empowers and engages staff to work in different ways by creating new multi-disciplinary teams; by redesigning jobs so that they are more rewarding, sustainable and efficient; and by implementing newer professional roles.
NHSE. 11
Figure 13 shows the logic model and Figure 14 shows the narrative developed by the project team for the focus group.
FIGURE 13.
Programme theory component M3: logic model.
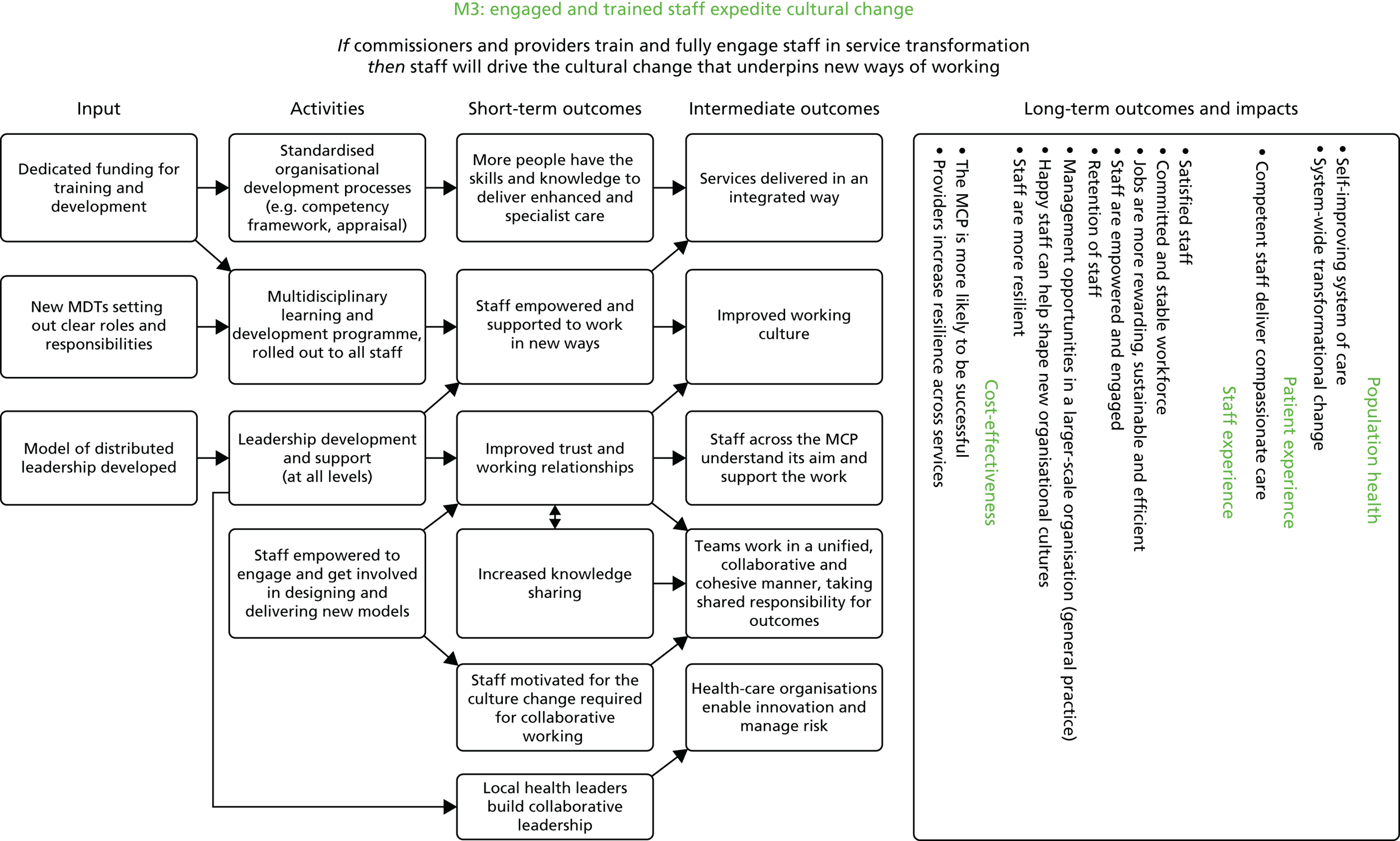
FIGURE 14.
Programme theory component M3: narrative.
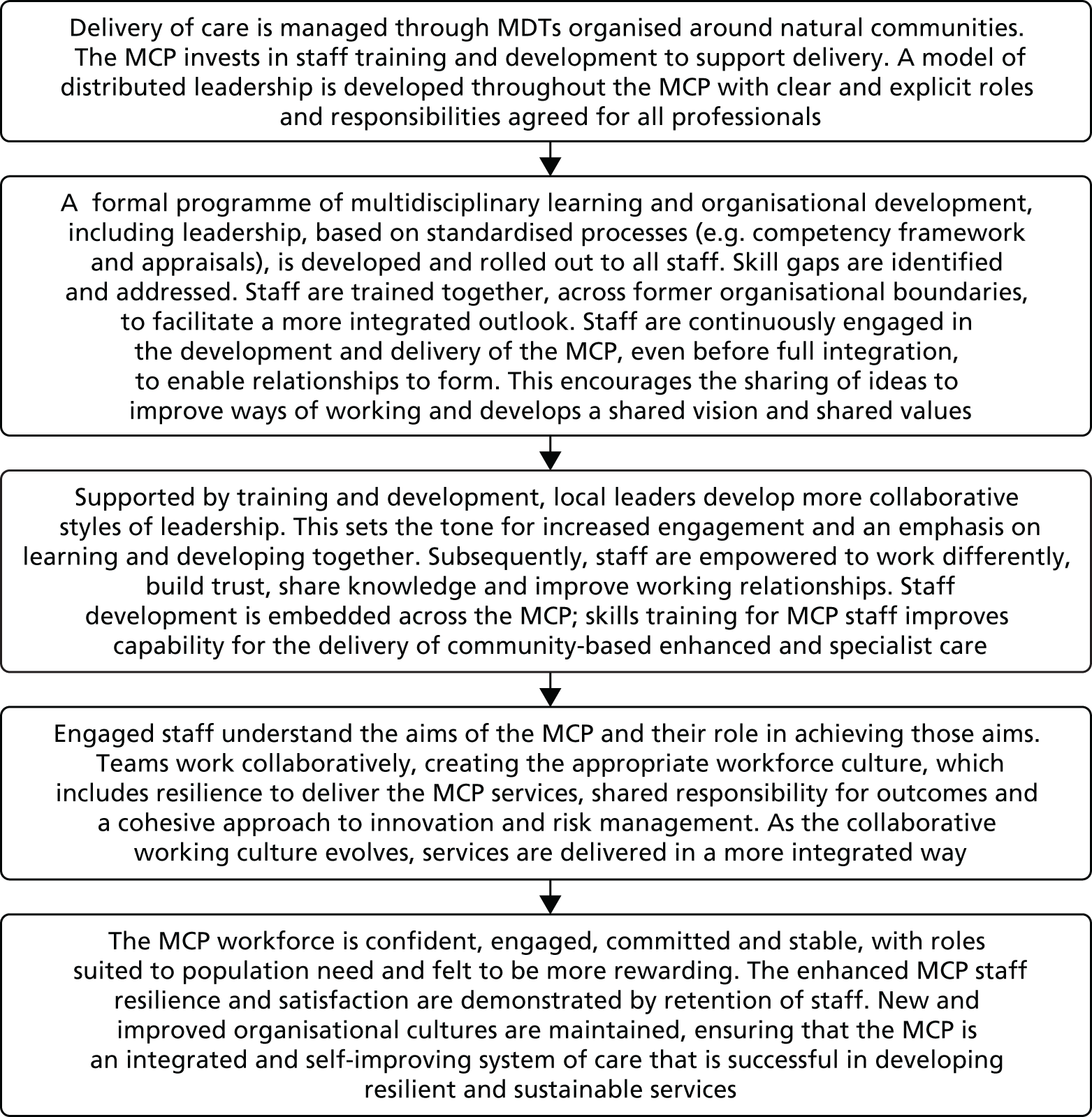
Investment in training and development is recognised as being important to the development of new and expanded roles and integrated roles, in particular, opening up leadership development to a wider audience and skills development for all those involved in delivering care closer to home. 140 This represents a vision in which staff development contributes to shared accountability, demonstrating the interdependencies between new contractual levers and cultural change. A focus on staff empowerment encourages individuals and teams to take responsibility for performance and outcomes, and to hold each other to account.
It is noticeable from the logic models and associated documents that vanguards recognise the importance of multidisciplinary development ahead of formal integration to prepare staff for new ways of working. This is evidenced by Stockport MCP, who held a series of engagement events with social work and district nursing staff to prepare for integrated working. 104
The vanguards are building on a history of integration programmes that are likely to offer learning on organisational development and cultural change to support transformation.
M4: system learning embeds and sustains transformational change
If MCPs learn and adapt quickly using evaluation/monitoring loops and knowledge-sharing then MCPs will sustain transformational change.
This programme theory component derives from the emphasis on the iterative and experimental approach of the MCP vanguards, with formative evaluation and system learning featuring prominently in vanguard plans. Recognising the level of ambition and complexity inherent within the New Care Models programme, NHSE has emphasised the importance of organisational learning and knowledge-sharing, in recognising that knowledge-sharing and organisational learning have not always been prioritised in earlier change programmes. 89
Figure 15 shows the logic model and Figure 16 shows the narrative developed by the project team for the focus group.
FIGURE 15.
Programme theory component M4: logic model.
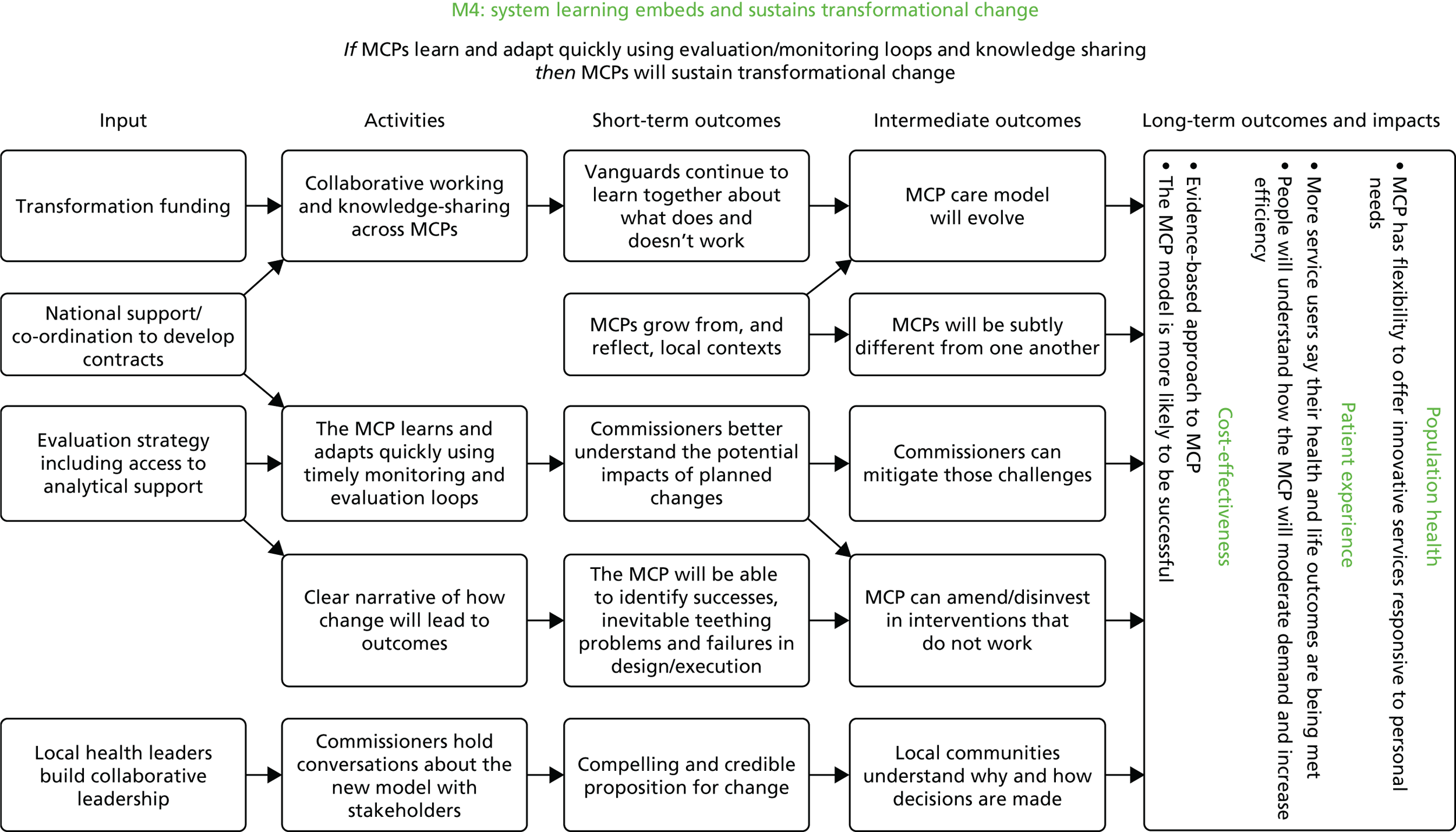
FIGURE 16.
Programme theory component M4: narrative.
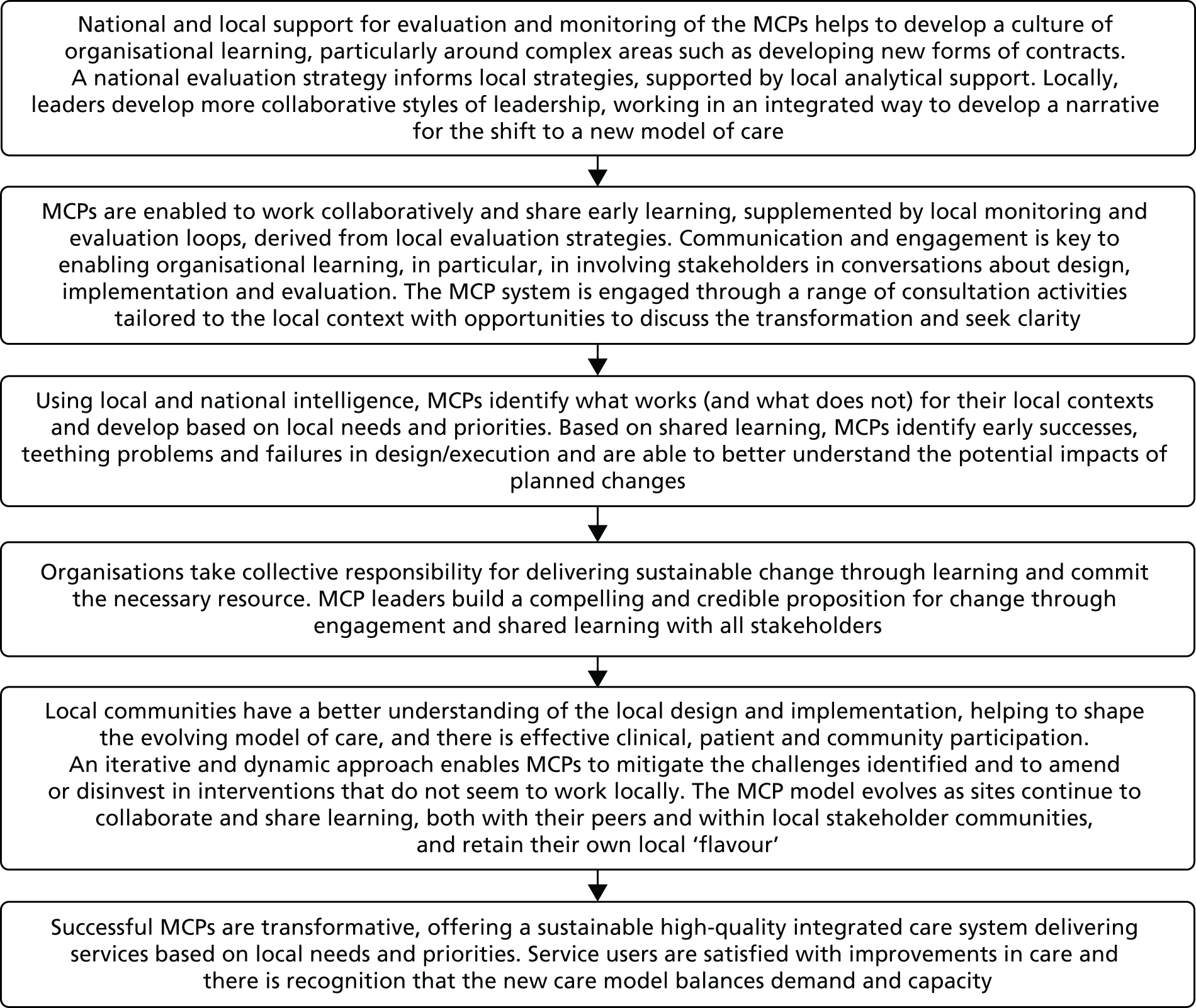
All vanguards are required to undertake local formative evaluation with the aim of informing local design and implementation, as well as future MCP models. 89 Rapid learning cycles and feedback loops are utilised to inform a more iterative approach to service design, implementation and evaluation. 141 Some models embody ambitions to develop as self-improving or learning health-care systems, working towards the creation of a self-improving system, to sustain a culture of improvement and innovation in a complex and uncertain environment. 130
In Chapters 7 and 8, we show that although complexity theory has influenced earlier service transformation,88,142 the emphasis on evaluation and shared learning in the New Care Models programme is relatively new to national policy. 143 As such, although there may be learning from earlier integration and transformation programmes, it is likely that this theory component will be informed by the international literature base. 144
M5: proactive population health is dependent on shared and linked data
If MCP staff are not able to access shared/linked data then patients will continue to experience fragmented care.
A key aim of the MCP model is to improve the co-ordination of care, notably through MDTs (see R1: community-based, co-ordinated care is more accessible and M2: multidisciplinary teams provide continuity for patients with long-term conditions/complex needs) working in ‘natural communities’. The delivery of this aim is dependent on systems and processes that enable information-sharing – a common thread in the design of MCP models. Shared and linked data could be seen as not merely enablers to integrated working, but as prerequisites. 145 The NHSE framework notes the importance of data in driving transformational change:
[The MCP model] is reliant on using high-quality business intelligence systems, with data that is [are] as real time as possible. Without these, an MCP is ‘flying blind’.
NHSE. 11
Several MCP vanguards have prioritised the use of information systems to support decision-making at both the patient and the population levels. Infrastructure becomes critical to enable information-sharing at the point of care and decision-making, with several MCPs describing information hubs; for example, Wakefield MCP’s105 hub is situated within a Response Centre, thus acting as a conduit across the local health and care system to enable predictive modelling and proactive care for patients at a high risk of hospital admission. This concept has evolved further to explicitly support MDTs through:
groups of staff known as ‘fusion cells’ whose job will be to pull together the threads of information about people and services in the area, including health and care services but also the West Yorkshire Fire and Rescue Service and police, for example.
NHS Confederation, NHS Providers, Local Government Association and NHS Clinical Commissioners146
In Chapter 7, we show that information-sharing represents a prominent theme of earlier integration efforts, such as the Integrated Care Pioneers programme,147 which has employed risk stratification, shared records and linked data to inform patient- and population-level decision-making. 126
Figure 17 shows the logic model and Figure 18 shows the narrative, developed by the project team for the focus group.
FIGURE 17.
Programme theory component M5: logic model. IT, information technology; JSNA, Joint Strategic Needs Assessment.
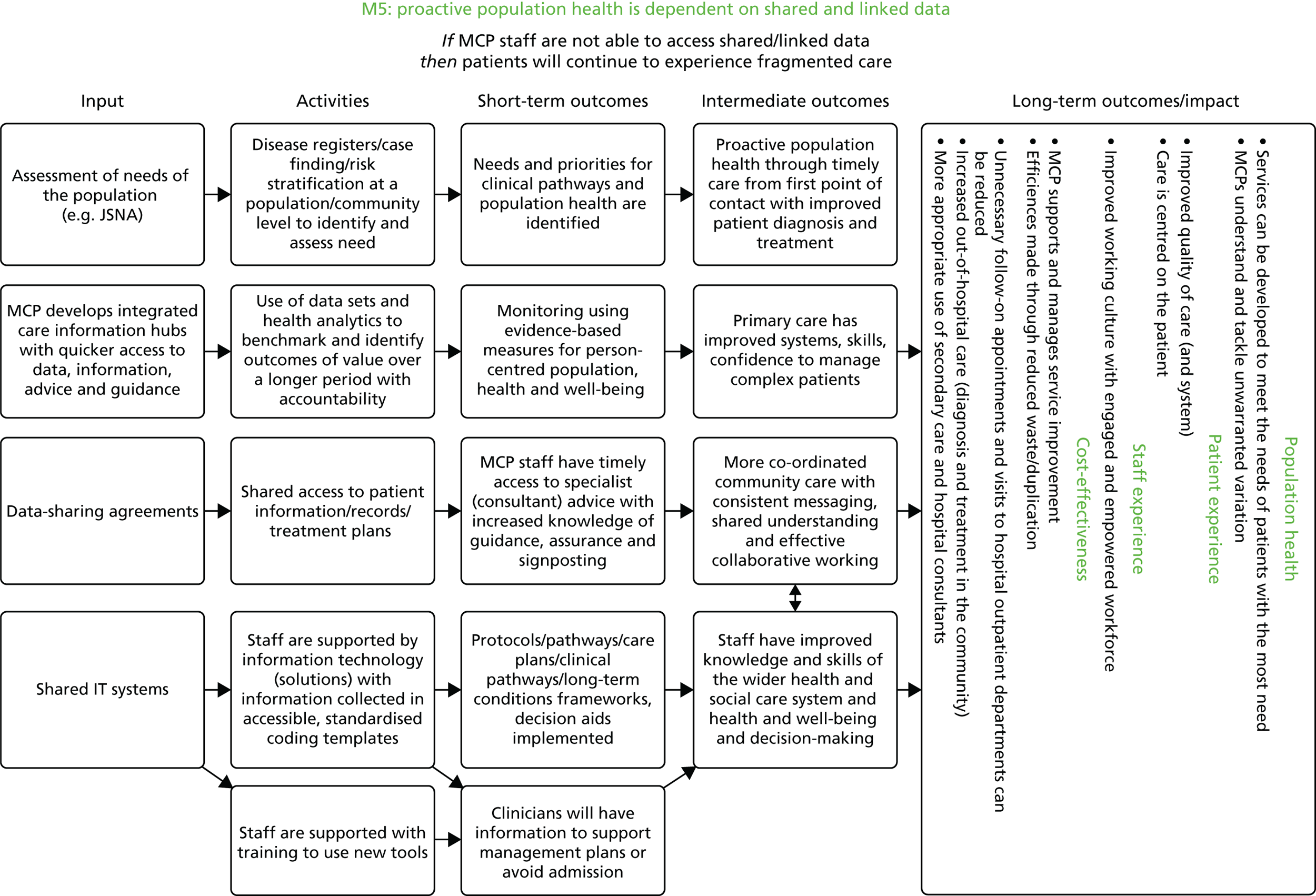
FIGURE 18.
Programme theory component M5: narrative. IT, information technology.

Chapter summary
In summary, this chapter expands on the eight programme theory components, providing a graphical representation, brief narrative and summary of the underlying theories of change as represented by the MCP vanguards and NHSE. For each of the theory components, we have indicated the relevant legacy models, offering experiential learning from within a NHS context, and from international models of care, offering transferable lessons.
Chapter 4 Community-based, co-ordinated care is more accessible
Introduction
This chapter examines the first of three theory components that were prioritised for realist review purposes:
If primary care provision is enhanced (new/expanded roles, additional services, hubs, extended hours) to deliver place-based services, then patients will access more care within community settings, rather than the hospital.
It begins by setting the evidence scene for the if statement, that is, the characteristics of enhanced primary care provision and its delivery in place-based settings. It then assesses the then statement in the literature, by describing access to care in community settings. Next, a brief description of the state of the evidence is provided for R1, which precedes the section for outcomes, delineated by the quadruple aim and unintended consequences. Subsequently, we describe the mechanisms as resources (of the intervention) and reasoning (stakeholder volition)76 for the patient, staff and system. When possible, we juxtapose the resources of the mechanisms with the context within which the theory component operates, together with the specific intervention outcomes. Finally, we provide a brief overview to capture the key aspects of R1.
Characteristics of community-based care and primary care access
The initiatives to enhance primary care provision in community settings, and to provide improved access to those services, have developed as a response to the ‘crisis’148 in general practice, characterised by the pressures of an increasingly complex and intense workload, recruitment difficulties and a drive for care closer to home. 149 Such challenges may be addressed through the enhancement of primary care, by which the system offers greater access to health and social care in community settings through:
-
creating new and expanded roles to increase the ability of primary care teams to deliver care150,151
-
increasing the provision of specialist care in community settings by providing direct care in the community or by supporting other staff in the extended primary care team151
-
care navigation to steer patients to appropriate care with the least number of contacts150
-
extending opening times at general practices to improve access to primary care150
-
increasing the use of technology to provide alternatives to face-to-face consultations. 150,151
In examining this theory component, we concentrate on points 1–3, given that points 4 and 5 are less relevant to the delivery of co-ordinated care. Chapter 7 and the theory component M5 also map some of the evidence around co-ordinated information systems, and upcoming research findings will shed more light on the potential benefits of alternative types of consultations. 152,153
To date, efforts to expand the primary care workforce have focused on upskilling the non-medical workforce, such as nurses32,154–157 and pharmacists,32,155,158–160 to substitute or supplement GP consultations. Other innovations in the UK include self-referral to allied health professionals, such as physiotherapists in community settings32,161,162 and paramedics undertaking home visits. 32,163 Expansion of primary care through the development of new roles in the UK is currently limited to the development of the physician associate role, borrowing from the physician assistant role in the USA. 164–166 This chapter focuses on medical roles, whereas Chapter 7 and theory component M2 provide more information on the expansion of primary care roles to include professionals contributing to social or holistic primary care services.
Access is subjective, determined by an individual’s priorities;167 however, three criteria have been identified as influencing a patient’s preferences for accessing primary care: (1) the ability to see a preferred GP or nurse,167–169 (2) the availability and proximity of care170 and (3) the timeliness of care. 170,171 We adopt the definition by Collaborations for Leadership in Applied Health Research and Care (CLAHRC) Greater Manchester, which characterises access to primary care by the responsiveness of primary health-care services to the needs of the population and the subsequent empowerment of individuals to use and benefit from health-care services. 172
Earlier models of providing specialist care in the community include interventions that involve the transfer of services where primary care substitutes for secondary care [e.g. GPs with specialist interests (GPwSIs)71,173,174 or the relocation of services from secondary care to primary care settings). 174–178 More recently, the ways in which specialist care is being implemented in primary care go beyond the ‘drag and drop’ approach of simply relocating a hospital outpatient clinic into a community setting; instead, methods that put education at the core alongside the redesign of the patient pathway and/or the role of the professional are becoming more established. 179 Examples included in a recent The King’s Fund report, Specialists in Out-Of-Hospital Settings: Findings from Six Case Studies,179 are outreach clinics jointly staffed by hospital consultants and other health-care professionals, consultant-run e-mail and telephone helplines, consultant participation in MDT meetings, consultant-run education sessions and consultants supporting staff to work in extended roles.
The evidence base
The evidence base for this theory component, R1, included limited review evidence and mainly consists of a limited number of small-scale evaluations comprising uncontrolled before-and-after studies or single-case studies (see Appendix 5). The review is based on four systematic reviews (including two with meta-analysis), eleven reviews, one realist review, one pragmatic randomised controlled trial, four mixed-methods studies, four qualitative studies, two observational studies, one cohort study, eight case studies, one briefing and one framework. Support for this component can therefore be considered to be moderate. Limitations of the evidence base mainly relate to the long-term impacts of enhanced primary care teams delivering care closer to home, resulting in a moderate level of uncertainty around the conclusions. Literature from the UK has been prioritised for relevance; when international examples are used, we have given precedence to countries with a similar primary care model to the UK, most notably in having a gatekeeper role. 180 Many studies are descriptive and focus on the implementation with limited sound evidence about effectiveness, and a few studies provide anticipated outcomes.
Outcomes
Population health
A systematic review154 of the substitution of physicians by nurses in primary care found inconclusive evidence on the effects of nurse-led care on quality-of-life measures for patients; the authors note that interpretation was difficult because of heterogeneous outcome reporting, valuation of resources and the small number of studies. The review154 did find nurse-led care to be associated with lower overall mortality, particularly when providing routine care and non-urgent visits. However, earlier reviews154,156 did not find mortality rates between physician and nurse-led care to differ, but did find demonstrable improvements in clinical parameters of chronic conditions by nurses compared with physicians. Similarly, interventions in which pharmacists supported GPs to optimise prescribing or patient medication use were reported to show a limited effect or no effect on outcomes related to quality of life; however, improvements in the management of chronic conditions and the attainment of health goals were observed. 158
Expanded primary care roles have been found to demonstrate an acceptable level of patient safety or better. Nurses have been reported to show no difference in appropriate diagnosis and prescribing in primary care compared with physicians,156 whereas pharmacist interventions in general practice clinics have been shown to improve the quality of prescribing and medication appropriateness. 158 The introduction of a self-referral pathway for physiotherapy has been reported to be clinically effective compared with usual care, and has been deemed to be safe. 162 The evidence about the appropriateness of care provided by physician associates is weak; however, where evidence exists, it is reported positively. 164,181 In general, studies reporting on the transfer of care from secondary to primary care have reported that the quality of care achieves an acceptable standard. 71,173,174 The safety of diagnostic services transfer is equivocal; a literature-mapping exercise175 found evidence that the quality (including diagnostic accuracy and the appropriateness of test ordering) and safety of diagnostic service provision in the community is mixed.
Cost-effectiveness
Evidence on the effect that expanded primary care roles have on health-care service use is underdeveloped, with most evidence reported in case studies including anecdotal claims. Reviews looking at the upskilling of non-physician clinicians, such as nurse practitioners154,156 and pharmacists,156 and the contribution of physician associates in primary care,181 report a dearth of economic data. Furthermore, much of what does exist is based on direct costs only (e.g. resource use, follow-up consultations, length of consultations and salary costs), with inconsistent evaluation approaches used across studies. 154
Single studies and case studies have painted a more positive picture. A cost-effectiveness analysis of the introduction of a self-referral pathway for physiotherapy reported that the service was cost-effective as a result of a reduction in the average number of patients attending and the wasted appointments by patients who do not initiate or actively commit to treatment. 161 The use of physician associates in UK settings has been found to have lower consultation costs than GPs, albeit with limitations, as costs considered only the time spent in consultation and no other factors, such as support time from GPs. 164 Case studies reporting on pharmacists working in general practice have shown some reduction in primary and secondary health-care usage when pharmacists work in general practice,32 and cost-savings through reduced locum costs. 182 Case study reports of paramedics working in primary care provide a more mixed picture. 163 Although a lower conveyance rate than for other paramedics has been reported, other accounts conclude that the cost-effectiveness remains uncertain, given the supervision time required and longer appointment times. 163 Many authors warn that the provision of care in the community may not be cheaper than outpatient services, and, in some cases, services may actually lead to increased costs. 174,183,184
Few economic evaluations exist regarding the transfer of services. Pawson et al. 71 conclude that there is little solid evidence that GPwSIs have reduced the outpatient workload, in regard to anecdotal claims of this reported in the literature. Furthermore, the evidence on cost-savings from the use of GPwSIs is mixed and based on inconclusive data. 71 This view is supported by a scoping review by Winpenny et al. ,174 who confirm inconclusive cost-effectiveness findings, with several studies suggesting that interventions might increase the cost of care provision. Reviews exploring the use of GPwSIs report that the higher cost of GPwSIs can be justified only if the increased cost can be offset against the benefit in improved access to health. 173,174
Similarly, shifted outpatient models are likely to be more expensive than hospital-based outpatient clinics,174 with the ‘drag and drop’ model that replicates the hospital model in different settings being an inefficient use of time and resources. 176 Few formal evaluations have been reported on more recent innovations, such as attaching a specialist to primary care, so that education is at the core of the model;174,179 however, currently, such services may appear to be costly. 174 Early evaluations of a specialist paediatric outreach clinic (monthly joint clinics between GPs and hospital-based general paediatricians) and MDT meetings held in GP practices are showing promising results. 185 Outpatient referrals have been reduced by avoiding appointments altogether through MDT discussions and improved care co-ordination, or by shifting the appointment from the hospital to the GP practice. 185 Furthermore, the joint GP consultant clinics have reduced the follow-up rate, which is attributed to the presence of the GP in the consultation, allowing a joint plan to be agreed, and the awareness of easy connectivity for further paediatric input, should it be needed. 185
Improved connectivity to specialist advice through the use of e-mail or telephone has shown a substantial opportunity to reduce the number of patients who are seen in outpatient clinics,174,186 support the GP’s management of the patient in primary care and identify potentially unnecessary referrals. 186 Similarly, where consultants have supported staff to work in extended roles through training sessions and ongoing support (telephone and by e-mail), a decrease in referrals has been reported, returning to pre-pilot levels after the pilot had finished. 187 Specialist advice can also help to guide the referral to the most appropriate specialist for patients who are not suitable for community-based care, assisting the patient in getting to the right professional first time, saving duplicate appointments. 186
Patient experience
In general, expanded primary care roles are associated with higher patient satisfaction for nurses,154 physician associates,164 self-referral physiotherapy services32,161 and pharmacists working in general practice. 182 A systematic review focusing on pharmacist services provided in general practice clinics found limited or no effect on outcomes relating to patient satisfaction; however, the included studies focused on interventions aimed at optimising prescribing and/or medication use, and may therefore not represent a direct substitution of the care received by GPs. 158 Patient experience in relation to the transfer of services from secondary care to primary care is consistently reported as being positive for receiving care closer to home,179,187 improved access and convenience,178 and a better overall experience (e.g. less intimidating than the hospital). 178,179 There may, however, be some instances that require a trade-off between the convenience of community-based care and the patient experience for some patient populations; for example, families with small children who enjoy the excitement and exclusivity that the children’s hospital provides, and where the absence of medical technologies decreases confidence in the quality of care provided. 178 This may be particularly noticed during symptomatic illness and the need for reassurance of a medical environment with immediate access to investigations. 178
Patient acceptance is generally high for nurses157 and physician associates164,181 used as substitutes for doctors; however, both alternatives report conditions for which patients would prefer to see a doctor. 157,181 Case study experience from pharmacists working in primary care in Cornwall has shown how pharmacists have been accepted with some patients, who now specifically book directly to see a pharmacist for medication issues. 182
Nurses more frequently provide advice and information to patients and can improve access to health-care services and treatments. 156 The introduction of a self-referral pathway for physiotherapy has also been reported to improve access by reducing waiting times,161,162 as has the introduction of GPwSIs. 71,173 However, evaluations of both services acknowledge that it is possible that times increase with longevity of the service,71 or expansion of the service without substantial resources. 161
Experience from the GP Access Fund pilots has found that patients of hub practices have benefited more from extended-access initiatives than those in other practices. 32 The introduction of specialist paediatric community care in London was reported to increase attendance because of decreases in ‘did-not-attend’ rates;185 however, a controlled evaluation of a relocated paediatric outpatient clinic in Birmingham found that higher attendance was associated only with shorter travel distance. 177 Children living in the most deprived areas were more likely to miss appointments. 177
Staff and provider experience
Both staff undertaking new roles and their colleagues have reported increased satisfaction. Case study accounts from a paramedic practitioner pilot found that paramedics were enthusiastic about career progression and development;163 however, it should be noted that paramedic practitioners offer a new way of working that is characterised by the development of a career framework. 188 Physicians and nurses also report consistently high levels of satisfaction in response to pharmacists159 and physician associates166,181 working in primary care, and GPs using consultant e-mail advice highly value the ease of access and efficiency of the response. 186 Physician associates have also proved to be a flexible workforce resource to cover the work of nurses in the case of absence. 189
The expansion of the primary care workforce might also help to relieve the pressure of GPs and free up time as shown in the case of pharmacists,182 nurses,32 paramedics32,163 and direct referral to a physiotherapist via trained care navigators. 32 Although the use of physician associates has been reported to have the potential to increase physician or practice productivity, it carries the associated risk that they will increase the workload of some staff, given the need for supervision and prescribing support in the UK. 181
Unintended consequences
The main reported unintended consequences of R1 are the loss of continuity, increased inequity, the burdening of the wider workforce, increased demand and cost, and workforce challenges.
If continuity of care is defined as ‘seeing the same health care provider every-time’,155 then the evidence suggests that practice-size expansion to include enhanced and/or new roles could potentially disrupt relational continuity. 156 Although some patients may value the new forms of access that larger-scale primary care can bring, others have expressed concerns over losing an ongoing, trusted relationship with their own GP and their own practice. Continuity of care is likely to be more important for elderly patients, those with long-term conditions and those with multiple morbidities, whereas patients with episodic or minor problems value access more highly. 168,169 Analysis of the 2009/10 English General Practitioner Patient Survey168 has, however, highlighted ‘the difficulty for practices in offering speedy access and continuity of care simultaneously’. Rosen et al. 190 warn that the benefits of larger-scale primary care need to maintain the expert generalist skills of general practice. New roles in primary care might best concentrate on areas where workload is high, such as acute ‘same-day’ workload in general practice, so that doctors can focus on complexity in their caseload. This has been demonstrated by physician associates181 and pharmacists. 182 Experience from a Child Health GP Hub system in west London found that, for economies of scale in the reductions in secondary care usage to be achieved, hubs must operate at a sufficiently large capacity of at least 15,000–20,000 people in the practice population and to engage enough professionals,185 while avoiding detrimental access to primary care. Imison et al. 184 point to evidence demonstrating that access to primary care is more sensitive to distance than the use of outpatient or acute services; therefore, more accessible outpatient services would insufficiently compensate for primary care access. A hub-and-spoke model, where the polyclinic acts as a central resource base in a co-ordinated network of practices,184 is proposed as a better strategy to provide equitable access. The subsequent experience of GP Access Fund pilots suggests that practices operating as a hub can offer more extended-access benefits than independent practices. 32
The opportunity for existing general practice staff to enhance their skill set is appreciated. However, without the ability to change their original role, the additional activity of the enhanced role makes it difficult to balance workload,32 in some cases leading to staff using their own time,187 which is ultimately unsustainable. 172 The appeal of an enhanced role may lead staff to pursue a specialist career and leave their original role,187 or lead to a depletion of their source professional role;163 in both cases, succession-planning is required, such that enhanced roles are within an overall career ladder. 163 Experience from Canada found that physician and nurse practitioners were reluctant to fully integrate the pharmacist’s role during the first year, when the service was referred to as a pilot project and the funding to support the service was therefore not permanent, as a result of concerns that they may become dependent on a new service that might not remain available the following year. 159
Introducing new services has the potential to induce demand,71 or there is potential for the new service to address a previously unmet need, if, for example, incentives encourage procedures that had not previously been available. 174 New or transferred services have the tendency to become supplementary rather than a substitute service. 151,163,172,174 This can create a situation in which the wrong case mix is addressed; staff may misuse new services and refer patients who ordinarily would have been managed by GPs;71,187 or patients seen in the new community-based services might then need to be referred to hospital174 or seen again in primary care. 151 In addition to increased demand through supplementary services, money might also be needed to backfill traditional posts if necessary. 187
Other reasons for the increase in service delivery costs include time spent supervising (including signing prescriptions for non-prescribing staff)154,163,164,166,181 or supporting staff;174,191 longer appointment lengths for new roles;156,164,192 more frequent patient contact;149,192 lower case mix;71,181 fewer patients seen than traditional services;174 loss of economies of scale;174 increased cost of staff, as they take on tasks that might traditionally be delegated;174,176 set-up costs, such as indemnity costs for new posts;32,163 and Care Quality Commission registration for hubs and federations. 32 These, along with administrative support and resources to ensure that protocols can be reliably followed, are aspects of cost that must be factored into any service confirmation. 174,187
Experience from the UK has shown that some of these new ways of working face challenges in their demands for the new and extended roles required by the workforce. A critical shortage of ANPs, coupled with a short time frame of the GP Access Fund pilots to train ANPs, meant that they faced challenges with recruitment and, subsequently, implementation. 32 Similarly, the low numbers of currently qualified physician associates in the UK is a limitation to the scope of use. 163,189 The capacity of some workforce groups may also be reduced as they face competing priorities, such as consultant 7-day working. 163,189
The pay of staff also needs to be considered; if it is too low in comparison with other specialties or primary care physicians, then recruitment of staff might also be difficult,155 and, conversely, where it is too high or ‘virtually the same as a GP’, this may affect commissioners’ decisions about the potential benefits. 172
Mechanisms
We have identified several mechanisms for R1 from the evidence base. In the following section, we categorise these as patient, staff and system factors, and make distinct the resource and reasoning aspects of mechanisms. 76
Patient factors
Improved utilisation of community-based health services (outcome) is dependent on the location of such services (resource); location is tailored to the characteristics of the population (context) with respect to travel distance, deprivation and ethnicity177 and how the care provided in community settings ‘fits into their lives’, meaning that there is consideration of patients’ or carers’ place, space and time and their emotional connection (‘at homeness’) with the location (reasoning). 178
Provided that patients are made aware of services (resource) involving new roles or ways of working in primary care (context), such as practice-based pharmacy and paramedic practitioners,163 and that they have sufficient time to experience this care or envisage it181,185 to build confidence (reasoning) to use this service in the future,185 they will accept the care from an alternative clinician (outcome). 182
Staff factors
Where new roles or ways of working are introduced (context), resources such as clinical champions of innovation,159,174,176,177,179,182 regulatory frameworks,156,163 training and development,156,179 clearly defined roles and responsibilities,156,176,179 an explicit case for change176 and dedicated change-management staff32,156,191 assisting with regular communication and engagement,32,191 can be facilitative. In turn, these resources can motivate professionals (reasoning) to embrace change through a better understanding of the new scope of their role, practice and organisation163,176 and an enhanced perception of the credibility, legitimacy and sustainability of new posts. 159,163,174,176 This results in enthusiasm and willingness to adopt new ways of working, including clinical buy-in,191 and combats resistance to change (outcome). 179
Embedding the new and expanded roles within primary care settings (context) requires time and/or funding (resources) to develop the role163 and upskill, as relevant, through training and education. 155,191 For example, hospital specialists can train clinicians in primary care to manage complex patients in the community. 179 Funding will also provide diagnostics in the community where necessary. 187 As for adopting new roles, the ability to embed new roles and the resources of funding and training provide primary care professionals with both the experience149 and the confidence (reasoning)179,186 to diagnose or treat more complex patients themselves in primary care, without onward referral to a hospital (outcome). 179,187 Similarly, notwithstanding limited evidence on care navigation in community-based settings, receptionists who are trained in care navigation (resource) and have increased awareness and knowledge of alternative services (reasoning), could facilitate a direct referral to new services, avoiding a GP consultation (outcome). This has been demonstrated in practice through the use of care navigators in the implementation of a ‘PhysioFirst’ service,32 and through the inclusion of consultations with pharmacists for telephone triage of same-day appointments. 182
Building staff confidence and empowerment can also lead to greater job satisfaction. Job satisfaction can be improved further (outcome) if regulations of the roles allow for greater autonomy and enhancement of the scope of the role (resource), so that professionals are empowered in their position (reasoning). This has been demonstrated by pharmacists working in a general practice who can prescribe,182 and also, conversely, through the inability of physician associates to currently prescribe as per the exclusion of physician associates from the regulatory framework for health-care professionals. 189
System factors
In the earlier section, Staff factors, we reported a dependency on staff willingness to adopt new ways of working and subsequent training to empower them to take on new tasks. In this section, we move on to consider the task-shifting phase. ‘Task shifting requires both willingness to give up tasks on physicians side as well as the ability and capacity to perform these tasks on non-physician health professionals side’. 155 A systematic review on the substitution of physicians by nurses in primary care found GPs unwilling to give up tasks, as demonstrated by a low level of clinical autonomy in nurses. 154 Similarly, Pawson et al. ,71 in their realist review on demand management, note ‘the lack of success of General Practitioners with Specialist Interests (GPwSIs) initiatives due to reluctance to let go by consultants’.
Where new ways of working are introduced (context), resources such as the negotiated division of labour,71 clearly defined roles and responsibilities,154 protocols that define practice boundaries155 and communication and engagement with the wider workforce179 can facilitate task-shifting (outcome). These resources, in turn, create an agreed and accepted case mix of patients to be treated in the community. 71,190 Preconceptions and attitudes of what professional roles entail are eliminated,154,179 enabling professionals to better understand and appreciate the role of each team player,155,159,193 which helps to diminish a fear of losing control or professional insecurities160,163,193 (reasoning).
With the introduction of new roles (context), resources such as co-location,159,193 electronic medical records193 and meetings193 can be facilitative. These resources, in turn, enable professionals to develop collaborative relationships and improve communication, trust and respect,159,185,190 resulting in improved delivery of community services (outcome). For instance, improved trust (context) will determine the level of support that staff in new roles receive (resource) as consultants accept the new service (reasoning),71 improving the safety and efficacy of the community-based services (outcome). 174
Mechanisms summary
From a patient perspective, improving the utilisation of community-based services can be enhanced if service locations are tailored to patients’ emotional connections, as well as developing patient confidence through greater awareness and experience.
From a staff perspective, overcoming resistance to change and the willingness to adopt new ways of working, along with maintaining new ways of working, are key considerations. In order to create a culture receptive to change, structured processes (e.g. regulatory frameworks, training and development programmes) need to be incorporated to develop staff confidence in the new way of working. Once staff have been encouraged to adopt new ways of working, investment is needed to embed such roles, so that primary care professionals have both the experience and the confidence to maintain the new way of working. Staff can further be empowered through autonomy and enhancement of the scope of the role, increasing staff resilience.
From a wider staff perspective, the introduction of new ways of working needs to be done in a structured systematic way, so that all stakeholders have confidence in the new way of working. Collaborative relationships and the promotion of new services will encourage their use.
Chapter summary
Of the characteristics of interest to this theory component (see Characteristics of community-based care and primary care access), some initiatives are relatively new, particularly in UK settings, and need further evaluation. Furthermore, a paucity of research data has also been noted for the more established enhanced primary care roles, such as advanced nurse or physician associate roles. 156 Upcoming evaluations, such as the second phase of the GP Access Fund,194 will help to develop the evidence base, as well as future evaluations of pilot programmes, such as the 3-year Clinical Pharmacists in General Practice phased pilot. 195
Notwithstanding the limited evidence base, we conclude that delivering new and expanded roles in primary care as part of the provision of more care in the community requires trust between professionals, alongside appropriate training and practical tools to trigger professional willingness to adopt new ways of working, such as task-shifting for community-based care. Subsequent embedding of the effective new ways of working has the potential to achieve the outcomes of better management of chronic conditions, a reduction in the number of secondary care referrals, improved health-care accessibility for patients and higher staff satisfaction for individuals performing new roles, as well as others benefiting from reduced pressure in the system. Cost-savings in this context may only be possible following the sustained implementation and stabilisation of increased demand, where the costs of training and additional community service provision are included.
Chapter 5 Place-based contracting and payment systems as a means to incentivise shared accountability
Introduction
This chapter explores the second of three theory components that were prioritised for realist review purposes:
If commissioners award place-based contracts (incorporating capitated budgets and risk-/gain-sharing) then providers will share accountability for population health, cost-effectiveness, patient experience and staff experience.
The chapter begins by setting the evidence scene for the if statement, that is, the characteristics of new forms of contracting and their contribution to place-based care, followed by an assessment of the then statement in the literature, by describing the outcomes associated with capitation, risk-/gain-sharing and financial incentives. Next, a brief description of the state of the evidence is provided for R2, which precedes the section for outcomes, delineated by the quadruple aim and unintended outcomes. Subsequently, we describe the mechanisms as resources (of the intervention) and reasoning (stakeholder volition) for patient, staff and system. When possible, we place the resources of the mechanisms alongside the context within which the theory component operates together with the specific intervention outcomes. Finally, we provide a brief overview to capture the key aspects of R2.
Characteristics of place-based contracting and payment systems
According to Andersson and Wikström,196 accountability in health care could be construed to incorporate ‘answerability, blameworthiness, liability and expectation of account giving’. Shared accountability, then, might be the product of integration, facilitated by a range of levers and incentives within new payment models designed to improve outcomes, reduce unnecessary expenditure and encourage place-based care: capitation; risk- and gain-sharing; differential outcome-based payments; and pay for performance. 119,120
Owing to its emphasis on collective accountability through long-term planning, aligned incentives and risk-/gain-sharing, an ‘accountable care’ model – loosely based on the ACO model from the USA – is seen as offering a balance of structured payment systems with the flexibility to adapt to local contexts. 119,120,126 Bringing together multiple services under a single contract and a capitated budget signals a shift in emphasis from activity to outcomes, theoretically offering health and care systems the ability to reduce supplier-induced demand, increase standardisation, share best practice, reduce variation and thus, improve productivity and overall value. 118,119,197 Furthermore, meeting the dual requirements of an integrated system that is cost-effective highlights the need for a population-level budget, with a focus on outcomes to enable greater attention on population prevention strategies. 118
The MCP framework,11 produced by NHSE, describes the ambition for a fully integrated MCP, incorporating capitation (the whole-population budget),198 risk-/gain-sharing and incentives (the MCP Improvement Payment Scheme, which replaces the QOF). 198 Capitation may involve pooling budgets across health and social care. 199 Vanguards are seeking longer-term contracts, of between 5 and 15 years,200 to enable longer-term planning and investment, allowing providers to spread the risk over a longer time frame and to address the wider determinants of health.
The King’s Fund recently undertook a series of interviews with vanguard sites to explore progress,200 noting that many of the commissioners are exploring capitation as an opportunity to abandon ineffective and perverse payment mechanisms. Risk- and gain-sharing is designed to ensure ‘that the payment system does not inhibit the path to transformational, system-wide change’ (contains public sector information licensed under the Open Government Licence v3.0),11 avoid perverse incentives and encourage public reporting on quality and costs. 118 Risk- and gain-sharing agreements have gained traction, demonstrated by the contract for musculoskeletal services in Bedfordshire. 201
The learning from current examples emphasises the time taken to design and embed new pathways and new ways of working, in addition to the implementation costs at the start of the contract,126,201 which is reflected in the NHSE draft MCP contract. 202 In the Bedfordshire example, the performance management starts after the first year of operation. The MCP framework suggests that the performance payment might amount to 10% of the total contract value. In a series of interviews with vanguard commissioners, Collins200 noted that the operational risks expected of providers may not reflect the reality of what is in their control, for example, in relation to unscheduled care and delayed transfers of care.
Advocates of outcome-based commissioning suggest that a focus on patient and population outcomes, rather than on process outcomes, will drive up the quality of care. Influenced by the concept of value-based health care,203 outcome-based commissioning gained attention through work in Milton Keynes. 118 Pay-for-performance incentives, a feature of outcome-based contracts, are used to drive productivity or quality. 204 The design and format of payments vary, typically based on units or thresholds, and may be paid retrospectively or prospectively. 205,206 The vanguards recognise the need for the alignment of incentives at different levels of the system, from the individual level to the service level. 200
Current commissioning practice typically involves the management of numerous contracts, ranging in value, for different community-based services. The lead provider model, potentially the vehicle for the fully or partially integrated MCP, has been promoted as enabling better management of pathways and offering clearer governance and accountability,201 and is the preferred model in several vanguards,200 with at least one vanguard working with a prime contractor, or systems integrator,207 to develop the model. The theoretical benefits of this approach include a lower administrative burden; greater co-ordination of specialist providers; and the facilitation of innovative approaches to care. 118 The alliance contract, the likely vehicle for engaging GPs in the partially integrated or virtual MCP,11 is considered to result in less disruption locally, but still requiring robust governance arrangements. 201
The evidence base
The evidence base underpinning R2 is characterised by limited empirical evidence, although there have been earlier reviews of available evidence; there are a number of commentaries, drawing on experiential evidence (case studies and informal evaluations). Details are provided in Appendix 6. The review is based on 12 reviews, 3 qualitative studies, 7 experimental studies, 8 official publications and 18 commentaries. Support for this component is therefore relatively weak. Limitations of the evidence base mainly relate to the heterogeneity of contracting models and variable reporting, resulting in a moderate level of uncertainty around the conclusions.
There has been substantial debate and commentary on contractual models within UK and international literature, but limited empirical studies that test and evaluate the theory, perhaps indicative of the challenges involved in measuring impact. Owing to the features of NHS funding and its flows, much of the international evidence base needs to be considered for its applicability to a NHS context. It has even been suggested that, given the significant variation, the labels used may be unhelpful, implying a level of consistency not visible in reality. 201 The evidence base, although limited, will help to articulate the theory and underlying assumptions of the MCP model. When appropriate, gaps in the knowledge base are highlighted, suggesting potential priorities for further research and evaluation.
Outcomes
Population health
Reviews197,208 of contracting arrangements in health and social care present a relatively mixed picture of the impact on population health outcomes, with those that had ‘well-developed and comprehensive pooling arrangements across a range of sources, creating large health and social care budgets’208 demonstrating positive impacts. The reviews found limited studies exploring the impact of contracts on the quality of care, and considerable variation in the measures used. The findings suggested that pooled resources might offer providers the ability to create a more holistic package of care that meets patients’ needs; however, this carries an associated risk that capitation might act as a perverse incentive, encouraging providers to sacrifice quality to reduce cost. The opportunity hinges on the availability of information on health needs, service utilisation and quality indicators. 197
Learning from legacy initiatives, such as the Better Care Fund, suggests that expectations on population health outcomes may be ambitious, failing to take into account the time taken to influence changes in behaviours and to demonstrate an impact on morbidity or mortality;209 a qualitative analysis of Better Care Fund implementations suggests that a time scale of ≥ 5 years is realistic. This same analysis notes how several local health economies chose to scale back ambitions, focusing on specific population groups to achieve short-term goals. Elsewhere, it is proposed that financial reform in health care could have a negligible or negative impact on health inequalities,210 although the evidence is limited.
Three Cochrane reviews204–206 have explored the effectiveness of financial incentives, which highlights the need for more robust evidence on the impact of financial incentives on patient outcomes. Although incentives seem to have some effect on the behaviours of health-care professionals, this may not necessarily translate into improvements in patient outcomes. 205 Capitation, fee for service and pay for performance were found by Yuan et al. 206 as likely to have little or no impact on health outcomes, leading to their conclusion that decision-makers should consider the selection of performance measures and targets, the availability of funding and the means to test the payment level needed to influence behaviour change. 206
Several MCP vanguards have expressed a commitment to develop new outcome frameworks for primary care, replacing the QOF. The QOF was established to drive up quality in primary care, but has since been criticised for (1) its failure to address multimorbidity;211 (2) encouraging an overly mechanistic approach to care, focusing on biomedical surveillance and neglecting self-management;212,213 (3) a focus on measurable, rather than truly improved, health outcomes;214 and (4) imposing barriers to case-finding, particularly in deprived practices, in which prevalence is higher. 211 The focus on single diseases211 may have inhibited a more holistic approach for comorbid patients. However, it has been argued215 that, although guidelines could be created for common comorbidities such as depression, the task would be overwhelming, because of the multitude of potential conditions and combinations.
A recent review216 suggests some lessons, relating to the QOF, which may usefully inform new outcome frameworks. The review found a limited effect on outcomes, including glycaemic control and high blood pressure, suggesting that impacts may be transient and may not lead to improvements in population-level morbidity and mortality. Attribution is problematic – typically many influences, such as housing, environmental factors and deprivation, will have contributed to these outcomes. 118,197,209,216,217 It has been argued that the long-term contracts being developed by MCPs may offer an opportunity to invest in interventions with partners to address these wider determinants. 11
Cost-effectiveness
The current focus on savings and reduced utilisation does not seem to be borne out in the literature. Findings regarding the cost-effectiveness of new contractual arrangements in earlier legacy initiatives have been mixed. A review208 of 34 schemes found only three that reported significant reductions in utilisation; 11 had no significant effect; and, for the remaining studies, results were mixed. Few studies have assessed the long-term impacts, making it difficult to draw conclusions on the sustainability of any reductions in service utilisation. 208 Notwithstanding several evaluations of integrated care contracts, such as Torbay and Wye Valley, the methodologies make it difficult to compare findings accurately. 197 It is possible that integration may help to identify unmet need, which may initially limit savings and tip resources towards acute-based care;208 in addition, the current climate of widespread provider deficit holds a risk that ‘crisis management’ may over-ride prevention. 197 Even when costs are reduced, it can be difficult to translate these into actual savings, without reducing provision or closing beds. 197
A commentary, by Humphries,218 argues that the Better Care Fund, designed to enable integration through pooling resources, ‘created risks as well as opportunities’, because of implicit assumptions ‘based on optimism rather than evidence’ about the savings that could be achieved. The ambition to deliver £511M of savings in 2015–16 was not attained, as a result of increased emergency admissions and delayed transfers of care. 209 Plans to reduce delayed transfers of care by 293,000 days in total actually resulted in an increase of 185,000 days and additional costs of £146M – approximately 75% of areas were unable to achieve the targeted reductions in delayed transfers of care. Similar numbers of local areas experienced increases in emergency admissions, leading to costs of £311M over the plans. Qualitative interviews suggest that the initial administration of the fund created a level of bureaucracy that affected capacity and existing integration schemes. 209 Similar comments about the administrative overhead have been made, by Allen and Petsoulas,219 about the Commissioning for Quality and Innovation scheme. The assumption that pooling resources will help to identify and address barriers to improvement fails to take account of the inevitable redundancy within any system. 217
Looking further afield, to understand what may be learnt from international systems of care, commentaries on the early ACOs in the USA point to mixed results on costs and health outcomes. 119,126,220 A difference-in-differences analysis221 suggests that the success of the ACO model may derive from the shift to lower-cost facilities and the emphasis on outcomes, rather than activity, based on learning from the Massachusetts-based initiative incorporating capitation and pay for performance. These changes are associated with reduced utilisation in some population groups. At this stage, given the maturity level of ACOs, it may be too early to see, where reductions in utilisation have been demonstrated, if these can be sustained over time. 126 Questions remain regarding the expectations of cost-savings from shifting care closer to home191,222 within a NHS context. An evaluation of the CMS Group Practice Demonstration Programme223 found significant reductions (US$500 per person per year) for the sickest patients (people receiving both Medicare and Medicaid support). The authors go on to speculate that ACOs may have a role in ‘slowing the rate of increase in health care spending and in bringing about some improvements in the quality of care’; however, they also point out that ‘if ACOs are to bring benefits then they will need a range of capabilities in order to manage cost and quality and to be able to implement what is known about the characteristics of successful integrated systems’. 223
Capitation and pay for performance were found to be ‘generally effective’, based on the findings from a Cochrane review. 204 In an outpatient setting, pay-for-performance incentives were associated with improvements in quality in outpatient settings, particularly in the use of tests and treatments for long-term conditions, but little or no difference to health outcomes or utilisation of services. 206 Learning from the QOF suggests that the effectiveness has been variable. The QOF has been associated with a small curb in the increase in emergency admissions216 for those conditions that are included in the framework. However, it is difficult to attribute any improvements to the QOF, given the multiple factors that may have contributed. A key criticism of the QOF is that the framework incentivises activity rather than quality. 204,224
Lessons from earlier initiatives suggest that potential savings could be limited by the time and set-up costs to design and implement new contracts, outcome frameworks and performance management systems. 201,225 There may be costs associated with data collection and management, actuarial analysis and training. It has been suggested that this work can take up to 2 years. 201,226
Patient experience
With the emphasis on outcome-based commissioning within MCP contracts, it could be argued that the use of financial incentives is geared more at improving productivity than quality. However, little evidence exists to support the notion that financial incentives will drive up quality without some investment of organisational development,205 particularly focusing on collaboration, communication and teamwork. 118 The review found little evidence on the impact of financial incentives on patient experience.
This is indicative of the challenge of defining and measuring outcomes that are meaningful from both a patient and service perspective118 and is a recurrent theme in the literature: ‘. . . complying to arrangements for patient empowerment and patient centredness will be challenging as these terms are not self-defining and there are a wide variety of approaches to achieving these goals, depending on how they are understood.’118
Staff and provider experience
The evidence base appears to focus on the experience of provider organisations rather than individual staff, suggesting a potential research gap.
For providers, there may be greater flexibility for investment within a pathway and over the lifetime of a contract, to manage risks and gains. 227 It has been argued that this creates an environment for innovation118 and enables a focus on the wider determinants of health.
The context in which MCPs will be operating presents challenges to commissioners and providers, in particular, political pressure to deliver change within time frames that have been described as idealistic; Burns and Pauly220 suggest that a time frame of 5–7 years is more realistic. Anecdotally, MCP teams are noting the time involved in building relationships and structures. In a conference presentation on new care models, Hopson226 noted that the logistics of getting out to talk to stakeholders (e.g. practices, local authorities) presented significant challenges to vanguard teams.
Unintended consequences
Elsewhere in this report, the issue of defining ‘place’ or ‘community’ is noted. Although many of the MCP vanguards refer to ‘natural communities’, the notion of ‘community’ is fluid and subjective (further described in Chapter 6). As with any boundary, there may be consequences from where contractual lines are drawn. For patients living near the boundaries, there may be impacts on patient choice and on the liability of the MCP, as suggested in the following commentary:
If a patient opts to seek care from a different provider outside the area, the local ACO would remain accountable for that individual’s care and bear all the costs. In addition, the ACO or other provider that receives this out-of-network patient would be remunerated depending on the level of success.
Reproduced from Ahmed et al. 119
Uncertainty exists regarding the tensions and trade-offs resulting from the shift of care from hospital to community settings, with speculation that organisations may act in their own interests rather than those of the overall system. 118 Conflicting policies may exacerbate this, as pointed out in the National Audit Office analysis of integrated care. 209 Although some areas (such as Salford and Northumberland)200 are making progress on pooling budgets, hurdles remain in pooling across health and social care, making it difficult to align incentives,208 and in transferring savings and risks across sectors. Those areas that are making progress are building on a history of collaborative working. 200 In the USA, there has been speculation228 that the ACO model, in its emphasis on consolidation and co-ordination, may inhibit those market forces/competition that are necessary in driving cost and quality improvement.
In addition, concerns have been expressed that the lead provider/contractor model, advocated in the fully and partially integrated MCP contracts, could have negative consequences, creating further distance between commissioners and providers and affecting clinical governance and patient safety. 118 The actions of individuals are also unpredictable; a review, by Billings and de Weger,118 points to earlier analysis of the effectiveness of incentives: ‘. . . although agents will often change their behaviour in response to sanction/reward mechanisms, this is not always in desired ways’. Outcome frameworks may risk focusing on process outcomes, rather than those that are more challenging to define. The implications for providers should also be considered – qualitative measures may involve new data collections and could incur more cost. 118
Learning from the ACO models in the USA, it has been noted that current savings typically derive from the first cohort, set up in 2012, demonstrating the time needed to deliver efficiencies/improved productivity. 229 Similarly, it seems unlikely that improvements to the quality or experience of care can be delivered in a matter of months. 221 This may translate into an optimism bias,201 whereby commissioners may develop contractual forms that do not have the support of providers and local communities. The challenge of designing a population-based capitated contract, in which subcontracted providers may hail from both the public and private sectors, should not be underestimated; ‘gains’ may be seen as profit for shareholders or reinvestment for improvements. 200 New guidance230 from NHS Improvement suggests that adjustments will be considered for agreed periods, to enable integrated working to become embeded.
There is a risk that incentives may reward inappropriate behaviours; for example, capitation could restrict access for some patients to some services;208 however, commissioners have the opportunity to set thresholds to mitigate this. The focus on reducing hospital utilisation may also have an impact on patient choice, if packages of care are focused around this aim to the exclusion of patient preferences. 208 In particular, it can be difficult to define outcomes relating to the experience of care.
The different contractual forms described in the MCP framework11 offer different combinations of risk and opportunity. Reviews of contracting arrangements have found that alliances (the vehicle for GP practices to join partially integrated MCPs) benefit from incentives to collaborate, improved relationships, active involvement of commissioners,201 information-sharing, reduced capital costs and better co-ordination. 225 However, some evidence suggests a high failure rate in alliances118 because of the conflict between competition and collaboration:
Alliance partnerships differ in the amount of pressure the firms feel to cooperate vs compete. These competitive forces are affected by contracts existing between the parties, the amount of product and service overlap, as well as the amount of trust in the relationship.
Reproduced from Billings and de Weger118
The lead provider model offers commissioners the opportunity to address pathways via one contract, as opposed to the multiple contracts currently in place. This raises questions on how group accountability for outcomes will be managed. It has been argued that incentives might result in unintended behaviours and outcomes. Incentivising case-finding could initially increase costs as unmet needs are identified. Professionals may be incentivised to focus their efforts on outcomes that are rewarded, thus neglecting other aspects of care. 205 Furthermore, there is an associated risk of ‘gaming’ unless robust information systems underpin performance management. 197,208 The availability of information is associated with the power balance between commissioner and provider; information asymmetry is a risk227 when commissioners are ‘price-takers rather than price-setters’,208 leading to inefficiencies in the contract.
As the theory behind longer-term, place-based and outcome-based contracts suggests that outcomes can be improved, recent examples – such as Hinchingbrooke231 and the UnitingCare contract in Cambridgeshire and Peterborough200,232–234 – have demonstrated the difficulty of pricing services previously procured on block contracts. The UnitingCare contract – a 5-year £725M contract awarded in 2014 for acute and mental health services for older people and community services across Cambridgeshire – failed, resulting in at least £16M in termination costs shared by the parent companies of the provider and the CCG. 200 The viability of the procurement, which stipulated a 10% reduction in costs over the course of the contract, was questioned. 233 In addition, the financial risk and value-added tax (VAT) implications were not sufficiently addressed. 232,233 The context of an existing unsatisfactory contract combined with local ambition to deliver to tight time scales influenced decision-making behaviours to prematurely sign the contract. 233 Potential implications may relate to circumstances in which commissioners prefer larger providers or partnerships, which offer greater financial resilience200 over smaller providers.
Mechanisms
We have identified several mechanisms for R2 from the evidence base. In the following section, we categorise these as staff and system factors and make distinct the resource and reasoning aspects of mechanisms. 76
Staff factors
It is widely recognised that the contracting arrangements alone are unlikely to deliver change without an explicit commitment to organisational development. 200,209 A culture of trust and collaboration (context), which takes time to develop, is needed to underpin the new ways of working (outcome) required of new contracting arrangements. A key theme to emerge from the literature is the mutually reinforcing relationship between structural interventions, for example, organisational forms (context) and governance structures (resource), and behavioural change [e.g. staff motivation (reasoning)] from staff engagement and development (resource), leading to a shift from siloed working (reasoning). 235 In addition to these cultural factors, specialist capacity and capability (resource), with clear roles and responsibilities in contract management and procurement,233,234 are underlined as critical to enabling new contracts. Investment to stimulate engagement and organisational development (resource) is considered imperative to improving the value of health care221 (outcome).
At an individual practitioner level, it has been argued that extrinsic incentives (resource) ‘may crowd out or reduce intrinsic motivation’204 (reasoning). 182,192,205 This reflects the logic of the value-based health-care movement203 that value should be defined by the customer (patient/local, community/clinicians). This might be facilitated by the co-production of incentives with clinicians and patients (resource) to focus performance around measures that are meaningful within local communities118 (outcome). There is also an argument for considering the appropriate ceiling216 and ‘strength’204 of incentives:
For example, a weak incentive to perform a valued behaviour may be more effective than a strong incentive to perform a behaviour that is not seen as important by the physician.
Reproduced from Flodgren et al. 204
System factors
Co-production (resource) encourages outcomes that are meaningful to patients, practitioners, local communities, providers and commissioners236 (outcome) which, in turn, depend on robust information11 (resource). Incomplete information, partly attributable to siloed working, was one of the issues identified in the analysis of the UnitingCare contract failure. 232 This approach suggests a focus on value rather than activity203 (context), presenting the challenge of translating a complex system of care into a set of measurable outcomes and indicators. 196 Accountability ‘as active inquiry over time: listening, asking questions and talking, as opposed to taking a snapshot’196,236 has the potential to build the relational behaviours (reasoning; see Chapter 6) that underpin the MCP vision.
Collaborative behaviours (outcome) and sustainable relationships (outcome) are dependent on trust (reasoning). 118,120,200,219,225 Contracts in the NHS depend on a level of flexibility (resource), which is challenging where relations are fragile or adversarial (context); Sanderson et al. 225 note the importance of relationships in building a shared sense of identity and values, which is particularly important in the context of agreeing opportunities for improvement or innovation and in determining what outcomes should be monitored.
Collaboration (reasoning) may be encouraged through a co-productive approach (resource), described in an ethnographic study196 as ‘social accounting [. . .] through the acknowledgement and enactment of multiple accountabilities and relationships’ – in recognition that changes to structure and process are not sufficient to facilitate a culture of shared accountability (outcome).
The effectiveness of incentives is explored by Mehrotra et al. 237 in their application of behavioural economics theory to the use of incentives. Although commissioners find the threat of penalties (resource) to be a useful incentive, not all of them act on the penalites219 (reasoning), citing the risk of impeding provider efforts to improve quality as one reason; thus, incentives may fail to influence individual practitioners’ behaviour118 (outcome). The unpredictability of behaviours also makes it difficult to ensure how measures influence individual practice. 212,238 Findings from The King’s Fund inquiry into the quality of general practice concluded that protected time (resource) is needed alongside incentives, to allow for reflection239,240 (reasoning). The co-production and testing of outcomes and incentives with stakeholders may help to ensure alignment with business plans and interagency strategies118,227 (context).
The readiness of organisations (context) to take on the role of lead provider has been questioned,118 with the suggestion that larger institutions providing secondary care may be in a more favourable position to take on the level of risk, particularly in areas that lack a strong GP federation. The need for investment in technology, information systems, governance, process re-engineering and cultural change (resource), and the resulting need for revenue streams to manage high set-up costs (context), may also favour larger institutions. 220 It has been suggested that implementation costs could outweigh potential savings. 118 Within a primary care context, there is a suggestion that the large multispecialty group practices in the USA are able to improve quality as a result of shared infrastructure; however, this has not been robustly tested. 241 It is likely that GP practices will vary in enthusiasm for existing contracts and readiness to give up existing contracts (reasoning) to participate in the partially or fully integrated model. 200 Readiness is dependent on a host of contextual factors,200 notably the strength of existing relationships across the health and care economy (context). It can be challenging to build collaborative system-wide relationships in a regulatory system built around the performance of separate organisations (context),200 and it is acknowledged that relationships will evolve over years rather than months. NHS Improvement and NHSE are jointly developing the Integrated Support and Assurance Process to support new care models. 230
The programme theory articulates the notion that new contracting and payment arrangements will incentivise shared accountability. However, it is clear from the evidence that consideration needs to be given as to how to encourage inclusivity (reasoning) through the co-production of outcomes (resource) and engagement in data collection196 (resource). An ethos of co-production combined with a long-term perspective (context) goes some way towards the vision of the culture of stewardship described by Gray242 (outcome).
Chapter summary
The review highlights significant gaps in the literature base, notably relating to patient and staff experience of introducing new contractual forms. There is limited empirical evidence, and much of the literature seems to be anecdotal or theoretical, based on limited case studies or informal evaluations, rather than robust research designs. This is indicative of the challenges of measuring and attributing outcomes to contractual forms; when studies have been able to explore outcomes, these often look at aspects of the MCP contractual model in isolation (e.g. incentives or capitation), rather than the overall approach.
The influence of contractual forms on population health seems to be mixed, which is suggestive of the impact of different local contexts. Findings suggest that a tension between incentives to compete and collaborate could lead to potential confusion within a system; however, there does seem to be potential to encourage more holistic care through pooling resources. Learning from other programmes of integrated care suggest that ambitions are often unrealistic, particularly with regard to the savings that can be achieved and the time scales of changing the behaviours within a system. Behaviours can be unpredictable, and there is a risk that well-intended incentives may result in inappropriate behaviours, for example, by prioritising productivity over quality.
From a system-wide perspective, new forms of contracting will need to be supported by an explicit programme of organisational development and the involvement of clinicians and patients in the development of outcomes and incentives. This cultural change is needed to ensure a shared understanding of value within the context of the local community, and to encourage the behaviours associated with new ways of working inherent in the new contract. Our analysis suggests that the involvement of clinicians in the development of incentive frameworks (context), with sufficient time for reflection and learning (resource) enables individuals to understand how their role contributes to patient outcomes (reasoning). Equally, engagement of patients and service users helps to define ‘shared accountability’ on clear measures of value (outcome). Investment in organisational development (resources) and robust high-quality information on cost and quality (resource) encourages trust and collaboration (reasoning), in turn enabling informed (re)investments (resourcing) and financial risk to be managed appropriately (outcome). This sharing of information and intelligence, which provides access to the same outcome data (resource), can facilitate joint accountability (outcome) for informed and consistent decisions (resourcing).
Chapter 6 Fostering relational behaviours builds resilience within communities
Introduction
This chapter explores the third of three theory components that were prioritised for realist review purposes (see Chapter 3 for more detail on how MCPs intended this theory component to work). It begins by setting the evidence scene for the if statement, focusing on the characteristics of relational behaviours and co-production followed by the then statement, describing how health and care services support local communities to build resilience. Next, a brief description of the state of the evidence is provided, which precedes the section for outcomes, delineated by the quadruple aim and unintended consequences. Subsequent to this, we describe the mechanisms as resources (of the intervention) and reasoning (stakeholder volition) for patient, staff and system. When possible, we place the resources of the mechanisms alongside the context within which the theory component operates together with the specific intervention outcomes. This narrative is followed by a summary of the extended advisory group discussions related to R3, highlighting aspects that further develop the theory components. Finally, we provide a brief overview to capture the key aspects of R3.
Characteristics of relational behaviours
Influenced by systems thinking, MCP vanguards recognise that health care is inexorably interconnected with other public services, support networks and local neighbourhoods. MCP vanguards express an ambition for a different relationship with local communities, in which patients and members of the public, along with community groups and local businesses, are more engaged in the design and delivery of health care. A sense of ‘co-ownership’ or ‘mutuality’ is described. This chapter focuses on the multifaceted approach, described by MCP vanguards in their logic models, to develop mutually beneficial relationships between service users, professionals, services and communities. Recognising these various dimensions, this chapter considers the breadth of this approach, illustrated by interventions referenced in the MCP logic models, at the individual (self-management and social prescribing) and community (co-production, community engagement and joint working) levels.
As referenced in Chapter 5, the concept of ‘community’ is fluid. A community may be defined by shared interests, needs or experiences (such as groups with similar health needs), or by common attributes such as place of residence, ethnicity, age and occupation. 243 Individuals are likely to belong to various ‘communities’, associated with specific identities such as race or religion, as well as interests, or by needs of health care244 or social care. An inherent tension in defining communities is in setting boundaries of inclusivity, thus determining who is or is not included. 245
To address the growing demand on services and the social burden of long-term conditions, national and local policies advocate interventions such as self-management, shared decision-making and social prescribing, with a focus on empowerment. Recognising that actively involved patients will need support networks, services are increasingly exploring joint working with voluntary and community services to build social capital, by engaging volunteers and peer-support workers. 246,247 The strategy of connecting patients to local support networks is at the core of social prescribing initiatives. 248
The changing relationship between health services and local communities is characterised by increased engagement, encompassing ‘a range of approaches to maximise the involvement of local communities in local initiatives to improve their health and wellbeing and reduce health inequalities’. 243 Engagement can help to identify and prioritise community needs and preferences as well as develop community assets that may support the design and delivery of services. 249 Building on engagement, co-production involves the ‘contribution of service users to the provision of services’,250 enabling service users to take an active role, challenging the perception of patients as passive recipients of care. Originating in the USA during the 1970s,251 co-production is increasingly adopted by services250,252 in the UK.
As the concept of co-production is increasingly applied within health care, guidance has developed. Six principles of co-production have been developed by Nesta: (1) building on people’s existing capabilities; (2) reciprocity and mutuality; (3) peer-support networks; (4) blurring distinctions of professionals and service users; (5) facilitation of networks, rather than delivering; and (6) recognising the importance of assets. 252 NHSE has published a set of six principles, developed by the Independent People and Communities Board, for new care models, focusing on the empowerment of patients and communities. 253
The move towards co-production and engagement is also reflected in increased collaboration with other public services, such as schools, fire services, police services and housing. For example, fire services are working with health and social care commissioners254 and, in Chapter 3, we shared details of an innovative competition, working with a local school, to engage young people in health care. This combination of activities is intended to improve community resilience, defined as the ability to withstand, adapt and recover, by individuals and communities. 255 Community resilience is increasingly being recognised as an important ingredient to the reduction of health inequalities. 255,256 The resilience of individual patients and their local communities is interdependent and access to social resources has been demonstrated to be critical to empowering patients to self-care. 257 The nature of the relationships between individuals and their neighbours, statutory authorities and voluntary groups has an impact on the quality of life, and the capacity, of the community to contribute to positive changes within the community. 258 Notable relevant policies in recent years include the ‘Big Society’ initiative,259 which sought to encourage individuals to take a more active role in their communities; and ‘Healthy Lives, Healthy People’,260 which aimed to empower local communities to adopt healthier behaviours. These policies have tended to focus on developing the assets and resources needed for a community to thrive: human capital (e.g. skills and education), social capital (e.g. social networks), built capital (e.g. access to amenities), natural capital (access to green space) and economic capital (e.g. income). 256,259 More recently, the Realising the Value programme249 has provided funding for a series of partnerships between health services and the voluntary sector.
The evidence base
The evidence base for R3 is varied, with limited review evidence available for the effectiveness of co-production and social-prescribing interventions, and several systematic reviews examining self-management interventions. Literature from the UK has been prioritised for relevance; when international examples are used, we have given precedence to countries with a similar primary care model to the UK. The dearth of evidence is reflected in the data set used for this review (11 systematic reviews; seven literature reviews; two qualitative studies; one quantitative study; one cost–benefit analysis; six evaluation reports; and six commentaries). Support for this component can therefore be considered to be moderate. Limitations mainly relate to the use of before-and-after methods, which are prone to bias, and variable reporting, resulting in a moderate level of uncertainty around the conclusions.
Much of the evidence relating to mutual beneficial professional relationships stems from case studies of health and social care integration programmes. Many studies examining co-production and social-prescribing initiatives are small in scale, descriptive and focus on implementation, with limited evidence on effectiveness. Such initiatives are relatively new to the UK and need further evaluation. Review evidence pertaining to self-management consists of international literature, often with a bias towards studies from the USA; many studies are limited in follow-up on outcomes, with an absence of evidence on outcomes for staff experience. Please refer to Appendix 7 for a list of studies included.
Outcomes
There are significant challenges in measuring the impact on community resilience of new models of care, not least that any impacts are likely to be long term in nature and evaluations can often indicate only proxy measures. An associated issue relates to the definition of measures and outcomes, which are meaningful to service users and communities. 261,262 As described in Chapter 5, this may present an opportunity for the co-creation of outcomes and measures. 262,263
Population health
Although there is some evidence of the impact of a higher level of participation (through co-production, volunteering, empowerment through self-management and social prescribing) on health and well-being outcomes, there are issues around heterogeneity, the quality of reporting, the lack of sufficient control comparison and short follow-up periods. 264,265 Evaluations have reported findings of varying quality, citing improvements in lifestyle changes, social isolation, reduced symptoms, health literacy, improved support for carers and improved independence. 33,132,265–272 From a service perspective, it has been suggested that co-production can help improve the quality of care. 273 Boyle and Harris274 suggest that participation in public services could help service users to develop a social network, building social cohesion, which may be key in supporting them to manage their condition(s). In a case study of an arts intervention for multisensory impairment, Vogelpoel and Jarrold270 hypothesise that interventions such as social-prescribing can help to address the needs of high-risk groups that are particularly hard to reach through traditional channels. However, the impact of poorly managed participation does not seem to be reported.
A key characteristic of the MCP model is the focus on social action. There is some evidence to suggest that involvement in public services, through volunteering or co-production, is associated with higher levels of health and well-being and can also have an impact on social outcomes within local communities. 256,275 A Cochrane systematic review276 examining community-driven interventions targeting racial and ethnic minority populations reported mixed results. Interventions led by community health workers were found to lead to changes in health status, but results were not consistent. Wider health and social care system interventions led to small changes in measures of health behaviour and health status.
These findings, although sometimes based on anecdotal evidence, suggest a need for a longer follow-up period, to understand how levels of engagement and health outcomes might change over time and the contextual factors that are likely to influence behaviours and, thus, the resilience of local communities.
Cost-effectiveness
The MCP focus on participation is based on a theory that service users who are supported and engaged will be better informed to make appropriate use of services and, in turn, better able to contribute to a mutually supportive network. However, there are considerable challenges in translating this to an impact on the cost-effectiveness of services, notably, the lack of robust measures and the difficulties of relating outcome measures to costs. 265,272,277 Few studies report costs, and even when costs are reported, it is often difficult to determine the cost of individual elements of services and interventions. 264 This is particularly challenging in services involving volunteers, whose unpaid contributions, training and support may be excluded from analysis. 132,264,269 Evidence suggests that higher engagement may lead to earlier intervention, which could help to prevent downstream costs. 272,274 A broader range of metrics may be more appropriate in assessing the impact of greater participation, including on admissions; workload in primary and community care; and the service-user and carer experience. 247
Several case studies suggest potential impacts on cost-effectiveness; for example, Boyle and Harris274 cite the Expert Patient programme, which reported a 7% reduction in GP consultations and 16% reduction in accident and emergency (A&E) visits. Partnership-working seems to be a key factor; large-scale self-management initiatives, involving national or regional authorities, were found to reduce admissions, deaths and time off work. 278 The Brighton and Hove social-prescribing pilot evaluation279 estimated potential savings of £1.36M per year of GP time. Several authors,33,280 however, caution that programmes often understate supplier-induced demand and overstate cost reductions, failing to account for set-up and operational costs appropriately:
The idea of self-management as a demand management strategy is also based on an assumption that utilisation behaviour is patient-led, when some aspects of utilisation (such as clinical attendance) are also a function of professional behaviours and may not be affected by changes in patients or carers.
Reproduced from Panagioti et al. 280
Dayson et al. 132 also point to the issue of scale, suggesting that, for some interventions, cost-effectiveness depends on a large critical mass of service users. There is also the potential to deliver improved cost-effectiveness through partnership-working with public health services; a recent study281 found a median return on investment (ROI) of public health interventions of ≈14.1. Health promotion interventions, including falls prevention and smoking cessation, delivered a median ROI of 2.2; health-care interventions, including disease management, offered a median ROI of 5.14. There may be potential for partnership-working across public services to address wider determinants of health; interventions were found to deliver a fivefold ROI. Partnership-working with the third sector may need specific consideration in terms of financial sustainability – the uncertainty around budgets, typical of the public sector, can have very far-reaching ramifications for small third-sector groups and for individual volunteers. 132
A case study282 reports on an instance of community engagement following a consultation to close a community hospital as a result of the recruitment and retention issues in primary care. The community, opposed to the closure, rallied to support GP recruitment, producing promotional materials to attract applicants to the area.
Patient experience
Reviews suggest that service users’ experience of participation in health care271 seems to be generally positive, reporting benefits relating to physical and emotional health and well-being, self-confidence, self-esteem, social relationships and their individual sense of empowerment. 267 However, the experience can prove to be negative for some service users. 267 Co-production is viewed by some service users as an opportunity to move ‘beyond token involvement and consultation towards more equitable power relations’ through ‘genuine collaboration’. 283
A greater role for third-sector and community groups may offer service users access to specialist knowledge, for example, on dementia,282 which could prove to be a valuable resource. 284 Where service users are actively engaged, they may also begin to contribute their knowledge; this is illustrated by del Castillo et al. ,282 in which patients with rare diseases collectively shared knowledge to support each other. Increased involvement of the third sector can also create and mobilise a body of volunteers, who can contribute to a more holistic care and support package, connecting service users to provide further support, complementing that provided through public services. 132,270 Farenden et al. 279 suggest that this collaboration adds value by spanning the gaps between services. This mutually supportive relationship is demonstrated in a Hospital to Home service,282 which recruited volunteers to support early discharge, reporting a statistically significant positive impact on patient experience, mood, anxiety levels, nutrition and hydration, and releasing nurses’ time to care. Similar findings are echoed by Maughan et al. ,33 who also cite ‘improved socialisation and occupational outcomes’.
Where service users are referred to social-prescribing programmes, the evidence suggests a mixed picture. Attendance varies considerably, with one review, which reported on two studies, reporting a 58% attendance rate and a 100% attendance rate, respectively. 265 An evaluation of a pilot reported that 101 out of 393 referred patients were unable to complete the package of support offered. 279 There are various possible reasons for low uptake suggested in various studies and evaluations, including inappropriate referrals, readiness to engage and logistical difficulties. High levels of satisfaction have been reported;265,279 an evaluation of a pilot service reported that service users felt that their needs were better understood. 279 A further theme to emerge from the research and evaluation is the sense of mutual support that service users can give and receive through initiatives such as social-prescribing. Vogelpoel and Jarrold270 describe the development of ‘supportive relationships […] where skills, practical advice and mutual support were shared’ between participants of an arts intervention for people with sensory impairment. Over time, this grew into a ‘genuine sense of community’, stemming from ‘a willingness to extend informal support to one another’.
Staff experience
The evidence base suggests that health-care workers have mixed experiences of initiatives such as social-prescribing, with some evaluations reporting relatively high levels of satisfaction,247,265,279 whereas others have reported a reluctance among primary care staff to get involved in non-medical aspects of care. 275 Potential reasons for this are explored in the literature, with suggestions that a medically oriented model of care (as opposed to a socially oriented model), as well as confidence in third-sector organisations, may influence perceptions of the value of social prescribing. 275
Conversely, volunteers and third-sector workers felt that they were able to spend more time with service users and could therefore offer a more intense level of help and support than those offered in primary care. 275 Pilot evaluations suggest that volunteer retention can remain relatively high when part of a formal structure. 279 In the Brighton and Hove pilot,279 volunteers gave an average of 7 hours per week during the first 12 months, totalling 5824 hours.
It has been suggested that a contract enabling collaboration across public sector and third-sector organisations could offer a balance of scale and infrastructure, with an expert understanding of communities, thus helping to create the conditions for a culture of improvement. 284 Some of the services that have been developed within the NHS have developed a ‘broker’ role, contracting with an umbrella third-sector organisation,132,269,279 offering a pragmatic option to commissioners and providers to manage relationships with multiple groups and organisations.
Unintended consequences
There are challenges in sustaining community involvement over time, and barriers such as the technical terminology used routinely in the NHS can act as a barrier to involvement. 285 There is some evidence of uneven representation or engagement across demographic groups, particularly from ethnic minorities and those with low levels of literacy. 256,286,287 Similar findings have emerged from initiatives aimed at individual service users, for example, social-prescribing. 132 This presents the risk of widening, rather than resolving, health inequalities. A universal community engagement intervention (covering both relatively advantaged and disadvantaged groups) risks increasing health inequalities. 264,266 Inequalities may also be widened when social networks benefit members of one particular group, but exclude others outside the group from sharing those resources. 264 As well as difficulties in recruiting patients and carers, it may also be difficult to retain them through the different stages of projects; for example, patients who are no longer using the service may decline further participation. 271
There is some debate regarding the extent to which service users may wish to engage in decisions about their care or about local services, with clear differences in expectations affecting willingness and capacity to engage in self-management and co-design. 261,288 A case study from the UK reports some reluctance to participate, with some patients stating that ‘it was the clinician’s role to manage their care’. 288 This is echoed in a recent review:
Not all patients have the desire or capacity to be active participants in coproducing their healthcare service. Sometimes patients are sick, and need a health professional to relieve a burden rather than enable self-care.
Batalden et al. 261
Howieson and Fenwick289 use the example of a patient’s right to choose their general practice to highlight that patient choice is generally not exercised. They also argue that the assumption that the public – with whom the NHS would be in collaboration – would be reasonable and open-minded and would have (and take) a holistic view of the health service and understand and appreciate the best way to allocate resources for health provision is very much open to debate.
Greater engagement may be experienced as burdensome by some, with the physical and mental health benefits of community engagement diluted by the stresses and strains associated with involvement for some participants. 267 Sorting helpful from available information is complex; diminishing the value of professional expertise by transferring care responsibility to patients and families could result in bad health outcomes. 261
Implementing community engagement among disadvantaged communities has highlighted complex challenges, such as poor health system infrastructure and service delivery, and poor staffing and resources. 266 Furthermore, these complex challenges often result in unmet community needs, causing community partners and study participants to feel dispirited, and compromise the potential for community engagement. 266 Clarke et al. 271 report that a lack of progress in community engagement projects can lead to frustration for both staff and patients. Programmes are likely to be considered ‘tokenistic’ in nature when suggestions are not acted upon,267 and compromise the trust and relationship-building purpose of community-engagement initiatives, resulting in poor individual health outcomes. 266
The role of social movements and third-sector organisations and groups in health care is growing. However, tensions can emerge from working across very different cultures and governance structures. The agile and dynamic nature of social movements can clash with the more structured approach of publicly funded services, and del Castillo et al. 282 recommend a considered approach with realistic expectations. Voluntary and community organisations, although able to mobilise volunteers, are limited by resource constraints. In the example of one social-prescribing pilot, it became clear that NHS-led time scales for roll-out across practices had not factored in time to cascade training and guidance around the availability of volunteers and the capacity of individual practices. 279
Where there is willingness to participate, there is potential for confusion regarding this new more participatory role for service users, as reported in a 2014 systematic review,290 which highlighted contradictory information and conflicting instructions about individuals’ needs, priorities and management strategies.
Self-management and social-prescribing programmes are based on implicit assumptions that improving health literacy and self-confidence will lead to long-term behaviour change, increasing independence and reducing service utilisation. However, as pointed out in a NIHR-funded systematic review,280 few trials and evaluations measure outcomes beyond 1 year, so the extent of ongoing support needed remains uncertain. This leads to the question of ‘whether or not the reductions in utilisation achieved are significantly greater than the service input required to maintain gains in knowledge, skills and confidence’. 280
Furthermore, Batalden et al. 261 highlighted experience from shared decision-making, demonstrating that, even after training, many patients and professionals in Scotland inconsistently apply newfound skills and orientation.
Service-user participation can help to identify unmet needs and gaps in service provision. In the short term, this may result in higher costs. 247 It is debatable as to the extent to which voluntary and community services have the capacity to offer help to people who do not meet thresholds for formal care, but who may benefit from social contact and low-level practical help. Conversely, service gaps were also thought to contribute to the inappropriate referral of service users with highly complex needs to a social-prescribing pilot: ‘some clients fall through the gaps’. 279 Service evaluations report on the impact of funding cuts and the uncertainty of future funding on the capacity of voluntary and community services, highlighting the risk of delays in agreeing contracts. 279 The impact on volunteers and service users can be significant, with longer waiting lists for support, reduced or closed services and low retention of volunteers being reported. 279 There is a risk that service users, who may be vulnerable, are left feeling ‘abandoned’291 and that other services, such as general practice, are placed under additional pressure. 279 In a competitive market, staff may be more likely to move on to new roles in the event of continued uncertainty regarding future funding. 279
There is also the potential to introduce unnecessary duplication and waste if roles and responsibilities are not explicitly clear – for example, various referral routes to social-prescribing support. 132
Mechanisms
Through the evidence base, several mechanisms have been identified for R3. We describe these in the following section as service users, staff and system factors, and make distinct the resource and reasoning aspects of mechanisms. 76
Service users
Patient mutuality and co-ownership in health-care services (context) require patients to be appropriately trained [e.g. in health literacy287,292 and self-management261 skills (resources)], improving their self-efficacy and confidence to manage their care292 (reasoning). More widely, low awareness of long-term conditions (context) could be improved by a stronger narrative (resource), informing ‘patient help-seeking behaviour and public perceptions of need’. 278 This can help individual service users, who are interested in getting more actively involved in decisions about their care, but is dependent on an understanding of the service user’s context (e.g. carer/family support)275 and a shared understanding291 (reasoning), which can help to develop confidence and personal resilience (reasoning):
Self-management was conceptualised by health care professionals as incorporating both a biomedical model of compliance and individual responsibility. Lay people understood self-management in wider terms, reflecting biomedical, psychological and social domains and different expectations of responsibility.
Sadler et al. 291
The willingness of service users to participate in social-prescribing programmes265,275 depends on an individual’s sense of confidence265,270 (reasoning), the relevance of the activities provided (reasoning),265 the individual’s literacy (context) and logistical issues, such as travel270 (resource). Facilitated support (resource) has been shown to be more effective in assisting people with wider social needs than simple signposting, and in one case study, maintaining follow-up (resource) ‘enabled participants to implement important choice-making and autonomy building processes’ (reasoning). 270 Greater confidence (reasoning) can help service users to make connections with their peers and to explore options for support (outcome). 270
Where community engagement is introduced (context), research should be conducted264,266 (resource) to build a clear understanding of the community and its resources293,294 (reasoning), which would then enable appropriate community resources to be mobilised264,266 (outcome). Coulter294 emphasises the importance of starting with a very clear sense of the local community, centred on the ability to describe target stakeholders and the value of engagement.
Through the successful mobilisation of appropriate community resources (context), the programme can be carefully designed, with community involvement and validation where possible264,266 (resource). Services can therefore be tailored to reflect community representation, not tokenism, such as through the cultural adaptation of programmes264,266,294 (resource); community resources, such as community leaders, outreach workers and lay workers,263,266,293 are used to facilitate and promote opportunities to relevant participants287 (resources). This increased awareness of authentic and credible programmes can enable people to identify with a community264,293 (reasoning), helping to remove barriers to participation and to empower citizens to become involved266,287,293 (outcomes).
The design of community engagement programmes (context) should include clearly defined roles and responsibilities,271 and training and support. 250,264,278,287,291,294 Methods of participation that address concerns and support requirements,287 facilitated or delivered by community representatives,264 can be facilitative. In turn, these resources can build the confidence of service users so that they become more aware of their contribution273 and expectations283,287 (reasoning), thus encouraging involvement263,267,287 (outcome).
To encourage service-user participation, incentives, such as financial rewards or recognition,264,273,283,287,294 support with practical issues such as time and transport287 (resource) or meetings to suit community members’ needs can help to engender a sense of trust and respect (reasoning) between patients and health professionals287,295 (resources). Methods for participation should be carefully selected so that they recognise patient abilities261,267 and give consideration to practical and logistical problems. 271,294 Recognising that service users differ in their preferences for involvement in decision-making, there should be an offer of alternative forms of participation (resource). 263,264,267,287 Carers, in particular, may need to be consulted, as there is some evidence to suggest that programmes of self-management and social-prescribing can assume a certain level of capacity among carers and can also cause confusion regarding responsibilities. 291 Delivery should be culturally relevant264,266 and goals should be realistic. 263,273 Communications should be clear and transparent (resource),264,294 using bidirectional communication when necessary,295 avoiding overloading service users,263,267 and making involvement an accessible and enjoyable experience264 (reasoning), thus encouraging commitment and retention266,283 (outcome):
. . . individuals are less likely to find community engagement a positive experience where consultation is the main method employed by professionals and no real power to effect change is ceded to community members.
Reproduced from Attree et al. 267
Staff factors
Where leaders have identified participation in decision-making and co-production of services as a priority (context), a clear case for change (resource)273,294 championed by confident leaders with the energy to innovate and motivate (reasoning)296 (resource) has been shown to facilitate cultural change (outcome):263,289
Some of the key challenges in co-production within health care are the different education, culture, philosophy and interaction models of different professional groups.
Reproduced from Philips and Morgan263
Practically, support for staff (resource) can encourage new ways of working (outcome) – for example, training using patient stories,261,263,265 time to develop and utilise skills,261,263,264,271,287,289,294 supportive tools and infrastructure,261,273,287,289 feedback33 and appropriate guidance274 – can motivate staff (reasoning) through understanding the case for new ways of working. 249,273 This also applies where volunteers are engaged in the delivery of services; evaluations demonstrate the importance of mentoring support, feedback and information-sharing (resource), to help volunteers to feel like a part of the team (reasoning). 33,275,279 A change in mindset to one that recognises service users as equal partners261,263,274,289 and diminishes the fear of losing status and control273,289 can help to develop confidence in ‘sharing power and accepting user expertise’287 (reasoning). Underpinning this is the challenge to build a sense of mutual trust266,275 (reasoning) across different cultures:
Co-production calls, instead, for a slower pace of sharing and producing knowledge and for open-ended, experimental forms of learning, critical thinking, and working together in health care and research.
Reproduced from Filipe et al. 283
Given that some local health economies may experience a high turnover of staff, there needs to be an ongoing programme of training and development to embed and sustain more participative decision-making. 278
Relevant policy and governance structures (resource) will need to support new ways of working, articulating the shared purpose, values and principles that emerge from joint working across the local health and care system. 249,261,263,271,273,286,292 On a practical level, this will help to clarify, for example, the referral criteria for social-prescribing support. 33,270 This can provide staff with clarity of purpose and expectations (reasoning), and provides assurance for system leaders through regular reviews of progress and impact. 263,274,283 This can encourage sustainable partnerships and collectively agreed, realistic outcomes (outcome).
System factors
In a MCP context, a co-production approach is intended to achieve a more participative relationship with individual service users and community groups, contributing to a system-wide impact. 250,261 Within public sector organisations, working with service users to understand their experiences (resource) has been shown to create a sense of urgency among staff to act, and served to legitimise (reasoning) the realisation of quality improvements to higher management bodies (reasoning). 297 To support greater levels of participation by service users in decisions about their own care and about services (outcome), a shift in the role of staff from ‘fixers to facilitators’ is required. 274 This shift balances power towards service users (reasoning) through front-line professionals who are trained (resource) and subsequently empowered (reasoning) to take on these new roles. 250 Management of expectations will be an important consideration in bringing together people with different motivations, cultural backgrounds and prior experience, coupled with realistic goals (resource):
. . . co-productive experiments are best seen as generative processes that are less about delivering predictable impacts and outputs and more about developing new communities, interactions, practices, and different modes of knowledge and value production.
Reproduced from Ryder268
Poortinga256 references the five capital model, which emphasises the importance of health services working with other public services and community groups to address the wider determinants of health:
. . . healthy neighbourhoods have a balanced combination of human capital (e.g. skills and education), social capital (e.g. social networks), built capital (e.g. access to amenities), natural capital (e.g. access to green space), and economic capital (e.g. income) resources.
Reproduced from Poortinga256
Social movements may be a route to encouraging open innovation to address specific community needs,282 but there is a risk that the bureaucracy inherent within the public sector can stifle smaller and more agile groups, which suggests a need for strong relationships to manage potential tensions in relation to priorities, governance and culture. 282 A useful early step may be to map community ‘asset’ or resources (resource),33,269 potentially via an umbrella third-sector organisation acting as a broker. 269,279
Although trust is often mentioned as important to building and maintaining strong relationships, there is also an argument that ‘distrust is not necessarily detrimental to community involvement and wellbeing’, helping to engender greater ‘political involvement’ or ‘critical trust’, encouraging individuals to get involved in decisions about local public services. 256
When working across multiagency sectors (context), time and space for learning,261,263,264,274,283,294 role definition,283,291 shared planning and values,261,284,294 external facilitators271,295 and administrative support264,295(resources) can be important enablers. Opportunities for face-to-face contact (resource), to build social connections, can help to develop trust (reasoning) across diverse services and groups;275 for example, across primary care and community groups, this can help to build the legitimacy of groups that may be unfamiliar to staff. Training (resource) may be needed at multiple levels of the local health-care system, including at the board level. 284 This can support the development of collaborative relationships and trust261,263,283 through a shared understanding and recognition of each other’s expertise and values. 250,261,283 External support (resource) can help to resolve tensions and conflicts,295 allowing critical inquiry and the confrontation of ideas283 (reasoning). This can help to create an environment of improved power-sharing250,266,271,274 and collective decision-making264 (outcome).
Chapter summary
The review highlights a number of gaps in the literature base, notably relating to the longer-term outcomes of self-management, social-prescribing and social action. There is limited empirical evidence, and much of the literature seems to be anecdotal or theoretical, based on limited case studies or informal evaluations, rather than robust research designs. This is indicative of the challenges of measuring and attributing outcomes to new ways of working; where studies have been able to explore outcomes, these often look at aspects such as patient or staff satisfaction.
There is some evidence to suggest that involvement in public services, for example, through volunteering, can lead to an improved sense of well-being. There are also suggestions that the involvement of volunteers and third-sector groups can help to build social cohesion, which increases the social support that people with long-term or complex conditions may access. Patient satisfaction levels seem to be positive, although there needs to be an acknowledgement that service users and carers will vary in their preferences for engagement and involvement in decision-making, whether about their own care or about services more widely. Staff satisfaction suggests a need for co-ordination, communication and engagement to build relationships. Cost-effectiveness has proved to be difficult to measure; some costs can be less visible and may not be included in an analysis. There is emerging evidence, however, that working with public health offers a ROI.
Mutually beneficial relationships to support co-production are dependent on effective community engagement, that is, actively involving service users, community groups and other members of the local community. This engagement can lead to more targeted self-management support and social-prescribing, encouraging healthier behaviours and helping to reduce social isolation. Organisational development, with a focus on interpersonal skills, can help to build confidence and motivate staff to establish the conditions for a culture of co-production and reciprocity. However, there is a risk that low representation from key groups may widen existing health inequalities.
Chapter 7 Programme theory maps
This chapter maps the evidence base pertaining to the remaining five programme theory components. These maps are intended to be indicative, rather than representing an exhaustive review of the literature base, providing a starting point for further exploration. The focus of the maps is on signposting the relevant wider literature bases, which offer valuable, transferable learning for the design, implementation and evaluation of population health-based models of care.
M1: collective responsibility improves quality and safety outcomes
As described in Chapter 3, integrated pathways feature as a focal point in MCP models, driving collective responsibility for quality and safety. Nationally, the Right Care programme is developing pathways to ‘support Local Health Economies to concentrate their improvement efforts on where there is greater opportunity to address variation and improve population health’ (contains public sector information licensed under the Open Government Licence v3.0). 298 Related closely to place-based contracting driving new outcome frameworks (R2) and more collaborative working (R3), this programme theory component relates to the alignment of processes, people and technology:
If providers share collective responsibility for outcomes through standard integrated pathways, then providers will improve the quality and safety of care.
The evidence map for this component of the programme theory is derived from five ‘sets’ of related evidence (Table 5). Three of these evidence sets relate to context and two relate to potential mechanisms:
-
care for long-term conditions and multimorbidity (context)
-
population-based approaches to primary and community care (context)
-
integrated and collaborative care (context)
-
quality improvement (mechanisms)
-
service development (mechanisms).
The three contextual evidence sets are primarily theoretical, whereas those relating to mechanisms are underpinned by varying levels of empirical and theoretical evidence.
| Focus | References |
|---|---|
| Care for long-term conditions and multimorbidity | Grant and Chika-Ezerihoa299 |
| Population-based approaches to primary and community care | Alderwick et al.,102 Collins139 and Tomlinson et al.300 |
| Integrated and collaborative care | Alderwick et al.,102 Collins,139 Tomlinson et al.,300 Threapleton et al.,301 Whittle and Hewison,302 Curry and Ham,303 McConnell et al.304 and Beenstock et al.305 |
| Quality improvement | Threapleton et al.,301 Whittle and Hewison,302 Chen et al.306 and Veenstra et al.307 |
| Service development | Grant and Chika-Ezerihoa,299 Curry and Ham,303 McConnell et al.,304 Beenstock et al.,305 Chen et al.306 and Veenstra et al.307 |
Outcomes relating to the quadruple aim
There is some evidence to suggest that integrated care pathways could contribute to improved health outcomes. A disease-management programme in Germany has established disease-specific objectives with defined treatment goals and specific criteria for referrals to secondary care. The programme has an emphasis on patient education and self-management. Patients choose a physician, who co-ordinates their treatment; the framework clearly sets out when specialists should be involved in patient care to avoid gaps in care provision. 303,308 Further afield, the shared guidelines and standard procedures of the Mayo clinic are considered to contribute to lower complications and improved clinical outcomes. 303,309 An end-to-end pathway may enable the focus on prevention common to many of the MCP logic models; one example suggests that integrated pathways may contribute to a reduced incidence of falls, following knee arthroplasty. 302 Although it is difficult to attribute population health outcomes to pathways, theoretically, integrated pathways may help to stimulate an environment that encourages communication, collaboration and peer review, thus leading to improvements in quality and safety. 303 Audit and feedback can strengthen the impact of integrated pathways, identifying what works in improving health outcomes and identifying problems that may indicate potential improvements or amendments to the pathway. 303,306
Integrated pathways, through reducing waste and duplication, could contribute to improved cost-effectiveness and lower unnecessary utilisation. The Nuka system of care, run by the Southcentral Foundation in Alaska, is credited with achieving improved quality for a lower cost, demonstrated by a decrease in unscheduled care alongside improved patient and staff satisfaction. 139 Integrated pathways have been used to enable a shift of care from hospital to community settings, demonstrated by the Veterans Home Administration, which measured fewer hospital bed-days and overall admissions. 303,310,311 Integrated pathways may also lay the foundations to introduce technology to support the delivery of care. Shared health records have a role in driving patient safety and adherence to guidance, supporting smoother discharge and transition between teams or services. 301 Telecare and telehealth can support more home-based care through remote monitoring and, in some contexts, has been found to contribute to reduced bed-days and increased patient satisfaction. 303,312 Opportunities exist to embed technology within pathways; for example, patient deterioration can trigger a responsive multidisciplinary package of care to avoid further decline, based on an agreed care plan facilitated by record-sharing. 303 Some countries have initiated condition-specific approaches, such as disease-management programmes in Germany, Sweden’s chains of care and Scotland’s managed clinical networks, finding the most impact on patients with long-term conditions. All of these approaches involve elements of integrated care, recognising the importance of co-ordinating care and working across systems, and creating pathways across traditional ‘single-disease’ pathways. 303
Unintended consequences
Integrated pathways are dependent on behaviour change and multidisciplinary working. However, behaviour can be unpredictable, with the risk that practice may not change in the way intended. This could lead to inconsistency, fragmentation and ‘disharmony’, ultimately affecting the safety and quality of care. 303 Integrated pathways intricately link the success or failure of providers, supporting a population health-based approach and shared accountability102 for outcomes, as illustrated by ACOs such as Kaiser Permanente. 303 There is, however, a risk that misaligned responsibilities between different professions, departments and organisations can prevent the effective integration of pathways,303,313 particularly beyond defined boundaries. 303,314 The intention to collaborate and consolidate brings potential benefits of economies of scale, but could backfire if the collective organisations are perceived as a monopoly, hindering competition; nonetheless, Curry and Ham303 suggest that competition and integration need not be mutually exclusive:
. . . there is no inherent contradiction between integration and competition provided that patients are able to exercise choice either within or between integrated care organisations.
Curry and Ham303
It could be argued that integrated pathways encourage a ‘cookie-cutter’ approach to patient care, failing to consider the individuality of patients – their needs, preferences and case mix. 299,302 The integrated pathway may also assume a level playing field in terms of infrastructure, which could, in reality, be strikingly different across settings. 299 This highlights a need for strategies to achieve closer co-ordination of care. 303
Mechanisms
A virtuous cycle, akin to the theory of the MCP model, could operate where clinicians and managers work more effectively across boundaries to attain financial and quality goals, which then improve cost-effectiveness, which can support investment in quality initiatives. 302 In such an environment, integrated care pathways can act as a focal point for clarifying and articulating the roles, responsibilities, processes and systems to underpin co-ordinated care, shared decision-making and care-planning. 302,303 This co-ordination can provide the stimulus for information-sharing, supporting patient-centred care. Where the design of integrated care pathways is based on engagement with patients and practitioners, patients may feel empowered and supported to maintain independence for longer. 102,301,303 Such engagement can also be instrumental in enabling access to a more holistic approach to care. 301 From a patient perspective, an integrated pathway can translate into a single point of entry, a single assessment and a personalised care plan, delivered by a MDT (see Chapter 7, M2: multidisciplinary teams provide continuity for patients with long-term conditions/complex needs), which can help to reduce the burden on carers and address unmet needs. 301,303 This co-ordinated standardisation can, in theory, address unwarranted variation, drive up quality and improve equity of access. 302 Patient satisfaction can be strengthened by the routine collection of patient-reported outcomes and regular patient feedback. 303,306
The process of developing integrated care pathways to incorporate shared values and goals can support the integration of teams and influence organisational culture and staff motivation, making it more likely that new processes will be embedded in routine practice. 301,304 Closer working and standard pathways can help to identify those patients with more complex needs who need specialist secondary care, and those who are better managed in the community. 303 Pathways informed by formal needs analysis – for example, Joint Strategic Needs Assessments – and community engagement can help to align the investment of resources within local communities,139,300,305 factoring in the wider determinants of health and significant risk factors specific to local communities. 102 This, in turn, can help to promote holistic and person-centred care and a sense of ‘shared ownership’, shared goals and incentives to address prevention. 139,303
Early engagement of staff will help to ensure that pathways are comprehensive and realistic,299 and can ‘offer an opportunity for professionals to renew their implicit rules for operation and shape collective meanings and objectives’. 302 Affording more opportunities for communication across teams302 can contribute to ‘an environment in which excellence in clinical care will flourish’. 307 Standardisation facilitates monitoring and evaluation;302 supported by transparent reporting, this can be a catalyst for quality improvement when larger teams are better able to exploit performance data for quality improvement, and to address wider issues, such as prevention and health promotion. 303 Benchmarking, using national audits and other tools, can help to demonstrate the impacts of changes to pathways and to highlight issues relating to demand and capacity. A culture of personal professional responsibility and innovation among health-care professionals can be encouraged through more autonomy. 301,304,307 Multidisciplinary training and development, with a focus on communication and trust, can encourage more collaborative working. 299,301,304,307 When individuals understand their contribution and that of others, pathways are more likely to be ‘owned’ by staff and successfully embedded in practice. 139,302 Problems can be identified and resolved collectively,301 thus developing a learning culture and a ‘continuous quality improvement “mind-set” ’. 307 Where a history of co-operation and trust pre-exists, this may be a smoother process; conversely, where relations are more adversarial, behavioural change is likely to require significantly more investment. 139,303 Cultural barriers, such as competitive funding, poor relationships between senior leaders and risk aversion can stifle innovation and motivation. 301 Local barriers and facilitators need to be considered, for example, around data-sharing. 102
Although engagement is to be encouraged, there is evidence to suggest that the design and testing of integrated care pathways may be better managed by small focused teams, which are sufficiently agile to make the decisions needed to progress, but also sufficiently connected to ensure staff commitment and confidence. 301 Pathways alone are unlikely to deliver significant transformation – delivery may be contingent on new or expanded roles within primary and community settings. 139 In areas where there are long-standing recruitment issues, integrated pathways could be hindered by key staff shortages that, without workforce planning and development, could serve to undermine morale. 302 Multidisciplinary working will need to be supported by organisational development, to tackle cultural aspects, contractual incentives to influence behaviours and operational logistics, such as systems to enable shared data,102,301 as demonstrated in Geisenger Health. 303 Information systems, in particular, may help to facilitate timely and efficient information flow, supporting knowledge-sharing, the spread of good practice, consistent standards and communication between generalists and specialists. 299,303 Shared governance can promote care standards, patient safety and professional competencies;301 conversely, instability can severely constrain the implementation of integrated pathways. 102,299,303
M2: multidisciplinary teams provide continuity for patients with long-term conditions/complex needs
Multidisciplinary working is core to the MCP model of care, underpinning care-planning and more proactive management of patients with long-term conditions and more complex needs, as described in Chapter 3. Specifically, this programme theory component relates to the impact on the continuity of care of MDTs:
If commissioners and providers train and fully engage staff in service transformation, then staff will drive the cultural change that underpins new ways of working.
Continuity denotes consistency and can be described from a patient perspective, entailing a continuous relationship, or from a provider perspective, entailing co-ordinated or seamless care. 315 It is a longitudinal concept, judged over time. 315 Informational continuity is an important element, dependent on shared records and information to ensure a full history. 316 Continuity is often described on a continuum with access, with suggestions that patients with long-term conditions prefer continuity of care, whereas patients with acute episodic needs prefer convenient access;316 it is unlikely to be so simplistic in practice, and will be influenced by contextual factors. Continuity has been associated with reduced unnecessary utilisation and improved prevention,316,317 so could be an important ingredient to achieving the quadruple aim through the use of MDTs. 318
The evidence map for this component of the programme theory is derived from five ‘sets’ of related evidence (Table 6). Three of these evidence sets relate to context and two to potential mechanisms:
-
management of long-term conditions (context)
-
population-based approaches to primary and community care (context)
-
integrated and collaborative care (context)
-
quality improvement in primary care (mechanisms)
-
team and organisational development (mechanisms).
The three contextual evidence sets are primarily theoretical, whereas those relating to mechanisms are underpinned by varying levels of empirical evidence.
| Focus | References |
|---|---|
| Management of long-term conditions | Kadam et al.,319 Kasteridis et al.,320 Powers et al.,321 Ruikes et al.,322 Thistlethwaite,323 Archer et al.,324 Bearne et al.,325 Chung et al.,326 Coventry et al.,327 Fortuna et al.,328 Glogowska et al.,329 Green et al.,330 Bonney et al.,331 Smith et al.,332 Tricco et al.,333 Hernández et al.,334 Huang et al.,335 Maneze et al.336 and Raine et al.337 |
| Population-based approaches to primary and community care | Kasteridis et al.,320 Powers et al.,321 Ruikes et al.,322 Thistlethwaite,323 Huang et al.,335 Kruis et al.,338 Loewenson and Simpson,339 Ouwens et al.,340 Stranges et al.,341 Kruis et al.,342 Nandram and Koster343 and Martínez-González et al.344 |
| Integrated and collaborative care | Goodwin et al.,239, Archer et al.,324 Bearne et al.,325 Chung et al.,326 Coventry et al.,327 Fortuna et al.,328 Glogowska et al.,329 Green et al.,330 Hernández et al.,334 Huang et al.,335 Maneze et al.,336 Raine et al.,337 Kruis et al.,338 Loewenson and Simpson,339 Ouwens et al.,340 Stranges et al.,341 Martínez-González et al.,344 Mulvale et al.,345 Morgan et al.,346 Parker and Fuller,347 van Dongen et al.348 and Gray et al.349 |
| Quality improvement in primary care | Goodwin et al.,239 Bonney et al.,331 Smith et al.,332 Tricco et al.,333 Mulvale et al.,345 van Dongen et al.,348 Powell et al.350 and Schepman et al.351 |
| Team and organisational development | Kruis et al.,342 Nandram and Koster,343 Morgan et al.,346 Parker and Fuller,347 Gray et al.,349 Powell et al.350 and Schepman et al.351 |
Outcomes relating to the quadruple aim
There is evidence to suggest that an integrated approach to care, via MDTs, is associated with improved outcomes for patients with long-term conditions or complex needs;340 however, the majority of studies focus on single conditions – for example, reduced glycated haemoglobin values/improved glycaemic control in diabetes,335,344 blood pressure control,328 treatment compliance,328,344 reduced depression and anxiety324,327,334,352 – and it is unclear if benefits are sustained over time. As with any package of interventions, attribution is a challenge and, typically, MDTs are implemented alongside programmes of self-management, case management and enhanced pathways. 340 It has been suggested that the ‘supportive network of professionals and peers’352 contributes to improved health and well-being. Additional evidence suggests that MDTs can facilitate disease management and encourage self-management,334 reflecting the common features of MDT working, including case management,351 care-planning,351 the promotion of self-management and medication adherence. 325,334,338,353
Conversely, there seems to be little or no impact of MDT-working on patient-reported outcomes, such as activities of daily living,338,353 functioning,322 quality of life322,325 and disability. 325 There may be limited benefits for older people with multimorbidity or frailty. 351 The extensivist model (based on the Care More model in the USA)321 is designed to provide more intensive support for older patients with very complex needs, and is being implemented as part of the MCP model in Fylde Coast. It can be challenging to measure the effectiveness of MDTs, notably the appropriate follow-up period within which to measure impact and the baseline (with a ‘ceiling effect’ of limited impact, whereby primary care was already well organised). 322
Patients with multiple conditions may find it challenging to manage the complexity of their conditions and to prioritise needs, particularly within the context of deprivation or social isolation. 336 It can be difficult to navigate the health and care system, and care packages developed by MDTs could be a critical element in improving support to patients and carers, as demonstrated in Torbay. 323 Patient involvement may be facilitated by certain roles within MDTs; one qualitative study354 reported perceived improvements in care co-ordination and problem-solving, following the inclusion of a nurse practitioner within the MDT. Trust was also greater, possibly resulting from more time spent with patients and more opportunities for communication. The value of a MDT is in the opportunity for interdisciplinary diversity, with multidisciplinary participation emphasised as a key benefit of MDT meetings,337 supporting a range of social functions such as peer support, team-building and bonding,337 which can, in turn, have an impact on health outcomes. 350
Several studies report reductions in service utilisation associated with integrated care via MDTs (hospital admission,326,334,355 A&E attendance,339 readmission341 and length of stay)326 with a potentially higher impact in those ‘with at least moderate disease’. 326 Few cost-effectiveness studies explore the effect of MDTs. Of those studies that do report costs, few have reported savings. 344 One cost-effectiveness study estimated330 a mean cost per QALY of £14,248, arguing that collaborative care is expected to be less costly and more effective.
Unintended consequences
Integrated governance frameworks have been used to clarify roles, responsibilities and reporting arrangements,345 and the principle of MDTs seems to be valued by professionals. 338 However, dissatisfaction and frustration can arise from perceptions of inequality and underinvestment in relationships,337,356 potentially leading to issues regarding team processes and structure, available resources and sharing of information. 315,337 This suggests that the reality of multidisciplinary working may diverge from the vision of increased co-ordination. Decision-making may even be impaired by the multidisciplinary approach, where the enabling cultural change (see Chapter 7, M3: engaged and trained staff expedite cultural change) has not occurred.
Attendance and participation at MDT meetings can be problematic as a result of workload pressures. An observational study,349 found that the number of participants ranged from 7 to 27, with an average of 14 participants; however, the mean number of people contributing was only three. There seem to be clear cultural differences across teams, with some dominated by relatively few people, and others demonstrating higher levels of participation. Medical dominance is perceived in some contexts to be a barrier to participants having an equal voice. 337,349 There may also be tensions from the underlying perspectives of different disciplines, which influence how practitioners perceive their role and relationship with patients. 337 Cancer Research UK found a relatively low level of verbal contribution from nurses in meetings,349 which could impact patient care if the nurse has greater contact with patients and greater familiarity with patient preferences. The report suggests that 10–15% of MDT recommendations are not implemented, partly because such preferences were not taken into account. 349 Contrary to this, Raine et al. 337 did not find a link between discussions on preferences and the decisions made. Preferences may change over time, with differing opinions on how this knowledge should be incorporated into care-planning. Interestingly, Raine et al. 337 found that those teams that were more medically dominated showed a stronger record of implementing decisions made. Implementation was found337 to be influenced by socioeconomic factors, which may have implications for the role of MDTs in building community resilience (see Chapter 6), and this is noted as an area that needs further investigation.
Significant variation in how MDTs operate reflects the different contexts within which teams are working. However, this could reflect a lack of clarity on best practice and a need for guidance. 337 Delays in decision-making have been reported, as a result of a lack of availability of key staff and/or information,337,349 with staff shortages being cited as having a strong effect on attendance. Notwithstanding attendance and participation barriers, the caseload of MDTs can have an impact on the quality of discussions. The Cancer Research UK study349 found that meetings lasted up to 5 hours; the mean length of patient discussions was 3.2 minutes, and over half of the discussions were < 2 minutes long.
Mechanisms
The professional composition of MDTs is variable and typically comprises three to eight members, with GPs and nurses most frequently represented. The inclusion of voluntary sector organisations (VSOs) in MDTs has recently increased, often to support self-management and more holistic care. 357 Involving other public services, such as housing, enables a care plan that addresses the wider determinants of health, and supports patient-focused goals to tackle social isolation. 358 Specialist nurse roles, with arguably more capacity than GPs, can help to support patient education329 by spending time with patients to personalise information. This could be of particular benefit to patients who may struggle with more generic approaches, for such reasons as language, learning difficulties and cognitive decline. The ‘drip feed’ of information can support a continuous relationship. 329 For patients with multimorbidities, decisions on the trade-offs between the benefits and harms of treatments can be supported by specialist roles. 329 Conversely, it has been argued that patients with very complex needs might need more support from GPs. 331
In bringing together multiple services, the role of care co-ordinator can be critical in tackling fragmentation,359 supporting relational continuity between the services and the patient; informational continuity between services and with the patient; ensuring accountability to the patient; and acting as the patient’s advocate to ensure patient-centred care. Nurses without advanced qualifications or advanced training have reported feeling ill equipped to take on the care co-ordination role, highlighting the importance of support (information systems, monitoring processes, guidelines), as well as training and development. 347
Space and time for informal communication and shared communication methods are identified as enablers,346 underpinning access to, and the exchange of, essential information and ideas. MDT working can be facilitated by a shared understanding and vision of integrated care,340,346 translated into clear, agreed objectives. 360 Operationally, explicit processes338,345,346 can help to clarify expectations; for example, mandating attendance in job descriptions, regular feedback on team performance, provision of administrative support and sharing of information with other practitioners involved in pathways. An absence of such clarity can have an impact on the implementation of decisions. 337 Organisational development can support the development of shared goals, values and outcome measures. 239
To effectively manage multimorbidity, interventions may offer greater benefit if targeted at specific combinations of common conditions or specific problems facing comorbid patients,332 highlighting the role of dedicated case managers. 327,333 Risk stratification and predictive modelling are often used to support case-finding,361 and several recent studies present alternative methods to predict future utilisation. 319,320 Sharing and access to patient records is critical in MDTs working across organisational boundaries to support clinical decisions and more holistic support. 323,343,345 The use of technology is variable,337 challenging information-sharing within current systems. The experience of the Buurtzorg model suggests that technology can underpin timely communication, operational transparency, knowledge-sharing and quality improvement, through team access to audit and performance data. 343,345
System leadership,346,362 with its attributes of building a common vision and engaging with colleagues and partners to build commitment, may act as a trigger to develop the collaborative culture that is key to MDTs. Maintaining a shared vision that is clearly communicated, alongside an explicit commitment to quality improvement through benchmarking and peer review, are considered to be essential to creating the environment for integrated working. 337
The vanguards seem to recognise that integrated working is unlikely to emerge simply by forming teams. Team development is needed at all levels of the system – not just at the executive level – and investment in organisational development is needed to underpin structural and cultural change. 360,363 Without explicit development, teams can lapse into ‘domain thinking’. 348 Specific training and development can help to define a shared language and strengthen relationships. 348 Development may involve coaching, leadership training, 360-degree feedback, personal development and action-learning sets. 364
Although not a multidisciplinary model, the underlying philosophy of the Buurtzorg model,55 with its emphasis on autonomy and empowerment, may offer valuable learning. Care is delivered by self-organising teams, typically comprising 8 to 12 nurses or health-care assistants. Teams are given the freedom to develop their own models for joint working with other professions. Value-based recruitment has created a virtuous cycle, in which the high levels of patient and staff satisfaction have attracted highly motivated individuals who perpetuate the cycle. The Buurtzorg mission is based on a shared sense of purpose, which ‘appeals to professional pride’, aimed at stimulating a culture of innovation and improvement. Teams are embedded within communities, developing detailed knowledge of their ‘clients’, their families and community resources; this informs problem-solving, and, in turn, helps to build the resilience of patients, families and communities. 343
The mix of professional backgrounds in MDTs can enable ‘participants to transcend their own professional roles and routines, leading to learning and a more collaborative environment’. 345 Support for reflection, innovation, open communication and supportive colleagues can create an environment in which participants feel part of the team, supporting a belief in interprofessional care. 345 On a practical level, a nominated lead to co-ordinate and chair meetings, supported by administrative resource, can help to nurture the team as it develops,345,348 with appropriate personal development. This need for development is emphasised by West et al. ,356 who note that leadership skills are unlikely to emerge from clinical experience alone and will need nurturing through training and support.
M3: engaged and trained staff expedite cultural change
Closely related to the emphasis on multidisciplinary working is the aspiration for a systematic approach to engagement and development of the workforce. This is referenced earlier in Chapters 4–6, demonstrating engagement and development as important enablers to new care models:
If commissioners and providers train and fully engage staff in service transformation, then staff will drive the cultural change that underpins new ways of working.
The evidence map for this programme theory component is derived from five ‘sets’ of related evidence (Table 7). Two of these evidence sets relate to context and three to potential mechanisms:
-
population-based approaches to primary and community care (context)
-
integrated and collaborative care (context)
-
quality improvement in primary and community care (mechanisms)
-
team and organisational development (mechanisms)
-
leadership development (mechanisms).
The two contextual evidence sets are primarily theoretical, whereas those relating to mechanisms are underpinned by varying levels of empirical evidence.
| Focus | References |
|---|---|
| Population-based approaches to primary and community care (context) | Roland et al.,365 Akhnif et al.366 and Perreira et al.367 |
| Integrated and collaborative care (context) | Ghate et al.362 Roland et al.,365 Donahue et al.,368 Fillingham and Weir,91 Smith et al.,369 Timmins,370 Frich et al.,371 Hardacre et al.,372 Rosenman et al.,373 West et al.374 and Willis et al.375 |
| Quality improvement in primary and community care (mechanisms) | Powell et al.,350 West et al.,364 Roland et al.,365 Apekey et al.376 and Lega et al.377 |
| Team and organisational development (mechanisms) | van Dongen et al.,348 Powell et al.,350 Roland et al.,365 Akhnif et al.,366 Perreira et al.,367 Lega et al.,377 McMullen et al.378 and Storey et al.379 |
| Leadership development (mechanisms) | van Dongen et al.,348 Ghate et al.,362 West et al.,364 Roland et al.,365 Donahue et al.,368 Fillingham and Weir,91 Smith et al.,369 Timmins,370 Frich et al.,371 Hardacre et al.,372 Rosenman et al.,373 West et al.,374 Willis et al.,375 Apekey et al.,376 McMullen et al.378 and Storey et al.379 |
Outcomes relating to the quadruple aim
Findings from the UK National Staff Survey suggest that staff engagement is the best overall predictor of NHS organisations’ outcomes (care quality and financial performance; patient satisfaction; staff absenteeism; and health and well-being). 374 The impact of staff experience on the quality and safety of care has been explored, following the Francis inquiry380 and the Berwick report,381 with suggestions that strong team-working and clear aims among staff can contribute to patient outcomes. 382,383 Engagement has also been linked with organisational productivity, quality of patient care, lower mortality rates and better financial performance. 383 In one study, practices demonstrating higher leadership scores were more likely to implement clinical improvements. 368
Leadership development, through training and increasing workforce capabilities, is seen as a particularly critical element of workforce development. Staff on leadership programmes, such as the Leadership Challenge programme, have reported improved organisational impact, including raised awareness of costs and cost-savings, as well as improved patient care. 364 The experience of staff is often linked to patient satisfaction. 350,360,374,384,385 Staff views of leaders are strongly related to patients’ perceptions of the quality of care. Where leadership enables effective team-working, health-care delivery is more effective, and organisations exhibit higher levels of innovation and patient satisfaction. 374 Team working, in particular, has been found to be a critical ingredient in high-quality care, particularly in relation to care for long-term conditions. 365
Higher levels of support for staff from managers has been associated with higher numbers of patients reporting better care. 350,374 Greater engagement has also been linked to safer patient outcomes and significant associations with patient satisfaction, patient mortality and infection rates. 385 When staff experience is positive, for example when they feel that they have ‘meaningful roles’, individual staff outcomes (e.g. job satisfaction) and organisational outcomes (e.g. absenteeism and staff turnover) have tended to improve. 350 Conversely, higher turnover may exist where working environments are perceived as negative, because of bullying, harassment and aggression. 350 A learning organisational culture, exemplified in many high-performing services, has been linked with organisational commitment, job satisfaction, innovation and performance. 366 Linking with the theory components M2 and M4, learning organisations typically demonstrate an effective use of data to reflect and learn from performance at the individual, team and organisation levels. 371
Unintended consequences
The criticisms of leadership development programmes, referenced earlier, can result in a process-driven and task-focused approach to change, which is incongruous with the system leadership style advocated for complex change. 362,373 There is a risk that organisational development cannot keep pace with the skills development needed to design, deliver and evaluate service transformation. On a broader scale, the ability of formal education to keep pace has been questioned. 386 For example, problem-based learning to develop emotional intelligence, strategic planning and organisational awareness will take time to establish.
An inevitable tension exists between the competing priorities of continuing to run existing services, while planning and commissioning new services. Focusing efforts on the development of selected cohorts could limit opportunities for ‘cultivating greater levels of understanding and communication networks across professional groups’,371 and runs the risk of developing subcultures of unnecessary variation. 350 Staff engagement is recognised as a critical enabler to service transformation,146 but in an environment of ambiguity, volatility, complexity and uncertainty,362 it can be challenging to maintain efforts in a meaningful way. 375
Mechanisms
Organisational development could usefully focus on empowering teams to explore opportunities to improve and innovate. Positive staff experience has been associated with the ability to contribute towards service and quality improvement at work and strong communication. 350 Clarity on the opportunities for involvement and engagement in change has been identified as ‘an important contextual element’. 375 Multidisciplinary learning, potentially working via networks, can help to cement the vision of integrated working365,378 and develop the adaptive skills needed to implement and evaluate service transformation. Leadership and quality improvement skills in primary care have been identified as a priority; team dynamics may also be influenced by value-based recruitment. 365
Leadership development often focuses on processes, targeting more senior or medical roles, thereby missing the opportunity to develop skills more widely. 371 Various groups within health care, notably primary care staff, have not engaged as much with leadership development, possibly because of capacity issues. 365 This points to an opportunity to engage more of the workforce in leadership development. A ‘learning organisation’ culture can be encouraged through processes and systems to support the sharing of knowledge, data and feedback. 364 With leadership support, including time for reflection, teams can be trained and empowered to audit and benchmark their performance, analyse problems and share knowledge. 364–366 For clinicians, autonomy may be a particularly important factor, enabling more collaborative and innovative behaviours. 379,387 Evidence suggests that learning and development should be seen as an ongoing commitment; incremental change to encourage continuous learning and improvement364,375 has been shown to sustain cultural change.
High levels of motivation are associated with higher levels of productivity, and tend to be reflected in positive relationships with patients/service users. 367 Motivation is influenced by levels of engagement and the working environment; continuous high pressure and evidence of discrimination are associated with lower levels of motivation and patient satisfaction. 350,382 A positive environment may be encouraged through clear goals382 and a systematic approach to learning and development. 366 The attributes of senior leaders are an important influence here, with a key role to play in inspiring collaborative working through fair-mindedness, the empowerment of staff, vision and organisational awareness:379,386 ‘capacity building and effective leadership development implies social systems to help build commitments among members of a community’. 386
Integrated care depends on a system perspective, and much has been written about system or collective leadership,362,369,370,374 where there is a ‘notional dispersal and sharing of leadership’. 379 Distributed leadership models, which allocate time and resources to staff engagement, can ‘create a shared sense of energy’,388,389 activating ‘a learner’s sense of psychological safety’. Involving people in projects can help to build the credibility of the change programme, demonstrating the feasibility of change and encouraging uptake, spread and sustainability. 366,375
Interpersonal skills are a critical element in creating ‘the foundation for making good ideas into tangible improvements’;372 this is especially the case with complex change, for which senior clinicians will need to influence others to contribute expertise and ideas. A longer-term view is needed to build the relationships that are needed to support complex change, and this will also help to develop insight to spot opportunities in an environment of ambiguity and uncertainty. 372 A key priority is to develop primary care staff, at all levels, to support quality improvement and innovation,365,376,377 with a clear role for mid-level managers in creating and sustaining change. 368,378
The pace and scale of change involved in new models has the potential to demotivate staff. Although evidence suggests that employing a range of staff can extend the current skill mix and improve working life, an accompanying risk of stress and anxiety highlights the importance of mutual support, which can be encouraged by team development. 365,367 It is important to staff that they feel that their roles make a difference to patient care, which increases their trust in their employer; a sense of shared values and a feeling of belonging can build mutual respect, which is particularly important in potentially stressful contexts. From these perceptions of trust and respect, motivation and satisfaction can increase, demonstrated by lower levels of staff turnover. Similarly, when staff feel like they are under less pressure, training and appraisals seem to increase in frequency. Personal experience is strongly affected by instances of negative behaviours – bullying, harassment, discrimination and aggression – particularly, when it is perceived that it is inadequately addressed, leading to low morale, and potentially increased absence, which affects patient satisfaction. 350,367
M4: system learning embeds and sustains transformational change
System learning is a thread that runs through several of the identified programme theory components, demonstrating its critical role in transformation. Evaluation and feedback loops are presented as underpinning new ways of working within enhanced primary care and MDTs, and informing strategic commissioning and place-based accountability:
If MCPs learn and adapt quickly using evaluation/monitoring loops and knowledge sharing, then MCPs will sustain transformational change.
System learning takes place at multiple levels, notably within MCPs, across the MCP vanguard sites, and, ultimately, through the lessons learnt, as they are shared within the overall health system. As ‘system-learning’ is a nebulous concept, Figure 19 is included to describe it, within the context of a logic model. The evidence map for this programme theory component is derived from six ‘sets’ of related evidence (Table 8). Three evidence sets relate to context and three to potential mechanisms:
-
large-scale transformational change (context)
-
population-based approaches to primary care (context)
-
complex adaptive systems (context)
-
learning theory (mechanisms)
-
quality improvement (mechanisms)
-
audit and feedback (mechanisms).
The three contextual evidence sets are primarily theoretical, whereas those relating to mechanisms are underpinned by empirical evidence.
FIGURE 19.
Logic model for programme theory component M4: system learning embeds and sustains large-scale transformational change (context).
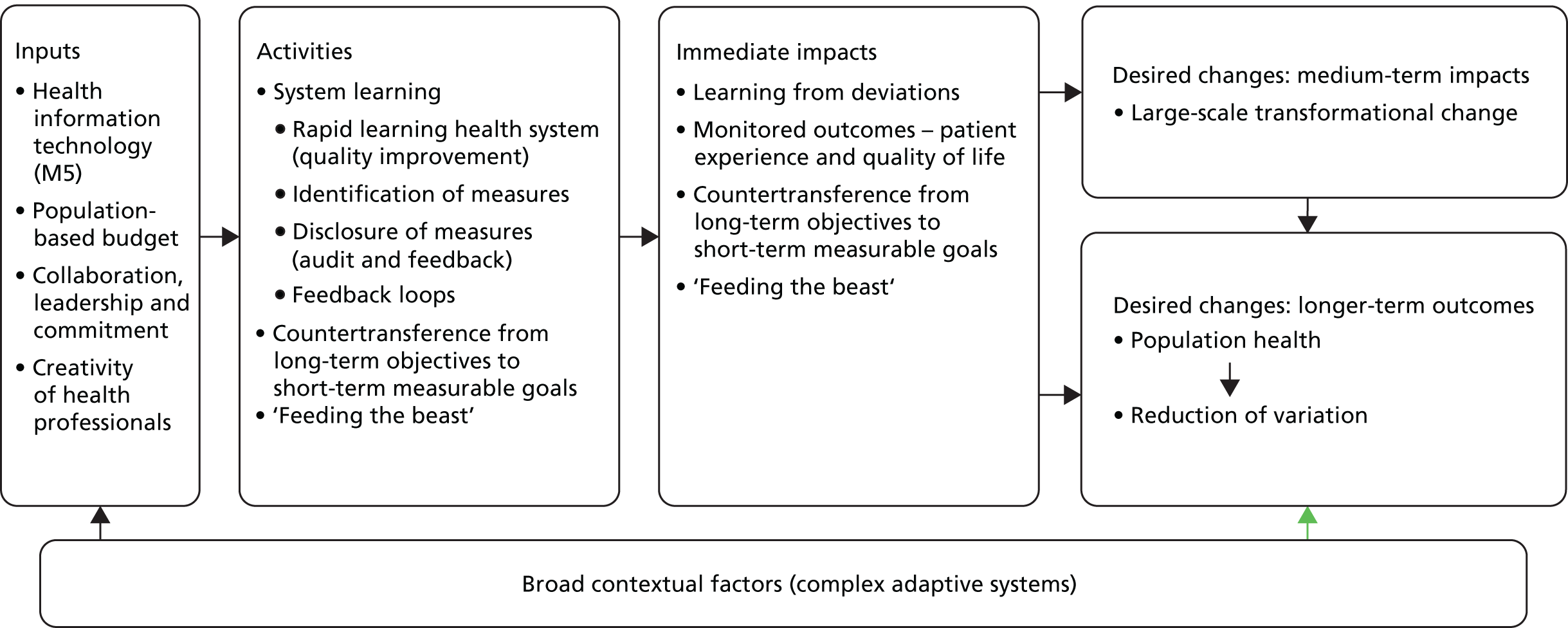
| Focus | References |
|---|---|
| Large-scale transformational change | Best et al.,88 Rosen et al.,190 Pettigrew et al.,390 Willis et al.391 and Swanson et al.392 |
| Population-based approaches to primary care | Rosen et al.,190 Sturmberg and Lanham,318 Pettigrew et al.390 and Stroebel et al.393 |
| Complex adaptive systems | Best et al.88 Sturmberg and Lanham,318 Willis et al.,391 Swanson et al.,392 Stroebel et al.,393 Hovlid et al.,394 and Fraser and Greenhalgh395 |
| Learning theory | Hovlid et al.,394 and Fraser and Greenhalgh395 |
| Quality improvement | Stroebel et al.393 and Taylor et al.396 |
| Audit and feedback |
Outcomes relating to the quadruple aim
In contrast to other programme theory components, the achievement of transformational change does not map directly to the quadruple aim. Instead, it is best seen as an intermediate outcome by which the medium- to long-term outcomes articulated by the quadruple aim might be achieved. An alternative view might locate transformational change as a subsequent context, within which the achievement of outcomes might be demonstrated through the monitoring of outcomes and the creation of feedback mechanisms.
Population health
A key underpinning theory to US ACOs is that the allocation of a population-based budget set against the delivery of agreed outcomes will provide the incentive for providers to invest in activities to encourage better health, thus reducing utilisation. 397 In their review of large-scale approaches to primary care, Pettigrew et al. 390 examined the claim that population health management enables improvements in the quality of care and reduces unwarranted variation. They presented four published observational before-and-after studies in support of this claim, concluding that the results appear promising, demonstrating a step-wise improvement in most, but not all, areas. 390 A qualitative study398 examined by the same authors390 evaluated quality and safety processes, and provided staff views on their job satisfaction and staff views on patient experience. Study results were equivocal, with evidence to suggest that cross-coverage and greater skill mix may inadvertently contribute to fragmentation of care and a loss of continuity of care. Pettigrew et al. 390 observed that, collectively, these studies support the theory that large-scale general practice collaborations may provide a better environment for standardisation of care, greater community resilience, investment in technology and improved access to care.
Other large-scale population-health providers exist across the globe (see Ewbank et al. 399 and Figure 16). Ribera Salud, a private service provider in Valencia, encapsulates the attitude of a population-health approach, focused on improving health outcomes for the whole population, while managing demand and achieving value for money. 399 This incentivises Ribera Salud to intervene at the most effective moment.
Cost-effectiveness
A supplemental theory underpinning US ACOs is that receipt of a population-based budget incentivises providers to shift care from higher-cost hospital sites to community-based settings. 397 Ribera Salud in Valencia was contracted to provide secondary care, extending the contract to primary care for financial reasons. 400 Overall, Ribera Salud has delivered care improvements at a 26% lower cost than providers within the wider Valencia region. 400
Pettigrew et al. 390 highlighted a lack of evidence to identify the characteristics (e.g. size, governance) of large-scale general practice that are likely to contribute to sustainability. Arguments for large-scale primary care organisations tend to rest on improved financial sustainability. Having reviewed the literature, Pettigrew et al. 390 concluded that further research is needed to evaluate the effects of general practice operating on a large-scale. In particular, such effects should be evaluated over the long term in relation to effects on the workforce, patient experience, clinical outcomes and costs.
Patient experience
A 15-month mixed-methods study showed that three-quarters of practices were now involved in bigger partnerships or federations,190 but this had a minimal impact on performance against a range of quality indicators, and patient satisfaction had fallen. 401 Rosen et al. 190 recommends a phased introduction of alternative contract models for large-scale general practice organisations and integration with community providers, citing a lack of evidence that large-scale general practice leads to improvements in the quality and value of care.
Staff/provider experience
Achieving population-based care within a NHS context requires practices to organise into larger-scale practices. The Primary Care Workforce Commission acknowledges that larger-scale general practice collaborations could enable the delivery of a wider range of services, offer better opportunities for staff development and training and allow more effective relationships with commissioners, specialists, hospitals and social services. 402 Mechanisms for achieving such improvements relate to ‘investing in technology, strengthening clinical governance, standardising procedures, performance monitoring and benchmarking, peer review and feedback, spreading best practice, and having a population-based approach to services’. 390
Unintended consequences
A counterargument to measurement activities is their counterproductive or unintended effects: ‘what gets measured influences behaviour’. 88,403 Transformational processes are less easily measured than transactional activities, possibly contributing to a countertransference from the longer-term objectives to short-term measurable goals. 88 Those working in health care split their time between the ‘two jobs’ of health care: ‘to do their work and to improve it’. 404 Many front-line staff face competing priorities, with associated undue effort in ‘feeding the beast’ through metrics and accounting for performance. 405 Metrics and learning, the third of five key components of accountable care (population; outcomes; metrics and learning; payments and incentives; and co-ordinated delivery), require both the means (i.e. metrics and processes) by which to monitor outcomes and the feedback loops required to learn from unintended outcomes. 406 All components are related in a closed-system feedback loop. 407 This principle has been fundamental to developments within the vanguard sites.
Leaders need time to realise the benefits from new models of care, not being accountable simply for short-term performance. Alderwick and Ham408 comment that the time needed to implement large-scale change in the NHS and to demonstrate its impact is often dramatically underestimated. 409 At the same time, expectations from new care models have been overestimated, requiring a more realistic appraisal from policy-makers and health service leaders. Feedback loops need to blend quantitative and qualitative data in order to ‘make sense of the transformation effort’. 88
Vize410 highlights a further paradox, namely that, at a time when increasing time, money and effort are being invested in integrated care, the system is experiencing pressures in funding research that explores the impact of integrated care on ‘costs, outcomes, and patients’ experiences’. Even when such evaluation activities are forthcoming, their results are not always used to transform practice.
A rapid realist review88 identified five ‘simple rules’ of large-scale transformational change. One rule involves establishing feedback loops: ‘Almost without exception, successful large-scale transformational efforts were recognized and sustained through the careful identification of measures and judicious disclosure of those measures to those both inside and outside the organization’. 88
Do feedback loops work under all circumstances and contexts? Best et al. 88 attributes success within transformational change to two factors: (1) leadership commitment to reporting performance throughout and outside the organisation, in order to effect transformation (a necessary accompaniment of Vanguard status);411 and (2) the quality of the supporting information infrastructure (see programme theory in Chapter 7, M5: proactive population health is dependent on shared and linked data) in order to effect the aggregation of data for audit and performance management. 412,413 The literature offers vigorous debate as to if and how NHS performance management systems are comparable to those of, for example, Kaiser Permanente. 414
Large-scale longitudinal case studies conducted across 12 health-care systems identified five interactive elements considered to be critical to successful transformational change. The elements include an impetus to transform, leadership commitment to quality and improvement initiatives that engage staff in meaningful problem-solving. Additional elements include alignment between organisational goals and resource allocation, and integration across traditional intraorganisational boundaries. 415
A systematic review416 of organisational change identified 56 recent studies, 13 of which were in health care. Limited differences were found between health care and other industry studies, suggesting a future productive line of inquiry. Published research reveals that transformational change is multifactorial, attesting to the need to adopt a complexity lens for evaluation. 416 A mixed-methods study of transformational change in the NHS, located in north-east England similarly revealed ‘a need to develop new methods to understand how change occurs, or fails, in complex settings like the NHS’. 417 In-depth mixed-methods case studies are required to supplement evidence synthesis work, such as our own report.
Complex adaptive systems (context)
Feedback loops are equally prominent within complex adaptive system (CAS) frameworks that seek to explain how transformation occurs. 394,418,419 A CAS is ‘a collection of individual agents with freedom to act in ways that are not always totally predictable, and whose actions are interconnected so that one agent’s actions changes the context for other agents’. 418 The influential Institute of Medicine report, Crossing the Quality Chasm,420 played a major role in recognising how a CAS’s lens can help in understanding how to improve and transform health systems. It reinforced the idea that health organisations operate within CASs,421 an idea further developed in a series of papers in the British Medical Journal. 418,422 In focusing not on organisational elements themselves, but on the interdependency of those elements, the CAS approach seems particularly well suited to the complexities of evaluating new care models. 423
Even though CASs are complex and unpredictable, they are open to the influence of simple rules that are sufficiently flexible to allow for adaptation. Rather than trying to manage the complex system through top-down large-scale transformation efforts, a CAS approach seeks to mobilise the natural creativity of health-care professionals to evolve, through system learning, locally owned solutions by which to achieve quality. 424
Complex adaptive systems, such as that within which integrated care operates,425,426 pose a further challenge with regard to evaluation; with so many different aspects to care, the system itself inevitably changes over time as practice develops. 410 Evaluators seek to measure a moving target.
Best et al. 427 employed an action research methodology to explore transformation within the British Columbia health system, using a systems-thinking perspective. Requirements for managing large-scale clinical change included creating a context to prepare clinicians for health system transformation initiatives; promoting shared clinical leadership; strengthening knowledge management, strategic communications and opportunities for networking; and clearing pathways through the complexity of a multilevel, dynamic system. More specifically, Sturmberg and Lanham318 identify future priorities for research into systems-thinking and complexity theory within general practice, ‘applying nonlinear dynamics and empirical modelling to patient care, and to organizing and developing local practices, engaging in community development, and influencing health care reform’.
Feedback loops can generate change or stability within a system. Where feedback loops generate change, two systems that initially are quite similar may develop significant differences over time. Even the same system, after the passage of time, may bear little resemblance to its previous configuration. Because the context for each CAS is unique, and each CAS is context dependent, each CAS is unique. 428 The implications for planning are far-reaching, requiring that notions of ‘control’ over the process of change should be avoided, as should language that emphasises ‘overcoming resistance’. 422,429 Instead, efforts should be directed towards iterative planning and practice cycles that acknowledge that successful action is less about meeting targets and more about shifting the system’s behaviour through generic guidance and steering mechanisms. Changing the principles by which people carry out their work is considered to be more important than attaining seemingly arbitrary predefined targets.
Complex adaptive systems require constant monitoring and adaptation if transformational change is to be achieved. CASs challenge the linear logic models utilised by the vanguards; they are ‘self-organizing and constantly adapting to change; they are driven by interactions between systems components and governed by feedback; and they are nonlinear and often unpredictable, with changes on one part of the system producing unexpected changes in other parts’. 430 Although the realist method offers one particular lens for exploring such complexity, further work is required to develop methods for the evaluation of real-world CASs. 431 The recognition of system complexity opens up the use of a diverse range of ‘systems-thinking tools’,432 which might include knowledge synthesis, concept-mapping, social network analysis, programme budgeting and marginal analysis and system dynamics modelling. 419
Mechanisms
Learning theory (mechanisms)
The link between system-thinking and learning theory is explicit:
Systems thinking is an iterative learning process in which we replace a reductionist, narrow, short-run, static view of the world with a holistic, broad, long-term, dynamic view, reinventing our policies and institutions accordingly.
Reproduced from Sterman429
The challenge for 21st-century health services is to ‘aim not merely for change, improvement, and response, but for changeability, improvability, and responsiveness’. 395 This requires a change from enabling not just competence, but also capability. Effective implementation requires a system-wide approach in which ‘the needed capabilities are combined, articulated and developed simultaneously in the same delivery system. Networks of providers will need to put energies and effort into the management of change and ensuring capabilities are embedded’. 220 Commentators recognise that needed capabilities are often in short supply and investment in leadership and organisation development is required if NHS providers are to be ready to take on additional risks and responsibilities. 433
System learning requires an environment within which individuals are able to develop sustainable abilities appropriate for a continuously evolving organisation395 and that enables organisations to capitalise on local knowledge to generate continuous improvements. 434 Such a supportive learning environment enables an organisation to harness relationships and the skills and capacities of individuals in the system. 88 A learning culture, focused on developing the capability, capacity and confidence of staff and service users, provides an environment for the collaborative problem-identification and solving, experimentation and evaluation that is key to addressing systemic issues. 435 The US ACO experience confirms that successful ACOs manufacture mechanisms and systems for learning (and then act on that learning). 126 Such learning systems must be agile in driving rapid quality improvements, as they empower staff and service users to address shortcomings in care. 126
‘Rapid-cycle’ evaluation is an identifying characteristic of many organisations that seek to achieve transformational change. 436 In a study of transformational change in acute care, Greenhalgh et al. 437 emphasise the criticality of ‘tools and techniques for quality improvement, including systematic data capture with rapid feedback loops (plan–do–study–act cycles)’. Rapid-learning cycles enable organisations, such as the ChenMed organisation, which offers high-quality primary care to older people in the USA, to test different ways of working across different contexts,117 tailoring approaches in the light of agile feedback. However, the evidence base for plan–do–study–act (PDSA) methods, notwithstanding their prominence in system transformation, modernisation and quality improvement, is equivocal at best. Few formal objective evaluations of their effectiveness have been conducted, and the achievements of PDSA approaches range from significant improvements in care and patient outcomes through to no improvement at all. 396 A systematic review of PDSA cycles in quality improvement found that many inherent advantages of the PDSA method, such as the facility for iterative learning, and the ability to build up to larger cycles from small-scale changes and capitalise on learning from abandoned cycles, remain underexploited. 396
In Saskatchewan, Canada, primary health-care teams were equipped with the tools and resources to allow them to understand, monitor and compare their own performance as part of the drive towards large-scale transformation. 391 Rather than reflecting a strong accountability structure, such tools place learning at the ‘forefront of the re-design process’;391 building in the capacity for rapid learning is likely to be equally critical to the development of integrated care in the NHS.
The link between individual and organisational learning requires the identification and negotiation of shared mental models. 438 Closely related is the concept of double-loop learning, which arises when such shared mental models enable action at an organisational level. 439 Whereas single-loop learning corrects any defect or mismatch between desired and actual outcomes without challenging any underlying assumptions, double-loop learning effects a more profound, longer-lasting and, thus, transformational change by changing not just the defect but also reconfiguring the underlying decision-making rules.
Research and evaluation consistently emphasise the importance of organisational and system architecture in supporting high performance in health care and other sectors. 440 Collins200 claims that how the vanguards work together as effective learning systems will prove to be critical to their success. Membership of the network of vanguards is predicated on a principle of ‘reciprocal benefit’;441 sharing of data and current practice in turn opens up the prospect of accessing the data and practice of other organisations and, thereby, accelerating the lessons learnt.
Quality improvement (mechanisms)
Within large-scale primary care, stronger performance monitoring and feedback has been cited as a way of improving clinical quality and removing variation. 390 Performance data on quality and cost are key to improvement at an overall practice and individual physician level. Rosen et al. 190 report that monitoring and improving quality represents a constant priority for the central management team, with significant resources allocated to identifying and addressing weak performance in individual practices and services. Dashboards and other performance management systems frequently feature in vanguard documentation. An internal modality report stated that the use of technology to centralise information across all sites and to improve monitoring systems had allowed leaders to hold partners to account for variations in quality and performance. 190 Fifteen indicators were used for monitoring the performance of the primary care organisations across four domains: (1) prescribing, (2) hospital activity, (3) the QOF and (4) patient satisfaction (the GP Patient Survey). 190
Variable results from quality improvement can be attributed, at least in part, to the fact that ‘improvement strategies typically treat practices as something . . . that can be independently isolated and “fixed”, and as such, optimally approach change through the implementation of sequential steps, or stages, to achieve a set objective.’393 Understanding primary care organisations as CASs would recognise their need for support in ‘achieving reflective, adaptive, and action-oriented approaches to managing the future’. This represents a different feedback culture from the current emphasis on ‘hard’ performance indicators. Sheaff et al. 442 describe ‘concertive control’, whereby members monitor each other’s work through peer pressure and peer review, using a combination of organisational culture and technical knowledge to implement collective decisions. Concertive control represents a natural evolution, as organisations move from hierarchical control to self-managing teams. 443 Rosen et al. 190 contrast a ‘directive’ model of change, whereby executive staff both determine the need for change and then facilitate staff to undertake it with a ‘consultative’ model of change, in which peer review and peer pressure are prominent. The latter model corresponds to ‘concertive control’ – exemplified by federations in which individual practices kept their own separate contracts. 442
Audit and feedback (mechanisms)
Evidence on the value of audit and feedback, although not exclusive to a primary care setting, is considered to be quite conclusive, albeit to modest effect. A Cochrane review444 of audit and feedback activity recorded ‘small but important’ improvements in professional practice. A cumulative meta-analysis by the same authors led them to question if allocating further resources to testing the effectiveness of audit would be worthwhile. 445 At least 20 systematic reviews report data on the use of audit and feedback in primary care. 446 Audit and feedback in primary care achieved only modest effects, with a median change of 1.3%. Many unanswered questions remain, for example on whether single or multiple component feedback mechanisms are more effective and exactly what the mechanisms are by which audit and feedback achieves its effect. A realist review of clinical audit by the University of Groningen447 suggests four mechanisms for audit: (1) those relating to continuous improvement, (2) the fact that the process is ‘bottom-up’, (3) the active involvement of professionals and (4) a miscellaneous category of other mechanisms.
M5: proactive population health is dependent on shared and linked data
Closely related to the new ways of working (R1 and M2) and system learning (M4) is the need for linked and shared data to inform decision-making and continuous improvement:
If MCP staff are not able to access shared/linked data, then patients will continue to experience fragmented care.
The evidence map (Table 9) for this programme theory component is derived from four ‘sets’ of related evidence. Three of these evidence sets relate to context and one to potential mechanisms:
-
population-based approaches to primary and community care (context)
-
evidence-informed commissioning/value-based health care (context)
-
integrated and collaborative care (context)
-
quality improvement in primary and community care (mechanisms).
The three contextual evidence sets are primarily theoretical, whereas those relating to mechanisms are underpinned by varying levels of empirical evidence.
| Focus | References |
|---|---|
| Population-based approaches to primary and community care | Tian et al.,448 House of Commons,449 The University of York450 and NHS RightCare451 |
| Evidence-informed commissioning/value-based health care | Hunter et al.417 and the House of Commons449 |
| Integrated and collaborative care | Winpenny et al.,174 Sheaff et al.452 and Rodgers et al.453 |
| Quality improvement in primary and community care | Winpenny et al.,174 Hunter et al.,417 Tian et al.,448 NHS RightCare,451 Sheaff et al.452 and Rodgers et al.453 |
Outcomes relating to the quadruple aim
The importance of information to assist with public health is well recognised. At the local level, data are used to target interventions and monitor population health. At the national level, information is used to make informed decisions about prioritisation, planning and commissioning. At the global level, information assists with the burden of disease and tackling global health threats. Routinely collected health data are not only used by public health agencies, but also for academic research and the development of technology. Large population-level data can help to accurately identify social inequities, and target specific groups and geographical and regional challenges, which can be addressed through evidence-based health interventions. 454 The Symphony Project in south Somerset is an example of the use of extensive data sets for the purpose of improving the integration of care. Data on utilisation, costs and patient characteristics have been combined with local intelligence to identify groups that would benefit the most from proactive care. 450 To this end, examples also exist in which segmentation analysis combined with ‘big data’ has divided patient populations into distinct groups, for needs-based targeting of care models and intervention programs. 455
Southampton City CCG is an example of an organisation that has used data to assist with the reduction of unwarranted variation in health care. NHS RightCare provided data that highlighted the key priority areas for the reduction of variation, which could increase the value of health care. The CCG used these data to target areas of concern for spend and quality indicators, which subsequently led to the development of an implementation plan to improve the management of gastrointestinal patients. 451 A UK study suggests that information on variations in costs, activity and outcome could be better exploited, perhaps indicating a need for tools to help understand the causes of variation in health-care delivery. 456 Despite the availability of data, however, data on disease surveillance, cause-specific mortality, intervention coverage and other vital statistics remain underused data sources,454 suggesting missed opportunities in discovery and innovation.
The potential for effective information-sharing to achieve cost-savings remains inconclusive. One systematic review concluded that there is sufficient evidence to suggest a reduction in costs through the use of electronic health records,457 whereas another study suggests that, although such cost-savings are achievable over a long period of time, there is a high degree of variation dependent on the practice setting. 458 The high costs of implementation can also function as a barrier to the uptake of electronic health records. 459 Such costs may also not be recovered. 460 Support for the cost-effectiveness of shared electronic health records remains limited and conflicting. 459
The government-anticipated ‘big data’ and the use of large data sets for the purposes of analysis have been promoted as potentially reducing costs, with an estimated £20B of benefit over a 5-year period for the central government. 449 This estimate was based on the understanding that the cost-effectiveness of services is, to some degree, dependent upon data transparency and effective data-sharing. 449 To this end, linked data have proved to be useful in exploring the utilisation and costs of services. Patient-level linked data have been used to explore the NHS and social care costs of the care pathway associated with elderly patients recovering from a fall in Torbay, Devon, UK. In this case, cost data patterns proved to be helpful in identifying and targeting patients to fall prevention services. 448
Information-sharing can help to improve patient–doctor interaction, including through the use of telephone, e-mail and web-based consultations, with tools such as webGP and askmyGP enabling patients to share information with clinicians to support clinical decision-making. 461 Modality, a super-partnership in Birmingham and Sandwell, and one of the MCP vanguards, operates a remote hub to support triage, self-management and same-day consultations, enabling 65% of health concerns to be dealt with remotely. 461 A similar system, based at south Somerset’s Symphony, one of the PACS vanguards, has established a web platform to enable patients to access their care plan, messaging capabilities (such as Skype™; Microsoft Corporation, Redmond, WA, USA), test results, information about their condition and telehealth functionality. The platform enables a ‘single view of clinical activity between the [integrated] hub and practices’, directly linked with the GP system. From an information governance perspective, such systems can also clarify permissions for sharing information with carers and family members, which can be useful in the event of a crisis or emergency or when the patient is reluctant to engage with technology. 462 Mobile phone applications are increasingly being used463 and may help to support patient empowerment and shared decision-making.
An earlier HSDR programme study452 explored continuity and co-ordination in primary care, including the impact of informational continuity. Up to half of the patients at all five sites studied described instances of information, regarding history, diagnosis and treatment, not being passed between providers. Patients reported correcting health worker omissions and out-of-date information, and having to repeat information to the next practitioner. In one instance, a district general hospital delayed action on an urgent GP referral, resulting in emergency admission of the patient 2 days later. Poor protocols for sharing data and unclear responsibilities were cited as contributing factors. Informational continuity seems to decline across traditional boundaries, with some patients with long-term conditions maintaining their own paper-based histories.
Effective communication, to share and link data, underpins multidisciplinary and collaborative working,174,453 and can range from a basic model through to a shared care record with e-referrals, e-prescribing and e-discharge. Data-sharing, enabled by telemedicine, allows GPs to access advice from specialists; examples include GPs working with dermatologists and ophthalmologists to share data and enable remote specialist consultation, with mixed results. 174 Informational continuity, through shared records across primary and secondary care, seems to show potential in improving decision support outside of specialist clinics. 174
Data-sharing is considered to be one of the key factors driving high-quality care for chronic conditions, with the potential to improve efficiency, drive up quality and reduce duplication. 453,464,465 The chronic illness care model466,467 encourages the use of information systems to facilitate data-sharing and communication across traditional boundaries, helping to translate knowledge into practice. One example demonstrates integrated medical records for frail elderly patients providing read–write access for all health professionals involved in care, as well as patients and carers. 452 Such systems can be built on to develop tools and dashboards to alert MDTs to patients at risk of admission417,452 and identify potential bottlenecks and delays. 417 In north London, an information technology tool was developed and used to support information storage, sharing and analysis to support integrated care programmes. 468 Information-sharing does, however, depend on data quality; GP systems and templates may enable standardised and complete data collection. 453,469
Unintended consequences
The push for data-sharing and health information exchange has given rise to concerns surrounding privacy, confidentiality and control of data about individuals,470 specifically, concerns around user trust, data privacy, transparency of data ownership and the potentially intrusive nature of data analytics. Poor communication and confusing messages can turn public and patient attitudes against the sharing of personal data, as demonstrated in the issues surrounding care data. 470 The risks and benefits should be clearly articulated, as should information on data governance and anonymisation techniques. 470 Data governance is likely to become an even more important issue, given the predicted rise in wearable technology and digital applications, which have the potential to link directly to records to support decision-making and remote monitoring. 461 Privacy terms and conditions are less clear, and the process for opting out is sometimes not explicit. 470
Inevitable concerns persist in relation to sharing data with patients and carers, with the ‘digital divide’ highlighting the socioeconomic disparities in access to technology,462 which can be exacerbated when patients with low educational attainment and health literacy rely on carers for information. NHSE ran a widening digital participation programme from July 2013 to April 2016, which provided digital health training to 221,941 people who were at a risk of being digitally excluded. 471
The focus on shared data and technology-driven data collection could unintentionally signal a shift away from the social contract that underpinned the traditional doctor–patient relationship,470 with criticisms regarding the ‘depersonalisation’ of care and risks to provider autonomy. 472 There is an additional risk that staff may feel that data collection is being driven by targets rather than patient-centred care. 417
Mechanisms
Facilitated by new ‘disruptive’ technologies enabling large data sets,470 real-time analytics can be a catalyst to drive population-based health care. Future iterations of clinical decision support systems are likely to enable data linking across sectors, enabling primary and secondary care clinicians to access data to inform decisions at key points in the pathway. 461 Currently, information exchange is constrained by such factors as local information governance protocols, incompatible information systems leading to duplication and rescanning, unreliable connectivity and inconsistent clinical coding. 452 Digital strategies should encompass a range of technologies to support data-sharing and co-ordinated multidisciplinary care; shared electronic records, used in combination with predictive analytics; telehealth; and patient-facing tools, such as portals. 469 Consideration needs to be given to infrastructure (e.g. data storage, real-time analytics and integration of distributed data sets);470 capacity and skills;470 and financial sustainability. 454,464 Some form of central administration is needed to ‘monitor, mediate and facilitate data-sharing across multiple stakeholder organisations’454 and to manage protocols, processes and data specifications. 470 At a national level, there is also a role to ensure interoperability between policies, systems, data standards and supporting market development,454,461 in order to avoid unnecessary variation472 and conflicting policies. 469,473
The sustainability of data innovations is dependent on demonstrating benefits for patients, commissioners and practitioners. 472 Data-sharing needs to be supported by cultural changes, such as multidisciplinary working and support for shared decision-making. 174,461 Innovations are also likely to be more acceptable if patients and staff have been engaged, and communication on the legal and ethics implications has been clear. 470
Both patients and health-care professionals will need support in developing the skills and knowledge to benefit from data-sharing. 470 Training centres specialising in big data (large linked data from electronic health records and health data collected by personal wearable devices) and open data (the sharing of data sets) can help services to reap the benefits from data-sharing to address population health needs. 470 In the absence of training, the ‘noise’ of large data sets may risk the misinterpretation and misuse of data. 470
Numerous barriers to technology transformation have been identified, including the absence of standards, significant variation in workflows, inefficiency of health information technology, incompatible legacy systems, incomplete information flows and poor system design. 452–454,472 An absence of incentives for data-sharing, opportunity costs and disagreements around the use of data can also hinder effective information exchange. 454 Poorly defined goals can result in uncertainty about what can be shared and which data need to be included,464 potentially leading to variation in the capability of organisations and services to share and act on data. 464 Relationships based on trust and collaboration will be key to overcoming structural, cultural and ethics barriers. 454
Chapter summary
The intention for these maps has not been to systematically cover all of the relevant literature. Indeed, it is clear that each of the evidence sets relating to the programme theory components holds the potential to sustain an in-depth analysis of empirical literature and the underpinning theory. The maps demonstrate the interdependencies between individual theory components. Structural developments, such as the introduction of MDTs and integrated pathways, are contingent on cultural change, which, in turn, needs to be stimulated through organisational development and system leadership behaviours. Staff autonomy and empowerment is identified as a critical thread in cultural change, associated with trust and collaboration. This shift to a more collaborative, population-based approach to health care can be hindered by misaligned systems and processes, and it is clear from the evidence base that shared data can offer the opportunity to improve the co-ordination and continuity of care for patients and to instigate improvement and innovation. System learning, within each vanguard and then across vanguards under the aegis of NHSE initiatives, can be demonstrated to be a key component of the New Care Models programme to a degree that has not typically been encountered with vanguard-type initiatives. Indeed, similarities can be detected with the Institute of Medicine’s Learning Health Care System model. 474 In particular, feedback loops built into audit and formative evaluation could potentially trigger a range of different mechanisms, variously interpreted as responses to transformational change, learning or quality improvement resources.
Chapter 8 Discussion
In this chapter, we bring together the findings from the realist reviews (R1–3) and maps (M1–5) of the programme theory components. The overlaps between them are discussed in the context of implications for research and practice. This provides the means by which we refine the policy and MCP vanguard programme theories (from NHSE MCP guidance and logic models, respectively) within the realist synthesis approach70 and propose a conceptual model for future accountable population-based integrated systems (Figure 20).
FIGURE 20.
A conceptual model encompassing the tangible features of a logic model with the more intangible resource and reasoning mechanisms.
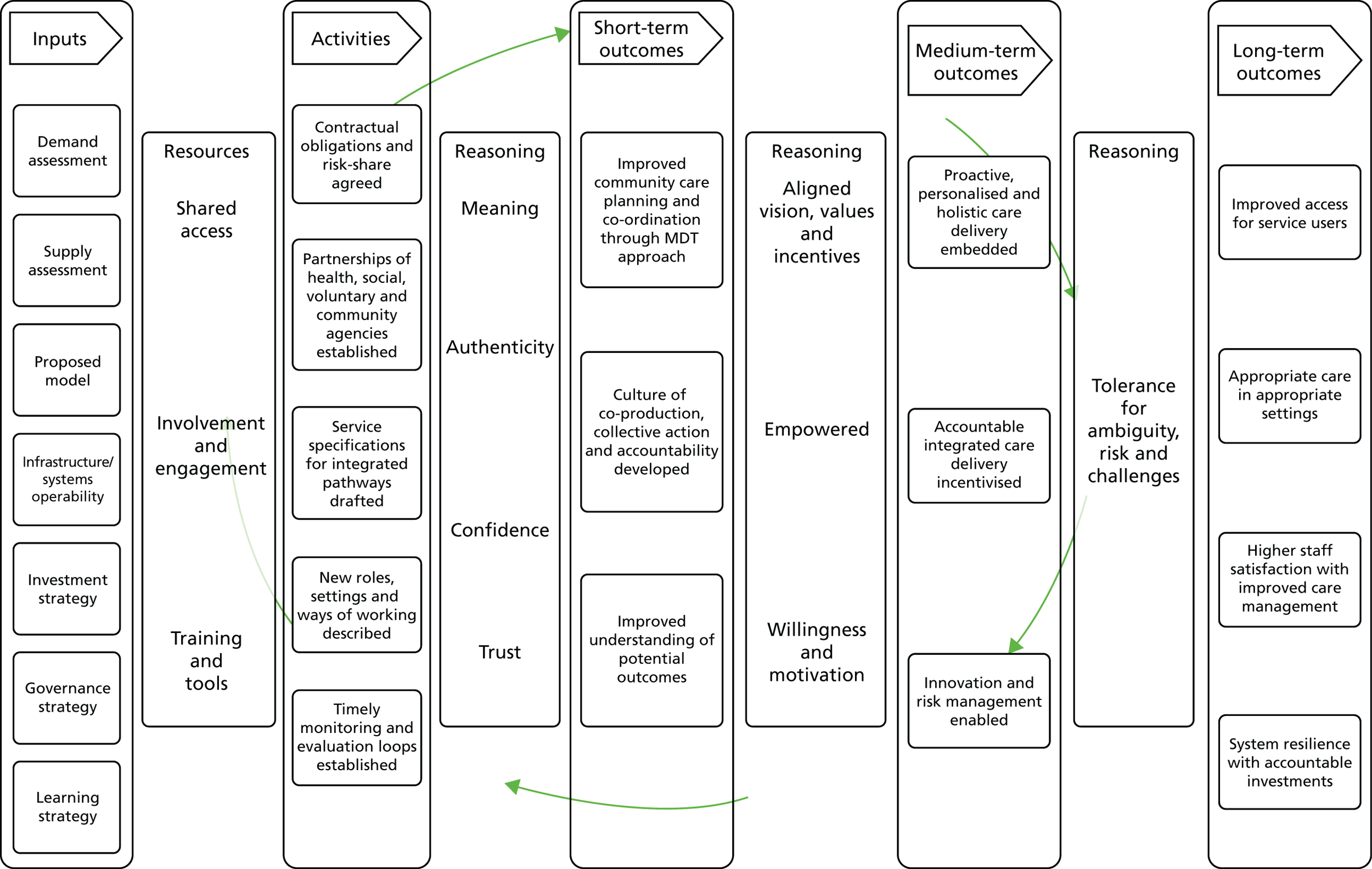
The review set out to address four research questions, which are discussed fully in the previous sections of this report:
-
What are the foremost theories of change inherent within the MCP model of care? In Programme theory components, we summarise each of the three prioritised components, the maps and the unintended consequences.
-
What seem to be the ‘active ingredients’ that should inform design of MCP models of care? The Implications for practice section below captures discussions from testing our emerging findings at a MCP stakeholder workshop and a dissemination activity with NHSE’s New Care Models programme teams. These have helped to refine our proposed active ingredients to support practitioners (Table 10).
-
What are the social and cultural conditions that influence (enabling and blocking) change within MCP models of care and how do these mechanisms operate in different contexts? In Implications for research, we frame the combined findings within a theoretical understanding by abstracting to relevant mid-range theories. This provides an explanatory framework to reinforce the conceptual model (see Figure 20).
-
What are the key knowledge gaps and uncertainties in relation to the design, implementation and evaluation of MCP models of care? The study strengths and limitations within Implications for research describe this aspect in more detail.
| Framework theme | What | How |
|---|---|---|
| Design |
|
|
| Delivery |
|
|
| Management |
|
|
| People and communities |
|
|
| Workforce |
|
|
| Technology |
|
|
| Leadership |
|
|
| Knowledge |
|
|
Programme theory components
The programme theory relates to activities, such as contracting, as well as behaviours, such as community involvement. The individual theory components were notable in their coverage of both interventions (what MCPs will do) and ways of working (how MCPs will design and deliver services). The evidence base is variable, characterised by limited empirical studies; experiential learning through informal case studies and before-and-after evaluations; and the transfer of lessons from international models to a NHS context. Our synthesis incorporated stakeholder engagement, via an advisory group and focus group (see Stakeholder engagement), which enabled sense-checking of emerging findings.
R1
The delivery of new and expanded roles in primary care, including access to specialist care in the community, requires a degree of trust between the different professionals. The provision of relevant training and practical tools in parallel can trigger professional willingness to adopt new ways of working or task-shifting. Once new professional roles and behaviours are effectively embedded, there is the potential to achieve the outcomes of better management of chronic conditions, a reduction in the number of secondary care referrals and cost-savings, following sustained implementation and stabilisation of increased demand (with the costs of training and additional community services provision accounted for).
R2
The opportunity for clinicians and patients to engage with providers and commissioners for accountable place-based contracting and payment systems requires the alignment of personal, professional and organisational values and incentives. Moreover, sufficient time needs to be allocated to learning and development, agreeing outcome frameworks and sharing access to robust high-quality information that includes cost and quality data. This will allow the building of trust, collaboration and shared decision-making for accountability across quadruple aim outcomes. Furthermore, through service users and a diverse group of professionals having the confidence to hold providers and commissioners to account, MCP leaders will be spurred to make informed (re)investments based on clear measures of value and appropriate management of financial risk.
R3
The development of mutually beneficial relationships with communities requires opportunities for equal and reciprocal engagement for all relevant health-care professionals and the local population. The provision of ongoing training, guidance, feedback and practical support for community-based working needs roles, responsibilities and expectations to be clearly articulated. Together, they can empower individuals with the confidence to contribute to decision-making or the sharing of experience and knowledge to inform the priorities for targeted preventative and holistic care. Consequentially, this encouragement of shared community ownership will result in improved health behaviours and increased social participation, and will engender community resilience.
M1–5
The maps further demonstrate the interdependencies between individual theory components at the individual, organisational and system levels. Professional autonomy and empowerment is critical for driving cultural change that is associated with trust and collaboration, particularly for structural developments of MDTs and integrated pathways. Cultural change needs to be stimulated through organisational development and system leadership behaviours that promote collaborative, population-based approaches to health care and aligned processes that support delivery. Shared data, in particular, offer the opportunity to improve the co-ordination and continuity of care at the individual and organisational levels, while MCP-wide learning can be accomplished through training and feedback loops, built into audit and formative evaluation, to support system learning and improvement.
Unintended system consequences
The concept of ‘community’, as we discuss in Chapter 6, is fluid and subjective and does not necessarily follow the boundaries set out by MCP designers. As a consequence, the drawing of contractual lines may effect patient choice and the liability of the MCP. 119 There are also organisational boundaries to consider. The shift of care from hospital to community settings is fraught with tensions and trade-offs, with speculation that organisations may act in their own interests rather than in the interests of the overall system,118 and this is not helped by the presence of conflicting policies. 209
A lack of representation or engagement with co-production activities by some groups in a community may result in increased health inequalities, as services are designed without them in mind. 286,287 In any case, any initiative must take care to be consistent in its information-sharing with service users; for example, receiving conflicting instructions about service users’ individual needs, priorities and management strategies in self-management would prevent the successful uptake of self-management initiatives. 290
Defining the continuity of care in community-based settings as ‘seeing the same health care provider every-time’155 poses a problem for access to an expanded primary care, as discussed in Chapter 4. MCP delivery by an enhanced team with more new roles has the potential to disrupt relational continuity156 for those service users who prefer an ongoing, trusted relationship with a specific professional over quick access. This means that an expanded primary care and community system will need to maintain both its connectivity to the local population and the generalism inherent in general practice;190 operate as hubs to offer more extended access;32 and have sufficient and appropriate staffing,185 which pays heed to workload,32,172 staff development163 and the status of innovation. 159 It is notable that those areas seen to be making the most progress are those building on a history of collaborative working;200 their learning is that it is difficult to develop accountable approaches without aligning incentives208 and transferring savings and risks across sectors. In any case, introducing new services has the potential to induce demand71 or incentivise use. 174 There is the potential to misuse new services71,187, or duplicate care at hospital174 or in primary care. 151
The findings from Chapter 5 suggest that the risks of increased costs187 cannot be overstated and include loss of economies of scale;174 set-up costs for new posts32,163 or registration for hubs and federations;32 and the associated administrative support and resource cost to ensure that system protocols are followed. 174,187 There is also the potential that a model focused on consolidation and co-ordination might inhibit those market forces/competition that are necessary to drive cost and quality improvement. 228
Quality of the evidence base
The evidence base identified varies from moderate (for R1 and R3) to relatively weak (for R2). There is a lack of robust, empirical evidence and the findings are therefore somewhat dependent on experiential evidence, informed by case studies and informal evaluations. The ‘intellectual heritage’ of the MCP models – earlier NHS integration programmes and international models of accountable care – offer some transferable findings, although the contexts differ significantly.
Application of theories to enhance the understanding of implications
Complex adaptive systems theory418 offers a conceptual lens to explore the MCP model. The focus within the CAS approach on the interdependency of elements in a system, and not the system itself, makes it particularly well suited to framing the complexities of integrated care at the core of the new models and, in time, evaluating it,423 in order to guide future policy and practice. 475 CASs are characterised by a range of features that are particularly relevant to the design, implementation and evaluation of the MCP model of care, including the following:
-
Feedback loops – these serve to feed back the output of a process, as an input, into the same system. 74 Positive feedback loops can be facilitative, for example, in the use of PDSA cycles in quality improvement processes. 396 Feedback loops are particularly pertinent to the commitment of new care models to shared and continuous learning and improvement (explored in our programme theory component M4). This capacity to learn, and to share learning, is dependent on positive feedback reinforcement when intended outcomes are being realised or corrective action following negative feedback from less desired outcomes. Thus, in a MCP-like system, feedback allows adaptation476 of delivery to align with the constantly shifting landscape. This is likely to be a critical factor, as new care models are rolled out and incorporated into sustainability and transformation plans or ACSs.
-
Connectivity – the manner in which agents in a system connect and interact, and gives rise to the behaviour of a CAS, highlighting the significance of these relationships over the agents themselves. As Plsek and Greenhalgh418 note, ‘the observable outcomes are more than merely the sum of the parts’. 418 This connectivity is a recurrent theme in the MCP programme theory. This includes practitioners connecting to adopt new roles and ways of working, building or strengthening relationships to co-ordinate care for the benefit of patients (R1). The involvement of service users and local communities in the design and delivery of care (R3) adds a further dimension of connectivity. The responsibility of delivering safe, appropriate and high-quality care is discharged through collective decision-making, with dependency on good communication and working relationships (M1 and M2). The importance of team-building and peer support is clear in a model that is built on interdisciplinary working (M2 and M3) and, on a broader level, also underpins the deployment of technology to support population health (M5).
-
Edge of chaos – a CAS approach seeks to draw out and mobilise the natural creativity of health-care professionals to adapt to circumstances and evolve. 418,477 This suggests that multidisciplinary delivery teams – which may comprise NHS practitioners and staff, independent and private contractors and third-sector groups – need the capacity and the capability to reflect and innovate. Capability will need to be built through organisational development, and capacity can be built through system learning and locally owned solutions to improve quality,424 contrary to an arguable emphasis on top-down large-scale transformation efforts. Crucially, this requires some experimentation and risk-taking to encourage learning from mistakes or failures, within clear boundaries for accountability. There may also be a need to allow tensions to play out, for instance, in R2, the contracting and payment mechanism for MCPs is necessarily at the edge of chaos, using the opposing forces of competition and co-operation to be mutually beneficial,478 in order to allow local sites to innovate for their accountable local place-based system.
Several theories may be usefully applied to enhance our understanding of complexity in practice, and a fuller discussion is included in Appendix 8, which offers some pointers regarding when further analysis may prove to be valuable. On a practical level, the ‘capability’, ‘opportunity’, ‘motivation’ and ‘behaviour’ (COM-B) model can be used to understand the implications for the design, implementation and delivery of MCPs. 479 New care models are built on the premise of changing behaviours at the individual (i.e. clinicians, support staff, service users, carers, system leaders), community and wider system levels. The COM-B model is based on the argument that an individual’s or group’s behaviour arises from capability, opportunity and motivation. We have mapped our key findings to the COM-B model to describe contextual factors that are likely to influence behaviour change (Figure 21). This has been expanded on in order to develop a set of ‘active ingredients’ to inform the wider roll-out of integrated models of care.
FIGURE 21.
Implementation theory applied to the MCP model. Adapted from Michie et al. 479 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
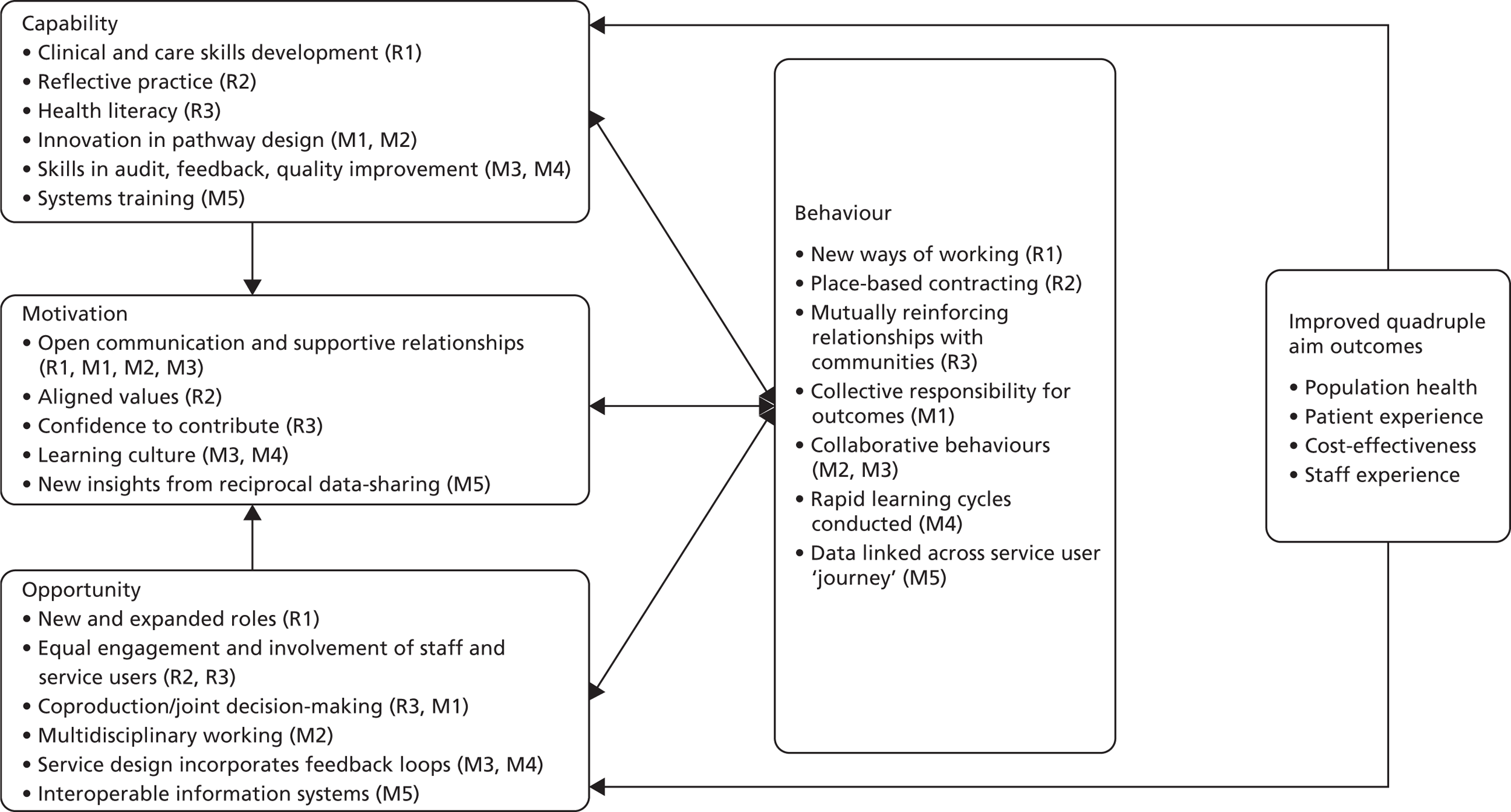
Study strengths and limitations
Strengths
The project team composition is relatively unique in being embedded in the NHS, with methodological support and mentoring from an academic partner. This model of co-production ensures a connectedness with current policy and practice, while maintaining methodological rigour. A key strength of this partnership is in harnessing existing links to connect with a range of stakeholders at a strategic and operational level. On a practical level, these links have helped in enabling early access to relevant NHS documents. The team is also well placed to translate emerging findings into language that resonates with key audiences and to relate findings to current service priorities. These findings are not limited to MCPs, but can apply to transformation or integrated care more generally.
Expertise in the principles of realist synthesis remains relatively scarce, although the approach is fast emerging as a response to the challenges of evaluating CASs. We were able to harness expertise acquired from prior involvement in other NIHR HSDR evidence syntheses, and from NIHR projects more generally, as well as borrowing heavily from the tools developed by other teams funded by the HSDR programme. Our methodology acknowledges the increasingly hybrid nature of current realist synthesis projects, spanning the published literature and stakeholder input. We believe that our methodology was genuinely innovative, by starting with the analysis of existing logic models, as well as by using a best-fit framework synthesis to produce a conceptual framework, not only for structuring our own analysis, but also as a potential vehicle for the evaluation of future service models. We benefited from pooling the expertise of three information specialists relating to the ‘realist search’ being captured by a book chapter being written concurrently with our own project,65 as well as from existing tools such as Pawson’s time and task template64 and data extraction forms developed by other teams. 70 The team has used the RAMESES training materials480 in expanding our realist synthesis capacity, and RAMESES guidance62 to ensure project outputs and high-quality reporting.
The close involvement of the advisory group has proven to be valuable in articulating and validating programme theories, and validating a clear, consensual basis on which to focus and target the synthesis strategy. The work with the advisory group helped to ensure that the prioritised in-depth realist reviews focused on the aspects likely to add the most value, while ensuring the relatively comprehensive coverage of the breadth of the MCP model, through the series of theory maps. To test and validate findings, the advisory group was expanded to form a broader focus group, involving additional key stakeholders identified during the project. The focus group provided a ‘reality check’ of our findings. A summary of discussions at the focus group and during interviews with advisory group members is included in the review chapters.
Patient and public involvement has been a key component of stakeholder engagement. In developing the review proposal, the team contacted local patient participation groups to invite feedback from current patients and members of the public. As Davies et al. 481 point out, patients and the public constitute a group that has been largely absent from the knowledge mobilisation literature. The project aimed to address this gap through the active involvement of service users. Two PPI representatives were appointed to the advisory group and have provided valuable input throughout, notably in the prioritisation of programme theories for review, reviewing emerging findings and advising on dissemination activities.
Communications and engagement are critical to producing outputs focused on relevant and actionable insights for our various stakeholder audiences. Recognising the importance, the team has been supported by dedicated and specialist communications support and expertise. The skills and experience have been valuable and have enabled stronger relationships with the communications team at NHSE, enabling wider reach to MCP sites and minimising the risk of overburdening them with ill-timed requests and information. The dedicated communications role, with a background in communicating complex research, might be a useful model for future projects.
See Appendix 9 for a summary of how the study has addressed the research objectives.
Limitations
The programme theory was substantially based on the MCP vanguards’ logic models, developed to support the submission of value propositions to bid for transformation funding. However, this approach was dependent on complete logic models being available and other national processes affected the production of the logic models. The team was able to access logic models for 12 of the 14 vanguards and, at this early stage, the format and granularity of the models were variable. The team subsequently used associated documentation available in the public domain, from the vanguard sites (e.g. consultation documents) and NHSE, to supplement the logic models. As the models have evolved significantly during the lifetime of the review, particularly regarding procurement and contracting, the team has endeavoured to keep up to date with emerging policy and guidance. However, given the rapid pace and scale of change, it is likely that the programme theory will continue to evolve subsequent to our analysis.
From a methodological perspective, we acknowledge that conducting a review against a backdrop of continual change, to add to the already-identified complexity associated with diverse contexts, was extremely challenging. Although the new care models are being intensively evaluated, and our networks identified relevant data as soon as these became available, we encountered a degree of prematurity within the specific context of a UK-focused evaluation. We sought to minimise the impact of this in two ways, by (1) exploring transferable lessons from international comparisons and UK legacy models and (2) seeking to identify generic lessons that may be used to explore future care models that seek to achieve large-scale transformational change within CASs. Although vanguard sites offered a ready-made source of what was intended to happen, there was little supporting detail on how this was to be achieved. In particular, individual sites lacked specificity about the perceived and actual intended impacts from the new care models, making inferences about mechanisms extremely problematic. However, we were able to use the composite picture, derived from 12 sites, to mitigate some of these difficulties, and we believe that our analysis was particularly strong in isolating unintended consequences. In particular, the embedded nature of our NHS-based team, continuous stakeholder engagement and telephone interviews with key informants added to the value of our inquiry.
Although the overall review draws on a broad evidence base, this predominantly derives from within the health sector. The team has made a concerted effort to explore social care and third-sector literature, but recognises that there may be valuable learning from other disciplines, for example, lessons from other public services or the private sector in relation to large-scale public-funded procurements. A realist review does not aim for the exhaustive searching of a systematic review and, therefore, it is possible that important papers have been missed. The iterative approach and stakeholder engagement has focused the search on the identification of key sources, but does not eliminate the risk of confirmation bias.
Implications for practice
Stakeholder engagement
At our stakeholder event in May 2017 (see Chapter 2) we tested our emerging findings across the programme theory components with stakeholders. We framed our discussion in the context of the observable progress at the MCP sites from the perspective of participants. The discussion content is summarised according to the relevant theory components below; there was of course overlap between the topics.
R1
There was much support for new ways of working; however, in the 2 years since the vanguards had been appointed (in March 2015), the substantial preparatory work was still to materialise into standardised improved access to health care. MCPs that had made progress were noted to have prior experience of collaborative working. As a consequence, these mature models had allowed for the development of trust (see Figure 20) between professionals over time. Conversely, where historical organisational partnership relationships were deemed to be poor, this had an impact on professional motivation and willingness to change. There was also a recognition of the potential widening of inequalities within sites as MCPs progress. For instance, patients at smaller practices were yet to benefit from some of the changes implemented at larger practices, the location of practices may prohibit access to improved estates, and access to specialist care in the community may not be available to all.
R2
The concerns within the literature base were reiterated by stakeholders – too much faith may be put in contractual processes and mechanisms, potentially neglecting the significant cultural change needed to support the effective implementation of capitation and risk-/gain-sharing. Five strategies were put forward to manage the inherent challenges: (1) the contract should be viewed as a system transformation enabler with a dependency on aligning strategic, operational and front-line behaviours; (2) a longer-term contract offered greater stability, with the ability to invest in organisational development, cultural change and underlying infrastructure to support system-wide transformation – this also negated the significant effort expended in reviewing and negotiating contracts on an annual basis and the resulting emphasis on short-term outcomes; (3) time scales for transformation, especially linked to payment mechanisms, had to be realistic, with a period of realignment and readjustment built in; (4) a rigorous governance structure articulating how shared resources are to be used, how decisions will be made and how risk is shared across the system should be transparent to all; and (5) MCP-wide difficult conversations, including clinicians and patients, regarding trade-offs across the system to facilitate improved prioritisation and decision-making.
Among all of this, the potential risks of destabilising current providers should contracts be awarded to new market entrants rather than incumbent providers needs to be monitored, in particular, the management of failure; participants made explicit references to the UnitingCare contract failure in this regard.
R3
The stakeholder discussions highlighted the challenge of defining communities on a place-based geographical basis; in practice, there were many layers and shifting boundaries within a community. Within this, there was a need to scope community assets and map the full range of organisations that could be included in delivering place-based accountable care. Resourcing of third-sector and voluntary organisations, both in terms of funding and the availability of staff or volunteers, was essential, with consideration of prevention and holistic care becoming increasingly important. Standardised training for this varying workforce needed to be delivered by the MCP to ensure a consistent, person-centred approach and appropriate skills and support for all.
Although co-production was seen as ‘a good thing’, the cynicism on the part of health professionals was discussed. The value of co-production was in need of promotion in a way that would appeal to clinicians. Within co-production approaches, there should be a focus on a short list of ‘outcomes that matter’. It was acknowledged that co-production, by definition, calls for difficult conversations regarding trade-offs across the system, but that these opportunities should be viewed as a means to engage clinicians and patients.
M1–M5
The interdependencies inherent within the MCP model were made clear. The discussion around ‘equal’ versus ‘collective’ responsibility, incorporating statutory duties and delegated responsibilities within a multiprovider model, found favour in the development of a combined reward system. This was proposed to encourage shared accountability in integrated pathways by ensuring ‘skin in the game’. In line with this, a culture of openness, transparency and honesty ‘a non-defensive system’ was required of a MCP, with processes for learning and feedback that also included tacit knowledge and acknowledgement of mistakes. The ‘fail fast learn fast’ principle was considered to be particularly pertinent to the pace of change within vanguards. Another contributor to collective responsibility is shared professional access to data; the current ‘brick wall’ between primary and secondary care should be a priority for MCPs to redress.
Similarly, the delivery of integrated pathways within ‘natural communities’ by MDTs needed to bear in mind the ‘communities within communities’ and the support networks available for patients with long-term or complex needs. As MDT working was gaining traction elsewhere, there were observable innovations emerging within MCP settings; for instance, one vanguard was using a MDT to support same-day access to acute episodic care, part of a two-pronged approach to reduce A&E attendances and increase resilience within general practice. A MDT need not be limited to clinical teams. Inclusion of non-clinical staff in system-wide pathway development would facilitate the necessary cultural change as part of a wider strategy of staff development, which includes leadership.
Dissemination
NHS England has signalled the intention for new care models to continue to evolve,57 with a commitment to developing ACSs, subsequently announced in eight areas, two of which include current MCP vanguards. 59 These ACSs will have responsibility for improving population health, developing horizontally and vertically integrated models of care, learning from the MCP and PACS vanguards. As the vanguards have evolved to fit within their local contexts, it is apparent that they share common characteristics, and any distinguishing characteristics between the two models become more blurred, as acute providers become more involved in MCPs and community providers in PACS. Using the best-fit framework as a structure, and informed by our mapping to the COM-B model (see Figure 21), we provide a quick-view summary of the key findings from our synthesis, extracting the interventions and mechanisms identified in the evidence as significant to the MCP model of care (see Table 10). We describe these conditions as ‘active ingredients’ that, although derived from a programme theory relating to the MCP model, will offer transferable insights to population health-based models of care in general. This table was refined as part of the dissemination activities, which included a presentation to the new care models team but also discussions with the wider Strategy Unit team and NHS colleagues interested in accountable integrated models of care.
Implications for research
Our review has identified considerable gaps and areas of uncertainty within the evidence base. The local and national evaluations of the New Models of Care vanguards may go some way to addressing some of these gaps. As ACSs (now referred to as integrated care systems by NHSE) start to emerge within England, building on the learning from the vanguards, further research is needed to provide actionable insights into the development of place-based population health management within the NHS.
To inform future research and evaluation, we have endeavoured to articulate those areas of uncertainty that could be considered a priority. We present these in the list below, which we prioritise by the potential scale of opportunity to influence policy and practice and the quality of currently available evidence:
-
Future research could usefully explore the medium- to long-term impact of enhanced primary care, particularly in relation to workforce recruitment and retention; workload; demand and capacity; quality of care; or access to care. Although there is some evidence relating to new and expanded roles in primary care, the quality is variable. In particular, there is a need for evaluation of the role of care navigator, common to several MCP vanguards. This is likely to be best served by a mixed-methods evaluation, including case studies, to measure quantitative impacts, such as emergency admissions, and qualitative impacts, such as perceived workload.
-
Given recent high-profile failures of large-scale contracts, there is a need for greater insight into the effects of longer-term contracts and associated procurement, on financial sustainability, patient experience and system capacity. In particular, economic evaluation could usefully explore the impact of risk- and gain-sharing on patient outcomes; the tension between competition and collaboration; and the contribution of contextual factors (e.g. historical relationships, financial deficit). There is also an opportunity to test the theory that newer contracting forms enable a greater focus on the wider determinants of health, potentially via organisational case studies.
-
The conditions to develop system capacity for rapid-cycle learning are central to the underpinning philosophies of the New Models of Care Programme. Our synthesis has highlighted the role of organisational development and the need for agile learning to enable continuous improvement. The evidence relating to system learning suggests that although PDSA cycles are common, implementation is variable and the evidence equivocal, pointing to a need for applied action research into the development of learning health systems. This should focus on improving our understanding of the conditions needed for successful continuous improvement and learning at a system level.
-
We found surprisingly few publications specifically on the role and experience of carers in relation to patient empowerment, suggesting a significant gap in the evidence base. It could be argued that the current emphasis on patient activation is based on assumptions on carer capacity and capability, yet little is understood about the needs and behaviours of this overlooked and heterogeneous group. Further research into the role of carers in self-care, shared decision-making and social-prescribing could usefully inform future policy and practice. Realist evaluation, with a focus on what works for whom in what circumstances, would offer useful insights into relevant mechanisms in different contexts.
-
There is a need for further insight into community perspectives on involvement in decisions about patient care, and the design, implementation and evaluation of new care models. Our analysis suggests that, despite an intention to address inequalities, there is a very real risk of widening existing gaps in provision. There is therefore a need for research to improve our understanding of how involvement affects individual patients, community groups and local charities; how initiatives such as social-prescribing, self-care and community participation can be sustained over time; and how these collectively might contribute to community resilience. This may benefit from further evidence synthesis, in the form of a systematic review, encompassing literature beyond health and social care.
In testing the programme theory of the MCP model, we have explored the potential unintended consequences. This is likely to be useful to policy-makers and strategic decision-makers, and we suggest that the complexity associated with the New Models of Care Programme warrants mixed-methods approaches to capture quantitative measures and qualitative perspectives of impact. There is also the potential to learn from other sectors, for example, how large-scale contract failures are managed in other public services.
Acknowledgements
We gratefully acknowledge the contributions and support of stakeholders and participants during the project:
-
the focus group attendees
-
the members of our project advisory group (see Appendix 1)
-
Laura Freeman, Julia Grace, Cara McDonagh, Peta Mylan, Sukhmeet Panesar, Charles Tallack, Louise Watson, Mike Lawrie, Dan Northam-Jones and the wider New Care Models programme and Operational Research teams, NHSE
-
Sharon Townsend and Deborah Mabbley for providing administrative support to the project
-
Lorna Crofts for her work in formatting the report
-
Louise Rowan and Katrina Wilcox for their work on communications and engagement
-
Peter Spilsbury and Fraser Battye for their support and advice
-
all of our colleagues at The Strategy Unit for their practical support.
Contributions of authors
Alison Turner was the principal investigator for the review and was involved in developing the programme theory, designing the search strategy and screening the search results. She led the synthesis of R2 and M2, contributed to the synthesis of R3, led on writing Chapters 3, 5, 6 and 7, and contributed to Chapter 8.
Dr Abeda Mulla was the co-applicant for the review, led the work to develop the programme theory and was involved in screening the search results. She led on Chapters 1 and 8 and contributed to Chapters 4 and 6.
Dr Andrew Booth was the co-applicant for the review, leading on the methodology and acting as a mentor to Alison Turner and Abeda Mulla. He wrote Chapter 2, led on the synthesis and writing of M4, co-authored Chapter 7 and advised on Chapters 3–8.
Shiona Aldridge was involved in developing the programme theory, designing the search strategy and screening the search results. She led the synthesis of R1 and led on the writing of Chapter 4. Shiona also contributed to the synthesis of R3 and to the writing of Chapter 6.
Sharon Stevens was involved in developing the programme theory, designing the search strategy and screening the search results. Sharon contributed to the synthesis of R3 and the writing of Chapter 6. She also contributed to the synthesis of M1, M2, M3 and M5.
Mahmoda Begum was involved in screening the search results and led the synthesis of M1 and M3, writing these sections of Chapter 7.
Anam Malik was involved in screening the search results and led the synthesis of M5, writing this section of Chapter 7. She also contributed to Chapter 1.
Other contributions from the project team
Peter Spilsbury chaired the project advisory group and the focus group, and commented on early findings and drafts of this report.
Fraser Battye deputised for Peter Spilsbury in the role of chairperson and acted as an expert advisor to the project, commenting on early findings and drafts of this report.
Sharon Townsend provided administrative support for the project and convened the project advisory group.
Lorna Crofts convened the focus group and supported the production of this report.
Data-sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Five Year Forward View. London: NHS England; 2014.
- The NHS and Social Care: Quality and Finance Briefing. London: Nuffield Trust; 2014.
- Emmerson C, Johnson P, Joyce R. IFS Green Budget 2017. London: Institute for Fiscal Studies; 2017.
- Managing the Care of People with Long–term Conditions. Second Report of Session 2014–15. London: The Stationery Office; 2014.
- Ham C, Walsh N. Lessons from Experience: Making Integrated Care Happen at Scale and Pace. London: The King’s Fund; 2013.
- Emergency Admissions to Hospital: Managing the Demand. London: National Audit Office; 2013.
- Care Closer to Home: Narrative Report. London: Royal College of Physicians; 2012.
- de Silva D. Evidence: Helping People Help Themselves. A Review of the Evidence Considering Whether it is Worthwhile to Support Self-Management. London: The Health Foundation; 2011.
- Ham C, Dixon A, Brooke B. Transforming the Delivery of Health and Social Care: The Case for Fundamental Change. London: The King’s Fund; 2012.
- Future Hospital: Caring for Medical Patients. London: Royal College of Physicians; 2013.
- The Multispecialty Community Provider (MCP) Emerging Care Model and Contract Framework. London: NHS England; 2016.
- Making Integrated Out-Of-Hospital Care a Reality. London: NHS Confederation; 2012.
- Ham C, Smith J, Eastmure E. Commissioning Integrated Care in a Liberated NHS. London: Nuffield Trust; 2011.
- NHS England Draft Contract for MCP documents. London: NHS England; 2016.
- New Care Models: Vanguards – Developing a Blueprint for the Future of NHS and Care Services. London: NHS England; 2016.
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 2014;12:573-6. https://doi.org/10.1370/afm.1713.
- Sikka R, Morath JM, Leape L. The Quadruple Aim: care, health, cost and meaning in work. BMJ Qual Saf 2015;24:608-10. https://doi.org/10.1136/bmjqs-2015-004160.
- New Care Models and Staff Engagement: All Aboard. London: NHS Confederation; 2016.
- Darzi A. High Quality Care For All. NHS Next Stage Review Final Report. London: Department of Health and Social Care; 2008.
- Integrated Care and Support: Our Shared Commitment. London: Department of Health and Social Care; 2013.
- Armitage GD, Suter E, Oelke ND, Adair CE. Health systems integration: state of the evidence. Int J Integr Care 2009;9:1-11. https://doi.org/10.5334/ijic.316.
- Nolte E, Pitchforth E. What is the Evidence on the Economic Impacts of Integrated Care?. Copenhagen: World Health Organization Regional Office Europe; 2014.
- Macadam M. Progress toward integrating care for seniors in Canada: ‘We have to skate toward where the puck is going to be, not to where it has been.’. Int J Integr Care 2011;11. https://doi.org/10.5334/ijic.563.
- Shaw S, Rosen R, Rumbold B. What is Integrated Care? An Overview of Integrated Care in the NHS. London: Nuffield Trust; 2011.
- Naylor C, Alderwick H, Honeyman M. Acute Hospitals and Integrated Care: From Hospitals to Health Systems. London: The King’s Fund; 2015.
- Cameron A, Lart R, Bostock L, Coomber C. Factors that promote and hinder joint and integrated working between health and social care services: a review of research literature. Health Soc Care Community 2014;22:225-33. https://doi.org/10.1111/hsc.12057.
- Four Nations United: Critical Learning from Four Different Systems for the Successful Integration of Social Care and Health Services. London: ADASS; 2013.
- Goodwin N, Dixon A, Anderson G, Wodchis W. Providing Integrated Care for Older People with Complex Needs: Lessons from Seven International Case Studies. London: The King’s Fund; 2014.
- Ling T, Brereton L, Conklin A, Newbould J, Roland M. Barriers and facilitators to integrating care: experiences from the English Integrated Care Pilots. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.982.
- Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care 2013;13. https://doi.org/10.5334/ijic.886.
- GP Access Fund. London: NHS England; n.d.
- Prime Minister’s Challenge Fund: Improving Access to General Practice: Second Evaluation Report to September 2015. London: NHS England; 2016.
- Maughan DL, Patel A, Parveen T, Braithwaite I, Cook J, Lillywhite R, et al. Primary-care-based social prescribing for mental health: an analysis of financial and environmental sustainability. Prim Health Care Res Dev 2016;17:114-21. https://doi.org/10.1017/S1463423615000328.
- Healthy Villages . Birmingham Healthy Villages 2013. http://nhsproviders.org/media/1814/birmingham-final-p.pdf (accessed 21 June 2017).
- Erens B, Wistow G, Mounier-Jack S, Douglas N, Jones L, Manacorda T, et al. Early evaluation of the Integrated Care and Support Pioneers Programme: Final Report. London: Policy Innovation Research Unit, London School of Hygiene and Tropical Medicine; 2016.
- National Evaluation of the Department of Health’s Integrated Care Pilots. Cambridge: RAND Corporation; 2012.
- Pioneer ACO Final Report. Baltimore, MD: Centers for Medicare and Medicaid Services; 2016.
- de Rosa Torner A. Lessons from Spain; The Alzira Model. London: The King’s Fund, International Integrated Care Summit; 2012.
- Gray B, Sarnak D, Burgers J. Home Care by Self-Governing Nursing Teams: The Netherlands’ Buurtzorg Model. New York, NY: The Commonwealth Fund; 2015.
- Hildebrandt H, Hermann C, Knittel R, Richter-Reichhelm M, Siegel A, Witzenrath W. Gesundes Kinzigtal Integrated Care: improving population health by a shared health gain approach and a shared savings contract. Int J Integr Care 2010;10. https://doi.org/10.5334/ijic.539.
- Southcentral Foundation . Nuka FY2015: Progress Report 2016. www.southcentralfoundation.com/wp-content/uploads/2017/01/Progress-Report_2016.pdf (accessed 15 June 2017).
- Making Change Possible: A Transformation Fund for the NHS. London: The Health Foundation; 2015.
- The Patient Protection and Affordable Care Act. Washington, DC: US Congress; 2010.
- Shortell SM, Colla CH, Lewis VA, Fisher E, Kessell E, Ramsay P. Accountable care organizations: the national landscape. J Health Polit Policy Law 2015;40:647-68. https://doi.org/10.1215/03616878-3149976.
- Centers for Medicare and Medicaid Services . Pioneer ACO Model Frequently Asked Questions 2017. https://innovation.cms.gov/initiatives/Pioneer-ACO-Model/Pioneer-ACO-FAQs.html (accessed 21 June 2017).
- Struckmann V, Boerma W, van Ginneken E. Innovating Care for People With Multiple Chronic Conditions in Europe 2015. www.nivel.nl/sites/default/files/bestanden/Rapport-State-of-the-Art-ICARE4EU.pdf (accessed 15 June 2017).
- Schulte T, Pimperl A, Fischer A, Dittmann B, Wendel P, Hildebrandt H. Ergebnisqualität Gesundes Kinzigtal–quantifiziert durch Mortalitätskennzahlen. Das Gesundheitswesen 2016;78. https://doi.org/10.1055/s-0036-1586652.
- Acerete B, Stafford A, Stapleton P. Spanish healthcare public private partnerships: the ‘Alzira model’. Crit Perspect Account 2011;22:533-49. https://doi.org/10.1016/j.cpa.2011.06.004.
- Acerete B, Stafford A, Stapleton P. New development: new global health care PPP developments – a critique of the success story. Public Money Manage 2012;32:311-14. https://doi.org/10.1080/09540962.2012.691315.
- Gottlieb K. The Nuka System of Care: improving health through ownership and relationships. Int J Circumpolar Health 2013;72. https://doi.org/10.3402/ijch.v72i0.21118.
- Goodwin N. Thinking differently about integration: people-centred care and the role of local communities. Int J Integr Care 2014;14. https://doi.org/10.5334/ijic.1736.
- Kreitzer MJ, Monsen KA, Nandram S, de Blok J. Buurtzorg Nederland: a global model of social innovation, change, and whole-systems healing. Glob Adv Health Med 2015;4:40-4. https://doi.org/10.7453/gahmj.2014.030.
- Monsen KA, de Blok J. Buurtzorg: nurse-led community care. Creat Nurs 2013;19:122-7.
- Moore A. At the vanguard of partnership working. Nurs Stand 2016;30:24-5. https://doi.org/10.7748/ns.30.26.24.s24.
- Buurtzorg . The History of Buurtzorg n.d. www.buurtzorg.com/about-us/history/ (accessed 21 June 2017).
- Nandram SS. Organizational Innovation by Integrating Simplification. New York, NY: Springer; 2015.
- Next Steps on the NHS Five Year Forward View. London: NHS England; 2017.
- Williams D. What’s New in Care Models. London: Health Service Journal; 2017.
- Brennan S. Simon Stevens Names the First ‘Accountable Care Systems’. London: Health Service Journal; 2017.
- Williams D, Brennan S. First Nine ‘Accountable Care Systems’ Revealed. London: Health Service Journal; 2017.
- Turner A, Mulla A, Booth A, Aldridge S, Stevens S, Battye F, et al. An evidence synthesis of the international knowledge base for new care models to inform and mobilise knowledge for multispecialty community providers (MCPs). Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0346-x.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Greenhalgh J, Dalkin S, Gooding K, Gibbons E, Wright J, Meads D, et al. Functionality and feedback: a realist synthesis of the collation, interpretation and utilisation of patient-reported outcome measures data to improve patient care. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05020.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: Sage; 2006.
- Booth A, Wright J, Briscoe S, Emmel N, Greenhalgh J, Manzano A, et al. Doing Realist Research. London: Sage; 2018.
- Booth A, Carroll C. How to build up the actionable knowledge base: the role of ‘best fit’ framework synthesis for studies of improvement in healthcare. BMJ Qual Saf 2015;24:700-8. https://doi.org/10.1136/bmjqs-2014-003642.
- Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-39.
- Carroll C, Booth A, Leaviss J, Rick J. ‘Best fit’ framework synthesis: refining the method. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-37.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-33.
- Pawson R, Greenhalgh J, Brennan C. Demand management for planned care: a realist synthesis. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04020.
- Rycroft-Malone J, Burton CR, Williams L, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04120.
- Denyer D, Tranfield D, Buchanan DA, Bryman A. The Sage Handbook of Organizational Research Methods. Thousand Oaks, CA: Sage Publications Ltd; 2009.
- Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist Synthesis: RAMESES Training Materials 2013. www.ramesesproject.org/media/Realist_reviews_training_materials.pdf (accessed 21 June 2017).
- Hewitt G, Sims S, Harris R. The realist approach to evaluation research: an introduction. Int J Ther Rehabil 2012;19:250-9. https://doi.org/10.12968/ijtr.2012.19.5.250.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Pawson R. Nothing as practical as a good theory. Evaluation 2003;9:471-90. https://doi.org/10.1177/1356389003094007.
- Rycroft-Malone J, Burton C, Hall B, McCormack B, Nutley S, Seddon D, et al. Improving skills and care standards in the support workforce for older people: a realist review. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005356.
- Saul JE, Willis CD, Bitz J, Best A. A time-responsive tool for informing policy making: rapid realist review. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-103.
- James K, Randall N, Haddaway N. A methodology for systematic mapping in environmental sciences. Environ Evid 2016;5. https://doi.org/10.1186/s13750-016-0059-6.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Clapton J, Rutter D, Sharif N. SCIE Systematic Mapping Guidance. London: Social Care Institute for Excellence; 2009.
- Funnell S, Rogers P. Purposeful Program Theory: Effective Use of Theories of Change and Logic Models. San Francisco, CA: John Wiley and Sons; 2011.
- Breuer E, Lee L, De Silva M, Lund C. Using theory of change to design and evaluate public health interventions: a systematic review. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0422-6.
- The Magenta Book: Guidance for Evaluation. London: HM Treasury; 2011.
- MCP Framework: Working Document. London: NHS England; 2016.
- Booth A, Sutton A, Papaioannou D. Systematic Approaches to a Successful Literature Review. London: Sage; 2016.
- Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q 2012;90:421-56. https://doi.org/10.1111/j.1468-0009.2012.00670.x.
- The Forward View into Action: New Care Models: Update and Initial Support. London: NHS England; 2015.
- Framework on Integrated, People-Centred Health Services. Geneva: World Health Organization; 2016.
- Fillingham D, Weir B. System Leadership: Lessons and Learning from AQuA’s Integrated Care Discovery Communities. London: The King’s Fund; 2014.
- Gough D. Weight of evidence: a framework for the appraisal of the quality and relevance of evidence. Res Pap Educ 2007;22:213-28. https://doi.org/10.1080/02671520701296189.
- Papaioannou D, Sutton A, Carroll C, Booth A, Wong R. Literature searching for social science systematic reviews: consideration of a range of search techniques. Health Info Libr J 2010;27:114-22. https://doi.org/10.1111/j.1471-1842.2009.00863.x.
- Oliver-Baxter J, Brown L, Bywood P. Integrated Care: What Policies Support and Influence Integration in Health Care in Australia. Adelaide, SA: Primary Health Care Research and Information Service; 2013.
- Williams I, Glasby J. Making ‘what works’ work: the use of knowledge in UK health and social care decision-making. Policy Soc 2010;29:95-102. https://doi.org/10.1016/j.polsoc.2010.03.002.
- Lorenc T, Clayton S, Neary D, Whitehead M, Petticrew M, Thomson H, et al. Crime, fear of crime, environment, and mental health and wellbeing: mapping review of theories and causal pathways. Health Place 2012;18:757-65. https://doi.org/10.1016/j.healthplace.2012.04.001.
- Health Research Authority, INVOLVE . Public Involvement in Research and Research Ethics Committee Review 2016. www.invo.org.uk/posttypepublication/public-involvement-in-research-and-research-ethics-committee-review/ (accessed 21 June 2017).
- Medical Research Council . Is My Study Research? n.d. www.hra-decisiontools.org.uk/research/ (accessed 30 May 2018).
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60. https://doi.org/10.1177/1356389016638615.
- Multi-Specialty Community Provider (MCP) Value Proposition Version 4. Rushcliffe: Principia; 2016.
- Malik A, Aldridge S, Crofts L, Callaghan D, Frith D. Scenario Analysis for Dudley’s Multispecialty Community Provider Strategy V1.1 Full Project Report. West Bromwich: The Strategy Unit; 2018.
- Alderwick H, Ham C, Buck D. Population Health Systems: Going Beyond Integrated Care. London: The King’s Fund; 2015.
- Ham C, Alderwick H. Place-Based Systems Of Care. London: The King’s Fund; 2015.
- Connecting Consultants and GPs. Stockport: Stockport Together; n.d.
- Esmond N, Fay M, Haining S, Thackray N. West Wakefield Health and Wellbeing Limited New Care Model Evaluation Programme Qualitative Evaluation Report. Newcastle: North of England Commissioning Support Unit; 2017.
- Ellins J, Griffith L, Rosen R, Miller R, Brown H, Smith J. Evaluation of the Connected Care Partnership Vanguard. Scoping and Early Findings Report. Birmingham: University of Birmingham and Nuffield Trust; 2017.
- University of Birmingham . An Evaluation of New Models of Care in Sandwell and West Birmingham n.d. www.birmingham.ac.uk/schools/social-policy/departments/health-services-management-centre/research/projects/2017/an-evaluation-of-new-models-of-care-in-sandwell-and-west-birmingham.aspx (accessed 20 November 2017).
- Jones C. West Wakefield Health and Wellbeing MCP Vanguard. Wakefield: West Wakefield Health and Wellbeing; 2015.
- Encompass MCP Value Proposition. Canterbury: Encompass; 2016.
- Evans R, McGovern R, Birch J, Newbury-Birch D. Which extended paramedic skills are making an impact in emergency care and can be related to the UK paramedic system? A systematic review of the literature. Emerg Med J 2014;31:594-603. https://doi.org/10.1136/emermed-2012-202129.
- Wickware C. Ambulance Trust Withdraws Paramedics from Home Visiting Service. London: Healthcare Leader; 2017.
- NHS Next Stage Review: Our Vision for Primary and Community Care. London: Department of Health and Social Care; 2008.
- Integrated Care and Support Pioneer Programme: Annual Report 2014. London: NHS England; 2014.
- Thorlby R, Smith J, Barnett P, Mays N. Primary Care for the 21st Century. London: Nuffield Trust; 2012.
- Ling K. How Neighbourhood Care in the Netherlands is Hitting the Right Note. London: NHS Confederation; 2015.
- Zanon E. Is Sweden’s Model of Integrated Care a Beacon of Light for the NHS?. London: NHS Confederation; 2015.
- Rosen R. Transforming General Practice: What are the Levers for Change?. London: Nuffield Trust; 2015.
- Billings J, de Weger E. Contracting for integrated health and social care : a critical review of four models. J Integr Care 2015;23:153-75. https://doi.org/10.1108/JICA-03-2015-0015.
- Ahmed F, Mays N, Ahmed N, Bisognano M, Gottlieb G. Can the Accountable Care Organization model facilitate integrated care in England?. J Health Serv Res Policy 2015;20:261-4. https://doi.org/10.1177/1355819615590845.
- Shortell SM, Addicott R, Walsh N, Ham C. The NHS Five Year Forward View: lessons from the United States in developing new care models. BMJ 2015;350. https://doi.org/10.1136/bmj.h2005.
- Dudley Clinical Commissioning Group . Multi-Specialty Community Provider (MCP) – Dudley 2017. www.contractsfinder.service.gov.uk/Notice/8840a0a4-d576-43ff-935f-4e1488073290 (accessed 23 June 2017).
- Dudley Multi Specialty Community Provider (MCP). Overview of MCP Role and Responsibilities and Purpose of Prior Information Notice (PIN). Dudley: Dudley CCG; 2016.
- Better Care Fund. Leeds: NHS England; n.d.
- Integrated Care Pioneers. Leeds: NHS England; n.d.
- NICE Quality and Outcomes Framework Indicator. London: NICE; n.d.
- Shortell S, Addicott R, Walsh N, Ham C. Accountable Care Organisations in the United States and England: Testing, Evaluating and Learning What Works. London: The King’s Fund; 2014.
- Zanon E. Germany’s Approach to Integrated Care is Delivering a Trio of Achievements. London: NHS Confederation; 2015.
- The Search for Low-Cost Integrated Healthcare. The Alzira Model – from the Region of Valencia. London: NHS Confederation; 2011.
- Schools App Challenge . Co-Designed Apps by Children, for Children n.d. http://schoolsappchallenge.com/ (accessed 4 June 2018).
- Dudley New Care Model: Developing a Multispecialty Community Provider Value Proposition. February 2016. Dudley: Dudley CCG; 2016.
- The Erewash Multispecialty Community Provider Value Proposition. Refreshed for 2016/17. Derby: Wellbeing Erewash; 2016.
- Dayson C, Bashir N, Pearson S. From Dependence to Independence: Emerging Lessons from the Rotherham Social Prescribing Pilot. Sheffield: Sheffield Hallam University; 2013.
- Horne M, Khan H, Corrigan P. People Powered Health: Health for People, By People and With People. London: Nesta; 2013.
- Service Scope and Service Model for Multi-Specialty Community Provider Document 12. Dudley: Dudley CCG; 2017.
- Freeman G, Hughes J. Continuity of Care and the Patient Experience. London: The King’s Fund; 2010.
- Red Zebra Community Solutions . Help and Support for the Voluntary and Community Sector in Kent n.d. www.redzebra.org.uk/ (accessed 30 May 2018).
- Value Proposition Version 1. Southern Hampshire: Better Local Care; 2015.
- Tanio C, Chen C. Innovations at Miami practice show promise for treating high-risk Medicare patients. Health Aff 2013;32:1078-82. https://doi.org/10.1377/hlthaff.2012.0201.
- Collins B. Intentional Whole Health System Redesign: Southcentral Foundation’s ‘Nuka’ System of Care. London: The King’s Fund; 2015.
- Sunderland All Together Better. Evaluation of ‘All Together Better’ MCP Vanguard Programme – Final Report. London: Cordis Bright; 2017.
- Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-117.
- Evidence Scan: Complex Adaptive Systems. London: The Health Foundation; 2010.
- Ham C, Berwick D, Dixon J. Improving Quality in the English NHS. London: The King’s Fund; 2016.
- Berwick D. How Are the New Care Model Vanguards Working to Improve Outcomes?. London: The King’s Fund; 2016.
- Ham C. The ten characteristics of the high-performing chronic care system. Health Econ Policy Law 2010;5:71-90. https://doi.org/10.1017/S1744133109990120.
- New Care Models and Prevention: An Integral Partnership. London: NHS Confederation; 2016.
- People Helping People. Year Two of the Pioneer Programme. London: NHS England; 2016.
- Dayan M, Arora S, Rosen R, Curry N. Is General Practice in Crisis?. London: Nuffield Trust; 2014.
- Baird B, Charles A, Honeyman M, Maguire D, Das P. Understanding Pressures in General Practice. London: The King’s Fund; 2016.
- General Practice Forward View. London: NHS England; 2016.
- The Future of Primary Care. Creating Teams for Tomorrow. Leeds: Health Education England; 2015.
- Roland M, Wilson E, Pitchforth E, Head F, Abel G, Newbould J. Tele-First: Telephone Triage As an Alternative to Face to Face Contact in General Practice. Protocol 2015. www.journalslibrary.nihr.ac.uk/programmes/hsdr/135940/#/ (accessed 21 June 2017).
- Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A. The potential of alternatives to face-to-face consultation in general practice, and the impact on different patient groups: a mixed-methods case study. Health Serv Deliv Res 2018;6. https://www.ncbi.nlm.nih.gov/books/NBK507060/.
- Martínez-González NA, Djalali S, Tandjung R, Huber-Geismann F, Markun S, Wensing M, et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-214.
- Freund T, Everett C, Griffiths P, Hudon C, Naccarella L, Laurant M. Skill mix, roles and remuneration in the primary care workforce: who are the healthcare professionals in the primary care teams across the world?. Int J Nurs Stud 2015;52:727-43. https://doi.org/10.1016/j.ijnurstu.2014.11.014.
- Laurant M, Harmsen M, Faber M, Wollersheim H, Sibbald B, Grol R. Revision of Professional Roles and Quality Improvement: A Review of the Evidence. London: The Health Foundation; 2010.
- Rashid C. Benefits and limitations of nurses taking on aspects of the clinical role of doctors in primary care: integrative literature review. J Adv Nurs 2010;66:1658-70. https://doi.org/10.1111/j.1365-2648.2010.05327.x.
- Tan EC, Stewart K, Elliott RA, George J. Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Social Adm Pharm 2014;10:608-22. https://doi.org/10.1016/j.sapharm.2013.08.006.
- Jorgenson D, Laubscher T, Lyons B, Palmer R. Integrating pharmacists into primary care teams: barriers and facilitators. Int J Pharm Pract 2014;22:292-9. https://doi.org/10.1111/ijpp.12080.
- Bradley F, Elvey R, Ashcroft DM, Hassell K, Kendall J, Sibbald B, et al. The challenge of integrating community pharmacists into the primary health care team: a case study of local pharmaceutical services (LPS) pilots and interprofessional collaboration. J Interprof Care 2008;22:387-98. https://doi.org/10.1080/13561820802137005.
- Mallett R, Bakker E, Burton M. Is physiotherapy self-referral with telephone triage viable, cost-effective and beneficial to musculoskeletal outpatients in a primary care setting?. Musculoskeletal Care 2014;12:251-60. http://dx.doi.org/10.1002/msc.1075.
- Salisbury C, Montgomery AA, Hollinghurst S, Hopper C, Bishop A, Franchini A, et al. Effectiveness of PhysioDirect telephone assessment and advice services for patients with musculoskeletal problems: pragmatic randomised controlled trial. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f43.
- Imison C, Castle-Clarke S, Watson R. Reshaping the Workforce to Deliver the Care Patients Need. London: Nuffield Trust; 2016.
- Drennan VM, Halter M, Joly L, Gage H, Grant RL, Gabe J, et al. Physician associates and GPs in primary care: a comparison. Br J Gen Pract 2015;65:e344-50. https://doi.org/10.3399/bjgp15X684877.
- Drennan VM, Halter M, Brearley S, Carneiro W, Gabe J, Gage H, et al. Investigating the contribution of physician assistants to primary care in England: a mixed-methods study. Health Serv Deliv Res 2014;2. http://dx.doi.org/10.3310/hsdr02160.
- Drennan V, Levenson R, Halter M, Tye C. Physician assistants in English general practice: a qualitative study of employers’ viewpoints. J Health Serv Res Policy 2011;16:75-80. https://doi.org/10.1258/jhsrp.2010.010061.
- Ware J, Mawby R. Patient Access to General Practice: Ideas and Challenges from the Front Line. London: Royal College of General Practitioners; 2015.
- Aboulghate A, Abel G, Elliott MN, Parker RA, Campbell J, Lyratzopoulos G, et al. Do English patients want continuity of care, and do they receive it?. Br J Gen Pract 2012;62:e567-75. https://doi.org/10.3399/bjgp12X653624.
- Anwar MS, Baker R, Walker N, Mainous AG, Bankart MJ. Chronic disease detection and access: does access improve detection, or does detection make access more difficult?. Br J Gen Pract 2012;62:e337-43. https://doi.org/10.3399/bjgp12X641456.
- Rose KD, Ross JS, Horwitz LI. Advanced access scheduling outcomes: a systematic review. Arch Intern Med 2011;171:1150-9. https://doi.org/10.1001/archinternmed.2011.168.
- Boyle B, Appleby J, Harrison A. A Rapid View of Access to Care. London: The King’s Fund; 2010.
- NHS Greater Manchester Primary Care Demonstrator Evaluation. Final Report. Manchester: NIHR CLAHRC Greater Manchester; 2015.
- Taneja A, Singh PP, Tan JP, Hill DG, Connolly AB, Hill AG. Efficacy of general practitioners with specialty interests for surgical procedures. ANZ J Surg 2015;85:344-8. https://doi.org/10.1111/ans.12721.
- Winpenny E, Miani C, Pitchforth E, Ball S, Nolte E, King S, et al. Outpatient services and primary care: scoping review, substudies and international comparisons. Health Serv Deliv Res 2016;4. http://dx.doi.org/10.3310/hsdr04150.
- Chambers D, Booth A, Baxter SK, Johnson M, Dickinson KC, Goyder EC. Evidence for models of diagnostic service provision in the community: literature mapping exercise and focused rapid reviews. Health Serv Deliv Res 2016;4. http://dx.doi.org/10.3310/hsdr04350.
- Heath G, Cameron E, Cummins C, Greenfield S, Pattison H, Kelly D, et al. Paediatric ‘care closer to home’: stake-holder views and barriers to implementation. Health Place 2012;18:1068-73. https://doi.org/10.1016/j.healthplace.2012.05.003.
- McLeod H, Heath G, Cameron E, Debelle G, Cummins C. Introducing consultant outpatient clinics to community settings to improve access to paediatrics: an observational impact study. BMJ Qual Saf 2015;24:377-84. https://doi.org/10.1136/bmjqs-2014-003687.
- Heath G, Greenfield S, Redwood S. The meaning of ‘place’ in families’ lived experiences of paediatric outpatient care in different settings: a descriptive phenomenological study. Health Place 2015;31:46-53. https://doi.org/10.1016/j.healthplace.2014.10.014.
- Robertson R, Sonola L, Honeyman M, Brooke B, Kothari S. Specialists in Out-Of-Hospital Settings: Findings from Six Case Studies. London: The King’s Fund; 2014.
- International Profiles of Health Care Systems. New York, NY: The Commonwealth Fund; 2017.
- Halter M, Drennan V, Chattopadhyay K, Carneiro W, Yiallouros J, de Lusignan S, et al. The contribution of physician assistants in primary care: a systematic review. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-223.
- Williams H, Stone M. The Benefits of Employing Pharmacists in GP Practices. Medeconomics; 2014.
- Bramwell D, Checkland K, Allen P, Peckham S. Moving Services Out of Hospital: Joining Up General Practice and Community Services?. London: Policy Research Unit in Commissioning and the Healthcare System; 2014.
- Imison C, Naylor C, Maybin J. Under One Roof: Will Polyclinics Deliver Integrated Care?. London: The King’s Fund; 2008.
- Montgomery-Taylor S, Watson M, Klaber R. Child Health General Practice Hubs: a service evaluation. Arch Dis Child 2016;101:333-7. https://doi.org/10.1136/archdischild-2015-308910.
- Montgomery-Taylor S, Cotton R, Manek N, Watson M, Klaber RE. Using an email advice line to connect care for children. Arch Dis Child 2015;100:600-1. https://doi.org/10.1136/archdischild-2015-308199.
- Pollard L, Rogers S, Shribman J, Sprigings D, Sinfield P. A study of role expansion: a new GP role in cardiology care. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-205.
- College of Paramedics . Paramedics Career Framework 2016. www.collegeofparamedics.co.uk/downloads/College_of_ParamedicsInteractiveCareer_Framework16.pdf (accessed 21 June 2017).
- Drennan V, Halter M, Brearley S, Carneiro W, Gabe J, Gage H. Investigating the contribution of physician assistants to primary care in England: a mixed-methods study. Health Serv Deliv Res 2014;2.
- Rosen R, Kumpunen S, Curry N, Davies A, Pettigrew L, Kossarova L. Is Bigger Better? Lessons for Large-Scale General Practice. London: Nuffield Trust; 2016.
- Imison C, Curry N, Holder H, Castle-Clarke S, Nimmons D, Appleby J, et al. Shifting the Balance of Care: Great Expectations. London: Nuffield Trust; 2017.
- Bienkowska-Gibbs T, King S, Saunders C, Henham M. New Organisational Models of Primary Care to Meet the Future Needs of the NHS: A Brief Overview of Recent Reports. Santa Monica, CA: RAND Corporation; 2015.
- Donnelly C, Brenchley C, Crawford C, Letts L. The integration of occupational therapy into primary care: a multiple case study design. BMC Fam Pract 2013;14. https://doi.org/10.1186/1471-2296-14-60.
- Collaborations for Leadership in Applied Health Research and Care Greater Manchester . Project: GP Access Fund Wave 2 Evaluation 2017. http://clahrc-gm.nihr.ac.uk/our-work/organising-healthcare/gp-access-fund-evaluation/ (accessed 21 June 2017).
- NHS England . Clinical Pharmacists in General Practice 2017. www.england.nhs.uk/gp/gpfv/workforce/building-the-general-practice-workforce/cp-gp/ (accessed 21 June 2017).
- Andersson J, Wikström E. Constructing accountability in inter-organisational collaboration: the implications of a narrow performance-based focus. J Health Organ Manag 2014;28:619-34. https://doi.org/10.1108/JHOM-10-2013-0220.
- Mason A, Goddard M, Weatherly H. Financial Mechanisms for Integrating Funds for Health and Social Care: An Evidence Review. York: University of York; 2014.
- GP Participation in a Multispecialty Community Provider. Supporting Document to Draft Multispecialty Community Provider Contract. London: NHS England; 2016.
- Multispecialty Community Providers (MCPs) and the NHS Commissioning System. Supporting Document to Draft Multispecialty Community Provider Contract. London: NHS England; 2016.
- Collins B. New Care Models: Emerging Innovations in Governance and Organisational Form. London: The King’s Fund; 2016.
- Addicott R. Commissioning and Contracting for Integrated Care. London: The King’s Fund; 2014.
- Multispecialty Community Provider (MCP) Financial Strategy. Supporting Document to Multispecialty Community Provider Contract. London: NHS England; 2016.
- Porter ME. What is value in health care?. N Engl J Med 2010;363:2477-81. https://doi.org/10.1056/NEJMp1011024.
- Flodgren G, Eccles MP, Shepperd S, Scott A, Parmelli E, Beyer FR. An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database Syst Rev 2011;7. https://doi.org/10.1002/14651858.CD009255.
- Scott A, Sivey P, Ait Ouakrim D, Willenberg L, Naccarella L, Furler J, et al. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database Syst Rev 2011;9. https://doi.org/10.1002/14651858.CD008451.pub2.
- Yuan B, He L, Meng Q, Jia L. Payment methods for outpatient care facilities. Cochrane Database Syst Rev 2017;3. https://doi.org/10.1002/14651858.CD011153.pub2.
- Shortt S. Greater Nottingham Accountable Care System n.d.
- Mason A, Goddard M, Weatherly H, Chalkley M. Integrating funds for health and social care: an evidence review. J Health Serv Res Policy 2015;20:177-88. https://doi.org/10.1177/1355819614566832.
- Health and Social Care Integration. London: National Audit Office; 2017.
- Bambra C, Garthwaite K, Hunter D. All things being equal: does it matter for equity how you organize and pay for health care? A review of the international evidence. Int J Health Serv 2014;44:457-77. https://doi.org/10.2190/HS.44.3.c.
- Dixon A, Khachatryan A, Wallace A, Peckham S, Boyce T, Gillam S. Impact of Quality and Outcomes Framework on Health Inequalities. London: The King’s Fund; 2011.
- Chew-Graham CA, Hunter C, Langer S, Stenhoff A, Drinkwater J, Guthrie EA, et al. How QOF is shaping primary care review consultations: a longitudinal qualitative study. BMC Fam Pract 2013;14. https://doi.org/10.1186/1471-2296-14-103.
- Blakeman T, Chew-Graham C, Reeves D, Rogers A, Bower P. The Quality and Outcomes Framework and self-management dialogue in primary care consultations: a qualitative study. Br J Gen Pract 2011;61:e666-73. https://doi.org/10.3399/bjgp11X601389.
- Calvert M, Shankar A, McManus RJ, Lester H, Freemantle N. Effect of the Quality and Outcomes Framework on diabetes care in the United Kingdom: retrospective cohort study. BMJ 2009;338. https://doi.org/10.1136/bmj.b1870.
- Roland M, Paddison C. Better management of patients with multimorbidity. BMJ 2013;346. https://doi.org/10.1136/bmj.f2510.
- Forbes L, Marchand C, Peckham S. Review of the Quality and Outcomes Framework in England: Final Report. London: Policy Research Unit in Commissioning and the Healthcare System; 2016.
- Dickinson H, Glasby J, Nicholds A, Sullivan H. Making sense of joint commissioning: three discourses of prevention, empowerment and efficiency. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-S1-S6.
- Humphries R. Integrated health and social care in England – progress and prospects. Health Policy 2015;119:856-9. https://doi.org/10.1016/j.healthpol.2015.04.010.
- Allen P, Petsoulas C, Ritchie B. Study of the Use of Contractual Mechanisms in Commissioning: Final Report. London: Policy Research Unit in Commissioning and the Healthcare System; 2015.
- Burns LR, Pauly MV. Accountable care organizations may have difficulty avoiding the failures of integrated delivery networks of the 1990s. Health Aff 2012;31:2407-16. https://doi.org/10.1377/hlthaff.2011.0675.
- Song Z, Safran DG, Landon BE, Landrum MB, He Y, Mechanic RE, et al. The ‘Alternative Quality Contract,’ based on a global budget, lowered medical spending and improved quality. Health Aff 2012;31:1885-94. https://doi.org/10.1377/hlthaff.2012.0327.
- Moving Healthcare Closer to Home: Summary. London: Monitor; 2015.
- Colla CH, Wennberg DE, Meara E, Skinner JS, Gottlieb D, Lewis VA, et al. Spending differences associated with the Medicare Physician Group Practice Demonstration. JAMA 2012;308:1015-23. https://doi.org/10.1001/2012.jama.10812.
- Gorman D, Horn M. Purchasing better, innovative and integrated health services. Intern Med J 2015;45:1205-10. https://doi.org/10.1111/imj.12929.
- Sanderson M, Allen P, Garnett E, Gill R. Alliance Contracting, Prime Contracting and Outcome Based Contracting: What Can the NHS Learn from Elsewhere? A Literature Review. London: Policy Research Unit in Commissioning and the Healthcare System; 2016.
- Hopson C. Next Steps for Delivering the New Models of Care and Vanguard Sites. London: Westminster Health Forum; 2016.
- Conrad DA. The theory of value-based payment incentives and their application to health care. Health Serv Res 2015;50:2057-89. https://doi.org/10.1111/1475-6773.12408.
- Baicker K, Levy H. Coordination versus competition in health care reform. N Engl J Med 2013;369:789-91. https://doi.org/10.1056/NEJMp1306268.
- West J. Next Steps for Delivering the New Models of Care and Vanguard Sites. London: Westminster Health Forum; 2016.
- Oversight of New Care Models. Key Issues: Your Questions Answered. London: NHS Improvement; 2017.
- An Update on Hinchingbrooke Health Care NHS Trust. London: The Stationery Office; 2015.
- Stout D. NHS England Review of Uniting Care Contract. The Key Facts and Root Causes behind the Termination of the UnitingCare Partnership Contract. London: NHS England; 2016.
- Investigation into the Collapse of the UnitingCare Partnership Contract in Cambridgeshire and Peterborough. London: National Audit Office; 2016.
- UnitingCare Partnership (UCP) Procurement Review. London: NHS England; 2016.
- Britnell M, Jamilkowski M, Kuehn J. Paths to Population Health. Achieving Coordinated and Accountable Care. London: Klynveld Peat Marwick Goerdeler; 2015.
- Lynn J, McKethan A, Jha AK. Value-based payments require valuing what matters to patients. JAMA 2015;314:1445-6. https://doi.org/10.1001/jama.2015.8909.
- Mehrotra A, Sorbero ME, Damberg CL. Using the lessons of behavioral economics to design more effective pay-for-performance programs. Am J Manag Care 2010;16:497-503.
- Crinson I, Gallagher H, Thomas N, de Lusignan S. How ready is general practice to improve quality in chronic kidney disease? A diagnostic analysis. Br J Gen Pract 2010;60:403-9. https://doi.org/10.3399/bjgp10X502100.
- Goodwin N, Dixon A, Poole T, Raleigh V. Improving the Quality of Care in General Practice: Report of an Independent Inquiry Commissioned by The King’s Fund. London: The King’s Fund; 2011.
- Sumner J. Next steps for Delivering the New Models of Care and Vanguard Sites. London; 2016.
- Weeks WB, Gottlieb DJ, Nyweide DE, Sutherland JM, Bynum J, Casalino LP, et al. Higher health care quality and bigger savings found at large multispecialty medical groups. Health Aff 2010;29:991-7. https://doi.org/10.1377/hlthaff.2009.0388.
- Gray M. A Culture of Stewardship. The Responsibility of NHS Leaders to Deliver Better Value Healthcare. London: NHS Confederation; 2015.
- Community Engagement: Improving Health and Wellbeing. London: NICE; 2017.
- Gowar C. Inclusive Communities: A Research Report 2014.
- Crow G, Mah A. Connected Communities. Conceptualisations and Meanings of ‘Community’: The Theory and Operationalization of a Contested Concept. Bristol: University of Bristol; 2012.
- Sellick V. People Helping People: Lessons Learned from Three Years Supporting Social Action Innovations to Scale. London: Nesta; 2016.
- Georghiou T, Ariti C, Davies M, Arora S, Bhatia T, Bardsley M, et al. Harnessing Social Action to Support Older People: Evaluating the Reducing Winter Pressures Fund. London: Nuffield Trust; 2016.
- Social Prescribing at a Glance: North West England. A Scoping Report of Activity for the North West. Manchester: Health Education England; 2016.
- Realising the Value: Ten Key Actions to Put People and Communities at the Heart of Health and Wellbeing. London: The Health Foundation, Nesta, NHS England; 2016.
- Realpe A, Wallace LM. What is Co-production?. London: The Health Foundation; 2010.
- Ostrom V, Ostrom E, Savas E. Alternatives for Delivering Public Services. Boulder, CO: West View Press; 1978.
- People Powered Health Co-Production Catalogue. London: Nesta; 2012.
- New Care Models: Empowering Patients and Communities – A Call to Action for a Directory of Support. London: NHS England; 2015.
- Working Together – How Health, Social Care and Fire and Rescue Services Can Increase their Reach, Scale and Impact Through Joint Working. London: NHS England; 2016.
- Wulff K, Donato D, Lurie N. What is health resilience and how can we build it?. Annu Rev Public Health 2015;36:361-74. https://doi.org/10.1146/annurev-publhealth-031914-122829.
- Poortinga W. Community resilience and health: the role of bonding, bridging, and linking aspects of social capital. Health Place 2012;18:286-95. https://doi.org/10.1016/j.healthplace.2011.09.017.
- Coventry PA, Small N, Panagioti M, Adeyemi I, Bee P. Living with complexity; marshalling resources: a systematic review and qualitative meta-synthesis of lived experience of mental and physical multimorbidity. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0345-3.
- Adapting to Change: The Role of Community Resilience. London: Young Foundation; 2012.
- Building the Big Society. London: The Stationery Office; 2010.
- Healthy Lives, Healthy People; Our Strategy for Public Health in England. London: The Stationery Office; 2010.
- Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-Arrigan L, et al. Coproduction of healthcare service. BMJ Qual Saf 2016;25:509-17. https://doi.org/10.1136/bmjqs-2015-004315.
- Boger E, Ellis J, Latter S, Foster C, Kennedy A, Jones F, et al. Self-management and self-management support outcomes: a systematic review and mixed research synthesis of stakeholder views. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0130990.
- Philips A, Morgan G. Co-production within health and social care – the implications for Wales?. Qual Ageing Older Adults 2015;15:10-2. https://doi.org/10.1108/QAOA-06-2013-0014.
- O’Mara-Eves A, Brunton G, McDaid D, Oliver S, Kavanaugh J, Jamal F, et al. Community engagement to reduce inequalities in health: a systematic review, meta-analysis and economic analysis. Public Health Res 2013;1.
- Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013384.
- Cyril S, Smith BJ, Possamai-Inesedy A, Renzaho AM. Exploring the role of community engagement in improving the health of disadvantaged populations: a systematic review. Glob Health Action 2015;8. https://doi.org/10.3402/gha.v8.29842.
- Attree P, French B, Milton B, Povall S, Whitehead M, Popay J. The experience of community engagement for individuals: a rapid review of evidence. Health Soc Care Community 2011;19:250-60. https://doi.org/10.1111/j.1365-2524.2010.00976.x.
- Ryder E. The Flexible Care Service: a third-sector service for older people with mental health needs. Br J Community Nurs 2015;20:30-4. https://doi.org/10.12968/bjcn.2015.20.1.30.
- Dayson C, Bashir N. The Social and Economic Impact of the Rotherham Social Prescribing Pilot: Main Evaluation Report. Sheffield: Sheffield Hallam University; 2014.
- Vogelpoel N, Jarrold K. Social prescription and the role of participatory arts programmes for older people with sensory impairments. J Integr Care 2014;22:39-50. https://doi.org/10.1108/JICA-01-2014-0002.
- Clarke D, Jones F, Harris R, Robert G. Collaborative Rehabilitation Environments in Acute Stroke (CREATE) team . What outcomes are associated with developing and implementing co-produced interventions in acute healthcare settings? A rapid evidence synthesis. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014650.
- Popay J, Whitehead M, Carr-Hill R, Dibben C, Dixon P, Halliday E, et al. The impact on health inequalities of approaches to community engagement in the New Deal for Communities regeneration initiative: a mixed-methods evaluation. Public Health Res 2015;3. https://doi.org/10.3310/phr03120.
- Voorberg WH, Bekkers VJJM, Tummers LG. A systematic review of co-creation and co-production: embarking on the social innovation journey. Public Manag Rev 2015;17:1333-57. https://doi.org/10.1080/14719037.2014.930505.
- Boyle D, Harris M. The Challenge of Co-Production. London: Nesta; 2009.
- White JM, Cornish F, Kerr S. Front-line perspectives on ‘joined-up’ working relationships: a qualitative study of social prescribing in the west of Scotland. Health Soc Care Community 2017;25:194-203. https://doi.org/10.1111/hsc.12290.
- Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner-Brown J, Krause LK. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst Rev 2015;6. https://doi.org/10.1002/14651858.CD009905.pub2.
- Rippon S, Hopkins T. Head, Hands and Heart: Asset-Based Approaches in Health Care. London: The Health Foundation; 2015.
- Taylor SJC, Pinnock H, Epiphaniou E, Pearce G, Parke HL, Schwappach A, et al. A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions: PRISMS – Practical systematic Review of Self-Management Support for long-term conditions. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02530.
- Farenden C, Mitchell C, Feast S, Verdenicci S. Community Navigation in Brighton & Hove. Evaluation of a Social Prescribing Pilot. Hove: Brighton and Hove Impetus; 2015.
- Panagioti M, Richardson G, Murray E, Rogers A, Kennedy A, Newman S, et al. Reducing Care Utilisation through Self-management Interventions (RECURSIVE): a systematic review and meta-analysis. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02540.
- Masters R, Anwar E, Collins B, Cookson R, Capewell S. Return on investment of public health interventions: a systematic review. J Epidemiol Community Health 2017;71:827-34. https://doi.org/10.1136/jech-2016-208141.
- del Castillo J, Khan H, Nicholas L, Finnis A. Health as a Social Movement: The Power of People in Movements. London: Nesta; 2016.
- Filipe A, Renedo A, Marston C. The co-production of what? Knowledge, values, and social relations in health care. PLOS Biol 2017;15. https://doi.org/10.1371/journal.pbio.2001403.
- Addicott R. Working Together to Deliver the Mandate: Strengthening Partnerships Between the NHS and the Voluntary Sector. London: The King’s Fund; 2013.
- Kovacs Burns K, Bellows M, Eigenseher C, Gallivan J. ‘Practical’ resources to support patient and family engagement in healthcare decisions: a scoping review. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-175.
- Cameron A, Bostock L, Lart R. Service user and carers perspectives of joint and integrated working between health and social care. J Integr Care 2014;22:62-70. https://doi.org/10.1108/JICA-10-2013-0042.
- Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf 2016;25:626-32. https://doi.org/10.1136/bmjqs-2015-004839.
- Tsegai A, Gamiz R. Messages for integration from working with carers. J Integr Care 2014;22:99-107. https://doi.org/10.1108/JICA-04-2014-0011.
- Howieson B, Fenwick C. A mutual health service in Scotland. Do we understand fully the leadership implications?. Leadersh Health Serv 2014;27:193-20. https://doi.org/10.1108/LHS-12-2012-0040.
- Liddy C, Blazkho V, Mill K. Challenges of self-management when living with multiple chronic conditions: systematic review of the qualitative literature. Can Fam Physician 2014;60:1123-33.
- Sadler E, Wolfe CD, McKevitt C. Lay and health care professional understandings of self-management: a systematic review and narrative synthesis. SAGE Open Med 2014;2. https://doi.org/10.1177/2050312114544493.
- The Future of People Powered Health. Insights from Leaders and Thinkers on How Digital and Social Innovation Can Contribute to Better Outcomes. London: Nesta; 2016.
- Bloomfield M, Cayton H. Community Engagement Report for the Health Foundation. London: The Health Foundation; 2009.
- Coulter A. Engaging Communities for Health Improvement: A Scoping Study for the Health Foundation. London: The Health Foundation; 2009.
- Brunton G, Caird J, Kneale D, Thomas J, Richardson M. Review 2: Community Engagement for Health Via Coalitions, Collaborations and Partners. A Systematic Review and Meta-Analysis. London: Evidence for Policy and Practice Information Centre; 2015.
- Seale B. Patients as Partners: Building Collaborative Relationships Among Professionals, Patients, Carers and Communities. London: The King’s Fund; 2016.
- Vennik F. Co-production in healthcare: rhetoric and practice. Int Rev Admin Sci 2015;82:150-68. https://doi.org/10.1177/0020852315570553.
- NHS England . NHS RightCare Pathways 2016. www.england.nhs.uk/rightcare/products/pathways (accessed 19 October 2017).
- Grant P, Chika-Ezerihoa I. Evaluating diabetes integrated care pathways. Pract Diabet 2014;31:319-22. https://doi.org/10.1002/pdi.1894.
- Tomlinson P, Hewitt S, Blackshaw N. Joining up health and planning: how Joint Strategic Needs Assessment (JSNA) can inform health and wellbeing strategies and spatial planning. Perspect Public Health 2013;133:254-62. https://doi.org/10.1177/1757913913488331.
- Threapleton DE, Chung RY, Wong SYS, Wong E, Chau P, Woo J, et al. Integrated care for older populations and its implementation facilitators and barriers: a rapid scoping review. Int J Qual Health Care 2017;29:327-34. https://doi.org/10.1093/intqhc/mzx041.
- Whittle C, Hewison A. Integrated care pathways: pathways to change in health care?. J Health Organ Manag 2007;21:297-306. https://doi.org/10.1108/14777260710751753.
- Curry N, Ham C. Clinical and Service Integration: The Route to Improved Outcomes. London: The King’s Fund; 2010.
- McConnell T, O’Halloran P, Porter S, Donnelly M. Systematic realist review of key factors affecting the successful implementation and sustainability of the Liverpool care pathway for the dying patient. Worldviews Evid Based Nurs 2013;10:218-37. https://doi.org/10.1111/wvn.12003.
- Beenstock J, Sowden S, Hunter DJ, White M. Are health and well-being strategies in England fit for purpose? A thematic content analysis. J Public Health 2015;37:461-9. https://doi.org/10.1093/pubmed/fdu073.
- Chen J, Ou L, Hollis SJ. A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-211.
- Veenstra GL, Ahaus K, Welker GA, Heineman E, van der Laan MJ, Muntinghe FL. Rethinking clinical governance: healthcare professionals’ views: a Delphi study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-012591.
- Nolte E, Knai C, McKee M. Managing Chronic Conditions: Experience in Eight Countries. Copenhagen: World Health Organization Regional Office Europe; 2008.
- McCarthy D, Mueller K, Wrenn J. Mayo Clinic: Multidisciplinary Teamwork, Physician-Led Governance, and Patient-Centered Culture Drive World-Class Health Care. New York, NY: Commonwealth Fund; 2009.
- Asch SM, McGlynn EA, Hogan MM, Hayward RA, Shekelle P, Rubenstein L, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Intern Med 2004;141:938-45. https://doi.org/10.7326/0003-4819-141-12-200412210-00010.
- Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manag Care 2004;10:828-36.
- Darkins A, Ryan P, Kobb R, Foster L, Edmonson E, Wakefield B, et al. Care Coordination/Home Telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health 2008;14:1118-26. https://doi.org/10.1089/tmj.2008.0021.
- Åhgren B. Chain of care development in Sweden: results of a national study. Int J Integr Care 2003;3. https://doi.org/10.5334/ijic.88.
- Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care – two essential elements of delivery-system reform. N Engl J Med 2009;361:2301-3. https://doi.org/10.1056/NEJMp0909327.
- Gulliford M, Naithani S, Morgan M. What is ‘continuity of care’?. J Health Serv Res Policy 2006;11:248-50. https://doi.org/10.1258/135581906778476490.
- Björkelund C, Maun A, Murante AM, Hoffman K, De Maeseneer J, Farkas-Pall Z. Impact of continuity on quality of primary care: from the perspective of citizens’ preferences and multimorbidity - position paper of the European Forum for Primary Care. Qual Prim Care 2013;21:193-204.
- Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data. BMJ 2017;356. https://doi.org/10.1136/bmj.j84.
- Sturmberg J, Lanham HJ. Understanding health care delivery as a complex system: achieving best possible health outcomes for individuals and communities by focusing on interdependencies. J Eval Clin Pract 2014;20:1005-9. https://doi.org/10.1111/jep.12142.
- Kadam UT, Uttley J, Jones PW, Iqbal Z. Chronic disease multimorbidity transitions across healthcare interfaces and associated costs: a clinical-linkage database study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003109.
- Kasteridis P, Street A, Dolman M, Gallier L, Hudson K, Martin J, et al. Who would most benefit from improved integrated care? Implementing an analytical strategy in South Somerset. Int J Integr Care 2015;15. https://doi.org/10.5334/ijic.1594.
- Powers BW, Milstein A, Jain SH. Delivery models for high-risk older patients: back to the future?. JAMA 2016;315:23-4. https://doi.org/10.1001/jama.2015.17029.
- Ruikes FG, Zuidema SU, Akkermans RP, Assendelft WJ, Schers HJ, Koopmans RT. Multicomponent program to reduce functional decline in frail elderly people: a cluster controlled trial. J Am Board Fam Med 2016;29:209-17. https://doi.org/10.3122/jabfm.2016.02.150214.
- Thistlethwaite P. Integrating Health and Social Care in Torbay. Improving Care for Mrs Smith. London: The King’s Fund; 2011.
- Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev 2012;10. https://doi.org/10.1002/14651858.CD006525.pub2.
- Bearne LM, Byrne AM, Segrave H, White CM. Multidisciplinary team care for people with rheumatoid arthritis: a systematic review and meta-analysis. Rheumatol Int 2016;36:311-24. https://doi.org/10.1007/s00296-015-3380-4.
- Chung LP, Lake F, Hyde E, McCamley C, Phuangmalai N, Lim M, et al. Integrated multidisciplinary community service for chronic obstructive pulmonary disease reduces hospitalisations. Intern Med J 2016;46:427-34. https://doi.org/10.1111/imj.12984.
- Coventry PA, Hudson JL, Kontopantelis E, Archer J, Richards DA, Gilbody S, et al. Characteristics of effective collaborative care for treatment of depression: a systematic review and meta-regression of 74 randomised controlled trials. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0108114.
- Fortuna RJ, Nagel AK, Rose E, McCann R, Teeters JC, Quigley DD, et al. Effectiveness of a multidisciplinary intervention to improve hypertension control in an urban underserved practice. J Am Soc Hypertens 2015;9:966-74. https://doi.org/10.1016/j.jash.2015.10.004.
- Glogowska M, Simmonds R, McLachlan S, Cramer H, Sanders T, Johnson R, et al. Managing patients with heart failure: a qualitative study of multidisciplinary teams with specialist heart failure nurses. Ann Fam Med 2015;13:466-71. https://doi.org/10.1370/afm.1845.
- Green C, Richards DA, Hill JJ, Gask L, Lovell K, Chew-Graham C, et al. Cost-effectiveness of collaborative care for depression in UK primary care: economic evaluation of a randomised controlled trial (CADET). PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0104225.
- Bonney A, Magee C, Pearson R. Cross-sectional survey of older patients’ views regarding multidisciplinary care for chronic conditions in general practice. Aust J Prim Health 2014;20:27-33. https://doi.org/10.1071/PY12101.
- Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 2012;345. https://doi.org/10.1136/bmj.e5205.
- Tricco AC, Antony J, Ivers NM, Ashoor HM, Khan PA, Blondal E, et al. Effectiveness of quality improvement strategies for coordination of care to reduce use of health care services: a systematic review and meta-analysis. CMAJ 2014;186:E568-78. https://doi.org/10.1503/cmaj.140289.
- Hernández C, Alonso A, Garcia-Aymerich J, Serra I, Marti D, Rodriguez-Roisin R, et al. Effectiveness of community-based integrated care in frail COPD patients: a randomised controlled trial. NPJ Prim Care Respir Med 2015;25. https://doi.org/10.1038/npjpcrm.2015.22.
- Huang Y, Wei X, Wu T, Chen R, Guo A. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis. BMC Psychiatry 2013;13. https://doi.org/10.1186/1471-244X-13-260.
- Maneze D, Dennis S, Chen HY, Taggart J, Vagholkar S, Bunker J, et al. Multidisciplinary care: experience of patients with complex needs. Aust J Prim Health 2014;20:20-6. https://doi.org/10.1071/PY12072.
- Raine R, Wallace I, Nic a’ Bháird C, Xanthopoulou P, Lanceley A, Clarke A, et al. Improving the effectiveness of multidisciplinary team meetings for patients with chronic diseases: a prospective observational study. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02370.
- Kruis AL, Boland MR, Assendelft WJ, Gussekloo J, Tsiachristas A, Stijnen T, et al. Effectiveness of integrated disease management for primary care chronic obstructive pulmonary disease patients: results of cluster randomised trial. BMJ 2014;349. https://doi.org/10.1136/bmj.g5392.
- Loewenson R, Simpson S. Strengthening integrated care through population-focused primary care services: international experiences outside the United States. Annu Rev Public Health 2017;38:413-29. https://doi.org/10.1146/annurev-publhealth-031816-044518.
- Ouwens M, Wollersheim H, Hermens R, Hulscher M, Grol R. Integrated care programmes for chronically ill patients: a review of systematic reviews. Int J Qual Health Care 2005;17:141-6. https://doi.org/10.1093/intqhc/mzi016.
- Stranges PM, Marshall VD, Walker PC, Hall KE, Griffith DK, Remington T. A multidisciplinary intervention for reducing readmissions among older adults in a patient-centered medical home. Am J Manag Care 2015;21:106-13.
- Kruis AL, Soljak M, Chavannes NH, Elkin SL. COPD multidisciplinary team meetings in the United Kingdom: health care professionals’ perceptions of aims and structure. COPD 2016;13:639-41. https://doi.org/10.3109/15412555.2015.1007930.
- Nandram S, Koster N. Organizational innovation and integrated care: lessons from Buurtzorg. J Integr Care 2014;22:174-84. https://doi.org/10.1108/JICA-06-2014-0024.
- Martínez-González NA, Berchtold P, Ullman K, Busato A, Egger M. Integrated care programmes for adults with chronic conditions: a meta-review. Int J Qual Health Care 2014;26:561-70. https://doi.org/10.1093/intqhc/mzu071.
- Mulvale G, Embrett M, Razavi SD. ‘Gearing Up’ to improve interprofessional collaboration in primary care: a systematic review and conceptual framework. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0492-1.
- Morgan S, Pullon S, McKinlay E. Observation of interprofessional collaborative practice in primary care teams: an integrative literature review. Int J Nurs Stud 2015;52:1217-30. https://doi.org/10.1016/j.ijnurstu.2015.03.008.
- Parker S, Fuller J. Are nurses well placed as care co-ordinators in primary care and what is needed to develop their role: a rapid review?. Health Soc Care Community 2016;24:113-22. https://doi.org/10.1111/hsc.12194.
- van Dongen JJ, Lenzen SA, van Bokhoven MA, Daniëls R, van der Weijden T, Beurskens A. Interprofessional collaboration regarding patients’ care plans in primary care: a focus group study into influential factors. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0456-5.
- Gray R, Gordon B, Meredith M. Meeting Patients’ Needs: Improving the Effectiveness of Multidisciplinary Team Meetings in Cancer Services. London: Cancer Research UK; 2017.
- Powell M, Dawson J, Topakas A, Durose J, Fewtrell C. Staff satisfaction and organisational performance: evidence from a longitudinal secondary analysis of the NHS staff survey and outcome data. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02500.
- Schepman S, Hansen J, de Putter ID, Batenburg RS, de Bakker DH. The common characteristics and outcomes of multidisciplinary collaboration in primary health care: a systematic literature review. Int J Integr Care 2015;15. https://doi.org/10.5334/ijic.1359.
- Thota AB, Sipe TA, Byard GJ, Zometa CS, Hahn RA, McKnight-Eily LR, et al. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med 2012;42:525-38. https://doi.org/10.1016/j.amepre.2012.01.019.
- Fens M, Vluggen T, van Haastregt JC, Verbunt JA, Beusmans GH, van Heugten CM. Multidisciplinary care for stroke patients living in the community: a systematic review. J Rehabil Med 2013;45:321-30. https://doi.org/10.2340/16501977-1128.
- Kilpatrick K, Jabbour M, Fortin C. Processes in healthcare teams that include nurse practitioners: what do patients and families perceive to be effective?. J Clin Nurs 2016;25:619-30. https://doi.org/10.1111/jocn.13085.
- Drewes HW, Steuten LM, Lemmens LC, Baan CA, Boshuizen HC, Elissen AM, et al. The effectiveness of chronic care management for heart failure: meta-regression analyses to explain the heterogeneity in outcomes. Health Serv Res 2012;47:1926-59. https://doi.org/10.1111/j.1475-6773.2012.01396.x.
- West M, Almo-Metcalfe B, Dawson J, Ansari WE, Glasby J, Hardy G, et al. Effectiveness of Multi-Professional Team Working (MPTW) in Mental Health Care. Southampton: National Institute for Health Research Service Delivery and Organisation Programme; 2012.
- Portillo MC, Regaira E, Pumar-Méndez MJ, Mujika A, Vassilev I, Rogers A, et al. Voluntary organizations and community groups as new partners in diabetes self-management and education: a critical interpretative synthesis. Diabetes Educ 2015;41:550-68. https://doi.org/10.1177/0145721715594026.
- Hunt L. Green Light for Greenwich: Integration and Older People’s Care. London: Chartered Society of Physiotherapists; 2014.
- Goodwin N, Sonola L, Thiel V, Kodner DL. Co-ordinated Care for People with Complex Chronic Conditions: Key Lessons and Markers for Success. London: The King’s Fund; 2013.
- West M, Dawson J. Employee Engagement and NHS Performance. London: The King’s Fund; 2012.
- Georghiou T, Steventon A, Billings J, Blunt I, Lewis G, Bardsley M. Predictive Risk and Health Care: An Overview. London: Nuffield Trust; 2011.
- Ghate D, Lewis J, Welbourn D. Systems Leadership: Exceptional leadership for Exceptional Times. Synthesis Paper. Nottingham: The Virtual Staff College; 2013.
- Woodford M. Integrating Health and Social Care in Herefordshire n.d. www.kingsfund.org.uk/sites/files/kf/Martin%20Woodford.pdf (accessed 23 May 2017).
- West M, Armit K, Loewenthal L, Eckert R, West T, Lee A. Leadership and Leadership Development in Health Care: The Evidence Base. London: The King’s Fund; 2015.
- Roland M, Barber N, Howe A, Imison C, Rubin G, Storey K. The Future of Primary Care: Creating Teams for Tomorrow. London: Health Education England; 2015.
- Akhnif E, Macq J, Idrissi Fakhreddine MO, Meessen B. Scoping literature review on the Learning Organisation concept as applied to the health system. Health Res Policy Syst 2017;15. https://doi.org/10.1186/s12961-017-0176-x.
- Perreira TA, Innis J, Berta W. Work motivation in health care: a scoping literature review. Int J Evid Based Healthc 2016;14:175-82. https://doi.org/10.1097/XEB.0000000000000093.
- Donahue KE, Halladay JR, Wise A, Reiter K, Lee SY, Ward K, et al. Facilitators of transforming primary care: a look under the hood at practice leadership. Ann Fam Med 2013;11:27-33. https://doi.org/10.1370/afm.1492.
- Smith J, Holder H, Edwards N, Maybin J, Parker H, Rosen R, et al. Securing the Future of General Practice: New Models of Primary Care. London: The King’s Fund and Nuffield Trust; 2013.
- Timmins N. The Practice of System Leadership: Being Comfortable with Chaos. London: The King’s Fund; 2015.
- Frich JC, Brewster AL, Cherlin EJ, Bradley EH. Leadership development programs for physicians: a systematic review. J Gen Intern Med 2015;30:656-74. https://doi.org/10.1007/s11606-014-3141-1.
- Hardacre J, Cragg R, Shapiro J, Spurgeon P, Flanagan H. What’s Leadership Got To Do With It? Exploring Links Between Quality Improvement and Leadership in the NHS. London: The Health Foundation; 2011.
- Rosenman ED, Shandro JR, Ilgen JS, Harper AL, Fernandez R. Leadership training in health care action teams: a systematic review. Acad Med 2014;89:1295-306. https://doi.org/10.1097/ACM.0000000000000413.
- West M, Eckert R, Steward K, Pasmore B. Developing Collective Leadership for Health Care. London: The King’s Fund; 2014.
- Willis CD, Saul J, Bevan H, Scheirer MA, Best A, Greenhalgh T, et al. Sustaining organizational culture change in health systems. J Health Organ Manag 2016;30:2-30. https://doi.org/10.1108/JHOM-07-2014-0117.
- Apekey TA, McSorley G, Tilling M, Siriwardena AN. Room for improvement? Leadership, innovation culture and uptake of quality improvement methods in general practice. J Eval Clin Pract 2011;17:311-18. https://doi.org/10.1111/j.1365-2753.2010.01447.x.
- Lega F, Prenestini A, Rosso M. Leadership research in healthcare: a realist review. Health Serv Manage Res 2017;30:94-104. https://doi.org/10.1177/0951484817708915.
- McMullen CK, Schneider J, Firemark A, Davis J, Spofford M. Cultivating engaged leadership through a learning collaborative: lessons from primary care renewal in Oregon safety net clinics. Ann Fam Med 2013;11:34-40. https://doi.org/10.1370/afm.1489.
- Storey J, Holti R, Hartley J, Marshall M, Matharu T. Methods of Mobilizing Clinical Engagement and Clinical Leadership in and around Clinical Commissioning Groups: State of the Art Literature Review and Research Agenda. Milton Keynes: The Open University; 2015.
- Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- A Promise to Learn – a Commitment to Act. Improving the Safety of Patients in England. London: Department of Health and Social Care; 2013.
- West M. Leading Cultures That Deliver High Quality Care n.d.
- Ham C. Leadership and Engagement for Improvement in the NHS: Together We Can. London: The King’s Fund on Leadership Review; 2012.
- Sinsky CA, Willard-Grace R, Schutzbank AM, Sinsky TA, Margolius D, Bodenheimer T. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med 2013;11:272-8. https://doi.org/10.1370/afm.1531.
- Dawson J, West M. A closer look at how we feel: the annual NHS staff survey reveals there is room for improvement, report Jeremy Dawson and Michael West. Nurs Standard 2012;26:62-3. https://doi.org/10.7748/ns.26.43.62.s55.
- Khoshhal KI, Guraya SY. Leaders produce leaders and managers produce followers. A systematic review of the desired competencies and standard settings for physicians’ leadership. Saudi Med J 2016;37:1061-7. https://doi.org/10.15537/smj.2016.10.15620.
- Miller R, Peckham S, Checkland K, Coleman A, McDermott I, Harrison S, et al. Clinical Engagement in Primary Care-Led Commissioning: A Review of the Evidence. London: Policy Research Unit in Commissioning and the Healthcare System; 2012.
- Harrison MI, Kimani J. Building capacity for a transformation initiative: system redesign at Denver Health. Health Care Manage Rev 2009;34:42-53. https://doi.org/10.1097/01.HMR.0000342979.91931.d9.
- Chreim S, Williams BE, Janz L, Dastmalchian A. Change agency in a primary health care context: the case of distributed leadership. Health Care Manage Rev 2010;35:187-99. https://doi.org/10.1097/HMR.0b013e3181c8b1f8.
- Pettigrew L, Mays N, Kumpunen S, Rosen R, Posaner R. Large-Scale General Practice in England: What Can We Learn from the Literature?. London: Nuffield Trust; 2016.
- Willis CD, Best A, Riley B, Herbert CP, Millar J, Howland D. Systems thinking for transformational change in health. Evid Policy 2014;10:113-26. https://doi.org/10.1332/174426413X662815.
- Swanson RC, Cattaneo A, Bradley E, Chunharas S, Atun R, Abbas KM, et al. Rethinking health systems strengthening: key systems thinking tools and strategies for transformational change. Health Policy Plan 2012;27:iv54-61. https://doi.org/10.1093/heapol/czs090.
- Stroebel CK, McDaniel RR, Crabtree BF, Miller WL, Nutting PA, Stange KC. How complexity science can inform a reflective process for improvement in primary care practices. Jt Comm J Qual Patient Saf 2005;31:438-46. https://doi.org/10.1016/S1553-7250(05)31057-9.
- Hovlid E, Bukve O, Haug K, Aslaksen AB, von Plessen C. Sustainability of healthcare improvement: what can we learn from learning theory?. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-235.
- Fraser SW, Greenhalgh T. Coping with complexity: educating for capability. BMJ 2001;323:799-803. https://doi.org/10.1136/bmj.323.7316.799.
- Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf 2014;23:290-8. https://doi.org/10.1136/bmjqs-2013-001862.
- Accountable Care Organisations: The Future of the NHS?. Manchester: National Health Executive; 2017.
- Baker R, Willars J, McNicol S, Dixon-Woods M, McKee L. Primary care quality and safety systems in the English National Health Service: a case study of a new type of primary care provider. J Health Serv Res Policy 2014;19:34-41. https://doi.org/10.1177/1355819613500664.
- Ewbank L, Hitchcock A, Sasse T. Who Cares? The Future of General Practice. London: Reform; 2016.
- The Search for Low-Cost Integrated Healthcare: The Alzira Model – from the Region of Valencia. Brussels: NHS European Office; 2011.
- Limb M. Scaled up general practice organisations do not provide better quality of care, report says. BMJ 2016;354. https://doi.org/10.1136/bmj.i4002.
- The Future of Primary Care: Creating Teams for Tomorrow. London: Primary Care Workforce Commission; 2015.
- Miller D. Going Lean in Health Care. Cambridge, MA: Institute for Healthcare Improvement; 2005.
- Batalden PB, Davidoff F. What is ‘quality improvement’ and how can it transform healthcare?. Qual Saf Health Care 2007;16:2-3. https://doi.org/10.1136/qshc.2006.022046.
- Allcock C, Dormon F, Taunt R, Dixon J. Constructive comfort: accelerating change in the NHS. Policy Anal 2015.
- McClellan M, Kent J, Beales S, Macdonnell M, Thoumi A, Shuttleworth B, et al. Accountable Care: Focusing Accountability on the Outcomes That Matter 2013. www.brookings.edu/research/accountable-care-focusing-accountability-on-the-outcomes-that-matter/ (accessed 21 June 2017).
- McClellan M, Kent J, Beales SJ, Cohen SI, Macdonnell M, Thoumi A, et al. Accountable care around the world: a framework to guide reform strategies. Health Aff 2014;33:1507-15. https://doi.org/10.1377/hlthaff.2014.0373.
- Alderwick H, Ham C. Sustainability and transformation plans for the NHS in England: what do they say and what happens next?. BMJ 2017;356. https://doi.org/10.1136/bmj.j1541.
- Bardsley M, Steventon A, Smith J, Dixon J. Evaluating Integrated and Community-Based Care. How Do We Know What Works?. London: Nuffield Trust; 2013.
- Vize R. Financial benefits of integration: a case of wishful thinking?. BMJ 2014;348. https://doi.org/10.1136/bmj.g3661.
- Loftus B. Putting Patients First: The Kaiser Permanente Experience n.d.
- Brokel JM, Harrison MI. Redesigning care processes using an electronic health record: a system’s experience. Jt Comm J Qual Patient Saf 2009;35:82-9. https://doi.org/10.1016/S1553-7250(09)35011-4.
- Brown T, Duthe R. Getting ‘lean’: hardwiring process excellence into Northeast Health. J Healthc Inf Manag 2009;23:34-8.
- Chen C, Garrido T, Chock D, Okawa G, Liang L. The Kaiser Permanente Electronic Health Record: transforming and streamlining modalities of care. Health Aff 2009;28:323-33. https://doi.org/10.1377/hlthaff.28.2.323.
- Lukas CV, Holmes SK, Cohen AB, Restuccia J, Cramer IE, Shwartz M, et al. Transformational change in health care systems: an organizational model. Health Care Manage Rev 2007;32:309-20. https://doi.org/10.1097/01.HMR.0000296785.29718.5d.
- Lee SY, Weiner BJ, Harrison MI, Belden CM. Organizational transformation: a systematic review of empirical research in health care and other industries. Med Care Res Rev 2013;70:115-42. https://doi.org/10.1177/1077558712458539.
- Hunter DJ, Erskine J, Hicks C, McGovern T, Small A, Lugsden E, et al. A mixed-methods evaluation of transformational change in NHS North East. Health Serv Deliv Res 2014;2.
- Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in health care. BMJ 2001;323:625-8. https://doi.org/10.1136/bmj.323.7313.625.
- Best A, Clark PI, Leischow SJ, Trochim WM. Greater Than the Sum: Systems Thinking in Tobacco Control. Rockville, MD: National Cancer Institute; 2007.
- Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
- Zimmerman B, Lindberg C, Plsek P. Edgeware: Lessons From Complexity Science for Health Care Leaders 1998.
- Plsek PE, Wilson T. Complexity, leadership, and management in healthcare organisations. BMJ 2001;323:746-9. https://doi.org/10.1136/bmj.323.7315.746.
- Edgren L. The meaning of integrated care: a systems approach. Int J Integr Care 2008;8. https://doi.org/10.5334/ijic.293.
- Lanham HJ, McDaniel RR, Crabtree BF, Miller WL, Stange KC, Tallia AF, et al. How improving practice relationships among clinicians and nonclinicians can improve quality in primary care. Jt Comm J Qual Patient Saf 2009;35:457-66. https://doi.org/10.1016/S1553-7250(09)35064-3.
- Edgren L, Barnard K. Complex adaptive systems for management of integrated care. Leadersh Health Serv 2012;25:39-51. https://doi.org/10.1108/17511871211198061.
- Tsasis P, Evans JM, Owen S. Reframing the challenges to integrated care: a complex-adaptive systems perspective. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.843.
- Best A, Berland A, Herbert C, Bitz J, van Dijk MW, Krause C, et al. Using systems thinking to support clinical system transformation. J Health Organ Manage 2016;30:302-23. https://doi.org/10.1108/JHOM-12-2014-0206.
- Begun J, Zimmerman B, Dooley K, Mick S, Wyttenbach M. Advances in Health Care Organization Theory. San Francisco, CA: Jossey-Bass; 2003.
- Sterman JD. Learning from evidence in a complex world. Am J Public Health 2006;96:505-14. https://doi.org/10.2105/AJPH.2005.066043.
- Best A, Saul JE. Systems thinking: a different window on the world of implementation and global exchange of behavioral medicine evidence. Transl Behav Med 2011;1:361-3. https://doi.org/10.1007/s13142-011-0050-2.
- Lamont T, Barber N, de Pury J, Fulop N, Garfield-Birkbeck S, Lilford R, et al. New approaches to evaluating complex health and care systems. BMJ 2016;352. https://doi.org/10.1136/bmj.i154.
- Willis CD, Mitton C, Gordon J, Best A. System tools for system change. BMJ Qual Saf 2012;21:250-62. https://doi.org/10.1136/bmjqs-2011-000482.
- Addicott R, Ham C. Commissioning and Funding General Practice: Making the Case for Family Care Networks. London: The King’s Fund; 2014.
- Senge P. The Fifth Discipline: The Art and Practice of the Learning Organization. London: Random House Business; 2006.
- Fillingham D, Jones B, Pereira P. The Challenge and Potential of Whole System Flow: Improving the Flow of People, Information and Resources Across Whole Health and Social Care Economies. London: The Health Foundation; 2016.
- Shrank W. The Center For Medicare and Medicaid Innovation’s blueprint for rapid-cycle evaluation of new care and payment models. Health Aff (Millwood) 2013;32:807-12. https://doi.org/10.1377/hlthaff.2013.0216.
- Greenhalgh T, Macfarlane F, Barton-Sweeney C, Woodard F. ‘If we build it, will it stay?’ A case study of the sustainability of whole-system change in London. Milbank Q 2012;90:516-47. https://doi.org/10.1111/j.1468-0009.2012.00673.x.
- Kim DH. The link between individual and organizational learning. MIT Sloan Manag Rev 1993;35:41-62.
- Argyris C, Schon D. Organizational Learning II. Theory, Method and Practice. Reading, MA: Addison-Wesley; 1996.
- Baker GR. High Performing Healthcare Systems: Delivering Quality by Design. Toronto, ON: Longwoods Publishing; 2008.
- Friedman CP, Wong AK, Blumenthal D. Achieving a nationwide learning health system. Sci Transl Med 2010;2. https://doi.org/10.1126/scitranslmed.3001456.
- Sheaff R, Child S, Schofield J, Dowling B, Pickard S, Mannion R. Understanding Professional Partnerships and Non-Hierarchical Organisations. Final Report. Southampton: National Institute for Health Research Service Delivery and Organisation programme; 2012.
- Barker JR. Tightening the iron cage: concertive control in self-managing teams. Admin Sci Quart 1993;38:408-37. https://doi.org/10.2307/2393374.
- Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;6. https://doi.org/10.1002/14651858.CD000259.pub3.
- Ivers NM, Grimshaw JM, Jamtvedt G, Flottorp S, O’Brien MA, French SD, et al. Growing literature, stagnant science? Systematic review, meta-regression and cumulative analysis of audit and feedback interventions in health care. J Gen Intern Med 2014;29:1534-41. https://doi.org/10.1007/s11606-014-2913-y.
- Lau R, Stevenson F, Ong BN, Dziedzic K, Treweek S, Eldridge S, et al. Achieving change in primary care – effectiveness of strategies for improving implementation of complex interventions: systematic review of reviews. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009993.
- Hut-Mossel L, Welker G, Ahaus K, Gans R. Understanding how and why audits work: protocol for a realist review of audit programmes to improve hospital care. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-015121.
- Tian Y, Thompson J, Buck D, Sonola L. Exploring the System-Wide Costs of Falls in Older People in Torbay. London: The King’s Fund; 2013.
- The Big Data Dilemma: Fourth Report of Session 2016–2016. London: The Stationery Office; 2016.
- The Importance of Multimorbidity in Explaining Utilisation and Costs Across Health and Social Care Settings: Evidence from South Somerset’s Symphony Project. York: University of York, Centre for Health Economics; 2014.
- NHS RightCare . Case Study: Tackling Unwarranted Variation and Maximising Value in Healthcare Using the NHS RightCare Approach 2017. www.hfma.org.uk/docs/default-source/our-networks/healthcare-costing-for-value-institute/case-studies/nhs-southampton-city-ccg-w-nhs-rightcare---hc4vi-case-study-january-2017.pdf?sfvrsn=2 (accessed 21 June 2017).
- Sheaff R, Halliday J, Ovretveit J, Byng R, Exworthy M, Peckham S, et al. Integration and continuity of primary care: polyclinics and alternatives – a patient-centred analysis of how organisation constrains care co-ordination. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03350.
- Rodgers M, Dalton J, Harden M, Street A, Parker G, Eastwood A. Integrated care to address the physical health needs of people with severe mental illness: a rapid review. Health Serv Deliv Res 2016;4.
- van Panhuis WG, Paul P, Emerson C, Grefenstette J, Wilder R, Herbst AJ, et al. A systematic review of barriers to data sharing in public health. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-1144.
- Vuik SI, Mayer EK, Darzi A. Patient segmentation analysis offers significant benefits for integrated care and support. Health Aff 2016;35:769-75. https://doi.org/10.1377/hlthaff.2015.1311.
- Schang L, Morton A, DaSilva P, Bevan G. From data to decisions? Exploring how healthcare payers respond to the NHS Atlas of Variation in Healthcare in England. Health Policy 2014;114:79-87. https://doi.org/10.1016/j.healthpol.2013.04.014.
- Uslu AM, Stausberg J. Value of the electronic patient record: an analysis of the literature. J Biomed Inform 2008;41:675-82. https://doi.org/10.1016/j.jbi.2008.02.001.
- Costs and Benefits of Health Information Technology: An Updated Systematic Review. Santa Monica, CA: RAND Corporation; 2009.
- Khangura S, Grimshaw J, Moher D. Evidence Summary: Electronic Health Records (EHRs). CIHR-Funded Knowledge to Action Research Group. Ottawa, ON: CIHR-funded knowledge to action research group; 2010.
- Miller RH, West CE. The value of electronic health records in community health centers: policy implications. Health Aff 2007;26:206-14. https://doi.org/10.1377/hlthaff.26.1.206.
- Castle-Clarke S, Kumpunen S, Machaqueiro S, Curry N, Imison C. The Future of Primary Care: New Models and Digital Requirements. London: Nuffield Trust; 2015.
- Wolff JL, Berger A, Clarke D, Green JA, Stametz R, Yule C, et al. Patients, care partners, and shared access to the patient portal: online practices at an integrated health system. J Am Med Inform Assoc 2016;23:1150-8. https://doi.org/10.1093/jamia/ocw025.
- Wildevuur SE, Simonse LW. Information and communication technology-enabled person-centered care for the ‘big five’ chronic conditions: scoping review. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.3687.
- Holmgren AJ, Adler-Milstein J. Health information exchange in US hospitals: the current landscape and a path to improved information sharing. J Hosp Med 2017;12:193-8. https://doi.org/10.12788/jhm.2704.
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002;288:1775-9. https://doi.org/10.1001/jama.288.14.1775.
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q 1996;74:511-44. https://doi.org/10.2307/3350391.
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff 2001;20:64-78. https://doi.org/10.1377/hlthaff.20.6.64.
- Greaves F, Pappas Y, Bardsley M, Harris M, Curry N, Holder H, et al. Evaluation of complex integrated care programmes: the approach in North West London. Int J Integr Care 2013;13. https://doi.org/10.5334/ijic.974.
- Castle-Clarke S, Kumpunen S, Machaqueiro S, Curry N, Imison C. Digital Requirements for New Primary Care Models. A Briefing for Clinicians and Managers. London: Nuffield Trust; 2016.
- Kostkova P, Brewer H, de Lusignan S, Fottrell E, Goldacre B, Hart G, et al. Who owns the data? Open data for healthcare. Front Public Health 2016;4. https://doi.org/10.3389/fpubh.2016.00007.
- Health and Digital: Reducing Inequalities, Improving Society – An Evaluation of the Widening Digital Participation Programme. London: Tinder Foundation; 2016.
- Phillips AB, Merrill JA. Innovative use of the integrative review to evaluate evidence of technology transformation in healthcare. J Biomed Inform 2015;58:114-21. https://doi.org/10.1016/j.jbi.2015.09.014.
- Winters S, Magalhaes L, Anne Kinsella E, Kothari A. Cross-sector service provision in health and social care: an umbrella review. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2460.
- Integrating Research and Practice: Health System Leaders Working Toward High-Value Care: Workshop Summary. Washington, DC: National Academies Press; 2015.
- Lipsitz LA. Understanding health care as a complex system: the foundation for unintended consequences. JAMA 2012;308:243-4. https://doi.org/10.1001/jama.2012.7551.
- Holland J. Hidden Order: How Adaptation Builds Complexity. New York, NY: Addison-Wesley; 1995.
- Lorenz E. The Essence of Chaos. London: UCL Press; 1993.
- Axelrod RM. The Evolution of Cooperation: Revised Edition. New York, NY: Basic Books; 2006.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist Synthesis: RAMESES Training Materials 2015. www.ramesesproject.org/Standards_and_Training_materials.php#rs_training (accessed 15 June 2016).
- Davies HTO, Powell AE, Nutley SM. Mobilising knowledge to improve UK health care: learning from other countries and other sectors – a multimethod mapping study. Health Serv Deliv Res 2015;3. http://dx.doi.org/10.3310/hsdr03270.
- Rosen R. Meeting Need or Fuelling Demand? Improved Access to Primary Care and Supply-Induced Demand. London: Nuffield Trust; 2014.
- Colla CH, Lewis VA, Shortell SM, Fisher ES. First national survey of ACOs finds that physicians are playing strong leadership and ownership roles. Health Aff 2014;33:964-71. https://doi.org/10.1377/hlthaff.2013.1463.
- Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0242-0.
- Zimmerman B, Lindberg C, Plsek P. A Complexity Science Primer: What is Complexity Science and Why Should I Learn About It. Irving, TX: VHA Inc.; 1998.
- Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing ‘neighborhood effects’: social processes and new directions in research. Annu Rev Sociol 2002;28:443-78. https://doi.org/10.1146/annurev.soc.28.110601.141114.
- Paina L, Peters DH. Understanding pathways for scaling up health services through the lens of complex adaptive systems. Health Policy Plan 2012;27:365-73. https://doi.org/10.1093/heapol/czr054.
- Perkins DD, Zimmerman MA. Empowerment theory, research, and application. Am J Community Psychol 1995;23:569-79. https://doi.org/10.1007/BF02506982.
- Kanter R. Men and Women of the Corporation. New York, NY: Basic Books; 1993.
- Larkin M, Cierpial C, Stack J, Morrison V, Griffith C. Empowerment theory in action: the wisdom of collaborative governance. Online J Issues Nurs 2008;13.
- Kluska KM, Laschinger HK, Kerr MS. Staff nurse empowerment and effort-reward imbalance. Nurs Leadersh 2004;17:112-28. https://doi.org/10.12927/cjnl.2004.16247.
- Mangold KL, Pearson KK, Schmitz JR, Scherb CA, Specht JP, Loes JL. Perceptions and characteristics of registered nurses’ involvement in decision making. Nurs Adm Q 2006;30:266-72. https://doi.org/10.1097/00006216-200607000-00011.
- Imison C, Sonola L, Honeyman M, Ross S, Edwards N. Insights from the clinical assurance of service reconfiguration in the NHS: the drivers of reconfiguration and the evidence that underpins it – a mixed-methods study. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03090.
- Tetlock PE. Accountability: the neglected social context of judgment and choice. Res Organ Behav 1985;7:297-332.
- Tetlock PE. The impact of accountability on judgment and choice: toward a social contingency model. Adv Exp Soc Psychol 1992;25:331-76. https://doi.org/10.1016/S0065-2601(08)60287-7.
- Frink DD, Hall AT, Perryman AA, Ranft AL, Hochwarter WA, Ferris GR, et al. Meso-level theory of accountability in organizations. Res Pers Hum Res Man 2008;27:177-245. https://doi.org/10.1016/S0742-7301(08)27005-2.
- Emanuel EJ, Emanuel LL. What is accountability in health care?. Ann Intern Med 1996;124:229-39. https://doi.org/10.7326/0003-4819-124-2-199601150-00007.
- Scott SV, Orlikowski WJ. Reconfiguring relations of accountability: materialization of social media in the travel sector. Account Org Soc 2012;37:26-40. https://doi.org/10.1016/j.aos.2011.11.005.
- Messner M. The limits of accountability. Account Org Soc 2009;34:918-38. https://doi.org/10.1016/j.aos.2009.07.003.
- Gittell JH, Kyriakidou O, Özbilgin M. Relational Perspectives in Organizational Studies: A Research Companion. Cheltenham: Edward Elgar Publishing; 2006.
- Gittell JH, Godfrey M, Thistlethwaite J. Interprofessional collaborative practice and relational coordination: improving healthcare through relationships. J Interprof Care 2013;27:210-13. https://doi.org/10.3109/13561820.2012.730564.
- West MA. Effective Teamwork: Practical Lessons from Organizational Research. Hoboken, NJ: John Wiley and Sons; 2012.
- Powell HA, Baldwin DR. Multidisciplinary team management in thoracic oncology: more than just a concept?. Eur Respir J 2014;43:1776-86. https://doi.org/10.1183/09031936.00150813.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. https://doi.org/10.1037/0033-295X.84.2.191.
- Billett S, Henderson A, Choy S, Dymock D, Beven F, Kelly A, et al. Change, Work and Learning: Aligning Continuing Education and Training. Adelaide, SA: National Centre for Vocational Education Research; 2012.
- Shrank WH, Saunders RS, McClellan M. Better evidence to guide payment reforms: recognizing the importance of perspective. JAMA 2017;317:805-6. https://doi.org/10.1001/jama.2017.0034.
- Callon M, Latour B. Don’t throw the baby out with the bath school! A reply to Collins and Yearley. Sci Pract Cult 1992;343.
- Latour B, Bijker W, Law J. Shaping Technology/Building Society: Studies in Sociotechnical Change. Cambridge, MA: MIT Press; 1992.
- Cresswell KM, Worth A, Sheikh A. Actor-Network Theory and its role in understanding the implementation of information technology developments in healthcare. BMC Med Inform Decis Mak 2010;10. https://doi.org/10.1186/1472-6947-10-67.
- Greenhalgh T, Stones R. Theorising big IT programmes in healthcare: strong structuration theory meets actor-network theory. Soc Sci Med 2010;70:1285-94. https://doi.org/10.1016/j.socscimed.2009.12.034.
- Sheaff R, Charles N, Mahon A. NHS commissioning practice and health system governance: a mixed-methods realistic evaluation. Health Serv Deliv Res 2015;3.
- Winpenny EM, Corbett J, Miani C, King S, Pitchforth E, Ling T, et al. Community hospitals in selected high income countries: a scoping review of approaches and models. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2463.
- Hovell MF, Wahlgren DR, Gehrman CA, DiClemente RJ, Crosby RA, Kegler MC. Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health. Hoboken, NJ: John Wiley and Sons; 2002.
- Butterfoss FD, Kegler MC, DiClemente RJ, Crosby RA, Kegler MC. Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health. Hoboken, NJ: John Wiley and Sons; 2002.
- Ehrlich C, Chester P, Kendall E, Crompton D. Implementing new models of integrated mental health care: what impacts effective performance?. Int J Integr Care 2017;17. https://doi.org/10.5334/ijic.3189.
- Knowles M. The Modern Practice of Adult Education: From Pedagogy to Andragogy 1980.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall, Inc; 1986.
- Friedkin NE, Johnsen EC. Social Influence Network Theory: A Sociological Examination of Small Group Dynamics. Cambridge: Cambridge University Press; 2011.
- Penrose ET. The Theory of the Growth of the Firm. New York, NY: John Wiley and Sons; 1959.
- Wernerfelt B. A resource-based view of the firm. Strateg Manage J 1984;5:171-80. https://doi.org/10.1002/smj.4250050207.
- Bass BM. From transactional to transformational leadership: learning to share the vision. Organ Dyn 1990;18:19-31. https://doi.org/10.1016/0090-2616(90)90061-S.
- Isaac Mostovicz E, Kakabadse NK, Kakabadse AP. A dynamic theory of leadership development. Leadersh Org Dev J 2009;30:563-76. https://doi.org/10.1108/01437730910981935.
- Kotter JP. Leading Change. Boston: Harvard Business School Press; 1996.
- Holmes BJ, Finegood D, Riley B, Best A, Brownson R, Colditz G, et al. Dissemination and Implementation Research in Health: Translating Science to Practice. New York, NY: Oxford University Press Inc.; 2012.
- Macfarlane F, Barton-Sweeney C, Woodard F, Greenhalgh T. Achieving and sustaining profound institutional change in healthcare: case study using neo-institutional theory. Soc Sci Med 2013;80:10-8. https://doi.org/10.1016/j.socscimed.2013.01.005.
- Fitzgerald L, McDermott A. Challenging Perspectives on Organizational Change in Health Care. Abingdon: Routledge; 2017.
- Hinings CR, Greenwood R. The Dynamics of Strategic Change. Hoboken, NJ: Wiley-Blackwell; 1989.
- Kanter RM, Stein B, Jick TD. Challenge of Organizational Change: How Companies Experience it and Leaders Guide it. New York, NY: Simon and Schuster; 2003.
- Pettigrew A. The Awakening Giant: Continuity and Change in Imperial Chemical Industries. Hoboken, NJ: Wiley-Blackwell; 1985.
- Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Upper Saddle River, NJ: FT Press; 2014.
- Gardner B, Whittington C, McAteer J, Eccles MP, Michie S. Using theory to synthesise evidence from behaviour change interventions: the example of audit and feedback. Soc Sci Med 2010;70:1618-25. https://doi.org/10.1016/j.socscimed.2010.01.039.
- Kluger AN, DeNisi A. The effects of feedback interventions on performance: a historical review, a meta-analysis, and a preliminary feedback intervention theory. Psychol Bull 1996;119:254-84. https://doi.org/10.1037/0033-2909.119.2.254.
- Rushmer RK, Cheetham M, Cox L, Crosland A, Gray J, Hughes L, et al. Research utilisation and knowledge mobilisation in the commissioning and joint planning of public health interventions to reduce alcohol-related harms: a qualitative case design using a cocreation approach. Health Serv Deliv Res 2015;3.
- Porter M. Towards a dynamic theory of strategy. Strateg Manage J 1991;12:95-117. https://doi.org/10.1002/smj.4250121008.
Appendix 1 Terms of reference for the project advisory group (June 2016)
Project advisory group: terms of reference
Aims and objectives of the project
The project is led by The Strategy Unit, NHS Midlands and Lancashire Commission Support Unit together with the School of Health and Related Research (ScHARR) University of Sheffield. Funded by the NIHR HSDR programme (project reference number 15/77/15), the project is concerned with combining existing knowledge of what works in integrated care with the intentions of the MCPs in developing innovative new care models. It is expected that this work will help MCPs to improve their models.
The aim of this synthesis is to provide decision-makers in health and social care with a practical evidence base relating to the MCP model of care. The synthesis, based on realist principles, will develop a ‘blueprint’, which articulates how and why MCP models work, to inform design of future iterations of the MCP model. 61
Specifically, the objectives of the synthesis are to:61
-
articulate the underlying programme theories behind the MCP model of care, by mapping the logic models of the MCP demonstrator sites, prioritising key theories for investigation
-
identify sources of theoretical, empirical and practice evidence to test the programme theories
-
appraise, extract and analyse evidence, reconciling confirmatory and contradictory evidence
-
develop the synthesis, producing a ‘blueprint’ to explain how the mechanisms used in different contexts contribute to outcomes and process variables
-
consult with key stakeholders from selected MCP demonstrator sites to validate findings and to test applicability to different contexts
-
finalise the synthesis, incorporating stakeholder feedback
-
disseminate the findings, preparing a series of practical tools to support knowledge mobilisation.
Terms of reference of the advisory group
This group has been established to provide the project with independent support and advice. Its objectives are to:
-
provide stakeholder perspectives on the scope of the synthesis and on emerging findings
-
inform the study design, including input into the search strategy
-
participate in strategic decisions about the project
-
advise on key policy, strategy and communication activities which may inform or impact this project
-
advise on the identification of key audiences and networks for dissemination activity
-
advise on dissemination formats, routes and activities
-
advise on interpretation of findings, to ensure relevance to stakeholders
-
support the translation of findings into actionable recommendations and tools for local health economies.
Membership
Members have been assembled to provide a range of experience and expertise, including New Care Model vanguard sites, NHSE, senior leaders in health and social care, public representation, academic partners and collaborators, communications expertise and project team members (Table 11).
| Name | Affiliation |
|---|---|
| Peter Spilsbury (chairperson) | Director, The Strategy Unit, MLCSU |
| Dr Sue Baxter | ScHARR, University of Sheffield and chief investigator of a project funded under the same call |
| Professor Simon Brake | Director of Primary Care, Sustainability & Integration, Coventry and Rugby CCG |
| Amanda Doyle | Accountable Officer/Chief Clinical Officer, Blackpool CCG |
| Bryan Gould | Patient and public representative |
| Julia Grace | Senior Strategic Account Manager, New Care Models programme – FYFV, NHSE |
| Paul Maubach | Chief Officer, Dudley CCG |
| Naresh Rati | Executive Director, Modality |
| Louise Rowan | Communications Consultant and Fellow |
| Kevin Rudge | Patient and public representative |
| Charles Tallack | Head of Operational Research and Evaluation, NHSE |
| Lorraine Thomas | Director of Strategy and Transformation, Birmingham Community Healthcare Foundation Trust |
| Project team | |
| Fraser Battye | The Strategy Unit, MLCSU |
| Dr Andrew Booth (co-applicant) | Reader in Evidence Based Information Practice and Director of Information, ScHARR, University of Sheffield |
| Dr Abeda Mulla (co-applicant) | Senior Consultant, The Strategy Unit, MLCSU |
| Alison Turner (chief investigator) | Head of Evidence Analysis, The Strategy Unit, MLCSU |
Working methods
It is expected that the advisory group will be convened on up to four occasions during the project, at the following key stages:
-
at the project start, to confirm the scope of the synthesis
-
during the analysis stage, to share and test emerging findings
-
ahead of stakeholder consultation, to consult on the draft conceptual model
-
at the project conclusion, to sign off the final report and dissemination outputs.
Electronic communication may be used between advisory group meetings.
Minutes will be taken at each meeting and will be shared with the NIHR HSDR programme and, potentially, more widely. The advisory group will be supported administratively by Sharon Townsend, Project Officer.
June 2016
Appendix 2 MEDLINE search strategy
MEDLINE
Date range searched: 2000–16.
Date searched: December 2016.
Search strategy
| # | Term |
|---|---|
| 1 | (“multispecialty community provider*”).ti,ab |
| 2 | (“primary care home*”).ti,ab |
| 3 | (vanguard* AND (model* ADJ5 care)).ti,ab |
| 4 | (“place-based”).ti,ab |
| 5 | COMMUNITY HEALTH PLANNING/ |
| 6 | (“integrated care pioneer*”).ti,ab |
| 7 | (“accountable care organi*ation*”).ti,ab |
| 8 | ACCOUNTABLE CARE ORGANIZATIONS/ |
| 9 | MODELS, ORGANIZATIONAL/ |
| 10 | (“primary care at scale”).ti,ab |
| 11 | (“primary care”).ti,ab |
| 12 | (“general practi*”).ti,ab |
| 13 | (“community care”).ti,ab |
| 14 | exp “COMMUNITY HEALTH SERVICES”/ |
| 15 | exp GENERAL PRACTICE/ |
| 16 | PRIMARY HEALTH CARE/ |
| 17 | “COMPREHENSIVE HEALTH CARE”/ |
| 18 | (federation* OR network* OR alliance* OR partnership* OR collaborat*).ti,ab |
| 19 | (11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17) |
| 20 | (18 AND 19) |
| 21 | (14 OR 15 OR 16 OR 17) |
| 22 | (18 AND 21) |
| 23 | (5 AND 19) |
| 24 | (7 OR 8) |
| 25 | (19 AND 24) |
| 26 | (9 AND 19) |
| 27 | PATIENT CARE TEAM/ |
| 28 | (multidisciplinary OR interdisciplinary OR “multi disciplinary” OR “inter disciplinary” OR integrate* OR collaborat*).ti,ab |
| 29 | (27 AND 28) |
| 30 | (19 AND 29) |
| 31 | (21 AND 29) |
| 32 | INTERDISCIPLINARY COMMUNICATION/ |
| 33 | PATIENT CENTERED CARE/ |
| 34 | DELIVERY OF HEALTH CARE, INTEGRATED/ |
| 35 | (“whole system” ADJ5 (change* OR transform* OR redesign*)).ti,ab |
| 36 | ((vertical OR horizontal) ADJ5 integrat*).ti,ab |
| 37 | (“health systems integrat*”).ti,ab |
| 38 | (32 OR 33 OR 34 OR 35 OR 36 OR 37) |
| 39 | (19 AND 38) |
| 40 | (21 AND 38) |
| 41 | (“case manag*”).ti,ab |
| 42 | CASE MANAGEMENT/ |
| 43 | PATIENT CARE PLANNING/ |
| 44 | (“case finding”).ti,ab |
| 45 | (“risk stratif*”).ti,ab |
| 46 | (“predictive model*”).ti,ab |
| 47 | (“population segment*”).ti,ab |
| 48 | ACTUARIAL ANALYSIS/ |
| 49 | (45 OR 46 OR 47 OR 48) |
| 50 | (41 OR 42 OR 43 OR 44 OR 49) |
| 51 | (19 AND 50) |
| 52 | (21 AND 50) |
| 53 | (31 AND 50) |
| 54 | (38 AND 50) |
| 55 | HEALTH SERVICES ACCESSIBILITY/ |
| 56 | “APPOINTMENTS AND SCHEDULES”/ |
| 57 | (access ADJ5 (extend* OR scale OR enhanc* OR improv*)).ti,ab |
| 58 | appointment* ADJ5 (extend* OR long*).ti,ab |
| 59 | (hour* ADJ5 (extend* OR enhanc* OR improv*)).ti,ab |
| 60 | (“same day appointment*”).ti,ab |
| 61 | (55 OR 56 OR 57 OR 59 OR 60) |
| 62 | (19 AND 61) |
| 63 | (21 AND 61) |
| 64 | (38 AND 61) |
| 65 | MOBILE APPLICATIONS/ |
| 66 | CONSUMER HEALTH INFORMATION/ |
| 67 | (“patient access” ADJ5 record*).ti,ab |
| 68 | (65 OR 66 OR 67) |
| 69 | (19 AND 68) |
| 70 | (21 AND 68) |
| 71 | (29 AND 68) |
| 72 | (38 AND 68) |
| 73 | DIAGNOSTIC SERVICES/ |
| 74 | AMBULATORY CARE/ |
| 75 | AMBULATORY CARE FACILITIES/ |
| 76 | (73 OR 74 OR 75) |
| 77 | (19 AND 76) |
| 78 | (21 AND 76) |
| 79 | ((outpatient* OR specialist*) ADJ5 (shift* OR transfer* OR relocat* OR substitut*)).ti,ab |
| 80 | (19 AND 79) |
| 81 | (21 AND 79) |
| 82 | (“care closer to home”).ti,ab |
| 83 | (extensivist*).ti,ab |
| 84 | (“community medical assessment*”).ti,ab |
| 85 | PATIENT NAVIGATION/ |
| 86 | (“directory of service*”).ti,ab |
| 87 | (“single point of access”).ti,ab |
| 88 | (signpost*).ti,ab |
| 89 | (navigat*).ti,ab |
| 90 | COMMUNITY INTEGRATION/ |
| 91 | COMMUNITY NETWORKS/ |
| 92 | COMMUNITY PARTICIPATION/ |
| 93 | COMMUNITY INSTITUTIONAL RELATIONS/ |
| 94 | (engag* ADJ5 (communit* OR volunteer* OR patient* OR people OR carer* OR public OR citizen* OR “service user*”)).ti,ab |
| 95 | (involv* ADJ5 (communit* OR volunteer* OR patient* OR people OR carer* OR public OR citizen* OR “service user*”)).ti,ab |
| 96 | (5 OR 8 OR 38) |
| 97 | (94 OR 95) |
| 98 | (96 AND 97) |
| 99 | CAREGIVERS/ |
| 100 | (carer OR carers).ti,ab |
| 101 | (99 OR 100) |
| 102 | “SELF-HELP GROUPS”/ |
| 103 | “SOCIAL SUPPORT”/ |
| 104 | (102 OR 103) |
| 105 | (101 AND 104) |
| 106 | (99 AND 100) |
| 107 | (104 AND 106) |
| 108 | SELF CARE/ |
| 109 | (“self care”).ti,ab |
| 110 | (“self management”).ti,ab |
| 111 | (“health coach*”).ti,ab |
| 112 | PATIENT PARTICIPATION/ |
| 113 | (108 OR 109 OR 110 OR 111 OR 112) |
| 114 | (29 AND 113) |
| 115 | (38 AND 113) |
| 116 | (“mutuality”).ti,ab |
| 117 | (5 AND 116) |
| 118 | (38 AND 116) |
| 119 | (91 OR 92 OR 93 OR 94 OR 95) |
| 120 | (116 AND 119) |
| 121 | (38 AND 119) |
| 122 | (5 AND 119) |
| 123 | (29 AND 119) |
| 124 | (8 AND 119) |
| 125 | VOLUNTARY HEALTH AGENCIES/ |
| 126 | SOCIAL CAPITAL/ |
| 127 | VOLUNTEERS/ |
| 128 | (“social movement*”).ti,ab |
| 129 | (“community asset*”).ti,ab |
| 130 | (“third sector”).ti,ab |
| 131 | (125 OR 126 OR 127 OR 128 OR 129 OR 130) |
| 132 | (5 AND 131) |
| 133 | (19 AND 131) |
| 134 | (21 AND 131) |
| 135 | (29 AND 131) |
| 136 | (38 AND 131) |
| 137 | INTERINSTITUTIONAL RELATIONS/ |
| 138 | (19 AND 137) |
| 139 | (29 OR 38) |
| 140 | (138 AND 139) |
| 141 | CONTRACTS/ |
| 142 | exp BUDGETS/ |
| 143 | RISK SHARING, FINANCIAL/ |
| 144 | (tariff*).ti,ab |
| 145 | (procur*).ti,ab |
| 146 | (141 OR 142 OR 143 OR 144 OR 145) |
| 147 | (5 AND 146) |
| 148 | (8 AND 146) |
| 149 | (38 AND 146) |
| 150 | (pool* ADJ5 budget*).ti,ab |
| 151 | (“capitated budget*”).ti,ab |
| 152 | (“provider partner*”).ti,ab |
| 153 | (“provider alliance*”).ti,ab |
| 154 | VALUE BASED PURCHASING/ |
| 155 | (147 OR 148 OR 149 OR 150 OR 151 OR 152 OR 153 OR 154) |
| 156 | HEALTH MANPOWER/ |
| 157 | LEADERSHIP/ |
| 158 | ORGANIZATIONAL CULTURE/ |
| 159 | (ma).fs |
| 160 | (workforce ADJ5 (capacity OR develop* OR model* OR train* OR plan* OR redesign*)).ti,ab |
| 161 | (156 OR 157 OR 158 OR 159 OR 160) |
| 162 | (29 AND 161) |
| 163 | (38 AND 161) |
| 164 | (“health champion*”).ti,ab |
| 165 | (“community anchor*”).ti,ab |
| 166 | (“lay worker*”).ti,ab |
| 167 | (“link worker*”).ti,ab |
| 168 | (“care navigator*”).ti,ab |
| 169 | (“outreach worker*”).ti,ab |
| 170 | (“care co-ordinator*”).ti,ab |
| 171 | (“support worker*”).ti,ab |
| 172 | (169 OR 171) |
| 173 | (29 AND 172) |
| 174 | (38 AND 172) |
| 175 | (19 AND 172) |
| 176 | (role* ADJ5 (new OR embed* OR emerg* OR extend* OR expand*)).ti,ab |
| 177 | (29 AND 176) |
| 178 | (38 AND 176) |
| 179 | (GPwSI* OR “GP with a special interest*” OR “practitioner with a special interest”).ti,ab |
| 180 | (specialist* OR consultant* OR paramedic* OR pharmacist* OR physiotherap*).ti,ab |
| 181 | (29 AND 180) |
| 182 | (19 AND 181) |
| 183 | (“values based recruitment”).ti,ab |
| 184 | PREVENTIVE HEALTH SERVICES/ |
| 185 | (29 AND 184) |
| 186 | (38 AND 184) |
| 187 | (“social prescri*”).ti,ab |
| 188 | (4 AND 9) |
| 189 | (4 AND 19) |
| 190 | (4 AND 5) |
| 191 | (4 AND 29) |
| 192 | (4 AND 38) |
| 193 | (4 AND 119) |
| 194 | (5 AND 24) |
| 195 | (9 AND 24) |
| 196 | (24 AND 38) |
| 197 | (24 AND 119) |
| 198 | (20 AND 61) |
| 199 | (20 AND 76) |
| 200 | (20 AND 79) |
| 201 | (20 AND 119) |
| 202 | (20 AND 131) |
| 203 | (20 AND 146) |
| 204 | (20 AND 161) |
| 205 | (20 AND 176) |
| 206 | (29 AND 38) |
| 207 | (19 AND 206) |
| 208 | (1 OR 2 OR 3 OR 6 OR 23 OR 25 OR 189 OR 190 OR 191 OR 192 OR 193) |
| 209 | (188 OR 194 OR 195 OR 196 OR 197 OR 208) |
| 210 | (38 AND 77) |
| 211 | (19 AND 163) |
| 212 | (5 AND 38) |
| 213 | (209 OR 212) |
| 214 | (“system leader*”).ti,ab |
| 215 | (“collective leader*”).ti,ab |
| 216 | (“collaborative leader*”).ti,ab |
| 217 | (“leadership development”).ti,ab |
| 218 | (214 OR 215 OR 216 OR 217) |
| 219 | (96 AND 218) |
| 220 | (“risk shar*”).ti,ab |
| 221 | (146 OR 220) |
| 222 | (96 AND 221) |
| 223 | (150 OR 151 OR 152 OR 153 OR 154 OR 222) |
| 224 | (“multi specialty community provider*”).ti,ab |
| 225 | (“multi-specialty community provider*”).ti,ab |
| 226 | (“multi-specialty community care”).ti,ab |
| 227 | (“multispecialty community care”).ti,ab |
| 228 | (“multi specialty community care”).ti,ab |
| 229 | (213 OR 227) |
| 230 | (53 OR 54 OR 64 OR 69 OR 70 OR 71 OR 72 OR 210 OR 80 OR 82 OR 83 OR 85 OR 86 OR 87 OR 88) |
| 231 | (162 OR 211 OR 219 OR 164 OR 165 OR 166 OR 167 OR 168 OR 170 OR 173 OR 174 OR 175 OR 177 OR 178 OR 179 OR 182 OR 183 OR 185 OR 186 OR 187) |
| 232 | (90 OR 107 OR 114 OR 115 OR 117 OR 118 OR 120 OR 121 OR 122 OR 123 OR 124 OR 132 OR 135 OR 136 OR 140) |
| 233 | (223 OR 229 OR 230 OR 231 OR 232) [DT 2000-2016] [Languages English] |
| 234 | (23 AND 38) |
| 235 | (29 AND 54) |
| 236 | (63 AND 64) |
| 237 | (19 AND 115) |
| 238 | (19 AND 121) |
| 239 | (19 AND 122) |
| 240 | (1 OR 2 OR 3 OR 6 OR 25 OR 189 OR 190 OR 191 OR 192 OR 193 OR 194 OR 195 OR 196 OR 197 OR 212 OR 227 OR 234) |
| 242 | (90 OR 107 OR 114 OR 117 OR 118 OR 120 OR 123 OR 124 OR 132 OR 135 OR 136 OR 140 OR 239) |
| 243 | (53 OR 69 OR 70 OR 71 OR 72 OR 210 OR 80 OR 82 OR 83 OR 85 OR 86 OR 87 OR 88 OR 235 OR 236) |
| 244 | (223 OR 231 OR 240 OR 242 OR 243) [DT 2000-2016] [Languages English] |
| 245 | (1 OR 2 OR 3 OR 6 OR 25 OR 189 OR 190 OR 191 OR 192 OR 193 OR 194 OR 195 OR 196 OR 197 OR 212 OR 227 OR 234) [DT 2000-2016] [Languages English] |
| 246 | (90 OR 107 OR 114 OR 117 OR 118 OR 120 OR 123 OR 124 OR 132 OR 135 OR 136 OR 140 OR 239) [DT 2000-2016] [Languages English] |
| 247 | (53 OR 69 OR 70 OR 71 OR 72 OR 210 OR 80 OR 82 OR 83 OR 85 OR 86 OR 87 OR 88 OR 235 OR 236) [DT 2000-2016] [Languages English] |
| 248 | (162 OR 211 OR 219 OR 164 OR 165 OR 166 OR 167 OR 168 OR 170 OR 173 OR 174 OR 175 OR 177 OR 178 OR 179 OR 182 OR 183 OR 185 OR 186 OR 187) [DT 2000-2016] [Languages English] |
| 249 | (150 OR 151 OR 152 OR 153 OR 154 OR 222) [DT 2000-2016] [Languages English] |
| 250 | (skype).ti,ab |
| 251 | (“demand management”).ti,ab |
| 252 | (“new ways of working”).ti,ab |
| 253 | (skype).ti,ab |
| 254 | (250 OR 251 OR 252 OR 253) |
| 255 | (96 and 254) |
| 256 | (96 and 254) [DT 2000-2016] [Languages English] |
| 257 | (“shared care record*”).ti,ab |
| 258 | (255 OR 257) |
| 259 | (255 or 257) |
| 260 | (255 or 257) [DT 2000-2016] [Languages English] |
Appendix 3 Grey literature sources
-
Health Foundation.
-
Health Service Journal.
-
The King’s Fund.
-
Local Government Association.
-
National Association of Primary Care.
-
National Voices (communities search).
-
Nesta (communities search).
-
NHS Clinical Commissioners.
-
NHS Confederation.
-
NHS England.
-
NHS Improvement.
-
NIHR Journals Library and Collaboration for Leadership in Applied Health Research and Care (www.clahrcprojects.co.uk/impact/projects).
-
Nuffield Trust.
-
Policy Research Unit in Commissioning and the Healthcare system (PRUComm).
-
Public Health England (communities search).
-
Pulse.
-
Royal College of General Practitioners.
-
Social Care Institute for Excellence Social Care Online.
Appendix 4 Data extraction form
Appendix 5 Table of included studies: R1
| Citation (including year of publication) | Country | Study type |
|---|---|---|
| Baird et al., 2016149 | UK | Mixed-methods analysis |
| Bienkowska-Gibbs et al., 2015192 | International | Literature review |
| Bradley et al., 2008160 | UK | Case study |
| Bramwell et al., 2014183 | International | Literature review |
| Chambers et al., 2016175 | International | Mapping and focused rapid review |
| College of Paramedics, 2016188 | UK | Framework |
| Donnelly et al., 2013193 | Canada | Case study |
| Drennan et al., 2011166 | UK | Qualitative study |
| Drennan et al., 2014189 | UK | Mixed-methods study |
| Drennan et al., 2015164 | UK | Observational study |
| Freund et al., 2015155 | UK | Literature review |
| Halter et al., 2013181 | International (46 out of 49 papers from the USA) | Systematic review |
| Heath et al., 2012176 | UK | Qualitative study |
| Heath et al., 2015178 | UK | Qualitative study |
| Imison et al., 2017191 | International | Review |
| Imison et al., 2008184 | International | Review |
| Imison et al., 2016163 | UK | Review |
| Jorgenson et al., 2014159 | Canada | Qualitative study |
| Laurant et al., 2010156 | International | Review |
| Mallett et al., 2014161 | UK | Cohort study |
| Martínez-González et al., 2014154 | International | Systematic review and meta-analysis |
| McLeod et al., 2015177 | UK | Observational study |
| Montgomery-Taylor et al., 2016185 | UK | Case study |
| Montgomery-Taylor et al., 2015186 | UK | Case study |
| Mott MacDonald and SQW, 201532 | UK | Case study |
| CLAHRC Greater Manchester, 2015172 | UK | Mixed-methods evaluation |
| Pawson et al., 201671 | International | Realist review |
| Pollard et al., 2014187 | UK | Case study |
| Primary Care Workforce Commission, 2015151 | International | Review |
| Rashid, 2010157 | UK | Integrative literature review |
| Robertson et al., 2014179 | UK | Case study |
| Rosen et al., 2016190 | UK | Mixed-methods evaluation |
| Rosen, 2014482 | UK | Briefing |
| Salisbury et al. 2013162 | UK | Pragmatic randomised controlled trial |
| Tan et al., 2014158 | International | Systematic review and meta-analysis |
| Taneja et al., 2015173 | International | Narrative systematic review |
| Williams and Stone, 2014182 | UK | Case study |
| Winpenny et al., 2016174 | International | Scoping review |
Appendix 6 Table of included studies: R2
| Citation (including year of publication) | Country | Study type |
|---|---|---|
| Addicott, 2014201 | UK | Commentary |
| Ahmed et al., 2015119 | UK | Commentary |
| Allen et al., 2015219 | UK | Evidence review |
| Andersson and Wikström, 2014196 | Sweden | Qualitative research |
| Baicker and Levy, 2013228 | USA | Commentary |
| Bambra et al., 2014210 | UK | Evidence review |
| Billings and de Weger, 2015118 | UK | Evidence review |
| Blakeman et al., 2011213 | UK | Qualitative study |
| Britnell et al., 2015235 | International | Commentary |
| Burns and Pauly, 2012220 | USA | Commentary |
| Calvert et al., 2009214 | UK | Retrospective cohort study |
| Chew-Graham et al., 2013212 | UK | Longitudinal qualitative study |
| Colla et al., 2012483 | USA | Quasi-experimental analysis |
| Collins, 2016200 | UK | Commentary based on qualitative analysis |
| Conrad, 2015227 | USA | Evidence review |
| Crinson et al., 2010238 | UK | Diagnostic analysis |
| Dickinson et al., 2013217 | UK | Evidence review |
| Dixon et al., 2011211 | UK | Summary of mixed-methods research |
| Flodgren et al., 2011204 | International | Review of systematic reviews |
| Forbes et al., 2016216 | UK | Evidence review |
| Goodwin et al., 2011239 | UK | Independent inquiry report |
| Gorman and Horn, 2015224 | Australia | Commentary |
| Gray et al., 2015349 | UK | Commentary |
| Hopson, 2016226 | UK | Commentary |
| House of Commons, 2015231 | UK | Government publication |
| Humphries, 2015218 | UK | Commentary |
| Imison et al., 2017191 | UK | Review |
| Lynn et al., 2015236 | USA | Commentary |
| Mason et al., 2014197 | UK | Evidence review |
| Mason et al., 2015208 | UK | Evidence review |
| Mehrotra et al., 2010237 | USA | Commentary |
| Monitor, 2015222 | UK | Summary of qualitative and quantitative analysis |
| National Audit Office, 2017209 | UK | Audit report |
| National Audit Office, 2016233 | UK | Audit report |
| NHS Improvement, 2017230 | UK | Policy/guidance |
| Porter, 2010203 | USA | Commentary |
| Price Waterhouse Coopers LLP, 2016234 | UK | Audit report |
| Roland and Paddison, 2013215 | UK | Commentary |
| Scott et al., 2011205 | International | Systematic review |
| Shortell et al., 201544 | UK | Commentary |
| Shortell et al., 2014126 | UK | Commentary |
| Song et al., 2012221 | USA | Difference-in-differences analysis |
| Stout, 2016232 | UK | Audit report |
| Sumner, 2016240 | UK | Commentary |
| Weeks et al., 2010241 | USA | Quantitative analysis |
| West, 2016229 | UK | Commentary |
| Yuan et al., 2017206 | International | Systematic review |
Appendix 7 Table of included studies: R3
| Citation (including year of publication) | Country | Study type |
|---|---|---|
| Addicott, 2013284 | UK | Commentary |
| Anderson et al., 2015276 | International | Systematic review (Cochrane) |
| Attree et al., 2011267 | International | Rapid review |
| Batalden et al., 2016261 | UK | Literature review |
| Bickerdike et al., 2017265 | UK | Systematic review |
| Bloomfield and Cayton, 2009293 | International | Commentary |
| Boger et al., 2015262 | International | Systematic review and mixed research synthesis |
| Boyle and Harris, 2009274 | International | Literature review |
| Brunton et al., 2015295 | International | Systematic review and meta-analysis |
| Cameron et al., 2014286 | UK | Case study |
| Clarke et al., 2017271 | International | Rapid review |
| Coulter, 2013294 | UK | Commentary |
| Cyril et al., 2015266 | International | Systematic review |
| Dayson et al., 2013132 | UK | Evaluation report |
| del Castillo et al., 2016282 | UK | Review |
| Farenden et al., 2015279 | UK | Evaluation report |
| Filipe et al., 2017283 | UK | Commentary |
| Georghiou et al., 2016247 | UK | Evaluation report |
| Howieson and Fenwick, 2014289 | UK | Commentary |
| Liddy et al., 2014290 | International | Systematic review |
| Masters et al., 2017281 | UK | Cost benefit analysis |
| Maughan et al., 201633 | UK | Observational study |
| Nesta, 2016292 | UK | Evaluation report |
| O’Mara-Eves et al., 2013264 | UK | Systematic review, meta-analysis and economic analysis |
| Ocloo and Matthews, 2016287 | UK | Review |
| Panagioti et al., 2014280 | International | Systematic review and meta-analysis (NIHR) |
| Philips and Morgan, 2015263 | International | Literature review |
| Poortinga, 2012256 | UK | Quantitative analysis |
| Popay et al., 2015272 | UK | Mixed-methods evaluation (NIHR) |
| Realpe and Wallace, 2009250 | UK | Commentary |
| Rippon and Hopkins, 2015277 | International | Research report |
| Ryder, 2015268 | UK | Case study |
| Sadler et al., 2014291 | International | Systematic review |
| Seale, 2016296 | UK | Guide |
| Taylor et al., 2014278 | International | Systematic review |
| Tsegai and Gamiz, 2014288 | UK | Case study |
| Vennik et al., 2015297 | The Netherlands | Qualitative research |
| Vogelpoel and Jarrold, 2014270 | UK | Case study |
| Voorberg et al., 2015273 | International | Systematic review |
| White et al., 2017275 | UK | Case study |
Appendix 8 Abstraction to middle-range theories
This appendix describes some of the theories, models and frameworks that we understood to contribute to our understanding of how the MCP model may work in practice and supports the discussion in Chapter 8. Theories, models and frameworks are distinct concepts, although the terms are often used interchangeably. Nilsen484 puts forward a ‘taxonomy that distinguishes between different categories of theories, models and framework’ for selection and application for researchers and practitioners. With respect to understanding and/or explaining what influences implementation outcomes, three categories are put forward:
-
determinant frameworks
-
classic theories
-
implementation models.
In Table 12, we describe some of the theories that could usefully contribute to our understanding of behaviour change within the context of the MCP model. We focus on the application of CASs theory as a lens through which to understand complex transformation; and the COM-B model to inform implementation.
| Programme theory component | Determinant framework: to provide a conceptual understanding | Classic theory: to explain social process | Implementation models: to provide a tool for action |
|---|---|---|---|
| R1: community-based, co-ordinated care is more accessible | CAS (connectivity) | (Structural) empowerment theories | COM-B |
| R2: place-based contracting and payment systems as a means to incentivise shared accountability | CAS (edge of chaos) | Accountability theory | |
| R3: fostering relational behaviours builds resilience within communities | CAS (connectivity) | Relational co-ordination | |
| M1: collective responsibility improves quality and safety outcomes | CAS (connectivity) | (Structural) empowerment theories | |
| M2: MDTs provide continuity for patients with long-term conditions and complex needs | CAS (connectivity) | Relational co-ordination | |
| M3: engaged and trained staff expedite cultural change | CAS (connectivity) | Relational co-ordination | |
| M4: system learning embeds and sustains transformational change | CAS (feedback loops) | Social learning theory | |
| M5: proactive population health is dependent on shared and linked data | CAS (connectivity) | Actor network theory |
Determinant framework
The determinant framework of CASs has emerged from our evidence base, offering a conceptual lens to explore the MCP model as a complex primary care-led and community-based integrated ACS. To frame this understanding for health-care systems, we adopted Plsek and Greenhalgh’s418 definition: ‘a complex adaptive system is a collection of individual agents with freedom to act in ways that are not always totally predictable, and whose actions are interconnected so that one agent’s actions changes the context for other agents’.
The use of the CAS lens to understand how to improve and transform health systems was introduced by Zimmerman et al.,485 and has subsequently been used to argue a need to ‘abandon linear models, accept unpredictability, respect (and utilise) autonomy and creativity, and respond flexibly to emerging patterns and opportunities’. 418 Kreitzer et al. 52 conceptualise the Dutch Buurtzorg model as a complex system, confirming a need to be ever ‘nimble and responsive’ to changing conditions.
The focus within the CAS approach on the interdependency of elements in a system and not the system itself makes it particularly well suited to framing the complexities of integrated care at the core of the new models and, in time, evaluating the new models,423 in order to guide future policies to avoid the unanticipated consequences. 475 The following subsections discussed some key features of CASs and their relevance to MCP theory components (see Table 12).
Feedback loops
The feedback loops serve to feed back the output of a process, as an input, into the same system. 74 In health-care studies, feedback loops between individuals and their community or environment have been assessed to determine how ‘neighbourhood effects’ or ‘place effects’ affect the individual’s health. 486,487 Feedback loops can generate change or stability in a system, depending on the relationships among different agents;422 positive feedback loops can be facilitative, for example, in the use of PDSA cycles in quality improvement processes. 396 Of our eight theory components, feedback loops are most useful in framing the necessary system learning (M4) through positive feedback reinforcement when intended outcomes are being realised, or taking corrective action following negative feedback from less-desired outcomes. Thus, in a MCP-like system, feedback allows the adaptation476 of the New Care Models programme delivery to align with the constantly shifting NHS landscape, for instance, allowing MCPs to be incorporated into sustainability and transformation plans or to begin journeys as ACSs, as vanguard evaluation findings are fed back.
Connectivity
The manner in which agents in a system connect and interact gives rise to the behaviour of a CAS, highlighting the importance of relationships between the agents over the agents themselves; as Plsek and Greenhalgh418 note, ‘the observable outcomes are more than merely the sum of the parts’. The capacity to connect and leverage social networks is described to be the most distinctive feature of the Buurtzorg model in the Netherlands, in which multilevel networks with intra- and interprofessional group connectivity coexist at local and national settings. 52
This connectivity is a recurrent theme in the MCP programme theory, occurring within components R1, R3, M1, M2, M3 and M5. This includes primary, community and specialist professionals connecting to adopt new roles and ways of working through building or strengthening relationships to co-ordinate care for the benefit of patients (R1). In R3, the inclusion of service users for co-production purposes adds a further dimension of connectivity.
In M1, the responsibility of delivering safe and high-quality care is discharged through collective decision-making with dependency on good communication and working relationships. In M2, interdisciplinary connectivity within a MDT offers shared decision-making and streamlined care for the benefit of the patient, and promotes team-building and peer support for the benefit of professionals.
The importance of connectivity for staff engagement is clear in M3; effective connectivity through sharing and leadership leads to improved staff engagement and workforce morale. Connectivity is also important with a technological interface, as the sharing of data by human agents brings about the intended change of proactive population health (M5).
Edge of chaos
The most productive state for a complex system is proposed to be at the ‘edge of chaos’, to allow for maximum variety and creativity, making it fundamentally unpredictable and, as such, it has to be observed over time. 418,477 A CAS approach seeks to draw out and mobilise the natural creativity of health-care professionals to adapt to circumstances and evolve. This requires system learning from locally owned solutions that are intended to achieve improved quality,424 rather than achieving this through top-down large-scale transformation efforts. Crucially, this requires risk-taking and learning from mistakes or failures (see Chapter 8, Stakeholder engagement), rather than national interventions to limit local risk-taking. There may also be a need to allow tensions to play out, for instance, in R2, the contracting and payment mechanism for MCPs is necessarily at the edge of chaos, using the opposing forces of competition and co-operation to be mutually beneficial,478 to allow local sites to innovate for their accountable local place-based system.
We have abstracted the resource and reasoning aspects of the intangible mechanisms (see Table 12) to six classic middle-range theories, in order to provide a rationale for the underlying social processes to inform future accountable population-based integrated care models. This is by no means an exhaustive search for middle-range theories, but a selection of six classic theories that can apply across system transformation, such as the introduction of a MCP.
Empowerment and structural empowerment theories
Empowerment occurs when individuals or communities have a degree of autonomy and self-determination to represent their interests in a responsible and self-determined way and act on their own authority. 488 Empowerment theory assumes that the experience, knowledge and skills of people can be harnessed to address issues. 488 The patient ownership and the relationship-based approach of the Nuka care model illustrates how shared responsibility and co-ownership can facilitate improved performance, community engagement and population health. 50
Similarly, Kanter’s489 theory of structural empowerment focuses on empowerment through access to information, resources, support and the opportunity to learn and develop. Empowered employees have a higher commitment to their organisation, are more accountable for their work and are better able to fulfil job demands in an effective manner. 490 Workplaces that facilitate access to resources have been shown to empower employees to accomplish their work more meaningfully. 491,492 Empowerment is a key aspect of stakeholder reasoning when moving from short-term outcomes to intermediate outcomes (see Figure 20). For example, in R1, empowered professionals are more likely to adopt new roles and task-shift to community-based, co-ordinated care delivery, through which they can access structural resources, such as regulatory frameworks,493 training and development179 and dedicated change management support. 191
In M1, population-based, integrated care for long-term conditions and multimorbidities builds on the involvement of patients in decision-making about their own lifestyle choices and self-care. Similarly, it is empowered staff who can draw on structures or resources of a credible integrated care model, and joint decision-making between staff in different services and good working relationships with other professionals are able to achieve the quality improvements of equitable access to services and streamlined patient journeys, including efficient discharges.
Accountability theory
Accountability is pervasive in social systems. 494,495 Frink et al. 496 argue for a meso-level conceptualisation to better understand the relevant context. Within health care, Emanuel and Emanuel497 put forward three essential components: (1) the loci of accountability – the number of different agencies that can be held accountable or hold others accountable; (2) the domains of accountability – the number of activities for which agents or agencies can be held accountable (professional competence, legal and ethics conduct, financial performance, safety and quality); and (3) the procedures of accountability, including formal and informal procedures for evaluating compliance and disclosing it.
Commentators on the German Gesundes Kinzigtal programme have illustrated that accountability comes through the locus of a ‘doctor of trust’ acting as a gatekeeper (previously unknown in the German health-care system) in co-ordinating care for complex conditions. In the MCP vanguards, primary care bolsters its gatekeeper function through appropriate referrals and providing continuity to ensure collective accountability.
The programme theory component of R2 proposes that place-based contracts and payment systems will incentivise shared accountability. The locus of accountability is likely to be at a system level for the domains of outcomes and assurance, but incentives may need to be tailored to organisational or service levels, with the necessary adaptation and feedback of a complex system. The process of accountability for MCPs is likely to require a co-productive approach of ‘social accounting’196 operating at several loci, such that the domains of accountability and the procedures take into account not just the structural transactional elements that lead to cost-effectiveness outcomes,498 but also the operational subculture. 499
Relational co-ordination theory
Relational co-ordination theory500 focuses on three attributes of relationships among members of a work process to support co-ordination and performance. These are shared goals over and above the specific goals of individuals; shared knowledge that helps individuals to see how their specific tasks fit within the whole process; and mutual respect, which helps individuals to view others’ work as credible. 500
The application of relational co-ordination to health care highlights the significance of relationships. 501 For example, the Buurtzorg model of care is based on the shared goal of ‘humanity over bureaucracy’ to provide a sustainable, holistic model of community care; this emphasises connectivity and mutual respect through shared knowledge within an autonomous team responsible of all aspects of care for a group of patients. 53 The theory component of M2 resonates strongly with the Buurtzorg model, in which the shared goal is one of co-ordinated patient-centred care through interprofessional delivery,345 the clarity of roles and support through reflective practice,345,502 emphasising team ‘belonging’. 315,329,502 The emphasis of the MCP on co-production and community resilience (R3) requires trust,266 ownership and confidence,263,274,287 enabling individuals to recognise their reciprocal roles286 and maintain mutually beneficial relationships. Staff who share a goal of working within a learning organisation or high-performing service (M3 and M4) are able to effectively use data to reflect and learn from performance, at the individual, team and organisation levels;371 a supportive environment in which staff take on new roles366 is linked to improved staff engagement and job satisfaction, as well as the organisational outcomes of reduced absenteeism and staff turnover. 503
Social learning theory
Social learning theory postulates that learning occurs through observation, imitation and modelling, and encompasses attention, memory and motivation. 504 A supportive learning environment enables an organisation to harness relationships and the skills and capacities of individuals in the system, and to respond to occupational innovations. 505 Learning through iterative evaluation is a core feature of MCPs. This theory encompasses both resources (training and tools) and reasoning (trust and confidence), as well as the activities associated with new ways of working and timely evaluation loops.
Many pioneer ACOs reported an iterative process of learning through experimentation and rapid-cycle changes in their approaches to care management, quality improvement and care transition efforts. 506 In keeping with the complex systems lens, their learning and feedback processes were not always formalised, but were through an ‘organically assembled collection of information sources’, including past experience of staff, multiple data analysis, expert advice from consultants, learning collaboratives with peer ACO organisations and partnerships with other providers. 506 These observations of pioneer ACOs can be imitated in the vanguards; building in the capacity for rapid learning and collaboration as learning systems is likely to be critical to embedding and sustaining the transformational change of the NHS new care models. 200 The ACO experience of developing mechanisms and systems for learning (and then acting on that learning) acknowledges the key role of performance data and individual physician-level learning and action. 126
Actor network theory
This theory considers networks to be made up of both people and technologies, and focuses on how these ‘actors’ behave as a result of their position in a network and the power that emerges from their dynamic configurations. 507,508 The theory provides a lens through which to view the role of technology in shaping social processes in a complex system. 509,510
In a new care model setting that depends on shared access to linked data (see Figure 20) for the delivery of proactive care (M5), the application of actor network theory is apt. The problem is that the sharing and linking of data are fraught with patient confidentiality and information governance issues,454 not to mention systemic and historical information technology compatibility issues. 511 Generating patient and professional interest is dependent on demonstrating benefits for each of these groups, which, for MCP purposes, would include the receipt (for patients) or delivery (for health-care professionals) of timely access to appropriate care. The theory highlights the importance of defining the role of each actor, from the professionals who enter the data to those who audit it, and the tools, ranging from electronic health records to big data repositories. Importantly, this also requires a defined goal for health information exchange. 464 There is a need to align with other cultural changes occurring, such as multidisciplinary working (M2), shared decision-making (M1)512 and training (M3) for patients and health-care professionals,470 to overcome technological and ethics barriers. 454
Further application of theory
Our evidence maps identified a great degree of overlap between the different foci. The links between quality improvement, audit and feedback are self-apparent, while quality improvement and the learning organisation are both categorised by an upwards spiral of individual and organisational development. Feedback is a key component of both transformational change and of quality improvement, and is also linked to the ideas of single-loop and double-loop learning rehearsed above. This interdependence is further emphasised by the presence of common theories (Table 13). For example, Lukas et al. ’s415 model is designed to offer a lens on transformational change within the context of CASs. Further work is required in order to explore the extent to which it might be helpful to engage with these large and significant bodies of theory within the context of system learning.
| Evidence base | Potential mid-range theories |
|---|---|
| M1–M5: population-based approaches to primary care (context) |
Behaviour ecological model513 Community coalition action theory514 |
| M1–M3 and M5: integrated and collaborative care (context) | Normalisation process theory515 |
| M1–M5: quality improvement in primary and community care (mechanisms) |
Adult learning theory516 Social cognitive theory517 Social influence network theory518 |
| M1: service development (mechanisms) | Resource-based view of the firm519,520 |
| M2 and M3: team and organisational development (mechanisms) | Resource-based view of the firm519,520 |
| M3: leadership development (mechanisms) |
Transformational leadership521 Dynamic theory of leadership development522 Kotter’s eight-stage change model523 |
| M4: large-scale transformational change (context) |
Behaviour change theory and the role of feedback524 Lukas et al. ’s415 organisational model for transformational change in health-care systems Neoinstitutional theory525 Organisational change theory526 |
| M4: CASs (context) |
Hinings and Greenwood’s527 model of change dynamics Kanter et al. ’s528 ‘big three’ model of organisational change528 Lukas et al. ’s415 organisational model for transformational change in health-care systems Pettigrew’s context/content/process model529 |
| M4: learning theory (mechanisms) |
Adult learning theory516 Experiential learning theory530 |
| M4: audit and feedback (mechanisms) |
Control theory531 Feedback intervention theory532 |
| M5: evidence-informed commissioning/value-based health care (context) |
Saliency and immediacy533 Three-way pull of competing demands – politics/influence (power), science and evidence (truth) and the public and acceptability (legitimacy)533 Dynamic theory of strategy534 |
Appendix 9 Revisiting the research objectives
This section summarises how the overall approach and findings relate to the objectives agreed at the outset of the review.
Articulate the underlying programme theories behind the multispecialty community provider model of care, by mapping the logic models of the 14 multispecialty community provider demonstrator sites, prioritising key theories for investigation
This review has articulated a programme theory, comprising eight components, based on the logic models and associated documents from the MCP vanguards and relevant documentation from NHSE. With the support of the project advisory group, the candidate theory components considered to be of greatest benefit for the realist review were prioritised.
Identify sources of theoretical, empirical and practice evidence to test the programme theories
As described in Chapter 2, the review has incorporated theoretical, experiential and empirical evidence, to capture and validate transferable learning to new models of care. This ‘blended’ evidence base provides important lessons in relation to the effectiveness of the interventions, but, in recognition of the inherent complexity and variation, also identifies practical insights to understand the mechanisms of change within the different contexts of the MCPs.
Appraise, extract and analyse evidence, reconciling confirmatory and contradictory evidence
The in-depth realist reviews (Chapters 4–6) provide an overview of the evidence base in relation to three of the core elements of the programme theory: (1) enhanced primary care, (2) new forms of contracting and (3) behaviours to develop community resilience. Theory component maps have been developed to provide an indicative summary of the relevant evidence bases that will inform the design, implementation and evaluation of integrated pathways, multidisciplinary working, organisational development, system learning and shared data.
Develop the synthesis, producing a ‘blueprint’ to explain how the mechanisms used in different contexts contribute to outcomes and process variables
The project team will be working with communications colleagues to develop tools to communicate the findings in accessible formats and with NHSE colleagues to translate findings into actionable insights. A model of the overall programme theory has been developed to summarise the key components of the theory of change underpinning the MCP model. A typology of interventions and mechanisms has also been created using the best-fit framework to facilitate communication with key audiences.
Consult with key multispecialty community provider stakeholders to validate the findings and to test their applicability to different contexts
The project team established an advisory group to provide the project with independent support and advice. Members were assembled to provide a range of experience and expertise, including new care model vanguard sites, NHSE, senior leaders in health and social care, public representation, academic partners and collaborators, communications expertise and project team members. The group was consulted specifically on four aspects of the review to:
-
confirm the scope of the synthesis
-
prioritise the programme theory components for review
-
test and validate the programme theory components as they evolved
-
test the emerging findings.
Working with the advisory group has been useful, not only in testing the approach and programme theories, but also in building awareness of relevant work within the New Care Models programme and the vanguard sites. For example, the team was able to secure early sight of an implementation matrix being developed by NHSE, which sets out the key characteristics and expectations of new models of care.
Finalise the synthesis, incorporating stakeholder feedback
The project team held a focus group, involving the project’s advisory group, to share and test emerging findings. When operational priorities prevented attendance, the team subsequently followed up with individuals either by telephone or in person. The range of perspectives – operational/strategic, clinical/non-clinical, current MCP/planned MCP – was particularly useful in testing the findings for a range of audiences. A summary of stakeholder feedback is provided in the review chapters, providing an insight into the implications of the findings for practice at the strategic and operational levels.
Disseminate the findings, preparing a series of practical tools to support knowledge mobilisation
The project team worked with a freelance consultant, with experience of supporting the communication of complex research, to provide dedicated specialist support and advice alongside an in-house communications team, with expertise in engaging staff across health and social care. Communication and engagement are embedded in the project from the outset, initially focused on further developing an existing network of contacts, to ensure the awareness of, and alignment with, national activities. Through these links, the review has had some coverage in NHSE’s regular communication with new care model sites. An early output was the advocates toolkit for use by the project team and advisory group members, to ensure consistent messages.
The project protocol was shared via the PROSPERO service and published in Systematic Reviews;61 further opportunities for publication are being explored. Abeda Mulla presented a poster on our innovative methodology – a combination of a realist synthesis with a best-fit framework synthesis – at the second International Conference on Realist Evaluation and Synthesis conference in October 2016.
A blog was established to share updates on the project (https://mcpsynthesis.wordpress.com/). The team has also raised awareness of the project via Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com), using a dedicated hashtag (#mcpsynthesis) from the @Strategy_Unit account. In September 2016, the review was promoted at the national NHS Expo event, organised by NHSE, with the aim of raising awareness of the synthesis and inviting delegates to participate, either through a focus group or by sharing local evaluations and other relevant materials.
The team presented at the Health Services Research Network conference in July 2017, and is exploring opportunities at academic and practitioner events to further share findings. The team is also co-ordinating discussions with related projects to identify opportunities to collaborate on dissemination.
Glossary
- Access
- A subjective concept, incorporating different aspects of care, including the availability of services (e.g. opening hours), accessibility (e.g. sensitivity to cultural needs) and convenience (e.g. location).
- Accountable care organisation
- An organisational form in which a group of providers agree to take responsibility for providing all care for a given population for a defined period of time under a contractual arrangement with a commissioner. Providers are held accountable for achieving a set of pre-agreed quality outcomes within a given budget or expenditure target.
- Advanced nurse practitioner
- A registered nurse who has acquired the expert knowledge base, complex decision-making skills and clinical competencies for expanded practice, the characteristics of which are shaped by the context and/or country in which s/he is credentialled to practice. A master’s degree is usually part of the criteria for entry-level advanced nurse practitioner roles.
- Alliance contracting
- An agreement between a set of providers and a commissioner to deliver services. All providers share the risk and responsibility for delivery and, unlike the lead provider model, are not co-ordinated by a prime contractor. As a result, there is a greater emphasis on internal governance.
- Allied health profession
- Health-care professions that are distinct from nursing, medicine and pharmacy. These include arts therapists, chiropodists/podiatrists, dietitians, occupational therapists, orthoptists, orthotists, paramedics, physiotherapists, prosthetists, radiographers, and speech and language therapists.
- Capitation
- Paying a provider or a group of providers to cover the majority (or all) of the care provided to a specified population across different care settings. The regular payments are calculated as a lump sum per patient.
- Care planning
- An approach to provide people with long-term conditions with an integrated and personalised care plan within a wider context of condition management that promotes risk stratification, targeted care and self-management.
- Case management
- Planning, co-ordinating, managing and reviewing an individual’s care. This involves a case manager/team assessing a patient’s needs, developing a care plan, organising the required care, monitoring the quality of care and maintaining contact with the patient and carer.
- Clinical Commissioning Group
- An organisation responsible for implementing the commissioning roles as set out in the Health and Social Care Act 2012 (Great Britain. Health and Social Care Act 2012. London: The Stationery Office; 2012). It does this by planning and designing local health services in England, then ‘commissioning’ or buying health and care services, including planned hospital care and urgent and emergency care.
- Community
- A group of people who have common characteristics or interests. Communities can be defined by: geographical location, race, ethnicity, age, occupation, a shared interest or affinity (such as religion and faith) or other common bonds, such as a health need or disadvantage.
- Community anchors
- Independent community-led organisations with multipurpose functions, which provide a focal point for local communities and community organisations, and for community services. They often own and manage community assets, and support small community organisations to reach out across the community.
- Community engagement
- A range of approaches to maximise the involvement of local communities in local initiatives to improve their health and well-being and reduce health inequalities. This includes needs assessment, community development, planning, design, development, delivery and evaluation.
- Community resilience
- A quality or state that produces good outcomes for individuals and communities, despite serious threats to their adaptation or development; these threats may arise both from shocks or emergencies and ongoing daily conditions of life.
- Complex adaptive systems
- A collection of individual agents with the freedom to act in ways that are not always totally predictable, and whose actions are interconnected, so that one agent’s actions change the context for other agents.
- Co-ordinated care
- Care organised around ‘natural communities’ or ‘hubs’ and delivered by multidisciplinary teams comprising generalists and specialists from the NHS, independent practice, social care, community services and third-sector services.
- eHealth
- Health-care practices supported by electronic processes and communication.
- Enhanced primary care
- An enhanced level of clinical and social support to enable individuals to receive a high level of clinical support while remaining in a community setting. This combines general practitioners, practice staff and community and specialist health staff working together, and includes primary care, community and district nursing, community, mental health services, community therapies, care navigation, social care, third-sector services and voluntary services.
- EuroQol-5 Dimensions
- A standardised instrument for measuring health outcomes.
- Feedback loops
- Feeding back the output of a process, as an input, into the same system.
- General Practitioner Access Fund (previously the Prime Minister’s Challenge Fund)
- A development fund helping to improve access to general practice and to stimulate innovative ways of providing primary care services. Schemes are chosen based on testing innovative ways of increasing access and delivering wider transformational change in general practice.
- General practitioner with a special interest
- An ‘extended clinical role’ largely based on traditional specialty-based areas, such as dermatology or minor surgery. This role was introduced following the NHS plan (Department of Health and Social Care. The NHS Plan: A Plan for Investment, a Plan for Reform. London: Department of Health and Social Care; 2000) to improve patient access to specialist care, and reduce waiting times and referrals.
- Information governance
- Management of information through standardised structures, policies, processes and controls.
- Informational continuity
- Information relevant to the patient is made available to the patient and the health-care provider, at the right place and at the right time, to support continuity of care.
- Integrated care
- An approach to an individual’s care that aims to address fragmentation in patient services and enable better co-ordinated care and continuity of care to improve patient experience and achieve greater efficiency of health delivery systems.
- Integrated care pathways
- Collaboration between health-care professionals that streamlines patient management with standardised treatment.
- Integration
- This relates to the methods and models at various levels (e.g. clinical, organisational, cross-sector) that aim to align services to improve outcomes. Integration involves collaborative working across services, organisations and sectors.
- Lead provider model (also known as prime provider model)
- One provider is given the responsibility, through a contract for subcontracting to other providers for the various aspects of care, to both deliver care and to ensure that all various aspects of care are fully integrated, bringing together the previously episodic providers of care into a single pathway.
- Logic models
- An outline of the inputs, processes, outputs and outcomes of a programme, presented in an accessible diagrammatic form, typically with accompanying notation and/or explanatory text.
- Macro-level integration (also known as system integration)
- When providers, either together or with commissioners, seek to deliver integrated care to the populations that they serve.
- Meso-level integration (also known as professional and organisational integration)
- When providers, either together or with commissioners, seek to deliver integrated care for a particular care group or populations with the same disease or conditions, through the redesign of care pathways and other approaches.
- Micro-level integration (also known as clinical integration)
- When providers, either together or with commissioners, seek to deliver integrated care for individual service users and their carers through care co-ordination, care planning, the use of technology and other approaches.
- Multispecialty community provider
- A model of care developed as part of NHS England’s Five Year Forward View (NHS England. Five Year Forward View. London: NHS England; 2014) and that is primary care-led and aims to provide more enhanced care, such as diagnostic services and outpatient clinics, in a community setting. Some also incorporate mental health services and social care.
- Mutualisation
- Ownership and accountability that passes from central government to the direct stakeholders of public services – those who work in them and those who benefit from them. There are two ways to do this. The first approach is to convert public services into non-profit enterprises, and the second approach is simply to get the public back into public services.
- NHS vanguard site
- Individual organisations and health and social care partnerships that were chosen by NHS England in 2015 to develop models to support the improvement and integration of services, with the aim of transforming how care is delivered locally.
- Outcome-based commissioning
- Designed to shift the focus from activities to results, and from how a programme operates to the good it accomplishes. The funding is to be given, not in terms of outputs achieved or processes to be followed, but in terms of what outcomes might be expected.
- Pay for performance
- A provider payment model that explicitly seeks to align payment incentives with health system objectives related to quality, care co-ordination, health improvement and efficiency by rewarding the achievement of targeted performance measures.
- Physician associate
- The physician associate is a new type of health professional, who works with the clinical team to provide quality health care across the NHS. Physician associates carry out defined duties under supervision to support, but not replace, doctors.
- Practice-based commissioning
- Front-line primary care service delivery (general practitioners, nurses and other health-care professionals) that holds the commissioning power to ‘buy’ health services for its population.
- Predictive analytics
- The use of data to make predictions about unknown events.
- Primary and acute care system
- A collaborative approach to improving patient care by creating new partnerships under a variety of frameworks to join up general practitioner, hospital, community and mental health services and provide new models of care delivery.
- Programme theory
- Describes the theory built into every programme, being expressed as ‘if we provide these people with these resources it may change their behaviour’ (Pawson R. Nothing as practical as a good theory. Evaluation 2003;9:471– 90).
- Quadruple aim
- Sometimes referenced as the triple aim plus one, this derives from the triple aim, an approach developed in the USA, to describe the ambition to drive improvement across three dimensions of health care: population health, patient experience and cost-effectiveness. The quadruple aim refers to the extension of this approach to incorporate staff/provider experience.
- Realist synthesis
- A theory-driven approach to summarising the literature that seeks to unearth ‘the unseen elements of a programme (the mechanisms) that leads to its success or failure’ [Rycroft-Malone J, Burton CR, Williams L, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. Health Serv Deliv Res 2016;4(12)].
- Real-time analytics
- The ability to use data for the purposes of analysis, as soon as these are available to the system.
- Risk- and gain-sharing
- A management method of sharing risks and rewards between members of a group by distributing gains and losses on a predetermined basis.
- Telecommunication
- Communication involving voice, data and video transmission, using information-transmitting technologies, such as the telephone and the internet.
- Teleconsultations
- A consultation involving a network or video link between the doctor and the patient.
- Teledermatology
- Telemedicine applied specifically for the subspecialty of dermatology.
- Teledermoscopy
- Telemedicine applied specifically for the subspecialty of dermoscopy.
- Telemedicine
- The use of telecommunications technology for remote diagnosis and treatment.
- Telemonitoring
- The ongoing assessment of a patient with a condition, using data collected remotely.
- Telepsychiatry
- Telemedicine applied specifically for the subspecialty of psychiatry.
- Value propositions
- Long-term ambitions in relation to achieving some form of the triple aim of better health, better care and better value.
- Virtual clinics
- Direct contact with a health-care professional by e-mail, telephone or video.
- Virtual health-related community
- Direct contact with other patients over the internet.
List of abbreviations
- A&E
- accident and emergency
- ACO
- accountable care organisation
- ACS
- accountable care system
- ANP
- advanced nurse practitioner
- CAS
- complex adaptive system
- CCG
- Clinical Commissioning Group
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMS
- Centers for Medicare and Medicaid Services
- COM-B
- ‘capability’, ‘opportunity’, ‘motivation’ and ‘behaviour’
- FYFV
- Five Year Forward View
- GP
- general practitioner
- GPwSI
- general practitioner with specialist interests
- HMIC
- Health Management Information Consortium
- HSDR
- Health Services and Delivery Research
- MCP
- multispecialty community provider
- MDT
- multidisciplinary team
- NHSE
- NHS England
- NIHR
- National Institute for Health Research
- PACS
- primary and acute care system
- PDSA
- plan–do–study–act
- PPI
- patient and public involvement
- QOF
- Quality and Outcomes Framework
- RAMESES
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
- ROI
- return on investment
