Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/10/42. The contractual start date was in January 2015. The final report began editorial review in February 2017 and was accepted for publication in October 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Jon Nicholl has previously written an article for a newspaper (The Mail on Sunday) on the same topic. No payment was made for this article. Suzanne Mason is a member of the Health Services and Delivery Research Commissioning Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Knowles et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Context to the reorganisation of emergency care in England
The modern day emergency department
Over the past 50 years in the UK, emergency medicine has emerged as a specialty and a unique discipline with its own body of knowledge. 1 Over the same period, there has been a dramatic rise in the number of emergency physicians, as well as in the number of visits by patients to emergency departments (EDs). 2 The ED [also known as the accident and emergency (A&E) department] is the ‘shop window’ of acute hospitals. It is the part of the hospital that is most closely in contact with the public as it offers the most informal access. It plays an important part in caring for the acutely ill and injured patients and has the ability to have a significant impact on the functioning of the wider hospital system. It is surrounded by substantial media interest, probably as a result of the perceived drama of emergency care. 3
Initially set up as ‘casualty units’, EDs have evolved and there are now four different types, with a type 1 ED being a 24-hour consultant-led service that deals with all types of accidents and emergencies, a type 2 ED being a single-specialty emergency unit (e.g. for dental emergencies), a type 3 ED being a minor emergency service and a type 4 ED being a walk-in centre (WIC).
Demand for emergency care
Emergency care in England is under continued pressure, with demand continuing to increase across the emergency care system. Ambulance service emergency call volumes have risen significantly in the last 10 years: from 5.6 million in 2004/54 to 9 million in 2014/15. 5 Although there has only been a small increase in type 1 ED attendances over a similar period, there have been large increases in the number of attenders at minor type 3 and 4 departments. 6 Of the patients attending a major ED, around one-quarter (26%) go on to be admitted to hospital,7 a statistic that increased from 23% in 2011. 8 The overall number of emergency admissions has continued to rise steadily over the past 5 years: from 5.3 million in 2010/119 to 5.7 million in 2015/16. 10
Despite the introduction of new urgent care services over the last 20 years, such as WICs, NHS Direct and NHS 111, these services appear to have had little impact on diverting demand away from emergency care. 11,12
The rise in demand for emergency care is not clearly understood. Many explanatory factors have been proposed, alone or in combination, including poor access to alternatives such as primary care, behavioural change in which patients more commonly expect immediate one-stop medical assessment and care, and an ageing population with more complex health needs. In addition, increased social mobility and a lack of robust social care structures make patients more likely to access emergency care rather than rely on their social networks. One result of the increasing number of emergency admissions globally has been increasingly long waiting times and crowding of ED in many countries, a problem that frequently attracts substantial attention from the press and public.
Emergency and urgent care services are also under unprecedented scrutiny. The NHS Commissioning Board is currently reviewing the model of urgent and emergency services in England. 13 The review will set out proposals to reorganise care that best meets the needs of patients, in a sustainable way. The first phase of this review has recently been completed and sets out a vision for redefining EDs into two types of emergency centre: ‘emergency centres’ and ‘major emergency centres’. 13 Proposals suggest that emergency centres will assess and initiate treatment, with the larger major emergency centres hosting specialist services. 13
Supply of emergency care
The Royal College of Emergency Medicine has cited ‘proper staffing’ as the single most important factor in providing a high-quality, timely and clinically effective service to patients. 14
The rising demand for emergency care comes at a time when EDs are facing a staffing shortage. It has been reported that EDs are understaffed by an average of 10%. 15 Although this is, in part, caused by rising demand, there are also problems in recruiting staff to, and retaining staff in, departments because of the increased pressure of the workload and work intensity. Anecdotal evidence exists of ED consultants leaving the NHS,16 citing increasing patient demand, a lack of resources and excessive time pressures as reasons for leaving the UK to continue a career in emergency medicine overseas. 15
Significant staffing shortages coupled with rising demand may have implications for the safety of patients. One solution to this may be to close some of the EDs facing such problems, or to suspend services during the night. Indeed, two NHS hospitals (County Hospital in Stafford and Fairfield General Hospital in Greater Manchester) have recently suspended ED services for children, citing that they could not run them safely. 17 Further restrictions on ED services in Grantham and Chorley have been attributed to a national shortage of skilled ED doctors. 18
History of closures
An accurate number of ED closures or downgrades in England could not be identified as there appears to be no definitive list of these departments. However, estimates suggest that there was a net reduction of 8% in the number of EDs providing care in the 10-year period leading up to 2011/12. 19 These departments are likely to have closed for reasons of safety, sustainability or affordability. No further evidence identifying ED closures, after 2012, was found. However, based on media reporting, we are aware of further closures between 2012 and 2017.
Recent media reporting of NHS sustainability and transformation plans (STPs) suggests that further closures and downgrades are being considered; around one-third of the 44 local STPs submitted indicate plans to reorganise emergency care in their respective geographical areas.
Existing evidence regarding closures (or closure-related evidence)
For many people living in areas affected by proposed or actual closures, this issue evokes strong feelings, as is demonstrated by local campaign groups that have formed to oppose closures. Despite this strong public interest, the evidence on whether or not closures are detrimental to local populations is limited and often conflicting.
Travelling longer distances to receive emergency care
There is large variation in the average home-to-hospital ‘straight-line’ distances in England, which range from 1.6 to 21.3 miles,19 with over half of the population living < 3.7 miles away from an ED. When an ED closes, some patients may have to travel further for emergency care, which may have an impact on their decision to access care. There is some evidence that those living closer to an ED are more likely to use the ED than those living further away. 20
There is some evidence that travelling further for care can lead to poorer clinical outcomes. This may be true because travelling further increases the amount of time before arriving at the ED.
Studies originating in the USA that focus on ED and trauma centre closures have looked at the impact on mortality. One study21 found that for those patients residing in an area of an ED closure and being admitted to a hospital, their odds of dying as an inpatient increased by 5% compared with patients living in an area not affected by an ED closure. Trauma centres in the USA have a high level of staffing and resources and are designed to deal with the most severely injured patients. One study22 focused on the change in journey time to the nearest trauma centre, following a trauma centre closure. For those who faced an increase in drive time to the nearest trauma centre, this was, on average, 47 minutes. The study showed a strong association between closures and increased inpatient mortality, with the odds increasing by 21% for those who had an increased journey time before receiving care. Conversely, those with a decrease in journey time had 17% lower odds of dying (compared with those experiencing no change in journey time). 22
Other studies have found that an increasing distance to hospital may have an adverse impact on patients with specific clinical conditions following an emergency incident. After a hospital or ED closure, patients suffering a myocardial infarction (MI),23,24 unintentional injury,25,26 stroke or sepsis have a greater risk of death if there is an increased distance to a hospital. Nicholl et al. 27 found that, for serious emergencies, particularly respiratory problems, a longer journey distance to hospital appeared to be associated with an increased risk of mortality.
Early administration of emergency treatments
Emergency treatments are usually more effective the earlier they are given to a patient. Tranexamic acid, given to bleeding trauma patients within 1 hour of injury, reduces deaths from bleeding by 5%, but the same treatment given 3 hours later is ineffective. 28 Evidence also suggests that patients suffering MI have higher mortality if primary angioplasty is delayed, even by short periods,29 and for patients suffering an acute ischaemic stroke, reducing the time to treatment has a positive impact on mortality. 30 Added to this, delays in the arrival at the ED may also delay the administration of effective analgesia for patients.
The impact of the hospital and staff providing emergency care
It is widely accepted that outcomes for certain conditions – particularly strokes, heart attacks and major trauma – are better when patients are treated in specialist centres than in general hospitals. This may be because specialist centres can provide different care, such as neurosurgery, or because they also provide better care. However, the extent of the benefit is unclear. With the increasingly widespread availability of primary angioplasty, for example, it is possible that the benefit of specialist care for heart attacks is diminishing. Furthermore, one systematic review31 found that patients with major trauma and moderate-to-severe head injury did not have improved clinical outcomes when treated in a specialist centre, although there was some evidence that patients who were treated following a stroke did have better outcomes. However, the authors acknowledge that these conclusions were based on poor-quality data. 31 The evidence relating to mortality and stroke care suggests that receiving care in a specialist centre32 or from a specialist clinician33 reduces the risk of dying, and the reorganisation of stroke care to specialist centres in London is widely credited with having significantly reduced stroke mortality there. 34
There is also some evidence that who provides care at the hospital where the patient arrives may determine patient outcomes. ED care provided under the supervision of senior doctors is more effective than care provided by less experienced doctors,35 and junior doctors have less confidence in their clinical skills. 36 There also appears to be some evidence to suggest that the presence of consultants working on the ED ‘shop floor’ during the night can reduce ED length of stay (LOS) and rates of admission. 37
Implications for ambulance services
Because ambulances take most patients to their nearest appropriate hospital, closing an ED and diverting all patients to more distant hospitals is likely to increase ambulance journey times. This may, in turn, reduce ambulance availability and, therefore, also adversely affect ambulance service performance.
With the increase in ambulance journeys to the neighbouring hospital, this may also have an effect on crowding within the neighbouring ED. 38 Such increases in attendance at the ED may then have negative repercussions for ambulance handover at the ED and this may also adversely affect ambulance service performance.
Importance of this study
There is little research evidence to support decisions about closing or retaining EDs. Currently, we know little about the impact that closures may have on the mortality of a local population, or the workload implications for local emergency care providers, or indeed if the hospitals that patients will be redirected to are sufficiently better than the ones where the ED has closed to compensate for the increased journey times. Closing EDs is not viewed positively by the public and patients, as demonstrated by campaign groups that have formed to prevent these closures. However, closures may not have the negative impact on patient outcomes that campaign groups suggest. With further ED closures planned, evidence to inform future decision-making is needed. Identifying any impact of closures on an emergency health-care system will help NHS providers and the public to assess the implications of closure on their local system and develop strategies to minimise any potentially adverse impact.
Model to assess the impact of emergency department closures
In order to inform our assessment of the impact of the closure or downgrading of an ED, we have developed a simple model of health-care pathways following an emergency incident that requires (i.e. with the capacity to benefit from) type 1 24/7 (24 hours a day, 7 days a week) ED care (Figure 1). In the model, patients who are having an emergency go directly to an ED, telephone 999 or contact another emergency service, or delay doing anything. The numbers choosing these options may be affected by the closure or downgrading of local EDs, but in this study we proposed to capture the impact only on the number of patients who go directly to an ED and on the number who call 999. The number of patients who choose other options is hard to obtain from routine sources. We have developed survey methods to assess these other impacts39,40 but these methods require before-and-after studies that we could not use (as the EDs included in our study had already closed).
FIGURE 1.
A model to assess the impact of ED closure.
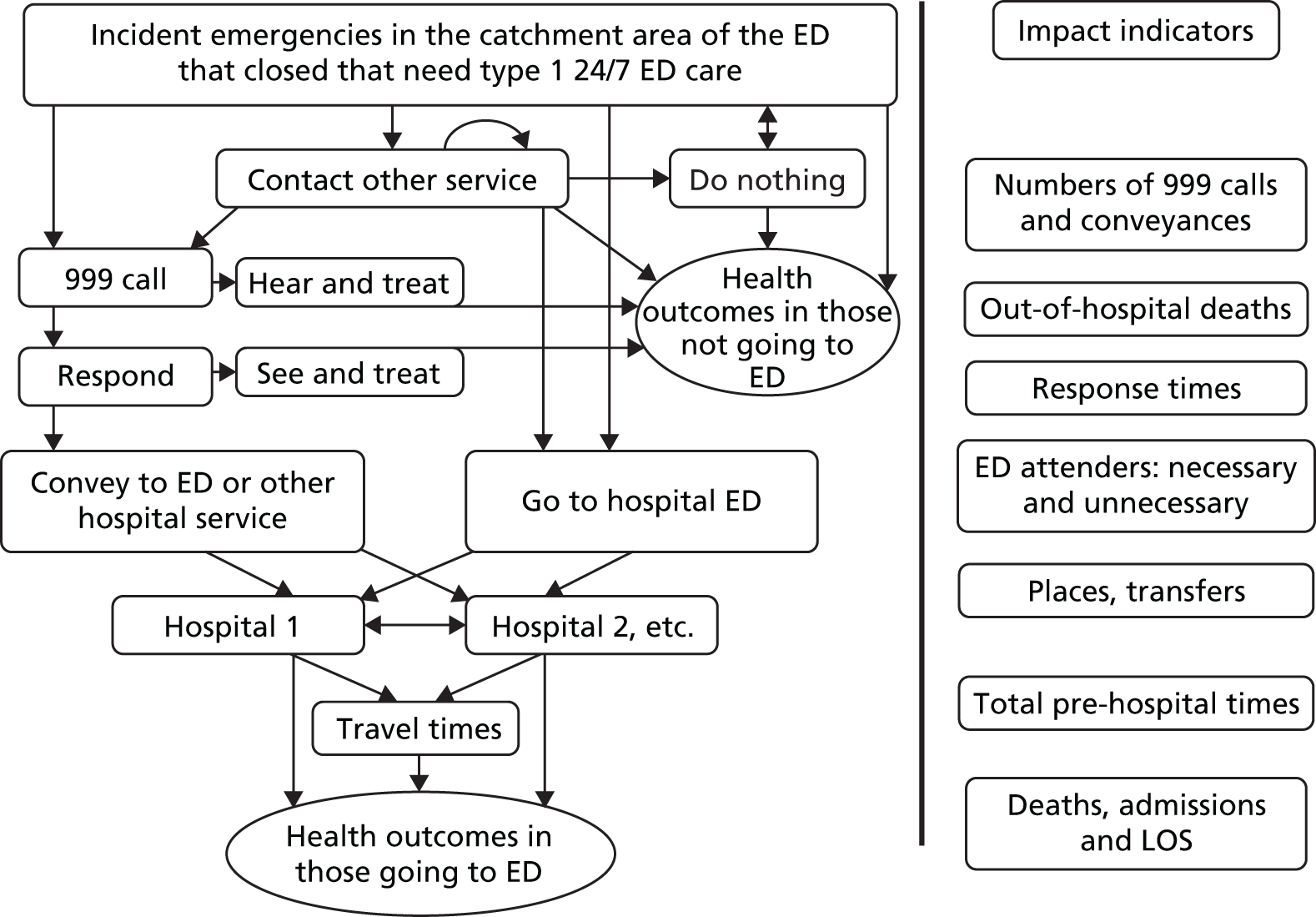
Those who choose to not go directly to an ED may also end up at the ED, but if they do not we assume that either they die (in which case we assume that they were patients who needed treatment in an ED) or their problem is resolved. We have looked at the impact on deaths in those patients who do not get to an ED as well as those who do. For all those who do end up at an ED, attendance may or may not have been necessary. NHS England has recently claimed that 40% of attendances at an ED may not have been necessary13 and, using a similar methodology based on our own work,41 we have looked at the effect of ED closures on the numbers of these minor attendances. The closure of an ED affects what hospital patients attend, which in turn, determines a number of factors including how long it took to get there, the number of emergency admissions and the quality of their hospital (ED and inpatient) care. These effects result in patient health outcomes, and we have investigated the impact on both the processes (travel times and admissions) and the outcomes (number of deaths and mean LOS in hospital).
Aims and objectives
The aim of this study was to establish the implications of closing or downgrading EDs on the population and emergency care providers and, in doing so, to provide the general public, the NHS and policy-makers with some evidence to inform decision-making about future ED closures.
Our specific objectives were to detect changes in:
-
the number of NHS ambulance service incidents, and time to take patients to hospital in our resident catchment populations following the closure or downgrading of an ED
-
emergency department attendance by our resident catchment populations following the closure or downgrading of an ED
-
emergency admissions in our resident catchment populations for all conditions, and certain conditions that are relatively rich in ‘avoidable emergency admissions’, following the closure or downgrading of an ED
-
mortality in emergencies in our resident catchment populations for certain serious emergency conditions (SECs) following the closure or downgrading of an ED.
Chapter 2 Study overview
Study design
A controlled interrupted time-series analysis42 of a series of impact measures was undertaken to detect the impact of ED closures on the resident catchment populations of five EDs that were closed or downgraded between 2009 and 2011.
Settings
The study settings are 10 geographical areas in England: five intervention areas where an ED closed or was downgraded between 2009 and 2011 and a control area for each intervention area. Each intervention area was defined by the catchment population of the ED that closed (see Chapter 4).
Patient and public involvement
The closure of EDs can provoke strong reaction from local groups. Prior to the inception of the study, a co-author (JN) had been approached by members of local campaign groups seeking research evidence with regard to the closure of EDs. This prompted our interest in developing this study. Engaging with these local groups in the development and conduct of this research was not desirable given concerns about impartiality. However, given the public interest in this area, the perspective of the public and patients was especially important.
The School of Health and Related Research (ScHARR) at the University of Sheffield has a large portfolio of emergency and urgent care research projects. In order to support patient and public involvement (PPI) activities across these projects, a PPI group, the Sheffield Emergency Care Forum (SECF), was established. This group provides direct support to research teams within ScHARR and also provides wider links to related PPI groups within the South Yorkshire comprehensive local research network and Healthwatch.
Members of the SECF contributed to the study. Enid Hirst, lay co-ordinator of the SECF, attended the management meetings during the project and Linda Abouzeid participated in the management meetings alongside her. Linda Abouzeid had no previous experience of PPI involvement in a research study and used this as a developmental opportunity. In addition, both Enid Hirst and Linda Abouzeid supported the collection of media material related to the closures and downgrades. John Bennett provided PPI input at the project advisory group meetings.
During the study, the PPI representatives were available to influence decisions being made about how to operationalise the research proposal and interpret the findings. The PPI group led the writing of the Plain English summary for this report, assisted in the construction of a wide-reaching dissemination strategy and will assist in writing further lay summaries of the findings for dissemination.
Ethics and governance
The study used anonymised routinely collected data. No primary data were collected as part of this study. We sought guidance from NHS Research Ethics Committee and were informed that this study did not require NHS ethics approval. However, approval was sought, and granted, from the ScHARR Research Ethics Committee for the use of secondary data. NHS permission was granted from all participating NHS ambulance trusts. Although the NHS ambulance services that were operating in the control areas selected were consulted on their inclusion in the study, NHS acute trusts were not. Hospital Episode Statistics (HES) data from these trusts were retrieved directly from NHS Digital (previously the Health and Social Care Information Centre). Therefore, we have not identified the control sites in this report.
Changes to the planned research
Most of the study was delivered as planned. However, it was not possible to deliver everything that was set out in the original proposal. The changes are summarised in Appendix 1.
Study settings and history of emergency care reorganisation
Five geographical areas were chosen as intervention areas in this study: Hemel Hempstead, Bishop Auckland, Rochdale, Newark and Hartlepool. The criterion for selection of an intervention site was that the closure or downgrade preceded 2012, to ensure that 24 months of follow-up data could be obtained. Some background information on each closure is provided in the following sections. Publicly available consultation documents and internet searches of media reports were sourced to inform this background.
Hemel Hempstead: a large town situated in southern England
Emergency service provision
Acute care
Hemel Hempstead Hospital forms part of West Hertfordshire Hospitals NHS Trust, along with two other acute hospitals: St Albans City Hospital and Watford General Hospital.
Ambulance care
Ambulance care for the residents of Hemel Hempstead is provided by the East of England Ambulance Service NHS Trust, which responds to more than 500,000 emergency incidents each year. 43
Background to the closure
A public consultation led to an announcement in November 2006 that the ED at Hemel Hempstead hospital was closing. 44 However, claims that the closure was based on a flawed consultation process led to a further consultation, Delivering Quality Care for Hertfordshire. This consultation process ran between June and October 2007, and was built on an argument that local clinicians had concerns that, unless acute and emergency hospital services in Hertfordshire were consolidated onto fewer hospital sites, these services would become substandard, unsustainable, unattractive to clinical staff and, ultimately, unsafe.
The consultation provided proposals for the reorganisation of care across the county of Hertfordshire affecting three NHS trusts, rather than Hemel Hempstead in isolation. Specifically in relation to Hemel Hempstead, these proposals suggested:
-
the commissioning of two local general hospitals to provide substantial centres of care for local communities in Hemel Hempstead and either Welwyn Garden City or Stevenage (East and North Hertfordshire and West Hertfordshire Primary Care NHS Trusts)
-
the establishment of eight urgent care centres (UCCs) to provide emergency care access for about two-thirds of patients who currently attend an A&E department (East and North Hertfordshire and West Hertfordshire Primary Care NHS Trusts)
-
the centralisation of children’s emergency services and children’s day surgery services at Watford General Hospital (West Hertfordshire Hospitals NHS Trust).
The ‘new’ service
The UCC opened in October 2008 and was positioned adjacent to the ED. The UCC and the ED ran alongside each other until the ED closed in March 2009. The UCC, led by general practitioners (GPs), is open 24/7. It was perceived that the UCC would care for 65% of those patients who had previously visited the ED in Hemel Hempstead.
Following the closure, it was expected that many patients would use the ED services at either Watford General Hospital or Luton and Dunstable University Hospital.
Perceived outcomes following the reorganisation
The consultation acknowledged that some members of the local population may find it difficult to see how travelling further for emergency care would ensure safer and higher-quality services overall, but it highlighted that this was the view of local NHS clinicians, as well as many national clinical experts in the UK and other countries. The document (no longer publicly available) cited a number of reasons for believing that acute and emergency services are best provided in a smaller number of specialist sites.
Delivering specialist care in specialist centres
Larger specialist units with skilled staff could save more lives; the document suggested that this had been shown to be true for a number of clinical conditions such as heart attacks and strokes.
Consolidation of technologies
The Queen Elizabeth II Hospital, Lister Hospital, Watford General Hospital and Hemel Hempstead Hospital each had one computerised tomography (CT) scanner. In order for the service to be truly sustainable, the consultation document suggested that a hospital needs to have at least two CT scanners on site. By consolidating emergency stroke services in fewer hospital sites in Hertfordshire, centres of excellence with sustainable CT services that are available on a 24-hour basis could be developed.
Increased consultant availability
Consolidating acute 24/7 services in two hospitals was intended to help to ensure that more patients benefit from increased consultant availability at each site. The consultation document suggested that the better availability of consultants would save more lives.
The consultation document (no longer publicly available) focused on improving outcomes for patients and achieving better efficiency. The overall message appeared to be focused on providing care closer to home when possible and the centralisation of services with the aim of providing safe and sustainable services.
Concerns raised by the local population and media
An internet search identified concerns that had been raised regarding the closure. Local MPs raised concerns regarding the increase in travel times to Watford General Hospital. Local media also reported an increase in the number of patients travelling from the Hemel Hempstead area to receive care at Watford General Hospital; there were reports that the number of patients had more than doubled from 879 in 2007 to 2205 in 2012. 45
Bishop Auckland: a market town in the north-east of England
Emergency service provision
Acute care
Bishop Auckland General Hospital forms part of County Durham and Darlington NHS Foundation Trust (CDDFT), along with two other acute hospitals: Darlington Memorial Hospital and the University Hospital of North Durham.
Ambulance care
Ambulance care for the residents of Bishop Auckland is provided by the North East Ambulance Service NHS Foundation Trust. The service provides care to a population of around 2.65 million people across a geographical area of approximately 3230 square miles; it responds to more than 230,000 emergency incidents each year. 43
Background to the closure
Following a period of public consultation, plans to close the ED were approved in September 2008. This had been preceded by a major review of the care provided at CDDFT (Seizing the Future),46 which aimed to provide:
Safe, sustainable and high quality services.
At the time of the review, all three acute hospitals within CDDFT were providing ED care, although trauma and emergency surgery patients were already being diverted away from Bishop Auckland General Hospital to the hospitals in Darlington or Durham.
The rationale for the reorganisation of emergency and urgent care was that the hospitals within this area were:
Small hospitals serving small populations.
and that there was a risk that safe care (including ED, acute and critical care) could not be sustained at the hospitals in Bishop Auckland and Darlington.
In summary, the review of the reorganisation of emergency and urgent care46 proposed:
-
the development of a 24-hour urgent care centre in Bishop Auckland
-
an expectation that the majority of ED care would be provided at Darlington Memorial Hospital and the University Hospital of North Durham.
The ‘new’ service
The ED was downgraded to a UCC in October 2009. The centre, led by GPs, is open 24/7 and deals with minor injuries and illnesses.
Following the downgrade, it was expected that many patients would use the ED services at either Darlington Memorial Hospital or the University Hospital of North Durham.
Perceived outcomes following the reorganisation
Trauma/emergency surgery
Bishop Auckland General Hospital had not undertaken trauma care or any unplanned surgery (i.e. no emergency surgery) for the 5 years following the local Darzi review. 47 Instead, care had been centralised in Darlington and Durham. Following the ED closure, it was anticipated that trauma patients (once stabilised) would be transferred to Bishop Auckland General Hospital for rehabilitation if this was closer to their home, rather than remaining in Darlington or Durham for the remainder of their inpatient stay.
Intensive care
Bishop Auckland General Hospital was struggling to recruit intensive care doctors to cover 24 hours a day. This was identified as a risk to patients. At the time, the most serious critically ill patients were being transferred to the Darlington or Durham hospitals.
Diagnostics
The review identified that it was difficult to provide the full range of 24/7 diagnostics when spread over the three hospitals and that centralisation of some diagnostics was desirable. The review identified an example of providing timely CT scans for stroke patients.
Staffing
The review highlighted that both hospitals (Bishop Auckland General Hospital and Darlington Memorial Hospital) did not meet the required number of emergency physicians recommended by the Royal College of Physicians.
Concerns raised by the local population and media
An internet search identified concerns that were raised regarding the closure. Both the local population and councillors raised concerns regarding the increase in travel times to Darlington or Durham, suggesting that this would pose a risk to health. This was of particular concern for those residents living in outlying areas, and it was suggested that these patients would need to travel an additional 14 miles to reach their nearest ED. However, the review undertaken by CDDFT46 stated that:
There is no evidence that patients are put at increased risk owing to longer journey times. In fact, the evidence shows that results for patients are better in bigger A&E departments.
Therefore, the review was suggesting that patient outcomes would improve as a result of the reorganisation.
Local campaigners also expressed concerns that the EDs in Durham and Darlington would have difficulties with absorbing the perceived additional caseload.
Rochdale: a market town in the north-west of England
Emergency service provision
Acute care
Rochdale Infirmary forms part of the Pennine Acute Hospitals NHS Trust, along with three other acute hospitals: North Manchester General Hospital, The Royal Oldham Hospital and Fairfield General Hospital.
Ambulance care
Ambulance care for the residents of Rochdale is provided by the North West Ambulance Service NHS Trust, which is the largest regional ambulance service in England. The service provides care to a population of around 7 million people across a geographical area of approximately 5400 square miles and it responds to > 770,000 emergency incidents each year. 43
Background to the closure
‘Healthy Futures’ was a public consultation/plan regarding the future of health services for adult care. It focused on the reorganisation of care in the north-east area of Greater Manchester. The basis for the reorganisation was to ensure that health services maintained a safe and sustainable approach to care and that care would be better situated in fewer hospital sites where resources and expertise could be concentrated. Local access to urgent care would be maintained.
In summary, the review of the reorganisation of emergency and urgent care proposed:
-
an expectation that the majority of ED care would be provided at The Royal Oldham Hospital, North Manchester General Hospital and Fairfield General Hospital
-
the development of a ‘locality hospital’ at Rochdale Infirmary; this hospital would provide planned care, outpatient care and diagnostic services, with urgent care delivered by a UCC located in the hospital site
-
the concentration of emergency surgery in The Royal Oldham Hospital and North Manchester General Hospital
-
that acute medicine would be provided at The Royal Oldham Hospital, North Manchester General Hospital and Fairfield General Hospital.
The consultation process was concluded in May 2006 and plans were approved in June 2007. However, there were claims that the public consultation was legally flawed. 48 The Healthy Futures programme was reviewed again in 2010 and approved in early 2011.
The ‘new’ service
The ED was downgraded to a UCC in April 2011. The centre is open 24/7, with services being delivered by experienced nurses, nurse practitioners and a GP. At the time of the downgrade, a 12-bed overnight and short-stay clinical assessment unit was opened at Rochdale Infirmary. This unit was intended for the treatment of patients who were referred directly by GPs, from the community or by the UCC.
Prior to the downgrade, the ED had been closed to ambulances during the night (18.00–08.00) since August 2010 because of staff shortages and related issues of patient safety.
Following the closure, it was expected that many patients would use the ED services at North Manchester General Hospital, The Royal Oldham Hospital or Fairfield General Hospital.
Perceived outcomes following the reorganisation
The UCC would not receive patients by emergency ambulance; patients would be transported to the nearest appropriate hospital. It was perceived that the UCC at Rochdale Infirmary would care for an estimated 85% of those patients who had previously used the ED in Rochdale.
Concerns raised by the local population and media
An internet search identified concerns that were raised regarding the closure. Following the closure, the chief executive of the Pennine Acute Hospitals NHS Trust acknowledged that the closure of the ED in Rochdale had caused operational pressure in the ED in Oldham. 49 The perception of why this had been problematic was that the closure in Rochdale had taken place earlier than was desirable and that it had been brought forward because of the unsustainability of the ED in Rochdale. In October 2011, five additional general medical beds were made available in The Royal Oldham Hospital to alleviate pressure within the hospital. 50
In 2012, it was reported that the closure of the ED in Rochdale had put pressure on services in the Royal Blackburn Hospital, which had led to a budget overspend. 51
Newark: a market town in the East Midlands of England
Emergency service provision
Acute care
Newark Hospital forms part of Sherwood Forest Hospitals NHS Foundation Trust, along with one other acute hospital: King’s Mill Hospital.
Ambulance care
Ambulance care for the residents of Newark is provided by the East Midlands Ambulance Service NHS Trust. The service provides care to a population of around 4.8 million people across a geographical area of approximately 6425 square miles; it responds to more than 600,000 emergency incidents each year. 43
Background to the closure
Newark’s Healthcare Review (no longer publicly available) formed the basis for a public consultation on the reorganisation of care in Newark in 2010. It was highlighted that the ED at Newark Hospital was not sustainable in terms of staffing or in the maintenance of skills among ED doctors. In addition, there were no intensive care beds or access to major surgical facilities on site, which affected the acceptance of medical emergencies. Therefore, it appears that ambulance patients with major injuries or conditions were already being diverted away from Newark Hospital prior to the consultation.
The consultation was challenged by members of the local population and was reviewed by a Nottinghamshire County Council committee. Two further appeals were dismissed.
In summary, the review of the reorganisation of emergency and urgent care proposed:
-
the development of a minor injuries unit (MIU) and UCC on site
-
that medical emergencies should no longer be accepted in Newark Hospital
-
the presence of a GP and emergency care practitioner in Newark Hospital
-
a reduction in the number of medical beds in Newark Hospital
-
an expectation that the majority of ED care would be provided in Lincoln County Hospital or King’s Mill Hospital.
The ‘new’ service
The ED was downgraded to a 24/7 MIU and UCC in April 2011.
Following the closure, it was expected that many patients would now use the ED services in King’s Mill Hospital or Lincoln County Hospital.
Perceived outcomes following the reorganisation
It was perceived that 85% of patients who were treated in the ED (pre closure) would continue to receive their care at the new MIU and UCC and that there would be a reduction in the number of emergency ambulance transfers from Newark Hospital to other hospitals, as patients would receive their care in the right place, first time. 52
Concerns raised by the local population and media
An internet search identified concerns that were raised regarding the closure. Local residents expressed concerns that current ambulance service provision would be insufficient to provide adequate response times and transport patients to another hospital in an emergency event.
A media report53 suggested that in Newark, following category A ambulance calls, it was taking a mean time of 90 minutes from the 999 call to the patient being handed over to an ED. In 10% of cases, the time was 150 minutes. A further media report54 suggested that there had been a 37% rise in death rates for emergency patients residing in areas with a Newark postcode.
Hartlepool: a coastal town in the north-east of England
Emergency service provision
Acute care
The University Hospital of Hartlepool (UHH) forms part of North Tees and Hartlepool Hospitals NHS Foundation Trust, along with one other acute hospital: the University Hospital of North Tees (UHNT).
Ambulance care
Ambulance care for the residents of Hartlepool is provided by the North East Ambulance Service NHS Foundation Trust. The service provides care to a population of around 2.65 million people across a geographical area of approximately 3230 square miles; it responds to > 230,000 emergency incidents each year. 43
Background to the closure
The Momentum: Pathways to Healthcare Programme was established in April 2007 and took a system-wide approach to the redesign of health care across primary, community and secondary care, which involved the development of new community facilities and the building of a new hospital in the North Tees and Hartlepool area. Part of the programme supported the development of a UCC (and the closure of the existing ED in UHH) in Hartlepool.
An attempt to close the ED took place in December 2010, but this was blocked when an independent review found that the public consultation process had lacked detail in relation to the reorganisation of ED care. A further independent review, in March 2011, subsequently recommended the closure of the ED. The review (External Review of Hartlepool Accident and Emergency Services, 14 March 2011; not publicly available) identified that local NHS managers and doctors supported the closure of the ED in UHH primarily because of safety concerns, citing (1) insufficient numbers of medical staff to cover the two rotas in UHNT and UHH and (2) limited overnight supervision of junior medical staff at UHH. The review highlighted that alternative options to closing the ED had been explored, including increasing the recruitment of medical staff (which was perceived as not being viable). An option to close the ED during the night had also been explored but it was felt that this would be confusing for patients and may increase safety concerns if patients arrived at the ED during the night (i.e. when it was closed).
In summary, the review of the reorganisation of emergency and urgent care proposed:
-
the development of a 24-hour urgent care centre in Hartlepool
-
that acute medicine would be provided at UHH for GP-referred cases only
-
an enhanced emergency admissions unit at UHH for assessing and potentially admitting patients with acute medical problems
-
an expectation that the majority of ED care would be provided at UHNT.
The ‘new’ service
The ED at UHH closed in August 2011. The One Life Urgent Care Centre in Hartlepool opened in the same month. The UCC was not based on the existing hospital site and is located approximately 2 miles away from the ED that closed. The centre provides a 24-hour MIU, a WIC that is open for 12 hours each day (08:00 to 20:00) and out-of-hours GP medical services.
Following the closure, it was expected that many patients would use the ED services at UHNT.
Perceived outcomes following the reorganisation
Prior to the closure, it was indicated by the trust annual report (not publicly available) that there were 40,000 annual attendances at the ED at UHH, and it set out how care for these patients would be redistributed after the closure of the ED. The perception was that the UCC would absorb 18,000 attendances, 7000 patients would be dealt with by the rapid assessment and treatment unit at UHH, 12,340 patients would self-present at the ED at UHNT and the remaining 2660 patients would be absorbed by other organisations.
Concerns raised by the local population and media
An internet search identified concerns that were raised regarding the closure. In 2015 (4 years after the closure), the North East Ambulance Service NHS Foundation Trust was asked if the closure of the ED in Hartlepool had increased delays in ambulance response times. The ambulance service responded that there was no link between the two55 and that additional (and continuing) ambulance resources had been put in place at the time of the closure to minimise the impact of the change in ambulance destination.
Control areas
For each intervention area, a control area was sought. Our intention was to analyse the national HES A&E data set in order to identify a control area that provided a close sociodemographic and socioeconomic match to its paired intervention site. However, because of concerns regarding data minimisation, NHS Digital requested that we select a maximum of three potential control areas for each intervention site, with a view to selecting one of these as the primary control area. The catchment areas for all EDs were to be calculated using the HES A&E data. Therefore, because we had to request these data before we could calculate the catchment area, we had to identify three geographical areas in England that we believed could provide a suitable match for each intervention area. Identifying potential control areas was further limited by our exclusion criteria. We selected potential control areas that did not share the same ambulance service with their prospective intervention areas and that did not share a geographical boundary with the catchment area of any other ED that had closed or was downgraded during the same data collection period.
Perhaps inevitably, there were some sociodemographic and socioeconomic differences between intervention areas and their controls (see Appendix 2), although the extent to which these differences may have differentially affected the time series of impact measures we have studied is uncertain.
Chapter 3 Documentary analysis
Background
Emergency and urgent health-care systems frequently develop to meet the changing needs of the population. We needed to account for any major changes to services in the emergency and urgent care system other than the ED closing in the intervention areas or any other major changes occurring in the control areas. We undertook documentary analysis for two reasons:
-
To inform the analysis of routine data by identifying ‘steps’ to be included within the statistical model. Our interpretation of important change included the introduction, closure or relocation of a service accessed by the general population (e.g. the relocation of a WIC, the introduction of NHS 111 or the closure of an ED).
-
To provide information that may help interpret the results from any of the impact measures included in the analysis.
The approach we took in identifying these changes was through the analysis of local NHS organisations’ annual reports in each of the geographical intervention and control areas that were selected. Major changes were likely to be recorded by local primary care trusts (PCTs), acute hospital trusts and ambulance service trusts.
Methods
We sought to collect information from the annual reports of a number of NHS organisations: PCTs, acute trusts and ambulance trusts. NHS annual reports cover a reporting period between April and March (i.e. 2011/12 reports cover the period between April 2011 and March 2012). We searched the website of each identified individual NHS trust for the period of 24 months before and the period of 24 months after closure for each intervention and control site in order to download the relevant report. If a report could not be located, we contacted the NHS organisation to request a copy. Once located, we read each annual report to identify any reported major changes to the emergency and urgent care system. We defined a ‘major change’ as anything that may have an impact on the way that the local general population used urgent and emergency care; for example, the introduction of the national non-urgent telephone number, ‘NHS 111’. We extracted information from the report and created a timeline for each intervention and control site, highlighting any important changes to the emergency and urgent care system or any reference to one of the group of conditions we have focused on that were identified as including potentially avoidable admissions or avoidable deaths. 56
Findings
In total, we identified and extracted information from 120 NHS annual reports. We located all of the annual reports (n = 90) for the NHS acute trusts and ambulance services that were identified (see Appendix 3).
The PCT reports were more problematic to locate. PCTs ceased to be operational in April 2013 and were replaced by clinical commissioning groups (CCGs). The majority of the reports that we sought to locate pre-dated 2013. PCT websites are no longer live; therefore, a search of the PCT website for the relevant report was not possible. We contacted CCGs in the hope that they may have historical copies of PCT reports but, given that not all CCGs are geographically coterminous with the PCT that they had replaced, many CCGs did not hold these reports. In addition, we also undertook a generic internet search and contacted The National Archives to identify any reports that had been archived. Despite these difficulties, we identified 68% (30/44) of the PCT/CCG reports that were identified.
Major changes to the emergency and urgent care system identified
Documentary analysis identified a small number of major changes to the emergency and urgent care system in each intervention and control site (see Appendix 4). In two of the control areas, no major changes to the emergency and urgent care system were identified. NHS 111 was introduced during the 48-month period we studied in six areas (three intervention and three control areas). In five areas (three intervention areas and two control areas), other changes to the system were identified, such as the opening or relocation of primary or urgent care centres. In one intervention area, in the months prior to the closure, emergency ambulances had been diverted away from the ED during the night. These changes could have had an impact on our findings, and thus we took account of these changes in the statistical model used in the analysis. In our analysis, we refer to these changes as ‘steps’.
Chapter 4 Calculation of the resident catchment population
Background
We sought to identify changes in local emergency care service activity and performance, and changes in the pattern of mortality among residents of the catchment areas where EDs had been closed. It was thus necessary to first identify the (geographical) catchment areas for EDs. The resident catchment population was defined as the population that was resident in the identified catchment areas.
A number of methods were identified and explored; these are detailed below.
Methods
The catchment area for each ED was defined by a set of small geographical areas, lower-layer super output areas (LSOAs). The Office for National Statistics (ONS) created LSOAs such that England was covered by non-intersecting LSOAs; all have similar population sizes (approximately 1500 residents in 2001) and all have internally homogeneous populations (assessed on a variety of census measures). There were two sets of LSOAs available: one derived from the 2001 UK census57 and one derived from the 2011 UK census. 58 The set of LSOAs derived from the 2001 census were used because these were readily available in the HES data sets.
Method 1: Hospital Episode Statistics accident and emergency attendance data
We identified this method in our protocol as our intended method of calculating resident catchment populations.
Using HES A&E attendance data, each LSOA was allocated to a single ED. For each LSOA, of all first attendances (in contrast to ‘follow-up attendances’) from the LSOA to any ED, the ED with most first attendances from the LSOA was selected. The LSOA that was recorded was that of the patient’s residence.
Method 2: Department for Transport road travel time data
A list of type 1 A&E department (ED) locations (in England, Wales and the south of Scotland) was prepared for the Department for Transport (DfT). Journey times were modelled by the DfT using their journey time statistics methodology59 (minute level accuracy), from the centroid of every LSOA in England to every listed ED. The DfT provided details of the 10 shortest travel times from each LSOA. For each LSOA, the ED with the shortest road travel time was selected.
Method 3: ambulance service dispatch data
Using ambulance service dispatch data, each LSOA was allocated to a single ED. For each LSOA, of all conveyances from the LSOA to any ED, the ED with most emergency conveyances from the LSOA was selected. The LSOA recorded was that of the location from where the patient was conveyed (the scene of the incident).
Method 4: ambulance service estimated catchment areas
Ambulance services were provided with a map of the area surrounding the relevant ED sites (and the road network) and were asked to draw a boundary (or boundaries) to indicate the area(s) in which they would most probably convey patients to the relevant EDs. The annotated maps were digitised and the set of LSOAs intersecting with the bounded area(s) were selected as the catchment area(s) for the ED(s).
Method 5: straight-line (Euclidean) distance
The straight-line distances from every LSOA centroid to every identified ED were calculated. For each LSOA, the ED with the shortest straight-line distance was selected.
Findings
Method 1: Hospital Episode Statistics accident and emergency attendance data
The project proposal stated that we would identify resident catchment areas using attendance data to each ED site from the HES A&E data set. It was found that the HES A&E data set only reliably records activity at the acute trust level,9 and so it was not possible to directly identify site-level activity for trusts operating more than one ED. It was only possible to use this method for one site. The project management team believed that it would be better to use a single, consistent method to identify catchment areas for all EDs.
Method 2: Department for Transport road travel time data (the selected method)
This method was possible for all areas and used a single, consistently recorded data source. An additional benefit was that the data included intuitive ‘dose’ data (the excess travel time from the LSOA to the next-nearest ED) for each of the LSOAs in the catchment area of the closure ED.
The identified ED closures did not take place simultaneously, thus catchment areas were calculated using the configuration of EDs 2 years prior to the closure of the relevant ED. In practice, this only required two different sets of ED catchment areas for all control and intervention areas.
Method 3: ambulance service computer-aided dispatch data
There were issues with smaller than anticipated numbers in the data set within a 1-year period for some LSOAs, and LSOAs that contained hospitals required corrections (as many of the ambulance conveyances from the LSOA were probably from the hospital to other hospital sites). Moreover, ambulance conveyances are likely to represent the more-severe attendances at an ED rather than attendances as a whole.
Method 4: ambulance service estimated catchment areas
The boundaries that were returned from ambulance services were of variable quality, with some services returning boundaries that formed catchment areas highly similar to those found using computer-aided dispatch (CAD) data (method 3). However, other services provided boundaries that produced catchment areas that varied markedly from those found using the CAD data (method 3). Possible reasons for such variation include staff turnover – some closures had taken place 6 years earlier.
Method 5: straight-line (Euclidean) distance
This method is similar to the DfT road travel time method but is not sensitive to unusual road geographies and so was considered inferior to the DfT method.
Method 6: Hospital Episode Statistics admitted patient care emergency admissions (not investigated)
It would be possible to uniquely identify hospital sites within the HES admitted patient care (APC) data set and to construct catchment areas by examining the residence location of emergency admission patients as opposed to A&E first attendance patients (method 1); however, there are some difficulties with this method.
-
Some trusts use multiple codes for the same site and these would all have to be mapped for all hospitals with significant numbers of emergency admissions.
-
Emergency admissions are not necessarily representative of ED use as emergency admissions are likely to represent more-severe cases and also include other, direct admissions that did not go through the ED.
The selected method
The project management group selected method 2, using DfT road travel times. This method relies on data that are independent of the system being measured. The method can be applied consistently across England and is robust to unusual geographies (e.g. estuaries and other concave coastlines). Furthermore, the method provides intuitive ‘dose’ data – the additional time to the next-nearest ED from LSOAs surrounding an intervention ED.
Chapter 5 The impact of emergency department closures on system performance and population outcomes
Methods
A number of impact measures were identified as being useful to help understand the impact that ED closures had had on the emergency care system and the local population. Measures were developed only if the research team felt that the measures could be calculated using routinely collected data held by ONS, HES or NHS ambulance services. We differentiated between primary and secondary measures. All primary measures were calculated when data were available. Secondary measures were calculated if (1) the primary measure had reliable data and (2) the result from the primary measure suggested that further investigation was required.
The measures, rationale for inclusion and data source are stated in Table 1. A detailed description of the methods that were used to calculate these measures is described in Appendix 5.
| Type of measure (data source) | Impact measuresa and the mean number of cases per month in the closure areas | Rationale for impact measure inclusion |
|---|---|---|
| Ambulance service (ambulance service CAD data) | Total number of emergency ambulance incidents: the mean number of incidents per month ranged from 1000 to 1756 | If an ED is not easily accessible for patients, ambulance call volumes may increase for patients without access to alternative transport. Conversely, ambulance call volumes may decrease if a patient chooses to use an alternative care provider closer to home rather than travel by ambulance to an ED further away (and have to find their own transport to return to their home) |
| Total number of emergency ambulance ‘Red’ incidents: ‘Red’ incidents is a term used by the ambulance service to categorise ‘life-threatening emergencies’; the mean number of ‘Red’ incidents per month ranged from 349 to 702 | ||
| Mean time from 999 call answered to arrival at hospital for ‘Red’ incidents | Ambulance journey times are likely to be longer from the catchment area to the now-nearest ED | |
| Mean time from 999 call answered to crew arrival at the scene | Although ambulance response times should not be affected by the closure of an ED, there is a possibility that ambulances may be further away from the catchment area after travelling to more distant EDs | |
| Mean time from 999 call answered to time conveying resource arrival at the scene | Although ambulance response times should not be affected by the closure of an ED, there is a possibility that ambulances may be further away from the catchment area after travelling to more distant EDs | |
| Mean time from conveying resource arriving at the scene to arrival at hospital | Ambulance journey times are likely to be longer from the catchment area to the now-nearest ED | |
| Mean time from ambulance arrival at hospital to time when ambulance is available for next job | Following ED closures, neighbouring EDs will receive patients. If the receiving EDs are having difficulties with managing this additional demand, one consequence may be an increase in the time taken for ambulance crews to hand over care to the ED | |
| Total number of emergency ‘Red’ hospital transfer incidents | Emergency transfers may decrease if, as anticipated, the patient is taken to the ‘right place, first time’52 | |
| Emergency ‘green’ incidents not conveyed to a type 1 or type 2 A&E department (ratio) | Ambulance services may increase their use of non-conveyance to minimise the potential impact of increased journey times on service performance measures | |
| Emergency and urgent care attendances (HES A&E data) | Total number of emergency and urgent care attendances at ED: the mean number of attendances per month ranged from 2682 to 4835 | Ease of access is a prominent determinant of ED attendance rates.21 Type 1 ED attendance may decrease because (1) patients choose not to travel further or (2) ambulance services increase their use of non-conveyance |
| Total number of attendances by mode of arrival (ambulance/other) | Changes in the total number of ED attendances may result either from changes in the numbers of patients self-referring to the ED or changes in ambulance service conveyance rates | |
| Total number of patients arriving at an ED who are discharged without treatment or investigation(s) that required hospital facilities (minor attendances): the mean number of minor attendances per month ranged from 844 to 2021 | Minor ED attendances are more likely to be affected by ED closures than all attendances and may decrease if patients choose to seek alternative care that is closer to home rather than travel further to an ED | |
| Proportion of attenders at ED who are admitted to an inpatient bed | The proportion of attenders who are admitted may change as a result of patients going to different EDs, or because discharging patients home from the ED may be more difficult as distances from the ED to patients’ homes increase | |
| Emergency hospital admissions (HES APC data) | Total number of emergency admissions: the mean number of emergency admissions per month ranged from 592 to 1245 | The emergency hospital admissions rate may be affected by (1) where a patient goes and (2) when they get there. Where they go may affect admissions because of differences between hospitals in admission rates and because of difficulties in discharging patients home from the ED who are at a non-local ED. If a patient delays seeking treatment or has increased travel time to hospital, this may lead to deterioration in their condition that may necessitate admission |
| Total number of potentially avoidable emergency admissions: the mean number of potentially avoidable emergency admissions per month ranged from 159 to 355 | A well-performing urgent and emergency care system might be expected to avoid some admissions for selected urgent care conditions (see Appendix 6).41 We know that ‘avoidable admission’ rates vary between hospitals,39 so admission rates could be affected by which hospital a patient goes to and also by delays in the patient arriving at hospital | |
| Mean LOS for emergency admissions | Increases in LOS may be affected by where patients are admitted and also may be an indicator of (1) condition severity or (2) difficulties in discharging patients to non-local services | |
| Total number of admissions to critical care | Admissions to critical care may be affected by where patients are admitted and may also indicate condition severity. The condition of patients with a delayed presentation may deteriorate and lead to critical care admission | |
| Death/risk of death (ONS mortality data and HES–ONS linked mortality data) | Total number of deaths from SECs occurring within 7 days: the mean number of deaths per month ranged from 24 to 41 | Mortality from SECs (see Appendix 7)56 may be affected by (1) where a patient goes (i.e. the quality of the emergency care hospital that the patient attends) and (2) how long they take to get there. If a patient delays seeking treatment or has increased travel time to hospital, this may have an adverse impact on mortality. We have focused on deaths within 7 days of the incident because later deaths are less influenced by the emergency care phase of treatment |
| CFRs for all SECs | The risk of death for a patient with a SEC (see Appendix 7) may be affected by (1) where the patient goes (i.e. the quality of the hospital that the patient attends) and (2) how long they take to get there. The ratio of deaths within 7 days to deaths plus emergency admissions for ≥ 2 days for patients who survived is an indicator of this risk41 | |
| Total number of out-of-hospital deaths from SECs: the mean number of out-of-hospital deaths per month ranged from 17 to 29 | Deaths occurring before hospital admission (which we have termed out-of-hospital deaths) from SECs (see Appendix 7) may be affected by how long it takes for the patient to get to hospital | |
| Total number of deaths from specific conditions occurring within 7 days (stroke/MI) | Evidence shows that treatment for specific emergency conditions, such as stroke and MI, is more effective the quicker it is administered. Travelling further to hospital may delay the onset of this treatment | |
| CFRs for specific conditions (stroke/MI) | Evidence shows that treatment for specific emergency conditions, such as stroke and MI, is more effective the quicker it is administered, but is also more effective at some hospitals than at others. Travelling further to hospital may delay the onset of this treatment but may improve care once the patient arrives at hospital |
Plan of analysis
For each of the five areas that we have studied where a local hospital ED was closed or downgraded, we have examined the impact of the closure on the performance of the emergency care system for the population resident in the catchment area of the hospital. We have used a controlled interrupted time-series approach. Specifically:
-
We have plotted monthly activity for each site and control pair over the 2 years before and the 2 years after the closure so that any change over time could be seen graphically. We have also fitted a locally weighted scatterplot smoothing curve through the series of 48 data points representing the monthly activity or performance at each site to help visualise whether or not there was any change at the time of closure.
-
We then fitted a time-series regression model to the time series for the closure area using a negative binomial model [for counts, this was run in Stata® (StataCorp LP, College Station, TX, USA)] and a Prais–Winsten model [for other types of data, this was run in R (The R Foundation for Statistical Computing, Vienna, Austria)] to test for preliminary evidence that activity or performance had changed at the time of ED closure (model 1). The time-series model fitted is an autoregressive [AR(1)] model (i.e. with a lag of one time period so that autocorrelation arises only from any linear dependence of each monthly value on the previous month’s value). The model consists of a seasonal effect, a linear time trend, a term for before and after the time when the site ED was downgraded or closed and a before-and-after step term for any other potentially important changes introduced at the site. The seasonal effect was a fixed-effect term with six levels representing pairs of months (January and February, March and April, etc.), which ensures that Easter always falls in the same season, and was included to help explain some of the variation in the data that was attributable to regular seasonal fluctuations in activity. A linear time trend was used because it accurately describes the long-term trend in ED use, ambulance service call volumes and emergency admissions to hospital and was also expected to adequately describe the short-term trend over 4 years. In addition, it was used, rather than a more complicated curve, in order to keep the model simple.
The other important changes that we have modelled include three types of event:
-
the introduction of NHS 111 covering the catchment area
-
the introduction or closure of any urgent care service, such as a WIC, in the catchment area
-
the introduction of ambulance diversion.
-
For the effect of closure and these other types of event, only a simple ‘step’ was included in the model. A term for any impact on the trend was not included, and so the step represents the estimated impact of the closure at the time of closure.
-
We then tested for changes in each closure site catchment area compared with its control site catchment area using time-series regression to test for the impact of the closure and obtain estimates [and confidence intervals (CIs)] of the impact (model 2). We used a simple model with three main elements:
-
The basic model, consisting of a linear trend in activity over the 48 months and the seasonal effects constrained to be the same in the closure and control areas, plus a site effect.
-
We then added site-specific effects for any potentially important changes other than the ED closure introduced during the 48 months. For example, in one of our control site catchment areas, a WIC was introduced prior to the time the ED closed in the closure area, which may have changed ED access volumes and times in the control site. To allow for any impact of this change, and other similar changes in either the closure or control area, we included site specific before-and-after terms in the models.
-
We then included a step term to model any change in activity or performance in both the closure and control site catchment areas at the time of the closure of the ED at the closure site. Lastly, we introduced an interaction term between the two-level site term and the two-level before-and-after closure step term, to model the effect of closure in the closure site relative to any change in the control site.
-
-
We undertook a third analysis by fitting a ‘dose model’ instead of the ‘step model’ described above (this is labelled as model 6). In this dose model, instead of modelling the average effect across the whole of the closure site’s catchment area, we made use of the fact that different parts of the catchment area might be differentially affected by the closure of an ED. We used data from DfT on the estimated travel times by road from the centroid of each LSOA in the catchment area of the closed ED to that ED, and from each LSOA to the next-nearest ED, to calculate the change in journey time from home to hospital, in an emergency, that was caused by closing the local ED. The changes in the DfT estimated travel times from the nearest ED, which is the one that closed, to the next-nearest ED for residents of LSOAs in the five catchment areas together are shown in Figure 2. There are about 100 LSOAs in each catchment area, and the change in time to hospital varies from 0 minutes to about 25 minutes, with a median change of 9 minutes, for these LSOAs.
FIGURE 2.
Change in time from LSOA to ED following ED closure, for residents of LSOAs in the catchment areas of EDs that closed.
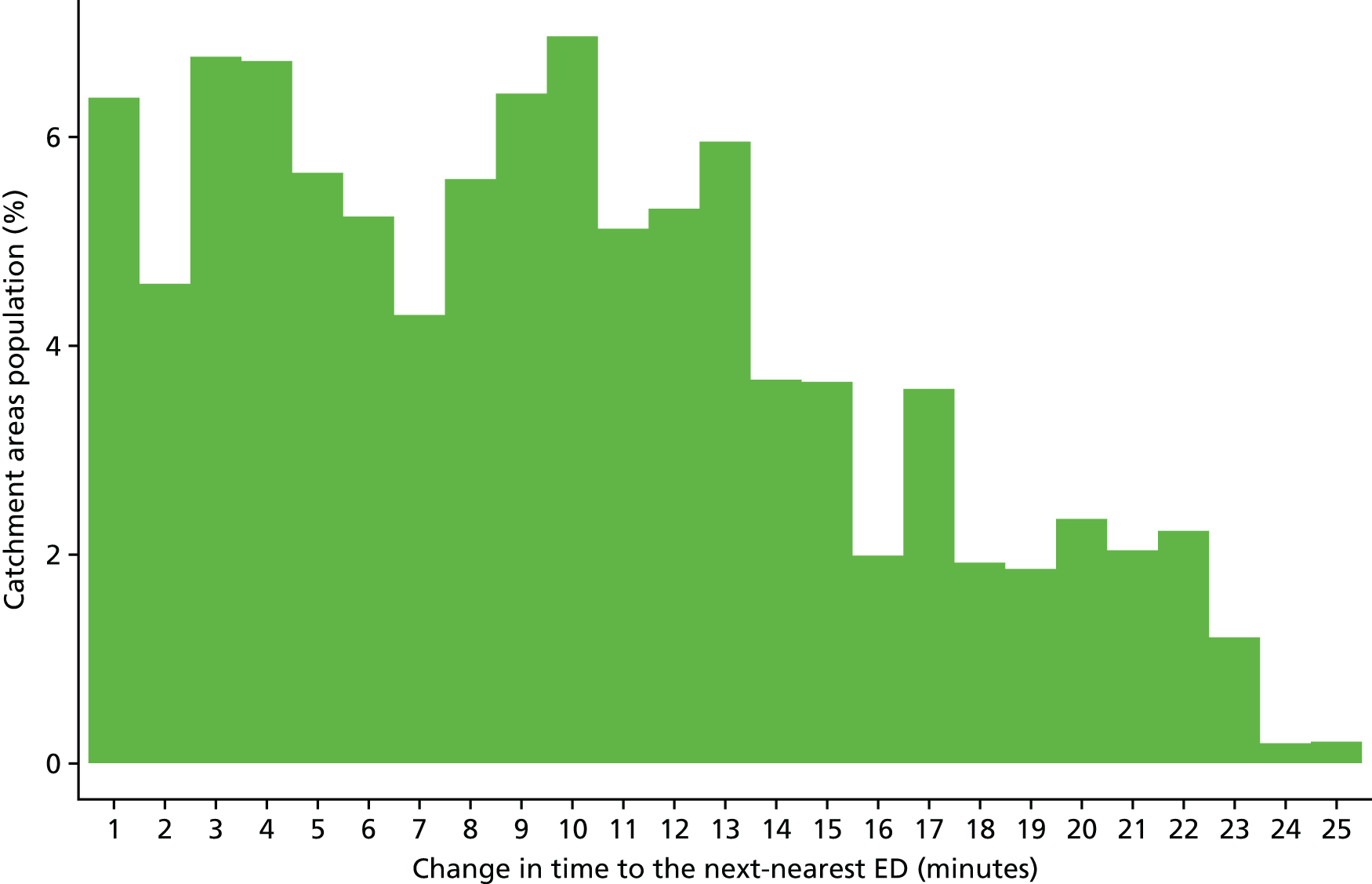
We have then simply dichotomised all of the LSOAs in the catchment area into high-dose areas (with a change in travel time above the median change in time) and low-dose areas (with a change below the median). We then fitted interrupted time-series models, as described in step 3 in the description of the time-series approach above, but compared high-dose and low-dose areas rather closure and control areas.
We took the approach of dichotomising the LSOAs by dose rather than examining the continuous relationship between dose and effect because for some outcomes there are too few data on performance and activity in each LSOA to fit models to the LSOA data.
-
Finally, for each of the activity and performance impact measures, we have combined the results from the five individual areas. We have done this for each of the three models previously described:
-
We have summarised the results of the individual site analyses that used an interrupted time-series model for the catchment area alone to estimate the impact of closure (model 1). We have used forest plots and estimated an overall effect by combining the individual site estimates using a random-effects meta-analysis. 60 We have reported the overall estimate and a 95% CI for this estimate, together with a p-value.
-
We have summarised the results of the five individual site analyses that compared the closure areas with their controls (model 2) using forest plots with an estimate of overall effect.
-
We have summarised the analyses of the models comparing the impact for residents of LSOAs that were expected to have had a relatively large change in the time to ED (high-dose areas) with areas that were expected to have had a relatively small change (low-dose areas), again using forest plots with an estimate of overall effect (these analyses are labelled model 6 in the plots). In each site, high dose and low dose have been defined differently, by the median change in time to ED estimated by the DfT for LSOAs in that area. These summaries may be combining heterogeneous effects and have also been combined using random-effects models that estimate the average effect across sites.
-
Data quality
In these analyses, we usually included 48 data points for monthly activity or performance in the 2 years before and the 2 years after closure or downgrading. However, inspection of the data shows that in some catchment areas there are missing or incorrectly reported values. What constitutes an incorrect or ‘outlier’ value is not well defined of course, but when the data show sudden, large and unexpected changes from one month to the next this usually represents a data error or change in reporting practice rather than a change in activity or performance. Accordingly, we have defined outlier data points as values that are > 3 standard deviations (SDs) away from the monthly average value. These data points have been dropped from the analysis and, in the models comparing the closure areas with control areas, the paired monthly value has also been omitted. If too many data points were missing or unreliable, we have omitted the whole analysis.
Presentation of results
The results are presented separately for each closure site for changes in each of the activity and performance impact measures described in Table 1, following the first four steps described in Plan of analysis:
-
a plot of the monthly activity or performance measure for closure and control areas for the 2 years before and the 2 years after the date of the closure
-
the results of the time-series regression model for the closure site (model 1)
-
the results for the step model comparing closure and control areas (model 2)
-
the results of the ‘dose’ model comparing the change in the measure for high-dose areas with the change for low-dose areas (model 6).
The negative binomial procedure models the log of the counts, and so we have reported the percentage change (and 95% CI and p-value) for these models, whereas the Prais–Winsten procedure models the absolute change in the measure. We have not reported statistical significance as such, but, rather, have described results with p-values of < 0.001 as presenting strong evidence, p-values of between 0.001 and 0.01 as presenting some evidence and p-values of > 0.01 as not providing any statistically reliable evidence.
The results for the individual areas are presented in Appendix 8. Here, the results for all areas combined (see Plan of analysis, step 5) are presented.
Data obtained
We obtained data from NHS Digital, ONS, DfT and a number of ambulance services.
We aimed to obtain data for the period from April 2007 to March 2014 (inclusive). In cases for which this was impossible or impracticable, we attempted to obtain data for the 4-year period evenly spanning the month of closure of the relevant ED.
The NHS Digital Hospital Episode Statistics admitted patient care data
The HES APC data were complete and reliable throughout the period of interest for all areas. We have examined all emergency admissions and those admissions in which the primary diagnosis was for a condition identified as an urgent emergency condition (see Appendix 6).
The NHS Digital Hospital Episode Statistics accident and emergency data
We were supplied with HES A&E data for the entire period of interest. However, data quality was variable and was especially poor in the reporting year 2007/8, but it improved over time. Incompleteness was a major issue throughout the period; it was apparent that particular EDs, UCCs, MIUs and WICs did not consistently report to the HES A&E data set. Only three sites (Rochdale, Newark and Bishop Auckland) reported sufficiently reliable data spanning the closure of the ED to analyse the changes in ED use by the catchment populations.
The Office for National Statistics death registration data
Death registration data were complete and reliable throughout the period of interest for all areas. It was noted that throughout the period of interest the ONS twice changed their method of coding underlying causes of death. However, we included deaths from SECs (see Appendix 7), in which the underlying cause or other cause of death was recorded as one of the identified conditions, so these changes have a negligible effect on the results.
The ONS death registration data and HES APC data were provided with a common, pseudonymised identifier, enabling records for the same individual in both data sets to be linked. Using these data sets, we defined the following:
-
In-hospital deaths within 7 days of the incident (taken to be the day of admission) for a SEC (see Appendix 7): deaths from a SEC that terminate an emergency admission of a duration of ≤ 7 full days.
-
Out-of-hospital deaths attributable to a SEC: deaths from a SEC not occurring during an emergency admission. Note that deaths occurring (1) prior to any contact with an emergency service (e.g. at home), (2) at the scene of the incident or in an ambulance, (3) in an ED prior to admission and (4) subsequent to being admitted to hospital and being discharged alive are all counted here as an ‘out-of-hospital death’ if their cause of death is recorded as a SEC.
The Department for Transport journey time data
The DfT journey time data were supplied for two time points, representing the relevant configurations of EDs 2 years prior to the closure of each ED studied. The DfT data were complete except for one LSOA centroid that was not mapped to the road network and for which no travel times could be calculated by the DfT. The ‘unconnected’ LSOA was surrounded on all sides by LSOAs with the same nearest ED, thus the nearest ED for the surrounding LSOAs was chosen as the nearest ED for the ‘unconnected’ LSOA. This single LSOA was omitted from LSOA-level analyses.
The ambulance service data
Data were obtained from the following ambulance services:
-
East Midlands Ambulance Service NHS Trust
-
East of England Ambulance Service NHS Trust
-
North East Ambulance Service NHS Foundation Trust
-
North West Ambulance Service NHS Trust
-
West Midlands Ambulance Service NHS Foundation Trust
-
Yorkshire Ambulance Service NHS Trust.
There were many difficulties in obtaining ambulance service data. Notable difficulties included:
-
ambulance service data are not recorded in a consistent format across NHS trusts
-
most ambulance services had made numerous major changes to their CAD systems during the period of the study.
In some control areas, the ambulance service data quality issues were so significant that it was not possible to use particular elements of the supplied data. In a minority of cases, there was an insufficient number of data or such extensive data quality issues that it was not possible to meaningfully analyse any of the data. One control site could not supply data on the number of 999 calls over the 4-year period, and most control sites could not provide reliable data on the times from call to hospital for 999 ‘Red’ calls. Thus, comparisons between closure sites and their control areas for the mean time it took for patients to get to hospital are missing. Details of the missing data are provided in Appendix 8.
Findings
Readers with a statistical background may wish to read Appendix 8, which presents the findings, by geographical area, of each impact measure that was calculated. In the interest of reader accessibility, we report the summaries of these analyses in this section.
Summary of findings by area
Hemel Hempstead
Following the closure, for residents of the ED catchment area in Hemel Hempstead:
-
There was some evidence of a large increase in the number of emergency ambulance incidents, but no statistically reliable evidence was found to suggest this regarding ‘Red’ incidents. No comparison could be made with the control area.
-
There was strong evidence of an increase in the time from 999 call to arrival at hospital. However, no comparison could be made with the control area.
-
There were data quality issues with the HES A&E extract. No reliable analyses could be undertaken on the emergency and urgent care service attendance measures.
-
There was strong evidence of a large decrease in the number of emergency hospital admissions. This decrease remained evident when compared with the control area.
-
There was strong evidence of a large decrease in the number of potentially avoidable hospital admissions, but only when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in LOS for those admitted to hospital as an emergency case.
-
There was no statistically reliable evidence to suggest a change in the number of deaths or ‘risk of death’ from the 16 SECs studied.
Comparing pre- and post-closure journey times to the nearest ED, for those experiencing a larger change in post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of emergency ambulance incidents when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There were data quality issues with HES A&E data and, therefore, no reliable analyses could be undertaken on the emergency and urgent care service attendance measures.
-
There was strong evidence of a large decrease in the number of emergency hospital admissions, but no statistically reliable evidence of a decrease in potentially avoidable hospital admissions, when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in LOS for those admitted as an emergency case when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the mortality measures when compared with those experiencing a smaller change in journey times.
Bishop Auckland
Following the closure, for residents of the ED catchment area in Bishop Auckland:
-
There was strong evidence of a large increase in the number of emergency ambulance incidents, and some evidence of a large increase in ‘Red’ incidents following the closure of the ED. These increases remained evident when compared with the control area.
-
There was strong evidence of an increase in the time from 999 call to arrival at hospital. This increase arose principally from an increase in the time from the scene of the incident to arrival at hospital. However, no comparison could be made with the control area.
-
There was strong evidence of a large decrease in the number of emergency and urgent care attendances. This appeared to be driven by a decrease in the number of attendances by patients arriving by ambulance. This decrease remained evident when compared with the control area. However, there may be a coding issue with these data.
-
There was strong evidence of a large decrease in the number of minor attendances at emergency and urgent care services. This decrease remained evident when compared with the control area. Again, there may be a coding issue with these data.
-
There was no statistically reliable evidence to suggest a change in the number of emergency hospital admissions.
-
There was some evidence of a large increase in the number of potentially avoidable hospital admissions, but only when compared with the control area.
-
There was some evidence of an increase in LOS for those admitted as an emergency case; this was no longer evident when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in death or ‘risk of death’ from the 16 SECs studied.
Comparing pre- and post-closure journey times to the nearest ED, for those experiencing longer post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of ambulance incidents when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large decrease in both overall emergency and urgent care attendances and minor attendances when compared with those experiencing a smaller change in journey times. However, there may be a coding issue with these data.
-
There was no statistically reliable evidence to suggest a change in emergency hospital admission measures when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in death or ‘risk of death’ when compared with those experiencing a smaller change in journey times.
Rochdale
Following the closure, for residents of the ED catchment area in Rochdale:
-
There was some evidence of a large increase in the number of emergency ambulance incidents, including ‘Red’ incidents. This increase was no longer evident when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the time from 999 call to arrival at hospital. No comparison could be made with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of emergency and urgent care attendances.
-
There was some evidence of a large decrease in the number of minor attendances at emergency and urgent care services, but this decrease was not evident when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of emergency hospital admissions.
-
There was some evidence of a large decrease in the number of potentially avoidable hospital admissions, and strong evidence when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in LOS for those admitted as an emergency case.
-
There was no statistically reliable evidence to suggest a change in the number of deaths or ‘risk of death’ from the 16 SECs studied.
Comparing pre- and post-closure journey times to the nearest ED, for those experiencing longer post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of emergency ambulance incidents when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of an increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in either total emergency and urgent care attendances, or minor attendances, when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the emergency hospital admission measures when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the mortality measures when compared with those experiencing a smaller change in journey times.
Newark
Following the closure, for residents of the ED catchment area in Newark:
-
There was strong evidence of a large increase in the number of emergency ambulance incidents, including ‘Red’ incidents. This increase was only evident when compared with the control area.
-
There was strong evidence of a large increase in the time from ambulance service 999 call to arrival at hospital, when compared with the control area. The increase appeared to be driven by an increase in the time from the scene of the incident to hospital.
-
There was some evidence to suggest an increase in the number of emergency and urgent care attendances, but this was not evident when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of minor attendances at emergency and urgent care services.
-
There was some evidence of an increase in the number of emergency hospital admissions when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of potentially avoidable hospital admissions.
-
There was no statistically reliable evidence to suggest a change in LOS for those admitted to hospital as an emergency case.
-
There was no statistically reliable evidence to suggest a change in death or ‘risk of death’ from the 16 SECs studied.
Comparing pre- and post-closure journey times to the nearest ED, for those experiencing longer post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of emergency ambulance incidents but there was some evidence of a large increase in ‘Red’ incidents when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the emergency and urgent care service attendance measures when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the emergency hospital admission measures when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the mortality measures when compared with those experiencing a smaller change in journey times.
Hartlepool
Following the closure, for residents of the ED catchment area in Hartlepool:
-
There was some evidence of an increase in the number of emergency ambulance incidents, and strong evidence of a large increase in ‘Red’ incidents, but only when compared with the control area.
-
There was strong evidence of an increase in the time from ambulance service 999 call to arrival at hospital, but only when compared with the control area. The increase appeared to be driven by an increase in the time from the scene of the incident to hospital.
-
There were no reliable data to inform the analysis of total emergency and urgent care service attendance. Analysis of this measure by mode of arrival indicated that there was strong evidence of a decrease in the number of attendances by patients arriving by ambulance. No comparison with the control area was possible.
-
There was some evidence of a large decrease in the number of emergency hospital admissions, and there was strong evidence of this when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of potentially avoidable hospital admissions.
-
There was strong evidence of an increase in LOS for those admitted to hospital as an emergency case but only when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in death or ‘risk of death’ from the 16 SECs studied.
Comparing pre- and post-closure journey times to the nearest ED, for those experiencing longer post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of emergency ambulance incidents, but there was some evidence of a large increase in ‘Red’ incidents when compared with those experiencing a smaller change in journey times.
-
There was some evidence to suggest an increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There were no reliable data to inform the analysis of emergency and urgent care service attendance. There was strong evidence of a decrease in the number of attendances by patients arriving by ambulance when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large decrease in total emergency hospital admissions, but there was no evidence to suggest a change in potentially avoidable admissions, when compared with those experiencing a smaller change in journey times.
-
There was no evidence to suggest a change in LOS for those admitted to hospital as an emergency case when compared with those experiencing a smaller change in journey times.
-
There was no evidence to suggest a change in the mortality measures when compared with those experiencing a smaller change in journey times.
Results: all areas
We have combined the results of the three types of analysis that we carried out for each impact measure in the individual areas:
-
We summarised the results of the individual site analyses that used an interrupted time series for the site catchment area alone to estimate the impact of closure (model 1). We have used forest plots, and estimated the average effect by combining the individual estimates weighted by the inverse of their standard errors. We have reported the overall estimate and a 95% CI for this estimate, together with a p-value.
-
We summarised the results of the five individual site analyses that compared the closure areas with their controls (model 2), also using forest plots with an estimate of the average effect.
-
We summarised the analyses of the models comparing the impact for residents of LSOAs that were expected to have had a relatively large change in time to travel to an ED (high-dose areas) with areas that were expected to have had a relatively small change (low-dose areas), again using forest plots with an estimate of the average effect (these analyses are labelled ‘model 6’ in the plots). In each site, high dose and low dose have been defined differently, by the median change in time to an ED estimated by the DfT for LSOAs in each study area. Therefore, these summaries may be combining heterogeneous effects.
A summary table of this analysis is presented at the end of this section (see Table 2). This table shows the direction of change for the population residing in the areas affected by ED closures.
Ambulance service performance
Total number of incidents following 999 calls to the ambulance service
Figure 3 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of incidents following 999 calls to the ambulance services for residents of the catchment areas of the EDs that closed.
FIGURE 3.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of ambulance service incidents in the catchment areas of the EDs that closed (model 1).
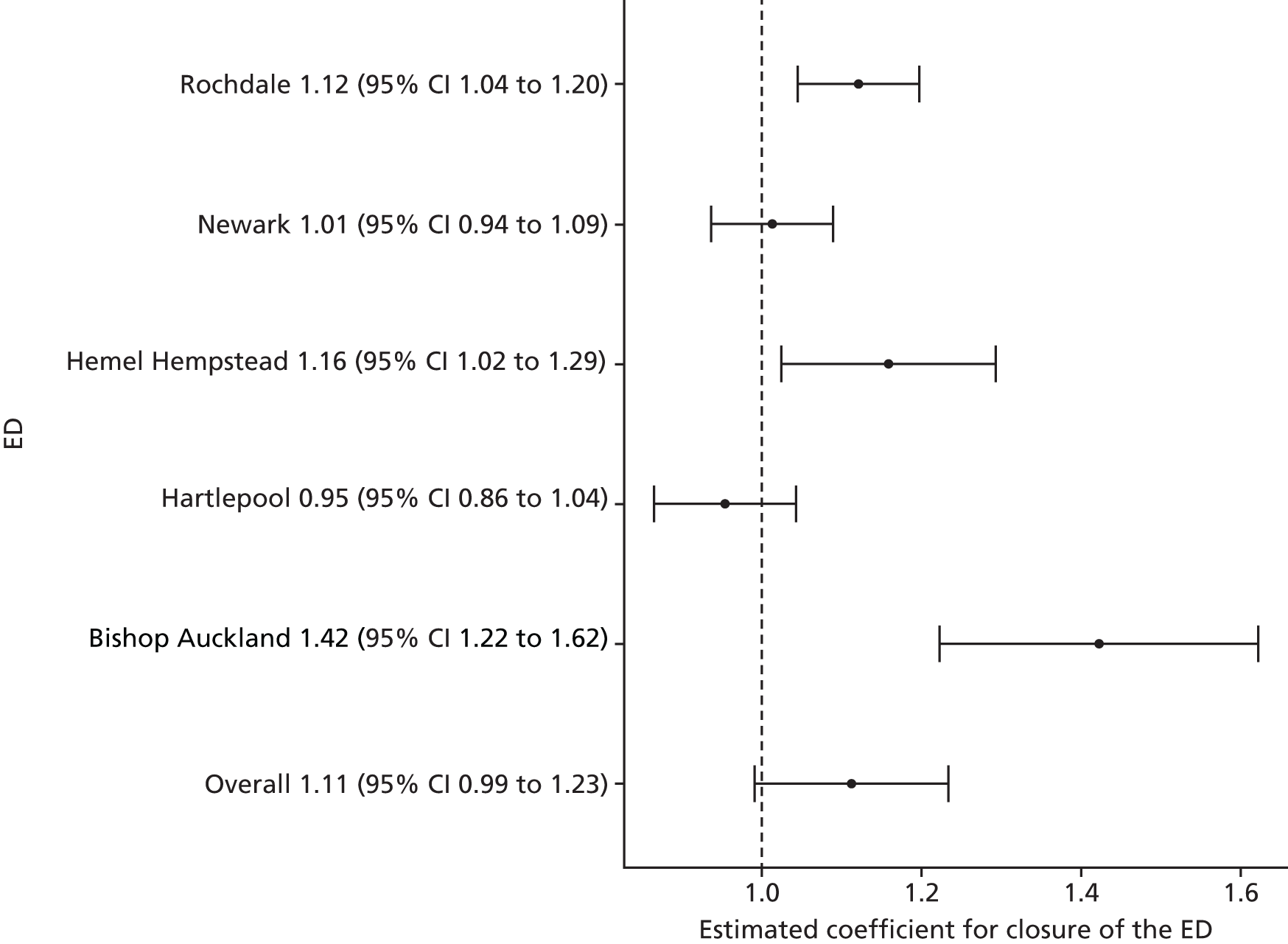
Over all areas, there was no statistically reliable evidence to suggest a change in the total number of ambulance incidents following closure of a local ED. The estimated effect was an increase of 11.2% (95% CI –1.0% to 23.4%; p = 0.07).
Figure 4 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of incidents following 999 calls to the ambulance services for residents of the catchment areas of the EDs that closed compared with their control areas.
FIGURE 4.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of ambulance service incidents in the catchment areas of the EDs that closed compared with their control areas (model 2).
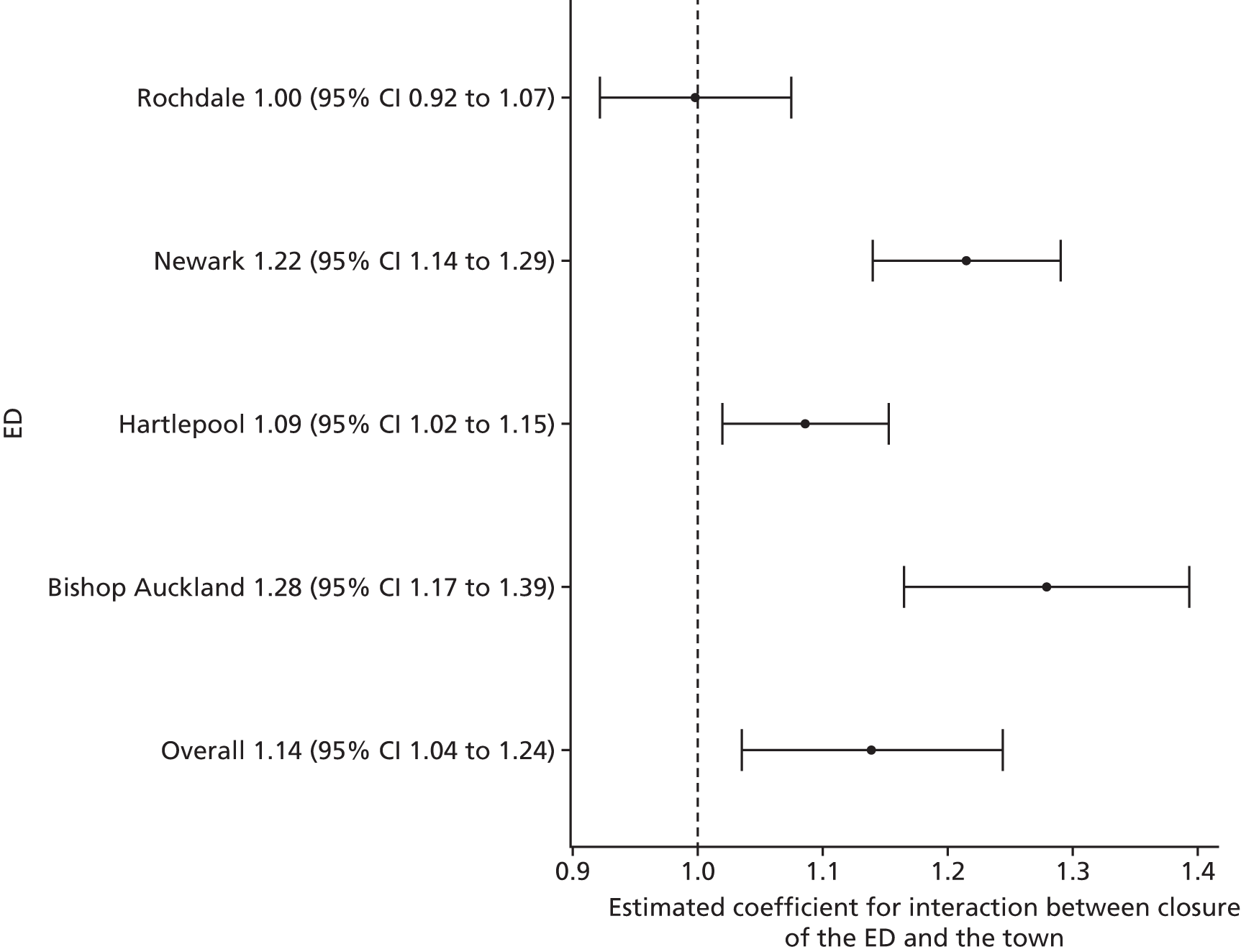
Compared with control sites, over all sites, there was some evidence of a large increase in the total number of ambulance incidents following the closure of a local ED. The estimated effect was an increase of 13.9% (95% CI 3.5% to 24.4%; p = 0.008).
Figure 5 summarises the results of the individual site analyses that compared the impact of the ED closure for residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 5.
The results of the individual site analyses that compared the impact of the ED closure on the number of ambulance service incidents for high-dose LSOAs with the impact in relatively low-dose LSOAs in that area (model 6).
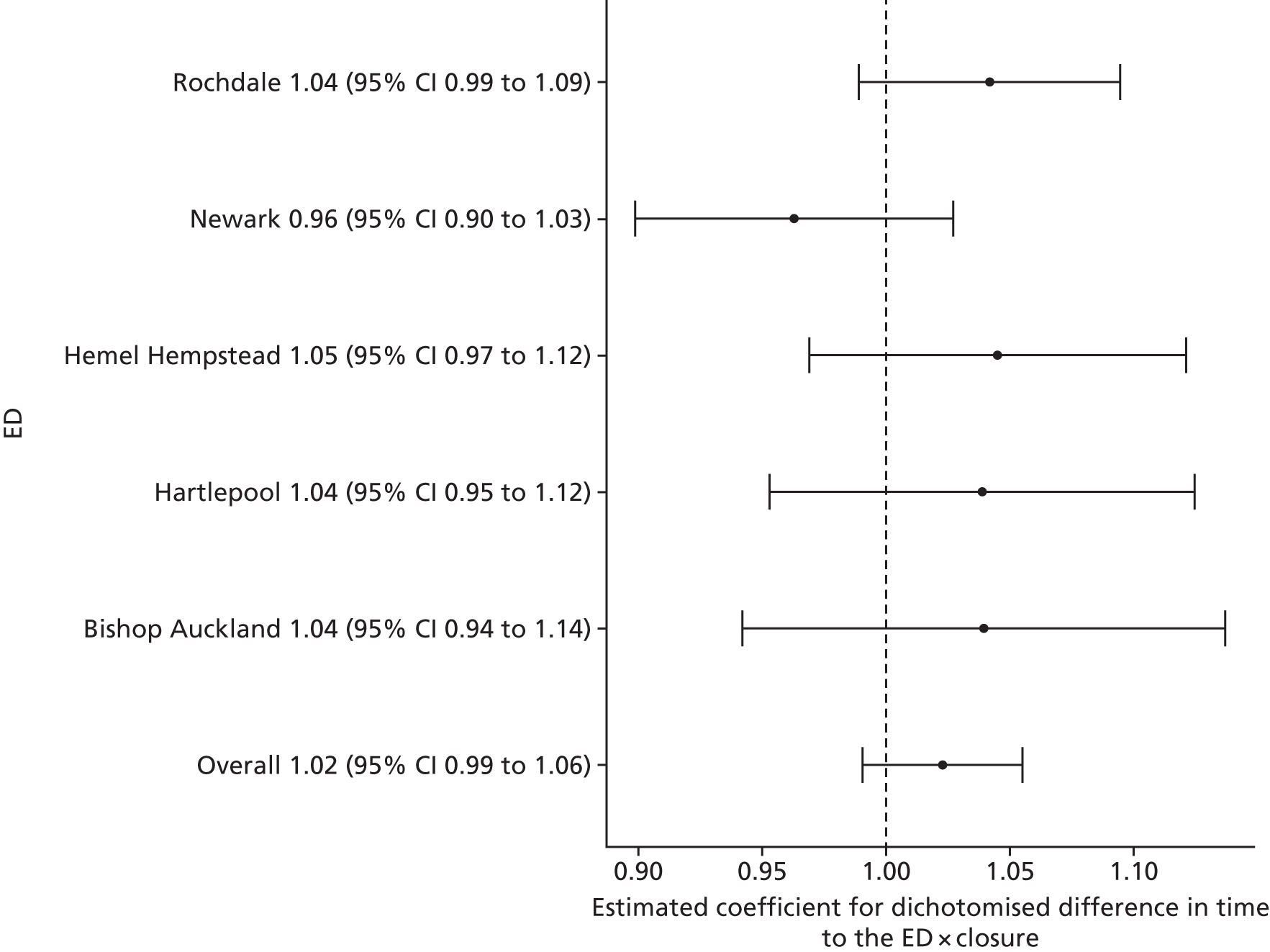
Over all sites, there was no statistically reliable evidence to suggest a change in the total number of ambulance incidents in high-dose areas compared with low-dose areas following the closure of the local ED. The estimated effect was an increase in high-dose areas relative to low-dose areas of 2.3% (95% CI –0.9% to 5.5%; p = 0.16).
Number of emergency ambulance ‘Red’ incidents
Figure 6 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of ambulance service 999 ‘Red’ incidents for residents of the catchment areas of the EDs that closed.
FIGURE 6.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of ambulance service ‘Red’ incidents in the catchment areas of the EDs that closed (model 1).
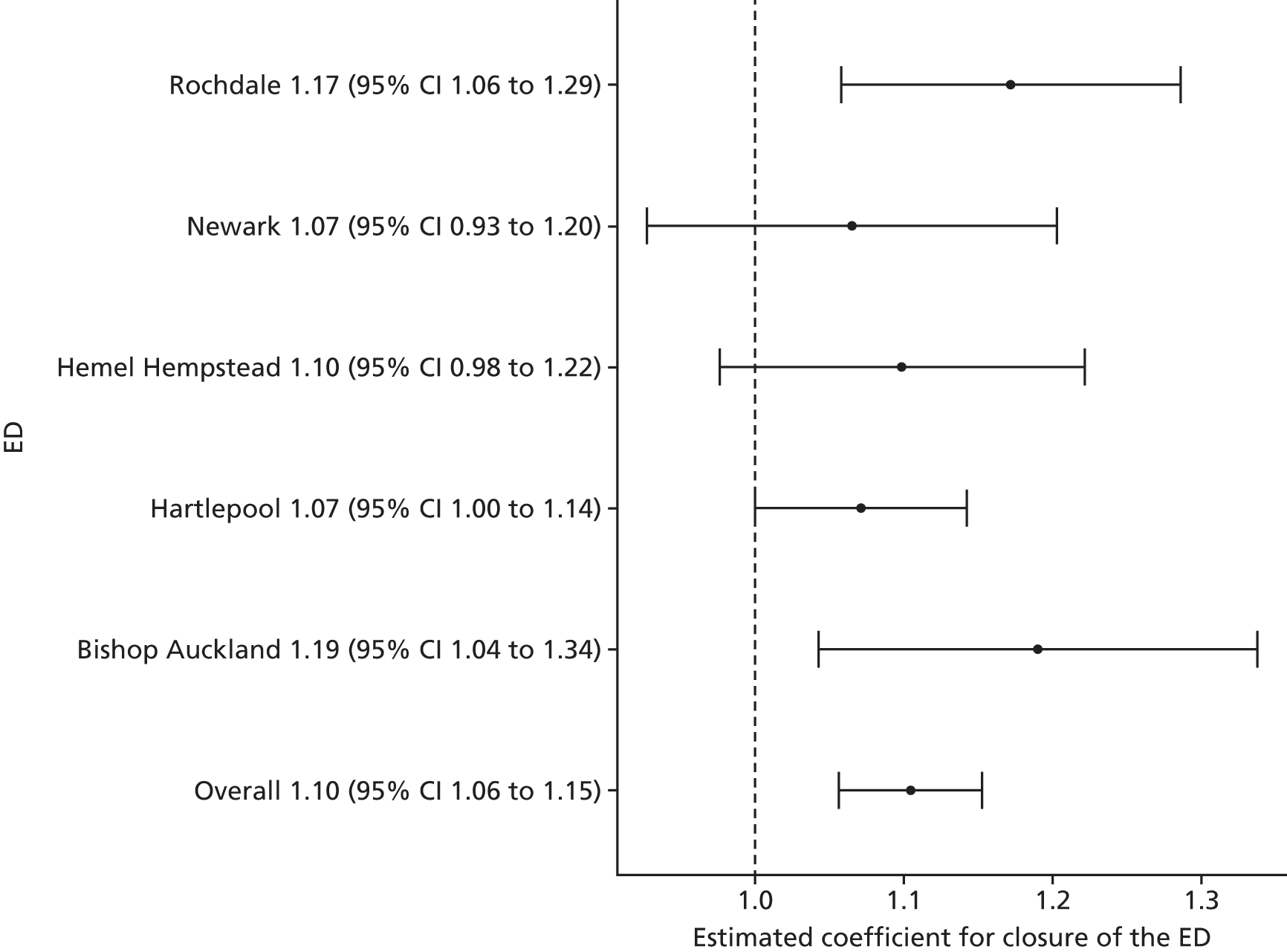
Over all sites, there was strong evidence of a large increase in the total number of ambulance ‘Red’ incidents following the closure of a local ED. The estimated effect was an increase of 10.5% (95% CI 5.7% to 15.2%; p < 0.001).
Figure 7 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of ambulance service 999 ‘Red’ incidents for residents of the catchment areas of the EDs that closed compared with the impact in their control sites. No comparison was possible for Hemel Hempstead because of poor-quality data.
FIGURE 7.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of ambulance service ‘Red’ incidents in the catchment areas of the EDs that closed compared with their control sites (model 2).
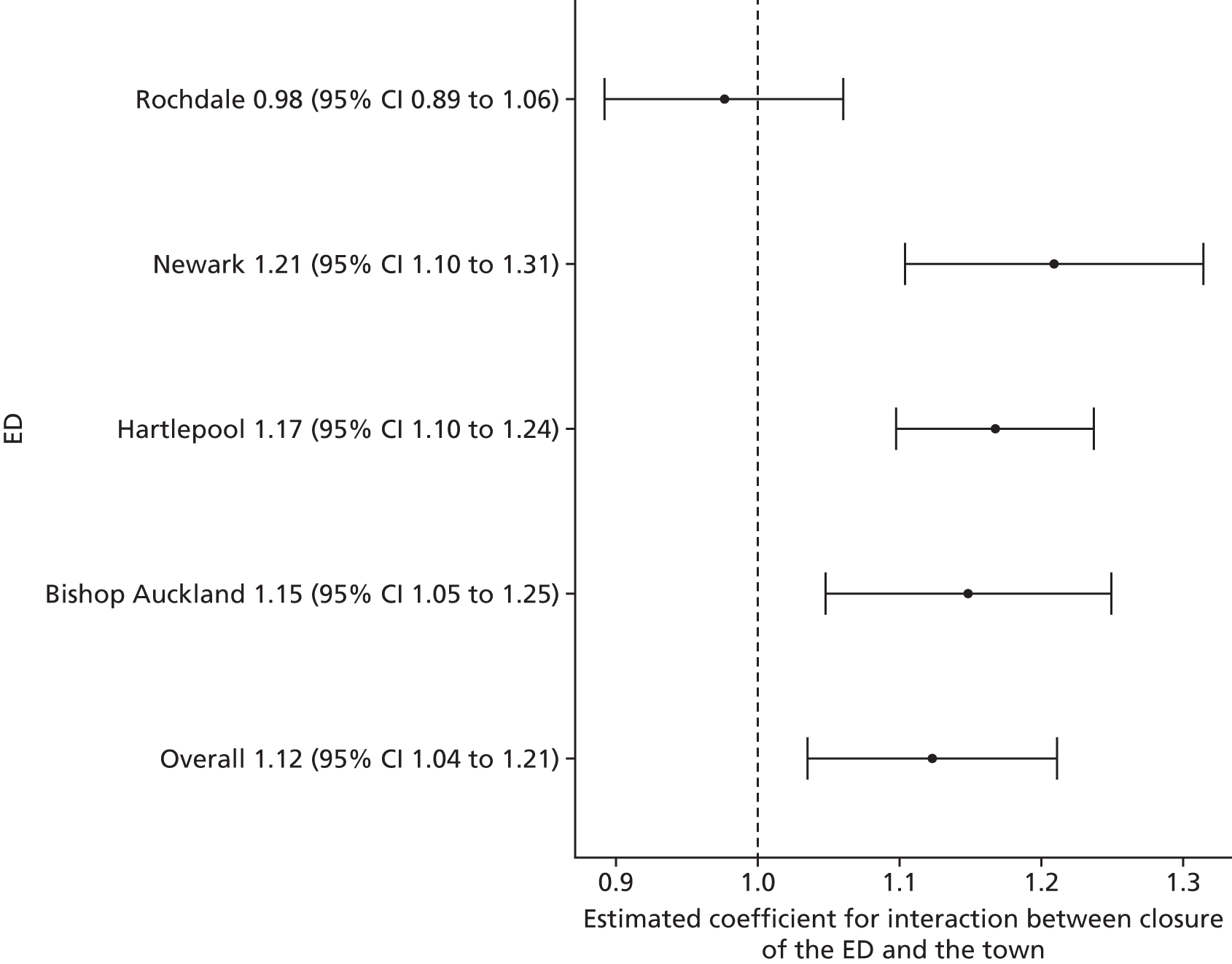
Compared with control sites, over all sites, there was some evidence of a large increase in the total number of ambulance ‘Red’ incidents following the closure of a local ED. The estimated effect was an increase of 12.3% (95% CI 3.5% to 21.1%; p = 0.006).
Figure 8 summarises the results of the individual site analyses that compared the impact of the ED closure on the number of ambulance service ‘Red’ incidents for residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 8.
The results of the individual site analyses that compared the impact of the ED closure on the number of ambulance service ‘Red’ incidents for high-dose LSOAs with the impact in relatively low-dose LSOAs in that area (model 6).
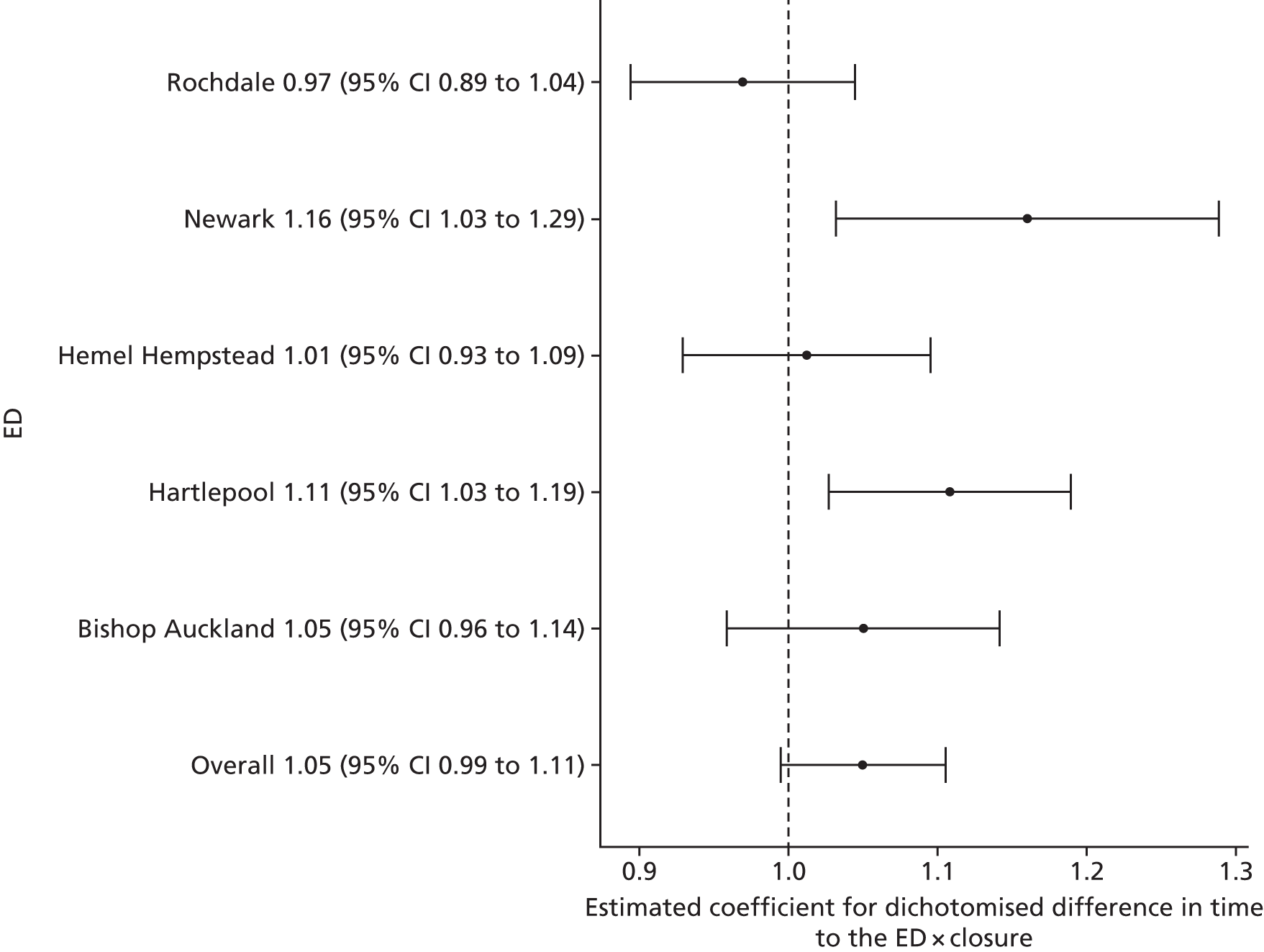
Over all sites, there was no statistically reliable evidence to suggest a change in the total number of ambulance ‘Red’ incidents in high-dose areas compared with low-dose areas following the closure of the local ED. The estimated effect was a small increase in high-dose areas relative to low-dose areas of 5.0% (–0.9% to 10.5%; p = 0.07).
Mean time from 999 call to arrival at hospital for ‘Red’ incidents
Figure 9 presents the results of the individual site analyses that estimated the impact of closing EDs on the mean time from 999 call to arrival at hospital, for ‘Red’ incidents, for residents of the catchment areas of the EDs that closed. In Rochdale, the time is measured from the time when the call was received, but in the other sites the time is measured from the time when the call was answered.
FIGURE 9.
The results of the individual site analyses that estimated the impact of the ED closure on the mean time from 999 call to arrival at hospital for ‘Red’ incidents in the catchment areas of the EDs that closed (model 1).
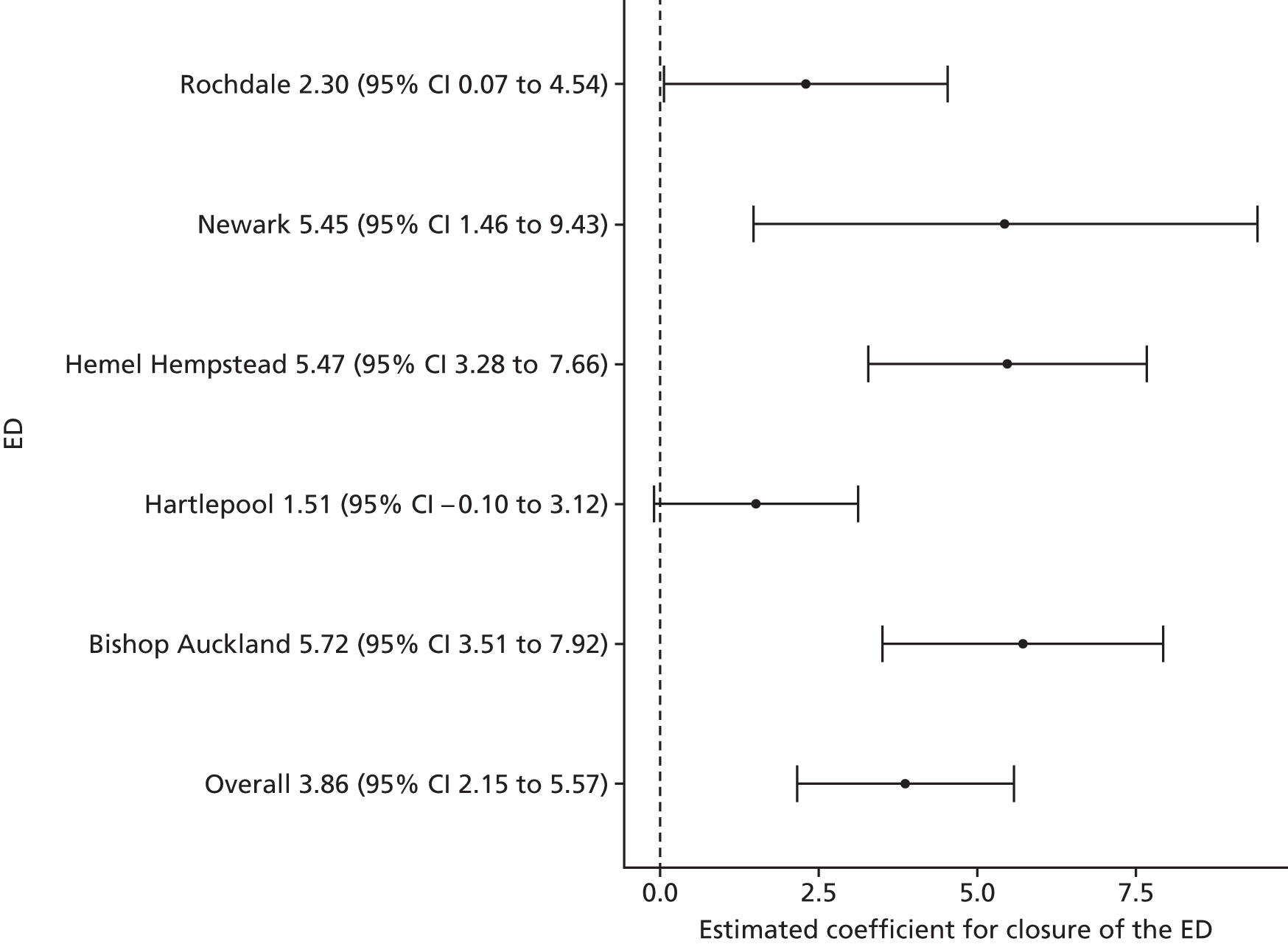
Over all sites, there was strong evidence to suggest a small increase in the mean time from 999 call to arrival at hospital following closure of a local ED. The estimated effect at the time of closure was an increase of 3.9 minutes (95% CI 2.2 to 5.6 minutes; p < 0.001).
Unfortunately, there were almost no useful data on journey times from control sites over the 4-year study period (see Appendix 8). There were no usable data from two of the control sites, only 3 years of data from two other sites and some erratic data for all 4 years from another control site. Overall, it has not been possible to summarise across sites the impact of ED closure on ambulance times from 999 call to arrival at hospital compared with the control sites.
Figure 10 summarises the results of the individual site analyses that compared the impact of the ED closure on the mean time from 999 call to arrival at hospital, for ‘Red’ calls, for residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 10.
The results of the individual site analyses that compared the impact of the ED closure on the mean time from 999 ‘Red’ call to arrival at hospital for residents of high-dose LSOAs with the impact in relatively low-dose LSOAs (model 6).
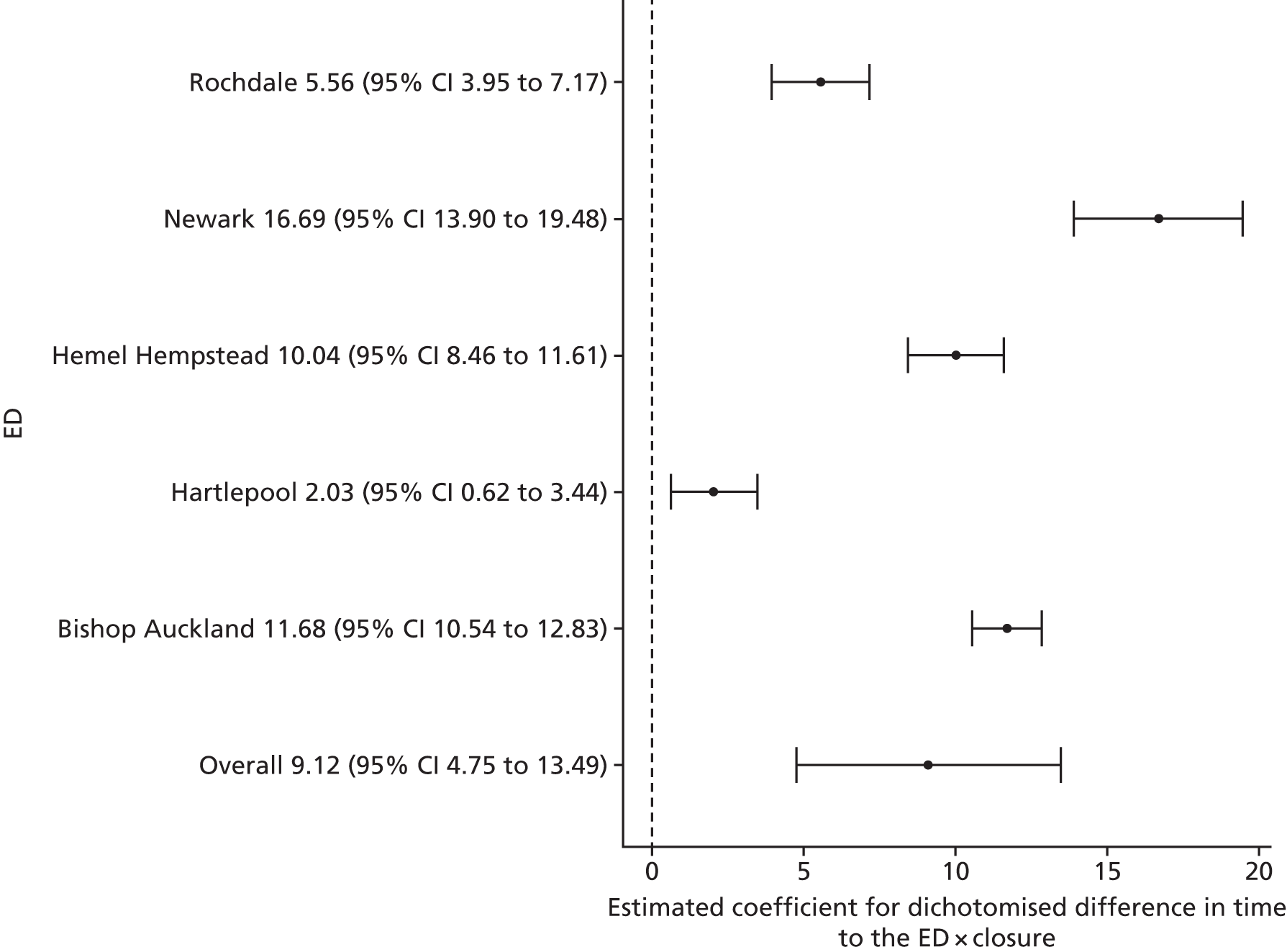
Over all sites, there was strong evidence of a large increase in the mean time to hospital following 999 ‘Red’ calls for residents of high-dose areas compared with low-dose areas following the closure of the local ED. The estimated effect was an increase in high-dose areas relative to low-dose areas of 9.1 minutes (95% CI 4.8 to 13.5 minutes; p < 0.001).
Emergency and urgent care attendances
Total number of emergency and urgent care attendances
Figure 11 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of emergency and urgent care attendances for residents of the catchment areas of the EDs that closed. Reliable data were only available for three of the five sites: Rochdale, Newark and Bishop Auckland.
FIGURE 11.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of emergency and urgent care attendances for residents of the catchment areas of the EDs that closed (model 1).
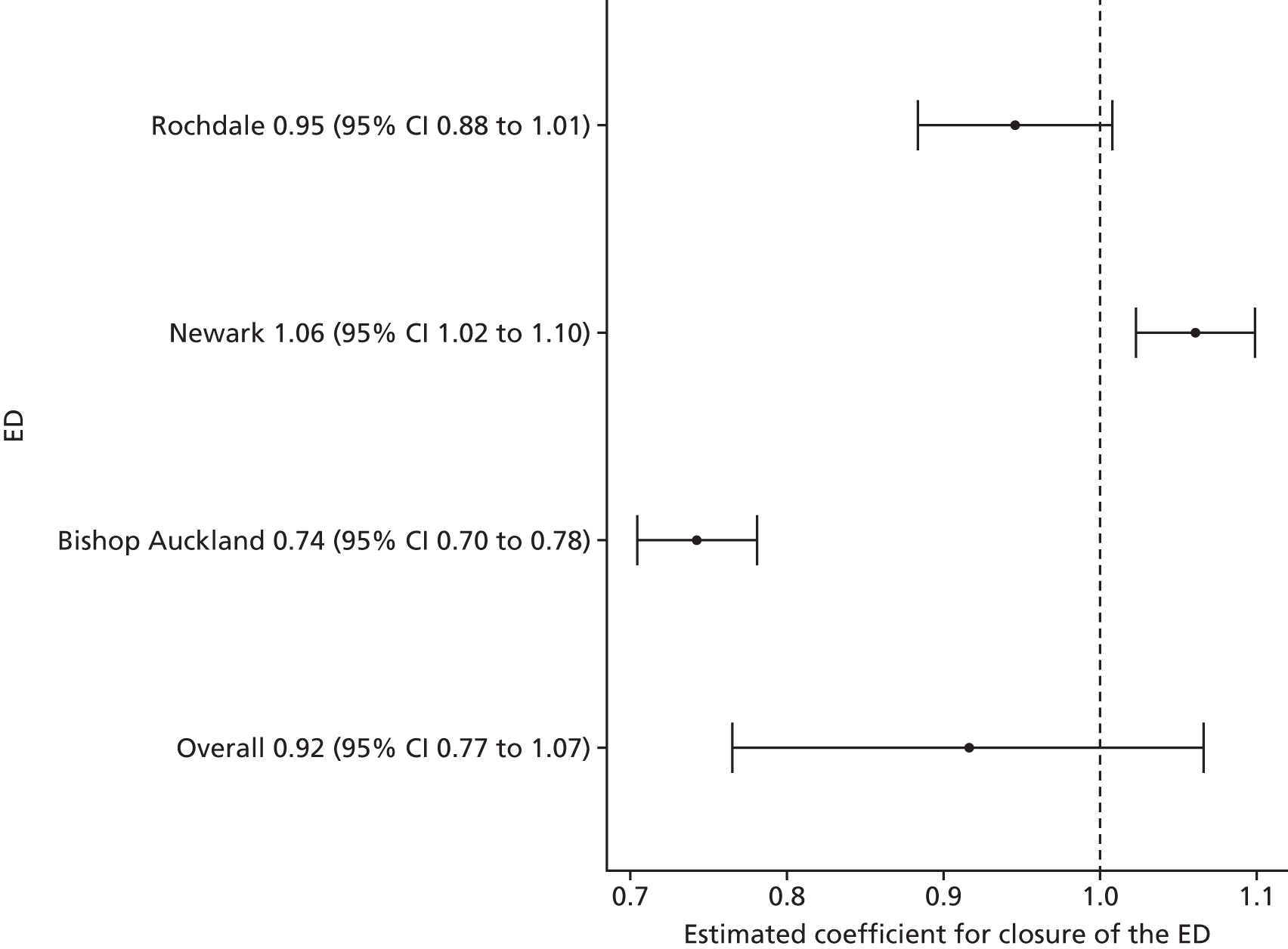
Over all sites, there was no statistically reliable evidence to suggest a change in the total number of emergency and urgent care attendances following the closure of a local ED. It was estimated that there was a reduction in the total number of emergency and urgent care attendances at the time of closure of –8.4% (95% CI –23.5% to 6.7%; p = 0.27).
Figure 12 presents the results of the individual site analyses that estimated the impact of closing the EDs on the number of emergency and urgent care attendances by residents of the catchment areas of the EDs that closed compared with the impact in their control sites. As before, results are only shown for the three sites with reliable data.
FIGURE 12.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of emergency and urgent care attendances for residents of the catchment areas of the EDs that closed compared with the impact in control areas (model 2).
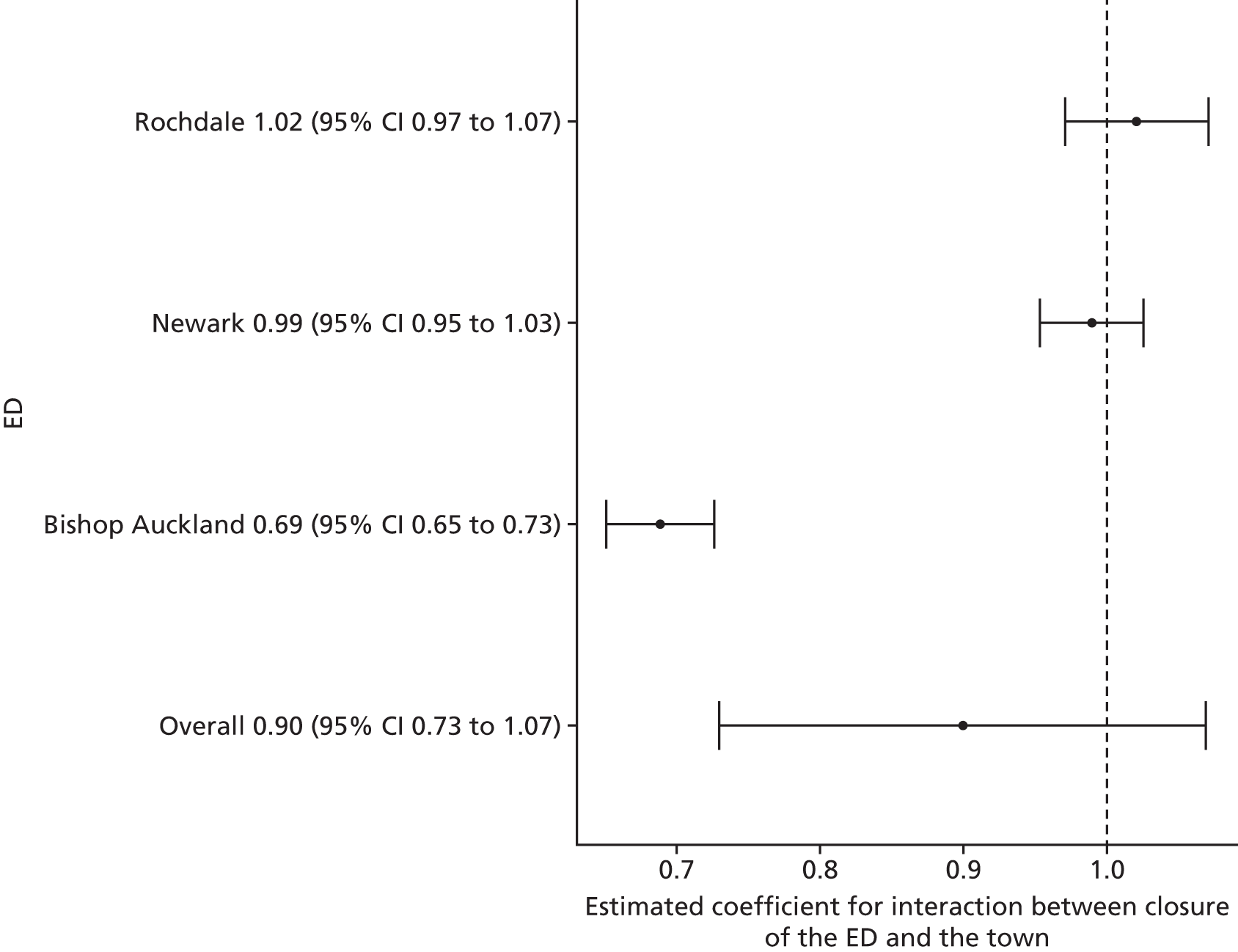
Compared with control sites, there was no statistically reliable evidence to suggest a change in the number of emergency and urgent care attendances following the closure of a local ED. Over all sites, it was estimated that there was a reduction in emergency and urgent care attendances at the time of closure relative to the control sites of –10.0% (95% CI –27.1% to 6.9%; p = 0.25).
Figure 13 summarises the results of the individual site analyses that compared the impact of the ED closure on the number of emergency and urgent care attendances by residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 13.
The results of the individual site analyses that compared the impact of the ED closure on the number of emergency and urgent care attendances for high-dose LSOAs with the impact in relatively low-dose LSOAs in that area (model 6).
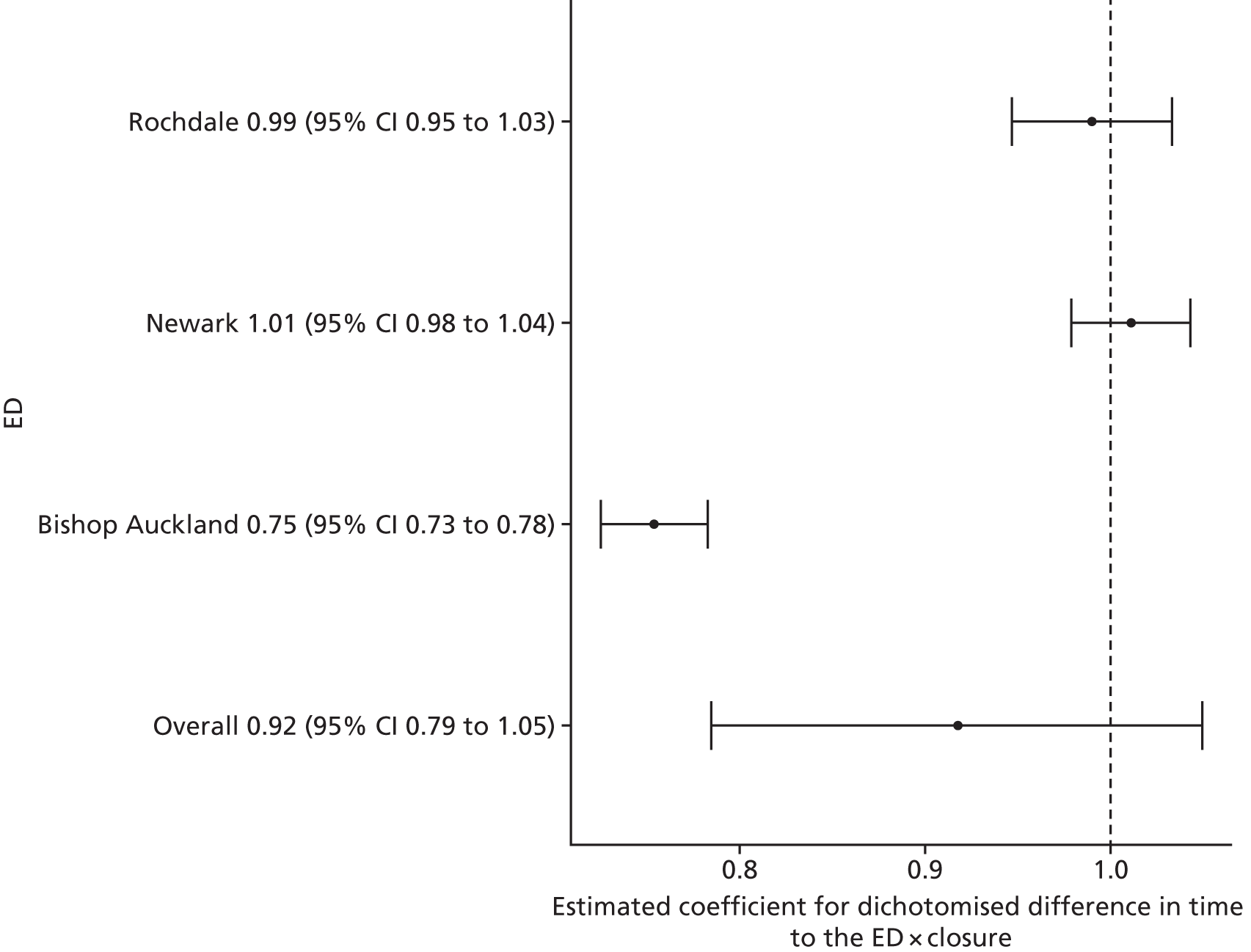
Over all three sites with usable data, there was no statistically reliable evidence to suggest a change in emergency and urgent care attendances following the closure of a local ED. It was estimated that there was a reduction of –8.3% (95% CI –21.5% to 5.0%; p = 0.22) in emergency and urgent care attendances in high-dose areas compared with low-dose areas following the closure of the local ED.
Minor attendances at an emergency or urgent care service
Figure 14 presents the results of the individual site analyses that estimated the impact of closing the EDs on the number of minor emergency and urgent care attendances for residents of the catchment areas of the EDs that closed. Minor emergency and urgent care attendances were defined as attenders who were discharged to home without any treatments or investigations that needed hospital attendance. Reliable data were only available for three of the five sites: Rochdale, Newark and Bishop Auckland.
FIGURE 14.
The results of the individual site analyses that estimated the impact of the ED closure on the number of minor emergency and urgent care attendances for residents of the catchment areas of the EDs that closed (model 1).
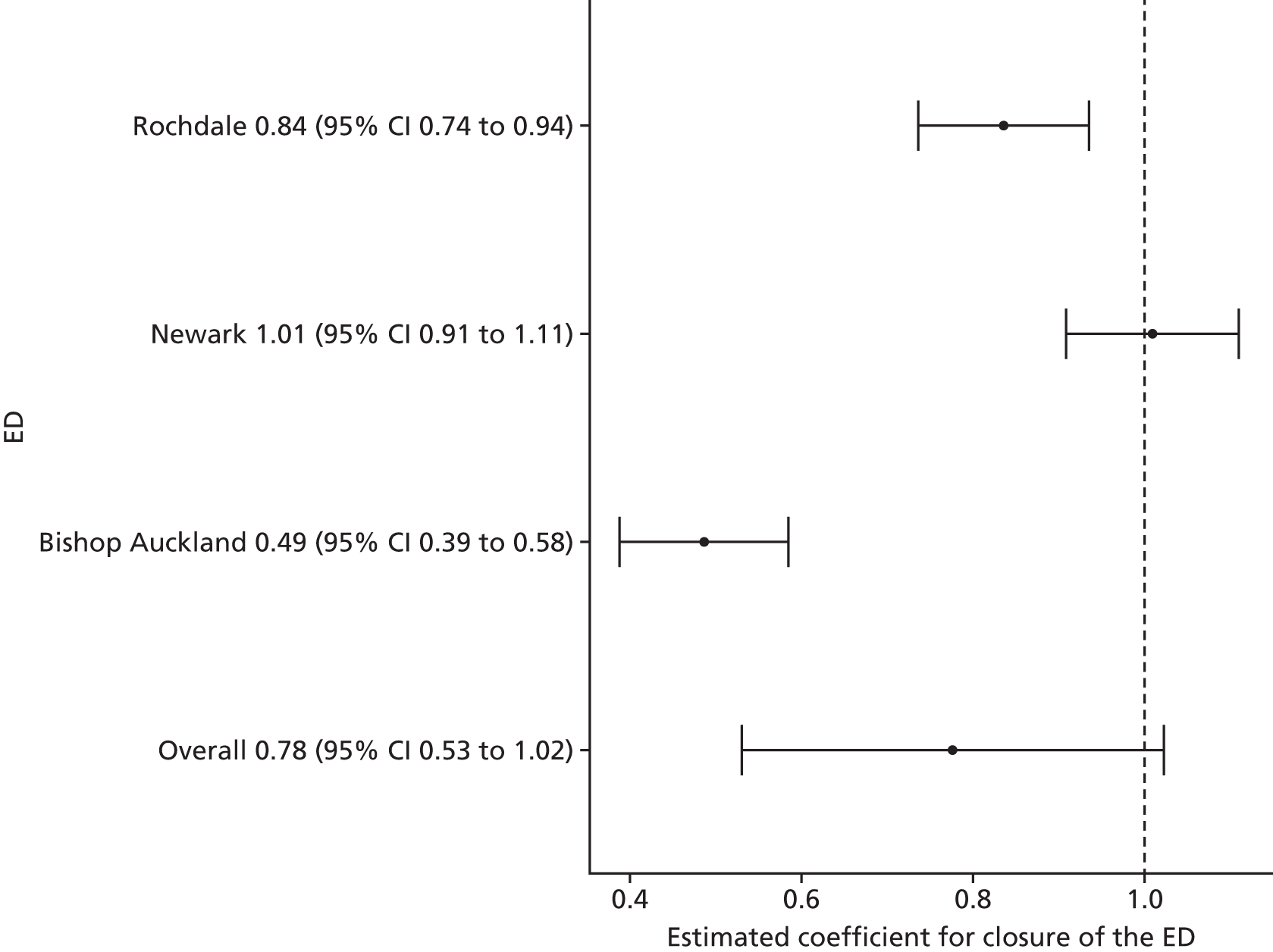
Over all three sites, no statistically reliable evidence was found to suggest a change in the number of minor emergency and urgent care attendances following the closure of a local ED. It was estimated that there was a reduction in the number of minor emergency and urgent care attendances at the time of closure by –22.3% (95% CI –47.0% to 2.3%; p = 0.08).
Figure 15 presents the results of the individual site analyses that estimated the impact of closing the EDs on the number of minor emergency and urgent care attendances by residents of the catchment areas of the EDs that closed compared with the impact in their control sites. As before, results are only shown for the three sites with reliable data.
FIGURE 15.
The results of the individual site analyses that estimated the impact of the ED closure on the number of minor emergency and urgent care attendances for residents of the catchment areas of the EDs that closed compared with the impact in their control areas (model 2).
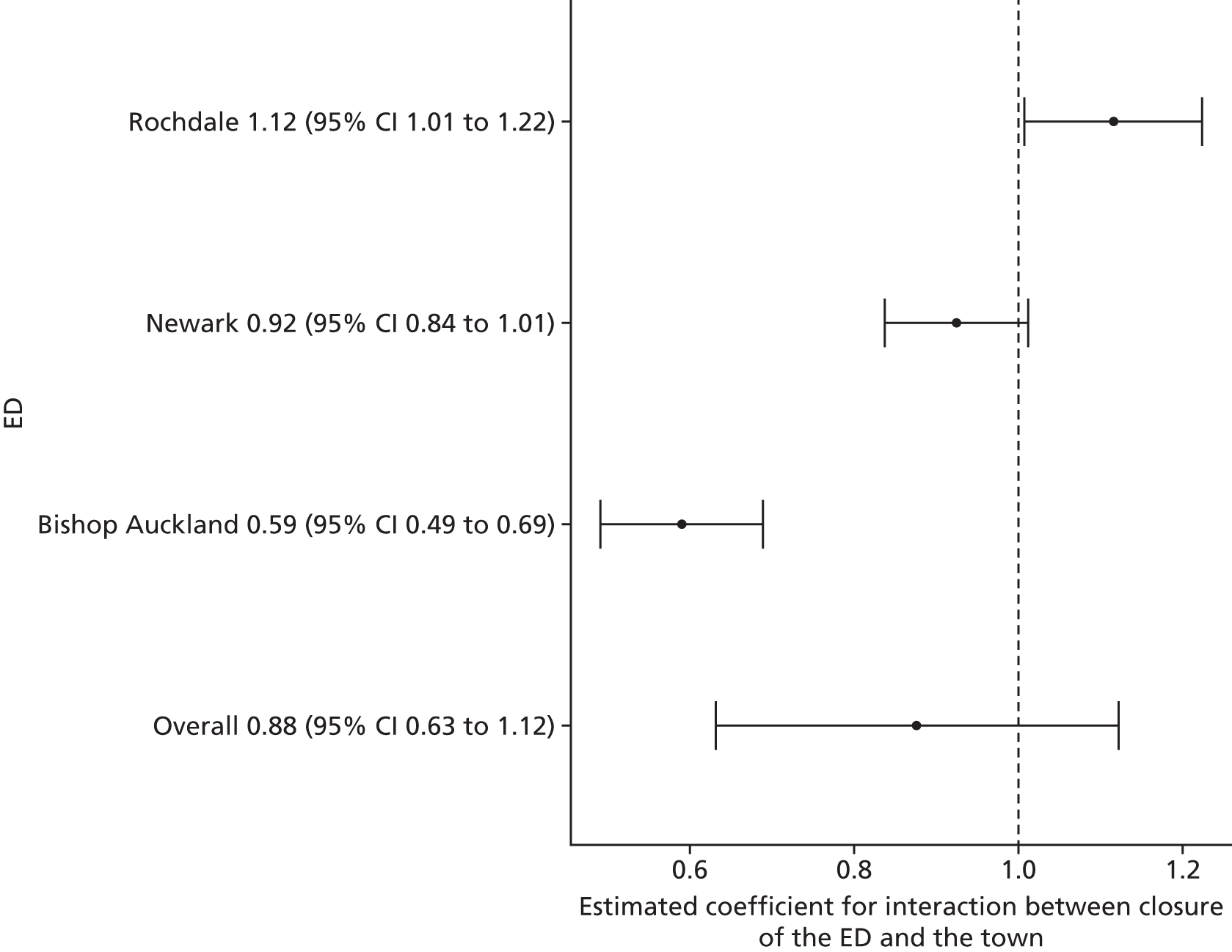
Compared with control sites, no statistically reliable evidence was found to suggest a change in the number of minor emergency and urgent care attendances following the closure of a local ED. It was estimated that there was a reduction in the number of minor emergency and urgent care attendances at the time of closure over all three sites relative to their control sites of –12.4% (95% CI –36.8% to 12.1%; p = 0.32).
Figure 16 summarises the results of the individual site analyses that compared the impact of the ED closure on the number of minor emergency and urgent care attendances by residents of relatively high-dose LSOAs in each ED catchment area with relatively low-dose LSOAs in that area.
FIGURE 16.
The results of the individual site analyses that compared the impact of the ED closure on the number of minor emergency and urgent care attendances for high-dose LSOAs with the impact in relatively low-dose LSOAs in that area (model 6).
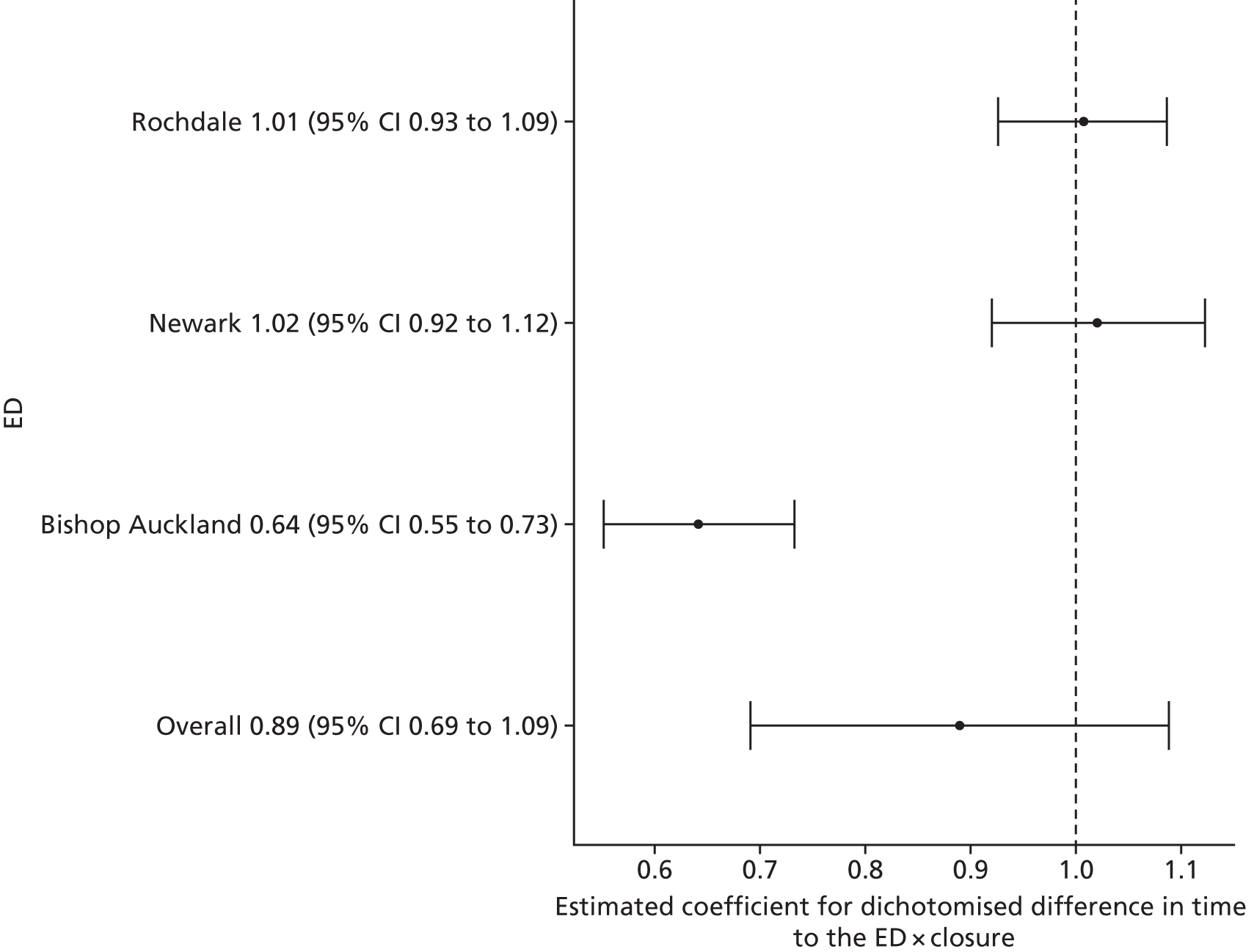
Over all three sites, no statistically reliable evidence was found to suggest a change in the number of minor emergency and urgent care attendances following the closure of a local ED. It was estimated that there was a reduction of –11.1% (95% CI –30.9% to 8.8%; p = 0.28) in minor emergency and urgent care attendances in high-dose areas compared with low-dose areas following the closure of the local ED.
Admissions
All emergency admissions
Figure 17 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of emergency admissions to hospital per month for residents of the catchment areas of the EDs that closed.
FIGURE 17.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of emergency admissions in the catchment areas of the EDs that closed (model 1).
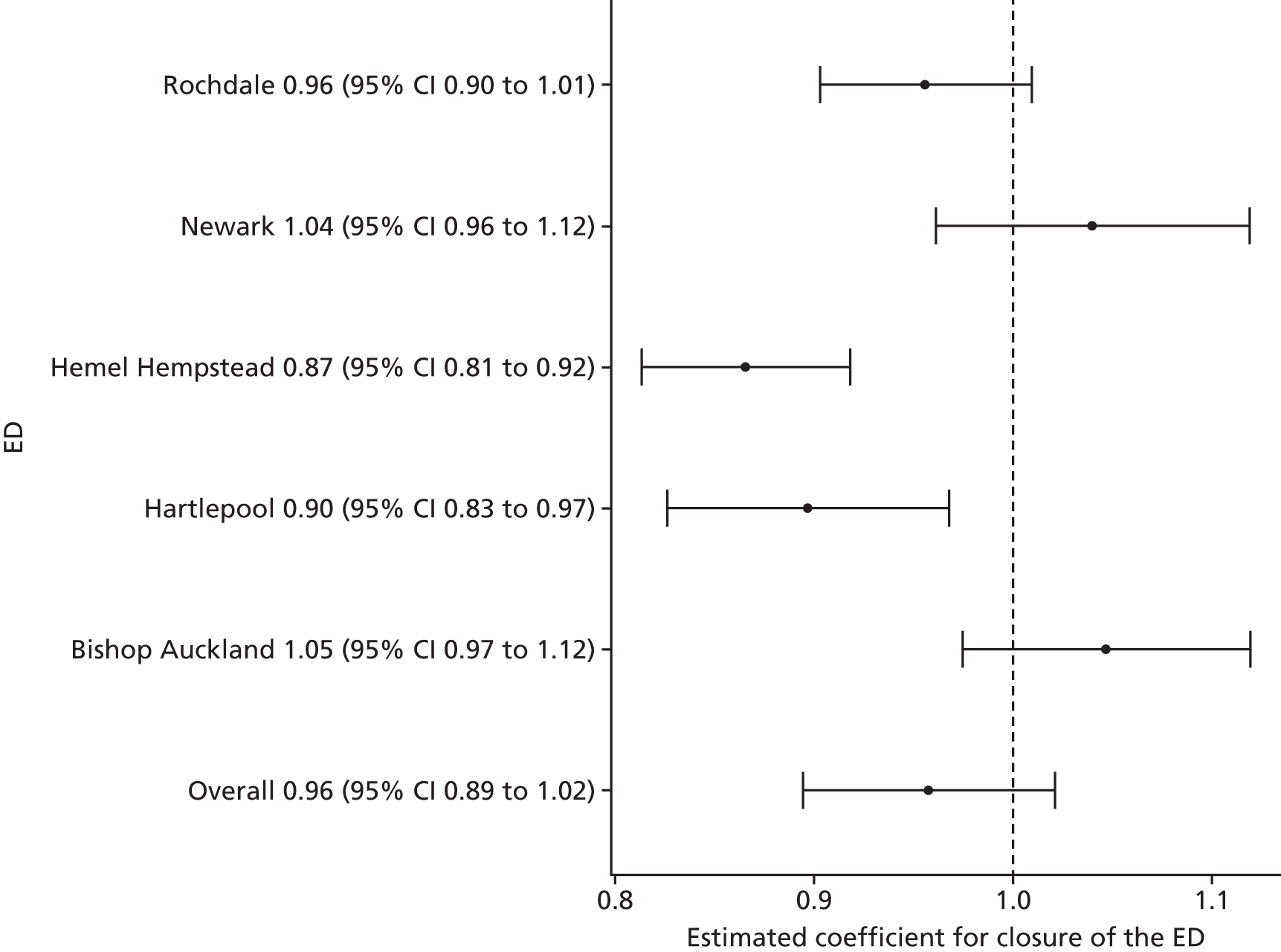
Over all sites, no statistically reliable evidence was found to suggest a change in the total number of emergency hospital admissions following the closure of a local ED. The estimated effect was a decrease of –4.3% (95% CI –10.6% to 2.1%; p = 0.19).
Figure 18 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of potentially avoidable emergency hospital admissions for residents of the catchment areas of the EDs that closed compared with the impact in their control sites.
FIGURE 18.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of emergency admissions in the catchment areas of the EDs that closed compared with the impact in their control areas (model 2).
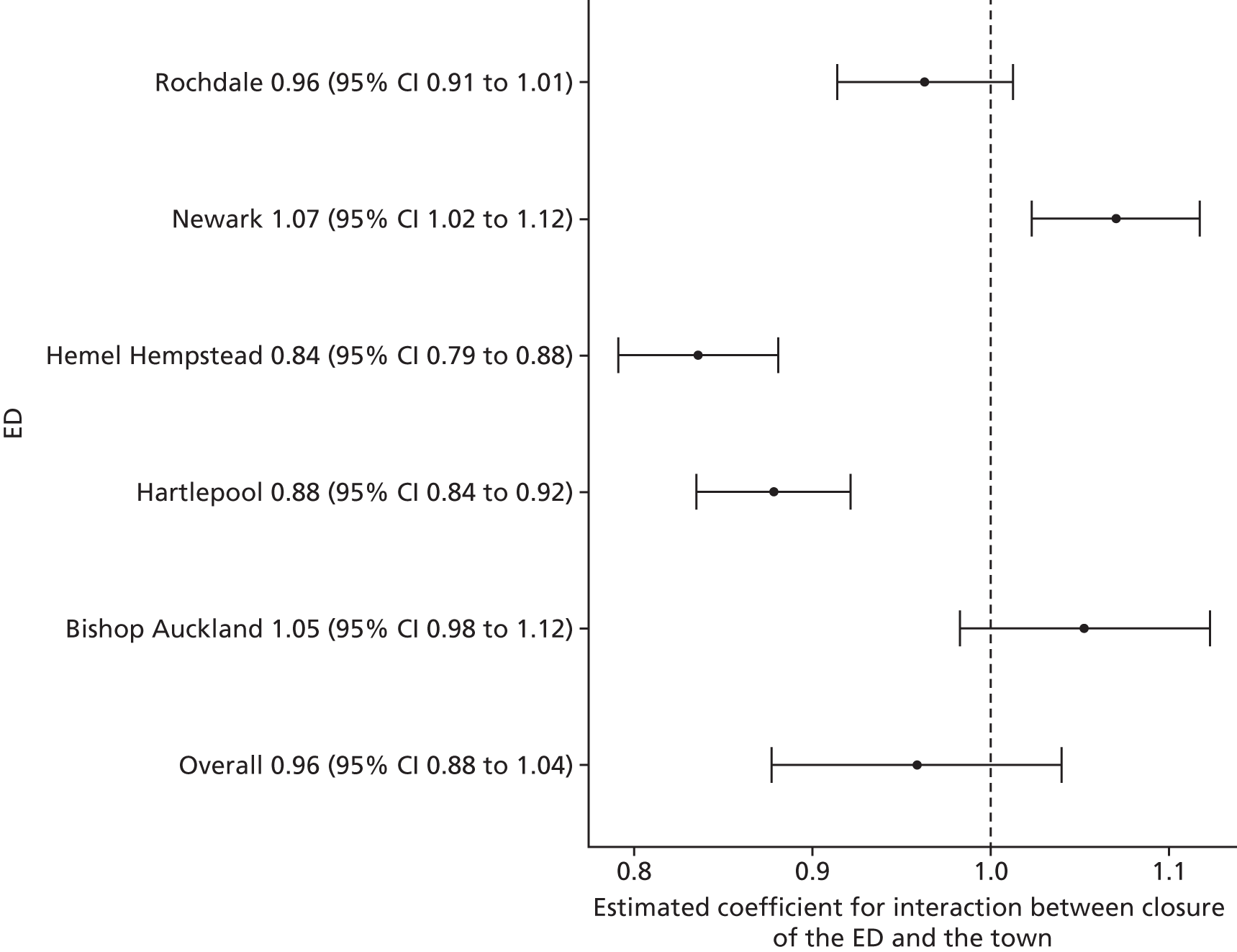
Compared with the control sites, over all sites, no statistically reliable evidence was found to suggest a change in the total number of emergency hospital admissions following the closure of a local ED. The estimated effect was a decrease of –4.2% (95% CI –12.4% to 3.9%; p = 0.31).
Figure 19 summarises the results of the individual site analyses that compared the impact of the ED closure on the number of emergency admissions for residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 19.
The results of the individual site analyses that compared the impact of the ED closure on the number of emergency admissions for relatively high-dose LSOAs with the impact in relatively low-dose LSOAs in that area (model 6).
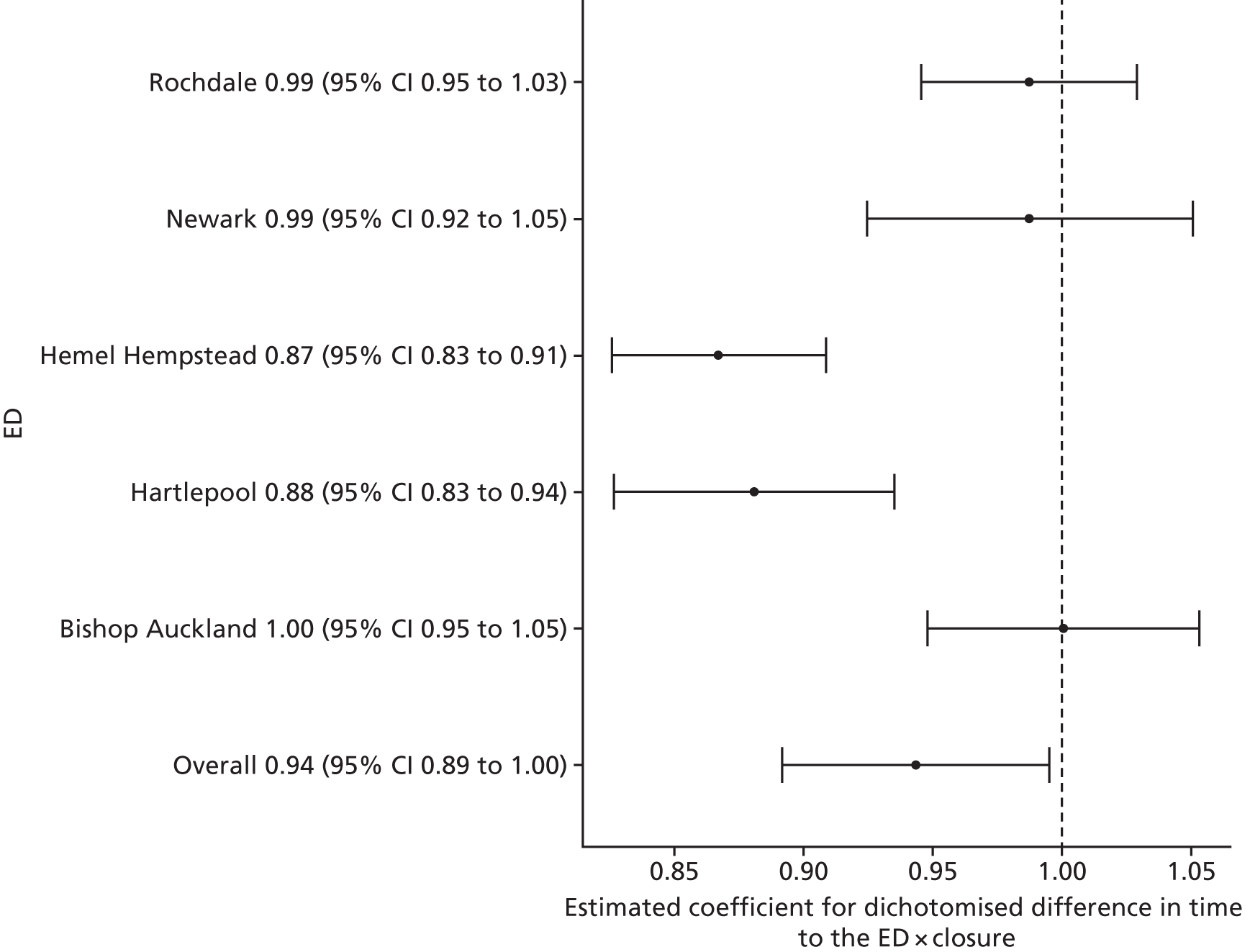
Over all sites, no statistically reliable evidence was found to suggest a change in the total number of emergency hospital admissions following the closure of a local ED. The estimated effect was a decrease in the high-dose areas relative to the low-dose areas of –5.7% (95% CI –10.8% to 0.5%; p = 0.03).
Potentially avoidable emergency admissions
Figure 20 presents the results of the individual site analyses that estimated the impact of closing the EDs on the number of potentially avoidable emergency admissions to hospital per month for residents of the catchment areas of the EDs that closed. These admissions were for any of the 14 conditions that were previously identified as rich in potentially avoidable admissions.
FIGURE 20.
The results of the individual site analyses that estimated the impact of the ED closure on the number of potentially avoidable emergency admissions in the catchment areas of the EDs that closed (model 1).
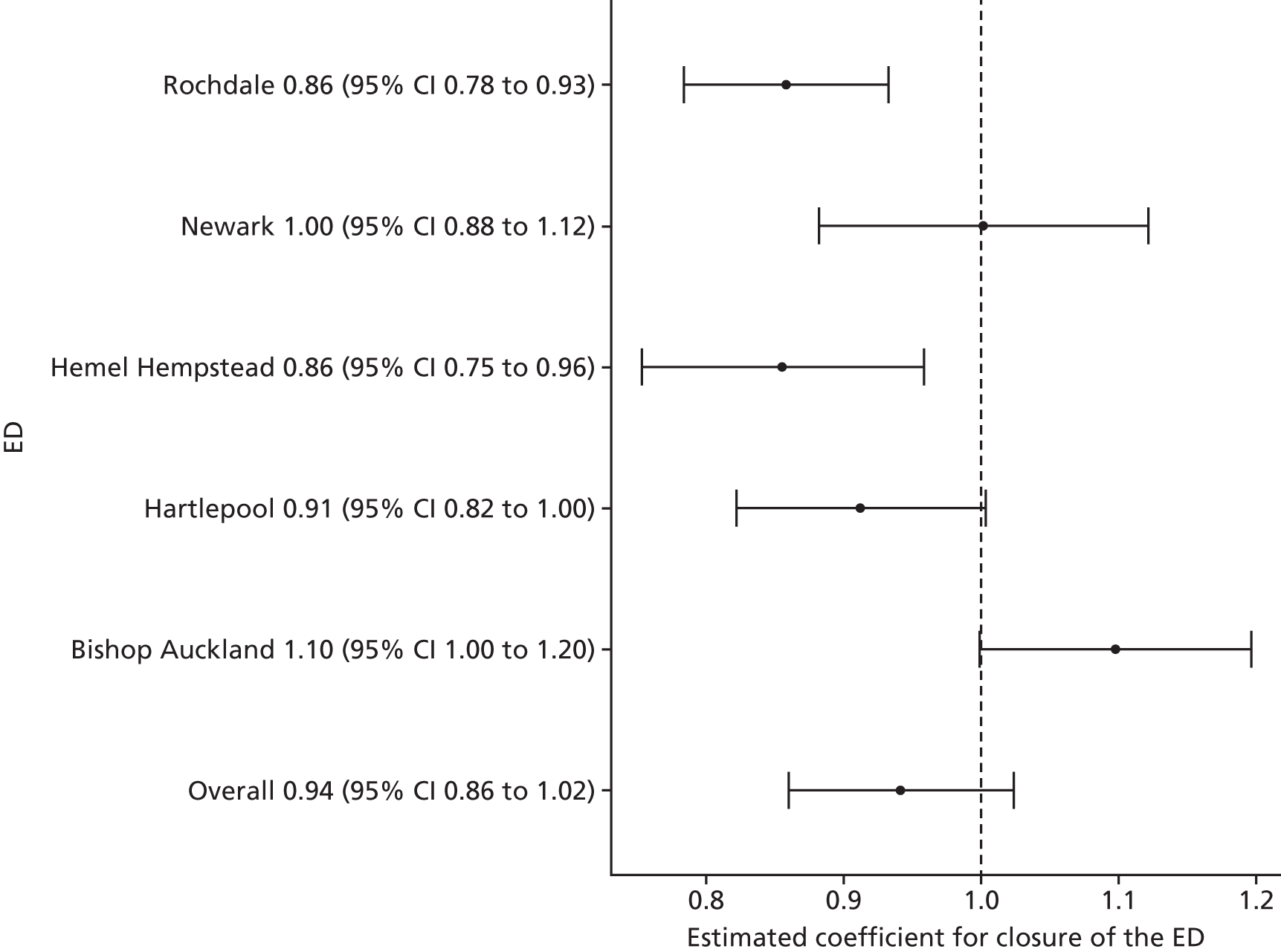
Over all sites, no statistically reliable evidence was found to suggest a change in the total number of potentially avoidable emergency hospital admissions following the closure of a local ED. The estimated effect was a decrease of –5.9% (95% CI –14.1% to 2.3%; p = 0.16).
Figure 21 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of emergency hospital admissions for residents of the catchment areas of the EDs that closed compared with the impact in their control sites.
FIGURE 21.
The results of the individual site analyses that estimated the impact of the ED closure on the number of potentially avoidable emergency admissions in the catchment areas of the EDs that closed compared with the impact in their control areas (model 2).
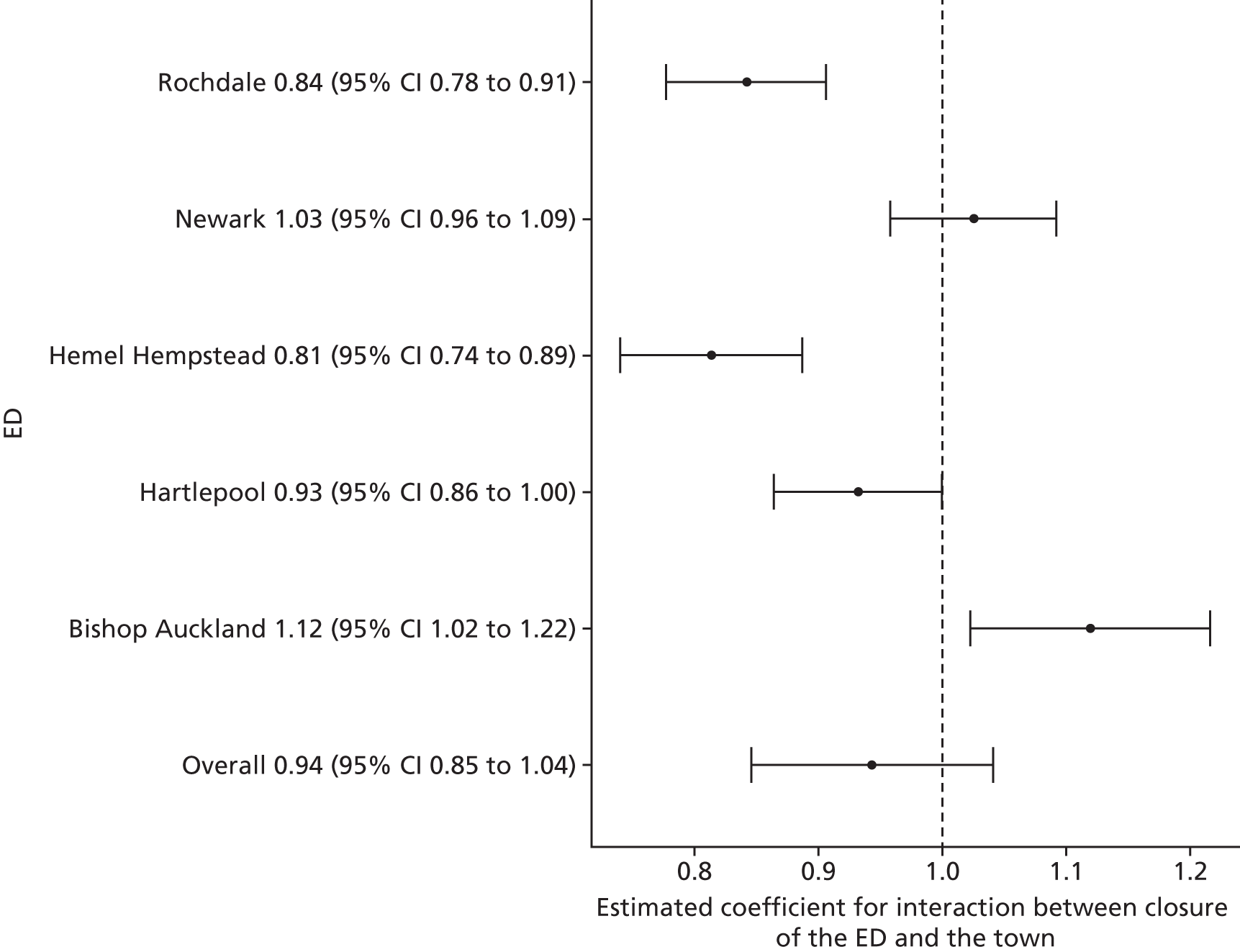
Compared with the control sites, over all sites, there was no statistically reliable evidence to suggest a change in the total number of potentially avoidable emergency hospital admissions following the closure of a local ED. The estimated effect was a decrease of –5.7% (95% CI –15.4% to 4.1%; p = 0.25).
Figure 22 summarises the results of the individual site analyses that compared the impact of the ED closure on the number of potentially avoidable emergency admissions for residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 22.
The results of the individual site analyses that compared the impact of the ED closure on the number of potentially avoidable emergency admissions for relatively high-dose LSOAs with the impact in relatively low-dose LSOAs in that area (model 6).
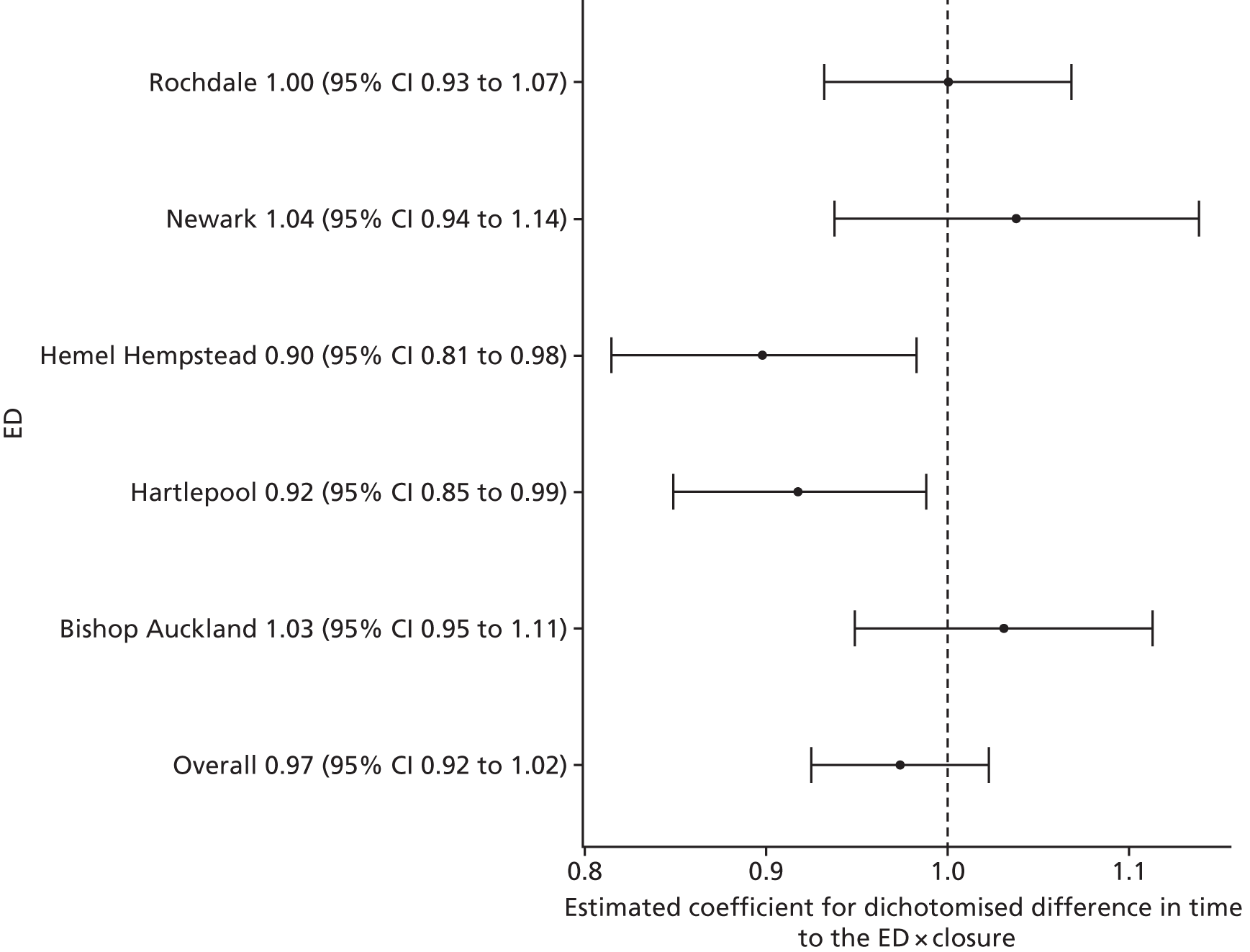
Over all sites, there was no statistically reliable evidence to suggest a change in the total number of potentially avoidable emergency hospital admissions following the closure of a local ED. The estimated effect was a decrease in the high-dose areas relative to the low-dose areas of –2.6% (95% CI –7.6% to 2.3%; p = 0.30).
Length of stay for emergency admissions
Figure 23 presents the results of the individual site analyses that estimated the impact of closing EDs on the mean LOS in hospital for emergency admissions for residents of the catchment areas of the EDs that closed.
FIGURE 23.
The results of the individual site analyses that estimated the impact of the ED closure on the mean LOS in hospital for residents of the catchment areas of the EDs that closed (model 1).
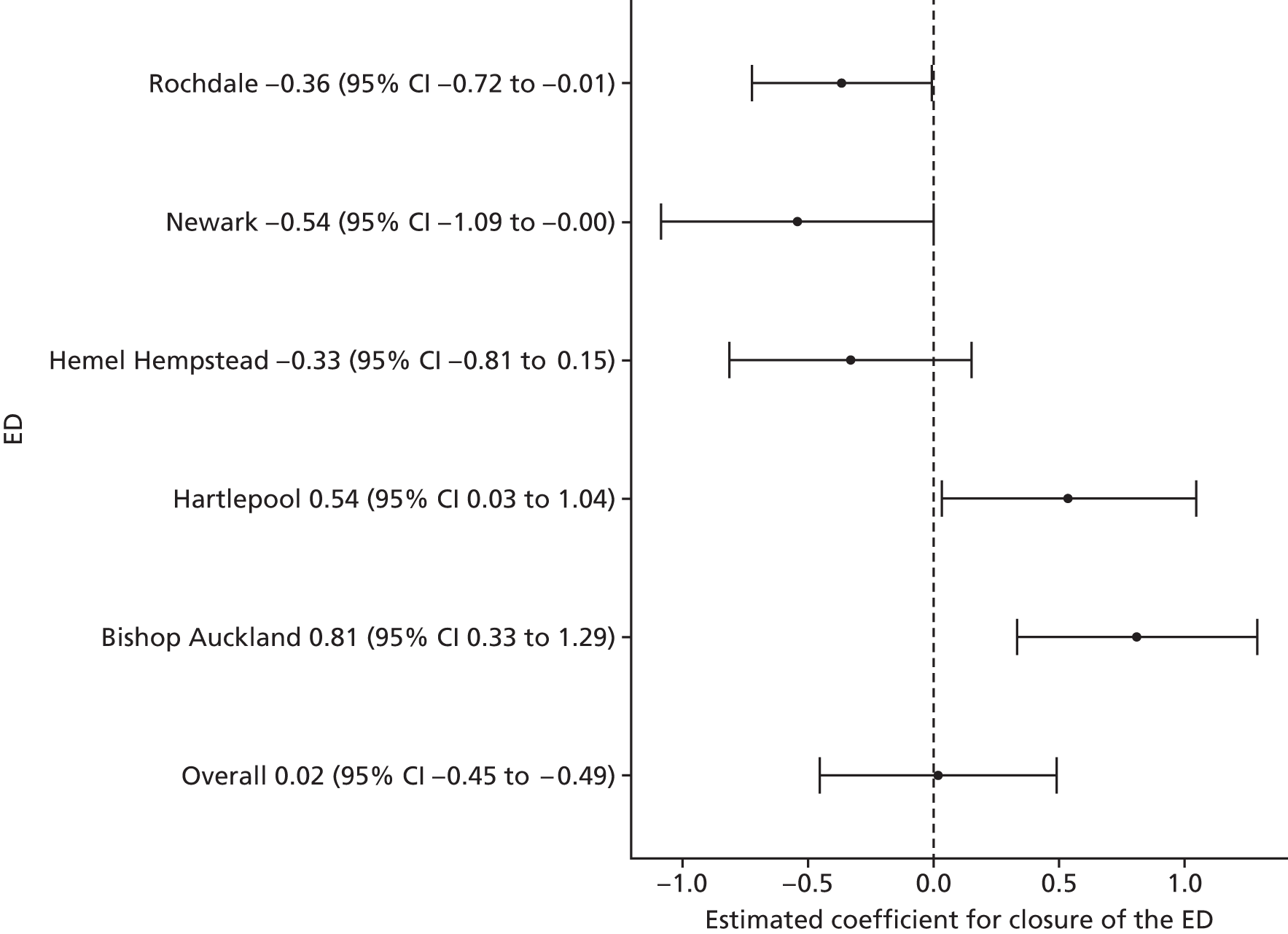
Over all sites, there was no statistically reliable evidence to suggest a change in the mean LOS following the closure of a local ED. The estimated effect was an increase of 0.02 days (95% CI –0.45 to 0.49 days; p = 0.94).
Figure 24 presents the results of the individual site analyses that estimated the impact of closing EDs on the mean LOS in hospital for emergency admissions for residents of the catchment areas of the EDs that closed compared with the impact in their control sites.
FIGURE 24.
The results of the individual site analyses that estimated the impact of the ED closure on the mean LOS in hospital for residents of the catchment areas of the EDs that closed compared with the impact in their control areas (model 2).
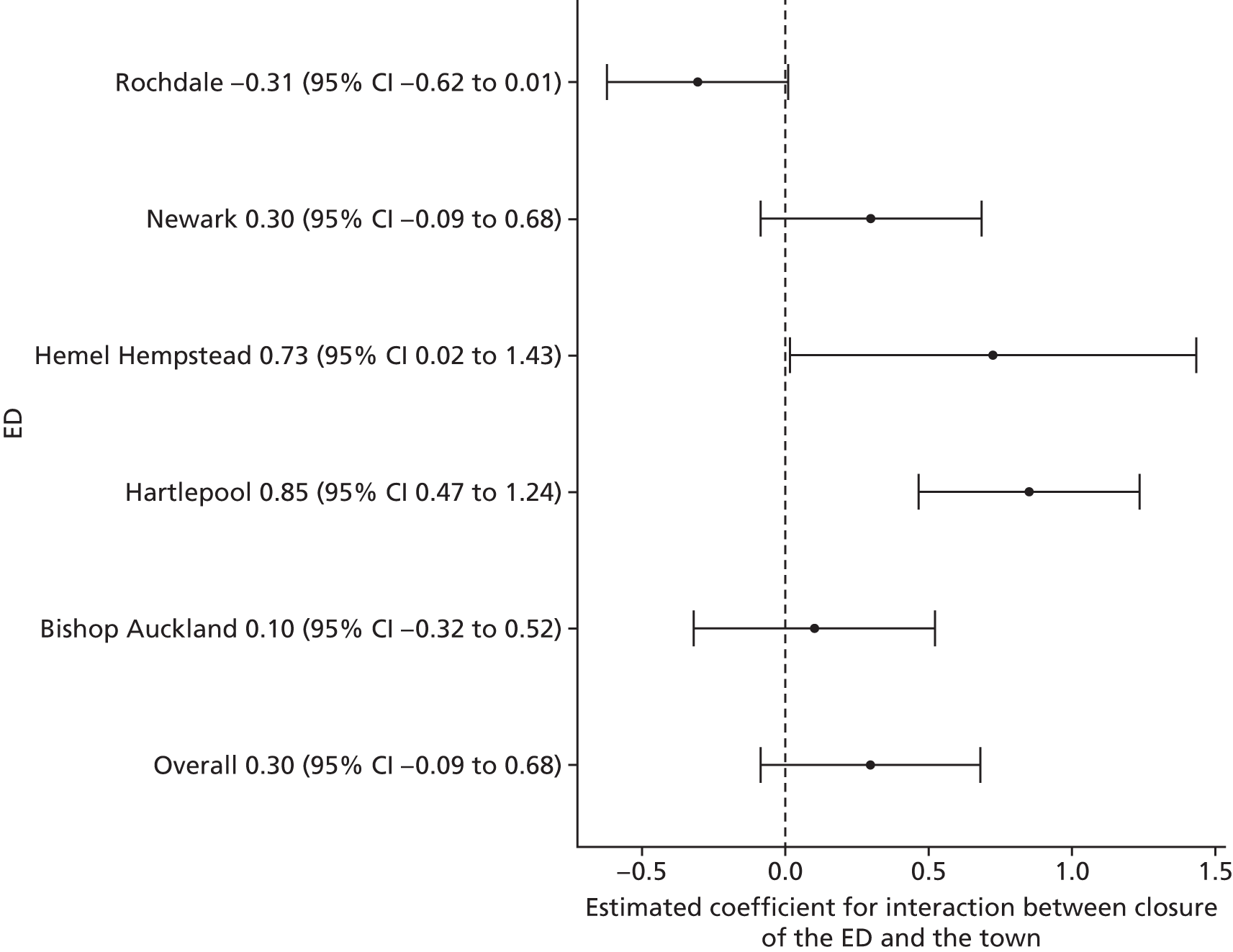
Compared with the control sites, over all sites, there was no statistically reliable evidence to suggest a change in the mean LOS following the closure of a local ED. The estimated effect was an increase of 0.3 days (95% CI 0.1 to 0.7 days; p = 0.13).
Figure 25 summarises the results of the individual site analyses that compared the impact of the ED closure on the mean LOS in hospital following emergency admissions for residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 25.
The results of the individual site analyses that compared the impact of the ED closure on the mean LOS in hospital for residents of high-dose LSOAs with the impact in relatively low-dose LSOAs (model 6).
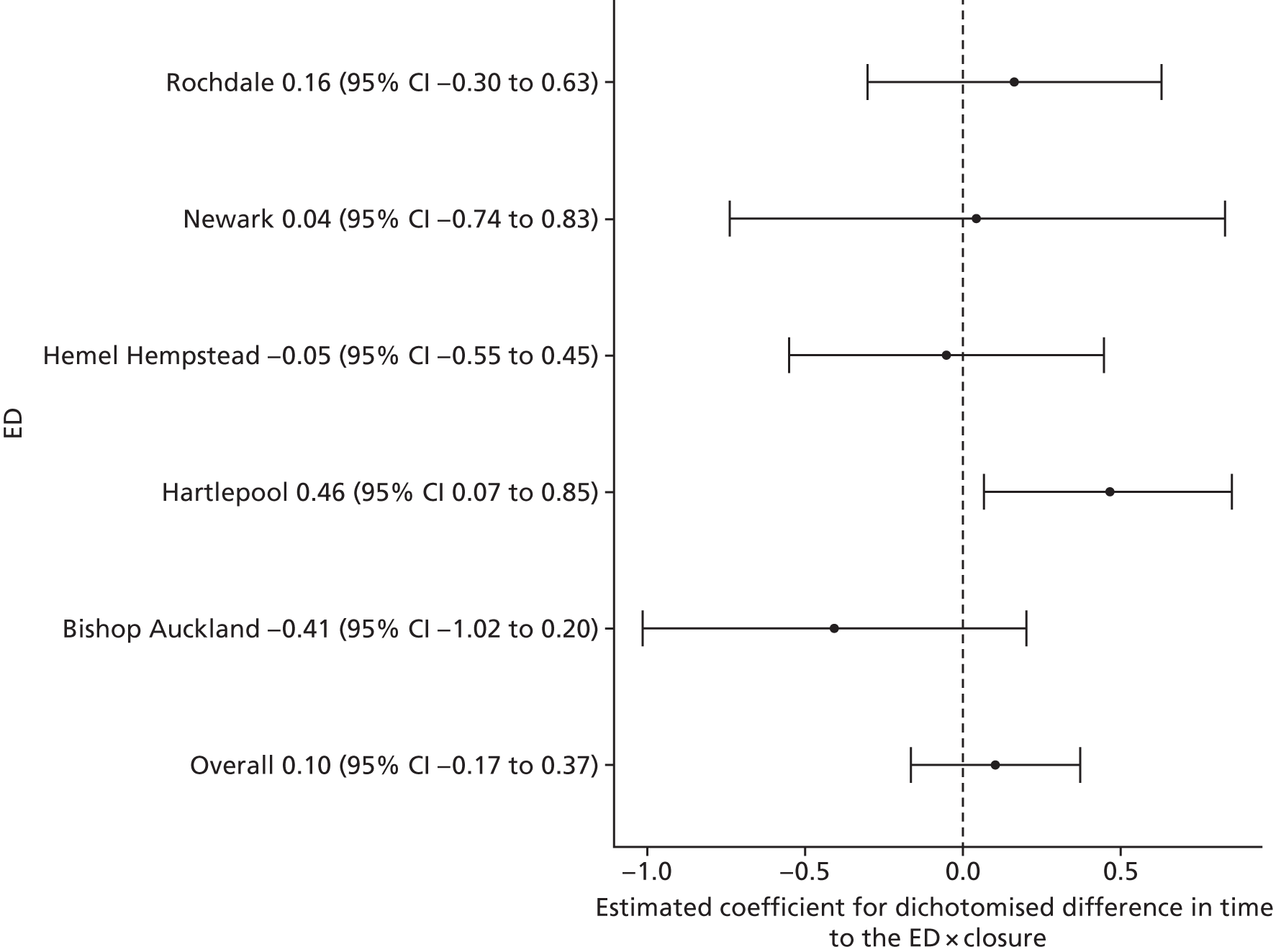
Over all sites, there was no statistically reliable evidence to suggest a change in the in mean time in hospital following emergency admissions for residents of high-dose areas compared with low-dose areas following the closure of the local ED. The estimated effect was an increase in the high-dose areas relative to the low-dose areas of 0.1 days (95% CI –0.2 to 0.4 days; p = 0.45).
Deaths
Out-of-hospital deaths from certain serious conditions
Out-of-hospital deaths may occur: at home prior to making contact with a service, in an ambulance on the way to hospital, in the ED prior to hospital admission, or when a patient is recorded as having a SEC incident and is admitted, discharged alive and subsequently dies without being readmitted.
Figure 26 presents the results of the individual site analyses that estimated the impact of closing the EDs on the mean number of out-of-hospital deaths from 16 emergency conditions per month for residents of the catchment areas of the EDs that closed.
FIGURE 26.
The results of the individual site analyses that estimated the impact of the ED closure on the number of out-of-hospital deaths in the catchment areas of the EDs that closed (model 1).
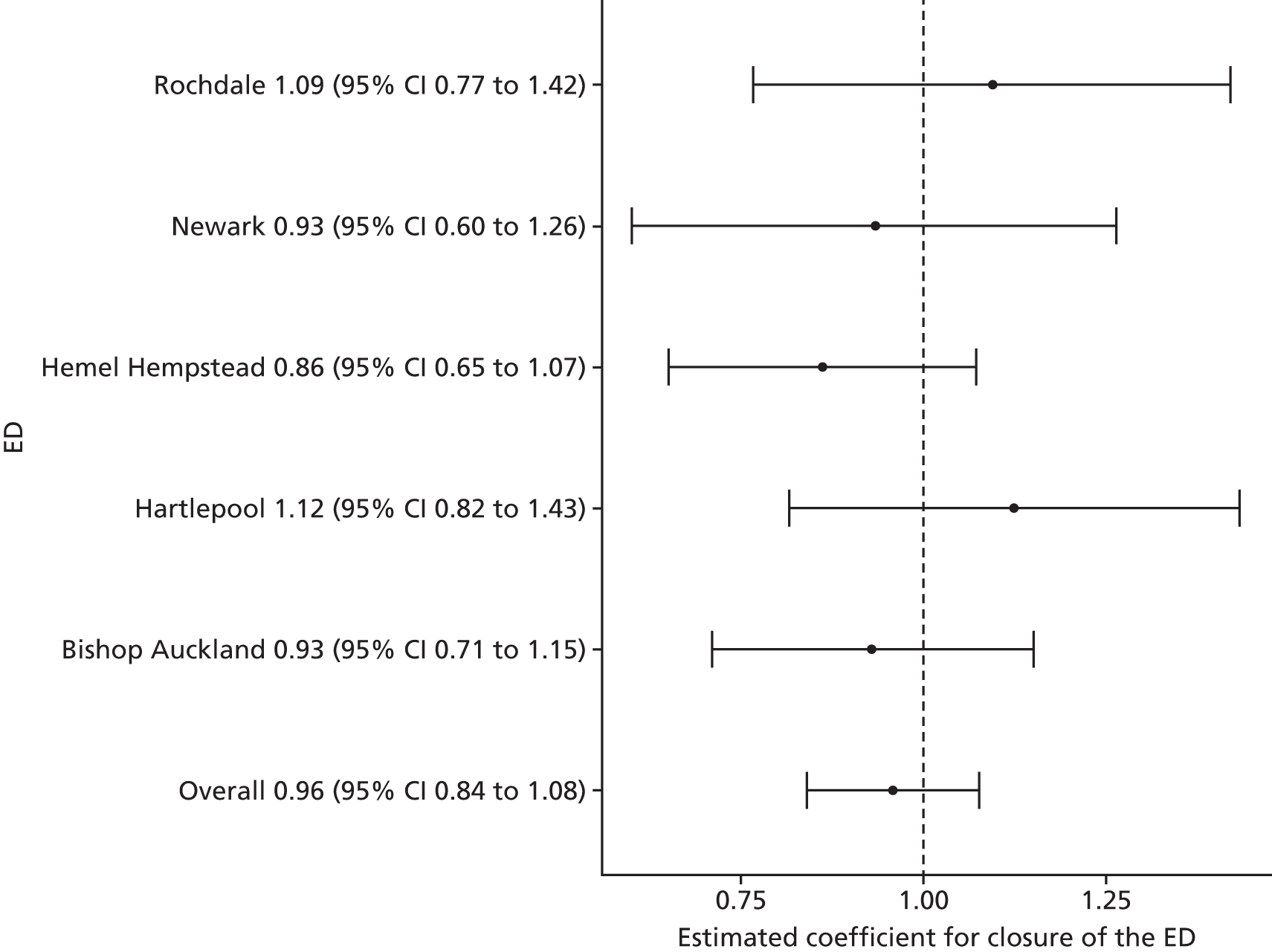
Over all sites, there was no statistically reliable evidence to suggest a change in the total number of out-of-hospital deaths following the closure of a local ED. The estimated effect was a decrease of –4.2% (95% CI –15.9% to 7.7%; p = 0.49).
Figure 27 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of out-of-hospital deaths that occurred within 7 days for these 16 emergency conditions for residents of the catchment areas of the EDs that closed compared with the impact in their control sites.
FIGURE 27.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of deaths within 7 days for 16 emergency conditions in the catchment areas of the EDs that closed compared with the impact in their control areas (model 2).
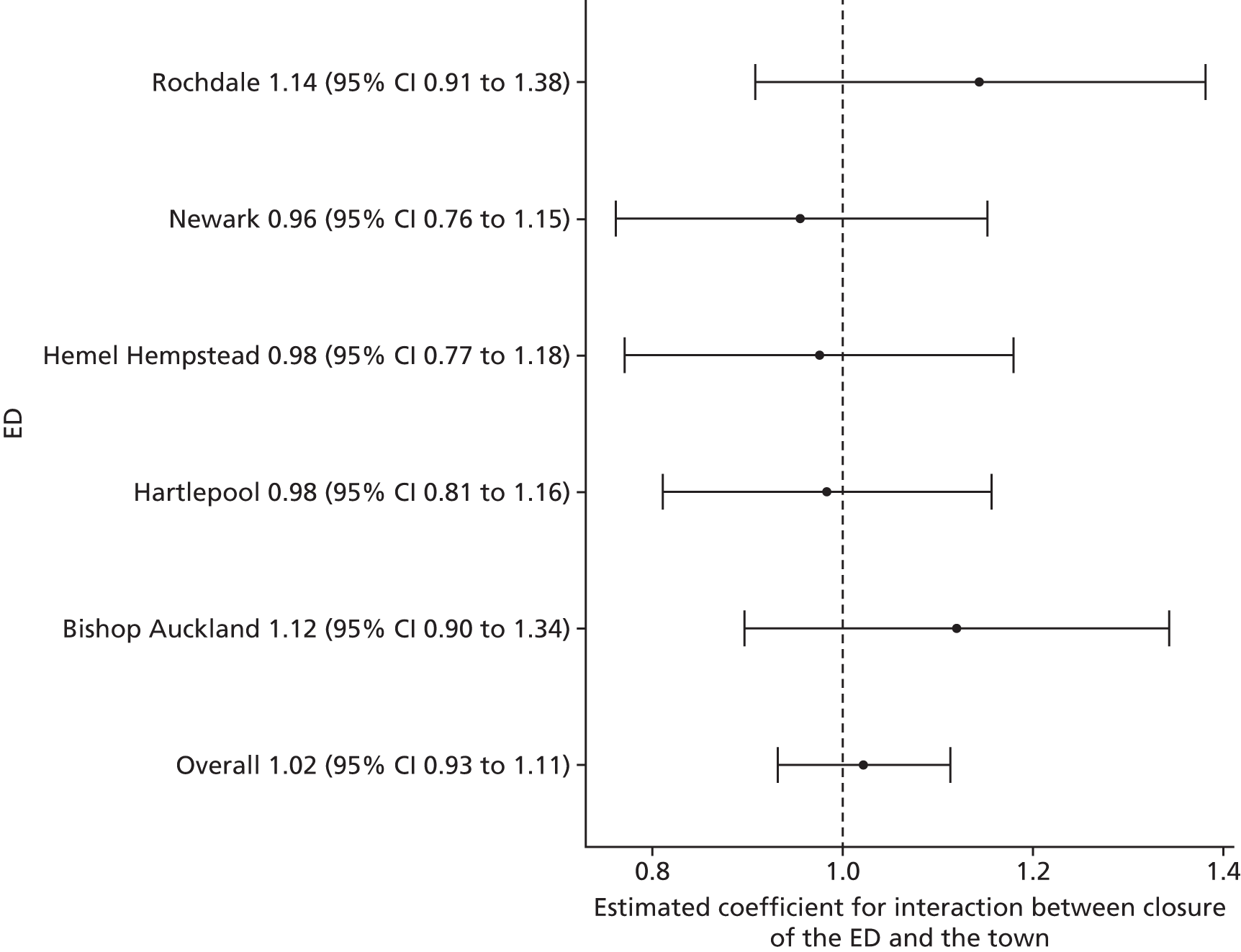
Compared with the control sites, over all sites, there was no statistically reliable evidence to suggest a change in the number of out-of-hospital deaths from SECs following the closure of a local ED. The estimated effect was a slight increase of 2.2% (95% CI –6.9% to 11.3%; p = 0.63).
Figure 28 summarises the results of the individual site analyses that compared the impact of the ED closure on the number of out-of-hospital deaths among residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 28.
The results of the individual site analyses that compared the impact of the ED closure on the number of out-of-hospital deaths among residents of relatively high-dose LSOAs with relatively low-dose LSOAs in that area (model 6).
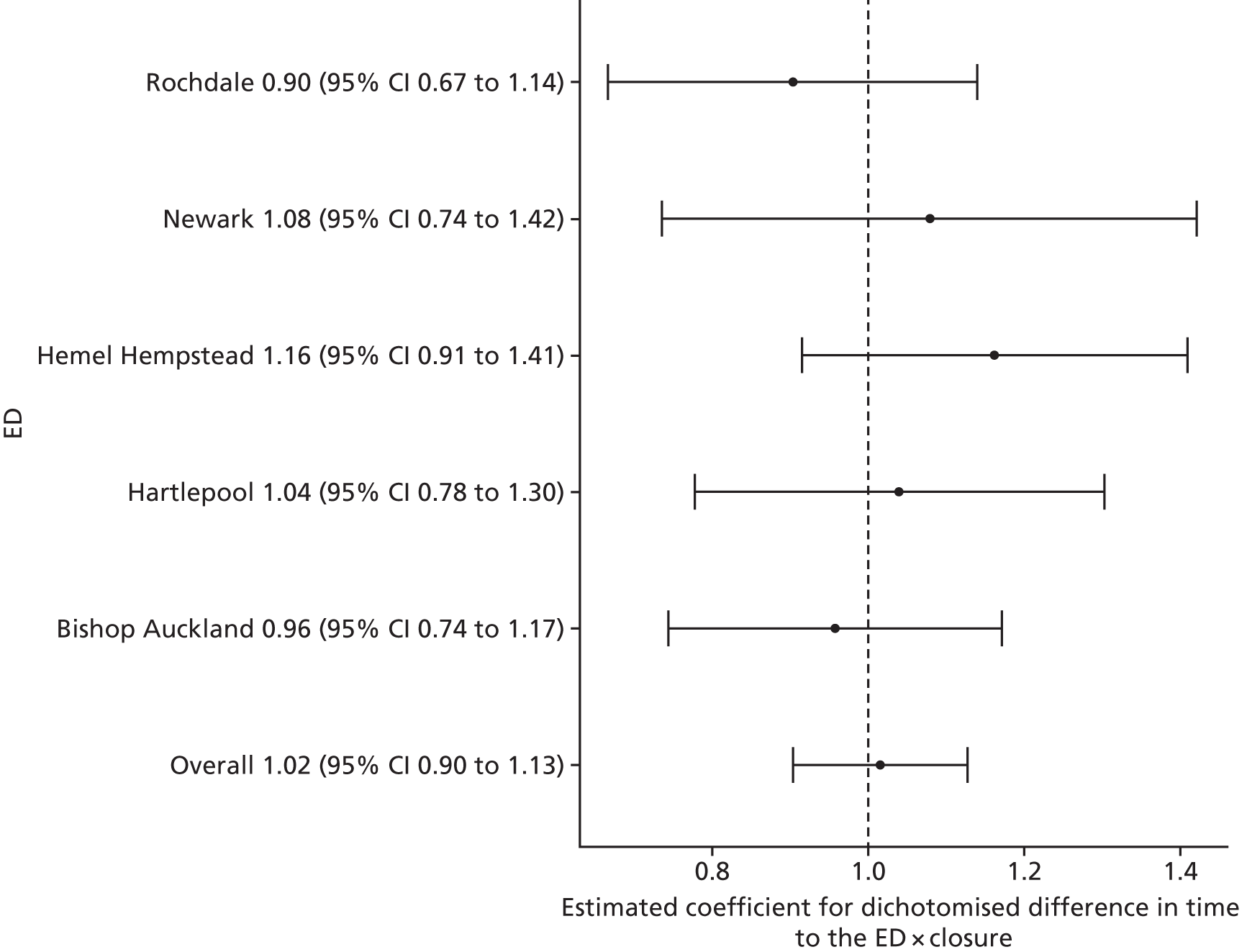
Over all sites, there was no statistically reliable evidence to suggest a change in the number of out-of-hospital deaths from emergency conditions in high-dose areas compared with low-dose areas following the closure of the local ED. The estimated effect was an increase in the high-dose areas relative to the low-dose areas of 1.6% (95% CI –9.7% to 12.8%; p = 0.78).
All deaths from certain serious conditions occurring within 7 days
Figure 29 presents the results of the individual site analyses that estimated the impact of closing the EDs on the mean number of deaths per month that occurred within 7 days from 16 emergency conditions for residents of the catchment areas of the EDs that closed.
FIGURE 29.
The results of the individual site analyses that estimated the impact of the ED closure on the number of deaths within 7 days of an emergency for residents of the catchment areas of the EDs that closed (model 1).
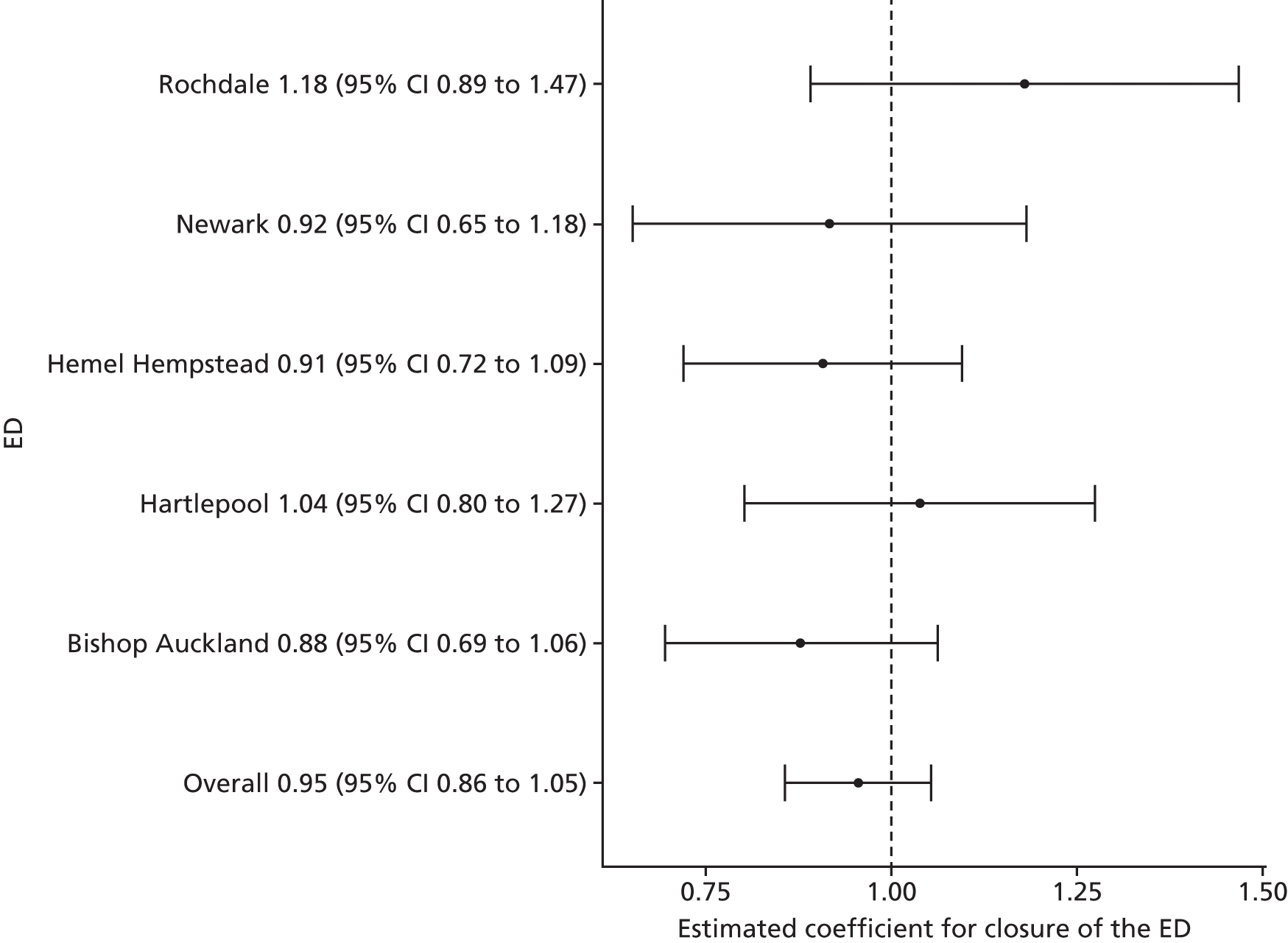
Over all sites, there was no statistically reliable evidence to suggest a change in the total number of deaths occurring within 7 days of emergencies following the closure of a local ED. The estimated effect was a decrease of –4.6% (95% CI –14.4% to 5.4%; p = 0.37).
Figure 30 presents the results of the individual site analyses that estimated the impact of closing the EDs on the total number of deaths that occurred within 7 days for these 16 emergency conditions for residents of the catchment areas of the EDs that closed compared with the impact in their control sites.
FIGURE 30.
The results of the individual site analyses that estimated the impact of the ED closure on the total number of deaths within 7 days for 16 emergency conditions in the catchment areas of the EDs that closed compared with the impact in their control areas (model 2).
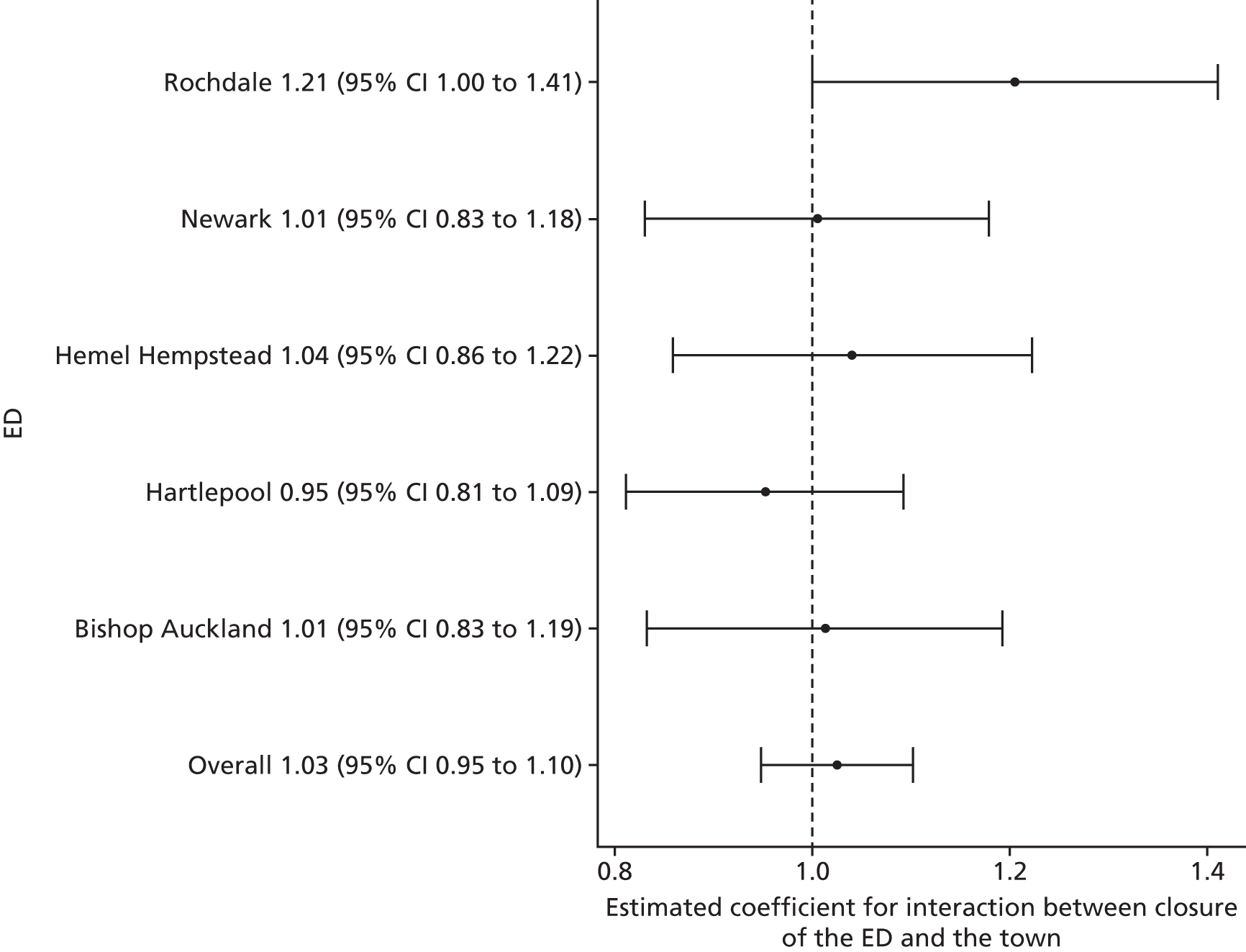
Compared with the control sites, over all sites, there was no statistically reliable evidence to suggest a change in the number of deaths within 7 days of emergencies following the closure of a local ED. The estimated effect was a slight increase of 2.5% (95% CI –5.2% to 10.2%; p = 0.52).
Figure 31 summarises the results of the individual site analyses that compared the impact of the ED closure on the number of deaths within 7 days of emergencies among residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 31.
The results of the individual site analyses that compared the impact of the ED closure on the number of deaths within 7 days of an emergency among residents of relatively high-dose LSOAs with the impact in relatively low-dose LSOAs in that area (model 6).
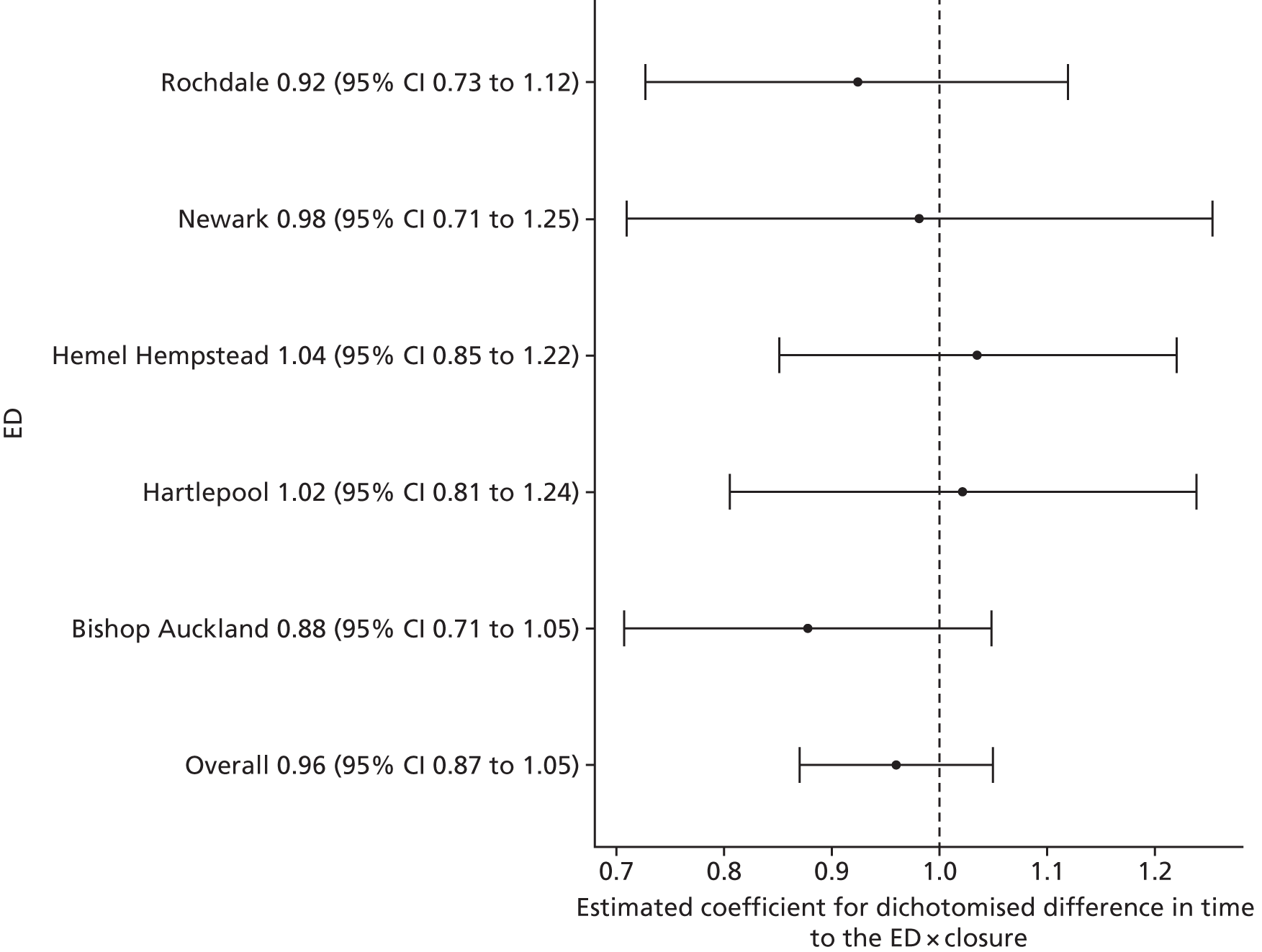
Over all sites, there was no statistically reliable evidence to suggest a change in the number of deaths within 7 days from emergency conditions in high-dose areas compared with low-dose areas following the closure of the local ED. The estimated effect was a change in the high-dose areas relative to low-dose areas of –4.0% (95% CI –13.0% to 5.0%; p = 0.39).
Case fatality ratios for all serious emergency conditions studied
Figure 32 presents the results of the individual site analyses that estimated the impact of closing the EDs on the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths plus admissions of patients who survived beyond 7 days for the 16 SECs in residents of the catchment areas of the EDs that closed.
FIGURE 32.
The results of the individual site analyses that estimated the impact of the ED closure on the case fatality ratio for 16 emergency conditions for residents of the catchment areas of the EDs that closed (model 1).
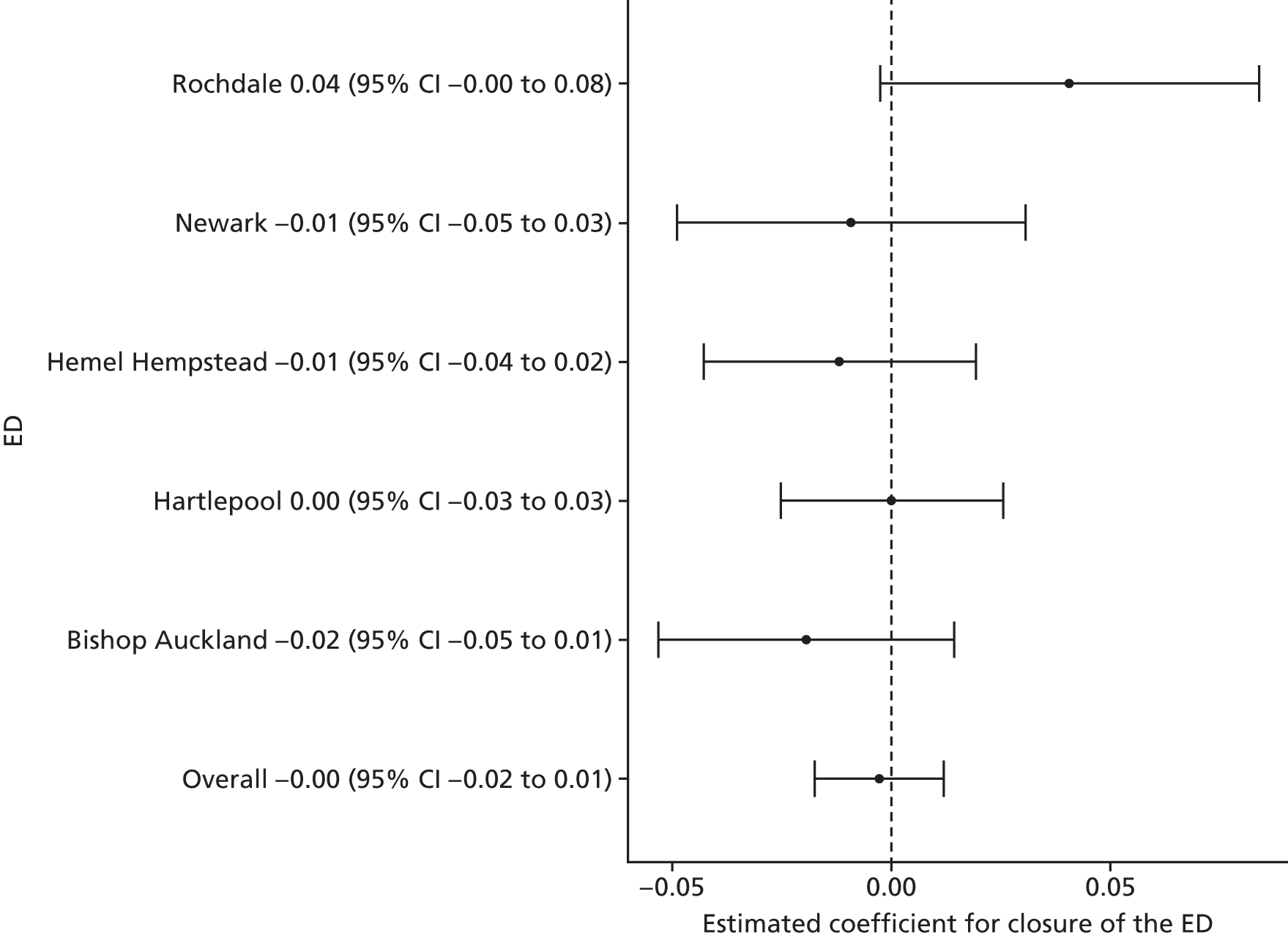
Over all sites, there was no statistically reliable evidence to suggest a change in the case fatality ratio (CFR) for deaths within 7 days of emergencies following the closure of a local ED. The estimated effect was a decrease of –0.003 (95% CI –0.017 to 0.012; p = 0.71), a decrease in the percentage of patients who died of just –0.3.
Figure 33 presents the results of the individual site analyses that estimated the impact of closing the EDs on the CFR for deaths within 7 days that were attributable to these 16 emergency conditions for residents of the catchment areas of the EDs that closed compared with the impact in their control sites.
FIGURE 33.
The results of the individual site analyses that estimated the impact of the ED closure on the CFR for deaths within 7 days for 16 emergency conditions in the catchment areas of the EDs that closed compared with the impact in their control areas (model 2).
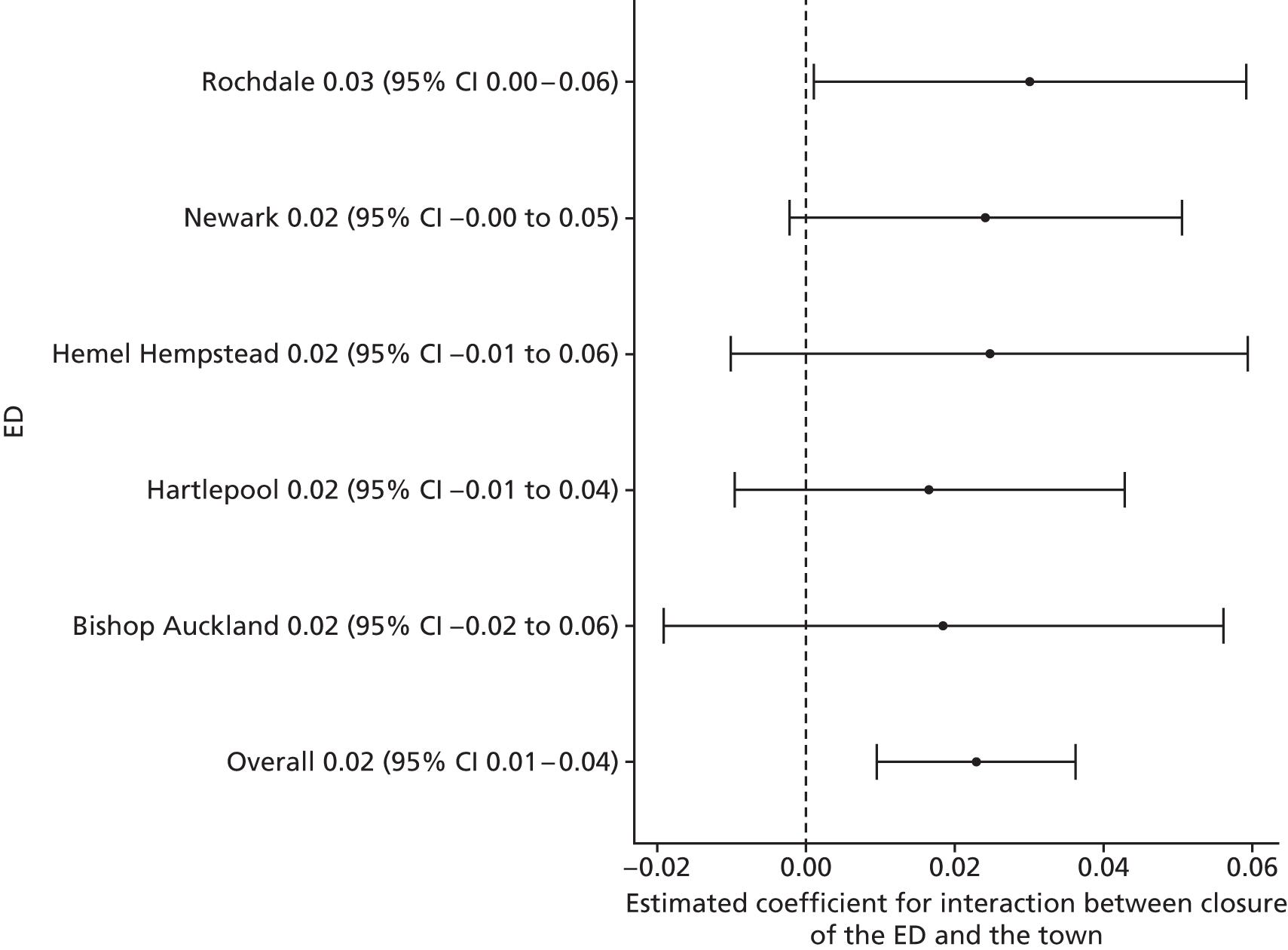
Compared with the control sites, over all sites, there was no statistically reliable evidence to suggest a change in the CFR for deaths within 7 days that were attributable to these 16 emergency conditions following closure of a local ED. The estimated effect was 0.023 (95% CI 0.009 to 0.036; p < 0.001), an increase of 2.3 in the percentage of patients who died.
Figure 34 summarises the results of the individual site analyses that compared the impact of the ED closure on the CFR for deaths for within 7 days or these 16 emergency conditions residents of relatively high-dose LSOAs in each ED catchment area with the impact in relatively low-dose LSOAs in that area.
FIGURE 34.
The results of the individual site analyses that compared the impact of the ED closure on the CFR for deaths within 7 days for 16 emergency conditions for residents of relatively high-dose LSOAs with the impact in relatively low-dose LSOAs in that area (model 6).
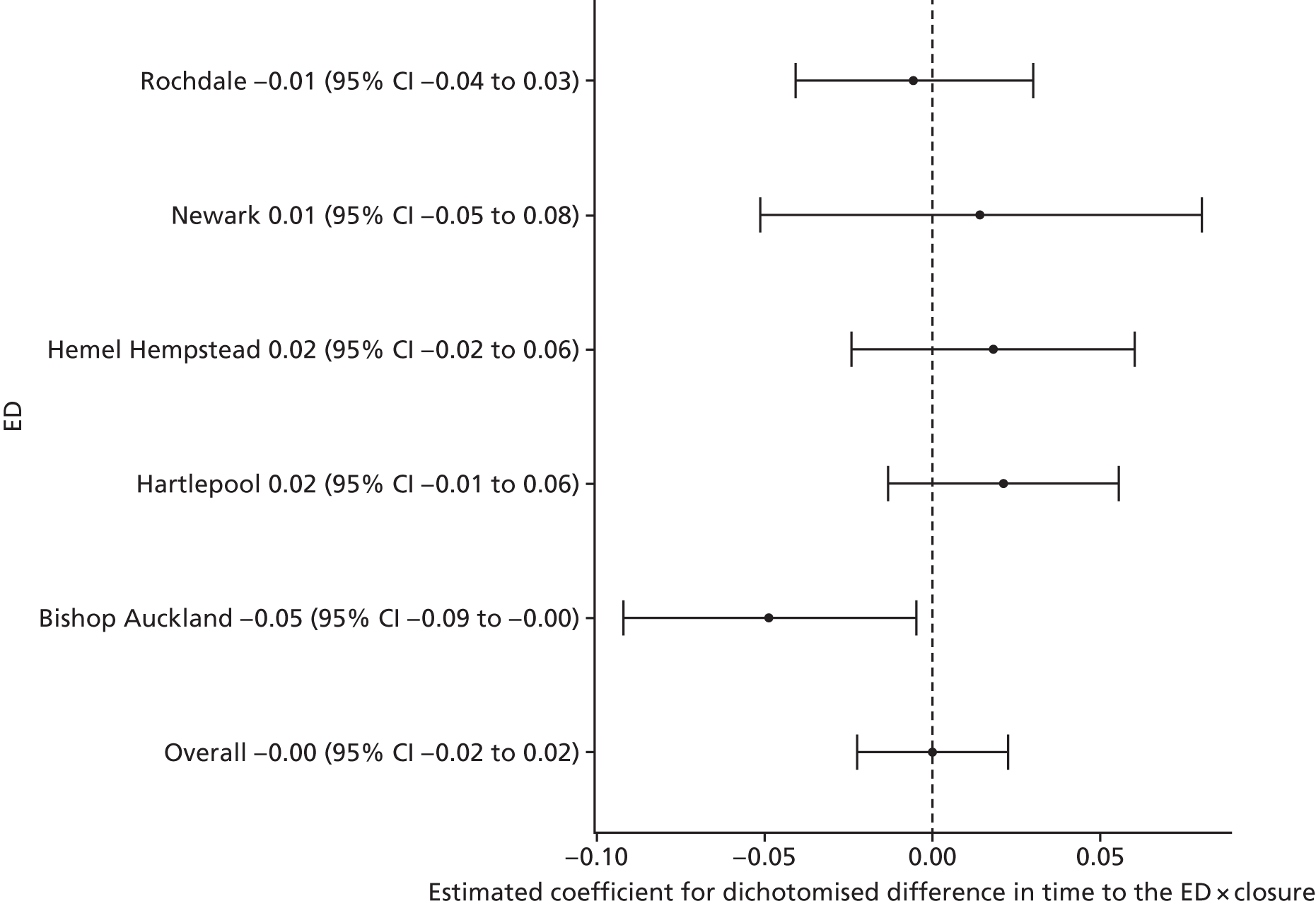
Over all sites, there was no statistically reliable evidence to suggest a change in the CFR for deaths within 7 days that were attributable to these 16 emergency conditions in high-dose areas compared with low-dose areas following the closure of the local ED. The estimated effect was a change in the high-dose areas relative to the low-dose areas of 0.000 (95% CI –0.023 to 0.023; p = 0.10); there was no change in the percentage of patients who died.
Table 2 provides a summary of the results.
| Impact measure | Model, effect (95% CI); p-value | ||
|---|---|---|---|
| 1: no control | 2: compared with control | 6: high-dose areas | |
| Total number of emergency ambulance incidents | Increase: 11.2% (–1.0% to 23.4%); 0.07 | Increase: 13.9% (3.5% to 24.4%); 0.008 | Increase: 2.3% (–0.9% to 5.5%); 0.16 |
| Total number of emergency ambulance ‘Red’ incidents | Increase: 10.5% (5.7% to 15.2%); < 0.001 | Increase: 12.3% (3.5% to 21.1%); 0.006 | Increase: 5.0% (0.9% to 10.5%); 0.07 |
| Mean time from 999 ‘Red’ call to arrival at hospital | Increase: 3.9 minutes (2.2 to 5.6 minutes); < 0.001 | No reliable data | Increase: 9.1 minutes (4.8 to 13.5 minutes); 0.001 |
| Total number of emergency and urgent care attendances | Decrease: –8.4% (–23.5% to 6.7%); 0.27 | Decrease: –10.0% (–27.1% to 6.9%); 0.25 | Decrease: –8.3% (–21.5% to 5.0%); 0.22 |
| Total number of minor attendances at an emergency and urgent care service | Decrease: –22.3% (–47.0% to 2.3%); 0.08 | Decrease: –12.4% (–36.8% to 12.1%); 0.32 | Decrease: –11.1% (–30.9% to 8.8%); 0.28 |
| Total number of emergency hospital admissions | Decrease: –4.3% (–10.6% to 2.1%); 0.19 | Decrease: –4.2% (–12.4% to 3.9%); 0.31 | Decrease: –5.7% (–10.8% to –0.5%); 0.03 |
| Total number of potentially avoidable emergency hospital admissions | Decrease: –5.9% (–14.1% to 2.3%); 0.16 | Decrease: –5.7% (–15.4% to 4.1%); 0.25 | Decrease: –2.6% (–7.6% to 2.3%); 0.28 |
| Mean LOS for emergency hospital admissions | Increase: 0.2 days (–0.45 to 0.49 days); 0.94 | Increase: 0.3 days (0.1 to 0.7 days); 0.12 | Increase: 0.1 days (–0.2 to 0.4 days); 0.45 |
| Total number of out-of-hospital deaths | Decrease: –4.2% (–15.9% to 7.7%); 0.49 | Increase: 2.2% (–6.9% to 11.3%); 0.63 | Increase: 1.6% (–9.7% to 12.8%); 0.78 |
| Total number of deaths occurring within 7 days post incident | Decrease: –4.6% (–14.4% to 5.4%); 0.37 | Increase: 2.5% (–5.2% to 10.2%); 0.52 | Decrease: –4.0% (–13.0% to 5.0%); 0.39 |
| CFR (7 days) | Decrease: –0.3% (–0.017% to 0.012%); 0.71 | Increase: 2.3% (0.009% to 0.036%); < 0.001 | No change: 0.0% (–0.023% to 0.023%); 0.10 |
Chapter 6 Discussion
Summary of findings
We evaluated the impact of ED closures and downgrades that took place between 2009 and 2011 in five areas of England. The main findings of the evaluation are discussed in this chapter.
The overall effect of closing emergency departments in the five areas studied
Given such a major reorganisation of emergency and urgent care, we might expect there to be some changes in emergency and urgent care activity. This was apparent for some measures of activity in some sites but the impact was not consistent.
When statistical analyses of the five ED closure areas were combined, there was some evidence of a large increase on average in the total number of 999 ambulance incidents and in the total number of ‘Red’ incidents in these areas. There was also evidence to suggest that ambulance journey times from emergency call to hospital had increased.
No consistent effects were found regarding the hospital impact measures. The model estimates suggested that, on average across the sites, there was a decrease in total attendance at an emergency or urgent care service, and also a decrease in those minor attendance patients who were discharged without treatment or investigations that required hospital facilities. However, the evidence was not statistically reliable. There was also some statistically unreliable evidence of a decrease on average across the sites in the number of emergency admissions and in those admissions that were ‘potentially avoidable’.
The estimates relating to the impact on mortality were much more consistent across sites, but they also found no statistically reliable evidence to suggest a change in the number of deaths following an ED closure in any site or on average across all sites. However, there was some evidence to suggest that, on average across the five sites, there was a small increase in an indicator of the ‘risk of death’ for specific emergency conditions when compared with the five control areas studied.
The effect of travel times to the nearest type 1 emergency department
These results for the whole catchment populations of the five sites were closely mirrored by the results we found when comparing populations living relatively close to or far away from the next nearest type 1 ED following ED closure. Perhaps not surprisingly given their distance to hospital, those living in the areas furthest away had a mean increase of 9 minutes longer in the time that it took from an ambulance 999 call being received to the patient arriving at hospital than in those living in less affected areas. This overall effect was also apparent in the analysis for each of the five individual areas included in this study.
However, this difference between high-dose areas and low-dose areas, which was very similar to the difference in travel times predicted by DfT for the whole catchment populations before and after closure of their nearest ED, did not translate into any consistent, reliable evidence of impact on the outcome measures.
In particular, there was no statistically reliable evidence to suggest a relative change in the number of deaths, or ‘risk of death’, in the population who were now living furthest away from the nearest type 1 ED, following an ED closure.
The effect on individual areas affected by emergency department closures
There was significant heterogeneity across the five areas with regard to the emergency care activity and performance impact measures. Although some of this heterogeneity may be attributable to differences and inconsistencies in data recording, it is likely that this points to real differences in terms of the impact that an ED closure has had in some areas compared with others. Investigating why these differences were found was beyond the remit of this study. However, the provision of services in the wider emergency and urgent care system, and their performance prior to an ED closure, combined with the NHS provider’s management of the reorganisation of care, may have influenced this.
This heterogeneity means that the summary effects we have reported should not be regarded as estimates of the ‘true’ effects of closing or downgrading EDs, but rather as estimates of the average effects across the five sites we have studied.
Despite the differences found across areas with regard to the emergency care measures, the findings from the mortality impact measures appeared to be consistent. This suggests that these measures represent reliable estimates and that emergency care systems can be robust in dealing with such large-scale reorganisation.
Implications
The impact measure that is probably of most importance to the public, health-care providers and policy-makers is mortality. The public, in particular, require reassurance that the closure or downgrade of an ED does not result in increased death rates within the population. In the five geographical areas studied here, we found no statistically reliable and consistent evidence of an increase in deaths within the population from SECs in the period following the reorganisation of care.
However, there are further implications to consider for the population, health-care providers and policy-makers. We highlight these in turn in the following sections.
Implications for the population
The reorganisation of care should be assessed based on the needs of the local population as a whole, and our research shows that the reorganisation of emergency care did not have a negative impact on each of the local populations studied as a whole. Of course, there may have been individuals, or incidents, in those populations for whom the effects are different from the average effect, but our research was not designed to explore individual experiences.
Continuity is important for the population. Four of the five areas studied replaced the ED with an urgent care facility on the hospital site of the ED. Therefore, in these areas, there was continuity for the population in terms of access to urgent care. In the remaining area (Hartlepool), the new urgent care facility was located within 3 miles of the ED that closed. Perhaps because of this, we found no reliable consistent evidence of a change in the use of emergency or urgent care. It is possible that those who really need ED care still go, albeit to a more distant ED, and others go to the new urgent care centres.
As expected, those in the population who had a longer journey time to a type 1 ED following the closure had an increased journey time to hospital when attending via ambulance. Increases in journey time to the ED are likely to be higher for those in the population who make their own way to the ED. Added to this, patients may be unfamiliar with the local area of the ‘new’ ED and the layout of the hospital site, which may increase their journey time from ‘door to door’. Although unlikely to be detrimental to health outcomes, some of the population may feel that this adds to their inconvenience when experiencing a health episode.
Over time, there have been significant advances in care and treatment for SECs. This has resulted in a decrease in the 30 day mortality rate in England for some SECs that we included in our study (such as MI and stroke). 61 We expected to see a downward trend for deaths in our study. Although the absolute numbers of deaths decreased, there was no strong statistical evidence to indicate that closing the EDs had any additional impact on this trend.
Of all of the mortality impact measures, only one finding provided reliable statistical evidence: the overall CFR for the 16 SECs in the areas of ED closure or downgrade when compared with the control areas. It is useful to examine changes in the risk of death rather than just changes in the number of deaths because the number of deaths changes according to the size of the population studied, the prevalence of the conditions in the population and may also depend on how conditions are coded. The CFR is an indicator of the risk of death, but it is not a direct measure of the risk (which is not available). It is the ratio of the number of deaths to the number of deaths plus survivors admitted to hospital for more than 2 days. As such, it can change if the number of deaths relative to the number of admissions changes, or if the number of admissions changes for reasons that are not attributable to changes in prevalence; for example, because the threshold for admitting patients for more than 2 days changes. The relatively small increase of 2.3% that we found in the CFR reassuringly did not translate to actual deaths, and it is possible that it reflects a change in admission practices rather than the risk of dying with a SEC.
We have only studied the impact of ED closure on the population residing within the catchment area of the ED that closed. However, an impact may be felt by patients in the catchment areas of neighbouring hospitals if patients in the area where the ED was closed are now accessing a type 1 ED in their area. For example, the chief executive of the NHS acute trust neighbouring the ED that closed in Rochdale (Pennine Acute Hospitals NHS Trust) perceived that the closure had put additional pressure on the type 1 ED in Oldham. 49 For patients, this may be felt by increases in waiting times and crowding. The data collected as part of the HES A&E data set did not allow us to identify individual EDs and, therefore, analysis of the impact on individual EDs was not possible.
The ED as a ‘brand’ is well established in the public mind, as a service that provides care for 24 hours a day ‘on demand’. Public perceptions may focus on a service that delivers safe care and saves lives. Although this is undoubtedly true, the EDs we studied were closed or downgraded on the basis of issues of staffing difficulties and associated safety. It is clearly unknown what potential impact the retention of these EDs would have had on the population if they had remained open.
Implications for health-care providers
Health-care providers clearly have to prepare for the consequences of any reorganisation of care.
Our study did not have a remit to identify what, if anything, providers and commissioners did in preparation for the closure to mitigate any unintended negative consequences of reorganisation. We would be surprised if service modifications had not been undertaken locally in preparation for the reorganisation (e.g. changes to service delivery within the ambulance service). NHS annual reports did not provide this information explicitly. We contacted each of the four NHS ambulance services (covering the five geographical areas where care was reorganised) to seek to establish if operational practice was changed in preparation for the closure. Given that the EDs were closed up to 8 years prior to this study, it was perhaps unsurprising that services were not able to identify staff that could help us with this query.
However, our data do suggest that some changes were ‘anticipated’ and some effects may have been delayed. For example, although the travel time data suggested that closing EDs would change journey times to hospital from people’s homes by about 10 minutes on average, the estimates from our models of the data from ambulance services on times from incident scenes only found an increase of 4 minutes on average across the sites. However, this is an estimate of the change at the time of closure and scrutiny of the data trends suggest that the ambulance services may have been anticipating the closures before they took place.
Impact on NHS ambulance trusts
Across England, ambulance service call volumes continue to rise. 62 Our study showed an increase in ambulance incidents, over and above the increase when compared with the control area. This suggests that the ED closures studied here may have contributed to an additional increase in incidents within these areas.
Our study was hindered by data quality issues in some of the time measures collected from ambulance services. Following the closure of an ED, ambulances will inevitably have to travel longer distances to reach the nearest type 1 ED. There is some suggestion that it took longer for patients to arrive at hospital following a 999 ambulance call, but the lack of control data for this measure does not lead us to assert this finding with confidence.
Despite the increase in the number of ambulance incidents, the data suggested that there might have been a decrease in the number of emergency and urgent care attendances. How was this higher number of ambulance service incidents dealt with if they did not result in transfer to an emergency or urgent care service? For a number of years, ambulance services in England have continued to increase the proportion of the calls that they deal with without conveying a patient to an ED (non-conveyance). 62 They have done this by providing advice over the telephone (‘hear and treat’), or discharge at the scene (‘see and treat’). It is possible that ambulance services in these five areas were utilising these non-conveyance practices successfully in order to limit any negative impact created by an increase in the number of incidents and longer journey times.
Impact on NHS acute trusts
As with ambulance service call volumes, there is also a national trend towards increasing numbers of attendances at EDs and emergency hospital admissions.
Our study found a decrease of around 10% on average across sites in the number of attendances at an emergency or urgent care service, and a decrease in the number of emergency hospital admissions of around 4%; however, these changes were not consistent and the evidence is not reliable.
These figures indicate that broadly similar numbers of patients who were attending an emergency or urgent care service or were admitted to hospital prior to the closure of the ED continued to do so post closure. In some of the areas studied, emergency hospital admissions were no longer accepted at the NHS acute trust (of the closure site) following the closure of the ED. Although difficult to ascertain from the documentary analysis, this appeared to be evident in Rochdale, where all emergency admissions appeared to be transferred to a neighbouring hospital, and to some extent in Hartlepool, where a reduced emergency admissions facility appeared to operate following the closure of the ED. Therefore, either all or some of the emergency admissions were transferred to a neighbouring acute hospital and an emergency admissions unit was effectively closed. Added to the existing emergency admissions population in the neighbouring hospital, this reorganisation creates an additional emergency admissions population for the neighbouring hospital and may increase the burden on this hospital.
With regard to attendance at an emergency or urgent care service, the implication of any additional workload is less likely to be evident. Unlike emergency admissions, in each of the areas where a type 1 ED closed, a replacement urgent care service was provided that would have been able to manage a proportion of the patients who were attending the ED before closure. These patients would not need to go to neighbouring EDs, and so we might expect that the impact of closing an ED is less for neighbouring EDs than for neighbouring emergency admission services.
In our study, emergency and urgent care attendances combined both type 1, 2, 3 and 4 ED attendances and those attendances recorded as ‘unknown’. We were unable to isolate type 1 attendances so we are unsure exactly what the impact for type 1 attendances that move to neighbouring EDs was. However, any increase in attendances at a neighbouring type 1 ED may then have implications for waiting times, crowding, staffing levels and, ultimately, safety.
We were unable to identify, through documentary analysis, how the neighbouring hospitals absorbed any increased workload and whether or not this had implications for their performance.
A final implication for NHS providers is the need to provide complete and high-quality routine data. Our analysis of routine data collected from some ambulance services and the HES A&E data set identified incomplete data extracts and inconsistencies in coding. If we are to track the impact of reorganisation in emergency care to inform health care in the future, it is important that NHS providers provide robust data to allow this.
Implications for policy-makers
The demand for emergency care shows no sign of abating. In a publicly funded health-care system, such as the NHS, services will inevitably be subject to rationalisation. Reorganisation of emergency care is often controversial and evokes strong reaction among local populations and the media. Much of the media interest following the recent announcement in STPs in England has centred on the reorganisation of emergency care and the suggestions that further EDs will be closed or downgraded. This study found that the closure of the five type 1 EDs in this study was associated with an increase in the number of ambulance incidents, but did not consistently affect the burden on the number of NHS beds overall or have a negative impact on the health of the population. However, even if the overall number of emergency admissions did not increase, the burden on individual neighbouring hospitals may have increased with unknown consequences.
Although our study highlights that there was no discernible negative impact of reorganising emergency care by closing EDs on average across the five areas we have studied, this finding may not translate to other areas where EDs are being considered for reorganisation. Our documentary analysis identified that all of the five EDs included in this study were closed on the basis of safety or a lack of staff to run these departments, suggesting that there were operational issues within these departments prior to the closure. Given this, patients with serious clinical conditions (such as MI, stroke or trauma) may have already been diverted away from the ED that closed to a regional specialist centre and, therefore, the EDs we studied may have been delivering care within a less clinically acute environment at the time of the closure.
Our evidence in this study is that changes to the average travel times of the magnitude that we found are not detrimental to the population as a whole. This suggests that any negative effects caused by an increased journey time to an ED can be offset by other factors (e.g. if the care received at the now-nearest hospital is more effective than that provided at the hospital where the ED closed). Therefore, operating fewer, larger centres for emergency care that are geographically dispersed may be achievable without harm. This could alleviate the current staffing shortages and might prevent any deterioration in the quality of care resulting from increasing demands. However, there are huge uncertainties about this, and, importantly, the selection of such centres would require careful consideration in terms of quality of care, staffing, distance to hospital for the catchment population affected by reorganisation, the needs of the local population and the current, or required, level of service provision elsewhere in the emergency and urgent care system.
‘Time’ versus ‘place’
In our original proposal, we planned to undertake some exploratory analysis to provide a better understanding of why any changes may have been detected. Change may be attributable to changes in how long it took a patient to get to hospital, but also attributable to which hospital the patient received treatment in. Hospitals vary in terms of performance (e.g. adherence to the ED 4-hour wait target and ‘in-hospital’ mortality rates). Undertaking this exploratory analysis requires the identification of individual hospitals. As highlighted earlier in this report, we were unable to identify individual hospitals and were therefore not able to undertake this exploratory work as planned.
We have compared the impact of the ED closures for residents living in parts of the catchment areas that were most affected in terms of journey time to an ED (high-dose areas) with the impact in the parts that were least affected (low-dose areas). These comparisons are directly focused on the impact of the change in journey time, which, on average across all areas, was about 10 minutes more in high-dose areas than in low-dose areas. These comparisons found no reliable and consistent evidence of an impact on mortality from emergency conditions. Because these comparisons are made within areas, so that other changes to the system affect everyone, they are particularly robust against confounding by other influences.
Statistical analyses
We have undertaken interrupted time-series analyses of a package of measures reflecting different aspects of the possible impact of closing EDs. Interrupted time-series analysis is generally regarded as one of the most robust approaches to non-randomised study designs, especially when control series are used to account for wider changes taking place during the period being studied. Of course, using control series in observational health service research studies means that the results are vulnerable to changes in the control area rather than changes in the intervention area. We have tried to guard against this by undertaking a documentary analysis to try to discover what changes happened in the control areas and to allow for these changes in our models. We have also compared our five intervention sites with five control sites. This means that the control series more closely reflects the overall national context.
A useful list of quality criteria highlights both the strengths and weaknesses in our data. 42 Two of the quality criteria that Ramsay et al. 42 identify are the intervention being introduced independently of other changes and the intervention being unlikely to affect data collection. Our study has been affected by both issues. However, we have attempted to allow for other changes in the models and, although we can see evidence that in some sites for some measures data collection has changed over the study periods, we have taken care to highlight this when it has been a problem.
The models we have used are quite simple (e.g. with linear trends, no change in trend, first-order lags and simple seasonality). Although refinements could be made, they often result in overparameterisation, difficulties in interpretation and misunderstanding of the results. Furthermore, it is not possible to undertake a sensitivity analysis to understand how vulnerable the results are to these model assumptions in a conventional way because we have conducted over 150 different analyses of 55 data sets. Varying some or all of the model assumptions might change some of these results but not others. One approach to this multiplicity problem is to just focus on a single, most important analysis or group of analyses. In our case, this could be the analyses of all deaths occurring within 7 days of the incident, compared with the controls, in each site and synthesised across all sites. We have not done this either, partly because alternative assumptions were not specified in our protocol, and because there is an element of data fishing in this approach, but mainly because such sensitivity analyses cannot change our conclusions. When the conclusion from statistical analysis using a model is that there is too much statistical uncertainty to reach a definitive conclusion, then a sensitivity analysis seeking to find whether or not there is also too much model uncertainty to reach a conclusion cannot help. Our conclusion, using the simple model prespecified in our protocol, is that, despite analysing data on more than 15,000 deaths across 4 years in 10 sites, there is no reliable evidence in these data that closing ED departments changed the death rates. A sensitivity analysis cannot change or undermine that conclusion.
We have examined five sites, 11 primary impact measures and three statistical models. We can be certain, therefore, that there is noise in our results as well as in the data. However, we have tried to be cautious about overinterpreting the results.
We have summarised the results for all five sites together by showing the site effects in forest plots and using random-effects meta-analyses to summarise the average effect across sites. The results of these analyses are estimates of the average effect across heterogeneous sites; they are not estimates of some common ‘true’ effect.
Strengths and limitations
Strengths
The study had various strengths:
-
This is the first study to look at the impact of closing or downgrading EDs in England.
-
Reorganisation of emergency care will continue. Part of this reorganisation will inevitably include the closure of further type 1 EDs. We have identified a series of impact measures, and a methodology, that can be used to look at the impact of closing further EDs.
-
This evaluation is based on a controlled interrupted time-series comparison of routine data. Regarding evidence, this is the most robust method when an experiment, such as a randomised controlled trial, cannot be used.
-
This evaluation is timely. Further closures or downgrades of EDs are imminent. This evaluation can inform policy-makers, the NHS and the general public when considering closures.
-
Routine data obtained for the mortality and hospital inpatient measures were based on robust routine data sets, and we can be confident of the reliability of the findings of these impact measures.
-
We attempted to reduce the impact of ‘noise’ (i.e. changes) in the emergency and urgent care system. Health care in England is constantly evolving to meet the needs of the patients it provides for. The emergency and urgent care system is no exception. We attempted to limit the impact that any changes in the system might have on our analysis by undertaking a documentary analysis of NHS provider annual reports. We believe that the documentary analysis highlighted a number of major changes in the emergency and urgent care system, such as the introduction of NHS 111, the introduction/relocation of primary and urgent care health centres and ambulance diversion to nearby EDs, which were subsequently accounted for in our analysis.
-
We have conducted a within-area analysis, comparing the impact of closure on those parts of the catchment areas of the EDs that closed that were most affected with those parts that were least affected by the change in journey time to a type 1 ED. These analyses are free from the effects of any ‘noise’, and provide robust evidence of the impact of changes in travel times alone.
Limitations
The limitations of this study are predominantly centred around the quality of routine data, which had an impact on our study methodology and subsequent analysis. These limitations are highlighted in the following sections.
Amendments to the original proposal
Issues with obtaining routine data and with the quality of the data received necessitated the adaptation of some of the methods we identified in our original proposal. These issues and adaptations are detailed in the following sections.
The inability to use Hospital Episode Statistics accident and emergency data to calculate the resident catchment areas of emergency departments
In our proposal, we described a method for calculating a resident catchment area for an ED using HES A&E routine data codes to identify the hospital rather than the trust in which the ED is situated. In analysis of 2011/12 data we found that, of 193 codes, 100 did not identify the hospital. Therefore, in over half of the codes, no individual ED could be identified.
The inability to calculate all of the impact measures identified
Given the historical nature of the data required for the time-series analysis, there were some issues with the reliability of some data. Although we collated and analysed data, the data were of insufficient quality to undertake any meaningful analysis for some of the secondary impact measures identified and, therefore, an analysis has not been presented in this report. The secondary impact measures that could not be analysed were:
-
component parts of the time when the ambulance call was received to the time of arrival at hospital
-
emergency ‘Red’ hospital transfer incidents
-
emergency ‘Green’ incidents in which the patient is not conveyed to a type 1 or type 2 A&E department (ratio)
-
the proportion of attenders at an ED who are admitted to an inpatient bed
-
the number of admissions to a critical care department.
Use of a 7-day period instead of a 3-day period to calculate mortality measures
We had originally planned that we would calculate mortality measures at 3 days. However, we found no evidence in the literature to suggest an optimum cut-off period for examining mortality in emergencies. Various time periods from 1 day to 30 days have been widely used. We wanted to use a short time period to reflect the focus on the emergency care system, but needed to recognise the importance of ‘place’ as well as ‘time’. We therefore decided to use a 7-day outcome period rather than a 3-day outcome period.
Data quality and completeness
Hospital Episode Statistics accident and emergency data
The submission of NHS provider data to HES records is compulsory. Prior to the start of this study, we were aware of data quality issues regarding the HES A&E data set. HES A&E data have been recorded since 2007. There is evidence of significant improvements that have been made to the data quality since then. However, evidence does suggest that there were discrepancies in HES attendance data in May 2011, which is within the data period for four of the five closure sites in our study. 63
Ambulance service data
There were some difficulties in obtaining reliable ambulance service data. Notable difficulties included (1) ambulance service data not being recorded in a consistent format across trusts and (2) most ambulance services making numerous major changes to their CAD systems over the period of the study.
In some ambulance services, data quality issues were so significant that it was not possible to use particular elements of the supplied data. In a minority of cases, data were missing or (as was the case in one control area) there were such extensive data quality issues that it was not possible to meaningfully analyse any of the data.
Mortality data
In our original proposal, we did not propose to dichotomise ‘in-hospital’ and ‘out-of-hospital’ deaths. However, we thought that this would be useful because deaths occurring prior to a patient arriving at hospital may be affected by increased travel times to hospital. Although the routine data obtained for the mortality measures are robust, we were unable to isolate the various scenarios in which people may die ‘out of hospital’. For example, in our study, ‘out-of-hospital’ deaths may occur at home prior to making contact with a service, in an ambulance on the way to hospital, in the ED prior to hospital admission or when a patient is recorded as having a SEC incident and are admitted, discharged alive and subsequently die out of hospital (i.e. without being readmitted). We estimate that the majority of these deaths occur within a pre-hospital setting. For some of these ‘out-of-hospital’ deaths, it is worth noting that there was little that the emergency care system could do to prevent this death (e.g. if a person died without making contact with an emergency service).
Selecting a 48-month time series
The analysis of data in the time series spanned the 24 months before and 24 months after the closure. It is likely that local health systems began to adopt different ways of providing care prior to the closure. We undertook documentary analysis to identify this, but it is possible that such changes in practices were not recorded in trust annual reports and took place prior to the closure date. It appears that some EDs were already operating at a ‘reduced’ care level prior to closure but it was not possible to establish this with any precise detail or certainty. Given that some of the EDs closed up to 5 years after their first public consultation regarding the reorganisation, there is a possibility that NHS providers within the emergency and urgent care system began to introduce small changes to their practice in anticipation of the closure ahead of our 24-month pre-closure time series.
We also found some evidence that ambulance services may have anticipated the closures, for example by transporting patients to other hospitals prior to the closure. Our analyses have focused on the impact at the time of the closure, not on the impact of the closure. Of course, there is a clear argument that this is what we should focus on because if the other changes were made prior to the closure then they could be made whether or not the ED closed, and so are not strictly a consequence of the closure.
Documentary analysis
Some PCT reports could not be found and, because of the disbanding of PCTs in 2013, it was not possible to contact these trusts to source annual reports that we could not find ourselves. However, of the PCT reports that were not located, we did source reports for the relevant NHS acute trusts and NHS ambulance trusts. Therefore, we believe that any significant reorganisation of care within the local emergency and urgent care system would have been identified in the annual reports of these trusts.
The primary remit of the documentary analysis was to inform the analysis of the routine data by identifying major changes to the emergency and urgent care system that affected the catchment populations of the ED that closed and its corresponding control area. The documentary analysis did not extend to any neighbouring areas where the population may have gone on to use NHS services following the reorganisation of care. Therefore, any perceived impact of closures that may have been reported in NHS annual reports in these neighbouring areas was not identified.
Conclusions
The impact measure that is probably of most importance to the public, health-care providers and policy-makers is mortality. The public, in particular, require reassurance that the closure or downgrade of an ED does not result in increased death rates within the population. In the five geographical areas studied here, we found no statistically reliable and consistent evidence of an increase in deaths within the population from SECs in the period following the reorganisation of care. This suggests that any negative effects caused by an increased journey time to an ED can be offset by other factors (e.g. if other new services are introduced and care is more effective than it used to be, or if the care received at the now-nearest hospital is more effective than that provided at the hospital in which the ED closed).
Given such a major reorganisation of emergency and urgent care, we might expect there to be some changes in emergency and urgent care activity. This was apparent in our study.
Across England, ambulance service call volumes continue to rise. Our study found some evidence of an increase in the number of ambulance incidents on average across the five sites, over and above the increase when compared with the control area. This suggests that the ED closures studied here may have contributed to an additional increase in workload within these areas.
As with ambulance service call volumes, there is also a national trend towards increasing numbers of attendances at EDs and emergency hospital admissions. However, our study found no statistically reliable and consistent evidence of an impact of the ED closures on hospital activity, although the direction of change pointed to a decrease in activity on average.
Implications for research
This study relied on obtaining reliable routine data. As noted earlier, some of our analysis was hampered by inconsistencies in recording and subsequent reliability of these data.
Ambulance service data
Interest in using NHS ambulance service routine data for research purposes has increased in recent years. In some ambulance services, we requested routine data regarding incidents dating back to 2007. Our study experienced difficulties in accessing some of this historical data in some services. A lack of consistency in variable labelling and coding was also noted across the six ambulance services supplying data for this study. This added a further layer of complexity for the study team as they prepared the data for analysis.
Hospital Episode Statistics data
Hospital Episode Statistics A&E data have been collected since April 2007. The onus is on the trusts providing care in EDs, UCCs, MIUs or WICs to self-identify and supply data to NHS Digital. Although the quality of these data has improved over time, our study found inaccurate recording within this data set as recently as March 2014. For example, in one of the areas where a type 1 ED was replaced with a type 3 ED (UCC), there is negligible recording of type 3 attendances following the ED closure, inaccurately indicating that there was little use of this UCC by the local population.
Since this study was conducted, the Emergency Care Data Set has been introduced. The Emergency Care Data Set aims to provide detailed ED data, collected in a consistent way, and will feed into HES A&E data. If implemented fully, this will improve the quality of HES A&E data.
The use of NHS provider routine data within research is increasing, and these data have great value when conducting studies such as ours. However, to improve the utility of these data, there is clearly a need to improve the consistency of coding and recording practices in order to optimise the benefit to research. Failing this, some indication of data quality prior to writing research proposals or conducting research may be desirable.
Recommendations for future research
Although our study has determined the impact of closing or downgrading EDs, we have identified opportunities for research to further inform reorganisation:
-
This study relied wholly on routine data and was designed to highlight the effects of ED closure rather than to provide an understanding of why the effects were evident. In order to further understand why an effect is apparent, it is often necessary to investigate this as the change happens in practice. Given that further ED closures are imminent, we see value in undertaking further data collection as reorganisation happens, in real time. We believe that there are four important questions to consider:
-
Why are there differences in impact in different places when EDs close?
-
What processes are used by commissioners and health-care providers to implement reorganisation in order to minimise any adverse effect on local populations and health services?
-
How do patients experience reorganisation? Do patients change their help-seeking behaviour following reorganisation and how does this affect their satisfaction with care?
-
What is the effect on neighbouring areas? Are hospitals able to absorb any additional workload? what are the implications for the population in these areas? Is there any impact on the workforce in these areas in terms of satisfaction?
-
-
Without doubt, emergency care is expensive. The average 2015/16 cost of an A&E attendance was £138 and the average cost of a non-elective inpatient stay was £1609. 64 The closure or downgrade of a type 1 ED may have financial implications both in and out of hospital. An economic evaluation to identify the cost consequences of such reorganisation on the emergency and urgent care system as a whole may be useful.
-
This study looked at the impact on emergency care performance only, namely in the ambulance service, in EDs and in terms of emergency admissions. Analysis of the wider health system should be considered (e.g. to understand if the reorganisation of care has any impact on primary care).
Acknowledgements
Richard Campbell provided administrative support to the study.
The DfT modelled LSOA journey times using the Journey Time Statistics methodology. 59
The NHS ambulance services in England provided routine data.
NHS Digital supplied HES data and ONS mortality data. We would particularly like to acknowledge Dave Cronin (NHS Digital), who was influential in facilitating this process.
The ONS supplied ONS mortality data.
Project advisory group: Matthew Cooke (chairperson), John Bennett, Alex Bottle, Andrew Hodge and Daniel Mason.
Contributions of authors
Emma Knowles (Senior Research Fellow, Health Services Research) led the study, contributed to the study design and the interpretation of the data and wrote the first draft of the report.
Neil Shephard (Medical Statistician, Clinical Trials) conducted the routine data analysis and contributed to drafts of the report.
Tony Stone (Research Assistant, Health Services Research) led the acquisition of the routine data, contributed to the interpretation of the data and to drafts of the report.
Lindsey Bishop-Edwards (Research Associate, Health Services Research) conducted the documentary analysis and contributed to drafts of the report.
Enid Hirst (PPI Representative, Sheffield Emergency Care Forum) contributed to the documentary analysis and to drafts of the report.
Linda Abouzeid (PPI Representative, SECF) contributed to the documentary analysis and to drafts of the report.
Suzanne Mason (Professor, Health Services Research) contributed to the interpretation of the data and to drafts of the report.
Jon Nicholl (Professor, Health Services Research) conceived the idea for the study, contributed to the study design, led the analysis of the data and contributed to the interpretation of the data and to drafts of the report.
Data sharing statement
The data analysed in this study were drawn from several routine sources including the ONS, HES (A&E attendance and APC) and NHS ambulance service CAD data sets. The conditions attached to the release of these data to the original authors mean that they cannot be shared further and data providers should be contacted directly for the release of further data sets.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Sakr M, Wardrope J. Casualty, accident and emergency, or emergency medicine, the evolution. J Accid Emerg Med 2000;17:314-19. https://doi.org/10.1136/emj.17.5.314.
- Nicholl J, Mason S. Return of the ‘corridors of shame’?. BMJ 2013;347. https://doi.org/10.1136/bmj.f4343.
- Schneider SM, Gardner AF, Weiss LD, Wood JP, Ybarra M, Beck DM, et al. The future of emergency medicine. Acad Emerg Med 2010;17:998-1003. https://doi.org/10.1111/j.1553-2712.2010.00854.x.
- Ambulance Service, England 2004–2005. London: NHS Digital; 2005.
- Ambulance Service, England 2014–2015. London: NHS Digital, Workforce and Facilities Team HSCIC; 2015.
- Appleby J. Are accident and emergency attendances increasing?. BMJ 2013;346. https://doi.org/10.1136/bmj.f3677.
- Morse A. Emergency Admissions to Hospital: Managing The Demand. London: National Audit Office, Department of Health; 2013.
- What’s Going on in A&E? The Key Questions Answered. London: The King’s Fund; 2016.
- Headline Figures, 2010–2011. London: NHS Digital; 2011.
- Provisional Monthly HES Data for Admitted Patient Care. London: NHS Digital; 2016.
- Munro J, Nicholl J, O’Cathain A, Knowles E. Impact of NHS direct on demand for immediate care: observational study. BMJ 2000;321:150-3. https://doi.org/10.1136/bmj.321.7254.150.
- Turner J, O’Cathain A, Knowles E, Nicholl J. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003451.
- Transforming Urgent and Emergency Care Services in England. London: NHS England; 2013.
- The Way Ahead 2008–2012. London: The Royal College of Emergency Medicine; 2008.
- BBC . A&Amp;E Consultants: Why We Left the NHS to Work Abroad 2013. www.bbc.co.uk/news/health-24396884 (accessed 17 July 2017).
- El-Sheikha S. Surprised an A&E is closing because of doctor shortages? We warned you we would leave – now it’s happening. The Independent 2016. www.independent.co.uk/voices/nhs-hospital-closing-accident-emergency-department-junior-doctors-contract-jeremy-hunt-theresa-may-a7185041.html (accessed 17 July 2017).
- Donnelly L. NHS takes axe to hospital units amid financial crisis. The Telegraph 2016. www.telegraph.co.uk/news/2016/08/25/glut-of-nhs-closures-ahead-warn-hospital-chiefs (accessed 27 June 2018).
- Donnelly L. NHS takes axe to hospital units amid financial crisis. The Telegraph 2016. www.telegraph.co.uk/news/2016/08/25/glut-of-nhs-closures-ahead-warn-hospital-chiefs/ (accessed 17 July 2017).
- Roberts A, Blunt I, Bardsley M. Focus On: Distance from Home to Emergency Care. London: The Nuffield Trust; 2014.
- Lee JE, Sung JH, Ward WB, Fos PJ, Lee WJ, Kim JC. Utilization of the emergency room: impact of geographic distance. Geospat Health 2007;1:243-53. https://doi.org/10.4081/gh.2007.272.
- Hull SA, Jones IR, Moser K. Factors influencing the attendance rate at accident and emergency departments in East London: the contributions of practice organization, population characteristics and distance. J Health Serv Res Policy 1997;2:6-13. https://doi.org/10.1177/135581969700200104.
- Hsia RY, Srebotnjak T, Maselli J, Crandall M, McCulloch C, Kellermann AL. The association of trauma center closures with increased inpatient mortality for injured patients. J Trauma Acute Care Surg 2014;76:1048-54. https://doi.org/10.1097/TA.0000000000000166.
- Shen YC, Hsia RY. Does decreased access to emergency departments affect patient outcomes? Analysis of acute myocardial infarction population 1996–2005. Health Serv Res 2012;47:188-210. https://doi.org/10.1111/j.1475-6773.2011.01319.x.
- Wei L, Lang CC, Sullivan FM, Boyle P, Wang J, Pringle SD, et al. Impact on mortality following first acute myocardial infarction of distance between home and hospital: cohort study. Heart 2008;94:1141-6. https://doi.org/10.1136/hrt.2007.123612.
- Buchmueller TC, Jacobson M, Wold C. How far to the hospital? The effect of hospital closures on access to care. J Health Econ 2006;25:740-61. https://doi.org/10.1016/j.jhealeco.2005.10.006.
- Liu C, Srebotnjak T, Hsia RY. California emergency department closures are associated with increased inpatient mortality at nearby hospitals. Health Aff 2014;33:1323-9. https://doi.org/10.1377/hlthaff.2013.1203.
- Nicholl J, West J, Goodacre S, Turner J. The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J 2007;24:665-8. https://doi.org/10.1136/emj.2007.047654.
- Crash-2 Collaborators, Roberts I, Shakur H, Afolabi A, Brohi K, Coats T, et al. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet 2011;377:1096-101. https://doi.org/10.1016/S0140-6736(11)60278-X.
- Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, et al. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ 2009;338. https://doi.org/10.1136/bmj.b1807.
- Saver JL, Fonarow GC, Smith EE, Reeves MJ, Grau-Sepulveda MV, Pan W, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013;309:2480-8. https://doi.org/10.1001/jama.2013.6959.
- Pickering A, Cooper K, Harnan S, Holmes M, Sutton A, Mason S, et al. Comparison of Direct Transfer to Specialist Care Centres with Delivery to the Nearest Hospital: A Systematic Review and Economic Evaluation. Final Report. London: NIHR Service Delivery and Organisation Programme; 2014.
- Palmer K. Reconfiguring Hosptial Services: Lessons from South East London. London: The King’s Fund; 2011.
- Smith MA, Liou JI, Frytak JR, Finch MD. 30-day survival and rehospitalization for stroke patients according to physician specialty. Cerebrovasc Dis 2006;22:21-6. https://doi.org/10.1159/000092333.
- Hawkes N. BMJ 2013;347. https://doi.org/10.1136/bmj.f4954.
- White AL, Armstrong PA, Thakore S. Impact of senior clinical review on patient disposition from the emergency department. Emerg Med J 2010;27:262-5. https://doi.org/10.1136/emj.2009.077842.
- Croft SJ, Mason S. Are emergency department junior doctors becoming less experienced in performing common practical procedures?. Emerg Med J 2007;24:657-8. https://doi.org/10.1136/emj.2006.045302.
- Christmas E, Johnson I, Locker T. The impact of 24 h consultant shop floor presence on emergency department performance: a natural experiment. Emerg Med J 2013;30:360-2. https://doi.org/10.1136/emermed-2012-201369.
- Sun BC, Mohanty SA, Weiss R, Tadeo R, Hasbrouck M, Koenig W, et al. Effects of hospital closures and hospital characteristics on emergency department ambulance diversion, Los Angeles County, 1998 to 2004. Ann Emerg Med 2006;47:309-16. https://doi.org/10.1016/j.annemergmed.2005.12.003.
- O’Cathain A, Knowles E, Maheswaran R, Turner J, Hirst E, Goodacre S, et al. Hospital characteristics affecting potentially avoidable emergency admissions: national ecological study. Health Serv Manage Res 2014;26:110-18. https://doi.org/10.1177/0951484814525357.
- Knowles E, O’Cathain A, Nicholl J. Patients’ experiences and views of an emergency and urgent care system. Health Expect 2012;15:78-86. https://doi.org/10.1111/j.1369-7625.2010.00659.x.
- Nicholl J, Coleman P, Jenkins J, Knowles E, O’Cathain A, Turner J. Emergency and Urgent Care Systems. Final report to Department of Health 2006–2010. Sheffield: Medical Care Research Unit; 2011.
- Ramsay CR, Matowe L, Grilli R, Grimshaw JM, Thomas RE. Interrupted time series designs in health technology assessment: lessons from two systematic reviews of behavior change strategies. Int J Technol Assess Health Care 2003;19:613-23. https://doi.org/10.1017/S0266462303000576.
- Ambulance Quality Indicators: System Indicators Time Series (to December 2016). London: NHS England; 2017.
- BBC . A&Amp;E Closure Decision Criticised 2006. http://news.bbc.co.uk/1/hi/england/beds/bucks/herts/6157852.stm (accessed 17 July 2017).
- Binnie A. Number of St Albans patients visiting Watford General Hospital quadruples in six years. St Albans &Amp; Harpenden Review 2013. www.stalbansreview.co.uk/news/10749666.Number_of_St_Albans_patients_visiting_Watford_General_quadruples_in_six_years/ (accessed 17 July 2017).
- Seizing the Future, a Public Consultation Document. Thirsk: NHS County Durham Foundation Trust; 2009.
- High Quality Care for All Workforce: NHS Next Stage Review Final Report. London: Department of Health and Social Care; 2008.
- Rochdale Online . Healthy Futures High Court Hearing Decision Delayed 2007. www.rochdaleonline.co.uk/news-features/2/news/2783/healthy-futures-high-court-hearing-decision-delayed (accessed 17 July 2017).
- Manchester Evening News . Health boss: Rochdale Infirmary closure left Oldham A&E struggling to cope. Manchester Evening News 2011. www.manchestereveningnews.co.uk/news/local-news/health-boss-rochdale-infirmary-closure-871301 (accessed 17 July 2017).
- Fitzpatrick K. Beds opened to cover Rochdale Infirmary A&E closure. Manchester Evening News 2011. www.manchestereveningnews.co.uk/news/local-news/beds-opened-to-cover-rochdale-infirmary-873514 (accessed 17 July 2017).
- Coyle S. Neighbouring East Lancashire feeling the strain of Rochdale Infirmary A&E closure. Manchester Evening News 2012. www.manchestereveningnews.co.uk/news/local-news/neighbouring-east-lancashire-feeling-the-strain-680010 (accessed 17 July 2017).
- Newark’s Healthcare Review. Nottingham: NHS Nottinghamshire County; 2010.
- Nottingham Post . Emergency care in Newark is near to collapse. Nottingham Post 2012. www.nottinghampost.com/emergency-care-newark-near-collapse/story-16871906-detail/story.html (accessed 17 July 2017).
- Rose D. Shocking Proof A&Amp;E Closures Cost Lives: Death Rate Jumps More Than a THIRD After Department Closes 2013. www.dailymail.co.uk/news/article-2323141/Shocking-proof-Accident-Emergency-closures-cost-lives-Death-rate-jumps-THIRD-department-closes.html (accessed 17 July 2017).
- Newman V. Ambulance bosses deny Hartlepool A&E closure is to blame for delays. Hartlepool Mail 2015. www.hartlepoolmail.co.uk/news/health/ambulance-bosses-deny-hartlepool-a-e-closure-is-to-blame-for-delays-1-7160430 (accessed 17 July 2017).
- Coleman P, Nicholl J. Consensus methods to identify a set of potential performance indicators for systems of emergency and urgent care. J Health Serv Res Policy 2010;15:12-8. https://doi.org/10.1258/jhsrp.2009.009096.
- 2001 Census. Newport: Office for National Statistics; 2001.
- 2011 Census. Newport: Office for National Statistics; 2011.
- Department for Transport . Journey Time Statistics Guidance n.d. www.gov.uk/government/publications/journey-time-statistics-guidance (accessed 21 March 2018).
- Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342. https://doi.org/10.1136/bmj.d549.
- HES: Deaths Within 30 Days of a Hospital Procedure or of an Emergency Admission to Hospital, Financial Year 2014/15. London: NHS Digital; 2016.
- NHS Ambulance Services. London: National Audit Office; 2017.
- Hughes G. A&E Quality Indicators. London: BMJ Publishing Group Ltd and the British Association for Accident & Emergency Medicine; 2012.
- Reference Costs 2015–16. London: Department of Health and Social Care; 2016.
- Rural and Urban Area Classification 2004: An Introductory Guide. Newport: Office for National Statistics; 2004.
- English Indices of Deprivation 2010. London: Ministry of Housing, Communities & Local Government; 2011.
- Hospital Episode Statistics. Leeds: NHS Digital; n.d.
Appendix 1 Changes to the planned study
| Plan | Change | Reason |
|---|---|---|
| Resident catchment population to be calculated using HES A&E data | Resident catchment population was calculated using DfT data | HES A&E data were initially explored, as identified in the protocol, but were found to inconsistently record the individual hospital where there were multiple EDs within a NHS acute trust. Therefore, individual EDs could not be identified for the majority of our chosen areas |
| ‘Step’ model analysis only | In addition, this included the ‘dose’ analysis | Different parts of the catchment area might be differentially affected by the closure of an ED. The dose analysis was able to capture the effects of a change in journey time to the nearest ED for residents of the catchment area |
| 3-day cut-off period for calculating mortality measures | 7-day cut-off period for calculating mortality measures | On investigation of the literature, we found no evidence to suggest an optimum cut-off period for examining mortality in emergencies. Various time periods from 1 day to 30 days have been widely used |
| Secondary impact measures not reported | ||
| Ambulance journey component times | Findings are not presented in the report | Data were collected, and measures were calculated. However, on investigation, there appeared to be inconsistencies in the data from some services. When the findings from the measure ‘mean time from 999 call answered to arrival at hospital’ required further investigation, we looked at the component times to further our understanding |
| Total number of emergency ‘Red’ hospital transfer incidents | Findings are not presented in the report | Data were collected, and this measure was calculated. However, on investigation there were an insufficient number of data points of sufficient quality to undertake any meaningful analysis |
| Emergency ‘green’ incidents not conveyed to a type 1 or type 2 A&E department (ratio) | Findings are not presented in the report | Data were collected, and this measure was calculated. However, on investigation there were an insufficient number of data points of sufficient quality to undertake any meaningful analysis |
| Total number of ED attendances by mode of arrival | Findings are not presented in the report | Data were collected, and this measure was calculated. This measure was reported if there appeared to be further investigation required in the overall ‘total number of ED attendances’ |
| Proportion of attenders at ED who are admitted to an inpatient bed | Findings are not presented in the report | Data were collected, and this measure was calculated. This was a ‘secondary’ measure. Given the number of measures already reported, we made the decision to not report this measure |
| The number of patients admitted to critical care | Findings are not presented in the report | Data were collected, and this measure was calculated. However, on investigation there were an insufficient number of data points of sufficient quality to undertake any meaningful analysis |
| Impact measures reported but with sites omitted from the combined analysis | ||
| Ambulance emergency incidents | Analysis does not include data from one control site | Incomplete or unreliable data were omitted |
| Ambulance call times | Analysis does not include data from five control sites | Incomplete or unreliable data were omitted |
| ED attendance | Analysis does not include data from two closure sites | Incomplete or unreliable data were omitted |
Appendix 2 Comparison of intervention sites and control sites: sociodemographic characteristics
| Site | Year of closure | Site type | Population size | Aged ≥ 65 years (%) | Most deprived quintile (%) | Rural (%) | Non-white (%) | Long-term illness (%) | Annual ED attendances (per 1000) (crude) | Annual deaths (per 100,000) (crude) | Annual SEC deaths (per 100,000) (crude) | SEC deaths (% of all deaths) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bishop Auckland | 2009 | Intervention | 145,000 | 17.9 | 38.1 | 47.3 | 1.2 | 23.9 | 250 | 1130 | 390 | 35.0 |
| Matched control | 131,000 | 19.1 | 25.5 | 57.6 | 1.4 | 21.2 | 213 | 1060 | 380 | 35.8 | ||
| Hemel Hempstead | 2009 | Intervention | 231,000 | 16.1 | 0.0 | 10 | 10.5 | 14.6 | 192 | 830 | 300 | 36.5 |
| Matched control | 252,000 | 17.5 | 1.9 | 24 | 11.0 | 16.0 | 229 | 900 | 310 | 34.1 | ||
| Newark | 2011 | Intervention | 125,000 | 19.4 | 9.1 | 67.4 | 3.1 | 18.5 | 253 | 940 | 280 | 29.6 |
| Matched control | 157,000 | 23.3 | 4.4 | 16.8 | 2.9 | 22.0 | 353 | 1170 | 370 | 31.8 | ||
| Rochdale | 2011 | Intervention | 154,000 | 14.4 | 45.8 | 4.3 | 21.3 | 20.4 | 441 | 860 | 270 | 31.5 |
| Matched control | 369,000 | 17.5 | 36.4 | 9.1 | 7.8 | 22.3 | 313 | 1020 | 310 | 30.0 | ||
| Hartlepool | 2011 | Intervention | 155,000 | 17.2 | 48.1 | 21.9 | 2.0 | 26.0 | 318 | 1000 | 280 | 27.9 |
| Matched control | 213,000 | 19.0 | 30.2 | 20.6 | 2.3 | 20.0 | 293 | 1020 | 360 | 35.4 |
Appendix 3 The NHS trust annual reports identified during documentary analysis
| Time period | Site | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bishop Auckland | Hartlepool | Hemel Hempstead | Newark | Rochdale | ||||||||||||||||||||||||||
| PCT/CCG | Acute trust | Ambulance trust | PCT/CCG | Acute trust | Ambulance trust | PCT/CCG | Acute trust | Ambulance trust | PCT/CCG | Acute trust | Ambulance trust | PCT/CCG | Acute trust | Ambulance trust | ||||||||||||||||
| C | I | C | I | C | I | C | I | C | I | C | I | C | I | C | I | C | I | C | I | C | I | C | I | C | I | C | I | C | I | |
| 2007/8 | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | – | – | – | – | – |
| 2008/9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | – | – | – | – | – |
| 2009/10 | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 2010/11 | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 2011/12 | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ |
| 2012/13 | – | – | – | – | – | – | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 2013/14 | – | – | – | – | – | – | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
Appendix 4 Steps identified and included in the analysis
| Catchment area | Date of change (relative month in the 48-month time series) | ||
|---|---|---|---|
| ED closure | Introduction of NHS 111 | Other major changea | |
| Bishop Auckland | 1 October 2009 (25) | 1 August 2010 (35) | N/A |
| Bishop Auckland control | N/A | N/A | N/A |
| Hartlepool | 1 August 2011 (25) | 1 April 2013 (45) | 1 May 2011 (22) |
| Hartlepool control | N/A | 1 November 2010 (16) | N/A |
| Hemel Hempstead | 1 March 2009 (25) | N/A | 1 October 2008 (20) |
| Hemel Hempstead control | N/A | N/A | N/A |
| Newark | 1 April 2011 (25) | N/A | N/A |
| Newark control | N/A | 1 March 2013 (48) | 1 June 2009 (03) |
| Rochdale | 1 April 2011 (25) | 1 March 2013 (48) | 1 August 2010 (17) |
| Rochdale control | N/A | 1 March 2013 (48) | 1 June 2009 (11) |
Appendix 5 Calculation of impact measures
Overview
Impact measures were calculated for each calendar month for each identified catchment area and for each LSOA within the catchment areas. No standardisation (age, deprivation, etc.) was applied as, within the time horizon of the indicators (4 years), population structure and case mix were unlikely to change significantly.
Data sources and data pre-processing
The NHS Digital Hospital Episode Statistics accident and emergency data
Data were provided by NHS Digital for most NHS (or NHS-commissioned) A&E care at the attendance level; one record was provided for each patient attendance at a major A&E department, single specialty A&E department (e.g. eye/ophthalmic A&E), UCC, WIC and MIU. The analysis includes attendances categorised as a ‘first attendance’ (i.e. it does not include follow-up attendances, planned or otherwise, or attendances for which this information is unknown). Figure 35 illustrates the inclusion procedure that was followed.
FIGURE 35.
Inclusion criteria and procedure for HES A&E data.
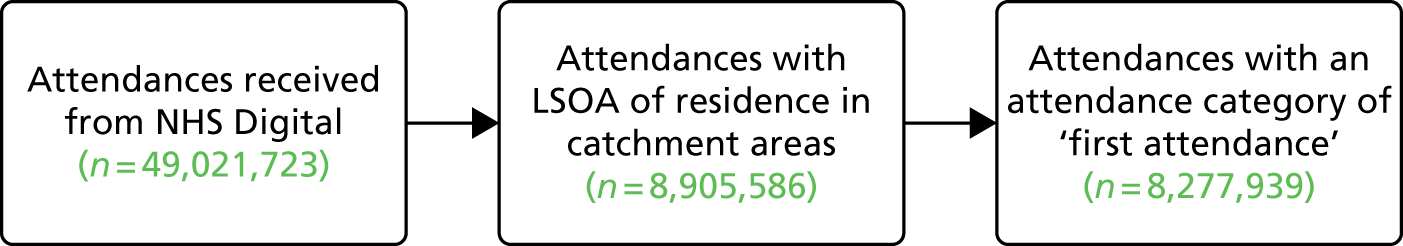
The NHS Digital Hospital Episode Statistics admitted patient care data
Data were provided by NHS Digital for all NHS (or NHS-commissioned) admitted/inpatient care at the episode level; data were in the form of a record of continuous care completed under the supervision of one consultant. Some patients were treated under the supervision of more than one consultant within a period of care; in addition, a small minority of patients had their care delivered by more than one hospital trust. The analysis was based on an analysis of the data at the continuous inpatient spell (CIPS) level. A CIPS is a record of a patient’s entire single period of care. CIPSs are formed by aggregating episodes within a patient’s single period of care regardless of whether that period of care was under the supervision of more than one consultant or provided by more than one trust. Figure 36 illustrates the procedure used to transform the data from episode level to a CIPS level. In the analysis, only CIPSs that commenced with an emergency admission were included, that is, a CIPS was included only if the method of admission for the first episode within the CIPS was recorded as one of the following HES codes:
21. Accident and emergency or dental casualty department of the health care provider
2A. Accident and emergency department of another provider where the patient had not been admitted (from 2013/14)
2B. Transfer of an admitted patient from another hospital provider in an emergency (from 2013/14)
2C. Baby born at home as intended (from 2013/14)
2D. Other emergency admission (from 2013/14)
28. Other methods such as:
-
admitted from the A&E department of another provider where they had not been admitted
-
transfer of an admitted patient from another hospital provider in an emergency
-
baby born at home as intended.
FIGURE 36.
Inclusion criteria and procedure for HES APC data.
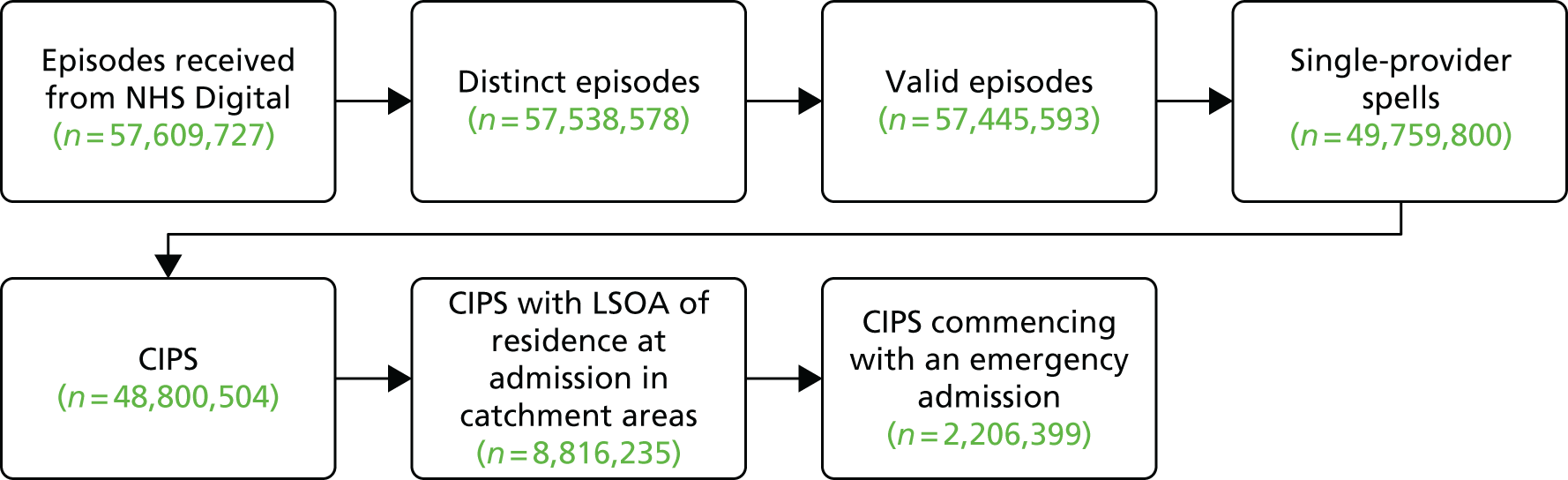
The NHS Digital Hospital Episode Statistics/Office for National Statistics death and birth records linked data
A bespoke data extract was supplied by NHS Digital, providing us with death record data for all individuals who appeared in the supplied HES APC and/or HES A&E data extracts and who had died within the study period. NHS Digital also supplied death record data for all individuals who had died while resident in any of our LSOAs of interest and within the study period but who did not appear in either the HES APC or HES A&E data extracts. In addition to an individual’s age at death, the data supplied included the date of death, all specified causes of death [using International Classification of Diseases, Tenth Edition (ICD-10), codes] and the LSOA of residence at the time of death. The death data were linked to the HES APC and A&E data using a common identifier (an encrypted HES ID), which was attached by NHS Digital.
The ambulance service data
Ambulance services supplied call-level data in a standardised form. These data included timestamps of call ‘events’ (‘call at switchboard’, ‘first resource on scene’, ‘conveying resource leaving scene’, ‘conveying resource arriving at a destination’, ‘conveying resource “going clear” ’, etc.) and the final disposition of each call (e.g. ‘conveyed to A&E’ or ‘hear and treat’). Durations of intervals calculated from the ambulance data that were not consistent with the expected sequence of events were excluded, in that negative values for the durations were excluded (e.g. when ‘call at switchboard’ had a later timestamp than that of ‘first resource on scene’). Corrections were applied to intervals calculated from timestamps that were potentially altered by adjustments for daylight saving time. Ambulance services also supplied the LSOA of the incident to which a resource (or resources) were sent or, if the call was resolved by telephone advice only, the LSOA from which the caller telephoned. Owing to the differences in how ambulance services calculate and record their data, for each identified catchment area only data from a single ambulance service – the service contracted to serve the majority of the population in that area (the majority provider) – were used to produce measures. The vast majority of the population of the identified catchment areas were resident inside the boundaries of the majority ambulance service provider (all sites had > 85% of their population served by the majority provider; two sites had > 97% of their population served by the majority provider).
Ambulance service
A detailed description of each measure is provided in Tables 7–29, providing a hypothesis, data source and the process for constructing each measure.
| Hypothesis | If an ED is not easily accessible for patients, ambulance call volumes may increase for patients without access to alternative transport. Conversely, ambulance incident volumes may decrease if a patient chooses to use an alternative care provider, closer to home, rather than travel by ambulance to an ED further away (and have to find their own transport to return to their home) |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Process | Count of all incidents within a geographical area defined as a LSOA and satisfying the following condition:
|
| Comment | |
| Hypothesis | If an ED is not easily accessible for patients, ambulance call volumes may increase for patients without access to alternative transport. Conversely, ambulance call volumes may decrease if a patient chooses to use an alternative care provider, closer to home, rather than travel by ambulance to an ED further away (and have to find their own transport to return to their home) |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Process | Count of all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | |
| Hypothesis | Ambulance journey times from the catchment area to the now-nearest ED are likely to be longer. In addition, although ambulance response times should not be affected by the closure of an ED, there is a possibility that ambulances may be further away from the catchment area after travelling to more distant EDs |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Process | The mean duration from the time when the call was answered to the first resource arriving at a destination (e.g. an ED) for all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | The first conveying resource was defined as the first resource to arrive at a type 1 or type 2 A&E department conveying a patient from the incident of the call; or, if there was no conveyance to a type 1 or type 2 A&E, the first conveying resource to arrive at any destination conveying a patient from the incident of the call |
| Hypothesis | Although ambulance response times should not be affected by the closure of an ED, there is a possibility that ambulances may be further away from the catchment area after travelling to more distant EDs |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Process | The mean duration from the time of the call to the first resource arriving at the scene for all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | |
| Hypothesis | Although ambulance response times should not be affected by the closure of an ED, there is a possibility that ambulances may be further away from the catchment area after travelling to more distant EDs |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Process | The mean duration from the time when the call was answered to the first conveying resource arriving at the scene for all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | The first conveying resource was defined as the first resource to arrive at a type 1 or type 2 A&E department conveying a patient from the incident of the call; or, if there was no conveyance to a type 1 or type 2 A&E, the first conveying resource to arrive at any destination conveying a patient from the incident of the call |
| Hypothesis | Ambulance journey times are likely to be longer from the catchment area to the now nearest ED |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Process | The mean duration from the first conveying resource arriving at the scene to the first resource arriving at a destination (e.g. an ED) for all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | The first conveying resource was defined as the first resource to arrive at a type 1 or type 2 A&E department conveying a patient from the incident of the call; or, if there was no conveyance to a type 1 or type 2 A&E, the first conveying resource to arrive at any destination conveying a patient from the incident of the call |
| Hypothesis | Following ED closures, neighbouring EDs will receive patients. If the receiving EDs are having difficulties with managing this additional demand, one consequence may be an increase in the time taken for ambulance crews to hand over care to the ED |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Process | The mean duration from the first conveying resource arriving at a destination (e.g. an ED) to the first conveying resource to ‘go clear’ (i.e. to be ready to attend another incident) for all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | The first conveying resource was defined as the first resource to arrive at a type 1 or type 2 A&E department conveying a patient from the incident of the call; or, if there was no conveyance to a type 1 or type 2 A&E, the first conveying resource to arrive at any destination conveying a patient from the incident of the call |
| Hypothesis | Emergency transfers may decrease if, as anticipated, the patient is taken to the ‘right place, first time’52 |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Process | Count of all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | |
| Hypothesis | Ambulance services may increase their use of non-conveyance to minimise the potential impact of increased journey times on service performance measures |
| Data source(s) | Bespoke incident-level data from NHS ambulance service trusts |
| Construction | |
| Numerator | Count of all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Denominator | Count of all incidents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Process | Ratio of numerator to denominator |
| Comment | |
Emergency and urgent care attendances
| Hypothesis | Ease of access is a prominent determinant of ED attendance rates.21 ED attendance may decrease because of (1) patients choosing to not travel further or (2) ambulance services increasing their use of non-conveyance |
| Data source(s) | NHS Digital HES A&E |
| Construction | |
| Process | Number of attendances of residents within a geographical area defined as a LSOA and satisfying the following condition:
|
| Comment | |
| Hypothesis | Changes in the total number of ED attendances may result from (1) changes in the numbers self-referring to an ED or (2) changes in ambulance service conveyance rates |
| Data source(s) | NHS Digital HES A&E |
| Construction | |
| Process | Number of attendances of residents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | |
| Hypothesis | Changes in total ED attendances may result either from changes in the numbers self-referring to ED or changes in ambulance service conveyance rates |
| Data source(s) | NHS Digital HES A&E |
| Construction | |
| Process | Number of attendances of residents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | |
| Hypothesis | The number of low-acuity attendances may decrease if patients choose to seek alternative care (e.g. GP services), closer to home, rather than travel further to an ED |
| Data source(s) | NHS Digital HES A&E |
| Construction | |
| Process | Number of attendances of residents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment | |
| Hypothesis | The proportion of attenders who are admitted may change as a result of patients going to different EDs or because discharging patients home from an ED may be more difficult as distances from the ED to a patient’s home increase |
| Data source(s) | NHS Digital HES A&E |
| Construction | |
| Numerator | Number of attendances of residents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Denominator | Number of attendances of residents within a geographical area defined as a LSOA and satisfying the following condition:
|
| Process | Ratio of numerator to denominator |
| Comment | |
Emergency admissions
| Hypothesis | The emergency hospital admissions rate may be affected by (1) where a patient goes and (2) when they get there. Where they go may affect admissions because of differences between hospitals in admission rates, and because of difficulties with discharging patients home from an ED if the patient is at a non-local ED. If a patient delays seeking treatment or has an increased travel time to hospital, this may lead to deterioration in their condition, which may necessitate admission |
| Data source(s) | NHS Digital HES APC |
| Construction | |
| Process | Number of CIPSs, commencing with an emergency admission, of residents within a geographical area defined as a LSOA |
| Comment | |
| Hypothesis | A well-performing urgent and emergency care system might be expected to avoid some admissions for selected conditions.41 We know that ‘avoidable admission’ rates vary between hospitals39 so admission rates could be affected by which hospital a patient goes to and also by delays in the patient arriving at hospital |
| Data source(s) | NHS Digital HES APC |
| Construction | |
| Process | Number of CIPSs, commencing with an emergency admission, of residents within a geographical area defined as a LSOA and satisfying the following condition:
|
| Comment | When required, the patient’s age is that recorded at the start of the first (admission) episode of the relevant CIPS |
| Hypothesis | Increases in LOS may be affected by where patients are admitted, and may be an indicator of (1) condition severity or (2) difficulties in discharging patients to non-local services |
| Data source(s) | NHS Digital HES APC |
| Construction | |
| Process | The mean LOS of all CIPSs, commencing with an emergency admission, of residents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment |
Length of stay of a CIPS is calculated in ‘nights’ (number of date changes) between (1) the earliest of the admission date or earliest episode start date and (2) the latest episode end date CIPSs with a LOS of 184 nights or more are excluded to avoid bias in the data. CIPSs that started within the period for which we have data but finished such that their discharge date was outside the period for which we have data would not be identified as being ‘finished’. Data are available for the period extending up to 183 nights (inclusive) after the end of the last month for which an indicator is required |
| Hypothesis | Admissions to critical care may be affected by where patients are admitted, and also indicate condition severity. The condition of patients with a delayed presentation may deteriorate and lead to critical care admission |
| Data source(s) | NHS Digital HES APC |
| Construction | |
| Process | Number of CIPSs, commencing with an emergency admission, of residents within a geographical area defined as a LSOA and satisfying the following condition:
|
| Comment | |
Number of deaths and risk of death
| Hypothesis | Mortality may be affected by (1) where a patient goes (i.e. the quality of the hospital that the patient attends) and (2) when they get there (i.e. increased time to treatment may have an adverse impact on mortality) |
| Data source(s) | Bespoke linked NHS Digital HES APC/ONS death registrations/ONS birth registrations |
| Construction | |
| Process | Number of deaths of residents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment |
A death is defined as having terminated a CIPS if the date of death is the day of discharge or is within the CIPS When required, the individual’s age is identified using the age at death as supplied by the ONS, which is based on the dates present on the birth and death registrations Some out-of-hospital deaths subsequent to an emergency admission may be because of the event (onset/incident of a condition) that caused the admission. It is, however, not possible to identify events per se, hence all out-of-hospital deaths have been included |
| Hypothesis | The CFR may be affected by (1) where a patient goes (i.e. the quality of the hospital that the patient attends), and (2) when they get there. If a patient delays seeking treatment or has an increased travel time to hospital, this may have an adverse impact on case fatality |
| Data source(s) | Bespoke linked NHS Digital HES APC/ONS death registrations/ONS birth registrations |
| Construction | |
| Numerator | Deaths from 16 SECs, out of hospital or within 7 days in hospital |
| Denominator | All deaths in the numerator and in addition to the following
|
| Process | Ratio of numerator to denominator |
| Comment |
A death is defined as having terminated a CIPS if the date of death is the day of discharge or is within the CIPS When required, the individual’s age is identified using the patient’s age as recorded at the start of the first (admission) episode of the relevant CIPS Length of stay of a CIPS is calculated in ‘nights’ (number of date changes) between (1) the earliest of the admission date or earliest episode start date and (2) the latest episode end date CIPSs with a LOS of 184 nights or more are excluded to avoid bias in the data. CIPSs that started within the period for which we have data but finished such that their discharge date was outside the period for which we have data would not be identified as being ‘finished’. Data are available for the period extending up to 183 nights (inclusive) after the end of the last month for which an indicator is required |
| Hypothesis | Mortality may be affected by changes in travel time to hospital. If travel time to hospital increases, patients may die before reaching (being admitted to) hospital |
| Data source(s) | Bespoke linked NHS Digital HES APC/ONS death registrations/ONS birth registrations |
| Construction | |
| Process | Number of deaths of residents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment |
Out-of-hospital deaths may occur: at home prior to making contact with a service, in an ambulance on the way to hospital, in the ED prior to hospital admission or when a patient is recorded as having a SEC incident and is admitted, discharged alive and subsequently dies without being readmitted When required, the individual’s age is identified using the age at death as supplied by the ONS, which is based on the dates present on the birth and death registrations Some out-of-hospital deaths subsequent to an emergency admission may be because of the event (onset/incident of a condition) that caused the admission. It is, however, not possible to identify events per se, hence all out-of-hospital deaths have been included |
| Hypothesis | Mortality may be affected by the hospital in which a patient receives treatment. The quality and availability of services at a hospital may have an impact on mortality |
| Data source(s) | Bespoke linked NHS Digital HES APC/ONS death registrations/ONS birth registrations |
| Construction | |
| Process | Number of deaths of residents within a geographical area defined as a LSOA and satisfying all of the following conditions:
|
| Comment |
A death is defined as having terminated a CIPS if the date of death is the day of discharge or is within the CIPS When required, the individual’s age is identified using the age at death as supplied by the ONS, which is based on the dates present on the birth and death registrations |
| Hypothesis | The CFR may be affected by (1) where a patient goes (i.e. the quality of the hospital that the patient attends) and (2) when they get there. If a patient delays seeking treatment or has an increased travel time to hospital, this may have an adverse impact on case fatality |
| Data source(s) | Bespoke linked NHS Digital HES APC/ONS death registrations/ONS birth registrations |
| Construction | |
| Numerator | Deaths from specific SECs that are identified as rich in avoidable deaths (stroke and MI), within 7 days in hospital |
| Denominator | All deaths in the numerator and, additionally:
|
| Process | Ratio of numerator to denominator |
| Comment |
A death is defined as having terminated a CIPS if the date of death is the day of discharge or is within the CIPS When required, the individual’s age is identified using the patient’s age as recorded at the start of the first (admission) episode of the relevant CIPS Length of stay of a CIPS is calculated in ‘nights’ (number of date changes) between (1) the earliest of the admission date or earliest episode start date and (2) the latest episode end date CIPSs of 184 nights or more are excluded to avoid bias in the data. CIPSs that started within the period for which we have data but finished such that their discharge date was outside the period for which we have data would not be identified as being ‘finished’. Data are available for the period extending up to 183 nights (inclusive) after the end of the last month for which an indicator is required |
Appendix 6 Urgent emergency conditions
The urgent emergency conditions used in the analysis of admissions are presented in Table 30. These conditions were identified in a Delphi study for use as indicators of the performance of emergency and urgent care systems because they are conditions that a well-performing emergency and urgent care system could manage out of hospital or in settings without admission to an inpatient bed. 56 Patients admitted to hospital with a primary diagnosis associated with one of these codes were included in the analysis of ‘potentially avoidable’ emergency admissions.
| Condition | ICD-10 codes |
|---|---|
| Hypoglycaemia | E10–E15, E161 and E162 |
| Acute mental health crisis | F00–F99 |
| Epileptic fit | G40 and G41 |
| Angina | I20 |
| Deep-vein thrombosis | I80–I82 |
| Chronic obstructive pulmonary disease | J40–J44 |
| Cellulitis | L03 |
| Urinary tract infection | N390 |
| Non-specific chest pain | R07.2–R07.4 |
| Non-specific abdominal pain | R10 |
| Pyrexial child (< 6 years) | R50 |
| Minor head injuries | S00 |
| Blocked catheter | T830 |
| Any external injury, and the cause is | |
| Falls (≥ 75 years) | W00–W19 |
Appendix 7 Serious emergency conditions
The SECs used in the analysis of deaths are presented in Table 31. These conditions were identified in a Delphi study for use as indicators of the performance of emergency care systems because they are conditions for which a well-performing emergency and urgent care system could improve chances of survival. 56 Deaths with an underlying or other recorded cause coded to one of the conditions in Table 31 were included in the analysis.
| Condition | ICD-10 codes |
|---|---|
| Septic shock | A40 and A41 |
| Meningitis | G01–G03, A39 and A32.1 |
| MI | I21–I23 |
| Cardiac arrest | I46 |
| Acute heart failure | I50 |
| Stroke/cerebrovascular accident | I61, I63, I64 and I62.9 |
| Ruptured aortic aneurysm | I71.0–I71.3, I71.5 and I71.8 |
| Asthma | J45 and J46 |
| Pregnancy and birth related | O00–O99 |
| Anaphylaxis | T780, T782, T805 and T886 |
| Asphyxiation | T17, T71 and R09.0 |
| Fractured neck of femur | S72 |
| Serious head injuries | S02–S09 |
| Any external injury, and the cause is | |
| Road traffic accidents | V00–V79, V802–V805, V821, V892, V830, V832, V833, V840–V843, V850–V853, V860–V863, V870–V878 |
| Falls (< 75 years) | W00–W19 |
| Self-harm | X60–X84 |
Appendix 8 Statistical analysis of individual sites
Note: readers without a statistical background may wish to bypass the statistics reported in the sections of this appendix entitled ‘Findings from individual activity and performance measures’ and instead look at the ‘Summary of findings’ sections and Figures 3–34 (to see any changes over time).
Hemel Hempstead
The ED at Hemel Hempstead Hospital was closed in March 2009. We have examined changes in activity and performance of the emergency care system for residents of the catchment area of Hemel Hempstead ED (HH ED) over the 2 years before and 2 years after this closure. We have also compared these changes with changes over the same 4-year period for residents of the catchment area of a control ED.
In the analysis of the impact of the closure of HH ED, there was one system change that was accounted for in addition to the closure, and no changes to the control site emergency care system were identified.
Hemel Hempstead ED catchment area changes accounted for in the analysis:
-
Introduction of an UCC in October 2008.
Control site ED catchment area changes accounted for in the analysis:
-
No important changes were identified in the control site catchment area.
Summary of findings
Following the closure, for residents of the ED catchment area in Hemel Hempstead:
-
There was some evidence of a large increase in the number of emergency ambulance incidents, but no statistically reliable evidence was found to suggest this regarding ‘Red’ incidents. No comparison could be made with the control area.
-
There was strong evidence of an increase in the time from 999 call to arrival at hospital. However, no comparison could be made with the control area.
-
There were data quality issues with the HES A&E extract. No reliable analyses could be undertaken on the emergency and urgent care service attendance measures.
-
There was strong evidence of a large decrease in the number of emergency hospital admissions. This decrease remained evident when compared with the control area.
-
There was strong evidence of a large decrease in the number of potentially avoidable hospital admissions, but only when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in LOS for those admitted to hospital as an emergency case.
-
There was no statistically reliable evidence to suggest a change in the number of deaths or risk of death from the 16 SECs studied.
In comparing pre- and post-closure journey times to the nearest ED, for those experiencing a larger change in post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of emergency ambulance incidents when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There were data quality issues with the HES A&E extract and, therefore, no reliable analyses could be undertaken on the emergency and urgent care service attendance measures.
-
There was strong evidence of a large decrease in the number of emergency hospital admissions, but no statistically reliable evidence of a decrease in potentially avoidable hospital admissions, when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in LOS for those admitted as an emergency case when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the mortality measures when compared with those experiencing a smaller change in journey times.
| Impact measure | Model, effect (95% CI); p-value | ||
|---|---|---|---|
| 1: no control | 2: compared with control | 6: high-dose areas | |
| Total number of emergency ambulance incidents | Increase: 15.9% (3.2% to 30.1%); 0.01 | No reliable data | Increase: 4.5% (–0.3% to 12.4%); 0.24 |
| Total number of emergency ambulance ‘Red’ incidents | Increase: 9.9% (–1.7% to 22.9%); 0.10 | No reliable data | Increase: 1.2% (–6.7% to 9.8%); 0.77 |
| Mean time from 999 ‘Red’ call to arrival at hospital | Increase: 5.5 minutes (3.3 to 7.7 minutes); < 0.001 | No reliable data | Increase: 10.0 minutes (8.5 to 11.6 minutes); < 0.001 |
| Total number of emergency and urgent care attendances | No reliable data | No reliable data | No reliable data |
| Total number of minor attendances at an emergency and urgent care service | No reliable data | No reliable data | No reliable data |
| Total number of emergency hospital admissions | Decrease: –13.4% (–18.5% to –8.0%); < 0.001 | Decrease: –16.4% (–20.8% to –11.8%); < 0.001 | Decrease: –13.3% (–17.3% to –9.0%); < 0.001 |
| Total number of potentially avoidable emergency hospital admissions | Decrease: –14.5% (–24.2% to –4.5%); 0.01 | Decrease: –18.6% (–25.6% to –11.0%); < 0.001 | Decrease: –10.1% (–18.1% to –1.4%); 0.03 |
| Mean LOS for emergency hospital admissions | Increase: 0.3 days (–0.2 to 1.0 days); 0.19 | Increase: 0.7 days (0.0 to 1.4 days); 0.05 | Decrease: –0.05 days (–0.1 to 0.5 days); 0.83 |
| Total number of out-of-hospital deaths | Decrease: –13.8% (–32.5% to 10.0%); 0.23 | Decrease: –2.4% (–20.8% to 20.2%); 0.82 | Increase: 16.2% (–6.1% to 43.7%); 0.17 |
| Total number of deaths occurring within 7 days post incident | Decrease: –9.3% (–26.2% to 11.5%); 0.36 | Increase: 4.0% (–12.6% to 23.9%); 0.66 | Increase: 3.6% (–13.3% to 23.7%); 0.70 |
| CFR (7 days) | Decrease: –1.2% (–4.3% to –1.9%); 0.46 | Increase: 2.5% (–1.0% to 5.9%); 0.17 | Increase: 1.8% (–2.4% to 6.0%); 0.40 |
Change in time to the next-nearest emergency department
Following the ED closure, the change in time to reach the next-nearest ED for the residents of the catchment area ranged from 0 to 19 minutes.
FIGURE 37.
Geographical map of Hemel Hempstead and surrounding EDs showing the change in time to the next-nearest ED. Map tiles by Stamen Design, under a Creative Commons Attribution license (CC BY 3.0; see https://creativecommons.org/license/by/3.0/). Data by OpenStreetMap, under ODbL. Contains National Statistics data © Crown copyright and database right 2016. Contains OS data © Crown copyright and database right 2016.
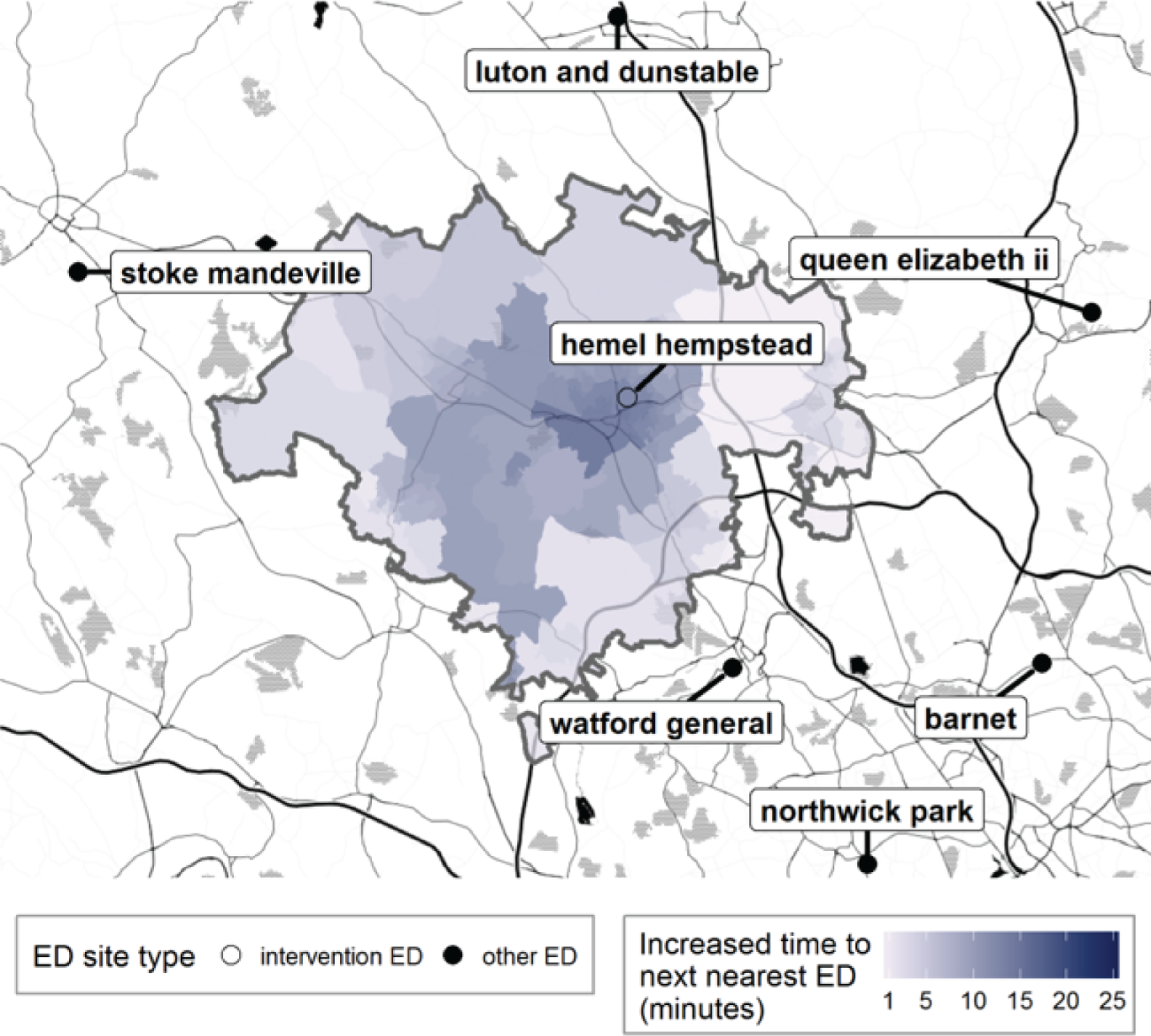
FIGURE 38.
Hemel Hempstead: change in time from LSOA to ED following ED closure, for residents of the catchment area of Hemel Hempstead Hospital ED.
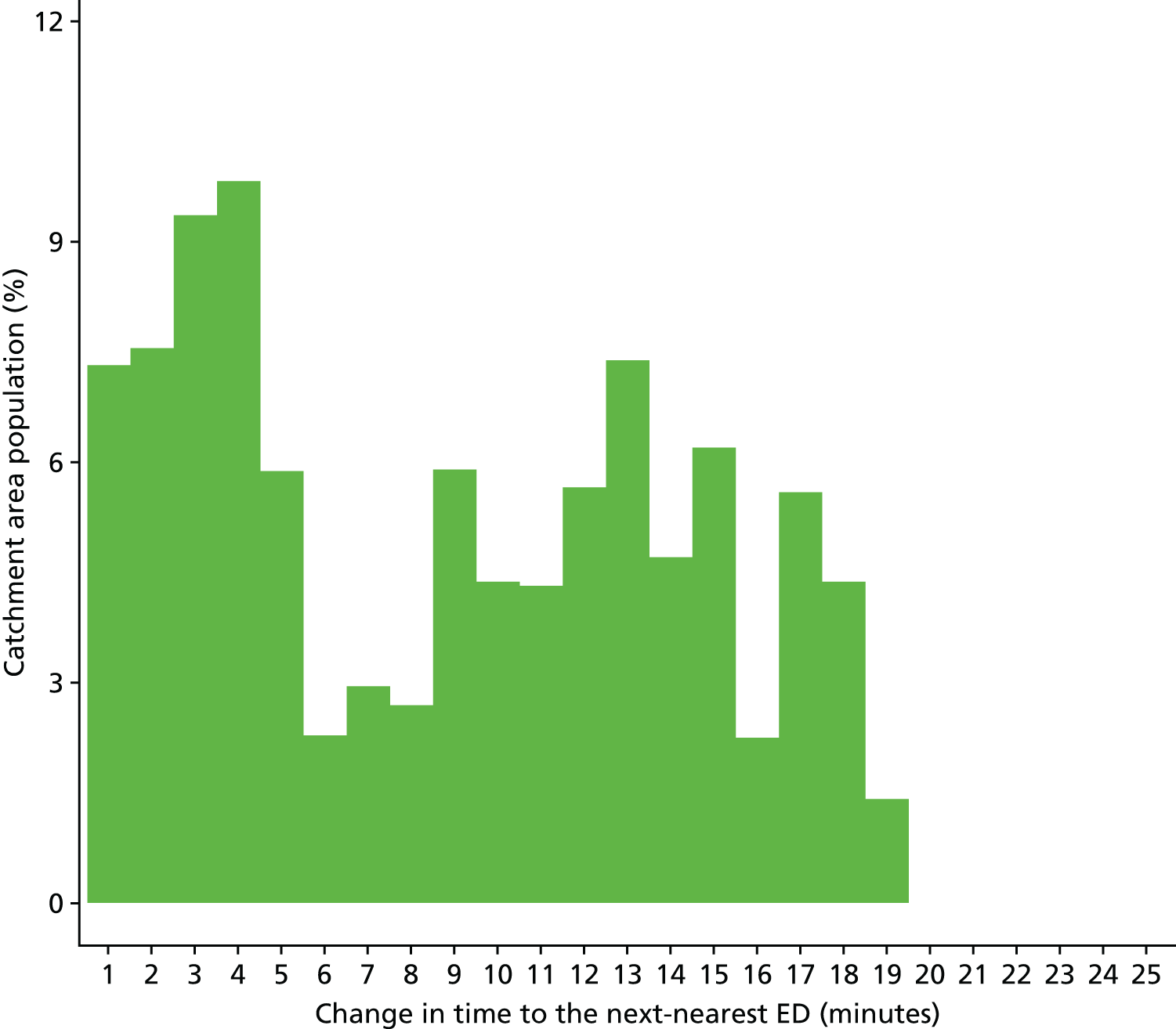
Findings from individual activity and performance measures
Ambulance service performance
Total number of incidents following 999 calls to the ambulance service
Plot of monthly activity
Figure 39 shows the total number of 999 incidents referred to the ambulance service from residents of the HH ED catchment area and the control area, for each month over the 2 years prior to and the 2 years after the date of the closure of Hemel Hempstead ED. There was a small change in the number of calls in HH. The number of incidents reduced by 3% from 1752 to 1697 per month. There were no useable data for the period preceding the closure from the control area.
FIGURE 39.
Total number of 999 incidents for residents of the Hemel Hempstead ED catchment area and the control area.
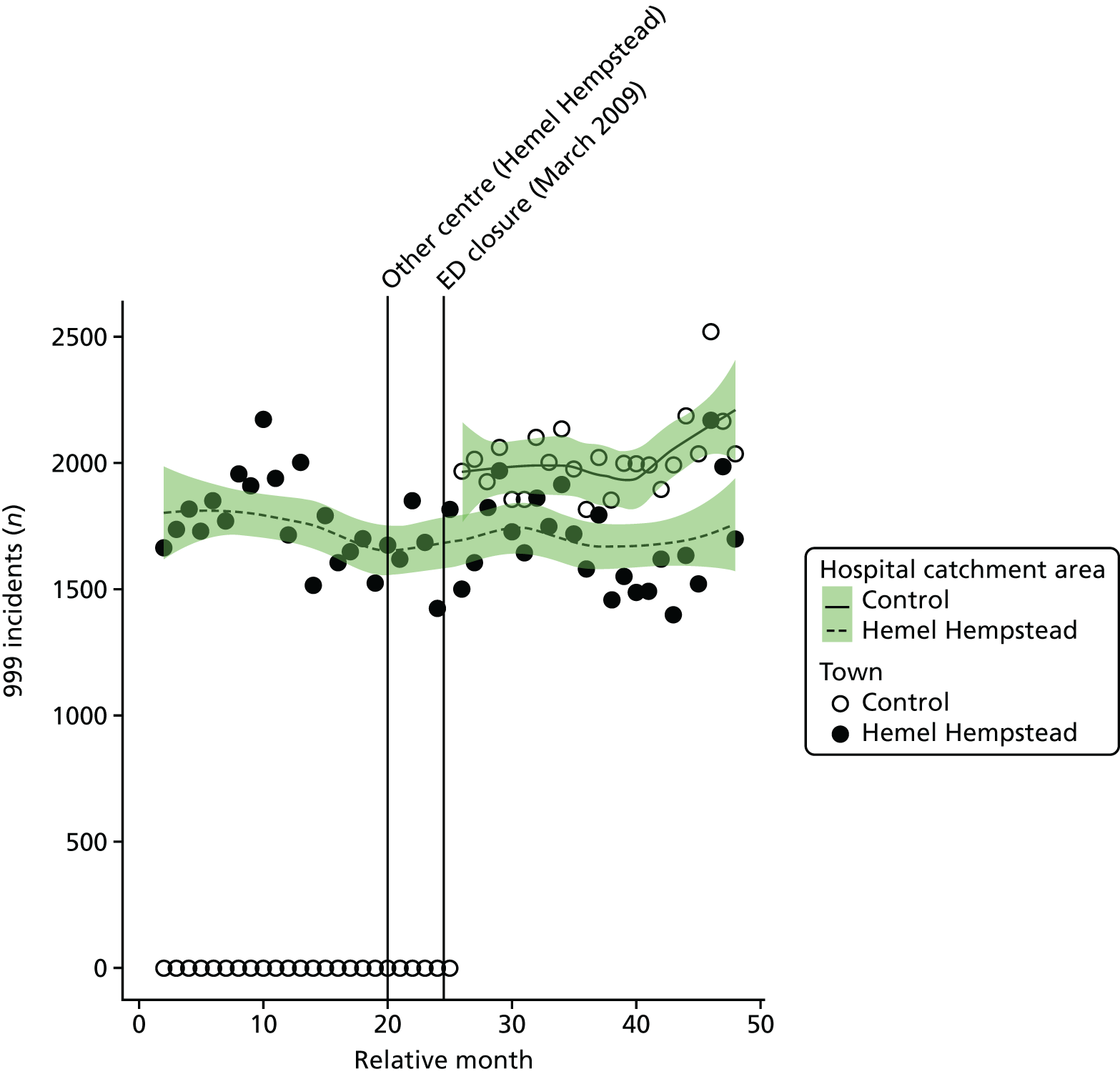
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of incidents each month for residents of the HH ED catchment area increased at the time of the closure by a mean of 15.9% (95% CI 3.2% to 30.1%; p = 0.01).
The emergency department closure and control area model
There were no useable data from before the closure date from the control area, and so this model could not be fitted.
Dose model
Figure 40 shows the mean number of incidents each month for residents of LSOAs that were expected to have a relatively large change (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) in time to an ED after the closure of the HH ED. The pattern of change in these two areas was similar, with a 5% reduction in low-dose areas and a 1% reduction in high-dose areas.
FIGURE 40.
Total number of 999 incidents for residents of areas in Hemel Hempstead that were expected to have a large change (high dose) and those expected to have a small change (low dose) in time to an ED.
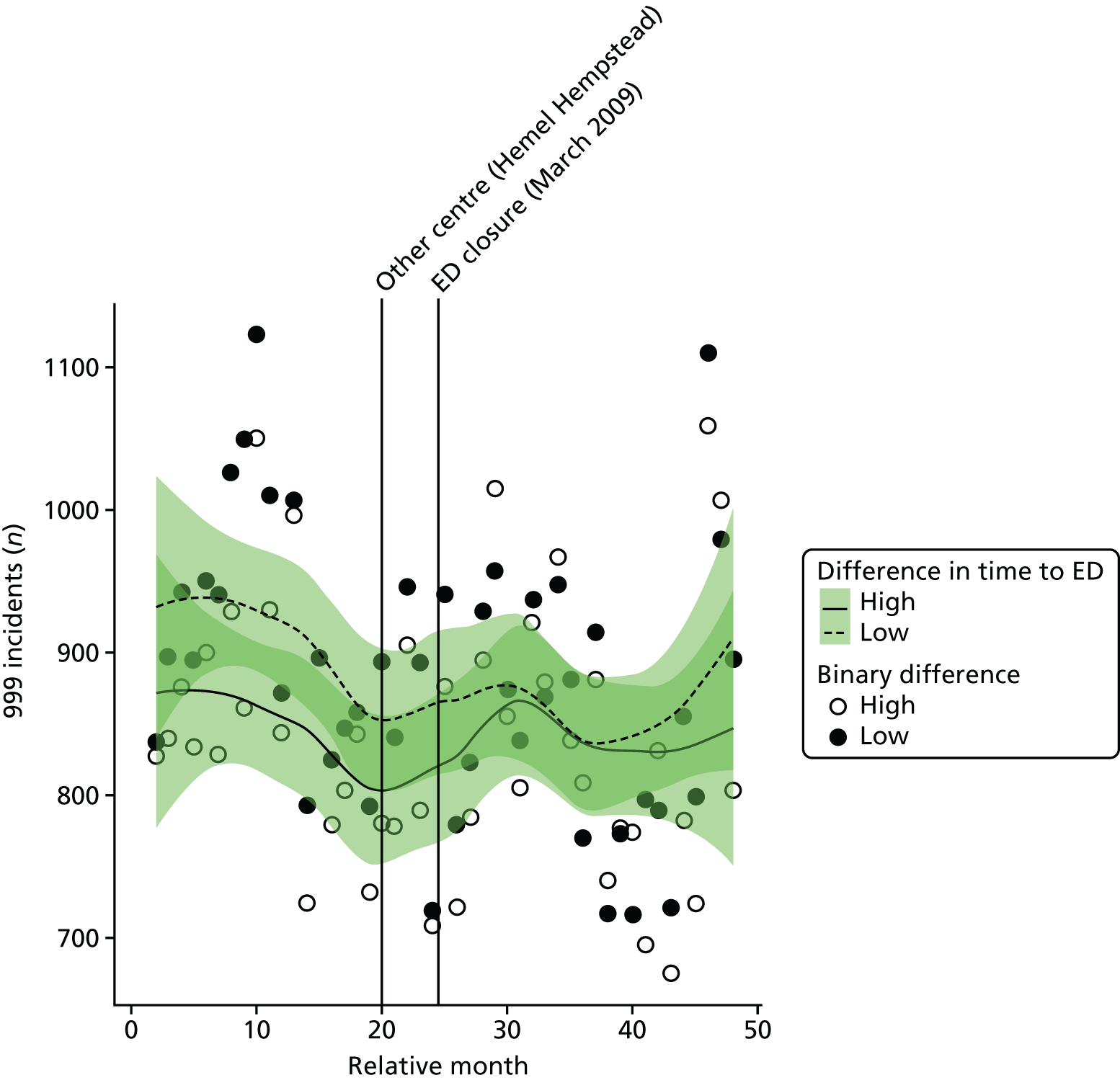
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of 999 incidents in high-dose areas relative to low-dose areas at the time of closure was 4.5% (95% CI –0.28% to 12.4%; p = 0.24).
Number of emergency ambulance ‘Red’ incidents received by the ambulance service
Plot of monthly activity
Figure 41 shows the number of the 999 incidents, classified as ‘Red’, to the ambulance service from residents of the HH ED catchment area and the control area for each month over the 2 years prior to and the 2 years after the date of the closure of the HH ED. Excluding the data from the 10 months when the incidents seem to have been coded differently, there was little evidence of any change in the number of ‘Red’ calls in HH. The number of ‘Red’ incidents went up by 9% from a mean of 610 per month to 663 per month in the HH ED catchment area. There were no useable pre-closure data from the control area.
FIGURE 41.
Number of ‘Red’ 999 incidents for residents of the Hemel Hempstead ED catchment area and the control area.

The emergency department closure area model
After allowing for seasonal effects, any long-term trend, and other known changes in the ED catchment area, the estimated number of ‘Red’ incidents each month for residents of the HH ED catchment area increased at the time of the closure by an average of 9.9% (95% CI –1.7% to 22.9%; p = 0.10).
The emergency department closure and control area model
There were no useable data from before the closure date from the control area, and so this model cannot be fitted.
Dose model
Figure 42 shows the mean number of ‘Red’ incidents each month for residents of LSOAs that were expected to have a relatively large change (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) in time to ED after the closure of the HH ED. The pattern of change in these two areas was very similar, with a 9% increase from 296 to 323 ‘Red’ incidents per month in high-dose areas, and an 8% increase from 314 to 340 in low-dose areas.
FIGURE 42.
Number of ‘Red’ 999 incidents for residents of areas in Hemel Hempstead that were expected to have a large change (high dose) and those expected to have a small change (low dose) in time to an ED.
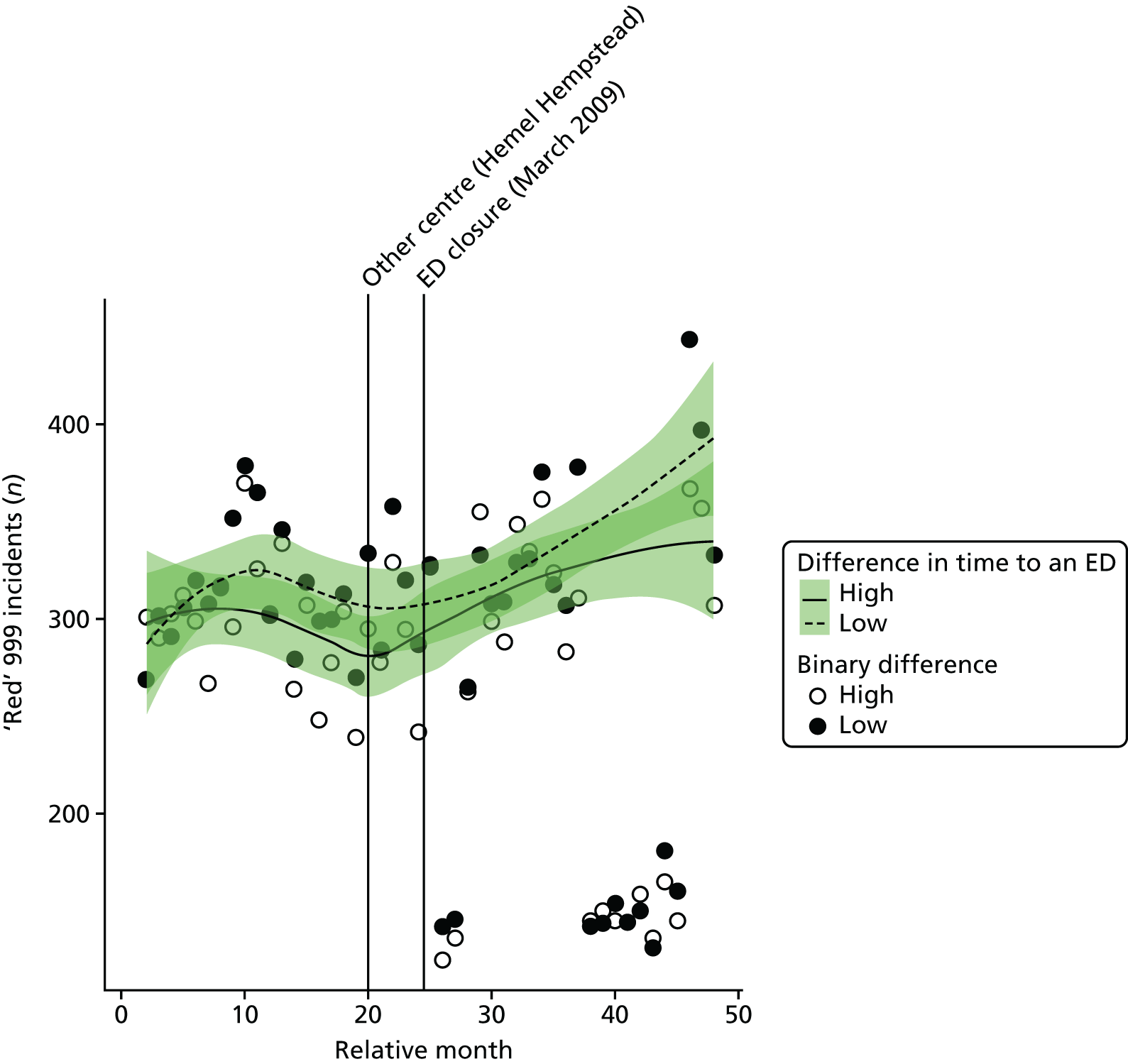
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend, and other known changes in the ED catchment area, the estimated increase in the number of 999 red incidents in high-dose areas relative to low-dose areas at the time of closure was 1.2% (95% CI –6.7% to 9.8%; p = 0.77).
Mean time from 999 ‘Red’ call to arrival at hospital
Plot of monthly activity
Figure 43 shows the mean time from 999 ‘Red’ call to hospital by ambulance for each month over the 2 years prior to and the 2 years after the closure of the HH ED.
The performance shows a clear increase in mean time from the call to arrival at hospital in the HH ED catchment area over the period spanning the closure of the ED. Prior to closure, the mean time to hospital was 45.9 minutes and after closure it was 55.4 minutes. However, it looks as though this increase had started prior to the closure. In the control site, data were obtained only for the period after the closure and no comparison can be made.
FIGURE 43.
Mean time from 999 ‘Red’ calls to arrival at hospital for residents of the Hemel Hempstead and control site ED catchment areas.
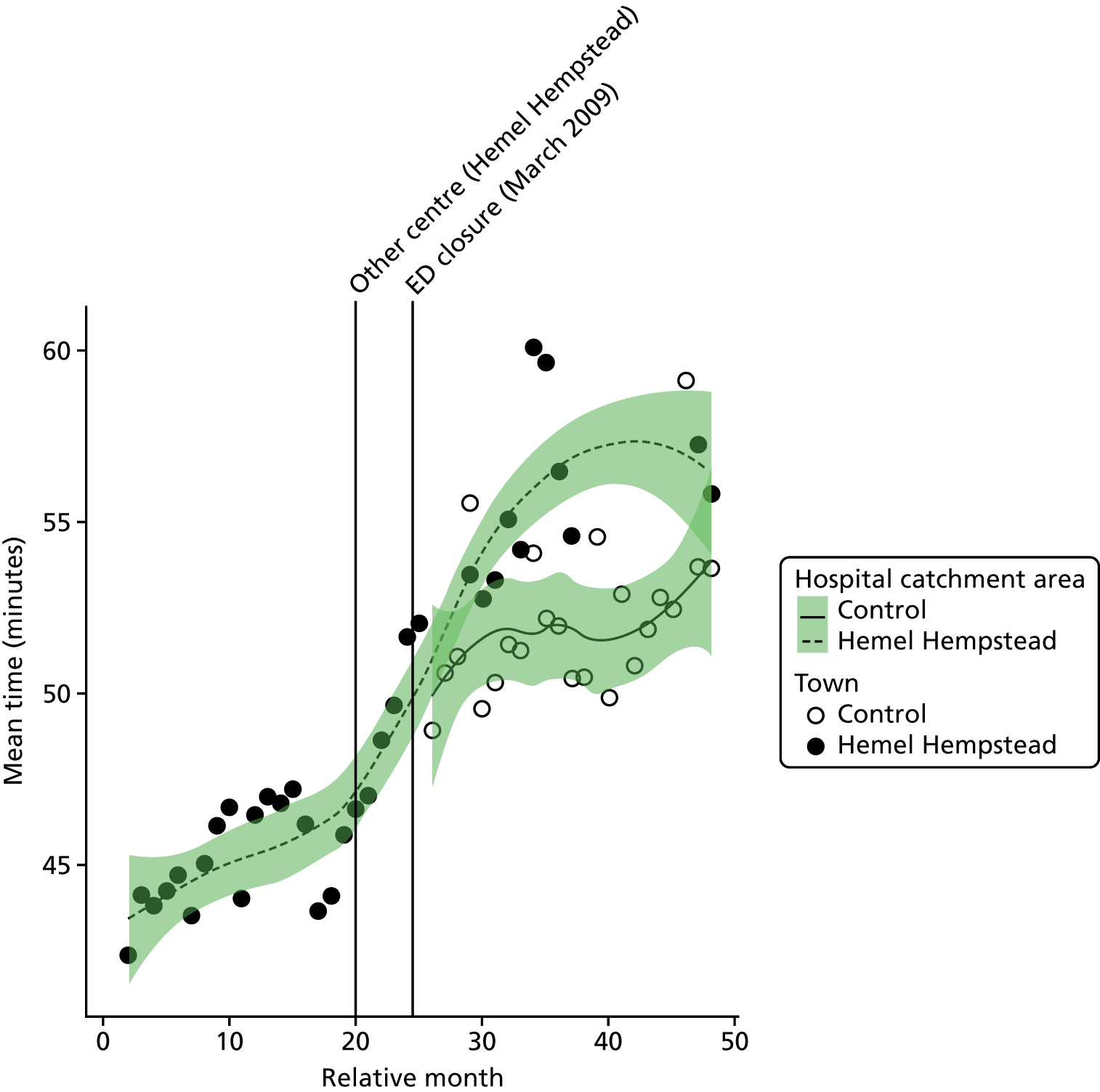
The emergency department closure area model
After allowing for seasonal effects, any long-term trend, and other known changes in the ED catchment area, the estimated mean time from call to arrival at hospital for 999 ‘Red’ calls in the ED catchment area increased at the time of the closure by an average of 5.5 minutes (95% CI 3.3 to 7.7 minutes; p < 0.001) compared with the pre-closure period.
The emergency department closure and control area model
Because no useable control site data could be obtained, no comparison with a control area has been made.
Dose model
Figure 44 shows the mean time from call to arrival at hospital for ‘Red’ calls made each month by residents of LSOAs that were expected to have a relatively large change in time to ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HH ED. The pattern of change in these two areas was quite different, as expected. High-dose LSOAs had an increase in mean time from the incident scene to the hospital of 15.6 minutes, and low-dose areas had an increase of just 5.4 minutes.
FIGURE 44.
Mean time from call to hospital for ‘Red’ calls for residents of areas in Hemel Hempstead that were expected to have a large change in time to ED (high dose) and those expected to have a small change (low dose).
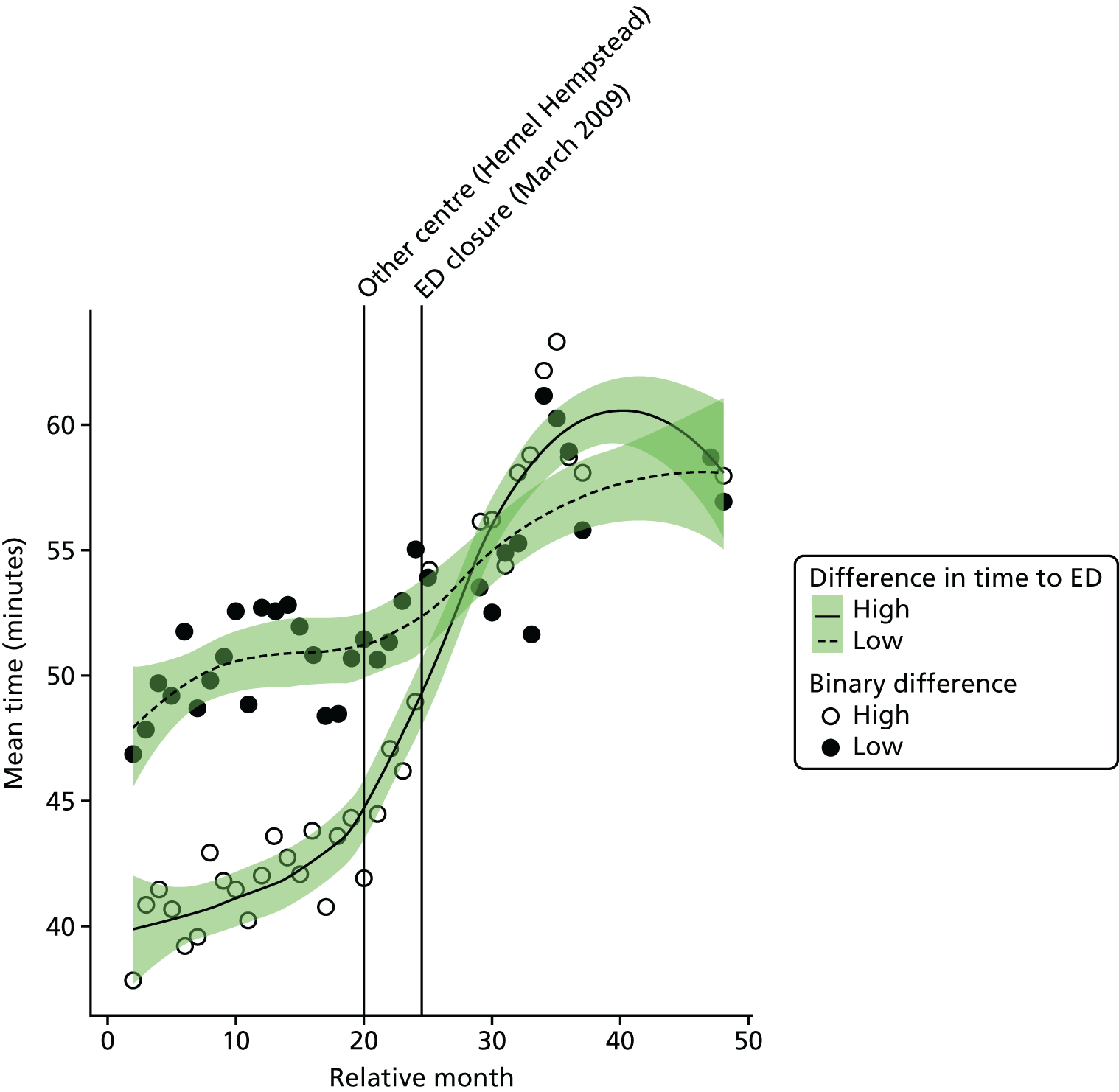
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend, and other known changes in the ED catchment area, the change in time from call to arrival at hospital that took place at the time of closure of the ED for residents of high-dose areas was estimated to be an extra 10.0 minutes (95% CI 8.5 to 11.6 minutes; p < 0.001).
Emergency and urgent care attendances
Figure 45 shows the total number of emergency and urgent care attendances (inclusive of A&E types 1–4 and attendances coded as ‘unknown’) by residents of the HH ED catchment area and the control site catchment area in each month of the 4-year study period.
FIGURE 45.
Total number of attendances at an ED by residents of the Hemel Hempstead and control ED catchment areas.
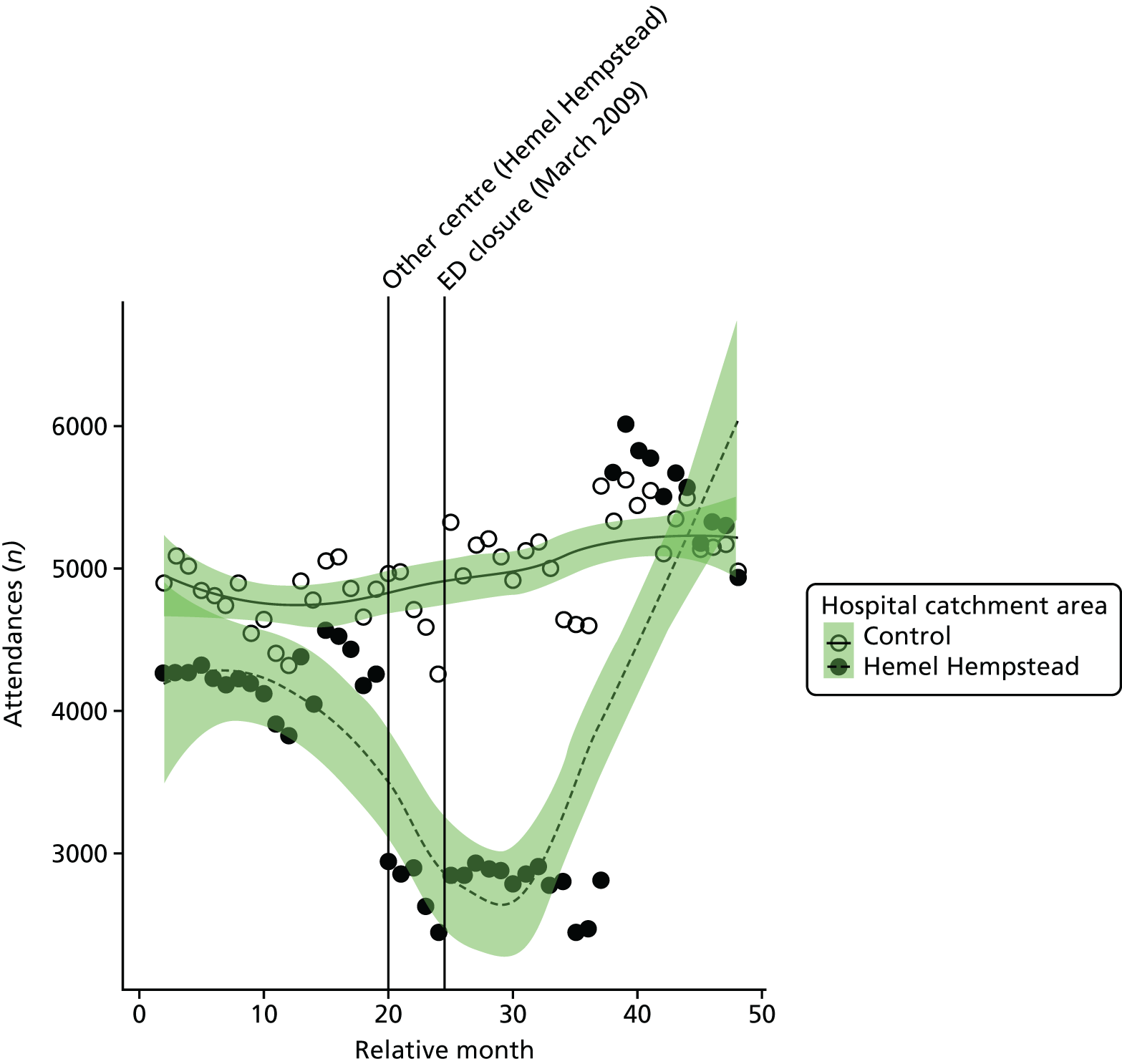
The data for emergency and urgent care attendances by residents of the HH ED catchment area are of poor quality, showing very large and sudden changes. These data effects are probably because of changes in recording practices at hospitals serving the HH ED catchment area rather than changes in attendance rate, so no further analyses have been carried out using these data.
Admissions
All emergency admissions
Plot of monthly activity
Figure 46 shows the total number of emergency admissions to any hospital by residents of the HH ED catchment area and residents of the control site catchment area in each month of the 4-year study period.
FIGURE 46.
Total number of emergency admissions of residents of the Hemel Hempstead ED catchment area and the control catchment area.
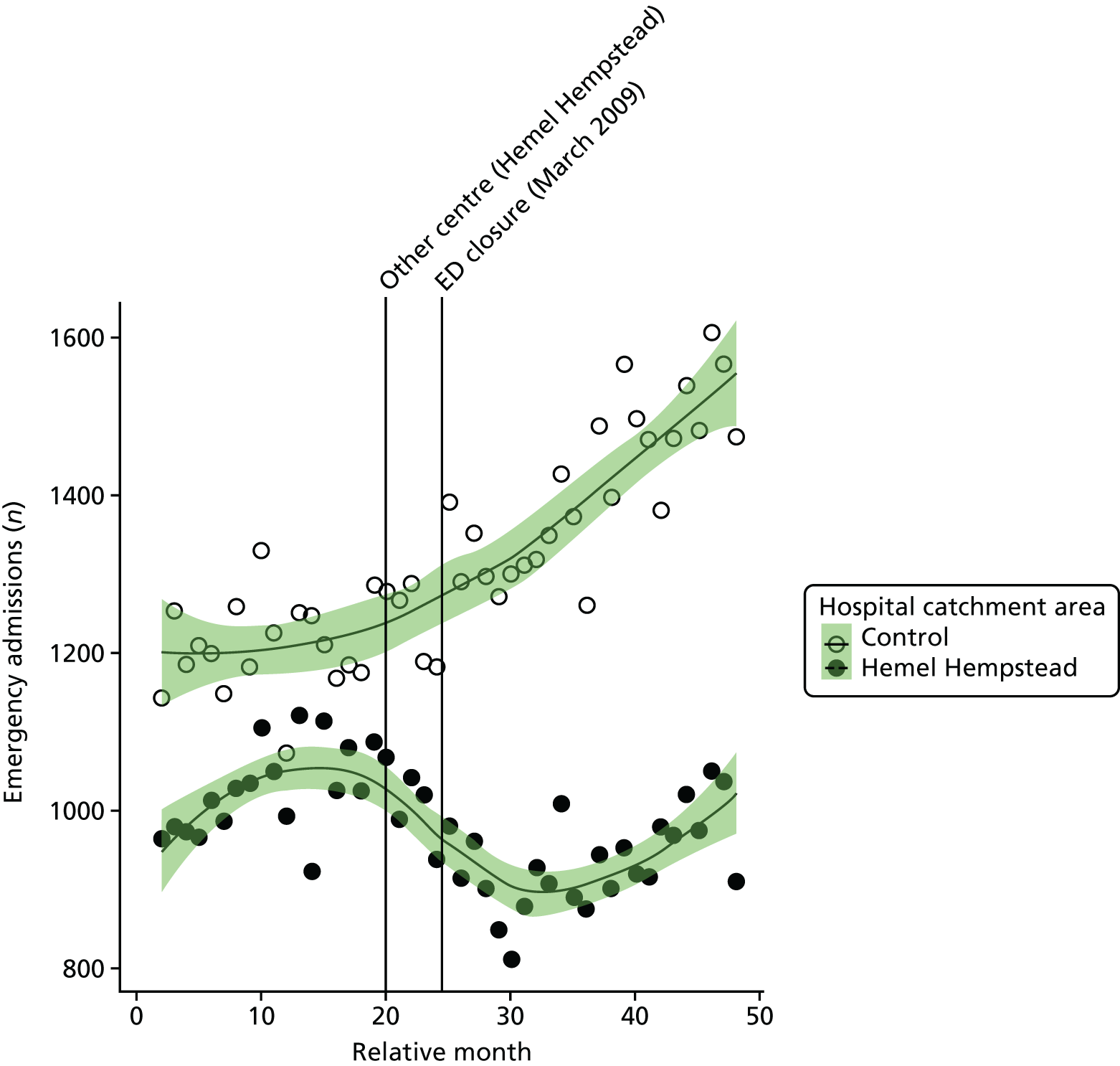
There is some suggestion that the number of admissions did change around the time of closure for residents of HH. In HH, there were, on average, 1023 emergency admissions per month prior to the closure and 937 post closure, a reduction of 8.4%. The control area shows a steady rise over the study period, increasing from 1214 to 1411 (an increase of 16.2%).
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of emergency admissions for residents of the catchment area of HH ED was –13.4% (95% CI –18.5% to –8.0%; p < 0.001).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly mean number of emergency admissions for residents of the catchment area of HH ED relative to the control site was –16.4% (95% CI –20.8% to –11.8%; p < 0.001).
Dose model
Figure 47 shows the mean number of emergency admissions each month made by residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HH ED. The pattern of change in these two areas was different, with a 14% decrease in high-dose areas, from 558 to 478 admissions per month, but only a 1% decrease from 464 to 459 in low-dose areas.
FIGURE 47.
Number of emergency admissions to hospital for residents of areas in Hemel Hempstead that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
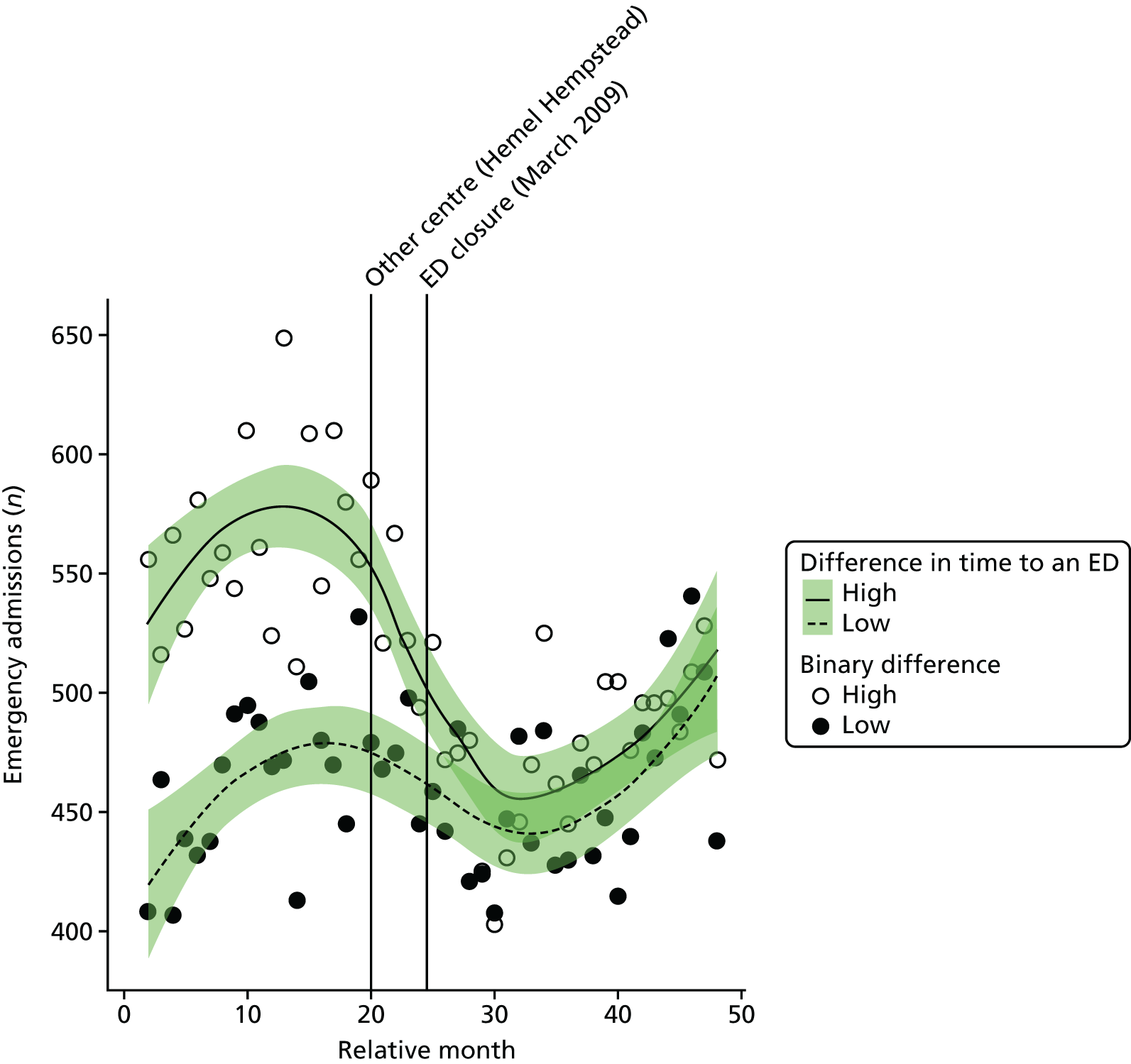
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of emergency admissions in high-dose areas compared with low-dose areas was –13.3% (95% CI –17.3% to –9.0%; p < 0.001).
Potentially avoidable emergency admissions
Plot of monthly activity
Figure 48 shows the number of potentially avoidable emergency admissions to any hospital by residents of the HH ED catchment area and residents of the control site catchment area in each month of the 4-year study period. The pattern of admissions from these 14 emergency conditions is very similar to the pattern for all emergency admissions, with some indication of changes in the numbers over the period spanning the ED closure. In the HH area, there were, on average, 269 avoidable emergency admissions per month prior to the closure and 236 post closure, a reduction of 12.2%. In the control area, there were, on average, 320 admissions per month prior to the closure date and 400 afterwards.
FIGURE 48.
Number of potentially avoidable emergency admissions of residents of Hemel Hempstead ED catchment area and the control catchment area.
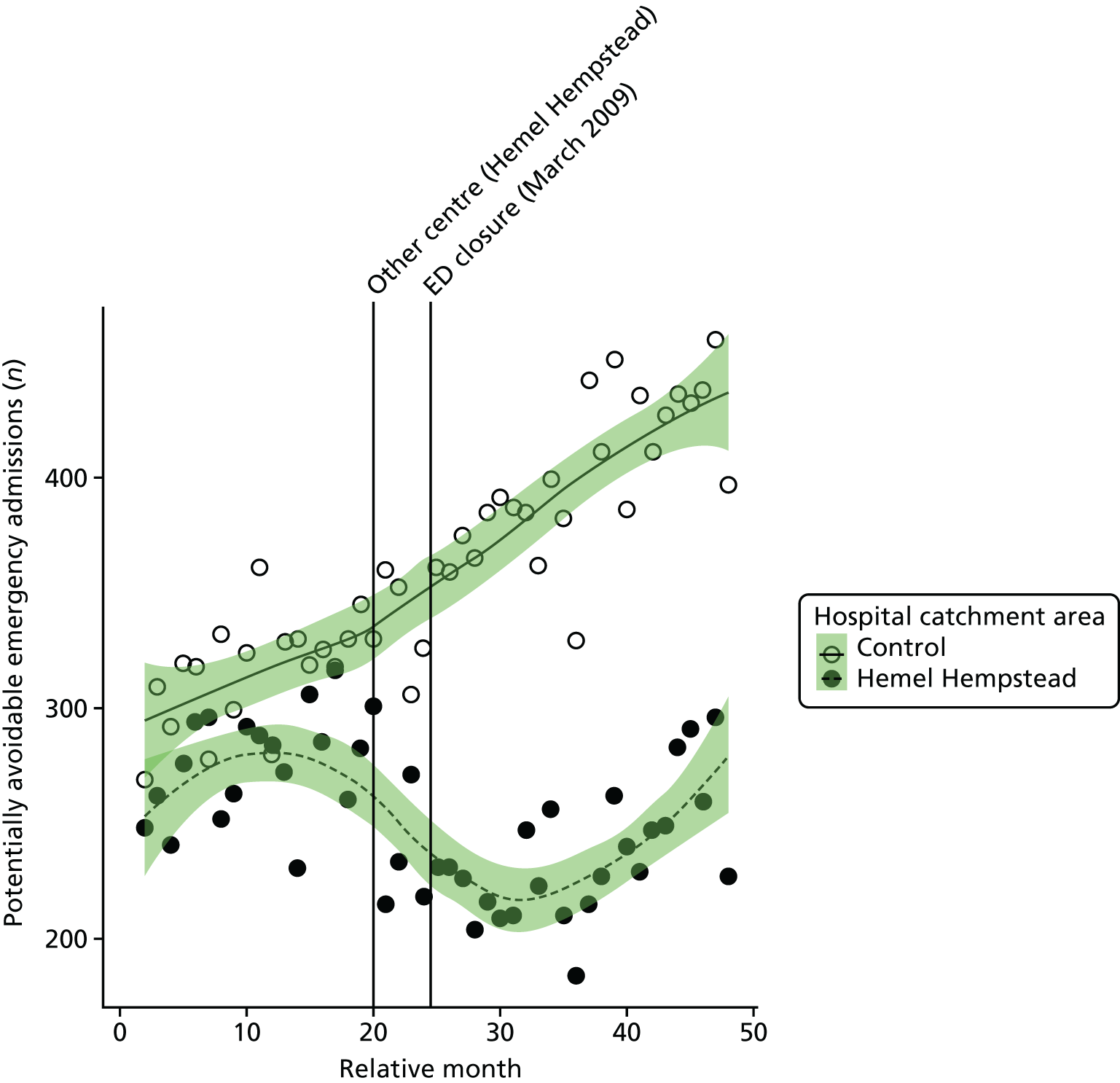
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of avoidable emergency admissions for residents of the catchment area of HH ED was –14.5% (95% CI –24.2% to –4.5%; p = 0.01).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change at the time of the closure in the monthly mean number of avoidable emergency admissions for residents of the catchment area of HH ED relative to the control site was –18.6% (95% CI –25.6% to –11.0%; p < 0.001).
Dose model
Figure 49 shows the mean number of potentially avoidable emergency admissions each month for residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HH ED. The pattern of change in these two areas was similar, with reductions of 16% in high-dose areas and 7% in low-dose areas.
FIGURE 49.
Mean number of potentially avoidable emergency admissions to hospital for residents of areas in Hemel Hempstead that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
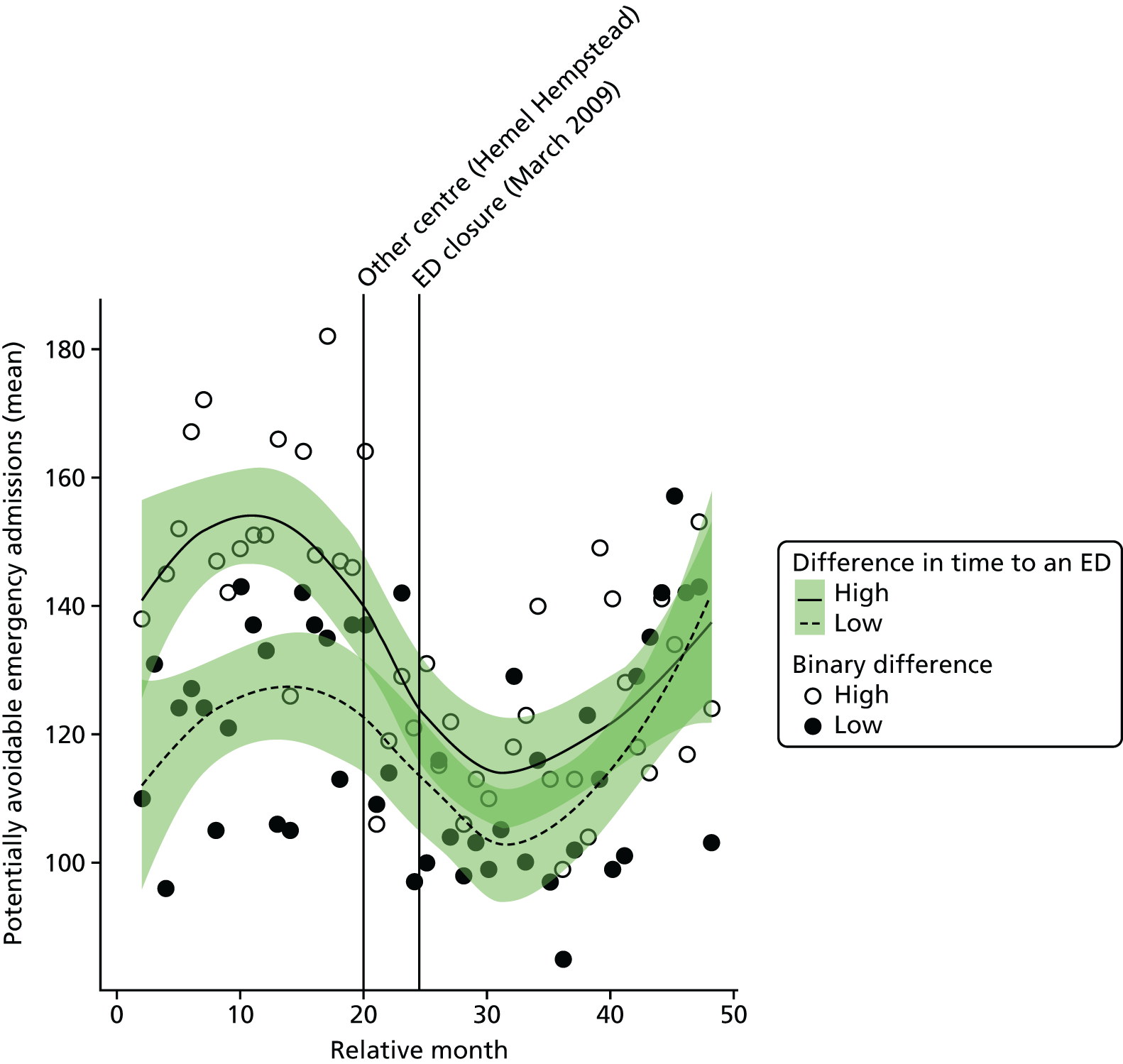
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the estimated number of emergency admissions in high-dose areas compared with low-dose areas was –10.1% (95% CI –18.1% to –1.4%; p = 0.03).
Length of stay for emergency admissions
Plot of monthly activity
Figure 50 shows the mean LOS in hospital of patients admitted as emergencies for residents of the HH ED catchment area and residents of the control site catchment area in each month of the 4-year study period. There was little change in HH, with the mean LOS increasing from 7.2 days before the closure to 7.5 days after the closure of the ED. In the control site, there was a decrease from 9.1 days before the closure to 8.3 days after the closure.
FIGURE 50.
Mean LOS for emergency admissions for residents of the Hemel Hempstead ED catchment area and the control area.
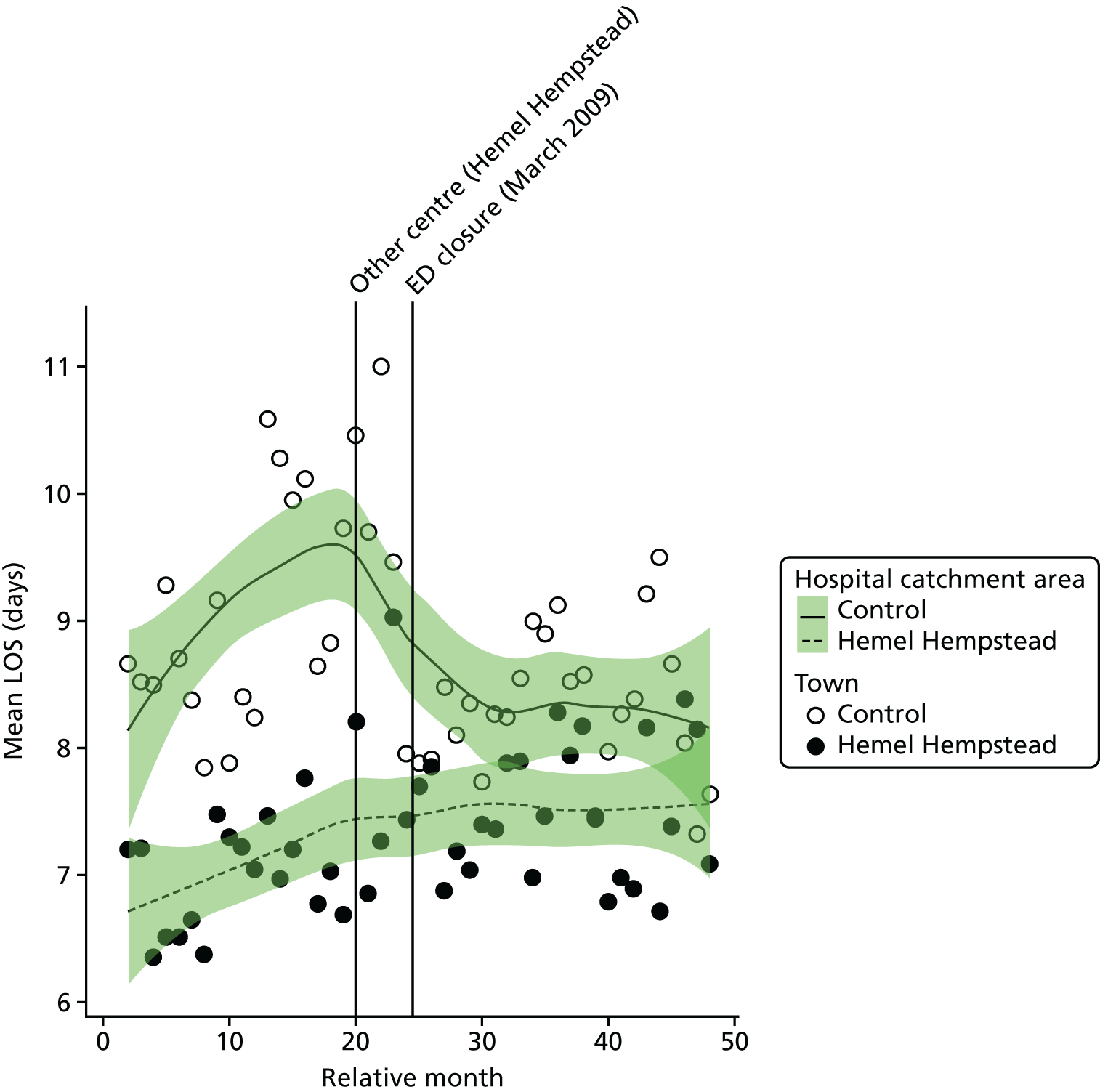
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the mean LOS for residents of the catchment area of HH ED was 0.33 days (95% CI –0.15 to 0.8 days; p = 0.19).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the change in mean length of stay for residents of the catchment area of HH ED at the time of the closure relative to the control site was 0.73 days (95% CI 0.02 to 1.4 days; p = 0.05).
Dose model
Figure 51 shows the mean LOS in hospital for emergency admissions for residents of LSOAs that were expected to have a relatively large change in time to ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HH ED. The pattern of change in these two areas was very similar, with almost no change in the LOS.
FIGURE 51.
Mean LOS in hospital for emergency admissions for residents of areas in Hemel Hempstead that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
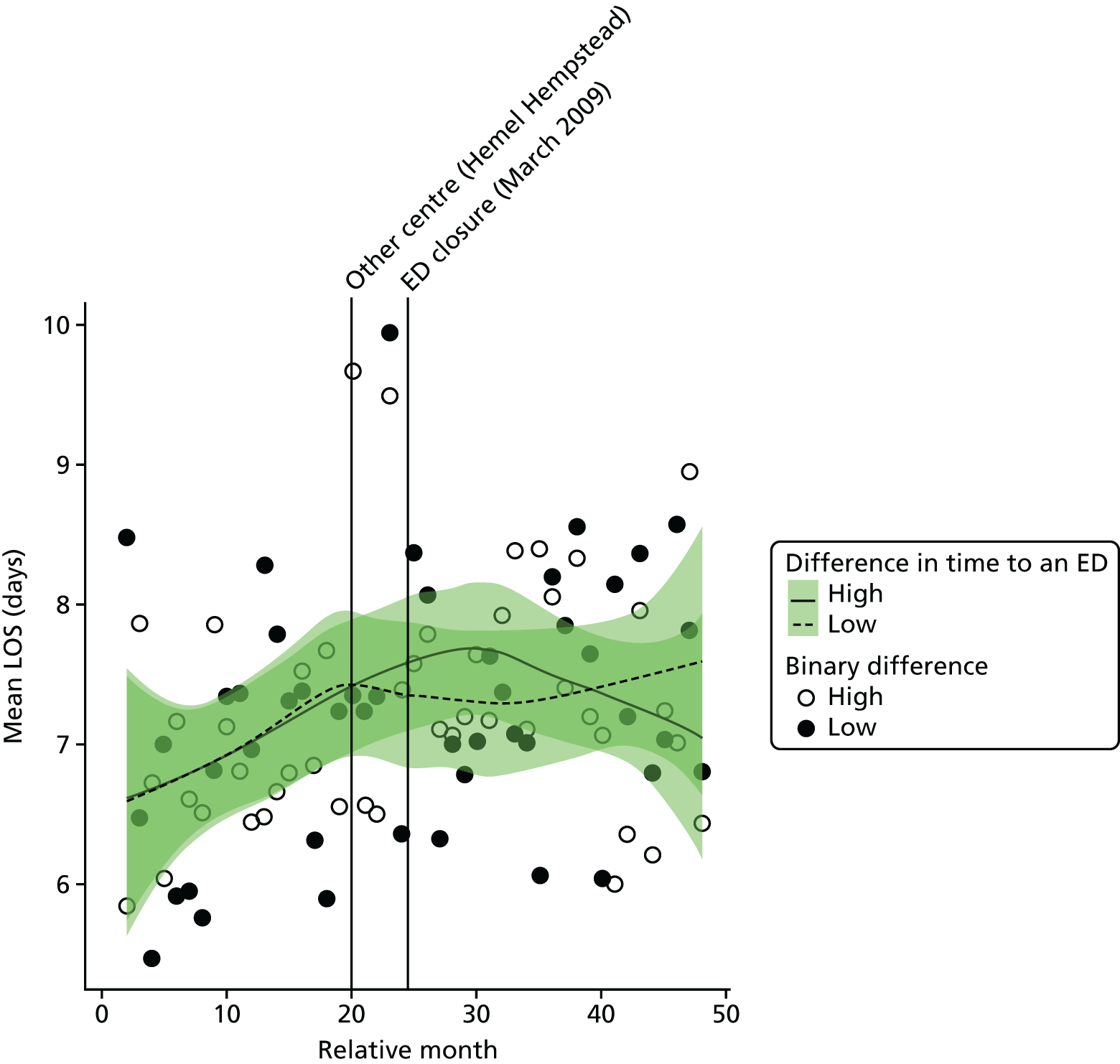
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the mean LOS for residents of high-dose areas was estimated to be –0.05 days (95% CI –0.55 to 0.45 days; p = 0.83).
Deaths
Out-of-hospital deaths from serious emergency conditions
‘Out-of-hospital’ deaths may occur at home prior to making contact with a service, in an ambulance on the way to hospital, in the ED prior to hospital admission or when a patient is recorded as having a SEC incident and is admitted, discharged alive and subsequently dies out of hospital without being readmitted.
Plot of monthly activity
Figure 52 shows the number of out-of-hospital deaths occurring before arrival at hospital from any of the 16 SECs we have focused on among residents of the HH ED catchment area and residents of the control site catchment area in each month of the 4-year study period. There is little indication of any significant change in these numbers. Among residents of the HH catchment area, there were, on average, 29.2 out-of-hospital deaths per month prior to the closure and 28.7 out-of-hospital deaths per month post closure, a reduction of –1.7%. In the control area, the monthly average number of out-of-hospital deaths decreased from 31.5 prior to the closure to 30.0 post closure.
FIGURE 52.
Number of out-of-hospital deaths for SECs for residents of the catchment areas of the Hemel Hempstead ED and the control ED.
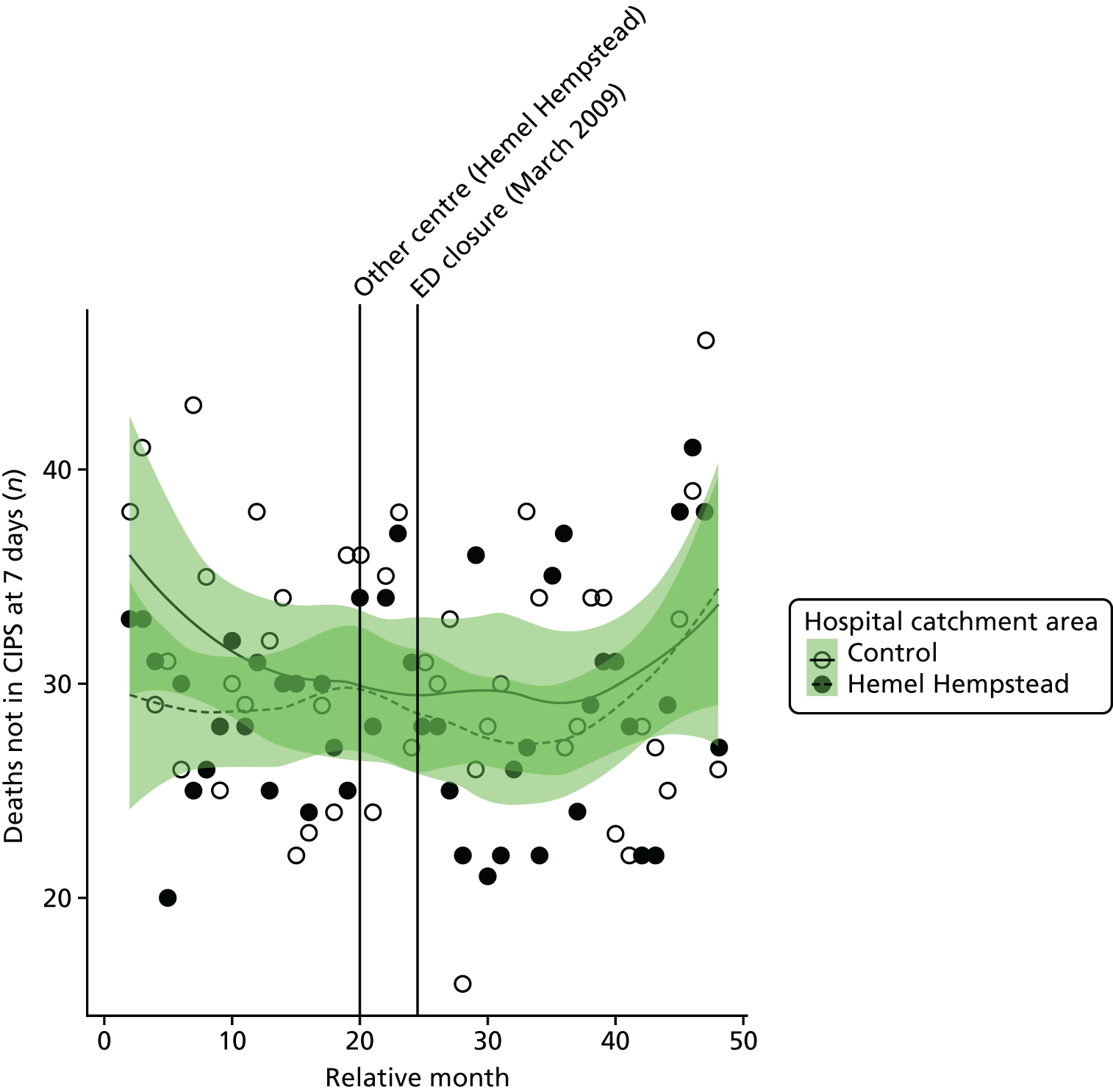
The emergency department closure area model
After allowing for seasonal effects, any long-term trend, and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of out-of-hospital deaths from the 16 SECs for residents of the catchment area of HH ED was –13.8% (95% CI –32.5% to 10.0%; p = 0.23).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, there was no detectable impact on the number of out-of-hospital deaths. The estimated change in the monthly mean number of deaths from emergency conditions occurring before arrival at hospital for residents of the catchment area of HH ED at the time of the closure relative to the control site was –2.4% (95% CI –20.8% to 20.2%; p = 0.82).
Dose model
Figure 53 shows the mean number of out-of-hospital deaths each month made by residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HH ED. The pattern of change in these two areas showed a small increase in high-dose areas, by 6% from an average of 14.0 out-of-hospital deaths per month pre closure to 14.9 out-of-hospital deaths per month post closure, and a small decrease in low-dose areas, by 9% from an average of 15.2 out-of-hospital deaths per month pre closure to 13.8 out-of-hospital deaths per month post closure.
FIGURE 53.
Out-of-hospital deaths from SECs for residents of areas in Hemel Hempstead that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
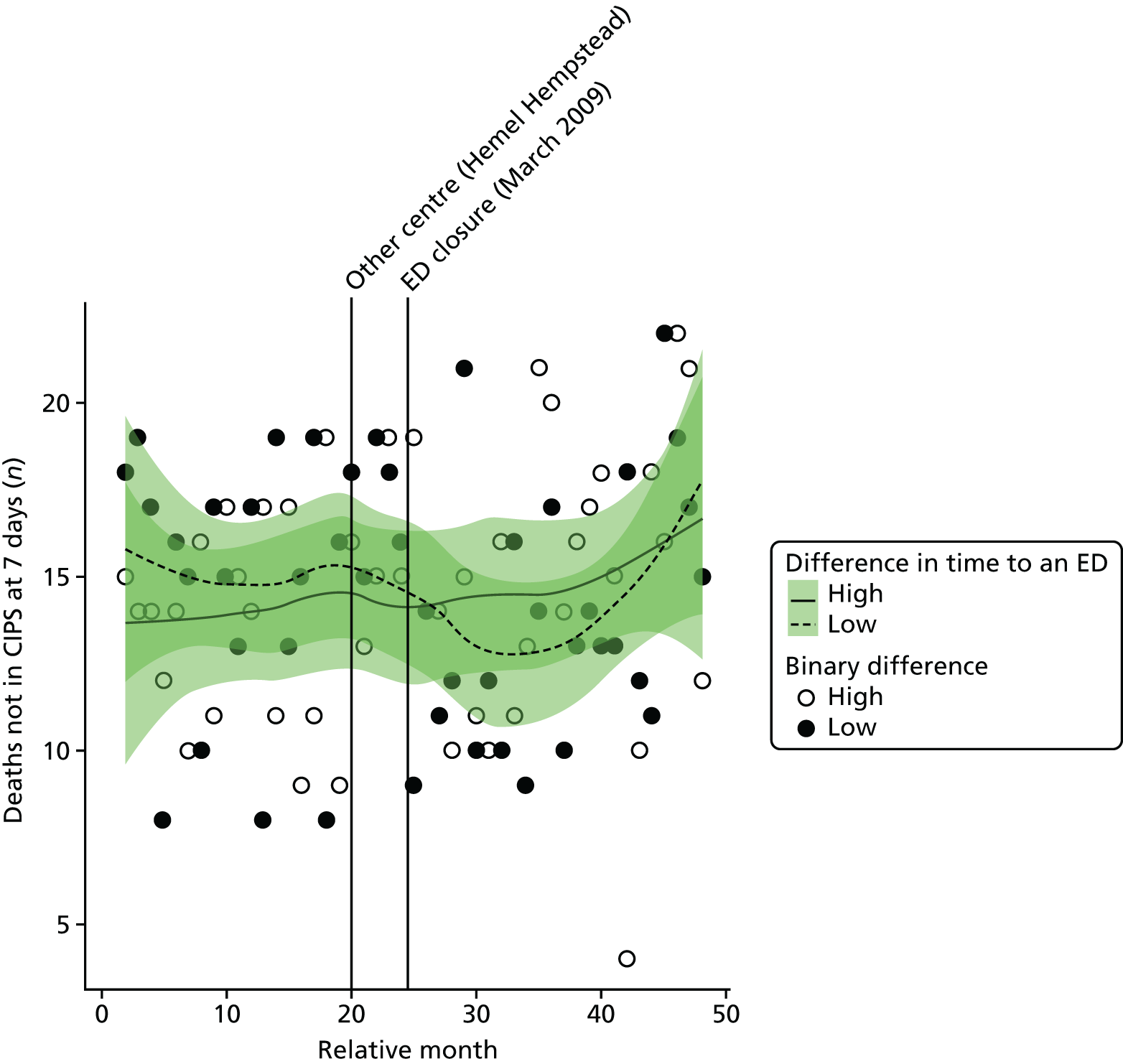
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, there was no reliable evidence of any difference between the areas. The estimated increase in the number of out-of-hospital deaths in high-dose areas compared with low-dose areas was 16.2% (95% CI –6.1% to 43.7%; p = 0.17).
All deaths from serious emergency conditions occurring within 7 days
Plot of monthly activity
Figure 54 shows the total number of deaths occurring up to 7 days post incident from the 16 SECs among residents of the HH ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These deaths may have occurred out of hospital or within 7 days of hospital admission. There is little indication of any significant change in these numbers. There were, on average, 42.3 deaths per month prior to the closure and 40.4 post closure, a reduction of 4.5%. In the control area, the monthly average number of deaths from SECs reduced by 6.4% from 48.6 to 45.5 deaths.
FIGURE 54.
Number of deaths from SECs occurring within 7 days of the incident for residents of the catchment areas of the Hemel Hempstead and control EDs.
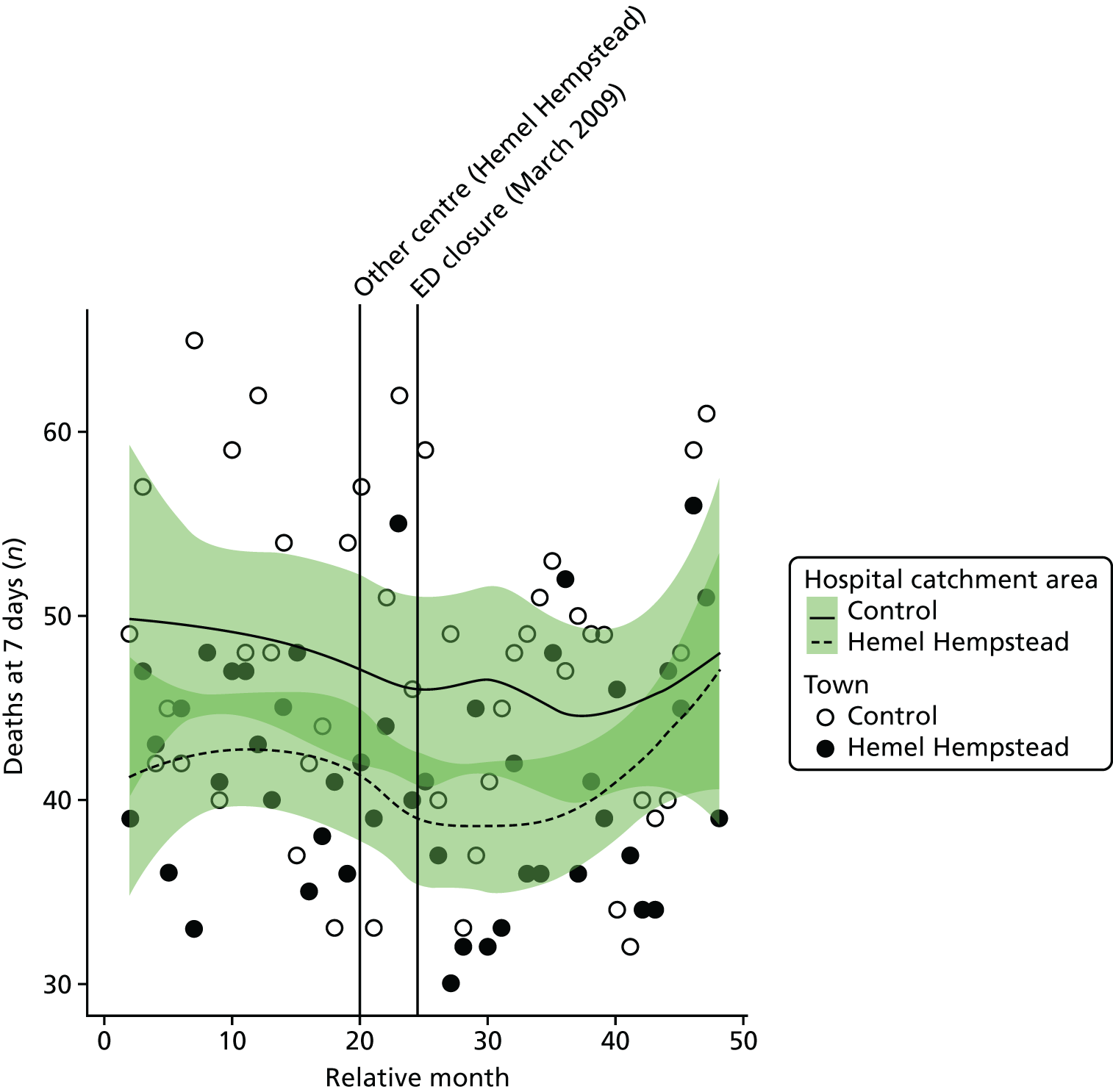
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of deaths from the 16 SECs for residents of the catchment area of HH ED was –9.3% (95% CI –26.2% to 11.5%; p = 0.36).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, there was no detectable effect of the closure on the number of deaths. The estimated change in the monthly mean number of deaths from the 16 emergency conditions occurring up to 7 days post incident for residents of the catchment area of HH ED at the time of closure relative to the control site was 4.0% (95% CI –12.6% to 23.9%; p = 0.66).
Dose model
Figure 55 shows the mean number of deaths occurring up to 7 days post incident each month among residents of the LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HH ED. The pattern of change in these two areas was very similar, with only very small changes in the number of deaths.
FIGURE 55.
Mean number of deaths within 7 days from SECs for residents of areas in Hemel Hempstead that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
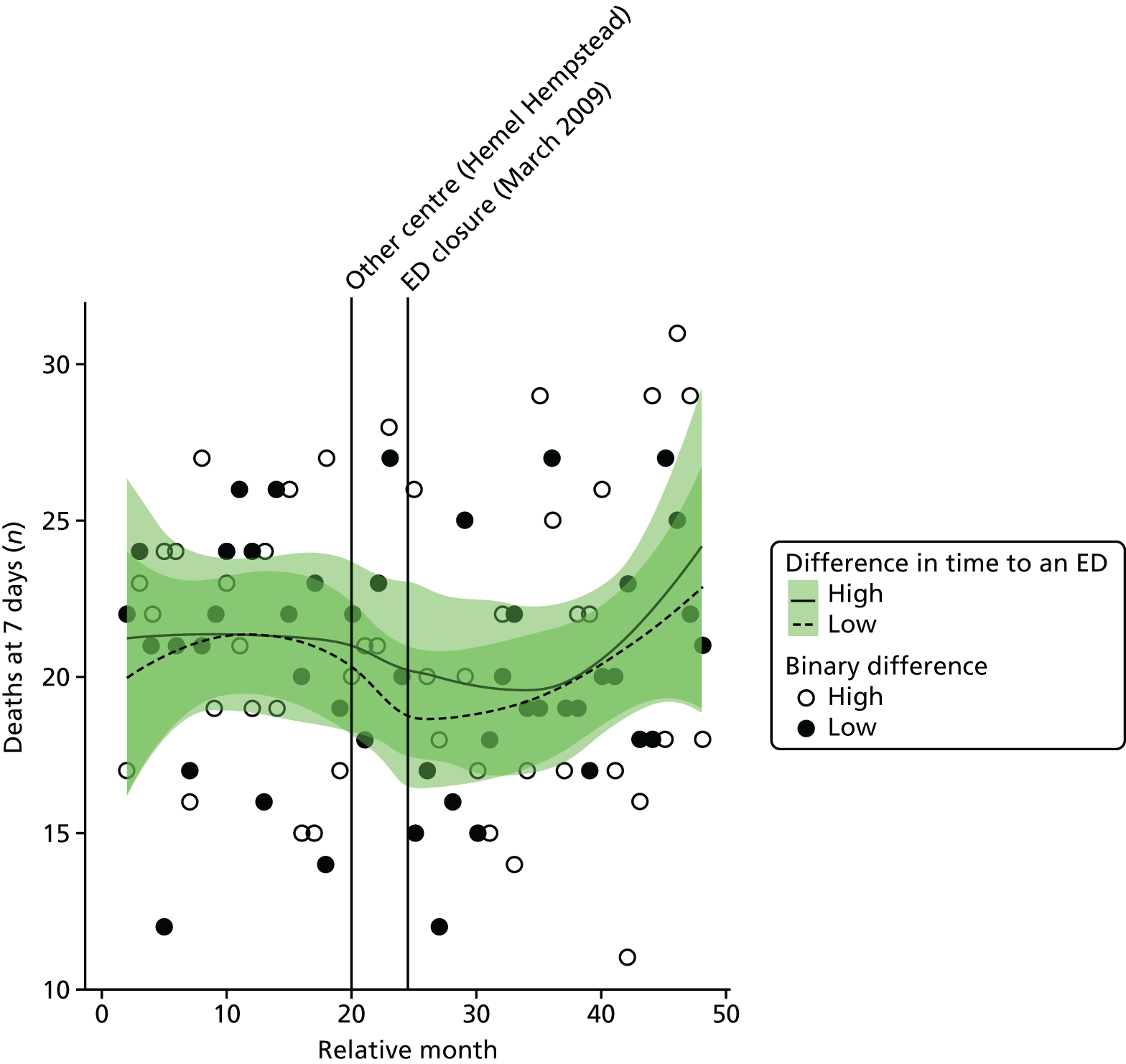
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of deaths from any of the 16 emergency conditions occurring within 7 days of the incident for residents of high-dose areas compared with low-dose areas was 3.6% (95% CI –13.3% to 23.7%; p = 0.70).
Case fatality ratios: all serious emergency conditions studied
Plot of monthly activity
Figure 56 shows the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths plus admissions for patients who survived beyond 7 days from the 16 SECs among residents of the HH ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These ratios reflect the risk of dying from these emergency conditions. There is little indication of any significant change in these ratios. In HH, over the 2 years before the closure, the average ratio was 0.282 (indicating that 28.2% of the patients died) and 0.275 afterwards, a reduction of 0.7 in the percentage of patients who died. In the control site, the average ratio changed from 0.271 to 0.255.
FIGURE 56.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident for residents of the catchment areas of the Hemel Hempstead and control EDs.
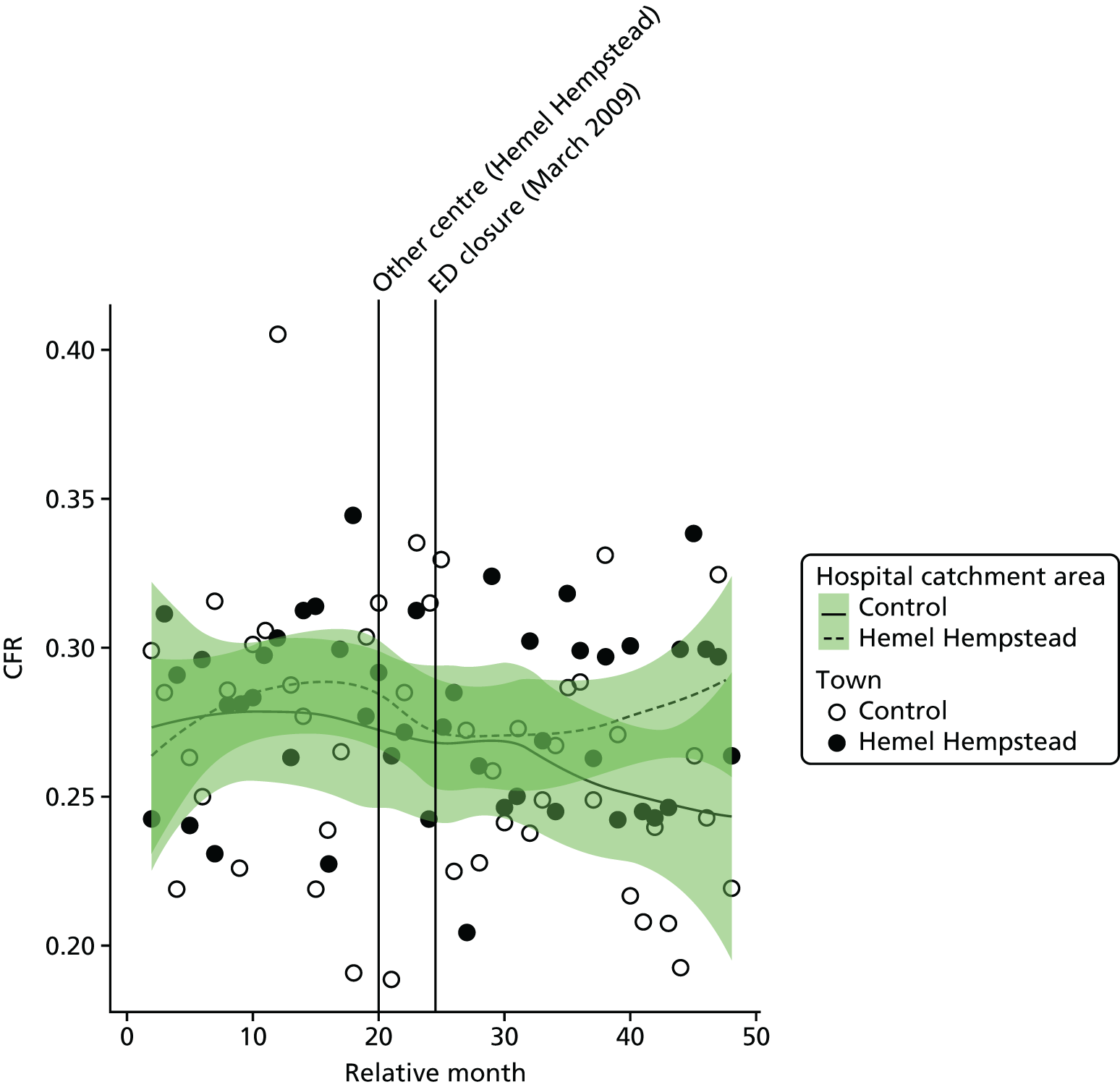
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the CFR for the 16 SECs for residents of the catchment area of HH ED was –0.012 (95% CI –0.043 to –0.019; p = 0.46); this is a reduction of 1.2 in the percentage of patients who died.
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly average CFR for residents of the catchment area of HH ED at the time of the closure relative to the control site was 0.025 (95% CI –0.010 to 0.059; p = 0.17); this is an increase of 2.5 in the percentage of patients who died.
Dose model
Figure 57 shows the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths, plus admissions for patients who survived beyond 7 days each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HH ED. There was little evidence of any significant change in either area.
FIGURE 57.
Case fatality ratio for deaths within 7 days from SECs for residents of areas in Hemel Hempstead that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
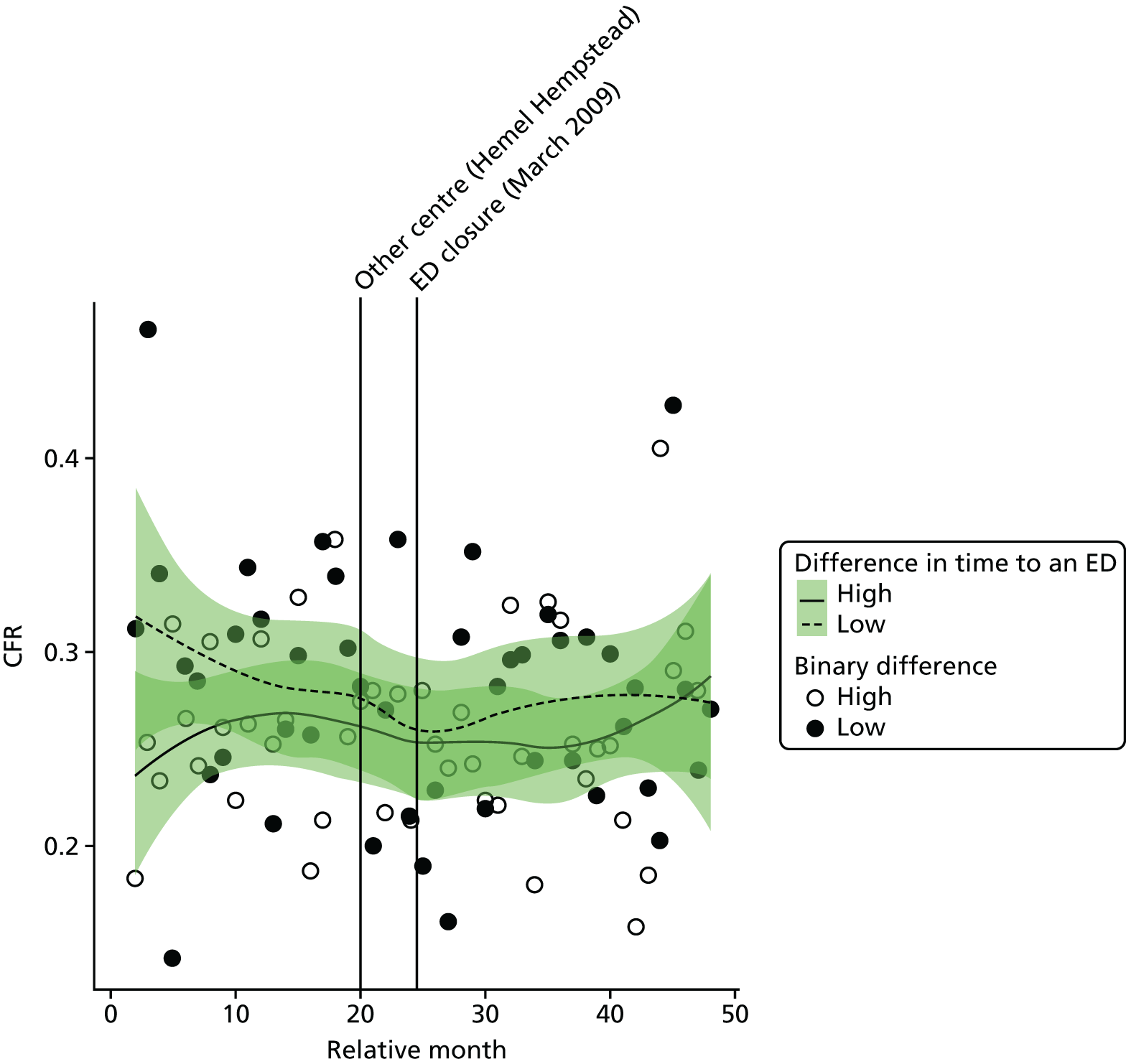
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the CFR for residents of high-dose areas compared with low-dose areas was 0.018 (95% CI –0.024 to 0.060; p = 0.40); this was an estimated increase of 1.8 in the percentage of patients who died.
Case fatality ratios: myocardial infarction and stroke
We have also examined the change in the CFRs for MI and for stroke separately (Tables 33 and 34). There was no evidence that the CFRs had changed for either of these conditions, and there was no evidence of any difference for residents of Hemel Hempstead and its control area, or for residents of high-dose areas of Hemel Hempstead and the low-dose areas.
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Hemel Hempstead | |||
| Low-dose areas | 0.353 (0.179) | 0.411 (0.217) | +5.8 |
| High-dose areas | 0.337 (0.147) | 0.324 (0.168) | –1.4 |
| Total | 0.336 (0.131) | 0.351 (0.105) | +1.5 |
| Control | 0.296 (0.080) | 0.333 (0.104) | +3.7 |
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Hemel Hempstead | |||
| Low-dose areas | 0.386 (0.134) | 0.372 (0.142) | –1.5 |
| High-dose areas | 0.347 (0.123) | 0.309 (0.149) | –3.8 |
| Total | 0.369 (0.087) | 0.340 (0.092) | –2.8 |
| Control | 0.400 (0.124) | 0.352 (0.086) | –4.8 |
Bishop Auckland
The ED at Bishop Auckland General Hospital (BA ED) was closed in October 2009. We have compared the changes in activity and performance of the emergency care system for residents of the catchment area of BA ED over the 2 years before and the 2 years after the closure with changes over the same 4-year period for residents of the catchment area of a control ED.
In the analysis of the impact of the closure of BA ED there was one system change that was accounted for in addition to the closure, and no changes to the control site emergency care system were identified.
Bishop Auckland ED catchment area changes accounted for in the analysis:
-
Introduction of NHS 111 in August 2010.
Control site ED catchment area changes accounted for in the analysis:
-
No other important changes were identified in the control site catchment area.
Summary of findings
Following the closure, for residents of the ED catchment area in Bishop Auckland:
-
There was strong evidence of a large increase in the number of emergency ambulance incidents and some evidence of a large increase in the number of ‘Red’ incidents following the closure of the ED. These increases remained evident when compared with the control area.
-
There was strong evidence of an increase in the length of time from 999 call to arrival at hospital. This increase arose principally from an increase in the time from the scene of the incident to arrival at hospital. However, no comparison could be made with the control area.
-
There was strong evidence of a large decrease in the number of emergency and urgent care attendances. This appeared to be driven by a decrease in the number of those attendances by patients arriving by ambulance. This decrease remained evident when compared with the control area. However, there may be a coding issue with these data.
-
There was strong evidence of a large decrease in the number of minor attendances at emergency and urgent care services. This decrease remained evident when compared with the control area. Again, there may be a coding issue with these data.
-
There was no statistically reliable evidence to suggest a change in the number of emergency hospital admissions.
-
There was some evidence of a large increase in the number of potentially avoidable hospital admissions, but only when compared with the control area.
-
There was some evidence of an increase in LOS for those admitted as an emergency case, which was no longer evident when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of deaths or risk of death from the 16 SECs studied.
In comparing pre- and post-closure journey times to the nearest ED, for those experiencing longer post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of ambulance incidents when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large decrease in both the number of overall emergency and urgent care attendances and the number of minor attendances when compared with those experiencing a smaller change in journey times. However, there may be a coding issue with these data.
-
There was no statistically reliable evidence to suggest a change in emergency hospital admission measures when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the number of deaths or risk of death when compared with those experiencing a smaller change in journey times.
| Impact measure | Model, effect (95% CI); p-value | ||
|---|---|---|---|
| 1: no control | 2: compared with control | 6: high-dose areas | |
| Total number of emergency ambulance incidents | Increase: 42.2% (23.6% to 63.6%); < 0.001 | Increase: 27.9% (17.0% to 39.9%); < 0.001 | Increase: 3.9% (–5.3% to 14.1%); 0.42 |
| Total number of emergency ambulance ‘Red’ incidents | Increase: 19.0% (5.1% to 34.7%); 0.01 | Increase: 14.9% (5.2% to 25.4%); 0.002 | Increase: 5.0% (–5.7% to 14.5%); 0.27 |
| Mean time from 999 ‘Red’ call to arrival at hospital | Increase: 5.7 minutes (3.5 to 7.9 minutes); < 0.001 | No reliable data | Increase: 11.7 minutes (10.5 to 12.8 minutes); < 0.001 |
| Total number of emergency and urgent care attendances | Decrease: –25.7% (–29.4% to –21.8%); < 0.001 | Decrease: –31.1% (–34.8% to –27.3%); < 0.001 | Decrease: –24.6% (–27.4% to –21.7%); < 0.001 |
| Total number of minor attendances at an emergency and urgent care service | Decrease: –51.4% (–60.3% to –40.5%); < 0.001 | Decrease: –40.9% (–50.0% to –30.2%); < 0.001 | Decrease: –35.8% (–44.3% to –26.1%); < 0.001 |
| Total number of emergency hospital admissions | Increase: 4.7% (–2.3% to 12.1%); 0.19 | Increase: 5.2% (–1.6% to 12.5%); 0.13 | Increase: 0.1% (–5.1% to 5.5%); 0.98 |
| Total number of potentially avoidable emergency hospital admissions | Increase: 9.8% (0.3% to 20.1%); 0.04 | Increase: 11.9% (2.7% to 22.0%); 0.01 | Increase: 3.1% (–4.8% to 11.6%); 0.45 |
| Mean LOS for emergency hospital admissions | Increase: 0.8 days (0.3 to 1.3 days); 0.002 | Increase: 0.1 days (–0.3 to 0.5 days); 0.64 | Decrease: –0.4 days (–1.0 to 0.2 days); 0.19 |
| Total number of out-of-hospital deaths | Decrease: –7.0% (–27.6% to 17.9%); 0.55 | Increase: 12.0% (–8.1% to 36.6%); 0.26 | Decrease: –4.2% (–23.4% to 19.8%); 0.71 |
| Total number of deaths occurring within 7 days post incident | Decrease: –12.2% (–28.8% to 8.1%); 0.22 | Increase: 1.3% (–15.2% to 20.9%); 0.89 | Decrease: –12.2% (–27.7% to 6.6%); 0.19 |
| CFR (7 days) | Decrease: –1.9% (–5.3% to 1.4%); 0.27 | Increase: 1.8% (–1.9% to 5.6%); 0.34 | Decrease: –4.8% (–9.2% to 0.5%); 0.03 |
Change in time to the next-nearest emergency department
Following the ED closure, the change in time to reach the next-nearest ED for the residents of the catchment area ranged from 0 to 22 minutes.
FIGURE 58.
Geographical map of Bishop Auckland and the surrounding EDs showing the change in time to the next-nearest ED. Map tiles by Stamen Design, under a Creative Commons Attribution license (CC BY 3.0; see https://creativecommons.org/licenses/by/3.0/). Data by OpenStreetMap, under ODbL. Contains National Statistics data. © Crown copyright and database right 2016. Contains OS data © Crown copyright and database right 2016.
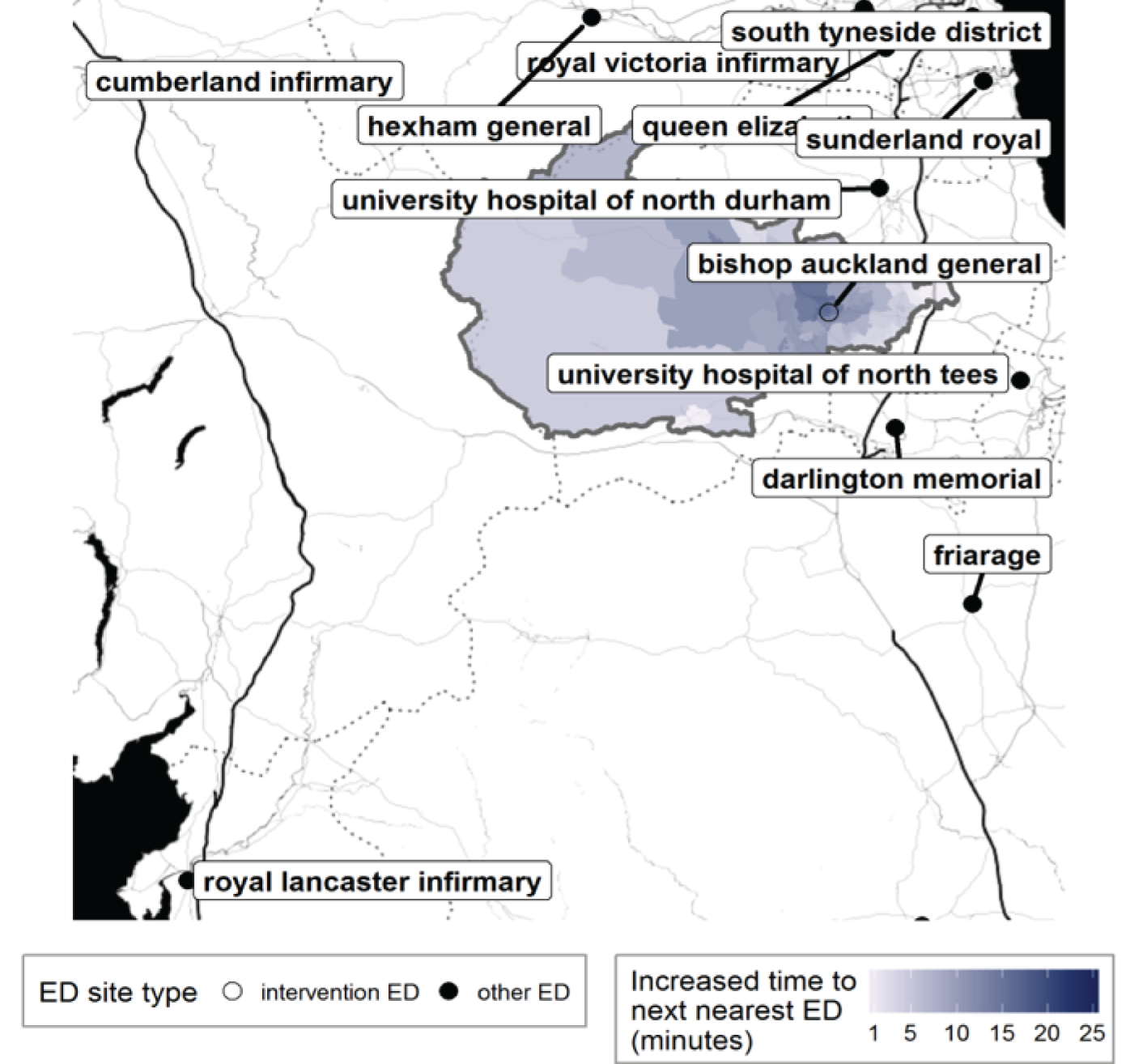
FIGURE 59.
Bishop Auckland: change in time from LSOA to an ED following ED closure, for residents of the catchment area of Bishop Auckland Hospital ED.
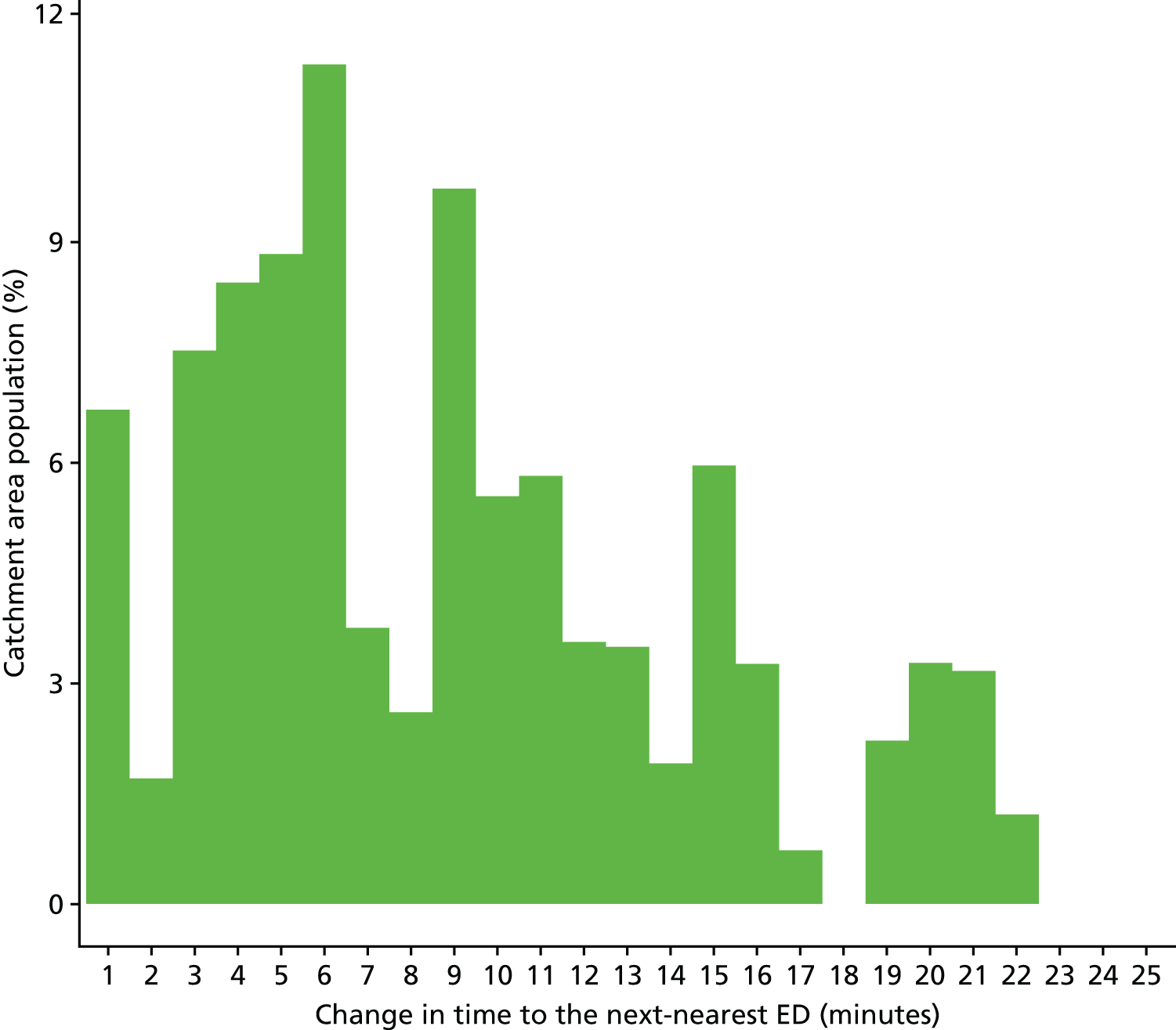
Findings from individual activity and performance measures
Ambulance service performance
Total number of incidents following 999 calls to the ambulance service
Plot of monthly activity
Figure 60 shows the total number of 999 incidents referred to the ambulance service from residents of the BA ED catchment area, and the control area, for each month over the 2 years prior to the closure of the BA ED and the 2 years after. There was an increase in the number of incidents in both areas. Incidents went up by 37% from an average of 1189 per month pre closure to 1624 per month post closure in the BA ED catchment area, and by 16% from 842 per month pre closure to 980 per month post closure in the control area.
FIGURE 60.
Total number of 999 incidents among residents of the Bishop Auckland ED catchment area and control area.
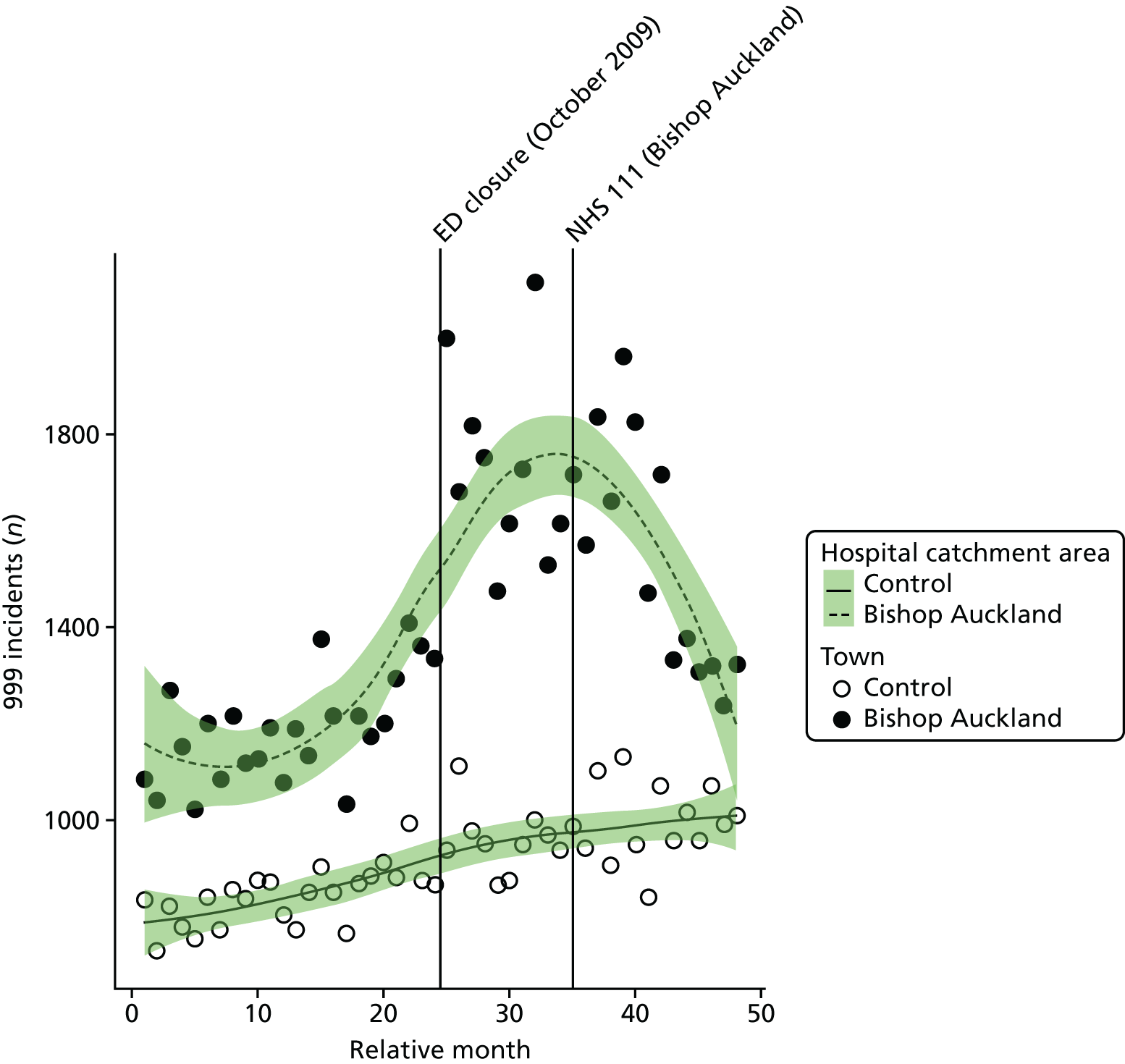
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of incidents each month for residents of the BA ED catchment area increased at the time of the closure by an average of 42.2% (95% CI 23.6% to 63.6%; p < 0.001).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of incidents each month for residents of the BA ED catchment area increased relative to the control area by an average of 27.9% (95% CI 17.0% to 39.9%; p < 0.001).
Dose model
Figure 61 shows the mean number of incidents each month made among residents of LSOAs that were expected to have a relatively large change in time to ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of BA ED. In high-dose areas, the number of incidents increased by 39% from 660 pre closure to 917 post closure, and in low-dose areas by 33% from 529 pre closure to 707 post closure.
FIGURE 61.
Mean number of 999 incidents among residents of areas in Bishop Auckland that were expected to have a large change in time to an ED (high dose) and a those expected to have a small change (low dose).
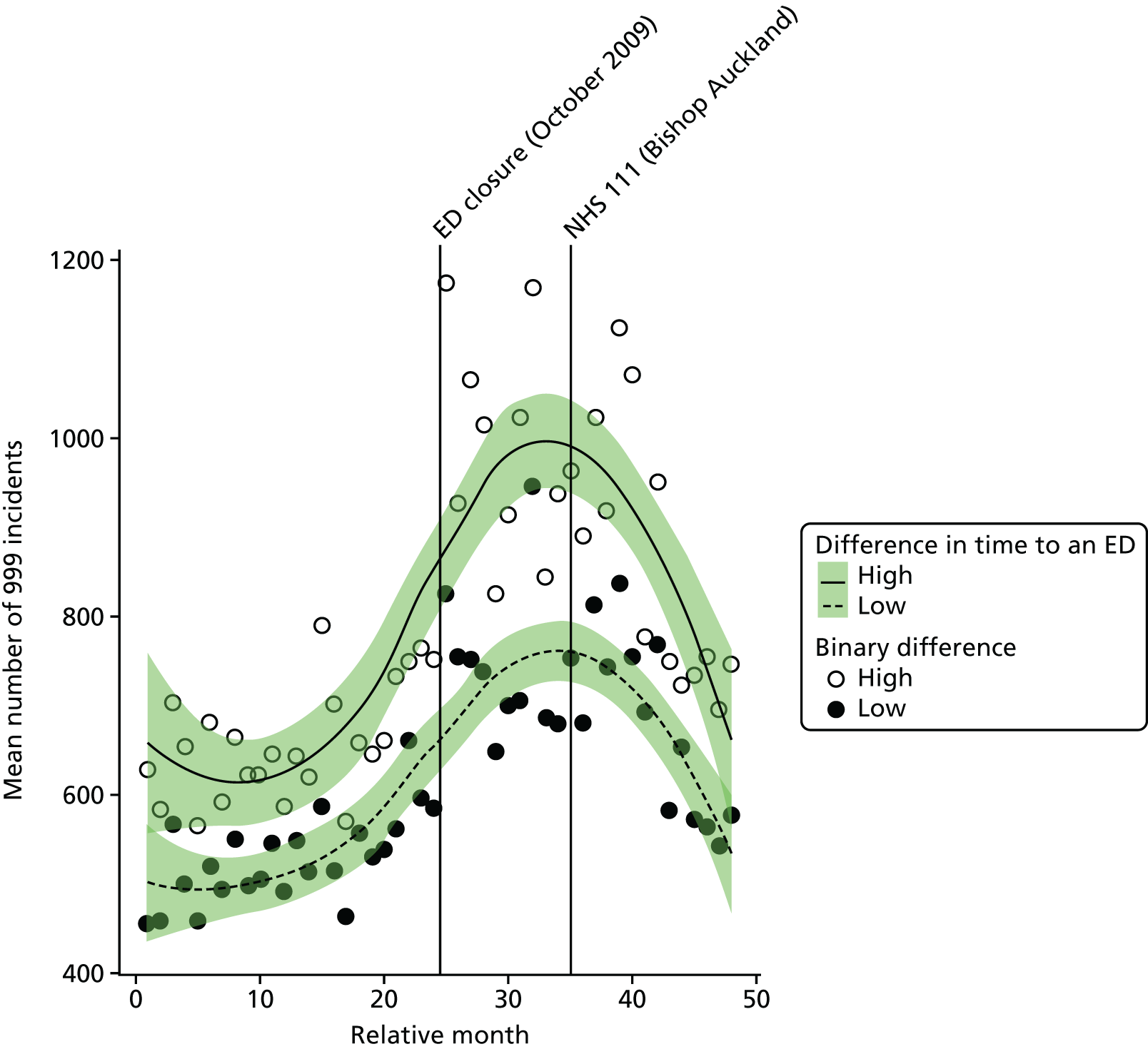
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, there was an increase in the number of incidents in high-dose areas relative to low-dose areas at the time of closure of 3.9% (95% CI –5.3% to 14.1%; p = 0.42).
Number of emergency ambulance ‘Red’ incidents
Plot of monthly activity
Figure 62 shows the number of ‘Red’ 999 incidents referred to the ambulance service from residents of the BA ED catchment area, and the control area, for each month over the 2 years prior to and the 2 years after the closure of the BA ED. There was a clear increase in the number of ‘Red’ incidents in both areas. Incidents increased by 43% from an average of 384 per month pre closure to 547 per month post closure in the BA ED catchment area, and by 31% from 328 pre closure to 429 post closure in the control area.
FIGURE 62.
Number of ‘Red’ 999 incidents among residents of the Bishop Auckland ED catchment area and control area.
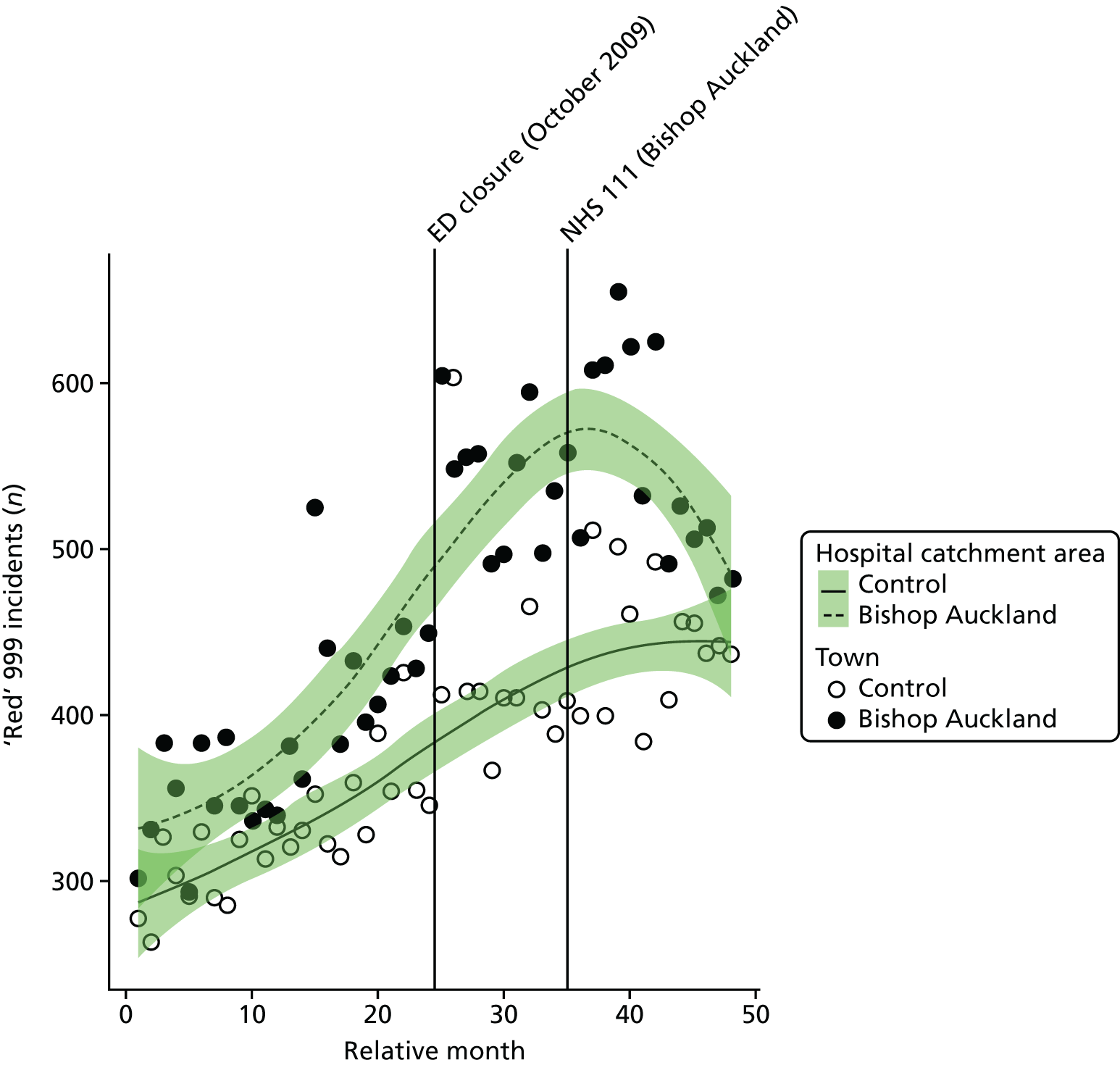
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of ‘Red’ incidents each month for residents of the BA ED catchment area increased at the time of the closure by an average of 19% (95% CI 5.1% to 34.7%; p = 0.01).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of ‘Red’ incidents each month for residents of the BA ED catchment area increased relative to the control area by an average of 14.9% (95% CI 5.2% to 25.4%; p = 0.002).
Dose model
Figure 63 shows the mean number of ‘Red’ incidents each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the BA ED. The pattern of change in these two areas is similar, with both showing a large increase. In high-dose areas, the number of ‘Red’ incidents increased by 46% from 209 pre closure to 305 post closure, and in low-dose areas by 39% from 175 pre closure to 243 post closure.
FIGURE 63.
Mean number of ‘Red’ 999 incidents for residents of areas in Bishop Auckland that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
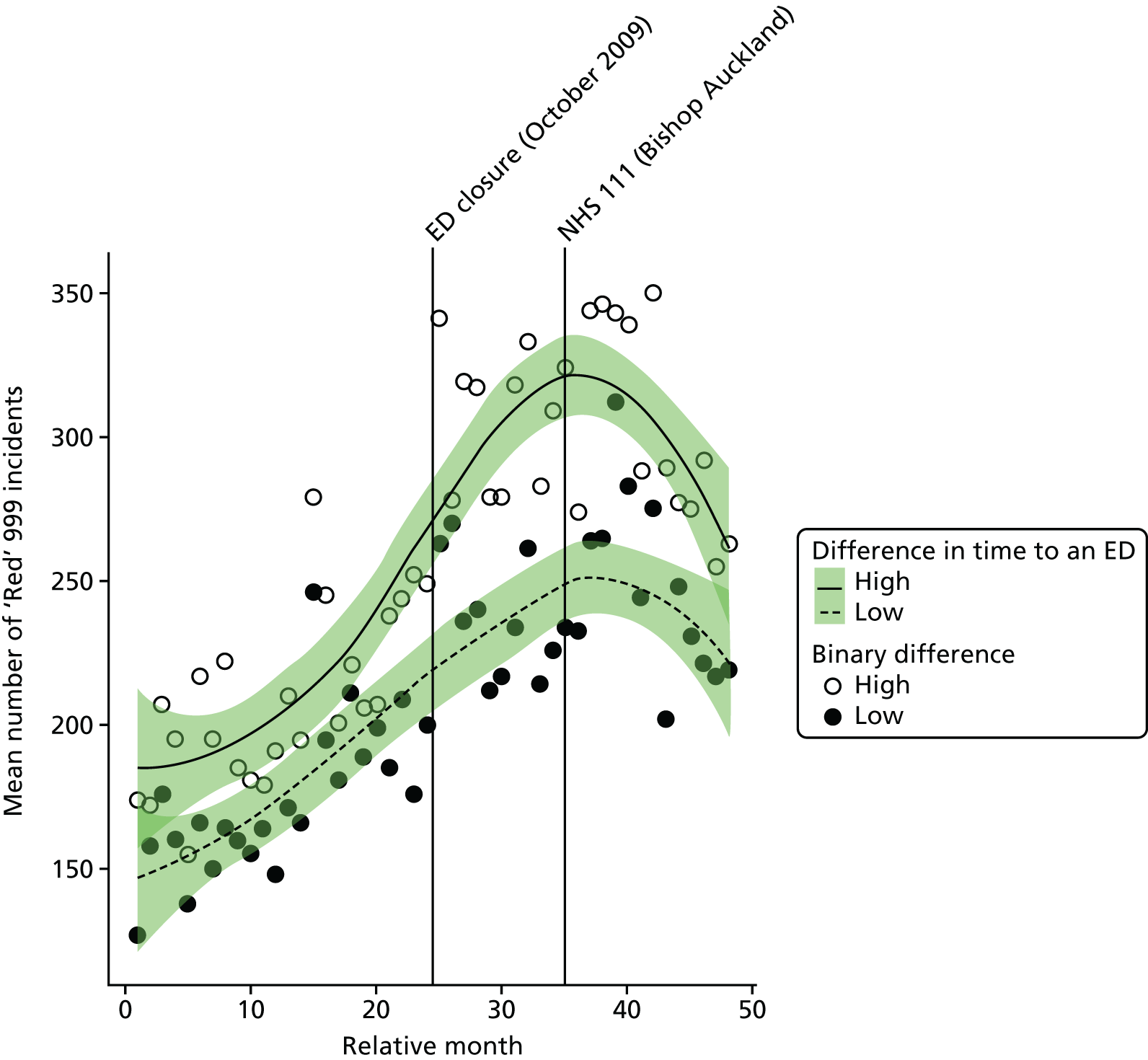
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the number of ‘Red’ incidents in high-dose areas relative to low-dose areas at the time of closure was 5.0% (95% CI –5.7% to 14.5%; p = 0.27).
Mean time from 999 call to arrival at hospital for ‘Red’ incidents
Plot of monthly performance
Figure 64 shows, for 999 ‘Red’ incidents, the mean time from call to arrival at hospital in each month over the 2 years prior to and the 2 years after the closure of the BA ED for residents of the BA ED catchment area and the control area. There was a clear increase in these times for residents of the BA ED catchment area from before the closure (monthly mean 42.3 minutes) to after the closure (monthly mean 55.0 minutes), an increase of 12.7 minutes on average. There were an insufficient number of data from the pre-closure period in the control area to make any useful comparison.
FIGURE 64.
Mean time from 999 ‘Red’ call to arrival at hospital for residents of the Bishop Auckland ED catchment area and the control area.
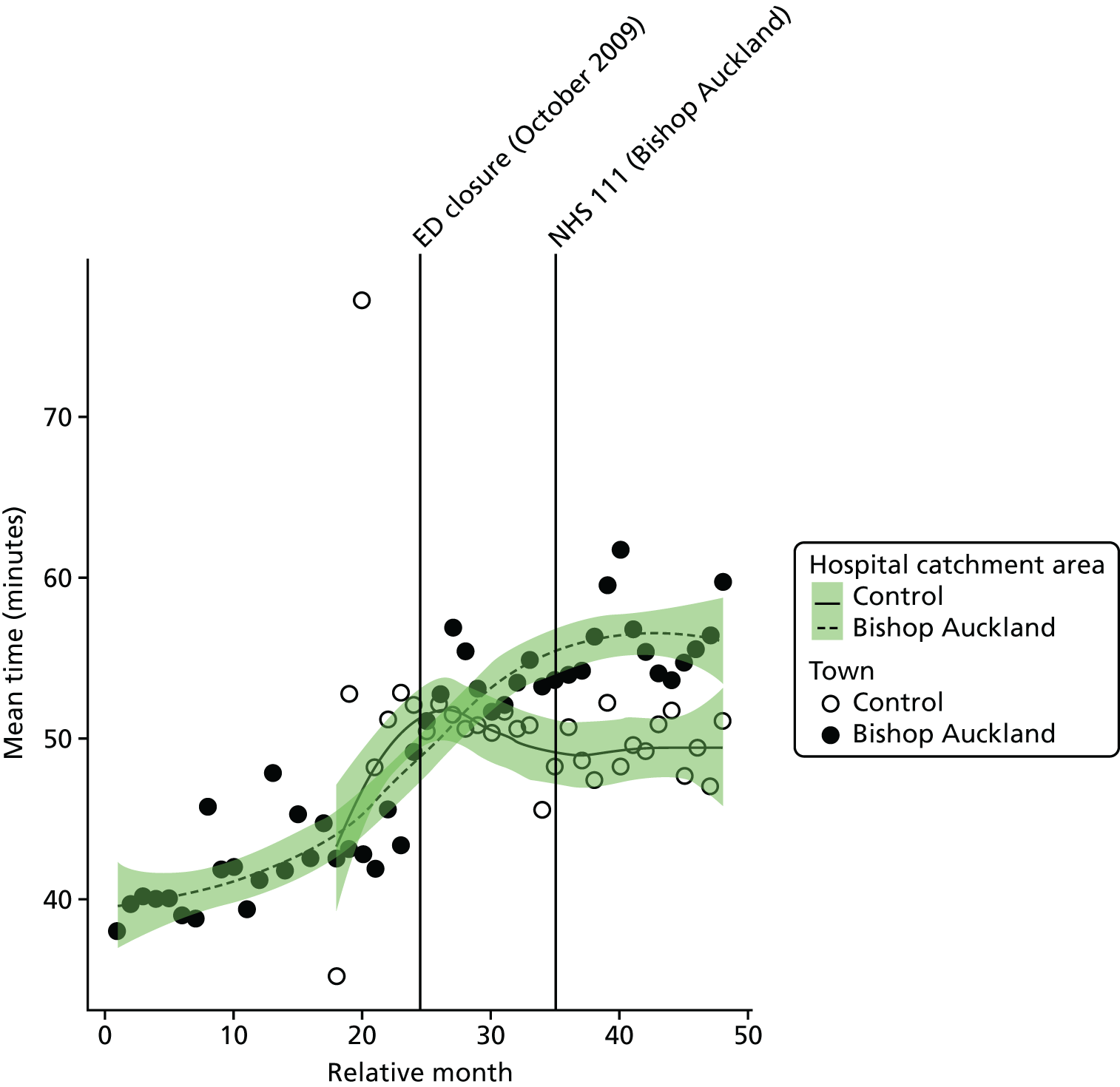
Examining the component times, it is clear that this increase arose principally from an increase in the time from the scene of the incident to arrival the hospital, not in the time from call to arrival at the scene. The mean time from call to arrival at hospital increased by 2.6 minutes after the closure, but the time from the scene of the incident to arrival at hospital increased by 10.0 minutes after the closure.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated mean time from call to hospital for 999 callers in the BA ED catchment area increased at the time of the closure by an average of 5.7 minutes (95% CI 3.5 to 7.9 minutes; p < 0.001), which is a 13.4% increase compared with the months before the closure.
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated post-closure increase from the call to arrival at the scene was 0.6 minutes, and the increase from the scene to arrival at the hospital was estimated to be 5.3 minutes.
The emergency department closure and control area model
Because no useable control site data on times could be obtained, no comparison with a control area has been made.
Dose model
Figure 65 shows the mean time from the scene of the incident to arrival at hospital for ‘Red’ incidents each month for residents of LSOAs that were expected to have a relatively large change in time to ED (high-dose areas) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of BA ED. As expected, the pattern of change in these two areas was different. High-dose LSOAs had a post-closure increase in mean time from the incident scene to arrival at hospital of 18.0 minutes, compared with an increase of 7.1 minutes in the low-dose areas. The increase seen in high-dose areas took place in the time from the incident scene to arrival at hospital (14.4 minutes) rather than in the time from the call to arrival at the scene (3.3 minutes).
FIGURE 65.
Mean time from scene of incident to arrival at hospital for ‘Red’ incidents for residents of areas in Bishop Auckland that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
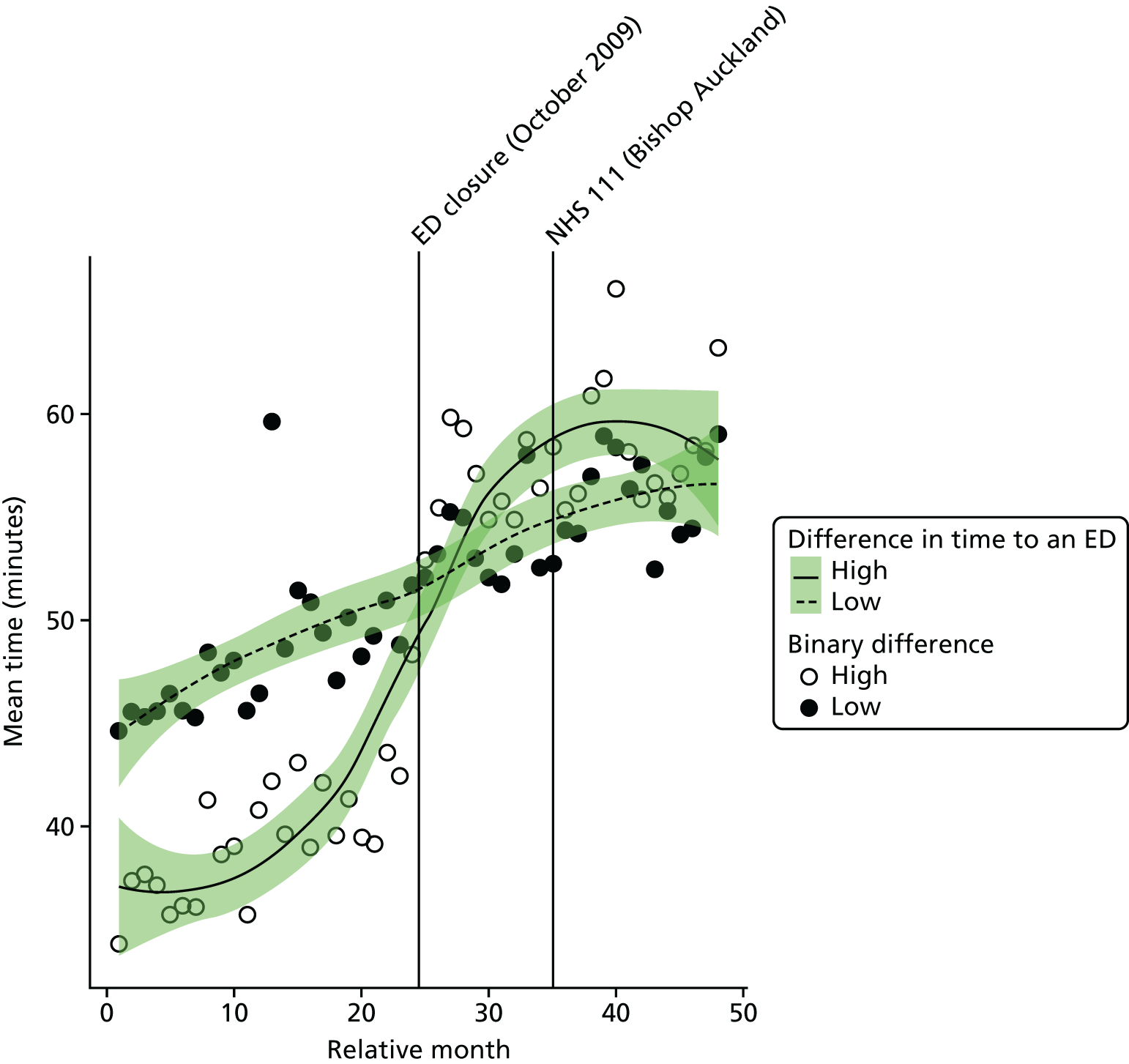
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in time from call to hospital for residents of high-dose areas was estimated to be an additional 11.7 minutes (95% CI 10.5 to 12.8 minutes; p < 0.001).
Emergency and urgent care attendances
Total number of emergency and urgent care attendances
Plot of monthly activity
Figure 66 shows the number of attendances at an ED (inclusive of A&E types 1–4 and attendances coded as ‘unknown’) among residents of the BA ED catchment area, and the control area, in each month over the 2 years prior to and the 2 years after the closure of the BA ED. There was a clear decrease in the number of attendances in BA. The number of attendances reduced by 22%, from an average of 3018 per month pre closure to 2345 per month post closure in the BA ED catchment area. In contrast, attendances rose by 15% from 2281 per month pre closure to 2612 post closure in the control area.
FIGURE 66.
Number of emergency and urgent care attendances among residents of the Bishop Auckland ED catchment area and the control area.
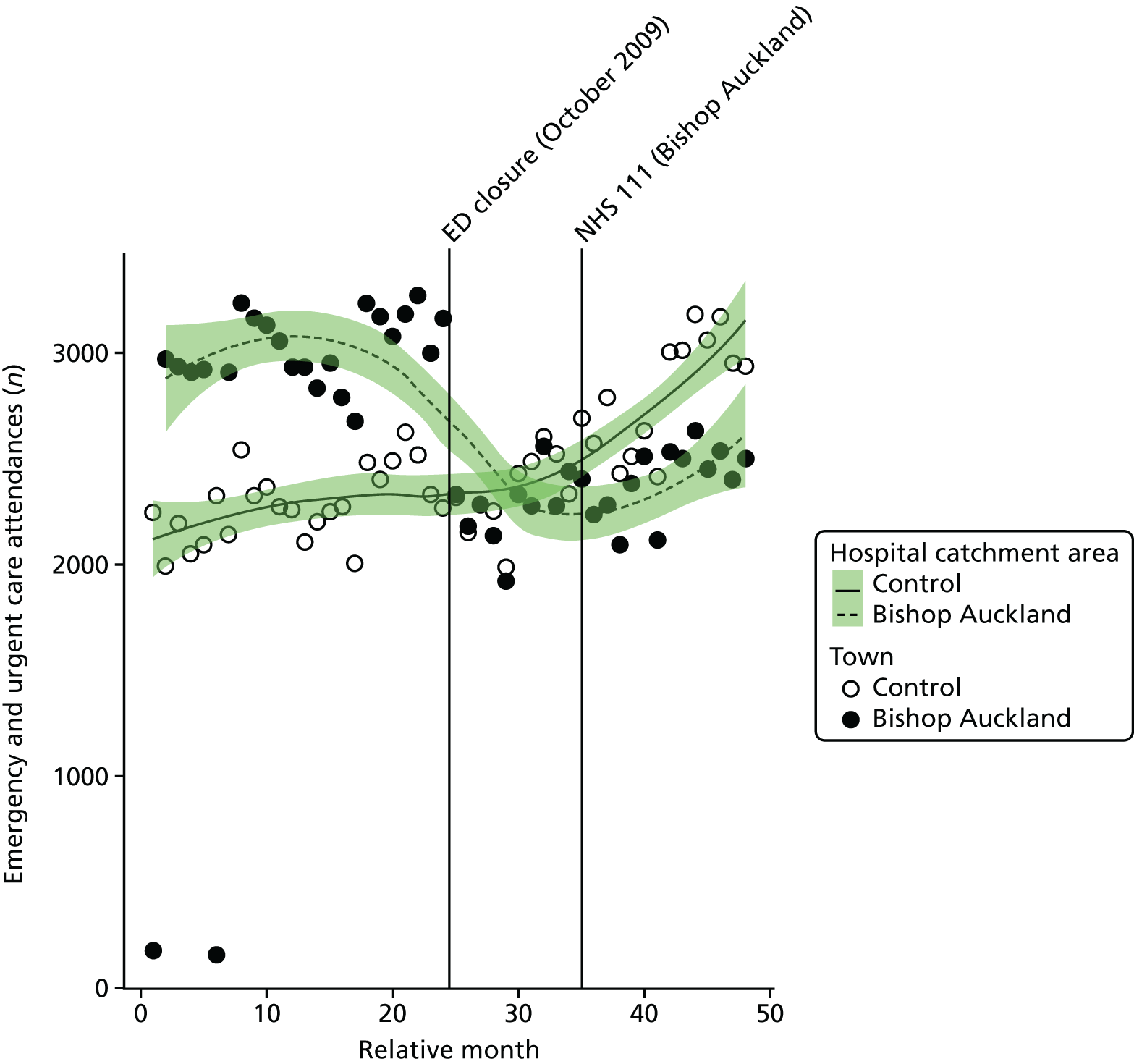
Examining the mode of arrival at the ED, it appears that the decrease in the number of attendances was only in attendances by patients arriving by ambulance, not by walk-in patients. The number of recorded ambulance attendances decreased by 1205 per month on average, but the number of recorded walk-in attendances increased by an average of 525 per month. In fact, examination of the data shows that it is possible that there has been some change in recording practice because the numbers of walk-in attendances show a sudden and unexplained rise in the last 9 months of the analysis period. However, even in the first year post closure, there was a small rise in the number of walk-in attendances; this was in clear contrast to the reduction in the recorded numbers of ambulance attenders.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of attendances each month for residents of the BA ED catchment area reduced at the time of the closure by an average of –25.7% (95% CI –29.4% to –21.8%; p < 0.001).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of emergency and urgent care attendances each month for residents of the BA ED catchment area changed relative to the control area by an average of –31.1% (95% CI –34.8% to –27.3%; p < 0.001).
Dose model
Figure 67 shows the mean number of attendances each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of BA ED. The pattern of change in these two areas was different, with a 32% decrease in the number of attendances among residents of high-dose areas from 1651 pre closure to 1118 post closure per month, and a smaller decrease of 10% from 1367 pre closure to 1227 post closure for low-dose areas
FIGURE 67.
Mean number of emergency and urgent care attendances among residents of areas in Bishop Auckland that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
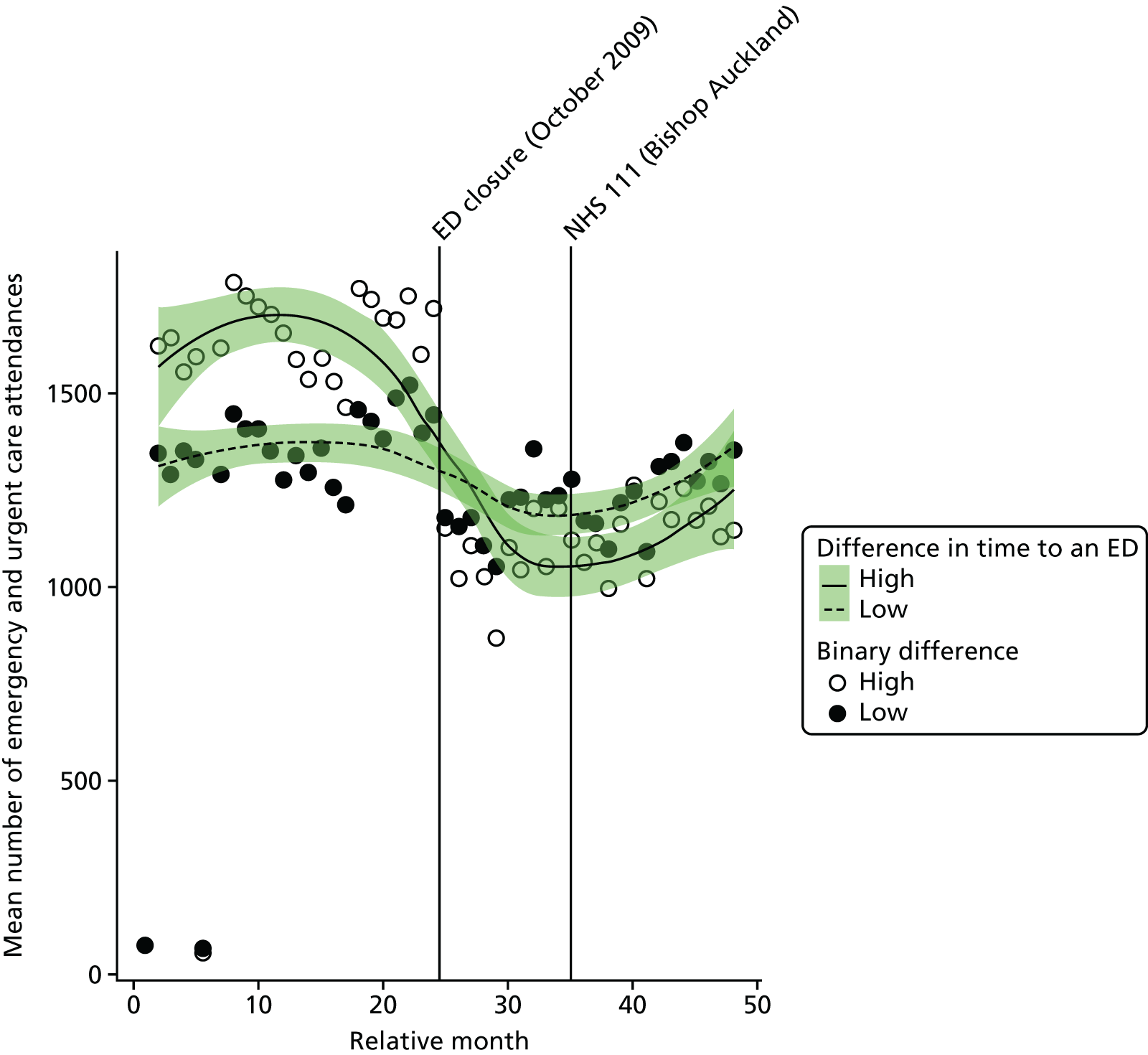
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the estimated number of emergency and urgent care attendances in high-dose areas compared with low-dose areas was –24.6% (95% CI –27.4% to –21.7%; p < 0.001).
Minor attendances at an emergency or urgent care service
Plot of monthly activity
We have examined the impact of the ED closure on the number of ‘minor’ attendances among patients who were discharged home without having had any treatment or investigation that needed attendance at hospital. Figure 68 shows the monthly number of these minor attendances among residents of the BA ED catchment area and the control area over the 2 years before and 2 years after the closure.
FIGURE 68.
Number of minor attendances at an emergency or urgent care service among residents of the Bishop Auckland ED catchment area and the control area.
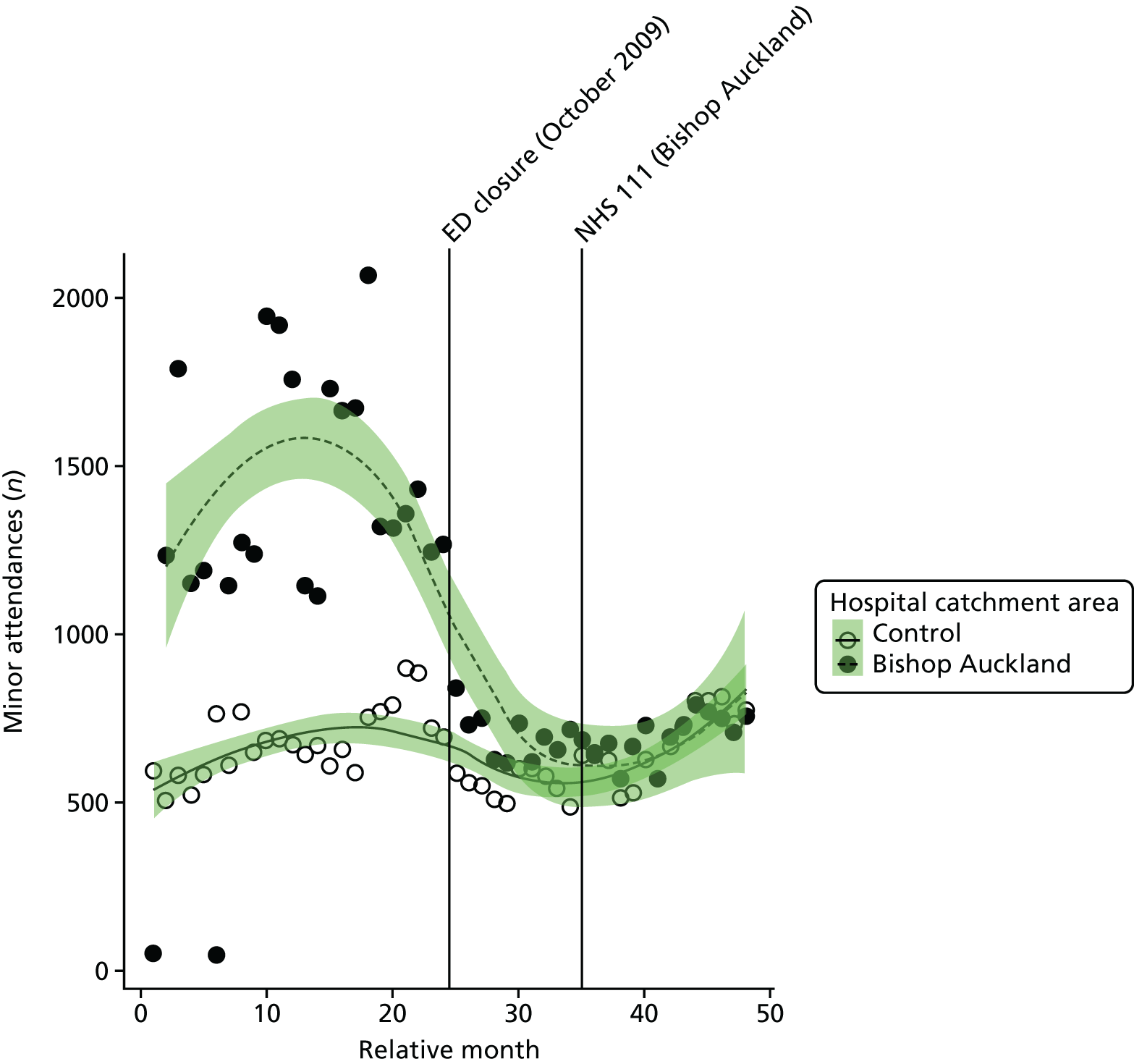
There was a clear decrease in the number of minor attendances among residents of BA. The number of minor attendances decreased by 52%, from an average of 1452 per month pre closure to 697 per month post closure in the BA ED catchment area. In contrast, minor attendances fell by only 8% from 678 per month pre closure to 623 post closure in the control area.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of minor attendances each month among residents of the BA ED catchment area changed at the time of the closure by an average of –51.4% (95% CI –60.3% to –40.5%; p < 0.001).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of minor emergency and urgent care attendances each month among residents of the BA ED catchment area changed relative to the control area by an average of –40.9% (95% CI –50.0% to –30.2%; p < 0.001).
Dose model
Figure 69 shows the mean number of minor emergency and urgent care attendances each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the BA ED. The pattern of change in these two areas showed a 61% decrease in the number of attendances for residents of high-dose areas from 829 per month pre closure to 320 per month post closure, and there was a smaller decrease of 40% from 622 per month pre closure to 377 per month post closure for low-dose areas.
FIGURE 69.
Mean number of minor attendances at an emergency or urgent care service among residents of areas in Bishop Auckland that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
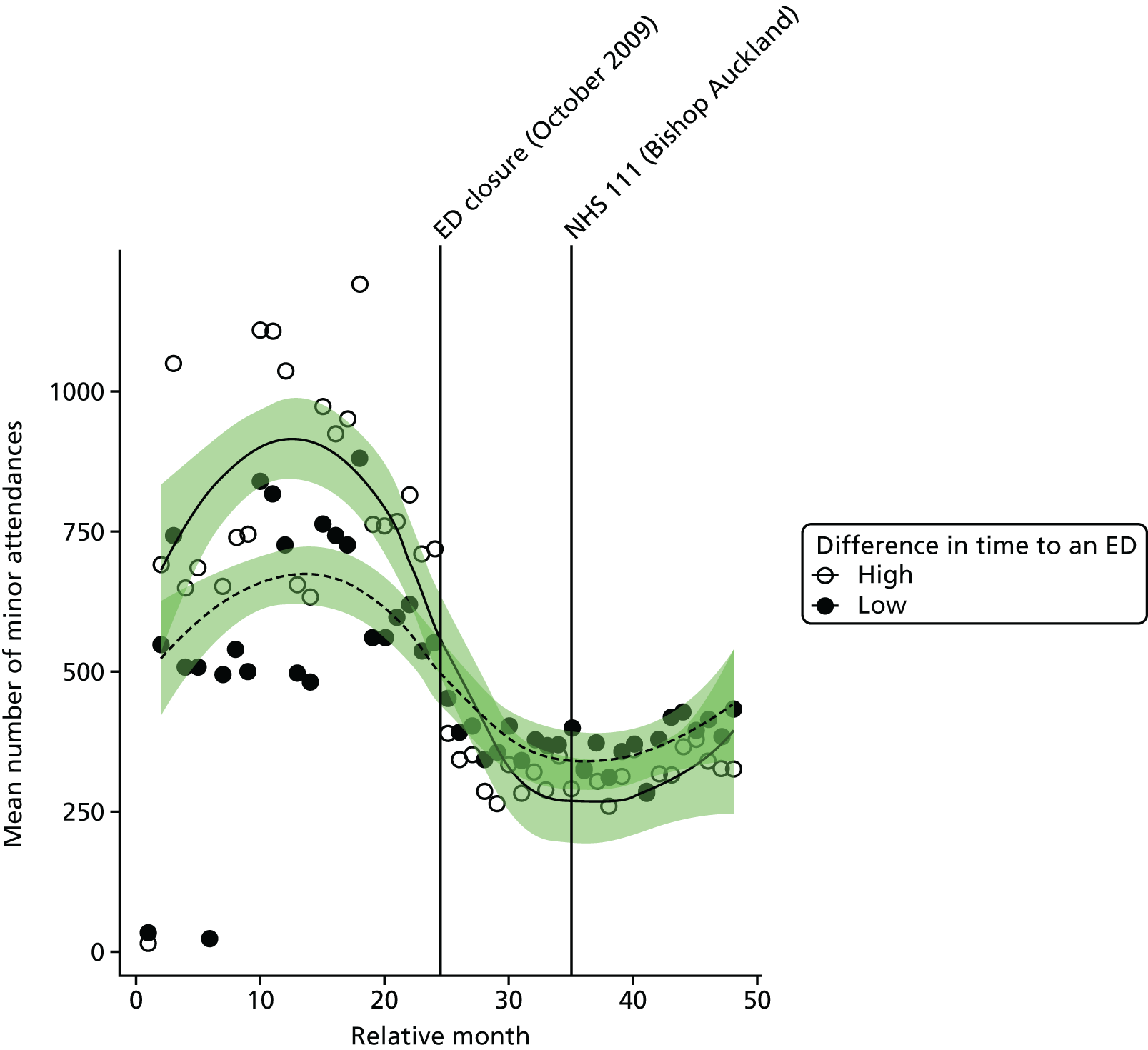
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of minor emergency and urgent care attendances in high-dose areas compared with low-dose areas was –35.8% (95% CI –44.3% to –26.1%; p < 0.001).
Admissions
All emergency admissions
Plot of monthly activity
Figure 70 shows the total number of emergency admissions to any hospital by residents of the BA ED catchment area and by residents of the control site catchment area in each month of the 4-year study period.
FIGURE 70.
Total number of emergency admissions among residents of the Bishop Auckland ED catchment area and the control catchment area.
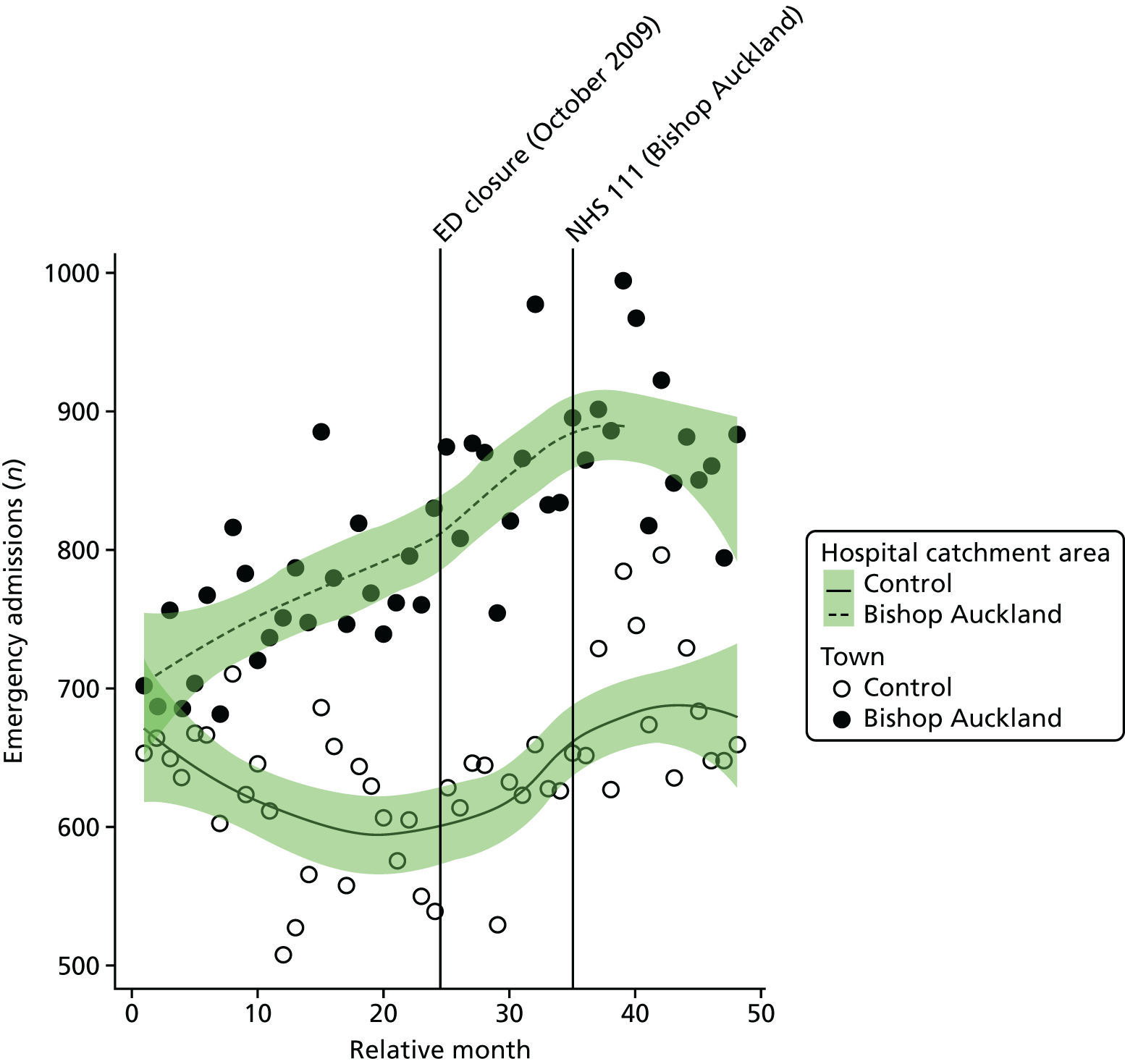
In BA, there were, on average, 758 emergency admissions per month prior to the closure and 870 post closure, an increase of 14.7%, but Figure 70 suggests that this reflected a steady increase during the study period. The control area also saw a small change over the period, increasing by 7.5% from 615 emergency admissions pre closure to 662 emergency admissions post closure.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend, and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of emergency admissions for residents of the catchment area of BA ED was 4.7% (95% CI –2.3% to 12.1%; p = 0.19).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly mean number of emergency admissions for residents of the catchment area of BA ED at the time of the closure relative to the control site was 5.2% (95% CI –1.6% to 12.5%; p = 0.13).
Dose model
Figure 71 shows the mean number of emergency admissions each month for residents of LSOAs that were expected to have a relatively large change in time to ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the BA ED. The pattern of change in these two areas was very similar, with a small increase of 14% in high-dose areas from 395 emergency admissions pre closure to 451 emergency admissions post closure per month, and there was also a 14% increase from 363 emergency admissions pre closure to 415 emergency admissions post closure per month in low-dose areas.
FIGURE 71.
Mean total number of emergency admissions among residents of areas of Bishop Auckland that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
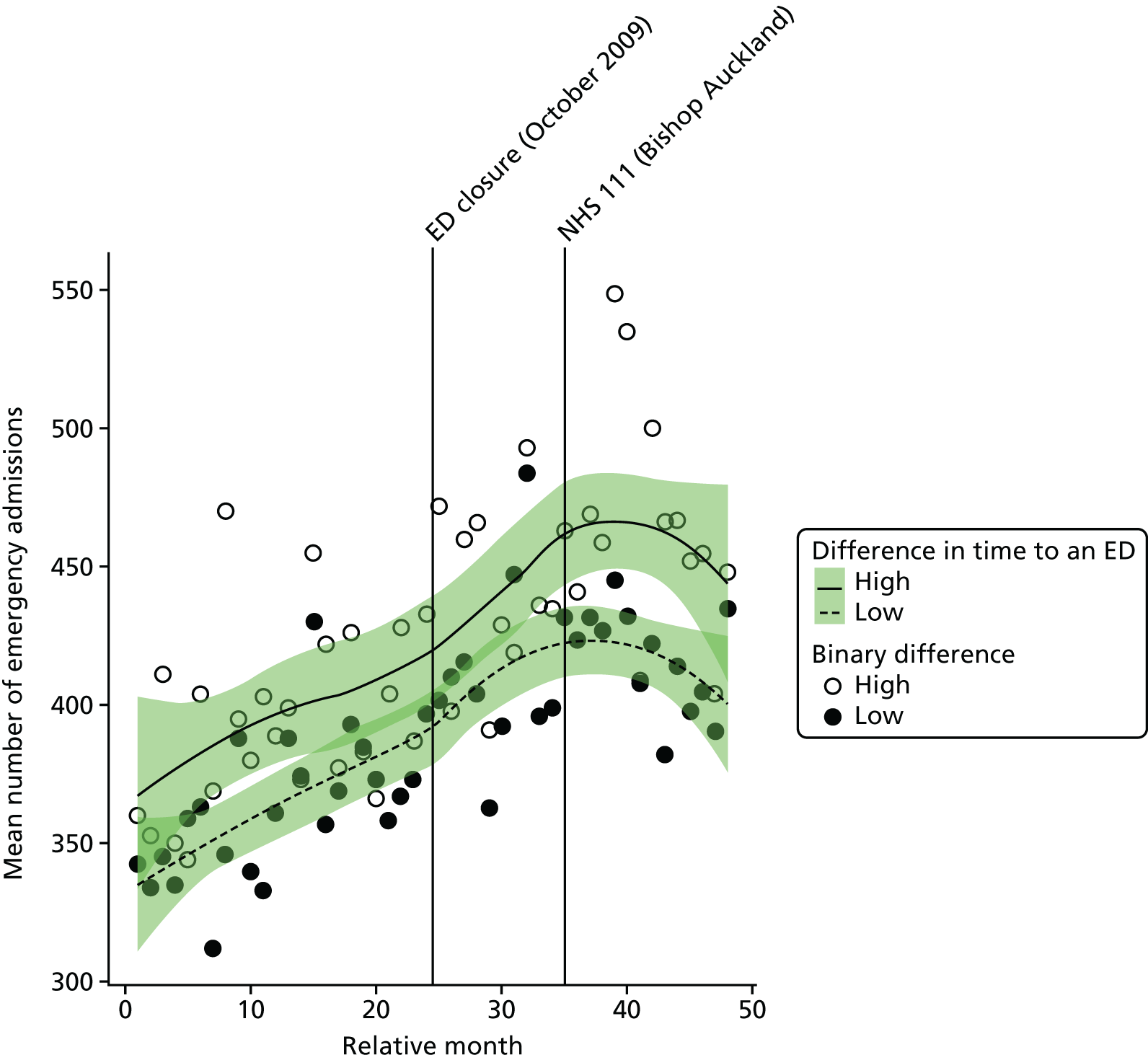
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of emergency admissions in high-dose areas compared with low-dose areas was 0.1% (95% CI –5.1% to 5.5%; p = 0.98).
Potentially avoidable emergency admissions
Plot of monthly activity
Figure 72 shows the number of potentially avoidable emergency admissions to any hospital among residents of the BA ED catchment area and among residents of the control site catchment area in each month of the 4-year study period. The pattern for admissions from these 14 emergency conditions is very similar to the pattern for all emergency admissions, with some indication of changes in the numbers over the period spanning the analysis of the ED closure. In the BA area, there were, on average, 200 avoidable emergency admissions per month prior to the closure and 247 post closure, an increase of 23.7%. In the control area, there were, on average, 183 avoidable emergency admissions per month prior to the closure date and 194 in the period after it.
FIGURE 72.
Number of potentially avoidable emergency admissions among residents of the Bishop Auckland ED catchment area and the control catchment area.
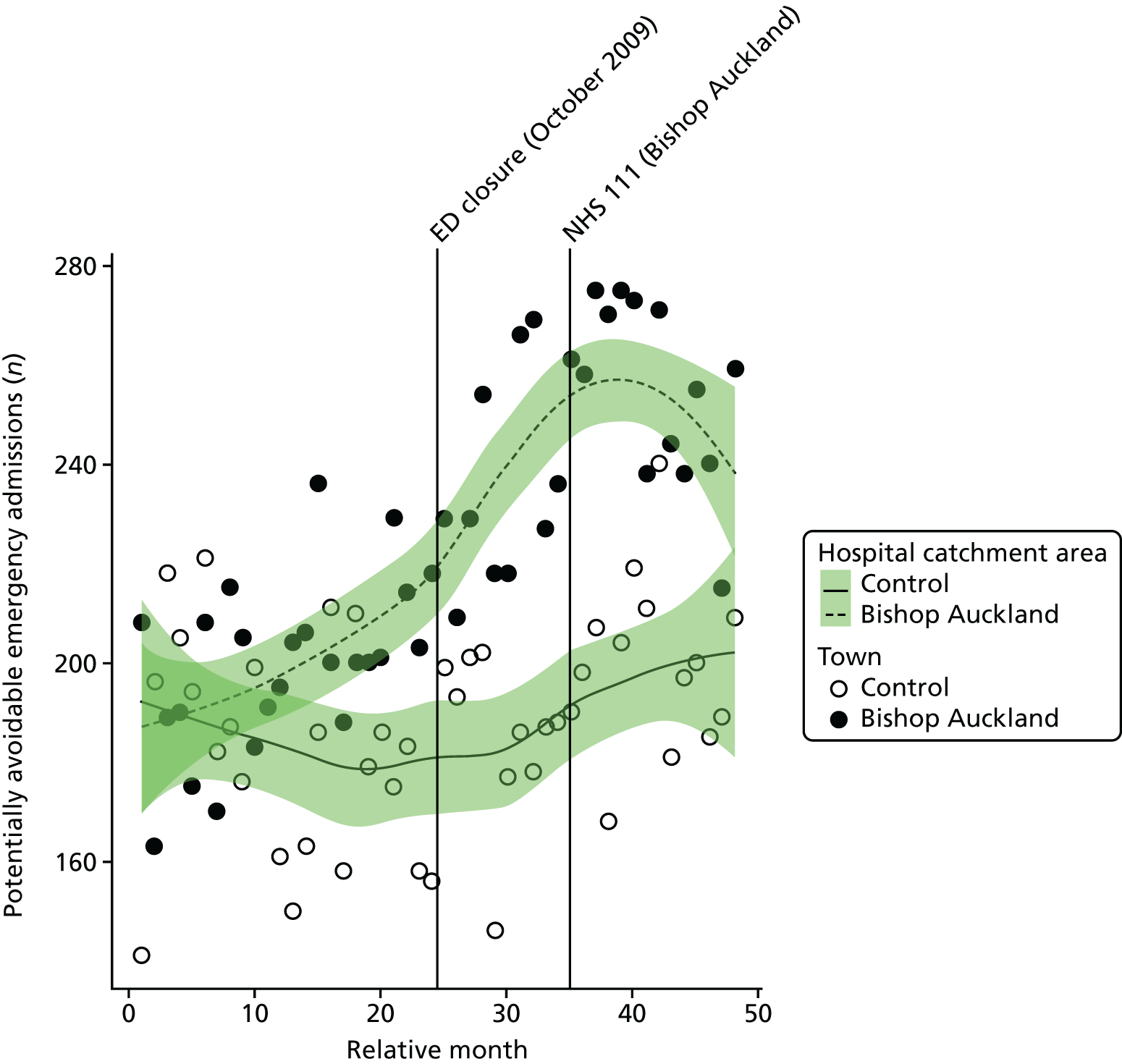
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of avoidable emergency admissions for residents of the catchment area of the BA ED was 9.8% (95% CI 0.3% to 20.1%; p = 0.04).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly mean number of avoidable emergency admissions for residents of the catchment area of the BA ED relative to the control site was 11.9% (95% CI 2.7% to 22.0%; p = 0.01).
Dose model
Figure 73 shows the mean number of potentially avoidable emergency admissions each month for residents of LSOAs that were expected to have a relatively large change in time to ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of BA ED. The pattern of change in these two areas was very similar, with an increase of 26% in high-dose areas from 103 admissions pre closure to 129 admissions post closure per month, and a 22% increase from 97 admissions pre closure to 118 admissions post closure per month in low-dose areas.
FIGURE 73.
Mean number of potentially avoidable emergency admissions among residents of areas of Bishop Auckland that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
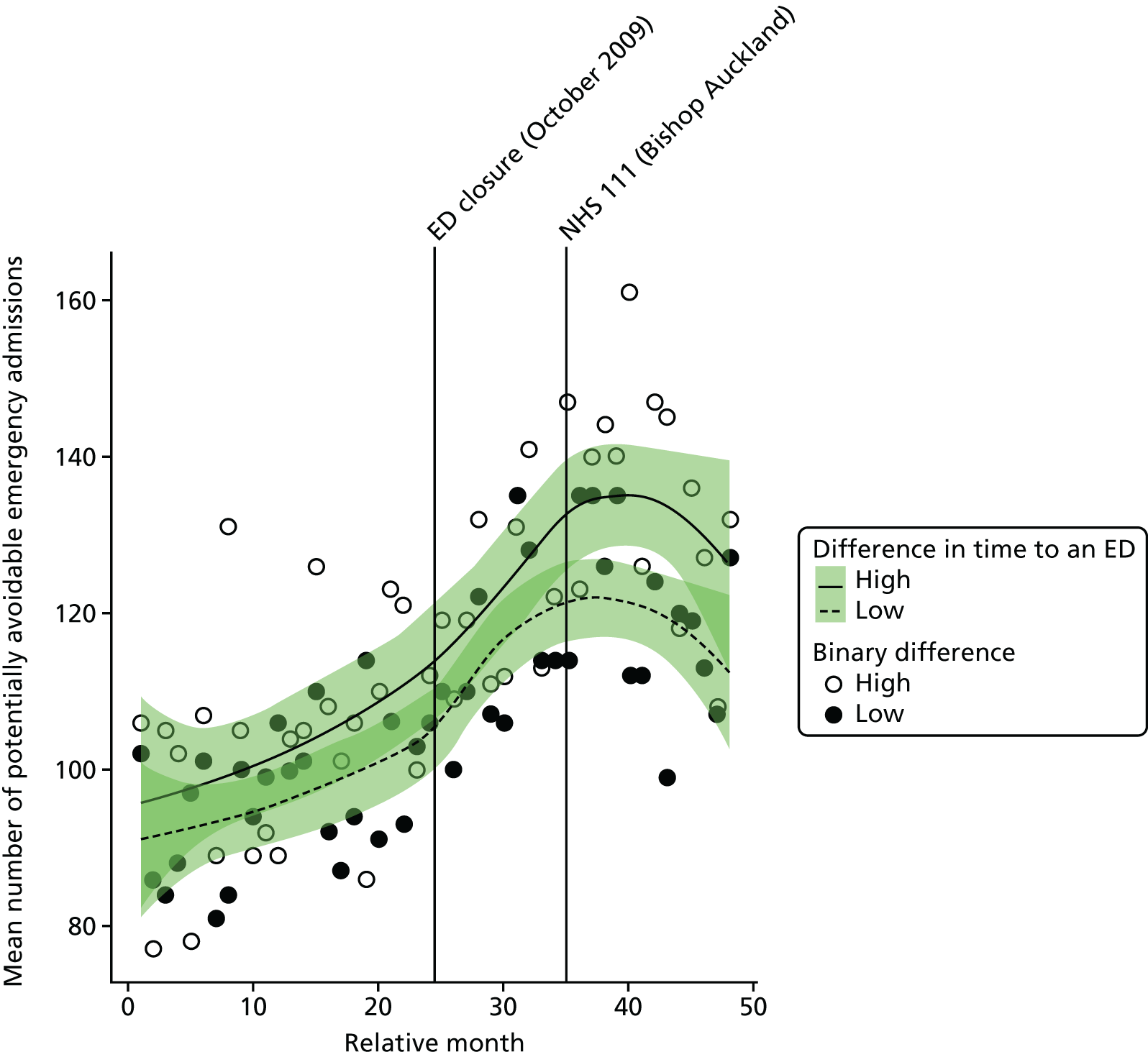
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of avoidable emergency admissions in high-dose areas compared with low-dose areas was just 3.1% (95% CI –4.8% to 11.6%; p = 0.45).
Length of stay for emergency admissions
Plot of monthly activity
Figure 74 shows the mean LOS in hospital for patients admitted as emergencies, among residents of the BA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. There was little change in BA, with the mean LOS increasing from 5.8 days before to 6.2 days after the closure of the ED. In the control site, the change was a similar small increase from 6.4 days before the closure to 6.7 days after the closure.
FIGURE 74.
Mean LOS for emergency admissions among residents of the Bishop Auckland ED catchment area and the control area.
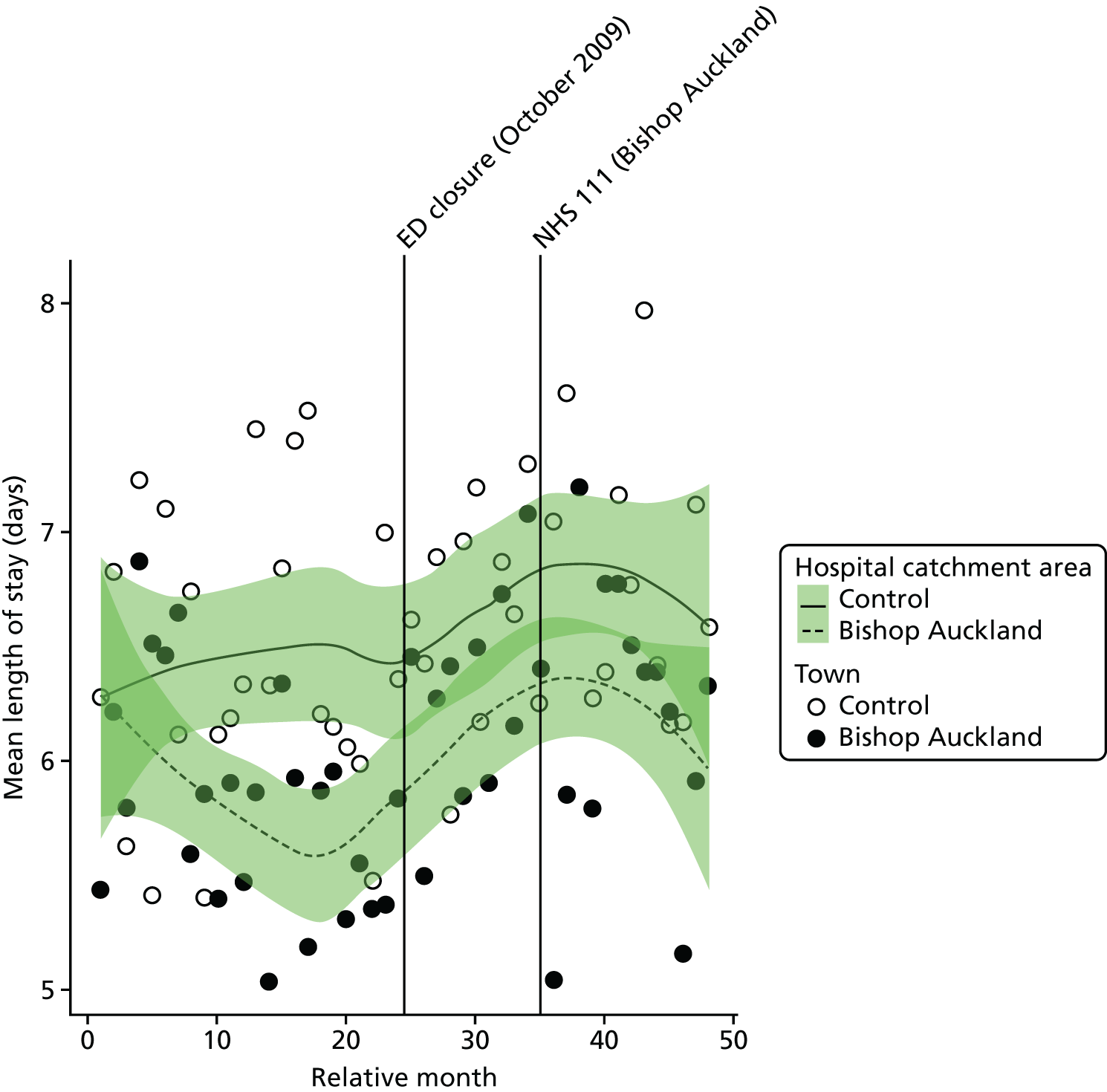
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the mean LOS for residents of the catchment area of the BA ED was 0.81 days (95% CI 0.33 to 1.29 days; p = 0.002).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly average LOS for emergency admissions among residents of the catchment area of the BA ED at the time of the closure relative to the control site was 0.10 days (95% CI –0.32 to 0.52 days; p = 0.64).
Dose model
Figure 75 shows the mean LOS for emergency admissions each month for residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the BA ED. The pattern of change in these two areas was similar, with an increase of 3% in high-dose areas from 5.7 days before the closure to 5.9 days after the closure, and an 11% increase from 5.1 days before the closure to 5.7 days after the closure in low-dose areas.
FIGURE 75.
Mean LOS for emergency admissions among residents of the areas in Bishop Auckland that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
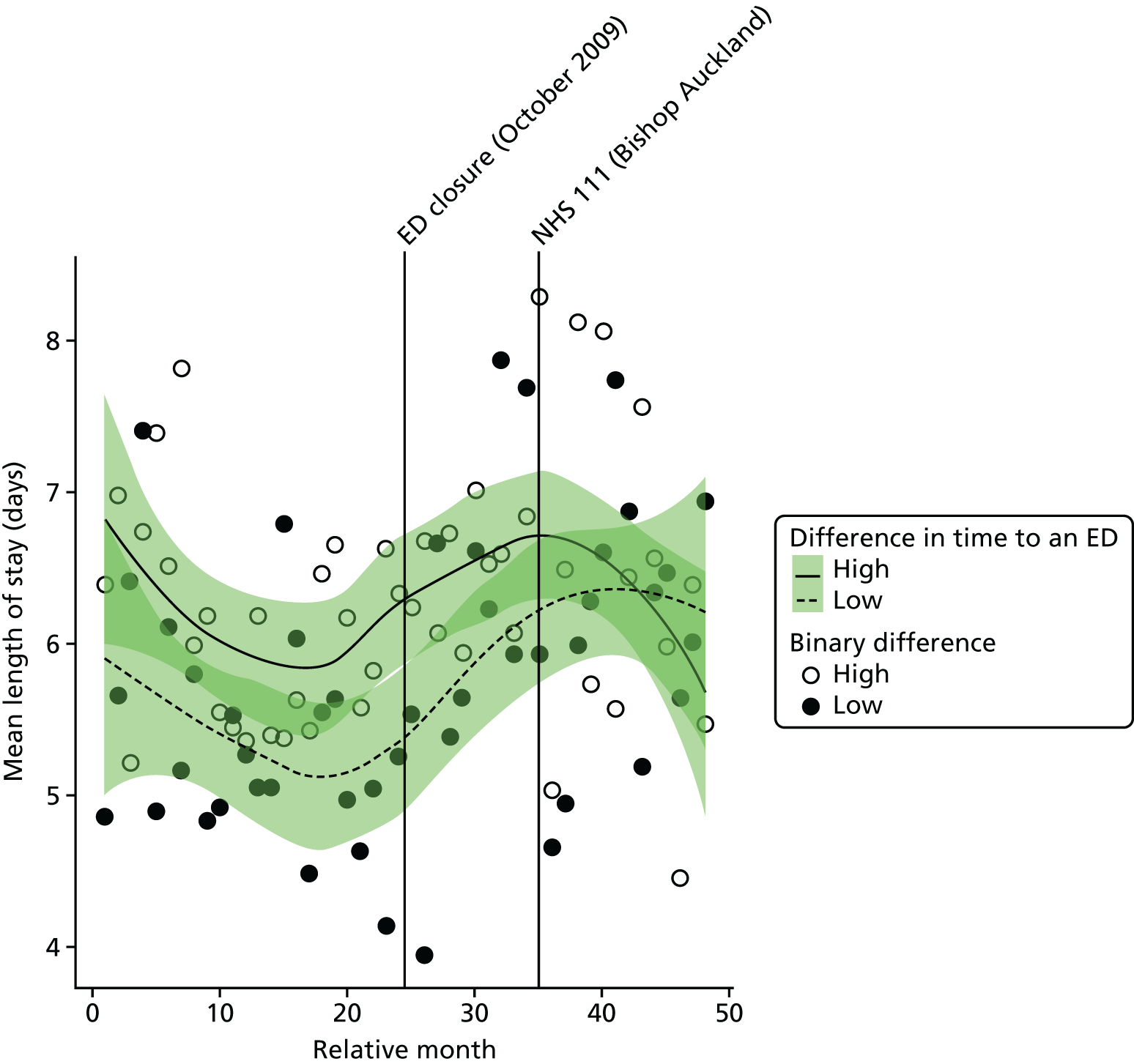
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the mean LOS for emergency admissions in high-dose areas compared with low-dose areas was –0.41 days (95% CI –1.0 to 0.2 days; p = 0.19).
Deaths
Out-of-hospital deaths from serious emergency conditions
‘Out-of-hospital’ deaths may occur at home prior to making contact with a service, in an ambulance on the way to hospital, in the ED prior to hospital admission or when a patient is recorded as having a SEC incident and is admitted, discharged alive and subsequently dies out of hospital without being readmitted.
Plot of monthly activity
Figure 76 shows the number of deaths occurring before arrival at hospital from any of the 16 SECs we have focused on among residents of the BA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. There was some indication of a change in these numbers. In residents of the BA catchment area, there were, on average, 28.6 deaths per month prior to the closure and 24.4 deaths post closure: a decrease of 14.7%. The monthly average also reduced in the control area, by 17% from 27.9 deaths pre closure to 23.1 deaths post closure.
FIGURE 76.
Number of deaths occurring out of hospital for SECs among residents of the catchment areas of Bishop Auckland and control EDs.
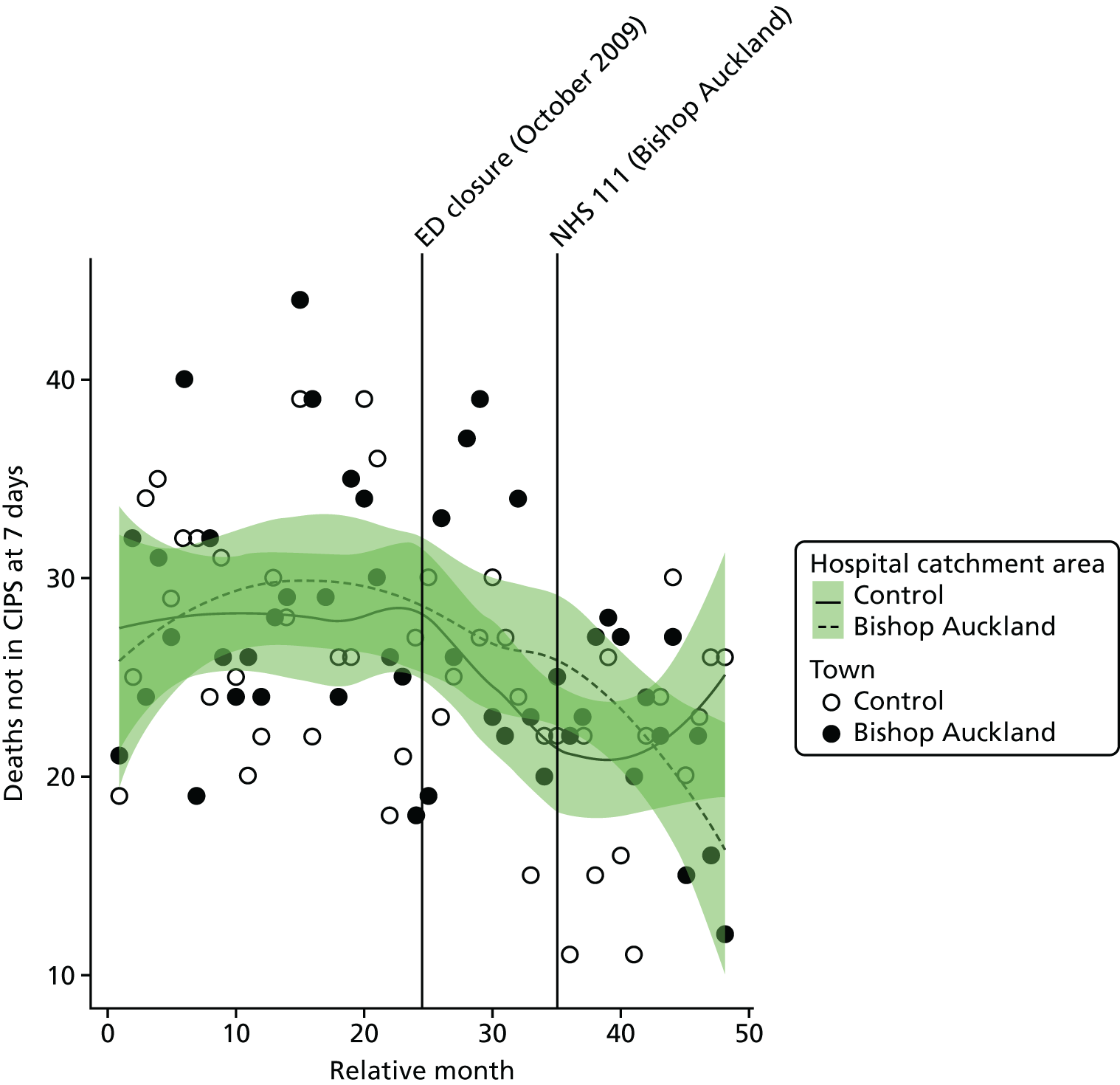
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of out-of-hospital deaths from the 16 SECs among residents of the catchment area of the BA ED was –7.0% (95% CI –27.6% to 17.9%; p = 0.55).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly mean number of emergency condition deaths occurring out of hospital for residents of the catchment area of the BA ED at the time of the closure relative to the control site was 12.0% (95% CI –8.1% to 36.6%; p = 0.26).
Dose model
Figure 77 shows the number of out-of-hospital deaths each month for residents of LSOAs that were expected to have a relatively large change in time to arrival at an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the BA ED. The pattern of change in these two areas was similar, with a 15% decrease in high-dose areas from an average of 15.7 pre-closure to 13.4 post-closure deaths per month, and a similar decrease of 11% from 12.4 pre-closure to 11.0 post-closure deaths in low-dose areas.
FIGURE 77.
Out-of-hospital deaths from SECs among residents of areas of Bishop Auckland that were expected to have a large change in time to arrival at an ED (high dose) and those expected to have a small change (low dose).
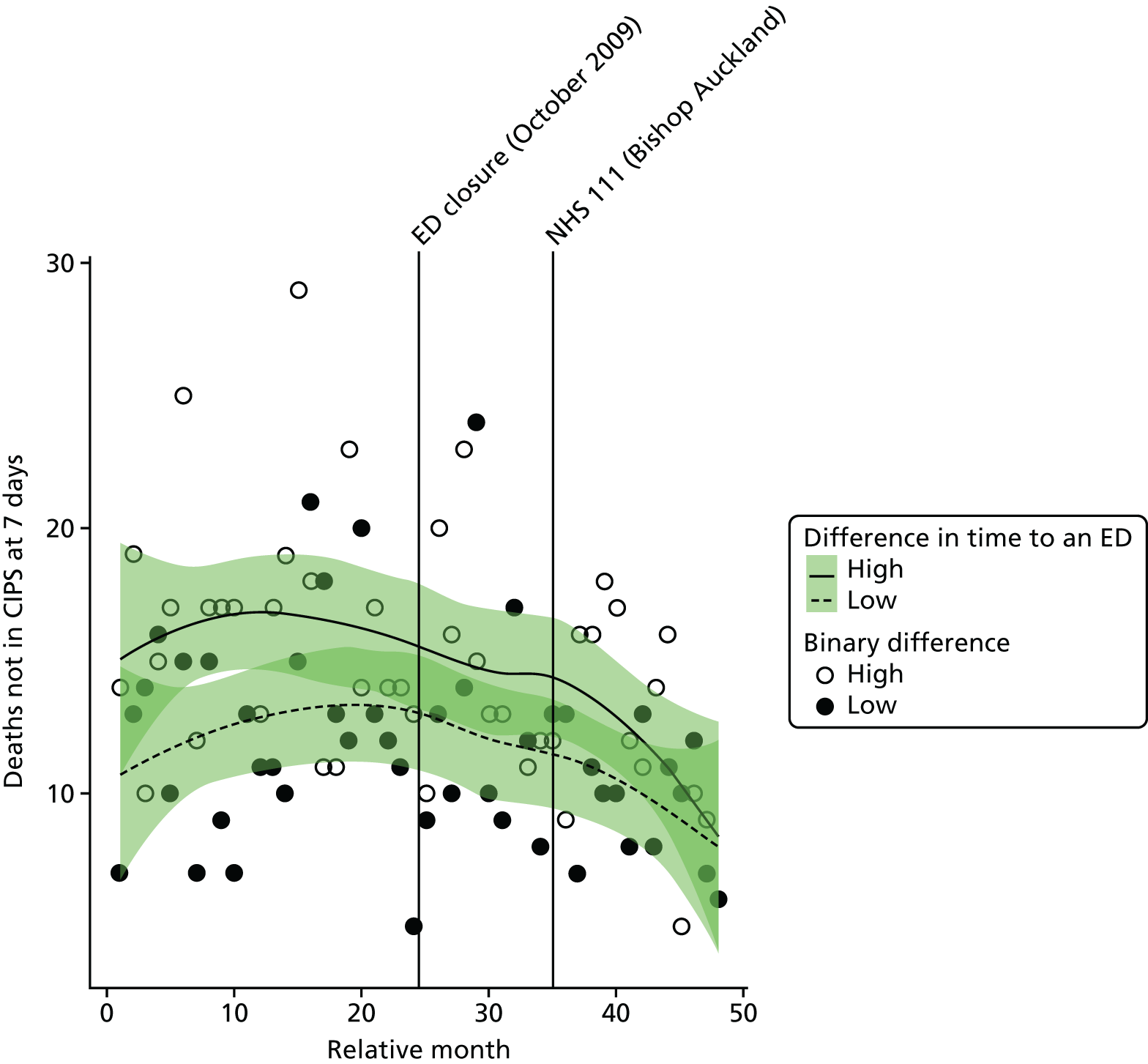
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of out-of-hospital deaths in high-dose areas compared with low-dose areas was –4.2% (95% CI –23.4% to 19.8%; p = 0.71).
All deaths from serious emergency conditions occurring within 7 days
Plot of monthly activity
Figure 78 shows the total number of deaths occurring up to 7 days post incident from the 16 SECs among residents of the BA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These deaths may have occurred before arrival at hospital or after admission to hospital within 7 days of admission. These numbers show the same pattern as that for deaths out of hospital. There were, on average, 39.1 deaths per month prior to the closure and 33.1 post closure, a reduction of 15.3%. In the control area, the monthly average reduced by 12.2% from 34.9 pre-closure to 30.6 post-closure deaths.
FIGURE 78.
Total number of deaths from SECs occurring within 7 days of the incident among residents of the catchment areas of the Bishop Auckland and control EDs.
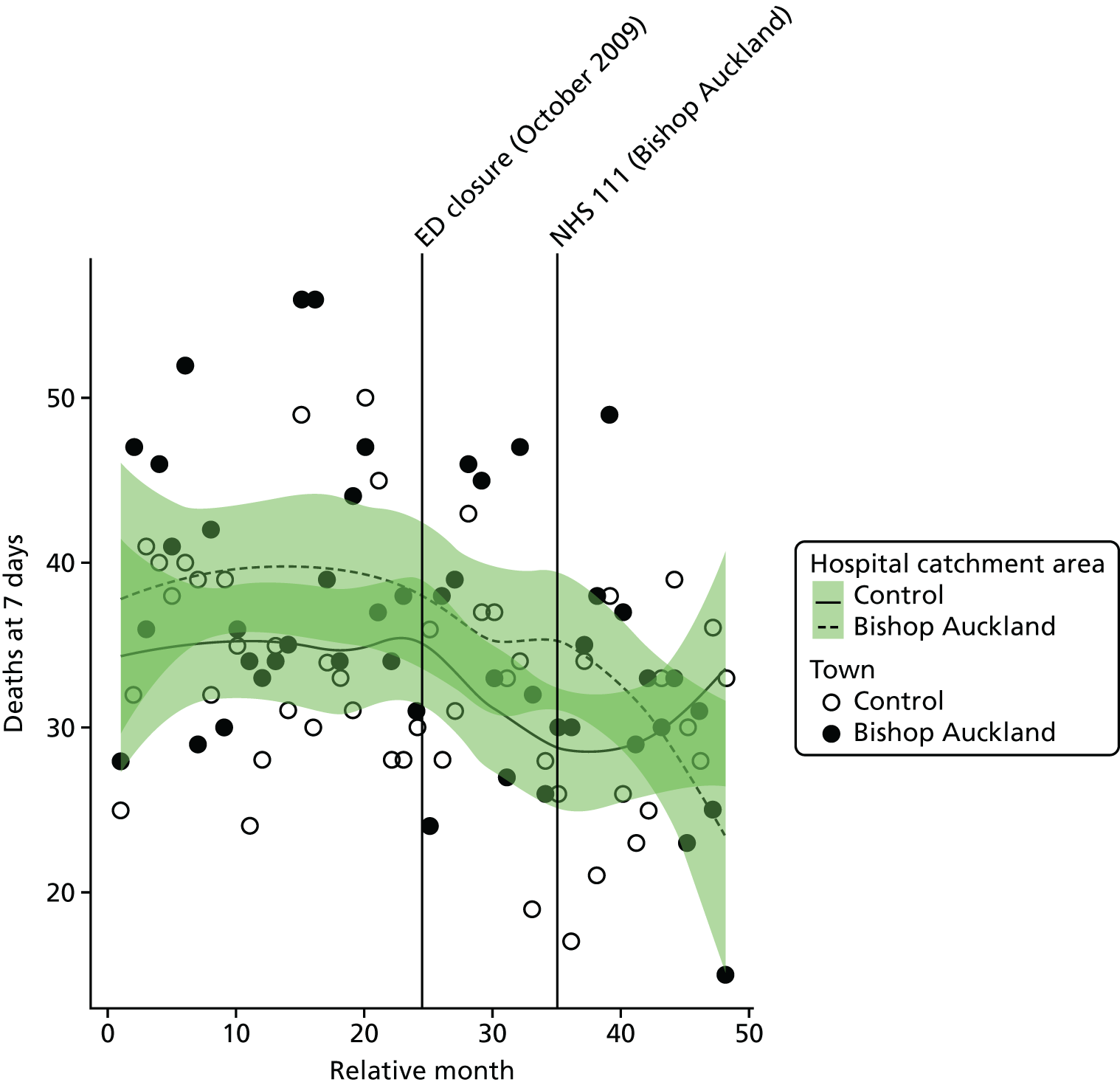
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of deaths within 7 days from the 16 SECs for residents of the catchment area of the BA ED was –12.2% (95% CI –28.8% to 8.1%; p = 0.22).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly mean number of deaths within 7 days from the 16 SECs for residents of the catchment area of the BA ED at the time of the closure relative to the control site was 1.3% (95% CI –15.2% to 20.9%; p = 0.89).
Dose model
Figure 79 shows the total number of deaths occurring up to 7 days post incident from the 16 SECs each month among residents of LSOAs that were expected to have a relatively large change in time to ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the BA ED. There was a decrease of 19%, from an average of 22.0 pre-closure to 17.9 post-closure deaths per month in high-dose areas, and a decrease of 8% from 16.5 pre-closure to 15.3 post-closure deaths in low-dose areas.
FIGURE 79.
Total number of deaths from SECs up to 7 days post incident among residents of areas of Bishop Auckland that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
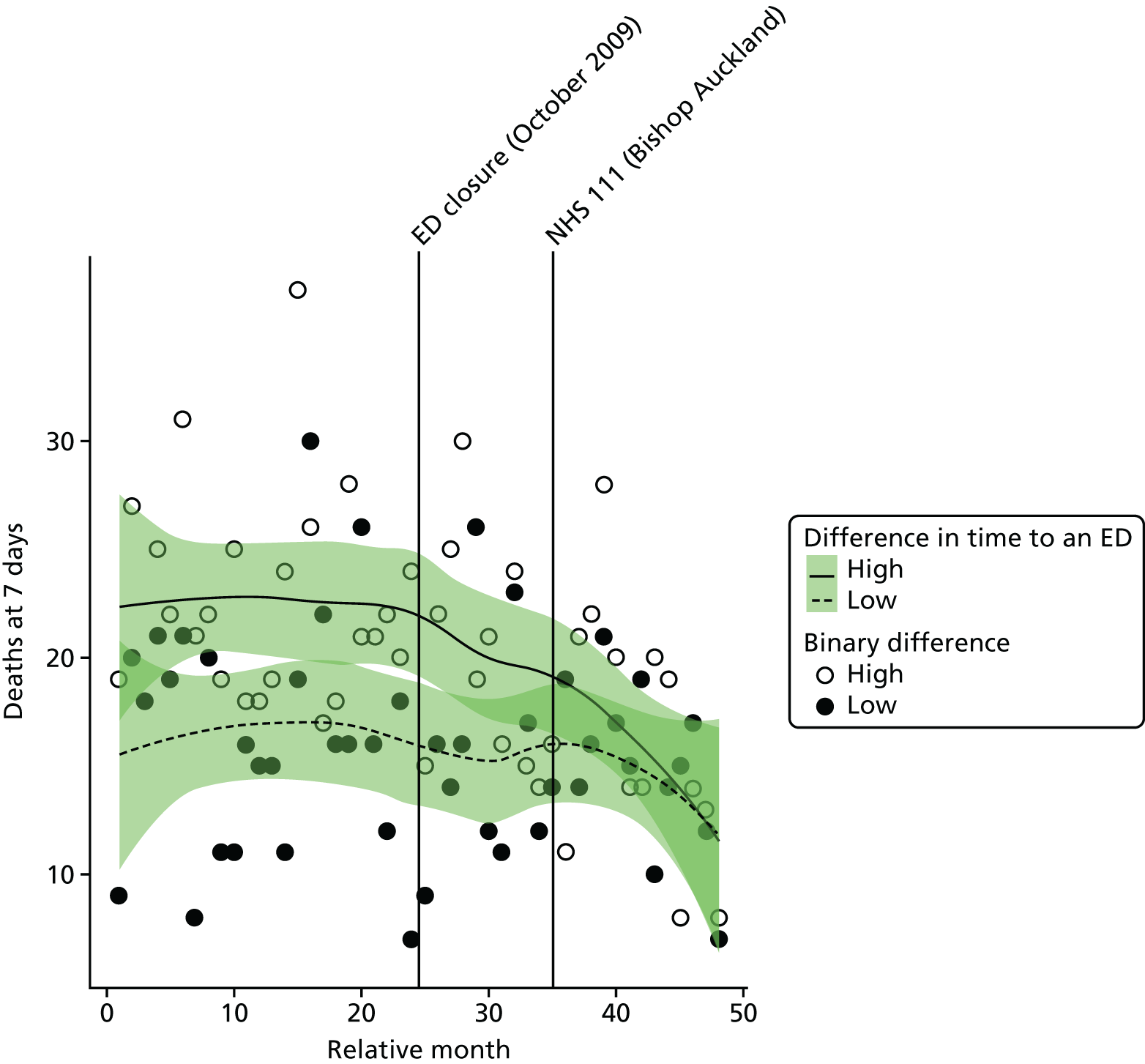
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of deaths among residents of high-dose areas compared with low-dose areas was –12.2% (95% CI –27.7% to 6.6%; p = 0.19).
Case fatality ratios: all serious emergency conditions studied
Plot of monthly activity
Figure 80 shows the ratio of the total number of deaths from the 16 SECs occurring up to 7 days post incident to the total number of deaths from the 16 SECs plus admissions for patients who survived beyond 7 days in residents of the BA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These ratios reflect the risk of dying from these emergency conditions. There is some indication of a change in these ratios. In BA, over the 2 years before the closure, the average ratio was 0.292 (indicating that 29.2% of the patients died), and it was 0.246 afterwards, a reduction of 4.6 in the percentage of patients who died. In the control site, the average ratio changed from 0.313 to 0.264.
FIGURE 80.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident among residents of the catchment areas of the Bishop Auckland and control EDs.
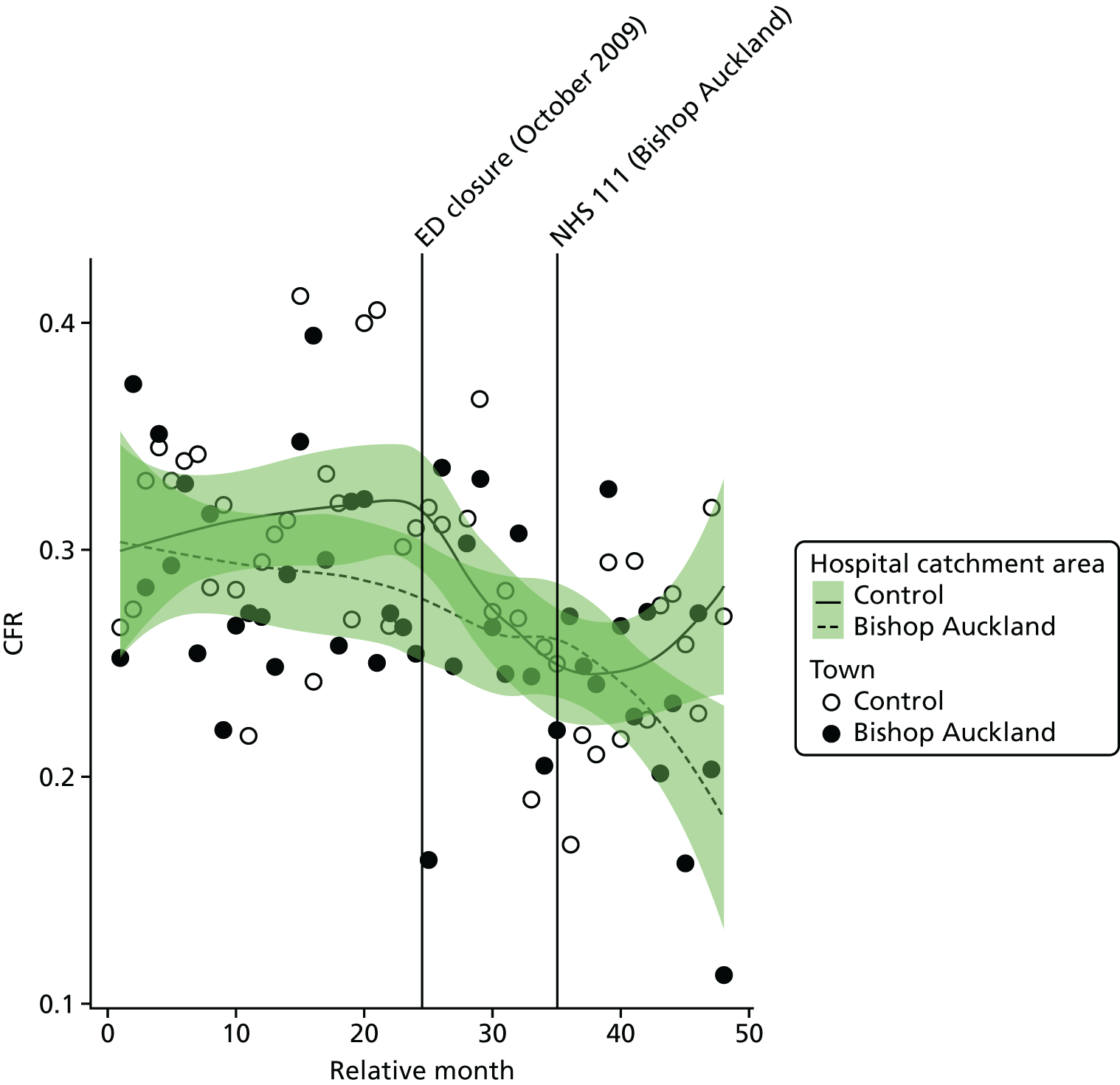
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the CFR for the 16 SECs for residents of the catchment area of the BA ED was –0.019 (95% CI –0.053 to 0.014; p = 0.27); this is a reduction of 1.9 in the percentage of patients who died.
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly average CFR for residents of the catchment area of the BA ED at the time of the closure relative to the control site was 0.018 (95% CI –0.019 to 0.056; p = 0.34); this is an increase of 1.8 in the percentage of patients who died.
Dose model
Figure 81 shows the ratio of the total number of deaths from the 16 SECs occurring up to 7 days post incident to the total number of deaths from the 16 SECs plus admissions for patients who survived beyond 7 days in residents of LSOAs that were expected to have a relatively large change in time to arrival at an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the BA ED. In high-dose areas, over the 2 years before closure, the average ratio was 0.310 (indicating that 31.0% of the patients died), and it was 0.237 afterwards, a reduction of 7.3 in the percentage of patients who died. In the low-dose areas, the average ratio changed from 0.265 to 0.242.
FIGURE 81.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident among residents of areas of Bishop Auckland that were expected to have a relatively large change in time to an ED (high dose) and those expected to have a small change (low dose).
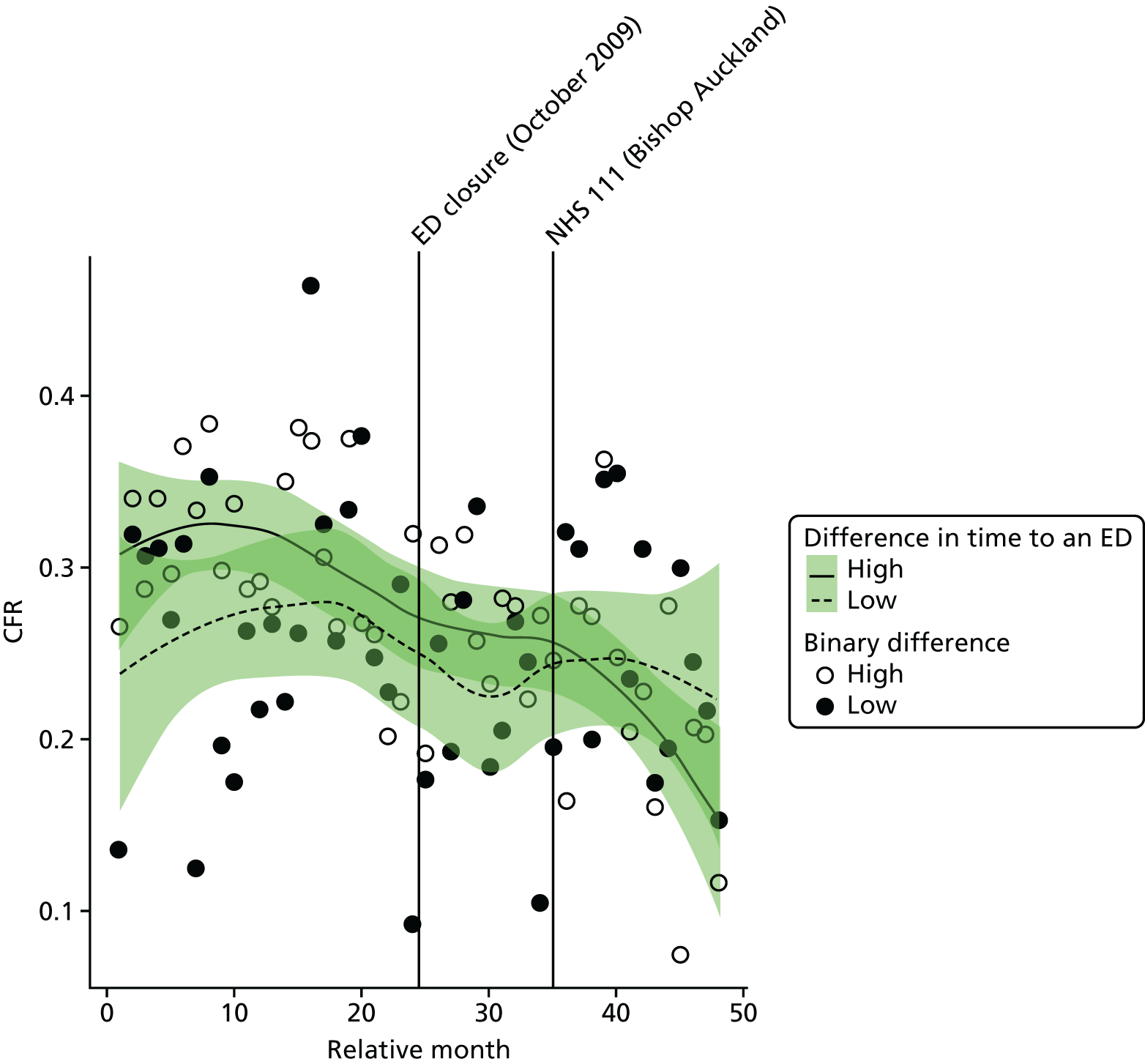
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the CFR in high-dose areas compared with low-dose areas was –0.048 (95% CI –0.092 to –0.005; p = 0.03), a reduction of 4.8 in the percentage of patients who died.
Case fatality ratios: myocardial infarction and stroke
We have also examined the change in the CFRs for MI and for stroke separately (Tables 36 and 37). There was little evidence that the CFRs had changed for either condition, and there was no evidence of any difference for residents of Bishop Auckland and its control area, or for residents of the high-dose areas of Bishop Auckland compared with the low-dose areas.
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Bishop Auckland | |||
| Low-dose areas | 0.290 (0.120) | 0.269 (0.124) | –2.1 |
| High-dose areas | 0.315 (0.114) | 0.291 (0.130) | –2.4 |
| Total | 0.306 (0.078) | 0.256 (0.095) | –5.0 |
| Control | 0.335 (0.130) | 0.252 (0.106) | –8.3 |
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Bishop Auckland | |||
| Low-dose areas | 0.469 (0.222) | 0.364 (0.170) | –10.6 |
| High-dose areas | 0.380 (0.342) | 0.342 (0.114) | –3.8 |
| Total | 0.416 (0.114) | 0.337 (0.114) | –7.9 |
| Control | 0.498 (0.129) | 0.370 (0.120) | –12.8 |
Rochdale
The ED at Rochdale Infirmary (RO ED) was closed in April 2011. We have examined the changes in activity and performance of the emergency care system for residents of the catchment area of RO ED over the 2 years before and the 2 years after the closure. We have also compared these changes with changes over the same 4-year period for residents of the catchment area of a control ED.
In the analysis of the impact of the closure of RO ED, there were four system changes that were accounted for in addition to the closure.
Rochdale ED catchment area changes accounted for in the analysis:
-
Introduction of an overnight ambulance diversion in August 2010.
-
Introduction of NHS 111 in March 2013.
Control site ED catchment area changes accounted for in the analysis:
-
Introduction of an UCC in June 2009.
-
Introduction of NHS 111 in March 2013.
Summary of findings
Following the closure, for residents of the ED catchment area in Rochdale:
-
There was some evidence of a large increase in the number of emergency ambulance incidents, including ‘Red’ incidents. This increase was no longer evident when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the time from 999 call to arrival at hospital. No comparison could be made with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of emergency and urgent care attendances.
-
There was some evidence of a large decrease in the number of minor attendances at emergency and urgent care services, but this decrease was not evident when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of emergency hospital admissions.
-
There was some evidence of a large decrease in the number of potentially avoidable hospital admissions and strong evidence when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the LOS for those admitted as an emergency case.
-
There was no statistically reliable evidence to suggest a change in the number of deaths or risk of death from the 16 SECs studied.
In comparing pre- and post-closure journey times to the nearest ED, for those experiencing longer post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of emergency ambulance incidents when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of an increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in either the total number of emergency and urgent care attendances or the total number of minor attendances, when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the emergency hospital admission measures when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the mortality measures when compared with those experiencing a smaller change in journey times.
| Impact measure | Model, effect (95% CI); p-value | ||
|---|---|---|---|
| 1: no control | 2: compared with control | 6: high-dose areas | |
| Total number of emergency ambulance incidents | Increase: 12.1% (4.7% to 20.0%); 0.001 | Decrease: –0.2% (–7.6% to 7.8%); 0.96 | Increase: 4.2% (–0.1% to 9.6%); 0.11 |
| Total number of emergency ambulance ‘Red’ incidents | Increase: 17.2% (6.3% to 29.2%); 0.001 | Decrease: –2.4% (–10.4% to 6.4%); 0.58 | Decrease: –3.1% (–10.4% to 4.8%); 0.43 |
| Mean time from 999 ‘Red’ call to arrival at hospital | Increase: 2.3 minutes (0.1 to 4.5 minutes); 0.05 | No reliable data | Increase: 5.6 minutes (4.0 to 7.2 minutes); < 0.001 |
| Total number of emergency and urgent care attendances | Decrease: –5.5% (–11.5% to 1.0%); 0.10 | Increase: 2.1% (–2.8% to 7.2%); 0.40 | Decrease: –1.0% (–5.2% to 3.4%); 0.64 |
| Total number of minor attendances at an emergency and urgent care service | Decrease: –16.4% (–25.8% to –5.8%); 0.003 | Increase: 11.6% (1.3% to 23.0%); 0.03 | Increase: 0.6% (–7.1% to 9.0%); 0.88 |
| Total number of emergency hospital admissions | Decrease: –4.4% (–9.6% to 1.1%); 0.11 | Decrease: –3.7% (–8.5% to 1.4%); 0.15 | Decrease: –1.3% (–5.4% to 3.0%); 0.55 |
| Total number of potentially avoidable emergency hospital admissions | Decrease: –14.2% (–21.3% to –6.4%); 0.001 | Decrease: –15.8% (–22.0% to –9.1%); < 0.001 | No change: 0% (–7.6% to 7.1%); 0.99 |
| Mean LOS for emergency hospital admissions | Decrease: –0.4 days (–0.7 to 0.01 days); 0.05 | Decrease: –0.3 days (–0.6 to 0.01 days); 0.06 | Increase: 0.2 days (–0.3 to 0.6 days); 0.50 |
| Total number of out-of-hospital deaths | Increase: 9.4% (–18.8% to 47.5%); 0.55 | Increase: 14.4% (–7.0% to 40.7%); 0.20 | Decrease: –9.6% (–30.5% to 17.4%); 0.45 |
| Total number of deaths occurring within 7 days post incident | Increase: 17.9% (–7.6% to 50.5%); 0.19 | Increase: 20.6% (1.7% to 42.9%); 0.03 | Decrease: –7.7% (–25.3% to 14.1%); 0.46 |
| CFR (7 days) | Increase: 4.1% (–0.2% to 8.4%); 0.07 | Increase: 3.0% (0.1% to 5.9%); 0.05 | Decrease: –0.5% (–4.1% to 3.0%); 0.76 |
Change in time to the next-nearest emergency department
Following the ED closure, the change in time to reach the next-nearest ED for the residents of the catchment area ranged from 0 to 14 minutes.
FIGURE 82.
Geographical map of Rochdale and surrounding EDs showing the change in time to the next-nearest ED. Map tiles by Stamen Design, under a Creative Commons Attribution license (CC BY 3.0; see https://creativecommons.org/licenses/by/3.0/). Data by OpenStreetMap, under ODbL. Contains National Statistics data. © Crown copyright and database right 2016. Contains OS data © Crown copyright and database right 2016.
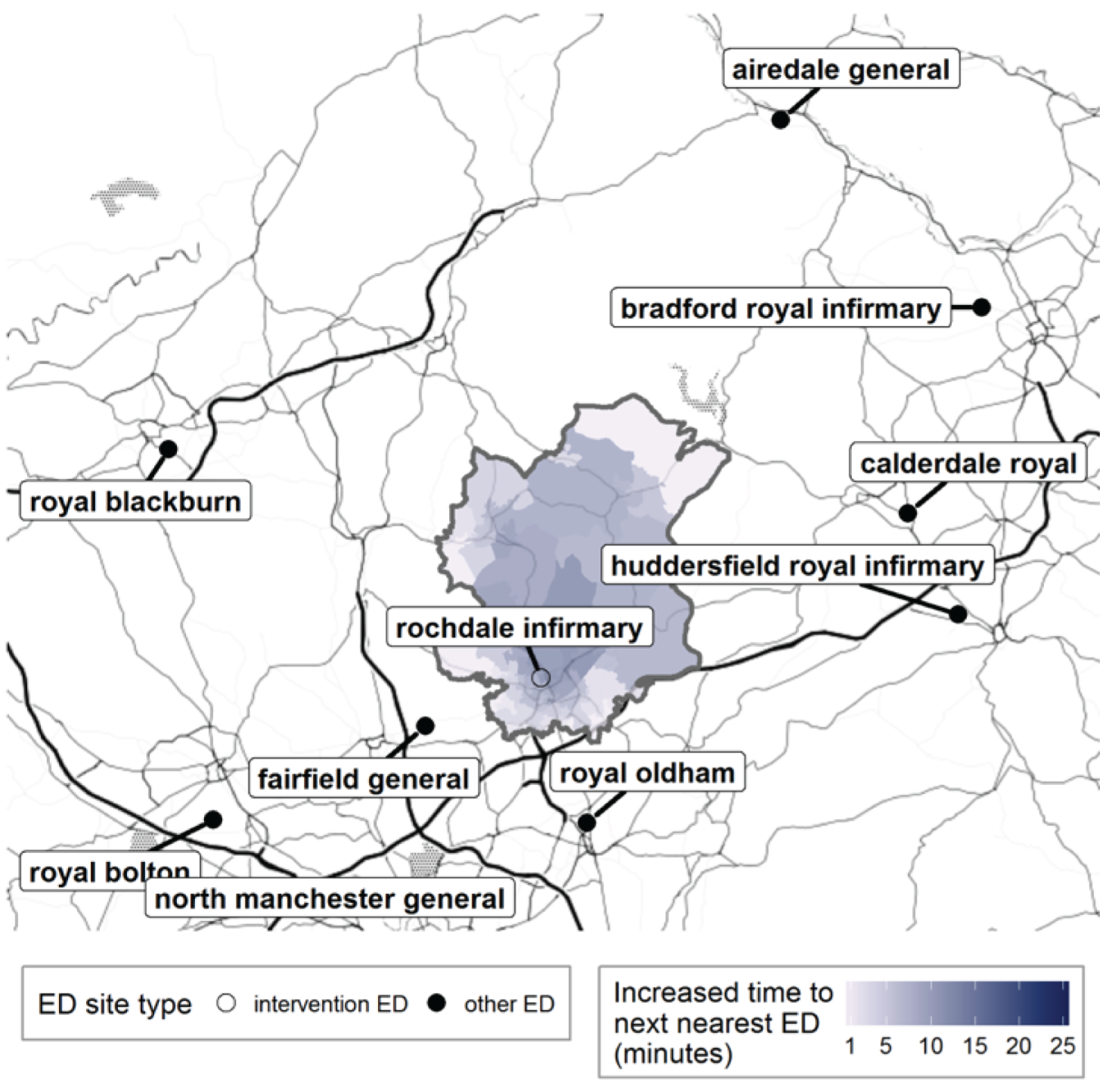
FIGURE 83.
Rochdale: change in time from LSOA to ED following ED closure, for residents of the catchment area of Rochdale Infirmary ED.
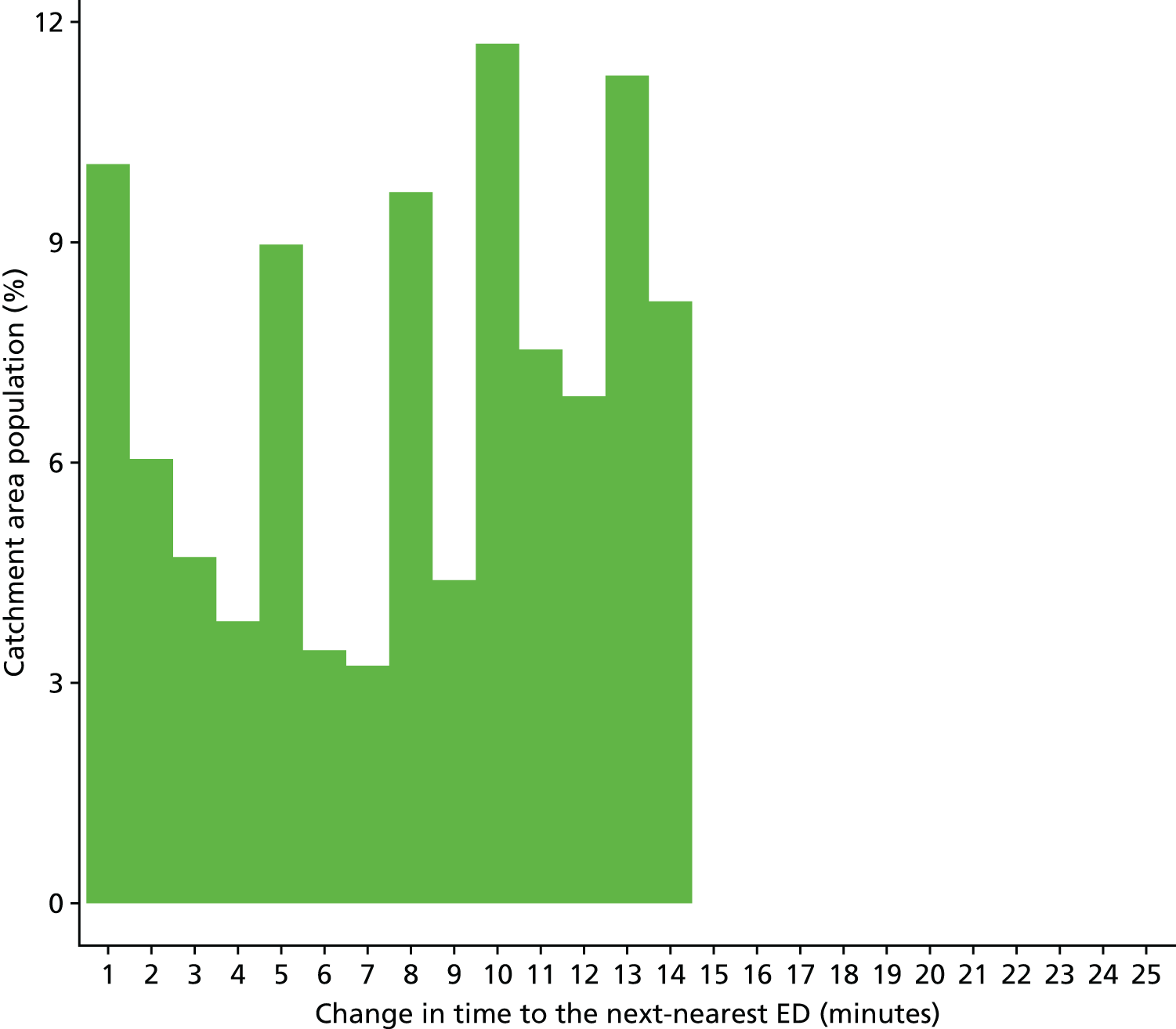
Findings from individual activity and performance measures
Ambulance service performance
Total number of incidents following 999 calls to the ambulance service
Plot of monthly activity
Figure 84 shows the total number of 999 incidents referred to the ambulance service from residents of the RO ED catchment area, and the control area, for each month over the 2 years prior to and the 2 years after the closure of the ED. There was a small increase in the number of incidents in both areas. The number of incidents went up by 4% from an average of 1479 per month pre closure to 1538 per month post closure in the RO ED catchment area, and also by 4% from 2987 per month pre closure to 3107 per month post closure in the control area.
FIGURE 84.
Total number of 999 incidents among residents of the Rochdale ED catchment area and the control area.
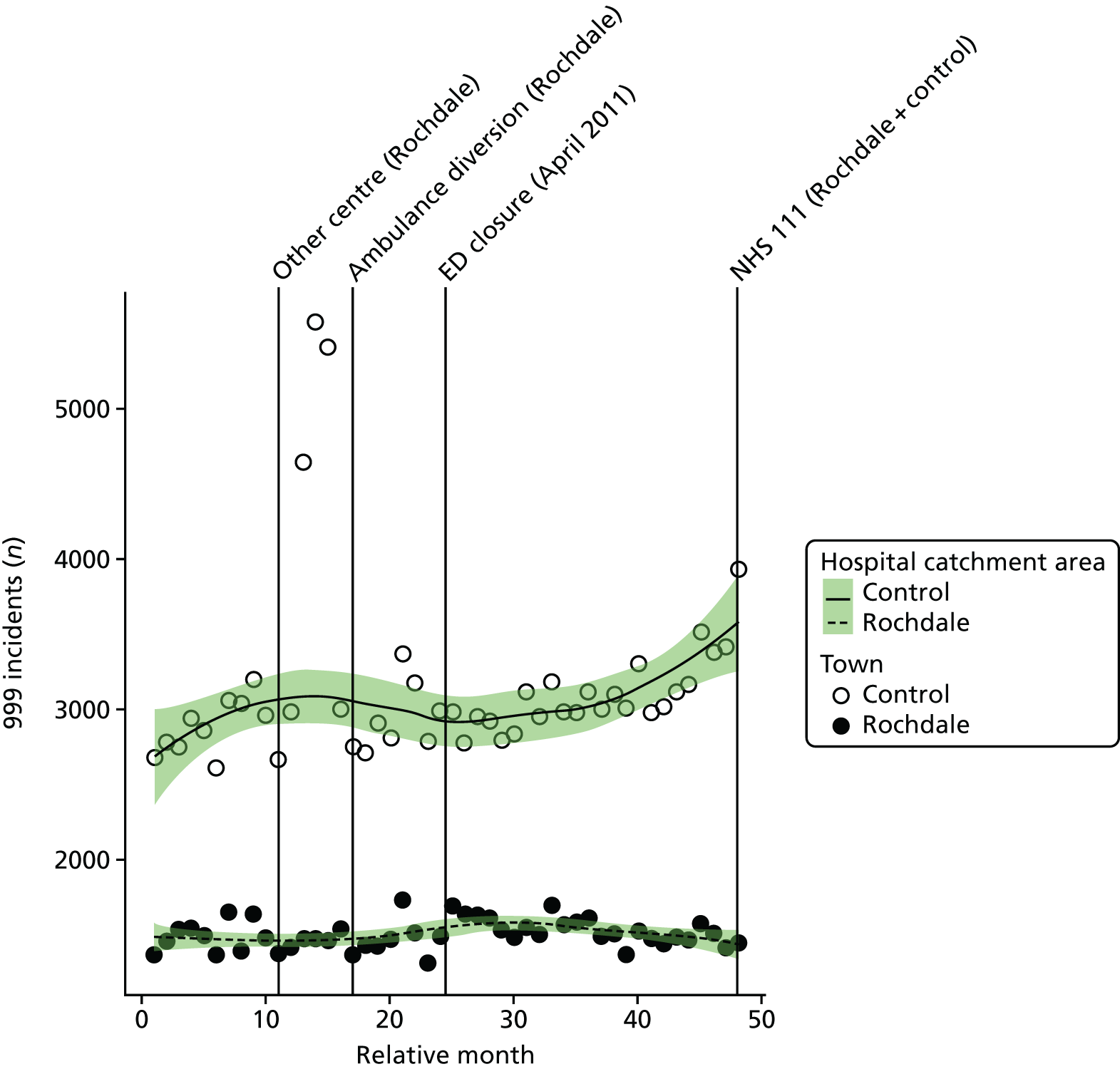
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of incidents each month for residents of the RO ED catchment area increased at the time of the closure by an average of 12.1% (95% CI 4.7% to 20.0%; p = 0.001).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of incidents each month for residents of the RO ED catchment area changed at the time of the closure relative to the control area by an average of –0.2% (95% CI –7.6% to 7.8%; p = 0.96).
Dose model
Figure 85 shows the mean number of incidents each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the RO ED. In high-dose areas, the number of incidents increased by 6% from 911 before the closure to 961 after the closure, and in low-dose areas by 1% from 569 before the closure to 577 after the closure.
FIGURE 85.
Mean number of 999 incidents among residents of areas in Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
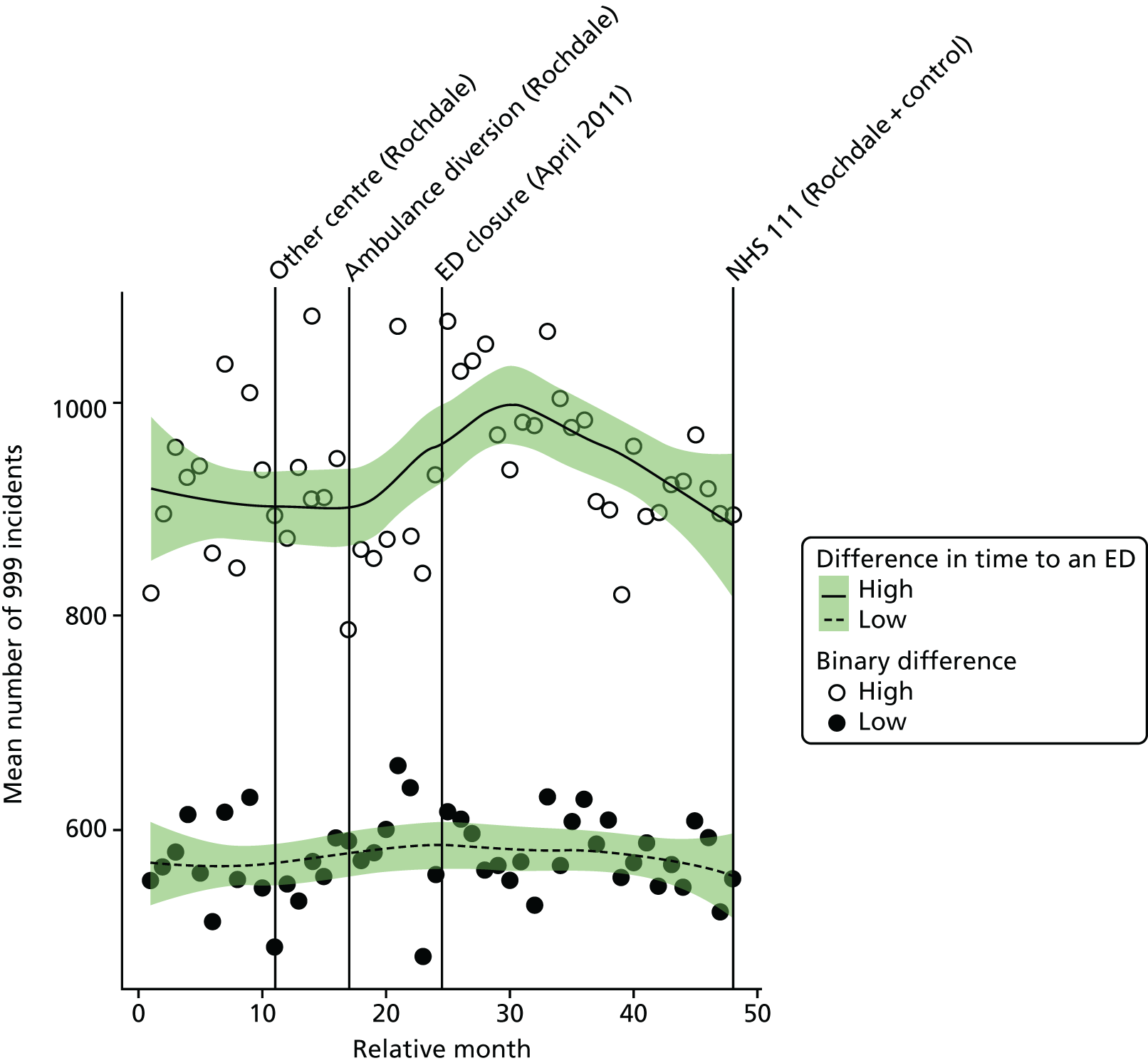
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the increase in the number of incidents in the high-dose areas relative to the low-dose areas at the time of the closure was 4.2% (95% CI –0.1% to 9.6%; p = 0.11).
Number of emergency ambulance ‘Red’ incidents
Plot of monthly activity
Figure 86 shows the number of 999 ‘Red’ incidents received by the ambulance service from residents of the RO ED catchment area and the control area, for each month over the 2 years prior to and the 2 years after the date of closure of the RO ED. There was a small increase in the number of ‘Red’ incidents in both areas. Incidents went up by 3% from an average of 581 per month pre closure to 597 per month post closure in the RO ED catchment area, and by 10% from 1332 per month pre closure to 1460 post closure in the control area.
FIGURE 86.
Number of ‘Red’ 999 incidents for residents of the Rochdale ED catchment area and the control area.
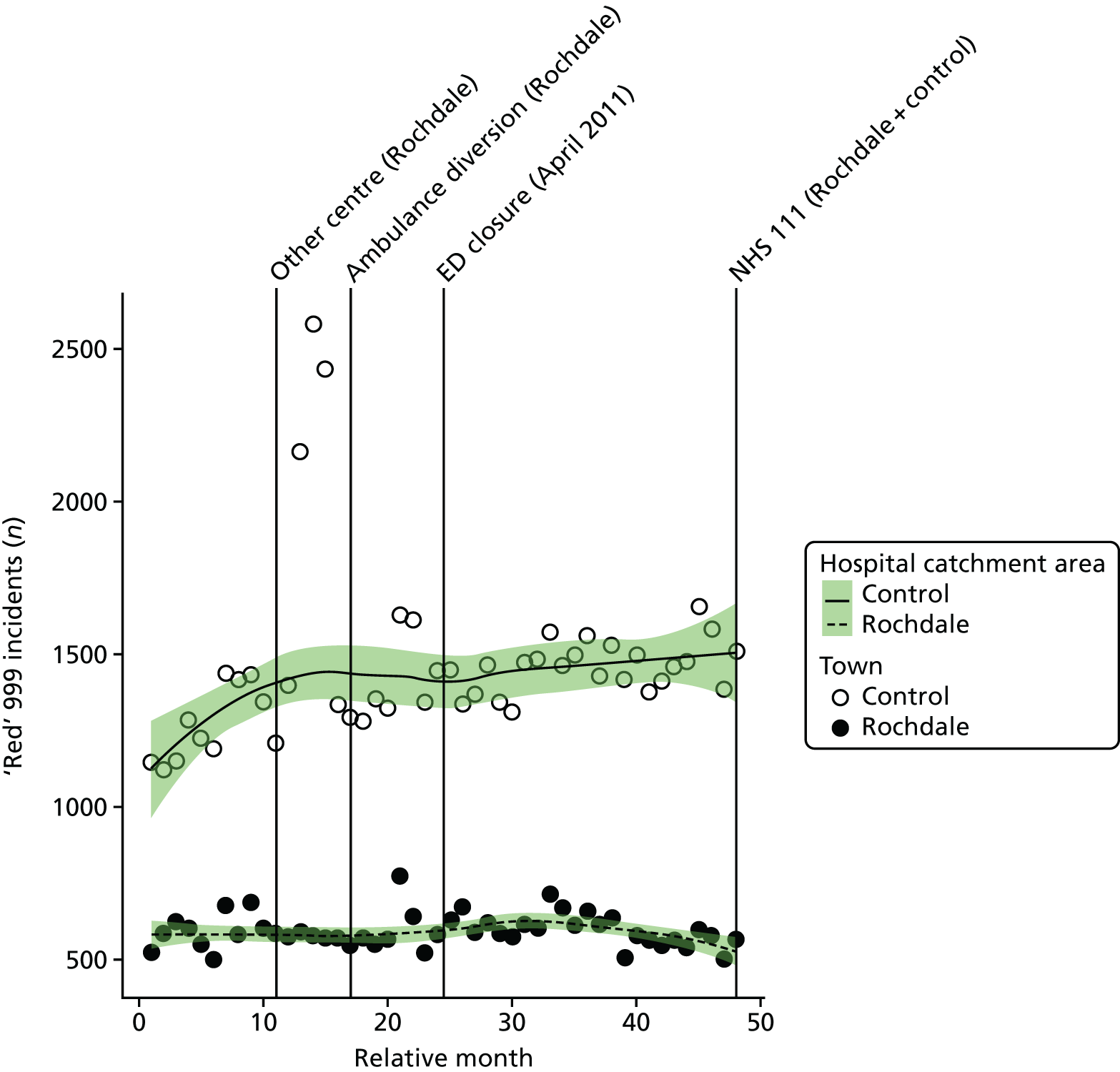
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of ‘Red’ incidents each month for residents of the RO ED catchment area increased at the time of the closure by an average of 17.2% (95% CI 6.3% to 29.2%; p = 0.001).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of ‘Red’ incidents each month for residents of the RO ED catchment area changed relative to the control area by an average of –2.4% (95% CI –10.4% to 6.4%; p = 0.58).
Dose model
Figure 87 shows the mean number of ‘Red’ incidents each month among residents of LSOAs that were expected to have a relatively large change in time to arrival at an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the RO ED. The pattern of change in these two areas suggests that there was little change in the mean number of ‘Red’ incidents in either area following the closure of the RO ED.
FIGURE 87.
Mean number of ‘Red’ 999 incidents among residents of areas in Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
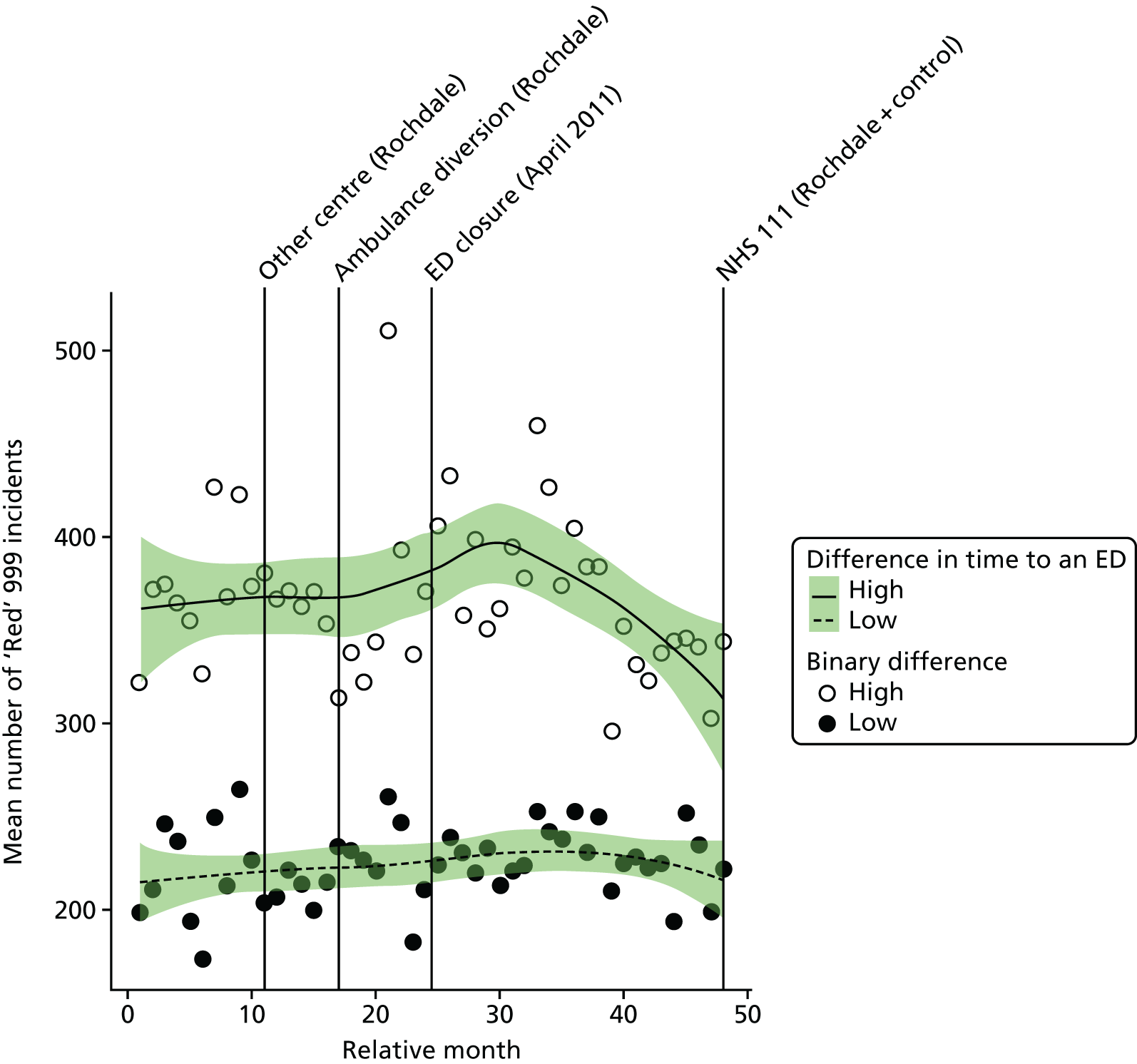
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the number of ‘Red’ incidents in the high-dose areas relative to the low-dose areas at the time of the closure was –3.1% (95% CI –10.4% to 4.8%; p = 0.43).
Mean time from 999 call to arrival at hospital for ‘Red’ incidents
Plot of monthly performance
Figure 88 shows the mean time from 999 ‘Red’ calls to arrival at hospital in each month over the 2 years prior to and the 2 years after the closure of the RO ED, for residents of the RO ED catchment area. For residents of Rochdale, these times have been measured from the time when the call was received at the switchboard to the time of arrival at hospital. In other areas, these times have been measured from when the call was answered, but this time was not available for all 4 years in Rochdale. There was an increase in these times for residents of the RO ED catchment area from before the closure (monthly mean 42.3 minutes) to after the closure (monthly mean 53.6 minutes): an increase of 11.3 minutes on average. There were no usable data from the control area on ambulance journey times.
FIGURE 88.
Mean time from 999 call to arrival at hospital among residents of the Rochdale ED catchment area.
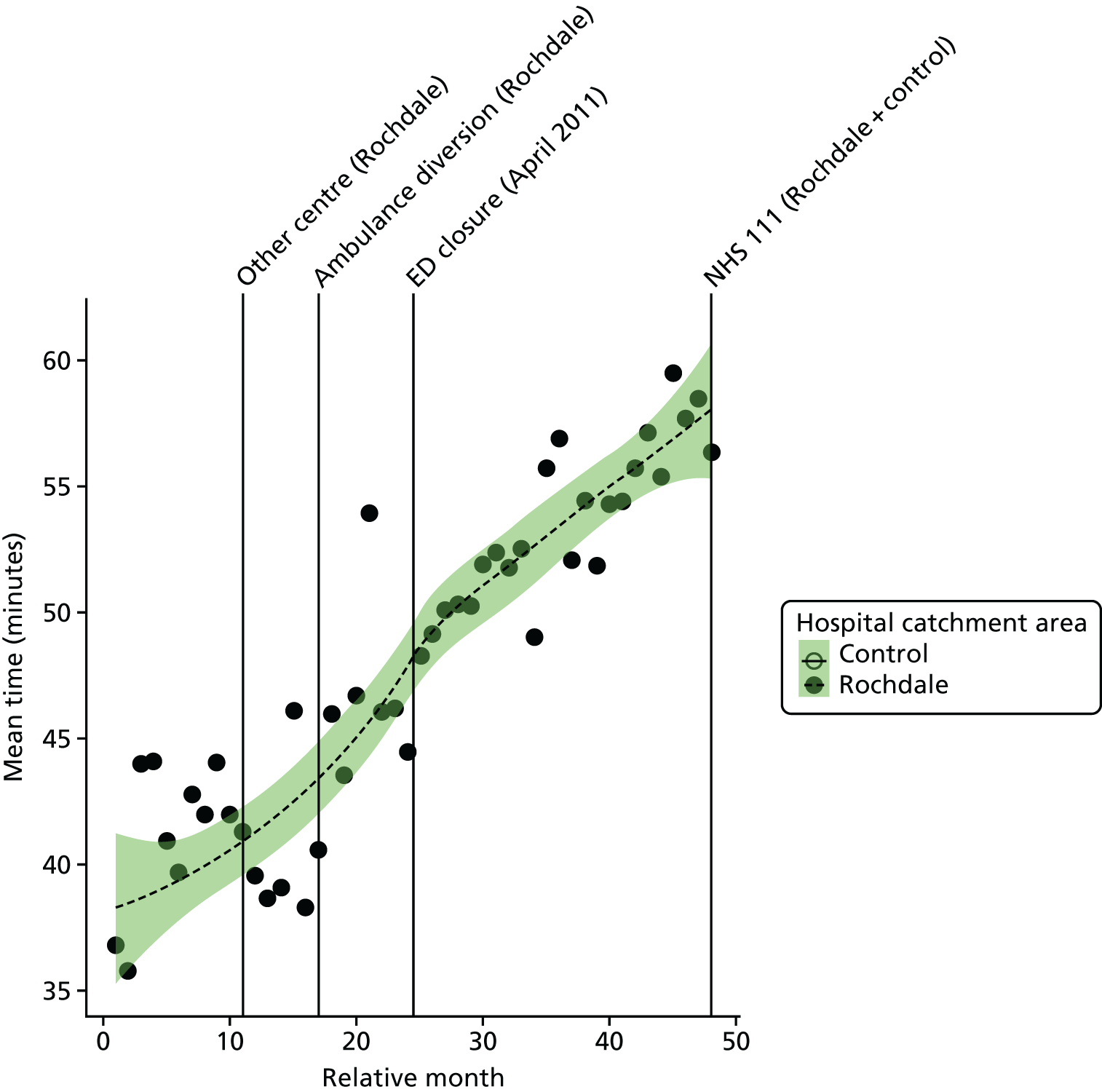
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated mean time from call to arrival at hospital for 999 callers in the RO ED catchment area increased at the time of the closure by an average of 2.3 minutes (95% CI 0.1 to 4.5 minutes; p = 0.05), which is a 5.4% increase compared with the 24 months before closure.
The emergency department closure and control area model
Because no useable control site data on times could be obtained, no comparison with a control area has been made.
Dose model
Figure 89 shows the mean time from call to arrival at hospital for ‘Red’ incidents each month made by residents of LSOAs that were expected to have a relatively large change in time to ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of RO ED. The pattern of change in these two areas was different, as expected. High-dose LSOAs had an increase in mean time from call to hospital of 14.8 minutes, but there was only a 9.2-minute increase in the low-dose areas.
FIGURE 89.
Mean time from call to arrival at hospital for 999 ‘Red’ incidents among residents of areas in Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
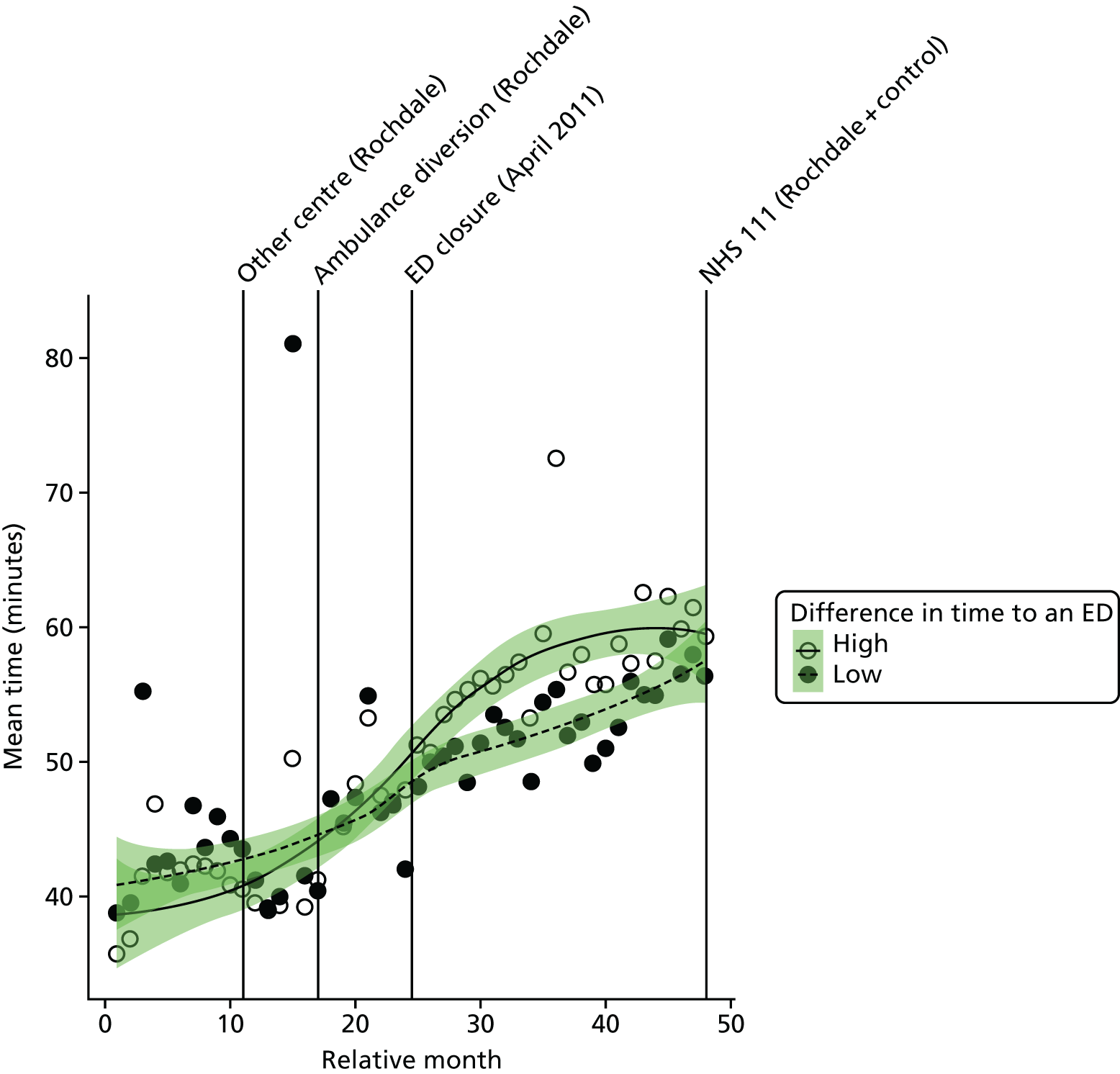
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in time from call to hospital for residents of high-dose areas was estimated an to be additional 5.6 minutes (95% CI 4.0 to 7.2 minutes; p < 0.001).
Emergency and urgent care attendances
Total number of emergency and urgent care attendances
Plot of monthly activity
Figure 90 shows the number of attendances at an ED (inclusive of A&E types 1–4 and attendances coded as ‘unknown’) by residents of the RO ED catchment area, and the control area, in each month over the 2 years prior to and the 2 years after the closure of the RO ED. There was an increase in the number of attendances in RO. Attendances went up by 7.5%, from an average of 5443 per month pre closure to 5853 per month post closure. The number of attendances also increased in the control area, by 4.2%, from 9539 per month pre closure to 9944 per month post closure.
FIGURE 90.
Total number of emergency and urgent care attendances among residents of the Rochdale ED catchment area and the control area.
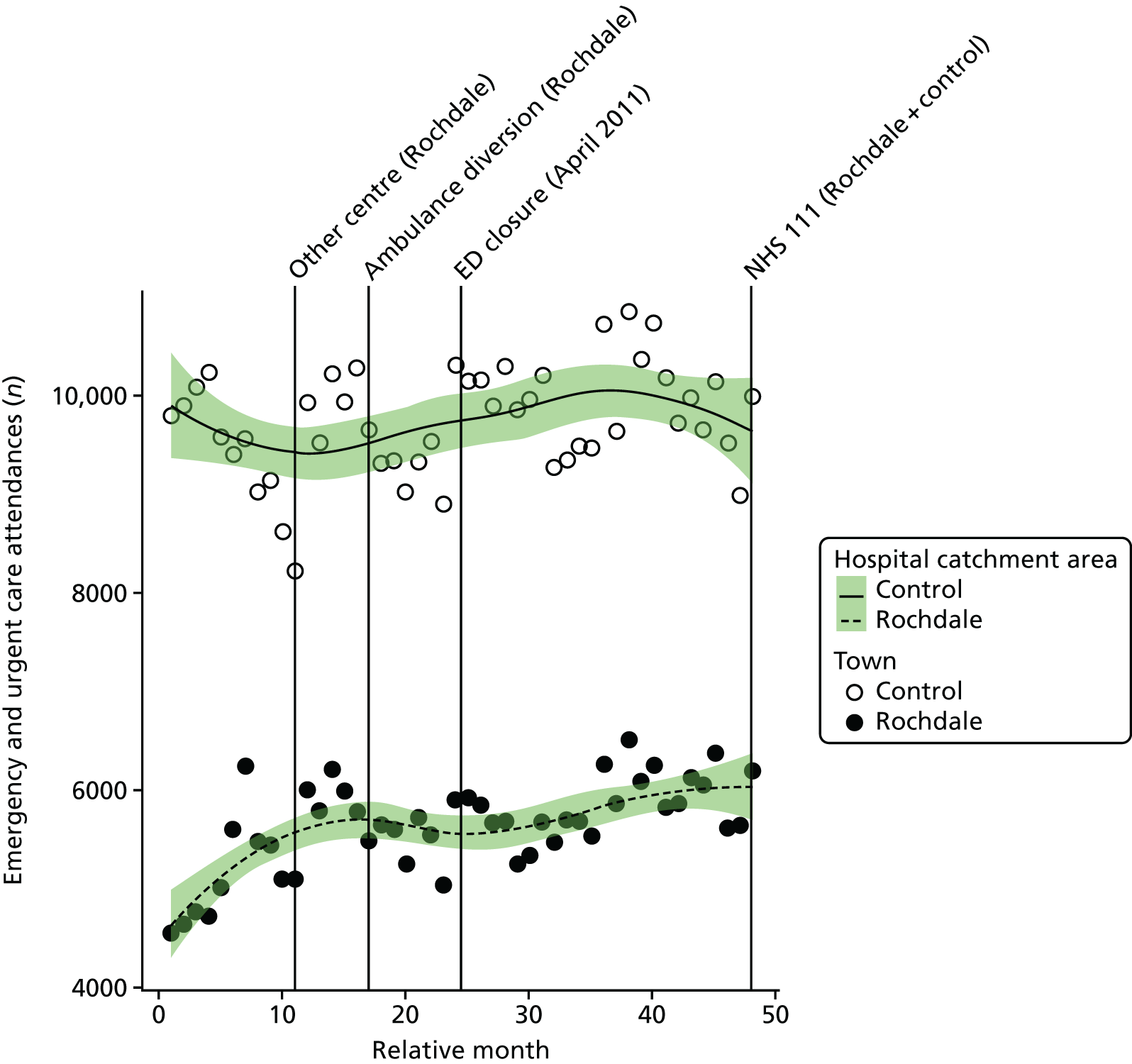
Examining the mode of arrival at the ED, it was found that the small increase in the number of attendances among residents of RO was split between an increase in those arriving by ambulance (6.6%) and in those arriving by other modes of travel (7.8%).
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the number of emergency and urgent care attendances each month among residents of the RO ED catchment area was estimated to have decreased at the time of the closure by an average of –5.5% (95% CI –11.5% to 1.0%; p = 0.10).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of emergency and urgent care attendances each month among residents of the RO ED catchment area increased at the time of the closure relative to the control area by 2.1% (–2.8% to 7.2%; p = 0.40).
Dose model
Figure 91 shows the mean number of emergency and urgent care attendances each month made by residents of LSOAs that were expected to have a relatively large change in time to arrival at an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the RO ED. The pattern of change in these two areas was the same, with a 7% increase in high-dose areas from 3351 pre-closure to 3588 post-closure attendances per month, and a similar increase, by 8%, from 2092 pre-closure to 2265 post-closure attendances per month in low-dose areas.
FIGURE 91.
Mean number of emergency and urgent care attendances among residents of areas in Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
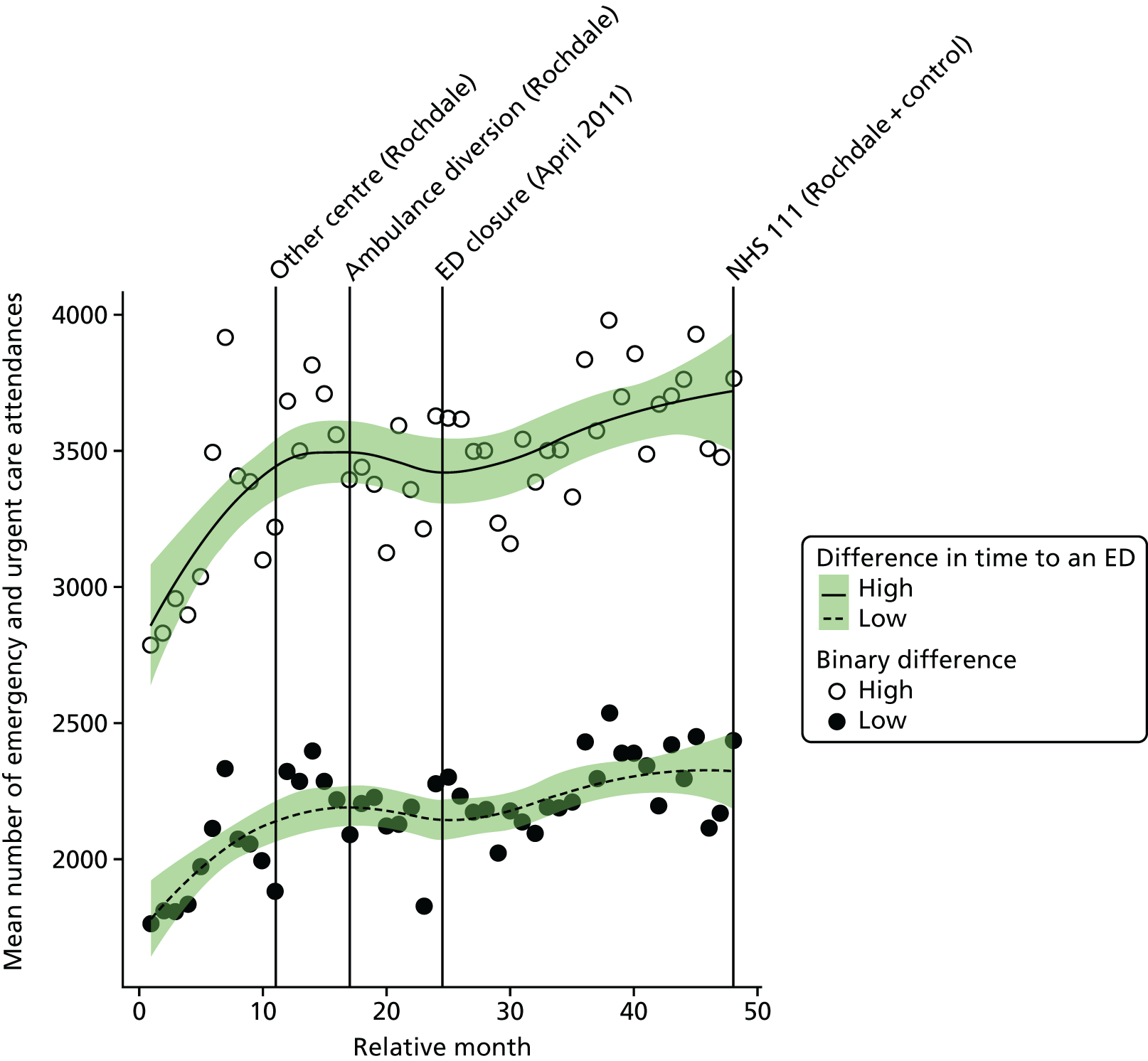
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the estimated number of emergency and urgent care attendances in high-dose areas compared with low-dose areas was just –1.0% (95% CI –5.2% to 3.4%; p = 0.64).
Minor attendances at an emergency or urgent care service
Plot of monthly activity
We have also examined the impact of the ED closure on the number of ‘minor’ emergency and urgent care attendances, defined as patients who were discharged home without having had any treatment or investigation that needed attendance at hospital. Figure 92 shows the monthly number of these minor attendances among residents of the RO ED catchment area and the control area over the 2 years before and the 2 years after the closure.
FIGURE 92.
Number of minor attendances at an emergency or urgent care service among residents of the Rochdale ED catchment area and the control area.
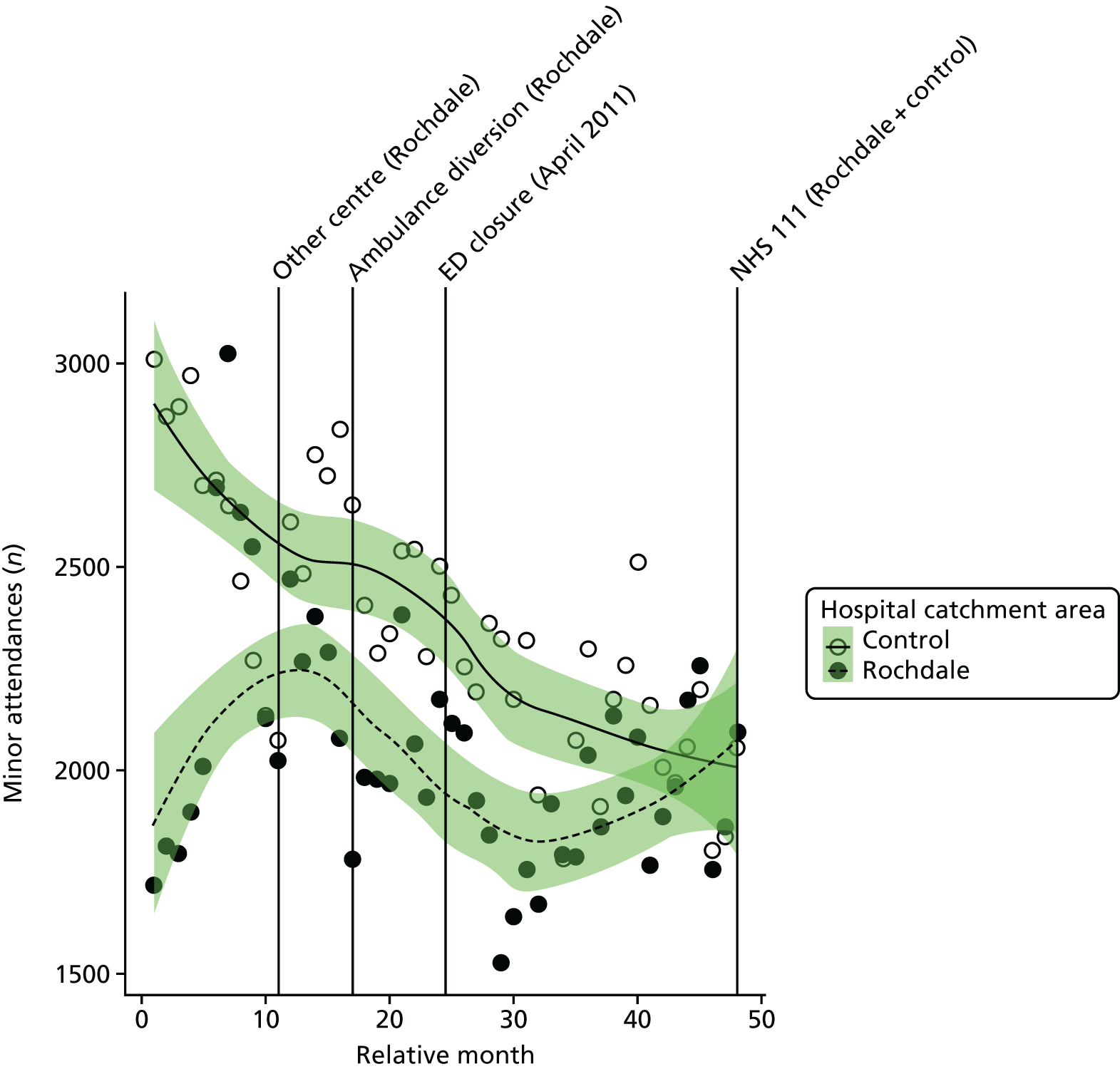
There was a decrease in the number of minor attendances among residents of RO. The number of minor attendances went down by 10%, from an average of 2131 per month pre closure to 1911 per month post closure. The number of minor attendances fell more sharply, by 17%, in the control area, from 2572 per month pre closure to 2167 per month post closure.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the number of minor attendances each month among residents of the RO ED catchment area was estimated to have changed at the time of the closure by an average of –16.4% (95% CI –25.8% to –5.8%; p = 0.003).
The emergency department closure and control area model
When the change in RO was compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of minor emergency and urgent care attendances each month among residents of the RO ED catchment area increased. Relative to the control area, at the time of the closure the number of attendances was estimated to have increased by an average of 11.6% (95% CI 1.3% to 23.0%; p = 0.03).
Dose model
Figure 93 shows the mean number of ‘minor’ emergency and urgent care attendances each month made by residents of LSOAs that were expected to have a relatively large change in time to ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of the RO ED. The pattern of change in these two areas was very similar, with an 11% reduction in the number of minor attendances in both the high-dose areas and the low-dose areas.
FIGURE 93.
Mean number of minor attendances at an emergency or urgent care service among residents of areas of Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
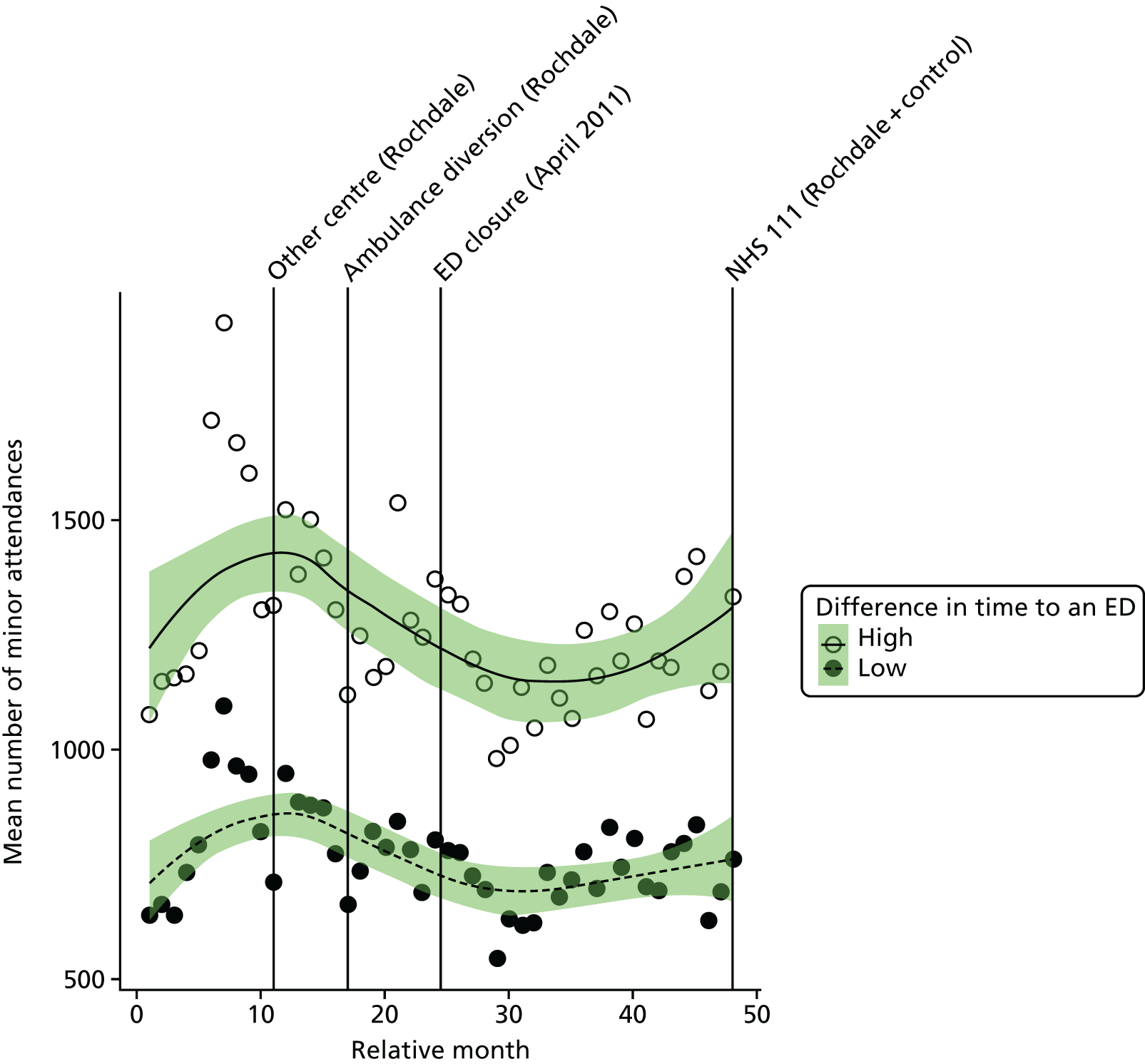
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of minor emergency and urgent care attendances in high-dose areas compared with low-dose areas was 0.6% (95% CI –7.1% to 9.0%; p = 0.88).
Admissions
All emergency admissions
Plot of monthly activity
Figure 94 shows the total number of emergency admissions to any hospital among residents of the RO ED catchment area and residents of the control site catchment area in each month of the 4-year study period.
FIGURE 94.
Total number of emergency admissions among residents of Rochdale ED catchment area and the control catchment area.
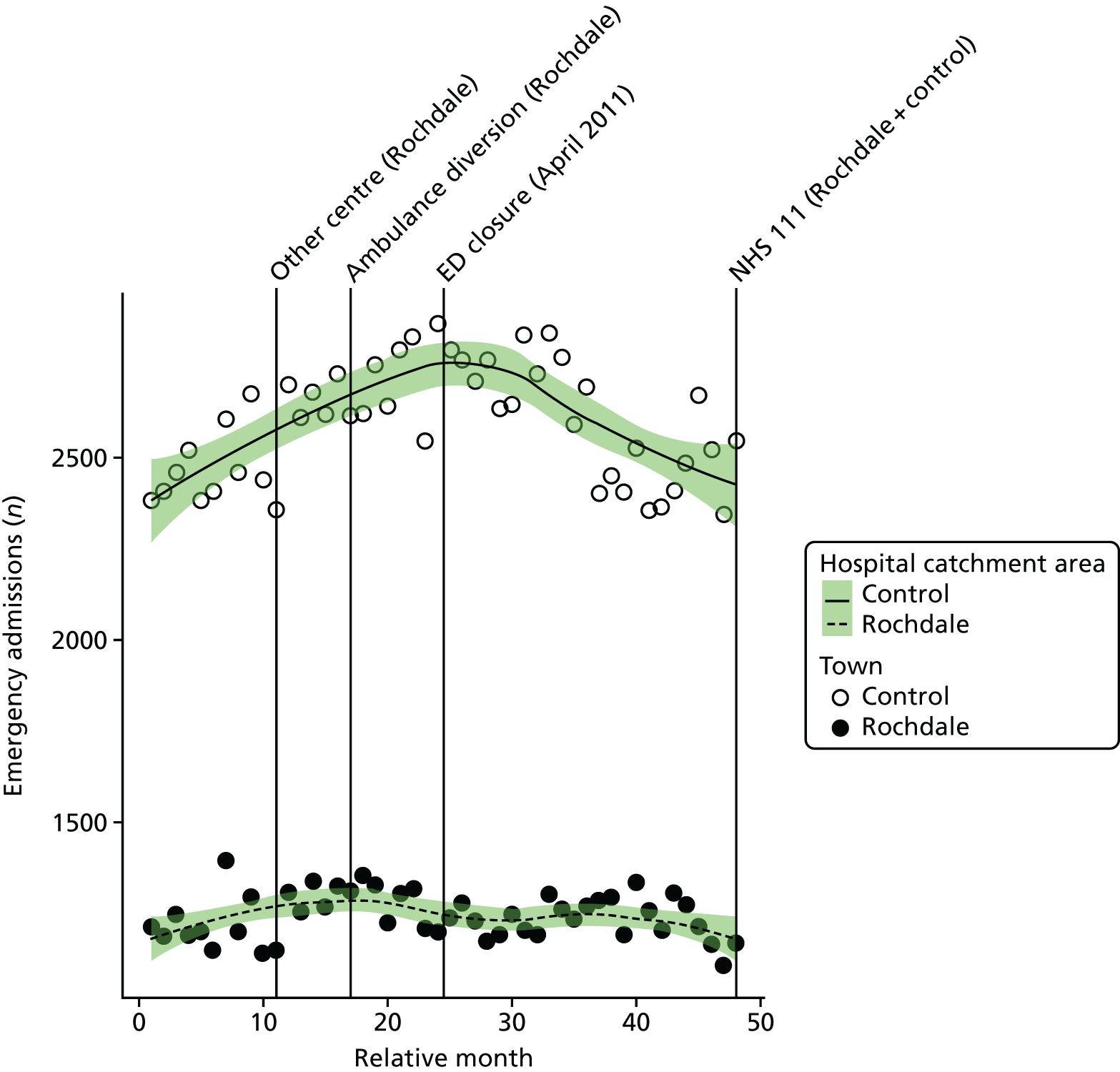
There is little evidence that the number of emergency admissions changed around the time of closure for residents of RO. In RO, there were, on average, 1255 emergency admissions per month prior to the closure and 1235 post closure: a decrease of –1.6%. The control area also showed little change over this period, with an increase from 2587 emergency admissions per month pre closure to 2594 emergency admissions per month post closure: an increase of just 0.3%.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of emergency admissions among residents of the catchment area of RO ED was –4.4% (95% CI –9.6% to 1.1%; p = 0.11).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change at the time of the closure in the monthly mean number of emergency admissions among residents of the catchment area of RO ED relative to the control site was –3.7% (95% CI –8.5% to 1.4%; p = 0.15).
Dose model
Figure 95 shows the mean number of emergency admissions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of RO ED. The pattern of change in these two areas was very similar, with a small reduction of 2% in the high-dose areas, from 757 pre-closure to 742 post-closure admissions per month, and a 1% reduction from 496 pre-closure to 493 post-closure admissions per month in the low-dose areas.
FIGURE 95.
Mean total number of emergency admissions among residents of areas of Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
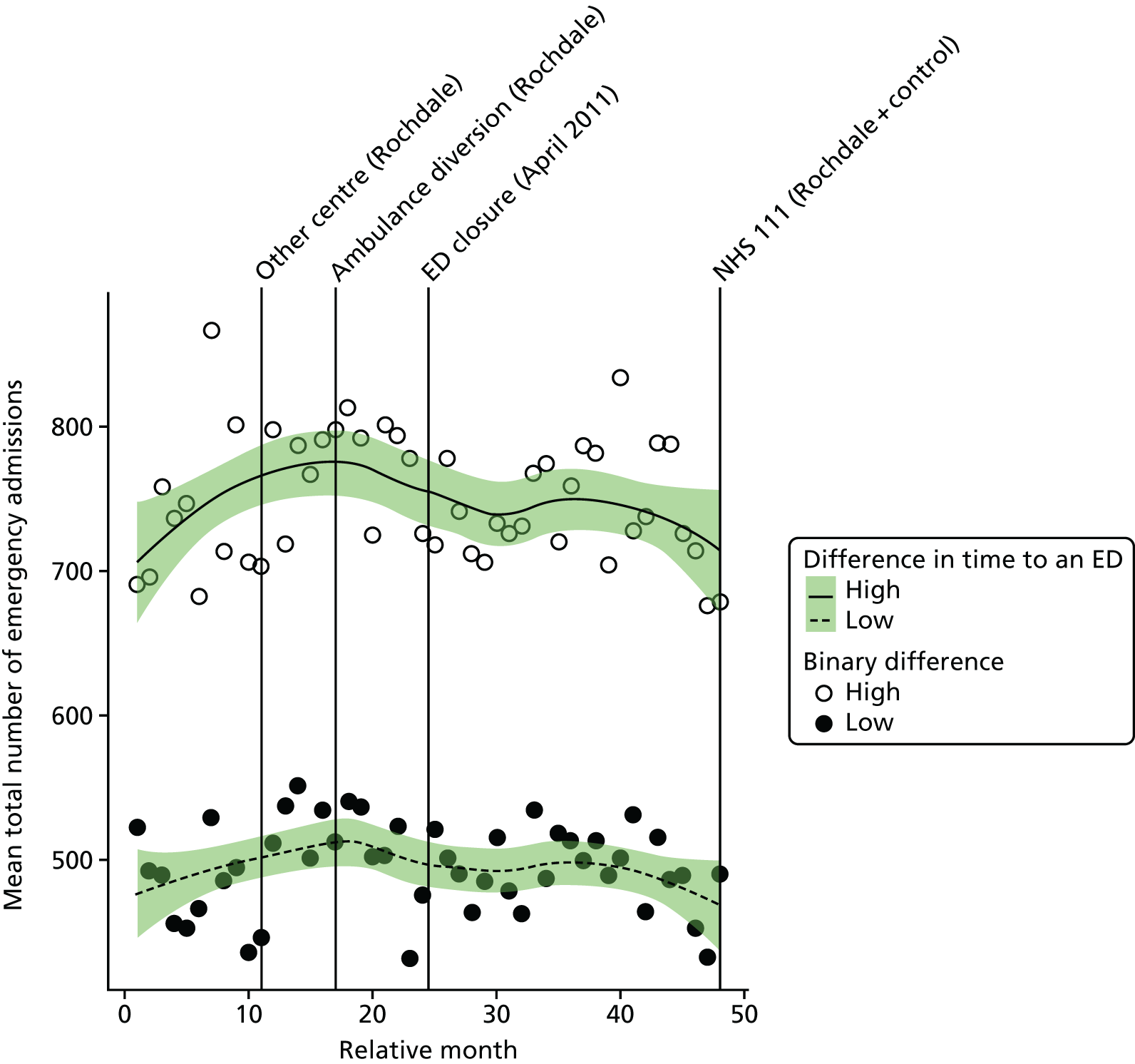
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of emergency admissions in the high-dose areas compared with the low-dose areas was –1.3% (95% CI –5.4% to 3.0%; p = 0.55).
Potentially avoidable emergency admissions
Plot of monthly activity
Figure 96 shows the number of potentially avoidable emergency admissions to any hospital among residents of the RO ED catchment area and residents of the control site catchment area in each month of the 4-year study period. The pattern for admissions from these 14 emergency conditions is similar to the pattern for all emergency admissions, but with some small changes in the numbers over the period spanning the ED closure in RO. In the RO area, there were, on average, 383 avoidable emergency admissions per month prior to the closure and 327 post closure: a decrease of 14.9%. In the control area, there were, on average, 721 emergency admissions per month prior to the closure date and 720 afterwards.
FIGURE 96.
Number of potentially avoidable emergency admissions among residents of Rochdale ED catchment area and the control catchment area.
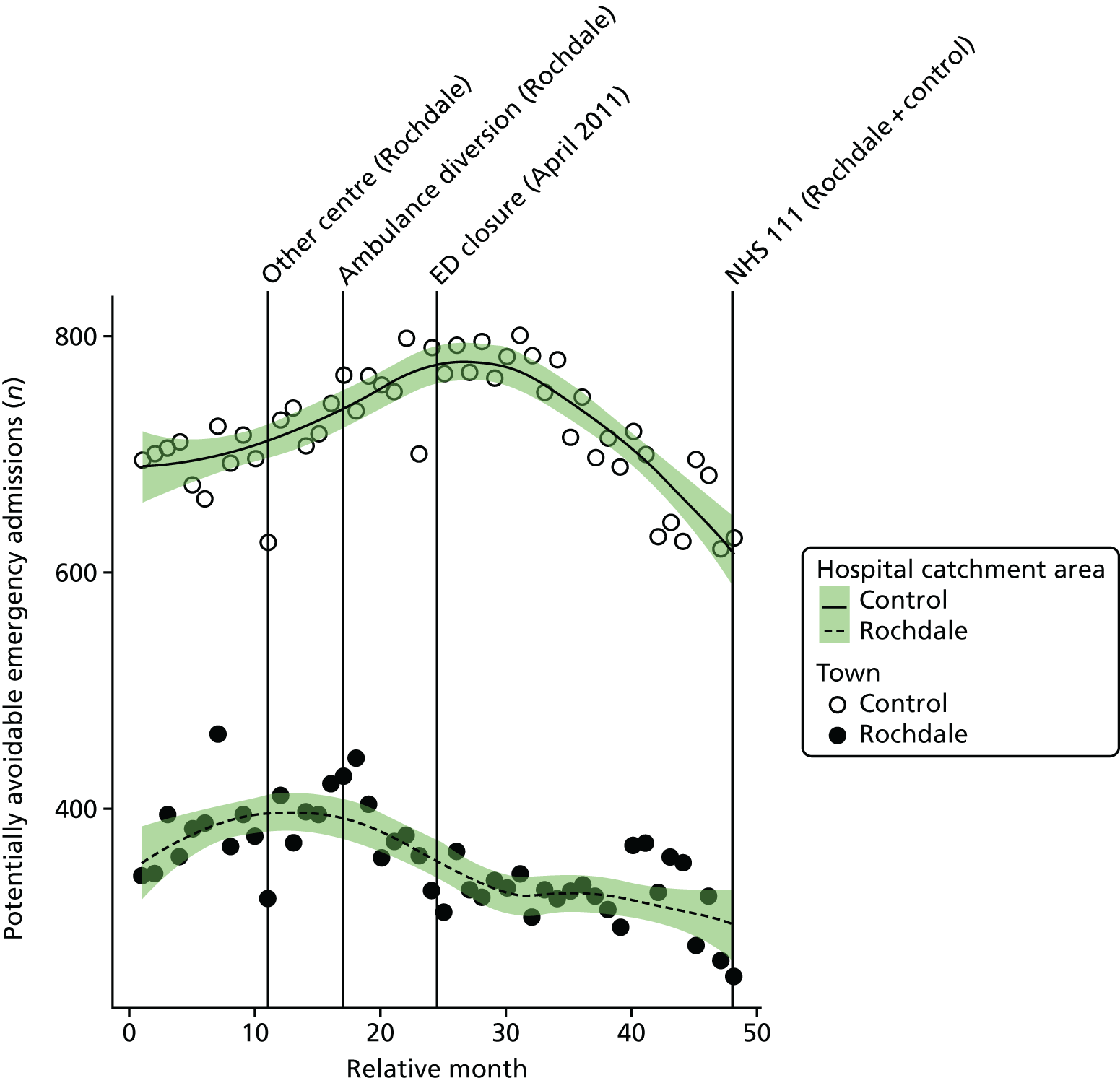
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of avoidable emergency admissions among residents of the catchment area of RO ED was –14.2% (95% CI –21.3% to –6.4%; p = 0.001).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly mean number of avoidable emergency admissions among residents of the catchment area of RO ED relative to the control site was –15.8% (95% CI –22.0% to –9.1%; p < 0.001).
Dose model
Figure 97 shows the number of potentially avoidable emergency admissions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of RO ED. The pattern of change in these two areas was the same, with a reduction of 15% in both the high-dose areas and the low-dose areas.
FIGURE 97.
Number of potentially avoidable emergency admissions among residents of areas of Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
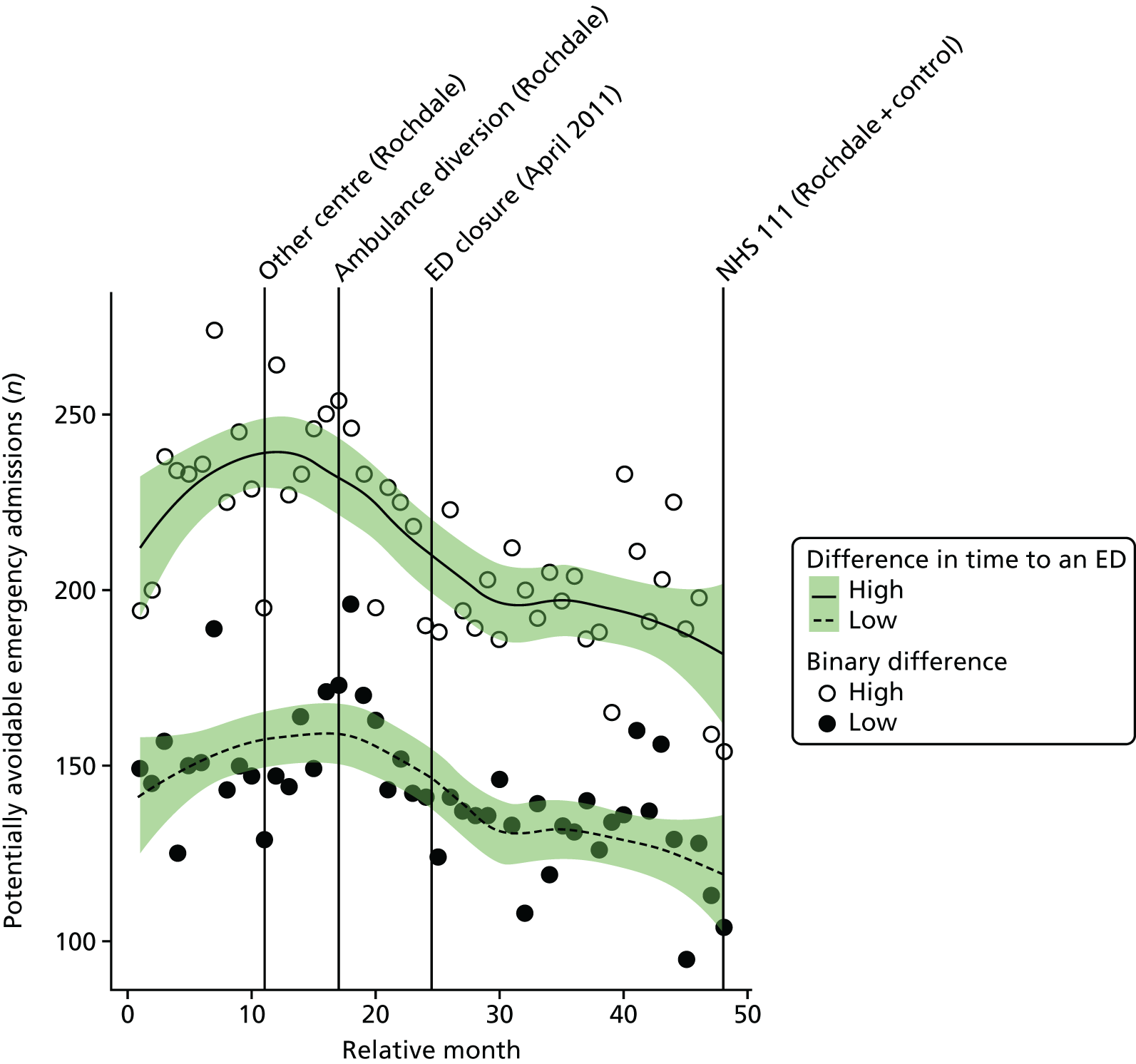
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of potentially avoidable emergency admissions in high-dose areas compared with low-dose areas was 0.0% (95% CI –7.6% to 7.1%; p = 0.99).
Length of stay for emergency admissions
Plot of monthly activity
Figure 98 shows the mean LOS in hospital for patients admitted as emergencies among residents of the RO ED catchment area and residents of the control site catchment area in each month of the 4-year study period. There was a small change in RO, with the mean LOS decreasing from 5.1 to 4.5 days before and after closure of the ED, respectively. In the control site, there was a smaller decrease, from 6.7 to 6.5 days before and after closure of the ED, respectively.
FIGURE 98.
Mean LOS for emergency admissions among residents of Rochdale ED catchment area and the control area.
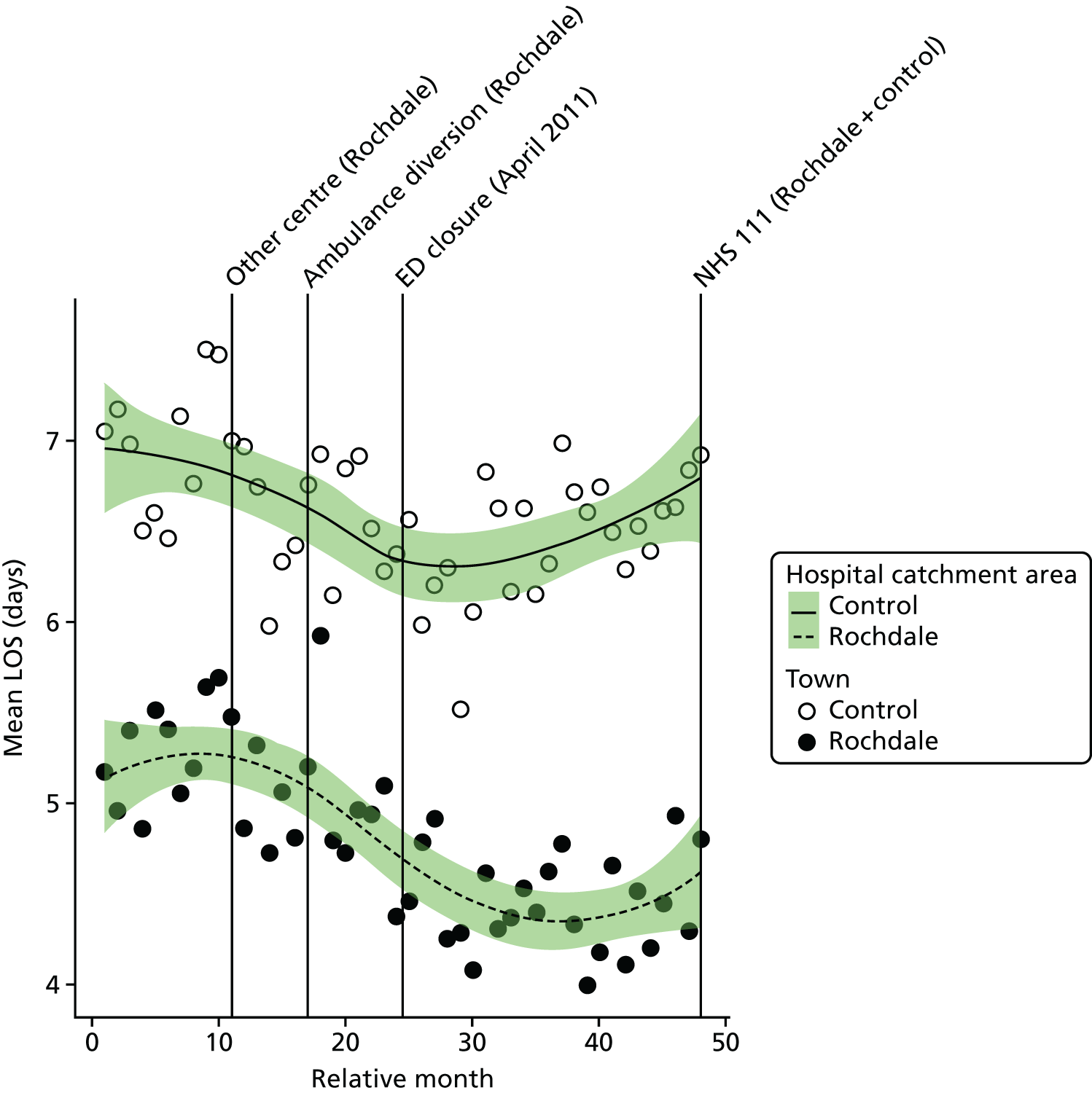
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the mean LOS among residents of the catchment area of RO ED was –0.36 days (95% CI –0.72 to 0.01 days; p = 0.05).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the mean length of stay for residents of the catchment area of RO ED at the time of the closure relative to the control site was –0.31 days (95% CI –0.62 to 0.01 days; p = 0.06).
Dose model
Figure 99 shows the mean LOS for emergency admissions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of RO ED. The pattern of change in these two areas was very similar, with a fall of 12% in the high-dose areas, from 5.2 days prior to the closure to 4.6 days after the closure, and a 15% reduction in the low-dose areas, from 5.2 days prior to the closure to 4.5 days after the closure.
FIGURE 99.
Mean LOS for emergency admissions among residents of areas in Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
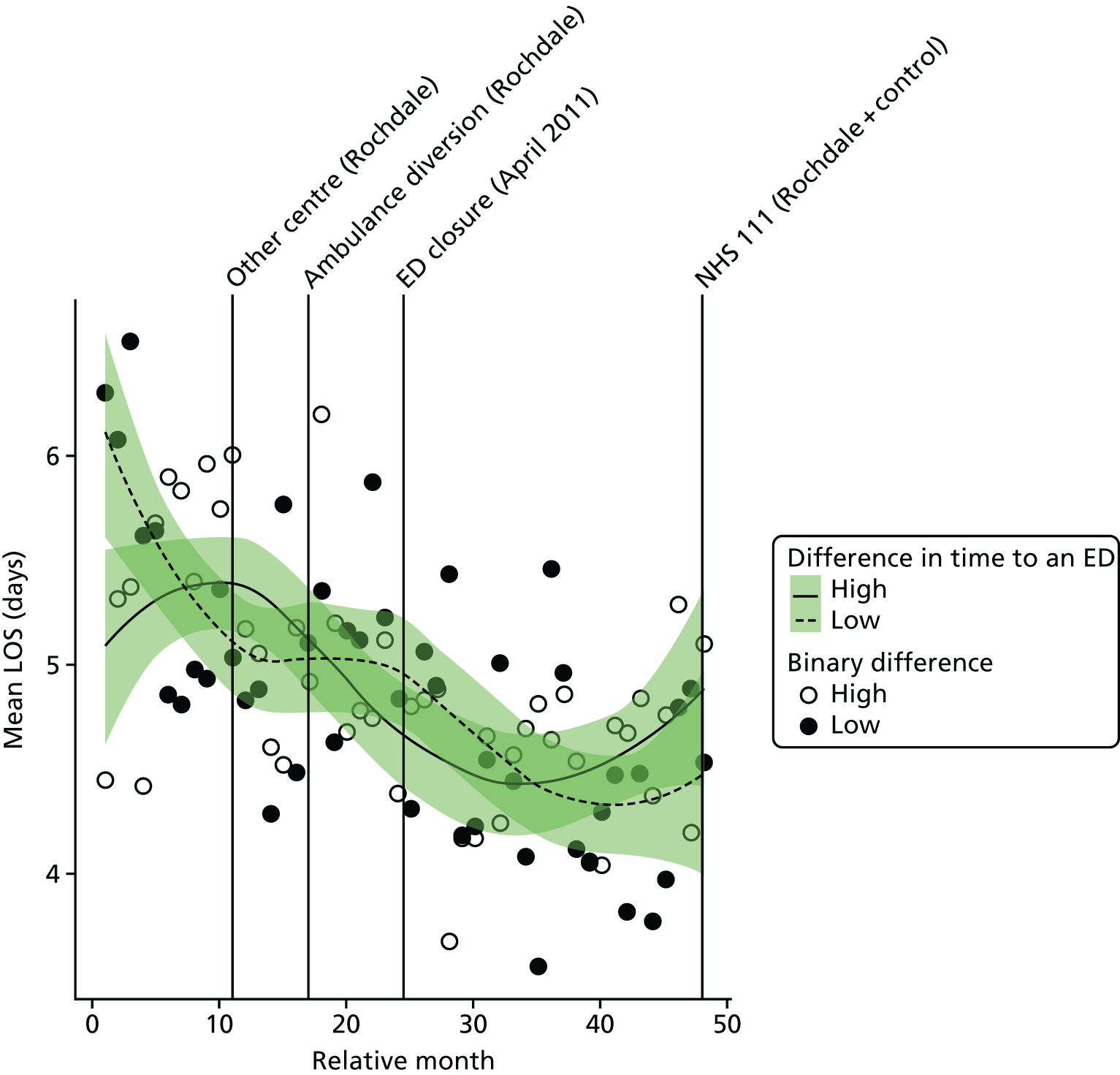
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the mean LOS for emergency admissions in the high-dose areas compared with the low-dose areas was 0.16 days (95% CI –0.3 to 0.63 days; p = 0.50).
Deaths
Out-of-hospital deaths from serious emergency conditions from certain serious conditions
‘Out-of-hospital’ deaths may occur at home prior to making contact with a service, in an ambulance on the way to hospital, in the ED prior to hospital admission or when a patient is recorded as having a SEC incident and is admitted, discharged alive and subsequently dies out of hospital without being readmitted.
Plot of monthly activity
Figure 100 shows the number of deaths occurring before arrival at hospital from any of the 16 SECs we have focused on in residents of the RO ED catchment area and residents of the control site catchment area in each month of the 4-year study period. In residents of the RO catchment area, there were, on average, 17.9 out-of-hospital deaths per month prior to the closure and 21.2 out-of-hospital deaths per month post closure: an increase of 18.1%. In the control area, the monthly average number of out-of-hospital deaths increased from 45.9 pre closure to 46.9 post closure.
FIGURE 100.
Number of deaths occurring out of hospital for SECs among residents of the catchment areas of the Rochdale and control EDs.
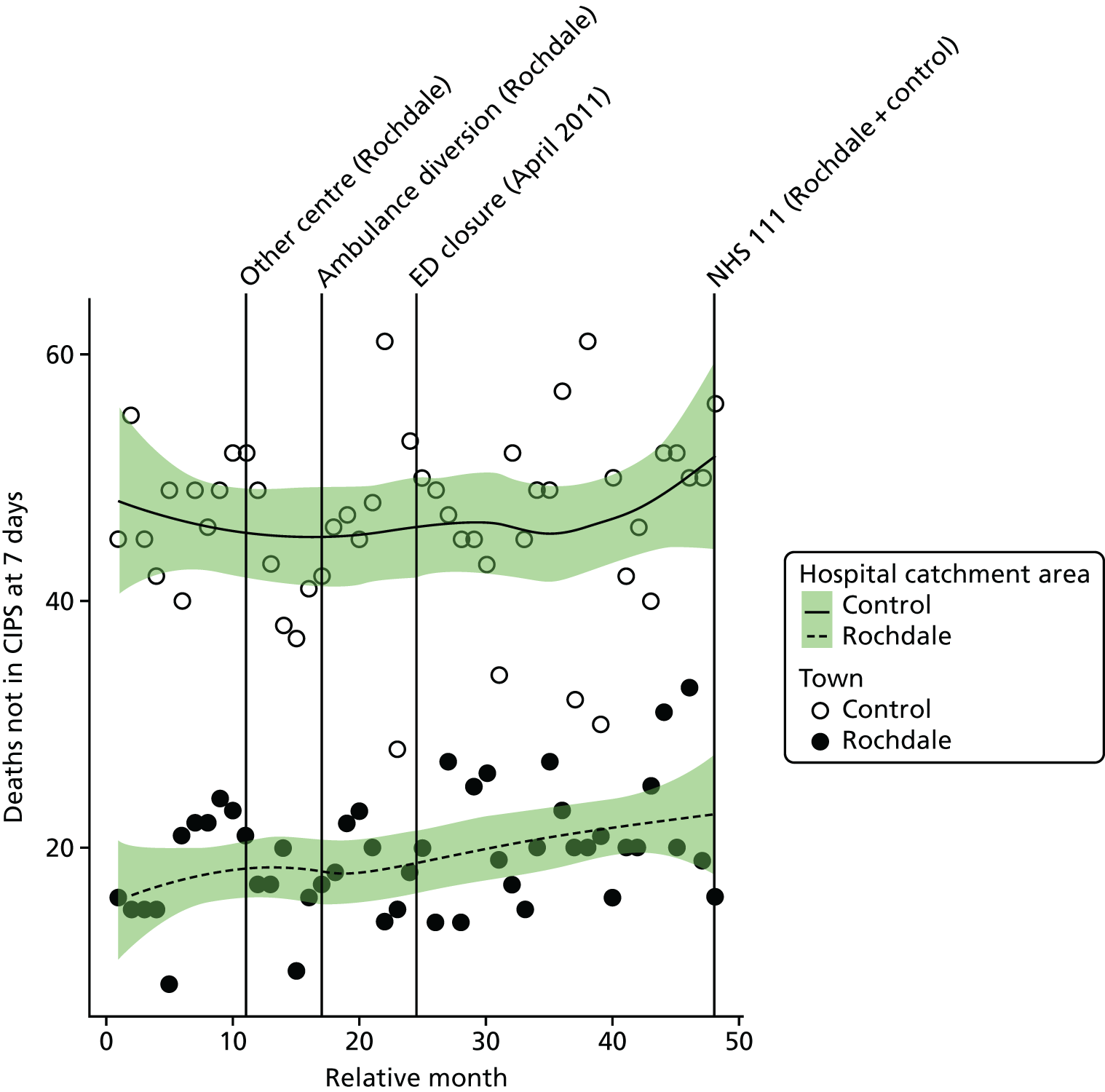
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the monthly mean number of out-of-hospital deaths from the 16 SECs among residents of the catchment area of RO ED was 9.4% (95% CI –18.8% to 47.5%; p = 0.55).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly mean number of emergency condition deaths occurring out of hospital among residents of the catchment area of RO ED at the time of the closure relative to the control site was 14.4% (95% CI –7.0% to 40.7%; p = 0.20).
Dose model
Figure 101 shows the number of out-of-hospital deaths each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of RO ED. The pattern of change in these two areas was similar, with a small increase of 10%, from 10.2 pre-closure to 11.3 post-closure deaths per month in the high-dose areas, and an increase of 22%, from 7.6 pre-closure to 9.3 post-closure deaths per month in the low-dose areas.
FIGURE 101.
Number of out-of-hospital deaths from SECs among residents of areas in Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
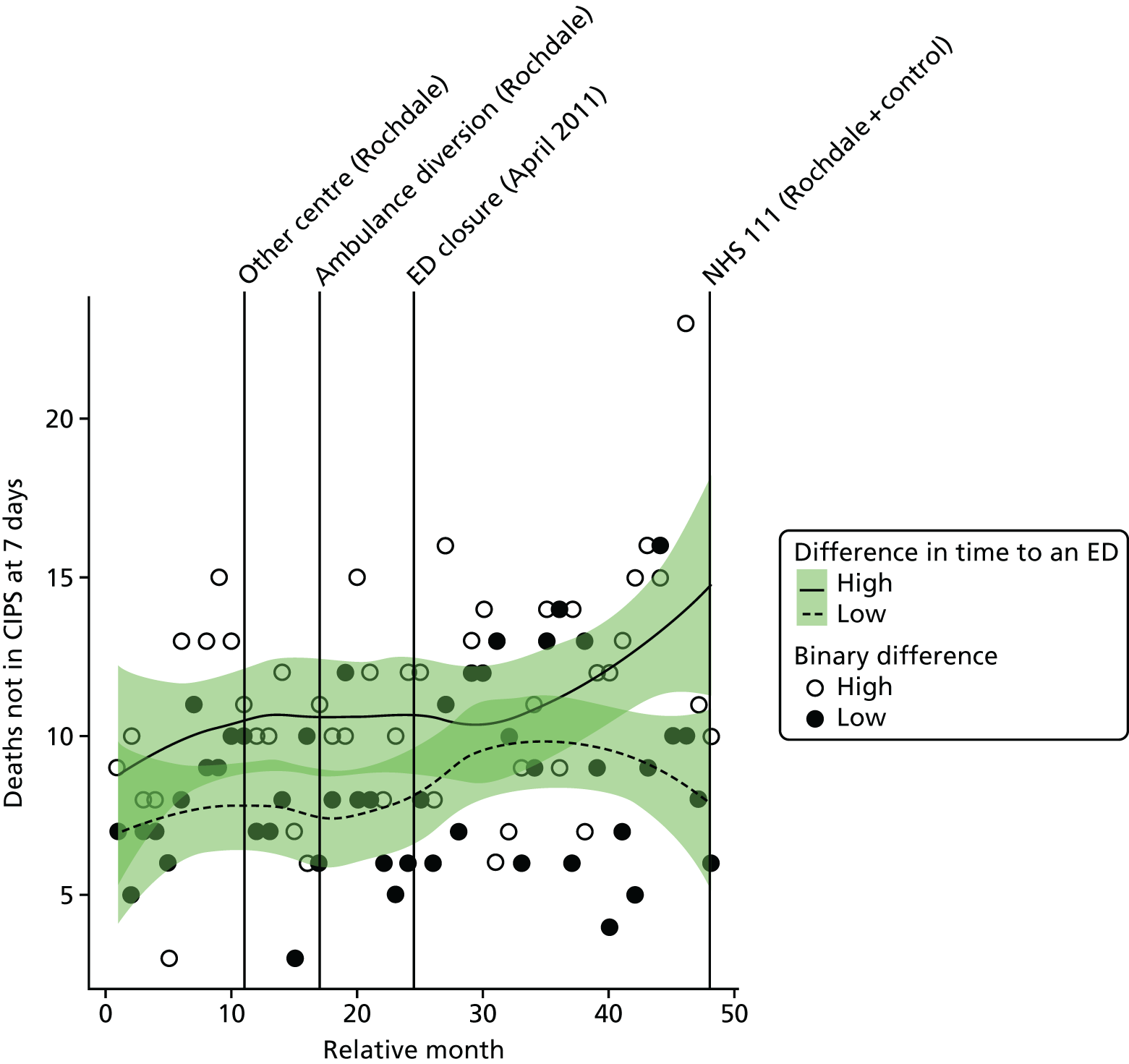
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of out-of-hospital deaths in the high-dose areas compared with the low-dose areas was –9.6% (95% CI –30.5% to 17.4%; p = 0.45).
All deaths from serious emergency conditions occurring within 7 days
Plot of monthly activity
Figure 102 shows the total number of deaths occurring up to 7 days post incident from the 16 SECs among residents of the RO ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These deaths may have occurred out of hospital or after hospital admission within 7 days. These numbers show a similar pattern as that for all out-of-hospital deaths. In the RO area, there were, on average, 27.1 deaths per month prior to the closure and 31.8 post closure: an increase of 17.4%. In the control area, the monthly average number of deaths decreased from 70.5 pre closure to 69.6 post closure.
FIGURE 102.
Total number of deaths from SECs occurring within 7 days of the incident among residents of the catchment areas of the Rochdale and control EDs.
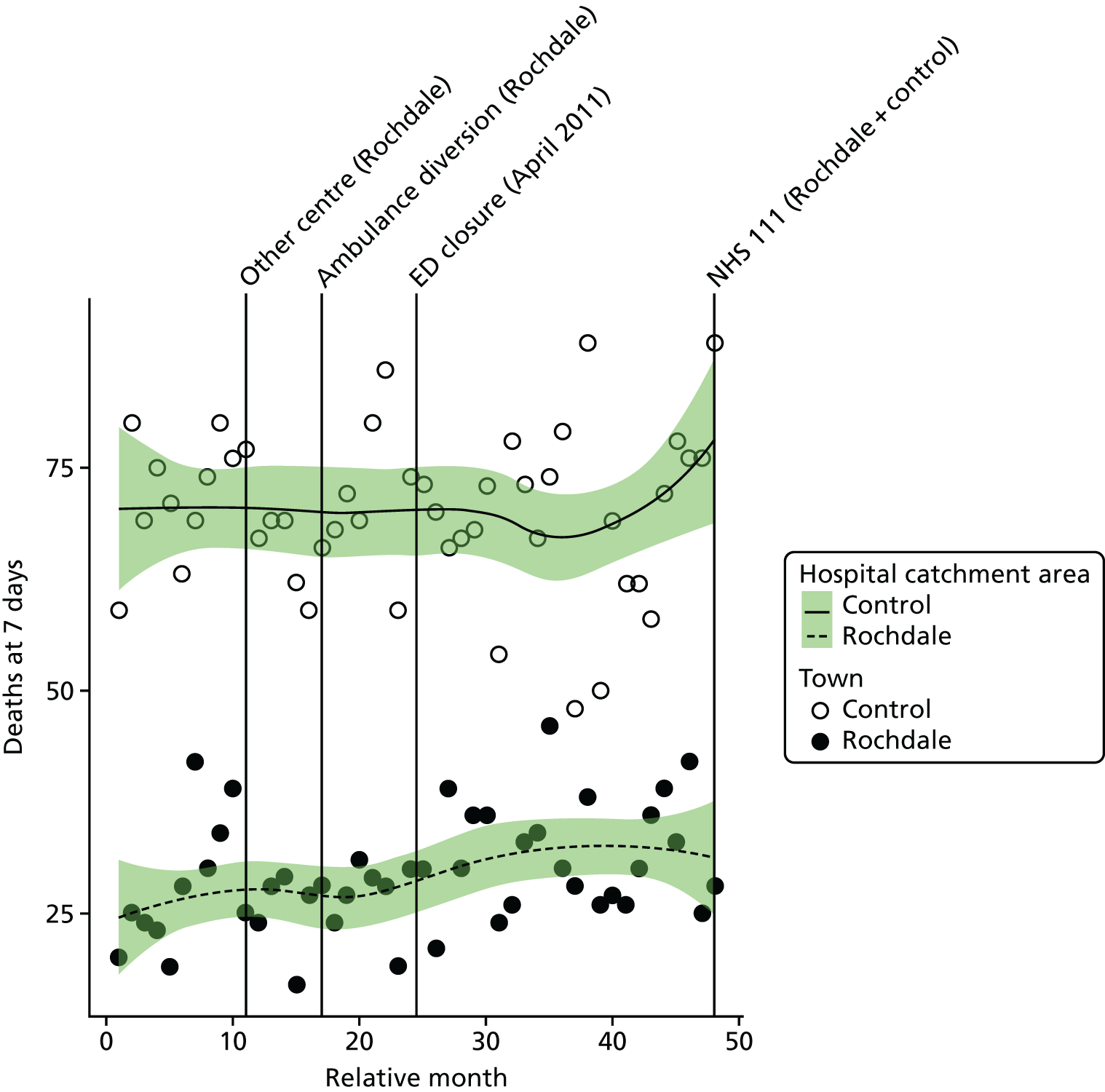
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the monthly mean number of deaths within 7 days from the 16 SECs among residents of the catchment area of RO ED was 17.9% (95% CI –7.6% to 50.5%; p = 0.19).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly mean number of deaths with 7 days from the 16 SECs for residents of the catchment area of RO ED at the time of the closure relative to the control site was 20.6% (95% CI 1.7% to 42.9%; p = 0.03).
Dose model
Figure 103 shows the total number of deaths occurring up to 7 days post incident from the 16 emergency conditions each month for residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of RO ED. The pattern of change in these two areas was similar, with a small increase of 13%, from 15.8 pre-closure to 17.9 post-closure deaths per month in the high-dose areas, and an increase of 22%, from 11.3 pre-closure to 13.9 post-closure deaths per month in the low-dose areas.
FIGURE 103.
Total number of deaths from SECs up to 7 days post incident among residents of areas in Rochdale that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
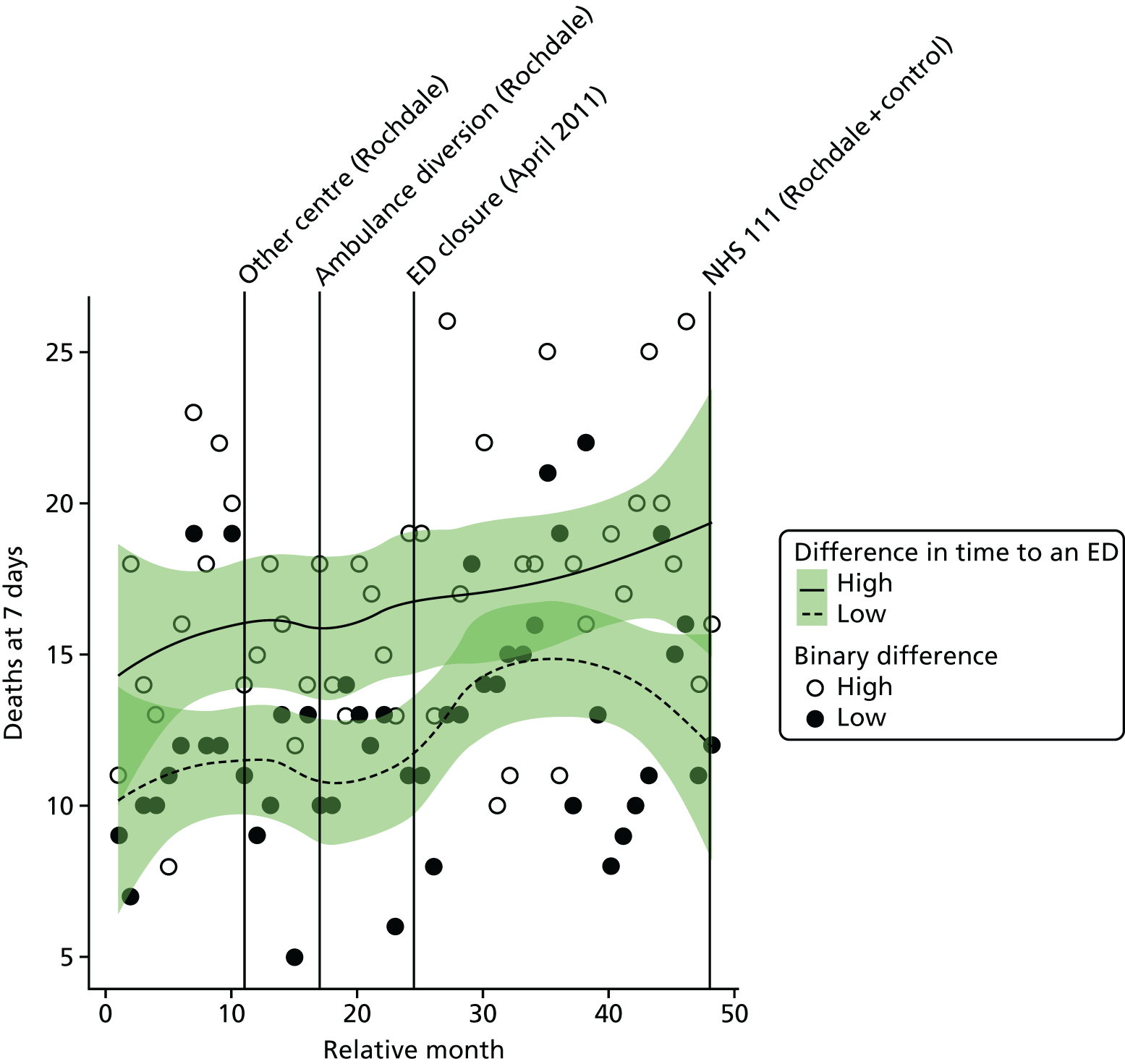
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of deaths in residents of high-dose areas compared with low-dose areas was –7.7% (95% CI –25.3% to 14.1%; p = 0.46).
Case fatality ratios: all serious emergency conditions studied
Plot of monthly activity
Figure 104 shows the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths plus admissions for patients who survived beyond 7 days from the 16 SECs among residents of the RO ED catchment area and residents of the control site catchment area. These ratios reflect the risk of dying from these emergency conditions. There is little indication of a change in these ratios. In RO, over the 2 years before the closure the average ratio was 0.212 (indicating that 21.2% of the patients died), and it was 0.242 afterwards: an increase of 3.0 in the percentage of patients who died. In the control site, the average ratio changed from 0.213 pre closure to 0.217 post closure.
FIGURE 104.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident for residents of the catchment areas of the Rochdale and control EDs.
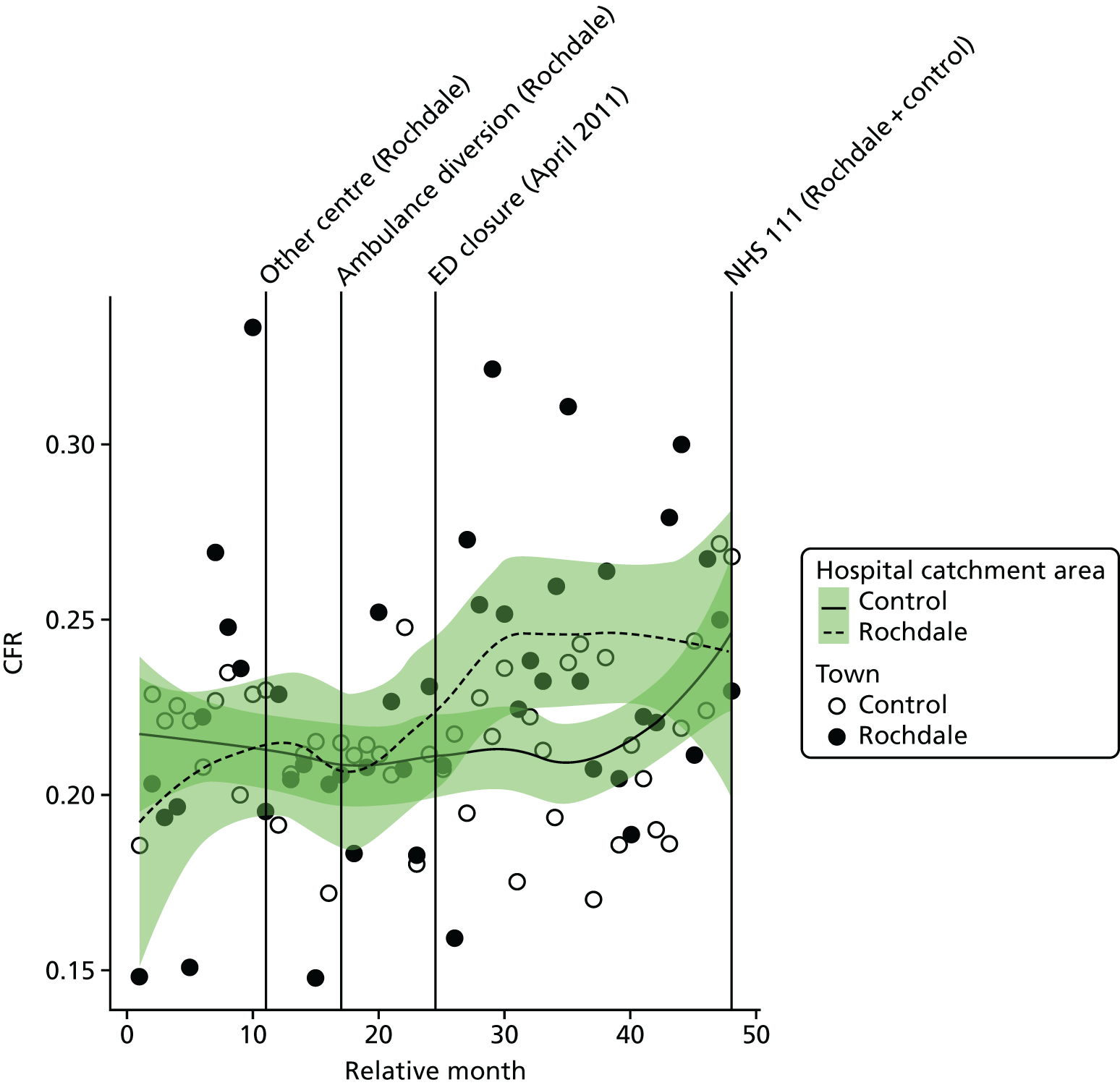
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the CFR for the 16 SECs among residents of the catchment area of RO ED was 0.041 (95% CI –0.002 to 0.084; p = 0.07); this is an increase of 4.1 in the percentage of patients who died.
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly average CFR for the 16 SECs among residents of the catchment area of RO ED at the time of the closure relative to the control site was 0.030 (95% CI 0.001 to 0.059; p = 0.05), indicating an increase of 3.0 in the percentage of patients who died.
Dose model
Figure 105 shows the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths plus admissions for patients who survived beyond 7 days from the 16 SECs among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of RO ED. The change in these ratios was very similar in the high-dose and low-dose areas. In high-dose areas, over the 2 years before the closure the average ratio was 0.205 (indicating that 20.5% of the patients died), and it was 0.238 afterwards: an increase of 3.3 in the percentage of patients who died. In the low-dose areas, the average ratio changed from 0.220 pre closure to 0.259 post closure.
FIGURE 105.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident among residents of areas in Rochdale that were expected to have a relatively large change in time to an ED (high dose) and those expected to have a small change (low dose).
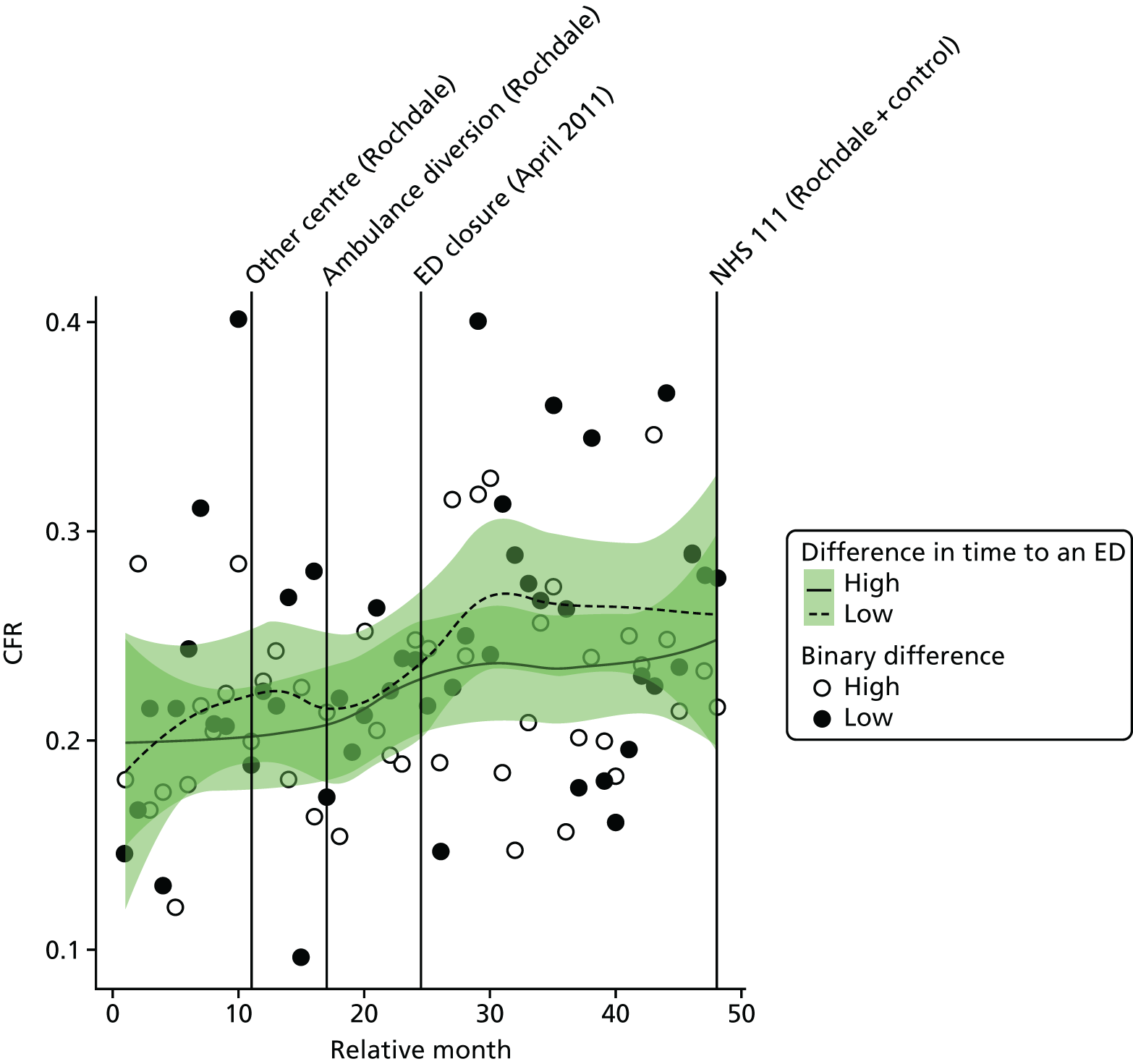
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the CFR in high-dose areas compared with low-dose areas was –0.005 (95% CI –0.041 to 0.030; p = 0.76).
Case fatality ratios: myocardial infarction and stroke
We have also examined the change in the CFRs for MI and for stroke separately (Tables 39 and 40). There was little evidence that the CFRs had changed for either condition, and there was no evidence of any difference for residents of Rochdale and its control area, or for residents of high-dose areas of Rochdale compared with the low-dose areas.
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Rochdale | |||
| Low-dose areas | 0.416 (0.123) | 0.401 (0.168) | –1.5 |
| High-dose areas | 0.363 (0.198) | 0.353 (0.152) | –1.0 |
| Total | 0.354 (0.133) | 0.362 (0.125) | –0.8 |
| Control | 0.226 (0.050) | 0.226 (0.070) | 0.0 |
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Rochdale | |||
| Low-dose areas | 0.376 (0.195) | 0.370 (0.145) | –0.6 |
| High-dose areas | 0.353 (0.152) | 0.390 (0.154) | +3.7 |
| Total | 0.365 (0.118) | 0.368 (0.129) | +0.2 |
| Control | 0.307 (0.065) | 0.317 (0.060) | +0.9 |
Newark
The Newark Hospital ED (NE ED) was closed in April 2011. We have compared the changes in activity and performance of the emergency care system for residents of the catchment area of NE ED over the 2 years before and the 2 years after the closure with changes over the same 4-year period for residents of the catchment area of a control ED.
In the analysis of the impact of the closure of NE ED, there were two system changes, both in the control area, that were accounted for in addition to the closure.
Newark ED catchment area other changes accounted for in the analysis:
-
No other changes were identified.
Control site ED catchment area other changes accounted for in the analysis:
-
Introduction of another UCC in June 2009.
-
Introduction of NHS 111 in March 2013.
Summary of findings
Following the closure, for residents of the ED catchment area in Newark:
-
There was strong evidence of a large increase in the number of emergency ambulance incidents, including ‘Red’ incidents. This evidence was only evident when compared with the control area.
-
There was strong evidence of a large increase in the time from ambulance service 999 call to arrival at hospital, when compared with the control area. The increase appeared to be driven by an increase in the time from the scene of the incident to the hospital.
-
There was some evidence to suggest an increase in the number of emergency and urgent care attendances, but this was not evident when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of minor attendances at emergency and urgent care services.
-
There was some evidence of an increase in the number of emergency hospital admissions when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of potentially avoidable hospital admissions.
-
There was no statistically reliable evidence to suggest a change in LOS for those admitted to hospital as an emergency case.
-
There was no statistically reliable evidence to suggest a change in the number of deaths or risk of deaths from the 16 SECs studied.
In comparing pre- and post-closure journey times to the nearest ED, for those experiencing longer post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of emergency ambulance incidents, but there was some evidence of a large increase in the number of ‘Red’ incidents when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the emergency and urgent care service attendance measures when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the emergency hospital admission measures when compared with those experiencing a smaller change in journey times.
-
There was no statistically reliable evidence to suggest a change in the mortality measures when compared with those experiencing a smaller change in journey times.
| Impact measure | Model, effect (95% CI); p-value | ||
|---|---|---|---|
| 1: no control | 2: compared with control | 6: high-dose areas | |
| Total number of emergency ambulance incidents | Increase: 1.3% (–6.0% to 9.2%); 0.74 | Increase: 21.5% (14.3% to 29.2%); < 0.001 | Decrease: –3.7% (–9.9% to 2.9%); 0.27 |
| Total number of emergency ambulance ‘Red’ incidents | Increase: 6.5% (–6.4% to 21.2%); 0.34 | Increase: 20.9% (10.8% to 31.9%); < 0.001 | Increase: 16.0% (3.9% to 29.6%); 0.008 |
| Mean time from 999 ‘Red’ call to arrival at hospital | Increase: 5.4 minutes (1.5 to 9.4 minutes); 0.01 | Increase: 21.2 minutes (16.5 to 25.8 minutes); < 0.001 | Increase: 16.7 minutes (13.9 to 19.5 minutes); < 0.001 |
| Total number of emergency and urgent care attendances | Increase: 6.1% (2.3% to 10.0%); 0.001 | Decrease: –1.0% (–4.6% to 2.7%); 0.59 | Increase: 1.1% (–2.1% to 4.3%); 0.51 |
| Total number of minor attendances at an emergency and urgent care service | Increase: 1.0% (–8.6% to 11.6%); 0.85 | Decrease: –7.5% (–15.8% to 1.6%); 0.10 | Increase: 2.1% (–7.3% to 12.6%); 0.67 |
| Total number of emergency hospital admissions | Increase: 4.0% (–3.6% to 12.2%); 0.31 | Increase: 7.0% (2.4% to 11.8%); 0.003 | Decrease: –1.2% (–7.3% to 5.2%); 0.70 |
| Total number of potentially avoidable emergency hospital admissions | Increase: 0.2% (–11.1% to 12.9%); 0.98 | Increase: 2.5% (–3.9% to 9.5%); 0.45 | Increase: 3.8% (–5.7% to 14.3%); 0.45 |
| Mean LOS for emergency hospital admissions | Decrease: –0.5 days (–1.1 to –0.0 days); 0.06 | Increase: 0.3 days (–0.1 to 0.7 days); 0.13 | Increase: 0.04 days (–0.7 to 0.8 days); 0.91 |
| Total number of out-of-hospital deaths | Decrease: –6.8% (–34.6% to 33.0%); 0.70 | Decrease: –4.4% (–22.0% to 17.3%); 0.67 | Increase: 7.9% (–21.5% to 48.3%); 0.64 |
| Total number of deaths occurring within 7 days post incident | Decrease: –8.3% (–31.4% to 22.5%); 0.56 | Increase: 0.5% (–15.4% to 19.4%); 0.95 | Decrease: –1.8% (–25.6% to 29.5%); 0.90 |
| CFR (7 days) | Decrease: –0.9% (–4.9% to 3.1%); 0.65 | Increase: 2.4% (–0.2% to 5.0%); 0.08 | Increase: 1.5% (–5.1% to 8.1%); 0.67 |
Change in time to the next-nearest emergency department
Following the ED closure, the change in time to reach the next-nearest ED for the residents of the catchment area ranged from 0 to 23 minutes.
FIGURE 106.
Geographical map of Newark and surrounding EDs showing the change in time to the next-nearest ED. Map tiles by Stamen Design, under a Creative Commons Attribution license (CC BY 3.0; see https://creativecommons.org/licenses/by/3.0/). Data by OpenStreetMap, under ODbL. Contains National Statistics data. © Crown copyright and database right 2016. Contains OS data © Crown copyright and database right 2016.
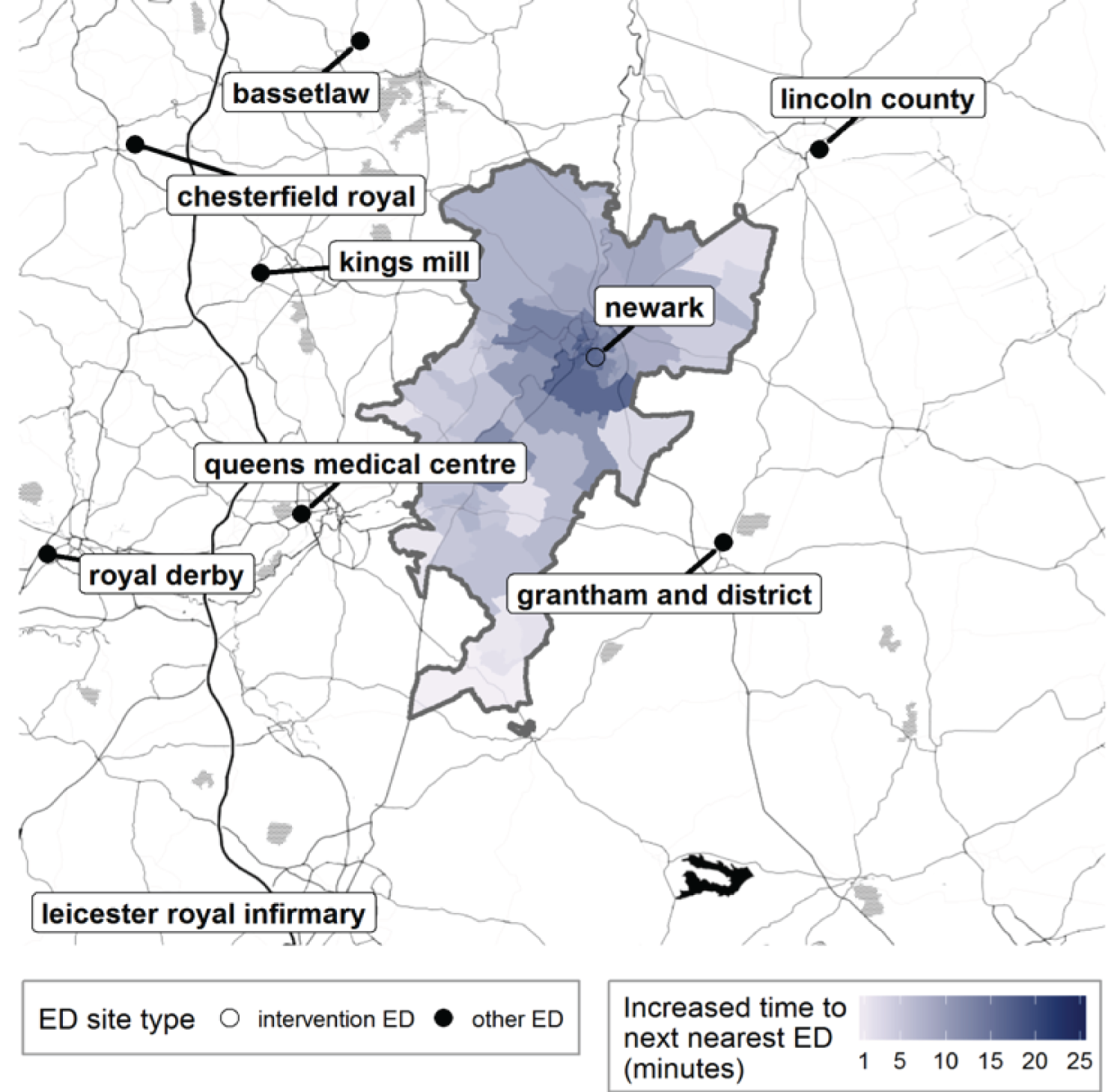
FIGURE 107.
Newark: change in time from LSOA to ED following ED closure, for residents of the catchment area of Newark Hospital ED.
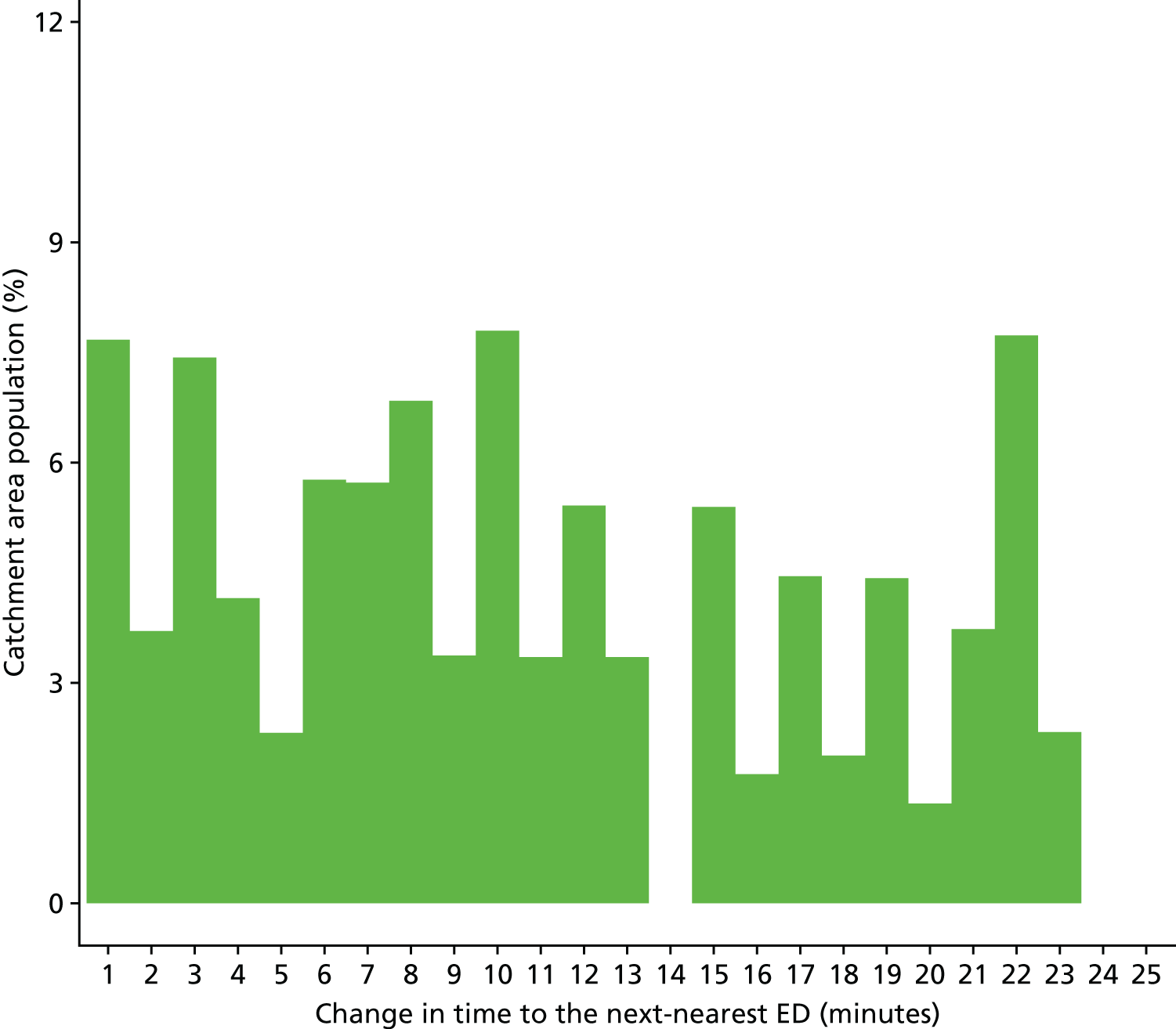
Findings from individual activity and performance measures
Ambulance service performance
Total number of incidents following 999 calls to the ambulance service
Plot of monthly activity
Figure 108 shows the total number of 999 incidents referred to the ambulance service from residents of NE ED catchment area, and the control area, for each month over the 2 years prior to and the 2 years after the closure of the NE ED. There were no usable data from the ambulance service in the NE ED catchment area for the first year. Incidents went up by 13% from an average of 946 per month pre closure to 1066 post closure in the NE ED catchment area, but fell by 7% from 1628 per month pre closure to 1511 per month post closure in the control area.
FIGURE 108.
Total number of 999 incidents among residents of the Newark ED catchment area and the control area.
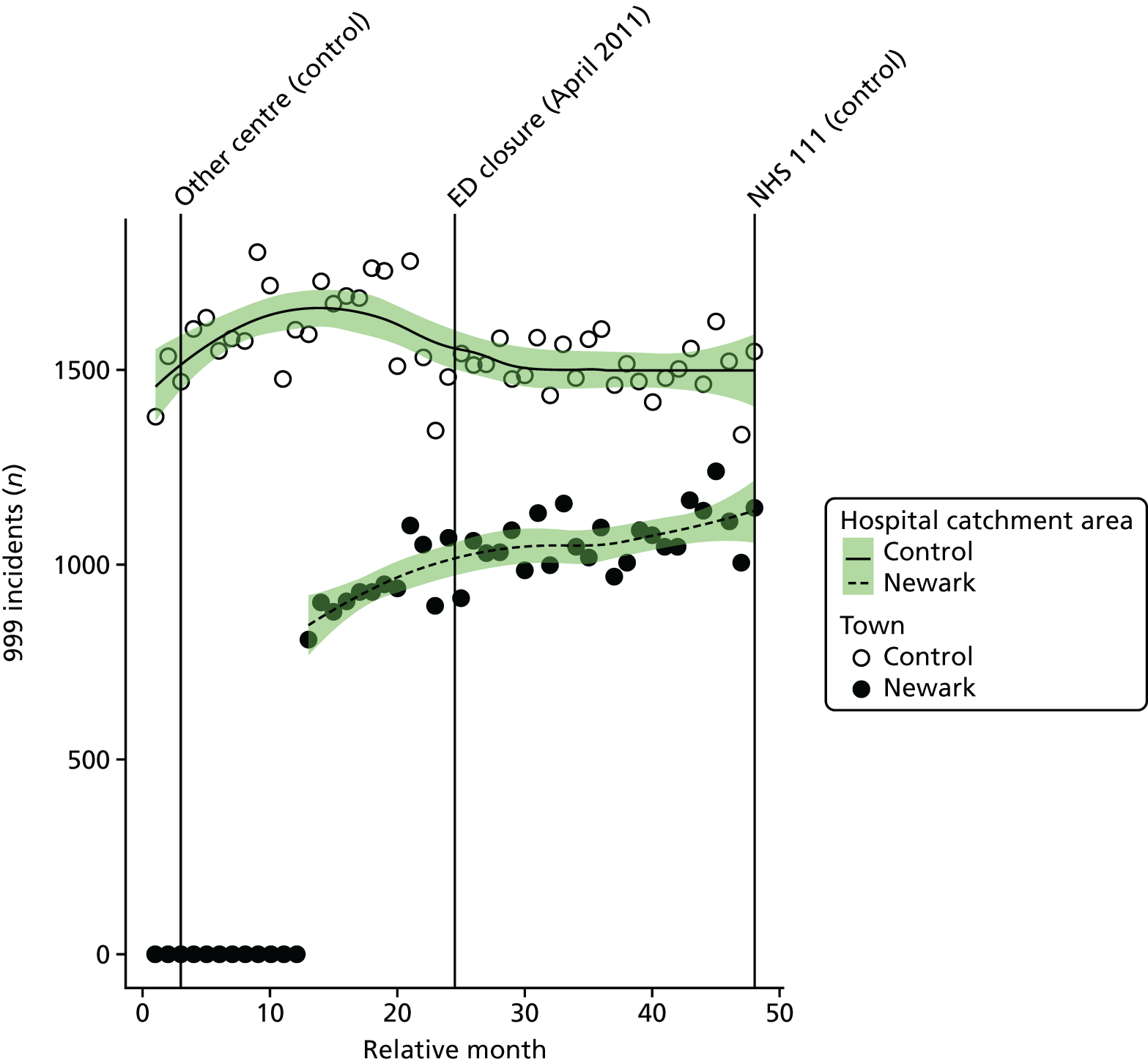
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of incidents each month for residents of the NE ED catchment area increased at the time of the closure by an average of 1.3% (95% CI –6.0% to 9.2%; p = 0.74).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment areas, the estimated number of incidents each month for residents of the NE ED catchment area increased at the time of the closure relative to the control area by an average of 21.5% (95% CI 14.3% to 29.2%; p < 0.001).
Dose model
Figure 109 shows the mean number of incidents each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. In high-dose areas, the number of incidents increased by 11%, from 574 pre closure to 637 post closure, and in low-dose areas the number of incidents increased by 15%, from 373 pre closure to 429 post closure.
FIGURE 109.
Mean number of 999 incidents among residents of areas in Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
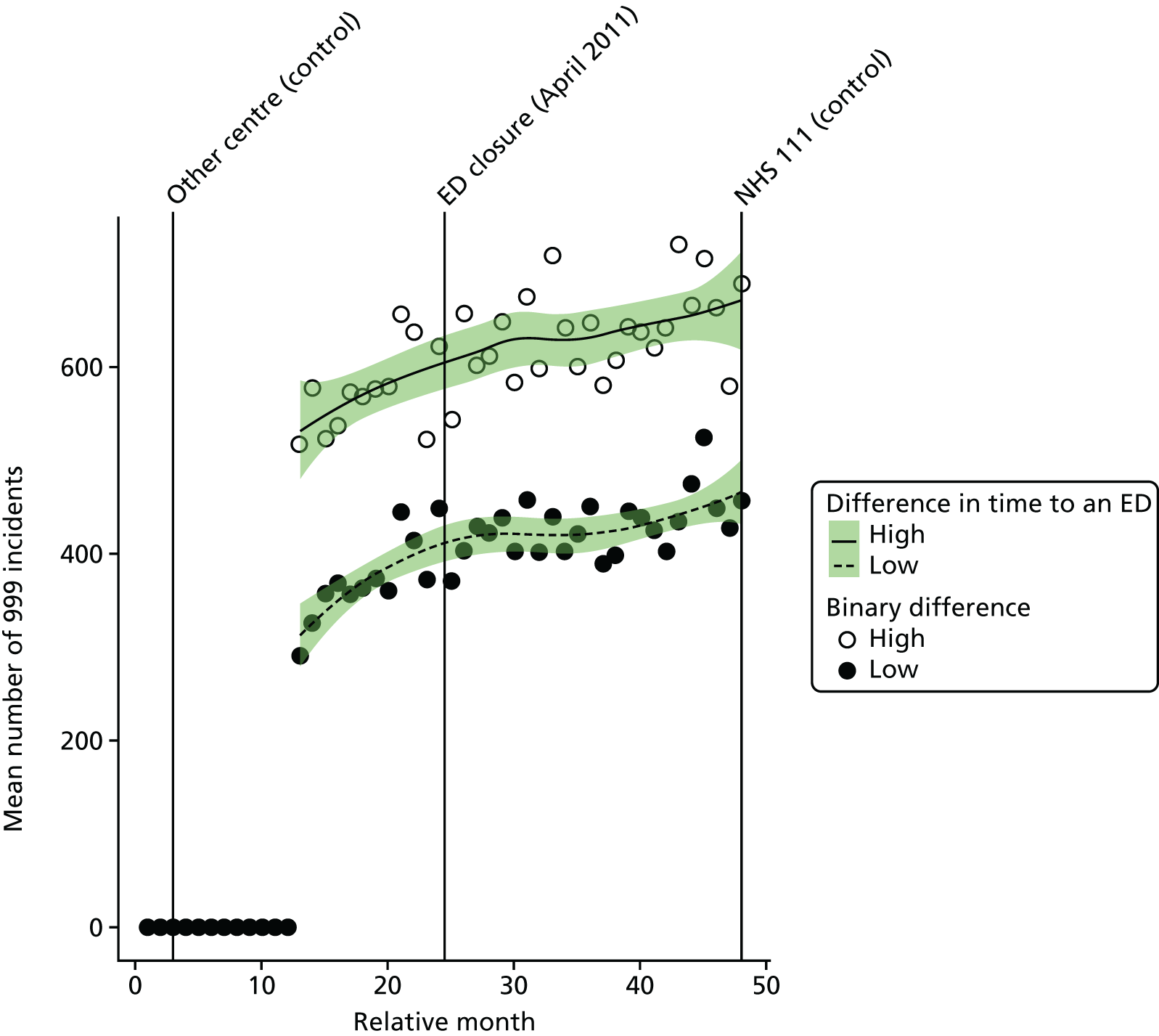
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the number of incidents in the high-dose areas relative to the low-dose areas at the time of the closure was –3.7% (95% CI –9.9% to 2.9%; p = 0.27).
Number of emergency ambulance ‘Red’ incidents
Plot of monthly activity
Figure 110 shows the number of ‘Red’ 999 incidents referred to the ambulance service from residents of the NE ED catchment area and the control area for each month over the 2 years prior to and the 2 years after the date of closure of the NE ED. There were no usable data from the ambulance service for the NE ED catchment area in the first year. The number of incidents went up by 9%, from an average of 334 per month pre closure to 364 per month post closure in the NE ED catchment area, and the number of incidents went down by 10% from 623 pre closure to 562 post closure in the control area.
FIGURE 110.
Number of ‘Red’ 999 incidents among residents of the Newark ED catchment area and the control area.
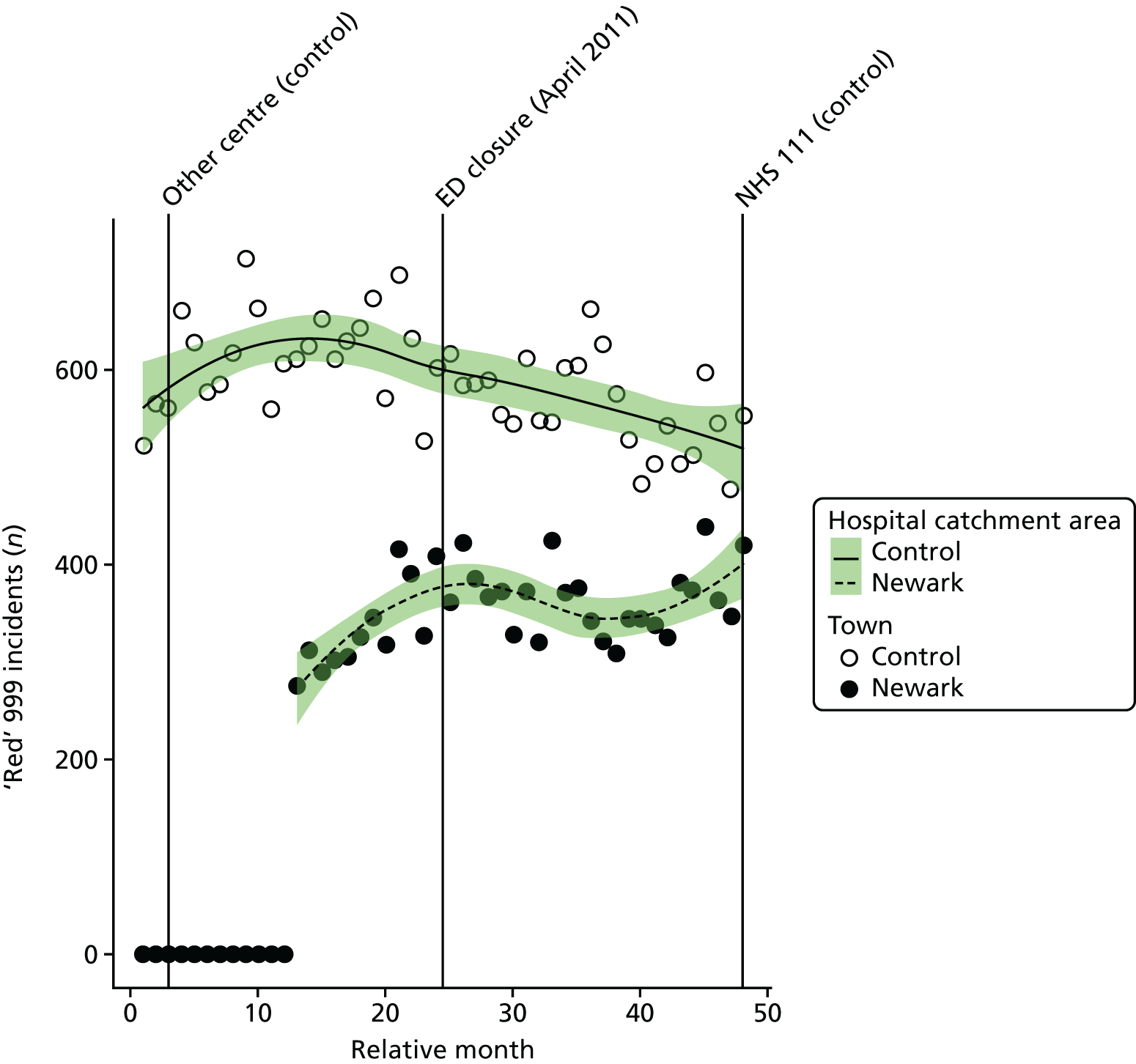
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the number of ‘Red’ incidents each month among residents of the NE ED catchment area increased at the time of the closure by an estimated 6.5% (95% CI –6.4% to 21.2%; p = 0.34).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment areas, the number of ‘Red’ incidents each month among residents of the NE ED catchment area increased at the time of the closure relative to the control area by an estimated 20.9% (95% CI 10.8% to 31.9%; p < 0.001).
Dose model
Figure 111 shows the mean number of ‘Red’ incidents each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. The pattern of change in these two areas was slightly different. There was no significant change in the number of incidents in low-dose areas, with the average monthly number of ‘Red’ incidents changing from 136 to 135, and there was a small increase in the average monthly number of ‘Red’ incidents from 198 to 229 in the high-dose areas.
FIGURE 111.
Number of ‘Red’ 999 incidents among residents of areas in Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
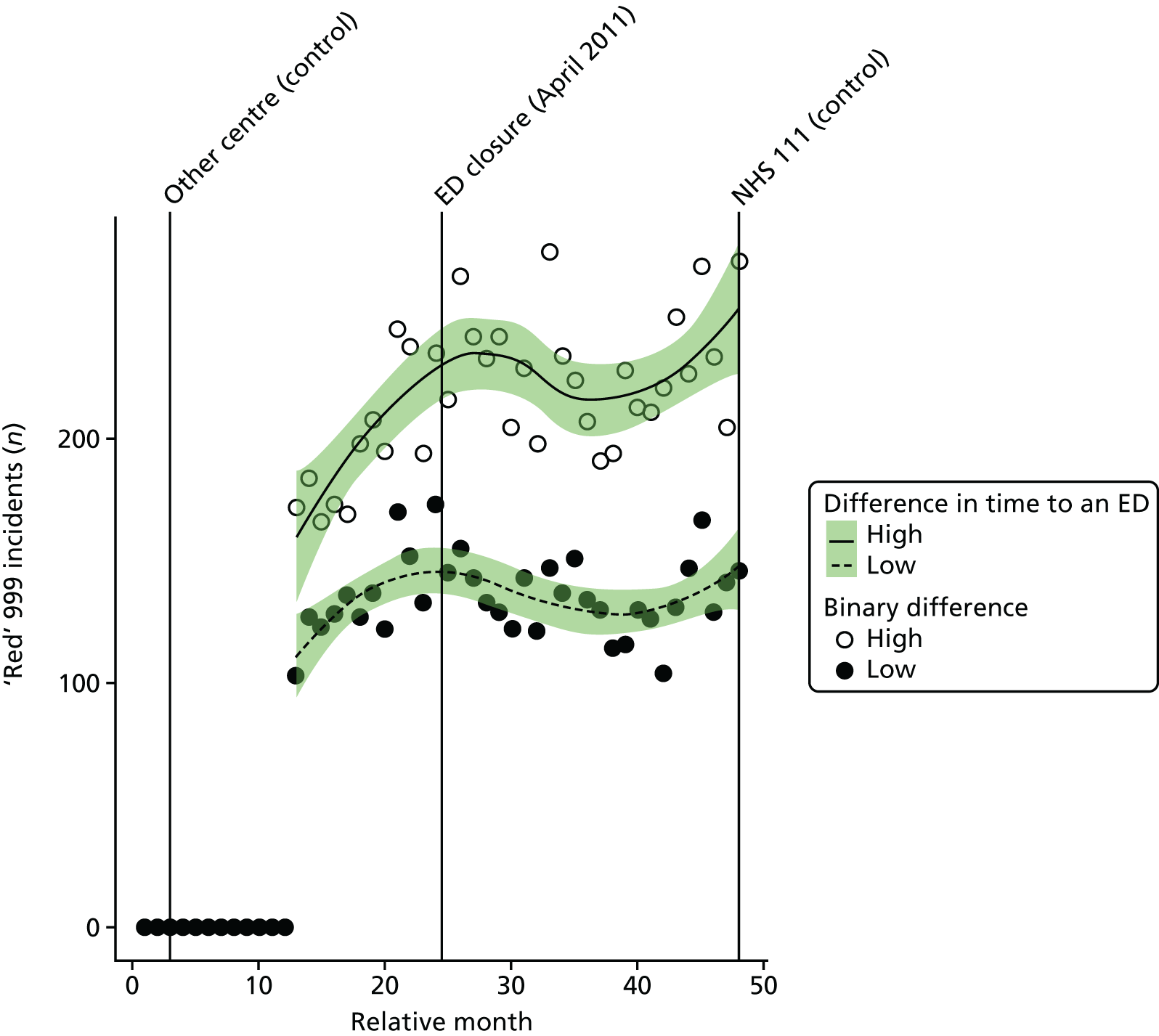
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the number of ‘Red’ incidents in high-dose areas relative to low-dose areas at the time of the closure was 16.0% (95% CI 3.9% to 29.6%; p = 0.008).
Mean time from 999 call to arrival at hospital for ‘Red’ incidents
Plot of monthly performance
Figure 112 shows the mean time for 999 ‘Red’ incidents from call to arrival at hospital in each month over the 2 years prior to and the 2 years after the closure of the NE ED for residents of the NE ED catchment area. There was a large increase in these times for residents of the NE ED catchment area from before the closure (monthly mean 66.7 minutes) to after the closure (monthly mean 81.8 minutes): an increase of 15.1 minutes on average. In contrast, in the control area these times fell by an average of 5.4 minutes. In the control area, some of the journey times that were recorded were very long. However, the median time also fell by 4.3 minutes.
FIGURE 112.
Mean time from 999 call to arrival at hospital for residents of the Newark ED catchment area and the control area.
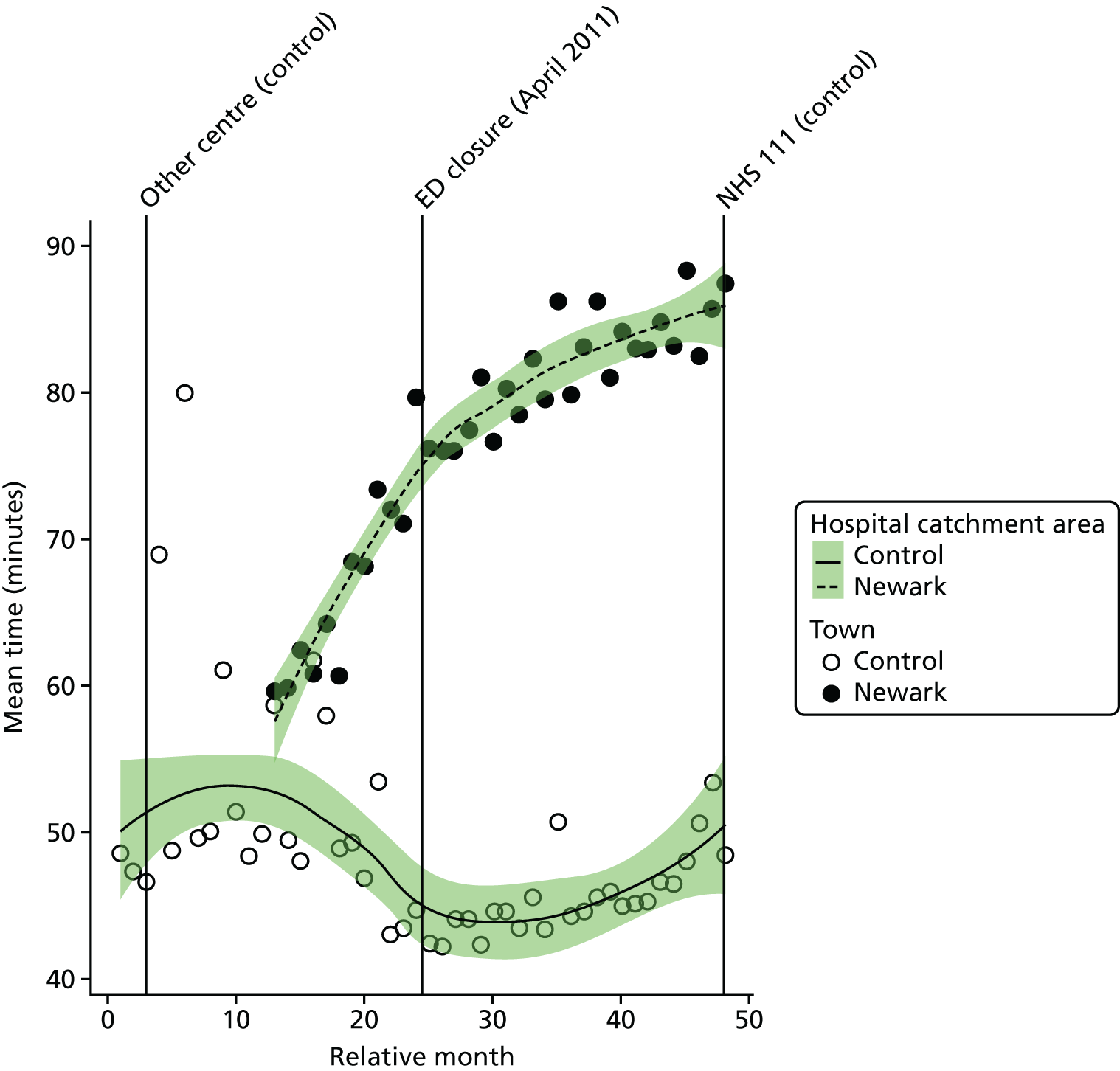
When examining the component times, it appears that the increase in the NE ED catchment area arose from an increase in the time from the incident scene to arrival at hospital, not in the time from the call to arrival at the scene. The mean time from the call to the incident scene increased by just 0.5 minutes, but the time from the scene to the hospital increased by 13.9 minutes.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated mean time from call to hospital for 999 ‘Red’ callers in the NE ED catchment area increased at the time of the closure by an average of 5.4 minutes (95% CI 1.5 to 9.4 minutes; p = 0.01), which is an 8% increase compared with the months before closure.
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change from the call to the incident scene was a decrease of –1.3 minutes, and from the incident scene to the hospital was an increase of –6.8 minutes.
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated mean time from call to arrival at hospital for 999 ‘Red’ incidents in the NE ED catchment area increased at the time of the closure by an average of 21.2 minutes (95% CI 16.5 to 25.8 minutes; p < 0.001) relative to the control area.
Dose model
Figure 113 shows the mean time from call to arrival at hospital for ‘Red’ incidents each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high-dose areas) and residents of LSOAs that were expected to have a relatively small change (low-dose areas) after the closure of NE ED. The pattern of change in these two areas was different, as expected. High-dose LSOAs had an increase in mean time from call to hospital of 21.5 minutes, but this was only 4.9 minutes in the low-dose areas.
FIGURE 113.
Mean time from call to arrival at hospital for ‘Red’ incidents among residents of areas in Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
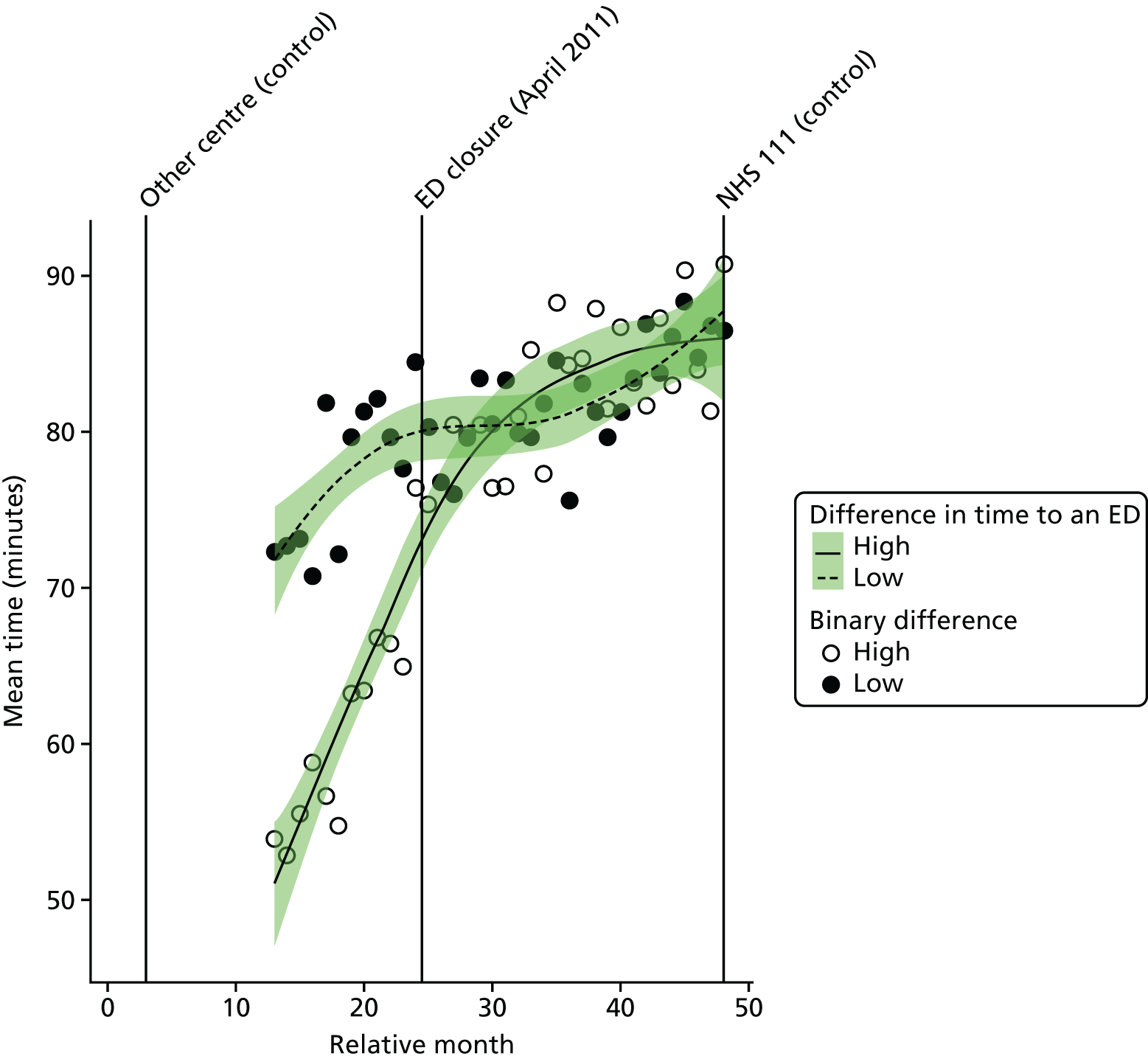
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the increase in time from call to arrival at hospital for residents of high-dose areas was estimated to be 16.7 minutes (95% CI 13.9 to 19.5 minutes; p < 0.001).
Emergency and urgent care attendances
Total number of emergency and urgent care attendances
Plot of monthly activity
Figure 114 shows the number of attendances (inclusive of A&E types 1–4 and attendances coded as ‘unknown’) at EDs by residents of the NE ED catchment area, and the control area, in each month over the 2 years prior to and the 2 years after the closure of the NE ED. There was an increase in the number of attendances by residents of both areas. Attendances went up by 10.9%, from an average of 2639 per month pre closure to 2926 per month post closure in the NE area, and by 12.3% from 4431 per month pre closure to 4976 per month post closure in the control area.
FIGURE 114.
Number of emergency and urgent care attendances among residents of the Newark ED catchment area and the control area.
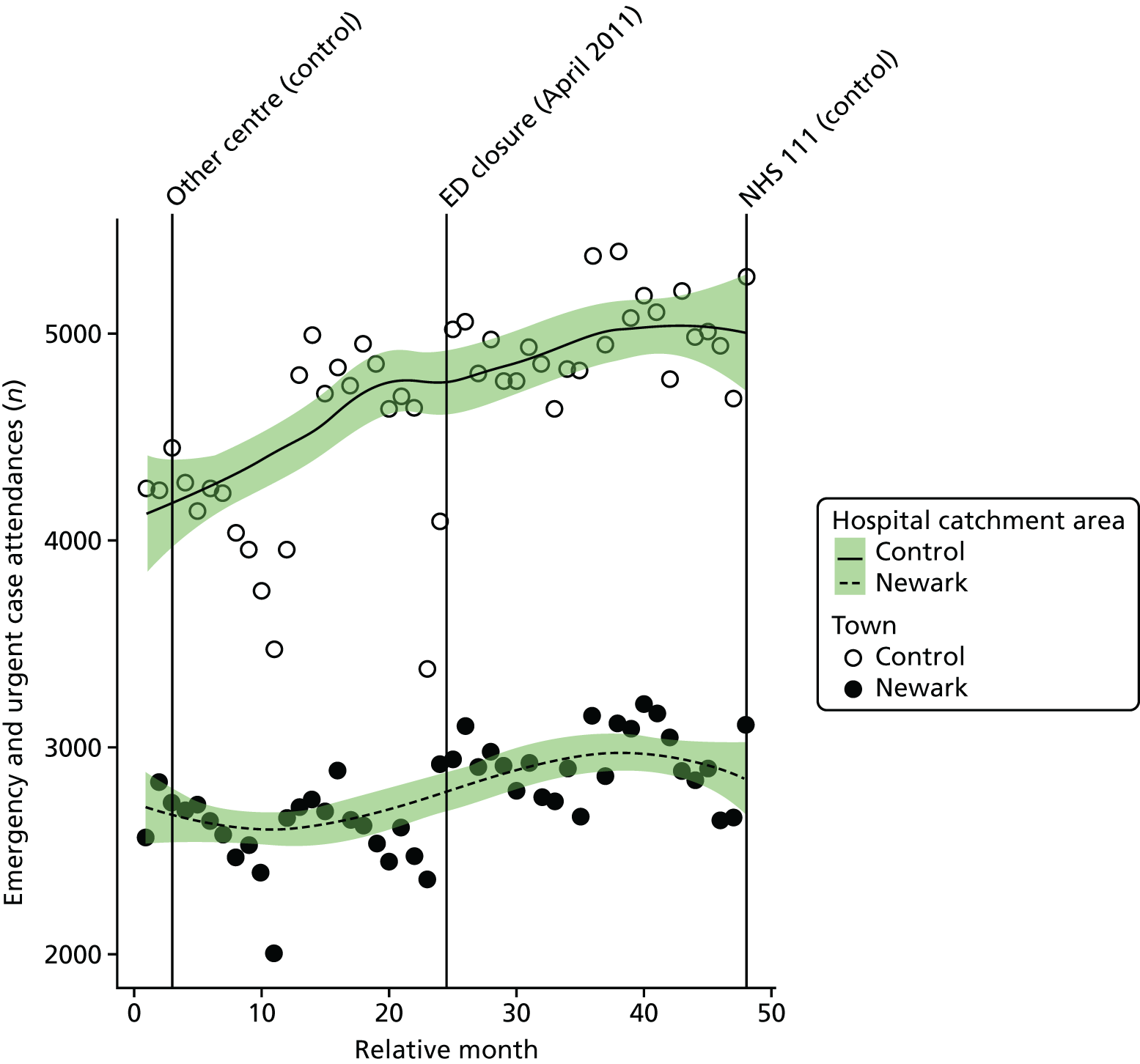
Examining the mode of arrival at the ED shows that the increase in the number of attendances by residents of the NE catchment area was equally split between an increase in those arriving by ambulance (12.0%) and in those arriving by other modes of travel (10.6%).
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of attendances each month among residents of the NE ED catchment area increased at the time of the closure by an average of 6.1% (95% CI 2.3% to 10.0%; p = 0.001).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment areas, the estimated number of emergency and urgent care attendances each month among residents of the NE ED catchment area changed at the time of the closure by –1.0% (95% CI –4.6% to 2.7%; p = 0.59).
Dose model
Figure 115 shows the mean number of attendances each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. The pattern of change in these two areas was similar, with an 11% increase in the number of attendances in high-dose areas, from an average of 1739 pre closure to 1935 post closure per month, and a similar increase in the number of attendances, of 10%, from 900 pre closure to 991 post closure in low-dose areas.
FIGURE 115.
Mean number of emergency and urgent care attendances among residents of areas of Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
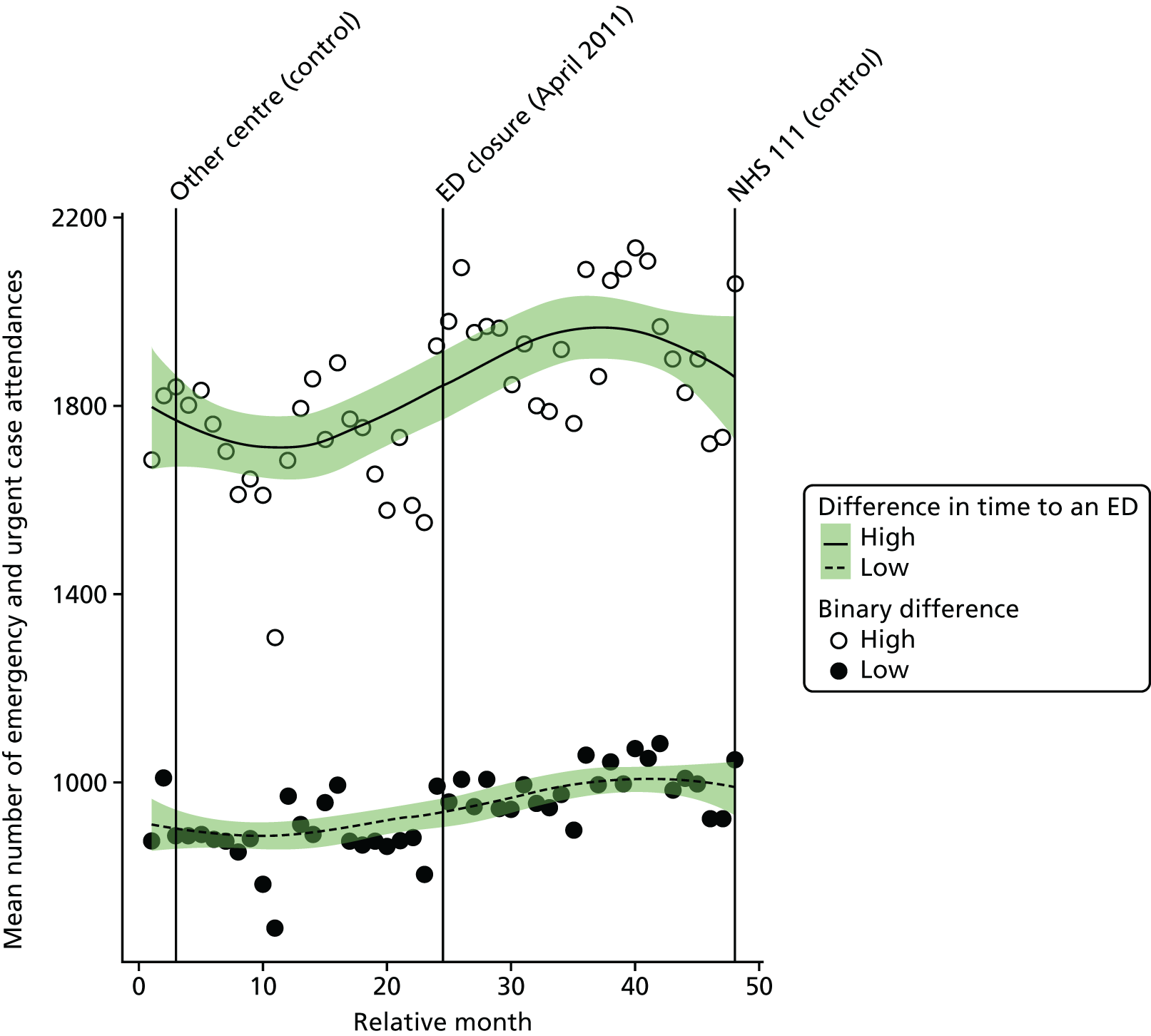
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of emergency and urgent care attendances in high-dose areas compared with low-dose areas was 1.1% (95% CI –2.1% to 4.3%; p = 0.51).
Minor attendances at an emergency or urgent care service
Plot of monthly activity
We have also examined the impact of the ED closure on the number of ‘minor’ attendances, defined as patients who were discharged home without having had any treatment or investigation that needed attendance at a hospital. Figure 116 shows the monthly number of these minor attendances among residents of the NE ED catchment area and the control area over the 2 years before and 2 years after the closure.
FIGURE 116.
Number of minor attendances at an emergency or urgent care service among residents of the Newark ED catchment area and the control area.
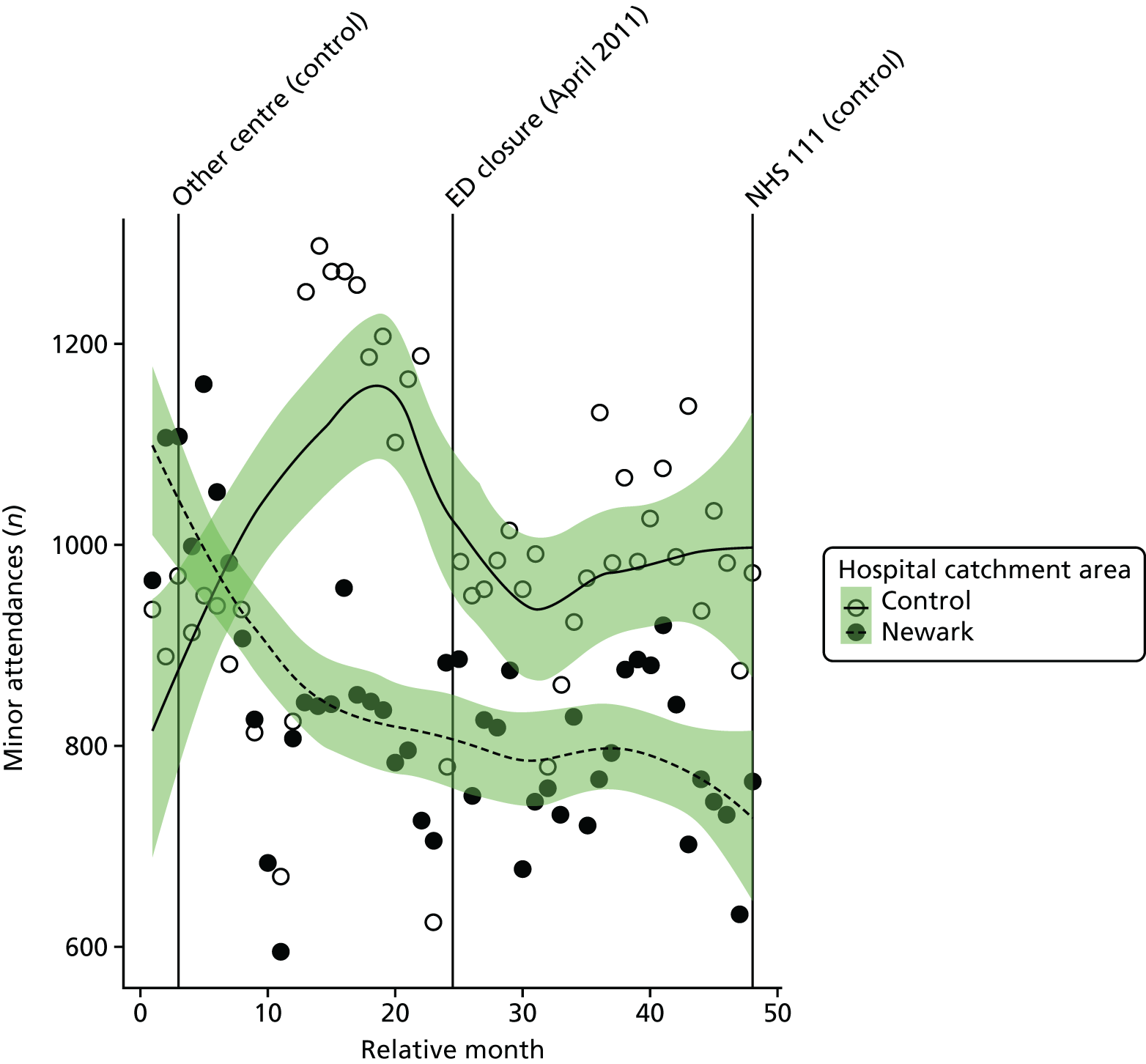
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of minor attendances each month among residents of the NE ED catchment area hardly increased at the time of the closure, increasing by an average of just 1.0% (95% CI –8.6% to 11.6%; p = 0.85).
In contrast to the results for all attendances, there was a small decrease in the number of minor attendances among residents of the NE ED catchment area. Minor attendances went down by 12.4%, from an average of 900 per month pre closure to 788 per month post closure among residents of the NE ED catchment area. The recorded numbers of minor attendances in the control area were erratic and the monthly average fell by 4.9% between 2 years before and 2 years after the closure of the ED.
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of minor emergency and urgent care attendances each month among residents of the NE ED catchment area was estimated to have fallen by an average of –7.5% (95% CI –15.8% to 1.6%; p = 0.10), but the erratic control data mean that this estimate is unreliable.
Dose model
Figure 117 shows the mean number of ‘minor’ emergency and urgent care attendances each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. The pattern of change in these two areas was similar, with a reduction of 12% in high-dose areas from an average of 656 pre-closure to 579 post-closure minor attendances per month, and a 14% reduction from 243 pre-closure to 210 post-closure minor attendances per month in low-dose areas.
FIGURE 117.
Mean number of minor attendances at an emergency or urgent care service among residents of areas of Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
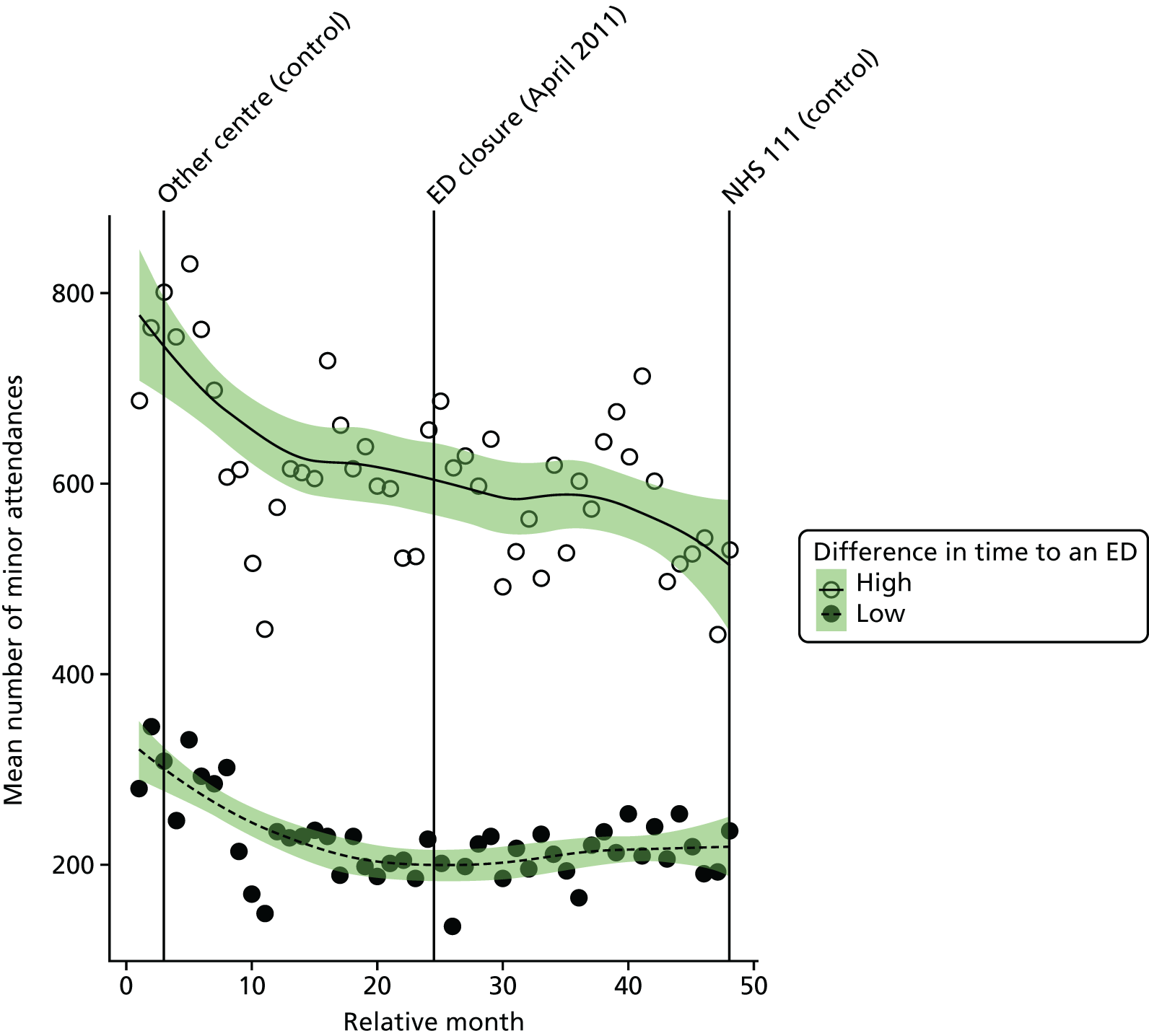
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of minor emergency and urgent care attendances in high-dose areas compared with low-dose areas was 2.1% (95% CI –7.3% to 12.6%; p = 0.67).
Admissions
All emergency admissions
Plot of monthly activity
Figure 118 shows the total number of emergency admissions to any hospital among residents of the NE ED catchment area and residents of the control site catchment area in each month of the 4-year study period.
FIGURE 118.
Total number of emergency admissions among residents of Newark ED catchment area and the control catchment area.
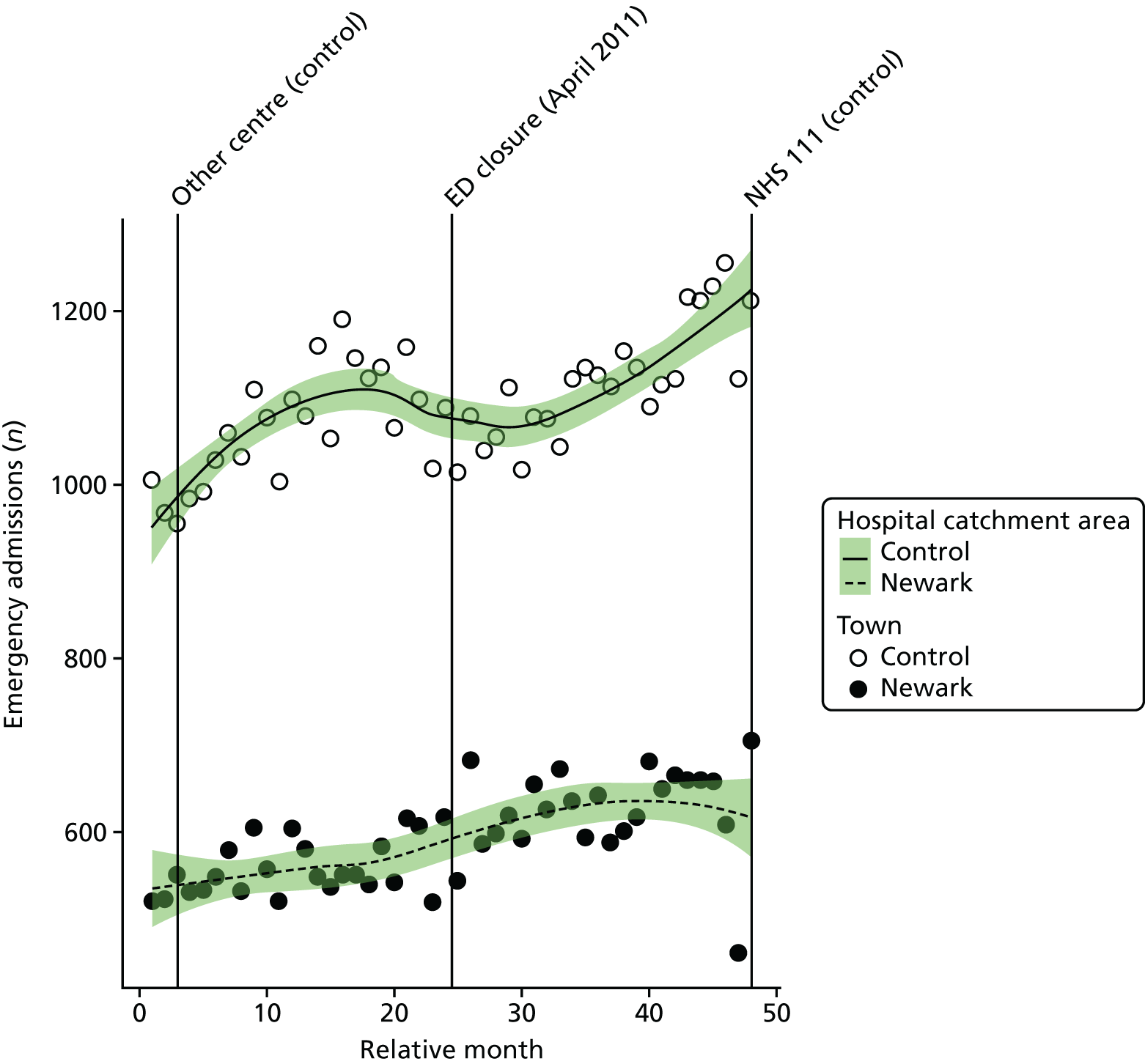
The number of emergency admissions changed around the time of closure for residents of NE, from an average 558 emergency admissions per month prior to the closure to 625 admissions per month post closure: an increase of 12.0%. The control area also showed a small change over the same period, with emergency admissions increasing from 1068 pre closure to 1119 post closure: an increase of 4.8%.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of emergency admissions among residents of the catchment area of NE ED was 4.0% (95% CI –3.6% to 12.2%; p = 0.31).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly mean number of emergency admissions among residents of the catchment area of NE ED relative to the control site was 7.0% (95% CI 2.4% to 11.8%; p = 0.003).
Dose model
Figure 119 shows the mean number of emergency admissions each month for residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. The pattern of change in these two areas was similar, with a small increase of 11% in high-dose areas, from an average of 326 pre-closure to 364 post-closure admissions per month, and there was a 13% increase, from 232 pre-closure to 262 post-closure admissions per month in low-dose areas.
FIGURE 119.
Mean total number of emergency admissions among residents of areas of Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
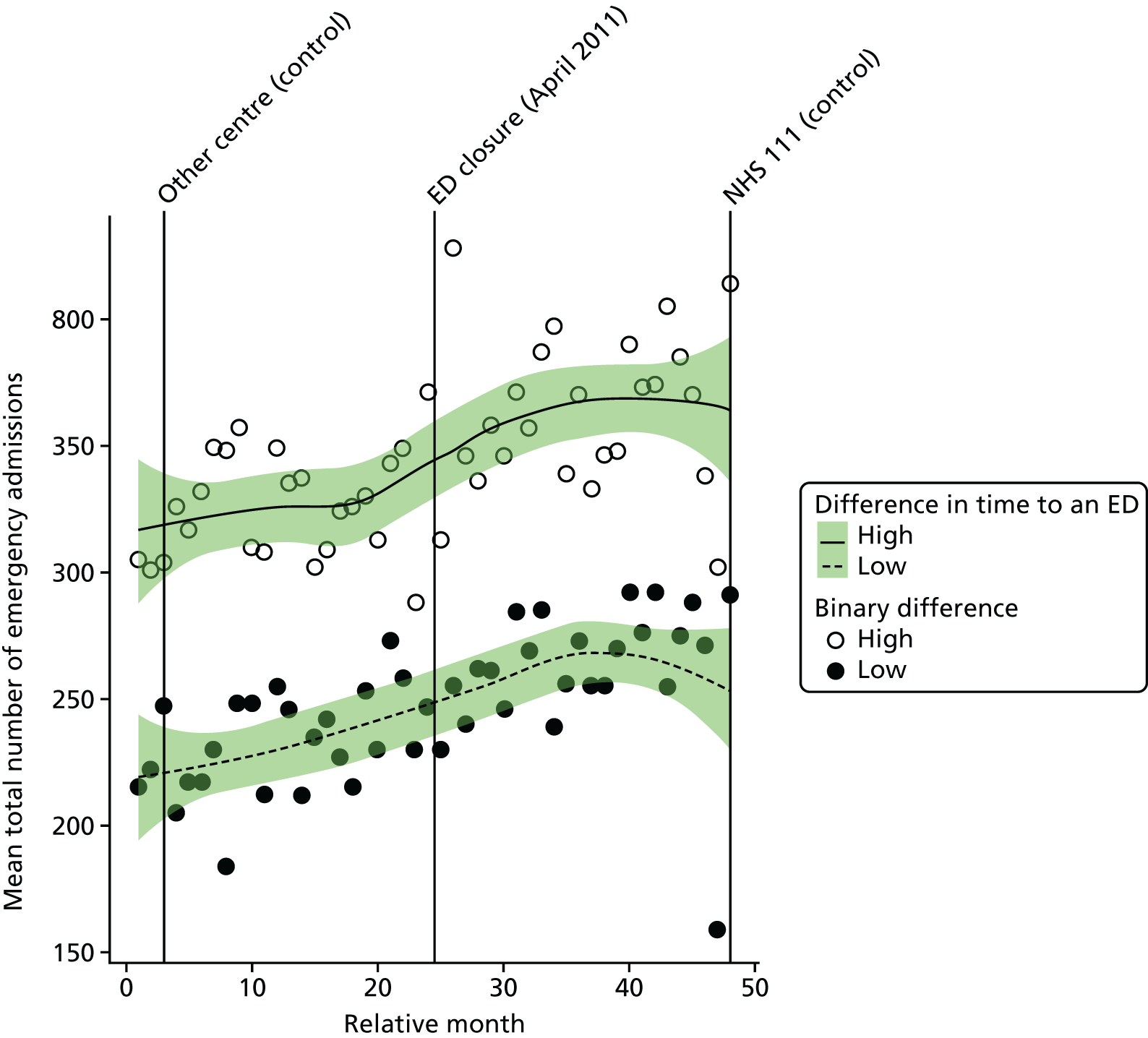
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of emergency admissions in high-dose areas compared with low-dose areas was –1.2% (95% CI –7.3% to 5.2%; p = 0.70).
Potentially avoidable emergency admissions
Plot of monthly activity
Figure 120 shows the number of potentially avoidable emergency admissions to any hospital among residents of the NE ED catchment area and residents of the control site catchment area in each month of the 4-year study period. The pattern for admissions from these 14 emergency conditions is similar to the pattern for all emergency admissions, but with some small changes in the numbers over the period spanning the ED closure in NE. In the NE area, there were, on average, 154 avoidable emergency admissions per month prior to the closure and 163 avoidable emergency admissions post closure: an increase of just 5.9%. In the control area, there were, on average, 326 admissions per month prior to the closure date and 335 admissions per month in the period after the closure.
FIGURE 120.
Number of potentially avoidable emergency admissions among residents of the Newark ED catchment area and the control catchment area.
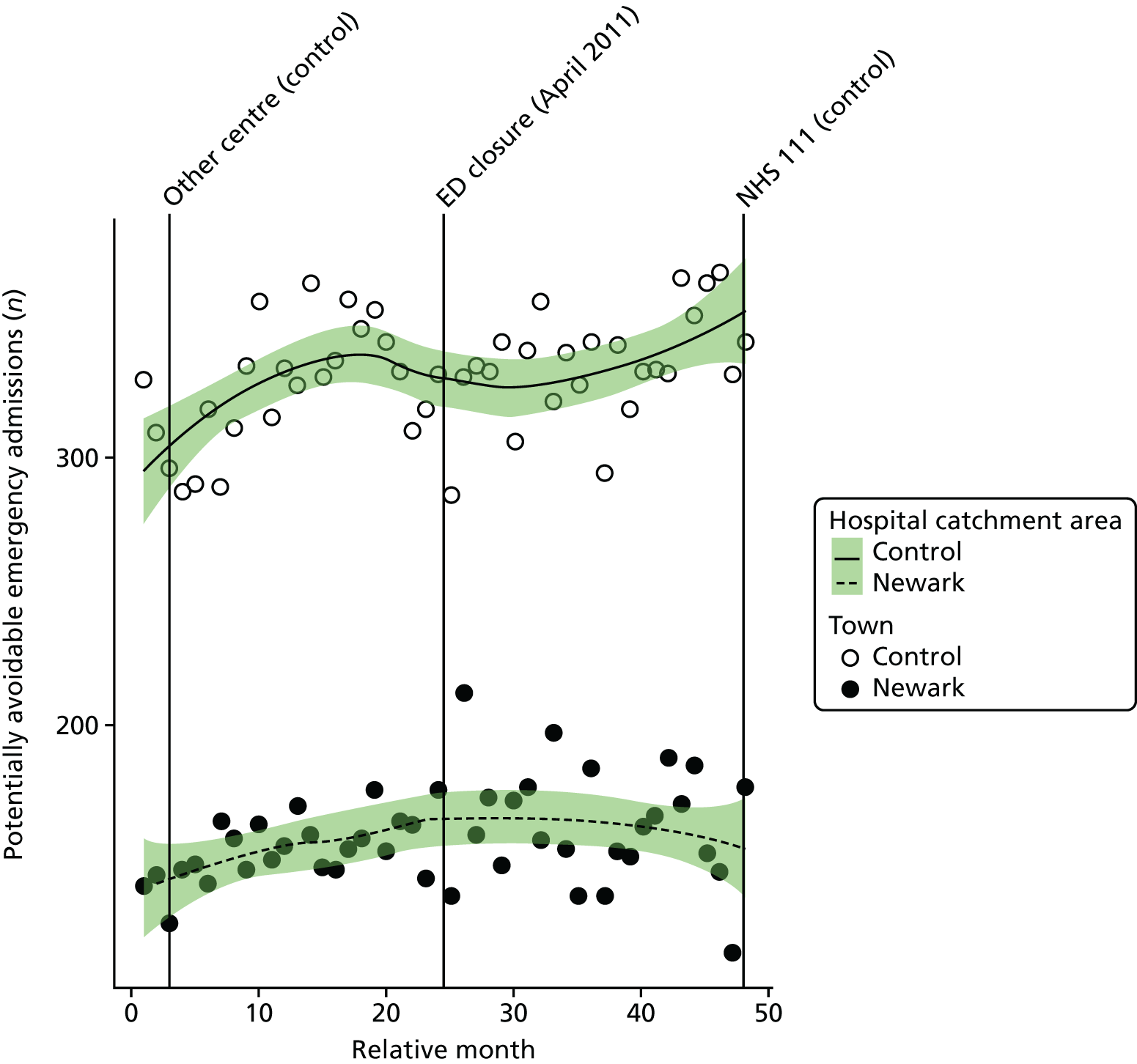
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the monthly mean number of avoidable emergency admissions among residents of the catchment area of NE ED was 0.2% (95% CI –11.1% to 12.9%; p = 0.98).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly mean number of avoidable emergency admissions among residents of the catchment area of NE ED relative to the control site was 2.5% (95% CI –3.9% to 9.5%; p = 0.45).
Dose model
Figure 121 shows the number of potentially avoidable emergency admissions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. The pattern of change in these two areas was, again, very similar, with a small increase of 7% in high-dose areas, from an average of 89 pre-closure to 96 post-closure admissions per month, and a 4% increase from 64 pre-closure to 67 post-closure admissions in low-dose areas.
FIGURE 121.
Number of potentially avoidable emergency admissions among residents of areas of Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
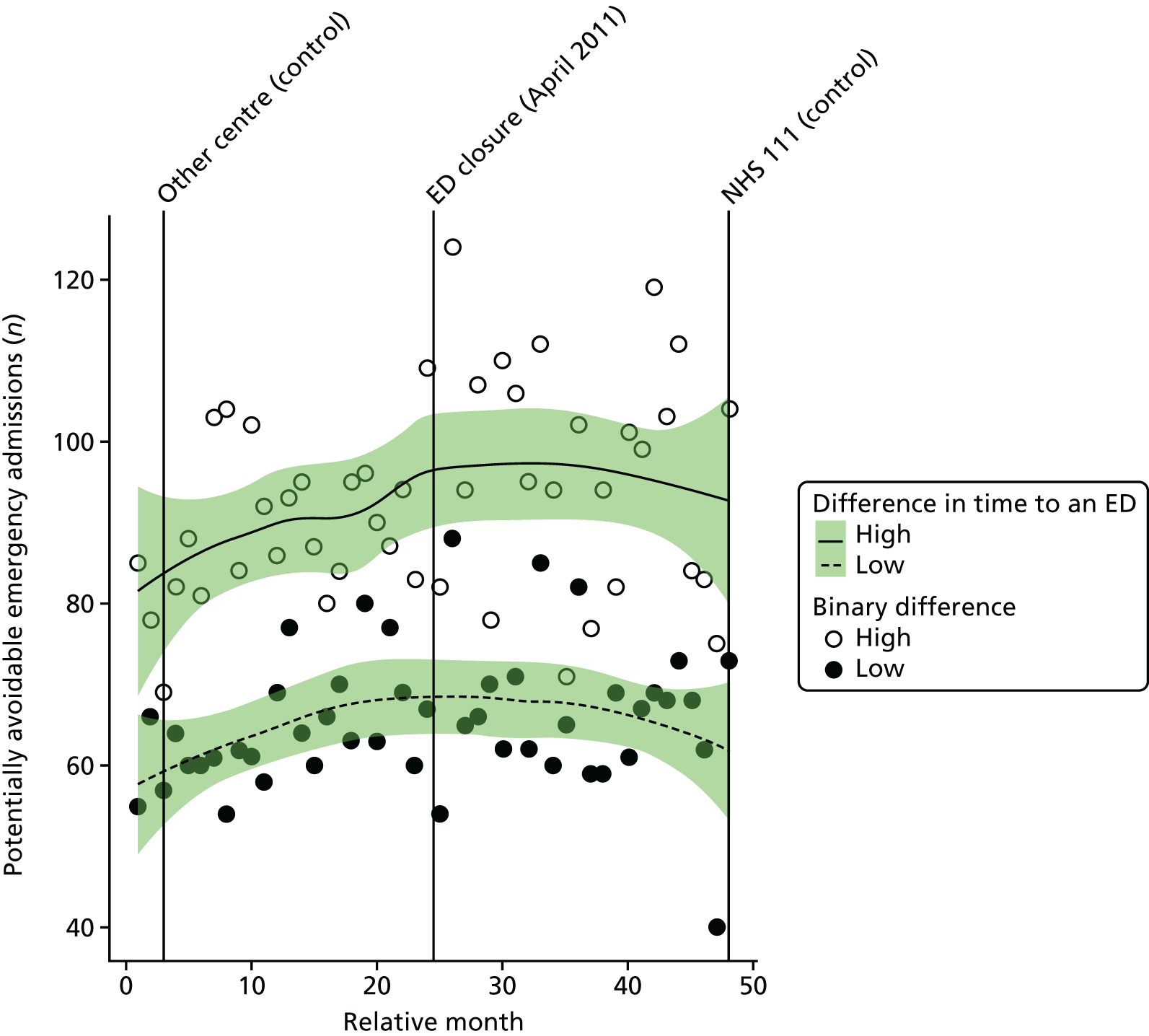
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the increase in the estimated number of potentially avoidable emergency admissions in high-dose areas compared with low-dose areas was 3.8% (95% CI –5.7% to 14.3%; p = 0.45).
Length of stay for emergency admissions
Plot of monthly activity
Figure 122 shows the mean LOS in hospital for patients admitted as emergencies among residents of the NE ED catchment area and residents of the control site catchment area in each month of the 4-year study period. There was a no change in NE, with the mean LOS being 7.3 days both before closure of the ED and after closure of the ED. In the control site, there was a small decrease in mean LOS, from 6.4 to 6.0 days.
FIGURE 122.
Mean LOS for emergency admissions among residents of the Newark ED catchment area and the control area.
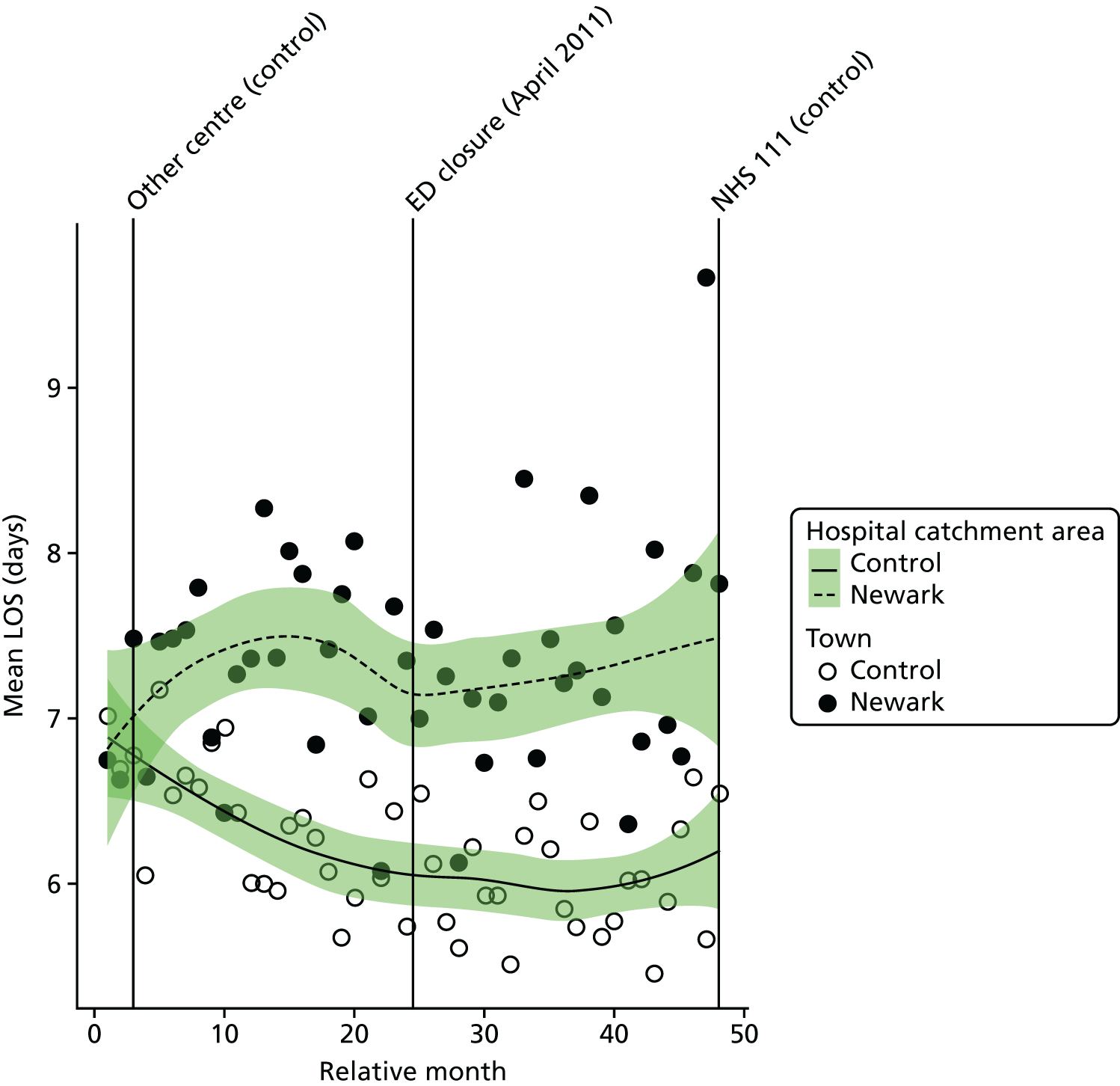
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the mean LOS for residents of the catchment area of NE ED was –0.54 days (95% CI –1.1 to 0.0 days; p = 0.06).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the mean length of stay for residents of the catchment area of NE ED at the time of the closure relative to the control site was 0.30 days (95% CI –0.1 to 0.7 days; p = 0.13).
Dose model
Figure 123 shows the mean LOS for emergency admissions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. The pattern of change in these two areas was very similar, with no significant change in either area.
FIGURE 123.
Mean LOS for emergency admissions among residents of areas of Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
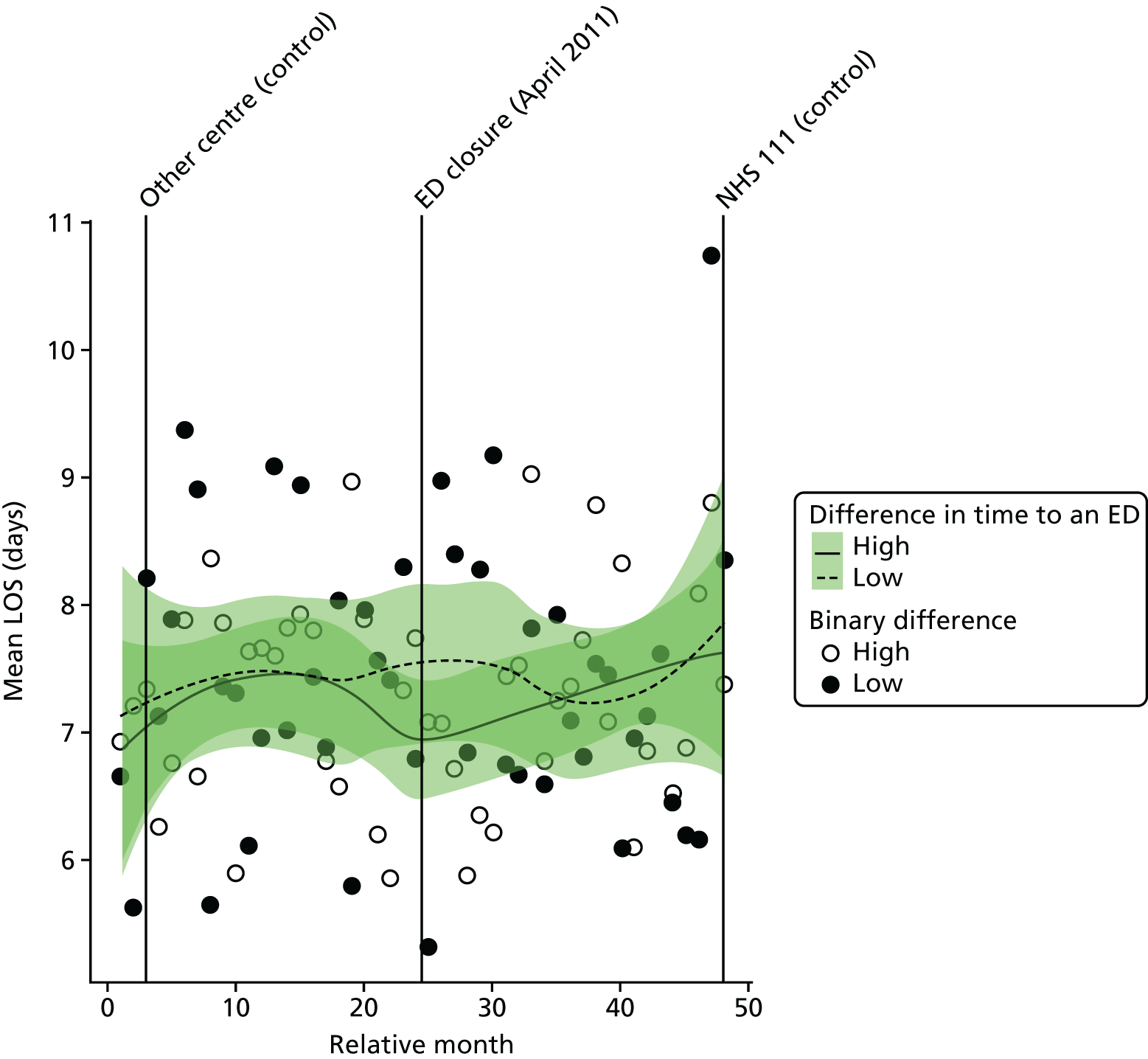
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the mean LOS for emergency admissions in high-dose areas compared with low-dose areas was 0.04 days (95% CI –0.73 to 0.82 days; p = 0.91).
Deaths
Out-of-hospital deaths from serious emergency conditions from certain serious conditions
‘Out-of-hospital’ deaths may occur at home prior to making contact with a service, in an ambulance on the way to hospital, in the ED prior to hospital admission or when a patient is recorded as having a SEC incident and is admitted, discharged alive and subsequently dies out of hospital without being readmitted.
Plot of monthly activity
Figure 124 shows the number of deaths occurring before arrival at hospital from the 16 SECs we have focused on among residents of the NE ED catchment area and residents of the control site catchment area in each month of the 4-year study period. There was little change in these numbers. In residents of the NE catchment area, there were, on average, 17.4 out-of-hospital deaths per month prior to the closure and 16.4 out-of-hospital deaths per month post closure: a decrease of 5.7%. In the control area, the monthly average number of out-of-hospital deaths changed from 26.3 pre closure to 25.5 post closure.
FIGURE 124.
Number of deaths occurring out of hospital for SECs among residents of the catchment areas of the Newark and control EDs.
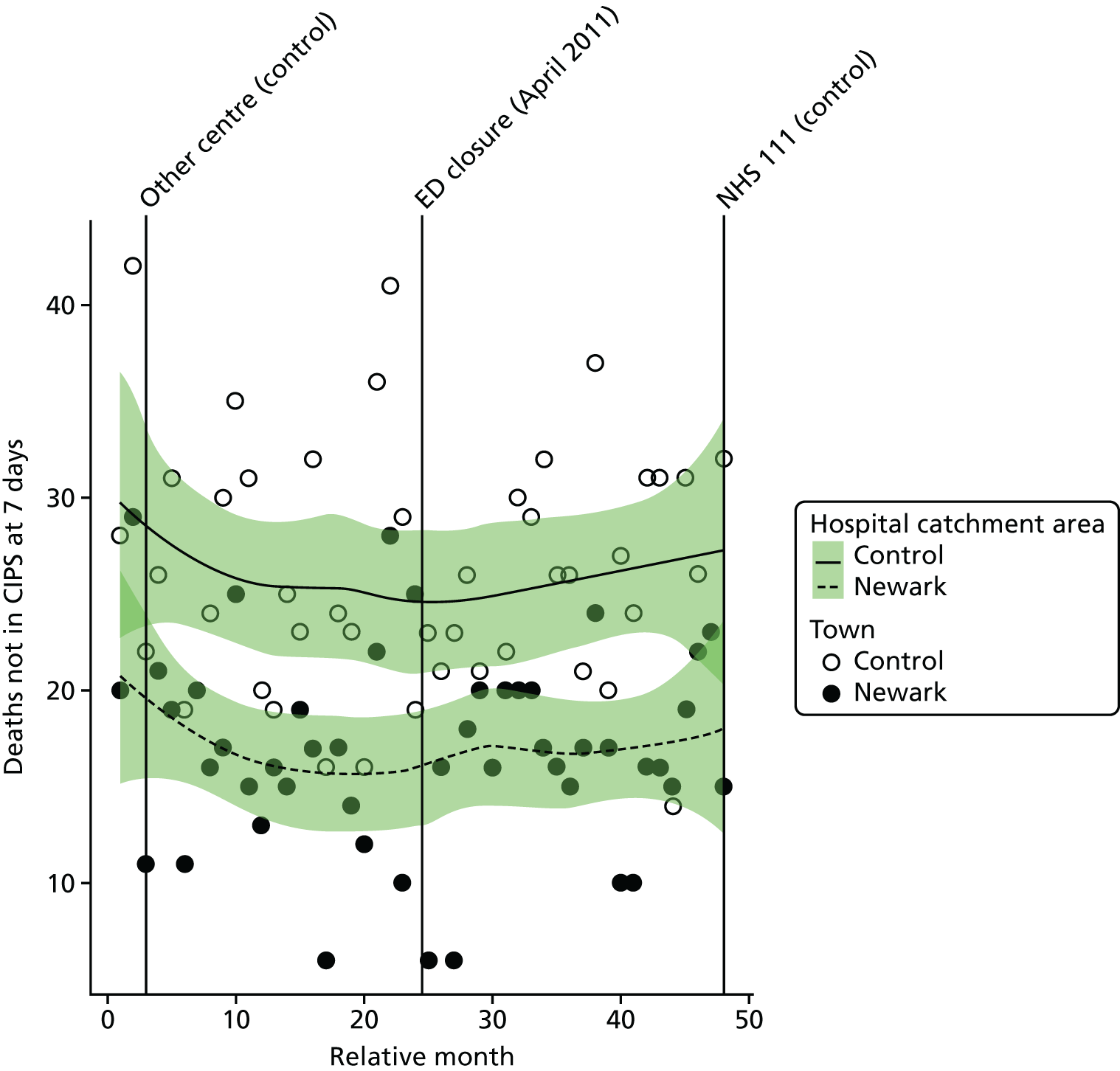
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of out-of-hospital deaths from the 16 SECs among residents of the catchment area of NE ED was –6.8% (95% CI –34.6% to 33.0%; p = 0.70).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly mean number of deaths from emergency conditions occurring out of hospital among residents of the catchment area of NE ED at the time of the closure relative to the control site was –4.4% (95% CI –22.0% to 17.3%; p = 0.67).
Dose model
Figure 125 shows the number of out-of-hospital deaths each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. The pattern of change in these two areas was a small increase of 1% in the high-dose areas, from an average of 8.4 pre-closure to 8.5 post-closure deaths per month, and there was a 7% decrease from 8.5 pre-closure to 7.9 post-closure deaths in low-dose areas.
FIGURE 125.
Number of out-of-hospital deaths from SECs among residents of areas of Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
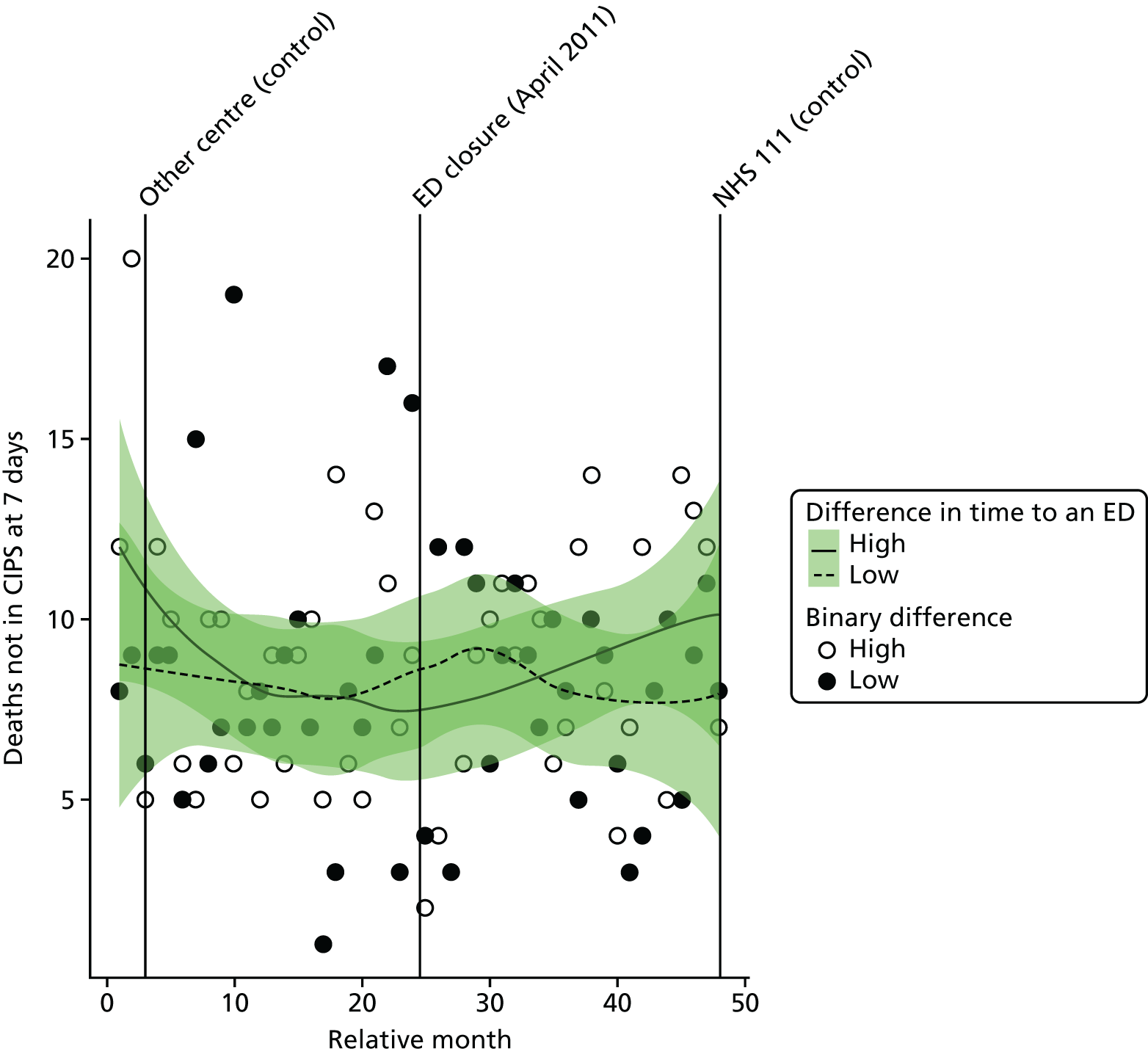
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of out-of-hospital deaths in high-dose areas compared with low-dose areas was 7.9% (95% CI –21.5% to 48.3%; p = 0.64).
All deaths from serious emergency conditions occurring within 7 days
Plot of monthly activity
Figure 126 shows the total number of deaths occurring up to 7 days post incident from the 16 SECs among residents of the NE ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These deaths may have occurred out of hospital or in hospital within 7 days of admission. These numbers show the same pattern as that for out-of-hospital deaths. There were, on average, 24.9 deaths per month prior to the closure and 23.8 deaths per month post closure: a decrease of 4.2%. In the control area, the monthly average fell from 39.3 deaths per month prior to the closure to 36.6 deaths per month post closure.
FIGURE 126.
Total number of deaths from SECs occurring within 7 days of the incident among residents of the catchment areas of the Newark and control EDs.
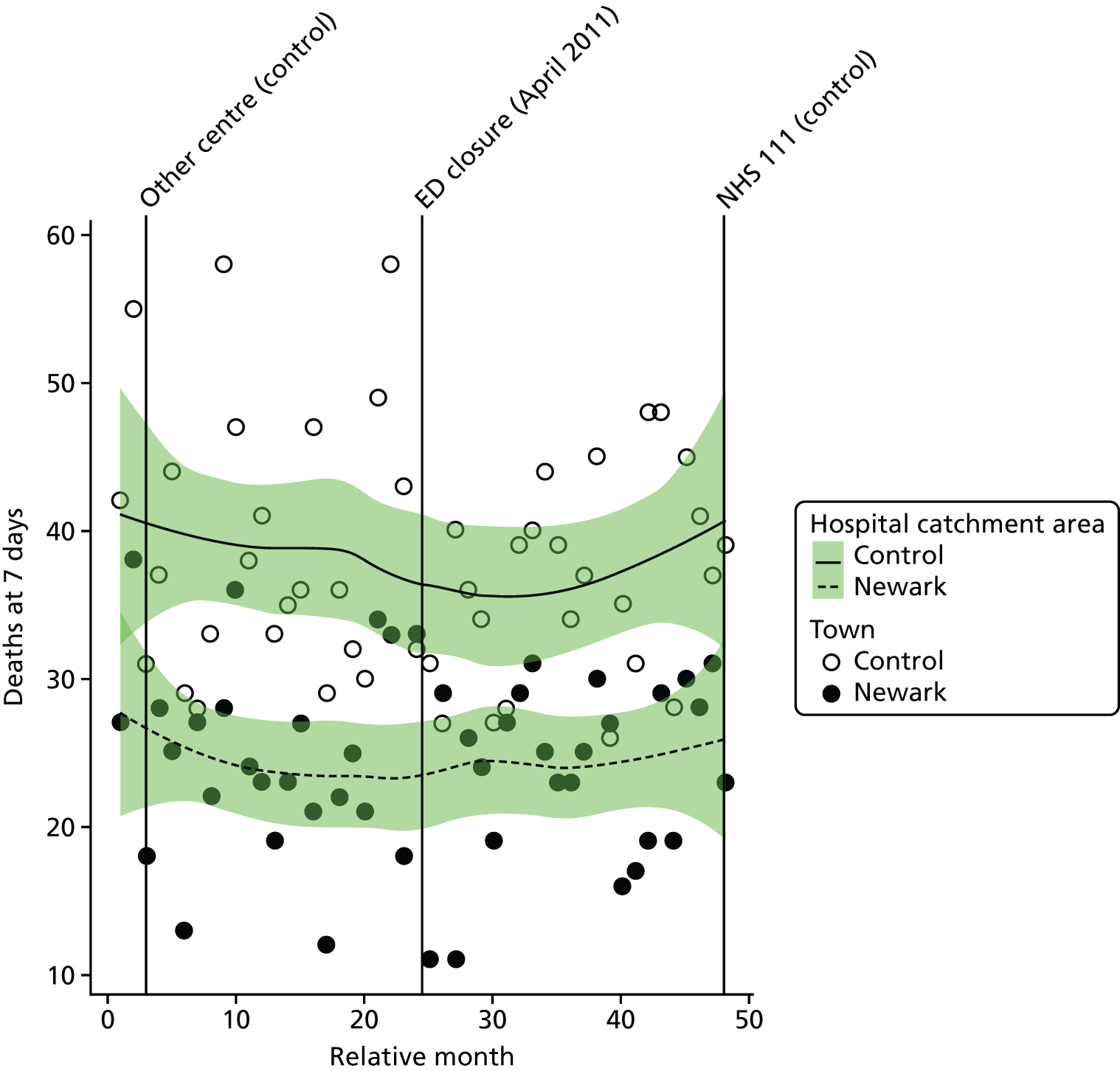
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of deaths within 7 days from the 16 SECs among residents of the catchment area of NE ED was –8.3% (95% CI –31.4% to 22.5%; p = 0.56).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly mean number of deaths within 7 days from the 16 SECs residents of the catchment area of NE ED at the time of the closure relative to the control site was 0.5% (95% CI –15.4% to 19.4%; p = 0.95).
Dose model
Figure 127 shows the total number of deaths occurring up to 7 days post incident from the 16 emergency conditions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. The pattern of change in these two areas was similar, with a small decrease of 5% in high-dose areas, from 13.8 pre-closure to 13.1 post-closure deaths per month, and a similar decrease, of 3%, from 11.1 pre-closure to 10.8 post-closure deaths in low-dose areas.
FIGURE 127.
Total number of deaths from SECs up to 7 days post incident among residents of areas of Newark that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
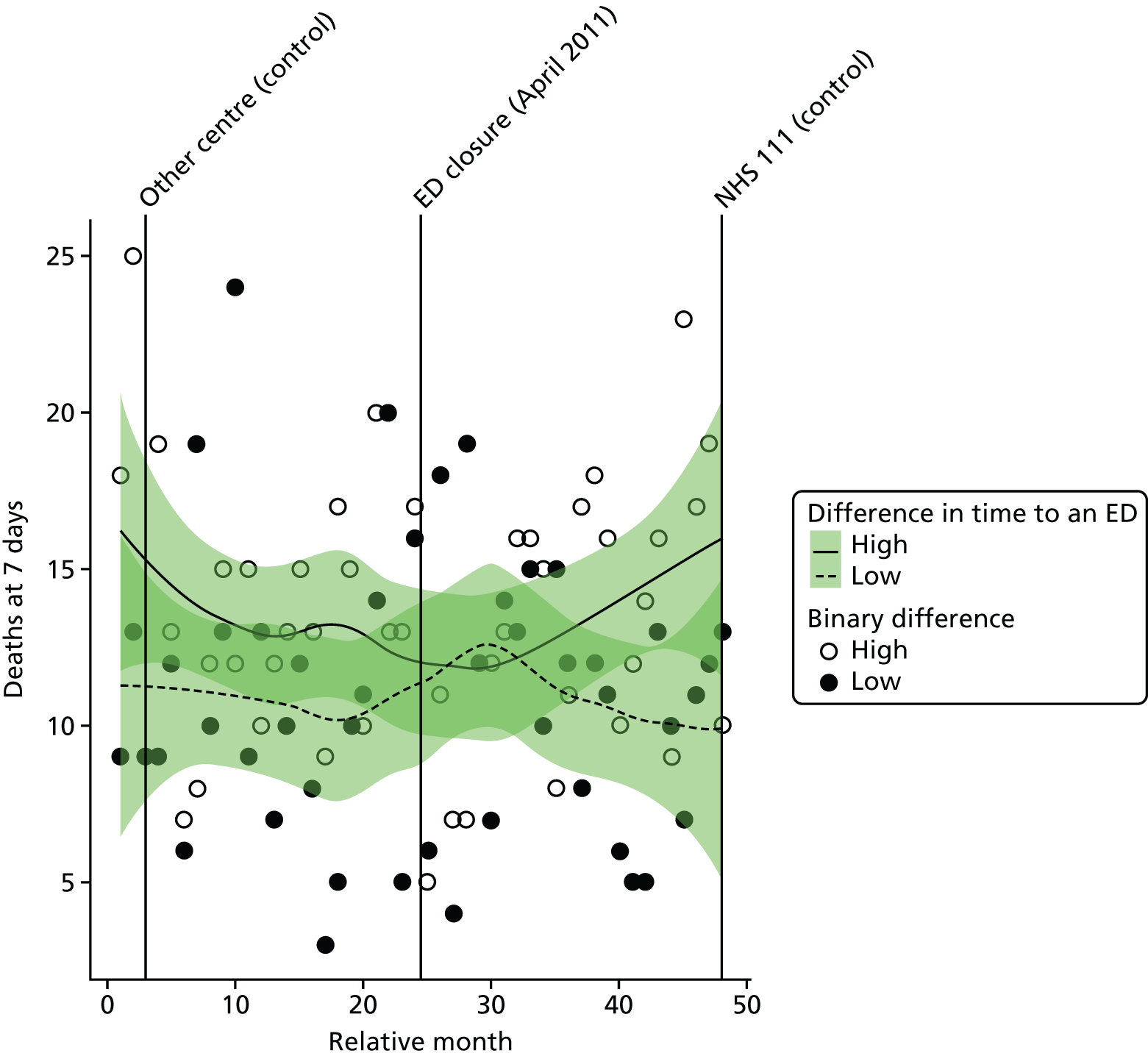
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of deaths among residents of high-dose areas compared with low-dose areas was –1.8% (95% CI –25.6% to 29.5%; p = 0.90).
Case fatality ratios: all serious emergency conditions studied
Plot of monthly activity
Figure 128 shows the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths plus admissions for patients who survived beyond 7 days from the 16 SECs among residents of the NE ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These ratios reflect the risk of dying from these emergency conditions. There is little indication of any significant change in these ratios. In NE, over the 2 years before the closure the average ratio was 0.252 (indicating that 25.2% of the patients died), and it was 0.254 in the period after the closure: an increase of 0.2 in the percentage of patients who died. In the control site, the average ratio changed from 0.268 pre closure to 0.244 post closure.
FIGURE 128.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident among residents of the catchment areas of the Newark and control EDs.
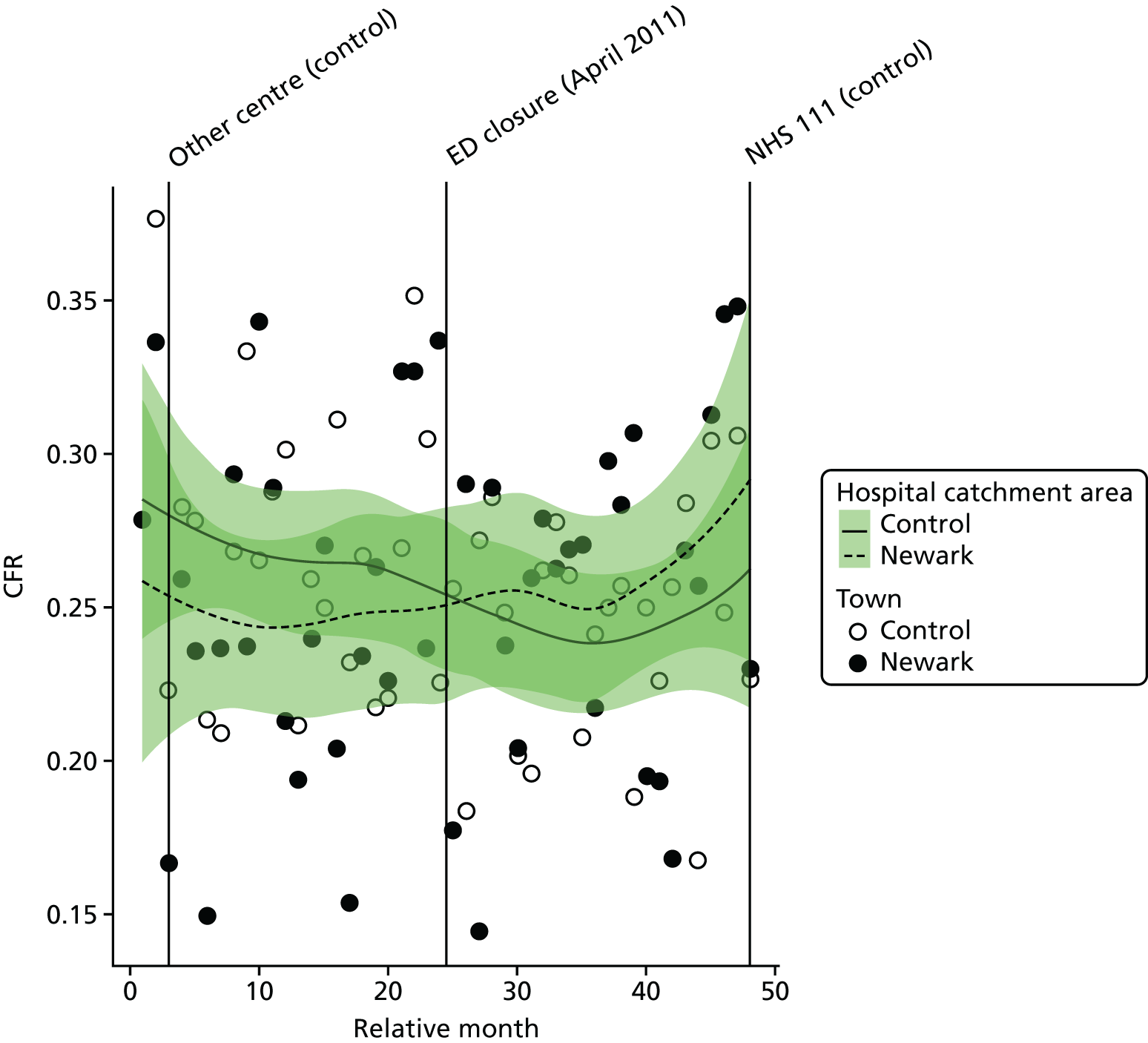
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the CFR for the 16 SECs for residents of the catchment area of NE ED was –0.009 (95% CI –0.049 to 0.031; p = 0.65); this is a decrease of –0.9 in the percentage of patients who died.
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly average CFR for the 16 SECs among residents of the catchment area of NE ED at the time of the closure relative to the control site was 0.024 (95% CI –0.002 to 0.050; p = 0.08); this is an increase of 2.4 in the percentage of patients who died.
Dose model
Figure 129 shows the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths plus admissions for patients who survived beyond 7 days from the 16 SECs among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of NE ED. In high-dose areas, over the 2 years before the closure the average ratio was 0.243 (indicating that 24.3% of the patients died), and it was 0.257 afterwards: an increase of 1.4 in the percentage of patients who died. In the low-dose areas, the average ratio changed from 0.263 pre closure to 0.262 post closure.
FIGURE 129.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident among residents of areas of Newark that were expected to have a relatively large change in time to an ED (high dose) and those expected to have a small change (low dose).
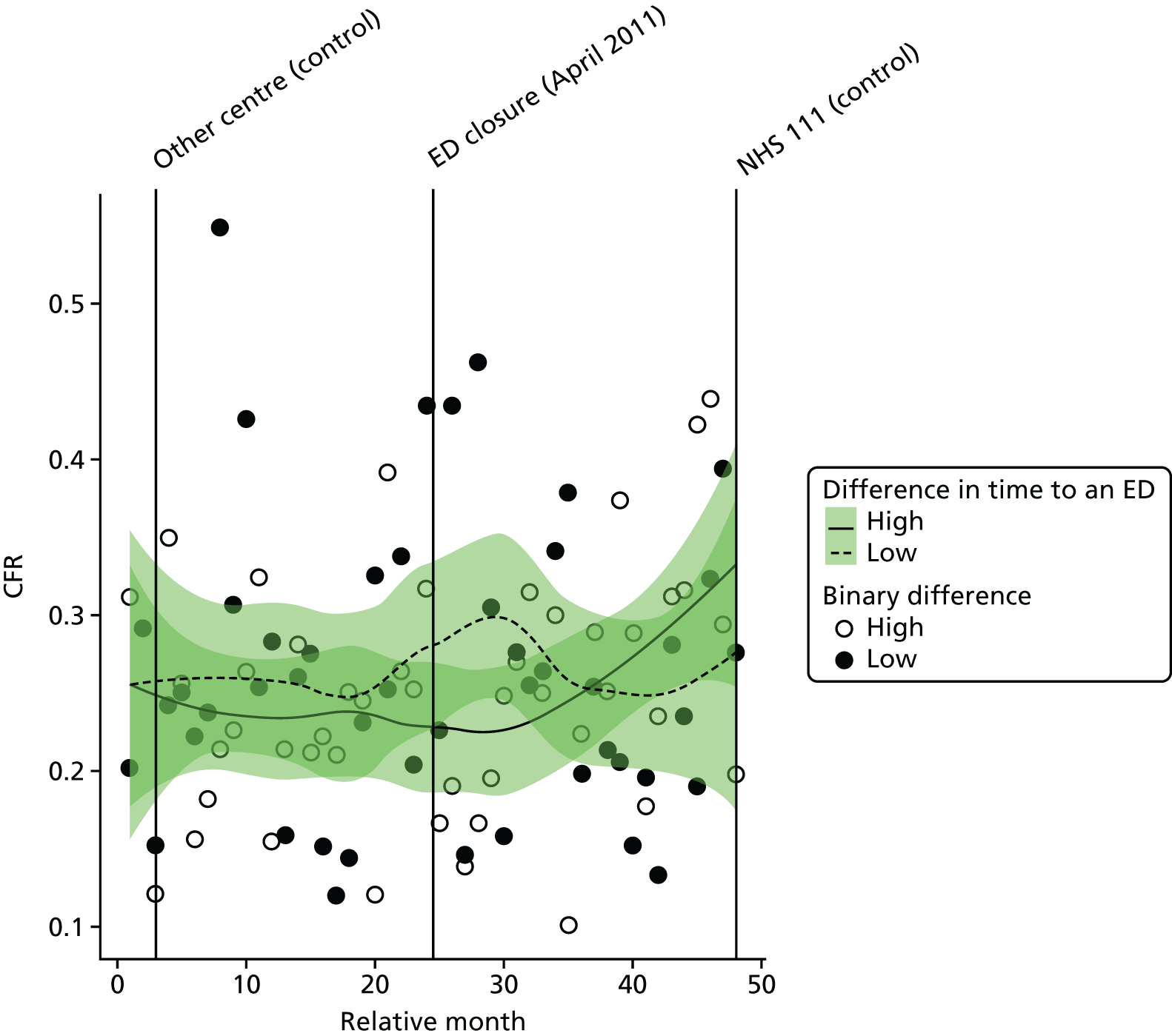
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the CFR in high-dose areas compared with low-dose areas was 0.015 (95% CI –0.051 to 0.081; p = 0.67).
Case fatality ratios: myocardial infarction and stroke
We have also examined the change in the CFRs for MI and for stroke separately (Tables 42 and 43). There was little evidence that the CFRs had changed for either condition, and there was no evidence of any difference for residents of Newark and its control area, or for residents of the high-dose areas of Newark compared with the low-dose areas.
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Newark | |||
| Low-dose areas | 0.294 (0.139) | 0.370 (0.160) | +7.5 |
| High-dose areas | 0.282 (0.151) | 0.319 (0.212) | +3.7 |
| Total | 0.259 (0.119) | 0.283 (0.104) | +2.4 |
| Control | 0.279 (0.095) | 0.276 (0.105) | –0.3 |
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Newark | |||
| Low-dose areas | 0.416 (0.186) | 0.404 (0.237) | –1.2 |
| High-dose areas | 0.326 (0.134) | 0.367 (0.155) | +4.1 |
| Total | 0.350 (0.118) | 0.352 (0.132) | +0.2 |
| Control | 0.367 (0.106) | 0.310 (0.088) | –5.8 |
Hartlepool
The ED at UHH (HA ED) was closed in August 2011. We have compared the changes in activity and performance of the emergency care system for residents of the catchment area of HA ED over the 2 years before and the 2 years after the closure with changes over the same 4-year period for residents of the catchment area of a control ED.
In the analysis of the impact of the closure of HA ED, there were two system changes that were accounted for in addition to the closure.
Hartlepool ED catchment area changes accounted for in the analysis:
-
Introduction of NHS 111 in April 2013.
Control site ED catchment area changes accounted for in the analysis:
-
Introduction of NHS 111 in November 2010.
A WIC in Hartlepool relocated in May 2011, just 3 months before the ED closure. This change is shown in all of the graphs below but it has not been modelled because the change happened so close in time to the ED closure that we cannot reliably separate the effects of the closure and this reorganisation. Therefore, the analysis assesses the joint effect of closing the ED and the associated reorganisation of urgent care services in Hartlepool in the summer of 2011.
Summary of findings
Following the closure, for residents of the ED catchment area in Hartlepool:
-
There was some evidence of an increase in the number of emergency ambulance incidents and strong evidence of a large increase in ‘Red’ incidents, but only when compared with the control area.
-
There was strong evidence of an increase in the time from ambulance service 999 call to arrival at hospital, but only when compared with the control area. The increase appeared to be driven by an increase in the time from the scene of the incident to arrival at hospital.
-
There were no reliable data to inform the analysis of total emergency and urgent care service attendance. Analysis of this measure by mode of arrival indicated that there was strong evidence of a decrease in the number of attendances by patients arriving by ambulance. No comparison with the control area was possible.
-
There was some evidence of a large decrease in the number of emergency hospital admissions, and there was strong evidence of this when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of potentially avoidable hospital admissions.
-
There was strong evidence of an increase in LOS for those admitted to hospital as an emergency case but only when compared with the control area.
-
There was no statistically reliable evidence to suggest a change in the number of deaths or risk of death from the 16 SECs studied.
In comparing pre- and post-closure journey times to the nearest ED, for those experiencing longer post-closure journeys:
-
There was no statistically reliable evidence to suggest a change in the number of emergency ambulance incidents, but there was some evidence of a large increase in ‘Red’ incidents when compared with those experiencing a smaller change in journey times.
-
There was some evidence to suggest an increase in the time from ambulance service 999 call to arrival at hospital when compared with those experiencing a smaller change in journey times.
-
There were no reliable data to inform the analysis of emergency and urgent care service attendance. There was strong evidence of a decrease in the number of attendances by patients arriving by ambulance when compared with those experiencing a smaller change in journey times.
-
There was strong evidence of a large decrease in total number of emergency hospital admissions, but no evidence to suggest a change in the number of potentially avoidable admissions, when compared with those experiencing a smaller change in journey times.
-
There was no evidence to suggest a change in LOS for those admitted to hospital as an emergency case when compared with those experiencing a smaller change in journey times.
-
There was no evidence to suggest a change in the mortality measures when compared with those experiencing a smaller change in journey times.
| Impact measure | Model, effect (95% CI); p-value | ||
|---|---|---|---|
| 1: no control | 2: compared with control | 6: high-dose areas | |
| Total number of emergency ambulance incidents | Decrease: –4.6% (–13.1% to 4.7%); 0.32 | Increase: 8.6% (2.2% to 15.5%); 0.008 | Increase: 3.9% (–4.3% to 12.8%); 0.36 |
| Total number of emergency ambulance ‘Red’ incidents | Increase: 7.1% (0.2% to 14.4%); 0.04 | Increase: 16.8% (10.0% to 23.9%); < 0.001 | Increase: 10.8% (3.0% to 19.2%); 0.006 |
| Mean time from 999 ‘Red’ call to arrival at hospital | Increase: 1.5 minutes (–0.1 to 3.1 minutes); 0.07 | Increase: 6.5% (4.5% to 8.5%); < 0.001 | Increase: 2.0 minutes (0.6 to 3.4 minutes); 0.006 |
| Total number of emergency and urgent care attendances (arriving by ambulance) | Decrease: –19.9% (–24.3% to –15.3%); < 0.001 | No reliable data | Decrease: –23.7% (–27.6% to –19.7%); < 0.001 |
| Total number of minor attendances at an emergency and urgent care service | No reliable data | No reliable data | No reliable data |
| Total number of emergency hospital admissions | Decrease: –10.3% (–17.1% to –2.9%); 0.007 | Decrease: –12.2% (–16.4% to –7.8%); < 0.001 | Decrease: –11.9% (–17.2% to –6.3%); < 0.001 |
| Total number of potentially avoidable emergency hospital admissions | Decrease: –8.8% (–17.4% to 0.7%); 0.07 | Decrease: –6.8% (–13.4% to 0.2%); 0.06 | Decrease: –8.2% (–14.9% to –1.0%); 0.03 |
| Mean LOS for emergency hospital admissions | Increase: 0.5 days (0.03 to 1.0 days); 0.04 | Increase: 0.9 days (0.5 to 1.2 days); < 0.001 | Increase: 0.5 days (0.07 to 0.9 days); 0.03 |
| Total number of out-of-hospital deaths | Increase: 12.4% (–14.5% to 47.9%); 0.40 | Decrease: –1.7% (–17.5% to 17.2%); 0.85 | Increase: 4.0% (–19.2% to 33.8%); 0.76 |
| Total number of deaths occurring within 7 days post incident | Increase: 3.8% (–17.3% to 30.3%); 0.75 | Decrease: –4.8% (–17.8% to 10.3%); 0.52 | Increase: 2.2% (–17.3% to 26.3%); 0.84 |
| CFR (7 days) | No change: 0% (–2.5% to 2.5%); 0.99 | Increase: 1.7% (–1.0% to 4.3%); 0.22 | Increase: 2.1% (–1.3% to 5.6%); 0.23 |
Change in time to the next-nearest emergency department
Following the ED closure, the change in time to reach the next-nearest ED for the residents of the catchment area ranged from 0 to 25 minutes.
FIGURE 130.
Geographical map of Hartlepool and surrounding EDs showing the change in time to the next-nearest ED. Map tiles by Stamen Design, under a Creative Commons Attribution license (CC BY 3.0; see https://creativecommons.org/licenses/by/3.0/). Data by OpenStreetMap, under ODbL. Contains National Statistics data. © Crown copyright and database right 2016. Contains OS data © Crown copyright and database right 2016.
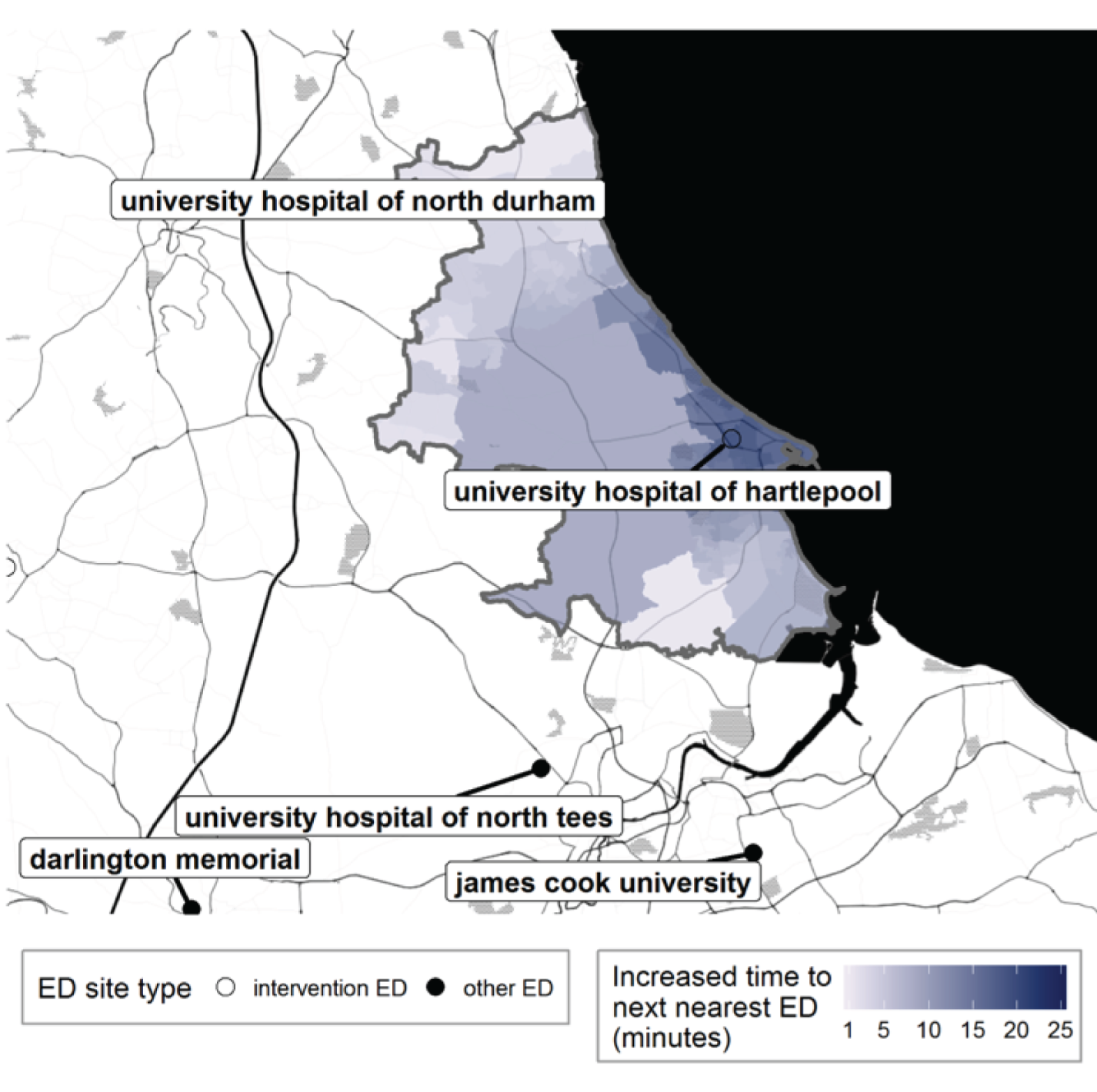
FIGURE 131.
Hartlepool: change in time from LSOA to ED following ED closure, for residents of the catchment area of University Hospital of Hartlepool ED.
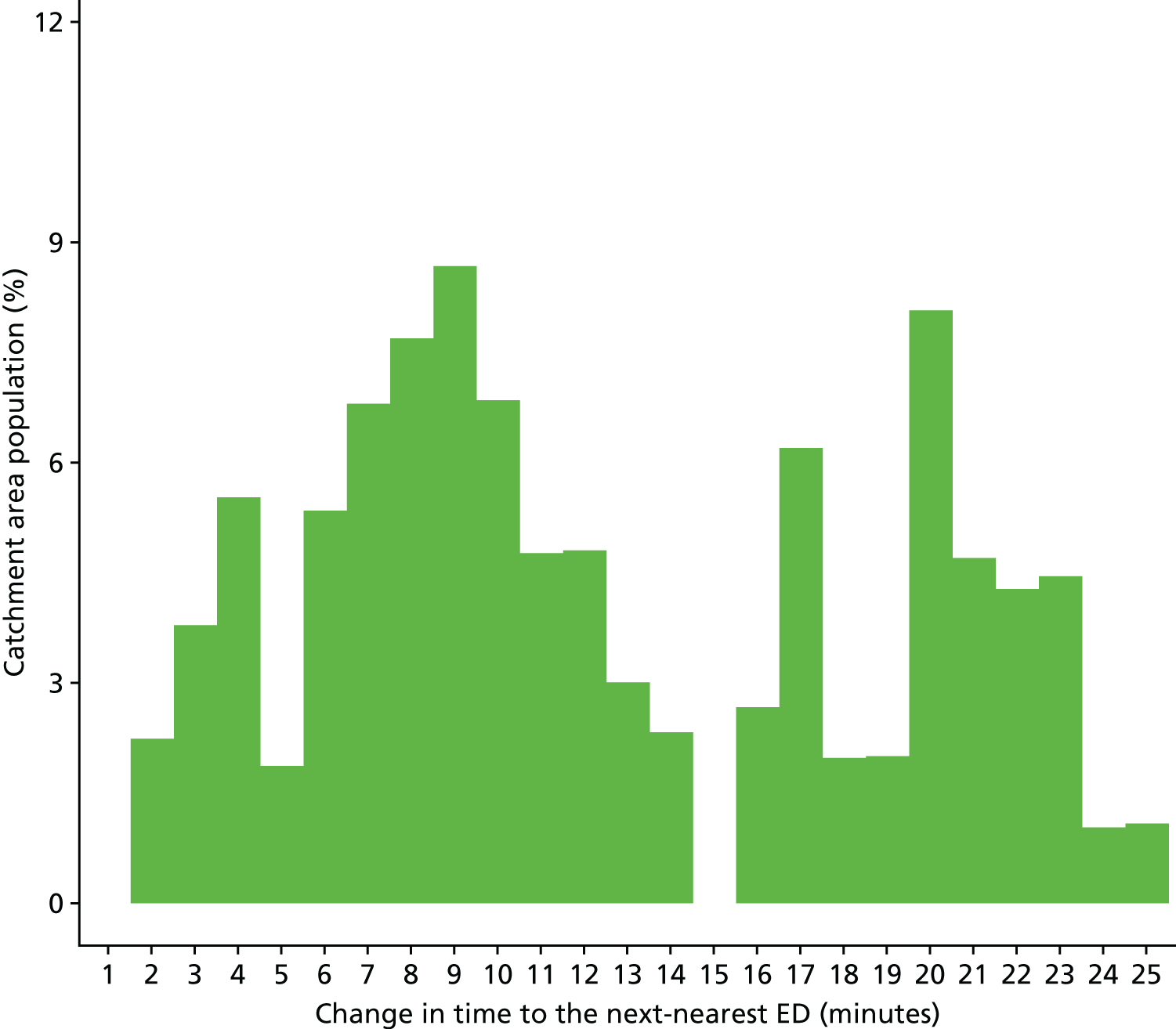
Findings from individual activity and performance measures
Ambulance service performance
Total number of incidents following 999 calls to the ambulance service
Plot of monthly activity
Figure 132 shows the number of 999 incidents referred to the ambulance service from residents of the HA ED catchment area for each month over the 2 years prior to and the 2 years after the date of closure of the HA ED. We had only data on incident volumes from the control ambulance service for 1 year prior to the date of closure. The number of incidents went up by 13%, from an average of 1653 per month pre closure to 1860 per month post closure in the HA ED catchment area, and by 5%, from 2270 per month pre closure to 2373 per month post closure in the control area.
FIGURE 132.
Total number of 999 incidents among residents of the Hartlepool ED catchment area and the control area.
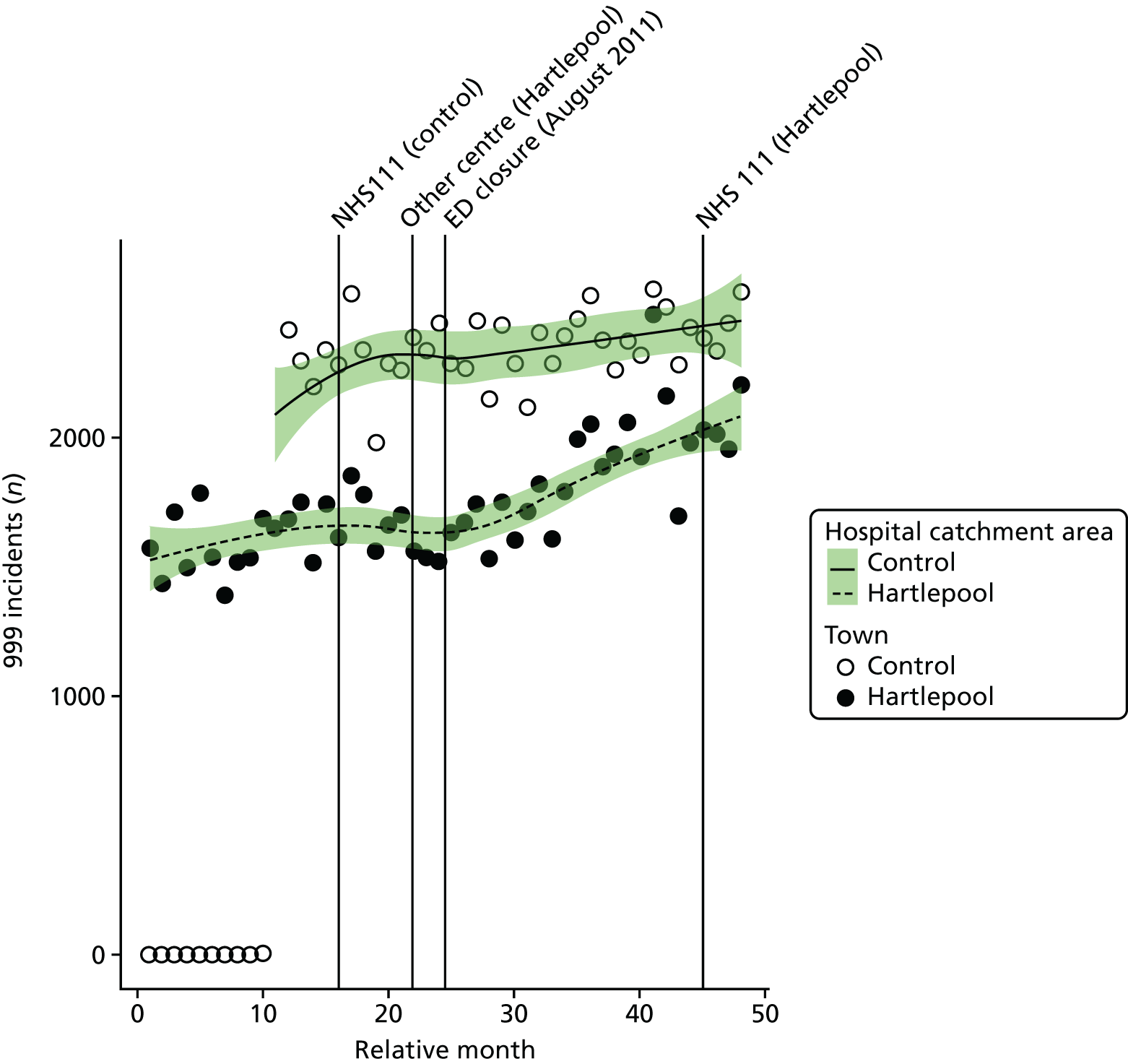
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of incidents each month among residents of the HA ED catchment area changed at the time of the closure by an average of –4.6% (95% CI –13.1% to 4.7%; p = 0.32).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of incidents each month among residents of the HA ED catchment area increased relative to the control area by an average of 8.6% (95% CI 2.2% to 15.5%; p = 0.008).
Dose model
Figure 133 shows the mean number of incidents each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HA ED. The pattern of change in these two groups of areas was similar. There was an increase in incident volumes in high-dose areas, with the average monthly number of incidents increasing by 15%, from 847 pre closure to 977 post closure, and there was a similar increase, of 11%, from 806 pre closure to 896 post closure in low-dose areas.
FIGURE 133.
Mean number of 999 incidents among residents of areas in Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
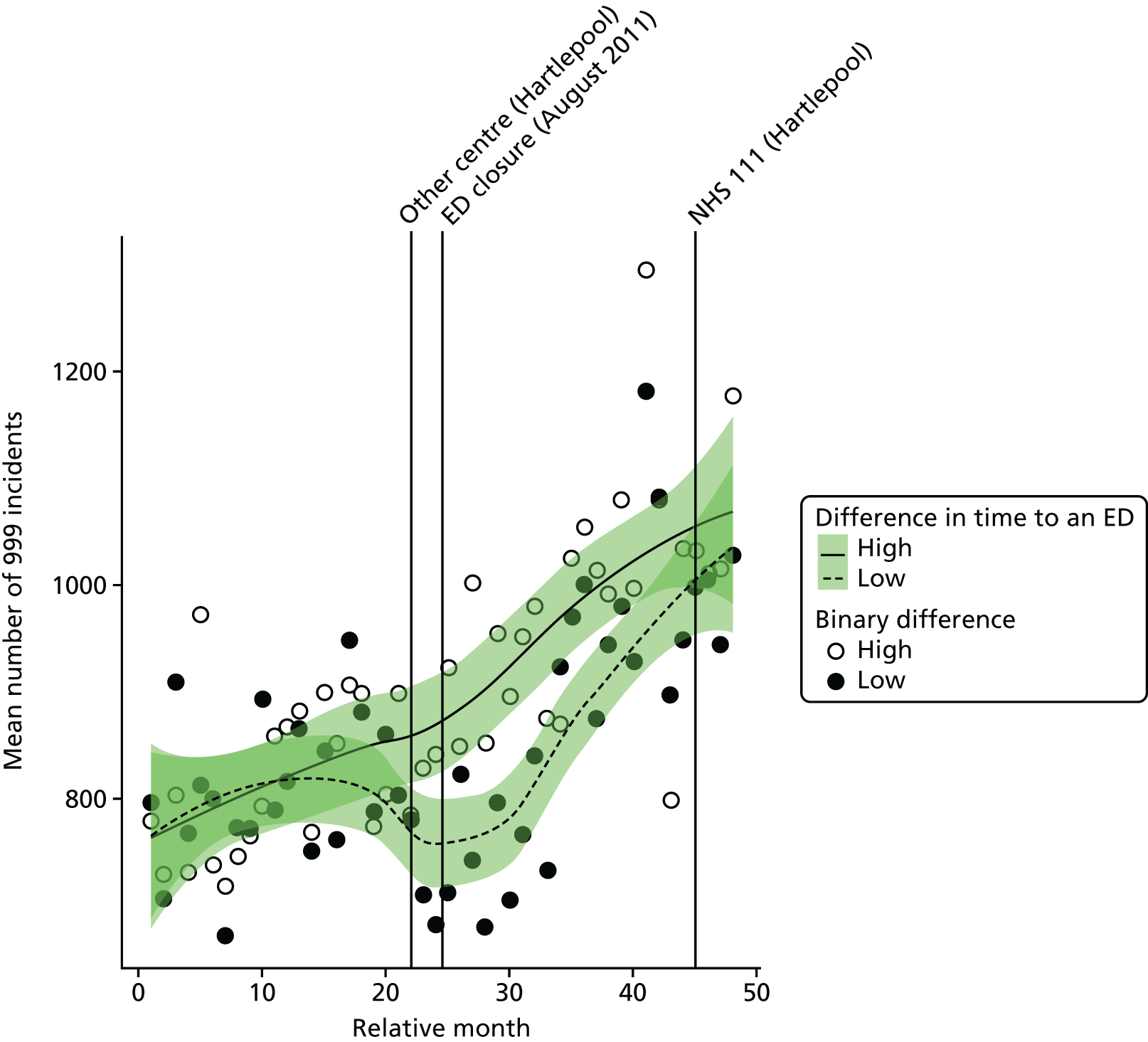
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the increase in the number of incidents in high-dose areas relative to low-dose areas at the time of closure was 3.9% (95% CI –4.3% to 12.8%; p = 0.36).
Number of emergency ambulance ‘Red’ incidents
Plot of monthly activity
Figure 134 shows the number of ‘Red’ 999 incidents referred to the ambulance service from residents of the HA ED catchment area, for each month over the 2 years prior to and the 2 years after the date of closure of the HA ED. We had only data on incident volumes from the control ambulance service for 1 year prior to the date of closure. The number of incidents increased by 29%, from an average of 613 per month pre closure to 791 per month post closure in the HA ED catchment area, and by 11%, from 836 pre closure to 928 post closure in the control area.
FIGURE 134.
Number of ‘Red’ 999 incidents among residents of the Hartlepool ED catchment area and the control area.
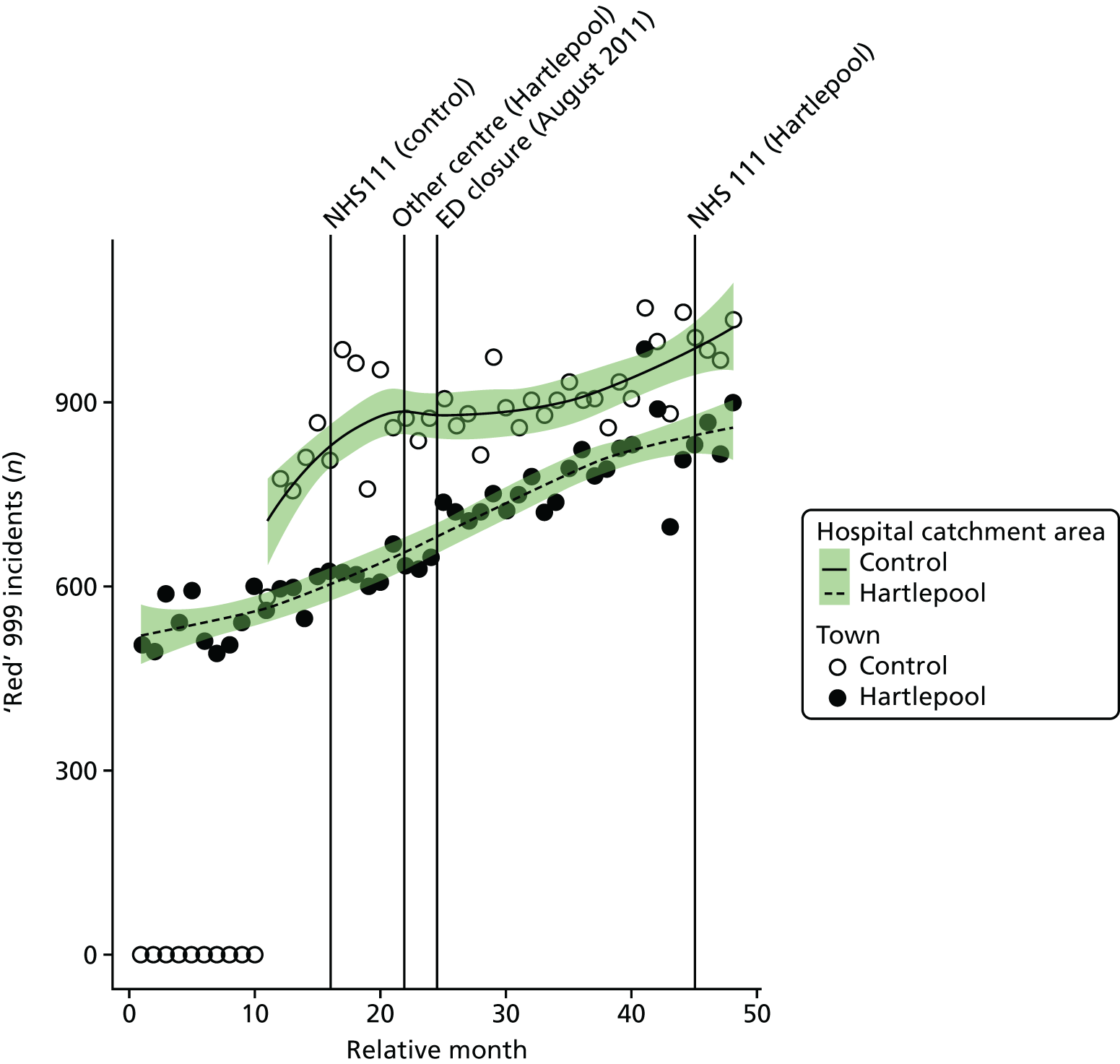
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of ‘Red’ incidents each month among residents of the HA ED catchment area increased at the time of the closure by an average of 7.1% (95% CI 0.2% to 14.4%; p = 0.04).
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of ‘Red’ incidents each month among residents of the HA ED catchment area increased relative to the control area by an average of 16.8% (95% CI 10.0% to 23.9%; p < 0.001).
Dose model
Figure 135 shows the mean number of ‘Red’ incidents each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HA ED. The pattern of change in these two groups of areas was similar. There was a large increase in incident volumes in high-dose areas, with the average monthly number of ‘Red’ incidents changing from 305 pre closure to 413 post closure, and there was a similar increase, from 308 pre closure to 378 post closure, in low-dose areas.
FIGURE 135.
Mean number of ‘Red’ 999 incidents among residents of areas in Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
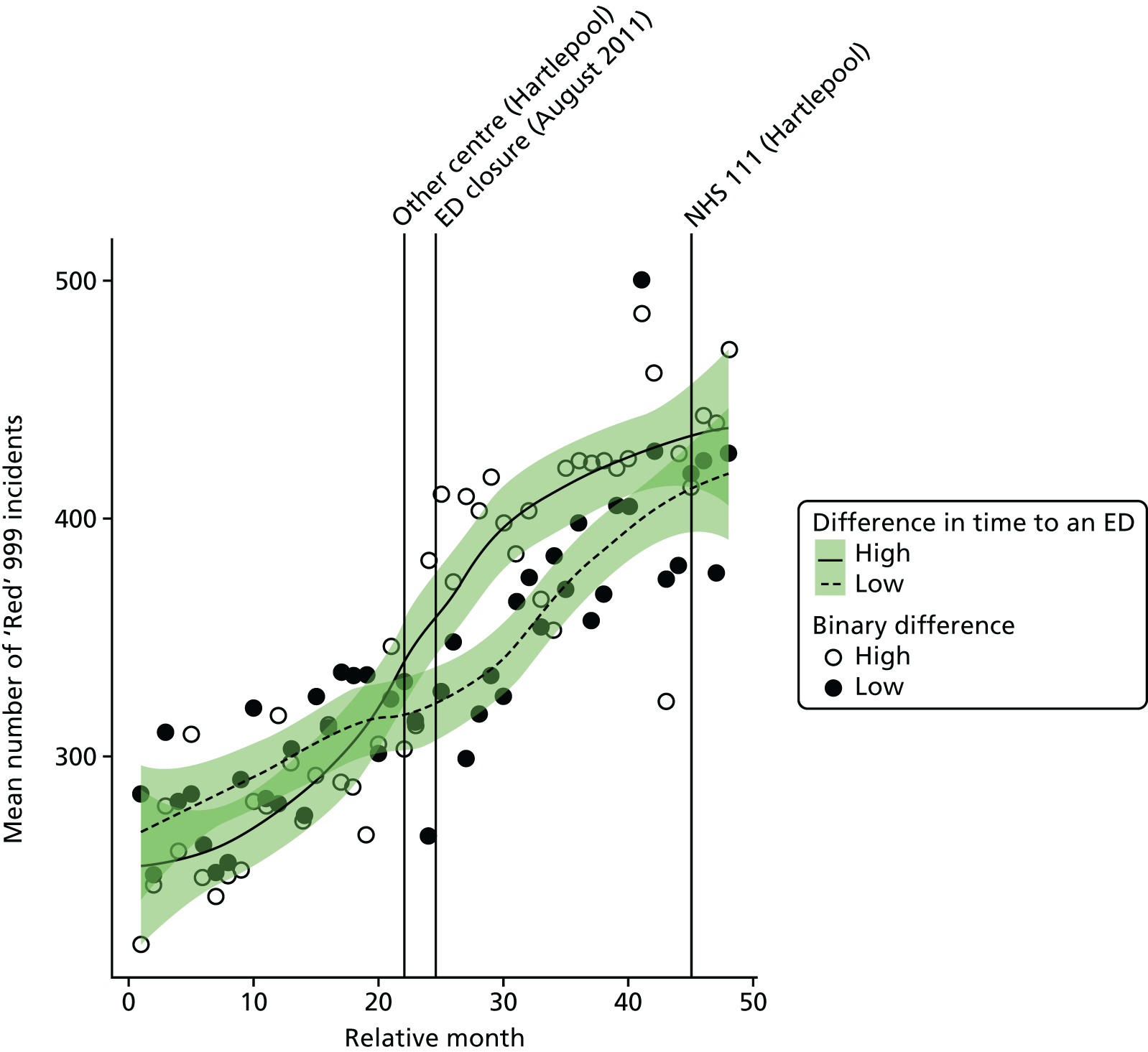
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the increase in the number of ‘Red’ incidents in high-dose areas relative to low-dose areas at the time of the closure was 10.8% (95% CI 3.0% to 19.2%; p = 0.006).
Mean time from 999 call to arrival at hospital for ‘Red’ incidents
Plot of monthly performance
Figure 136 shows the mean time from 999 ‘Red’ call to arrival at hospital in each month over the 2 years prior to and the 2 years after the closure of the HA ED for residents of the HA ED catchment area. There was an increase in these times for residents of the HA ED catchment area from before the closure (monthly mean 45.7 minutes) to after the closure (monthly mean 54.8 minutes): an increase of 9.1 minutes on average. There were useable data from the control area on ambulance journey times for 1 year before the closure date only, and these data showed a smaller increase, from an average of 51.1 minutes to 53.3 minutes over this year.
FIGURE 136.
Mean time from 999 call to arrival at hospital for residents of the Hartlepool ED catchment area and the control area.
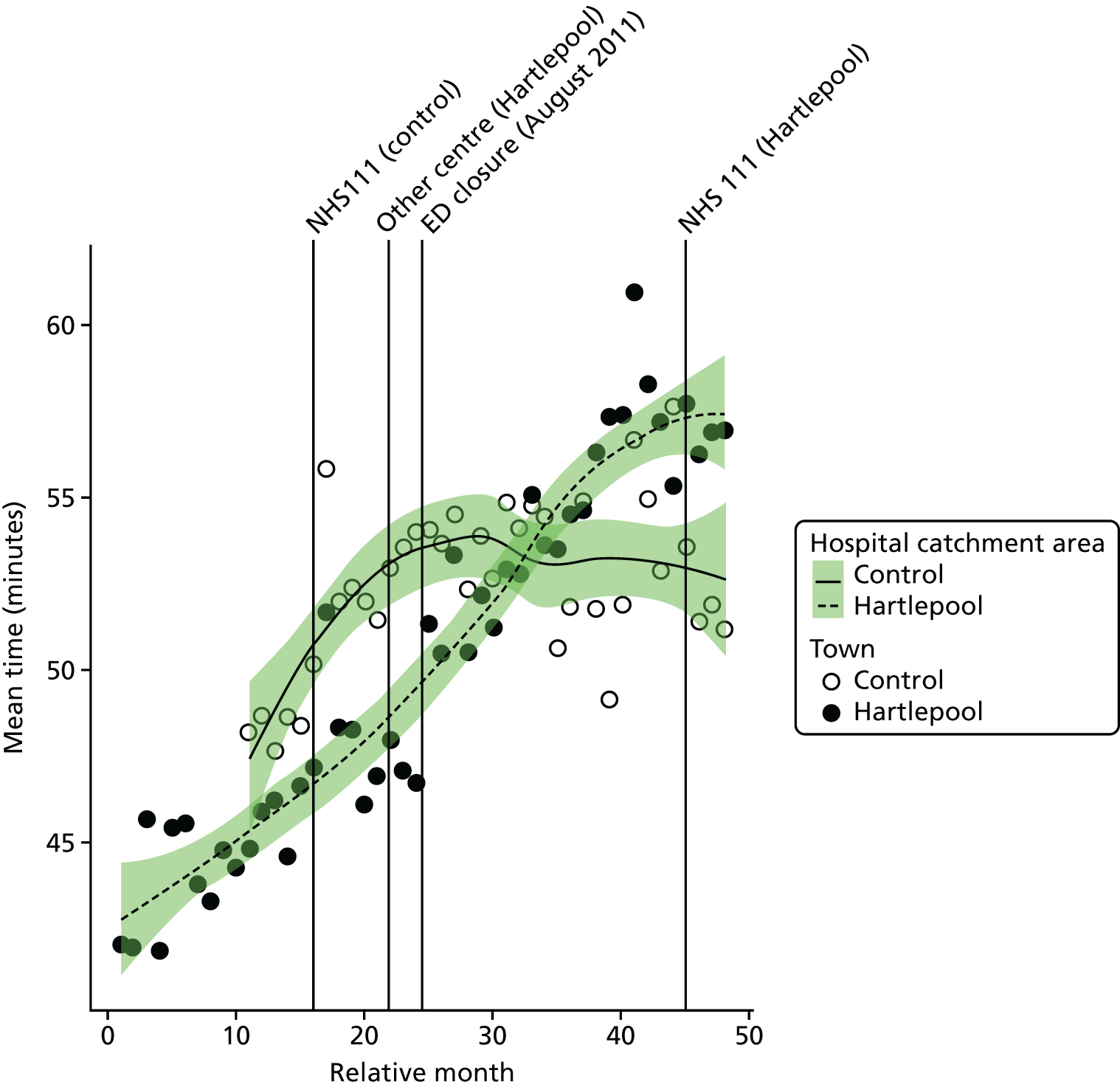
Examining the component times, it appears that the increase in the HA area arose principally from an increase in the time from the incident scene to arrival at hospital. The mean time from the call to the incident scene increased by 3.2 minutes, but the time from the incident scene to hospital increased by 5.9 minutes.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated mean time from call to hospital for 999 callers in the HA ED catchment area increased at the time of the closure by an average of 1.5 minutes (95% CI –0.1 to 3.1 minutes; p = 0.07).
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in time from call to incident scene was a decrease of 0.73 minutes, and the change from incident scene to hospital was an increase of 3.4 minutes.
The emergency department closure and control area model
Compared with the control area, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated mean time from call to arrival at hospital for 999 callers in the HA ED catchment area increased at the time of the closure by an average of 6.5 minutes (95% CI 4.5 to 8.5 minutes; p < 0.001).
Dose model
Figure 137 shows the mean time from call to arrival at hospital for ‘Red’ incidents each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high-dose areas) and residents of LSOAs that were expected to have a relatively small change (low-dose areas) after the closure of HA ED. The pattern of change in these two areas was similar. High-dose LSOAs had an increase in mean time from call to hospital of 9.9 minutes, and there was an increase of 8.0 minutes in the low-dose areas.
FIGURE 137.
Mean time from call to arrival at hospital for ‘Red’ incidents among residents of areas in Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
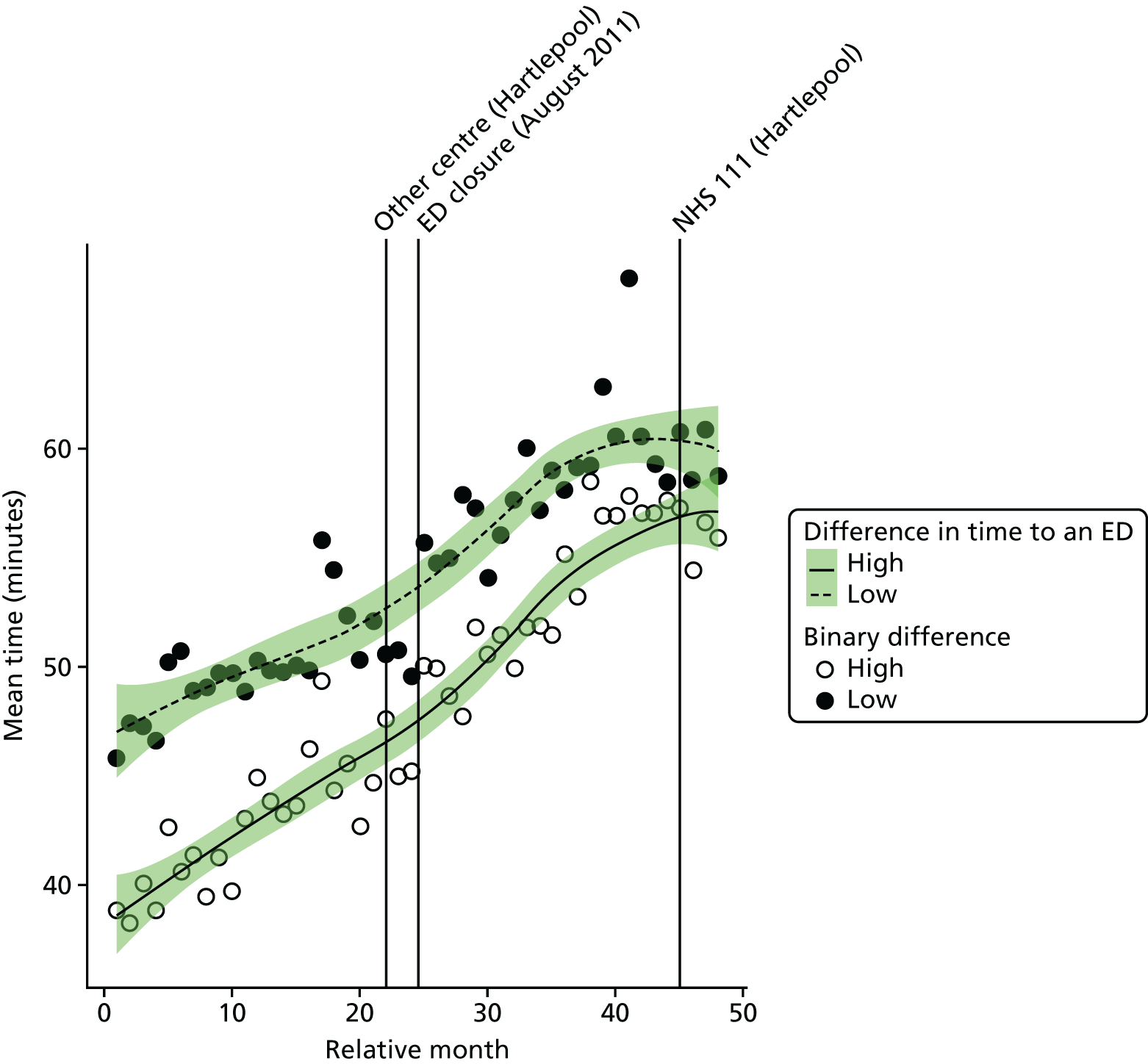
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the increase in the mean time from call to hospital for residents of high-dose areas at the time of the closure was estimated to be 2.0 minutes (95% CI 0.6 to 3.4 minutes; p = 0.006).
Emergency and urgent care attendances
Total number of emergency and urgent care attendances
Plot of monthly activity
Figure 138 shows the number of attendances at an ED (inclusive of A&E types 1–4 and attendances coded as ‘unknown’) among residents of the HA ED catchment area, and the control area, in each month over the 2 years prior to and the 2 years after the closure of the HA ED.
FIGURE 138.
Number of emergency and urgent care attendances among residents of the Hartlepool ED catchment area and the control area.
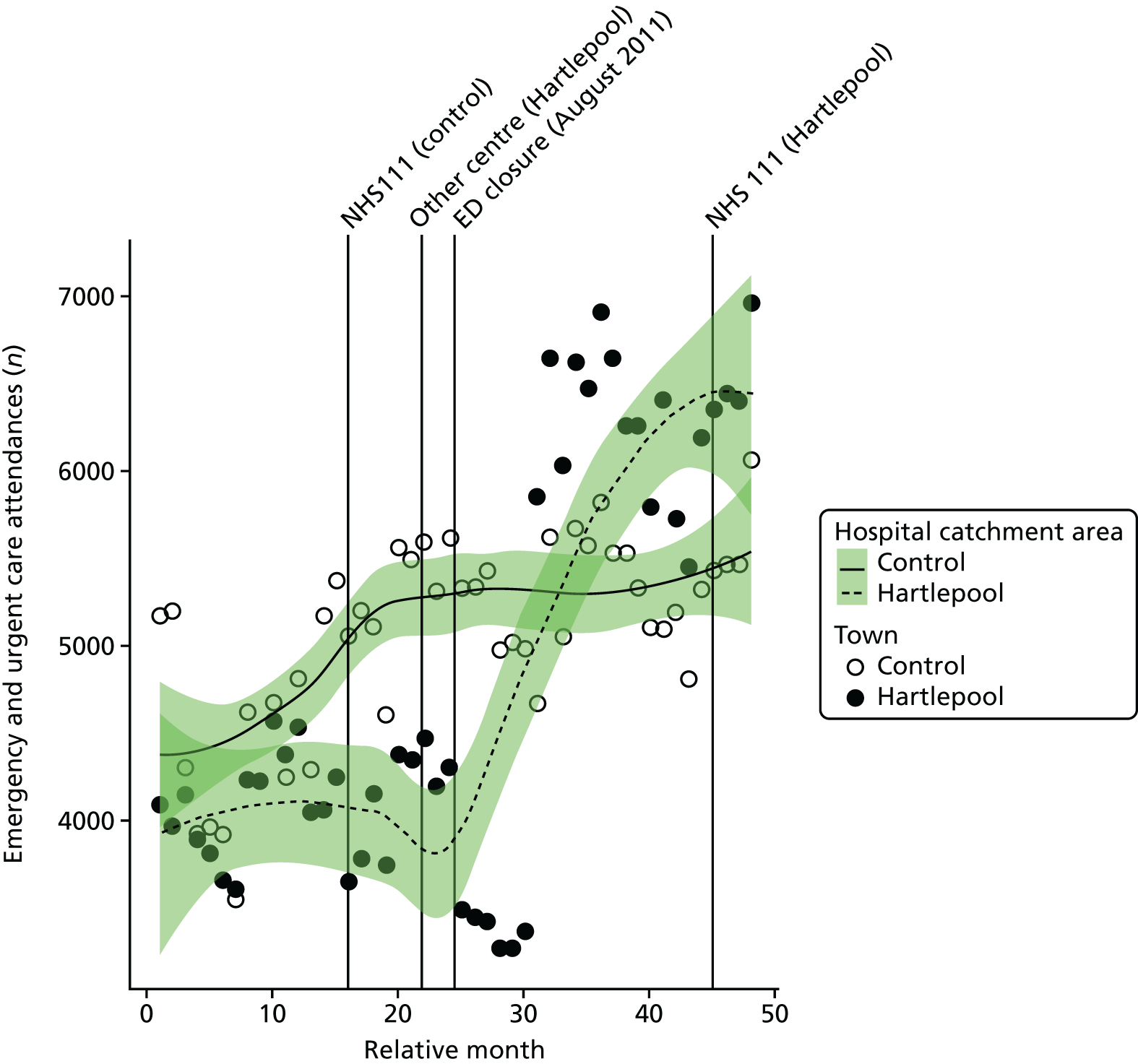
There was a decrease in the recorded number of attendances in the 6 months post closure, followed by a large and sudden increase in the recorded number of attendances in February 2012. This increase may have been the result of changes in data recording in an UCC in Peterlee. Unfortunately, we cannot reliably separate the impact of this change in data recording from the impact of the ED closure on overall attendance numbers or attendances for minor conditions. However, we have been able to examine the impact of the ED closure on the numbers of attendances at emergency and urgent care services for patients arriving by ambulance, which should exclude most UCC-type attenders.
Number of emergency and urgent care attendances for patients arriving by ambulance
Plot of monthly activity
Looking at attendances by residents of the HA ED catchment area who arrived by ambulance (which should exclude nearly all UCC patients), there was some suggestion that the number of attendances at an ED by patients arriving by ambulance decreased at the time of the closure of the HA ED (see Figure 139). The number of attendances by patients arriving by ambulance went down by 7%, from 887 per month pre closure to 824 per month post closure. It appears that there may have been a data recording problem for arrivals by ambulance in the control area and no comparisons have been made with this area.
FIGURE 139.
Number of emergency and urgent care attendances among residents of the Hartlepool ED catchment area and the control area for patients arriving by ambulance.
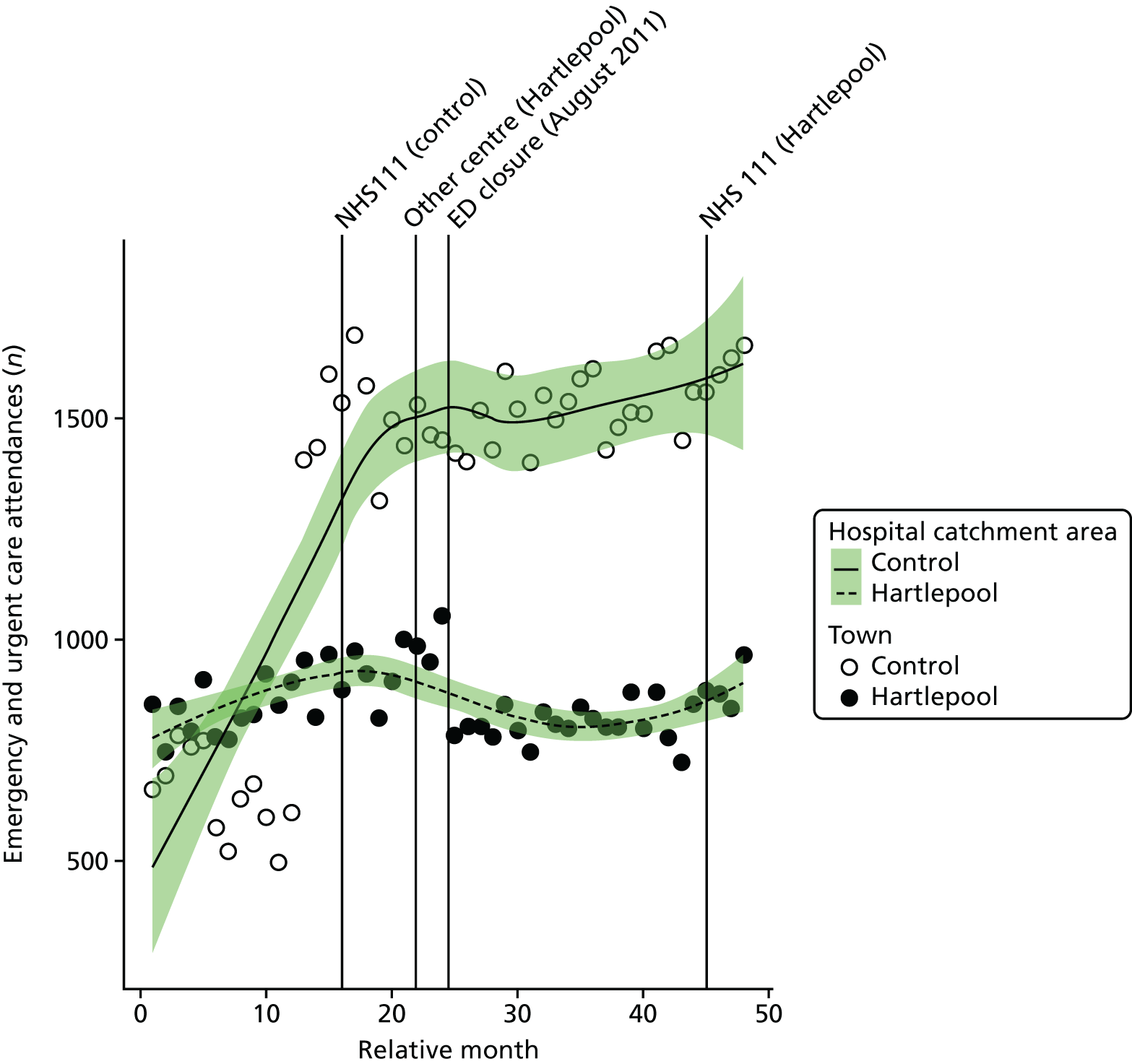
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated number of attendances by ambulance each month among residents of the HA ED catchment area decreased at the time of the closure by an average of –19.9% (95% CI –24.3% to –15.3%; p < 0.001).
The emergency department closure and control area model
No comparison with the control area was possible.
Dose model
Figure 140 shows the mean number of attendances each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HA ED. The pattern of change in these two areas was distinctly different. There was a much bigger change in the high-dose areas, which saw a reduction of –19% in the number of attendances arriving by ambulance, compared with a reduction of –7% in low-dose areas.
FIGURE 140.
Mean number of emergency and urgent care attendances for patients arriving by ambulance among residents of areas of Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
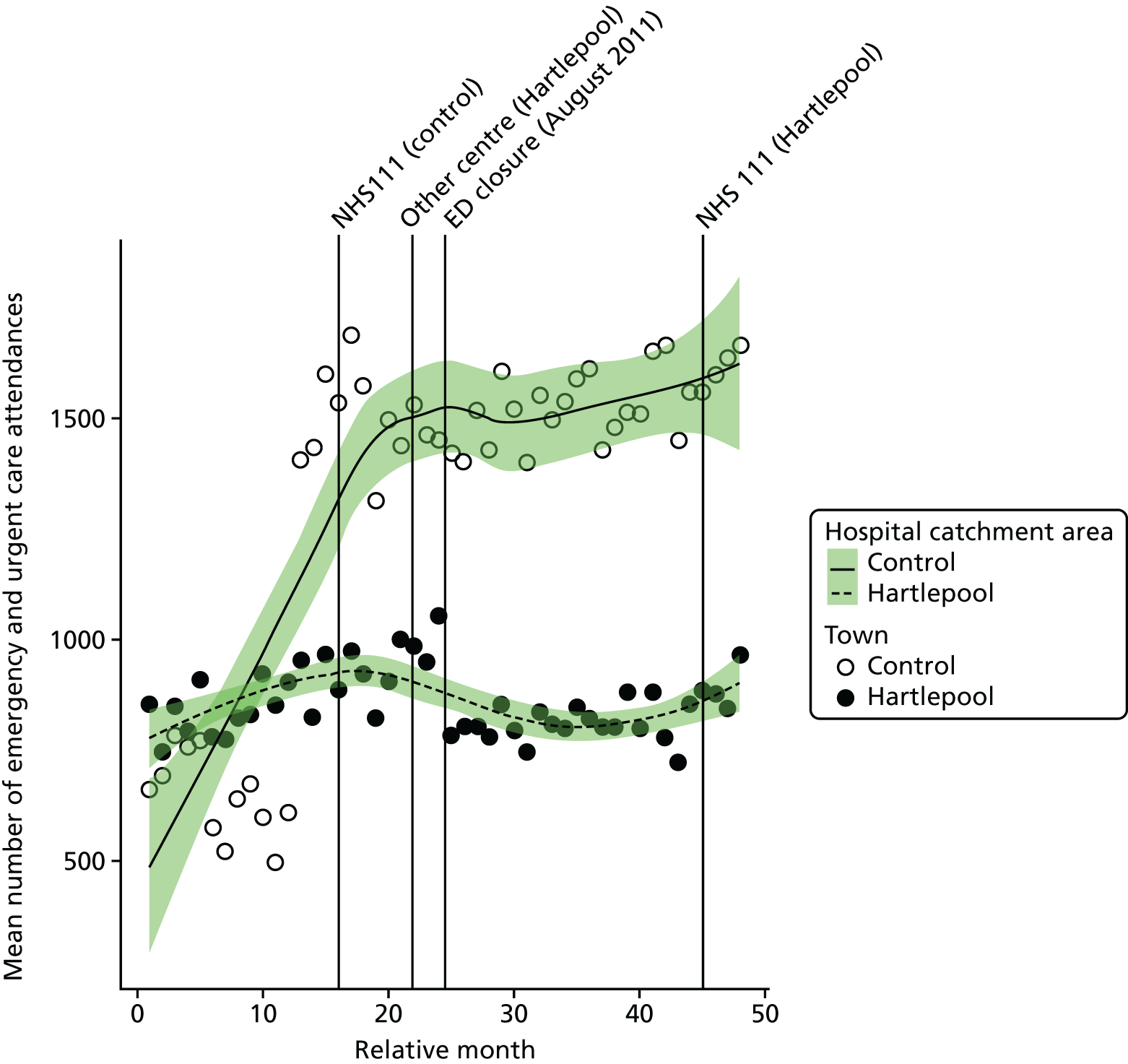
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the estimated number of attendances by patients arriving by ambulance in high-dose areas compared with low-dose areas was –23.7% (95% CI –27.6% to –19.7%; p < 0.001).
Admissions
All emergency admissions
Plot of monthly activity
Figure 141 shows the total number of emergency admissions to any hospital among residents of the HA ED catchment area and among residents of the control site catchment area in each month of the 4-year study period.
FIGURE 141.
Total number of emergency admissions among residents of the Hartlepool ED catchment area and the control catchment area.
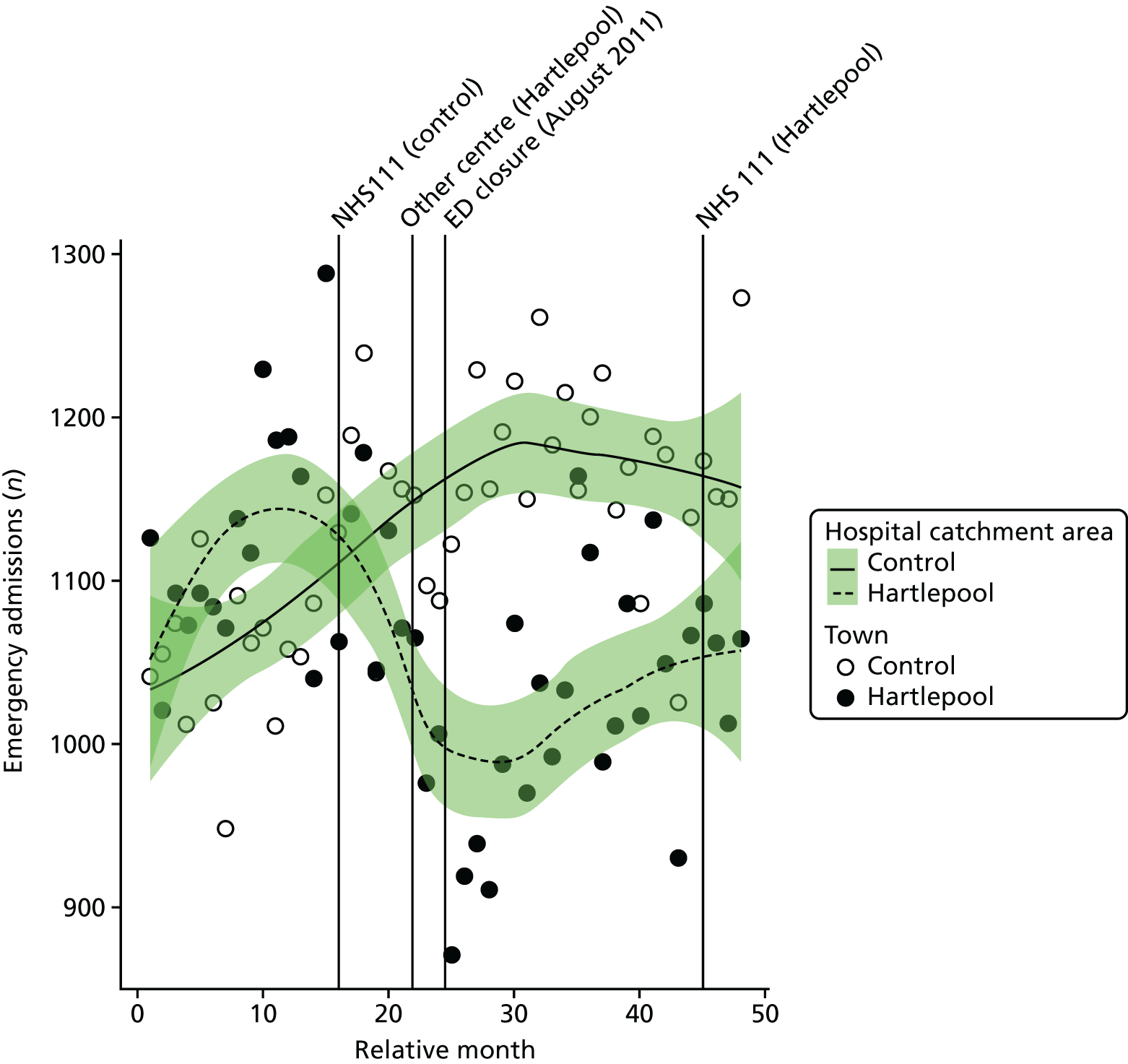
The number of emergency admissions changed slightly around the time of the closure for residents of HA. There were, on average, 1108 emergency admissions per month prior to the closure and 1029 post closure: a decrease of –7.7%. The control area showed the opposite effect, with a small increase over this period, from 1089 pre-closure to 1172 post-closure admissions per month: an increase of 7.7%.
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the monthly mean number of emergency admissions among residents of the catchment area of HA ED was –10.3% (95% CI –17.1% to –2.9%; p = 0.007).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly mean number of emergency admissions among residents of the catchment area of HA ED relative to the control site was –12.2% (95% CI –16.4% to –7.8%; p < 0.001).
Dose model
Figure 142 shows the mean number of emergency admissions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HA ED. The pattern of change in these two areas was similar, with a small reduction in high-dose areas, from 579 pre-closure to 509 post-closure admissions per month, and there was almost no change in low-dose areas, from 507 pre-closure to 503 post-closure admissions per month.
FIGURE 142.
Mean total number of emergency admissions among residents of areas of Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
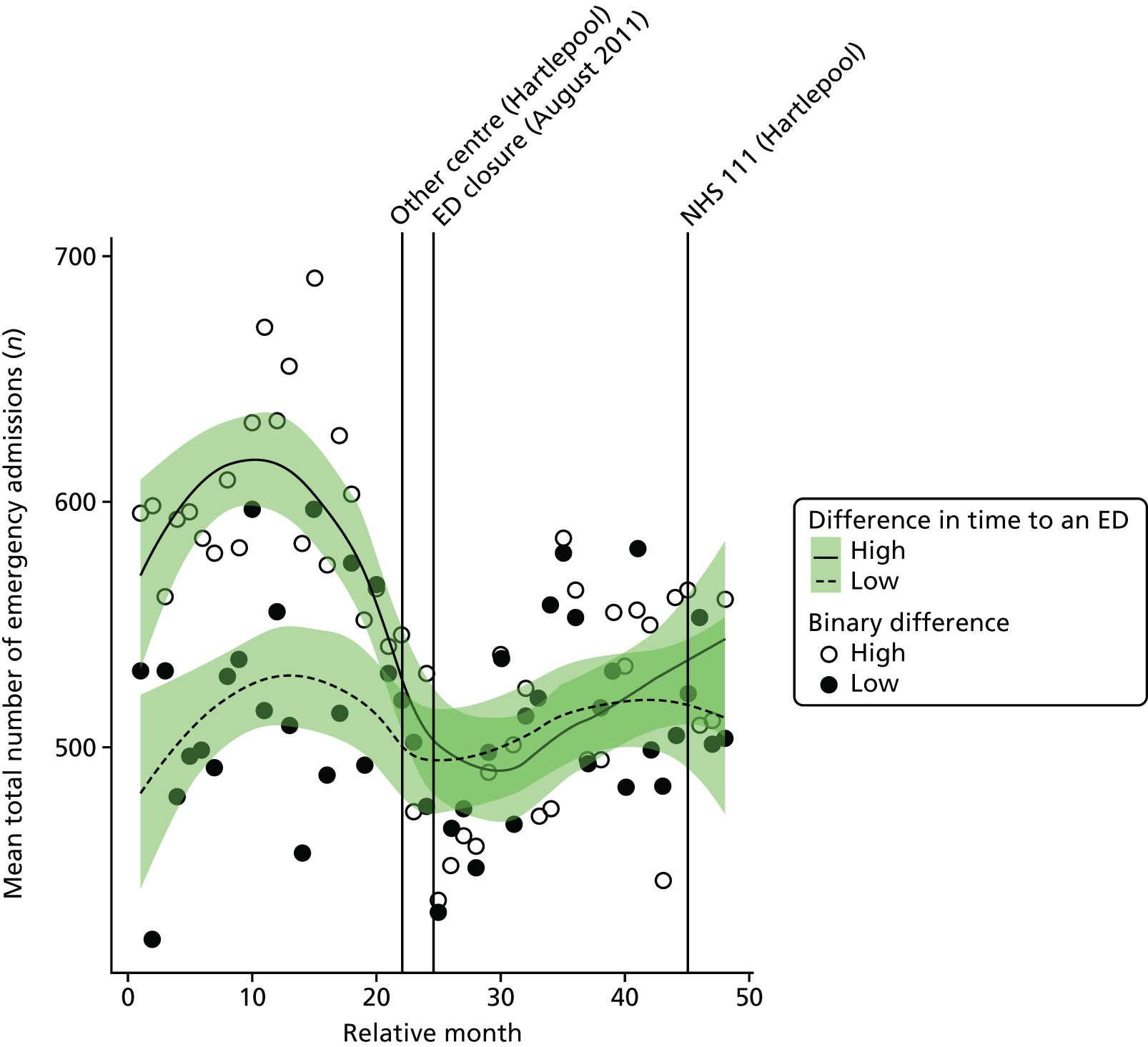
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change in the number of emergency admissions in high-dose areas compared with low-dose areas was –11.9% (95% CI –17.2% to –6.3%; p < 0.001).
Potentially avoidable emergency admissions
Plot of monthly activity
Figure 143 shows the potentially avoidable emergency admissions to any hospital among residents of the HA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. The pattern for admissions from these 14 emergency conditions is similar to the pattern for all emergency admissions, but with some small changes in the numbers over the period spanning the ED closure in HA. In the HA area, there were, on average, 315 avoidable emergency admissions per month prior to the closure and 287 post closure: a decrease of 8.9%. In the control area, there were, on average, 312 admissions per month prior to the closure date and 320 in the period after the closure.
FIGURE 143.
Number of potentially avoidable emergency admissions among residents of the Hartlepool ED catchment area and the control catchment area.
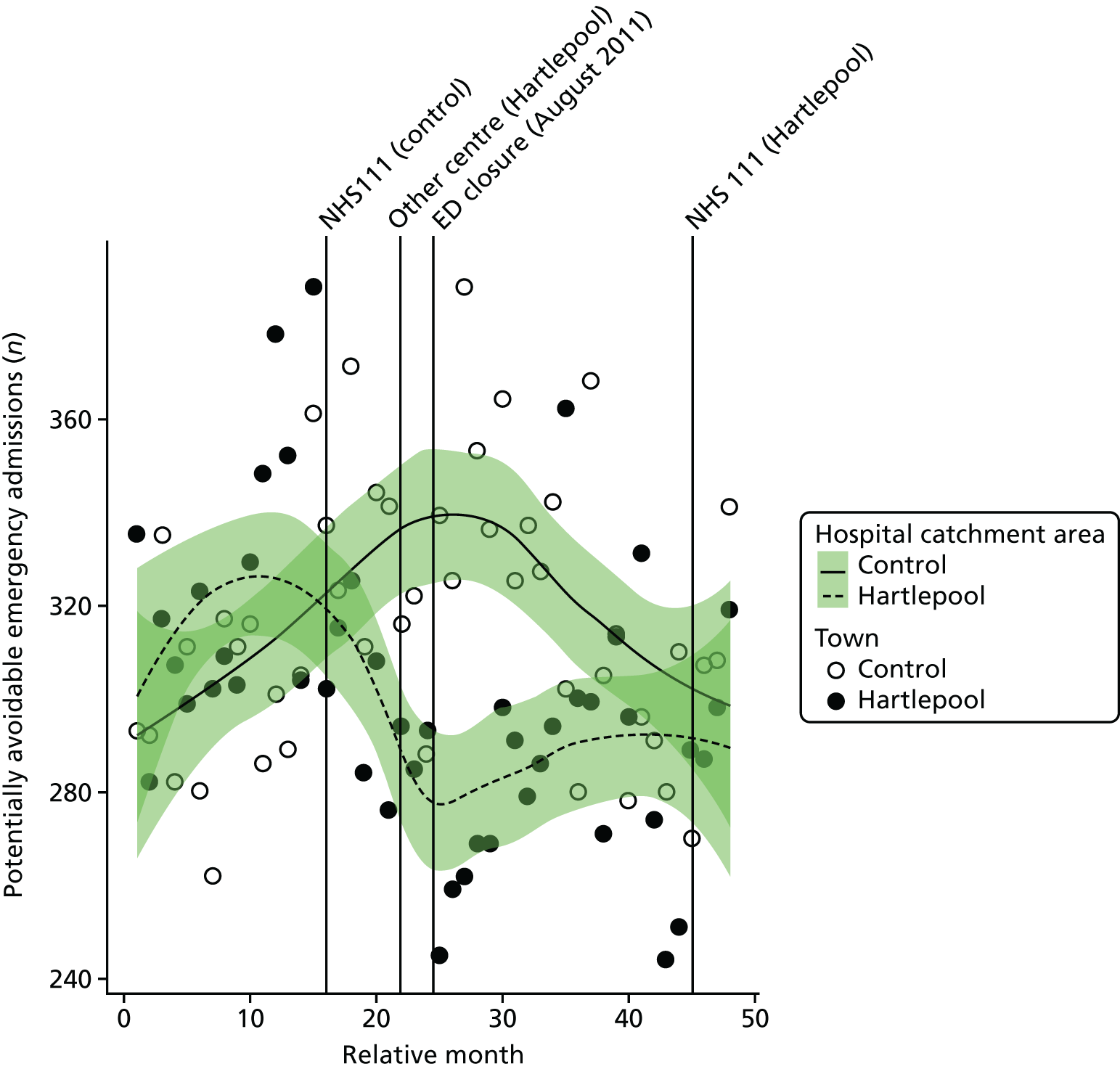
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of closure in the monthly mean number of avoidable emergency admissions for residents of the catchment area of HA ED was –8.8% (95% CI –17.4% to 0.7%; p = 0.07).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly mean number of avoidable emergency admissions among residents of the catchment area of HA ED relative to the control site was –6.8% (95% CI –13.4% to 0.2%; p = 0.06).
Dose model
Figure 144 shows the number of potentially avoidable emergency admissions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HA ED. The pattern of change in these two areas was very similar to the pattern for all emergency admissions, with a small reduction of 14% in high-dose areas, from 168 pre-closure to 148 post-closure avoidable admissions per month, and there was almost no change in the low-dose areas, from 145 pre-closure to 139 post-closure avoidable admissions per month.
FIGURE 144.
Number of potentially avoidable emergency admissions among residents of areas of Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
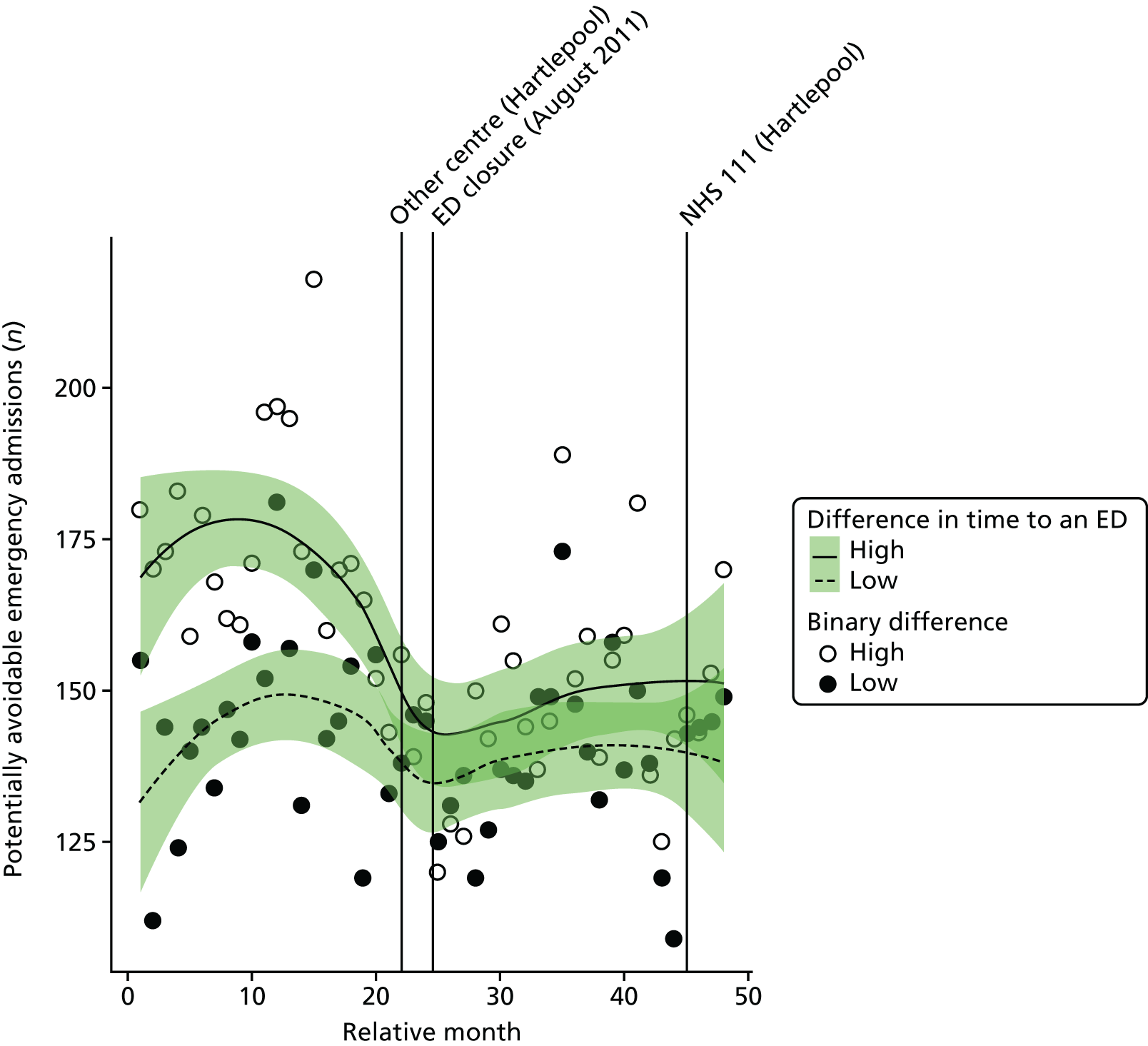
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the change in the estimated number of potentially avoidable emergency admissions in high-dose areas compared with low-dose areas was –8.2% (95% CI –14.9% to –1.0%; p = 0.03).
Length of stay for emergency admissions
Plot of monthly activity
Figure 145 shows the mean LOS in hospital for patients admitted as emergencies among residents of the HA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. There was a small change in HA, with the mean LOS increasing from 5.2 to 5.9 days before and after the closure of the ED, respectively. In the control site, there was almost no change, with a decrease from 7.2 to 7.1 days before and after the closure of the ED, respectively.
FIGURE 145.
Mean LOS for emergency admissions among residents of the Hartlepool ED catchment area and the control area.
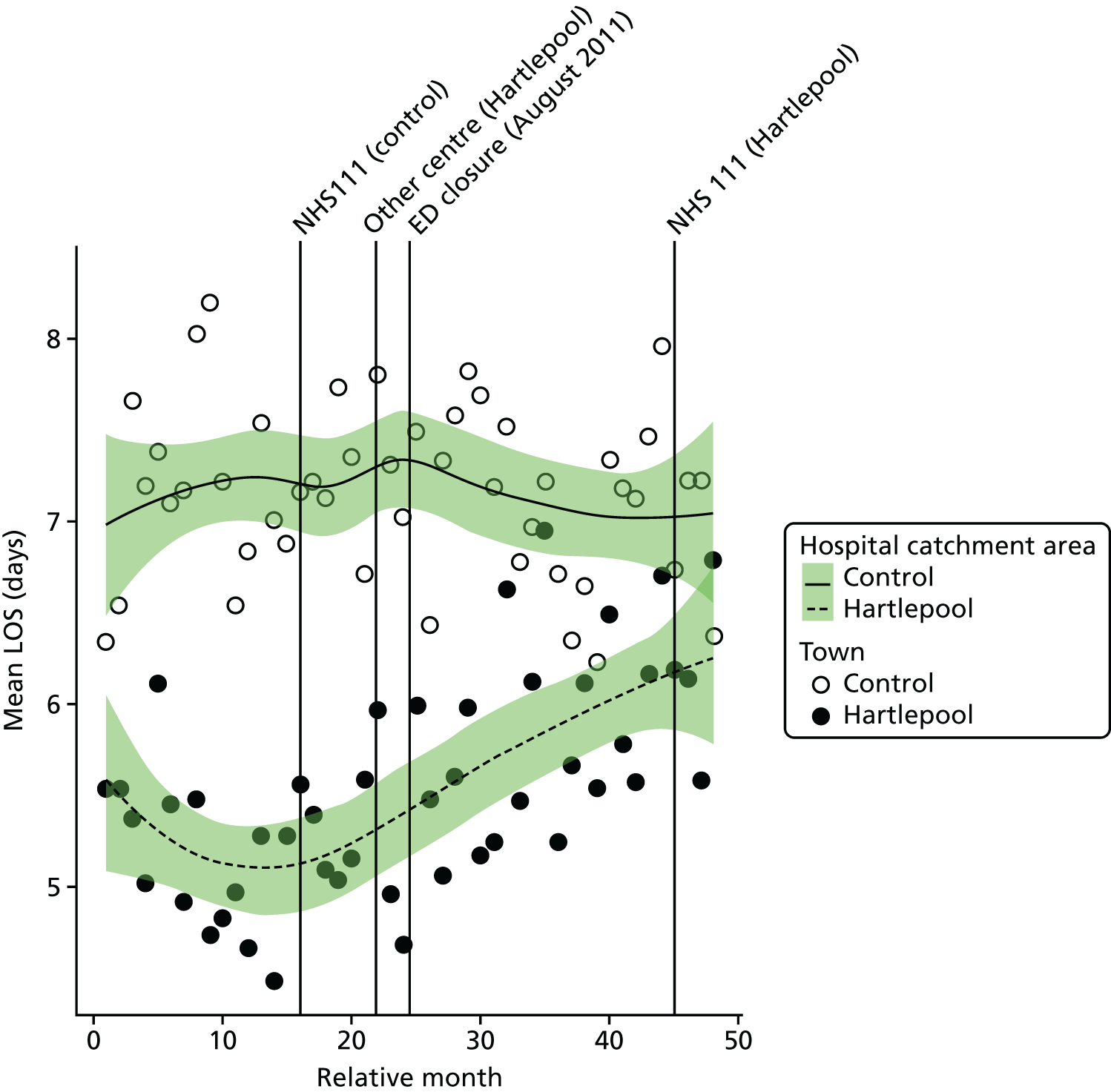
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the mean LOS among residents of the catchment area of HA ED was 0.54 days (95% CI 0.03 to 1.04 days; p = 0.04).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the mean length of stay for residents of the catchment area of HA ED at the time of the closure relative to the control site was 0.85 days (95% CI 0.47 to 1.24 days; p < 0.001).
Dose model
Figure 146 shows the mean LOS for emergency admissions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HA ED. There was an 18% increase in LOS in high-dose areas, from 5.1 days pre closure to 6.0 days post closure, and a 9% increase from 5.2 pre closure to 5.7 days post closure in low-dose areas.
FIGURE 146.
Mean LOS for emergency admissions among residents of areas of Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
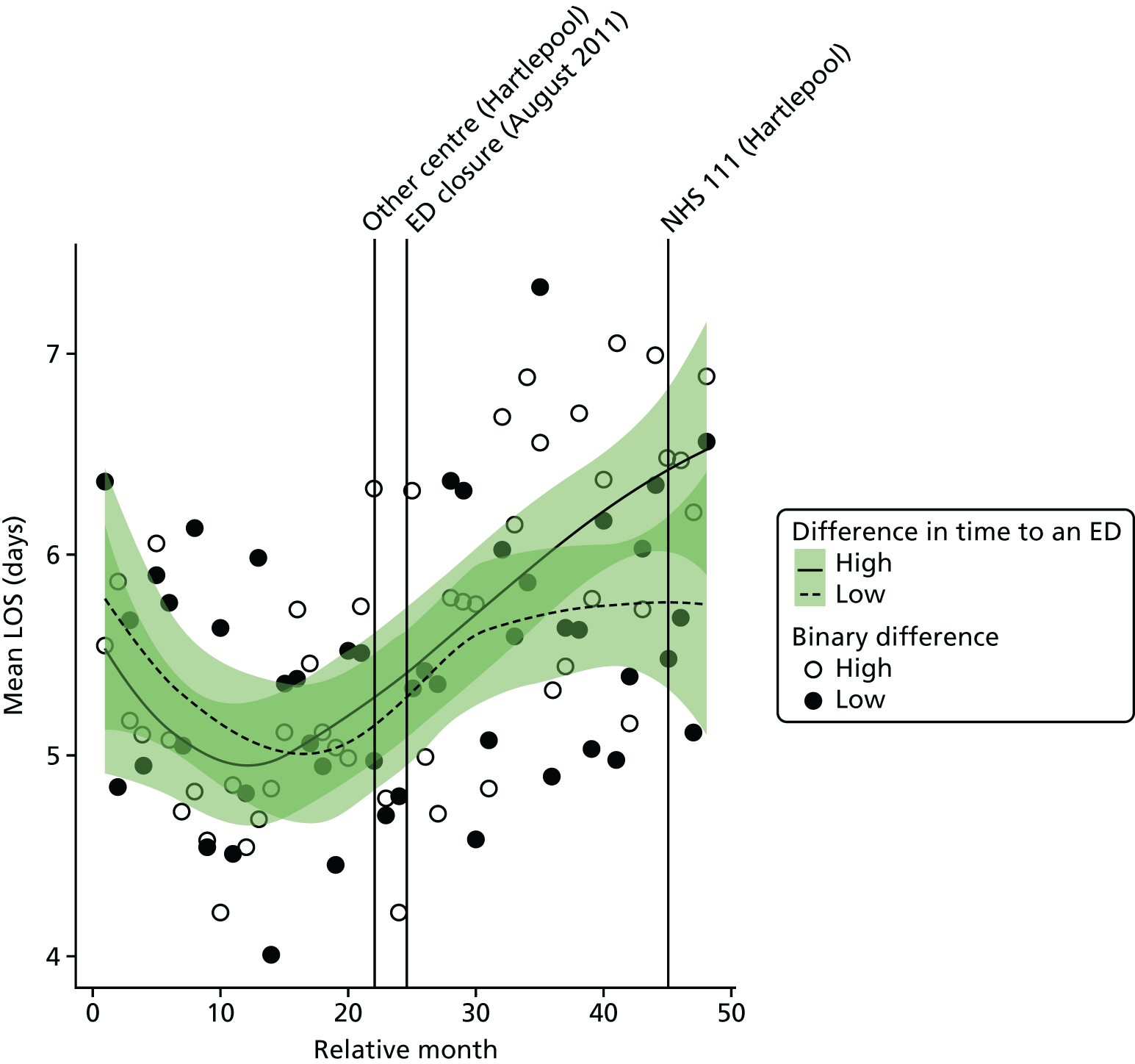
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the mean LOS for emergency admissions in high-dose areas compared with low-dose areas was 0.46 days (95% CI 0.07 to 0.85 days; p = 0.03).
Deaths
Out-of-hospital deaths from serious emergency conditions from certain serious conditions
‘Out-of-hospital’ deaths may occur at home prior to making contact with a service, in an ambulance on the way to hospital, in the ED prior to hospital admission or when a patient is recorded as having a SEC incident and is admitted, discharged alive and subsequently dies out of hospital without being readmitted.
Plot of monthly activity
Figure 147 shows the number of deaths occurring before arrival at hospital from the 16 SECs we have focused on, among residents of the HA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. Among residents of the HA catchment area, there were, on average, 21.0 deaths per month prior to the closure and 19.4 post closure: a decrease of 7.7%. In the control area, the monthly average decreased by 6.3%, from 34.5 deaths per month prior to the closure to 32.4 post closure.
FIGURE 147.
Number of deaths occurring out of hospital for SECs among residents of the catchment areas of the Hartlepool and control EDs.
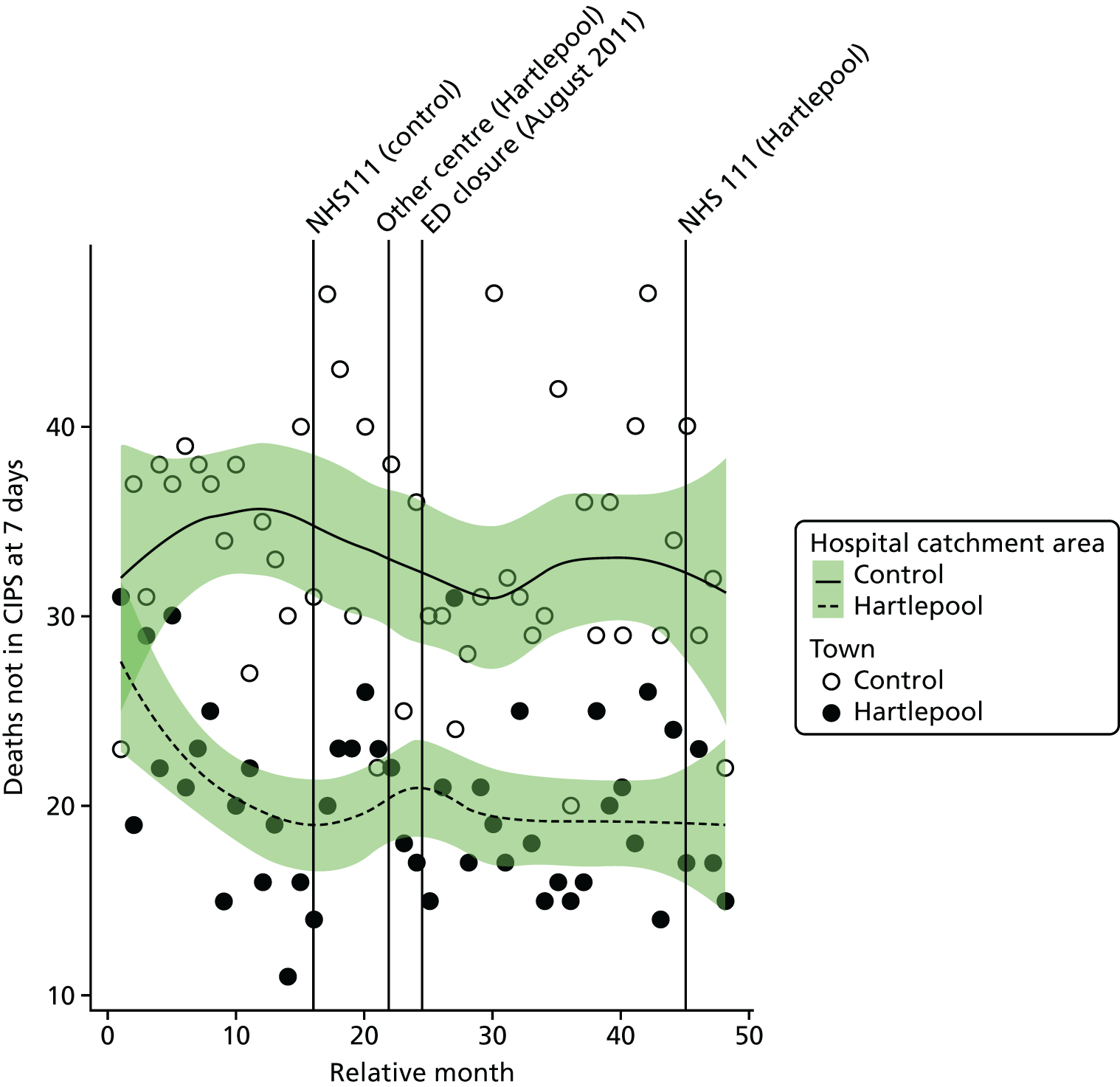
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the monthly mean number of out-of-hospital deaths from the 16 SECs among residents of the catchment area of HA ED was 12.4% (95% CI –14.5% to 47.9%; p = 0.40).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly mean number of deaths from emergency conditions occurring out of hospital among residents of the catchment area of HA ED at the time of the closure relative to the control site was –1.7% (95% CI –17.5% to 17.2%; p = 0.85).
Dose model
Figure 148 shows the number of out-of-hospital deaths each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HA ED. The pattern of change in these two areas was similar, with a small decrease of 6% in high-dose areas from an average of 10.6 pre-closure to 10.0 post-closure deaths per month, and there was a decrease of 10% from 10.5 pre-closure to 9.5 -post closure deaths per month in low-dose areas.
FIGURE 148.
Number of out-of-hospital deaths from SECs among residents of areas of Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
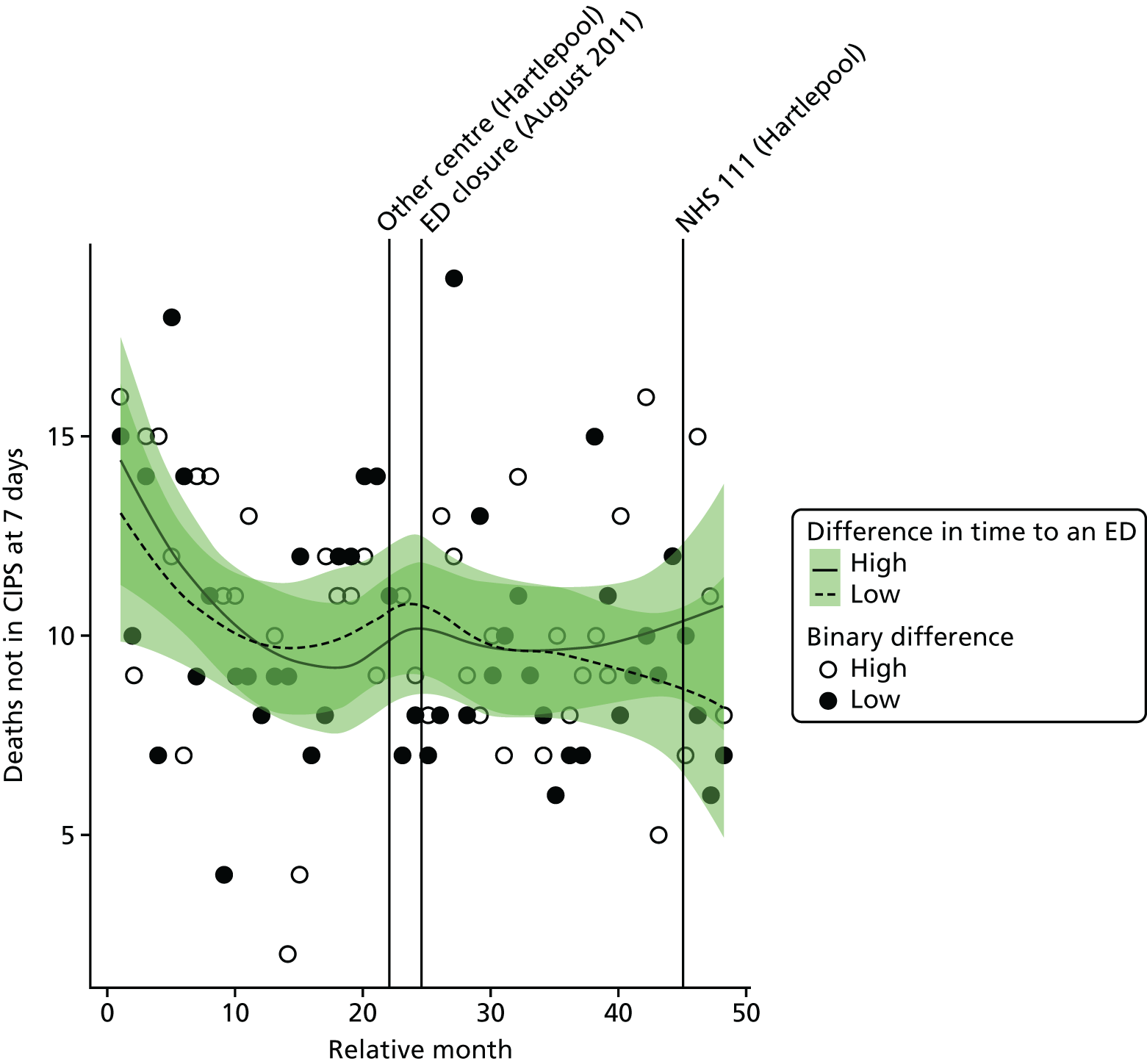
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of out-of-hospital deaths in high-dose areas compared with low-dose areas was 4.0% (95% CI –19.2% to 33.8%; p = 0.76).
All deaths from serious emergency conditions occurring within 7 days
Plot of monthly activity
Figure 149 shows the total number of deaths occurring up to 7 days post incident from the 16 SECs among residents of the HA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These deaths may have occurred out of hospital or in hospital within 7 days of admission. These numbers show a similar pattern as that for deaths that were out of hospital. There were, on average, 30.4 deaths per month prior to the closure and 27.9 deaths per month post closure: a decrease of –8.2%. In the control area, the monthly average decreased by –6.0%, from 51.4 deaths per month prior to the closure to 48.3 deaths per month post closure.
FIGURE 149.
Total number of deaths from SECs occurring within 7 days of the incident among residents of the catchment areas of the Hartlepool and control EDs.
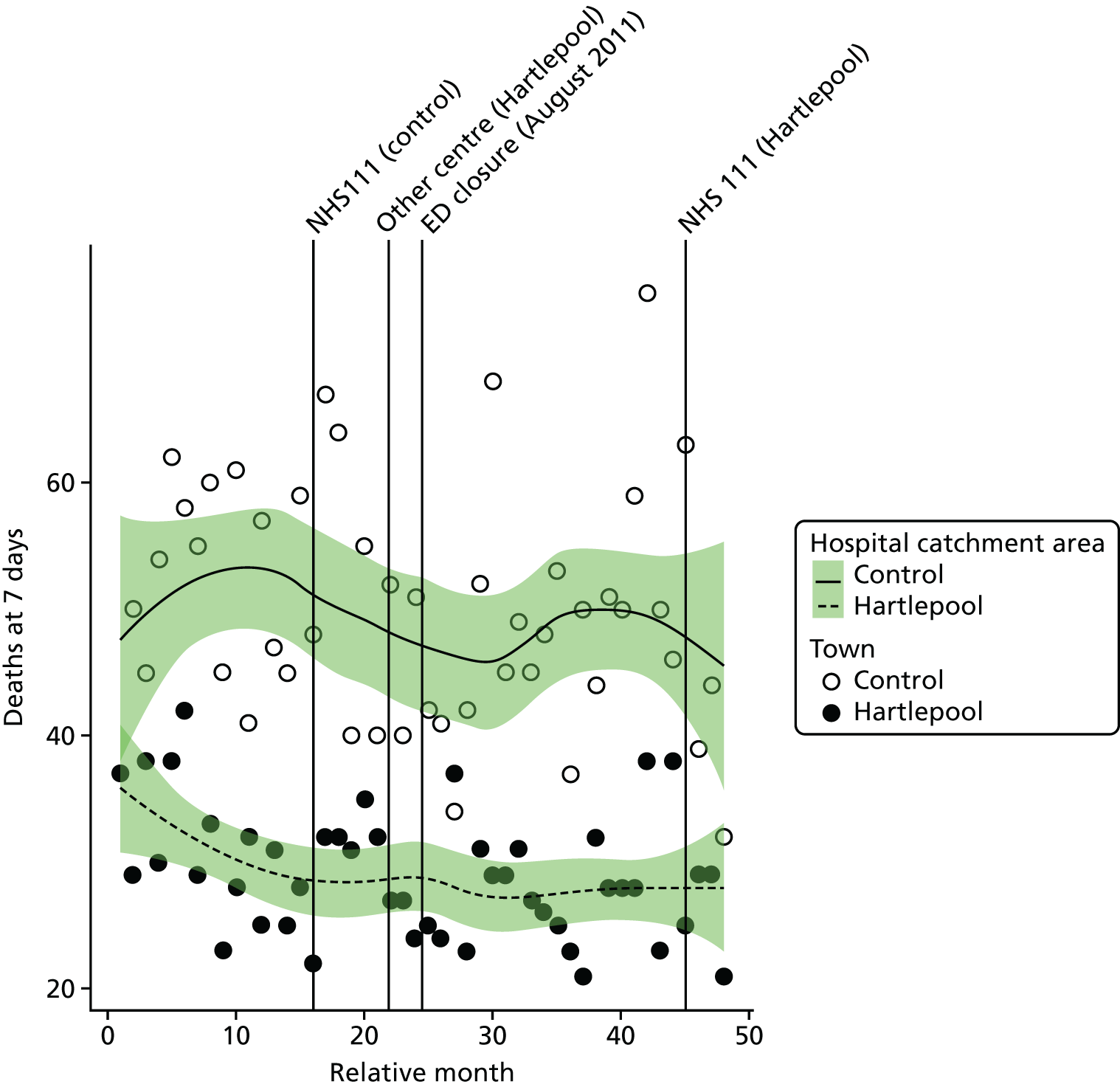
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase at the time of the closure in the monthly mean number of deaths within 7 days from the 16 SECs among residents of the catchment area of HA ED was 3.8% (95% CI –17.3% to 30.3%; p = 0.75).
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated change in the monthly mean number of deaths within 7 days from the 16 SECs for residents of the catchment area of HA ED at the time of the closure relative to the control site was –4.8% (95% CI –17.8% to 10.3%; p = 0.52).
Dose model
Figure 150 shows the total number of deaths occurring up to 7 days post incident from the 16 emergency conditions each month among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of HA ED. The pattern of change in these two areas was similar, with a small reduction in the average monthly number of deaths in both areas, from 15.1 deaths prior to the closure to 14.3 deaths post closure in high-dose areas, and from 14.7 deaths prior to the closure to 13.6 deaths post closure in low-dose areas.
FIGURE 150.
Total number of deaths from SECs up to 7 days post incident among residents of areas of Hartlepool that were expected to have a large change in time to an ED (high dose) and those expected to have a small change (low dose).
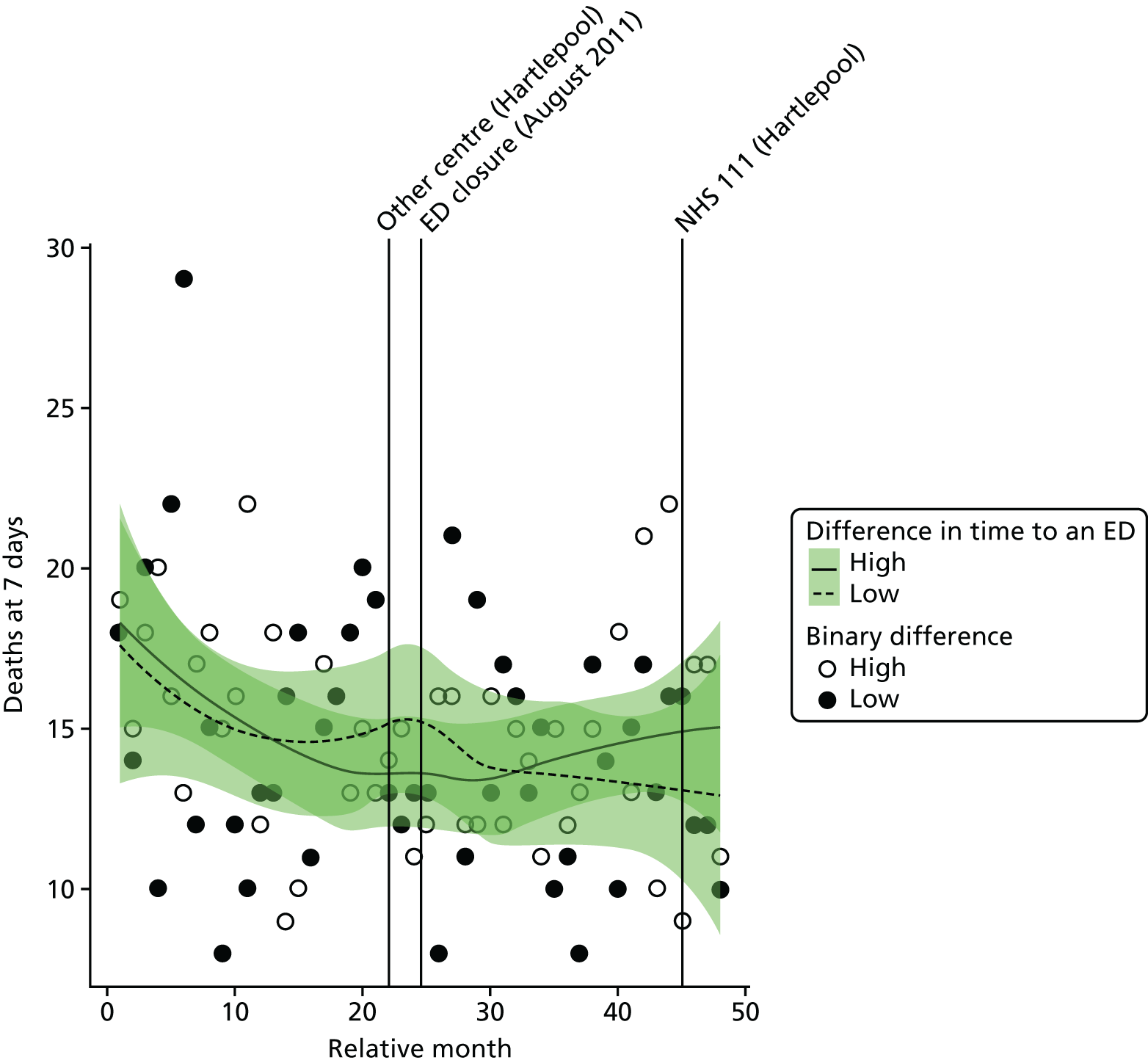
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the number of deaths among residents of high-dose areas compared with low-dose areas was 2.2% (95% CI –17.3% to 26.3%; p = 0.84).
Case fatality ratios: all serious emergency conditions studied
Plot of monthly activity
Figure 151 shows the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths plus admissions for patients who survived beyond 7 days from the 16 SECs among residents of the HA ED catchment area and residents of the control site catchment area in each month of the 4-year study period. These ratios reflect the risk of dying from these emergency conditions. In HA, over the 2 years before the closure the average ratio was 0.198 (indicating that 19.8% of the patients died) and it was 0.194 in the period after the closure: a reduction of just 0.4% in the percentage of patients who died. In the control site, the average ratio fell from 0.275 pre closure to 0.249 post closure.
FIGURE 151.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident among residents of the catchment areas of the Hartlepool and control EDs.
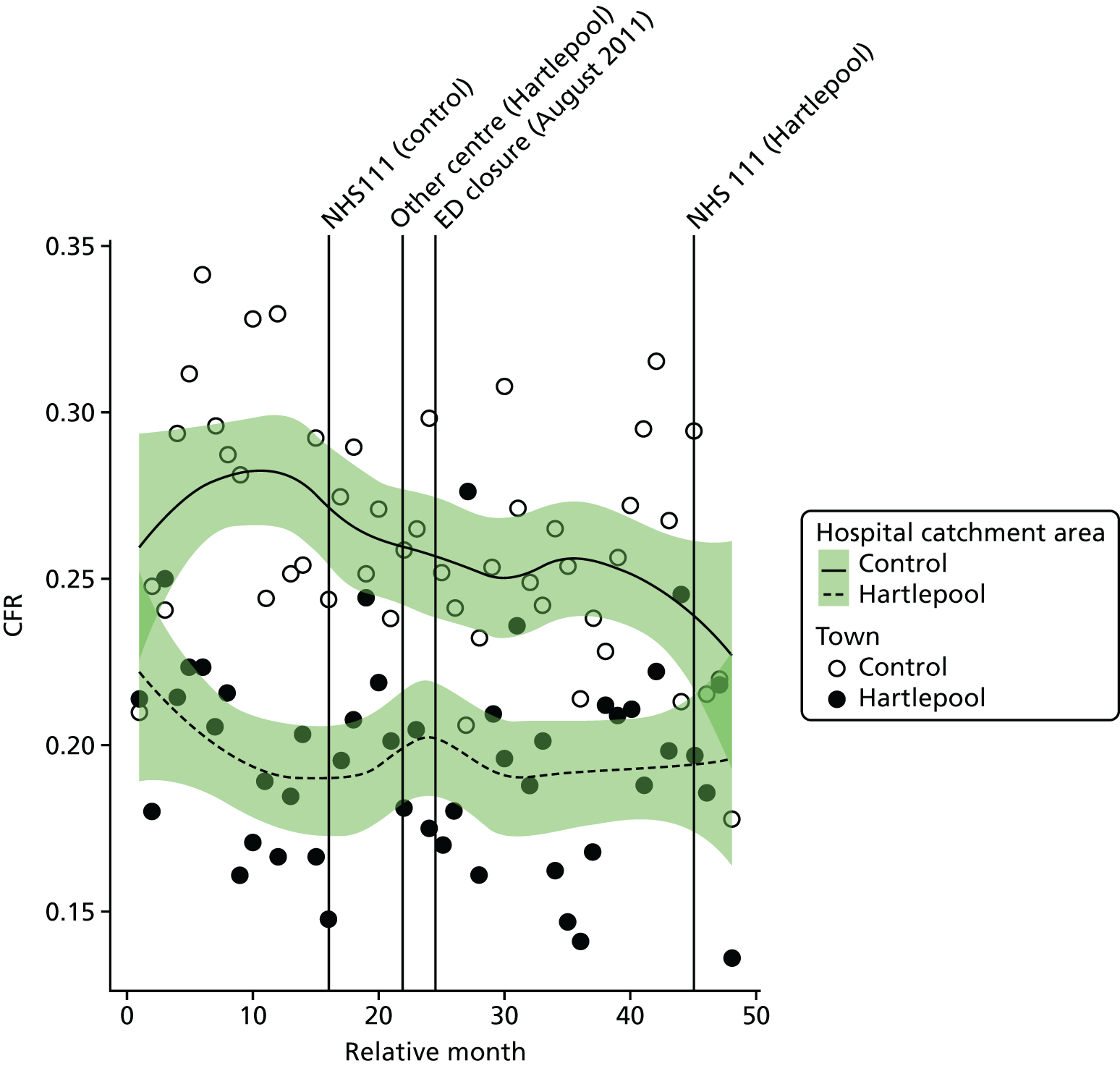
The emergency department closure area model
After allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated change at the time of the closure in the CFR for the 16 SECs among residents of the catchment area of HA ED was 0.00 (95% CI –0.025 to 0.025; p = 0.99), indicating that there was no change at all in the percentage of patients who died.
The emergency department closure site and control area model
Compared with the control site, after allowing for seasonal effects, any long-term trend and other known changes in the two catchment areas, the estimated increase in the monthly average CFR for the 16 SECs among residents of the catchment area of HA ED at the time of closure relative to the control site was 0.017 (95% CI –0.010 to 0.043; p = 0.22), indicating an increase of 1.7 in the percentage of patients who died.
Dose model
Figure 152 shows the ratio of the total number of deaths occurring up to 7 days post incident to the total number of deaths plus admissions for patients who survived beyond 7 days from the 16 SECs among residents of LSOAs that were expected to have a relatively large change in time to an ED (high dose) and residents of LSOAs that were expected to have a relatively small change (low dose) after the closure of Hartlepool ED. In high-dose areas, over the 2 years before closure the average ratio was 0.178 (indicating that 17.8% of the patients died) and it was 0.192 in the period after the closure: an increase of 1.4 in the percentage of patients who died. In the low-dose areas, the average ratio decreased slightly from 0.198 pre closure to 0.192 post closure.
FIGURE 152.
Case fatality ratio for deaths from SECs occurring within 7 days of the incident among residents of areas in Hartlepool that were expected to have a relatively large change in time to an ED (high dose) and those expected to have a small change (low dose).
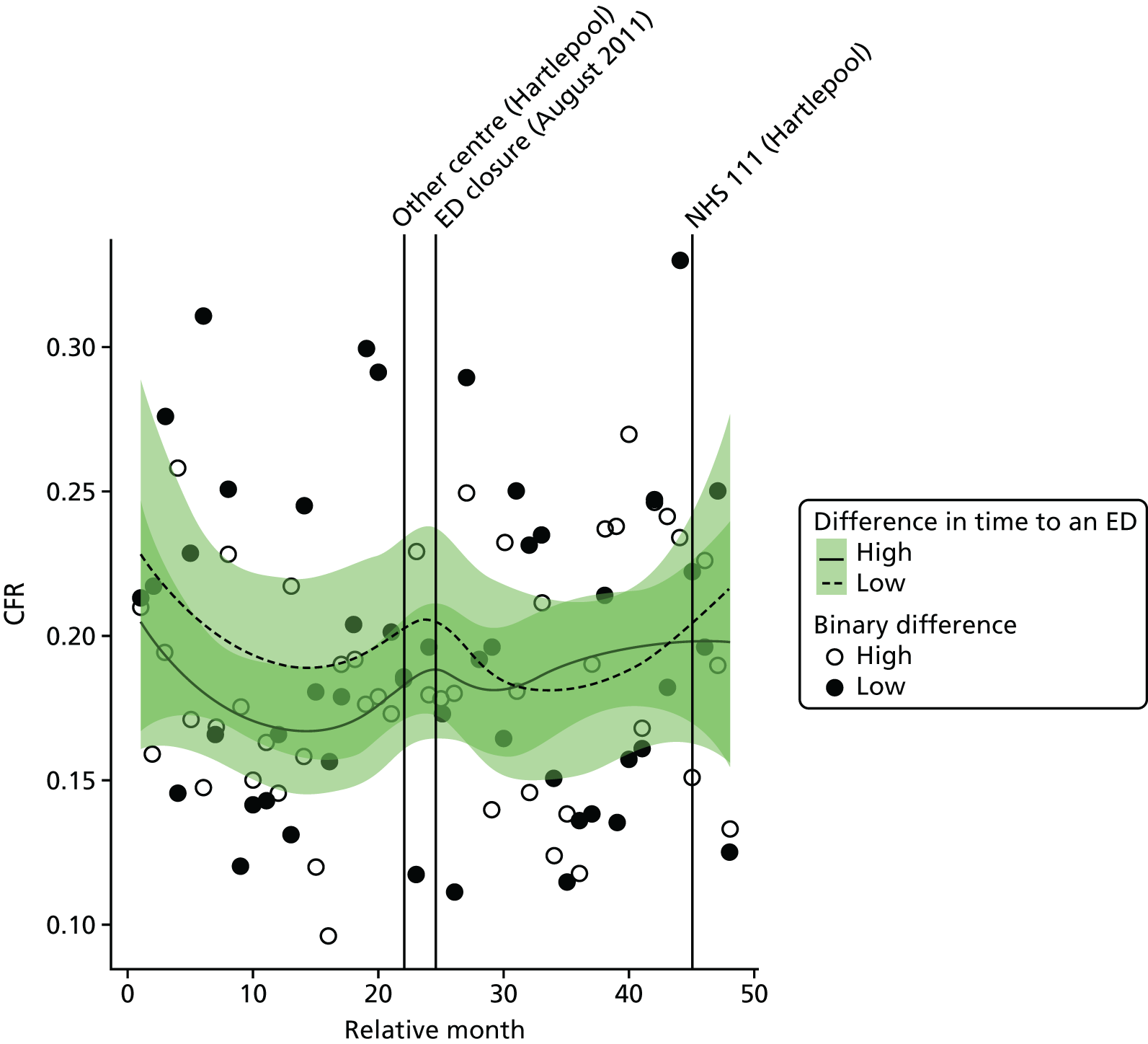
Compared with the low-dose areas, after allowing for seasonal effects, any long-term trend and other known changes in the ED catchment area, the estimated increase in the CFR in high-dose areas compared with low-dose areas was 0.021 (95% CI –0.013 to 0.056; p = 0.23).
Case fatality ratios: myocardial infarction and stroke
We have also examined the change in the CFRs for MI and for stroke separately (Tables 45 and 46). There was little evidence that the CFRs had changed for either condition, and there was no evidence of any difference for residents of Hartlepool and its control area, or for residents of the high-dose areas of Hartlepool compared with the low-dose areas.
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Hartlepool | |||
| Low-dose areas | 0.223 (0.090) | 0.230 (0.119) | –0.6 |
| High-dose areas | 0.277 (0.132) | 0.272 (0.119) | –0.5 |
| Total | 0.241 (0.102) | 0.232 (0.100) | –0.9 |
| Control | 0.385 (0.078) | 0.372 (0.086) | –1.3 |
| Area | CFRs | Change in the % of patients who died | |
|---|---|---|---|
| Pre closure, mean (SD) | Post closure, mean (SD) | ||
| Hartlepool | |||
| Low-dose areas | 0.347 (0.194) | 0.338 (0.151) | –0.9 |
| High-dose areas | 0.309 (0.123) | 0.346 (0.162) | +3.6 |
| Total | 0.309 (0.101) | 0.316 (0.106) | +0.7 |
| Control | 0.467 (0.130) | 0.379 (0.069) | –8.8 |
Glossary
- Ambulance conveyance
- Transport of patients to an emergency department by ambulance.
- Ambulance diversion
- An agreed diversion of ambulance patients to other emergency departments.
- Case fatality ratio
- The ratio of the number of deaths from a disease to the number of deaths plus admissions of patients diagnosed with the disease who survive over a certain period of time. It is an indicator of the risk of death.
- Category A ambulance call
- A call that should be responded to within 8 minutes (national targets apply).
- Critical care
- A branch of medicine concerned with life support for critically ill patients.
- Crowding
- According to the the Royal College of Emergency Medicine (Crowding in Emergency Departments. The Royal College of Emergency Medicine; 2014. URL: https://secure.rcem.ac.uk/code/document.asp?ID=6296), in the case of an emergency department, crowding is present if ‘ambulances cannot offload, there are long delays for high acuity patients to see a doctor, there are high rates of patients with a “Left before being seen” code, there are more trolley patients in the emergency department than there are cubicle spaces, or if patients are waiting more than two hours for an in-patient bed after a decision to admit has been made.’ Quotation reproduced with the permission of the Royal College of Emergency Medicine.2014Royal College of Emergency Medicinehttps://secure.rcem.ac.uk/code/document.asp?ID=6296
- Department of Health and Social Care
- The government department that is responsible for public health issues and that exists to improve the health and well-being of people in England.
- Emergency admission
- An admission that is unpredictable and occurs at short notice because of clinical need.
- Emergency department
- Also known as accident and emergency, an emergency room or casualty department, a medical facility specialising in acute care for patients who present without prior appointment, either by their own means or by ambulance.
- Locally weighted scatterplot smoothing curve
- A statistical method to, in this case, create a smooth trend line through the time-series data.
- Lower-layer super output area
- Non-intersecting small areas of geography of approximately equal population size that cover England. They are defined using census data to be internally homogeneous.
- Minor attendance
- Emergency department attenders who are discharged without treatment and/or investigations that require hospital facilities.
- Minor injuries unit
- A walk-in service provided in some hospitals, providing treatment for minor injuries such as laceration and fractures.
- Negative binomial model
- A statistical tool for analysing count data such as the monthly number of deaths.
- NHS Sustainability and Transformation Plans
- Five-year plans covering all aspects of NHS spending in each of the 44 geographical areas covering England. Plans were developed locally, by NHS organisations and local authorities with guidance from NHS England and other national NHS bodies.
- Out-of-hospital death
- A death occurring before hospital admission.
- Prais–Winsten
- A procedure that is designed to account for autocorrelation when analysing time-series data.
- Royal College of Emergency Medicine
- The body responsible for setting standards of training and administering examinations in emergency medicine for the award of Fellowship and Membership of the College as well as for recommending trainees for a certificate in completion of training in emergency care.
- Type 1 emergency department
- A consultant-led accident and emergency department with major resuscitation facilities available at all times.
List of abbreviations
- A&E
- accident and emergency
- APC
- admitted patient care
- BA ED
- Bishop Auckland emergency department
- CAD
- computer-aided dispatch
- CCG
- clinical commissioning group
- CDDFT
- County Durham and Darlington NHS Foundation Trust
- CFR
- case fatality ratio
- CI
- confidence interval
- CIPS
- continuous inpatient spell
- CT
- computerised tomography
- DfT
- Department for Transport
- ED
- emergency department
- GP
- general practitioner
- HA ED
- University Hospital of Hartlepool emergency department
- HES
- Hospital Episode Statistics
- HH ED
- Hemel Hempstead emergency department
- ICD-10
- International Classification of Diseases, Tenth Edition
- LOS
- length of stay
- LSOA
- lower-layer super output area
- MI
- myocardial infarction
- MIU
- minor injuries unit
- NE ED
- Newark Hospital emergency department
- ONS
- Office for National Statistics
- PCT
- primary care trust
- PPI
- patient and public involvement
- RO ED
- Rochdale Infirmary emergency department
- ScHARR
- School of Health and Related Research
- SD
- standard deviation
- SEC
- serious emergency condition
- SECF
- Sheffield Emergency Care Forum
- STP
- sustainability and transformation plan
- UCC
- urgent care centre
- UHH
- University Hospital of Hartlepool
- UHNT
- University Hospital of North Tees
- WIC
- walk-in centre
