Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/04/33. The contractual start date was in November 2015. The final report began editorial review in November 2016 and was accepted for publication in May 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Mannion et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Whistleblowing: a complex and contested issue
Employee whistleblowing – loosely, the raising of concerns or speaking up about unsafe, unethical or poor-quality care by employees to persons able to effect action – has emerged as a central issue in debates over quality and safety in many health systems. 1 In the English NHS, recent inquiries and reports into poor standards of care have highlighted the vital contribution that whistleblowing can play in the detection and prevention of harm to patients. 2 Yet, for all its importance, the act of whistleblowing is no simple issue3 and is fraught with ambiguity. For example, individual whistleblowers may be perceived as heroes by some (for championing patients’ interests, promoting better care and challenging management) but may be seen as villains by others (for denigrating services and damaging professional and organisational reputations). Indeed, in the popular media whistleblowers are often portrayed either as ‘courageous employees’ who act to maintain standards at great personal cost or as ‘disloyal malcontents’ who ‘snitch’ or ‘grass’ on colleagues and pursue their own interests regardless of the dysfunctional consequences for individuals and organisations. Moreover, it would be naive to assume that all whistleblowers are necessarily motivated entirely by genuine concerns about patient care. Some may be motivated in addition by work grievances or personality clashes; in the extreme, concerns may even be of a malicious nature. In fact, clear delineation between such labels is problematic. Whistleblowing may arise out of complex and contested circumstances, as what is ‘safe’ and what is ‘acceptable’ (in terms of quality) are disputable. Therefore, binary distinctions (such as hero/villain, loyal/disloyal and warranted/unwarranted) are often unhelpful, and disguise the complexity and ambiguity of whistleblowers and whistleblowing.
When concerns are raised, it is also important that organisations respond positively, learn from any mistakes of the past and put in place effective policies to prevent such mistakes from happening again. Unfortunately, in the NHS there have been all too many high-profile examples of front-line staff raising serious concerns that have not been adequately dealt with by the organisation. Patients have suffered as a result, and staff, too, may have been harmed from the direct and indirect consequences of their raising concerns. As Sir Robert Francis’ independent review, Freedom to Speak Up, concluded:
. . . there is a culture within many parts of the NHS which deters staff from raising serious and sensitive concerns and which not infrequently has negative consequences for those brave enough to raise them.
However, whistleblowing always happens in a deeply cultural and highly situated organisational and policy context, and involves managing ambiguity and handling contestation. Whistleblowing policies thus need very careful design, implementation and enacting to protect those raising legitimate concerns, as well as offering support in cases of fallout from more doubtful or even vexatious whistleblowing.
Numerous surveys across different professional groups confirm significant shortcomings (or, at least, perceptions of significant shortcomings) in the protection and support offered to whistleblowers seeking to raise legitimate concerns about poor or unsafe patient care in the NHS. A possible reason for this is the widely held perception among health professionals that they will be victimised, ostracised or bullied if they raise concerns about colleagues or poor standards of care. 4 This is not a new development. More than a decade ago, the report following the Bristol Royal Infirmary Inquiry recognised that many staff, particularly junior staff, remained silent in the face of poor care or wrongdoing as they feared raising concerns and/or challenging superiors because of the possible repercussions:
There is a real fear among staff (particularly among junior doctors and nurses) that to comment on colleagues, particularly consultants, is to endanger their future work prospects. The junior needs a reference and a recommendation; nurses want to keep their jobs. This is a powerful motive for keeping quiet.
These concerns remain current. The 2015 NHS Staff Survey (NSS) found that, when asked whether or not their organisation treated staff involved in near misses, errors and incidents fairly, fewer than half (43%) of staff reported that this was the case. In addition, only half (50%) of staff reported that feedback was given by their organisation about any changes that had been made in response to the reported error or incident. 6 In 2013, the Royal College of Nursing polled its members, with almost one-quarter (24%) saying that they had been warned off or discouraged from whistleblowing and 45% saying that, even after they had spoken out, their employer had taken no action. Similarly, a survey of doctors undertaken in 2012 by the Medical Protection Society reported that only 11% of respondents said that they would be confident in the process if they were to blow the whistle, and 49% of doctors reported that ‘fear of consequences’ is why the whistleblowing process is ineffective. Only one-third (33%) of doctors who had blown the whistle said that colleagues supported their decision and < 40% felt that their concerns had been addressed (with, as a result, 18% feeling isolated, 14% moving location or job and 12% reporting health issues). 4
That there should be so much uncertainty and disquiet about speaking out should not come as a surprise. Local discursive practices (e.g. on the nature of success, failure, risk and performance) and local operational contingencies (such as resource constraints, service rivalries and stakeholder pressure) will have a powerful influence on the willingness of employees to raise concerns and the ability and willingness of employers to respond appropriately. Of course, whatever the local contingencies and discourses, these play out within a larger political, policy and legal context, and it is to these that we now turn.
Policy and legal context
Currently, protection for whistleblowers in England is enshrined entirely within an employment context and is contained in the Employment Rights Act (ERA)7 as amended by the Public Interest Disclosure Act 1998 (PIDA)8 (see Chapter 5, which contains a fuller overview of the legal framework related to whistleblowing in England). PIDA was passed to protect whistleblowers in the wake of the Bristol paediatric cardiac surgery scandal and provides legal protection against detriment for workers who raise concerns in the public interest (also known as making a disclosure) about a danger, risk, malpractice or wrongdoing in the workplace that affects others. For a whistleblower to be protected, the disclosure must be in the public interest, the worker must have a reasonable belief that the information shows the occurrence, or likely occurrence, of one of the categories of wrongdoing listed in the legislation, and the concern must be raised in the correct way. This is now enshrined in the NHS Constitution,9 which mandates that:
-
staff should raise concerns at the earliest opportunity
-
NHS organisations should support staff by ensuring that their concerns are fully investigated and that there is someone independent, outside their team, who can provide support
-
there is a legal right for staff to raise concerns about safety, malpractice or other wrongdoing without suffering any detriment.
Whistleblowing policies have been mandated and promoted for many years outside any strict legal framework – for example by health-care employers, regulators and professional associations – aimed particularly at securing safe and effective services. Professional bodies, including the Royal College of General Practitioners and the UK Nursing and Midwifery Council (NMC), have professional codes that place obligations on registrants to report untoward incidents to their employers, and they have produced guidance for doctors, nurses, midwives and students raising concerns about quality of care. In 2012, NHS Employers launched the Speaking Up Charter,10 which encouraged NHS organisations to pledge publicly a commitment to creating cultures and policies that support staff in raising concerns and a continuous review and evaluation of such policies to ensure that they remain effective. The Department of Health and Social Care (DHSC) has also commissioned a whistleblowing helpline that provides free advice and support to staff on whether or not and how to raise concerns at work. Since 2015, a statutory duty of candour has operated that requires NHS bodies and all Care Quality Commission (CQC)-registered providers (rather than individuals) to be open and honest when an unintended or unexpected incident has resulted in, or could result in, death, moderate or severe physical harm, or prolonged psychological harm. In such instances, providers must notify the patient involved, offer an apology and follow up the incident in writing.
The report of the independent Freedom to Speak Up review, chaired by Sir Robert Francis,2 identified 20 principles and associated actions that should underpin whistleblowing polices in the NHS and recommended that the Secretary of State for Health should review, at least annually, the progress made in their implementation. These principles and actions include:
-
a common policy and procedure for raising concerns, including better investigations and promoting a model of good practice in the handling of concerns
-
training for managers and all staff in the raising and handling of concerns
-
cultural change towards creating more open, transparent and learning cultures that value communication and staff engagement
-
Freedom to Speak Up guardians to be appointed to each NHS organisation, supported by an independent national officer (INO)
-
legal changes to antidiscrimination laws to protect whistleblowers from discrimination in recruitment
-
additions to the list of prescribed persons to whom protected disclosures can be made.
In July 2015, the Secretary of State for Health confirmed the steps to be taken to develop a culture of safety, including the appointment of a national guardian alongside a local guardian in every NHS trust, with the goal of promoting the raising of concerns across the NHS. Although all NHS organisations are now required to have policies and procedures in place that urge staff to ‘speak up’ when necessary, there is no requirement for uniformity, and, as noted by Francis,11 different sources of guidance express themselves differently and there is, therefore, a risk that such a plethora of information, advice and guidance may be confusing for staff working in the NHS. For example, staff may not know where to go for the best advice or if, having spoken to a particular organisation, they still need to report their concerns elsewhere.
Aims and objectives of this study
Against this background, it is clear that there are serious uncertainties and challenges in relation to current whistleblowing and speaking up policies in the NHS. Our study addresses these concerns with the aim of developing theoretically grounded and evidence-informed guidance to assist policy-makers, managers and others responsible for designing/implementing effective whistleblowing and speaking up policies.
The specific objectives were to:
-
explore the main strands of the academic and grey literature on whistleblowing and related concepts such as employee silence, and to identify the key theoretical and conceptual frameworks that inform the understanding of employee whistleblowing
-
synthesise empirical evidence from different industries, sectors and countries with regard to the organisational processes, systems, incentives and cultures that serve to facilitate (or impede) employees raising legitimate concerns
-
examine the legal framework for whistleblowing in relation to health care as a mechanism for promoting (or inhibiting patient safety) and review the approaches to whistleblowing in relation to European Union member states and consider what lessons can be learnt at a domestic level from such comparisons
-
distil the lessons for whistleblowing policies and practice from the findings of formal Inquiries into serious failings in NHS care
-
ascertain the views, expectations and experiences of a range of key stakeholders, including service user and carer representatives, about the development of effective whistleblowing policies in the NHS and use these views to help structure and inform the desk research set out above
-
on the basis of findings relating to points 1–5, develop theoretically grounded and evidence-informed practical guidance for policy-makers, managers and others with responsibility for designing and implementing effective whistleblowing policies in the NHS.
Project overview and reporting structure
Full details of the methods used at each stage of the project are reported within the corresponding chapters, which broadly correspond to the six core objectives as set out above. In essence, the study comprised four distinct but overlapping strands:
-
a series of linked narrative literature reviews of the theoretical and empirical literature related to raising concerns, speaking up and whistleblowing across a range of sectors and contexts
-
an overview of the legal issues related to whistleblowing in an international context
-
a review of formal inquiry and government documents related to previous failings of NHS care
-
scoping interviews with key informants.
Throughout the project (completed in 1 year), the whole project team met extensively to discuss the emerging findings from each strand and to ensure that these emerging findings informed and complemented the ongoing work. In that sense, the work reported under separate chapter headings, although having a distinct focus that maps to the core objectives, has been informed by the parallel stands of work reported elsewhere. Supporting this, the scoping interviews with key informants were developed and implemented early in the project and helped to structure and inform the main desk research.
The chapters reporting the key aspects of the research are as follows:
-
Chapter 2 – the conceptual underpinnings of whistleblowing
-
Chapter 3 – empirical evidence on whistleblowing
-
Chapter 4 – the main whistleblowing inquiries and formal responses to inquiry recommendation
-
Chapter 5 – the legal underpinnings of whistleblowing
-
Chapter 6 – key informant interviews.
In compiling this report, we have sought to produce a synthesis that embraces the complexities and ambiguities associated with developing an understanding of whistleblowing and related policies in the context of health-care services, and to identify the different narratives and contours of debate in an inclusive and holistic manner, interweaving and interlinking common themes across the various strands of the study and thereby building a rich picture of whistleblowing across diverse sources of evidence. The final chapter (see Chapter 7) continues this integrative process and draws out the conclusions and research implications.
Chapter 2 The conceptual underpinnings of whistleblowing
Introduction
Any study intending to explore whistleblowing in the NHS requires an understanding of the conceptual underpinnings of whistleblowing and the key theoretical and methodological debates within whistleblowing research. This chapter, therefore, begins the process of unpacking what is meant by whistleblowing and introduces some of the sources of the ideas, conceptual underpinnings and different approaches to understanding whistleblowing and related terms such as ‘speaking up’. The material draws on the systematic literature review detailed in Chapter 3 (see that chapter for an account of the methods by which the literature was uncovered and collated), as well as from the accumulated expertise of the research team and from discussions with leading researchers in the field.
The chapter is structured as follows. We begin by outlining how whistleblowing has developed as a distinctive field of enquiry, and explore how whistleblowing and related concepts such as speaking up have been defined in the literature. We then review the main theoretical perspectives on whistleblowing that have been seen in the literature, and examine emerging perspectives that have the potential to develop our understanding further. We then rehearse the key methodological challenges involved in whistleblowing research, before drawing out some of the implications of these for more thorough NHS-specific research.
The emergence of whistleblowing as a field of study
Whistleblowing was first brought to wide public awareness in the 1970s, and has become progressively more high profile. The release of the Pentagon Papers in 1971 was not the first example of whistleblowing, but it was arguably the first to be widely known. There are three competing explanations for the origins of the term ‘whistleblowing’, and these provide useful insights into the tensions and ambiguities that still surround the practice. The most frequently encountered explanation is that it comes from an analogy with police officers blowing a whistle, to attract the attention of an individual to whom the officer wished to speak, or to bring other officers in the vicinity to the scene (in the days before mobile communications). Another suggested analogy is with the use of a whistle by referees in sport to call a halt to a game after a foul has been committed.
A third, perhaps less likely, but nonetheless intriguing, explanation, is that the term derives from 19th century US legislation that required train drivers to sound a whistle when they approached crossings. Failure to do so could lead to fines, and, moreover, citizens calling attention to these failures could receive payment for doing so. Indeed, in the US legal system it remains the case that those blowing the whistle on financial irregularities can sometimes stand to gain personally from the reporting of such wrongdoing. This articulation of whistleblowing speaks to the still-current concern that whistleblowers might be motivated by personal gain. Taken together, then, these putative etymologies describe whistleblowing variously as an act of calling for help, crying foul or informing the authorities (perhaps) for personal gain.
The academic interest in whistleblowing followed its greater public profile, with a handful of seminal articles published between 1983 and 1985 proving influential (see Chapter 3, Literature review methods). From the outset, whistleblowing research was inherently multidisciplinary, with scholars from law, management, public administration, sociology and psychology all interested in the phenomenon. An unusual feature of the whistleblowing field is the relative lack of definitional debates. Over 30 years ago, Near and Miceli12 defined whistleblowing as ‘the disclosure by organization members (former or current) of illegal, immoral, or illegitimate practices under the control of their employers, to persons or organizations that may be able to effect action’. This definition quickly gained almost universal acceptance and application, and remains the standard definition. The surprising lack of debates on definition among whistleblowing researchers stands in stark contrast to debates within wider society concerning the purpose and value of whistleblowing, the motivation of whistleblowers and the circumstances under which they should receive legal protection for their actions. The last issue is key: prospective whistleblowers are likely to be less concerned about how academics define whistleblowing, and more concerned about how the law defines it and whether or not they can expect protection under the law for their actions. 13
The debate continues as countries around the world consider enacting whistleblowing protection legislation or revising existing laws.
Raising concerns, speaking up or blowing the whistle?
Academics typically define a given social phenomenon more narrowly and precisely than the way in which lay people talk about the phenomenon. Whistleblowing represents an unusual reversal of that pattern, as the most widely used definition12 incorporates behaviour that most employees or citizens would be unlikely to label whistleblowing. Park et al. ,14 who developed a typology of whistleblowing based on a decision tree, illustrate this. They suggest that individuals who have decided to raise concerns face three key choices: to raise issues (1) informally or formally, (2) anonymously or on the record and (3) internally or externally. This typology suggests eight types of whistleblowing, only some of which would fit with how most people would understand the concept. For example, before deciding to blow the whistle employees usually find themselves trying to work out exactly what is happening, often through engaging in dialogue with colleagues. 15 Such behaviour could be consistent with the informal/identified/internal whistleblowing pathway,14 but it seems unlikely that staff would perceive such conversations as a form of whistleblowing. Table 1 details how the Park et al. 14 typology might translate into a health-care context.
| Type of whistleblowing | Examples |
|---|---|
| Informal | |
| Anonymous, internal | Unsigned note sent to a manager in the internal mail; telephone call to HR (or similar) giving no name |
| Anonymous, external | Tip-off to a journalist; anonymous web postings |
| Identified, internal | Discussing one’s concerns with a colleague |
| Identified, external | Posts on social media criticising one’s employer |
| Formal | |
| Anonymous, internal | Leaving a message on a drug error hotline |
| Anonymous, external | Medication error reporting programmes |
| Identified, internal | Raising concerns with a Speaking Up guardian |
| Identified, external | Raising concerns with a regulator; approaching a MP; speaking to a journalist |
Notwithstanding the Park et al. 14 typology detailed above, the academic literature has traditionally focused on a dichotomous choice between whistleblowing and silence; that is, when faced with wrongdoing, an employee makes a conscious choice either to remain silent or to act by raising concerns. 16 Yet, as highlighted by Jones and Kelly,17 this simplistic dichotomy obscures a range of alternative strategies to whistleblowing that may be just as effective in identifying and preventing wrongdoing. Such strategies might include interpersonal approaches such as the use of humour or sarcasm to signal discontent, or informal and off-the-record discussions with managers and employees. Jones and Kelly17 suggest that these ‘informal and circumlocutory’ channels of communication may be valuable organisational mechanisms for addressing poor standards of care. Indeed, they argue that these can prove more effective than formal reporting systems, as they are more likely to circumvent the ‘deaf effect’ (see below). This fits with the current emphasis in NHS policy debates on ‘raising concerns’ and ‘speaking up’, rather than whistleblowing per se, consistent with our observations in Chapter 3 that the relevant literature within health care tends to emphasise voice behaviours rather than formal whistleblowing.
Francis11 notes that many staff appear unhappy with the term whistleblowing, hence the suggestion that terms like ‘raising concerns’ and ‘speaking up’ are to be preferred. However, it is useful to think of raising concerns, speaking up and whistleblowing as a continuum, even though, arguably, all can be subsumed under the academic definition of whistleblowing. We can differentiate between them in various ways, but it may be most useful to think about how employees might distinguish between them. An employee who has concerns about a particular issue that affects quality and safety of patient care might ‘raise concerns’ with their line manager, possibly informally. If they get no response, they may choose to ‘speak up’, potentially talking again to the same manager, but this time more formally and perhaps making clear that they expects their concerns to be a matter of record. If the issue is still not resolved, they may choose to ‘blow the whistle’ to someone more senior, or perhaps go outside the organisation.
From an employee perspective, the act of ‘raising concerns’ may be relatively low risk, something that might be done routinely, perhaps even just in passing (e.g. ‘I think the new health-care assistant is a little brusque with the older patients’). Speaking up is more serious: the very phrasing implies raising one’s voice or breaking a silence. The perceived level of risk may not be very great; in some cases the employee may only risk feeling foolish if they are mistaken, although their concern about this may, in itself, be enough to ensure that they remain silent. 15 Whistleblowing is a more significant act, to which the organisation may respond negatively. Alford18 has argued that whistleblowers are defined post hoc, by the organisation’s response to their action. Using the NHS terminology, someone who thought they were just ‘raising concerns’ or ‘speaking up’ can discover that they are a whistleblower if the organisation responds negatively. The general perception among NHS staff and the wider public is that NHS whistleblowers tend to fare badly,19 so staff thinking about speaking up may, from the outset, be concerned that they will receive a very negative response. This may lead individuals with relatively low-level concerns to refrain from raising them.
In a health-care context, another important distinction between raising concerns/speaking up and whistleblowing may be the focus of the concern. The classic definition of whistleblowing specifies that it is about ‘illegal, immoral or illegitimate practices’. 20 Many issues that could affect care quality and patient safety, and about which we would hope staff would raise any concerns, do not necessarily come under any of those headings. Staffing levels, poor practice or poor performance (e.g. from a colleague dealing with personal problems) are all issues that could have a detrimental effect on patient care, but that staff would probably not view as ‘wrongdoing’ (see below for a more detailed discussion). Nevertheless, such issues may eventually lead to whistleblowing if they are not properly addressed. If a junior doctor raised concerns about a colleague’s confidence in dealing with challenging patients, they are clearly not concerned about ‘illegal, immoral or illegitimate’ behaviour. However, if those concerns are not addressed, and problems continue, a decision to speak to someone more senior about the issue is implicitly speaking up about the failure to address the problem. Such action is more consistent with whistleblowing. This is a subtle but important point that is often missed: whistleblowers are often described as blowing the whistle about a specific issue (e.g. poor practice), but they are often effectively blowing the whistle on management’s failure to act once made aware of the original issue.
Recent discussion of speaking up2,21,22 has tended to frame the problem in terms of creating environments in which staff feel more able to voice their concerns. Yet, as Francis11 and Kelly and Jones19 observe, in many scandals staff had voiced their concerns; the problem was getting someone to listen.
This is consistent with the ‘deaf effect’, a term originally coined by Keil and Robey23 to describe the reluctance of senior managers to hear, accept and act on challenging observations from lower down the organisation. Vandekerckhove et al. 24 suggest that researchers need to pay more attention to the question of how recipients of whistleblowing respond, and in particular to ‘hearer action’, which we might view as the antithesis of the deaf effect. Whereas it is widely recognised that it takes a degree of courage for someone to blow the whistle, it is less immediately obvious that it may also take courage for a manager to take on board the issues and act on them. Just as the whistleblower knows that the line manager may not want to hear bad news, so the line manager knows that more senior management may be similarly reluctant to be informed of breaches or the requirements of remediation. Whistleblowing recipients in management roles know that their actions in raising the whistleblower’s concerns may receive a negative response and may even lead to the sort of retaliation and victimisation that can sometimes be experienced by whistleblowers themselves. For this reason, Vandekerckhove et al. 24 suggest that there is a need for research into ‘hearer courage’ to understand ‘which managers have the courage to hear, under which circumstances, and with regard to which wrongs’ (p. 316). The same issues may pertain to the new Speaking Up guardian roles in the NHS, for whom a whistleblower’s report may feel like the whistleblower taking a burden off their own shoulders and placing it on the guardian’s.
Our analysis of the various public inquiries (see Chapter 4) suggests that senior management may sometimes also suffer from ‘collective myopia’,25 a shared inability to see a problem. This is potentially more problematic than the deaf effect, as it leaves those in management positions genuinely unable to see what the whistleblower is trying to bring to their attention. This could lead an individual to proceed from raising concerns to speaking up to internal whistleblowing, not in search of ‘someone willing to listen’ but in search of ‘someone able to see’. However, the NHS can be viewed as a single large organisation in many ways, and criticisms of regulator responses to cases such as that at the centre of the Mid Staffordshire NHS Foundation Trust Public Inquiry11 suggest that even when the individual goes outside the immediate organisation, they may still find people unable to see/unwilling to listen. There is a sense in which raising concerns and speaking up in health care adhere to both organisational ‘etiquette’ and the hierarchical chain of command, which inevitably means that management can choose to ignore the issue. There is also a sense that individuals may feel that they have done their duty in raising the issue. 26 Blowing the whistle, especially externally, raises the stakes and is much harder to ignore.
Blowing the whistle on what?
Central to whistleblowing research has been the idea of wrongdoing, a catch-all term that includes everything from persistent acts of minor incivility to multibillion-pound corruption. Within any given organisation, there are various types of wrongdoing on which an individual might feel it necessary to blow the whistle. The focus of the present project is on issues pertaining to the quality and safety of patient care, but it is worth examining the ways in which perceptions of the nature of the wrongdoing might affect whistleblowing. The bulk of whistleblowing research has been concerned with pecuniary wrongdoing such as fraud and corruption, in which there is, in principle, a final legal judgement to be obtained as to whether or not wrongdoing has occurred. In contrast, issues around safety and quality can be much more ambiguous, a point illustrated by two cases that form part of NHS folklore on whistleblowing: the ‘Graham Pink case’27 and Bristol Royal Infirmary. 5
The Graham Pink case is generally remembered as an archetypal whistleblowing narrative. Pink (a nurse) raised concerns with the hospital’s management about dangerously low staffing levels; management would not listen and did not act, so Pink ‘blew the whistle’ and was eventually removed from his post for his trouble. Vinten28 suggests a somewhat different interpretation, arguing that there was ample evidence that management took Pink’s concerns seriously and investigated, but found staffing levels to be appropriate. Pink’s colleagues on the unit agreed with the management’s assessment, but were unable to get this message across to the Royal College of Nursing, who found Pink’s account more compelling against a backdrop of concerns about government policy in the NHS. The Pink case revolved around an issue – staffing levels – about which there was (and is) considerable scope for experienced practitioners to reach very different views. Although there will be a level of staffing that everyone would agree is unsafe, it has proved difficult to develop an evidence-based metric to calculate minimum safe staffing levels and appropriate skill mix. 29
The tragic events surrounding infant heart surgery at Bristol Royal Infirmary might appear to be more amenable to an evidence-based analysis, given that the extensive use of clinical audit data allows comparisons of performance over time and between units. Yet, as Weick and Sutcliffe30 observe, even with such extensive data there is still a need for organisations to make sense of the data, and all sense-making is intentional and social. There was clearly a desire at Bristol Royal Infirmary to believe that the unit was performing acceptably, and management and senior clinicians interpreted the data in terms of a learning curve. They focused on evidence that the unit was improving, and overlooked evidence that it was still underperforming relative to comparable units and that it was improving only slowly.
As the analysis of public inquiries shows (see Chapter 4), issues that appear unambiguous after the event may have seemed open to interpretation of the event at the time. This creates a challenge for policy-makers: we are generally dealing not with malevolent individuals or corrupt systems, but with individuals and systems that are failing in some way, and resistant to hearing the messages about that failure. As the whole premise of whistleblowing is ‘wrongdoing’, and wrongdoing appears a moral appellation, people are reluctant to use the term and recipients are reluctant to hear it. This underlines the importance of developing a greater understanding of hearer courage, particularly in a NHS context.
The inherent ambiguity of many of the situations complained about at the heart of whistleblowing in the NHS draws further attention to the importance of definitional issues. Brown et al. 31 suggest that wrongdoing be defined as ‘when a person or organisation does things that are unlawful, unjust, dangerous or dishonest enough to harm the interests of individuals, the organisation or wider society’. This definition is both more precise and more encompassing than the traditional ‘illegal, immoral or illegitimate practices’,20 and would certainly cover actions/omissions that could have a negative impact on care quality and safety.
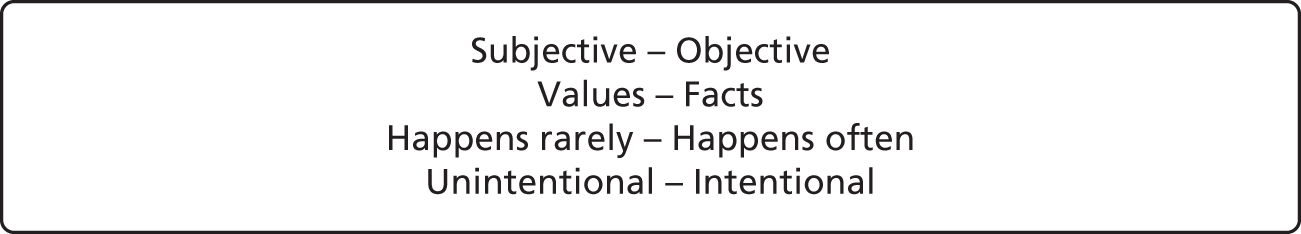
Taking this further, Skivenes and Trygstad32 suggest that there are six ‘intrinsic dimensions’ that affect individuals’ assessment ‘of an alleged act or practice of wrongdoing and the degree of importance (or seriousness) of an act of wrongdoing’ (p. 97). These dimensions are (1) whether the perception of wrongdoing is subject or objective, (2) whether it relates to values (such as dignity) or facts (such as clinical outcomes), (3) the frequency of the wrongdoing (e.g. a rare occurrence or an ongoing problem), (4) whether or not the wrongdoing was intentional, (5) whether or not there is a public interest dimension and (6) the persons/groups affected (e.g. are they vulnerable?). In a NHS context, the final two dimensions are arguably ‘fixed’; the activities of the service always have a public interest dimension, and patients are by definition vulnerable persons even if they would not in the normal course of life be viewed in those terms. It is therefore only the first four dimensions that influence whether or not a situation is assessed as wrongdoing, and, if so, how serious it is (Figure 1; Table 2 provides some simple vignettes that illustrate the opposite ends of these dimensions).
| Example | Assessment against dimensions noted in Figure 1 |
|---|---|
| An Asian man is being admitted to a ward. He is very friendly and chats non-stop to the ward team. The member of staff dealing with his admission asks the nurse in charge which bed to put him in; she points to a bay opposite ward control where three white patients are sitting quietly by their beds, and says ‘Put him in there, he’ll add a bit of colour to the place’. The patient does not say anything, although the nurse thinks he looks rather surprised. She is also surprised, as she feels that the remark was racist, although she has never heard her colleague say anything like that before | Subjective, based on values, a one-off occurrence, (probably) unintentional |
| A long-serving surgeon has a particular way in which he likes to undertake a certain surgical procedure, which differs from that of the other surgeons on the unit and from guidance issued by NICE 3 years ago. This has been raised with him, but he simply states that his approach leads to better outcomes from the patient. The clinical outcomes data do not support his assertion | Objective, based on facts, a repeated occurrence and intentional |
The main purpose of the two examples in Table 2 is to illustrate the assessment dimensions, but vignettes like these are also useful in allowing us to place ourselves in the place of staff observing possible wrongdoing.
Outsider whistleblowing?
The classic definition of whistleblowing is that it is an action taken by current or former members of an organisation. The term ‘member’ is not explicitly defined, but it has generally been taken to mean organisational members or employees. 33 This excludes many individuals who may have links with an organisation and be in a position to observe, and raise concerns about, wrongdoing within the organisation. Miceli et al. 34 note that many significant ‘whistleblowing’ cases reported in the press are technically not examples of whistleblowing, as the person who raised the concerns was not a current or former member of the organisation in question. Acknowledging that these cases are, nevertheless, important, and deserving of further study, the authors propose the term ‘bell-ringing’ to describe the raising of concerns by outsiders. Although we acknowledge the logic of this attempt to bring definitional clarity to this new offshoot of the whistleblowing field, it is difficult for academics to impose such definitional precision retrospectively, once a term is out in the public domain and being used ‘wrongly’. Culiberg and Mihelic33 suggest that rather than framing the issue in terms of whistleblowing versus bell-ringing, it might be more useful to refer to insider versus outsider whistleblowing.
Outsider whistleblowing is potentially a more significant issue for health care than for any other sector. Examples of potential outsider whistleblowers would include patients, relatives and visitors, suppliers, professionals working in other organisations [e.g. social workers and general practitioners (GPs)], clinical tutors and contractors. Outsider whistleblowers might be assumed to be freer to speak up than staff, yet all of these individuals may have reasons to be reluctant to blow the whistle. Patients, relatives and visitors are obvious examples: all are likely to have concerns about the potential for the patient to suffer reprisals for raising concerns. In addition, outsider whistleblowers themselves can be targeted; a recent radio programme discussed the apparent rise in care homes ‘banning’ visitors and relatives who had raised concerns about care. As the model of delivery for NHS services becomes more complex, involving a greater range of non-NHS organisations, there is a need to think carefully about the role of outsider whistleblowers, and how they might be encouraged and supported. This may be particularly important for employees of other organisations, as they are presently unlikely to enjoy any legal protection under PIDA.
Theoretical perspectives on whistleblowing
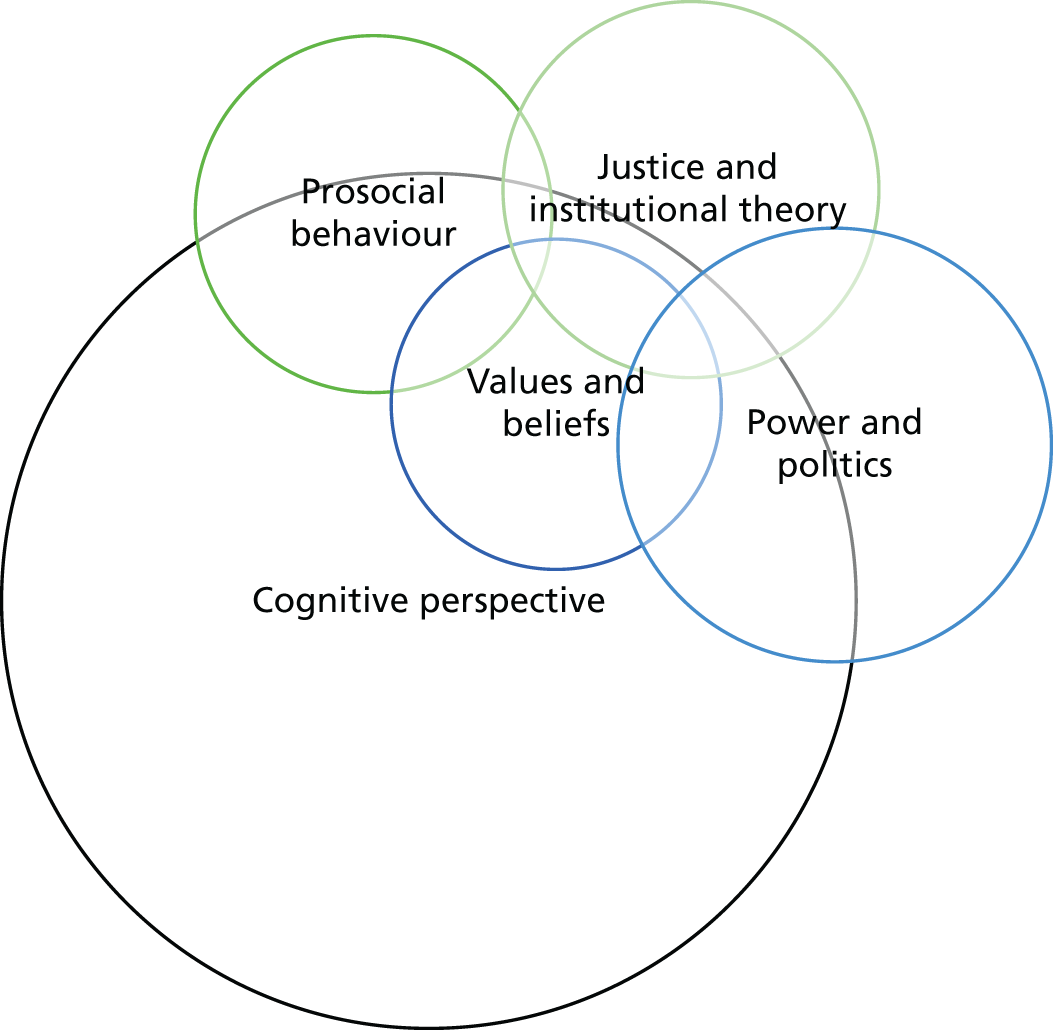
Given the interdisciplinary nature of whistleblowing research, it is perhaps unsurprising that our review of the literature, as with previous reviews (e.g. Kelly and Jones19), did not identify a universal or shared underpinning theoretical framework for whistleblowing research. We can, however, identify a number of different theoretical perspectives that provide useful lenses through which to view the phenomenon (Figure 2). Note that these are not distinct ‘schools of thought’, and researchers often borrow ideas from several perspectives in developing their research. The figure should be viewed as a useful heuristic, rather than a strict mapping of the position of each perspective on some notional x- and y-axes.
FIGURE 2.
Theoretical perspectives on whistleblowing.
In their seminal paper, from which much other work has derived its definition of whistleblowing, Near and Miceli20 identified the steps involved in the whistleblowing process (Table 3). This framework has been widely used in whistleblowing research. At one level, it is simply a description of a sequence of events, but, by emphasising decisions, the framework reinforces a focus on decision-making, which in part explains the dominance of the cognitive perspective in the whistleblowing literature.
| Step 1 | Step 2 | Step 3 | Step 4 |
|---|---|---|---|
| Observer’s decision 1: is the observed activity illegal, immoral or illegitimate? | Observer’s decision 2: should the activity be reported? | Organisation’s decision 1: should the action be halted? | Organisation’s decision 2: should the whistleblower be punished? |
Taking each of the perspectives shown in Figure 2 in turn, we can see that each has distinctive foci of interest, and that each brings to the fore specific insights about the whistleblowing process.
Cognitive perspective
The cognitive view within psychology has been a major influence on whistleblowing research. Considering its relevance to the understanding of how stakeholders respond to misconduct, Barnett35 highlights two key assumptions, namely that ‘people cannot attend to all the stimuli competing for their limited attention’ and ‘factors particular to the person and the situation influence how one allocates his or her attention and responds to stimuli’. Many whistleblowing researchers emphasise the importance of the decision-making process that takes place after an event of potential wrongdoing is witnessed, typically at stage 2 of Near and Miceli’s12 model of the whistleblowing process. The implication is that observers consciously weigh the factors for and against blowing the whistle, such as wanton violation of rules and laws, negligence in a duty of care or abuse of power. However, a cognitive perspective recognises that the decision to blow the whistle is also influenced by factors of which the individual may be largely unaware. Research from this perspective explores whistleblowing as a deed that results from the confluence of an individual’s values and beliefs, and the context in which a problematic act occurs, that is, what behaviours ‘fit’ within the potential whistleblower’s personal paradigm. Whistleblowing research adopting a cognitive perspective recognises that, although the observer may not be fully aware of all of the various influences on their decision, such influences must be accounted for if our understanding of the topic is to be improved. 15,36
Values and beliefs
Research adopting this perspective is concerned with how externally derived values and beliefs influence whistleblowing. These values and beliefs may come from macro-level societal-level influences (e.g. religious teachings or national culture) or by more meso- or micro-level influences, such as the local organisational culture, rules and regulations, or the influence of dominant team leaders. A key assumption is that guidance relating to what is right and wrong is a principal driver of whistleblowing behaviour. This guidance is potentially captured by organisational policies, but also by the teachings and traditions from other occupations. There is a connection here with the cognitive view through cultural influence. However, with the values and beliefs perspective, the distinction is that other parties create the influence on whistleblowing for the individual, whereas the cognitive view presents the influences on the whistleblowing decision as being internally constructed, albeit influenced by a myriad of other overlapping factors. In Figure 2, we located the values and beliefs perspective wholly inside the cognitive perspective, reflecting the fact that values and beliefs can be viewed as an influence on the decision-making process. Thus, religious beliefs may have a strong influence on what individuals perceive as wrongdoing, and their perceptions of their own responsibilities as observers of this wrongdoing, but ultimately the individual still has a decision to make.
For example, Rothwell and Baldwin,37 examining whistleblowing in police agencies in Georgia, USA, noted that uniformed staff, in spite of close personal relationships with colleagues, were more likely than civilian employees to blow the whistle on wrongdoing, suggesting that the external values and formal regulation associated with uniformed service were important. Indeed, Alford38 discusses the threat posed to organisations by the ‘ethical autonomy’ (cf. Kant) of their members. Organisations, therefore, would find work from this perspective useful, as it could provide clues as to how to inculcate values and beliefs that the organisation and wider society deem appropriate to encourage whistleblowing behaviour when necessary. The review by Trevino et al. 39 contributes to this perspective by exploring individual behaviours that were judged as ethical or otherwise when measured against the norms in which those behaviours occur. Sekerka et al. 40 note that organisations typically encourage individuals to behave ethically by imposition of external ‘rules and legal standards’, rather than by encouraging professional moral courage. One of the key insights of this perspective is the importance of setting out clear rules, standards and norms regarding what employees are expected to do if they encounter wrongdoing.
Justice and institutional theories
This perspective considers the impact that the legal system and organisational rules and regulations have on the whistleblowing process. Embedded within the concept of ‘justice’ is that of ‘fairness’, and although recognising the importance of the topic, a number of authors emphasise the range of perceptions of fairness as a factor in whistleblowing. For example, Alleyne et al. ,41 following Rawls,42 suggest that ‘justice is seen as fairness when the allocation of resources in society is considered rationally as advantageous or disadvantageous’. They suggest that perception of injustice is a key driver of the act of whistleblowing, a view supported by Near et al. 43 Gundlach et al. 44 note that ‘looking fair may be more important than being fair’, and, for this reason, there is clear overlap with other theoretical perspectives, given that the cognitive perspective relies on individual perceptions, and what is perceived as prosocial behaviour will vary from one context to another. This raises the difficult question of perception of fairness, a perception that inevitably interacts with national differences. In this review, we have focused on Western cultures, as this is where the bulk of whistleblowing research has been undertaken. However, given the marked cultural and national diversity of the NHS workforce, there is potential for considerable cultural differences in attitudes towards whistleblowing, which may be highly significant.
Within the more institutionalist strand of this perspective, recent research has specifically examined how institutional mechanisms in public sector organisations influence whistleblowing. 45,46 This work has been outside health care and the outside the UK, but could be very relevant to the NHS, particularly in terms of understanding the institutional processes by which policy-makers influence the process (cf. Blenkinsopp and Snowden47).
Power and politics
This perspective explores the impact that power and political actions in all organisations have on whistleblowing. In their seminal work, Near and Miceli20 emphasise the importance of power in the construction of their model of the whistleblowing process, and retaliation from organisations towards whistleblowers can be viewed as a response to the threat they pose to organisational power. 48 Avakian and Roberts49 suggest that ‘Our analysis indicates that the imbalance of power results from the way the whistleblower exercises the hidden knowledge in unexpected ways’. This links to recent work from a Foucauldian perspective, which introduces the concept of parrhesia to whistleblowing research. 50,51 Foucault used this term to describe ‘a specific modality of truth-telling (veridiction) that emerges in the context of asymmetrical power relations’. 51 This line of work offers valuable insights into the various difficulties faced by individuals seeking to raise concerns about matters that are (usually) factual and provide management with information that would appear useful (see Weinstein52 and Alford38 for non-Foucauldian approaches to this issue).
Near et al. 43 also explore the interface between theories of power and justice theory, and comment that when organisations deliberately provide their own legal protection (and hence power) to a ‘role-prescribed whistleblower’ (e.g. internal auditors), positive outcomes for both the whistleblowers and their organisations are experienced. Pittroff53 supports the view of the centrality of power to successful implementation of a whistleblowing system within an organisation, stating that ‘implementation of internal [whistleblowing] systems is ostensibly driven by power theories’.
It is clear, therefore, that the papers exploring whistleblowing through focusing on the influence of power and politics have a major role to play in developing our understanding of the topic. This perspective may be especially relevant to the NHS, which is very hierarchical in nature, with considerable variations in power between different occupational groups and different levels, and the added complication of a further powerful hierarchy above the chief executive, who is ultimately accountable to the Secretary of State for Health and Social Care.
Prosocial theory
The final theme to emerge from our review relates to works that explore the desire to ‘do good for others’ by blowing the whistle. Typically, such papers explore the concept of whistleblowing as an act that benefits the welfare of others both inside and outside the organisation, even though there may be an element of self-interest driving their decision to expose wrongdoing. As Dozier and Miceli54 state, ‘[whistleblowing] is more appropriately viewed as ‘prosocial’ behaviour, involving both selfish (egotistic) and unselfish (altruistic) motives on the part of the actor’. This creates a managerial dilemma; Dungan et al. 55 state that ‘people are moral hypocrites – espousing moral values when judging others, while actively ignoring when self-interest is at stake’. The same authors point to scientific evidence that suggests that prosocial behaviour is intrinsically rewarding, and, for this reason, imply that a natural positive predisposition towards whistleblowing exists. This is important to any attempt to support the reporting of wrongdoing, and perhaps has the potential to challenge a common organisational perception of whistleblowers as ‘trouble causers’.
Alternative perspectives
The work considered in each of the subsections above demonstrates where authors have adopted a particular stance on the topic, and we believe that different and productive interpretations of whistleblowing can be generated by adopting different stances and using different lenses. As whistleblowing becomes more high profile, and researchers from other academic fields become interested in exploring the concept, we are witnessing the publication of articles that examine whistleblowing from new and illuminating perspectives.
Through an examination of language
The definitional complexities alluded to above draw attention to the importance of clarity in the language used, but also the influence of language on how whistleblowing situations are framed. We might describe the same behaviour as ‘raising concerns about an issue affecting patient safety’ or ‘blowing the whistle on poor practice’, but the former phrasing may be more acceptable to staff and management, and more likely to lead to change. It is, therefore, important to consider the language used in and around the act of whistleblowing, with sensitivity to style and content. Contu56 argues that looking at how the language used to explore a whistleblowing event evolves over time ‘opens up an appreciation of the ethical and political valence of the process of whistleblowing’.
Through an examination of sense-making
The sense-making perspective57 offers potentially valuable insights. Its relevance to health care has been acknowledged, as Weick and colleagues have examined ‘high reliability organisations’; for analyses directly relevant to the NHS, see Weick and Sutcliffe30 and Weick et al. 58 Blenkinsopp and Edwards15 drew on the sense-making perspective to develop the concept of ‘cues for inaction’. They suggest that clinical staff are very aware of the risks of whistleblowing (or even of just raising concerns) but are also aware of their responsibility for the patient (under codes of conduct and NHS policies). Caught between a ‘rock and a hard place’, they are motivated to find ways of making sense of the situation that allow them to stay silent. The challenge for organisations is to find ways to create ‘cues for action’, and reduce or even eliminate possible cues for inaction.
Given the diversity of conceptual lenses open to researchers, and the diverse insights thus available to date, future empirical work on whistleblowing in the NHS should carefully exploit the conceptual diversity for fresh insightful gains.
Methodological issues in whistleblowing research
Whistleblowing is an inherently difficult phenomenon to study. Although the act of whistleblowing involves bringing a situation to the attention of others, in most cases that does not bring it to wider attention; cases in which the situation becomes a matter of common knowledge within the organisation will be the exception rather than the rule, and the proportion of cases in which the situation comes to wider public attention is tiny. These high-profile cases of whistleblowing can provide researchers with valuable insights, but the sensitivity of such cases make it difficult to gather data, especially if the situation is the subject of investigations (criminal, disciplinary, fitness to practice) or other legal processes (e.g. negligence claims). A further barrier to data gathering can arise in cases in which the whistleblower’s employment is terminated through the employer and employee reaching a settlement agreement that includes non-disclosure clauses.
Despite these difficulties, researchers have developed various approaches to investigate whistleblowing. Olsen59 identifies the main research methodologies used in whistleblowing research as experimental studies (e.g. Burton and Near60), content analysis of legal cases and press coverage (e.g. Brewer61), analysis of government data (e.g. records of whistleblowers contacting government agencies), qualitative case studies, surveys using hypothetical scenarios and surveys of actual whistleblowing. These last three have been by far the most widely used, and below we consider each in turn (the specific findings emerging from each of these methodological traditions are covered more fully in Chapter 3; here we concentrate on highlighting differences in methodological approach).
Qualitative research
Some of the earliest studies of whistleblowing were qualitative or even journalistic examinations of specific whistleblowing cases,28,62 including biographical and autobiographical accounts of whistleblowers (e.g. Robison, Watkins26). More recent work in this vein includes more theoretically informed analyses of cases. 15,18,30
Surveys using hypothetical situations
This is the most widely used approach in whistleblowing research. The most common research design is cross-sectional, generally using whistleblowing intentions as the dependent variable, as intentions to perform a given behaviour are generally regarded as a good predictor of future behaviour. 63 A typical design would present participants with one or more vignettes describing a situation that might be viewed as wrongdoing and asking how likely they would be to report it. Inviting individuals to imagine what they would do in a given situation is problematic, as it relies on the participant being able to make a realistic appraisal of what they might do in a situation that may be very unfamiliar to them. It does, however, allow researchers to gather data on a range of permutations. A good example for health care is offered by Lawton and Parker,64 who produced nine vignettes which varied across two dimensions: adherence to protocols (compliance, deliberate violation, and improvisation in the absence of a protocol) and outcome for the patient (good, poor or bad).
Surveys of actual whistleblowing
Bjørkelo and Bye65 suggest that approaches to measuring actual whistleblowing can be categorised as having a behavioural versus operational definition. Behavioural approaches (e.g. US Merit Systems Protection Board survey) ask individuals about whether or not they have observed wrongdoing (from a list of examples) and whether or not they reported it, whereas an operational definition approach offers participants an explicit definition of whistleblowing and asks whether or not they have blown the whistle. The behavioural approach has the advantage of providing insights into how frequently wrongdoing is encountered, and what proportion of people blow the whistle on it. However, it assumes that the types of wrongdoing listed are ‘illegal, immoral or illegitimate’ in similar ways across all settings and cultures. The operational approach avoids this difficulty, but leaves us unsure how to categorise those respondents who report that they have not blown the whistle.
Reviews of whistleblowing research59 indicate problems with identifying variables that consistently predict key outcomes (e.g. the decision to blow the whistle, whether or not the action succeeds, whether or not the whistleblower suffers retaliation). We suggest that it is not that the field has been unable to identify key factors, but that contextual differences have a significant impact. Tolstoy once wrote that ‘Happy families are all alike; every unhappy family is unhappy in its own way’,66 and whistleblowing involves very unhappy (organisational) families. Although it would normally be impractical to develop frameworks tailored to specific organisational contexts, there is nonetheless a tradition of looking at this issue for key occupational groups (e.g. auditors) or sectors (e.g. financial services). For an organisation the size of the NHS, it could be feasible to develop a model of what works specifically in that setting. What would be required is research that builds on existing models of whistleblowing to identify how these models apply in the specific context of the NHS, and it is to this that we turn in the next section.
Concluding remarks: further exploration of whistleblowing in the NHS
In this final section, we consider how existing theory and research might be translated into a more thorough and conceptually rooted exploration of whistleblowing in the NHS. We start by considering how much the NHS context matters. We noted above that there are some translational issues in applying insights from mainstream whistleblowing research to health care, because so much of the literature focuses on wrongdoing such as fraud and corruption. However, having acknowledged that health care is different from many other industries, we also need to consider whether or not there are factors associated specifically with the NHS that make it different again.
The first point to note is that the NHS has a uniquely dominant position in health care, different from health-care arrangements in other developed countries. The NHS is monolithic and comprises a large number of organisations (and different types of organisation), each legally a separate employer. However, the reality of ‘working for the NHS’ means that blowing the whistle on wrongdoing in one NHS organisation risks not only retaliation from that organisation, but also an effective ‘blacklisting’ from employment elsewhere in the NHS. Despite some expansion in private health care, the NHS remains the major employer for most health-care professionals, so being excluded from the NHS almost amounts to being excluded from health-care employment. A related point is that in the NHS, linked by formal and informal networks, staff may have concerns about their ability to find an ‘honest broker’, with some former whistleblowers recalling being shocked at how little support they received from professional bodies, regulators, and even unions.
Within the wider literature on organisational citizenship behaviour, there is a small body of research exploring the influence of organisational politics, and in particular employees’ ‘perception of organisational politics’. 67 When organisations are perceived to be highly political, there may be a perception that things are done not for maximum effectiveness and efficiency, but for self-serving reasons. This creates a perception of organisational politics (POP), which is defined as ‘an individual’s subjective evaluation about the extent to which the work environment is characterised by co-workers and supervisors who demonstrate . . . self-serving behaviour’. 68 POP affects our confidence in the organisation following its own policies and procedures, which would clearly make prospective whistleblowers less confident in speaking up.
All organisations are, to some extent, political (with a small ‘p’), but public sector organisations are also political with a big ‘P’, with the NHS arguably the most political of all. Therefore, for the NHS we can envisage a wider notion of POP, in which it may include a perception that the wider health-care system is affected by politicking (even if a specific individual’s work is perceived not to be). This can create situations in which staff perceive that management’s response will be driven by political concerns [e.g. about how a particular issue might play out with politicians (local and national)], rather than by what is in the best interest of patients.
The specific NHS context, then, highlights specific concerns that are not always fully addressed in the existing whistleblowing literature. The variety of conceptual lenses through which whistleblowing has been viewed does, however, provide fresh opportunities to bring these specific contextual issues to the fore through a range of methodologically diverse projects. What follows next, in Chapter 3, is an exploration of what is already known empirically about whistleblowing from diverse contexts including, but not restricted to, those involving patient care.
Chapter 3 Empirical evidence on whistleblowing
Introduction
In the previous chapter, we explored the wide variety of ways in which whistleblowing has been conceived and defined within the theoretical and conceptual literature. In this chapter, we draw on the theoretical insights gleaned to critically review empirical research on whistleblowing undertaken in both health-care and non-health-care contexts. The chapter begins with a description of the innovative methodology used to establish a broad bibliography that formed the basis of the review. We then present a thematic narrative analysis of the literature uncovered. The remaining sections then describe the empirical research findings with regard to the external, internal and personal factors that have influenced whistleblowing, and the evidence on the range of organisational responses to whistleblowing.
Literature review methods
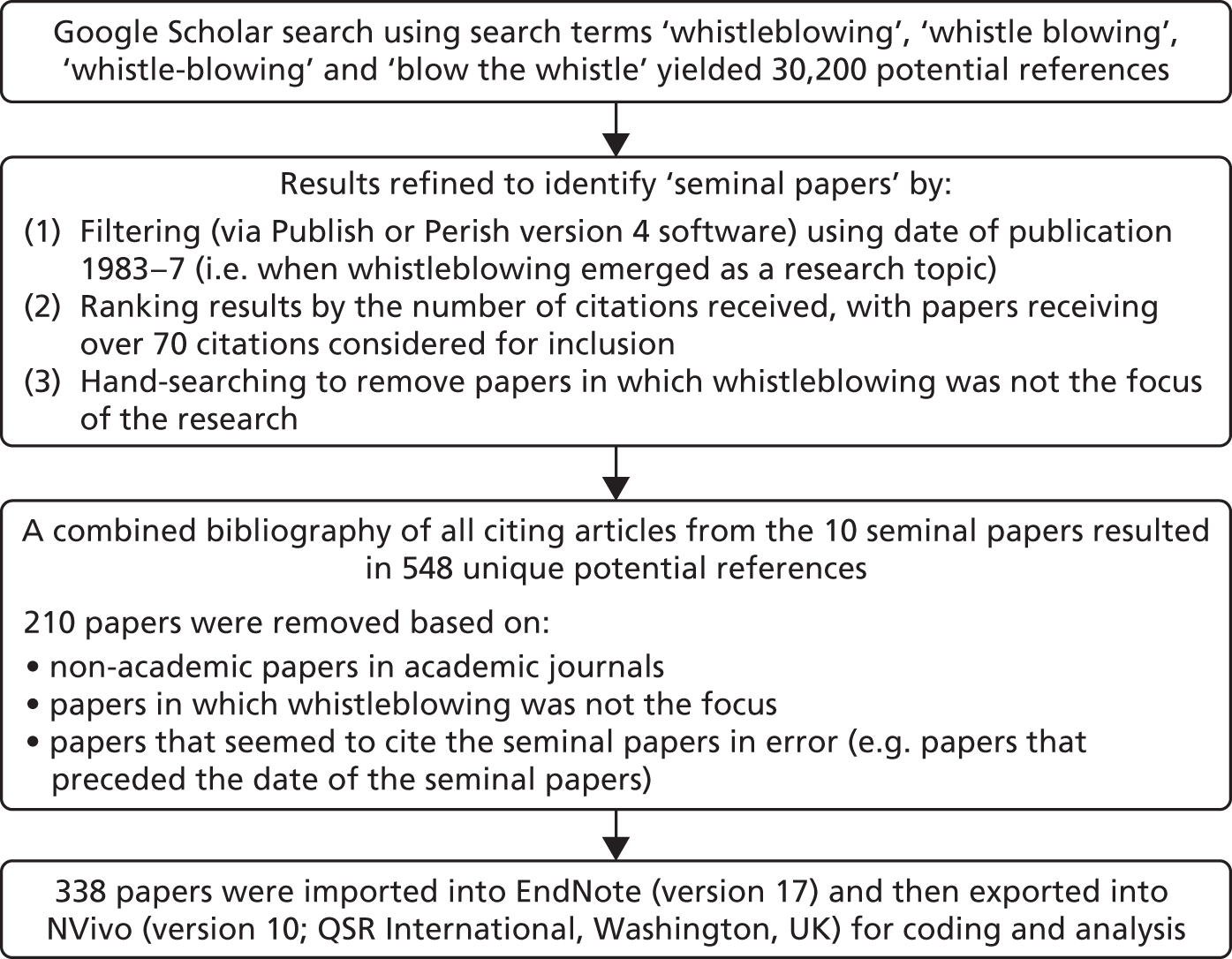
The literature that underpinned both this chapter and Chapter 2 aimed to identify the key theoretical and conceptual frameworks that might inform an understanding of employee whistleblowing in health-care contexts, and also sought to explore the empirical evidence as to how and why whistleblowing plays out as it does. In doing so, we aimed to produce a synthesis that embraced the complexities and ambiguities associated with whistleblowing first introduced in Chapter 1. We detail the review process below; for a schematic overview, see Figures 5 and 6.
Systematic reviews are an established means of summarising available research. A number of approaches are available, and selection depends on the review’s aims and the nature of the evidence to be explored. 69 In developing a protocol for the review, we were guided by the principles advocated by Denyer and Tranfield70 and Macpherson and Jones,71 although some important adaptations were required. Although we undertook a systematic approach to literature sampling and reviewing, we did not evaluate evidence from studies in the manner of a Cochrane review. There are two reasons for this. First, the whistleblowing literature is very diffuse: indeed, some of the relevant literature may not even be labelled as whistleblowing (e.g. research on incident reporting, employee voice and silence). Although there may be valuable insights to be gained from these diverse sources, it would be difficult to achieve a clear synthesis of such widely dispersed and divergently framed research. Second, there are very few studies that gather direct evidence on whistleblowing. The topic is very sensitive, and whistleblowers who agree to participate in research could put themselves at risk of retaliation, professional sanctions or even prosecution. To avoid these problems, empirical researchers have typically explored participants’ responses indirectly, through, for example, hypothetical scenarios. Such studies can clearly be evaluated in terms of the rigour of their research design, and the findings do offer important insights to practitioners and policy-makers, but it would be difficult to utilise the kind of formal weighting of the evidence required for a Cochrane-style review.
We began by searching Google Scholar (Google, Inc., Mountain View, CA, USA) using the search terms ‘whistleblowing’, ‘whistle blowing’, ‘whistle-blowing’ and ‘blow the whistle’, but this yielded an unmanageable 30,200 references. We reviewed a sample of these references to try to refine the search, and also to develop inclusion and exclusion criteria to produce a more practicable bibliography. This proved difficult for two reasons. First, whistleblowing research is undertaken by scholars coming from a range of disciplines. It is, therefore, difficult to use disciplinary markers (e.g. journal title or subject-specific databases) to narrow the search. Second, Google Scholar does not allow one to narrow searches to terms found in an article’s abstract and/or keywords. Unable to identify a bibliographic database that could address both of these issues, we sought to create our own de facto database. Academic fields often develop from an initial burst of research activity, and we observed that whistleblowing research had emerged in the early 1980s and developed rapidly. Later research invariably draws on at least one of these early articles, if only to cite the now widely agreed definition of whistleblowing established by these seminal papers. A comprehensive list of papers citing these key early articles would, therefore, provide us with a manageable database of potentially relevant papers that could then be readily searched, browsed and reviewed.
To identify the seminal articles, we searched Google Scholar for work on whistleblowing published before 1985. A 1983 article by Near and Jensen72 appears to represent the earliest example of published whistleblowing research; there are prior scholarly works, both books and articles, some of which have been widely cited (e.g. Westin et al. 73) but they do not represent the headwaters of the subsequent stream of whistleblowing research. Taking 1983 as our starting point, and observing how rapidly the field developed, we undertook a second search of Google Scholar for papers published between 1983 and 1987. We allowed this window because the time delay in academic publishing could mean that articles published in 1987 were written much earlier, and therefore without the authors being aware of key articles written around the same time. Using the ‘Publish or Perish’ software (Harzing AW, 2007; https://harzing.com/resources/publish-or-perish; accessed 3 December 2015) to generate a hierarchy of papers, we ranked the various papers by citation, and observed a natural break after 11 articles: the 11th article on the list had 73 citations, compared with the 12th, which had only 34. As a check on the rigour of this selection of key articles, we repeated the exercise using two other bibliographic databases, Scopus and EBSCOhost, which between them also cover a range of other databases (Academic Search Premier, Business Source Premier, CINAHL complete, ERIC, MEDLINE, PsycARTICLES and PsycINFO). All 11 seminal papers appeared in EBSCOhost, with five of them also found in Scopus. The ranking within the 11 papers was slightly different from that in Google Scholar, but they were still clearly the most highly cited early papers. When reviewing the citations for each article, we identified that one of these, Dworkin and Near,74 represented something of an outlier, so we excluded it from our list (it was cited predominantly in relation to legal proceedings, rather than research on whistleblowing, and the few non-legal citations of the paper were to be found in the citation lists for one or more of the other articles). The 10 remaining ‘seminal papers for whistleblowing research’ are listed in Table 4.
| Citations | Authors | Title | Year | Publication |
|---|---|---|---|---|
| 546 | Near and Miceli12 | Organizational dissidence: the case of whistle-blowing | 1985 | Journal of Business Ethics |
| 395 | Dozier and Miceli54 | Potential predictors of whistle-blowing: a prosocial behaviour perspective | 1985 | Academy of Management Review |
| 321 | Miceli and Near75 | The relationship among beliefs, organisation position, and whistle-blowing status: a discriminant analysis | 1984 | Academy of Management Journal |
| 271 | Miceli and Near76 | Characteristics of organizational climate and perceived wrongdoing associated with whistle-blowing decisions | 1985 | Personnel Psychology |
| 175 | Near and Miceli20 | Retaliation against whistleblowers: predictors and effects | 1986 | Journal of Applied Psychology |
| 160 | Greenberger et al.77 | Oppositionists and group norms: the reciprocal influence of whistle-blowers and co-workers | 1987 | Journal of Business Ethics |
| 154 | Brabeck78 | Ethical characteristics of whistle blowers | 1984 | Journal of Research in Personality |
| 146 | Near and Miceli79 | Whistle-blowers in organizations: dissidents or reformers? | 1987 | Research in Organizational Behavior |
| 96 | Near and Jensen72 | The whistleblowing process: retaliation and perceived effectiveness | 1983 | Work and Occupations |
| 73 | Jensen80 | Ethical tension points in whistleblowing | 1987 | Journal of Business Ethics |
This process, then, led to a set of 10 papers that could be seen as seminal to the field. Our next step involved combining the citations from these 10 papers into a single bibliography of works relating to the development of whistleblowing as a research field, starting with the most cited paper (Near and Miceli12) and working down the 10 papers in order of number of citations. The articles citing each seminal paper were downloaded into EndNote [Clarivate Analytics (formerly Thompson Reuters), Philadelphia, PA, USA], using the links provided in Scopus and EBSCOhost. The process by which the bibliography was created is outlined in Figure 3.
FIGURE 3.
Selection process for general literature on whistleblowing.
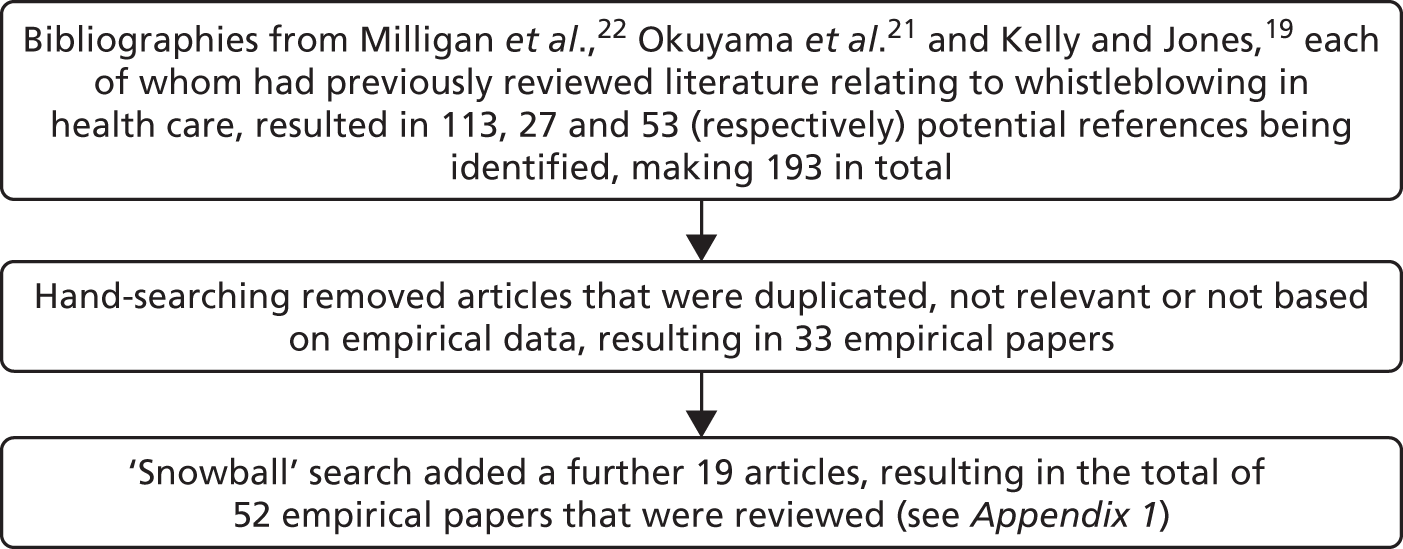
The review process produced a working bibliography of a manageable size, allowing us to review each article in terms of its relevance to the objectives of the project. Although this methodology generated a strong general academic literature, it was recognised that some more recent empirical health-care research papers may not be found using this route. In recognition of this, the papers from the bibliographies of three recent literature reviews in related fields (Milligan et al. ,22 Okuyama et al. 21 and Kelly and Jones19) were converted into an ‘empirical health care’ bibliography (Figure 4). Papers were selected based on an academic judgement of their relevance to this report. Further health-care papers were added via ‘snowballing’ from the initial sources. The most significant papers from the bibliography are summarised in Appendix 1, Tables 8 and 9.
FIGURE 4.
Selection process for empirical papers in health care.
The whistleblowing literature uncovered
Wide dispersal of the whistleblowing literature
The academic whistleblowing literature appears to be very widely dispersed across diverse journals. Within the general literature reviewed, 188 different journals published one or more of the 338 whistleblowing papers uncovered that had been published since 1983. The Journal of Business Ethics was by far the largest contributor of articles, with some 62 papers published here. In contrast, no other single journal accounted for whistleblowing papers numbering into double figures. The empirical health-care literature uncovered (52 papers) was also very widely spread across diverse journals (42 outlets in total). The most common source for these papers was Nurse Education Today, but even this accounted for only eight papers.
Growth in academic publications on whistleblowing
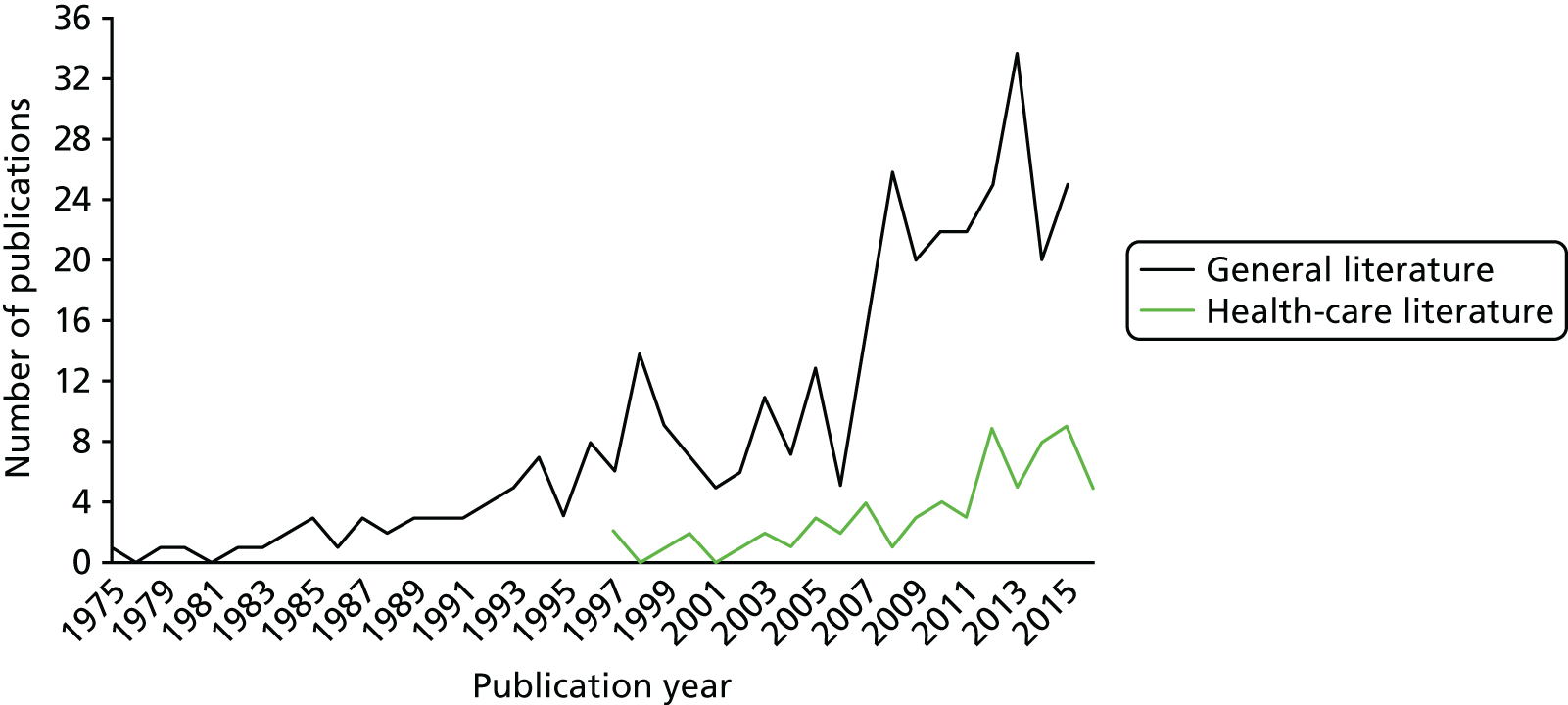
Both the general literature and the specific empirical health-care studies show a marked increase in publication volume since the mid-2000s (Figure 5). The general literature in particular has seen increases to 20–25 new publications per year for each of the past 7–8 years, with the health-care-specific literature contributing 6–8 new papers per year in the same period. (NB owing to the timing of this report, the figures for publications in 2016 account for only the first 6 months of that year.)
FIGURE 5.
Publications on whistleblowing by year since 1975.
Limitations by place of study and participants included
In terms of research specifically on whistleblowing in health care, it is striking the extent to which the UK (29% of papers published) and Australia (27% of papers) dominate the literature, with a relative lack of research emanating from the USA (9.5% of papers). Similarly, about 1 in 10 health-care papers came from Canada (9.5%), with the rest of the world making up only one-quarter of the publications uncovered (25%). Although this pattern undoubtedly reflects a bias in our bibliography towards English-language publications, nonetheless, given the scale and contested nature of US health care, the relatively small research contribution from here is, perhaps, surprising. The domination in this data set of just two countries (the UK and Australia) is a potentially limiting factor in terms of gaining insights into ways in which different health-care systems approach the issue.
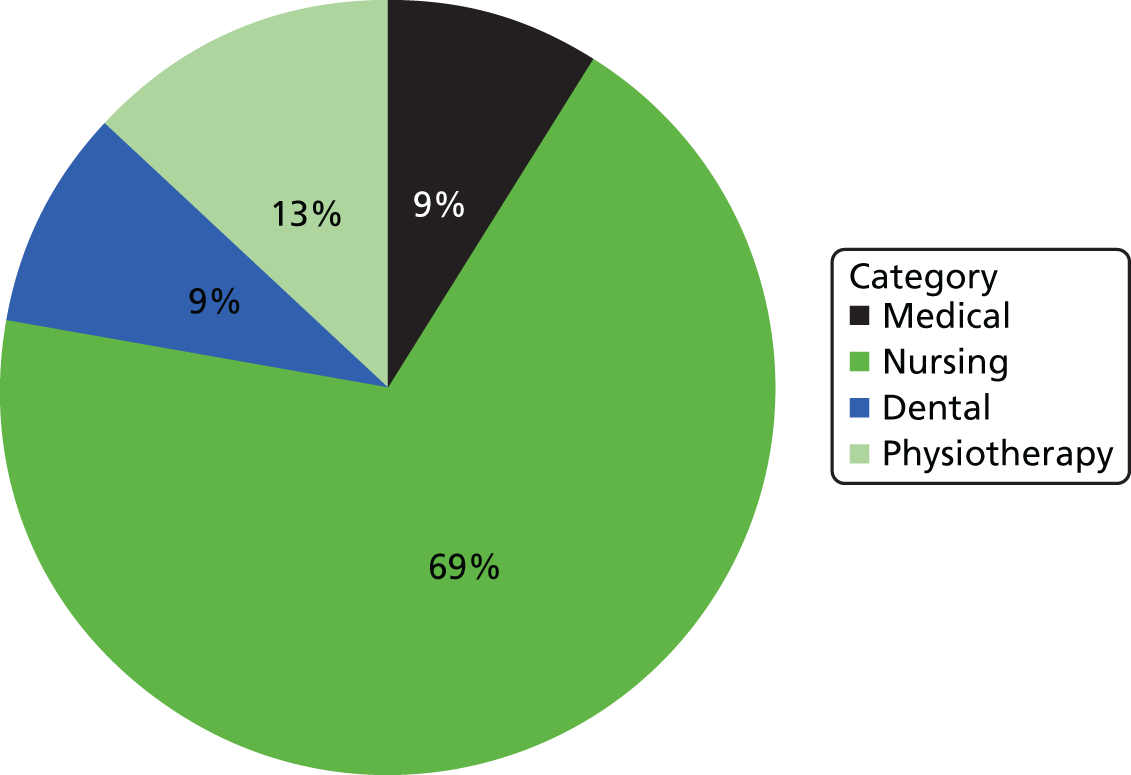
A further potential limitation is that the health-care literature uncovered relates primarily to whistleblowing by nurses: nurses and student nurses account of > 80% of participants in the studies reviewed (Figure 6). Moreover, most of the reported studies leave unspecified the specialty of the nurses under study (64%; Figure 7). Over one-quarter of the health-care studies (29%) used students as study participants (Figure 8), and these were mainly student nurses (69%) with relatively few student doctors included (9%). Furthermore, it is interesting to note that only two authors (Beckstead81 and Monrouxe et al. 82) made an attempt to distinguish between male and female participants, with only Monrouxe et al. 82 commenting on any significant differences between the sexes (specifically, in relation to noting the apparently raised emotions in women after witnessing poor patient care).
FIGURE 6.
Percentage of health-care studies involving different professions.
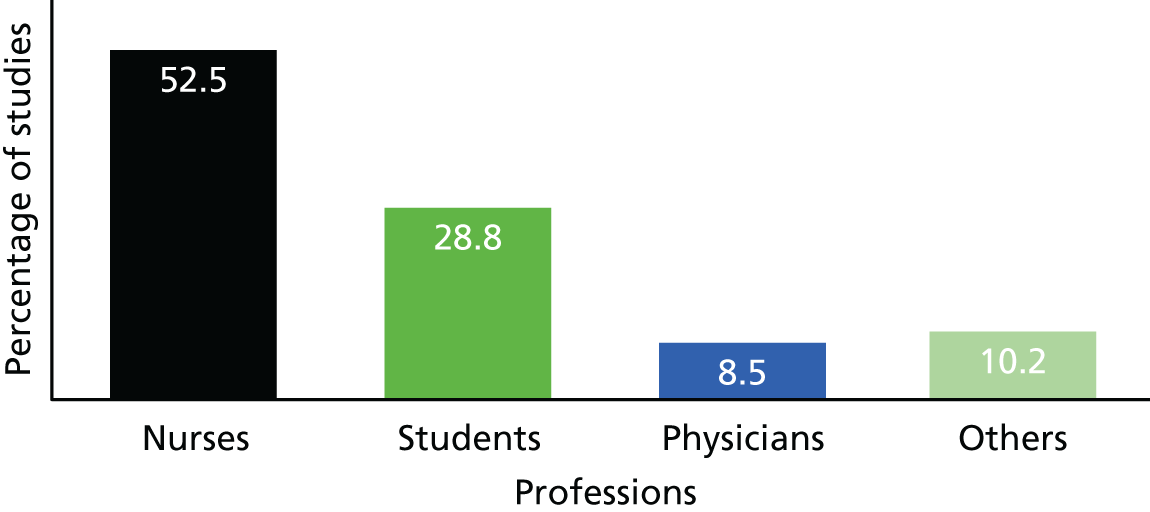
FIGURE 7.
Percentage of health-care studies involving different nursing specialties.
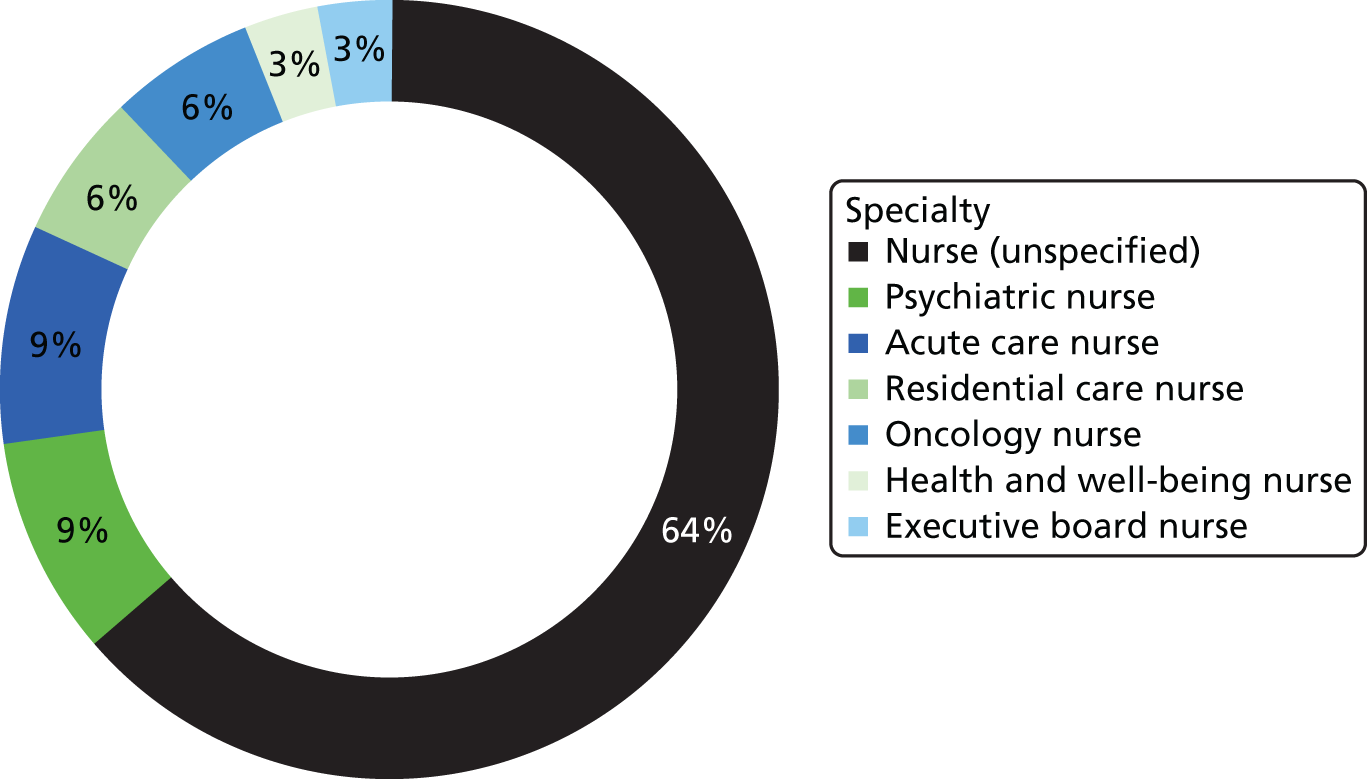
FIGURE 8.
Percentage of health-care studies involving different student categories.
Limited interconnectivity between the general whistleblowing literature and the health-care-specific literature
Perhaps surprisingly, only 15 papers in the general literature review related to health care, of which six presented original empirical research into whistleblowing in health care. We consider this to be one of the most significant findings of our review, as it highlights the extent to which whistleblowing research in health care has developed separately from the wider development of the field, and therefore has not drawn on the theoretical and empirical insights of mainstream whistleblowing research.
Exploring the factors affecting whistleblowing
Whistleblowing has been widely recognised as a complex and contested phenomenon. 44,77,83–86 Numerous factors are recognised as having influence on the whistleblowing process, and that process itself has been structured into five ‘stages’ by Near and Miceli. 12 Table 5 details these stages, and notes the key empirical literature that addresses aspects of these stages: from recognising an event or situation as problematic; through decisions to take action (or not); the actions taken (internally and externally); the organisational responses to these actions; and, finally, the whistleblower’s assessment of those responses (and, potentially, future actions by the whistleblower). In that sense, then, the staged model by Near and Miceli12 might also be thought of as a potentially continuing cycle of response, interpretation and action.
| Stage 1: potential whistleblower recognises event as problematic | Stage 2: decides on action to take | Stage 3: takes action (or not) to report internally or externally | Stage 4: organisation (or other stakeholder) responds to whistleblower’s actions | Stage 5: whistleblower assesses organisational response and decides on what (if anything) to do next |
|---|---|---|---|---|
| Ahern and McDonald87 | ||||
| Attree88 | ||||
| Beckstead81 | ||||
| Bellefontaine89 | ||||
| Bickhoff et al.90 | ||||
| Black91 | ||||
| Bradbury-Jones et al.92 | ||||
| Bradbury-Jones et al.93 | ||||
| Espin and Meikle94 | ||||
| Firth-Cozens et al.95 | Firth-Cozens et al.95 | |||
| Fledderjohann and Johnson36 | ||||
| Gould and Drey96 | Gould and Drey96 | |||
| Greaves and McGlone97 | ||||
| Grube et al.84 | ||||
| Hutchinson and Jackson98 | Hutchinson and Jackson98 | |||
| Ion et al.86 | Ion et al.86 | |||
| Ion et al.99 | ||||
| Jackson and Raftos100 | ||||
| Jackson et al.101 | ||||
| Jackson et al.102 | ||||
| Jackson et al.101 | ||||
| Jones and Kelly17 | ||||
| Jones et al.103 | ||||
| Kent et al.104 | ||||
| Killam et al.105 | ||||
| Killam et al.106 | ||||
| Kingston et al.107 | Kingston et al.107 | |||
| Ko and Yu108 | ||||
| Law and Chan109 | ||||
| Levett-Jones and Lathlean110 | ||||
| McCann et al.111 | ||||
| McDonald and Ahern112 | ||||
| McDonald and Ahern113 | ||||
| Mansbach et al.114 | ||||
| Monrouxe et al.82 | ||||
| Moore and McAuliffe115 | Moore and McAuliffe115 | |||
| Newton et al.116 | ||||
| Ohnishi et al.117 | ||||
| Peternelj-Taylor118 | ||||
| Prang and Jelsness-Jorgensen119 | ||||
| Schwappach and Gehring120 | ||||
| Schwappach and Gehring121 | ||||
| Stevanin et al.122 | ||||
| St Pierre et al.123 | ||||
| Tella et al.124 | ||||
| Throckmorton and Etchegaray125 | ||||
In this section, then, we surface the most significant of the factors that have been suggested as influencing the whistleblowing process as these have emerged in the empirical health-care literature. To facilitate the ordering of our findings, we have categorised the factors affecting whistleblowing into three broad areas, although there is necessarily a degree of overlap among these:
-
the external context – including the role of regional and national cultures; the law and legal frameworks; professional standards, including ethical codes and guidelines; and economic and financial influences
-
the internal context – including organisational culture and climate; education and training; peer pressure and local relationships; local leadership and management; and boundary definitions (i.e. what is seen to count as ‘wrongdoing’ or unacceptable practice)
-
personal factors – including personal traits and characteristics; and the position and role in the organisation occupied by the would-be whistleblower.
In the following sections, we take each of these broad areas in turn.
External context
Here we consider aspects of the environment that are external to the organisation, and over which organisational members typically have little control.
Regional and national culture
Much has been written in the management and organisation studies literature on the regional and national cultural dimension of power relations,126,127 and there has been mainstream work on the relevance of national culture to whistleblowing (e.g. Park et al. 14). In a health-care context, Ohnishi et al. 117 note the significant impact of national culture in their research with psychiatric nurses in Japan, and Cheng et al. 128 compared British and Chinese students (from various disciplines) and noted that ‘individuals from collectivist cultures are less likely to be whistleblowers, and less accepting of whistleblowing behaviour, than individuals from individualistic cultures’.
Throughout its history the NHS has benefited from drawing upon the talents of a global workforce, some coming from nations where speak up behaviour is less culturally acceptable and/or environments in which speaking up is viewed as very risky. It is important that these potential differences are taken into account in the design of speak up arrangements, and in the induction and training given to staff. However, there is little empirical research in the field of health care specifically examining nationality as a factor in whistleblowing. Tella et al. 124,129 found that UK nursing students considered themselves better prepared for reporting on problems in relation to patient safety than their Finnish counterparts, and Tabak et al. 130 noted that knowledge of the concept of whistleblowing was relatively underdeveloped in Israel compared with the UK, although it was reported that the same moral imperative to care for patients existed in both countries. Skivenes and Trygstad131 discussed research carried out by the Norwegian government on whistleblowing in the broader public sector, which suggests that, in contrast to the findings of many international studies, Norwegians generally had very positive experiences of whistleblowing, reporting constructive responses when reporting problems to employers. The authors posit that this was because of the strong emphasis in Norwegian culture on collective arrangements, and the creation of clear reporting structures that encourage an open and honest culture for communicating problems to senior managers.
The law and legal frameworks
Whereas the complexity of the legal perspective on whistleblowing is addressed in Chapter 5, in this section, we consider the impact of the presence (or absence) of legal frameworks on whistleblowers and whistleblowing. Research in the USA by Miceli and Near48 suggests that the introduction of new laws in the 1980s that supported the protection of whistleblowers against retaliation from employers actually had little impact on reducing the occurrence of employer retaliation. Interestingly, however, a later large-scale survey study of US employees found that the threat of retaliation did not, in fact, discourage whistleblowing; instead, it encouraged reporting to external agencies able to effect action, rather than to internal organisational members who may have been able to rectify the perceived wrongdoing but who may also have been tempted to ‘kill the messenger’. 132 Such counterintuitive behaviour may have resulted from a belief that ‘the law will protect me’, or might have been driven by other factors. Legal protection for actual and potential whistleblowers in the UK is enshrined in PIDA,8 and this is discussed at length in Chapter 5.
In the health-care literature, the question of legal protection and responsibilities for whistleblowers did not feature heavily in empirical studies. Greaves and McGlone97 reported interviews with public sector workers in Australia (including nurses), and some of the participants perceived laws that protect whistleblowing as ‘meaningless’. Similarly, the literature review by Delk133 suggests that although a comprehensive legal framework may, in theory, provide health-care whistleblowers with protection against employer retaliation, in reality the nature and diversity of retaliatory acts available to organisations against those who blow the whistle means that legal safeguards seem to offer little deterrent.
Professional standards, including ethical codes of practice and guidelines
In accountancy, the existence of organisational whistleblowing policies and procedures has been perceived to increase the likelihood of internal reporting of wrongdoing. 134 In health care, the situation is more ambiguous: Klaas et al. 135 considered the impact of formal whistleblowing policies and processes within organisations, and reported that such formal instruments were likely to make whistleblowing appear to be a strategy of last resort, as it could be perceived as an open challenge to the authority of management. However, the existence of clear professional standards and guidelines has been found to be an important factor in supporting whistleblowing in health care in a number of empirical studies86,95,101,102,136 and particularly in nursing rather than other health-care professions. However, Hutchinson and Jackson98 noted that the entrenched behavioural patterns within health-care organisations are often at odds with the officially espoused organisational approach, and Jones and Kelly17 reported that formal procedural approaches were ‘neutralised’ by organisational cultures that opposed ‘voice’. Interestingly, Newton et al. ,116 in a study involving 374 acute care nurses, found that nurses often took independent action to address poor care rather than pursue official channels of compliant. McCann et al. 111 observed a similar phenomenon, whereby, in response to more challenging performance targets amid a reduction in resources, both front-line and mid-management employees resorted to ‘a form of “street-level bureaucracy” – a situation in which traditional professional norms are reasserted informally in ways that often transgress prescribed performance systems’.
Economic and financial influences
There appear to be no studies within health care of whistleblowing over financial wrongdoing, whereas in the mainstream literature this is the most common form of wrongdoing studied. The main financial dimension in health-care research, albeit limited, was a focus on the pressure to achieve financial targets and job security. Similarly, there was little attention afforded to potential variations in approaches to whistleblowing between the public, private and voluntary sectors providing health care, with the literature rarely making a distinction between these groups. The evidence from McCann et al. 111 highlights the impact of austerity measures in the NHS on whistleblowing, and more specifically on voice: given the difficulties of meeting more challenging targets with fewer resources, the authors report that NHS staff often resort to ‘under-the-radar’ tactics to deliver the quality of care that they feel meets their professional standards, while avoiding the potential risks associated with ‘speaking up’. Set against the backdrop of austerity in the NHS described by Hyde137 and McCann et al. ,111 it can be seen how pressure to meet business targets begins to undermine nurses’ confidence in their judgement on what is an acceptable level of care, and thereby modify their behaviours in response. Given the increasing financial constraints in the NHS that throw job security into sharper relief, staff are less likely to blow the whistle when doing so brings them to the attention of management, which may result in retaliatory action. 113
Keil et al. 138 suggest that whistleblowers engage in a holistic cost–benefit analysis when deciding whether or not to blow the whistle and, therefore, financial incentives may encourage whistleblowing. However, Gino et al. 139 suggest that economic incentives and competitive pressures may result in workers abandoning their ethical standards. Similarly, examining the reporting of fraud, Brink et al. 140 found that offering an incentive increased internal reporting, and decreased external reporting of wrongdoing. However, in the NHS, providing financial incentives to staff to report concerns about patient safety or poor care quality would go against the norms of NHS culture. In addition, if health-care workers fear being perceived by their peers as having reported for personal gain, offering incentives may unintentionally reduce reporting, or weaken the whistleblower’s credibility if an ‘offender’ challenged their evidence.
Internal context
In this section, factors internal to the organisation that influence whistleblowing are considered. These factors can be, to a greater or lesser extent, influenced by the deliberate actions of key members of the organisation, and include an organisation’s culture and climate, education and training, peer pressure and relationships, leadership and management, and where the boundary is drawn between good and unsafe care.
Organisational culture and climate
The significance to whistleblowing of organisational culture has attracted much attention, as has the way in which employees experience this culture (i.e. organisational climate). While investigating whistleblowing in financial auditing, Hooks et al. 141 commented that organisational culture had a greater influence on the decision to blow the whistle than (for example) the social influences, personal characteristics and responsibilities of the observer, or the characteristics of the wrongdoing itself. Kaptein142 explored a range of factors incorporated into the ‘ethical culture’ of an organisation, and noted that careful management of these factors could ‘enhance the self-correcting capacity of the organisation’.
Hutchinson and Jackson98 reported that many nurses experienced a contrast between the actual culture and espoused mission of the organisation voiced by senior management and expressed in official documents. Jones and Kelly17 highlighted how formal procedural approaches to encouraging open reporting of concerns gave way to ‘[a] process of socialisation and habituation in the workplace’, in other words, organisational culture ‘trumps’ organisational procedures in influencing whether or not staff feel that it is safe and useful to report concerns about the quality of care. However, Kingston et al. 107 formed a different view, noting that the culture in nursing encouraged compliance with formal rules and protocols, whereas the ‘medical’ culture encouraged dealing with incidents informally and ‘off-the-record’. Ahern and McDonald87 found that nurses who blew the whistle on wrongdoing had a belief system that privileged their role as ‘patient advocate’ (see Personal factors).
Those nurses who had witnessed wrongdoing but did not report it were more likely to believe that they were equally as responsible to their colleagues and their employer as they were to the patient. Ion et al. 99 suggests that a ‘blame culture’ exists within student nursing, and Prang and Jelsness-Jorgensen119 found that organisational culture was perceived as a barrier to reporting concerns. The work by St Pierre et al. 123 supports this view, finding that, in simulated critical situations, nurses were rarely likely to challenge decisions that they believed to be dangerous, with justifications for that silence including a lack of knowledge of whistleblowing procedures and a perceived inability to challenge superiors. The authors argue that this points towards an organisational culture that suppresses voice and erodes the confidence of nursing staff in their own judgement. We return to this theme in Personal traits and characteristics.
Education and training
The health-care literature thoroughly covers the part played by training nurses in reporting wrongdoing. Indeed, student nurses are in a good position in terms of identifying poor-quality or unsafe care92 in that as students they will have recently been trained to identify good and poor practice, and may not yet have been socialised into a particular organisational culture. For example, Killam et al. 105,106 observed how students on clinical placements are often well aware of unsafe clinical practices. However, as junior members of the clinical staff they may lack the experience and confidence necessary to raise concerns with their superiors. 104 Bradbury-Jones et al. 92 noted how, in this respect, training and education can increase nurses’ confidence and willingness to report and challenge poor practice. Similarly, Law and Chan109 emphasise the value of formal mentoring of graduate nurses in order to enhance their understanding of what constitutes good-quality (and poor-quality) care and to raise their confidence in reporting concerns. By contrast, Tella et al. 124,129 explored the views of British and Finnish nursing students and noted that in both groups that there was a clear preference for learning in a formal environment rather than in a clinical setting. The authors suggest that the workplace environment may ‘cloud’ nurses’ judgement of what constitutes unsafe care. Johnstone and Kanitsaki143 suggest that nurses and others need to ‘learn from practice errors and to use the lessons learned to help prevent future errors from occurring’, and so encourage educators to present raising concerns in a positive light.
Peer pressure and relationships
Many authors report that (both internal and external) whistleblowers often suffer deterioration in their relationships with their peers, irrespective of whether or not the concerns reported are genuine and legitimate. 81,113,133 The formal process of investigating a concern is often traumatic for complainants and for subjects of complaints, as well as for bystanders. 88,101,102,112,113,115,119,144 Jackson et al. 145 explored this issue, interviewing both whistleblowers and targets of whistleblowing. They found that ‘whistle-blowing had a profound and overwhelmingly negative effect on working relationships’,145 with collegial and interprofessional relationships damaged, and those involved suffered bullying and exclusion. Bystanders were not immune to the impact of poorly managed whistleblowing, and could also suffer from a decline in peer relationships. 145
Bradbury-Jones et al. 93 noted that the fear of failing their placement assessment often deters health-care students from speaking up when they see poor-quality care, and these authors cited the influential work by Hirschman,146 who argues that exercising ‘voice’ with peers can have a negative outcome if that voice is perceived as being too ‘loud’. Bradbury-Jones et al. 93 described the impact of this fear as encouraging ‘exit’ by student nurses, implying a withdrawal from the potential whistleblowing situation, rather than from the organisation. These authors went on to consider how students found ways to raise concerns, or ‘negotiated’ a way to give voice to their concerns, and how this approach could be supported. In doing so, the authors recognised the weakness of the idea of a binary choice between ‘voice’ and ‘silence’, and discussed how student nurses explored different ways of raising concerns so that they could satisfy their recognised duty to speak up while avoiding appearing ‘cocky’, that is, being perceived as having a ‘voice’ that was too loud. This ‘exit’ versus ‘voice’ continuum is displayed in Figure 9.
FIGURE 9.
The exit–voice continuum.
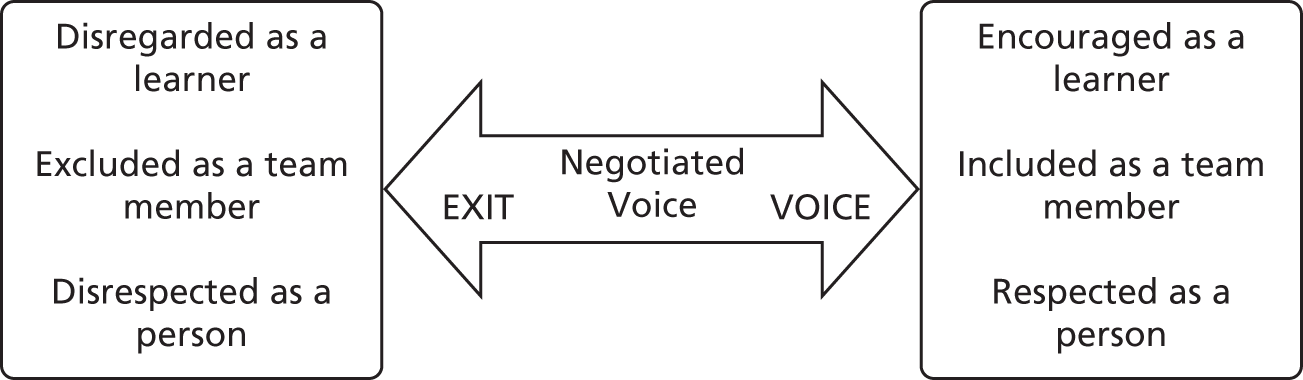
Leadership and management
The mainstream whistleblowing literature includes a number of studies that focus directly on the role of leadership and management in encouraging or inhibiting whistleblowing; there are no comparable studies in health care. Culiberg and Mihelic33 report on a number of studies that highlight the importance of ethical leadership and positive leader–member relationships in promoting ethical behaviour, specifically with regard to whistleblowing. Goldberg147 notes that the typical reactions to whistleblowing result in a loss of ‘moral leadership’ (more so than appointed leadership) from health-care organisations. Hutchinson and Jackson98 suggest that the very nature of the public sector predisposes health-care organisations to favour an authoritarian leadership style in which bullying and intimidation of staff can thrive and leads to a punitive culture that discourages public sector employees from whistleblowing.
Many studies have found that nurses lack confidence in the reporting systems put in place by management and that this acts as a barrier to reporting poor care. 85,88,91 Cleary and Doyle148 describe a NHS report that highlighted a sharp contrast between the positive perceptions of senior executives regarding the ease of reporting wrongdoing and subsequent action, and the actual difficulties reported by nurses. Similarly, Jackson et al. 101 report that health-care managers were often perceived to have not dealt with complaints appropriately, and comment that a more responsive and inclusive style of management would improve standards of care. 47
Jackson and Raftos100 highlight nurses’ perceptions of the barriers and obstacles put in place by management that discourage the reporting of concerns internally. The authors argue that such defensive behaviour among managers can serve to drive some nurses to report externally (although probably more to simply remain silent). Furthermore, the perception by employees that management will fail to respond positively to concerns is frequently cited in the literature as a key reason why health-care workers do not to speak up when faced with unsafe care. 88,91,95,100,107 However, this finding is in contrast to Moore and McAucliffe,115 who found that nurse managers appeared to be more likely to report poor care than nurses themselves, a finding supported by Schwappach and Gehring121 and Throckmorton and Etchegaray. 125 Milligan et al. ,22 drawing on research by Espin and Meikle94 with health-care students, note that some of the barriers created by senior managers could be overcome by creating a more clearly defined ‘reporting ladder’ (p. 27) that facilitates the recognition of a clear path through which concerns could be raised in organisations.
In the first study of its kind, Mannion et al. 149 explored the relationship between hospital board governance and patient safety in the NHS. They found a statistically significant relationship between particular (self-reported) board competencies and whistleblowing-related questions in the annual NSS. In particular, there was an association between board competencies and staff’s reported willingness to report errors and incidents as well as staff perceptions that their organisation would take positive action if they did report problems requiring attention. This study draws attention to the wider governance context as well as local management and leadership in supporting the reporting of front-line concerns.
Boundary definitions
The difficulty in identifying actions and behaviours that constitute ‘wrongdoing’ receives considerable attention in the literature, particularly in that relating to student nursing. Enabling trainee health-care workers to judge where the line is drawn in terms of delineating poor care from adequate care is considered fundamental to nurse training, with many authors contributing to the general discussion on this. 96,104,122,124,129 Ion et al. 86 argue that student nurses often lack confidence in their own judgement, and Bickhoff et al. 90 note the importance of linking nurse training to nurses’ own moral code and previous life experiences as a benchmark for judging poor-quality care. The issue of boundaries is also addressed by Prang and Jelsness-Jorgensen,119 who claim that, in addition to poor organisational culture and support, a lack of clarity around routines and processes was a barrier to speaking up. Jones and Kelly17 note that the ‘incremental expansion of normative boundaries’ leads to a gradual shift in what is perceived as acceptable behaviour, adding further to local ambiguity and uncertainty.
Personal factors
Factors that are specific (but not unique) to an individual but that may influence whistleblowing behaviour are presented in the following section. The literature here uncovers and explores various factors grouped under the following broad headings: personal traits and characteristics; and position and role in the organisation.
Personal traits and characteristics
Ohnishi et al. 117 note the large personal challenge of blowing the whistle: ‘The social significance of belonging to a group, the psychological pain of disloyalty, obedience to the chain of command, fear of being exposed as the whistleblower, and fear of accusation and retribution all hinder whistleblowing’. Indeed, the authors draw attention to the complexity of social, ethical and personal forces at work in these situations. Clearly, speaking up and whistleblowing are acts that cannot be untaken lightly by any organisation member.
Many empirical studies highlight the importance of nurses’ self-image and perceived duty as patient advocates. 85,87,90,91,102 This advocacy role has been recognised as a crucial part of a nurses’ training,109,122,124 and perceived as fundamental to helping nurses recognise when care is poor. Ion et al. 99 note the natural human tendency to describe oneself in the most positive light, leading whistleblowers to claim to be strong characters, whereas non-whistleblowers blame factors outside their control for their failure to report, perhaps suggesting that, at some level of consciousness, nurses understand and believe that their primary responsibility is to the patient. 150 Peternelj-Taylor118 supports this view, and implies that there is a possible naivety among nurses who believe that organisations will respond to reports of wrongdoing in an ethical matter consistent with their ‘nurse as patient advocate’ ideals. The author goes on to emphasise that to be able to speak out about wrongdoing in the health-care sector requires resilience, confidence and moral courage. This view is supported by several empirical studies, including Bickhoff et al. 90 and Monrouxe et al. 151 In addition, Bellefontaine89 notes that a strong student–mentor relationship and supportive university representatives are key to giving student nurses the personal confidence and information necessary to speak up about concerns around patient safety.
Work by Schwappach and Gehring120 raises an interesting point relating to nurses being concerned about how to raise concerns, rather than whether to raise them. This perhaps suggests that a person with a reflective, reflexive personality would be more predisposed to blow the whistle than individuals who are less self-aware. Although a number of the empirical studies recorded a predominance of women included (mirroring health-care professions more widely), there was little attempt to differentiate the sexes with regard to whistleblowing responses. Fledderjohann and Johnson,36 working with the general public, noted that men were less likely to report child neglect, and Monrouxe et al. 82 found that men were less likely to classify themselves as distressed after witnessing poor patient treatment. However, Kent et al. 104 found that sex, age and ethnicity had little or no influence on the willingness of student nurses to speak up. There clearly remains much to uncover here regarding personal predisposing factors to whistleblowing.
Position and role in the organisation
A number of papers highlight differences in willingness to speak up between individuals in different roles and positions within health-care organisations: St Pierre et al. 123 noted that, in critical situations, nurses rarely challenged potentially dangerous decisions made by their superiors, in this case anaesthetists. Moore and McAuliffe115 found that nurse managers were more likely than staff nurses to report poor care. Throckmorton and Etchegaray125 contradict this finding to some extent, reporting that although (perhaps not surprisingly for a postal questionnaire) 99% of nurses claimed that they would report incidents that they felt would result in moderate to severe injury or death, error reporting was more likely to come from nurses who were operationally closer to the patient, and from nurses who were less well established in their roles. The lack of a managerial role for doctors and nurses appears to reduce the likelihood that they will be willing to speaking up when confronted with poor or unsafe care. 121
Responses to whistleblowing
In many articles, the fear of reprisal is cited as a central cause of failure to report wrongdoing. Typically, the anticipated retaliation has its source as the organisational formal and informal apparatuses, but also may include the fear of actions of peers, and the whistleblowers’ own inner personal turmoil as they try to balance ‘doing the right thing’ against loyalty to their peers, to the organisation and, potentially, to their profession. It is to these issues that we now turn.
Responses from organisations
The employing organisation’s responses (both positive and negative) to whistleblowers have a great bearing on the entire whistleblowing process. Indeed, the lack of response (i.e. a change in poor practice or the addressing of wrongdoing) is widely cited as a key reason for a decision not to report. 100,107,115,150 Although this could perhaps be seen as an attempt by non-reporting observers to justify the lack of action, given the risks associated with whistleblowing, one would expect that seeing a positive response from the organisation would support the further reporting of wrongdoing. 112 Fear of retaliation by the organisation emerged as a significant barrier to speaking up,88,93,133 yet there has been a dearth of research exploring the proportion of whistleblowing that actually results in retaliation, or of positive responses to the raising of concerns. It is quite plausible that highly publicised but isolated incidents of the mistreatment of whistleblowers have a disproportionate impact on the level of apprehension that is experienced among general employees. This underlines the need for a clearer picture of what health-care professionals (and the public) understand by the terms whistleblowing and raising concerns, and a clearer sense of what might happen as a consequence of those actions.
Responses from peers
Whistleblowers report the potential for reprisals from peers as a major factor in their decision-making process, with McDonald and Ahern112 reporting ‘unofficial’ (i.e. not initiated by the organisation) reprisals on whistleblowers from their colleagues taking the form of pressure to resign, social rejection, being treated as a traitor and having their career progression halted. Attree88 discusses ‘negative social outcomes, alienation and withdrawal of peer support’ as the experience of some whistleblowers, and both Peters et al. 144 and Bickhoff et al. 90 report bullying and exclusion from social groups. Jackson et al. 145 offer a slightly different perspective, noting how nurses desire to blend in with their colleagues and to conform to group norms, and depend on those norms to report, or not report, wrongdoing. Law and Chan109 raise a further dimension to peer responses to whistleblowing, specifically the extent to which peers naturally support colleagues who report wrongdoing, and consider the use of peers as mentors in these situations.
Responses from non-whistleblowing observers of wrongdoing
Newton et al. 116 suggest that there are many ‘under-the-radar’ responses to the observation of poor care that manifest as changed behaviours in those directly or indirectly affected by the wrongdoing; their response to an observation may be to take their own action (i.e. outside their normal channels) to address the problem and alleviate the moral distress they feel as a result of observing poor care. For example, rather than blow the whistle, nurses may address problems by ‘contacting other healthcare team members, making referrals and coordinating care with other departments such as home care and hospice, as well as initiating contact with groups such as professional regulatory bodies or unions’. Newton116 suggests that nurses are ‘silenced’ by organisations, but are not always ‘silent’; that is, if they are not listened to by the relevant authorities, or are told to be quiet, they may elect to address the poor care directly and unofficially, rather than risk suffering the negative responses to whistleblowing from organisation or peers that so many nurses seem to anticipate.
In discussing a study that involved interviewing practising oncology doctors and nurses, Schwappach and Gehring120 uncovered a range of non-verbal communication signals that were exchanged between colleagues in an attempt to avoid compromising patient safety. However, this behaviour was moderated by the degree of severity of the risk to the patient, with greater risk garnering more overt and more direct ‘voice’. This suggests that bystanders’ (in)actions may be an important consideration alongside the actions/voice of putative whistleblowers themselves. Perceptions of wrongdoing may also be important: Mansbach et al. 114 found that physiotherapy students tended to view management wrongdoing as more serious than practitioner wrongdoing, whereas qualified practitioners took the opposite stance.
McDonald and Ahern112 found that the indecision around whether or not to blow the whistle on poor care caused nurses moral anguish, with the most effective response to alleviate these symptoms being to take problem-focused action, and the least effective being avoidance and denial. Monrouxe et al. 82 looked more closely at the anguish caused to observers of wrongdoing (irrespective of whether or not they blow the whistle) and highlighted the finding that male medical students claimed to be less distressed by observation of poor-quality care than their female counterparts. Interestingly, the authors also found that increased exposure to poor care apparently increased distress levels, which runs counter to what might have been expected given the findings from other studies that suggest that as nurses become more socialised members of an organisation, they become less likely to notice or become desensitised to poor care, and, therefore, become less minded to report such cases. 17,110 Blenkinsopp and Edwards15 commented on the emotional response of failing to speak up, noting ‘strong negative emotions, including anger, fear and cynicism . . . driven by fear of the consequences of speaking up’ (p. 187). Greaves and McGlone97 go further, reporting on the long-term damage done to a whistleblower’s mental health as a result of the reprisals exacted by their employing organisations. Similarly, Peters et al. 144 emphasised the negative impact of whistleblowing incidents on the emotional health of those involved, particularly if the ensuing investigations are protracted.
Concluding remarks
This chapter concludes our review of the theoretical and empirical literature on whistleblowing. We move next to an analysis of key Inquiry reports into serious failings in NHS care, beginning with the Bristol Royal Infirmary Inquiry report and covering the causes of concern, the main recommendations of the inquiry, the response to recommendations and the fate of the whistleblower.
Chapter 4 The main whistleblowing inquiries and formal responses to inquiry recommendations
Introduction
This chapter focuses on distilling the key lessons for whistleblowing policy and practice from an analysis of the findings of formal inquiries into serious failings in NHS care. It reviews inquiries dating back to the Bristol Royal Infirmary5 and moving through Ayling,152 Kerr/Haslam,153 Shipman154 and Francis155–159 to the Francis Freedom to Speak Up review. 2 The starting point was chosen on the grounds that Bristol was the first major inquiry since PIDA, that it featured a clearly identified ‘whistleblower’ and that it discussed issues that foreshadow those in subsequent inquiries, such as the importance of ‘culture’ and the duty of candour. In addition, this chapter examines the responses of the main stakeholders to the respective Inquiry reports, including the government, the Health Select Committee, and health-care ‘producer’ organisations such as the Royal College of Nursing and the General Medical Council (GMC).
For each Inquiry report, information is presented on the following issues.
-
Who (if anyone) was the whistleblower?
-
How and why did they ‘blow the whistle’?
-
What factors did or could facilitate or inhibit the action?
-
What organisational actions were taken as a result?
-
What were the consequences for the whistleblower?
For each response to the inquiry, attention is focused on the recommendations of that inquiry.
As the inquiries contain thousands of pages, the traditional historical ‘reading’ of the documents160 would have been problematic. Instead, electronic searches of the documents were performed using thematic coding in a deductive and inductive sense through keywords from the conceptual and theoretical work of the earlier chapters, and arising inductively from the documents. The most obvious search term is ‘Whistle*’, but other terms used included ‘Concern’, ‘Bully*’, ‘Victim*’, ‘Intimidat*’, ‘Reprisal’, ‘Silen*’, ‘Fear’ and ‘Speak*’. These sections (and surrounding paragraphs, together with any signposted links) were then explored in more detail. This chapter provides a summary of the inquiries and responses, followed by a discussion of the emerging themes.
The formal NHS inquiries from the Kennedy report onwards
Each of the key inquiries is now taken in turn, with a structured summary provided of the events underpinning the inquiry and the matters arising that are directly relevant to whistleblowing. Appendices 2 and 3 provide fuller details of these inquiries (and, indeed, of the formal responses made to the recommendations for each inquiry).
Kennedy5
Kennedy5 reported on a public inquiry, set up in 1998, that examined the management of the care of children receiving complex cardiac surgical services at Bristol Royal Infirmary between 1984 and 1995, which particularly focused on the high mortality rates of two main surgeons, Mr Wisheart and Mr Dhasmana. The surgeons and the chief executive officer (CEO), Dr Roylance, were found guilty of serious professional misconduct in 1998. The Inquiry report stated that it would be reassuring to think that the situation could not happen again, but ‘we cannot give that reassurance. Unless lessons are learned, it certainly could happen again’ (p. i).
Blowing the whistle
The main whistleblower was Dr Steve Bolsin. Soon after his appointment as consultant anaesthetist in September 1988, Dr Bolsin began to have concerns about the duration of operations and the consequent effect on outcomes (p. 136). He began to gather data in 1989 and attempted to raise concerns through a number of internal and external routes. However, these actions had little impact, and in January 1995 the death of 18-month-old Joshua Loveday following surgery led to an external inquiry.
Factors
The report pointed to a ‘club culture’, an imbalance of power with too much control in the hands of a few individuals (p. 2). Many staff, particularly junior staff, remained silent in the face of poor care as they were fearful of raising concerns and/or challenging superiors because of possible repercussions: ‘There is a real fear among staff (particularly among junior doctors and nurses) that to comment on colleagues, particularly consultants, is to endanger their future work prospects’ (p. 2). The report regards it as ‘significant’ that nursing staff did not bring concerns to senior figures. This was not a result of ‘any lack of concern, but illustrating a larger truth of the hierarchical system that made it difficult for nursing staff to voice concerns and be heard’ (p. 175). In short, nursing staff were ‘let down by a culture that excluded them’ (p. 176).
Consequences for the whistleblower
Although there is nothing in the report on this issue, other sources (e.g. Hammond and Bousfield161) record that Dr Bolsin was described as ‘the most hated anaesthetist in Europe’ and found himself unemployable in the NHS. He left the UK in 1995 to work in Australia, but in 2013 he was awarded the Royal College of Anaesthetists medal in recognition of the work that he has done to promote safety in anaesthesia (p. 8). 162
Consequences for the NHS
The report presented 198 recommendations, under the following themes: respect and honesty; a health service that is well led; competent health-care professionals; the safety of care; care of an appropriate standard; public involvement through empowerment; and the care of children. Although there was no explicit recommendation on whistleblowing, a number of recommendations foreshadowed some of those of later reports, such as ‘a duty of candour’ to patients (recommendation 33), a framework of regulation independent of government (recommendations 39 and 40), doctors’ Code of Professional Practice incorporated in the contract of employment (recommendation 45), a regulatory body, and a professional code of practice for health-care managers (recommendation 91), a national reporting system (recommendations 109–112), and incentives to encourage the reporting of sentinel events (recommendations 113–118). However, more generally, stress was placed on changing the ‘culture of the NHS’.
Quotations in this sections are reproduced from Kennedy. 5 © Crown copyright. Contains public sector information licenced under the Open Government Licence v3.0.
Ayling152
In 1998, Clifford Ayling was arrested and charged with indecently assaulting former patients. In 2000, he was convicted on 12 counts of indecent assault relating to 10 female patients, and sentenced to 4 years’ imprisonment. His name was placed indefinitely on the sex offender’s register under the Sex Offenders Act 1997. 163 In 2001, the professional conduct committee of the GMC determined that Ayling’s name should be erased from the medical register.
Blowing the whistle
Ayling worked in hospitals and as a GP. In the hospital setting there were a number of concerns, but only two complaints, ‘which is indicative of the contemporaneous culture within the profession to rely upon informal mechanisms for raising concerns about a colleague’ (p. 37). Midwife Delphine Bentley wrote a complaint in 1984, which appeared to result in no action. In 1980, Sister Penny Moore reported Ayling for masturbating while carrying out a vaginal examination on a young woman.
Ayling became a GP in 1981 and remained in general practice until 2000. In 1991, a patient made a complaint to Kent Police about the way he had examined her at his surgery. The Crown Prosecution Service took the decision not to prosecute, but the incident was brought to the attention of the Family Health Services Authority by a letter from the Kent Police. Ayling was ultimately tried and convicted of indecent assault against the patient in 2000 (p. 63).
From 1985 until 2000, a succession of patients transferred from Ayling’s practice to a neighbouring surgery, with many female patients referring to his apparent misconduct in the context of breast and vaginal examinations (p. 65). In 1988, Dr Anderson contacted his medical defence organisation, and in 1993 Dr Pickering approached Kent Local Medical Committee, but these did not result in any action. Both Dr Anderson and Dr Pickering worked at a neighbouring practice and had received requests for patients to be transferred from Ayling’s practice.
Factors
The report pointed to the ‘individuals who could and should have acted on the information then available’ (p. 109), and identified a number of missed opportunities between 1971 and 1998. It discussed a number of issues, such as clinical freedom and self-regulation; staff hierarchies; lack of openness; a failure to hear; lack of clear professional guidance; preference for the use of informal systems; lack of information sharing or ‘corporate memory’; barriers to making complaints; the lack of gathering and sharing ‘soft’ information; and a lack of procedures for raising concerns. However, the single most important barrier to staff, such as nurses and midwives, formally expressing their concerns about Ayling was ‘the absence of any formal procedure for doing so’ (p. 138). The inquiry quoted some optimistic witnesses who considered that things had changed for the better in terms of speaking up about any concerns, and stated that ‘NHS staff are increasingly willing to speak up for patient safety, even at some personal risk’ (p. 159).
Consequences for the whistleblower
There appear to have been no consequences for the whistleblowers.
Consequences for the NHS
The report produced 19 recommendations on ‘sexualised behaviour’ (recommendations 1 and 2), ‘listening and hearing’ (recommendations 3 and 4), ‘complaints procedures’ (recommendation 5), ‘tracking repeated complaints and concerns’ (recommendations 6–8), ‘sole practitioners’ (recommendations 9 and 10), ‘chaperones’ (recommendations 11–13), ‘local medical committees’ (recommendations 14 and 15) and ‘criminal investigations’ (recommendations 16–19). Only one of these (recommendation 2) was concerned with whistleblowing: ‘we recommend that local policies within all NHS trusts for reporting staff concerns (whistleblowing) should specifically identify “sexualised behaviour” as appropriate for reporting within the confidence of this procedure’ (p. 22).
Quotations in this sections are reproduced from Ayling. 152 © Crown copyright. Contains public sector information licenced under the Open Government Licence v3.0.
Kerr/Haslam153
This inquiry was concerned with understanding the problem of the sexual abuse of psychiatric patients by William Kerr and Michael Haslam at Clifton Hospital, York. In 2000, Kerr was convicted of one count of indecent assault, and in 2003 Haslam was convicted of four counts of indecent assault (p. 4). This was ‘a story of management failure, failed communication, poor record keeping and a culture where the consultant was all-powerful’. It argued that many ignored warning signs or dismissed rumours, and that some chose to remain silent when they should have been raising their voices (p. 5). Moreover, it pointed out that the failure to react and investigate emerged as a common theme in reports such as Shipman,154 Ayling152 and Neale164 (pp. 466–7). This report struck an optimistic tone, claiming to detect a significant change – beginning in the 1990s and carrying through to the present day – in both attitudes and systems. However, it concluded that change of culture was at the heart of real change.
Blowing the whistle
The main whistleblower was Deputy Sister Linda Bigwood, but others who raised concerns included Stephen Brooks, a community psychiatric nurse, and Dr Christopher Simpson, a newly appointed consultant psychiatrist. The inquiry also discussed the GP whistleblowers Dr Wade (on Kerr in 1979), Dr Moroney (on Haslam in 1987) and Dr Moran (on Haslam in 1988) (p. 431), but these GPs who took action to pursue concerns ‘represented the minority’.
In 1983, Bigwood pursued her concerns about Kerr’s alleged sexual misconduct towards a number of patients with the hospital authorities, the district health authority and, beyond that, the regional health authority. However, an inquiry focused on the messenger rather than the message, and, despite letters and meetings setting out Bigwood’s concerns over a period of almost 5 years and involving the most senior NHS managers, no investigation was ever made into Kerr’s practice. The inquiry noted that in the period before 1983, of the 30 concerns alleged to have been raised about Kerr, all but one (below) ‘fell on deaf ears’ (p. 7). The failure of the local GPs to respond is a striking feature of the Kerr story (p. 12).
In 1988, Patient B7 informed Brooks that she had had problems with Haslam and was frightened to see him, and later told Brooks that she had told her GP, Dr Moran, of these problems. Moran and Brooks informed Dr Kennedy, the CEO of the district health authority. However, little was done until the end of 1997, when Professor Sir Liam Donaldson, the then regional director of the NHS Executive of Northern and Yorkshire, set up the ‘Manzoor Inquiry’ into the allegations of sexual misconduct against Haslam between 1984 and 1988, which led to Haslam’s dismissal in September 1998.
Factors
The report pointed to an ‘unhealthy’ culture in which professionals were reluctant to take action against consultants, through either a misguided sense of loyalty or fear of confrontation. It categorised the root causes of this comprehensive failure to attend to patient concerns under five headings: organisational, cultural, structural, professional practice and individual failings. It points to the key factors explaining GPs’ lack of response: the ‘old-boy network’ or professional loyalty, the isolation of GPs, a tolerance of sexualised behaviour, insufficient expertise in psychiatry, confidentiality, the power of consultants, and an ambivalent attitude to relationships between doctors and patients. Rather unusually, compared with other reports, the inquiry stresses the importance of individual ‘agency’ as opposed to collective ‘structural factors’.
Consequences for the whistleblower
Dr Simpson appeared not to have suffered any detriment, but Bigwood, like many other so-called ‘whistleblowers’, suffered professional detriment (p. 8). She was moved from an acute admissions ward to a geriatric ward, which she viewed as a demotion, and she felt that she was being punished for raising a patient’s disclosure (p. 181).
Consequences for the NHS
The inquiry recommended that the DHSC should review the effectiveness of whistleblowing policies and initiatives within NHS-funded organisations (p. 29); that the NHS should adopt and reinforce the recommendations in the Manzoor report (Manzoor Z, NHS Executive Northern and Yorkshire, unpublished) and in ‘Making Amends’ (CMO 2003);165 that there should be a duty of candour imposed on, and accepted by, NHS staff (p. 36); and that all Strategic Health Authorities (SHAs) should set up a staffed telephone helpline, where anonymised (or identified) concerns could be received and processed (p. 66). The inquiry stated that there must be a ‘change of ethos’, but noted that it is one thing for a policy to be put in place and quite another to establish a culture that supports, enables and encourages staff to raise their concerns (p. 664).
Quotations in this sections are reproduced from The Kerr/Haslam Inquiry. 153 © Crown copyright. Contains public sector information licenced under the Open Government Licence v3.0.
Shipman154
The Shipman Inquiry report154 consists of six volumes, with the main material about whistleblowing in volume 5. Harold Shipman was a GP who was convicted in 2000 of murdering 15 patients, and of forging a will. The inquiry identified 215 victims, but ‘the true number is far greater and cannot be counted’154 (volume 1, p. 202).
Blowing the whistle
The Shipman Inquiry tried to avoid using the expression ‘whistleblowing’ whenever possible (p. 319). It noted that there were a number of missed opportunities to raise concerns in 1976 and in 1994, and that over the years some people (e.g. two home helps, a taxi driver and a niece of one of the victims) had concerns, but did not report them. Funeral director Mrs Deborah Bambroffe mentioned these concerns to GP Dr Susan Booth, which contributed to the raising of anxieties within Brooke Practice, which led, some time later, to GP Dr Linda Reynolds’ report to the coroner. He, in turn, passed the information to the police, but the first police investigation concluded that the concerns were without foundation. In short, the inquiry considered that before March 1998 when Dr Reynolds reported her concerns, very few people had had any concerns about Shipman (p. 24). It considered that none of these people were ‘whistleblowers’ per se, as they did not work in the same organisation as Shipman but were merely voicing their concerns to those who they felt were the appropriate authorities. Another feature that set these people apart from the typical ‘whistleblower’ was that most of them were far from confident that their concerns were justified (volume 5, p. 318). 154
Factors
The inquiry pointed to factors that may inhibit reporting, including the unclear duty to report; the fear of being accused of disparagement; the ‘one-off’ or ‘genuine’ mistake; the insufficiency of evidence; ignorance of procedures; the fear of being seen as a troublemaker or ‘maverick’; the fear of recriminations; a concern that making a report might lead to proceedings for defamation; and a feeling of impotence grounded in the belief that, even if the report is made, nothing will be done about it. There is a tendency for attention to be focused on the messenger rather than on the message and the ‘whistleblower’ may suffer reprisals (p. 320).
Consequences for the whistleblower
There appeared to be no consequences for the whistleblowers.
Consequences for the NHS
In contrast to many other inquiries, this inquiry stressed the role of ‘raising concerns’: ‘I believe that the willingness of one health-care professional to take responsibility for raising concerns about the conduct, performance or health of another could make a greater potential contribution to patient safety than any other single factor’154 (p. 23). The inquiry made a total of 190 recommendations. The most relevant appear to include the need for a general practice whistleblowing policy; that primary care trusts should provide information and training about whistleblowing policies directly to practice staff; and the provision of a telephone helpline. The inquiry appeared to be rather optimistic about the future, mentioning ‘radical changes within the NHS’ since Shipman’s arrest.
Quotations in this section are reproduced from The Shipman Inquiry. 154 © Crown copyright. Contains public sector information licenced under the Open Government Licence v3.0.
Francis 2010155,156
Concerns about mortality and the standard of care provided at the Mid Staffordshire NHS Foundation Trust resulted in an investigation by the Healthcare Commission (HCC), which published a highly critical report in March 2009, followed by two reviews commissioned by the DHSC. 155,156
Blowing the whistle
The main material on whistleblowing was given in a section covering pages 279–91. It stated that whistleblowing could take many forms, including passing information to management or colleagues in the same organisation or, in some cases, to some external body or individual or even the media (p. 279). The inquiry was made aware of the facts of only three whistleblowing reports: a consultant who submitted a memorandum to the parliamentary Health Select Committee, and later to the HCC in 2008; allegations of poor care in ward 3 made by a nurse and a health-care support worker; and allegations of falsification of patient documentation in order to avoid the breach of targets in accident and emergency (A&E) departments, and a more general allegation of bullying and harassment made in 2007 against two sisters working in A&E. It concluded that ‘all give cause for concern as to whether individuals who blow the whistle are properly looked after and whether the concerns they raise are properly pursued’ (p. 281), and that ‘the experiences of those involved in these three episodes arising out of raising serious concerns is not encouraging’ (p. 291).
Factors
The inquiry pointed to an organisational culture that included a culture of bullying, target-driven priorities, disengagement from management, low staff morale, isolation, lack of candour, acceptance of poor behaviours, reliance on external assessments, and denial (p. 152). It stated that fear manifested itself in the reluctance of staff, particularly nursing staff, to come forward to the inquiry (p. 166), and that the experience of staff who had raised concerns about colleagues suggests that trust management appeared keener to protect the subject of the concern rather than the informant (pp. 174–5).
Consequences for the whistleblower
In the three whistleblowing cases discussed above, respectively, a consultant was suspended, allegations made in 2005 that closely matched the 2010 inquiry’s main findings were dismissed, and the whistleblower left the trust. The inquiry stated that the handling of these cases was unlikely to encourage others to come forward, and the responses to the investigation of the concerns raised had been ineffective (p. 20).
Consequences for the NHS
The inquiry produced 18 recommendations, but only one focused on whistleblowing. Recommendation 8 states that ‘The Board should give priority to ensuring that any member of staff who raises an honestly held concern about the standard or safety of the provision of services to patients is supported and protected from any adverse consequences, and should foster a culture of openness and insight’ (p. 27). It stated that there was a ‘very real reluctance’ to raise concerns, linked to the ‘widespread belief that the protections offered are theoretical rather than real’. It continued that ‘The most important factor in changing this will not be a new system or policy of protection for whistleblowers, but the fostering of a culture of openness, self-criticism and teamwork’ (p. 409).
Quotations in this section are reproduced from Francis. 155,156 © Crown copyright. Contains public sector information licenced under the Open Government Licence v3.0.
Francis 2013157–159
The Conservative Secretary of State for Health in the coalition government, Andrew Lansley, asked Francis to undertake a wider public inquiry, with three reports resulting from this. 157–159
Blowing the whistle
This included a mix of the same cases as the 2010 inquiry (with names and more details) and some new cases. It discussed doctors who sought to raise issues of concern, but they ‘fared little better than the nurses’ (p. 238).
Factors
There appear to be three main factors why whistleblowing was ineffective. First, the trust had an atmosphere of not welcoming criticism, and the consultants were completely disenfranchised. Second, there was a ‘culture of fear’. Third, although the evidence supports what was heard during the first inquiry regarding the disengagement of doctors, it does not explain why no clinician appears to have taken his or her concerns outside the trust to a regulator, the PCT or the SHA.
Consequences for the whistleblower
Helene Donnelly felt that the atmosphere in the department continued to be poisonous, and she left in 2008. Her experience illustrates one reason why staff may have been deterred from seeking to exploit the so-called protection available to whistleblowers (pp. 235–7). She was subsequently awarded an OBE and is the Ambassador for Cultural Change in Staffordshire and Stoke-on-Trent Partnership NHS Trust. It appears that some staff who made complaints had been suspended pending the inquiry and were so traumatised that they left the trust to work elsewhere (pp. 65–66). The suspension of Dr Singh ‘would have discouraged colleagues from getting involved’ (p. 176). However, Dr Turner experienced no recriminations from within the trust (p. 241).
Consequences for the NHS
The term ‘whistleblowing’ did not feature in the recommendations, which favoured cultural rather than legal remedies: ‘the solution lies in creating the right culture, not in focusing on improvements to whistleblowing legislation, important though such protection is’ (p. 242). The closest approximation was recommendation 12, reporting of incidents of concern relevant to patient safety: compliance with fundamental standards or some higher requirement of the employer needs to be not only encouraged but insisted on. Staff are entitled to receive feedback in relation to any report they make, including information about any action taken or reasons for not acting (p. 243).
Quotations in this section are reproduced from Francis. 157–159 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Summary of findings from the formal inquiries
As Table 6 shows, the inquiries were of different types and focused on different sectors. Not all gave a clear definition of whistleblowing, and the definitions given varied. In many cases there was no clear internal management response, and only Francis11 led to responses by external professional bodies.
| Inquiry | Type | Sector | Definition of whistleblowing | Internal management response | Professional body response |
|---|---|---|---|---|---|
| Kennedy5 | Public inquiry | Acute | Dr Bolsin was not a whistleblower, as, had PIDA been in force, it would not have applied to him, as his disclosures would not have qualified as a ‘qualifying statement’ | No clear response | No clear response |
| Ayling152 | Independent statutory (non-public) inquiry | Acute | No clear definition | In 1998 EKHA became involved in the police investigation | No clear response |
| Neale164 | Independent statutory (non-public) inquiry | Acute | No clear definition | Disciplinary hearing in 1995; negotiated severance package; subsequently employed by two hospitals; alert letter sent by RHA in 1998 | No clear response |
| Kerr/Haslam153 | Independent statutory (non-public) inquiry | Mental health | No clear definition | In 1997 RHA set up an inquiry into Haslam | No clear response |
| Shipman154 | General practice |
The inquiry tried to avoid using the expression ‘whistleblowing’ whenever possible There were no ‘whistleblowers’ per se, as they did not work in the same organisation as Shipman |
No clear response | No clear response | |
| Francis155,156,159 | Independent (non-public) inquiry | Acute | Whistleblowing can take many forms | No clear response | No clear response |
| Francis11 | Public inquiry | Acute | No clear definition | No clear response | BMA; RCN; GMC |
Table 7 summarises the answers to the main research questions. It shows a variety of whistleblowers who took a number of internal and external different routes to raise concerns. There is little on factors that facilitated action, but the overarching factor that inhibits action is broadly concerned with organisational culture. Not all whistleblowers suffered detriment, but in some cases the consequences for them were significant. Finally, only eight of the total of about 820 recommendations in all of the inquiries are directly concerned with whistleblowing.
| Inquiry | Who? | How? | Why? | Factors | With what effect to the individual? | With what effect to the NHS? |
|---|---|---|---|---|---|---|
| Kennedy5 | Dr Steve Bolsin | Various routes within Bristol Royal Infirmary and wider NHS | Concern that operations were taking a long time, and mortality rates were high | ‘Club culture’; ‘culture of fear’ | ‘Unemployable’ in NHS; moved to Australia | 198 recommendations |
| Ayling152 | Sister Penny Moore; Midwife Delphine Bentley; GPs Dr Pickering and Dr Anderson | Report/complaint | Unclear |
Clinical freedom and self regulation; staff hierarchies; lack of openness; a failure to hear; lack of clear professional guidance; preference for the use of informal systems; lack of information sharing or ‘corporate memory’; barriers to making complaints; and the lack of gathering and sharing of ‘soft’ information However, the single most important barrier was the absence of any formal procedure for reporting concerns |
Unclear | 19 recommendations |
| Neale164 | None | NA | NA | NA | NA | 27 recommendations |
| Kerr/Haslam153 | GP Dr Mathewson, in Northern Ireland in 1964; Deputy Sister Linda Bigwood; GPs Dr Wade (on Kerr in 1979), Dr Moroney (on Haslam in 1987) and Dr Moran (on Haslam in 1988); Community Psychiatric Nurse Stephen Brooks | Unclear | Unclear |
‘Unhealthy’ culture Key factors explaining GPs’ lack of response: the ‘old-boy network’ or professional loyalty; the isolation of GPs; tolerance of sexualised behaviour; insufficient expertise in psychiatry; confidentiality; the power of consultants; and an ambivalent attitude to relationships between doctor and patient Stressed the importance of individual, ‘agency’ as opposed to collective, structural factors |
Deputy Sister Bigwood felt that she suffered professional detriment | 74 recommendations |
| Shipman154 | GP from neighbouring practice, Dr Linda Reynolds |
Report to coroner Resulted in police investigation that cleared Shipman |
Concerns of large numbers of deaths, and nature of deaths | Fear of being accused of disparagement; the ‘one-off’ or ‘genuine’ mistake; the insufficiency of evidence; ignorance of procedures; the fear of being seen as a troublemaker or ‘maverick’; the fear of recriminations; a concern that making a report might lead to proceedings for defamation; a feeling of impotence that nothing will be done about it; and fear that the ‘whistleblower’ may suffer reprisals | No apparent negative repercussions | 190 recommendations |
| Francis155,156,159 | Three main whistleblowers: consultant, nurse and health-care support worker, and nurse | Reports/complaints | Unclear | An organisational culture that included a culture of bullying, target-driven priorities, disengagement from management, low staff morale, isolation, a lack of candour, an acceptance of poor behaviours, a reliance on external assessment, and denial | Left employment | 18 recommendations (including one on whistleblowing: recommendation 8) |
| Francis11 | Named whistleblowers from the 2010 inquiry, with more detail | Reports/complaints | Unclear | Atmosphere of not welcoming criticism; consultants completely disenfranchised; ‘culture of fear’ | Left employment | 290 recommendations |
Formal responses to whistleblowing inquiries
This section now follows through from each of the inquiries to the formal responses to the recommendations made by the government and other formal bodies.
Secretary of State for Health (Bristol)
The government166 accepted most of the Kennedy5 recommendations. It was stated that:
Bristol was a turning point in the history of the NHS.
p. 13. 166
However, the government also argued that the organisational or institutional fix for the problems identified in Bristol had already been carried out: the Commission for Health Improvement (CHI); the National Institute for Health and Care Excellence (NICE); the National Patient Safety Agency (NPSA); the National Clinical Assessment Authority (NCAA); the National Service Frameworks; the NHS Modernisation Agency; and the establishment of a new Council for the Quality of Health Care and a new Council for the Regulation of Health Care Professionals (pp. 3–4). 166
However, Kennedy set out a vision in which the patient should be at the heart of the NHS (p. 14),5 which is associated with recommendations 33–36. In particular, the government agreed recommendation 33 on ‘a duty of candour’, meaning that a duty to tell a patient if adverse events have occurred must be recognised as owed by all those working in the NHS to patients (p. 34). 166 Recommendations 106–112 focused on a single national system of reporting adverse events. Recommendations 113–118 were concerned with the reporting of sentinel events. However, the government rejected recommendations 45–46, that codes of professional conduct should be included in the contracts of employment for health professionals, as this was already implicit in employment contracts: ‘we do not believe that we need to go further’ (p. 106). 166 The government agreed ‘in part’ with recommendation 91, that managers as health-care professionals should be subject to the same obligations as other health-care professionals, including being subject to a regulatory body and professional code of practice. The government did not think that it was practicable to establish self-regulation for senior managers.
Home Secretary and Secretary of State for Health (Shipman)
The government167 stressed the acknowledgement of the Shipman Inquiry that the NHS today was in many ways very different from the NHS in which Shipman practised. The response then focused on issues in the fifth report of the use of routine monitoring data and of responding to complaints and concerns. It agreed with most of the 190 recommendations of the Shipman Inquiry. In particular, it noted that it recommended a number of improvements both to encourage the raising of complaints and concerns and to ensure that primary care organisations took effective action on them. These key proposals included PCTs treating expressions of concern as seriously, and in the same way, as complaints; health-care organisations (including general practices) clarifying the arrangements for raising concerns about fellow professionals; and strengthening the statutory protection for whistleblowers. However, it did not consider that PIDA should be amended. It stated that the crucial first step in any system for managing professional performance is the initial identification of cause for concern. In the case of Shipman, a number of potential clues were missed, and similar lessons emerge from the Ayling and Kerr/Haslam inquiries of failure to recognise the significance of concerns expressed (p. 22).
Secretary of State for Health (Safeguarding Patients)
This response168 set out the action that the government proposed taking regarding the four reports on the abuse of trust by health professionals: the Shipman Inquiry’s fifth report, and the reports of the Ayling, Neale and Kerr/Haslam Inquiries. It is noted that although the nature of the abuse differs among the four reports, the underlying question is the same in each case: why did the NHS at the time fail to identify the risk and take the appropriate action to protect patients (p. 5)?
The response noted that, between them, the reports contain a total of 228 recommendations (p. 8). The government agreed that complaints (from patients or their representatives) and concerns (from fellow professionals) can provide vital information in identifying potential risks to patient safety (p. 9). It proposed that all organisations providing services to the NHS should have a written policy setting out the procedures to be followed by staff wishing to raise concerns (p. 52). However, the government was not convinced by Shipman Inquiry recommendation 37, of considering amending PIDA, as staff who disclose concerns to the HCC are already protected by PIDA, as the commission was now a ‘prescribed person’ as a result of the Health and Social Care (Community Health and Standards) Act 2003. 169
House of Commons Health Committee
These reports170,171 considered that the NHS remained largely unsupportive of whistleblowing, and recommended that the DHSC bring forward proposals on how to improve this situation. The key tasks of the government were to ensure that the NHS develops a culture of openness and ‘fair blame’; strengthens, clarifies and promulgates its whistleblowing policy; and provides leadership that listens to and acts on staff suggestions for service changes to improve efficiency and quality (p. 7).
The committee stated that an important measure of an organisation’s safety culture is how it treats ‘whistleblowing’ (i.e. ‘spontaneous reporting outside normal channels by individual members of staff’) (p. 50)172 as a last resort in order to draw attention to unsafe care. It noted that ‘In one sense, “whistleblowing” can be seen as evidence of a failure to learn – people are far more likely to pursue channels outside their own organisation if there has been a failure to act on or even acknowledge concerns raised internally. To many a perceived need for external whistleblowing is in itself a sign that organisational culture is seriously awry’ (p. 64) (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). 172 Despite the ‘theoretical’ protection of PIDA, in practice it seemed that many NHS staff feared the consequences of whistleblowing, and the fear of victimisation may well have been a factor inhibiting staff from whistleblowing at the trust (p. 89). The committee recommended that Annex 1 of the Health Service Circular, HSC 1999/198, The Public Interest Disclosure Act 1998 – Whistleblowing in the NHS173 be recirculated to all trusts for dissemination to all their staff as a matter of urgency.
Secretary of State for Health (Mid Staffordshire NHS Foundation Trust)
The government174 stated that a toxic culture was allowed to develop unchecked that fostered the normalisation of cruelty and the victimisation of those brave enough to speak up. For far too long, warning signs were not seen or were ignored or dismissed (p. 5). The government stated that it would listen to staff who were worried about the quality of care, praising them for speaking up, even if a concern was misplaced (p. 11).
The government noted in its response that it intended to create the role of Chief Inspector of Hospitals, and that this individual would be ‘the nation’s whistleblower’ (p. 17). It stressed the Francis themes of ‘openness, transparency and candour’ (p. 22), and supported Francis’ recommendation on ‘gagging clauses’ (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). It stated that it had already taken a series of steps to enhance the protections available to whistleblowers, including staff contracts, the NHS Constitution, issuing new guidance to employers and extending the national helpline to include staff in social care settings for the first time. In 2013, the Secretary of State for Health wrote to all trusts reminding them again of their obligations to have (PIDA-compliant) whistleblowing policies (p. 47). The government agreed an amendment to the Enterprise and Regulatory Reform Bill, securing PIDA protections for all NHS staff. However, the government rejected Francis’ recommendation of an independent authority to which staff could turn when their own organisation is not listening (p. 50).
British Medical Association (Mid Staffordshire NHS Foundation Trust)
The British Medical Association (BMA)175 stated that it would do all it could to work with others in developing a new culture in the NHS to prevent similar catastrophes from happening again. However, the BMA did not believe that pursuing the recommendation in the report to move to a statutory duty of candour was the right way forward. Rather, there was a need to address the underlying culture in the NHS, which can prevent doctors from reporting concerns, and to look at alternative ways of ensuring that doctors feel able to report their fears, such as a separate reporting route parallel to management.
Royal College of Nursing (Mid Staffordshire NHS Foundation Trust)
The RCN176 revised and publicised its ‘whistleblowing’ guidance for members and reviewed the way it supported them to raise concerns (p. 10). It noted that the terms ‘openness, transparency and candour’ in the Francis report (2013) were wide-ranging, and applied to everything from informal feedback from patients and their families up to and including whistleblowing (p. 23). It pointed out that nursing staff tended to view whistleblowing as a high-risk, low-benefit action (p. 26).
Nursing and Midwifery Council (Francis)
The NMC177 did not explicitly mention whistleblowing. However, it pledged that it would undertake a planned review of the Code and other practice standards, including clear duties of nurses and midwives in relation to complaints handling, communication with patients and raising concerns, in the following year. At a recent listening event, there was some support for a statutory duty of candour but also considerable concern about the consequences of introducing criminal sanctions (p. 14). The response did not support the recommendation that the NMC should be tasked directly with investigating systems issues, as the boundaries of the distinct roles and responsibilities of professional and systems regulators should not be blurred (p. 24).
General Medical Council (Mid Staffordshire NHS Foundation Trust)
The GMC178 stated that in 2012 it launched a confidential helpline for doctors concerned about patient safety, and an online tool to guide them through the process of raising concerns, together with new guidance on raising and acting on concerns about patient safety (p. 5).
Clwyd and Hart
Recommendations in Clwyd and Hart179 focused on four areas for change: improving the quality of care; improving the way complaints are handled; ensuring independence in the complaints procedures; and whistleblowing (p. 32). It needed to be clearly stated how whistleblowers were to be protected, and gagging clauses should not be allowed in staff contracts (p. 34).
Berwick
Berwick180 contained no explicit discussion of whistleblowing. However, it noted that clear warning signals were not heeded (p. 4). It stated that the most important single change was that the NHS should become a system devoted to continual learning and improvement of patient care (p. 5). It produced 10 recommendations, including learning, transparency and patient and carer voice, but nothing on whistleblowing. Its main message was that:
In the end, culture will trump rules, standards and control strategies every single time, and achieving a vastly safer NHS will depend far more on major cultural change than on a new regulatory regime.
p. 11. 180
Keogh
Similarly, Keogh181 contained nothing that explicitly referred to whistleblowing. However, it noted that all 14 trusts had recommendations in their action plans on workforce issues, with four taking forward actions to improve whistleblowing policies (p. 22).
House of Commons Health Committee
The Health Committee report182 wanted to establish a culture that is comfortable with challenge, arguing that the responsibility for establishing a truly open managerial and professional culture that would make the role of the whistleblower redundant lies with each trust board. The section on the Francis report and whistleblowers focused on Helene Donnelly. It considered that, despite the existence of whistleblowing policies, she was not given adequate support when she attempted to raise concerns, which gave little encouragement to other potential whistleblowers to come forward.
In evidence to the committee, Robert Francis182 stated that it has been remarked that he had not made any recommendations specifically called ‘whistleblowers’. He considered that, whatever the system in place, it would not be easy for staff to raise concerns that are not accepted by those for whom they work. Although theoretical protection is provided by PIDA, this is unlikely to be of much reassurance to staff who have to face the wrath of their colleagues. He concluded that:
whistleblowing is only necessary because of the absence of systems and a culture accepted by all staff which positively welcomes internal reporting of concerns. If that culture is absent, then raising concerns external to the system is bound to be a difficult and challenging matter exposing the whistleblower to pressure from colleagues. Therefore, the solution lies in creating the right culture, not in focusing on improvements to whistleblowing legislation, important though such protection is.
The committee observed that the government claimed in its initial response to the Francis Report that it had already taken a number of steps to enhance protection available to whistleblowers. However, although the government’s actions were welcome, as far as they went, the committee agreed with Francis that a legislative solution focused on protecting whistleblowers was missing the point:
whatever legislation you have about whistleblowers, so-called, it will not in itself stop the sorts of things that the Stafford whistleblowers had to put up with from their colleagues, so-called, in the ward.
The committee agreed with Francis’ recommendation of a change in the culture.
Dalton and Williams
This report183 stated that, put simply, candour means the quality of being open and honest (p. 2). Its first recommendation stated that a duty of candour required a culture of candour. The report that it had many parallels with Berwick,180 and wanted to build on his recommendations and reaffirm that a culture of openness and honesty required a full commitment from health and care organisations to create and maintain effective systems of learning and improvement (p. 6). However, even in a culture of greater candour, effective whistleblowing and complaints systems would continue to be vital parts of an open and transparent culture that is committed to improvements in safety and quality (pp. 14–15).
Secretary of State for Health (Mid Staffordshire NHS Foundation Trust)184
The Secretary of State for Health184 made clear that so-called ‘gagging orders’ are unacceptable, and claimed that all health-care professionals would be protected by the provisions of PIDA. It was vital that whistleblowing was taken seriously: in legislation, inspection and education and training. The government also acted on compromise agreements.
Secretary of State for Health (Mid Staffordshire NHS Foundation Trust)185
The second volume of the Secretary of State for Health’s response185 provided a detailed response to each of the 290 recommendations made by the inquiry across every level of the system. It made clear which recommendations were accepted and by whom, and what progress was being made towards their implementation. The DH was to lead the system in providing an annual report on progress across the system each autumn (p. 4), and the Health Select Committee in 2013 confirmed that it agreed with the inquiry that it should monitor the implementation of all of its recommendations.
The government accepted recommendation 2 on a shared culture; accepted, in principle, recommendation 7, that all NHS staff should be required to enter into an express commitment to abide by the NHS values and the Constitution, both of which should be incorporated into the contracts of employment; and accepted recommendation 12, that the reporting of incidents of concern relevant to patient safety needs to be insisted on. It accepted, in principle, recommendation 98, that reporting to the National Reporting and Learning System of all significant adverse incidents should be mandatory on the part of trusts. It accepted most of the recommendations on openness, transparency and candour, but accepted in principle recommendation 178 on incorporating the NHS Constitution into contracts of employment, and recommendation 181 on a statutory obligation to observe a duty of candour for health-care providers, and for registered medical practitioners and registered nurses and other registered professionals. However, it did not accept recommendation 183 of making it a criminal offence to make untruthful statements, although it agreed ‘with the intention behind this recommendation’.
Secretary of State for Health (Francis inquiries)
The government stated that the online supporting annex to this document186 set out, in detail, the substantial progress made regarding the 290 recommendations of the public inquiry. However, although this is important:
perhaps the most important point is that the ongoing need to change the culture in the NHS to one of patient-centred, continual improvement in care and safety.
p. 17. 186
It noted that the CQC and its chief inspectors would report annually to the Secretary of State for Health with their assessment of how well the NHS was doing in taking forward the recommendations on both the public inquiry and the Freedom to Speak Up review (p. 20). 2
Whistleblowing plays an important role in raising issues and holding organisations to account across many sectors of life, such as the aviation and off-shore oil industries, as well as the NHS. The government has introduced a number of measures to make it easier for those working in the NHS to raise concerns, including ‘unequivocal guidance’, adding new bodies to the Prescribed Persons list, applying the concept of vicarious liability to the whistleblowing legislative framework, and writing in March 2014 to all chairpersons in NHS trusts and foundation trusts in England, to reiterate the vital importance of fostering a culture of openness and transparency in the NHS in which concerns about care can be raised, investigated and acted on (p. 31). Finally, the Secretary of State for Health commissioned Francis to carry out an independent Freedom to Speak Up review (below).
Francis
Francis2 stated:
I would have liked to report to you that there was in fact no problem with the treatment of ‘whistleblowers’ and their concerns. Unfortunately, this is far from the case. The effect of the experiences has in some cases been truly shocking, and lives can be ruined by poor handling of staff who have raised concerns.
p. 5. 2
He went on:
There is a need for a culture in which concerns raised by staff are taken seriously, investigated and addressed by appropriate corrective measures.
p. 6. 2
Francis pointed to:
a remarkable consistency in the pattern of reactions described by staff who told of bad experiences.
p. 8. 2
Although PIDA theoretically provides protection for whistleblowers, this legislation was limited in its effectiveness. At best, it provided a series of remedies after detriment, including loss of employment, had been suffered. The review included two recommendations, 20 principles and 38 actions (p. 22).
Francis cited the words of Dame Janet Smith in the Shipman fifth report (see Chapter 7, Research objective 4: learning from the findings of formal inquiries), that professionals raising concerns ‘could make a greater potential contribution to patient safety than any other single factor’ (above), adding that her statement rang as true now as it did then. He reported that in recent years there had been a number of reviews that had considered whistleblowing or related issues in the NHS and other sectors [e.g. Francis;11,155,156 National Audit Office;187,188 Public Concern at Work (PCAW);162 Department for Business, Innovation and Skills189].
He pointed to the complexity of the current legal whistleblowing position, and noted that the law seeking to protect whistleblowers is cast entirely in an employment context (p. 49). From the evidence, the following themes emerged: the need for culture change; improved handling of cases; measures to support good practice; particular measures for vulnerable groups; and extending legal protection (p. 88). There was near-universal agreement that the most important factor affecting people’s willingness to speak up or raise concerns is the culture of the organisation (p. 94).
Francis considered whether or not the term ‘whistleblowing’ itself contributed to the barriers, and gave serious consideration to recommending that the term ‘whistleblower’ should be dropped (p. 100). He concluded that, although the existing legislation is weak, he did not recommend a wholesale review of the ERA 1996, but considered that there are two steps that should be taken: extending the list of prescribed persons to ensure that NHS workers are protected if they raise a concern with any relevant person/body, and extending statutory protection to all students studying for a career in health care rather than just student nurses. In addition, consideration needed to be given to extending discrimination law to protect those who make a protected disclosure from discrimination either in the ERA 1996190 or in the Equality Act 2010191 or to finding an alternative means to avoid discrimination on these grounds (p. 192).
Hooper
Hooper192 was an independent review for the GMC of how it engages with individuals who regard themselves as whistleblowers. Like Francis, Hooper cited Dame Janet Smith (2005) in the Shipman fifth report (above) (p. 2). He stated that there was considerable evidence that, in the workplace, whistleblowers may well suffer, or believe that they will suffer, reprisals at the hands of an employer or fellow workers (p. 5). Hooper was concerned that employers may use the process of making an allegation to the GMC about a doctor’s fitness to practise as an act of retaliation against a doctor who had raised concerns (p. 7). He made a total of eight recommendations to reduce ‘retaliation by referral’, including declaring if the doctor being referred had raised concerns about patient safety or the integrity of the system, and fully training investigators to understand ‘whistleblowing’, particularly in the context of the GMC and the NHS; and a simple, confidential and voluntary online system to record concerns, run by an organisation independent of the regulators.
House of Commons Health Committee193
This report193 stated that the treatment of whistleblowers remained ‘a stain on the reputation of the NHS’ (pp. 3–4). PIDA was a deterrent rather than a remedy, and that if an employee had to have recourse to PIDA’s provisions then his or her prospects were already substantially impaired (p. 35).
The solution appeared to mean establishing a reporting culture that paralleled the open reporting culture in other safety-critical sectors such as aviation and nuclear energy: in which ‘the concept of the whistleblower is quite simply redundant’ (p. 36). It recommended that there should be a programme to identify whistleblowers who have suffered serious harm and whose actions are proven to have been vindicated, and provide them with an apology and practical redress (p. 36).
Secretary of State for Health
This government response194 stated that the shocking evidence amassed by Francis2 detailed the price paid by far too many NHS staff who spoke up with concerns about the quality of care. It agreed with Francis’ recommendation of a support scheme to help whistleblowers to find alternative employment if they can demonstrate that they are having difficulty finding employment as a result of raising concerns.
The DHSC accepted Francis’2 two overarching recommendations, and consulted on a package of measures to implement these (p. 15). The consultation showed that most responses supported the Freedom to Speak Up guardian role, while the majority of these supported the INO role hosted by the CQC (p. 18). It favoured Francis’2 recommendation that the Freedom to Speak Up guardian should be appointed by the chief executive of the organisation to act in a genuinely independent capacity, and should raise concerns with the trust’s chief executive or the board. However, the government recommended that the guardian be able to raise concerns with the INO if they had lost confidence, or if they considered that good practice had not been followed, in how the organisation handled concerns (p. 28).
Concluding remarks
Despite the thousands of pages and hundreds of recommendations, and assurances of learning over a period of nearly 15 years, there remain many cases of institutional failings (e.g. PCAW162) and poor treatment of whistleblowers (e.g. Hammond and Bousfield,161 Sawer and Donnnelly195). Although it is difficult to firmly establish the impact of any changes associated with the inquiries, the conclusion perhaps mirrors the verdict of Ashton196 that PIDA’s achievements in effecting a tangible, sustainable cultural shift towards transparency in the UK workplace appear incremental at best.
In the following chapter, we move on to review the legal framework for whistleblowing, which underscores the fragmented legal background against which these cases unfolded.
Chapter 5 The legal underpinnings of whistleblowing
Introduction
In this chapter, we move on to consider the legal basis of whistleblowing. We begin by examining the employment law perspective of whistleblowing in the NHS and explore the situations in which breaking a duty of trust and confidence can be held to be justifiable and safeguarded first at common law and then under specific provisions of the ERA 19967 as amended by PIDA8 and subsequent legislation. We note the problems with both the substantive law and with its implementation. Second, we consider the question of human rights and freedom of speech in the NHS and the potential but also the problem in bringing such rights challenges. Third, the chapter considers whistleblowing from regulatory and open government perspectives within the NHS. Finally, drawing on international comparisons, the chapter considers some alternative legal and regulatory approaches that could be taken. This does not attempt to provide a wholly comprehensive overview of comparative approaches given the scope of this issue and the diversity of questions addressed in the literature, but it is informed by existing work in the area (e.g. discussion in Council of Europe,197 Osterhaus and Fagan,198 Dworkin and Brown199 and Fasterling200). It should be noted that there is no specific comparable legislation in another jurisdiction applicable in the context of health care; rather, selected examples of approaches are utilised to suggest possible alternative models that might be taken forward in the future.
The research methods employed involved searches being undertaken of primary legal sources (i.e. statutory and case law materials). Secondary literature searches were undertaken in legal databases Lexis® (LexisNexis, London, UK), Westlaw (Thomson Reuters, CA, USA), HeinOnline (William S Hein & Co Inc., Buffalo, NY, USA) and Google Scholar (Google Inc., Mountain View, CA, USA). Reference was also made to published books and edited collections.
Context and structure
There has been major recent controversy concerning whistleblowing in the NHS, but in fact legal controversy in this area stretches back many decades. In 1967, in the context of conditions in mental health hospitals, the then Minister of Health, Kenneth Robinson, when asked whether or not he would safeguard whistleblowers from victimisation, responded, ‘yes certainly’. 201 Yet nearly 50 years later whistleblowing and whistleblowing safeguards remain a major problem for the NHS. More recent legal developments concerning whistleblowing in the NHS can be seen as deriving from the case of Graham Pink, a nurse at Stockport General Infirmary, who blew the whistle on poor patient care at the hospital in the late 1980s. 202 Pink was disciplined for breach of patient confidentiality when relatives claimed that they could identify their elderly family members from the descriptions given. It led to an employment tribunal case that was eventually settled by the NHS body on the basis of escalating costs. 203 This was followed by findings at the Ashworth Special Hospital Inquiry that staff at who had spoken out had been threatened and victimised. 204 Numerous whistleblowing cases and developments across a range of areas led to the establishment of the organisation PCAW, which provides support for whistleblowers. In 1992, there was an unsuccessful attempt to introduce statutory safeguards in the form of the NHS Freedom of Speech Bill introduced by Derek Fatchett MP (Member of Parliament). 205 Although this was a time of major controversy in relation to NHS whistleblowing, there were also major controversies surrounding standards in public life and safety in transport in the workplace, as exemplified by the Nolan Report, the Clapham Junction Rail Crash Report and the Piper Alpha disaster (paragraphs 1 and 03–1.1.2). 206 Legislation providing some protection for whistleblowers was finally enacted in 1998 in the form of PIDA,8 and we explore these provisions below.
Writing in the US context in 2012, Robert Vaughan suggested that there were four perspectives in whistleblowing law that had an impact on legal standards and protections. 207 Although these typologies do not totally translate owing to jurisdictional differences, nonetheless these can be seen as reflected in relation to how whistleblowing in the NHS context is viewed. The first of these typologies is that of employment law. As we will see, much of the discussion in England and Wales concerns employment law itself and, indeed, that is the perspective of the Freedom to Speak Up report. 2 Second, Vaughan sets out an open-government perspective. In relation to the NHS, this can be seen as whistleblowing facilitating decision-making processes in the public sector in the public interest. Third, whistleblowing can be considered from a market or regulatory perspective: seen as facilitating professional regulation (e.g. blowing the whistle on poor performance by clinicians). Finally, it can be seen from a human rights perspective. Of course, although these are separate perspectives they are nonetheless inter-related. An employment perspective can incorporate a human rights perspective; a regulatory perspective can incorporate an open-government/decision-making basis.
This chapter proceeds as follows: first, we explore employment law and blowing of the whistle in the public interest, and in particular the role of PIDA. 16 We then look at a human rights perspective on whistleblowing, before taking a regulatory perspective that has come much to the fore with the Freedom to Speak Up report of 2015. 2 The chapter rounds off with a discussion of some of the implications of this legal background for whistleblowing in the NHS.
Employment law and blowing the whistle in the public interest: the Public Interest Disclosure Act 1998
Introduction
The PIDA8 was enacted in 1998, some 3 years before the Bristol Royal Infirmary Inquiry Report was published. The 1998 Act was reformed by the Enterprise and Regulatory Reform Act 2013. 208 The employer–employee relationship is one of trust and confidence. 206 Such a duty is implied in the employment relationship. 209,210 In addition, employment contracts may include specific confidentiality clauses. The emphasis is, therefore, on non-disclosure rather than on freedom of expression. However, the law sanctions departure from the standard boundaries of the employment relationship in certain situations in which this is in the public interest. 211 Today, individuals who have blown the whistle and suffered adverse consequences in the employment relationship may be safeguarded through being able to institute proceedings in employment law for unfair dismissal. Here, first we consider those situations in employment law cases in which the court may be prepared to hold that employees may, in fact, have a duty to disclose. Second, we consider the application of PIDA8 provisions that amended the ERA 19967 and safeguard what are known as ‘protected disclosures’ by employees.
In the past, the courts have considered whether or not an employee could have a duty to raise concerns. In Bell v Lever Bros, the House of Lords rejected a claim that an employee could be placed under a duty to disclose information. 212 However, subsequently it was held that there was a distinction between an employee reporting his own wrongdoing and having an obligation to report the wrongdoing of others. 213 The court also held that a distinction could be drawn between reporting past wrongdoing and reporting ongoing wrongdoing. In Rochern an obligation was placed on Roques, a senior employee who became aware of the fact that employees within the organisation had set up rival companies while still employed by the original employer to act in competition with that organisation. 206 That case concerned an individual reporting subordinates, but the court has also confirmed that this can extend to reporting superiors. 214 The seriousness of the wrongdoing is important here in determining whether or not there is an obligation. 215,216 There have also been some indications that the court may be prepared to find that an employee should disclose their own wrongdoing. 217 This could mean that there was no real distinction between drawing attention to your own wrongdoing, as opposed to that of others, and being seen as part of the developing case law concerning the duty of trust and confidence in the employment relationship. There may also be duties placed on an employer to investigate wrongdoing in an organisation. 214 The notion of such positive employment duties to raise concerns could, of course, have very broad implications; however, to date it appears that such legal principles have not been utilised further in general, either by the court or in the specific context of disclosure in the NHS.
In examining the scope of the PIDA legislation, we will now focus on several distinct areas: the employees who come under the scope of the Act, the types of disclosures that are protected and the actors to whom disclosures can lawfully be made. We will then consider the role of contractual confidentiality clauses (so-called ‘gagging clauses’), before looking at the remedies available when detriment has been suffered and the impact of the legislation in relation to whistleblowing in health care.
Employees under the Public Interest Disclosure Act
The ERA 19967 safeguards disclosures made by a range of employees. ‘Employees’ refers to those in a contractual relationship and also would include, for example, nurses employed via an agency working for the NHS. 218,219 The PCAW Whistleblowing Commission has suggested that the legislation should be extended to incorporate others such as applicants for jobs, student health professionals, volunteers and interns, and non-executive directors. 162 The scope of the legislation was extended to include primary health-care professionals, such as GPs and nurses, by amendments made to the ERA 1996 by the Enterprise and Regulatory Reform Act 2013, section 20. 208 Similarly, the Freedom to Speak Up report2 supported an extension to job applicants and to students. Nursing students have now been included via regulations amending the primary legislation in 2015. 220 However, this does not appear to apply to all students.
Blacklisting was a concern raised by the PCAW Commission and in Freedom to Speak Up. 2,162 As of 2010, legislation has provided protection for trade unionists from blacklisting. 7,221 In addition, following the FTSU report, section 149 of the Small Business, Enterprise and Employment Act 2015222 inserts a new section, 49B, into the ERA 2006, providing that the Secretary of State may make regulations prohibiting a NHS employer from discriminating against a job applicant when it appears to the prospective employer that the applicant has made a ‘protected disclosure’ under the Act. An action will be discriminatory when the employer refuses the application or ‘in some other ways treat the applicant less favourably than is or would be the case in relation to other applicants in relation to this contract/post or office’ [section 49B(3) ERA 1996]. 7 This is potentially a very important provision if it operates correctly in addressing concerns around the ‘blacklisting’ of whistleblowers.
Protected disclosures
The ERA 19967 safeguards what are known as ‘protected disclosures’. These are defined under section 43A as:
a qualifying disclosure (as defined by section 43B) which is made by a worker in accordance with any of sections 43C to 43H.
Section 43B then goes on to set out what constitutes such ‘qualifying disclosures’:
In this Part a ‘qualifying disclosure’ means any disclosure of information which, in the reasonable belief of the worker making the disclosure, [is made in the public interest and] tends to show one or more of the following
that a criminal offence has been committed, is being committed or is likely to be committed,
that a person has failed, is failing or is likely to fail to comply with any legal obligation to which he is subject,
that a miscarriage of justice has occurred, is occurring or is likely to occur,
that the health or safety of any individual has been, is being or is likely to be endangered,
that the environment has been, is being or is likely to be damaged, or
that information tending to show any matter falling within any one of the preceding paragraphs has been, or is likely to be deliberately concealed.
A disclosure of information is not a qualifying disclosure if the person making the disclosure commits an offence by making it.
It should be noted from the outset that the courts have taken a purposive approach and that the aim of the Act is to facilitate responsible whistleblowing. 223,224 However, as Lewis et al. 206 have noted, ‘responsible whistleblowing may in some cases be in tension with the legislative objective of encouraging those in a position to sound the early alarm to come forward and do so to an appropriate person’. The words ‘is made in the public interest’ were included in section 43B in the amendments made to the 1998 Act by the Enterprise Regulatory Reform Act (ERRA) 2013 in 2013. The Act excludes matters of personal rather than public interest. The PCAW Commission expressed concern at this inclusion of ‘public interest’ into this provision, as it could result in unpredictability and a consequent increase in litigation (p. 17). 162 Lewis has argued that it may be difficult to hold that a belief is reasonable in the case of whistleblowers who act alone. 225
However, initial judicial determination suggests that a public interest requirement itself may not be difficult to establish. Ashton196 suggests that it would be rarely the case that a workplace matter would solely affect one employee as opposed to having broader implications. It is anticipated that the Court of Appeal will provide useful guidance in the appeal in Chesterton. This was originally due to be heard in the Court of Appeal in 2016, but the hearing was postponed. 226 In relation to failing to comply with a legal obligation under section 43B, this does not extend to something that may be a moral rather than a legal obligation, or to general allegations, for example that an employee ‘is concerned with financial probity’ [see Lewis et al. 206 at paragraph 3.82 and Sim v Manchester Action on Street Health (EAT/10085/01)227]. Section 43B also makes reference to disclosure of health and safety risks. Although trivial concerns are not excluded, the nature of those concerns will be noted in determining whether or not they fall within the statutory provision. 228
The 2013 legislative amendments have removed the requirement that the disclosure was in ‘good faith’ following recommendations in the Shipman report. 154 Ashton notes that this had proved difficult in relation to litigation196 and that, as Lewis et al. 206 have commented, ‘the public interest in encouraging the disclosure of concerns may be no less compelling because there are ulterior motives’. Nonetheless, as Ashton196 comments, an element of good faith remains in relation to remedies, as a tribunal has a statutory power to reduce a remedy by up to 25% if the disclosure is not made in good faith [ERRA 2013, sections 18(4)–(5)].
A qualifying disclosure refers to information disclosed by a worker in accordance with sections 43C to 43G. A disclosure may fall within this provision in a situation in which the belief is shown later to be incorrect. 229 There is some judicial guidance in relation to the operation of this provision. When a worker believes that a criminal offence has been committed and such a belief is ‘objectively reasonable’, the possibility that the belief is wrong or that the information does not concern a criminal offence will not, by itself, mean that the belief is unreasonable. 229 This test has both a subjective and an objective element. 224 In addition, the employment appeal tribunal in Geduld v Cavendish Munro Professional Risks Management Ltd230 stated that there was a difference between the communication of ‘information’, which is protected under the Act, and making what are ‘allegations’. In that case, Mr Justice Slade indicated that ‘health and safety requirements are not being complied with’, which would be unprotected allegations. In contrast, ‘to say the wards of the hospital have not been cleaned for two weeks and sharps were left lying around’ is information that is protected under the legislation. Further consideration of what constitutes ‘information’ was subsequently provided in the case of Kilraine v London Borough of Wandsworth in 2016231 and see also discussion in Aamod and Paulin. 232 Here, Mr Justice Langstaf stressed that there is not a ‘ready-made’ distinction between what constitutes information and what amounts to allegations. He noted that the sole issue is whether or not this is disclosure of information. 231
The PCAW Commission suggested that it would reduce uncertainty if the government or the employment appeal tribunal provided guidance as to what constituted the public interest (p. 18). 162 We return to the question of the efficacy of the provision of further formal guidance and/or a statutory Code of Practice below.
Actors to whom disclosures can lawfully be made
The Act operates to safeguard, and thus effectively privilege, what Lewis et al. 206 class as ‘three tiers’ of disclosure. First, protected disclosures include disclosure to an employer (section 43C). This is unsurprising, as it retains disclosure within the relationship of trust and of confidence. Disclosure to a legal advisor is also included (section 43D). This is in line with the special position accorded to lawyer–client disclosures more generally in English law through the doctrine of legal professional privilege. This provision does not include disclosure to persons who may be performing related advice functions [e.g. trade union representatives (p. 23)]. 162 Disclosure to Ministers of the Crown is also safeguarded in this way (section 43E), as is finally disclosure to what is known as a ‘prescribed person’, as set out in Regulations (section 43F). Included in this category are the CQC, NHS Commissioning Board, NHS Trust Development Authority and Health and Safety Executive [Public Interest Disclosure (Prescribed Persons) Order 2014: SI No 2418] and Monitor and Healthwatch [Public Interest Disclosure (Prescribed Persons) (Amendment) (No 2) Order 2015]. In addition, other health-care regulators such as the General Chiropractic Council, General Dental Council, General Pharmaceutical Council and Health and Care Professions Council are included. A new section, 43FA, also provides for the production of regulations by the Secretary of State requiring a prescribed person to produce an annual report in relation to disclosures made to them by workers. Such reports, however, would not require detailed information that would allow workers or employees be identified from it.
The Act thus operates to facilitate internal organisational disclosure. As the Handbook on the NHS Constitution for England notes, those individuals who raise reasonable concerns internally will be protected. 233 They are also expected to raise such concerns as soon as possible. But if this were all, the legislation would be of limited use. The Act goes beyond this and does sanction external disclosures under two further provisions: sections 43G and 43H.
First, section 43G outlines further criteria for disclosure, including, but not necessarily, in a situation in which the employee has already raised concerns internally but, for example, nothing has happened and the situation that led to the original disclosure (e.g. poor standards of health care) is continuing (this section was amended by the Enterprise and Regulatory Reform Act 2013). 208 It states that disclosures may be made when a worker reasonably believes that the information/allegation is substantially true, that disclosure is not for personal gain, that it is in all circumstances reasonable to disclose and that the criteria set out in section 43G(2) are complied with. These criteria are that the worker has reasonable belief when the disclosure is made that they would be subject to detriment from the employer. The second provision is when there is no prescribed person to disclose to and the worker reasonably believes that, if they disclose to their employer, evidence will be concealed or destroyed, or they have previously disclosed what is substantially the same information either to the employer or externally under the provisions in section 43F (discussed below). Here the onus is placed on the employee to demonstrate reasonable belief that he or she believes this to be true. The section does not protect disclosures that are made for personal gain. This disclosure must be reasonable; relevant factors include to whom the disclosure is made, the seriousness of the matter, whether or not it is ongoing and whether or not it has been made in breach of a duty of confidentiality [section 43G(3)(d)]. So, for example, if a health-care professional had disclosed confidential patient information, this would be relevant. 234 Vickers suggests that, in such a situation, although ‘disclosure to the press would be very difficult to justify; disclosure to another medical practitioner may be acceptable’. 234
Third, in addition to section 43G, there is a further provision that sanctions directly blowing the whistle outside the organisation. Section 43H provides that, in cases of disclosure of exceptionally serious failure, there is no need to go through internal procedures before disclosing. The worker must reasonably believe that the information disclosed or the allegations made are substantially true; in addition, the disclosure must not be made for personal gain, and the failure must be exceptionally serious. In these circumstances it is reasonable to make the disclosure, taking into account to whom it is made. Vickers suggests that workers who disclose such things as malpractice and incompetence or who disclose in situations such that adequate care cannot be given will come within the provisions. 234
The Act provides that the employee has a right not to be subject to detriment from his specific disclosure [section 47(B), ERA 2006]. 7 What constitutes detriment is not defined in the legislation. Freedom to Speak Up2 gives as examples ‘bullying, harassment or victimisation’ (paragraph 2.2.7). Some judicial guidance has been given on this point. 235 It is suggested that it will be construed at least as wide as, and possibly wider than, the meaning given to detriment under the Equality Act 2010191 (paragraph 7.13). 206 This does not only relate to detriment from an employer but has also been extended to cover detriment by a colleague (section 19 of ERRA and overturns decision in Fecitt & Others v NHS Manchester [2011] EWCA Civ 1190). 236 It does not apply only to employment but to the ‘employment field’ and this will include, for example, provision of a reference after employment. 237 In ascertaining detriment, an action would be a detriment only if both this employee was actually disadvantaged and in this situation a reasonable employee would be disadvantaged. 238 It also extends to disclosures not made to the current employer. 239 Although threats of detriment are not explicitly included in the legislation, it is envisaged that they would be implicitly included (paragraph 7.14). 206
The Act imposes a vicarious liability on employers and also a personal liability on workers. When a worker is dismissed and this is because of a protected disclosure, or the protected disclosure is the principal reason for the dismissal, this will be an unfair dismissal under section 103A. The causation tests for detriment and dismissal are different, in detriment the test being more favourable for whistleblowing claimants. It has been suggested that these provisions should be amended to bring the test for dismissal in line with the test for detriment.
Contractual confidentiality clauses
One point of controversy for some time has been the use of contractual confidentiality clauses that are inserted with the aim of stopping further disclosure by an employee; these are at times referred to as ‘gagging clauses’. 240 The report on the Mid Staffordshire Inquiry commented that use of such ‘disparagement clauses’ is widespread and that:
Any clause restricting an individual’s liberty to make a disclosure or imposing a duty of confidentiality should be limited to the minimum necessary to protect the public interest and not the reputation of any organisation or individual.
p. 1458.
The Mid Staffordshire report recommended that gagging clauses should be prohibited in relation to health-care organisations, regulators and commissioners to the extent to which these prohibit what is bona fide disclosure of public interest questions of safety of care. However, there are examples of continued use as in relation to a whistleblowing NHS consultant in the Baby P case, in which multiple opportunities were missed by health and social care agencies and Great Ormond Street Hospital to intervene and stop cruelty and neglect. 241 In 2013, the Secretary of State for Health, Jeremy Hunt, told the press that gagging orders in the NHS would be banned. 242 However, the use of gagging clauses continued. 196 The amended section 43J of ERA 2006190 now provides that:
Any provision in an agreement to which this section applies is void in so far as it purports to preclude the worker from making a protected disclosure.
This section applies to any agreement between a worker and his employer (whether a worker’s contract or not), including an agreement to refrain from instituting or continuing any proceedings under this Act or any proceedings for breach of contract.
This does not mean that such a clause could not be inserted into a contract, but it is suggested that if there was a breach of a clause relating to a protected disclosure this would not be enforceable. 243 This still means that an employee would need to use legal remedies to ultimately enforce their rights here. In addition, as Freedom to Speak Up notes, the provision does not ‘cover clauses that impose on either or both parties to the agreement or contract a duty to maintain confidentiality in other respects, such as in relation to financial details or the personal details of third parties‘ (paragraph 2.2.11). 2 Freedom to Speak Up states that it had not seen any settlement agreements that were not compliant with the law but did see some that seemed ‘unnecessarily draconian or restrictive’ and that ‘there is an atmosphere of fear and confusion surrounding the obligations of confidentiality in such agreements so as to make them a deterrent against public interest disclosures even where they do not have that effect in law’ (paragraphs 7.4.20 and 7.4.21). 2 The report recommended that such clauses should be:
drafted in a way that is easily understood by both parties and are genuinely in the public interest.
Paragraph 7.4.26. 2
However, this raises the question of whether or not such clauses can ever be seen to be in the public interest, an issue we return to below.
Remedies
Actions under the ERA may be brought against the employer or an employee who is claimed to be responsible for the detriment suffered. When a worker has not been dismissed, a declaration can be sought to establish that the complaint was justified along with compensation. Dismissal as a result of a protected disclosure will constitute an unfair dismissal. 222 If the worker is found to be unfairly dismissed, then they can be awarded compensation, and an order may be made for their reinstatement. Historically, reinstatement is rare and, moreover, employers are not required to comply with this, but should they not do so a further award of compensation may be made save where they can demonstrate that it is not practicable to do this (S117). 7 Freedom to Speak Up commented that it was not practicable to force individuals to be reinstated but that the NHS ‘has a moral obligation to support those staff whose performance is sound but who have suffered as a result of speaking up.’ (paragraph 9.10). 2 The extent to which this can be effectively achieved, however, remains an issue.
Impact of the legislation in relation to whistleblowing in health care
Although legislation provides some safeguards for those who ‘blow the whistle’ in the NHS, this is not by any means a panacea for facilitating whistleblowing in practice. 244 Although the legislation has been in existence for some 18 years in practice, how effective has it been in the health-care context? In relation to the impact of the Act in general, commentators have been equivocal, with suggestions that it has led to limited change. 196 In some contexts, it has been suggested that the legislation is more deterrent than remedy (paragraph 107). 245 Gobert and Punch246 comment that for the honest and well-meaning whistleblower the Act may be seen as ‘a trap’. Not only are organisations effective at intimidating troublemakers but, in addition, finding new employment for the whistleblower – even if they are ultimately vindicated – may prove very difficult indeed. It remains to be seen whether or not the new provisions aimed at addressing blacklisting in the NHS will remedy this situation.
There is also a perception that, although groundbreaking in its time, the legislation is dated and has been overtaken in the approach taken in other jurisdictions. Blueprint has argued that, set against international standards addressing coverage, protection and disclosure to remedies and relief administration and engagement drawn up by international organisations and NGOs with whistleblower protection, the PIDA provisions contain only 37% of the standards (pp. 15–17). 247 Enforcing the legislation is also a problem. The introduction in July 2013 of fees for claimants bringing employment tribunal proceedings has led to a significant drop in the number of cases (paragraph 2.2.9). 2 The cost of upfront lawyer fees may prove a considerable deterrent to taking a case forward with ‘typical’ legal costs of between £800 and £2500, and in some cases much higher (p. 35). 247 Measures inhibiting access to justice in this way deterring whistleblowers may ultimately result in the NHS having less opportunity to learn from its mistakes.
In the context of health care specifically, the impact of the legislation is difficult to properly assess for a number of reasons. Although some cases have been litigated, these may be seen as the tip of the iceberg. In a case with a strong claim, the parties would be encouraged to settle rather than taking the litigation forward in tribunal. It is uncertain how many such settlements have been reached by various NHS bodies during the period the Act has been in force. Inevitably, the use of the legislation itself at tribunal demonstrates failure: it shows that raising concerns has not been respected within the institution. Statistics from the Ministry of Justice indicate that the proportion of total claims successful at hearing have varied between 3% and 5%. 162 The vast majority of claims are either settled at Acas (www.acas.org.uk/; accessed 5 July 2018) or withdrawn or privately settled. 196 Greater information may be available in the future. S. 148 of the Small Business, Enterprise and Employment Act 2015222 provides that there is a power for the Secretary of State to require certain bodies listed on the Public Interest Disclosure (Prescribed Persons) Act 2015248 to provide annual reports in relation to disclosures by workers. Further requirements in relation to this disclosure are to be set out in regulations. This may enhance transparency and also identify problems (e.g. if there are a large cluster of such cases in particular NHS bodies).
Whistleblowing: a human rights perspective
Another perspective that can be taken on whistleblowing is that of human rights. 207 Here we consider the potential impact of fundamental rights considerations from the perspective of the European Convention on Human Rights (ECHR), which is now enshrined in domestic law following the Human Rights Act 1998. 249 Three human rights are particularly pertinent in this context: Article 8 (the right to privacy), Article 9 (freedom of conscience, religion and belief) and Article 10 (the right to free speech). It should be noted from the outset that none is an absolute right: all are expressed in qualified terms with reference to the rights and freedoms of others, the protection of health or morals or the reputation or rights of others. This is important when, as below, we examine the interpretation of these provisions. Freedom to Speak Up, despite its title, did not frame its discussion in terms of fundamental human rights in general nor in relation to freedom of speech – this is in contrast to, for example, the Fatchett Freedom of Speech in the NHS Bill produced in 2012, and to the approach of the Council of Europe, which we turn to consider next.
Council of Europe and whistleblowers
In 2014, the Council of Europe issued a recommendation on the protection of whistleblowers. 250 It viewed whistleblowing as a ‘safe alternative to silence’ and as something that could ‘reinforce the value of facilitating channels to report risk or wrongdoing’ (p. 14). 251 Nonetheless, whistleblowing was also regarded as a balancing exercise between employers’ rights and interests and the rights of the public to know when their interests were at risk or when laws were broken (p. 15). 251 The Council of Europe sees whistleblowing as aligned with the work of the Group of States against Corruption, which monitors the corruption-prevention standards of the Council of Europe. 251,252
The Council of Europe defines a ‘whistleblower’ as ‘any person who reports or discloses information on a threat or harm to the public interest in the context of their work-based relationship whether it be in the public or private sector’ [Appendix to Recommendation CM/Rec (2014) 7, paragraph a]. 251 It provides that normative, institutional and judicial frameworks should be designed with the aim of facilitating public interest reports and disclosure. This should extend to all persons in both the public and the private sector, and extend beyond, in some cases, those in a current employment relationship. It is recommended that member states undertake a review of law, professional codes and internal rules to ascertain the scope of a possible normative framework and provides guidance on what this can include. The emphasis is on proportionate measures. Channels for reporting structures should also be established concerning both internal and external disclosures, including those to the press or MPs (paragraph 11)251 (see Appendix 3). The recommendation also provides that, in general, whistleblowers should be entitled to have their confidentiality maintained ‘subject to fair trial guarantees’. Moreover, safeguards should be given against retaliation, either direct or indirect, against whistleblowers (paragraph 21). 251
The recommendation noted above illustrates the multidimensional elements of whistleblowing and the danger in this being seen in the legal context largely through the prism of employment law rather than in relation to the broader frameworks/norms within which disclosures may take place. As we have seen above, although existing law goes some way to address these issues, there remain real concerns as to the practical effectiveness of existing protections. Furthermore, domestic law falls far short of the normative framework suggested here and there needs to be a more thorough overview of such frameworks at the national level.
Human rights, whistleblowers and the NHS
To what extent does the Human Rights Act 1998 today have an impact on the position of whistleblowers in health care? The Human Rights Act is directly applicable to the NHS, which is a public body (S.6). 249 There are three human rights that may be of particular importance here: Article 10, which sets out the right to freedom of expression; Article 8, the right to privacy; and Article 9, the right to safeguard freedom of conscience, religion and belief. Freedom of expression is an international common right, and European Convention on Human Rights Article 10 (2) is known as a ‘qualified right’. The courts will examine the speech and determine whether or not it is proportionate [Handysides v UK (1976) EHRR 77]. 253 Factors that the court will consider in ascertaining this will include the employee’s job, their conduct while employed, the circumstances in which the disclosure is made and the nature of the information disclosed (p. 131). 234
The ECHR has noted the need to protect whistleblowers under Article 10 in Guija v Moldova. 254 Here the Court held that the dismissal of a civil servant who had disclosed two confidential letters from the office of public prosecutor to the press did constitute a breach of Article 10, and Castells v Spain255 stated that government should be subject to very tight scrutiny not simply by the legislature or judiciary but also by media or the public. In some instances the public interest will be sufficiently strong to outweigh the duty of confidence. 255
Although the court held that disclosure should initially be undertaken internally to a person’s superior or to a competent body, it was recognised that external public disclosure could be undertaken as a last-resort measure. They took into account what could be the chilling effect of the individual’s dismissal that might stop others reporting misconduct. 256,257
The question of confidentiality and whistleblowing in relation to the vulnerable arose in Heinisch v Germany, in which the ECHR recognised that whistleblowing involved balancing of interests of employer and employee and public policy concerns. 258 Mrs Heinisch was a nurse in a state-operated nursing home. She disclosed the mistreatment of elderly patients, and she was dismissed. After litigation in Germany with no success, she succeeded before the ECHR. The ECHR noted that freedom of expression had been held applicable in the context of employment. 259,260 It held that the interference with freedom of expression was a legitimate aim of protecting the rights and freedoms of others, in this case the employer, but in the circumstances the interference here with Article 10 was not proportionate and public interest in details about limitations in state-owned company institutional care for elderly people is more significant in a democratic society than safeguarding the state-owned company's interests and business reputation. 258
A fundamental human-rights-based employment policy based on concerns for procedural fairness and for free speech might have interesting longer term consequences for perceptions of whistleblowing in the workplace. It appears, however, that currently the courts and employment tribunals have not been willing to recognise free speech provisions in relation to actions under Part IVA of the Employment Act 1996261 and the Freedom to Speak Up approach itself is one of an employment law driven rather than fundamental human rights driven perspective.
A further possibility is the development by the courts of whistleblowing as part of a right to safeguard individual conscience. This could potentially be seen as part of Article 9 of the ECHR, which safeguards freedom of conscience, religion and belief. Domestic principles of English law provide no general recognition for conscientious objection. However, two specific statutory safeguards do exist in relation to abortion and reproductive technology treatment and embryo research (section 4 of the Abortion Act 1967,262 section 38 Human Fertilisation and Embryology Act 1990,263 as amended). Both provisions can be seen in the light of the considerable sensitivity and different cultural and religious positions concerning the status of the embryo and the fetus. In the context of Canada and the Canadian Charter of Rights and Freedoms and its reference to conscience it has been suggested that there is the possibility of utilising a strongly developed freedom of conscience to provide further safeguards to the position of whistleblowers. 264 English law has, however, yet to follow such an approach, and it remains very uncertain whether or not this would be developed by the courts. 265
Third, whistleblowing in the NHS can be viewed through the perspective of individual patient’s rights to privacy and confidentiality. This was a major issue in the Pink litigation referred to above. Professional–patient confidentiality is expressly safeguarded by health-care professionals’ ethical codes. 266,267 In English law, respect for patient confidentiality is underpinned by Article 8 of ECHR, the right to privacy and also safeguarded through the operation of what is called the equitable remedy of breach of confidence. This was confirmed by the House of Lords in the case of Campbell v Mirror Group Newspapers Limted (MGN). 268 In this case a three-part test was established. First, is there a reasonable expectation that the information is to be kept confidential? Second, would disclosure be ‘highly offensive to a person of ordinary sensibilities’? Third, is the information ‘obviously private’? In practice, although there was a new test, this did not change the essence of protection for health-care professional–patient information, which has always be recognised as ‘both private and confidential’.
This duty is based in equity but there is a separate tort relating to the misuse of private information. 269 However, our focus here is on the equitable remedy of breach of confidence. Health-care confidentiality has never been regarded in law as absolute; it is a balancing exercise between the public interest in confidentiality and the public interest in disclosure. 270 Furthermore, Article 8 is what is known as a ‘qualified right’, namely qualified by reference to public health, national security and the prevention of crime and disorder. Thus, disclosing information, even patient-sensitive information, may be justifiable when it is in the public interest to do so. Disclosure may be in the public interest to stop the abuse of a particular patient and also justifiable because that disclosure may avert future harm to patients. In addition, disclosure may be seen as justified in relation to individual freedom of expression claims. 271 Finally, confidential information may be disclosed expressly in the public interest because this is sanctioned by statute.
Whistleblowing and the open government and regulatory perspective: speaking up in the public interest
There is a final perspective in relation to whistleblowing in the NHS, which relates to two categories in Vaughan’s207 typology, namely open government and a regulatory perspective. Raising concerns can be seen as a means of highlighting defective standards of professional practice and poor patient care and, thus, can be linked to professional discipline and to reducing the prospect of such harms in the future. This can be seen as a professional practice obligation. It can also be regarded as an obligation within the terms and conditions of employment. Reporting systems are increasingly a feature of the NHS. This can be seen partly as a matter of addressing patient safety, partly as a question of general efficiency and accountability, and partly as a matter of open government in that transparency can be seen ultimately as necessary to ensure adherence to the statutory obligations placed on NHS actors and organisations under the NHS Act 2006. 272 NHS bodies are also now required to ensure that board-level directors are fit and proper persons for their role. 273 Freedom to Speak Up stresses the need for transparency for individuals and the organisation (paragraph 7.4). 2
There are a series of bodies that regulate health care. The CQC has extensive powers in relation to the inspection of health and social care facilities. Further oversight is provided by the NHS Trust Development Authority, which monitors NHS trust performance and undertakes appointments including those of chairpersons and non-executive members to NHS trusts (paragraph 2.4.12). 2 As we have seen above, in relation to the discussion in the context of human rights, in addition health professionals may be mandated under their professional codes to raise concerns and whistleblowers may refer concerns to professional statutory regulatory bodies such as the GMC and the Nursing and Midwifery Council, which may result in professional disciplinary proceedings. The GMC has itself instituted the Hooper Review, into the handling of the cases of whistleblowing doctors, which reported in 2015. 192 In addition, it has produced whistleblowing guidance. 274 Raising concerns can also be seen as part of a process of reporting risks to patient safety through other means such as the operation of health and safety law. So, for example, the Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 2013 require employers to report and keep records of work-related accidents that lead to death or serious injury.
Procedures enabling internal whistleblowing
Vickers, writing in 1999, suggested that the 1998 Act ‘creates a clear incentive to employers to provide good internal procedures to enable concerns to be raised within the organisation’ (p. 129). 234 Without such procedures, external disclosure is more likely to be reasonable at tribunal. Internal procedures can facilitate effective regulation and accountability. There is a long history of whistleblowing procedures in the NHS. 275 Relevant here is the NHS Constitution for England. Section 1B of the NHS Act 2006 provides that:
In exercising functions in relation to the health service, the Secretary of State must have regard to the NHS Constitution.
The NHS Constitution for England contains an obligation to:
raise any genuine concern you may have about a risk, malpractice or wrongdoing at work (such as a risk to patient safety, fraud or breaches of patient confidentiality), which may affect patients, the public, other staff or the organisation itself, at the earliest reasonable opportunity.
p. 15. 275
The House of Lords Select Committee report in 2013, After Francis: Making a Difference, called for the CQC to see if arrangements were in place for staff members who wanted to raise concerns during a CQC inspection. 276 The National Audit Office report into out-of-hours GP services by Serco in March 2013 stated that the DHSC should require NHS organisations to publish their whistleblowing policies.
Freedom to Speak Up recommended the creation of a new INO, which would be:
resourced jointly by national systems regulators and oversight bodies and authorised by them to carry out the functions described in this report.
p. 18, paragraph 7.6.11. 2
The INO was to:
review the handling of concerns raised by NHS workers where there is reason to believe that there has been a failure to follow good practice, particularly failing to address dangers to patient safety or causing injustice to staff
where this has occurred, to advise the relevant NHS organisation to take appropriate and proportionate action, or to recommend to the relevant systems regulator or oversight body that it make a direction requiring such action.
p. 19, paragraph 7.6.12. 2
The INO would not replace existing remedies, nor was it expected to review or investigate ‘historic cases’ (paragraph 7.6.13). 2 The aim was not for them to take up cases themselves but, for example, to invite others to take them up. It would not have binding powers and would not be ‘strictly comparable’ with an ombudsman (paragraph 7.6.15). 2 It was not an appeal body; rather, its role would be to advise organisations as to action to be taken. It would have wide discretion (paragraph 7.6.15). 2
Following Freedom to Speak Up, a National Guardian’s Office was established (www.cqc.org.uk/content/national-guardians-office; accessed 5 July 2018). This is operated from within the CQC rather than, as Freedom to Speak Up suggested, by a series of regulators. Location within the CQC has advantages in that it roots this within a body integrally concerned with NHS standards and in promoting processes within the NHS. It can be seen in line with the Freedom to Speak Up recommendation not to have something that would be cumbersome and bound by ‘legalistic process’ (paragraph 78). 2 However, it could also be argued that a totally independent body could be a better approach to signal that this issue is being taken seriously. It appears that the guardian office will selectively review cases and provide recommendations but very much following the recommendations of Freedom to Speak Up will not review historic cases nor initiate investigations. 277
The National Guardian’s Office got off to a somewhat problematic start. Dame Eileen Sills, Chief Nursing Officer of Guy’s and St Thomas’ NHS Foundation Trust, left in March 2016 after only 2 months in the role, which she explained was incompatible with her day job. 278 This was followed by the resignation of David Bell, the deputy guardian, in April 2016. 279 A new whistleblowing guardian, Dr Henrietta Hughes, a GP and NHS England Medical Director for North Central and East London, was appointed on a 4-day-per-week basis while keeping jobs as a GP and a GP appraiser. This appointment sparked controversy, first because it was not full-time and second because a representative from NHS England was on the board that had appointed her. 280
In April 2016, the Freedom to Speak Up: Raising Concerns (whistleblowing) policy for the NHS was published. 281 This emphasises that concerns could be raised about ‘risk malpractice and wrongdoing’ (p. 4)in relation to services that are delivered or commissioned (see Appendix 3). It stresses that:
If you raise a genuine concern under this policy, you will not be at risk of losing your job or suffering any form of reprisal as a result.
NHS England. 281
The guidance also stresses that there will be no toleration of harassment/victimisation/bullying. Concerns can be raised confidentially (p. 4). 281 It applies to current and former NHS workers and those who work for independent organisations providing NHS services. The aim is to include ‘agency workers, temporary workers, students, volunteers and governors’ (p. 5). 281 Processes for raising concerns are set out; this may be with the line manager or, when not appropriate or in a situation in which there has been no resolution, with the Freedom to Speak Up guardian or risk management team. There is a third stage, which is to raise concerns with the executive or non-executive director with responsibility for whistleblowing (p. 5). 281 The aim is to record concerns and respond within 2 days. If an individual has been unable to resolve it speedily, then there will be a ‘proportionate investigation’. This will involve a person ‘suitably independent (usually from a different part of the organisation) who has been properly trained’. The aim is that this will be objective. If individuals are not comfortable raising concerns internally they can raise matters with a number of external listed bodies as appropriate (p. 7). 281 The guidance makes reference to the existing law and notes that people may seek independent advice from ‘the Whistleblowing Helpline for the NHS and social care, Public Concern at Work or a legal representative’ (p. 8). 281
The NHS Contract 2016/17 stated that Freedom to Speak Up guardians were to be appointed in NHS trusts by 1 October 2016 (www.cqc.org.uk/content/national-guardians-office; accessed 5 July 2018). By January 2017, guardians had been appointed in 86% of trusts. 282 The National Guardian’s Office was to support their work. The guardians’ declared ‘purpose’ is:
to support the organisation in becoming a more open and transparent place to work, where all staff are actively encouraged and enabled to speak up safely.
Health and Social Care Act 2008. 273
The key principles include that they should be impartial and able to hold trusts to account in relation to developing a culture for speaking up and actions to make improvements. They are to be empowered, visible, influential, knowledgeable, inclusive, credible, empathetic, trusted, resilient, forward thinking, supported and effective. These are demanding criteria and clearly these will be challenging roles. Delilah Hesling, the UK’s first Patient Safety Ombudsman, commenting on the Freedom to Speak Up guardian, stated that she found her role difficult, although she was operating with the support of her chief executive. It was reported that there could be obstruction from managers and that staff were initially unwilling to come forward. She suggested that guardians needed ‘teeth’ if they were to be effective, but at present they had not been given such enforcement powers,283 and the new whistleblowing guardian, Henrietta Hughes, has stated that she does not think that such ‘teeth’ are necessary. 284 A question remains as to whether or not without real enforcement powers, ultimately the role will have traction. Cotton285 has also suggested that the role of ‘leadership buy-in’ here is crucial and suggests that, without this:
individual guardians will go the way of decades of diversity and equality reps: burnt out and bullied into silence themselves.
Cotton. 285 This article is published under the Creative Commons Attribution-No Derivatives 4.0 International (CC BY-ND 4.0)
One further practical challenge is that the NHS is increasingly using a myriad of different providers to provide NHS services. If care providers are, for example, GPs and consultants operating as locums, nurses brought in from private agencies or private sector providers who are operating under a specific contract to provide a range of services such as operations, what impact might this have on their willingness to raise concern and their awareness of the whistleblowing procedures and processes in operation? There may be a need to raise awareness of these issues in a diverse workforce, some of whom may not have received their professional training in the UK. It is clear from recent evidence of implementation of legislation in another context, that of the Mental Capacity Act 2005 from the House of Lords Select Committee Report in 2013, that without continuing information and training health-care professionals are likely to remain unaware of the applicable legal frameworks. 276
Freedom to Speak Up suggested that mediation and dispute resolution techniques could assist in resolution of disputes (paragraph 53). 2 It proposed that resources should be available to NHS bodies to undertake alternative dispute resolution methods to address concerns and build up trust and that mediation be undertaken by trained experts (paragraph 53). 2 Mediation can be considerably less costly than judicial determination and may provide more flexible resolution (p. 52). 244 However, there are some potential disadvantages with alternative dispute resolution approaches. As Lewis244 notes, employees may regard mediators as ‘authority figures’ who are, thus, much more likely to side with the employers. With both mediation and arbitration, there is the danger that matters can be resolved and buried away from the public gaze if the whistleblowing concerned is about addressing cultural and system changes more broadly rather than simply an issue to be mediated/resolved/contained at an individual level. This raises fundamental questions of professional and institutional responsibility as well as of free speech, and needs a much more comprehensive structural approach to ensure that findings from whistleblowing processes are fed through the system so that lessons can truly be learnt.
The duty of candour
The notion of a duty of candour goes back many years. In 1987, Sir John Donaldson, the Master of the Rolls, stated that in professional negligence cases, in particular those concerning medical negligence, there is a duty of candour and this can be seen as a part of the general duty of care arising in the doctor–patient, NHS body–patient relationship. 286
This statement was, however, not binding on subsequent courts. A duty of candour was advocated in 1995 in a British Medical Journal article by Jean H Ritchie QC and Sally C Davies, then a consultant haematologist and later Chief Medical Officer. 287 The duty of candour was also proposed in the Bristol Royal Infirmary Inquiry report. 5 A campaign for the introduction of a statutory duty was undertaken by Will Powell, the father of Robbie Powell from Ystradgynlais. Robbie had Addison’s disease; he was treated by five doctors in the fortnight before his death and was found to have died as a result of neglect. 288 Support for a duty of candour was contained in the Donaldson report Making Amends and included in the recommendations in the Mid Staffordshire Inquiry Report (paragraph 22.164). 289 Some notification duties already existed in relation to adverse incidents, for example the CQC, which considered in inspections whether hospital systems informed patients or others of adverse incidents that had arisen in relation to their care and that could have caused harm. 290 This is included in the standard contract between NHS clinical providers and commissioners. Hospitals are also required to report serious untoward incidents to the CQC without delay in circumstances in which patients have died as a result of circumstances that cannot be reasonably attributed to the condition of the patient or when there has been an untoward incident that has harmed a patient or shortened a patient’s lifespan [National Health Service (CQC) Regulations291 and see Newdick and Danbury292 p. 958].
Following Freedom to Speak Up, section 81 of the Care Act 2014293 provides the Secretary of State for Health with power to make regulations concerning the duty of candour:
[W]here an incident of a specified description affecting a person’s safety occurs in the course of the person being provided with a service.
Care Act 2014. 293
As the explanatory notes to the legislation state:
This duty will mean that such providers will be required to ensure that patients and service users are told when something unexpected or unintended occurs in the course of their care or treatment, helping to ensure that honesty and transparency are the norm in every organisation overseen by the CQC.
Care Act 2014. 293
This provision now has to be read in conjunction with regulation 20 of the Health and Social Care Act 2008 (Regulated Activities)277 Regulations 2014. It places a statutory obligation on the registered person where such a safety incident has arisen to inform the relevant person that this has taken place and provide support. It sets out the manner in which this should be done including the fact it must be given in person and include an apology and a written record of other enquiries that are to be undertaken, and this must be followed by a formal written notification of information given, the apology, further enquiries, etc. (see Appendix 3). Further guidance as to how this should operate has been provided by the GMC and Nursing and Midwifery Council (see Appendix 3).
The scope, operation and effectiveness to date of the duty of candour have been questioned. The emphasis is on apology in relation to individual failings, not in relation to apologies for systems failings or, indeed, the failure of other persons. Nor is it directed at situations in which a patient’s condition worsens owing to natural progression, but Oliver argued that these situations could cause distress and the conditions for complaint. 294 He argued that although an apology did not constitute an acceptance of liability, it remained questionable whether or not health-care professionals would accept that this was, in fact, the case. He stressed that the organisation must provide support to professionals. Oliver noted that the NMC/GMC guidance focuses on doctors and nurses, but that although other health professionals and NHS managers could play an important part in determining care conditions, they were not necessarily the subject of registration or ethical codes. 294 He argued that ‘for faults at the organisational or system level, the organisation or systems leaders should apologise including the Health Secretary himself’. 294
The operation of the duty in practice to date has been questioned. A recent report by the Action Against Medical Accidents, reviewing CQC inspections of 90 trusts, highlighted major concerns regarding trusts that were failing to address the duty of candour or that were superficial in the manner in which they had done so, and that there was evidence of inconsistent implementation across England (p. 15)295 and lack of adherence to the duty. 296 Following the Action Against Medical Accidents report, Robbie Powell’s father, Will Powell, noted the problems with the existing legal position and stated that what was needed was a free-standing duty of candour. 297
As we have seen, failure to raise concerns can be seen as part of the professional obligations of health-care professionals. Freedom to Speak Up recognises that managers should be accountable but is somewhat equivocal as to how this can be achieved. 2 Evidence to Freedom to Speak Up in 20152 suggested that there should be a degree of statutory regulation of NHS managers. Freedom to Speak Up stated that the duty of candour and Fit and Proper Person Test for Directors could provide a greater means of promoting accountability (paragraph 7.5.13). 2 However, it noted uncertainty and that this should be kept under review (paragraph 7.5.14),2 but Francis ‘was not convinced that the time is right’ for a comparable system of regulation for managers (paragraph 7.5.15). 2
Concluding remarks
Legislative protection for whistleblowers has improved to some extent during the last 3 years through targeted protection for whistleblowers such as some students and job applicants. This will be assisted by having greater provision of information in relation to statutory requirements regarding the disclosure of such cases to certain bodies. A broader culture of transparency and accountability may also be facilitated through the statutory duty of candour. However, although some reframing of the legislation may indeed be beneficial, and is to be welcomed, nonetheless expectations should not be raised unduly here. The legislation, inevitably, has practical limitations because in reality only a small fraction of employees who are successful at tribunal are ever reinstated. Experience in jurisdictions such as the USA before the introduction of PIDA8 indicated that, in reality, whistleblowing employment law can be seen only as a last resort, a measure utilised when it is too late to ‘shut the stable door’. The movement towards establishing Guardians may facilitate and improve the situation in relation to whistleblowing but, as currently constructed, Guardians have a very challenging, and possibly unsustainable, role. Blowing the whistle in different areas of health care (e.g. in a hospital compared with in primary care) gives rise to different challenges. In addition, there is little attempt at present to fully reconcile the professional practice obligations of health-care professionals such as doctors and nurses with not only the duty to be frank and open but also the idea that there may be a case for a duty to blow the whistle. Twenty-four years on from the Fatchett Bill, there has been no attempt to provide comprehensive statutory regulatory coverage for whistleblowers in the NHS. Whistleblowing does not seem cast as a human right or as a tool of open government and effective regulation. Moreover, as Lewis et al. have noted, ‘since disclosure by a whistleblower might prevent a disaster or perpetuation of fraud the question arises as to whether there should also be a duty to blow the whistle and investigate the concerns once they have been raised’. 206 It is suggested that the time has come for the government to explore further the effectiveness of whistleblowing law in general and the legal rights and duties of whistleblowers in the NHS in particular.
Chapter 6 Key informant interviews
Introduction
In this chapter, we present the findings from interviews undertaken to gain the contemporary views of key informants on the design of current whistleblowing and speaking up policies and initiatives in the NHS. The key messages from the interviews informed our team discussions that underpinned the integration and interpretation of the findings relating to the wider objectives in the study, as well as providing important steering to the analyses in the other main chapters. We begin with an overview of the methods used in the key informant interviews, before presenting the main themes that emerged. The final section draws together the key findings and offers some suggestions for future policy development in this area.
Methods
We selected for interview a purposive sample of 16 individuals holding key positions with regard to NHS whistleblowing policy, namely informants occupying roles with specific involvement or knowledge of whistleblowing policy formulation and delivery in the NHS (listed in Box 1). The interviews were semistructured, and were based on an interview guide drawn up after early literature reading and after discussions across the (highly experienced) research team. Interviewer questioning and prompts asked participants about:
-
contemporary issues related to the implementation of whistleblowing policies
-
perceived problems with current approaches
-
proposed solutions to overcoming any perceived difficulties.
-
Representatives from the DHSC (n = 2).
-
The two key regulators: Monitor (merged into NHS Improvement during fieldwork) and the CQC (n = 2).
-
Professional and workforce representation through Unite, the GMC and NHS Professionals (n = 3).
-
Workforce development representation through NHS Employers (n = 1).
-
Patient/user perspectives through Action Against Medical Accidents and Point of Care Foundation (n = 3).
-
Policy delivery perspectives from the Whistleblowing Helpline and PCAW (n = 3).
-
Legal perspective from Capsticks legal firm (n = 1).
-
A leading academic in the field of whistleblowing policy (n = 1).
Following in the tradition of other patient safety research projects,298–300 the key informant strand of the present study adopted a narratological approach to data collection and analysis. In this regard, Waring299 summarises how storied accounts often help actors give meaning to complex and emotional situations through the development of plotlines, which are sometimes ordered and linear, but are more often fragmented and complex. In our data collection and analysis, we sought to weave together these storied accounts into a series of interconnected and overlapping narratives that connected to wider debates relating to the design and implementation of whistleblowing and speaking up policies in the NHS. The NVivo computer software program was used to support the coding of information and focused on surfacing current policy problems, solutions and recommendations with regard to improving whistleblowing policies in the NHS. The interviews were carried out between January and June 2016. Ethics and research governance arrangements were approved by the Health Research Authority (IRAS 189539). Informed consent was provided along with assurances that anonymity would be assured. In respect to the wishes of interviewees, quotations have been anonymised.
Emerging narrative storylines
Here we present the key narrative lines voiced about the features of an effective whistleblowing policy. Initially, the findings draw attention to key problems and challenges in relation to how whistleblowing is currently framed and conceived of in the NHS. This is followed by a section that details the alternative framings for whistleblowing in the NHS contributed by key informants. We then pay particular attention to current initiatives to implement the speaking up agenda in the NHS. Sections then follow that document the views of key informants regarding implementation of whistleblowing policies. The final section presents views on how the current whistleblowing agenda for the NHS may be improved, including more training and guidance in relation to whistleblowing policies and better use of data to track actions and responses over time.
Current problems facing whistleblowing in the NHS
Key informants described a range of problems and challenges in relation to current whistleblowing policies in the NHS. Central to these were widespread negative perceptions about the way in which the term has traditionally been used in the NHS. These challenges were clustered into two broad narratives: how speaking up in the NHS is synonymous with a ‘climate of fear’; and the limitations of existing legal protection for those speaking up about poor practice. Each is now discussed in turn.
A climate of fear
Interviewees offered a range of insights into current problems and challenges associated with the ways in which whistleblowing has traditionally been framed in the NHS. Many informants thought that, historically, the NHS had been poor in encouraging, responding to and managing employee whistleblowing concerns. The events at Mid Staffordshire NHS Foundation Trust hospital were cited by some informants as a case in point, in that they highlighted an organisation that did not listen to patients and staff when legitimate concerns were raised and that managers would often dismiss such concerns or ‘scapegoated’ those individuals raising them. Informants presented the key policy challenge as one of providing better protection for those ‘brave’ enough to speak up about problems with patient care. Many informants believed that whistleblowing had become synonymous with high-profile negative cases that were widely documented in the media, with those raising concerns often facing ‘frightening’ repercussions from managers and colleagues for their actions:
You heard of chief execs whistleblowing or doctors whistleblowing and being suspended from work for huge amounts of time and then losing their jobs. And those high-profile cases stick in people’s minds.
Every day across the NHS thousands of cases where people raise concerns, often purely on a one-to-one basis . . . obviously, we don’t hear about them. All we hear about through the media are those horror cases of which there are far too many. Where individuals have been very clearly, you know suffered detriment as a result of raising, in good faith, concerns about what they’ve seen in the service.
The poor treatment of individuals who had blown the whistle had led to ‘campaigns’ from some employees who were angry about the way they and their colleagues had been dealt with by the NHS:
You’ve got cases where the system has got it wrong and where the evidence has been considered and weighed, in the way that employment tribunals do, they’ve determined that. And then you’ve got others which have been to employment tribunals and lost, been to courts and still lost and still maintain that they were right and everybody else was wrong. We’ve had people whose careers have been destroyed . . . it’s the absence of transparency and the way that the culture would close in and around whistleblowers.
There are people who raise concerns who may have genuinely raised concerns don’t like the answer they get. And then go on a crusade to crucify the people they work with.
Interviewees suggested that it was the combination of these elements that had created a ‘culture of fear’ in the NHS, with staff often unsure about the extent to which they would be supported and their identities protected if they did raise concerns. The fear of negative reprisals and even dismissal – often alongside a sense that nothing would be done – were thought to be having a negative impact on the willingness of staff to speak up about poor care.
The limits to legal protection
Alongside the current climate of fear, interviewees described how the inappropriate treatment of whistleblowers was exacerbated by an inadequate legal framework. Since 1998, PIDA8 (see Chapter 4) has provided the legal framework for tribunal outcomes and awards to those who had been ‘victims’ by exercising their whistleblowing rights:
[PIDA] is there to protect genuine people who suffer from, you know, genuine detrimental dismissal because they’ve raised concerns. I mean it’s very . . . The legislation is very broad. So it doesn’t take you much to get over the legal tests in terms of becoming a whistleblower . . .
Although PIDA was raised as helpful in supporting those speaking up about poor care, some had concerns about how it was used to protect those in the NHS. Central to these were the emotional and practical difficulties of going through PIDA:
One of the challenges remains the current system of paying to go to an employment tribunal, and it’s a shame when it has to come to an employment tribunal, and part of our role is to keep people on the right side of the legislation, so that isn’t the case.
The protection for individuals has always got a question mark against it because some organisations might take the view, ‘oh, it’s going to cost us £140,000, that’s worth it, let’s get rid of him or her’, so there’s that element to it.
PIDA is not what some people think it is, is it? It’s a remedy after the facts really, isn’t it? The use of the term ‘protected disclosure’ is potentially a bit misleading because some people see it as you’ll be able to protect me and no one will be able to do anything to hurt me or cause me detriment, whereas it doesn’t really work like that, does it?
Informants also raised questions about PIDA being ‘synonymous with employment’, at the expense of clinical and safety issues that were often at the root of the problems being raised. There were also thought to be difficulties about being protected by the legal framework ‘the further away you go from the employer’:
I think this is one of the challenges around this, which is this mixture of employment and clinical safety issues that gets put in the washing machine and spun round in a certain way, in a quite tricky and very, very difficult way.
It’s a balancing act in the law, but it means that it’s very complex and actually there’s lots of problems with the way the law’s drafted at the moment.
Based on these concerns, many informants believed that the key policy challenge was to create a conducive climate within NHS organisations in which staff no longer felt the need to go outside their organisation to report problems. Informants described a need to encourage discussions and situations in which externalising or moving into ‘the formal stages’ of legal action did not need to happen:
I think if you have to call someone a whistleblower, then it’s already gone wrong . . . I think you’ve already, sort of, lost the battle.
Reframing the debate from whistleblowing to one of raising concerns
A key narrative emerging from the interviews was the call for a change in the nature of the current debates surrounding whistleblowing. It was thought that ‘opening up’ whistleblowing to ‘new conversations’ was needed to ensure that whistleblowing concerns were acted on without fear of bullying or persecution. A central driver for creating these new conversations was seen to be the work carried out by the Francis inquiry and the subsequent report into whistleblowing practice. The work of Sir Robert Francis was attributed with setting out a new agenda surrounding whistleblowing to one more clearly focused on quality and safety. The subsequent review and report into whistleblowing, Freedom to Speak Up, was cited as a significant milestone in helping to redefine the debate away from ‘whistleblowing’ to one of ‘raising concerns’. It was thought that this report was clear in setting out how whistleblowing needed to cover more than protected disclosures. The subsequent development of national whistleblowing policy has sought to build on this agenda in the promotion of whistleblowing as one about raising concerns:
I think one of the aims of having a national whistleblowing policy is to normalise raising of concerns and so it’s less of a case of something being a protected disclosure or not, but making sure that the general premise is if you’re worried about something, you should say something. And if that happens then the need to, for example, to maybe go outside the organisation or the need to think about whether you need to make a protected disclosure, i.e. you need that protection, is reduced because this is just normal behaviour. This is just an expected behaviour.
Raising concerns was the preferred term for the key informants, as it was thought that this ‘softened’ the tone and made the action potentially more accessible and ‘doable’ for employees. This term provided a more helpful way of ‘normalising’ any whistleblowing action and concerns. Key to this was a change in mindset away from seeing whistleblowing as an issue worked through ‘bureaucratic policy and procedures’ to one of becoming ‘absolutely standard practice’:
You want to encourage them [staff] to raise anything as opposed to debating whether or not it’s serious enough. So, you know it’s helpful in say raising concerns to capture all.
It’s so emotive to talk about whistleblowing and it sounds like an unusual activity. I mean I’d like us to stop talking about whistleblowing and just talk about raising concerns.
We all are striving to overcome [the view] that people think it’s a big deal to raise a concern. It’s just done as a routine, you know part of the day-to-day interaction of people working alongside each other with the aim of providing a decent standard of care.
Formulating whistleblowing policy
Those directly involved in the formulation of whistleblowing policy described the creation of a ‘broad front’ policy agenda promoting the need among staff to raise concerns. Recent developments in this area included the introduction of a new training curriculum for staff to increase awareness and offer guidance regarding whistleblowing. An employment support scheme was also being introduced to support whistleblowers back into work as well as acting as a supporting mechanism for whistleblowers in ‘fear of their jobs’. Although these initiatives were touched on, much of the attention and impact given to current policy concerned the appointment of a national guardian and the creation of a network of local guardians. These were seen as significant policy developments, with interviewees outlining both opportunities and challenges when implementing and supporting these roles. Policy-makers noted how the introduction of the national guardian role should have a range of associated functions, involving providing an oversight role and making sure that whistleblowing issues are handled appropriately; being a platform for disseminating knowledge about what works well in whistleblowing policy; and providing guidance to local guardians by offering peer support and training:
It sends a message . . . that it’s important that people can raise concerns safely and those that run the systems are concerned that those systems support them to do that . . . I think those messages play a really important role in changing culture . . . Because it’s saying that those who design the system think this is important.
Local guardians were described as being central to the current approach. Policy-makers presented these roles as a ‘step forward’ in demonstrating that whistleblowing would be taken seriously at a local level through creating the conditions for people to speak out:
[The role is saying] we’re investing time and money in it and if you’ve got issues about safety about quality about fraud, whatever it might be, that you want to raise, here’s a vehicle through which you can do it.
Informants outlined a number of attributes that guardians would require in terms of mediation, listening and communication. A knowledge of risk management and governance processes, as well as a familiarity with ‘speaking to senior people’, was also required in the role:
[Local guardians] have to be trusted and respected and seen as a sort of, safe space, and a confidential space by people who want to raise concerns. But they also have to have you know, the ear and the confidence of senior management in an organisation so that the concerns that are raised with them are listened to and can be acted upon.
I think they should be trusted. I think they should be respected. People should feel that they are part of the solution and they’re not part of a closed culture. I think when we’ve asked whistleblowers, they’ve said that they don’t think that the local guardian can be in HR [Human Resources] and this is the connection with employment issues.
Implementation of whistleblowing policy
Policy-makers described how recent whistleblowing policies represented a genuine attempt by the government to stimulate culture change and transformation at the local level. Building on Freedom to Speak Up, the policy approach advocated a much more ‘bottom-up’ and ‘local approach’:
One size doesn’t fit all. We’re very conscious of not being prescriptive in what needs to happen. But I think the report made loud and clear the issues that we really do have to address in some way, shape or form. And it can’t be ignored. So, we need to get better at what we’re doing.
I don’t think you can shove this in from a national level. I think it’s got to be owned at the local level. If people do this because they’ve got to do then I think we’re in danger of hitting a target, but completely missing the point. And this will not be the panacea anywhere, but actually the purpose is to begin to change the tenor of the debate taking place and the behaviours that are occurring. For me, that’s what culture is: it’s a mixture of behaviours and discussion. And if we’re going to change that, you can’t sit in offices in London and Birmingham and Newcastle and Manchester and affect what they’re going to do in Norwich and Newquay quite frankly . . . it is that mixture of national leadership, providing a framework, but local action.
The policy approach taken was described as having a ‘trickle-down effect’. As a result, it was thought that it was the role of boards to recognise the serious nature of the proposals and set the mood accordingly within their trusts:
We think openness, we think responding to people who raise concerns with . . . Well in an open way, in a kind of collegiate way really, is absolutely essential and that’s the message that they [boards] should be seeking to promulgate . . . really and down through the organisation.
It’s a question of leadership within the trust, you know, you’ve got to have chief executive who literally goes around and she or he will be saying every month, going around and seeing the staff, ‘do make sure that I want to see and hear about any of your concerns’. It’s got to be as simple as that.
Implementation challenges facing current policy
Our interviewees voiced support and optimism regarding the current policy agenda. However, there were particular issues flagged up in terms of how far this policy agenda would be implemented with the current demands and financial pressures facing the NHS.
Bottom up or top down?
Although a ‘bottom-up’ approach was favoured, informants presented a range of barriers that might impede the achievement of this goal. Given current demands and pressures, some interviewees thought that there was a danger of the policy being interpreted as ‘something new that “needs to be dumped on top” ’. In contrast, the bottom-up flexible approach espoused by policy-makers was susceptible to a lack of full implementation. Such an approach had ‘no guarantees’ of being successful in terms of delivering the culture change being called for:
What we see a lot of is that people on front-line teams often feel very disempowered generally. They sort of wait – they feel that they can’t – that they need orders almost to do – or permission to do things . . . it’s an environment in which even some of the most highly qualified, highly trained, clever people don’t take initiative. So it’s a – there’s a tremendously difficult landscape to do this work on.
Although there was clear support for national and local guardians, some interviewees did express concerns about how far these new roles would impact on changing entrenched behaviour and practice in NHS organisations. Indeed, some informants were very sceptical about the extent to which the national guardian would be able to influence local practice. Concerns were also raised about how far local guardians would be able to fully exercise their duties within a service under severe financial pressures. Possible problems were also raised in relation to the lack of legal authority associated with the role:
You’ve got to have someone there who’s doing it full time and is sitting there wearing legal armour and not just the ability to phone up someone and say, ‘oh, I hear it’s not too good in your trust’.
Informants also voiced a range of potential issues regarding the assumed impartiality of local guardians. One suggested option was to have the guardian role located outside the formal NHS management structure:
For local guardians, there is an issue for us . . . that the local guardian is still going to be employed by the trust for which they are the local guardian. Well, you know, bit difficult, then isn’t it?
Important gaps in current policy were also noted. Social care remained ‘an important piece of the jigsaw’ that was relatively underdeveloped. It was thought that the nature of social care organisations posed a range of challenges for the creation of environments that were conducive to staff raising concerns:
In social care, in small teams, the infrastructure often isn’t there to support people through this exercise . . . they’re small organisations and people feel very, very vulnerable. They’re not a big machine like the NHS with . . . behind it, the infrastructure, such as big HR [human resources] systems and that sort of thing, so it is an important piece of the jigsaw, and sometimes I think one that we forget about.
To ensure policy success, there were calls for a stronger, ‘top-down’ approach. Although various measures were thought to have the potential to nurture virtuous culture change, concern remained that these needed to be more robustly implemented:
The policy is right and some of the things that we’ve put in place are right but it’s actually seeing them used and put into practice . . . It’s this following through on policy and regulations to actually seeing regulatory action to make it stick that are the things that we think’s missing.
Gagging orders were raised as a case in point. Although the Secretary of State for Health and Social Care had stated that there would not be compromise agreements on gagging orders, in practice these were still taking place:
Gagging clauses, ministers have written out saying they disapprove of them, it shouldn’t be happening but it should really be mandated.
Financial context
There were mixed views about the extent to which the current financial pressures affected whistleblowing. Some believed that the financial circumstances had the potential to discourage people to ‘step out of line’:
If you’ve got a trust who has financial . . . well they’ve all got financial pressures but is struggling . . . or, you know, running at a deficit . . . they’ve then got CQC who are coming to do an inspection because, you know, they were rated as inadequate 6 months ago . . . I do wonder whether that’s the environment . . . that trust and the staff are working in is probably not conducive to raising concerns because everybody is so focused on the task in hand it’s just like right let’s do this move on to the next thing.
A policy context of ‘targets and terror’ was thought by some to provide a negative context that did not encourage staff to speak up when they had concerns. In such a situation it was thought that NHS managers were often placed in a difficult position because of competing priorities: ‘squeezed from the top in relation to budgets and squeezed from the bottom in relation to staff’:
I think the real issue is politics here isn’t it in that hospitals come under pressure. I’m being very blunt . . . Come under pressure to deliver targets which put pressure on people. I mean things get . . . It means that things go wrong.
Others noted that all whistleblowing issues should be dealt with appropriately, regardless of financial constraints:
I think the pressures have been there all the time. They don’t go away. Organisations have to face cuts. They have done for many, many years. So this is no different. And I don’t think that can be used as an excuse not to do this and get this right.
In the face of severe financial pressures, it was suggested that the raising concern agenda could be framed as a way to save money. Intervening at the early stage of concerns could prevent employment tribunals and ‘getting into a high-profile cases’:
You know if you nip this in the bud you know and you look at your early interventions systems and working with staff to find the solutions then this doesn’t become a big issue any more. It becomes just a normal part of employment. So it is normal conversations and, you know staff are responsible for the solution, not just the managers.
Legal protection
Informants raised concerns that the current policy agenda had not sufficiently addressed the area of legal protection. Alongside the changes being made, some interviewees suggested that policy needed to further support legislative change, particularly the need for full legal protection. It was also noted that the NHS could also usefully look to other countries, such as Australia and Ireland, that gave ‘clear messages’ to staff regarding statutory provisions. Without such mandatory procedures, it was thought that current policy would not translate into action:
What’s the missing part of the fabric on this is the legal framework extending to someone who has got real, legal authority to come in to say to the chief executive of the trust, ‘this is what I’ve been told by two or your staff, what the hell’s going on here?’. And being able to get full disclosure on what’s going on. All that kind of thing, which you’d see as part of a very effective role which, so long as the legal part of that armour isn’t there, will always be missing.
It was noted that the raising concerns agenda needed to make more of a direct reference to whistleblowing. Whistleblowing as a term did not feature in Freedom to Speak Up; as a result, there was a danger that it remained outside the discussion:
Lawyers will still call it whistleblowing. The media will still call it whistleblowing. Staff will have this perception that whistleblowing is something out of the ordinary. But, you know, all your ordinary is called something else and it doesn’t cross-reference to it, and I think that can – there’s a danger that you entrench the negative views and you entrench the sense that whistleblowing is toxic, negative, or where nothing’s being done and nobody’s listening. And of course there’s an element of, yes, you’re trying to put in a process that deals with those more difficult scenarios, but don’t sort of completely divorce it from business as usual.
It was thought that there was an opportunity to strengthen the legal framework in the national guardian role:
With a guardian, you know, great idea, could be very effective but with no legal authority, no legal levers that it can pull . . . there is that – I think that’s a missing part of the whole sort of fabric of what we’ve got with whistleblowing because there is no doubt that where we’ve got difficult trusts which try to hide what’s going on . . .
Improving whistleblowing practice
Alongside the views and expectations regarding current policy, a number of interviewees were keen to outline areas in which the NHS could improve the translation of whistleblowing policy into practice. Although the raising concerns agenda was largely supported, interviewees described how a key challenge lay in changing practice. The majority of NHS trusts had whistleblowing policies in place, as reflected in the NSS results, yet further work was needed to translate policy into practice:
It isn’t just what you say in your policy, it’s how you operate the policy and how you are seen to be reviewing it and questioning it and working out whether it is effective . . . it’s not just having a policy. The NHS would tick all the boxes and would have done for 5 or 10 years on having a policy.
To reframe how whistleblowing is understood and dealt with in the NHS, a range of supporting factors were outlined by informants as being critical to its success. Chief among these was a focus on internal organisational dynamics regarding how the organisation responds to whistleblowing. A proactive, ongoing approach was thought to be required to promote continuous quality improvement:
It’s not just a case of listening to a concern and saying thank you very much and not doing anything with it . . . it’s supporting that person throughout the whole process because they can be subject to bullying. We know that’s happened. And it’s something that we need to get better at identifying and nipping in the bud very quickly . . . it’s about the whole rounded package.
The challenge for managers was raised here in responding to concerns quickly to prevent escalation. Further management guidance and training was needed to support the whistleblower and the wider team in terms of what to do and who to go to:
The management culture seems to be critical. So a culture that genuinely encourages challenge in the pursuit of safety and has a management style that is open and listening.
It was also thought that some managers required more sensitivity when working with professional groups. Care needed to be taken with how any issues were discussed with professional groups to ensure that raising concerns was done appropriately, with clear feedback processes in place:
The investigation itself can have a significant impact . . . regardless of the outcome. And therefore what doctors have said is, well, that’s all very well, but that will have a significant impact on my career. And there is a fear of that and therefore it is an effective tool to silence whistleblowers, etc., etc.
Further training was thought to be required needed to educate staff about confidentiality and anonymity. Although interviewees reported that the current helplines appeared be working as a ‘safe space’ where people could explore options, issues regarding confidentiality and anonymity remained a ‘massively misunderstood area’:
I don’t think people understand what that means in practice. I don’t think people, particularly staff, but also managers, understand where the difficulties are with that and how in some circumstances it’s not possible to be anonymous or it’s not possible for your identity to be protected and therefore to be reporting something confidentially.
Interviewees described how improvements to whistleblowing practice could be achieved through further analysis and ‘triangulation’ of organisational intelligence:
What we need to describe is a virtuous circle around raising concerns. So we need some hard and fast measures to look across the system and I think the best one we’ve got is the staff survey but it’s far from perfect.
How do you prove, how do you prove that your organisation has got that open culture? . . . we’ve changed legislation, you know, we’ve done lots of different things but how at a grass-roots level, at a local level are you going to be able to measure that your organisation is OK? I don’t know how you measure that . . .
It’s how you understand the data you’re being given and how you take that forward and how that is built into your organisational development plan. So that thing about continuous review . . . The key bit that is missing out of policy so far. You know the key principles . . . organisations need to adopt in regards assessing where the organisation is and you know what they need to do to make it better.
Some informants believed that better use of existing data sources would provide a number of opportunities and serve as an ‘early warning system’, highlighting where problems in the whistleblowing system were located. It was noted that the NSS results could provide a baseline measure for viewing any improvements made. In addition, interviewees suggested other measures that could be used as indicators to capture and triangulate a view of whistleblowing. These included statistically significant changes in the following performance indicators:
-
number of disciplinary incidents and grievances
-
fraud and corruption returns from NHS Protect
-
safeguarding information
-
benchmarks for openness and transparency
-
serious incidents
-
patient complaints
-
inpatient survey results (how much people feel engaged in their care)
-
Friends and Family Test.
The triangulation of such indicators was thought to provide a better way forward to understand whistleblowing patterns and improvements across the NHS in terms of translating data analysis into positive action; it was suggested that the introduction of local guardians provided an opportunity to develop these arrangements. Their role had the potential to make appropriate links within the organisation, collect the relevant evidence, and co-ordinate a ‘real-time alert system’ that would be reported for consideration to NHS trust boards:
Boards will be getting that, and I’d like to think that there was somewhere that the monitoring of whistleblowing could be standardised so that you can see a story being told . . . we can find the story that fits the picture, and I think there needs to be something that pulls that information almost by routine together.
Suggestions were also put forward about the need to capture and publicise ‘successful’ resolutions in whistleblowing cases. This would involve developing case studies of staff raising concerns that have been handled in an appropriate way and led directly to service improvements:
I think that the biggest message that will come out is when organisations start to use examples of where it has worked, so that people see folk get on in their careers because they’ve changed the attitude. So I think there’s a challenge there to be set almost, for the NHS, to start picking up people who have perhaps progressed their career because they’ve almost bucked the system and moved on.
Concluding remarks
Our interviews with key informants have provided a range of views on and insights into current whistleblowing policies in the NHS. The findings draw attention to the challenging and problematic ways in which whistleblowing is currently framed (tending to reinforce a ‘climate of fear’), as well as the difficulties associated with implementing the legal framework, PIDA. They also drew attention to how the current policy agenda assumes that ‘raising concerns’ is the key mechanism by which whistleblowing policy and practice can be improved. Although there is clear support for the approach being taken, problems were raised with regard to how far the measures can be achieved solely through a ‘bottom-up’ approach. In setting out future developments and recommendations, informants pointed to the need for further training and guidance for NHS staff at all levels of the hierarchy, particularly about how best to handle staff concerns. The informants also highlighted the need for more creative ways of using existing performance measures and data that are routinely collected in the NHS, in particular the information contained in the annual NSS. It was thought that nationally collected data sets could be better combined and synthesised as a way of triangulating and highlighting statistical patterns and trends in whistleblowing over time. Such information could be used to track the impact of new policy initiatives on the ability and willingness of NHS staff to raise concerns and staff perceptions on whether or not they felt confident that their organisation would respond appropriately if they did. This could, it was thought, serve as an ongoing ‘organisational barometer’ to gauge the extent to which the NHS was moving towards more openness in its reporting cultures.
Chapter 7 Conclusions and research implications
Introduction
As the NHS struggles to respond to periodic crises in health-care delivery, more interest is being shown in supporting front-line staff in getting their voices heard and making sure that organisations respond appropriately when genuine concerns are raised. Although many concerns about poor-quality or unsafe care are dealt with satisfactorily, there is compelling evidence to suggest that in many parts of the NHS staff feel unable to speak up, and when they do speak up there is a prevailing culture in the NHS ‘which not infrequently has negative consequences for those brave enough [to raise concerns]’ (p. 1). 2 This is despite the existence of employment legislation (mainly PIDA; see Chapter 5) that offers protection for whistleblowers and a plethora of national and local initiatives and guidance designed to support front-line staff in raising concerns and providing advice to organisations on how best to respond.
Against this background, we wanted to strengthen the theoretical and empirical evidence base underpinning whistleblowing policy and practice in the NHS. Drawing on a rich stream of academic research within and beyond health care (see Chapters 2 and 3), an analysis of NHS inquiries (see Chapter 4) and a critical review of the legal framework surrounding whistleblowing (see Chapter 5) underpinned by interviews with core NHS stakeholders (see Chapter 6), our work has sought to surface the challenges and opportunities for improved action on front-line concerns. In this final chapter, we draw together the main findings and conclusions of the study and look forward at the emerging research agenda in this vitally important but under-researched area.
A reminder of the ambitions of this study
In the design of this study we have sought to generate new knowledge and evidence to support improved whistleblowing policies in the NHS. The specific objectives were to:
-
explore – in an integrative and interdisciplinary way – the main strands of the academic and grey literature on whistleblowing and related concepts such as employee silence, and so to identify the key theoretical and conceptual frameworks that inform contemporary understanding of employee whistleblowing
-
synthesise the empirical evidence from different industries, sectors and countries with regard to the organisational processes, systems, incentives and cultures that serve to facilitate (or impede) employees raising legitimate concerns
-
examine the legal framework for whistleblowing in relation to health care as a mechanism for promoting (or inhibiting) patient safety and review the approaches to whistleblowing in relation to European Union member states and consider what lessons can be learnt at the domestic level from such comparisons
-
distil the lessons for whistleblowing policies and practice from the findings of formal inquiries into serious failings in NHS care
-
ascertain the views, expectations and experiences of a range of key stakeholders, including service users and carer representatives, about the development of effective whistleblowing policies in the NHS and to use these views to help structure and inform the desk research set out above
-
on the basis of findings relating to points 1–5, to develop theoretically grounded and evidence-informed practical guidance for policy-makers, managers and others with responsibility for designing and implementing effective whistleblowing policies in the NHS.
Members of the research team liaised throughout the literature review process to discuss and synthesise the emergent findings and ensure that insights were shared and integrated across the work packages. These discussions across, for example, policy, organisation behaviour and law aided a more integrative and interdisciplinary set of understandings as outlined in preceding chapters. For example, the review of conceptions and theories of whistleblowing informed the analysis of the Inquiry reports and the content of the key informant interviews, and the key informant interviews provided many departure points for assembling and interpreting the academic work emerging from across diverse disciplines.
In the rest of this chapter, we summarise the main findings of the research relating to each of these objectives and identify the research issues arising from the study. We take the first two objectives together, as they are highly inter-related and are informed by the same literature review. The key messages from the stakeholder interviews have been reported in Chapter 6 and have informed our interpretation of the findings relating to the other objectives as well as providing important steering to the analyses in the other main chapters.
Research objectives 1 and 2: identifying key conceptual issues and empirical findings
In Chapters 2 and 3, we outlined how whistleblowing has developed as a distinct field of academic enquiry and identified the seminal publications that have influenced and shaped the contours of debate in this area. An important finding from our review of the literature is that whistleblowing research in health care has developed separately and has therefore not drawn on the theoretical and empirical insights of mainstream whistleblowing research published in the management and organisation literature. We reviewed the different theoretical approaches that have been used in the management and social sciences literature as conceptual lenses to understand whistleblowing. The key conceptual and empirical issues uncovered by our review, with practical import for understanding, designing and improving whistleblowing and speaking up policies in the NHS, include the following important observations.
Silence and voice
There is no simple dichotomous choice between whistleblowing and silence (the collective-level phenomena of doing or saying very little in response to significant problems or issues facing an organisation). Policy prescriptions have tended to conceive the issue of raising concerns about unsafe or poor-quality care as a simple (individual) choice between deciding to ‘blow the whistle’ or determining to remain silent. Yet research suggests that such simple dichotomies are unhelpful; for example, health-care professionals may raise concerns internally within the organisation in more informal ways before (or instead of) utilising whistleblowing processes. Before coming to any decision on whether or not to blow the whistle, employees usually find themselves trying to work out exactly what is happening, often through engaging in dialogue with colleagues and seeking a ‘second opinion’. Other informal strategies may include the use of humour or sarcasm to signal discontent or the use of ‘off-the-record’ discussions with managers and employees. This kind of behaviour is framed sometimes as a prelude to whistleblowing and sometimes as a substitute. It also draws attention to the fact that the process of raising concerns about unsafe care may be largely hidden from view (apart from those participating directly in the dialogue) and may therefore not readily be identifiable as voicing concern, much less ‘whistleblowing’.
Such a view highlights the different routes through which health-care employees are able to articulate their ‘voice’ and challenges the pejorative notion, often promoted in the media, that health-care professionals are culpable bystanders who tolerate poor standards of care and are ‘silent witnesses’ to malpractice and mistreatment. Silence or voice, then, is not a binary choice but more of a spectrum. It is also about more than just individuals: it is collective and cultural (see later discussion of culture in this chapter).
Hearing and acting
Effective voicing of concerns is but the first stage in reshaping better safer health care: those with influence have to hear, and they have to act. In this regard we discussed the ‘deaf effect’, a concept that has been used in the management and organisation literature to describe the reluctance of senior managers to hear, accept and act on concerns by those raised by employees lower down the hierarchy. In some cases it is clear that senior players seek to ostracise and isolate individuals by undermining their concerns. In extreme cases, health-care professionals have been disciplined, suspended or reported for misconduct to professional bodies on pretexts derived from a very particular and partisan reading and framing of events. In an intensely hierarchical organisation such as the NHS, entrenched status and power differences between different professional and occupational groups (e.g. between nurses and doctors or between front-line staff and managers) that have been affirmed over decades and woven into the fabric of health-care delivery can serve to limit or attenuate the development of open reporting cultures.
Any articulation of a whistleblowing strategy must deal with the challenging organisational dynamic of resistance to bad news, especially by those in positions of power who may already be vested in narratives of success. Just as whistleblowers’ actions may be complex, variably motivated, ambiguous and contested, so too can be the responses of those in authority (within and outside the organisation) when confronted with new information and demands for action. Although an unwillingness to hear and resistance to change are commonplace, other responses may be seen: from shifts in attitudes and understanding to direct actions; from actions that support beneficial change to those that denigrate and damage the whistleblowers. Thus, we need as sophisticated an understanding of these response dynamics as we do of the dynamics of whistleblowing itself.
In this respect, the work of Dixon-Woods et al. 301 can be used to shed light on this issue. On the basis of empirical work in the NHS, the study grouped senior management’s responses into two broad categories of behaviour: ‘problem-sensing’ and ‘comfort-seeking’. Problem-sensing was assessed to occur when senior managers actively sought out problems in their organisations using a blend of hard and soft intelligence. 302 Comfort-seeking arose when managers sought information from only a range of limited sources and had a preoccupation with compliance, meeting external requirements and receiving positive news that served to provided ‘reassurance that all was well’. Managers actively disassociated themselves from issues raised by front-line staff and perceived any reported problems as ‘whining or disruptive behaviour’. Such comfort-seeking (as opposed to problem-seeking) behaviours among senior managers in the NHS may, therefore, serve to support the ‘deaf effect’. 148 Senior management may sometimes also suffer from ‘collective myopia’,25 a shared inability to see a problem. This is potentially even more problematic than the deaf effect as it leaves those in management positions genuinely unable to see what the whistleblower is trying to bring to their attention. Moreover, powerful systematic biases in group and team decision-making, including Groupthink, can serve to suppress the willingness of health-care professionals to report, hear and respond to concerns about unsafe care. 303,304
Interactional processes
Linked to the above is the recognition that whistleblowing is an interactional process and not just a one-off act by an identifiable whistleblower. The process is better seen as a dynamic and recursive interaction between whistleblower and recipient: it is not just that the speaker requires the courage to speak up but also the recipient(s) need to hear what is being said and to take appropriate action. 24 Most previous research and policy around whistleblowing have focused on the whistleblower, in particular the factors that inhibit whistleblowing and determine who has ‘the courage’ to speak up and under what circumstances. This has traditionally led to policies and interventions designed to lower the speaker-courage threshold in health-care contexts, such as legal protection, anonymous reporting channels and attempts to nurture ‘no-blame’ cultures. However, more focus needs to be placed on why some managers respond effectively and others do not, and the personal and organisational factors that can contribute to lowering the hearer-courage threshold.
Taking this one step further, attention should also be extended to understanding ‘protector courage’, whereby managers make an effort to protect whistleblowers from adverse consequences. According to Vandekerckhove et al. ,24 protector courage is, thus, ‘a way of understanding which managers have the courage to stand up for, or organise interventions around those who blow the whistle within areas under their influence or control in order to reduce or combat the familiar risks of retaliation, conflict or suspicion of the reporting action’ (p. 321). Managers able to effect hearer action may not always be in a position to support protector action and vice versa. An understanding of how, when and why NHS managers can take on such roles and the organisational factors that support (or impede) them is central to the design of better whistleblowing policies in the NHS.
Whistleblowing, or bell-ringing?
As conceived in the academic literature as well as in wider public understanding, whistleblowing usually describes internal organisational members raising concerns to those who can effect action. However, ‘bell-ringing’, or outsider whistleblowing, is also a possibility, and is potentially a more significant issue for health care than for any other sector. Examples of potential outsider whistleblowers include patients, relatives and visitors, or suppliers, consultants and professionals working in other organisations (e.g. social workers, GPs or management consultants). As the NHS becomes ever more diverse in terms of collaboration with other sectors (public, private, third sector), and as social media and information-sharing technologies become more developed, external staff are increasingly exposed to, and in a position to speak up about, poor-quality care. Indeed, staff from other sectors and those from other countries may bring very different values and beliefs (for good or ill) regarding what constitutes unsafe care and this may influence the NHS staff with whom they collaborate. Our review of the literature also uncovered evidence that health-care staff coming from different countries can have very different values regarding whether or not and when it is appropriate to blow the whistle.
Policy impacts on local judgements
Notions and assumptions about what is deemed to be good or substandard care, and therefore on decisions to speak up, are not only shaped locally but also influenced by the national context including current government policy, the action of interest groups, ethical codes and guidelines promoted by professional bodies, and care standards expected by national regulators. For example, in the current financial climate in the NHS some services may be withdrawn and staff levels reduced, posing new challenges to local perceptions of care adequacy.
However, as highlighted by Hyde,137 it is unlikely that reductions in care delivery will benefit patients; but when is it deemed by staff to be unacceptable practice? When, precisely, should staff raise the alarm when the level of care has deteriorated? In such situations, the best course of action is not always apparent. In addition, in an era of austerity, increasing financial constraints and job insecurity in the NHS, many staff may be reluctant to raise concerns because of potential retaliatory action by management. Any consideration of whistleblowing policy in the NHS must, therefore, be alert to the influence of such background factors on employees’ willingness to speak up and the responses of organisations when they do.
Personal factors in raising concerns
There is mixed evidence on the role and impact of personal factors in raising concerns. For example, in terms of length and security of tenure, some studies have found that the more embedded and socialised into a particular culture staff are, the less likely they are to spot poor practice and report it (perhaps because of personal and social links with colleagues). Other studies have shown that newly qualified nurses are in a position to blow the whistle because of their increased knowledge and confidence as to what constitutes poor care. Similarly, the evidence is mixed on whether nurses who, over time, become more socialised and integrated members of the organisation are less likely (through de-sensitisation) or more likely (through better organisational knowledge and developed networks) to detect and report poor care. These issues are under-researched in the NHS context and require detailed local study.
Key practice action points arising from research objectives 1 and 2
-
Managers should not be resistant to ‘bad news’ and should endeavour to seek out problems in their organisations using a blend of hard data and soft intelligence. Finding ways to encourage this will be a key challenge for management education and leadership training.
-
NHS organisations should nurture cultures that are supportive of staff raising concerns and respond positively to such concerns when they are raised; greater attention should be paid to communicating such changes in culture to care staff.
-
Particular attention should be focused on ensuring that staff are not penalised or ‘scapegoated’ for raising legitimate concerns (or perceived to be); particular attention will need to be paid to the effect that singular breaches of this will have on undermining leadership pronouncements of open cultures.
-
Whistleblowing policies should take into consideration how reporting channels are opened up to external staff, how organisations respond to external concerns, and the influence of external staff and those from other countries on the values that underpin health-care delivery, including the reporting of clinical incidents.
Research objective 3: the legal frameworks for whistleblowing
In this section, we reflect on the current position and consider alternative approaches that may be taken to the statutory basis and regulation of whistleblowing. Sir Robert Francis, in Freedom to Speak Up,2 after stating that he did not regard the current legislation adequate, went on to say:
The legislation applies to all employers, not only those in the NHS, so it would not be appropriate to make recommendations for amendment which might impact on other sectors in ways that I am not aware of.
p. 22, paragraph 95. 2
In contrast, other reports have been prepared to engage with reform of the law in this area (e.g. PCAW162 and Blueprint247). A number of avenues are open for future legal protection in relation to whistleblowing. These are set out below.
Oversight from an independent agency
As part of a review of the law in this area, one approach is the creation of a specific national independent whistleblowing agency, either a freestanding body or within an existing agency (Lewis;305 Blueprint, pp. 27–8247). Blueprint has suggested that such a body could receive and investigate whistleblowing disclosures, collect information in relation to workplace disclosures and have powers to obtain information from regulators for subsequent action. It could issue penalties when organisations did not follow up in relation to information disclosure, order the cessation of retaliation against a whistleblower and be able to order compensation and order reinstatement. In addition, it could provide advice and support to whistleblowers, monitor and review frameworks, and raise public awareness about such issues.
Savage and Hyde306 support such an approach in principle; however, as they then comment, the ‘prevailing political climate appears to be against the creation of a regulatory body to specifically cater to whistleblowing disclosures’. There are some further practical challenges here. First, the remit of such a body would be vast, so vast that it is reasonable to ask would it be ultimately bound to fail? It would require a robust, independent permanent chairperson and secretariat who would have sufficient time to address to their tasks. Proper resourcing would be needed to ensure that it could operate effectively. The interface between its operation and that of other regulators would need very careful clarification to ensure that information was disclosed appropriately. Research undertaken of national regulators has highlighted existing inconsistencies in the way in which these operate to handle concerns and it would be important to ensure that such inconsistencies were not further replicated in the way in which any national body might operate. 306 The ability to require reinstatement would go to the heart of the employment relationship. Historically, reinstatement is very rarely possible and would be unlikely to be ordered by the courts. This is related to practical issues given that by the time the issue is dealt with by the legal system the employment relationship is likely to have broken down to such an extent that the relationship of trust and confidence that exists in relation to the employment relationship is unlikely to be satisfactorily re-established, or to be re-established only in very rare cases. At national level, such a general agency would thus require careful consideration; within the NHS a whistleblowing agency may have more traction. The Guardian’s Office goes some way towards this, but it is non-statutory and would need considerable restructuring to bring it in line with Blueprint’s proposals.
Statutory requirement to establish whistleblowing procedures
The establishment and maintenance of whistleblowing procedures could be made a legal requirement. In the Republic of Ireland, the Protected Disclosures Act 2014307 places a specific requirement on public bodies to create and maintain procedures for employees to make protected disclosures and to provide them with information concerning this. Ministers can issue guidance to the bodies on their obligations under this section. The public body is also under a duty to submit an annual report in relation to the number of protected disclosures made to it. This could also be accompanied by the production of a Code of Practice. The PCAW Commission proposed that PIDA could be amended to provide that the Secretary of State, after consultation, could issue a code of practice on whistleblowing to taken into account by courts and tribunals (p. 12, paragraph 49). 162 Such a code could also assist in framing requirements for whistleblowing guidance within the NHS itself.
Early-stage protection for whistleblowers
It has been suggested that whistleblowers should be able to apply for whistleblower status to receive early-stage protection (p. 55). 247 Currently, under section 128 of the ERA 2006, an employee can apply to an employment tribunal and ask for an order that they can remain employed. This maintains the contractual arrangement while waiting for the whistleblower’s case to be determined. However, as Blueprint has noted, this has limited utility: whistleblowers must act within 7 days, it is expensive, and employers cannot be forced to allow the whistleblower to continue working (pp. 5–6). 247 The ERA does not stop retaliation against a whistleblower at that stage, cases may take around 20 months to conclude and such litigation is costly. 247 In contrast, the law on whistleblower protection in the institutions of Bosnia and Herzegovina provides that employees can be given whistleblowing status through pre-emptive action by applying to the Agency for Prevention of Corruption and the Coordination of Fight Against Corruption. The agency has to respond to the request within 30 days. If such status is given, it prevents action being taken against an employee who has reported corruption under the law (p. 13). 247 It is not clear to date the extent to which this has been used in the health-care context in Bosnia, although it appears to have been used effectively in the context of corruption (p. 55). 247 Blueprint suggests that such a system could be established so that whistleblowers could apply for a Whistleblower Protection Certificate with the aim of stopping further retaliation. The whistleblower could apply to an independent agency for such a certificate or to the Department for Business, Innovation and Skills (p. 55). 247 They propose that, where there is evidence that an organisation has ignored such a certificate in three or more instances or has undertaken aggressive retaliation against whistleblowers, the organisation should be required to appoint a whistleblowing monitor to produce a plan for improving whistleblowing protection in the workplace and produce an annual report for regulators (p. 55). 247
Incentives for whistleblowing
One possible approach that can be taken to encourage whistleblowers to come forward, supported by Blueprint, is the provision of financial incentives, whether in the form of proportion of fines levied or other financial benefits obtained as a result of their disclosure (p. 26). 247 They suggest that the absence of such incentives ‘significantly reduces the ability of a whistleblower to be encouraged to come forward and in turn be rewarded for the risk undertaken’ (p. 26). 247 Incentives have been used in other contexts, notably in the USA,199,308 where the Dodd–Frank Wall Street Reform and Consumer Protection Act 2010309 provides substantial incentives of between 10% and 30% of monies of > US$1M recovered by the government as a consequence of an enforcement action (p. 254). 13 The use of incentives and facilitating whistleblowing can be seen as the aftermath of the failure of the Madoff Ponzi scheme (p. 673). 199 Incentivising whistleblowing in this way in the context of health care is likely to prove extremely controversial. It is also predicated on an assumption that individuals working in the NHS would be motivated by such financial incentives, something that may be less applicable than in other areas. PCAW commented that incentives could be seen as inconsistent with current culture and the moral stance of whistleblowers, and could undermine the credibility of witnesses in subsequent legal proceedings and be seen as inconsistent with the current compensatory regime (paragraph 60). 162 Freedom to Speak Up stated that there was no demand for such incentives, that these would not increase the number of persons coming forward and that they could cause resentment (paragraph 5.7.4). 2 The report noted that representatives from other sectors whom the report team had met did not offer financial incentives (paragraph 5.7.5),2 and cited research, produced by the Financial Conduct Authority, that they would ‘be unlikely to increase the number of quality disclosures made to them’ (paragraph 5.7.6). 2 The introduction of such incentives would require careful consideration. However, although it may not be thought to be easily transferable as a model in relation to standard health and social care whistleblowing, in contrast such a model could be applicable more directly if the whistleblower was, for example, exposing major fraudulent conduct by senior NHS management and, consequently, saving the NHS major sums of money.
Confidentiality/gagging clauses
The question of confidentiality or so-called ‘gagging’ clauses was discussed in Chapter 5. These clauses may be seen as valid and appropriate from an employment law perspective but are considerably less so from a freedom of speech approach to whistleblowing or from a regulatory approach. It remains very questionable as to the extent to which such clauses are ever appropriate in the public sector and, as noted, the Secretary of State for Health and Social Care has previously indicated that these would be banned. Further work and/or guidance in this area may be necessary.
Using the criminal law to protect whistleblowers
The legislation in England and Wales does not provide for criminal penalties against those who commit reprisals against whistleblowers. In contrast, such provisions do apply in relation to certain other jurisdictions. 310 For example, section 1107 of the US Sarbanes–Oxley Act 2002311 provides that it is an offence to knowingly and with intent retaliate or take action harmful to another person. This includes the interference with a person’s lawful employment or livelihood if they have provided a law enforcement officer with information that is truthful concerning the commission, or possible commission, of a federal offence. The section provides for the imposition of a fine or of a period of imprisonment of up to 10 years. The extent to which this can, however, be seen in terms of discrete whistleblower protection or rather as an extension of more general offences concerning obstruction of justice has been questioned.
The criminal law could be used to provide specific protection for whistleblowers who blow the whistle in relation to gross negligence manslaughter and are called to give evidence in a subsequent criminal trial. In relation to prosecutions of this nature, such whistleblowers could be classed as ‘intimidated witnesses’ and given greater protection at a criminal trial in terms of the manner in which they gave evidence. 310 The further engagement with the criminal law in this way is a question that has much broader implications than this report.
Making additional compensation claims available to whistleblowers
In addition to providing redress in employment law, another approach taken in the Republic of Ireland is that of providing additional compensation claims for whistleblowers. The Protected Disclosures Act 2014312 provides that if a person causes detriment (including intimidation, harassment, discrimination or injury) to another person who has undertaken a protected disclosure, then the person seeking protected disclosure will have a right of action in tort against the person who has caused the detriment (section 13). 307 The Act gives express immunity for liability in relation to civil actions in a situation in which an individual makes a protected disclosure save in relation to a defamation action. It also provides for a ‘qualified privilege’ in relation to defamation law and that a whistleblower’s identity can be safeguarded in certain situations. It is too early to assess properly the impact of these provisions, but such an approach may also assist whistleblowers who are prepared to come forward in the future.
None of the potential avenues for legal innovation laid out above offer simple or swift remedial action to a patched and patchwork legal system. Nonetheless, they do set out avenues for future discussion, consultation and empirical research, hopefully before new legislative proposals are brought forward.
Key practice action points arising from research objective 3
-
The legal framework surrounding whistleblowing is likely to change in the near future (possibly, but not necessarily, along the lines suggested above) and it is incumbent on managers to keep abreast of developments so that local whistleblowing and speaking up policies are continually updated and aligned with any changes in the law.
-
The potential deficiencies and deficits of the existing legal frameworks should be openly acknowledged and ‘worked around’ with due consideration of the needs of an open culture – and should not be used ‘tactically’ to depress open reporting or excuse managerial inaction on such reporting.
Research objective 4: learning from the findings of formal inquiries
In Chapter 4 we presented the findings of our analysis of Inquiries dating back to the Bristol Royal Infirmary5 through Ayling,152 Kerr/Haslam,153 Shipman,154 Francis155,156 and Francis11 to the Freedom to Speak Up review. 2 A number of issues arise from these analyses of the inquiries and response reports, which are now outlined.
Diverse definitions of whistleblowing
First, and as highlighted in Chapter 2, there is no clear and universally accepted definition of whistleblowing. Indeed, the Shipman Inquiry tried to avoid using the expression ‘whistleblowing’ whenever possible (319),154 and Francis2 considered replacing the term. Francis2 presented a broad definition as ‘a person who raises concerns in the public interest’. Hooper192 defined it as ‘the raising of a concern, either within the workplace or externally, about a danger, risk, malpractice or wrongdoing that affects others’ (p. 1). Hooper continued that it is sometimes said that a whistleblower is a person who raises concerns externally, but ‘this is not right’. Many persons who raise concerns do not necessarily, at the time of raising the concerns, see themselves as whistleblowers. They are likely to come to regard themselves as whistleblowers only if they suffer detriment as a result of raising the concerns or if no action is taken on their concerns (p. 2). The Shipman Inquiry considered that none of these persons who raised concerns were ‘whistleblowers’ per se, as they did not work in the same organisation as Shipman (p. 318). The Bristol inquiry did not appear to recognise Dr Steve Bolsin as a whistleblower, as it is stated that had PIDA been in force it would not have applied to Dr Bolsin because he did not make a ‘qualifying statement’ (160). 5 So, there appear to be three dimensions to whistleblowing contained in formal Inquiry reports: (1) whether or not the person works for the organisation; (2) whether they raise concerns internally or externally (or escalate from internal to external, if the internal route produces no results); and (3) whether or not they are a whistleblower in the strict legal sense of the term and are making a ‘qualifying statement’.
Few specific recommendations on whistleblowing
It is perhaps surprising, given their subject matter, but there is little specific discussion of, or recommendations concerning, whistleblowing across these inquiries. The inquiries focus (perhaps disproportionately) on patient complaints rather than on employee voice. However, the Shipman Inquiry stated that ‘I believe that the willingness of one healthcare professional to take responsibility for raising concerns about the conduct, performance or health of another could make a greater potential contribution to patient safety than any other single factor’ (p. 23)160 (subsequently cited in Hooper192 and Francis2). Similarly, as Niall Dickson, CEO of the GMC, put it in 2012: ‘The eyes and ears of health professionals are often the most valuable means of protecting patients and ensuring high quality care’. 192 Of some 820 recommendations across all of the inquiries reviewed, only eight are directly concerned with whistleblowing. Even the Shipman Inquiry, which stressed the role of health professionals in raising concerns, had only 3 of its 190 recommendations focused on whistleblowing.
System failures rather than individual shortcomings
It was notable that most inquiry accounts focused on the ‘system’ rather than on the people within it: structural and collective, rather than agency or individual, explanations. However, Kerr/Haslam153 contrasted the action of the first ‘whistleblower’ in the case of Kerr, Dr Mathewson, a GP practising in Northern Ireland, who gave evidence at a disciplinary tribunal in 1964, with the result that Kerr’s career in Northern Ireland came to an end, with the inaction of GPs in England: ‘it is a sad fact . . . that once in England there was not a single GP who displayed the fortitude of Dr Mathewson in pursuing any one of the many complaints against William Kerr to the logical conclusion of any form of disciplinary’ (p. 446; © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). 153 As the counsel for the patients put it to the inquiry: ‘for the main part, we do not say they are system failures, they are personality failures, where patients were so short-changed by individuals, not by the system: the system worked in 1966 [a reference to Northern Ireland], the system could have worked if individual doctors, GPs, had taken extra steps’ (volume 2, pp. 801–2; © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). 153
Cultural change over legal safeguards
The most consistent remedy drawn out from inquiry recommendations has been cultural reform and renewal rather than legal safeguards. Inquiries since Kennedy5 have consistently argued in favour of ‘culture change’ (without specifying in any detail how this was to be achieved). For example, Francis155,156 pointed to the problem of organisational culture and considered that ‘the most important factor in changing this will not be a new system or policy of protection for whistleblowers, but the fostering of a culture of openness, self-criticism and teamwork’ (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). Francis11 cited Ken Lownds of Cure the NHS that regardless of protective legislation and policies it was the culture that mattered. Without a positive culture, it would never be easy to raise concerns. Francis considered that whistleblowing was only necessary because of the absence of systems and a culture accepted by all staff that is receptive to internal reporting of concerns. ‘Therefore, the solution lies in creating the right culture, not in focusing on improvements to whistleblowing legislation, important though such protection is’ (p. 242; © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). 11
Similarly, whether expressed in terms of ‘a system devoted to continual learning’179 (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0) or ‘a culture which is comfortable with challenge’182 (© Parliamentary Copyright. Contains Parliamentary information licensed under the Open Parliament Licence v3.0. www.parliament.uk/site-information/copyright-parliament/open-parliament-licence/) it has been claimed that ‘culture change’ would make the role of the whistleblower redundant. Similar points are made by the government: although progress on Francis’ 290 recommendations were important, ‘perhaps the most important point is that the ongoing need to change the culture in the NHS to one of patient-centred, continual improvement in care and safety’ (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). 186 That cultural change is as unproblematic as such pronouncements seem to suppose has, however, received some considerable challenge. 313
The Francis public inquiry,11 like the Kennedy inquiry at Bristol more than a decade earlier, went to considerable trouble to try to understand the meaning of culture in a health-care context. Yet the subtlety of some of the supporting evidence to the inquiry was not matched by the same degree of nuance in the inquiry’s recommendations about culture, which are somewhat aspirational and broad brush. 313 By finding fault with culture and providing prescriptions for change, Francis made several assumptions that require examination. First, he presupposes that we can identify and assess common aspects of culture as well as identify which aspects are supportive of or inimical to high-quality care. Second, he assumes that these aspects of culture can be purposely changed, that any changes will lead to improvements and that the costs and dysfunctions from such prescriptive changes will be outweighed by the benefits. Finally, although acknowledging that culture may vary ‘from organisation to organisation and from department to department’, Francis emphasises the need for ‘a positive and common culture throughout’. This presumes that common cultures are possible and desirable even in systems as large and distributed as the NHS. However, much research shows more complex and nuanced relations between cultures, practices and outcomes than implied by Francis and other inquiries. 314
Reinvention and retreads
Evident from these Inquiry reports is a high degree of ‘reinventing the wheel’, with some return to similar solutions over time: a situation described as ‘Groundhog Day’ as recommendations from previous Inquiries become recycled. 315 The clearest example of this is the repeated identification of culture as both culprit and solution to periodic failings in the quality of care in the NHS (discussed above). A further example is the term ‘duty of candour’, which appeared in Kennedy5 through Kerr/Haslam,153 to Francis,11 Dalton and Williams183 and the DHSC. 275 However, this term appears to be rather widely and vaguely defined, and it remains to be seen what sanctions may be applied to those who fail to display their statutory duty of candour in future.
Similarly, there has been a repeated emphasis on reissuing policies and guidelines despite scant evidence that these have much effect. 153,154,168,170,171 Indeed, Francis11 noted that the Mid Staffordshire Trust had actually had a policy on whistleblowing since 2001 but events exposed the ‘hollowness’ of that policy. Perhaps in earlier periods, one major problem may have been that many staff were not fully aware of whistleblowing policies or procedures. For example, the single most important barrier to staff such as nurses and midwives formally expressing their concerns about Ayling was the absence of any formal procedure for doing so. 152 However, it now seems that that there is a problem of ‘bridging the gap’ between being aware of issues and being willing to blow the whistle (see Chapter 2).
Although some recommendations of the inquiries have been implemented (see Appendix 2), the impact of these changes remains unclear, and there is not yet any coherent body of case law on the impact of the ERRA 2013208 (see also Chapter 5; and Ashton196).
Optimism over improvements
Many of the reports appear to be somewhat optimistic that ‘things are getting better’, that institutions, policies and procedures are in place that will not allow earlier problems to recur. 152,154 Governments tend to argue that ‘much has changed’ since the incidents took place and that remedial policies have been put into place. 166,186 However, although there have been some positive changes,196 there is a concern that the pattern in health care will follow that of child abuse inquiries: that lessons have been learnt and it will never occur again – until the next time.
Overall, the impression gained across these inquiries is one of missed opportunities and failed learning. Indeed, the word ‘hindsight’ was used 456 times in the testimony to the Francis public inquiry. 316 In terms of whistleblowing and speaking up, the NHS appears to have much to learn in becoming a learning organisation. 317 At times the NHS appears to be an organisation without much of a memory: ‘sorry’ may be the hardest word but learning and implementation seem to be the hardest activities. 317
Key practice action points arising from research objective 4
-
Many of the larger-scale and more prominent NHS failures could have been dealt with more effectively and more timely if local managerial cultures were more appropriately attuned to ‘hear’ signals of challenge, highlighting the importance of open cultures.
-
The challenge is for local management and leadership to create open and responsive cultures. The evidence indicates that at national/policy level actions in response to manifest failures are often both slow and lacking specificity in relation to local contexts.
-
Recommendations from NHS inquiries need careful interpretation and implementation at the local level, as not all recommendations will be appropriate or useful for particular organisations or different circumstances and staff.
Directions for future whistleblowing research in health care
Taken together, the arguments emerging through the various strands of this work highlight the need for a new socially situated research agenda, not just of whistleblowing as aberrant activity but of the full range of organisationally embedded communications, sense-making, judgement-forming and responses. Although some form of whistleblowing – and the social, legal and structural arrangements in support of it – may always be necessary, a better understanding of these organisationally situated dynamics may, paradoxically, enable a diminution of its prominence. 314 Given this, we now explore some of the directions such a revitalised research agenda might take.
Exploring the ‘deaf effect’, hearer courage and hearer protection
Most previous research has focused on whistleblowers themselves, and there is a paucity of evidence on the nature of the managerial and organisational responses to those raising serious concerns in health-care contexts. Future research could, therefore, usefully explore the personal and organisational factors that appear to support (or impede) appropriate (or inappropriate) responses from managers across a range of health-care contexts. In particular, the factors associated with hearer courage and hearer protection need to be explored so that lessons can be transferred across the NHS. As whistleblowing is a dynamic and recursive process (not a singular event), any research in this area needs to be alert to this dynamic and recognise that such a process is mutually constituted. In doing so, the creation of socially situated perceptions, and the discourse(s) that support and/or impede these, will be crucial. The unit of analysis, then, becomes the unfolding interactional process, not the whistleblower or responding manager per se. It could also be productive to investigate the informal measures taken by health-care professionals to address poor care, and to consider the factors that lead workers to follow this route rather than more formal signals to (internal or external) authority.
Progression from raising concerns to whistleblowing
In Chapter 2, we proposed a distinction between raising concerns, speaking up and whistleblowing. There is a need for work that examines whether or not this proposed framework is robust, and that clarifies the relationship between raising concerns, speaking up and whistleblowing. For example, should these acts be viewed as a chronological sequence through which staff may progress in highlighting problems, or are they essentially separate, distinct and discrete phenomena?
An important issue is to identify how interventions aimed at strengthening one element affect the others. It seems intuitively appealing to focus on encouraging raising concerns, partly because this may ensure that problems are addressed earlier, but also because we might assume a greater willingness to raise concerns will flow through into greater willingness to speak up and blow the whistle if needed. However, our review of the health-care literature on whistleblowing suggests that negative responses to whistleblowers make staff less willing to raise concerns. It may be that the best way to ensure that the majority of staff are prepared to raise concerns is to publicly support and protect the minority who do blow the whistle. Linked to this, there is an obvious need for research on the implementation and effectiveness of the local Speaking Up guardians and the national guardian. How are different NHS organisations introducing these new roles and what is their impact on reshaping organisation strategies, structures, incentives and cultures with regard to raising concerns and speaking up?
Cultural and interpersonal differences
The NHS is one of the most culturally and ethnically diverse organisations in the world, and so there is a pressing need to explore how cultural differences in values, beliefs and attitudes towards whistleblowing affect the willingness of staff to raise concerns, and also the willingness of managers and organisations to respond. The existing literature has barely begun the task of theorising cultural, gendered, experience-led or personality-related drivers of local actions and reporting.
For example, one of the most striking findings from the literature review is that nurses who perceive themselves as first and foremost the patient’s advocate are inherently more likely to blow the whistle than those who perceive patients as just one of several stakeholders to whom they have obligations (it would be useful to see whether or not this pattern might also be observed among other health-care professionals). In the modern NHS, HR policy and practice is frequently directed towards gaining commitment and engagement from staff that might unintentionally reinforce the perception that their obligations to the organisation over-ride or trump their obligations to the patient. Senior management then may be able to influence this by emphasising the extent to which staff are empowered to put the patient first. This provides just one example of an area ripe for further empirical work and subsequent guidance.
Research on other health professionals
Recognising that much of the literature is focused on nurses, and particularly on student nurses, it would be valuable to explore whistleblowing beliefs, practices and experiences of non-nursing health-care workers more comprehensively. An important area for research should be an examination of the influence of professional standards, codes and guidelines, as these are a powerful influence on voice behaviour. There is some suggestion that the code of practice onus placed on nurses to ensure that patients do not come to harm leads to them taking independent action to resolve issues of poor care, avoiding the risks (to them) of whistleblowing but also potentially increasing risk to patient safety (as underlying problems are not brought to management attention). Future whistleblowing research needs to be sensitive not only to the local context and wider policy background, but also to the details of professional socialisation and regulatory wrap-arounds.
Theory of planned behaviour
Park and Blenkinsopp,318 Bjorkelo and Bye65 and Vanderkerkchove et al. 24 have all suggested the theory of planned behaviour63 as a general model for whistleblowing research. One of the key insights of this model is that the relationship between attitudes towards an action (in this case whistleblowing), intention to act and, finally, acting is influenced by perceived behavioural control (i.e. whether or not the individual believes he or she could, in principle, carry out the action) and subjective norms (i.e. the individual’s beliefs about what significant others would think of them undertaking the action). Perceived behavioural control and subject norms are both implicitly ‘composite’ variables. To illustrate, in measuring subjective norms Park and Blenkinsopp318 asked participants what five groups might think of their behaviour: family members, co-workers, immediate supervisors, friends and neighbours. It is clearly possible for these groups to have different views about the behaviour and also for the would-be whistleblower to weight these views differently (e.g. he or she may be largely unconcerned about the views of co-workers, but place great weight on what family members think). Similarly, among the various factors that might affect perceived behavioural control, there may be one or two key elements that are most significant. There is a need then for further research in NHS settings to understand the factors that influence perceived behavioural control and subjective norms, which may vary considerably between occupations, units and organisations.
Better use of data
We have alluded to the considerable ambiguity and interpretation around whether a particular situation is a quality and safety problem or just acceptable variation in level of service. Given the number of data now collected by the NHS, and the increasingly sophisticated ways in which they can be analysed, it ought to be possible to reduce this ambiguity but also, potentially, to reduce the need for whistleblowing; potential problems may be detectable as trends in the data, making the service less reliant on staff bringing it to management’s attention. The use of evidence such as clinical audit data to reduce the need for whistleblowing, and also the ambiguity around whether or not a particular practice or situation is acceptable, could, therefore, be a topic for translational research. In addition, the annual NSS collects data on staff perceptions in relation to whistleblowing and organisational responses when concerns are raised; these could be exploited to look at trends over time and across services and staff groups to highlight potential system weaknesses. Early quantitative work in this area using NSS data has identified a statistically significant association between hospital-board-level competencies and the willingness of staff to report concerns, as well as staff perceptions that their organisation will respond positively when they do. 319
Types of wrongdoing
Wrongdoing covers a range of issues, ranging from financial mismanagement to physical abuse and, in the extreme, murder. Future research should aim to highlight how the type of wrongdoing affects the willingness of staff to speak up, as well as the response from health-care organisations. There are differences, for example, in practice and theory when it comes to the issue of speaking up about ‘everyday’ poor practice due to mistakes, low staffing on wards, exhaustion and unpleasant working cultures, and speaking up about ‘extreme’ predatory or abusive individuals.
Media coverage
The political sensitivity of the NHS, and the media scrutiny it attracts, raises the stakes for senior management in responding to problems raised by staff. It would, therefore, be useful to examine how the interaction of media coverage and the efforts of NHS organisations to manage this coverage influence managerial responses to whistleblowing, including hearer courage and hearer protection, as outlined above. The aim would be to identify ways to ‘lower the stakes’ for management, making it easier for them to acknowledge and address problems. Comparative research would be particularly revealing here, as the NHS is an outlier in terms of the level of scrutiny it receives from the media compared with health care in other countries.
Research design
As with all research, a robust and rigorous study design enhances the credibility of findings, and future research into whistleblowing and speaking up in the NHS would benefit from a number of design and methodological features.
-
Future studies should be mixed method and multidisciplinary/interdisciplinary in design, drawing on a range of appropriate quantitative and qualitative methods. Detailed ethnographic and autobiographical approaches would seem particularly suitable for exploring many of the sensitive and contextual specific issues related to whistleblowing and speaking up in complex and fast-changing health-care settings.
-
As the phenomena under study are essentially dynamic (performance, reporting and organisational responses), a longitudinal study will offer important additional insights over cross-sectional designs. For example, a longitudinal statistical analysis of the NSS could be used to uncover changes in reporting practices and organisational responses, over time, as policies change. Longitudinal qualitative work could also assesses the long-term career consequences for whistleblowers and those health-care services that have been subject to concerns.
-
Investigating the nuances surrounding whistleblowing in different health-care settings would require researchers to gain very substantial access to organisations in order to be able to investigate whistleblowing in context. This could involve ‘co-production’ of research with those NHS organisations that recognise that they have particular problems in terms of employee voice or a history of inappropriate responses when legitimate concerns have been raised. Similarly, there may be benefit in researching ‘positively deviant’ organisations, that is, those that have a history of responding quickly and positively to genuine concerns.
-
Data relating to the whistleblowing and speaking up questions contained in the NSS could be used to identify potential organisational case study sites that appear to have particular problems in terms of staff raising concerns, as well as those organisations that appear to perform better in this respect.
-
An analysis of NSS whistleblowing data could also be used to track the longitudinal impact of new policy initiatives on the willingness of staff to raise concerns and staff perceptions on whether or not they feel confident that their organisation would respond appropriately if they did. Such an analysis could then be used to gauge the extent to which the NHS is moving towards more openness in its reporting cultures.
Study limitations
As with all research projects, it is important to acknowledge the limitations of the study. The first relates to the linked narrative literature reviews that examined peer-reviewed studies written in English. Although every effort was made to capture all of the relevant papers in relation to the published theoretical and empirical work in this area, using comprehensive search strategies, some may have been missed owing to poor indexing across disparate disciplines. The predominance of nursing students’ studies found in the literature necessarily skews the field, by focusing on a group that is important (and numerous) but not necessarily typical. Second, our review of Inquiry reports and related documents was on a purposeful sample of material, and if our scope had been wider we may have drawn into the analysis materials that offered divergent perspectives from the ones reviewed. Third, our review of the legal literature was necessarily selective, given the amount of work in this area, and this may have had an impact on our findings. Finally, we interviewed only a small number of interviewees (at one point in time) as part of the empirical part of the stakeholder interviews, and our findings may have been different if we had included a larger sample or different individuals with wider roles and responsibilities.
Concluding remarks
Current policy prescriptions that seek to develop better whistleblowing policies and nurture open reporting cultures are in need of a more secure evidential base. In this review, we have drawn on a rich stream of academic research and documentary and legal analysis with the aim of sharpening the thinking around the nature of whistleblowing and related concepts in health-care settings. Although we have set out a wide range of issues that need consideration in developing whistleblowing policies, it is beyond the remit of this research to convert these concerns into specific recommendations of the ways in which current policies can be improved: that is a process that needs to be led from elsewhere, in the light of this new evidence summary, and in full partnership with the service. It is our view, however, that there is still much to learn regarding this important, but under-researched, area of health policy and management practice, and to this end we have highlighted a number of important gaps in knowledge that are in need of more sustained research.
Acknowledgements
The financial support of the National Institute for Health Research Health Services and Delivery Research programme is acknowledged (project code 14/04/33).
We would like to thank the members of our project advisory board for their helpful advice, guidance and support: Pam Alonzo, Gerry Armitage, Malcolm Bocock and Martin Marshall. We are also grateful to the key informants who agreed to be interviewed for the study. Our sincere thanks also go to Sam Bereket, Legal Officer at PCAW, for reading an earlier version of Chapter 5, and to Aled Jones for identifying some of the empirical articles. We are very grateful to Evelina Balandyte for her excellent administrative and secretarial support throughout the project.
Public and patient involvement
We interviewed patient representatives as part of the key informant interviews, and two patient and public representatives, Pam Alonzo and Malcolm Bowcock, were members of the project advisory board and helped to shape the research design and interpret the emerging findings from the study.
Contributions of authors
Professor Russell Mannion (University of Birmingham) has a background in health services research. He led the project, was the first author of the final report and participated in all aspects of the research.
Professor John Blenkinsopp (University of Birmingham) has a background in management studies. He was the second author of the final report and a co-applicant, and he led the review of the conceptual and empirical literature.
Professor Martin Powell (University of Birmingham) has a background in health and social policy. He was the third author of the final report and a co-applicant, and he led the review of the Inquiry reports.
Professor Jean McHale (University of Birmingham) has a background in law. She was the fourth author of the final report and a co-applicant, and she led the legal review and analysis.
Dr Ross Millar (University of Birmingham) has a background in health services research. He was the fifth author of the final report and a co-applicant, and he led and conducted the key informant interviews.
Dr Nicholas Snowden (University of Hull) was the sixth author of the final report, compiled the bibliography and conducted the narrative review of the empirical literature.
Professor Huw Davies (University of St Andrews) has a background in health services research. He was the seventh author of the final report and provided methodological advice and guidance throughout the project.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Braithwaite J, Matsuyama Y, Mannion R, Johnson J. Healthcare Reform, Quality and Safety: Perspectives, Participants, Partnerships and Prospects in 30 Countries. Abingdon: Ashgate Publishers; 2015.
- Francis R. Freedom to Speak Up: An Independent Review into Creating an Open and Honest Reporting Culture in the NHS. London: The Stationery Office; 2015.
- Mannion R, Davies HT. Cultures of silence and cultures of voice: the role of whistleblowing in healthcare organisations. Int J Health Policy Manag 2015;4:503-5. https://doi.org/10.15171/ijhpm.2015.120.
- Whistleblowing Doctors Afraid to Speak Out. London: MPS; 2012.
- Kennedy I. The Report of the Public Inquiry into Children’s Heart Surgery at the Bristol Royal Infirmary 1984–95. Learning from Bristol. London: The Stationery Office; 2001.
- NHS Staff Survey 2015. London: NHS England; 2016.
- Employment Rights Act 1996. London: The Stationery Office; 1996.
- Public Interest Disclosure Act 1998. London: The Stationery Office; 1998.
- The NHS Constitution for England. London: DHSC; 2015.
- NHS Speaking Up Charter. London: NHS Employers; 2015.
- Francis R. The Mid Staffordshire NHS Foundation Trust Public Inquiry (Chaired by Robert Francis QC) Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Near JP, Miceli MP. Organizational dissidence: the case of whistle-blowing. J Bus Ethics 1985;4:1-16. https://doi.org/10.1007/BF00382668.
- Lewis D, Brown AJ, Moberly R, Brown AJ, Lewis D, Moberly R, et al. The International Handbook on Whistleblowing Research. Cheltenham: Edward Elgar Publishing; 2014.
- Park H, Blenkinsopp J, Oktem MK, Omurgonulsen U. Cultural orientation and attitudes towards types of whistle-blowing: a comparison of Turkey, South Korea and the UK. J Bus Ethics 2008;82:929-39. https://doi.org/10.1007/s10551-007-9603-1.
- Blenkinsopp J, Edwards MS, Zerbe WJ, Charmine EJ, Härtel, Ashkanasy NM. Emotions, Ethics and Decision-Making (Research on Emotion in Organizations, Volume 4). Emerald Group Publishing Limited; 2008.
- Teo H, Caspersz D. Dissenting discourse: exploring alternatives to the whistleblowing/silence dichotomy. J Bus Ethics 2011;104:237-49. https://doi.org/10.1007/s10551-011-0906-x.
- Jones A, Kelly D. Whistle-blowing and workplace culture in older peoples’ care: qualitative insights from the healthcare and social care workforce. Sociol Health Ill 2014;36:986-1002. https://doi.org/10.1111/1467-9566.12137.
- Alford CF. Whistleblowers: Broken Lives and Organizational Power. Ithaca, NY: Cornell University Press; 2001.
- Kelly D, Jones A. When care is needed: the role of whistleblowing in promoting best standards from an individual and organizational perspective. Qual Ageing Older Adults 2013;14:180-91. https://doi.org/10.1108/QAOA-05-2013-0010.
- Near JP, Miceli MP. Retaliation against whistle blowers: predictors and effects. J Appl Physiol 1986;71:137-45. https://doi.org/10.1037/0021-9010.71.1.137.
- Okuyama A, Wagner C, Bijnen B. Speaking up for patient safety by hospital-based health care professionals: a literature review. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-61.
- Milligan F, Wareing M, Bhandol J, Pappas Y, Randhawa G, Preston-Shoot M. Supporting Nursing, Midwifery and Allied Health Professional Students to Raise Concerns with the Quality Of Care: A Systematic Literature Review. University of Bedfordshire, Council of Deans of Health; 2016.
- Keil M, Robey D. Blowing the whistle on troubled software projects. Commun ACM 2001;44:87-93. https://doi.org/10.1145/367211.367274.
- Vandekerckhove W, Brown AJ, Tsahuridu E, Brown AJ, Lewis D, Moberly R, et al. International Handbook of Whistleblowing Research. Cheltenham: Edward Elgar Publishing; 2014.
- Chikudate N. Collective myopia and disciplinary power behind the scenes of unethical practices: a diagnostic theory on Japanese organization. J Manage Stud 2002;39:289-307. https://doi.org/10.1111/1467-6486.00293.
- Robison R, Vinten G. Whistleblowing: Subversion or Corporate Citizenship?. London: Paul Chapman Publishing; 1994.
- Vinten G, Vinten G. Whistleblowing: Subversion or Corporate citizenship?. London: Palgrave Macmillan; 1994.
- Vinten G. Asset protection through whistleblowing. J Asset Protect Financ Crime 1994;2:121-31. https://doi.org/10.1108/eb025641.
- Masnick K, McDonnell G. A model linking clinical workforce skill mix planning to health and health care dynamics. Hum Resour Health 2010;8. https://doi.org/10.1186/1478-4491-8-11.
- Weick KE, Sutcliffe KM. Managing the Unexpected: Assuring High Performance in an Age of Complexity. San Francisco, CA: Jossey-Bass; 2001.
- Brown AJ, Vandekerckhove W, Dreyfus S, Ala’I P, Vaughn R. International Reader on Transparency. Cheltenham: Edward Elgar Publishing; 2014.
- Skivenes M, Trygstad SC, Brown AJ, Lewis D, Moberly R, Vandekerckhove W. International Handbook on Whistleblowing Research. London: Edward Elgar Publishing; 2014.
- Culiberg B, Mihelic KK. The evolution of whistleblowing studies: a critical review and research agenda. J Bus Ethics 2017;146:787-803. https://doi.org/10.1007/s10551-016-3237-0.
- Miceli MP, Dreyfus S, Near JP, Brown AJ, Lewis D, Moberly RE. International Handbook on Whistleblowing Research. Edward Elgar Publishing; 2014.
- Barnett M L. Why stakeholders ignore firm misconduct: a cognitive view. J Manage 2014;40:676-702. https://doi.org/10.1177/0149206311433854.
- Fledderjohann J, Johnson DR. What predicts the actions taken toward observed child neglect? The influence of community context and bystander characteristics. Soc Sci Q 2012;93:1030-52. https://doi.org/10.1111/j.1540-6237.2012.00859.x.
- Rothwell GR, Baldwin JN. Whistle-blowing and the code of silence in police agencies: policy and structural predictors. Crime Delinq 2007;53:605-32. https://doi.org/10.1177/0011128706295048.
- Alford CF. Whistle-blowers: how much we can learn from them depends on how much we can give up. Am Behav Sci 1999;43:264-77. https://doi.org/10.1177/00027649921955254.
- Trevino LK, Weaver GR, Reynolds SJ. Behavioral ethics in organizations: a review. J Manage 2006:951-90. https://doi.org/10.1177/0149206306294258.
- Sekerka L, Bagozzi R, Charnigo R. Facing ethical challenges in the workplace: conceptualizing and measuring professional moral courage. J Bus Ethics 2009;89:565-79. https://doi.org/10.1007/s10551-008-0017-5.
- Alleyne P, Hudaib M, Pike R. Towards a conceptual model of whistle-blowing intentions among external auditors. Br Account Revi 2013;45:10-23. https://doi.org/10.1016/j.bar.2012.12.003.
- Rawls J. A Theory of Justice. Cambridge, MA: Harvard University Press; 1971.
- Near JP, Dworkin TM, Miceli MP. Explaining the whistle-blowing process: suggestions from power theory and justice theory. Organ Sci 1993;4:393-411. https://doi.org/10.1287/orsc.4.3.393.
- Gundlach MJ, Douglas SC, Martinko MJ. The decision to blow the whistle: a social information processing framework. Acad Manage Rev 2003;28:107-23. https://doi.org/10.5465/amr.2003.8925239.
- Pillay S, Reddy PS, Morgan D. Institutional isomorphism and whistle-blowing intentions in public sector institutions. Pub Manage Rev 2017;19:423-42. https://doi.org/10.1080/14719037.2016.1178322.
- Skivenes M, Trygstad SC. Whistleblowing in local government: an empirical study of contact patterns and whistleblowing in 20 Norwegian municipalities. Scand Polit Sstud 2016;39:264-89. https://doi.org/10.1111/1467-9477.12066.
- Blenkinsopp J, Snowden N. What about leadership?: Comment on ‘cultures of silence and cultures of voice: the role of whistleblowing in healthcare organisations’. Int J Health Policy Manag 2015;5:125-7. https://doi.org/10.15171/ijhpm.2015.193.
- Miceli MP, Near JP. The incidence of wrongdoing, whistle-blowing, and retaliation: results of a naturally occurring field experiment. Employee Respon Rights J 1989;2:91-108. https://doi.org/10.1007/BF01384940.
- Avakian S, Roberts J. Whistleblowers in organisations: prophets at work?. J Bus Ethics 2012;110:71-84. https://doi.org/10.1007/s10551-011-1148-7.
- Vandekerckhove W, Langenberg S. Can we organize courage? Implications from Foucault’s parrhesia. Electron J Bus Ethics Organ Stud 2012;17:35-44.
- Weiskopf R, Tobias-Miersch Y. Whistleblowing, parrhesia and the contestation of truth in the workplace [published online ahead of print July 12 2016]. Organ Stud 2016. https://doi.org/10.1177/0170840616655497.
- Weinstein D. Bureaucratic Opposition: Challenging Abuses at the Workplace. New York, NY: Pergamon Press; 1979.
- Pittroff E. Whistle-blowing systems and legitimacy theory: a study of the motivation to implement whistle-blowing systems in German organizations. J Bus Ethics 2014;124:399-412. https://doi.org/10.1007/s10551-013-1880-2.
- Dozier JB, Miceli MP. Potential predictors of whistle-blowing. a prosocial behavior perspective. Acad Manage Rev 1985;10:823-36. https://doi.org/10.5465/amr.1985.4279105.
- Dungan J, Waytz A, Young L. Corruption in the context of moral trade-offs. J Interdiscipl Econom 2014;26:97-118.
- Contu A. Rationality and relationality in the process of whistleblowing: recasting whistleblowing through readings of Antigone. J Manage Inquiry 2014;23:393-406. https://doi.org/10.1177/1056492613517512.
- Weick KE. Sensemaking in Organizations. Thousand Oaks, CA: Sage Publications; 1995.
- Weick KE, Sutcliffe KM, Obstfeld D. Organizing and the process of sensemaking. Organ Sci 2005;16:409-21. https://doi.org/10.1287/orsc.1050.0133.
- Olsen J, Brown AJ, Lewis D, Moberly R, Vandekerckhove W. International Handbook on Whistleblowing Research. Cheltenham: Edward Elgar Publishing; 2014.
- Burton BK, Near JP. Estimating the incidence of wrongdoing and whistle-blowing: results of a study using randomized response technique. J Bus Ethics 1995;14:17-30. https://doi.org/10.1007/BF00873732.
- Brewer GA. Incidence of Whistleblowing in the Public and Private Sectors. Athens, GA: Department of Political Science, University of Georgia; 1996.
- Hunt G. Whistleblowing in the Health Service: Accountability, Law and Professional Practice. London: Edward Arnold; 1995.
- Ajzen I. The theory of planned behaviour. Organ Behav Hum Dec 1991;50:179-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- Lawton R, Parker D. Barriers to incident reporting in a healthcare system. Qual Saf Health Care 2002;11:15-8. https://doi.org/10.1136/qhc.11.1.15.
- Bjørkelo B, Bye HH, Brown AJ, Lewis D, Moberly R, Vandekerckhove W. International Handbook on Whistleblowing Research. Cheltenham: Edward Elgar Publishing; 2014.
- Tolstoy L. Anna Karenina. London: Penguin; 2000.
- Randall ML, Cropanzano R, Borman CA, Birjulin A. Organizational politics and organizational support as predictors of work attitudes, job performance, and organizational citizenship behavior. J Organ Behav 1999;20:159-74. https://doi.org/10.1002/(SICI)1099-1379(199903)20:2<159::AID-JOB881>3.0.CO;2-7.
- Ferris RG, Harrell-Cook G, Dulebohn JH. Organizational politics: the nature of the relationship between politics perceptions and political behavior. Res Sociol Organ 2000;17:89-130. https://doi.org/10.1016/S0733-558X(00)17004-1.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Southampton: National Institute for Health Research; 2006.
- Denyer D, Tranfield D, Bryman DABA. The Sage Handbook of Organizational Research Methods. Thousand Oaks, CA: Sage Publications Ltd; 2009.
- Macpherson A, Jones O. Editorial: strategies for the development of International Journal of Management Reviews. Int J Manage Rev 2010;12:107-13. https://doi.org/10.1111/j.1468-2370.2010.00282.x.
- Near JP, Jensen TC. The whistleblowing process: retaliation and perceived effectiveness. Work Occupation 1983;10:3-28. https://doi.org/10.1177/0730888483010001001.
- Westin AF, Kurtz HI, Robbins A. Whistle blowing: Loyalty and Dissent in the Corporation. New York, NY: McGraw-Hill; 1981.
- Dworkin TM, Near JP. A better statutory approach to whistle-blowing. Bus Ethics Q 1997;7:1-16. https://doi.org/10.2307/3857229.
- Miceli MP, Near JP. The relationships among beliefs, organizational position, and whistle-blowing status: a discriminant analysis. Acad Manage J 1984;27:687-705.
- Miceli MP, Near JP. Characteristics of organizational climate and perceived wrongdoing associated with whistle-blowing decisions. Pers Psychol 1985;38:525-44. https://doi.org/10.1111/j.1744-6570.1985.tb00558.x.
- Greenberger DB, Miceli MP, Cohen DJ. Oppositionists and group norms: the reciprocal influence of whistle-blowers and co-workers. J Bus Ethics 1987;6:527-42. https://doi.org/10.1007/BF00383744.
- Brabeck MM. Ethical characteristics of whistle blowers. J Res Person 1984;18:41-53. https://doi.org/10.1016/0092-6566(84)90037-0.
- Near JP, Miceli MP. Whistle-blowers in organizations: dissidents or reformers?. Res Organ Behav 1987;9:321-68.
- Jensen JV. Ethical tension points in whistleblowing. J Bus Ethics 1987;6:321-8. https://doi.org/10.1007/BF00382941.
- Beckstead JW. Reporting peer wrongdoing in the healthcare profession: the role of incompetence and substance abuse information. Int J Nurs Stud 2005;42:325-31. https://doi.org/10.1016/j.ijnurstu.2004.07.003.
- Monrouxe LV, Rees CE, Dennis I, Wells SE. Professionalism dilemmas, moral distress and the healthcare student: insights from two online UK-wide questionnaire studies. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-007518.
- Henik E. Mad as hell or scared stiff? the effects of value conflict and emotions on potential whistle-blowers. J Bus Ethics 2008;80:111-19. https://doi.org/10.1007/s10551-007-9441-1.
- Grube JA, Piliavin JA, Turner JW. The courage of one’s conviction: when do nurse practitioners report unsafe practices?. Health Commun 2010;25:155-64. https://doi.org/10.1080/10410230903544944.
- Firtko A, Jackson D. Do the ends justify the means? Nursing and the dilemma of whistleblowing. Aust J Adv Nurs 2005;23:51-6.
- Ion R, Smith K, Nimmo S, Rice AM, McMillan L. Factors influencing student nurse decisions to report poor practice witnessed while on placement. Nurs Educ Today 2015;35:900-5. https://doi.org/10.1016/j.nedt.2015.02.006.
- Ahern K, McDonald S. The beliefs of nurses who were involved in a whistleblowing event. J Adv Nurs 2002;38:303-9. https://doi.org/10.1046/j.1365-2648.2002.02180.x.
- Attree M. Factors influencing nurses’ decisions to raise concerns about care quality. J Nurs Manag 2007;15:392-40. https://doi.org/10.1111/j.1365-2834.2007.00679.x.
- Bellefontaine N. Exploring whether student nurses report poor practice they have witnessed on placements. Nurs Times 2009;105:28-31.
- Bickhoff L, Levett-Jones T, Sinclair PM. Rocking the boat – nursing students’ stories of moral courage: a qualitative descriptive study. Nurse Educ Today 2016;42:35-40. https://doi.org/10.1016/j.nedt.2016.03.030.
- Black LM. Tragedy into policy – a quantitative study of nurses attitudes toward patient advocacy activities. Am J Nurs 2011;111:27-35. https://doi.org/10.1097/01.NAJ.0000398537.06542.c0.
- Bradbury-Jones C, Irvine F, Sambrook S. Empowerment of nursing students in clinical practice: spheres of influence. J Adv Nurs 2010;66:2061-70. https://doi.org/10.1111/j.1365–2648.2010.05351.x.
- Bradbury-Jones C, Sambrook S, Irvine F. Nursing students and the issue of voice: a qualitative study. Nurs Educ Today 2011;31:628-32. https://doi.org/10.1016/j.nedt.2010.10.030.
- Espin S, Meikle D. Fourth-year nursing student perceptions of incidents and incident reporting. J Nurs Educ 2014;53:238-43. https://doi.org/10.3928/01484834-20140217-04.
- Firth-Cozens J, Firth RA, Booth S. Attitudes to and experiences of reporting poor care. Int J Health Governance 2003;8:331-6. https://doi.org/10.1108/14777270310499423.
- Gould D, Drey N. Student nurses’ experiences of infection prevention and control during clinical placements. Am J Infect Control 2013;41:760-3. https://doi.org/10.1016/j.ajic.2013.01.025.
- Greaves R, McGlone JK. The health consequences of speaking out. Soc Med 2012;6:259-63.
- Hutchinson M, Jackson D. The construction and legitimation of workplace bullying in the public sector: insight into power dynamics and organisational failures in health and social care. Nurs Inq 2015;22:13-26. https://doi.org/10.1111/nin.12077.
- Ion R, Smith K, Moir J, Nimmo S. Accounting for actions and omissions: a discourse analysis of student nurse accounts of responding to instances of poor care. J Adv Nurs 2016;72:1054-64. https://doi.org/10.1111/jan.12893.
- Jackson D, Raftos M. In uncharted waters – confronting the culture of silence in a residential care institution. Int J Nurs Pract 1997;3:34-9. https://doi.org/10.1111/j.1440-172X.1997.tb00068.x.
- Jackson D, Peters K, Andrew S, Edenborough M, Halcomb E, Luck L, et al. Understanding whistleblowing: qualitative insights from nurse whistleblowers. J Adv Nurs 2010;66:2194-201. https://doi.org/10.1111/j.1365-2648.2010.05365.x.
- Jackson D, Peters K, Andrew S, Edenborough M, Halcomb E, Luck L, et al. Trial and retribution: a qualitative study of whistleblowing and workplace relationships in nursing. Contemp Nurs 2010;36:34-4.
- Jones A, Lankshear A, Kelly D. Giving voice to quality and safety matters at board level: a qualitative study of the experiences of executive nurses working in England and Wales. Int J Nurs Stud 2016;59:169-76. https://doi.org/10.1016/j.ijnurstu.2016.04.007.
- Kent L, Anderson G, Ciocca R, Shanks L, Enlow M. Effects of a senior practicum course on nursing students’ confidence in speaking up for patient safety. J Nurs Educ 2015;54:12-5. https://doi.org/10.3928/01484834-20150218-04.
- Killam LA, Montgomery P, Raymond JM, Mossey S, Timmermans KE, Binette J. Unsafe clinical practices as perceived by final year baccalaureate nursing students: Q methodology. BMC Nurs 2012;11. https://doi.org/10.1186/1472-6955-11-26.
- Killam LA, Mossey S, Montgomery P, Timmermans KE. First year nursing students’ viewpoints about compromised clinical safety. Nurs Educ Today 2013;33:475-80. https://doi.org/10.1016/j.nedt.2012.05.010.
- Kingston MJ, Evans SM, Smith BJ, Berry JG. Attitudes of doctors and nurses towards incident reporting: a qualitative analysis. MJA 2004;181:36-9.
- Ko Y, Yu S. The relationships among perceived patients’ safety culture, intention to report errors, and leader coaching behavior of nurses in Korea: a pilot study. J Patient Saf 2017;13:175-83. https://doi.org/10.1097/PTS.0000000000000224.
- Law BY, Chan EA. The experience of learning to speak up: a narrative inquiry on newly graduated registered nurses. J Clin Nurs 2015;24:1837-48. https://doi.org/10.1111/jocn.12805.
- Levett-Jones T, Lathlean J. Don’t rock the boat – nursing students’ experiences of conformity and compliance. Nurse Educ Today 2009;29:342-9. https://doi.org/10.1016/j.nedt.2008.10.009.
- McCann L, Granter E, Hassard J, Hyde P. ‘You can’t do both – something will give’: limitations of the targets culture in managing UK health care workforces. Hum Resource Manage 2015;54:773-91. https://doi.org/10.1002/hrm.21701.
- McDonald S, Ahern K. Whistleblowing – effective and ineffective coping responses. Nurs Forum 1999;34:5-13. https://doi.org/10.1111/j.1744-6198.1999.tb01165.x.
- McDonald S, Ahern K. The professional consequences of whistleblowing by nurses. J Prof Nurs 2000;16:313-21. https://doi.org/10.1053/jpnu.2000.18178.
- Mansbach A, Melzer I, Bachner YG. Blowing the whistle to protect a patient: a comparison between physiotherapy students and physiotherapists. Physiotherapy 2012;98:307-12. https://doi.org/10.1016/j.physio.2011.06.001.
- Moore L, McAuliffe E. Is inadequate response to whistleblowing perpetuating a culture of silence in hospitals?. Clin Govern: Int J 2010;15:166-78. https://doi.org/10.1108/14777271011063805.
- Newton L, Storch JL, Makaroff KS, Pauly B. ‘Stop the noise!’ From voice to silence. Nurs Leadersh 2012;25:90-104. https://doi.org/10.12927/cjnl.2012.22828.
- Ohnishi K, Hayama Y, Asai A, Kosugi S. The process of whistleblowing in a Japanese psychiatric hospital. Nurs Ethics 2008;15:631-42. https://doi.org/10.1177/0969733008092871.
- Peternelj-Taylor C. Whistleblowing and boundary violations: exposing a colleague in the forensic milieu. Nurs Ethics 2003;10:526-37. https://doi.org/10.1191/0969733003ne634oa.
- Prang IW, Jelsness-Jorgensen LP. Should I report? A qualitative study of barriers to incident reporting among nurses working in nursing homes. Geriatr Nurs 2014;35:441-7. https://doi.org/10.1016/j.gerinurse.2014.07.003.
- Schwappach DL, Gehring K. ‘Saying it without words’: a qualitative study of oncology staff’s experiences with speaking up about safety concerns. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013–004740.
- Schwappach DL, Gehring K. Silence that can be dangerous: a vignette study to assess healthcare professionals’ likelihood of speaking up about safety concerns. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0104720.
- Stevanin S, Bressan V, Bulfone G, Zanini A, Dante A, Palese A. Knowledge and competence with patient safety as perceived by nursing students: the findings of a cross-sectional study. Nurs Educ Today 2015;35:926-34. https://doi.org/10.1016/j.nedt.2015.04.002.
- St Pierre M, Scholler A, Strembski D, Breuer G. Do residents and nurses communicate safety relevant concerns?: simulation study on the influence of the authority gradient. Der Anaesthesist 2012;61:857-66.
- Tella S, Smith NJ, Partanen P, Jamookeeah D, Lamidi ML, Turunen H. Learning to ensure patient safety in clinical settings: comparing Finnish and British nursing students’ perceptions. J Clin Nurs 2015;24:2954-64.
- Throckmorton T, Etchegaray J. Factors affecting incident reporting by registered nurses: the relationship of perceptions of the environment for reporting errors, knowledge of the nursing practice act, and demographics on intent to report errors. J Perianesth Nurs 2007;22:400-12. https://doi.org/10.1016/j.jopan.2007.09.006.
- Hofstede G. Cultures and Organizations, Software of the Mind: Intercultural Cooperation and its Importance for Survival. London: McGraw-Hill; 1994.
- Trompenaars FJ, Masthoff ED, Van Heck GL, De Vries J, Hodiamont PP. Relationships between social functioning and quality of life in a population of Dutch adult psychiatric outpatients. Int J Soc Psych 2007;53:36-47. https://doi.org/10.1177/0020764006074281.
- Cheng X, Karim KE, Lin KJ. A cross-cultural comparison of whistleblowing perceptions. Int J Manage Dec Mak 2015;14:15-31. https://doi.org/10.1504/IJMDM.2015.067374.
- Tella S, Smith NJ, Partanen P, Turunen H. Learning patient safety in academic settings: a comparative study of Finnish and British nursing students’ perceptions. Worldviews Evid Based Nurs 2015;12:154-64. https://doi.org/10.1111/wvn.12088.
- Tabak N, Reches R, Wagner N. Whistle-blowing knowledge and attitude of Israeli nurses. Med Law 1997;16:541-55.
- Skivenes M, Trygstad SC. When whistle-blowing works: the Norwegian case. Hum Relat 2010;63:1071-97. https://doi.org/10.1177/0018726709353954.
- Miceli MP, Near JP, Dworkin TM. A word to the wise: how managers and policy-makers can encourage employees to report wrongdoing. J Bus Ethics 2009;86:379-96. https://doi.org/10.1007/s10551-008-9853-6.
- Delk KL. Whistleblowing – is it really worth the consequences?. Workplace Health Saf 2013;61:61-4. https://doi.org/10.3928/21650799-20130129-03.
- Seifert DL, Sweeney JT, Joireman J, Thornton JM. The influence of organizational justice on accountant whistleblowing. Account Org Soc 2010;35:707-17. https://doi.org/10.1016/j.aos.2010.09.002.
- Klaas BS, Olson-Buchanan JB, Ward AK. The determinants of alternative forms of workplace voice: an integrative perspective. J Manage 2012;38:314-45. https://doi.org/10.1177/0149206311423823.
- Orbe MP, King G. Negotiating the tension between policy and reality: exploring nurses’ communication about organizational wrongdoing. Health Commun 2000;12:41-6. https://doi.org/10.1207/S15327027HC1201_03.
- Hyde P. A wicked problem? Whistleblowing in healthcare organisations comment on ‘cultures of silence and cultures of voice: the role of whistleblowing in healthcare organisations’. Int J Health Planning Manage 2016;5:267-9. https://doi.org/10.15171/ijhpm.2016.01.
- Keil M, Tiwana A, Sainsbury R, Sneha S. Toward a theory of whistleblowing intentions: a benefit-to-cost differential perspective. Decision Sci 2010;41:787-812. https://doi.org/10.1111/j.1540-5915.2010.00288.x.
- Gino F, Moore DA, Bazerman MH, Kramer FM, Tenbrunsel AE, Bazerman MH. Social Decision Making: Social Dilemmas, Social Values, and Ethical Judgments. New York, NY: Psychology Press; 2009.
- Brink AG, Jordan Lowe D, Victoravich LM. The effect of evidence strength and internal rewards on intentions to report fraud in the Dodd-Frank Regulatory Environment. J Pract Theory 2013;32:87-104. https://doi.org/10.2308/ajpt-50449.
- Hooks KL, Kaplan SE, Schultz JJ. Enhancing communication to assist in fraud prevention and detection. Auditing 1994;13:86-117.
- Kaptein M. From inaction to external whistleblowing: the influence of the ethical culture of organizations on employee responses to observed wrongdoing. J Bus Ethics 2011;98:513-30. https://doi.org/10.1007/s10551-010-0591-1.
- Johnstone MJ, Kanitsaki O. The ethics and practical importance of defining, distinguishing and disclosing nursing errors: a discussion paper. Int J Nurs Stud 2006;43:367-76. https://doi.org/10.1016/j.ijnurstu.2005.04.010.
- Peters K, Luck L, Hutchinson M, Wilkes L, Andrew S, Jackson D. The emotional sequelae of whistleblowing: findings from a qualitative study. J Clin Nurs 2011;20:2907-14.
- Jackson D, Hickman LD, Hutchinson M, Andrew S, Smith J, Potgieter I, et al. Whistleblowing: an integrative literature review of data-based studies involving nurses. Contemp Nurs 2014;48:240-52. https://doi.org/10.1080/10376178.2014.11081946.
- Hirschman AO. Exit, Voice, and Loyalty: Responses to Decline in Firms, Organizations, and States. Cambridge, MA: Harvard University Press; 1970.
- Goldberg R. The whistle-blower in healthcare. Healthcare Q 2007;10. https://doi.org/10.12927/hcq. 18792.
- Cleary SR, Doyle KE. Whistleblowing need not occur if internal voices are heard: from deaf effect to hearer courage: comment on ‘cultures of silence and cultures of voice: the role of whistleblowing in healthcare organisations’. Int J Health Pol Manage 2016;5:59-61. https://doi.org/10.15171/ijhpm.2015.177.
- Mannion R, Freeman T, Millar R, Davies H. Effective board governance of safe care: a (theoretically underpinned) cross-sectioned examination of the breadth and depth of relationships through national quantitative surveys and in-depth qualitative case studies. Health Serv Deliv Res 2016;4.
- Moore L, McAuliffe E. To report or not to report? Why some nurses are reluctant to whistleblow. Clinic Govern: Int J 2012;17:332-42. https://doi.org/10.1108/14777271211273215.
- Monrouxe LV, Rees CE, Endacott R, Ternan E. ‘Even now it makes me angry’: health care students’ professionalism dilemma narratives. Medic Educ 2014;48:502-17. https://doi.org/10.1111/medu.12377.
- Pauffley A. Committee of Inquiry. Independent Investigation into How the NHS Handled Allegations About the Conduct of Clifford Ayling. London: DHSC; 2004.
- The Kerr/Haslam Inquiry. London: Her Majesty’s Stationery Office; 2005.
- Smith J. The Shipman Inquiry. Six Volumes. London: Her Majesty’s Stationery Office; n.d.
- Francis R. Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust January 2005–March 2009: Volume 1. London: The Stationery Office; 2010.
- Francis R. Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust January 2005–March 2009: Volume 2. London: The Stationery Office; 2010.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. Volume 1: Analysis of Evidence and Lessons Learned (Part 1). London: The Stationery Office; 2013.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. Volume 2: Analysis of Evidence and Lessons Learned (Part 2). London: The Stationery Office; 2013.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. Volume 3: Present and Future Annexes. London: The Stationery Office; 2013.
- Powell M. The changing blueprints of the British NHS: the White Papers of 1944 and 1989. Health Care Anal 1994;2:111-17. https://doi.org/10.1007/BF02249732.
- Hammond P, Bousfield A. Shoot the messenger. Private Eye 2011.
- The Whistleblowing Commission, Report on the Effectiveness of Existing Arrangements for Workplace Whistleblowing in the UK. London: PCAW; 2013.
- Sex Offenders Act 1997. London: The Stationery Office; 1997.
- Committee of Inquiry. To Investigate how the NHS Handled Allegations about the Performance and Conduct of Richard Neale. London: The Stationery Office; 2004.
- Making Amends. A consultation paper setting out proposals for reforming the approach to clinical negligence in the NHS. A report by the Chief Medical Officer. London: DHSC; 2003.
- Learning from Bristol: The Department of Health’s Response to the Report of the Public Inquiry into Children’s Heart Surgery at the Bristol Royal Infirmary 1984–1995. London: The Stationery Office; 2002.
- Learning from Tragedy, Keeping Patients Safe. Overview of the Government’s Action Programme in Response to the Recommendations of the Shipman Inquiry. London: The Stationery Office; 2007.
- Safeguarding Patients. The Government’s Response to the Recommendations of the Shipman Inquiry’s fifth report and to the recommendations of the Ayling, Neale and Kerr/Haslam Inquiries. London: The Stationery Office; 2007.
- Health and Social Care (Community Health and Standards) Act 2003. London: The Stationery Office; 2003.
- Patient Safety. Sixth Report of Session 2008–09. Volume I. Report, Together with Formal Minutes. London: The Stationery Office; 2009.
- Patient Safety. Sixth Report of Session 2008–09. Volume II. Oral and Written Evidence. London: The Stationery Office; 2009.
- Donaldson L. An organisation with a memory. Report of an expert group on learning from adverse events in the NHS chaired by the Chief Medical Officer. London: TSO; 2000.
- HSC 1999/198. The Public Interest Disclosure Act 1998 – Whistleblowing in the NHS. London: The Stationery Office; 1998.
- Patients First and Foremost The Initial Government Response to the Report of The Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Parliamentary Briefing. Recommendations of the Francis Report into the Mid-Staffordshire NHS Foundation Trust. London: BMA; 2013.
- Mid Staffordshire NHS Foundation Trust Public Inquiry Report Response of the Royal College of Nursing. London: RCN; 2013.
- NMC Response to the Francis Report. London: NMC; 2013.
- The General Medical Council response to the report of the Mid-Staffordshire NHS Foundation Trust Public Inquiry. London: GMC; 2013.
- Clwyd A, Hart T. A Review of the NHS Hospitals Complaints System – Putting Patients Back in the Picture. London: DHSC; 2013.
- Berwick D. A Promise to Learn – A Commitment to Act, Improving the Safety of Patients in England, National Advisory Group on the Safety of Patients in England. London: DHSC; 2013.
- Keogh B. Review into the Quality of Care and Treatment Provided by 14 Hospital Trusts in England: Overview Report. London: NHS England; 2013.
- After Francis: Making a Difference, Third Report of Session 2013–14. London: The Stationery Office; 2013.
- Dalton D, Williams N. Building a Culture of Candour – A Review of the Threshold for the Duty of Candour and of the Incentives for Care Organisations to be Candid. London: Royal College of Surgeons; 2014.
- Hard Truths. The Journey to Putting Patients First. Volume One of the Government Response to the Mid Staffordshire NHS Foundation Trust Public Inquiry: Response to the Inquiry’s Recommendations. London: The Stationery Office; 2014.
- Hard Truths. The Journey to Putting Patients First. Volume Two of the Government Response to the Mid Staffordshire NHS Foundation Trust Public Inquiry: Response to the Inquiry’s Recommendations. London: The Stationery Office; 2014.
- Culture Change in the NHS: Applying the Lessons of the Francis Inquiries. London: The Stationery Office; 2015.
- Government Whistleblowing Policies. London: National Audit Office; 2014.
- Making a Whistleblowing Policy Work. London: National Audit Office; 2014.
- Whistleblowing Framework: Call for Evidence – Government Response. London: Department for Business, Innovation and Skills; 2014.
- Employment Rights Act 2006. London: The Stationery Office; 2006.
- Equality Act 2010. London: The Stationery Office; 2010.
- Hooper A. The Handling by the General Medical Council of Cases Involving Whistleblowers. London: GMC; 2015.
- Complaints and Raising Concerns. Fourth Report of Session 2014–15. London: The Stationery Office; 2015.
- Learning not Blaming: The Government Response to the Freedom to Speak Up Consultation, the Public Administration Select Committee Report ‘Investigating Clinical Incidents in the NHS’, and the Morecambe Bay Investigation. London: The Stationery Office; 2015.
- Sawer P, Donnelly L. Meet the NHS whistle-blowers who exposed the truth. Daily Telegraph 2015.
- Ashton J. 15 years of whistleblowing protection under the Public Interest Disclosure Act 1998: are we still shooting the messenger?. Ind Law J 2015;44:29-52. https://doi.org/10.1093/indlaw/dwu029.
- Parliamentary Assembly . Report of the Council of Europe Committee on Legal Affairs and Human Rights, Protection of Whistleblowers 2009.
- Osterhaus A, Fagan C. Alternative to Silence: Whistleblower Protection in 10 European Countries. Berlin: Transparency International; 2009.
- Dworkin TM, Brown AJ. The money or the media? Lessons from contrasting developments in US and Australian whistleblowing laws. Seattle J Soc Just 2013;11:653-71.
- Fasterling B, Brown AJ, Lewis D, Moberly R, Vandekerckhove R. International Handbook on Whistleblowing Research. Cheltenham: Edward Elgar Publishing; 2014.
- Hilton C. Whistle-blowing and duty of candour in the National Health Service: a ‘history and policy’ case study of the 1960s and 2010s. J R Soc Med 2016;109:327-30. https://doi.org/10.1177/0141076816658787.
- McHale JV. Whistle blowing in the NHS. J Soc Welf Fam Law 1992;363:59-68.
- Jones J. NHS ‘whistle-blower’ wins £11,000 damages: health authority pulls out of tribunal brought by former nurse. The Independent 1993.
- Blom-Cooper L. Report of the Inquiry into Complaints About Ashworth Special Hospital. London: The Stationery Office; 1994.
- McHale JV, Hunt G. Whistleblowing in the Health Services. Edward Arnold; 1994.
- Lewis J, Bowers J, Fodder M, Mitchell J. Whistleblowing Law and Practice. Oxford: Oxford University Press; 2012.
- Vaughan R. The Success and Failures of Whistleblower Laws. Cheltenham: Edward Elgar Publishing; 2012.
- Enterprise and Regulatory Reform Act 2013. London: The Stationery Office; 2013.
- Faccenda Chicken Ltd V Fowler and Others 1986.
- Ticehurst and Another V British Telecommunications Plc 1992.
- Initial Services Ltd V Putterill 1968.
- Bell V Lever Bros Ltd 1932.
- Sybron Corporation V Rochem 1984.
- RBG Resources PLC (In Liquidation) V Rastogi and Others 2005.
- Lister V Hesley Hall Ltd 2001.
- Stag Line Ltd V Tyne Shiprepair Group Ltd. The Zinnia 1984.
- Item Software (UK) Ltd V Kouroush Fassihm, Andy Liddiardrams, International Ltd Isograph Ltd 2003.
- Breakley P. Legal update employment. New Law J 2016;167.
- McTigue V University Hospital Bristol NHS Foundation Trust n.d.
- Protected Disclosures (Extension of Meaning of Worker) Order 2015/491. London: The Stationery Office; 2015.
- Employment Relations Act 1999 (Blacklists) Regulations 2010. London: The Stationery Office; 2010.
- Small Business, Enterprise and Employment Act 2015. London: The Stationery Office; 2015.
- BP Plc V Elstone and Petrotechnics Limited 2010.
- Babula V Waltham Forest College 2007.
- Lewis D. Is a public interest test for workplace whistleblowing in society’s interest?. Int J Law Manage 2015;57:141-58. https://doi.org/10.1108/IJLMA-10-2014-0056.
- Smith I. Legal update employment. New Law J 2015;165.
- Sim V Manchester Action on Street Health n.d.
- Easwaran V St George’s University of London n.d.
- Darnton V University of Surrey 2003.
- Cavendish Munro Professional Risks Management Ltd V Geduld 2010.
- Kilraine V London Borough of Wandsworth 2016.
- Aamod A, Paulin M. Blowing in the wind. New Law J 2016;166.
- Handbook on the NHS Constitution for England. London: DHSC; 2015.
- Vickers L. Freedom of Speech in the NHS. J Soc Welf Fam Law 1999;21:121-34. https://doi.org/10.1080/09649069908410560.
- Moyhing and Another V Barts and London NHS Trust 2006.
- NHS Manchester V Fecitt &Amp; Others 2011.
- Woodward V Abbey National Plc 2006.
- De Souza V Automobile Association 1986.
- BP Plc V Elstone &Amp; Petrotechnics Ltd 2010.
- Gornall J. The price of silence. BMJ 2009;339. https://doi.org/10.1136/bmj.b3202.
- Confidentiality Clauses and Special Severance Agreements – Public Accounts Committee. London: The Stationery Office; 2013.
- Chapman J. Victory for NHS whistleblowers: after Daily Mail campaign, Health Secretary bans gagging orders on NHS staff. Mail Online 2013.
- Pyper D. House of Commons Briefing Paper; Whistleblowing and Gagging Clauses 2016.
- Lewis D. Resolving whistleblowing disputes in the public interest: is tribunal adjudication the best that can be offered?. Ind Law J 2013;42:35-52. https://doi.org/10.1093/indlaw/dwt001.
- Complaints and Raising Concerns: Fourth Report of Session 2014–5. London: The Stationery Office; 2015.
- Gobert J, Punch M. Whistleblowers, the public interest and the Public Interest Disclosure Act. Mod Law Rev 2000;63. https://doi.org/10.1111/1468-2230.00249.
- Wolfe S, Worth M, Dreyfus S, Brown A. Blueprint for Free Speech Breaking the Silence: Strengths and Weaknesses in G20 Whistleblower Protection Laws 2015. www.blueprintforfreespeech.net (accessed 1 May 2018).
- Public Interest Disclosure (Prescribed Persons) Act 2015. London: The Stationery Office; 2015.
- Human Rights Act 1998. London: The Stationery Office; 1998.
- Recommendation CM/REC(2014)7 of the Committee of Ministers to Member States on the Protection of Whistleblowers. Strasbourg: Council of Europe; 2014.
- Council of Europe . Explanatory Memorandum of Recommendation CM Rec 2014.
- Civil Law Convention on Corruption. Strasbourg: Council of Europe; 2006.
- Handysides V The United Kingdom 1981.
- Guija v Moldova. Strasbourg: Council of Europe; 2008.
- Castells v Spain. 1992.
- Bucur and Toma v Romania. Strasbourg: Council of Europe; 2014.
- Matúz v Hungary. Strasbourg: Council of Europe; 2014.
- Heinisch V Germany 2011.
- Kudeshkina V Russia 2009.
- Vogel V Germany 1995.
- Fasterling B, Lewis D. Leaks, legislation and freedom of speech: how can the law effectively promote public interest whistleblowing?. Ind Labour Rev 2014;153:71-92. https://doi.org/10.1111/j.1564-913X.2014.00197.x.
- Abortion Act 1967. London: Her Majesty’s Stationery Office; 1967.
- Human Fertilisation and Embryology Act 1990. London: Her Majesty’s Stationery Office; 1990.
- Haigh R, Bowal P. Whistleblowing and freedom of conscience: towards a new legal analysis. Dalhouisie Law J 2015;35:89-125.
- Montgomery J. Conscientious objection: personal and professional ethics in the public space. Med Law Rev 2015;23:200-2. https://doi.org/10.1093/medlaw/fwv013.
- Confidentiality. London: GMC; 2009.
- The Code: Professional Standards of Practice and Behaviour for Nurses and Midwives. London: Nursing and Midwifery Council; 2015.
- Campbell V Mirror Group Newspapers Ltd (MGN) 2004.
- Vidal-Hall and Others V Google Inc 2014.
- W V Edgell 1990.
- Douglas, Zeta Jones, Northern and Shell Plc V Hello! Limited (No.1) 2001.
- National Health Service Act 2006. London: The Stationery Office; 2006.
- Health and Social Care Act 2008. London: The Stationery Office; 2008.
- Whistleblowing Policy. London: GMC; 2015.
- Introducing the Statutory Duty of Candour: A Consultation on Proposals to Introduce a New CQC Registration Regulation. London: DHSC; 2014.
- Mental Capacity Act 2005: Post-legislative Scrutiny. London: The Stationery Office; 2014.
- Hazell W. Whistleblower Guardian will not be an investigation body. Health Service Journal 2016.
- Quinn B. NHS’s first ‘national guardian’ resigns after two months. The Guardian 2016. www.theguardian.com/society/2016/mar/08/nhs-national-guardian-resigns-post-eileen-sills (accessed 1 May 2018).
- Gregory A. Second whistleblowing tsar departs as Office of National Guardian sinks further into ‘crisis’. The Mirror 2016.
- Gregory A, Keegan S. Jeremy Hunt warned that second whistleblowing Tsar is not independent enough. The Mirror 2016.
- NHS England . Freedom to Speak Up Guardians: Purpose and Key Principles of the Role 2016.
- Hughes H. First 100 Days Report. CQC; 2017.
- Moore A. Blowing the whistle on bad practice. Nurs Stand 2015;30:22-3. https://doi.org/10.7748/ns.30.15.22.s26.
- Smyth C. Happiness is the best medicine, grumpy doctors and nurses told. The Times 2016.
- Cotton E. NHS guardians won’t help whistleblowers unless they’re protected from bullying too. The Conversation 2015. https://theconversation.com/nhs-guardians-wont-help-whistleblowers-unless-theyre-protected-from-bullying-too-37543 (accessed 1 May 2018).
- Naylor V Preston Area Health Authority 1987.
- Ritchie JH, Davies SC. Professional negligence: a duty of candid disclosure?. BMJ 1995;310:888-9. https://doi.org/10.1136/bmj.310.6984.888.
- Powell V United Kingdom 2000.
- The Mid Staffordshire NHS Foundation Trust . Report of the Mid-Staffordshire NHS Foundation Trust Public Inquiry n.d. http://webarchive.nationalarchives.gov.uk/20150407084003/http://www.midstaffspublicinquiry.com/ (accessed August 2018).
- Guidance About Compliance – Essential Standards of Quality and Safety. London: CQC; 2010.
- National Health Service . Care Quality Commission (Registration) Regulations 2009 2009.
- Newdick C, Danbury C. Culture, compassion and clinical neglect: probity in the NHS after Mid Staffordshire. J Med Ethics 2015;41:956-62. https://doi.org/10.1136/medethics-2012-101048.
- Care Act 2014. London: The Stationery Office; 2014.
- Oliver D. The hardest word: managers and leaders should say sorry too. BMJ 2015;351. https://doi.org/10.1136/bmj.h3644.
- Blythe H. Regulating the Duty of Candour. London: Action against Medical Accidents; 2016.
- Paduano M. Family not told of cancer op error at Coventry hospital. BBC News 2016. www.bbc.co.uk/news/uk-england-coventry-warwickshire-37365233 (accessed 1 May 2018).
- Action Against Medical Accidents . Care Quality Commission Told It ‘Must Improve’ on Duty of Candour 2016. www.avma.org.uk/news/care-quality-commission-told-it-must-improve-on-duty-of-candour/ (accessed 1 May 2018).
- Millar R, Freeman T, Mannion R. Hospital board oversight of quality and safety: a stakeholder analysis exploring the role of trust and intelligence. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0771-x.
- Waring JJ. Constructing and re-constructing narratives of patient safety. Soc Sci Med 2009;69:1722-31. https://doi.org/10.1016/j.socscimed.2009.09.052.
- Currie G, Brown AD. A narratological approach to understanding processes of organizing in a UK Hospital. Hum Relat 2003;56:563-86. https://doi.org/10.1177/0018726703056005003.
- Dixon-Woods M, Suokas A, Pitchforth E, Tarrant C. An ethnographic study of classifying and accounting for risk at the sharp end of medical wards. Soc Sci Med 2009;69:362-9. https://doi.org/10.1016/j.socscimed.2009.05.025.
- Goddard M, Mannion R, Smith PC. Assessing the performance of NHS hospital trusts: the role of ‘hard’ and ‘soft’ information. Health Policy 1999;48:119-34. https://doi.org/10.1016/S0168-8510(99)00035-4.
- Janis IL. Groupthink: Psychological Studies of Policy Decisions and Fiascoes. London: Houghton Mifflin; 1982.
- Mannion R, Thompson C. Systematic biases in group decision making: implications for patient safety. Int J Qual Health Care 2014;26:606-12. https://doi.org/10.1093/intqhc/mzu083.
- Lewis D. Ten years of Public Interest Disclosure Act 1998 claims; what can we learn from statistics and recent research?. Ind Law J 2010;39:325-8. https://doi.org/10.1093/indlaw/dwq018.
- Savage A, Hyde R. The response to whistleblowing by regulators: a practical perspective. Legal Stud 2015;35:408-29. https://doi.org/10.1111/lest.12066.
- Republic of Ireland . The Protected Disclosures Act 2014 n.d.
- Faunce T, Crow K, Nikolic T, Morgan FM, Brown AJ, Lewis D, et al. International Handbook on Whistleblowing Research. Cheltenham: Edward Elgar; 2014.
- United States . Dodd–Frank Wall Street Reform and Consumer Protection Act 2010 2010.
- Spencer M, Spencer J, Brown AJ, Lewis D, Moberly R, Vandekerckhove R. International Handbook on Whistleblowing Research. Cheltenham: Edward Elgar; 2014.
- Sarbanes–Oxley Act 2002.
- Doherty M, Ryan R, Thusing G, Forst G. Whistleblowing a Comparative Study. Springer; 2016.
- Davies HT, Mannion R. Will prescriptions for cultural change improve the NHS?. BMJ 2013;346. https://doi.org/10.1136/bmj.f1305.
- Mannion R, Davies H, Ferlie E, Montgomery K, Reff Pedersen A. Oxford Handbook of Health Care Management. Oxford: Oxford University Press; 2016.
- Powell M, Mannion R, Exworthy M, Mannion R, Powell M. Dismantling the NHS: Evaluating the Impact of Health Reforms. Bristol: Policy Press; 2016.
- Taylor EZ, Curtis MB. Whistleblowing in audit firms: organizational response and power distance. Behav Res Account 2013;25:21-43. https://doi.org/10.2308/bria-50415.
- Powell M, Mannion R, Braithwaite J, Matsuyama Y, Mannion Johnson RJ. Healthcare Reform, Quality and Safety. Farnham: Ashgate; 2015.
- Park H, Blenkinsopp J. Whistle-blowing as planned behaviour: a survey of South Korean police officers. J Bus Ethics 2009;85:545-56. https://doi.org/10.1007/s10551-008-9788-y.
- Mannion R, Davies HT. Whistleblowing in the wind towards a socially situated research agenda: a response to recent commentaries. Int J Health Pol Manage 2016;5:395-6. https://doi.org/10.15171/ijhpm.2016.34.
- Alford CF. What makes whistleblowers so threatening?: comment on ‘cultures of silence and cultures of voice: the role of whistleblowing in healthcare organisations’. Int J Health Policy Manag 2015;5:71-3. https://doi.org/10.15171/ijhpm.2015.183.
- Bolsin S, Faunce T, Oakley J. Practical virtue ethics: healthcare whistleblowing and portable digital technology. J Med Ethics 2005;31:612-18. https://doi.org/10.1136/jme.2004.010603.
- Elcock K. Raising concerns in an open culture. Br J Nurs 2013;22. https://doi.org/10.12968/bjon.2013.22.19.1140.
- Johnstone MJ. Patient safety ethics and human error management in ED contexts. Australas Emergency Nurs J 2007;10:13-20. https://doi.org/10.1016/j.aenj.2006.09.002.
- White SM. Confidentiality, ‘no blame culture’ and whistleblowing, non-physician practice and accountability. Best Pract Res Clin Anaesthesiol 2006;20:525-43. https://doi.org/10.1016/j.bpa.2006.09.002.
- The NHS Plan 2010. London: The Stationery Office; 2000.
- High Quality Care For All: NHS Next Stage Review Final Report. London: The Stationery Office; 2008.
- EUR-Lex . Access to European Union Law n.d. https://eur-lex.europa.eu/content/legal-notice/legal-notice.html (accessed July 2018).
- Whistleblowing in Europe: Legal Protections for Whistleblowers. London: Transparency International; 2013.
- Investigating Clinical Incidents in the NHS, Sixth Report of Session 2014–15. London: The Stationery Office; 2015.
- Deckert K, Sweeney M, Thüsing G, Forst G. Whistleblowing: A Comparative Study. New York, NY: Springer International Publishing; 2016.
- Guyer TM, Peterson NF. The Current State of Whistleblowing Law in Europe: A Report by the Government Accountability Project 2013. www.whistleblower.org/sites/default/files/TheCurrentStateofWhistleblowerLawinEurope.pdf (accessed 1 May 2018).
- Krause R, Thüsing G, Forst G. Whistleblowing: A Comparative Study. Springer International Publishing; 2016.
- Laleta S, Smokvina V, Thüsing G, Forst G. Whistleblowing: A Comparative Study. Springer International Publishing; 2016.
- Inquiries Act 2005. London: The Stationery Office; 2005.
- HC Deb 2009. https://hansard.parliament.uk/commons/2009-05-12/debates/09051228000018/Whistleblowers (accessed July 2018).
- General Medical Council . Good Medical Practice n.d. www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice (accessed 18 May 2017).
- Dehn G, Calland R. Whistleblowing Around the World: Law, Culture and Practice. Pretoria: IDASA Publishers; 2004.
- Kirkup B. The Report of the Morecambe Bay Investigation. London: The Stationery Office; 2015.
Appendix 1 Summary of key publications from the empirical and theoretical literature on whistleblowing and speaking up
| Authors, country, journal | Health-care sector | Context (aims) | Method of investigation | Summary of findings | |
|---|---|---|---|---|---|
| 1 | Ahern and McDonald,87 Australia, Journal of Advanced Nursing | Nursing | To explore the beliefs of nurses who wrestled with ethical dilemmas |
Empirical A statistical analysis of responses to a questionnaire containing ‘belief statements’; 95 responses from whistleblower and non-whistleblower nurses |
Whistleblowers believed in primacy of their role as patient advocate. Non-whistleblowers believed that they were equally responsible to the patient, physician and employer |
| 2 | Attree,88 UK, Journal of Nursing Management | Nursing (medical, surgical and older people) | To explore factors that influence nurses’ decisions to raise concerns about standards of practice |
Empirical Grounded theory. Qualitative data were taken from semistructured interviews with 142 practising nurses, theoretically sampled from three acute NHS trusts in England |
Fear of repercussions, retribution, labelling and blame for raising concerns, about which they predicted nothing would be done, were disincentives to raising concerns. Reporting was perceived as a high-risk/low-benefit action. Nurses lacked confidence in reporting systems |
| 3 | Beckstead,81 USA, International Journal of Nursing Studies | Nursing | To analyse the thinking processes nurses use when making decisions to report peer wrongdoing, particularly relating to substance abuse |
Empirical Scenario-based behavioural questionnaire issued to 113 female and seven male nurses |
Working under the influence of any type of substance considered a very serious offence. Combination of ‘incompetence’ and ‘substance-abuse’ cues occurred in complex ways, possibly due to education and practice |
| 4 | Bellefontaine,89 UK, Nursing Times | Student nursing | To explore the factors that influence nursing students in reporting concerns about practice |
Empirical Qualitative study, using a phenomenological approach. Semistructured interviews with six student nurses |
Four main themes were identified: the student–mentor relationship in clinical placement; actual or potential support provided by both the practice area and university; students’ own personal confidence and professional knowledge base; and fear of failing clinical placements |
| 5 | Bickhoff et al.,90 Australia, Nurse Education Today | Student nursing | How nursing students demonstrate moral courage when in whistleblowing situations, and factors that encouraged or inhibited their willingness to speak up |
Empirical Qualitative descriptive study. Thematic analysis of interview data from 10 nursing students attending an Australian university |
Of importance are patient-advocate identity, linking to knowing one’s own moral code and previous life experiences; consequences for both patient and participant; impact of key individuals; and picking battles carefully |
| 6 | Black,91 USA, American Journal of Nursing | Nursing | Nurses’ experiences with workplace attitudes towards patient advocacy activities |
Empirical Postal questionnaire, resulting in quantitative analysis of 564 responses from Nevada State registered nurses |
One-third of respondents reported failing to report conditions potentially harmful to patients: key drivers were fear of retaliation and belief that reporting would not change the situation |
| 7 | Bradbury-Jones et al.,92 UK, Nurse Education Today | Student nursing | A study exploring the empowerment of nursing students in clinical practice |
Empirical Longitudinal study underpinned by hermeneutic phenomenology. 13 first-year nursing students recruited using a purposive sampling strategy. Annual, in-depth interviews over 3 years |
The nurses’ education process resulted in a feeling of greater empowerment. External spheres influence the extent to which nursing students are likely to experience increased knowledge and confidence, and thus empowerment. However, nursing students use a number of strategies to promote their own empowerment in clinical practice |
| 8 | Bradbury-Jones et al.,93 UK, Nurse Education Today | Student nursing | Explore the phenomenon of ‘voice’ and the extent to which nursing students are able to exercise voice during their clinical practice experiences | As above | In situations that called for nursing students to ‘speak up’ they did one of two things: exit (typically metaphorically) or voice. However, there was bridging of these actions in the form of ‘negotiating voice’, where participants were conscious of their own attempts to explore how to raise concerns in different ways so that their voice was ‘heard’, and without suffering retaliation |
| 9 | Espin and Meikle,94 Canada, Journal of Nursing Education | Student nursing | Investigate perception of (and reporting of) events potentially harmful to patients in fourth-year nursing students |
Empirical Data from 10 fourth-year students who were individually interviewed after reading each of five risk scenarios |
Students noted scope of practice, professional roles, and presence or absence of harm as important in their decision-making process Authors mention a ‘reporting ladder’ as a mechanism through which a report can be escalated |
| 10 | Firth-Cozens et al.,95 UK, Clinical Governance: An International Journal | Nursing, hospital doctors, GPs | To expose causes of under-reporting of errors, and suggest improvements |
Empirical Statistical analysis of questionnaire-based survey of 342 nurses, 201 hospital doctors and 81 GPs |
Willingness to report poor care was higher than imagined, particularly in nursing. Need for clear guidance both on what should be reported and the systems for doing so. Need to ensure ‘safety’ of reporters, and that change occurs in response to reporting |
| 11 | Fledderjohann and Johnson,36 USA, Social Science Quarterly | Child protection agencies | The influence of community context and bystander characteristics on actions taken towards observed child neglect |
Empirical Large telephone survey of general public (3679 respondents). Statistical analysis of results |
At the individual level, age, gender, place of residence and sentinel status were all found to have a significant effect on bystanders’ willingness to report observed child neglect |
| 12 | Gould and Drey,96 UK, American Journal of Infection Control | Student nursing | Understand nursing students’ experiences of infection control in the clinical setting |
Empirical 488 responses to online survey |
Students demonstrated sound understanding of infection control and were able to identify lack of compliance on the basis of preclinical classroom instruction. A culture of blame was observed between different groups of staff. In the few cases where they challenged poor practice, students had been penalised |
| 13 | Greaves and McGlone,97 Australia, Social Medicine | Various public sector roles, including nursing | Explore the health consequences of speaking out |
Empirical Narrative enquiry using 11 unstructured interviews |
Whistleblowers found laws to be ‘meaningless’ and organisational procedures to be ineffective in providing protection. As a result of reporting, health and careers were ruined, but self-respect was maintained |
| 14 | Grube et al.,84 USA, Health Communication | Nursing | Discover when and why nurses report unsafe patient practices when they see them |
Empirical Quantitative analysis of 330 questionnaires |
Probability of reporting unsafe practices increases (1) as the frequency of unsafe practices increases and (2) when nurses have a strong role identity and strong organisational role identity. However, the highest probability for reporting occurs when both organisation and nurse role identities are low |
| 15 | Hutchinson and Jackson,98 Australia, Nursing Inquiry | Public sector, focusing on health and social care | Illuminate the connections between bullying, abuse of power and institutional failures |
Empirical Cross-sectional survey (n = 3345) from public sector organisations in one state of Australia. Covered public sector health and non-health organisations |
Need to understand the practices of power in public sector institutions. Bullying as an indicator of broader institutional failings. Contrast between culture and espoused organisational mission |
| 16 | Ion et al.,86 UK, Nurse Education Today | Student nursing | Understand the influences on student decisions on whether or not to report poor clinical practice that is a result of deliberate action and that is witnessed while on placement |
Empirical Qualitative interviews with 13 pre-registration (adult and mental health) nursing students from the UK. Age range from 20 to 47 years |
Drivers for ‘voice’ were own moral position and professional code of conduct Drivers for ‘silence’ were perceived threat of retaliation, lack of confidence in own judgement, and unfamiliar procedures and process |
| 17 | Ion et al.,99 UK, Journal of Advanced Nursing | Student nursing | Improve understanding of lack of reporting of poor care |
Empirical Discourse analysis of semistructured interviews with 13 pre-registration (adult and mental health) nursing students from the UK. Age range from 20 to 47 years |
Both reporters and non-reporters construct narratives that present themselves in a positive light: reporters lay claim to positive character strength and commitment; non-reporters blame factors outside their control |
| 18 | Jackson and Raftos,100 Australia, International Journal of Nursing Practice | Residential care nurses | Exploration of experiences of whistleblowers |
Empirical, drawing on feminist research theory Data collected via field notes taken from serial interviews with three nurses |
Three distinct emotional phases occurred as the decision to whistleblow externally was taken: trepidation and optimism as incident was reported internally; barriers and obstacles from management; disillusionment and defeat due to lack of change, resulting in external whistleblowing |
| 19 | Jackson et al.,101 Australia, Contemporary Nurse | Nursing | To present and describe the effects of whistleblowing episodes on the workplace relationships of the nurses involved |
Empirical Qualitative narrative inquiry. 18 participants with direct experience of whistleblowing as whistleblowers, bystanders or subjects of complaint |
Whistleblowers can lose their employment, be bullied, excluded and unsupported by management and colleagues, and have their collegial professional relationships destroyed |
| 20 | Jackson et al.,100 Australia, Journal of Advanced Nursing | Nursing | Explore the reasons behind the decision to blow the whistle and provide insights into nurses’ experiences of being whistleblowers |
Empirical Qualitative narrative inquiry. Data from 11 nurse whistleblowers (as in Jackson et al. , 2010101) |
Whistleblowing was highly stressful for blowers, who wrestle to reconcile their fear of reprisals (organisational and individual) against their indignation at perceived wrongdoing. Nurses are driven to whistleblow by perceived duty of care for patients. Clarity needed regarding the role nurses have as patient advocates. Need for clearer opportunities to voice concerns, a timely and appropriate response from health-care systems, and a safe environment in which to raise concerns |
| 21 | Jackson et al.,100 Australia, Contemporary Nurse | Nursing | Effects of whistleblowing on workplace relationships |
Empirical Qualitative narrative enquiry, drawing on face-to-face or telephone interview data from 18 nurses who had been involved as whistleblower, bystander or subject of complaint |
Whistleblowing resulted in hostility at work, manifesting as damaged collegial and interprofessional relationships, bullying and exclusion. Whistleblowers, bystanders and subjects of complaints were all potentially affected |
| 22 | Jackson et al.,145 Australia, Contemporary Nurse | Nursing | To summarise and critique the research literature about whistleblowing and nurses. | Integrative literature review of 15 empirical papers, capturing data from seven countries | Nurses have a key role to play in maintaining practice standards and in reporting care that is unacceptable. However, the repercussions to nurses who raise concerns are insupportable |
| 23 | Jones and Kelly,17 UK, Sociology of Health & Illness | Care of Elderly People | Explore employee perceptions of whistleblowing in in care for the elderly settings, & identify alternative strategies to whistleblowing |
Empirical. Qualitative study, deploying interview and focus group techniques with 60 participants from various elderly care settings |
Formal procedural approaches adopted by organisations in order to facilitate raising of concerns are largely neutralised by ‘[a] process of socialisation and habituation in the workplace’ – these everyday behaviours are the key to improving the reporting culture |
| 24 | Jones et al.,103 UK, International Journal of Nursing Studies | Executive board nurses | Explore the experiences of nurse executives, particularly in relation to ensuring that their views and concerns about quality and safety are taken into account at board level |
Empirical Purposive sample comprised 40 executive board nurses. Semistructured interviews followed by thematic analysis |
Two successful strategies for raising concerns and tackling ‘groupthink’ at board level were exposed: to ‘brief’ (i.e. exchange information pre board meeting) and build relationships; preparing and delivering a credible, evidence-based case |
| 25 | Kent et al.,104 UK, Journal of Nursing Education | Student nursing | Effects of a course and placement aimed at increasing nursing students willingness to speak up for patient safety |
Empirical Quantitative survey (H-PEPSS) on 63 student nurses. Testing was pre and post a short course on raising concerns/challenging authority figures |
No significant relationships were found with regard to age, gender or ethnicity on the expressed possibility of raising concerns. An increase in confidence in speaking up was found in the post-test (p = > 0.001), but no increase in willingness to challenge someone in authority |
| 26 | Killam et al.,105 Canada, BMC Nursing | Student nursing | Perception of unsafe clinical practices by final-year baccalaureate nursing students |
Empirical Q methodology: 59 fourth-year students sorted 43 theoretical statement cards, descriptive of unsafe clinical practice |
Final-year nursing students perceive that deficits in knowledge, patient-centred practice, professional morality and authenticity threaten safety in the clinical learning environment |
| 27 | Killam et al.,106 Canada, Nurse Education Today | Student nursing | Perception of unsafe clinical practices by first-year baccalaureate nursing students |
Empirical Q methodology: 64 first-year students sorted 43 theoretical statement cards that described of unsafe clinical practice |
Viewpoints included an overwhelming sense of inner discomfort, practising contrary to conventions, lacking in professional integrity and disharmonising relations. Overall, a consensus viewpoint described exonerating the clinical educator as not being solely responsible for clinical safety |
| 28 | Kingston et al.,107 Australia, Medical Journal of Australia | Consultants, registrars, resident medical officers, senior nurses, junior nurses | (1) To examine the attitudes of medical and nursing staff towards reporting incidents (adverse events and near-misses), and (2) to identify measures to facilitate incident reporting |
Empirical Qualitative, semistructured questions were given to five focus groups, one each for consultants, registrars, resident medical officers, senior nurses and junior nurses, a total of 14 medical and 19 nursing staff from three public hospitals |
Nurses reported more habitually than doctors because of a culture that provided directives, protocols and the notion of security (by following prescribed processes). The medical culture favoured dealing with incidents ‘in house’, and was less reliant on directives. Barriers to reporting incidents included time constraints, unsatisfactory processes, deficiencies in knowledge, cultural norms, inadequate feedback, beliefs about risk and a perceived lack of value in the process |
| 29 | Ko and Yu,108 Republic of Korea, Journal of Patient Safety | Nursing | Explore the correlations among nurses’ perceptions of patient safety culture, their intention to report errors, and leader coaching behaviours |
Empirical The views of a total of 289 nurses from five Korean hospitals were assessed using self-report instruments. Data were statistically analysed |
Coaching behaviour by senior nurses led to an improvement in patient safety culture and intention to report errors |
| 30 | Law and Chan,109 Hong Kong, Journal of Clinical Nursing | Graduate nurses | To explore the process of learning to speak up in practice among newly graduated registered nurses |
Empirical Stories of experiences of speaking up emerged naturally during repeated unstructured interviews with 18 new graduates |
Speaking up is helped by (1) more than one-off training and safety tools, (2) mentoring of speaking up in the midst of good and bad educative experiences and (3) making public spaces safe for telling secret stories |
| 31 | Levett-Jones and Lathlean,110 UK and Australia, Nurse Education Today | Student nursing | Examined nursing students’ experience of relationship between belongingness, conformity and compliance when undertaking clinical placements |
Empirical Mixed-methods case study; 18 third-year nursing students from two universities in Australia and one in the UK were interviewed, and the data were thematically analysed |
Three subthemes emerged: don’t rock the boat, getting the registered nurses offside and speaking up Students described how and why they adopted or adapted to the teams’ and institution’s values and norms, rather than challenging them, believing that this would improve the likelihood that they would be accepted and included by the nursing staff |
| 32 | Mansbach et al.,114 Israel, Physiotherapy | Physiotherapy students and physiotherapists | Investigation into misconduct reporting tendencies of student physiotherapists vs. practitioners |
Empirical A total of 227 participants in two groups (126 students and 101 practitioners) were presented with two vignettes: one describing a colleague’s misconduct and the other describing a manager’s misconduct. They were then asked to make a decision about whistleblowing |
Both students and practitioners viewed misconduct that had an impact on patient welfare as being serious, and were prepared to act. Students perceived managers’ misconduct as more serious, and preferred to report externally (possibly because of a lack of understanding of the personal consequences of doing so). Practitioners saw colleagues’ misconduct as more serious and preferred to report internally. The results suggested that older participants, and more experienced participants, were less likely to report misconduct |
| 33 | McCann et al.,111 UK, Human Resource Management | Front-line and mid-management NHS employees | Explore the impact of metrics-based target systems on patient care and staff morale |
Empirical Ethnographic study of four NHS organisations over 3 years |
The challenge of reconciling the increasing demand for economic efficiency alongside improving patient outcomes resulted in ‘street-level bureaucracy’, a situation in which traditional professional norms are reasserted informally in ways that often transgress prescribed performance systems |
| 34 | McDonald and Ahern,112 Australia, Nursing Forum | Nursing | What are the coping responses of nurses who identified misconduct at work, and what responses were considered effective? |
Empirical Descriptive survey design, resulting in analysis of 95 postal questionnaires completed by whistleblowers and non-whistleblowers. Response rate of 20% |
Most effective responses (in terms of avoiding feelings of moral anguish) were problem-focused actions, but require personal attributes of conviction, self-confidence and assertiveness. Least effective were avoidance and denial |
| 35 | McDonald and Ahern,113 Australia, Journal of Professional Nursing | General and mental health nursing | Uncover the professional consequences of reporting misconduct or remaining silent for nurses |
Empirical Data were taken from 1999 study112 |
Official reprisals included demotion (4%), reprimand (11%) and referral to a psychiatrist (9%). Unofficial professional reprisals included threats (16%), rejection by peers (14%), pressure to resign (7%) and being treated as a traitor (14%). 10% reported a halted career |
| 36 | Monrouxe et al.,151 UK, Medical Education | Medical students (29 dentistry, 13 nursing, 12 pharmacy and 15 physiotherapy) | To examine dental, nursing, pharmacy and physiotherapy students’ narratives of professionalism dilemmas: the types of events they encounter (‘whats’) and the ways in which they narrate those events (‘hows’) | A qualitative cross-sectional study; 69 health-care students participated in group/individual narrative interviews, resulting in 226 personal incident narratives that were analysed and coded | By focusing on common professionalism issues (including whistleblowing and challenging) at a conceptual level, health-care students can share experiences through narratives. The role-playing of idealised actions (how students wish they had acted) can facilitate synergy between personal moral values and moral action enabling students to commit and recommit to professionalism values together |
| 37 | Monrouxe et al.,82 UK, BMJ Open | Medical students (study 1), and nursing, dentistry, physiotherapy and pharmacy students (study 2) | To understand the prevalence of health-care students’ witnessing or participating in something that they think is unethical (professionalism dilemmas) during workplace learning |
Empirical Two cross-sectional online questionnaires; 2397 medical students (67.4% female) and 1399 other health-care students (81.1% female) |
Students commonly encountered student abuse and patient dignity and safety dilemmas. Men were more likely to classify themselves as experiencing no distress; women were more likely to classify themselves as distressed. While some evidence suggested more exposure to unethical behaviour resulted in less distress, other evidence suggested distress increased with increased exposure |
| 38 | Moore and McAuliffe,115 Ireland, Clinical Governance: An International Journal | Acute nursing | Examination of experiences of those who have observed and reported poor care, and the consequences of doing so |
Empirical Exploratory quantitative study, using data from 152 anonymous questionnaires (26% response rate) |
A total of 88% of respondents had observed poor care in the previous 6 months, with 70% of these reporting it. Nurse managers were more likely to report than staff nurses. Only one in four was satisfied with how reports of poor care were dealt with. Fear of retribution and perceived improbability of change were barriers to reporting |
| 39 | Moore and McAuliffe,150 Ireland, Clinical Governance | Nursing (acute) | Explore why some health-care professionals report incidents and others fail to do so | Data as in Moore and Auliffe115 | Key findings as above, with addition that the ‘best interests of the patient’ was the key driver for reporting |
| 40 | Newton et al.,116 Canada, Nursing Leadership | Acute care nursing | To understand nurses’ response to being unable to blow the whistle (i.e. being silenced) |
Empirical Qualitative and quantitative postal survey of 374 nurses (22% response rate) |
Nurses took independent action to address the poor care, rather than pursue official complaint channels, or to resort to whistleblowing, raising questions regarding empowerment and control of health-care employees |
| 41 | Ohnishi et al.,117 Japan, Nursing Ethics | Psychiatric nursing | Unveil the process of whistleblowing |
Empirical In-depth semistructured interviews with two psychiatric nurses who blew the whistle on one Japanese case |
National/social culture has a significant impact on willingness to blow the whistle Blowers required more clarity on boundaries of acceptable behaviour Whistleblowing process is influenced by complex social, ethical, personal, organisational and professional forces |
| 42 | Orbe and King,136 USA, Health Communication | Nursing | Explores the ways in which registered nurses communicate about organisational wrongdoing |
Empirical Critical incidents were gathered from 202 registered nurses. An analysis was conducted through a phenomenological process of description, reduction and interpretation |
Five themes emerged as central to responses of policy violations and personal ethics in the workplace: (1) perceptions of wrongdoing, (2) upholding the ideals of the profession, (3) clarity and evidence of wrongdoing, (4) consequences of reporting and (5) workplace dynamics |
| 43 | Peternelj-Taylor,118 Canada, Nursing Ethics | Psychiatric nursing | Discuss consequences of whistleblowing |
Empirical Single case study |
Speaking out requires resilience, confidence and moral courage. Clear ethical models and faith that organisations will respond provide support for speaking up |
| 44 | Peters et al.,144 Australia, Journal of Clinical Nursing | Nurse health and well-being | Illuminate the emotional sequelae of whistleblowing |
Empirical Qualitative narrative enquiry. Interview data were from 14 nurses who were either whistleblowers or subjects of whistleblowing complaints |
Emotional health was significantly compromised as a result of the whistleblowing incident. The protracted nature of resultant enquiries intensified the emotional health consequences |
| 45 | Prang and Jelsness-Jorgensen,119 Norway, Geriatric Nursing | Residential care nurses | Explore the barriers to incident reporting in nursing homes compared with in hospitals |
Empirical Semistructured interviews with 13 nurses working in nursing homes. Qualitative thematic analysis of data |
Organisational barriers were (1) lack of support and culture, (2) unclear outcomes and (3) unclear routines Individual barriers were (1) fear of vilification and conflicts, (2) lack of technological confidence and knowledge, (3) time and (4) assessment of degree of severity |
| 46 | Schwappach and Gehring,120 Switzerland, BMJ Open | Experienced oncology doctors and nurses | To explore the experiences of staff regarding communicating safety concerns and to examine the situational factors and motivations surrounding the decision whether and how to speak up | Semistructured interviews with 32 experienced oncology health-care professionals. Interviewees were self-selected | Participants commonly experienced situations that raised concerns and required questioning, clarifying and correcting. Non-verbal communication was often used to signal safety concerns. Speaking up behaviour was strongly related to a clinical safety issue. Most episodes of ‘silence’ were connected to hygiene, isolation and invasive procedures. However, medication doubts and concerns were readily raised by all. Nearly all interviewees, particularly lower-ranking nurses, were concerned with ‘how’ to raise concerns |
| 47 | Schwappach and Gehring,121 Switzerland, PLOS ONE | Experienced oncology doctors and nurses | To investigate the likelihood of speaking up about patient safety in oncology and to clarify the effect of clinical and situational context factors on the likelihood of voicing concerns | A total of 1013 nurses and doctors in oncology rated four clinical vignettes describing co-workers’ errors and rule violations in a self-administered factorial survey | While dealing with hypothetical situations, clinicians’ willingness to speak up about patient safety is surprisingly high, but is considerably affected by contextual factors. Physicians and nurses without managerial function report substantial discomfort with speaking up |
| 48 | St Pierre et al.,123 Germany, Der Anaesthesist | Nurses and anaesthetists | Investigate the impact of organisational hierarchy on the voicing of concerns in critical situations |
Empirical 18 nurses and 59 anaesthetists took part in seven simulated critical situations |
Nurses rarely (one in four) challenged decisions they believed to be dangerous for the patient: 37% could give no reason for this, 35% felt that they lacked knowledge and 12% did not feel able to challenge their superiors |
| 49 | Stevanin et al.,122 Italy, Nurse Education Today | Student nursing | Assess students’ perceptions of their knowledge about and competence regarding patient safety |
Empirical A total of 574 students responded to an Italian version of the Health Professional Education in Patient Safety Survey |
29% of students had witnessed a safety ‘incident’, and in 96% of these incidents students observed an ‘adverse event’ form being completed. Most students considered themselves to have a high degree of knowledge and competence regarding patient safety. Classroom and clinical settings for learning were of equal value |
| 50 | Tabak et al.,130 Israel, Medicine and Law | Nurses | Investigate the meaning, concept and attitude of nurses to whistleblowing |
Empirical Questionnaire distributed to 110 registered nurses |
Of the nurses, 70% did not know the meaning of whistleblowing, but 77% were motivated to report on negligence. Most (58%) recognised the threat to their career of reporting and saw whistleblowing as a last resort; 95% noted the need for clearer reporting standards and open communication channels |
| 51 | Tella et al.,124 Finland/UK, Journal of Clinical Nursing | Student nursing | Explore and compare Finnish and British nursing students’ perceptions of their learning about patient safety in clinical settings |
Empirical A questionnaire-based cross-sectional comparative study of 195 Finnish and 158 British student nurses |
British students perceived themselves to have been better prepared for reporting on patient safety by their training than their Finnish peers. Both groups valued formal learning over clinical settings for developing knowledge of patient safety |
| 52 | Throckmorton and Etchegaray,125 USA, Journal of PeriAnesthesia Nursing | Nursing | Explore nurses’ willingness to report (i.e. voice) errors of varying degrees of severity and the factors that impacted that intent |
Empirical Anonymous postal questionnaires: 411 responses (64% response rate). Saying you would report and reporting are very different |
A majority of nurses were willing to report all levels of errors. Primary position, reasons for not reporting, and years since initial licensure were predictors of intent to report incidents with scenarios that involved no or minimal injury to patients; 99% indicated that they would report incidents resulting in moderate to severe injury or death |
| Author/publication | Profession | Focus of paper | Type of paper | Key conclusions |
|---|---|---|---|---|
| Alford,320 USA, International Journal of Health Policy and Management | Non-specific | Highlight the need for support for whistleblowers | Discussion paper | Importance of lowering the barriers to whistleblowing |
| Bolsin et al.,321 Australia, Journal of Medical Ethics | Generic health care | Considers the importance of consideration of whistleblowing in medical ethics training |
Theoretical paper Considered literature and experience from health-care ethics education |
Health-care whistleblowing should become an essential part of health-care training. Self-reporting via portable digital technology could help to develop a non-punitive, personal development-orientated culture |
| Delk,133 USA, Workplace Health and Safety | Nursing (occupational health) | Provide a guide to the legal protection afforded to whistleblowers in different states in USA | Literature review (of state law) | State law provides significant theoretical protection, but such measures fail to combat the reality of retaliation on whistleblowers by peers and organisations who typically have negative perceptions of the act |
| Elcock,322 UK, British Journal of Nursing | Student nursing | Explore how student nurses are able to raise concerns | Discussion paper | Students are well placed to notice poor care and bad practice, but need (1) to feel welcome and secure in their work placement, (2) to know how to report these concerns and (3) to feel safe in doing so |
| Firtko and Jackson,85 Australia, Australian Journal of Advanced Nursing | Nursing | Discuss dilemmas, repercussions and definitions of whistleblowing in relation to nursing, and explore the role of the media | Review of literature | Implies that whistleblowing occurs only when reporting is to a person or body not normally involved in the organisation’s normal problem-solving strategy. Nurses’ advocacy role is vitally important, and must be protected |
| Goldberg,147 Canada, Healthcare Quarterly | Generic health care | Discuss the barriers to whistleblowing in health care | Discussion paper | Seeing whistleblowing as opportunities to learn requires cultural change in organisations |
| Johnstone and Kanitsaki,143 Australia, International Journal of Nursing Studies | Nursing | Understand issues surrounding self-reporting of nursing errors | Discussion paper | A ‘nursing error’ is poorly defined in the literature. Consequences of self-reporting are often severe, causing under-reporting, and should be viewed as opportunities to learn |
| Johnstone,323 Australia, Australasian Emergency Nursing Journal | Nursing (emergency room) acute?? | Discuss the incidence and impact of preventable adverse events in emergency-room contexts, and the development of a ‘culture of safety’, drawing lessons from other hazardous industries | Discussion paper |
Failure rates in other hazardous industries are significantly lower (notwithstanding the fact that emergency-room ‘normal’ is to service high-risk ‘customers’) ‘Culture of safety’ can be encouraged by deploying a systems approach to clinical risk management |
| Kelly and Jones,19 UK, Quality in Ageing and Older Adults | Care of older people | Understand the process of whistleblowing and its role in maintaining care standards | Literature review |
No widely accepted theoretical framework or conceptual underpinning for whistleblowing An imposed, rather than chosen, route to raise concerns The term has attracted overwhelmingly negative connotations |
| Mannion and Davies,3 UK, International Journal of Health Policy and Management | Generic health care | Highlight that safer health care requires cultures that support whistleblowing |
Theoretical paper Considered literature and experience from health-care research |
Whistleblowing is a complex and ambiguous phenomenon, and cannot be guaranteed simply by managerial decree or policy-making |
| Mannion and Davies,319 UK, International Journal of Health Policy and Management | General health care | Highlight emerging issues relating to the challenge of whistleblowing in health care | Discussion/response paper | Need for a new, socially situated research agenda to address communication, sense-making and judgement-making in health care and (more widely) that will result in a reduced need for whistleblowing |
| Skivenes and Trygstad,131 Norway, Human Relations | Public sector | Explore the findings of a Norwegian government report on whistleblowing in the public sector | Secondary research | Findings from the study contrast with those of international research, showing Norwegian experiences of whistleblowing to be significantly more positive than in many other countries. Structures that favour a communication culture are (in part) seen as responsible |
| White,324 UK, Best Practice & Research Clinical Anaesthesiology | General health care | Discuss the development of the law and ethics in the area of whistleblowing | Discussion paper |
Error is inevitable in large, complex organisations By causing fear of personal reprisal, ‘blame culture’ leads to institutional secrecy, and reduces the reporting of medical error, making its repetition more likely. Centralised, voluntary, transparent, ‘blame-free’ error-reporting systems improve (patient) safety Whistleblowing is morally justifiable if it forces remedial action to prevent violations and, therefore, further identifiable patient harm |
Appendix 2 Summary of key recommendations from the Inquiry reports
This appendix draws together and summarises the key recommendations contained within the Inquiry reports, beginning with the Kennedy report.
Kennedy5
The report presented 198 recommendations under the following themes: respect and honesty; a health service that is well led; competent health-care professionals; the safety of care; care of an appropriate standard; public involvement through empowerment; and the care of children.
Although there was no explicit recommendation on whistleblowing, the most relevant recommendations appear to be the following:
R33 – ‘a duty of candour’, meaning a duty to tell a patient if adverse events have occurred must be recognised as owed by all working in the NHS to patients
R39 – the framework of regulation must consist of two organisations: a Council for the Quality of Health Care (including CHI, NICE and the proposed National Patient Safety Agency), and a Council for the Regulation of Healthcare Professionals) including the GMC and the NMC) (in effect this is the body referred to in the ‘NHS Plan’325 as the Council of Healthcare Regulators
R40 – the two organisations must be independent of government and report both to the DH and to Parliament
R45 – the doctors Code of Professional Practice, as set down in the GMC’s ‘Good Medical Practice’ should be incorporated in the contract of employment between doctors and trusts
R46 – The relevant codes of practice for nurses, for professions allied to medicine and for managers should be incorporated into their contracts of employment with hospital trusts or primary care trusts.
R91 – managers as healthcare professionals should be subject to the same obligations as other healthcare professionals, including being subject to a regulatory body, and professional code of practice
R106 – We support and endorse the broad framework of recommendations advocated in the report ‘An Organisation with a Memory’ by the Chief Medical Officer’s expert group on learning from adverse events in the NHS. The National Patient Safety Agency proposed as a consequence of that report should, like all other bodies which contribute to the regulation of the safety and quality of healthcare, be independent of the NHS and the DH
R107 – Every effort should be made to create in the NHS an open and non-punitive environment in which it is safe to report and admit sentinel events
R109–112 – there should be a national reporting system
R113–118 – there should be incentives to encourage the reporting of sentinel events, including:
R113 – the reporting of sentinel events must be made as easy as possible, using all available means of communication (including a confidential telephone reporting line)
R114 – members of staff in the NHS should receive immunity from disciplinary action by the employer or by a professional body if they report a sentinel event to the trustor to the national database within 48 hours, except where they themselves have committed a criminal offence
R115 – members of staff in the NHS who cover up a sentinel event may be subject to disciplinary action by their employer or their professional body
R116 – the opportunity should exist to report a sentinel event in confidence.
Kennedy. 5
Secretary of State for Health (2002)166
R33 – A duty of candour, meaning a duty to tell a patient if adverse events have occurred, must be recognised as owed by all those working in the NHS to patients.
We agree. The broader implications for clinical negligence legislation will be addressed in the CMO’s work on clinical negligence, leading to a White Paper early in 2002.
R39 – The framework of regulation must consist of two overarching organisations, independent of government, which bring together the various bodies which regulate healthcare. A Council for the Quality of Healthcare should be created to bring together those bodies which regulate healthcare standards and institutions (including for example, the Commission for Health Improvement (CHI), the National Institute for Health and Care Excellence (NICE) and the proposed National Patient Safety Agency). A Council for the Regulation of Healthcare Professionals should be created to bring together those bodies which regulate healthcare professionals (including, for example, the GMC and the Nursing and Midwifery Council); in effect, this is the body currently referred to in ‘The NHS Plan’ as the Council of Healthcare Regulators. These overarching organisations must ensure that there is an integrated and co-ordinated approach to setting standards, monitoring performance, and inspection and validation. Issues of overlap and of gaps between the various bodies must be addressed and resolved.
We agree. Proposals for the creation of the Council for the Regulation of Health Care Professionals were published for consultation in August 2001. They are designed to replace the current fragmented arrangements and to lead to more effective co-ordination and clearer accountability mechanisms. We plan to legislate to effect the changes in the NHS Reform and Health Care Professions Bill.
R40 – The two Councils should be independent of government and report both to the DH and to Parliament. There should be close collaboration between the two Councils. The DH should establish and fund the Councils and set their strategic framework, and thereafter periodically review them.
We agree in principle. We will establish and fund a new administrative Council for Quality of Health Care in 2002 to ensure co-ordination between the Council for the Regulation of Health Care Professionals and other organisations with an interest in service quality, including NICE, CHI, NCAA and the NPSA. This will be at arm’s length from the Department of Health. The Council for the Regulation of Health Care Professionals will be independent and report to Parliament.
R45 – The doctors’ Code of Professional Practice, as set down in the GMC’s ‘Good Medical Practice’, should be incorporated into the contract of employment between doctors and trusts. In the case of GPs, the terms of service should be amended to incorporate the Code.
We reject. The standard documentation for consultants’ appraisal – a contractual requirement from April 2001 – already explicitly includes the headings set out in the GMC’s Good Medical Practice. The same principles will apply to other NHS doctors including GPs where appraisal is under negotiation.
R46 – The relevant codes of practice for nurses, for professions allied to medicine and for managers should be incorporated into their contracts of employment with hospital trusts or primary care trusts.
We agree in principle. Contracts of employment for health care professionals are already based on the premise that they are properly registered with their regulatory body. Many contracts include this specific provision but it is implicit in all contracts of employment.
R71 – In addition, a single body should be charged with the overall co-ordination of the various professional bodies and with integrating the various systems of regulation. It should be called the Council for the Regulation of Healthcare Professionals. (In effect, this is the body currently proposed in ‘The NHS Plan’, and referred to as the Council of Healthcare Regulators.)
We agree. Proposals for a Council for the Regulation of Health Care Professionals were set out in a consultation document Modernising Regulation in the Health Professions, published in August 2001 and we have introduced legislation to give these effect.
R106 – We support and endorse the broad framework of recommendations advocated in the report ‘An Organisation with a Memory’ by the Chief Medical Officer’s expert group on learning from adverse events in the NHS. The National Patient Safety Agency proposed as a consequence of that report should, like all other bodies which contribute to the regulation of the safety and quality of healthcare, be independent of the NHS and the DH.
We reject the recommendation that the NPSA should be outwith the NHS. It was established in July 2001 as a Special Health Authority. This provides the independence necessary to give the Agency credibility with patients and the public while ensuring it has the confidence of health care staff and is able to work closely with the NHS.
R107 – Every effort should be made to create in the NHS an open and non-punitive environment in which it is safe to report and admit sentinel events.
We agree. The work of the NPSA together with the clinical governance initiative and the Department’s Risk Management System aims to develop a ‘just culture’ where non-punitive reporting of adverse incidents will help to improve patient safety.
R109 – There should a single, unified, accessible system for reporting and analysing sentinel events, with clear protocols indicating the categories of information which must be reported to a national database.
We agree. The new national reporting system will be rolled out early in 2002.
R113 – The reporting of sentinel events must be made as easy as possible, using all available means of communication (including a confidential telephone reporting line).
We agree. The aim is that most reports of adverse incidents to the NPSA will be transmitted electronically. A free-phone confidential telephone line will also be established.
R114, 115 and 117 – Members of staff in the NHS should receive immunity from disciplinary action by the employer or by a professional body if they report a sentinel event to the trust or to the national database within 48 hours, except where they themselves have committed a criminal offence.
Members of staff in the NHS who cover up or do not report a sentinel event may be subject to disciplinary action by their employer or by their professional body.
There should be a stipulation in every healthcare professional’s contract that sentinel events must be reported, that reporting can be confidential, and that reporting within a specified time period will not attract disciplinary action.
We agree in principle, unless for example a criminal offence has been committed, and will be exploring, through the work of the CMO’s Committee on Clinical Negligence, how this can be introduced.
R116 – The opportunity should exist to report a sentinel event in confidence.
We agree. Information reported to the NPSA will be held in confidence.
Secretary of State for Health. 166
Secretary of State (2007)168
Shipman, Fifth Report
R15a – Concerns expressed about a GP by someone other than a patient or patient’s representative (e.g. by a fellow healthcare professional) should be dealt with in the same way as patient complaints. Such concerns should be investigated (where necessary) by the inter-PCT investigation team.
Agree.
R15b – . . . or, in a case raising difficult or complex issues, by the Healthcare Commission. Consideration should be given to amending the relevant provisions of the draft Complaints Regulations to permit the Healthcare Commission to accept and investigate concerns referred to it by a PCT or healthcare body without the need for a reference from the Secretary of State for Health.
See R13 – Accept may be need to help healthcare organisations with the more complex investigations but do not accept that an automatic referral to Healthcare Commission would be helpful.
R17 – In order to ensure that, so far as possible, complaints about healthcare can reach the appropriate destinations, there should be a ‘single portal’ by which complaints or concerns can be directed or redirected to the appropriate quarter. This service should also provide information about the various advice services available to persons who are considering whether and/or how to complain or raise a concern. Advice must be provided for persons who are concerned about the legal implications of raising a concern.
Accept need for support for patients who are unsure where to make a complaint. Preferred solution is to introduce standards so that all bodies receiving complaints will forward to right recipient and tell complainant what they have done.
R33 – PCTs should keep a separate file for each individual GP on their lists. That file should hold all material relating to the doctor which could have any possible relevance to clinical governance. If a doctor moves from one PCT to another, the file (or a copy of it) should be sent to the new PCT.
Accept in principle, and will take forward in discussion with stakeholders.
R34a – Every GP practice should have a written policy, setting out the procedure to be followed by a member of the practice staff who wishes to raise concerns, in particular concerns about the clinical practice or conduct of a healthcare professional within the practice. Staff should be encouraged to bring forward any concerns they may have openly, routinely and without fear of criticism.
All NHS organisation should have such a policy; will discuss with stakeholders how best to carry forward.
R34b – In the event that a member of the staff of a GP practice feels unable to raise his/her concern within the practice, s/he should be able to approach a person designated by the PCT for the purpose. The contact details of that person should appear in the written policy. The designated person should make him/herself known to all practice staff working in the PCT area. PCTs should ensure, through training, that practice staff understand the importance of reporting concerns and know how to do so.
Accept in principle that an appropriate channel for such concerns should be available. Either the PCT or SHA may have a role; will discuss further with stakeholders.
R35 – The written policy should contain details of organisations from which staff can obtain free independent advice. If the ‘single portal’ is created, in whatever form, the policy should set out contact details of that also.
Agree.
R37 – Consideration should be given to amending the Public Interest Disclosure Act 1998 in order to give greater protection to persons disclosing information, the disclosure of which is in the public interest.
Not persuaded that change to PIDA is needed. Will work with NHS organisations to draw up protocols under Act which will give equivalent protection to that sought by Inquiry.
R38 – Written policies setting out procedures for raising concerns in the healthcare sector should be capable of being used in relation to persons who do not share a common employment.
Agree.
R39 – There should be some national provision (probably a telephone helpline) to enable any person, whether working within heath care or not, to obtain advice about the best way to raise a concern about a healthcare matter and about the legal implications of doing so. It might be possible to link this helpline with the ‘single portal’ previously referred to.
We will discuss with SHAs and PCTs the best way of providing a locally or regionally based helpline for health service staff, or members of the general public, who want confidential advice about raising concerns. This could be linked to the service described in the response to recommendation 34.
Secretary of State for Health. 168
Ayling152
(Recommendations not numbered in original report.)
R2 – In parallel with this, we recommend that local policies within all NHS Trusts for reporting staff concerns (whistleblowing) should specifically identify sexualised behaviour as appropriate for reporting within the confidence of this procedure.
We will follow up this recommendation.
R8 – We recommend that the regular reports on patient complaints and concerns made to NHS Trust Boards and other corporate governance bodies should be structured to provide an analysis not only of trends in subject matter and clinical area but also to indicate whether a named practitioner has been the subject of previous complaints.
We agree that clinical governance staff in healthcare organisations should analyse data on complaints and concerns in order to identify any ‘clusters’ relating to individual health professionals. We would not necessarily expect the individuals to be named in reports to Trust Boards unless further investigation confirmed that there was significant cause for concern. For doctors, the local clinical governance team will also wish to discuss with the GMC affiliate.
Neale164
R25 – The National Patient Safety Agency should take the lead in developing adverse event reporting systems. Data taken from complaints should be integrated with and/or read alongside other data from such sources as confidential reports on near misses, patient satisfaction surveys and clinical and medical audit.
The government agrees that it is vital for local information systems to be able to integrate information from different sources such as complaints, clinical audit, patient satisfaction surveys and adverse incident reports, in order to identify clusters of indicators which might point to poor professional performance or systems failures. Some PCTs have developed impressive ‘practice profile’ systems of this kind.
At present the NPSA’s core role is to collect patient safety incident data from local reporting systems and other sources through the National Reporting and Learning System and the Patient Safety Observatory. The Observatory analyses these incident data alongside other national level data relevant to safety, e.g. clinical negligence claims from the NHS Litigation Authority. In the light of the recent report Safety First the Department of Health and NPSA are reviewing the future role of NPSA and of local patient safety action teams in encouraging the development of integrated local systems.
R27 – Statutory provision should be made to encourage the reporting of adverse events.
The government agrees the importance of encouraging health professionals to report any concerns about the safety of services but considers that this is better promoted by professional ethical guidance rather than through statutory provision. A proposed ‘duty of candour’ was rejected by Parliament during debate on the 2006 NHS Redress Act.
Kerr/Haslam168
(Recommendations not numbered in original.)
R8 – The Department of Health should develop and publish a specific policy, with practical guidance on implementation, to guide NHS managers in their handling of allegations or disclosure of sexualised behaviour.
The Department of Health accepts these recommendations and is asking Council for Healthcare Regulatory Excellence to progress them as part of the project referred to in para 6.4 of this response.
R23 – The Department of Health should urgently investigate and report upon the need for a co-ordinated method of mandatory data collection and mandatory recording, in relation to the area of abuse of patients by mental healthcare professionals.
The Department of Health will encourage the professional regulators to carry out a retrospective analysis of recent fitness to practice cases to determine in what proportion boundary violations have been a factor.
R27 – Within 12 months of publication of this Report, the Department of Health should issue guidance as to how and where any disclosure or complaint of abuse by another healthcare professional made to a doctor or nurse should be recorded (if at all) in the patient’s medical records, and elsewhere.
Agree in principle. The Department of Health will work with stakeholders to develop guidance on the content of the files to be held by healthcare organisations relating to the performance of individual professionals, including complaints and concerns. It would not normally be appropriate for such information to be held in the patient’s clinical records and the Department will consider, as part of the wider review of the complaints system, whether further guidance is needed on this point.
R30 – The current regulations relating to complaints procedures should be amended to enable any person with a concern about the safety and effectiveness of the NHS to be allowed more readily to use the NHS complaints procedure.
The government agrees that the complaints procedure should be as simple as possible for patients and their representatives to use; this is one of the key principles of the review of the complaints system described in chapter 5 of this response. For people with a generalised rather than personal concern about safety and effectiveness of the NHS a number of possible routes are available, including the PALS services.
R31 – The Department of Health review the effectiveness of whistleblowing policies and initiatives within NHS-funded organisations.
The government fully agrees the need to support healthcare workers who wish to raise concerns about the services in which they work or the performance of individual professionals.
R32 – As a matter of some urgency the NHS should clarify the context of the positive obligation of NHS staff to inform NHS management of concerns in relation to the suspicion of the abuse of patients.
This principle is already covered in ethical guidance from the professional regulators and from NCAS [National Clinical Assessment Service]. We will discuss with the professional regulatory bodies and universities how this duty can be further emphasised especially in undergraduate education.
R37 – Front-line staff who receive complaints about issues which compromise patient safety – whether or not in the confines of a therapeutic disclosure – should be under an express obligation to report that matter to a complaints manager (in or beyond their own organisation) whether or not they work for the organisation named in the complaint.
R57 – In line with the recommendations of the Shipman Inquiry, a centralised database [should] be set up which is capable of recording a range of information about the performance of individual doctors.
Agree in principle. For doctors, the GMC register will act as the central depository of information on the registration status of doctors, together with any related information including disciplinary action by employers and alert notices. See Trust, assurance, safety.
R70 – The NHS should adopt and reinforce the recommendations in the Manzoor Report and in Making Amends, that there should be a duty of candour imposed on, and accepted by, NHS staff. This duty would mean that there is a responsibility to be proactively informative with patients and with their relatives and carers.
Members of the medical, nursing and midwifery professions are already under a professional obligation to inform patients when things go wrong during treatment. The Government made clear in debates on the NHS Redress Act why it did not consider it appropriate to impose a statutory duty on top of these professional obligations, and the Shipman Inquiry came to a similar conclusion in their Fifth Report. We will discuss with the Council for Healthcare Regulatory Excellence and the other regulators whether a similar approach could be adopted for the other health professions.
R73 – All Strategic Health Authorities should set up a manned telephone Helpline (perhaps called a ‘PatientLine’), where anonymised (or identified) concerns could be received and processed. Any information received through the Helpline should be logged and received in confidence (unless there is express identification of the caller), and if there is sufficient information disclosed, should be discussed with the relevant NHS Trust or PCT. Consideration should be given as to how this information could best be collated either regionally or nationally.
The government believes that staff with concerns over patient safety issues should be invited in the first instance to share their concerns in confidence with local management. We recognise however that there are situations (not just in primary care) in which staff feel unable to raise their concerns with the organisation in which they work. In these circumstances, the PCT or SHA may have a role to play; we will explore this in more detail with stakeholders.
Home Secretary and Secretary of State for Health167
The government proposes:
to issue guidance on the level at which complaints should be investigated, in particular ensuring that those which may raise more general issues about the performance or conduct of health professionals are investigated at a sufficient level of seniority, and that complaints from more vulnerable people who may find it difficult to articulate their true concerns are taken seriously
to place a responsibility on PCTs to maintain an overview of complaints against GPs, including where necessary taking over the investigation of complaints even where they were lodged with the practice in the first instance, as recommended by the Shipman Inquiry154
to work with the NHS to build capacity and skills in practices, PCTs and hospital trusts to investigate serious allegations, including collaboration between PCTs where this would help to concentrate skills and experience
to develop more robust arrangements for the performance management of complaints handling in healthcare organisations.
Underpinning these specific measures, the Government proposes, as Parliamentary time allows, to strengthen the statutory responsibility for quality of healthcare organisations, including a specific responsibility for ensuring that lessons are learnt from medical errors and complaints. This fulfils recommendations from the Shipman Inquiry and from the CMO’s review.
In relation to the inquiry’s fifth report, the action set out in the Government’s formal response Safeguarding patients and in the White Paper on professional regulation Trust, assurance and safety (see Annex B for detailed references) should be seen as a single programme of action. The overall objective must be to ensure patient safety, and to reassure the public that in future any behaviour by health professionals which puts that safety at risk will be swiftly identified, investigated, and dealt with. Although the broad thrust of the action programme is clear, many issues of detail remain which the Department of Health will need to discuss with patient, NHS, and professional groups. The Department will
in due course publish an integrated action plan setting out a timetable for all the action envisaged in the two documents; and
establish a national advisory group with all relevant stakeholders to advise the Department on implementation.
As the Shipman Inquiry noted, it will never be possible to give absolute assurances against the possibility of criminal action like that perpetrated by Shipman. The Government believes however that the actions summarised in this paper
represent a proportionate response to the challenges posed by the Shipman case
will make it highly unlikely that any future criminal could go long without being detected; and
will achieve this without putting undue obstacles in the way of that overwhelming majority of health professionals who want to give the best possible service to their patients.
Francis156
R6 – The Board should review the Trust’s arrangements for the management of complaints and incident reporting in the light of the findings of this report and ensure that it:
provides responses and resolutions to complaints which satisfy complainants;
ensures that staff are engaged in the process from the investigation of a complaint or an incident to the implementation of any lessons to be learned all part of the recommendation;
minimises the risk of deficiencies exposed by the problems recurring; and
makes available full information on the matters reported, and the action to resolve deficiencies, to the Board, the governors and the public.
R7 – Trust policies, procedures and practice regarding professional oversight and discipline should be reviewed in the light of the principles described in this report.
R8 – The Board should give priority to ensuring that any member of staff who raises an honestly held concern about the standard or safety of the provision of services to patients is supported and protected from any adverse consequences, and should foster a culture of openness and insight.
R9 – In the light of the findings of the Next Stage Review,326 the Secretary of State and Monitor should review the arrangements for the training, appointment, support and accountability of executive and non-executive directors of NHS trusts and NHS foundation trusts, with a view to creating and enforcing uniform professional standards for such posts by means of standards formulated and overseen by an independent body given powers of disciplinary sanction.
R11 – The Board should review the management structure to ensure that clinical staff and their views are fully represented at all levels of the Trust and that they are aware of concerns raised by clinicians on matters relating to the standard and safety of the service provided to patients.
Francis (2013, volume 3)159
This is complex and contains multiple clauses (e.g. R1 has 4 parts; R2 has 5 requirements).
R2 – The NHS and all who work for it must adopt and demonstrate a shared culture in which the patient is the priority in everything done.
R7 – All NHS staff should be required to enter into an express commitment to abide by the NHS values and the Constitution, both of which should be incorporated into the contracts of employment.
R12 – Reporting of incidents of concern relevant to patient safety, compliance with fundamental standards or some higher requirement of the employer needs to be not only encouraged but insisted upon. Staff are entitled to receive feedback in relation to any report they make, including information about any action taken or reasons for not acting.
R98 – (National Patient Safety Agency functions) Reporting to the National Reporting and Learning System of all significant adverse incidents not amounting to serious untoward incidents but involving harm to patients should be mandatory on the part of trusts.
R109–122 – Effective Complaints handling (but not staff concerns).
R173–184 – Openness, transparency and candour (Openness – enabling concerns and complaints to be raised freely without fear and questions asked to be answered; Transparency – allowing information about the truth about performance and outcomes to be shared with staff, patients, the public and regulators; Candour – any patient harmed by the provision of a healthcare service is informed of the fact and an appropriate remedy offered, regardless of whether a complaint has been made or a question asked about it.)
R173 – Every healthcare organisation and everyone working for them must be honest, open and truthful in all their dealings with patients and the public, and organisational and personal interests must never be allowed to outweigh the duty to be honest, open and truthful.
R178 – The NHS Constitution should be revised to reflect the changes recommended with regard to a duty of openness, transparency and candour, and all organisations should review their contracts of employment, policies and guidance to ensure that, where relevant, they expressly include and are consistent with above principles and these recommendations.
R179 – ‘Gagging clauses’ or non disparagement clauses should be prohibited in the policies and contracts of all healthcare organisations, regulators and commissioners; insofar as they seek, or appear, to limit bona fide disclosure in relation to public interest issues of patient safety and care.
R180 – Guidance and policies should be reviewed to ensure that they will lead to compliance with Being Open, the guidance published by the National Patient Safety Agency.
R181 – A statutory obligation should be imposed to observe a duty of candour:
On healthcare providers who believe or suspect that treatment or care provided by it to a patient has caused death or serious injury to a patient to inform that patient or other duly authorised person as soon as is practicable of that fact and thereafter to provide such information and explanation as the patient reasonably may request;
On registered medical practitioners and registered nurses and other registered professionals who believe or suspect that treatment or care provided to a patient by or on behalf of any healthcare provider by which they are employed has caused death or serious injury to the patient to report their belief or suspicion to their employer as soon as is reasonably practicable. The provision of information in compliance with this requirement should not of itself be evidence or an admission of any civil or criminal liability, but non-compliance with the statutory duty should entitle the patient to a remedy.
Francis. 11
Secretary of State for Health185
This document accepted recommendation 2 on a shared culture; accepted in principle recommendation 7, that all NHS staff should be required to enter into an express commitment to abide by the NHS values and the Constitution, both of which should be incorporated into the contracts of employment; and accepted recommendation 12, that reporting of incidents of concern relevant to patient safety needs to insisted on. It accepted in principle recommendation 98, that reporting to the National Reporting and Learning System of all significant adverse incidents should be mandatory on the part of trusts. It accepted most of the recommendations on openness, transparency and candour, but accepted in principle recommendation 178 on incorporating the NHS Constitution into contracts of employment, and recommendation 181 on a statutory obligation to observe a duty of candour on health-care providers, and on registered medical practitioners and registered nurses and other registered professionals. However, it did not accept recommendation 183 of a criminal offence for any registered medical practitioner, or nurse, or allied health professional or director of an authorised or registered health-care organisation to make untruthful statements, although it agreed ‘with the intention behind this recommendation’.
The document makes clear which recommendations have been accepted and by whom and what progress is being made towards their implementation. The DHSC will lead the system in providing an annual report on progress across the system each autumn. The Health Select Committee confirmed in its third report, After Francis: Making a Difference,182 published in September 2013, that it agreed with the inquiry’s recommendation that it should monitor the implementation of all of Francis’ recommendations:
R2 – The NHS and all who work for it must adopt and demonstrate a shared culture in which the patient is the priority in everything done.
Accepted.
We are putting in place legal changes that place a statutory duty of candour on healthcare providers and which create a new offence of providing false or misleading information. We believe that the combination of positive reinforcement of the value of openness with sanctions for the most serious failings in candour and honesty will support the NHS to become a far more open culture than the one examined by the Inquiry’s report.
R7 – All NHS staff should be required to enter into an express commitment to abide by the NHS values and the Constitution, both of which should be incorporated into the contracts of employment.
Accepted in principle.
R12 – Reporting of incidents of concern relevant to patient safety, compliance with fundamental standards or some higher requirement of the employer needs to be not only encouraged but insisted upon. Staff are entitled to receive feedback in relation to any report they make, including information about any action taken or reasons for not acting.
Accepted.
R98 – Reporting to the National Reporting and Learning System of all significant adverse incidents not amounting to serious untoward incidents but involving harm to patients should be mandatory on the part of trusts.
Accepted in principle. Reporting of patient safety incidents involving severe harm and death is already mandatory nationally under the Care Quality Commission regulations and these incidents are actively reviewed by NHS England as well as being shared with the Care Quality Commission. The Government’s current policy is not to introduce a mandatory reporting system at this stage however the Government does agree there should be a new duty on providers to be candid to patients (as set out in recommendation 174) and more should be done to promote the reporting of all patient safety incidents among healthcare professionals (as set out in recommendation 181). The National Reporting and Learning System already receives over 1.2 million incident reports a year and NHS England continues to encourage increased reporting from across the healthcare system. Indicator 5.1 of the NHS Outcomes Framework requires that the NHS continues to increase the numbers of incidents that are reported to the National Reporting and Learning System as this is a good indication of the development of a mature patient safety culture where organisations are open about incidents. NHS England will continue to drive the development of the safety culture within the NHS, not least by implementing relevant recommendations from the Berwick report. Organisations should routinely collect, analyse and respond to local measures that serve as indicators of the level of quality and safety of healthcare, including the voices of patients and staff, staffing levels, the reliability of critical processes and other quality metrics. As stated in recommendation 97, the Chief Inspector of Hospitals’ assessment will include an inspection for patient safety which will inform the ratings of all NHS providers and the Care Quality Commission and NHS England will work closely together to share information, including reported incidents from the National Reporting and Learning System, to support Care Quality Commission’s surveillance and inspection.
Secretary of State for Health. 185
Openness, transparency and candour
The Inquiry identified the principles of openness, transparency and candour as the ‘cornerstone of healthcare’.
The Government has introduced a new statutory duty of candour on providers that will ensure patients are given the truth when things go wrong, and that honesty and transparency are the norm in every organisation.
In April, the Enterprise and Regulatory Reform Act 2013202 strengthened the position of whistleblowers so that an individual now has the right to expect their employer to take reasonable steps to prevent them suffering detriment from a co-worker as a result of blowing the whistle. The Government now requires the inclusion of an explicit clause in compromise agreement to make it clear that staff can make a protected disclosure in the public interest, and the Care Quality Commission is using staff surveys and the whistleblowing concerns it receives as part of the data in its new intelligent monitoring system. Since September the Care Quality Commission’s new inspection system includes discussions with hospitals about how they deal with, and handle, whistleblowers.
R173 – Every healthcare organisation and everyone working for them must be honest, open and truthful in all their dealings with patients and the public, and organisational and personal interests must never be allowed to outweigh the duty to be honest, open and truthful.
Accepted.
R174 – Where death or serious harm has been or may have been caused to a patient by an act or omission of the organisation or its staff, the patient (or any lawfully entitled personal representative or other authorised person) should be informed of the incident, given full disclosure of the surrounding circumstances and be offered an appropriate level of support, whether or not the patient or representative has asked for this information.
Accepted.
Secretary of State for Health. 185
The Secretary of State for Health legally required NHS England to insert a contractual duty of candour into the NHS Standard Contract in 2013–14. This means that NHS Trusts and Foundation Trusts are contractually required to operate a duty of candour. The contract also refers organisations to the Being Open framework that was first produced by the National Patient Safety Agency.
The Government has also introduced in the Care Bill a new requirement for a statutory duty of candour and this will be included as a new registration requirement for health and social care providers registered with the CQC.
R178 – The NHS Constitution should be revised to reflect the changes recommended with regard to a duty of openness, transparency and candour, and all organisations should review their contracts of employment, policies and guidance to ensure that, where relevant, they expressly include and are consistent with above principles and these recommendations.
Accepted in principle.
While we generally agree with the importance of these recommendations, The NHS Constitution focuses specifically on setting out the values of the NHS along with the rights and pledges to patients and staff, and their responsibilities. As it is not intended to address organisational reporting processes and interactions with regulatory bodies, it is not considered appropriate to reflect these issues in The NHS Constitution. We do not think that including a duty of openness, transparency and candour into contracts of employment is relevant, not least because of the difficulty in defining these terms for contractual purposes.
R179 – ‘Gagging clauses’ or non disparagement clauses should be prohibited in the policies and contracts of all healthcare organisations, regulators and commissioners; insofar as they seek, or appear, to limit bona fide disclosure in relation to public interest issues of patient safety and care.
Accepted. We understand the critical importance of fostering and sustaining an open culture in which concerns about care can be raised, investigated and acted upon without fear of retribution. Our policy is clear that any attempts to prevent individuals from speaking out in the public interest will not be tolerated. NHS guidance has been consistently clear that local policies should prohibit the inclusion of confidentiality clauses in contracts of employment and compromise agreements which seek to prevent an individual from making a disclosure in accordance with the Public Interest Disclosure Act (PIDA). We are, however, also aware that some confidentiality clauses that may make some people feel as though they are being ‘gagged’ even though they are not. Such clauses, although not illegal, may have what is known as a ‘chilling effect’ on some people. We now therefore require the inclusion of an explicit clause in the compromise agreement to make it absolutely clear to staff signing an agreement that they can make a disclosure in the public interest in accordance with PIDA, regardless of what other clauses may be included in the agreement.
R180 – Guidance and policies should be reviewed to ensure that they will lead to compliance with Being Open, the guidance published by the National Patient Safety Agency.
Accepted.
R181 – A statutory obligation should be imposed to observe a duty of candour:
On healthcare providers who believe or suspect that treatment or care provided by it to a patient has caused death or serious injury to a patient to inform that patient or other duly authorised person as soon as is practicable of that fact and thereafter to provide such information and explanation as the patient reasonably may request.
On registered medical practitioners and registered nurses and other registered professionals who believe or suspect that treatment or care provided to a patient by or on behalf of any healthcare provider by which they are employed has caused death or serious injury to the patient to report their belief or suspicion to their employer as soon as is reasonably practicable. The provision of information in compliance with this requirement should not of itself be evidence or an admission of any civil or criminal liability, but non-compliance with the statutory duty should entitle the patient to a remedy.
Accepted in principle.
The Government agrees that the professional values of individual clinicians are critical in ensuring an open culture in which mistakes are reported, whether or not they cause actual harm. General Medical Council, Nursing and Midwifery Council and other professional regulators will be working to agree consistent approaches to candour and reporting of errors, including a common responsibility across doctors and nurses, and other health professions to be candid with patients when mistakes occur whether serious or not, and clear guidance that professionals who seek to obstruct others in raising concerns or being candid would be in breach of their professional responsibilities.
R183 – It should be made a criminal offence for any registered medical practitioner, or nurse, or allied health professional or director of an authorised or registered healthcare organisation:
knowingly to obstruct another in the performance of these statutory duties;
to provide information to a patient or nearest relative intending to mislead them about such an incident;
dishonestly to make an untruthful statement to a commissioner or regulator knowing or believing that they are likely to rely on the statement in the performance of their duties.
Not accepted, however we agree with the intention behind this recommendation.
Secretary of State for Health. 185
Appendix 3 Legal review
This appendix provides additional supporting material for the legal review contained in Chapter 5.
Extract from the Employment Rights Act 2006190
s43G A qualifying disclosure is made in accordance with this section if –
S43G (a) . . .
(b) [the worker] reasonably believes that the information disclosed, and any allegation contained in it, are substantially true,
(c) he does not make the disclosure for purposes of personal gain,
(d) any of the conditions in subsection (2) is met, and
(e) in all the circumstances of the case, it is reasonable for him to make the disclosure.
(2) The conditions referred to in subsection (1) (d) are –
(a) that, at the time he makes the disclosure, the worker reasonably believes that he will be subjected to a detriment by his employer if he makes a disclosure to his employer or in accordance with section 43F,
(b) that, in a case where no person is prescribed for the purposes of section 43F in relation to the relevant failure, the worker reasonably believes that it is likely that evidence relating to the relevant failure will be concealed or destroyed if he makes a disclosure to his employer, or
(c) that the worker has previously made a disclosure of substantially the same information –
(i) to his employer, or
(ii) in accordance with section 43F.
(3) In determining for the purposes of subsection (1) (e) whether it is reasonable for the worker to make the disclosure, regard shall be had, in particular, to –
(a) the identity of the person to whom the disclosure is made,
(b) the seriousness of the relevant failure,
(c) whether the relevant failure is continuing or is likely to occur in the future,
(d) whether the disclosure is made in breach of a duty of confidentiality owed by the employer to any other person,
(e) in a case falling within subsection (2)(c)(i) or (ii), any action which the employer or the person to whom the previous disclosure in accordance with section 43F was made has taken or might reasonably be expected to have taken as a result of the previous disclosure, and
(f) in a case falling within subsection (2) (c) (i), whether in making the disclosure to the employer the worker complied with any procedure whose use by him was authorised by the employer.
Employment Rights Act 2006. 190
Extracts from the Council of Europe recommendation CM/REC (2014)
Council of Europe250
The normative framework should reflect a comprehensive and coherent approach to facilitating public interest reporting and disclosures.
8. Restrictions and exceptions to the rights and obligations of any person in relation to public interest reports and disclosures should be no more than necessary and, in any event, not be such as to defeat the objectives of the principles set out in this recommendation.
9. Member States should ensure that there is in place an effective mechanism or mechanisms for acting on public interest reports and disclosures.
10. Any person who is prejudiced, whether directly or indirectly, by the reporting or disclosure of inaccurate or misleading information should retain the protection and the remedies available to him or her under the rules of general law.
11. An employer should not be able to rely on a person’s legal or contractual obligations in order to prevent that person from making a public interest report or disclosure or to penalise him or her for having done so.
Channels for Reporting and Disclosure should be established and should comprise:
– reports within an organisation or enterprise (including to persons designated to receive reports in confidence);
– reports to relevant public regulatory bodies, law enforcement agencies and supervisory bodies;
– disclosures to the public, for example to a journalist or a member of parliament.
Whistleblowers should be entitled to have the confidentiality of their identity maintained, subject to fair trial guarantees.
21. Whistleblowers should be protected against retaliation of any form, whether directly or indirectly, by their employer and by persons working for or acting on behalf of the employer. Forms of such retaliation might include dismissal, suspension, demotion, loss of promotion opportunities, punitive transfers and reductions in or deductions of wages, harassment or other punitive or discriminatory treatment.
European Union statements concerning treatment of whistleblowers in European Union institutions
Obligations are placed on officials or civil servants within the EU requiring them to report fraud, corruption and other illegal activities. There are positive obligations to disclose and also protections given to those who make such disclosures.
Regulation No 31 (EEC), 11 (EAEC), laying down the Staff Regulations of Officials and the Conditions of Employment of Other Servants of the European Economic Community and the European Atomic Energy Community327
Any official who, in the course of or in connection with the performance of his duties, becomes aware of facts which give rise to a presumption of the existence of possible illegal activity, including fraud or corruption, detrimental to the interests of the Union or of conduct relating to the discharge of professional duties which may constitute a serious failure to comply with the obligations of officials of the Union shall without delay inform either his immediate superior or his Director-General or, if he considers it useful, the Secretary-General, or the persons in equivalent positions, or the European Anti-Fraud Office (OLAF) direct.
Information mentioned in the first subparagraph shall be given in writing.
This paragraph shall also apply in the event of serious failure to comply with a similar obligation on the part of a Member of an institution or any other person in the service of or carrying out work for an institution.
2. Any official receiving the information referred to in paragraph 1 shall without delay transmit to OLAF any evidence of which he is aware from which the existence of the irregularities referred to in paragraph 1 may be presumed.
3. An official shall not suffer any prejudicial effects on the part of the institution as a result of having communicated the information referred to in paragraphs 1 and 2, provided that he acted reasonably and honestly.
4. Paragraphs 1 to 3 shall not apply to documents, deeds, reports, notes or information in any form whatsoever held for the purposes of, or created or disclosed to the official in the course of, proceedings in legal cases, whether pending or closed.
EUR-Lex. 255 Reproduced with permission. © European Union, http://eur-lex.europa.eu/, 1998–2018
Article 22b goes on to provide that:
1. An official who further discloses information as defined in Article 22a to the President of the Commission or of the Court of Auditors or of the Council or of the European Parliament, or to the European Ombudsman, shall not suffer any prejudicial effects on the part of the institution to which he belongs provided that both of the following conditions are met:
(a) the official honestly and reasonably believes that the information disclosed, and any allegation contained in it, are substantially true; and
(b) the official has previously disclosed the same information to OLAF or to his own institution and has allowed OLAF or that institution the period of time set by the Office or the institution, given the complexity of the case, to take appropriate action. The official shall be duly informed of that period of time within 60 days.
EUR-Lex. 255 Reproduced with permission. © European Union, http://eur-lex.europa.eu/, 1998–2018
In 2013 the European Parliament called on the European Commission to introduce a legislative proposal to create effective and comprehensive protection for whistleblowers in both the public and private sectors. Although there have been subsequent calls for the EU to take forward such proposals, this has not happened to date, although there is some recognition of whistleblowing by, for example, the EU ombudsman.
Comparative whistleblowing approaches in European countries
Although, as set out above in this appendix, there have been recommendations at EU and Council of Europe level, to date European nation states’ approaches are governed by their domestic jurisprudence. A comprehensive overview and analysis of the state of whistleblowing laws in G20 countries is given by Wolfe et al. 247 and that of European countries by Transparency International. 328 Here we explore some notable examples of the different approaches taken to whistleblowers across European states to provide potentially useful comparisons with/contrasts to the UK position. The focus here on European states reflects the fact that Council of Europe member states are affected by the same fundamental human rights norms as stated in the Council of Europe Convention on Human Rights. What is striking is the diversity in approaches across states. Transparency International, in a report published in 2013, divided EU countries into three categories. 328 The first were those countries with advanced protection. These include the UK, Luxembourg, Romania and Slovenia. Today the Republic of Ireland can also be included in that list with its Protected Disclosures Act 2014, aspects of which are considered below and in the main body of this report. The second category concerns partial protection provided for whistleblowers in a countries laws; this includes countries such as Austria, Belgium, France and Germany. The third category comprises countries where there is no protection for whistleblowers or, where such protection exists, it is exceedingly limited in nature. Within each category, the application of applicable legal principles may also be affected by questions of existing substantive law, including such things as fundamental principles of human rights. What is notable is that the UK provides a much more comprehensive framework than is the case in relation to many other European states.
In relation to the first category, the UK’s PIDA was the first major piece of legislation in this area. The first protection in continental Europe was that provided in Romania in 2004, where a Whistleblower Protection Act was enacted that applies to government employees. In 2010, Hungary passed legislation that governs whistleblowing in both public and private sectors. In Ireland, broad legislation was enacted in 2014 that is modelled on the UK approach but goes considerably beyond it in scope and in the level of safeguards provided to those who blow the whistle. 186 The backdrop to the Irish legislation was that of high-profile scandals in relation to clergy, banking, police and health care. Ireland now has legislation that provides some safeguards to whistleblowers in the form of the Protected Disclosures Act 2014,307 which amends the Unfair Dismissal Act 1977. 329 There are notable similarities to the approach taken in the UK legislation but also some sharp differences, as the Act provides greater safeguards not only in relation to unfair dismissal but also in relation to other forms of litigation; these are discussed in Chapter 5 of the report.
The second category noted above concerns partial protection; this operates, for example, in France, where there are a series of limited safeguards in specific contexts. 330 Here, between 2007 and 2014, five separate pieces of legislation were adopted in relation to public and private sectors facilitating some disclosures in the context of grave risks to health, environment and matters of corruption. There is now a new law known as Sapin 2 (Act is No 2016–1691 of 9 December 2016). This strengthens the law concerning corruption. Chapter II of the Act provides enhanced protection for whistleblowers who revealing crimes, breach of ratified and approved international commitments or serious breaches of law or serious threats/harms to the public interest. In addition, although French civil servants are obliged in law to disclose crimes and other offences, when they have knowledge of them, to the state prosecutor, at the same time there are no specific protections given to them, which has led to individuals losing employment or to those who remain in employment being ostracised. 328 Protection is given in French labour law to disclosures in the context of corruption and, in addition, the courts have protected whistleblowers through the use of freedom of expression principles. 330 However, in some instances, data protection provisions have been used to inhibit whistleblowing. 330
In Austria, the Public Service Law has since 2012 contained specific protection from discrimination provisions, which are the first specific provisions in relation to whistleblowing. In addition, the Labour Law safeguards employees from dismissals that have the effect of violating Austria’s basic social principles, which include the principle of freedom of speech. 328 In Bosnia and Herzogovina, the Law on Whistleblower Protection in the Institutions of Bosnia-Herzegovina includes a provision enabling employees to be given whistleblowing status through pre-emptive action by applying to the Agency for Prevention of Corruption and Co-ordination of Fight Against Corruptions, which has to respond to the request within 30 days. If such status is given, then this prevents a state institution from undertaking action against an employee who has reported corruption under the law. This is a potentially powerful provision and there is nothing comparable currently in UK law.
In Germany, there are conflicting attitudes to whistleblowers and indeed historically very negative language has been used to describe whistleblowers. 331,332 As noted in the main text of the report, whistleblowers have brought ECHR challenges under Article 10. Article 4 of the Grungesetz – the Constitution – provides that there is a freedom of conscience, of information and of expression with a right to petition. This includes rights to bring requests to complaints to government agencies. There is a constitutional principle of indirect third-party effect, such that a court would be required to make reference to human rights provisions when they are interpreting general Civil Code clauses. In addition, it has been said that the Labour Act provides that discrimination should be forbidden by a certain allowed exercises of rights. However, there are rights to disclose externally [e.g. in the area of health and safety law [section 17(2) 1, Employment Protection Act)]. Other protections also exist in relation to, for example, information being provided to external authorities in the context of money laundering. 332 In Croatia, there is no general whistleblowing law at present, but certain specific protections are given to those who reveal corruption. 333
Finally, there remain some member states, such as Portugal, where there is minimal or non-existent protection. 328 It appears that in relation to these European countries to date, none has any extensive empirical research on the impact of whistleblowing specifically in the health-care context.
Extracts from Schedule 1 of the Human Rights Act 1998249
The Articles set out below are from Schedule 1 of the Human Rights Act and are relevant provisions of the Council of Europe Convention on Human Rights. Section 3 of the Human Rights Act 1998 provides that legislation must be interpreted and given effect to in a manner compatible with Convention rights.
Quotations in this section are reproduced from the Human Rights Act 1998. 249 © Crown copyright. Contains public sector information licenced under the Open Government Licence v3.0.
Article 8
Right to respect for private and family life
Everyone has the right to respect for his private and family life, his home and his correspondence.
There shall be no interference by a public authority with the exercise of this right except such as is in accordance with the law and is necessary in a democratic society in the interests of national security, public safety or the economic well-being of the country, for the prevention of disorder or crime, for the protection of health or morals, or for the protection of the rights and freedoms of others.
Article 9
Freedom of thought, conscience and religion
Everyone has the right to freedom of thought, conscience and religion; this right includes freedom to change his religion or belief and freedom, either alone or in community with others and in public or private, to manifest his religion or belief, in worship, teaching, practice and observance.
Freedom to manifest one’s religion or beliefs shall be subject only to such limitations as are prescribed by law and are necessary in a democratic society in the interests of public safety, for the protection of public order, health or morals, or for the protection of the rights and freedoms of others.
Article 10
Freedom of expression
Everyone has the right to freedom of expression. This right shall include freedom to hold opinions and to receive and impart information and ideas without interference by public authority and regardless of frontiers. This Article shall not prevent States from requiring the licensing of broadcasting, television or cinema enterprises.
The exercise of these freedoms, since it carries with it duties and responsibilities, may be subject to such formalities, conditions, restrictions or penalties as are prescribed by law and are necessary in a democratic society, in the interests of national security, territorial integrity or public safety, for the prevention of disorder or crime, for the protection of health or morals, for the protection of the reputation or rights of others, for preventing the disclosure of information received in confidence, or for maintaining the authority and impartiality of the judiciary.
If there is breach of one of the substantive articles of the Convention, as set out above and there is in addition an allegation of discrimination then an additional claim may also be brought under Article 14 as set out below.
Article 14
Prohibition of discrimination
The enjoyment of the rights and freedoms set forth in this Convention shall be secured without discrimination on any ground such as sex, race, colour, language, religion, political or other opinion, national or social origin, association with a national minority, property, birth or other status.
The duty of candour
Extracts from Regulation 20 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014273
(1) [Registered persons] must act in an open and transparent way with relevant persons in relation to care and treatment provided to service users in carrying on a regulated activity.
(2) As soon as reasonably practicable after becoming aware that a notifiable safety incident has occurred a [registered person] must –
(a) notify the relevant person that the incident has occurred in accordance with paragraph (3), and
(b) provide reasonable support to the relevant person in relation to the incident, including when giving such notification.
(3) The notification to be given under paragraph (2)(a) must –
(a) be given in person by one or more representatives of the [registered person],
(b) provide an account, which to the best of the [registered person’s] knowledge is true, of all the facts the [registered person] knows about the incident as at the date of the notification,
(c) advise the relevant person what further enquiries into the incident the [registered person] believes are appropriate,
(d) include an apology, and
(e) be recorded in a written record which is kept securely by the [registered person].
(4) The notification given under paragraph (2)(a) must be followed by a written notification given or sent to the relevant person containing –
(a) the information provided under paragraph (3)(b),
(b) details of any enquiries to be undertaken in accordance with paragraph (3)(c),
(c) the results of any further enquiries into the incident, and
(d) an apology.
(5) But if the relevant person cannot be contacted in person or declines to speak to the representative of the [registered person] –
(a) paragraphs (2) to (4) are not to apply, and
(b) a written record is to be kept of attempts to contact or to speak to the relevant person.
(6) The [registered person] must keep a copy of all correspondence with the relevant person under paragraph (4).
Health and Social Care Act 2008. 273
Guidance on the duty of candour has been produced by the GMC and Nursing and Midwifery Council. 267,274 This emphasises that patients must ‘be fully informed’ about their care (paragraph 6). 267,274 The statements in relation to information provision reflect existing law concerning consent to treatment. It stipulates that it is relevant where something has gone wrong and harm has resulted (paragraph 8). 267,274 Onus is placed on the health professional or on someone in their team to speak to the patient; the guidance notes that ‘the most appropriate team member will usually be the lead or accountable clinician’ (paragraph 9). 267,274 This should be done as soon as possible and, moreover, the guidance states that:
You should share all you know and believe to be true about what went wrong and why, and what the consequences are likely to be. You should explain if anything is still uncertain and you must respond honestly to any questions. You should apologise to the patient.
When patients do not want more information, this option should still be raised with the patient. Their wishes should be respected ‘as far as possible’ and their decision should be recorded (paragraph 12). 267,274 It is also the case that individuals are not expected to take responsibility for things that are not their fault, but there is an expectation that an individual will receive an apology from an appropriate team member. This could lead to interesting and difficult dynamics in relation to who provides the apology if a range of different people’s actions have contributed to the harm caused (paragraph 15). 267,274 The guidance states that patients expect three things in relation to an apology:
a. what happened
b. what can be done to deal with any harm caused
c. what will be done to prevent someone else being harmed.
At the same time it states that this does not constitute legal liability (paragraph 14). 267,274 It may also amount to evidence of insight at a professional practice panel (paragraph 14). 267,274 While it is suggested that a formulaic response to apologising is not being encouraged, the guidance does provide some structured criteria in relation to apologies such as comprehensible information, delivered in a manner respecting of privacy/dignity as appropriate and that a personalised approach can be ‘more meaningful’ rather than a ‘generalised expression of regret’ (paragraph 16). 267,274 The guidance also notes the need to be open and honest in relation to those close to the patient if the patient has died or harm of such a severe nature has been suffered such that they are unlikely to regain decision making capacity (paragraph 17). 267,274 Emphasis again is placed on appropriate sensitivity being used and appropriate support being given (paragraphs 18 and 19). 267,274 The guidance makes reference to the ‘near miss’, which is defined as being ‘an adverse incident that had the potential to result in harm but did not do so’ (paragraph 20). 267,274
The guidance states that professional judgement is to be exercised as to whether or not patients are told but that there can be some circumstances in which if patients are not told then this could damage their trust and confidence in the team (paragraphs 20 and 21). 267,274 It is likely that these could prove challenging questions for clinical teams in the future. The guidance makes express reference to the need to encourage ‘a learning culture by reporting errors’ (paragraph 22 onwards). 267,274 It is stated that:
When something goes wrong with patient care, it is crucial that it is reported at an early stage so that lessons can be learnt quickly and patients can be protected from harm in the future.
Moreover, it is stated that health-care organisations are required to have policies in relation to the reporting of adverse incidents and near misses (paragraph 23). 267,274 The guidance notes existing reporting systems (paragraph 24);267,274 these are referenced above in relation to health and safety considerations. The guidance notes the need for organisation support, and critically states that:
Your organisation should support you to report adverse incidents and near misses routinely. If you do not feel supported to report, and in particular if you are discouraged or prevented from reporting, you should raise a concern in line with our guidance.
This demonstrates that raising issues under the duty of candour will necessitate internal whistleblowing. Moreover, the guidance goes on to state:
You must not try to prevent colleagues or former colleagues from raising concerns about patient safety. If you are in a management role, you must make sure that individuals who raise concerns are protected from unfair criticism or action, including any detriment or dismissal.
Essentially, the guidance means that the GMC and NMC are recognising the need to safeguard those who blow the whistle. Furthermore, specific responsibilities are placed on those nurses, midwives and doctors with management responsibilities, as well as on ‘senior or high profile clinicians’ (paragraphs 29 and 30). 267,274 Here, duties are set out very clearly:
Senior clinicians have a responsibility to set an example and encourage openness and honesty. In reporting adverse incidents and near misses. Clinical leaders should actively foster a culture of learning and improvement.
If you have a management role or responsibility, you must make sure that systems are in place to give early warning of any failure, or potential failure, in the clinical performance of individuals or teams. These should include systems for conducting audits and considering patient feedback. You must make sure that any concerns about the performance of an individual or team are investigated and, if appropriate, addressed quickly and effectively.
The onus is, thus, on the management in terms of both setting the tone and developing culture, but in addition, and importantly, making sure that the appropriate systems are in place. This again illustrates that health professionals in such a situation have a dual role: as health professionals with responsibility in relation to their professional code and as employees who are managers.
Appendix 4 Summaries of key Inquiry reports
This appendix provides a summary of inquiries and reports, from Bristol Royal Infirmary5 to the Francis2 Freedom to Speak Up review, and the responses of the main stakeholders to these reports. For each report, information is presented on issues such as who was the whistleblower, how and why did they ‘blow the whistle’, what factors did or could facilitate or inhibit the action and what were the consequences for the whistleblower? For each response, attention is focused on the recommendations of the associated inquiry.
Kennedy
This was a public inquiry set up in 1998,5 with the terms of reference to inquire into the management of the care of children receiving complex cardiac surgical services at Bristol Royal Infirmary between 1984 and 1995; to make findings as to the adequacy of the services provided; to establish what action was taken both within and outside the hospital to deal with concerns raised about the surgery; to identify any failure to take appropriate action promptly; to reach conclusions from these events; and to make recommendations that could help to secure high-quality care across the NHS (p. 1). In particular, it examined high mortality rates, focusing on two main surgeons, Mr Wisheart and Mr Dhasmana. It was estimated that during the period 1991–5, between 30 and 35 more children aged under 1 year died after open-heart surgery in the Bristol unit than would be expected had the unit been typical of other paediatric cardiac surgery (PCS) units in England at the time (p. 2). The report stressed that it is ‘not an account of bad people’ (p. 1), but a ‘tragedy born of high hopes and ambitions and peopled by dedicated hard-working people’ (p. i). However, Mr Wisheart, Mr Dhasmana and CEO Dr Roylance were found guilty of serious professional misconduct in 1998 (p. 25). The report stated that it would be reassuring to think that it could not happen again. ‘We cannot give that reassurance. Unless lessons are learned, it certainly could happen again’ (p. i).
Blowing the whistle
The main whistleblower was Dr Steve Bolsin, a consultant anaesthetist. However, the term ‘whistleblower’ was mentioned only once, where it was stated that had PIDA been in force it would not have applied to Dr Bolsin as he did not make a ‘qualifying statement’ (p. 160). Dr Bolsin was appointed as consultant anaesthetist in September 1988, and soon began to have concerns about the duration of operations and the consequent effect on outcomes (p. 136). Dr Bolsin began to gather data in 1989. He wrote to Dr Roylance in 1990, with copies sent to the Chair of the Health Authority and the Chair of Her Majesty’s Courts service. Dr Bolsin was called to Mr Wisheart’s office and rebuked for taking information about PCS to ‘outsiders’, including apparently the CEO. A copy was also sent to the chairperson of the division of anaesthetics, Dr Williams, who stated that ‘No one supported the way in which Steve Bolsin had raised the issue but all were fully supportive of his efforts to obtain appropriate data to assess the situation more accurately in an endeavour to improve results’. At a meeting in 1991, Dr Bolsin said that he was told to ‘keep his head down’ (p. 138). In 1991, he showed his data to Professor Prys-Roberts (Professor of Anaesthesia, and later President of the Royal College of Anaesthetists 1994–7), who advised him to collect more data. In 1993, a report was shared with colleagues in the Department of Anaesthesia, but not with the surgeons Mr Wisheart or Mr Dhasmana. In the autumn of 1991, Dr Bolsin spoke to the director of anaesthetics and medical director of a neighbouring hospital, Dr John Zorab, who sent a letter to Sir Terrence English, President of the Royal College of Surgeons of England (1989–92) (p. 139). In 1992, Private Eye published articles about the Bristol PCS. A concerned parent read the article and contacted the NHS Management Executive. Mr Wisheart drafted a letter stating that results at Bristol were good. In April 1992, Dr Bolsin met Dr Phil Hammond, whom he regarded as a ‘concerned trainee GP’, and who was, unknown to Bolsin at that time, the author of the Private Eye articles (p. 141). In late 1993, Bolsin spoke to Dr Jane Ashwell, a senior medical officer at the DHSC (p. 145), and in July 1994 Dr Bolsin gave data to Dr Peter Doyle, a senior medical officer at the DHSC, who ‘did not look at the data’ and ‘filed the document’ (p. 148). In December 1994, 18-month-old Joshua Loveday was scheduled to have a switch operation performed by Mr Dhasmana. On 6 January 1995, Professor Angelini tried to persuade Mr Wisheart that it would not be wise for the operation to go ahead, which he claims was the first time that he recalls an open expression of concern about PCS. A clinical meeting on 11 January decided that the operation should go ahead, and on 12 January Joshua Loveday died following surgery (p. 149). Later in January, an external independent inquiry was set up. In February, Mr Wisheart claimed he first heard about Dr Bolsin’s audit data (p. 150).
The report examined ‘Dr Bolsin’s actions’ (pp. 159–62). In 1988, he approached the problem as a clinical issue within his own division. In 1990, in a ‘rather oblique’ approach, he sent a letter to the CEO. In 1991 he raised his concerns at a meeting of cardiac anaesthetists who ‘were supportive of his concerns, though critical of the manner of his approach’. In late 1991, his concerns became known to anaesthetists outside University Hospitals Bristol NHS Foundation Trust; to Dr Phil Hammond in April 1992; to surgical colleagues other than those whose work gave rise to his concerns in 1993; and to senior medical officers in the DHSC in 1993–5. The report stated that Dr Bolsin’s role has been lionised by those who were critical of the PCS service, and attacked by those who support the Bristol surgeons. He did not follow the ‘Three Wise Men’ route advised by the DHSC, which is ‘not surprising’ as this route was perceived as dealing primarily with individual clinicians whose performance was affected by problems such as ill health, and Mr Wisheart would have been one of the ‘Three Wise Men’. It concluded that ‘In addition to the contacts Dr Bolsin made, there was no other obvious route for raising questions about quality of care’.
Factors
The report pointed to a ‘club culture’, an imbalance of power with too much control in the hands of a few individuals (p. 2). Career development depended on ‘fit’ within the club rather than performance, and any challenge to policy was regarded as disloyalty (p. 201). It discussed the structural and individual elements of hierarchies that prevented open discussion (pp. 161–2). This included the difficulty of an anaesthetist being critical of a surgeon, particularly a senior figure such as Mr Wisheart. ‘In our view, the possibility of such open discussion was barred by the firmly held views of Mr Wisheart’. For example, one witness reported that when Professors Angelini and Farndon tried to raise concerns with Mr Wisheart, he spoke to them ‘like a couple of schoolboys’ (p. 161). He encountered the ‘territorial loyalties and boundaries within the culture of medicine and the NHS, and also the realities of power and influence’ (p. 161). It was ‘understandable’ that Dr Bolsin did not approach Mr Wisheart, a senior figure of whom he was in some awe, and probably some fear. However, it was less clear and ‘unfortunate’ why he did not approach Mr Dhasmana. In general, Dr Bolsin’s path was therefore ‘understandable’, and ‘in summary, while Dr Bolsin’s actions may not always have been the wisest, and sometimes he gave mixed signals . . . he persisted, and was right to do so’.
More widely, other anaesthetists shared his concerns, and a number of attempts were made to bring those concerns to the attention of Dr Roylance and Mr Wisheart, by the anaesthetists clinical director, Dr Monk (p. 173). According to Kennedy,5 many staff, particularly junior staff, remained silent in the face of poor care or wrongdoing as they were fearful of raising concerns and/or challenging superiors because of the possible repercussions: ‘There is a real fear among staff (particularly among junior doctors and nurses) that to comment on colleagues, particularly consultants, is to endanger their future work prospects. The junior needs a reference and a recommendation; nurses want to keep their jobs. This is a powerful motive for keeping quiet’ (p. 273).
The report regarded it as ‘significant’ that it was not heard that concerns were brought to senior figures by the nursing staff. This was not due to ‘any lack of concern; but illustrating a larger truth of the hierarchical system that made it difficult for nursing staff to voice concerns and be heard (p. 175). For example, one witness described a ‘culture of fear’, with Director of Operations and Nursing Advisor, Mrs Maisey, being described as ‘the Rottweiler of the Trust’ (p. 171). In short, nursing staff were let down by a culture that excluded them (p. 176).
Consequences for the whistleblower
There is nothing in the report on this issue. According to Hammond and Bousfield,161 Dr Bolsin was a hero; yet the medical and managerial establishments turned against him for exposing how dangerous and self-protective they were. They continued that Bolsin, a leading thinker in patient safety, would have been a huge asset to the NHS had he not been ostracised and briefed against. At a European cardiac surgeons meeting, he was described as ‘the most hated anaesthetist in Europe’ and found himself unemployable in the NHS. He left the UK in 1995 to work – very successfully – in Australia. At a patient safety conference on 23 October 2013, Dr Bolsin was awarded the Royal College of Anaesthetists Medal in recognition of the work that he has done to promote safety in anaesthesia. 162
Consequences for the NHS
The report presented 198 recommendations, with the caveats that ‘there are no right answers; just, perhaps, less wrong answers’, ‘cultural and institutional change takes time and can be slow’, and ‘there are no quick fixes’. The recommendations were classified under the following themes: respect and honesty; a health service that is well led; competent health-care professionals; the safety of care; care of an appropriate standard; public involvement through empowerment; and the care of children. Although there was no explicit recommendation on whistleblowing, a number of recommendations foreshadowed some of those of later reports, such as ‘a duty of candour’ to patients (recommendation 33), a framework of regulation independent of government (recommendations 39–40), doctors’ Code of Professional Practice incorporated in the contract of employment (recommendation 45), a regulatory body, and professional code of practice for health-care managers (recommendation 91), a national reporting system (recommendations 109–112), and incentives to encourage the reporting of sentinel events (recommendations 113–118).
More generally, stress was placed on changing the ‘culture of the NHS’. For example, the culture of the future must be a culture of safety and quality and a culture of openness and accountability (p. 13). Learning from error rather than seeking a person to blame had to be the priority (p. 11). However, although there were flaws with the hospital, its organisation and culture and the wider NHS, there were individuals who ‘should and could’ have behaved differently (p. 9). Finally, there had to be more openness (p. 3). Although the term was not used, the importance of ‘soft’ evidence or intelligence was stressed. Concerns, albeit without ‘hard evidence’, had been raised as early as 1986–7, with Emeritus Professor Andrew Henderson distributing a letter at a meeting of the South Glamorgan Health Authority that ‘it is no secret that their [UBH’s paediatric cardiac] surgical service is regarded as being at the bottom of the UK league for quality’ (p. 134), and in June 1987 BBC Wales broadcast the programme ‘Heart Surgery – The Second Class Service’ (p. 135). The hospital’s own data showed the unit’s high mortality figures, but these were disregarded or explained away. In short, Bristol was ‘awash with data but was, at the same time, singularly uninformed’ (p. 176).
In 2001 the Secretary of State for Health announced the setting-up of three separate, independent statutory inquiries,152,153,164 none of which was to be held in public, which became known as the ‘three inquiries’. They had broadly similar terms of reference, which required in each case an investigation of how the NHS locally had handled complaints about the performance and/or conduct of the doctors.
Quotations in this section are reproduced from Kennedy. 5 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Ayling152
This was one of the three inquiries announced in 2001, and on 6 September 2002 the Secretary of State for Health announced that Anna Pauffley QC (later The Honourable Mrs Justice Pauffley) would chair this inquiry. In 1998, Clifford Ayling was arrested and charged with indecently assaulting former patients. In 2000, he was convicted on 12 counts of indecent assault, relating to 10 female patients, and sentenced to 4 years’ imprisonment. His name was placed indefinitely on the Sex Offender’s Register under the Sex Offenders Act 1997. In 2001, the professional conduct committee of the GMC determined that Ayling’s name should be erased from the Medical Register.
Blowing the whistle
Ayling worked in hospitals and as a GP. Although some midwives at Thanet had concerns during 1975–88, only one written record of staff complaints was found, which is indicative of the contemporaneous culture within the profession to rely on informal mechanisms for raising concerns about a colleague (p. 37). Midwife Delphine Bentley wrote a complaint in 1984, but it would appear that this resulted in no action of any kind. It appears that the serious failure of the senior staff and management at Thanet and King’s College Hospital to recognise and address concerns about Ayling’s conduct resulted from inadequate communication within the professional hierarchies (p. 43). There was also an incident at Thanet Antenatal Clinic in 1980 when, according to Sister Penny Moore’s account, she was called urgently by a nurse chaperone at a postnatal examination, and, on entering the room, found Ayling masturbating while carrying out a vaginal examination on a young woman. She asked the patient’s consultant, Mr Fullman, to come to the hospital immediately and told him that she did not want Ayling at the clinic again. However, some time later, the other consultant, Mr Paterson, reintroduced Ayling to the clinic. The report considers that the incident reported by Penny Moore clearly warranted an immediate investigation and action at the highest level, including – if substantiated – dismissal and referral to both the police and the GMC. This could have ended Ayling’s career 20 years before he finally ceased to practise. ‘We deplore that fact that no such investigation was undertaken’ (p. 45).
Ayling became a GP in 1981, and remained in general practice until 2000. In 1991 a patient made a complaint to Kent Police about the way he had examined her at his surgery. Ayling was ultimately tried and convicted of indecent assault against the patient in 2000. In 1991 the Crown Prosecution Service took the decision not to prosecute, but brought to the attention of the Family Health Services Authority by a letter from Kent Police (p. 63). The report stated that it was clear that the incident had not been taken sufficiently seriously by the Family Health Services Authority’s senior management and that there had been a significant failure on their part to ensure appropriate investigative or supervisory action (p. 64).
From 1985 until Ayling’s conviction in 2000, a succession of patients transferred from his practice to a neighbouring surgery. It turned out that many female patients referred, in more or less explicit terms, to apparent misconduct by Ayling in the context of breast and vaginal examinations (p. 65). Two partners, Dr Pickering and later Dr Anderson, conducted the ‘transfer interviews’ (p. 66). It was not until late 1993 that Dr Pickering decided to approach the Kent Local Medical Committee, after further discussions with his partners. A few months later, he was told that there was no need for the committee to do anything, as the William Harvey Hospital, which employed Ayling as a part-time clinical assistant, had received complaints of a similar nature and was taking action (p. 69). By 1998 Dr Anderson had become sufficiently concerned to telephone his Medical Defence Organisation. He was told that, unless a patient came forward to complain, there was little he could do. He subsequently spoke to Dr Snell, the European Kidney Health Alliance’s medical advisor, on 5 November 1998, and thereafter became involved in the ongoing police investigation (p. 71).
Factors
The report pointed to the ‘individuals who could and should have acted on the information then available’, and identified a number of missed opportunities from 1971 until 1998 when concerns and complaints about Ayling might have been acted on (p. 109). It looked at some of the underlying causes within the culture and systems of the NHS in those years, which seem to us to be as significant in the creation of the missed opportunities and perhaps even more so than the actions of individuals at the time.
It stated that patients were reluctant to complain, and there was an almost complete lack of support available to patients who might have wanted to raise a concern. Doctors were believed over patients or other staff: the fear that patients had, namely that their word would not be believed, was not unjustified (p. 113). There was a lack of a truly inquisitive or inquisitorial approach, as well as a defensive response to complaints, which was a product of a culture that saw complaints as a challenge, rather than a source of information and an opportunity to learn from that information (p. 113).
It discussed a number of issues such as clinical freedom and self regulation; staff hierarchies; lack of openness; a failure to hear; lack of clear professional guidance; preference for the use of informal systems; lack of information sharing or ‘corporate memory’; barriers to making complaints – staff and colleagues; the lack of gathering and sharing ‘soft’ information; and lack of procedures for raising concerns.
However, the single most important barrier to staff such as nurses and midwives formally expressing their concerns about Ayling was the absence of any formal procedure for doing so (p. 138), and it was not until 1993 that formal guidance was given to the NHS on concerns at work. Until 1995, the GMC route was ambiguous and suggested that reporting concerns about a fellow doctor should be tempered with caution about denigration and defamation (p. 138). Moreover, a repeated theme during the inquiry was the need to capture ‘soft’ or informal information that fell short of a formal complaint, and an ‘open and fair culture’ would have encouraged staff to speak up about the activities they had witnessed (p. 155).
The inquiry quoted some optimistic witnesses who considered that things had changed for the better in terms of speaking up about any concerns, and stated that ‘whilst substantial improvement is still needed, NHS staff are increasingly willing to speak up for patient safety, even at some personal risk’. However ‘it would take considerable courage on their part to use a whistleblowing policy, especially in light of the reported accounts we heard of Ayling’s aggressive denial of questionable conduct and practice (p. 159). Moreover, ‘the impact of the Government’s plans and investment in health services has dramatically altered the landscape of the NHS. At an organisational level, it is almost unrecognisable as the NHS in which Ayling practised’. However, it was too early to conclude that, if individual patients should encounter another Ayling, particularly in the general practice setting, the improved systems were yet fully developed that would enable their concerns to be heard and acted on (p. 163).
Consequences for the whistleblower
There appeared to be no consequences for the whistleblower.
Consequences for the NHS
The report produced 19 recommendations on ‘sexualised behaviour’ (recommendations 1–2), ‘listening and hearing’ (recommendations 3–4), ‘complaints procedures’ (recommendation 5), ‘tracking repeated complaints and concerns’ (recommendations 6–8), ‘sole practitioners’ (recommendations 9–10), ‘chaperones’ (recommendations 11–13), ‘local medical committees’ (recommendations 14–15) and ‘criminal investigations’ (recommendations 16–19). Only one of these (recommendation 2) was concerned with whistleblowing: ‘we recommend that local policies within all NHS Trusts for reporting staff concerns (whistleblowing) should specifically identify ‘sexualised behaviour’ as appropriate for reporting within the confidence of this procedure’ (p. 22).
Quotations in this section are reproduced from Ayling. 152 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Neale164
In 1985 Richard Neale was erased from the Canadian Medical Register following a disciplinary hearing, but in 1984 he was offered employment by the Yorkshire Regional Health Authority, working at Friarage Hospital and Darlington Memorial Hospital, and, after reorganisation in 1992, by Northallerton Health Services NHS Trust, where later that year he was appointed Clinical Director of Obstetrics and Gynaecology. In 1993, media stories revealed that he had been struck off in Canada in 1985, and had been involved in an incident at a public toilet in Richmond, Yorkshire, for which he had been cautioned by the police. In December 1993 Dr Richard Peterson headed an investigation panel into these disclosures, resulting in Neale being demoted from his post as clinical director. In 1995 the trust decided to set up a disciplinary hearing into various allegations concerning his conduct and activities. It was decided to negotiate a severance package, and he left the trust’s employment after a year’s sabbatical, but was subsequently employed by two hospitals in Leicester and the Isle of Wight.
The Regional Chief Medical Officer, Liam Donaldson, first became aware of clinical concerns about Richard Neale in late January 1998, when a BBC regional television programme made revelations about Neale involving women who had been treated by him in North Yorkshire. On 12 June 1998, an alert letter was sent out by the Northern and Yorkshire Regional Office to NHS health authority and trust chief executives about Richard Neale, at the instigation of Professor Donaldson and Dr Cresswell. On 25 July 2000, the GMC erased Richard Neale’s name from the Register (p. 15).
Blowing the whistle
Although there was a paper on whistleblowing shared with other inquiries, and a seminar on supporting staff in raising concerns about colleagues, the inquiry contained little on whistleblowing.
Factors
The report stated that both the system and those working in it were not operating as effectively as they should have been to guarantee patient confidence and patient safety.
The report considered that between 1985 and 1997 there were systems failures within the employment and complaints procedures within the NHS, and, very importantly, failures within other professional bodies on which the NHS was dependent. A sense of complacency undoubtedly contributed to what occurred, and there remained an urgent need for a root-and-branch change in attitudes and culture within the NHS. However, the most perplexing aspect was that Neale had been struck off in Canada, but was able to retain his licence to practise medicine in the UK (p. 13).
The 1995 investigation covered a number of concerns: inappropriate leave, lack of supervision of junior staff, clinical mismanagement and working relationships with colleague. The 2004 report concluded that staff were, to a considerable degree, in awe of Mr Neale and felt unable to challenge his clinical competence even if they had had grounds to do so. His personality made him difficult to challenge (p. 180).
The trust pointed to the ‘cardinal rule’ of going through the proper channels ‘. . . you must resist the temptation to do things by the back door!!’ The report considered that this could be viewed as an inhibiting message to staff faced with problems about a more senior member of staff and reflected a culture described by many staff of a reticence to raise concerns about Neale, which would make it extremely difficult for patients to raise concerns or complaints, and echoes a comment heard in the evidence: ‘we have no complaints at the Friarage’ (p. 199).
Consequences for the whistleblower
There appears to be no whistleblower.
Consequences for the NHS
The report produced 27 recommendations, but none had much relevance to whistleblowing. However, it appeared to suggest the optimistic message that, even before the inquiry began, many of the wider lessons had been learnt and change had been implemented (p. 180).
Quotations in this section are reproduced from the Richard Neale Inquiry. 164 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Kerr/Haslam153
This report was concerned with understanding the problem of the sexual abuse of psychiatric patients. William Kerr started working as a locum senior house officer in psychiatry at Clifton Hospital in York in 1965, was appointed as consultant in 1967 and retired in 1988. The first complaint against Kerr in North Yorkshire was in 1965, his very first year in the post, and evidence received indicated that 38 former patients claimed that they had made disclosures to NHS staff of sexualised behaviour by William Kerr before his retirement. Not one of these led to any investigation of his practice (p. 6).
Michael Haslam took up his post as consultant in psychological medicine at Clifton Hospital, York, and Harrogate District Hospital in 1970. In 1974, the first complaint (of which the inquiry was aware) concerning Michael Haslam was brought to the attention of a local GP (p. 8). The inquiry received evidence indicating that at least eight patients had, during Haslam’s time in York, raised concerns about his alleged sexual advances towards them (p. 294). In 2000, Kerr was convicted (in his absence, on a Trial of the Facts) of one count of indecent assault, and in 2003 Haslam was convicted of four counts of indecent assault (a conviction of rape was quashed on appeal) (p. 4).
The inquiry posed the central questions:
-
How could it be that the voices of the patients and former patients of William Kerr and Michael Haslam were not heard?
-
Why were so many opportunities to respond and investigate missed?
-
How could it happen that the abuse of patients, evidenced by the convictions of William Kerr and Michael Haslam, went undetected for so long? (pp. 4–5).
The report stated that the story was one of management failure, failed communication, poor record-keeping and a culture in which the consultant was all-powerful. It argued that many ignored ‘warning bells’ or dismissed rumours, and some chose to remain silent when they should have been raising their voices. Although the majority stood back, there were, as in all such stories, some who stepped forward, but even those lone voices were not heard. Above all it was an account of psychiatric patients, many in number, whose concerns and complaints fell on ‘deaf ears’ (p. 5).
The inquiry stated that the overall picture was one of failure, or missed opportunities, over a number of years. The first serious investigation into William Kerr’s practice was in 1997, almost 10 years after he had left the NHS. In relation to Michael Haslam, the Manzoor inquiry took place in 1998, again almost 10 years after he left the North Yorkshire NHS. Moreover, a failure to react and investigate has emerged as a common theme in reports such as Shipman,154 Ayling152 and Neale164 (pp. 466–7).
However, the report also struck an optimistic tone, claiming to detect a significant change – beginning in the 1990s and carrying through to the present day – in both attitudes and systems. Many professionals who gave evidence to the inquiry describing their response to concerns and complaints in the 1970s and 1980s stated that they would act differently now. Not only was there a willingness to change, but there are now in place systems throughout the NHS – some say too many – that treat the patient as consumer, entitled to be dissatisfied and to express their dissatisfaction (p. 16). Colleagues reporting concerns about fellow colleagues has become much more widely accepted as a result of the Bristol Royal Infirmary inquiry and of the multiple deaths of vulnerable older patients in the case of Harold Shipman (p. 663), and that there have been signs that professional loyalty as previously understood is no longer an acceptable barrier to protecting patient safety (p. 664).
However, the report concluded that change of culture is at the heart of real change. Whatever the systems in place, if those who operate them at all levels are not focused on patient safety, then other factors, other pressures, will prevail (p. 808). Individuals with the attitudes and responses reflected in some of the evidence given to the inquiry create a culture that is infectious and leave a legacy that cannot be changed overnight (p. 811). The inquiry feared that all of its concerns had not been addressed: ‘There may have been recent wake-up calls – recognised in this and several other Inquiries. But the tendency of institutions to develop a culture of accepting, or denying the existence of, the unacceptable has not fundamentally changed’ (p. 810).
Blowing the whistle
The most determined and persistent whistleblower was Deputy Sister Linda Bigwood. However, others who raised concerns included Community Psychiatric Nurse Stephen Brooks, and newly appointed consultant psychiatrist at the Friarage Hospital in Northallerton, Dr Christopher Simpson, in October 1987. The inquiry also discussed GPs, each of whom to a greater or lesser extent sought to pass on their concern and, in modern terminology, ‘blow the whistle’: Dr Wade (on Kerr in 1979), Dr Moroney (on Haslam in 1987) and Dr Moran (on Haslam in 1988) (p. 431). These clear instances of GPs taking action to pursue concerns ‘represented the minority’; the more characteristic picture was of GPs who were well aware of patient concerns about the practices of Kerr and/or Haslam, and did nothing or very little (p. 415). The inquiry suggest some temporal dimension in that the responses of Doctors Moroney and Moran to a complaint about Michael Haslam show a markedly different approach from that of many of the GPs who were the recipients of concerns a decade or more earlier (p. 439).
Kerr
In 1983 an account of an alleged sexual relationship between a psychiatric patient, Patient A17, and her treating consultant, William Kerr, was disclosed to Deputy Sister Bigwood: not by way of complaint, but as part of the patient’s life story. Unlike so many of her colleagues, she was not prepared to ‘turn a blind eye’, and pursued her concerns about Kerr’s alleged sexual misconduct towards not only Patient A17 but a number of patients, with the hospital authorities, the district health authority and, beyond that, with the regional health authority.
Perhaps as a result of COHSE’s involvement, the focus was on ‘the grievances of Linda Bigwood’, and there was a failure to focus on the patient safety issues raised by the extremely serious allegations against William Kerr. In concentrating on the messenger, the substance of the message was both lost and ignored (p. 189). An inquiry, chaired by Mr Ray Wilk, the director of nursing services (mental illness), entirely excluded from its remit the most concerning aspect of Linda Bigwood’s complaint, namely that a consultant psychiatrist was allegedly sexually abusing his female patients and that knowledge of these allegations was widespread among other health-care professionals (p. 236). Despite letters and meetings setting out Bigwood’s concerns over a period of almost 5 years and involving the most senior NHS managers, and despite the support of her union representatives, no investigation was ever made into Kerr’s practice.
This can be contrasted with the complaint against Michael Haslam in 1974, when Patient B1 informed her GP, Dr Foggitt, that (allegedly) she had been having an affair with Michael Haslam. However, in a pattern that echoed the response to complaints regarding Kerr, this was never pursued either by the patient herself or by Dr Foggitt as a formal complaint or as an issue that needed to be reported to health service management (p. 9). The report continues that the stories of Haslam and Kerr, perhaps inevitably, overlap. Indeed, Linda Bigwood, whose efforts as a whistleblower were concentrated on William Kerr, also brought concerns about Michael Haslam to the attention of management (p. 10).
The report noted that a significant number of concerns, whether or not raised as formal complaints, were voiced but not heard. In the period before 1983, of the 30 concerns alleged to have been raised about William Kerr all but one fell (below) on deaf ears (p. 7). It stated that the response of GPs, who in many instances were the first and often only recipient of concerns expressed by patients of Kerr and Haslam, was varied (p. 11). The first complaint concerning Haslam of which the inquiry was aware was communicated to Dr Foggitt. In the same way as GPs had failed to forward their concerns about Kerr to any higher authority, Dr Foggitt (although he took steps to refer his patient, Patient B1, to another consultant) did not seek to inform the authorities of Haslam’s alleged sexual relationship with Patient B1. However, the later complaints against Haslam, arising in 1987 and 1988, provoked a very different response from Dr Moroney and Dr Moran, which is perhaps explicable by the gradual change of culture that had occurred by this stage (p. 12).
The failure by the local GPs to respond is a striking feature of the William Kerr story (p. 12). One of the potentially most alarming aspects of Linda Bigwood’s written complaint was the suggestion that rumours of William Kerr’s alleged abuse of female patients were well known to GPs in Harrogate, to the extent that some would no longer refer young female patients to him (p. 209). The report found only one instance of a GP, Dr Wade, taking any active steps to pursue a complaint about Kerr in 1979 (p. 12). This was the case of Patient A222. However, ‘it is one of the great ironies in this account that the consultant to whom Dr Wade chose to speak about his concerns regarding William Kerr was Michael Haslam’. Perhaps unsurprisingly, given his attitude to sexual contact between patients and doctors, Haslam did not take the matter any further (p. 7).
What was revealed by the Patient A17 story was a disturbing picture of inaction, or part action, amounting in the end to a total failure by hospital staff and administrators to investigate the allegations against William Kerr (despite Linda Bigwood’s dogged pursuit of the issue). As was later recognised by the health authorities in written submissions to the inquiry, Bigwood was ‘courageous, persistent and determined in her fight to have a proper investigation into Patient A17’s allegations to her’. The inquiry concluded that Bigwood deserved a better hearing (p. 175).
Haslam
On 26 September 1988, Patient B7 informed community psychiatric nurse Stephen Brooks that she had had problems with Michael Haslam and was frightened to see him. Brooks was clear in his evidence that he had a duty to take this matter further and that he explained this duty to Patient B7. This is in marked contrast to the evidence of some other witnesses, who told us that they felt so constrained by patient confidentiality that they could not pass on the concerns. The clarity of Brooks’ evidence as to his duty to inform where there is potential risk to patients serves to highlight the confusion which then (and probably now) exists as to what should be done in such circumstances (p. 342).
On 28 September 1988, Patient B7 told Brooks that she had told her GP, Dr Moran, that Haslam had been unprofessional and that she ‘just froze’. Dr Moran spoke to his GP partners and contacted Brooks. Moran and Brooks met on 29 September 1988 to discuss the matter and took the decision to inform Dr Kennedy, CEO of the DHA (p. 343). Dr Kennedy later returned Dr Moran’s telephone call and Dr Moran formed the impression that a decision had been taken that Haslam would be asked to resign. However, Patient B7 did not want to take the matter further (p. 344). At the criminal trial, Patient B7 indicated that that she considered that her complaint would be considered by the ‘authorities at Bootham Park’ and that the police would be involved (p. 346).
At the end of 1997, Professor Sir Liam Donaldson, then Regional Director NHS Executive Northern and Yorkshire, set up an inquiry into the allegations of sexual misconduct against Haslam between 1984 and 1988, chaired by Mrs Zahida Manzoor, Regional Chairperson, NHS Executive Northern and Yorkshire (p. 384). Haslam was dismissed from his post at South West Durham Mental Health NHS Trust in September 1998 following the production of the Manzoor Report (p. 393). The police had decided not to proceed with laying charges against Haslam, but in September 1997 the police reopened their investigations in relation to Haslam on receipt of further evidence from Patient B7. Owing to Patient B7’s reluctance to proceed to give evidence in court, the police were forced to discontinue their investigations in November 1997, without laying charges (p. 395).
However, the report points to the first ‘whistleblower’. In 1964, Dr Mathewson, a GP practising in Northern Ireland, ignored express pressure that he should not give evidence against a colleague, and pursued a complaint by a young female patient against Kerr. Dr Mathewson gave evidence at a disciplinary tribunal, with the result that Kerr’s career in Northern Ireland came to an end. It is a sad fact not only that Kerr was able to evade the consequences of the disciplinary hearing by relocating to England, but that once in England there was not a single GP who displayed the fortitude of Dr Mathewson in pursuing any one of the many complaints against William Kerr to the logical conclusion of any form of disciplinary (p. 446).
Factors
The report pointed to an ‘unhealthy’ culture in which professionals were reluctant to take action against consultants, through either a misguided sense of loyalty or fear of confrontation. Administrators felt powerless, and devised mechanisms to protect themselves, rather than the patients or those who raised concerns. Sadly, some of the failure arose because it was easier, and perhaps professionally safer, to do little or nothing at all (p. 13). The report categorised the root causes of this comprehensive failure to attend to patient concerns under five headings: organisational, cultural, structural, professional practice and individual failings. It pointed to the key factors explaining GPs’ lack of response: the ‘old-boy network’ or professional loyalty; isolation of GPs; tolerance of sexualised behaviour; insufficient expertise in psychiatry; confidentiality; the power of consultants; and an ambivalent attitude to relationships between doctors and patients.
Rather unusually, compared with other reports, the inquiry stressed the importance of individual ‘agency’ as opposed to collective, structural factors. It stated that it accepted as broadly correct the following summary from the submissions made on behalf of the health authorities:
The reason why a consultant was able to continue in practice and assault his patients . . . was a mixture of a flawed structure, poor procedures, systems failures, individual and collective failures in an institution that was created at a time when to most, if not all, people the idea that patients might need protection from doctors was unthinkable.
pp. 214–15
However, with different emphasis on ‘individual and collective failures’, this summary broadly accords with the submissions made on behalf of the former patients of both Kerr and Haslam (volume 2, p. 801). As the counsel for the patients put it to the inquiry:
For the main part, we do not say are system failures, they are personality failures, where patients were so short-changed by individuals, not by the system: the system worked in 1966 [a reference to Northern Ireland], the system could have worked if individual doctors, GPs, had taken extra steps.
Volume 2, p. 802153
Consequences for the whistleblower
Shortly after she had passed on Patient A17’s disclosure, Linda Bigwood was informed that she was to be moved from Ash Tree House Ward, an acute admissions ward, to Rosedale Ward, a geriatric ward. She viewed this move as a demotion and felt that she was being punished for raising Patient A17’s disclosure (p. 181).
The inquiry pointed to ‘some courageous individuals’ who spoke out and raised their concerns. Some did so being new into their jobs and not steeped in the culture of ‘the way we do things around here’, such as Dr Simpson, a new consultant psychiatrist, who was able to raise concerns and suffer no detriment to his position. Others, such as Linda Bigwood, were not so fortunate (volume 2, p. 664). Bigwood – as with many other so-called ‘whistleblowers’ – in personally raising the issue of how the complaints were handled suffered professional detriment (p. 8).
Consequences for the NHS
The report recommended that the DHSC should review the effectiveness of whistleblowing policies and initiatives within NHS-funded organisations (p. 29); that the NHS should adopt and reinforce the recommendations in the Manzoor report and in Making Amends; that there should be a duty of candour imposed on, and accepted by, NHS staff (p. 36); and that all SHAs should set up a manned telephone helpline, through which anonymised (or identified) concerns could be received and processed (p. 66).
It stated that health professionals acting as Linda Bigwood did should be regarded as people to be treated positively and given support. They are not threats to the NHS, but the essential catalysts that will bring about better patient care and better patient protection (p. 20). There must be a ‘change of ethos’, which can be promoted in three ways: education, promoting the obligation to speak out and promoting knowledge and skills. Patient safety requires a culture in which speaking out (whether or not categorised as whistleblowing) is welcomed. The NHS must fully support its staff, who in turn must be left in no doubt that the culture of turning a blind eye is unacceptable, and that to stay silent may be to perpetuate and thus participate in wrongdoing. There should be no career detriment for those who speak out to promote patient safety (p. 21). Enabling staff to feel able to raise these concerns constructively, so that something is done and they (as the whistleblower) are not victimised either by the individual they raise concerns about or the wider staff team, remains a challenge in the modern-day NHS. It is one thing for a policy to be put in place and quite another to establish a culture that supports, enables and encourages staff to raise their concerns (p. 664).
Quotations in this section are reproduced from The Kerr/Haslam Inquiry. 153 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Shipman154
The Shipman Inquiry consists of six reports, with the main material about whistleblowing in volume 5. Harold Shipman was a GP who was convicted in 2000 of murdering 15 patients, and of forging a will. However, the inquiry identified 215 victims, but ‘the true number is far greater and cannot be counted’154 (volume 1, p. 202). It considered that:
it is deeply disturbing that Shipman’s killing of his patients did not arouse suspicion for so many years. Had it not been for Shipman’s grossly incompetent forgery of Mrs Grundy’s will, it is by no means clear that his crimes would ever have been detected.
Volume 1, p. 200154
When it came to light at his trial that, in 1976, Shipman had been convicted of offences of forgery, unlawful possession pethidine and obtaining pethidine by deception, ‘many people began to ask how it was that he had been able to return to unsupervised general practice in 1977, just over a year later’, and how his repeated killing of patients had escaped the notice of the authorities. From 1977, Shipman worked at the Donneybrook practice in Hyde, Greater Manchester, until in late 1991 he set up as a single-handed practitioner (volume 5, p. 1).
Blowing the whistle
The inquiry tried to avoid using the expression ‘whistleblowing’ wherever possible (p. 319). It noted that there were a number of missed opportunities to raise concerns. In 1976, the GMC allowed Shipman to continue to practise. In 1994, Shipman gave a gross overdose of diamorphine to a 46-year-old patient, who later died in Tameside General Hospital. Both of the consultants in charge did not report the event and ‘must be criticised’ for their failure to report Shipman’s actions, but this is ‘tempered’ because the culture within the profession at the time was that to report a colleague was ‘not done’, and many doctors throughout the country would have failed to act, as these two doctors did. Moreover, it was most unlikely that Shipman would have been erased from the medical register (p. 22). Over the years some people (e.g. two home helps, a taxi driver and a niece of one of the victims) had concerns, but did not report them. ‘There must not be a word of criticism of these people for what, on the face of it, appears to be failure to raise serious concerns in the appropriate quarter’ (p. 319). 154 The only other person who had attempted to raise a concern was Mrs Christine Simpson, the resident manager of Ogden Court, a sheltered housing development in Hyde, who in 1995 or 1996 tried to alert her line manager (p. 24). Funeral director Mrs Deborah Bambroffe mentioned concerns to GP Dr Susan Booth, which contributed to the raising of anxieties within the Brooke Practice and led, some time later, to GP Dr Linda Reynolds’ report to the Coroner. He passed the information to the police. Unfortunately, the first police investigation resulted in the conclusion that the concerns were without foundation. Dr Reynolds made her report to the Coroner based on two particular grounds for concern: the large number of cremation Forms B, and the unusual characteristics of deaths, namely that the deceased persons were elderly women who had been found dead at home, apparently alone and fully dressed, and did not appear to have been ill (volume 2, p. 1). In short, the inquiry considered that before March 1998, when Dr Reynolds reported her concerns, very few people had had any concerns about Shipman (p. 24). The inquiry considered that none of these persons were ‘whistleblowers’ per se, as they did not work within the same organisation as Shipman, but were merely voicing their concerns to those who they felt were the appropriate authorities. Another feature that set those people apart from the typical ‘whistleblower’ was the fact that most of them were far from confident that their concerns were justified (volume 5, p. 318).
Factors
The inquiry reviewed the history of the raising of concerns in the health sector (including DHSC guidance in 1993; a checklist from the second Nolan Report of 1996; and fresh DHSC guidance in 1999, following the coming into force of PIDA) and considered that further impetus towards a culture of open reporting within the NHS came from the report of the Bristol inquiry (pp. 329–31).
It noted that although it had always been possible for a doctor who was concerned about the treatment given to a patient by another doctor to report his or her concerns about that treatment to an appropriate authority, the culture was that it was ‘not done’. Even with revised GMC guidance in the early 1990s, ‘the old culture lingered on’. The inquiry was told that the culture had not changed until the events that had occurred at Bristol Royal Infirmary came to light, but ‘[e]vidence received by this Inquiry suggests that, in some quarters, it survives even today’ (p. 20).
Evidence given to the inquiry suggested that nurses faced particular difficulty in reporting concerns about doctors, although they had found it rather easier to report concerns about members of their own profession. Both the Bristol Inquiry report and the Ledward Inquiry report said that the culture in medicine inhibited the proper reporting of concerns by nurses about doctors (p. 336).
The inquiry pointed to factors that may inhibit reporting, including the unclear duty to report; the fear of being accused of disparagement; the ‘one-off’ or ‘genuine’ mistake; the insufficiency of evidence; ignorance of procedures (p. 288–300); the fear of being seen as a troublemaker or ‘maverick’; the fear of recriminations; a concern that making a report might lead to proceedings for defamation; and a feeling of impotence grounded in the belief that, even if the report is made, nothing will be done about it. ‘Such fears may be well founded’ as the experience of Dr Stephen Bolsin (Bristol, above) ‘demonstrated how serious the consequences of raising concerns can be’ (p. 319). There was a tendency for attention to be focused on the messenger rather than on the message, and the ‘whistleblower’ may suffer reprisals (p. 320).
Consequences for the whistleblower
There appear to be no consequences for the whistleblowers.
Consequences for the NHS
In contrast to most of the others, this inquiry stressed the role of ‘whistleblowers’:
I believe that the willingness of one healthcare professional to take responsibility for raising concerns about the conduct, performance or health of another could make a greater potential contribution to patient safety than any other single factor.
p. 23154
The inquiry made a total of 190 recommendations. The most relevant appeared to include the need for a general practice whistleblowing policy; that PCTs should provide information and training about whistleblowing policies directly to practice staff; and the provision of a telephone helpline.
It stated that although practice staff technically enjoy the protection of PIDA, there were two potential problems. First, it was unclear if raising concerns to the PCT was a ‘protected route’, and PIDA should be amended to clarify this. Second, as working relationships within the practice may break down, the right to retain employment was an empty one, and the PCT should assist the employee to find a post in another practice wherever possible (pp. 285–6).
There should be some provision (probably a telephone helpline) to enable any person, whether or not working within health care, to obtain advice about the best way to raise a concern about a health-care matter and about the legal implications of so doing (p. 1093).
The report appeared to be rather optimistic about the future. Since Shipman’s arrest, there have been radical changes within the NHS: the introduction of National Service Frameworks; the CHI (later the Commission for Healthcare Audit and Inspection, now the HCC); and the NCAA (p. 10). It stated that there were signs that the culture of mutual self-protection had changed, although the process was by no means complete (p. 23). It continued that, since 1998, there had been a considerable change of attitude towards those who want to raise a concern about some aspect of health care. All NHS bodies now have a ‘whistleblowing’ policy that advises employees how to raise a concern and gives an assurance that concerns will be given serious consideration and that there will be no victimisation even if the concern turns out to be unfounded. PIDA provided a measure of protection against victimisation for all employees who raise concerns. In addition, independent advice was now provided by a charitable body, PCAW. Nevertheless, more needed to be done (p. 25):
It appears to me that the position of any person seeking to raise a concern is now very much better than it was even six years ago, when the PIDA was passed. I think that the PIDA has been of great value, both in the relief it has provided for individuals and also in changing general attitudes. However, I am sure that more remains to be done.
p. 339154
Quotations in this section are reproduced from The Shipman Inquiry. 154 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Francis155,156
Concerns about mortality and the standard of care provided at the Mid Staffordshire NHS Foundation Trust resulted in an investigation by the HCC, which published a highly critical report in March 2009, which was followed by two reviews commissioned by the DHSC. This inquiry, focusing on the period from 2005 to 2009, was set up by the Labour Secretary of State for Health, Andy Burnham, in July 2009. Its terms of reference were:
-
to investigate any individual case relating to the care provided by Mid Staffordshire NHS Foundation Trust between 2005 and 2008 that, in its opinion, caused concern and to the extent that it considered appropriate
-
in the light of such investigation, to consider whether any additional lessons were to be learnt beyond those identified by the inquiries conducted by the Healthcare Commission, Professor Alberti and Dr Colin-Thomé; and, if so
-
to consider what additional action was necessary for the new hospital management to ensure that the trust was delivering a sustainably good service to its local population
-
to prepare and deliver to the Secretary of State a report of its findings.
Although the government resisted calls for a full public inquiry, it stated that if the chairperson considered that he needed powers to compel the attendance of witnesses, then it had the power to convert the inquiry under the Inquiries Act 2005 (p. 29). 334
Blowing the whistle
The main material on whistleblowing is given in a section covering pages 279–91. It stated that whistleblowing could take many forms, including passing information to management or colleagues within the same organisation or, in some cases, to some external body or individual or even the media (p. 279).
According to the Director of HR, Norma Sadler, there were only 10 incidents in the 6 years that she was in post (from 2000 to 2006) and some of these were not, in fact, whistleblowing. The inquiry was aware of the facts of only three whistleblowing reports (below). ‘All give cause for concern as to whether individuals who blow the whistle are properly looked after and whether the concerns they raise are properly pursued’ (p. 281).
The first case concerned a consultant who, on 30 May 2008, submitted a memorandum to the Parliamentary Health Select Committee, and later to the HCC, in which he outlined his attempts over many years to raise concerns. On 30 March 2009, 1 day after the publication of the HCC report, he was suspended by Dr Suarez, the outgoing medical director, on the grounds of an allegation that he had behaved in an intimidating manner towards a colleague and a patient (p. 282). One of the first actions taken by the new medical director, Dr Obhrai, was to remove the suspension. The inquiry noted the ‘unhappy coincidence, to say the least, in the correlation between the timing of the publication of the HCC report, and his suspension in circumstances which have later been found to be unjustified’ (p. 283).
The second case was drawn to the attention of the inquiry by the whistleblower, the external investigator and Cure the NHS, but not the trust. The complaint concerned allegations of poor care in ward 3 and was made by a nurse and a health-care support worker. They raised concerns about the management of the ward and identified particular members of staff. Both had left the hospital, having made the allegations under the whistleblowing policy at a formal meeting with the director of human resources on 21 July 2005 (p. 284). The former finance director, Mr Newsham, who was at that time acting chief executive, along with Ms Brisby, former chairperson of the trust, commissioned an external investigation, in part it seems because the whistleblowers did not want the director of clinical standards to be involved. Mr Newsham received the report after Mr Yeates took over as chief executive, and handed the report to him. The inquiry considered that the report ‘came to a number of damning conclusions’ (p. 285), (such as an increase in the death rate, poor staffing levels, and poor governance arrangements across the directorate and trust), but there did not appear to have been any discussion by the board of the serious issues raised. ‘It is striking that the investigator’s conclusions closely mirror the findings of the HCC and the evidence collated in this Inquiry’s report’ (pp. 286–7).
The third case occurred on 28 October 2007, concerning an allegation of falsification of patient documentation in order to avoid the breach of targets in A&E, and a more general allegation against two sisters working in A&E of bullying and harassment. This was also drawn to the inquiry’s attention by Cure the NHS. The two nurses against whom the principal allegations were made were suspended from duty, and the directorate manager for surgery was appointed to investigate, who concluded that there was no case to answer on the principal allegation (p. 288). A further investigation took place into the more general complaints of bullying and harassment and into allegations of specific incidents of harassment following the whistleblowing report. The notes of the investigatory interviews conducted by the external investigating officer appear to corroborate the whistleblower’s allegation that staff had been instructed to lie about 4-hour waiting times. The two members of staff who were subject to the complaint were reinstated to work in A&E, with no explanation being given to the whistleblower, who later stated that her experience of the process was a principal reason why she left the employment of the hospital (p. 289). The inquiry concluded that the conclusions the fabrication issue were ‘generous’ and the report did not explain why the evidence from witnesses other than the principal whistleblower ‘did not lead to a more critical conclusion’. Moreover, an ‘inadequate degree of protection was given to the whistleblower’ and ‘clear and cogent evidence that record fabrication was habitual’ did not lead to a general investigation and audit of records (p. 290). The inquiry’s overall comment was that ‘the experiences of those involved in these three episodes arising out of raising serious concerns is not encouraging’ (p. 291).
Factors
The inquiry pointed to an organisational culture which included: a culture of bullying; target-driven priorities; disengagement from management; low staff morale; isolation; lack of candour; acceptance of poor behaviours; reliance on external assessments; and denial (p. 152). It stated that fear had also manifested itself in the reluctance of staff, particularly nursing staff, to come forward to the inquiry (p. 166), and that the experience of staff who had raised concerns about colleagues suggested that trust management appeared more keen to protect the subject of the concern rather than the informant (p. 174–5).
Although protecting whistleblowers has been a concern of public policy for a number of years (p. 279), and although the trust has had a policy on whistleblowing since 2001 (p. 280), there remained a ‘very real reluctance’ on the part of staff at all levels of seniority in raising concerns (p. 409). The 2008 version of trust policy stated that its aim ‘is to encourage staff to raise concerns about possible malpractice in the Trust at an early stage and in the right way, and that the Trust Board ‘is committed to developing a climate of openness and free expression whereby concerns about the delivery of patient care, financial malpractice, or other wrong doing is welcomed, appreciated and acted upon positively’.
Consequences for the whistleblower
In the three whistleblowing cases discussed above, a consultant was suspended; allegations made in 2005 that closely matched the 2010 inquiry’s main findings were dismissed; and the whistleblower left the trust. The executive summary stated that the few instances of reports by whistleblowers of which the inquiry was made aware suggested that the trust had not offered support and respect to those who took this step. The handling of these cases was unlikely to encourage others to come forward, and the responses to the investigation of the concerns raised have been ineffective (p. 20).
Consequences for the NHS
The Inquiry produced 18 recommendations, but only one focuses on whistleblowing. Recommendation 8 states that ‘The Board should give priority to ensuring that any member of staff who raises an honestly held concern about the standard or safety of the provision of services to patients is supported and protected from any adverse consequences, and should foster a culture of openness and insight’ (p. 27).
The inquiry stated that there was a ‘very real reluctance’ to raise concerns, linked to the ‘widespread belief that the protections offered are theoretical rather than real’. It continued that ‘The most important factor in changing this will not be a new system or policy of protection for whistleblowers, but the fostering of a culture of openness, self-criticism and teamwork’. This requires ‘leadership by example at all levels as well as a reinforcement of the formal protections available’ (p. 409). It argued that no employee should suffer any adverse consequences from management or colleagues for raising or reporting, whether internally or externally, concerns relating to the standard and safety of care provided to patients based on a reasonably held belief, even if an investigation subsequently concludes that there are no grounds for such a concern. It should be a disciplinary offence for any member of management or a colleague to act in a way which is prejudicial to the continued employment of that employee or detrimental to his or her well-being because of the raising or reporting of such concerns (p. 410).
Quotations in this section are reproduced from Francis. 155,156 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Francis157–159
The Conservative Secretary of State for Health in the coalition government, Andrew Lansley, decided that this inquiry should be a public inquiry under the Inquiries Act 2005. 334 In his view, the previous reports were clear that the following existed: a culture of fear in which staff did not feel able to report concerns; a culture of secrecy in which the trust board shut itself off from what was happening in its hospital and ignored its patients; and a culture of bullying, which prevented people from doing their jobs properly. Yet how these conditions developed had not been satisfactorily addressed (pp. 15–16).
Blowing the whistle
This included a mix of the same cases as the 2010 Inquiry (with names and more detail) and some new cases. The first case concerned Dr Pradip Singh, a Consultant Gastro-Enterologist, who was suspended on 30 March 2009 on the grounds of an allegation that he had behaved in an intimidating manner towards a colleague and a patient. The second case of the 2010 Inquiry concerned the report of 2005 by Robina Barry, a clinical psychologist, who was Director of Psychological Therapies for South Staffordshire Healthcare NHS Trust. The third case of the 2010 Inquiry concerned Helene Donnelly’s complaint. It was disclosed that Ms Donnelly felt the atmosphere was so unpleasant she approached the RCN for assistance and was offered advice by the RCN’s Regional Officer. Unknown to her, he was also advising and representing the nurses who were the subject of the complaint. She described him as being ‘dismissive’ of her complaints, and his advice was that she should ‘keep her head down’. Effectively he told her there was little that could be done (p. 109).
The 2013 inquiry discussed doctors who sought to raise issues of concern, but they ‘fared little better than the nurses’ (p. 238). Dr Daggett, a consultant physician at the trust from 1982 until his retirement in July 2010, produced a quantity of letters he had written to management from 2001 to 2008 (p. 175). Dr Singh told the inquiry that he had continuously raised concerns. Mr David, a consultant surgeon, stated that he and others had raised their concerns in the only way available to them, via the directorate structure, but the response came back that management said that things would improve once Foundation Trust status had been obtained (pp. 176–7). Dr Turner, then a specialist registrar in emergency medicine, was ‘one of the few medical practitioners to raise concerns’ in 2008 to Deanery staff visiting the trust to review junior doctor training, clinical placements and supervision (p. 120). He later stated that ‘On arrival at Stafford I found the Emergency Department to be an absolute disaster. Its culture was unlike any other I had worked in despite being in the NHS for 25 years’ (p. 121). Although he had not seen the HCC letter before the inquiry, Dr Turner thought that the concerns described in the letter of 23 May exactly reflected his own concerns about A&E. Dr Turner told the inquiry that he had tried to raise his concerns with his educational supervisor but ‘got nowhere’. He raised concerns at a meeting of the Royal College of Emergency Medicine at some point during 2008. He telephoned the HCC twice without a response. On the third attempt there was a reaction and in due course he was interviewed as part of their investigation (p. 121–2). Dr Turner said that it should not have been down to him, a trainee, to take on the burden of challenging the trust leadership (p. 217).
The second and third volume are concerned with the wider NHS, and say little about whistleblowing. However, there were accusations of a culture of bullying in the CQC and the DHSC. A headline in the Independent on 15 August 2012 was ‘Exclusive: NHS watchdog claimed that whistleblower Kay Sheldon was “mentally ill” ‘ (volume 2, p. 989). The tone of a letter from the chairperson of the CQC to all staff left little doubt as to the board’s view of Ms Sheldon’s decision to give evidence, and clearly implied that she was undermining the organisation. Looked at from the perspective of a CQC employee, it seemed unlikely that any member of staff reading this letter could be left reassured about the CQC’s approach to whistleblowing and, by implication, the response they would get should they ever wish publicly to raise concerns of their own (volume 3, p. 1470). The chairperson of CQC said that she liked to think that the issues at the trust would have been detected earlier by the CQC’s processes, with one reason being ‘the importance accorded to whistleblowers’. This may seem a little ironic given CQC’s reaction to its own whistleblower (volume 2, p. 1003).
Consultancy reports found ‘a shame and blame culture of fear’ in the the DHSC and the NHS (volume 2, p. 1282). Although the evidence before the inquiry did not justify a conclusion that there is in fact a culture within the department that could properly be described as one of bullying, it is possible to see how this could be interpreted further down the hierarchy as such (volume 2, p. 1347). Finally, a ‘whistleblowing’ e-mail to NPSA in 2004 from a senior staff nurse who may have been working at the trust appeared not to have produced any response (volume 2, p. 1193).
Factors
There appeared to be three main factors why whistleblowing was ineffective. First, Dr Singh felt inhibited in raising concerns directly because he felt that the trust had an atmosphere of not welcoming criticism, and that the consultants were completely disenfranchised. Dr Daggett told the inquiry that there were four or five consultants who tended to raise complaints, but they were seen as ‘naughty boys’ (pp. 238–9).
Second, there was a ‘culture of fear’. Dr Singh took ‘the path of least resistance’, stating that there were veiled threats that he should not ‘rock the boat’ at his stage in life because, for example, he needed discretionary points or to be put forward for clinical excellence awards. The inquiry states that his evidence highlights how easy it is for conscientious professionals to find reasons not to ‘rock the boat’ and the need for very robust support to enable and empower even senior consultants to raise important issues and to persist in doing so (p. 177). He told the inquiry that if he had persisted in raising concerns ‘I would have then ended up becoming either a stroke or a heart attack, and being on the road [i.e. out of a job, linked to ‘the excuse for destroying your career’] . . . I am brave . . . But I’m not Nelson Mandela . . .’ (p. 239). The inquiry stated that the impression given by this witness was of a professional who felt that he had done his best to raise issues, but when that failed to have any effect he became disillusioned and gave up, focusing on getting on with his job, in part for fear of the effect on his career of continuing to make a fuss. Dr Singh’s feelings in this regard were likely to have been influenced by his experience in March 2009 of having been suspended following an incident in which he complained to nursing staff about not being accompanied on a ward round (pp. 239–40).
Third, while the evidence supported what was heard during the first inquiry regarding the disengagement of doctors, it does not explain why no clinician (even among those who did raise matters internally) appears to have taken his or her concerns outside the trust to a regulator, the PCT or the SHA. Dr Daggett’s explanation was that at the time he had no understanding of the roles of these various bodies (p. 238) (although Dr Turner did contact the HCC).
Consequences for the whistleblower
Helene Donnelly told the inquiry that ‘People saying that they know where I live, and basically threats to sort of my physical safety were made, to the point where I had to at the end of a shift . . . at night would have to have either my mum or my dad or my husband come and collect me from work because I was too afraid to walk to my car in the dark on my own’ (p. 236). She felt that the atmosphere in the department continued to be poisonous, and left in 2008 (p. 111). The inquiry stated that such treatment was likely to deter others from following her example. Since she left the trust remaining colleagues told her they had felt deterred from raising concerns because of what happened to her. Her evidence exposed the hollowness of the promises in the whistleblowing policy. The experience of Helene Donnelly illustrated one reason why they may have been deterred from seeking to exploit the so-called protection available to whistleblowers (pp. 235–7). Helene Donnelly has since been awarded an OBE, and is Ambassador for Cultural Change at Staffordshire and Stoke-On-Trent Partnership NHS Trust.
In a letter of 2009, Robina Barry reported that the staff who had made the complaints that led to her investigation had been suspended pending the inquiry and were so traumatised that they had since left the trust to work elsewhere (pp. 65–6). The story of Dr Pradip Singh (his suspension was in 2009) ‘would have discouraged colleagues from getting involved’ (p. 176). However, it is fair to record that Dr Turner experienced no recriminations from within the trust since he communicated his concerns to the HCC. His promotion to consultant confirms that (p. 241).
Consequences for the NHS
The term ‘whistleblowing’ did not feature in the recommendations, which favoured cultural rather than legal remedies. The closest approximation was recommendation 12: reporting of incidents of concern relevant to patient safety, compliance with fundamental standards or some higher requirement of the employer needs to be not only encouraged but insisted on. Staff are entitled to receive feedback in relation to any report they make, including information about any action taken or reasons for not acting (p. 243).
Much was said at this inquiry about ‘whistleblowing’. The experiences described here do not suggest that, whatever system is in place, it would be easy for staff to raise concerns that are not accepted by those for whom they work. Theoretical protection is provided by PIDA, but this is unlikely to be of much reassurance to staff who have to face the wrath of their colleagues. Julie Bailey thought that nursing staff would be ‘petrified’ to come forward (p. 241). Ken Lownds of Cure the NHS made the point that, regardless of protective legislation and policies, it was the culture that mattered. Without a positive culture it would never be easy to raise concerns. Peter Walsh of Action against Medical Accidents made a similar point. They are correct: whistleblowing is necessary only because of the absence of systems and a culture accepted by all staff which positively welcomes internal reporting of concerns. If that culture is absent then raising concerns external to the system is bound to be a difficult and challenging matter exposing the whistleblower to pressure from colleagues. Therefore, the solution lies in creating the right culture, not in focusing on improvements to whistleblowing legislation, important though such protection is (p. 242). 182
Quotations in this section are reproduced from Francis. 157–159 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Responses
Secretary of State for Health
According to the Secretary of State for Health,166 Alan Milburn, the Kennedy report provided a powerful analysis of the flaws and failures of the organisation and culture, not only at the Bristol Royal Infirmary in the years in question, but of the wider NHS at that time. Kennedy acknowledged the progress that had been made in recent years, and the vision and initiatives of the NHS Plan325 had set clearly on the road that Kennedy described. However, Kennedy also provided a bigger ambition of building a new culture, of trust not blame, within the NHS, which is a challenge that the government accepted. It accepted most of the recommendations, with work underway to implement them.
The main document pointed to the establishment since 1997 of new independent standard setting and inspecting bodies: the CHI and NICE, as well as the National Patient Safety Agency (NPSA) and the NCAA to tackle poor clinical practice where it had been identified. It also pointed to national standards in place for the first time through National Service Frameworks, and help for NHS organisations to improve performance through the NHS Modernisation Agency. Finally, the NHS Plan325 sought to build on these developments to give a new direction to the health service (p. 2). The document pointed to the establishment of a new Council for the Quality of Healthcare and a new Council for the Regulation of Health Care Professionals (pp. 3–4). In other words, the organisational or institutional fix for the problems identified in Bristol had already been carried out.
It stated that ‘Bristol was a turning point in the history of the NHS’ (p. 13; © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). Kennedy set out a vision in which the patient should be at the heart of the NHS (p. 14). This included ‘responding to patients when things go wrong’, receiving an explanation and apology when things go wrong, with complaints being dealt with swiftly and thoroughly (p. 34). This was associated with Recommendations 33–36. In particular, the government agreed recommendation 33: a duty of candour, meaning a duty to tell a patient if adverse events have occurred, must be recognised as owed by all those working in the NHS to patients (p. 34). Recommendations 106–112 focused on a single national system of reporting adverse events. Recommendations 113–118 were concerned with the reporting of sentinel events. However, it rejected recommendations 45–46, that codes of professional conduct should be included in the contracts of employment for health professionals, as compliance with professional codes of conduct were therefore already implicit in employment contracts: ‘we do not believe that we need to go further’ (p. 106). The government agreed ‘in part’ with recommendation 91: managers as health-care professionals should be subject to the same obligations as other health-care professionals, including being subject to a regulatory body and professional code of practice. The government did not think it was practicable to establish self-regulation for senior managers. They agreed that the standards expected of senior NHS managers should be explicit, but favoured a code of conduct, stronger performance management and tighter contracts rather than regulation.
The Kennedy report found that the NHS was still failing to learn from things that go wrong and that the prevailing blame culture is a major barrier to openness and learning. The response states that ‘An Organisation with a Memory’172 ‘was a turning point’ (although two turning points in consecutive years seems a little excessive) as, for the first time in 50 years, attention was drawn to the scale of unintended harm to patients from potentially avoidable error in the health care system (p. 68).
Quotations in this section are © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Home Secretary and Secretary of State for Health
The preface to this report167 stated that ‘one of the questions that have been continuously debated in the years since Shipman was convicted is why did nobody in authority realise what was going on?’ (p. 3; © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). The government stressed the acknowledgement of the Shipman Inquiry that the NHS today is in many ways very different from the NHS in which Shipman practised. The priority now must be to ask how Shipman’s crimes could have gone undetected for so long and why a number of potential warning signals were ignored or overlooked (p. 5). It continued that the inquiry found that he did let his guard slip on a number of occasions, leaving clues that could and should have been picked up at an earlier stage (p. 7).
The response then focused on issues in the fifth report of the use of routine monitoring data and of responding to complaints and concerns. It noted that complaints from patients, and expressions of concern from fellow professionals, are potentially a rich source of information to help health-care organisations detect early signs of poor or malicious performance in health professionals. In Shipman’s time there were already avenues open to complaints from patients, and from 1987 onwards doctors had an explicit ethical duty to report any concerns about their colleagues, but these potential safeguards were ineffective for various reasons (p. 10).
The response agreed with most of the 190 recommendations of the Shipman Inquiry. In particular, it noted that it recommended a number of improvements both to encourage the raising of complaints and concerns and to ensure that primary care organisations took effective action on them. These key proposals included that PCTs should treat expressions of concern as seriously, and in the same way, as complaints; that health-care organisations (including general practices) should clarify the arrangements for raising concerns about fellow professionals; and that the statutory protection for whistleblowers should be strengthened. However, it did not consider that PIDA should be amended.
The response surveyed some of the changes that had already taken place in the NHS since Shipman’s day, concluding that ‘If the processes and attitudes described had been in place then, it is very likely that Shipman’s misdeeds would have been detected far earlier’167 (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). However, the government accepted that more needed to be done to embed these processes and, more importantly, to achieve the change in culture needed to instil a true patient focus throughout the NHS (p. 10).
The response stated that the crucial first step in any system for managing professional performance is the initial identification of cause for concern. In the case of Shipman, a number of potential clues were missed, and similar lessons emerged from the Ayling and Kerr/Haslam inquiries of failure to recognise the significance of concerns expressed, coupled – in Ayling’s case – with the failure of different NHS organisations to combine the information that they had (p. 22). To identify potential performance issues, clinical governance units in PCTs and specialist trusts needed to work with two different kinds of information: indicators of clinical processes and outcomes; and information derived from complaints from patients and carers, expressions of concern from fellow professionals, and information from other organisations that have employed the professional (p. 22). It continued that both the Shipman and the Ayling cases demonstrated that the safety of patients may depend on joining up pieces of ‘soft’ information that, individually, would not justify taking action. In addition, where, following a fair and thorough investigation, a complaint has been upheld and action taken – for instance, where this has led to formal disciplinary action or, for doctors, the issuing of a ‘recorded concern’ – this is information that could well be relevant to handling any further complaints or concerns (p. 22). Subject to consultation, the government proposed to ensure widespread dissemination of the arrangements to enable fellow professionals or members of the general public to raise concerns, including arrangements to cater for situations in which the person raising the complaint feels unable to go to their own management or organisation (pp. 23–4).
Secretary of State for Health
This response168 set out the action that the government proposed taking in response to four reports relating to the abuse of trust by health professionals – the Shipman Inquiry’s fifth report, and the reports of the Ayling, Neale and Kerr/Haslam inquiries. It was noted that although the nature of the abuse differed between the four reports, the underlying question was the same in each case: why did the NHS at the time fail to identify the risk and take the appropriate action to protect patients? (p. 5). Together the reports provided an account of complaints and concerns, the failure to join up information available in different organisations, and the failure to investigate serious allegations with an appropriate degree of rigour – as well some specific issues relating to recruitment processes, maintaining appropriate boundaries between professionals and their patients, and the need for particular precautions in relation to vulnerable patients such as those suffering from mental illness (p. 6). It stated that this document should be read in conjunction with the White Paper Trust, Assurance and Safety: The Regulation of Health Professionals in the 21st Century, which deals with similar issues from the perspective of professional regulation. Action arising from the two documents was to be carried forward as a single, integrated work programme (p. 7).
It noted that, between them, the reports contain a total of 228 recommendations (p. 8). The government agreed that complaints (from patients or their representatives) and concerns (from fellow professionals) can provide vital information in identifying potential risks to patient safety (p. 9). Many of the detailed recommendations in the Shipman Inquiry’s fifth report are either addressed directly in the White Paper or will fall to the regulators for the individual professions to take forward in the light of the general framework that it sets out (p. 14). The response claimed that clinical governance included learning from patients’ complaints and expressions of concern from professionals (p. 17), while promoting active learning from mistakes requires moving from a ‘blame culture’ to a ‘safety culture’ in which clinical staff are encouraged to report errors and near misses so that learning can take place (p. 20).
The response stated that complaints from patients and concerns from fellow professionals may be the first signals drawing attention to deficient care or abuse of patients (p. 43). It agreed with Shipman Inquiry recommendation 15, that concerns expressed about a GP by someone other than a patient or patient’s representative (e.g. by a fellow health-care professional) should be dealt with in the same way as patient complaints. Both the Shipman and the Ayling cases demonstrate how harm to patients could have been averted at a much earlier point if concerns of this kind had been taken seriously (p. 51).
It supported Shipman Inquiry recommendation 34, that every general practice should have a written policy about raising concerns. It also supported Shipman recommendation 39 and Kerr/Haslam recommendation 73 of a telephone helpline, and of a DHSC review of the effectiveness of whistleblowing policies and initiatives within NHS-funded organisations (although there does not appear to be any record of this initiative).
It stated that it fully agreed with the need to support and protect all those wishing, in good faith, to raise concerns about the actions of a health-care colleague. They should be invited in the first instance to share their concerns in confidence with local management and with their professional regulator, even though (as with patient complaints) it may subsequently be necessary for them to make specific allegations if their concerns are to be further investigated. While these principles may be particularly important in primary care – where staff may be working with little other support closely alongside the colleague whose performance or behaviour is giving cause for concern – it considered that they should apply to staff working in all health-care settings. It therefore proposed that all organisations providing services to the NHS should have a written policy setting out the procedures to be followed by staff wishing to raise concerns, and we discussed with stakeholders how this might best be achieved (p. 52). It continued that it would discuss with the professional regulatory bodies and universities how the current ethics guidance from the GMC and the other regulators of the duty of all health professionals to raise any concerns they have about the conduct, health or performance of a fellow professional, especially where this could put the safety of patients at risk, can be further emphasised. However, the government was not convinced by Shipman Inquiry recommendation 37 of considering amending PIDA as staff who disclosed concerns to the HCC are already protected by PIDA, as the Commission is now a ‘prescribed person’ as a result of the Health and Social Care (Community Health and Standards) Act 2003. 169 It proposed working with NHS organisations to draw up protocols under the Act that will provide further protection (e.g. for staff bringing concerns to the attention of the GMC). It supported Shipman Inquiry recommendation 38, that written policies setting out procedures for raising concerns in the health-care sector should be capable of being used in relation to persons who do not share a common employment (p. 53).
The government fully shared the Shipman Inquiry’s belief that information is the key to enabling NHS employers and PCTs to protect patients from unacceptable professional performance. The Ayling, Neale, Kerr and Haslam cases illustrated the same point: there were enough clues potentially available to indicate serious problems at a much earlier stage, yet the information was not ‘joined up’ and no effective action was taken. This partly reflected the then prevailing culture, in which it was almost unthinkable that health professionals would deliberately set out to harm their patients. Even more, however, it reflected the fact that NHS organisations did not have the systems and processes to ensure that the relevant information was brought together and critically scrutinised. It supported Shipman Inquiry recommendation 33, that PCTs should keep a separate file for each individual GP on their lists, and the Ayling recommendation of a formal declaration of any other concurrent employment, and of Kerr/Haslam of DHSC guidance as to how and where any disclosure or complaint of abuse by another health-care professional made to a doctor or nurse should be recorded in the patient’s medical records (p. 62).
House of Commons Health Committee
The House of Commons Health Committee170,171 considered that NHS remained largely unsupportive of whistleblowing, with many staff fearful about the consequences of going outside official channels to bring unsafe care to light. It recommended that the DHSC bring forward proposals on how to improve this situation. The key tasks of the government were to ensure that the NHS developed a culture of openness and ‘fair blame’; strengthened, clarified and promulgated its whistleblowing policy; and provided leadership that listens to and acts on staff suggestions for service changes to improve efficiency and quality and, by the provision of examples and incentives, encourages and enables staff to implement practical and proven improvements in patient safety (p. 7). It was noted that, since 2000, the DHSC has sought to move the NHS away from a ‘blame culture’ (p. 17).
The committee stated that an important measure of an organisation’s safety culture is how it treats ‘whistleblowing’, that is, the ‘spontaneous reporting outside normal channels by individual members of staff’ (p. 50; © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0)325 as a last resort in order to draw attention to unsafe care. It noted that ‘In one sense, ‘whistleblowing’ can be seen as evidence of a failure to learn—people are far more likely to pursue channels outside their own organisation if there has been a failure to act on or even acknowledge concerns raised internally. To many a perceived need for external whistleblowing is in itself a sign that organisational culture is seriously awry’ (p. 64; © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). 325 It continued that managers and boards in NHS bodies have a duty to heed whistleblowers and afford them protection from victimisation for raising genuine matters of concern. In theory, such protection exists under PIDA;8 it is reinforced in the NHS by executive guidance, issued in 1999, requiring appropriate local policies and procedures, and is also reiterated in the draft NHS Constitution. Yet, in practice, it seemed that many NHS staff fear the consequences of whistleblowing. (p. 89). However, the Secretary of State for Health, Alan Johnson, referred to ‘the mystery of Stafford being the absence of any whistleblower’ as he considered that adequate legal protection for whistleblowers existed. Whistleblowing is necessary due to the lack of systems and a culture that welcomes reporting of concerns. This means that the solution may require creating the correct culture rather than in changing whistleblowing legislation. 335 However, the committee stated that fear of victimisation may well have been a factor inhibiting staff at the trust from whistleblowing (p. 89). It pointed to evidence from the Royal College of Nursing arising from a survey of its members according to which:
-
78% of respondents said that they would be concerned about victimisation, personal reprisals or a negative effect on their career if they were to report concerns to their employers
-
21% had been discouraged from reporting, or told directly not to report, concerns at their workplace
-
64% did not feel confident that their employer would protect them if they spoke up
-
99% of registered nurses understood their professional responsibility to report worries about patient safety, but fears about personal reprisals meant that only 43% would be confident to report concerns without thinking twice
-
71% said that their employers had not taken immediate action to resolve the situation after concerns had been reported
-
35% said that no action was ever taken by employers after concerns had been reported
-
45% did not know if their employer had a whistleblowing policy.
The committee recommended that the DHSC bring forward proposals on how to improve whistleblowing, and that it give consideration to the model operated in New Zealand, where whistleblowers can complain to an independent statutory body. It recommend that Annex 1 of the Health Service Circular, HSC 1999/198, ‘The Public Interest Disclosure Act 1998 – Whistleblowing in the NHS’173 be recirculated to all trusts for dissemination to all their staff as a matter of urgency.
It was unconvinced of the case for a full public inquiry into Mid Staffordshire NHS Foundation Trust, given that the work that has already been done by the HCC, Professor Sir George Alberti and Dr David Colin-Thomé, and the likely further disruption to the trust. However, it saw merit in the idea, recommended to it by the RCN, of holding hearings in private to allow members of staff to give evidence confidentially to discover how the state of affairs had progressed so far without detection by the trust board.
In the second volume,171 the committee considered oral evidence from Dr Daggett and written evidence from Dr Pradip Singh from the Mid Staffordshire NHS Foundation Trust. The Shadow Secretary of State for Health, Andrew Lansley, raised the issue of whistleblowing: none of the reviews provided any answers on whistleblowing, and there were no mentions of the inadequacy of whistleblowing procedures, or questions raised about why staff inside Stafford Hospital did not feel that they could speak out and stop what was going on. He stated that he received evidence that potential whistleblowers at Stafford received intimidating rebuttals from the hospital’s legal team. It was vital to get to the bottom of this mystery through an investigation of whistleblowing procedures, and the manner in which staff who attempted to raise their concerns were treated.
Secretary of State for Health
The government174 stated that a toxic culture was allowed to develop unchecked that fostered the normalisation of cruelty and the victimisation of those brave enough to speak up. For far too long, warning signs were not seen, or were ignored or dismissed. Regulators, commissioners, the SHA, the professional bodies and the DHSC did not identify problems early enough, or, when the problems were clear, take swift action to tackle poor care (p. 5). It stated that it would listen to patients who raised concerns, respond to them and learn from them. It would listen to staff who were worried about the quality of care and praise them for speaking up, even if a concern was misplaced (p. 11). It intended to create the role of chief inspector of hospitals. Just as Ofsted (Office for Standards in Education, Children’s Services and Skills) acts as a credible, respected and independent arbiter of the best and the worst in schools, the chief inspector would shine a light on how hospitals were serving patients, becoming ‘the nation’s whistleblower’, naming poor care without fear or favour from politicians, institutional vested interests or through loyalty to the system rather than the patients that it served (p. 17). The response also pointed to Francis’ five key themes, under which the majority of his recommendations sit: values and standards; openness, transparency and candour; leadership; compassion and care; and information. The theme of ‘openness, transparency and candour’ included strengthening the protection and support available to whistleblowers, including a right to raise concerns within staff contracts; and the amendment of the NHS Constitution to include explicit rights and pledges on whistleblowing (p. 22). The government supported Francis’ recommendation that any ‘gagging clause’ that seeks to limit legitimate disclosure of problems with patient safety and care should be prohibited, stating that the era of gagging NHS staff from raising their real worries about patient care must come to an end. Staff who show the professionalism and personal courage to speak out in the public interest – which is difficult even in an open culture – must be celebrated and rewarded, even if, following investigation the concern turns out to be misplaced. It was stated that the government had already taken a series of steps to enhance the protections available to whistleblowers, including a right to raise concerns within staff contracts; amending the NHS Constitution to include explicit rights and pledges on whistleblowing; issuing new guidance to employers; and extending the national helpline to include staff in social care settings for the first time. In addition, the annual NSS asks staff if they are aware of how to raise a concern, if they feel safe to do so and if they believe that their organisation would take action on a concern. On 15 February 2013, the Secretary of State for Health wrote to all trusts reminding them again of their obligations to have (PIDA-compliant) whistleblowing policies and asking that they ‘check that the confidentiality clauses in your contracts (and compromise agreements with departing employees) do indeed embrace the spirit of [this] guidance’ (p. 47; © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). The government agreed an amendment to the Enterprise and Regulatory Reform Bill, securing PIDA protections for all NHS staff by adding other NHS contractual arrangements to the extended definition of ‘worker’ in section 43K of the ERA 1996. It recently welcomed proposals from the Department for Business, Innovation and Skills to introduce vicarious liability into employment law to provide even greater whistleblower protections, meaning that if staff who raise concerns about poor care are harassed by their colleagues, their employer is liable for this conduct (p. 49). However, the government rejected Francis’ recommendation for an independent authority to which staff could turn when their own organisation is not listening, but would work to ensure all organisations work together to learn from whistleblowers and make sure that action is taken when people raise concerns (p. 50). Finally, the DHSC established an independent review to consider the handling of concerns and complaints,179 which includes the handling of concerns raised by staff, including the support of whistleblowers (p. 52).
British Medical Association
The BMA175 stated that it would do all it could to work with others in developing a new culture in the NHS to prevent similar catastrophes from happening again. There had to be an urgent shift towards more openness, transparency and candour throughout the NHS that values learning from mistakes and that puts the patient at the centre of the health service. A shift in culture was needed to end the climate of fear, bullying and harassment that can stop clinicians from speaking out against poor care. However, the BMA did not believe that pursuing the recommendation in the report to move to a statutory duty of candour was the right way forward. There were already clear professional duties on doctors to raise and act on concerns about patient safety. A further ‘blunt’ instrument of legislation could create the wrong sort of culture change, encouraging defensive practice rather than a professional commitment to openness and partnership.
The report raised the responsibility on individuals and organisations to raise concerns about patient safety and poor standards of care. There were already very clear professional duties on doctors, outlined in the GMC’s guidance, Good Medical Practice,336 to be open and honest with patients if things go wrong and to raise and act on concerns about patient safety. The BMA believed that more could and must be done to promote and monitor these duties, while also removing any barriers to doctors fulfilling these obligations. The BMA welcomed the report’s findings that NHS organisations must do more to listen and act on the concerns of staff. Placing a corresponding duty on health-care providers ‘to listen’ could send a positive and reassuring sign to staff that they will be heard without fear of punitive action. However, the report stated that existing obligations on individuals to report concerns did not go far enough in enforcing the need for staff to disclose important information. The report made two key recommendations: a statutory obligation to observe a duty of candour, and the introduction of criminal sanctions against those obstructing the duty of candour. The BMA was concerned that moves to a statutory duty of candour may create a negative culture of fear, encouraging defensive practice rather than a professional commitment to openness and partnership. Moreover, the practical difficulties in enforcing a statutory duty of candour must also be considered. Rather, there was a need to address the underlying culture in the NHS, which can prevent doctors reporting concerns, and to look at alternative ways of ensuring that doctors feel able to report their fears, such as a separate reporting route parallel to management.
It would need to reflect on and consider the 290 recommendations in the report, and in particular those that deal with NHS culture, medical training, regulation, data and information very carefully, and would respond in detail to specific recommendations in due course.
Royal College of Nursing
The RCN176 revised and publicised its whistleblowing guidance for members and reviewed the way it supported them to raise concerns. It stated that the role of a chief inspector of hospitals could be an important step towards redressing the past imbalance between financial measures and quality, experience and care measures. Future work needed to focus on developing competence in and understanding of the continuum of information from informal satisfaction ratings, through structured gathering of experiential data, right up to the appropriate escalation of serious concerns via formal complaints and ‘whistle blowing’ (p. 22). It noted that the term ‘openness, transparency and candour’ in the Francis report17 was wide-ranging, and applied to everything from informal feedback from patients and their families up to and including whistleblowing (p. 23). It pointed to limited international evidence that, in situations where all staff have a legal duty to report poor care or unprofessional behaviour through the available reporting structures, a more open and transparent culture results, particularly around whistleblowing, and nursing staff tend to view whistleblowing as a high-risk, low-benefit action. Nurses blow the whistle as a last resort in their role as advocates for patients and promoters of patient safety. Descriptions of the experiences of nurse whistleblowers show that whistleblowing is a stigmatised activity carried out at considerable personal expense to the individual and with negative ramifications for the organisation (p. 26).
Nursing and Midwifery Council
The NMC177 did not explicitly mention whistleblowing. However, it pledged that it would undertake a planned review of the Code and other practice standards, including clear duties on nurses and midwives in relation to complaints handling, communication with patients and raising concerns, in the next year. It would ensure that these duties were highlighted in the revised Code, which would form the benchmark for appraisals and revalidation. It would also take more immediate steps to raise awareness of these duties and our guidance on raising concerns among nurses, midwives and the public (p. 12). The Code also placed a clear obligation on nurses and midwives to act without delay if they believed that they, a colleague or anyone else may be putting someone at risk (p. 13). At a recent listening event for a large group of stakeholders, there was some support for a statutory duty of candour but considerable concern about the consequences of introducing criminal sanctions (p. 14). It did not support the recommendation that the NMC should be tasked directly with investigating systems issues, as the boundaries of the distinct roles and responsibilities of professional and systems regulators should not be blurred (p. 24).
General Medical Council
The GMC178 stated that in 2012 it launched a confidential helpline for doctors concerned about patient safety, aimed at those who wanted advice and support about guidance or who felt they could raise a concern locally. It also produced an online tool to guide people through the process of raising concerns, and produced new guidance on raising and acting on concerns about patient safety, which the GMC sent to every doctor in the UK (p. 5). It considered that proactive steps needed to be taken to encourage openness on the part of trainees and to protect them from any adverse consequences in relation to raising concerns, and believed that some good progress has been made in this area, including through the inclusion of a patient safety question in the National Training Survey, the development of new guidance on raising concerns and the introduction of the new confidential helpline for doctors (pp. 6–7).
Clwyd and Hart
One of the inquiry’s179 terms of reference included the handling of concerns raised by staff, including the support of whistleblowers (p. 7). It noted that few organisations provided evidence on whistleblowing, although there was support from some for a Duty of Candour (p. 25).
Its recommendations focused on four areas for change: improving the quality of care; improving the way complaints are handled; ensuring independence in the complaints procedures; and whistleblowing (p. 32). It needed to be clearly stated how whistleblowers were to be protected, and gagging clauses should not be allowed in staff contracts (p. 34).
It noted that the question of whistleblowing was raised occasionally by both staff and patients during the review. It welcomed the Secretary of State’s decision to ban the practice of so-called ‘gagging’ clauses, as such clauses have in the past obliged clinical and other staff to be silent about practices that endanger patient safety. However, it was aware of repeated concerns about a number of unresolved questions surrounding this issue. These concerns related first to securing justice for past whistleblowers whose careers have been seriously jeopardised and who have suffered financially as a result of drawing attention to malpractice. It urged the DHSC to undertake the review of such cases with a view to both learning lessons for the future and undertaking restorative justice for those individuals affected. Second, there remained disquiet about the opportunities available for staff to be heard when they believe that there is bad practice both within hospitals and in the wider regulatory system. There was uncertainty, too, about what employment protection was genuinely to be offered to future whistleblowers who reveal their concerns externally to regulators, or the press and media, for example (p. 37).
It believed that much more needed to be done to avoid the need for whistleblowing in the future, and to protect those who, with justification, speak out, when there is no other means of drawing attention to situations in which patient safety is threatened (p. 38). Its recommendations included:
-
clear guidance for staff on how they should report concerns, including access to the chief executive on request
-
a board member with responsibility for whistleblowing should be accessible to staff on a regular basis
-
a legal obligation to consider concerns raised by staff, and to act on them if confirmed to be true
-
in assessing the complaints systems of hospitals, the CQC should investigate the ease with which staff can express concerns and how whistleblowing is responded to where it has taken place
-
the CQC itself should designate a board member with specific responsibility for whistleblowing, and ensure that it acts on intelligence received from whistleblowers.
It noted that although this was not the first report on complaints handling, and a great deal was known about what needs to be done, the challenge is to ensure the implementation of the recommendations so that they lead to real improvements for patients (p. 39).
Berwick
Berwick180 contained no explicit discussion of whistleblowing. However, it noted that in some instances, including in Mid Staffordshire NHS Foundation Trust, there were many clear warning signals that were not heeded, especially the voices of patients and carers (p. 4). It stated that the most important single change in the NHS in response to this report would be for it to become, more than ever before, a system devoted to continual learning and the improvement of patient care, top to bottom and end to end (p. 5). It produced 10 recommendations, including learning, transparency, and patient and carer voice, but nothing on whistleblowing. However, it noted that everyone, including staff, should be free to state openly their concerns about patient safety without reprisal, and that there was no place for compromise agreements (‘gagging clauses’) that prevent staff from discussing safety concerns (p. 10). Its main message was that ‘In the end, culture will trump rules, standards and control strategies every single time, and achieving a vastly safer NHS will depend far more on major cultural change than on a new regulatory regime’ (p. 11; quotations in this section are © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). All NHS staff should raise concerns to their colleagues and superiors and be welcomed in so doing. This vigilance could not come from regulation. It required culture change and therefore countless, consistent and repeated messages and deeds over a period of years. It meant living the values of the NHS Constitution. Goals and incentives should be clear, fully aligned and focused on the interests of patients, with a high level of coherence across the system as a whole. The best way to reduce harm was for the NHS to embrace wholeheartedly a culture of learning (p. 14). It needed to promote leadership behaviours that reduced risk and made health care more safe: expecting and insisting on transparency, welcoming warnings of problems; recognising that the most valuable information is about risks and things that have gone wrong; hearing the patient voice, at every level, even when that voice is a whisper; and seeking out and listen to colleagues and staff (p. 14). Everyone should ‘be a quality inspector’, never knowingly passing on a defect, error or risk to a colleague or patient, putting things right where possible, and reporting everything, especially where help is needed to put it right (p. 23).
Keogh
Similarly, Keogh181 contained nothing explicitly on whistleblowing. It stated that, during several of the reviews, staff came forward to tell the review teams about their concerns in confidence. These staff felt unable to share their anxieties about staffing levels and other issues with their senior managers, which suggested that staff engagement at some of the trusts was not good. All 14 trusts had recommendations in their action plans relating to workforce issues, with four trusts taking forward actions to improve whistleblowing policies (p. 22).
House of Commons Health Committee
The committee182 wanted to establish a culture that is comfortable with challenge, arguing that the responsibility for establishing a truly open managerial and professional culture, which would make the role of the whistleblower redundant, lies with each trust board.
The section ‘The Francis Report and whistleblowers’ focused on Helene Donnelly. It considered that, despite the existence of whistleblowing policies, no adequate support was given to Donnelly, who attempted to raise concerns about poor practice in the A&E department at Stafford General Hospital. Although her concerns were investigated, the way in which the investigation was conducted gave little encouragement to other potential whistleblowers to come forward. There was scant regard for the complainant’s anonymity, and no formal determination was made as to whether or not her allegations were accepted. She was provided with no adequate support, endured harassment from colleagues and eventually left the trust.
It considered that the Francis report11 described a culture in which medical professionals felt inhibited in raising concerns for a number of reasons: they considered that such concerns would not be acted on effectively, feared negative repercussions from colleagues or feared victimisation by management. A greater priority was instinctively given by managers to issues surrounding the behaviour of the complainant, rather than the implications for patient safety raised by the complaint.
In evidence to the committee, Robert Francis stated that it has been remarked that he had not made any recommendations specifically called ‘whistleblowers’. He considered that, whatever system was in place, it would not be easy for staff to raise concerns that are not accepted by those for whom they work. Although theoretical protection was provided by PIDA, this was unlikely to be of much reassurance to staff who had to face the wrath of their colleagues. He concluded that:
Whistleblowing is only necessary because of the absence of systems and a culture accepted by all staff which positively welcomes internal reporting of concerns. If that culture is absent then raising concerns external to the system is bound to be a difficult and challenging matter exposing the whistleblower to pressure from colleagues. Therefore the solution lies in creating the right culture, not in focusing on improvements to whistleblowing legislation, important though such protection is.
The committee observed that the government claimed, in its initial response to the Francis report, that it had already taken a number of steps to enhance protection available to whistleblowers. Contracts of NHS staff would include a right to raise concerns; the NHS Constitution was amended to include explicit rights and pledges on whistleblowing; fresh guidance on the subject was issued to employers; the national whistleblowing helpline was extended to include staff in social care settings; whistleblowing questions were included in the NSS; and an amendment to the Enterprise and Regulatory Reform Act 2013208 extended protection under the ERA 19967 (as amended by PIDA) to all categories of NHS staff. That Act also introduced a provision aimed at preventing the victimisation of whistleblowers by, in certain circumstances, extending to employers the liability for detriment caused to a whistleblowing employee by a colleague.
The committee considered that the government’s actions were welcome, as far as they went, but, as Francis suggested, a legislative solution focused on protecting whistleblowers was missing the point: whatever legislation there was about whistleblowers, so-called, it would not in itself stop the sorts of things that the Stafford whistleblowers had to experience from their colleagues in the ward. It may help at an employment tribunal later down the line, but it would not help at the time. What was required was to find a means of making it the normal thing to do to raise concerns about what was going on in the hospital and, if necessary, about colleagues.
The committee agreed with Francis’ recommendation of a change in the culture, whereby it would be easier, and more palatable, to raise a genuine concern than not to do so, although it recognised that there could be serious consequences for individuals who do raise their concerns. The management of each provider of NHS care had an unequivocal obligation to establish a culture in the organisation within which issues of genuine concern could be raised freely. Disciplinary procedures, professional standards hearings and employment tribunals were not appropriate forums for constructive airings of honestly held concerns about patient safety and care quality.
The committee agreed with Francis that providers of health and care, as well as their regulators, should be required to be open and transparent. Non-disparagement, or ‘gagging’, clauses, which inhibit the free discussion of issues of care quality and patient safety, were unlawful. No NHS body should be party to such an agreement or should seek to enforce an agreement in a way which inhibited the free discussion of such issues.
An Annex considered the case of Mr Gary Walker, the former chief executive of the United Lincolnshire Hospitals NHS Trust from October 2006 to February 2010, who was dismissed by the trust on grounds of gross misconduct and then lodged a claim for unfair dismissal with the employment tribunal. The case was settled outside the tribunal in October 2011, when Mr Walker and the trust entered into a compromise agreement to settle the claim. Mr Walker stated to the committee that in entering into this compromise agreement he had been ‘gagged’ by ULHT. In questioning, Andrew George MP noted that ‘culture of fear’, arguing that although there may be a duty of candour, that candour can be career limiting. David Bowles (former chairperson of United Lincolnshire Hospitals NHS Trust) mentioned the 2009 NHS Confederation report, which talked about a climate of fear, intimidation and bullying, while the 2008 reports (IHI) talked about the public humiliation of CEOs as being the main improvement tool.
Dalton and Williams
The report183 stated that, put simply, candour means the quality of being open and honest (p. 2). Its first recommendation stated that a duty of candour required a culture of candour, and, over the long term, it encouraged the government to consider how it could ensure that the legal system was most able to support such a culture (p. 4). The report stated that it had ‘many parallels’ with Berwick,180 and wanted to build on his recommendations and reaffirm that a culture of openness and honesty required a full commitment from our health and care organisations to create and maintain effective systems of learning and improvement (p. 6). It continued that leadership was vital. A consistent and visible commitment to support and learning rather than blame and punishment from the leaders of health and care organisations and from regulators is likely to lead to a far greater willingness from staff to act in a candid manner when something goes wrong (p. 14). However, even in a culture of greater candour, effective whistleblowing and complaints systems would continue to be vital parts of an open and transparent culture that is committed to improvements in safety and quality (pp. 14–15). The report continued that fulfilling the duty of candour should be statutory rather than discretionary or voluntary. 183 Its hope was that organisations respond to this signal wholeheartedly, and make a reality of candour for themselves and the people they serve, and that they do this not simply because the law is changing, but because they see the value of it for the people who use their services. Bare compliance and vague endorsement would not be sufficient: a determination to really tackle the challenges would be required (p. 19).
Department of Health and Social Care
The document275 stated that the introduction of a statutory duty of candour would be a major step towards implementing a key recommendation from the Francis inquiry (p. 6). It noted that Berwick also recommended that, for serious incidents, CQC regulations should require that the patient or carer affected by a safety incident is notified and supported. However, it did not subscribe to an ‘automatic’ duty of candour, whereby patients are told about every error or near miss, as this would lead to defensive documentation and large bureaucratic overheads that detract from patient care (p. 8).
Secretary of State for Health and Social Care
The Secretary of State for Health and Social Care184,185 made clear that so-called ‘gagging orders’ were unacceptable. NHS staff would be able to raise concerns about patient care in the knowledge that they would be listened to and their views would be welcomed. The new chief inspector of hospitals would judge whether the culture of the organisation actively promoted the benefits of openness and transparency; and staff could now blow the whistle to their health and care professional regulatory bodies. All health-care professionals would be protected by the provisions of PIDA. Compromise agreements had to include an explicit clause that made clear that nothing within the agreement prevented disclosure under the Act. NHS England was to develop a Friends and Family Test for staff, and the ‘Cultural Barometer’ was piloted and evaluated before a further roll-out (p. 16). Complaints and concerns from patient groups and whistleblowers could trigger regulatory action under Monitor’s new Risk Assessment Framework, introduced in October 2013 (p. 34).
It was vital for whistleblowing to be taken seriously: in legislation, inspection and education and training. The Enterprise and Regulatory Reform Act 2013208 strengthened the position of whistleblowers so that an individual now had the right to expect their employer to take reasonable steps to prevent them suffering detriment from a co-worker as a result of blowing the whistle. The CQC was using staff surveys and the whistleblowing concerns it receives as part of the data in its new intelligent monitoring system to guide it about which hospitals to inspect. Since September 2013, the CQC’s new inspection system included discussions with hospitals about how they deal with whistleblowers (p. 48). The Care Bill stated that, as a registration requirement with the CQC, providers must be open with patients about care failings. ‘The duty should drive an open culture throughout organisations, including its staff, so we do not believe an individual obstruction offence is necessary at this time. In addition to candour at the organisational level, it was vital to ensure that individuals live up to their professional obligations to be candid’184 (p. 48) (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0).
It argued that many of the measures set out in this response were designed to ensure that the NHS was a genuinely open and transparent culture, a culture that would make whistleblowing far less necessary than at present. There would always, however, be a need to ensure that staff who have concerns are able to raise them. NHS staff should feel free and able to raise their real concerns about patient care, and the era of gagging staff must come to an end. The government has acted to ensure that this becomes a reality by:
-
extending to all health-care professionals the protections of PIDA by the Enterprise and Regulatory Reform Act, which received Royal Assent in April 2013
-
giving the new chief inspector of hospitals an important role in ensuring that hospital inspections are not just seen as a ‘tick-box’ exercise by judging whether or not the culture of the organisation actively promotes the benefits of openness and transparency
-
enabling staff to blow the whistle to health and care professional regulatory bodies as of 1 October 2013
-
backing the Whistleblowing Helpline’s refresh of the Speak Up for Healthy NHS guidance, as recommended in its ‘Bridge the Gap’ campaign report of July 2013. 184
The government also acted on compromise agreements, updating guidance in March 2013 to make clear that where a compromise agreement is used it must include an explicit clause stating that nothing within the agreement prevents an individual from making a protected disclosure under PIDA. NHS Employers provided guidance in 2013 suggesting some model confidentiality clauses and model wording for the explicit clause now required in NHS compromise agreements.
The second volume185 provided a detailed response to each of the 290 recommendations made by the inquiry across every level of the system. It made clear which recommendations were accepted and by whom, and what progress was being made towards their implementation. The DHSC was to lead the system in providing an annual report on progress across the system each autumn (p. 4), and the Health Select Committee confirmed that it agreed with the inquiry’s recommendation that it should monitor the implementation of all of its recommendations.
The government accepted recommendation 2 on a shared culture; accepted in principle recommendation 7, that all NHS staff should be required to enter into an express commitment to abide by the NHS values and the Constitution, both of which should be incorporated into the contracts of employment; and accepted recommendation 12, that the reporting of incidents of concern relevant to patient safety needs to insisted on. It accepted in principle recommendation 98, that reporting to the National Reporting and Learning System of all significant adverse incidents should be mandatory on the part of trusts. It accepted most of the recommendations on openness, transparency and candour, but accepted in principle recommendation 178 on a incorporating the NHS Constitution into contracts of employed, and recommendation 181 on a statutory obligation to observe a duty of candour on health-care providers, and on registered medical practitioners and registered nurses and other registered professionals. However, it did not accept recommendation 183 for it to be a criminal offence for any registered medical practitioner, nurse, allied health professional or director of an authorised or registered health-care organisation to make untruthful statements, although it agreed ‘with the intention behind this recommendation’.
Secretary of State for Health
The foreword186 by Jeremy Hunt states that ‘Almost the first thing I did when I was appointed as Health Secretary was to read Sir Robert Francis QC’s initial report on the scandal at Mid Staffordshire NHS Foundation Trust. I was profoundly shocked by what I read’ (p. 3). However, he continued that:
a lot has changed since then. While there is much to celebrate, there is no reason for complacency. Changing culture takes time, and we have only just started on the journey. We have also raised our ambition – not only to prevent a repeat of the events at Mid Staffordshire, but also to become the first healthcare system in the world that truly embraces the standards of safety common in the airline, nuclear and oil industries. That means creating a learning culture in which doctors, nurses and front-line staff always feel able to speak out if they have concerns about safety or care. One of the four pillars of our response is to get the culture right: more accountability for patients, more transparency over outcomes and a commitment to put patients in the driving seat for any decisions taken about them.
p. 4. 186
One of the more shocking aspects of the events at Mid Staffordshire NHS Foundation Trust was the way in which a whole system failed to notice what was happening at the hospital for such an extended period of time (p. 10). The CQC was regarded as ‘the nation’s whistleblower’, with the independence and expertise to speak up when services are poor, and to quickly identify failure (p. 12). The document used data from the NSS to show that the percentage of staff who spoke positively about the quality and openness of their work and organisation, and who responded that ‘The care of patients/service users is my Trust’s top priority’ and ‘When errors, near misses or incidents are reported, my Trust takes action to ensure that they do not happen again’, had broadly increased since 2010. So when NHS staff speak up, it is critical that the system listens with humility and responds with conviction. Since the publication of the public Inquiry report, and with a new willingness at the centre of the health and care system to hear the reality of failings, the voice of a substantial group of NHS people who have spoken up and suffered as a result has become all the more insistent. Although since 2010 the government had put in place a range of new measures to strengthen the voice of people who speak up for patients, known as ‘whistleblowers’, there was still a strong sense that the NHS had yet to turn the cultural corner and face up consistently and with humility to the hard truths spoken by its staff (p. 16).
The government stated that the online supporting annex to this document set out in detail the substantial progress made against the 290 recommendations of the public inquiry. However, although this is important, ‘perhaps the most important point is that the ongoing need to change the culture in the NHS to one of patient-centred, continual improvement in care and safety’ (p. 17). It noted that the CQC and its chief inspectors would report annually to the Secretary of State for Health with their assessment of how well the NHS was doing in taking forward the recommendations on both the public inquiry and the Freedom to Speak Up review (p. 20).
It was claimed that ‘since the publication of the Public Inquiry report the landscape of policy and legislation to ensure safe, effective, respectful and compassionate care has been transformed’. The inspection regime has been overhauled, and a programme of robust, expert, thorough and independent inspection has now been rolled out across health and social care services in England. New sanctions, fundamental standards, and tighter and tougher accountability have brought a harder edge to the assurance of good care. The beginning of a revolution in transparency about quality of care is brought the power of open access to comparative data to bear on the priorities and consciousness of those who govern and lead in health and social care (p. 30).
It continued that, although these changes were necessary, they were insufficient on their own to secure the consistency of experience and reliability of care that patients should be able to take for granted, and that staff are striving to provide. The remaining critical component was culture. Since the publication of the public Inquiry report, the NHS had undoubtedly made progress in strengthening its culture, but a great deal more remained to be done. In an organisation as large and as complex as the NHS, no matter how strong the professional instinct to do the right thing, and no matter how powerful the impulse to care, there were inevitably times when it might feel easier to conceal mistakes, to deny that things had gone wrong and to slide into postures of institutional defensiveness. So it was vital that leaders were alert to the risks and actively work to promote the culture of openness, learning, and professional and institutional humility, which is the absolute bedrock of safe care. The most important resource available to the NHS was its staff, and one of the key lessons of the public inquiry, but also of the work of the Keogh Review and of the new, rigorous inspections undertaken by the CQC, was the importance of listening to staff (p. 30).
There were, of course, always situations when the ‘normal channels’ were not effective or appropriate, and an individual feels obliged to ‘blow the whistle’. Whistleblowing played an important role in raising issues and holding organisations to account across many sectors of life, such as the aviation and off-shore oil industries, as well as the NHS. Although there were some areas of good practice in the NHS, all too often staff raising concerns felt that they were not taken seriously, and those who blew the whistle could feel isolated and undermined (p. 31). The government was determined that the NHS should be the safest and most transparent health-care system in the world. To achieve this, individuals must feel safe to raise the alarm about matters which are in the public interest and be confident that action will be taken when concerns are raised (p. 31). The public inquiry exposed a toxic and intimidating management culture, which deterred staff from raising concerns. When concerns were raised in good faith, they were ignored, and staff were vilified for speaking up. There was an instinct to deny rather than to learn, to defend rather than to improve (p. 31). The government introduced a number of measures to make it easier for those working within the NHS to raise concerns. These included:
-
issuing unequivocal guidance to NHS organisations that all their contracts of employment should cover staff whistleblowing rights
-
the publication of new guidance by the whistleblowing helpline in March 2014
-
adding the health and social care regulatory bodies, NHS Trust Development Authority and auditors of foundation trusts to the Prescribed Persons list, increasing the number of organisations to which staff can blow the whistle
-
applying the concept of vicarious liability to the whistleblowing legislative framework, which means that when there is any bullying or harassment of a whistleblower by a fellow worker, this is treated as being done by the employer
-
the Secretary of State writing, in March 2014, to all chairpersons in NHS trusts and foundation trusts in England to reiterate the importance of fostering a culture of openness and transparency in the NHS, in which concerns about care can be raised, investigated and acted on (p. 31).
The Secretary of State for Health commissioned Francis to carry out the independent Freedom to Speak Up review to provide independent advice and recommendations on creating a more open and honest reporting culture in the NHS. The review was asked to identify measures to help to foster a culture of reporting and in future better protect people who do speak out about patient safety, as well as learning lessons from the existing culture in the NHS by listening to those who have experiences to share, both positive and negative. The aim was to learn from other areas where safety is vital – such as aviation, nuclear power and the oil industry – about how to foster a culture in which it is simply the norm to flag up problems, risks and mistakes as they occur and in which everyone – from the CEO to the cleaners – does the right thing without hesitation and without fear of comeback. The review2 is being published alongside this report,186 and the Secretary of State for Health will set out the government’s response (p. 32).
Quotations in this section are reproduced from Culture Change in the NHS186 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Francis
In his letter to Secretary of State, Francis2 stated that:
[P]art of the progress since the Public Inquiry is an increasing recognition of the contribution staff can make to patient care through speaking up. However you identified a continuing problem with regard to the treatment of staff who raise genuine concerns about safety and other matters of public interest, and the handling of those concerns. You asked me to conduct an independent review and to make recommendations for improvement in this area. A listening system is a safer system. Organisations which ignore staff concerns, or worse, victimise those who express them are likely to be dangerous places for their patients . . . I would have liked to report to you that there was in fact no problem with the treatment of ‘whistleblowers’ and their concerns. Unfortunately this is far from the case. This is a ‘serious issue’ that requires ‘urgent attention’. There was near unanimity among staff, managers, regulators and leaders who assisted the Review that action needs to be taken. In our trust survey, over 30% of those who raised a concern felt unsafe afterwards. Of those who had not raised a concern, 18% expressed a lack of trust in the system as a reason, and 15% blamed fear of victimisation. This is unacceptable. Each time someone is deterred from speaking up, an opportunity to improve patient safety is missed.
pp. 4–5. 2
The effect of the experiences has in some cases been truly shocking. We heard all too frequently of jobs being lost, but also of serious psychological damage, even to the extent of suicidal depression. In some, sad, cases, it is clear that the toll of continual battles has been to consume lives and cause dedicated people to behave out of character. Just as patients whose complaints are ignored can become mistrustful of all, even those trying to help them, staff who have been badly treated can become isolated, and disadvantaged in their ability to obtain appropriate alternative employment. In short, lives can be ruined by poor handling of staff who have raised concerns (p. 5). There is a need for a culture in which concerns raised by staff are taken seriously, investigated and addressed by appropriate corrective measures. Above all, behaviour by anyone which is designed to bully staff into silence, or to subject them to retribution for speaking up must not be tolerated. The measures recommended in this report are largely about doing better what should already be done. They build on the progress made in implementing the culture change started following the earlier report. Francis set out 20 Principles which he believed should guide the development of a consistent approach to raising concerns throughout the NHS, while leaving scope for flexibility for organisations to adapt them to their own circumstances. The overarching Principle is that every organisation needs to foster a culture of safety and learning in which all staff feel safe to raise a concern.
p. 6. 2
In the executive summary, Francis pointed to ‘a remarkable consistency in the pattern of reactions described by staff who told of bad experiences’2 (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). Whistleblowers provided convincing evidence that they had raised serious concerns that not only were rejected but were met with a response that focused on disciplinary action against them rather than any effective attempt to address the issue they raised. It was concluded that there was a culture within many parts of the NHS that deterred staff from raising serious and sensitive concerns and that, not infrequently, has negative consequences for those who raise them (p. 8).
He argued that the legal and policy framework surrounding whistleblowing is not easy to understand and has many layers. The legislation which theoretically provides protection for whistleblowers is contained in the ERA 1996, as amended by PIDA. Where a worker makes a protected disclosure, he/she has a right not to be subjected to any detriment by his employer for making that disclosure. However, for a number of reasons this legislation was limited in its effectiveness. At best the legislation provided a series of remedies after detriment, including loss of employment, has been suffered. The legislation was limited in its applicability, and does nothing to remove the confusion that exists around the term ‘whistleblowing’, which does not appear in it at all. In recent years there has been a range of measures which may encourage, or impose a responsibility on staff to speak up. These include introduction of a new Statutory Duty of Candour, the Fit and Proper Person Test and (CQC’s new inspection and ratings regime (pp. 9–10).
He defined a whistleblower, in the context of the NHS, as:
a person who raises concerns in the public interest. For the purpose of concerns relating to the NHS, and in particular patient safety concerns, the term ‘whistleblower’ is used in this report to apply to those who speak up when they see something wrong usually relating to patient safety but also to the integrity of the system.
p. 221. 2
Francis stated that over 600 individuals and 43 organisations wrote in response to the review‘s invitation to contribute and over 19,500 responded to the staff surveys sent out by independent researchers. He continued that they met with over 300 people through meetings, workshops and seminars, held four seminars in different parts of the country with a cross section of invited delegates to consider different stages of the process of raising concerns and potential solutions, and commissioned independent qualitative and quantitative research (p. 10).
It was suggested that some may not be comfortable seeking advice from a Freedom to Speak Up guardian if, for example, they are from a different professional background. There should therefore be a range of others to whom people can go for advice and support. This should include at least one executive director, which may be the person responsible for safety and/or the medical director; at least one nominated manager in each department; and one external organisation, such as the Whistleblowing Helpline (p. 16).
It was the responsibility of boards to ensure that there is no victimisation of or retaliation against whistleblowers, and they should be held to account for it (p. 18). The review highlighted the lack of any co-ordination between the various regulators in their approach to whistleblowing (p. 19). The legislation applied to all employers, not only those in the NHS, so it would not be appropriate to make recommendations for amendment which might have an impact on other sectors in ways that I am not aware of. However I am particularly concerned by one aspect of the legislation, which is that it does nothing to protect people who are seeking employment from discrimination on the grounds that they are known to be a whistleblower. This is an important omission which should be reviewed, at least in respect of the NHS. I invite the Government to review the legislation to extend protection to include discrimination by employers in the NHS, if not more widely, either under the Employment Rights Act 1996 or under the Equality Act 2010 (p. 22).
The review included two recommendations, 20 principles and 38 actions (p. 22).
The main reports opened with the words of the statement of Dame Janet Smith in the fifth report on the Shipman Inquiry:154 ‘I believe that the willingness of one healthcare professional to take responsibility for raising concerns about the conduct, performance or health of another could make a greater potential contribution to patient safety than any other single factor’ (© Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0). Francis added that this statement still rang true. Staff who raise concerns about any issues of patient safety can, and do, save lives. When a NHS worker speaks up, they are making a vital contribution to the quality and safety of patient care (p. 30). Francis reported that in recent years there had been a number of reviews that considered whistleblowing or related issues in the NHS and other sectors (e.g. Francis;11,155,156,159 National Audit Office;187,188 PCAW;162 Department for Business, Innovation and Skills189), while other relevant reviews include Berwick,180 Clwyd and Hart179 and Dalton and Williams. 183
Francis considered that each of these reports considered measures that contributed to an open and honest culture, including organisational transparency and leadership. There were also a number of reviews that took place in parallel to this review, the findings and recommendations of which were likely to be relevant to the issues considered in this report, including the Assurance Report by Kate Lampard CBE on the Jimmy Savile Investigations; Lord Rose’s review of NHS leadership; the GMC’s review of whistleblowing by Sir Anthony Hooper; and the Health Select Committee’s Inquiry on complaints and raising concerns,245 which was published after completion of the Francis report (p. 34).
Francis stated that the Enterprise and Regulatory Reform Act 2013 introduced significant changes to the 1996 Act. In particular, it introduced vicarious liability for the bullying or harassment of whistleblowers (p. 40). He also discussed the NHS Constitution, the statutory duty of candour, and the Fit and Proper Persons Test. He continued that there was a risk that such a plethora of information, advice and guidance, and the various ways it could be obtained, might be confusing for NHS workers who have concerns. They might not know where to go for the best advice or whether, having spoken to any particular organisation, they still need to report their concerns elsewhere; or whether even speaking to that organisation affected their rights under the 1996 Act. There was also the risk of conflicting advice, including different definitions of the term ‘whistleblowing’ (p. 43).
Francis also pointed to the complexity of the current position. The quantity of activity in the fields of legislation, policy and guidance indicated a continuing institutional recognition that more needed to be done to support the freedom of staff to speak up, and concern that the measures already in place were insufficient. He felt that this had resulted in a somewhat piecemeal and reactive approach to this issue and, moreover, that the law seeking to protect whistleblowers was cast entirely in an employment context (p. 49).
Unsurprisingly, given the nature of this review, positive experiences of whistleblowing were a small minority. They were generally attributed to working in an organisation with a culture of openness, having a good knowledge of whistleblowing policies and procedures, feeling supported during the process and maintaining good working relationships with colleagues (p. 53).
The hostile culture was likely to have been reinforced by the negative language often used in reference to speaking up. Contributors described how those who raised a concern, whether internally or externally, were often seen as ‘troublemakers’ or ‘backstabbers’. Some suggested that different words should be used, such as ‘raising concerns champion’. At the seminars conducted as part of the background to the Francis Report, there was widespread confusion about the meaning of the term ‘whistleblowing’ and its relationship to a protected disclosure, but there was agreement that the term had negative connotations. It was stressed that people who raise concerns did not always think of themselves as whistleblowers, and some contributors wanted the words whistleblower and whistleblowing changed (p. 57). Although the majority of staff were aware of their local whistleblowing policies and procedures, a significant minority were not (p. 58).
From the evidence, the following themes emerged: the need for culture change; improved handling of cases; measures to support good practice; particular measures for vulnerable groups; and the extension if legal protection (p. 88):
Only if the good intentions of any law are matched by a change in culture can a safe alternative to silence be created.
Dehn and Calland, p. 94337
There was near-universal agreement that the most important factor affecting people’s willingness to speak up or raise concerns was the culture of the organisation (p. 94).
Francis considered whether the term ‘whistleblowing’ itself contributed to the barriers. He saw three problems. First, there is confusion about what qualifies as whistleblowing. Some people consider whistleblowing to be concerned with criminal wrongdoing such as fraud rather than relating to a patient safety concern. Some consider it applied when escalating a concern outside the normal management chain, or about a more senior colleague. Some believe that it only applied to raising a concern outside the organisation, or even that it was limited to disclosure to the media or otherwise into the public domain. Second, the complexity of the legislation and confusion among contributors about what constitutes a ‘protected disclosure’ was unhelpful. Third, the term had negative connotations (p. 100).
He gave serious consideration to recommending that the term ‘whistleblower’ should be dropped. Although he still had reservations about the term, he was persuaded that it was so widely used, and in so many different contexts, that this would probably not succeed. Instead, he felt that the focus should be on giving the term a more positive image, believing that the measures recommended in the report would do much to promote the acceptance of ‘whistleblowing’ as normal and positive behaviour in health care (p. 100).
He concluded that, although the existing legislation is weak, he did not recommend a wholesale review of the 1996 ERA for two reasons:
First, he did not think that legislative change could be implemented quickly enough to make a difference to those working in the NHS today. What is needed is a change in the culture and mindset of the NHS so that concerns are welcomed and handled correctly. If this can be achieved, fewer staff will need recourse to the law. Second, this Review is concerned only with the position of disclosures made within one part of the public sector, the NHS. The Act covers all forms of employment, whether in the public or private sectors. There may well be different considerations in other fields.
However, he did consider that there were two steps that should be taken. First, extending the list of prescribed persons to ensure that NHS workers are protected if they raise a concern with any relevant person/body. There are some surprising omissions from this list: most notably clinical commissioning groups and NHS England, as commissioners of services, are not included. A wide variety of bodies responsible for training are not included and among scrutiny bodies neither Healthwatch England nor local Healthwatch, unless by implication from the fact the former is a subcommittee of CQC, are included.
Second, he proposed extending statutory protection to all students studying for a career in health care rather than just student nurses. The government’s response to its ‘Whistleblowing Framework Call to Evidence’ indicates that it might consider extending the scope to ‘other student arrangements similar to student nurses’. In his view, there is a compelling case for taking this step. In addition, he stated that consideration needed to be given to extending discrimination law to protect those who make a protected disclosure from discrimination either in the ERA 1996 or the Equality Act 2010 or to finding an alternative means to avoid discrimination on these grounds.
Francis concluded that it was clear that the concerns that had led to the setting-up of the review were justified. What was needed was not radical, but rather a careful and committed application of the principles of a culture of safety and learning. His report set out 20 principles that:
when implemented together with the measures already being progressed following my previous report into the failings at Mid Staffordshire, will, I believe, go a long way to reduce the number of upsetting cases and deliver the open and honest culture that staff in the NHS need. Each principle was accompanied by recommended actions.
p. 197. 2
Recommendation 1: All organisations which provide NHS healthcare and regulators should implement the Principles and Actions set out in this report in line with the good practice described in this report.
Recommendation 2: The Secretary of State for Health should review at least annually the progress made in the implementation of these Principles and Actions and the performance of the NHS in handling concerns and the treatment of those who raise them, and report to Parliament.
p. 197. 2
Finally, Annex B set out actions by organisation.
Hooper
This was an independent review192 for the GMC of how it engaged with individuals who regarded themselves as whistleblowers. Whistleblowing was defined as ‘the raising of a concern, either within the workplace or externally, about a danger, risk, malpractice or wrongdoing which affects others’ (p. 1). The report presented the definition from Francis2 of ‘a person who raises concerns in the public interest’. Hooper192 added that:
It is sometimes said that a whistleblower is a person who raises concerns externally, that is, with persons other than his or her employer. This is not right. Many persons who raise concerns do not necessarily, at the time of raising the concerns, see themselves as whistleblowers. They may, at that time, be ignorant of the protections afforded to persons who raise such concerns. They are likely to come to regard themselves as whistleblowers if they suffer detriment as a result of raising the concerns or if no action is taken on their concerns.
p. 2. 192 Reproduced with permission
Hooper cited Dame Janet Smith154 in the fifth Shipman report:
I believe that the willingness of one healthcare professional to take responsibility for raising concerns about the conduct, performance or health of another could make a greater potential contribution to patient safety than any other single factor.
p. 2. 154 © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0
It was stated that the GMC recognised the vital importance of raising concerns. He discussed paragraphs 24 and 25 of Good Medical Practice,336 which state that:
You must promote and encourage a culture that allows all staff to raise concerns openly and safely. You must take prompt action if you think that patient safety, dignity or comfort is or may be seriously compromised.
Failure to comply with paragraphs 24 or 25 may amount to ‘misconduct’ and a finding that a doctor’s fitness to practise is impaired. Good Medical Practice states in paragraph 6 that: ‘Serious or persistent failure to follow this guidance will put your registration at risk’ (p. 3; reproduced with permission). 336
According to the chief executive of the GMC, Niall Dickson:
We know that many front line staff can feel under enormous pressures and that the culture of the institutions in which they work is vital in creating the conditions for openness and honesty – not a blame culture but a learning culture. And that means everyone in the healthcare team feeling able to raise concerns. The feedback we have received suggests there is some way to go in this – some doctors are not confident they would be supported if they raised a concern, while others need to know where to take their concerns. The awful reality that emerged from Mid Staffs and indeed other inquiries was that doctors knew about our guidance but were not empowered by it. They felt it was acceptable to ‘walk by the other side of the ward’ knowing that there was unsafe and unacceptable practice going on. We must all do what we can to make sure that does not happen again. The joint statement we have signed, is an important milestone and makes it clear that the professional duty of candour sits with every healthcare professional, regardless of their field of practice.
p. 4. © GMC. 336 Reproduced with permission
There was considerable evidence that, in the workplace, persons who raise concerns about a danger, risk, malpractice or wrongdoing that affects others may well suffer, or believe that they will suffer, reprisals at the hands of an employer or fellow workers (p. 5). Hooper stated that reprisals may take many forms. The effect of the reprisals on individuals at work and at home is likely to be devastating. Doctors who have devoted their lives to the care of others face the prospect of their careers being brought to an end. One of the consequences may be that the doctor against whom the retaliatory measures are being taken becomes clinically depressed. Their depression may then be used as justification for further action against them. It was self-evident that the fear of suffering reprisals acted as a powerful disincentive to raising concerns, as did also a belief that the concern will be ignored. The attainment of the objective of patient safety therefore required that the risk of reprisals was reduced or eliminated, and that concerns were not ignored (p. 6). Hooper was concerned that employers may use the process of making an allegation to the GMC about a doctor’s fitness to practise as an act of retaliation against a doctor because they have raised concerns or, simply, as an inappropriate alternative to dealing with the matter in house. If that happened, the GMC would unwittingly become the instrument of the employer in its campaign against the doctor (p. 7).
The evidence from ‘Patients First’174 to the Francis review11 offered support for the proposition that some employers use referral to punish healthcare professionals who raise concerns, which has been termed ‘retaliation by referral’ (p. 8). Hooper therefore made a total of eight recommendations to reduce these, including declaring if the doctor being referred has raised concerns about patient safety or the integrity of the system, and fully training investigators to understand ‘whistleblowing’, particularly in the context of the GMC and the NHS; and a simple, confidential and voluntary online system to record concerns, run by an organisation independent of the regulators. In December 2012, when the GMC launched a helpline, Mr Dickson said:
The eyes and ears of health professionals are often the most valuable means of protecting patients and ensuring high quality care.
p. 20192 Reproduced with permission
Except where otherwise stated, quotations in this section are © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
House of Commons Health Committee
The Committee193 stated that:
Just as we expect the NHS to respond in a timely, honest and open manner to patients or families raising complaints or concerns, we should expect the same for staff. The treatment of whistleblowers remains a stain on the reputation of the NHS and has led to unwarranted and inexcusable pain for a number of individuals. The treatment of those whistleblowers has not only caused them direct harm but has also undermined the willingness of others to come forward and this has ongoing implications for patient safety. Although the committee was clear that professionals have a duty to put patients first and to come forward with their concerns, it recommended that those who had suffered harm as a result of doing so and whose actions were proven to have been vindicated should be identified and receive an apology and practical redress.
pp. 3–4. 193
The CEO of the GMC, Mr Dickson, freely acknowledged that there were instances in which a trust could seek to use a referral as retaliation against a registrant raising legitimate concerns about practices in the trust, and stated that ‘there is history around this of individuals who are classic whistleblowers’ (p. 32).
The government argued that whistleblowers are protected from detriment by PIDA, but evidence from PCAW and others argued that PIDA was a deterrent rather than a remedy, and that if an employee had to have recourse to PIDA’s provisions then his or her prospects were already substantially impaired (p. 35). The committee had stated previously that employment tribunals and related fora were no place for honestly held concerns about patient safety and similar issues to be debated. 182 A means had to be found for health and care service workers to be able to speak up safely about professional concerns (p. 35).
The committee’s position had long been that there was an unambiguous professional duty on professional registrants to speak up, but that equally that there was a similar duty on employers to establish an open culture that encouraged concerns to be raised and acted to address and resolve them, rather than punishing the person raising them (p. 35).
The Francis review was welcome:
As the treatment of whistleblowers is a stain on the reputation of the NHS and has led to unwarranted, inexcusable pain for the courageous individuals affected. The aim for an NHS complaints and raising concerns system must be to establish a reporting culture in the health and care sector which parallels the open reporting culture on other safety-critical sectors such as aviation and nuclear energy: one in which the concept of the whistleblower is quite simply redundant.
p. 36. 193
The failure to deal appropriately with the consequences of cases where staff have sought protection as whistleblowers had caused people to suffer detriment such as losing their job and, in some cases, being unable to find similar employment. This undermined trust in the system’s ability to treat whistleblowers with fairness. This lack of confidence about the consequences of raising concerns was seen to have implications for patient safety (p. 36).
The committee expected the NHS to respond in a timely, honest and open manner to patients, and the same had to be expected for staff. It recommended that there should be a programme to identify whistleblowers who have suffered serious harm and whose actions were proven to have been vindicated, and provide them with an apology and practical redress (p. 36).
House of Commons Public Administration Select Committee
The government329 accepted Francis’ recommendation that trusts should appoint a person to receive concerns and offer advice, to ensure that cases are properly investigated and issues are addressed without repercussions for the person who raised an issue: Freedom to Speak Up guardians. The Secretary of State for Health and Social Care explained that these people would be ‘part of the organisation but just there, so that, if you do not want to tell your line manager, you have someone else you can talk to in the Trust’. There was also to be, he explained, a national Freedom to Speak Up guardian, ‘so there is someone outside the hospital if you ultimately needed it’ (p. 6; © Parliamentary Copyright. Contains Parliamentary information licensed under the Open Parliament Licence v3.0. www.parliament.uk/site-information/copyright-parliament/open-parliament-licence/).
South West Whistleblowers Health Action Group told the committee that:
[T]he department was ‘currently part of the problem’: In 2000 the Department of Health published ‘An organisation with a memory’. The fact that the Committee is carrying out an inquiry into complaints and clinical failure nearly 15 years after this report was produced is a testament to the failure of the Department of Health and Governments since 2000 to drive forward improvements.
p. 12. 329
The committee stated that the Department for Transport’s Air Accidents Investigation Branch came up frequently in the evidence, and much of the commentary was very positive (p. 34). The Secretary of State for Health explained how things work in air accident investigation: every single death is investigated by the Air Accidents Investigation Branch, and every single death is avoidable. In that industry, as in the nuclear industry and the oil industry, the presumption is zero deaths, and so, when there is a death, it immediately triggers a process. The Secretary of State for Health told the committee that the ‘processes that we are trying to create have been modelled on those in the airline industry, which are designed to make it incredibly easy for pilots to speak up’329 (© Parliamentary Copyright. Contains Parliamentary information licensed under the Open Parliament Licence v3.0. www.parliament.uk/site-information/copyright-parliament/open-parliament-licence/).
The Secretary of State told the committee that he and Mike Durkin of NHS England put together a report containing data on ‘whether trusts have an open and honest reporting culture’, which showed that around 20% of trusts did not have this. Mr Hunt said that there should ultimately be no need for whistleblowers, because ‘we should have a culture where people want to find out that things have gone wrong and why they have gone wrong, and to learn from them. You only have whistleblowers when you have a system which is not doing that’ (p. 37)329 (© Parliamentary Copyright. Contains Parliamentary information licensed under the Open Parliament Licence v3.0. www.parliament.uk/site-information/copyright-parliament/open-parliament-licence/).
The committee welcomed the proposal for Freedom to Speak Up guardians recently accepted by the government, but in order for them to be effective, the information given to guardians had to be protected from disclosure, so that information could not be used to publish or penalise those making whistleblowing reports to guardians; that would require legislation (p. 50). It also welcomed the decision of the Secretary of State for Health to invite Mike Durkin to look at the possibility of setting up a new independent patient safety investigation body to conduct clinical investigations. This would not solve all of the problems identified, but was an essential step. It was struck by the fact that no public inquiry into an aviation accident had taken place since the 1970s, for which just such a body exists in the form of the Air Accidents Investigation Branch. The present situation in the NHS, where investigations of clinical incidents and complaints were tangled together and often prove hard for the patient and their family to navigate, needed to be replaced by a more rational and easy-to-understand system. The committee therefore concluded there was a need for a new, permanent, simplified, functioning, trusted system for swift and effective local clinical incident investigation conducted by trained staff, so that facts and evidence could be established early, without the need to find blame, and regardless of whether a complaint had been raised. This would greatly reduce or remove the need for costly major inquiries into clinical failure (p. 50).
Some quotations in this section are © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
Secretary of State for Health
This was a response194 to the Freedom to Speak Up consultation associated with Francis,2 the Public Administration Select Committee329 report Investigating Clinical Incidents in the NHS, and the Morecambe Bay Investigation. 338
It was stated that the evidence amassed by Francis2 detailed the price paid by far too many NHS staff who spoke up with concerns about the quality of care. Those who should have listened to those concerns – and acted on them- responded instead in many cases with evasiveness and hostility (p. 4). The response continued that a lot was asked of the people who worked in the NHS, but they should never be put in a position where they had to choose between telling the truth and keeping their job. Francis heard troubling accounts of whistleblowers who struggled to find alternative employment after raising their concerns. In line with his recommendation, the response agreed that NHS England, Monitor and the NHS Trust Development Authority should devise a support scheme to help whistleblowers who can demonstrate that they were having difficulty finding employment as a result of raising concerns to find alternative employment. Furthermore, a regulation-making power was enacted to prohibit discrimination by prospective NHS employers against a job applicant on the grounds that the applicant appeared to have made a protected disclosure. Regulations to implement this prohibition were to be made (p. 11).
The DHSC accepted Francis’2 two overarching recommendations, and consulted on a package of measures to implement them (p. 15). The consultation showed that most responses supported the role of the Freedom to Speak Up guardian, while the majority of these supported the INO role hosted by CQC (p. 18). The government proposed that:
-
the CQC should consult in summer 2015 on how the INO role would be implemented, taking into account principle 15 and its associated actions in the Freedom to Speak Up report
-
the INO should be appointed by the CQC by December 2015. Once in place the INO was to produce guidance on local implementation of the Freedom to Speak Up guardian role and how this role would develop
-
Health Education England should produce guidance on the training that would be needed for the Freedom to Speak Up guardian role
-
the department would share the responses to this consultation with the relevant organisations and the INO to help inform the guidance they will develop.
Local NHS organisations were expected to take forward the actions in an effective, proportionate and affordable manner (p. 21). The document considered whether the Freedom to Speak Up guardian should report to the board of the organisation that appointed them, or directly to the INO. It favoured Francis’11 recommendation that the Freedom to Speak Up guardian should be appointed by the chief executive of the organisation to act in a genuinely independent capacity, and should raise concerns with the trust’s chief executive or the board. However, the government recommended that the Freedom to Speak Up guardian be able to raise concerns with the INO if they had lost confidence, or if they considered that good practice had not been followed, in how the organisation was handling concerns (p. 28).
Professional codes are guidance on behaviour and how to deal with particular situations such as communication with patients, delegation, seeking consent, treating people with dignity, and what to do if a professional has witnessed something about which they have concerns. The response stated that Professor Sir Bruce Keogh was currently considering the professional codes, including how they covered the issue of raising concerns, and was to report back shortly (p. 36).
The Freedom To Speak Up report proposed legislative change in principle 20 concerning legal protection. Since the publication of the report, a regulation making power was added to the Small Business, Enterprise and Employment Act 2015222 to prohibit discrimination against whistleblowers (or applicants believed by the prospective employer to have been whistleblowers) when they apply for jobs with prescribed NHS employers (p. 36). The Act also introduced a regulation-making power to impose a duty on prescribed persons (such as the CQC, Monitor and the professional regulatory bodies) to report annually on whistleblowing disclosures made to them. Going forward, taking account of the Freedom To Speak Up report’s proposal, it was intend that further organisations would be added to the Prescribed Persons Order (p. 36).
The government also considered the PASC329 report. It accepted the recommendation of the committee to create a new independent patient safety investigation body to conduct investigations in the NHS: the Independent Patient Safety Investigation Service (p. 39). The committee had considered that information given to the Freedom to Speak Up guardians must be protected from disclosure, which requires legislation. However, the government claimed that the committee was mistaken: as Freedom to Speak Up guardians would be employees of their organisations, existing legislation would apply to them. When a whistleblower makes a protected disclosure to a Freedom to Speak Up guardian who is also an employee of the whistleblower’s employer, they would potentially be making a protected disclosure to their employer under existing legislation. Therefore, the whistleblower has a statutory right not be subjected to any detriment by their employer and there is no intention to make new or amend existing legislation (p. 50).
The government expected all NHS organisations to have in place whistleblowing policies that were compliant with the ERA 1996, as amended by the PIDA, and with best practice. In addition, it supported a free helpline, run by Mencap, that provides independent and confidential advice to staff in the NHS and social care who want to raise a concern but are unsure how to do so or what protections they have in law if they do so. The whistleblowing helpline also gives employers advice on best practice in implementing whistleblowing policies that are compliant with the Employment Rights Act 1996 (p. 50). 192 It noted that, in March 2014, revised NHS and Social Care Whistleblowing Guidance was published, aimed at staff and employers (www.wbhelpline.org.uk/resources/raising-concerns-at-work/) (p. 50).
Finally, the government responded to the Kirkup338 report on Morecambe Bay. Kirkup produced four recommendations on openness and transparency (recommendations 24–27). The government accepted recommendation 24 on a duty of candour. Similarly, it accepted recommendation 26 by accepting in principle the recommendations of Francis: ‘We commend the introduction of a clear national policy on whistleblowing. As well as protecting the interests of whistleblowers, we recommend that this is implemented in such a way that ensures that systematic and proportionate response is made by Trusts to concerns identified. Action: The Department of Health’ (pp. 76–7).
Quotations in this section are © Crown copyright. Contains public sector information licensed under the Open Government Licence v3.0.
List of abbreviations
- A&E
- accident and emergency
- BMA
- British Medical Association
- CEO
- chief executive officer
- CHI
- Commission for Health Improvement
- CMO
- Chief Medical Officer
- CQC
- Care Quality Commission
- DHSC
- Department of Health and Social Care
- ECHR
- European Convention on Human Rights
- ERA
- Employment Rights Act
- ERRA
- Enterprise Regulatory Reform Act
- GMC
- General Medical Council
- GP
- general practitioner
- HCC
- Healthcare Commission
- HR
- Human Resources
- INO
- independent national officer
- MP
- Member of Parliament
- NCAA
- National Clinical Assessment Authority
- NCAS
- National Clinical Assessment Service
- NICE
- National Institute for Health and Care Excellence
- NMC
- Nursing and Midwifery Council
- NPSA
- National Patient Safety Agency
- NSS
- NHS Staff Survey
- PALS
- Patient Advice and Liaison Service
- PCAW
- Public Concern at Work
- PCS
- paediatric cardiac surgery
- PCT
- primary care trust
- PIDA
- Public Interest Disclosure Act 1998
- POP
- perception of organisational politics
- RCN
- Royal College of Nursing
- SHA
- Strategic Health Authority