Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/130/33. The contractual start date was in April 2014. The final report began editorial review in February 2017 and was accepted for publication in September 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Matt Sutton serves on the Health Services and Delivery Research (HSDR) Commissioning Board (commissioned and researcher led). Mark Hann has a role with the National Institute for Health Research (NIHR) Research Design Service. Rachel Meacock serves as an associate member of the HSDR Commissioning Board (commissioned and researcher led). Mark Sidaway and John Ainsworth report grants from the NIHR and the Medical Research Council (MRC) during the conduct of the study. Ruth Boaden is Director of the NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRC) Greater Manchester, which is hosted by Salford Royal NHS Foundation Trust, one of the organisations that comprise the Salford Integrated Care Programme (SICP), the subject of the research in this report. In addition, Ruth Boaden holds an honorary (unpaid) contract at Salford Royal NHS Foundation Trust as an Associate Director; however, her CLAHRC role does not involve any relationship with the SICP/integrated care organisation. Ruth Boaden is also a member of the NIHR HSDR Commissioning Board (commissioned and researcher led). Both Iain Buchan and Siobhan Reilly have received grants from MRC. Katherine Checkland reports grant income from the NIHR Policy Research Programme.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Bower et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Long-term conditions and integrated care
The burden of disease worldwide is shifting to long-term conditions. 1,2 Although advances have been made in effective service delivery, major challenges remain, namely projected increases in populations aged ≥ 65 years, the increases in demand associated with an ageing population and government pressure for major efficiency savings.
Current services are organised around single conditions, but many people have more than one (multimorbidity), which means that care is often fragmented and unresponsive to needs. Patient and policy consultation around care for long-term conditions has repeatedly emphasised the need for ‘integration’. 3–5
What is integrated care?
There is a significant body of literature on integration, but a lack of consensus around definition; one review found 175 definitions. 6 A number of different perspectives are possible on the meaning of integration, including managerial, health systems, social science and patient perspectives. 7 The British Medical Association8 has highlighted that integration is a nebulous term, associated with wide-ranging definitions and processes. Analysts have distinguished between different dimensions of integration:9
-
Types of integration – functional (key support and functions, i.e. human resources and financial management), organisational (contracting or strategic alliances between different organisations), professional (joint working, alliance and strategic contracting between professionals) and clinical (co-ordination of patient care services).
-
Breadth of integration – this includes both vertical (bringing together organisations at different hierarchical levels) and horizontal (bringing together organisations that are on the same working level) integration.
-
Degree of integration – full integration or more limited collaboration of services, working practices or organisations.
-
Process of integration – this includes structural (alignments of tasks, functions and activities), cultural (values, norms and working practices) and social (the strengthening of social relationships between individuals) integration.
Models of implementing integration are also diverse. Health and social care systems are complex, with multiple providers and different levels of demand on the system, and so integration is likely to be equally variable. 9 A review referred to three different models of integration:6
-
System level – the focus here is on organisational change, whereby leadership plays a pivotal role in performance.
-
Programme or service level – the emphasis here is to try to improve the patient outcomes by providing more co-ordinated care.
-
Progressive/sequential models – integration is not a specific goal but is a means to try to improve health-care performance in general.
Some partners have adopted a person-centred definition of integrated care, focusing on the ways in which care is experienced by patients. 5 This definition is supported by a number of ‘I statements’, which set out what integrated care should feel like to those in receipt of it. It is suggested that delivering care in this way will fulfil a number of goals (e.g. people feeling more confident to manage their conditions, improved sharing of decisions and relationships, and better sharing of information with the patient and among different services), which will in turn lead to improved outcomes (such as fewer admissions and, crucially, lower costs). However, it has been suggested that a person-centred model of integration might be better achieved through policy innovations such as personal health budgets and direct payments (allowing individuals to join up services in ways that make sense to them), rather than organisational and professional integration. 10 Such a conception has been supported by recent qualitative work within integrated care pilots (ICPs). 11
What is the review evidence for the benefits for ‘integrated care’?
There have been a variety of reviews and syntheses around the effectiveness and cost-effectiveness of integrated care. A ‘stocktake’ of the integrated care literature in 2009 found discussions to be dominated by potential benefits, with a lack of clarity over definitions and standardised outcomes. 6 Although the scope of the literature has improved since that time, there is still a lack of clarity over the main findings in this area.
A metareview12 (or ‘review of reviews’) that included 27 separate reviews explored integrated care for adults across a range of long-term conditions. The authors coded 10 key principles of integration and reported a range of positive outcomes across the reviews, including in relation to hospital admissions (in heart failure and diabetes mellitus), adherence to guidelines [diabetes mellitus, chronic obstructive pulmonary disease (COPD) and asthma] and quality of life (diabetes mellitus). Reductions in costs were far less frequently reported. Another review13 of integrated delivery systems found 25 reports, with the majority showing an increase in quality of care associated with integration. Again, there was more limited evidence showing reductions in utilisation associated with integration. A recent ‘review of reviews’14 on integrated care for chronic diseases synthesised data from 50 reviews, which included a wide range of interventions (e.g. case management, variants of the chronic care model,15 multidisciplinary teams and self-management). As with other reviews, there was evidence of positive impacts in many outcomes, but results were not consistent, and the authors again highlighted the gap between the importance of the concept of integration in health policy and the strength of the evidence concerning its benefits.
Although comprehensive, these very broad reviews necessarily include a very wide range of patients and interventions and, therefore, can lack precision. Other reviews in the literature have had a more restricted scope in terms of interventions, populations and outcomes, providing greater specificity over outcomes. A review of integration at the primary–secondary care interface found 10 studies that demonstrated some benefits in terms of process of care (care delivery, disease control), but these generally did not extend to clinical outcomes and were achieved at some increase in costs. 16 A review of co-ordinated and integrated care for the frail elderly found nine studies, with a slim majority reporting improved outcomes and reduced health-care utilisation, but with few data on the effects on caregivers. 17
Case management is a popular method of integration, and a review18 of case management for older people found that the majority of trials showed no reduction in admission rates compared with usual care. A review19 of case management for at-risk patients in primary care reported 36 studies, but the only consistent benefits were in terms of patient satisfaction, with no demonstrable benefit in utilisation, costs or mortality. In contrast, a review20 of hospital-initiated case management for heart failure reported reductions in readmissions and length of stay, although those benefits did not translate to reduced costs. Interventions initiated from the community were less prevalent and showed less evidence of benefit.
A number of previous reviews have suggested that the economic benefits of integrated care are less consistently demonstrated than impacts on the process or quality of care. A review21 restricted to the economic impacts of integrated care identified 19 studies of relevance. As well as identifying a lack of clarity about definitions, the evidence was mixed, with some positive findings; generally, however, the evidence was characterised as ‘weak’. A review22 focused on integrating funding for health and social care found 38 studies. Health outcomes were frequently assessed, but evidence of benefits were limited and only a minority of studies found reduced secondary care costs.
The evidence is clearly mixed. 23 There is a significant amount of evidence, such that a number of studies have used a metareview method, which is an efficient instrument for summarising large numbers of data, but not a very precise method of quantifying gain or assessing patterns in the data, or identifying fruitful approaches to integration. Interpreting the reviews is a challenge because of the complexity of the concept of integrated care and the different scope of the reviews, which is clearly demonstrated in the different numbers of studies included in each review. However, the overall impression is that benefits are inconsistent and most regularly associated with process measures (e.g. quality of care). When impacts on admissions are reported, they are most likely to be related to certain conditions (such as heart failure), rather than demonstrated across broader groups of long-term conditions. Reductions in utilisation may not translate to reduced costs, which may reflect the fact that integrated care is associated with its own costs; benefits of reduced utilisation in one part of the system may be lost when other costs are taken into account. 24 Cost savings may require radical changes such as closing hospital beds,25 which may be unpopular and difficult to implement. 23
Recent empirical evaluations in the UK
The previous section has outlined reviews of the effects of integrated care and highlighted the inconsistency in the evidence. The reviews have been international in scope. Although that brings major benefits in terms of the size and scope of the evidence, it does lead to additional complications in interpretation. Integrated care may have different meanings in different health systems, and the comparator conditions may also vary widely. It is generally accepted that context is an important moderator of the effects of complex interventions,26–28 and the context in which integrated care is introduced may also be very different. 25 This section has a focus on empirical evaluations conducted in the UK.
The Evercare evaluation29 explored the case management of older people at high risk of emergency hospital admission. Although not a formal integrated care intervention, it shares a number of features in terms of the eligible population and the nature of the intervention. Evaluation showed no effects on admissions or other outcomes, although the service was popular with patients and carers. 30
The Partnerships for Older People Projects involved a wide range of community- and hospital-facing services, with a significant focus on prevention. Evaluation using data from the British Household Panel Survey suggested some improvements in quality of life, although the comparator was not particularly strong in methodological terms. Although overall analyses31 suggested that the investment led to savings, more detailed analyses32 of a subgroup of services found no evidence of reductions in hospital admissions, and even suggested some increases.
An early pilot scheme in England33 involved the establishment of 16 ICPs. It should be noted that although these were all introduced into a single health-care system, the pilots did vary, being based on local circumstances in which the care included in the ‘integration’ project was dependent on the local context. Overall, the evaluation found that there was an increase in emergency admissions in the pilot areas and there was mixed evidence about whether or not the ICPs were able to reduce costs. Among the 16 ICPs, case management was perceived to be the best option for reducing secondary care costs (a net reduction in combined inpatient and outpatient costs were reported). Such comparisons lack the rigour of randomisation. The findings were also difficult to interpret as the key outcomes that the services were trying to change (emergency admissions) showed increases in activity, whereas reductions occurred in untargeted elective services. Assessments of patients were also conducted as part of the evaluation of the ICPs. Patients reported that they were more likely to be told that they had a care plan, to feel clear about follow-up arrangements and to know whom to contact, and were less likely to report problems with medication. All of these are relevant outcomes of an integrated care initiative. However, somewhat surprisingly, they also reported being less likely to see the health professional of their choice, being less involved in decisions about their care and being less likely to report that their preferences had been taken into account. Again, all these are relevant outcomes for a person-centred integrated care service. The fact that patients reported reductions in some patient experience measures and improvements in others highlights the difficulties of improving outcomes in this area. 33
The North West London Integrated Care Pilot was a large-scale programme that had an initial focus on people with diabetes mellitus and patients aged > 75 years. The intervention involved information technology to support case finding and multidisciplinary groups (MDGs) to deliver care planning. Although implementation was generally successful (albeit somewhat delayed) and there were some impacts on process of care (including rates of care planning), a matched controls analysis of effects showed no impact on emergency admissions, although the analysis was judged to be preliminary. 34,35
There was also a call for ‘ambitious and visionary’ local areas to become integrated care pioneers, with 14 sites starting in one wave in 2013 and another 11 sites starting in a second wave in 2015. 36 Pioneers were tasked with the conventional outcomes of integration initiatives (improved patient experience, outcomes and financial efficiency), with expert support and some very limited additional funding. Early results from the pioneers (largely on the basis of interviews and self-reports from stakeholders) found a common focus on a particular cohort (older, multimorbid or frail patients) and a wide range of potential interventions (including interventions focused on those in need, as well as longer-term prevention work).
Early evaluation has identified a number of barriers to and facilitators of progress, leading to slow progress and a reining in of ambitions concerning any rapid demonstration of improved outcomes. Patient experience was judged to be the area in which initial gains were most likely to be made. The authors of the report into the pioneers highlighted the ‘integration paradox’, whereby financial and other service pressures both increase the pressure for integration (to manage those pressures) and act as a barrier to its effective implementation. 37
In some ways, the evidence from the UK studies is less positive than the international literature. Although some positive impacts have been observed, these have been matched by some negative findings (including increases in admissions and reductions in some aspects of patient experience). It is not clear why this should be. The UK has a fairly strong primary care system with which patients are generally highly satisfied. 38 It is possible that changes that lead to disruption in existing arrangements can cause difficulties for patients, even if the intention is to improve integration.
Summary
Integration remains a cornerstone of current health policy, but evidence concerning the benefits of integration, optimal methods of achieving it and the factors that influence success is still limited. The identification of models of integration in the UK that are feasible, sustainable and cost-effective remains a priority.
In that context, the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme advertised a call for ‘ambitious research studies assessing the cost-effectiveness of new and innovative models of care or clinical pathways for people with long term conditions. The aim is to generate high-impact research which will provide commissioners and providers with useful evidence when re-designing services’. 39
The Salford Integrated Care Programme (SICP) was judged to be ‘a new and innovative model of care . . . for people with long term conditions’. 39 The aims of the SICP were to improve integration of care to provide better health and social care outcomes, improved experience for services users and carers, and reduced health and social care costs.
The broad aims of Comprehensive Longitudinal Assessment of Salford Integrated Care (CLASSIC) were to assess the clinical effectiveness and cost-effectiveness of the SICP, with the following research questions.
Implementation
-
How do key stakeholders (commissioners, strategic partners) view the SICP, what do they expect from it and how is it aligned with their objectives and incentives?
-
What is the process of implementation of two key aspects of the SICP [the MDGs and the integrated contact centre (ICC)]?
Outcomes
-
What is the impact of the MDGs on the outcomes and costs of people with long-term conditions?
-
What is the impact of health coaching in the ICC on the outcomes and costs of people with long-term conditions?
Chapter 2 Salford Integrated Care Programme: an overview
Context
The setting was Salford in the north-west of England. At the time of CLASSIC, the population of Salford was 234,916 (of whom 34,000 were aged ≥ 65 years). There are comparatively high levels of deprivation (Salford is one of the 20 local authorities with the highest proportion of areas in the most deprived decile) and illness (22.8% living with a long-term illness, compared with a national rate of 17.9%) (SICP unpublished internal briefing document).
The health and social care system in Salford is largely coterminous, with one local government partner (Salford City Council), a single health commissioner [Salford Clinical Commissioning Group (CCG)], a mental health provider (Greater Manchester West) and a provider of acute and community services (Salford Royal Foundation Trust). Salford contains 52 general practices in eight neighbourhoods.
Salford Integrated Care Programme
The SICP is a large transformational project designed to achieve integration between health and social care to achieve the ‘triple aim’: delivering better health and social care outcomes, improving the experience of service users and carers, and reducing costs.
There is strong history of local integrated working. In 2007, Salford introduced Salford’s Health Investment For Tomorrow programme, a ‘whole economy’ approach to care pathway redesign and the transfer of care from secondary care into community and primary care.
In 2011, Salford Royal Foundation Trust was approached by the Advancing Quality Alliance (AQuA, a quality improvement organisation) and asked to participate in an integrated care programme along with the Salford CCG and Salford City Council (SICP unpublished internal briefing document). With time, a working group developed a case for change and from May 2012 formal governance was established for the SICP. The initial plan was for three programmes:
-
the promotion of local community assets to support increased independence
-
the establishment of an ICC to provide navigation and support
-
the formation of MDGs supporting older people at most risk.
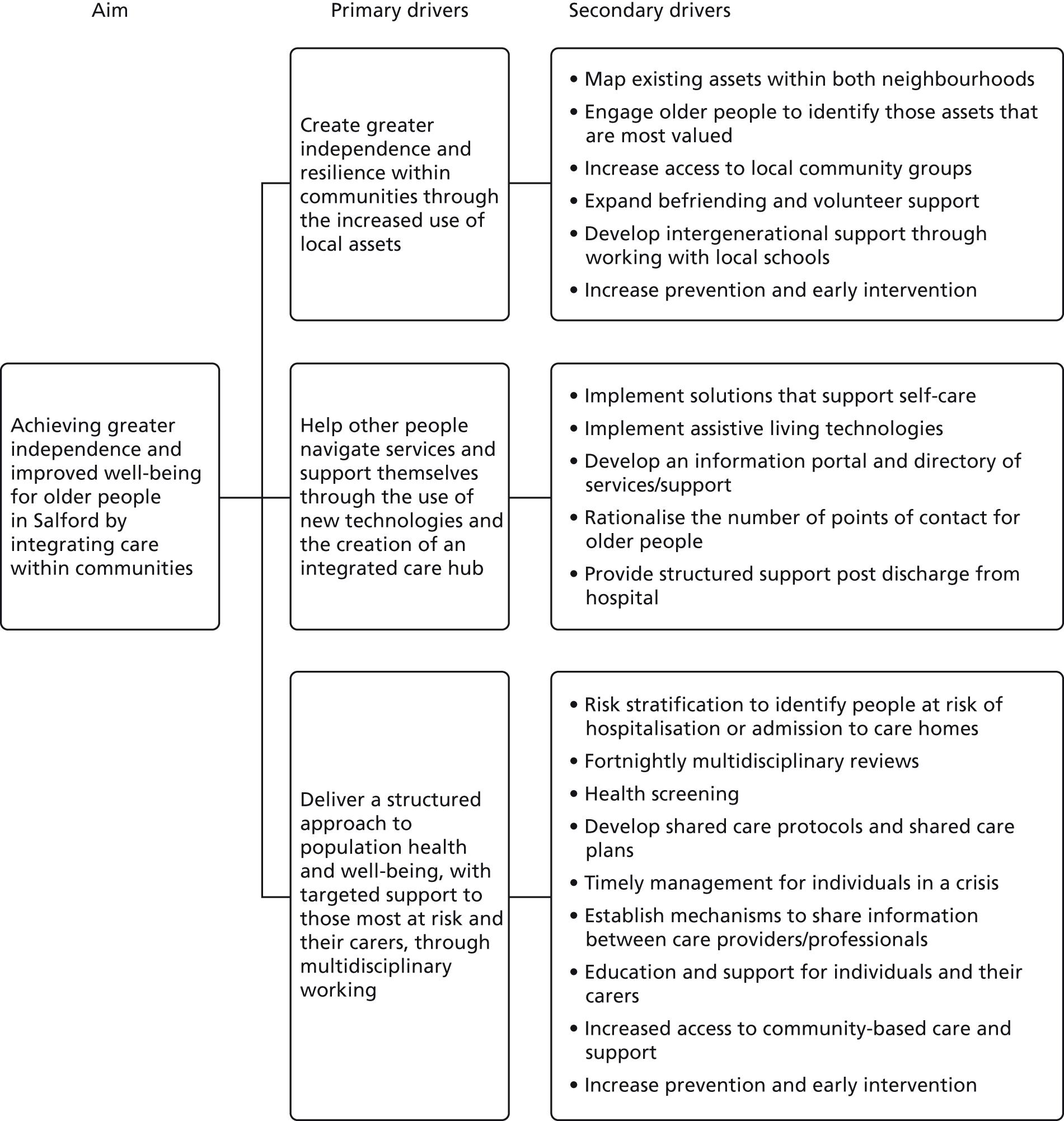
The SICP model and operational plan (Figure 1) outlines aims and ‘primary’ and ‘secondary’ drivers. There are seven improvement measures for the SICP for 2020: (1) reduced emergency admissions and readmissions, (2) reduced permanent admissions to residential and nursing care, (3) improved quality of life for users and carers, (4) an increased proportion of people supported to manage their own condition, (5) increased satisfaction with care and support provided, (6) increased flu vaccine uptake and (7) an increased proportion of people who die at home (or in their preferred place).
FIGURE 1.
Salford Integrated Care Programme and programme ‘drivers’. Reproduced with permission from Salford Together from SICP background briefing materials.
As discussed in Chapter 1, one of the drivers of integrated care was the patient perception that care was not ‘joined up’, which led to the production of a number of ‘principles’ of integrated care designed to enhance the patient experience of care. 3–5 To enhance that ‘patient-centred’ perspective, SICP implementation was based on a fictional character (Sally Ford) and her family. Sally Ford is a 78-year-old woman, who is divorced with no children and experiencing average health. She has family consisting of siblings and their partners, who all experience varying levels of health. The aged > 65 years population was categorised into four different levels of health need (Table 1).
| Level of ‘Sally’ | Level descriptor |
|---|---|
| ‘Able Sally’ | Able to support and sustain own health and well-being needs |
| ‘Needs some help Sally’ | Likely to have contact with at least one service agency. A need for education/intervention to enable self-management. Lower level of social care needs. Provides informal care to another individual. Early diagnosis of dementia |
| ‘Needs some more help Sally’ | Regular visits from health (including mental health) and/or social care services. Intermediate care/reablement. Meets social care eligibility criteria,5 receives formal or informal care |
| ‘Needs a lot of help Sally’ | Needs 24/7 care either in a residential, nursing or EMI home, or at home with high level of need (e.g. often over a 24-hour period) |
The SICP was to be delivered in five phases:
-
phase 1 – refine scope and prepare for implementation (completed)
-
phase 2 – neighbourhood ‘tests of change’ (completed)
-
phase 3 – interim review of impact (scheduled January to March 2014)
-
phase 4 – extend to other neighbourhoods/city wide (April 2014 onwards)
-
phase 5 – formal evaluation (April 2014 to March 2019).
Three core mechanisms of integration were included in the specification of the SICP (Box 1).
This was designed to take advantage of the knowledge and experience of older residents, involving them in local service improvement and strengthening communities. Despite the high levels of deprivation in Salford, there were a number of local assets, which included volunteers, green spaces, leisure centres and local clubs. Better access to these assets could help people engage in healthy behaviour and improve quality of life.
Integrated contact centreThe aim of the centre of contact was to support older people and carers managing long-term conditions by better integrating health and social care functions. This would be achieved by co-locating staff from both adult social care, district nursing and intermediate care.
The centre was expected to provide a number of functions, including support for self-management and links with the ‘community assets’ workstream.
The centre would also provide a range of specific services, including follow-up and support to particular groups of patients (such as those requiring intermediate care following hospital discharge); advice and support for those with long-term conditions, including support for patients with depression via health coaching; and the promotion of self-management via telehealth.
Multidisciplinary groupsMultidisciplinary groups were to be organised around a ‘neighbourhood’ model of federated practices, based on GP clusters that already existed in Salford.
Each group would hold a register of people aged ≥ 65 years, and would use risk stratification tools to assess risk of hospitalisation and care home admission. Support will be based on those identified needs. Patients judged to be at high risk would receive further support from multidisciplinary groups, who would use shared care protocols and care plans to co-ordinate care delivery.
The SICP also involves a wider range of mechanisms. The local health improvement agency [Haelo; see www.haelo.org.uk/ (accessed 3 April 2018)] conducted interim evaluation work alongside CLASSIC, and their report included a schematic, which detailed the full range of mechanisms within the SICP as well as some indication of the relative scope of investment in each (Figure 2).
FIGURE 2.
Schematic showing range of SICP activities. Reproduced with permission from Haelo (Haelo, Salford Integrated Care Programme: Summary and Lessons Learned, 2016, internal report). CRM, customer relationship management; QA, quality assurance; SCR, shared care record; SIRP, single integrated referral point; W2W, Ways to Well-being.
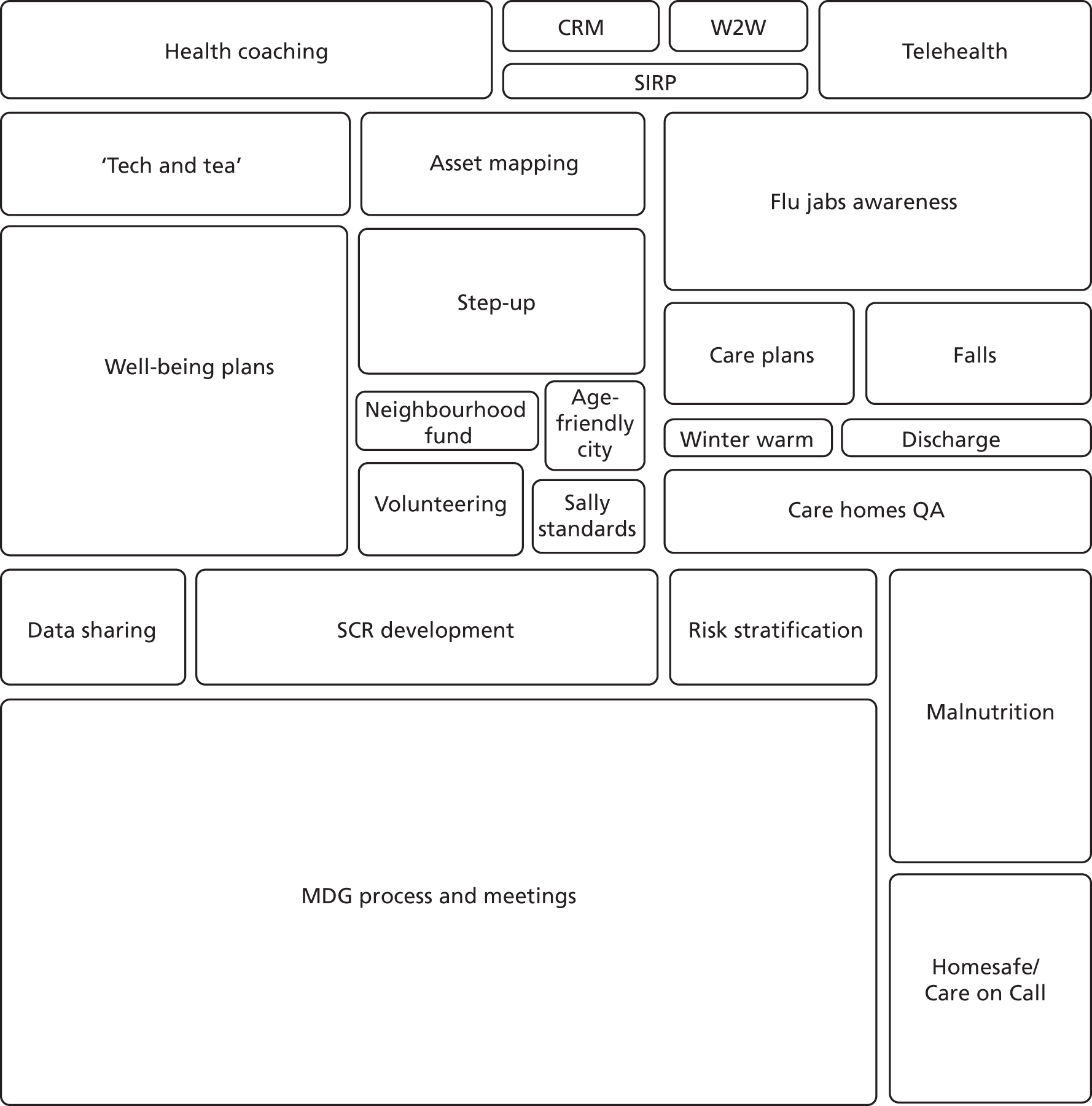
Two mechanisms were a core focus for the CLASSIC study: MDGs and ‘health coaching’ via the ICC. The MDGs were developed by the SICP team, and we describe their broad nature shortly, with data on their implementation and effects discussed in Chapters 11 and 13. Health coaching via the ICC was developed based on existing local services, but the precise model used was led by the academic team and evaluated through a formal trial. For this reason, the detailed description of the health coaching is provided as part of the trial description in Chapter 8.
Multidisciplinary groups
To describe MDGs, we have drawn on a published descriptive framework40 (Table 2) and mapped the groups in the SICP. There are features of the SICP model that may facilitate effectiveness. At a system and organisational level, the impact of the groups is potentially enhanced by the partnership underlying the SICP model (the CCG, city council, acute trust and mental health trust sharing risk and benefits), the alignment of goals and frameworks that this may achieve, and the potential for effective and co-ordinated leadership. Engagement of general practices should be facilitated by the proposed structure of the groups and the involvement of the CCG as a core partner organisation. The importance of self-management is reflected in the interface between the groups and other core aspects of the SICP (community assets and health coaching). A focus on ‘continuous quality measurement and improvement’ has been identified as an important success factor, and the local development of the model is supported by quality improvement teams to assess the model through small-scale ‘tests of change’.
| General description | Objectives | Development stage | Target population | Population coverage |
|---|---|---|---|---|
| MDGs provide targeted support to older people who are most at risk and have a population focus on screening, primary prevention and signposting to community support | The aim is to achieve greater independence and improved well-being for those aged ≥ 65 years by integrating care within communities. The focus is on reviewing and problem-solving complex cases, providing anticipatory care plans and assisting with navigation through the health and social care system | Piloted in two sites, with support from a quality improvement team and regular use of PDSA cycles to develop model | Older people with long-term conditions and social care needs | All older people in local area, although focus is on certain levels of need |
| Caseload | Funders | Breadth and degree of integration | Shared medical records | Risk stratification |
| Each group holds a register of all people who are aged ≥ 65 years. The register is based on the ‘list’ of the practices that are members of the group | Funding comes from the SICP. The four statutory partners (CCG, council, acute trust and mental health trust) have all formally signed up to the SICP and delegated authority to a board | Horizontal integration with some vertical integration based on improvements in co-ordination between primary and acute providers, and between health and social care professionals | Local integrated records provide unique linked primary care and secondary care data. Current linkage with social care less well developed | Uses a four-strata model of risk, with the role of the MDGs focused on those identified at levels 3 and 4 and at risk of escalation |
| Providers | Single point of referral | Patient eligibility criteria | Single assessment | Care planning |
| GP/nurse (with link to community geriatrician when required), social care worker (link into housing and health trainers when required), district nurse (link to hospital and discharge support), mental health, OT and administrator | Patients identified by risk stratification tool complemented by professional judgement, as well as direct referral from members of the MDG | As identified by risk stratification tool or professional judgement, based on risk of hospital emergency admission (and readmission) and admission to care homes | Yes | An integrated care plan is agreed with each individual. Content varies depending on risk and need, but includes a focus on primary and secondary prevention. All individuals are reassessed with frequency determined by level of risk |
| Care co-ordinator/case manager | Multidisciplinary team | Financial and non-financial incentives | Self-management support | Carer assessment and support |
| A small number of individuals with the most complex needs will be discussed at a MDG meeting to help plan and co-ordinate their care. Individuals are assigned a key worker to support their needs. The key worker will be identified based on who is likely to have most input into care for that individual patient | Yes | Partners have signed up to a high-level risk and benefits sharing agreement. As part of the SICP, the partners are exploring pooled budgets for health and social care, a joint venture/alliance contract and a capitation funding model | Provide links to ICC (including care navigation and health coaching) and community assets strands of the SICP (including self-help groups in the community) | Although carer needs may be part of the person-centred assessment and care planning, formal involvement of carers is not prioritised at present |
| Voluntary sector and peer support | Co-production | |||
| Although not a formal part of the MDG remit, the voluntary sector and peer support were identified as important issues in the early piloting and may be involved through MDG links to the community assets theme | Patient involvement has not been a high priority in the design of the MDGs, although there has been input from patients in some of the higher-level learning sessions in the development of the SICP |
Chapter 3 CLASSIC evaluation methods: an overview
Methodological frameworks
Integrated care raises major challenges for evaluation, reflecting the general pressure within health services research whereby increasingly complex service redesign requires rapid and rigorous evaluation. 41,42
The evaluation of health technologies has been heavily influenced by the Medical Research Council (MRC) Complex Interventions Framework,43 and each of the mechanisms of integration in the SICP (MDGs, health coaching, community assets) would probably meet the conventional definition of a ‘complex intervention’ (i.e. ‘interventions with several interacting components’).
The SICP itself may be best characterised as a ‘large-scale transformation’, defined as ‘interventions aimed at co-ordinated, system-wide change affecting multiple organizations and care providers, with the goal of significant improvements in . . . outcomes’. 44 ‘Complex interventions’ are nested within the SICP, but the large-scale transformation is not simply the sum of those interventions, but instead involves wider structural, organisational and cultural changes, which may serve to help or hinder the translation of individual mechanisms of integration into improved outcomes.
To answer our research questions, we adopted a mixed-methods approach using conventional health services research methods:
-
We used qualitative methods (interviews and observations) to explore the implementation of the SICP, both at the level of leadership and management of the major organisations involved (implementation 1), and at the level of managers and clinicians involved in the everyday delivery of the intervention (implementation 2).
-
We used analysis of routine data sets [Hospital Episode Statistics (HES)] and appropriate comparators and non-randomised methodologies45 to explore effects of the SICP on outcomes (‘outcome 1’).
-
We conducted a formal randomised controlled trial (RCT) within the cohort (‘outcome 2’).
In addition, to provide flexibility to assess a variety of aspects of the SICP, we also adopted a patient cohort. This cohort provided an assessment of patient-reported outcomes (health, quality of life and experience of services), which are missing from many integrated care evaluations that use routine data.
The planned cohort also provided an opportunity to explore the innovative cohort multiple randomised controlled trial (cmRCT) design, which at that point had not received significant practical application. 46 In this design, a large population cohort is recruited and followed over time. As well as providing an assessment of the impact of the SICP over time, natural variation in the exposure of patients within the cohort to different mechanisms of integration allowed more sophisticated modelling of effects.
In addition, the cmRCT provided a good conceptual ‘fit’ for the evaluation of health coaching within the CLASSIC study. One of the criticisms of RCTs is that they test innovations in a very selected group of patients, which then fail to ‘scale’ because of low rates of acceptability among the wider population. Pragmatic trials are in part a response to this, but they are still selective, as patients are selectively recruited on the basis of their willingness to engage with the intervention. A pragmatic trial may show effects, but can still be unacceptable to many patients who refuse to engage.
This is less of a problem in the evaluation of interventions where patients are seeking help. However, it has less relevance when an intervention involves services proactively identifying patients on the basis of risk. In the cmRCT, engagement in the wider population is, in principle, built into the design, alongside the usual impact of variable adherence (which is already built in to pragmatic trials).
The cmRCT was felt to be a relevant test of health coaching as applied in integrated care as a population health strategy, aimed in a preventative capacity for those at risk of poor outcomes (rather than a population identified on the basis of previous high utilisation).
Conceptual frameworks
A number of conceptual frameworks are of relevance. First, we drew on realist evaluations,28,47 which move beyond simple questions concerning whether or not an intervention ‘works’ to a more detailed assessment of ‘context’, ‘mechanism’ and ‘outcome’:
The complete realist question is: ‘What works, for whom, in what respects, to what extent, in what contexts, and how?’ In order to answer that question, realist evaluators aim to identify the underlying generative mechanisms that explain ‘how’ the outcomes were caused and the influence of context.
The process of a realist evaluation involves developing initial programme theories, conducting empirical work to test those theories and then analysing the relationships between context, mechanism and outcome to provide insights for those commissioning programmes.
An understanding of context is thus critical, as context can function to make particular mechanisms more or less potent. However, context is a complex concept. 26,27 An analysis49 of the process of managing ‘strategic change’ highlighted the importance of what was being implemented (content – equivalent to realist ‘mechanisms’), how this implementation was being undertaken (process) and the context surrounding change, with a distinction between ‘inner context’ (including concepts such as strategy and culture) and ‘outer context’ (the wider economic, political and social situation). This work also identified a number of features relating to a ‘receptive context’ for change:
-
quality and coherence and policy
-
availability of key people leading change
-
intensity and scale of long-term environmental pressure
-
supportive organisational culture
-
effective managerial–clinical relations
-
co-operative interorganisational networks
-
simplicity and clarity of goals and priorities
-
fit between the change agenda and the locale.
There is already a significant body of literature on large-scale change. As noted previously, a model of ‘large-scale change’ has been developed, which summarises five ‘rules’ underlying such transformations. 44
-
‘engage individuals in leading the change efforts’, highlighting the importance of both ‘designated’ and ‘distributed’ leadership
-
‘establish feedback loops’ concerning the collection and use of measures of progress (which can both help and hinder transformation)
-
‘attend to history’, in the sense of understanding previous efforts at change and their implications for current programmes
-
‘engage physicians’, as they are likely to be crucial to transformation efforts owing to their relative power and autonomy
-
‘involve patients and families’ to enhance outcomes.
In the area of integrated care, previous analyses have outlined important issues that need to be considered. A systematic review50 of factors that supported successful integration of health and social care for people with long-term conditions found seven studies and limited evidence overall, but highlighted a number of themes:
-
colocation of staff and teamwork
-
integrated organisations
-
management support and leadership
-
resources and capacity
-
information technology.
The evaluation of the SICPs also included a detailed analysis of > 200 interviews conducted to drive a ‘bottom-up’ model of barriers to and facilitators of integration,51 many of which were felt to be common to any large-scale change:
-
structure and characteristics of organisations and interventions:
-
size and complexity of the intervention
-
information technology
-
relationships and communication
-
professional engagement and leadership, credibility and shared values
-
-
contextual factors:
-
public service bureaucracy
-
resources allocated to the programme
-
external policy reform
-
organisational culture.
-
As noted earlier, the ‘large-scale transformation’ of the SICP has complex interventions nested within it, which can be viewed as distinct health technologies using a more granular approach. The development and analysis of health technologies can draw on a number of conceptual frameworks, which often relate to the particular logic model underlying an intervention.
For example, normalisation process theory (NPT)52,53 offers a framework to investigate how complex interventions become embedded and become sustainable over time, based on four generative mechanisms: (1) coherence (what is the work to be done?), (2) cognitive participation (participants have to ‘buy in’ to the work, individually and collectively), (3) collective action (what work has to be done to enact and enable new practices?) and (4) reflexive monitoring (what work can be done to help appraise new practices?).
The analysis of complex interventions within the SICP can also draw on frameworks more specifically related to the particular interventions under test. In the current context, this would include psychological models of behaviour change underlying self-management, which use related concepts such as self-efficacy and patient activation54 to understand the mechanisms by which patients undertake self-management. It can also include clinically focused models, such as ‘patient centredness’,55 to explore how mechanisms of integration impact on patient experience of care, as discussed in Chapter 1.
Timeline
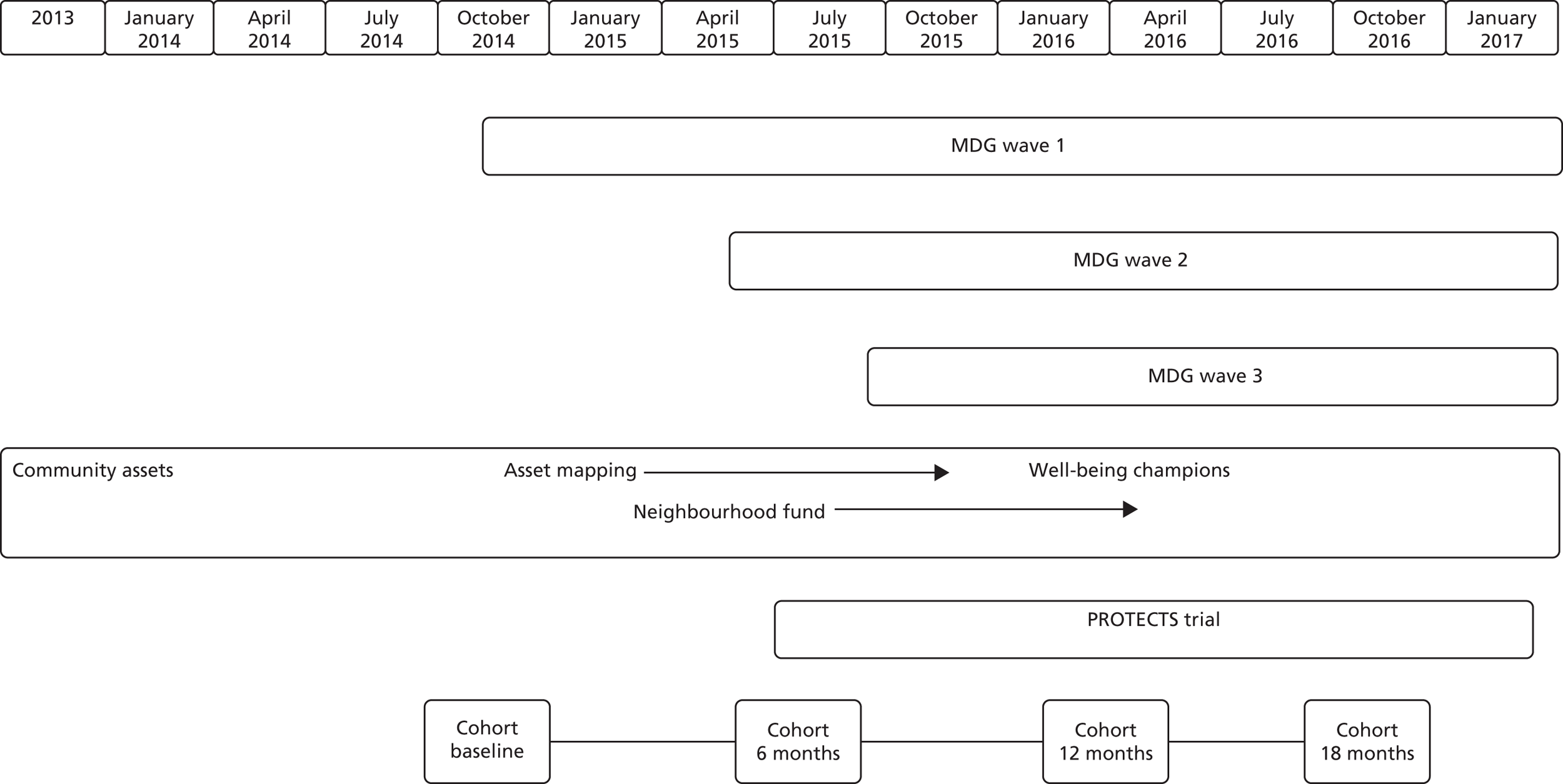
An illustrative timeline of SICP and CLASSIC activities is provided in Figure 3.
FIGURE 3.
Illustrative timeline of the SICP. PROTECTS, Proactive Telephone Coaching and Tailored Support.
Patient and public involvement in SICP and CLASSIC
Funding bodies require patient and public involvement (PPI) to ensure that research is relevant for its intended beneficiaries and that it prioritises issues of importance.
Where applied health research involves the development of interventions, and PPI is often focused on ensuring that those interventions are sensitised to the needs of patients. In the case of CLASSIC and the SICP, the interventions within the SICP involved patient input to the service development outside the formal research context of CLASSIC.
We now describe patient involvement in the initial development of the SICP and the more conventional PPI within the design and delivery of CLASSIC.
Public involvement in the SICP
The SICP aimed to improve person-centred care. Public engagement was undertaken throughout its formation (2011–12), via engagement activities undertaken by public governors and links with existing organisations (Salford Link Project and HealthWatch). As the SICP aimed to integrate health and social care, the programme was able to draw on existing reference groups.
Engagement with the wider community was required and in July 2012 an event was held with older people, which identified their priorities:
-
reducing emergency and permanent admissions to nursing and residential homes
-
enabling people to have more control over daily life
-
improving satisfaction with care
-
supporting people to die in their place of choosing.
Having developed these priorities, a ‘driver diagram’ was used to promote the SICP.
Public involvement was also used to modify the concepts behind ‘Sally Ford’, a character developed to help provide patient focus. By being able to comment on various iterations, group members aimed to make ‘Sally Ford’ more representative.
Additional input meant that ‘Sally Standards’ developed, which outlined how older people could help health and social care providers achieve their outcomes by taking a more active role in their own health and well-being. These underpinned the ‘My Well-being Plan’ developed in collaboration with the community assets team. Public involvement was central to the community assets workstream, with a mapping exercise identifying the unmet need for social groups for older people within neighbourhoods. Older people were encouraged and supported to apply for funding to set up and run local groups themselves. The community assets workstream was steered by its own patient group (the Community Assets Work Stream Group), who began their work by asking three simple questions: (1) ‘What motivates you?’, (2) ‘What makes you feel good?’ and (3) ‘How do you find out about things?’. This identified potential barriers (which included limited physical activity, lack of access to information, not eating well and being socially isolated), thereby forming the focus for ongoing work.
Patient and public involvement in CLASSIC
Ahead of our original NIHR application submission, we consulted with members of a Citizen Scientist Project (www.citizenscientist.org.uk; accessed 16 August 2018) based at Salford Royal NHS Foundation Trust, and other interest groups. In April 2013 we held an engagement event to discuss strategies to ensure older people’s active involvement in CLASSIC. This event highlighted the need for telephone support, engagement through social events (not just written materials) and the importance of peer networks in dissemination of information. The event also helped inform the development of the CLASSIC health coaching intervention.
The CLASSIC Study Advisory Group was formed following assistance from the engagement in research manager from the trust who attended our initial Study Steering Committee. The CLASSIC study was promoted on the Citizen Scientist website, which included an advert for advisory group members. For further meetings, two members of Primary Care Research in Manchester Engagement Resource (PRIMER) [http://research.bmh.manchester.ac.uk/PRIMER (accessed 3 April 2018)] (a local PPI group of long standing) were recruited specifically to work with the CLASSIC team. Its remit included overseeing management of the research, providing a patient voice and commenting on the emerging results and dissemination strategy.
Specific patient and public involvement activity within workstreams
CLASSIC cohort
Our researchers presented the cohort to a local group. In response to their feedback, we made changes to the survey, including increasing font size and type; improving questionnaire layout; providing an indication of time to complete; providing an explanation of why we are asking the questions; adding a statement regarding confidentiality, especially around data sharing; including examples of question completion; providing name and telephone details of a contact to assist with completion; and adding free-text boxes to enable people to add their own comments. The group also provided a ‘critical friend’ approach to letters and participant information sheets being developed to send to potential participants.
In March 2015, we presented to the PRIMER group, and its members provided advice on encouraging people to stay in the cohort and around how we fed back the results from CLASSIC. It was agreed that providing ongoing incentives would help retain participants.
Health coaching
At the meeting in March 2015, PRIMER members discussed the health coaching model, providing guidance on participant recruitment and retention with the telephone-based intervention.
Members of local groups were consulted in 2015 about recruitment methods and gave feedback that many older people were unlikely to answer their telephone to an ‘unknown’ caller. It was therefore agreed that a letter would be sent to potential participants, which included the telephone number that they would be called from, helping increase uptake.
Dissemination of CLASSIC evaluation results
Our two PPI representatives (PB and MM) have commented on the summary findings from the CLASSIC study and assisted with the Plain English summary. Dissemination is ongoing, and we anticipate writing a summary piece in collaboration with our PPI representatives for inclusion on the website (via the SICP communications team) and for inclusion in a local newsletter.
Our website [www.classicsicp.org.uk (accessed 3 April 2018)] will be a repository for publications arising from the CLASSIC study.
Chapter 4 Methods of the CLASSIC cohort
Practice recruitment
Ethics approval was obtained from the National Research Ethics Service (NRES) North West Lancaster (Research Ethics Committee reference 14/NW/0206).
Not all practices were invited to participate as they either had low numbers of patients aged ≥ 65 years or were affiliated with care homes with high numbers of dementia patients. Forty-seven practices were invited and 33 (70%) agreed to participate.
We used FARSITE [a tool for recruitment to research; see http://nweh.co.uk/products/farsite (accessed 18 May 2018)] to generate a list of eligible patients. Each practice was then asked to identify patients meeting exclusion criteria (i.e. in palliative care, those with conditions that reduce capacity to consent).
Practices did not receive incentives but did receive support costs to reimburse their time.
Patient recruitment and retention
Eligible participants were those aged ≥ 65 years and registered as having at least one long-term condition at a general practice.
A total of 12,989 patients were eligible and surveyed through general practice between November 2014 and February 2015. If they did not respond, they were sent a reminder and a second copy of the questionnaire 3 weeks later. Participants were offered an incentive of a £10 voucher.
Response was taken to indicate consent to further surveys at 6, 12 and 18 months.
To increase retention, patients were called by a researcher to offer completion of the questionnaire over the telephone. Patients were offered a £5 gift voucher for the completion of the 12- and 18-month follow-ups.
Cohort measures
The following list of measures was used in one or more of the surveys (Table 3).
-
Baseline assessment included sociodemographic questions from the General Practice Patient Survey,56 including sex, age, work situation and qualifications; ethnicity using 17 2011 Census categories;57 a single-item health literacy measure;58 a measure of the number and impact of long-term conditions;59 and use of local community assets. 60
-
The Patient Assessment of Chronic Illness Care (PACIC),61 which includes items in five subscales (patient activation, delivery system design and decision support, goal-setting, problem-solving, and co-ordination); we used the short 11-item version. 62
-
The Patient Activation Measure (PAM) of patient knowledge, skills and confidence in self-management for long-term conditions;54,63 we used the short 13-item version. 64
-
The Summary of Diabetes Self-Care Activities (SDSCA) measure assesses the number of days per week on which respondents engage in healthy and unhealthy behaviours. 65
-
The Multimorbidity Illness Perceptions Scale (MULTIPleS) assesses patient experience of managing multimorbidity;66 we used 16 items from the MULTIPleS.
-
The Quality, Innovation, Productivity and Prevention (QIPP) measure of personalised long-term condition care. 67
-
The ENRICHD Social Support Instrument (ESSI). 68
-
The EuroQol-5 Dimensions (EQ-5D) measure of health-related quality of life;69 we used the new EuroQol-5 Dimensions, five-level version (EQ-5D-5L). 70
-
The Mental Health Inventory – 5 (MHI-5) is a five-item scale that measures general mental health. 71
-
The ICEpop CAPability measure for Older people (ICECAP-O) index of capability measures quality of life for people aged ≥ 65 years in terms of attachment, security, role, enjoyment and control. 72
-
The World Health Organization Quality of Life-BREF (WHOQOL-BREF) 26-item measure of global quality of life across four domains (physical health, psychological health, social relationships and environmental), as well as a single-item scale. 73
-
Health-care utilisation, based on our previous studies;74 continuity of care and care planning from the General Practice Patient Survey;56 and patient experience of safety from the ICPs evaluation.
-
We also used single-item measures assessing other issues, including items assessing issues of interest to stakeholders (e.g. internet use and accommodation).
| Baseline | Follow-up time point | ||
|---|---|---|---|
| 6 months | 12 months | 18 months | |
|
|
|
|
We used a short assessment for carers, including EQ-5D, Patient Health Questionnaire-9 items, ICECAP-O and the Modified Caregiver Strain Index. 75 Carer data are presented in Appendix 1.
Chapter 5 Methods of implementation 1
Implementation 1 was designed to address the following research question:
How do key stakeholders (commissioners, strategic partners) view the SICP, what do they expect from it and how is it aligned with their objectives and incentives?
The specific objectives were to explore and understand:
-
how commissioners view the programme, what they expect from it and how it is seen in terms of their performance objectives
-
how the programme is viewed by strategic partners such as the local authority and how it is sustained under financial pressure
-
how the programme affects the work of the two foundation trusts, in particular how the integrated community and acute provider adapts to reductions in inpatient activity
-
how the programme affects primary care, in particular general practice
-
the extent to which the financial incentives (explicit and implicit) in the local health and social care system are aligned with the ambitions of the programme.
A qualitative approach was adopted to understand how the SICP was developed and how organisations were working together to transform care. Fieldwork took place from November 2014 to September 2016. Data collection included approximately 56 hours of non-participant observations of SICP programme meetings. A researcher attended meetings, including the Alliance Board, Study Steering Group and MDG meetings.
In addition, 28 interviews were carried out with professionals working across the four key stakeholder organisations associated with the SICP. Initially, 22 interviews were carried out in late 2014/early 2015 and six follow-up interviews were carried out with key stakeholders in 2016 to see how the SICP had developed, the factors that influenced the SICP and the relationships across the four key stakeholder organisations (Table 4). Documents, including operational plans and business cases, were collected from the SICP and relevant meetings to provide context.
| Data collection method | Number of interviews | Further information |
|---|---|---|
| Interviews | 28 in total (22 plus six follow-up interviews) |
|
| Observations | 19 (around 56 hours) | Observations included:
|
The data from interviews and observations were coded in the same way and analysis of the data was facilitated by the computerised data analysis package NVivo version 10 (QSR International, Warrington, UK). Initial coding was carried out using a priori codes derived from our existing understanding of the issues associated with commissioning complex programmes. These were supplemented by inductive coding arising from the data. Analytical memos were written and discussed to develop a collective understanding of the issues represented in the data.
Findings relating to the commissioning of the programme were shared with the wider research team and further explored in interviews with those responsible for the implementation of the project.
Chapter 6 Methods of implementation 2
Implementation 2 was designed to address the following research questions.
Multidisciplinary groups:
-
What are the characteristics and composition of the groups?
-
How do the groups function as teams and in collaboration with other providers?
-
How well do the groups achieve fidelity to the original SICP model?
-
What are the key barriers to and facilitators of effective functioning and outcomes?
-
How is the work of the groups experienced by patients and carers?
Integrated contact centre:
-
What services are provided by the centre and which staff provide those services?
-
What is uptake and usage of the ICC services?
-
What are the key barriers to, and facilitators of, effective functioning and outcomes?
-
How are ICC services experienced by patients and carers?
Methods and analysis
As discussed in Chapter 3, we drew on the realist model and the ‘five simple rules of large-scale transformation’ (designated and distributed leadership, presence and use of feedback, attention to historical factors, provider engagement, and PPI)7 as a framework to understand the process of implementation of these two aspects of the SICP. We also drew on NPT and psychological models of self-management and patient centredness to guide analysis.
Study methods: multidisciplinary groups
Multidisciplinary group fieldwork took place from March to December 2015, with fieldwork largely based on non-participatory attendance at neighbourhood MDG meetings. Data collection included 72 hours observing MDG meetings, with sequential fortnightly observations in one neighbourhood MDG for each of the three waves of roll-out (Table 5). Additional observations were undertaken at other meetings supporting the MDG process (including the working group meetings, joint chairpersons’ meetings and administrator meetings) as well as engagement events. Further observations were conducted with MDG nurse and social care co-chairpersons to outline how the work of referring and prioritising patients for discussion and pre-MDG meetings was enacted.
| Data collection method | Number | Further information |
|---|---|---|
| Interviews | 37 |
|
| Observations | 36 (approximately 72 hours) | Observations included:
|
By agreement, field notes made during the MDG meetings did not contain any identifiable patient data. Initials, sex and the general practice were recorded, permitting further questioning around individual cases with the relevant general practitioners (GPs) and to identify potential patients to be invited to participate in qualitative interviews.
Thirty-two face-to-face interviews were carried out with professionals participating in the MDG meetings or those whose work was associated with them. Maximum variation sampling was used to ensure that representatives from all staff groups participating in MDGs were interviewed.
We used routine data (workload and throughput, patient characteristics, links with other services) to contextualise our data. Operational documents were collected from the MDG processes and meetings around them and used to provide information about the implementation.
Study methods: integrated contact centre
Fieldwork took place between October 2015 and July 2016, during which time the single integrated referral point (SIRP) was based within a Salford City Council facility. Colocation with the council corporate team unfortunately meant that permission to carry out observational work within the SIRP was declined. Data collection was therefore based mainly on interviews with 11 ICC staff during which in-depth descriptions of their work were provided in lieu of observations (Table 6).
| Data collection method | Number | Further information |
|---|---|---|
| Interviews | 17 |
|
| Observations | 5 (approximately 11 hours) | Observations included:
|
We explored the various services provided by the centre through individual interviews with participating staff and managers to assess the development of the service over time, how fidelity to the model was achieved and the potential for unintended consequences. We used routine data reported by respondents (workload, patient characteristics, referrals) to contextualise the data.
We described the characteristics of the centre, its staffing and technology, and how the existence and function of the centre is communicated to patients. At the level of the patient, we described the interaction between the staff and patients, through individual interviews with six patients/carers who had direct experience. Observations included 11 hours of non-participant observations of meetings directly related to the centre, including a short visit to the SIRP, observing the locality base, a care homes meeting and initial engagement events promoting the wider SICP. In addition, documents providing evidence of the implementation process and allowing a comparison with the initial plans for the ICC at the start of the SICP were collated. Health coaching data are presented in Appendix 2.
Qualitative analysis methods
Qualitative data from both the ICC and MDG observations and interview transcripts were organised using NVivo 10. Techniques from grounded theory were used for the thematic analysis. 76 Analytical memos were written and discussed to develop a collective understanding of the issues represented in the data. Members of the qualitative team met monthly to discuss emerging themes and to agree subthemes.
Normalisation process theory was used as a starting point to inform the original topic guide used in the qualitative interviews. We considered how data mapped onto the framework, and although there were some connections between concepts, these were limited. We therefore adopted a more responsive approach, using iterative sampling and analysis of data until no new information emerged. This prevented the background framework from constraining the interviews and allowed us to learn from, and develop, the topic guide as the interviews were conducted.
Qualitative data from both the ICC and MDGs observations and interview transcripts were organised using NVivo 10. We conducted a thematic analysis drawing on some techniques from a grounded theory approach, including open coding and the creation of analytical memos as a basis for iterative analysis and sampling as outlined previously. Members of the qualitative team met monthly to discuss emerging themes and subthemes, any unusual cases and to agree the final stage of ‘selective’ coding. These processes of coding and iterative analysis enabled core themes to emerge inductively from the data consistent with a grounded theory approach. 76
Chapter 7 Methods of outcomes 1
A core SICP aim was to reduce emergency admissions. Although all mechanisms of integration in the SICP have a potential role in reducing admissions, the MDGs are most clearly focused on providing a rapid reduction in the use of hospital services through intervention with patients at high risk of admission.
Multidisciplinary groups and linked case management interventions have an important place in the NHS as a core mechanism of integration. Since the Evercare pilots,29,30 studies have cast some doubt on the evidence that this model can achieve reductions in hospital admissions. 18,19,33,77,78 However, an unpublished survey of CCGs reported that 80% included some variant in their integration plans. 79 There are a number of different models of MDGs and some of the ways in which they vary are outlined in Table 2. In line with the realist model (see Chapter 3), there is also an argument that the general case management ‘mechanism’ is effective only in certain contexts, such as a history of previous joint working among staff in an integrated care service.
Methods
The SICP was targeted at all general practices. Therefore, the primary analysis for the effects of the MDGs compared data from practices in Salford with suitable comparators in other parts of England. However, the introduction of MDGs was staged, and we used this to assess any differential impact relating to the staged introduction.
We adopted lagged dependent variable approaches to estimate the effect of the MDGs. 80 This approach does not require assumptions of parallel trends between intervention and comparator groups imposed by a difference-in-differences specification. The lagged dependent variable approach uses a fixed vector of lagged values of the outcomes prior to the intervention as explanatory variables. The analysis is conducted only on the time points following the intervention. 80
If the parallel trends assumption does not hold, the lagged dependent variable approach is less prone to bias and is more efficient than alternatives such as the creation of synthetic controls. 80 The superiority of the lagged dependent variable approach is increased when data are available on more pre-intervention periods, as is the case in this setting.
Data
Data were HES from NHS Digital, stratified by financial quarter and general practice (financial years 2009/10–2015/16), for populations aged ≥ 65 years:
-
the number of accident and emergency (A&E) attendances per person
-
the number of A&E attendances referred by health and social care providers per person
-
the number of self-referred A&E attendances per person
-
the number of emergency admissions per person
-
the number of emergency admissions via A&E per person
-
the number of direct emergency admissions per person
-
the number of ambulatory care-sensitive emergency admissions per person
-
the proportion of patients discharged to usual place of residence.
We also obtained general practice patient registration lists for persons aged ≥ 65 years from two sources: (1) the Personal Demographic Service for the financial years 2009/10 and 2010/11 and (2) NHS Digital for the financial years 2013/14 to 2015/16. For the financial years 2008/9, 2011/12 and 2012/13, we used the closest year of data available.
Intervention sites
Practices in Salford CCG were all considered to be the intervention site, but we also identified distinct subgroups (non-adopters, early adopters and late adopters). Non-adopters (n = 5) were excluded from the analysis, leaving three intervention sites:
-
9 early adopters, classified as starting the intervention in April 2014
-
32 later adopters, classified as starting the intervention in April 2015
-
41 adopters, classified as starting the intervention in April 2015.
Comparator sites
Four comparator sites were used outside Salford CCG (Table 7):
-
all practices in Greater Manchester excluding Salford (‘Greater Manchester’)
-
practices in two CCGs to the west of Greater Manchester (‘West’)
-
practices in nine CCGs to the west of Greater Manchester [‘West (extended)’]
-
all practices in England excluding Salford (‘England’).
| Control group | List of CCGs | Number of practices |
|---|---|---|
| Greater Manchester | Bury, Central Manchester, North Manchester, South Manchester, Stockport, Tameside and Glossop, Bolton, Wigan, Heywood Middleton and Rochdale, Trafford, and Oldham | 418 |
| West | Warrington, and Knowsley and St Helens | 89 |
| West (extended) | Warrington, Knowsley and St Helens, West Lancashire, Vale Royal, Halton, Southport and Formby, South Sefton, Wirral, and Liverpool | 339 |
| England | All CCGs in England except Salford | 7434 |
Regressions
In total, we estimated 96 models (Table 8). We weighted all analyses by population size and used robust standard errors to allow for heteroscedasticity. We included proportions of the total practice population aged 65–74, 75–84 and ≥ 85 years as additional controls.
| Intervention site | Comparator site | Outcome |
|---|---|---|
| Early adopters | Greater Manchester | A&E attendances per person |
| Late adopters | West | A&E attendances referred by health/social care per person |
| All adopters | West (extended) | Self-referred A&E attendances per person |
| England | Emergency admissions per person | |
| Emergency admissions via A&E per person | ||
| Direct emergency admissions per person | ||
| Ambulatory care-sensitive emergency admissions per person | ||
| Proportion discharged to usual place of residence |
Robustness
An additional three models were estimated for the primary outcome (emergency admissions per person). For the first test of robustness, we omitted the data for the first financial year (2009/10). We omitted the first four quarters of data owing to small denominators in the general practice list sizes for the comparators ‘West’, ‘West (extended)’ and ‘England’.
For the second test of robustness, we limited the analysis to the period following the 2011 Census. The 2011 Census resulted in a recalibration of practice populations and may have affected the intervention sites in a different way from the comparators.
For the final robustness analysis, we used a difference-in-differences specification. Our models for difference-in-differences analysis control for Index of Multiple Deprivation,81 quarterly time dummies and proportion of practice list size of certain ages (65–74, 75–84 and ≥ 85 years). Difference-in-differences is not used for the primary analysis as this method relies on the parallel trends assumption. Parallel trends assumption requires that both intervention and comparator sites must have parallel trends pre intervention; violations will result in biased estimated treatment effects.
Chapter 8 Methods of outcomes 2
The ICC involves a number of services, but a key one is health coaching in long-term conditions:
Health coaching involves ‘a regular series of phone calls between patient and health professional . . . to provide support and encouragement to the patient, and promote healthy behaviours such as treatment control, healthy diet, physical activity and mobility, rehabilitation, and good mental health’.
McLean et al. 82
Table 9 shows key dimensions of health coaching interventions. 83–86
| Populations | Identification of patients | Technology | Responsiveness | Model |
|---|---|---|---|---|
| Coaching can be preventative or target those with existing conditions. If the latter, this can involve those with a specific disorder, a range of conditions or multimorbidity. Other methods of targeting include a focus on high health-care users or those at a high risk of admission | Patients can come to health coaching through self-referral, identification through routine consultations (or post discharge) or the use of formal risk stratification models | Technology can involve conventional telephone and mobiles, or enhancements such as telemonitoring, videophone, automated telephone support, SMS or combinations of technologies | Coaching can recruit patients through referral from services, or proactively identify patients ‘at need’ or ‘at risk’. The delivery of the coaching itself can be more or less scripted | A variety of models of coaching can be used, based on counselling, CBT, self-management and self-efficacy, or motivational interviewing |
| Target | Practitioner | Intensity | Care context | |
| The targeted outcomes for coaching can include education and information, decision-making, motivation and self-efficacy, self-care behaviours, health-care utilisation, mental health and substance abuse | Coaching can be delivered by peers, trained non-clinical staff, clinicians, or may be automated to various degrees | The intensity of coaching may vary in terms of the length and number of calls per week, the overall duration of contacts and the use of ‘booster’ sessions | Coaching can be used as part of a ‘stand-alone’ intervention, or delivered as part of wider programme of care. Linkage to other services (such as primary care) may also vary |
What is the evidence for health coaching?
A number of reviews have tried to assess the overall evidence. A review87 of the effects of health coaching on adults with chronic disease found 13 studies in a broad range of populations and conditions. Only a minority used telephone health coaching. Benefits were reported for a variety of outcomes, with the most consistent results for weight, physical activity and health status. However, the studies included adults of a range of ages rather than older people. A second review85 found 30 studies of health coaching for long-term conditions and, again, reported evidence of positive effects on a range of outcomes (including self-efficacy, satisfaction and health status). An integrative review88 of qualitative and quantitative research found 15 studies and rated 40% as showing improvement in one or more health behaviours. A review84 specific to telephone coaching services for people with long-term conditions found 34 eligible studies, focused on diabetes mellitus or cardiovascular conditions. Most reported some outcomes in favour of health coaching, although reporting of cost outcomes was rare. The variation in the numbers of included studies in reviews highlights variable definitions in this area, but the overall evidence suggests an intervention that is promising but far from proven.
Other recent studies in the last 5 years also give a mixed picture. A quasi-experiment89 exploring the impact of telephone health coaching on care utilisation reported no impact on emergency admissions, but found savings of US$412 in total costs per person, largely through reduced outpatient and inpatient expenditures. Again, the sample was adults and only a small proportion were aged ≥ 65 years. A second quasi-experiment88 in an adult Medicaid population found the opposite: health coaching was not associated with changes in a range of utilisation measures and expenditures, but did reduce emergency department use. A recent evaluation90 of the Birmingham OwnHealth health coaching service in 2698 patients and matched controls explored impacts of a service targeted at people with heart failure, coronary heart disease, diabetes mellitus or COPD. The analysis found no reductions in utilisation with a nurse-led health coaching service, although other outcomes (such as empowerment and quality of life) were not measured. A large (n = 1535) study of health coaching in patients aged ≥ 45 years with one of three long-term conditions and unmet treatment goals found that blood pressure control improved in the intervention group, but found no other benefits on primary end points. 91 A small (n = 43) study92 of health coaching for older patients with multimorbidity in nursing homes in Korea reported benefits in self-management, self-efficacy and health status. A trial93 of 232 patients with long-term conditions and depression found that coaching added only short-term benefits over access to a self-care intervention in an older population (mean age 55 years). A cluster trial94 of 473 patients receiving a practice nurse-based health coaching intervention found no benefits over usual care on glycated haemoglobin (HbA1c) outcomes. A trial of patients95 with coronary heart disease in university teaching hospitals receiving telephone coaching found a significant impact on total cholesterol outcomes at 6 months compared with controls. The PACCTS (Pro-active call centre treatment support) study96 randomised 591 patients with type 2 diabetes mellitus to telephone support from paraprofessionals and found significant changes in only a subgroup of those with poor glucose control at baseline. A trial97 in 436 older patients with chronic kidney disease (CKD) found that coaching by paraprofessionals and supported by a bespoke website led to improvements in health-related quality of life and blood pressure control, and was highly likely to be cost-effective.
The overall picture on the effectiveness of health coaching is complex. There are a number of positive evaluations, but the studies have included a very mixed group of patients and interventions. Clearly, further research is required to assess the impact of this promising intervention and its place in integrated care for long-term conditions, especially given the limited evidence base in multimorbidity,98 which is highly prevalent in patients aged ≥ 65 years. 1
The CLASSIC Proactive Telephone Coaching and Tailored Support (PROTECTS) trial was a pragmatic, individual-level randomised trial to evaluate the clinical effectiveness and cost-effectiveness of telephone coaching.
Eligibility criteria
All patients were aged ≥ 65 years, had two or more existing long-term conditions and were assessed as needing some assistance with self-management. We included the following self-reported conditions: asthma, back pain, cancer, CKD, COPD, diabetes mellitus, heart disease, heart failure, irritable bowel syndrome (IBS), osteoarthritis, osteoporosis, rheumatic disease, rheumatoid arthritis, stroke and thyroid problems.
We assessed self-management with the PAM, and included those with PAM levels of 2 or 3 (Table 10).
| Level | Description |
|---|---|
| 1 | Patients do not feel in charge of their own health and care, with low confidence in their ability to manage health and few problem-solving skills or coping skills |
| 2 | May lack basic knowledge about their long term-condition(s) and have low confidence in their ability to manage health, with limited knowledge about appropriate treatments and self-management behaviours. Patients expect their health and social care professionals to be in charge in terms of making decisions |
| 3 | Patients have basic facts relating to their long term-condition(s) and appropriate treatments. Patients will have some experience and success in making changes to self-management behaviour, as well as some confidence in handling limited aspects of their health |
| 4 | Patients have made most of the necessary behaviour changes, although they may face difficulty in maintaining behaviours over time or during times of stress |
Interventions
The intervention was health coaching, as defined previously. 82 We describe the intervention according to the TIDieR (Template for Intervention Description and Replication) guidelines99 in Table 11 and show a schematic of the process in Figure 4. The intervention was based on three mechanisms: (1) health coaching, (2) social prescribing and (3) low-intensity support for low mood. Social prescribing is linking patients and resources in the wider community. 100,101 Low-intensity support for low mood includes the assessment of common mental health problems, simple lifestyle advice and behavioural techniques to manage mood, and appropriate risk protocols. 102,103
| TIDieR category | Description of PROTECTS |
|---|---|
| What |
Telephone health coaching: the core telephone and health coaching materials include telephone and associated patient tracking and management software, and scripts for lifestyle support around diet, exercise, smoking and alcohol Social prescribing: advisors had access to local resources in Salford through the Ways to Well-being site Support for low mood: around three core areas (assessment of symptoms, advice and behavioural activation, risk assessment) |
| Who | The intervention was delivered by a health advisor (Agenda for Change band 4 worker) with essential skills in working with information technology and communication, as well as experience of working with the general public, good time management and an ability to work flexibly and under time pressure. The health advisors were supported by specialist nurses and managers within the ICC, with additional advice around mental health and social prescribing from the academic team |
| How and where | The health coaching was delivered via telephone from a central facility |
| When and how much | Proactive, monthly calls of around 20 minutes were made for a period of 6 months, with the option for additional calls to deal with complex patients or issues of risk |
| Tailoring | Health coaching staff were trained to customise the pace and detail of the call to the social context of the individual patient. Provision of support for low mood and access to community resources was provided when appropriate |
| Modifications | There were no major changes to the delivery of the intervention through the study |
| How well | The fidelity of the intervention was assessed by qualitative work with patients and staff and ensured by ongoing clinical supervision |
FIGURE 4.
Schematic of health coaching process. PLANS, Patient-Led Assessment for Network Support.
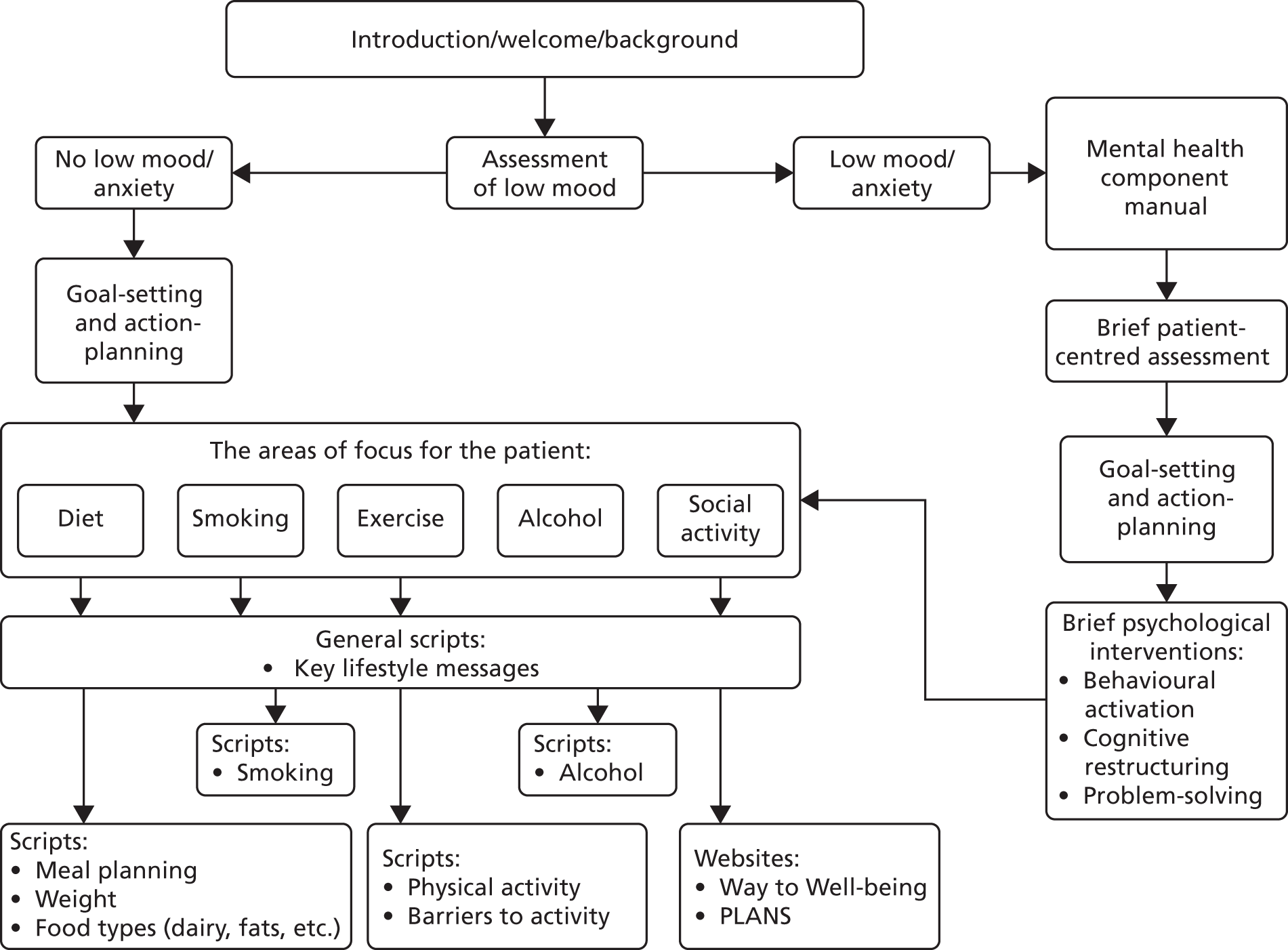
Training and supervision
The intervention was delivered by a health advisor (Agenda for Change band 4) who was already delivering health coaching to patients with diabetes mellitus or pre-diabetes mellitus. Training focused on the additional skills needed when dealing with a wider range of long-term conditions and dealing with low mood. A session on long-term conditions was run by a GP from the CLASSIC team, to help prepare for potential queries. Advisors were encouraged to refer people to the NHS Choices website.
Advisors were trained in detecting and working with participants with low mood over a 2-day training session with further updates over time. They were given the opportunity to role play low mood assessments and delivering interventions.They also received a comprehensive manual to aid them in delivery of the low mood component.
The advisors received clinical supervision (initially fortnightly, then monthly from applicant KL) by group for 1 hour. They had an opportunity to discuss challenging calls and risk issues. They were supported in making decisions about how to progress the intervention for each patient who identified as having low mood and in delivering structured low mood intervention such as behavioural activation. The advisors had contact details for the supervisors for immediate concerns.
Outcomes
The PROTECTS trial was a cmRCT,20 for which a large population cohort is recruited and followed systematically over time. Participants were followed up as detailed in Chapter 7. Outcomes used in the PROTECTS trial were prespecified in an analytic plan (see Appendix 1, Tables 52–61).
We set up an appropriate Study Steering Committee for CLASSIC, but as the study was based on modification of an existing service, for which the likely risks are minimal, a Data Monitoring Committee was not used. 104
Procedures
Recruitment and assignment of interventions
Participants were enrolled through the CLASSIC cohort. In a standard trial, patients receive information and then provide informed consent to participate. At that point, they are randomised. A significant drawback is that patients are told about different treatments in the different arms (including any new treatment), but only half the patients are randomised to that new treatment. This can cause dissatisfaction.
In the cmRCT, patients eligible for the trial are identified from the cohort and randomly selected. Patients who are randomly selected for usual care continue to be followed up in the cohort and are not informed about the trial or the randomisation. Patients who are randomised to the new treatment are then contacted and offered the treatment. They still provide consent to the new treatment and can decide whether or not they wish to receive it. If patients agree to the new treatment, they are provided with the new treatment and continue to be followed up in the cohort. If patients decide that they do not wish to receive the new treatment, they continue to receive usual care and continue to be followed up in the cohort.
We piloted these procedures in 50 patients to test the rate of uptake of the new treatment.
After assessment of eligibility, we selected patients randomly for health coaching or usual care using appropriate central randomisation through a clinical trials unit to ensure concealment of allocation. In this pragmatic evaluation, there was no blinding of patients or providers. All outcomes were either self-reported or routine data.
Sample size and analysis
At the time of study development there were no bespoke methods for powering cmRCTs, and, following existing cmRCTs, we used conventional methods. We powered the study to have 80% power (α = 5%) to detect a standardised effect size of 0.25 on any continuous outcome measure. Allowing for 25% attrition among participants – and assuming that outcome measures at baseline correlate 0.5 with their follow-ups – 504 patients were needed (252 per arm).
The initial uptake rate was lower than anticipated; hence, we selected a further 252 patients to be offered the intervention. However, within the cmRCT framework all 504 patients offered treatment remained in the treatment group in analysis, including those who declined. In consequence, the effect size between arms detectable at 80% power was 0.39 among those consenting to treatment.
Analysis followed intention-to-treat principles and a prespecified analysis plan (see Appendix 1). In summary, we report the trial and analysis in accordance with the updated Consolidated Standards of Reporting Trials (CONSORT) standards and utilising the extension for pragmatic trials. The main test of the intervention was that the overall main effect of the intervention is zero. Condition group was used as a binary variable. Continuous outcomes were assessed using linear regression, controlling, where appropriate, for baseline values of the respective outcome. Outcomes measured using ordinal scales were treated as continuous variables. Results for non-normal variables (skew or kurtosis > 1.0) were confirmed using bootstrap analysis. Baseline values of outcomes and design factors were included in all analyses. Some additional covariates were prespecified.
Owing to implementation delays, no patient was offered treatment up to 6 months after the baseline assessment and for some the offer was not made until month 12 or later. This caused variations in the duration of time before start of the treatment, ranging from 259 to 513 days. Length of follow-up from the end of treatment to 20-month follow-up was similarly variable. Thus, the trial is considered to have run for > 20 months, with patients receiving treatment at any time within that period.
The cmRCT design provides an estimate of the mean effect in people offered treatment. Compared with a pragmatic trial, which provides an estimate of the mean effect in people agreeing to treatment, the effect is ‘diluted’ by the proportion of patients in the treatment arm who do not consent to treatment. An estimate of the effect size in patients consenting to treatment was obtained through application of a complier-average causal effect (CACE) analysis. 105,106 CACE does not increase the power to detect an effect.
Economic analysis
The economic analysis aimed to assess the incremental cost-effectiveness of health coaching compared with usual care.
The primary outcome measure for the economic evaluation was health-related quality of life measured by the EQ-5D-5L,107 a new version developed as a result of concerns over the lack of sensitivity to change of the original. Published English general population preference weightings70 were used to convert responses to a single utility index for each time point.
This was combined with in-hospital mortality information taken from the secondary care utilisation data, applying a utility value of zero to all patients on death. Quality-adjusted life-years (QALYs) were calculated using the ‘area under the curve’ method, assuming linear extrapolation of utility between time points. QALYs experienced in the second year of the trial were discounted at an annual rate of 3.5%, as specified by the National Institute for Health and Care Excellence (NICE) in its reference case. 108
Resource utilisation and costs
Resource utilisation and costs were calculated from the perspective of the UK NHS. Patient-level utilisation data were collected from two sources. Information on GP contacts in the previous 6 months was collected from cohort data at 6, 12 and 18 months. Hospital utilisation data were extracted from linked administrative patient records provided by the NHS, divided into emergency admissions (short stays, ≤ 5 days; long stays, > 5 days), elective admissions, elective day cases, outpatients and A&E attendances.
Utilisation data were combined with relevant unit cost data for the price year 2014/15 to calculate total costs. Unit costs not available for this price year were inflated to 2014/15 prices using the Consumer Price Index. 109 Costs occurring in the second year were discounted at a rate of 3.5%. 108
Unit cost figures were sourced from the Personal Social Services Research Unit’s (PSSRU’s) unit costs of health and social care (2015)110 and national NHS reference costs. 111
Health coaching costs
Costs were estimated combining the cost of training and supervising staff, materials and delivery of the health coaching sessions. The intervention was offered to all participants randomly selected, although only 189 received at least one call and were used to estimate costs.
Missing data
Data required for QALY and cost calculation were missing in a small number of cases (n = 2), and were imputed. Missing information on age and sex was sourced from administrative data (sex, n = 6; age, n = 35) or imputed (missing age n = 30), to ensure independence from allocation. 112
For missing EQ-5D-5L and resource use data, we used multiple imputation by chained equations to generate 50 imputed data sets, assuming that the data were missing at random. The independent variables specified in the imputation models were age, sex, treatment arm and baseline EQ-5D-5L. To account for non-normality, predictive mean matching was used to ensure values observed in the original data set. Multiple imputation was conducted using Stata’s ICE package and analysis using Stata’s MI package (version 14.2; StataCorp LP, College Station, TX, USA).
Cost–utility analysis
The economic analysis estimates the incremental cost-effectiveness of the offer of health coaching compared with usual care at standard UK willingness-to-pay thresholds.
The primary analysis was based on a comparison on the full sample with multiple imputation. A sensitivity analysis was performed using only the complete-case sample (health coaching n = 206, usual care n = 378). Analysis used Stata version 14.
The incremental cost-effectiveness ratio (ICER) was calculated, adjusting for age, sex and baseline EQ-5D-5L index score. 113 To assess uncertainty surrounding the estimates and to account for the typically skewed nature of cost data, incremental costs and QALYs were bootstrapped using pairwise bootstrapping with replacement using 10,000 replications. Cost-effectiveness planes plot these 10,000 bootstrap replications of the ICER estimates to illustrate the uncertainty around the point estimate of the ICER in probabilistic terms. Finally, cost-effectiveness acceptability curves (CEACs) were plotted to represent graphically the probability of the intervention being cost-effective across a range of cost-effectiveness thresholds.
Chapter 9 Results of the CLASSIC cohort
Figure 5 shows the flow of patients into the cohort.
FIGURE 5.
Flow of patients in the cohort.
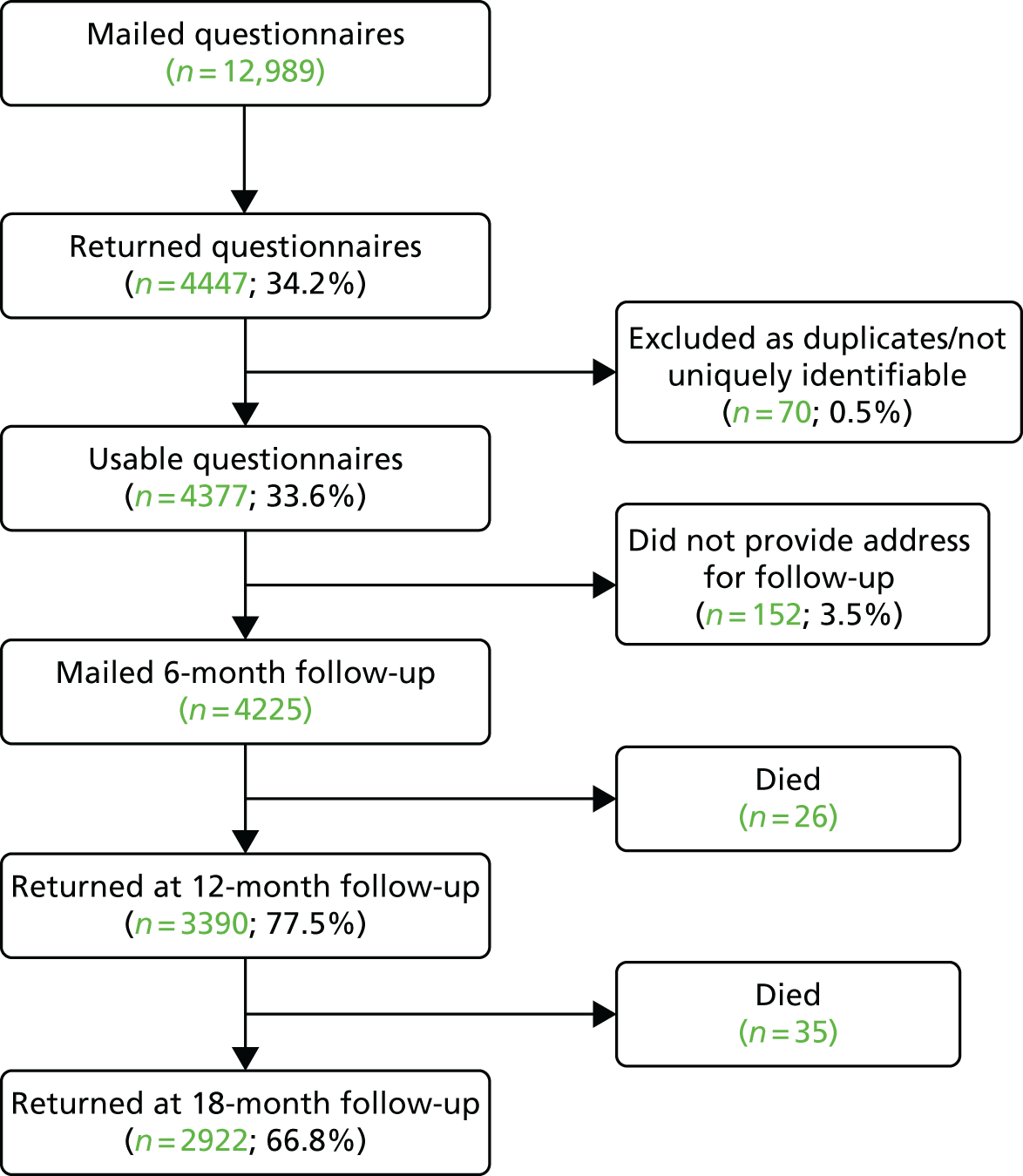
Owing to current word limits on the report, we do not present detailed descriptive data on the cohort and restrict the main presentation to quasi-experimental analyses of SICP mechanisms of integration (community assets and care plans).
We present basic descriptive data on patient experience items in Appendix 3. Analyses using the cohort data to explore other aspects of care for older people can be found in published papers,114,115 and more will be reported in due course.
A limitation of existing analyses of integrated care is that they are too large in scope or rapid in delivery to allow setting up data collection to capture effects, restricting analyses to routine data that lack patient-reported outcomes. The CLASSIC trial used the cmRCT design to develop a cohort, which provided the ‘context’ into which the SICP and its mechanisms of integration would be introduced. The cohort had two functions:
-
to provide a sampling frame for the cmRCT within CLASSIC for formal experimental analyses (full details are provided in Chapters 8 and 13)
-
to provide a sample of the total eligible population of older people, which could be used to track the impact of mechanisms of integration on patients through variation in exposure to those mechanisms among patients in the cohort.
This chapter will focus on the second function. Two mechanisms of integration suited to evaluation through the cohort are community assets and care plans. Community assets were a specific mechanism of integration within the SICP, with its own dedicated workstream (see Chapter 2, Box 1). Care plans have long been seen as critical to effective management of long-term conditions,15,116 and a major feature of health policy in the UK. 117 We assessed use of both community assets and care plans in the cohort and used variation in use to explore their impact on patient outcomes.
Community assets
In 2010, the UK government stressed the need for a ‘Big Society’, whereby individuals engage more with the facilities in their local community. A critical component was community assets, defined as:
. . . the collective resources which individuals and communities have at their disposal, which protect against negative health outcomes and promote health status.
Community assets (such as charity, voluntary or community groups) may have a role in improving health and reducing inequalities. Reviews119–121 and qualitative work suggest that community assets improve health,122 but quantitative evidence is sparse.
The community assets workstream of the SICP was not a primary focus of the CLASSIC research programme. The community assets workstream involved a number of different parts, including increasing voluntary work, delivery of well-being plans, digital inclusion, falls prevention and malnutrition awareness. A community assets working group brought together multiple partners locally as well as older people to develop better co-ordination of current assets. We used the cohort to answer the following research questions:
-
How do people in the cohort use community assets and how does that change over time?
-
Is community asset use associated with outcomes (quality of life and health-care utilisation)?
Care plans
Care plans are seen as critical to quality care for long-term conditions,15,117 but, despite their importance in policy, implementation is inconsistent. 74,123 In the SICP, care plans were important in both the MDG (shared care plans) and community asset (well-being plans) workstreams.
We used the CLASSIC cohort to answer the following research questions:
-
What is the prevalence of self-reported care plans in the cohort and how does that change over time?
-
Is the self-report of a care plan associated with outcomes (feelings that care is integrated, patient activation and health-care utilisation)?
Methods
Details of the CLASSIC cohort are provided in Chapter 4.
Community asset use
Individuals were asked ‘Have you attended or used any of the following community groups, activities and services in the last 6 months?’ and provided with the following options: (1) trade unions, (2) group for the elderly or older people (e.g. lunch club), (3) environmental groups, (4) youth groups (e.g. Scouts, Guides), (5) parent–teacher association or school association, (6) Women’s Institute, Townswomen’s Guild or women’s groups, (7) residents’ group or neighbourhood watch, (8) social club (including working men’s clubs, Rotary Clubs), (9) education, arts, music or singing groups, (10) sports club, gym, exercise or dance groups, (11) religious group or church organisation, (12) other group or organisation and (13) charity, voluntary or community group. This represented only a part of the SICP community assets programme.
An individual was classified as using community assets if they ticked ‘yes’ to one or more. The list of assets was less comprehensive in waves 2 and 3, as it included only (2) and (8)–(12). However, results were robust to these changes.
We obtained the costs of outpatient attendances, ambulance use and A&E visits from NHS reference costs,111 and cost of a GP visits from a PSSRU costs publication. 110 In 2014/15 prices were as follows: GP appointment £65.00, outpatient attendance £134.22, ambulance callout £96.35 and A&E visit £131.92.
Analytic methods
How do people in the CLASSIC cohort use community assets and how does that change over time?
We present descriptive data from the cohort on community asset use over time.
-
Is community asset use associated with quality of life and health-care utilisation?
We used variation in use of community assets to explore its causal impact. In the absence of randomisation, determining causal associations is complex, as cross-sectional associations may reflect reverse pathways (health influencing asset use rather than vice versa) or unmeasured confounders. We conducted the following analyses:
-
examined cross-sectional associations between asset use and outcomes (quality of life, health-care utilisation), controlling for measured confounders
-
used an instrumental variable approach (using distance to community assets as an instrument) to test whether or not the association was maintained, to provide a more rigorous test of a causal relationship
-
used longitudinal data to assess whether or not change in asset use was associated with outcomes.
Associations between asset use and outcomes
We compared quality of life, health-care utilisation and costs between users and non-users of community assets. We estimated three multivariate models for quality of life and utilisation, including community asset use and:
-
sex, age and socioeconomic characteristics only
-
sex, age, socioeconomic characteristics and the presence of 23 long-term conditions
-
sex, age, socioeconomic characteristics and the presence of 23 long-term conditions limiting activity.
We combined the effects on health-related quality of life and costs to produce estimates of the societal value of 1 year’s participation in community assets using the net benefit framework. 124 This net benefit combines both the benefit and the cost into one single metric. For example, it would be better equipped to deal with a scenario in which an individual’s health improved at the same time as they used more NHS resources (i.e. having higher costs). This involves multiplying EQ-5D scores by a value for a QALY and subtracting the annual cost of health-care utilisation. We use a range of threshold values (£20,000, £30,000 and £12,936)125 and multiplied 6-month costs to obtain annual costs. Net benefit was then used in three further regression models, which included sex, age, socioeconomic characteristics and 23 long-term conditions limiting activities.
Instrumental variable analyses
We received council data containing postcodes of community assets (May 2014–15). These assets were defined by the council as:
. . . buildings or amenities that play a vital role in local life . . . community centres, libraries, swimming pools, village shops, markets or pubs.
We included a range of asset types (‘health and well-being’, ‘skills and training’, ‘food’, ‘outdoor space’, ‘physical exercise’, ‘religious’, ‘shopping’, ‘social’, ‘volunteering’ and ‘other’), but excluded those coded as ‘older teenage’.
Data from patient postcodes enabled the calculation of distance between households and assets, by translating postcodes to co-ordinates and calculating distances using the Stata® (StataCorp, College Station, TX, USA) ‘vincenty’ command via the law of cosines. We calculated (1) the minimum distance to the nearest asset (in miles) and (2) the number of assets within a given radius (1, 2, 5, 10, 15 and 20 miles).
As noted earlier, regression of community asset use on outcomes can produce bias via reverse causality. To overcome this bias, we used an instrumental variables approach, defined as ‘an analytical technique, traditionally used in non-randomised research studies, which uses a variable associated with the factor under study but not directly associated with the outcome variable or any potential confounders’. 127 Instruments are variables that are related to asset use, but not directly to outcomes. We used the distance to nearest asset and the number of assets in a certain radius as instruments. We argue that the way in which assets impact on health is through use only. That is, the distance to an individual’s nearest asset can affect their health only if that individual then uses that asset. Just because an individual lives close to an asset is not sufficient for their health to improve, they must make use of that asset.
Instrumental variable models have two stages:
-
the prediction of asset use conditional on minimum distance and number of assets in the radii (and other cofounders)
-
effect of asset use on health (the first stage prediction of asset use is used in the second stage).
As asset use is binary, we used linear regression with endogenous treatment effects:128,129
-
we estimated three separate multivariate models for the EQ-5D score, which included asset use and sex, age and socioeconomic characteristics only
-
sex, age, socioeconomic characteristics and the presence of 23 long-term conditions
-
sex, age, socioeconomic characteristics and the presence of 23 long-term conditions limiting activity.
We then estimated the same models for utilisation (GP, outpatient and total costs). Finally, we combined the effects on quality of life and costs to produce estimates of societal value.
Longitudinal analyses
We estimated the effect of asset use using a matched control group analysis,130 whereby the effect is defined as the mean difference between the observed and the imputed potential outcome for each individual. We use nearest ‘neighbour matching’ to impute potential outcomes, which takes an average of the outcome of similar subjects that are not treated. We further matched on baseline EQ-5D to better capture baseline health. As well as considering the effects of starting asset use, we estimate effects of stopping. We estimated short- (baseline to 6 months) and long-term (baseline to 12 months) effects (Table 12) of starting and stopping use of assets.
| Follow-up point | Start | Stop | ||
|---|---|---|---|---|
| Treatment | Control | Treatment | Control | |
| Short term | NY | NN | YN | YY |
| Long term | NYY | NNN | YNN | YYY |
In all models, we matched on baseline age, sex, living arrangements and the presence of limiting conditions. We additionally matched on baseline EQ-5D scores in a later specification. For utilisation and net benefits outcomes, we further matched on baseline levels of these outcomes.
Care plans
The analysis of the effects of care plans used analogous methods to the assessment of community assets, using change in use of care plans over time to explore potential impacts on patient outcomes.
The measure of care plans was the question ‘Do you have a written care plan?’ at baseline and 18 months.
Outcomes were:
-
patient perception of integration; we used a single item from the unpublished QIPP measure, ‘Do you think the support and care you receive is joined up and working for you’, scored on a four-point Likert scale
-
patient activation as measured by the PAM (see Chapter 4)
-
EQ-5D.
Results
Participation in community assets
Fifty per cent (1829/3686) of respondents at baseline reported using community assets. Most reported using one, and those using at least one community asset reported use of an average of two assets.
Table 13 shows participation over time among those reporting data at three waves of the cohort.
| Status of use at each point (baseline, 6 and 12 months) | n (%) |
|---|---|
| YYY | 990 (40) |
| YYN | 49 (2) |
| YNY | 250 (10) |
| YNN | 94 (4) |
| NYY | 178 (7) |
| NYN | 72 (3) |
| NNY | 124 (5) |
| NNN | 700 (29) |
Associations between community asset use and outcomes
On average, community asset users had an EQ-5D score of 0.690 compared with 0.596 for non-users (difference 0.094; p < 0.001) (Table 14). Table 14 shows that there were few differences between the two groups in other characteristics, but 9% of community asset users had university qualifications, compared with 4% of non-users.
| Variable | No use | Use | Difference | 95% CI |
|---|---|---|---|---|
| Health-related quality of life | ||||
| EQ-5D health utility index | 0.596 | 0.690 | 0.094 | 0.0767 to 0.1107 |
| Health-care utilisation | ||||
| GP visits (6 months) | 3.252 | 2.927 | –0.326 | –0.5191 to –0.1320 |
| Hospital outpatient (6 months) | 2.456 | 2.159 | –0.297 | –0.5180 to –0.0760 |
| Ambulance call outs (6 months) | 0.418 | 0.218 | –0.200 | –0.3353 to –0.0637 |
| Visits to casualty (6 months) | 0.556 | 0.439 | –0.117 | –0.2040 to –0.0299 |
| Total cost (£) of care (6 months) | 544.77 | 447.83 | –96.94 | –161.25 to –32.64 |
| Demographic characteristics | ||||
| Female | 0.505 | 0.521 | 0.015 | –0.0169 to 0.0477 |
| Aged 65–69 years | 0.296 | 0.289 | –0.006 | –0.0358 to 0.0229 |
| Aged 70–74 years | 0.257 | 0.275 | 0.017 | –0.0115 to 0.0456 |
| Aged 75–79 years | 0.202 | 0.223 | 0.021 | –0.0053 to 0.0475 |
| Aged 80–84 years | 0.136 | 0.124 | –0.012 | –0.0339 to 0.0096 |
| Aged ≥ 85 years | 0.109 | 0.0894 | –0.020 | –0.0390 to –0.0003 |
| Education | ||||
| School-level qualifications | 0.153 | 0.317 | 0.164 | 0.1373 to 0.1910 |
| College-level qualifications | 0.0390 | 0.122 | 0.083 | 0.0658 to 0.1005 |
| University-level qualifications | 0.0423 | 0.0861 | 0.044 | 0.0286 to 0.0602 |
| NVQ and trade qualifications | 0.211 | 0.258 | 0.047 | 0.0196 to 0.0743 |
| Professional qualifications | 0.136 | 0.239 | 0.102 | 0.0771 to 0.1272 |
| Living arrangements | ||||
| Lives alone | 0.351 | 0.354 | 0.002 | –0.0285 to 0.0333 |
| Lives with spouse | 0.568 | 0.591 | 0.023 | –0.0090 to 0.0549 |
| Lives with other | 0.131 | 0.103 | –0.028 | –0.0488 to –0.0074 |
| Health conditions | ||||
| Asthma | 0.152 | 0.139 | –0.013 | –0.0358 to 0.0099 |
| Cancer | 0.0780 | 0.0795 | 0.002 | –0.0156 to 0.0191 |
| Back pain/sciatica | 0.342 | 0.304 | –0.037 | –0.0676 to –0.0072 |
| Bronchitis/COPD | 0.170 | 0.115 | –0.056 | –0.0784 to –0.0333 |
| Kidney disease | 0.0542 | 0.0345 | –0.021 | –0.0344 to –0.0077 |
| Colon/irritable bowel | 0.141 | 0.157 | 0.016 | –0.0071 to 0.0388 |
| Congestive heart failure | 0.0618 | 0.0422 | –0.019 | –0.0336 to –0.005 |
| Diabetes mellitus | 0.234 | 0.201 | –0.034 | –0.0607 to –0.0075 |
| Hard of hearing | 0.412 | 0.409 | –0.001 | –0.0331 to 0.0304 |
| Heart disease/angina | 0.247 | 0.221 | –0.024 | –0.0514 to 0.0032 |
| High blood pressure | 0.532 | 0.530 | –0.003 | –0.0356 to 0.0289 |
| High cholesterol | 0.454 | 0.441 | –0.013 | –0.0454 to 0.0188 |
| Osteoarthritis | 0.304 | 0.317 | 0.015 | –0.0154 to 0.0444 |
| Osteoporosis | 0.141 | 0.116 | –0.026 | –0.0479 to –0.0047 |
| Overweight | 0.404 | 0.405 | 0.001 | –0.0304 to 0.0329 |
| Poor circulation in legs | 0.409 | 0.328 | –0.079 | –0.1101 to –0.0480 |
| Rheumatoid arthritis | 0.169 | 0.110 | –0.058 | –0.0804 to –0.0358 |
| Rheumatic disease | 0.0347 | 0.0302 | –0.004 | –0.0158 to 0.0070 |
| Stomach problem/ulcer, etc. | 0.241 | 0.249 | 0.009 | –0.0186 to 0.0369 |
| Stroke | 0.0726 | 0.0680 | –0.005 | –0.0214 to 0.0116 |
| Thyroid disorder | 0.112 | 0.131 | 0.019 | –0.0025 to 0.0398 |
| Problems with vision | 0.470 | 0.446 | –0.022 | –0.0545 to 0.0098 |
| Other health condition | 0.0856 | 0.0965 | 0.011 | –0.0080 to 0.0292 |
| Sample size | 1857 | 1829 | ||
On average, community asset users had visited a GP three times in the previous 6 months, 0.33 visits fewer than non-users (p < 0.001). Community asset users reported an average of 2.2 hospital outpatient appointments in the last 6 months, 0.3 visits fewer than non-users. Users also reported fewer ambulance call-outs and casualty visits. The average health-care costs over a 6-month period in users was £97 (p = 0.003) lower than non-users (£448 vs. £545).
Instrumental variable models
Table 15 shows the average distance, with users of assets closer to assets [difference –0.026, 95% confidence interval (CI) –0.039 to –0.013]. There is little difference in the number of assets within given radii for users and non-users, suggesting that asset availability is not responsible for the higher quality of life in users.
| Characteristic | Overall | No use | Use | Difference | 95% CI |
|---|---|---|---|---|---|
| EQ-5D score | 0.644 | 0.597 | 0.692 | 0.094 | 0.770 to 0.112 |
| Minimum distance | 0.156 | 0.169 | 0.143 | –0.026 | –0.039 to –0.013 |
| Number of assets within | |||||
| 1 mile | 96.544 | 97.608 | 95.471 | –2.137 | –6.441 to 2.167 |
| 2 miles | 278.739 | 272.519 | 285.016 | 12.497 | 2.230 to 22.695 |
| 5 miles | 826.0645 | 828.641 | 823.464 | –5.178 | –18.450 to 8.144 |
| 10 miles | 1085.808 | 1086.171 | 1085.442 | –0.729 | –2.368 to 0.911 |
| 15 miles | 1102.481 | 1102.406 | 1102.558 | 0.152 | –0.011 to 0.315 |
| 20 miles | 1107.455 | 1107.456 | 1107.455 | –0.001 | –0.058 to 0.057 |
| Number of individuals | 3470 | 1743 | 1727 | ||
We ran regressions with different combinations of distance and radii variables. All met validity tests:
-
instruments predict asset use (first stage chi-squared statistic of 316.47; p < 0.0001)
-
they are not overidentified, as shown by a Sargan score of 1.425 (p = 0.84).
The best-fitting model using Bayesian information criterion131 was one with five instruments: (1) distance to nearest asset, (2) this distance squared, (3) number of assets within a 1-mile radius, (4) number of assets within a 10-mile radius and (5) number of assets within a 15-mile radius. Table 16 presents results from the regression. Column 1 shows the first-stage results. Longer distances to the nearest asset reduce the probability of use (as expected). If the distance to the nearest asset increases by 1 mile, then individuals are 66% less likely to use assets. The number of assets in a local area is statistically significant only if that area is defined as within a 15-mile radius. In second stage results (the effects of asset use on quality of life), we observe a significant positive effect of use. Controlling for health conditions and their effects on activity reduces the effect, but it remains statistically significant.
| Analysis | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Model specification | Probit | OLS | OLS | OLS |
| Dependent variable | Asset use | EQ-5D | EQ-5D | EQ-5D |
| Controlling for | Socioeconomic characteristicsa | Socioeconomic characteristicsa |
Socioeconomic characteristicsa Presence of health conditions |
Socioeconomic characteristicsa Limiting health conditions |
| Community asset use | 0.226*** (0.163 to 0.290) | 0.177*** (0.093 to 0.260) | 0.137*** (0.051 to 0.224) | |
| Distance to nearest community asset | –0.659** (–1.096 to –0.222) | |||
| Distance to nearest community asset squared | –0.758*** (–1.160 to –0.357) | |||
| Number of assets in a 1-mile radius | 0.000768 (0.000 to 0.002) | |||
| Number of assets in a 10-mile radius | 0.0008 (–0.000 to 0.000) | |||
| Number of assets in a 15-mile radius | 0.0552*** (0.028 to 0.083) | |||
| Observations | 3470 | 3470 | 3470 | 3470 |
In analyses of the effects of asset use on utilisation and costs, asset use does reduce health-care utilisation and total costs, but the reductions are not statistically significant (Table 17).
| Dependent variable (second stage) | Coefficient | 95% CI | p-value |
|---|---|---|---|
| GP visits | –1.13 | –2.769 to 0.509 | p = 0.177 |
| Hospital (OP) | –1.09 | –2.621 to 0.437 | p = 0.162 |
| Total costs | –183.10 | –434.195 to 68.015 | p = 0.153 |
| Net benefit £12,936 | 2288.30*** | 1067.941 to 3508.697 | p < 0.001 |
| Net benefit £20,000 | 3264.20*** | 1473.523 to 5054.834 | p < 0.001 |
| Net benefit £30,000 | 4665.90*** | 2061.963 to 7269.757 | p < 0.001 |
Using the current NICE threshold values of £20,000–30,000 per QALY, we estimated that the net benefits of community asset use were £3624.20 (95% CI £1473.52 to £5054.83) to £4665.90 (95% CI £2061.96 to £7269.78) per participant per year (see Table 17). Using the threshold value proposed by Claxton et al. 125 gave a net benefit estimate of £2288.30 per participant per year (95% CI £1067.94 to £3508.70).
Longitudinal analyses: short-term effects (0–6 months)
We present a range of models estimating the effects of starting to use assets (Table 18), with the primary analysis being ‘nearest neighbour with five matches’ (see Table 18). Starting using assets increases EQ-5D scores (0.058, 95% CI 0.031to 0.085), but has no significant effect on GP or hospital outpatient visits. Analysis of net benefit showed large and statistically significant gains at all three thresholds.
| Difference | Treatment effect | p-value | 95% CI | Matching variable | Matching technique |
|---|---|---|---|---|---|
| EQ-5D score | 0.035 | p = 0.044 | 0.001 to 0.070 | (a) | Nearest neighbour with one match |
| EQ-5D score | 0.040 | p = 0.012 | 0.008 to 0.070 | (b) | Nearest neighbour with one match |
| EQ-5D score | 0.058 | p < 0.0001 | 0.031 to 0.085 | (b) | Nearest neighbour with five matches |
| EQ-5D score | 0.017 | p = 0.026 | 0.002 to 0.033 | (b) | Propensity score match with five matches |
| Number of GP visits | 0.238 | p = 0.421 | –0.342 to 0.819 | (c) | Nearest neighbour with five matches |
| Number of hospital (OP) visits | 0.321 | p = 0.341 | –0.339 to 0.980 | (c) | Nearest neighbour with five matches |
| Total NHS costs | 33.03 | p = 0.510 | –65.35 to 131.42 | (c) | Nearest neighbour with five matches |
| Net benefit £12,936 | 751.50 | p < 0.0001 | 349.30 to 1153.70 | (c) | Nearest neighbour with five matches |
| Net benefit £20,000 | 1197.86 | p < 0.0001 | 631.68 to 1764.03 | (c) | Nearest neighbour with five matches |
| Net benefit £30,000 | 1829.82 | p < 0.0001 | 1019.89 to 2639.75 | (c) | Nearest neighbour with five matches |
Table 19 shows effects for stopping asset use, whereby the reduced benefits associated with stopping were smaller than the benefits of starting and the change in net benefit was not statistically significant.
| Difference | Treatment effect | p-value | 95% CI | Matching variable | Matching technique |
|---|---|---|---|---|---|
| EQ-5D score | –0.036 | p = 0.006 | –0.061 to –0.010 | (a) | Nearest neighbour with one match |
| EQ-5D score | –0.020 | p = 0.064 | –0.041 to 0.001 | (b) | Nearest neighbour with one match |
| EQ-5D score | –0.019 | p = 0.033 | –0.037 to –0.002 | (b) | Nearest neighbour with five matches |
| EQ-5D score | –0.014 | p = 0.064 | –0.029 to 0.001 | (b) | Propensity score match with five matches |
| Number of GP visits | –0.210 | p = 0.125 | –0.478 to 0.058 | (c) | Nearest neighbour with five matches |
| Number of hospital (OP) visits | –0.018 | p = 0.912 | –0.3412 to 0.305 | (c) | Nearest neighbour with five matches |
| Total NHS costs | –10.09 | p = 0.708 | –62.84 to 42.65 | (c) | Nearest neighbour with five matches |
| Net benefit £12,936 | –185.11 | p = 0.190 | –461.90 to 91.68 | (c) | Nearest neighbour with five matches |
| Net benefit £20,000 | –297.21 | p = 0.143 | –694.89 to 100.46 | (c) | Nearest neighbour with five matches |
| Net benefit £30,000 | –455.91 | p = 0.119 | –1029.36 to 117.54 | (c) | Nearest neighbour with five matches |
Longitudinal analyses: long-term effects (0–12 months)
Table 20 shows long-term effects of asset use were similar to the short term. Effects on health-care utilisation remained non-significant, but net benefit increases were significant.
| Difference | Treatment effect | p-value | 95% CI | Matching variable | Matching technique |
|---|---|---|---|---|---|
| EQ-5D score | 0.043 | p = 0.045 | 0.001 to 0.086 | (a) | Nearest neighbour with one match |
| EQ-5D score | 0.042 | p = 0.005 | 0.01 to 0.071 | (b) | Nearest neighbour with one match |
| EQ-5D score | 0.050 | p = 0.001 | 0.022 to 0.078 | (b) | Nearest neighbour with five matches |
| EQ-5D score | 0.037 | p = 0.007 | 0.010 to 0.064 | (b) | Propensity score match with five matches |
| Number of GP visits | –0.693 | p = 0.168 | –1.679 to 0.292 | (c) | Nearest neighbour with five matches |
| Number of hospital (OP) visits | –0.122 | p = 0.438 | –0.431 to 0.187 | (c) | Nearest neighbour with five matches |
| Total NHS costs | –84.38 | p = 0.065 | –173.89 to 5.14 | (c) | Nearest neighbour with five matches |
| Net benefit £12,936 | 859.02 | p < 0.0001 | 444.01 to 1274.03 | (c) | Nearest neighbour with five matches |
| Net benefit £20,000 | 1235.96 | p < 0.0001 | 642.07 to 1829.85 | (c) | Nearest neighbour with five matches |
| Net benefit £30,000 | 1769.56 | p < 0.0001 | 913.00 to 2626.12 | (c) | Nearest neighbour with five matches |
The effects of stopping asset use were not statistically significant for EQ-5D and health-care utilisation, and were significant only in terms of net benefit, whereby the reductions were considerably larger in the longer term than the short term (Table 21).
| Difference | Treatment effect | p-value | 95% CI | Matching variable | Matching technique |
|---|---|---|---|---|---|
| EQ-5D score | –0.054 | p = 0.124 | –0.124 to 0.015 | (a) | Nearest neighbour with one match |
| EQ-5D score | –0.033 | p = 0.119 | –0.074 to 0.008 | (b) | Nearest neighbour with one match |
| EQ-5D score | –0.041 | p = 0.038 | –0.079 to –0.002 | (b) | Nearest neighbour with five matches |
| EQ-5D score | –0.020 | p = 0.342 | –0.060 to 0.021 | (b) | Propensity score match with five matches |
| Number of GP visits | 0.370 | p = 0.215 | –0.215 to 0.956 | (c) | Nearest neighbour with five matches |
| Number of hospital (OP) visits | 0.317 | p = 0.391 | –0.408 to 1.041 | (c) | Nearest neighbour with five matches |
| Total NHS costs | 51.72 | p = 0.412 | –71.76 to 175.20 | (c) | Nearest neighbour with five matches |
| Net benefit £12,936 | –668.20 | p = 0.044 | –1319.24 to –17.16 | (c) | Nearest neighbour with five matches |
| Net benefit £20,000 | –976.60 | p = 0.044 | –1928.47 to –24.74 | (c) | Nearest neighbour with five matches |
| Net benefit £30,000 | –1413.19 | p = 0.046 | –2803.06 to –23.31 | (c) | Nearest neighbour with five matches |
Use of care plans
The numbers of people reporting a care plan increased over time (baseline 6.4%, 12 months 8.9%, 18 months 10.7%). A similar pattern was observed when restricted to people with data at all three time points (baseline 5.4%, 12 months 8.5%, 18 months 10.4%).
We used a quasi-experimental approach and estimated the effect associated with gaining a care plan. As before, we used the nearest neighbour matching method to match older people who gained a care plan to similar individuals who did not get a plan between baseline and 18 months.
In all models the outcome is either perceptions of integration, patient activation or quality of life at 18 months. We tested the following models:
-
model 1 – matched on age, sex and living arrangements at baseline, 1 : 1 matching
-
model 2 – model 1 plus presence of limiting health conditions at baseline, 1 : 1 matching
-
model 3 – model 2 plus baseline value of outcomes, 1 : 1 matching
-
model 4 – model 3, 5 : 1 matching
-
model 5 – model 3, propensity score matching.
Results
Gaining a care plan was associated with significant increases in the proportion of patients reporting that their care was ‘joined up and working’ (Table 22). There were no associations between gaining a care plan and either patient activation (Table 23) or quality of life (Table 24).
| Dependent variable | Coefficient | 95% CI | p-value |
|---|---|---|---|
| Perceptions of integration (model 1) | 0.172 | 0.089 to 0.254 | p = 0.000 |
| Perceptions of integration (model 2) | 0.187 | –0.097 to 0.277 | p = 0.000 |
| Perceptions of integration (model 3) | 0.128 | 0.038 to 0.218 | p = 0.005 |
| Perceptions of integration (model 4) | 0.169 | 0.088 to 0.250 | p = 0.000 |
| Perceptions of integration (model 5) | 0.124 | 0.041 to 0.208 | p < 0.004 |
| Dependent variable | Coefficient | 95% CI | p-value |
|---|---|---|---|
| Patient activation (model 1) | 0.228 | –2.25 to 2.71 | p = 0.857 |
| Patient activation (model 2) | 1.796 | –1.32 to 4.91 | p = 0.259 |
| Patient activation (model 3) | 0.218 | –2.38 to 2.81 | p = 0.979 |
| Patient activation (model 4) | –1.96 | –4.40 to 0.48 | p = 0.869 |
| Patient activation (model 5) | –1.96 | –4.40 to 0.48 | p = 0.116 |
| Dependent variable | Coefficient | 95% CI | p-value |
|---|---|---|---|
| EQ-5D (model 1) | –0.028 | –0.07 to 0.01 | p = 0.199 |
| EQ-5D (model 2) | 0.136 | –0.021 to 0.0 | p = 0.452 |
| EQ-5D (model 3) | 0.018 | –0.01 to 0.05 | p = 0.230 |
| EQ-5D (model 4) | 0.032 | –0.01 to 0.06 | p = 0.005 |
| EQ-5D (model 5) | –0.027 | –0.62 to 0.01 | p = 0.140 |
Summary
We used cohort data to assess the causal relationship between care plans, use of community assets and patient outcomes.
Only a minority of patients reported a care plan at baseline. The numbers doubled over the period of the cohort, although the rates remained small (around 10%). Reporting a care plan was associated with increased feelings that care was integrated, but did not affect patient activation or quality of life. These broad outcomes are similar to a smaller cross-sectional study conducted as part of the evaluation of the North West London Integrated Care Pilot. 132
Self-reported use of care plans may not always accord with service measures. For many older patients, care plans are a relatively new clinical tool, and our previous work has highlighted the potential difficulty of measuring the presence or absence of care plans. 133 Although the rate of care plans reported here accords with other studies,74 it is possible for care plans to be created for patients who may either be unaware of the care plan or unfamiliar with the terminology used. Nevertheless, awareness of the plan and full involvement in the production of the plan is supposedly an important part of the process.
Asset use was associated with quality of life in cross-sectional analyses, and the relationship remained significant in analyses using instrumental variables and longitudinal approaches. Although confidence in the internal validity of that causal relationship cannot approach that of a formal randomised trial, the analyses make a significant contribution to the literature concerning the health benefits of asset use.
It is noteworthy that the benefits (and net benefits) of asset use are largely restricted to improvements in quality of life, as impacts on utilisation were small and largely non-significant.
There are methodological limitations to consider. The cohort was self-selected and attrition further reduced the sample size and representativeness. All measures were self-reported, which is appropriate for feelings of integration, activation and quality of life, but potentially less accurate for health-care utilisation. There is evidence that self-reports are reasonably accurate compared with routine data on utilisation,134 and since the analysis is largely focused on associations rather than absolute levels, the overall results may be reasonably robust to any self-report bias.
We highlight two issues in relation to the measurement of assets.
First, we used a simple binary measure of asset use, without any details as regards the amount or pattern of use. Although a more detailed assessment of asset use would have been preferable, our survey was limited in space to reduce respondent burden, and a more detailed measure was not possible. Further research using more detailed measures of asset use may report different findings, but we would expect the relationships demonstrated with a less precise measure to be conservative.
Second, we used a generic measure of community asset use. There is a lack of consensus over the scope of the term. Also, understanding among patients of the meaning of terms and how they relate to assets they use are likely to be complex. We used a scale that has been used before, but which was not directly linked to the interventions undertaken by the SICP community assets programme, which included a range of other activities (including well-being champions, volunteers in care homes, well-being plans, digital inclusion, falls prevention and malnutrition awareness). This is because the exact nature of those programmes was not clear when the cohort started, and it was felt that using specific terms for the assets used by the SICP would be potentially unreliable as they might not be known to patients. Therefore, linking changes in overall asset use (the 6% increase in those reporting use at waves 1 and 3) with the specific SICP investments is open to challenge. We can be more confident that changes in asset use over time are driving changes in health outcomes, but can only infer that the benefits seen here are only caused by the SICP.
Chapter 10 Results of implementation 1
Introduction
The aims and objectives of implementation 1 are detailed in Chapter 5. When these objectives were formulated, we assumed that the commissioning of the SICP would be stable over time, and that it would be possible to trace links between commissioning, overall project governance and outcomes. We intended to use a realist framework to structure the research,47,135 exploring contexts and mechanisms that appeared to support outcomes. However, in practice, the local and national commissioning context has been rapidly changing throughout the study, making it difficult to locate stable elements in the commissioning of the programme.
A number of national and local policy changes are relevant here. Local health-care organisations had an opportunity in 2014 to apply to be vanguard sites, which provided additional funding to test new ways of providing services. Salford took advantage of this, becoming a vanguard site in 2015. This brought with it new funding, new requirements for reporting and accountability and catalysed the expansion of the programme into integrated care for adults, including several service transformation plans and the establishment of an integrated care organisation (ICO). In addition, organisations within Greater Manchester took on a degree of devolved responsibility for health and social care, adding a new layer of local governance and rapidly evolving organisational structures. 136,137 These changes will be discussed in more detail in the rest of this chapter, but of relevance here is their impact on the original intention to pursue a realist approach. In the realist methodology, researchers define and refine programme theories about the contexts and mechanisms by which policy programmes have an effect. However, the rapid evolution of the commissioning context identified above made it impossible to identify any stable contextual conditions or mechanisms relating to the commissioning of the SICP. As each element of the programme was explored, and candidate mechanisms identified, the context changed, with new structures, governance procedures and commissioning mechanisms. Furthermore, we found little clear linkage between the commissioning, governance and oversight of the programme and the actual activity on the ground, with the three SICP mechanisms of integration continuing to be rolled out in ways that appeared to be little affected by higher-level organisational and governance changes. Seeking linkage between mechanisms and outcomes was therefore not fruitful.
Finally, realist evaluation seeks to identify local programme theories underlying change programmes before exploring in depth the contexts and mechanisms. This assumes that, once identified, programme theories remain relatively fixed, with deeper exploration aimed at identifying new mechanisms or clarifying contexts, with the final outcome being a modification or clarification of how and why the programme theory applies or does not apply. In applying this framework to our case we suggest that the development of the ICO was in fact underpinned by an entirely different programme theory than the SICP. The ‘decoupling’ that we identified between the commissioning and the implementation of the programme may stem from this change in underpinning theory. Together, these three factors rendered the realist evaluation approach unhelpful and have made it difficult to draw clear conclusions about the impact of the commissioning of the programme.
In this chapter, therefore, we start by providing a descriptive account of the changes affecting SICP commissioning and management, including the development and implementation of the SICP, the development of the ICO and the latest move towards an integrated care system (ICS). We provide an account of the programme-level factors that facilitated introduction of the SICP and its maintenance over time. We structure this with reference to the factors supporting large-scale health system change. 44,138 We then provide a brief account of evidence relevant to our original study objectives and finish by discussing the wider implications.
Section 1: commissioning and programme governance
Early development of programme commissioning and governance
Understanding the commissioning and funding of the SICP is not straightforward, as the programme was implemented and developed in a changing policy context. However, there are two core commissioning processes underlying the SICP: (1) national Section 75 funding and the associated Better Care Fund (BCF) and (2) the local Alliance Agreement.
Since 2006, local authorities and NHS commissioners have been able to pool aspects of their budgets to support joint initiatives, under Section 75 of the National Health Service Act 2006. Historically, these initiatives have been small scale (e.g. focused on joint commissioning for children with learning difficulties). Generally known as ‘Section 75 funding’, this continues to be the statutory underpinning for the funding of the SICP and the developing ICS.
In order to promote greater integration, in 2013 the Department of Health and Social Care announced the BCF,139 an ongoing national programme available to local authorities and NHS commissioners to jointly plan and deliver integrated services, with an initial intention that £3.8B of health and social care funding would be pooled from April 2015. The BCF did not introduce any new legislation; Section 75 remained the statutory mechanism. Local health commissioners were required to identify elements of their existing budgets to pool with local authority budgets. It was assumed by policy-makers that the costs of integrated services would be covered by the savings generated by a reduction in hospital admissions.
The BCF was announced after the start of the SICP. The SICP commissioning partners (CCG and council) had already agreed to pool £98M under Section 75. The BCF process (compulsory for all CCGs and local authorities) required them to submit plans to NHS England and the Local Government Association.
In response, the CCG identified £20M of its £98M pooled budget as its BCF contribution. There were problems with the BCF application, locally and nationally. 139 Locally, the situation was complicated by the existence of the wider agreement to pool a larger budget. This meant retrofitting existing plans to fit BCF requirements and submitting further evidence to satisfy the national process. In addition, there were specific problems surrounding the expectations about estimated reductions in hospital use:
We have been through the assurance process for the BCF; we have been approved with support. This is the second best rating. We have received a number of risk issues that we need to respond to by the end of November, several of them relate to each other. ID 6 spoke to the BCF and is working with the [S]ICP steering and finance steering group, the risks have now been reduced to 10. We are pleased that our plans to reduce emergency admissions have been accepted. Nationally they wanted to reduce emergency admissions by 3.5%, we put forward that we should reduce them by 1% locally. This suggestion looked like a sticking point but it has been accepted.
ID 16 senior city council manager
Taking the Section 75 and BCF funding together, the total SICP funding started out as £98M, rising to £112M in the financial year 2015/16. The CCG contributed two-thirds and the city council one-third. Before agreements were made, a process of mapping was carried out between the council and CCG, focusing on current services for the health and social care in older people. They specifically looked at services that were in scope (at least 50% of the service had to contribute to the care of older people); any services that were deemed in scope had to be 100% within the programme to ensure that the governance arrangements were adequate. This Section 75 pooled budget arrangement was different from any previous historical budget sharing, as the operational management of the budget was governed by an Alliance Agreement, which included both commissioners and providers. The service provision included in the budget was:
-
acute and community health via the foundation trust (£50M)
-
care services provided or subcontracted by the city council (£30M)
-
CCG expenditure including continuing health care and hospice (£10M)
-
older people’s mental health services from the mental health trust (£8M).
Although the providers were not funding the SICP, contingencies for a partner organisation’s cost improvement programme were included within the contract. As part of the contract setting, providers had their contracts reduced through tariff arrangements, to ensure that they achieved cost reductions.
The traditional approach to commissioning involves a ‘commissioning cycle’: assessing population need, assessing current service availability and suitability, designing appropriate services to meet needs, assessing the availability of relevant providers and procuring the service, managing demand and monitoring performance (see http://commissioning.libraryservices.nhs.uk/commissioning-cycle; accessed 18 May 2018).
The SICP worked differently. It did not matter whether partners were commissioners or providers: both were equally involved in the decision-making:
I think it’s having a bit of faith and constantly when people raise that, just really assuring them that . . . and I can’t remember at the beginning how many times I said this is a partnership approach, it’s a partnership approach. Because people used to say things like oh well, it shouldn’t be Salford Royal dictating how that happens. Well, it isn’t Salford Royal, it’s a partnership and we’re in the room, we get listened to. And it was just constantly reassuring. And it was a different way of working actually, it wasn’t a commissioner led . . . and it was just constantly reminding people this isn’t commissioner led. It’s a partnership and we have to give and take and compromise.
ID 6 senior CCG manager
In the early phases of the SICP, when contractual decisions were being made, providers were present as members of the Alliance Board, and perceived as experts who can offer useful information, even when the service being discussed was to be provided by a different organisation. This dynamic shifted the balance of the commissioning process:
Then we’ll have individual service contracts, so the CCG or the council will then go away and have contracts in place with the relevant provider organisation. Because it might not be Salford Royal or GMW [Greater Manchester West] that’s the provider. So GMW and provider when they’re in the room are from the alliance perspective, are giving their expert opinion in terms of what will work and how we will deliver the model to achieve the outcomes, not as an organisation we can do that and we want the contract to deliver that. Some instances they will have the contract, in other instances they won’t have the contract.
ID 11 senior CCG manager
Alliance Agreement
In addition to Section 75, the SICP was also underpinned by an Alliance Agreement. This outlined how decisions were made and the governance mechanisms which applied. The document articulated how the organisations would work together as a system of both commissioners and providers. Although sometimes referred to as the ‘Alliance Contract’, it was technically not a contract, as the provisions were not specific enough to be legally enforceable:
I mean if anything on reflection I think the Alliance Contract is about publicly saying, we’re going to work together. Contractually in blunt terms it’s probably not worth the paper it’s written on, if you know what I mean? It’s the principle of it.
ID 15 senior mental health trust manager
The document can be seen as a set of guidelines for behaviour. The document outlined the terms of the agreement (initially 3 years 5 months, with the option for a further 3 years). Such an extension would have to be agreed by all parties (except the general practice provider). The agreement included provision for an annual review, which was intended to ensure that the SICP was delivering its objectives. The Alliance Agreement was not a definitive document; many issues remained to be clarified and it simply set out the process by which such decisions will be made in the future. For example, clause 15 outlined that a framework for risk and benefit sharing needed to be developed. Timelines were included, highlighting when tasks needed to be carried out, but these lacked specificity about who should performing those roles. Furthermore, the document lacked specificity in terms of situations in which conflicts or disagreements may have arisen. The Alliance Agreement proposed a risk and benefit sharing framework, which would outline procedures if the pooled budget faced either an over- or under-spend (Alliance Agreement, internal report).
It was acknowledged that it was impossible to prespecify all possible future scenarios, with the Alliance Board seen as the forum in which any problems would be discussed:
. . . and the reality is, when issues do arise, the situation for each one is different and the factors for creating is different. So the Alliance Board use a forum for those conversations.
ID 5 SICP programme manager
Overall, the agreement could be seen as an agreement to agree at some point in the future, rather than an actual contract. The most specific aspect of the agreement was the scheme of delegation for decision-making (see Appendix 4, Table 61), which clearly defined what decisions could be made within the structure of the SICP without each decision having to be taken back to each partner organisation.
Alongside the Alliance Agreement, there was a detailed ‘service and financial plan’, which provided a breakdown of the pooled budget, with additional detail regarding the investment and disinvestment of services, BCF plans and the general models for implementation.
Although not a legal contract, respondents stated that the process of developing the agreement had been as important in supporting the early development of the programme as the details of the agreement itself. Simply knowing that there was a formal process of sign-up, with clear governance processes, allowed the key organisations to feel secure in decision-making. Presenting the details in the form of an Alliance Agreement made their declarations ‘official’ and provided legitimacy. The process of developing the Alliance Agreement allowed the key stakeholder organisations time and resources to think about what they wanted to achieve, outlining risks and benefits for the organisations:
But the benefit of the Alliance Agreement was primarily the process we went through to agree it. It was refining a shared vision. It was having the difficult conversations about, you know, what are our anxieties, what do we want to achieve. It codified the things we were setting out to do and our expectations of each other.
ID 4 senior foundation trust manager
Furthermore, individuals stated that part of the value of the contract was that the act of signing a document makes the stakeholder organisations more likely to work through issues when disagreements arose:
So it’s a big deal, you know, you sort of owe the other stakeholders once you’ve agreed this. Because people will walk away without any of that control, they always have, and will do. So hence there has to be an overbearing focus on governance, it dominates everything.
ID 3 senior CCG manager
During the period in which the Alliance Agreement was in place, no significant conflicts or disagreements arose. Therefore, the Alliance Agreement arrangement was never tested. It was acknowledged that, in part, this was because a financial buffer had been put in place, limiting the financial risk:
Yeah, so there was some slippage created and that balanced it out last year and then a couple of other things happened this year, so they knew that they’d got underspend within the Alliance budget . . .
ID 5 SICP programme manager
Towards an integrated care organisation
Not long after the SICP was established, moves began towards a formal ICO (mooted in CCG documents from July 2014). This would achieve two things:
-
move beyond the ‘partnership’ model underpinning the SICP, moving staff from the council social care team into the foundation trust alongside community services colleagues
-
extend the population covered to all adults.
The logic underlying this was not clear. In interviews, respondents simply characterised this as ‘the obvious next step’, without clearly explaining why:
I mean, obviously, one of the things that we’ve got to do in terms of the programme, I mean, we’ve moved onto the ICO rather than the integrated care programme but it makes sense because it’s the next step really.
ID 2 senior city council manager
This respondent spoke of greater ‘efficiency’, without clarifying what this might mean and how it might be achieved:
The agreement that was reached as the system was that the ICO itself needs to have benefits in and of itself, so it has to be more efficient to have more people together, so having social workers working in the same teams employed by the same body as district nurses, has to be more efficient. You have to be able to reduce some duplication etc., so the ICO has a target for efficiency. It comes as a result of bringing staff closer together.
ID 25 senior foundation trust manager
An ‘outline case’ briefing document was used internally to provide information for those involved in discussions about the ICO (Box 2). This document set out the advantages of integrated care and suggested that a more formal integrated organisation could overcome deficiencies in the partnership model:
4.6: although care can be integrated without creating an ICO, the advantage of this approach is that a single organisation with one funding envelope, a single set of goals and one vision for Salford’s health and social care economy is able to avoid many of the problems of fragmentation experienced in virtually integrated systems.
4.7: those areas that have sought to integrate services without some form of structural or functional integration have frequently experienced a number of difficulties in making integration ‘stick’. There typically include:
-
inability to align service delivery ‘on the ground’
-
organisational and professional silos
-
inconsistent operational procedures and policies
-
fragment information technology, information and reporting systems
-
different approaches to managing performance, risk and governance.
However, no evidence was forthcoming about the existence of these problems in Salford. Indeed, interviews with senior leaders in all organisations had emphasised the strength of the partnership model. The focus appeared to be on anticipating and preventing future problems. Thus, at an engagement event to promote the ICO idea, the focus was on the ICO as an obvious step in order to cement the gains made to date:
We are motivated by success and we have a really strong shared vision for the future. We want to harness what we have got and maximise benefits. All the main organisations have agreed to go a step further so that we can deliver services to all adults in an integrated way; integration will be delivered by an ICO or a lead provider organisation. This is a really big step and change but we will be working with the same outlines as we did for older people. Our vision is to deliver care in a different way, centred on individual needs to maximise the benefits.
ID 6 senior CCG manager engagement event
During interviews, individuals were asked what the ICO could offer that the SICP could not, especially as the programmes of work were essentially unchanged, other than expanded age coverage. The ICO was described as a structural mechanism enabling the transformation that the SICP was trying to deliver:
It’s structural [ICO] . . . by structural I mean employment, legal, etc. The integrated care programme is about transformation, so it’s about doing things differently . . . setting up a preventative way of working, supporting people to support themselves, etc., so clear goals and aims and all the rest of it. The ICO is an enabler to that, so by bringing staff together by removing barriers, by having one team Salford, it would be easier then to transform the work what we do, to deliver the goals of the [S]ICP.
ID 25 senior foundation trust manager
The SICP and ICO were not described as separate entities. Instead, the SICP was perceived to outline the strategy for the programme of work, whereas the ICO has been introduced as a mechanism to deliver the strategy:
. . . but the programme I suppose is a strategy and the ICO is actually the operational delivery, I suppose that’s one way, but they kind of knit it together, they’re not two distinct entities, if you like.
ID 17 senior mental health trust manager
The ICO was described as a way of providing a single leadership structure, which provided the co-ordination of services and reduces fragmentation. Although partnership working was perceived to be good locally, the single leadership structure of the ICO was an opportunity to better co-ordinate care. The ICO was identified as a means to examine care pathways more closely to ensure that there was one service for patients:
That’s four different hand-offs along a pathway. You know, it enables Salford Royal to look at it and go, d’you know what, it makes sense to have one service. People’s experiences is one experience, so . . .
ID 2 senior city council manager
One possible explanation for the decision to establish the ICO lay in the broader NHS. In 2014, NHS England published its Five year Forward View. 140 Central was a call for NHS and social care organisations to develop ‘new models of care’.
Five new models were proposed:
-
primary and acute care systems (PACS), bringing together acute hospitals with primary, community and social care providers
-
multispecialty community providers (MCPs), in which all types of community providers work together with their social care counterparts
-
extended care in care homes, in which local primary and community care providers work together with private- and council-funded care homes to improve care for patients
-
urgent and emergency care, in which different combinations of providers work together across a geographical area to rationalise and improve urgent and emergency care
-
acute care systems, in which providers of acute care work together to rationalise and improve provision of more specialised services.
Volunteer groups of providers (designated as ‘vanguards’) were invited to come forward to test these ‘new care models’, and would be provided with additional funding and support.
This provided an opportunity for the SICP, as national policy supported existing local plans. There had already been discussions about how the SICP could be extended and the model embodied in the SICP (close collaboration between a foundation trust, CCG, general practice providers, and the local authority commissioners and providers of social care) already met many PACS requirements. As the vanguard was aligned with existing local plans, linkage would offer additional financial support, as well as access to a network of providers undertaking a similar journey.
A second motivation lay in the more general environment for large providers. A 2014 review of provider activity and development for the Department of Health and Social Care141 highlighted both the need for innovation in the provision of care and the need for a facilitative regulative structure at national-level supporting providers looking to innovate. The report advocated allowing innovative providers to move ahead rapidly, with light touch regulation and support. The development of ICOs was one of the innovations advocated. The opportunity to be seen as at the leading edge of developments was attractive.
Thus, 2015 saw the introduction of a PACS vanguard with an intention to integrate primary and acute care systems, joining up general practice, hospital, community, social care and mental health services for adults. The ICO was to be established as the ‘prime provider’ of services across Salford, bringing the adult services provider arm of the city council into the foundation trust and subcontracting with other providers (such as non-specialist services at the main mental health trust) for a range of services.
The application set out what the vanguard hoped to achieve, building on the ‘successful’ elements of the SICP, aligned to a federated model of general practice. As discussed above, the ICO/vanguard included the transfer of adult social care from the city council to foundation trust, including the contracts for adult social care homes and domiciliary care. Furthermore, the contract for mental health services for adults and older people was also transferred to the foundation trust, which could be subcontracted to the mental health trust.
The practical issues associated with ICO set up were considerable. The aim was to bring together local adult health, social, mental health and acute care into one place, underpinned by a single health and social care contract for the ICO. For the foundation trust to take on this new role, a large number of staff moved across from council to trust under Transfer of Undertakings in Public Employment (TUPE) legislation:
We’ve been working on what we call an ‘on-boarding process’, so to welcome 400 people into the new organisation, they have to learn new systems for time recording, sequence recording – all sorts of things – e-learning. But that’s just the practical side of things . . . The other part of my role is around the business strategy side. I’ve been involved in the development of various legal agreements, contracts, and risk share agreements, which is hell of a lot of work, just to make sure that organisationally we understand the relationships for the future and there’s no barriers that could be created because we didn’t clearly articulate what the arrangement was, so . . . I think that’s quite a strength for Salford and has been for some time, that we’ve got a group of senior managers across the organisations that get together and think those agreements through in a very methodical way.
ID 6 senior CCG manager
Integrated care organisation implementation was rhetorically designated as a ‘safe landing’. It was agreed by all stakeholders that, for the future success of the ICO, the initial phase was to implement the ICO, transfer staff across and take on the responsibility without initially making any changes to how people work and how services are delivered. The stakeholders wanted to continue to work in partnership and not produce additional risk:
. . . the phrase we use is, safe landing, so nothing should change. The people who are receiving services . . . nothing should change because there should be a smooth transition, so that we’re not creating any risk in the system, but having said that, it is obviously different as well, so you’ve got to get it right for staff and so on. It is a period of change and we’ve been really clear and all partners have agreed that, yeah it will take a few months for that to bed down, but everybody should sort of move in to their new roles if you like, but also we’re all still here, we’re all still a partnership.
ID 25 senior foundation trust manager
Ongoing commissioning of integration: the ‘integrated care system’
As we have seen, the local and national policy context was constantly shifting, requiring those involved with integration services to adapt. The most recent change was the devolution of responsibility for health and social care to Greater Manchester in the devolution settlement. 136 This required all boroughs to produce a locality plan, setting out how health and social care services will work together and providing an opportunity for leaders to develop an overarching narrative, which pulled all the various initiatives together into a coherent whole.
Leaders now talked about an ICS, which aimed to make sense of the changes that have occurred and generate organisational and public ‘buy-in’. The partnership underlying integrated care was rebadged, with the overall aim of improving the health of the population through integrated care. The vision was expressed in the concepts of ‘start well’, ‘live well’ (addressed by the ICO, focusing on the adult population) and ‘age well’ (addressed by the SICP, people > 65 years of age).
The ultimate aim of the ICS was to link general practice more closely with the other stakeholder organisations to deliver services in a neighbourhood model. This would involve general practices working more closely together to provide services across a geographical footprint covering 30,000–50,000 people. To facilitate this, a general practice provider organisation would bring practices together and form a single body with which the ICO could contract and interact. How this would work in practice, and what the relationship would be between general practices and the ICS, remained unclear.
To support these developments, new governance and contractual mechanisms have been required.
In our initial interviews, it was suggested that the Alliance Agreement would form the basis for the ongoing developments. However, once it had been decided to move towards an ICO, a new governance structure was necessary. The ICO formally came into being in July 2016. The new ICS was focused on the integration agenda for the whole of the adult population, which included the original SICP. The new pooled budget covered £246M of expenditure.
The areas of work for the adult population were said to be based on learning from the SICP and will continue to include the programmes of work (community assets, MDGs and ICCs). The focus of the adult population will be across several key priority areas including:
-
vulnerable adults
-
long-term conditions
-
mental health (drug and alcohol dependency in particular)
-
dementia
-
mental and physical needs.
The aim of the ICS was to bridge a projected £6M financial gap over a 5-year period through service redesign. A new service and financial plan was devised for the whole adult population based on a pooled budget between CCG and council from 2016 to 2021. The budget included all adult social care, learning disabilities, community equipment, foundation trust hospital care, foundation trust community services, adult (non-specialist) mental care services (hospital and community), A&E, continuing health care and NHS funded care, and some CCG grants/contracts for non-NHS providers.
The plan for the ICS was developed in phases:
-
Phase 1 – in March 2016, an initial review of the commissioning intentions within the older people’s financial plan was conducted.
-
Phase 2 – in May/June 2016, a stocktake of the workstreams within the SICP was carried out, to set a clear work plan for 2016/17; pre-planned city council and CCG workstreams and service reviews were documented alongside the vanguard proposals.
-
Phase 3 – the amalgamation of the workstreams above, outlining the outcomes of the plan, shared programme risks and the process by which the plan will be delivered and monitored.
For the ICS to operate, commissioning intentions across Salford have been consolidated over a number of workstreams. The consolidation included:
-
older people’s service and financial plan 2014/15–2017/18
-
existing or preplanned city council or CCG workstreams and reviews
-
aspirations within Salford PACS (the vanguard application).
To oversee the ICS a new governance structure was developed to replace the Alliance Agreement and Alliance Board from June 2016 (see Appendix 4, Figure 13). There are now two new committees: (1) the Advisory Board for Integrated Care, which has a similar membership to the Alliance Board, bringing together commissioners and providers, and (2) an Integrated Adult Health and Care Commissioning Joint Committee (ICJC; see Appendix 4, Figure 14), which involved only commissioners. This was necessary to allow commissioners to make joint decisions about the pooled commissioning budget:
So it was felt to be more appropriate for us to move from an alliance of the two providers and two commissioners to the two commissioners making all the decisions about the pooled budget, the commissioning budget by agreeing a service and financial plan and keeping that as a commissioner only decision-making process . . . Now in reality there’s no way because of our history in Salford we would just go in a dark room and write that as commissioners and present it to the providers, it would still be an iterative process. So we’ve established two groups, there’s the decision-making board, which is a joint committee between the council and the CCG, and then there’s an Advisory Board which is quite similar to the old Alliance Board . . . But they do not have any decision-making. But if they felt really, really strongly about something it is going to have an influence on it, they might not be the decision-makers but it will have an influence. And if we reach a stage where we’ve got the Advisory Board saying one thing and the decision-makers say another then we’re in a bad place really so we have to sort that out.
ID 6 senior CCG manager
The ICJC would oversee the pooled budget across the council and CCG, whereas the Advisory Board has responsibility for the additional investment that has been received from the devolved Greater Manchester transformation fund to support the vanguard.
Devolution added another layer of complexity. The first year of being a nationally designated vanguard saw additional funding to support the work. This was non-recurrent, intended to support ‘transformational’ activity by, for example, allowing investment in infrastructure or to support ‘double running’. In the second year, vanguards were required to submit a further value proposition, setting out what additional funding they required. However, the Greater Manchester Devolution Partnership had negotiated a transformation fund with the Treasury, and it was decided that Greater Manchester’s allocation of vanguard funding was included in this total. The rebidding process caused delays and complications, but, under the transformation fund, Salford accessed £18.2M over a 3-year period:
But because GM [Greater Manchester] has a 5-year funding pot, we were able to secure commitment for more than a single year. So we put forward an application, as I say, over 3 years, so we’ve got a 3-year investment plan, which matches with the 5-year disinvestment plan. And our ICO and the arrangements that we’re establishing, and this investment and disinvestment, makes a contribution to closing Salford locality plans projected funding gap.
ID 4 senior foundation trust manager
However, ongoing funding depended on demonstrating impact:
We always have healthy debates here. We need to demonstrate that we are doing what we said or else GM will terminate the funding.
ID 4 senior foundation trust manager (September Advisory Board)
The contractual mechanism was a so-called ‘prime provider’ contract between commissioners and providers. This form was relatively new and untested in the NHS. A single large organisation is designated as the ‘prime provider’ for a range of services. This provider is then responsible for providing those services, either themselves, or by subcontracting with other providers. The foundation trust was the ‘prime provider’, with the scope of services covered including care for the entire adult population. Thus, the foundation trust will be contracted to provide acute and community care, subcontracting for mental health services. Under this contract, commissioners set the overall strategy and the prime provider was then responsible for service delivery within the specified budget, as well as the quality of subcontracted services. The contract will usually include a range of incentives and risk-sharing provisions. The original intention was that the foundation trust would also subcontract for some services provided by general practices, via a primary care provider organisation. However, this proved difficult.
General practice was an important strand in the initial vanguard plan:
The vision is that general practice, at a neighbourhood level, will collaborate and embrace all community-based health and social care services for a defined population. This includes other primary care based services; pharmacists, dentists and opticians, as well as community and voluntary organisations. It is expected that all care that doesn’t require hospital facilities will be based and managed in the neighbourhood and for pathways of care crossing into hospital to be better for patients. Personalised care planning will benefit from a multiprofessional approach, drawing in specialist expertise and resources as needed.
Vanguard value proposition, internal primary care document
However, interviewees acknowledged that, in developing the ICO, less attention had been paid to engaging with primary care in the development of this vision. General practices, although engaged in the SICP via their participation in MDGs, remained largely detached from the broader ICO development:
So I think . . . well, some obviously GP practices no matter how often you try and talk to them they don’t really have time to listen, do they, really? They weren’t necessarily listening and then there were lots of misunderstanding about what we were doing and then jump to [conclusions] . . . and everything felt like two steps forward, one back and everything.
ID 6 senior CCG manager
An intensive programme of engagement work was launched in spring 2015. Conducted by the CCG, the intention was to encourage member practices to become more involved with the integration agenda. Later, this included the appointment of an external consultant (January 2016), who engaged with local GPs. This engagement highlighted the lack of connection between the broader agenda of the ICS and the wider NHS, and the day-to-day reality of GPs’ working lives:
What was immediately clear is actually GPs were largely disengaged from most of the process that had been going on. So by that what I mean is actually most people were unable to articulate what a vanguard was, nearly everyone was unable to articulate what the ICO was. Very few people had heard of Five Year Forward Views and the like, and actually when you started to talk about the context of integration in general practice, most of the stuff that the GPs wanted to know was ‘is this going to relieve my workload, is this going to help me with my workforce’, and occasionally ‘is this going to help me with my premises, which is also under pressure.’. So, once again, it wasn’t that GPs were pulling against the idea of an ICO, it’s just it wasn’t relevant to their day jobs.
ID 26 independent GP
Summary: commissioning integrated care
As we have highlighted, the development of the SICP and the ICO fundamentally changed the relationship between commissioners and providers. Rather than commissioners identifying needs, specifying services to meet those needs and then procuring relevant services, commissioners and providers in Salford are working in partnership, co-designing services. This was clearly seen during the fieldwork; when observing the Alliance Board meetings, an observer would not be able to tell which participants are providers and which commissioners. The commissioners, any more than any other partner, do not set the terms of the discussion, and there is no ‘challenge’ from commissioners. Rather, the focus is on a partnership approach. This raises questions about the longer-term development of the commissioner role, as it seems likely that future service developments will be provider led. In addition, as a prime provider, the foundation trust will be commissioning and contracting for mental health services on behalf of the CCG, leading to potential longer-term complications around conflicts of interest:
There is the potential the SRFT [Salford Royal Foundation Trust] will change as they commission services as they will have different agendas, will the CCG pass on that infrastructure / resource? We need to be clear what the purpose of the CCG is. The CCG may choose to commission PC [primary care] and they still have an acute agenda, but for MH [mental health] this will be delegated to the ICO. There will be potential conflicts of interest with the roles of commissioning and providing. They need to be clear what the commissioning agenda is and what is the provider agenda is. This is difficult as there is an invisible wall where commissioning ends and providing starts. For example if in the future in the MDGs, SRFT feel that GMWFT [Greater Manchester West Foundation Trust] aren’t providing mental health to the standard they expect, they may challenge as a commissioner but then we could argue that there aren’t enough district nurses which is a problem for them as a provider.
ID 17 senior mental health trust manager
Furthermore, the development of this strong partnership gave providers in the room some power over other (non-partner) providers locally. Contractual arrangements with these other providers were discussed at partnership meetings, and this could give foundation trusts an advantage. Although this can be viewed as potentially detrimental with regard to competition, it could also be argued that having the high-level people sitting around a table offers a forum in which commissioners and providers can have discussions beyond the SICP to bring about change, and that this may be more effective than competition as a means of improving services. For example, at one Alliance Board there was a need for the CCG to commission more beds at the trust:
We’ve invested in SR [Salford Royal] for 18-month contract for beds, etc. whilst the review is worked through. For community equipment we have supported the business case in principal, we need some more information. The good news is that this is major investment area for the programme.
ID 11 senior CCG manager
When the ICO was in development there seemed to be a need to re-establish a distinction between the commissioner and provider roles. During interviews, key stakeholders were asked why the roles were being separated. It was explained that it was a request of the commissioners and was required if they would be working in a prime provider model.
I think there’s a lot going to one place, so I think commissioners needed a way of holding that to account, so I think that’s one thing. I think the second thing is that the city council’s obviously changing its role . . . moving from being a direct deliverer of services to being a commissioner of services, so I think the view was that was part of the process of allowing the city council to move into its new role of being a strategic commissioner.
ID 25 senior foundation trust manager
-
The change in the relationship was described as a mechanism to clarify roles and responsibilities. However, the new arrangements do not override all of the partnership working that has been established:
So that’s slightly delineates responsibilities more, you know, it’s much clearer now. Salford Royal is responsible for making integrated care happen through a supply chain. And the commissioners have the responsibility for commissioning from Salford Royal as the prime provider, the range of integrated care services and outcomes that they want to achieve. That doesn’t mean that we’ve reverted to just a contractual relationship, you know, but that world exists in parallel – and I mean that in a good way – to one where we are sitting down as partners and debating what is it that we want to do.
ID 4 senior foundation trust manager
During an observation of the Advisory Board there was an acknowledgement that there were a number of committees that were commissioner or provider only. However, the majority were still perceived to be following a partnership model of working:
There are other sources of finances separate from here. In terms of the governance, I think it is important that we are still all working in partnership other than a couple of committees.
ID6 senior CCG manager
The consequences of the new working relationships are unclear. However, observations of the workings of the Advisory Board suggested that the separation between the commissioners and providers has led to additional complexities being introduced into the structure of the partnership and the financing of specific projects. The Advisory Board has the decision-making responsibility for the non-recurrent investment funds allocated to the ICO from the transformation fund, whereas the ICJC will oversee the pooled recurrent budget across the council and CCG for the adult population. Although they are clearly separate ways of funding programmes of work, it was identified that some specific programmes of work will obtain funding from both budgets. This will impact on how and where decisions are made, underlining the need to tightly manage communication.
These complexities will arise in other vanguard sites as they establish new models of care. There is work being undertaken by the national team responsible for vanguard development to support them as they navigate the new relationships required. The test will most likely come if a prime provider fails to deliver the outcomes for which they are contracted.
At the onset of this research it was assumed that the commissioning of the programme would be stable, and that it would be possible to explore the relationship between SICP progress and success and the mechanisms used to commission it. In reality, partly owing to the ambitions of those leading the programme, and partly in response to conditions in the wider NHS, the commissioning and governance structures associated with integrated care were in constant flux. It is therefore very difficult to make links between programme commissioning and governance, the extent to which implementation has been successful and the achieved outcomes. Although the structures and governance of the SICP were changing in the fundamental ways, the work of the SICP has continued more or less unchanged. A ‘stocktake’ determined that there was as yet no evidence that the programme will meet the initial agreed targets (e.g. reduce hospital admissions), but no specific changes were suggested other than to continue with the ICO implementation.
In the next section we explore the factors that seem to have supported or inhibited setting up the SICP.
Section 2: understanding system change
As discussed in Chapter 3, a review of major health system change identified ‘five rules’, which support successful change;44 these were subsequently modified. 138 Four of these modified rules of the greatest relevance to this chapter are set out in Table 25.
| Rule | Adapted rule |
|---|---|
| Blend designated leadership with distributed leadership | System-wide authority is needed to align multiple stakeholders over a large scale and encourage clinical commitment to system-wide improvement goals |
| Establish feedback loops | Feedback may need to be combined with other tools to encourage behaviour change (e.g. financial incentives) |
| Attend to history | Contextual factors can be a barrier to implementing lessons learned; political authority may be needed to challenge the existing context and enable more radical forms of transformation |
| Engage physicians | Need to involve a range of stakeholders in planning major system change and have a system-wide governance structure to align their interests |
Rule 1: blend designated with distributed leadership
The SICP was strongly led from the top, including strong representation from senior managers on the Alliance Board. Furthermore, there had been stability among these managers. The foundation trust initially took an overall lead given the disestablishment of PCTs and creation of CCGs; as well as initially driving the agenda, it was also prepared to commit more resources.
Furthermore, senior leaders were prepared to commit significant amounts of time. Weekly meetings were held between key people involved with the development of the programme:
And I think one of the things I learnt from the programme is that momentum of meeting weekly, being really disciplined in doing the work and meeting weekly really started to pay off quite quickly, in that it really got the momentum going in that project . . . So it sounded really over the top to me, weekly, it really did. But I think as long as you don’t set yourself massive tasks during the intervals, or give yourself dates to do certain things.
ID 6 senior CCG manager
At the same time, a robust management structure was also developed, with strong commitment from the middle management in partner organisations:
So we’ve got some executive and chief officer leadership, there’s some sort of second line reports beneath that level where there’s some dedicated time, and that’s largely about kind of the governance of the programme through the finance and steering group now. There’s a dedicated project team, and then we’ve got some operational capacity, so people in city council, in Salford Royal mostly, a little bit in GMW [Greater Manchester West] where we’ve released capacity, we’ve said, actually, this is really important to us . . .
ID 4 senior foundation trust manager
This structure included a clear system of delegated decision-making. This was important in supporting the day-to-day running of the programme. Our interviews suggest that, in the early stages, close partnership working between senior leaders from both the commissioners and providers was important in deciding what the interventions should be and in getting the programme running. This was particularly important in the time and effort invested in developing the Alliance Agreement.
Working together to produce an agreement supported the partners in developing a trusting relationship, which in turn supported the development of the programme as a whole. Once implementation was under way, however, the focus of these senior leaders on the Alliance Board shifted towards the development of the ICO and the vanguard, leaving the middle-level managers to get on with the day-to-day tasks required to run the programme. The scheme of delegation allowed the middle tier of managers to operate with some freedom within the confines of their delegated authority, in keeping with the need to allow those below the most senior level of management to provide local leadership. 44 The leadership for the integration agenda as a whole has remained the same throughout the development and implementation of the SICP, ICO and ICS. The same people representing the four key stakeholder organisations have been involved with the partnership, which has enabled trust and consistency to be developed. This has allowed individuals to carry out the work required of them, rather than working on establishing relationships and trust across the organisations.
Alongside this, the programme was set up with designated managerial time and support, further facilitating ‘distributed’ leadership. Thus, for example, initial work on the programme was carried out with support from an independent innovation and improvement centre.
Rule 2: establish feedback loops
‘Feedback loops’ about performance are an important determinant of success in large-scale change. However, although helpful, other tools to support behaviour change – such as financial incentives – may be important. 138 The SICP was set up with clear performance goals, centring on reduction in admissions and the improvement in patient experience. The Alliance Board received regular reports about performance against these metrics. However, delays in establishing elements of the programme allowed those involved to develop a narrative which emphasised the longer-term nature of expected improvements:
. . . and what people have fed back to me is that it has taken longer than was anticipated to implement, . . . the point at which people say yes, this is up and running and people . . . it’s embedded, it’s become the way of doing things, you would then start to see something . . . some impact, so that’s . . . and I think from what I understand there are starting to be some initial . . . [impacts].
ID 5 SICP programme manager
There were also concerns about the data that was being used to monitor the programme indicators:
Another measure, not a local measure but certainly it gets a lot of national attention and is one of the Better Care Fund measures is our delayed transfers of care. That has significantly reduced since we’ve been doing this programme, however, I am dubious about the data quality of that particular measure and this goes back many, many years in that it is open to a little bit of interpretation when that’s a delayed discharge.
ID 6 senior CCG manager
The governance structures of the Alliance Agreement were such that the Alliance Board – with the senior leaders – was the primary reporting forum for such data. Although the boards of the individual organisations each received progress reports from the Alliance Board, ownership of the performance metrics sat with the Alliance Board. At the same time as these somewhat disappointing metrics were being reported, the Alliance Board was undertaking the complex work of establishing the ICO. This brought about considerable changes to the working lives of those affected, in particular city council staff. As we have seen, motivating such staff and making the considerable changes needed required enthusiasm and momentum to be generated, which in turn required a positive narrative of success. Thus, in engagement events, a positive message about the achievements of the SICP was required. It is possible that this inhibited more critical reflection on progress.
This suggests a further mechanism, which may be important in the operation of feedback loops. The presence of the most senior leaders from the partnership organisations on the Alliance Board was very helpful in establishing the programme. However, as implementation proceeded, it is possible that the fact that ownership of performance metrics sat at Alliance Board level acted to limit independent or critical scrutiny by the boards of the constituent organisations. Thus, our study suggests that, although a strong governance structure is important in establishing a programme such as this, which requires joint working across organisational boundaries, it is also probably important that the individual boards retain ownership of the performance of the collaboration, and that those in receipt of the information are not limited in their ability to respond by the demands of implementation.
The SICP did not establish any specific incentive mechanisms at programme level beyond the overall incentive that if savings were made they could be reinvested in relevant services. As we have seen, the Alliance Agreement made reference to the establishment of risk and benefit sharing mechanisms, but these were not formally elucidated. In the other workstreams, incentives for engagement were indirect, couched in terms of the ability to provide a better service.
Rule 3: attend to history
Our interviewees and those we observed in meetings clearly expressed the opinion that the establishment of the SICP owed much to local history, highlighting longstanding collaborative working and working relationships over a considerable period of time:
So in Salford, we’ve got a very strong record in terms of joint working. So from a commissioner-only perspective between the council and the PCT [primary care trust] that was and the CCG, we’ve got a track record of pooled budgets and the council taking lead for commissioning on services and CCG for the others. So we already had pooled budgets in place for immediate care, for the equipment service, for learning difficulties. And we’ve got joint appointments. So we’ve got a pool of commissioning managers that work across the council and the CCG as well. So we’ve got some very good examples of how we’ve worked collectively as commissioners. So we’ve got that history.
ID 11 senior CCG manager
At the same time, it was acknowledged that the geographical and organisational context (shared boundaries and similar geographical coverage) was important. Moreover, this has been stable for many years:
Salford has quite a reputation for being a very strong partnership-focused district, and if you were to look at the underpinning behind that there are a number of aspects that I think it’s fair to say are drivers for it, so it’s had a stable boundary, so it hasn’t had to go through constant upheaval in terms of boundary changes like Lancashire or other districts have had with bits of it coming in and going out.
ID 10 city council public health
Unlike the earlier study,138 there was no clear evidence that this strong shared historico-geographical context acted to limit the ambition for significant change.
Rule 4: engage physicians
In keeping with the model of major system change,138 we found that engagement must include a much broader range of stakeholders than simply physicians. In the early phases of the SICP there had been some engagement work with community service providers, social care staff and some interested GPs to define the model. Wider engagement was carried out with staff affected by the ICO. Interviews suggested that such outreach work had been fairly successful in generating a shared sense of purpose. Thus, interviews with individuals across the stakeholder organisations, revealed a consistent view about the programme. The development of the SICP was about developing a system of work rather than a series of initiatives:
So I suppose part of this is an all-system approach to seeing that the right people get the right service at the right time. So that is the aim of just enough support, I suppose.
ID 9 city council manager
Individuals in the CCG and the council highlighted the need to focus on prevention:
You’ve got an acute sector that has a very, very unusual leadership style, which basically I think recognised very early on that growing the acute economy was not the future, so a sense that you could not build a sustainable model for Salford Royal on the basis of just hoovering up additional acute activity, but recognising that it needed to think about new areas of business, new models of delivery, get away from simply acute focus care and begin to think about where it could operate full pathways into the communities – only into some of those areas where you might be talking about preventative types of activities.
ID 10 city council public health
However, as we have indicated, engagement of the broader population of local general practices was limited, and this limited the ability of the ICO to deliver its more ambitious plans for primary care. General practices remained independent contractors and, although practices are members of the CCG, it is not clear what this ‘membership’ really means. 142 The local experience suggests that CCG status as a membership organisation does not mean that CCG leaders can speak unequivocally on behalf of the members. The CCG was a key partner, but GPs were more detached:
Salford who had basically done a lot of work on the ICO but were finding that general practices’ role within the ICO was probably actually further away than it had ever been, but with the failure of their local [in inverted commas] GP federation to engage, but also the fact that actually general practice had very different priorities.
ID 26 independent GP
General practice engagement proved problematic in two ways. First, as discussed in implementation 2 (see Chapter 11), in the early stages of MDG development, general practice involvement was not always easy to obtain:
I can talk from personal experience about my practice, my practice is one of the practices involved in the MDGs and our experience has not been positive so far of MDG working, in that we don’t feel we’ve got anything out of it, we don’t feel it’s reduced admissions, readmissions or anything, so I expect it to be quite negative. To such an extent that the partner who’s going stopped going so our practice hasn’t been involved and we’re the only practice in [the neighbourhood] that hasn’t been involved.
ID 14 CCG GP
General practitioners struggled to take time out of practice, and good engagement was obtained only when reimbursement was increased. Second, GP engagement in the ICO was also limited. Investigation by an independent consultant revealed significant pressures:
Then actually that was quite revealing in itself in that there was this perception that GPs were not engaging, well actually it was just the fact that they weren’t informed and it wasn’t that no one was trying to tell them, it was just once again that some of them are actually worried about their very survival beyond the end of this year, so people start talking about stuff that’s going to be happening in the next few years, it sort of becomes abstract for them.
ID 26 independent GP
They also expressed concerns that the foundation trust was becoming too dominant:
I know, and people keeping asking why SRFT [Salford Royal Foundation Trust] are in charge of the neighbourhoods. I’ve said that SRFT are not, this is a partnership. So in terms of primary care, we have suggested that people who join the neighbourhood groups can be represented on the ICO group.
ID 6 senior CCG manager
These findings suggest that the need identified for ‘system-wide authority’ invested in individuals or groups in order to align multiple stakeholders138 may be difficult when general practices need to be engaged in a change programme.
More widely, there were also some issues with engagement with other stakeholders.
For example, some of those working in community assets found that they were isolated from the rest of the programme and experienced confusion around the terminology (often medicalised) used by others in the SICP:
To come in cold and then try and understand what it was about and then try and develop well what does . . . because in the end community assets is a bit, I don’t know, I suppose it sits outside slightly or did sit outside slightly. In the early days people really thought about what that would mean or how that might fit within the programme, people were still perhaps thinking about services, so the council services, about hospital provision, they were thinking much more along those lines. Whereas this project’s grown and developed and community assets have been able to influence a bit more, people are now starting to think about well actually the priority is what can we support to enable people to stay at home and live their lives.
ID 12 voluntary sector
Rule 5: engage with patients and the public
This issue is covered in implementation 2 (see Chapter 11) and in PPI (see Chapter 3).
Section 3: answering study questions
In this section we briefly summarise the evidence relating to our original objectives. The intention here is to bring together the evidence that we have presented in the previous sections in summary form in order to answer our initial research questions, before putting these in context with reference to other research and our analytical framework in the Discussion.
How do commissioners view the programme, what they expect from it and how it is seen in terms of their objectives?
It was envisaged that the SICP would be seen by the CCG as something they were commissioning, alongside other programmes. In practice, however, CCG leaders were committed to the programme as equal partners. The SICP was seen by the CCG as essential to contain costs and improve quality, and there was a significant commitment to partnership working, whereby the needs of individual organisations were subsumed to the needs of the programme.
However, the development of the ICO and the institution of a ‘prime provider’ contract led to the establishment of formal governance arrangements which reintroduced a separation between commissioners and providers. At the time of data collection, the implications of these changes to the governance and the formal ICO arrangements were still unknown. In particular, it will be interesting to see whether or not the reintroduction of a separation between commissioners and providers leads to a different approach to outcomes and performance management.
How is the programme viewed by strategic partners such as the local authority and how is it sustained under financial pressure?
History played a pivotal role in encouraging the main stakeholder organisations to develop the SICP and the Alliance Agreement. Positive experiences of working together in the past enabled them to develop the SICP and recognised that they all had a vested interest in the programme. All stakeholders discussed the potential difficult decisions that would need to be made. However, they believed that the organisations were willing to face organisational challenges without walking away from the programme. The collective success of SICP was deemed to be more important than individual organisational gains.
The financial pressures that were being faced by all organisations provided an incentive to senior leaders to support their organisations to work differently. Although the foundation trust and CCG were perceived to have a strong financial position, there was recognition that all organisations were working together, and, therefore, the shrinking local authority budget was not considered to inhibit partnership working. However, it remains to be seen in the longer term whether or not developing financial pressures affect the work of the ICO.
The role of Greater Manchester West Foundation Trust (GMWFT) in the SICP was different from the other three stakeholder organisations. GMWFT provided services to a wider geographical footprint, and its interaction with the programme was perceived to be more distant at times. For example, GMWFT did not have as many staff working on the SICP or attending high-level meetings. This different relationship was also identifiable in the move towards the ICO. GMWFT did not have a formal role within the organisation, and its services were to be subcontracted by the prime provider.
The local development of SICP was further supported by national policy and an appetite to introduce new models of care (vanguards), which provided Salford with an opportunity to get additional investment into the local health and social care economy. Moreover, the vanguard status also gave Salford organisations the prospect of recognition as exemplars of new approaches to service delivery. The decision to move to a formal ICO was made collectively by all stakeholder organisations. We were unable to find any evidence that this decision was based upon an appraisal of the impacts of the SICP; the focus appeared to be on the prevention of future problems rather than evidence of SICP success.
Overall, the programme involved a strong partnership between all the organisations involved. All stakeholders that we interviewed expressed their commitment. However, the question as to how the SICP figured in the broader strategic plans of the stakeholder organisations was reduced in relevance by the decision to move towards an ICO. It is possible that the early decision to move towards an ICO was prompted, in part, by financial pressures, but this was not clearly articulated by those involved.
How does the programme impact on the work of the two foundation trusts, in particular how the integrated community and acute provider adapt to reductions in inpatient activity?
This question presupposed that acute hospital activity would be reduced. In practice this has not happened (see Chapter 12).
How does the programme impacts on primary care, in particular general practice?
We have described and explained how the SICP, overall, struggled to engage with general practices, and we have considered some of the underlying causes of this, as well as identified solutions.
How far are the financial incentives (explicit and implicit) in the local health and social care system aligned with the ambitions of the programme?
The SICP did not put in place any specific incentive schemes, other than direct payments to GPs to take part in MDG work and the implicit incentive that any money saved could be reinvested in services. The initial funding for GPs was not deemed to be adequate to cover their costs and time; therefore, additional funding was required by the CCG to ensure GP commitment. The CCG funded local GPs through a local enhanced service for patients with long-term conditions. It was found in implementation 2 (see Chapter 11) that GPs were being funded twice – both by the local enhanced service and through the SICP – for doing similar work. This demonstrates how the objectives of the CCG mirrored that of the SICP, but also highlights difficulties associated with engaging GPs. Over and above the GP-related work, we did not see any evidence of reliance on specific financial incentives to implement SICP, other than the general incentive that it was argued that the programme would improve the sustainability of the local health economy.
Discussion
This chapter has explored the initial establishment and the early operation of the SICP, the introduction of the ICO and a move towards an ICS. The governance arrangements in Salford have been changing rapidly. This makes it difficult to identify specific commissioning mechanisms that could potentially underpin ‘success’. Indeed, we found a disconnect between commissioning and governance activity and the implementation of programmes of work on the ground. This is an important finding. In addition, we have highlighted the factors supporting the development of the programme and explored the nature of the commissioning and contracting involved. In this final section we will consider the wider lessons arising from the commissioning and implementation of the programme to date.
What type of integration does the SICP represent?
As discussed in the initial literature review (see Chapter 1), there are many different ways of defining integrated care. Bringing together our observational evidence, interviews and documentary analysis, we have identified two somewhat different ‘programme theories’. Figure 6 sets out our interpretation of the theory underlying the SICP as it was conceived. Figure 7 sets out our interpretation of the programme theory underpinning the latest developments.
FIGURE 6.
Overall programme theory underlying SICP (initial thinking). LA, local authority; SRFT, Salford Royal Foundation Trust.
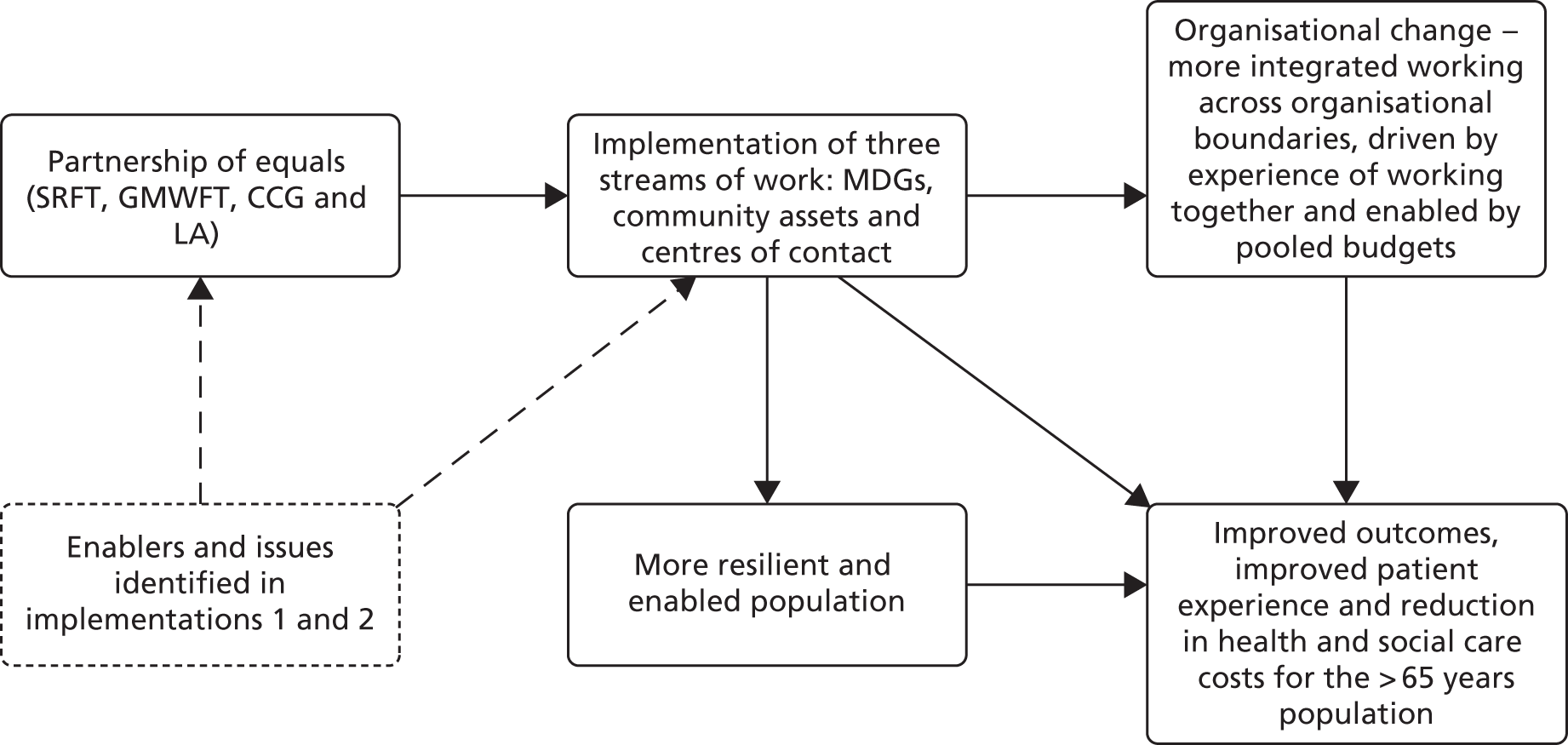
FIGURE 7.
Overall programme theory underlying Salford ICO/ICS (from July 2016).
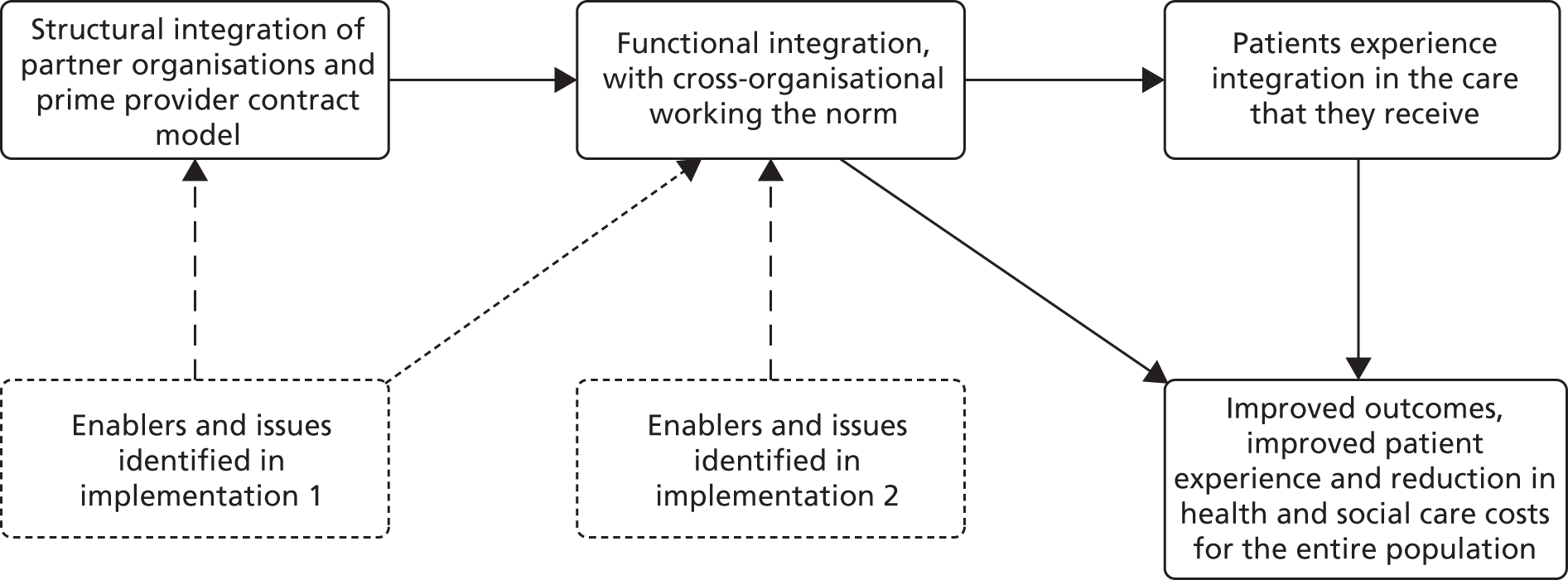
In its initial phases, the SICP was underpinned by a strong ideal of partnership working. The three programmes of work were identified as targets for service change and it was assumed that the experience of working together would break down organisational barriers and support wider improvement. At the same time, the programmes of work would support local people in becoming more resilient. This suggests a model of integration in which the focus is on functional and service-level integration, in which staff from different organisations work together across organisational boundaries. From this perspective, the integration of systems [such as information technology (IT) or financial systems] develops out of what is required to make collaborative working possible.
For the ICO (and subsequently the ICS), those involved told us that closer structural integration (with organisations either subsumed into the foundation trust or subcontracted by them) would lead to the embedding of functional integration, in which working together across organisational and professional boundaries would become the norm, leading to better outcomes and patient experience. This view of integration assumes that the integration of systems, financial flows and management systems is a prerequisite for integrated working. In this model, integrated organisations and systems come first, with integrated working flowing from this. The initial vision underpinning the SICP focused on the value that would be derived from the functional integration associated with the three programmes of work. By contrast, the vision underpinning the ICO suggests that, to be successful, such functional integration requires structural integration.
Our study, which has finished just as the development of the ICO is coming to fruition, cannot adjudicate between these two approaches. Indeed, it could be argued that these changing underlying assumptions and beliefs simply reflect the changing context of the NHS. This includes two important macro-level pressures: the national drive towards the formation of new models of care under the vanguard programme, in which elements of structural integration, although not essential, are encouraged; and a worsening financial environment in which all NHS and social care commissioners and providers are struggling to balance budgets. In this environment, the creation of larger, more streamlined organisations which are able to reduce duplication may seem an attractive proposition, regardless of the impact on the delivery of more integrated care.
Supporting and commissioning large-scale service change: comparison with other research
We have used the published framework for understanding large-scale system changes. 44,143 This proved valuable in analysing our findings, and our evidence confirms and amplifies the importance of some elements embodied in the framework.
First, the local experience highlighted the value of the clear scheme of delegation, which allowed middle-level managers to exercise local leadership within delegated resources. This allowed the programme to be implemented while senior leaders were engaged in developing the next phase.
Second, our study reaffirmed the importance of history and geography in providing a context within which change programmes can be implemented. This included good personal relationships, which had developed over many years, and a local geography, which allowed coherence around a core group sharing the same geographical footprint. Although some senior personnel did change towards the end of our fieldwork period, respondents were clear that the trust developed by working together on complex agreements over time was a vital ingredient in its ability to implement the ICO.
Third, our study suggested an interesting nuance in the need to establish feedback loops, particularly in the context of an evolving programme. The establishment of an Alliance Board, which included the most senior leaders from the contributing organisations, may have acted to limit the scrutiny of outcomes. Our study suggests that, although the establishment of a strong governance structure for a collaborative venture is important, it is probably also important that the individual boards of the collaborating organisations retain ownership and scrutiny. In establishing feedback loops, it is thus important that those in receipt of the information are not limited in their ability to respond by the demands of implementation.
Finally, our study re-emphasised the need to engage with stakeholders. Although some emphasise the need to engage with a wide range of local stakeholders,143 the local experience suggested that engagement of GPs had a specific impact. The plans involving general practice included in the ICO vanguard application remain some way from fruition and have required an intensive process of engagement.
Looking at previous research, the most comprehensive analysis is that of the ICPs undertaken by RAND. 51 In Table 26, we compare the findings. The RAND report also highlighted potential ‘enablers’ to integrated care, which are compared in Table 27.
| RAND report: activities required for integration success | Comparisons with SICP |
|---|---|
Building governance and performance management systems:
|
In Salford they had Alliance Contract which formed the governance of the SICP:
|
Making and developing the local business case for integrated care:
|
The potential benefits of the SICP were worked out by the main partners in collaboration and with the support of a local quality improvement organisation:
|
Changing attitudes and behaviours:
|
Engagement:
|
Developing the necessary infrastructure (including IT):
|
Salford infrastructure:
|
Establishing supportive financial systems and incentives:
|
Finance:
|
| RAND report enablers | What happened in Salford? |
|---|---|
| Strong leadership was repeatedly cited as key to the success of pilots. Existing personal relationships between individuals also helped pilots to make rapid progress | Strong leadership was perceived to be a key enabler to the success of the SICP. Leadership was delivered by all organisations involved, which meant that the programme had a consistent story across the partnership. There have been few staff changes across the organisations which meant that individuals and organisations had established relationships, enabling them to work together rather than getting to know each other |
| The larger and more complex the intervention, the harder it was to implement the desired changes . . . the scale and complexity of the integrating tasks were often greater than anticipated. This varied from site to site | The initial focus of the SICP was relatively modest, limiting coverage to older people and focusing on just three workstreams: MDGs, ICCs and developing community assets. Within this, the roll out of some elements (e.g. MDGs) has been cautious and slow, seeking to minimise the complications associated with large-scale change. The ICO, by contrast, is intended to deliver change on a much wider scale, although it is not yet clear what this will look like in practice |
| Values and professional attitudes were of great importance to the success of pilots, with shared values, a collective communicated vision and efforts to achieve widespread staff engagement cited as strong facilitating factors. Where key staff groups were not engaged (e.g. GPs), it was difficult to make progress. It was much easier to make progress where staff could see clear benefits that would result from the changes proposed and where they felt involved in the development of new services | At the top level of the organisation, strong leadership has enabled shared values to be developed at the highest levels within these organisations. The SICP has a communication workstream, which enables each organisation to deliver a consistent story about the programme. However, difficulties with engaging GPs, district nursing and social workers at MDG level were experienced within the programme. For social work and district nursing there were capacity issues in terms of staffing to ensure that they could attend MDG meetings. For GPs, although financially incentivised to attend MDGs, they were being asked to discuss patients who did not belong to their practice and categorise patients for the MDGs |
| Changing staff roles presented challenges. Where individual staff roles or professional identity was threatened, this was a barrier to integration. If education and training specific to the changed service was provided, this increased the chance of success. Changes to staff employment involving TUPE regulations were a major barrier to change | Not much discussion about staff roles was seen in the early stages of the SICP. However, the profile of this issue was raised when discussions with staff began about the ICO at the engagement event. The move to a lead provider organisation has implications for city council staff moving into SRFT. Staff roles, working practices and professional identity are potential issues for staff and the development of the ICO |
| Unrelated organisational changes were a particular challenge, as was the bureaucratic nature of NHS and local government processes. IT was commonly cited as a barrier to change. Financial constraints, such as unexpected budget changes, were also major barriers | The SICP was also affected by wide contextual changes, particularly financial challenges, and the need to respond to policy initiatives such as the vanguard programme IT was seen as a strength of the SICP. Salford already has the Salford Integrated Record, so sharing information is perceived to be a strength of the local working practices. The SICP aimed to develop this further by introducing a shared care record for patients. This record would be filled out with the patients and discussed at MDGs. It would allow mental health services, social work, district nursing, secondary care and primary care (people directly involved with the MDG) to access the information. There are still a number of issues in this area that are being developed by the SICP |
| Some barriers related to national policies, processes or legislation. For example, the financial structures of primary care, secondary care and social care in England make it a complex, time-consuming and sometimes impossible task to pool budgets for joint initiatives | The financial and organisational structures of primary care were partly responsible for the difficulty found in engaging GPs. Pooling budgets was not seen as problematic, although it is not yet clear how the new prime provider contract will work in practice. The development of health and social care devolution in Greater Manchester also altered the context, requiring Salford organisations to focus on ensuring that their ongoing strategy fits within the overall Greater Manchester Strategy. Further decisions about providing the ICO with additional support funding will be made at the Greater Manchester level |
Taken together, it can be seen that the SICP fulfils many of the conditions highlighted by the RAND report as underpinning the successful programmes, and this could be said to be reflected in the success in establishing the three programmes of work making up the SICP (albeit more slowly than intended).
Emerging metrics that suggested that targets were not being met were not acted on, and we have already highlighted the failure to fully engage with GPs. Furthermore, as we have highlighted, the goals of the programme continued to develop while it was being implemented, making it difficult to assess fully the impact of these issues. RAND highlighted the impact of increasing scale and complexity, and it remains to be seen how the wider changes enacted under the ICO play out.
Evidence relating to the potential transferability of the SICP
This evaluation is intended to generate learning that could be applied to other areas, and we have tried to do this by using and building on existing frameworks for understanding major system change. However, local contexts and relationship dynamics are perceived by those involved as the key ingredients enabling the development and implementation of the programme:
The programme itself didn’t come from thin air. The programme came from personal relationships built up over a programme of time across organisations, and so there was an awful lot of good [learning disabilities service] . . . So they had something they could see and was tangible within Salford, that they thought, ‘yeah, well if it can work there, it can work on a lot bigger scale, because we’ve seen the benefits for the individuals concerned who receive the service’.
ID 9 city council manager
Thus, the approach taken in the SICP will not necessarily suit all populations. A key early stage in the local journey was to explore the widely praised ‘Torbay model’ of integrated care. 144 Local leaders told us that, although successful in Torbay, on closer review the local population needs were different and therefore tailored solutions were required:
I think that Torbay/Sally Ford storyline is one that illustrates the limitations of thinking that you can do lift and drop. Populations are different. There are aspects of these things which you can mirror, and I’m sure when you talk to the people who are in the detail they will talk about the way in which they’ve looked at some of the work that Torbay did . . . There’s a sense for me about constantly reminding people about the population demographics.
ID 10 city council public health professional
So in Torbay, they are gentrified, relatively affluent, moved to the area, usually short on family connections or they were distant, and quite often are healthy till later in life because of their financial status as much as anything; whereas Sally Ford has quite often lived on the streets she was born in, has a big family network, is considerably impoverished, by comparison to Mrs Smith, and ends up with a long-term condition probably 10 years earlier than her, so the whole pressure in the system is different but also the ways of managing it are very different, because she has a community network of support that we can tap into and use. In Torbay, they didn’t.
ID 10 city council public health professional
Concluding remarks
In our early chapters, we highlighted the complexity of integrated care. The goal of integrated care is generally to improve patients’ experience of care, with less duplication and fewer ‘hand-offs’ between different organisations. There is an underlying assumption that this will, in turn, lead to better outcomes at reduced costs. Although the initial work done by the SICP included the development of a clear model of the needs of the population, the programme of work in Salford focused on interventions that were relatively modest in their scope and reach. However, as we have demonstrated, even these relatively modest interventions required a complicated, multilevel and continually evolving structure to oversee, commission and manage. Furthermore, even before the programme was fully established, it was decided that working together in partnership would not be enough and that structural integration was required.
Evaluating such a programme is extremely difficult, as it requires the evaluators to try to unpick and differentiate between the impact of interventions, whether or not interventions were implemented as planned and the factors affecting that implementation. Failure to meet objectives might reflect an inappropriate intervention, a failed implementation or a changed context. It was hoped that the design of this evaluation, exploring implementation at the system/commissioning as well as the operational level, might help to unpick this complexity. However, although we have been able to highlight some issues that have been important in supporting this change programme and which are relevant to wider issues of system change, the continually changing oversight and commissioning of the programme makes it very difficult indeed to know which aspects of this helped, which hindered and what would be necessary for anyone trying to replicate the programme.
Chapter 11 Results of implementation 2
Integrated contact centre
We provide a description of the service, followed by a discussion of:
-
a summary of major issues in implementation and relationships to known drivers of change
-
patient experience.
Description of the integrated contact centre
Although the SICP focused on those aged ≥ 65 years, the ICC was developed around an existing ‘all-adult’ service and was not restricted to older people, although they formed the bulk of the caseload. The ICC initially comprised three strands: SIRP, health coaching and telehealth. Although health coaching was part of the ICC, the results of the health coaching are presented in Chapter 13. Telehealth (based on text messaging) aimed to affect admission rates by providing monitoring equipment and links to the ICC, but the SICP did not renew the licence.
Single integrated referral point
The SIRP aimed to manage referrals into health (excluding general practice) and social care via a single number, to enhance perceptions of integration and ease navigation. During fieldwork, the three teams were receiving calls to their own numbers, which were then rerouted; this later changed to two numbers [adult social care contact team (ASCCT) and intermediate care numbers being combined with district nurses (DNs) retaining their own number]. Having an integrated team triaging and responding to calls meant that needs could be dealt with more appropriately:
The goal that we’re working towards is a model whereby it doesn’t matter which service you ring in for . . . and the response that you will get will be the right response for what you’re ringing in for. So you might ring in for a social worker, but you actually might get an OT [occupational therapist] . . . [my] mum’s had a fall, she needs a social worker, she needs support at home. And actually she might not do, what she might need is some rehab, some enablement.
ID 82, manager
Most SIRP staff were administrators from three teams working centrally in a single base (Table 28).
| Team | Function |
|---|---|
| ASCCT |
|
| DN |
|
| Intermediate care | The work undertaken by the administrative team includes:
|
Adult social care contact team
Staff had one half-day per week for handling e-mail enquiries and a further half-day for dealing with alerts concerning people coming into hospital or who have a planned discharge with social care implications. This provided a break from the general call-handling work, although staff highlighted call variety compared with their role title:
You don’t know what the call’s going to be about. It could just be transferring the call through to somebody or it could be a referral. It could be an appropriate adult [safeguarding], which takes about an hour to deal with . . . If a carer has been to a client and they’ve not been able to get any answer at their home so we have to then follow up to find out where the person is.
ID 10474, ASCCT
Two advanced practitioners and 11 occupational therapists and community assessment officers worked alongside, allowing staff answering calls to pass referrals on to colleagues and avoiding the need for assessment and support from locality teams. When a request was made for social worker involvement, staff completed a needs assessment by telephone and passed to the locality team if required. The ASCCT has been functioning in this way since 2011.
District nurse team
The SIRP was the main contact point for district nursing. As a result of calls, messages were relayed to nurses in each locality base. Managers saw benefit in the ICC being able to answer calls to the nurse service where callers had previously only been able to leave messages:
. . . from the DN side I would say it’s working for the people [patients] because initially the phone never got answered. You used to phone a district nurse, you kind of accepted you were getting an answering machine. Whereas now the majority of them calls you get to speak to a person, and I can only think that must be a benefit.
ID 10429, manager
Attempts were made to incorporate clinicans from district nursing and intermediate care who would provide clinical input to SIRP staff to manage more calls in-house, which was seen as preferable to telephoning nurses for advice, as they were frequently out on visits. If patients or carers were not happy discussing medical issues with ‘admin’ staff, the DN called patients back.
Intermediate care
Access to intermediate care was via the single entry point (SEP), which had two administrative workers plus a clinician based within the SIRP. In contrast to callers to adult social care and district nursing, callers included health professionals. Intermediate care had around 100 beds based in three units providing rehabilitation and assessment. Although units did not have a permanent medical presence, they were regularly visited by geriatricians and a GP.
Uptake and usage of the integrated contact centre
Calls were tracked to ensure that targets set by the council in terms of response time, satisfaction and call volume were met. Initially the corporate target of answering 70% calls within 30 seconds was used, but the emphasis for SIRP was on the quality of the call. For adult social care staff, call handling was reviewed every 3 months by managers. All SIRP staff had access to data on call numbers and response times. Reports from the date we interviewed SIRP staff showed that 672 calls were received by the three colocated teams (between 07.00 and 18.00).
Issues in implementation and relationships to known drivers of change
We initially used the ‘five simple rules’ (see Chapter 3) as a framework to understand ICC implementation. In terms of the ‘simple rules’, the core issues facing the ICC related to mission and vision (a function of ‘designated and distributed leadership’). The ICC demonstrated the greatest level of change and disagreement between partners as to what should be included, and what might be considered separate. During ICC development, additional projects (care homes HomeSafe and out of hours, all involving telephony) were incorporated into the ICC model along with ‘Ways to Well-being’ for signposting callers. Incorporating these additional projects within the ICC led to a complex business case, prolonging discussions around funding:
The centre of contact [ICC] is a concept more than an actual place for the programme, because the actual workstream has involved that many different things in order to pull everything together to have one contact centre, centre of contact would become completely unworkable.
ID 82, manager
Although some staff believed the ICC remit was too large, others felt that integrating the workstreams was necessary to achieve its aims:
. . . things have slowed down and stopped because people have started to think ‘actually we need to join these things together’. People are going off and doing wonderful work but because it’s so huge, . . . are automatically going off and working in silos, and I don’t know how we overcome that.
ID 10479, manager
Examples of the success of such linkage were reported:
There’s been five referrals [to the wellbeing project] from here [SIRP] up to now . . . He first met up with [community assets worker] . . . [he was] very closed, hood, hat covering his face, very quiet and reserved. He’s now walking round, enjoying life, wearing a flat cap. He’s just completed a 5-day computer course. They’re looking at him going on and becoming a well-being plan champion.
ID 10479, manager
In terms of ‘presence and use of feedback’, measurement of performance was something that was naturally possible for the ICC, although that focused on measures of call volume and handling efficiency, an important part of a system designed to improve patient experience, but is only a very partial view of the process. Although call quality was assessed as part of staff management, such data were more difficult to capture.
Finally, ‘patient involvement’ was an important issue. A key function of the ICC was patient centred – to make navigation easier and create the perception of a ‘joined up’ service. The ICC involved introducing new ways of working, which could complicate access for those who had already navigated previous systems. We now explore these issues further.
Other barriers to, and facilitators of, effective functioning and outcomes
As well as the analysis of the ‘five simple rules’, we also identified additional factors of relevance to the implementation of the ICC.
Colocation
Staff from all three services were colocated, interspersed within two banks of desks. Physical proximity helped them learn informally about colleagues’ work:
. . . you, kind of, want to listen to what their call is because you know you’re going to be dealing with those calls so you want to pick up and see what they do but most of the time you’re on the phone anyway.
ID 10474, ASCCT
Ultimately, staff felt that the integrated approach would improve responsiveness:
. . . eventually when it’s one number that will be even better because sometimes they do ring through and they’ve got a social care query and they might have a district nurse query as well so we will be able to deal with that all at once . . . I’ll just ask the person next to me rather than giving the number to ring somewhere else you’d just deal with that yourself and ask your colleague or leave a message with them.
ID 10474, ASCCT
Staff felt that colocation was essential to support the SIRP administrative team in call management:
I think it works at the moment for social care staff. I don’t think it’s working as well for the district nurse staff. And if we are integrated they’d have to put more professionals with us, and they’d maybe then need to rotate them, I don’t know. But it would need people here so that you’ve got some back up.
ID 10474, ASCCT
Central integration versus fragmenting existing local teams
Although part of the SICP, administrative staff were employed by different employers (adult social care by the council and DNs by the trust). When located separately, the fact that SIRP staff were employed on different pay scales and bands did not cause issues. Since July 2016, the employer of council staff working for the SICP has been the ICO (see Chapter 10), with human resources undertaken by the trust as ‘lead provider’:
. . . the other problem we’ve got at the moment is we’re persistently talking about three groups of people doing the same job, and them three groups of people are all on different pay grades, and how do we move that forward?
ID 10479, manager
Administrative staff from NHS services contrasted their experiences with those of their social care colleagues who had been in place for 5 years and who had managers within the same open-plan office, providing regular opportunities for team and one-to-one meetings. District nursing and intermediate care managers were based off-site. This meant that staff often sought advice from social care managers:
. . . they’ve got their bosses, they’ve got four bosses on the floor . . . We’ve nobody, and we feel a little bit hurt and deserted really. I know they’re contactable by e-mail but it’s not the same . . .
ID 10477, DN administrator
District nursing and intermediate care reported some loss of sense of being part of a team:
I get a lot of hostility at the moment as well because they’re rushed off their feet . . . they’re not fully aware and understand what we do really. We were taken for granted when we were with them [in the locality bases], we were always there; also part of the team. I don’t feel a part of any team now, I don’t feel . . . I hope I make a difference but I don’t feel . . . I’m just a faceless person looking at a screen now . . .
ID 10477, DN administrator
Centralising the SIRP created difficulties for services elsewhere. Removing DN administrative staff meant that new ‘housekeeper’ posts had to be created at each locality base to replace some of the functions that were too costly for band 5 nurses. Having at least one DN within the SIRP supported administrative decision-making and enabled calls to be dealt with in-house, but was viewed as unsustainable in the long term:
. . . there was a district nurse based here with a very specific role and purpose for triage . . . She’d already stopped about three or four calls going through to the team at like half nine, quarter to ten in the morning, which might not sound a lot, but she’s probably done a lot more by then, and that was really successful . . . I think there was the will, but there wasn’t the staff to dedicate a district nurse from here.
ID 10479, manager
Loss of a sense of ‘team’ was also true of intermediate care staff when community rehabilitation, the SEP administrative team, rapid response and the intermediate care units were in separate locations:
. . . even though we’re based with the Salford council, and integrating with them [at SIRP], . . . from our point . . . we’re merging more with Salford council team, but our own team seem to be separated quite a lot.
ID 10476, intermediate care administrator
Similarly, for intermediate care, relocating the clinician away from SIRP meant that administrative staff could not physically pass on messages. As the clincian spent a large amount of time on the telephone, it was difficult for staff to relay messages. Although other SIRP administrative staff relayed messages via e-mail, the consensus was that it was easier to give out direct numbers and suggest that people contact staff themselves, contrasting with the ethos of SIRP. Staff felt that, over time, this might mean that calls that should be routed through the SIRP would bypass them:
. . . we’ve found it a bit harder taking messages, because she likes phone call messages . . . because she’s on the phone so often, she can’t check her e-mails as often, so it’s not great really, with her not being here, for that reason . . . so I’d rather just give [her] number out to that person . . .
ID 10476, administrator
Centralising the contact service aimed to make access easier, but it also created issues when people were referred for multiple assessments: a person might require an occupational therapy and social work assessment and their carer might require a carer’s assessment. This was recorded as three separate referrals. The process was being streamlined to ensure that, to avoid duplication, a single assessment was conducted by the most appropriate person:
I was thinking, ‘hang on a minute, this one person has been contacted three times in 2 days by three different people in the same office.‘. What that person on the end of the phone must have been thinking’s going on here I’ve no idea, because if it was me I’d be like, ‘hello, are you talking to each other?’. So we’ve worked on changing that now and it does work a lot better.
ID 10479, manager
A 3-day test of change was conducted to try to rectify this. It found that colocation of a DN or intermediate care clinician alongside their administrative counterparts from SIRP was helpful in providing clinical advice and led to more calls being dealt with in-house, although this was not sustainable because of staffing shortages. One proposed solution was for clinicians to work on a rotation basis, enabling them to gain experience of SIRP work:
. . . a good mentor is being with nurses . . . I’ve picked up an awful lot of information. I don’t give clinical information out, but I do understand what their procedures are, and what they do now, it’s invaluable that.
ID 10477, DN administrator
Mental health involvement
A lack of representation from mental health within the SIRP created issues. Concerns about mental health were raised with social care via the ICC, either through referrals or through welfare notices from the police or ambulance service:
. . . if something comes through here and it’s mental health we can’t simply say ‘oh, well, we’ll assign that to mental health’ because it doesn’t work, and if we just sent things to them via their generic inbox which may or may not be manned you’ve got no guarantee that’s going to be picked up . . . all we can do here is notify the GP and see if they want to consider referring them to mental health . . . an awful lot of people have said, ‘well, why don’t we just triage mental health here’ . . .
ID 10479, manager
Two main issues seem to have influenced this: (1) the contractual agreements concerning what the mental health trust would provide and (2) the fact that, although the team will assess people, any mental health issues attributable to functional illness are discharged back to GP care without the requirement for the mental health trust to provide any intervention:
I had a meeting with the commissioners and the managers in the old person’s mental health teams and it soon transpired that historical agreements of what GMW were going to provide in terms of social care, with GMW restructuring over the years, agreements no longer were fit for purpose. They no longer fit the service like it is today.
ID 10479, manager
Although the mental health trust was one of the four integrated organisations, its staff were not transferring across to the ICO and it was undergoing its own organisational change.
Complex information technology systems
An issue faced by the SICP in general, but which particularly affects the ICC, is that the NHS and council each invested in different IT systems. Although integration of health and social care services was the primary aim, call handlers were required to work with multiple IT systems.
The trust had developed a system enabling its electronic patient record (EPR), which held hospital data to link with data from primary care via the Salford integrated record interface prior to the SICP. This was then used to develop the shared care record (SCR), which supported the sharing of information at MDG meetings. Although facilitating the MDG meetings, the summary SCR was not available to staff within SIRP. Meetings in spring 2016 showed that links between the SICP on a wider level were being considered, with a suggestion that, if a person known to MDGs telephoned SIRP and consequently had a SCR, their care co-ordinator could be contacted and updated with any relevant details. Subsequent to this, plans were discussed that ICC telephone triage would be used to manage telephone referrals from patients and carers wishing to self-refer to MDGs.
How was the integrated contact centre experienced by patients and carers?
The patients and carers interviewed appreciated the care provided by both district nurses and social care, but reported frustration at having to call the SIRP frequently to get cases reopened:
. . . at the moment me mum’s off social services’ books, but she’ll be back on them by now because of this bed situation [levered provision at home] that has kicked off today . . . So she’s off the books and then she’s back on and then she’s off the books and she’s back on. It just means I’ve got to keep ringing them when . . . I ring them when we need them and they respond. They’re great, you know. And I know it’s a numbers game and it’s about making it look as if they’re managing better than they are . . . They’re very responsive. They are good. When they say they’ll get back to you, they get back to you.
ID 9776, carer
Some people reported difficulties communicating with the DN service. Although the ICC provided a mechanism for calls to be answered (as opposed to previous systems, in which the majority of calls went to an answer machine), patients were frustrated at not being able to get their queries answered:
. . . I had a clash. So I needed to ring . . . it was the clinic number. But it went to a central something. Now, so I tried Thursday and spoke to somebody, and nobody ever came back to me. I tried Friday about three times. Oh, I’ll post it on the board and I’ll send a message, and all this jazz.
ID 13029, patient
Patients and carers hoped to be given an approximate time for visits. During observations at locality bases we identified some patients calling multiple times to ensure that they had not been overlooked. Each time a caller spoke to a member of the administrative staff from the ICC, a message had to be logged, creating issues for patients having to ‘re-tell their story’ (one of the alleged benefits of integrated care). As a result, patients and carers found alternative ways to communicate:
I know that they’ve changed the system at the contact centre . . . and that’s been, in my view, quite disastrous. . . . where, say she’s had a hospital appointment on a Tuesday, I’ve rung and I’ve left a message for the district nurses and said, ‘you know, she’s going to be out so don’t come or come in the morning.’. And in the old system that message got through because you were basically ringing their office. Three times now, that message hasn’t got through and the district nurses have turned up when my mum’s been out. So they’ve had a wasted journey and me mum hasn’t had her dressing changed. So now what I do is I leave a little note for the district nurse, you know. So she comes on a Tuesday, if we’re not going to be in on a Friday afternoon, I leave a note in what we call the nurse’s box, where she keeps all her dressings and that works. So the nurses pass the message on between them . . . once it became clear that that wasn’t working I just thought, well, they always go in the box. And so I leave them notes and they sometimes leave me notes . . . But that shouldn’t have to happen.
ID 9776, carer
The SIRP staff expected that people calling a central number would be happier knowing to whom they were speaking, but even when people asked for a specific member of the contact team by name, calls were not always transferred:
With us just having one number now, rather than one when we were in different places, it’s easier now with just the one number to come through to so they know who they’re ringing . . . There’s certain people who do phone up and ask for particular staff but you just deal with that yourself. You just deal with a call rather than transfer it to your colleague.
ID 10474, ASCCT
Some respondents reported feeling better connected when calling the locality base previously, as it meant that they dealt with a smaller number of people answering their calls and so were able to develop relationships over time.
Multidisciplinary group
We initially provide a description of the MDGs, followed by a discussion of:
-
major issues in implementation and relationships to known drivers of change
-
patient experience.
Multidisciplinary groups served eight neighbourhoods based on electoral wards (Table 29). A separate MDG existed for patients registered with a ‘care homes practice’ (85% of care home residents).
| Neighbourhood | Population (n) | Population aged ≥ 65 years (n) | % |
|---|---|---|---|
| Broughton, Lower Kersal and Irwell Riverside | 34,687 | 4431 | 12.8 |
| Claremont, Weaste and Seedley | 21,357 | 3707 | 17.5 |
| Eccles, Barton and Winton | 34,564 | 6401 | 18.5 |
| Irlam and Cadishead | 19,157 | 3659 | 19.0 |
| Ordsall and Langworthy | 18,959 | 3413 | 18.0 |
| Swinton North, Swinton South and Pendlebury | 33,492 | 8195 | 24.5 |
| Walkden, Boothstown, Ellenbrook and Worsely and Little Hulton | 34,124 and 19,763 | 4230 and 1076 | 9.8 |
| Care home’s medical practice | 1089 | 962 | 88.3 |
| All Salford | 217,192 | 36,074 | 16.6 |
Description of the service
An operational document set out the MDG vision, model and process of service delivery. Core membership included MDG administrators, a social worker (joint chairperson), a DN (joint chairperson), a GP, a mental health lead, a community psychiatric nurse, a consultant psychiatrist, a practice nurse and a geriatrician. The document also suggested wider MDG membership if direct care or support for the individual was required, including a health improvement officer, mental health practitioners (community occupational therapist, social worker, clinical psychologist), a pharmacist, a rapid response team, a housing officer, intermediate care workers and third-sector staff.
Observations at MDG meetings and analysis of the attendance registers collated by the CCG showed that similar membership and attendance existed across all the neighbourhoods (see Appendix 4, Table 63).
The first three staff roles were funded to varying degrees by SICP. One-hundred per cent of the time of administrative and nursing leads was funded, with social care leads funded 50% for MDG work and retaining caseloads for the other 50% of their funding. This meant that nursing leads had more time available for MDG work. This led to tensions when this was seen to be at the expense of direct work with patients:
They see us on a computer and say, well, that’s not a nursing task. When I input it [SCRs] on the iPad [Apple Inc., Cupertino, CA, USA], I used to sit out in the car park because you can still get Wi-Fi there, but nobody can see you. But it’s almost like a dirty little secret doing admin when you’re a nurse, because you should be attending to patients.
ID 59, nursing lead
These frustrations led to the team leader for the MDG nurses arranging a single central workspace for all nurses in one locality base.
The pre work for MDGs was a vital part of the process, and the nursing and social care leads were responsible for ensuring that links between health and social care records were added to the SCR. In some MDGs, nursing and social care staff sat together each using their own system, with the nursing chairperson also inputting data into the SCR. In other neighbourhoods, the nursing chairpersons travelled to the locality bases to work collaboratively, combining this with ‘safety huddles’ to reduce travel. If this was not possible, two nurse co-chairpersons tended to prepare the SCR for their patient caseload then e-mail it to their co-chairperson for their input, before forwarding to others.
The nursing co-chairpersons continue to attend ‘safety huddle’ meetings in the locality bases. At these meetings the local district nursing teams discussed patients they were concerned about, and nurses visiting the same patient shared their expertise. ‘Safety huddles’ enabled the nurses to promote the benefit of MDG working, accepting referrals on behalf of patients who might benefit from discussion within MDGs:
We’ve had some difficulties in describing what the [MDG nursing] role is, so we’ve had some . . . not issues, but the question from district nursing is around, well, what exactly is it you’re doing? Now, at this point, we’re just going to a time where you can see that clinical duties will be part of the role, it was almost as if we had to step out of them initially and to try and find out how we would fit.
ID 62, MDG nursing co-chairperson
In contrast, social care leads remained embedded within their locality teams and retained a small yet complex caseload. Similarly, they were keen to promote the benefits of MDGs among colleagues, and one way was getting colleagues to shadow them at meetings:
We have monthly team meetings . . . I update my team about what we’re doing. I like to keep people informed because they might find themselves as care co-ordinator so it is important for me they understand the work of the MDG and also I am trying to get them involved by getting them one by one to attend the MDG with me, so that will give them a better understanding when I’m asking for information or asking them to do things then they will understand why.
ID 58, MDG social care lead
Weekly micro-coaching meetings at the nurse base were delivered by a facilitator from the quality improvement team. Social care chairpersons were invited to participate, although only half were present at the session observed.
General practitioners were reimbursed for MDG attendance by Salford CCG, with the CCG eventually agreeing to pay for 7 hours, including pre and post work. Practice nurses attending the MDGs were not reimbursed, although in some cases they deputised for the GPs and often shared the pre and post work, particularly when they had more frequent patient contact:
. . . we tend to split the list between us and we each take the patients that we have more information on and know best. There’s quite a lot of work to do after the meetings too and its especially important when we have discussed patients that our colleagues have referred to MDG that we write up the outcomes from the meetings quickly so they know exactly what the outcomes are.
ID 15, practice nurse
Project managers and administrators pointed out that single-handed GPs were keen for support from colleagues. Even where differences existed, this did not affect the functioning of the meetings:
. . . they’re really good groups now. They work quite well together. And the key is regular attendance really from the same people, because you can’t build a forum of trust with new faces all the time, can you? . . . we’ve had the same faces over and over, and we can be really open and honest about the conversations that we have with our colleagues, and then we all agree what’s recorded formally and put into the shared care record.
ID 55, project manager
Practice nurse input was highly regarded by the MDG team, with practice nurses often seeing patients over a prolonged period while providing long-term care.
Multidisciplinary groups chose to involve practice managers in different ways. Initially, they provided a critical function in terms of assisting with allocating ‘Sally’ levels to patients. Some accompanied their GP to meetings or deputised. MDG meetings were seen as a clinical arena for discussing patient care, and it was expected that their input would cease once MDGs became established:
. . . in the newer [MDG] meetings I can forgive it, because a lot of it is about the system and the processes, so what’s risk stratification, what’s the next steps, we need to code them, we need to refer them into choose and book . . . [But] we are experiencing more and more practice managers at MDGs at the moment, and I’m not particularly comfortable with it . . . Then it was fed back to me that actually we could do with practice managers being put on there [SCR access list], because if you want information copied from one clinical system into another, who’s going to sit there and do that?
ID 55, project manager
In many neighbourhoods, the geriatricians were appointed later, and only at pilot sites were they involved at an early stage. Even once identified, staff shortages and increasing demand limited their input:
. . . recruiting has been difficult across each of the different services . . . only three geriatricians qualified last year . . . I know that there’s a geriatrician coming to those [two MDG] areas in August, September time . . . because they are hospital-based staff really, they could, and it’s not the same as having them there in the forum for conversation, but they could liaise with us via the shared care record.
ID 55, project manager
The geriatricians’ role within the MDG was viewed as key, with high expectations about the value of their input. GPs saw the geriatricians as a key reason to engage:
I think once the geriatrician is involved, and we establish good links with him, I think it could actually be much more stimulating, and much more rewarding, in terms of educating us, and improving our standards of care. But, obviously, we’ve spent 6, 7 months without anybody . . .
ID 70, GP
During observations, the geriatricians were able to access hospital patient data, enriching the discussions with information not contained in the SCR. They were involved in many key actions and frequently advised GPs on medication reviews:
. . . earlier we were discussing a case where a lady had a rapid deterioration of a wound and I asked if she might be diabetic. The geriatrician was able to pull up her blood glucose results confirm she hadn’t been tested and sent a message for this to be done. MDG reviews mean more people can contribute to a possible solution that may otherwise have not been considered.
ID 15, practice nurse
Involvement of mental health professionals could be an issue owing to resource limitations:
I think there’s buy-in from mental health . . . you know what they’re able to deliver is fairly limited and the need is massive . . . mental illness, it goes on over a period of time and, sort of, we’re so far off anticipating what the need might be, because we’re worried about putting more need [support] in there than what’s required.
ID 89, geriatrician
Process and content of multidisciplinary group meetings
Patients were stratified into four groups of ‘need’ to allow services to be better matched. Patients receiving three or more visits per week from district nursing and/or social care teams (around 3100 patients) were deemed most likely to benefit from MDGs. Practices had voluntarily participated in an exercise to identify the 2% of their population at greatest risk of admission (national ‘enhanced service’). Although existing algorithms existed [e.g. Patients at Risk of Rehospitalisation (PARR), PARR+] to identify patients at risk, dissatisfaction led to new ones being developed to code patients to ‘Sally’ levels (Table 30 and Appendix 4, Figure 15).
| MDG (aged ≥ 65 years) | Wave | General practices | Training started | Embedding (SCR created) | Functioning (achieve mean) | Average number of patients discussed (per 2-week MDG) | Number (%) of MDG patients as reviews | Green statusa | Number of patients discussed (% of level 2 + level 3)b |
|---|---|---|---|---|---|---|---|---|---|
| Eccles and Monton | 1 | 6/7 | March 2014 | 23 January 2015 | 3 April 2015 | 10 | 4 (40.0) | 235 (54.5) | |
| Swinton and Pendlebury | 1 | 4/5 | March 2014 | 23 January 2015 | 6 March 2015 | 13 | 6.5 (50.0) | 331 (61.4) | |
| Ordsall and Langworthy | 2 | 5/5 | 15 January 2015 | 12 February 2015 | 13 March 2015 | 11 | 6 (54.5) | 10 August 2015 (83.6) | 238 (78.5) |
| Irlam and Cadishead | 2 | 4/5 | 13 January 2015 | 13 February 2015 | 13 March 2015 | 10 | 5 (50.0) | 250 (100.0) | |
| Claremont and Weaste | 3 | 6/6 | 3 March 2015 | 3 April 2015 | 3 April 2015 | 10 | 5 (50.0) | 7 September 2015 (80.8) | 197 (72.4) |
| East Salford (Broughton) | 3 | 6/10 | 10 March 2015 | 27 March 2015 | 8 April 2015 | 12 | 2 (17.0) | 5 October 2015 (84.0) | 157 (32.2) |
| Little Hultonc | 3 | 6/6 | 12 March 2015 | 22 May 2015 | 19 June 2015 | 5 | 2 (40.0) | 127 (85.2) | |
| Walkden, Worsley and Boothstownc | 4/4 | 27 March 2015 | 24 April 2015 | 8 | 3.5 (43.7) | 10 August 2015 (85.8) | 220 (93.2) | ||
| Total | 41/49 (83.7) | 79 | 34 (43.0) | 1651 (62.8) |
Although there were tensions between the amount of work and pre work provided by various parties, there was mutual respect for the different perspectives provided. During interviews, the concept of teams tended to be reserved for each group’s specialty, and team working seemed more limited at the MDG meeting itself. An exception was where the nursing and social care co-chairpersons worked closely together and formed strong dyads.
An electronic SCR was used to enable information to be shared between the relevant statutory agencies, and these were projected during MDG discussions. The majority of SCRs were initially created by the MDG nurses, with input being provided by the social care chairperson and then being sent onto GPs, practice nurses and mental health staff. An agreed shared care plan within the SCR was then developed based on MDG discussion.
Initially, there was an emphasis on the creation of the SCR, and targets to encourage this could have affected the quality of data they contained. A working group was set up to look at content of the SCR, especially when there was an expectation that a summary SCR (in the form of a plan) would be shared with patients:
. . . we’ve, kind of, learned about the shared care record, about the data and how to look through it quickly and how working alongside the social worker with their system open and shared care record, how together, you know, you can get really good quality information, it’s much quicker to do it that way, so more timely.
ID 62, nurse lead
. . . the patients eventually, they’re going to be getting a copy of this . . . you don’t want to write anything that’s going to upset them. There’s a lot of debate at the moment about what we should be writing, and we’ve had a few little working groups about trying to standardise documentation.
ID 59, nurse lead
By the end of observations, SCRs were still not being shared with patients. Patients often had not been told they had been assigned a care co-ordinator and did not have their contact details.
Summary of major issues in implementation and relationships to known drivers of change
We used the ‘five simple rules’44 (see Chapter 3) as a framework to understand implementation.
Involvement of general practitioners
In terms of the factors identified by the ‘five simple rules’, one of the core issues facing the MDGs related to GP involvement. Initial participation was not always enthusiastic; not all practices took part, and identifying a GP to be the MDG lead was difficult for some practices. Incentives were required, although over time the involvement of GPs grew (as did that of practice nurses). The SICP delivered a somewhat unique neighbourhood model (compared with a practice-based one), which meant that GPs were exposed to MDG work around patients in other practices, which might be seen as inefficient, although it could have advantages.
Two MDG managers visited practices to explain the MDG concept and worked with practice managers and a GP lead at each site to encourage engagement. As a result, most practices in Salford agreed to participate, although some delayed joining owing to staffing and/or relocation issues:
I don’t remember being made to feel compelled to do it, I could be wrong . . . for me, we had to try it, so I went in thinking, ‘I’ll give you 6 months, at the very most I’ll give you 6 months.’. I went in with a very negative attitude. Fortunately, I didn’t allow my head to rule my heart and I started being a bit more open about it . . .
ID 85, practice staff
Practices agreeing to participate met together and underwent three training sessions initially. The first meeting introduced MDGs and how they operated. The second planned to carry out a Belbin assessment of all the team members to identify strengths and weaknesses and to facilitate better project working. At this second meeting the process to refer patients and the SCR were demonstrated. At the third training meeting, practices were each asked to identify one patient as a trial run for MDG discussion. In the MDG meetings that followed, practices were asked to refer other patients into the system (initially two or three patients per practice and then five patients per practice).
There were competing initiatives with these groups of patients, such as those run by the CCG:
[Long-term conditions] creates a lot of work. It’s a local initiative and the CCG want us to review patients twice yearly who have a LTC [long-term condition]. Discussion re[garding] symptoms, medication, health promotion advice and agree an action plan with them. If the individual has a respiratory condition or diabetes they receive an action plan for this and a LTC action plan. This is a lot of duplication and the process is time consuming. Reviews have become a tick-box exercise and the discussion about agreed actions is comprised due to time constraints.
ID 15, practice nurse
Measurement
The second simple rule related to measurement. Again, the MDGs had ready indices to assess progress and care delivery (such as numbers of SCRs). The initial risk stratification identified 3100 people potentially requiring discussion at MDGs, creating a tension between creating SCRs (to meet targets) and collecting data of sufficient quality to aid care co-ordination and planning.
One of the main ways in which learning was shared across the neighbourhoods was through the ‘MDG joint chairpersons’ meeting. MDG project managers led this meeting, which managed issues and facilitated learning. The number of level 3 patients with SCRs was fed back in terms of their achieving red, amber or green status. This feedback aimed to encourage a sense of competition between the neighbourhoods, but also highlighted difficulties when individual practices had not met the requirement of creating SCRs for 80% of their identified level 3 patients. In addition to this in-depth monitoring, which was updated on a weekly basis, ‘dashboards’ were created, which allowed interrogation of the data by individual practices.
Patient involvement
The NHS National Collaboration for Integrated Care and Support4 adopted a narrative definition of what integrated care should feel like for the patient [e.g. ‘I can plan my care with people who work together to understand me and my carer(s), allow me control, and bring together services to achieve the outcomes important to me’]. Recent qualitative work has highlighted some of the dimensions of this experience, identifying six themes around person-centeredness (holism, naming, heed, compassion, continuity of care, and agency and empowerment) and exploring the patient experience of being ‘unseen’ by their practitioners. 11
In principle, there are two key processes by which MDGs may help deliver patient-centred care. The first is care planning, which involves an assessment of the needs of the individual patient and the development of an individualised care plan reflecting the patient’s personal circumstances and needs. Second is care co-ordination, which is the process of helping patients to navigate services by enhancing communication and providing advocacy. Nevertheless, there are potential tensions between patient-centred care and MDG working. Core features of patient-centred care include detailed knowledge of the patient (and application to decision-making) and an effective ‘therapeutic relationship’, both of which may be more difficult to achieve in the context of team-based care. A patient seeing a variety of health professionals may feel less able to build up a relational continuity. 145 Patient involvement can be difficult in the context of MDGs and team-based clinical decision-making.
Multidisciplinary group guidance indicated that patients and carers should be contacted and a discussion had with them ahead of MDG discussions. In reality, the pressure to create a SCR and wider service pressures meant this rarely happened. Virtually all MDG staff interviewed felt that consent should be sought ahead of discussion:
I think the idea is that if they’re open to a particular worker within social services that we would have that discussion with them, if they’ve got district nurses going in regularly that they would or that if they are regular visitors to the GP that they would . . . I guess it’s sort of one of them where ideally the care co-ordinator would be in place and it would be that person that would then go and have that discussion with them and give them the feedback from the meeting and everything.
ID 60, social care lead
In December 2015, the CCG launched standards for services across practices, with guidance regarding consulting patients ahead of MDG discussions and feeding back outcomes. However, observations at MDG meetings showed that the discussions were of patients receiving feedback in the future.
We identified three core themes concerning how MDGs delivered patient-centred care:
-
structure of MDGs and person-centred care
-
processes within MDGs supporting person-centred care
-
barriers to the delivery of person-centred care.
The structure of multidisciplinary groups and person-centred care
The SICP used the ‘Sally Ford’ character to highlight the issues faced by older people. The multidisciplinary nature of MDGs provided a platform for a biopsychosocial assessment. By working together, health and social care professionals better appreciated each other’s roles. A second critical structural support was the creation of the SCR, which used data from the existing locally integrated primary, secondary and clinical settings, and into which social care staff could input data. The SCR was displayed during the discussion for each patient and updated with outcomes and actions arising.
Processes within multidisciplinary groups supporting person-centred care
All staff viewed the MDGs as an opportunity to share knowledge and provide a more holistic approach to care provision:
It’s bringing everything together so that we’re truly thinking more holistically about a person and considering not just individual kind of professional service-specific issues but seeing the overview and what might really matter to a person or what might be a priority and then coming up with an action plan that actually meets that.
ID 56, project manager
Although colocated previously, the arrangement whereby MDGs were co-chaired by staff from district nursing and social care provided greater insights into each other’s work and changes to practice:
. . . I’ve seen where there have been suspicions between health and social care, and crucially where people have different priorities . . . the pressure on hospital beds, which means people need to be discharged . . . Now having a better understanding around how the social care, how we do things that will help them to understand that it’s not as straightforward to just discharge somebody. We need to discharge and ensure that they are safe wherever they are going, and I think that wider integration [including psychological, medical and community services] can help address that.
ID 58, social care lead
Multidisciplinary group discussions yielded rapid solutions, particularly when local authority-commissioned social care packages required amendments. Small changes, termed ‘tinkering at the edges of care’,146 enabled patients to attend one-off hospital appointments and also regular exercise classes:
. . . we were saying about this fellow going at night to [a hospital] appointment, and I was saying about the care agency going in later, the social workers can arrange that; and she said, ‘but they finish at 8 o’clock’; so everything I was saying was being answered really negatively . . . But then we realised that maybe . . . the evening district nurses could go and put him in bed that night.
ID 70, nurse
Knowledge of patients’ interests helped MDGs find some solutions to frequent hospital attendance:
. . . one time the [MDG] nurse was in the house, [the patient] went in the other room and rang an ambulance, this gentleman. [Then] it’s somebody who just thought . . . ‘such a person’s not rang, what’s going on?’. [Then] . . . somebody realising that whenever, say, the tennis was on or the Olympics, he never went into A&E. He never rang A&E, he never went in. Then the practice nurse must have had a conversation with the son and he might have just said, he really loves sport. His son went out and bought him a Freeview box and it’s got sports channels on. Since that date, he’s never had an admission to A&E.
ID 63, administrator
A second process concerned MDGs sharing knowledge from health and social care perspectives about local services, encouraging a broader approach to meeting patient needs. Although time-consuming, MDG meetings provided a forum for professionals to learn about services available. GPs found it difficult to keep abreast of service changes, especially those delivered by non-statutory organisations:
. . . some of the other GPs . . . they’ve said, ‘oh well, I’ve learnt that there’s this service or that service.’. But they’ve learnt about maybe a handful of services in coming up to a year of . . . a part of the MDG you’ve got to ask is that actually a good educational use? . . . A lot of those services I knew about before . . . [It’s] hard to look at all your e-mails ’cause you get bombarded with so many, it’s easy to miss a service or you read one you think, ‘oh, that sounds fantastic’ and then you forget about it ’cause you won’t refer to it very much.
ID 79, GP
Multidisciplinary groups could also support person-centred care by involving those best known to the patient. A professional already known to the patient was usually assigned to the role of care co-ordinator, and the details of all those involved in their care were recorded in the SCR, pulling data from many agencies into a single source to aid care co-ordination.
Continuity of care was seen as vital to having effective knowledge of patients and their families, with GPs being seen as key. Despite this in-depth knowledge, the geriatricians were continuing to see patients face to face during assessments, and they questioned whether or not admissions can really be avoided. Geriatricians suggested that more proactive care planning, by GPs in particular, is required to reduce future admission rates and support more appropriate (rather than earlier) discharge for those who are hospitalised:
They [GPs] know them inside out, yet, they’re not necessarily thinking about what might tip them into, you know, non-elective emergency responses . . . but they [GPs] may not see that there’s any other alternative.
ID 89, geriatrician
Barriers to person-centred care
Although consultations during the development of the SICP had included patients and carers, MDG discussions did not directly include them:
. . . why wouldn’t they want to be involved? What is being discussed there that the person and their families wouldn’t find relevant, appropriate or interesting? . . . and is that right and what is the purpose of those [MDGs] if it’s, if it’s not to engage, you know, . . . [Is this] a process for just professionals to speak short hand about, together, about the integrated care management of a person and the contact with the person takes place elsewhere, possibly?
ID 81, third sector staff
Observations showed that although GPs fed back the outcome of MDG meetings to their patients, patients did not always agree to the suggestions made. This was especially true when MDGs recommended memory or social care assessments, which caused anxiety.
Aspects of MDGs limited the degree to which patient-centred care could be delivered. Nurses recognised the value of visiting patients at home, building a relationship and getting quality information to inform care planning, but flagged up difficulties with this when workload pressures limited the information supplied by colleagues:
. . . we need to be taking the patients that we’re seeing for MDG, to go and meet them, . . . to actually have a good picture of how they live and what’s going on, and the dynamics of families, and just get an overall picture. Because you can’t [get that] from looking at a screen.
ID 59, MDG nurse
Some questioned the utility of the SCR:
I can’t tell you how annoying I find that . . . It’s not a plan. There is no care plan. It is a record of information about a person . . . There are no directions on that record that give you a prescription for treatment. So it’s not a care plan . . . And as nurses, we pick up on that, they don’t.
ID 93, nurse
Towards the end of our observations, there was a change in MDG discussions, which coincided with the inclusion of a ‘summary of existing risks and issues’ on the SCR, which helped generate a more proactive care planning approach.
How is the work of the multidisciplinary groups experienced by patients and carers?
Patients and carers knew little about the SICP or the MDGs. Of those who did, many had been directly involved in the initiative through the Older People’s Partnership Board or the Citizens Reference Group.
This lack of awareness, combined with shared care plans not being shared with patients, meant that people were unlikely to know that they were part of a MDG. As patients were not routinely consulted ahead of MDG meetings, this limited the number of interviews that we were able to undertake.
Among those who were interviewed, there was limited evidence of active ‘case management’, and any care co-ordination seemed to focus on integrating records from health and social care via the SCR. Most patients could not identify a ‘care co-ordinator’.
Most GPs (during interviews and at MDG meetings) said that they would tell patients about discussions with colleagues if they saw the patient, but would not make a specific telephone call to discuss the MDG. If patients ended up being referred to health improvement services, then the GP would put the referral on hold while they confirmed that the patient was happy for their details to be shared:
The [GP] did mention it to me once I think, something about she’d been talking and she was going to put my name forward, something to do with this kind of thing [MDG], yeah . . . you can only give it a try and if you think it’s going to do you good well you’ll do it, won’t you?
ID 69, patient
Some patients don’t even know they are being discussed. I will try to contact patients or ask when I see them about discussing them at an MDG, but sometimes if we can’t contact them and there is a pressing issue that needs discussing we will have the meeting and then afterwards I will talk to them about it.
ID 15, practice nurse
There were examples of patient involvement in MDGs. An 80-year-old woman with a history of frequent A&E visits arising from repeated falls had lost confidence and was no longer going out of her flat, citing fears about using her stairlift. She gave consent to be discussed at MDG by her GP, who was concerned about the changes occurring:
I’ve known her for nearly 20 years, and she lives in a sheltered housing complex. She used to go and visit her mates [in another housing scheme], and get involved in all this social stuff . . . I also know she’d lost her confidence after various falls, and she wasn’t going out . . . she’s scared to leave her front door. I have a very good idea about what the patients I know very well want.
ID 70, GP
I had about five or six [falls], from last Christmas, in the flat and everywhere, you know, and I’ve lost my confidence . . . I’d left my [care on call] band in the bathroom . . . You know, if I fall I can ring them right away, . . . So sometimes I was sitting here 2 or 3 . . . about 3 hours before anybody came . . .
ID 69, MDG patient
Prior to the MDG discussion, the GP requested a change of housing. Once relocated to a bungalow in the same complex, she was assessed for, and received, mobility equipment from the rehabilitation team and was able to re-engage with other residents after the health improvement team invited all residents to attend a meeting.
It is possible that limited patient involvement limits the benefits of MDG work and the creation of relevant care plans. The process to refine the shared care plan, however, took far longer than anticipated, and there were many issues around what format the plan should be in so it could be shared with patients:
. . . we were discussing the logistics of how printing off a copy of the shared care plan for the patient and how that’s difficult at the moment. It doesn’t look nice. It’s not very ergonomic. It’s not very user friendly at all. In fact it’s horrible.
ID 55, project manager
. . . the patients eventually, they’re going to be getting a copy of this, . . . you don’t want to write anything that’s going to upset them. There’s a lot of debate at the moment about what we should be writing, and we’ve had a few little working groups about trying to standardise documentation.
ID 59, MDG nurse
Patients and carers were often overwhelmed by the sheer number of services they received. Where carers were aware of the MDGs and knew the appointed care co-ordinator, they were happy to remain involved in making arrangements:
[Mum] had visits from nurses, doctors, hospitals, GPs, physiotherapists, dieticians, intravenous teams, and others . . . care agency, et cetera, so her house is like Waterloo Station. It’s very busy . . . [If you’ve got a hospital visit] I phone [the care agency] usually a couple of days before, and say, my mum’s got a hospital visit on whatever day. Can you leave her in the wheelchair in the morning, and don’t do her lunch. I’ll do her lunch when I bring her back. So . . . and that always works. I don’t want to do that sort of stuff through a [care] co-ordinator. I’m happy to . . . on day-to-day issues like that, that’s fine.
ID 1, carer
Some carers felt too much was sometimes being done to patients in the NHS, which was unnecessary:
The NHS has a concept of ‘doing things to the older person’ . . . It pathologizes. It treats people as patients ‘cause that’s how they present rather than standing back a bit . . . older people tend to be hypochondriacs and they’re costing the NHS a lot of money. So rather than not constantly respond to them as patients, we might be sensible to stand back and actually talk to them a bit.
ID 33, carer
Chapter 12 Results of outcome 1
This chapter presents analysis of the effects of the SICP on hospital admissions in intervention and comparator sites. We use the label ‘intervention’ to refer to the data from the Salford sites and ‘comparators’ to reflect those sites outside Salford. It is important to note the meaning of those labels. We use data from Salford as a whole, on the basis that the population has been exposed to the effects of the SICP. The SICP involves a number of mechanisms of integration (MDGs, ICC, community assets). The mechanism most clearly linked to reductions in hospital admissions is the MDGs. However, not all patients in Salford have been managed by a MDG, and some will have been exposed to other mechanisms. The analysis presented here is not a test of the specific impact of MDGs on admissions among those managed by the teams. Rather, it is a broader test of the impact of the SICP across Salford, with an assumption that any effect largely reflects the operation of the MDGs. In addition, many sites in England have their own versions of MDGs. 79 Therefore, the comparison presented here explores whether or not the SICP is having an effect on admissions across the Salford population compared with the general trend (including integrated care initiatives outside Salford).
Descriptive data on population sizes, attendances and admissions from 2009/10 until 2015/16 for all adopters for the intervention and comparator groups are shown in Appendix 4, Table 64, together with data on non-adopters and the comparator sites.
We found that practice registrations of people aged ≥ 65 years increased over time, with an increase of 19% when looking at all areas in England (including Salford). Around 11–12% of the population aged ≥ 65 years in Salford are not registered to practices that are within the SICP.
Between 2009/10 and 2015/16, there was an overall increase in the number of A&E attendances, with the West comparator having the highest proportion of people aged ≥ 65 years attending A&E. Between 2009/10 and 2015/16, the number of emergency admissions increased almost in line with the rise in the population; as a result, the proportion of the population admitted to hospitals under an emergency largely remained constant or showed small reductions at all sites.
The proportion of patients discharged to usual place of residence fell in all intervention and comparator sites over time; the lowest proportion was among patients registered to general practices in Salford. The proportion of patients who were admitted with an ambulatory care-sensitive condition increased between 2009/10 and 2015/16.
Population-weighted mean values of the outcomes and explanatory variables and age bands are shown for all intervention and comparator groups (Table 31).
| Outcomes and characteristics | Site | ||||||
|---|---|---|---|---|---|---|---|
| Intervention | Comparator | ||||||
| Early | Late | All | Greater Manchester | West | West (extended) | England | |
| Outcomes (rates) | |||||||
| A&E attendances per person | 0.107 | 0.126 | 0.119 | 0.110 | 0.124 | 0.112 | 0.090 |
| A&E attendances referred by health/social care providers per person | 0.060 | 0.066 | 0.064 | 0.027 | 0.037 | 0.032 | 0.032 |
| Self-referred A&E attendances per person | 0.042 | 0.051 | 0.048 | 0.059 | 0.075 | 0.065 | 0.045 |
| Discharged to usual place of residence | 0.027 | 0.029 | 0.028 | 0.047 | 0.076 | 0.079 | 0.063 |
| Ambulatory care-sensitive conditions admissions per person | 0.038 | 0.044 | 0.042 | 0.038 | 0.038 | 0.036 | 0.031 |
| Emergency admissions per person | 0.069 | 0.081 | 0.077 | 0.066 | 0.072 | 0.070 | 0.058 |
| Emergency admissions via A&E per person | 0.062 | 0.073 | 0.069 | 0.055 | 0.054 | 0.051 | 0.044 |
| Direct emergency admissions per person | 0.005 | 0.006 | 0.006 | 0.009 | 0.014 | 0.016 | 0.011 |
| Patient age (proportion) | |||||||
| Aged 65–74 years | 0.093 | 0.086 | 0.089 | 0.092 | 0.099 | 0.100 | 0.101 |
| Aged 75–84 years | 0.056 | 0.059 | 0.058 | 0.053 | 0.061 | 0.064 | 0.062 |
| Aged ≥ 85 years | 0.019 | 0.035 | 0.029 | 0.020 | 0.021 | 0.023 | 0.026 |
| Observations (n) | 252 | 896 | 1148 | 11,760 | 2492 | 9436 | 207,984 |
The proportion of patients aged ≥ 65 years is higher in the population of England as a whole than in the intervention sites. Age distributions of > 85-year-olds show that the population in the intervention sites is, on average, older than the population of England. The exception is the early adopters, among whom the age distribution is younger.
Rates of all versions of A&E attendances and emergency admissions are higher in the intervention sites than in all of England, with the exception of direct emergency admissions. There are lower rates of patients who return to their usual place of residence in the intervention sites than in all of England. Early adopters have lower rates of all outcomes than late adopters. A&E attendances from health and social care referrals are much higher in the intervention sites (6.4%) than in comparator sites (3.2%).
Population-weighted mean values
Regression results
Table 32 shows the results comparing all adopters with the four comparator sites. Graphs of trends for all outcomes are also provided (see Appendix 4, Figures 16–23).
| Comparisons and outcomes | Site | |||
|---|---|---|---|---|
| Greater Manchester | West | West (extended) | England | |
| Early implementers | ||||
| A&E attendances | 0.005* | 0.006* | 0.005* | 0.006*** |
| A&E attendances: health and social care referral | 0.002 | 0.005* | 0.006** | 0.004** |
| A&E attendances: self-referral | 0.004*** | 0.005 | 0.002* | 0.003*** |
| Discharged to usual place of residence | –0.011*** | –0.036*** | –0.028*** | –0.012*** |
| Avoidable admissions (ACSC) | 0.002* | 0.003** | 0.003** | 0.002** |
| Emergency admissions | 0.006*** | 0.004** | 0.004*** | 0.006*** |
| Emergency admissions: via A&E | 0.009*** | 0.011*** | 0.009*** | 0.010*** |
| Emergency admissions: direct | –0.001*** | –0.007*** | –0.006*** | –0.002*** |
| Late implementers | ||||
| A&E attendances | 0.006** | 0.008* | 0.002 | 0.005** |
| A&E attendances: health and social care referral | 0.005** | 0.005** | 0.008*** | 0.007*** |
| A&E attendances: self-referral | 0.004** | –0.001 | –0.000 | 0.002 |
| Discharged to usual place of residence | –0.004* | –0.006 | –0.009** | –0.004** |
| Avoidable admissions (ACSC) | –0.001 | 0.000 | –0.000 | –0.001 |
| Emergency admissions | 0.003* | –0.001 | –0.001 | 0.002 |
| Emergency admissions: via A&E | 0.005*** | 0.005** | 0.002 | 0.004** |
| Emergency admissions: direct | –0.000 | –0.003* | –0.002* | –0.001** |
| All implementers | ||||
| A&E attendances | 0.008*** | 0.010*** | 0.005* | 0.008*** |
| A&E attendances: health and social care referral | 0.006*** | 0.007*** | 0.009*** | 0.008*** |
| A&E attendances: self-referral | 0.004*** | 0.000 | 0.001 | 0.002* |
| Discharged to usual place of residence | –0.003 | –0.005 | –0.008** | –0.005*** |
| Avoidable admissions (ACSC) | 0.000 | 0.001 | 0.001 | 0.000 |
| Emergency admissions | 0.005*** | 0.002 | 0.001 | 0.003** |
| Emergency admissions: via A&E | 0.007*** | 0.008*** | 0.004*** | 0.006*** |
| Emergency admissions: direct | –0.000 | –0.002 | –0.002** | –0.001*** |
We focus on the comparisons using the largest numbers of observations: all adopters compared with the rest of England. We find that the intervention sites showed increased numbers of A&E attendances, by 0.008 per quarter per person. Between 1 April 2015 and 31 March 2016, the intervention sites saw 1063 (95% CI 664 to 1462) more A&E attendances.
We find that the intervention sites showed a similar absolute effect on health and social care referrals to A&E, which also increased by 0.008 per person per quarter. This represents an increase of 1063 (95% CI 797 to 1462) in the number of attendances over the same period. Self-referred A&E attendances had a more modest increase of 0.002 per person per quarter, which represents an increase of 266 (95% CI 0 to 532) A&E attendances.
We find that the intervention was associated with an increase in emergency admissions of 0.003 per person per quarter, which represents an increase of 399 (95% CI 133 to 664) additional emergency admissions between 1 April 2015 and 31 March 2016. Emergency admissions via A&E increased by 0.6%, an increase of 797 (95% CI 399 to 1063) admissions. We found a fall in direct emergency admissions by 0.001 per person per quarter, resulting in a fall of 133 (95% CI 0 to 133) admissions. The effect of the intervention on avoidable emergency admissions is not statistically significant.
We found that the intervention led to a decrease in the number of patients who are discharged to the usual place of residence of 0.005%. The intervention resulted in a larger relative decrease in the number of patients returning to their usual place of residence among early implementers (0.012%) than among late implementers (0.004%).
Results using Greater Manchester, West and West (extended) show similar results to using all of England as the comparator group, when focusing on all results from all implementers. The signs of the coefficients remain the same for all estimated effects of the intervention along with similar absolute magnitudes. The small differences in estimate effects are explained by the changes in the sample size.
Robustness checks
Reducing the pre-intervention period by removing the first four and first eight financial quarters of the sample produced results that were consistent with the results obtained using data from the full sample (Table 33). We find that emergency admissions increased by 0.003 and 0.004 per person per quarter for models removing the first four and eight quarters, respectively.
| Intervention effect | Site, emergency admissions | |||
|---|---|---|---|---|
| Greater Manchester | West | West (extended) | England | |
| All years | 0.005*** | 0.002 | 0.001 | 0.003** |
| 2009/10 | 0.005*** | 0.001 | 0.001 | 0.003** |
| 2010/11 | 0.005*** | 0.002 | 0.001 | 0.004** |
| Differences in differences | 0.003 | 0.039 | 0.013 | 0.004 |
The results from the difference-in-differences estimator were not statistically significant. However, the point estimate of the effect of the intervention using all of England as the comparator group is identical to the main results. Therefore, both difference-in-differences and lagged dependent variable approaches resulted in impacts of similar magnitude, but the lagged dependent variable generates a more precise estimate.
Conclusion
Our findings suggest that, compared with the general trend, the SICP led to increases in the number of A&E attendances, particularly for those referred from health and social care providers. We also find that the intervention led to increases in the number of emergency admissions, mostly driven by admissions through A&E. Although we find increases in emergency admission, we did not find a statistically significant effect on ambulatory care-sensitive admissions. Increases in hospital utilisation may have been the result of integrated care increasing contact with health-care professionals. This assumption is made more plausible when considering that the SICP had no effect on ambulatory care-sensitive conditions, which is a better indicator of GP care quality. We find that fewer patients have been discharged to usual place of residence; possible explanations for this may be that the increase in integration in health and social care has resulted in patients being discharged into care more easily.
These results were robust to the use of other methods for estimating the impact of the programme and also reducing the time period. Removing the first four or eight quarters of data did not affect the results.
As noted in the earlier summary of previous integrated care initiatives in the UK, a number of studies of similar case management schemes have found either no impact on hospital utilisation29 or increases in some types of utilisation. 32,33 Chapter 11 discusses in more detail the activities of the MDGs, which may provide insights into the mechanisms underlying the particular pattern of results, which are then considered in more detail in the discussion.
Chapter 13 Outcome 2 (health coaching randomised trial and cost-effectiveness analysis)
Recruitment and retention
Patient flow is outlined in Figure 8. In total, 1306 patients met the eligibility criteria and 504 were selected for health coaching. Rates of follow-up for the various outcome measures are shown in Figure 8. There was evidence of an imbalance in attrition, with slightly higher rates of loss among patients selected for the intervention.
FIGURE 8.
The PROTECTS trial CONSORT diagram. QoL, quality of life; SD, standard deviation. Reproduced from Panagioti et al. 147 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
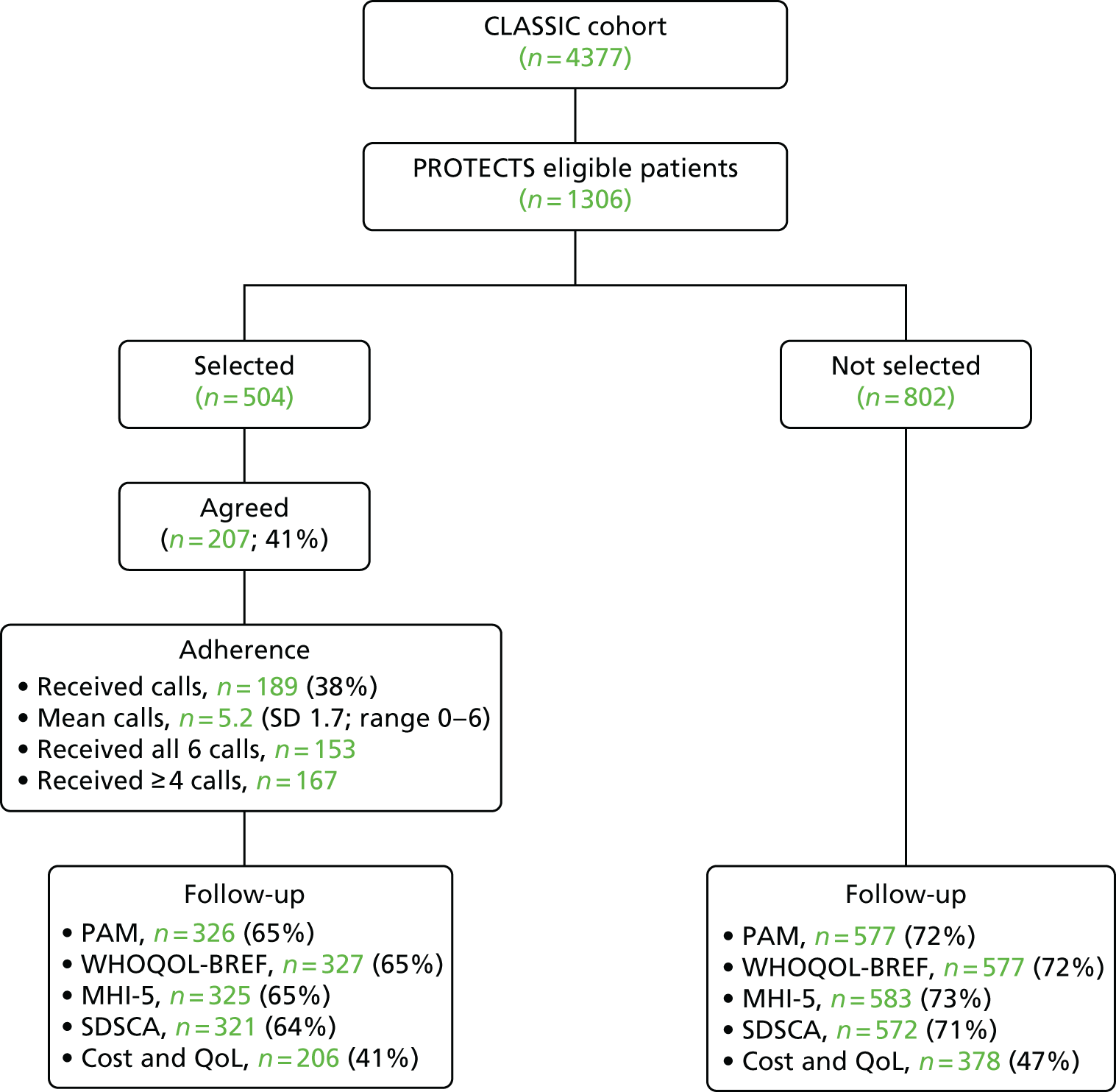
Table 34 shows the table of baseline characteristics comparing patients selected for the health coaching with those eligible but not selected, as a check on the success of the randomisation.
| Characteristic | Selection | Total (n = 1306) | |
|---|---|---|---|
| Not selected (n = 802) | Selected (n = 504) | ||
| Mean (SD) age (years) | 74.2 (6.4) | 75.4 (6.8) | 74.7 (6.6) |
| Age (years) in categories, n (%) | |||
| 65–69 | 216 (26.9) | 115 (22.8) | 331 (25.3) |
| 70–79 | 385 (48.0) | 230 (45.6) | 615 (47.1) |
| 80–98 | 155 (19.3) | 140 (27.8) | 295 (22.6) |
| Sex, n (%) | |||
| Female | 441 (55.0) | 270 (53.6) | 711 (54.4) |
| Male | 357 (44.5) | 232 (46.0) | 589 (45.1) |
| Health literacy, n (%) | |||
| Never | 536 (66.8) | 322 (63.9) | 858 (65.7) |
| Rarely | 100 (12.5) | 57 (11.3) | 157 (12.0) |
| Sometimes | 87 (10.9) | 63 (12.5) | 150 (11.5) |
| Often/always | 59 (7.4) | 44 (8.7) | 103 (7.9) |
| Living status, n (%) | |||
| Live with partner or others | 509 (63.5) | 315 (62.5) | 824 (63.1) |
| Live alone | 288 (35.9) | 188 (37.3) | 476 (36.5) |
| Education, n (%) | |||
| No qualifications | 352 (43.9) | 221 (43.9) | 573 (43.9) |
| School-level qualifications | 68 (8.5) | 56 (11.1) | 124 (9.5) |
| College degree or higher | 349 (43.5) | 191 (37.9) | 540 (41.4) |
| Mean (SD) chronic conditions | 6.8 (2.6) | 6.8 (2.5) | 6.8 (2.6) |
| Mean (SD) Index of Multiple Deprivation | 31.0 (18.8) | 33.0 (18.6) | 31.8 (18.7) |
| Employment, n (%) | |||
| Retired or not economically active | 748 (93.3) | 472 (93.7) | 1220 (93.4) |
| Working or other | 39 (4.7) | 23 (4.6) | 62 (4.8) |
| Ethnicity, n (%) | |||
| White | 786 (98.0) | 489 (97.0) | 1275 (97.6) |
| Non-white | 11 (1.37) | 12 (2.4) | 23 (1.8) |
| Mean (SD) number of GP visits in past 6 months | 3.1 (2.0) | 3.0 (1.9) | 3.1 (1.9) |
| Mean (SD) patient activation score | 57.8 (6.0) | 57.6 (5.6) | 57.8 (5.9) |
| Mean (SD) quality-of-life score (physical health) | 55.3 (19.8) | 54.0 (18.8) | 54.8 (19.4) |
| Mean (SD) number of depressive symptoms | 65.3 (21.3) | 65.3 (21.8) | 65.3 (21.3) |
| Possible depression diagnosis, n (%) | |||
| Depression | 371 (46.3) | 227 (45.0) | 598 (45.8) |
| No depression | 426 (53.1) | 265 (52.9) | 691 (52.9) |
| Mean (SD) number of self-care activities | 3.8 (0.9) | 3.8 (0.9) | 3.8 (0.9) |
Consent to participate in health coaching
Signed consent to the offer of health coaching among those eligible was initially 41% (207/504), although only 189 actually received calls (38%). Logistic regression exploring baseline factors associated with consent to health coaching is presented in Table 35. In multivariate analyses, only younger age and higher education predicted consent to take up the health coaching intervention.
| Baseline characteristic | Model | |||
|---|---|---|---|---|
| Univariate | Multivariate | |||
| Regression coefficient (95% CI) | p-value | Regression coefficient (95% CI) | p-value | |
| Age | 0.06 (–0.09 to –0.04) | 0.00 | 0.08 (–0.14 to –0.03) | 0.00 |
| Sex | ||||
| Male | 1 | 1 | ||
| Female | 0.10 (–0.26 to 0.46) | 0.58 | 0.31 (–0.29 to 0.91) | 0.31 |
| Health literacy | ||||
| Never | 1 | 1 | ||
| Rarely | –0.63 (–1.24 to –0.02) | 0.04 | –0.59 (–1.30 to 0.13) | 0.11 |
| Sometimes | –0.62 (–1.20 to –0.03) | 0.04 | –0.71 (–1.85 to 0.43) | 0.22 |
| Often/always | –0.76 (–1.46 to –0.06) | 0.03 | –1.05 (–2.05 to –0.05) | 0.04 |
| Living status | ||||
| Live with partner or others | 1 | |||
| Live alone | –0.15 (–0.53 to 0.22) | 0.42 | 0.28 (–0.46 to 1.03) | 0.46 |
| Education | ||||
| No qualifications | 1 | 1 | ||
| School-level qualifications | 0.57 (–0.02 to 1.17) | 0.06 | –0.02 (–1.21 to 1.17) | 0.98 |
| College degree or higher | 0.82 (0.42 to 1.22) | 0.00 | 1.10 (0.48 to 1.72) | 0.00 |
| Patient safety incidents | ||||
| No incident | 1 | 1 | ||
| Incident | –0.15 (–0.76 to 0.47) | 0.64 | 0.60 (–0.49 to 1.68) | 0.28 |
| Health-care access in past 12 months | ||||
| No | 1 | 1 | ||
| Yes | –0.14 (–0.65 to 0.37) | 0.58 | –0.52 (–1.62 to 0.57) | 0.35 |
| Number of chronic conditions | 0.02 (–0.05 to 0.10) | 0.49 | 0.05 (–0.09 to 0.20) | 0.5 |
| Patient activation | 0.02 (–0.01 to 0.05) | 0.16 | 0.03 (–0.02 to 0.07) | 0.25 |
| Depression | 0.01 (0.00 to 0.02) | 0.03 | 0.02 (0.00 to 0.03) | 0.06 |
| Quality of life (physical health) | 0.00 (0.00 to 0.01) | 0.33 | –0.01 (–0.03 to 0.01) | 0.28 |
| Quality of life (social relationships) | 0.00 (–0.01 to 0.00) | 0.33 | 0.01 (–0.01 to 0.03) | 0.42 |
| Quality of life (environmental) | 0.01 (0.00 to 0.02) | 0.18 | –0.01 (–0.03 to 0.02) | 0.68 |
| Self-care | 0.02 (–0.19 to 0.22) | 0.87 | –0.20 (–0.58 to 0.17) | 0.29 |
| Social support | –0.03 (–0.05 to 0.00) | 0.05 | –0.02 (–0.09 to 0.05) | 0.55 |
| PACIC total | 0.07 (–0.12 to 0.26) | 0.46 | 0.24 (–0.07 to 0.55) | 0.14 |
| Satisfied with GP care | 0.07 (–0.06 to 0.20) | 0.28 | 0.07 (–0.12 to 0.26) | 0.49 |
| Number of GP visits in past 6 months | –0.08 (–0.19 to 0.03) | 0.16 | –0.03 (–0.20 to 0.14) | 0.74 |
| Access to community assets | 0.11 (–0.04 to 0.26) | 0.16 | 0.10 (–0.07 to 0.28) | 0.25 |
The process of health coaching in patients who consented
The defined ‘dose’ of the PROTECTS intervention was monthly calls of around 20 minutes for a period of 6 months, with the option for additional calls to deal with complex patients or issues of risk.
A total of 189 out of 504 (38%) people who were randomised to the health coaching intervention agreed to take part and were referred to the health coaching team from July 2015 to March 2016. In terms of adherence, 167 out of 189 (88%) participants who consented to the intervention received four or more telephone calls.
Results on primary and secondary outcomes at follow-up
Table 36 shows the patient-reported outcomes for patients selected for the intervention and those not selected. There were no significant differences on any primary or secondary outcome.
| Outcome | Intervention, mean (SD); n | Control, mean (SD); n | Comparison | CACE estimates, adjusted difference in means (95% CI) | |
|---|---|---|---|---|---|
| Adjusted difference in means (95% CI) | p-value | ||||
| Primary outcome | |||||
| Patient activation (PAM) | 62.88 (14.39); 326 | 61.92 (13.24); 577 | 1.44 (–0.46 to 3.33) | 0.133 | 3.69 (–1.17 to 8.53) |
| Quality of life: physical health (WHOQOL-BREF) | 55.74 (19.15); 327 | 55.41 (18.72); 577 | 1.62 (–0.32 to 3.56) | 0.099 | 4.15 (–0.82 to 9.12) |
| Secondary outcome | |||||
| Depression (MHI-5) | 75.74 (16.40); 325 | 74.29 (17.26); 583 | 1.00 (–1.25 to 3.26) | 0.373 | 2.56 (–3.20 to 8.36) |
| Self-care (SDSCA) | 3.49 (1.09); 321 | 3.54 (1.10); 572 | –0.04 (–0.19 to 0.11) | 0.58 | –0.10 (–0.49 to 0.28) |
In the CACE analyses, effect sizes were higher, but none of the outcomes showed significant benefits to health coaching (see Table 36).
Sensitivity analyses provided no evidence for the results being substantively influenced by model assumptions (Table 37).
| Outcome | Comparison | |||
|---|---|---|---|---|
| After removal of covariates except baseline outcome | Following multiple imputation | |||
| Adjusted difference in means (95% CI) | p-value | Adjusted difference in means (95% CI) | p-value | |
| Primary outcome | ||||
| Patient activation (PAM) | 0.94 (–0.89 to 2.77) | 0.306 | 0.91 (–0.82 to 2.63) | 0.288 |
| Quality of life: physical health (WHOQOL) | 1.06 (–0.68 to 2.80) | 0.223 | 0.83 (–0.77 to 2.43) | 0.294 |
| Secondary outcome | ||||
| Depression (MHI-5) | 1.00 (–1.26 to 3.26) | 0.376 | 1.01 (–0.71 to 2.73) | 0.238 |
| Self-care (SDSCA) | –0.05 (–0.18 to 0.08) | 0.580 | –0.04 (–0.15 to 0.08) | 0.525 |
Economic results
Complete-case analysis requires data on age and sex at baseline, and EQ-5D-5L responses and resource utilisation at all four time points. Complete data necessary for the economic analysis were available for 45% of the sample (584/1306).
Table 38 presents the baseline characteristics of the full sample compared with the complete-case sample.
| Characteristic | Sample | |||||||
|---|---|---|---|---|---|---|---|---|
| Full (n = 1306) | Complete case (n = 584) | |||||||
| Usual care (n = 802) | Health coaching (n = 504) | Usual care (n = 378) | Health coaching (n = 206) | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age (missing, n) | 74.2 (22) | 6.40 | 75.4 (8) | 6.8 | 73.63 | 6.00 | 74.37 | 6.05 |
| Baseline EQ-5D-5L index (missing, n) | 0.70 (12) | 0.24 | 0.68 (16) | 0.25 | 0.71 | 0.23 | 0.70 | 0.24 |
| Male, % (missing, n) | 45 (0) | 46 (0) | 47 | 50 | ||||
Resource utilisation and costs: health coaching
The resources required to deliver health coaching are presented in Table 39. They consisted of training sessions on intervention delivery, staff supervision, information materials for staff and patients, and the cost of coaching sessions.
| Cost and unit estimation | 2014/15 value (£) | Notes |
|---|---|---|
| Formal PROTECTS training sessions | ||
| Main training: facilitators | 1385.60; 2 full days (16 hours) | 2 full-day sessions by researchers (one professor, one research associate), based on mid-points of University of Manchester bands 9D and 6 pay scales |
| Main training: staff time | 1856.00; 2 full days | Based on the attendance of four coaches |
| Total costs for session 1 | 3241.60 | |
| Long-term conditions training: facilitators | 560.00 (4 hours) | Half-day training session facilitated by GP |
| Long-term conditions training: staff time | 464.00 (4 hours) | Based on the attendance of four health coaches |
| Total cost | 1024.00 | |
| Additional training sessions | ||
| Additional session 1 | 214.40 | 90-minute session (one research associate) for four coaches |
| Additional session 2 | 344.30 | 90-minute session (two research associates, one professor) for four coaches |
| Additional session 3 | 254.79 | 90-minute session (two research associates) for four coaches |
| Additional session 4 | 254.79 | 90-minute session (two research associates) for four coaches |
| Additional session 5 | 214.40 | 90-minute session (one research associate) for four coaches |
| Total cost | 1282.67 | |
| Supervision | 2633.80 | Six 1-hour sessions in year 1 and seven 1-hour sessions in year 2 (one professor and two research associates) supervising four coaches |
| Production of manual | 11.40 | Printing one manual and one script per coach |
| Patient paperwork | 1.03 | Printing for progression recording and information sheets and postage |
| Delivery of PROTECTS | ||
| Call 1 | 22.08 | 25-minute call and 15 minutes of preparation by health coach |
| Call 2 | 16.70 | 20-minute call and 10 minutes of preparation by health coach |
| Call 3 | 15.51 | 18-minute call and 10 minutes of preparation by health coach |
| Call 4 | 15.51 | 18-minute call and 10 minutes of preparation by health coach |
| Call 5 | 15.51 | 18-minute call and 10 minutes of preparation by health coach |
| Call 6 | 13.73 | 15-minute call and 10 minutes of preparation by health coach |
| Unanswered/rescheduled | 4.83 | 10 minutes of staff time by health coach. Average one per participant |
| Average cost of health coaching | 148.27 per patient | Based on costs of training and delivery during the study period |
The main training session was delivered by project staff and lasted 2 full days. A second half-day training session focusing on long-term conditions was delivered by a GP. There were five additional training sessions, again delivered by project staff, each lasting 90 minutes. Thirteen 1-hour supervision sessions were conducted with project staff. Manuals and scripts for health coaches and information sheets and notes pages were printed for participants. Telephone coaching calls lasted between 15 and 25 minutes, with an additional 10–15 minutes of staff preparation before or after the call. On average, each participant had one unanswered or rearranged call, which utilised an additional 10 minutes of staff time. The average cost per individual receiving the full course of health coaching (six calls) was £148.27, of which £44.38 related to training, supervision and paperwork and £103.89 related to delivery of health coaching.
Additional resource utilisation over trial follow-up
In addition to the direct costs of the health coaching, the economic analysis also considered wider NHS resource utilisation. Table 40 reports the average utilisation by resource category for the complete-case sample, separated by treatment arm, and summarised as the mean number of contacts with each service per individual.
| Type of service | Usual care (n = 378) | Health coaching (n = 206) | ||
|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | |
| Baseline to 6 months | ||||
| Secondary care contact | ||||
| Emergency short stay | 0.063 | 0.039 to 0.088 | 0.058 | 0.026 to 0.091 |
| Emergency long stay | 0.026 | 0.009 to 0.044 | 0.024 | 0.003 to 0.045 |
| Day case | 0.172 | 0.104 to 0.240 | 0.112 | 0.059 to 0.165 |
| Elective admission | 0.024 | 0.008 to 0.039 | 0.029 | 0.002 to 0.056 |
| Outpatient | 4.992 | 4.162 to 5.823 | 6.553 | 4.977 to 8.130 |
| A&E attendance | 0.156 | 0.110 to 0.203 | 0.131 | 0.083 to 0.179 |
| GP appointments | 3.111 | 2.791 to 3.431 | 3.039 | 2.641 to 3.437 |
| 7–12 months | ||||
| Secondary care contact | ||||
| Emergency short stay | 0.050 | 0.027 to 0.074 | 0.039 | 0.006 to 0.072 |
| Emergency long stay | 0.040 | 0.010 to 0.069 | 0.019 | 0.000 to 0.038 |
| Day case | 0.127 | 0.069 to 0.185 | 0.053 | 0.017 to 0.090 |
| Elective admission | 0.029 | 0.009 to 0.049 | 0.029 | 0.002 to 0.056 |
| Outpatient | 4.595 | 3.650 to 5.540 | 6.403 | 5.126 to 7.680 |
| A&E attendance | 0.159 | 0.108 to 0.209 | 0.097 | 0.041 to 0.153 |
| GP appointments | 2.783 | 2.527 to 3.039 | 3.058 | 2.696 to 3.421 |
| 13–18 months | ||||
| Secondary care contact | ||||
| Emergency short stay | 0.132 | 0.091 to 0.174 | 0.068 | 0.028 to 0.108 |
| Emergency long stay | 0.045 | 0.022 to 0.068 | 0.034 | 0.009 to 0.059 |
| Day case | 0.196 | 0.107 to 0.284 | 0.180 | 0.105 to 0.254 |
| Elective admission | 0.040 | 0.020 to 0.059 | 0.063 | 0.027 to 0.099 |
| Outpatient | 7.185 | 6.064 to 8.307 | 9.893 | 8.570 to 11.217 |
| A&E attendance | 0.275 | 0.207 to 0.343 | 0.170 | 0.112 to 0.228 |
| GP appointments | 2.865 | 2.599 to 3.131 | 2.922 | 2.543 to 3.302 |
Although there was variation in the use of services over time and between treatment arms, some consistent patterns can be seen. The most frequently utilised category across both treatment groups was outpatient appointments, followed by GP appointments.
The average number of emergency admissions (short stays) and A&E attendances was lower for the health coaching arm at all three time points, with the differences between the treatment arms increasing over time. The health coaching arm also had lower emergency admissions (long stays) and day cases at all three time points. Elective admissions and outpatient appointments were higher at all three time points among the health coaching arm, with the difference in outpatient appointments increasing over time.
Resource use was higher at 18 months than it had been at 12 months for all resource use categories in both treatment arms. However, in the health coaching arm, emergency admissions, day cases, outpatient appointments and A&E attendances fell at 12 months compared with 6 months, before rising again. Although emergency admissions (short stays), day cases and outpatient appointments also fell in the usual care arm, no such drop was observed for emergency admissions (long stays) or A&E attendances, with use rising at each consecutive time point in the usual care arm.
Overall, there was a pattern of greater use of emergency care among the usual care arm, whereas health coaching patients utilised more planned services.
To cost both arms, unit costs were applied to individual utilisation. Table 41 presents a list of all unit costs used, together with their source. Table 42 combines the resource utilisation of the complete-case sample with the unit costs to obtain the average costs associated with this resource utilisation over the trial period.
| Item | Unit cost (£) | Unit | Source | Details |
|---|---|---|---|---|
| Secondary care | ||||
| Emergency short stay | 608.00 | Per stay | PSSRU UCHSC110 | Non-elective inpatient stay (short stay), average cost per episode |
| Emergency long stay | 2863.00 | Per stay | PSSRU UCHSC110 | Non-elective inpatient stay (long stay), average cost per episode |
| Elective admission | 3405.00 | Per stay | PSSRU UCHSC110 | Elective inpatient stay, average cost per episode |
| Day case | 704.00 | Per day case | PSSRU UCHSC110 | Day case, weighted average of all stays |
| Outpatient | 112.00 | Per attendance | PSSRU UCHSC110 | Outpatient attendances, weighted average of all (consultant and non-consultant led) |
| A&E attendance | 132.00 | Per attendance | NHS reference costs 111 | A&E attendance |
| Primary care | ||||
| GP | 44.00 | Per visit | PSSRU UCHSC110 | GP visits: surgery (11.7 minutes) |
| Unit costs associated with the health coaching | ||||
| Health coach | 29.00 | Per hour | PSSRU UCHSC110 | Agenda for Change band 4 mid-point. Cost per working hour |
| Research associate (grade 6) | 26.93 | Per hour | University pay scales | Mid-point of grade 6, including national insurance, pension, leave and sick pay |
| Professor (grade 9D) | 59.67 | Per hour | University pay scales | Mid-point of grade 9D, including national insurance, pension, leave and sick pay |
| GP | 140.00 | Per hour | PSSRU UCHSC110 | Per hour of GMS activity, with qualification costs |
| Call costs | 0.29 | Per minute | BT consumer price guide | BT local call domestic rate |
| Printing | 0.05 | Per page | ||
| Postage | 0.53 | Per item posted | Royal Mail | Second class stamp |
| Type of service | Sample group | |||
|---|---|---|---|---|
| Usual care (n = 378) | Health coaching (n = 206) | |||
| Mean (£) | 95% CI (£) | Mean (£) | 95% CI (£) | |
| Secondary care cost | ||||
| Emergency short stay | 146.87 | 112.25 to 181.48 | 98.95 | 64.27 to 133.63 |
| Emergency long stay | 313.76 | 190.97 to 436.54 | 219.08 | 101.92 to 336.24 |
| Day case | 343.61 | 212.29 to 474.93 | 238.36 | 166.87 to 309.86 |
| Elective admission | 310.71 | 203.04 to 418.38 | 405.96 | 201.93 to 609.99 |
| Outpatient appointment | 1851.42 | 1605.13 to 2097.70 | 2521.95 | 2139.57 to 2904.32 |
| A&E attendance | 76.66 | 62.69 to 90.63 | 51.79 | 39.33 to 64.24 |
| Mean total costs of secondary care contacts | 3043.02 | 2626.02 to 3460.03 | 3536.09 | 2979.87 to 4092.31 |
| GP appointments | 381.14 | 350.96 to 411.32 | 392.50 | 351.72 to 433.28 |
| Health coaching costs | 79.29 | 69.59 to 88.99 | ||
| Mean total cost | 3424.16 | 2999.98 to 3848.34 | 4007.88 | 3444.57 to 4571.18 |
The most costly category of resource use was outpatient appointments, followed by elective admissions and GP appointments. These are all planned care services, the costs of which were higher in the health coaching group. Conversely, the costs of emergency admissions (short and long stays), day cases and A&E attendances were higher in the usual care group. Overall, mean costs were higher in the health coaching group (£4000.88) than in the usual care group (£3424.16).
Intervention costs in the health coaching averaged £79.29. This was lower than the £148.27 estimated for full treatment because not all individuals took up the offer or completed the full course.
Outcomes
Table 43 summarises the EQ-5D-5L utility scores at each time point and the total QALYs gained over the 18-month follow-up period for the complete-case sample. On average, patients who received health coaching reported slightly lower health-related quality of life at baseline than those who received usual care (mean utility 0.696 and 0.708, respectively). This value fell steadily over the follow-up period in the usual care group, reaching 0.664 at the 18-month follow-up, but in the health coaching group remained relatively unchanged at the end of follow-up, at 0.691. The mean unadjusted QALYs for usual care and health coaching over the study period were 1.105 and 1.124, respectively.
| Time point | Sample group | |||||||
|---|---|---|---|---|---|---|---|---|
| Usual care (n = 378) | Health coaching (n = 206) | |||||||
| Mean | SD | Minimum | Maximum | Mean | SD | Minimum | Maximum | |
| Baseline | 0.708 | 0.230 | –0.180 | 1.000 | 0.696 | 0.236 | –0.102 | 1.000 |
| 6 months | 0.691 | 0.247 | –0.185 | 1.000 | 0.709 | 0.228 | 0.018 | 1.000 |
| 12 months | 0.685 | 0.254 | –0.246 | 1.000 | 0.694 | 0.237 | –0.000 | 1.000 |
| 18 months | 0.664 | 0.264 | –0.180 | 1.000 | 0.691 | 0.260 | 0.000 | 1.000 |
| QALYs | 1.105 | 0.374 | –0.290 | 1.723 | 1.124 | 0.355 | 0.055 | 1.683 |
Cost-effectiveness analysis: full sample with imputation
Table 44 presents the adjusted estimates of the effect of the offer of health coaching on the incremental costs and QALYs over and above usual care in the full sample with imputed data. This analysis controls for age, sex and baseline utility. Health coaching is associated with a mean incremental total cost increase of £150.583 (95% CI –£470.611 to £711.776) and a mean incremental QALY gain of 0.019 (95% CI –0.006 to 0.043).
| Health coaching (n = 503) over usual care (n = 802) | Mean | Bootstrapped standard error | Bootstrapped 95% CI |
|---|---|---|---|
| Incremental cost (£) | 150.583 | 316.941 | –470.611 to 771.776 |
| Incremental QALYs | 0.019 | 0.012 | –0.006 to 0.043 |
| ICER (£) | 8049.96 |
Although there are no statistically significant differences in either costs or QALYs, the point estimate of the ICER is £8049.96 per QALY. This would represent a cost-effective intervention with respect to the standard cost per QALY threshold of £20,000–30,000. However, it is important to consider the uncertainty surrounding this estimate.
The cost-effectiveness plane plots the 10,000 bootstrap replications of incremental cost and QALY estimates to illustrate uncertainty in probabilistic terms (Figure 9). The replications are clustered predominantly in the north-east quadrant, reflecting a positive health gain at an increased cost. Health coaching resulted in an incremental QALY gain in 94% of bootstrap replications and costs were higher than usual care in 69% of replications.
FIGURE 9.
Cost-effectiveness plane: full sample with imputed data. Reproduced from Panagioti et al. 147 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
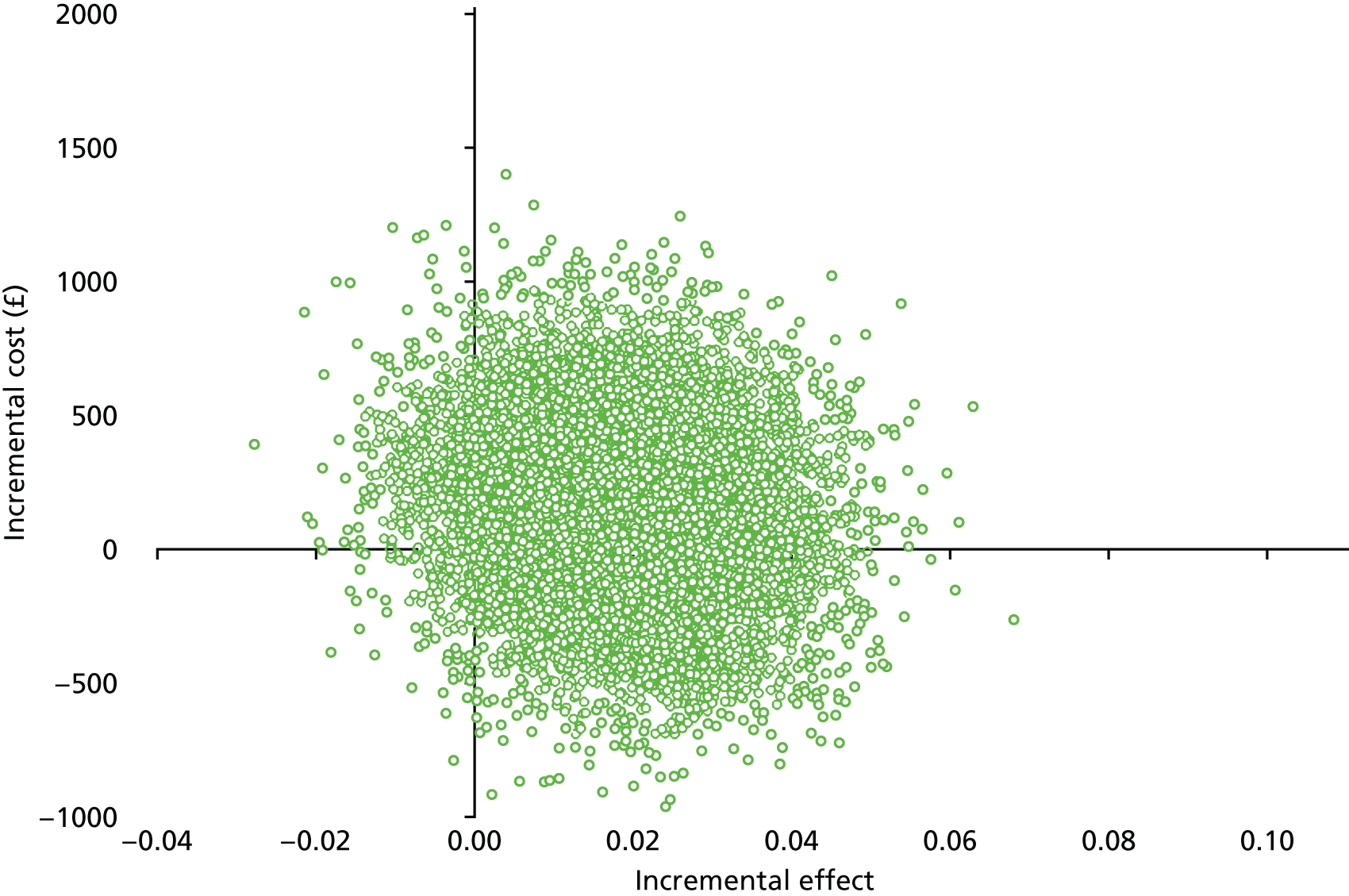
The CEAC (Figure 10) demonstrates how the probability that health coaching is cost-effective increases with the decision-maker’s willingness to pay. At the lower bound threshold of £20,000 per QALY, there is a 70.2% probability of health coaching being cost-effective. This rises to 79.0% at the upper bound of £30,000. Compared with usual care, health coaching is likely to be cost-effective in ≥ 50% cases if decision-makers are willing to pay ≥ £8180 for 1 QALY.
FIGURE 10.
Cost-effectiveness acceptability curve: full sample with imputed data. Reproduced from Panagioti et al. 147 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
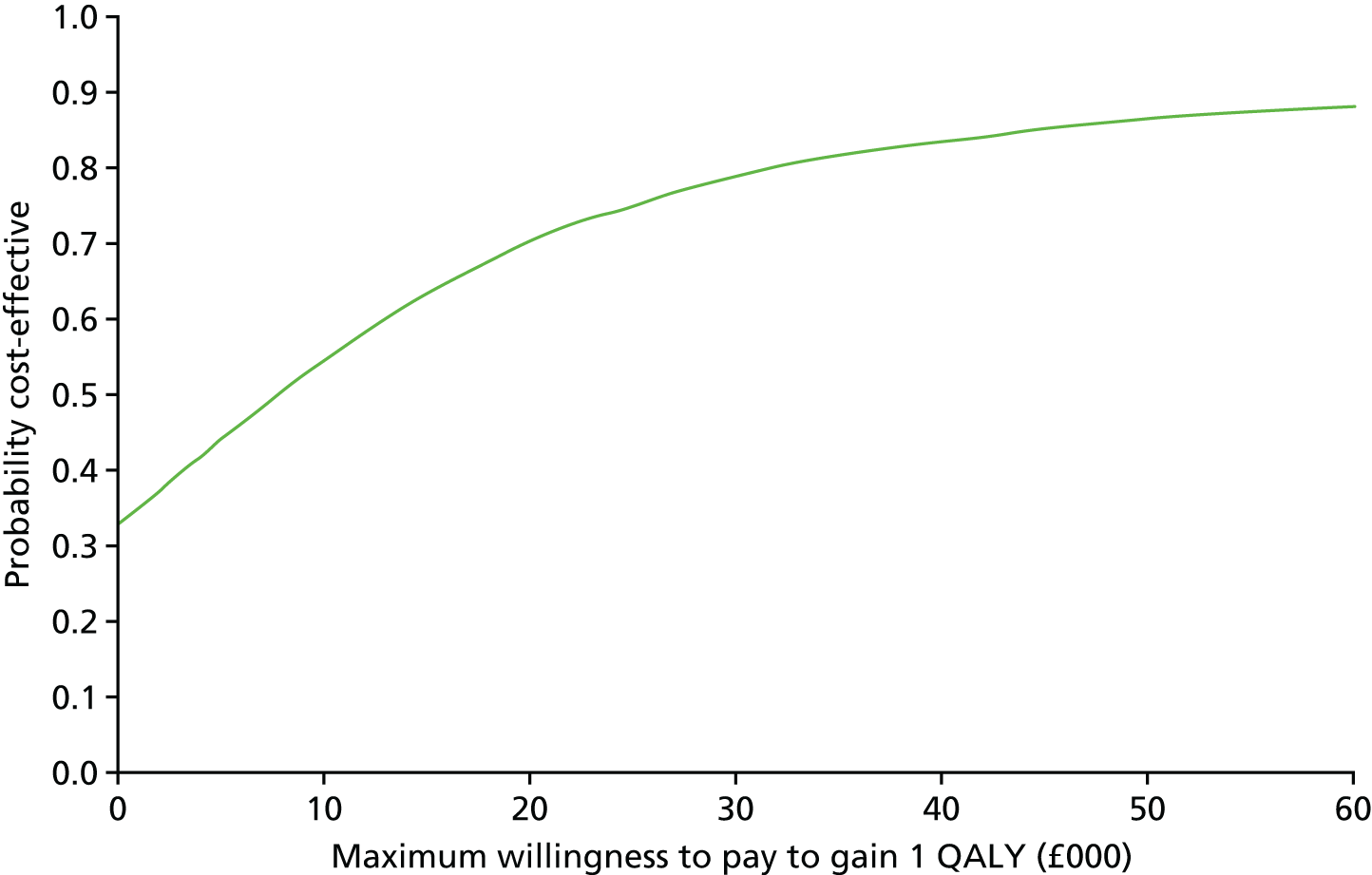
Cost-effectiveness analysis: complete-case analysis
Table 45 presents the adjusted estimates of the effect of the offer of health coaching on the incremental costs and QALYs over and above usual care in the complete-case sample.
| Health coaching (n = 206) over usual care (n = 378) | Mean | Bootstrapped standard error | Bootstrapped 95% CI |
|---|---|---|---|
| Incremental cost (£) | 497.99 | 350.6141 | –189.19 to 1185.19 |
| Incremental QALYs | 0.037 | 0.017 | 0.004 to 0.070 |
| ICER (£) | 13,506.27 |
Health coaching is associated with a mean incremental cost of £497.99 (95% CI –£189.19 to £1185.19). Although higher than the incremental cost associated with health coaching in the full sample with imputation, this difference in cost between arms still does not reach statistical significance. The incremental QALY estimate is also higher, at 0.037 (95% CI 0.0037 to 0.070), indicating that there was a significant QALY gain associated with health coaching among the complete-case sample. This results in an ICER of £13,506.27 per QALY, which is again below the lower bound of recommended cost-effectiveness thresholds.
It is again important to examine the uncertainty around these point estimates in probabilistic terms.
Figure 11 shows that the bootstrapped replications are again clustered predominantly in the north-east quadrant. There is notable shift north above the x-axis and to the right of the y-axis compared with the full sample with imputation, as even more of the replications now fall into this quadrant, representing incremental increases in both costs and QALYs above usual care. Health coaching was more costly in 92.5% of replications and led to an incremental QALY gain in 98.6% of replications. The CEAC illustrates that, at the lower bound (£20,000/QALY), there is a 67.2% probability that health coaching is cost-effective, rising to 82.0% at the upper bound of £30,000 per QALY (Figure 12). Compared with usual care, health coaching is likely to be cost-effective in ≥ 50% cases if decision-makers are willing to pay ≥ £13,570 for 1 QALY.
FIGURE 11.
Cost-effectiveness plane: complete-case sample.
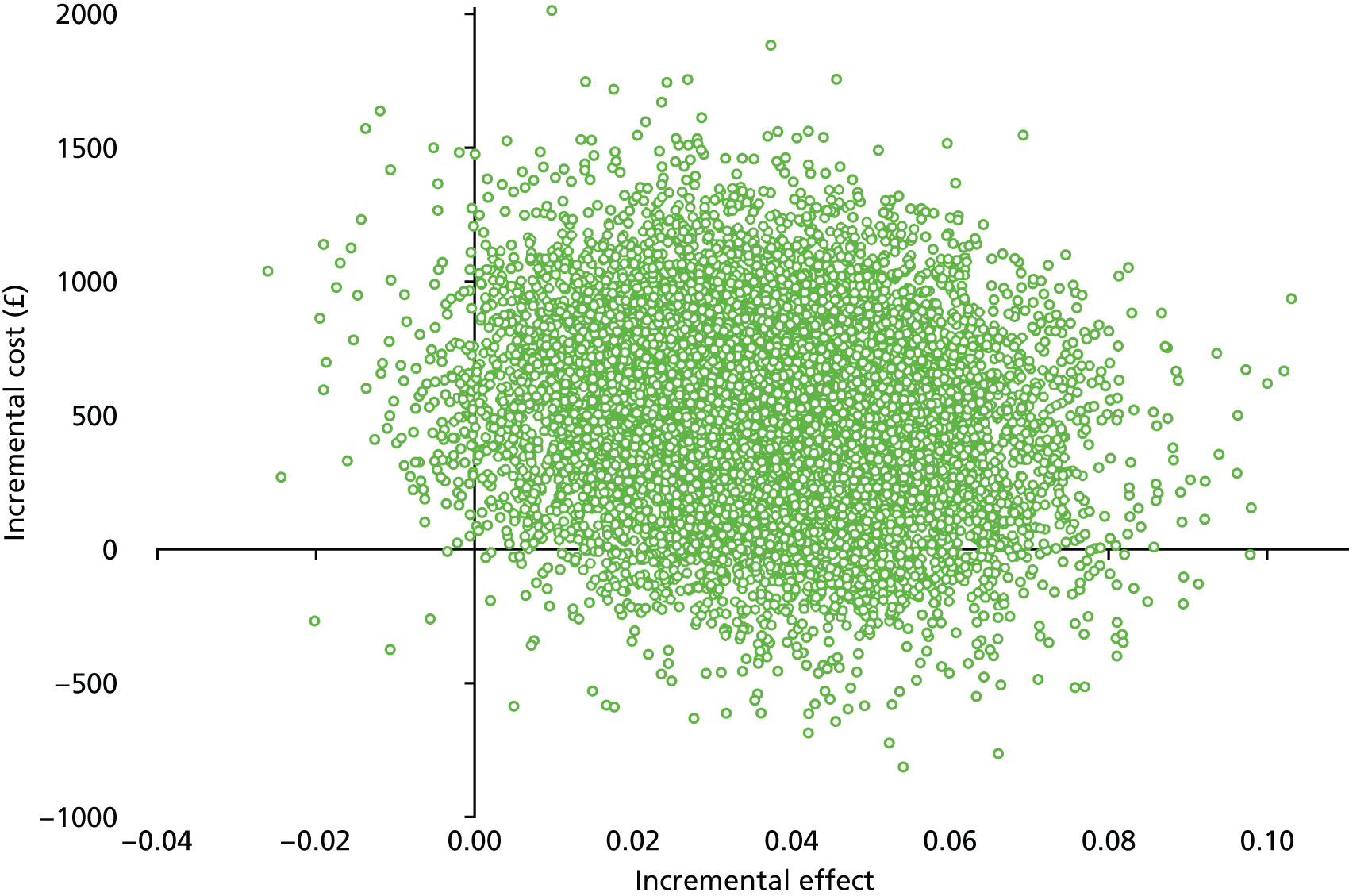
FIGURE 12.
Cost-effectiveness acceptability curve: complete-case sample.
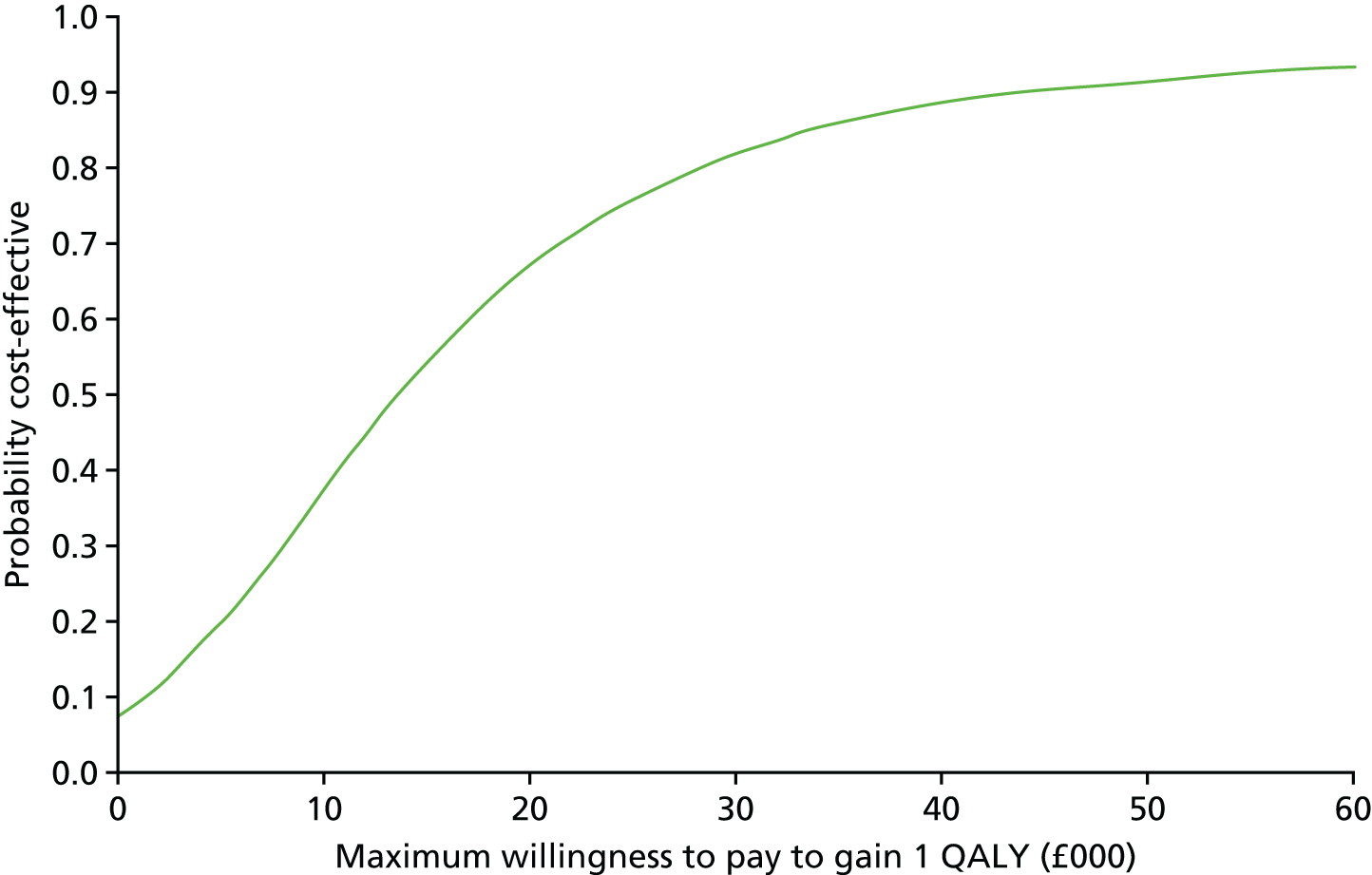
Discussion
The economic analysis suggested that health coaching resulted in an incremental increase in both costs and QALYs. When a QALY is valued at £20,000, the primary analysis suggests that there is a 70% probability that health coaching is cost-effective.
We used administrative records to fully capture secondary care utilisation, relying on self-reported data for GP appointments only. This thorough examination of resource utilisation patterns showed that individuals in health coaching had a higher utilisation of planned services and lower use of emergency hospital services than those in usual care.
The cmRCT estimates represent the mean effect of the offer of treatment, rather than the effect of treatment on those receiving treatment. The estimates are diluted further by the use of data collected at fixed time intervals. As the start of treatment varied greatly between individuals, the treatment effect is diluted by the inclusion of this pre-treatment period. The estimates presented therefore represent a very conservative estimate of the impact of health coaching.
A major criticism of conventional trials is that they show the effectiveness of an innovation in a very selected group of patients, but fail to ‘scale’ because of issues such as low rates of acceptability among the wider population and differences between those who take part in trials and those eligible for the intervention. 148 Low uptake is not a problem in trials – variable uptake and adherence is inherent in pragmatic trials, by design, on the assumption that utilising interventions in routine settings will be accompanied by these issues, and that the estimates of effect generated are those that are most relevant to NHS decision-makers. 149 The PRagmatic Explanatory Continuum Indicator Summary (PRECIS)-2 tool for the assessment of pragmatic trials has a specific rating of the measures in place to ensure adherence, with the highest scores for those with no special measures in place. 150
However, conventional pragmatic trials are still selective, as patients are randomised on the basis of their initial willingness to engage with the intervention. In a cmRCT, acceptability in the wider population is built into the design, alongside the usual impact of variable adherence. In such a context, it is very challenging to show benefit, but it was felt that the design was a relevant test of health coaching as applied in an integrated care system as a population health strategy, reaching out to patients assessed as in need, but who may not necessarily be looking for self-management support.
Chapter 14 Discussion
Summary of the principal findings
As noted earlier, the original research call was for ‘ambitious research studies assessing the cost-effectiveness of new and innovative models of care or clinical pathways for people with long term conditions. The aim is to generate high-impact research which will provide commissioners and providers with useful evidence when re-designing services’. 39
The broad aims of the CLASSIC study were to meet this brief, assessing, in detail, the process of implementation of the new SICP and the degree to which it was influenced by the local and national context, and to complement this with a detailed analysis of the impact of the SICP on patients and its clinical effectiveness and cost-effectiveness. The CLASSIC study had the following research questions:
-
How do key stakeholders (commissioners, strategic partners) view the SICP, what do they expect from it and how is it aligned with their objectives and incentives?
-
What is the process of implementation of two key aspects of the SICP: the MDGs and ICC?
-
What is the impact of the MDGs on the outcomes and costs of people with long-term conditions?
-
What is the impact of health coaching from the ICC on the outcomes and costs of people with long-term conditions?
As an overview, the results presented in this report could characterise the SICP as showing rapid progress in terms of organisational integration, with slower implementation of the planned mechanisms of integration. At this point in time, there is limited evidence of patient benefit, in terms of either reach (the numbers of patients receiving exposure to mechanisms of integration) or impact (the size and scope of the benefits reported).
Our interviews with stakeholders made it clear that the development of the SICP (and the ICO) was facilitated by strong partnerships between organisations, local geography and a history of local joint working. The initial governance model (an Alliance Board and Alliance Agreement) ensured that the initial impetus was sustained despite the complexities of the integration process. The Alliance Agreement did not represent a legally enforceable contract and was not ‘tested’ during the development of the SICP, nor have applications of this model been formally evaluated. 151 Nevertheless, the process was important in cementing partnerships. Managerial work associated with implementing the ICO may have distracted attention from operational detail, but the structures in place to manage the SICP (operational managers and management groups) meant that the programme continued to be implemented even as the ICO drew in attention and resources. The failure to fully engage primary care providers (in particular GPs) is perhaps the most obvious limitation of the early implementation. The creation of the Salford GP provider organisation in mid-2016 (towards the end of the research) provided new opportunities for the development of effective ways of working with the ICO, but has occurred fairly late in the delivery of the CLASSIC research programme.
As befits a ‘large-scale service transformation’, the SICP delivered integration of various types and levels. 6,9 System-level integration was well developed, with functional and structural integration in pooling health and social care budgets, the Alliance Agreement and development of the ICO. ‘Service-level’ integration was observed in the ICC and the MDGs, although the speed of development trailed somewhat behind the system level. This may reflect the changes in the programme theory outlined in Chapter 10, that is, a move towards a logic that closer structural integration would lead to functional integration, in which working together across organisational and professional boundaries would become the norm, leading to better outcomes and patient experience, rather than the mechanisms of integration being the primary driver of change. Whether or not structural integration will deliver those benefits152 and whether the additional focus on structure facilitates or delays patient benefit remains to be seen.
Implementation of the mechanisms of integration in the SICP
As noted earlier, the progress on structural integration through the SICP to the ICO was not closely connected to the delivery of integrated care services, and the various management processes put in place by the SICP ensured that progress continued on delivery. The next section will consider how much progress was achieved in delivering the planned mechanisms of integration.
The MDGs were the largest mechanism in terms of scope and resource, and the most rapidly implemented (with some delays around planned pilots and ‘tests of change’). There were some significant challenges in implementation (owing to issues with engaging with GPs), dealt with in time through relevant contractual arrangements. SICP staff involved in the MDG process reported that consistent input from all professional groups was achieved around August 2016, when it might be said that the complete model was in place, placing it towards the end of the CLASSIC study timeline and thus limiting our ability to assess impact of the complete model given the data that were available.
Multidisciplinary group meetings were generally well attended, and staff were broadly positive about the model. They reported some issues with what was perceived to be slow progress, as well as a focus on patients at certain levels of need who may have fewer opportunities to experience proactive care. These concerns echoed the general debate about risk stratification of patients and about where resources are best placed to generate real gains in health and reductions in utilisation. 78
Early implementation in MDGs focused on process measures (such as creation of records). Actions arising from the MDGs were often relatively limited, echoing similar interventions elsewhere in the UK. 153 Although ‘care co-ordinators’ were allocated to patients being discussed by MDGs, interviews with patients and carers showed that MDG discussions were taking place without their involvement. As MDGs were quickly implemented across the locality, we could not conduct a formal experiment. We compared admissions in Salford with those in other areas, which showed little difference from the national trend, with the strongest evidence suggesting an increase in emergency admissions. The SICP is not the only integrated care initiative to report such outcomes. 33 There is a legitimate question as to when the MDGs could reasonably expect to see effects on utilisation, and the timing of the full implementation may have reduced the ability to show benefits of MDGs in the CLASSIC timeline. Further analysis can continue to explore utilisation to see if the initial effects change over time.
The ICC faced some significant challenges in implementation and clarity of vision. Patients’ experiences of the ICC were mixed, which in part reflected the need to adapt to new ways of engaging with services. It was not clear that the centre was functioning to enhance patient experience of an integrated service, although colocation was noted by staff to be a potentially important mechanism of integration in terms of understanding roles and identifying new possibilities for support, which suggests that initial benefits may be focused on staff rather than patients. 153 Such benefits in the process of care are likely to show benefits in patient outcomes over the longer term, if at all.
We conducted a formal trial of a health coaching intervention within the ICC. Patients using the service reported that it was acceptable and useful. Impacts on self-management and self-reported health were small, but the economic analysis suggested a reasonable probability that the intervention was cost-effective at conventional levels of willingness to pay. However, the intervention delivered improved health-related quality of life at an additional cost, and did not reduce utilisation overall (although the pattern of use suggested less use of emergency care and more use of planned appointments).
The SICP sought to increase access to community assets, and we saw a small increase in reported use of assets plausibly attributable to the SICP. Asset use was associated with better quality of life, when accounting for other factors, but impacts on utilisation were not significant. As with coaching, and in line with other quality improvement projects in integrated care, improving outcomes seems easier to deliver than reductions in utilisation. 154,155
Overall, the SICP made some modest improvements in outcomes to some patients, including patient experience and quality of life, although the numbers impacted were relatively small and the magnitude of the benefits was limited. There was much less evidence that the programme was leading to reductions in health-care utilisation.
Interpretation of the findings: overall
As noted in Chapter 1, there is a fairly large body of international literature on integrated care, and this has demonstrated some benefits of this model, although effects are somewhat inconsistent and impacts on economic outcomes are difficult to demonstrate consistently. However, there are issues concerning the interpretation of that very broad set of studies and applying the results to the particular context of the NHS. Empirical studies of integrated care in the NHS have demonstrated more modest impacts. A key motivation for the present study was to explore whether or not a particular model of integration (the SICP) delivered in a receptive context49 could demonstrate improved outcomes. Overall, the results suggested that the receptive local context facilitated moves to structural integration, but it is not clear if benefits translated to the delivery of the specific mechanisms of integration, which faced the challenges and delays that have been reported in other evaluations. 36,37 There were initial indicators of benefits among a modest proportion of patients (increases in reports of community assets and care plans, themselves associated with improved outcomes).
Interpretation of the findings in the context of the wider literature: multidisciplinary groups
Multidisciplinary groups (and linked case management interventions) have a peculiar place as mechanisms of integration in the NHS. They are very common, with a survey of CCG plans finding that around 80% included some form of MDG. 79 Nevertheless, since Evercare,29,30 evidence that this model can reliably reduce hospital admissions is weak. 18,19,33,77,78,156 The recent National Audit Office report stated that:
While popular approaches, such as multi-disciplinary teams focusing on patients with multiple and complex needs, may improve the care experience for a minority of patients, the evidence to date does not suggest that they will achieve the widespread efficiencies and outcomes needed in the current financially constrained times.
A realist model would hypothesise that the mechanism of MDGs might activate only in certain contexts. We identified a number of contextual factors that might be present in the SICP, including the partnership underlying the SICP, high-quality IT, the potential for self-management support via the interface between MDGs and other mechanisms of integration in the SICP, support for MDG development through quality improvement and ‘tests of change’, and the use of a ‘neighbourhood’ model for MDGs. Although many of these contextual facilitators are plausible effect modifiers, there is no strong evidence either way as to their actual impact.
The quantitative analysis was unambiguous in showing that the introduction of the MDGs failed to reduce admissions, with the strongest evidence showing an increase. This core result was robust to a variety of analytical models, comparators and the staging of the MDGs, and reflects similar outcomes found in previous work. 33
There are a number of possibilities that account for this lack of effect:
-
MDGs are not effective. As noted, the lack of effect demonstrated here is not unusual. 19 There are potential competing interventions to reduce admissions, such as enhanced continuity of care,157 although they are more difficult to test in a controlled fashion.
-
MDGs are effective, but are so widespread that showing differences for an intervention in any one area compared with comparators is difficult (as noted, most CCGs include the intervention in some form). The SICP MDGs may be unable to outperform similar interventions elsewhere, rather than being ineffective per se.
-
The contextual facilitators we describe are incorrect or ineffective. We did not find strong evidence that IT was a strong facilitator of the MDGs, linkage to other parts of the SICP (such as community assets) to support self-management was limited, GP engagement was variable and the advantages of the neighbourhood model not fully articulated or observed.
-
MDGs are effective if targeted. Critics suggest that excessive focus on ‘high utilisers’ means that interventions are provided to a patient group that is both too small to show meaningful change in admissions and impervious to change because of the severity of their conditions. 78 A variety of risk algorithms have been used worldwide, but these were not adopted here, which may have attenuated effects, although there is little strong evidence that particular algorithms are effective. Targeting of specific groups and specific contexts, such as hospital-led case management for heart failure, may increase impact but clearly restricts the scope of benefits. 20 It is interesting to note that the health coaching intervention (which is based on an assessment of patient activation, not future risk of admission) actually led to reductions in emergency care use, providing some support to the idea that a focus on prevention among larger groups of lower-risk patients may be an alternative strategy (although the evidence here is also weak).
-
The evaluation of MDGs was too early to show benefits. A significant focus of the early work on MDGs was on forming the groups, identifying patients, developing ways of working and organising required systems. The numbers of patients managed by MDGs and the various performance indicators in place may have led to a focus on certain aspects (such as the creation of records), to the detriment of others (such as referral to other parts of the SICP to support self-management). Analysis of the work of similar teams in north-west London also found improved collaboration, but a lack of actions to take forward,158 as well as suggestions that the benefits might be more apparent for professionals (via shared learning) than patients. 153 There was some evidence that MDG function improved over time. Improved patient outcomes may become apparent only later.
-
Patient involvement in MDGs was insufficient. There were aspirations for patients to be involved (such as being informed that they were subject to a discussions and involvement in care planning). However, the numbers of patients to be managed and pressure of performance targets may have limited scope for patient involvement. There may be aspects of integrated care that can be achieved without significant patient involvement (such as better co-ordination between agencies) and through which patient benefits may accrue, even if integration is ‘behind the scenes’. The empirical evidence that the effects of MDGs are multiplied by effective patient involvement is not strong. However, there is an argument that some of the potential benefits of MDGs are lost without that involvement. Recent research has outlined some of the ways in which they could contribute and the barriers to them doing so. 159
Interpretation of the findings in the context of the wider literature: health coaching
Compared with MDGs, health coaching is focused on patients lower down the ‘risk pyramid’, with a simpler intervention focused on improving self-management. The benefits of such an intervention on high-cost health-care utilisation (such as admissions) is likely to be deferred in time, as patients are not at high risk. However, such prevention models may be more effective in the longer term, as the numbers of patients in this group are so much higher and their potential to benefit from intervention may be greater. 160,161
Of course, realising those benefits requires two features: (1) a significant level of uptake of the intervention among patients with needs who are not necessarily seeking help and (2) enduring impact on health attitudes and behaviour which will translate to longer-term benefits, especially in relation to care utilisation.
We did not demonstrate significant impacts on patient-reported outcomes, despite largely positive assessments from patients in the qualitative research. An important limit on effectiveness was the low uptake among patients. In terms of uptake, the levels found (40%) are reasonable, given that this was not a help-seeking group and the invitation came from outside usual services routes (such as GPs). This suggests a willingness to take part in such ‘preventative’ interventions among an older population with long-term conditions. It is, of course, important to remember that the CLASSIC cohort was itself selected, in that patients had to agree to be part of it.
The cmRCT estimates the effect of being selected for treatment, regardless of whether or not that offer is taken up. This is different from a conventional trial, in which patients who do not give consent are excluded from the trial and the effect being estimated is that of randomisation to treatment. Therefore, demonstrating effectiveness in a cmRCT is even more challenging than in a conventional pragmatic trial, as the cmRCT faces loss of potency through variability in quality of delivery and adherence as well as overall uptake, as opposed to the former alone in a pragmatic trial.
We argue that the treatment effect estimated is an appropriate one for health coaching, as it is a model of integrated care designed to be proactive, using identification of patients in the community according to external criteria rather than their own help-seeking, and designed to achieve population benefit. However, it cannot be assumed that the rates of consent in PROTECTS would generalise to delivery in routine practice. 162
The economic analysis suggested that the intervention was likely to be cost-effective, delivering modest improvements in quality of life at some increased overall cost. The methods of the cost-effectiveness analysis are not based on notions of clinical or statistical significance. Decisions to adopt one intervention over another are based on the expected cost-effectiveness of the interventions and the probability of making the correct decision. 163
Interpretation of the findings in the context of the wider literature: community assets
Although there is a consensus that community assets improve health, the experimental literature around assets and related interventions, such as social prescribing, is limited. 164 We found a small increase in use of assets among cohort participants and found that increases in asset use were related to improvements in quality of life, but not care utilisation. It is possible that benefits in quality of life have a longer-term impact on utilisation, in line with the prevention model underlying some discussions of integrated care. 160
Strengths and weaknesses of the CLASSIC study
There is an increasing recognition that the scale and pace of reform and reorganisation in the NHS calls for new methods of evaluation that balance rigour with speed and responsiveness. 41
Our broad methods were conventional, using routine data and non-randomised comparisons to assess causal relationships, allied to detailed descriptive and qualitative research to provide depth, explore context and assess mechanisms. 29,30,33,51
The use of the cmRCT represented a methodological innovation. The cohort provided an ongoing assessment of patient experience (absent from assessments based on routine data only), eased recruitment of the trial sample and allowed modelling of the impact of mechanisms of integration, such as community assets, by providing a measurement framework into which interventions were introduced, rather than measurement following the intervention. The cohort also provided the opportunity to produce a variety of papers related to the general management of patients with multiple long-term conditions. 114,115 Attempts were made to run additional trials, but funding bids were not successful.
It had been hoped that mechanisms of integration in the SICP could have been allocated in ways that allowed more scope for causal inference (such as ‘stepped’ allocation). In reality, the practical demands of the programme were such that the only ‘staging’ of change involved the early introduction of the MDGs in two neighbourhoods, driven by a desire to pilot the service.
The challenges faced in the delivery of the SICP are not dissimilar to many of these reported in the wider literature, with slower than anticipated implementation a common feature of integrated care evaluations that causes difficulties for the timing of any evaluation. 165 As noted previously, the impact of investment in community assets, delivery of care plans and significant engagement by MDGs with large numbers of patients had yet to materialise, and thus clear evidence of benefit may be deferred. As noted in Chapter 2, the formal ‘end date’ for evaluation of the SICP is 2019–20. The original CLASSIC bid was for 5 years, and extending the evaluation could assess longer-term effects.
We took a population perspective, exploring the effects of the mechanisms of integration on a large cohort (for self-reported outcomes) and the population of Salford (for hospital utilisation), rather than a more restrictive view exploring effects on those patients who were specifically targeted by particular SICP mechanisms. The latter approach may be more likely to show impacts, as there is a direct link between the mechanisms and the outcome. However, the restricted view would ignore wider effects; for example, MDGs might generate benefits by focusing on a sample of patients, with worse outcomes among those who are not targeted and thus receive less attention.
Although some outcomes may take time to become apparent, some previous evaluations of integrated care have reported impacts on issues such as patient experience at an earlier stage. 33 We found only limited evidence of such impacts here, with the most notable change being in reports of written care plans and access to community assets. Although there were initial concerns among the research team that the SICP may have been implemented before the necessary ethical and governance arrangements were in place for CLASSIC, in reality, the introduction of CLASSIC proceeded at a pace that may have been too rapid for the benefits of the SICP to be evident.
The combination of the population perspective and the timing of the SICP and CLASSIC mean that the limited impacts shown at this point are provisional; the SICP has not demonstrated significant population-level impacts at this point in its development. It remains to be seen if those effects will become apparent in time.
The CLASSIC study does represent a single-site evaluation, with consequent limits on external validity. We have provided as detailed a description as possible of the local context (within the limits of the report format) to enhance interpretation. Of course, there is no consensus on the numbers of sites and amount of variation between sites that would allow stronger statements about generalisability in the context of ‘large-scale transformation’.
The study was premised to a degree on the idea that the local context provided a particularly fruitful one for integration. The health and social care system was largely coterminous (with one council, one commissioner, one mental health provider and one principal provider of acute and community health), and included a long history of partnership working and an integrated care record. If the overall outcomes had been more positive, then a debate would have ensued about the ability to replicate it in other settings. Given the more modest impacts, despite the context, the interpretative task is different. In the realist model, mechanisms of integration will show more or less potency in certain contexts. We have outlined the ways in which the chosen site was one in which integration was enabled by history and geography. The fact that there was only limited evidence of improved patient outcomes could be seen as a challenge for the realist model, as mechanisms of integration should arguably be more potent – more modest effects might be expected in areas with a less amenable context, such as multiple providers and more complex interorganisational relationships. This will be most evident in comparative data that uses external locations, as external sites may potentially lack both the ‘mechanism of integration’ and the contextual enabler. Of course, an alternative interpretation is that the effective mechanisms of integration are yet to be identified.
Meaning of the study: possible explanations and implications for clinicians and policy-makers
The SICP has been implemented consistent with the original vision. However, there has been more rapid success in establishing new integrated structures, rather than delivering mechanisms of integration at the level of services which impact on patients.
As with many integrated care transformations, it has proved challenging to deliver transformation in care, which means that the evaluation data reported here may be premature. It is still not clear if greater improvements in outcome will flow from integrated structures.
The failure to evidence improvements in patient outcomes may reflect a number of issues. Although the chosen mechanisms of integration were broadly supported by existing reviews (in the case of health coaching), or consistent with wider service activity (in the case of MDGs), there is still limited evidence about each. The ‘decoupling’ of the system and service-level integration means that the SICP is not wedded to these particular mechanisms. The potential for improved integration in the ICO (such as staff working in a common organisation) could support other mechanisms of integration.
The data would suggest that there is an urgent need to develop and evaluate new mechanisms that could be deployed from integrated organisations. It is also possible that more modest ambitions than the ‘triple aim’ (better outcomes, enhanced experience, lower costs) need to be set for those interventions, given the difficulties in achieving health gain without increasing cost. 24 Other writers have emphasised more radical changes to the approach, such as an additional focus on prevention,79 and the recent plan for health and social care under the devolved arrangements in Greater Manchester suggests a preventative focus, allied to a drive to ‘enhance our primary care services, with local GPs driving new models of care and local care organisations forming to include community, social care, acute, mental health services, the full range of third-sector providers and other local providers such as schools’. 161 The Salford vanguard (see Chapter 10) is one of the new organisations mooted in the plan.
The SICP has introduced new services, but it is not clear that the scale or ‘dose’ of the programme is sufficient to have an impact on wider population health. To talk of a ‘dose’ of integrated care may seem inappropriate, as it suggests that the complexity of the SICP can be reduced to a simple measure. Nevertheless, considerations of ‘dose’ may have some utility. Box 3 outlines some relevant data. These are crude indicators of ‘dose’, and ignore wider changes in the structure and organisation of care that may not be immediately apparent or easily measured. Examples would include MDGs that impact on general ways of working, with the potential to impact on all patients. However, some issues are worth noting. The programme that involved the largest numbers of patients (community assets, of relevance to all patients and most relevant to the larger numbers of patients at lower levels) showed only limited evidence of direct engagement with patients in the study period. This is supported by analyses in Chapter 9, which showed that large numbers of older people reported engagement with assets at baseline (unlikely to have been affected by the SICP), with only small changes over the timeline of the programme. The numbers directly affected by the ICC were more significant, and the impacts were more likely to translate to immediate benefit. Nevertheless, the proportion of patients was still relatively small. Finally, the MDGs delivered a ‘mechanism of integration’ to a relatively large number of patients, especially in proportion to those at levels 2 and 3 who were eligible. Nevertheless, as detailed earlier, actual MDG activity with respect to many patients was limited, with minimal patient involvement and small changes in care delivery.
Analyses conducted by Haelo as part of a mid-term assessment of the SICP, and of data collected by the CLASSIC team, provide the following indicators of ‘dose’.
In terms of community assets, £100,000 funding was provided for 19 groups, and 53 ‘well-being champions’ were enlisted. Well-being plans were created for 435 Salford residents, and 24 ‘tech and tea’ events to improve older people’s access to technology were run and included 76 older people.
In terms of interventions within the ICC, 236 were on simple telehealth (‘Flo’), before that service was suspended, and 733 were on care call, including 197 on PROTECTS.
MDGs discussed 1651 patients, out of a population of 36,074, 4.5% of the total number of > 65-year-olds and 63% of patients at levels 2 and 3.
Although the data related to dose are only indicative and do not cover all the changes made as part of the SICP, they suggest that, although many older people may have received some form of integration, the dose at the level of the population may have been limited.
Unanswered questions and future research
Demonstrating significant health benefits from integrated care interventions remains a significant challenge. In part this represents difficulties in defining integration of care in a way that makes it amenable to evaluation. When integrated care programmes are part of a larger-scale transformation of services, there are additional complexities around the timing of evaluation. The enormous challenges associated with integration at scale do suggest that benefits may be deferred. However, if evaluation is delayed, then services may already be so committed to a model that responding to the results of the evaluation may be difficult. Identification of comparators (and keeping them from adopting new services rapidly) is also made more problematic.
Some of the results reported here are in line with other evaluations of integrated care: slower than anticipated progress on aspects of the programme36,37 and limited impacts of interventions on patient experience and admissions (including increases in some outcomes). 33 In Chapter 2, we hypothesised that context would be a significant enabler in the SICP, given the long history of joint working, but the context seems to have facilitated the speed of higher-level organisational change, rather than enhancing the delivery of mechanisms of integration and consequent impact on patient outcomes. Although there is consensus in the health services research literature as to the importance of context,166,167 the ways in which it interacts with discrete interventions and impacts on patient outcomes are less well understood. A recent exploration of the context–mechanism–outcome relationships in integrated care for diabetes mellitus reported many barriers involving organisational issues (such as deficits in IT and provider self-management support skills), whereas facilitators more often involved social issues (such as involvement in staff in decision-making, leadership and culture). 168
The future research questions around MDGs are complex, as there is now a weight of evidence suggesting limited benefits, despite the popularity of the model. 79 Within the SICP, and integration initiatives more generally,36,37 the usual patient under consideration is an older patient with multimorbidity. One of the barriers faced by integration initiatives is that, despite large amounts of evidence about the challenges faced by these patients,169 the evidence base concerning interventions that demonstrably improve the care of multimorbidity is very poor,98 as highlighted by the recent NICE guidelines,170 with consequent funding calls from NIHR. Indeed, there is a debate about whether the concept of multimorbidity is optimal, or whether a focus on frailty would be better, as the populations captured under these terms are related but not identical. 171 The success or otherwise of integrated care may be dependent on the development of that evidence base.
It is possible that the model needs improved targeting of patients or disease subgroups to demonstrate effectiveness, although there is the challenge of identifying suitable subgroups. Although the targeting of patients at high risk has face validity, effectiveness will be dependent on the ability of services to make significant improvements to their care without increasing the risk of other patients who are not targeted. The best way to undertake risk stratification and the types of patients who should be targeted remains controversial,78 and the field awaits the results of trials of different methods. 172
One of the limitations of risk stratification models is that they only identify risk and do not necessarily drive intervention (which has been called the ‘impact’ of such prognostic tools). 173 There is clearly a role for further detailed qualitative examination of the actions generated by such multidisciplinary working, given the findings of this study and those of others that suggested limited impacts on patient care. 132,153 It is important to explore if these limited impacts reflect the nature of work in these groups, the amount of support that these patients are already receiving and the limitations in available resources to manage problems that have been identified through multidisciplinary meetings. Nevertheless, the weight of evidence would suggest a more limited role for the model in integrated care and the consequent need to identify alternative mechanisms.
Health coaching is in a somewhat similar position as an evidence-based intervention, as early reviews of small studies in particular groups showed promise,85,87 whereas larger, more pragmatic evaluations suggested more modest gains. 90 Overall, the evidence seems stronger than that for MDGs, although the search for a reliable model of coaching that can be implemented at scale remains. The benefits reported here, although cost-effective at conventional levels of willingness to pay, would not translate to savings for commissioners or providers. This means that the model may have a limited role in achieving the sorts of reductions in health-care utilisation that are critical to many integrated care initiatives. Nevertheless, the positive patient experience (as reported in Appendix 2) and the changes in patterns of resource utilisation (see Chapter 13) should not be discounted.
The data suggest a role for community assets in generation of gains in quality of life. Further quantitative exploration is required to assess longer-term benefits, especially longer-term impacts on utilisation, which may be generated by short-term improvements in quality of life. It would also be useful to explore the patient and contextual factors that drive asset use and that influence the level of benefit derived by older patients. For example, many social prescribing schemes have a focus on mental health, in terms of both inclusion criteria and measurement of outcomes. Appropriate qualitative methods might be employed to explore the factors underlying access to assets (beyond the effects of proximity explored in Chapter 9), and the psychological and social mechanisms by which they achieve their effects (such as improvements in self-efficacy or activation, reductions in loneliness or improved social support).
Community asset interventions as described here are linked to social prescribing interventions, which have received recent interest from policy-makers,174 although the evidence base remains weak. 164 Social prescribing schemes are generally based on a GP referral mechanism, which differs from the broader community assets intervention employed in the SICP. The relative impact of the different schemes could be usefully explored. Referral through a GP may well increase access to assets in principle, and provide greater linkage to other aspects of management of long-term conditions through an effective primary care-based care planning process. However, enthusiasm for such schemes may be highly variable among GPs. There is a useful debate to be had about the amenability of such schemes to formal test, compared with the quasi-experimental models employed here, but examples of randomised evaluation do exist. 175
As noted previously, it remains an open question whether or not health impacts from community assets convert to genuine savings in care utilisation. Although the ‘triple aim’ remains part of the vision of integrated care, the pattern of results reported here (achieving improved outcomes at increased cost) is less likely to be sustainable.
The use of the cmRCT design in the CLASSIC programme has identified a number of issues with the design, including the management of low levels of uptake among patients and the logistics of follow-up. As more trials utilise the design, synthesis of the findings will be required to better understand the advantages and disadvantages of the model and how it can best be used to meet the challenges of evaluation in the NHS in years to come. 41
Although many integrated care initiatives share common mechanisms (especially variants of the MDG), there is no reason why a wider variety of interventions might be employed and tested within the context of integrated services. For example, many integration initiatives have an initial focus on prevention36,37 and future work could explore preventative interventions that could be facilitated through integrated services to improve the outcomes of older people.
Summary
The SICP has been implemented in a way that is consistent with the original vision for services, built around three main mechanisms of integration. Although the SICP has been successful in establishing new integrated structures, the progress at a system level has not been matched by such rapid progress in terms of delivery of integrated services. The SICP has introduced new services, but it is not clear if the scale of the programme is sufficient at this point in time to make an impact on population health.
The greatest resource and fastest progress has involved MDGs, with the ICC facing the greatest challenges to implementation.
In terms of the outcomes reported in the CLASSIC timeline, patient experience is only one of the core outcomes of the SICP, and there was little evidence that a sample of older patients in Salford were experiencing care as feeling more ‘joined up’ at this point of the evaluation of the SICP.
The evaluation of individual components of the SICP (MDGs, health coaching, community assets) suggests only limited evidence of benefits, focused around quality of life, even in the facilitative context of a system with a significant history of joint working and supportive structures for organisational integration.
As with many integrated care transformations, the evaluation data reported here may be ‘early’ in terms of the evolution of new services for which benefits may be delayed. Whether or not better outcomes will flow from these new integrated structures remains to be seen.
Acknowledgements
The authors would like to thank the patients who took part in the research and contributed through PPI activities, and the staff within Salford Together who generously gave of their time to participate. ‘Salford Together’ is a partnership of Salford City Council, NHS Salford CCG, Salford Royal NHS Foundation Trust, Greater Manchester Mental Health NHS Foundation Trust and Salford Primary Care Together.
We would also like to express our special thanks to Christine Camacho, who was instrumental in the development of CLASSIC and securing the grant, and to Caroline Gardner, for all her help and support with the cohort. We would also like to express our thanks to the members of the Study Steering Committee for their advice and support throughout.
Contributions of authors
Peter Bower was an applicant on the original submission and contributed to the design; designed and delivered the cohort; was involved in implementation 1 and implementation 2, the design and delivery of the health coaching trial and the effectiveness analyses of outcome 2; co-ordinated writing the report; and is guarantor.
David Reeves was an applicant on the original submission and contributed to the design, designed and delivered the cohort, was involved in the design and delivery of the health coaching trial and in the effectiveness analyses of outcome 2, and co-ordinated writing the report.
Matt Sutton was an applicant on the original submission and contributed to the design, designed and delivered the cohort, was involved in outcome 1, and co-ordinated writing the report.
Karina Lovell was an applicant on the original submission and contributed to the design, and was involved in the design and delivery of the health coaching trial.
Amy Blakemore was involved in implementation 2, was involved in the design and delivery of the health coaching trial, and wrote sections of the report.
Mark Hann designed and delivered the cohort and was involved in the effectiveness analyses of outcome 2.
Kelly Howells designed and delivered the cohort, was involved in implementation 2, was involved in the design and delivery of the health coaching trial, and wrote sections of the report.
Rachel Meacock was involved in the cost-effectiveness analyses of outcome 2.
Luke Munford led the analyses of the data in Chapter 9 and wrote sections of the report.
Maria Panagioti led analyses of the cohort and was involved in the effectiveness analyses of outcome 2.
Beth Parkinson was involved in the cost-effectiveness analyses of outcome 2.
Lisa Riste designed and delivered the cohort, was involved in implementation 2 and the design and delivery of the health coaching trial, and wrote sections of the report.
Mark Sidaway designed and delivered the cohort, and was involved in the design and delivery of the health coaching trial.
Yiu-Shing Lau was involved in outcome 1 and wrote sections of the report.
Lynsey Warwick-Giles was involved in implementation 1.
John Ainsworth was an applicant on the original submission and contributed to the design, and assisted in the use of routine data in the cohort and outcome 2.
Thomas Blakeman was an applicant on the original submission and contributed to the design, and was involved in the design and delivery of the health coaching trial.
Ruth Boaden was an applicant on the original submission and contributed to the design, was involved in implementation 1 and co-ordinated writing the report.
Iain Buchan was an applicant on the original submission and contributed to the design, and assisted in the use of routine data in the cohort and outcome 2.
Stephen Campbell was an applicant on the original submission and contributed to the design, and was involved in ongoing analyses of the cohort.
Peter Coventry was an applicant on the original submission and contributed to the design, and was involved in implementation 2 and the design and delivery of the health coaching trial.
Siobhan Reilly was an applicant on the original submission and contributed to the design and was involved in implementation 2.
Caroline Sanders was an applicant on the original submission and contributed to the design and was involved in implementation 2.
Suzanne Skevington was an applicant on the original submission and contributed to the design, and designed and delivered the cohort.
Waquas Waheed was an applicant on the original submission and contributed to the design and was involved in ongoing analyses of the cohort.
Katherine Checkland was an applicant on the original submission and contributed to the design, was involved in implementation 1, and co-ordinated writing the report.
Publications
Blakemore A, Hann M, Howells K, Panagioti M, Sidaway M, Reeves D, et al. Patient activation in older people with long-term conditions and multimorbidity: correlates and change in a cohort study in the United Kingdom. BMC Health Serv Res 2016;16:582.
Cotterill S, Howells K, Rhodes S, Bower P. The effect of social pressure on retention in a longitudinal health questionnaire: an embedded randomised controlled retention trial. Trials 2017;18:341.
Munford LA, Sidaway M, Blakemore A, Sutton M, Bower P. Associations of participation in community assets with health-related quality of life and healthcare usage: a cross-sectional study of older people in the community. BMJ Open 2017;7:e012374.
Panagioti M, Blakeman T, Hann M, Bower P. Patient-reported safety incidents in older patients with long-term conditions: a large cross-sectional study. BMJ Open 2017;7:e013524.
Warwick-Giles L, Checkland K. Integrated care: using ‘sensemaking’ to understand how organisations are working together to transform local health and social care services. J Health Organ Manag 2017;32.
Panagioti M, Reeves D, Meacock R, Parkinson B, Lovell K, Hann M, et al. Is telephone health coaching a useful population health strategy for supporting older people with multimorbidity? An evaluation of reach, effectiveness and cost-effectiveness using a ‘trial within a cohort’. BMC Med 2018;16:80.
Reeves D, Howells K, Sidaway M, Blakemore A, Hann M, Panagioti M, Bower P. The cohort multiple randomized controlled trial design was found to be highly susceptible to low statistical power and internal validity biases. J Clin Epidemiol 2018;95:111–119.
Riste LK, Coventry PA, Reilly ST, Bower P, Sanders C. Enacting person-centredness in integrated care: a qualitative study of practice and perspectives within multidisciplinary groups in the care of older people [published online ahead of print 13 July 2018]. Health Expect 2018.
Stokes J, Riste L, Cheraghi-Sohi S. Targeting the ‘right’ patients for integrated care: stakeholder perspectives from a qualitative study. J Health Serv Res Policy 2018;1:1355819618788100.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Please note exclusive use will be retained until the publication of major outputs. Access to anonymised data may be granted following review and is subject to appropriate agreements being in place.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Barnett B, Mercer S, Norbury M, Watt G, Wyke S, Guthrie B. The epidemiology of multimorbidity in a large cross-sectional dataset: implications for health care, research and medical education. Lancet 2012;380:37-43. https://doi.org/10.1016/S0140-6736(12)60240-2.
- The Global Burden of Disease: 2004 Update. Geneva: WHO; 2009.
- National Voices . Principles for Integrated Care n.d. www.nationalvoices.org.uk/publications/our-publications/principles-integrated-care (accessed 7 February 2017).
- National Voices . A Narrative for Person-Centred Coordinated Care n.d. www.nationalvoices.org.uk/sites/default/files/public/publications/narrative-for-person-centred-coordinated-care.pdf (accessed 7 February 2017).
- National Collaboration for Integrated Care and Support . Integrated Care: Our Shared Commitment n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/287815/DEFINITIVE_FINAL_VERSION_Integrated_Care_and_Support_-_Our_Shared_Commitment_2013-05-13.pdf (accessed 7 February 2017).
- Armitage GD, Suter E, Oelke ND, Adair CE. Health systems integration: state of the evidence. Int J Integr Care 2009;9. https://doi.org/10.5334/ijic.316.
- Goodwin N. Understanding integrated care. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2530.
- What is Social Care, and How Can Health Services Better Integrate with It?. London: BMA; 2014.
- Nolte E, McKee M. Caring for People with Chronic Conditions. A Health System Perspective. Berkshire: Open University Press; 2008.
- Glasby J. If integration is the answer, what was the question? What next for English health and social care partnerships?. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2535.
- Greenfield G, Ignatowicz AM, Belsi A, Pappas Y, Car J, Majeed A, et al. Wake up, wake up! It’s me! It’s my life! Patient narratives on person-centeredness in the integrated care context: a qualitative study. BMC Health Serv Res 2014;14. https://doi.org/10.1186/s12913-014-0619-9.
- Martínez-González NA, Berchtold P, Ullman K, Busato A, Egger M. Integrated care programmes for adults with chronic conditions: a meta-review. Int J Qual Health Care 2014;26:561-70. https://doi.org/10.1093/intqhc/mzu071.
- Hwang W, Chang J, Laclair M, Paz H. Effects of integrated delivery system on cost and quality. Am J Manag Care 2013;19:e175-84.
- Damery S, Flanagan S, Combes G. Does integrated care reduce hospital activity for patients with chronic diseases? An umbrella review of systematic reviews. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011952.
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA 2002;288:1909-14. https://doi.org/10.1001/jama.288.15.1909.
- Mitchell GK, Burridge L, Zhang J, Donald M, Scott IA, Dart J, et al. Systematic review of integrated models of health care delivered at the primary–secondary interface: how effective is it and what determines effectiveness?. Aus J Prim Health 2015;21:391-408. https://doi.org/10.1071/PY14172.
- Eklund K, Wilhelmson K. Outcomes of coordinated and integrated interventions targeting frail elderly people: a systematic review of randomised controlled trials. Health Soc Care Community 2009;17:447-58. https://doi.org/10.1111/j.1365-2524.2009.00844.x.
- Huntley A, Thomas R, Mann M, Huws D, Elwyn G, Paranjothy S, et al. Is case management effective in reducing the risk of unplanned hospital admissions for older people? A systematic review and meta-analysis. Fam Pract 2013;30:266-75. https://doi.org/10.1093/fampra/cms081.
- Stokes J, Panagioti M, Alam R, Checkland K, Cheraghi-Sohi S, Bower P. Effectiveness of case management for ‘at risk’ patients in primary care: a systematic review and meta-analysis. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0132340.
- Huntley AL, Johnson R, King A, Morris RW, Purdy S. Does case management for patients with heart failure based in the community reduce unplanned hospital admissions? A systematic review and meta-analysis. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010933.
- Nolte E, Pitchforth E. What is the Evidence on the Economic Impacts of Integrated Care?. Copenhagen: European Commission, European Observatory on Health Systems and Policies; 2014.
- Mason A, Goddard M, Weatherly H, Chalkley M. Integrating funds for health and social care: an evidence review. J Health Serv Res Policy 2015;20:177-88. https://doi.org/10.1177/1355819614566832.
- Goddard M, Mason AR. Integrated care: a pill for all ills?. Int J Health Policy Manag 2016;6:1-3. https://doi.org/10.15171/ijhpm.2016.111.
- Panagioti M, Richardson G, Murray E, Rogers A, Kennedy A, Newman S, et al. Reducing Care Utilisation through Self-management Interventions (RECURSIVE): a systematic review and meta-analysis. Health Serv Deliv Res 2014;2.
- Health and Social Care Integration. London: National Audit Office; n.d.
- Bate P. Context is Everything. London: The Health Foundation; 2014.
- Øvretveit J. How Does Context Affect Quality Improvement?. London: The Health Foundation; 2014.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Gravelle H, Dusheiko M, Sheaff R, Sargent P, Boaden R, Pickard S, et al. Impact of case management (Evercare) on frail elderly patients: controlled before and after analysis of quantitative outcome data. BMJ 2007;334. https://doi.org/10.1136/bmj.39020.413310.55.
- Sheaff R, Boaden R, Sargent P, Pickard S, Gravelle H, Parker S, et al. Impacts of case management for frail elderly people: a qualitative study. J Health Serv Res Policy 2009;14:88-95. https://doi.org/10.1258/jhsrp.2008.007142.
- Windle K, Wagland R, Forder J, D’Amico F, Janssen D, Wisstow G. National Evaluation of Partnerships for Older People: Final Report. London: Personal Social Services Research Unit; 2009.
- Steventon A, Bardsley M, Billings J, Georghiou T, Lewis G. An Evaluation of the Impact of Community-Based Interventions on Hospital Use: A Case Study of Eight Partnership for Older People Projects (POPP). London: Nuffield Trust; 2011.
- Roland M, Lewis R, Steventon A, Abel G, Adams J, Bardsley M, et al. Case management for at-risk elderly patients in the English integrated care pilots: observational study of staff and patient experience and secondary care utilisation. Int J Integr Care 2013;12.
- Evaluation of the First Year of the Inner North West London Integrated Care Pilot. London: Nuffield Trust; 2013.
- Curry N, Harris M, Gunn L, Pappas Y, Blunt I, Soljak M, et al. Integrated care pilot in north west London: a mixed methods evaluation. Int J Integr Care 2013;13. https://doi.org/10.5334/ijic.1149.
- Erens B, Wistow G, Mounier-Jack S, Douglas N, Jones L, Manacorda T, et al. Early Evaluation of the Integrated Care and Support Pioneers Programme: Final Report. London: Policy Innovation Research Unit; 2016.
- Erens B, Wistow G, Mounier-Jack S, Douglas N, Manacorda T, Durand M, et al. Early findings from the evaluation of the integrated care and support pioneers in England. J Integr Care 2017;25. https://doi.org/10.1108/JICA-12-2016-0047.
- Burt J, Campbell J, Abel G, Aboulghate A, Ahmed F, Asprey A, et al. Improving patient experience in primary care: a multimethod programme of research on the measurement and improvement of patient experience. Programme Grants Appl Res 2017;5. https://doi.org/10.3310/pgfar05090.
- Commissioning Brief (12/130) Evaluating New Models of Care for People with Longterm Conditions. Southampton: NIHR Health Services and Delivery Research programme; 2013.
- Goodwin N, Sonola L, Thiel V, Kodner D. Co-Ordinated Care for People With Complex Chronic Conditions: Key Lessons and Markers for Success 2013. www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/co-ordinated-care-for-people-with-complex-chronic-conditions-kingsfund-oct13.pdf (accessed 7 February 2017).
- Raine R, Fitzpatrick R, Barratt H, Bevan G, Black N, Boaden R, et al. Challenges, solutions and future directions in the evaluation of service innovations in health care and public health. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04160.
- Lamont T, Barber N, de Pury J, Fulop N, Garfield-Birkbeck S, Lilford R, et al. New approaches to evaluating complex health and care systems. BMJ 2016;352. https://doi.org/10.1136/bmj.i154.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q 2012;90:421-56. https://doi.org/10.1111/j.1468-0009.2012.00670.x.
- Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health 2012;66:1182-6. https://doi.org/10.1136/jech-2011-200375.
- Relton C, Torgerson D, O’Cathain A, Nicholl J. Rethinking pragmatic randomised controlled trials: introducing the ‘cohort multiple randomised controlled trial’ design. BMJ 2013;340.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications Ltd; 2011.
- Better Evaluation . Realist Evaluation n.d. www.betterevaluation.org/en/approach/realist_evaluation (accessed 17 July 2018).
- Pettigrew A, Ferlie E, McKee L. Shaping Strategic Change: Making Change in Large Organisations, the Case of the NHS. London: Sage Publications Ltd; 1992.
- Mackie S, Darvill A. Factors enabling implementation of integrated health and social care: a systematic review. Br J Community Nurs 2016;21:82-7. https://doi.org/10.12968/bjcn.2016.21.2.82.
- Ling T, Brereton L, Conklin A, Newbould J, Roland M. Barriers and facilitators to integrating care: experiences from the English integrated care pilots. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.982.
- May C, Murray E, Finch T, Mair F, Treweek S, Ballini L, et al. Normalization Process Theory On-Line Users’ Manual and Toolkit 2010. www.normalizationprocess.org (accessed 17 February 2011).
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-29.
- Hibbard J, Gilburt H. Supporting People to Manage Their Health: An Introduction to Patient Activation. London: The King’s Fund; 2014.
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med 2000;51:1087-110. https://doi.org/10.1016/S0277-9536(00)00098-8.
- Campbell J, Smith P, Nissen S, Bower P, Elliott M, Roland M. The GP Patient Survey for use in primary care in the National Health Service in the UK – development and psychometric characteristics. BMC Fam Pract 2009;10. https://doi.org/10.1186/1471-2296-10-57.
- 2011 Census Aggregate Data. Essex: UK Data Service; 2016.
- Morris NS, MacLean CD, Chew LD, Littenberg B. The single item literacy screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract 2006;7. https://doi.org/10.1186/1471-2296-7-21.
- Bayliss E, Ellis J, Steiner J. Subjective assessments of comorbidity correlate with quality of life health outcomes: initial validation of a comorbidity assessment instrument. Health Qual Life Outcomes 2005;3. https://doi.org/10.1186/1477-7525-3-51.
- Bajekal M, Purdon S. Social Capital and Social Exclusion: Development of a Condensed Module for the Health Survey for England. London: National Centre for Social Research; 2001.
- Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Med Care 2005;43:436-44. https://doi.org/10.1097/01.mlr.0000160375.47920.8c.
- Gugiu PC, Coryn C, Clark R, Kuehn A. Development and evaluation of the short version of the Patient Assessment of Chronic Illness Care instrument. Chronic Illn 2009;5:268-76. https://doi.org/10.1177/1742395309348072.
- Hibbard J, Stockard E, Mahoney E, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005-26. https://doi.org/10.1111/j.1475-6773.2004.00269.x.
- Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the Patient Activation Measure. Health Serv Res 2005;40:1918-30. https://doi.org/10.1111/j.1475-6773.2005.00438.x.
- Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care 2000;23:943-50. https://doi.org/10.2337/diacare.23.7.943.
- Gibbons CJ, Kenning C, Coventry PA, Bee P, Bundy C, Fisher L, et al. Development of a multimorbidity illness perceptions scale (MULTIPleS). PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0081852.
- Year of Care . Year of Care: Report of Findings from the Pilot Programme 2011. www.yearofcare.co.uk/sites/default/files/images/YOC_Report%20-%20correct.pdf (accessed 6 September 2017).
- Mitchell P, Powell L, Blumenthal J, Norten J, Ironson G, Pitula C, et al. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. J Cardiopulm Rehabil 2003;23:398-403. https://doi.org/10.1097/00008483-200311000-00001.
- Euroqol Copyright Group . Euroqol – a new facility for the measurement of health related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England [published online ahead of print 22 August 2017]. Health Econ 2017. https://doi.org/10.1002/hec.3564.
- Berwick DM, Murphy JM, Goldman PA, Ware JE, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care 1991;29:169-76. https://doi.org/10.1097/00005650-199102000-00008.
- Flynn T, Chan P, Coast J, Peters T. Assessing quality of life among British older people using the ICEPOP CAPability (ICECAP-O) measure. Appl Health Econ Health Policy 2011;9:317-29. https://doi.org/10.2165/11594150-000000000-00000.
- Skevington S, Lotfy M, O’Connell K. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial – a report from the WHOQOL group. Quality Life Res 2013;13:299-310. https://doi.org/10.1023/B:QURE.0000018486.91360.00.
- Reeves D, Hann M, Rick J, Rowe K, Small N, Burt J, et al. Care plans and care planning in the management of long-term conditions in the UK: a controlled prospective cohort study. Br J Gen Pract 2014;64:e568-75. https://doi.org/10.3399/bjgp14X681385.
- Cartwright M, Hirani S, Rixon L, Beynon M, Doll H, Bower P, et al. Effect of telehealth on quality of life and psychological outcomes over 12 months (Whole Systems Demonstrator telehealth questionnaire study): nested study of patient reported outcomes in a pragmatic, cluster randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.f653.
- Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine; 1967.
- Stokes J, Kristensen SR, Checkland K, Bower P. Effectiveness of multidisciplinary team case management: difference-in-differences analysis. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010468.
- Roland M, Abel G. Reducing emergency admissions: are we on the right track?. BMJ 2012;345. https://doi.org/10.1136/bmj.e6017.
- Stokes J, Checkland K, Kristensen SR. Integrated care: theory to practice. J Health Serv Res Policy 2016;21:282-5. https://doi.org/10.1177/1355819616660581.
- O’Neill S, Kreif N, Grieve R, Sutton M, Sekhon JS. Estimating causal effects: considering three alternatives to difference-in-differences estimation. Health Serv Outcomes Res Methodol 2016;16:1-21. https://doi.org/10.1007/s10742-016-0146-8.
- Ministry of Housing, Communities & Local Government . English Indices of Deprivation 2015. GOV. UK 2015. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 16 August 2018).
- McLean S, Protti D, Sheikh A. Telehealthcare for long term conditions. BMJ 2011;342. https://doi.org/10.1136/bmj.d120.
- Lin W, Chien H, Willis G, O’Connell E, Rennie K, Bottella H, et al. The effect of a telephone-based health coaching disease management program on Medicaid members with chronic conditions. Med Care 2012;50:91-8. https://doi.org/10.1097/MLR.0b013e31822dcedf.
- Hutchison AJ, Breckon JD. A review of telephone coaching services for people with long-term conditions. J Telemed Telecare 2011;17:451-8. https://doi.org/10.1258/jtt.2011.110513.
- Dennis SM, Harris M, Lloyd J, Powell Davies G, Faruqi N, . Do people with existing chronic conditions benefit from telephone coaching? A rapid review. Aust Health Rev 2013;37:381-8. https://doi.org/10.1071/AH13005.
- McCall N, Cromwell J. Results of the Medicare health support disease-management pilot program. N Engl J Med 2011;365:1704-12. https://doi.org/10.1056/NEJMsa1011785.
- Kivelä K, Elo S, Kyngäs H, Kääriäinen M. The effects of health coaching on adult patients with chronic diseases: a systematic review. Patient Educ Couns 2014;97:147-57. https://doi.org/10.1016/j.pec.2014.07.026.
- Olsen JM, Nesbitt BJ. Health coaching to improve healthy lifestyle behaviors: an integrative review. Am J Health Promot 2010;25:e1-e12. https://doi.org/10.4278/ajhp.090313-LIT-101.
- Jonk Y, Lawson K, O’Connor H, Riise KS, Eisenberg D, Dowd B, et al. How effective is health coaching in reducing health services expenditures?. Med Care 2015;53:133-40. https://doi.org/10.1097/MLR.0000000000000287.
- Steventon A, Tunkel S, Blunt I, Bardsley M. Effects of telephone health coaching (Birmingham OwnHealth) on hospital use and associated costs: cohort study with matched controls. BMJ 2013;347. https://doi.org/10.1136/bmj.f4585.
- Patja K, Absetz P, Auvinen A, Tokola K, Kytö J, Oksman E, et al. Health coaching by telephony to support self-care in chronic diseases: clinical outcomes from The TERVA randomized controlled trial. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-147.
- Park YH, Chang H. Effect of a health coaching self-management program for older adults with multimorbidity in nursing homes. Patient Prefer Adherence 2014;8:959-70. https://doi.org/10.2147/PPA.S62411.
- McCusker J, Cole MG, Yaffe M, Strumpf E, Sewitch M, Sussman T, et al. A randomized trial of a depression self-care toolkit with or without lay telephone coaching for primary care patients with chronic physical conditions. Gen Hosp Psychiatry 2015;37:257-65. https://doi.org/10.1016/j.genhosppsych.2015.03.007.
- Blackberry ID, Furler JS, Best JD, Chondros P, Vale M, Walker C, et al. Effectiveness of general practice based, practice nurse led telephone coaching on glycaemic control of type 2 diabetes: the Patient Engagement and Coaching for Health (PEACH) pragmatic cluster randomised controlled trial. BMJ 2013;347. https://doi.org/10.1136/bmj.f5272.
- Vale MJ, Jelinek MV, Best JD, Dart A, Grigg L, Hare D, et al. Coaching patients on achieving cardiovascular health (coach): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med 2003;163:2775-83. https://doi.org/10.1001/archinte.163.22.2775.
- Young R, Taylor J, Friede T, Hollis S, Mason J, Lee P, et al. Pro-active call center treatment support (PACCTS) to improve glucose control in type 2 diabetes: a randomized controlled trial. Diabetes Care 2005;28:278-82. https://doi.org/10.2337/diacare.28.2.278.
- Blakeman T, Blickem C, Kennedy A, Reeves D, Bower P, Gaffney H, et al. Effect of information and telephone-guided access to community support for people with chronic kidney disease: randomised controlled trial. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0109135.
- Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 2016;3. https://doi.org/10.1002/14651858.CD006560.pub3.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- South J, Higgins T, Woodall J, White P. Can social prescribing provide the missing link?. Prim Health Care Res Develop 2008;9:310-18. https://doi.org/10.1017/S146342360800087X.
- Brandling J, House W. Social prescribing in general practice: adding meaning to medicine. Br J Gen Pract 2009;59:454-6. https://doi.org/10.3399/bjgp09X421085.
- Lovell K, Bower P, Richards D, Barkham M, Sibbald B, Roberts C, et al. Developing guided self-help for depression using the Medical Research Council complex interventions framework: a description of the modelling phase and results of an exploratory randomised controlled trial. BMC Psychiatry 2008;8. https://doi.org/10.1186/1471-244X-8-91.
- Lovell K, Richards D. A Recovery Programme for Depression 2007. www.rethink.org/resources/r/recovery-programme-for-depression-booklet-april-2012 (accessed 7 February 2017).
- European Medicines Agency . Guideline on Data Monitoring Committees n.d. www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003635.pdf (accessed 17 July 2018).
- Dunn G, Emsley R, Liu H, Landau S, Green J, White I, et al. Evaluation and validation of social and psychological markers in randomised trials of complex interventions in mental health: a methodological research programme. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19930.
- Dunn G, Maracy M, Dowrick C, Ayuso-Mateos JL, Dalgard OS, Page H, et al. Estimating psychological treatment effects from a randomised controlled trial with both non-compliance and loss to follow-up. Br J Psychiatry 2003;183:323-31. https://doi.org/10.1192/bjp.183.4.323.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Developing NICE Guidelines: The Manual. Process and Methods Guides. London: NICE; 2014.
- Guide to the Methods of Technology Appraisal 2013. Manchester: NICE; 2013.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research, Unit, University of Kent; 2015.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2014 to 2015 2015. www.gov.uk/government/publications/nhs-reference-costs-2014-to-2015 (accessed 7 February 2017).
- Faria R, Gomes M, Epstein D, White I. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. PharmacoEconomics 2014;32:1157-70. https://doi.org/doi:10.1007/s40273-014-0193-3.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- Blakemore A, Hann M, Howells K, Panagioti M, Sidaway M, Reeves D, et al. Patient activation in older people with long-term conditions and multimorbidity: correlates and change in a cohort study in the United Kingdom. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1843-2.
- Panagioti M, Blakeman T, Hann M, Bower P. Patient-reported safety incidents in older patients with long-term conditions: a large cross-sectional study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013524.
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA 2002;288:2469-75. https://doi.org/10.1001/jama.288.19.2469.
- Darzi A. High Quality Care for All: NHS Next Stage Review; Final Report. London: Department of Health and Social Care; 2008.
- McLean J. Asset Based Approaches for Health Improvement: Redressing the Balance 2011. www.gcph.co.uk/assets/0000/2627/GCPH_Briefing_Paper_CS9web.pdf (accessed 7 February 2017).
- Kretzmann J, McKnight JP. Assets-based community development. Nat Civic Rev 1996;85:23-9. https://doi.org/10.1002/ncr.4100850405.
- Mathie A, Cunningham G. From clients to citizens: asset-based community development as a strategy for community-driven development. Develop Pract 2003;13:474-86. https://doi.org/10.1080/0961452032000125857.
- Whiting L, Kendall S, Wills W. An asset-based approach: an alternative health promotion strategy?. Community Pract 2012;85:25-8.
- Dobrof J, Heyman JC, Greenberg RM. Building on community assets to improve palliative and end-of-life care. J Soc Work End Life Palliat Care 2011;7:5-13. https://doi.org/10.1080/15524256.2011.548044.
- Burt J, Roland M, Paddison C, Reeves D, Campbell J, Abel G, et al. Prevalence and benefits of care plans and care planning for people with long-term conditions in England. J Health Serv Res Policy 2012;17:64-71. https://doi.org/10.1258/jhsrp.2011.010172.
- Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making 1998;18:68-80. https://doi.org/10.1177/0272989X98018002S09.
- Claxton K, Martin S, Soares M, Rice N, Spackman E, Hinde S, et al. Methods for the estimation of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19140.
- The Stationery Office . Localism Act 2011 2011. www.legislation.gov.uk/ukpga/2011/20/pdfs/ukpga_20110020_en.pdf (accessed 7 February 2017).
- Sussman JB, Hayward RA. An IV for the RCT: using instrumental variables to adjust for treatment contamination in randomised controlled trials. BMJ 2010;340. https://doi.org/10.1136/bmj.c2073.
- Heckman JJ. Dummy endogenous variables in a simultaneous equation system. Econometrica 1978;46:931-59. https://doi.org/10.2307/1909757.
- Maddala GS. Limited-Dependent and Qualitative Variables in Econometrics. Cambridge: Cambridge University Press; 1983.
- Steffens NK, Cruwys T, Haslam C, Jetten J, Haslam SA. Social group memberships in retirement are associated with reduced risk of premature death: evidence from a longitudinal cohort study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010164.
- Schwarz G. Estimating the dimension of a model. Ann Statist 1978;6:461-4. https://doi.org/10.1214/aos/1176344136.
- Mastellos N, Gunn L, Harris M, Majeed A, Car J, Pappas Y. Assessing patients’ experience of integrated care: a survey of patient views in the North West London Integrated Care Pilot. Int J Integr Care 2014;14. https://doi.org/10.5334/ijic.1453.
- Newbould J, Burt J, Bower P, Blakeman T, Kennedy A, Rogers A, et al. Experiences of care planning in England: interviews with patients with long term conditions. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-71.
- Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA, Lorig KR. Self-reports of health care utilization compared to provider records. J Clin Epidemiol 2001;54:136-41. https://doi.org/10.1016/S0895-4356(00)00261-4.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage Publications Ltd; 2013.
- Walshe K, Coleman A, McDonald R, Lorne C, Munford L. Health and social care devolution: the Greater Manchester experiment. BMJ 2016;352. https://doi.org/10.1136/bmj.i1495.
- Checkland K, Segar J, Voorhees J, Coleman A. ‘Like a circle in a spiral, like a wheel within a wheel’: the layers of complexity and challenge for devolution of health and social care in Greater Manchester. Representation 2015;51:453-69. https://doi.org/10.1080/00344893.2016.1165514.
- Turner S, Ramsay A, Perry C, Boaden R, McKevitt C, Morris S, et al. Lessons for major system change: centralization of stroke services in two metropolitan areas of England. J Health Serv Res Policy 2016;21:156-65. https://doi.org/10.1177/1355819615626189.
- National Audit Office . Planning for the Better Care Fund 2014. www.nao.org.uk/report/planning-better-care-fund-2/ (accessed 7 February 2017).
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 23 August 2017).
- Dalton D. Examining New Options and Opportunities for Providers of NHS Care: The Dalton Review 2014. www.gov.uk/government/uploads/system/uploads/attachment_data/file/384126/Dalton_Review.pdf (accessed 7 February 2017).
- Checkland K, Coleman A, McDermott I, Segar J, Miller R, Wallace A, et al. Exploring the Early Workings of Emerging Clinical Commissioning Groups: Final Report. Manchester: Policy Research Unit in Commissioning and the Healthcare System; 2012.
- Turner S, Goulding L, Denis J, McDonald R, Fulop N. Major system change: a management and organisational research perspective. Health Serv Delivery Res 2016;4.
- Thistlewaite P. Integrating Health and Social Care in Torbay 2011. www.kingsfund.org.uk/sites/default/files/integrating-health-social-care-torbay-case-study-kings-fund-march-2011.pdf (accessed 16 August 2018).
- Rhodes P, Campbell S, Sanders C. Trust, temporality and systems: how do patients understand patient safety in primary care? A qualitative study. Health Expectations 2015;19:253-63. https://doi.org/10.1111/hex.12342.
- Mol A. The Logic of Care: Health and the Problem of the Patient. New York, NY: Routledge; 2008.
- Panagioti M, Reeves D, Meacock R, Parkinson B, Lovell K, Hann M, et al. Is telephone health coaching a useful population health strategy for supporting older people with multimorbidity? An evaluation of reach, effectiveness and cost-effectiveness using a ‘trial within a cohort’. BMC Med 2018;16. https://doi.org//10.1186/s12916-018-1051-5.
- Treweek S, Dryden R, McCowan C, Harrow A, Thompson AM. Do participants in adjuvant breast cancer trials reflect the breast cancer patient population?. Eur J Cancer 2015;51:907-14. https://doi.org/10.1016/j.ejca.2015.01.064.
- Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, et al. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ 2008;337. https://doi.org/10.1136/bmj.a2390.
- Loudon K, Treweek S, Sullivan F, Donnan P, Thorpe KE, Zwarenstein M. The PRECIS-2 tool: designing trials that are fit for purpose. BMJ 2015;350. https://doi.org/10.1136/bmj.h2147.
- Billings J, de Weger E. Contracting for integrated health and social care: a critical review of four models. J Integr Care 2015;23:153-75. https://doi.org/10.1108/JICA-03-2015-0015.
- Janse B, Huijsman R, de Kuyper RDM, Fabbricotti IN. Do integrated care structures foster processes of integration? a quasi-experimental study in frail elderly care from the professional perspective. Int J Qual Health Care 2016;28:376-83. https://doi.org/10.1093/intqhc/mzw045.
- Kassianos AP, Ignatowicz A, Greenfield G, Majeed A, Car J, Pappas Y. ‘Partners rather than just providers . . .’: a qualitative study on health care professionals’ views on implementation of multidisciplinary group meetings in the North West London Integrated Care Pilot. Int J Integr Care 2015;15. https://doi.org/10.5334/ijic.2019.
- Powell Davies G, Harris M, Perkins D, Roland M, Williams A, Larsen K, et al. Coordination of Care Within Primary Health Care and with Other Sectors: A Systematic Review. Acton, ACT: Australian Primary Care Research Institute; 2006.
- Powell Davies G, Williams AM, Larsen K, Perkins D, Roland M, Harris MF. Coordinating primary health care: an analysis of the outcomes of a systematic review. Med J Aust 2008;188:65-8.
- Lewis G, Georghiou T, Steventon A, Vaithianathan R, Chitnis X, Billings J, et al. Impact of ‘Virtual Wards’ on Hospital Use: A Research Study Using Propensity Matched Controls and a Cost Analysis. Final Report. Southampton: NIHR Service Delivery and Organisation programme; 2013.
- Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data. BMJ 2017;356. https://doi.org/10.1136/bmj.j84.
- Harris M, Greaves F, Gunn L, Patterson S, Greenfield G, Car J, et al. Multidisciplinary integration in the context of integrated care – results from the North West London Integrated Care Pilot. Int J Integr Care 2013;13. https://doi.org/10.5334/ijic.1146.
- Gowing A, Dickinson C, Gorman T, Robinson L, Duncan R. Patients’ experiences of a multidisciplinary team-led community case management programme: a qualitative study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012019.
- Goldberg D. Goldberg III: Can the NHS Deliver Integration? Lessons from Around the World 2014. www.good-governance.org.uk/services/goldberg-iii-can-the-nhs-deliver-integration-lessons-from-around-the-world/ (accessed 23 August 2017).
- Taking Charge of our Health and Social Care in Greater Manchester: the Plan. Manchester: Greater Manchester Combined Authority; 2015.
- Pate A, Candlish J, Sperrin M, Van Staa TP. Cohort multiple randomised controlled trials (cmRCT) design: efficient but biased? A simulation study to evaluate the feasibility of the Cluster cmRCT design. BMC Med Res Method 2016;16. https://doi.org/10.1186/s12874-016-0208-1.
- Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ 1999;18:341-64. https://doi.org/10.1016/S0167-6296(98)00039-3.
- Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013384.
- Wistow G, Gaskins M, Holder H, Smith J. Putting Integrated Care into Practice: The North West London Experience. London: LSE and Nuffield Trust; 2015.
- Howarth E, Devers K, Moore G, O’Cathain A, Dixon-Woods M. Contextual issues and qualitative research. Health Serv Deliv Res 2016;4.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process Evaluation of Complex Interventions: Medical Research Council Guidance. London: Medical Research Council; 2015.
- Busetto L, Luijkx KG, Elissen AMJ, Vrijhoef HJM. Context, mechanisms and outcomes of integrated care for diabetes mellitus type 2: a systematic review. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-015-1231-3.
- Sinnott C, Mc Hugh S, Browne J, Bradley C. GPs’ perspectives on the management of patients with multimorbidity: systematic review and synthesis of qualitative research. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003610.
- Multimorbidity: Clinical Assessment and Management. London: NICE; 2016.
- Villacampa-Fernández P, Navarro-Pardo E, Tarín JJ, Cano A. Frailty and multimorbidity: two related yet different concepts. Maturitas 2017;95:31-5. https://doi.org/10.1016/j.maturitas.2016.10.008.
- Hutchings HA, Evans BA, Fitzsimmons D, Harrison J, Heaven M, Huxley P, et al. Predictive risk stratification model: a progressive cluster-randomised trial in chronic conditions management (PRISMATIC) research protocol. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-301.
- Moons KG, Altman DG, Vergouwe Y, Royston P. Prognosis and prognostic research: application and impact of prognostic models in clinical practice. BMJ 2009;338. https://doi.org/10.1136/bmj.b606.
- Wilson P, Booth A. Evidence to Inform the Commissioning of Social Prescribing. York: Centre for Reviews and Dissemination; 2015.
- Grant C, Goodenough T, Harvey I, Hine C. A randomised controlled trial and economic evaluation of a referrals facilitator between primary care and the voluntary sector. BMJ 2000;320:419-23. https://doi.org/10.1136/bmj.320.7232.419.
Appendix 1 The PROTECTS analysis plan (8 November 2016)
This document specifies the planned statistical analysis of the PROTECTS (Proactive Telephone Coaching and Tailored Support) RCT to assess the effectiveness of the PROTECTS intervention. Note that the below does not include analysis to address economic evaluation of the intervention, nor the qualitative analysis of processes and meaning for patients.
Type of study
The trial is a pragmatic, two-arm, cohort multiple randomised controlled trial (cmRCT). Randomisation was undertaken at patient level. Data was collected at baseline (0 months), 6, 12 and 20 months.
Objectives
Main analysis
The main analysis is principally concerned to test for a treatment effect between the two trial arms on each primary and secondary outcome variable at the 20-month follow-up.
Sample and power
All patients included in CLASSIC were aged 65+ as this is the scope of the Salford Integrated Care Programme (SICP). For inclusion in CLASSIC PROTECTS, patients had to meet the following two criteria:
-
Have 2 or more existing long-term conditions.
-
Have been assed assessed as needing some assistance with self-management at baseline CLASSIC cohort assessment (classified in level 2 and 3 of the Patient Activation Measure).
After applying these two inclusion criteria, 1306 patients from the CLASSIC cohort met the eligibility criteria for PROTECTS. In line with previous cmRCTs of similar interventions, we applied a 1 : 1 allocation and we estimated a required sample of 504, or 252 per arm. The calculation also assumed an attrition rate of 25% across the trial and a conservative correlation of 0.5 between baseline and follow-up outcome scores. Based on the power calculation, we randomly selected 252 eligible patients to be offered the intervention. However, due to a high rate of non-consent we later took a top-up sample of a further 252 patients who were also offered the intervention, giving a treatment group of 504 and a control group of 802.
For each outcome in this analysis plan, the sample will be all patients who were eligible at baseline.
Analysis populations
Intention to treat. Analyses are performed by the treatment assigned to the patient.
General issues of analysis
We will report the trial and analysis according to updated CONSORT standards, including full details of use of the various telephone coaching components, linking to analysis of patient data in Implementation 2 to contextualise the quantitative findings. We will utilise the extension for pragmatic trials.
The main test of the intervention will be the test that the overall main effect of the intervention is zero. Condition group will be used as a binary variable.
Binary outcomes will be analysed using logistic regression and continuous outcomes using linear regression, controlling, where appropriate, for baseline values of the respective outcome. Outcomes measured using ordinal scales will be treated as continuous variables. The sample size is large enough to justify this. However, results for non-normal variables (skew or kurtosis > 1.0) will be confirmed using bootstrap analysis.
Baseline values of outcomes and design factors will be included in all analyses. Some additional covariates will be pre-specified.
Design-specific issues to be considered in analysis
Sample selection
The sample size and power calculation described above were undertaken under the assumption that all 252 patients offered the treatment would consent to receive it, whereas only 100 (40%) actually did. To account for this, the treatment was offered to a further ‘top-up’ sample of 252 patients of which 107 consented, producing an overall consent rate of 41% (207/504). Under the cmRCT design all 504 patients selected for treatment remain in the treatment arm for analysis. This includes 51 patients who could not be contacted and hence were never offered the intervention. To exclude these would risk introducing bias.
Definition of baseline and principal follow-up
The baseline for all patients will be time zero and the measures taken at that time point. Although no patient received treatment until after the 6-month follow-up, the measures at that point were post-randomisation for half of the sample and therefore potentially affected by arm allocation. The principal follow-up will be the 20-month time point. This will ensure that all patients across both arms have equal length of time duration between baseline and follow-up. We consider this to be the approach with least chance of selection bias under the null hypothesis.
Timing of treatment
Due to implementation delays, no patient was offered treatment before 6 months after the baseline assessment and for some the offer was not made until month 12 or later. This caused variations in the duration of time before start of the treatment, ranging from 259 to 513 days. Length of follow-up from end of treatment to 20-month follow-up was similarly variable. Thus the trial is considered to have run over the 20-month period, with individual patients receiving treatment at any time within that period.
Treatment effect estimation
The cmRCT design provides an estimate of the mean effect in people offered treatment. Compared to a pragmatic CRT, which provides an estimate of the mean effect in people agreeing to treatment, the effect is ‘diluted’ by the proportion of patients in the treatment arm who do not consent to treatment. An estimate of the effect size in patients consenting to treatment can be obtained through application of a Complier Average Causal Effect (CACE) analysis, and we will undertake that here. We note however, that CACE does not increase the power to detect an effect.
1. Main analyses of primary outcomes
Research hypotheses to be tested
There are no overall significant differences in the primary outcomes between intervention and control groups at 20 months.
-
Patient Activation Measure. A standardised spreadsheet in excel is used to score the PAM. Overall score (0–100) on the PAM scale where higher scores indicate high patient activation. A total score will be generated where participants answer at least 10 out of the 13 PAM questions. The continuous scores are categorised into four levels for descriptive purposes using the standardised spreadsheet. Higher scores indicate higher patient activation.
-
Quality of life – physical health domain. Physical health domain of the World Health Organization Quality of Life instrument (WHOQOL-100). WHOQOL is a 26-item measure which includes two items on general overall QoL and health, plus 24 which are scored in four QoL domains: physical, psychological, social relationships and environmental QoL. Facets are scored from 1 to 5, and higher scores indicate better QoL. Domain scores are transformed onto a scale from 0 to 100.
Statistical methods to be employed
Test of the intervention
The overall effect of the intervention will be tested by the main effect of treatment group from the regression analysis.
The primary analysis will be a complete-cases analysis and we will support this with a main sensitivity analysis that uses multiple imputation to include cases with missing baseline or follow-up data.
Analysis method
Multiple regression analysis of complete cases. Baseline data was collected for all the primary outcomes.
Dependent variable: primary outcome at 20 months.
Independent variables: trial arm, baseline value of primary outcome, pre-specified covariates.
Level of significance: 0.05.
Alternative tests if distribution assumptions are violated
Regression with bootstrapping.
Adjustments of significance and confidence levels due to multiplicity of outcomes
Each primary outcome addresses a different hypothesis and therefore adjustment for multiple testing will not be applied.
Sensitivity analysis
See relevant section below.
3. Analyses of secondary outcomes
Research hypotheses to be tested
There are no significant differences in the secondary outcomes between trial arms. Secondary outcomes include a number of outcomes at 20-month outcomes.
Depression measure
The MHI-5 is a five-item scale that measures general mental health, including depression, anxiety, behavioural–emotional control and general positive affect. The standardised score ranges from 0 to 100; scores below 60 indicate probable depression.
Baseline Summary of Diabetes Self-Care Activities
A 7-item measure which assesses the number of days per week respondents engage in healthy and unhealthy behaviours (i.e. eating fruit and vegetable, eating red meat, undertaking exercise, drinking alcohol, and smoking).
Statistical tests to be employed
Baseline data were available for all the secondary outcomes.
Analysis of secondary outcomes
Patient-level multiple regression analysis of complete cases.
Dependent variable: secondary outcome.
Independent variables: trial arms; baseline value of secondary outcome; pre-specified covariates.
Level of significance: 0.05.
Adjustment of significance and confidence levels due to multiplicity of outcomes
The analysis of secondary outcomes is regarded as exploratory and therefore not subjected to adjustment for multiple testing.
Alternative tests if distribution assumptions are violated
Regression with bootstrapping.
Sensitivity analysis
See relevant section below.
5. Sensitivity analyses
All the above analyses will be subjected to three sensitivity analyses.
The first (and main) sensitivity analysis will repeat the primary analyses using multiple imputation to include cases with missing baseline or follow-up data (see below).
The second sensitivity analysis will assess the robustness of the main analysis results to changes in the regression model. This analysis will remove the pre-specified covariates from the model (but still include the outcome at baseline).
A (provisional) third sensitivity analysis will examine the results after excluding patients with very short time intervals between the date receiving the first intervention phone call and return of the 20-month questionnaires. This is provisional because we will precede this by an analysis to examine the variation in times and only proceed with the sensitivity analysis if there are substantial numbers with intervals of < 6 months.
6. Treatment of missing data
For the main sensitivity analysis, missing data values for variables at baseline and follow-up will be substituted using chained-equation multiple imputation (MI) procedures. We will apply multiple imputation to baseline and 20-month variables with missing values by the chained equations approach using scores on all primary and secondary outcome measures (at baseline and follow-up). We will use 20 multiple imputation sets, as this will provide appropriate stability of results. Cases for whom imputation of baseline values is not possible (e.g. where the entire baseline questionnaire is missing) will be excluded.
7. Distributional tests
We will examine the distributional properties of each outcome variable. Variables for which skewness or kurtosis > 1.0 will be analysed using a bootstrap method. We will not do tests for normality because the large sample size makes these likely to be significant even for small deviations from normality.
8. Bootstrapping
Bootstrapping of p-values and CIs will be applied for outcome variables with skew > 1.0 or kurtosis > 1.0. In these cases the bootstrapped estimate of standard error will be used. Prior to any bootstrapping a set of pseudorandom numbers will be generated (depending upon how many outcomes have skew or kurtosis > 1.0) using random.org to act as seeds for each bootstrap analysis.
9. Choice of covariates
The covariates to be included in all primary and secondary analyses will be selected in the below manner.
First, the baseline values of the outcome that is the focus of each analysis will be included as co-variates. Second, a set of pre-specified covariates will automatically be included. The categorisation of variables (e.g. age, number of long-term conditions) is based upon examination of the distributions of these variables at baseline. These variables will be included in all primary and secondary analyses to reduce bias resulting from missing data.
| Pre-specified covariates | Description |
|---|---|
| Sex |
Question A1GENDER Coded as Male or Female |
| Age |
Question A2AGE Recoded as Agecat2 65–69; 70–79; 80–98 |
| General Practice ID | GP practice ID number |
| Health literacy (baseline) | A single 1–5-item health literacy measure |
| Baseline social support (ESSI) (from baseline) | The ESSI is a 7-item scale. A total score is calculated by summing all individual items; a higher score indicates greater social support |
| Baseline patient activation | PAM total continuous score |
| Baseline depression |
MHI-5 Coded as probable depression > 60; no depression < 60 |
| Baseline Quality of life | WHOQOL physical health domain |
| Pre-specified covariates | Description |
|---|---|
| Sex |
Question A1GENDER Coded as Male or Female |
| Age |
Question A2AGE Recoded as Agecat2 65–69; 70–79; 80–98 |
| General Practice ID | GP practice ID number |
| Health literacy (baseline) | A single 1–5-item health literacy measure |
| Baseline social support (ESSI) (from baseline) | The ESSI is a 7-item scale. A total score is calculated by summing all individual items; a higher score indicates greater social support |
| Baseline patient activation | PAM total continuous score |
| Baseline depression |
MHI-5 Coded as probable depression > 60; no depression < 60 |
| Baseline Quality of life | WHOQOL physical health domain |
| Pre-specified covariates | Description |
|---|---|
| Sex |
Question A1GENDER Coded as Male or Female |
| Age |
Question A2AGE Recoded as Agecat2 65–69; 70–79; 80–98 |
| General Practice ID | GP practice ID number |
| Health literacy (baseline) | A single 1–5-item health literacy measure |
| Baseline social support (ESSI) (from baseline) | The ESSI is a 7-item scale. A total score is calculated by summing all individual items; a higher score indicates greater social support |
| Baseline patient activation | PAM total continuous score |
| Baseline depression |
MHI-5 Coded as probable depression > 60; no depression < 60 |
| Baseline Quality of life | WHOQOL physical health domain |
| Pre-specified covariates | Description |
|---|---|
| Sex |
Question A1GENDER Coded as Male or Female |
| Age |
Question A2AGE Recoded as Agecat2 65–69; 70–79; 80–98 |
| General Practice ID | GP practice ID number |
| Health literacy (baseline) | A single 1–5-item health literacy measure |
| Baseline social support (ESSI) (from baseline) | The ESSI is a 7-item scale. A total score is calculated by summing all individual items; a higher score indicates greater social support |
| Baseline self-care activities | SDSCA total |
| Baseline depression |
MHI-5 Coded as probable depression > 60; no depression < 60 |
| Baseline Quality of life | WHOQOL physical health domain |
| Primary outcome (all at 20 months) | Description |
|---|---|
| Patient Activation Measure | A standardised spreadsheet in excel is used to score the PAM. Overall score (0–100) on the PAM scale where higher scores indicate high patient activation. A total score will be generated where participants answer at least 10 out of the 13 PAM questions. The continuous scores are categorised into four levels for descriptive purposes using the standardised spreadsheet. Higher scores indicate higher patient activation |
| Quality of life – physical health domain | Physical health domain of the World Health Organization Quality of Life instrument (WHOQOL-100). WHOQOL is a 26-item measure which includes two items on general overall QoL and health, plus 24 which are scored in four QoL domains: physical, psychological, social relationships and environmental QoL. Facets are scored from 1 to 5, and higher scores indicate better QoL. Domain scores are transformed onto a scale from 0 to 100 |
| Secondary outcome | Description |
|---|---|
| Depression measure | The MHI-5 is a five-item scale which measures general mental health, including depression, anxiety, behavioural-emotional control and general positive affect. The standardised score ranges from 0 to 100; scores below 60 indicate probable depression |
| Baseline SDSCA | A 7-item measure which assesses the number of days per week respondents engage in healthy and unhealthy behaviours (i.e. eating fruit and vegetable, eating red meat, undertaking exercise, drinking alcohol, and smoking) |
Pre-specified covariates
| Pre-specified covariates | Description |
|---|---|
| Sex |
Question A1GENDER Coded as Male or Female |
| Age |
Question A2AGE Recoded as Agecat2 65–69; 70–79; 80–98 |
| General Practice ID | GP practice ID number |
| Health literacy (baseline) | A single 1–5-item health literacy measure |
| Baseline social support (ESSI) (from baseline) | The ESSI is a 7-item scale. A total score is calculated by summing all individual items; a higher score indicates greater social support |
| Baseline patient activation | PAM total continuous score |
| Baseline depression |
MHI-5 Coded as probable depression > 60; no depression < 60 |
| Baseline Quality of life | WHOQOL physical health domain |
| Pre-specified covariates | Description |
|---|---|
| Sex |
Question A1GENDER Coded as Male or Female |
| Age |
Question A2AGE Recoded as Agecat2 65–69; 70–79; 80–98 |
| General Practice ID | GP practice ID number |
| Health literacy (baseline) | A single 1–5-item health literacy measure |
| Baseline social support (ESSI) (from baseline) | The ESSI is a 7-item scale. A total score is calculated by summing all individual items; a higher score indicates greater social support |
| Baseline patient activation | PAM total continuous score |
| Baseline depression |
MHI-5 Coded as probable depression > 60; no depression < 60 |
| Baseline Quality of life | WHOQOL physical health domain |
| Pre-specified covariates | Description |
|---|---|
| Sex |
Question A1GENDER Coded as Male or Female |
| Age |
Question A2AGE Recoded as Agecat2 65–69; 70–79; 80–98 |
| General Practice ID | GP practice ID number |
| Health literacy (baseline) | A single 1–5-item health literacy measure |
| Baseline social support (ESSI) (from baseline) | The ESSI is a 7-item scale. A total score is calculated by summing all individual items; a higher score indicates greater social support |
| Baseline patient activation | PAM total continuous score |
| Baseline depression |
MHI-5 Coded as probable depression > 60; no depression < 60 |
| Baseline Quality of life | WHOQOL physical health domain |
| Pre-specified covariates | Description |
|---|---|
| Sex |
Question A1GENDER Coded as Male or Female |
| Age |
Question A2AGE Recoded as Agecat2 65–69; 70–79; 80–98 |
| General Practice ID | GP practice ID number |
| Health literacy (baseline) | A single 1–5-item health literacy measure |
| Baseline social support (ESSI) (from baseline) | The ESSI is a 7-item scale. A total score is calculated by summing all individual items; a higher score indicates greater social support |
| Baseline self-care | SDSCA total |
| Baseline depression |
MHI-5 Coded as probable depression > 60; no depression < 60 |
| Baseline Quality of life | WHOQOL physical health domain |
Appendix 2 Qualitative study on health coaching
Observation work
Eight observation sessions were undertaken in March–July 2016, which covered 31 intervention calls ranging from session 1 to session 7. Observations captured only the health coaches’ side of the conversation, but notes were available during the call and the coaches were able to clarify issues immediately after the call.
All seven participants observed during sessions 6 and 7 were willing to be interviewed about their experience of receiving the health coaching. Further participants were selected at random and asked to return a reply slip if they were willing to be interviewed.
Qualitative interviews were conducted with 22 participants:
-
seven participants who completed all six sessions of the PROTECTS intervention
-
three who dropped out after starting the intervention
-
two who did not begin health coaching.
Participant characteristics are listed in Table 56.
| Interview ID | PROTECTS ID | n sessions completed | Health coach (initials) | Age (years) | Sex | Marital status | Number of LTCs | Baseline scores | |
|---|---|---|---|---|---|---|---|---|---|
| PAM | Probable depression (MHI-5) | ||||||||
| 1 | 767 | 6 | JN | 73 | Male | M | 11 | 3 | Yes |
| 2 | 1721 | 6 | JJ | 77 | Female | S (D) | 10 | 3 | Yes |
| 3 | 1462 | 6 | JN | 76 | Female | M | 3 | 3 | 0 |
| 4 | 1451 | 6 | JJ | 67 | Male | M | 6 | 3 | Yes |
| 5 | 958 | 6 | JN | 68 | Female | M | 4 | 3 | 0 |
| 6 | 2885 | 6 | SW | 69 | Female | S (D) | 2 | 2 | Yes |
| 7 | 2147 | 6 | SW | 73 | Male | M | 6 | 3 | 0 |
| 8 | 1068 | 6 | JN | 73 | Female | 5 | 2 | 0 | |
| 9 | 1264 | 6 | JN | 73 | Female | S (D) | 15 | 3 | 0 |
| 10 | 1053 | 6 | JJ | 74 | Female | 8 | 2 | Yes | |
| 11 | 974 | 6 | JN | 86 | Male | 5 | 3 | 0 | |
| 12 | 3372 | 6 | SW | 80 | Female | 2 | 3 | Yes | |
| 13 | 1315 | 6 | JN | 80 | Female | 8 | 2 | 0 | |
| 14 | 2552 | 6 | JN | 69 | Female | 4 | 3 | Yes | |
| 15 | 2038 | 6 | SH | 85 | Male | S (W) | 10 | 2 | Yes |
| 16 | 134 | 6 | SH | 69 | Female | 3 | 3 | Yes | |
| 17 | 3064 | 6 | SH | 80 | Male | M | 5 | 4 | 0 |
| 18 | 3517 | 2 | SH | 70 | Female | 14 | 3 | 0 | |
| 19 | 1946 | 2 | SH | 77 | Female | 4 | 3 | Missing | |
| 20 | 848 | 3 | JJ | 83 | Female | 11 | 2 | 1 | |
| 21 | 1865 | 0 | – | 90 | Female | S (W) | 6 | 3 | 0 |
| 22 | 3666 | 0 | – | 80 | Female | S | 9 | 3 | 1 |
Qualitative themes
We present the main themes arising from the PROTECTS interviews:
-
initial engagement with the PROTECTS intervention
-
experience of core features of the PROTECTS intervention –
-
format of the intervention
-
developing the relationship
-
providing information to participants
-
-
activating the patient
-
managing multimorbidity
-
assessing and working with low mood.
Initial engagement with the Preactive Telephone Coaching and Tailored Support intervention
Preactive Telephone Coaching and Tailored Support is a proactive intervention provided to older people who report multiple long-term conditions and moderate levels of activation, rather than any expression of specific or immediate clinical need. Therefore, the process by which people become engaged (or not) is important.
There was a basic understanding that the invitation to health coaching was linked in some way to people completing questionnaires as part of our cohort for older people. Invitation letters were sent via the patient’s practice, and this led a number of people to feel they had been ‘specially selected’ by their GP. One lady invited to take part reported asking her GP about how it might benefit her and the GP saying he did not think it would:
. . . whilst I was with [my] doctor, I mentioned it and he said oh he didn’t think it would be of any use to me because my cholesterol’s fine, my blood pressure’s fine and he said I don’t seem to put weight on from the dieting point of view.
PROTECTS 16, F69
She went on to complete the health coaching and was supported by the health coach to rejoin a slimming club and lost 5 lbs. She had previously discussed weight loss with her GP and was upset that many of her clothes no longer fitted her.
Many people were not entirely sure how it would help them, but chose to participate and remain in the study for a variety of reasons, including altruism; some people were keen to take part in something specifically designed for older people and many had been part of research studies previously (with Salford being particularly active in recruiting patients though its Citizen Scientist panel). People used their past experience of research to inform their decision to participate:
But I’ve always volunteered because I always think . . . I just think any sort of research, any sort of survey, it might not help me but in the future it will help other people.
PROTECTS 19, F77
I’ve been involved in research since I was 50. Initially it was memory . . . occasionally I get surveys which I fill in, how do you feel today on a scale of 1–10 and things like this. So I’ve always been interested, and I’m on the panel for Salford Royal.
PROTECTS 13, F80
This is why I was a bit dubious. I really didn’t understand what it [health coaching] would mean. But then when I thought about it, coming from a doctor’s side background, I suppose, I thought I might have had an idea that it might be about what you eat and exercise and just things in general. And then once [health coach] explained that it was for research purposes, and that you were hoping to roll it out if it was a success, that they needed people from all, that I didn’t consider myself in need really, but yeah, I’m quite happy to do it, not a problem.
PROTECTS 5, F68
Most participants enjoyed the sessions and felt they had gained something from the process, but almost universally suggested it might have been more appropriate and beneficial for people struggling with illness or who were isolated. Some participants were already active (e.g. regularly playing golf, eating healthily), so did not feel they would benefit from joining an exercise group. This is illustrated by the two examples below where participants who had friends and were not lonely felt guilty that the health coaching they received could have helped others more:
If I was on my own, you’d almost welcome that contact from someone prepared to talk and listen and give advice. My guilty feeling is maybe that time could be spent better with someone who needs it, but that someone might not always be there.
PROTECTS 4, M67
I thought if somebody was living on their own and alone it would benefit them enormously, but I’m out and about quite a lot so that side of it I didn’t think was of benefit to me . . . I just think like if I was lonely that call could be like a lifeline to you, couldn’t it?
PROTECTS 12, F80
For some, the health coaching came at difficult times and this was the reason for them dropping out of receiving the intervention (after two sessions), whereas others interviewed could not remember choosing to opt out (after three sessions):
. . . all this has been going on while my husband was very poorly and I had district nurses and doctors and Macmillan nurses, you know, and I had the family coming. I was just absolutely . . . I think that’s why [I stopped having the health coaching], yeah.
PROTECTS 19, F77
I don’t remember, actually saying, you know, ‘knock me off’ [health coaching] . . . Whether you think it’s worth continuing with it, or not, because of the situation, you know, with being a little bit further away from the centre of Salford, where, obviously, the connection is probably needed more than . . .
PROTECTS 20, F83
We also interviewed two people who were offered health coaching but did not return consent forms so did not receive calls. Neither remembered receiving the invite but, when asked, both provided reasons why it might not have appealed to them. The first person was very self-sufficient and thought she would probably know more than the coaches from her background in pharmacy and working in a GP surgery herself:
No, I haven’t had anything like that [invitation to health coaching]. The last thing I had was one of the big forms [questionnaires] to fill in and send back to the university . . . Well, because all these things they keep telling us, I know anyway . . . my husband was a pharmacist and I was involved in the business. And I’ve always been interested in medicine . . . I qualified as an apothecary, and I used to work from the doctor’s surgery over in Huddersfield, years and years ago. So I’ve always been interested in medical things, yeah.
PROTECTS 21, F90
The second person was extremely busy, acting as an advocate for her disabled daughter. She appeared very focused on physical illness and was unsure how a health coach could help her:
If I’m saying to this person how’s your health been? Well, I haven’t been too good, what are they actually going to do for me? Is it going to be useful for me?
PROTECTS 22, F80
Experience of the PROTECTS intervention
There are several core features of the PROTECTS intervention. The target population comprises patients with multiple long-term conditions and moderate levels of ‘patient activation’. The intervention is short and time limited, and delivered by telephone. The health coaches provided a seventh session for seven participants whom they felt needed this. The core intervention mechanisms are health coaching, social prescribing and low-intensity support for low mood. We now explore these features.
Format of the intervention
Participants liked the length of the sessions and the fact that they were monthly. The length of call was about right, although some suggested that calls could have been more frequent, especially for those with more complex needs. For others, a frequency of once a month allowed them to fit in other commitments because they were anxious not to miss a call if possible:
Once a month is OK. Because sometimes I have different appointments, and I don’t want to let anybody down, or I go out when it’s sunny and things like that, and I try to be back by 1 o’clock [this was the time of her monthly call] . . . I try to be back and I’m worried in case I can’t get back . . . The only time I didn’t [have the call], because I was literally in hospital, the emergency hospital, you know?
PROTECTS 2, F77
One participant said the information he received from the health coaches for his diabetes mellitus was better than that provided when he was initially diagnosed, and felt this was because of the time he spent speaking with the health advisor. He suggested that older people struggle to remember advice and the coaches help remind people of the right approach to take with their health:
I mean they may have mentioned, you know, eat this, eat that, and that; but not in detail like the lady on the phone . . . no, I don’t think they did. Can’t remember. But they seem to have more time than this lot, you see, don’t they?. . . Because you go to see the practice nurse and I think you’re only allowed about 5–10 minutes or something like that.
PROTECTS 11, M86
Most participants were happy to receive health coaching by telephone, but participants with few friends thought face-to-face delivery could be a way of meeting and talking to other people:
It would be nice, because it breaks your day as well, especially if it’s in the winter when it’s dark very early, and you’re miserable and can’t go out, and nobody around, no friends.
PROTECTS 2, F77
. . . we just rambled a lot of the time but I don’t feel . . . it’s not a criticism, it was supportive, but that’s all you can ask for really, and I think I would personally, because we talked a lot, I would have liked to have met [her].
PROTECTS 12, F80
Despite enjoying the coaching, many participants felt they were not deserving and that it would have been better targeted at people who were more ill or isolated or suffering from depression:
I enjoyed talking to [health coach] and looked forward to her calls but I felt, because I feel it would benefit people that are living alone, I felt I was robbing somebody of the benefit. So that’s the only thing, I wouldn’t object to her still calling me.
PROTECTS 12, F80
. . . I was willing to talk to anybody but I don’t know about other people if they were iller or, you know, if they were poorly more or not, you see? Some people might not like that, . . . older people might have appreciated whoever calls, . . . I probably think it helped with it being the same person because you’re not going over the same stuff, are you, again?
PROTECTS 7, M73
Developing the relationship
As noted earlier, health coaching is defined as ‘a regular series of phone calls between patient and health professional . . . to provide support and encouragement to the patient, and promote healthy behaviours such as treatment control, healthy diet, physical activity and mobility, rehabilitation, and good mental health’. 5
The health coaches explained the importance of building this relationship, especially during the initial call:
. . . whatever message I’m going to deliver I’ve still got to build that side of it first or else I feel they won’t really listen. I’ve got to listen to them and they’ve got to listen to me, so I have to build up the relationship . . . Even the tone of your voice, which you will notice in that bit of building a relationship, it’s . . . I don’t like to say win a person over, but I think in some ways whatever direction you’re going in it has to be that, it’s that first impression of you to them and them to you isn’t it?
Health coach
Developing a relationship with participants was a core part of the intervention. All participants described the health coaches as warm and empathetic. There was agreement that it was preferable if a single health coach made all six calls. One of our health coaches retired during the intervention period and, despite trying to ensure that she had completed all calls, a small number of participants had to be transferred to an alternative health coach:
Oh I don’t think they could relate with different people. You build up a relationship. We just did. I felt quite comfy, quite comfy.
PROTECTS 1, M73
During observations it was clear that the health coaches had formed good rapport with their participants. In only one instance was a participant referred to by their title rather than their first name. Negotiating what people wanted to be called was always addressed during the first call, and in many cases the name we had been given was the not the name that the participant preferred to be known by.
The health coaches were not provided with any information from the CLASSIC questionnaire and they were all in agreement during the focus group that they preferred not to access hospital data at the first call to avoid making assumptions about patients.
Most people enjoyed the conversational approach adopted by the health coach, with some describing their calls as akin to a ‘chat’ or ‘a talk with a friend’. For others, the calls appeared to have more structure. This was true from observations, with the health coaches typically starting out asking how the person was, but invariably following this up with a reminder from the previous session and a plan for what they thought might be useful for that particular call. They were very keen to get agreement from people on what to discuss and were flexible where needed:
I started talking on what she’d asked me to do or what she talked about and I would answer like I’m talking to you now, that whatever she was talking about I would talk about, you know?
PROTECTS 7, M73
She just told me she was like a carer or whatever, and would I mind to talk to her, and things like that you know? If I need anything, how I feel. I feel very lonely, that’s one thing, I’m very lonely, . . . and I would chat to her for half an hour . . .
PROTECTS 2, F77
The health coaches could meet a variety of functions depending on patient circumstance. Many of those interviewed found talking to someone outside their family helpful, particularly around health issues, when they did not want to cause worry:
. . . it’s as if because she was a stranger, you’d tell a stranger something that you wouldn’t tell your family . . .
PROTECTS 9, F73
You could talk to them [the health coach] more about different things, you know? I don’t like complaining to my son and my daughter, I’m not well or something, because they will get fed up with me. And I’m not really complaining to them, I don’t. I keep it for myself, and that’s the trouble sometimes.
PROTECTS F77
Alternatively, the role of the relationship within health coaching was important in the case of isolated patients. Often, as people age, their circle of friends can became smaller and some who have poor mobility can became isolated and lose their sense of community. People who move into smaller ‘retirement’ communities or sheltered accommodation can often support each other, but they can also then feel impending loss as friends around them die.
The health coach was viewed as helpful to many lonely older people, and some coaches tried to reconnect some people with their community via participation in local activities, although often ill health meant this was difficult:
I have one friend, she lives in Yorkshire . . . So I’ve got no friends [locally], and then I said, ‘if I would just have somebody, to go out for a coffee, or a lunch or something’ . . . [she asked] have I made any progress going to meet some people, but I couldn’t because of my eyes.
PROTECTS 2, F77
I had one lady . . . she had lost her husband for like 2 years before, but it was still quite raw for her and also she felt that she had to be strong for the rest of the family, because the girls were upset, her daughters were upset, so she didn’t want to cry in front of them. But, sometimes she did get upset when she was talking about her husband and things like that on the phone to me.
Health coach
Providing information to participants
Although developing the relationship was crucial, health coaching involved promotion of lifestyle change. The health coaches used two main strategies to deliver key health messages, conveying them verbally over the telephone and then directing participants to websites (NHS Choices and Patient) to reiterate their message.
Information was sent by post to participants who did not have internet access or if people did have the internet but were confused by the array of information available. In addition to condition-specific information and support groups, other groups for older people (such as falls prevention and healthy ‘hips and hearts’ classes) were also introduced, in many cases starting with an introduction to exercise through the armchair exercise leaflet:
. . . it’s better if you hear it from a health professional because, you know, I’ve begun to see that the internet can be as big a problem as it is an asset, because there’s so much information on there.
PROTECTS 3, F76
Participants liked the fact that information was provided in a friendly way. Others thought that the friendliness of the delivery might detract from the messages that the coaches were trying to convey:
She explained who she was, where she was from. Came across very friendly, sometimes people can come across a bit dictatorial, you know, but she was very approachable, I found her. She encouraged you to talk about anything you were worried about, not just within her range. We used to have a little chat about all sorts. So that, in itself, I think broke a barrier, she didn’t just come across as, well I’m here now, I’m on the phone, and this is what you should be doing today, you should be eating so many vegetables, and change your fats and your margarine. You know what I mean? The way she came across, I thought, was excellent, yeah, full of praise for her.
PROTECTS 5, F68
I would say that if the advice had come from [health coach] I would feel that it was more a friend advising me rather than a doctor, not that the advice was any the less important . . . because a friend, well, it can go in one ear and out the other but if a doctor tells you something I think you pay more attention, especially somebody of my generation because doctors and policemen were important people in those days, I don’t think they are now.
PROTECTS 12, F80
The health coaches’ previous roles working with patients with diabetes mellitus and pre-diabetes mellitus means they were used to giving dietary advice and had existing scripts advising people about the various food groups and also portion size. Some of these scripts were adjusted for this intervention, but on observation some of the ‘world’ foods being suggested (chapatti and couscous) did not appear well matched to the age of the participants.
The health coaches were seen as a trusted source of information and, in particular, told people with diabetes mellitus of their expertise in this area. In some cases they identified patients who were taking medications incorrectly and were able to help them rectify this:
I was taking them [tablets] at the wrong time on the . . . I was taking them, one, one, one, something like that, after meals. She [health coach] said, no, two in the morning after your breakfast, and then two after your tea . . . And she said, if you do have anything, like fruit, make sure you have it immediately after your meal, because if you leave it till the afternoon, like you say with a biscuit, it spikes up again. Is that correct? . . . I’ve stuck to that religiously . . . Anyway it brought it [HbA1c] down from 70-something, . . . brought it right down to 56 or 57 . . . Well, they’re looking at [aiming for] something in the 40s . . . Well, they’re the experts, aren’t they? You know, they’re talking to people all the time; I’m sort of here on my own.
PROTECTS 11, M86
Written information was always offered to participants and, if accepted, was sent to participants through the post on the same day. If information required participants to get to support groups and courses they were given information on public transport and the local ring and ride service.
The health coaches always started out their calls by checking that the participant had received the information posted out to them, if they had time to read it and if they had then either started using the information or were planning to in the future:
She asked me to go the heart care, the heart care club, Salford Heart Care Club, and I said yes I would when me sister got better but she’s not going to get no better. But I will go especially . . . if I can spare the time.
PROTECTS 9, F73
Even participants whose health problems interfered with their ability to undertake suggestions were keen not to let the coach down. One lady who started a computer course had to discontinue after cataract surgery, but was determined to restart the course when fully recovered:
I joined a computer course, ’cause I’m so terrible, and I’ve got an iPad but I don’t know how to use it. And I was there 5 weeks, it should be an 8-week course I think. And I had to leave because I couldn’t see any more in the eye, it was just before the [cataract] operation, and I said, ‘well I can’t see what they’re doing there, and it’s no good for me’.
PROTECTS 2, F77
Although most coaches focused on one area (Table 57), there were some participants were helped in a number of areas:
I found it very useful, because, you know, going over the different food groups, and exercise, and relaxation, and sleep, I mean, we discussed all of that.
PROTECTS 3, F76
| Areas addressed during coaching | n |
|---|---|
| Behavioural activation | 46 |
| Cognitive restructuring | 23 |
| Problem-solving | 24 |
| Diet | 79 |
| Smoking | 9 |
| Exercise | 70 |
| Alcohol | 9 |
| Social prescribing | 31 |
Some of the health coaches focused on more areas with an individual during the health coaching (Table 58). Data need to be treated cautiously as the two coaches with the lower average number were the two coaches who did not complete sessions with participants owing to retirement.
| Health coach | Average number of areas addresseda |
|---|---|
| 1 | 1.86 |
| 2 | 1.89 |
| 3 | 1.39 |
| 4 | 0.55 |
Other patients felt that they already knew much of the advice being given, although this still did not deter them from completing the intervention:
Virtually everything that we discussed, I knew. But that sounds a bit big-headed I know . . . but it’s not intended to be, it’s absolutely no reflection on the lady that interviewed me, she was doing what she had to do. And I think this is where sadly you’re not going to pick up the people that you need to pick up . . . I’d agreed to take part, and I know you could stop at any time, but I thought, well, that’s not productive if I stop it, because I thought, well, there might be some evaluation of the project and I could then give an evaluation.
PROTECTS 13, F80
Activating the patient
Patient activation was a primary outcome of the PROTECTS study. Patient activation refers to a patient’s understanding of their own role in the health-care process and their level of knowledge, skill and confidence in managing their own health.
Patients were recruited into the PROTECTS trial on the basis of a having a moderate score (level 2 or 3) on the PAM. A PAM level of 2 or 3 reflects that a patient has some understanding of his or her own role in the management of their long-term condition and is somewhat motivated to make changes to their lifestyle, but requires some support to do so.
Patients in PROTECTS talked about how the health coaches had supported them to increase their knowledge, skill and confidence in managing their health. Many patients described how the health coaches had helped them to seek help from their GP as well as other support available from within their local community:
. . . with [health coach] I’ve got enough confidence to go to my doctor and say I’m not happy, which I suppose a lot of people aren’t, they’ll just accept it or sulk. I have a whinge if I don’t think I’m getting a, you know – well, if I don’t think I’m being treated fairly.
PROTECTS 4, M67y
The health coaches frequently advised participants to return to their GP for a review of their medication and, with their support, participants described taking action earlier that they would have done before, and feeling more confident to do so:
I’d been . . . I changed tablet, depression tablets, and my daughter, and everyone, was saying to me, you’re not yourself, [patient name], but of course when you’re . . . when you’ve got depression you’re really inside yourself. It’s like a glass, you just . . . you know, even though you know it there’s nothing you can do about it. So it was with her [health coach] persuasion and telling me to get back to the doctor straightaway it was because of her. I think I would have gone on for months and months longer if she hadn’t.
PROTECTS 6, F69
One of the ways in which health coaches were able to activate patients was by increasing their knowledge of healthy eating. Many patients talked about how they had changed their diet as a result of the intervention:
She did tell me she said that I’m eating the right stuff, the lettuce and that and she said don’t eat . . . don’t drink the orange juice because two little oranges are better than one orange juice sort of thing. I thought ‘alright then I’ll eat accordingly’.
PROTECTS 9, F73
The dietary advice patients received was described as useful and different from health care that they had received in the past, whe they did not remember diet being discussed:
It was different health advice than I’ve received in the past. Because nobody had ever discussed diet with me before, so, you know, that was useful.
PROTECTS 15, M85
Some talked about the knowledge around diet and their health having resulted in weight loss and how this had affected their mood and quality of life:
They [health coaches] taught me about my health, how to be more healthy, and I told them that I was going to lose weight, and they said ‘well, that is very, very good’, and she advised me on the benefits of healthy . . . which obviously has worked because I’ve lost all this weight . . . I’m happy now, honestly. I can do things . . . I can even get in and out the car which used to be hard for me. And the kids, we have the grandkids all weekend and I can play with them.
PROTECTS 18, F70
In some cases patients also talked about the changes they had made having an impact on their health outcomes, such as reduced cholesterol:
But yeah, I was genuinely surprised that just with a little bit of effort; you can make a big change can’t you? And so when my cholesterol had come down .2 I said to the doctor, ‘well I have been really, really trying,’ and I’m desperately trying, . . .
PROTECTS 5, F68
If people lived with partners (or in some cases grandchildren), dietary changes were often at household level rather than restricted to the participant themselves. It may be therefore that the health coaching intervention had spill-over effects.
Although most accounts were positive, on occasion patients were reluctant to change some of their dietary habits, especially if they saw a particular food as a treat, although they were happy to swap other food items:
But the thing is I won’t go off me butter, I like me butter me, I like butter and it makes no difference what you’re telling me I’ll still eat the butter. She said, ‘go on this low fat.’ I said, ‘no I’m sorry love I’m stopping on me butter. I don’t get many treats in life.’.
PROTECTS 9, F73
As well as advice on diet, there were also examples of health coaches encouraging patients to take opportunities to increase their exercise within their daily routine, such as walking to the next bus stop instead of standing and waiting for the bus:
This business of walking further along, if I walk down Lancaster Road and I don’t see any buses and a bus is coming when I get there, I’ll get on it, but if I don’t see a bus when I get to the bus stop I will walk to the next one. Invariably it passes me, in which case I get there and I don’t see another one so I walk to the next one, but I find that I’m running . . . I’m not walking any further. And another thing, I do get up in the morning and I’ll do my hoovering and I’ll prepare the tea and I’ll do my washing and I’ll do . . . but if I sit down in the afternoon I could doze off, so I’ll do something. I’ll write a letter or I’ll do my ironing.
PROTECTS 8, F73y
This was the case for patients who had also reported experiencing significant symptoms of low mood and had previously found it hard to get out:
And it’s like I say, even if, you know, I’m not going to do anything special. I’ll jump on a bus and go for a ride and things like that rather than sit and mope. I find now that I don’t want to sit in now. Well I’ve got into a habit now of doing things instead of sitting there. So what she said to me has gone in, you know, because I do feel as if I want to do things now which I didn’t do before.
PROTECTS 10, F74y
One lady with low mood whose mobility was limited and used a scooter outside her home was encouraged by the health coaches to move from passive to a slightly more active form of exercise. She ultimately hoped to return to a healthy hips and hearts class run locally:
Well [health coach] sent me her information [on armchair exercises]. You know what they do, and it’s the same thing. Yeah, I’ve got the elastic bands and . . . Yes, I do that now, and I’ve got this [vibration plate exerciser] as well, this is good.
PROTECTS 6, F69
Patients also talked about how the health coaches had increased their knowledge about their own medication and they gave examples of how they had improved their skills in managing their own medication regimes. One man with diabetes mellitus talked about sugar levels being very high and how the health coach had identified he was taking his diabetic medication at the wrong time of day:
Anyway, but with the help of that lady from Hope Hospital, Salford Royal, that rang me, I was taking them at the wrong time on the . . . I was taking them, one, one, one, something like that, after meals. She said, no, two in the morning after your breakfast, and then two after your tea . . . And what else was it? I’ve always liked fruit and veg, well, yeah, I do. And she said, if you do have anything, like fruit, make sure you have it immediately after your meal, because if you leave it till the afternoon, like you say with a biscuit, it spikes up again . . .
PROTECTS 11, M86
Participants described the techniques that the health coaches used to engage them and increase their level of activation:
I told her what I did and some days you do what you think is right but it turns out it isn’t, so then I think, ‘oh, blow everything, why do I bother?’. For a couple of days and then I think, ‘no, come on, pull yourself together’. So I spoke to her about that and she didn’t say, ‘well, you should stick to what you’re trying to do instead of thinking, “oh, blow it all” ’she just said, ‘as long as you go back to it’. So, as I say, there was nothing dictatorial about it, you’ve got to do this and you’ve got to do that, but the support was there.
PROTECTS 12, F80
When patients talked about experiencing barriers to behaviour change the health coaches suggested alternatives to support them in achieving the change. They also encouraged them to set realistic and achievable goals and used problem-solving techniques to help them overcome challenges:
I said, I don’t like eating fruit in cold weather, I know it’s silly, but I eat loads of fruits in summer time, but she suggested ways of doing things, like fruits salads, and so on, and so forth. Then, about walking, she said, ‘well, set yourself a small goal’, because, of course, [grandson] can walk now, and he walks with his mum and his dad with the dogs. He was my real catalyst for keep walking, but I had a spell, when I had painful knees, and all sorts, and I just didn’t. So, I started back doing that again, and realised how much better it makes you feel . . .
Managing multimorbidity
All patients in PROTECTS had self-reported two or more long-term conditions in the cohort baseline questionnaire. The management of multiple conditions can complicate care, although many long-term conditions lead to common challenges around self-management. The number of conditions reported ranged from 2 to 19, with some participants struggling to remember them all:
I’ve got bronchitis and asthma, epilepsy, I’ve had strokes, five strokes I’ve had . . . What else have I got? I’m sure I’ve got something else. Nineteen things I’ve wrong with me I’ve got anyway, that’s all I can think of . . .
PROTECTS 9, F73
The initial call with the health coach tended to be longer than average (30–40 minutes) and covered a lot of background about the patient’s long-term conditions and the type of issues that the health coaching intervention would cover. Some patients spoke only about the conditions affecting them at that particular time and did not disclose what they considered ‘old’ conditions unless currently affected by them:
. . . she didn’t know [about the falls], because that was before I talked to [her] . . . she kept asking me how I feel, and if I feel any better, how is my foot, how is my eyes?
PROTECTS 2, F77
One patient was discussed by her health coach at supervision and it was not until her final session that she discussed receiving 90% burns as a child aged 7 years. Although not actively avoiding the subject, the coach felt disappointed that they had not explored this during earlier sessions:
She asked about me asthma and bronchitis . . . she didn’t ask about me my burns it was me that opened my mouth about me burns.
PROTECTS 9, F73
For many people, illness was part of the ageing process and people with long-term conditions tended to be accepting of them and viewed medication use as inevitable:
Atrial fibrillation. Hypertension. Basically those are the two main ones. Oh, apart from being deaf and I’m wearing hearing aids, but I don’t really call that a medical condition to be honest, that’s just old age . . . I take my medication regularly . . . I’d forgotten about that, I had a stroke about 8 years ago and I was put on Warfarin, and I’ve been on it ever since, so I’ll be on it for the rest of my life. But I go roughly about every 3 months to the blood clinic and they check what the INR [international normalized ratio] should be. So yeah, I’m monitored really as far as my health is concerned. Then every – oh, you forget these things, I’ve got CKD, but nearly everybody’s got that about my age, and that’s a urine check every 12 months.
PROTECTS 13, F80
Although most long-term conditions reported by participants were common (diabetes mellitus, hypertension, arthritis, heart disease, stroke, etc.) there were some relatively unusual conditions (PROTECTS 14 – bronchiectasis, giant cell arteritis), which the health coaches sought information on to be better able to support their patients:
I was going to the doctors for a long time with this fibromyalgia thing and keep going and getting different tablets, because he said we have to try different things. I never mentioned the IBS . . . [with the health coach] each time we just spoke about general health and she persuaded me to go to the doctors, because I’d not been for years about my IBS. ‘Well, I just thought, well, he’s told me what it is, I’ve just got to get on with it’, and I was. But it was quite bad, so [she] said, ‘go back and tell him and ask him’, she said, ‘if you don’t tell him, he won’t know’, so fair enough . . . [tablets] it does help, but I still have issues, but the pains, it did help with that . . .
PROTECTS 14, F69
Here they encouraged the patient to re-engage with the GP and to discuss medication and a dietitian referral to help with her IBS symptoms, which were starting to prevent her leaving the house.
Assessing and working with low mood
During the first appointment, the health coaches asked the patients if they had ever experienced low mood. The coaches felt that most people, even those struggling with low mood, were unlikely to disclose their feelings until they had developed a certain level of trust:
. . . most of them are saying their mood is OK. Now, I’ve got a couple [with low mood], I know that, and one of them is the patient that I’m due to ring next week. Because I’m unsure myself, and I will be literally working from the manual. But because it’s a study and that person has agreed to do it, the confident bit in me is able to say ‘this is what . . .’. You know what I mean? I’m going to be led by that manual and work from it, and I’m hoping that I can say to the patient this is what we’re going to do. So ask me again later . . . He was the one that I know I’ve to focus on, not looking back because that’s sort of with regret, and if we look to the future, which we did, it frightens him. But I’ve got to work on being in the present moment, being in the day.
Health coach 2
Even when participants suggested they might have low mood on occasion, they did not want to discuss it with their health coach. Sometimes this was simply a choice to underplay their symptoms, but others actively avoided talking about low mood even when they knew they had a problem:
She said, ‘do you get depressed?’, and I said, ‘I don’t really’. Sometimes you feel a bit down with your health, you know what I mean, but I didn’t go desperate about it, you know what I mean?
PROTECTS 7, M73
This lady explained how she had purposively described her love of music and line dancing in great detail to her health coach as a way of avoiding some of the discussion around her mood, which she preferred not to talk about. Like many older people she was also heavily involved in the lives of her children and grandchildren and worried about them thus also helping distract thoughts away from herself:
I think mainly I was upbeat, not her fault I was upbeat, we talked mainly about my line dancing because I do love it, I love music I adore music . . . I’m the sort of person I don’t need anyone else to judge me, I’m my own judge and jury and I know when I’m doing something wrong, when I’m not doing something I am my own judge and jury . . . I think this is mainly why I dwell a lot on other people, because I don’t have time to think about myself, I don’t have time I’m too busy, so I dwell on everybody else’s problems . . .
PROTECTS 16, F69
Others participants talked about having ‘occasional’ low mood but were keen to say they had never been depressed, and others that loneliness and long-term conditions contributed to them feeling ‘down’:
I’m not down on the floor never have been, I pick myself up, dust myself down and start all over again. That’s what I had to do in the very beginning and what I’m doing now. No reason why but I’ve never been that way inclined. I’ve had some downers but I’ve not been down there long, pick yourself up.
PROTECTS 9, F73
I didn’t know whether I would get any benefit from it but I thought, well, if there’s somebody that I can have a moan to about, I’m feeling fed up today, it’s a good thing . . . I can be quite positive and if I do feel down I just keep myself quiet, as I say, I go in and shut my door and forget about everybody and everything for a couple of days and then get myself a kick up the bum and off we go again . . . I might have told her if I do get depressed this is how I deal with it, yes, but I know it was mentioned but not because I was feeling depressed at the time . . . she was just saying, have you tried such and such a thing? I can’t remember any of them . . .
PROTECTS 12, F80
Three of the participants interviewed had either previously had, or were currently experiencing, depression. They described the darkness they felt, but were keen to reiterate that the antidepressants they took were the lowest possible dose:
I am on Mirtazapine now, just the lowest dose . . . I was for months like that. It was horrible and it was abs . . . and all I could do was just sit here and I just . . . I didn’t even know what it was but I just felt in this dark, dark tunnel . . . I did go to [my] doctor and I started crying, I said, ‘I don’t know what’s the matter with me’, and I’m still on them, only the lowest dose and I like I said I am terrified of that happening again.
PROTECTS 16, F69
Although not finding previous cognitive–behavioural therapy helpful, this lady valued the health coaching particularly because it provided her with someone to talk to who was non-judgemental:
One week I had to put people that I would hold in high esteem then sort of go down the ladder to where I would position myself. And in the end I didn’t really feel very good about myself and where I needed . . . because I don’t have anyone to talk to, to keep it all inside to myself and . . . I don’t have anyone that I feel . . . I’ve no immediate family, sister or whatever that I can . . . no. No one that I can offload onto.
PROTECTS 16, F69
People found it helpful to be given a different approach to some of their frustrations and the coaches encouraged people to make time for things they found important:
. . . she, sort of, gave me another way of looking at things, you know . . . when I said about having no time to do this, and she said, ’well, have you thought why you haven’t got any time, you know, it’s changing the focus of how you’re looking at things.’. I’d maybe make a statement about something and she’d say, ‘well, have you tried doing this, or, have you tried . . .’. When I asked her about things she was very helpful, and making me look at things in a different way, and attempting to do things differently, like, my exercise and rest.
PROTECTS 3, F76
Appendix 3 Descriptive data from the cohort
| Characteristic | Number of patients | Mean number of patients | SD |
|---|---|---|---|
| Age (years) | 4098 | 75 | 6.8 |
| PAM score | |||
| Baseline | 3539 | 60.83 | 15.4 |
| 6-month follow-up | 2795 | 60.33 | 20.0 |
| MHI-5 | 4123 | 67.1 | 22.6 |
| n | % | ||
| Sex | |||
| Male | 2024 | 45.8 | |
| Female | 2316 | 52.4 | |
| Long-term condition(s) | |||
| One | 1115 | 25.5 | |
| Two or more | 2631 | 60.1 | |
| Ethnicity: white British | 4123 | 95.4 | |
| Living status: living alone | 1594 | 36.9 | |
| Employment status: retired/not economically active | 3985 | 93.8 | |
| Health literacy | |||
| Never needs help | 2974 | 70.3 | |
| Rarely needs help | 427 | 10.1 | |
| Sometimes needs help | 455 | 10.8 | |
| Often needs help | 158 | 3.7 | |
| Always needs help | 215 | 5.1 | |
| Social support: good social support | 2755 | 66.4 | |
| Variable | Mean % |
|---|---|
| Do you have a written care plan? | |
| Baseline | Yes, 5.4 |
| Follow-up | Yes, 10.4 |
| Were you involved as much as you wanted to be in decisions about your care or treatment? | |
| Baseline | Almost always, 49.7 |
| Follow-up | Almost always, 47.6 |
| Have you had enough support from your health and social care team to help you manage your health? | |
| Baseline | Almost always, 54.4 |
| Follow-up | Almost always, 49.4 |
| Do you think the support and care you receive is joined up and working for you? | |
| Baseline | Almost always, 50.2 |
| Follow-up | Almost always, 45.3 |
| Baseline patient activation level | |
| 1 | 13.0 |
| 2 | 17.3 |
| 3 | 48.0 |
| 4 | 21.7 |
| Follow-up patient activation level | |
| 1 | 12.6 |
| 2 | 14.2 |
| 3 | 43.9 |
| 4 | 29.3 |
Appendix 4 Additional tables and figures
| Level | Responsibility | Scope |
|---|---|---|
| 1 | Partners of the Alliance Agreement to endorse |
|
| 2 | Alliance Board to endorse |
|
| 3 | Steering and Finance Group to endorse |
|
| 4 | Senior commissioning managers |
|
| 5 | Service managers |
|
FIGURE 13.
Salford ICS governance infrastructure (version 0.15). GMW, Greater Manchester West.
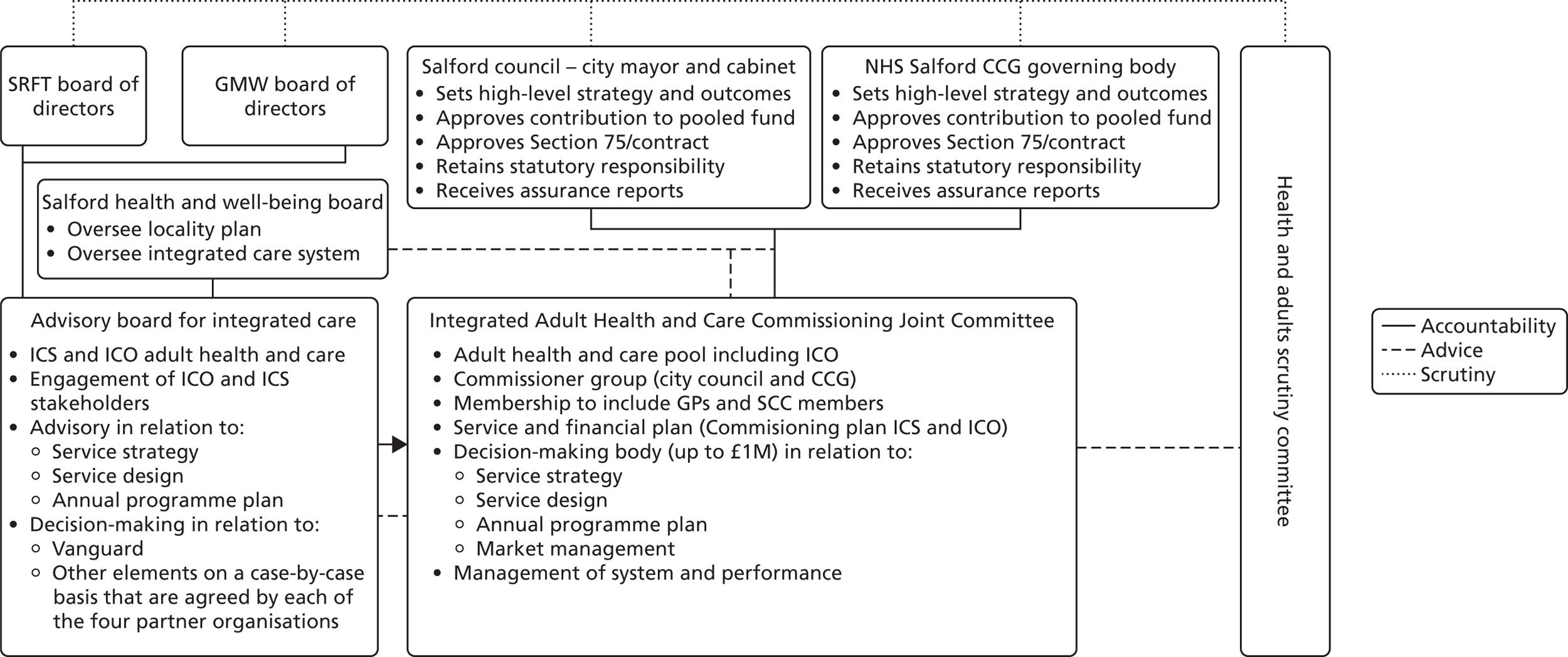
| Advisory Board | ICJC |
|---|---|
| Membership: GMWFT, SCC, SCCG and GP providers | Membership: city council and CCG |
| Four CCGs, four councils, five trusts, one mental health trust and four genral practices (quorate if third of membership is there – with one member of each organisation needing to be in the room) | Nine CCGs (chief accountable officer, clinical lead for quality and safety, clinical lead for planning and partnerships, a five clinical leads from each of the neighbourhoods) and six CCs (all councillors) (quorate third membership with at least three members from each organisation present). If no agreement is met it can be put to the vote, if no decision can be made it must go back to the respective organisations |
| They have no decision powers in their own rights but they have been delegated by their respective organisations | Non-voting: two CCGs, three CCs and public health |
| There to recommend the strategic direction for integration for adult services in Salford (ICO and SICP) | City council and CCG delegate their functions to the committee, accountable to the CCG and the city council |
| Advise on strategy and the development on an annual work programme | Decisions must adhere to city council key decisions and constitution |
| Partners must consider issues that arise for resolution | Core principles are the same as the advisory board |
| Able to develop task-and-finish groups | Support provided by integrated communication and engagement team under the management of the CCG |
| Eleven core principles | Work is to be scrutinised by the scrutiny committee |
| Decision-making processes are in line with city council duties for transparency | The ICJC will monitor actual income and expenditure in relation to the pooled fund |
| They will take vanguard decisions where consensus can be found – if not, decisions go back to respective organisations | |
| Provide advice to the ICJC |
FIGURE 14.
Commissioning and contracting in the ICO.
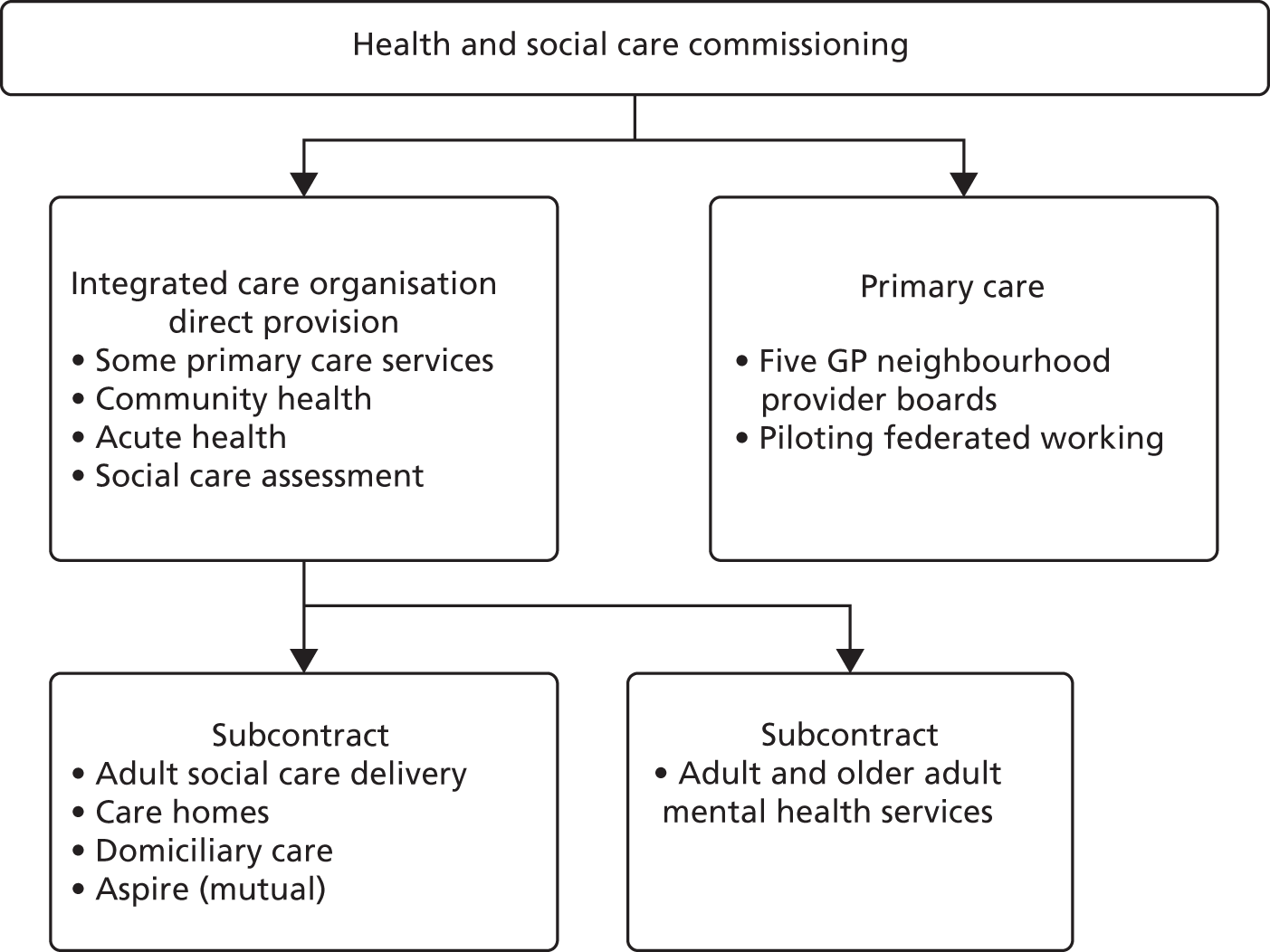
| MDG neighbourhood | Staff | |||||||
|---|---|---|---|---|---|---|---|---|
| MDG administrator | Nursing lead | Social care lead | GP | Geriatrician | Mental health lead | Health improvement | Other | |
| Eccles | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Swinton | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | Physiotherapist |
| Ordsall and Langworthy | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | Assistant practice manager |
| Irlam and Cadishead | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Claremont and Weaste | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Broughton | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | Two practice managers |
| Little Hulton and Walkden, Worsley and Boothstown | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Care homes’ practice | ✗ | ✗ | ||||||
FIGURE 15.
General practice READ coding flow chart for risk stratification. LCS, locally commissioned service; LTC, long-term condition; SC, social care, SRFT, Salford Royal Foundation Trust.
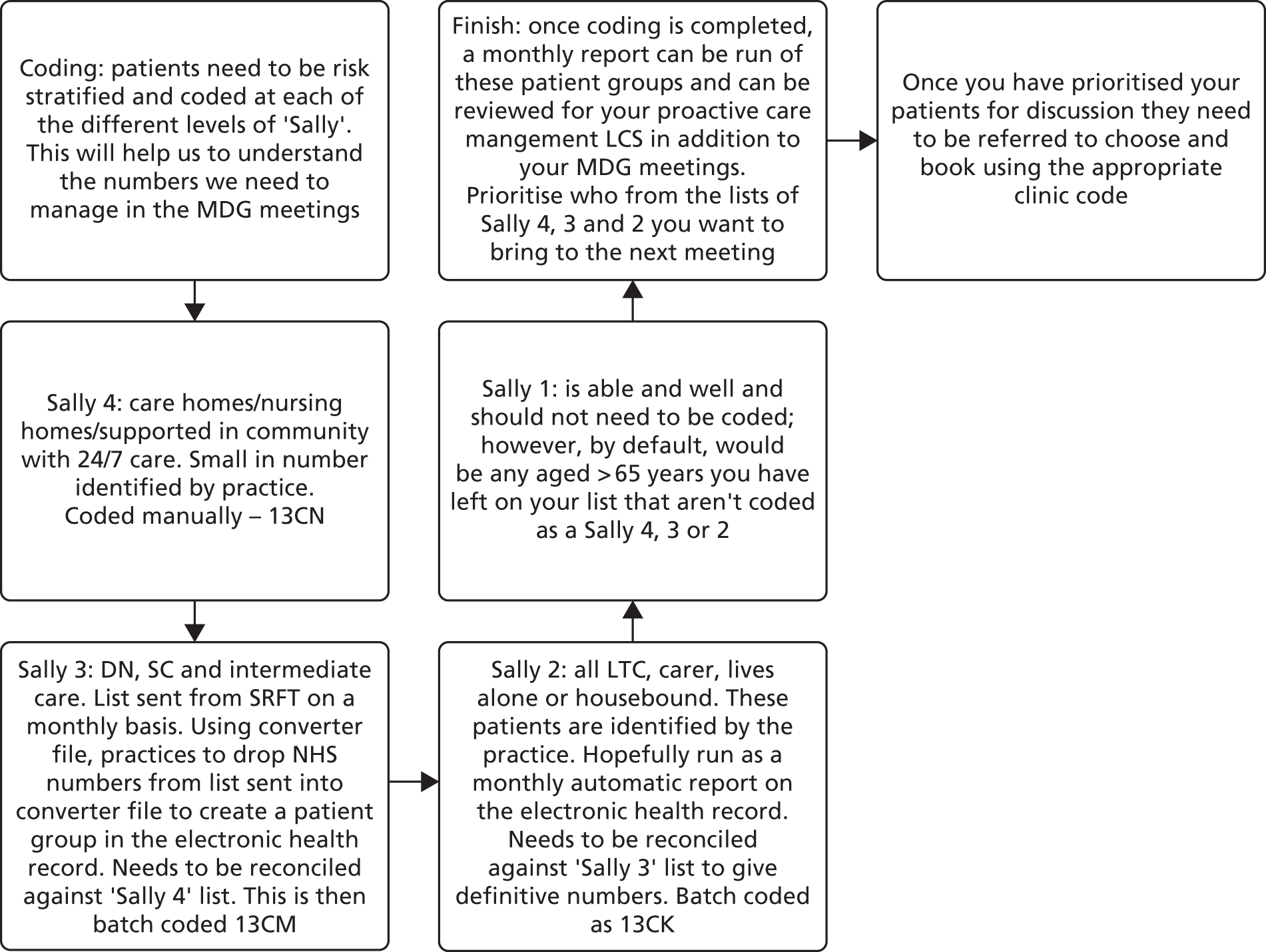
| Outcome | Financial year | ||||||
|---|---|---|---|---|---|---|---|
| 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | |
| Population aged ≥ 65 years | |||||||
| All adopters | 28,517 | 28,618 | 31,872 | 31,872 | 31,872 | 32,286 | 33,222 |
| Non-adopters in Salford | 3522 | 3985 | 4159 | 4159 | 4159 | 4198 | 4256 |
| Greater Manchester | 340,462 | 349,627 | 383,905 | 383,905 | 383,905 | 393,279 | 402,740 |
| West | 84,143 | 85,659 | 94,479 | 94,479 | 94,479 | 96,685 | 99,057 |
| West (extensive) | 309,955 | 314,846 | 345,070 | 345,070 | 345,070 | 353,030 | 360,812 |
| England | 8,123,925 | 8,326,125 | 9,186,494 | 9,186,627 | 9,186,627 | 9,446,649 | 9,695,384 |
| Activity | |||||||
| A&E attendances | |||||||
| All adopters | 13,773 | 13,466 | 13,450 | 14,547 | 15,328 | 15,939 | 17,368 |
| Non-adopters in Salford | 1792 | 2018 | 1773 | 1995 | 2076 | 1968 | 2093 |
| Greater Manchester | 146,380 | 150,906 | 156,499 | 170,149 | 169,873 | 179,593 | 184,135 |
| West | 43,406 | 32,385 | 40,341 | 51,511 | 47,693 | 52,256 | 53,750 |
| West (extensive) | 133,359 | 128,111 | 144,699 | 164,946 | 157,782 | 162,936 | 171,080 |
| England | 2,668,409 | 2,854,846 | 3,086,040 | 3,304,093 | 3,385,248 | 3,619,570 | 3,797,749 |
| A&E attendances via health/social care providers | |||||||
| All adopters | 6999 | 6888 | 6891 | 7664 | 8701 | 8823 | 9940 |
| Non-adopters in Salford | 943 | 1107 | 944 | 1024 | 1154 | 1084 | 1184 |
| Greater Manchester | 24,751 | 27,946 | 40,638 | 40,235 | 42,954 | 49,080 | 54,448 |
| West | 17,626 | 13,762 | 12,848 | 14,788 | 11,960 | 12,995 | 13,347 |
| West (extensive) | 35,772 | 34,431 | 37,447 | 46,540 | 43,386 | 49,878 | 52,507 |
| England | 917,870 | 988,768 | 1,055,553 | 1,131,851 | 1,220,757 | 1,344,607 | 1,427,631 |
| Self-referred A&E attendances | |||||||
| All adopters | 5749 | 5431 | 5663 | 5991 | 5768 | 6409 | 6868 |
| Non-adopters in Salford | 732 | 735 | 710 | 869 | 807 | 810 | 856 |
| Greater Manchester | 78,941 | 81,581 | 76,472 | 88,585 | 92,696 | 101,947 | 98,375 |
| West | 21,477 | 14,684 | 23,588 | 32,870 | 30,979 | 34,228 | 35,785 |
| West (extensive) | 77,957 | 74,195 | 77,460 | 96,046 | 90,887 | 96,336 | 100,522 |
| England | 1,342,737 | 1,442,371 | 1,566,318 | 1,662,172 | 1,674,445 | 1,792,195 | 1,868,641 |
| Ambulatory care-sensitive admissions | |||||||
| All adopters | 4699 | 4679 | 4837 | 5181 | 5498 | 5788 | 5875 |
| Non-adopters in Salford | 613 | 675 | 607 | 643 | 709 | 661 | 718 |
| Greater Manchester | 50,018 | 54,300 | 54,207 | 57,115 | 59,024 | 62,059 | 63,014 |
| West | 12,254 | 13,154 | 13,518 | 14,745 | 14,575 | 15,240 | 14,775 |
| West (extensive) | 43,296 | 46,397 | 47,104 | 50,756 | 50,372 | 53,687 | 52,807 |
| England | 952,360 | 1,030,319 | 1,059,630 | 1,134,286 | 1,172,250 | 1,247,939 | 1,286,611 |
| Emergency admissions | |||||||
| All adopters | 8873 | 8885 | 9179 | 9293 | 9889 | 10,595 | 10,528 |
| Non-adopters in Salford | 1153 | 1337 | 1143 | 1177 | 1274 | 1246 | 1243 |
| Greater Manchester | 93,616 | 97,336 | 97,691 | 101,088 | 102,017 | 106,256 | 102,727 |
| West | 25,190 | 25,534 | 25,736 | 27,183 | 26,827 | 28,213 | 27,311 |
| West (extensive) | 90,223 | 92,033 | 91,039 | 95,033 | 95,255 | 100,882 | 98,871 |
| England | 1,930,040 | 1,990,658 | 2,026,958 | 2,112,316 | 2,145,995 | 2,263,568 | 2,263,252 |
| Emergency admissions via A&E | |||||||
| All adopters | 7945 | 8011 | 7918 | 8179 | 8944 | 9831 | 9813 |
| Non-adopters in Salford | 1032 | 1212 | 996 | 1046 | 1143 | 1165 | 1174 |
| Greater Manchester | 76,643 | 80,713 | 78,596 | 83,283 | 84,881 | 89,445 | 86,961 |
| West | 19,631 | 18,880 | 19,722 | 21,094 | 20,106 | 20,556 | 20,387 |
| West (extensive) | 63,899 | 65,312 | 65,534 | 69,426 | 68,888 | 74,125 | 74,101 |
| England | 1,370,849 | 1,449,396 | 1,507,621 | 1,603,257 | 1,635,783 | 1,743,323 | 1,750,642 |
| Direct emergency admissions | |||||||
| All adopters | 709 | 638 | 927 | 933 | 744 | 593 | 550 |
| Non-adopters in Salford | 88 | 78 | 103 | 97 | 102 | 59 | 50 |
| Greater Manchester | 12,895 | 12,559 | 14,837 | 13,928 | 12,985 | 12,557 | 11,571 |
| West | 3778 | 5102 | 4976 | 5059 | 5770 | 6691 | 5894 |
| West (extensive) | 20,518 | 21,235 | 21,232 | 21,492 | 22,789 | 23,396 | 21,310 |
| England | 446,796 | 430,329 | 409,049 | 394,515 | 390,317 | 390,830 | 383,971 |
| Population weighted rates | |||||||
| A&E attendances | |||||||
| All adopters | 0.121 | 0.118 | 0.106 | 0.114 | 0.120 | 0.123 | 0.131 |
| Non-adopters in Salford | 0.127 | 0.127 | 0.107 | 0.120 | 0.125 | 0.117 | 0.123 |
| Greater Manchester | 0.107 | 0.108 | 0.102 | 0.111 | 0.111 | 0.114 | 0.114 |
| West | 0.129 | 0.095 | 0.107 | 0.136 | 0.126 | 0.135 | 0.136 |
| West (extensive) | 0.108 | 0.102 | 0.105 | 0.120 | 0.114 | 0.115 | 0.119 |
| England | 0.082 | 0.086 | 0.084 | 0.090 | 0.092 | 0.096 | 0.098 |
| A&E attendances referred by health/social care providers | |||||||
| All adopters | 0.061 | 0.060 | 0.054 | 0.060 | 0.068 | 0.068 | 0.075 |
| Non-adopters in Salford | 0.067 | 0.069 | 0.057 | 0.062 | 0.069 | 0.065 | 0.070 |
| Greater Manchester | 0.018 | 0.020 | 0.026 | 0.026 | 0.028 | 0.031 | 0.034 |
| West | 0.052 | 0.040 | 0.034 | 0.039 | 0.032 | 0.034 | 0.034 |
| West (extensive) | 0.029 | 0.027 | 0.027 | 0.034 | 0.031 | 0.035 | 0.036 |
| England | 0.028 | 0.030 | 0.029 | 0.031 | 0.033 | 0.036 | 0.037 |
| Self-referred A&E attendances | |||||||
| All adopters | 0.050 | 0.047 | 0.044 | 0.047 | 0.045 | 0.050 | 0.052 |
| Non-adopters in Salford | 0.052 | 0.046 | 0.043 | 0.052 | 0.049 | 0.048 | 0.050 |
| Greater Manchester | 0.058 | 0.058 | 0.050 | 0.058 | 0.060 | 0.065 | 0.061 |
| West | 0.064 | 0.043 | 0.062 | 0.087 | 0.082 | 0.089 | 0.090 |
| West (extensive) | 0.063 | 0.059 | 0.056 | 0.070 | 0.066 | 0.068 | 0.070 |
| England | 0.041 | 0.043 | 0.043 | 0.045 | 0.046 | 0.047 | 0.048 |
| Ambulatory care-sensitive admissions | |||||||
| All adopters | 0.041 | 0.041 | 0.038 | 0.041 | 0.043 | 0.045 | 0.044 |
| Non-adopters in Salford | 0.044 | 0.042 | 0.036 | 0.039 | 0.043 | 0.039 | 0.042 |
| Greater Manchester | 0.037 | 0.039 | 0.035 | 0.037 | 0.038 | 0.039 | 0.039 |
| West | 0.036 | 0.038 | 0.036 | 0.039 | 0.039 | 0.039 | 0.037 |
| West (extensive) | 0.035 | 0.037 | 0.034 | 0.037 | 0.036 | 0.038 | 0.037 |
| England | 0.029 | 0.031 | 0.029 | 0.031 | 0.032 | 0.033 | 0.033 |
| Emergency admissions | |||||||
| All adopters | 0.078 | 0.078 | 0.072 | 0.073 | 0.078 | 0.082 | 0.079 |
| Non-adopters in Salford | 0.082 | 0.084 | 0.069 | 0.071 | 0.077 | 0.074 | 0.073 |
| Greater Manchester | 0.069 | 0.070 | 0.064 | 0.066 | 0.066 | 0.068 | 0.064 |
| West | 0.075 | 0.075 | 0.068 | 0.072 | 0.071 | 0.073 | 0.069 |
| West (extensive) | 0.073 | 0.073 | 0.066 | 0.069 | 0.069 | 0.071 | 0.069 |
| England | 0.059 | 0.060 | 0.055 | 0.057 | 0.058 | 0.060 | 0.058 |
| Emergency admissions via A&E | |||||||
| All adopters | 0.070 | 0.070 | 0.062 | 0.064 | 0.070 | 0.076 | 0.074 |
| Non-adopters in Salford | 0.073 | 0.076 | 0.060 | 0.063 | 0.069 | 0.069 | 0.069 |
| Greater Manchester | 0.056 | 0.058 | 0.051 | 0.054 | 0.055 | 0.057 | 0.054 |
| West | 0.058 | 0.055 | 0.052 | 0.056 | 0.053 | 0.053 | 0.051 |
| West (extensive) | 0.052 | 0.052 | 0.047 | 0.050 | 0.050 | 0.052 | 0.051 |
| England | 0.042 | 0.044 | 0.041 | 0.044 | 0.045 | 0.046 | 0.045 |
| Direct emergency admissions | |||||||
| All adopters | 0.006 | 0.006 | 0.007 | 0.007 | 0.006 | 0.005 | 0.004 |
| Non-adopters in Salford | 0.006 | 0.005 | 0.006 | 0.006 | 0.006 | 0.004 | 0.003 |
| Greater Manchester | 0.009 | 0.009 | 0.010 | 0.009 | 0.008 | 0.008 | 0.007 |
| West | 0.011 | 0.015 | 0.013 | 0.013 | 0.015 | 0.017 | 0.015 |
| West (extensive) | 0.017 | 0.017 | 0.015 | 0.016 | 0.017 | 0.017 | 0.015 |
| England | 0.014 | 0.013 | 0.011 | 0.011 | 0.011 | 0.010 | 0.010 |
| Discharge to usual place of residence | |||||||
| All adopters | 0.031 | 0.027 | 0.036 | 0.035 | 0.027 | 0.021 | 0.021 |
| Non-adopters in Salford | 0.028 | 0.020 | 0.030 | 0.029 | 0.025 | 0.015 | 0.016 |
| Greater Manchester | 0.051 | 0.048 | 0.055 | 0.049 | 0.045 | 0.043 | 0.040 |
| West | 0.061 | 0.077 | 0.077 | 0.072 | 0.079 | 0.087 | 0.076 |
| West (extensive) | 0.082 | 0.082 | 0.080 | 0.079 | 0.079 | 0.078 | 0.071 |
| England | 0.077 | 0.071 | 0.066 | 0.062 | 0.058 | 0.056 | 0.055 |
FIGURE 16.
Trends in A&E attendances in Salford and England.
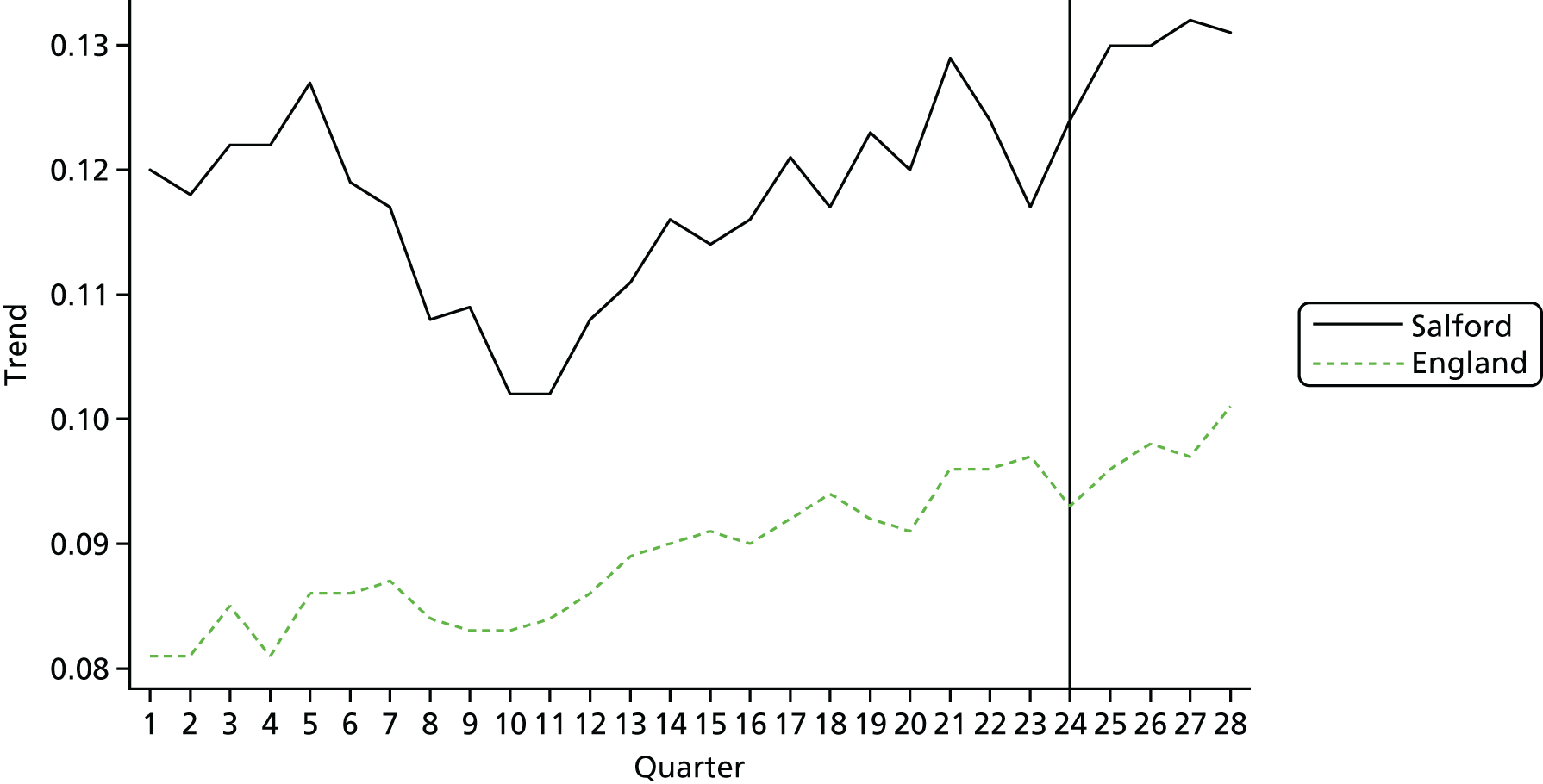
FIGURE 17.
Trends in A&E attendances (health and social care) in Salford and England.
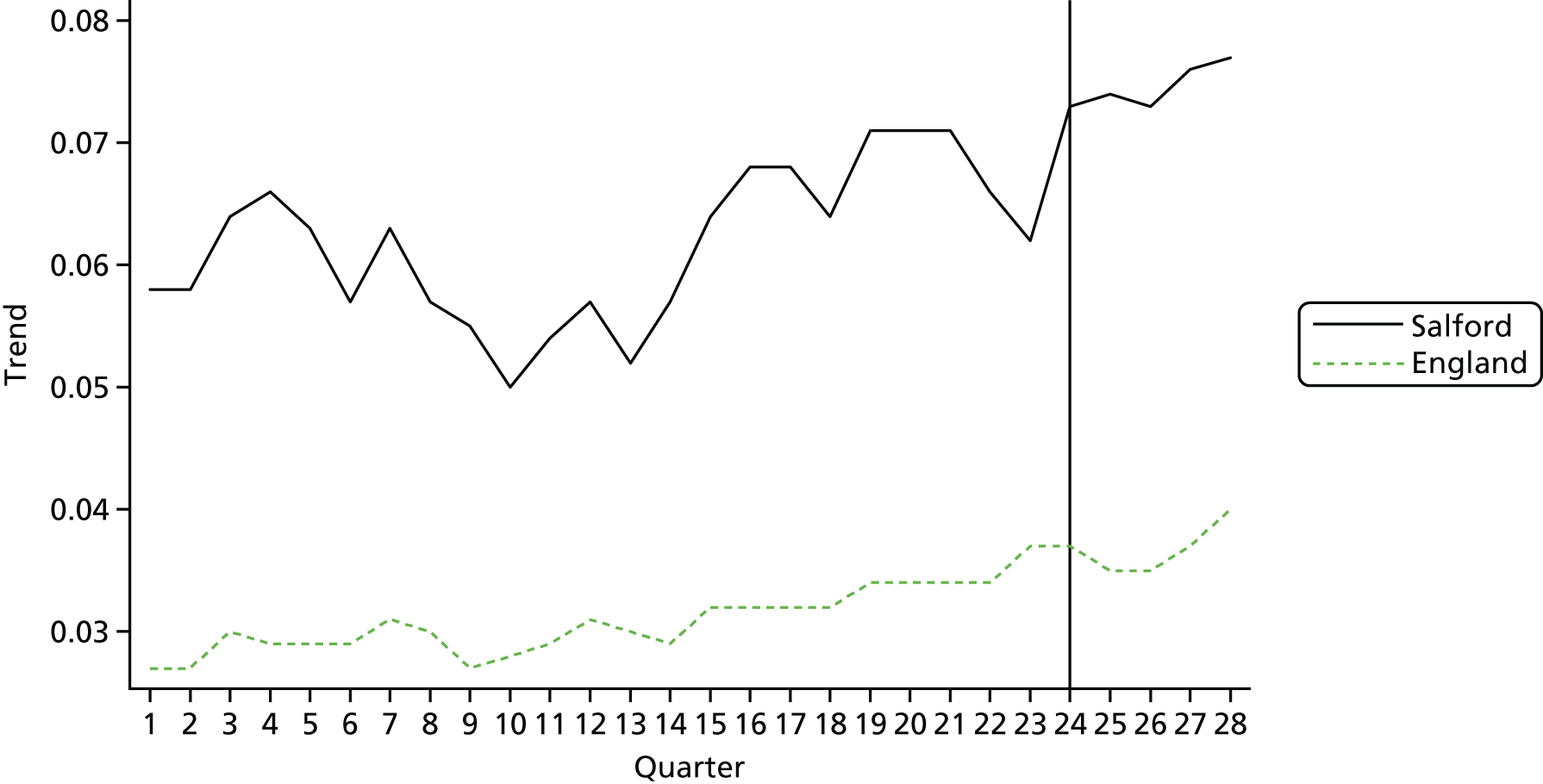
FIGURE 18.
Trends in A&E attendances (self-referral) in Salford and England.
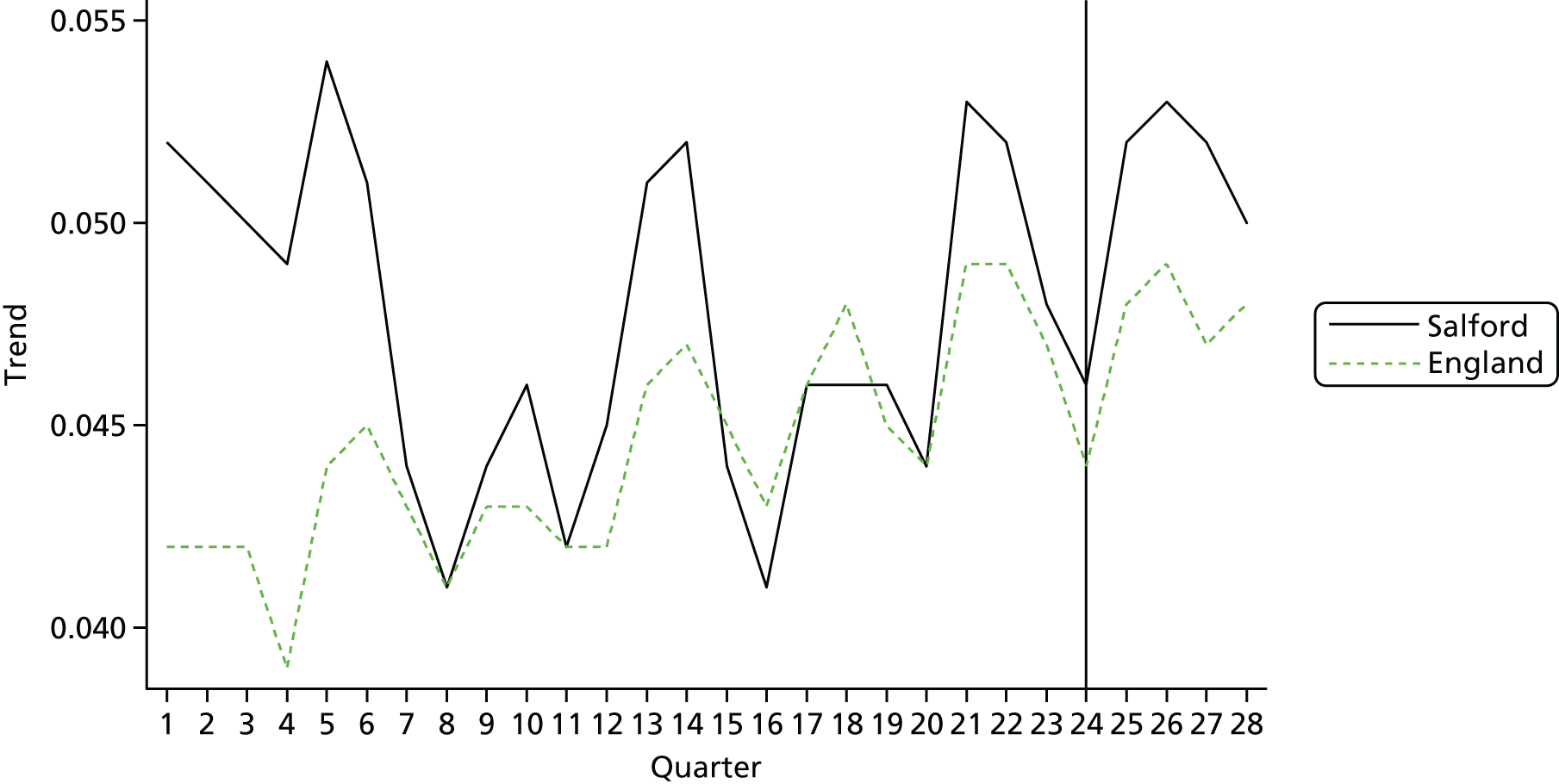
FIGURE 19.
Trends in discharge to usual place of residence in Salford and England.
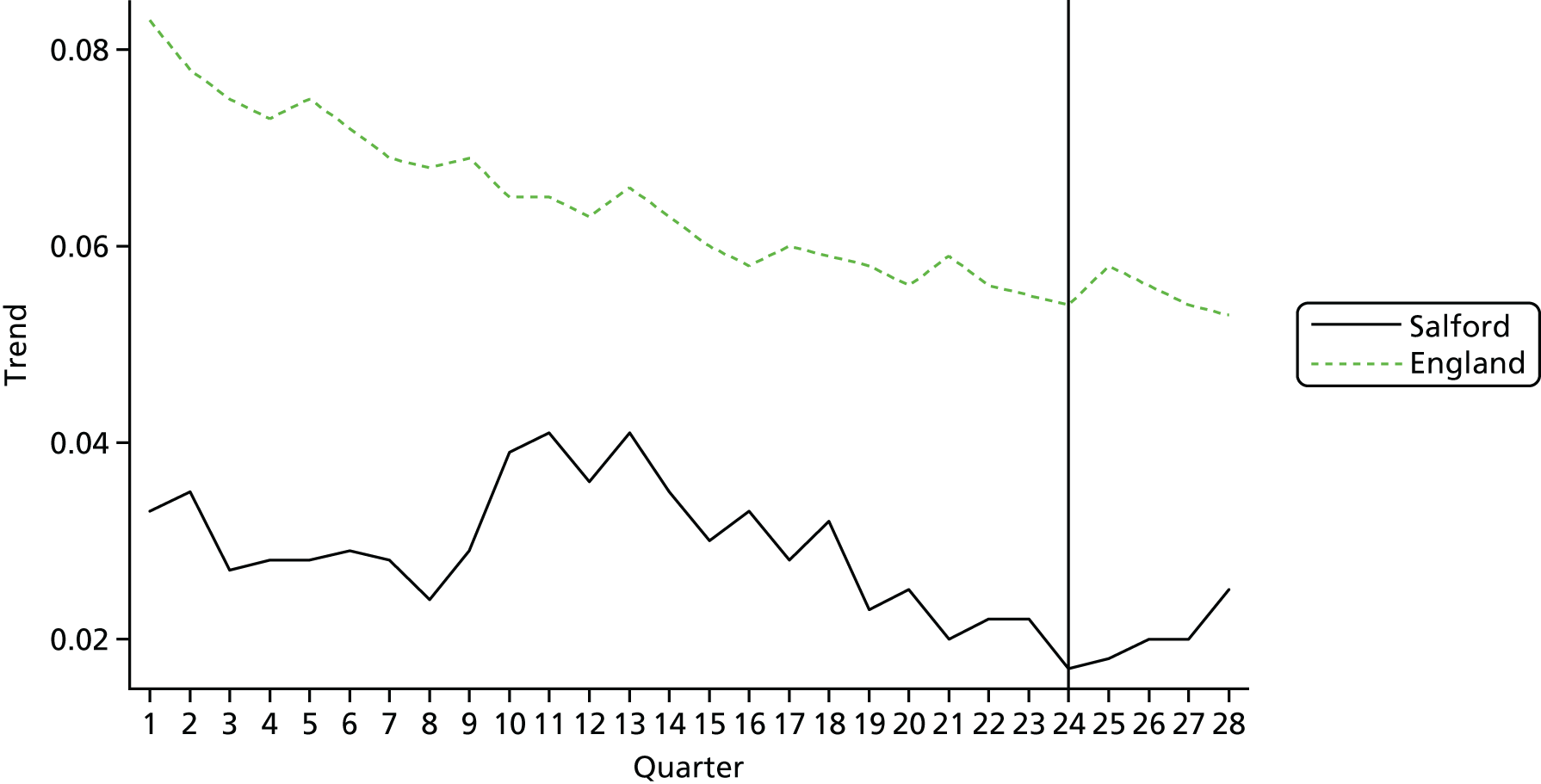
FIGURE 20.
Trends in avoidable admissions in Salford and England.
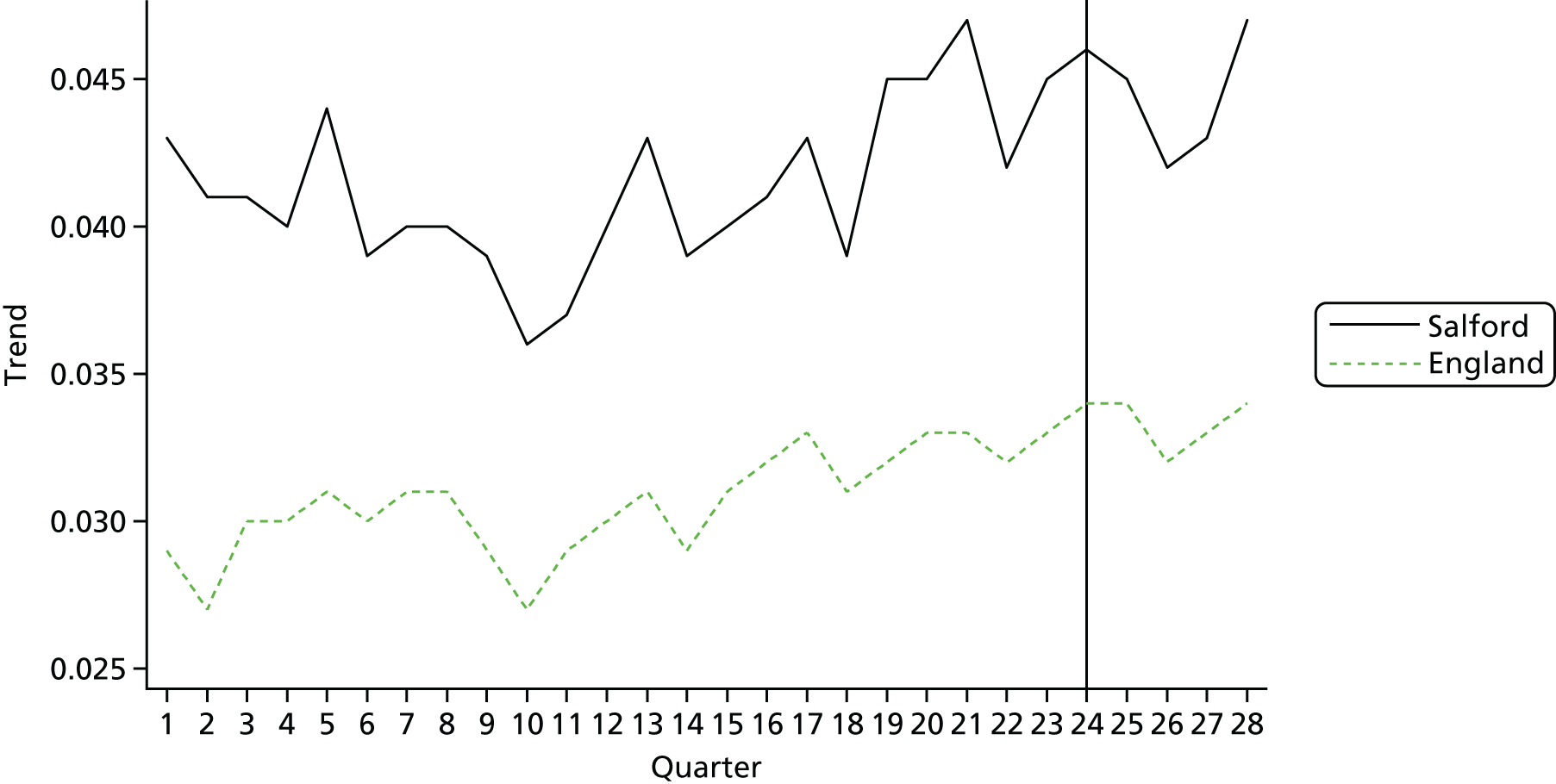
FIGURE 21.
Trends in emergency admissions in Salford and England.
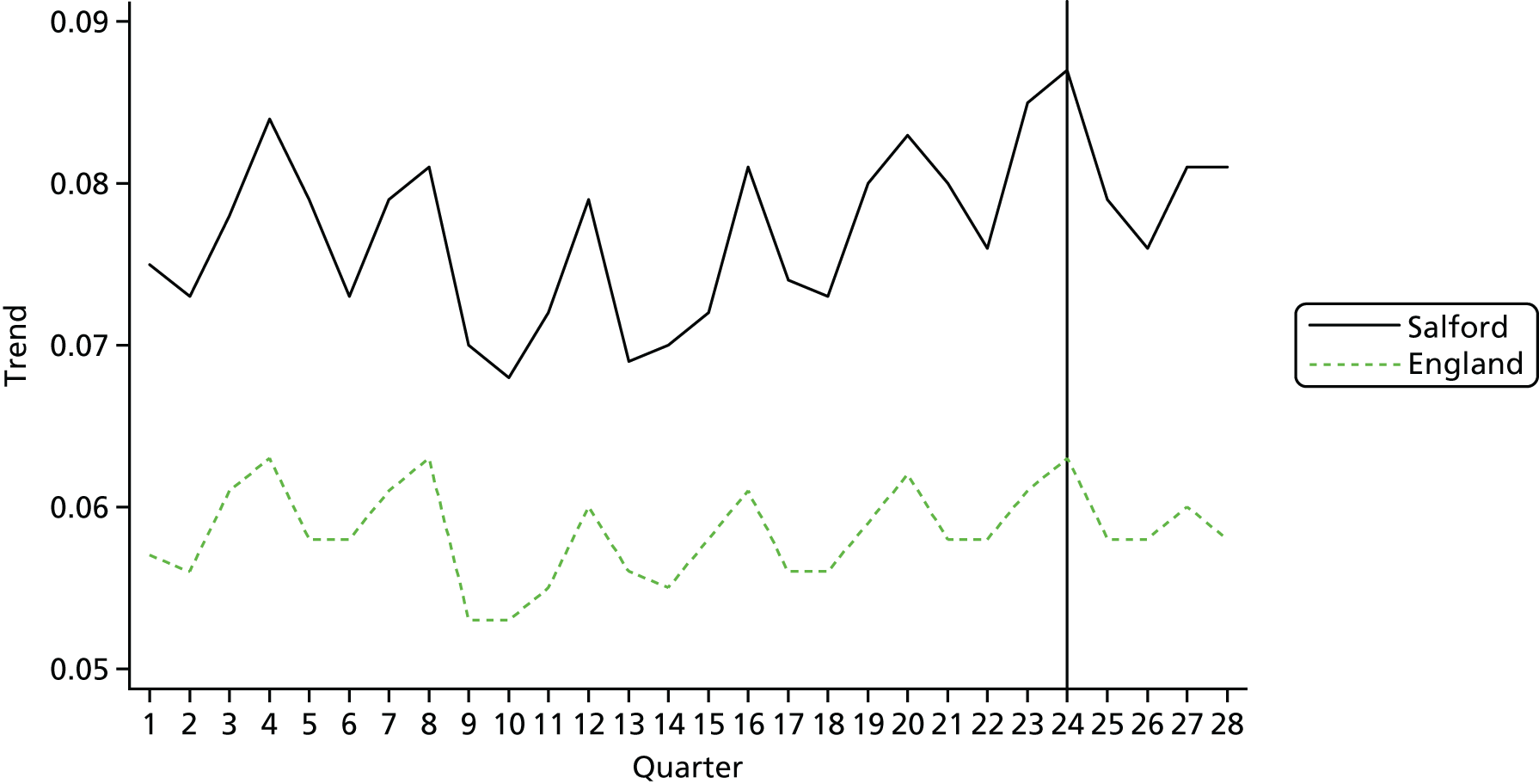
FIGURE 22.
Trends in emergency admissions via A&E in Salford and England.
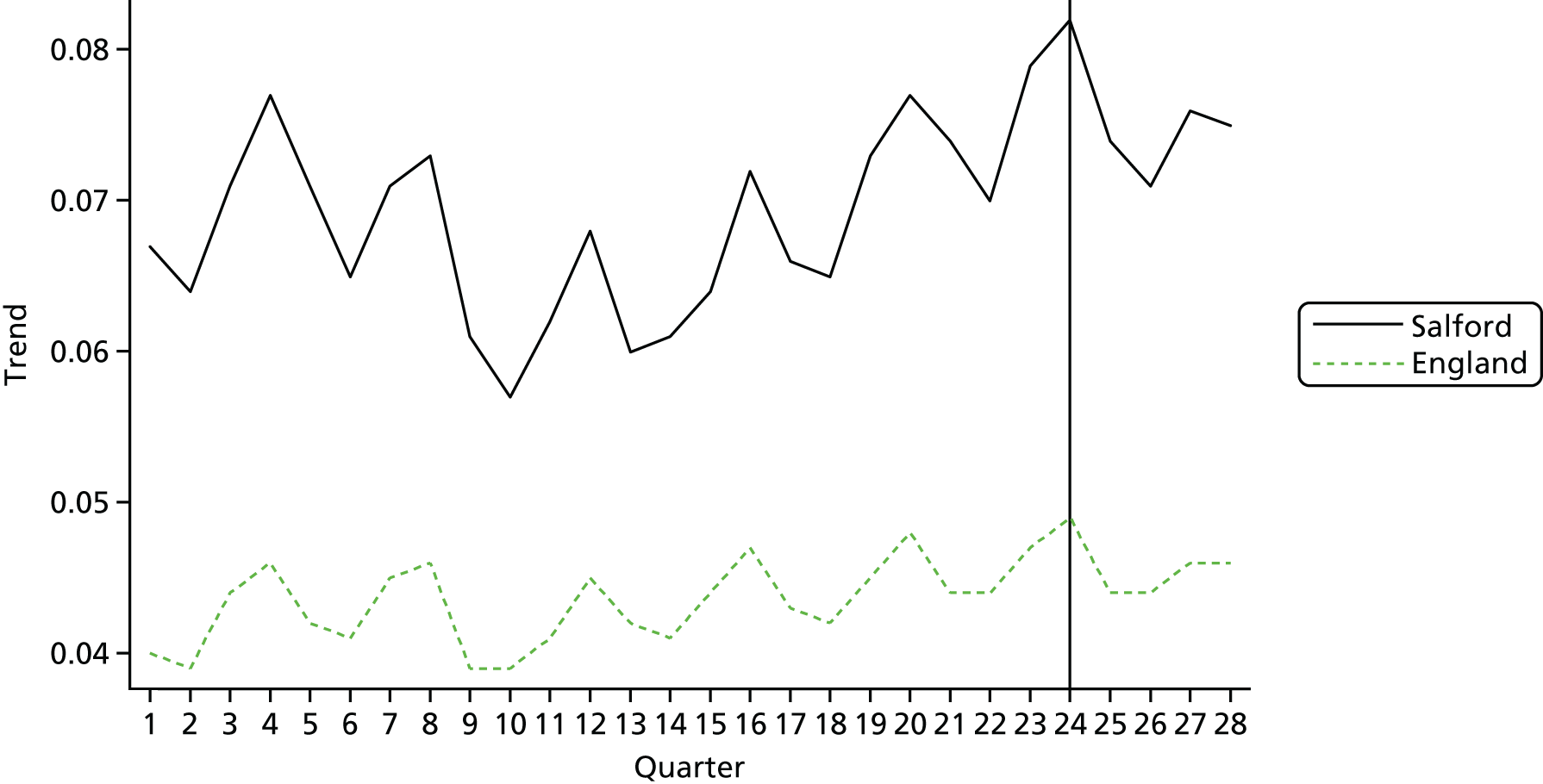
FIGURE 23.
Trends in emergency admissions (direct) in Salford and England.
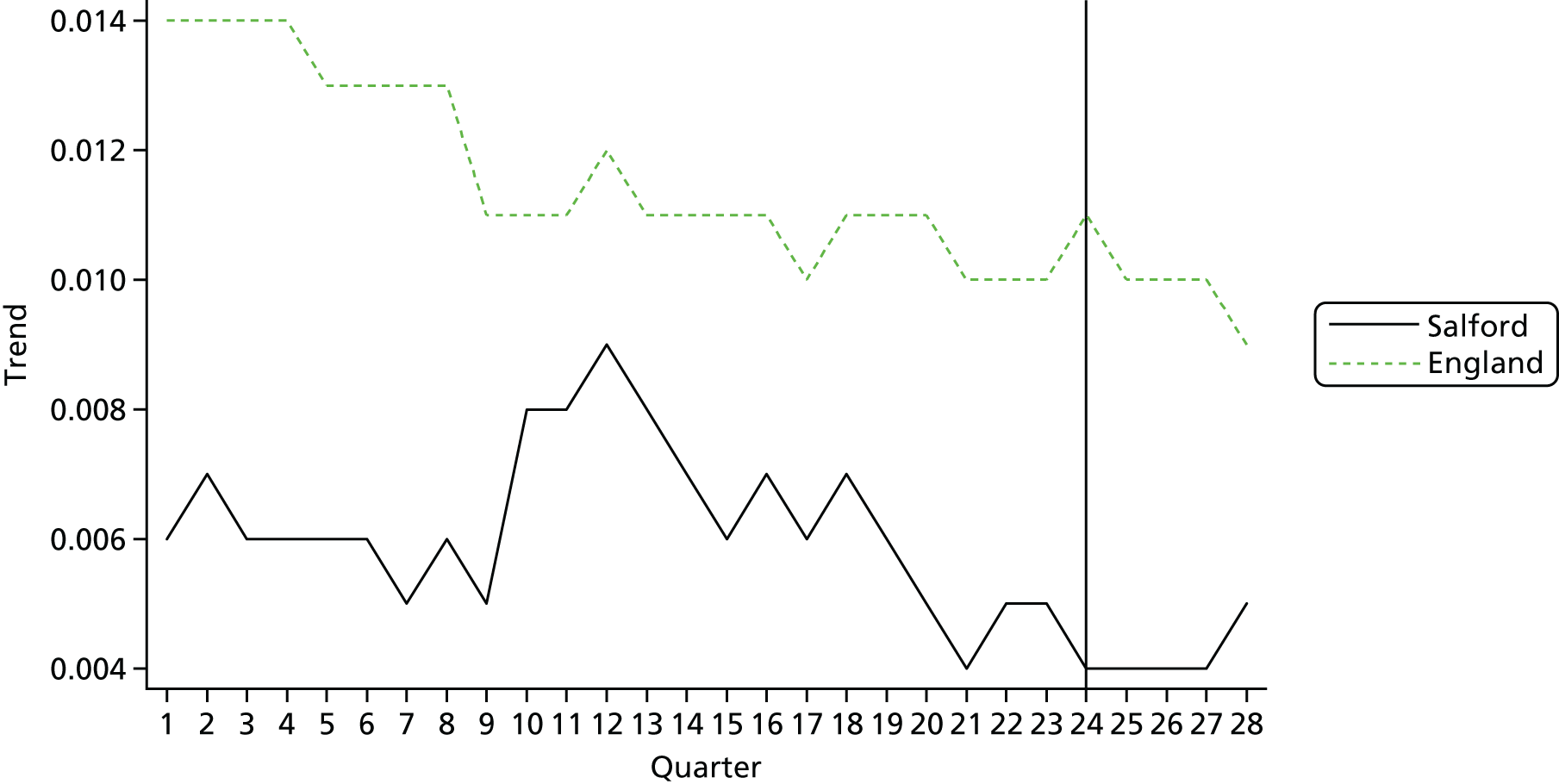
Appendix 5 Carer data
As part of the baseline cohort survey, patients were asked if they had an informal carer (such as a family member). They were also asked to provide contact details if they would be willing to complete a short questionnaire on their experiences of being a carer. In total, 297 patients supplied details and 231 carers returned a survey.
We collected information on a range of carer characteristics in the questionnaire:
-
demography, including age, sex, ethnicity, employment and relationship with patient
-
EQ-5D-5L, a generic measure of health-related quality of life
-
ICECAP-O index of capability measures quality of life for people aged ≥ 65 years
-
modified Caregiver Strain Index of stress and burden.
Results
Table 65 summarises the findings.
| Demographic variable | Number of patients | Mean number of patients | SD | % |
|---|---|---|---|---|
| Age (years) | 231 | 62.7 | 18.2 | – |
| Sex | ||||
| Male | 85 | 36.8 | ||
| Female | 141 | 61.0 | ||
| White British | 220 | 95.2 | ||
| Live with spouse/partner | 179 | 77.5 | ||
| Retired/not economically active | 128 | 55.4 | ||
| Number of long-term conditions | 166 | 1 | 0.10 | |
| Relationship with patient | ||||
| Spouse/partner | 122 | 52.8 | ||
| Daughter/son | 62 | 26.8 | ||
| Friend | 29 | 12.6 | ||
| EQ-5D-5L | ||||
| I have no problems walking about | 127 | 55.0 | ||
| I have slight problems walking about | 53 | 22.9 | ||
| I have moderate problems walking about | 34 | 14.7 | ||
| I have severe problems walking about | 11 | 4.8 | ||
| I am unable to walk about | 4 | 1.7 | ||
| I have no problems washing or dressing myself | 198 | 85.7 | ||
| I have slight problems washing or dressing myself | 20 | 8.7 | ||
| I have moderate problems washing or dressing myself | 7 | 3.0 | ||
| I have severe problems washing or dressing myself | 3 | 0.4 | ||
| I am unable to wash or dress myself | 6 | 2.6 | ||
| I have no problems doing my usual activities | 108 | 46.8 | ||
| I have slight problems doing my usual activities | 61 | 26.4 | ||
| I have moderate problems doing my usual activities | 46 | 19.9 | ||
| I have severe problems doing my usual activities | 9 | 3.9 | ||
| I am unable to do my usual activities | 1 | 0.9 | ||
| I have no pain or discomfort | 63 | 27.3 | ||
| I have slight pain or discomfort | 84 | 36.4 | ||
| I have moderate pain or discomfort | 62 | 26.8 | ||
| I have severe pain or discomfort | 17 | 7.4 | ||
| I have extreme pain or discomfort | 1 | 0.4 | ||
| I am not anxious or depressed | 102 | 44.2 | ||
| I am slightly anxious or depressed | 83 | 35.9 | ||
| I am moderately anxious or depressed | 32 | 13.9 | ||
| I am severely anxious or depressed | 7 | 3.0 | ||
| I am extremely anxious or depressed | 4 | 1.7 | ||
| Caregiver Strain Index Score | 223 | 7.60 | 5.23 | |
| ICECAP-O | ||||
| I can have all the friendship and love I want | 8 | 3.5 | ||
| I can have a lot of the friendship and love I want | 35 | 15.2 | ||
| I can have a little of the friendship and love I want | 48 | 20.8 | ||
| I cannot have any of the love and friendship I want | 138 | 59.7 | ||
| I think about the future without any concern | 36 | 15.6 | ||
| I can think about the future with only a little concern | 69 | 29.9 | ||
| I can think about the future with some concern | 83 | 35.9 | ||
| I think about the future with a lot of concern | 42 | 18.2 | ||
| I am able to do all the things that make me feel valued | 6 | 2.6 | ||
| I am able to do many of the things that make me feel valued | 49 | 21.2 | ||
| I am able to do a few of things that make me feel valued | 104 | 45.0 | ||
| I am able to do all the things that make me feel valued | 71 | 30.7 | ||
| I can have all the enjoyment and pleasure that I want | 7 | 3 | ||
| I can have a lot of the enjoyment and pleasure that I want | 81 | 35.1 | ||
| I can have a little of the enjoyment and pleasure that I want | 95 | 41.1 | ||
| I cannot have any of the enjoyment and pleasure I want | 47 | 20.3 | ||
| I am able to be completely independent | 6 | 2.6 | ||
| I am able to be independent in many things | 36 | 15.6 | ||
| I am able to be independent in a few things | 87 | 37.7 | ||
| I am unable to be independent at all | 102 | 44.2 | ||
The results show that 72% of carers had their own health problems and had at least one long-term condition.
The EQ-5D shows that some of the carers experienced problem walking and carrying out their daily activities and their own age-related health may be a factor contributing to their stress.
The Caregiver Strain Index showed that a mean value of 7.60, showing that the majority of carers are ‘highly stressed’. The EQ-5D shows that 56% of carers experience some form of anxiety or depression; however, there appeared to be no relationship between number of long-term conditions and caregiver strain.
Analysis of ICE-CAP suggests that carer stress may be related to the lack of control and independence carers have.
Appendix 6 Abstracts of the four main studies in CLASSIC
Implementation 1: how do key stakeholders view the SICP, what do they expect from it, and how is it aligned with their objectives and incentives?
Background
Implementing integrated care is a complex task, with many stakeholders involved in developing new collaborations. The process of implementation is influenced by local context, including history, geography and existing relationships.
Objective(s)
How do key stakeholders (commissioners, strategic partners) view the SICP, what do they expect from it, and how is it aligned with their objectives and incentives?
Design
A qualitative approach was adopted involving non-participant observations of meetings, interviews with managers and professionals working across the four key stakeholder organisations, and review of documents.
Participants
Foundation Trust senior and programme managers; CCG GPs and senior managers; Council staff, including senior management and public health; GP provider organization; mental health trust senior managers.
Results
We sought to trace links between programme commissioning, governance and outcomes. However, in practice, the commissioning context was rapidly changing. During the study, there was implementation of the SICP, the development of an Integrated Care Organisation (ICO – with staff moved from council to trust, and extension of the model to a wider population) and finally moves towards an Integrated Care System (ICS). We found few links between the commissioning, governance and oversight of these programme and the SICP, with the three mechanisms of integration continuing to be implemented, little affected by these higher level developments.
The SICP built on existing collaborations and was based on a shared vision developed over time. Positive experiences of working together in the past enabled senior managers to develop the SICP and all recognised that they had a vested interest in the programme. The geography of Salford was also a factor, with organisations all covering a similar footprint. The initial governance model included an Alliance Board, with an associated Alliance Agreement. This was non-binding, but regarded as valuable in establishing trust. A clear system of delegated decision making was important in supporting the programme.
The development of the SICP was further supported by national policy and an appetite to introduce new models of care (‘Primary and Acute Care Systems’ as part of the vanguards) which provided opportunities for additional investment. The decision to move to a formal ICO was made collectively by all stakeholder organisations, but was not based upon an appraisal of SICP impacts.
Primary care engagement is a significant issue, as a ‘Primary and Acute Care System’ depends on close collaboration between primary and secondary care. Although primary care providers were engaged in the SICP, initial engagement was challenging. The creation of the Salford GP provider organisation towards the end of the study provided new opportunities for collaboration with the ICO.
CCG leaders were committed to the SICP as equal partners, but the development of the ICO led to the establishment of formal governance arrangements which reintroduced a separation between commissioners and providers.
Limitations
Changes in the commissioning context made it difficult to trace links between commissioning, overall programme governance and outcomes.
Conclusions
Initially, the SICP was underpinned by a strong ideal of partnership working. There was an assumption that the experience of working together would break down organisational barriers and support wider improvement. At the same time, the three SICP programmes of work around integration would support local people in becoming more resilient. This suggests a model of integration in which the focus was on functional and service-level integration.
For the ICO (and subsequently the ICS), respondents reported that they believed that closer structural integration, would lead to the embedding of functional integration, in which working together across organisational and professional boundaries would become the norm, leading to better outcomes and patient experience. This view of integration assumes that the integration of systems, financial flows and management systems is a prerequisite for integrated working. It is not yet clear how far these assumptions will be realised in practice.
Future work
It will be important to continue to assess the success of the SICP to explore whether that closer structural integration builds on the modest outcomes of the early phases of the SICP.
Implementation 2: what is the process of implementation of two key aspects of the SICP (the multidisciplinary groups and the integrated contact centre)?
Background
Multidisciplinary groups are designed to improve integration of care for patients at higher levels of need, through identification and proactive management of patients at high risk of hospital admission or other outcomes. It is one of the most popular models of integrated care in England. The international evidence for multidisciplinary groups is mixed.
The person-centred definition of integrated care focuses on the experience of patients, and one of the common experiences reported by older people is that their health and social care is not ‘joined up’. In the SICP, the integrated contact centre was designed to be a central point of contact for older people with health and social care needs, to help better integrate health and social care services, as well as providing access to support and advice.
Objective(s)
How were the multidisciplinary groups and the integrated contact centre implemented in practice?
Design
For analysis of multidisciplinary groups, data collection included observing meetings and interviews with professionals and patients. For analysis of the integrated contact centre, data collection involved interviews with staff and patients.
Participants
Health and social care staff involved in multidisciplinary groups and the integrated contact centre, and patients with experience of these services.
Results
Multidisciplinary group meetings were generally well attended by the appropriate mix of health professionals. However, securing the involvement of GPs was more challenging, and was facilitated through local contracting.
Clinical staff reported some issues with slow progress, and considered at times there was focus on patients at certain levels of need who were already well supported, compared to more ‘unstable’ patients with greater opportunities for proactive care.
There was a significant focus on process measures (such as the numbers of ‘shared care’ records created), and actions arising from the groups were sometimes limited because of the short time slots allocated for discussion. Actions involved chasing up outstanding results and referrals; health improvement work, mental health, carer assessments; ‘tweaking’ existing health and social care packages; supply of equipment; and supporting housing requests.
‘Care co-ordinators’ were allocated to each patient discussed, but patients and carers did not recall details of co-ordinators. We identified a number of ways in which the multidisciplinary groups could support ‘person-centred care’. The multidisciplinary nature of groups provided a platform for a biopsychosocial assessment, a better appreciation of staff roles and expertise, and more effective sharing of information about local services and assets. The shared care record could also provide useful data about patients. Barriers to person-centred care included a lack of direct patient involvement.
The integrated contact centre faced some major delays in set-up, although the centre was dealing with a significant call volume when operating fully. Colocation of staff was seen as a key advantage in meeting the aims of the integrated contact centre, but IT issues and a lack of mental health involvement were significant challenges. On the basis of interviews with a small number of patients, experience of the centre was mixed, which in part reflected the need to adapt to a new way of engaging with services.
Limitations
Much of the research concerned early implementation of these services. We were only able to interview small numbers of patients with experience of these services.
Conclusions
Implementation of these mechanisms of integration faced significant challenges. The multidisciplinary team model has potential to improve collaborative relationships and to provide opportunities for more effective interventions for patients, but it is less clear how the model can improve patient experience of an integrated service.
Future work
More research is required to better understand how multidisciplinary groups can better target patients in need, and can better deliver care which combines effects on care utilisation with improved patient experience.
Outcomes 1: what is the impact of multidisciplinary groups on the outcomes of people with long-term conditions?
Background
Multidisciplinary groups and related interventions (‘case management’) are a common model of integrated care, focussed on the identification and proactive management of patients at high risk of hospital admission. However, evidence for their effectiveness in reducing service use is weak.
Objective(s)
To assess the effectiveness of multidisciplinary groups in the SICP on hospital use, compared to external comparator sites.
Design
We used non-experimental methods, comparing data from the SICP with suitable comparators in other parts of England. We used lagged dependent variable approaches to estimate the effect of the multidisciplinary groups. This approach does not require an assumption of parallel trends between intervention and comparator groups imposed by a difference-in-differences specification.
Participants
Older people aged 65+.
Interventions
Multidisciplinary groups caring for older people.
Main outcome measures
Numbers of: A&E attendances per person; A&E attendances referred by health and social care providers per person; self-referred A&E attendances per person; emergency admissions per person; emergency admissions via A&E per person; direct emergency admissions per person; ambulatory care-sensitive emergency admissions per person; proportion of patients discharged to usual place of residence.
Data sources
Data were Hospital Episode Statistics from NHS Digital, stratified by financial quarter and general practice.
Results
In the comparisons using the largest numbers of observations (all SICP practices versus the rest of England), we found that the SICP showed increased numbers of A&E attendances (by 0.008 per quarter per person), representing 1063 (95% CI 664 to 1462) more A&E attendances (between April 1 2015 to March 31 2016).
The SICP showed a similar absolute effect on health and social care referrals to A&E (increase of 0.008 per person per quarter) representing an increase of 1063 (95% CI 797 to 1462) attendances over the same period. Self-referred A&E attendances had a more modest increase (0.002 per person per quarter), representing 266 (95% CI 0 to 532) A&E attendances.
We found that the SICP was associated with an increase in emergency admissions of 0.003 per person per quarter, representing 399 (95% CI 133 to 664) additional admissions. Emergency admissions via A&E also increased by 0.6% (797 admissions, 95% CI 399 to 1063). We found a fall in direct emergency admissions by 0.001 per person per quarter (133 admissions, 95% CI 0 to 133). The effect of the SICP on avoidable emergency admissions was not statistically significant.
Limitations
The comparisons did not have the benefit of randomisation. We used data from the SICP as a whole. Not all older patients in the SICP were managed by a multidisciplinary group (although some will have been exposed to other SICP mechanisms of integration). The analysis is thus a broad test of the impact of the SICP, and explores whether the SICP is effective compared to the general trend (including integrated care initiatives outside Salford).
Conclusions
Our findings suggest increases in the number of A&E attendances, particularly from health and social care providers. We also found that the intervention led to increases in the number of emergency admissions, mostly through A&E. Increases in hospital utilisation may have been the result of integrated care increasing contact with health and social care professionals.
Future work
There is a need to explore longer term effects, as any benefits may be delayed. There is a need to understand why multidisciplinary groups do not reliably reduce health-care use to support development of more effective models.
Outcomes 2: what is the impact of health coaching on the outcomes and costs of people with long-term conditions?
Background
Innovative ways of delivering care are needed to improve outcomes for older people with multimorbidity. These innovations need to be delivered ‘at scale’ to help the population of older people in a sustainable way. The evidence on health coaching is complex, and further research is needed to assess its contribution to care for older people with multimorbidity.
Objectives
To estimate the effectiveness and cost-effectiveness of health coaching on the outcomes and costs of people with long-term conditions.
Design
The trial was a pragmatic trial, using the cohort multiple RCT design. A large population cohort was recruited. A trial was then conducted within the cohort. Eligible patients were selected at random for the intervention or usual care. Only those patients selected for the intervention were offered the intervention, mimicking the consent process in routine care.
Participants
Older people (aged 65+) with two or more long-term conditions, and needing some assistance with self-management based on a validated measure of ‘patient activation’.
Interventions
The intervention was health coaching, delivered by a professional with previous experience of coaching in diabetes mellitus, working in the SICP integrated contact centre. Additional training focussed on managing a wider range of long-term conditions, as well as depression and anxiety.
Main outcome measures
Patient activation, quality of life, depression and self-management behaviour.
Data sources
We used hospital use data from the NHS (around 90% of total costs), combined with self-report data on primary care use.
Results
1306 older people were eligible, and we selected 504 for ‘health coaching’. 41% accepted the offer, and 80% of those received 4+ sessions.
In the intention-to-treat analysis, those selected for health coaching did not differ on any primary or secondary outcome from those receiving usual care. Effects in those accepting the intervention were also not statistically significant. Patients selected for health coaching reported lower levels of emergency care, but an increase in elective services. Health coaching was associated with improvements in QALYs (mean incremental QALY gain of 0.018, 95% CI –0.0051 to 0.042) at increased cost (mean incremental total cost increase of £145.13, 95% CI –£489.37 to £779.64). The overall cost per QALY was £7887, with a 70–79% probability of being cost effective at cost per QALY thresholds of £20,000–30,000. Results were similar in patients with complete data.
Limitations
The design estimates the effect of being selected for treatment, regardless of whether treatment is accepted. Therefore, demonstrating effectiveness in this design is even more challenging than a conventional pragmatic trial. The cmRCT design raised other methodological challenges.
Conclusions
We found that health coaching was associated with small and non-significant benefits in patient reported outcomes, but that improvements in quality of life were sufficient to make the intervention likely to be cost-effective. Health coaching among patients with multimorbidity may have value as a way of improving quality of care, but may not be an effective strategy for reducing overall use of health care.
Future work
Further work is needed to enhance the effectiveness and acceptability of health coaching.
List of abbreviations
- A&E
- accident and emergency
- AQuA
- Advancing Quality Alliance
- ASCCT
- adult social care contact team
- BCF
- Better Care Fund
- CACE
- complier-average causal effect
- CCG
- Clinical Commissioning Group
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CKD
- chronic kidney disease
- CLASSIC
- Comprehensive Longitudinal Assessment of Salford Integrated Care
- cmRCT
- cohort multiple randomised controlled trial
- CONSORT
- Consolidated Standards of Reporting Trials
- COPD
- chronic obstructive pulmonary disease
- DN
- district nurse
- EPR
- electronic patient record
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- ESSI
- ENRICHD Social Support Instrument
- GMWFT
- Greater Manchester West Foundation Trust
- GP
- general practitioner
- HbA1c
- glycated haemoglobin
- HES
- Hospital Episode Statistics
- HSDR
- Health Services and Delivery Research
- IBS
- irritable bowel syndrome
- ICC
- integrated contact centre
- ICECAP-O
- ICEpop CAPability measure for Older people
- ICER
- incremental cost-effectiveness ratio
- ICJC
- Integrated Adult Health and Care Commissioning Joint Committee
- ICO
- integrated care organisation
- ICP
- integrated care pilot
- ICS
- integrated care system
- ISRCTN
- International Standard Randomised Controlled Trial Number
- IT
- information technology
- MCP
- multispecialty community provider
- MDG
- multidisciplinary group
- MHI-5
- Mental Health Inventory – 5
- MRC
- Medical Research Council
- MULTIPleS
- Multimorbidity Illness Perceptions Scale
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- NRES
- National Research Ethics Service
- NVQ
- National Vocational Qualification
- PACIC
- Patient Assessment of Chronic Illness Care
- PACS
- primary and acute care systems
- PAM
- Patient Activation Measure
- PARR
- Patients at Risk of Rehospitalisation
- PPI
- patient and public involvement
- PRIMER
- Primary Care Research in Manchester Engagement Resource
- PROTECTS
- Proactive Telephone Coaching and Tailored Support
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QIPP
- Quality, Innovation, Productivity and Prevention
- RCT
- randomised controlled trial
- SCR
- shared care record
- SD
- standard deviation
- SDSCA
- Summary of Diabetes Self-Care Activities
- SEP
- single entry point
- SICP
- Salford Integrated Care Programme
- SIRP
- single integrated referral point
- TIDieR
- Template for Intervention Description and Replication
- TUPE
- Transfer of Undertakings in Public Employment
- WHOQOL
- World Health Organization Quality of Life
- WHOQOL-BREF
- World Health Organization Quality of Life-BREF
