Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/5001/62. The contractual start date was in May 2013. The final report began editorial review in March 2017 and was accepted for publication in August 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Edge et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
Schizophrenia and psychoses
Schizophrenia is a syndrome of psychotic disorders. Psychoses/psychotic disorders are severe mental illnesses (SMIs) characterised by delusions, hallucinations, changes in behaviour and related problems of cognition, thoughts and emotions. In their 2012 systematic review, Kirkbride et al. 1 reported the pooled annual incidence of psychotic disorders as 32 cases per 100,000 and of schizophrenia as 15 per 100,000.
Although the incidence of psychotic disorders was once believed to be similar across all populations, Kirkbride et al. ’s1 findings confirm those of studies in the last decade,2–7 indicating that rates of psychoses among Black and minority ethnic (BME) populations are significantly higher than in comparison populations among whom they reside. Overall, evidence suggests that rates of schizophrenia are 5.6 times greater in Black Caribbean people than in White British people [95% confidence interval (CI) 3.4 to 9.2]. Elevated rates were also reported in Black African [relative risk (RR) 4.7, 95% CI 3.3 to 6.8; I2 = 0.47] and Asian groups (RR 2.4, 95% CI 1.3 to 4.5; I2 = 0.42). The Aetiology and Epidemiology of Schizophrenia and Other Psychoses study8 of populations in London, Bristol and Nottingham reported even higher incidence rates among African-Caribbean people (71/100,000 per year). This equates to a risk of diagnosis that is ninefold higher than in the White British population (incidence rate ratio 9.1, 95% CI 6.6 to 12.6).
Schizophrenia and related psychoses are associated with considerable personal, economic and societal burdens. It is estimated that the total annual cost of a broadly defined schizophrenia (non-affective psychoses) is £8.8B. 1 Forty per cent (£3.5B) of this cost is attributable to service use, 47% (£4.1B) to lost employment and 13% to informal care (£1.2B). Although it is not entirely clear why some BME groups are at greater risk of psychosis, it is suggested that ‘urbanicity’, discrimination and socioeconomic disadvantage are important contributory factors. 9,10
African-Caribbean people, schizophrenia and UK mental health services
African-Caribbean people’s elevated risk in the UK is accompanied by poorer utilisation of services and worse clinical and non-clinical outcomes, especially among young men. 2,3,11,12 African-Caribbean people’s experience of specialist mental health services is also poor. 6,13–15 Characterised by delayed access, despite multiple attempts at help-seeking, their care pathways are more adverse than those of their White British counterparts. 15 For example, they are less likely to access specialist services via general practitioners and more likely to do so via the police and criminal justice system,15–17 with high rates of detention under the Mental Health Act 2007. 18 African-Caribbean family members disproportionately report involving the police because they are unable to gain timely access to support from specialist services. 19 This is important because delayed access to diagnosis and treatment increases the duration of untreated symptoms and the illness acuity on contact with services. 20,21
Once in specialist services, African-Caribbean people experience more coercive care than White British people, including higher rates of seclusion and restraint, plus higher mean doses of psychotropic medication and related side effects. 13,15 They are also less likely to be offered psychological therapy, and they experience worse clinical outcomes, such as longer inpatient stay and higher rates of relapse and readmission. 8,13 The Centre for Mental Health22 described African-Caribbean people’s experience of mental health services as a vicious ‘circle of fear’ involving delayed engagement/non-engagement, adverse care pathways, coercive treatment and inferior outcomes. These experiences, combined with perceptions of services as institutionally racist, reinforce African-Caribbean service users’ and families’ fear, mistrust and avoidance of statutory mental health services. 14,22–24 Delayed access to care also creates considerable family tension, conflict and increased burden on carers, which can result in family breakdown. Lack of access to family support and social contact is, in turn, associated with service users’ social isolation and increased risk of relapse. 25
Family intervention and schizophrenia
Family intervention (FI) is a psychosocial treatment with a strong evidence base of clinical effectiveness. 26,27 Since the findings from the first UK trial of FI for schizophrenia were published in 1982, research has consistently shown that undertaking FI with service users diagnosed with schizophrenia and their families improves outcomes. 9,27–30 For example, in their Cochrane review, Pharaoh et al. 26 reported that FI improved medication compliance, self-management and problem-solving, which were associated with reduced risk of psychotic relapse. In a meta-analysis of randomised controlled trials (RCTs),27 FI plus medication yielded better outcomes than medication alone. In addition to decreasing or preventing relapse, improving service users’ social functioning and enhancing their quality of life, a key aim of FI is to reduce carer burden and ill-health. 31
Although there are a number of approaches to FI, they share common core components such as psychoeducation, problem-solving, stress and crisis management, enabling carers to practise good self-care. 26,27 The core principles of FI models include a holistic approach to care and treatment, establishing therapeutic alliance, addressing family tension and setting reasonable and achievable goals and expectations. The National Institute for Health and Care Excellence (NICE)30 recommends at least 10 sessions of FI for people with schizophrenia diagnoses who are in contact with their families. Few services provide FI for the general population. 32 At a time of significant financial pressures on the NHS and related reduction in staff numbers, perceptions of FI as time and labour intensive and, therefore, costly, mean that FI practitioners are rarely given time to practise. 33
Family intervention and African-Caribbean people
Commenting on care providers’ inconsistent and ineffective response to inequalities in the care and the treatment of African-Caribbean people diagnosed with schizophrenia, NICE11 specifically recommends FI for African-Caribbean people with schizophrenia. The unavailability of FI might disproportionately affect BME service users in general, as they are known to have inferior access to psychological therapies. 15 African-Caribbean service users are likely to have even poorer access to FI owing to high levels of family disruption.
In community consultation to develop this study, African-Caribbean people expressed dissatisfaction with the lack of access to psychological therapy and expressed a strong desire for culturally appropriate ‘talking treatments’. They also wanted to develop better understanding of schizophrenia and improve relationships within families, between African-Caribbean communities and with mental health services.
However, lack of research into the feasibility of delivering psychological therapies in general, and FI in particular, to African-Caribbean people means that it is unclear if the benefits of FI are generalisable to members of this ethnic group. 26 Furthermore, it is unclear if a standard approach to the content and delivery of FI would be acceptable to service users and families whose relationship with mental health services and health-care professionals is characterised by a lack of trust.
In response to concerns and dissatisfaction within African-Caribbean communities, and in response to NICE guidelines,11 we undertook to culturally adapt an evidence-based, cognitive–behavioural model of FI, which was developed by co-applicants Barrowclough and Tarrier. 34 This model was selected because previous work by the principal investigator (PI)35,36 and others37,38 has suggested that African-Caribbean people’s models of mental illness and related attributions require cognitive–behavioural interventions such as FI to be culturally adapted for this group. Additionally, the evidence-based model was developed and is the model of choice in Manchester Mental Health and Social Care NHS Trust (MHSCT), where the study was conducted.
Overview of study
This mixed-methods study was designed to culturally adapt an existing model of FI to make it more specific to the needs of African-Caribbean service users diagnosed with schizophrenia and their families. Our study aimed to address four research questions.
Research questions
-
How can existing evidence-based FI be culturally adapted for African-Caribbean people with schizophrenia and related disorders?
-
Is it feasible for culturally adapted FI to be delivered in hospital and community settings?
-
Can ‘proxy families’ serve as acceptable alternatives where families are unavailable?
-
Will culturally adapted FI be acceptable to service users, families and health professionals?
Aims and objectives
Study aims
-
Assess the feasibility of culturally adapting, implementing and evaluating an innovative approach to FI among African-Caribbean service users with schizophrenia and their families across a range of clinical settings.
-
Test the feasibility and acceptability of delivering Culturally adapted Family Intervention (CaFI) via ‘proxy families’ where families are not available.
Study objectives
-
Involve key stakeholders (service users, families and clinicians) in culturally adapting an existing FI for African-Caribbean people diagnosed with schizophrenia.
-
Produce a manual to support the delivery of the intervention.
-
Identify client- and family-centred outcomes and quality-of-life outcomes.
-
Identify and address the training needs of therapists and ‘proxy families’.
-
Test the feasibility of delivering culturally adapted FI among African-Caribbean people in hospital and community settings.
-
Test the feasibility of recruiting and ‘proxy families’ and delivering the intervention via both.
-
Test the feasibility of recruiting participants in hospital and community settings.
-
Compare recruitment and retention in different clinical settings.
-
Identify outcome measures for future randomised studies and assess the feasibility of collecting them.
-
Assess the acceptability of the intervention to key stakeholders: service users, their families and mental health professionals.
Overview of design and methods
Following the Medical Research Council’s framework for developing complex interventions,39 we used a mixed-methods approach to design and test the feasibility of delivering CaFI for African-Caribbean service users and their families. The study was conducted in three distinct but related phases.
Phase 1: culturally adapting the intervention
The purpose of this phase of the study was to identify the elements of the existing FI model to be culturally adapted, determine how such modifications would be achieved, identify and agree on suitable outcome measures and identify training needs associated with delivery of the intervention. This aspect of the study was conducted in the following three subphases.
Phase 1A: literature review
An initial literature search, undertaken while developing the study, revealed that there was an insufficient number of studies to allow us to conduct a systematic review on culturally adapted psychosocial interventions specifically for African-Caribbean people diagnosed with schizophrenia. We undertook a scoping review40,41 of theoretical and intervention papers, using broad search terms and searching reference lists of key papers, to determine issues of importance in relation to culturally adapting psychosocial interventions. As we found only one trial relating to cultural adaptation and African-Caribbean people, we widened our scope to include other ethnic and cultural groups. Consequently, we undertook a systematic literature review of culturally adapted psychosocial interventions for schizophrenia to provide a cultural adaptation framework to inform our theoretical model of adaptation (see Chapter 2). Our framework was then used to inform the process of culturally adapting the intervention in collaboration with key stakeholders (phases 1B and 1C).
Phase 1B: focus groups
Guided by phase 1A findings, we designed topic guides/interview schedules to enable us to collect qualitative data from key stakeholder groups. First, we conducted three focus groups comprising (i) current and/or former service users, (ii) families, carers and advocates and (iii) health professionals. A fourth, ‘mixed’, focus group, drawn from these three groups, enabled us to resolve any differences between groups and to validate findings from the first three stakeholder focus groups.
Service users were all of African-Caribbean descent, including those who self-identified as ‘Black British’ or of ‘mixed’ heritage but had at least one parent or grandparent of African ancestry who originated from the Caribbean. Other participants came from a range of ethnic backgrounds, including South Asian and White British. The sample was also diverse in terms of age, gender and professional background, thereby providing a range of perspectives on how best to culturally adapt Barrowclough and Tarrier’s model of FI34 and the training that might be needed to enable family therapists to deliver the intervention. Focus groups also explored the feasibility of using ‘proxy families’, individuals who would work with service users who did not have access to families to enable them to participate in CaFI. The training needs of therapists and Family Support Members (FSMs) (‘proxy families’ was used in our original proposal to describe people who would support service users to receive the intervention in the absence of families; this was changed to FSMs during phase 1B of the study) were also discussed. The data were analysed using framework analysis,42 enabling the exploration of both a priori topics and emergent themes in relation to our research questions: specifically, content, outcomes and delivery of the intervention.
Phase 1C: consensus conference
Subsequent to the focus groups, we held a consensus conference43 of ‘experts’ by experience (service users and carers) and by profession (health-care professionals, academics, advocates) and other key stakeholders such as the police. The purpose of the consensus conference was to synthesise findings from the literature review (phase 1A) and focus groups (phase 1B) to agree the content of the culturally adapted FI and the manual to support its delivery. Participants in the consensus conference (experts by experience/profession and other key stakeholders) also agreed on outcome measures and the training needs of the therapists and FSMs.
Phase 2: training
The purpose of the training phase was to recruit and train therapists and FSMs to undertake their role in CaFI, ensuring that we addressed the training needs identified during phase 1 of the study. Underpinned by outcomes from phase 1, we worked with our service users and carers and Just Psychology,44 a Manchester-based social enterprise that specialises in cultural diversity, to develop bespoke cultural competency training for CaFI therapists, co-therapists and FSMs. We also employed Meriden Family Programme45 to deliver bespoke training on culturally specific family work for the therapists. In line with NICE recommendations, to deliver cultural competence training at both organisational and individual levels, we planned to deliver competency sessions in a range of clinical settings, reflecting areas of recruitment into our study. However, organisational issues meant that this was not possible. Instead, we delivered a trust-wide clinical seminar for all staff and delivered presentations to promote the study and cultural awareness among clinical leads, health-care professionals, and service user and carer groups in the NHS and in third-sector organisations.
Phase 3: feasibility study
Phase 3A: delivering and evaluating the intervention
The third and final phase involved testing the feasibility and acceptability of delivering CaFI in hospital and community settings across the then largest mental health trust in Manchester: Manchester Mental Health and Social Care NHS Trust (MHSCT) [this trust has since merged with Greater Manchester and is now called Greater Manchester Mental Health NHS Foundation Trust (GMMH)]. We elected to test CaFI in a range of settings to determine whether or not the intervention could be delivered in different clinical contexts and at varying levels of illness acuity and chronicity. Data on uptake, attrition and engagement (including number of completed sessions and reasons for non-completion) were the primary means of assessing feasibility. The key objectives of this phase of the study were to:
-
test the feasibility of delivering CaFI to African-Caribbean service users and their families
-
test the feasibility of recruiting families and FSMs and of delivering the intervention via both
-
test the feasibility of recruiting participants in hospital and community settings
-
compare recruitment and retention in different clinical settings
-
identify suitable primary and secondary outcome measures and the feasibility of collecting them –
-
estimate the parameters for designing future RCTs, including:
-
recruitment, retention, attrition and follow-up response rates
-
characteristics of outcome measures and estimating the standard deviation (SD) and intracluster correlation to enable future sample size calculation
-
-
-
assess the acceptability of the intervention with key stakeholders – service users, their families, FSMs and mental health professionals using in-depth qualitative interviews (see Chapter 7).
Phase 3B: fidelity study
Adherence to the therapy manual and delivery of the intervention was tested by an independent review of 10% of randomly selected CaFI sessions. The first subscale of the fidelity measure comprised a modified version of the Cognitive Therapy Scale for Psychosis. 46 We included a second subscale to provide a descriptive account of the manual components covered in the selected sessions, which included two items from the Family Interventions in Psychosis-Adherence Scale (FIPAS). 47 The third and final subscale was developed to rate the degree of cultural awareness or competencies of the therapists. This subscale was based on the manual and existing cultural competency questionnaires and literature. To help to ensure treatment fidelity and maintain the quality of therapy, digital recordings of sessions were discussed in clinical supervision. The clinical supervisor also rated a therapy session for each therapy pair every 6 months using the fidelity scale and gave detailed feedback.
Service user, carer and community involvement
We have chosen to entitle this section ‘service user, carer and community involvement’ rather than use the most commonly used term, ‘service user and public involvement’, based on the preferences of carers/relatives, community members and service users who constitute our Research Advisory Group (RAG).
What does involvement in CaFI mean?
Having the active involvement of service users, carers/relatives and members of the public was to improve the quality, governance, feasibility and practicality of our research by:
-
including the perspective of African-Caribbean people in the development, management and oversight of the project
-
ensuring that cultural competency training included service user, carer and community member perspectives
-
ensuring that recruitment and consent processes were appropriate for service users and families (family members and ‘FSMs’)
-
ensuring that our communication with the families and ‘FSMs’ was accessible and acceptable
-
discussing and agreeing suitable forms of dissemination with service users and families, drawing on their knowledge and expertise to identify and access suitable outlets.
CaFI Research Advisory Group
The purpose of CaFI’s RAG was to maximise the involvement of service users, carers, families and members of the community in our research. Our RAG panel consists of eight people of African-Caribbean background (six women and two men) who are passionate about making a difference to the lives of African-Caribbean people living with mental health problems in their local community and across the UK.
Research Advisory Group meetings were held (two or three times per year; eight meetings in total) during the 3 years and were chaired by a co-applicant, Paul Grey, who has lived experience and expert knowledge in the area. As a former Delivering Race Equality in Mental Health Care Ambassador, Paul has a wealth of experience delivering seminars and conferences and advising policy-makers and service providers on the mental health of BME communities and their experience of services. He also has > 20 years’ experience of using mental health services.
The RAG advised and supported the team in developing research materials [such as the participant information sheet (PIS) and adverts], as well as advising on appropriate recruitment and dissemination strategies. The RAG also helped to refine the therapy manual, in particular the ‘ethos of delivery’, and co-produced and delivered the training programmes during phase 2. They also participated in the dissemination of our work through conference presentations.
Community launch events
To generate awareness and engage the local community, we hosted two community-level launch events in areas of high population density of African-Caribbean people, both within the MHSCT footprint in South Manchester [Levenshulme Inspire Community Centre (25 October 2013) and Moss Side Leisure Centre (30 October 2013)]. During the events, the PI and research project manager (RPM) delivered presentations to:
-
outline the study’s rationale, aims and objectives
-
highlight opportunities to get involved, including becoming RAG members and FSMs
-
gauge the level of interest and willingness among eligible individuals; we provided food and drink as we know this to be important for socialising and building relationships in African-Caribbean cultures. 48
Altogether, the events were attended by around 100 people, including community members, service representatives, service users, carers, family members, and health and social care professionals. Anecdotal feedback from attendees was extremely positive and many were keen to get involved and support the research, as participants, advisors or collaborators. The majority of attendees left their details so that they could be contacted for further information. Following the event, the RPM was invited to present the CaFI study at third-sector organisations and to host a stall at the African & Caribbean Mental Health Services (ACMHS) Mental Health and Well-being Day (18 October 2013), to further promote the study. The event provided a platform for us to strengthen collaborations with Black-majority churches, community groups and agencies, including the ACMHS, Just Psychology,44 Manchester BME Network,49 Black Health Agency,50 Manchester Carers Forum,51 ReThink: Manchester Carers in Action,52 Self-Help Services,53 Service User Voices54 and Bluesci. 55
Ethics approval
The CaFI study was approved by North West Greater Manchester East National Research Ethics Service Ethics Committee (13/NW/0571).
Report outline
The remaining chapters detail the cultural adaptation process and feasibility testing of an evidence-based FI to ensure its cultural specificity for African-Caribbean service users and their families.
Chapter 2 reports on our systematic review of the current literature on cultural adaptation of psychosocial interventions for schizophrenia and psychosis, identifying key components of our culturally adapted framework.
Chapters 3 and 4 detail the process of co-production by which the extant model of FI was culturally adapted in collaboration with African-Caribbean service users, families and community members, alongside health-care professionals, using focus group and consensus methodologies.
Chapter 5 describes the development and delivery of training for family therapists, co-therapists and FSMs (‘proxy families’) based on the recommendations of key stakeholders in the first phase of the study (see Chapters 3 and 4) and the available literature (see Chapter 2).
Chapter 6 reports the feasibility trial to test our CaFI across a range of clinical and community settings, involving service users with different severity of illness and levels of acuity/chronicity. A novel aspect of the trial involved testing the feasibility of delivering the intervention via FSMs in the anticipated absence of families owing to high levels of family disruption. In this chapter, we also report findings from our embedded fidelity study.
Chapter 7 reports on the acceptability of the intervention from the perspectives of service users, their families, FSMs, therapists and key workers of service users who participated in CaFI.
Chapter 8 presents a discussion of our findings in relation to the available evidence and the original study aims and objectives. While highlighting strengths and limitations of our study, we also suggest implications for policy, practice and future research. We conclude by making recommendations on the basis of our findings.
Chapter 2 Review of the literature
Introduction
Phase 1A consisted of a structured background review of current literature on culturally adapted psychosocial interventions in schizophrenia and psychosis. We initially conducted a broad scoping review40 of existing literature to establish key issues and gaps in knowledge relating to the cultural adaptation of psychological interventions. This provided a useful ‘map’ of the breath of research in relation to the size and scope of existing primary and secondary studies where evidence is limited. 56
Our initial search, using broad search terms (i.e. terms relating to African-Caribbean and culturally adapted intervention and schizophrenia), yielded one trial adapting cognitive–behavioural therapy (CBT) for African-Caribbean culture, but adaptations were reported across multiple minority ethnic groups and were not specific to this group. 57,58 We found no studies of adapted FI for African-Caribbean people in the UK.
Despite the limited work in the African-Caribbean population, there are an increasing number of studies reporting on psychosocial interventions adapted for other ethnic and cultural groups. A systematic review of the existing research in this area was therefore carried out to inform our theoretical model of adaptation and provide a framework of the nature of adaptations to guide research and practice. A thematic analysis59 was undertaken to provide a narrative summary of the key issues that informed the qualitative components of this phase of the study.
Aims and objectives
Phase 1 research question
How can existing evidence-based FI be culturally adapted for African-Caribbean people with schizophrenia and related disorders?
Background
There have been a number of systematic reviews on cultural adaptations of mental health interventions. 60–65 Across these studies, meta-analytic effect sizes have been mostly moderate (range 0.41–0.72) in favour of culturally adapted interventions, which is comparable with those reported in reviews of non-adapted interventions in ‘Western populations’. 66 For example, Griner and Smith62 conducted a meta-analysis of 76 studies and found a moderate effect size (d = 0.45) for culturally adapted treatments targeting various mental health problems. However, the majority of systematic reviews have been heterogeneous, including mixed diagnostic and ethnic samples. Moreover, the reviews tend to focus on outcomes and few make efforts to systematically analyse the nature of cultural adaptations to provide a framework or model of adaptation that is grounded in empirical evidence.
Chowdhary et al. 61 examined both the nature and the effectiveness of adapted psychological treatments for depression. They reported a large effect size (standard mean difference –0.72) for depressive symptoms based on findings from 16 out of 20 reviewed RCTs. Chowdhary et al. 61 systematically identified the nature of treatment adaptations for depression through the application of Bernal and Sáez-Santiago’s67 framework, which has eight components:
-
language
-
therapist matching
-
cultural symbols or metaphors
-
cultural knowledge or content
-
treatment conceptualisation
-
treatment goals
-
treatment methods
-
treatment context.
Using this framework, common adaptations across the reviewed studies were mostly within the language, therapist and context dimensions. However, Chowdhary et al. 61 highlighted the small number of included studies, incompleteness of data and significant heterogeneity relating to diverse contexts and designs, which prevented comparisons of different types of interventions or adaptations. Additionally, they did not comment on the usefulness of Bernal and Sáez-Santiago’s67 framework in terms of its applicability to either their study sample or to other mental health conditions.
Bhui et al. 68 reviewed a wide range of interventions designed to improve therapeutic communications between BME service users and clinicians in psychiatric services. This included 21 articles of multiple intervention types, of which culturally adapted psychotherapies, ethnographic and motivational assessment were found to be effective and preferred by patients and carers. Meta-analytic effect sizes showed benefits for a range of different outcomes, including symptoms and medication adherence (high-quality trials; d = 0.18–0.75). Thematic analyses identified common components of the interventions across the reviewed studies, which were classified using Tseng’s framework69 and categorised into three broad subthemes:
-
patient, including understanding causal explanations and belief systems, pre-therapy preparation, and improving accessibility and training
-
patient and professional, including ethnic matching
-
adaptation of therapy, including changes to structure and content, technical delivery/structure of therapy, working with social systems, and facilitating empowerment and engagement.
Their inclusion criteria were broad in scope and included various study designs, service users diagnoses and interventions that targeted several ethnic groups. Bhui et al. ’s68 review found no differences in symptomatic or service user-reported outcomes for adapted interventions generalised across mixed ethnic samples58 when compared with homogenous ethnic samples,70 but as this was based on findings from two studies no firm conclusions can be inferred about the need for ethnic specificity in adapting interventions. Bhui et al. 68 called for more clinical trials in the UK and the USA, economic evaluations and tests of the effectiveness of specific intervention components.
Evidence-based psychosocial interventions for schizophrenia spectrum diagnoses originally developed in Europe or the USA are important elements of therapy that require adaptation for both minority ethnic groups in Western countries and majority ethnic groups in non-Western countries. Despite the increasing number of trials on culturally adapted interventions in schizophrenia,71 there have been no attempts to summarise this work, and the developing literature in schizophrenia71 has not yet been reviewed systematically. Doing so may enable us to identify common processes within adaptation that could guide future research on adapted psychosocial interventions. A number of frameworks have been developed to provide guidance on cultural adaptations to treatments,67,69,72,73 but none of these approaches focuses on psychosocial interventions in schizophrenia and their application across different ethnic and cultural groups in this area is questionable.
This study aims to:
-
analyse the nature of cultural adaptations of psychosocial interventions in schizophrenia
-
develop a framework to guide the adaptation of evidence-based interventions for different ethnic and cultural contexts.
Method
The systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 74
Search strategy
On 3 March 2016, the RPM conducted an electronic database search of Ovid MEDLINE, EMBASE, PsycINFO and Web of Science. Databases were searched from inception and no date or language restrictions were specified (see Appendix 1 for the full search strategy and search terms). The titles and abstracts were downloaded into EndNote X8 Management software (version 8; Clarivate Analytics, Philadelphia, PA, USA) and duplicates were removed. The RPM (AD) and research assistant (RA) (SB) independently screened the articles for eligibility using the following inclusion and exclusion criteria.
Inclusion and exclusion criteria
Inclusion criteria
-
Studies of any controlled trial design evaluating an adapted evidence-based psychosocial intervention for a specific subculture or ethnic group.
-
Studies reporting on interventions adapted for a minority ethnic population in a Western country or any non-Western population.
-
Studies in which 100% of participants were adults (aged ≥ 18 years) and had a diagnosis of schizophrenia or a related diagnosis [Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) schizophrenia or International Classification of Diseases, Tenth Edition (ICD-10) F20–29: schizophreniform disorder, schizoaffective disorder, delusional disorder or psychosis not otherwise specified].
-
Peer-reviewed articles available in English.
Exclusion criteria
-
Studies in which adaptations were not made for a specific subculture or ethnic group but were generalised across multiple groups (and no findings were available by group, despite contacting the authors).
-
Studies evaluating interventions without specific adaptations for culture, including no change (i.e. assessing the same intervention in a different subculture or ethnic group), direct translation to the language of the population of interest, or adapting for some other characteristic such as age or location (e.g. rural vs. urban needs).
-
Studies testing a novel intervention developed specifically for a particular subculture or ethnic group without an adaptation of an existing evidence-based intervention.
-
Interventions that were neither evidence-based nor psychosocial (e.g. service provision such as assertive community treatment).
-
Non-evaluative unpublished studies (e.g. literature reviews, conference papers, qualitative studies and case studies).
Selection of studies
Full-text papers of potentially relevant articles were accessed and screened by the RPM (AD) and RA (SB). Authors were contacted with requests for English versions of non-English citations and citations that could not be accessed. Interlibrary loans were also sought for inaccessible papers. Reference lists of full-text articles and systematic literature reviews were screened to identify any additional papers not picked up in the search. Key experts were contacted and received the full reference lists to identify any missing studies. All uncertainties or disagreements relating to the eligibility of articles were resolved via discussion with a co-applicant and senior researcher (RD).
Data extraction
Descriptive characteristics of eligible studies were recorded in a data extraction spreadsheet. To address the research question regarding the nature of cultural adaptations, all adaptations to interventions described in the papers were summarised in a second spreadsheet. When there was limited information, corresponding authors were contacted and adaptations were extracted from any additional literature or notes provided by the authors.
Data synthesis
A thematic analysis59 was used to evaluate the nature of cultural adaptations across the reviewed studies. A number of frameworks have been developed to provide guidance on cultural adaptations to treatments67,69,72,73,75 and two of these have been applied to data in recent reviews. 61,68 The thematic analysis was applied inductively to the extracted data to generate themes and subthemes of adaptations emerging from their current application in the field, rather than to deductively apply an existing model to the data.
Results
Included studies
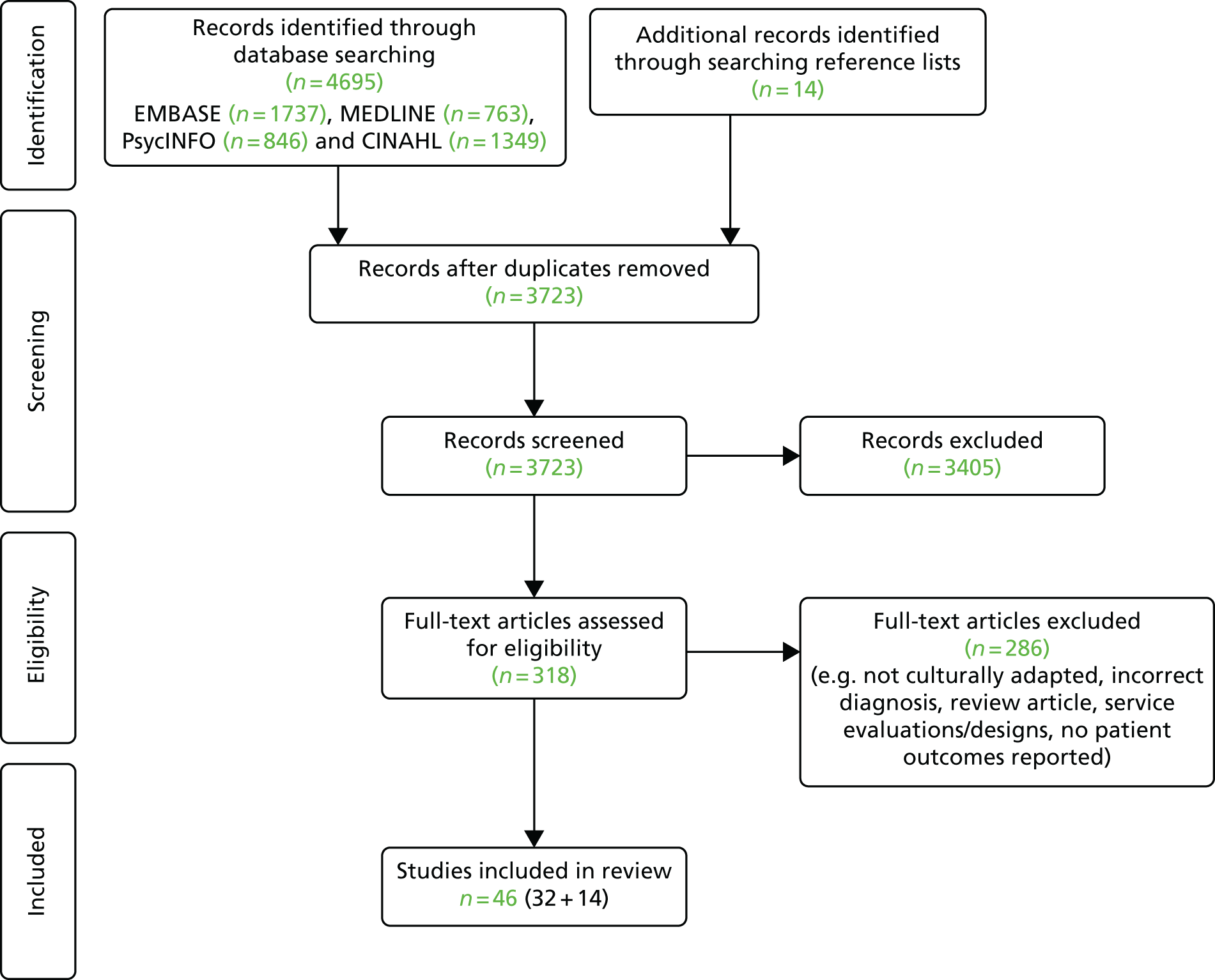
The database search returned 4695 results, providing 3723 unique citations after duplicates were removed. Titles and abstracts were screened and a further 3405 articles were excluded. Full texts of the remaining 318 articles identified as potentially relevant were accessed and examined against the eligibility criteria. Of these, 32 were included in the review. An additional 14 articles were identified for inclusion through e-mailing authors and searching reference lists of the full-text papers. The study selection process is presented in the PRISMA flow diagram shown in Figure 1.
FIGURE 1.
The PRISMA flow diagram. CINAHL, Cumulative Index to Nursing and Allied Health Literature.
Study characteristics
In total, 46 papers reporting 43 individual trials with 7828 participants were included. The characteristics of the reviewed studies are detailed in Appendix 2. Studies comprised 31 RCTs, 12 cluster RCTs, two non-randomised pilot studies and one block RCT. The mean age of service users ranged between 24 and 57 years and, among the studies that reported gender (n = 38), 42% were female. Sample sizes varied across the studies, ranging from six76 to 3082,77 with a mean of 182. All studies included samples of service users who had a diagnosis of schizophrenia spectrum disorder, usually defined using DSM-IV and ICD-10 screening criteria.
Three RCT papers included participants who had been reported in an earlier paper: one paper78 reported 24-month follow-up data of a subsample of an earlier RCT;77 one study79 used the same sample as an earlier paper;80 and one three-armed RCT81 included a subsample of participants reported in an earlier two-armed RCT. 82 Of the 39 studies reporting attrition, the range was from zero83–85 to 43.4%. 86 Attrition was < 15% in 25 studies83–85,87–108 and > 40% in three studies. 86,109,110 Attrition was not reported in seven studies. 71,76,87,111–114
Intervention characteristics
The characteristics of the culturally adapted psychosocial interventions assessed in the reviewed studies are described in Appendix 3. Interventions were delivered in 13 countries. The majority (74%, n = 34) were conducted in Asia (25 in China,77–80,83,84,87,89,94,96–98,100–102,104–110,113–115 two in each of Pakistan,71,92 Taiwan, Province of China,88,116 and India86,112 and one in each of Iran,91 Saudi Arabia76 and Malaysia93). Nine studies (20%) were conducted in the Americas (six in the USA,81,82,85,99,117,118 two in Mexico119,120 and one in Brazil95), and one study (2%) was conducted in each of Italy,90 Australia1 and Egypt. 111 Most interventions (85%, n = 39) were adapted for a majority non-Western population and seven studies (15%) were adapted for a minority population.
Around half of the studies (54%, n = 25) were FIs consisting of a psychoeducational or mutual support component. FIs varied across the studies in terms of their components and the evidence-based models from which they were adapted (see Appendix 3). The majority (88%, n = 2277–80,83–87,89–91,94,98,100,101,104,105,114,115,117,118) involved group family therapy sessions; only three FIs93,96,97 consisted of just individual sessions. In 12 of the FIs studies (48%),80,83,84,87,89,94,98,101,104,105,115,117 all of the sessions were designed for the family members and service users to attend together. In five studies, service users attended at least part of the intervention (25–86% of the sessions) and in the remaining eight studies77–79,85,86,90,91,114 only family members were invited. Ten (22%) studies evaluated some form of cognitive therapy, consisting of three social cognitive skills training,81,82,102 one social cognitive remediation therapy,111 three CBTs,71,92,107 two metacognitive training110,112 and one integrated psychological therapy (IPT). 95 Family members attended two71,121 of the CBT interventions; the remaining eight81,82,95,102,110–112,122 cognitive interventions were for service users only. Three studies73,109,113 were combined interventions comprising components adapted from multiple Western therapy manuals and theoretical frameworks; two of these were symptom-coping programmes and one included family therapy sessions. Five studies99,106,108,119,120 assessed social skills training (SST). Family members attended four of the SST interventions. Of the remaining interventions, two were illness management and recovery (IMR) programmes88,116 and one was a mindfulness-based psychoeducation programme,103 both of which were for service users only.
The majority of interventions (59%, n = 2771,79,80,82–86,88,91,92,94,96–98,101,103–105,107–109,111–113,116,119) were delivered in clinical settings. Six interventions81,90,99,106,114,117 were delivered in community settings and four87,89,93,115 delivered sessions in both clinical and community settings. Nine studies did not report intervention setting. 76–78,95,102,106,110,118,120 The duration of interventions ranged from 3 weeks88 to 2 years,77,78,89,90 with a mean of 8 months. The majority of the interventions were led by mental health professionals (80%, n = 37); five of these (all assessing group FIs) were co-facilitated by a family member participating in the study. Five studies did not specify therapist training (see Appendix 3).
Cultural adaptations of interventions
Culturally adapted themes
Details of extracted themes of cultural adaptation with examples from the reviewed studies are described in Appendix 4. To summarise, nine overarching themes were generated inductively from the reviewed interventions: language; concepts; family; communication; content; cultural norms and practices; context and delivery; therapeutic alliance; and treatment goals. Appendix 5 presents the frequency of each theme against each of the reviewed studies.
Language
Adaptations for language were reported in all studies (n = 46). These took the form of translating the original intervention into the national or local language91,112,114,115 and included local colloquialisms and idioms to improve cultural relevance and acceptability. 71,92,111 For example, So et al. 110 replaced the word ‘Stalinism’ with ‘Communism’ and incorporated colloquial Cantonese words to make the metacognitive training programme better suited to Chinese culture. Additionally, specific terminology was exchanged for more culturally appropriate words (e.g. replacing ‘module’ with ‘treatment areas’),119 and efforts were made to remove jargon and formal terms. 92
Concepts
The majority of interventions (78%, n = 36) were adapted to incorporate culturally appropriate presentations of concepts, with consideration of culture-specific belief systems, enhanced mental health stigma and low levels of education. This included working with alternative explanatory models to the ‘biopsychosocial’ model commonly held in Western countries, including the attribution of mental illness to spiritual or supernatural agents,93,117 predestination and fate91 and an imbalance of yin and yang forces during adolescence. 83 Some studies reported the inclusion of spiritual factors in formulations and discussion of locally held beliefs in psychoeducation sessions. 71,92 Mental health stigma was addressed by sharing personal stories and recovery narratives for normalisation and by holding group forums for participants to discuss their concerns. 80,88,94,109 Owing to a lack of mental health knowledge and low education levels in certain cultural contexts, adaptations were made to alter the complexity and amount of psychoeducation or therapy material provided to make it more manageable for service users and families. 82,85,95
Family
Most interventions (76%, n = 35) were adapted to acknowledge the pivotal role of the family in service users’ care and recovery, as well as culturally distinct family structures and processes. Adaptations included efforts to engage the family and encourage their active and continued involvement throughout the intervention71,90 (e.g. by offering additional sessions or informal home visits for family members and maintaining contact after treatment). 85,89,115,118 Modifications were made to accommodate more interdependent family structures and those that valued familial responsibility and collectivism over individualism. 94,96 These took the form of involving family members in decision-making and assessing the needs of the family as a whole (e.g. placing focus on medication adherence as an action that would benefit the family unit rather than the individual). 81,82,117 Further considerations included being sensitive to culture-specific family roles and expectations, such as in hierarchical families where younger generations are expected not to question their elders. 80,91,119
Communication
Twenty-two (48%) studies71,79–82,84,85,92–94,96–99,101,103,104,107,117–120 reported adaptations to integrate culturally specific ways of communicating and learning in the sessions. This included the use of culturally appropriate methods for dealing with conflict and problem-solving. For example, acknowledging that Chinese people do not tend to openly talk about their concerns and prefer to manage problems through reparative action and touch,80,84,94,97,98 and balancing the concepts of assertiveness and expression of one’s needs in the West with mutual respect and avoidance of confrontation in more family dominant cultures. 71,82,85 Further cultural considerations were made in relation to the disclosure of private information, such as the irrelevance of confidentiality due to the close nature of families,119,120 and reluctance to openly discuss family matters. 98 Additionally, culturally appropriate teaching methods were used in the sessions, for example encouraging collaboration and active participation in more passive cultures,82,99 or facilitating practical rehearsals or using visual aids rather than talking. 97,118
Content
Around half of the interventions (43%, n = 20) were modified by the adding or removing of content. Specific content was removed from original intervention manuals93,95,110,111,119 because it was culturally irrelevant. For example, So et al. 110 removed the Western conspiracy theory about Paul McCartney’s death from their module ‘jumping to conclusions’ in their Chinese metacognitive therapy for delusions (MCTd). Content was also removed due to limited access to appropriate technology or materials; for example, Valencia et al. 119 omitted video-assisted modelling used in the original American SST123 owing to limitations with the Mexican version, and Gohar et al. 111 omitted Arabic video materials from the ‘mentalizing component’ of cognitive remediation. Additional components were also added to intervention manuals to make them more culturally relevant. 93
Cultural norms
Adaptations were made to incorporate culture-specific norms and practices in 31 (67%) studies. 71,76,79–82,84–86,90–94,97–99,101,103–105,107–109,111,113–115,117,119,120 Interventions were modified to accommodate spiritual or religious practices and means of coping, such as the use of traditional healers, religious texts and prayer. 71,76,115 Culturally relevant activities (e.g. karaoke, t’ai chi and mah-jong,113 and Baduanjin relaxation exercises)85 and scenarios were also integrated into interventions (e.g. the use of traditional folk stories and religious characters in role plays, recordings and videos). 71,76,106 Recognising the social structures of certain cultures, additional efforts were made to build social networks and mutual support through group meetings, workshops/seminars and social gatherings outside therapy. 85,100,114 Studies also reported the use of peer leaders to deliver sessions alongside mental health professionals to facilitate community support and shared experiences. 97
Context
Almost half of the studies (48%, n = 2271,77,78,83,85,86,88–92,96,97,100,108,109,111,114–116,119,120) reported adaptations to facilitate feasibility in a particular cultural context by addressing specific cultural norms or organisational barriers due to lack of commitment, funding or resources. 85,88,96 Adaptations included delivering interventions at accessible locations where there were sufficient resources,90,96 offering flexibility in scheduling sessions71,109 and changing the duration of treatment. 85,88 Furthermore, the format of delivery was selected based on cultural appropriateness, including whether to see service users and family together or separately85,86,90 and the use of group versus individual interventions. 80,101
Therapeutic alliance
Adaptations to improve therapeutic alliance were present in 28% (n = 1381,82,85,86,91,93,99,102,115,117,119,120,124) of the studies. These included matching therapists and clients for ethnicity and other characteristics such as age, gender or language to enhance acceptability and shared cultural experiences. 91,115 A few studies reported on the training or supervision of therapists to improve their cultural competency. 99,117 Other studies reported on modifications to build rapport, trust and engagement, for example therapists adopting an informal approach by engaging in small talk and warm-up activities before the intervention99,102,119 and presenting appropriate forms of self-disclosure from their own lives to facilitate a more personalised therapeutic relationship. 119
Treatment goals
Treatment goals were modified in 13 studies79–82,84,86,94,98,101,104,117,119,120 (28%) to develop formulations that were realistic and congruent with cultural values. In some studies, this involved developing shared goals to meet the needs of the family unit and managing expectations of different family members, for example the tendency to expect immediate and practical help from close relatives in Chinese cultures. 79,80
Culturally adapted framework
To develop our evidence-based cultural adaptation framework (Box 1), these nine components were further refined by discussion within the team to increase their cultural specificity for African-Caribbean people. Our six-item framework is modelled on the Department of Health and Social Care’s ‘Six Cs for Caring’125 to increase accessibility to health-care professionals.
-
Concepts.
-
Cultural norms and practices.
-
Culturally relevant content.
-
Communication and language.
-
Context.
-
Cultural competence of practitioners.
Discussion
We conducted the first review of current evidence on the nature of culturally adapted psychosocial interventions in schizophrenia. We were interested in interventions originally developed in the West (Europe or the USA) and adapted for minority ethnic groups in Western countries and majority ethnic groups in non-Western countries. Our systematic search identified 46 articles comprising 43 individual controlled trials with 7828 participants.
Our framework highlights agreement regarding what constitutes adaptation for culture. All studies reported adaptations to language, which included direct translation and/or modifications to incorporate local colloquialisms and acceptable terminology. The majority of studies made adaptations in the domains of concepts, family, and cultural norms and practices. This included the consideration of culturally distinct belief systems, causal models of illness and methods of coping (e.g. spiritual/religious), incorporation of culturally specific activities and stories, involving the family in treatment and decision-making, and acknowledging culturally distinct familial structures such as those that are interdependent and hierarchical. Other common adaptations were to recognise different forms of communication and tackling problems, such as the use of practical aids rather than open discussion, removal of culturally irrelevant content (e.g. local celebrities, technology), and changing the delivery (e.g. location) to recognise contextual barriers. Common adaptations were also made to improve engagement and therapeutic alliance, including ethnic matching of therapists to clients, training therapists in cultural competency, integrating ‘warm-up’ (social) activities and small talk, and developing shared treatment goals. As previously reported in relation to adapted treatments for depression,61 authors did not report changes to the core components of the interventions but rather to their delivery to improve acceptability and feasibility in a specific cultural context, thus adhering to their underlying theoretical models.
Although these studies provide evidence of what to culturally adapt, there remains limited guidance on how to do so. Thematic analyses of cultural adaptations reported in each of the reviewed studies produced a framework comprising six essential components of cultural adaptation that may serve as a benchmark for future adaptations (see Box 1). In Chapters 3 and 4, we provide details of how we applied our framework to produce CaFI.
Conclusion
We have updated the field by empirically deriving a framework from existing trials of adapted treatments in schizophrenia. We used this framework as a guide to culturally adapt FI for African-Caribbean people. Our framework requires further refinement and testing. However, it provides the basis for a useful evidence-based tool to guide clinicians and researchers in the development and reporting of adapted psychosocial interventions in schizophrenia.
Chapter 3 What does cultural adaptation look like and how is it applied?
Introduction
Using findings from the current literature (phase 1A), we developed a cultural adaptation framework and applied it systematically to an extant FI model in collaboration with key stakeholder groups.
Historically adversarial relationships between NHS mental health services, African-Caribbean service users and their families,10,14,23,122 meant that co-producing CaFI with key stakeholders was essential for its credibility both among the African-Caribbean community and health-care professionals.
Co-producing CaFI involved three separate but inter-related phases:
Aims and objectives
How can existing evidence-based FI be culturally adapted for African-Caribbean people with schizophrenia and related disorders?
Phase 1 study objectives
-
Involve key stakeholders (service users, families and clinicians) in culturally adapting an existing FI for African-Caribbean people with schizophrenia (phases 1B and 1C).
-
Produce a manual to support delivery of the intervention (phase 1C).
-
Identify client and family centred outcomes and quality-of-life outcomes (phases 1B and 1C).
-
Identify therapist and FSM training needs (phases 1B and 1C).
Phase 1A: literature review findings
The Chapter 2 literature review generated components of culturally adapted psychosocial interventions. These became the framework for culturally adapting FI (see Box 1).
Working with members of our RAG of eight African-Caribbean service users and carers, we utilised these criteria to pinpoint and develop supporting materials for the cultural adaptation focus groups. For example, the importance of communication and language – going beyond mere translation, involves actively excluding culturally offensive language and incorporating concepts and phrases familiar to members of the ‘in group’. In CaFI, this includes words like ‘obeah’ (a term used in the Caribbean, particularly in Jamaica, denoting folk magic sorcery and witchcraft, and akin to ‘evil eye’; it embodies practices by which supernatural powers are invoked to achieve personal protection and/or the destruction of enemies) and reference to ‘the system’ [shorthand for powerful institutions (such as mental health care and the police) that many African-Caribbean people associate with oppression and institutional racism]. We also sought to address stereotypes and misconceptions such as highlighting the heterogeneity of the Caribbean islands.
Phase 1B: focus groups
The purpose of the focus groups was to ascertain participants’ perspectives on:
-
the perceived need for FI in this ethnic group
-
how FI might be culturally adapted
-
the potential benefits of CaFI
-
an appropriate means of evaluating potential benefits and outcomes
-
how to engage and recruit service users and families into therapy
-
maximising family retention in the study.
Methods
Study design
This was a cross-sectional qualitative cohort study using focus group methodology with key stakeholders. We conducted three separate stakeholder focus groups for service users, carers and advocates, and health professionals. We convened a purposefully selected ‘mixed’ group (comprising stakeholders from the initial focus groups) to verify emergent themes and agree the items to be taken to the consensus conference (phase 1C), where final decisions about CaFI’s content, delivery and associated training were made.
Participants and recruitment procedures
We used novel recruitment strategies building on the PI’s community engagement work at community mental health conferences and with service users (at the request of our service users, this term is used in preference to ‘patient’ throughout the report) and Patient and Public Involvement (PPI) events supported by National Institute for Health Research’s (NIHR’s) Research Design Service’s bursary award. Potential participants were recruited via events in accessible venues, such as churches and community centres. Information was also posted in community newspapers and the Manchester Evening News and the study was presented during live phone-in discussions about mental health and illness on local radio stations instigated by the PI. The PI and RPM made presentations to service user and carer forums, Community Mental Health Teams (CMHTs) and voluntary sector organisations, including our collaborating partner ACMHS. Advertisement posters/flyers (see Appendix 6 for service user example) were also placed strategically at various community locations and sites within the host NHS trust (MHSCT). Recruitment information was also made available via the ‘Get Involved’ page of the Researching African Caribbean Health website [URL: http://research.bmh.manchester.ac.uk/ReACH/getinvolved (accessed 2 December 2017)], which we created for this study.
Inclusion criteria
Service users
-
Current female and male service users, including those receiving treatment from CMHTs or on community treatment orders (CTOs) who clinical teams considered well enough to participate.
-
Former female and male service users who, although not on active treatment, might be subject to periodic reviews by mental health teams and/or in receipt of support from voluntary sector agencies such as ACMHS.
-
Aged ≥ 18 years, who self-identified as being of ‘African-Caribbean origin’, including ‘Black British’ and ‘mixed’ African-Caribbean.
Carers and advocates
Carers (including paid support workers, family and friends) and advocates (such as ACMHS) with experience of working with African-Caribbean people. Unlike service users, carers and advocates could be from any ethnic/cultural background.
Clinical staff
We sought to include as wide a range of professions with differing levels of experience/expertise as possible, including nurses, occupational therapists (OTs), psychologists, psychiatrists and social workers.
Study participants
Participants were service users (n = 10), health professionals (n = 7) and carers and advocates (n = 14). The ‘mixed’ focus group comprised purposefully selected individuals from the previous three stakeholder groups (n = 11). Service users all had ICD-10 F20–F29126 or DSM-IV127 schizophrenia diagnoses. Health professionals included social workers, OTs and registered mental health nurses (RMNs). Carers and advocates were predominantly family members [spouses or partners, siblings, and parents (mostly mothers)] and voluntary sector provider representatives such as ACMHS.
Procedures and materials
Interested individuals who contacted the research team were provided with PISs (see Appendix 7 for service user example), tailored for each stakeholder group and given at least 48 hours to decide whether or not to opt into the study. Potential participants met with the RPM to address any queries and complete consent forms (see Appendix 8 for service user example).
Reflecting the differing perspectives of the stakeholder groups, separate topic guides (see Appendix 9 for service user example) were developed for each focus group based on the literature review (phase 1A) and information generated in discussions with former service users and carers when developing the study. Topic guides and supporting materials were refined via consultation with our RAG.
Each focus group commenced with context setting and establishing ground rules to help create a ‘safe space’ for individuals to talk about potentially sensitive and/or distressing experiences in relation to schizophrenia and mental health care, and to ensure that all participants were afforded the opportunity for their voices to be heard.
Demographic information (age, gender, ethnicity, marital and employment status, postcode and religion) were collected and consent regarding recording and data usage confirmed. Strategies for dealing with distress were also outlined and sources of available support provided (see Appendix 10). All focus groups were facilitated by the PI, supported by the RPM.
Data collection
Initial focus groups
Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) presentations were used to outline the background to the study, the purpose of the focus group, session content and process (see Appendix 11 for service user example).
To collect data, we worked systematically through the topic guide (see Appendix 9), as follows:
-
We explored participants’ experiences of services and perceptions of the need for ‘talking treatments’ in general and CaFI in particular.
-
We gave participants the opportunity to discuss the impact of schizophrenia on the family, cultural models of mental illness and past experiences and perceptions of services and psychological therapies.
-
We presented individual components (Box 2) of the extant evidence-based FI model34 and invited participants to comment on (a) the face validity of the different components and (b) what, if anything, needed to be done to improve their cultural appropriateness – that is, to make the existing components more ‘African-Caribbean specific’ for service users and their families.
-
We sought participants’ views on additional African-Caribbean-specific topics to be included in CaFI.
-
We explored participants’ views about the delivery of CaFI. Specifically:
-
factors related to delivery (number, duration and location of sessions)
-
ethnic matching of therapists and families
-
communication and language use in a therapeutic context
-
suggestions for culturally relevant materials to support delivery
-
factors that might encourage or hinder engagement.
-
-
We identified relevant and important outcome measures from participants’ perspectives.
-
We ascertained participants’ views about maximising recruitment and retention and minimising attrition during the trial phase of the study (phase 3).
-
We sought participants’ views about the involvement of FSMs/’proxy families’ (trusted individuals who would support service users’ participation in the absence of families).
-
We asked participants to comment on the perceived training needs both of FSMs and CaFI therapists.
-
We invited participants to contribute additional information they considered important, but which had been omitted from the topic guide or not covered during discussion.
-
Service user assessment:
-
current and past episodes of illness
-
functioning
-
strengths and resources
-
relationships.
-
-
Family assessment.
-
Psychoeducation.
-
Stress management and coping.
-
Problem-solving and goal-planning.
‘Mixed’ focus groups
To validate findings from the first three stakeholder focus groups and resolve any differences between groups, we conducted a fourth ‘mixed’ focus group comprising purposely selected representatives (n = 11) from the initial focus groups. Participants were tasked with agreeing the essential components of a culturally specific FI to be taken forward to the consensus conference. A topic guide (see Appendix 12 for ‘mixed focus group’ topic guide), based on findings from the three previous focus groups, was used to facilitate data collection.
In common with previous sessions, the ‘mixed’ focus group commenced with the moderator (PI) outlining its purpose and addressing ethical issues. Findings from the earlier focus groups were presented in a structured format using a PowerPoint presentation (see Appendix 13 for ‘mixed focus group’ presentation slides). Additional information was presented on flip-charts or as printed materials. This approach enabled participants to address anomalies/inconsistencies and to resolve differences between groups through discussion using a range of techniques, including ranking, voting and visual models, without losing focus. For example, in relation to therapeutic alliance, we shared findings from previous research about ‘ethnic matching’ and ‘cultural competence’ to facilitate discussion about the utility in delivering CaFI. We also shared materials, including our draft ‘Lay guide to schizophrenia and psychosis’, as well as inviting participants to suggest other resources that could improve the cultural specificity of CaFI’s content and delivery.
All focus groups were digitally recorded and data managed in accordance with The University of Manchester’s data protection policy and management plan and the host trust’s research and development (R&D) policy.
Data analysis
The data were transcribed, checked for accuracy, and identifying material was removed and analysed using framework analysis42 by the RPM and PI, with input from the wider team and qualitative methods experts independent of the team. Framework analysis is a systematic process of data analysis that allows for inclusion of both a priori and emergent themes and concepts. 128,129 A framework approach was particularly suited to our study as there were specific topics we wanted to explore, such as the content and delivery of the intervention, as well as ascertaining participants’ views about key issues, such as the utility of the intervention and recommendations for maximising uptake.
The interconnected stages of framework analysis include familiarisation (through the reading and re-reading of the transcripts), coding, framework development, charting and indexing. This was used to guide data analysis from initial management through to the development of explanatory accounts. Data verification strategies included peer and participant review to examine and verify themes, findings and conclusions. For example, two other experienced qualitative researchers (Baker and a qualitative methods specialist independent of the research team), rigorously reviewed the research process and emergent findings identified by the PI and RPM. In addition, findings were shared with the wider research team and Research Management Group (RMG). The ‘mixed’ focus group served as a means of ‘member checking’ or ‘respondent validation’, were participants were given the opportunity to comment on the validity of findings. These are recognised methods of ensuring ‘trustworthiness’ of the data and subsequent findings. 130,131 NVivo version 10 (QSR International, Warrington, UK) was used to support data management and analysis.
Findings
Presented here are the findings from the fourth ‘mixed’ focus group. They represent the synthesis of data generated from all four phase 1 focus groups, underpinned by the literature. Illustrated by participants’ verbatim quotations, the findings are presented in three overarching themes that reflect the research objectives for this phase of the study, that is, participants’ views on how to make the (1) content, (2) outcomes and (3) delivery of the intervention culturally appropriate for African-Caribbean people.
Theme 1: content of the intervention
Participants did not suggest that any of the current FI content (outlined in Box 2) was irrelevant. Instead, they suggested additional African-Caribbean-specific elements (summarised below) in relation to the different components of FI.
Service user assessment
Participants stated that racism and discrimination should be explicitly explored (Box 3), highlighting the effect of ‘current and previous episodes of illness’ experiences on mental health and help-seeking:
There’s massive talk of institutionalised racism in so many different areas, whether that’s education, crime and other areas. We know it can’t be separate from the health area as well so there has to be an acknowledgement that it’s there.
Male advocate
-
Racism and discrimination.
-
Models of mental health and illness.
-
Prescribed and illicit drugs.
-
Culturally relevant markers of social functioning.
-
Recovery and the future.
-
Family structures and dynamics.
Service users’ ‘models of mental illness’, including spirituality and religious affiliation, the significance of wellness and well-being and perceptions of mental illness as deviance, were regarded as areas of particular relevance for African-Caribbean people and of difference from other ethnic groups:
I remember working in a mental health system and every time I came across somebody from a BME culture, particularly Caribbean, when they had a mental health issue, the family wasn’t saying that they’re not well; they would say ‘they got in with the wrong crowd’ . . . the family would say ‘my brother is strong, he is very intelligent, he got in with the wrong crowd’. So the mental illness is associated with being deviant instead of being associated as being an illness.
Male advocate
There was near-unanimous agreement that service user assessment should include open discussion on beliefs about and experiences of psychotropic ‘medication’, including side effects as well as the relationship between psychotic symptoms and illicit drugs use:
I’ve been on medication for some time and I remember at one stage I was using cannabis and alcohol at the same time and I had a word with someone in authority about it and they said, ‘what you’re doing, you’re self-medicating, because the medication that you’re supposed [to take] . . . is not having its desired effect. So you’re self-medicating’.
Female service user
Social functioning, including developing/regaining social skills and the ability to ‘mix with people’ and establish new relationships, was regarded as especially important for a group with high levels of social isolation linked to stigma. Participants spoke about therapists’ need to be particularly aware of the cultural symbolism of food. For many African-Caribbean people, an individual’s ability to care for and nurture themselves and others is an important indicator of effective social function:
I cook right; chicken, fish, healthy food, food in the oven. My mum comes and I give her food, my sister, I give them food and make sure they’re all okay. They’re very, very grateful. Mum’s very happy with me.
Female service user
African-Caribbean-specific additions to the ‘strengths and resources’ component included a ‘future-focused’, recovery-based approach. Work, studies and entrepreneurship were regarded as significant markers of recovery and enhanced self-esteem:
There’s too much emphasis on ‘illness’ and ‘episodes’. I’d like to have more well-being and self-esteem . . . it’s about also drawing on what is it like for them when they have got their full well-being.
Male carer
Although regarded as a potentially important resource, spirituality was a source of ambivalence. Participants warned against reifying or essentialising the relationship between African-Caribbean people and religious institutions, as interactions with such organisations were not always positive:
They talk about certain things happening in church, and ‘when you get unwell you turn to the church’, but I’ve been taken out of free [three] churches . . .
Male service user
Therapists’ awareness of family structures and dynamics (including age and gender hierarchies) within African-Caribbean families, and how these ‘relationships’ might play out in therapy, was highlighted. Although this could be said of any ethnic group, participants felt that family tension and conflict were especially pertinent for African-Caribbean people owing to delayed access to care and lack of understanding of symptoms:
When you are not ill, [there] maybe a lot of things that you do within the family that’s no problem . . . when you get ill you can’t do those things and not being able to do those things brings accusations that maybe ‘before you do this but now you don’t want to do this’ and that beings lots of tension and argument and can bring lots of problems, because they don’t understand . . .
Female service user
Therapists should also explore perceptions/experiences of services’ seemingly arbitrary and inflexible approaches to engaging with service users’ networks, which contribute to difficulties in maintaining relationships:
Last time I was in [hospital], a lady came to see me, who wasn’t my wife, and they said that she had to have 5 years’ relationship before the doctor would give her permission to find out if I was OK or not.
Male service user
Family assessment
Although participants felt the content of the current FI model was entirely relevant, they also emphasised the significance of African-Caribbean beliefs about mental illness and the impact of service users’ experiences and difficulties on carers and family members (Box 4):
. . . you also have to aware of the belief system within a family, because you might meet up from the spiritual aspect of it where this is caused ‘because someone did this to me’ . . . back home [Caribbean] we call it Obeah . . . and if you come up against that you’re going to have to be prepared for that and how to deal with it.
Female carer
. . . involve other siblings and family members and also recognise their needs so they will understand better why a particular member of the family needs more support instead of creating resentment between the family members.
Male carer and former service user
-
Beliefs about mental illness.
-
Impact of service users’ experiences and difficulties on carers and family members.
-
Concerns about confidentiality and risks associated with disclosure.
Participants highlighted the importance of being able to explore the history of predominantly negative experiences of services during therapy, without these being pathologised, minimised or dismissed. Past experiences of feeling excluded from decision-making and restricted access to information should be addressed in CaFI:
. . . when they are having a meeting for the care plans I’m not there, even though I’m down as the main carer, because apparently he says he doesn’t want me to be there. But how can you care for someone if you don’t know what you’re caring for?
Female carer
Concerns about confidentiality and cultural sanctions accompanying the risk of disclosure and negative perceptions of help-seeking from statutory services (as indicative of ‘not coping’) had potentially adverse consequences for their families, which made them reluctant to share information with health-care professionals:
I’ve been brought up ‘don’t speak to them. Don’t speak to social services. Don’t give them too much information’ . . . So it’s ‘how honest you can be?’ . . . because I’m scared, if I’m to be honest, they might think ‘you ain’t coping, you ain’t managing this situation so now we’ll get these [social services] involved’.
Male carer
Families’ reluctance to disclose information or seek help was endorsed by health-care professionals who reported that lack of trust within the African-Caribbean community represented a significant barrier to therapeutic engagement. Therapists therefore need to specifically explore this during assessment and recognise how this might impact formulations about families’ needs/presenting issues:
I run support groups across Manchester for carers and one of them is at the [place name] and that was the hardest group to sustain and to gain trust with . . . maybe it’s because I’m White and I’m going in to a predominantly Black community but also I find that the carers between them, they lack trust and they’re not willing to share as much information, they’re not as open, and that’s just from my perspective.
Female health-care professional (emphasis in bold)
Psychoeducation or ‘shared learning’
In the original FI model, psychoeducation focuses on fostering understanding schizophrenia, explaining illness models and available treatments, and exploring beliefs about the illness. The process involves educating families about ‘helpful’ beliefs about impact and course of illness and how to change ‘unhelpful’ beliefs (e.g. that service users can control symptoms).
Participants identified a number of African-Caribbean-specific additions to CaFI (Box 5). The majority centred on communication and advocacy. For example, participants suggested incorporating information on how ‘the [mental health] system’ works, including the roles of core multidisciplinary team members such as social workers, RMNs, psychiatrists and psychologists:
. . . educate people around the difference between a psychiatrist and a psychologist, because talking therapy is a psychological intervention, whereas medication is a psychiatric intervention, and a lot of us don’t know the difference. So a lot of people might be fearful of a psychologist because they think that if they go to see a psychologist they’re going to end up being medicated, which isn’t necessarily so.
Male carer and former service user
-
How the mental health ‘system’ works.
-
Police involvement including differences between the UK and the Caribbean.
-
Models of mental illness.
-
Awareness of resources (e.g. support groups, hearing voices movement).
-
Stigma, including stigma-reduction strategies.
-
Medication: how it affects the brain, side effects, physical effects, anxiety.
-
Illicit drugs (e.g. cannabis use): use as self-medication, challenge stereotype.
-
Challenging misconceptions (e.g. mental illness as weakness/deviance).
Informing service users and carers about their rights in relation to the Mental Health Act (‘sectioning’),132 visiting hospitalised relatives, legal representation and carer assessment was regarded as particularly pertinent to African-Caribbean people, who consistently reported a lack of awareness:
I think maybe empowering them to find out what their rights are, to ask the professionals involved, you know, ‘as a family, is there any support for us?’ ‘What are my rights in respect of attending a ward round or being there when the care plan is being done?’
Female health-care professional
What about understanding the rights, you know, to be sectioned and what the rights are when you’re picked up by the police and taken to hospital. What rights have you got? I don’t think people understand that. And if you get sectioned . . . What are the rights in them situations?
Female service user
Participants expressed concerns that information-seeking and advocacy could be perceived negatively by professionals (as challenging ‘the system’), with potentially deleterious consequences for care and recovery:
Because there’s fear in consequences. He felt if he challenged his psychiatrist too much then he wouldn’t go to this hostel as soon as he thought he would, and that was his thing, ‘I can’t rock the boat’.
Male advocate
Because fear of such consequences meant that African-Caribbean service users were particularly less likely to ‘rock the boat’, it was agreed that therapists should explicitly address people’s fears during CaFI. It was also felt that therapists should also enable service users to assert themselves if attempts at advocacy invoked adverse responses from staff and to cope with any negative aftermath.
Given African-Caribbean people’s greater likelihood of entering mental health services via the criminal justice system, it is perhaps unsurprising that the role of the police, and the associated negative stereotypes of Black men, in particular, was considered an essential component of CaFI:
They are stereotyping . . . ‘the Black man is aggressive and violent’. That’s why they call the police, because they know the Black man is ill and aggressive and violent, that’s another stereotype. That’s why the police are involved sometimes.
Male service user
Challenging misconceptions, especially associations between deviant behaviours and onset of mental illness and the extent to which symptoms were under service users’ control, was especially pertinent to African-Caribbean families:
I know people who have said ‘no, she’s not ill, she’s just playing games’ or ‘she’s messing around’ or ‘she just wants her own way’ or ‘he just wants his own way’. So it’s about how you get that across to let them understand that it is an illness that this person has.
Male advocate
Stress management and coping
The stress management and coping component (Box 6) of Barrowclough and Tarrier’s FI model34 examines current stresses within the family, with particular emphasis on service user-focused situations that the family finds difficult to cope with, such as aggressive behaviour or suicide risk.
-
Managing conflict and conflict resolution.
-
‘Two-way support’: service user as carer and vice versa.
-
Relapse prevention.
-
Crisis planning.
-
Focus on holistic approach to wellness and well-being.
To improve cultural specificity, participants suggested placing greater emphasis on strategies for dealing with conflict and achieving resolutions and acknowledging the situation from both service user and carer/family perspectives. In a community where cultural mores inhibit ‘talking your business’ outside the family,35,36 it was suggested that therapists’ ability to help families acknowledge experiences of illness and impacts of symptoms were especially germane:
On this ‘coping’, for me, I think it’s about acknowledging, especially with hearing voices, that that service user is hearing those voices [instead of] . . . ‘No you’re not! That’s stupid, you’re not!’ . . . I think what I’m trying to say is recognising that, acknowledging is a [form of] coping, because . . . if you don’t acknowledge, you don’t cope, do you?
Health-care professional (emphasis in bold)
Acknowledging that service users were often also carers, and vice versa, and developing strategies to address the dynamics of this ‘two-way support’, was an important aspect of managing stress and enabling families to cope:
I think also we need to acknowledge blurred lines between the service user and carer, because sometimes . . . it might be in the forefront that the carer is the carer but, if you scratch underneath the surface, what you might find is the service user is caring for the carer because they might have a lot of physical complex health needs . . .
Male service user and carer
It’s like with me . . . my dad, 30 years ago, was a younger man, and now he’s become an older man, he’s getting dementia, but he was my next of kin. So now it’s a case of me trying to help him, and I’m not well and he’s not well . . .
Male service user
African-Caribbean people experience more negative care pathways. Participants stated that relapse prevention (specifically, the identification and management of early warning signs) and crisis planning to promote more positive access to care and support were essential elements of stress management and coping:
I have a friend and when she’s going into a crisis the neighbours obviously know there’s something wrong and they usually phone the police and it ends up a really negative situation. So what happens if somebody’s at home with their family and they’re not well and they’re going into a crisis? What does the family do? How do they respond? What should they do? Who do they phone?
Female advocate
Participants reiterated that all aspects of CaFI, but perhaps especially stress management and coping, should have a clear focus on wellness, well-being and a ‘holistic’ approach to coping, including the use of alternative therapies:
But the other thing that I found to myself is that holistic things like massage, acupuncture, Reiki, aromatherapy; things like that have helped me to cope, and even as what [name] was saying, I just got a thing to go to the gym myself.
Male service user
Problem-solving and goal-planning
The extant FI model outlines 10 steps that the service user, family and therapist work through to solve problems and achieve agreed goals. These were presented to focus group members using a visual representation created by the CaFI team to explain the process (Figure 2).
FIGURE 2.
Worked example of problem-solving and goal-planning.
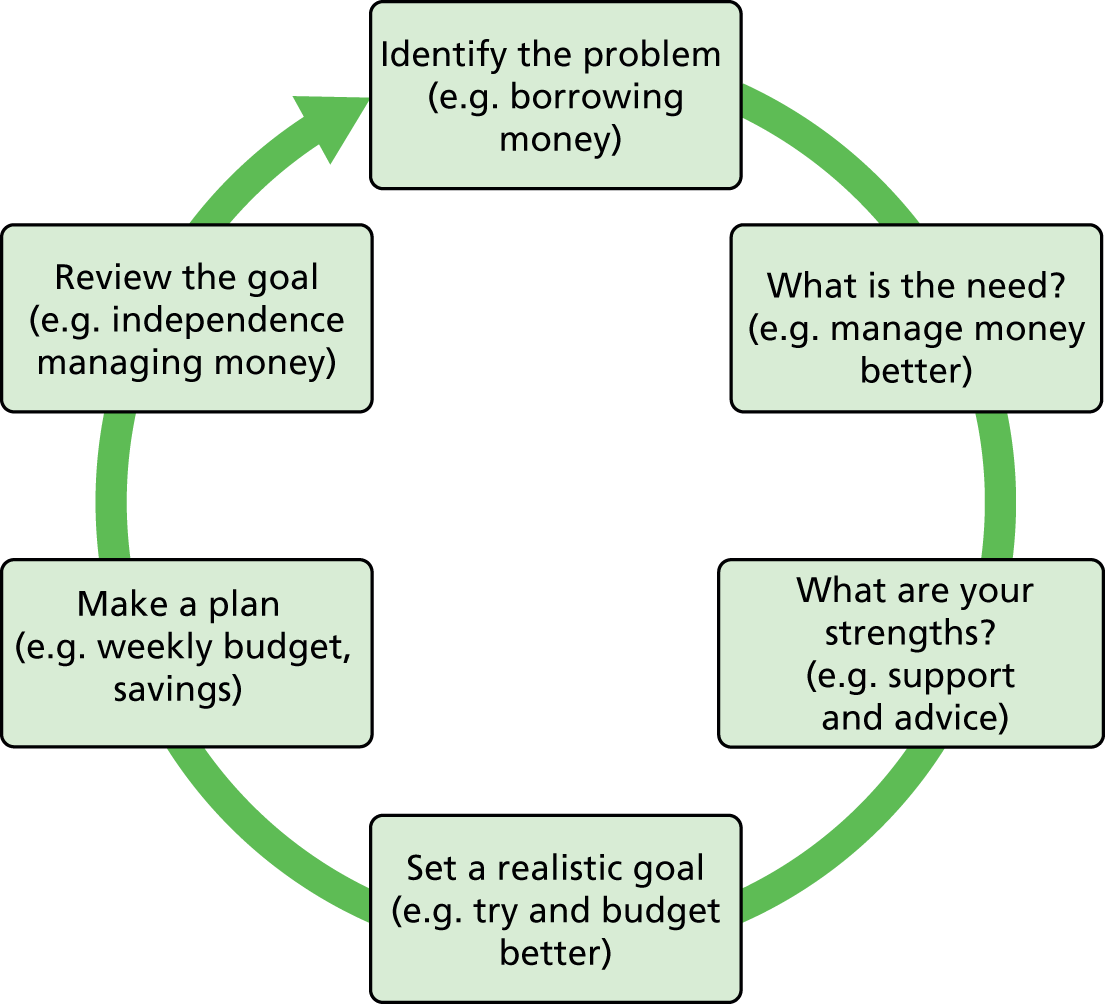
Participants thought that this was helpful: they liked breaking goals into small, achievable steps, solution-focused approaches and focusing on progress versus failure; and creating opportunities to celebrate even small successes was especially welcomed. They believed that this approach could have a significant influence on family conflict resolution and confidence building in African-Caribbean families:
I think what this does is really kind of gets the family to realise, and also the service user, how resourceful they are to find a solution to their problem . . . So, in one way, it develops confidence that ‘I have got the resources’.
Male carer
I think also if it does break down at any point I think it would be useful to focus on how far you’ve travelled and the positive rather than the negative . . . you’ve got so far round that circle and that’s a very positive step and if you focus on that, then maybe next time you’ll get past that place and on to the next stage.
Female carer
Although participants liked the process, their responses highlighted the need to develop a range of culturally appropriate tools to support delivery of the intervention. For example, although some participants liked the visual representation (see Figure 2), others suggested that it could be interpreted as ‘going round in circles’ and that perhaps a more linear representation might suit some families (the availability of resources for supporting delivery is explored further in Theme 3: delivery of CaFI):
. . . as a flow chart and that does work because then you do exactly what you’re saying, you do feel like you’ve got to the end and the solution is at the end.
Female health-care professional
Theme 2: desired outcomes and measures
In our original application, we identified (from existing literature) outcome measures to be feasibility tested during the trial (phase 3). Mindful that some of these measures might lack cultural specificity and the reported service experiences of this ethnic group, we gave stakeholders the opportunity to (a) identify the most relevant service user and family-centred outcomes and (b) agree the primary and secondary outcome measures that they considered most relevant for a future RCT of CaFI.
We shared copies of potential measures with participants and sought their opinions about which were most relevant to African-Caribbean people.
Participants expressed concerns about the number of measures, the length of some and the cultural appropriateness of all. There was agreement that outcomes were an important aspect of testing any intervention.
Increased knowledge was regarded as particularly beneficial for families and carers because ‘knowledge is power’ (female carer). Participants suggested that more culturally appropriate tools were needed and endorsed our decision to update the Knowledge About Psychosis Interview (KAPI),133 itself derived from Barrowclough and Tarrier’s Knowledge About Schizophrenia Interview (KASI). 34,134 Although the KAPI is used in the current study, we have validated a new Knowledge About Psychosis (KAP) measure and developed and validated a culturally adapted version specifically for African-Caribbean people (Culturally-adapted Knowledge about Psychosis; CaKAP) for use in future trials (paper under review).
Other desired family outcomes included:
-
better attitude towards wellness and recovery
-
improved stress management and coping
-
feeling more supported
-
having better access to resources (both NHS and community level).
Desired service user outcomes included:
-
developing better family relationships (e.g. better attitude, less perceived criticism)
-
measurable changes that might indicate moving towards recovery such as:
-
reduction in symptoms
-
less reliance on medication
-
fewer hospital admissions:Female health-care professional
I suppose what we could measure would be things like less admission to hospital and less reliance on medication [agreement].
-
Participants also spoke about potentially negative or harmful outcomes to avoid, such as a breakdown in trust between families and therapists, and carers feeling less supported. Accordingly, measures to assess therapeutic alliance were endorsed. A breakdown in family relations that leads to service users’ alienation from their families and increased isolation was regarded especially negatively:
I suppose becoming more alienated from your family, [agreement] that’s got to be one that you want to avoid but it might actually be as a result of the family therapy.
Female health-care professional
It was agreed that all measures should be accessible (using visual representations vs. written information where possible), and should be capable of collecting data longitudinally to evaluate CaFI’s impact over time and in other contexts:
. . . there needs to be some way of evaluating it and seeing what works and what can be changed, because you could be asked to deliver it in London next year or something, you never know.
Female service user
These discussions culminated in the decision to take a number of measures to the Consensus Conference for a final decision about the measurement of CaFI outcomes (see Chapter 6, Methods).
Theme 3: delivery of CaFI
We invited participants to comment on what, if anything, needed to be done to ensure that the delivery of CaFI was culturally appropriate for African-Caribbean people. Stakeholders’ views were also sought on key issues to support the delivery of CaFI, including the training needs of therapists and ‘proxy families’. Three subthemes emerged from respondents’ views on the delivery of CaFI: (1) ‘ethos of delivery’, (2) ‘therapists’ knowledge and skills’ and (3) ‘practical issues’.
Ethos of delivery
Participants felt that the way that CaFI was delivered would make it truly African-Caribbean specific. Here, they placed greatest emphasis on the relationships between the therapists, service users and families. They advocated an explicitly collaborative ‘shared learning’ approach. CaFI’s ethos of delivery should be a three-way process whereby therapists’ acquisition of culturally relevant knowledge is as important as service users and families learning about psychosis and family work. Much of this could be regarded as good clinical practice. In CaFI, a participant stated that an important aspect is the therapist’s skill in being explicit and deliberate in seeking to understand African-Caribbean culture(s) and willingness to share his or her own background to identify similarities and differences. This approach was seen a crucial step in building trust by reducing social distance, flattening hierarchies and fostering engagement:
‘I’ve got something to learn from you, but you’ve also got something to learn from me’ . . . it’s like flattening it out [the] power, because they’ve got a massive amount of power that is mostly misused . . .
Female advocate
I think it’s really important for people to feel like they have power in this situation, that they have some level of control, because I think quite often, particularly in mental health services, people feel very powerless, and we talk about our person-centred approach and partnership and I see quite often that that is in reality . . . So I think, in this instance of family therapy [CaFI], if somebody comes in and feels like ‘actually my voice is really going to be heard and I can actually affect some change for myself’ then that would maybe lead to it being more productive.
Female health-care professional
Therapists’ knowledge and skills
Participants felt that therapists would need to have excellent therapeutic skills and the ability to engage service users and families so that they could build trusting relationships and work effectively with members of this community. Being person centred and focusing on strengths were regarded as essential. In addition to being clinically competent, therapists would need to be culturally competent or, at the very least, ‘culturally aware’. This would enable a better understanding of service users and families’ perspectives and avoid misconceptions and potential pathologising of cultural norms and experiences, especially in relation to issues such as spirituality and beliefs:
It needs to be a skilled therapist and using a person-centred approach so that it’s focusing on the person . . . it’s not about tick-box questions, it’s about building the relationship and using things like, let’s say, motivational interviewing, which is focusing on the positive things in a person’s life, the strengths and so on, and I think that really is key . . .
Male advocate
I would like to strongly advocate that we need to have cultural sensitivity and cultural competence in the therapists, because when people talk about certain things from their spiritual context, from their faith context, from their cultural context, sometimes they’re given bizarre looks, and it’s not that they’re being bizarre, it’s part of their belief.
Male carer and former service user
Cultural competency generated discussions about ‘ethnic matching’ of therapists and families. Some participants felt that membership of the same ethnic group would enhance the therapeutic relationship, particularly in establishing trust early in the relationship:
. . . I think if the person was Jamaican and they were speaking to someone who is Jamaican, I think they would have similarities there instantly and be able to open up in different ways about their backgrounds and their specific cultures. Instantly there’s unsaid things that you have in common, like the food you eat or the music you listen to, and that cultural ethic is what you have.
Male carer
Others strongly disagreed suggesting that ethnic matching was based on erroneous assumptions of intraethnic similarities that failed to take account of significant within-group differences, including between people from the Caribbean. Instead, these participants suggested that the therapists’ self-awareness coupled with self-awareness and reflective practice were more significant than ethnic matching:
I’m not necessarily saying in terms of White or Black but, ‘how does your role or identity and how you got there influence whether you can do things?’ . . . So to me, it’s not the cultural awareness, it’s like ‘do you know yourself particularly well?’ ‘Do you understand that your power balance/imbalance with the person you’re working with has an impact on the way you work?’
Male advocate
Practical considerations
Participants highlighted a number of practical issues in delivery of CaFI. These included having choice and flexibility in:
-
where CaFI would be delivered
-
when CaFI would be delivered
-
how CaFI would be delivered.
Number and duration of session
For example, although participants agreed that hour-long sessions would be ‘about right’, there was concern that the proposed number of sessions (10) might not be sufficient as several sessions might be needed to establish trust, an issue particular relevance to African-Caribbean people:
No, I think it’s just not enough. I think given the experiences that are so longstanding, that people have been in services for such a long time but have never had any opportunity to have talking therapies before, I think those [things] would suggest that, actually, it might take people longer to get used to that way of working . . .
Female health-care professional
Therapy resources
There was general agreement that materials should ideally include:
-
audio-visual formats such as Eleanor Longden’s TED Talk135 about her experiences of services and recovery
-
other internet resources
-
information in DVD or audio format to ensure inclusion of people who might not have ready access to the internet:Male advocate
So you talked earlier about sending out the assessment prior to so they can have a look at that . . . Can it be sent out in a DVD form for those who are not that comfortable with reading so they can watch it on the TV? Can it be done in audio form so that if they’ve got a disability?
‘Proxy families’ (family support members)
Responses to the concept of involving ‘trusted individuals’ in delivering CaFI, thus enabling service users to access the intervention in the absence of families, were somewhat ambivalent. Some participants welcomed the idea:
What you said is absolutely brilliant, because . . . I think it actually allows those people to also have access to the services that don’t have real blood families but they might have another form of family.
Male carer
Others raised concerns about confidentiality and trust, issues that were regarded as having particular salience for African-Caribbean people. However, giving service users’ ability to choose ‘trusted individuals’ to work with made this less problematic:
If you are going to choose other people to be part of your family then obviously it means that you do trust them already . . . because if you didn’t trust them, you wouldn’t have trust in them to be part of your family anyway.
Service user
Language use
Language use and terminology were also regarded as especially important within this community. Participants advocated language that would demystify the mental health ‘system’. Avoiding jargon and acronyms such as ‘CTO’ would enable families to feel included in discussion and decision-making. Participants also stressed the need for clear, accessible, non-stigmatising language, including rejecting the term ‘psychoeducation’:
. . . what I don’t want is, to be honest, ‘psychoeducation’ because that would make me straightway think negative and put me off . . .
Female service user
. . . ‘psycho’ is such a negative term that we hear all the time, so we don’t want to call it ‘psycho’. It puts people off.
Male carer
Alternatives to the term ‘proxy family’ that emerged from previous groups were discussed and narrowed to nine options (Box 7), which were subsequently taken to the consensus conference for final decision-making.
-
Adopted families.
-
Befriending.
-
Nominated families.
-
Chosen families.
-
Substitute families.
-
Support families.
-
Alternative families.
-
Surrogate families.
-
Family support.
Discussion
We achieved our main aim of demonstrating how an existing evidence-based FI model could be culturally adapted for African-Caribbean people with schizophrenia and related disorders and their families. In doing so, we met our study objectives:
-
partnering with service users, families and clinicians to co-produce a culturally adapted FI for African-Caribbean people
-
identifying components of the therapy manual to support CaFI’s delivery
-
identified preferred client- and family-centred outcomes
-
identified therapist and FSM training needs and how to address them.
Using our cultural adaptation framework, derived from our systematic review of the literature, we presented the current FI model34 and asked focus group participants to:
-
comment on its face validity
-
identify how it could be adapted to meet the culturally specific needs of African-Caribbean people.
It proved feasible to collaborate with key stakeholders to agree key components of the culturally adapted measure. This is important in terms of establishing CaFI’s validity and credibility both within a community that is suspicious of mental health services and among health professionals who would be tasked with its delivery. Although members of the focus groups were able to identify the cultural adaptation elements of the intervention, we are mindful that participants were a self-selected group whose views might not reflect those of other stakeholders. Nevertheless, the successful engagement of service users, their families, community members and health professionals to work together demonstrates the level of commitment to improving mental health care for this group.
Overall, the extant FI model34 was well received. Respondents’ adoption of the current model is in line with previous cultural adaptation studies, which indicate that adaptations that improve cultural specificity versus changes to core components of interventions are required. 61,136
To culturally adapt CaFI for African-Caribbean people, respondents proposed that:
-
the greatest adaptation should be in its ‘ethos of delivery’ and that this would ultimately rely on therapists’ cultural competency and skills
-
culturally adapting the ‘psychoeducation’ component would involve a clear focus on ‘shared learning’ and inclusion of ‘communication and advocacy’, specifically:
-
teaching families how ‘the system’ works
-
enhancing families’ assertiveness and advocacy, to improve communication and interaction with services
-
improving the understanding of the role of the key mental health care professionals and the police
-
increasing service users and carers’ knowledge of available resources and how to access them.
-
Service user and carer participants spontaneously raised the issue of evaluating the intervention, highlighting the need for measures that would facilitate longitudinal data collection to demonstrate change over time. All agreed that, standardised measures (e.g. rating symptoms) notwithstanding, the most important outcome would be rates of relapse and readmission. This makes good sense within a group who are disproportionately admitted as psychiatric inpatients. Given that the rationale for FI is to create more benign family environments, thus reducing family tension and conflict and the risk of relapse, this also seems an eminently suitable outcome to measure in future trials. Although it proved feasible to collect these data, we experienced significant challenges in doing so (see Chapter 6). These included missing ethnicity data and incomplete information as the basis for rating relapse. Given the reduction in bed numbers, hospital admissions may be less valid a measure in current services than previously assumed. The feasibility of these recommendations should be investigated further to inform decisions about the primary and secondary outcomes of future trials.
Respondents indicated that cultural competency should be at the core of therapists’ training to enable them to deliver CaFI. This generated discussion and debate about ‘ethnic matching’ of therapists and families. Citing the lack of ethnic diversity among therapists, participants suggested that ethnic matching was not only impractical but also potentially undesirable. It was felt that all therapists should be trained to deliver culturally appropriate care. Moreover, they suggested that ‘ethnic matching’ demonstrates a lack of awareness of the diversity within, as well as between, groups. Presumed homogeneity based on skin colour or ethnic origin was regarded as erroneous and potentially harmful – especially for a group already disenfranchised within mainstream mental health services.
Conclusion
In summary, we have demonstrated the feasibility of recruiting and partnering with key stakeholders to identify elements of cultural adaptation to be applied to an extant FI model in the consensus conference. To do so, we utilised the literature to develop a cultural adaptation framework (see Chapter 2) and applied it systematically with focus group members in a transparent co-production process designed not only to ensure the cultural specificity of CaFI, but also to establish its credibility among key stakeholders. According to respondents’ accounts, this was crucial for uptake and implementation in services.
Chapter 4 Developing CaFI: a consensus conference
Introduction
We held a 1-day consensus conference, inviting experts by experience and profession to synthesise data from phases 1A and 1B (see Chapters 2 and 3). Through discussion,137 ‘experts’ resolved areas of disagreement considered key to modifying the intervention. 138,139 Consensus was reached on:
Methods
Consensus methods are used in health service research when there is complexity and little previous work. 43 Historically, decisions in health care were made informally, an approach criticised for lack of scientific credibility, rationality and authority. 140 Consensus methods provide a mechanism for improving informal group decisions. 141 There are a number of approaches to building consensus, the most common being (1) Delphi studies,142 (2) nominal group technique143 and (3) consensus development conferences or panels, commonly referred to as ‘consensus conferences’ or ‘expert consensus conferences’. 43
Participant recruitment
Despite ongoing debate about the expertise of experts,144 defining participants by expertise remains an essential feature of consensus methods. 43 A cohort of local, regional and national experts (n = 24) was identified using a range of approaches.
Academics were recruited based on their track record of conducting and publishing national and international research pertaining to African-Caribbean people with schizophrenia and cultural adaptation.
Current and former service users who regarded themselves as being from African-Caribbean backgrounds (‘Black British’ and ‘mixed’ heritage) were recruited from the University of Manchester’s Service User Research Group, ACMHS, MHSCT and service user forums.
Carers and advocates were recruited from a number of Manchester carer forums and third-sector organisations. To ensure as broad a range of consensus as possible, we also recruited members of voice hearing networks and the ‘antipsychiatry’ movement.
Health professionals were identified by their expertise in working with BME groups in general and African-Caribbean people in particular. We specifically involved individuals with expertise in FI.
Police representation was provided by contacting Greater Manchester Police.
Procedures and materials
Interested individuals were provided with the PIS (see Appendix 14) and met with the RPM to determine eligibility, discuss their involvement and address any queries. Individuals were given at least 48 hours to make a decision about their participation before meeting with the RPM to sign a consent form (see Appendix 8 for service user example).
A full-day consensus conference was co-facilitated by the PI, RPM and co-applicant (JB) at the University of Manchester.
The day was divided into three sessions reflecting the emergent themes from focus groups (phase 1B). Accompanying discussions focused on the cultural specificity of the proposed intervention to agree:
-
content
-
outcome
-
delivery.
Findings from phases 1A and 1B were presented to the consensus panel using PowerPoint presentations (see Appendix 15), which also outlined:
-
the rationale for the study
-
the overview of the work conducted to date (phases 1A and 1B)
-
the purpose and structure of the consensus conference
-
an explanation of how ‘consensus’ would be determined.
Turning Point (version 5.3.1., Turning Technologies, Belfast, UK), an interactive audience response system, was used to facilitate data collection. Embedded within the PowerPoint slides, the easy-to-use polling software enabled participants to respond to questions using their handsets (‘clickers’), generating ‘real-time’ data. ‘Real-time’ voting and analysis was chosen in preference to other consensus methods such as the Delphi, which can lack transparency and is comparably slower. 145 As votes were instantly translated into on-screen graphs, they were viewed by participants and used to generate further discussion and resolution when needed (e.g. when ranked items received the same score).
Reflecting our co-production approach, the views of ‘experts by experience’ (service users, carers and the community) were considered as important as expertise by professional standing. 144 Each expert had one vote per item. All votes were considered equal and no individual had a casting vote. Voting ceased when all experts had voted.
Data collection
The findings from the focus groups were presented to the experts for consideration of the extent to which the proposed adaptations would improve the cultural specificity of FI for African-Caribbean people. For each aspect of the intervention, experts were shown the current content of FI alongside the additional elements focus group members identified as key to improving its cultural specificity (see Chapter 3). Consensus was reached via two methods: (1) discussion and (2) subsequent voting.
Discussion
Discussion, occurring in small groups of four to six and two larger groups (each comprising half the participants), preceded each round of voting. Small groups were a means of ensuring that dissenting and less dominant voices were enabled to contribute and to identify important issues that might have not previously been considered. Group discussions were recorded, transcribed and later revisited by the research teams to ensure that stakeholders’ disagreements and the process of resolution were documented. During discussions, participants were asked to record important items about cultural adaptation that were missing from those identified by focus groups via a series of Post-it® notes (3M, Berkshire, UK). Thirty-four Post-it notes were collected and discussed to determine whether or not they should be added to those generated from phase 1B prior to consensus being sought on agreed items.
Voting
Voting followed each round of discussion. Participants rated their responses to items that emerged from the focus groups and literature by ranking, ‘yes/no’ responses, or on seven-point Likert scales. In relation to Likert scaling, we decided to include a ‘neutral’ mid-point to enable voting by participants who did not feel strongly about a topic. 146 Votes were presented back to the experts via graphical representation (bar charts), displaying numbers and percentages embedded within the PowerPoint. The presentation (see Appendix 15) was saved to capture votes for further analysis.
To familiarise participants with the voting system and stimulate discussion, we commenced the day by asking participants to vote ‘true/false’ in relation to the statement, ‘[T]here’s no such thing as African-Caribbean culture’.
Data analysis
As consensus does not necessarily denote full agreement,43 we agreed that consensus would constitute ‘near-unanimous agreement’ achieved by:
Results
Participants
The final sample comprised 22 experts (24 were recruited but two were unable to attend on the day). Participants included ‘experts by experience’ [services users and carers (n = 5); carers and advocates (n = 9), including the third sector and church] and ‘experts by profession’ [(n = 7) including academics, police, health professionals and service managers with expertise in schizophrenia in the African-Caribbean population].
Cultural specificity
Table 1 shows that experts achieved near-unanimous consensus (between 81% and 95%) that all items generated by the focus groups and the literature would improve the cultural specificity of CaFI for African-Caribbean people: specifically, its content, outcome and delivery.
| CaFI component | Response, % (n) | Missing data, % (n) | ||||||
|---|---|---|---|---|---|---|---|---|
| Strongly agree | Agree | Somewhat agree | Neutral | Somewhat disagree | Disagree | Strongly disagree | ||
| Service user assessment (four sections) | ||||||||
| Current and past episode of illness | 40.9 (9) | 18.1 (4) | (0) | 4.5 (1) | (0) | 4.5 (1) | (0) | 31.8 (7) |
| Functioning | 45.4 (10) | 27.2 (6) | 4.5 (1) | 4.5 (1) | (0) | 4.5 (1) | (0) | 13.6 (3) |
| Strengths and resources | 54.5 (12) | 22.7 (5) | (0) | 4.5 (1) | (0) | (0) | (0) | 18.1 (4) |
| Relationships | 54.5 (12) | 22.7 (5) | 4.5 (1) | 9 (2) | (0) | (0) | (0) | 9 (2) |
| Family assessment | 36.3 (8) | 45.4 (10) | 4.5 (1) | 9 (2) | 4.5 (1) | (0) | (0) | – (0) |
| Stress management, problem-solving and coping | 54.5 (12) | 31.8 (7) | 4.5 (1) | 4.5 (1) | 4.5 (1) | (0) | (0) | – (0) |
Content
Service user assessment
Table 1 shows that consensus of between 85% and 95% was reached that all proposed additional items would improve the model’s cultural appropriateness. The highest level of agreement was in relation to ‘strengths and resources’, on which 67% of experts ‘strongly agreed’ and a further 28% ‘agreed’ that the items presented would make CaFI culturally specific for African-Caribbean people. There was no disagreement, with one individual (5%) recorded as ‘neutral’.
Family assessment
This item yielded the greatest dispersion of views. One expert ‘agreed somewhat’, two were ‘neutral’ and one ‘disagreed’ that the proposed adaptation would make this aspect of the intervention more culturally appropriate. This reflects experts’ discussions in which participants stated that issues such as family structure and hierarchy, causes of family tension (blame, criticism, rivalry) and previous experiences of services were common to all ethnic groups. However, consensus was reached that the suggested items were sufficiently specific to African-Caribbean families to warrant their inclusion (81% agreement).
Psychoeducation
This aspect of FI generated the greatest number of recommended additional items from the focus groups (eight in total). Items considered especially relevant for African-Caribbean people included:
-
better understanding of how the mental health ‘system’ works
-
information about rights in relation to police involvement
-
effects of stigma (within families, communities and wider society)
-
challenging stereotypes and misconceptions
-
understanding psychotropic medication – how it works, side effects
-
understanding the relationship with illicit drug use and medication/illness progression
-
culturally specific models of mental illness
-
better awareness of available resources (community and NHS).
Experts ranked these items numerically so that those ranked more important were assigned higher numbers. The cumulative value of rankings for each of the content areas is represented in Figure 3 by the weighted count. Figure 3 shows that items were ranked fairly evenly, with ‘how the “system” works’ (15%), ‘models of illness’ (15%) and ‘medication’ (14%) rated the top three most important aspects of psychoeducation in CaFI. Illicit drug use (8%) was ranked lowest.
FIGURE 3.
Ranked importance of additional ‘psychoeducation’ content.
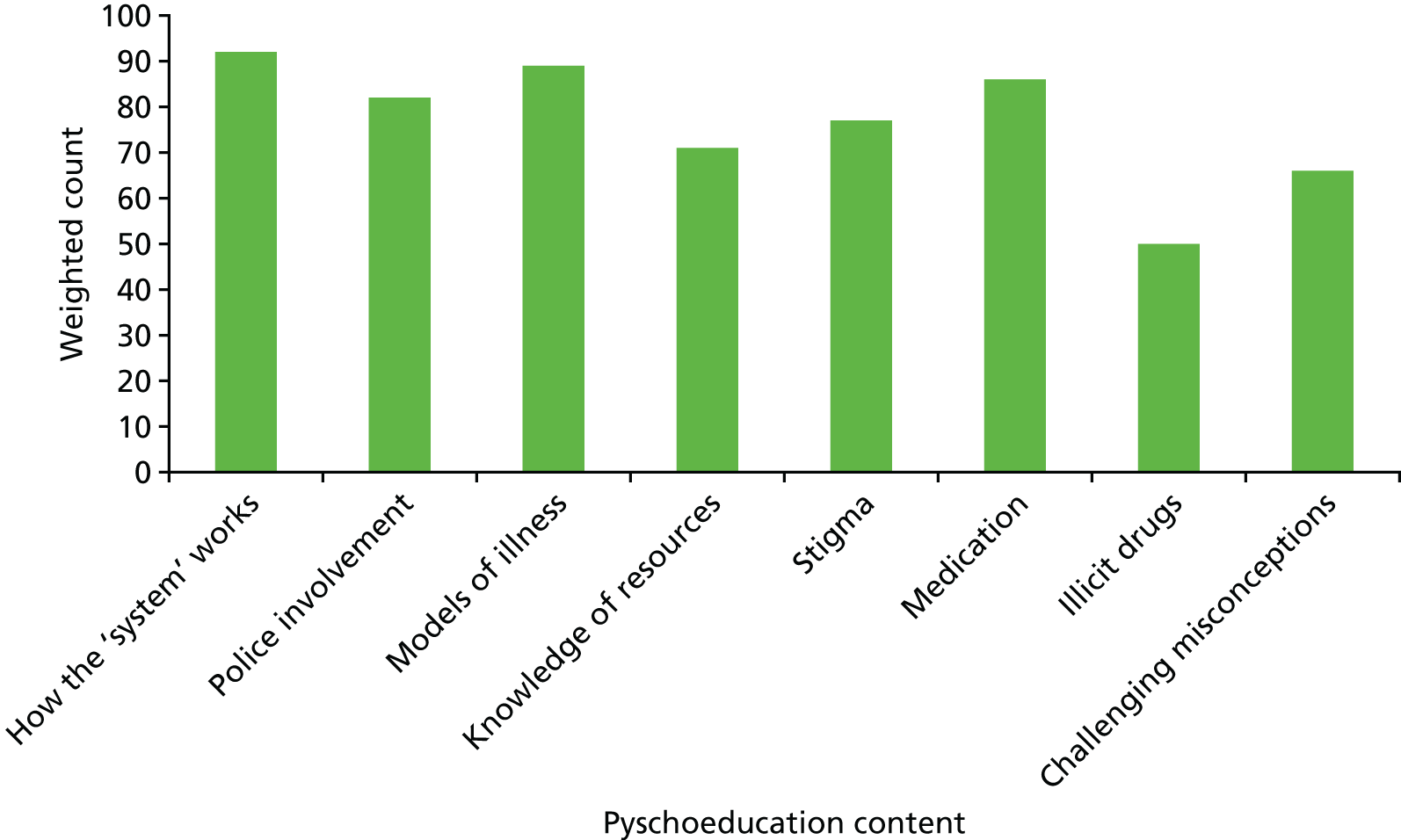
Focus group members indicated a strong dislike of the term ‘psychoeducation’. Experts chose ‘shared learning’ (Figure 4) from the available options (6 out of 21 voters, 29%). As ‘mental (ill) health awareness’ was voted a close second (5 out of 21 voters, 24%), further discussion ensued from which shared learning received the most votes by a show of hands (n = 15).
FIGURE 4.
Votes for preferred alternatives to psychoeducation.
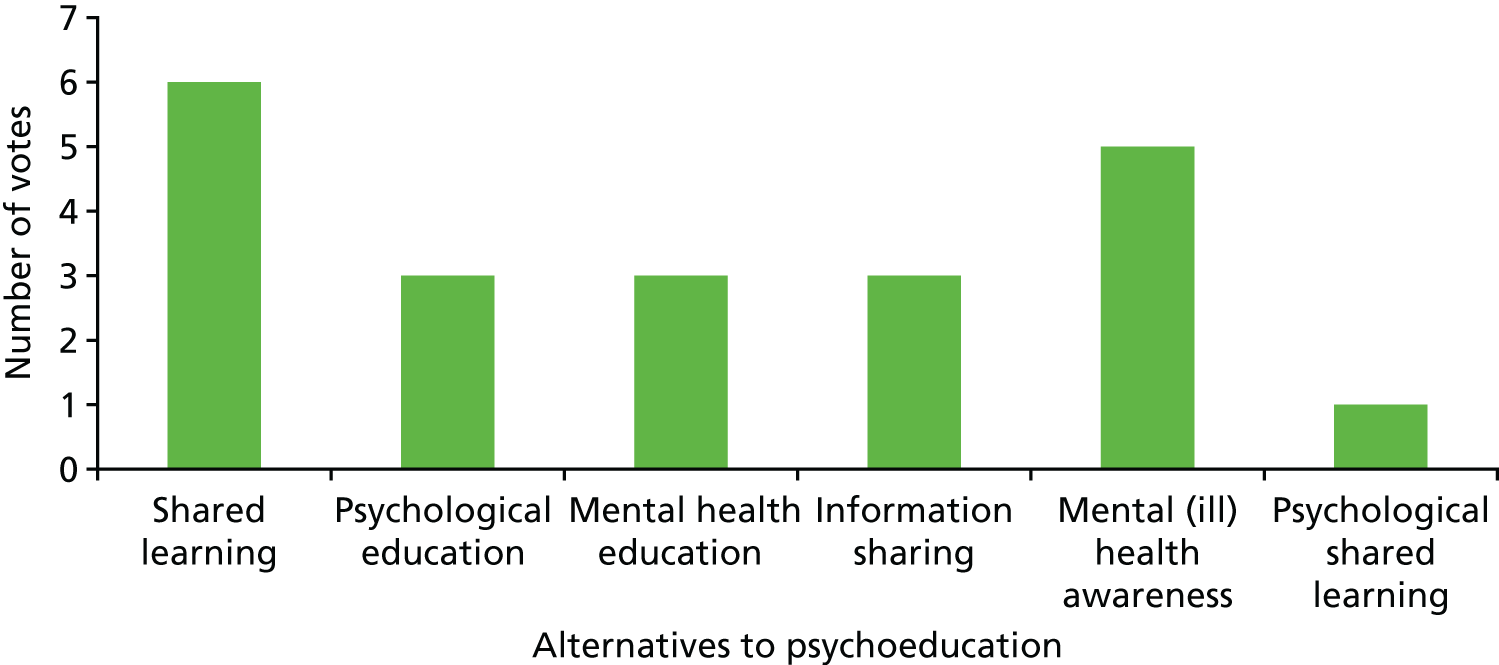
Stress management and coping
Additional items identified in phase 1B included managing conflict between service users and relatives (specifically in relation to ‘sectioning’) and between families and health-care professionals. Carers’ rights and responsibilities, as well as acknowledging carer burden and the fact that some people are simultaneously service users and carers, were regarded as important additions. Relapse prevention, crisis planning and developing more positive ways of coping were also suggested. There was 87% agreement among experts that these items would improve cultural relevance for African-Caribbean people.
Problem-solving and goal-planning
Experts were shown the diagram used to illustrate the 10 steps that service users, families and therapists work through to identify problems, goals and rewards (Table 2). As with focus group members, experts agreed that this was a good model. They also agreed that additional items, such as contingency planning, highlighting resources and focusing on progress versus failure, were important. In relation to the latter, celebrating success along the ‘journey’ to acknowledge even small steps was suggested as an important means of maintaining focus and momentum.
| Session number | Session content |
|---|---|
| 1 and 2 | Engagement and assessment |
| 3 and 4 | Shared learning |
| 5 and 6 | Communication |
| 7 and 8 | Stress-management, coping and problem-solving |
| 9 and 10 | Staying well and maintaining gains |
Although focus group members endorsed Specific, Measurable, Achievable, Realistic and Timely (SMART) goals, experts recommended they should be made ‘SMARTER’ by adding ‘Evaluated’ and ‘Rewarded’. It was agreed that evaluating and rewarding goals should occur on a session-by-session basis, accompanied by evaluation of goal achievement against between-session tasks. End-of-therapy evaluation was regarded as important for reviewing and agreeing how to maintain gains.
At the end of this process, agreement was reached through discussion that the content of the 10 CaFI sessions would be as outlined in Table 2. However, in line with good clinical practice, experts highlighted that this should not be regarded as a linear process. Rather, the order and pace of delivery should reflect the needs of individual service users and their families.
Outcomes
Focus group members identified 10 desired outcomes. For CaFI, the top five outcomes were ranked as ‘better familial relationships’, ‘health and well-being’, ‘social functioning’, ‘reduction in relapse and readmission’ and ‘relatives’ positive attributions and attitudes towards illness’. As shown in Figure 5, several of the outcomes had similar weighted counts, indicating that most were deemed important by experts. This is reflected in this quote from one expert about the difficulty of ranking inter-related items:
I’m a bit torn between ‘social functioning’ . . . and also ‘coping with stress’ because I think with these topics some of them go hand-in-hand. But I think coping with stress is fundamental to staying well and hopefully not becoming unwell again, not being readmitted and also with activity and how you’re doing on a day-to-day basis so I don’t know which one’s [to rank] one and two really.
FIGURE 5.
Ranked importance of potential outcomes from the CaFI.
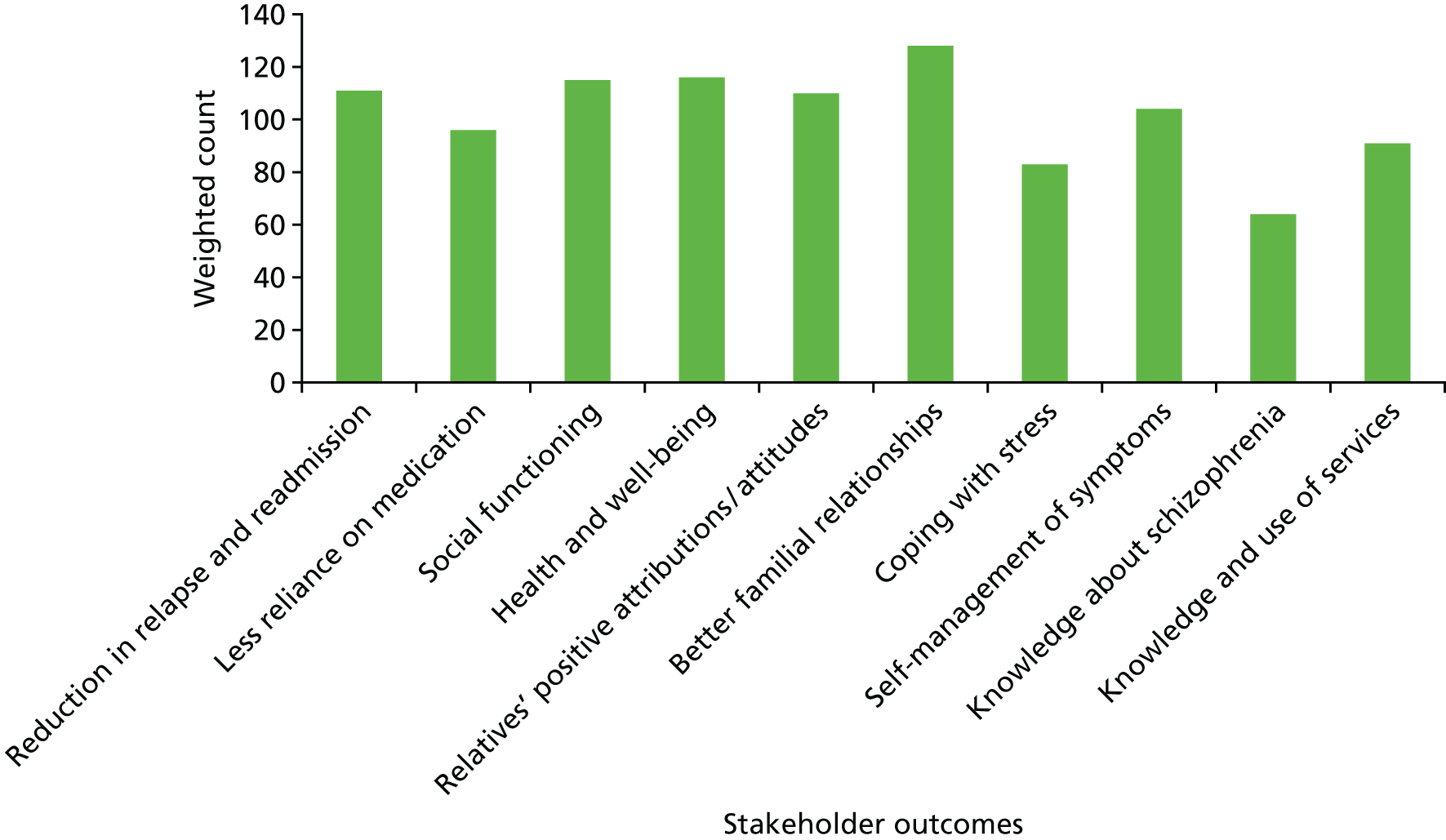
‘Knowledge about schizophrenia’ received the lowest ranking. Although some experts felt that this was an important outcome to measure, others disagreed:
The problem that I have with this is that it implies that if you rank something 10 or whatever it implies that you have fairly neutral feelings about it. I would actually positively object to knowledge about schizophrenia being an outcome measure in a study like this . . .
Following further discussion, experts agreed that in future studies, to examine CaFI’s effectiveness, ‘reduction in relapse and readmission’ should be a primary outcome and ‘relatives’ attributions and attitudes’ a secondary outcome. Interestingly, although originally ranked last, ‘knowledge about schizophrenia’ was agreed to be an important outcome that should be considered, with the proviso that a culturally valid version would be developed.
Delivery
In the final consensus conference session, experts were tasked with agreeing:
-
how best to adapt the delivery (vs. content) of FI to ensure that it suited the needs of African-Caribbean people
-
key approaches to supporting delivery of the intervention
-
training needs of therapists and ‘proxy family’ members.
Experts agreed that these three objectives were inextricably linked. Consequently, much of their discussion focused on CaFI’s ‘ethos of delivery’ and therapists’ ability to establish and maintain therapeutic relationships with members of this community in the context of a history of fear and mistrust of services.
‘Ethos of delivery’
Revisiting earlier discussion about ‘psychoeducation’, experts endorsed the overarching ethos of delivery as one of ‘shared learning’. Building on focus group discussions, they agreed that ‘shared learning’ must be a ‘three-way process’, involving service users, carers and therapists in mutual exchange of information. Experts agreed that the main aims of CaFI should be:
-
facilitating positive family relationships/interactions that enhance mental well-being for relatives and service users
-
enabling families to optimise interactions with services to foster engagement, thereby improving access, experiences and outcomes.
To achieve these aims, experts concluded that therapists must work collaboratively with families to realise the following related objectives, as detailed in the therapy manual (see Appendix 16):
-
develop more helpful explanations for symptoms (e.g. viewing service users’ experiences as ‘symptoms’ of mental illness vs. ‘deviance’)
-
facilitate better communication in the family (e.g. improve active listening)
-
develop more effective coping and stress management strategies, including self-monitoring
-
improve problem-solving skills using appropriate tools and resources (e.g. case studies and vignettes, exemplars from a weekly report from family)
-
promote recovery and relapse prevention, including identifying ‘relapse signature’
-
improve understanding of how ‘the system’ works and strategies for engaging and communicating with mental health services and partner agencies
-
promote strategies for engaging and communicating with mental health services and partner agencies.
Therapists’ cultural awareness, knowledge and skills
Although all items in Box 8 were regarded as important for delivering CaFI, experts agreed that a crucial aspect of delivery would be therapists’ cultural awareness and insights into the potential impact on engagement and alliance of their:
-
background (e.g. ethnicity, faith, social class, sexual orientation)
-
beliefs (potential misconceptions about ‘African-Caribbean culture’)
-
experiences (e.g. working transculturally).
-
Ethos: focus on ‘wellness’.
-
Therapists’ cultural awareness.
-
Therapeutic relationship – power balance and building trust.
-
Illness models/spirituality and belief systems.
-
Shame and stigma.
-
Family dynamics and structure.
-
Social networks and significant others.
-
Help-seeking and care pathways.
-
Importance of choice and flexibility (vs. resources).
-
Language and communication.
This led some experts to suggest that therapists should have personal experience of African-Caribbean communities either as members themselves or through close personal contacts:
The first thing is to recruit therapists from the community, that’s the first thing. The second thing is if you’re not recruiting therapists from the community, to recruit therapists who have personal experience in the community or they have friends . . .
Academic professor
There were, however, dissenting voices. Some experts felt strongly that all therapists should be equipped to work with any individual, irrespective of their background versus ‘training up’ individuals to work with particular groups:
I find it offensive that we’re in this day and age and you think that only certain groups of people need to be aware of the groups of people that they’re working with. Large numbers of Black and minority ethnic groups are in mental health services so therefore it’s everyone’s responsibility.
Health-care professional (emphasis in bold)
Others suggested that an important aspect of a ‘shared learning’ approach would be enabling African-Caribbean people to raise White professionals’ awareness of the impact of additional dimensions of power (rooted in the historic legacy of colonialism and slavery) on the therapeutic relationship when working with African-Caribbean clients:
I think in terms of experiential work people from Black communities [we] have a very important role in changing the sensitivities of White professionals who may well not be aware of the power implications and the power differentials and how those are sedimented historically in our shared histories of colonialism and all the rest of it.
Advocate
Therapist training
As with focus group members, experts felt that a prerequisite for working with this community was having high levels of skill and expertise in family work, as the issues being brought to therapy were likely to be complex and potentially deeply ingrained because of long delays in receiving care and negative experiences.
Cultural competence training would be required to ensure therapists develop the confidence to explore issues that affect members of this community, such as racism and discrimination, which some therapists might find personally challenging. Training should address both contemporary and historical aspects that affect this community. These include the history and heterogeneity of the Caribbean islands as well as patterns of migration. In addition, knowledge and awareness of disproportionately high rates of schizophrenia diagnosis (and related theories), together with reports of negative experiences and outcomes for African-Caribbean people, were regarded as vital to enable therapists to understand the high levels of mistrust within this community and to work effectively to develop trusting relationships with families.
When asked how therapists should be trained, experts suggested that bespoke training needed to be commissioned as few mainstream NHS therapists would have the cultural competency required. They advocated the involvement of service users and carers in designing and delivering the training. It was acknowledged that it would be difficult to evaluate the effectiveness of such training in the absence of a cultural competence framework. They endorsed our proposed fidelity study (see Chapter 6, Fidelity study) and the collection of qualitative data from the perspectives of service users, family members and ‘proxy’ family members and therapists.
Family support member/’proxy family’ training
Experts concluded that the purpose of training (see Chapter 5, Family support members) for ‘proxy family’ members was not to develop expert knowledge in psychosis and schizophrenia. Instead, it was agreed that a basic introduction to serious mental illness in general and to schizophrenia in particular was appropriate because many family members had at least some knowledge about mental illness. Furthermore, it was felt that this level of knowledge was required for interested individuals to make informed choices about becoming FSMs (‘proxy family’ members).
In addition, experts suggested that FSM training should focus on key aspects of governance (e.g. confidentiality, health and safety) and measures to safeguard their own mental health and well-being, alongside clarifying the scope and nature of the role and boundary-setting.
Evaluation of consensus conference
Amorphous processes such as consensus conferences may achieve high degrees of statistical consensus without reaching ‘genuine agreement’. 149 Understanding the differing positions and degrees of polarisation/agreement between experts by experience versus profession may be more significant than statistical consensus. 150 We were unable to explore such differences on the day. Providing a period of discussion prior to voting enabled ‘outliers’ to voice their views and ensured that dissenters did not withdraw from the process. 151,152 Nevertheless, it is possible that items achieving statistical consensus represented the safer ‘middle ground’ of opinion. Using predetermined questions/items based on findings from the literature review and focus groups might have made disagreement difficult for some members of the conference.
Feedback and evaluation indicate that this was not the case here. At the end of the consensus conference, we asked participants if they had been able to contribute to consensus-making. Of the 16 evaluations returned, 94% (n = 15) agreed/strongly agreed that they had ‘been able to contribute views and ideas’, that ‘their views had been heard and valued’ and that the ‘people here today were the right group to develop talking therapy for African-Caribbean people’. When asked whether or not any other voices should have been included, 50% agreed/strongly agreed and 43.8% disagreed. Participants suggested that there should have been greater involvement of the criminal justice system and psychiatry. Both groups were represented on the day. This may reflect our decision to use only first names (vs. professional titles or labels) to reduce social distance between conference members and minimise the influence of social and professional hierarchies.
Discussion and conclusions
Our expert consensus conference marked the culmination of a process involving three inter-related studies to determine how to adapt FI to increase its cultural specificity for African-Caribbean service users diagnosed with schizophrenia and their families. This is important because, although previous studies had identified components of the cultural adaptation process, none had identified how these should be applied.
Having identified essential components of cultural adaptation, we applied them systematically to the content of an existing FI model, seeking key stakeholders’ views about what was needed to improve its cultural specificity for African-Caribbean people. Findings from current literature (phase 1A) and focus groups (phase 1B) were synthesised and presented to a range of experts in a specially convened consensus conference in which they agreed the content, outcome measures and mode of delivery of our CaFI. These experts by experience and profession achieved robust consensus (≥ 80% agreement) on all aspects on the intervention.
A central feature of this co-production approach was achieving genuine service user and community engagement and ‘buy-in’ to the process of developing CaFI. This was a significant achievement given the endemic barriers to fear, mistrust and lack of engagement153 within this community. It was important that the panel included African-Caribbean ‘experts by profession’ such as psychologists, counsellors, psychotherapists, RMNs and voluntary sector organisations. We also invited those with ‘antipsychiatry’ views and members of voice-hearing networks to ensure that consensus reflected the widest possible range of stakeholder perspectives.
Participants were indeed very robust in sharing their views, particularly in relation to the validity of concepts like ‘schizophrenia’. Other areas of contention concerned questions about the pros and cons of ‘ethnic matching’ of therapists and families and whether or not training therapists in ‘cultural competency’ is achievable. Participants debated the value of endorsing such concepts in the absence of frameworks to evaluate them. These discussions and the fact that we were able to resolve them through debate, demonstrate our success in managing difference to achieve genuine consensus on key CaFI deliverables. Specifically, we:
-
agreed content of CaFI and the basis of the therapy manual to support its delivery (see Appendix 16 for summary of therapy components)
-
identified primary, secondary and other desired outcomes
-
identified training needs of therapists and ‘family support’ members as the basis for co-producing bespoke training with service users and carers.
The cultural adaptation process we have described was undertaken with African-Caribbean service users, families and community members in collaboration with health-care professionals. Our approach has significance for developing interventions with other marginalised communities. Co-producing interventions with, versus for, marginalised groups has the potential to reduce barriers to mistrust and improve uptake and engagement of evidence-based care, thus reducing inequalities.
Chapter 5 Therapist and family support member training
Introduction
This chapter reports the recruitment and training of therapists to deliver CaFI (phase 2). We also report the recruitment and training of FSMs. These were service user peers and community volunteers who worked alongside service users wishing to receive CaFI, but who were unable to nominate family members to participate with them.
Aims and objectives
Phase 2 study objective
To address the training needs of therapists and FSMs identified during phases 1B (focus groups) (Box 9) and 1C (expert consensus conference) (Box 10).
-
High levels of skill and expertise in family work to enable them to manage complex and potentially deeply ingrained needs and problems.
-
Cultural competence training to develop the confidence to explore sensitive and potentially personally challenging issues such as racism and discrimination.
-
Awareness and understanding of contemporary and historical factors that affect the African-Caribbean community in the UK, including patterns of migration.
-
Knowledge and awareness of the evidence base related to schizophrenia and African-Caribbean people, such as:
-
disproportionately high rates of schizophrenia diagnosis
-
reports of negative experiences and outcomes for African-Caribbean people.
-
-
Basic introduction to SMIs in general and schizophrenia in particular.
-
Clinical governance issues such as confidentiality and health and safety.
-
Clarifying the scope and nature of the FSM role and boundary-setting.
-
Safeguarding their own mental health and well-being.
-
Mechanisms for therapist pairs to support one another and work together.
-
Ways to learn about a person’s culture and demonstrate cultural competency.
-
Knowledge about carer assessments and support for carers.
-
Managing the definition and misconception of ‘carer’.
-
Referring service users who are on your clinical team or caseload.
-
Explaining the difference between research and therapy to families.
-
How to build trust in a relatively short intervention.
-
How to end the therapeutic relationship after ten sessions.
-
How to keep the family engaged and manage disengagement.
-
How to manage individual and shared family assessments in 10 sessions.
-
How to work with and involve FSMs during the sessions.
-
How to deliver all (relevant) material in 10 sessions.
-
How to be flexible but maintain fidelity to the manual.
-
How to manage service user in care management/service (e.g. acute to community).
-
How to encourage the family to generalise and use skills outside sessions.
Therapist training
As recommended by consensus conference experts [phase 1C (see Chapter 4)], we developed bespoke training programmes in collaboration with Just Psychology44 and Meriden Family Programme45,154 to address therapists’ and FSMs’ training needs:
-
‘Cultural competency’ training for both therapists and FSMs was delivered by Just Psychology, a Manchester-based Community Interest Company specialising in the delivery of culturally sensitive training and psychological therapy.
-
We commissioned Meriden Family Programme to provide additional training for CaFI therapists only in ‘FIs and cultural competence’. Meriden Family Work Programme is:Mission statement, 2009. Reproduced with permission155
-
. . . a training and organisational development programme, which has been promoting the development of family-sensitive, evidence-based mental health services since 1998.
-
The overall aim of the Programme is to ensure that service users and families have access to family sensitive services and evidence based interventions. This is achieved by training clinical staff, service users and carers in the skills needed to work with families, and to ensure that workers are able to implement these interventions following receipt of training through influencing management and creating a supportive host culture in the organisation.
-
As NICE advocate cultural competence training at both organisational and individual levels, we also delivered a 1-day ‘cultural competency’ workshop to health and social care professionals working in acute, rehabilitation and community services at MHSCT. This afforded opportunities to engender cultural awareness at the trust and promote the study within the participating clinical teams.
Training content
Cultural competency and family work
Key components of the training delivered by Just Psychology and the Meriden Family Programme included:
-
core competences to work effectively with families experiencing schizophrenia and psychosis156
-
current legislation and how it relates to clinical practice (such as The Equality Act in 2010,132 Protected Characteristics132, NHS Knowledge Skills Framework157 and Public Sector Equality Duty132)
-
cultural awareness and family work practice (e.g. the potential impact of culture and family experience on CaFI’s delivery)
-
relationship between racism, discrimination, adversity and mental illness
-
effect of power and prejudice in building trusting therapeutic relationships.
Throughout the training programme, the RPM recorded therapists’ perceptions of additional training needs and specific competencies for delivering CaFI (see Box 10). These were used to enhance training in using the CaFI therapy manual. Therapists were also asked to note any learning outcomes that they felt had not been achieved during training so that they could be addressed in supervision where necessary.
CaFI manual
Therapists received half-day training in the delivery of the CaFI manual facilitated by the research team (PI, RPM and clinical supervisor), including:
-
the background/context of CaFI, including an introduction to the historical, cultural and social context of African-Caribbean mental health in the UK and the rationale for developing CaFI
-
a research protocol to familiarise therapists with the development of CaFI and the feasibility trial
-
delivering therapy in research and versus clinical settings
-
CaFI’s ‘ethos of delivery’
-
CaFI sessions/components and related resources (including in-session tasks/activities, homework)
-
practical considerations relating to supervision and the delivery of CaFI.
(See Appendix 17 for training slides.)
All therapists were provided hardcopies of the CaFI manual and resources. We also developed a therapy research protocol (see Edge et al. 158) to provide information and guidance on:
-
CaFI outcome measures
-
therapy session measures (feedback sheets, therapeutic alliance)
-
supervision and fidelity to the manual
-
CaFI therapy files (manual contents and resources for data management and storage).
Supervision
All therapists received hourly supervision fortnightly with lead and co-therapist pairs by the same supervisor who was a member of the RMG and was involved in the development of the therapy manual and therapist training in the manual. The supervisor was a clinical psychologist, accredited CBT therapist and experienced trial therapist in psychological therapy for SMI and in the supervision of psychological therapists in the NHS. A significant part of supervision focused on adherence to the model and manual. The research team (PI, RPM and clinical supervisor) also facilitated two group supervision sessions for therapists to share good practice and to discuss and problem-solve common issues/barriers relating to delivering the sessions.
Therapist recruitment
First wave of recruitment
We recruited three therapist dyads [lead therapist (NHS Agenda for Change band 7) and co-therapists (NHS band 4)] to deliver up to 300 hours of therapy to 30 families (30 × 10-hourly sessions) across acute, rehab and community settings over a 12-month intervention period. Our original proposal was to recruit clinical psychologists as lead therapists. Unable to do so within our host NHS trust, we recruited lead therapists with experience of family work within the trust, comprising one social worker and two OTs working in CMHTs and rehabilitation units. Each had undertaken training in a CBT-based model of FI which we had culturally adapted through training in advanced psychosocial interventions for psychosis. Co-therapists comprised two support workers and an assistant psychologist, all working in CMHTs. Therapists delivered CaFI as part of their current caseload at MHSCT, thus allowing us to explore the feasibility of embedding CaFI within the mainstream services.
Second wave of recruitment
The host trust, MHSCT, underwent considerable financial and service upheaval during the study, which affected the job roles and workloads of a significant number of staff. By the end of the study, MHSCT had merged with Greater Manchester West NHS Foundation Trust (GMW) to form Greater Manchester Mental Health NHS Foundation Trust.
Although it had been agreed with managers that therapists would be released for one clinical session per week (4 hours/half-day) to undertake the CaFI work, this proved to be difficult. In practice, therapists were attempting to deliver CaFI alongside their caseload due to staff pressures. They reported lacking the capacity to manage an increased caseload and deliver the 10 CaFI sessions within the agreed therapy window of 20 weeks.
Having successfully recruited service users and families to the feasibility trial (phase 3; see Chapter 6), somewhat ironically, we had to slow recruitment from this ‘hard-to-reach’ group due to therapists’ lack of capacity, creating a waiting list. Mindful that delays in accessing CaFI could reinforce negative perceptions of services resulting in the disengagement and withdrawal, we undertook the following actions:
-
facilitated group supervision to better understand the factors contributing to a lack of capacity and how best we could support therapists to continue delivering CaFI
-
recruited additional therapists from other Greater Manchester NHS trusts to deliver CaFI to service users on the waiting list
-
extended the recruitment and intervention period to enable service users on the waiting list to receive CaFI
-
extended recruitment to a neighbouring trust (GMW) to explore the feasibility of rolling CaFI out at an alternative site.
Six months into the intervention period, we recruited four additional lead therapists and four co-therapists to support the delivery of CaFI to people on the waiting list. The lead therapists comprised three clinical psychologists working in three different Greater Manchester NHS trusts (GMW, Pennine Care NHS Foundation Trust and Central Manchester University Hospitals NHS Foundation Trust) and one mental health nurse/clinical practice lead in a MHSCT rehab unit who had received training in advanced psychosocial interventions for psychosis. The four co-therapists comprised an assistant psychologist, two support workers and one postgraduate researcher (delivering FI to parents experiencing psychosis as part of doctoral study).
The second wave of therapists received copies of the manual and supporting materials. They also received training in using the manual from the research team. Owing to time and other resource constraints, they did not complete the Just Psychology and Meriden Family Programme training programmes. Instead, therapists were provided with copies of all training materials and listened to audio-recordings of the training sessions.
Family support members
Recruitment
We successfully recruited 13 FSMs as a result of our extensive engagement and publicity strategies during study phases 1 and 2. Advertisement was conducted via the community launch events, local media (community radio, newspaper), distributing posters/flyers (see Appendix 18), and delivering presentations at local third-sector organisations and locations frequented by large numbers of African-Caribbean people, such as ‘Black-majority churches’. Recruitment materials provided contact details of the research team. Potential FSMs met with the research team for an informal interview to determine their suitability for the role and were fully briefed about the study. The RPM worked through the PIS (see Appendix 19) with the FSMs before obtaining informed consent to participate. Nine out of the 13 recruited FSMs took part in the feasibility study (see Chapter 6, Results for FSM sample characteristics).
Training content
To address the training needs of FSMs, we developed a bespoke training programme based on key components identified during phase 1 (see Box 9) and drew on expertise within the research and training teams.
Family support members completed a Disclosure and Barring Service and other relevant checks (e.g. MHSCT’s confidentiality agreement, occupational health), in line with NHS policies and procedures for working with service users at trust sites. FSMs received 1-day ‘cultural competency’ training delivered by Just Psychology. Key components of the training included developing awareness and understanding of:
-
schizophrenia and psychosis, and specific issues affecting African-Caribbean people
-
diversity in African-Caribbean cultures
-
the impact of racism and discrimination on mental health
-
mental health legislation, including The Equality Act (2010)132
-
how to build relationships with family members
-
how to build relationships with staff.
Family support members received an additional 2-hour training session facilitated by the research team (PI and RPM), which comprised:
-
background/context of CaFI
-
CaFI research protocol
-
practical considerations relating to the FSM role
-
expectations and skills/qualities for FSM role
-
supervision and peer (FSM) support.
Supervision
As FSMs were essentially volunteers and included former service users, it was important that they were provided with strategies for accessing support and retaining appropriate boundaries. FSMs received monthly group supervision from the clinical supervisor (KB) to share their experiences and discuss any concerns, barriers or risk issues relating to supporting the service user through the intervention. FSMs also had the opportunity to contact or meet with the clinical supervisor independently between these sessions. During the initial CaFI session, therapists were required to agree on the boundaries and expectations of the FSM–service user relationship in collaboration with the FSM and the service user.
Clinical teams
Cultural competency workshop
To increase cultural awareness within the trust, CaFI co-applicant and internationally leading expert on mental health and diversity, Professor Dinesh Bhugra, delivered a 2-hour ‘cultural competency workshop’ to health-care professionals working in the participating teams at MHSCT. The aim was to facilitate organisational change by increasing staff confidence in working effectively with service users from different cultural backgrounds. The event was also used as a vehicle to raise awareness of and promote recruitment for the CaFI study.
We originally planned to conduct three separate workshops within individual teams but this was impeded by the limited capacity of individual teams to host such events. Anecdotal feedback from trust staff suggested that facilitating one larger event with a keynote speaker would be more appropriate and would maximise attendance.
Staff participation
Key trust staff and service leads were invited to attend through targeted e-mails to ensure that the training was delivered to provide the greatest impact at MHSCT. Out of the 30 people who registered, 17 attended; we received two apologies for absences due to unforeseeable circumstances on the day. The remaining 11 people did not attend despite e-mail prompts leading up to the event asking delegates to give up their places to people on the waiting list if they were no longer able to attend. Attendees were three service managers, one consultant mental health nurse, two psychiatrists, two clinical psychologists, one OT, one assistant psychologist, five social workers, one Professor of Mental Health Nursing and one R&D staff member.
Training evaluation
Meriden Family Programme training
Method
Five therapists (first wave of recruitment; see Training content) attended and evaluated the Meriden Family Programme training day. Evaluation forms were completed at the end of the day (see Appendix 20).
Results
All therapists rated both the content and presentation of the training as excellent on a five-point Likert scale from zero (very poor/inadequate) to four (excellent). General written feedback included positive comments on:
-
the usefulness of sharing personal accounts and experiences of family work in practice
-
the clear and comprehensive presentation and user-friendly handouts
-
the relevance of the training despite differences in the model used [behavioural family management (BFM) vs. CBT] and that attendance at the Meriden Family Programme week-long course would have been helpful.
Just Psychology cultural competency training
Method
Six therapists (first wave of recruitment; see Training content) and nine FSMs attended and evaluated the cultural competency training. Questionnaires were completed before and after training days to assess change in self-reported knowledge and confidence relating to the training content. Different questionnaires were developed for FSMs (see Appendix 21) and therapists (see Appendix 22) to reflect the different topic areas and role requirements.
Family support members were asked to rate their knowledge and understanding of:
-
schizophrenia and psychoses
-
issues relating to mental health care for African-Caribbean people in the African-Caribbean culture
-
the impact of racism/discrimination on mental health
-
developing supportive relationships and boundaries with service users and staff
-
sources of support for themselves and service users.
They were also required to rate their confidence in:
-
working effectively with African-Caribbean service users
-
discussing issues relating to ethnicity, racism or discrimination with service users, family members or staff.
Therapist questionnaires included two of the above seven items (four and seven) and additional items to rate their:
-
confidence in their ability to build therapeutic relationships with African-Caribbean service users and families
-
awareness and knowledge of ‘cultural competence’ and how it relates to their work.
These items were rated on 11-point Likert scales from zero (‘not very good’) to 10 (‘excellent’). Finally, in the post-training questionnaires, both FSM and therapist attendees were asked to rate the training in terms of:
-
content
-
presentation
-
level of difficulty.
Participants were also asked to provide written open-ended feedback about what they liked/did not like about the training and suggestions for future training events.
Results
Both therapist and FSM training days were evaluated favourably by attendees in terms of the content, delivery and level of understanding. Comparisons of pre- and post-questionnaire scores suggested that the training was beneficial in increasing cultural awareness, with scores on all items increasing for both FSM and therapist groups. Positive written feedback included:
-
the interactive nature of the sessions
-
sharing personal stories
-
skilled trainers and the training resources used.
Negative feedback related to overdominant voices and lack of practical skills with service users. Suggestions included delivering the training over 2 days (rather than 1 day), to allow more in-depth discussion for each of the topics. The Just Psychology trainers commented on the varied levels of knowledge and experience within each of the groups, which was reflected in contradictory feedback about the content and pace of the training. Recommendations from the Just Psychology evaluation report (see Appendix 23) included facilitating reflective supervision, peer support and further ‘on-the-job’ training.
Research team training
Method
Following the therapist and FSM training delivered by the research team, attendees were asked to complete a short five-item evaluation form. This consisted of two closed-response questions in which attendees were asked to rate the training, in terms of the quality of the presentation and information, on a scale of one (‘very poor’) to five (‘very good’), followed by three open-response questions which asked attendees to record what aspects of the training were useful, what improvements could be made and any additional comments. A second measure asked attendees to rate (on a scale of 1–10) how confident they felt undertaking their role as therapists or FSMs in the delivery of CaFI, where one was ‘not confident at all’ and 10 was ‘very confident’.
Results
Therapists
All six therapists completed the evaluation forms. The feedback for the therapist training was positive, with attendees rating the quality of the presentation as ‘good’ (n = 3, 50%) or ‘very good’ (n = 3, 50%) and the quality of the information as ‘good’ (n = 2, 33.3%) or ‘very good’ (n = 4, 66.7%). Self-reported confidence ratings also improved by 25% following training (mean scores 5.67–7.67). Feedback on what aspects were useful included the quality of the manual and resource packs, learning about the historical background of the study and the supervision format. Suggested improvements included having the opportunity to work through some of the in-session resources.
Family support members
Six out of the eight FSMs who attended training completed evaluation forms. Half of the FSMs (n = 3) rated the quality of presentation as ‘good’ and the other half as ‘very good’. Two-thirds rated the quality of the information given as ‘very good’ (n = 4) and one-third (n = 2) rated the information as ‘good’. FSMs’ confidence ratings increased by 38% after the training session (mean scores 5.50–8.50). Feedback about the usefulness of training included:
-
greater understanding of what is expected of a FSM and the role
-
learning about the historical background of the study
-
reassurance that the FSM role does not require advanced knowledge about the topic.
Family support member feedback suggested that there should have been more time for discussion around the topic areas.
Clinical teams cultural competency workshop
Method
Before the workshop, attendees were asked to rate four items from one (not very good) to 10 (excellent):
-
level of confidence in working effectively with people from cultural backgrounds different from their own
-
awareness and knowledge of cultural issues in mental health
-
ability to form therapeutic relationships with people from different cultural backgrounds
-
awareness of ‘cultural competence’ and how it applies to their work as mental health practitioners.
Respondents were also asked an open-ended question about any learning outcomes that they would like the seminar to cover.
Following the seminar, an evaluation form was administered that included the same four questions as the one that had been distributed before the event. The change in mean scores for self-reported cultural competence pre to post training is reported in the Table 3.
| Question | Before training (n = 18) | After training (n = 18) | Mean difference | SD | t-value |
|---|---|---|---|---|---|
| How confident do you currently feel about your ability to work effectively with people experiencing mental health problems whose cultural background is different from yours? | Mean = 6.31 | Mean = 7.75 | 1.44 | 1.93 | 2.978** |
| How would you rate your current awareness and knowledge of issues relating to the impact of culture on mental health? | Mean = 6.19 | Mean = 7.81 | 1.62 | 2.42 | 2.687* |
| How confident do you currently feel about your ability to build a therapeutic relationship with individuals with mental health problems whose background is dissimilar from yours? | Mean = 6.63 | Mean = 7.75 | 1.12 | 1.93 | 2.334* |
| How would you rate your current awareness and knowledge of ‘cultural competence’ and how this applies to your work? | Mean = 5.81 | Mean = 7.56 | 1.75 | 2.35 | 3.976** |
The post-training evaluation form also included a feedback section that asked attendees to rate the seminar on a Likert scale from one (very poor) to five (very good), in terms of its content/information and presentation/delivery. Figure 6 shows the proportion of responses in relation to the content of the training and Figure 7 shows the proportion of responses in relation to the delivery of the training. Four additional open-response questions asked attendees:
-
what they liked about the training and what aspects of it were useful
-
what they liked least about the training and what improvements could be made
-
to provide suggestions for future training events
-
for any additional comments or feedback.
FIGURE 6.
Health-care professionals’ feedback in relation to the workshop content/information.
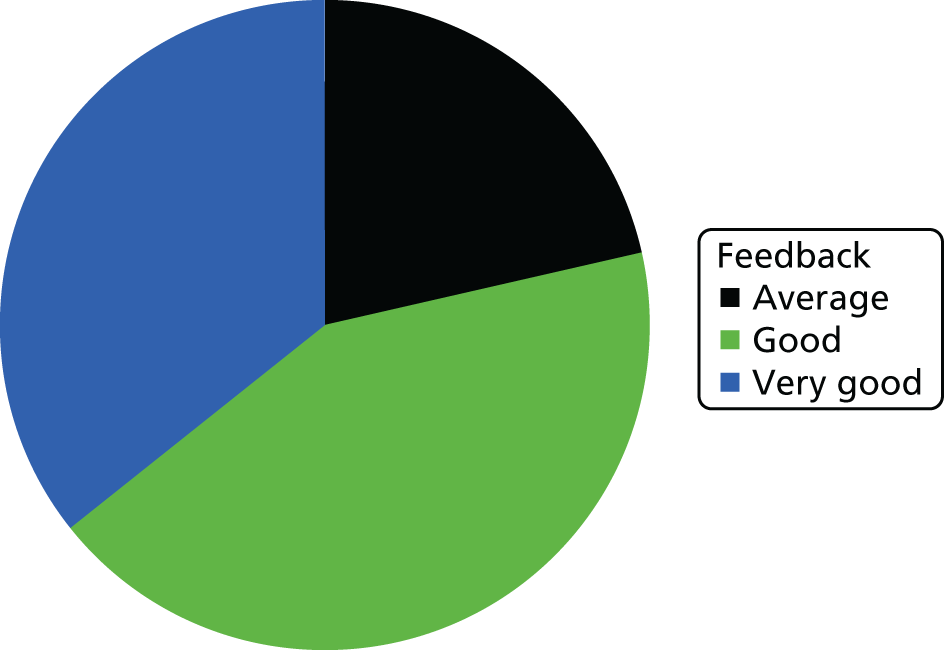
FIGURE 7.
Health-care professionals’ feedback in relation to the workshop presentation/delivery.
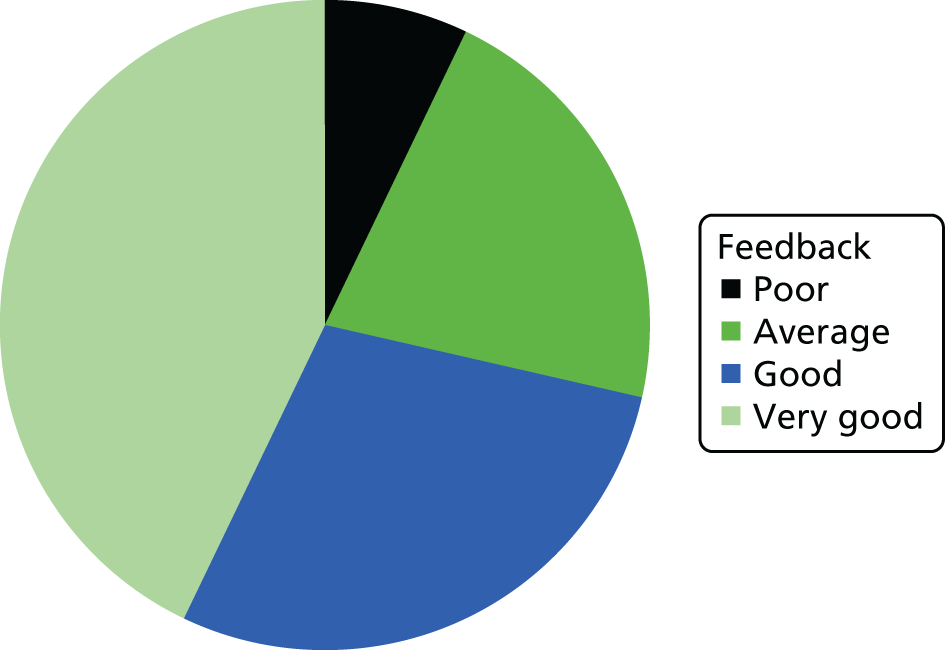
The responses to these open-ended questions have been collated and are presented in Table 3.
A paired samples t-test was conducted to allow comparison of the ratings from the pre- and post-workshop questionnaires. As detailed in Table 3, there was a significant difference pre to post training for each of the four items, which suggests that health-care professionals’ self-reported cultural competency improved following the workshop. Mean scores for attendees’ self-reported measure of cultural competence significantly improved for each of the four items, suggesting that the workshop was successful in increasing awareness and knowledge of the impact of culture on mental health and the application of cultural competence in mental health care, and improving staff members’ confidence in working effectively and building therapeutic relationships with people whose cultural background is dissimilar to their own.
Figure 6 shows that the majority of attendees rated the content of the training as either ‘good’ or ‘very good’, with none of the attendees rating the content lower than average. The mean response was 4.14 out of a possible 5, suggesting that the group as a whole thought that the content of the training was good.
Figure 7 demonstrates that the majority of responses in relation to the presentation and delivery of the training were ‘good’ to ‘very good’. The mean response across the group was 4.07 out of a possible 5, suggesting that the majority of the group were satisfied with the way in which the information was delivered.
In the open-ended questions regarding attendees’ views on the workshop, most reported that 2 hours was not long enough to cover such a large topic in a satisfactory level of detail, with some suggesting that future sessions addressing culture and mental health (rather than just ‘ethnic diversity or cultural competency’) would be beneficial. Positive feedback included the importance and relevance of the workshop content relating to cultural identities, explanatory models for mental illness and cultural awareness, the opportunity to learn from a world expert and the interactive nature of the seminar.
Discussion
In partnership with key stakeholders (service users, family and community members, and health-care professionals), we identified and addressed the training needs of the therapists and FSMs to support delivery of CaFI. Focus group members (phase 1B) and consensus conference experts (phase 1C) identified therapists’ cultural competency alongside excellent clinical skills and positive personal attributes as essential for effective delivery of CaFI.
Stakeholders highlighted the need to commission bespoke training given the intervention’s cultural specificity and lack of cultural competency in NHS training. The European Psychiatry Association guidance suggests cultural competency training whereby practitioners view service users’ behaviour in the context of their own culture whilst also acknowledging their own values and prejudices – an approach that is integral to good clinical practice. 159 Nevertheless, cultural competency is rarely included in health-care professionals’ training, and there remains a lack of understanding about how to implement or evaluate its effectiveness. 160
Mindful of these issues, we sought the views and opinions of experts by experience and profession (see Chapter 4), who strongly advocated involvement of service users and carers in designing and delivering therapist and FSM training. In the absence of a cultural competence framework to evaluate the effectiveness of such training,160 these experts endorsed our proposed fidelity study (see Chapter 6) and collection of qualitative acceptability data from the perspectives of service users, family members, FSMs and therapists (see Chapter 7). Focus group and consensus conference members also endorsed NICE recommendations for cultural competence training at both an organisational and individual level to promote embedding it into everyday practice.
We commissioned external partners to deliver training, sharing findings from phase 1 with facilitators to ensure the identified training needs were fully integrated. Additionally, our service users and carers both influenced the content and participated in the delivery of training. This is in-keeping with our co-production philosophy: genuine partnership working, in which service users’ and carers’ views and experiences are as valued as those of other experts. We also delivered training to FSMs. In practice, this was more ‘awareness raising’ that formal training per se. This was in line with stakeholder views that FSMs should receive sufficient information to enable informed consent to participate, compliance with clinical governance and self-care.
Our training was rated highly with attendees consistently reporting increased confidence after training. Additionally, the training appeared to have enhanced therapeutic engagement as suggested by our fidelity study findings (see Chapter 6). This is in line with findings from a recent systematic review which reported that cultural competence training is an effective means of enabling health-care professionals to provide culturally competent care, which increases ethnic minorities’ satisfaction with services. 160
This was not entirely reflected in the trial and related acceptability study. Non-psychologist lead therapists, who received the full package of training, reported lack of confidence when delivering CaFI, and carers rated them lower than psychologists in some aspects of delivery. However, analyses indicated that this was an issue of clinical capacity versus cultural competency, reflecting non-psychologists’ lack of opportunity to practise FI skills due to demanding caseloads and the need to prioritise emergencies over routine care.
Although these issues might have been exaggerated because of significant organisational challenges within the host trust, they have been previously highlighted32,161,162 as serious barriers to implementing FI. This is important because FI is known to be clinically effective and cost-effective. Yet service users and their families are unable to access FI as part of routine care owing to lack of suitably qualified and experienced therapists.
Lack of access to evidence-based interventions disproportionately affects ethnic minorities. Embedding cultural competence in organisational structures represents a comprehensive response to improving the effectiveness of mental health care. 159 To achieve these aims, we aimed to address competence at both individual and organisational levels. We conclude that work is urgently needed to strengthen the evidence base on the effectiveness of cultural competency. To do so, a framework for delivering and evaluating cultural competency training is urgently needed.
Chapter 6 Feasibility trial
Introduction
In this chapter we report on phase 3 of the study, which was concerned with the feasibility of delivering and evaluating the CaFI intervention. Acceptability will be addressed in Chapter 7.
Aims and objectives
The CaFI feasibility study (phase 3) addressed the second of four research questions:
Is it feasible for culturally adapted FI to be delivered in hospital and community settings to African-Caribbean service users and their families?
Phase 3 study objectives
-
To test the feasibility of delivering culturally adapted FI among African-Caribbean people in hospital and community settings.
-
To test the feasibility of recruiting family members and ‘proxy families’ and delivering the intervention via both.
-
To test the feasibility of recruiting participants in hospital and community settings.
-
To compare recruitment and retention in different clinical settings.
-
To identify outcome measures for future randomised studies and assess the feasibility of collecting them.
-
To assess the acceptability of the intervention to key stakeholders, including service users, their families and mental health professionals (see Chapter 7).
Methods
Design
A feasibility cohort study incorporating a qualitative component.
Sample size
Over 9 months, we planned to recruit and consent a convenience sample of 30 participants via MHSCT and community referral. An audit of MHSCT data via the trust clinical information system (AMIGOS 3.0; Usable Systems, Dyfed, UK) at one time point (18 February 2015), indicated that there were 290 service users meeting our inclusion criteria. We estimated around 200 potential participants would be well enough to participate, of whom 150 would be eligible and 20% (n = 30) would opt in to the study. Thirty service users are sufficient to examine the feasibility of delivering the intervention across a range of service user and family types.
Participant inclusion/exclusion criteria
Service users
-
African-Caribbean descent (including those who self-identified as ‘Black British’, ‘African-Caribbean’ or ‘mixed’ African-Caribbean, but who had at least one African-Caribbean parent or grandparent).
-
Diagnosis of schizophrenia or related diagnoses (ICD-10 F20–29/DSM-IV). 126,127
-
Receiving treatment through psychiatric (acute or rehabilitation) inpatient services or community services within MHSCT (and later GMW).
-
Aged ≥ 18 years.
-
Assessed by key workers as having the capacity to consent and participate.
-
Sufficient understanding of English language to complete measures.
-
No significant cognitive impairment implicated in aetiology (e.g. organic disorder).
-
No high risk to self or others as assessed by care teams.
Family members
Family members and FSMs did not have to be of African-Caribbean origin but were required to be at least 18 years old and have sufficient understanding of the English language to be able to give written, informed consent and complete measures.
Family support members
Recruited FSMs had to attend an informal interview for eligibility and successfully complete relevant checks (see Chapter 5, Therapist recruitment).
Participants and recruitment procedures
Service users
Service users were recruited via their care teams or self-referral. Recruitment at MHSCT was slower than anticipated and, therefore, we expanded recruitment to a second site, GMW (see Second wave of recruitment).
African-Caribbean people remain in inpatient services for longer than their White British counterparts,13,15 so implementation of CaFI in acute as well as community settings might improve engagement and outcome. Therefore, we recruited participants from acute wards, rehabilitation units and community settings to include service users at differing levels of acuity and chronicity, and assess the feasibility of delivering CaFI across different clinical environments.
Advertisement posters and flyers (see Appendix 24) were placed in MHSCT sites that were accessible to service users and in community locations. NIHR Clinical Research Network (CRN) clinical studies officers (CSOs) supported recruitment by helping to identify and recruit suitable participants. CSOs and RAs visited teams at CMHTs and inpatient services to present the study and inform clinical staff about the inclusion criteria. Recruitment packs, including the study PIS (see Appendix 21), were posted to service users who were well enough [following risk assessment from care co-ordinator (CC)/clinical team], had the capacity to consent and gave permission for their contact details to be handed to the research team. The CSO/RA followed this up with a telephone call (at least 24 hours later). Interested service users were invited to meet with the RA to receive further information about the study and ask any questions. During the meeting, service users were asked to self-ascribe their ethnicity (as this is often recorded incorrectly in case notes) and provide written informed consent. Consenting participants were invited to complete baseline assessments in the initial meeting or an additional meeting. Figure 8 shows the Consolidated Standards of Reporting Trials (CONSORT) flow diagram163 that details CaFI service user participant flow163 and the progress of service user participants through the study.
FIGURE 8.
The CONSORT flow diagram: CaFI service user participant flow. Reproduced from Edge et al. 158 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The figure includes minor formatting changes to the original text.
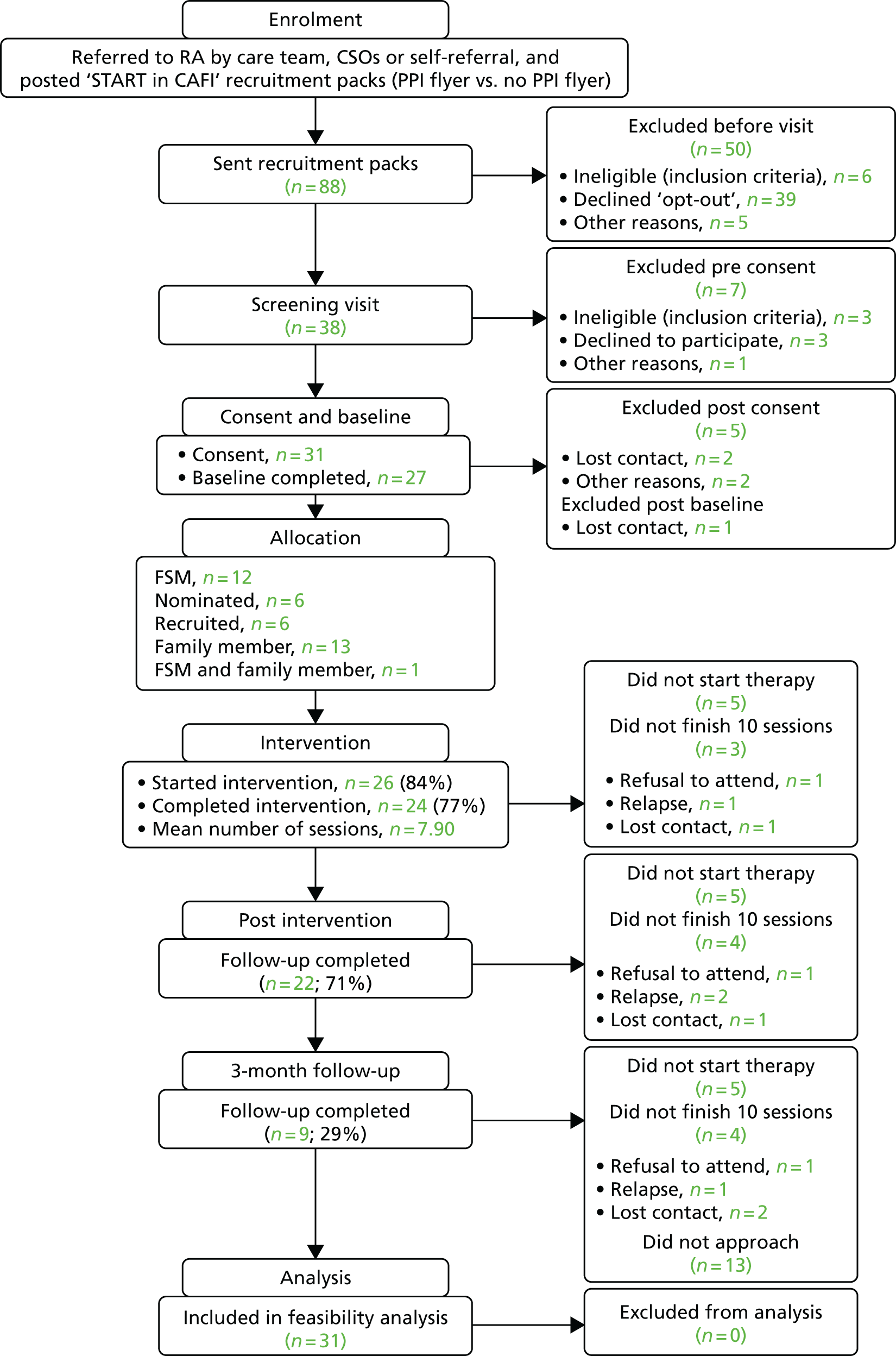
There were four ways in which service users were identified for referral into the CaFI study:
-
CRN face to face – CSOs were located at different NHS settings and spoke to service users and clinical staff about the CaFI study, alongside other studies they were recruiting to. They recorded names and contact details of service users who met the criteria and were willing to be approached by the research team for further information. This information was then passed to the RPM/RA.
-
CaFI research visit teams – RAs/CSOs regularly presented the CaFI study to clinical and management teams in various NHS settings. CCs approached the service users about the study and passed on the contact details of eligible service users who were willing to be approached to the RPM/RA.
-
E-mails to CCs based on electronic case notes – the trust recruitment facilitator/information technology manager screened the clinical information system (AMIGOS) and generated a list of CCs of those service users who met the study eligibility criteria. RAs/CSOs sent e-mails to CCs asking if they would approach the service users on their caseload to see if they would be happy to be contacted by the research team.
-
Direct contact from referrer – CCs heard about the study through adverts (via NHS staff intranet, daily mail, posters/flyers at trust sites), presentations at team meetings or ‘word of mouth’; and contacted the research team directly with names of interested service users.
Family members
Family members were recruited via service users (and their care teams) or self-referral. Posters and flyers advertising the study were placed in appropriate locations in MHSCT settings (e.g. visiting/relatives’ rooms and noticeboards) and community settings such as local community centres, carer support groups and churches. Previous patient and public involvement work with African-Caribbean communities indicates that churches play an important role in terms of community cohesion and knowledge transfer. Working with ‘Black-majority’ churches is therefore an innovative and culturally sensitive approach to recruitment within this ethnic group. Where service users were recruited first, we sought permission to contact their families and invite them to participate. Interested family members were also able to self-refer directly to the research team or via care teams. Permission was sought for the CSO/RA to contact service users to confirm interest in the study and receive the PIS by post. The CSO/RA contacted family members by telephone (at least 24 hours later) to arrange an initial appointment, during which informed consent was taken and baseline assessments were conducted for those opting in.
Family support members
Family support members were recruited in one of two ways.
-
Service user nominated: service users could nominate trusted individuals, such as friends, support workers or a religious leader. The CSO/RA confirmed with service users that their nominated FSMs were aware of the study and happy to be approached. Recruitment, consent and baseline assessments were conducted following the procedure for family members described above.
-
Recruited: service users who were unable to nominate anyone but wished to participate were given the opportunity to select FSMs from a pool of nine community volunteers who were specifically recruited for this study (see Chapter 5, Therapist recruitment for recruitment and training of recruited FSMs). To match recruited FSMs to service users, FSMs were asked to provide a brief biography (a maximum of one A4 sheet) describing who they were (i.e. their name, background, hobbies and interests) and why they wanted to participate in CaFI. This information, together with an introductory meeting facilitated by the FSM, enabled service users to choose who they wanted to work with (e.g. they might have wanted to work with someone of a different gender). Once the FSM was matched to a service user, another meeting was scheduled to conduct baseline assessments.
Intervention
In phase 1, we designed the CaFI intervention comprising 10 sessions as follows (see Appendix 16 for description of manual components):
-
sessions 1 and 2 – engagement and assessment
-
sessions 3 and 4 – shared learning
-
sessions 5 and 6 – communication
-
sessions 7 and 8 – stress management, coping and problem-solving
-
sessions 9 and 10 – staying well and maintaining gains.
Quantitative data collection
Feasibility of recruitment and delivery
We assessed the feasibility of delivering CaFI using the following outcomes:
-
recruitment (number approached vs. number consented)
-
attendance (number of sessions attended)
-
attrition (number of dropouts at each time point)
-
retention (the proportion of participants who complete therapy sessions)
-
completeness of outcome measurement.
Data were collected on reasons for ineligibility and non-consent, including anonymous information on gender, ethnicity and date of birth for those who were approached but did not consent to take part across different referral sites (inpatient, community, third sector) and sources (CRN, research team, self-referral, clinical referral).
Outcome measures for future randomised controlled trial design
To identify outcome measures for future RCTs and assess the feasibility of collecting them, participants (service users and family members/FSMs) completed a range of quantitative outcome measures at baseline, post intervention and at the 3-month follow-up. These measures were conducted by the RPM and trained RAs who were independent of the delivery of the therapy. When participants left the intervention early, we attempted to gather data on outcomes at the time of their exit and at the 3-month follow-up.
Service user and family member/family support member outcome measures
Tables 4 and 5 show the service user assessment schedule and the family member/FSM assessment schedule used in the study respectively.
| Assessment tool | Brief description | Time point | |||
|---|---|---|---|---|---|
| Duration (minutes) | Baseline | Post CaFI | 3-month follow-up | ||
| Sociodemographic | Sociodemographic | 5 | ✗ | ||
| PANSS | Symptoms | 30–40 | ✗ | ✗ | ✗ |
| PSP | Personal and social functioning | 5 | ✗ | ✗ | |
| PCS | Perceived criticism | 5 | ✗ | ✗ | ✗ |
| BIPQ | Illness beliefs | 5 | ✗ | ||
| EQ-5D | Economic evaluation | 5 | ✗ | ✗ | ✗ |
| WAI short form | Working alliance/engagement | 5 | ✗ | ✗ | ✗ |
| Qualitative interview | Acceptability and feasibility | 30–45 | ✗ | ||
| Total time burden (minutes) | 60–80 | 45 | 80–95 | ||
| Session feedback forms | Acceptability | 5 minutes at end of each session | |||
| WAI short form (session 3) | Therapeutic alliance | 5 minutes complete during session 3 | |||
| Relapse | Mirror image protocol design: hospital admissions and change in care management | 0 minutes (undertaken by independent review at 3-month follow-up) | |||
| Assessment tool | Brief description | Time point | |||
|---|---|---|---|---|---|
| Duration (minutes) | Baseline | Post CaFI | 3-month follow-up | ||
| Sociodemographic | Sociodemographic | 5 | ✗ | ||
| GHQ short form | Stress/burden | 5 | ✗ | ✗ | ✗ |
| KAPI relativesa | KAP | 15–30 | ✗ | ✗ | ✗ |
| BIPQa | Illness beliefs | 5 | ✗ | ||
| EQ-5D | Economic evaluation | 5 | ✗ | ✗ | ✗ |
| Qualitative interview | Acceptability and feasibility | 30–45 | ✗ | ||
| Total time burden (minutes) | 35–50 | 25–40 | 55–70 | ||
| WAI short form (session 3) | Therapeutic alliance | 5 minutes complete during session 3 | |||
| Session feedback forms | Acceptability | 5 minutes at end of each session | |||
Psychosis symptom severity (service users)
The Positive and Negative Syndrome Scale (PANSS)164 is a widely used 30-item semistructured interview designed to assess positive, negative and general symptoms in service users with schizophrenic spectrum diagnoses. The PANSS has good psychometric properties of reliability and validity and is sensitive to change. 165 Trained RAs rated the PANSS. High levels of inter-rater reliability were found between the four RAs’ PANSS scores. The average measure intraclass correlation coefficient (ICC) was excellent for PANSS positive (ICC 0.986, 95% CI 0.961 to 0.996), negative (ICC 0.976, 95% CI 0.934 to 0.994), general (ICC 0.975, 95% CI 0.931 to 0.994) and total (ICC 0.985, 95% CI 0.958 to 0.996).
Social functioning (service users)
The Personal and Social Performance Scale (PSP)166 is a 100-point, observer-rated, single-item scale. The scale measures social functioning across the past month in four areas: socially useful activities (including work and study), personal and social relationships, self-care, and disturbing and aggressive behaviours. It is reliable, valid, sensitive to change and correlates with PANSS scores. 167 Ratings were made by trained RAs on the basis of service users’ reports of symptoms, service users’ behaviour during PANSS interviews and reports from care staff and significant others. PSP data were collected at baseline and at the 3-month follow-up only.
Perceived criticism (service users)
The Perceived Criticism Scale (PCS)168 is a four-item self-report measure of service user perceptions of relatives’ criticism. It provides an efficient way of assessing negative aspects of the psychosocial environment. The PCS is a reliable and valid measure169 and perceived criticism has been shown to predict symptom course, treatment outcome and relapse in schizophrenia. 169,170 Service users were asked to complete this measure in relation to their family member/FSM. If there was more than one family member/FSM taking part in the intervention, the service user was asked to rate the person who was currently the most important to them and with whom they shared the closest relationship.
Knowledge About Psychosis (family members/nominated family support members)
The KAPI133 is a revised version of the KASI. 34 The KAPI was not conducted with recruited FSMs at baseline as they had limited knowledge of the service user’s problems before the intervention.
Family stress/burden (family members/family support members)
The 12-item General Health Questionnaire (GHQ)171 is one of the most widely used and valid measures of emotional distress and is frequently used to detect the risk of psychiatric morbidity. It was used as a measure of burden and general stress among family members and FSMs.
Working alliance (service users, family members/family support members)
The Working Alliance Inventory (WAI) short form172 is a 12-item self-report measure of the quality of staff–service user relationships and comprises three subscales: agreement on goals; agreement on tasks and emotional bond. The WAI short form has good psychometric properties. 173 Working alliance has also been shown to influence outcome in therapy. 174–176 Service users completed the WAI in relation to their key worker at the three assessment time points. Service users and family members/FSMs also completed the WAI in relation to the therapist dyad at the end of session 3.
Healthy utility index (service users, family members/family support members)
The EuroQol-5 Dimensions, five-level version (EQ-5D-5L)177 is a generic preference-based self-report measure of health-related quality of life which covers five domains: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Individuals’ responses to the EQ-5D-5L can be used to calculate a single index utility value from a tariff derived from UK population-based valuation studies. These utility values are used to calculate quality-adjusted life-years within economic evaluations. The EQ-5D-5L has been validated in diverse populations178 and is recommended by NICE. 179 We assessed the feasibility of using the EQ-5D-5L as a utility measure in a formal cost–utility analysis as part of a future definitive RCT.
Relapse measure
Reduction in relapse was analysed using two recognised methods:180
-
number and duration of inpatient admissions identified from hospital notes
-
number and duration of exacerbations of symptoms lasting longer than 2 weeks and leading to a change in service user management, such as increased observation and/or medication change by clinical team as assessed by hospital case notes (when symptom exacerbation preceded hospitalisation, only one relapse was recorded).
Discharge rates and hospital admissions were recorded, as was whether service users were discharged to higher- or lower-intensity services. For each participant, we used a ‘mirror image protocol’ to identify and compare relapse events for CaFI participants during two time periods:
-
The time from the individual’s first CaFI session until the date when case notes were accessed [time point 1 (TP1)].
-
A pre-intervention period, matched to the same length [time point 2 (TP2)]. For those participants who did not start therapy, the date of consent was used rather than the first therapy session. Relapse was rated retrospectively by two independent raters (JM and AS).
Hospital admissions
Using the aforementioned ‘mirror image protocol’ design, an independent rater recorded admissions data from electronic case notes on the number of hospital admissions, their dates, and the length of inpatient stay (days) during two time periods (TP1 and TP2) for the MHSCT service users (n = 29). Data were also gathered for two matched samples of Black and White British participants to draw comparison with controls receiving usual care versus CaFI. Participants were matched on diagnosis, gender, age and NHS setting.
Additional service user and family member/family support member measures
The following measures are not outcome measures but may be controlled for in future RCTs. Descriptive data will be reported in the results.
Sociodemographic questionnaire
A self-report sociodemographic questionnaire to collect data on key variables, such as age, gender, ethnic group and religion, was completed by service users, family members and FSMs. Additional questions for service users included diagnosis, country of origin, relationship with family member/FSM, length of time since first contact with services, inpatient history and medication.
Illness beliefs (service users, family members/nominated family support members)
A 12-item modified version of the Brief Illness Perception Questionnaire (BIPQ)181 was used to assess illness perceptions in service users and family members/nominated FSMs at baseline. The BIPQ, like the original Illness Perception Questionnaire,182 from which it was derived, was designed for physical health problems but can be adapted for mental health problems. 183 Modifications of this study were consistent with previous adaptations for mental health184 and included replacing the word ‘illness’ with ‘mental health problems’ and adding three items that assessed the following: personal effort (how much effort the individual was making to help them get well), cause internal (the extent to which the symptoms were caused by the individual’s behaviour) and self-blame (the extent to which the individual was to blame for their mental health problems). Scores on 11 illness perception items can be summed to compute a total score, with higher scores indicating a more negative model of illness. The BIPQ has demonstrated good reliability and validity181 and has previously been used in psychosis research. 185
Staff outcome measures
Working alliance (key workers, therapists)
The key worker assessment schedule and the therapist assessment schedule are presented in Tables 6 and 7 respectively. The staff version of the WAI short form173 was completed by key workers in relation to the service user at the three assessment time points. Items were identical to those of the service user measure but were reworded to reflect staff members’ perspectives. The lead therapist and co-therapists also completed the WAI in relation to the service user and each family member/FSM at the end of session 3. The WAI has previously been used with key workers and therapists. 186–188
| Assessment tool | Time point | |||
|---|---|---|---|---|
| Duration (minutes) | Baseline | Post CaFI | 3-month follow-up | |
| Referral information and demographic | ||||
| Sociodemographic | 10 | ✗ | ||
| WAI short form | ||||
| Working alliance | 5 | ✗ | ✗ | ✗ |
| SES | ||||
| Service engagement | 5 | ✗ | ✗ | ✗ |
| Qualitative interview (n = 10) | ||||
| Acceptability and feasibility | 30–45 | ✗ | ||
| Total time burden (minutes) | 20 | 10 | 40–55 | |
| Assessment tool | Time point | |||
|---|---|---|---|---|
| Duration (minutes) | Baseline | Post CaFI | 3-month follow-up | |
| Qualitative interview | ||||
| Acceptability and feasibility | 30–45 | ✗ | ||
| WAI short form (session 3) | ||||
| Therapeutic alliance | 5 minutes complete during session 3 | |||
| Total time burden (minutes) | 50 | |||
Service engagement (key workers)
The Service Engagement Scale (SES)189 is a 14-item self-report measure assessing participants’ engagement with services from a key worker perspective. The measure has four subscales: availability, collaboration, help-seeking and treatment adherence. The SES has been validated in a psychosis sample and has evidence of good psychometric properties. 189
Data analysis
Quantitative data were analysed using Stata® 14 (StataCorp LP, College Station, TX, USA). Data analysis followed a predetermined statistical analysis plan (see Appendix 25) drawn up by the trial statistician and agreed with the research team.
We present descriptive statistics on our primary outcome of recruitment, consent, demographics, adherence, missing or incomplete scales and attrition of participants, including an exploratory analysis of factors affecting adherence and attrition (using univariate associations with failure to complete).
We examined the characteristics of the various outcome measures to consider which might be appropriate in a future trial and estimated variability to inform sample size calculation.
The EQ-5D-5L scores were used to calculate a health utility index,190 commonly used in cost–utility analyses of definitive RCTs. This made its distribution of interest in understanding the scale’s suitability for a larger trial recruiting from this population. As a secondary analysis, the hypothesis that the intervention would improve health utility index over time in all participants was tested by comparing scores before and after the intervention. Given that the data were skewed and that there were theoretical, prima facie reasons that CaFI might work differently when service users worked with family members rather than with FSMs, the hypothesis was tested using t-tests, bootstrapped with 200 repetitions from separate strata for dyads with family members and those with FSMs. This analysis was performed for both service users and participants, without correction for multiple testing given its exploratory nature. 191
Relapse data were unavailable for definitive analysis, but readmission data from the trial participants and the two groups of matched controls were summarised to examine the proportions readmitted over follow-up; the number and length of readmissions; and the difference in these data between groups and within individuals between TP1 (before the start of intervention) and TP2 (after the start of admission). Each time period was defined as a ‘mirror image’ that is the duration of TP2 was the period from recruitment to data collection at the end of the trial and TP1 was defined as an identical duration before recruitment. As a series of secondary analyses, the number and duration of admissions during TP1 and TP2 were compared between groups and a survival analysis comparing time to first admission during TP2 between groups was conducted. These analyses tested the hypotheses that (1) CaFI would lead to a reduction in the number, total duration and hazard of admissions; and (2) these changes would be greater than any changes in the populations from which the matched samples were drawn. The comparison allowed for identification of trends in admission that were common to the intervention and control groups. Again, for such exploratory analyses, there was no correction for multiple testing. 191
Results
We present results on:
-
the recruitment of service users and family members/FSMs
-
the baseline characteristics of participants
-
the attendance at sessions and completion of therapy
-
the assessment of the outcome measures for use in a future trial.
Recruitment
Service user recruitment
Overall, 97 recruitment packs were sent to a total of 88 individuals (some people were sent packs twice as they did not receive the first). The mean age of the 88 service users we approached was 40.92 years (SD 13.53 years; n = 67) and there were nearly three times as many men as women [men, n = 60 (68.18%); women, n = 21 (23.86%)]. The remaining had missing responses.
Methods of recruitment
Various methods of recruiting participants were attempted. Direct CSO/CRN contact was the most successful approach (n = 36, 40.91%), followed by visits to clinical teams by the CaFI researchers (n = 28, 31.82%). Less successful approaches via services were through CCs (n = 13, 14.77%) and direct referrals from health-care staff (n = 11, 12.50%) (total n = 88).
Eligibility
Of the 88 service users to whom recruitment packs were sent, 74 (84%) were eligible, nine were ineligible (they did not meet the inclusion criteria), and for five there were insufficient data to determine their eligibility. Of those who were ineligible, three were assessed as lacking capacity, one was deemed too high risk, and one had a diagnosis that did not meet the study’s inclusion criteria. Two participants were not of African-Caribbean ethnicity and for two there was no reason for ineligibility recorded.
Compared with those who were not eligible to join the study, the eligible service users were slightly younger [35 (SD 16.54) years vs. 41 (SD 13.49) years] and were just as likely to be male (74.32% were male vs. 71.43% in the ineligible group). Service users from rehabilitation units were more likely to be ineligible than those from other settings as can be seen in Table 8.
| Characteristic | Eligibility, n (%) | |
|---|---|---|
| Eligible | Ineligible | |
| Age (years), mean (SD) | 35.99 (16.54) | 41.14 (13.49) |
| Gender (male) | 55 (74.32) | 5 (71.43) |
| Setting | ||
| CMHT | 36 (38.65) | 4 (44.44) |
| Acute inpatient | 25 (33.78) | 2 (22.22) |
| EIS | 8 (10.81) | 0 |
| Rehabilitation unit | 4 (5.41) | 3 (33.33) |
| Third sector | 1 (1.35) | 0 |
Consent
Out of 74 eligible service users approached, 31 (42%) consented to join the study and 43 declined to participate. Reasons for opting out were obtained from 24 service users, the most common being that they were not interested or did not have enough time.
Compared with the non-consenters, those who joined the study were slightly older (mean age of 43 years vs. 39 years) and slightly less likely to be male (68% male vs. 75%). Consenters were less likely to come from acute inpatient wards (19.35% of consenters vs. 40.38% of non-consenters) and more likely to be from CMHTs (64.52% of consenters vs. 38.46% of non-consenters).
Of the 31 service users who consented to the study, 28 (90.3%) were from MHSCT and three (9.7%) were from GMW.
Most service users were recruited from community settings (n = 21, 67.74%), which includes CMHTs (n = 17), third-sector organisations (n = 1) and Early Intervention Services (EIS) (n = 3). Fewer patients were recruited from rehabilitation settings (n = 7), including rehab unit/wards (n = 4), nursing homes (n = 1) and supported housing (n = 2). Only three patients were recruited from acute inpatient settings.
Family member and family support member recruitment
Eleven of the recruited FSMs were able to complete the necessary checks and other processes to allow them to participate in the feasibility study (see Chapter 5, Therapist recruitment). Nine of these eventually participated, either being matched with service users before therapy started or replacing relatives/FSMs who had dropped out during therapy. It was not known in advance how many service users would work with nominated or recruited FSMs or, indeed, if FSMs would be needed or accepted.
Of those who started the therapy (n = 26), 13 service users (50%) participated with family members. Two service users participated with two relatives each. The remaining 11 took part with one relative each. One service user attended sessions with both a family member and a nominated FSM. There were 16 relatives in total: seven mothers, two fathers, three spouses, one aunt, one daughter, one brother and one sister.
Fifteen FSMs participated (seven nominated and eight recruited). Six (19.35%) were nominated by service users and comprised three CCs, two key workers and one friend. Six (19.35%) service users participated in CaFI with recruited FSMs. Four service users started with one recruited FSM and two started with two recruited FSMs.
Six service family members/FSMs dropped out during therapy, which led to the recruitment of an additional six participants to replace the dropouts (see Changes in family members/family support members during therapy for more detail).
Baseline characteristics
Service users
We report the baseline characteristics of service users in Tables 12–14.
Missing data
Data on gender, age and ethnicity were provided by all 31 participants. The remaining variables were available for 26–28 participants.
Personal characteristics
The patient sample (n = 31) was predominantly male (n = 21, 67.74%) with a mean age of 43 (range 17–81, SD 13.77) years. All were Black and 17 (54.84%) were African-Caribbean, 6 (19.35%) were mixed White and African-Caribbean, 4 (12.90%) were Black British, three (9.68%) were of other mixed background and one (3.23%) was of other Black background. The majority (n = 22, 78.57%) were born in England and 6 (21.43%) were born in the Caribbean. Most had some form of religious affiliation (n = 22, 81.48%), principally Christian (n = 17, 77%).
Employment and education
More than half (n = 14, 51.85%) of the service users were either long-term sick or registered disabled. Seven were unemployed, two were volunteers, two were students and one was retired. None was in work. The majority (n = 23, 85.19%) held qualifications at GCSE level or higher, including three (14.8%) who had Advanced levels (A levels) and one (3.7%) who had a degree-level qualification.
Family and living arrangements
Most of the service users were single (n = 21, 80.77%), one was married and two were cohabiting. Just over half of service users (n = 15, 53.57%) had children. Over half (n = 15, 55.56%) lived alone; the rest lived with partners or spouses (n = 3, 11.1%), parents (n = 3, 11.1%) and other family members (n = 2, 7.4%).
Mental health status: service users
All service users had schizophrenia spectrum diagnoses, bar three participants with first episode psychosis recruited from EIS (psychiatrists confirmed that these service users had non-affective psychosis and were on the schizophrenia spectrum). The age at which they first received treatment ranged between 11 and > 30 years.
Family members/family support members
We report the baseline characteristics of 36 out of the 37 family members (n = 16) and FSMs (n = 21) who took part in the study in Tables 16–18.
Missing data
Data on gender, religion, employment status and children were provided by all 36 participants. The remaining variables were available for 18–35 participants.
Personal characteristics
Twenty-nine of the 36 family member/FSM participants were female (80.56%) and seven (19.44%) were male. Most participants (58.33%) self-identified as being of African-Caribbean background and 14 (38.89%) as White British. The majority of relatives/FSMs described themselves as having a religion, including 21 (58.33%) Christian, three Muslim and one Buddhist. Eleven (30.56%) participants were not religious (Table 9).
| Characteristic | Frequency, n (%) |
|---|---|
| Gender (male) (n = 36) | 7 (19.44) |
| Ethnicity (n = 36) | |
| White British | 14 (38.89) |
| Black/African-Caribbean | 9 (25) |
| Black British | 4 (11.11) |
| Any other mixed/multiple ethnic background | 3 (8.33) |
| White and Black Caribbean | 2 (5.56) |
| Asian British | 2 (5.56) |
| Any other Black/African/Caribbean background | 1 (2.78) |
| White Irish | 1 (2.78) |
| Religion (n = 36) | |
| Christian | 21 (58.33) |
| No religion | 11 (30.56) |
| Muslim | 3 (8.33) |
| Buddhist | 1 (2.78) |
| Other | 0 |
Employment and education
Almost half (47.23%) of the relatives/FSMs were employed full- or part-time. Seven were unemployed. Five were students, four were unemployed, and the rest were retired (n = 3), long-term sick (n = 3), volunteers (n = 2) and looking after the family/home (n = 2). The majority (n = 33, 91.67%) held qualifications at GCSE level or higher, including six (16.67%) who had A levels and 12 (33.33%) who had a degree-level qualification.
Family and living arrangements
Most of the relatives/FSMs were single (n = 18, 51.43%), seven (20%) were married, five (14.29%) were cohabiting, four (11.43%) were separated and one was widowed. The majority (69.44%) had children. One-quarter (n = 9, 25.71%) lived alone; the rest lived with partners or spouses (n = 13, 37.14%), parents (n = 2, 5.71%) or other family members (n = 10, 28.57%).
Feasibility of CaFI delivery
Of the 31 service users recruited into the study, 27 completed the baseline outcome measures and 26 started CaFI by attending at least one therapy session. Twenty-four family units completed all 10 therapy sessions.
Completion of treatment
CaFI comprised 10 sessions. We define ‘completion’ of treatment in three ways.
First, either the participant and/or a family member/FSM attend all 10 sessions. This flexibility was acceptable because some sessions can be beneficial if only service user or family member attends. By this definition, 24 out of 31 (77.42%) family units completed treatment. This is the definition we have adopted for the CONSORT diagram. Completion rates did not vary by clinical setting (Table 10).
| Treatment completion | Acute | Rehab | Community | Third sector | Total |
|---|---|---|---|---|---|
| Recruited | 6 | 1 | 23 | 1 | 31 |
| Completed (10/10) | 5 (83.33%) | 0 | 19 (82.61%) | 0 | 24 (77.42%) |
Second, completion by the service user. Twenty service users (64.52% of those recruited) completed all 10 sessions. Twenty-three (74.19%) service users attended at least eight sessions.
Third, attendance by a family member/FSM at all 10 sessions although not necessarily the same individual family member/FSM at every session. Thirteen family members/FSMs (41.94%) completed treatment by this definition.
Service users attended a mean of 7.74 (SD 3.81) sessions out of 10 and family members/FSMs attended a mean of 6.87 (SD 3.85) sessions. The mean number of sessions attended by family units (i.e. the service user, relative/FSM or both) was 7.90 (SD 3.96) out of 10.
The number of family units, service users and FSMs attending by session did not vary greatly between sessions, other than a slight tailing off over time. Of the 26 family units starting therapy, only two did not complete the full 10 sessions (one missed the final session and another missed session 8 and the final session) (see Changes in family members/family support members during therapy for details of withdrawals/attrition). We compared completion for family units who were treated by psychologists with those who were not and found no difference.
Therapy length and time of sessions
A therapy window of 20 weeks to complete 10 hour-long therapy sessions was set a priori and 13 out of 21 completing family units completed treatment in this time. The mean time to complete treatment was 23.27 (SD 9.87) weeks, with a minimum completion time of 11 weeks and a maximum of 51 weeks.
On average, each session lasted 62.45 (SD 11.36) minutes.
The average completion time was 16.92 (SD 4.15) weeks for psychologists, compared with 29.62 (SD 9.92) weeks for non-psychologists.
Outcome measures for a future randomised controlled trial
We report on (1) data completeness, (2) variability, (3) distribution and (4) change in outcomes.
Data completeness (missing data)
The responses to each measure are summarised in Table 11. As the questionnaires were administered by the RAs, there were few missing responses and little variation in response rates.
| Outcome measure | Time point, n (%) | ||
|---|---|---|---|
| Baseline (N = 27) | Post intervention (N = 22) | 3-month follow-up (N = 9) | |
| PANSS positive | 26 (96.3) | 22 (100) | 9 (100) |
| PANSS negative | 26 (96.3) | 22 (100) | 9 (100) |
| PANSS general | 26 (96.3) | 22 (100) | 9 (100) |
| PANSS total | 26 (96.3) | 22 (100) | 9 (100) |
| PSP total | 26 (96.3) | – | 9 (100) |
| PCS item 1 | 24/24 (100)a | 22 (100) | 9 (100) |
| PCS item 2 | 24/24 (100)a | 22 (100) | 9 (100) |
| WAI total | 27 (100) | 18 (81.81) | 9 (100) |
| EQ-5D | 27 (100) | 22 (100) | 9 (100) |
| BIPQ total | 27 (100) | – | – |
Service users
Service users were asked to complete all measures, but those working with recruited FSMs did not complete the PCS if they had not yet met the recruited FSM. Of the 31 service users recruited to the CaFI study, 27 completed baseline assessments, 22 completed assessments post intervention and nine completed assessments at the 3-month follow-up (see Table 11). We were unable to approach most service users at 3 months owing to delays in therapy delivery and data collection assessments (see Therapy delivery and Chapter 5, Therapist recruitment).
We achieved very high rates of data collection on all measures. Only one person missed PANSS and PSP measures at baseline. Two people did not complete the PCS at baseline as they had not yet met the FSMs. Four people did not complete the WAI post intervention (one did not complete the full measure and three had missing items). The common missing item was ‘I believe she/he likes me’ (service users often reported feeling uncomfortable responding to this item).
Family members/family support members
All family members/FSMs were asked to complete the quantitative assessments at baseline, post intervention and at the 3-month follow-up. Of the 37 family members/FSMs recruited to the CaFI study, 36 completed baseline measurements. Twenty-five completed post-intervention assessments (of whom 21 completed EuroQol-5 Dimensions), and nine completed assessments at the 3-month follow-up.
The recruited FSMs completed the GHQ but did not complete the KAPI and the BIPQ at baseline, as they did not know the service user. Furthermore, the medication subscale on the KAPI was not relevant for two service users who were currently not taking medication and, therefore, this subscale score was replaced with the mean subscale score. This meant that only 24 family members/nominated FSMs completed the KAPI and the BIPQ at baseline. We achieved very high rates of data collection on all measures.
Key workers
Of the 27 service users who completed the baseline assessments, all of their corresponding key workers agreed to complete the outcome measures. Twenty-eight key workers completed assessments at baseline, 23 completed assessments post intervention and 10 completed assessments at the 3-month follow-up.
The completion rates for individual measures were higher for the WAI than for the SES. This was because key workers reported being unable to answer some WAI items because they were not relevant to their relationship with their clients. Three service users’ key workers changed during the therapy and, therefore, the post intervention and follow-up assessments were completed by a different key worker.
Variability in outcome measures
We report the variability of the various outcomes measures for use in estimating the sample size for a future RCT (Table 12).
| Group | Outcome measure | n | SD |
|---|---|---|---|
| Service users | PANSS positive | 57 | 6.21 |
| PANSS negative | 57 | 4.29 | |
| PANSS general | 57 | 8.53 | |
| PANSS total | 56 | 15.54 | |
| PSP total | 29 | 15.43 | |
| PCS item 1 | 55 | 2.68 | |
| PCS item 2 | 55 | 2.83 | |
| WAI total | 52 | 15.70 | |
| BIPQ total | 27 | 16.91 | |
| FSMs | GHQ total | 61 | 5.84 |
| KAPI total | 46 | 3.66 | |
| BIPQ total | 22 | 18.73 | |
| Key workers | WAI total | 57 | 10.19 |
| SES total | 52 | 9.17 |
Change in outcome measures
As a feasibility pilot, the study is not powered to estimate changes in health outcome and it does not include a control group as comparison.
We originally planned (as outlined in the statistical analysis plan; see Appendix 25) to present the trajectories of each individual, from baseline to 3-month follow-up, and explore the patterns of missing data. This would have allowed us to assess whether missing outcomes were related to the trajectory of the individual, or whether they were missing at random. However, this was not conducted because only 9 out of the 31 family units completed the 3-month follow-up assessments. This is partly attributed to the fact that 13 families could not be approached for 3-month assessment visits as a result of delays in the therapy delivery and hence in data collection periods (see Chapter 5, Therapist recruitment). We cannot know whether or not these 13 participants would have completed the final set of outcome measures. The remaining nine families dropped out (see Therapy delivery).
Healthy utility index
We assessed the feasibility of administering the EQ-5D-5L177 utility measure to service users and FSMs/family members for a formal cost–utility analysis in a future definitive RCT.
Service users
Descriptive statistics for the EQ-5D-5L responses are shown in Table 13. Because data were available for only nine service users at the 3-month follow-up (see Outcome measures for a future randomised controlled trial), only the first two time points’ data are presented here. The reasons for the low proportion followed up at the final assessment are discussed in Withdrawals/attrition from therapy. EQ-5D-5L scale completion was 100% for those who were seen.
| Item rating | Baseline (n = 27) | Post intervention (n = 22) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | |
| No problems, n | 18 | 18 | 9 | 12 | 11 | 15 | 17 | 15 | 13 | 13 |
| Slight problems, n | 5 | 5 | 9 | 9 | 5 | 4 | 1 | 4 | 3 | 2 |
| Moderate problems, n | 2 | 3 | 5 | 3 | 6 | 1 | 4 | 1 | 3 | 5 |
| Severe problems, n | 2 | 1 | 2 | 1 | 4 | 2 | 0 | 1 | 3 | 1 |
| Extreme problems, n | 0 | 0 | 0 | 2 | 1 | 0 | 1 | 1 | 0 | 1 |
| EQ-5D-5L utility score | ||||||||||
| Mean (SD) | 0.74 (0.28) | 0.82 (0.18) | ||||||||
| Median (quartiles) | 0.82 (0.67, 0.95) | 0.92 (0.73, 1.00) | ||||||||
At each time point, the EQ-5D-5L health utility score190 was substantially positively skewed: the most frequently reported level was ‘no problems’ for all five of the domains at baseline and at post intervention. Perhaps unsurprisingly, mobility and self-care were the two items for which most individuals reported having ‘no problems’ at baseline. Pain/discomfort and anxiety/depression were the only items on which any individuals reported having ‘extreme problems’. Post intervention, self-care was the item for which most individuals reported having ‘no problems’, followed by mobility and usual activities. Between baseline and post intervention, the most substantial change appears to have occurred in the usual activities item.
The range of scores at baseline was –0.20 to 1.00 and at the end of the intervention was 0.11 to 1. The mean EQ-5D-5L utility index was 0.74 at baseline, rising to 0.82 post intervention. Health utility index scores improved significantly after intervention (mean difference 0.09, 95% CI 0.02 to 0.17; p < 0.05, bootstrapped t-test). Although those with family members involved already reported their health state as better at baseline, the differences in health utility index between the 16 service users entering the intervention with family members (median 0.88; quartiles 0.71, 0.98; mean 0.71; SD 0.31) and the 11 with FSMs (median 0.67; quartiles 0.58, 0.83; mean 0.67; SD 0.23) were non-significant (mean difference –0.12, 95% CI –0.32 to 0.08; p > 0.05). In any case, both of these groups showed a trend to improve their utility score, although those with FSMs improved more (median score 0.89; quartiles 0.54, 1.00; mean 0.88; SD 0.26) than those with family members (median 0.94; quartiles 0.79, 1.00; mean 0.84; SD 0.25), who had less scope to improve. There was no significant difference between the two groups in the final score (mean difference 0.06, 95% CI –0.16 to 0.28; p > 0.05, bootstrapped t-test).
Family members/family support members
The range of health utility index scores at baseline was 0.31 to 1.00 and after intervention was 0.47 to 1.00. At both baseline and post intervention, health utility scores for family members/FSMs were negatively skewed, even more than for service users (see Table 13). Health utility index did not improve significantly after the intervention (mean difference 0.05, 95% CI –0.02 to 0.12; p > 0.05). This was the case both for those who were family members and for those who were FSMs (Tables 14 and 15). Given the high scores at baseline (e.g. > 25% scoring a maximum of 1.00, most family members scoring > 0.96), it was difficult for the intervention to produce any meaningful improvement.
| Item rating | Baseline (n = 36) | Post intervention (n = 21) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | |
| No problems, n | 25 | 32 | 28 | 17 | 21 | 16 | 18 | 14 | 11 | 13 |
| Slight problems, n | 4 | 1 | 2 | 8 | 8 | 2 | 1 | 3 | 5 | 6 |
| Moderate problems, n | 5 | 3 | 6 | 6 | 6 | 3 | 1 | 3 | 4 | 1 |
| Severe problems, n | 2 | 0 | 0 | 3 | 1 | 0 | 1 | 1 | 1 | 1 |
| Extreme problems, n | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| EQ-5D-5L utility score | ||||||||||
| Mean (SD) | 0.85 (0.20) | 0.86 (0.16) | ||||||||
| Median (quartiles) | 0.93 (0.78, 1.00) | 0.92 (0.82, 1.00) | ||||||||
| Family group variable | Baseline | Post intervention |
|---|---|---|
| FSMs, median (quartiles) | 0.90 (0.74, 1.00) | 0.93 (0.74, 1.00) |
| Family member, median (quartiles) | 0.97 (0.86, 1.00) | 0.92 (0.92, 0.94) |
Relapse rates
Relapse measure
At the time of writing, data for the comprehensive assessment of relapse180 remain to be finalised. As not all relapse data were collected owing to the hospital merger, this work is ongoing. Data regarding relapse will be available and presented in future trial publications. For the report, relapse data will therefore be presented for the audit at MHSCT only. Not all relapse data were collected owing to the hospital merger. This work is ongoing. Data will be included in the main trial outcome paper (in preparation).
Hospital admissions
For all three groups (CaFI service users, matched Black and White British controls), the mean period of assessment before and after the intervention was 313 (SD 142) days. The number of inpatient days was skewed. Before intervention, the overall median stay across all groups was 0 (quartiles 0, 0; range 0–733) days. Afterwards, the overall median was also 0 (quartiles 0, 0; range 0–168) days; this did not differ significantly over time across groups (p > 0.05, Wilcoxon matched-pairs signed-rank test), despite a noticeable shortening of maximum admission length (Table 16).
| Group | Inpatient days before intervention, median (range) | Number of admissions before intervention | Inpatient days after intervention, median (range) | Number of admissions after intervention | ||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 0 | 1 | 2 | |||
| CaFI participants | 0 (0–588) | 22 | 4 | 1 | 0 (0–160) | 23 | 3 | 1 |
| White controls | 0 (0–366) | 24 | 2 | 1 | 0 (0–104) | 23 | 4 | 0 |
| Black controls | 0 (0–733) | 24 | 3 | 0 | 0 (0–168) | 24 | 3 | 0 |
There were no significant differences between the groups in the number of admissions in the control period before the intervention started (p > 0.05, Fisher’s exact test) or in the length of inpatient stay (p > 0.05, Kruskal–Wallis test). Nor did time to relapse differ between the groups (p > 0.05, Cox regression model stratified by gender and controlling for age; Figure 9).
FIGURE 9.
Kaplan–Meier survival estimates. Survival time (days) without relapse before intervention across groups. BC, Black Caribbean; WB, White British.
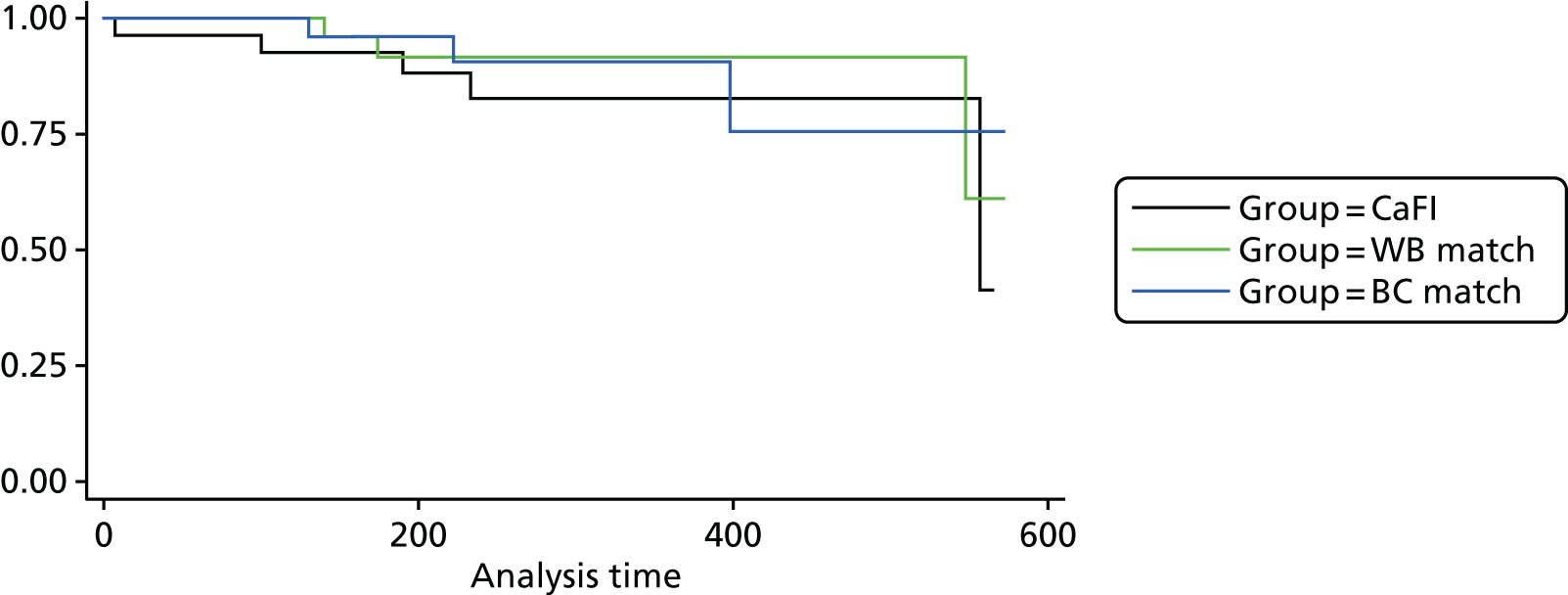
There were no significant differences between the groups in the number of admissions in the period after intervention started (p > 0.05, Fisher’s exact test; see Table 16). This did not represent a signficant decrease in the number of admissions for the CaFI group (p > 0.05, Wilcoxon matched pairs signed-rank test) or the two control groups (p > 0.05 and p > 0.05). Nor did days in hospital differ signficantly across all groups (p > 0.05, Wilcoxon), between groups (p > 0.05, Kruskal–Wallis test) or over time for any of the groups (p > 0.05, p > 0.05, p > 0.05 for the CaFI group, White and Black controls, respectively, Wilcoxon test).
Time to admission after the intervention did not differ signficantly between groups (p > 0.05, Cox regression model stratified by gender and controlling for age). Controlling for length of survival in the previous period by adding this to the model (adjusting for differences between individuals, and hence groups, in propensity to be admitted) made almost no difference (p > 0.05 between groups).
Therapy delivery
Withdrawals/attrition from therapy
Of the 31 service users who consented to the study, five dropped out pre intervention, four pre baseline and the remaining one post baseline. Out of these, the research team lost contact with three, one reported not feeling well enough to take part and one did not feel able to commit to the study due to new work commitments.
Of the 26 service users and respective family members/FSMs who started the therapy, three service users dropped out during therapy and did not re-engage. Out of these, one service user disengaged after session 3 (but their two family members continued with the therapy) and two service users dropped out after session 9; one service user relapsed and one agreed but did not attend the final session. In addition, one family member dropped out after session 1 due to a family bereavement and two FSMs (one nominated and one recruited) dropped out at session 4 because they could not be contacted after session 3.
Post intervention, four service users dropped out. Two did so following relapse, one refused to complete assessments and one could not be contacted. One family member and one nominated FSM were lost post intervention, one did not complete the assessments because their relative had relapsed shortly after the intervention and the research team were unable to contact the nominated FSM after the service user had completed therapy. All seven recruited FSMs who finished therapy completed post-intervention assessments. Two staff members did not complete post-intervention assessment: one did not want to because the client had relapsed and they had not been in contact with them for a while; and the other staff member was unavailable because of illness.
Thirteen family units were not approached to complete 3-month follow-up assessments as a result of delays in therapy delivery (see Chapter 5, Therapist recruitment). Of the participants approached, one service user dropped out as they no longer wished to be contacted, one refused to complete assessments and two did not complete assessments owing to relapse. In addition, one nominated FSM did not complete follow-up assessments as they could not be contacted. All staff members and recruited FSMs who were approached completed the 3-month follow-up assessments.
Changes in family members/family support members during therapy
Six service users changed family members/FSMs during the study, but these changes were addressed early on in therapy. Two service users nominated their key workers to participate with them, but these key workers dropped out post baseline as they changed their place of work before the therapy started. One of these service users subsequently took part with a recruited FSM and the other took part with their CC. Two service users initially opted to take part with family members but then changed to take part with FSMs post baseline. One experienced a breakdown in their relationship with their family member before therapy started, so a FSM was recruited, who joined from session 3. The other family member withdrew owing to a family bereavement after session 1; there was then a suspension of therapy and the service user started therapy again from session 1 with a recruited FSM. Of the remaining two participants, one changed to a different recruited FSM from session 7 following a period of disengagement resulting from the service user’s alcohol misuse and the other service user changed from two recruited FSMs to a nominated FSM following a breakdown in therapy after session 3 (this service user used subsequently resumed therapy from session 1 with two new therapists).
Two other service users experienced a suspension in therapy and did not change family member/FSMs but changed therapists. One service user disengaged at session 5 and re-engaged at session 7 following a pause in therapy. The other disengaged after session 1 because he did not feel comfortable working with male therapists, and the family restarted therapy after being allocated female therapists.
Adverse events
There were seven adverse events and one serious adverse event, none of which was related to the intervention. In the case of the serious adverse event, the participant relapsed and was hospitalised post intervention (shortly after session 10). The seven adverse events all occurred during the intervention. One was related to alcohol misuse, one was related to drug misuse and three were related to an exacerbation of mental health problems during the therapy, which resulted in hospitalisation, a prolongation of hospitalisation or an increased involvement of the care team. Of the remaining two, one was due to the participant becoming unresponsive during a therapy session and one was related to the therapists’ concerns regarding the service user’s risk to others. Two adverse events resulted in a suspension of therapy until the service users were stable enough to continue with therapy and one service user did not continue with therapy after their adverse event.
Fidelity study
Method
The CaFI fidelity measure is a modified version of the subscale of the Cognitive Therapy Scale for Psychosis,46 which has been adapted for this study to account for the presence of two therapists and the relatives. Seven items were used: agenda setting, feedback, understanding, interpersonal effectiveness, collaboration, homework, and quality of CBT techniques. The second subscale includes components that map directly on to the CaFI therapy manual, along with two additional items from the FIPAS:47 reducing criticism and conflict; and reducing overinvolvement. The third and final subscale comprised six items that rated the degree of cultural awareness or competencies of the therapists during the session. This subscale was based on the manual and existing cultural competency questionnaires and literature192–196 (see Appendix 26 for the CaFI fidelity measure).
Fidelity was assessed by independent ratings of 10% of semi-randomly selected sessions, ensuring equal spread across therapist pairs and session number. This was achieved by initially randomly choosing a recording for each therapist pair from the sessions remaining unsampled and randomly selecting a recording. We randomly sampled from all remaining recordings until we had reached the desired 10%. Treatment fidelity and quality were also monitored via discussion of audio-recordings of sessions in supervision. Every 6 weeks therapists also submitted a session to the clinical supervisor who rated the recording using the fidelity scale and gave feedback to the therapists.
Results
Overall, therapists scored well on part I of our scale, which reflected skills in CBT for psychosis (Table 17). Scores on the understanding, collaboration and interpersonal effectiveness items were particularly high, whereas feedback and homework items were lower.
| Subscale | Range | Mean | SD |
|---|---|---|---|
| Part I | |||
| Agenda | 1–6 | 4.60 | 1.50 |
| Feedback | 1–6 | 3.85 | 1.31 |
| Understanding | 3–6 | 5.60 | 0.88 |
| Interpersonal effectiveness | 5–6 | 5.65 | 0.49 |
| Collaboration | 3–6 | 5.00 | 0.86 |
| Homework | 0–6 | 2.65 | 1.66 |
| Quality of CBT | 2–6 | 4.05 | 1.15 |
| General total | 19–40 | 31.25 | 5.95 |
| Part III | |||
| Cultural awareness total | 3–6 | 4.90 | 0.91 |
Part II of the fidelity scale reflects the nature of topics covered within sessions, as opposed to the quality of delivery. All of the components of the manual were represented at least once, with the exception of three subcomponents (plans are put in place to reward and evaluate goals; goals are evaluated and rewarded when achieved; and help family to tolerate slow change within sessions). The independent rater also noted that it was not possible to rate the expressed emotion items on the content fidelity scale when family members were not present. Subcomponents related to communication and to helping the family formulate their own role in maintaining stress and the service user’s problems in a non-judgemental way seemed to be particularly well represented at least on the basis of the random selection of recordings rated (Table 18). Although, the independent rater noted that when family members were not present during sessions, the therapy was more akin to individual CBT than FI, and some aspects of family work during the sessions were not listed in the content part of the fidelity scale (Box 11).
| Items | Frequency, n (%) | |
|---|---|---|
| CaFI manual item | ||
| Assessment and engagement | ||
| Establish ground rules | 1 | 5 |
| Establish personal accounts of psychosis and treatment | 1 | 5 |
| Identify areas of need and priorities for the family and service user | 2 | 10 |
| Therapists specifically identify strengths and resources within the family | 2 | 10 |
| Agreed SMART goals that closely relate to identified needs and problems | 3 | 15 |
| Plans are put in place to reward and evaluate goals | 0 | 0 |
| Shared learning | ||
| Identify what the family want to know more about | 3 | 15 |
| Offer information/education | 4 | 20 |
| Answer questions raised by the family | 1 | 5 |
| Provide written information | 2 | 10 |
| Explain terminology and avoid use of jargon | 2 | 10 |
| Communication | ||
| Help family members to listen to each other, not allowing individuals to talk over each other | 3 | 15 |
| Identify positive and negative approaches to communication | 9 | 45 |
| Support and encourage families to express their needs to each other | 9 | 45 |
| Facilitate better ways of negotiating needs to services | 6 | 30 |
| Stress management, coping and problem-solving | ||
| Normalise stressful feelings in response to schizophrenia and psychosis | 5 | 25 |
| Help the family formulate their own role in maintaining stress and service user’s problems in a non-judgemental way | 8 | 40 |
| Help families break out of vicious cycles by changing their own thoughts, feelings and behaviours | 5 | 25 |
| Help families support service users in making changes in functioning by setting SMART goals | 2 | 10 |
| Goals are evaluated and rewarded when achieved | 0 | 0 |
| Staying well and maintaining gains | ||
| Help the family identify signs of relapse and coping strategies, including action plans in relation to early warning signs of crises | 4 | 20 |
| Help the family reflect on and consolidate their learning, including ideas about how any gains can be maintained or generalised to other goals | 4 | 20 |
| Help the family prepare for and deal with any difficult feeling in relation to ending therapy | 1 | 5 |
| Use the goodbye letter to communicate any positive experiences of working with the family and highlight strengths of the family unit or service user | 1 | 5 |
| FIPAS item | ||
| Reducing criticism and conflict | ||
| Defuse any anger | 4 | 20 |
| Reframe negative comments | 6 | 30 |
| Set appropriate limits | 3 | 15 |
| Model positive communication | 7 | 35 |
| Help family to tolerate slow change within sessions | 0 | 0 |
| Reducing overinvolvement | ||
| Identity and address overinvolvement | 4 | 20 |
| Normalise carer’s grief, guilt, loss, anxiety and related feelings | 4 | 20 |
| Set tasks to minimise independence in the context of involvement (within cultural norms) | 1 | 5 |
-
In some instances normalising occurred, but this was not necessarily about psychosis or schizophrenia, but about other issues more generally. Although still relevant and appropriate to discuss the issues, it was not related to psychosis, so the rater felt that they could not rate it under the relevant item in part II.
-
Stress management: the client and therapist might have been talking about stress but it was not in the context of psychosis so the rater could not rate this under stress management (even though it was still relevant to be talking about more general stress).
-
Understanding the role of worry and anxiety was discussed in a session. It seemed relevant but there was nowhere to specifically rate this.
-
The session might have focused on expressing needs, but it was not, at times, necessarily about expressing needs to other family members or services.
-
In one session the issue was about communication; however, it was about communication not necessarily with services/family but past communication problems (e.g. their time at school, etc.). There was not anywhere obvious to rate this; however, it was deemed relevant.
-
The session might have been talking about a toxic relationship with a family member; however, the discussion in the session was not necessarily around how to communicate better with that family member; rather it was more of a tirade about all the problems the client has with the toxic family members. It seemed relevant (although a little unfocused) to let the client talk about this and get it off his chest and thus could be rated for fidelity, but then the therapist did not necessarily do anything active with the information.
-
Some sessions focused on understanding voices and ways of coping with these (e.g. smoking), but there was nowhere obvious to rate this although deemed relevant.
Part III of the fidelity scale reflects cultural competence. At least half the sessions rated demonstrated evidence of aspects of cultural competence assessed. In fact, four out of six competencies assessed were evident in all, or nearly all, of the sessions rated (Table 19). The independent rater did, however, note that part III of the fidelity subscale was particularly difficult to rate. Without detailed information about the families, it was difficult to know whether cultural awareness or a cultural narrative should have been present but was missed, or if it was appropriately omitted.
| Cultural awareness item | Frequency, n (%) |
|---|---|
| Therapists demonstrate knowledge of or enquire about the client’s culture | 10 (50) |
| Therapists show awareness of the uniqueness of families or clients and heterogeneity of African-Caribbean people; avoiding common misconceptions | 20 (100) |
| Therapists respect different roles or hierarchies within the family and are sensitive to familial rules of communication | 19 (95) |
| Therapists demonstrate awareness of social conventions and hospitality (e.g. dealing appropriately with offers of drinks or food) | 18 (90) |
| Therapists address cultural issues that the family bring to the therapy (e.g. explanatory models/illness beliefs, including spiritual/religious beliefs); experiences of racism and discrimination; and experiences of services | 11 (55) |
| Therapists acknowledge that their personal biases and values may differ from those of the client and/or how these may influence perceptions of the client/family problems identified in therapy or the therapeutic relationship | 19 (95) |
The Barrowclough and Tarrier197 FI model clearly influenced the therapists’ practice. Non-psychologists had limited experience implementing psychological therapies with complex client groups, and so struggled in formulating this complexity and intervening in a less circumscribed idiosyncratic way. The clinical psychologists were more experienced in formulating and adapting to complexity. Although they clearly drew on the Barrowclough and Tarrier FI model,197 they also drew on other areas of expertise. For example, one lead therapist specialised in child and family work outside the study and another therapist was carrying out a more specialist course in cognitive analytic therapy. The independent rater also noted that therapists from non-psychological backgrounds tended to conceptualise psychosis in medical terms and used illness model language which did not necessarily facilitate discussion about other ways of thinking about mental health, such as including cultural appraisals and psychological factors.
Discussion of fidelity findings
Overall, fidelity assessment demonstrated that therapists were able to deliver therapy to protocol with good evidence of core skills in CBT for psychosis, as well as cultural competency and coverage of core components of the manual. A few exceptions may require increased emphasis in future training and supervision protocols, including opportunities for feedback, setting and/or reviewing homework, and reviewing and rewarding goals. The independent rater also highlighted some aspects of therapy that were evident in the recordings but were not listed in the second part of the fidelity scale, such as addressing problems not related to psychosis, managing communication outside the family and services, and understanding voices and ways of coping with these (see Box 11), which suggests that iterations of the measure may need to be more comprehensive. Expressed emotion items were not rated when the family were absent, which may also suggest that future iterations of the measure should include the clause ‘rate only if family member present’ prior to the expressed emotion items. Independent raters in future trials may benefit from more detailed information about family background and context to facilitate rating cultural competency subscales. Further consideration should be given to the role of FSMs and how to better utilise this resource within sessions.
Although we did not systematically assess therapists’ effects on the fidelity ratings because of the small number of therapist pairs, observations in supervision did suggest that therapists who had completed a doctorate in clinical psychology and were routinely providing therapy within other roles within the NHS, were more skilled in formulating and working with complex issues that presented in therapy. Observations by the independent rater also noted that non-psychologists presented a more medicalised concept of psychosis, which may partly reflect the predominance of this model within mental health services, but is nonetheless inconsistent with the ethos of the family therapy we aimed to deliver in the trial. Taken together, these findings highlight the benefits of the therapy being delivered by individuals with more specialised training in therapy or providing more intensive training and supervision to less-experienced staff.
Conclusions
Summary of findings
We successfully recruited our target of service users to CaFI, slightly exceeding our recruitment goal of 30. We recruited an additional participant because one had withdrawn before we ended the recruitment period and we had 30 spaces for therapy.
We also successfully allocated at least one family member or FSM to each service user. Half the service users who started therapy nominated a member of their family to join them in the CaFI intervention; around one-quarter (23%) nominated someone else known to them and one-quarter selected someone from the pool of recruited FSMs. One (4%) attended with both a family member and a nominated FSM. In a few cases, service users selected a relative or CC (nominated FSM) to take part with them, but they could not work with the service user because of a reported lack of interest or work commitments. There were a couple of cases where service users started the sessions with their chosen relative/FSM but certain circumstances (e.g. bereavement) meant that the relative/FSM dropped out of therapy. In both situations, service users were given the opportunity to work with a recruited FSM, which highlights the benefits of this approach as it enabled service users to receive CaFI who otherwise would not have access to the intervention.
As might be expected, the most successful method of identifying potential participants was face to face, with either the CRN CSO staff approaching service users or the CaFI researchers visiting clinical staff in their work setting; three-quarters of recruitment was done face to face with service users or clinical staff. Recruiting NHS service users can be a convoluted process as researchers must go through the service users’ CCs who have limited capacity to support research studies and refer service users on their caseload. In the present trial, this proved to be a lengthy process and led to delays in reaching those service users who were interested in the research or receiving complimentary therapy. Often RAs were required to wait for a couple of months before they could attend clinical team meetings and CCs would not respond to e-mails or return telephone calls. The CRN CSOs working in inpatient and rehab wards were, however, able to access service users face to face, which highlights the need for CRN support in mental health trials.
Most people (84%) who were identified proved to be eligible for the study. Reasons for ineligibility included lacking capacity, assessed as being ‘high risk’ and not being of African-Caribbean origin. NHS staff often incorrectly referred people of Black African ethnicity, which may highlight problems with the recruitment materials and language use (i.e. anecdotal feedback suggests that ‘Black Caribbean’ is less confusing than ‘African-Caribbean’, which could be mistaken for both Black African and Black Caribbean). It may also point to a lack of cultural understanding among clinical professionals about the diversity of Black cultures and the ethnic background of their clients. The research team have previously conducted audits at the host NHS trust (MHSCT) and found that ethnicity is often recorded incorrectly. The conversion rate from eligibility to consent was 42%, and the most common reasons for not providing consent were lack of interest, being too busy, or it being the wrong time. Compared with non-consenters, those who consented to the study were slightly older and more likely to be women.
In our study protocol,158 we planned to recruit from three types of setting: community settings, rehabilitation units and acute inpatient settings, with 10 services users in each setting. We successfully recruited from all three settings, but the spread across them was unequal: 21 were living in community settings (17 CMHTs, three EIS and one third sector), seven in rehabilitation units (including 24-hour staffed supported housing and hospital units) and three in acute inpatient wards. This may be an accurate reflection of the distribution of people meeting the criteria in these different settings. However, there were high numbers of referrals via the CRN from acute inpatient settings, presumably because the CSOs were located in these settings and could approach service users face to face and monitor new referrals. We found these acute settings more difficult to recruit from, because people tended to go in and out of them quite quickly, and some service users had moved on by the time we contacted them for the consent visit. Others were too ill to participate or lacked capacity to provide informed consent. In such cases, RAs/CSOs would approach the service user once the CC confirmed that they were well enough. It may therefore be helpful to gauge interest from service users receiving acute care, but to engage them in therapy only when deemed appropriate and when they have the capacity to participate.
Of the service users who entered the study, two-thirds were male and all were of African-Caribbean origin; the mean age was 43 years. Reflecting national census data,14 most were born in the UK (79%), with around one-third being of mixed ethnic background, one of the fastest growing ethnic categories. Most were single (81%) and over half lived alone (56%), reflecting previous reports of the impact of schizophrenia on social networks. 198 This finding also perhaps underscores the need to identify FSMs to work alongside service users who may be socially isolated. All but three service users had schizophrenia spectrum diagnoses; these people were recruited from EIS and, therefore, had not yet received a diagnosis (but this was confirmed by a psychiatrist to be non-affective psychosis).
Of the 31 service users who consented to take part in the study, 27 completed the baseline measures and 26 started CaFI. Among the 26 family units who started therapy, there was a high completion rate: 24 (92.31%) completed treatment, with completion defined as attendance at all 10 sessions by the service user, the family member or both. The mean number of sessions attended by family units was 7.74 (SD 3.81) out of 10 sessions. The number of family units who completed CaFI within the expected therapy window of 20 weeks was 12 out of 24 (50%) and the mean time to complete therapy was 23.27 weeks.
The therapy was delivered by therapist pairs, of which three were led by psychologists and four were led by CCs. Completion rates were the same for psychologists (12/13) and non-psychologists (12/13). The time taken to complete the therapy was longer for the non-psychologists (29.62 weeks) than the psychologists (16.92 weeks). These findings are supported by literature on the implementation of FI, which suggests that therapists need to have ring-fenced time rather than taking on therapy as part of their care co-ordination role. 33,161
The outcome measures are suitable for use in a future clinical trial, but they may need some adjustment for skewness. We were successful in collecting outcome measures from therapists and for most of the service users and family members who completed each stage of the trial. We report the variability of the measures for use in estimating sample size for a future trial.
Recommendations for the design of a future trial
-
The identification of service users to approach for the trial took more time than we had anticipated. Although face-to-face approaches are more labour intensive, a future trial should concentrate on these methods of recruitment, as they were the most successful in this feasibility trial. This is perhaps because of previous adverse relationships and limited experience or knowledge of therapy in this group.
-
Consent rates were fairly high in community settings, but gaining consent was much more difficult in acute settings as a result of high turnover, acute mental health state and lack of capacity. A future trial involving acute and rehabilitation settings should identify greater numbers of service users to allow for this drop-off. Recruitment efforts at acute sites should involve gauging interest of eligible participants and following them up when they are deemed well enough to engage in therapy.
-
We were able to recruit families, nominated FSMs and a pool of recruited FSMs. All three types of families were taken up by service users, demonstrating the feasibility of delivering CaFI with FSMs. The findings from the fidelity study suggest that further work is needed to determine whether or not this represents a different intervention. Nevertheless, it is important to note that half of the service users who started therapy would not have been able to participate without FSMs, suggesting a role that FSMs may have for other socially isolated groups beyond CaFI (e.g. the forensic population).
-
Most family units completed CaFI, which suggests that it was acceptable, and this is reinforced by the acceptability findings that will be discussed in Chapter 7. However, only half completed treatment within the therapy window of 20 weeks and, in particular, therapy delivered by non-psychologists took a longer time, suggesting that in a future trial we may need to consider additional training and supervision if non-psychologists are to deliver the intervention. We need to take greater measures to ensure that staff members have ring-fenced time to provide therapy, which involves them taking a reduced caseload of care co-ordination clients. Although this ring-fenced time was agreed by managers at the outset as part of the present study, these boundaries were not always adhered to. This was partly because therapy was only a small part of each of the initial lead therapists’ role, and all therapists were still trying to engage a relatively large caseload of other clients.
-
Although reasonable levels of fidelity were achieved, qualitative feedback from supervision suggested that, compared with less experienced therapists, those who were more experienced in delivering therapy as part of their routine job roles demonstrated greater skill in case formulation and working with the complexity presented by some of the families in the study. This suggests that future studies need to recruit experienced therapists or provide more intensive training and supervision to less experienced staff. Although these training requirements have implications for delivery in the NHS, it is noteworthy that the psychologists in the study were all relatively newly qualified (< 3 years post qualification) and had worked at no higher than band 7 in their other posts.
-
The methods of data collection adopted in this feasibility trial achieved high rates of completion at baseline and post intervention. We also achieved a high proportion of responses at 3 months post intervention, although the number of participants who reached that point before the trial ended was small (due to delays in therapy delivery) and, as such, not all participants could be approached for 3-month follow-up assessments. This suggests that the outcome measures were acceptable and feasible to collect from service users, families, FSMs and key workers.
-
One of the anticipated outcomes of CaFI is an improvement in the relationship between the service user and their key worker, and this should be measured as one of the outcomes of a future RCT. However, we identified that 3 out of the 31 services users in this feasibility study changed their key worker during therapy and, therefore, the post-intervention and follow-up assessments were completed by a different key worker. Further thought is needed about how this discrepancy can be assessed in future trials. Additionally, some items on the WAI were not deemed acceptable by service users and key workers, which led to missing total scores. Future trials should identify whether or not these items should be included and how to manage missing data for single items.
Chapter 7 Acceptability
Introduction
In this chapter, we assess CaFI’s acceptability to African-Caribbean service users, their families, FSMs and health professionals. This embedded, mixed-methods acceptability study addresses our final study objective and two of our four research questions:
-
Can FSMs (‘proxy families’) serve as acceptable alternatives where families are unavailable?
-
Will CaFI be acceptable to service users, families and health professionals?
Aims and objectives
To assess the acceptability of the intervention to key stakeholders, including service users, their families and mental health professionals.
Study design
We utilised mixed methods to assess the acceptability of the intervention as follows.
-
Longitudinal quantitative data were collected at the end of every session on the elements of CaFI that worked well and elements which did not using therapy feedback sheets.
-
The quality of therapeutic relationships was assessed, the WAI173 was completed after the third therapy session.
-
Qualitative interview data on participants’ views of CaFI were collected in individual, semistructured interviews on completion of therapy.
Therapy feedback sheets
Procedures and materials
Service users and family members/FSMs completed feedback sheets (see Appendix 27) to capture immediate responses and to assess the acceptability of each CaFI session and of the intervention overall. Feedback sheets included six statements, four of which were positively worded:
-
‘I learned something new today’.
-
‘I know where to get more information’.
-
‘I have a better relationship with my relative’.
-
‘I am more able to say what my needs are’.
To check engagement with the measure, two negatively worded items were included:
-
‘I am more worried about my ability to cope’.
-
‘The session was not useful’.
Two additional items sought participants’ views on the length of sessions and their feelings about attending the next session.
Data collection
Feedback sheets were distributed by therapists. They were completed by each individual, placed in sealed envelopes, labelled with identification numbers and returned to the therapists, who passed them to the RPM/RA for analysis. This was intended to maximise data capture and reassure participants about confidentiality.
Data analysis
Using descriptive statistics, data were analysed separately for services users and family members/FSMs, overall ratings (across all sessions), by therapist type, by clinical setting and by session number.
Results
Data completeness
Feedback sheets were completed by service users for 194 (84.35%) out of the 230 sessions and by family members/FSMs for 183 (83.18%) out of the 220 sessions they attended.
Overall acceptability
Service users
Service users’ feedback was largely positive (Table 20). The proportion of answers from service users who ‘agreed’ or ‘strongly agreed’ with positively scored items ranged from 82.87% to 91.24%. Less than 3% ‘disagreed’ or ‘strongly disagreed’ for all items. On the reverse-scored items, the proportion that ‘disagreed’ or ‘strongly disagreed’ was 73.26% and 81.58%, respectively. There were more negative responses to these items. Twenty-six (13.91%) service users ‘agreed’ or ‘strongly agreed’ that they had worried about their ability to cope and 22 (11.58%) that sessions had not been useful. It is possible that negative scoring caused confusion, as suggested by the high proportion of positively scored items, but we cannot assume this.
| Item | Response, n (%) | Total, n (%) | ||||
|---|---|---|---|---|---|---|
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | ||
| Learned something new | 89 (45.88) | 88 (45.36) | 14 (7.22) | 2 (1.03) | 1 (0.52) | 194 (100) |
| Know more about where to get information | 75 (39.47) | 93 (48.95) | 18 (9.47) | 4 (2.11) | 0 | 190 (100) |
| Better relationship with relative | 76 (41.99) | 74 (40.88) | 26 (14.36) | 4 (2.21) | 1 (0.55) | 181 (100) |
| More worried about ability to cope | 10 (5.35) | 16 (8.56) | 24 (12.83) | 88 (47.06) | 49 (26.20) | 187 (100) |
| Session was not useful | 6 (3.16) | 16 (8.42) | 13 (6.84) | 75 (39.47) | 80 (42.11) | 190 (100) |
| More able to say what needs are | 74 (38.54) | 97 (50.52) | 16 (8.33) | 3 (1.56) | 2 (1.04) | 192 (100) |
| Mostly positive | Neutral | Mostly negative | ||||
| Feelings about attending next session | 138 (75) | 40 (21.74) | 6 (3.26) | 184 (100) | ||
| Too long | Right length | Too short | ||||
| Feelings about length of session | 2 (1.05) | 170 (89.01) | 19 (9.95) | 191 (100) | ||
The proportion of service users who felt ‘mostly positive’ about attending the next session was 75%, with 21.74% neutral and 3.26% mostly negative. In relation to the length of sessions, 89.01% found them ‘about the right length’, 1.05% indicated that they were ‘too long’ and 9.95% said that they were ‘too short’.
Family members/family support members
Family members’ and FSMs’ responses were broadly positive (Table 21), although they were markedly less positive than those of service users. On the four positively worded items, the proportion that ‘agreed’ or ‘strongly agreed’ ranged from 51.96% to 86.82%. The proportion that ‘disagreed’ or ‘strongly disagreed’ was < 4% for all answers, reflecting a higher proportion of neutral answers than among service users.
| Item | Response, n (%) | Total, n (%) | ||||
|---|---|---|---|---|---|---|
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | ||
| Learned something new | 62 (34.07) | 96 (52.75) | 18 (9.89) | 5 (2.75) | 1 (0.55) | 182 (100) |
| Know more about where to get information | 18 (10.06) | 75 (41.90) | 70 (39.11) | 16 (8.94) | 0 | 179 (100) |
| Better relationship with relative | 35 (20.00) | 90 (51.43) | 45 (25.71) | 4 (2.29) | 1 (0.57) | 175 (100) |
| More worried about ability to cope | 4 (2.30) | 2 (1.15) | 53 (30.46) | 50 (28.74) | 65 (37.36) | 174 (100) |
| Session was not useful | 6 (3.30) | 12 (6.59) | 21 (11.54) | 67 (36.81) | 76 (41.76) | 182 (100) |
| More able to say what needs are | 23 (12.99) | 85 (48.02) | 65 (36.72) | 3 (1.69) | 1 (0.56) | 177 (100) |
| Mostly positive | Neutral | Mostly negative | ||||
| Feelings about attending next session | 142 (82.08) | 28 (16.18) | 3 (1.73) | 173 (100) | ||
| Too long | Right length | Too short | ||||
| Feelings about length of session | 1 (0.56) | 168 (93.33) | 11 (6.11) | 180 (100) | ||
Responses to reverse-scored items were also positive. The proportions that ‘disagreed’ and ‘strongly disagreed’ were 66.04% (coping) and 78.57% (helpfulness of session), with 3.45% and 9.89%, respectively, agreeing/strongly agreeing. In common with the service users, it is possible that the reverse-scored items were misunderstood. Although it may be possible to feel, for example, that the session was not useful, while also reporting a range of positive outcomes on other items, the inconsistency is clear.
The majority of family members/FSMs (82.08%) were positive about attending future sessions, higher than among services users. Regarding the length of the sessions, 93.33% of family members/FSMs felt that they were ‘about the right’, again higher than service users. Only one person (0.56%) reported that the session was ‘too long’.
Acceptability by therapist type
Therapeutic engagement affects the progress and effectiveness of interventions. 124 To compare therapy feedback scores between CaFI participants who worked with lead psychologists and those who worked with non-psychologists, we calculated the percentage of responses rated ‘positive’. We then compared the rate of positive responses between the two therapist types. Responses were classed as ‘positive’ if respondents:
-
agreed/strongly agreed with positive statements
-
disagreed/strongly disagreed with negative statements
-
were ‘mostly positive’ about attending the next session
-
felt that sessions were the ‘right length’.
There was no difference in service users’ rating of the sessions according to therapist type. Service users’ were as likely to rate psychologists positively (n = 75, 83.28%; feedback sheets) as they were to rate non-psychologists postitively (n = 119, 84.94%). Despite a slightly lower level of positive responses overall, a greater proportion of service users rated psychologists positively against the first six items (47.39% vs. 28.54% for non-psychologists). These items included increased ability to access information and improved relationship with relatives.
Family members/FSMs rated psychologists’ delivery of CaFI (n = 96, 78.73%) more positively than delivery by non-psychologists (n = 87, 68.86%).
Acceptability by clinical setting
Culturally adapted Family Intervention was delivered in three clinical contexts:
-
acute inpatient wards
-
rehabilitation units
-
community settings.
We calculated the proportion of service users and family members’/FSMs’ positive responses by clinical setting, applying the same criteria used to calculate responses by therapist type.
The highest proportion of positive responses was recorded by service users in rehabilitation settings (95.24%). Responses (n = 8) were too few to draw any conclusions. Those who received CaFI in community settings returned more positive ratings (n = 145, 88.92%) than those in inpatient wards (n = 41, 81.80%).
In contrast, family members were less likely to rate CaFI positively when it was delivered in rehabilitation (n = 8, 75%) than when it was delivered in community settings (n = 137, 87.14%). Delivery in acute inpatient settings (n = 37, 70.90%) received the lowest proportion of positive responses.
Acceptability by session number
Information about the acceptability of individual CaFI sessions is important because this will inform further revision of the intervention. We calculated the percentage of ‘positive’ responses separately for services users and family members/FSMs.
The proportion of positive responses was fairly consistent across the 10 sessions, ranging from 77.72% to 90.68% for service users and from 65.46% to 80.36% for family members/FSMs. There was no clear pattern of positive responses increasing or decreasing over the 10 sessions. Family members/FSMs generally rated sessions less positively than service users. Although 9 out of the 10 sessions were rated positively by > 75% of service users, only half received that rating by family members/FSMs.
Among both groups, the first session yielded the lowest proportion of positive responses: 77.72% for services users and 65.46% for family members/FSMs. Session 9 (90.6%) received the highest rating from service users and session 10 (80.3%) received the highest rating from family members/FSMs.
Working alliance
Procedures and materials
To measure the quality of the therapeutic relationship,175 the WAI173 (see Chapter 6, Outcome measures for a future randomised controlled trial) was completed by all session attendees at the end of the third therapy session.
Lead therapists and co-therapists individually completed separate key worker versions of the WAI in relation to the service user and each family member/FSM. Each service user and family member/FSM completed the client version of the WAI in relation to the therapist dyad (i.e. both lead and co-therapist).
Data collection
The WAIs were completed by each individual and placed in sealed envelopes labelled with identification numbers. Therapists then passed them to the RPM/RA for analysis (upholding confidentiality).
Results
Working Alliance Inventory: service users
The service user WAI was completed by 18 (58.06%) service users, 19 (61.29%) lead therapists and 14 (45.16%) co-therapists.
Service users’ mean WAI rating of the relationship with their therapy team was 68.28 (SD 13.71). The corresponding WAI rating by the lead therapist was 63.58 (SD 8.73) and by the co-therapist was 62.93 (SD 7.86).
Working Alliance Inventory: family members/family support members
The family member/FSM WAI was completed by 17 (54.84%) family members/FSMs, 14 (45.16%) lead therapists and 14 (32.25%) co-therapists. Family members’/FSMs’ mean WAI score was 68.71 (SD 11.85). The corresponding WAI rating by lead therapists was 63.07 (SD 8.40) and by co-therapists was 61.30 (SD 14.36).
Quantitative findings summary and conclusions
We achieved very high response rates. Service users and family members/FSMs completed feedback sheets on 84.35% and 83.18% of sessions, respectively. Participants were asked to rate all of the CaFI sessions they attended in relation to whether or not by the end of each session they:
-
had learnt something new
-
knew more about where to get information
-
had better relationships with relatives
-
were more able to articulate their needs.
Two negatively worded items related to whether or not the session:
-
made them more worried about their ability to cope
-
had not been useful.
Respondents were also asked to rate:
-
therapists
-
setting (community, acute inpatient wards, rehabilitation units)
-
individual sessions.
Between 83% and 91% of service users rated CaFI positively overall. Ratings were lower for family members or FSMs than for service users (51 vs. 86.82%). Given consistent reports of non-engagement among African-Caribbean service users and their families,23,199 these are important findings. They suggest that even service users with chronic symptoms found CaFI acceptable. Lower ratings by families and FSMs might reflect ambivalence to their role in therapy as highlighted in qualitative interviews.
Most respondents (89.01% of service users and 93.33% of families/FSMs) felt that 1 hour was about the right length for sessions. Acceptability of CaFI was maintained across all 10 sessions without any appreciable change over time. Although service users gave all but one session positive ratings in excess of 75%, only half of the sessions achieved ratings at this level from family members/FSMs. The first session received the lowest rating from both groups. This is perhaps not surprising in an ethnic group with reported reluctance to ‘talk your business’36 and who have had little previous access to psychological therapy. The first session, therefore, might have been particularly anxiety provoking.
Although all clinical settings achieved at least 70% positive rating, there were mixed views about the most acceptable location for CaFI delivery. Service users in rehabilitation settings rated the intervention more positively, whereas families/FSMs rated community settings more positively. It may be that service users perceived the intervention as potentially improving their ability to transition from services into the community and/or improve their social function in current contexts. Less positive ratings of inpatient settings by families and FSMs might reflect discomfiture with this environment, particularly among FSMs for whom this might have been their first experience of these settings.
Delivery of CaFI by psychologists or non-psychologists made no difference to the acceptability among service users, but family members/FSMs reported higher rates of acceptability when it was delivered by a psychologist (78.73% vs. 68.86%). Although both types of therapists were able to engage families, psychologists were rated as delivering specific components of CaFI more effectively. This is important because ability to access information, improve family relationships and better articulate their needs were key issues highlighted during the cultural adaptation process (see Chapters 3 and 4).
To assess the quality of therapeutic engagement, service users, family members/FSMs and therapists completed the WAI173,200 after the third CaFI session. Response rates were low compared with data collection in other aspects of CaFI. Between 32.25% and 61.29% of completed measures were returned for analysis. This was partly because of difficulties retrieving the data from therapists, meaning that some data were received too late for these analyses. Anecdotal evidence from therapists and FSMs indicate that some service users and family members had difficulty reading the measure. It was also suggested that some service users were uncomfortable completing feedback sheets in the presence of therapists and/or were reluctant to return forms via therapists. This may reflect deeply entrenched concerns about confidentiality in this community36 and concerns about the consequences of being seen to challenge ‘the system’ as expressed during focus group discussion (see Chapter 3).
High therapeutic alliance scores were achieved (ranges: 63–68 service users, 61–69 family members and 61–63 therapists). A systematic review of therapeutic alliance in psychological therapies for psychosis201 reported weighted WAI averages 64.51 (range 63.70–70.8) for clients and 61.26 (range of average 60.75–64.2) for therapist. This suggests that the WAI scores in the current trial were comparable to WAI scores in previous therapy trials for psychosis. Given African-Caribbean service users’, families’ and community members’ fear and mistrust of services,23 this level of therapeutic engagement was unexpectedly high. It augurs well for future trials of CaFI.
In conclusion, high levels of positive feedback and therapeutic engagement provide evidence that:
-
CaFI, as we delivered it, was acceptable to service users and family members/FSMs in terms of both content and length of session
-
delivery was acceptable across community and inpatient settings
-
delivery was acceptable via both psychologists and non-psychologists
-
non-psychologists might require additional training to improve the experience for family members/FSMs in relation to accessing information and ability to express their needs.
Qualitative interview data
Participants
To gain deeper insight into the acceptability of the intervention to service users, families, FSMs and therapists, we aimed to conduct qualitative interviews with all study participants. A sample of key workers from acute, rehabilitation and community settings was also purposively selected for interview. This approach enabled maximum variation in the sample in terms of profession, gender, clinical setting, retention in CaFI (i.e. those who completed the sessions and those who withdrew) and familial relationship type (family member/FSM).
Procedures
As qualitative follow-up interviews were ethically approved as part of the feasibility study, participants’ consent was obtained as part of this study before baseline assessments were carried out (see Chapter 6). The therapists informed the RPM/RA when the final sessions were planned so that post-intervention assessments could be scheduled in advance and process consent could be obtained via telephone.
Consenting participants were offered the choice of completing interviews during the post-intervention assessment or at an alternative date within the 3-month follow-up period. Service user, family and FSM participants received £10 for taking part in the interview.
All interview data were stored and managed in accordance with the University of Manchester’s Data Protection Policy and Management Plan and MHSCT’s R&D policy.
Materials
We developed study-specific interview schedules (see Appendix 28 for service user example) tailored to explore each group’s perspectives on different aspects of the study, including:
-
perceptions of the need and benefits of CaFI
-
usefulness, cultural specificity and accessibility of CaFI and supporting materials
-
content and delivery of CaFI sessions
-
perceived barriers to/facilitators of implementation
-
views and experiences of training/supervision
-
views and experiences on the role of FSMs
-
participating in research versus therapy.
Using predominantly open-ended questions in a semistructured interview format allowed us to explore aspects of the intervention that participants particularly liked or disliked and areas where improvements should be made. Interviews were conducted by the RPM/RA.
Data analysis
Interviews were digitally recorded, transcribed, checked for accuracy and analysed using framework analysis. 42 Thematic analysis had originally been proposed. However, as the data were intended to address a priori topics, a deductive approach was more appropriate. 202 The RPM and RA read and re-read the transcripts (familiarisation) before completing coding. To ensure data quality, a 10% sample was reviewed by the PI and discrepancies were resolved through discussion.
A coding framework was developed by clustering similar codes into preliminary themes and subthemes. These were reviewed by the wider research team and an independent qualitative methodologist. This framework was then applied across the entire data set, charting, indexing and annotating themes. This resulted in a refined (conceptual) framework, illustrated by particularly relevant quotes, which was examined by the research team and an independent qualitative expert for goodness of fit and the final theoretical framework agreed. Mapping the data onto the framework facilitated synthesis, interpretation and ‘auditability’. 128 Transparency of these processes attest to the ‘trustworthiness’ of findings. 203
NVivo 10 software (QSR International, Warrington, UK) was used to support data management and analysis. To preserve participants’ anonymity, illustrative quotations are presented using truncated study identification numbers.
Results
Sample characteristics
Forty-six out of the 52 participants who were approached completed qualitative interviews (88.46% response rate). In total, 22 service users, 12 family members and 14 FSMs (seven recruited, seven nominated) agreed to be interviewed within 3 months following delivery of CaFI. Among those families who started therapy (n = 26), four service users, one nominated FSM and one recruited FSM did not complete interviews. Two service users refused for their interviews to be recorded, one service user was too unwell (relapsed) and one service user and two FSMs could not be contacted. Demographic information for service users, FSMs and relatives can be found in Chapter 6, Baseline characteristics.
Thirteen therapists also completed interviews. One therapist could not complete the interview because of relocation. We successfully recruited purposively selected 10 key workers to complete interviews: eight CCs, one nurse and one psychiatrist. Seven were female and three were male. Nine out of the 10 key workers were from community settings, reflecting the mix of clients.
Given the centrality of the care co-ordination role, these participants were regarded as ‘key informants’121,204 in relation to CaFI’s acceptability and potential implementation among frontline NHS staff. We sought their views on:
-
the need for CaFI
-
the potential benefits/disbenefits of the intervention
-
the perceptions of whether or not it had made any actual difference to their clients
-
if CaFI should be rolled out across the organisation and wider NHS
-
the perceptions of barriers to implementation.
Results are reported separately for service users, family members, FSMs, therapists and key workers, reflecting their different roles and perspectives. Given previous engagement challenges, the findings in relation to services users are presented in greater detail than those of other participants.
Acceptability to service users
Meeting needs and benefits
All service user participants felt CaFI had at least partially met their needs. Specific benefits included:
-
increased confidence and self-esteem
-
greater insight into illness
-
improved symptoms
-
improved knowledge and understanding of services
-
better communication with family and health professionals
-
improved coping skills, including to ability to draw on personal and community resources.
It’s woken me up to my illness really. I’ve been in and out of hospital for about 12 to 13 years now. That’s half my life really. I felt if I opened up about my illness . . . my voices would get worse but they’re not getting worse. I’ve got them on lock down basically I’ve got them on a hush, on block. I’m blocking them out and I thought ‘if I opened up about it then it would make it worse’ but it didn’t. I felt good.
SU521
Service users also reported improvement in symptoms such as sleep problems and paranoia:
One week when they came in and spoke about helping me with my sleep problems, they told me not to drink after a certain time. [Therapist name] gave me meditation that I put on my phone to help me sleep.
SU502
. . . I’m not as paranoid now, when I used to speak to other members of my family I used to be quite paranoid . . .
SU506
Perceived benefits resulted in self-reported improved quality of life, including engaging in meaningful activity and starting new relationships:
. . . At the end of it [CaFI] she [therapist] told me about a position within the services that I could do. Befriending or something like that, which gimme a lot of confidence . . . made me feel valued as opposed to just persecuted all the time . . .
SU503
OK, can you think of any other changes that you’ve not mentioned that came about as a result of taking part in the therapy?
Erm, I got a boyfriend! [Laughs.]
Cultural specificity
Responses to the cultural specificity of the intervention were mixed. Some agreed that African-Caribbean people’s needs differed from those of other ethnic groups:
Caribbean people . . . they are different in many ways like White people or even Chinese or Asian.
SU503
Other respondents highlighted the need to treat all people as individuals, including recognising the diversity within, as well as between, ethnic groups:
I’m not Black. I’m mixed. You know there’s a difference. You’ve got White, you’ve got Black, you’ve got mixed so I suppose it’s good to have a mixed-race person in the study . . . You hear a lot of negative propaganda about Black people being killed in mental health care and in police stations . . . you don’t really hear it about mixed-race people . . .
SU509
Session content and supporting materials
Participants liked the session content and supporting materials such as the information booklet about schizophrenia and psychoses produced by the CaFI team (see Acknowledgements, Publications):
I think it was quite good, it tells you what causes psychosis . . . I’m not schizophrenic but I suffer from psychosis so I read up some information about them so it was quite helpful knowing about psychosis and what causes it and treatments.
SU506
In line with findings from the feedback sheets, most participants felt the number of sessions was ‘about right’, but there was some variation in responses. However, some people reported that it took ‘a good few sessions to open up’ (SU509) and establish trust with therapists, so 10 sessions were not quite enough. Yet one participant felt that she had ‘talked about everything’ by session 8. Consequently, the last two sessions where ‘they were wrapping up . . . was a little bit boring’ (SU509).
Flexibility and choice
Service users valued flexibility and choice in the delivery of CaFI sessions, especially in terms of time and location:
Most of them [were] in the afternoon because I used to have problems waking up in the morning so I think I’ve never had sessions in the morning, it’s always been 2, 3, 4 o’clock, which suited me better.
SU506
Whereas some participants welcomed the opportunity to have sessions in new environments:
I don’t really have any experience of anyone who does go to university. I thought it would be a good way to apply myself to having a level of university understanding . . . so it’s been great . . . really having to work in university and travel from there to here. I get to sit here and do this and gain from it, learn from it.
SU522
Others particularly valued the delivery of CaFI in their own homes:
I don’t drive, so it’s a bit difficult to get to some places . . . you feel more comfortable when you’re at home and people with illnesses can’t go certain places or they get paranoid, I tend to get quite paranoid and anxious when I’m going places that I don’t know, so coming here is a lot better.
SU506
Perceptions of therapists
Service users were overwhelmingly positive about the therapists: ‘some of the finest people I’ve ever met’ (SU522). Even the one service user who felt therapists were unable to understand his needs because they had not experienced ‘breakdown’ (SU507) acknowledged that they were ‘trying to get me better’ and that ‘in good time’ they achieved a measure of success, including developing a coping strategy of ‘what to do and what not to do’ that proved beneficial: ‘that’s helped me so much’ (SU507).
Participants valued therapists’ non-judgemental approach. This created a sense of safety, enabling being heard by family members – sometimes for the first time:
. . . my mother is really confrontational and she’s really abusive, and with [therapist names] sat there she couldn’t be so directly abusive and confrontational, she had to take into regard what I was saying . . . she had to come in and listen to what I was saying and what I felt. So it was good because she had to listen to what I was saying.
SU522 (emphasis in bold)
This female service user (who had been so withdrawn that she would not leave her flat) wished she could maintain contact with her lead therapist beyond the intervention:
I wished she [lead therapist] wasn’t the therapist. I really wanted to say, ‘come on you know let’s get our gladrags on and go out for a drink together’. Like, I did talk to her that much. I’d like to go out for a drink with her and just enjoy myself.
SU509 (emphasis in bold)
Most people thought that the lead and co-therapist working together was beneficial: ‘obviously two is better than one and . . . they were quite professional and I preferred the two than the one’ (SU 506). Not everyone was convinced, however:
Sometimes it was hard to talk to both [lead therapist name] and [co-therapist name] because I just wanted to get [lead therapist name] by herself and have a really good chat to her . . .
SU509
Perceptions of family support members
The FSM role was generally regarded positively. One service user commenced CaFI with a family member who could not continue due to bereavement. Unable to nominate an alternative, he was matched with a recruited FSM:
Yeah it was good because she knows a bit about mental illness. She’s doing a degree in psychology and I thought it was really good that she came and helped me as a family support member . . . I feel that she was appropriate, she was good. She’s Afro-Caribbean as well so she understands certain things.
SU506
In contrast, another service user ‘wasn’t totally comfortable with it’ and ‘wasn’t disheartened’ when her friend (nominated FSM) ‘sort of let everybody down’ by not completing agreed sessions as she felt the context impeded natural interaction:
I felt that she was holding back, you know. I’d prefer her to just let go and just say everything she felt about her experiences of me.
SU509
Would you recommend CaFI?
All service users said that they would recommend CaFI to someone they knew and that it should be rolled out across the NHS:
I would do, yeah. I really would, I really would. I think it should get spread all over the United Kingdom. I think it really should, ‘cause I think it’s really helpful. It’s helped me a lot.
SU521
It was a really good experience and I’d advise anyone to do it and I’d do it again tomorrow! Thanks for letting me be a part of the CaFI study . . . It’s really helped me . . . I’m a lot happier now than I was when I started, a lot more confident . . .
SU509 (emphasis in bold)
One participant made the distinction between participating in CaFI and participating in the trial, which he found somewhat onerous:
Yeah, but I’d recommend them to the CaFI itself rather than the strategy because first there’s interviews . . . then there’s the therapy, then there’s interviews of the results . . .
SU518
Acceptability to family members
Meeting needs and benefits
Overall, family members felt that participating in CaFI had been a positive, ‘eye-opening’ and ‘fulfilling’ (R5261) experience that either met or exceeded their needs. The greatest perceived benefit was improved insight into the illness:
I gained something from it. For people that don’t understand [schizophrenia], if they go through the therapy sessions, then it would open their eyes and help them understand and help them better deal with their relative or friend . . .
R5111
Participants identified positive changes both in themselves and in service users, including:
-
improved mood
-
learning more constructive ways of communicating with service users and health professionals
-
improved problem-solving skills
-
better relationship with service users.
The last is exemplified by this participant’s quotation which notes a decline in arguments between her and her son (service user):
We haven’t been having as many arguments. Well, we have arguments, but not as many.
R5171
Personal benefits to family members included improved stress management:
It teaches you how to manage stress differently and I suppose, when I was a bit stressed, I had to look at things . . . you have to take a step back and look at things.
R5051
However, this participant reported that reacting to a crisis quicker as a result of CaFI ended in frustration, reinforcing her view that there was little point in engaging early with ‘useless’ services:
I think it made me want to react quicker . . . rather than trying to cope with [service user] and deal with it at home. I tried to do what I had learnt and react quicker and get help with it quicker, but I was right. As usual, the services are useless. So there’s no point in learning it, there’s no point in reacting quicker because they [services] don’t react properly.
R5041
Cultural appropriateness
Participants perceived CaFI as beneficial and capable of meeting the needs of their families. However, they questioned the validity of having an intervention for all African and Caribbean people, highlighting the differences within this group and between other Black populations:
. . . people are different you know, all people different . . . I’m West Indian, I have an African Somali friend and we are different, you know, in many ways. I could tell you how Jamaicans think and work but I couldn’t tell you if other Caribbean or African countries do things the same because in Africa they do things different from us.
R5261
Session content and supporting materials
Session content was mostly rated positively. ‘Shared learning’ and ‘communication’ were perceived by the majority of participants as particularly helpful – specifically, learning constructive ways to communicate and clarify misunderstandings:
He [service user] was always angry because . . . he thought that I was the one who got him sectioned so we didn’t communicate very well until near the very end when he realised I can’t actually get him sectioned.
R5221
However, some participants reported that, having evolved their own ways of coping with stress, they found stress management sessions somewhat redundant:
I’ve learnt to deal with stress as I’ve gone along, there’s been a lot to deal with [service user] so I’ve always learnt to just cope so it didn’t really help to that [extent] because I could always already sort of cope.
R5221
Flexibility and choice
There was no consensus on the duration of individual sessions. Four participants agreed that 1 hour was ‘about right’, but five participants would have preferred sessions longer (90 minutes was most frequently recommended). Some people thought 10 sessions were ‘about right’, however, four participants would have preferred more than 10 (suggested range 12–20 sessions):
Yeah I wish they were a bit longer . . . Because sometimes you might have only just got to topic that you might have to finish quickly or say at the beginning if you just briefly mention it, but obviously can only do the hour so . . . I think about an hour and a half, because by the time you’ve taken your coats off and you call [service user] down to get settled then you’ve probably lost about 20-odd minutes to be honest.
R5171
All family members agreed that service users’ homes was the preferred location for delivering CaFI:
Being here [service user’s home] made it better for [service user] because it’s comfortable.
R5041
Yeah I think for [service user] it was more comfortable and relaxed for him to be on his own where he was familiar with his surroundings rather than us having to go off to somewhere maybe it made it more informal, rather than us having to travel somewhere. I think it was better.
R5191
Perceptions of therapists
All FSM participants reported liking the therapists as people, as well as liking their therapeutic approach:
They were both lovely. Yeah, they were both absolutely lovely and they were so knowledgeable that everybody should have one. They should be someone like [those] two available to every patient.
R5041
I’ve never actually been in a session like that so I couldn’t really compare but I thought they had a good approach.
R5191
The majority preferred two therapists over one, citing co-therapists’ supportive role in delivery, which allowed the lead therapist to focus on delivery:
[ . . . ] it give the lead person the opportunity to be talking and making eye contact with me and stuff like that, whilst the second person will be taking all the notes, so I think it’s better for two.
R5111
Would you recommend CaFI?
All family members said that they would recommend CaFI to anybody they knew who might be experiencing similar issues:
If I knew anybody – yeah, definitely! Yeah, because I think that . . . you know, not everyone’s mental health problem is the same as [service user’s name] and I would imagine it would be helpful for them yeah definitely.
R5031
Acceptability to family support members
Meeting needs and expectations
Most participants said that their expectations of CaFI were at least partly met. All but one FSM perceived that the intervention met the needs of African-Caribbean families. The participant who considered that CaFI did not meet the service user’s needs felt that there was not enough time or culturally appropriate resources to address past experiences of racism:
I definitely think it’s a good thing that that there’s a therapy that’s been adapted for African-Caribbean people erm and I do think that’s more likely to meet the needs of that community, but with [service user], probably not. But then again because he brought up issues of racism, this particular therapy may have been much more appropriate and may have met his needs in a better way.
R527110
Perceived benefits
Most FSMs felt that CaFI had benefited service users. Observed changes in service users included:
-
increased self-awareness and self-confidence
-
improved mood, communication and self-care skills
-
reduced self-blame for illness
-
changed outlook on the future.
Family support members also identified personal benefits from taking part. The most frequently mentioned benefit was increased confidence in relating to persons with mental illness through getting to know service users and learning more about their illness:
I’d say just listening to [service user’s] personal experiences and reading . . . I’ve read information before on psychosis, but actually seeing someone talking about it. It’s just so different and means so much more. So, yeah, I feel like I understand a lot more, more aware.
R523112 (emphasis in bold)
Cultural specificity
Although some FSMs gained greater awareness of important issues within African-Caribbean communities, such as faith and the role of the church, most could not identify specifically culturally adapted elements in CaFI’s delivery. Consequently, the intervention was perceived as being suitable for all families with mental illness independent of their cultural heritage:
It meets the needs of all people. I don’t know whether there was anything specific about it . . . it didn’t feel culturally adapted. It felt appropriate, but it didn’t feel that there were any sort of special considerations made due to erm [service user’s name] having an Afro-Caribbean background.
R5201
Perceptions of the family support member role
Family support members regarded participation in CaFI as a ‘good learning experience’ (R506111; R5251; R523112). However, although training and support (individual and group supervision) were consistently considered ‘good’ and ‘helpful’, uncertainty about FSMs’ roles and responsibilities was a recurrent theme:
But to go in as an artificial family support member, at times I felt really insecure because I felt like ‘what am I actually contributing?’ ‘What actual difference am I making?’ ‘Would it make a difference if I didn’t turn in today?’
R502102
Family support members also expressed uncertainty about meeting and working with the service users, especially in their homes and parts of the city unfamiliar to them:
I was a bit nervous at the start just because I would be meeting someone new and I didn’t really know how they would behave. I was going to a new area of Manchester that I’d never been before and into like into the house of a complete stranger.
R506111
Perceptions of CaFI sessions
Family support members identified a range of aspects of CaFI that they particularly liked, such as:
-
ice-breaker game in the initial sessions
-
guided imagery and relaxation
-
‘shared learning’
-
self-esteem work.
Less positively, some FSMs reported that the sessions should have been longer as sessions sometimes felt ‘a bit rushed’ or over-ran:
Sometimes it does feel a bit rushed . . . I do think, at first, we were going a little bit overtime . . . and, towards the end, I think they were trying to tighten it up which is totally understandable . . . so, I think having a bit more time to get the formalities and pleasantries and catching up bits out of the way first and then really getting to the therapy work would have been useful.
R510103
Family support members reported that miscommunication with therapists was a source of frustration:
. . . [I] left a message on their voicemail like ‘I’m not going to be here on the session’. When I went back the following week, they weren’t there and I didn’t know. Then [service user name] said ‘oh it’s not on this week’.
R515105
Perceptions of therapists
Despite some challenges with communication and involvement with therapists, FSMs gave mostly positive feedback on therapists who were perceived as competent, easy to work with, supportive and knowledgeable:
Nice person and I think he has a way obviously has a way in his capacity of working with people in mental health different form of mental healths he knew his work really.
R518105
She [lead therapist] was really friendly, very approachable. I felt like I could like talk to her about things. Very, sort of, down to earth I’d say . . . She’d sort of talk about her own life in the therapy sessions and she didn’t see herself as sort of above anyone, which is nice.
R506111
Would you recommend CaFI?
All participants would recommend CaFI, suggesting that they perceived the intervention to be beneficial and a good use of their and the service users’ time:
It’s been enjoyable. You know, we had our laugh, it’s an eye-opener, and I just hope that, you know, we can continue to get the help and support we need, at least from yourselves, or anyone else official. And it’s brought us closer. There’s been no tears today, just been no sadness. You know, that’s been ended up happiness. That’s a good thing. I enjoyed it, really.
R5211
Acceptability to therapists
Therapy manual and supporting materials
The CaFI therapy manual was positively received by all therapists. In particular, they valued its structured format coupled with its flexibility in delivery. This enabled them to tailor sessions to meet the needs of individual service users and their families. However, it was suggested that this degree of flexibility might not suit all therapists:
I guess on the flipside . . . some people might not like that flexibility and want it a bit more structured. But my personal opinion was that the manual’s flexibility was great because it allowed space to work with other things that came in so it didn’t feel as you were taking part in a research study . . . It felt more reflective I guess of what we might do in clinical practice.
T208
Therapists also commented positively on the supporting materials. According to T208, ‘quite a few of the resources were brilliant’. Relapse prevention, stress management, problem-solving and the ‘goodbye letter’ were cited as especially valuable. All therapists said that they had continued to use elements of the manual and supporting materials in their everyday practice and had shared them with colleagues:
I’ve used loads of it in my day job sort of thing. I’ve used loads of it and when people [other colleagues] have seen they have been, ‘ooh what’s this relapse thing you’ve got’, you know, they like it. I’ve used it twice today already!
T201
Working cross-culturally and clinical supervision
Although indicating that communication was ‘probably the most important bit’ of CaFI (T201), therapists found engaging service users and families in discussion around culture challenging:
So a couple of times he was like, ‘why do you keep bringing it up?’ Like I was obsessed with it [laughs] but that’s what he kind of made me feel.
T208
One therapist felt there might be generational differences in perceptions of cultural issues. She contrasted her experiences of working with service user A, an older person for whom culture was ‘the dominant theme in his life’. Racism, negative experiences of society and the NHS and references to spirituality were ‘very pronounced and comes into our sessions all the time’ with younger clients:
With [service user B], who’s younger, it felt like a real big theme but it wasn’t really talked about, he didn’t talk about it or raise it as an issue and it almost felt difficult to bring it in. The other person I worked with [service user C], it didn’t come in and I asked her about it directly about culture and she was just like ‘I’m just like everyone else’. So it felt like ‘oh, I’ve offended her’.
T210
This experienced FI therapist’s responses highlighted ‘inexperience in working with a culturally specific model’ (T210). Additionally, communication sessions were impeded by the unavailability of culturally appropriate resources for people from this ethnic background, especially if they did not read well:
I felt like ‘I don’t think I have the tools to work with somebody who can’t read very well and struggles with written documents, or somebody who is of Caribbean descent’ . . . So, I wonder if having more tools that were more specific would be useful, or creating them. It would be really great to have people doing the communication skills who were of Caribbean or African descent or a recording of the session, or something like that.
T210
Inexperience in working cross-culturally and lack of opportunity to practise and develop FI skills was a recurring theme among the non-psychologists. Feeling like ‘a novice’ while delivering CaFI was anxiety-provoking, increasing workload by the sense of needing to ‘over-plan’:
If you’re a novice you overplan and you try to really anticipate everything that could go wrong. Where, if you’re a bit more experienced with something, you don’t need to do that because you feel more confident to let the session go.
T201
In this context, access to regular clinical supervision was regarded as especially valuable:
Supervision was really helpful. It made us see things from a different perspective. It helped us to sort of plan and structure the next session so, yeah, I thought it was good.
T202
Number, length and duration of CaFI sessions
Therapists generally felt that the number (10) and length (1 hour) of sessions and duration of therapy (20 weeks) were ‘about right’. However, they also reported having insufficient time to plan so that preparation sometimes felt ‘bit of a squash and a squeeze’ (T210). Although 10 sessions were felt to be adequate, at least one therapist felt that (reflecting good clinical practice) follow-up sessions should have been offered post intervention:
. . . [In] clinical practice, if I was using this model, I’d probably add in a follow-up, revisiting the family after a period of time, that’s what a lot of therapists will do. They’ll end and then have a follow-up in 3 months’ time or 6 months’ time . . . I’d probably do that where it felt appropriate for the family and revisit skills and maybe be able to offer up to, I don’t know, 20 sessions if that’s needed.
T210
Therapists agreed that, in principle, a 20-week therapy window offered sufficient flexibility to complete sessions. Weekly or fortnightly sessions were considered ideal, but having an extended therapy window would increase scope to manage planned absences (such as holidays) and unforeseen circumstances (such as sickness and emergencies). In practice this was sometimes difficult to achieve. On occasion, this was due to families forgetting or cancelling sessions. In other instances, competing clinical priorities superseded involvement in CaFI:
So, how do you find managing it [CaFI] alongside your role?
Really difficult, really difficult – because you can’t prioritise it . . . [if] you’ve got somebody in an emergency situation, you just have to cancel the family. You have to. You can’t prioritise it.
Should CaFI be rolled out?
Some respondents agreed that CaFI and other culturally adapted interventions should be made available to the wider NHS, particularly in areas with high density of ethnic minorities:
Yeah, absolutely [it] should be rolled out. Ideally, culturally adapted interventions generally should be [available], particularly in certain areas . . . you know, where there are big communities of a particular culture, of a particular ethnicity, where the intervention might be more specific or more culturally involved to be effective . . . So I could easily, I could see it being rolled out, absolutely.
T208
However, the same therapist also highlighted the inherent tensions in commissioning and delivering culturally adapted interventions in a multicultural society:
I’m just thinking about commissioners [laughs]. They’d be like ‘well, that’s fine to have one for African-Caribbean cultures but how many of those live in Salford and how many of those are accessing services? That costs money. I think the idea of adapting something culturally is absolutely great because it personalises everything and makes it more specific . . . but . . . does there need to be something different for every culture?
T208
Acceptability to key workers
Meeting needs and benefits
Key workers agreed that there was a need for CaFI, citing lack of access to psychology and their inability to work with families due to time and workload pressures:
He was on the waiting list to see our psychologist when this [trial] came up and it was very, very pertinent to him . . . he was very keen to have that sort of approach and it involved his family which I thought was really, really helpful because his family struggle to deal with his issues and things. I thought the chance for them all to be together in a room and actually hear each other’s side of things would be really helpful . . .
KW5031
Like service users, key workers reported a range of benefits, including:
-
improvement in symptoms
-
greater compliance with medication
-
better engagement with families and service users, specifically, reconnecting ‘complex’ clients and their families where relationships had broken down; key workers suggested that FSMs could be a potential means of reconnecting service users with their communities where they had ‘burnt their bridges’ (KW5181) with families
-
becoming more positive and aspirational, for example, working towards achieving life goals such as starting a family and enrolling in college:KW5031
To be able to enrol in college . . . his willingness to talk to his mum a bit more . . . Those are the two things I probably have noticed that happened during [CaFI] and afterwards ‘cos he was really cagey about telling his mum anything but he has actually been quite open with her . . .
Relationships between relatives and staff also improved:
She [partner] would speak with me about his mental illness which she wouldn’t before . . . she could be, in the past, quite derogatory about him like ‘oh he’s gone mad again’ and, y’know, that kind of comment but she was very much more like ‘oh nobody understands mental illness’ and a bit more supportive of him really.
KW5021
However, as illustrated by this quotation about a service user’s change of environment and social networks, it was sometimes difficult to attribute improvements solely to CaFI:
. . . he’s slowly engaged a little bit more now, and his drug-seeking behaviour seems slightly reduced and he’s not made any attempts to abscond which was a constant problem while he was at Manchester.
KW5181
Cultural specificity
As they were not directly involved in delivery, most key workers felt unable to comment on this aspect of the intervention. However, one participant highlighted apparent conflation of ethnic labels and cultural identity:
. . . My understanding of it was that it was culturally adapted and I guess there are some people that their culture plays a big part of in their life but there [are] some service users that fall under this category simply by being ethnically African-Caribbean but, maybe culturally, they are not and I think there is a distinction.
KW5171
Barriers to implementation
Respondents suggested that services users’ mental state and families’ willingness to engage in therapy were potentially important implementation barriers. The most frequently cited barriers, however, were financial and service pressures which curtailed their capacity to deliver therapeutic interventions. Key workers felt that these barriers emanated from senior leadership and commissioner levels rather than from managers and front-line staff:
Most managers, most teams would see it as a positive thing which would actually enhance what we give, y’know, what we offer people rather than an issue of resources.
KW5171
Would you recommend CaFI?
All respondents said they would recommend CaFI to service users, families and colleagues. CaFI was considered ‘a very good idea’ (KW5181) that would address a gap in service. For this reason, key workers felt it should ‘be for everyone’ (KW 5171), irrespective of ethnic or cultural background.
Discussion
Culturally adapted Family Intervention proved acceptable to service users, families, FSMs and health professionals. Many of the key outcomes identified by stakeholders in co-producing CaFI (see Chapters 3 and 4) were among its reported benefits, including:
-
greater insight into illness by service users, families and FSMs
-
reduction in symptoms such as paranoia and sleep problems
-
better engagement in treatment, including medication adherence
-
improved social function, problem-solving and coping skills
-
increased confidence and self-esteem
-
improved knowledge and understanding of services
-
better communication with family and health professionals.
All groups reported that CaFI had met service users’ needs and, to a lesser extent, those of their families. For example, the proportions of service users who ‘agreed’ or ‘strongly agreed’ that they had learned something new (91%), knew more about sources of information (88%), had developed better relationships with their relatives (83%) and felt more able to express their needs (89%), were greater among service users than families. Corresponding positive ratings among family members/FSMs were 87%, 52%, 71% and 61%, respectively.
Ability to access information and to have their needs met was identified as an important outcome by carers and families in CaFI’s development. Acceptability findings indicate frustration that, having acquired/enhanced advocacy skills, family members’ attempts to access help and support were thwarted by services that remained insufficiently responsive – leading one participant to brand them ‘useless’. Nevertheless, 82% felt positively about attending the next session. This is counter to African-Caribbean people’s labelling as ‘hard to reach’. However, it is in line with findings from the Aetiology of Schizophrenia and Other Psychoses study, which reported African-Caribbean people’s multiple attempts to seek help but failure to gain timely access to services. 15–17
It is noteworthy that key workers, who were not directly involved in delivery of CaFI, reported improved communication between family members and also between family members, service users and themselves. Better communication between service users, families and mental health professionals marks an important shift in engagement within this triad. Participants’ reports suggest that aspirations of the intervention improving African-Caribbean people’s assertiveness and advocacy skills alongside gaining insight into how ‘the system’ works had been met. After decades of adversarial relationships,199 achieving any degree of rapprochement between members of this community and mental health services is a significant achievement. Further work is needed to identify whether or not specific elements of CaFI (such as the ‘shared learning’ ethos of delivery versus specific content) contributed to these positive outcomes and whether/how they can be replicated elsewhere.
We have demonstrated the feasibility and acceptability of delivering CaFI in acute wards (including psychiatric intensive care units), rehabilitation units and community settings. Service users’ ratings of the different clinical settings were consistently higher than those of family members/FSMs. This was most marked in relation to inpatient settings, which was rated positively by 82% of service users, compared with 71% of families/FSMs. Such a positive acceptability rating is an important achievement in a group with high levels of family disruption. Acute settings can be disturbing environments for those unfamiliar with them. It might therefore be anticipated that this would be reflected in FSMs’ ratings of these settings. However, qualitative analyses showed that they also reported discomfiture about visiting service users’ homes, especially when in areas of the city they were unfamiliar with. This may reflect the ethnocultural diversity of the group and the unfamiliarity of some FSMs with areas of high ethnic density. Our ability to deliver CaFI across all levels of services holds particular salience for this group, who have significantly longer lengths of hospitalisation than other ethnic groups. 30 Commencing FI and working more closely with health professionals to enable earlier discharge might be both cost-effective and clinically effective. Economic evaluation as part of a fully powered trial would be an important addition to the evidence base.
Therapeutic alliance is an essential element of effective psychological interventions of this nature. Service users, family members, FSMs and therapists completed the WAI200,205 after the third CaFI session to assess the alliance between them. Although response rates were lower than on other aspects of the study (32–61%), they were at least comparable with WAI scores in previous therapy trials for psychosis, but therapists’ ratings were slightly lower than service users’ ratings. This may be attributed to therapists’ tendencies to draw comparisons to alliance with other service users when making ratings. 201 Doing so with this group is problematic, given limited evidence about therapeutic alliance among African-Caribbean people diagnosed with schizophrenia and their families. Lack of access to psychological therapy, power differences and promotion of CaFI’s cultural appropriateness could have contributed to service users being less critical of therapy relationships than therapists. Qualitative research nested in a future trial would enable further in-depth exploration of these issues.
Family members/FSMs reported higher rates of acceptability when CaFI was delivered by psychologists (79%) than when it was delivered by non-psychologists (69%). In particular, families gave lower ratings to non-psychologists’ ability to support development of their advocacy and information-gathering skills compared with psychologists. Non-psychologists were band 6 Agenda for Change and psychologists were band 7, as stated in our original protocol and recommended by NICE. Differences in therapists’ skills and levels of experience might have contributed to this finding as suggested by non-psychologists’ reports that they lacked confidence in delivering FI due to inability to practise. The difficulties we experienced in recruiting suitably qualified and experienced therapists (see Chapter 5) are not new. Despite evidence of FI’s clinical effectiveness and cost-effectiveness, services’ inability to implement NICE guidelines161 persist. However, as outlined in Chapter 5, staff recruitment difficulties were compounded in CaFI by serious financial and organisational challenges within the trust that hosted our study.
Arguably the most novel aspect of our study was the involvement of FSMs. NICE30 recommends FI for service users in contact with their families. As African-Caribbean people experience high levels of family disruption and estrangement from their families, we encouraged service users who wanted to participate in CaFI to nominate ‘trusted individuals’ to work alongside them. 158 When this was not possible, service users could choose from a bank of FSMs recruited for the study. Without the involvement of FSMs, 40% of service users in our sample would not have been able to receive CaFI. If NICE recommendations about FI30 are not to reinforce inequality of access, we must evolve new ways of working with those service users who are the most marginalised and socially isolated if recovery and restoration to their families and communities are to be more than rhetoric. In this context, key workers’ suggestions that FSMs could form a ‘bridge’ between service users, their families and communities is worthy of further investigations.
Both families and FSMs reported positive personal benefits of involvement in CaFI, including improved understanding and knowledge of psychosis and schizophrenia. However, there was ambivalence about FSMs and a lack of clarity about their roles. The somewhat mixed response to FSMs among service users and families may reflect differences in FSMs’ backgrounds. Some FSMs were university students undertaking related degrees (psychology or mental health nursing) and others had related professional backgrounds (counselling, former social worker, CC). The remainder were lay members of the public. This range of experiences in general and of mental illness in particular, coupled with a lack of family ties for service users, is likely to have affected FSMs’ role in the therapeutic process. Therapists questioned whether or not FSM involvement represented a different intervention. Owing to lack of emotional involvement, it was argued that their involvement rendered CaFI more like a culturally adapted form of CBT than FI. This observation was reflected in independent rating of fidelity to the delivery of CaFI (see Chapter 6).
There were important differences between the groups in perceptions of CaFI’s benefits for service users and for the participants themselves. Family members were more conservative in their estimation of personal benefits and also reported fewer positive changes in service users compared with FSMs. It may be that FSMs were more highly motivated to participate due to a special interest in psychological interventions, which would likely influence perceptions of its utility and acceptability. Although it could be argued that family members would naturally be highly motivated to take part to improve outcomes for their relatives and families, their ratings and views might have reflected greater scepticism about potential or actual benefits based on previous negative experiences.
All groups said that they would recommend CaFI to others and suggested that it should be rolled out across the NHS. However, participants raised questions about CaFI’s cultural specificity compared with good clinical practice and working with service users and families as individuals. Although acknowledging the need to improve schizophrenia care for African-Caribbean people in the context of inferior care and adverse relationships with mental health services, they suggested that the benefits of CaFI should be available to everyone. An intriguing finding is the extent to which this was endorsed by service users, family members and FSMs, all of whom advocated that perceived benefits should be available to all ethnic groups. This may reflect the independent rater’s observations that several participants appeared to be more motivated by altruism (engaging in research to improve care for everyone), compared with receiving therapy. This has potential implications for CaFI’s implementation and should be explored in future studies.
Although participants believed that CaFI should be rolled out across the NHS, they questioned the viability of having this as one of a range of culturally adapted interventions that would be required to meet the needs of a multicultural society. This is an important consideration, particularly given the financial pressures within health and social care. We recommend that further empirical and theory-building work is undertaken to refine and trial both our cultural adaptation framework and CaFI to better inform commissioning intentions and meet the needs of all groups.
Conclusion
In conclusion, we have demonstrated that:
-
CaFI is acceptable to service users and family members/FSMs, in terms of content, length and duration of sessions
-
delivering CaFI in acute, rehabilitation and community settings is acceptable to key stakeholders
-
delivery by psychologists and non-psychologists is acceptable to service users and their families; however, psychologists’ effectiveness was rated more positively by carers than non-psychologists, suggesting NICE’s recommendations for band 7 therapists may be especially pertinent for a group with high levels of complexity
-
CaFI can be delivered via FSMs in the absence of families, albeit with some ambivalence (questions remain about whether or not FSMs is a different intervention)
-
CaFI has begun to influence wider service delivery as CaFI therapists were using the manual and supporting materials in everyday practice and sharing them with colleagues; this provides further evidence of its acceptability beyond those directly involved in the study and the need for CaFI or ‘CaFI-like’ psychosocial interventions
-
all groups would recommend CaFI to others they knew and for roll out across the NHS; however, further work is needed to:
-
clarify its culturally specific components
-
develop more culturally relevant supporting materials
-
compare the clinical effectiveness and cost-effectiveness of delivery via psychologists and non-psychologists
-
determine the role of FSMs
-
consider whether or not a culturally adaptable (vs. adapted) intervention is needed.
-
Chapter 8 Discussion
Chapter overview
We have demonstrated the feasibility of:
-
co-producing a culturally adapted version of an extant, evidence-based model of FI197 in partnership with African-Caribbean service users, their families and health-care professionals
-
implementing this new intervention (CaFI) in community and inpatient mental health services using a RCT methodology
-
delivering CaFI in the absence of families via FSMs.
We have also demonstrated CaFI’s acceptability to African-Caribbean service users, their families, FSMs, therapists and other health-care professionals. Thus, we have successfully answered all our research questions and achieved all the aims of our study.
In the context of historically adverse relationships between African-Caribbean people and mental health services, characterised by fear, mistrust and avoidance,6,22,206 these are significant achievements.
The discussion that follows focuses on the cultural adaptation and co-production processes, and the feasibility of implementing and evaluating CaFI in today’s NHS. We shall highlight strengths and limitations of the study, including the generalisability of findings. We conclude by considering the implications for clinical practice and future research of such an approach both within the African-Caribbean community and in the broader context of BME groups across the NHS.
Discussion of findings
Developing CaFI
We have provided evidence on how to successfully culturally adapt FI for African-Caribbean people diagnosed with schizophrenia and related disorders (research question 1) using co-production approaches. This is important because although a number of previous studies have developed cultural adaptation frameworks,69,136 none has been explicit about the process.
First, our systematic review207 identified key components of adapting psychological interventions for minority groups. We used these to develop our cultural adaptation framework comprising:
-
concepts
-
cultural norms and practices
-
culturally relevant content
-
communication and language
-
context
-
cultural competence of practitioners.
Second, in key stakeholder focus groups, these concepts were applied systematically to the content and delivery of the extant FI34 model that we sought to culturally adapt.
Third, the final model was agreed in a consensus conference comprising ‘experts’ by experience and profession. As in previous studies,61,136 respondents did not suggest changes to the core components of the intervention. Rather, they highlighted additional factors to improve the cultural specificity of its content, acceptability and the feasibility of its delivery. Experts also identified the training needs of CaFI therapists and FSMs together with suggestions for how these might be met.
In developing CaFI, the ‘psychoeducation’ component of the intervention underwent the greatest change from current FI. The most significant change in this regard was adopting an explicit ‘shared learning’ ethos of delivery (vs. ‘psychoeducation’). ‘Shared Learning’ goes beyond good clinical practice, acknowledging therapists’ need to acquire/develop culturally appropriate knowledge and understanding,159 as well as families’ learning about schizophrenia and psychoses. This approach was advocated by stakeholders explicitly to address the power imbalance in therapy and to reduce social distance and hierarchy between therapists and families. Other major adaptations included adding specific communication and advocacy sessions to help families understand their rights and to improve interaction with services. These adaptations were regarded as especially pertinent for fostering therapeutic engagement with African-Caribbean people, given consistently reported delayed engagement or non-engagement with services. 30
The therapy manual and supporting materials were designed to raise therapists’ awareness of what it means to be a person of African-Caribbean origin living with a schizophrenia diagnosis in the UK. The manual therefore includes information about the location, customs and cultural diversity of the Caribbean islands (‘there’s no such thing as Caribbean culture’), as, during focus groups, health professionals identified this as a gap in their knowledge. The manual also supported exploration of issues that many African-Caribbean people associate with onset of psychoses, including experiences of everyday discrimination and institutional racism. 23,208
Issues of race and racism were integral to many African-Caribbean service users’ and families’ illness models. According to them, and to health professionals in our study, racism often remained ‘the elephant in the room’ (an obvious problem or risk no one wants/feels able to discuss) during therapy and encounters with health-care professionals more generally. This is because African-Caribbean people fear that raising racism might be either regarded as evidence of paranoia or interpreted as attacking health-care staff. From staff’s perspective, they reported a lack of skill in addressing this sensitive and potentially personally challenging issue. Understanding the relationship between African-Caribbean people’s illness models and their experiences therefore provides an important context for deeper understanding of contextual factors and establishing therapeutic alliances with people who, understandably, may be anxious and/or appear avoidant in therapy.
Can new interventions in family intervention be delivered in today’s NHS?
An important element of any feasibility process is understanding if and how new interventions can be delivered in the services for which they are designed. Psychological therapies have become well evidenced and NICE recommended in recent years in mental health broadly and in schizophrenia and psychosis specifically. 30,58 Notwithstanding the evidence of its efficacy and cost-effectiveness, FI provision within mental health services is inconsistent. 161,162 This is partly because FI is perceived as being labour intensive and, therefore, expensive despite being contrary to the evidence, suggesting failure to take into account the financial, social and psychological cost of the burden of care experienced by families. 209
In the CaFI study, we encountered challenges in recruiting suitably qualified and experienced FI therapists (Agenda for Change band 7) as recommended by NICE11 in the host trust. We subsequently recruited band 6 (advanced practitioner) non-psychologists ‘with experience of FI’. Having recruited CCs as therapists, we found that they were delivering CaFI alongside their routine roles and responsibilities without agreed protected time. This often meant prioritising clinical responsibilities over delivering the intervention, causing delays in delivering sessions and the ironic situation whereby our ‘hard-to-reach’ group of service users and families were being placed on a waiting list to receive therapy. As a result, we employed newly qualified band 7 clinical psychologists from other Greater Manchester trusts on a sessional basis to fill the gap in local provision. The fact that we were able to retain service users, families and FSMs despite these delays bears testament to the high levels of engagement and commitment to receiving the intervention that we had achieved.
Although exacerbated by the organisational and financial issues affecting our host trust, our findings highlight previous concerns about the ongoing lack of suitably qualified therapists to deliver FI in the NHS,161 despite NICE guidance. 30 The fact that we were able to recruit staff from neighbouring trusts does indicate that this may a feature of service configuration versus actual numbers of available therapists. In the absence of clear information about the availability of FI therapists across the country, we advocate that future trials consider alternative approaches to lack of trained FI therapists in the NHS such as using clinical psychology and psychiatry trainees to deliver psychosocial interventions. This proposal would have the additional benefit of building NHS capacity by creating a broader pool of available FI therapists.
Our experience of delivering CaFI raises concerns about the implementation of new and, indeed, existing, interventions in the NHS. We acknowledge that the financial constraints and service pressures we encountered within our host NHS trust, resulting in its dissolution and merger with a neighbouring organisation, were extreme. Although NICE guidance30 is likely to influence future practice, current evidence suggests that barriers to implementing psychological interventions are widespread and apparently entrenched across the NHS. 210 It is noteworthy that we encountered additional barriers such as missing data and inaccuracies in recording information, including ethnicity and assessment of relapse. Given that the NHS has a statutory Public Sector Equality Duty to provide services equitably,132 it is difficult to understand why these data were not routinely collected, especially given policies aimed at ‘DRE [Delivering Race Equality] in mental health’. 206 The NHS equality and diversity mapping exercise (2017) should provide more up-to-date information about the organisational capacity to deliver against the various mandated equality and diversity standards across England. We also advocate process evaluation and inclusion of implementation science in future trials to evaluate the extent to which the challenges we faced are being addressed by NICE guidance and related commissioning. Additionally, as some of the data inaccuracies related to mislabelling African service users as Caribbean, recruitment into future trials including both African and Caribbeans might be less problematic in terms of data accuracy.
The implications of increasing financial constraints and service pressures for our study and future studies in this domain are various if such interventions are to be taken forward based on successful cost-effectiveness and clinical effectiveness evidence. Not only do such interventions require impetus and support from local commissioning, local services and manpower also need forward planning to ensure the availability of therapists of sufficient seniority to supervise more junior clinicians should such an intervention be taken forward with successful cost-effectiveness and clinical effectiveness evidence. In other words, new interventions must be commissioned and specifically planned with specialist training and clear career pathway development considered from the outset. This means that investment in FI cultural adaptation and in future full-scale trials needs to be considered in the longer-term plans of those commissioning and delivering local mental health services.
Implementing and evaluating CaFI
We achieved our primary outcome of recruiting to target. Of 74 eligible service users, 31 (42%) consented (exceeding our original expectations that 1 : 3 would participate). We also achieved a high retention rate. Twenty-four of the 26 recruited family units that commenced CaFI (92%) completed therapy despite significant organisational service barriers that resulted in service users and families being on a waiting list for some time. This is a major achievement in this group, whose engagement with services has been poor historically and who are under-represented in research.
Our success is at least partly attributable to novel ways of engaging with this community. These include hosting events in ‘Black-majority churches’ and community centres, publishing articles about Black mental health in local newspapers and instigating discussions about mental health via ‘phone-ins’ on local radio. Going into this community and asking them to identify their research priorities and how to address them enabled us to co-produce a solutions-focused research.
It is noteworthy that, despite decades of previous research identifying the lack of access to psychological therapy and family disruption in this community, CaFI marks the first attempt to develop a culturally appropriate intervention. Although the fact that the PI was a member of the African-Caribbean community might have facilitated access, this alone cannot account for the high levels of engagement (especially as the remainder of the research team and all but two of the therapists were White).
All service users, families and therapists found CaFI acceptable and would recommend it to others. Service users and family members were especially positive about the ‘shared learning’ ethos of delivery and opportunities to acquire/enhance communication and advocacy skills. They also commented positively on the therapists’ personal qualities and self-disclosure. Willingness to share their own personal experiences was important for trust building and normalisation of experiences. This is especially important for members of this ethnic group given previously reported lack of discussion about mental illness among community members due to misconceptions, stigma and cultural taboos about ‘talking your business’. 35,36
Only one FSM dissented from the overwhelmingly positive evaluation, indicating that, from the their perspective, CaFI had not met the needs of one service user. According to the FSM, the service user, who had deep-rooted fears of services due to experiences of racism, perceived the therapy content to be ‘White’. Specifically, the FSM did not believe that CaFI addressed the issue of racism sufficiently. Although this was not reflected in qualitative interviews with other participants (including the service user in question) in the acceptability study (see Chapter 7), it raises an important issue about whether this FSM’s perception of CaFI’s as ‘White’ related to its content or to the fact it was delivered by White therapists.
Our exploration of ‘ethnic matching’ of therapists and families reflect previously reported ambivalence about if and to what extent shared ethnicity between therapists and clients affects the nature of therapeutic engagement. 211 Although conceding the potential value of ‘ethnic matching’ for some families, participants concluded that this was impracticable in a NHS in which the majority of therapists are White or Asian. Moreover, endorsing findings from a meta-analysis which reported almost no benefit to treatment outcomes from racial/ethnic matching of clients with therapists,211 they suggested that the most important factor in therapeutic alliance was establishing trust as the basis of open communication.
Culturally adapted Family Intervention therapists reported that they valued the opportunity to gain in-depth knowledge about and experience of working with members of an ethnic group known to have complex needs. This enabled them to utilise both advanced and newly acquired skills. Although those who received the full training package (all non-psychologists) reported significant increase in cultural awareness and confidence (see Chapter 5), this was not reflected in the trial or acceptability data. Psychologists, although more recently qualified than non-psychologists, were more likely to deliver CaFI within the therapy window and were more positively rated by family members. This may reflect clinical psychologists’ greater familiarity with the model from which CaFI was derived and more advanced training such as cognitive analytic therapy, which afforded greater flexibility and skills to work with complex client groups. However, lack of protected therapy time and competing clinical priorities undoubtedly contributed to non-psychologists’ self-reports of sometimes insufficient time to reflect, plan and prepare for sessions.
It is also noteworthy that the clinician who independently rated CaFI sessions (see Chapter 6) noted that non-psychologists tended to conceptualise psychosis using ‘illness model language’, which did not facilitate discussion about cultural appraisals or alternative models of mental illness. This is important because this and previous studies36,212 indicate that, in common with other BME groups, African-Caribbean people’s conceptualisations often differ from those of White Westerners, who make up the majority of NHS therapists. Cultural competence and ‘psychological mindedness’ are therefore important considerations for delivering CaFI and other interventions, suggesting that capacity building is warranted if such interventions are to be delivered by non-psychologists.
Across all groups, the most frequently mentioned benefits derived from CaFI were improved understanding of schizophrenia and psychosis and communication between service users and health-care professionals, as well as with their families (see Chapter 7). Some CCs also reported improved communication with families. For example, one CC reported that a service user’s partner had begun to engage with her for the first time and was demonstrably more supportive and less dismissive of his illness. This is important given the well documented lack of engagement and adverse relationships between mental health services and African-Caribbean people. We know that this leads to increased carer burden, more family conflict (often resulting in families involving the police) and service access via adverse care pathways. 8,16
Delayed access is also costly for the NHS. The mean inpatient stay of African-Caribbean people is around 2.5 times longer than that of their White British contemporaries. The former also are more frequently hospitalised and more likely to be released on costly CTOs. 11 Improved communication between service users, their families and health-care professionals might facilitate earlier access to care, with an associated reduction in costs. Our findings suggest that evaluation of the clinical effectiveness and cost-effectiveness of culturally specific interventions, such as CaFI, in fully powered trials is warranted.
An important finding from our acceptability study was participants’ view that CaFI should be rolled out across the NHS and made available to all ethnic groups versus limiting its perceived benefits to African-Caribbean people. Participants further suggested that, as it was not feasible to implement different culturally adapted versions of FI for each ethnic/cultural group in the UK, a culturally adaptable form should be developed. This marks an interesting and important departure from the increasing number of culturally adapted psychological interventions. 58,61,213
Although culturally adaptable approaches were more often suggested by African-Caribbean service users and health-care professionals, they were also endorsed by other participants. Given recent changes in the UK population’s ethnic make-up,214 NICE guidance on implementing FI30 and the changing commissioning landscape, a culturally adaptable FI is appealing. However, the service barriers we experienced, principally a service virtually denuded of FI expertise, would need to be addressed for the benefits of CaFI and other forms of family work to be fully realised.
Study outputs
We have produced a series of new resources that can fill a gap for new practice and capacity building in NHS:
Service user, carer and community involvement
A major strength of this study was the collaboration with key stakeholders to co-produce the intervention. Service user involvement in identifying our research question, study design and membership of the research team has been acknowledged at a national level with the NIHR Mental Health Research Network’s 2014 award for outstanding contribution to patient and public involvement.
This level of engagement marked the culmination of several years of the PI’s work within this community, for example, delivering community mental health conferences to raise awareness of mental illness and to counter stigma. During one of these conferences, our service user co-investigator spoke openly about his experiences of being ‘sectioned’, police involvement in his care and several episodes of hospitalisation. The fact that he is now a church minister and married with children gave credibility to his assertion that recovery is possible. It also countered the tendency of some community members to attribute mental illness to deviance and/or demonic possession. Such open dialogue and self-disclosure is rare in a community renowned for unwillingness to discuss mental health issues. 36
A long history of negative experiences of mental health care has made members of the African-Caribbean community fearful of engaging with mental health services and practitioners. 23 Service user participants’ narratives indicate that many of them have experienced adverse care pathways and coercive care. For example, one service user (a single parent with no family locally) spoke about being ‘sectioned’ while her children were at school. She reported that six police vehicles came to her home, reinforcing negative associations among her neighbours between mental illness and dangerousness and deviance. She is now actively engaged in research and training health professionals based on her experience.
Families also spoke about routinely being excluded from care planning and feeling unable to advocate on behalf of service users (see Chapter 3). Nevertheless, motivated by a strong desire to improve mental health care, they were willing to help develop and test culturally appropriate ‘talking treatment’, the absence of which they highlighted as a significant gap in service provision during our community engagement events. In particular, they raised concerns about White therapists being able to understand African-Caribbean people’s cultural norms and the context of their lived experiences, which many associated with elevated rates of schizophrenia diagnosis within their community. A therapy that makes explicit such issues and provides cultural competency training for therapists was regarded by study participants (including service providers) and wider community as much needed and long overdue.
African-Caribbean service users, their families and community members have been actively involved in every stage of the research process:
-
participating in community conferences and focus groups to identify research priorities
-
developing the research questions and grant application
-
as co-applicants and collaborators on the CaFI study
-
serving as members and chairpersons of the RMG, RAG and the Study Steering Committee (SSC)
-
disseminating findings at conferences and co-authoring publications.
Our RAG was particularly actively involved in all aspects of developing CaFI. We sought their advice on strategies to maximise recruitment and retention and feedback on all study materials, including recruitment information and materials to support delivery of the intervention. This authentic partnership was integral to establishing CaFI and the study’s credibility in the African-Caribbean community. 217 African-Caribbean people’s involvement in determining the content of the therapy, developing and delivering therapists’ training, co-producing study materials and research management (RAG, RMG, SSC), undoubtedly contributed to our success in recruiting above target in our feasibility trial.
Community engagement also facilitated successful recruitment of FSMs, ‘trusted individuals’ who ‘came alongside’ service users to enable them to access CaFI in the absence of families. Service users who could not nominate family members could nominate friends, key workers or others to participate in CaFI with them. When individuals were unable to nominate anyone, they were able to select from a group of individuals recruited to fulfil this role, subsequent to police and other relevant checks. Recruited FSMs provided one-page profiles and met service users to facilitate the ‘matching’ process. Half of the service users (n = 13, 50%) would not have been able to participate without this wholly novel aspect of our study.
There were reservations and lack of clarity about the role of community-based FSMs in delivering CaFI. Although conceding that many service users would not have been able to access the therapy without them, therapists reported that their involvement meant some sessions were more akin to individual CBT than FI. Greater success was reported where FSMs were CCs or key workers as they could support service users in addressing issues related to the delivery of their care. This should be incorporated into future trials. Further work is needed to determine if, as suggested by some participants, community-based FSMs could form a ‘bridge’ to reconnect service users to their families and wider communities. For example, service users spoke movingly about the normalising and enabling effect of working with FSMs such as being able to go to the barber shop and eat in a café. Another service user who had severed all ties with his family had begun to reconnect with them via FSM’s acquaintance with members of his extended family.
Strengths and limitations
This study had several unique strengths:
-
The qualitative methods (focus groups and expert consensus conference) we employed were essential for establishing CaFI’s credibility with service users, their families and NHS professionals who would commission and deliver it.
-
Working collaboratively with members of the African-Caribbean community required high levels of engagement to build trust and develop an authentic partnership with health-care professionals.
-
Service users and carers, ‘experts by experience’, worked alongside ‘experts by profession’ (health and care staff, academics, advocates, voluntary sector agencies, police), in a non-hierarchical way to develop CaFI. The significance of having their voices heard and expertise by experience acknowledged cannot be overstated for a group so often labelled ‘hard to reach’, but who regard themselves as ‘seldom heard’.
-
We developed a cultural adaptation framework that we applied systematically to an evidence-based model of FI, demonstrating, we believe for the first time, how to culturally adapt an intervention compared with focusing on what to adapt.
-
The multidisciplinary composition of the research team and health professionals (social workers, OTs, psychologists, RMNs, psychiatrists) involved in CaFI’s development and testing is an additional strength of the study. This enabled a range of different perspectives to be considered, including ‘antipsychiatrists’, voice hearing network members and people committed to abolishing the schizophrenia label. The fact that consensus was reached on the content, delivery and desired outcomes of receiving CaFI by such a diverse group is a key strength of the intervention, facilitating its acceptability and implementation.
The main limitation in terms of developing and undertaking the research in this fashion is that the process was time and labour intensive. Community engagement requires significant investment of time, personal and professional resources. We are also mindful that although we successfully engaged a range of African-Caribbean service users, families and community members, their views (which underpin much of CaFI) might not reflect those of the entire constituency; in particular, service users with the most limited social function or family/community members whose experience of stigma and fear of sanctions, for example, might have hindered participation. Trialling the intervention and undertaking process evaluation in other geographical locations and clinical settings, including forensic services wherein African-Caribbean people are over-represented, would provide opportunities to address these limitations.
Another limitation of the study is that the initial cohort of CaFI therapists’ training in cultural awareness and confidence building was not delivered to subsequent therapists. Instead, they received detailed orientation to the study and guidance in using the therapy manual from the PI, clinical supervisor and RPM. This was due to the service delivery issues at the host NHS trust highlighted earlier in the report (see Chapter 5, Therapist recruitment, First wave of recruitment). Although delivering the same training to all therapists would have improved consistency of approach, our response to the service delivery issues encountered serendipitously enabled us to collect acceptability data on delivering CaFI by both psychologists and non-psychologists and to undertake initial assessment of the potential impact of training.
Clinical implications
-
Delivering individualised, person-centred care in a multicultural context requires a highly skilled, culturally competent workforce – especially when working with high levels of complexity such as chronic SMI coupled with family disruption.
-
From a practical perspective, delivering psychosocial interventions such as CaFI via the broadest possible group of health professionals would make the best use of resources and potentially facilitate FI becoming part of routine practice. However, this would have implications for the availability of local clinicians with the capacity to supervise therapists less experienced or with less time to practise FI, such as allied health professionals.
-
Developing the confidence to work flexibly requires time and opportunities to develop expertise. We found that, though less experienced in terms of length of service, psychologists were better able than non-psychologists to respond to the ‘live’ challenges with which families presented versus ‘overpreparing’. They were also significantly more able to deliver the intervention within the 20-week therapy window.
-
Lack of opportunity to practise FI was frequently cited by both non-psychologists and service users’ CCs. Time pressures and competing priorities meant that FI was often spoken of as something aspirational rather than an evidence-based, clinically effective intervention. Having a dedicated therapist to deliver the intervention might provide one way forward and might not result in additional costs. In our study, there was no difference between psychologists and non-psychologists costs. Moreover, an investment in developing more culturally competent therapists might reap dividends in terms of improved outcomes, including reduced relapse and readmission costs. This can be explored further in a RCT of clinical effectiveness and cost-effectiveness.
-
Service delivery issues gain particular salience when considered in the context of the need to provide evidence-based care at a time of increasing mental health needs coupled with significant financial challenges.
Implications for health service and delivery
-
Our study provides evidence that it is feasible to culturally adapt and implement FI with the group of service users who experience the most serious and persistent disparities in schizophrenia care in the UK and with whom services have struggled to engage over many decades. Our findings suggest that it might be possible to develop similar interventions with other underserved groups such as refugees and migrant workers.
-
NICE recommends FI. We contend that steps could be taken to ensure that FI is sufficiently culturally adaptable to meet the needs of an increasingly diverse society.
-
Current NICE guidelines indicate that FI need only be offered to people in regular contact with their families. This would mean that around half of our African-Caribbean sample would not have been eligible for FI. This has the potential to exacerbate disparities in accessing evidence-based psychological therapies experienced by Black, Asian and minority ethnic groups. It also has important public health implications for this and other groups of service users such as people seeking asylum and the forensic population who, despite significant need, would not be eligible to receive FI.
-
Moreover, although FI has a strong evidence base, this is not yet the case for culturally adapted interventions like CaFI. This is important because commissioners require evidence of cost effectiveness and clinical-effectiveness to determine whether specifically culturally adapted FI is warranted or, as has been suggested by our study participants, more culturally adaptable approaches are required.
-
Delivering person-centred care in a multicultural context requires new service provision, especially in an economically challenged NHS. For example, unlike African-Caribbean people, who are an established group, many recent migrants to the UK have experienced significant levels of trauma, often arriving in the UK without families. Meeting their needs will require a highly skilled and responsive workforce together with novel approaches such as working with FSMs.
-
Our findings suggest that there is potential for FSMs (particularly key workers/CCs) to participate in delivery of FI. Community-based FSMs might facilitate reconnection of services users with their families and communities. This might be especially salient for recent migrants fleeing conflict and other marginalised groups.
-
Delivering FI in a multicultural context requires effective cultural competence training and measures to demonstrate proficiency. What this would look like and how it can be sustained in a financially straitened NHS requires investigation based on further evidence of cost-effectiveness and clinical effectiveness.
-
Developing expertise to effectively deliver culturally adaptable psychological interventions by a wider range of health-care professionals appears to be an imperative.
-
Low-cost psychological interventions that can be developed in future may include educational and culturally adapted service materials to support embedding culturally appropriate approaches in routine practice.
-
The availability of accurate ethnicity data and clinical information, such as relapse indicators, is urgently needed in services.
Research recommendations
-
Test the CaFI model in multicentre trial. Our study proved feasible in central Manchester. As population demographics, service models and commissioning practices vary across the country, research is needed to assess its clinical effectiveness and cost-effectiveness in a range of different contexts. Including process evaluation to identify implementation barriers and strategies to overcome them within a trial would enable us to evaluate the feasibility of embedding CaFI in routine practice across the country without the need for further preparatory work.
-
High levels of engagement and trust building were integral to our success in recruiting and retaining participants, despite organisational challenges. We recommend that this approach is replicated and fully costed in future trials.
-
Trial CaFI alongside culturally adapted versions for other ethnic groups. As recommended by our stakeholders, developing a ‘culturally adaptable’ model makes good sense in a multicultural society. Trials involving other ethnic groups could identify the key components that constitute a robust culturally adaptable model. Such a model could potentially have international utility.
-
Develop a proficiency framework to assess cultural competence. Despite bespoke training delivering self-reported improved cultural awareness and confidence, this was not borne out in practice. This suggests that a framework to assess cultural proficiency is needed.
-
Further work is needed to examine the role of FSMs, without whom, half the service users in our study would not have been able to access CaFI. Although delivery via CC/key worker FSMs was positively evaluated (e.g. enabling service users to address difficulties in relation to their care), our findings suggest that involvement of FSMs may be a related but different intervention from extant FI. Process evaluation and further work to understand the mechanisms of this aspect of the intervention within a trial would help to determine how the role of FSMs might be developed and deployed (e.g. using peer support workers alongside CCs/key workers). Undertaking this work within a trial, would also help to determine whether or not FSMs would prove cost-effective and clinically effective and, therefore, commissionable as part of an innovative approach to service delivery.
Conclusions
Equality of access to care and treatment is a founding principle of the NHS. Nevertheless, despite numerous policy initiatives and recommendations from bodies such as NICE,11,30 the mental health care of African-Caribbean people continues to be suboptimal. Lack of access to evidence-based care and to psychological interventions in particular has been identified by NICE and the Department of Health and Social Care over many years. 30,153,206 This is now urgently needed, not least to enable service providers and commissioners to fulfil their public sector equality duty under The Equality Act. 132
Despite the African-Caribbean community being labelled ‘hard to reach’, we have successfully partnered with members’ community to culturally adapt an extant model of FI. Our findings provide evidence that delivery of CaFI in hospital and community settings is possible, despite considerable service barriers. CaFI is acceptable to all key stakeholder groups who recommended that it should be implemented in the NHS. This is important because acceptability of any new intervention is fundamental to its implementation and embedding in routine practice.
Considering UK mental health care delivered in a multicultural context, we suggest that the learning from CaFI should be applied to developing new ways of working with minority ethnic communities. We advocate going beyond cultural adaptation for individual groups to developing culturally adaptable models capable of meeting the needs of all groups. Measures to evaluate the cultural competence of both individual practitioners and services are warranted.
To increase the feasibility of doing so, our findings suggest that further work is needed to evaluate the clinical effectiveness and cost-effectiveness of this and other culturally adapted interventions. The capacity of services to deliver culturally appropriate care will also require investment in data recording and retrieval as well as training and workforce planning.
Acknowledgements
We wish to acknowledge the contributions of the following:
Ms Sophie Baker (RA; phase 3) supported the RPM with data collection and analyses and contributed to drafting sections of the report.
Professor Christine Barrowclough contributed to study design, and provided expertise in the model of FI that was culturally adapted and the KASI, which she co-devised.
Professor Dinesh Bhugra provided expertise in transcultural psychiatry and delivered the trust-wide cultural competency workshop.
Patrick Cahoon (MMHSCT Lead for Service User and Carer Engagement) provided support with accessing service user and carer groups and facilitated access to services.
Reverend Paul Grey contributed to the study design, advised on all phases of the study, chaired the RAG and was a member of RMG and SSC.
Mr Calvin Heal (RA to Dr Sarah Cotterill) performed quantitative analyses and contributed to the write-up of Chapter 6.
Professor Shon Lewis contributed to the development of the study and provided senior oversight and advice throughout.
Professor Nicholas Tarrier contributed to study design, and provided expertise in the model of FI that was culturally adapted and the KASI, which he co-devised.
We should also like to thank the members of our RAG for their invaluable contribution:
-
Ms Yvonne Thomas
-
Mr Anthony Stephens
-
Ms Natasha Penniston
-
Mrs Michelle Ayavoro
-
Ms Sonia Linday
-
Rev Paul Grey (chairperson)
-
Mrs Mary Maynard
-
Mrs Daisy Barratt.
Thanks also to our collaborators:
-
ACMHS, Manchester
-
Karina Lovell (Professor of Mental Health, University of Manchester)
-
Nusrat Husain (Professor of Psychiatry, University of Manchester)
-
Kevin Ronan (Foundation Professor in Psychology at Central Queensland University, Australia)
-
Rachel Meacock [Research Fellow (Health Economics), University of Manchester]
-
Dr Judith Richardson (Deputy Medical Director and Programme Director, Quality and Leadership, NICE).
Finally, we wish to thank BioMed Central for their permission to include aspects of the published CaFI protocol:
Edge D, Degnan A, Cotterill S, Berry K, Drake R, Baker J, et al. Culturally-adapted Family Intervention (CaFI) for African-Caribbeans diagnosed with schizophrenia and their families: a feasibility study protocol of implementation and acceptability. Pilot Feasibility Stud 2016;2:39.
Contributions of authors
Dr Dawn Edge (PI, Senior Lecturer) devised and oversaw the study; managed the RPM; led the phase 1 qualitative data collection (focus groups and consensus conference); co-analysed all qualitative data; led the writing of Chapters 1, 3, 4, 7 and 8 and contributed to others; and co-authored the published protocol and conference proceedings. She provided the final approval of the version to be published and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ms Amy Degnan (RPM) conducted the literature review; co-analysed the qualitative data for the focus groups and acceptability study; led the write-up of Chapters 2 and 5; and contributed to the write-up of Chapters 1, 3, 5, 6 and 7. She was responsible for managing and preparing the qualitative and quantitative data for every phase and she co-authored the published protocol.
Dr Sarah Cotterill contributed to the conception of the study; wrote the data management plan; conducted the quantitative analyses; led the write-up of Chapter 6; contributed to Chapter 8; critically reviewed other chapters for intellectual content; and co-authored the published study protocol.
Dr Katherine Berry (Senior Lecturer, Clinical Psychologist) led the development of the therapy manual; contributed to the therapist training in the manual; contributed to the development of the fidelity scales and study design; supervised the therapists and FSMs; and co-authored the published study protocol.
Dr John Baker contributed to study design; co-facilitated consensus conference and analysed qualitative data; contributed to writing Chapters 3 and 4; critically reviewed other chapters for intellectual content; and co-authored the published study protocol.
Dr Richard Drake contributed to study design, analysis of quantitative data (specifically the relapse rating and health utility measure) and co-authored published study protocol. Oversaw and contributed to writing the systematic review (see Chapter 2).
Professor Kathryn Abel contributed to study design and interpretation of the study; critically revised the report for important intellectual content; provided senior oversight of the project; and co-authored the published study protocol.
Publications
Peer-reviewed publications
Edge D, Degnan A, Cotterill S, Berry K, Drake R, Baker J, et al. Culturally-adapted Family Intervention (CaFI) for African-Caribbeans diagnosed with schizophrenia and their families: a feasibility study protocol of implementation and acceptability. Pilot Feasibility Stud 2016;2:39.
Degnan A, Baker S, Edge D, Nottidge W, Noke M, Press CJ, et al. The nature and efficacy of culturally-adapted psychosocial interventions for schizophrenia: a systematic review and meta-analysis. Psychol Med 2017:1–14.
Edge D, Grey P. An assets-based approach to co-producing Culturally-adapted Family Intervention (CaFI) with African-Caribbeans diagnosed with schizophrenia and their families. Ethn Dis 2018; in press.
Peer-reviewed conference contributions
Edge D, Stephens A, Thomas Y. Overcoming Challenges: Innovative Solutions in Public Involvement in Research. NIHR Research Design Service North West Patient and Public Involvement (and Engagement) Conference, Manchester, 2016.
Edge D, Degnan A. Service Users, Carers and Healthcare Professionals’ Perceptions and Experiences of Mental Health Services for African-Caribbean People Diagnosed with Psychosis: A Qualitative Study. Division of Clinical Psychology Annual Conference, Liverpool, 2017.
Invited conference contributions
Edge D. Culturally-adapting Family Intervention (CaFI) for African-Caribbeans Diagnosed with Schizophrenia: An Assets-Based Approach to Co-Production. World Psychiatric Conference International Congress, Cape Town, South Africa, 2016.
Edge D, Thomas Y. Cultural Adaptation, Implementation and Evaluation of Family Intervention for African-Caribbean Service Users with Schizophrenia in Secondary Care. NIHR/Medicines and Healthcare products Regulatory Agency, Nottingham, 2014.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J, et al. Incidence of schizophrenia and other psychoses in England, 1950–2009: a systematic review and meta-analyses. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0031660.
- Fearon P, Kirkbride J, Morgan C, Dazzan P, Morgan K, Lloyd T, et al. Incidence of schizophrenia and other psychoses in ethnic minority groups: results from the MRC AESOP Study. Psychol Med 2006;36:1541-50. https://doi.org/10.1017/S0033291706008774.
- Fearon P, Kirkbride J, Morgan C, Dazzan P, Morgan K, Lloyd T, et al. Ethnic minority groups, particularly African-Caribbean and black African groups, are at increased risk of psychosis in the UK: incidence of schizophrenia and other psychoses in ethnic minority groups: results from the MRC AESOP study. Evid Based Ment Health 2007;10. https://doi.org/10.1136/ebmh.10.3.95.
- Nazroo J, King M, Sproston K, Nazroo J. Psychosis – Symptoms and Estimated Rates. London: The Stationery Office; 2002.
- Takei N, Persaud R, Woodruff P, Brockington I, Murray RM. First episodes of psychosis in Afro-Caribbean and white people. An 18-year follow-up population-based study. Br J Psychiatry 1998;172:147-53. https://doi.org/10.1192/bjp.172.2.147.
- Morgan C, Kirkbride J, Mallett R, Hutchinson G, Fearon P, Morgan K, et al. Social isolation, ethnicity, and psychosis: findings from the AESOP first onset psychosis study. Schizophr Bull 2005;31.
- Cantor-Graae E, Selten JP. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry 2005;162:12-24. https://doi.org/10.1176/appi.ajp.162.1.12.
- Morgan C, Dazzan P, Morgan K, Jones P, Harrison G, Leff J, et al. First episode psychosis and ethnicity: initial findings from the AESOP study. World Psychiatry 2006;5:40-6.
- Morgan C, Abdul-Al R, Lappin JM, Jones P, Fearon P, Leese M, et al. Clinical and social determinants of duration of untreated psychosis in the AESOP first-episode psychosis study. Br J Psychiatry 2006;189:446-52. https://doi.org/10.1192/bjp.bp.106.021303.
- Morgan C, Fisher H, Hutchinson G, Kirkbride J, Craig TK, Morgan K, et al. Ethnicity, social disadvantage and psychotic-like experiences in a healthy population based sample. Acta Psychiatr Scand 2009;119:226-35. https://doi.org/10.1111/j.1600-0447.2008.01301.x.
- Schizophrenia: The NICE Guideline on Core Interventions in the Treatment and Management of Schizophrenia in Adults in Primary and Secondary Care (Updated Edition). National Clinical Guideline Number 82. London: The British Psychological Society and The Royal College of Psychiatrists; 2009.
- Sharpley M, Hutchinson G, McKenzie K, Murray RM. Understanding the excess of psychosis among the African-Caribbean population in England. Review of current hypotheses. Br J Psychiatry Suppl 2001;40:s60-8. https://doi.org/10.1192/bjp.178.40.s60.
- Bhui K, Stansfeld S, Hull S, Priebe S, Mole F, Feder G. Ethnic variations in pathways to and use of specialist mental health services in the UK. Systematic review. Br J Psychiatry 2003;182:105-16. https://doi.org/10.1192/bjp.182.2.105.
- National Mental Health and Learning Disability Ethnicity Census: Count Me In 2010. London: CQC and National Mental Health Development Unit, DHSC; 2010.
- Morgan C, Mallett R, Hutchinson G, Leff J. Negative pathways to psychiatric care and ethnicity: the bridge between social science and psychiatry. Soc Sci Med 2004;58:739-52. https://doi.org/10.1016/S0277-9536(03)00233-8.
- Morgan C, Mallett R, Hutchinson G, Bagalkote H, Morgan K, Fearon P, et al. Pathways to care and ethnicity. 1: sample characteristics and compulsory admission. Report from the AESOP study. Br J Psychiatry 2005;186:281-9. https://doi.org/10.1192/bjp.186.4.281.
- Morgan C, Mallett R, Hutchinson G, Bagalkote H, Morgan K, Fearon P, et al. Pathways to care and ethnicity. 2: source of referral and help-seeking. Report from the AESOP study. Br J Psychiatry 2005;186:290-6. https://doi.org/10.1192/bjp.186.4.290.
- Mental Health Act 2007. London: The Stationery Office; 2007.
- Shefer G, Rose D, Nellums L, Thornicroft G, Henderson C, Evans-Lacko S. ‘Our community is the worst’: the influence of cultural beliefs on stigma, relationships with family and help-seeking in three ethnic communities in London. Int J Soc Psychiatry 2013;59:535-44. https://doi.org/10.1177/0020764012443759.
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry 2005;62:975-83. https://doi.org/10.1001/archpsyc.62.9.975.
- Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry 2005;162:1785-804. https://doi.org/10.1176/appi.ajp.162.10.1785.
- Keating F, Robertson D, McCulloch A, Francis E. Breaking the Circles of Fear: A Review of the Relationship Between Mental Health Services and African and Caribbean Communities. London: The Sainsbury Centre for Mental Health; 2002.
- Keating F, Robertson D. Fear, black people and mental illness: a vicious circle?. Health Soc Care Community 2004;12:439-47. https://doi.org/10.1111/j.1365-2524.2004.00506.x.
- Mclean C, Campbell C, Cornish F. African-Caribbean interactions with mental health services in the UK: experiences and expectations of exclusion as (re)productive of health inequalities. Soc Sci Med 2003;56:657-69. https://doi.org/10.1016/S0277-9536(02)00063-1.
- Del Vecchio V, Luciano M, Sampogna G, De Rosa C, Giacco D, Tarricone I, et al. The role of relatives in pathways to care of patients with a first episode of psychosis. Int J Soc Psychiatry 2015;61:631-7. https://doi.org/10.1177/0020764014568129.
- Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database Syst Rev 2010;12. https://doi.org/10.1002/14651858.CD000088.pub3.
- Pilling S, Bebbington P, Kuipers E, Garety P, Geddes J, Orbach G, et al. Psychological treatments in schizophrenia: I. meta-analysis of family intervention and cognitive behaviour therapy. Psychol Med 2002;32:763-82. https://doi.org/10.1017/S0033291702005895.
- Addington J, Collins A, McCleery A, Addington D. The role of family work in early psychosis. Schizophr Res 2005;79:77-83. https://doi.org/10.1016/j.schres.2005.01.013.
- Onwumere J, Smith B, Kuipers E, Morgan C, Bhugra D. Principles of Social Psychiatry. Sussex: John Wiley & Sons, Ltd; 2010.
- Psychosis and Schizophrenia in Adults: Treatment and Management. NICE Clinical Guidelines. London: NICE; 2014.
- Lobban F, Postlethwaite A, Glentworth D, Pinfold V, Wainwright L, Dunn G, et al. A systematic review of randomised controlled trials of interventions reporting outcomes for relatives of people with psychosis. Clin Psychol Rev 2013;33:372-82. https://doi.org/10.1016/j.cpr.2012.12.004.
- Haddock G, Eisner E, Boone C, Davies G, Coogan C, Barrowclough C. An investigation of the implementation of NICE-recommended CBT interventions for people with schizophrenia. J Ment Health 2014;23:162-5. https://doi.org/10.3109/09638237.2013.869571.
- Bucci S, Berry K, Barrowclough C, Haddock G. Family interventions in psychosis: a review of the evidence and barriers to implementation. Aust Psychol 2016;51:62-8. https://doi.org/10.1111/ap.12172.
- Barrowclough C, Tarrier N. Families of Schizophrenic Patients: Cognitive Behavioural Interventions. London: Chapman & Hall; 1992.
- Edge D, Mackian SC. Ethnicity and mental health encounters in primary care: help-seeking and help-giving for perinatal depression among black Caribbean women in the UK. Ethn Health 2010;15:93-111. https://doi.org/10.1080/13557850903418836.
- Edge D, Rogers A. ‘Dealing with it’: black Caribbean women’s response to adversity and psychological distress associated with pregnancy, childbirth, and early motherhood. Soc Sci Med 2005;61:15-2. https://doi.org/10.1016/j.socscimed.2004.11.047.
- Arthur CM, Hickling FW, Robertson-Hickling H, Haynes-Robinson T, Abel W, Whitley R. ‘Mad, sick, head nuh good’: mental illness stigma in Jamaican communities. Transcult Psychiatry 2010;47:252-75. https://doi.org/10.1177/1363461510368912.
- Jackson D, Heatherington L. Young Jamaicans’ attitudes toward mental illness: experimental and demographic factors associated with social distance and stigmatizing opinions. J Commun Psychol 2006;34:563-76. https://doi.org/10.1002/jcop.20115.
- Developing and Evaluating Complex Interventions: New Guidance. London: MRC; 2008.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-69.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Black N, Pope C, Mays N. Qualitative Research in Health Care. London: BMJ Books/Blackwell; 2006.
- Just Psychology. n.d. www.justpsychology.co.uk/ (accessed 1 October 2015).
- The Meriden Family Programme n.d. www.meridenfamilyprogramme.com (accessed 1 October 2015).
- Haddock G, Devane S, Bradshaw T, McGovern J, Tarrier N, Kinderman P, et al. An Investigation into the psychometric properties of the Cognitive Therapy Scale for Psychosis (Cts-Psy). Behav Cogn Psychoth 2001;29:221-33. https://doi.org/10.1017/S1352465801002089.
- Onwumere J, Kuipers E, Gamble C, Jolley S, Smith B, Rollinson R, et al. Family interventions in psychosis: a scale to measure therapist adherence. J Fam Ther 2009;31:270-83. https://doi.org/10.1111/j.1467-6427.2009.00466.x.
- Reynolds T. Family and community networks in the (re) making of ethnic identity of Caribbean young people in Britain. Community Work Fam 2006;9:273-90. https://doi.org/10.1080/13668800600743586.
- Manchester BME Network n.d. www.manchesterbmenetwork.co.uk/ (accessed 21 March 2017).
- The Black Health Agency n.d. www.thebha.org.uk/ (accessed 21 March 2017).
- Manchester Carers Forum n.d. www.manchestercarersforum.org.uk/ (accessed 21 March 2017).
- Rethink Manchester Carers in Action n.d. http://rmcia.blogspot.co.uk/ (accessed 21 March 2017).
- Self-Help Services n.d. www.selfhelpservices.org.uk/ (accessed 21 March 2017).
- Patient Voices n.d. www.patientvoices.org.uk/ (accessed 21 March 2017).
- Bluesci Support n.d. www.bluesci.org.uk/ (accessed 21 March 2017).
- Grant M, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Lib J 2009;26:91-108. https://doi.org/10.1111/j.1471-1842.2009.00848.x.
- Rathod S, Kingdon D, Phiri P, Gobbi M. Developing culturally sensitive cognitive behaviour therapy for psychosis for ethnic minority patients by exploration and incorporation of service users’ and health professionals’ views and opinions. Behav Cogn Psychoth 2010;38:511-33. https://doi.org/10.1017/S1352465810000378.
- Rathod S, Phiri P, Harris S, Underwood C, Thagadur M, Padmanabi U, et al. Cognitive behaviour therapy for psychosis can be adapted for minority ethnic groups: a randomised controlled trial. Schizophr Res 2013;143:319-26. https://doi.org/10.1016/j.schres.2012.11.007.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Benish SG, Quintana S, Wampold BE. Culturally adapted psychotherapy and the legitimacy of myth: a direct-comparison meta-analysis. J Couns Psychol 2011;58:279-89. https://doi.org/10.1037/a0023626.
- Chowdhary N, Jotheeswaran A, Nadkarni A, Hollon S, King M, Jordans M, et al. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: a systematic review. Psychol Med 2014;44:1131-46. https://doi.org/10.1017/S0033291713001785.
- Griner D, Smith TB. Culturally adapted mental health intervention: a meta-analytic review. Psychother Theor Res Pract Train 2006;43. https://doi.org/10.1037/0033-3204.43.4.531.
- Huey SJ, Polo AJ. Evidence-based psychosocial treatments for ethnic minority youth. J Clin Child Adolesc Psychol 2008;37:262-301. https://doi.org/10.1080/15374410701820174.
- Smith TB, Rodríguez MD, Bernal G. Culture. J Clin Psychol 2011;67:166-75. https://doi.org/10.1002/jclp.20757.
- Hodge DR, Jackson KF, Vaughn MG. Culturally sensitive interventions and health and behavioral health youth outcomes: a meta-analytic review. Soc Work Health Care 2010;49:401-23. https://doi.org/10.1080/00981381003648398.
- Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull 2008;34:523-37. https://doi.org/10.1093/schbul/sbm114.
- Bernal G, Sáez-Santiago E. Culturally centered psychosocial interventions. J Community Psychol 2006;34:121-32. https://doi.org/10.1002/jcop.20096.
- Bhui K, Aslam W, Palinski A, McCabe R, Johnson M, Weich S, et al. Interventions to improve therapeutic communications between Black and minority ethnic patients and professionals in psychiatric services: systematic review. Br J Psychiatr 2015;207:95-103. https://doi.org/10.1192/bjp.bp.114.158899.
- Tseng W-S. Handbook of cultural psychiatry. Int Rev Psychiatr 2001;14:71-3.
- Alvidrez J, Arean PA, Stewart AL. Psychoeducation to increase psychotherapy entry for older African Americans. Am J Geriatr Psychiatry 2005;13:554-61. https://doi.org/10.1097/00019442-200507000-00003.
- Habib N, Dawood S, Kingdon D, Naeem F. Preliminary evaluation of culturally adapted CBT for psychosis (CA-CBTp): findings from developing culturally sensitive CBT project (DCCP). Behav Cogn Psychother 2015;43:200-8. https://doi.org/10.1017/S1352465813000829.
- Barrera M, Castro FG. A heuristic framework for the cultural adaptation of interventions. Clin Psychol 2006;13:311-16. https://doi.org/10.1111/j.1468-2850.2006.00043.x.
- Hwang WC. The Formative Method for Adapting Psychotherapy (FMAP): a community-based developmental approach to culturally adapting therapy. Prof Psychol Res Pr 2009;40:369-77. https://doi.org/10.1037/a0016240.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339. https://doi.org/10.1136/bmj.b2535.
- Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training. Clin Psychol Sci Pract 2006;13:295-310. https://doi.org/10.1111/j.1468-2850.2006.00042.x.
- Wahass S, Kent G. The modification of psychological interventions for persistent auditory hallucinations to an Islamic culture. Behav Cogn Psychoth 1997;25:351-64. https://doi.org/10.1017/S1352465800018750.
- Zhang M, Yan H. Effectiveness of psychoeducation of relatives of schizophrenic patients: a prospective cohort study in five cities of China. Int J Ment Health 1993;22:47-59. https://doi.org/10.1080/00207411.1993.11449246.
- Zhang M, He Y, Gittelman M, Wong Z, Yan H. Group psychoeducation of relatives of schizophrenic patients: two-year experiences. Psychiatry Clin Neurosci 1998;52:S344-S7. https://doi.org/10.1111/j.1440-1819.1998.tb03264.x.
- Chien WT, Chan SW, Thompson DR. Effects of a mutual support group for families of Chinese people with schizophrenia: 18-month follow-up. Br J Psychiatry 2006;189:41-9. https://doi.org/10.1192/bjp.bp.105.008375.
- Chien WT, Chan SW. One-year follow-up of a multiple-family-group intervention for Chinese families of patients with schizophrenia. Psychiatr Serv 2004;55:1276-84. https://doi.org/10.1176/appi.ps.55.11.1276.
- Mausbach BT, Bucardo J, McKibbin CL, Goldman SR, Jeste DV, Patterson TL, et al. Evaluation of a culturally tailored skills intervention for Latinos with persistent psychotic disorders. Am J Psychiatr Rehabil 2008;11:61-75. https://doi.org/10.1080/15487760701853102.
- Patterson TL, Bucardo J, McKibbin CL, Mausbach BT, Moore D, Barrio C, et al. Development and pilot testing of a new psychosocial intervention for older Latinos with chronic psychosis. Schizophr Bull 2005;31:922-30. https://doi.org/10.1093/schbul/sbi036.
- Chan SW, Yip B, Tso S, Cheng BS, Tam W. Evaluation of a psychoeducation program for Chinese clients with schizophrenia and their family caregivers. Patient Educ Couns 2009;75:67-76. https://doi.org/10.1016/j.pec.2008.08.028.
- Chien WT, Thompson DR, Norman I. Evaluation of a peer-led mutual support group for Chinese families of people with schizophrenia. Am J Community Psychol 2008;42:122-34. https://doi.org/10.1007/s10464-008-9178-8.
- Kung WW, Tseng Y-F, Wang Y, Hsu P-C, Chen D. Pilot study of ethnically sensitive family psychoeducation for Chinese-American patients with schizophrenia. Soc Work Ment Health 2012;10:384-408. https://doi.org/10.1080/15332985.2012.678570.
- Kulhara P, Chakrabarti S, Avasthi A, Sharma A, Sharma S. Psychoeducational intervention for caregivers of Indian patients with schizophrenia: a randomised-controlled trial. Acta Psychiatr Scand 2009;119:472-83. https://doi.org/10.1111/j.1600-0447.2008.01304.x.
- Zhang M, Wang M, Li J, Phillips MR. Randomised-control trial of family intervention for 78 first-episode male schizophrenic patients. An 18-month study in Suzhou, Jiangsu. Br J Psychiatry Suppl 1994;24:96-102.
- Lin EC-L, Chan CH, Shao W-C, Lin M-F, Shiau S, Mueser KT, et al. A randomized controlled trial of an adapted illness management and recovery program for people with schizophrenia awaiting discharge from a psychiatric hospital. Psychiatr Rehabil J 2013;36. https://doi.org/10.1037/prj0000013.
- Xiong W, Phillips MR, Hu X, Wang R, Dai Q, Kleinman J, et al. Family-based intervention for schizophrenic patients in China. A randomised controlled trial. Br J Psychiatr 1994;165:239-47. https://doi.org/10.1192/bjp.165.2.239.
- Carrà G, Montomoli C, Clerici M, Cazzullo CL. Family interventions for schizophrenia in Italy: randomized controlled trial. Eur Arch Psychiatry Clin Neurosci 2007;257:23-30. https://doi.org/10.1007/s00406-006-0677-z.
- Koolaee AK, Etemadi A. The outcome of two family interventions for the mothers of schizophrenia patients in Iran. Int J Soc Psychiatry 2009;56:634-46. https://doi.org/10.1177/0020764009344144.
- Naeem F, Saeed S, Irfan M, Kiran T, Mehmood N, Gul M, et al. Brief culturally adapted CBT for psychosis (CaCBTp): a randomized controlled trial from a low income country. Schizophr Res 2015;164:143-8. https://doi.org/10.1016/j.schres.2015.02.015.
- Razali SM, Hasanah CI, Khan A, Subramaniam M. Psychosocial interventions for schizophrenia. J Ment Health 2000;9:283-9. https://doi.org/10.1080/713680246.
- Chien WT. Effectiveness of psychoeducation and mutual support group program for family caregivers of Chinese people with schizophrenia. Open Nurs J 2008;2:28-39. https://doi.org/10.2174/1874434600802010028.
- Zimmer M, Duncan AV, Laitano D, Ferreira EE, Belmonte-de-Abreu P. A twelve-week randomized controlled study of the cognitive-behavioral Integrated Psychological Therapy program: positive effect on the social functioning of schizophrenic patients. Rev Bras Psiquiatr 2007;29:140-7. https://doi.org/10.1590/S1516-44462006005000030.
- Li Z, Arthur D. Family education for people with schizophrenia in Beijing, China: randomised controlled trial. Br J Psychiatry 2005;187:339-45. https://doi.org/10.1192/bjp.187.4.339.
- Chien WT, Lee IY. The schizophrenia care management program for family caregivers of Chinese patients with schizophrenia. Psychiatr Serv 2010;61:317-20. https://doi.org/10.1176/ps.2010.61.3.317.
- Chien WT, Chan SWC. The effectiveness of mutual support group intervention for Chinese families of people with schizophrenia: a randomised controlled trial with 24-month follow-up. Int J Nurs Stud 2013;50:1326-40. https://doi.org/10.1016/j.ijnurstu.2013.01.004.
- Kopelowicz A, Zarate R, Smith VG, Mintz J, Liberman RP. Disease management in Latinos with schizophrenia: a family-assisted, skills training approach. Schizophr Bull 2003;29:211-27. https://doi.org/10.1093/oxfordjournals.schbul.a006999.
- Ran M-S, Xiang M-Z, Chan CL-W, Leff J, Simpson P, Huang M-S, et al. Effectiveness of psychoeducational intervention for rural Chinese families experiencing schizophrenia. Soc Psychiatry Psychiatr Epidemiol 2003;38:69-75. https://doi.org/10.1007/s00127-003-0601-z.
- Chien WT, Thompson DR. An RCT with three-year follow-up of peer support groups for Chinese families of persons with schizophrenia. Psychiat Serv 2013;64:997-1005. https://doi.org/10.1176/appi.ps.201200243.
- Wang Y, Roberts DL, Xu B, Cao R, Yan M, Jiang Q. Social cognition and interaction training for patients with stable schizophrenia in Chinese community settings. Psychiatry Res 2013;210:751-5. https://doi.org/10.1016/j.psychres.2013.08.038.
- Chien WT, Lee IY. The mindfulness-based psychoeducation program for Chinese patients with schizophrenia. Psychiatr Serv 2013;64:376-9. https://doi.org/10.1176/appi.ps.002092012.
- Chien WT, Norman I, Thompson DR. A randomized controlled trial of a mutual support group for family caregivers of patients with schizophrenia. Int J Nurs Stud 2004;41:637-49. https://doi.org/10.1016/j.ijnurstu.2004.01.010.
- Chien WT, Wong KF. A family psychoeducation group program for Chinese people with schizophrenia in Hong Kong. Psychiatr Serv 2007;58:1003-6. https://doi.org/10.1176/ps.2007.58.7.1003.
- Lak DC, Tsang HW, Kopelowicz A, Liberman RP. Outcomes of the Chinese Basic Conversation Skill Module (CBCSM) for people with schizophrenia having mild to moderate symptoms and dysfunction in Hong Kong. Int J Psychiatr Clin Prac 2010;14:137-44. https://doi.org/10.3109/13651500903569613.
- Li Z-J, Guo Z-H, Wang N, Xu Z-Y, Qu Y, Wang X-Q, et al. Cognitive–behavioural therapy for patients with schizophrenia: a multicentre randomized controlled trial in Beijing, China. Psychol Med 2015;45:1893-905. https://doi.org/10.1017/S0033291714002992.
- Weng Y-z, Xiang Y-q, Liberman RP. Rehab rounds: psychiatric rehabilitation in a Chinese psychiatric hospital. Psychiat Serv 2005;56:401-3. https://doi.org/10.1176/appi.ps.56.4.401.
- Guo X, Zhai J, Liu Z, Fang M, Wang B, Wang C, et al. Effect of antipsychotic medication alone vs combined with psychosocial intervention on outcomes of early-stage schizophrenia: a randomized, 1-year study. Arch Gen Psychiatry 2010;67:895-904. https://doi.org/10.1001/archgenpsychiatry.2010.105.
- So SH, Chan AP, Chong CS, Wong MH, Lo WT, Chung DW, et al. Metacognitive training for delusions (MCTd): effectiveness on data-gathering and belief flexibility in a Chinese sample. Front Psychol 2015;6. https://doi.org/10.3389/fpsyg.2015.00730.
- Gohar SM, Hamdi E, El Ray LA, Horan WP, Green MF. Adapting and evaluating a social cognitive remediation program for schizophrenia in Arabic. Schizophr Res 2013;148:12-7. https://doi.org/10.1016/j.schres.2013.05.008.
- Kumar D, Zia Ul Haq M, Dubey I, Dotivala KN, Veqar Siddiqui S, Prakash R, et al. Effect of meta-cognitive training in the reduction of positive symptoms in schizophrenia. Eur J Psychother Couns 2010;12:149-58. https://doi.org/10.1080/13642537.2010.488875.
- Mann SKF, Chong BBW. The effect of symptoms coping program in reducing psychotic symptoms and enhancing functions in Chinese with schizophrenia. Am J Psychiatr Rehabil 2004;7:69-82. https://doi.org/10.1080/15487760490465013.
- Xiang M, Ran M, Li S. A controlled evaluation of psychoeducational family intervention in a rural Chinese community. Br J Psychiatr 1994;165:544-8. https://doi.org/10.1192/bjp.165.4.544.
- Bradley GM, Couchman GM, Perlesz A, Nguyen AT, Singh B, Riess C. Multiple-family group treatment for English- and Vietnamese-speaking families living with schizophrenia. Psychiatr Serv 2006;57:521-30. https://doi.org/10.1176/ps.2006.57.4.521.
- Lin EC, Shao WC, Chan CH, Shiau S, Wang HS, Huang SC. A pilot study of an illness management and recovery program in discharged patients with schizophrenia. J Nurs Res 2013;21:270-7. https://doi.org/10.1097/jnr.0000000000000004.
- Kopelowicz A, Zarate R, Wallace CJ, Liberman RP, Lopez SR, Mintz J. The ability of multifamily groups to improve treatment adherence in Mexican Americans with schizophrenia. Arch Gen Psychiatry 2012;69:265-73. https://doi.org/10.1001/archgenpsychiatry.2011.135.
- Shin SK, Lukens EP. Effects of psychoeducation for Korean Americans with chronic mental illness. Psychiatr Serv 2002;53:1125-31. https://doi.org/10.1176/appi.ps.53.9.1125.
- Valencia M, Rascon ML, Juarez F, Escamilla R, Saracco R, Liberman RP. Application in Mexico of psychosocial rehabilitation with schizophrenia patients. Psychiatry 2010;73:248-63. https://doi.org/10.1521/psyc.2010.73.3.248.
- Valencia M, Rascon ML, Juarez F, Murow E. A psychosocial skills training approach in Mexican out-patients with schizophrenia. Psychol Med 2007;37:1393-402. https://doi.org/10.1017/S0033291707000657.
- Gilchrist VJ, Crabtree BF, Miller WL. Doing Qualitative Research. Thousand Oaks, CA: Sage; 1992.
- BME Groups and Mental Health: Presentation and Evidence to the Centre for Social Justice Mental Health Review, 18 October 2010. London: Department of Health and Social Care; 2010.
- Liberman RP. Dissemination and adoption of social skills training: social validation of an evidence-based treatment for the mentally disabled. J Ment Health 2007;16:595-623. https://doi.org/10.1080/09638230701494902.
- Berry K, Gregg L, Hartwell R, Haddock G, Fitzsimmons M, Barrowclough C. Therapist-client relationships in a psychological therapy trial for psychosis and substance misuse. Drug Alcohol Depend 2015;152:170-6. https://doi.org/10.1016/j.drugalcdep.2015.04.006.
- Compassion in Practice. London: DHSC; 2012.
- The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992.
- Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2000.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Ritchie J, Lewis J. Qualitative Research Practice. A Guide for Social Science Students and Researchers. London: Sage; 2005.
- Gibbs G. Analyzing Qualitative Data. Los Angeles, CA: Sage; 2007.
- Gibson W, Brown A. Working with Qualitative Data. Los Angeles, CA: Sage; 2009.
- The Equality Act. London: The Stationery Office; 2010.
- Smith G, Higgs A, Gregory K. An Integrated Approach to Family Work for Psychosis: A Manual for Family Workers. London: Jessica KIngsley Publishers; 2007.
- Barrowclough C, Tarrier N, Watts S, Vaughn C, Bamrah JS, Freeman HL. Assessing the functional value of relatives’ knowledge about schizophrenia: a preliminary report. Br J Psychiatry 1987;151:1-8. https://doi.org/10.1192/bjp.151.1.1.
- Longden E. Eleanor Longden: The Voices in My Head 2013. www.ted.com/talks/eleanor_longden_the_voices_in_my_head (accessed 1 March 2014).
- Bernal G, Jimenez-Chafey MI, Rodriguez MMD. Cultural adaptation of treatments: a resource for considering culture in evidence-based practice. Prof Psychol Res Pr 2009;40:361-8. https://doi.org/10.1037/a0016401.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy 2005;10:45-53. https://doi.org/10.1177/135581960501000110.
- Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. London: Sage; 2007.
- Creswell JW, Plano Clark VL, Gutmann ML, Hanson WE, Tashakkori A, Teddlie C. Handbook of Mixed Methods in Social and Behavioral Research. Thousand Oaks, CA: Sage; 2003.
- Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CF, Askham J, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess 1998;2.
- Bowling A. Research Methods in Health: Investigating Health and Health Services. Buckingham: Open University Press; 2002.
- Dalkey N, Helmer D. An experimental application of the Delphi method to the use of experts. Manag Sci 1963;9:458-67. https://doi.org/10.1287/mnsc.9.3.458.
- Delbecq A, Van de Ven A. A group process model for problem identification and program planning. J Appl Behav Sci 1971;7:467-92. https://doi.org/10.1177/002188637100700404.
- Baker J, Lovell K, Harris N. How expert are the experts? An exploration of the concept of ‘expert’ within Delphi panel techniques. Nurse Res 2006;14:59-70. https://doi.org/10.7748/nr2006.10.14.1.59.c6010.
- Beech B. The Delphi approach: recent applications in health care. Nurse Res 2001;8:38-4. https://doi.org/10.7748/nr2001.07.8.4.38.c6164.
- Aday AL. Designing and Conducting Health Surveys: A Comprehensive Guide. San Francisco, CA: Jossey-Bass Inc.; 1996.
- O’Brien AP, O’Brien AJ, Hardy DJ, Morrison-Ngatai E, Gaskin CJ, Boddy JM, et al. The New Zealand development and trial of mental health nursing clinical indicators: a bicultural study. Int J Nurs Stud 2003;40:853-61. https://doi.org/10.1016/S0020-7489(03)00074-9.
- Salmond SW. Orthopaedic nursing research priorities: a Delphi study. Orthop Nurs 1994;13:31-45. https://doi.org/10.1097/00006416-199403000-00006.
- Sackman H. Delphi Critique: Expert Opinion, Forecasting, and Group Process. Lanham, MD: Lexington Books; 1975.
- Critcher C, Gladstone B. Utilizing the Delpi technique in policy discussion: a case study of a privatised utility in Britain. Publ Adm 1998;76:431-49. https://doi.org/10.1111/1467-9299.00110.
- Jones J, Hunter D, Pope C, May N, Pope C, May N. Qualitative Research in Health Care. London: BMJ Publishing Group; 2000.
- Mullen PM. Delphi: myths and reality. J Health Organ Manag 2003;17:37-52. https://doi.org/10.1108/14777260310469319.
- Count Me In 2010: Results of the 2010 National Census of Inpatients and Patients on Supervised Community Treatment in Mental Health and Learning Disability Services in England and Wales. London: CQC; 2011.
- Falloon I, Fadden G, Mueser K, Gingerich S, Rappaport S, McGill C, et al. Family Work Manual. Birmingham: Meriden Family Programme: Birmingham & Solihull Mental Health NHS Foundation Trust; 2014.
- Meriden Family Programme . About Us n.d. www.meridenfamilyprogramme.com/about (accessed 1 February 2017).
- Rumrill PD, Fitzgerald SM, Merchant WR. Using scoping literature reviews as a means of understanding and interpreting existing literature. Work 2010;35:399-404. https://doi.org/10.3233/WOR-2010-0998.
- NHS Knowledge and Skills Framework (NHS KSF) and The Development Review Process. London: Department of Health; 2004.
- Edge D, Degnan A, Cotterill S, Berry K, Drake R, Baker J, et al. Culturally-adapted Family Intervention (CaFI) for African-Caribbeans diagnosed with schizophrenia and their families: a feasibility study protocol of implementation and acceptability. Pilot Feas Stud 2016;2. https://doi.org/10.1186/s40814-016-0070-2.
- Schouler-Ocak M, Graef-Calliess IT, Tarricone I, Qureshi A, Kastrup MC, Bhugra D. EPA guidance on cultural competence training. Eur Psychiatry 2015;30:431-40. https://doi.org/10.1016/j.eurpsy.2015.01.012.
- Govere L, Govere EM. How effective is cultural competence training of healthcare providers on improving patient satisfaction of minority groups? A systematic review of literature. Worldviews Evid Based Nurs 2016;13:402-10. https://doi.org/10.1111/wvn.12176.
- Berry K, Haddock G. The implementation of the NICE guidelines for schizophrenia: barriers to the implementation of psychological interventions and recommendations for the future. Psychol Psychother-T 2008;81:419-36. https://doi.org/10.1348/147608308X329540.
- Fadden G. Implementation of family interventions in routine clinical practice following staff training programs: a major cause for concern. J Ment Health 1997;6:599-612. https://doi.org/10.1080/09638239718464.
- Moher D, Schulz KF, Altman DG, Group C. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 2001;357:1191-4. https://doi.org/10.1016/S0140-6736(00)04337-3.
- Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76. https://doi.org/10.1093/schbul/13.2.261.
- Kay SR, Opler LA, Lindenmayer JP. Reliability and validity of the positive and negative syndrome scale for schizophrenics. Psychiatry Res 1988;23:99-110. https://doi.org/10.1016/0165-1781(88)90038-8.
- Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand 2000;101:323-9.
- Patrick DL, Burns T, Morosini P, Rothman M, Gagnon DD, Wild D, et al. Reliability, validity and ability to detect change of the clinician-rated Personal and Social Performance scale in patients with acute symptoms of schizophrenia. Curr Med Res Opin 2009;25:325-38. https://doi.org/10.1185/03007990802611919.
- Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. J Abnorm Psychol 1989;98:229-35. https://doi.org/10.1037/0021-843X.98.3.229.
- Renshaw KD. The predictive, convergent, and discriminant validity of perceived criticism: a review. Clin Psychol Rev 2008;28:521-34. https://doi.org/10.1016/j.cpr.2007.09.002.
- Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry 1998;55:547-52. https://doi.org/10.1001/archpsyc.55.6.547.
- Goldberg D, Williams P. A User’s Guide to the General Health Questionnaire. Windsor: National Foundation for Educational Research/Nelson; 1988.
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. J Couns Psychol 1989;36:223-33. https://doi.org/10.1037/0022-0167.36.2.223.
- Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychol Assess 1989;1. https://doi.org/10.1037/1040-3590.1.3.207.
- Horvath AO, Bedi RP, Norcross JC. Psychotherapy Relationships that Work: Therapist Contributions and Responsiveness to Patients. New York, NY: Oxford University Press; 2002.
- Horvath AO, Luborsky L. The role of the therapeutic alliance in psychotherapy. J Consult Clin Psychol 1993;61:561-73. https://doi.org/10.1037/0022-006X.61.4.561.
- Norcross JC. Psychotherapy Relationships that Work: Therapist Contributions and Responsiveness to Patients. New York, NY: Oxford University Press; 2002.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 2013;22:1717-27. https://doi.org/10.1007/s11136-012-0322-4.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013. www.nice.org.uk/article/pmg9/chapter/5-the-reference-case (accessed 6 February 2015).
- Barrowclough C, Tarrier N, Lewis S, Sellwood W, Mainwaring J, Quinn J, et al. Randomised controlled effectiveness trial of a needs-based psychosocial intervention service for carers of people with schizophrenia. Br J Psychiatry 1999;174:505-11. https://doi.org/10.1192/bjp.174.6.505.
- Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosomat Res 2006;60:631-7. https://doi.org/10.1016/j.jpsychores.2005.10.020.
- Addington J, Graham H, Copello A, Birchwood M, Mueser KT. Substance Misuses in Psychosis: Approaches to Treatment and Service Delivery. Chichester: Wiley; 2003.
- Lobban F, Barrowclough C, Jones S. Assessing cognitive representations of mental health problems. II. the illness perception questionnaire for schizophrenia: relatives’ version. Br J Clin Psychol 2005;44:163-79. https://doi.org/10.1348/014466504X19785.
- Lobban F, Solis-Trapala I, Tyler E, Chandler C, Morriss RK, Group E. The role of beliefs about mood swings in determining outcome in bipolar disorder. Cognitive Ther Res 2013;37:51-60. https://doi.org/10.1007/s10608-012-9452-9.
- Broadbent E, Kydd R, Sanders D, Vanderpyl J. Unmet needs and treatment seeking in high users of mental health services: role of illness perceptions. Aust N Z J Psychiatry 2008;42:147-53. https://doi.org/10.1080/00048670701787503.
- Berry K, Barrowclough C, Wearden A. Attachment theory: a framework for understanding symptoms and interpersonal relationships in psychosis. Behav Res Ther 2008;46:1275-82. https://doi.org/10.1016/j.brat.2008.08.009.
- Degnan A, Seymour-Hyde A, Harris A, Berry K. The role of therapist attachment in alliance and outcome: a systematic literature review. Clin Psychol Psychother 2014;23:47-65. https://doi.org/10.1002/cpp.1937.
- Owens KA, Haddock G, Berry K. The role of the therapeutic alliance in the regulation of emotion in psychosis: an attachment perspective. Clin Psychol Psychother 2013;20:523-30. https://doi.org/10.1002/cpp.1793.
- Tait L, Birchwood M, Trower P. A new scale (SES) to measure engagement with community mental health services. J Ment Health 2002;11:191-8. https://doi.org/10.1080/09638230020023570-2.
- Devlin N, Shah K, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Sheffield: School of Health and Related Research (ScHARR); 2016.
- Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology 1990;1:43-6. https://doi.org/10.1097/00001648-199001000-00010.
- Gurpinar-Morgan A. What is cultural competence and how might clinical psychology training equip psychologists to work with ethnic diversity?. Clin Psychol Forum 2012.
- Kohn LP, Oden T, Muñoz RF, Robinson A, Leavitt D. Adapted cognitive behavioral group therapy for depressed low-income African American women. Community Ment Health J 2002;38:497-504. https://doi.org/10.1023/A:1020884202677.
- LaFromboise TD, Coleman HL, Hernandez A. Development and factor structure of the Cross-Cultural Counseling Inventory – Revised. Prof Psychol Res Pract 1991;22:380-8. https://doi.org/10.1037/0735-7028.22.5.380.
- Sue S, Zane N, Nagayama Hall GC, Berger LK. The case for cultural competency in psychotherapeutic interventions. Annu Rev Psychol 2009;60:525-48. https://doi.org/10.1146/annurev.psych.60.110707.163651.
- Zayfert C. Culturally competent treatment of posttraumatic stress disorder in clinical practice: an ideographic, transcultural approach. Clin Psychol Sci Pract 2008;15:68-73. https://doi.org/10.1111/j.1468-2850.2008.00111.x.
- Barrowclough C, Tarrier N. Families of Schizophrenic Patients: Cognitive Behavioural Intervention. London: Chapman & Hall; 1992.
- Randolph ET, Mueser KT, Tarrier N. Handbook of Social Functioning in Schizophrenia. Needham Heights, MA: Allyn Bacon; 1998.
- Bhui K, McCabe R, Weich S, Singh S, Johnson M, Szczepura A. THERACOM: a systematic review of the evidence base for interventions to improve therapeutic communications between black and minority ethnic populations and staff in specialist mental health services. Syst Rev 2013;2. https://doi.org/10.1186/2046-4053-2-15.
- Munder T, Wilmers F, Leonhart R, Linster HW, Barth J. Working Alliance Inventory – Short Revised (WAI-SR): psychometric properties in outpatients and inpatients. Clin Psychol Psychother 2010;17:231-9.
- Tryon G, Collins BS, Felleman HE. A meta-analytic examination of client–therapist perspectives of the working alliance. Psychother Res 2007;17:629-42. https://doi.org/10.1080/10503300701320611.
- Burnard P. A method of analysing interview transcripts in qualitative research. Nurse Educ Today 1991;11:461-6. https://doi.org/10.1016/0260-6917(91)90009-Y.
- Ritchie J, Spencer L, O’Connor W. Carrying out Qualitative Analysis. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Marshall MN. Sampling for qualitative research. Fam Pract 1996;13:522-5. https://doi.org/10.1093/fampra/13.6.522.
- Johansen R. Working Alliance and Service Engagement in Early Schizophrenia Spectrum Disorders 2013.
- Delivering Race Equality in Mental Health Care: An Action Plan for Reform Inside and Outside Services and the Government’s Response to the Independent Inquiry into the Death of David Bennett. London: DHSC; 2005.
- Degnan A, Baker S, Edge D, Nottidge W, Noke M, Husain N, et al. The nature and efficacy of culturally-adapted psychosocial interventions in schizophrenia: a systematic review and meta-analysis. Psychol Med 2017:1-14.
- McKenzie K, Bhui K. Institutional racism in mental health care. BMJ 2007;334:649-50. https://doi.org/10.1136/bmj.39163.395972.80.
- Fadden G. Family intervention in psychosis. J Ment Health 1998;7:115-22. https://doi.org/10.1080/09638239818166.
- Ince P, Haddock G, Tai S. A systematic review of the implementation of recommended psychological interventions for schizophrenia: rates, barriers, and improvement strategies. Psychol Psychother Theor Res Pract 2016;89:324-50. https://doi.org/10.1111/papt.12084.
- Cabral RR, Smith TB. Racial/ethnic matching of clients and therapists in mental health services: a meta-analytic review of preferences, perceptions, and outcomes. J Couns Psychol 2011;58:537-54. https://doi.org/10.1037/a0025266.
- Bhui K, Morgan N. Effective psychotherapy in a racially and culturally diverse society. Adv Psychiatr Treat 2007;13:187-93. https://doi.org/10.1192/apt.bp.106.002295.
- Husain N, Chaudhry N, Durairaj SV, Chaudhry I, Khan S, Husain M, et al. Prevention of: self harm in British South Asian women: study protocol of an exploratory RCT of culturally adapted manual assisted Problem Solving Training (C-MAP). Trials 2011;12. https://doi.org/10.1186/1745-6215-12-159.
- National Records of Scotland; Northern Ireland Statistics and Research Agency (2016): 2011 Census Aggregate Data. London: Office for National Statistics; 2016.
- Degnan A, Edge D, Abel KM, Berry K, Drake R, Ashworth M. Lay Guide to Schizophrenia and Psychosis. Manchester: Manchester Mental Health and Social Care NHS Trust; 2014.
- Degnan A, Berry K, James S, Edge D. Development, validation and cultural-adaptation of the knowledge about psychosis questionnaire for African-Caribbean people in the UK. Psychiatry Res 2018;263:199-206. https://doi.org/10.1016/j.psychres.2018.03.013.
- Edge D, Grey P. An assets-based approach to co-producing Culturally-adapted Family Intervention (CaFI) with African-Caribbeans diagnosed with schizophrenia and their families. Ethn Dis 2018.
- McFarlane WR, Deakins SM, Gingerich SL, Dunne E, Horen B, Newmark M. Multiple-Family Psychoeducational Group Treatment Manual. New York, NY: New York State Psychiatric Institute; 1991.
- McFarlane WR, Hornby H, Dixon L, McNary S, McFarlane WR. Multifamily Group Treatment for Severe Psychiatric Disorders. New York, NY: Guilford; 2002.
- Care Management in Early Psychosis: A Handbook. Melbourne, VIC: EPPIC; 2001.
- Posner CW, Wilson KG, Kral MJ, Lander S, Mcllwraith RD. Family psychoeducational support groups in schizophrenia. Am J Orthopsychiatry 1992;62:206-18. https://doi.org/10.1037/h0079337.
- Galinsky MJ, Schopler JH. Support Groups: Current Perspectives on Theory and Practice. New York, NY: Harworth Press; 1995.
- Wilson J. How to Work with Self-help Groups: Guidelines for Professionals. Aldershot, UK: Arena; 1995.
- McFarlane WR, Lukens E, Link B, Dushay R, Deakins SA, . Multiple-family groups and psychoeducation in the treatment of schizophrenia. Arch Gen Psychol 1995;52:679-87. https://doi.org/10.1001/archpsyc.1995.03950200069016.
- Bae SW, Kung WWM. Family intervention for Asian Americans with a schizophrenic patient in the family. Am J Orthopsychiatry 2000;70:532-41. https://doi.org/10.1037/h0087789.
- Anderson CM, Reiss DJ, Hogarty GE. Schizophrenia and the Family: A Practitioner’s Guide to Psychoeducation and Management. New York, NY: Guilford Press; 1986.
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1992;149:936-43. https://doi.org/10.1176/ajp.149.7.936.
- Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, . Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry 2004;161:1-56.
- Meissen GJ, Volk F, Lavoie F, Borkman T, Gidron B. Self-help and Mutual Aid Groups: International and Multicultural Perspectives. New York, NY: Haworth; 1995.
- Toseland RW, Rossiter CM. Group interventions to support family caregivers: a review and analysis. Gerontologist 1989;29:438-4. https://doi.org/10.1093/geront/29.4.438.
- Powell TJ. Understanding the Self-help Organization: Framework and Findings. Thousand Oaks, CA: Sage Publications; 1994.
- Horan WP, Kern RS, Tripp C, Hellemann G, Wynn JK, Bell M, et al. Efficacy and specificity of social cognitive skills training for outpatients with psychotic disorders. J Psychiatr Res 2011;45:1113-22. https://doi.org/10.1016/j.jpsychires.2011.01.015.
- Lehman AF, Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB, Goldberg R, et al. The schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull 2004;30:193-217. https://doi.org/10.1093/oxfordjournals.schbul.a007071.
- Kingdon D, Turkington D. Cognitive-Behavioral Therapy of Schizophrenia. Hove: Lawrence Erlbaum; 1994.
- Stengard E. Educational intervention for the relatives of schizophrenia patients in Finland. Nord J Psychiatry 2003;57:271-7. https://doi.org/10.1080/08039480310002093.
- Falloon IRH, Lansky MR. Family Therapy and Major Psychopathology. New York, NY: Grune & Stratton, Inc; 1981.
- Liberman RP, Corrigan PW. Designing new psychosocial treatments for schizophrenia. Psychiatry 1993;56:238-49. https://doi.org/10.1080/00332747.1993.11024640.
- Liberman RP, Wallace CJ, Blackwell G, Eckman TA, Vaccaro JV, Kuehnel TG. Innovations in skills training for the seriously mentally ill: The UCLA Social and Independent Living Skills Modules. Innovations and Research 1993;2:43-60.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- Leff J. Family work for schizophrenia: practical application. Acta Psychiatr Scand 2000;407:78-82. https://doi.org/10.1034/j.1600-0447.2000.00013.x.
- Moritz S, Woodward TS. Metacognition Study Group: Metacognitive Training for Patients with Schizophrenia (MCT) Manual. Hamburg: VanHam Campus Verlag; 2007.
- McFarlane WR. Multifamily Groups in the Treatment of Severe Psychiatric Disorders. New York, NY: Guilford Press; 2002.
- Liberman RP. Social and Independent Living Skills: Basic Conversation Skills Module. Los Angeles, CA: UCLA Clinical Research Center for Schizophrenia & Psychiatric Rehabilitation; 1990.
- Falloon IR, Boyd JL, McGill CW. Family Care of Schizophrenia: A Problem-solving Approach to the Treatment of Mental Illness. New York, NY: Guilford Press; 1984.
- Leff J, Kuipers L, Berkowitz R, Sturgeon D. A controlled trial of social intervention in the families of schizophrenic patients: two year follow-up. Br J Psychiatry 1985;146:594-600. https://doi.org/10.1192/bjp.146.6.594.
- Goldstein MJ, Hand I, Hahlweg K. Treatment of Schizophrenia: Family Assessment and Intervention. New York, NY: Springer-Verlag; 2012.
- Gingerich S, Mueser KT. Illness Management and Recovery Implementation Resource Kit (Revised ed.). Rockville: Center for Mental Health Services. Substance Abuse and Mental Health Services Administration; 2010.
- Alford GS, Fleece L, Rothblum E. Hallucinatory delusional verbalizations modification in a chronic schizophrenia by self-control and cognitive restructuring. Behav Modifi 1982;6:421-35. https://doi.org/10.1177/014544558263007.
- Garety PA, Kuipers L, Fowler D, Chamberlain F, Dunn G. Cognitive behavioural therapy for drug-resistant psychosis. Br J Med Psychol 1994;67:259-71. https://doi.org/10.1111/j.2044-8341.1994.tb01795.x.
- Lamontagne Y, Audet N, Elie R. Thought-stop for delusions and hallucinations: a pilot study. Behav Psychother 1983;11:177-84. https://doi.org/10.1017/S0141347300006601.
- Meichenbaum D, Cameron R. Training schizophrenics to talk to themselves: a means of developing attentional control. Behav Ther 1973;4:515-34. https://doi.org/10.1016/S0005-7894(73)80003-6.
- Bandura A, Mays V, Albee G, Schneider S. Prevention of AIDS: Psychological Approaches. Newbury Park, CA: Sage; 1989.
- Lalonde P, Shriqui CL, Nasrallah HA. Contemporary Issues in the Treatment of Schizophrenia. Washington, DC: American Psychiatric Press, Inc; 1995.
- Bernheim K, Lehman A. Working with Families of the Mentally Ill. New York, NY: Norton; 1985.
- Lukens E, Thorning H, Williams J, Ell K. Breakthroughs in Mental Health Research: Implications for Social Work Practice. Washington, DC: NASW Press; 1998.
- Wallace CJ, Liberman RP, MacKain SJ, Blackwell G, Eckman TE. Effectiveness and replicability of modules for teaching social and instrumental skills to the severely mentally ill. Am J Psychiatry 1992;149:654-8. https://doi.org/10.1176/ajp.149.5.654.
- Liberman R.P. Recovery from Disability. Manual of Psychiatric Rehabilitation. Arlington, VA: American Psychiatric Publishing; 2008.
- Bentall R, Haddock G, Slade P. Cognitive behaviour therapy for persistent auditory hallucinations: from theory to therapy. Behav Ther 1994;25:51-66. https://doi.org/10.1016/S0005-7894(05)80145-5.
- Nelson H, Thrasher S, Barnes T. Practical ways of alleviating auditory hallucinations. BMJ 1991;302. https://doi.org/10.1136/bmj.302.6772.327.
- Roberts DL, Penn DL, Combs DR. Social Cognition and Interaction Training (SCIT): Group Psychotherapy for Schizophrenia and Other Psychotic Disorders, Clinician Guide. New York, NY: Oxford University Press; 2015.
- Liberman RP, DeRisi WJ, Mueser K. Social Skills Training for Psychiatric Patients. Norwood, MA: Allyn & Bacon; 1989.
- Brown GW, Birley JLT, Wing JK. Influence of family life on course of schizophrenic disorders: a replication. Br J Psychiatry 1972;121:241-58. https://doi.org/10.1192/bjp.121.3.241.
- Falloon JRH, McGill CW, Boyd JL, Pederson J. Family management in the prevention of morbidity of schizophrenia: social outcome of a two-year longitudinal study. Psychol Med 1987;17:59-66. https://doi.org/10.1017/S0033291700012988.
- Abramowitz IA, Coursey RD. Impact of an education support group on family participants who take care of their schizophrenic relatives. J Consult Clin Psychol 1989;57. https://doi.org/10.1037/0022-006X.57.2.232.
- Vaughan K, Doyle M, McConaghy N, Blaszczynski A, Fox A, Tarrier N. The Sydney intervention trial: a controlled trial of relatives counselling to reduce schizophrenic relapse. Soc Psychiatry Psychiatr Epidemiol 1992;27:16-21. https://doi.org/10.1007/BF00788951.
- Leff J, Berkowitz R, Shavit N, Strachan A, Glass I, Vaughn C. A trial of family therapy versus a relatives’ group for schizophrenia: two-year follow-up. Br J Psychiatry 1990;157:571-7. https://doi.org/10.1192/bjp.157.4.571.
- Falloon IR, Boyd JL, McGill CW, Williamson M, Razani J, Moss HB, et al. Family management in the prevention of morbidity of schizophrenia: clinical outcome of a two-year longitudinal study. Arch Gen Psychiatry 1985;42:887-96. https://doi.org/10.1001/archpsyc.1985.01790320059008.
- Tarrier N, Barrowclough C, Vaughn C, Bamrah JS, Porceddu K, Watts S, et al. Community management of schizophrenia: a two-year follow up of a behavioural intervention with families. Br J Psychiatry 1989;154:625-8. https://doi.org/10.1192/bjp.154.5.625.
- Leff JP, Kuipers L, Berkowitz R, Eberlein-Vries R, Sturgeon D. A controlled trial of social intervention in schizophrenic families. Br J Psychiatry 1982;141:121-34. https://doi.org/10.1192/bjp.141.2.121.
- Vaughn CE, Leff JP. The influence of family and social factors on the course of psychiatric illness: a comparison of schizophrenia and depressed neurotic patients. Br J Psychiatry 1976;129:125-7. https://doi.org/10.1192/bjp.129.2.125.
- McFarlane MR. Family Therapy in Schizophrenia. New York, NY: Guilford Press; 1982.
- Goldstein MJ. Schizophrenia Treatment, Management and Rehabilitation. New York, NY: Grune & Stratton, Inc; 1984.
- Roder V, Müller DR, Brenner HD, Spaulding WD. Integrated Psychological Therapy (IPT): For the Treatment of Neurocognition, Social Cognition, and Social Competency in Schizophrenia Patients. Cambridge, MA: Hogrefe Publishing; 2010.
- Naeem F, Habib N, Gul M, Khalid M, Saeed S, Farooq S, et al. A qualitative study to explore patients’, carers’ and health professionals’ views to culturally adapt CBT for psychosis (CBTp) in Pakistan. Behav Cogn Psychother 2016;44:43-55. https://doi.org/10.1017/S1352465814000332.
- Shankar R, Menon MS. Development of a framework of interventions with families in the management of schizophrenia. Psychosoc Rehabil J 1993;16:75-91. https://doi.org/10.1037/h0095673.
- Lopez SR, Kopelowicz A, Canive J, Lefley HP, Johnson DL. Family Interventions in Mental Illness: International Perspectives. Westport, CT: Praeger; 2002.
- Li Z. The Effect of a Nurse Initiated Patient Family Education Strategy on People With Schizophrenia in Beijing 2003.
- Valencia M, Rascon ML, Quiroga H. Research contributions to psychosocial and familial treatment of schizophrenic patients. Salud Ment 2003;26:1-8.
- Valencia M, Moriana JA, Kopelowicz A, Lopez SR, Liberman RP. Social-Skills training for Spanish-speaking persons with schizophrenia: experiences from Latin America, Spain, and the United States. Am J Psychiatr Rehabil 2015;18:209-46.
- Naeem F, Waheed W, Gobbi M, Ayub M, Kingdon D. Preliminary evaluation of culturally sensitive CBT for depression in Pakistan: findings from Developing Culturally-sensitive CBT Project (DCCP). Behav Cogn Psychother 2010;39:165-73. https://doi.org/10.1017/S1352465810000822.
- Meredith WH, Abbott DA, Tsai R, Ming ZF. Healthy family functioning in Chinese cultures: an exploratory study using the Circumplex Model. Int J Sociol Fam 1994;24:147-5. https://www.jstor.org/stable/23029805.
Appendix 1 Search strategy for the systematic review of culturally adapted psychosocial interventions for schizophrenia
Cumulative Index to Nursing and Allied Health Literature, PsycINFO, MEDLINE and EMBASE: total records, n = 4695.
Date searched: 9 March 2016.
PsycINFO (via OvidSP)
Date range searched: 1806 to March week 1 2016.
Records: n = 846.
Search strategy
-
exp schizophrenia/ or exp psychosis/
-
(psychotic or schizo* or psychosis or psychoses).sh.ti.ab.hw.id [subject heading, title, abstract, heading word, key concepts]
-
((chronic* or sever*) adj5 mental* adj5 (ill* or disorder*)). sh.ti.ab.hw.id.
-
or/1-3
-
exp ethnology/ or exp culture (Anthropological) / or exp racial and ethnic groups/ or exp racial and ethnic differences/ or exp cross-cultural differences/ exp sociocultural factors/ or exp cultural sensitivity/ or exp acculturation/ or exp minority groups
-
(ethnic* or ethnolog* or cultur* or acculturation or rac* or minorit* or transcultur* or sociocultur*).sh.ti.ab.hw.id.
-
((cultur* adj3 (identity or cross or specific or sensiti* or relevant or adapt* or competen* or divers*)).sh.ti.ab.hw.id.
-
((ethnic or racial) adj3 (identity or group or minorit* or difference or variation or divers*)). sh.ti.ab.hw.id.
-
or/5-8
-
exp cross-cultural treatment/ or exp psychosocial rehabilitation/ or exp mental health services/ or exp psychotherapy/ or exp behaviour therapy/ or exp sociotherapy
-
((psychological or psychosocial or psychiat* or clinical) adj5 (intervention or therap* or rehabilitation or treatment or care)).sh.ti.ab.hw.id.
-
((cognitive or behav* or famil* or systemic or social* or education*) adj5 (intervention or therap* or rehabilitation or treatment or training or skill*)).sh.ti.ab.hw.id.
-
((cognitive or behav*) adj5 (remediat*).sh.ti.ab.hw.id.
-
((evidence based or empirically supported) adj5 (intervention or therap* or treatment)). sh.ti.ab.hw.id.
-
or/10-14
-
exp clinical trials/ or exp treatment effectiveness evaluation/
-
exp experimental controls
-
(controlled or clinical) adj3 (trial). sh.ti.ab.hw.id.
-
(random* or control* or trial or condition or assigned or group). sh.ti.ab.hw.id.
-
or/ 16-19
-
4 and 9 and 15 and 20
MEDLINE (via OvidSP)
Date range searched: 1946 to February week 4 2016.
Records: n = 763.
Search strategy
-
exp schizophrenia/ or exp psychotic disorders/
-
(psychotic or schizo* or psychosis or psychoses).ab.hw.kf.ti.kw [abstract, subject heading word, keyword heading word, title, keyword heading]
-
((chronic* or sever*) adj5 mental* adj5 (ill* or disorder*)).ab.hw.kf.ti.kw
-
or/1-3
-
exp culture/ or exp ethnology/ or exp acculturation/ or exp cross-cultural comparison/ or exp cultural characteristics/ or exp cultural diversity/ or exp ethnic groups/ or minority groups
-
(ethnic* or ethnolog* or cultur* or accultur* or rac* or minorit* or transcultur* or sociocultur*).ab.hw.kf.ti.kw
-
(cultur* adj3 (identity or cross or specific or sensiti* or relevant or adapt* or competen* or divers*)). ab.hw.kf.ti.kw
-
((ethnic or racial) adj3 (identity or group* or minorit* or difference or variation or divers*)). ab.hw.kf.ti.kw
-
or/5-8
-
exp rehabilitation/ or exp mental health services/ or exp psychotherapy/ or exp behaviour therapy
-
((psychological or psychosocial or psychiat* or clinical) adj5 (intervention or therap* or rehabilitation or treatment or care)). ab.hw.kf.ti.kw
-
((cognitive or behav* or famil* or systemic or social* or education*) adj5 (intervention or therap* or rehabilitation or treatment or training or skill*)). ab.hw.kf.ti.kw
-
((cognitive or behav*) adj5 (remediat*). ab.hw.kf.ti.kw
-
((evidence based or empirically supported) adj5 (intervention or therap* or treatment)). ab.hw.kf.ti.kw
-
or/10-14
-
exp clinical trial/ or exp controlled clinical trial/ or exp randomized controlled trial
-
exp random allocation/ or exp double-blind method/ or exp single blind method/ or exp control groups
-
(controlled or clinical) adj3 (trial). ab.hw.kf.ti.kw
-
(random* or control* or trial or condition or assigned or group). ab.hw.kf.ti.kw
-
exp feasibility studies/ exp pilot projects/ exp intervention studies
-
or/16-20
-
4 and 9 and 15 and 21
EMBASE (via OvidSP)
Date range searched: 1980 to week 10 2016.
Records: n = 1737.
Search strategy
-
exp schizophrenia/ or exp psychosis/
-
(psychotic or schizo$ or psychoses or psychosis).ti.hw.ab.kw.sh [title, heading words, abstract, key word, subject headings]
-
((chronic$ or sever$) adj5 mental$ adj5 (ill$ or disorder$)).ti.hw.ab.kw.sh [title, heading words, abstract, key word, subject headings]
-
or/1-3
-
exp ethnology/ or exp ethnic group/ or exp cultural factor/ or exp minority group/ or exp cultural anthropology/ exp ethnic and racial groups/ exp cultural competence
-
(ethnic$ or ethnolog$ or cultur$ or accultur$ or rac$ or minorit$ or transcultur$ or sociocultur$).ti.hw.ab.kw.sh
-
(cultur$ adj3 (identity or cross or specific or sensiti$ or relevant or adapt$ or competen$ or divers$)).ti.hw.ab.kw.sh
-
((ethnic or racial) adj3 (identity or group$ or minorit$ or difference or variation or divers$)).ti.hw.ab.kw.sh
-
or/5-9
-
exp psychiatric treatment/ or exp psychotherapy/ or exp sociotherapy/ or exp mental health services/ or exp psychosocial rehabilitation/ or exp behaviour therapy
-
((psychological or psychosocial or psychiat$ or clinical) adj5 (intervention or therap$ or rehabilitation or treatment or care)). ti.hw.ab.kw.sh
-
((cognitive or behav$ or famil$ or systemic or social$ or education$) adj5 (intervention or therap$ or rehabilitation or treatment or training or skill$)). ti.hw.ab.kw.sh
-
((cognitive or behav$) adj5 (remediat$). ti.hw.ab.kw.sh
-
(evidence based or empirically supported) adj5 (intervention or therap$ or treatment). ti.hw.ab.kw.sh
-
or/10-14
-
exp clinical trials (topic)/ or exp controlled clinical trial/ or exp randomized controlled trial
-
exp randomisation/ or exp control group
-
(controlled or clinical) adj3 (trial). ti.hw.ab.kw.sh
-
(random$ or control$ or trial or condition or assigned or group).ti.ab
-
exp intervention study/ exp pilot study/ exp feasibility study
-
or/ 16-20
-
4 and 9 and 15 and 21
Cumulative Index to Nursing and Allied Health Literature (via EBSCOhost)
Records: n = 1349.
MH = exact subject heading; MM = exact major subject heading; TX = keyword.
Search strategy
-
(MH “Schizophrenia+”) OR (MH “Psychotic Disorders+”)
-
TX=(psychotic OR schizo* OR psychosis OR psychoses)
-
TX=((chronic* OR sever*) N5 mental* N5 (ill* OR disorder*))
-
OR/1-3
-
(MH “Culture+”) OR (MM “Acculturation”) OR (MM “Cultural Diversity”) OR (MM “Ethnic Groups”) OR (MM “Ethnology”) OR (MM “Minority Groups”) OR (MM “Cultural Competence”)
-
TX=(ethnic* OR ethnolog* OR cultur* OR accultur* OR rac* OR minorit* OR transcultur* ORsociocultur*)
-
TX=(cultur* N3 (identity OR cross OR specific OR sensiti* OR relevant OR adapt* OR competen* OR divers*))
-
TX=((ethnic OR racial) N3 (identity OR group* OR minorit* OR difference OR variation OR divers*))
-
OR/5-8
-
(MH “Rehabilitation, Psychosocial+”) OR (MH “Mental Health Services+”) OR (MH “Psychotherapy+”) OR (MH “Behavior Therapy+”)
-
TX= ((psychological OR psychosocial OR psychiat* OR clinical) N5 (intervention OR therap* OR rehabilitation OR treatment OR care))
-
TX=((cognitive OR behav* OR famil* OR systemic OR social* OR education*)N5 (intervention OR therap* OR rehabilitation OR treatment OR training OR skill*))
-
TX=((cognitive OR behav*) N5 (remediat*))
-
TX=((“evidence based” OR “empirically supported”) N5 (intervention OR therap* OR treatment))
-
OR/10-14
-
(MH “Clinical Trials+”) OR (MM “Double-Blind Studies”) OR (MM “Intervention Trials”) OR (MM “Triple-Blind Studies”) OR (MM “Therapeutic Trials”) OR (MM “Single-Blind Studies”) OR (MM “Randomized Controlled Trials”)
-
(MM “Random Assignment”) OR (MM “Control Group”)
-
TX=((controlled OR clinical) N3 (trial))
-
TX=(random* OR control* OR trial OR condition OR assigned OR group)
-
TX= (“intervention study” OR “pilot study” OR “feasibility study”) OR MH “Feasibility Study”
-
OR/16-20
-
4 and 9 and 15 and 21
Appendix 2 Characteristics of studies included in the systematic review of culturally adapted interventions (n = 46)
| Author (year) | Study arms (n) | Sample characteristic | Study setting | Study design | Patient outcome measures (time point) | Attrition: time point, n (%) | Key finding(s) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Adapted intervention(s) | Comparison group(s) | Gender, n (M/F) | Mean age (years) | Diagnosis (diagnostic tool) | Chronicity/duration illness (years) | ||||||
| Bradley et al. (2006)115 | MFGT, 30 | Standard care – enhanced, 29 | Total, 50 (15/35); MFGT, 25 (7/18); CG, 25 (8/17) | MFGT, 33.6; CG, 34 | DSM-IV; outpatient diagnosis schizophrenia by psychiatrist | HAs 12 months pre intervention: MFGT, 0.60; CG, 0.29 | Community mental health programme of the Inner West Mental Health Service Royal Melbourne Hospital and participant home | RCT | BPRS; SANS; HoNOS; QOL (baseline, post intervention); relapse rates (post intervention, 18 months post intervention) | 18 months post intervention: total, 9/59 (15.3); MFGT, 5/30 (16.7); CG, 4/29 (13.8) |
Significant reduction found between baseline and post-intervention BPRS symptom scores for MFGT but no difference for the CG Relapse rates at end and 18 months post intervention were significantly lower for MFGT than for the CG |
| Carrà et al. (2007)90 | IG, 50; IG + SG, 26 | Standard care, 25 | Total, 101 (73/28); IG, 50 (35/15); IG + SG, 26 (22/4); CG, 25 (16/9) | IG, 29.9; IG + SG, 29.6; CG, 29.9 | DSM-IV; schizophrenia case notes screened by RAs | IG, 9.6; IG + SG, 11.3; CG, 10.3 | Family advocacy and support agency, Association for Research on Schizophrenia, Milan | RCT | Treatment compliance; relapse rates, HA rates; GAS; employment rates (baseline, 12 months and 24 months post intervention) | 24 months post intervention: total, 6/101(5.9); IG, 3/50 (6); IG + SG, 2/26 (8); CG, 1/25 (4) | Compliance with standard community care significantly higher at 12 months post intervention in the IG + SG group than in the CG |
| Chan et al. (2009)83 | PE, 36 | Standard care – enhanced, 37 | Total, 73 (48/25); PE, 36 (26/10); CG, 37 (22/15) | PE, 34.2; CG, 36.3 | DSM-IV; outpatient diagnosis schizophrenia by psychiatrist | PE, 10.2; CG, 10.5 | Psychiatric outpatient department of a regional mental health hospital in Hong Kong | Cluster RCT | BPRS; ROMI; ITAQ; SES (baseline, post intervention, 6 months and 12 months post intervention) | No attrition | Significant improvements over time found for the PE group in BPRS, ROMI and ITAQ scores. Significant group differences were found for BPRS at 6 months, ROMI at post intervention and at 6 months post intervention and the ITAQ at 6 and 12 months post intervention |
| Chien (2008)94 | PESG, 34 | Standard care – enhanced, 34 | Total, 68; NR | PESG, 37.3; CG, 28.8 | DSM-IV; schizophrenia diagnosis | 2.5 | Two psychiatric outpatient clinics, Hong Kong | Cluster RCT |
SLOF (baseline, 1 and 12 months post intervention) Number and duration of HAs (6 months pre intervention, over 9-month intervention period, 12 months post intervention) |
12 months post intervention: total, 5/68, (7.4); PESG, 3/34 (8.8); CG, 2/34 (5.9) | PESG showed significant improved level of functioning (SLOF) from baseline to 6 months post intervention when compared with the CG |
| aChien and Chan (2004)80 | MSG, 32; PE, 33 | Standard care – enhanced, 31 | Total, 96 (62/34); MSG, 32 (20/12); PE, 33 (20/13); CG, 31 (22/9) | MSG, 32.3; PE, 29.1; CG, 33.8 | DSM-IV; schizophrenia diagnosis | Just over 2 years (range: 6 months–5 years) | Two psychiatric outpatient clinics, Hong Kong | Cluster RCT |
BPRS; SLOF; (baseline, 1 week and 12 months post intervention) Number and duration of HAs (pre-intervention, over 6-month intervention period, 12 months post intervention) |
12 months post intervention:total, 7/96 (7.3); MSG, 4/32 (12.5); PG, 2/33 (6.1); CG, 1/31 (3.2) | MSG participants reported significant reduction in rehospitalisation compared with the PE group and the CG and greater improvement in all three subscales of SLOF (self-maintenance, social functioning and community living skills) |
| Chien and Chan (2013)98 | MSG, 45; PE, 45 | Standard care – enhanced, 45 | Total, 135 (84/51); MSG, 45 (28/17); PE, 45 (27/18); CG, 45 (29/16) | MSG, 24.3; PE, 25.2; CG, 26.2 | DSM-IV; schizophrenia diagnosis | Majority 1–2 years for all three groups | Two psychiatric outpatient clinics, Hong Kong | Cluster RCT |
BPRS; SLOF (baseline, 1 week, 12 and 24 months post intervention) Number and duration of HAs (9 months pre intervention, 1 week, 12 and 24 months post intervention) |
24 months post intervention: total, 7/135 (5.2); MSG, 2/45 (4.4); PG, 3/45 (6.7); CG, 2/45 (4.4) | At 12 and 24 months post-intervention time points compared with the CG BPRS score decreased significantly and the SLOF score for the MSG group increased significantly. Scores also decreased at 12 and 24 months post intervention when compared with the PE group. The average length of rehospitalisations was significantly lower in the MSG than the CG at all post-intervention time points |
| a Chien et al. (2006) 79 | MSG, 32; PE, 33 | Standard care – enhanced, 31 | Total, 96 (64/32); MSG, 32 (20/12); PE, 33 (22/11); CG, 31 (22/9) | MSG, 27.3; PE, 27.8; CG, 28.8 | DSM-IV; outpatients case note diagnosis schizophrenia | About 2 years (range 6 months–3 years) | Two psychiatric outpatient clinics, Hong Kong | Cluster RCT |
BPRS; SLOF; (baseline, 6 and 18 months post intervention) Number and duration of HAs (6 months pre intervention, 6 and 18 months post intervention) |
18 months post intervention: total, 7/96 (7.3); MSG, 2/32 (6.3); PE, 2/33 (6.1); CG, 3/31 (9.7) | Readmissions to hospital in the MSG group reduced significantly more than the other two groups from baseline to 18 months post intervention. Level of functioning in the MSG group improved significantly from baseline to 18 months post intervention compared with the other two groups. Patient functioning in the PE group also improved over time and significantly more than the CG |
| Chien and Lee (2010) 97 | SCMP, 46 | Standard care – enhanced, 46 | Total, 92; NR | NR | DSM-IV; schizophrenia diagnosis | NR | Three psychiatric outpatient clinics, Hong Kong | RCT |
BPRS; SLOF; (baseline, 1 and 15 months post intervention) Number and duration of HAs (6 months preceding intervention, 1 and 15 months post intervention) |
15 months post intervention: total, 3/92 (3.3); SCMP, 2/46 (4.3); CG, 1/46 (2.2) | There were significant differences between the SCMP group and the CG with patients’ functioning and number and length of rehospitalisations at 1 and 15 months post intervention, although patients’ functioning and number and length of rehospitalisations in the SCMP group only significantly improved at the 15 months post-intervention time point |
| Chien and Lee (2013) 103 | MBPP, 48 | Standard care – enhanced, 48 | Total, 96 (53/43) | 25.8 | DSM-IV; schizophrenia diagnosis | NR | Three psychiatric outpatient clinics, Hong Kong | RCT |
BPRS; SLOF; SSQ; ITAQ (baseline, 3 and 18 months post intervention) Number and duration HAs (6 months preceding intervention, 3 and 18 months post intervention) |
18 months post intervention: total, 6/96 (6.3); MBPP, 3/48 (6.3); CG, 3/48 (6.3) | There were significant differences between the MBPP group and the CG related to patients’ insight into illness, symptom severity, functioning and number and length of rehospitalisation at 3 and 18 months post intervention. MBPP participants’ symptom severity, illness insight and length of rehospitalisation improved significantly at 3 and 18 months post intervention, but functioning and number of rehospitalisation only significantly improved 18 months post intervention |
| Chien et al. (2004)104 | MSG, 24 | Standard care – enhanced, 24 | Total, 48 (27/21); MSG, 24 (14/10); CG, 24 (13/11) | MSG, 39.9; CG, 36.3 | DSM-IV; schizophrenia diagnosis | Approximately 2 years | Two psychiatric outpatient clinics | Cluster RCT | Duration of HAs (3 months preceding intervention, over the 3-month intervention period and 3 months post intervention) | No attrition | In the MSG group there was a significant decrease in the duration of patient rehospitalisation at 3 months post intervention compared with the CG |
| Chien and Thompson (2013) 101 | FPGP, 35 |
CG1 standard care – enhanced, 35; CG2 psychoeducation, 36 |
Total, 106 (66/40); FPGP, 35 (21/14); CG1, 36 (23/13); CG2, 35 (22/13) | FPGP, 26.3; CG1, 28.2; CG2, 27.2 | DSM-IV; schizophrenia diagnosis | 2.5 years (range 6 months–6 years) | Three psychiatric outpatient clinics, Hong Kong | RCT |
BPRS; SLOF; (baseline, 1 week, 18 and 36 months post intervention) Number and duration of HAs (6 months preceding intervention, 1 week, 18 and 36 months post intervention) |
36 months post intervention: total, 12/106 (11.3); FPGP, 4/35 (11.4); CG1, 3/36 (8.3); CG2, 5/35 (14.3) | Functioning improved significantly at 1 week and 18 months post intervention. Rehospitalisation of FPGP patients decreased significantly at the three respective time points in number and duration compared with CG1 and decreased significantly at 1 week and 18 months post intervention when compared with CG2. In the FPGP group there was a significant difference between patients’ SLOF score compared with the PE group and the CG |
| Chien et al. (2008) 84 | MSG, 38 | Standard care – enhanced, 38 | Total, 76 (32/44);MSG, 38 (17/21); CG, 38 (15/23) | MSG, 25.3; CG, 25.6 | DSM-IV; schizophrenia diagnosis | MSG, 2.7; CG, 2.6 | Two psychiatric outpatient clinics, Hong Kong | RCT |
BPRS (baseline, 1 week and 12 months post intervention) Number and duration of HAs (6 months preceding intervention, 1 week and 12 months post intervention) |
No attrition | In the MSG group the duration of patients’ rehospitalisation decreased significantly at 12 months post intervention |
| Chien and Wong (2007) 105 | PE, 42 | Standard care – enhanced, 42 | Total, 84 (51/33) | 28.8 | DSM-IV; schizophrenia diagnosis | 3.6 | Two psychiatric outpatient clinics, Hong Kong | RCT |
BPRS; SLOF; (baseline, 1 week and 12 months post intervention) Number and duration of HAs (6 months preceding intervention, 1 week and 12 months post intervention) |
12 months post intervention: total, 7/84 (8.3); PE, 3/42 (7.1); CG, 4/42 (9.5) | In the PE group number of patients’ rehospitalisation improved significantly at 1 week and 12 months post intervention. However, patients’ functioning and length of rehospitalisation only significantly improved at 12 months post intervention |
| Gohar et al. (2013) 111 | SCST, 22 | Non-adapted SCST | Total, 42 (34/8); SCST, 22 (16/6); CG, 20 (18/2) | SCST, 33.0; CG, 31.0 | DSM-IV SCID I; schizophrenia diagnosis | SCST, 11.8; CG, 8.4 | Outpatient clinic of the psychiatry and addiction hospital of Kasr Al-Ainy hospitals, Cairo university, Egypt | RCT | PANSS; MSCEIT; TMT Part A and Digit Symbol Substitution Test; the Digit Span Task from the Wechsler Memory Scale; the Proteus Maze Task; (baseline, post intervention) | NR – but tables suggest no attrition | SCST showed significant improvements in social cognition compared with the CG. On the MSCEIT, the SCST group showed significant improvements on the total score and branches 1 (emotion perception) and 4 (managing emotions) |
| Guo et al. (2010) 109 | CT, 633 | Medication, 635 | Total, 1268 (698/570); CT, 633 (344/289); CG, 635 (354/281) | CT, 26.1; CG, 26.4 | DSM-IV SCID I; schizophrenia/schizophreniform diagnosis rated by investigators or trained staff; PANSS total score < 60 | CT, 2.1; CG, 2 | Ten clinical sites in China (six university clinics and four province mental health agencies) | RCT |
PANSS; ITAQ; GAS; ADL; SF-36 (baseline, 3 and 6 months post intervention) Rates of treatment discontinuation (assessed every 2 weeks by a RA and monthly by a psychiatrist) |
12 months post intervention: total, 524/1268 (41.3); CT, 227/633 (35.9); CG, 338/635 (46.8) | Risk of relapse and readmission was lower in the CT group. Change in ITAQ scores was greater in the CT group than the CG. GAS and ADL scores were also greater over time for the CT group. the CT group also scored higher on four domains of the SF-36 (role-physical, general health, vitality and role-emotional) |
| Habib et al. (2015) 71 | CaCBTp, 21 | Standard care – medical consultation, 21 | Total, 42 (25/17); CaCBTp, 21(11/10); CG, 21 (14/7) | CaCBTp, 33.5; CG, 30.2 | DSM-IV-TR; inpatient; schizophrenia diagnosis | CaCBTp, 8.8; CG, 8.6 | Psychiatric inpatient clinic, Lahore, Pakistan | RCT | PANSS; PSYRATS; SAI (baseline, post intervention) | NR | CaCBTp group demonstrated significantly greater improvement on PANSS positive, negative and general symptoms and PSYRATS hallucinations, delusions and insight post intervention |
| Koolaee and Etemadi (2009) 91 | BFM, 21; PE, 21 | Standard care – enhanced, 20 | Total, 55 (40/15) | NR | DSM-IV; schizophrenia diagnosis | ≤ 3 years | Psychiatric outpatient clinic in Tehran, Iran | RCT |
BPRS (baseline, 3 and 6 months post intervention) Number and duration of HAS (preceding 3 months, baseline, 3 and 6 months post intervention) |
Post intervention: total, 7/62 (11.3); BFM group, 3/21 (14.3); PE, 2/21 (9.5); CG, 2/20 (10) | PE and BFM groups exhibited significantly greater reduction in positive symptoms at 3 and 6 months post intervention compared with the CG. PE-positive symptoms reduced significantly from baseline to 6 months post intervention when compared with BFM. Hospitalisation data NR |
| Kopelowicz et al. (2003) 99 | ST, 45 | Standard care, 47 | Total, 92 (62/30); ST, 45 (30/15); CG, 47 (32/15) | ST, 37.6; CG, 39.1 | DSM-IV; schizophrenia/schizoaffective diagnosis; one or more episodes of treatment in an inpatient facility, ≥ 1 week duration in previous 12 months | NR | Community mental health centre, Los Angeles, CA, USA | RCT | PANSS; HA rates; ILSS; QOLI; ROMI; MMM + generalisation assessments; SMM + generalisation assessments (baseline, post intervention and 6 months post intervention); medication adherence (monthly) | 6 months post intervention: total, 8/102 (7.8); ST, 6/45 (13.3); CG, 2/47 (4.3) | ST participants showed significantly reduced positive, negative and total symptoms post intervention which were maintained at 6 months post intervention. In the ST group there was also a significant main effect on skill acquisition for medication and symptom management skills. The ST group showed significantly improved level of functioning compared with the CG at post intervention. There was also significantly lower rehospitalisation rates in the ST group from baseline to follow-up compared with the CG |
| Kopelowicz et al. (2012) 117 | MFG-A, 64; MFG-S, 54 | Standard care, 60 | Total, 174 (114/60); MFG-A, 64 (43/21); MFG-S, 53 (36/17); CG, 57 (35/22) | MFG-A, 32.6; MFG-S, 29.6; CG, 32.8 | DSM-IV structured clinical interview; schizophrenia/schizoaffective diagnosis | NR | Two community mental health centres, Los Angeles, CA, USA | RCT |
BPRS (baseline, post intervention and 12 months post intervention); medication compliance (baseline, 4 and 8 months post baseline, post intervention, 6 and 12 months post intervention) HA rates (4 and 8 months post baseline, post intervention, 6 and 12 months post intervention) |
12 months post intervention: total, 33/178 (18.4); MFG-A, 10/64 (15.6); MFG-S, 13/54 (24.1); CG, 10/60 (16.7) | At post intervention, the MFG-A group demonstrated significantly higher medication adherence than the MFG-S group or the CG. The MFG-A participants had a longer time to first hospitalisation and were less likely to be hospitalised than those in the MFG-S group and the CG |
| Kulhara et al. (2009) 86 | PE, 38 | Standard care – enhanced, 38 | Total, 76 (42/34); PE, 38 (17/21); CG, 38 (25/13) | PE, 31.1; CG, 31.6 | DSM-IV; structured interview; schizophrenia diagnosis | PE, 4.7; CG, 5.1 | Department of psychiatry of a tertiary care hospital in North India | RCT |
PANSS; WHODAS (baseline, 1, 2, 3, 4, 5, 6 and 7 months post baseline; post intervention) Relapse (over the 9-month intervention period) |
Post intervention: total, 33/76 (43.4); PE, 15/38 (39.5); CG, 18/38 (47.4) | There was a significantly greater decline in monthly PANSS scores in the PE group on all three subscales in comparison with the CG. The only patient outcome showing a significant difference from baseline to post intervention was disability level, with the PE, group showing significantly lower levels of disability at post intervention than the CG |
| Kumar et al. (2010) 112 | HMCT, 8 | Standard care, 8 | Total, 16/0; HMCT, 8/0; CG, 8/0 | HMCT, 31.5; CG, 34.1 | ICD-10; patient diagnosis paranoid schizophrenia | HMCT, 7.6; CG, 6.5 | Inpatient hospital, central institute of psychiatry, Ranchi, India | RCT | PANSS (baseline, 2 week post baseline, post intervention) | NR | The HMCT group demonstrated a significantly greater reduction in positive symptoms post intervention compared with the CG |
| Kung et al. (2012)85 | FP, 9 | ‘Comparison group’ no details | Total, 12; FP, 9; CG, 3 | MFPG, 34.2; CG, 50.6 | ‘Schizophrenic form of disorder’ | NR | Psychiatric outpatient clinics | Non-RCT | BPRS; SANS; SLOF; WQOL (baseline, 3 months post baseline, post intervention, 3 months post intervention) | No attrition | In the MFPG group, BPRS and SANS scores showed significant improvement at post intervention and 3 months post intervention. The SLOF score was in the opposite direction than expected but consistent with the previous within group scores recorded at baseline, post-intervention and 3 months post-intervention |
| Lak et al. (2010) 106 | CBCSM + SGT, 35; CBCSM, 35 | ‘Placebo’ education and rehabilitation programme, 36 | Total, 106 (53/53); CBCSM + SGT, 35 (18/17); CBCSM, 35 (17/18); CG, 36 (18/18) | CBCSM + SGT, 38.3; CBCSM, 44.5; CG, 43.2 | ICD-10; schizophrenia diagnosis, free-from positive symptoms as indicated by BPRS score > 72 | CBCSM + SGT, 15.6; CBCSM, 18.3; CG, 18.9 | NR | RCT | BPRS; GAF; VSSS; ASSEI; PWI (baseline, post intervention, 3 and 6 months post intervention) | 6 months post intervention: total, 10/106 (9.4); CBCSM + SGT, 4/35 (11.4); CBCSM, 6/35 (17.1); CG, 0/36 (0) | Post intervention, the CBCSM + SGT group and the CBCSM group scored significantly higher than the CG in social skills. At 6 months post intervention, social skills of the CBCSM + SGT group were better than the CBCSM group and the CG |
| Li and Arthur (2005) 96 | FE, 46 | Standard care, 55 | Total, 101 (43/58); FE, 46 (18/28); CG, 55 (25/30) | NR | CCMD-II-R; inpatient diagnosis schizophrenia | NR | Non-acute inpatient hospital, Beijing, China | Cluster RCT | BPRS; GAS; KASI; NOSIE; relapse rates; medication compliance (baseline, post intervention, 3 and 9 months post intervention) | 9 months post intervention: total, 12/101 (11.9); FE, 3/46 (6.5); CG, 9/55 (16.4) | FE group showed significantly greater improvements in symptom severity, knowledge and overall functioning at 9 months post intervention compared with the CG |
| Li et al. (2015) 107 | CBT, 96 | Supportive therapy (TE), 96 | Total, 192 (72/120); CBT, 96 (32/64); CG, 96 (40/56) | CBT, 29.3; CG, 33.4 | SCID; DSM-IV; Axis I schizophrenia by research psychiatrists | CBT, 7.6; CG, 8.8 | Three specialised psychiatric hospitals, Beijing | Cluster RCT | PANSS; SAI; PSP (baseline, 12, 24, 36, 60 and 84 weeks post baseline) | 84 weeks post baseline: total, 25/192 (14.6); CBT, 11/96 (11.5); CG, 14/96 (14.6) | Both groups had a significant decrease in all PANSS symptoms, SAI insight and PSP social functioning post intervention (24 weeks), which were maintained up to 84 weeks post baseline. Compared with the CG, CBT showed significantly greater reductions in PANSS total and positive symptoms and PSP functioning scores from 36 weeks post baseline |
| Lin et al. (2013) 88 | IMR, 48 | Standard care, 49 | Total, 97 (62/35); IMR, 48 (30/18); CG, 49 (32/17) | IMR, 35.3; CG, 35.2 | DSM-IV; schizophrenia/schizoaffective diagnosis | IMR, 11.8; CG, 11.2 | Acute inpatient ward in two hospitals in Taiwan | RCT | BPRS; KI; DAI-30; SAI-E (baseline, post intervention and 1 month post intervention) | 1 month post intervention: total, 14/97 (14.4); IMR, 4/48 (8.3); CG, 10/49 (20.4) | The IMR group showed significantly greater improvements at post intervention and 1 month post intervention than the CG in BPRS negative symptoms, insight, illness management knowledge and attitudes towards medication |
| Lin et al. (2013)116 | IMR, 26 | N/A | Total: IMR, 26 (18/8) | 36.38 | DSM-IV; schizophrenia/schizoaffective diagnosis | NR | Six psychiatric acute wards at a psychiatric hospital in the department of psychiatry, Taiwan | Non-RCT | BPRS; KFI; DAI-30; SAI-E (baseline, post intervention) | NR | Participants improved in each psychopathology domain post intervention; however, only the change in the affective domain was significant |
| Mann and Chong (2004)113 | SCP, 25 | Education programme, 25 | Total, 50 (38/12) | 44.4 | DSM-IV; schizophrenia diagnosis with active positive psychotic symptoms ≥ 1 year assessed by psychiatrist | Average length of stay in hospital: 26.2 months (range 12–68 months) | Inpatient psychiatric hospital, Hong Kong | RCT | PANSS; LSP (baseline, post intervention and 1 month post intervention) | NR | Post-intervention, there was a significant improvement in PANSS scores for SCP and CG. However, this returned back to baseline level at 1 month post intervention |
| bMausbach et al. (2008)81 | PEDAL, 21 | CG1 FAST (non-adapted PEDAL), 15; CG2 support group (TE), 23 | Total, 59 (35/24); PEDAL, 21 (11/10); CG1, 15 (10/5); CG2, 23 (14/9) | PEDAL, 50.7; CG1, 47.4; CG2, 47.3 | DSM-IV; diagnosis of schizophrenia, schizoaffective or psychotic mood disorder | PEDAL, 23.5; CG1, 24.5; CG2, 23.8 | Board and care facilities, San Diego country and mental health clinics near the USA–Mexico border | Block RCT | PANSS; UPSA; SSPA; MMAA; QWB (baseline, post intervention) | Post intervention: total, 10/59 (16.9); PEDAL, 3/21 (14.3); CG1, 2/15 (13.3); CG2, 5/23 (21.7) | PEDAL group showed a significant improvement on the UPSA compared with those in CG1 and CG2. The PEDAL group had significantly higher SSPA scores at post intervention compared with CG1, but not CG2. The PEDAL group also made significantly fewer medication errors at post intervention than CG2 |
| Naeem et al. (2015) 92 | CaCBTp, 59 | Standard care, 57 | Total, 116 (70/46); CaCBTp, 57 (39/18); CG, 59 (31/28) | CaCBTp, 31.7; CG, 31.1 | ICD-10 RDC; diagnosis of schizophrenia or related disorder | CaCBTp, 4.7; CG, 5.8 | Psychiatric outpatient clinics, Karachi, Pakistan | RCT | PANSS; PSYRATS; SAI (baseline, post intervention) | Post intervention: total, 14/116 (12.1); CaCBT, 6/59 (10.1); CG, 8/57 (14) | At post intervention the CaCBTp group showed significantly greater improvements compared with the CG, in PANSS positive and negative symptoms and general psychopathology, PSYRATS delusions and hallucinations and insight |
| b Patterson et al. (2005) 82 | PEDAL, 21 | Support group, (TE) 8 | Total, 29 (14/15); PEDAL, 21 (11/10); CG, 8 (3/5) | PEDAL, 46.8; CG, 57.3 | DSM-IV; case note diagnosis of schizophrenia/schizoaffective disorder | Age of illness onset (years): PEDAL, 28.3; SG, 43.5 | Psychiatric clinics, San Diego, CA, USA | Cluster RCT | PANSS; UPSA; MMAA; SSPA; QWB (baseline, post intervention, 6 and 12 months post intervention) | 12 months post intervention: total, 5/21 (23.8); PEDAL, 5/21 (23.8); CG, no attrition | At 6 months post intervention the PEDAL had a significantly greater UPSA score than the CG. However, no significant differences were found between the groups at 6 and 12 months post intervention. At 12 months post intervention, the PEDAL group performed significantly better than the CG. The CG also had significantly lower PANSS ratings than the PEDAL group at 12 months post intervention |
| Ran et al. (2003)100 | FIG, 132 | CG1 medication treatment, 110; CG2 no intervention, 115 | Total, 326 (128/198); FIG, 126 (44/82); CG1, 103 (48/55); CG2, 97 (36/61) | FIG, 43.5; CG1, 42.4; CG2, 44.8 | ICD-10 and CCMD-II-R schizophrenia diagnosis | FIG, 11.6; CG1, 10.6; CG2, 12.3 | NR | Cluster RCT | PSE; GPISS; SDSS; medication compliance; relapse rate (baseline, post intervention) | Post intervention: total, 22/326 (6.7); FIG, 1/127 (0.8): CG1, 2/105 (1.9); CG2, 18/115 (15.7) | At post intervention, FIG treatment compliance was significantly higher than that in CG1 and CG2. There was no significant difference of clinical outcomes between FIG group and CG1, whereas the percentage of full recovery and significant improvement in FIG and CG1 was significantly higher than that in CG2. The relapse rate in FIG was significantly lower than CG1 |
| Razali et al. (2000)93 | CMFT, 80 | BFT, 86 | NR | NR | DSM-IV; diagnosis schizophrenia | CMFT, 13.7; CG, 14.2 | Outpatient hospital, University Hospital (USM) Kota Bharu, West Malaysia | RCT | BPRS; GAF; SBS; relapse rates; HA rates; medication compliance (baseline, 6 and 12 months post baseline) | 6 and 12 months post baseline: total, 23/166 (13.9); CMFT, 6/80 (7.5); CG, 17/86 (19.8) | At 12 months post baseline the CMFT group showed significant improvements in all variables compared with the CG |
| Shin and Lukens (2002) 118 | PE, 24 | Supportive therapy (TE), 24 | Total, 48 (20/28); PE, 24 (7/17); CG, 24 (13/11) | PE, 39.5; CG, 34.7 | DSM-IV; diagnosis of schizophrenia, schizoaffective, or schizophreniform disorder rated by psychiatrist |
Number of hospitalisations: PE, 2.7; CG, 1.2 Time since last hospitalisation (months): PE, 7.2; CG, 12.7 |
Outpatient mental health clinic, Queens, New York, NY | RCT | BPRS; SDS (baseline, post intervention) | NR (tables suggest no attrition) | At post intervention, the PE, group demonstrated significantly reduced symptom severity and perception of stigma in comparison with the CG |
| So et al. (2015) 110 | MCTd, 23 | Standard care – medication consultations, 21 | Total, 44 (24/20); MCTd, 23 (12/11); CG, 21 (12/9) | MCTd, 32.4; CG, 35.6 | Case note diagnosis schizophrenia, four or more PANSS delusions items | Number of hospitalisations: MCTd, 1.6; CG, 0.9 | Outpatient clinic, Hong Kong | RCT | PANSS; PSYRATS (baseline, post intervention and 1 month post intervention); WAIS (baseline or pre intervention only) | 1 month post intervention: total, 18/44 (40.9) MCTd, 10/23 (43.5); CG, 8/21 (38.1) | At post intervention there was a large effect size of improvement for the MCTd group’s PANSS positive scores, PANSS delusions score, PSYRATS delusions and PSYRATS delusional conviction |
| Valencia et al. (2007) 120 | PSST, 49 | Standard care – medication consultations, 49 | Total, 82 (64/18); PSST, 43 (31/12); CG, 39 (33/6) | PSST, 29.7; CG, 30.1 | DSM-IV and CIDI schizophrenia diagnosis with clinically stable psychotic symptoms (≥ 60 PANSS score) | Age of illness onset (years): PSST, 21.3; CG, 21.2 | Psychiatric outpatient hospital, Mexico | RCT | PANSS; PSFS; GAF (baseline, post intervention); relapse rates; HA rates; medication compliance; therapeutic adherence (over 12-month intervention period) | Post intervention: total ,16/98 (16.3) PSST, 6/49 (12.2); CG, 10/49 (20.4) | At post intervention, the PSST group showed significantly improved symptomatology scores on total score, positive and negative symptoms and GPS compared with the CG with large effect sizes for both groups. Significant improvements were also observed in the PSST group for all areas of psychosocial functioning and in the GPFS compared with the CG, and also with global functioning. During the intervention the PSST group had a significantly higher level of compliance with medication, therapeutic adherence and a significantly lower relapse rate than the CG |
| Valencia et al. (2010) 119 | PSST, 54 | Standard care – medication consultations, 53 | Total, 83 (60/23); PSST, 47 (34/13); CG, 36 (26/10) | PSST, 29.9; CG, 29.5 | DSM-IV and CIDI schizophrenia diagnosis | Age of illness onset (years) PSST, 22.4; CG, 21.1 | National institute of psychiatry outpatient clinic, Mexico City | RCT | PANSS; GAF (baseline, post intervention); relapse rates; HA rates; adherence to medication (over 12-month intervention period) | Post intervention: total, 24/108 (22.2); PSST, 7/54 (13); CG, 17/54 (31.5) | At post intervention, the PSST group exhibited significantly improved symptomatology, adherence to medication, attendance at appointments, social functioning, relapse and rehospitalisation rates |
| Wahass and Kent (1997)76 | MPI, 3 | Standard care – medication consultation, 3 | Total, 6 (6/0); MPI, 3 (3/0); CG, 3 (3/0) | MPI, 31.3; CG, 34.0 | ICD-10; schizophrenia diagnosis | Experiencing persistent auditory hallucinations for at least 4 years | NR | RCT | SAHI; 10-cm VAS to measure hallucination severity; two VAS to measure anxiety and depression in response to voices (baseline, post intervention, 3 months post intervention) | NR – tables suggest no attrition | Symptom ratings improved for two participants in the MPI group, but there were no changes in the third participant. The third patient also reported that the loudness of his voices increased over time |
| Wang et al. (2013)102 | SCIT, 22 | Standard care – medication consultations, 17 | Total, 39 (20/19); SCIT, 22 (12/10); CG, 17 (8/9) | SCIT, 43.9; CG, 40.9 | DSM-IV; schizophrenia diagnosis | NR | NR | RCT | PANSS; WAIS; PSP; FEIT; computerised version of the Eyes Task; Attributional Style Questionnaire (baseline, 6 months post intervention) | 6 months post intervention: total, 4/43 (9.3); SCIT, 0/22 (0); CG, 4/21 (19) | The SCIT group showed a significant improvement in emotion perception, theory of mind, attributional style and social functioning compared with the CG |
| Weng et al. (2005)108 | MRP, 62 | Standard care – enhanced, 62 | Total, 124; MRP, NR; CG, NR | NR | DSM-III-R; schizophrenia diagnosis | NR | Anding psychiatric hospital inpatient ward, Beijing | RCT | BPRS; NOSIE; SDSS; relapse and HA rates (every 2 weeks during intervention, monthly post intervention up to 12 months post intervention) | 12 months post intervention: total, 2/124 (1.6); MRP, 1/62 (1.61); CG, 1/62 (1.61) | BPRS, NOSIE, SDSS relapse and rehospitalisation rates improved significantly in the MRP group from baseline to post intervention and from post intervention to 12 months post intervention |
| Xiang et al. (1994)114 | PFI, 36 | Medication treatment, 41 | Total, 77; PFI, 36; CG, 41 | PFI, 40.5; CG, 41.2 | Schizophrenia and affective psychoses | 15.3 | Three rural townships of Xinjin county, China | RCT | PSE; SDSS; medication compliance rates (baseline, post intervention) | NR | Medication compliance was significantly higher in the PFI group than in the CG post intervention. In addition, the total rate of improvement in clinical state and level of social functioning was significantly higher in the PFI group than in the CG post intervention |
| Xiong et al. (1994)89 | FIG, 34 | Standard care – medication treatment, 29 | Total, 63 (43/20) | 31 | DSM-III-R; schizophrenia assessed on admission | 7.5 | Psychiatric outpatient clinic and home visits | RCT | BPRS; SAPS; SANS; GAF; SDSS; number and duration of HAs; relapse rates; medication compliance (baseline, 6, 12 and 18 months post intervention) | 18 months post intervention: total, 4/63 (6.3); FIG, 2/34 (5.9); CG, 2/29 (6.9) | Duration of rehospitalisation significantly shorter for FIG group at 12 and 18 months, and fewer relapsed at 12 months than the CG. BPRS, GAF and SDSS scores at 12 months and SAPS, BPRS, GAF and SDSS scores at 18 months showed significantly greater improvements in FIG group |
| cZhang and Heqin (1993)77 | FE, 2076 | Standard care, 1016 | Total, 3082 (1821/1261); FE, 2076 (1239/837); CG, 1016 (582/424) | FE, 40.3; CG, 40.8 | CCMD-II; schizophrenia diagnosis | FE, 15.1; CG, 15.5 | NR | Cluster RCT | Study-specific questionnaire; symptoms, recovery, relapse and duration of hospitalisation; WHO-DAS (baseline, 6 and 12 months post intervention) | NR | At post intervention, participants in the FE group showed a higher rate of recovery or stabilisation of condition; a greater reduction in exacerbation of both positive and negative symptoms, relapse rates, number institutionalised, duration of hospitalisation, plus total and factor score on the WHO-DAS |
| Zhang et al. (1994) 87 | FIG, 42 | Standard care, 41 | NR | FIG, 23.5; CG, 24.1 | Chinese Medical Association (1985): first admission patients with a diagnosis of schizophrenia | NR | Psychiatric outpatient clinic and family home | RCT | BPRS; GAS; HA rates (baseline; post intervention; 3, 6, 9, 12, 15 and 18 months post intervention) | 18 months post intervention: total, 5/83 (6); FIG, 3/42 (7.1); CG, 2/41 (4.9) | At 18 months post intervention, participants in the FIG group who were not readmitted had less severe psychiatric functioning and higher overall functioning compared with members of the CG who were not readmitted. The proportion of patients who were readmitted to hospital was significantly greater among those in the CG in comparison with participants who received the FIG |
| cZhang et al. (1998)78 | FE, 682 | Standard care, 355 | Total, 1037 (642/395); FE, 682 (420/262); CG, 355 (222/133) | FE, 38.3; CG, 39.0 | CCMD-2; schizophrenia diagnosis | FE, 7.3; CG, 7.7 | NR | Cluster RCT | Study-specific questionnaire to assess severity of the illness and symptoms, relapse, duration of HAs; WHO-DAS (baseline, 6, 12 and 24 months post baseline) | 24 months post baseline: total, 236/1284 (18.4); FE, 169/851 (19.9); CG, 67/433 (15.5) | At 24 months post baseline, those in the FE group showed a higher rate of recovery and stabilisation of the condition; a lower rate of exacerbation of symptoms and a reduction in annual relapse rates and annual times institutionalised in comparison with the CG |
| Zimmer et al. (2007)95 | IPT, 23 | Standard care – medication consultation, 43 | Total, 56 (42/14); IPT, 20 (17/3); CG, 36 (25/11) | IPT, 36.1; CG, 39.3 | ‘Schizophrenia outpatient database’ | IPT, 15.3; CG, 17.1 | Schizophrenia outpatient programme of the Hospital de Clínicas de Porto Alegre | RCT | MMSE; GAF; SOFAS; WHOQOL-BREF; SAS (baseline, post intervention) | Total, 4/56 (7.1); NR by group | At post intervention, the IPT group demonstrated significantly improved scores on cognition in the domains of spatiotemporal orientation, memory, social adjustment, leisure/social life, family relations, overall functioning, social occupational functioning and quality of life in the psychological domain |
Appendix 3 Characteristics of interventions included in the systematic review of culturally adapted psychosocial interventions for psychosis
| Author (year) | Target population | Intervention model | Intervention delivery | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | Adapted for (minority/majority) | Subculture | Adapted from (western model/theory) | Intervention type | Intervention attendees | Modality (individual/group) | Number of sessions, frequency and duration | Duration of intervention | Therapy setting | Therapist training | |
| Bradley et al. (2006)115 | Australia | Minority | Vietnamese | Multiple family psychoeducational group treatment manual218 | FI (MFGT) | Caregivers and patients | Group | 26 sessions, every 2 weeks | 12 months | Clinical + community | Primary therapists and support facilitators. Training initially provided by a 3-day national workshop conducted by William McFarlane |
| Carrà et al. (2007)90 | Italy | Majority | Italian | Psychoeducational multifamily groups219 | FI (IG; IG + SG) | Caregivers | Group |
IG: 24-weekly meetings (1.75 hours’ duration) SG: 48-weekly sessions (1.5 hours’ duration) |
24 months | Community | Two specifically trained psychiatrists not involved in patients’ community standard care |
| Chan et al. (2009)83 | China | Majority | Chinese | Care management in early psychosis handbook220 | FI (PE) | Family caregivers and patients | Group | 10-weekly sessions | 3 months | Clinical | A mental health nurse with > 15 years of working experience in community mental health setting |
| Chien (2008)94 | China | Majority | Chinese |
Psychoeducation: family psychoeducational support groups221 Mutual support: support groups theory and practice;222 and how to work with self-help group guidelines223 |
FI (PESG) | Primary caregiver, patient and other family members | Group | 18 sessions (2 hours’ duration) | 9 months | Clinical | Research psychiatric nurse, psychiatrist, research nurse, clinical psychologist and nurse researcher |
| aChien and Chan (2004)80 | China | Majority | Chinese |
Psychoeducation: multiple family groups and psychoeducation224 Mutual support: FI for Asian-Americans225 |
FI (MSG; PE) | Family caregivers and patients | Group |
MSG: 12 sessions every 2 weeks (2 hours’ duration) PE: 12 sessions bi-weekly (2 hours’ duration) |
6 months | Clinical | MSG: peer leader trained by researchers; PE: two psychiatric nurses experienced in psychiatric rehabilitation programmes |
| aChien and Chan (2013)98 | China | Majority | Chinese |
Psychoeducation: multiple-family groups and psychoeducation224 Mutual support: FI for Asian-Americans225 |
FI (MSG; PE) | Family caregivers and patients | Group | MSG; PE: 14 sessions, every 2–3 weeks (2 hours’ duration) | 9 months | Clinical |
MSG: a peer leader trained by researchers PE: psychiatric nurse experienced in psychoeducation and group therapy or guest speakers (i.e. mental health professionals) |
| aChien et al. (2006)79 | China | Majority | Chinese |
Psychoeducation: practitioner’s guide to psychoeducation and management226 Mutual support: support groups theory and practise222 FI for Asian-Americans225 |
FI (MSG; PE) |
MSG: family caregivers PE: family caregivers and patients |
Group | MSG; PE:12 bi-weekly sessions (2 hours’ duration) | 6 months | Clinical |
MSG: family carer assisted by a group facilitator (a trained psychiatric nurse) PE: two trained psychiatric nurses |
| Chien and Lee (2010)97 | China | Majority | Chinese | Multifamily groups219 | FI (SCMP) | Family caregivers and patients | Individual | 14 sessions, every 2 weeks (2 hours’ duration) | 7 months | Clinical | A case manager who received 3 days of formal training from the researchers |
| Chien and Lee (2013)103 | China | Majority | Chinese |
Meditation-based stress reduction programme227 Practice guidelines228 |
Psychoeducation – mindfulness based (MBPP) | Patients | Group | 12 sessions bi-weekly (2 hours’ duration) | 4 months | Clinical | NR |
| aChien et al. (2004)104 | China | Majority | Chinese | Support group intervention studies for family caregivers,222,229,230 with the phased development reflecting accepted good practice231 (Wilson, 1995223) | FI (MSG) | Family caregivers and patients | Group | 12-weekly sessions (2 hours’ duration) | 3 months | Clinical | The principal researcher, an experienced psychiatric nurse and group worker and a peer leader, elected by the group participants |
| Chien and Thompson (2013)101 | China | Majority | Chinese | Modified from author’s previous work79,80,84 | FI (FPGP) | Family caregivers and patients | Group | 14 sessions every 2–3 weeks (2 hours’ duration) | 9 months | Clinical | Trained research nurse |
| aChien et al. (2008)84 | China | Majority | Chinese | Support groups theory and practice (Galinsky and Schopler, 1995);222 how to work with self-help group guidelines (Wilson, 1995223) | FI (MSG) | Family caregivers and patients | Group | 12 sessions (2 hours’ duration) | 6 months | Clinical | Two family carers. One researcher who was a registered psychiatric nurse and an experienced group worker, acted as a participant and resource person for the group |
| Chien and Wong (2007)105 | China | Majority | Chinese | Multifamily groups219 | FI (FPGP) | Family caregivers and patients | Group | 18 sessions every 2 weeks (2 hours’ duration) | 9 months | Clinical | Psychiatric nurse trained in a 3-day workshop that was held by a family therapist and the researchers |
| Gohar et al. (2013)111 | Egypt | Majority | Egyptian | Social cognitive skills training232 | Social cognitive skills training (SCST) | Patients | Group | 16 sessions, twice per week (1 hour of duration, separated by a break) | 2 months | Clinical | Group leader (first author) who received in-person, supervised training from the developers of SCST in the USA |
| Guo et al. (2010)109 | China | Majority | Chinese | The schizophrenia patient outcomes research team manual233 | Combined intervention – family (CT) | Family caregivers and patients | Group | 48 sessions, once per month. Four group treatments on the same day (1 hour of duration) | 12 months | Clinical | Therapists, MD or PhD qualified with clinical experience |
| aHabib et al. (2015)71 | Pakistan | Majority | Pakistani | CBT manual234 | Cognitive – family (CaCBTp) | Patients and family members | Individual | 16 sessions, once or twice per week (approximately 1 hour of duration) | 4–6 months | Clinical | The first author, a psychologist with a post-graduate diploma and training in CBTp |
| Koolaee and Etemadi (2009)91 | Iran | Majority | Iranian |
Psychoeducation guidelines235 (Anderson et al. , 1986)226 BFM group intervention adapted from communication and problem-solving skills training236 |
FI (BFM; PE) | Mothers of the patients | Group | BFM; PE: 12 sessions, once per week (2 hours’ duration) | 3 months | Clinical | A researcher |
| Kopelowicz et al. (2003)99 | USA | Minority | Mexican-American, other Central American and Caribbean | SST237,238 | Skills training – family (ST) | Family members and patients | Group | Four sessions per week (1.5 hours’ duration) | 3 months | Community (CMHC) | Trainers (whose disciplines included nursing, psychology and social work) |
| Kopelowicz et al. (2012)117 | USA | Minority | Mexican-American |
Multifamily groups219 Theory of planned behaviour239 |
FI (MFG-S; MFG-A) | Family members and patients | Group | Two sessions per month (1.5 hours’ duration) | 12 months | Community (CMHC) | Bilingual/bicultural clinicians. psychiatrists, psychologists, or social workers with 1 year of experience conducting family groups and trained in the standard MFG and the MFG-A manual |
| Kulhara et al. (2009)86 | India | Majority | Indian | Family psychoeducational interventions (e.g. Leff 2000240) | FI (PE) | Caregivers | Group | One session per month (40–60 minutes’ duration) | 9 months | Clinical | Two mental health professionals trained for 2 months by consultant psychiatrists, by didactic lectures and ‘hands-on’ experience with patients and their families |
| Kumar et al. (2010)112 | India | Majority | Indian | Metacognitive training manual241 | Cognitive (HMCT) | Patients | Group | Two sessions per week (45–60 minutes’ duration) | 1 month | Clinical | NR |
| bKung et al. (2012)85 | USA | Minority | Chinese |
Family psychoeducation model (Anderson et al. , 1986)226 Problem-solving multifamily group (McFarlane, 2002)242 |
FI (MFPG) | Caregivers | Group | 12 sessions once every 2 weeks (2 hours’ duration) | 6 months | Clinical | One agency employer with a master’s degree in counselling psychology and 4 years of full-time clinical experience and the PI and first author, with a master’s and a doctorate in social work and 9 years of full-time clinical experience |
| Lak et al. (2010)106 | China | Majority | Chinese | UCLA social and independent living skills: basic conversation skills module243 | Skills training (CBCSM; CBCSM + SGT) | Patients | Group | 15 sessions, three per week (1 hour of duration) | 5 weeks | NR | Trainer who followed the instructions and guidelines of the trainer’s manual |
| Li and Arthur (2005)96 | China | Majority | Chinese | Family psychoeducational interventions (e.g. Anderson et al. 1986;226 Falloon, 1984;244 Leff, 1985;245 Goldstein et al., 1986;246 and Barrowclough and Tarrier, 199234) | FI (FE) | Patient and family | Individual | 8 hours with the patient and 36 hours with the family; 2 hours per month for 3 months for patient and family together | NR | Clinical | First author, a nurse with experience in FI and experienced registered nurse RAs educated to diploma or degree level |
| Li et al. (2015)107 | China | Majority | Chinese | Cognitive therapy234 | Cognitive (CBT) | Patients | Individual | 12 sessions in first 12 weeks, three booster sessions in subsequent 12 weeks (40–50 minutes’ duration) | 6 months | Clinical | Six experienced therapists (psychiatrists or psychologists) experienced using psychotherapy; trained in the application of cognitive therapy for psychosis and experienced in the application of CBT for psychosis using a translated Kingdon and Turkington234 manual |
| bLin et al. (2013)88 | Taiwan | Majority | Taiwanese | The US substance abuse and mental health administration’s evidence-based IMR programme | IMR programme | Patients | Group | Six sessions twice per week (1.5 hours’ duration) | 3 weeks | Clinical | The first author, an assistant professor and affiliated head nurse |
| aLin et al. (2013)116 | Taiwan | Majority | Taiwanese | IMR implementation resource kit247 | IMR programme | Patients | Group | Two sessions per week (1.5 hours’ duration) | 3 weeks | Clinical | A clinician |
| Mann and Chong (2004)113 | China | Majority | Chinese | Delusional verbalisation;248 CBT;249 thought stopping;250 and attentional control251 | Combined intervention (SCP) | Patients | Group | Six sessions | NR | Clinical | NR |
| aMausbach et al. (2008)81 | USA | Minority | Latino | Social cognitive theory252 | Social cognitive skills training (PEDAL) | Patients | Group | Sessions once per week (approximately 2 hours’ duration) | 6 months | Community – board and care facilities | NR |
| aNaeem et al. (2015)92 | Pakistan | Majority | Pakistani | CBT manual234 | Cognitive – family (CaCBTp) | Family members and patients | Individual | Six sessions for the patient (plus their carer who acted as a co-therapist), plus one session for the whole family | Approximately 4 months | Clinical | Three experienced psychology graduates trained by the first author |
| aPatterson et al. (2005)82 | USA | Minority | Latino | Social cognitive theory252 | Social cognitive skills training (PEDAL) | Patients | Group | 24 semi-weekly, sessions (2 hours’ duration) | 6 months | Clinical | Bilingual/bicultural group leader (with a masters- or doctorate- level degree) |
| Ran et al. (2003)100 | China | Majority | Chinese | The psychoeducational family approach (Anderson et al. 1986)226 and the vulnerability–stress model253 | FI (FIG) | Family and patients ‘encouraged’ to attend | Individual and group. Family education: once per month. Multiple family workshops: once every 3 months | Sessions once per month (approximately 1.5–3 hours’ duration) | 9 months | Community | Trained psychiatrists and village doctors. Village doctors did not get the same training as psychiatrists, but assisted with the interventions |
| Razali et al. (2000)93 | Malaysia | Majority | Malaysian | Behavioural family therapy244 | FI (CMFT) | Family members and patients | Individual | 30- to 45-minute sessions. Two additional home visits every 6 months | 12 months | Clinical and community (outpatient hospital and two additional home visits) | Experienced research psychiatrist/first author with specialised training |
| Shin and Lukens (2002)118 | USA | Minority | Korean-American | Psychoeducation and family therapy studies (Anderson et al., 1986;226 McFarlane et al., 1995;224 Bernheim and Lehman, 1985;254 Lukens and Thorning, 1998;255 and Falloon et al., 1984)244 | FI (CSPE) | Patients and family members (were offered parallel sessions) | Group | 10 sessions, once per week (90 minutes’ duration) | 10 weeks | NR | First author, a Korean-speaking psychiatric social worker |
| So et al. (2015)110 | China | Majority | Chinese | Metacognitive training241 | Cognitive (MCTd) | Patients | Group | Four sessions, once per week (1 hour of duration) | 1 month | NR | A clinical psychologist who specialises in psychosis and received metacognitive training from the original authors of metacognitive training |
| aValencia et al. (2007)120 | Mexico | Majority | Mexican | Psychosocial treatments;237 social and instrumental skills modules256 | Skills training and FI (PSST) | Patients and family members | Group | 48 sessions (time limit of 1 hour 15 minutes per week) | 12 months | NR | Two psychologists (postgraduates in clinical psychology) |
| aValencia et al. (2010)119 | Mexico | Majority | Mexican | Psychosocial treatments237 (Liberman 2008)257 | Skills training and FI (PSST) | Patients and family members | Group | 40 sessions (1 hour 30 minutes’ duration) | 12 months | Clinical | Two clinical psychologists at the master s and doctorate levels |
| Wahass and Kent (1997)76 | Saudi Arabia | Majority | Saudi Arabian | Coping strategy enhancement (e.g. Barrowclough and Tarrier, 199234); focusing strategy (e.g. Bentall and Slade, 1996258); distraction techniques (e.g. Nelson et al., 1991259) | Combined intervention (MPI) | Patients | Individual | Maximum of 25 sessions, three times per week (1 hour of duration) | 9 weeks | NR | A therapist who has attended several courses and workshops organised in the UK |
| Wang et al. (2013)102 | China | Majority | Chinese | Social cognition and interaction training manual260 | Social cognitive skills training (SCIT) | Patients | Group | 20 sessions, once per week | 20 weeks | NR | Six qualified psychiatric counsellors who had been trained by one of the SCITs developers (DR) |
| Weng et al. (2005)108 | China | Majority | Chinese | SST for psychiatric patients261 | Skills training (MRP) | Patients and key family members (for some sessions) | Group | NR | 2 months | Clinical | NR |
| Xiang et al. (1994)114 | China | Majority | Chinese | FIs (e.g. Brown et al, 1972;262 Leff et al., 1985;245 and Falloon et al. 1987263) | FI (PFI) | Family members | Group | NR | 4 months | Community | Village doctors |
| Xiong et al. (1994)89 | China | Majority | Chinese | Educational approaches;264 relatives’ groups;265 family therapy;266 behavioural treatments;267,268 and multicomponent psychosocial treatment245 | FI (FIG) | Family members and patients (if clinical condition stable enough) | Individual and group | Counselling sessions, once per month (45 minutes’ duration); family group, once per month (90 minutes’ duration); plus individual sessions with patient, leaders of patient work staff and family members | 12–24 months | Clinical and community (clinic and home visits) | A therapist |
| aZhang and Heqin (1993)77 | China | Majority | Chinese | Family psychoeducation approaches (e.g. Brown et al., 1972;262 Leff et al., 1982;269 and Vaughn and Leff, 1976270) | FI (FE) | Family members | Group |
First 5 weeks: four lectures and one group discussion (weekly) 2–6 months: four lectures and one group discussion (monthly) 7–12 months: two lectures and one group discussion (every 2 months) |
24 months | NR | Trained psychiatrists or nurses |
| Zhang et al. (1994)87 | China | Majority | Chinese | Family psychoeducation approaches (e.g. McFarlane, 1982;271 and Goldstein, 1984272) | FI (FIG) | Family members and patients | Individual and group |
Family group session: 3 months after discharge Families subsequently offered individual or group sessions every 3 months depending on whether or not they had ‘complex or common problems’ |
18 months | Clinical and community (clinic and home visits) | Counsellors |
| aZhang et al. (1998)78 | China | Majority | Chinese | Family psychoeducation approaches (e.g. Brown et al., 1972;262 Leff et al., 1982;269 and Vaughn and Leff, 1976270) | FI (FE) | Family members | Group | 14 sessions (1 hour of duration): 10 in the first year, four in the second year | 24 months | NR | Trained psychiatrists or nurses |
| Zimmer et al. (2007)95 | Brazil | Majority | Brazilian | IPT273 | Cognitive (IPT) | Patients | Group | 12 sessions, once per week (1 hour of duration) | 3 months | NR | A clinical psychologist previously trained by the IPT author |
Appendix 4 Description and examples of themes of cultural adaptation
| Theme | Subthemes | Description | Examples |
|---|---|---|---|
| Language: incorporating literal translation and culturally specific forms of expression and dialect | Direct translation | Translation of materials into national language or use of interpreters |
p. 523115 Use of an interpreter:p. 523115 The intervention:p. 3284p. 13111Koolaee and Etemadi, 2010, p. 63891 The intervention:p. 267117p. 153112p. 92582p. 1127118p. 752102 |
| Local dialect | Incorporating local dialect, colloquialisms and idioms |
p. 14111 |
|
| Concepts: culturally appropriate presentation of concepts, with consideration of culture-specific belief systems, mental health stigma and levels of education | Explanatory models | Adapting intervention to work with culture-specific explanatory models of mental illness |
p. 525115p. 7483p. 20571p. 1191Anahita Khodabakhshi Koolaee, Faculty of Counselling and Family, Department of Family Counselling, Social Welfare & Rehabilitation University, Tehran, Iran, and Ahmad Etemadi, Faculty of Counselling, Department Psychology & Education, Allameh Tabatabaee University, Tehran, Iran, 2011, personal communicationp. 21499p. 268117Parmanand Kulhara, Department of Psychiatry, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigah, India, 2009, personal communicationp. 38885Mann and Chong, 2004, p. 72113p. 14692 The lack of a correct recognition of mental illness is a serious problem for relatives of persons with schizophrenia in rural areas. They usually believe in witchcraft, and accept the notion that mental illness cannot be cured and that medication has no effect on the illness and only wastes family moneyp. 28493pp. 1126–7118(Habib et al. , 2015;71 Naeem et al., 201592) as cited in Naeem et al., (2016) p. 44274 All psychologists agreed that therapy should be adapted to suit local needs, such as taking culture and religion into account, as these affect patients’ views on illness origins and treatment. Although one psychologist emphasised the positive influence of religious beliefs on mental health, the remainder considered them to be detrimental71,92,274(Habib et al. , 201571; Naeem et al. , 201592) as cited in Naeem et al., (2016) p. 52274 Participants:p. 545114 |
| Stigma | Addressing issues of mental health stigma in culturally appropriate ways (e.g. avoiding Western/psychiatric diagnostic labels, sharing personal stories for normalisation) |
p. 3284 The intervention included:p. 3484p. 127880p. 132898p. 133198 Intervention included:p. 1000101p. 897109p. 27488Ester Ching-Lan Lin, Department of Nursing, National Cheng Kung University, Tainan, 2013, personal communicationp. 249119p. 545114 |
|
| Limited mental health knowledge and education | Adapting intervention to acknowledge low education levels and lack of mental health education in different cultural contexts (e.g. due to cultural group norms; and tendencies for lack of schooling and education in local area) |
Wai-Tong Chein, Nethersole School of Nursing, Chinese University of Hong Kong, China, 2016, personal communicationp. 1191Alex Kopelowicz, David Geffen School of Medicine, University of California, Los Angeles, 2012, personal communicationp. 38785p. 38885p. 38885Ester Ching-Lan Lin, personal communicationp. 52582p. 92582 The intervention was:p. 70100p. 545114pp. 239–4089 Some families believe social factors cause mental illness. They become controlling and overprotective in trying to keep the patient safe. Other families deny that the patient has a mental health problem and think the behaviour is out of choice, causing hostility towards the patient from relatives87Marilene Zimmer, Schizophrenia Program, Hospital de Clinicas de Porto Alegre (HCPA), Porto Alegre (RS), Brazil, 2007, personal communication |
|
| Family: consideration of family involvement, structure and dynamics and specific roles and expectations | Family involvement | Acknowledging the importance of the family unit in the recovery process and encouraging their active and continued involvement throughout the intervention (e.g. provision extra sessions, extra efforts to engage and maintain contact) | In Asian cultures, the family is a crucial social structure. [T]he burden of illness becomes a joint family obligation, with multiple members engaged in treatment. In contrast, Western values emphasize individualism – for example, protecti[ng the individual’s rights] to privacy and confidentiality as well as independent livingp. 529115Family joining sessions were conducted informally on an outreach basis in the homes of the Vietnamese families to maximize the likelihood that families would engage with the service and to provide an opportunity to include as many family members as possiblep. 525115In Italy, since the deinstitutionalization of the ‘70s [. . .] effective treatment systems for severe psychiatric disorders ha[ve] been balancing community-and-hospital-based mental health care [. . .] There has been an increasing acknowledgment of the importance of families in terms of [. . .] their therapeutic potential and the burden they carryp. 2490The content of the program was designed according to the preference and perceived needs of patient-caregiver dyads, and the case managers put much emphasis on addressing their cultural issues in family caregiving rolep. 31897‘Family members are actively involved in patient care in Pakistan, and therefore the intervention involved the family members in the treatment plan from the beginningp. 20371We chose a family approach because living with supportive relatives increases medication adherence, and interventions that give relatives information about the illness and teach them coping and problem-solving skills reduce relapses and rehospitalizationspp. 265–6117This high level of involvement of Indian families in the patients care is partly because of their preference, and partly because of the inadequacy of the mental-health set-upp. 47386Most families actively want to be involved in all aspects of their relatives wellbeing and problems.’ (Kulhara et al., 2009)As cited in Shankar & Menon, (1993) p. 77275To engage families, especially in the initial stage, in-home single-family sessions were offered in order to involve more relativesp. 388–985Over 80% of Latinos with schizophrenia live with their families (Guarnaccia & Parra, 1996) [. . .] therefore, including families was relevant to the task of maximizing the generalization of skills to the home environment (Kopelowicz et al., 2003; Kopelowicz et al., 2012)As cited in Lopez, Kopelowicz and Canive (2002) p. 71276After completing these sessions, skills trainers visited patients and families at their homes to review progress and help solve problems that arose (Kopelowicz et al., 2003; Kopelowicz et al., 2012)As cited in Lopez, Kopelowicz and Canive (2002) p. 72276Because of the importance of la familia (the family) in Mexican-American culture, the PEDAL intervention was adapted to help individuals work with family members for transportation needs rather than help them to utilize public transportation or to travel independentlypp. 72–381The ultimate social goal of family members of people with schizophrenia in China is to develop a sustainable family based support system for the dysfunctional individual (Xiong et al., 1994), problem solving and communication skills education was emphasized in this study. In this study the aim was to finish the main content of the education programme in the hospital, and connect with the families after the patients were discharged because few nurses work in community settings and the community mental health services were not sufficiently well developed(Li & Arthur, 2005)96 as cited in Li (2003)277To reinforce the interventions, parallel sessions, also conducted in Korean, were offered to family members of all participantsp. 1127118Nearly 80% of Hispanic Americans with Schizophrenia live with their families (Guarnaccia & Parra, 1996) in Mexico city, it is over 90%Valencia et al., 2003278Because of the importance of family cohesion and joint decision making in China, the key family members of patients were involved in some of the training sessions with patients when the topics were use of medication and an emergency plan for relapse preventionp. 402108The cultural and legal obligations of parents towards disabled children continue until the child is married, when the responsibility is transferred to the patient’s spouse. Disabled children who never marry are usually cared for by their parents until the parents diep. 240114Attention must be paid to the needs of family members, for whom care of a mentally ill person may constitute a considerable burden. They need community support, appropriate education, accessibility to professional consultation, and, in some cases, financial aidp. 4877In China, unlike the West, the societal and legal expectations are that the family members will care for these disabled individuals indefinitely, regardless of the emotional and economic burdenp. 10187 |
| Family structure | Adapting for culture-specific family structures. Nuclear/individualistic or extended/collectivist family structures | In treating Chinese families, it is important to recognize, respect and utilize the culture-specific family structures, functions and processes, such as the extended family structure with close linkage and interrelationships, interdependence and a strong sense of filial responsibility, collective identity and tangible supportp. 3094The program adopted a few strategies to address traditional Chinese cultural tenets. The first stage (orientation and engagement) focused on understanding strong interdependence, collective actions and decisions about family issues, acceptance of roles, and filial obligation of caregiving, respect for elders, and other traditional Chinese beliefsp. 31897The MBPP also adopted several strategies to address traditional Chinese cultural tenets. For instance, the first stage focuses on understanding strong interdependencep. 377103The program used a culturally sensitive family intervention model, which considered many of the cultural tenets that were taught by Confucius (for example, valuing collectivism over individualism and giving great importance during the needs assessment to family and kinship ties) in respect to family relationships and value orientationp. 1004105Given the centrality of the family unit in decision making for Mexican Americans, (Sabogal et al., 1987) the focus was on the approval or disapproval of family members for taking medication and the patient’s motivation to comply with those perceived wishesp. 268117All 3 groups reinforced the importance of Mexican cultural values and concepts, such as familismo (i.e., placing family over the individual), respeto (i.e., respect for older persons)p. 92582[. . .] handling medications involved a sense of ‘orgullo’ (i.e., pride) for many patients, owing to a desire to alleviate symptoms in order to contribute to the family. Thus, [. . .] treatment regimens w[ere] modified to include the potential benefits of medication adherence to the family system (versus the benefits of independence)p. 92682The success of our programme may also be attributed to the extended family system among the Malays’ (Yusof, 1976)p. 28893Commitment to the extended family is often valued more than individual autonomy among first and second generation Mexican-American families. The higher value placed on interdependence by Latinos may clash with the norms inherent in evidence-based practices designed in the United Statesp. 249119 | |
| Family roles and responsibilities | Demonstrating an awareness of culture-specific family roles and responsibilities (e.g. hierarchical roles, respect for elders, gender roles, expectations of specific family members) | Chinese families suggested that the younger generations are not supposed to question or challenge the decisions of their elders, which appear to run contrary the purpose of family intervention in promoting collaboration through mutual concern and discussion. This typical strong parental power in Chinese family may produce resentment and un-cooperation from the elder family member, who would perceive the younger group members or the therapist as a threat to their authority (Fung & Ma, 1997). There is a need to consider and adopt the specific Chinese culture for establishing a helping relationship in family interventions, for example, emphasis on mutual respect and equal position but not be rigidly confined to the passive reception of teaching and information by the familiesWai-Tong Chein, personal communicationMothers were the focus of this study because, in Iranian families, it is usually the mothers who show most interest in patient care. Even when patients are married and then divorce, mothers again take responsibility for the patients and sometimes the grandchildrenKoolaee and Etemadi, 2010, p. 63691In all modules, gender-appropriate activities were substituted, and modifications were made with regard to culturally expected roles in our scenarios and examples (cooking and house chores for women; working on the car and yard maintenance for men)p. 92682Proper distance and respectfulness were employed to address the participants who were older than the group facilitators due to Latinos emphasis on respect and hierarchiesp. 92682Consideration of Malay cultural values e.g. training to communicate assertively and establishing eye contact with the elderly (especially one’s parents) are regarded as disrespectful in the Malay culturep. 28893Fathers with traditional values and expectations also hew to the macho image as well as to the stigma of mental illness; hence, it takes special efforts, such as phone calls and home visits, by leaders of skills-training groups to gain the support of fathers in reinforcing homework assignments(Valencia et al., 2007;120 Valencia et al., 2010119) as cited in Valencia et al., (2015) p. 236279 | |
| Cultural norms and practices: adapting for cultural-specific values and social norms, religious/spiritual beliefs and practices, and incorporating culturally relevant social activities | Culturally specific practices and coping methods | Adapting intervention to accommodate cultural-specific beliefs, local practices and traditions, and coping methods (e.g. local remedies, prayer, spiritual/religious leaders, places of worship, experiences of symptoms) |
p. 525115p. 20471Habib et al. , 201571; Naeem et al., 201592) as cited in Naeem et al., 2010, p. 168280 Guidelines for therapists:p. 28593p. 35276p. 35276p. 35376 Designing the intervention to accommodate religious practice:p. 35576pp. 355–676pp. 355–676 |
| Culturally relevant activities and scenarios | Incorporating culturally relevant activities and scenarios (e.g. social activities, local stories, traditional characters) | For 5 sessions, relaxation exercises, including the Chinese Eight Elegant Movements (Baduanjin) were introduced and practiced at the end of the sessionp. 39085The CBCSM used local cultural scenarios as role-play activities and had video demonstrations performed by local actors. For example, ‘yum cha’ (tea gathering at the Chinese restaurant) was used to replace the party situation as it is a common local gathering activity for practicing conversationp. 140106Participants were encouraged to participate in culturally relevant activities like playing Mahjon, doing Tai Chi and singing KaraokeMann and Chong, 2010, p. 73113Identified scenarios that were deemed culturally neutral or more relevant to the local Hong Kong Chinese service usersp. 5110 | |
| Community and social networks | Building social networks and actively encouraging social and community support inside and outside the therapeutic setting (e.g. engaging families through social gatherings and offerings; use of peer-led sessions; providing opportunities for bonding) |
Giuseppe Carrà, Department of Mental Health Sciences, Royal Free and University College Medical School, London, UK, 2007, personal communicationp. 2490p. 3294 The intervention included:p. 3494 The use of ‘peer leaders’:Chien et al. , 2006, p. 4382 The intervention focused on:p. 37797p. 897109p. 21499pp. 388–985p. 70100p. 1127118p. 1127118 |
|
| Communication: culturally specific forms of communication, problem-solving and learning styles | Openness and disclosure | Adapting for cultural differences in open expression of emotion and/or disclosure of patient’s private information (e.g. sharing confidential information, reassurance to openly discuss problems) |
Wai-Tong Chien, personal communication Group instructor reinforced:pp. 32–384p. 132898 Intervention consisted of:p. 31897p. 377103Marcelo Valencia, School of Medicine, National University of Mexico, Mexico City, 2007, 2010, personal communication |
| Strategies for conflict resolution and problem-solving | Adapting for cultural-specific ways of communicating to resolve problems (e.g. preferences for direct/reparative actions vs. emotional reassurance; practical assistance vs. talking; avoiding confrontation; assertiveness) | There is a need to adapt the family intervention that has originated in the West to take into account Chinese ways of communication (as characterized by an emphasis on mutual respect and positive action for family members rather than talkingp. 3094The content of the program was designed according to the preference and perceived needs of patient-caregiver dyads, and the case managers put much emphasis on addressing their cultural issues in family caregiving role, effective communication, and resolving conflicts, as well as hands-on practical experiencesp. 31897Chinese people tend to show mutual concern and support by [meeting] each other’s actual needs[,] they are reluctant to seek profession help. Therefore, [. . .] care-giving and therapies which emphasize practical assistance and problem solving [are valued over] psychological reassurance and [. . .] expression of feelingsp. 12384Family involvement, differing patterns of communications (for example concept of assertiveness outside the West) should be important in adapting therapy for local clients in Pakistanp. 20671Patients were excluded from the multifamily group, since caregivers are likely to be inhibited in discussing their frustrations about their ill member due to cultural tendencies to avoid direct family confrontation in front of many non-family membersp. 38885Problem solving and communication skills education was emphasized in this study(Li and Arthur, 2005)96 as cited in Li (2003)277Emphasis on assertiveness in these modules struck a careful balance between respeto/formalidad (i.e., respect and formality) and encouraging patients to clearly state their needsp. 92682The programme such as training to communicate assertively and establishing eye contact with the elderly (especially one’s parents) are regarded as disrespectful in the Malay culturep. 28893Addition of coping strategies consistent with Islamic doctrine to the coping strategy enhancement component (Tarrier et al., 1990) of the interventionp. 35576 | |
| Teaching and learning styles | Adopting approach to teaching and delivery that accommodates culture-specific ways of learning (e.g. directive vs. collaborative; didactic vs. dialectic; active vs. passive) | Given the Chinese caregivers tendency to prefer a more hands-on and practical experience, they were invited to conduct behavioural rehearsals of coping strategies and skills in resolving conflicts within the familyp. 31897The active-directive teaching style, [which is central to] social skills training was modified to [facilitate greater] spontaneity [by] the patients. Because many patients do not respond to direct questions with direct answers, trainers were instructed to ‘stick with the patient’ longer than in conventional training sessions(Kopelowicz et al., 2003)99 as cited in Lopez and Kopelowicz (2002) p. 71276Also, the need to be an active participant in treatment was encouraged to overcome the tendency for members of a patriarchal culture to accept without question the counsel of authority figures like physicians (Zea et al., 1997)(Kopelowicz, 2003;99 Kopelowicz et al., 2012117) as cited in Lopez and Kopelowicz (2002) p. 71276This study integrated Chinese [. . .] values and practices into [. . .] CBT. For example, [a] hierarchical approach to the doctor–patient relationship could [enable early engagement with the CBT therapist]. However, the emphasis then needed to shift [later] to a more collaborative relationship, [. . .] encourag[ing] the patient[’s] contributi[on] to the therapyp. 1901107One of the psychologists talked about patients not being comfortable with downward arrow technique and Socratic dialogue. Most of them said cultural adaptation of CBT for psychosis patients expect a directive style rather than collaborative style(Habib et al., 2015;71 Naeem et al., 201592) as cited in Naeem et al., 2016, pp. 50–51274Patients also like a directive style and probably don’t feel comfortable when a collaborative style is used(Habib et al., 2015;71 Naeem et al., 201592) as cited in Naeem et al., 2010, p. 171280Korean clients are likely to feel more comfortable with a didactic format than with an interactive situation, because the former is less conducive to experiential types of sharing that require self-disclosure. Their culturally determined respect for experts and authority may help facilitate both the educational process and the therapeutic alliancep. 1126118Visual aids, including charts and handouts, were used to reinforce the didactic materialsp. 1127118Family members reported that their [. . .] relatives were uncomfortable with written material [(e.g.] writing exercises during sessions[/]homework assignments[)]. Instead, patients considered that therapy was for talking and learning[,] not for written activities that reminded them of school [. . .] Therefore, the skills trainers switched to oral exercises and assignments(Valencia et al., 2007;120 Valencia et al., 2010119) as cited in Valencia et al., (2015)279 p. 222 | |
| Context and delivery: adapting the delivery of the intervention to accommodate, contextual issues (e.g. lack of commitment, funding or resources) to facilitate feasibility in particular cultural context | Location of intervention | Delivery of sessions at an accessible and culturally appropriate location |
Giuseppe Carrà, personal communicationp. 402108(Li and Arthur, 2005)96 as cited in Li (2003)277p. 20171 Delivering the intervention in patients’ homes:p. 74100p. 544114p. 24089 |
| Flexibility in scheduling sessions | Flexibility in scheduling of therapy sessions to accommodate culture (e.g. frequency, time, intensity) | To encourage participation, all of the clients and caregivers were phoned once a week to keep them engaged during the 3 months of the PEP [Psychoeducation programme]. [. . .] [P]articipants were further reminded to attend [. . .] sessions 1 day in advance; repeat sessions were made available [. . .]; and the program was conducted on the weekendsp. 6883We designed this comprehensive psychosocial intervention to be delivered on the same day once a month mainly owing to the care structure in China, the potential time and cost burden to patients and their family members, and the feasibility of adoption by other care settingsp. 897109Providing psychological treatment during the inpatient phase might offer improved opportunities (Naeem, Gobbi, Ayub and Kingdon, 2010)p. 20171Attendance was facilitated by presentation, in each neighbourhood, of each lecture twice, once during the day and the other in the evening. Unlimited time was allowed for discussion and questions after each lectureZhang and Heqin, 1993, p. 5077 | |
| Mode of intervention | Modality of treatment to accommodate culture (e.g. group or individual; patient and/or caregiver attendees) | We didn’t include the patient, as Italian culture hardly allows an open expression of feelings re the ill relative in front of other people not belonging to the familyGiuseppe Carrà, personal communicationTraditional therapist-led single-family therapy that focuses on the psychological problems of the patient or family members may not be easily accepted by Chinese families because of their reluctance to reveal private thoughts and feelings in front of others, especially a therapist or someone not familiar to them . . . Therefore, it may be difficult to build rapport between the therapist and the family in the traditional family therapy session (Fung & Ma, 1997)Wai-Tong Chein, personal communicationMultiple family sessions gave them the opportunity to speak about their children with each other, which they felt was neededp. 1191Patients were excluded from the multifamily group, which was different from McFarlane’s (2002) model since caregivers are likely to be inhibited in discussing their frustrations about the ill member due to cultural tendencies to avoid direct confrontation within family in front of many ‘outsiders’ (Bae & Kung, 2000)p. 38885Patients were addressed separately, they were not required to attend the intervention sessions, because some caregivers felt that they would be unable to discuss their problems freely in the patient’s presencep. 47486 | |
| Length of intervention | Duration of treatment to accommodate cultural or contextual barriers | Although the multiple-family group intervention is generally used for two years, funding constraints necessitated a briefer interventionp. 524115The number of sessions had been reduced from 18 to 14 two-hour sessionsp. 31897Psychosocial interventions have become more popular in recent decades in China, but the number of well-trained therapists remains limited in many Chinese psychiatric settings. More frequent therapy sessions could be not only difficult for patients and family members but also hard for many psychiatric settings to adoptp. 897109The final adaptation was that the duration of the intervention was only 6 months in comparison to the usual 9–24 months. This is because many Chinese immigrants are reluctant to commit to long-term psycho-social treatments primarily because many of them are involved in low paying jobs with long work hourspp. 388–985A similar contextual barrier was the particular difficulty in organisations that are not fully committed to recovery, because IMR redistributes power to clients within a wider recovery paradigm, they suggested that this barrier should be the key priority in IMR implementation. Therefore, instead of fully complying with the standardized 9-month toolkit, a brief IMR was pragmatically developed to benefit patients living with various degrees of deinstitutionalization and cultural stigmatizationEster Ching-Lan Lin, personal communicationThe intervention is ongoing rather than time limited, because stopping it would mean the termination of any regular follow-up carep. 24089 | |
| Content: addition or removal of specific content | Addition of specific content | Adding culturally relevant content/materials to the intervention manual |
Giuseppe Carrà, personal communication Chan et al. 83 incorporated sessions about diagnostic labels and biochemical factors and laws in relation to mental health care in Hong Kong:p. 7583 Chien94 added a module to their mutual support intervention for family members to discuss:p. 3394 Chien and Chan98 added:p. 133298 Chien and Thompson101 added:p. 1000101p. 14111 The intervention included a session to address:and emphasised marriage as a primary concern because,(Shankar and Menon, 1993)275 as cited in Kulhara et al. (2009)86Parmanand Kulhara, personal communicationp. 153112p. 28493p. 753102 |
| Removal of specific content | Removing culturally irrelevant content/materials from the intervention manual | Modified some written vignettes describing emotions as they relate to pets, as it is not common in Egyptian culture to have a dog or cat in one’s homep. 14111We used most of the picture (e.g., faces, social scenarios), video, and auditory stimuli from the original version but excluded some that were not well suited to Egyptian culture. For example, we excluded pictures and videos that depicted unfamiliar recreational activities (e.g., American football or drinking alcohol beverages)p. 13111We omitted communication skills training as this is the least important among the three core components of the standard model. This is supported by the finding that generally the carers of Malay schizophrenic patients could tolerate negative symptoms of schizophrenia (Salleh, 1994)p. 28493For example, JTC [jumping to conclusions] was illustrated in the original MCT using the conspiracy theory about Paul McCartney’s death. This was substituted by a classic local myth about keeping pregnancy secretive during the first trimester so as to avoid a miscarriagep. 5110Only six of the seven learning activities used in the United States were used for Mexican patients. Video-assisted modelling was not used since skills training technology in Spanish had not been developed in Mexico. To overcome this obstacle, therapists demonstrated the skills to be learned during sessionsValencia et al., 2007;120 Valencia et al., 2010119 as cited in Valencia et al. (2015) p. 222279Another adaptation was the images used, as in Brazil, they do not have snow, trains and a very small number of patients can travel by planeMarilene Zunimer, personal communication | |
| Therapeutic alliance: consideration of therapist qualities/characteristics, approach and cultural competency training to improve engagement and alliance | Therapists and client matched for characteristics | Therapists matched for characteristics (e.g. ethnicity, age, gender, language spoken, etc.) | Vietnamese primary therapists were consistent for two intakes of the two cultural groupsp. 524115Cultural adaptations of the program included the use of Vietnamese speaking staff for all aspects of service provision within the programp. 525115Use of a female therapist for Iranian intervention designed for mothersAnahita Khodabakhshi Koolaee and Ahmad Etemadi, personal communicationAdditional cultural adaptations included the use of indigenous, bilingual, and bicultural staff of the community mental health center as skills trainers, the participation of family members (rather than clinicians) as ‘generalization aides’p. 21499As the participants in the study spoke either Mandarin or Cantonese, and some were more fluent in English, trilingual clinicians were soughtp. 39085 |
| Therapist ‘cultural competency’ training | Therapists received some form of cultural competency training and supervision | Trainers:. . . were all trained to meet cultural sensitivity standards outlined by the State of California and based on sound empirically-based principles (Rogler et al., 1987; Wallen, 1992)(Kopelowicz et al., 2003;99 Kopelowicz et al., 2012117) as cited in Lopez, Kopelowicz and Canive (2002) p. 71276Facilitators of these treatments should be educated and familiar with the relevant cultural values of the consumerp. 7381The treating clinicians needed special training because psychiatrists and psychiatric nurses in China have no experience in the evaluation and management of the family and social problems faced by mentally ill patientsp. 24089 | |
| Therapeutic approach | Therapeutic approach adapted to build rapport and trust between therapist and patient/family unit (e.g. informal, warm-up activities/ice breakers, personalised, general conversation, self-disclosure) | Skills trainers used an informal, personal style with patients and relatives that included the sharing of food and encouragement of ‘small talk’ before and after training sessions, made to encourage warm interactions between trainers, patients and relatives, thereby increasing retention in the study and increasing effectivenessp. 21499During the engagement, phase attempts were made to build a positive therapeutic alliance with the family. Preliminary information (oral/printed) about schizophrenia was provided. All this was done in a no fault atmosphere i.e. without attaching blame to anyone, especially the familyp. 47486Intervention focused on establishing trust relationship with patient and family, before identifying their individual needsp. 34096Accepting the patient’s interpretation of his or her illness to strengthen the therapeutic relationshipp. 28893Adaptations to Mexican culture included the therapists beginning the sessions by engaging in platica (small talk) with the patients which built trustp. 253119In addition, therapists offered their patients appropriate forms and amounts of self-disclosure from their own lives which generated a sense of personalismo or a personal orientation to therapeutic relationships that has been shown to improve the effectiveness of interventions with Latinos (Sue et al., 1991)p. 253119Each session began with a short warm-up activity (about 5 min), which was designed to create a more relaxed atmospherep. 753102 | |
| Treatment goals: formulating treatment goals and encouraging outcomes that are realistic, culturally relevant and tailored to the family | Intervention goals and expectations of outcome | Ensuring treatment expectations are realistic and modifying treatment goals to ensure culturally relevant (e.g. collaborative/shared goals; cultural values emphasised) |
p. 127880(Meredith et al. , 1994;281 Bae & Kung, 2000)225. (Chien, Chan & Thompson, 2006, p. 44)79p. 999101p. 268117 Content of sessions included:p. 47486p. 6681 The treatment goals were based on:p. 92582(Valencia et al. , 2007;120 Valencia et al., 2010119) as cited in Valencia et al., (2015) p. 230276 |
Appendix 5 Cultural adaptations emerging from thematic analysis of psychosocial interventions for psychosis
| Author (year) | Theme | Number of adaptations reported | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Language | Concepts | Family | Cultural norms | Communication | Context and delivery | Content | Therapeutic alliance | Treatment goals | ||
| Bradley et al. (2006)115 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | |||
| Carrà et al. (2007)90 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | ||||
| Chan et al. (2009)83 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | ||||
| Chien (2008)94 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| aChien and Chan (2004)80 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| aChien and Chan (2013)98 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| aChien et al. (2006)79 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| Chien and Lee (2010)97 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||
| Chien and Lee (2013)103 | ✗ | ✗ | ✗ | 3 | ||||||
| aChien et al. (2004)104 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| Chien and Thompson (2013)101 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| aChien et al. (2008)84 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| Chien and Wong (2007)105 | ✗ | ✗ | ✗ | ✗ | 3 | |||||
| Gohar et al. (2013)111 | ✗ | ✗ | ✗ | ✗ | 4 | |||||
| Guo et al. (2010)109 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | ||||
| aHabib et al. (2015)71 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | |||
| Koolaee and Etemadi (2009)91 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | |||
| Kopelowicz et al. (2003)99 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | |||
| Kopelowicz et al. (2012)117 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| Kulhara et al. (2009)86 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |
| Kumar et al. (2010)112 | ✗ | ✗ | 2 | |||||||
| bKung et al. (2012)85 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| Lak et al. (2010)106 | ✗ | 2 | ||||||||
| Li and Arthur (2005)96 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | ||||
| Li et al. (2015)107 | ✗ | ✗ | ✗ | ✗ | 3 | |||||
| aLin et al. (2013)88 | ✗ | ✗ | ✗ | ✗ | 4 | |||||
| bLin et al. (2013)116 | ✗ | ✗ | ✗ | ✗ | 4 | |||||
| Mann and Chong (2004)113 | ✗ | ✗ | ✗ | 3 | ||||||
| aMausbach et al. (2008)81 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| aNaeem et al. (2015)92 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | |||
| aPatterson et al. (2005)82 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| Ran et al. (2003)100 | ✗ | ✗ | ✗ | ✗ | 4 | |||||
| Razali et al. (2000)93 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | ||
| Shin and Lukens (2002)118 | ✗ | ✗ | ✗ | ✗ | 5 | |||||
| So et al. (2015)110 | ✗ | ✗ | 3 | |||||||
| aValencia et al. (2007)120 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 8 | |
| aValencia et al. (2010)119 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 8 |
| Wahass and Kent (1997)76 | ✗ | ✗ | 2 | |||||||
| Wang et al. (2013)102 | ✗ | ✗ | ✗ | 3 | ||||||
| Weng et al. (2005)108 | ✗ | ✗ | ✗ | ✗ | 4 | |||||
| Xiang et al. (1994)114 | ✗ | ✗ | ✗ | ✗ | ✗ | 4 | ||||
| Xiong et al. (1994)89 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | ||||
| aZhang and Heqin (1993)77 | ✗ | ✗ | ✗ | ✗ | 4 | |||||
| Zhang et al. (1994)87 | ✗ | ✗ | ✗ | 3 | ||||||
| aZhang et al. (1998)78 | ✗ | ✗ | ✗ | ✗ | 4 | |||||
| Zimmer et al. (2007)95 | ✗ | ✗ | ✗ | 3 | ||||||
| Total | 46 | 36 | 35 | 27 | 22 | 22 | 20 | 13 | 13 | |
Appendix 6 Phase 1 service user recruitment poster
Appendix 7 Phase 1 service user participant information sheet
Appendix 8 Phase 1 service user consent form
Appendix 9 Service user focus group topic guide
Appendix 10 Help in a crisis information sheet
Appendix 11 Service user focus group PowerPoint presentation slides
Appendix 12 Mixed focus group topic guide
Appendix 13 Mixed focus group presentation slides
Appendix 14 Consensus conference participant information sheet
Appendix 15 Consensus conference PowerPoint presentation slides
Appendix 16 Components of the CaFI therapy manual
Appendix 17 Therapist training slides for the delivery of the CaFI manual
Appendix 18 Family support member recruitment poster
Appendix 19 Phase 3 participant information sheet
Appendix 20 Meriden Family Programme training evaluation form
Appendix 21 Just Psychology cultural competency training family support workers’ feedback questionnaire
Appendix 22 Just Psychology cultural competency training therapist feedback questionnaire
Appendix 24 Phase 3 service user recruitment poster
Appendix 25 Statistical analysis plan
Appendix 26 CaFI fidelity measure
Appendix 27 Feedback sheets
Appendix 28 Qualitative follow-up interview schedule: service users
Appendix 29 Histograms of the outcome measures
FIGURE 10.
Histograms showing distribution of all appropriate outcome measures: service users. WAICV, Working Alliance Inventory Client Version. The figures show the distribution of service users’ (a) PANSS general score; (b) PANSS total score; (c) PSP total score; (d) WAICV total score; (e) PCS question 1; and (f) PCS question 2.
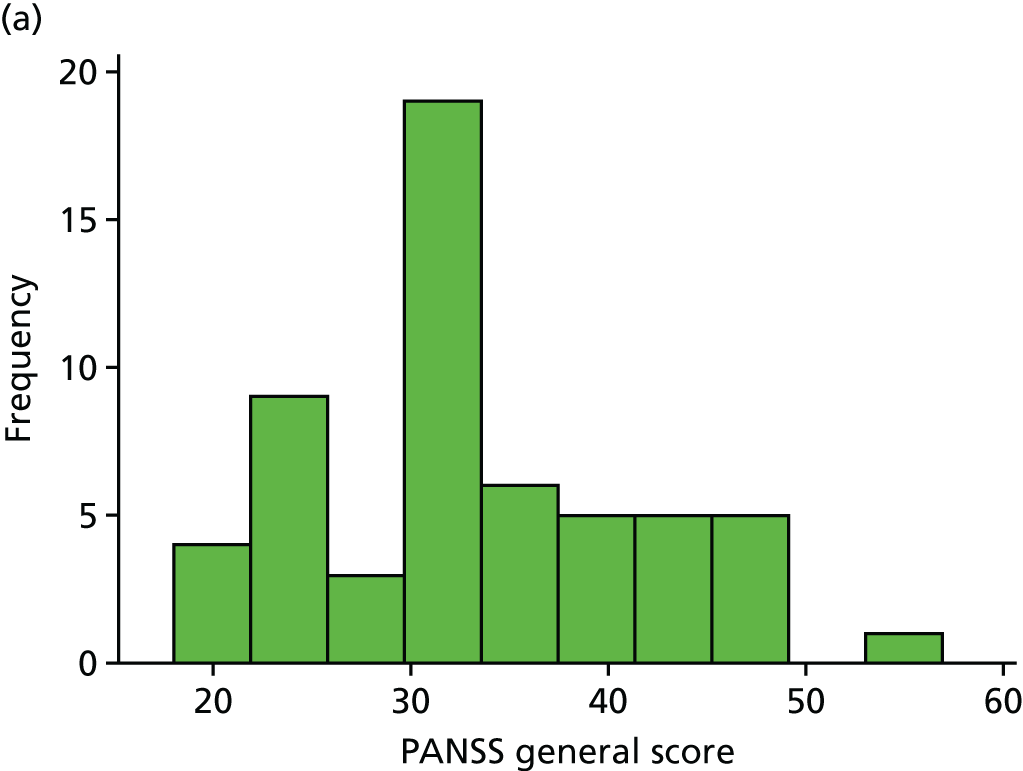
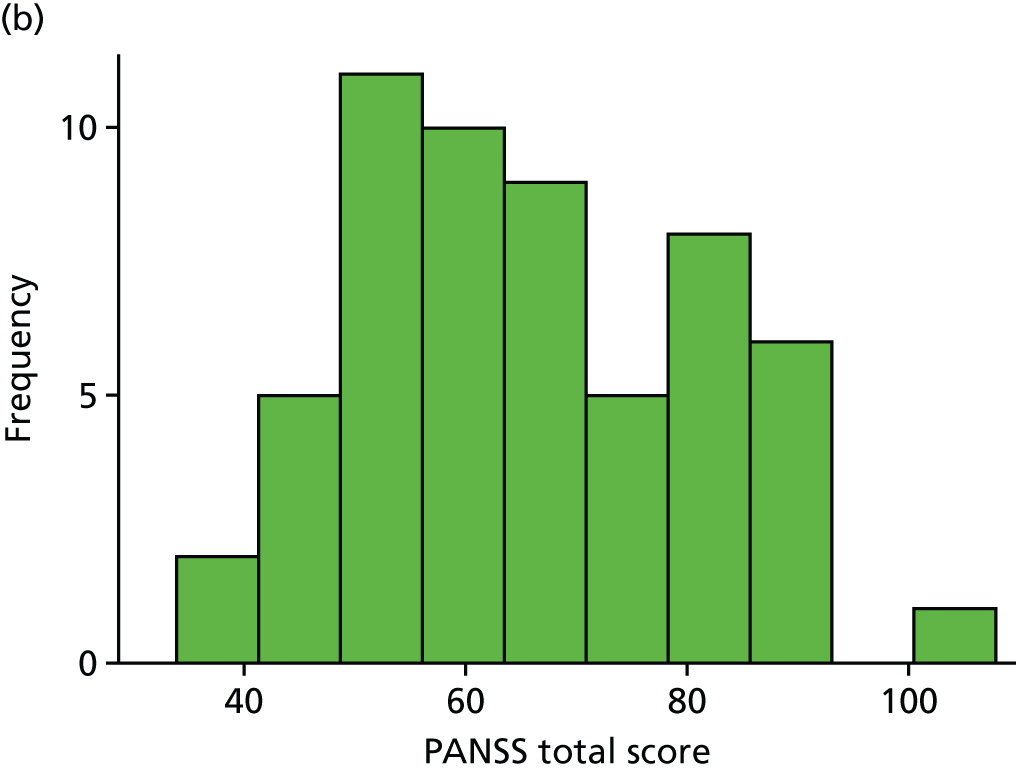
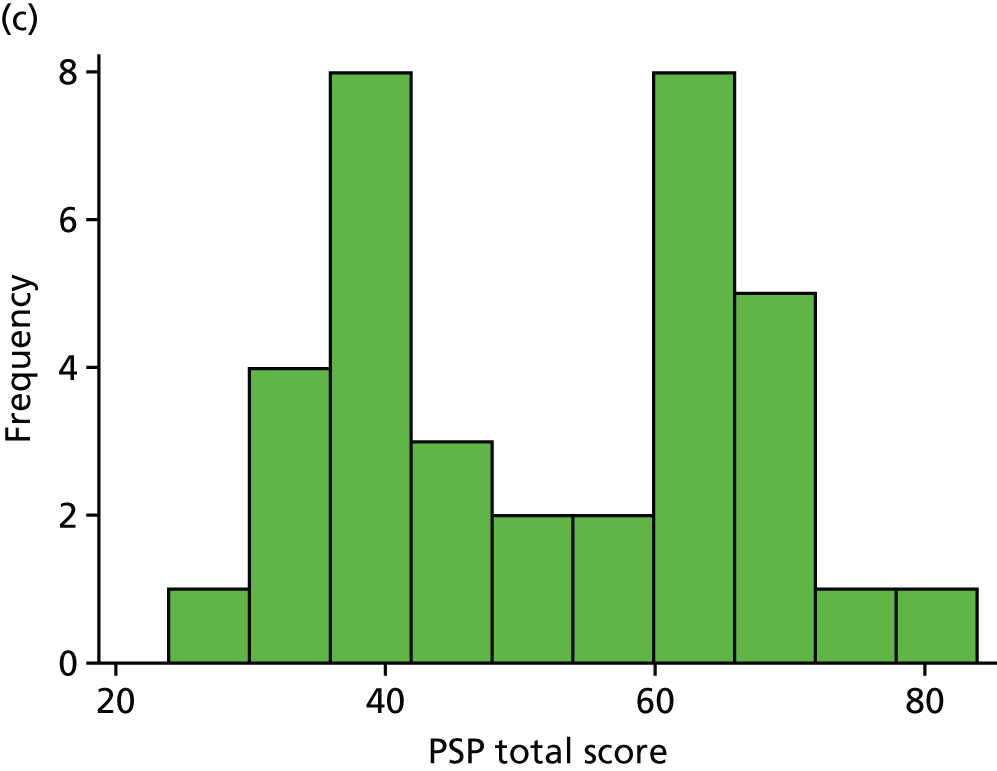
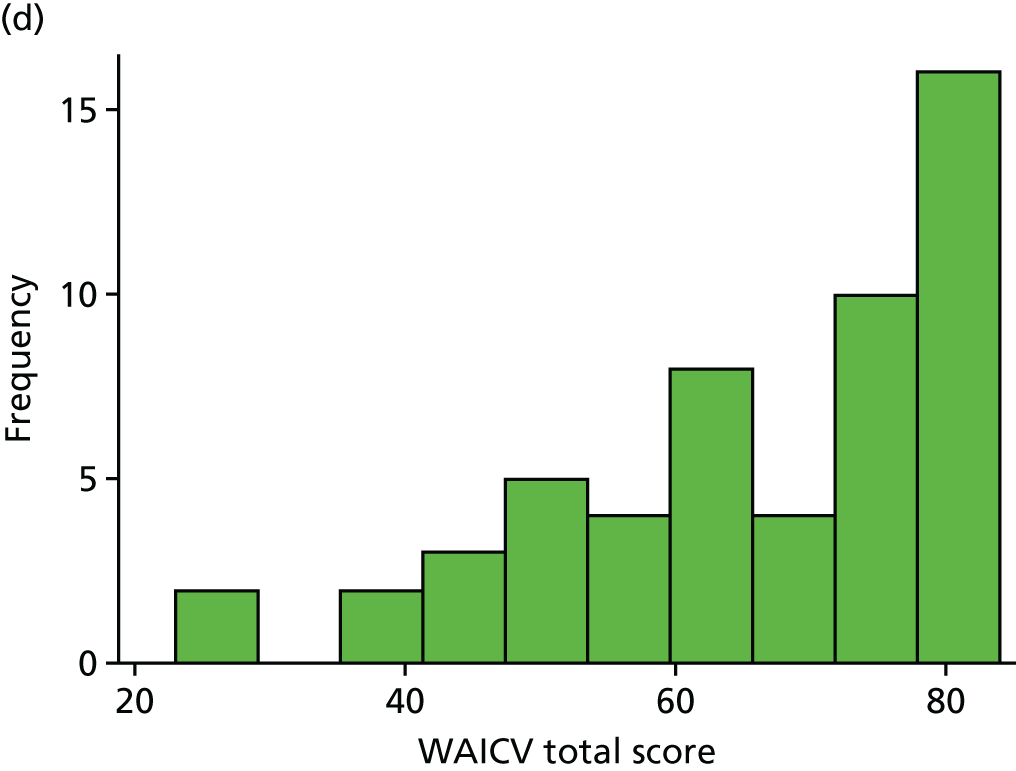
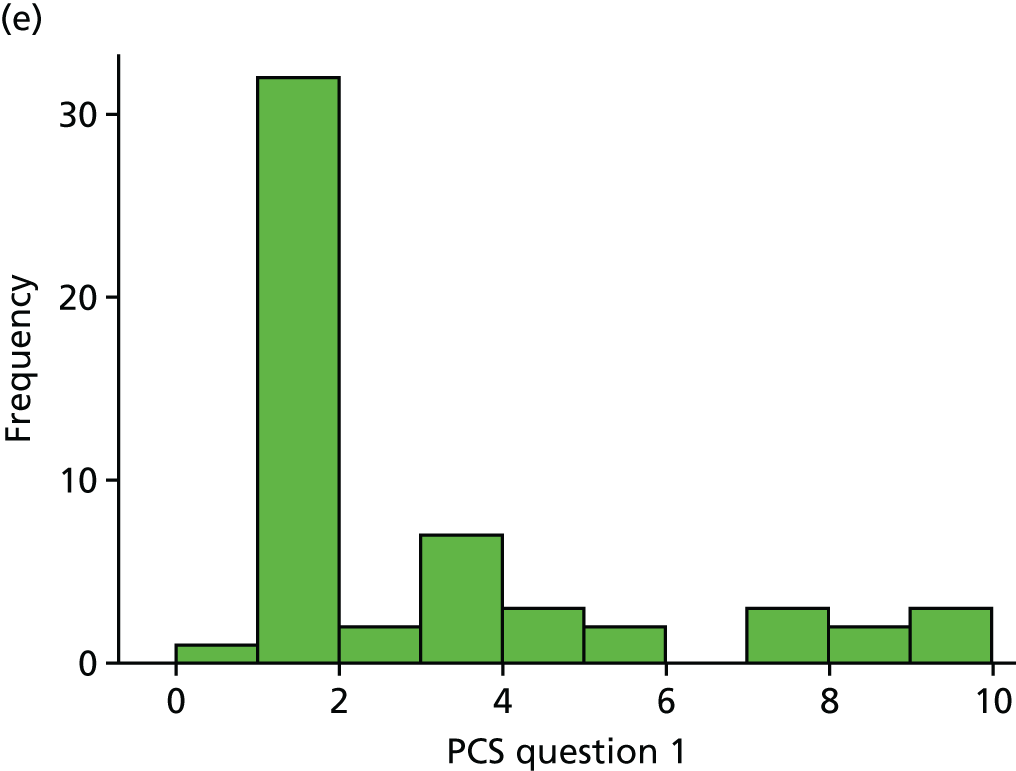
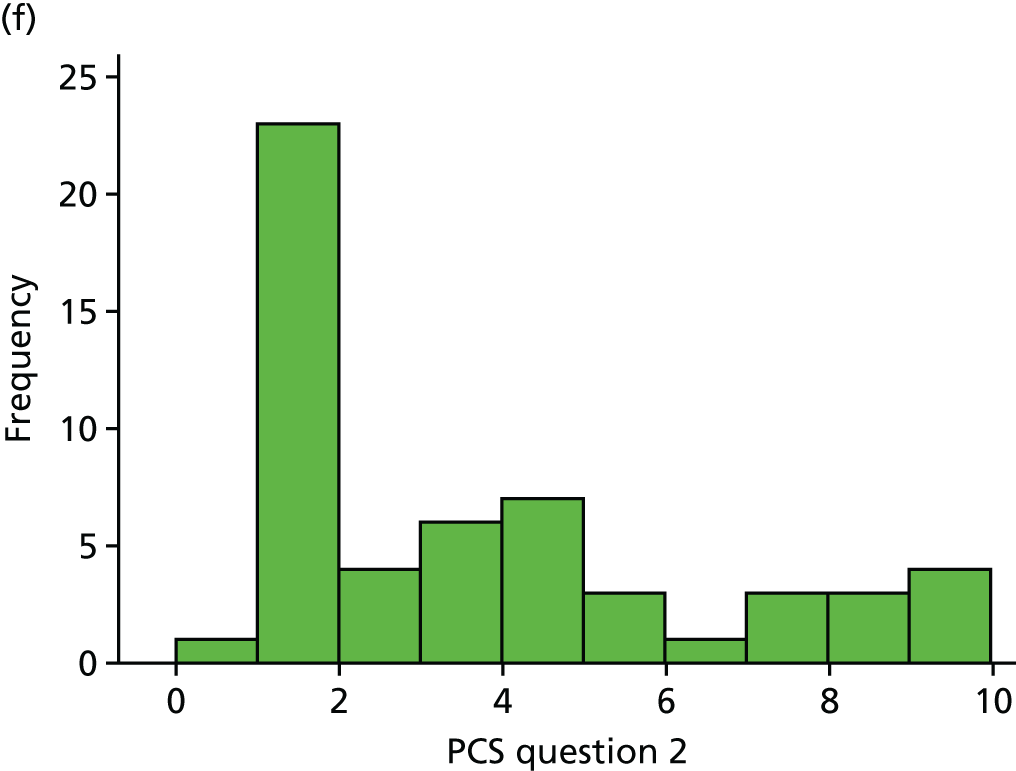
FIGURE 11.
Histograms showing distribution of all appropriate outcome measures: family members/FSMs.
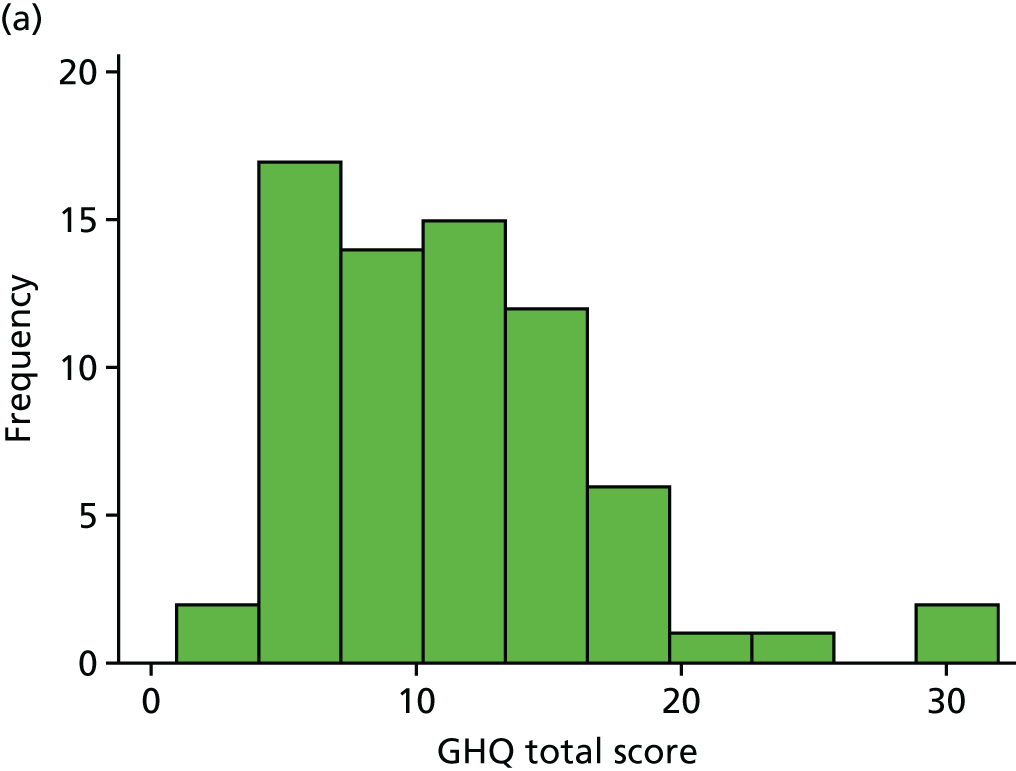
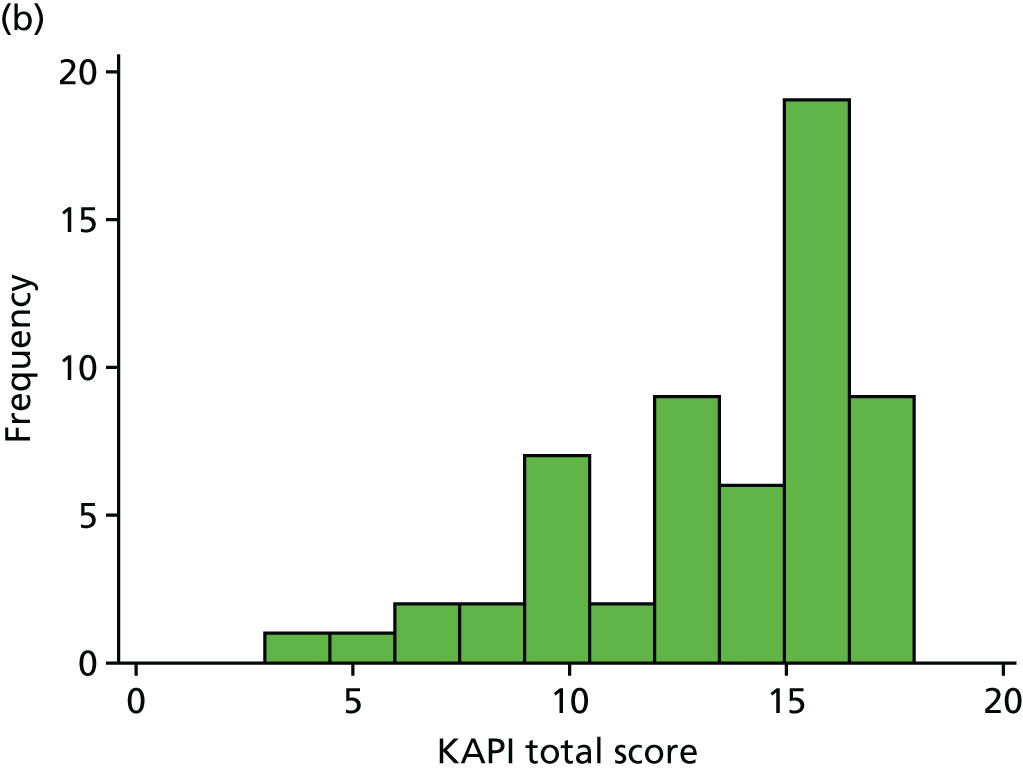
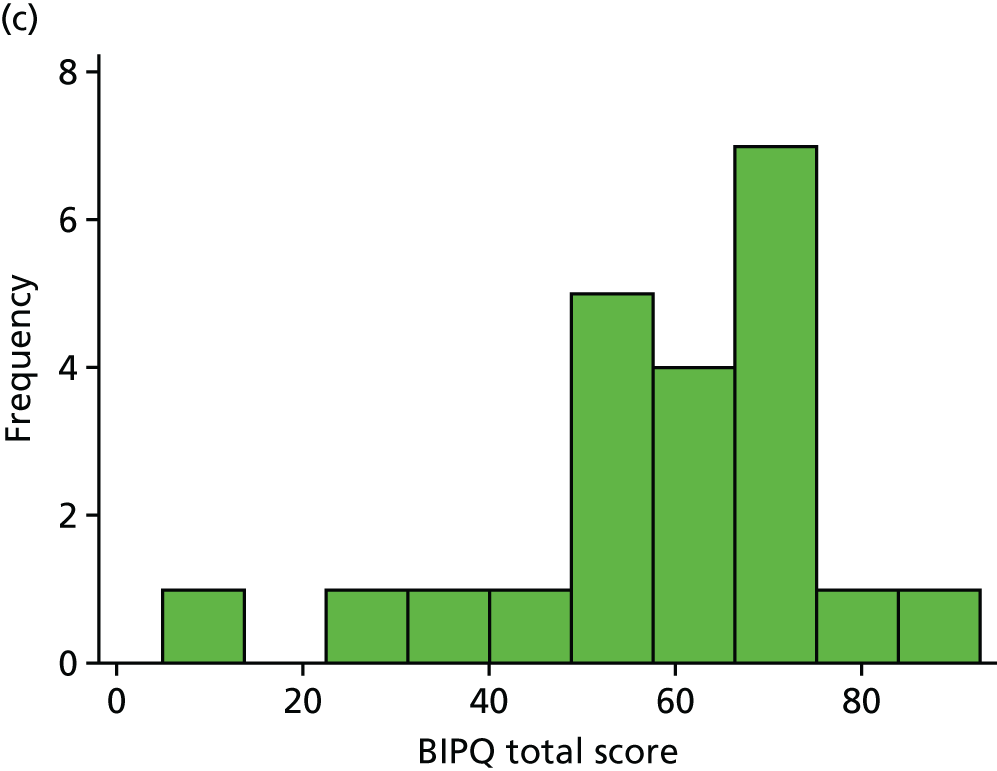
FIGURE 12.
Histograms showing distribution of all appropriate outcome measures: key workers.
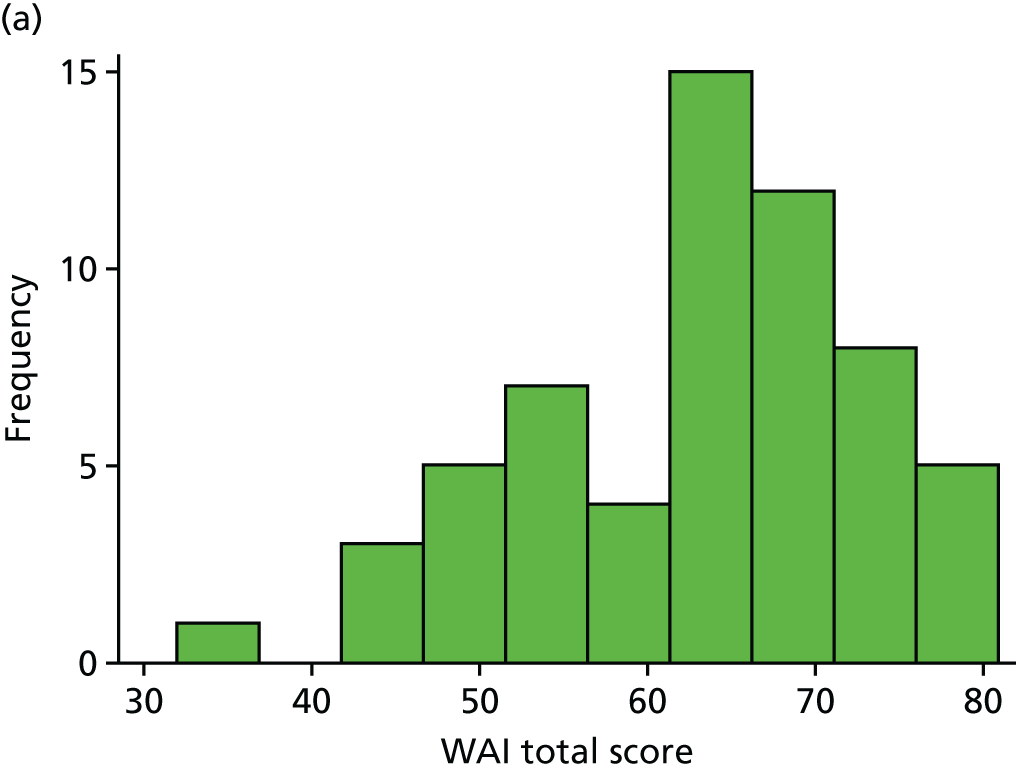
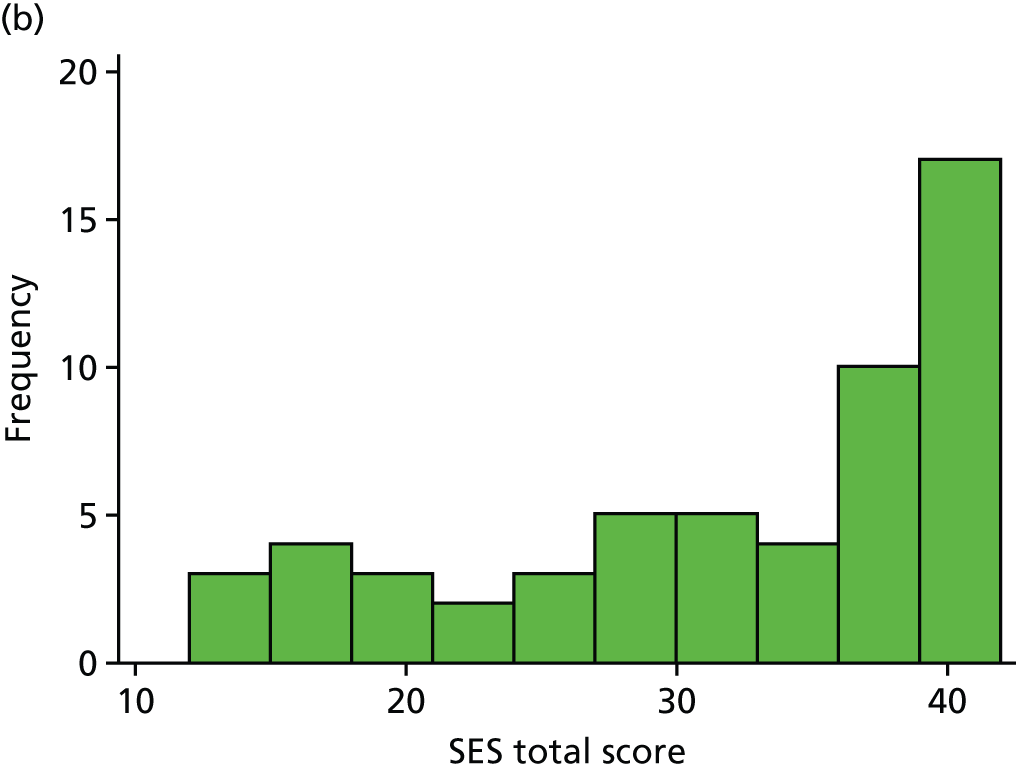
List of abbreviations
- ACMHS
- African & Caribbean Mental Health Services
- A level
- Advanced level
- BFM
- behavioural family management
- BIPQ
- Brief Illness Perception Questionnaire
- BME
- Black and minority ethnic
- CaFI
- Culturally adapted Family Intervention
- CaKAP
- Culturally adapted Knowledge about Psychosis
- CBT
- cognitive–behavioural therapy
- CC
- care co-ordinator
- CI
- confidence interval
- CMHT
- Community Mental Health Team
- CONSORT
- Consolidated Standards of Reporting Trials
- CRN
- Clinical Research Network
- CSO
- clinical studies officer
- CTO
- community treatment order
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- EIS
- Early Intervention Services
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FI
- family intervention
- FIPAS
- Family Interventions in Psychosis-Adherence Scale
- FSM
- family support member
- GCSE
- General Certificate of Secondary Education
- GHQ
- General Health Questionnaire
- GMW
- Greater Manchester West NHS Foundation Trust
- ICC
- intraclass correlation coefficient
- ICD-10
- International Classification of Diseases, Tenth Edition
- IMR
- illness management and recovery
- IPT
- integrated psychological therapy
- KAP
- Knowledge About Psychosis
- KAPI
- Knowledge About Psychosis Interview
- KASI
- Knowledge About Schizophrenia Interview
- MCTd
- metacognitive therapy for delusions
- MHSCT
- Manchester Mental Health and Social Care NHS Trust
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OT
- occupational therapist
- PANSS
- Positive and Negative Syndrome Scale
- PCS
- Perceived Criticism Scale
- PI
- principal investigator
- PIS
- participant information sheet
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PSP
- Personal and Social Performance Scale
- RA
- research assistant
- RAG
- Research Advisory Group
- RCT
- randomised controlled trial
- R&D
- research and development
- RMG
- Research Management Group
- RMN
- registered mental health nurse
- RPM
- research project manager
- SD
- standard deviation
- SES
- Service Engagement Scale
- SMART
- Specific, Measurable, Achievable, Realistic and Timely
- SMI
- severe mental illness
- SSC
- Study Steering Committee
- SST
- social skills training
- TP1
- time point 1
- TP2
- time point 2
- WAI
- Working Alliance Inventory
