Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/194/20. The contractual start date was in April 2016. The final report began editorial review in October 2017 and was accepted for publication in March 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
At the time of receiving funding for this project, Jo Rycroft-Malone was the Director of the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme and a member of the NIHR Journals Library Board. Christopher Burton was a member of the HSDR Commissioning Board during the project funding stage.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Burton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction and background
Ensuring patient safety and the delivery of good-quality care within the NHS in the UK is a political and societal imperative. Effective staffing levels are associated with improved patient outcomes. 1 The Francis report highlighted the detrimental impacts of low staffing within the Mid Staffordshire NHS Foundation Trust. 2 Further reviews into quality and safety within NHS England set out the requirements for appropriate levels of staffing and the need for transparency of reporting and clear pathways for action where deficits occur. 3,4 Ensuring the right staff, with the right skills, in the right place was an action area in the nursing, midwifery and care staff vision for health Compassion in Practice,5 with expectations for getting staffing right set out by the National Quality Board (NQB) framework in 2013. 6 This was updated in 2016,7 following the National Institute for Health and Care Excellence (NICE)’s staffing guidelines in adult inpatient and maternity settings8,9 and the Carter report,10 which called for standardisation in the approaches to managing staffing deployment and the recommendation of care hours per patient day (CHPPD) for consistency of recording and evaluating data.
Workforce planning and deployment tools and technologies (WPTs) are available to support NHS managers in their decision-making and oversight of staffing. These technologies generally employ top-down (e.g. benchmarking), bottom-up (e.g. modelling) or consensus approaches, which are reliant on judgement. 11 Compassion in Practice5 and the NQB guidance7 both refer to the importance of using evidence-based workforce tools for sensitive workforce measures and indicators of quality, safety and productivity, such as the Safer Nursing Care tool,12 the integrated Patient Acuity Monitoring Systems, HealthRoster, SafeCare (Allocate) and the Establishment Genie tool,13 which are all endorsed by NICE. The importance of developing local good-quality dashboards, which provide real-time staffing-related data, is also emphasised. 7,10 Lord Carter noted that digital systems, such as electronic rostering systems (e-rosters) and electronic staff records, are underinvested in. 10 He recommended that cultural change and communication plans are utilised to resolve underlying process or policy issues related to integrating WPTs within organisations. 10 In addition, WPTs need to be used in conjunction with the application of professional judgement, to interpret data, take account of context and patient needs and make informed decisions on day-to-day skill mix requirements. 7 The implementation of WPTs is therefore shaped through the capabilities, capacities and local knowledge of NHS managers. WPTs can provide good-quality data on the nursing workforce, which is vital for planning and deployment;14 however, there are many challenges.
Nurse staffing is an area of high cost in the NHS, reported as being £18.8B in 2014–15,15 particularly with the high demand for nursing and the accompanying increasing agency care costs since the Francis report. 10 Nurse staffing shortages are usually cyclical; 11 however, the current situation appears to be more entrenched, hampered by economic crisis, austerity and barriers to migration. 16 Potentially, recruitment may be further inhibited with the approaching exit of the UK from the European Union. The Health Foundation highlights how one in three new nurse registrations in 2013–14 were of nurses from European Union countries. 17 In addition, the workforce is ageing, bringing the prospect of further losses as a result of retirement rates. 18 The loss of the bursary in England for student education may further affect the already high attrition rates, with a 23% drop in university applications for 2017. 19 This crisis in staffing is set against the backdrop of increasing demands being placed on the NHS and changing patient and rising public expectations. 20
Matching staffing resources and patient needs
Workforce planning and deployment tools and technologies can support NHS managers to match nursing staff to patient requirement, in order to facilitate safe care. Safety is one dimension of good professional practice that is inextricably linked to good-quality care. 21
Having sufficient staff has an intuitive appeal for a positive impact on quality, and evidence does suggest that appropriate staffing is linked to good-quality patient care. 22 This is underpinned by the findings of Ball et al. 23 that 74% of registered nurses (RNs) reported care being left undone on their last shift, which was halved when the RN cared for six or fewer patients, compared with those who cared for 10 or more patients. Some of the evidence indicates that patient outcomes are compromised when there is a reduction in nurse-to-patient ratios, with adverse outcomes in nurse-sensitive indicators. 24,25 Having lower levels of RNs does adversely affect various quality outcomes, for example medication errors and wound infections. 24 Trinier26 noted a statistically significant association between nursing workload hours and patient care errors in paediatric critical care; evidence also suggests that lower staffing levels in the emergency department are associated with patients leaving without being seen and reduced care time. 27 The literature review of 35 studies by Griffiths et al. 28 found mixed evidence on RN staffing numbers for hospital-acquired infections and pressure ulcers, but clear evidence on the positive impact of staffing numbers for reducing falls and length of stay. However the authors commented that, as the analysis in these studies was mainly cross-sectional, no causal inference can be drawn. 28 An evidence review on nurse staffing levels, quality and outcomes of care in NHS hospitals concluded that lower nurse staffing levels are associated with worse patient outcomes in general acute wards and some patient groups; however, the identification of a threshold for safe staffing was difficult, with significant differences noted only when comparisons were made between the best-staffed wards and the worst-staffed wards. 29
Clinical areas with higher nurse staffing levels demonstrate lower patient mortality rates. 25,28,30,31 A systematic review by Kane et al. 25 found that the death rate decreased by 1.98% for every additional total nurse hour per patient day [95% confidence interval (CI) 0.96% to 3%], although this did not significantly change the mortality rate. The effect size for every additional full-time equivalent of a RN per patient day was far greater in surgical patients; the relative risk reduction in mortality was 16% for surgical patients compared with 9% for patients in the intensive care unit (ICU). A further study also found that an increase in nursing workload increased the likelihood of patient mortality within 30 days of admission by 7% [odds ratio (OR) = 1.068%, 95% CI 1.031% to 1.106%]. 32 In their systematic review of 50 studies, Kitson et al. 22 affirmed a clinical and statistical association between increased registered nurse staffing resources and better patient outcomes.
A diluted skill mix may compromise quality outcomes. Kitson et al. 22 suggest that increased RN numbers compared with increased numbers of less-qualified staff decrease the number of adverse events. A further study concluded that a richer RN skill mix may reduce the number of several types of adverse event, including failure to rescue. 33 Griffiths et al. 34 found that lower numbers of health-care support worker (HCSW) staffing were associated with lower mortality rates (risk ratio 0.95, 95% CI 0.91 to 1.00; p = 0.0). Within the Australian context, investigations on nursing care hours per day have not addressed skill mix issues;35 although McGillis Hall et al. 24 found that fewer RNs in the skill mix used more nursing hours. Furthermore, Ball et al. 36 found no impact of HCSW staffing on care left undone in England, and this trend was also noted in Sweden, with little effect being found from HCSW staffing on missed nursing care compared with increasing RN numbers. 23 Although this study did note the contextual difference, with 31% of direct care being provided by English nurses compared with 19% being provided by Swedish nurses, Ball et al. 23 concluded that:
If missed care is regarded as an inverse measure of productivity, it is unlikely that substitution would be an efficient approach to reducing it because the marginal gains from increased RN staffing are so much higher than for assistants.
Ball et al. 23
The Australian Nursing Federation goes further, highlighting that catastrophic and expensive problems can accrue from reducing the proportions of the most highly educated nurses in health-care settings. 37
Griffiths et al. 1 highlighted that, although there are plans in England to increase the number of unregistered support workers, research does not support HCSW staffing as a substitute for RNs. In England, the new associate nurse role may have an impact on skill mix, although its effect has yet to be evaluated. NHS England advises ‘temperature checks’ to assess any changes in RN contact time and their impact on patients, with changes in skill mix being one indicator of this. 38 Certainly, WPTs are a means of determining staffing and skill mix levels and the impact of these on patient outcomes.
Although there appears to be convincing evidence for the positive effects of RN levels and skill mix on patient care quality and safety outcomes, Griffiths et al. 1 highlight that there is a lack of high-quality studies on outcomes in relation to staffing. Furthermore, evidence suggests that nursing sensitivity indicators that are used to measure quality outcomes lack consistency, and variability in the measurement of unfinished care can have an adverse impact on the transferability of findings. 39–41 Kitson et al. 22 recommended the development of standardised metrics. Studies often focus on negative outcomes or adverse events (e.g. falls) rather than positive issues or process measures, such as adherence to care pathways or communication. 39 In addition, there may be discrepancies between staffing data and real-time staffing. 1 However, it is important to note that WPTs can play an important role in the standardisation of staffing data for effective evaluation and benchmarking.
Although patient outcomes appear to be linked to levels of nurse staffing, the evidence may fail to account for confounding variables, such as medical care, geography, the use of temporary staff and other factors. The presence of medical staff appears to be an important factor. Griffiths et al. 34 found that RN levels were significantly associated with reduced mortality rates for medical patients; there was also a significant positive relationship between patient outcomes and the numbers of doctors, although the levels of HCSW staffing had no benefits for patient mortality. 34 The availability of medical and nursing staff increased survival rates in critical care. 30 Furthermore, skill mix may be related not only to RN levels, but also to the qualities and capabilities of a nurse and their educational levels and work patterns. This information can be available for the NHS manager through WPTs. In addition, WPTs can convey data on temporary staffing. This may be the organisation’s own employees (bank) or external staff (agency), or those doing overtime. Float nurses move between clinical areas to cover staffing shortfalls. Temporary nurses may not have the skills and knowledge required for the assigned clinical area, but poor perceptions of agency nurses in relation to good-quality care may be unfounded. 42,43 Dall’Ora and Griffiths44 found mixed evidence for temporary staff, overtime and floating, with little evidence being specific to UK settings; some evidence suggests possible risks with temporary staffing, whereas other studies suggest that temporary staffing may compensate for nurse deficiencies, although effectiveness may be compromised and this would come at a higher cost. 44 Float pools may decrease overtime costs and reduce agency costs, but the economic evidence is limited. 44
Nurses’ education levels and hours worked also appear to influence the quality of care. Higher proportions of nurses with a bachelor’s degree appear to reduce the effect of low nurse staffing levels on clinical care left undone;45 similarly, graduate nurses improve patient outcomes (this was found in surgical patients aged > 50 years, in 300 settings in nine European countries). 32 However, an increased use of overtime is associated with adverse patient outcomes. 44 An evidence review on 12-hour shifts found an established link between adverse patient and staff well-being and increased daily and weekly working hours. 46 A recent study also found that nurses associated shifts of > 12 hours with poor ratings of the quality care and higher ratings of care left undone. 47 WPTs can establish ‘rules’ for working hours and highlight infringements to help the NHS manager deploy effectively.
The care environment and safe staffing
Organisational characteristics, the clinical environment, patient requirements and models of staffing appear to influence safe staffing and patient outcomes. Nurse staffing can have different effects in different hospital settings, so the effect of an additional nursing hour may have dissimilar effects. 48 Patient and hospital characteristics, including the hospital’s commitment to the quality of medical care, are likely to be contributing factors to patient outcomes, with surgical patients being the most sensitive to nurse staffing and the most likely to have improved outcomes as staffing levels and skill mix improve. 48 Ball et al. 23 note the differences in the RN role, which varies with context, commenting that:
A complex set of inter-related factors are associated with care left undone.
Ball et al. 23
Organisational factors also seem to influence the impact of staffing levels. A review of management approaches to staffing found that the presence of supervisory roles and training improved both patient and staff outcomes, as did organisational factors associated with Magnet programmes. 49 Magnet status is associated with transformational leadership, empowerment, professional practice, innovations and improvements. 49 Certainly, strong and clear clinical leadership is an expectation for high-quality care in relation to staffing. 7 A systematic review on models for staffing hospital units found that the introduction of specialist nurses and support may improve patient outcomes and certain models of nursing care, such as primary care and self-scheduling, may improve staff-related outcomes. 50 The impact of WPTs may also be contingent on organisational factors, which may have an impact on their implementation.
Contextual factors, such as hospital location, have an impact on staffing; after controlling for patient care unit type, hospital complexity and unit bed size, Kane et al. 25 found that hospitals located in areas with a lower RN supply employ fewer RNs and more second-level RNs. 25 RN staffing levels decrease as the supply of RNs in the surrounding geographic area decreases. 51 Hurst52 compared patient outcomes with ward layout, finding that the level of direct patient care was higher in Nightingale wards (for which there were higher quality scores), but that it was ‘racetrack’ wards, with a central nursing station, that were the most effective for nurse and patient outcomes. Bay wards could generate heavier workloads, with peaks and troughs of staff presence. 52
The evidence on the impact of nurse staffing has a focus on acute adult care, with evidence for safe staffing in other areas still emerging. The evidence on staffing levels and outcomes for mental health nursing is contradictory and complicated by the day-to-day allocation of staff resources to wards with more seriously ill patients. 53 A review on safe staffing and mental health further highlighted that there were no robust empirical studies to underpin policy for the complex issue of safe staffing in this area. 54 Likewise, recent reviews have also concluded that there is no substantive evidence to guide staffing in learning disabilities or caseload management in the community;55,56 safe staffing in care homes also lacks robust evidence. 57
Safe staffing and cost-effectiveness
Reports and guidance highlight the importance of making the best use of resources for financial sustainability, through efficient staff deployment and minimising agency use. 7,10 WPTs have an important role in budget management, through the potential articulation of staffing costs and spending requirements. Despite the potential for decreased costs resulting from improved patient outcomes, there appears to be cost implications for a richer RN mix. Wage growth for RNs in California, after mandated staffing levels, increased more than in other states, although the impact of the nurse shortage was proposed as one alternative explanation for the increase. 58 One review analysed four cost–benefit studies and five cost-effectiveness studies and found mixed results, and so was unable to draw conclusions around whether or not changing staffing levels and/or skill mix was a cost-effective intervention. 59 Griffiths et al. 28 reviewed five non-UK studies, finding inconsistencies in outcome and nurse staffing measures, with some of the secondary data analysis hampering the conclusions. One American study that was reviewed modelled scenarios to demonstrate that raising the number of RN nursing hours without increasing the total number of nursing hours may lead to net savings as a result of improved patient outcomes. 60 However, Griffiths et al. 28 noted that increasing nursing staffing costs may not be offset by better patient or system outcomes and concluded that the studies reviewed were of limited value for decision-making in the NHS.
Staff satisfaction
NHS Providers indicate that growing demand in NHS England and staff shortages mean that NHS roles are becoming more pressured, with staff being increasingly overworked and stressed. After surveying chief executives, it found that 55% indicated that they were worried that their trusts did not have the right numbers, quality and mix of staff to deliver high-quality care, and that most expect the situation to deteriorate. 61 Given that nurses constitute the majority of the workforce, this has implications for nurse well-being and, importantly, organisational recruitment and retention. When nurses are more satisfied with their working environment, they appear to be less likely to leave, which has a positive impact on staffing levels. Nurse satisfaction appears to be linked to perceptions of safe staffing levels; acute care hospital nurses link higher staffing levels to better patient safety. 62 Nurses also report being able to act as safe practitioners on the days when there are lower patient-to-nurse ratios (p = 0.011). 63
Conversely, when nursing staff are dissatisfied, they are more likely to leave organisations or have more absences from work, which further contributes to existing staffing deficits. The RN4CAST study surveyed nurses from 10 countries and found that nurse dissatisfaction and an intention to leave their job were linked to perceptions of inadequate nurse staffing, high patient-to-nurse ratios and quality and safety issues. 64 Staff dissatisfaction was also apparent when nurses felt that staffing levels were insufficient to produce good-quality care and that there was a lack of opportunity for their development. 65 A low level of occupational satisfaction has been linked to the rationing of care (because of limited resources, such as time, staffing or skill mix); this affects the perceptions of the quality of care that nurses could offer patients. 66 Poor perceptions of the workplace culture were also found to create dissatisfaction, particularly when associated with negative attitudes towards nursing management. 67
Workforce flexibility is important; WPTs can facilitate the identification of staffing resources across the organisation, enabling NHS managers to use their professional judgement to move staff when there are staffing shortages. When nurses are required to float to other areas, this may cause them dissatisfaction. Nurses can perceive that they lack the appropriate knowledge and skills for effective patient care. 68 Dziuba-Ellis68 argued that nurses should be competent to float to similar clinical areas and should be supported to do so. Shift patterns and allocation may also be another source of nurse dissatisfaction. Dall’Ora and Griffiths46 found evidence of risks to staff well-being with working long hours, both daily and weekly, with potentially reduced efficiency on longer shifts. They conclude that, although some staff members prefer 12-hour shifts, the net effect on nurse retention is unclear and there is no economic evidence of the consequences of 12-hour shifts. They recommended that staff should be encouraged to take planned breaks and suggested that fixed shift patterns may reduce risks and improve patient safety.
Increased work pressure from staff shortages, sickness and absences has been described as a downwards spiral, as the remaining nurses come under more pressure and are more likely to leave. 11 The intention of nurses to leave is particularly linked to burnout. 64 Retention and recruitment strategies to ensure nurse satisfaction, linked to career development, are vital components to improve nurse staffing. 7 Increasing staffing levels can have a positive effect; when nurses’ workloads adhered to the California-mandated ratios, the level of nurses’ job dissatisfaction was lower and they reported consistently better quality of care. 69 The creation of supportive environments and the engagement of nursing staff are recommended. 67 Nursing staff had more positive perceptions when they worked in areas that enabled participation in hospital affairs, with good leadership and nurse–physician relationships; positive perceptions of the work environment were linked to a 30% reduction in the intention to leave (OR = 0.57, 95% CI 0.53 to 0.63). 64 It is important that RNs work in an environment in which they feel safe and confident when providing care. 62 Acute organisations with Magnet characteristics were associated with supportive environments and had increased levels of nurse satisfaction and retention compared with other organisations. 49,70 However, financial constraints have the potential for worsening nurses’ level of dissatisfaction, linked to pay. Between 2010–11 and 2020–21, the pay of NHS staff will have declined in real terms by at least 12%. 17 In addition, the Health Foundation points to a lack of a coherent workforce strategy with regard to the integration of funding plans and service delivery models, instead citing piecemeal policy-making on pay and the use of the nursing workforce. 17
Patient and public experience
NHS Providers are required to actively seek the views of patients, carers and staff to determine the impact of their staffing policies, in order to understand the links between staffing and patient experiences and outcomes. 7 Nurse staffing levels and skill mix do appear to have an impact on patient experience, particularly in the hospital setting. Patient care experience is reported to be better in hospitals with a higher level of nurse staffing and a more favourable work environment, in which less clinical care is left undone. 45 Higher levels of rationing care decreased the odds of patient satisfaction (OR = 0.276, 95% CI 0.113 to 0.675). 71 Recent high-profile failures linked to staffing may have implications for patients’ perceptions of their safety associated with safe staffing. The inability to summon staff, owing to a lack of staff presence, made patients feel unsafe in the clinical environment; this was linked to perceptions that the area was short-staffed. 72 Evidence also suggests that the public is concerned about the dilution of skills; for example, the Patients Association in response to the Safe Nurse Staffing Levels (Wales) Bill highlighted concerns about an imbalance between the substitution of health-care assistants for registered nurses in care delivery. 73
Openness has been a major theme of recent policy reform in England, following a lack of transparency and secrecy in recent high-profile failures. This requirement for openness links to staffing levels. 74 Trusts have a legal duty of candour under the Health and Social Care Act regulations75 and are required by NHS England and the Care Quality Commission to display actual staff levels against planned levels outside wards. 76 Staffing levels can therefore be compared between organisations and publicly scrutinised, and WPTs can provide the staffing data required for comparison. However, there is concern that the methods of comparison, such as league tables, may focus on appearance rather than improvement. 74 It is unclear how staffing data will have an impact on public confidence and patient experience.
Legislation, policy and guidance
Safe staffing is a legislative requirement under the Health and Social Care Act regulations75 and one of the fundamental standards of quality and safety monitored and reported on by the Care Quality Commission. However, there is a lack of consensus about whether legislation, mandates within policy or guidance are the best means of ensuring safe staffing levels. Even within the devolved UK nations, there are different approaches; to date, only in Wales has legislation been adopted, with the Nurse Staffing Levels (Wales) Act 2016. 77 Scotland aims to enact similar legislation. 78
A key point of contention is in mandating nurse-to-patient ratios. The Royal College of Nursing has called for mandated staffing levels. 79 However, although Griffiths et al. 1 acknowledge that many sources of evidence suggest that policies are effective in increasing staffing levels, they also state that:
It is difficult to make direct conclusions about the impact of mandatory staffing policies because of the complex inter relationship between changes in staffing levels and system wide changes including patient case mix and other safety initiatives.
Griffiths et al. 1
Compliance with mandated nurse-to-patient ratios in California did appear to have some impact on preventing adverse patient events. 80 However, the Californian nurse-to-patient ratios did not account for nurse competency, and mandated levels also brought unanticipated effects, such as the increased length of emergency department waits, as nursing staff were called in when patient numbers increased. 80 It was suggested that the richer skill mix with mandated ratios reduced the level of appropriate task delegation to support workers. 80 However, there was no evidence that reductions in the number of support workers increased nurses’ workloads in California. 69 The increased use of agencies to fulfil legislative requirements has been found to affect care continuity, which may present an increased patient risk. 81 Furthermore, mandated nurse levels may increase agency costs. In England, since 2016, Monitor for the NHS Improvement programme has placed mandatory caps on agency pay, but evidence suggests that trusts are exceeding this cap. 82
Given the lack of clarity on mandated nurse-to-patient ratios, countries within the UK have explored other means of achieving evidence-based safe staffing through policy and guidance. NICE produced guidance on adult inpatient wards and midwifery. 8,9 The NQB and NHS Improvement 2016 guidance also focused on adult inpatient care. 83 Guidance on learning disabilities, mental health and adult community nursing services is in consultation. 84–86 Although NICE guidance on adult safe staffing8 identified that a threshold of more than eight patients per nurse was linked to increased patient risk, there was a recognition that no one nursing staff-to-patient ratio can be applied across the whole range of wards to assure patient safety.
Following Lord Carter’s recommendations,10 England has adopted nursing CHPPD to identify the number of staff required and staff availability in relation to the number of patients. It is calculated by adding RN hours to HCSW hours and dividing the total by every 24 hours of inpatient admissions; this is a more flexible approach to respond to patient demand in different settings, because, although an average of 9.1 hours of care is provided by RNs and HCSWs per patient day, this figure varies from 6.33 to 15.48 hours. 10 Similar approaches to nursing hours per day have been used in Western Australia, New Zealand and South Africa, with some success. 7 Kane et al. 25 found that this approach did reflect the average level of staffing across a 24-hour period, but did not reflect fluctuations in patient census and scheduling patterns in different shifts; in addition, it did not account for other nursing activities, such as meetings and administration. 25 Northern Ireland also adopted a non-prescriptive approach, with a focus on staffing ranges associated with specific environments, while allowing for a flexible approach to a range of factors, such as absence or sick leave. 87 Scotland uses the Nursing and Midwifery Workload and Workforce Planning Toolkit, which has evolved from a whole-systems approach to developing and testing nurse staffing tools, based on triangulation using professional judgement and local indicators of quality. 88 Wales is following a similar route to develop tools to support the implementation of the Nurse Staffing Levels (Wales) Act 2016. 77
The Health Foundation commented that the guidance in England is a relatively ‘light touch’ in comparison with developments in other countries. 89 In England, the NQB7 supports a triangulated approach to staffing decisions to ensure that the right staff with the right skills are at the right place and point in time. This approach is based on patients’ needs, acuity and risks, which should be monitored to provide appropriate judgements about delivering safe, sustainable and productive staffing. A core component of the expectation of having the right staff is evidence-based WPTs integrated with professional judgement and real-time information on skill mix, staff competencies and staff availability. NHS providers are required to display actual staffing levels against planned staffing levels outside wards, in addition to publishing data comparing actual staffing levels with planned staffing levels, with 6-monthly staffing establishment reviews. 76 Therefore, the accurate measurement of real-time and prospective staffing is essential; data will also be benchmarked against that of other organisations. WPTs are therefore central to the process of measurement, data transparency and decision-making for the achievement of safe staffing in the UK.
Workforce planning and deployment tools and technologies
Workforce planning and deployment tools and technologies can capture data for comparison and enable the transparency of resources and requirements, in addition to modelling solutions to enhance decisions on safe staffing. The Health Foundation indicated that multiple approaches have been used for determining staff levels in NHS trusts, some locally developed and others developed using proprietary systems or professional judgement; however, there has been no recent evaluation of the effectiveness of these approaches or practitioners’ perceptions of them. 90 Tools also need to be aligned with rostering and matched to staff availability in order to be effective. 90
The National Institute for Health and Care Excellence has endorsed staffing tools and recommends resources to support senior nurses to review, plan and budget staffing on adult inpatient wards. The NQB emphasised the need to have an agreed local quality dashboard to triangulate comparative data on staffing, skill mix and other quality metrics; this dashboard should have CHPPD. 7 WPTs can therefore provide data to contribute to benchmarking and the evaluation of organisational outcomes. However, Griffiths et al. 1 suggested that the evidence is unclear on the use of tools to match nurse staffing levels to individually assessed patient needs. Furthermore, the use of modelling technology to aid with the decision process and prediction of staffing need may also require further clarity; modelling studies on the floating of temporary staff to develop solutions have produced mixed results. 44
Most WPTs in NHS England are designed for use in acute care settings. Tools for community caseloads have been developed that are context specific, but their effectiveness is yet to be substantiated. 56 There is also a lack of evidence for the effectiveness of WPTs in learning disabilities and in care-home settings. 55,57 The Health Foundation suggests that more evidence is required on both the effectiveness and the use of tools. 90 They indicate that the fragmented evidence from the English NHS is able neither to provide a solid platform on which to base any universal approach to determining nurse staffing, nor even to indicate best practice in the use of available tools in many care settings. 90
Buchan et al. ,17 also for the Health Foundation, advocated the use of technology to support local decision-making, but emphasised that tools can be effective only if staff fully understand their use and are able to respond to live data; they linked this to empowering people to make staffing decisions, but highlighted the need for training and development. 17
Summary
In the wake of high-profile reviews of breakdowns in health-care quality and evidence that links nurse staffing with patient safety outcomes, delivering safe staffing is a political and professional imperative. A wide range of WPTs are available to support NHS managers to link staffing resources to patient and service demands. The application of these WPTs, in combination with professional judgement, appears to promote effective staffing, principally by providing predictions and rules about staffing requirements in relation to patient need. However, these are one part of a complex system of organisational and other work associated with delivering safe staffing. There are many influences on the system for good-quality care delivery and NHS managers have to make difficult decisions amid multiple demands within limited time frames. Understanding how managers can use WPTs successfully in this system, including the influences on implementation and the impacts on patients and staffing, is therefore an important area for research. This synthesis aims to summarise what is known about how WPTs can support NHS managers’ staffing work. Through ongoing stakeholder engagement, it will be ensured that what is known is contextualised within the systems and policy context shaping this issue within the NHS.
Review question and aims
This evidence synthesis has engaged stakeholders to produce an evidence-based realist programme theory that explains the successful implementation and impact of nursing WPTs by NHS managers. This programme theory will complement the evidence base about the validity and reliability of WPTs and guide the development of management training programmes and implementation.
The research question asked the following: ‘NHS managers’ use of workforce planning and deployment technologies and their impacts on nursing staffing and patient care: what works, for whom, how and in what circumstances?’
The main objectives of the study were to:
-
identify the different WPTs used to deploy the nursing workforce, paying attention to the ways in which these are assumed and observed to work
-
explore the range of observed impacts of these technologies in different health-care settings and other public services, paying attention to contingent factors
-
investigate ways that can help NHS managers to identify, deploy and evaluate the nursing workforce resource in order to have the greatest impact on patient care
-
generate actionable recommendations for management practice and organisational strategy
-
contribute to a wider understanding of the nature of the nursing workforce, nursing work and the quality of patient care.
Chapter 2 Methods
Introduction
The methods used for the evidence synthesis drew on the team’s previous experience of realist synthesis89,91 and adhered to established realist principles and publication standards. 92,93 The synthesis followed four phases, but, unlike the linear process of the traditional systematic review, a realist synthesis adopts a more iterative process because it is theory driven. In this synthesis, as the programme theory emerged from the review of the literature and stakeholder involvement, the search process went back and forth to further develop and refine the programme theory. This meant that there were some intersecting elements within the four phases of the study. This chapter captures the iterative processes that guided the realist synthesis by offering detailed descriptions of the areas of evidence from stakeholders and literature and interview data. The Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) publication standards for realist review have been used to structure the report. 93
Stakeholder engagement, including patient and public involvement
Stakeholder engagement is integral in realist work. The realist synthesis approach is based on negotiation between stakeholders and reviewers to develop the programme theory of the area for review; as such, stakeholder engagement is a key component. 94 For this review, stakeholder engagement was designed to help the research team to elaborate on review context, inform the programme theory development and interpretation and advise on the dissemination of findings. The review team followed a recognised systematic approach to stakeholder identification to ensure that the most appropriate people were contributing to the synthesis. 95 Stakeholders comprised NHS managers, RNs and patient and public involvement (PPI); in addition, the review team referred to an advisory group.
The NHS managers contributed multiple perspectives on nurse staffing, as their roles included nurses at the strategic level, directors of nursing, lead nurses, matrons, ward managers and team leaders. Engagement with this group helped to illuminate key concepts within the system of nurse workforce planning and deployment and refine the development of programme theories. The group members also offered information on the use of WPTs. The study engaged with members of the public, patients and carers. One PPI representative had previous experience in realist synthesis. The impacts of this engagement included the development of the review’s theoretical territory, assessment of the relevance of the context–mechanism–outcome (CMO) threads from a patient perspective and the conceptualisation of impacts that are important to patients, family and carers.
The project advisory group included key senior strategic stakeholders. Many of these stakeholders held a remit for strategy and policy development and had high levels of experience in workforce planning design and delivery within nursing and other health-care spheres. Group membership represented key influential organisations; this included nurse representatives in government from some UK countries, representatives from unions and professional bodies, chief nurses from large health-care organisations and representatives from nurse educational bodies. Group membership also included non-nurse health-care professionals who had expertise in workforce planning, policy and strategy (see Appendix 1). The project advisory group met every 6 months to advise on current strategy, policy, evidence and developments in WPTs. This group received detailed information on the development and progress of the study and offered advice on the dissemination of findings.
Stakeholder engagement was embedded throughout the synthesis as follows:
-
Phase 1 –
-
Two co-production workshops with NHS managers.
-
Two PPI co-production workshops.
-
These workshops (1) sought to establish a detailed understanding of the essential elements surrounding the planning and deployment of nursing staff and (2) aimed to facilitate an understanding of the complex issues that NHS managers have to consider in order to make effective staffing decisions.
-
-
The advisory group meeting sought to expand on understanding of the planning and deployment of nursing staff from a broader, strategic perspective. This meeting guided the team’s understanding of the evidence base for WPTs.
-
Ten semistructured interviews with a purposive sample of NHS managers to expand on themes from co-production workshops and capture variations in workforce planning systems across organisational settings.
-
-
Phase 2 –
-
The Advisory group meeting facilitated prioritisation of programme theory areas and informed and guided the development of CMO configurations.
-
-
Phase 3 –
-
Wechat#WeNurses Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) chat to gather nurse stakeholders’ perspectives.
-
Eleven think-aloud interviews to refine emerging programme theories.
-
A final advisory group meeting to refine the emerging programme theory and advise on the dissemination of findings in October 2017.
-
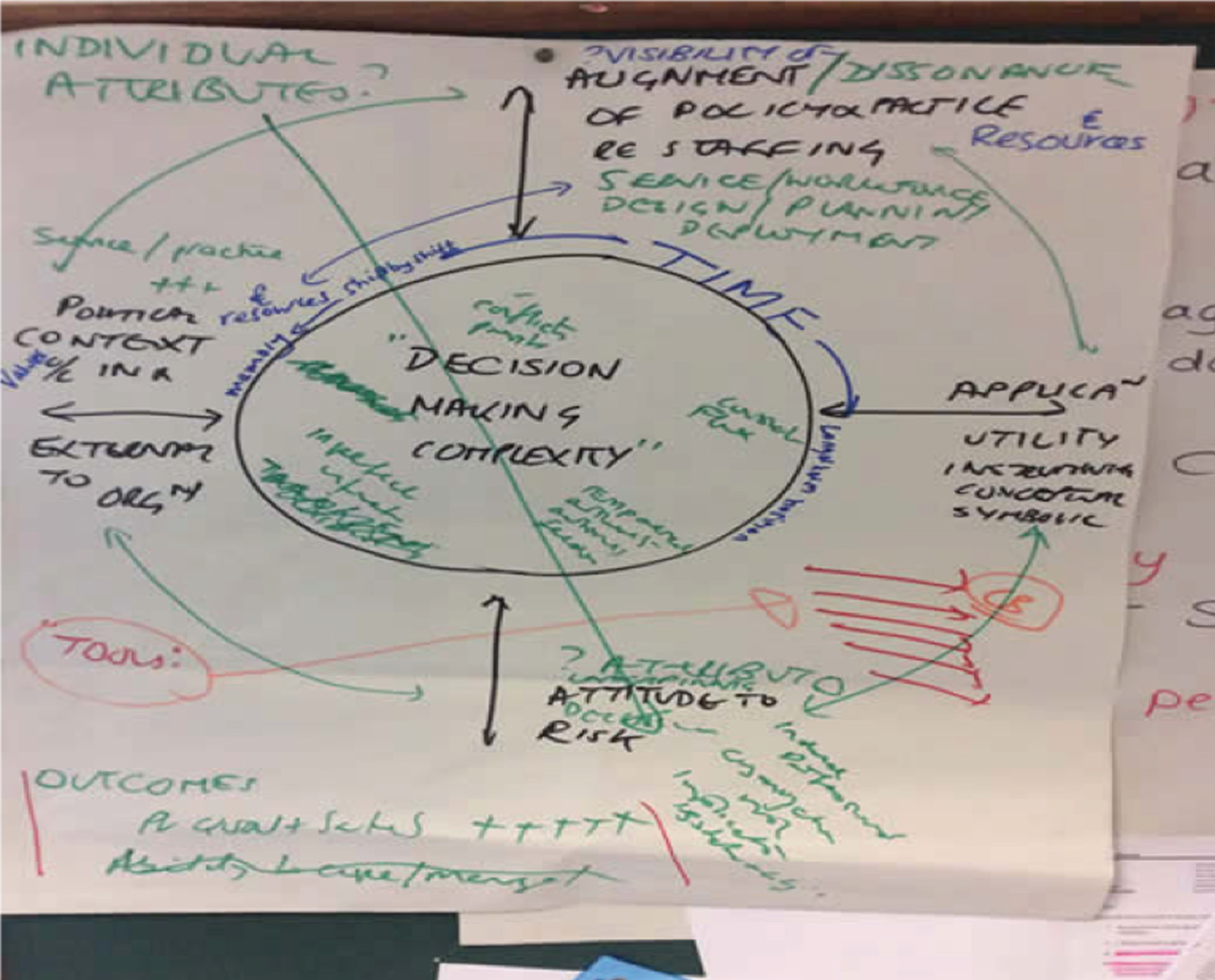
In addition, monthly project team meetings were held. Two PPI representatives accepted an invitation to join the project team, attended the monthly meetings and are co-authors of this report. Supplementary project team meetings were also held. In phase 1, the project team held a theory-building workshop to discuss the initial programme theories, based on the data gathered during the co-production workshops and the exploratory scope of the literature. Figure 1 illustrates the developmental process and formulation of ideas from this workshop. Additional workshops were held for data extraction, analysis and synthesis and to develop the CMO configurations.
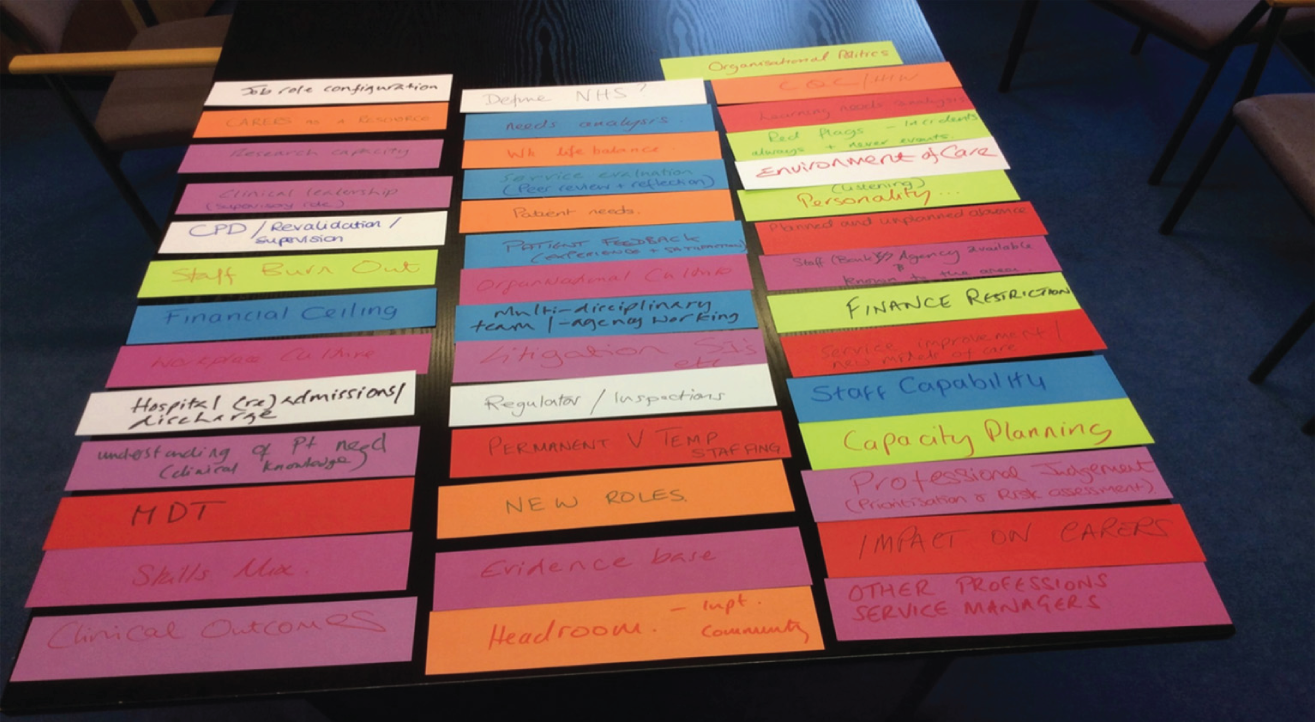
FIGURE 1.
An output from the project team’s theory-building workshop.
Rationale for using realist synthesis
Realist synthesis methodology is a theory-driven approach that draws on a heterogeneous evidence base to establish whether or not interventions work, how, in what contexts and for whom. 94,96 It offers the potential to provide practical solutions to, and/or explanations about, challenging problems and issues.
The system of nurse workforce planning and deployment is dynamic and multifaceted, involving many components and influential stakeholders who often have differing, often conflicting, needs. Workforce planning and deployment occurs in health settings characterised by fluctuating demands and requirements; the implementation, use and impacts of nursing WPTs appear to be complex and contingent on organisational context and managers’ expertise. Adopting a realist synthesis approach enabled the consideration of additional contextual influences on the implementation and impact of WPTs at different levels within the health-care system.
Within this realist synthesis, the analytical task was to construct, test and refine a programme theory of causal explanations about what works about WPTs and how NHS managers can be supported to use them. These causal explanations are expressed as plausible hypotheses or relationships between CMOs to show how certain contexts have triggered mechanisms to generate an observed outcome pattern or not. Therefore, a realist synthesis produces recommendations; for example, in situations (context) a complex intervention modified in this way (mechanism), may be appropriate in achieving x, y, z (outcomes). 97 In this review, theory development work was undertaken in phases 1 and 2 to articulate theories about what aspects of WPTs work, for whom and the conditions that may make these successful.
The study was interested in identifying the full range of the potential impacts of WPTs, which may extend beyond health care. These impacts relate to evidence about workforce (e.g. staff satisfaction) and organisation theories (e.g. organisational learning). Impact was conceptualised as a continuum, ranging from conceptual to instrumental or direct impacts, and therefore from awareness, knowledge and understanding, attitudes and perceptions to changes in behaviour. 98
An initial overview of the theoretical territory was developed, drawing largely on seminal theories and key evidence in relation to workforce planning systems and implementation. This guided the scoping review of the evidence and consultation with stakeholders (Table 1). This theoretical territory provided a provisional (hypothetical) explanation of what works and the impact of WPTs by investigating the literature and evidence from separate but interlinked disciplines, around two theory areas: the elements of workforce planning systems and their implementation. This guided the iterative searches.
|
Workforce planning systems (Theoretical domains that may explain how systems work) |
Implementation (Theoretical domains that may explain how the implementation of systems may be related to impacts) |
|---|---|
|
The identification of patient needs and acuity99,100 The nature of nursing work101 Workforce planning strategies (supply- vs. needs-based)102,103 Contracting and rostering practices33,104–106 Deployment, skill mix and nursing workload tools11 |
Technology adoption109 Professional decision-making and judgement110 Organisational and other contextual influences – structural factors affecting the implementation of learning and practices111–113 Organisational learning and knowledge management114 |
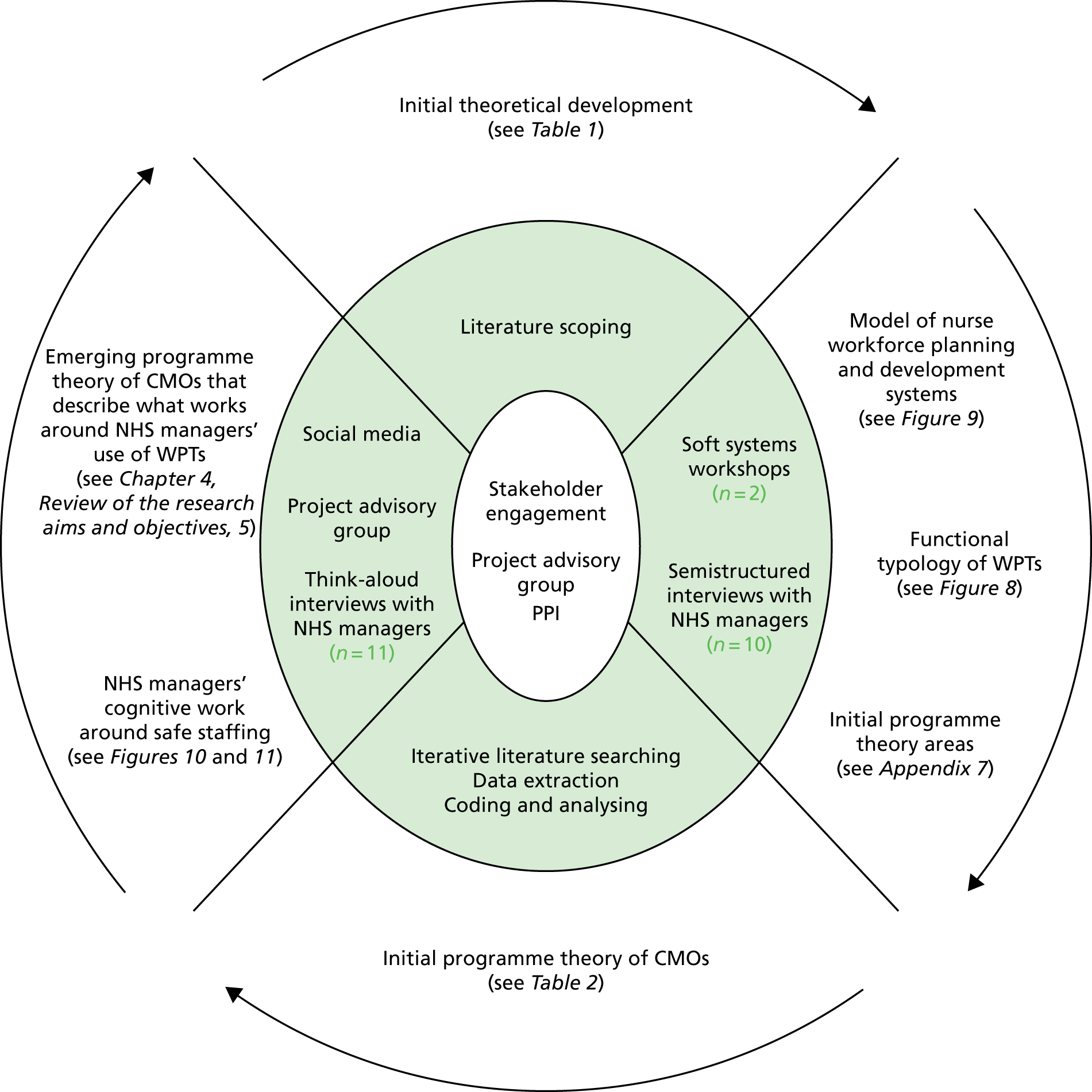
Programme theory development and refinement involved a number of interconnected processes (Figure 2). Figure 2 represents the centrality of stakeholder engagement throughout realist work, whereby stakeholders provided a sense check on the wider political, organisational and professional context of the synthesis, support for the interpretation of findings and advice on the dissemination and knowledge mobilisation activities. In this case, stakeholders included patient and public representatives who provided advice throughout the synthesis, concentrating particularly on the issues of disclosure of staffing to patients and families. Distributed around the core of stakeholder engagement are the methods that were adopted within the synthesis and their associated products. The methods are presented in more traditional sequential phases within this report, but in practice, there was considerable overlap between them.
FIGURE 2.
Synthesis map.
Phase 1: initial programme theory development
This was conducted from April 2016 to December 2016. Programme theory development (i.e. the hypotheses of what works for whom, how and in what context) is fundamental to realist synthesis. Using the theoretical territory as a basis, eight initial theory areas about ‘what works’ were developed with stakeholders through the co-production workshops, semistructured interviews, the advisory group engagement and the scope of the literature.
Initial scope of the literature
To guide the development of the initial programme theory, an exploration of the literature was conducted to help delineate how WPTs are supposed to work in particular contexts and to identify potential barriers to, and enablers of, their successful implementation. The study engaged with an information scientist (BH) with previous experience of realist synthesis, to help clarify the breadth of the resources available to support this synthesis. Scoping searches were conducted between May and September 2016. This scoping involved targeted searches of PubMed, MEDLINE and the Cumulative Index to Nursing and Allied Health Literature (CINAHL), a search for major reviews by The Cochrane Library and NICE and a search of the grey and allied literature included in key areas relevant to the expertise and networks of the research team (e.g. from UK mental health services). In addition, several health human resources and human resource management journals were searched. Further texts were gained from citation tracking. References were drawn on that were cited in the Royal College of Nursing guidance on safe nurse staffing levels in the UK and the Shelford Group Safer Nursing Care tool implementation guidance11,12 and a search was conducted for citations in identified articles via the Web of Science citation indices. Similarly, references were searched from an evidence review completed for NICE, Effectiveness of Management Approaches and Organisational Factors on Nurse Staffing Sensitive Outcomes;49 this resulted in the identification of six key articles that facilitated an understanding of the system complexity for this evidence synthesis. 118–123 Further scoping searches identified a further 11 sources of evidence from the literature. 124–134 Some of this literature was also identified in later targeted searches.
Conceptualising a model of nursing workforce planning and deployment
To illuminate the complexity of the contexts of the systems in which WPTs are used, soft systems methodology was used within the stakeholder co-production workshops. The format of the workshops, guided by soft systems methodology, was designed to understand the systems in which workforce deployment and planning operate through the co-production of a root definition. Soft systems methodology offers an epistemological approach for analysing complex, real-world issues, which may integrate multiple cognitive, social and cultural perspectives. 135 The methodology is appropriate for the examination of implementation challenges. 136 In addition, it is compatible with a realist approach for mapping complex programmes. 137 This approach accepts that issues that surround complex interventions and their implementation may be contested because of multiple stakeholder perspectives, which makes sense-making difficult. The relationship and synergy between people, systems, WPTs and resources around nurse workforce planning and deployment, can therefore be described as a soft, human adaptive system, which is open to differing perspectives and values about its purpose and impact. Data were explored using the six dimensions of a soft system (worldview, transformation, customers, owners, environment and actors), culminating in a narrative of the system of nurse workforce planning and deployment.
The two co-production workshops with NHS managers comprised a purposive sample of, in one case, 14 participants and, in the other, 17 participants from across NHS organisations and professional bodies within the UK, and combined a range of discussion and practical activities. Using techniques from LEGO® SERIOUS PLAY® (The LEGO Group, Billund, Denmark), individual models of the system of workforce planning and deployment of nurse staffing were constructed and important aspects from each individual model were then combined to create one overall collaborative nurse workforce planning and deployment model. Participants were required to offer explanatory accounts of the components they brought to the collaborative model; in this way, a root definition of the system was created that articulated multiple perspectives (see Appendix 2). Using the same technique, the initial PPI stakeholder groups (of seven participants) were asked to convey their ideas of what makes a good nurse manager (Figure 3). This knowledge contributed to the development of a root definition of a nurse workforce planning and deployment system. A second workshop explored the perceptions of staffing within the NHS. Seven PPI stakeholders participated and discussions centred on how staffing levels made visible by the organisation influence patients’ and their relatives’ perception of care, particularly when there are deficits (see Appendix 3).
FIGURE 3.
Patient and public involvement collaborative LEGO model of a ‘good’ nurse manager. This represents that nurse managers need to have good communication skills (represented by the bridge and chain) and take a high-level view of staffing needs. They should have compassion, courage and the leadership skills required for safe staffing. They need to value people, develop good ideas and remember the past (this is represented by being caught in the web).

Semistructured telephone interviews
Ten interviews were audio-recorded and built on the co-production workshops to explore variations in workforce planning systems across organisational settings and health services. The interview schedule consisted of 11 key themes, structured around the theory areas from the co-production workshops and the initial scoping review of the literature (see the interview material document at www.journalslibrary.nihr.ac.uk/programmes/hsdr/1419420/#/). Several themes intended to build an understanding of how WPTs are assumed to work, the impact of WPTs in different health-care settings and their predictive reliability. Interviews lasted approximately 30 minutes. Participants were recruited from NHS organisations from three sites, two of which were in large cities and one of which was in a smaller city within a rural area. Table 2 provides details on participants’ roles. An e-mail invitation to take part in the study was sent out to potential participants with a participant information sheet (see www.journalslibrary.nihr.ac.uk/programmes/hsdr/1419420/#/). Written consent was sought prior to participation (see www.journalslibrary.nihr.ac.uk/programmes/hsdr/1419420/#/). The data from the interviews further contributed to the emerging specifications of the systems of nurse workforce planning and deployment and a functional typology of WPTs.
| Participant | Role | Setting |
|---|---|---|
| 1 | Ward Manager | Hospital |
| 2 | Assistant Director of Nursing | Hospital |
| 3 | Matron Surgical Wards | Hospital |
| 4 | Improvement Advisor (staffing) | Hospital and community |
| 5 | Corporate Matron (staffing) | Hospital |
| 6 | Ward Manager | Hospital |
| 7 | Lead Nurse | Community hospital |
| 8 | Lead Nurse | Hospital |
| 9 | Lead Nurse | Hospital |
| 10 | Matron | Hospital |
Identification of theory areas
Based on the information from the stakeholder work gathered in phase 1, a complex, multifaceted system of nurse workforce planning and deployment emerged with explanations of the role and functions of WPTs. From this, the project team identified eight theory areas for the main searches of this evidence synthesis; these were operationally defined (see Appendix 4). These theory areas comprised the elements described by stakeholders as having an important influence on NHS managers’ use of WPTs within the system of nurse workforce planning and deployment.
Phase 2: the searching processes
In phase 2, from September 2016 to August 2017, the searching process involved identifying evidence relevant to the programme theory. The aim of this process was to gather the most relevant evidence to support or contradict initial ideas within the programme theory. Adhering to the realist approach, the search strategy was broad and extensive and a number of iterative searches were designed as the understanding of the programme theory developed.
In the first instance, the searches targeted evidence specific to the nursing workforce across hospital, community and third-sector care in the context of UK-based and comparable health systems. It was theorised that there would be transferable lessons from other public services for which the challenges of workforce planning and workforce developments are similar. Later searches were conducted to test the impacts of WPTs in related service fields, for example, in social care and policing, in which there are comparable workforce planning requirements. We drew on the direct experience of the project team in the identification of programmes to implement WPTs within UK mental health services. These included the All Wales Mental Health Acuity Group Project Report138 of the piloting of an acuity tool in six health boards. In addition, snowballing techniques and citation searching (pearling) were used; expertise was also solicited from the project steering group and other key researchers and organisations, to ensure that evidence that might be relevant but not visible through traditional searching methods was not missed.
Purposive searches
In total, 11 iterative searches were conducted. These evolved as the programme theory emerged from the review of the literature (Figure 4). For each search, bibliographic databases that were relevant to the topic were selected, and searches were translated for each database to use relevant keywords and make use of available thesauri. Search terms were identified from early scoping work, theory development and stakeholder engagement, and were built on and developed iteratively as common terms were identified from the selected literature (see Appendix 5).
FIGURE 4.
The iterative search process selection and appraisal of documents. ASSIA, Applied Social Sciences Index and Abstracts; DARE, Database of Abstracts of Reviews of Effects; HTA, Health Technology Assessment; NHSI, National Health Service Improvement; QNI, Queen's Nursing Institute; RCNI, Royal College of Nursing, (RCNi) is a wholly owned subsidiary of the Royal College of Nursing. a, Google Inc., Mountain View, CA, USA.
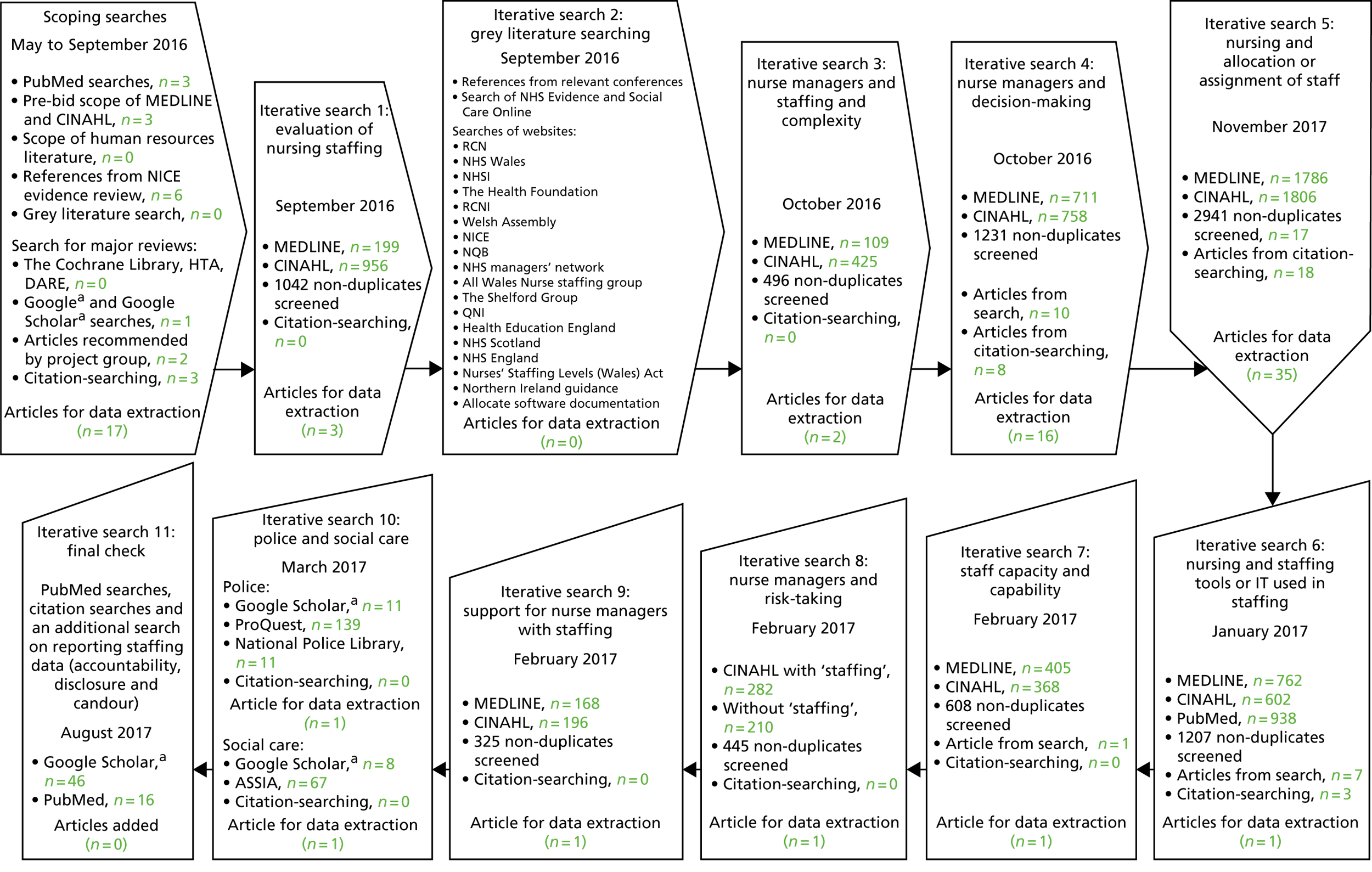
During the early scoping searches, a broad range of databases were used including The Cochrane Library, NHS Centre for Reviews and Dissemination, the Database of Abstracts of Reviews of Effects, the Health Technology Assessment database, PubMed, MEDLINE via EBSCOhost (1950 to March 2017) and CINAHL. Later, the purposive searches on nursing managers’ use of workforce tools and staffing management concentrated on the use of the MEDLINE via EBSCOhost (1950 to March 2017), CINAHL and PubMed databases. Additional specific databases were added for the searches of social care staffing management and for the police sector.
Only one search limit was applied: a date limit of 1983 to the March 2017. In 1983, the NHS Management Inquiry was commissioned to evaluate methods of estimating staffing levels and the classification of workload analysis approaches. 139 Backward reference searching was used to identify any works of relevance to this study that were cited in the selected articles. Forward reference searching was used to identify any newer works of relevance to this study that cited the selected articles.
Initially, the study sought to identify any studies that evaluated the effectiveness of nursing staffing models in the UK (iterative search 1). As the programme theory developed, the literature searches were designed around the complexity of nurse staffing (iterative search 3), a number of searches focused on the nurse managers themselves and how they make decisions (iterative search 4) and take risks (iterative search 8) and the support available to them (iterative search 9). Iterative search 5 was designed to focus on the practicalities of allocating staff to staffing structures, and iterative search 6 was designed to gather evidence on the different tools and information technology (IT) used for staffing management. Iterative search 7 was designed to capture any evidence on how information about the capacity and capability of staff is considered when allocating shifts and planning a rota (see Appendix 6 for an example of a search strategy).
Iterative search 2 focused on the grey literature, such as workforce planning project reports relating to national and local initiatives and evaluative information about these initiatives that is held in the public domain. The project team searched examples of development programmes across multiple services (adult, mental health, learning disability and community) on the evaluation of the use of WPTs. The grey literature search also explored policy, evidence to government, NHS organisational strategies and the reports of workforce technology projects and programmes. None of the pieces of evidence identified in this search was included in the final synthesis; however, the review of the grey literature informed the team’s understanding of the system’s complexity and highlighted contextual influences on the implementation and impact of WPTs.
In order to investigate WPTs in use in the social care sector, a search was designed for the Applied Social Sciences Index and Abstracts database on the ProQuest platform. For evidence from the police sector, the National Police Library at the College of Policing was contacted and the librarian provided the team with some references from a search of their library catalogue. This was also supplemented with a search of Google Scholar (Google Inc., Mountain View, CA, USA) and the databases available via the Bangor University ProQuest subscription.
Inclusion and exclusion criteria
A systematic process developed by the team in a recently completed realist synthesis was followed to determining relevance. 89 Consistent with Pawson’s suggestion,94 the test for inclusion involved:
-
linkage with the programme theory and explanatory potential
-
discernible ‘nuggets’ of evidence within the source material
-
evidence of trustworthiness.
Reports of WPTs, such as workforce planning, workforce measurement, workforce management, patient acuity and dependency, staffing ratios, professional judgement and skill mix, were included. Evidence on settings was also searched, recognising the shifting patterns of health care and the importance of enabling patient flow and quality across systems of care. As the programme theory developed, a functional typology of WPTs used in safe staffing was developed to encompass tools that (1) help to summarise and aggregate information, (2) aid communication and (3) support standard setting and quality assessment (see Table 4).
In a realist synthesis, evidence is excluded only if it does not relate to, or inform the development of, the programme theory; however, in this review, evidence was not included that had limited transferability to the NHS, such as nursing workforce issues within low-income countries. Evidence was included only if it was generated from different international contexts in comparable health systems in high-income countries. Discrepancies in opinions on the relevance of evidence were resolved through discussion among the project team. Title sifting was cross-checked across four team members (SD, AJ, LW and AM). Levels of agreement among reviewers were scored for 10% of the total titles.
Data extraction, analysis and synthesis process
This aspect of the review process is resource intensive and is reliant on discussion and deliberation, including consultation with a wider group of stakeholders. In a realist evidence synthesis, bespoke data extraction forms are developed to guide the decision-making process for extraction. 94 Based on the initial programme theory of WPTs, a bespoke extraction form was developed, based on the eight theory areas, to interrogate the literature and data were extracted only if the evidence met the test of relevance for the programme theory (see Appendix 7). The theory areas and their sub-elements, specified within the data extraction form, were transposed into ATLAS.ti code manager version 7.5.10 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany). A total of 90 sources from the literature were entered into ATLAS.ti for coding. Additional codes were also identified (see Appendix 8). The coding of a selection of included data was validated by three members of the project team (SD, CRB and AJ). Three sources of evidence were not able to be coded; therefore, the final selection was 87 sources of literature. This incorporated many types of published evidence, including qualitative interviews, quasi-experimental studies, surveys, evaluations and audits, case studies, frameworks and guidance, theoretical conceptualisations, literature and evidence reviews (see Appendix 9). Commentary evidence was included because it was felt that it was credible and critical to theory development, as it was provided by those directly engaging with WPTs in the field. Following data extraction, the eight theory areas guided the data analysis process. Within each of the eight theory areas and their coded sub-elements, the data were organised into themes (see Appendix 10). Appendix 11 offers an example of the thematic development within theory area 6.
The relationships between CMOs were analysed from the extracted information. This involved organising extracted data into evidence tables to represent the different bodies of literature. Using abduction and retroduction across the evidence themes,140 WPTs were reconceptualised from different angles to identify the underlying structures and emerging demiregularities (patterns) around plausible CMOs, seeking confirming and disconfirming evidence. Linking these demiregularities to develop the initial programme theory provided an explanation of the implementation, utilisation and impacts of nurse WPTs. The resultant seven hypotheses act as synthesised statements of findings around which a narrative can be developed that summarises the nature of the CMO links and the specific characteristics of the evidence underpinning them.
Phase 3: testing and refining the initial programme theory
Advisory group
The initial CMOs were developed by two members of the project team (CRB and LW) and were reviewed extensively in an advisory group meeting in May 2017. This process sought to clarify, develop and refine the CMOs.
Think-aloud interviews
To further enhance the trustworthiness of the resultant hypotheses and to facilitate the development of a final review narrative, 11 audio-recorded telephone interviews were conducted with NHS managers between July and August 2017. Participants were purposively sampled to obtain different perspectives that were relevant to the review question, including different national contexts and service settings (Table 3). Participants were recruited from four sites (three large cities and one smaller city surrounding a rural area). Interviews lasted approximately 30 minutes. In addition to exploring the synthesis findings, the interviews included a think-aloud technique, whereby NHS managers were given information and asked to describe their ‘thinking work’ around a nurse staffing scenario, validated by the project advisory group (see the interview material document at www.journalslibrary.nihr.ac.uk/programmes/hsdr/1419420/#/). This is a recognised technique for determining the information behind decision-making and judgements,141 which was considered to be a key focus for the operationalisation of the emerging programme theory. The technique illuminates the cues, priorities and strategies that are being considered at a particular point in time. It can identify the rationale and inference being drawn in that moment and can be used to test hypotheses;142 specifically, it was used to test and refine the seven CMOs.
| Participant | Role | Setting |
|---|---|---|
| 1 | Matron | Hospital |
| 2 | Specialist Practitioner | Community |
| 3 | Matron | Community |
| 4 | Ward Manager | Hospital |
| 5 | Unit Manager | Hospital |
| 6 | Team Leader | Community |
| 7 | Team Leader | Community |
| 8 | Corporate Matron | Hospital |
| 9 | Matron | Hospital |
| 10 | Matron | Hospital |
| 11 | Unit Manager | Hospital |
WeNurses Twitter chat
A Wechat#WeNurses Twitter chat was held in July 2017 to capture the stakeholder perspective on the use of tools and technology for nurse staffing deployment. This opportunity facilitated the refinement of the understanding of the complexity of NHS managers’ roles in managing the staffing resources day by day and tested the CMOs (see Appendix 12).
Changes to the protocol
Amendments to the protocol were granted in phase 3 of the review. These amendments related to the process of audio-recording verbal consent for telephone interviews with NHS managers in place of written consent and changes to the interview process for the second stage of the telephone interviews, in which the submitted interview schedule was replaced by a think-aloud scenario.
Ethics approval
Ethics approval was granted by the Bangor University Healthcare and Medical Sciences Academic Ethics Committee to conduct up to 10 semistructured telephone interviews in phase 1. Following amendments to the protocol, the team also gained ethics approval for the think-aloud interview technique, to seek audio-recorded verbal consent in phase 3 and to increase the number of interview participants.
Chapter 3 Findings
The system of nurse workforce planning and deployment
A root definition of the nurse workforce deployment and planning system in which NHS managers were working with WPTs was developed in the co-production workshops using soft systems methodology. 135 This offered a representation of the activities embodied in the system through exploring six dimensions (worldview, transformation, customers, owners, environment and actors) that, when combined, offered explanations of the purposeful activity of the system of nurse workforce planning and deployment. As the advisory group activity demonstrated (Figures 5 and 6), the system is complex, with multiple players and components, and interlinks with layers of different systems, such as social care.
FIGURE 5.
Members from the advisory group were asked to consider the influences on the system of nurse workforce planning and deployment.
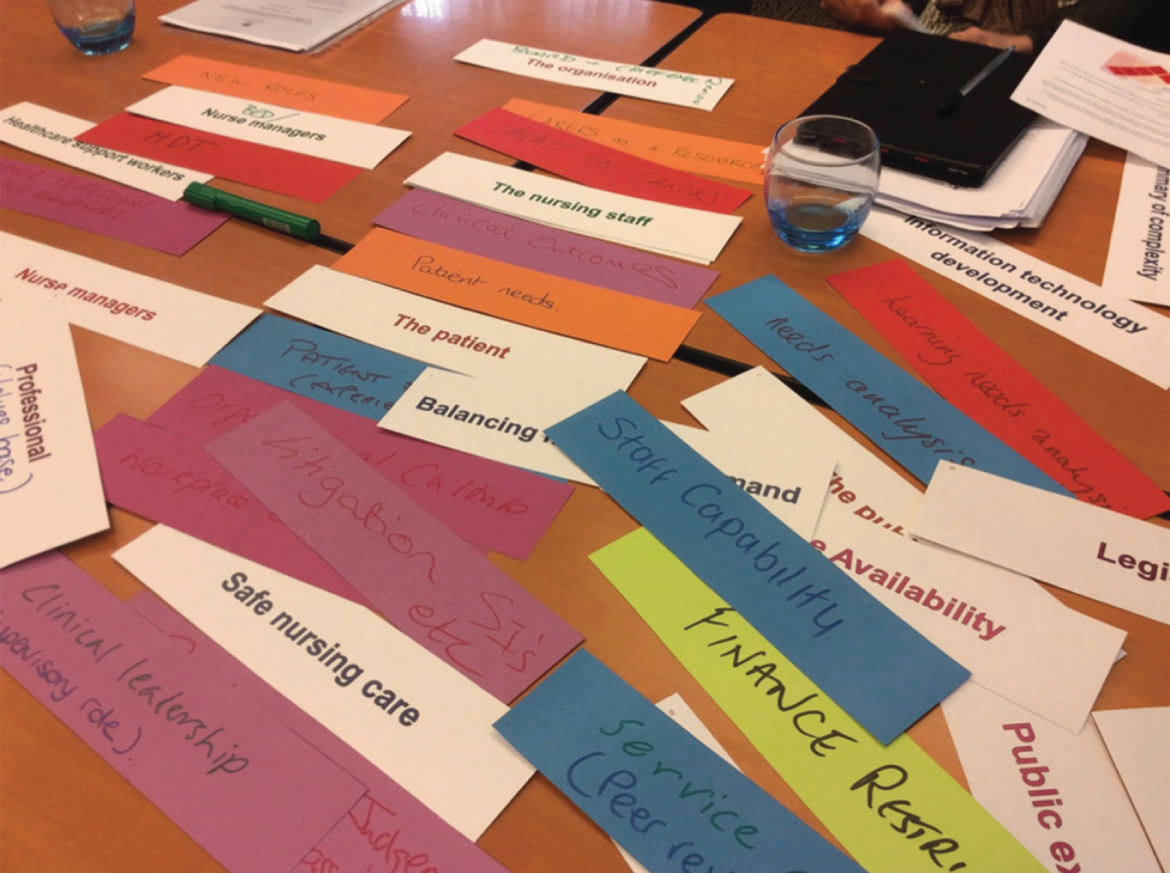
FIGURE 6.
The final list compiled by the advisory group of influences on the system of nurse workforce planning and deployment.
In soft systems methodology, the first dimension is the worldview. All stakeholder group members emphasised that the worldview, or core purpose, of the system of nurse workforce planning and deployment is that health-care organisations should provide good-quality care, so that patients are safe. Patient-centred care was described as:
. . . the pinnacle of organisational prioritisation.
NHS manager, group 2
Legislation, evidence-based guidance and corporate requirements for quality assurance exerted powerful influences on the worldview of nurse staffing. The NHS manager groups offered insight into how differing approaches within the UK had affected guidance and NHS managers’ work around staffing planning and deployment. WPTs may facilitate the transparency of data for aggregation and benchmarking between and within organisations, which are key improvement drivers for good-quality care delivery. Nurse regulation was also recognised as an important influence for the worldview. NHS manager groups noted that nurses have a duty of care. Professional care was also linked to individual appraisal of risk, through aligning staffing levels with patient need. The feedback from the advisory and NHS manager groups suggested the potential for dissonance between nurses’ professional values and organisational attitudes to costs and risk.
Transformation, or the system’s purposeful activity, is to achieve good-quality, safe, patient-centred care, mediated through effective planning and deployment of nurse staffing that is appropriate to patient need. A clear vision and a common frame of reference are required to achieve effective nurse staffing. This has to be achieved efficiently; all stakeholder groups inevitably linked staffing to finance, budgets and effective use of resources. The ability to see the ‘financial flows’ is important for budgeting, so data are required. In addition, when balancing need and demand, data can act as a currency to be used in pursuit of transformation:
What can we do differently? Via monitoring through some kind of system so we can see what has worked and what hasn’t and identify where there’s an issue and where we can get help from.
NHS manager, group 1
Workforce planning and deployment tools and technologies are useful for the provision of transparent and aggregated data, so they need to be developed to produce a system ‘that works for us’ (NHS manager, group 2). However, different drivers can produce competing priorities. Adherence to legislation, mandates and evidence-based guidance was considered to be non-negotiable by the advisory and NHS manager groups; however, discussions reflected the fact that adherence was complicated by staff shortages, financial pressures and increased demands. Although all participants agreed that strategic and legal requirements for safe staffing were vital, there was a gap noted between expectation and delivery in the current financial climate. The nursing stakeholder groups discussed the balance between organisational safety and risk management and emphasised the need for systems to have a safety net, ‘to catch people if they miss’ (NHS manager, group 1). A key long-term transformational goal is that nurses are satisfied with the system. NHS manager groups emphasised how this can positively influence the organisational reputation, leading to good levels of recruitment and retention of nursing staff.
There were multiple customers of the system identified by stakeholders. These included nursing staff, patients and members of the public, other health and social care organisations, such as care homes, and IT businesses. NHS manager groups indicated the importance of valuing and developing existing staff, working innovatively and creatively, often in redefining or developing new roles to ensure effective recruitment and retention. All stakeholder groups referred to the impact of the Francis Inquiry and its contribution to articulating the link between inadequate staffing and poor patient outcomes. 2 The powerful influence of patient and public expectations was emphasised by the NHS manager group’s feedback. This was strongly linked to organisational reputation and patient and public confidence in the quality and safety of the care delivered.
Owners were identified as NHS trusts and also legislators, policy-makers, budget holders, regulators and commissioners. NHS trusts have to ‘make do with what they have got’ (NHS manager, group 1). However, all stakeholder groups noted that this has to be balanced with the organisation’s attitude to risk management and the requirements for safe staffing. There were strong associations emphasised between finance, corporate reputation and workforce well-being, recruitment and retention. The advisory group noted that when finance had an adverse impact on nurse staffing, this had a contributory effect to negative nursing outcomes, with poor staff satisfaction, retention and recruitment, leading to poor organisational reputation. If health-care organisations are known for having safe staffing levels, this has a positive impact on patient and public confidence.
There were multiple environment factors that NHS manager stakeholders and the advisory group highlighted as being influential; for example, clinical settings and local geography could exert influences on demand and resource availability. Some clinical areas suffer from shortages of staff; this may be attributable to a lack of nurses with specific qualifications for particular roles. Geography can influence the nature of demand; this may be related to socioeconomic influences, urban or rural settings; geography could also impact on the availability of nurses. Public expectations exert a strong influence, fuelled by the local and national media, which in turn could have an impact on organisational reputation. Organisational context was also highlighted as an important influence on safe staffing. All stakeholders expected NHS organisations to support nurses for professional development. NHS manager stakeholders and the advisory group felt that organisations should facilitate training and education so that nurses can provide evidence-based care and utilise WPTs; therefore, access to IT support was felt to be important. PPI stakeholders expressed concern over bursary changes in England and the lack of professional development:
The problem lies in retaining nurses in the UK once they have qualified. The structure and opportunities for nursing overseas are much greater.
PPI stakeholder, group 2
All stakeholder groups reflected on the challenges encountered by NHS managers to ensure safe staffing, owing to a range of organisational factors, such as poor organisational processes (e.g. changes to planned procedures, powerful others with different political agendas, financial constraints and organisational pressures). There was a strong feeling that the organisation should support NHS managers’ decisions around staffing and recognise the need for a positive organisational learning culture, in which nurses are listened to and developed for their complex role of managing safe staffing. The NHS managers and PPI stakeholder groups felt that managers needed to be assertive in order to confront and challenge organisational deficits.
The actors within the system were identified as nurse managers, RNs, HCSW and IT staff: ‘There is a wealth of resources within the staff’ (NHS manager, group 1). The NHS manager groups also noted significant and powerful others, such as finance directors, physicians and bed managers. All of the stakeholders discussed how powerful senior managers may not appreciate staffing issues on the ground; this was particularly emphasised by PPI stakeholders with regard to non-nurse managers:
The managers are in their ivory tower, and think everything is coming up roses.
PPI stakeholder, group 1
Staff shortages were noted to be a key adverse influence on the ability to deliver safe care. There was acknowledgement that nursing staff do have situated expertise, related to a particular environment or patient group, but that organisational requirements demand flexible staff who can work well in different clinical areas. However, nurses are reluctant to move out of their usual environment when there are shortages, citing their duty to deliver the best care. The advisory and NHS manager groups emphasised nurses’ fears of not reaching the expected standards in new clinical environments. In addition, the role of agency nurses was noted as a potential risk or limitation for safe staffing, as their qualities are often unknown or untested. The high cost of agency nurses was also viewed as having a negative impact on finances and staffing outcomes. Potential innovation with non-nursing roles and the new associate nurse role in England was commented on by the NHS manager and advisory groups; the group members were neutral on the potential impact of future changes on staffing skill mix. PPI stakeholders felt that there was a gap where the enrolled nurses’ role had been. Although the need for collective responsibility for safe staffing was articulated by the advisory and NHS manager groups, the managers’ role was thought to be pivotal to the entire system:
They are the cogs; managers are integral to making things happen, getting things done.
NHS manager, group 1
NHS managers make the decisions needed to balance patient requirements with real-time resource availability, all within a dynamic, unpredictable care environment. The advisory group emphasised the difficulties of contending with planned versus unplanned care. The system is in constant flux because of changing requirements, from patient acuity, dependency or the need for escort duty to one-to-one care. NHS managers need to be aware of organisational context and the influence of other systems, such as human resources and primary care.
A vital part of the NHS managers’ role around safe staffing is to allocate a nurse with the appropriate skills and knowledge to match patients’ unique requirements. This requires professional judgement based on knowledge of clinical need and understanding of organisational objectives, organisational systems and processes and patient flow, plus understanding nurses’ capacity and capabilities:
It’s not about numbers of nurses, what keeps the place safe is good decision making and having just enough staff to act on decision-making.
NHS manager, group 1
WPTs may help NHS managers to make safe staffing decisions as they provide information on resource availability, patient flow and patient need. However, the NHS manager and advisory groups emphasised that data had to be up to date. Technology for communication is vital to ensure the validity of data, but often NHS managers need to corroborate the clinical situation by being there in person. NHS managers indicated that the data from WPTs facilitate professional judgements for safe staffing decisions. One stakeholder asked:
Can these judgements be captured in such a way that they inform long term decisions about, this is the demand I’ve got and this is the kind of staff I’ve got and how does that compare to other parts of the system to see if we’re using the resource properly?
NHS manager, group 1
The root definition highlighted the interplay between the system, the delivery of nursing care and the role of WPTs. The system should reflect the organisation of nursing care, as there is an alignment of a system of nursing with a system of technology, coupled with NHS managers who are:
Adept at decision-making, driven by patient-centred values.
NHS manager, group 2
In the NHS manager stakeholder groups, the system of safe staffing was visually interpreted through LEGO SERIOUS PLAY to formulate collaborative models (Figure 7).
FIGURE 7.
A nurse manager stakeholder LEGO SERIOUS PLAY model of the system of nurse workforce planning and deployment. This model depicts how managers should have many roles, but have a raised or helicopter view of the system. Cogs and links ensure effective communication, so that nurses are deployed effectively, dependent on the patient need and the nurses’ capacity. There should also be links to what has worked before and efficient management of resources.
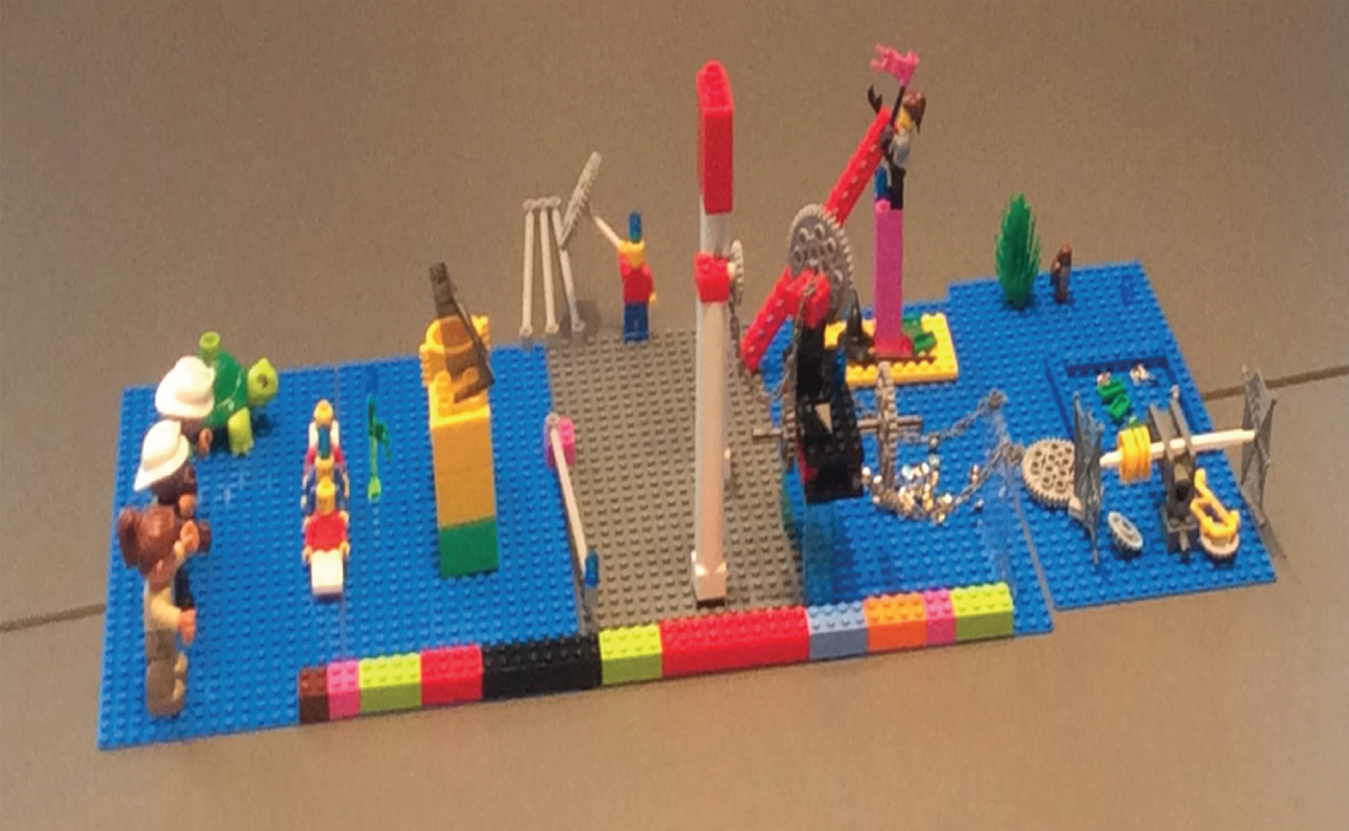
Themes from the phase 1 interviews
Understanding the system
NHS managers were aware that they were working within a complex system and that they needed to understand its demands and resources. The delivery of patient safety and good-quality care was their key priority, underpinned by the evidence base for safe staffing and focused by national standards for good-quality care. NHS managers acknowledged the increasing pressures from expanding demand and financial constraints. They understood the requirements to ‘flex up’ (increase staffing levels) because of unscheduled care and the numbers of patients generally, with higher acuity and complex needs:
So, my remit is to make sure that they [nurses] escalate that to the right people, to the right agendas, so that procedurally, when there are unscheduled care pressures, everybody has to change the pace of work not just, operational nursing, medical or therapy staff.
Site 1, participant 3
NHS managers discussed how the system also had to contend with a reduction in RNs, as nurses were retiring but not being replaced in sufficient numbers. This often prompted the dilution of skill mix through substitution with non-registered staff. NHS managers acknowledged the development of new roles, such as the associate nurse role in England, and, in some instances, welcomed this as a new way of potentially delivering good-quality care:
Everybody knows the staffing pressures in the organisation and the NHS as a whole. We know that we are working tremendously hard to improve those staffing numbers, and equally we’re looking at diverse roles as well, at trying to support . . . so thinking outside the box really.
Site 3, participant 3
The NHS managers’ work in safe staffing
NHS managers understood that their role with regard to staffing deployment is complex. They were conscious of their responsibility as decision-makers and acknowledged that this could sometimes be stressful, as they were accountable for balancing risk and safety:
What we can see is where we have increases in personal demand, we have reductions in core staffing, what you find then is . . . that . . . potentially even an increase in throughput, what you find then is there’s decision-making going on which is to increase staff, close the intake, move some things through, alter some activity, and it’s that decision-making which is really the thing that creates the level of safety.
Site 1, participant 4
NHS managers felt that they needed to be comfortable in justifying their staffing decisions in the light of patient requirements. They understood patients’ clinical needs and anticipated how these related to staffing requirements. They discussed their local knowledge of the organisation, clinical areas and staff capacity and capability:
So it’s important to know your staff really . . . and what skills they have, and how, probably, they sometimes work with each other.
Site 3, participant 1
Teamwork and planned meetings to determine demand and resource allocation, for example, bed meetings, were features of the nurse manager’s staffing work:
Staffing is always discussed at the end of bed meetings as well, just to say look, this is where . . . from an operational point of view, this is where our pressure points are, have we got the staff in place to support these? So, it’s knitted together very, very tightly.
Site 3, participant 3
The importance of communication
You’ve got to juggle the staff, you’ve got to juggle the patients, and you’ve got to juggle upward and downward messages, you know?
Site 2, participant 2
Communication with a range of staff, and for the escalation of concerns to senior managers, was an essential factor in safe staffing. NHS managers at all levels (e.g. matrons, lead nurses) had a physical presence in clinical areas, although for some lead nurses this was less often. This was to liaise with staff, make a first-hand assessment of the situation and assess the nurses’ ability to cope. This presence also enabled them to offer support and determine if redeployment was required:
And you can get the feel of the place . . . And it does take some footfall, so I’ll walk 15,000 steps on a late shift. But then I know that everyone is safe. And they appreciate it, they appreciate you going in and saying hello.
Site 3, participant 2
Many participants felt that they offered an independent, objective view to balance more emotional responses to system pressures. They had to understand the environment and culture to implement the staffing decisions they made, particularly if they were asking ‘difficult questions’ or negotiating the redeployment of staff. They related their own management skills to their experience:
Probably what I’ve got better at is at asking people to move and encouraging them to move, and . . . being able to charm people are probably the things I’ve got better at, rather than being able to ascertain where needs more support.
Site 3, participant 2
Valuing nurses
There was an overwhelming sense that nurses should be valued, respected and supported. Maintaining staff satisfaction was important, but this had to be balanced against patient needs. NHS managers wanted to ensure that junior staff were developed, particularly if they were in management roles. Staff development was also an important part of recruitment and retention:
I’ve started some forums for nursing assistants. I’ve started forums for junior staff nurses. I’m starting a band 6 development programme; starting surgical skills training. Since I’ve got to the division I’m on a mission to . . . I want to keep them engaged, want to keep them interested.
Site 3, participant 2
Patient and public satisfaction
NHS managers understood the importance of listening to staff and patient concerns, particularly in dealing with patients and the public when complaints were linked to staffing. Here, focused communication was used to determine a satisfactory outcome; often this meant managing expectations and setting realistic goals:
Because, unfortunately, that’s where a number of complaints come from, because (1) we haven’t communicated properly with families, and (2) we just haven’t had the right staffing infrastructure in place to deliver on what was expected from that family.
Site 3, participant 3
We try and avoid complaints getting to a formal stage, so at the point of a family complaining, going to X [formal complaints system], either the ward manager or the matron would go in and meet with the family and try and resolve those issues.
Site 3, participant 4
Seeing the bigger picture
NHS managers set great importance on seeking out appropriate information about demand and resources within the organisation as a whole; this was used alongside their professional judgement for effective staffing decisions:
So, the information goes to the senior management team for the hospital and the Trust so that they’ve got an understanding of what’s happening within the hospital, as well as whoever the on-call manager may be, and then the department managers as well also receive a copy of that. So, we’re going to the computer three times a day to input that information anyway and to send out.
Site 3, participant 4
The use of workforce planning and deployment tools and technologies
A range of components were considered for staffing decisions, for example the bed state, patient acuity levels and the number of nurses. NHS managers valued WPTs if these made data on patient need and resources transparent for decision-making; for example, WPTs were useful when they could match patient acuity and dependency data (e.g. early warning scores) with staffing requirements. In some instances, they could track both patients and nurses through the system. WPTs linked important components of staffing data, such as annual leave, sickness and payroll. They facilitated comparisons of costs and budgets. Some rostering technology also provided rules on, for example, skill mix and numbers on annual leave:
It [electronic rostering] does bring an awful lot of benefits around HR [human resource] management, and just having all the information in one place about your staff, annual leave management, time owing management, it’s all so much better . . . and completely traceable; whereas before it was quite difficult to manage.
Site 3, participant 4
Senior managers scrutinised data from WPTs for evaluation, to formulate evidence for establishment setting. Comparison and benchmarking enabled learning from other areas. Data could also be used for reviewing staffing levels where there had been complaints or clinical incident reporting. WPTs enhanced communication in many instances by making needs and resources visible:
And then that gets uploaded into a report, which is very clever and it allows us to view fill rate, overall fill rate, how many agency staff we’ve got on duty at any one time. And then it picks up, it allows us to pick up comments that the wards give us. So, it’s real time, it’s ward to board, anyone in the Trust can access it . . . from the Chief Exec down to a nursing . . . HCA [health-care assistant] on a ward.
Site 2, participant 1
However, some NHS managers indicated that WPTs were not used to full capacity for evaluation and suggested that this was an area for development. Senior NHS managers also found that technology highlighted whether or not managers were compliant and engaged with electronic staffing tools. NHS managers also had a role in encouraging their staff to engage with WPTs to ensure compliance with data input.
Real-time data
NHS managers generally embraced the use of WPTs, but only when they felt that the data were credible and reliable. Data were valued if these were real-time data. NHS managers often valued data from personal communication above data from WPTs and used paper records or computer printouts of current data on staffing and patient requirements, admissions and discharges, but checked these for accuracy by walking around the wards. They suggested that occasionally they were frustrated with technological difficulties with WPTs and how inputting data could be time-consuming. Some senior NHS managers reflected that it had been difficult to embed their use into practice, as other nurse managers were initially reluctant to engage and learn the skills required. In some instances, data had to be accessed in terminals away from the clinical area; NHS managers valued data that could be accessed anywhere, particularly via handheld devices.
The NHS manager’s role in facilitating the use of workforce planning and deployment tools and technologies
NHS managers recognised that they had a leadership role to engage staff to utilise WPTs effectively, and to develop the nursing staff’s skills for effective decision-making. Many felt that this was about setting standards and indicating expectations. This was particularly noted in ensuring that data input was a true reflection of the staffing requirements. Some participants suggested that it was important to liaise with nurses in areas where WPTs were to be introduced, so that they were user-friendly. Organisational support was important for the provision of dedicated staff with IT and nursing expertise to lead on training and education. This needed to be readily available, either virtually or in person. In addition, in order to ensure effective nurse development, all NHS managers reflected that they needed to know their staff and identify gaps in their skill set, via performance review. Nurturing staff was a key theme. This was facilitated through spending time with them, role modelling, mentoring, coaching and promoting access to leadership programmes and peer support:
So it took us about 6 months, really, to get people confident in the work of the systems, and just working with them while they were working the systems, just to give them the confidence and the knowledge.
Site 1, participant 3
The functional typology of nursing workforce planning and deployment tools and technologies
A range of WPTs were identified through the co-production stakeholder workshops, interviews with NHS managers, the advisory group and the review of the literature. An analysis of the primary reasons for the use of WPTs, and a consideration of their different functions and application, emerged from soft systems mapping work, the themes from the interviews and discussions with stakeholders; this facilitated the organisation of WPTs into explanatory types. The functional typology of four categories (summarising and aggregation; communication; workforce allocation; and standard setting and quality assurance) demonstrated that WPTs could have multiple functions and belong to different categories (Table 4). Stakeholders identified that some WPTs (e.g. care bundles) may not be immediately associated with staffing, but emphasised that making nurse-sensitive outcomes evident, through the use of care bundles and other quality of care tools, can aid safe staffing work. The link between safe staffing and nurse-sensitive quality outcomes is supported by the evidence. 1,23,25,28,34,36
| Primary function is | |||
|---|---|---|---|
| To summarise and aggregate information | Communication | Safe nursing workforce allocation | Standard setting and quality assurance |
| Electronic roster (e.g. allocate, can integrate budgets, staffing template, staff qualifications and annual leave and assessments and payroll) | Bed meetings – to review bed state, admissions, patient acuity (organisation/department) | Staffing systems and professional judgement tools (e.g. RAFAELA, Department of Veteran Affairs staffing methodology, Scottish toolkit) | Safe staffing templates/calculations (e.g. Safer Nursing Care tool, nursing care hours per day) |
| Spreadsheets/databases for resource management [e.g. Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) for budgets] and budget reports | Desktop computers/laptops | Establishment setting tools, (e.g. Safer Nursing Care tool) | Nursing-sensitive quality indicators |
| Social media [e.g. closed Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com)] | |||
| Patient electronic records [e.g. EMIS Web 5.4 (EMIS, health, UK) and Chameleon InforFlex version 5 (Chameleon Management Services Ltd, UK)] | Tablets/handheld devices | Acuity and dependency assessments (e.g. early warning scores) | Organisational strategies (e.g. human resource, finance, recruitment and retention) |
| Open/bid shift self-rostering technology, with apps | |||
| Risk assessments | Text (e.g. text burst to all staff) | Caseload tools [e.g. eCAT (version 4; Yarra Software Ltd, Belfast, UK)] | Policy or mandates linked to legislation |
| Bed state reporting – elective and emergency admissions, patient flow | Personal communication alerts/mobile phones | Nurse allocation tools (e.g. Synergy model) | Individual performance reviews and development plans |
| Handovers | Patient feedback/evaluations and complaints | ||
| Patient flow systems – transfers in and out, caseloads | Safety Huddle systems | Paper roster/e-roster [e.g. Health Roster version 10 (Allocate Software plc, Sydney, NSW, Australia)] | Quality and safety audits |
| Incident reports | Staffing meetings – to review staffing allocation | Written bed state/spreadsheet | Evidence-based guidance |
| Electronic staff records | Apps [e.g. the Safe Staffing APP version 1 (Nottingham University Hospitals NHS Trust, Nottingham UK)] | Electronic staff records | Staff feedback |
| Clinical information systems [e.g. Bedman electronic nursing information system, version 1 (Central Manchester University Hospital NHS Foundation Trust, Manchester, UK)] | Electronic whiteboards | Automated time and attendance tool | Care bundles, pathways and care plans |
| System tracking | Teleconference | Decision-making tools [e.g. CLASSICA version 1 (Ruland RM, RAVN IH; Oslo, Norway), dashboards] | Benchmarking standards (e.g. the modern hospital) |
| Data warehouse/dashboards | Board rounds – to review bed state, admissions, patient acuity (clinical area) | MISs (e.g. NMMDS) | National and local dashboard for evaluation between clinical areas/organisations |
| Caseload review | Dashboards | Risk assessment tools | Safety standards |
| Podcasts/e-learning to educate managers | Self-rostering technology [e.g. BidShift® version 3.2 (San Diego, CA, USA)] | ||
Synthesising the elements of the system of nurse workforce planning and deployment
The system of nurse workforce planning and deployment emerged as being dynamic, complicated and ultimately complex (Figure 8). Stakeholders provided a range of perspectives and articulated multiple influences on the system and the varied expectations from it. However, patient safety and good-quality care was a common frame of reference in all stakeholder groups and the interviews. Extensive stakeholder engagement revealed the system’s essential elements. The system is multidimensional, with interactions between different levels and processes within health organisations and external organisations. The system’s essential elements go beyond the mere availability of resources to be influenced by social, political and economic context. These influences are defined and shaped by the different expectations of the system. Financial considerations dominate, but stakeholders agreed that this was not at the expense of how the system produced safe, good-quality care.
FIGURE 8.
The model of nurse workforce planning and deployment.
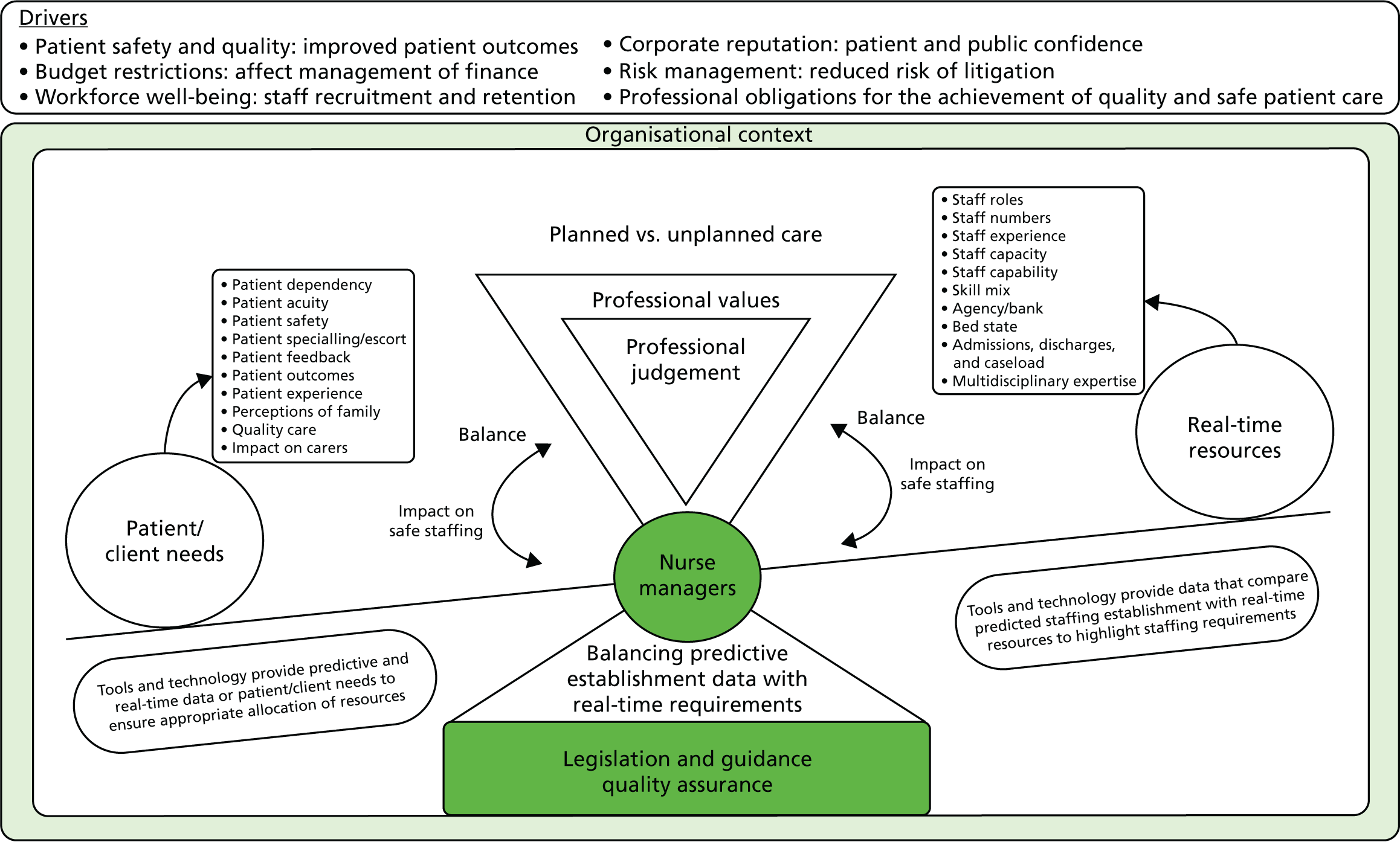
Patient needs dictate how the system responds. The system has elements of predictability (e.g. booked procedures), but also elements that, although anticipated to some degree, cannot be controlled (e.g. winter influenza causing increased demand). The system has to be flexible, although stakeholders indicated that sometimes it can be unwieldy because of a lack of resources or when organisational priorities, or processes, work to counteract seamless staffing planning and deployment.
The system relies on individuals and groups working in synergy, with organisational aims for safe staffing supporting their endeavours. Staff well-being is an essential component of the system – without this, safe patient care cannot be perpetuated by the system. The system sees interaction, and sometimes dissonance, between staff who may have different priorities, with the potential for different perspectives between clinicians and non-clinicians, influenced by professional value.
Managing the system requires expertise and a broad range of skills, particularly leadership. NHS managers understand how different layers within the system interact and may assist, or hamper, their complex task in ensuring safe staffing. NHS managers are equipped to manage the system through understanding how individuals and groups work within it. Experience of the system can facilitate understanding about those individuals who are powerful and can provide resources or other forms of help, and the capacities and capabilities of nursing staff.
Workforce planning and deployment tools and technologies have the potential to assist NHS managers to manage the complex system of nurse staffing planning and deployment, when the data these provide are credible. WPTs can provide objective data on patient needs and resource availability to contribute to safe staffing decisions. Furthermore, WPTs can enhance communication within the system. However, NHS managers need to bring their subjective understanding on the system for effective decision-making using WPTs.
Following stakeholder engagement activities, the system of nurse workforce planning and deployment was articulated into a dynamic systems model, which reflects its complexity. It illustrates the NHS manager as the lynchpin of the system, being supported by WPTs, in their use of professional judgement to balance patient needs and resources. The model depicts the manager at the centre of the see-saw, weighing up the best options to promote safe, good-quality patient care through the use of WPTs.
Context–mechanism–outcome configurations
Following stakeholder engagement, the emerging explanations on the system of nurse workforce planning and deployment were inter-related to the findings from the evidence synthesis of the literature. The realist synthesis of this accumulated evidence sought to identify contingencies and make inferences to present theoretical explanations on how NHS managers can be supported to use WPTs. This necessitated moving from descriptive accounts of findings to the identification of CMO configurations to illustrate the programme theory of NHS managers’ use of WPTs. This followed an analytical process, which offered emerging theoretical explanations of what works, for whom, how and in what circumstances. Seven conjectured CMO configurations emerged from this iterative process (Box 1).
-
When there is positive reinforcement of proximal (e.g. staff flexibility) and distal (e.g. social factors/organisational reputation) aspects of the staffing system (context), WPTs enable better forecasting of real-time and future demands (mechanisms), resulting in better staff outcomes (outcome).
-
When and where there is alignment between relevant organisational strategies (context), it enables NHS managers to use the tools and technology as levers for change or negotiation (mechanism), promoting the patient safety agenda within the organisation (outcome).
-
When there is visible support for managers, skill development and leadership (context), the tools and technology empower NHS managers to make sense of complex data (mechanism), increasing the likelihood of staffing skills being in the right place (outcome).
-
When managers possess the key attributes of leadership and ‘know their staff’ (context), and when tools and technology help to make resources visible (mechanism), NHS managers have greater influence on their safe staffing work (outcome).
-
When the culture within the organisation is supportive and includes a culture of evaluation (context), NHS managers are able to work together using standardised data from tools and technology (mechanism), to learn together about safe staffing (outcome).
-
When there is partnership in design with the users of staffing tools and technology (context), and when NHS managers see tools as being fit for purpose (mechanism); tools and technology are placed close to the decision-making point (outcome).
-
When there is the organisational propensity and policy around disclosure of staffing levels (context), communication is balanced between candour and refining the message (mechanism) to ensure the confidence of patients and families (outcome).
Together these CMOs constitute the programme theory of what works to support NHS managers to use WPTs. The CMOs are described in the following sections. These narratives provide an evidence-based explanatory account of how NHS managers can be supported to use WPTs and the contingent factors that may facilitate, or impede, this support and the implementation of WPTs. However, it is acknowledged that the term ‘nurse manager’ often lacked specification in the literature. In realist synthesis, the underpinning rationale for CMOs can be established from several sources of evidence. These descriptive accounts draw on excerpts from the published literature, co-production stakeholder workshops, the advisory group and interviews with NHS managers to offer illustrative explanations on salient issues.
System integration and workforce planning and deployment tools and technologies (context–mechanism–outcome 1)
When there is positive reinforcement of proximal (e.g. staff flexibility) and distal (e.g. social factors/organisational reputation) aspects of the staffing system (context), WPTs enable better forecasting of real-time and future demands (mechanisms), resulting in better staff outcomes (outcome).
Context and mechanism
The complexity of establishing staffing requirements has been characterised as subjective, contentious, political and time dependent. 143
It appears that, when NHS managers are encouraged to be responsive to staffing demands, it is vital that they understand the different levels of the staffing system and how proximal and distal aspects are in synergy. When a complex staffing system is working well because it responds effectively to real-time demand (proximal factor), this can create a positive reinforcement of distal aspects, such as upholding organisational reputation and enhancing recruitment (distal factors), creating a positive cycle so that nurses can be matched to demand. For responsive decision-making, NHS managers need to understand the essential factors of the staffing system and the interactions between them. Certainly, knowledge of the clinical environment, patient needs, organisational structures and processes is important for effective rostering and patient–nurse allocation. 129,131,144–152 Wilson and Weiss153 indicated similarities in police staffing and suggested that staffing must also account for broad local factors, such as geography and organisational changes. The NHS manager stakeholder group feedback indicated that there is little control of the work coming in, but that it is important to understand the system as a whole and recognise different needs.
Organisational factors and patient flow
Understanding the staffing system’s organisational processes and context is essential for NHS managers’ effective responsiveness to real-time and future need. The synthesis of the literature indicated how various organisation process factors had an impact on staffing resources and care delivery. 124,128,131,143,145,149,154–162 For example, nurse managers need knowledge of patient procedures and hospital/unit policies. 149 Nurse managers also need an understanding of specific organisational processes and organisation of work, for decisions on staffing. 161 These may be unique to each clinical area. Berkow et al. 152 assessed Chief Nursing Officers’ (CNOs’) staffing decisions in four unit types (paediatrics, the emergency department, general medicine and intermediate care) and found that CNOs from similar hospitals prioritised staffing for clinically similar units differently, suggesting that there are clinical and operational differences between similar organisations. 152
The NHS manager stakeholder group feedback highlighted that managers need to understand the system and how to effectively and efficiently move people through it. NHS Education for Scotland gave the example of knowing how many elective cases the ward area will receive and indicated the importance of attending to local context; including the local models of care, the turnover/throughput and the ward climate. 131 The advisory group emphasised the importance of being able to respond to planned and unplanned care. A key factor is admissions and discharges to ensure that there are enough beds. 131,145,151,161,163 The allocation of staff based on organisational processes is also related to the time and day of the week. 158 For example, Kontio et al. 151 found that managers in a cardiac unit made staffing decisions that were dependent on task prioritisation related to booked and emergency procedures; these were also based on the peaks and bottlenecks in the system.
Harris and McGillis Hall133 emphasised the importance of consideration of nursing structures, processes and nursing roles for staffing decisions. Decisions on skill mix should be determined not only in relation to patient need but also in the light of a ward’s or unit’s objectives. 131 Nurse licensure, which is linked to competence and the level of support staff, is also an important consideration for nurse-to-patient allocation for nurse managers. 158,164 Decisions about staffing need to relate the complexities of care to staff competencies, plus support within the environment. 144 However, Flynn and McKeown165 suggested that nurse managers believe that an appropriate skill mix has a high ratio of RNs to health-care assistants. Berkow et al. 152 found that RN experience and nurse-to-patient ratios were the most important factors for CNOs in units characterised by high rates of admission, discharge and transfer. 152
Evidence from the synthesis of the literature therefore emphasised the importance of responsive decision-making to ensure that staffing meets workload, as a result of patient flow. 151,156,158 This suggested synergy between proximal parts of the system, including the flow of patients, staffing and the nature of the work and its organisation. For example, Allen158 illustrated how this differed between clinical areas and offered the example of episodic care units in which task-orientated nursing work fitted with workload completion. In these contexts, workflow maintenance was only identified in episodic care units, reflecting the high volume of patients that are seen each day. A focus on making nurse-patient assignments that assist in the movement of patients through the unit is required.
Data for in-the-moment decision-making
When NHS managers understand the complexity and dynamicity of the staffing system, they can use data from WPTs for responsive decision-making and to enable better forecasting. Interview participants and evidence from the synthesis of the literature emphasised the importance of real-time data for decision-making on staffing:155,156,166–170
Having a real-time tool to stay on track on a daily and even hourly basis also makes a big difference in how well staffing matches demand.
Barton168
Evidence strongly suggested that WPTs can provide real-time data for decision-making. 151,161,168,169,171,172 Interview participants also indicated that real-time staffing resources were made visible by WPTs, so that staff could be redeployed to meet patients’ needs:
So, if you come on and you’re a nurse short, . . . you can connect the dots and see where, and then you’ll e-mail that ward sister direct and say is there any chance I can borrow a member of staff. And it works quite well . . . but we do use it all the time, people always look at each other’s [staff levels].
Site 2, participant 1
However, evidence sources emphasised that WPTs are effective only if the data input is up to date:167,173,174
It is inevitable that changes will be made to the active roster and essential that these changes are made in ‘real time’. Real-time data maintenance of the IRS [integrated rostering system] facilitates Senior Nursing Managers to accurately identify actual staffing levels throughout the hospital.
p. 99, Kerr and Timony167
The NHS managers’ role is intrinsic to real-time data collection. Wilson et al. 150 found that managers were actively involved and engaged with the workflow activities, so they knew the staffing information status of the unit by checking on patients and staff nurses:
This behavior helped the effective charge nurses to be prepared for the next admissions, know which nurse can take the next patient, be aware of the acuity level of the patients, and comprehensively have a hand on the pulse of the unit.
Wilson et al. 150
There was strong evidence from the interviews that NHS managers also did ‘walk-arounds’ in hospital settings to check that the data from WPTs were up to date:
You would go on and you would find the centralised data with all of it on there, I would then print that off and I would then walk the wards and double check the numbers match up with what is on there.
Site 3, participant 2
One participant indicated how inputting data on staffing levels had become embedded practice:
The thing is, if somebody hasn’t done it another person will spot it straight away, they’ll say ‘Well it looks like you’ve got five today’, ‘Oh no, she’s off sick’. So, it tends to be a habit for people to keep it up to date.
Site 2, participant 1
Data from patient dependency/acuity classification tools or technology are vital for forecasting real-time staffing requirements. Many sources of evidence indicated that managers use these scoring tools to match up staffing effectively; these scores are linked to workload. 124,125,127,129,130,133,144,147,151,175–180 Nagy and Nathan181 were able to use scheduling technology to identify appropriately skilled nurses, as it articulated experience and credentials. Botter173 proposed that a patient classification system was useful to predict real-time and future staffing levels, particularly when decision-makers were familiar with the daily activities of the clinical area. Data may come from other sources; Diers et al. 154 found that nurse managers kept a ward document or ‘brain’, which detailed patient factors (e.g. leaving the ward for tests), and this information was not in the computerised system. These nurse managers could not be dissuaded from using this information source, so it was eventually encouraged alongside the tool. Interview participants also indicated how NHS managers used knowledge of patient flow and acuity to determine staffing need; this also prompted the redeployment of staff:
. . . it fluctuates every day. And then what we do is we offset that with acuity of the ward. So, for example, X ward may have four registered nurses on this morning, but actually they’ve not got that many sick patients today, they’ve got delayed discharges, so they don’t need four registered nurses. Whereas the diabetes ward, for example, actually they’ve had a lot of sick patients overnight, they need a bit more help, so let’s move a registered nurse from that ward to that ward to try and help them.
Site 3, participant 3
The NHS manager stakeholder groups highlighted that there is often a wealth of skills on site; they emphasised the importance of a flexible workforce, in which staff are happy to be redeployed and have a good understanding of how each ward/clinical area works. Interview participants indicated the importance of the provision of staff in accordance with extra need, for example one-to-one supervision, and how technology could be used to specify for codes to ensure that agency or bank nurses had specific skills in line with patient requirements; extra staff were then distributed in accordance with need:
So if we need to book agency or check shifts or whatever, we tend to use our [handheld] devices to do that. So, everybody will put up their agency shift on the device and know exactly what position they’re in at that moment in time. Because sometimes we do need agency, but sometimes . . . we’ll share the agency round.
Site 2, participant 1
So, that’s a person who’s been booked a special, and we try to do it out of our own staff, you know, so that the patient is familiar with the member of staff. So, we might book agency, but they might go and work on the floor . . .
Site 3, participant 3 (talking about the one-to-one supervision of patients with dementia)
The interviews therefore suggested that NHS managers use WPTs to identify immediate need and use their professional judgement to distribute staff for effective patient care. van Oostveen et al. 178 argued that a computerised decision support system can never fully replace professional insight and decisions may need to be adjusted by nurse managers.
Data for forecasting future demands
When NHS managers understand the complexities of the staffing system and how proximal and distal aspects inter-relate, WPTs can articulate future requirements. There was evidence of how WPTs could be utilised to forecast the need for long-term workforce planning. 168,182 Ruland171 indicated how WPTs can provide prognostic data. This can also enable trend analysis. 131,154 WPTs can also predict costs associated with their staffing decisions,134,151,171,172,174,183 or they can be useful for the development of ‘what-if’ staffing scenarios, to determine potential financial and patient outcome feedback. 134 Therefore, computerised decision support systems can:
. . . facilitate the evaluation of the impact, adequacy and relative benefits of alternative nurse organization processes and structures.
Maenhout and Vanhoucke184
Anderson et al. 134 illustrated this by indicating how the use of a dashboard meant that managers would be able to forecast:
. . . the impact of various staffing patterns on patient outcomes and costs rather than staffing to keep costs down on a shift-by-shift basis. Managers will be able to predict the ‘true’ costs associated with staffing decisions and their impact to the bottom line.
Anderson et al. 134
Workforce planning and deployment tools and technologies may therefore assess multiple dimensions of the staffing system to determine future need. van Oostveen et al. 124 suggested that the Professional Assessment Of Optimal Nursing Care Intensity Tool (which assesses the optimal nursing care intensity for a clinical area) can highlight non-patient factors that may affect workload (e.g. organisational issues). The NHS Education for Scotland toolkit131 suggested how to determine numbers and skill mix in the light of demand and budget to ensure good-quality care. It identified the importance of workload measurement, to assess activity, capacity, demand and capability, and highlighted the professional judgement approach, acknowledging subjective judgements from nurse leaders in particular areas. Furthermore, Dent130 suggested that part of staffing planning was a focus on recruitment and retention and highlighted the importance of incorporating fatigue management guidelines when forecasting staffing:
These guidelines provide a strategy that recognizes and manages the potential negative consequences of sleep deprivation and sustained work hours on patient outcomes and staff wellbeing models of care on nursing outcomes.
Dent130
Workforce planning and deployment tools and technologies effectively drive the management of staffing establishments, for example through rostering. 129,185 Barton168 described how an acuity application technology linked to national benchmarks was used to set overall staffing parameters by unit and helped to adjust skill mix. Kane179 used technology for caseload analysis in the community for skill mix and numbers. There is some indication that establishment setting using WPTs has to consider the local organisational needs of the staffing system. Local knowledge of the clinical area/care setting is also deemed to be important when implementing WPTs. 127,175,178 Fenton and Casey147 emphasised that the Safer Nursing Care tool must relate to local factors and be used in combination with nurses’ professional judgement. 147 Taylor et al. 127 illustrated this point:
Each unit must define its needs using standardized approaches, and learn to argue the importance of the recommendations that they, as experts in the micro-system in which they provide care, consider optimal levels of staffing for safe patient care.
Taylor et al. 127
When WPTs forecast future need, responsive decisions can result from this. One interview participant reflected how the application of the Safer Nursing Care tool identified an increase in patient dependency and acuity, and thus establishment figures were adjusted accordingly. Interview participants associated the achievement of staffing establishments with the provision of good-quality care, but noted the importance of maintaining this level:
Now when I’m at template it’s three trained on a long day, so they get that better quality, and, safety in an afternoon with the extra trained, so that we have benefitted there, but that’s fine while you’ve got (pause) all your vacancies filled, isn’t it?
Site 1, participant 1
The budgeted establishment includes an allowance for the fact that staff hours are not necessarily just to fulfil demand, and this is called headroom; this is usually 22–25% of the budgeted establishment. 129 Drake further explained how staffing establishments must allow for headroom or time out; this includes:
. . . additional staff to allow for staff unavailability due to annual leave, sickness, study leave, parenting, etc.
Drake143
Headroom may also factor in meal breaks and seasonal pressure. In addition, making provision for headroom is a key performance indicator in England. 129 Many authors have highlighted how headroom must be factored in for staffing allocation. 129,159,186 Local flexibility associated with this headroom is an important proximal aspect of the staffing system associated with staff satisfaction, but with plausible repercussions for distal aspects, such as recruitment and retention. Murtola et al. 186 indicated how headroom must be incorporated into technology. Drake143 noted how headroom allowances are often lost because of budget when there are nurse-to-patient ratios.
Outcomes
Workforce planning and deployment tools and technologies can be used by NHS managers to forecast real-time and future demands so that they can respond effectively to deploy staff. This can have a positive impact on nursing outcomes, when there is positive reinforcement of proximal and distal aspects of the staffing system. Nursing outcomes, such as nurse satisfaction, recruitment and retention, appear to be linked to the impact of organisational factors on staffing. The data from the synthesis of the literature mainly examine nursing outcomes within hospital settings, with some preliminary evidence on long-term care and a lack of evidence in primary care. 133 The evidence suggested that organisations need to be responsive to staffing needs in order to have a positive impact on staff outcomes. The structural features of the organisation, organisational processes and outcomes appear to have an impact on staff outcomes. 184 When there is reinforcement of responsiveness to staffing needs, as part of the proximal staffing system, this appears to have a positive impact on recruitment, retention and satisfaction. Fairbrother et al. 121 found reduced vacancy rates when the model of care was team nursing, although the results were not significant (U = 10.0; p = 0.20). Team-based models of care have also been linked to increased job satisfaction. 120,121 In addition, Magnet hospitals associated with high levels of nurse support increased nurse satisfaction. 119,123 Educational support appears to be fundamental for the facilitation of nurse satisfaction with organisational factors. ‘Train the trainer’ programmes also increased nurse levels of satisfaction with teamworking. 120 Furthermore, nurse managers’ responses appear to strongly influence the environment or climate of care to improve nurse satisfaction. 149,187,188
The nurse manager’s ability to creatively problem solve and develop relationships with staff can positively influence the practice environment and nurses’ job satisfaction.
Zori et al. 188
The interview participants noted that they strove to make clinical areas attractive to potential staff and invested in current staff, often through development and education programmes, to promote retention. Some participants reflected that models of nursing care are changing with the development of new roles, such as the nurse associate role in England, prompting staff to be more innovative in their approach to care provision and mitigate nurse dissatisfaction with staffing deployment, through developing and reviewing different roles.
Understanding the proximal and distal aspects of the staffing system meant that there had to be a balance between staff satisfaction and ensuring safe staffing. There was an understanding of the synergy between proximal and distal staffing systems so that nurses did not feel disempowered. Both the PPI and NHS manager stakeholder groups highlighted the importance of valuing and respecting staff with regard to staffing decisions. The NHS manager stakeholder groups and interview participants emphasised the importance of working with staff to ensure flexibility. One participant indicated the level of engagement work needed across one clinical directorate to respond to real-time and future needs for a flexible workforce:
Staff were very much ‘This is my ward and I’m not leaving it’. It took them a while. So, . . . to overcome that, we’ve done quite a lot of work. So, we did a lot of time-out days, right at the beginning, but we also did all our training together.
Site 2, participant 1
The NHS manager stakeholder groups and interview participants also emphasised how effective communication helped to prevent nurse dissatisfaction when redeployment was required:
We’re very lucky as a team that we’re constantly talking to the staff so we’re making them aware of the . . . you know, the organisational pressures, what . . . you know, we’re not moving these staff unnecessarily, there is clinical need and priority to have to move them. So, to be fair, they’re very, very good.
Site 3, participant 3
NHS managers’ proximal decision-making around staffing deployment may have a positive impact on nursing outcomes. Good nurse–patient allocation/assignments improve organisational reputation, making the hospital a better employer. 178 Allen158 indicated that an equitable nurse-to-patient workload decreases burnout, and this influences satisfaction and reduces the nursing shortage. Furthermore, the manager’s role in rostering may have a direct impact on hospital performance,185 and rostering can have an impact on staff welfare and satisfaction. 131,155,181 The quality of management decisions therefore appear to affect staff outcomes related to job satisfaction and satisfaction about care standards. 131
The interview participants strongly indicated how recruitment, rostering and nurse–patient allocation was a priority to ensure both good patient outcomes and good nurse outcomes:
Well I think if you get your staffing right you’re 99% there, aren’t you? . . . To me, the two most important things of my job is recruitment and rostering. Patient safety is embedded in those two things. So, if you can get those two basics right, you know, if you can get your recruitment right in the first place and get your rostering right, and make sure it feels safe, because half the battle is your staff feeling safe.
Site 2, participant 2
The impact of tools and technology on nursing outcomes
Successful data information management tools may affect staff satisfaction. 151 Pruinelli et al. 175 suggested that the Nursing Management Minimum Data Set (NMMDS) can result in improved patient and staff outcomes:
These data are instrumental in supporting effective work-force management practices and in developing effective staff recruitment and retention strategies.
Pruinelli et al. 175
Crist-Grundman and Mulrooney169 indicated that technology can have a positive impact on nurses’ work–life balance. Maenhout and Vanhoucke184 suggested that electronic nurse scheduling should avoid unhealthy shift patterns (e.g. too many consecutive nights or too few days off):
The quality of a nurse roster is also measured in terms of personnel job satisfaction which is related to the working atmosphere, the fairness among nurses, the compliance with nurses’ wishes and requests and the healthiness of nursing schedules.
Maenhout and Vanhoucke184
Self-rostering has emerged as a result of shortages in nurses and difficulties in recruitment. 157 Davidhizar et al. 189 suggested that staff satisfaction increases when staff members control the assignment/allocation structure. Self-rostering technology enables staff to see which shifts are available online and select suitable shifts to work. Both Valentine et al. 190 and Brown191 reported increased staff satisfaction, recruitment and retention with self-rostering technologies. They found that it improved staff satisfaction through offering flexibility and choice in staff schedules. Brown191 described this as ‘empowering’ staff. Valentine et al. 190 indicated how accessing shift availability online at home was useful, as nurses wanted to work in specific areas, usually their own unit; the results were positive, as improved staff satisfaction resulted in increased staff retention.
In relation to positive reinforcement of the distal staffing system, NHS manager stakeholder groups highlighted that organisational reputation is important for recruiting staff and for people within the organisation. All interview participants emphasised how the retention of staff and recruitment were important priorities and how WPTs articulated data for understanding:
We’ve been doing quite a lot of work in terms of retention and trying to understand what gives us our turnover, you know. We’re no different in terms of our turnover; we’re no different from any other organisations, any large organisations of the same size and amount of nursing staff. So, we have a turnover at 10% or 11%, you know, but given the numbers of staff that we do employ, that’s quite considerable every month, you know, or in a year, you know. So, we’re doing quite a lot of work to try and understand trajectories and what does that . . . the impact that that does have on morale and wellbeing of our staff, you know.
Site 2, participant 2
In addition, WPTs can improve operational efficiencies and reduce staffing and agency costs, with Brown191 reporting a reduction of 50% in agency costs and better-quality care. Junttila et al. 192 indicated how nursing satisfaction could be captured with technology to enhance decision-making on staffing. They note that measurements on job satisfaction are rarely stored in databases, and these data could form part of a nursing management information data set.
When there may be misalignment
Proximal aspects of the staffing system, particularly management responsiveness, can be adversely affected without real-time data. Sources of evidence indicated how a lack of real-time data had an adverse impact on decision-making on staffing. 151,159,162 Kontio et al. 151 discussed the outcome of a lack of data on participants in their study:
This information would have helped them to estimate patient flow and thereby allocate staff better. They also lacked information about the bottlenecks in the process; therefore, they were not able to manage the process in real time. Furthermore, information on patient priority was not available in real time.
Kontio et al. 151
Some interview participants also noted how data from WPTs were not always up to date:
. . . so if somebody’s phoned in sick overnight . . . it won’t have been updated so it won’t be correct. So, the ring round is really important. With the best will in the world, the data . . . is only as good as the people that are inputting it.
Site 3, participant 1
Interview participants also highlighted when poor data input may impede the use of WPTs:
. . . to be honest, it doesn’t matter how good your systems are, if you put rubbish in you’ll get rubbish out.
Site 2, participant 1
Furthermore, Hockley and Boyle166 pointed out that any reliance on manual data input carries risks arising from time pressures on staff, human error, or the deliberate manipulation of data. Other barriers to effective real-time forecasting were apparent. NHS managers have little control of the distal environment (e.g. workforce availability) in which staffing decisions are made, and this causes demand-driven roster changes. 143 Some evidence from the literature and interview participants noted that, rather than being able to respond to need, managers had to make do with the staffing resources available. 158,164 Rischbieth160 cautions that rapid decision-making with limited resources may result in adverse patient-, staff- or system-related incidents. Allen,158 on interviewing nurse managers, uncovered a degree of pragmatism associated with making the best use of available staffing resources against a sliding scale of the attainment of ‘best care’.
. . . when you’ve got wards on minimum numbers it can be quite challenging at times. And, like I say, the only impact I can do on that is to try and do the best I can with the staff I’ve got. I’m not a magician, I can’t create staff out of . . . do you know what I mean?
Site 2, participant 2
Poor rostering practice can lead to staff dissatisfaction, absenteeism and a high level of nurse turnover. 143,151,156,163,178,185,189,193 Changes in the stability of nursing personnel, skill mix or decreasing nursing numbers may also affect patient outcomes:133
. . . poor rostering decision making can deleteriously affect the key performance areas of service delivery both clinical care and the patient experience), resource utilization, and staff morale and retention.
Silvestro and Silvestro185
Davidhizar et al. 189 indicated how changes in shift patterns or length, and moving staff to another area when there are staff shortages, increase unsafe patient care conditions. They indicate that the requirement placed on nurses to work shifts and unsocial hours is a major contributor to job dissatisfaction and burnout. Low RN ratios may have an impact on satisfaction levels. Tran et al. 122 found few differences in satisfaction levels with nursing care delivery models, but satisfaction with co-workers was reduced in a shared care in nursing model with increased proportions of second-level RNs and nursing assistants. van Oostveen et al. 132 found that staff dissatisfaction was linked to a desire for more autonomy and perceptions of a lack of authority. This may also be related to shift patterns:
Nurses are particularly frustrated when they feel a lack of input into decisions about their work and their schedules.
Davidhizar et al. 189
Drake162 emphasised that requests can be rejected if they conflict with the needs of the ward, but equally found that when a large number of requests were assigned to the roster before other duties, this reduced the number of consecutive shifts available, making rostering some shift patterns more difficult.
In addition, allocation does not always take into account nurses’ preferences for specific areas; many nursers consider themselves to be specialists despite the assumptions of others that ‘a nurse is a nurse’. 189 Interview data indicated that the redeployment of staff to cover for sickness and absence is a source of nurse dissatisfaction, particularly when staff are moved to different specialties that are short-staffed. Staff redeployment to cover staff shortages worsened the cycle of staffing deficits:
There is no doubt that there is some kind of link between the number of staff moves that occur and the sickness that is happening, because . . . staff are employed to work with one team, and they like to work with one team . . .
Site 3, participant 3
van Oostveen et al. 178 found that nurses were less satisfied about their patient assignment following the implementation of a computerised decision support system tool, as the choice of allocation to patient was lessened. However, Drake,162 on reviewing an electronic roster system, found that many areas avoided using an auto-roster in order to honour staffing requests. One interview participant indicated that the technology could be developed further, for example to incorporate agency into e-rostering or a staffing skills function.
Poor resource management may lead to the inefficient use of resources, such as overstaffing of the ward, not using staff members’ full contracted hours or mismanaging annual leave so that shifts are not covered;185,194 it may also result in excessive bank and agency costs. 171,185,193 Furthermore, poor management may have an adverse impact on organisational reputation, with a negative effect on recruitment. 185 Certainly, poor nurse satisfaction and morale appear to lead to high rates of nursing turnover134,185 and absenteeism. 185,193 There are organisational costs associated with high rates of nursing turnover. 144 Subirana et al. 128 proposed that in their realist logic model of nurse staffing and nurse outcomes, nurses’ perception of staffing inadequacy can lead to emotional exhaustion, burnout, job dissatisfaction and poor retention. High rates of turnover and absenteeism are associated with inadequate staffing. 134 Poor perceptions of staffing levels also reduced staff morale in police organisations. 153 However, Flynn and McKeown165 suggested that there is a small evidence base for staffing levels and adverse nurse outcomes.
Many stakeholders and all of the interview participants acknowledged problems in the distal elements of the system, which affected recruitment and retention. In semi-rural areas, nurses were unlikely to apply from outside the area; conversely, in urban settings within small geographical areas, there were high levels of competition for available staff, with several organisations trying to attract staff to work for them. Participants did not anticipate improvements in staffing levels:
But we still have vacancies; we still have staff turning over. You know yourself, the retirement age . . . particularly, for example, district nursing, we know that almost half the workforce is going to retire in the next 5 years.
Participant 3, site 3
One participant noted that retention had an impact on recruitment:
And there’s a correlation on wards that have higher amount of vacancies and higher turnover, so you know, you’d argue what comes first, it’s chicken and egg stuff isn’t it, you know? But we do have some wards that are unable to retain staff because of the vacancy rate, you know.
Site 2, participant 2
When recruitment and retention is a problem, the effectiveness of WPTs may be hampered. Taylor et al. 127 found that the staffing methodology recommendations for staffing and filling vacancies could not be realised because of recruitment and retention problems.
Alignment of organisational strategies over workforce planning and deployment tools and technologies (context–mechanism–outcome 2)
When and where there is alignment between relevant organisational strategies (context), it enables NHS managers to use tools and technology as levers for change or negotiation (mechanism), promoting the patient safety agenda within the organisation (outcome).
Context and mechanism
Multiple organisational strategies may influence NHS managers’ work in safe staffing deployment (Box 2). The evidence suggested that multiple organisational strategies underpin quality care and patient outcomes, and these can align to have an impact on safe staffing. Murtola et al. 186 suggested that strategy relates to organisational long-term goals, such as mission and vision. McIntyre129 noted that there are multiple influences on staffing deployment, such as service transformation, national policy, local care needs and staff supply. These influences and others are incorporated into organisational strategic aims for effective, efficient, good-quality care. The evidence from the synthesis suggested that when organisational strategies align to consistently promote good-quality patient care, this conveys certain organisational expectations on NHS managers to deliver safe staffing. 126,127,129,131,144,168–170,184,185,190,193 NHS manager stakeholder groups and interview participants felt that it is essential that NHS managers understand the strategic perspective and how this has an operational impact on multiple organisational systems.
-
Long-term overarching strategy: including vision and mission. 186
-
Financial: to ensure cost-effectiveness and efficiency. 126,127,129,131,133,144,156,158,160,170,176,184,185,190,193,195
-
Quality: linked to national standards and legislation on quality and patient safety. 126,127,130–132,156,183
-
Professional: regulatory processes from the professional body. 130,145,177
-
Human resource: employer requirements linked to staff well-being. Roster policies, family-friendly policies and use of agency and bank nurses. 129,130,143,146,147,155,157,169,177,184,185,189,195,196
-
Patient and public: linked to good-quality care safety, transparency and patient satisfaction. 165,166
Many sources linked strategic requirements to legislation. 126,130,133,145,146,177 Health and safety legislation linked to good-quality care and patient safety was found to be an important influence on the protection of the workforce177 and the enhancement of recruitment and retention,146 and on nurse staffing ratios or levels. 133 Legislative requirements also have an impact on organisational strategy and policy, leading to mandates on staffing methods or tools,126,127,130–132,190 thus influencing nurse managers’ priorities. 145 For example, the national strategy and policy in Finland mandated the use of patient classification systems, such as the Oulu system, within the RAFAELA staffing system, to determine nursing care intensity and optimum staffing ratios. 132 National guidance also influences organisational strategies. In England, NICE guidance has endorsed the Safer Nursing Care tool to calculate nursing establishment in acute adult settings. 147 Many interview participants indicated how this guidance had influenced hospital strategy, but also how this was an evolving process, as further strategic requirements emerged:
So, we use the safe staffing tool at the moment we do, yes, and we use the acuity and dependency, which is part of the safe staffing tool to set up that establishment. But, as you know, there is a shift at the moment in terms of e-roster [electronic rostering system] to move, to look at care hours per patient per day.
Site 3, participant 3
Professional regulation further influences staffing and affects organisational strategies. 145,177 Several interview participants indicated how the emergence of new roles had been embraced at a strategic level. Many commented on the new nurse associate role in England and its potential impact on future establishment levels. The NHS manager stakeholder groups and interview participants also commented on the importance of a strategy for recruitment and retention to ensure safe staffing:
The staff need to know what our recruitment plans are, the staff need to know what our retention plans are. They need to know that we are proactively trying to do things to support them and improve the situation.
Site 3, participant 2
Furthermore, organisational strategies need to be aligned at a local level; managerial decisions from different departments can have an impact on nurse staffing. For example, the literature noted how theatre schedules could be altered without notifying nurse managers so that they could provide sufficient staff in response:132,154
Our workload is determined by the physicians’ operating programme. We do not know how many resources we will need for the next week. We just respond afterwards. (Head nurse, 16).
van Oostveen et al. 132
The interview participants highlighted similar issues. The participants reflected the need to respond to strategic plans for service reorganisation and how this had implications for staffing:
. . . so they’ve got 16 beds that admit elective orthopaedic patients . . . but that ward was closed, but it’s re-providing unscheduled care pressure so outliers are going there, so that’s given us another 16 beds. However, because of staffing problems on the general orthopaedic ward what we’ve done is had to redeploy the staff from the ring-fenced ward.
Site 1, participant 3
In addition, interview participants commented on the importance of achieving strategic aims in good-quality care through nursing metrics evaluation and how this linked to safe staffing:
I’ve been asked to look at an increase in falls in the trust and correlation between staffing numbers.
Site 2, participant 1
And you do feedback, even though it’s short staffed, if you find that things haven’t been done, do you still go back to the staff? Yes we do, we discuss it in our safety briefing every morning, what we’re trying to strive for with our work, our compliance; even though when it’s busy we still have to achieve these standards to give the best care.
Site 1, participant 1
Financial strategy, linked to resource availability, underpinned all other organisational strategies related to staffing and quality care. 129,131,133,144,158,160,170,176,184,185,190,195 The evidence strongly suggested that strategic aims for the delivery of safe, good-quality care had to be considered in the light of financial strategy:
Patient safety during hospitalization requires deliberate planning to deploy resources that best meet patient needs in a cost effective way.
Pappas176
The interview participants indicated that the achievement of strategic aims for good-quality care and patient safety was tempered by the awareness of financial strategy:
I think the focus is always on safety. We haven’t got a limitless pot though have we? . . . so we have to manage our resources. . . . It is a balance, and we scrutinize our bank and agency spend every week, or what we’ve used and what we’re predicting to use.
Site 3, participant 1
Data to negotiate for change
Where and when the alignment of organisational strategies occurs, nurse managers are able to use the data from WPTs to demonstrate the reality of practice in comparison with strategic expectations. 126,127,129,131,144,169,192 These staffing data enable NHS managers to advocate and negotiate for a change in systems or resources, to ensure that staffing deployment achieves the organisational goals. The advisory group highlighted that, within organisations, many people can influence staffing decisions, such as doctors, financial managers and bed managers, and these powerful others may adversely affect nursing decisions. Eduardo et al. 148 indicated that nurse managers have to confront organisational barriers, owing to conflicting political goals from disparate groups:
The major forms of political intervention in decision-making arise from hierarchical power, financial control needed to implement the strategic decisions, and the influence on and the power of veto.
The evidence suggested that WPTs may empower NHS managers, as they provide additional weight to managers’ arguments to justify changes to staffing. 129,161,168,179 Eduardo et al. 148 suggested that decision-makers respond to policy and strategic aims. Therefore, it would appear that when WPTs provide data for the achievement of policy and strategy, they confer leverage to the NHS managers’ opinions. One manager with a strategic remit indicated what he had observed when NHS managers came to understand the utility of data from WPTs:
But it’s something else, you know, when you talk about it, it’s actually quite . . . quite invigorating, when you see a group of ward managers spend 3 hours together going through data and making decisions to change how they’re doing things tomorrow.
Site 1, participant 4
NHS managers need data for different purposes (e.g. strategic, financial). 180 Murtola et al. 186 indicated how managerial decision-making in hospitals occurs at strategic, tactical and operational levels. The strategic level is concerned with long-term goals and the tactical level is concerned with the achievement of short-term gaols, such as resource distribution, operational concerns and daily activities. Murtola et al. 186 suggested that nurse managers are generally involved in tactical and operational decisions. The evidence from the data also reflected that there are different information needs at different levels within the organisation. 131,180,182,186,197 Kivinen and Lammintakanen182 found the need for multifaceted information and more detailed information for different user groups with a management information system (MIS).
The interview participants also articulated the need for different information depending on their role. Ward managers and matrons were interested in real-time and retrospective staffing numbers in relation to patient acuity and dependency; they had a strong awareness of the financial data related to staffing in their specific areas. Matrons and lead nurses also reviewed this information, but from a broader perspective; in addition, they needed to link these data to other strategic areas, such as patient experience and workforce retention. This reflected the findings of Murtola et al. 186 that upper levels of management are generally interested in information about the quality of care and costs, with middle managers needing information about care processes and resources.
Workforce planning and deployment tools and technologies provide data to justify and rationalise the utilisation of resources and to convey the reality of managing the service related to resource availability. 131,144,161 The data from WPTs may make nursing care visible, providing objective evidence of staffing needs and how staff may best be deployed throughout the organisation. 168,179,192 The interview participants indicated how negotiation for tactical and operational decisions for changes, to ensure safe staffing in the short term, happen on a day-to-day basis, particularly the need to move staff. When using data from WPTs, interview participants indicated that they use their professional judgement and skills to negotiate staff moves:
Well obviously I negotiate it, we work as a team on the ward so moving people around on the ward if need be is not a problem.
Site 3, participant 4
The evidence suggested that data from WPTs can be used to achieve long-term strategic goals in quality care. 168,192 Junttila et al. 192 indicated how information from different tools within a nursing MIS was found:
. . . to be useful in redefining care profile of ward units and reallocation of nursing resources.
Junttila et al. 192
Barton et al. 168 discussed how one organisation used technology to determine staffing numbers and patient acuity, which provided data to set staffing parameters linked to national standards; this enabled the adjustment of staff numbers and skill mix, in alignment with budgetary information:
These data allow us to ensure each unit’s direct care staff stays right-sized during the course of the year, and it helps us justify the need for additional nurses.
Barton168
The interview participants also indicated that data from WPTs provided evidence for change to achieve strategic goals on good-quality care:
It provides evidence and backup that is so needed, that is saying actually, ‘look, this care of the elderly ward had this number of dependency 12 months ago, over a period of 12 months we’ve gone to this number of dependency’. So, we know that we’ve got to review the establishment of this ward because there’s been such a significant shift.
Site 3, participant 3
Therefore, through the use of WPTs, and the data they collate, NHS managers may be empowered to make changes or make the case for changes. van Oostveen et al. 132 found that the data from nursing workload measurement tools:
. . . creates possibilities for better positioning of nurses in hospitals and further professionalization in terms of enhanced authority and autonomy.
van Oostveen et al. 132
Kane179 found that team leaders who engaged with the Electronic Caseload Analysis Tool (eCAT) started to challenge the caseload data, as the tool enabled an objective and systematic review of equity within caseload allocation. On introducing a staffing technology that integrated patient acuity with staffing availability, Barton found that:
Nurse managers were hungry for data, and when they saw how the information generated by the system could help them improve staffing, they became enthusiastic supporters.
Barton168
Therefore, data from WPTs, such as rosters, can influence change129,164 through the reallocation of resources,169,192 and redefining care profiles of clinical areas. 192 Several interview participants commented on the need for innovation, as the functionality of existing staffing systems did not reflect the reality of staffing availability. The development of new roles was a key area for change:
Obviously, we’ve recently commenced the nursing associate role, and we also have assistant practitioners on the wards. So, it was about kind of thinking about your nursing team differently, what skills can other people bring into that team, rather than the old, traditional registered nurse, non-registered nurse.
Site 3, participant 3
Outcomes
Many sources of evidence linked staffing to quality and safety. 128,132,133,158,161,165,166,176,180,184,198 Effken et al. 145 indicated the challenges that nurse managers face in solving problems related to patient safety, quality and satisfaction and finance and staffing. All stakeholder feedback strongly emphasised that patient-centred care is the priority. When there is alignment of strategies in support of safe staffing, this facilitates the nurse managers’ use of data from WPTs to make an impact on patient care quality and safety outcomes:131,132,149,159,187
At the end of the day, if the ward needs it, we have to have it and I can justify why I used, why I spent it.
Site 1, participant 1
When there may be misalignment
Information is power, but only if there’s a process in place to interpret the data and then make policy and procedure decisions based on the evidence the system provides.
Crist-Grundman and Mulrooney169
The evidence highlighted areas in which there was misalignment between financial and other organisational strategies related to budget restrictions; this had the potential to adversely affect the effective use of WPTs;126,127,160 this was also the case for police staffing. 153
Robinson et al. 126 and Taylor et al. 127 reviewed the implementation of the Veterans Health Administration’s mandated staffing methodology. They categorised organisations on their implementation (by scoring on integration with budget, implementation of directive elements, engagement of leadership and use of data to support the process) and found that organisations with a low level of implementation did not have the flexibility within the budget to employ the recommended increase in staffing numbers. Conversely, if the budget provision is not sufficient to staff a unit as required then units could go over budget. 129 Given the strong links between staffing and patient outcomes, misalignment between financial and other organisational strategies may present:
. . . a danger that bottom-line fiscal improvements may occur at the expense of poor patient outcome in the longer term, thereby negating the presumed cost efficiencies.
Rischbieth160
Misalignment of financial strategy with staffing requirements was also articulated in the interviews:
And we get frustration from the ward managers, and they know what to do, but they have to go through in their own organisations to get . . . additional staffing, or to provide a business case for replacing the nurse that they’ve always had in their establishment who’s currently vacant. It takes 12 months to get a new nurse in post after one leaves. So, all these kinds of things, the organisations are almost set up to do exactly the opposite thing from what the ward managers know, but can’t quite articulate.
Site 1, participant 1
Furthermore, Murtola et al. 186 suggested that nurse managers are generally involved in tactical and operational decisions; however, most WPTs focus on strategic and tactical decision-making, with little evidence of support for operational decision-making. 186 Possibly, WPTs do support strategy when it is aligned, but do little to help articulate day-to-day operational requirements. Finally, when strategic requirements are ‘top down’, this may impede the implementation of WPTs because of a lack of ownership:
I think that maybe the deployment stuff, for me, I think having things that are thrust upon us from a governmental point . . . you know, so things like, say, staffing was . . . was very much thrust upon us, and so I don’t know whether the embedding, or the implementation was as nurse-driven as it should have been, and I think if you have things that are more driven . . . that are all accepted and better driven because of need, not just because we have been told to, I think we would have got better engagement, and I think that’s been a challenge.
Site 3, participant 2
Supporting the NHS manager to use workforce planning and deployment tools and technologies (context–mechanism–outcome 3)
When there is visible support for managers, skill development and leadership (context), WPTs empower NHS managers to make sense of complex data (mechanism), increasing the likelihood of staffing skills being in the right place (outcome).
Context and mechanism
Support and skills development
Several sources of evidence indicated the importance of the investment of time and resources to support nurse managers to successfully use WPTs, for effective and efficient staffing deployment decisions. 126,127,134,162,174,199 Examples that demonstrated this investment, and which may support NHS managers to develop the knowledge and skills required to use WPTs, are summarised in Box 3.
-
Expert support.
-
Mentoring.
-
Training.
-
Leadership programmes.
-
Workshops.
-
Peer support.
-
Leadership at all levels.
-
Practical guidance.
-
Examples of good practice.
-
Open channels of communication at all levels.
-
Action-learning sets.
It is important for managers to feel that they are supported in their decision-making on staffing deployment. 128,163 The evidence showed that support for managers in their decisions on safe staffing was visible in multiple ways. The evidence suggested that a key method of support was the presence of a dedicated support team. 124,126,154,179,191,194,200 This team could be strategic, encompassing managers and finance and information specialists. 174,195,199 A support team could also provide more practical advice on WPTs. Junttila et al. 192 highlighted the need for an information analyst with clinical expertise to produce reports, identify trends and recognise new information needs. Many interview participants commented on the helpful role of e-roster support teams; often this was online or via telephone:
I think the organisation invested very well into e-rostering, it had a good team, a good strong team putting it in, and they’ve sustained it by keeping a good helpdesk and a good turnover. If you’ve got a problem they’ll sort it for you quite quickly.
Site 2, participant 3
He can access our rosters remotely from there, so if there is a problem and we can’t do it he’ll do it then and there and then we just click refresh and carry on then.
Site 1, participant 1
The evidence indicated that support via personal contact is useful. Robinson et al. 126 found that the presence of a dedicated and knowledgeable staff was an important factor in support for the Veterans Health Administration staffing methodology processes. Staff had a specific remit to support the staffing methodology and acted as a resource for managers:
Our SM [staffing methodology] Coordinator . . . did an outstanding job with it . . . she found ways of taking stuff and making it to the point where the staff who lacked the expertise or the knowledge or skill set could really . . . digest it.
Robinson et al. 126
Interview participants acknowledged that face-to-face support was also very useful:
When I came into post we were still doing the daily drop-in sessions, teasing out problems really, snag lists; that sort of thing. I ended up going for a one to one session with X, . . . I booked it in, just so I knew what I was talking about.
Site 3, participant 4
If the ward manager or deputy is struggling with something and can’t remember how to do something, they can just pick up the phone and somebody’ll say ‘I’ll pop down there now and do it with you’ so next time they’ll be able to do it.
Site 1, participant 3
Also related to the Veterans Health Administration staffing methodology, Robinson et al. 126 and Taylor et al. 127 used unit and organisational expert panels for support. Taylor et al. 127 reported the use of expert users from other organisations to help with training. Organisations with a good reputation for e-roster such as Portsmouth Hospital, were chosen to demonstrate practice and tools to others. 129 Diers et al. 154 used a ‘buddy’ system; one interview participant also highlighted the importance of such a system:
I mean it’s a way of working together isn’t it, and to bringing people on. So, a new ward sister would always be buddied up with another ward sister, a more experienced one, to make sure they’re okay.
Site 2, participant 1
Research evidence suggested that it is vital that NHS managers have support to develop the skills and knowledge to equip them to deal with the challenges within their role, including decision-making around safe staffing. Shirey et al. 187 found that stress and organisational complexity has a negative impact on managers’ cognitive decision-making and recommended various means of support, including formal programmes for professional development and the creation of a supportive environment. The evidence suggested that supportive environments can be fostered by an organisation. Magnet hospitals appear to increase nurses’ perceptions of support; these are organisations in which professional models of nursing are promoted to enhance innovation and nursing autonomy. 118,119 One interview participant explained how her organisation facilitated support for NHS managers around safe staffing decisions:
So they’ll have support from their managers, and we’ve recently gone through an organisational restructure, so last year, that makes sure that we do have adequate nursing support, and we’ve put in extra posts to do that.
Site 2, participant 2
Peer support within the organisation also appears to be important for NHS managers. All of the stakeholder feedback highlighted how NHS managers should have compassion and empathy for each other and that there should be open channels of communication at all levels. One interview participant’s comments illustrated this:
My role is about maintaining positivity at the end of the day and, as I say to the matrons, you know, come in the office by all means, close the door, rant and rave and shout and say whatever you like, but when you go out there, you go out to the coal face, you know, you put your smile on your face and we deliver that positive encouragement to the teams as best we can. We know it’s hard, we know it’s not perfect by any stretch of the imagination, but what they want to see is, is they want to see the senior nurses out there on the wards supporting and helping, doing their best to try and get where they can.
Site 3, participant 3
Visible support is linked to investment in the development of NHS managers’ skills and knowledge. Feedback from the NHS manager stakeholder groups indicated that it is essential for NHS managers to understand the organisational model of staffing deployment and its impacts. Interview participants indicated how teamwork on staffing helped to develop a common understanding:
I think everybody knows what the expectations are to be honest.
Site 2, participant 2
The availability of training and education on WPTs was highlighted by many sources as being essential, so that nurse managers could input, collect and analyse data and understand how to use the technology effectively. 124–127,129,131,143,147,150,154,156,162,171,173,174,179,182,191,192,195,198–203
The evidence also suggested that training and education is important for the development of nurse managers’ skills for decision-making processes related to their role generally148,149,187,188 and in relation to staffing decisions. 153,174 Training and education can promote skills in organisation, critical thinking149,188 and human relations, such as communication and team-building,149 negotiation and conflict mediation148 and skills in technical competence. 149 Zori et al. 188 suggested that emotional and social intelligence skills can be developed through educational strategies. Interview participants also explained how some areas used mentorship programmes and action-learning sets to develop NHS managers’ skills. Leadership and the ability to work as a team are essential competencies for the nurse manager149 and are vital for staffing decisions. 163,167,186,189,199,202 The development of leadership and teamwork skills can be facilitated through train-the-trainer programmes. 120 Interview participants also found formal leadership programmes useful:
Well it’s given us a bit of ownership, and helped us with our leadership skills, maybe, to realise what our skills are and how to sort of improve them and how to, staff engagement and discussing and doing practical things like that. We’ve had practical sessions on, appraisals, managing the roster was another one, all very practical tools that we can use day-to-day, and of course it helped the networking with other managers, other hospitals and sites as well, and you realise you’re not the only one we all have the same problem.
Site 1, participant 1
Targeted training and education on WPTs appears to be important for all levels of the organisation. 126,127,174,179,195,200 The evidence suggested that nurse managers also have a role in the training and education of their staff; Lammintakanen et al. 197 found that in the introduction of electronic information systems:
Learning and using the information systems was supposed to take place in a positive and encouraging atmosphere. The nurse managers’ duty was to promote such an atmosphere, which also allowed learning by trial and error.
Lammintakanen et al. 197
Some interview participants who were senior managers stated that they mentored or coached more junior managers:
I’ll sort of show somebody three times, you do it on the fourth time; it’s that sort of coaching really just to get the confidence going.
Site 1, participant 3
Furthermore, Allen164 highlighted the importance of educating staff nurses on what to expect about how their patient allocation will be made. Bonner et al. 156 also suggested that staff need education in order to understand the constraints under which the decisions are made.
Consistency and standardisation in training for WPTs also had an impact on staffing deployment. 147,164,167,200 In addition, the training may clarify what can be expected from their use; Flynn et al. 203 commented on the need to:
. . . explain through the education and training sessions that the purpose of the workload and workforce planning tools was not necessarily to create additional capacity, but to obtain the most out of existing resources.
Flynn et al. 203
There were examples of the need for continuous repeated training and motivational sessions for some WPTs, for example the RAFAELA system (a workforce planning tool),124,125 and also for automated rostering. 167 Training took many forms for both managers and nurses. Anderson et al. 125 used exercises for a patient classification tool and NHS Education for Scotland used work-based activities within their toolkit. 125,202,203 Wallace and Pierson195 found that managers were positive about a scheduling programme of resources and tools, and found workshops helpful. They requested more scheduling guidance and an online discussion forum. Kane179 described regional user forums for the development eCAT, the community caseload technology. Diers et al. 154 and Ruland171 both noted the importance of financial training. There was some evidence that training aimed to provide additional technical skills or focus on those who lacked IT skills. 174,179 Kane179 found that those who had better IT skills were initially more likely to engage with a staffing technology, but:
Some users who perceived themselves ‘not good with computers’ were anxious at the start of the training, but most became so interested in the reports that they were inspired to learn more.
Kane et al. 179
Many interview participants indicated that they had received training in use of WPTs, particularly e-roster. However, some studies’ findings suggested that education and training alone are not sufficient and other factors are inter-related, such as the credibility of the support team and good leadership. 126 van Oostveen et al. 124 also concluded that although training and education are essential, preparatory work is needed on the social context to facilitate nurses’ acceptance of staffing tools.
Leadership
Strong nurse leadership appears to be important for effective nurse staffing. 126,129,134,143,146,169,199,200 All stakeholder groups highlighted the need for strong leadership and felt that a good leader will offer a shared vision and people will follow them. NHS manager stakeholder group feedback referred to leaders as ‘flying the flag for nursing’. This may be linked to the use of data from WPTs as political levers for change or negotiation. Drake143 further illustrated how leadership was important for roster management:
Directors of Nursing explained their relationship with ward staff in terms of patronage, often citing examples of, ‘fighting for resources’ or, ‘confronting non-nursing staff’ on behalf of the ward staff.
Drake143
Szumlas204 also suggested that effective leadership is important for recognition of nurse capacity to align staffing skills and competence with patient need. Supportive leadership also appears to be important to drive staff engagement with WPTs. One interview participant indicated how she gave practical help:
We’ve had a day training to learn how to e-roster. To be honest, I, as a ward sister at the time, as a matron now, I will still go and spend time with a ward manager on e-rostering, to teach them some of the tricks.
Site 2, participant 1
The importance of the nurse executive and other corporate-level roles in driving staff engagement with WPTs, through the provision of time and resources to embed their use, was also evident. 126,129,134,143,147,169,200 Douglas199 highlighted how WPTs should be at the top of the nurse executive’s priorities and that their experience and wisdom could influence success. Robinson et al. 126 found that organisations that were categorised as being at a high level for implementing a staffing methodology all had nurse director support, which ensured consistency and staff development at all levels. Senior nurse managers can also influence the type of training and education that managers receive. 150
The evidence suggested that leadership should be shared at different levels of the organisation to promote collaboration in the use of WPTs. 126,127,129,147,163,166,182,190,197,200 An aligned approach appears key to the facilitation of local clinical and human resource ownership. 129 This may also facilitate political leverage, negotiation and change. 166
A standardised team approach appears to be important in implementing new technology. 200 NHS manager stakeholder feedback, interview participants and many sources from the literature indicated how leadership delegation, collaboration and teamwork is essential:124,126,127,130,131,134,169,174,179,200,205
Obviously, we’re very lucky in my division that I have X care as well, that sits in my division, so the lead nurse for X care, we’re constantly talking, saying ‘Do you need staff? Do we need staff? How do we support each other? What do we do?’ So, the matrons will do that kind of at grass-roots level. They will move the staff and they will make the decisions based on the acuity of the ward at the time.
Site 3, participant 3
Integration of data for sense-making
The value of technology is its ability to capture and process large amounts of data and to display data in meaningful ways that optimize communications, support collaboration, drive informed decision making and maximize resource use.
Crist-Grundman and Mulrooney169
The integration of data from WPTs can empower managers to understand the link between the nursing workforce and the delivery of care on patient outcomes and identify potential problems. 206 Data can be integrated from multiple sources and tools,129,180,183 and can be used for multiple purposes. 180 Many sources noted that in order for nurse managers to make effective decisions, data needed to be presented in a format that they could understand. 175,180,183 Hyun et al. 180 suggested that data presentation should be in a standardised and user-configurable way, to allow for sophisticated processing and data-mining. 180 Pruinelli et al. 175 noted that unless data are integrated and extracted in a meaningful way:
. . . nurse leaders will struggle to achieve better patient, nurse, and financial outcomes.
Pruinelli et al. 175
There are many examples of the integration of different types of staffing data through the use of WPTs. Some approaches to data integration followed a data warehouse model, which is a single source of information relevant to staffing deployment collated in one tool or visual dashboard. 134,174,175,192 The evidence demonstrated how multiple sources of data had been integrated; for example, Kerr and Timony167 integrated a rostering system with patient dependency, the hospital information system and the payroll. 167 Junttila et al. 192 integrated nurse-sensitive indicator data with staffing and rostering. Robinson et al. 126 found that a staffing methodology was implemented effectively when integrated into the budgeting process. Data have also been integrated on admissions and discharges,192 caseload179 and the environment of care. 175 Many sources of evidence indicated the importance of having information on nurses’ characteristics (qualifications, skills competence and training requirements). 128,133,144,151,152,157,158,160,164,174,175,180,181,184,189,191,198 Rostering can also integrate data on annual leave and sickness. 129 Valentine et al. 190 integrated data on shift availability, tracking and incentives when introducing an ‘Openshift’ (self-rostering) technology. Similarities were also noted in other organisational staffing, with the need for the integration of an extensive series of factors for complex police staffing decisions, such as current police workload based on individual and group performance, and demand and performance indicators. 153
Technology is reported to be important for identifying data for effective nurse–patient allocation. 151,170,175,181,184,186,192 The integration of data appears to facilitate NHS managers’ understanding of resource availability. Pruinelli et al. 175 noted that prior to the development of the NMMDS, data related to nurses’ qualifications and licensure were found in disparate systems (e.g. human resources or unit manager’s records) and were difficult to access quickly. 175 The integration of data may also enable managers to identify potential problems, barriers and causes of unsatisfactory resource management. 171,172,206
Integration of the data to determine staffing demand
Determining staffing demand is complex; the integration of data from WPTs may empower NHS managers to make sense of the staffing need and have a positive impact on decision-making. Patient acuity and dependency were consistently key factors in the consideration of staffing deployment. 158,163,183,207,208 WPTs can integrate patient need with staffing resources:
I think what the electronic systems have started to do, and I think there is certainly scope for improvement in this, is accurately kind of . . . weigh up the acuity and dependency of the patients that we are seeing versus the number of staff rostered on duties.
Site 3, participant 3
One interview participant indicated how she used patient observation data, whereby acuity scores are entered on handheld devices, and aligned these with staffing availability:
I would make sure . . . that there’s no-one that’s sick who hasn’t been picked up, or make sure we’ve got enough people on there.
Site 3, participant 2
This participant explained how the system also indicated how many observations had not been done and this could suggest the need for support, as people are ‘struggling to get everything done’.
Hyun et al. 180 cautioned that it is not sufficient to use patient acuity data alone. For a data warehouse approach, Frith et al. 183 recommended multiple sources of information to determine prospective staffing decisions; these included patient factors, such as acuity, but also staffing factors such as skill mix, nursing characteristics and unit and hospital factors. 183 In a concept analysis, Cathro163 highlighted fifteen factors that have an impact on decision-making for nurse allocation; patient acuity and patient need factors were the most important, but other influential factors were regulatory and safety issues, continuity of care, anticipated flow and nursing factors.
Integration of the data for a triangulated approach
When nurse managers have effective support and facilitation of skills and knowledge development, they appear to be empowered to use tools effectively to understand the complexity of the problems they face. 145 The triangulated approach, consisting of the use of evidence-based tools, comparison with peers and the application of professional judgement, can be facilitated when data are integrated for effective decision-making. The evidence strongly suggested that the integration of data, including triangulating judgement with WPTs, enabled decision-making about safe staffing. 124–126,129,131,133,134,145–147,151,154,159–162,166–175,177,179–183,187,190–192,194,199,204,206,208–210
There were also examples of integrated data decision support tools, including CLASSICA MIS (version 1; Ruland RM, RAVN IH; Oslo, Norway)171,172 and the Dynamic Network Analysis Decision Support tool (DyNADS) (version 1; Effken et al. , AZ, USA). 145 According to Effken et al. ,145 tools can stimulate higher-level thinking, and, as managers are able to see the bigger picture, they do not seize on quick solutions that may not be effective in the long term. Tools do this as they:
. . . deal with multifactorial problems in ways that synthesize the disparate issues nurse managers encounter into higher level concepts and allow them to test hypotheses about the kinds of solutions they might implement in a safe, virtual environment.
Effken et al. 145
Importantly, in using their professional judgement for decision-making, managers need to critically interpret WPTs on patient data in order to align staffing allocation with patient needs. 131,158,163,176,178 van Oostveen et al. 178 indicated that a computerised decision support system:
. . . can never completely replace human insight. The nurse-to-patient assignment generated by the ILP [integer linear programme] model is a proposal that has to be assessed and, if necessary, adjusted by one or more nurses to obtain the final nurse-to-patient assignment.
van Oostveen et al. 178
Outcomes
Ensuring the efficient deployment of staffing skills, in the right place, is complicated. When nurse managers were visibly supported to develop knowledge and skills, and there is effective leadership, this had a positive impact on their engagement with and understanding of the data from WPTs;126,127,134,143,174,199 this facilitated effective decision-making for safe staffing deployment:
We rely on these systems to improve our ability to assure the right resources are assigned to the right situations that result in the best possible quality, safety, and financial outcomes.
Douglas199
The evidence indicated the importance of matching nurse characteristics, such as education and skills, with patient need. 134,158,160,174,184,189 However, multiple factors, such as finance and organisational requirements, also have an impact on efficiency in safe staffing. When nurse managers have effective support and leadership, this has a positive impact on their understanding and use of integrated data from WPTs to ensure appropriate and efficient deployment. For example, many sources of evidence indicated that managers use scoring tools to match up staffing effectively; these scores are linked to workload. 124,125,127,129,130,133,144,147,151,175–180
Furthermore, WPTs can have a positive impact on finance when data are integrated on resource availability in alignment with the budget. This results in efficient resource management leading to cost reduction, as a greater understanding of staff availability can reduce overtime and agency costs. 126,127,134,157,166,168,170–172,175,176,183,190,191,194,199,206 To conclude, although WPTs can facilitate sense-making of complex data, NHS managers require effective leadership and support to develop the skills and knowledge required to empower them to effectively interpret data from WPTs for safe staffing deployment.
When there may be misalignment
Poor understanding of WPTs can impede their use. 124–126,151,155,208 Evaluation studies found that poor understanding impeded knowledge on how and when to report data, and this had an impact on decision-making;134 poor understanding also conferred a lack of confidence in the data. 127 This appeared to be linked to a lack of resources and a dedicated support team126,193 and a lack of time to develop skills. 185 Poor access to training also appears to impede the use of WPTs. 125,126,185,193,208 However, van Oostveen et al. 124 and Anderson et al. 125 found that, even when training was provided, it lacked success in some areas. Kivinen and Lammintakanen182 found that some managers criticised the educational content for being too technically oriented. In relation to the nurse manager’s role in general, Eduardo et al. 148 found a mismatch in training received on decision-making and what is expected from hospital managers’ performance. Some interview participants indicated that WPTs were not used to their full capacity, often because of a lack of training:
They do put in acuity data and all that stuff, and their numbers, and all that numbers in, that does go in electronically and that goes onto e-rostering and to safe care. But that’s not what I would use, or anyone else would use, to allocate staff. Whether that is the intention of it I don’t know. It certainly isn’t being used for that, and it isn’t anywhere that close to being used for that at this present time.
It’s just not fit for purpose?
It’s taken a lot of embedding, and with the . . . so I don’t think . . . I don’t think that . . . maybe that is what it’s meant to be used for, but I’ve certainly never seen that being . . . we’ve not been taught how to do that, we’ve not been given reports from that or anything along those lines.
Poor leadership appears to also have a negative impact on nurse managers’ use of WPTs. 126,127,182 Poor leadership manifested when leaders lacked commitment to the implementation of WPTs; often they did not value them and failed to communicate effectively or to commit to providing training programmes. 126 Hockley and Boyle166 highlighted a lack of engagement by senior management in the adoption of IT solutions in England, despite established safety and efficiency benefits. Certainly, the evidence strongly suggested that weak leadership caused delays in the implementation of WPTs. 126,127,173,174 Robinson et al. 126 found that in organisations with a low level of implementation, leaders were sceptical and had not bought into the staffing methodology. Stable leadership also appears to be important, as Anderson et al. 125 indicated how a shift in leadership impeded the use of a tool. One interview participant indicated that restructuring within the organisation could impede nurses’ use of data effectively from tools:
Well they’re devolving it to an operational level, which is fine, and I think it needs to be at that level, but they’ve not allowed a period of transition of knowledge and competencies.
Site 1, participant 3
Integration of workforce planning and deployment tools and technologies with organisational knowledge and NHS managers’ capabilities (context–mechanism–outcome 4)
When managers possess key attributes of leadership and ‘know their staff’ (context), and when tools and technology help to make resources visible (mechanism), managers have greater influence in their safe staffing work (outcome).
Context and mechanism
Harris and McGillis Hall133 indicated that decision-making about staffing is optimised when:
. . . it reflects strong nursing leadership to promote professional nursing autonomy and collaborative relationships.
Harris and McGillis Hall133(p. 26)
Leadership attributes
The stakeholder feedback strongly suggested that NHS managers should be good leaders; this was also suggested in some of the literature, for example, Connelly et al. 149 However, sometimes the published evidence did not distinguish between the terms ‘managers’ and ‘leaders’, or define the range of associated roles. 130,144,146,183,199,204,205 All of the stakeholder feedback strongly conveyed that NHS managers should be approachable and good listeners, but emphasised that having authority was vital. For PPI stakeholders, it was important that NHS managers had worked their way up through the system, so that they knew different roles and understood them. All of the stakeholder group feedback highlighted that NHS managers should also be compassionate and caring. Being supportive also appears to be an important attribute. 128 NHS manager stakeholders strongly emphasised the importance of having knowledge, wisdom and credibility and of understanding the system. The evidence also suggested that integrity and personal credibility is essential:148,188,201
Nurse managers who are able to provide guidance for addressing issues and problems in a credible manner may create a feeling of trust and safety in staff RNs and a subsequent perception of support from their nurse manage.
Zori et al. 188
Being resourceful and decisive appears to be important for nurse managers when making decisions on staffing deployment;150 the NHS manager stakeholder feedback also indicated that such attributes were essential. Furthermore, the published evidence, the NHS manager stakeholder feedback and the advisory group feedback suggested that flexibility is an important leadership attribute for safe staffing,143,150,188 as it is an important quality for NHS managers in order to deal with the unexpected:
. . . when charge nurses are flexible, they can quickly make adjustments to imbalances in available staffing and changes in patient’s acuity or census to prevent a breach in patient safety, and detect which patients or nurses need the most help.
Wilson et al. 150
There was agreement between all stakeholders and from the published evidence that nurse managers have an important role, outlined in the responsibility and accountability that they have for safe staffing work. 126,127,129,143,162,163 With the introduction of a staffing methodology, Taylor et al. 127 emphasised the responsibility of the nurse executive and Robinson et al. 126 found that areas with high levels of implementation demonstrated leadership accountability. Managers have to take responsibility for rostering,129,143,162 with Cathro163 stating that charge nurses are accountable for decisions on nurse allocation. Both Robinson et al. 126 and McIntyre129 emphasised that accountability and responsibility are important at all levels of nurse management. Furthermore, all stakeholder groups highlighted that NHS managers should take responsibility. Taking ownership and engaging with safe staffing appear to be important attributes of leadership:126,149
The charge nurse role is critical because of current staffing issues, the use of agency and/or foreign nurses, and the need for a proficient nurse to be accountable for issues arising in the unit. In short, charge nurses must take ownership for all unit activities.
Connelly et al. 149
Leadership skills
Leadership skills appear to be important for effective rostering and allocation to ensure patient safety. 163,167,186,189,199,202 Important leadership qualities for effective staffing deployment include interpersonal skills,128,149,190,201 with the ability to be a tactful communicator being a fundamental leadership skill for the deployment of staff:
Effective charge nurses used their communication skills to elicit information to obtain nuanced factors that may influence staffing decisions. They regularly moved beyond simply using the prescheduled nurse–patient ratio to meet the intra shift staffing demands.
Wilson et al. 150
The literature indicated that nurse managers have to communicate effectively to negotiate with nursing staff, other professions or departments to ensure that they have the right numbers of nursing staff on duty each day. 130,149 One nurse manager explained that negotiation skills are important for staffing deployment when staff need to be moved:
. . . it’s about focusing on what . . . the reason we’re here isn’t it? It’s about actually all the patients under our care, you know, are our responsibility, and that shouldn’t matter which area they are, you know really. It’s that we have to provide the care, don’t we? And any team at any time could go under the same problems, so each sort of area will have its problems at different times around staffing, and one team may have supported another area at a time when they were short. So, it’s probably appealing to the better nature of people, you know, to provide the service that we need to.
Site 3, participant 1
The ability to think critically is an important leadership skill. 131,148–150,188 This was emphasised in the NHS manager stakeholder feedback. Leaders need to have organisational and co-ordination skills;126,149,190 they need to be skilled in planning131,149 and collaboration,131,133 and they need to be able to set expectations, monitor and evaluate. 126,129,176,199,204 Furthermore, leaders need to be competent in IT as they set an example for their employees:
‘I had to do it myself, too. My own example was a good incentive. You sit beside the employee on the computer all day if needed.’
Lammintakanen et al. 197
The nature of leadership work
Being a visible presence was emphasised as an important part of leadership for NHS managers in all stakeholder groups, with many examples in the interviews of NHS managers being present on each ward daily to assess staffing requirements and to support other nurses or nurse managers:
Then I have a slow walk round the wards; check on all the ward sisters, if they’re in. Just a general feel for the wards really.
Site 2, participant 1
Using communication skills at all levels is an important part of the NHS manager’s leadership role. The NHS manager stakeholder feedback reiterated the importance of negotiation and of clear communication channels with different people in different levels within the system. Crist-Grundman and Mulrooney169 also indicated that leaders must engage at all levels. For the NHS manager stakeholder groups and the interview participants, communication and negotiation were linked to knowing the system and understanding the bigger picture. Having a broad perspective on staffing throughout the organisation, and not within only one clinical area, was also evident in the literature:150,201
. . . the matrons will come on and we will move staff because we’ve obviously taken that helicopter view of all nine wards and recognise that some wards need some additional support.
Site 3, participant 3
With regard to the attribute of flexibility, Burns205 proposed that leaders should focus on action rather than design and avoid excess control to:
. . . create environments that allow complex adaptive systems to explore, self-organize, and create successfully.
Burns205
However, Burns205 found that, although leaders strongly agreed that health care is chaotic and complex, they did not agree with principles and statements that encourage minimal specifications, uncertainty or becoming comfortable with tension and paradox and managing with freedom and intuition. 205 Health-care managers preferred strong direction and control. Although stakeholder feedback with NHS manager groups reflected the importance of innovation and of generating new of ways of working, there was also a strong focus on the need for knowing the parameters, barriers and risks, suggesting the need for clear boundaries. Having a ‘safety net’ with the NHS manager acting as a gatekeeper was a consistent theme in the NHS manager stakeholder groups’ feedback. Seeking staff feedback and acting on it to improve the service was a theme from all of the stakeholder work. Gaining feedback from patients ‘to know their needs’ was emphasised within the PPI stakeholder groups. NHS manager stakeholder groups emphasised the managers’ role in advocating for the patient when making staffing decisions.
Knowing staff
Understanding the knowledge, skills and competence of the staff appeared to be a requirement for effective nurse rostering and patient–nurse allocation. 129,131,146,150–152,207 This included an understanding of non-registered staff competencies. 131 This information may be gained from various sources, including paper and electronic staff records, but can often be based solely on the manager’s personal knowledge of the individual nurse,151 as illustrated by one interview participant:
I’ve just got all my experience and knowledge of my own staff, and knowledge of the patients at the time, really.
Participant 1, site 1
Having knowledge on nurses’ education and skills is essential for safe staffing allocation;128,133,144,151,152,157,158,160,164,174,175,180,181,184,189,191,198 however, the development of this knowledge may be dependent on features of an organisation such as its size and complexity. However, some sources of evidence suggested that nurse managers also need to know about nurses’ capacity, so that skills and competencies can be aligned effectively with patient need;143,150,204 particularly as nurses may be viewed as an expert in one setting and a novice in another. 133 Berkow et al. 152 found that nurses linked expertise to experience of the patient group or setting:
On units where patients are at high risk of deteriorating rapidly, participants overwhelmingly agreed that experience is the most valuable staffing enhancement because experienced nurses were believed to provide faster differential diagnosis and intervention.
Berkow et al. 152
Allen164 found that one study participant summed up competence in the nurse as ‘Can he/she handle that acuity?’. Knowing staff may require many sources of information. One participant in Drake’s study on rostering indicated that managers needed to know the staff circumstances, such as whether they needed money or time off. 143 van Oostveen et al. 178 felt that the mental and physical health and other duties of nurses could be incorporated into a computerised decision tool for making patient assignments, as they found that:
. . . nurses are significantly influenced by each other’s emotional commitment, private circumstances, and mental load.
van Oostveen et al. 178
The NHS manager stakeholder groups and interview participants also strongly indicated the importance of knowing the team, through managing personalities, building team loyalty and playing to the teams’ strengths:
You just know who can deal with what because you can have a very experienced nurse that might not cope at all well with any kind of pressure, or stress, but you might have a more newly qualified nurse who’s very, calm, safe, and practical, do you know what I mean?
Site 1, participant 1
Knowing the team was linked to being a visible, supportive presence:
I know every single person on the wards, right the way from the housekeeper, to the domestics, to the ward manager, you know, and it’s about going round, making sure that everybody is okay, everybody is safe. If people have complaints and concerns you’re listening to them, you’re doing your best to action, and communicating. And that’s what I say to the matrons, you need to be visible, you need to be out there, you need to be in with the team, you need to be talking to the staff.
Site 3, participant 3
Importantly, nurse managers need to understand the capacity of temporary staff. 149,151,160 In relation to risk management in ICUs, Rischbieth160 pointed out that managers must decide whether or not to engage staff without knowing their capacity:
If their dilemma results in a decision to just take anyone or just do without, this may immediately expose that ICU to an increased risk of potential problems.
Rischbieth160
Local knowledge was linked to being resourceful, as it means that managers know where the resources are, how to use them to get things done and how to identify who can help. 149,150 The importance of being resourceful was echoed in the NHS manager stakeholder group feedback. Some sources suggested that experience is important for understanding and knowing staff:134,151
Experienced nurse managers possess insights into the relationship between the numbers and characteristics of nursing staff and patient outcomes.
Anderson et al. 134
Effken211 suggested that, although nursing intuition has been perceived as an integral part of clinical expertise, it is information based. Kontio et al. 151 found that managers emphasised that their tacit knowledge, gained from experience, influenced their decision-making when information was not available from information systems; this may be linked to professional judgement. According to one manager:
I make decisions daily on allocating staff to different posts. I don’t get any supporting information from any information systems; rather, I do this based on my own experience.
Kontio et al. 151
Visibility of real-time resource
The published evidence and stakeholder feedback emphasised that WPTs may be a resource for knowing staff capacity and capabilities. The literature highlighted the need for visibility and transparency of data. 161,162,179 Staffing software should be able to quickly find additional staff for changing staffing needs. 170 Many sources demonstrated that WPTs can provide data on real-time resources. 151,168,172,181,194 Nagy and Nathan181 found that a staff scheduling system made data visible, for example, on hours worked and staff availability. Ruland and Ravn172 found that a nursing MIS provided information on costs, activity and staffing, and Wadsworth and Kurilla194 found that an automated attendance system enabled managers to react to staffing levels in real time.
Technology was also important to identify information on education and skills. 151,170,181,184,186 Although management staff have an extensive personal knowledge of staff characteristics, this information should be in electronic format for use in decision-making about staffing:151,183
‘I have the staff competencies in my memory, but these should also be in an information system where all of the training sessions that an employee has taken are recorded. There could also be an employee self-evaluation of his/her competencies.’
Kontio et al. 151
One interview participant has found that an e-roster helps her to understand nurse competencies effectively:
So, each person had a competency attached to them on the system. So, if you hover over the name on e-roster you can see whether they can be in charge, you can also see what abilities they have, so whether they can give non-invasive ventilation.
Site 2, participant 1
However, for one interview participant, personal knowledge of staff does need to be complemented by the technology to facilitate complex decision-making:
So that the correct grades of staff are on, and how many they’ve got on, and there is a way of looking at it and they’ll tell you, you know, it will tell you if it’s, if it’s staffed safely, or if the finance is over, or if there’s too many on annual leave and stuff.
Do you find that useful?
Yes. No but it’s really, again, about knowing your staff anyway knowing the competency of the staff you’ve got working and who they are.
You think it’s a bit more than just having the right grade and the right numbers?
Oh, yeah, yeah, you give, you’ve got to know your staff and know the capabilities and it’s getting to know them and their working really, you know? Like, just a band 5 they could be, it depends what they, what sort of training and everything, and how, you know competent they are, and if they could be in charge of the ward.
In conjunction with professional judgement, WPTs can therefore facilitate the visibility of staffing resources for decision-making. 151,175,183 Pruinelli et al. 175 found this with the nursing minimal management data set; McIntyre advocated that the live roster should be used in handover and bed meetings;129 Kontio et al. 151 highlighted the importance of data for managers’ decision-making, for example, in finding out staff availability when there is an urgent need to cover a shift. Crist-Grundman and Mulrooney169 reported that technology enables the availability of data at any time and anywhere, which facilitates analysis for decision-makers. One interview participant offered an example of how technology can give real-time information:
As they’ve embedded e-roster within the practice of the day, and constantly referring back to it and utilising it within the day.
Site 3, participant 4
Furthermore, technology and tools can provide graphical displays to make data visible:126,129,134,151,154,168,174,175,181,183,206,212
A dashboard provides graphic representations of data in real time that can assist the nurse leader to make staffing decisions, monitor productivity, and track the effects of staffing on patient outcomes.
Frith et al. 183
Interview participants explained that when technology is used to input patient observations and critical illness scores, managers can remotely access data to gain an overview of patient acuity levels. Interview participants also indicated that WPTs can offer transparency and visibility of resources:
I’ve got an overview of exactly what’s needed and what’s available across the patch.
Site 3, participant 2
It’s much more visible. It’s much more measurable, you know so, for instance, we can say to people right, you all need to get your rosters in 6 weeks in advance and this is the cut off, you know, so everyone can work to that. So, it helps with temporary staff planning as well. So, if you do plan 6 weeks in advance as required by the trust it means that you can get your requests out. It’s much, much tighter with payroll, you know, you rarely have any queries, whereas years ago you used to have lots and lots of queries.
Site 3, participant 5
Therefore, WPTs may enhance decision-making. Anderson et al. 134 indicated that intuitive judgements that contribute to staffing decisions are subjective:
The experienced manager can intuitively predict the outcomes of staffing levels or skill mix; however, this decision-making process has disadvantages. It takes time to develop expertise, and decisions based on intuition are difficult to justify.
Anderson et al. 134
Anderson et al. 134 indicated that a dashboard will provide the manager with an ‘objective alternative to that innate sense developed through experience’. However, one interview participant pointed out that data from technology can only complement the manager’s skills and knowledge:
The same way that I think standing in a ward, feeling the ward, is the most important thing you can do about staffing. So, I don’t think . . . all the technology in the world is good, maybe you could call it icing on the cake, but I certainly don’t think we should ever take . . . have that instead of, it’s got to enhance it.
Site 3, participant 2
Outcomes
The visibility of data on resource availability can increase NHS managers’ impact on safe staffing when managers demonstrate key attributes of leadership and know their staff.
Allen158 found that the starting point for matching nurses to patients was determining staffing numbers; the author highlighted the importance of allocating staff who had the competence to keep the patient flow going, particularly in clinical areas in which assisting in the movement of patients through the unit was vital. NHS manager stakeholder feedback indicated that unlocking the potential of people was an important leadership role, which empowered staff and was linked to good-quality care. Bonner et al. 156 described the process of the assessment of skill mix and numbers for each shift as ‘an onerous one’. However, having real-time data can make a difference to matching staffing to demand,168 particularly in safety-critical environments. 166
Managers need to critically interpret WPTs on patient data in order to align staffing allocation with patient needs. 131,158,163,176,178 When data are visible, this enables NHS managers to respond flexibly to patient need. When WPTs facilitate the visibility of resources, this can be matched to performance metrics and finance. 131,134,168,206 Anderson et al. 134 suggested that dashboards improve resource visibility and metrics for performance improvement, and this can be linked to monetary reward. Finn206 found that the use of an e-roster improved the understanding of staff availability, bank and agency use, and this reduced staffing costs. Barton found that technology resulted in more effective resource management, as resources were made visible:
The managers often didn’t know what resources were available hospital wide. For example, a unit might order contract labor from an agency when float nurses were idle.
Barton168
Likewise, McIntyre’s129 guidance indicated that an effective roster provides an opportunity to respond to real-time staffing challenges by providing an overview of staffing across organisational units.
When there may be misalignment
Some of the evidence suggested that ineffective leadership attributes may impede safe staffing work. According to Anderson et al. ,125 a shift in leadership impeded the use of a tool, suggesting the importance of a consistent approach. Several sources found that poor leadership was a barrier to the implementation of WPTs. 126,127,173,174 Furthermore, the evidence suggested that some managers fail to use WPTs to full capacity to make needs and resources visible. Finn206 found that an e-roster was challenging for some managers, with some preferring manual methods over the automated function. Some staff members reported that e-rosters are made too far in advance, and others felt that they had lost the personal touch in allocation/requests. This was also noted by Drake:
Some Ward Managers viewed it favourably, while others felt that it removed the ‘human’ aspect of rostering and often produced unworkable patterns.
Drake162
There was also a suggestion by interview participants that WPTs were not used to their maximum capacity, for example, for understanding staff skills:
Would it be useful to have that on that e-rostering system so you could track that? I know some systems will tell you somebody’s experience, whether they can, you know . . .?
Yeah, I think probably that . . . I think probably there is a bit of that on there already; I just don’t think people use it.
Furthermore, despite the visibility of needs and resources, in some instances, WPTs may not facilitate NHS managers’ work on safe staffing. A study on a workforce measurement system found that nurses (including nurse managers) felt that they were filling in bits of paper but not seeing any benefit from it; this suggested that, on a day-to-day basis, the staffing changes resulting from the system were not welcomed:
If the system indicates that there is a surplus of nurses for the current workload, nurses will be sent out to float on other units; however, if it identifies a need for more staff, rarely will this result in extra staff support being provided to the unit.
Hall et al. 144
Organisational learning and workforce planning and deployment tools and technologies (context–mechanism–outcome 5)
When the culture within the organisation is supportive and includes a culture of evaluation (context), NHS managers are able to work together using standardised data from tools and technology (mechanism), to learn together about safe staffing (outcome).
Context and mechanism
The included evidence indicated the importance of a culture in which WPTs are implemented. 166,171,173,182,190 Botter173 also noted the importance of understanding the culture on the use of information, and found that data generated from a patient classification tool were used differently in different clinical areas and this was influenced by organisational and cultural factors. Organisational culture can also influence access to information and how it is used for decision-making. 182 The NHS manager stakeholder groups also highlighted the importance of who gets to see the staffing-related data and of it being utilised effectively. Kivinen and Lammintakanen182 described an information culture as one that recognises the value and use of information in achieving operational and strategic success, and suggested that, when an information culture is part of the organisation’s culture, information:
. . . forms the basis of organizational decision-making and information technology is an enabler for effective information management.
Kivinen and Lammintakanen182
When the organisational culture is supportive, this appears to have a positive impact on NHS managers’ staffing work and may positively influence their use of WPTs. Shirey et al. 187 found that positive and supportive cultures facilitated managers to handle their own workload, thrive in their complex roles, initiate innovation and challenge situations. All of the stakeholder feedback strongly indicated that a supportive and positive environment is one in which nurses are listened to and feel empowered. The interview participants suggested that a supportive culture has a positive impact on teamwork to facilitate safe staffing, as people ‘tend to look after each other’ (site 2, participant 2).
Organisational context and management approaches may influence a positive work culture. When management approaches centre on team-based models of care, as opposed to individual patient allocation, this has been associated with increased levels of nurse satisfaction and retention. 121 However, Tran et al. 122 found that shared care and patient allocation models of nursing care prompted similar levels of nurse satisfaction; they found that some nurse team leaders in shared care felt that their role was stressful, owing to the extra responsibility and challenges of negotiation with co-workers. It is noteworthy that NHS managers are also required to take responsibility and negotiate to facilitate safe staffing decisions. When management approaches support professional models of nursing care, with more nurses with higher levels of formal education, nurses feel more supported in their professional practice. 123 Lacey et al. 119 found that Magnet hospital programmes to promote professional practice are associated with a positive organisational culture; when nurses feel more supported, they are more likely to stay within the organisation. However, Lacey et al. 119 did find that the perception of support from nurse managers was low and felt that this was because nurse managers were spread too thinly; they indicated that it is important that nurses have access to nurse managers for staffing issues. Subirana et al. 128 formulated a realist logic model to determine the links between staffing and nursing outcomes; they proposed that the presence of a supportive nurse manager is related to positive nursing and patient outcomes. The interviewed participants reiterated how access to managerial support is important for NHS managers who make staffing decisions. One lead nurse explained when the matrons sought support from her:
We’re constantly talking, so I know every move that goes on. I obviously don’t do the move myself, because that’s the matron’s role to do that. They would escalate to me if there was a problem in terms of ‘we don’t have anybody, what do we do?’.
Site 3, participant 2
Furthermore, the organisational culture may have an impact on managers’ decision-making. Shirey et al. 187 found that nurse managers’ decision-making on a range of factors, including staffing issues, was consistent with the organisational culture and norms:
If organizational leadership supported communication and patient safety, nurse managers aligned their decisions to be consistent with communication and patient safety.
Shirey et al. 187
Shirey et al. 187 found that in the more supportive organisational cultures, nurse managers were less likely to make fear-driven decisions. The advisory group reiterated that decision-makers can feel supported and confident to make decisions if the culture is positive. They noted that, although organisational values and culture influence staffing decisions, these in turn are influenced by legislation, mandates, guidance and patient expectations.
A culture of evaluation
The implementation of a critical system does not end when the technology goes ‘live,’ rather it is an evolving journey, where the expectation of use is clearly communicated and practiced; where configurations and practices are re-evaluated as goals are achieved and new challenges are faced.
Crist-Grundman and Mulrooney169
The evidence supported the importance of evaluating the use of WPTs. 124,126,129,131,148,172,174,190,195,199 Robinson et al. 126 categorised organisations based on their implementation of a staffing methodology and found that, in organisations in which there was a high level of implementation, staffing data were fed back to the units. Formal staff feedback appeared to be important. 195,199 There were many examples of gaining staff feedback when WPTs were trialled. 124,127,144,146,161,174,176,179,192,197 Staff satisfaction surveys with scheduling practices were recommended. 189 One organisation surveyed staff on self-scheduling technology and found that 75% of staff viewed it positively, with 87% finding it easy to use and 68% commenting that they had received fewer calls asking them to come in for work. 191
All of the stakeholder groups emphasised the importance of gaining feedback from staff on planning and deployment and having open communication channels to facilitate this, with NHS managers having an important role in listening to staff. The advisory group emphasised the importance of an evaluation culture for a positive learning climate and organisational learning. The NHS manager stakeholder groups suggested that reflection was vital to learn for the future through determining what has worked, and innovating and making changes when necessary. Acknowledging when good work has been done, giving praise and celebrating success were also important. PPI feedback also reiterated the importance of listening to, and gaining feedback from, patients.
A standard approach to articulate needs and resources
An organisational culture that values engagement and learning may be strengthened when this is informed by standardised, credible data on needs and resources. Standardised data facilitate organisational learning through evaluation and comparison. The data from WPTs make needs and resources visible for evaluation in the light of planning and deployment outcomes; for example, Anderson et al. 134 indicated that their staffing tool, which used a dashboard format, aimed to:
. . . make current, relevant data available to nurse managers at the unit level and integrate evidence on staffing with patient and organizational outcomes.
Anderson et al. 134
When the organisational culture values information, technology facilitates its use for organisational decision-making. 182 Diers et al. 154 suggested that the technology may equip managers:
. . . with powerful tools for retrospective analysis of process management.
Diers et al. 154
E-rostering facilitated measurement of, and understanding about, staffing deployment. 206 Data from WPTs enable retrospective review to evaluate staffing levels124,170,175 and to identify the need for further resources. 168 When there is visibility and standardisation of data, this enables monitoring for cost, efficiency and quality purposes. 129,175 Importantly, this facilitates financial review. 194,210 This means that the impact of bank/agency spend is visible,129,206 as is the difference between actual staffing and predicted staffing:206
It’s all tracked . . . tracked on the system, so you can see at any point exactly where everybody is. So financially you can follow the trail.
Site 2, participant 1
Some sources emphasised a need for a standard approach for ease of measurement for comparison and for adherence to legislation, mandates or guidance. 124,126–128,131,147,175,183,195,199,206 Taylor et al. 127 emphasised the need for a standard approach, through which staffing methods are mandated. Fenton and Casey147 emphasised the importance of validating data and ensuring consistency for the Safer Nursing Care tool. Using a standard approach for a patient dependency tool was found to be a reliable method for delivering evidence-based workforce plans. 206 Furthermore, van Oostveen et al. 124 pointed out that a standard approach to a staffing system facilitated comparison:
. . . the RAFAELA system offers a fully Information and Communication Technology supported and uniform system for all clinical nursing wards, which facilitates a clear communication about nursing care intensity on all management levels throughout the hospital, and even on regional and national levels.
van Oostveen et al. 124
One interview participant reported that data from WPTs enabled comparisons in English providers:
. . . and we upload that as part of the Unify process. And that is then seen on the model hospital, and that allows us to benchmark with other organisations.
Site 2, participant 1
The evidence suggested that benchmarking data can confer organisational benefits. In a study by Robinson et al. ,126 a participant from an organisation categorised as medium for achievement in implementing WPTs said that the staffing methodology was a really good tool for benchmarking and that it was useful in the achievement of good-quality care. Benchmarking data can ensure data credibility for the calculation of costs per patient-day in organisations in which there are similar financial systems. 183 Finn206 found that, according to data from the e-roster, staffing unavailability or headroom was comparable to that reported in other organisations, at 28.8%. Fagerström and Rauhala210 found differences between organisations in costs and nursing workloads when applying the RAFAELA tool and suggested that the findings offer opportunities for organisational learning.
Outcomes
When an organisation’s culture is supportive and values evaluation, WPTs can produce standardised data on needs and resources to enable learning about safe staffing. Lammintakanen et al. 197 commented that:
Electronic information systems were seen as a shared effort of learning and development of practices among nurses and nurse managers.
Lammintakanen et al. 197
One interview participant indicated that she would monitor how other sites had implemented technology for e-rostering to determine staff capabilities:
But I think there are other areas that are building on reports that they’re going to be getting, and as they produce those reports and we see how useful they are I think we will be able to say that looks great, let’s do it that way. So, when we see more benefits coming out of it I don’t think it will be a big leap to go and say right, I want to do that now . . .
Site 3, participant 3
Data from evaluations can identify where quality improvements need to be made133,145,174 in line with agreed national standards. 147 Anderson et al. 134 indicated that data in the form of scorecards or dashboards are increasingly being used to improve performance. Juntilla et al. 192 reported that an evaluation of a data warehouse approach identified primary data errors, van Oostveen et al. 124 suggested that further education is required following the evaluation of the implementation of a tool, and Fenton and Casey147 claimed that evaluation of the results of the Safer Nursing Care tool could lead to changes in staffing establishment numbers. Furthermore, learning about safe staffing following the evaluation of WPTs can result in the formulation of action plans to improve their use and to deploy staffing more effectively. 129,195,200
Learning about safe staffing can also be facilitated through the comparison of data. The evidence suggested that data can be used for benchmarking between organisations. 124,126,129,131,147,171,179,180,182,183,210 Data can also be used for organisational benchmarking with similar organisations. 124,126,127,131,147,168,175,180,183,203,206 This includes using comparative data across specialties and different localities to promote learning. 131,210
Adaptation and refinement of WPTs may also ensue following learning about safe staffing. The evidence indicated how changes were made following trials and pilots: 124,126,174
The Dashboard is a work in progress. Many of the indicators that had originally been established were refined and will be revised based on suggestions from project participants and tested across the [organisation name].
Fram and Morgan174
Continuous evaluation is recommended, and this can contribute to the formalisation of organisational processes, which are important for nurse managers:129
. . . to determine what data they will generate from the system and what will be done with that data. Information is power, but only if there’s a process in place to interpret the data and then make policy and procedure decisions based on the evidence the system provides.
Crist-Grundman and Mulrooney169
When there may be misalignment
In less supportive work cultures, nurse managers were less empowered to challenge situations:
. . . a fear of punitive action prompted nurse manager silence.
Shirey et al. 187
If an organisation appears to be less supportive and does not have an evaluation culture, learning about safe staffing may be impeded. In the first instance, this may impede the implementation of WPTs to enable learning; Botter173 noted that the lack of a supportive culture impeded the use of a patient classification tool. Silvestro and Silvestro185 found that a lack of sharing of good practice, with no feedback loops between ward performance and ward objectives, hampered good practice with regard to rostering. When evaluation does occur, it is important to use findings to promote learning. Kane179 indicated how stakeholder feedback was not acted on in the trial period for a community tool, as the team leaders felt that stakeholders (caseload holders) were not fully engaged in the process. Kane179 reflected that this was a missed opportunity:
. . . to advance the knowledge of caseload analysis at all levels of the service.
Kane179
Some evidence suggested that evaluations are not effective. Murtola et al. 186 found that evaluations of information systems were mainly based on staff feedback of usability, but the authors felt that this was not focused on effectiveness or the impact on decision-making. van Oostveen et al. 124 found that, despite gaining positive staff feedback on the applicability and usability of the RAFAELA system, staff did not implement this system effectively. Furthermore, cross-organisation comparison is not always welcomed. One interview participant was concerned that comparison with other organisations may have the potential to reduce staffing:
. . . because we’re actually . . . we’ve got a very richness to our skill mix and we’ve got a very good fill rate, so there’s a fear that when we benchmark with other organisations, similar organisations, we might be seen as being much better than others in terms of staffing. And we’re slightly concerned about what NHSI [NHS Improvement] will say if a range, or a suitable range . . . for this type of ward, and if we’re over that what does that mean on our current staffing. So, I think they would be our concerns, you know.
Site 2, participant 1
Co-design of workforce planning and deployment tools and technologies (context–mechanism–outcome 6)
When there is partnership in design with the users of staffing tools and technology (context), and when NHS managers see tools as being fit for purpose (mechanism), tools and technology are placed close to the decision-making point (outcome).
Context and mechanism
Several sources within the synthesis of the literature indicated the importance of collaboration and partnership to design or select a staffing tool or technology. 126,127,131,134,146,147,154,169–171,174,175,183,190–192,194,195,197,199,200,203,208,209 Collaboration and partnership appear to be generally important for the NHS managers’ role around safe staffing. Dent130 emphasised that a shared vision is important for improved nurse staffing. Effective communication between nurses and other relevant groups appears to be important for partnership approaches to nurse staffing. In nursing, a team approach to care can promote communication. 121 Interview data and NHS manager stakeholder feedback emphasised that effective communication is important to manage the ever-changing environment for staffing:
So, we’re constantly talking, constantly kind of chatting about it, because it changes all the time. With, you know, in excess of four hundred staff it’s constantly moving, staff are going off sick, staff are returning to work, you know, it is always changing. Every shift, it changes.
Site 3, participant 3
The NHS manager feedback and the PPI stakeholder feedback revealed that managers need to be effective networkers. Szumlas204 suggested that nurse managers can create a culture of partnership and accountability to ensure staffing excellence through ‘consistency, dialogue, and idea and data sharing’. Effective collaboration and partnership in the design, selection and development of WPTs can promote shared accountability and ensure that systems are ‘simple and efficient to adopt and use’. 169
The synthesis of evidence strongly suggested that collaboration with multiple groups is essential for the achievement of an acceptable system, with collaboration being important for technology design. 209 Key stakeholders need to work together to design and develop WPTs. These groups include nurses and nurse managers from all levels of the organisation,126,146,154,168,175,192,199,203 expert panels,126,127,146,175 IT specialists,147,192,200 finance partners,174,195 human resource personnel,168,195 administrative staff195 and researchers. 146,171 Furthermore, linking with vendors or industry is important to develop systems that fulfil organisational requirements. 170,175,191,192,197,199,208 Douglas199 indicated that external technology consultants may be useful, but emphasised that it is important for nurse leaders to engage with the process and not to leave it up to the consultant.
The literature strongly recommends a prominent role for nurses, both nurse managers and staff nurses, in the developmental process. 174,190,194 Douglas199 advocated the formation of a multidisciplinary staffing committee with strong nurse representation to drive selection and implementation strategies, but noted that it is important that nursing staff (and not only the IT department) take ownership of the tools. 199 Robinson et al. 126 also found that a staffing methodology was more likely to be implemented if staff were included in the process. Collaboration with clinical nurse experts appears to be important in order to ensure the inclusion of data that influence nurse staffing. 146,192 Junttila et al. 192 used a nursing expert group, consisting of nurse directors, head nurses, experts in clinical nursing and hospital informatics, to determine management information needs in designing an information system for a hospital data warehouse approach. This integrated different sources of information of relevance for staffing decisions. Valentine et al. 190 reported that collaboration on the development of the OpenShift self-roster tool (Red Hat, Inc., Raleigh, NC, USA), for staff to self-select shifts, involved multiple partners across departments, from top leadership to front-line staff. Wadsworth and Kurilla194 included nurses in the selection decision for a staffing tool in a Magnet-designated hospital with a collaborative, inclusive philosophy:
. . . so before the final decision was made, we knew it was important to let the nurses weigh in. We asked them to also score the vendors and share their opinions. Their judgments aligned well with the opinions of the evaluation team.
Wadsworth and Kurilla194
Different formats for collaboration have been used to select, develop or design WPTs. Fasoli et al. 146 used an interdisciplinary team, comprising clinical experts, leaders and researchers, to develop a staffing methodology. Barton168 reported that a cross-disciplinary team of finance and human resources representatives, nursing unit managers and the staffing director collaborated in the development of a new staffing programme technology and suggested that this team approach was a major factor in its success. Diers et al. 154 used a pilot group of 14 nurse managers with operational experts, finance experts and computing experts to design a system of user-defined decision support tools. There were many examples in the literature of different processes for collaboration in the design, development and selection of WPTs. Wallace and Pierson195 established a corporate working group: the Best Practice Scheduling Task Force. Pruinelli et al. 175 pointed out that the NMMDS was developed via expert review panels, focus groups and national Delphi surveys to identify the core variables needed by managers to make decisions. The Scottish toolkit was formulated following a national conference to consider the workload and workforce tools that are appropriate for Scotland. 203 The evidence from interview participants also indicated the importance of collaboration. One interview participant believed that partnerships between NHS managers and IT teams help to ensure that the e-roster is fit for purpose:
And they meet on a fortnightly basis with one of the lead nurses, who goes through it with them, with the e-roster team. And with the work with the e-roster team, and getting the rules set correctly in the background on e-roster, the ward managers are actually finding it much more helpful now.
Site 3, participant 4
Defining need for staffing decisions
The evidence indicated that a key purpose of collaboration is to define need and establish goals for WPTs. 125,127,134,146,171,178,195,199 Other requirements included identification of the critical data elements and sources of data. 125,134 Douglas199 advocated gaining a clear understanding of the organisation’s current staffing and scheduling practices before choosing a tool:
This will formalize the picture of what is working and what needs to be fixed. It will also set in motion the involvement and support that will be needed later. From your assessment of current state, identify the goals you want to achieve.
Douglas199
The NHS manager needs to have information on multiple elements to make safe staffing decisions; these relate to the wider systems in which WPTs need to operate. According to Kivinen and Lammintakanen,182 the use of IT to aid operational decision-making, such as around staffing, is challenging, as health-care environments are complex because:
. . . rapid changes in the operating context and characteristics such professional culture, complex organization structure and management system.
Kivinen and Lammintakanen182
Burns205 suggested that health-care organisations are made up of complex adaptive systems whose evolvement cannot be predicted. Therefore, it is unsurprising that nurse staffing is also complex, given the number of inter-related systems and elements that need to be considered. For example, Dent130 formulated nine principles that relate to staffing decisions, with each of these being linked to different organisational systems, such as finance and staff recruitment. Pruinelli et al. 175 also explained how the NMMDS combines information of different systems, such as human resources and staffing systems, with electronic health records and information on the clinical area. This information is used to support the decision-making process and measure the impact on patient outcomes.
A collaborative approach can result in an enhanced understanding of the systems and elements that have an impact on staffing decisions. In developing a new scheduling scheme, one task force group devised a questionnaire for clinical managers and clerics involved in scheduling, in order to understand the ‘reality of scheduling on the front line’. 195 Fasoli et al. 146 reported on a consensus approach for the Department of Veteran Affairs to determine design principles for a nationally standardised nurse staffing methodology; following an evidence review and brainstorming session with an expert panel, indicators were agreed on to reflect nursing work, patient-centred variables, nursing characteristics and unit and hospital attributes. Also in relation to the Veteran Affairs staffing methodology, Taylor et al. 127 highlighted that this collaborative process helped to develop nurse-sensitive indicators, in the light of unit workload and patient group, to generate nursing full-time equivalent requirements. Kivinen and Lammintakanen182 also advocated collaborative discussion for nurse management systems, in order to identify the information requirements of different groups of managers and to establish common concepts and meaning; this was to promote more effective use of the information. van Oostveen et al. 178 found that there were different information requirements for different clinical areas, although patient acuity was consistently the most important. Furthermore, interview participants highlighted that collaborative processes were needed to ensure that nursing needs were firmly embedded within WPTs:
So, the e-roster team are from an IT background and I think that was the problem really to start with.
So, it was just really not understanding the needs for that . . . for being a nurse?
Partly. And I think for the ward managers, who did the work with them at the time, not recognising the importance of all the information they needed to provide. And I think it’s only when you start using the system that you realise that it is essential to get that information absolutely accurate at the beginning.
Partnership for trial, adaptation and innovation
Probably the strongest aspect of the project was its collaborative nature, as staff nurses and management staff worked together on a matter of high importance to both, providing valuable recommendations for shared nursing and interprofessional planning, Dashboard development and project management.
Fram and Morgan174
Collaboration appears to be important for the trial and adaptation of WPTs. 147,163,174,190,191 This can mean that WPTs can be effectively adapted for specific groups of patients or clinical areas,163 or that elements can be refined or added in order to improve validity. 174 Valentine et al. 190 discussed how a self-rostering technology was customised to organisational needs. In addition, for a specific self-rostering system [BidShift (Cerner, North Kansas City, MO, USA)], Brown191 charted how collaboration with the vendor resulted in a trial and eventual acceptance of differential shift payment incentives for hard-to-fill shifts. Furthermore, effective communication appears to be essential to the process of engaging and collaborating with staff to work in partnership to develop WPTs:
Developing a solid communications plan at the beginning of the project helped solidify the necessary relationships and environment for moving the project forward.
Valentine et al. 190
Engaging nursing staff to collaborate was an important part of implementing a self-rostering system; it was reported that regular communication, with the opportunity given to staff to ask questions about the new system, resulted in staff feeling that they had ownership in the process. 191 Fenton and Casey147 gave an example of a health organisation in which:
The trust gained the cooperation of staff by involving nursing staff from the outset, and encouraging open discussion of the advantages and disadvantages of using the tool.
Fenton and Casey147
The importance of trialling WPTs is evident in the literature,124,127,144,146,161,174,176,179,192,197 with stakeholder engagement and feedback being recommended by many sources. 126,127,144,174,179 Ruland171 used multidisciplinary team focus groups to design a staffing tool and emphasised that end-users need to have the time to identify and communicate their requirements clearly to system designers to promote continuous learning. Collaborative partnerships led to identification of areas for further development of the design of WPTs. Adaptation and tailoring to need were recommended or evident in many sources of evidence124,126,127,144,147,163,171,176,179,186,200,202,203,208 Murtola et al. 186 suggested that systems should be flexible so that they can be modified on the basis of user need. A collaborative process for a practical guide for patient assignments resulted in local area and population modifications in order to support the flexibility of the tool. 163 Robinson et al. 126 found that managers made recommendations for improving a staffing methodology tool, such as adding family leave. Fram and Morgan174 indicated the importance of acting on feedback for a dashboard project that displayed integrated staffing data for retrospective and projected views for staffing decisions:
The Dashboard is a work in progress. Many of the indicators that had originally been established were refined and will be revised based on suggestions from project participants and tested.
Fram and Morgan174
Effective collaboration may also result in innovation and in-house design. There are some examples in the evidence of the development of in-house staffing WPTs. 154,161,174,176 Fram and Morgan174 found that a collaborative approach to the dashboard project resulted in a practical tool that facilitated learning, as participants gained an appreciation of the depth of knowledge required for decisions on staffing numbers. Wyatt and Healey161 developed a system to escalate and monitor clinical capacity (STEAM) for children’s services; staff reported satisfaction with the tool, as they felt more in control, supported and confident in contacting senior staff. Diers et al. 154 reported how the user-defined data analysis and reporting tool was collaboratively designed to fit the way nurse managers think about the work; nurse managers were quick to understand the system and the importance of their role for valid data input. Pappas et al. 176 discussed how a collaboration of clinical nurses led to the design of a patient risk assessment tool. This emphasised the importance of closer nursing surveillance, as patients at higher risk of experiencing clinical events could be assigned nurses to mitigate the risk. The impact was an improvement in nursing-sensitive indicators and cost-savings, particularly in end-of-shift overtime. Pappas et al. 176 reported that in using the tool, nurses felt empowered, as patients’ clinical conditions were factored into staffing decisions and the nurse was placed in the pivotal role for decision-making. In addition, one interview participant spoke of how their organisation had designed its own staffing software; the software was nationally acclaimed and indicated staffing requirements for NHS managers:
We developed it in-house, so it was quite cheap. All the wards have iPads [Apple Inc., Cupertino, CA, USA], and on the iPad they have an app [application] that allows them to put in actual staffing compared to planned staffing.
Site 2, participant 1
Collaboration for communication and decision-making
In enhancing NHS managers’ understanding of staffing needs and resources, WPTs are proximal to decision-making processes. An increased understanding of staffing resources and requirements is facilitated through communication. Some evidence from the literature suggested that embedding WPTs in local practices and systems can promote collaboration through enhancing communication about nursing care. 151,175,186,199,209 The widespread use of handheld computer devices, e-mail, text messaging and other communication devices to alert NHS managers to staffing issues was evident from stakeholder feedback and interview participants. There were also examples in the literature of the integration of communication technology in order to enhance staffing decisions. A nursing management data set system was integrated with communication and alerting devices to ensure effective communication. 175 Kontio et al. 151 indicated that instant messages and text messages ensure timely data-sharing and support effective communication within organisations.
van Oostveen et al. 132 also noted that effective staffing systems may enhance communication for nurses:
Nurses desired a valid nursing care intensity system as an interdisciplinary and objective communication tool that makes nursing care visible and creates possibilities for better positioning of nurses in hospitals and further professionalization in terms of enhanced authority and autonomy.
van Oostveen et al. 132
Good decision-making is fundamental for effective staffing, and collaboration also appeared to be important for decision-making. 159 Data from WPTs inform decision-making. 171–174,180,182,184,186,210,212 Kivinen and Lammintakanen182 indicated that technology is important for managing information to use in decision-making by nurse managers in their daily work. Effken et al. 212 indicated that computerised decision support tools may facilitate nurse managers’ decision-making:
. . . by encouraging systemic, systematic, efficient decisions based on, not only a careful assessment of the nature and causes of the problem, but also an evaluation of alternative solutions to achieve the desired outcome.
Effken et al. 212
When there has been partnership and collaboration in the design of WPTs, the data are usable and near to the decision. 171,173 Following collaboration in the development of a patient classification system, Botter173 concluded that its primary purpose was to generate information for decisions about the provision of available nursing resources. Nurse managers used this patient classification tool for decision-making in changing or unusual situations. In addition, following partnership in development, Ruland171 felt that the CLASSICA decision support system offered a better understanding of financial processes that were proximal to the decision-making process. The advisory group indicated that data from WPTs inform decisions; managers triangulate different data sources to make professional judgements on skills, attributes and skill mix to get the right nurse for the patient. The ability to integrate professional judgement with technology was also reflected in the in-house designed app discussed by one interview participant:
But the key thing about it is it allows them to add in whether they, in their professional judgement, so that’s the nurse in charge, not admin, not matron, but in the nurse in charge, to say whether they feel safe or not.
Site 2, participant 2
One interview participant commented on the process of integrating decision-making with data from a tool:
. . . our view is always that it requires a common-sense approach when you’re looking at the Safe Nursing Care tool anyway. So, it gives you raw numbers but you need to ask some questions behind it . . . to then be able to make decisions based on staffing. So, I don’t think the systems necessarily help us to make decisions about staffing, but they certainly allow us to access the information we need about the staffing . . . to make those decisions.
Site 3, participant 4
Collaboration for a user-friendly system
Technology can be used to help NHS managers with decision-making with the aim of improving quality and safety outcomes, but it must fit into nurse managers’ workflow and be easy to use. 145 For decision-making, data should be presented in a format that can be understood. 183 The evidence suggests that, when a collaborative process has been instigated, systems can be selected and adapted to be user-friendly. 170,172,183,190,192,197,202,203 It was recommended that a collaborative process for tool selection should focus on user-friendly technology, with automated and balancing functions and intuitive software for use. 170 Following a collaborative process to develop a nursing MIS (CLASSICA),171 Ruland and Ravn172 found that nurse managers reported a high level of satisfaction with this information system, including the perceived ease of use. Junttila et al. 192 also used a collaborative process to implement and evaluate a nursing MIS and were able to make recommendations to increase its usefulness for the nurse decision-making process using a data warehouse model. Flynn et al. 203 charted how the collaborative process for WPTs in Scotland culminated in a suite of tools for selection, to be used alongside professional judgement. Evaluation of these tools showed fitness for purpose, but also areas for refinement, with Kellagher et al. 202 reporting user satisfaction and skills development on staffing and budgeting, following the pilot studies. One interview participant indicated that an e-roster had been made more user-friendly by users working in partnership with the IT team:
It’s easier to use now since it’s been updated. It was much harder before, it was a lot more time-consuming to do small tasks on it. So it’s, more, a lot more user-friendly now, the new version we’ve got.
Site 1, participant 1
Outcomes
NHS managers who find WPTs useful exhibit a change in their thinking, and this has an impact on how the WPTs are used, placing them close to the decision-making point. The literature contains examples of managers’ attitudes towards WPTs changing as they come to understand their utility for staffing decisions. Kane179 found that managers using an eCAT tool started to challenge the caseload data. The tool enabled this to be done in an objective and systematic way, in order to facilitate equity of caseload allocation within the team with. Diers et al. 154 found that managers grasped the ideas from decision support systems and wanted to use the technology. In a pilot on the implementation of the Scottish toolkit, Kellagher et al. 202 found that managers understood finance and human resource issues, developed budgeting skills and felt empowered to challenge staffing resources and change their ways of working. Furthermore, it was found that managers thought that electronic information systems strengthened their role and enabled them to fulfil their tasks more easily. 197 Finn206 observed that with an e-roster:
Ward managers have informally reported staff spending an increased amount of time with patients due to better allocation of leave, greater transparency of rosters, challenging historic working practices, accurate recording of under/over-contracted hours and reviewing of break and shift times.
Finn206
Furthermore, Effken et al. 145 suggested that decision support tools allow nurses to test their hypotheses about staffing solutions in a safe virtual environment. Effken et al. 145 proposed that decision support tools may facilitate the evaluation of decisions and considerations of alternatives to facilitate more long-term solutions rather than just satisficing:
By stimulating higher level thinking, managers might be less likely to engage in ‘fire stomping’ or jump to quick solutions without considering the larger picture.
Effken et al. 145
When there may be misalignment
Some of the evidence suggested that the utility of WPTs is hampered when nurses have not been involved in the collaborative process effectively. Murtola et al. 186 discussed this issue:
But still a discrepancy exists between the information systems needed by nurse managers and the existing ones. One possible explanation for this is that nurse managers might not have been able to communicate their needs.
Murtola et al. 186
Other reasons for a lack of effective collaboration are also evident in the data. Fram and Morgan174 found ongoing challenges in scheduling regular dashboard project development meetings in order to engage nurses, as nurses were unable to leave the wards because of staffing shortages. A lack of understanding within partnerships may be another issue; one interview participant expressed the belief that ineffective collaboration resulted in poor nurse allocation:
That was all part of the problem to start with really, about getting that information right about the department, so what are the skills that your staff should have in that department, and identifying the skills that the staff then do have. Initially, I think perhaps a lack of understanding on the e-roster team’s perspective . . . and working with the ward managers, it wasn’t . . . it wasn’t as accurate as it needed to be. So, it would be rostering staff on together that didn’t cover the skills that needed to be covered. But it was really about the rules in the background, it wasn’t about the actual system that was a problem.
Site 3, participant 4
Weak partnerships may hamper staff engagement with WPTs. In a pre-implementation study of the RAFAELA tool in the Netherlands, van Oostveen et al. 132 found that, despite the reliability and validity of the tool, it was not well accepted by nurses. van Oostveen et al. 132 felt that they should have focused more on a social context, such as strategies to enhance team functioning. Poor interprofessional communication may also be a problem; Lammintakanen et al. 197 found that a lack of collaboration between medicine and nursing impeded the use of WPTs. Kivinen and Lammintakanen182 also found that a lack of collaboration resulted in a failure to identify information needs at different levels of management; this had an impact on data utility for staffing decisions:
This emerged from descriptions that the information needs of managers working in different positions and units were not sufficiently identified and discussed and middle and front-line managers especially argued that MIS [Management Information Systems] do not enhance their daily work and decision making.
Kivinen and Lammintakanen182
Workforce planning and deployment tools and technologies and involving patients (context–mechanism–outcome 7)
When there is the organisational propensity and policy around disclosure of staffing levels (context), communication is balanced between candour and refining the message (mechanism) to ensure the confidence of patients and families (outcome):
I’m not sure really how much the public do realise . . . what a fine line it is to safely manage and run the ward to be honest with you . . . with staffing levels. I’m not sure how much they . . . do know.
Site 1, participant 1
Context and mechanism
Following reports on high-profile care failings,2,3 there are policy requirements in England and the rest of the UK to provide real-time quality assurance data on staffing levels for central scrutiny, such as the UNIFY safe staffing data collection in England. NHS organisations also have a legal duty of candour under the Health and Social Care Act regulations;75 current staffing levels should be displayed at the entrance to wards and departments, where the information can be viewed by patients and the public. 76 Hockley and Boyle166 indicate how WPTs have the potential to provide clarity on the reporting of these data, and highlight views from senior nurses about increasing public confidence, which may accrue from the availability of data. 166
Perspective of safe staffing
According to Flynn and McKeown,165 staffing and skill mix are central issues for health service governance, service users and the recruitment, retention and well-being of nurses across different sectors; however, they note that staffing levels and skill mix have to be defined in terms of sociocultural, political, economic, professional and service user contexts, with conflicts between the perceptions of safe staffing in different groups. From an organisational perspective, Flynn and McKeown165 suggest that directors of finance may have a different view of safe staffing from nurses. Effken expands on the theme of different perspectives, pointing out that professionals are the primary workers for care delivery and may take a role in organisational management:
This means that the primary workers have considerable latitude in how the organization’s work is conducted and also that the primary workers are more likely to have humanitarian values that may conflict with the organization’s commercial or financial goal.
Effken209
The evidence from the literature linked staffing to quality and safety. 128,132,133,158,161,162,164,165,167,176,180,198 Subirana et al. 128 linked safe staffing to patient outcomes for quality and safety, but pointed out that quality in elements of nursing care is multidimensional and difficult to distinguish from the overall health-care system. Flynn and McKeown165 commented that quality and safety in staffing are key areas for scrutiny from the public:
. . . there is a growing influence of service user movements in health and social care, which are perhaps equally interested in the impact of nurse staffing levels and skill mix on quality of care.
Flynn and McKeown165
The interview participants also noted that patients and the public are interested in staffing issues and link staff numbers with the quality of care:
So, now people are . . . are more aware that the . . . when you look round the ward and you’re looking at the number of staff, that that somehow equates to whether or not your mum and dad are being looked after properly. But what there is at the moment is that there is an incredible absence of understanding about what that actually means.
Site 1, participant 4
Understanding the public’s perception around safe staffing levels is complex. Flynn and McKeown165 suggest that service users have changing expectations and the nursing profession needs to determine appropriate levels of nursing care in the light of patient outcomes. One PPI stakeholder termed their perspectives on staffing shortages in stark terms:
If you are supposed to have four people on an ICU unit and you only have two, people are going to die.
PPI stakeholder
Furthermore, in the interview data, participants indicated how patient perspectives on staffing may differ from establishment-level interpretation:
Well it’s quite interesting patient perceptions really because that, we do an audit, the quality and safety audit every month, and, we’re only struggling with staffing in the last, this couple of months really, we’re quite lucky otherwise that we have been fully staffed, but the patients will always comment in the feedback, ‘I feel they need more staff, there’s not enough of them’, so they obviously feel that we need more.
Site 1, participant 1
Low or unsafe staffing levels have been linked with adverse patient and organisational outcomes. 144 The public may therefore lack confidence in organisations that have gained a reputation for poor patient outcomes that are linked to unsafe staffing levels. Certainly, Hockley and Boyle166 highlighted that recent reports on care failings related to the Mid Staffordshire enquiry centred on staffing issues, although the political focus was still at the micro level (nurse–patient interface) rather than the macro level (organisational processes). 2,166 Flynn and McKeown165 suggested that patient groups may join resistive alliances with nurses to challenge organisational practices on staffing. The public may also perceive that poor staffing is a consequence of underfunding and/or poor management:
When I have gone round visiting patients I have never heard a complaint about the nurse, I have heard complaints about management and short staff. From what I have come across there is always a lot of sympathy for the nurse, however at the same time, the patients anxiety levels must be raised if they know there is a shortage of staff.
PPI stakeholder
Barton168 suggested that administrators balance cost, quality, satisfaction and staffing. Balance is also referred to in the literature related to other public services; Wilson and Weiss153 commented on the sensitive balance between funding for staffing and public satisfaction in the police. The PPI stakeholder feedback reflected an understanding of the need to save money, but also strongly asserted that the NHS needs money.
Safe staffing, accountability and risk
Accountability and responsibility were linked to safe staffing;126,127,129,130,143,162,163 this can be seen to be intrinsic to organisational and professional objectives for the achievement of good-quality care. The staffing roster links to the mission of the organisation:
. . . every patient should be assured that there be skilled, adequate staff to provide safe, competent care.
deSilva et al. 170
Wallace and Pierson195 underlined that nurse managers have ultimate accountability for staff scheduling and are aware of the links between staffing deficits and patient outcomes. Furthermore, nurses are professionally accountable for raising concerns when patients are at risk, with professional bodies driving for a culture of openness and transparency to facilitate staff to speak out on safety concerns. 166 The advisory group commented that the organisational culture for managing risk may be at odds with professional values. As noted, nurse dissatisfaction with care standards may have an impact on organisational recruitment and retention, which further compounds poor staffing levels128,134,185,193 and potentially has an adverse impact on the organisational reputation. 185
Staffing skill mix may have more resonance with nurses than staffing numbers in relation to safety and risk management. Flynn and McKeown165 suggested that a diluted skill mix may present a threat to the professional concept of the nurse, with nurses being concerned with protecting the position of the nurse from encroachment by health-care assistants or other health-care practitioners. Skill mix remains a contentious issue for its impact on patient outcomes. 133 Nevertheless, for the public, the visibility of staffing numbers may be a source of comfort:
At the [University hospital in England] it was so marvellous to see more staff. You could tell the nurses weren’t under pressure.
PPI stakeholder
However, in the case of RNs, staffing levels may still be seen as unsafe if support workers or agency nurses are used to make up the numbers. The evidence suggested that an increasing use of agencies may have an impact on patient safety outcomes,133,160 and can have an impact on efficiency and continuity of care issues. 129 Conversely, low staffing levels may increase the use of an agency in nursing, despite the adverse financial impact of agency costs. 129,157,170,181,184,185,190,191 Wilson and Weiss153 also noted this phenomenon in the police literature. Rischbieth160 reported that nurse managers in intensive care felt pressurised to use agency nurses without knowing their capabilities for such a specialised area, and proposed that this may pose a risk. 160 Davidhizar et al. 189 found that nurses and nurse organisations often oppose ‘floating’ or working in an understaffed area, as it may put them in litigious or vulnerable situations, as nurses may not perceive that they have the relevant expertise required for optimal patient care. Consequently, high staff numbers may be reassuring for some patients, but suboptimal skill mix or capability may have an impact on nurses’ confidence levels and potentially on patient outcomes.
Many authors have described how staffing is integral to risk management. 150,160,176,198 Clark et al. 193 saw rostering as a strategic issue and suggested that unfilled shifts are a risk, with the potential for negative consequences. Safe staffing is part of both organisational and professional risk management. 193 According to Rischbieth,160 organisational attendance to risk and associated issues of patient safety is paramount, in the light of increased patient acuity and global nurse shortages. 160 Corporate indicators to gauge risk were apparent in the data; for example, Fram and Morgan174 discussed how a traffic light system was used in a dashboard to determine if key staffing data were acceptable at corporate levels, with red indicating when the levels were above or below the acceptable targets. Rapala198 stated that:
Certain interventions must be put into place to manage that risk, and staffing effectiveness is a critical part of clinical risk management.
Rapala198
The evidence from the literature shows that nurse managers focus on potential risks that could have an impact on patient safety. 150,176 Allen158 discussed how nurse managers make decisions on nurse–patient allocation while understanding the impact on patient safety. Shirey et al. 187 found that nurse managers considered how their decisions would have an impact on patients’ safety and their satisfaction with quality standards. Wilson et al. 150 described how nurse managers anticipate and manage staffing imbalances, such as high patient-to-nurse ratios, in relation to patient acuity:
This chronic wariness is defined as preoccupation with failure, in that at any moment a latent problem may erupt.
Wilson et al. 150
The evidence thus suggests that nurse managers are preoccupied with the potential risks from inadequate nurse staffing and their impact on patient care. One interview participant indicated that staffing deficits had an impact on the quality of care delivery:
. . . they [nurses] don’t have the time, they just have to get through, get the basics done for the shift and don’t always have that extra time to sit with them and do those extra things, and you do see the standard, the standard of paperwork, that drops when you go through periods like this and the acuity’s high, so it does have an impact.
Site 1, participant 1
Patient and public involvement stakeholder group members identified the possible detrimental impacts of staffing shortages on patients:
If patients see that the ward is over stretched, it would have to increase the stress levels of both patients and relatives I would think.
PPI stakeholder
I think that one thing that we have not been discussing is ‘the guilt of the patient.’ If patients were lying in bed knowing the ward is short staffed, would you feel guiltily asking for something? That could play on the minds of some people who don’t want to be a nuisance, especially those of the ‘older’ generation! We would just probably lie there, wet the bed or anything rather than ask for help.
PPI stakeholder
Disclosure of data on staffing and the manager’s role
Staffing data have not always been found to be robust, owing to the dynamic clinical environment; some authors noted a difference between the roster and the reality of staffing levels. 143,166 In a study in Malaysia, Drake143 found potential differences between rules on shifts and staffing and reality:
. . . published rosters were approved as safe and fair, but the actual safety, fairness and cost-effectiveness of the worked roster were unknown.
Drake143
Organisations do have requirements for public disclosure for scrutiny to determine financial processes and facilitate comparison with other organisations. One interview participant commented on this disclosure of data (all trusts in England are required to upload every month, through UNIFY, data on actual staffing and planned staffing):
And it’s about ensuring that trusts measure in the same way, and that they upload their data to be visible to NHSI and to the public.
Site 2, participant 2
It has been suggested that the use of WPTs may provide more accurate data. 131,166 According to Hockley and Boyle,166 that reliable systems to record workforce timekeeping will potentially have an impact on safety and efficiency and monitoring routine staffing data should be tied to visions for good-quality patient care. One interview participant held that a range of data relating to risk management, quality improvement and patient satisfaction and staffing can be accessed via technology:
When we receive complaints, all that is held at a central point, either through [patient feedback system] or through our formal complaints department, . . . we encourage our nursing staff to submit incident forms when the staffing is suboptimal . . . within the department, to the point that they feel it’s impacting on the ability to provide care to the standard that we’d want to. So that information is then accessible to us by being drawn together, and requesting that information through the systems that it’s held.
Site 3, participant 4
When organisations are required to be candid about staffing levels, it is at the ward or department interface that patients and the public will encounter indications of staffing levels:
So, we have our data at the door, the information is out . . . is available for visitors, parents, on a daily basis of what our staffing levels should be and what we’ve actually achieved for the day.
Site 3, participant 4
However, public perceptions may go beyond numbers to satisfaction with experience. Both the interview participants and the PPI stakeholders noted that ward activity has an impact:
All I would say, if your staff is running round . . . the perception is that it’s unsafe . . .
Site 2, participant 2
Managers forget that [hospital] patients are there 24 hours a day, they don’t need to be told they are short staffed, they can see they are short staffed because they are running around like headless chickens. Patients are underestimated in that sense, they have got nothing else to do but look at around at the staffing and they can see if they are short staffed.
PPI stakeholder
Nurses, and nurse managers in particular, are likely to be the source of communication with patients and the public on staffing levels and, as such, represent the organisation. PPI stakeholder feedback indicated that NHS managers should have good customer service skills, but acknowledged that conveying information about staffing shortages is sensitive:
Staff need to be prepared if a patient or their relatives asks about staffing. They need to be aware of how they communicate so they don’t make patients fearful. Provide reassurance, ‘yes we are short staffed but we are here if you need us so please ask if you need us’. Better to tell on person-by-person basis, it’s more personal.
PPI stakeholder
Shirey et al. 187 found that nurse managers comply with organisational aims:
Nurse managers quickly learned to go with the desired agenda.
Shirey et al. 187
Despite having a duty of candour, imposed by both professional and organisational requirements, nurse managers are likely to be mindful of patient experience and expectations for good-quality care. Shirey et al. 187 also noted that ward managers tend to customise messages to staff from senior management to frame issues in such a way that they will be well received. Although the framing of messages on staffing to patients is thus a possibility when staffing deficits occur, it may be argued that a lack of transparency of communication does not meet professional obligations. However, the duty of candour may possibly have limits in order to preserve the organisational reputation and ensure patient confidence. Certainly, the evidence noted that nurses can ‘game’ to achieve higher staffing numbers. 125,143 Anderson et al. 125 found that nurses using a patient classification system did not score nursing intensity as low during periods with low activity for fear of management sanctions. One interview participant described how nurse managers ‘cheated brilliantly’ as they used the data from WPTs to determine where they could find staff without declaring:
So, they’ll ring each other up and they’ll say ‘How are you doing?’, and they’ll say ‘Well I’ll send you a registered nurse and you send me an NA [HCSW], because I’ve got this . . . something special in the cubicle and you’ve got this other thing. But I’m going to go to admissions for a bit, but we won’t tell the bed managers we just . . . we just won’t . . . won’t affect your admissions if you can take them for the next couple of hours’. ‘Yeah, yeah, we can do that’, and you think . . .
Site 1, participant 4
However, Shirey et al. 187 found that nurse managers recognised that their actions had consequences, particularly in negative working cultures, where they identified unspoken lines of how far they could challenge staffing decisions. 187
The NHS manager stakeholder groups, the advisory group and the interview feedback suggested that NHS managers work hard at ensuring that patients and their family members have confidence in the system, through the use of effective communication and acting on patient feedback:
We have a system called ‘Tell us today’, we have the X [patient feedback system] department, and we have a formal complaints process. And, as ward managers and matrons, we try and meet with families just to check that everything is okay, by going round the ward. And if parents are raising that concern then we will . . . we will look at the care that’s being provided.
Site 3, participant 4
Furthermore, the interview participants identified the importance of paying attention to patient concerns around staffing and how this is often related to the expectations of patients or their families not being matched by the service provided, which culminates in potential complaints:
So, we would have then a very transparent conversation with the family about what is achievable and how we can . . . how we can achieve it, but actually then work with them and monitor that . . . that with them over the next few days to make sure we’re achieving it to a standard that they feel is okay.
Site 3, participant 4
In some respects the patients often focus on staffing as an issue, but it’s not necessarily staffing, and it’s about engaging patients to see ‘well this is how it should be with the set amount of staff we’ve got’.
Site 1, participant 3
Outcomes
The patient experience is a key priority as part of a drive for improved quality and safety,145 with NHS Education for Scotland131 stating that management decisions on staffing can be judged in terms of patient outcomes and patient satisfaction with nursing care. Allen158 indicated that a key priority for decision-making on the nurse–patient assignment was to ensure the best possible experience for patients and families. The data from the literature indicated that ensuring patient satisfaction was important for nurse managers:145,158
Managers spent much time daily checking in with patients and assuring their positive experience in the hospital because improving patient satisfaction was paramount.
Effken et al. 145
All of the stakeholders, and also interview participants, highlighted the major importance of gauging patients’ and families’ satisfaction in relation to staffing. For them the patient is the top priority. They highlighted that the patient should be the focus. Interview participants identified the importance of ensuring that the patient experience was good, and this was often linked to safe staffing:
. . . in our establishment reviews, we would take into account the . . . the friends and family element of what somebody’s saying about a ward. So, on paper we might say this looks okay, but a divisional nurse would say ‘But our patient experience or family experience is not so good’, and this is the justification of why you might need an additional role, or . . . additional numbers.
Site 2, participant 2
When there may be misalignment to the context–mechanism–outcome
Some evidence from the literature suggested that inadequate staffing levels are correlated with poor patient satisfaction. 134,145 The interview data aligned with this evidence:
We do get complaints about it, and we do get comments made. I mean you get those who will say ‘Oh, you’re all so really busy and I know you’re trying your best’, and then . . . you’ll get your families who really feel that care is being . . . compromised as a result of the nursing staff being busy.
Site 3, participant 2
However, interview data also indicated that some complaints, in which poor staffing was cited as an issue related to the quality of care, were often not substantiated when WPT data were reviewed:
In many now, what we do with complaints, if they, they do mention staffing, there’s about two that went out last week actually, it’s just, that’s why I can remember it quite clear, where they contributed the staffing, when I looked at the staffing they were actually above their template staffing. So they may have perceived it to be an issue, but it was necessarily wasn’t an issue.
Site 1, participant 3
Some stakeholder feedback suggested that displays of staffing numbers outside wards have little impact on the confidence of patients and the public:
If I was to arrive on a ward, having waited for 12 months to have knee replacement or hip replacement, and I see they are one staff member down, it would make no difference whatsoever.
PPI stakeholder
These display boards offer no context, what does that mean, how does that affect the quality of care? I wouldn’t know what the ramifications were. It’s a meaningless number.
PPI stakeholder
However, the majority of the PPI stakeholders strongly felt that displays indicating real-time staffing deficits were not a positive factor and that they would have a negative impact on public confidence:
If I saw a sign like that [indicating staff below establishment] that automatically means that there may well be a lowering of the quality of the care. It can’t mean anything else. Its common sense isn’t it.
PPI stakeholder
I think it raises more anxiety, I understand this idea for staffing levels to be visible, but I think the very idea of it being visible will raise people anxiety levels.
PPI stakeholder
I don’t see the benefit in telling the patients that you are short staffed, I imagine that would be counterproductive, because not only have you got the physical health to consider you have the patients mental health as well. If they really aren’t very well, they don’t need to hear that – I think it’s a bad idea.
PPI stakeholder
Summary of context–mechanism–outcome configurations
Although the CMO configurations have been explained individually, together they interconnect to generate a set of contingencies that can work to support the NHS manager to use WPTs. The alignment of organisational strategies and the integration of organisational systems are important factors for the effective implementation of WPTs. This facilitates synergy between proximal and distal decision-making, organisational learning and the provision of support for NHS managers in their learning for safe staffing decisions involving patients. Collective action through collaboration underpins the way in which the CMOs work; it also facilitates the co-design of WPTs so that they are fit for purpose. When the CMOs are integrated around collaborative and connected processes, they interact so that NHS managers are supported to implement WPTs effectively and this can have an impact on organisational outcomes, including the patient experience.
Programme theory evaluation: think-aloud interviews data analysis
To evaluate the programme theory further, the final set of stakeholder interviews focused on the specification of the cognitive processes around safe nurse staffing and determining their congruence to the evidence synthesis and developed CMOs (see Chapter 2, Phase 3: testing and refining the initial programme theory, Think aloud interviews). The mapping of the cognitive processes formed a sequential account of participants’ priorities and considerations in response to the staffing scenario (see the interview material at www.journalslibrary.nihr.ac.uk/programmes/hsdr/1419420/#/). Five core processes emerged (Figure 9).
FIGURE 9.
The cognitions within the five sequential processes.
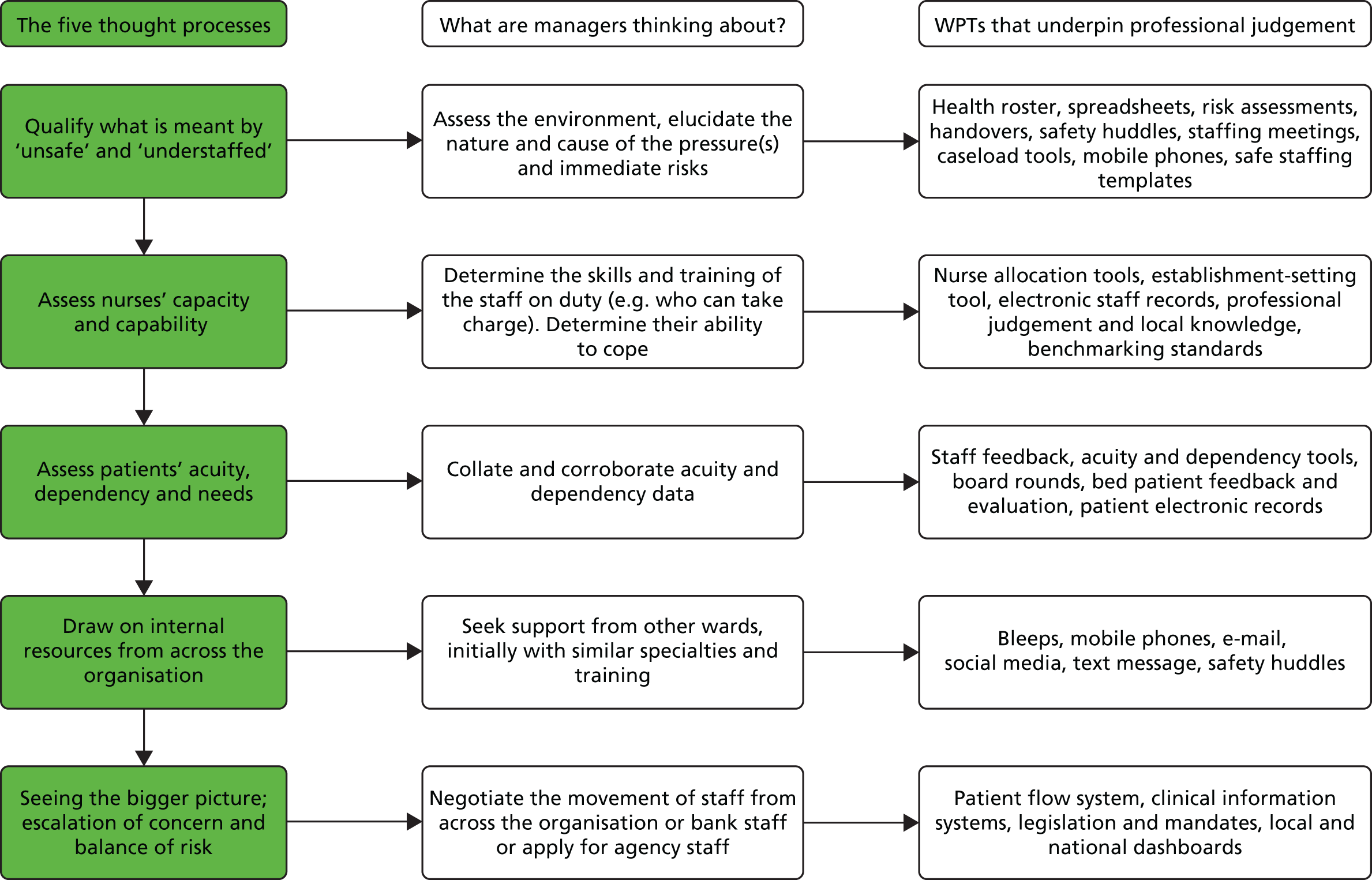
Figure 9 illustrates the NHS manager cognitions embedded within each process, as they navigate through the complexity of the dynamic system of nurse staffing and deployment. Each process demonstrates how NHS managers seek to corroborate staffing data through first-hand assessment of patient need and staffing resources. They apply their professional judgement, encompassing local and clinical understanding, to make, negotiate and communicate safe staffing decisions driven by patient-centred, good-quality care. WPTs are a feature within these processes, providing essential data and enhancing communication to facilitate NHS managers in their safe staffing work. In the following section, a narrative account of NHS managers’ cognitive processes for safe staffing is considered in relation to the CMOs. This facilitates interrogation of the programme theory to enhance the understanding of what works to support NHS managers in their use of WPTs.
1. Qualify what is meant by ‘unsafe’ and ‘understaffed’
Managers initially sought to clarify what is meant by ‘unsafe’ and ‘understaffed’. NHS managers’ assessment of safety revolved around elucidating the nature and cause of the pressure(s), to determine if staffing levels had fallen and/or to determine changes in patient needs:
The first thing I’d be thinking about is, is wanting to know specifically more about why it’s unsafe, what are the risks, what are the specific risks.
Site 3, participant 5
In most cases, the managers reported that this necessitated visiting the ward and assessing the environment. Participants emphasised their sense of responsibility and accountability for safe staffing:
I would have to assess it myself before I could action anything, because obviously I am accountable and I would have to account for my actions.
Site 3, participant 3
Accountability and responsibility related to several CMOs; in particular, CMO 2 was linked to organisational strategic requirements for the promotion of the patient safety agenda. NHS managers focused on the potential risk ensuing from inadequate staffing levels and how this could affect patient care. The data supported CMO 2, because when organisational strategies align to promote safe staffing, they convey certain expectations on the NHS manager to ensure that this occurs. NHS managers understood that organisational strategies underpin good-quality care outcomes and felt obligated to uphold them:
We obviously respond to any new policy and strategy coming, and obviously, we have to adhere to those policies. So, it’s my role to really understand how we might use them and implement them within the trust.
Site 2, participant 2
NHS managers understood that a safety agenda is embedded within strategies, and this influenced their priorities for safe staffing. Establishment data from WPTs provide the leverage for negotiation or change in the light of organisational strategic goals:
A tool gives some consistency of approach and it’s only if you’ve got something objective and you can articulate clearly what the risk is that the best decision can be made.
Site 3, participant 5
Accountability and responsibility are also reflected in CMO 1, in which proximal and distal aspects of the staffing system need to integrate, so immediate staffing decisions have a positive impact on organisational reputation and future safe staffing. Safe staffing is integral to risk management and WPTs make needs and resources visible and highlighted staffing deficits, as articulated in CMO 4. NHS managers were strongly aware of the risks from staffing deficits in relation to patient outcomes and were mindful of their professional obligation to address safety concerns. Furthermore, this sense of accountability and responsibility links to CMO 7, as NHS managers understood their duty of care for transparent communication with patients and the public. In support of CMO 7, there was a strong focus on reinforcing patient confidence in the organisation’s ability to deliver safe, good-quality care. One participant stated that they would:
. . . reassure the patient’s relative or the patient that the nurse in charge of the ward has made an assessment and deems it to be safe.
Site 2, participant 2
Furthermore, NHS managers emphasised that the application of professional judgement is essential to interpret data from WPTs on patient needs and resources related to safety. Some NHS managers implied that they had ‘a gut feeling’ about whether or not wards were safe; although this may be linked to intuition, it is more likely to have its basis in the clinical expertise and local knowledge, articulated in CMO 4, that is integral to professional judgement. The WeChat#WeNurses audience emphasised that professional judgement is essential for safe staffing and suggested that it can be developed within supportive environments; this corroborates CMO 3, in which visible support for managers to develop skills can facilitate sense-making of data from WPTs for safe staffing decisions.
2. Assess nurses’ capacity and capability
The next priority of NHS managers is to ascertain the skills and training of their staff on duty; the aim here is to relate the real-time skill mix to the establishment figures articulated by the WPTs. This involves:
. . . looking at what skills the staff have got, what banding are they . . . making sure that each bay of patients has got a nurse in, so that your nurse-to-patient ratios aren’t massive.
Site 3, participant 5
Managers considered the competence of the RNs, for example who can take charge, who can administer intravenous medication, and equally of those in vital support roles, such as HCSWs, discharge co-ordinators and administrative staff. Determining the skill mix required to meet patient needs is vital, and this emerged as an important theme in WeChat#WeNurses. Furthermore, NHS managers need to know the capacity of their staff to cope under certain pressures; this often subjective understanding relates to their professional judgement and ‘knowing their staff’, as articulated within CMO 4. NHS managers recognised the skills of their team and were able to manage personalities and balance skill sets to ensure safe staffing deployment. In support of CMO 4, NHS manager participants reported that they used their local knowledge and the data from WPTs on real-time staffing resources to make decisions:
We can identify that we want a nurse in charge to be on duty, so the e-roster will flag up if there isn’t a nurse that we deem capable to be in charge. So, to some degree, you can then put it into the pattern that, say, you wanted three nurses who have the capacity to be in charge, that will give you some assurance that you’ve got the right skill mix on duty.
Site 3, participant 6
When participants used data from WPTs with their local knowledge, they did so in consideration of staffing outcomes. This corroborates CMO 1, in which proximal and distal decision-making need to align to have a positive impact on staffing outcomes. Through knowing their staff, NHS managers consider staff well-being and their concerns for safe care:
Because it’s very easy to go it’s OK, there’s six nurses, but it’s all about the quality of those nurses and actually are they trained to look after the patients that you’ve got. There are a lot of complex patients out there who need a wide variety of skills, we can’t just treat nurses as numbers, and they’ve got to be a nurse that’s trained to look after that patient.
Site 3, participant 5
NHS managers explained that they observe staff to see if they are coping and use their leadership skills to offer support and guidance. They emphasised the importance of working with nurses to evaluate the situation and to develop perspective and problem-solving abilities. They recognised that being supportive, compassionate and caring instils trust and respect, which helps to foster collaborative relationships for flexible staff deployment. This supports the importance of leadership attributes for greater influence on safe staffing, as articulated in CMO 4:
There is a particularly poorly patient that’s making her feel so on edge. And does she need extra support?
Site 2, participant 2
NHS managers acknowledged the importance of the investment of time and resources to support nurses and managers in their role; these elements were surfaced in CMO 3 and CMO 5, in which a supportive culture is important to enable learning about safe staffing:
If I didn’t feel, after what she’d told me, it was unsafe, because sometimes it’s about ‘do you think you’re unsafe or are you extremely busy?’ because there is a difference. So, it’s about using that as an opportunity just for them to reflect.
Site 2, participant 6
If they needed any further training, if we hadn’t highlighted it in their PDR, [professional development review] we would see how we could support them through that so they didn’t feel that they weren’t supported.
Site 3, participant 1
In support of CMO 1, the NHS managers articulated that their real-time proximal decisions, although predominantly driven by patient safety, reinforced distal safe staffing systems. Therefore, participants realised that their assessment of staffing capacity and capability had a strong influence not only on immediate patient safety but also on future effects on the organisational reputation and public confidence referred to in CMO 7.
3. Assess patient acuity, dependency and needs
The interview participants indicated that WPTs that offered accurate data on patient acuity, dependency and need enabled them to form a real-time account of staffing requirements in the light of patient need; this sense-making of complex data supports CMO 3. Participants suggested that WPTs can provide information for effective staffing decisions, such as whether to visit a patient in the community:
We also have what we call Chameleon, which is attached to the hospital so if one of our patients is in hospital and hasn’t come home we can see they had their bloods done this morning then we know they are still in hospital and we can see what their blood results are. It’s a really good system actually.
Site 3, participant 1
So, you would use the acuity and dependency scoring tool, so you’d say well, on this 28-bedded ward I’ve got so many level 1As and 1Bs, which would automatically go yes, that’s going to be tough.
Site 2, participant 2
However, the NHS managers articulated how they used the objective data on patient need and applied their professional judgement to inter-relate this to staffing decisions:
We’ve got an in-house system called Bed Man, so, that gives you patient demographic information, but also what’s going on with those patients at a glance. . . . I can use my sort of clinical judgement to see what’s going on with that patient.
. . . we have quite a pragmatic approach that we’ll look at each individual case and look at the staffing required from that.
Site 3, participant 6
The interview participants recognised that ineffectual staffing decisions based on data from WPTs that make no allowance for professional judgement can have repercussions for organisational morale, nurse satisfaction and retention. This underpins the importance of managers’ understanding of how proximal and distal decisions have an impact on the staffing system, as illustrated in CMO 1, and also supports CMO 5, in which a collaborative approach to the design of WPTs can facilitate usability:
Having been a ward sister and now a matron, there is nothing more patronising than a manager coming along and saying well I have gone onto my tool and you don’t need, you can manage on that number, but what that tool probably won’t pick up is the variance in acuity.
Site 1, participant 1
4. Draw on immediate internal resources from across the organisation
NHS managers reflected that, when staffing deficits are made visible by WPTs, they would initially harness the resources they have immediately available to them. Data from WPTs can make resources visible, as articulated in CMO 3, and this information can be used alongside professional judgement. Depending on the nature and cause of the pressure, NHS managers explained that:
. . . there are things that staff can do to make it better.
Site 1, participant 1
NHS managers explained that they use leadership strategies, which could involve implementing tactical or creative solutions, strategically switching and amending shifts:
Sometimes, it’s about maybe you need to cohort the confused patients into one bay, and then you can have one health-care assistant in that bay and alternate with another health-care assistant overnight.
Site 1, participant 1
NHS manager participants indicated that they used core leadership attributes, such as critical thinking, resourcefulness and decisiveness, when making decisions on staffing using WPTs; this affirms CMO 4. This process also interlinks with CMO 1, showing that a staffing system that makes efforts to respond to demand can positively reinforce distal aspects, such as the organisational reputation and integrity. NHS managers would think about seeking support from wards where staff have similar specialties and training to move staff, in order to ensure an effective skill mix, rather than just focusing on numbers. Good negotiation skills are critical in this process and part of the range of leadership skills needed, as highlighted in CMO 4.
Likewise, NHS managers’ flexibility to work clinically and ensure their physical presence on the ward increases their integrity and credibility as a leader; and offers a role-model for a flexible workforce. NHS managers’ ability to show support clinically for their team permitted greater influence in their safe staffing work and also supports the nature of leadership work in CMO 4:
The ward managers don’t routinely work clinically, but often they will flex in and do some work on the wards, you know, if need be, and that helps . . . well, two things, they can be a good role model, it’s clinical credibility, and also its maintaining patient safety.
Site 3, participant 6
Resourcing staff requires the alignment of organisational strategies, as articulated in CMO 2. When WPTs provide data for strategy achievement, they give leverage to NHS managers’ opinions, empowering managers’ negotiation for changes to staffing:
My plan is to try and get a registered mental health nurse onto the ward to support the staff because we do really struggle. Having that tool [Safer Nursing Care tool] will give us a better case, better argument to get that.
Site 1, participant 1
Central to this stage is the need for a flexible and supportive workforce. Building trust and collaboration across teams is an important agenda for managers, and reiterates CMO 5, which highlights the value of fostering a supportive culture:
Our vision is to try and make it a respiratory unit and over the last few years that is what we have been working on, so even the Christmas party, we would all go together and be together, and it’s evident from the internal staff rotations across to the other team wards for a few weeks, that we all feel quite comfortable with each other so it much easier to say ‘oh could you go opposite and help out for 2 hours’, it’s a little bit more flexible.
Site 4, participant 1
This theme also resonates with CMO 1, in which NHS managers’ efforts to build compassion and empathy within their team can have positive influences system integration to impact positively on staff satisfaction, retention and recruitment. Furthermore, the collaborative processes evident in the data appear to articulate the organisational learning on safe staffing in support of CMO 5.
NHS manager participants indicated that they valued WPTs for accessing staffing resources. The WeChat#WeNurses audience also reflected that WPTs made staffing data available quickly for remote access; they indicated that innovative collaborative practice had resulted in the development of WPTs that are user-friendly, and which connected staff looking for shifts and facilitated real-time shift swap. This theme is exemplified in CMO 6, and shows that tools need to be fit for purpose, designed with the users in mind, to influence managers’ attitudes and change how WPTs are used:
. . . yeah, it’s fantastic, it’s so useful and we are already planning for quite far in advance . . . it’s really visual and quite easy to use, it’s easy to manage staffing hours, staff can the obviously view the e-roster on employee online for themselves or they can do that on their phone its very user friendly . . . I would never go to work and not go on it and update it with something.
Site 4, participant 1
Conversely, the interview and WeChat#WeNurses audience indicated that WPTs are not always user-friendly, and do not always reflect patient acuity or connect demand to capacity effectively. The problem of a lack of up-to-date information was highlighted. The WeChat#WeNurses audience emphasised that nurse involvement in the creation of technology is therefore vital for effectiveness in supporting practice, which again supports CMO 6. NHS managers and the WeChat#WeNurses audience emphasised that the most important factor is the application of WPTs through professional judgement.
5. Seeing the bigger picture; escalation of concerns and balancing the risk
When immediate internal resources do not fulfil staffing requirements, NHS managers escalate their concerns to senior managers and engage with those who have a strategic and clinical overview of the organisation to see if there is latitude for movement of staff from diverse areas, or if they need to use external staff. Participants noted that WPTs can make staffing resources visible, in support of CMO 4. They suggested that WPTs that fit into their workflow and which are user-friendly and easy to navigate enhance communication to escalate staffing requirements and promote shared accountability. Seeing the bigger picture is critical during this process and is reliant on NHS managers’ understanding of the clinical environment, patient group needs and the organisational structures and procedures, which are incorporated into CMO 1 and are imperative for responsive decision-making for real-time and future need:
So, if a matron is running a group or orthopaedic wards then you sort of manage them together, so you make sure that every ward is safe. . . . failing that, you could then go wider and look at the whole trust and see, or campus, and see who we could move.
Site 2, participant 2
However, there was some indication that WPTs were fit for purpose at the senior management level, but not for others. This underpins the need for partnership in design within CMO 6, so that the WPTs fulfil different requirements at different levels within the organisation:
Personally, I think the staff on the ground could do without it [the WPTs]. I would say for more senior management position to get more of a strategic overview, I think it’s imperative that there is some kind of standardised tool. We could do with something to be able to demonstrate to the organisation the lay of the land really out here, actual teams, workloads, and ratios.
Site 3, participant 2
Often, requests for additional staff within this process required justification based on professional judgement:
If we wanted additional staff members above and beyond our establishment we would have to get a matron approval so the next level approval to say, for example, we have got four really confused patients all wondering, one has fallen over, we need someone to sit in that bay or have a supervised bay or one to one, ‘Can we have an extra staffing member?’
Site 3, participant 1
NHS managers explained that they sought evidence from WPTs for in-the-moment decision-making (expected patient flow and discharges) and for forecasting future demands (patient dependency/acuity classification data) and associated cost:
I mean the other thing that we do look at number of patients in the ED [emergency department]. So, what the patient flow is throughout the hospital, you know. So, that’s something that’s done at quite a high level. And then the other things that we’ve got is we use a system, a software system called Nerve Centre which allows us to predict discharges.
Site 2, participant 2
This process is elucidated in CMO 1, and shows that managers who understand the complexity and dynamicity of the system can use data from WPTs for responsive decision-making. WPTs are also used to specify for codes to ensure that agency staff have specific skills depending on patients’ requirements:
We use a lot of agency staff at the moment, we book people who have a 04 code which mean they have emergency experience even if it is not at our trust.
Site 2, participant 1
Furthermore, the data suggest that within this process, NHS managers consider both immediate and future demands and how they can respond effectively to attain the best outcomes (which supports CMO 1), and that they under-score when managers are responsive and show agility and flexibility to staffing demands. This can create positive reinforcement of distal aspects, such as the organisational reputation and recruitment. Furthermore, this relates to a culture of evaluation for organisational learning, as articulated in CMO 5:
We sort out the immediate situation, but then we have to look at long term, is this something that’s going to be a recurrent problem, if so, what we can do about it, how do we manage that situation? Who needs to be aware of that situation that’s senior to us, or who needs to be aware of that situation that’s involved with that patient, and how do we manage the more long term then?
Site 3, participant 4
The NHS managers highlighted the need to be transparent and honest about staffing levels with patients and families, while carefully addressing any concerns, to ensure confidence in their service. They indicated that they take care to be sensitive and sympathetic to the apprehensions of patients and families, especially when there are deficits in staffing levels; emphasising that the training, experience and skill mix of their establishment is sufficient to meet patient need. This staffing work in balancing candour and refining communication supports CMO 7:
I would say ‘we would normally plan to have seven on, but unfortunately today, because of unforeseen circumstances we’ve only got six. However, we’ve got a really experienced team on, we’ve looked at the patient allocation accordingly, we’ve got additional people round if we need them . . . if you’ve got any concerns please come and talk to me.’
Site 3, participant 6
NHS managers used data from WPTs to highlight to patients or the public that their resources are sufficient to meet demands:
It’s about assessing skill mix, assessing experience, assessing acuity. So, occasionally you could say ‘Well actually we have got less staff, but we are safe because of these . . .’ the things that I’ve just mentioned, you know?
Site 2, participant 2
Summary
The data from the think-aloud interviews in phase 3 were found to resonate with all CMOs, reinforcing the idea that they combine to explain the programme theory of what works to support NHS managers’ use of WPTs. This was corroborated by the WeChat#WeNurses discussion. This evidence further supports the integrity and accuracy of the explanations offered within the evidence synthesis.
Chapter 4 Conclusions, implications and recommendations
Introduction
This evidence synthesis has resulted in an explanatory account of the organisational and developmental interventions that can support NHS managers to use WPTs in order to ensure effective staffing. It has drawn on a comprehensive range of evidence and included extensive stakeholder engagement in order to formulate a rich description of the system of nurse workforce planning and deployment and to generate seven CMOs, which combine to form an explanatory programme theory. Together, the system and the interaction between the CMOs convey the complexity of the task NHS managers have when making nurse staffing decisions. This chapter considers how the findings address the study’s aims and objectives and draws on illustrative mid-range theories to illuminate the programme theory. The implications for practice are examined and a quality assurance framework is proposed for the development and use of WPTs. Finally, recommendations for future research are presented.
Review of the research aim and objectives
The aim was to engage stakeholders to produce an evidence-based, realist theory to explain the successful implementation and impact of WPTs by NHS managers. The following sections discuss how the findings meet the study’s five objectives.
1. To identify the different workforce planning and deployment tools and technologies used to deploy the nursing workforce, paying attention to the ways in which they are assumed, and are observed, to work
A range of WPTs were identified in the functional typology (see Chapter 3, The functional typology of nursing workforce planning and deployment tools and technologies). The evidence suggests that WPTs work by making data visible so that patient need can be matched to staffing resources. 124,125,127,129,130,133,134,144,147,151,175–180 The ability of WPTs to integrate relevant data for understanding complex issues in staffing (e.g. data on staffing skills and patient need) facilitates sense-making for effective decisions. 126,129,134,167,169,175,180,183,192,206 This can ensure that the right resources are assigned for efficiency quality and safety. 199 The findings indicated that WPTs can be used to forecast real-time and future demand for financial and resource planning. 125,151,168,171,172,174,182 The evidence also suggested that, when there is a standardised approach to the use of WPTs, the data produced can be used for evaluation and comparison against organisational and national standards required by legislation, mandates or guidance. 124,126–128,131,147,175,183,195,199,206 Thus, data from WPTs can be used to identify areas in which improvements need to be made for quality improvement and for the achievement of organisational goals. 133,145,147,174
The evidence suggested that there is a diverse range of WPTs. Patient dependency and acuity assessment tools and e-rostering were more prevalent in acute adult settings, with limited evidence for managers’ use of community caseload technology. 179 There was evidence that some organisations embraced technology and used it to its full capacity, for example e-roster, self-roster apps and electronic bed management systems. However, there was also evidence of reliance on written rosters or bed states, with some resistance to the adoption of technology noted in the literature. 132,143,178,182,197 Disparities in the use of WPTs were also evident within different clinical areas in the same organisations. It would appear that there is little consistency between health organisations in how they select or implement WPTs; this may become more standardised with the advent of recent guidance for benchmarking. 10 Legislation, mandates and strategy appear to strongly influence the implementation of WPTs. 132,147
WPTs have to be based on up-to-date data in order to be valuable for real-time decision-making. 155,166–170 When WPTs were embedded in organisations, inputting data in a timely fashion was the accepted practice;126,206 however, stakeholders suggested that, when staffing was reduced, updating data was not a priority. Many of the managers emphasised that they valued ‘the walk-around’ in hospital settings to obtain up-to-date information, falling back on traditional paper methods, rather than relying on data from technology. This highlights the dynamic and complicated nature of health care and how managers need to have confidence in the data underpinning staffing decisions. 127 Even when WPTs were acknowledged to identify needs and resources accurately, the evidence supports the importance of using professional judgement and human insight,178 which was described by a manager as ‘feeling the ward’. Managers need to critically interpret data from WPTs for safe staffing decisions131,158,163,176,178 and know their staff to determine whether or not staff can cope with particular situations and to identify the best staff to move when shortages occur, in order to ensure patient safety and good-quality care. These decisions use clinical and personal knowledge of nurses and organisational processes beyond the skills, attributes and numbers identified by WPTs. Furthermore, NHS managers act as a supportive presence to ensure the best outcomes for both patients and staff. They prioritise patient needs, but are mindful of balancing these with long-term requirements, with an understanding of how staff satisfaction relates to retention and recruitment:
We sort out the immediate situation, but we have to look at the long term.
Phase 3, site 3, participant 4
2. To explore the range of observed impacts of these technologies in different health-care settings and other public services, paying attention to contingent factors
The majority of evidence available related to adult acute settings. The effective implementation of WPTs can have a positive impact on organisational strategic aims for efficiency and good-quality care. A standardised approach facilitates monitoring for cost, efficiency and quality. 129,175 The increased understanding of staffing availability and the use of temporary staff articulated by WPTs can also result in cost-savings. 190,191,206 WPTs provide standardised data for comparison and benchmarking within the organisation and against other organisations. 124,126,127,129,131,147,168,171,175,180,182,183,206,210 Data from WPTs can therefore be used to set staffing parameters. 168 WPTs can collate data to provide evidence for the achievement of organisational aims in good-quality care in the light of national standards,168,192 to result in organisational learning. Furthermore, WPTs can produce visible staffing data for patients and public scrutiny. The impact of this lacks clarity; staffing levels may be meaningless for some patients, and for others, these may cause anxiety.
When WPTs offer credible real-time data, they are able to support managers in their decision-making role through the articulation of the availability of staff skills;128,133,144,151,152,157,158,160,164,174,175,180,181,184,189,191,198 identifying patient acuity and dependency;158,163,183,207,208 and matching patient scores to workload. 124–126,129,130,133,144,147,151,175–180 WPTs can also be used by managers to forecast future demand based on current patient data. 134,151,168,171,172,174,182,183 The project team found evidence that high levels of vacancies have an adverse impact on staff morale in nursing143,151,156,163,178,185,189,193 and in the police. 153 When WPTs enhance effective rostering, this can have a positive impact on recruitment and retention169,189–191 as poor rostering practice can result in staff dissatisfaction. It is a balance to ensure safe staffing and maintain staff well-being. Auto-rostering may offer parity in staffing allocation, and self-rostering offers staff more control. 143,190,191
The integration of data enables managers to have an understanding about the complexity of staffing needs and requirement. WPTs can present the bigger picture,145 offering a ‘helicopter view’. When WPTs are used effectively, they may empower managers to make changes. 129,132,169,179,192 The stakeholder work suggested that data can be used to argue for more resources, as managers were aware of their professional accountability for safety and communicated risk to secure safe staffing. Data from WPTs can enhance communication and provide managers with the evidence to negotiate for resources and justify staffing decisions. 131,132,144,169,179,192
The evidence emphasised the importance of the alignment of organisational strategies for safe staffing. 126,127,129,131,144,168–170,184,185,190,193 Perhaps unsurprisingly, there was strong evidence that when there was misalignment between financial and other organisational strategies related to budget restrictions, this could have an adverse impact on the effective use of WPTs;126,127,160 this was echoed in police staffing. 153 If WPTs identify the need for resource investment and this is not forthcoming, staff are unlikely to value their use. 126,144 Poor understanding of WPTs also impedes their use,125,126,132,151,155,208 and can be linked to a lack of alignment of strategies, which results in underinvestment in support or training for WPTs. 126,127 Furthermore, organisational systems need to be integrated so that real-time decisions are in synergy with long-term planning strategies, particularly around recruitment and retention, for the efficient deployment of WPTs, so that flexible staffing resources are available. One manager conveyed that the two most important things in her job were recruitment and rostering, as they were embedded with patient safety.
3. To investigate ways that can help NHS managers to identify, deploy and evaluate the nursing workforce resource to have the greatest impact on patient care
Both organisational support and effective leadership have key roles to play in NHS managers’ use of WPTs. 124–126,129,134,143,147,151,155,169,200,208 These are linked to the alignment of strategies and system integration. The findings suggested that organisational factors can work to support or impede NHS managers’ use of WPTs, so a collaborative culture and a standardised team approach are needed. 132,200 Professional judgement is inherently important to safe staffing decisions. It can be postulated that this may be developed in organisations that adhere to ‘Magnet values’, as these offer a supportive, collaborative organisational culture in which staff feel valued and professional development is facilitated. 118,119 Organisational investment in resources for WPTs has a positive effect in facilitating the provision of specialist support, education and training. 126,127,134,174,199
The findings indicated the importance of organisational collaboration and partnership to develop or select WPTs. 126,127,131,134,146,147,154,169–171,174,175,183,190–192,194,195,197,200,203,208,209 Collaboration can result in WPTs that fulfil organisational goals and that are user-friendly and fit for purpose. Data need to be presented in an understandable way, as there are different information needs at different managerial levels. 131,180,182,186,197 A robust evaluation culture supports organisational and individual learning around WPTs and safe staffing. 124,126,129,131,148,172,174,190,195,199 The interview participants were aware of WPT-related developments in other clinical areas and hoped to learn from them.
The evidence strongly suggested that NHS managers can be supported to use WPTs through training, expert support, peer support, mentoring and feedback. 126,127,174,179,195,199,200 An individualised approach to training appears to be effective when staff are not confident with IT. 179 Staffing decisions are complex, so not only do NHS managers need to have a clinical understanding of patient needs, they also need to have support to develop their knowledge of the clinical environment, patient group needs and the organisational structures and processes, as this is important for effective rostering and patient–nurse allocation. 129,131,144–152 NHS managers also need to draw on a range of leadership, communication and negotiating skills. The evidence suggested that managers need training and education on staffing decisions,150,174 but that this should be linked to the development of leadership skills163,167,186,189,199,202 and financial skills. 154,171 Furthermore, it appears that given the requirements for transparency of public data, NHS managers need guidance on how to convey staffing data to address patient and public concerns.
4. To generate actionable recommendations for management practice and organisational strategy
The cumulative findings provide orientation for approaches to supporting NHS managers’ use of WPTs through surfacing the knowledge and understanding of what helps to develop management practice and how safe staffing can be underpinned by organisational strategy.
For the effective operationalisation of WPTs within the complicated, dynamic, health-care environment, the findings suggest that the alignment of organisational strategies helps to support safe staffing and the implementation of WPTs. Pivotal to this alignment is a financial strategy that works as a foundation for real-time patient safety but also acknowledges the need for investment and long-term planning for staff well-being. Organisational investment to embed WPTs, through training and support, appears to be fundamental to an effective financial strategy, particularly as WPTs have a key role in the achievement of financial efficiency. 10,129,166 When the financial strategy is supportive of immediate and future safe staffing, this facilitates the alignment of other strategies, such as those on quality and recruitment.
The evidence indicated that the integration of organisational systems can reinforce a seamless approach to real-time and distal safe staffing decisions. The alignment of organisational strategies will contribute to a synergistic approach to system integration and the operationalisation of WPTs. When organisational systems are integrated, WPTs can be used to their maximum capacity, as staff will be equipped with the knowledge and skills to use them and be empowered to make effective decisions on safe staffing in the light of organisational processes and patient flow.
Collaboration and partnership are central to this process, so that staff from different strata of the organisation understand and facilitate the NHS managers’ role and contribute to organisational aims for good-quality care. Collaboration is also an important feature to ensure that WPTs are fit for purpose for NHS managers at different levels of the organisation. The alignment of organisational strategy and system integration can promote the collaboration needed for the co-design, implementation and evaluation of WPTs. This can ensure that they are appropriate for organisational processes and user-friendly. In this way, WPTs can help to achieve organisational outcomes.
Finally, the evidence suggested that organisations need to invest in education and support for NHS managers to develop the leadership skills and knowledge required to make and communicate safe staffing decisions. Although training, access to resources and expert support in the use of WPTs appears to be fundamental to this process, a more individualised approach, such as through mentoring and feedback from senior staff, appears to offer NHS managers the level of support needed for many of the challenging staffing situations they face.
5. To contribute to the wider understanding of the nature of the nursing workforce, nursing work and the quality of patient care
The programme theory, which is a cumulation of the seven CMO configurations, offers an evidence-based explanatory account of what works to support NHS managers in the use of WPTs. Although this programme theory is specific to the use of WPTs, the CMOs refer to concepts that can be transferred across to other service contexts to support workforce managers to deploy staff effectively and efficiently. It is important to acknowledge the evidence on patient safety, as the effective use of WPTs has a contribution to make to monitoring and evaluating staffing against safety objectives, all of which have emerged as a focus for prioritisation. 2,4 The evidence from the synthesis suggests the need for inter-related data, and this is echoed within the patient safety literature. 213 The Vincent et al. 214 framework for safety measurement and monitoring indicates five stages: (1) past harm, (2) reliability, (3) sensitivity to operations, (4) anticipation and preparedness and (5) integration and learning. Each of these have resonance with the findings; the synthesis indicates that WPTs are used to determine staffing levels and skill mix when harm has occurred. WPTs need to have real-time data for reliability, but can then facilitate system flexibility (or sensitivity to operations). Finally, the findings suggested that WPTs have been linked to organisational planning (for preparedness) and learning.
When the CMOs configure effectively, change occurs at the individual and/or organisational levels. Mid-range theories have been drawn on to offer an explicit understanding of the contingent processes underlying these changes. 109,215–241 These may point to perspectives that provide a new lens on the use of WPTs that could be pursued in future research. The theories that relate to the CMO configurations have been organised into five conceptual themes and summarised in Table 5, with further detail given in Appendix 13. Some of these mid-range theories are more dominant than others and have relevance across CMOs.
| Conceptual area | Relevant theories | Application to WPT |
|---|---|---|
| Professional judgement | Intuition (Dreyfus and Dreyfus,229 Benner230); rationality (Bayes’ theorem231,232); social judgement theory (Brunswick233); cognitive continuum (Hammond et al.234) | These theories explain the influence of environment and experience on managers’ judgement when using WPTs; and how judgements may alternate between analytical and intuitive |
| Decision-making | Bounded rationality (Simon235); the theory of planned behaviour (Ajzen236); behavioural theories of the firm (Cyert and March237); game theory (Von Neumann and Morgenstern238) | Different perspectives are offered on the influences on decision-making, such as intention, negotiation of goals, satisficing or gaming |
| Capability | Self-efficacy (Bandura225); emotional intelligence (Goleman226); transformational leadership (Bass227); authentic leadership (Avolio et al.228) | Collectively, these theories offer an understanding of the influences on managers’ capabilities and capacities, particularly with regard to effective leadership skills |
| Complexity | Chaos theory (Rickles et al.215); systems theory (von Bertalanffy216); complexity (Zimmerman et al.217); contingency theory (Fielder218); actor–network theory (Latour219) | These theories relate to the complicated and complex dynamic environment for safe staffing and consider how systems and groups may interact, depending on circumstances and the influence of leadership |
| Knowledge transfer/implementation and change | Social learning theory (Bandura221); diffusions of innovations (Rogers109); organisational readiness (Weiner222); organisational knowledge creation (Nonaka and Von Krogh223); organisational learning (Argyris and Schon224) | The effective implementation of WPTs depends on individual and organisational learning; these theories offer an understanding of how knowledge can be transferred for learning to occur |
| Information systems | Human–computer interaction (Jacko and Stephanidis239); safety-critical systems (Perrow220); social construction of technology (Bijker et al.240); computer-supported co-operative work (Ackerman241) | For WPTs to be successfully implemented, an understanding is needed of the influences on the interaction between technology, systems and managers. These theories offer an insight into how managers may use WPTs within complex contexts |
Context–mechanism–outcome 1: system integration and workforce planning and deployment tools and technologies
The theories categorised under complexity are relevant to system integration to explain how dynamic system processes may interact and influence the actions and reactions of individuals and groups within networks. 215–219 The safety-critical theory, although it has a focus on high-risk industries, also offers an insight into human factors and safety in complex systems. 220
Context–mechanism–outcome 2: alignment of organisational strategies over workforce planning and deployment tools and technologies
Theories of complexity and knowledge transfer underpin the importance of the alignment of strategies. 215–219,221–224 Theories of complexity consider system interaction and system complexity versus system order. They may explain how people react to complex organisational contexts, so that they may integrate systems and learn and transfer knowledge on WPTs, so that staffing is safe and effective.
Context–mechanism–outcome 3: supporting the NHS manager to use workforce planning and deployment tools and technologies
Theories of knowledge transfer and capability are most illustrative of how managers can be supported to develop knowledge and skills on WPTs. 109,221–228 Knowledge transfer theories suggest that social processes can impede, or propel, knowledge absorption and implementation. These are linked to theories that explain individual’s capabilities and propensity to act and lead. Social learning theory offers an understanding on how capabilities can be developed. 221
Context–mechanism–outcome 4: integration of workforce planning and deployment tools and technologies with organisational knowledge and NHS managers’ capabilities
Theories on professional judgement and decision-making have a strong impact on CMO 4, but theories of capability are also relevant. 229–238 These theories examine the knowledge and understanding of probabilities (often through the use of modelling technology) needed to make safe staffing decisions, and they explain how managers are influenced by experience, the environment and social interaction.
Context–mechanism–outcome 5: organisational learning and workforce planning and deployment tools and technologies
Theories of knowledge transfer, implementation and change dominate organisational learning on the use of WPTs. 109,221–224 These theories explore and clarify how new knowledge and processes can be adopted by individuals and groups. The theory of organisational learning explains the importance of reflection, which can be linked to evaluation and feedback on the implementation of WPTs. 224
Context–mechanism–outcome 6: co-design of workforce planning and deployment tools and technologies
Theories on information systems underpin co-design and explain its importance for effective implementation and the use of technology. 220,239–241 Theories of knowledge transfer, implementation and change are also of relevance here, as co-design is strongly linked to knowledge creation and learning for the effective use of WPTs and development. 109,221–224
Context–mechanism–outcome 7: workforce planning and deployment tools and technologies and involving patients
Theories of professional judgement and decision-making strongly influence how managers use data from WPTs to communicate to patients. 229–238 Theories of individual capabilities, particularly emotional intelligence, also underpin the nuanced decisions and judgements made. 225–228
Review strengths and limitations
Strengths
A major strength of this synthesis was its methodological approach. A realist synthesis was eminently suited to the complexity of nurse workforce planning and deployment as it acknowledges contingencies within structures and processes that can impact on a range of outcomes. 92 A more traditional review would have a chief focus on outcomes, rather than exploring important contextual influences that may impede or trigger the mechanisms that influence outcomes. In adhering to realist principles, a theory-driven approach was followed to develop the programme theory, constituting seven CMO configurations. This explanatory account offers an insight into what works to support NHS managers to use WPTs and offers some consideration of the factors that may impede their use. The development of a functional typology of WPTs further enhances the understanding of the complexity of safe staffing. The use of the think-aloud technique in phase 3 articulated the decision-making processes undertaken by NHS managers; this refined and corroborated the emerging programme theory.
A realist synthesis embraces an eclectic approach to the range and quality of evidence for review, placing emphasis on evidence that is relevant to the emerging programme theory;94 unlike the traditional systematic review, quality is judged on this relevance. Therefore, the focus was on credible ‘nuggets’ of information that shed light on the programme theory, rather than criteria of validity and reliability within evidence hierarchies. By paying close attention to different perspectives from the published literature and stakeholder work, the review was iterative and accumulative; these processes were captured transparently within the description of the methods in Chapter 2.
A further strength of the realist approach was the inclusion of extensive stakeholder work embedded within the synthesis. A broad range of stakeholders participated, from NHS managers, experts in NHS staffing and PPI representatives with more extensive engagement through to people in a Twitter chat in phase 3 that was hosted by the chairperson from the advisory group. Their involvement and perspectives improved the trustworthiness of the findings by enhancing its credibility. They have also helped to mobilise knowledge from the synthesis as part of the review process. A more traditional systematic review may have impeded the understanding of nuanced factors, for example those relating to professional judgement.
Limitations
As this was a synthesis, the project team relied on scientific papers and reports, which often lacked detail on how managers applied their professional judgement in conjunction with the data from WPTs to make staffing decisions; consequently, the stakeholder engagement was amended to explore this further through a limited number of think-aloud interviews. The evidence about how managers develop skills in the communication of staffing levels to patients, the public and carers was very limited. Furthermore, the synthesis materials were often unclear about nurse managers’ roles within the organisational structure, their professional backgrounds or their capabilities. More of a range of relevant literature from the police and other public services was anticipated; however, extensive searching of relevant databases and using personal contacts did not surface significant evidence. There is also acknowledgement that in searching for ‘nuggets’ of explanatory evidence, the synthesis may have failed to track down all of the relevant literature; however, an extensive review of the literature within phase 1 sought to minimise omissions. It is also acknowledged that participants in the stakeholder engagement activities may have presented idealised versions of reality. However, the purpose of this engagement was to add depth to the reported evidence rather than to generate new findings per se.
The iterative nature of a realist review can present challenges in articulating and justifying the nuanced decisions made on which threads to pursue when developing the programme theory. It is acknowledged that the study, in focusing on NHS managers’ use of WPTs, examined only one part of the system of nurse workforce planning and deployment. However, Chapter 2 attempted to provide a transparent account of the approach. The decision-making process is the result of the uniqueness of the team, but can be viewed with confidence given the experience of the team members in realist methodology (CRB, JRM, LW, DF and BH). The study project team met monthly throughout the 18-month study period and offered a team-based approach to decisions; this was further guided by the advisory group; for example, the group suggested that balancing risks should be examined in safe staffing. The PPI group members articulated the importance of public scrutiny on staffing numbers for patients and carers.
Implications for practice
To support learning and improvement from this synthesis, a quality assurance framework was constructed (Figure 10) to serve as a heuristic way to summarise the key areas for creating the conditions to support NHS managers in the use of WPTs for safe staffing decisions.
FIGURE 10.
Quality assurance framework to support managers’ use of WPTs.
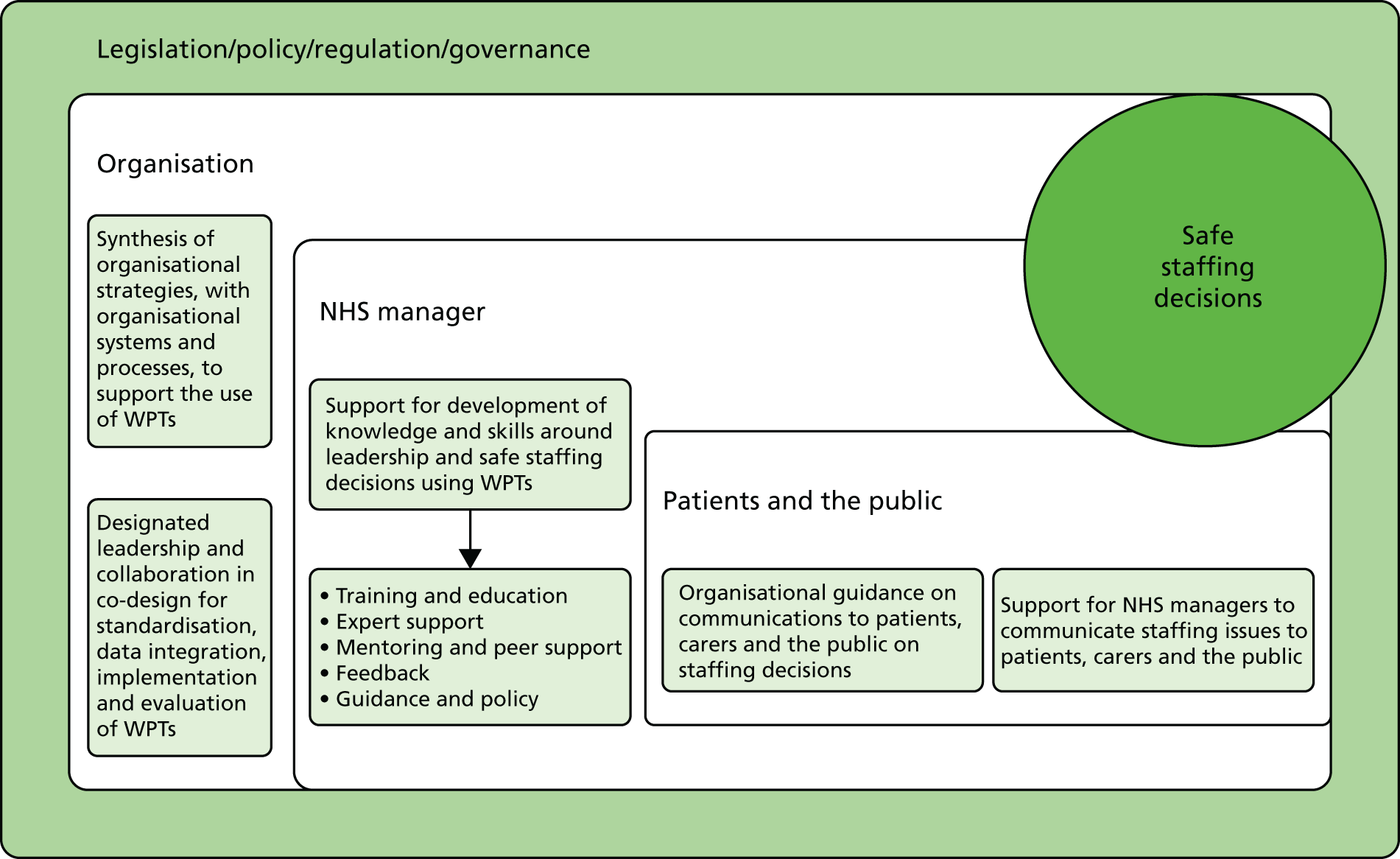
The evidence synthesis strongly suggests that the way in which NHS managers use WPTs is contingent on organisational factors and attention should be paid to ensure that managers are aware of their wider organisational system that surrounds workforce deployment. This system is multilayered and includes legislation, policy, regulation and other governance, over which managers may not have influence. Understanding the consequences of these and their local implementation within organisations will be key. Often, these consequences may be embedded in different organisational strategies, and senior management should ensure that these are sufficiently aligned around effective nurse staffing and care quality. Organisations will benefit from a collaborative and standardised approach to the implementation of WPTs, particularly if the organisation is to learn about ‘what works’ in its approach to nurse staffing.
Commitment from senior leadership is vital to ensure that organisational strategies work towards the same organisational goals for safe staffing and these are underpinned by supportive organisational systems and processes. Organisational staffing policies, for example on rostering, are essential for a synergistic approach. Collaboration and partnership from leaders, at all levels of the organisation, can ensure that WPTs are designed to be fit for purpose and user-friendly within different levels of the organisational systems. WPTs that integrate information on patient needs and staffing resources with costs facilitate efficient and effective decision-making. WPTs need to be embedded within the organisation’s systems and operations effectively, so that data are in real time and are credible. Collaboration within and across organisations is also vital for evaluation; here, organisations could focus on the fit between the use of data from WPTs and the organisational systems that have an impact on processes, patient flow and human resource management. The evidence indicates that organisations need to pay attention to system flexibility and responsiveness, so that the data from WPTs are used effectively. It appears to be essential that NHS managers who use these data to make real-time staffing decisions are part of these collaborative processes.
NHS managers have a challenging task in making effective decisions on staffing, and they need training and organisational support to develop their knowledge and skills in the effective use of WPTs. Expert support, from staff with IT skills and senior managers, has a positive impact. Importantly, the data for WPTs need to be applied using professional judgement and effective leadership skills. The synthesis suggests that organisations should focus on professional development programmes to develop these skills. Mentorship, peer support and feedback can also enhance the knowledge and local understanding gained through experience. Attention can be given to the development of communication and negotiation skills.
The transparency of staffing data for public scrutiny will have an impact on patients, the public and carers, but there is a limited evidence base on how staffing decisions may best be communicated by NHS managers. Clear organisational policies on communicating staffing levels and clear processes for communication with patients and the public may support NHS managers. Communication of staffing levels will go beyond numbers on notice boards outside clinical areas. However, this is an area where managers need additional support and advice, and further research is required to underpin this.
Recommendations for future research
The findings highlight a number of implications for future research to further evaluate the programme theory and enhance the understanding of NHS managers’ use of WPTs for safe staffing decisions. The evidence base on the use of professional judgement in the decision-making processes and how these are integrated into managers’ daily work could be broadened to offer greater insight into how effective judgements can best be developed. The findings also suggest that longitudinal studies are needed on the impact of co-design to facilitate the development of WPTs and effective implementation. Furthermore, studies could examine the best format for education programmes to prepare NHS managers for their safe staffing role. Further investigation of patient and public preferences for disclosure around staffing, including risks, benefits and consequences for professional staff, is required. Finally, studies could explain the communication processes that help NHS managers to inform patients, carers and the public on staffing decisions.
Conclusion
This realist evidence synthesis has constructed a programme theory of what works to support NHS managers in the use of WPTs, to determine what works for whom, how and in what circumstances. The synthesis concentrated on surfacing the explanatory detail of the complexity of the system of nurse staffing and focused on its dynamic nature. It has constructed the evidence base through scrutiny of the relevant published literature and extensive stakeholder engagement to produce actionable recommendations underpinned by mid-range theories. The synthesis approach helpfully facilitated the iterative development and evaluation of the programme theory following the integration of the evidence from the literature and stakeholder insights into NHS managers’ use of WPTs. The quality assurance framework is transferable and may provide a useful guide for organisational leaders in diverse services in which safe staffing decisions are essential for quality outcomes. The study offers an insight into the preparatory work and ongoing support required for the implementation of WPTs and their effective use by NHS managers.
Acknowledgements
The project team would like to acknowledge the contribution and support of the NHS managers and PPI stakeholders who participated in the co-production workshops. The team would also like to acknowledge the contribution of the NHS managers who participated in the phase 1 and phase 3 interviews.
The team is particularly indebted to Professor Jean White, who chaired the advisory group and led on the WeChat Twitter forum.
Many people engaged in a variety of different meetings and activities across the life of the project, and the team is grateful for their support: Professor Cheryl Lenney, Dr Theresa Shaw, Professor Angela Hopkins, Professor Elizabeth Robb, Professor Donna Kinnair, Anne Pearson, Angela Reed, Tina Donnelly, Dr Tim Devanney, Dianne Murray, Helen Whyley, Pippa Ford, Dr Sally Gosling, Rachel Finn and Jim Murray. The team is also grateful to Nyree Hulme for her administrative assistance in the preparation of this report.
Contributions of authors
Christopher R Burton (Noreen Edwards Chair of Rehabilitation and Nursing Research) was the chief investigator and led the study design, chaired the monthly research team meetings and was involved in all aspects of the review process, including the advisory group and co-production workshops. He is the lead author on this report.
Jo Rycroft-Malone (Pro-Vice Chancellor Research and Impact) was a co-applicant and advised on study design, attended the monthly project meetings and was involved in all aspects of the review process and the preparation for this report.
Lynne Williams (Senior Lecturer) was a co-applicant and was involved in all aspects of the review design and process, attended the monthly project meetings and co-facilitated the co-production workshops. She was involved in the preparation for this report.
Siân Davies (Lecturer in Adult Nursing) took day-to-day responsibility for the project management and for the review process, co-facilitated stakeholder and advisory group meetings, was involved in all aspects of the review process and co-led the preparation of this report.
Anne McBride (Senior Lecturer in Employment Studies) was a co-applicant and advised on human resource management. She was involved in the study design, the monthly project meetings and all aspects of the review process and the preparation for this report.
Beth Hall (Research Support Librarian and Academic Support Librarian) was a co-applicant and was involved in study design; she attended monthly project meetings, led the information searching, retrieval and organisation and gave feedback and participated in the preparation of this report.
Anne-Marie Rowlands (Assistant Director of Nursing) was a co-applicant and was involved in study design and advised on NHS nurse workforce management. She was involved in the monthly project meetings and participated in the advisory group and aspects of the review process and in the preparation for this report.
Adrian Jones (Clinical Academic Lead) advised on NHS nurse workforce management in relation to workforce management in mental health. He was involved in the monthly project meetings, the advisory group and all aspects of the review process and preparation for this report.
Denise Fisher was a co-applicant and lay research team member. She was involved in study design, provided feedback in project meetings and contributed to the stakeholder co-production workshops, the advisory group and all aspects of the review process, including the glossary of terms and preparation for this report.
Margaret Jones was a lay research team member and advised on the carers’ perspective. She participated in monthly project meetings and a stakeholder co-production workshop and participated in the preparation for the final report.
Maria Caulfield (Research Officer) led on the think-aloud interviews. She participated in monthly project meetings and the advisory group meetings and participated in the preparation for the final report.
Publication
Burton C, Rycroft-Malone J, Williams L, Davies S, McBride A, Hall B, et al. Managers’ use of nursing workforce planning and deployment technologies: protocol for a realist synthesis of implementation and impact. BMJ Open 2016;6:e013645.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Griffiths P, Ball J, Drennan J, Dall’Ora C, Jones J, Maruotti A, et al. Nurse staffing and patient outcomes: strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for the National Institute for Health and Care Excellence Safe Staffing guideline development. Int J Nurs Stud 2016;63:213-25. https://doi.org/10.1016/j.ijnurstu.2016.03.012.
- Francis R. Report of Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary. London: The Stationery Office; 2013.
- Keogh B. Review into the Quality and Care and Treatment Provided by 14 Hospital Trusts in England: Overview Report. London: NHS England; 2013.
- Berwick D. A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England. London: Department of Health and Social Care; 2013.
- Commissioning Board Chief Nursing Officer and Department of Health and Social Care Chief Nursing Adviser . Compassion in Practice. Nursing, Midwifery and Care Staff: Our Vision and Strategy 2012. www.england.nhs.uk/wp-content/uploads/2012/12/compassion-in-practice.pdf (accessed September 2017).
- How to Ensure the Right People, with the Right Skills, Are in the Right Place at the Right Time a Guide to Nursing, Midwifery and Care Staffing Capacity and Capability. London: NQB; 2013.
- Supporting NHS Providers to Deliver the Right Staff, with the Right Skills, in the Right Place at the Right Time. Safe Sustainable and Productive Staffing. London: NQB; 2016.
- Safe Staffing for Nursing in Adult Inpatient Wards in Acute Hospitals. London: NICE; 2014.
- Safe Midwifery Staffing for Maternity Settings. London: NICE; 2014.
- Lord Carter of Coles . Operational Productivity and Performance in English NHS Acute Hospitals: Unwarranted Variations. An Independent Report for the Department of Health 2016. www.gov.uk/government/uploads/system/uploads/attachment_data/file/499229/Operational_productivity_A.pdf (accessed September 2017).
- Guidance on Safe Nurse Staffing Levels in The UK. London: Royal College of Nursing; 2010.
- Safer Nursing Care Tool. Implementation Resource Pack. London: The Shelford Group; 2013.
- Safe Staffing for Nursing in Adult Inpatient Wards in Acute Hospitals: Establishment Genie. London: NICE; 2017.
- Ball J, Catton H. Planning nurse staffing: are we willing and able?. J Res Nurs 2011;16:551-8. https://doi.org/10.1177/1744987111422425.
- Lord Carter of Coles . Review of Operational Productivity in NHS Providers, Interim Report 2015. www.hsj.co.uk/Journals/2015/06/11/e/v/i/Lord-Carter-interim-report-June-2015.pdf (accessed September 2017).
- Buchan J, O’May F, Dussault G. Nursing workforce policy and the economic crisis: a global overview. J Nurs Scholarsh 2013;45:298-307. https://doi.org/10.1111/jnu.12028.
- Buchan J, Seccombe I, Gershlick B, Charlesworth A. In Short Supply: Pay Policy and Nurse Numbers. London: The Health Foundation; 2017.
- Buchan J, Seccombe I. A Decisive Decade: The UK Nursing Labour Market Review. London: Royal College of Nursing; 2011.
- Universities and Colleges Admissions Service (UCAS) . UK Application Rates by the January Deadline 2017. www.ucas.com/file/92746/download?token=4Ij-BMlr (accessed September 2017).
- The Future is Now. London: The King’s Fund; 2015.
- Scott C. Setting Safe Nurse Staffing Levels. An Exploration of the Issues. London: Royal College of Nursing; 2003.
- Kitson A, Wiechula R, Conroy T, Athlin AM, Whitaker N. The Future Shape of the Nursing Workforce: A Synthesis of the Evidence of Factors that Impact on Quality Nursing Care. Adelaide, SA: University of Adelaide; 2013.
- Ball JE, Griffiths P, Rafferty AM, Lindqvist R, Murrells T, Tishelman C. A cross-sectional study of ‘care left undone’ on nursing shifts in hospitals. J Adv Nurs 2016;72:2086-97. https://doi.org/10.1111/jan.12976.
- McGillis Hall L, Doran D, Pink GH. Nurse staffing models, nursing hours, and patient safety outcomes. J Nurs Adm 2004;34:41-5. https://doi.org/10.1097/00005110-200401000-00009.
- Kane R, Shamlyian T, Mueller C, Duval S, Wilt TJ. Nurse Staffing and Quality of Patient Care. Rockville, MD: Agency for Healthcare Research and Quality; 2007.
- Trinier RM. Nursing Workload and Its Relationship to Patient Care Error in the Paediatric Critical Care Setting 2016.
- Recio-Saucedo A, Pope C, Dall’Ora C, Griffiths P, Jones J, Crouch R, et al. Safe staffing for nursing in emergency departments: evidence review. Emerg Med J 2015;32:888-94. https://doi.org/10.1136/emermed-2015-204936.
- Griffiths P, Ball J, Drennan J, James l, Jones J, Recio-Saucedo A, . The Association Between Patient Safety Outcomes and Nurse Healthcare Assistant Skill Mix and Staffing Levels and Factors that May Influence Staffing Requirements. Southampton: Centre for Innovation and Leadership in Health Sciences, University of Southampton; 2014.
- Griffiths P, Ball J. Nurse Staffing Levels, Quality and Outcomes of Care in NHS Hospital Wards: What Does the Evidence Say?. Southampton: University of Southampton Health Work Evidence Brief; 2017.
- West E, Barron DN, Harrison D, Rafferty AM, Rowan K, Sanderson C. Nurse staffing, medical staffing and mortality in Intensive Care: an observational study. Int J Nurs Stud 2014;51:781-94. https://doi.org/10.1016/j.ijnurstu.2014.02.007.
- Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med 2011;364:1037-45. https://doi.org/10.1056/NEJMsa1001025.
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 2014;383:1824-30. https://doi.org/10.1016/S0140-6736(13)62631-8.
- Twigg D, Duffield C, Bremner A, Rapley P, Finn J. Impact of skill mix variations on patient outcomes following implementation of nursing hours per patient day staffing: a retrospective study. J Adv Nurs 2012;68:2710-18. https://doi.org/10.1111/j.1365-2648.2012.05971.x.
- Griffiths P, Ball J, Murrells T, Jones S, Rafferty AM. Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: a cross-sectional study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-008751.
- Twigg D, Duffield C, Bremner A, Rapley P, Finn J. The impact of the nursing hours per patient day (NHPPD) staffing method on patient outcomes: a retrospective analysis of patient and staffing data. Int J Nurs Stud 2011;48:540-8. https://doi.org/10.1016/j.ijnurstu.2010.07.013.
- Ball JE, Murrells T, Rafferty AM, Morrow E, Griffiths P. ‘Care left undone’ during nursing shifts: associations with workload and perceived quality of care. BMJ Qual Saf 2014;23:116-25. https://doi.org/10.1136/bmjqs-2012-001767.
- Why Investing in Nursing Makes Sense. Melbourne, VIC: Australian Nursing Federation; 2009.
- Safer Staffing: A Guide to Care Contact Time. London: Chief Nursing Officer England, NHS England; 2014.
- Savitz LA, Jones CB, Bernard S, Henriksen K, Battles JB, Marks ES, et al. Acute Care Settings. Advances in Patient Safety. Rockville, MO, USA: Agency for Healthcare Research and Quality; 2005.
- Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, et al. Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. Int J Nurs Stud 2007;44:175-82. https://doi.org/10.1016/j.ijnurstu.2006.08.003.
- Jones TL, Hamilton P, Murry N. Unfinished nursing care, missed care, and implicitly rationed care: state of the science review. Int J Nurs Stud 2015;52:1121-37. https://doi.org/10.1016/j.ijnurstu.2015.02.012.
- Manias E, Aitken R, Peerson A, Parker J, Wong K. Agency-nursing work: perceptions and experiences of agency nurses. Int J Nurs Stud 2003;40:269-79. https://doi.org/10.1016/S0020-7489(02)00085.8.
- Aiken LH, Xue Y, Clarke SP, Sloane DM. Supplemental nurse staffing in hospitals and quality of care. J Nurs Adm 2007;37:335-42. https://doi.org/10.1097/01.NNA.0000285119.53066.ae.
- Dall’Ora C, Griffiths P. Flexible Nurse Staffing in Hospital Wards: The Effects on Costs and Patient Outcomes?. Southampton: University of Southampton Health Work Evidence Brief; 2017.
- Bruyneel L, Li B, Ausserhofer D, Lesaffre E, Dumitrescu I, Smith HL, et al. Organization of hospital nursing, provision of nursing care, and patient experiences with care in Europe. Med Care Res Rev 2015;72:643-64. https://doi.org/10.1177/1077558715589188.
- Dall’Ora C, Griffiths P. Nursing Shift Work in Hospitals What Are the Effects on Patient and Employee Outcomes?. Southampton: University of Southampton Health Work Evidence Brief; 2017.
- Ball J, Day T, Murrells T, Dall’Ora C, Rafferty AM, Griffiths P, et al. Cross-sectional examination of the association between shift length and hospital nurses job satisfaction and nurse reported quality measures. BMC Nurs 2017;16. https://doi.org/10.1186/s12912-017-0221-7.
- Kane R, Shamlyian T, Mueller C. The association of registered nurse staffing levels and patient outcomes. Med Care 2007;45:95-1204. https://doi.org/10.1097/MLR.0b013e3181468ca3.
- Simon M, Ball J, Drennan J, Jones J, Recio-Saucedo A, Griffiths P. Effectiveness of Management Approaches and Organisational Factors on Nurse Staffing Sensitive Outcomes. Southampton: Centre for Innovation and Leadership in Health Sciences, University of Southampton; 2014.
- Butler M, Collins R, Drennan J, Halligan P, O’Mathúna DP, Schultz TJ, et al. Hospital nurse staffing models and patient and staff-related outcomes. Cochrane Database Syst Rev 2011;7. https://doi.org/10.1002/14651858.CD007019.pub2.
- Blegen MA, Vaughn T, Vojir CP. Nurse staffing levels: impact of organizational characteristics and registered nurse supply. Health Serv Res 2008;43:154-73. https://doi.org/10.1111/j.1475-6773.2007.00749.x.
- Hurst K. UK ward design: patient dependency, nursing workload, staffing and quality – an observational study. Int J Nurs Stud 2008;45:370-81. https://doi.org/10.1016/j.ijnurstu.2006.09.007.
- Bowers L, Crowder M. Nursing staff numbers and their relationship to conflict and containment rates on psychiatric wards – a cross sectional time series poisson regression study. Int J Nurs Stud 2012;49:15-20. https://doi.org/10.1016/j.ijnurstu.2011.07.005.
- Lawes A, Marcus L, Piling S. What Staffing Structures of Mental Health Services Are Associated With Improved Patient Outcomes? 2017. https://improvement.nhs.uk/uploads/documents/NCCMH_Literature_Review_Mental_Health_Final.pdf (accessed September 2017).
- Mafuba K, Gates B, Sivasubramanian M. Report of a Mixed Methods Systematic Review of the Literature to Inform the Development of Safe Sustainable Staffing Improvement Resource in Learning Disability (LD) Services for NHS Improvement. London: University of West London and NHS improvement; 2016.
- Jackson C, Wright T, Martin A. Safe Caseloads for Adult Community Nursing Services – An Updated Review of the Evidence 2016. https://improvement.nhs.uk/uploads/documents/Final_Version_Managing_Safe_Caseloads.pdf (accessed September 2017).
- Mitchell G, Cousins C, Burrows R, Cousins G. A review of safe-staffing models and their applicability to care homes. J Nurs Manag 2017;25:157-62. https://doi.org/10.1111/jonm.12450.
- Mark B, Harless DW, Spetz J. California’s minimum-nurse-staffing legislation and nurses’ wages. Health Aff 2009;28:w326-34. https://doi.org/10.1377/hlthaff.28.2.w326.
- Twigg DE, Myers H, Duffield C, Giles M, Evans G. Is there an economic case for investing in nursing care – what does the literature tell us?. J Adv Nurs 2015;71:975-90. https://doi.org/10.1111/jan.12577.
- Needleman J, Buerhaus PI, Stewart M, Zelevinsky K, Mattke S. Nurse staffing in hospitals: is there a business case for quality?. Health Aff 2006;25:204-11. https://doi.org/10.1377/hlthaff.25.1.204.
- The State of the NHS Provider Sector. London: NHS Providers; 2016.
- Smeds Alenius L, Tishelman C, Runesdotter S, Lindqvist R. Staffing and resource adequacy strongly related to RNs’ assessment of patient safety: a national study of RNs working in acute-care hospitals in Sweden. BMJ Qual Saf 2014;23:242-9. https://doi.org/10.1136/bmjqs-2012-001734.
- Louch G, O’Hara J, Gardner P, O’Connor DB. The daily relationships between staffing, safety perceptions and personality in hospital nursing: a longitudinal on-line diary study. Int J Nurs Stud 2016;59:27-3. https://doi.org/10.1016/j.ijnurstu.2016.02.010.
- Heinen MM, van Achterberg T, Schwendimann R, Zander B, Matthews A, Kózka M, et al. Nurses’ intention to leave their profession: a cross sectional observational study in 10 European countries. Int J Nurs Stud 2013;50:174-84. https://doi.org/10.1016/j.ijnurstu.2012.09.019.
- Bakker D, Conlon M, Fitch M, Green E, Butler L, Olson K, et al. Canadian oncology nurse work environments: part I. Nurs Leadersh 2010;22:50-68. https://doi.org/10.12927/cjnl.2010.21597.
- Papastavrou E, Andreou P, Vryonides S. The hidden ethical element of nursing care rationing. Nurs Ethics 2014;21:583-93. https://doi.org/10.1177/0969733013513210.
- Hahtela N, Paavilainen E, McCormack B, Slater P, Helminen M, Suominen T. Influence of workplace culture on nursing-sensitive nurse outcomes in municipal primary health care. J Nurs Manag 2015;23:931-9. https://doi.org/10.1111/jonm.12237.
- Dziuba-Ellis J. Float pools and resource teams: a review of the literature. J Nurs Care Qual 2006;21:352-9. https://doi.org/10.1097/00001786-200610000-00013.
- Aiken LH, Sloane DM, Cimiotti JP, Clarke SP, Flynn L, Seago JA, et al. Implications of the California nurse staffing mandate for other states. Health Serv Res 2010;45:904-21. https://doi.org/10.1111/j.1475-6773.2010.01114.x.
- Aiken LH, Clarke SP, Sloane DM. International Hospital Outcomes Research Consortium . Hospital staffing, organization, and quality of care: cross-national findings. Int J Qual Health Care 2002;14:5-13. https://doi.org/10.1093/intqhc/14.1.5.
- Ausserhofer D, Schubert M, Desmedt M, Blegen MA, De Geest S, Schwendimann R. The association of patient safety climate and nurse-related organizational factors with selected patient outcomes: a cross-sectional survey. Int J Nurs Stud 2013;50:240-52. https://doi.org/10.1016/j.ijnurstu.2012.04.007.
- Kenward L, Whiffin C, Spalek B. Feeling unsafe in the healthcare setting: patients’ perspectives. Br J Nurs 2017;26:143-9. https://doi.org/10.12968/bjon.2017.26.3.143.
- The Patients Association Response to the National Assembly for Wales on the Issue of Safe Nurse Staffing Levels 2015. www.patients-association.org.uk/. /2015/. /Patients-Association-Welsh-Assembly (accessed September 2017).
- Martin GP, Chew S, Palser TR. The personal and the organisational perspective on iatrogenic harm: bridging the gap through reconciliation processes. BMJ Qual Saf 2017:1-3. https://doi.org/10.1136/bmjqs-2017-006914.
- Health and Social Care Act. Regs 2014. Regulation 18: Staffing. London: The Stationery Office; 2014.
- Guidance Issued on Hard Truths Commitments Regarding the Publishing of Staffing Data. London; 2014.
- Nurse Staffing Levels (Wales) Act 2016. London: The Stationery Office; 2016.
- Safe and Effective Staffing in Health and Social Care. Executive Summary. Edinburgh: NHS Scotland; 2017.
- Mandatory Nurse Staffing Levels. London: Royal College of Nursing; 2012.
- Donaldson N, Shapiro S. Impact of California mandated acute care hospital nurse staffing ratios: a literature synthesis. Policy Polit Nurs Pract 2010;11:184-201. https://doi.org/10.1177/1527154410392240.
- Burnes Bolton L, Aydin CE, Donaldson N, Brown DS, Sandhu M, Fridman M, et al. Mandated nurse staffing ratios in California: a comparison of staffing and nursing-sensitive outcomes pre- and postregulation. Policy Polit Nurs Pract 2007;8:238-50. https://doi.org/10.1177/1527154407312737.
- What Has the Impact Been of Recent Caps on NHS Agency Staff Spend?. London: The King’s Fund; 2016.
- NHS Improvement . Safe Staffing for Adult Inpatients in Acute Care: A Guide to Help Standardise Staffing Decisions in Adult Inpatient Wards in Acute Hospitals 2016. https://improvement.nhs.uk/resources/safe-staffing-improvement-resources-adult-inpatient-acute-care/ (accessed September 2017).
- Safe, Sustainable and Productive Staffing: An Improvement Resource for Learning Disability Services. London: NQB; 2017.
- Safe, Sustainable and Productive Staffing: An Improvement Resource for Mental Health. London; 2017.
- Safe, Sustainable and Productive Staffing: An Improvement Resource for the District Nursing Service. London: NQB; 2017.
- Delivering Care: Nurse Staffing in Northern Ireland. Section 1. Belfast: Department of Health, Social Services and Public Safety; 2014.
- NHS Scotland . Workforce Planning n.d. www.knowledge.scot.nhs.uk/workforceplanning/resources/nursing-and-midwifery-workload-and-workforce-planning-tools.aspx (accessed September 2017).
- Rycroft-Malone J, Burton CR, Williams L, Edwards S, Fisher D, McCormack B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. Health Serv Deliv Res 2016;4.
- In Short Supply: Pay Policy and Nurse Numbers – Nurse Staffing. London: The Health Foundation; 2017.
- McCormack B, Rycroft-Malone J, Decorby K, Hutchinson AM, Bucknall T, Kent B, et al. A realist review of interventions and strategies to promote evidence-informed healthcare: a focus on change agency. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-107.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications; 1997.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. J Adv Nurs 2013;69:1005-22. https://doi.org/10.1111/jan.12095.
- Pawson R. Evidence-based Policy: A Realist Perspective. London: Sage Publications; 2006.
- Post JE, Preston LE, Sachs S. Managing the extended enterprise: the new stakeholder view. Calif Manag Rev 2002;45:6-28. https://doi.org/10.2307/41166151.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-33.
- Greenhalgh T, Wong G, Westhorp G, Pawson R. Protocol – realist and meta-narrative evidence synthesis: evolving standards (RAMESES). BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-115.
- Nutley SM, Walter I, Davies HT. Using Evidence: How Research Can Inform Public Services. Bristol: Policy Press; 2007.
- Malloch K, Conovaloff A. Patient classification systems, part 1: the third generation. J Nurs Adm 1999;29:49-56. https://doi.org/10.1097/00005110-199907000-00013.
- Van Slyck A, Johnson KR. Using patient acuity data to manage patient care outcomes and patient care costs. Outcomes Manag Nurs Pract 2001;5:36-40.
- Allen D. The Invisible Work of Nurses: Hospitals, Organisation and Healthcare. New York, NY: Routledge; 2014.
- Villarreal MC, Keskinocak P. Staff planning for operating rooms with different surgical services lines. Health Care Manag Sci 2016;19:144-69. https://doi.org/10.1007/s10729-014-9307-x.
- Sibbald B, Shen J, McBride A. Changing the skill-mix of the health care workforce. J Health Serv Res Policy 2004;9:28-3. https://doi.org/10.1258/135581904322724112.
- Burke EK, De Causmaecker P, Berghe GV, Van Landeghem H. The state of the art of nurse rostering. J Scheduling 2004;7:441-99. https://doi.org/10.1023/B:JOSH.0000046076.75950.0b.
- Duffield C, Diers D, O’Brien-Pallas L, Aisbett C, Roche M, King M, et al. Nursing staffing, nursing workload, the work environment and patient outcomes. Appl Nurs Res 2011;24:244-55. https://doi.org/10.1016/j.apnr.2009.12.004.
- Blay N, Duffield CM, Gallagher R, Roche M. Methodological integrative review of the work sampling technique used in nursing workload research. J Adv Nurs 2014;70:2434-49. https://doi.org/10.1111/jan.12466.
- Boxall P, Purcell J. Strategy and Human Resource Management. Basingstoke: Palgrave Macmillan; 2011.
- Working Together for Health: The World Health Report. Geneva: World Health Organization; 2006.
- Rogers EM. Diffusion of Innovations. New York, NY: Free Press; 2003.
- Thompson C, Dowding D. Clinical Decision Making and Judgement in Nursing. London: Churchill Livingstone; 2009.
- Easterby-Smith M. Disciplines of organizational learning: contributions and critiques. Hum Relat 1997;50:1085-113. https://doi.org/10.1177/001872679705000903.
- Raelin JA. Work-based learning in practice. J Workplace Learn 1998;10:280-3. https://doi.org/10.1108/13665629810236183.
- Dewing J, McCormack B, Manley K, Wilson V. International Practice Development in Nursing and Healthcare. Oxford: Oxford Blackwell; 2008.
- French B, Thomas LH, Baker P, Burton CR, Pennington L, Roddam H. What can management theories offer evidence-based practice? A comparative analysis of measurement tools for organisational context. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-28.
- Rycroft-Malone J, Harvey G, Seers K, Kitson A, McCormack B, Titchen A. An exploration of the factors that influence the implementation of evidence into practice. J Clin Nurs 2004;13:913-24. https://doi.org/10.1111/j.1365-2702.2004.01007.x.
- Ferlie E, Crilly T, Jashapara A, Trenholm S, Peckham A, Currie G. Knowledge mobilization in healthcare organizations: a view from the resource-based view of the firm. Int J Health Policy Manag 2015;4:127-30. https://doi.org/10.15171/ijhpm.2015.35.
- Crilly T, Jashapara A, Trenholm S, Peckham A, Currie G, Ferlie E. Knowledge Mobilisation in Healthcare Organisations: Synthesising Evidence and Theory Using Perspectives of Organisational Form, Resource Based View of the Firm and Critical Theory. Southampton: National Institute for Health Research Health Services and Delivery Research programme; 2013.
- Kooker BM, Kamikawa C. Successful strategies to improve RN retention and patient outcomes in a large medical centre in Hawaii. J Clin Nurs 2011;20:34-9. https://doi.org/10.1111/j.1365-2702.2010.03476.x.
- Lacey SR, Cox KS, Lorfing KC, Teasley SL, Carroll CA, Sexton K. Nursing support, workload, and intent to stay in Magnet, Magnet-aspiring, and non-Magnet hospitals. J Nurs Adm 2007;37:199-205. https://doi.org/10.1097/01.NNA.0000266839.61931.b6.
- Kalisch BJ, Xie B, Ronis DL. Train-the-trainer intervention to increase nursing teamwork and decrease missed nursing care in acute care patient units. Nurs Res 2013;62:405-13. https://doi.org/10.1097/NNR.0b013e3182a7a15d.
- Fairbrother G, Jones A, Rivas K. Changing model of nursing care from individual patient allocation to team nursing in the acute inpatient environment. Contemp Nurse 2010;35:202-20. https://doi.org/10.5172/conu.2010.35.2.202.
- Tran DT, Johnson M, Fernandez R, Jones S. A shared care model vs. a patient allocation model of nursing care delivery: comparing nursing staff satisfaction and stress outcomes. Int J Nurs Pract 2010;16:148-58. https://doi.org/10.1111/j.1440-172X.2010.01823.x.
- Dubois CA, D’amour D, Tchouaket E, Clarke S, Rivard M, Blais R. Associations of patient safety outcomes with models of nursing care organization at unit level in hospitals. Int J Qual Health Care 2013;25:110-17. https://doi.org/10.1093/intqhc/mzt019.
- van Oostveen CJ, Ubbink DT, Mens MA, Pompe EA, Vermeulen H. Pre-implementation studies of a workforce planning tool for nurse staffing and human resource management in university hospitals. J Nurs Manag 2016;24:184-91. https://doi.org/10.1111/jonm.12297.
- Anderson MH, Lønning K, Fagerström L. Testing reliability and validity of the Oulu patient classification instrument – the first step in evaluating the RAFAELA system in Norway. Open J Nurs 2014;4:303-11. https://doi.org/10.4236/ojn.2014.44035.
- Robinson CH, Annis AM, Form ANJ, Krein SL, Yankey N, Duffy SA, et al. Factors that affect implementation of a nurse staffing directive: results from a qualitative multi-case evaluation. J Adv Nurs 2016;72:1886-98. https://doi.org/10.1111/jan.12961.
- Taylor B, Yankey N, Robinson C, Annis A, Haddock KS, Alt-White A, et al. Evaluating the Veterans Health Administration’s staffing methodology model: a reliable approach. Nurs Econ 2015;33:36-40.
- Subirana M, Long A, Greenhalgh J, Firth J. A realist logic model of the links between nurse staffing and the outcomes of nursing. J Res Nurs 2014;19:8-23. https://doi.org/10.1177/1744987113481782.
- McIntyre L. Good Practice Guide: Rostering 2016. https://improvement.nhs.uk/uploads/documents/Rostering_Good_Practice_Guidance_Final_v2.pdf (accessed September 2017).
- Dent B. Nine principles for improved nurse staffing. Nurs Econ 2015;33:41-4.
- Nursing and Midwifery Workload and Workforce Planning Learning Toolkit. Edinburgh: NHS Education for Scotland; 2013.
- van Oostveen CJ, Mathijssen E, Vermeulen H. Nurse staffing issues are just the tip of the iceberg: a qualitative study about nurses’ perceptions of nurse staffing. Int J Nurs Stud 2015;52:1300-9. https://doi.org/10.1016/j.ijnurstu.2015.04.002.
- Harris A, McGillis Hall L. Evidence to Inform Staff Mix Decision-Making: A Focused Literature Review. Ottawa, ON: Canadian Nurses Association; 2012.
- Anderson EF, Frith KH, Caspers B. Linking economics and quality: developing an evidence-based nurse staffing tool. Nurs Adm Q 2011;35:53-60. https://doi.org/10.1097/NAQ.0b013e3182047dff.
- Checkland P. Systems Thinking, Systems Practice. Chichester: John Wiley & Sons; 1999.
- Dopson S, Fitzgerald L. Knowledge to Action? Evidence-Based Healthcare In Context. Oxford: Oxford University Press; 2005.
- Dalkin S, Lhussier M, Williams L, Burton CR, Rycroft-Malone J. Exploring the use of Soft Systems Methodology with realist approaches: a novel way to map programme complexity and develop and refine programme theory. Evaluation 2018;24:84-7. https://doi.org/10.1177/1356389017749036.
- Rudd L, Watkins A, Wyatt M, Jones A. All Wales Mental Health Acuity Programmes: Results of a National Pilot. Presented to the All Wales Mental Health Senior Nurse Advisory Group; 2016.
- Griffiths R. NHS Management Inquiry Report. London: Department of Health and Social Services; 1983.
- Meyer SB, Lunnay B. The application of abductive and retroductive inference for the design and analysis of theory-driven sociological research. Sociol Res Online 2012;18:1-11. https://doi.org/10.5153/sro.2819.
- Bucknall T, Aitken L, Gerrish K, Lacey A. The Research Process in Nursing. London: John Wiley & Sons; 2010.
- Payne JW. Thinking aloud: insights into information processing. Psychol Sci 1994;5:241-8. https://doi.org/10.1111/j.1467-9280.1994.tb00620.x.
- Drake RG. The nurse rostering problem: from operational research to organizational reality?. J Adv Nurs 2014;70:800-10. https://doi.org/10.1111/jan.12238.
- Hall LM, Pink L, Lalonde M, Murphy GT, O’Brien-Pallas L, Laschinger HK, et al. Decision making for nurse staffing: Canadian perspectives. Policy Polit Nurs Pract 2006;7:261-9. https://doi.org/10.1177/1527154406297799.
- Effken JA, Brewer BB, Logue MD, Gephart SM, Verran JA. Using Cognitive Work Analysis to fit decision support tools to nurse managers’ work flow. Int J Med Inform 2011;80:698-707. https://doi.org/10.1016/j.ijmedinf.2011.07.003.
- Fasoli DR, Fincke BG, Haddock KS. Going beyond patient classification systems to create an evidence-based staffing methodology. J Nurs Adm 2011;41:434-9. https://doi.org/10.1097/NNA.0b013e31822edd8e.
- Fenton K, Casey A. A tool to calculate safe nurse staffing levels. Nurs Times 2015;111:12-4.
- Eduardo EA, Peres AM, de Almeida Mde L, Roglio Kde D, Bernardino E. Analysis of the decision-making process of nurse managers: a collective reflection. Rev Bras Enferm 2015;68:582-8. https://doi.org/10.1590/0034-7167.2015680414i.
- Connelly LM, Yoder LH, Miner-Williams D. A qualitative study of charge nurse competencies. Medsurg Nurs 2003;12:298-305.
- Wilson DS, Talsma A, Martyn K. Mindful staffing: a qualitative description of charge nurses’ decision-making behaviors. West J Nurs Res 2011;33:805-24. https://doi.org/10.1177/0193945910396519.
- Kontio E, Lundgren-Laine H, Kontio J, Korvenranta H, Salanterä S. Information utilization in tactical decision making of middle management health managers. Comput Inform Nurs 2013;31:9-16. https://doi.org/10.1097/NXN.0b013e318261f192.
- Berkow S, Jaggi T, Fogelson R, Katz S, Hirschoff A. Fourteen unit attributes to guide staffing. J Nurs Adm 2007;37:150-5. https://doi.org/10.1097/01.NNA.0000262737.00662.f9.
- Wilson JM, Weiss A. Police staffing allocation and managing workload demand: a critical assessment of existing practices. Policing 2014;8:96-108. https://doi.org/10.1093/police/pau002.
- Diers D, Torre C, Heard DM, Bozzo J, O’Brien W. Bringing decision support to nurse managers. Comput Nurs 2000;18:137-44.
- Bonner R, Beaumont R, Smith B. Understanding rostering. Part 1. The rights and wrongs of rostering. Aust Nurs J 1995;2:18-20.
- Bonner R, Beaumont R, Smith B. Understanding rostering. Part 2. The rights and wrongs of rostering. Aust Nurs J 1995;2:28-31.
- Bonner R, Beaumont R, Smith B. Understanding rostering. Part 3. How a roster is developed. Aust Nurs J 1995;2:40-2.
- Allen SB. The Nurse–Patient Assignment: Purposes, Decision Factors and Steps of the Process 2012.
- Siirala E, Peltonen LM, Lundgrén-Laine H, Salanterä S, Junttila K. Nurse managers’ decision-making in daily unit operation in peri-operative settings: a cross-sectional descriptive study. J Nurs Manag 2016;24:806-15. https://doi.org/10.1111/jonm.12385.
- Rischbieth A. Matching nurse skill with patient acuity in the intensive care units: a risk management mandate. J Nurs Manag 2006;14:397-404. https://doi.org/10.1111/j.1365-2934.2006.00622.x.
- Wyatt M, Healey K. Managing capacity and workload in children’s services. Paediatr Nurs 2005;17:31-4. https://doi.org/10.7748/paed2005.07.17.6.31.c1031.
- Drake RG. The ‘Robust’ roster: exploring the nurse rostering process. J Adv Nurs 2014;70:2095-106. https://doi.org/10.1111/jan.12367.
- Cathro H. A practical guide to making patient assignments in acute care. J Nurs Adm 2013;43:6-9. https://doi.org/10.1097/NNA.0b013e3182785fff.
- Allen SB. The nurse–patient assignment: purposes and decision factors. J Nurs Adm 2015;45:628-35. https://doi.org/10.1097/NNA.0000000000000276.
- Flynn M, McKeown M. Nurse staffing levels revisited: a consideration of key issues in nurse staffing levels and skill mix research. J Nurs Manag 2009;17:759-66. https://doi.org/10.1111/j.1365-2834.2009.01023.x.
- Hockley T, Boyle S. NHS Safe Staffing: Not Just a Number. London: London School of Economics and Political Science; 2014.
- Kerr F, Timony Y. Review of an automated rostering system from a nurse manager’s perspective. Stud Health Technol Inform 2009;146:96-102.
- Barton NS. Matching nurse staffing to demand. Nurs Manage 2011;42:36-9. https://doi.org/10.1097/01.NUMA.0000392986.20185.fa.
- Crist-Grundman D, Mulrooney G. Effective workforce management starts with leveraging technology, while staffing optimization requires true collaboration. Nurs Econ 2011;29:195-200.
- deSilva A, Smith K, Jayawardena S. Demand a staff scheduling system that is easy to use, empowers your staff, AND slashes budgets!. CARING Newsletter 2005;20:6-11.
- Ruland CM. Developing a decision support system to meet nurse managers’ information needs for effective resource management. Comput Nurs 2001;19:187-93.
- Ruland CM, Ravn IH. Usefulness and effects on costs and staff management of a nursing resource management information system. J Nurs Manag 2003;11:208-15. https://doi.org/10.1046/j.1365-2834.2003.00381.x.
- Botter ML. The use of information generated by a patient classification system. J Nurs Adm 2000;30:544-51. https://doi.org/10.1097/00005110-200011000-00010.
- Fram N, Morgan B. Ontario: linking nursing outcomes, workload and staffing decisions in the workplace: the Dashboard Project. Nurs Leadersh 2012;25:114-25. https://doi.org/10.12927/cjnl.2012.22801.
- Pruinelli L, Delaney CW, Garciannie A, Caspers B, Westra BL. Nursing management minimum data set: cost-effective tool to demonstrate the value of nurse staffing in the big data science era. Nurs Econ 2016;34:66-71.
- Pappas S, Davidson N, Woodard J, Davis J, Welton JM. Risk-adjusted staffing to improve patient value. Nurs Econ 2015;33:73-8.
- Carter KF, Burnette HD. Creating patient–nurse synergy on a medical–surgical unit. Medsurg Nurs 2011;20:249-54.
- van Oostveen CJ, Braaksma A, Vermeulen H. Developing and testing a computerized decision support system for nurse-to-patient assignment: a multimethod study. Comput Inform Nurs 2014;32:276-85. https://doi.org/10.1097/CIN.0000000000000056.
- Kane K. Capturing district nursing through a knowledge-based electronic caseload analysis tool (eCAT). Br J Community Nurs 2014;19. https://doi.org/10.12968/bjcn.2014.19.3.116.
- Hyun S, Bakken S, Douglas K, Stone PW. Evidence-based staffing: potential roles for informatics. Nurs Econ 2008;26:151-8.
- Nagy KA, Nathan SK. Scheduling out of control? Consider workforce management options. Nurs Manage 2010;41:52-3. https://doi.org/10.1097/01.NUMA.0000388301.69975.df.
- Kivinen T, Lammintakanen J. The success of a management information system in health care – a case study from Finland. Int J Med Inform 2013;82:90-7. https://doi.org/10.1016/j.ijmedinf.2012.05.007.
- Frith KH, Anderson F, Sewell JP. Assessing and selecting data for a nursing services dashboard. J Nurs Adm 2010;40:10-6. https://doi.org/10.1097/NNA.0b013e3181c47d45.
- Maenhout B, Vanhoucke M. Analyzing the nursing organizational structure and process from a scheduling perspective. Health Care Manag Sci 2013;16:177-96. https://doi.org/10.1007/s10729-013-9222-6.
- Silvestro R, Silvestro C. Towards a model of Strategic Roster Planning and Control: an empirical study of nurse rostering practices in the UK National Health Service. Health Serv Manage Res 2008;21:93-105. https://doi.org/10.1258/hsmr.2008.007025.
- Murtola L-M, Lundgrén-Laine H, Salanterä S. Information systems in hospitals: a review article from a nursing management perspective. Int J Networking and Virtual Organisations 2013;13:81-100. https://doi.org/10.1504/IJNVO.2013.058441.
- Shirey MR, Ebright PR, McDaniel AM. Nurse manager cognitive decision-making amidst stress and work complexity. J Nurs Manag 2013;21:17-30. https://doi.org/10.1111/j.1365-2834.2012.01380.x.
- Zori S, Nosek LJ, Musil CM. Critical thinking of nurse managers related to staff RNs’ perceptions of the practice environment. J Nurs Scholarsh 2010;42:305-13. https://doi.org/10.1111/j.1547-5069.2010.01354.x.
- Davidhizar R, Dowd SB, Brownson K. An equitable nursing assignment structure. Nurs Manage 1998;29:33-5. https://doi.org/10.1097/00006247-199804000-00010.
- Valentine NM, Nash J, Hughes D, Douglas K. Achieving effective staffing through a shared decision-making approach to open-shift management. J Nurs Adm 2008;38:331-5. https://doi.org/10.1097/01.NNA.0000323941.04888.ed.
- Brown EV. Shifting priorities. A Georgia healthcare enterprise uses bid shifting technology to reduce agency labor costs and maximize nurse staffing efficiency. Health Manag Technol 2007;28.
- Junttila K, Meretoja R, Seppälä A, Tolppanen EM, Ala-Nikkola T, Silvennoinen L. Data warehouse approach to nursing management. J Nurs Manag 2007;15:155-61. https://doi.org/10.1111/j.1365-2834.2007.00690.x.
- Clark A, Moule P, Topping A, Serpell M. Rescheduling nursing shifts: scoping the challenge and examining the potential of mathematical model based tools. J Nurs Manag 2015;23:411-20. https://doi.org/10.1111/jonm.12158.
- Wadsworth B, Kurilla ML. An automated solution for managing your workforce. Nurs Manage 2009;40:49-51. https://doi.org/10.1097/01.NUMA.0000356637.33834.00.
- Wallace LA, Pierson S. A case study: the initiative to improve RN scheduling at Hamilton Health Sciences. Nurs Leadersh 2008;21:33-41. https://doi.org/10.12927/cjnl.2008.20285.
- Baker RL, Tindell S, Buckley Behan D, Turpin PG, Rosenberger JM, Punnakitikashem P. Phase I: creating an electronic prototype to generate equitable hospital nurse-to-patient assignments. Comput Inform Nurs 2010;28:57-62. https://doi.org/10.1097/NCN.0b013e3181c0472c.
- Lammintakanen J, Saranto K, Kivinen T. Use of electronic information systems in nursing management. Int J Med Inform 2010;79:324-31. https://doi.org/10.1016/j.ijmedinf.2010.01.015.
- Rapala KG. Staffing excellence: moving from retrospective to prospective management of risk. Nurs Econ 2011;29:211-14.
- Douglas K. What every nurse executive should know about staffing and scheduling technology initiatives. Nurs Econ 2011;29:273-5.
- Scott K, Van Norman J. Managing the complexity of a system wide electronic medical record design and implementation: lessons for nurse leaders. Nurs Adm Q 2009;33:109-15. https://doi.org/10.1097/NAQ.0b013e3181a10c64.
- Silvestro R, Silvestro C. An evaluation of nurse rostering practices in the National Health Service. J Adv Nurs 2000;32:525-35. https://doi.org/10.1046/j.1365-2648.2000.01512.x.
- Kellagher M, Simpson J, Flynn B, Armstrong D. Workload and workforce planning: developing a learning toolkit. Nurs Manag 2010;17:32-4. https://doi.org/10.7748/nm2010.04.17.1.32.c7646.
- Flynn B, Kellagher M, Simpson J. Workload and workforce planning: tools, education and training. Nurs Manag 2010;16:32-5. https://doi.org/10.7748/nm2010.03.16.10.32.c7612.
- Szumlas S. Leveraging staff nurse engagement to design effective patient care assignments. Nurse Leader 2013;11:46-9. https://doi.org/10.1016/j.mnl.2012.12.001.
- Burns JP. Complexity science and leadership in healthcare. J Nurs Adm 2001;31:474-82. https://doi.org/10.1097/00005110-200110000-00011.
- Finn R. Does staff eRostering boost patient outcomes?. Nurs Times 2013;109:20-1.
- Bostrom J, Suter WN. Charge nurse decision making about patient assignment. Nurs Adm Q 1992;16:32-8. https://doi.org/10.1097/00006216-199201640-00007.
- Perroca MG, Ek AC. Utilization of patient classification systems in Swedish hospitals and the degree of satisfaction among nursing staff. J Nurs Manag 2007;15:472-80. https://doi.org/10.1111/j.1365-2834.2007.00732.x.
- Effken JA. Different lenses, improved outcomes: a new approach to the analysis and design of healthcare information systems. Int J Med Inform 2002;65:59-74. https://doi.org/10.1016/S1386-5056(02)00003-5.
- Fagerström L, Rauhala A. Benchmarking in nursing care by the RAFAELA patient classification system – a possibility for nurse managers. J Nurs Manag 2007;15:683-92. https://doi.org/10.1111/j.1365-2934.2006.00728.x.
- Effken JA. Informational basis for expert intuition. J Adv Nurs 2001;34:246-55. https://doi.org/10.1046/j.1365-2648.2001.01751.x.
- Effken JA, Verran JA, Logue MD, Hsu YC. Nurse managers’ decisions: fast and favoring remediation. J Nurs Adm 2010;40:188-95. https://doi.org/10.1097/NNA.0b013e3181d40f7c.
- Hogan H, Olsen S, Scobie S, Chapman E, Sachs R, Vincent C, et al. What can we learn about patient safety form information sources within an acute hospital: a step on the ladder of integrated risk management. Qual Saf Health Care n.d.;17:209-15.
- Vincent C, Burnett S, Carthey J. Safety measurement and monitoring in healthcare: a framework to guide clinical teams and healthcare organisations in maintaining safety. BMJ Qual Saf 2014;23:670-7. https://doi.org/10.1136/bmjqs-2013-002757.
- Rickles D, Hawe P, Shiell A. A simple guide to chaos and complexity. J Epidemiol Community Health 2007;61:933-7. https://doi.org/10.1136/jech.2006.054254.
- von Bertalanffy L. General System Theory: Foundations, Development, Applications. New York, NY: George Braziller; 1968.
- Zimmerman B, Lindberg C, Plsek P. Edgeware: Insights From Complexity Science for Health Care Leaders. Irving, TX: VHA, Inc.; 1998.
- Fielder F. Contingency model of leadership effectiveness. Adv Exp Soc Psychol 1964;1:149-90. https://doi.org/10.1016/S0065-2601(08)60051-9.
- Latour B. Reassembling the Social: An Introduction to Actor-Network-Theory. Oxford: Oxford University Press; 2005.
- Perrow C. Normal Accidents, Living with High Risk Technologies. New York, NY: Basic Books; 1984.
- Bandura A. Social Learning Theory. New York, NY: General Learning Press; 1977.
- Weiner BJ. A theory of organizational readiness for change. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-67.
- Nonaka I, Von Krogh G. Perspective – tacit knowledge and knowledge conversion: controversy and advancement in organizational knowledge creation theory. Organ Sci 2009;20:635-52. https://doi.org/10.1287/orsc.1080.0412.
- Argyris C, Schon DA. Organisational Learning. A Theory of Action Perspective. Reading, MA: Addison-Wesley; 1978.
- Bandura A. Self-efficacy mechanism in human agency. Am Psychol 1982;37:122-47. https://doi.org/10.1037/0003-066X.37.2.122.
- Goleman D. Leadership that gets results. Harv Bus Rev 2000.
- Bass BM. Leadership and Performance Beyond Expectations. New York, NY: Free Press; 1985.
- Avolio B, Luthans F, Walumbwa FO. Authentic Leadership: Theory-building for Veritable Sustained Performance. Lincoln, NE: Gallup Leadership Institute, University of Nebraska; 2004.
- Dreyfus H, Dreyfus S. Mind Over Machine. New York, NY: Free Press; 1982.
- Benner P. From Novice to Expert. Excellence and Power in Clinical Nursing Practice. Menlo Park, CA: Addison-Wesley; 1984.
- Bayes T. An essay towards solving a problem in the doctrine of chances. Phil Trans 1763;53:370-418.
- Laplace PS. Théorie Analytique des Probabilités. Paris: Courcier; 1812.
- Brunswick E. Organismic achievement and the environment probability. Psych Rev 1943;50:255-72. https://doi.org/10.1037/h0060889.
- Hammond KR, Hamm RM, Grassia J, Pearson T. Direct comparison of the efficacy of intuitive and analytical cognition in expert judgement. IEEE Trans Cybern 1987;17:754-70.
- Simon H, Greenberger M. Computers, Communication and the Public Interest. Stanford, CA: Stanford University Press; 1971.
- Ajzen I. The theory of planned behaviour. Organ Behav Hum Decis Process 1991;50:179-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- Cyert R, March J. Behavioural Theory of the Firm. Oxford: Blackwell; 1963.
- Von Neumann J, Morgenstern O. Theory of Games and Economic Behaviour. Princeton, NJ: Princeton University Press; 1944.
- Jacko J, Stephanidis C. Human-Computer Interaction: Theory and Practice (Part 2), Volume 2. HCI International Conference Proceedings. Boca Raton, FL: CRC Press; 2003.
- Bijker WE, Hughes TP, Pinch T. The Social Construction of Technological Systems: New Directions in the Sociology and History of Technology. Cambridge, MA: Massachusetts Institute of Technology (MIT); 1987.
- Ackerman MS. The intellectual challenge of CSCW: the gap between social factors and technical feasibility. Hum Comput Interact 2000;15:179-203. https://doi.org/10.1207/S15327051HCI1523_5.
- Curnock E, Ferguson J, McKay J, Bowie P. Healthcare Improvement and Rapid PDSA Cycles of Change: A Realist Synthesis of the Literature. Glasgow: Patient Safety Multi-Professional Steering Group of NHS Education for Scotland; 2012.
Appendix 1 Advisory group members and affiliations during the study
8 November 2016; 17 May 2017; 6 October 2017.
| Advisory group member | Affiliation |
|---|---|
| Professor Jean White CBE | CNO for Wales |
| Diane Murray | Associate CNO, Scottish Government |
| Professor Cheryl Lenney | Chief Nurse, Manchester University NHS Foundation Trust |
| Mrs Philippa Ford MBE MCSP | Public Affairs and Policy Manager for Wales, The Chartered Society of Physiotherapy |
| Dr Theresa Shaw | Chief Executive Foundation of Nursing Studies |
| Dr Tim Devanney | Health Education England |
| Mrs Anne Pearson | Director of Programmes, The Queen’s Nursing Institute |
| Mrs Tina Donnelly CBE, FRCN DL | Director of the Royal College of Nursing, Wales |
| Mrs Angela Reed | Senior Professional Officer, Northern Ireland Practice and Education Council for Nursing and Midwifery |
| Ms Ann Casey | Senior Clinical Workforce Lead, NHS Improvement and Assistant Chief Nurse, University College London |
| Dr Adrian Jones | Clinical Academic Lead, Betsi Cadwaladr University Health Board |
| Professor Elizabeth Robb OBE | Chief Executive of The Florence Nightingale Foundation, then Independent Healthcare Consultant |
| Dr Sally Gosling | Assistant Director, Practice and Development, The Chartered Society of Physiotherapy |
| Dame Professor Donna Kinnair | Director of Nursing, Policy and Practice, Royal College of Nursing |
| Professor Angela Hopkins | Honorary Professor, Bangor University |
| Professor Janice Sigsworth | Director of Nursing, Imperial College Healthcare NHS Trust |
| Ms Gail Adams | Head of Nursing, Unison |
Appendix 2 NHS manager co-production workshops
-
The patient is at the ‘top’. Patient-orientated, patient-centeredness/patient values.
-
Safe, effective, good-quality care – this is mediated by decision-making. Quality of patient care as a predictor of staffing. Need for balance.
-
Evidence base – ensuring that the service is effective.
-
Cost/resources/money – the manager can use financial flow, this underpins everything. Strategic commissioning.
-
The bigger picture. External factors: Department of Health and Social Care, political, regulatory, environment and public influences.
-
Managing expectations with regard to quality of care and safe practice. Collective responsibility.
-
Engage in safety. Makes sure that no one falls through the ‘safety net’. The manager acts as a gatekeeper. Safe deployment of staff. Determining the impact of decisions/models of deployment – on day-to-day activity, on patient safety. Red flags. The need to articulate the language of harm-free care. Risk appetite related to quality. ‘Are you safe or unsafe?’
-
Clear and shared vision. Targets but a common goal. Collectively. The NHS manager is aware of the purpose with regard to care and can manage aims. Synergy between the visions. A whole-system approach – interdependency. Nothing is in isolation.
-
A lean safe/flexible system.
-
The authority has credibility (either the leader or the plan).
-
A systems view. A broad view is required of the multiple layers and other systems that have an impact. A wider perspective is needed on other wards/areas/infrastructures. Links with other areas and services. Extends to different areas. Awareness of corporate-level services. Strategic/operational perspective. Different levels of the system [e.g. chief executive/higher level for staff deployment (finance team)/front-line staff – matron and ward managers]. The flow of the system.
-
The manager is immersed in the system, but only part of the system. The manager needs to flexibly engage with the wider teams.
-
The system could be a philosophy of nursing/holistic care. Use of different models of care.
-
Systems may not be in synergy.
-
A changeable setting. Flexibility is needed. Freeing up ‘head room’ to deal with the unexpected.
-
Competing priorities – the need to process different information.
-
The influence of skill mix.
-
Integration of nursing services.
-
Forward planning – future ideas/people challenges. New ways of working that learn from the past.
-
Determining which data are required, who gets to see the data and where they go. Real-time information heralding a response. Use of mortality data as an indicator for staffing. Difficulties in benchmarking using staffing and mortality data.
-
The ability to manage new initiatives.
-
Use of tools constructively in a positive way to underpin the philosophy of care.
-
Understanding of parameters (not necessarily complex). There are barriers but everything can be sorted.
-
The need for a clear pathway to all strategic points – key points/direction.
-
Communication channels with the team and beyond. Different languages for different people and layers of the system.
-
Transformation (e.g. shift away from tasks).
-
Professional outcomes.
-
Organisational reputation on recruitment for staffing and on people within the organisation.
Has knowledge, wisdom and credibility.
Has the clinical skills/is a role model.
Understands systems and staffing changes.
The ability to use professional judgement.
Can make decisions.
Can juggle competing demands.
Multitasks.
Has a nurturing attitude.
Is a chameleon, wears different hats simultaneously.
Has a hard hat for when it gets tough.
Is open and transparent.
Listens.
Has the optimism to go forward/positive forward thinking.
Can manage/lead change.
Is prepared for the unexpected.
Cautious.
Has sensibility.
Takes responsibility.
Fairness.
Consistent.
Open-minded.
Understands risk.
Has skills to manage difficult situations.
Has fun and ‘formal’ modes.
Flying the flag for nursing.
Strong and firm leadership.
Knows when to ‘shout’.
Flexible.
Understands the deployment model and the consequences of the model.
Can use the toolkit.
Critical thinker.
Prioritises.
Can manage and channel resources.
Can deliver hard, unwelcomed messages.
Can build bridges and watches for anyone pulling through.
Knows the barriers and when it is unsafe.
The conductor of the orchestra – to make a nice sound at the right time.
Can advocate for patients and staff.
Can negotiate.
Kind, helpful/caring.
Celebrates success.
Managing the teamLeads from the front.
Brings themselves into the team.
Knows the team: knows the skill mix, plays to strengths, the right individual for the right time, builds loyalty, keeps the team together.
Can develop the team.
Manages personalities.
Can unlock the potential linked to quality. Can identify the stars of the team.
-
Staff are empowered.
-
A culture that is system wide.
-
A flexible system – ‘wriggle room’ to deal with the unexpected.
-
Data should feed into the whole system.
-
There is control.
-
Staff are resilient.
-
Staff learn.
-
Staff are listened to.
-
Leadership from the top.
-
Training for pathways.
-
Critical thinking.
-
Staff are empowered.
-
A culture that is system wide.
-
A flexible system – ‘wriggle room’ to deal with the unexpected.
-
Data should feed into the whole system.
-
There is control.
-
Staff are resilient.
-
Staff learn.
-
Staff are listened to.
-
Leadership from the top.
-
Training for pathways.
-
Critical thinking.
-
Data are not always fed back. Real-time information is required, otherwise this has a negative impact.
-
The variation in data: acuity/demand/competing functions.
-
Financial restrictions.
-
Complex environments – the speed of change, ‘juggling with jelly’.
-
Managing situations.
-
Lack of resilience.
-
Rigidity.
-
Stress.
-
Patient need should be the focus and not numbers.
-
Inadequate infrastructure.
-
Is nursing a service or a profession?
-
The ultimate approval for finance to support implementation may not be forthcoming or delayed. We cannot finalise that process.
Appendix 3 Patient and public representation workshops
-
The managers are in their ivory tower, and think everything is coming up roses. They need to get down and see what is happening beneath him – getting down to grass roots ‘ladder’. Listening to get the story and then back to the ivory tower to make a plan. The managers need to understand the system.
-
The manager should be a trained nurse and aware of current affairs – up to date – read a lot. The lion. The cobweb signifies what used to happen – the past. Qualities associated with nursing, seeing the world through nursing eyes, caring and compassionate. The chain symbolises a bridge for people working together.
-
Leadership – needs a sword to take away the bad wood. Clinicians practice that they insist on continuing. The book is evidence – need to save a fortune (refers to the Carter report10). People will follow a good leader. You’ve got to lead from the front. People will follow when they are confident in the leader ‘come down from the ivory tower’.
-
Model conveys hospital floor and wards. The manager is raised, not in an ivory tower but has a little bit of status. Chains = everybody should feel they can approach the person (communication). This is about back to basics – ‘ears’ are important for communication, as the manager should listen. The manager has got to have been through the system ‘nursing service’. A sunflower is used to convey how they should radiate warmth and approachability. They need to have customer service skills.
-
The patient is the skeleton (ill), they are chained to whatever the health service provides, to whatever storm waves arise. The manager wears different hats as they have gone through the system breaking down barriers between the manager and the patient. There is a lack of contact; listening and knowing the patients’ needs is important.
-
The manager should be at ground level. Everything needs to be transparent showing the wood from the trees. They should break barriers to achieve excellence (the goal). The manager should have loyalty from the unit or division.
-
Managers need to be visible and listen – the chain is two-way communication. Things should not be brushed under the carpet. All points of view need to be heard. Make sure they talk to you to resolve things.
-
Managers need status. They need to be ready for battle – they should be allowed to manage. They need to take it forward but not alone – they need to network. Health and social care should be seamless. The aim is excellence, perfection, so the ground workers can be the best that they can be.
-
Managers should have common sense. They should care, they should make a difference. They should be compassionate and take responsibility.
-
Managers need to have pride and set standards by example. They should be caring and not too busy to deal with things.
-
Managers need to smile and have experience, look smart and be trained.
-
They need to be approachable and not cold.
-
They need to be understanding, take responsibility and have authority. Not micro manage.
-
They should be ward leaders and a registered nurse.
-
Are there advantages of ward based training compared to academic based training, is one more useful than the other? Should ward training be prioritised so ‘students learn as they go’, therefore, when they qualify they are of ‘more immediate use’ on the ward.
-
If someone is progressing to be a Nurse Manager, you would want them to have an academic background and training so they are intellectually astute but it’s important to acknowledge that this doesn’t always marry well with a good bed side manner.
-
The training pathway means nurses specialise and become very knowledgeable in one area of care, nevertheless this can often mean in a hospital nurses have limited transferability to be moved, so you may get the scenario where you have too many staff on a particular ward and hardly any on another. ‘If you go into a cardiac arrest unit, or ICU or high dependency wards, they are usually very well staffed. It is the wards, which I called the “hospice wards” “care of the elderly” etc. It is those, which I feel, are not staffed; I don’t know why it is. You chat to the manager on the ward, and they say they are really under pressure’.
-
There is a tangible void left from removing the state enrolled nurse (SEN) role from the training pathway. Is there an easier way for healthcare assistances to progress through the system? How does the introduction of a healthcare assistance on grade 4 support the system if they aren’t a registered nurse? How does this compare to the role of a SEN and should they bring back the SEN?
-
For those nurses who would like to continue nursing and providing care to patients on a ward, there is little career progression available. Historically, the career pathway for nurses is out of nursing into administration and management.
-
What is the methodology for increasing their earning so they don’t have to leave the nursing role to progress, will this help retention levels and avoid the vacuum of nurses which ultimately impacts on patient care.
-
Those applying to be a nurse are no longer under the bursary scheme. The premise for abolishing the bursary scheme was that more nurses could apply because the bursaries weren’t limited. What has been the effect on applications?
-
A key problem lies in retaining nurses in the UK once they have qualified. The structure and opportunities for nursing overseas are currently very attractive.
-
Low staffing levels affect more rural hospitals. It very difficult to get agency staff in rural areas. Therefore, staff are asked to work extra shifts, they become exhausted and then become ill and sickness increases and the cycle continues.
-
Wards are not operating at full capacity because they are short staffed. Beds are being closed because of this. For example, in X hospital 50% of beds are down because they haven’t got the staff, they have never had full occupancy because they have never had the staffing levels to do it.
-
Red tape and paperwork is a huge hindrance for nurses. Despite having solid care plans in place, if they aren’t being delivered to the patients, then it is pointless. The staff are going home feeling frustrated because they can’t get round to delivering care and the patients suffer.
-
It’s not just the nurses’ or doctors’ fault; the management structure is huge and top heavy. The whole process is to blame and problems are symptomatic of the system itself. For example, people go to A&E [accident and emergency] because they can’t get doctors’ appointments, consequently, in many A&E wards there is little to no movement, because every bay is blocked with patients resulting in considerable delays and chaotic scenes.
-
All PPI group members were in accordance in challenging the rationale and purpose of displaying staffing levels. What is the psychology behind this method and what does it aim to achieve?
-
No context to given to these display boards. The skill mix on the ward carries more weight than simply displaying numbers.
-
Especially if the template is lower than planned, how staff communicate this fact to patients and/or relatives is critical in reassuring patients that they are safe and that the care they are receiving is adequate.
-
The visibility of nurses on the ward is key in preserving the perception of care. When relatives come to visit, what is important for them is to know who is the nurse caring for their family member and how can they contact them. This information needs to be displayed clearly.
The job needs what the job needs, so if they enforce the health and safety aspect, then if they are below staff they are operating illegally so they have to do something about it?
What is the psychology behind this? You don’t need to see doctors with their ‘L plates’ displayed on their coats, you do not need to see things like that. So what is the point, whose bright idea it is to display this information?
Numbers do not necessarily mean very much. I do not think it just numbers, it is actually skill mix which is important.
As a family member, if a relative of mine was in hospital, and they said ‘okay we are two nurses down’, I would say well could I stay? Rather than being told to leave at the end of visiting time, I would want to stay to make sure my significant other was okay.
Because we are in culture of ‘claiming’, people could photograph it (staffing board) and put in a claim.
When you ring the bell, you do not know who your nurse is. Communication is a problem. I understand that you cannot look at everybody all the time, but I wish there was somebody moving around, circulating the wards, to see if people where okay.
If they trained more caring nurses, and ensure that that caring element was there, I think that would help [in reassuring patients who someone is there].
I have noticed the wards which staff are short in are the ones with elderly patients in. Whether it is because they have to work much harder on those wards I don’t know or they get depressed.
I do not think it’s good when a visitor/relative is attending the ward and asks a nurse about their family member and they say ‘oh sorry they aren’t one of my patients’. That does not inspire confidence. It would be helpful for relatives to know which nurse is looking after their family member.
Because of the bay system if the nurse isn’t in the bay you don’t see them. Some patients have said, ‘I haven’t seen a nurse for ages, I have been ringing the bell and I haven’t seen anybody’ and others will say ‘oh the nurses don’t seem to have stopped’ but I don’t think either of those examples inspire confidence in the system, because they are either ‘not here’ or ‘busier over there’.
They are experimenting in [X hospital] now where they have got rid of the nursing station, and there are little nursing station in the bay, which I think is much better because you know who is nurse is then because they are in your bay.
‘There are lots of people hanging round the desk’, but they do not know who they are. I noticed in a [hospital] they had the desk by the units, which I think is a smashing idea because you can always call somebody then.
[Desks by the units] helps get rid of the impression that the nurses are ‘teenage girls having a chat and a laugh’ and telling each other what they did last night while you lie there sick.
Appendix 4 Theory areas
Operational definitions
| The worldview on staffing deployment (meta-explanations) | Organisational influences, context and responses to staffing deployment and evaluation | Influences of clinical need | Technologies and tools for articulating predictive and real-time data on patient needs |
|---|---|---|---|
Legislation, mandates, guidance:
|
Organisational culture and attitude to risk management:
|
Patient dependency and acuity:
|
Data for risk management (red flags and staffing):
|
Patient safety and quality outcomes:
|
Leadership and powerful others:
|
Quality care, patient safety:
|
Visibility of quality care and safety outcome data for evaluation and comparison:
|
Risk management-reduced risk of litigation:
|
Organisational investment in the system and support for users:
|
Patient feedback and experience:
|
Standard approach to compilation of patient dependency and acuity data:
|
| Professional obligations for achievement of quality and safe patient care | Organisational feedback and evaluation:
|
Impact on carers:
|
|
| Corporate reputation – patient and public confidence | Organisational trial, adaptation and innovation of technologies and tools | Public perceptions:
|
|
Workforce well-being – staff recruitment and retention:
|
|||
| Budget restrictions – effective management of finance |
| Resource availability | Day-to-day management of resources (with/without technology) | Nurse managers’ values and use of professional judgement | Impact of managers’ day-to-day work in balancing resources and demand |
|---|---|---|---|
| Staff roles, skill mix, staff numbers | Standardised approach for establishment setting in accordance with budget | Leadership skills:
|
Improved patient safety and quality outcomes |
Staff experience, capacity, capability:
|
Rule-setting system (e.g. skill mix, staffing requests and adaptation for patient needs)
|
Fairness; risk assessment:
|
Staff satisfaction, recruitment and retention:
|
Bed state, admissions, discharges:
|
Integration and visibility of complex data for comparison of patient needs and staffing requirements in the light of real time resources:
|
User perceptions of technologies and tools (complexity/simplicity/trustworthiness):
|
|
Bank/agency availability and costs:
|
Data for evaluation: comparison of clinical areas’ actual staffing needs compared with predicted needs:
|
Local knowledge; staff capabilities and environment of care:
|
Cost reduction:
|
Clinical environment and geography:
|
Comparison between clinical areas:
|
Professional values:
|
Improved organisational reputation:
|
Staff requirements (shift requests):
|
Flexibility and adaptability | ||
| Experience | |||
| Confidence | |||
| Clinical understanding of patient acuity/dependency – linked to experience |
Appendix 5 Search terms
Search terms used to identify the literature
A selection of different terms were used for each iterative search.
Nurses
-
Free-text keywords: nurs* or RN
-
Medical subject heading (MeSH) headings: Nurses, Nursing, ‘Specialties, Nursing’, Nurses, Nursing Staff, Nursing Manpower.
Nurse managers
-
Free-text keywords: ‘Nurse manager*’, ‘Nurse administrator*’, ‘ward sister*’, ‘ward manager*’, ‘charge nurse*’, ‘nurse supervisor*’, ‘nurse leader*’, ‘community manager*’, ‘community nurse manager*’, ‘clinical area manager*’, ‘nurse executive*’, ‘nurse director*’, ‘nurse in charge’, ‘head nurse’, matron*, ‘shift supervisor*’, ‘Patient care manager*’, ‘Middle manager*’
-
MeSH headings: Nurse Administrators, ‘nursing, supervisory’, ‘nursing management’, ‘nurse managers’.
Staffing
-
Free-text keywords: assignment, allocation, caseload, workload, ‘nurse:patient ratio*’, ‘nurse-patient ratio*, scheduling, reallocation, ‘time allocation*’, staffing, manpower, workforce, ‘skill mix’, ratio, roster, deployment
-
MeSH headings: Personnel Staffing and Scheduling, Workload, staffing, shiftwork, shift workers, nurse-patient ratio, skill mix, Health Manpower, workforce, nursing manpower.
Evaluation of tools (iterative search 1)
-
Free-text keywords: evaluation, effectiveness
-
MeSH headings: program evaluation.
Complexity (iterative search 3)
-
Free-text keywords: Complex*.
Nurse managers’ decision-making (iterative search 4)
-
Free-text keywords: ‘decision aid*’, ‘decision making’, ‘decision support*’, ‘choice behaviour*’, ‘choice behavior*’, ‘decision behaviour*’, ‘decision behavior*’
-
MeSH headings: ‘decision support techniques’, choice behaviour, ‘decision making’, ‘decision support systems, clinical’, Decision Support Systems, Management.
Allocation or assignment of nursing staff (iterative search 5)
-
Free-text keywords: assignment*, allocation, caseload, workload, ‘nurse:patient ratio*, ‘nurse-patient ratio*’, scheduling, reallocation, ‘time allocation*’.
Staffing tools or information technology used in staffing (iterative search 6)
-
Free-text keywords: tool*, technolog*, ‘decision making’, triangulation, ‘professional judgement’, acuity
-
MeSH headings: Personnel Staffing and Scheduling Information Systems.
Capacity and capability of staff (iterative search 7)
-
Free-text keywords: (‘personal capacity’, ‘work capacity’, capability, competence, experience, ability
Risk taking (iterative search 8)
-
Free-text keywords: ‘risk taking’ OR ‘risk assessment’ OR ‘risk taker’ OR ‘risk propensity’ OR ‘risk management’)
-
MeSH headings: ‘Risk-Taking’, ‘Risk Management’, ‘Risk Assessment’, Attitude to Risk.
Support for nurse managers (iterative search 9)
-
Free-text keywords: leadership, ‘professional development’, ‘managerial competence’, self-efficacy, ‘self efficacy’, ‘leadership development’, ‘staff development’, ‘professional development’, confidence
-
MeSH headings: ‘Staff Development, Leadership.
Appendix 6 Example search strategy
Iterative search 5: allocation or assignment of nursing staff
Search performed in MEDLINE (via EBSCOhost, from 1950 to current):
-
(MH ‘Personnel Staffing and Scheduling’)
-
AB ( assignment* or allocation or caseload or workload or ‘nurse:patient ratio*’ or ‘nurse-patient ratio*’ or scheduling or reallocation or ‘time allocation*’ ) OR TI ( assignment* or allocation or caseload or workload or ‘nurse:patient ratio*’ or ‘nurse-patient ratio*’ or scheduling or reallocation or ‘time allocation*’ )
-
(MH ‘Specialties, Nursing+’) OR (MH ‘Nursing’) OR (MH ‘Nurses+’) OR (MH ‘Nursing Staff, Hospital’) OR (MH ‘Nursing Staff’) OR (AB ( nurs* or RN ) OR TI ( nurs* or RN ) )
-
(MH ‘Workload’)
-
(1 and 2 and 3) or (4 and 2 and 3)
-
Post 1983 = 1786 results, search run on 9 November 2016
-
Seventeen articles chosen for inclusion and another 17 articles from citation-searching on these articles.
Appendix 7 Data extraction form
This is a new form that draws on items embedded within two published forms, Curnock et al. 242 and Rycroft-Malone et al. 96 [© Rycroft-Malone et al. ; licensee BioMed Central Ltd 2012. This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited].
Appendix 8 Additional codes
-
Organisational factors.
-
Communication and collaboration.
-
Flexibility in the system.
-
Negotiation.
-
Reactive decision-making vs. planned decisions.
-
Seeing the big picture.
-
System complexity.
-
The need for policy and regulations.
-
Effects of managers’ work around staffing.
-
Data, real-time availability.
-
Gaming.
-
Whole-system approach.
-
Decision-making.
Appendix 9 Evidence table
| Authors | Publication details | Country of origin | Type of study | Description and findings | Key areas, limitations and CMO contributions |
|---|---|---|---|---|---|
| Allen158 | The Nurse–Patient Assignment: Purposes, Decision Factors and Steps of the Process. PhD thesis. Columbia, SC: University of South Carolina; 2012 | USA | Qualitative | This study sought to identify purposes, decision factors and steps of the process. Fourteen charge nurses representing 11 nursing units of a suburban hospital were interviewed | Offers useful considerations on allocating nurses – some detailed quotes on nuanced judgements (e.g. nursing characteristics and patient requirements) |
| Allen164 | The nurse–patient assignment: purposes and decision factors. J Nurs Adm 2015;45:628–35 | USA | Qualitative | Article based on the above 2012 thesis158 further highlights 14 purposes of charge nurses when making allocation and considers these from the perspective of factors related to the nurse, the patient and the environment | Maps out key factors that influence charge nurses when making nurse–patient allocations. Based on evidence from the 2012 thesis158 |
| Anderson et al.134 | Linking economics and quality: developing an evidence-based nurse staffing tool. Nurs Adm Q 2011;35:53–60 | USA | Description of the development of a staffing tool | Discusses challenges in developing an integrated dashboard that can model decisions on staffing in relation to budget and patient outcomes and how this can offer objective data for decision-making | Describes some of the implementation challenges and the importance of organisational support and leadership. Reports midway through the project |
| Anderson et al.125 | Testing reliability and validity of the Oulu patient classification instrument – the first step in evaluating the RAFAELA system in Norway. Open J Nurs 2014;4:303–11 | Norway | Assessment of inter-rater reliability and prospective descriptive study | Determined the efficacy of triangulation of several tools under the RAFAELA system measuring:
|
Implementation factors explored on leadership, education and training and how this related to standard approaches to classification. One area avoided giving low nursing intensity scores fearing management sanctions. Some brief data imply that managers should understand the limitations of tools and the potential for gaming |
| Baker et al.196 | Phase I: creating an electronic prototype to generate equitable hospital nurse-to-patient assignments. Comput Inform Nurs 2010;28:57–62 | USA | Pilot study to evaluate nurse use of nurse-to-patient allocation technology | Pre and post surveys for RN students to determine the functionality and practicality of this prototype, with some comparison to manual methods. Found that the lack of bias and the speed of the system were favoured, but participants requested additions of multiple diagnoses, patient acuity and experience level of the nurse | Participants do not seem to be nurse managers and there were pre and post question changes, but the study does give information of how nurses value components for allocation with some insight on user perceptions |
| Barton168 | Matching nurse staffing to demand. Nurs Manage 2011;42:36–9 | USA | Commentary by nurse director | Charts the development, implementation and impact of a nurse staffing technology. This was a team approach and offered data for planning and cost-savings | Offers insight into the context and the practical application of the technology in one organisation; some detail, but superficial in some areas and potential for bias |
| Berkow et al.152 | Fourteen unit attributes to guide staffing. J Nurs Adm 2007;37:150–5 | USA | Qualitative, structured interviews with 32 chief nurses | Participants allocated the budget on a unit-by-unit basis across four distinct nursing workforce characteristics:
|
Proposed 14 attributes for prioritising staffing; however, there was some lack of consensus over prioritisation, even in similar settings. The authors acknowledge that this was a hypothetical exercise. Offers insight into the influence of context on managers’ decisions |
| Bonner et al.155 | Understanding rostering. Part 1. The rights and wrongs of rostering. Aust Nurs J 1995;2:18–20 | Australia | Commentary by managers | Breaks down elements into ‘inputs, outputs, process’. Highlights multiple methods [e.g. fixed, staff request and demand driven (computer led)] | Authors have management experience of rostering and its influencing factors. Emphasis on the importance of feedback |
| Bonner et al.156 | Understanding rostering. Part 2. The rights and wrongs of rostering. Aust Nurs J 1995;2:28–31 | Australia | Commentary | Reviews how resource availability and system constraints affect rostering. Some examination of calculation of numbers | Offers perspective of the system and influences, but little reference to evidence |
| Bonner et al.157 | Understanding rostering. Part 3. How a roster is developed. Aust Nurs J 1995;2:40–2 | Australia | Commentary | Compares shift work to other industries, looks at roster design (e.g. self and request). Considers experience and changes related to supply of nurses. Looks at ‘rules’, equity and other influences | Considers personal perspectives, but these were related to experience, and highlights important influencing factors |
| Bostrom et al.207 | Charge nurse decision making about patient assignment. Nurs Adm Q 1992;16:32–8 | USA | Mixed-methods, interviews and survey | An exploration of the factors that nurses consider in making patient assignments. Six nurses were interviewed from one hospital to identify 19 decision-making influences, which were constructed into a questionnaire. A total of 271 were returned. Decision-making applied to Benner’s novice to expert. Patient acuity was most prioritised | Considers diversity in decision-making and the influence of context. Considers clinical judgement and how experts may not be able to define the decision-making process as it has been internalised |
| Botter173 | The use of information generated by a patient classification system. J Nurs Adm 2000;30:544–51 | USA | Qualitative | A case study approach: 67 participants (staff nurse managers, administrators and nurse executives) in one acute hospital. Observations were also made and there was a document review. Reports the findings, describing how and why information is obtained from a patient classification system (Medicus) is used in hospital decision-making and discusses the implications for nurse administrators | Useful for perceptions on the use of data from a tool and its use at different organisational levels, plus what impedes its use |
| Brown191 | A Georgia healthcare enterprise uses bid shifting technology to reduce agency labor costs and maximize nurse staffing efficiency. Health Manag Technol 2007;28:18, 20–2 | USA | Commentary by a journal editor | Explains how an organisation introduced bid-shifting technology to reduce agency labour costs and maximise nurse staffing efficiency. It considers how implementation is facilitated and how nurses and managers were educated on the system | Details on the implementation of an electronic staffing system and what worked to support this, but less emphasis on the manager’s role in decision-making. An outsider’s perspective |
| Burns205 | Complexity science and leadership in healthcare. J Nurs Adm 2001;31:474–82 | USA | Survey | Proposes the theory that reactive decisions and planning should be balanced in the light of complexity. Survey explores managers’ perspectives; this indicated that managers were often more comfortable with planning | Links complexity theory to health organisations. Suggests that linear and prescriptive decision-making is not feasible, but managers often avoid experimentation and intuition. Survey data lack contextual details |
| Carter and Burnette177 | Creating patient–nurse synergy on a medical–surgical unit. Medsurg Nurs 2011;20:249–54 | USA | Evaluation of a tool | Evaluation of a synergy model that matches patient dependency and acuity with nurse’ competence and abilities. Some feedback on the impact on patient outcomes and staff satisfaction. Gives tools to demonstrate how factors are calculated | The tool is evaluated by its designers; potential for biasOf interest here is the focus on staff capability and competence and how this is applied to patient demand |
| Cathro163 | A practical guide to making patient assignments in acute care. J Nurs Adm 2013;43:6–9 | USA | A framework development for nurse–patient assignment | Following a concept analysis of the charge nurse role, a framework to guide the process of patient assignments. Highlights key components needed for decision-making and the need for policies and leadership skills development plus leader support for charge nurses | Useful for the consideration of factors related to regulation, safety, patient acuity and planned and unplanned patient flow. Framework not tested |
| Clark et al.193 | Rescheduling nursing shifts: scoping the challenge and examining the potential of mathematical model based tools. J Nurs Manag 2015;23:411–20 | England | Literature review and consultation with nurse managers | This identified rescheduling issues and existing mathematic modelling tools. The consultation exercise in four NHS trusts examined the challenges associated with rescheduling. Focused on reactive shift rescheduling and how this is complex for the manager, more so that scheduling explores the potential for modelling tools | Highlights how poor rescheduling can result in disruption to planned nursing shifts, which may have a negative impact on the quality and cost of patient care, nursing morale and retention. Has a focus on a lack of technological support; proposes that modelling may help |
| Connelly et al.149 | A qualitative study of charge nurse competencies. Medsurg Nurs 2003;12:298–305 | USA | Qualitative | The study identified charge nurse competencies through 42 interviews in a military hospital. A total of 54 competencies were identified in four categories: clinical/technical, critical thinking, organisational and human relations skills. Emphasis on collaboration | Looks at the characteristics of an effective charge nurse. Highlights the operational skills required for workforce management and some strategies for development. No focus on decision-making |
| Crist-Grundman and Mulrooney169 | Effective workforce management starts with leveraging technology, while staffing optimization requires true collaboration. Nurs Econ 2011;29:195–200 | USA | Commentary by a strategist and nurse informatics specialist | Reviews development and use of technology for staffing through offering evidence of their organisations’ positive experiences in cost-savings and implementation | Focuses on the use of technology and considers potential problems, such as staff working excessive hours. Also useful on the need for collaboration and leadership |
| Davidhizar et al.189 | An equitable nursing assignment structure. Nurs Manage 1998;29:33–5 | USA | Commentary from nurse academics | Identifies conflicts involved with the nursing assignment structure and its implications for nursing managers’ decision-making | Considers support to facilitate nurse autonomy and the manager’s role |
| Dent B130 | Nine principles for improved nurse staffing. Nurs Econ 2015;33:41–4, 66 | USA | Commentary by a health organisation’s senior vice president | Indicates how staffing is managed flexibly in his organisation. Considers group decision-making on establishment figures, the flexibility of the workforce, rule-setting to prevent nurse fatigue, tools and technology | Considers relevant factors for staffing decisions, but does not focus on implementation or what supports managers to make decisions |
| deSilva et al.170 | Demand a staff scheduling system that is easy to use, empowers your staff, AND slashes budgets! CARING Newsletter 2005;20:6–11 | USA | Commentary by nursing informatics company managers | Commentary on how workforce deployment tools can help. Offers guidance on what is required from a tool and how tools can be optimally used and when decisions are made outside these systems. Refers to companies producing tools that may not be suitable | Potential for bias because the authors are company representatives; however, discusses influencing factors and context (e.g. staff satisfaction/regulation). Dispels myths and highlights problems between vendors and users |
| Diers et al.154 | Bringing decision support to nurse managers. Comput Nurs 2000;18:137–44 | USA | Report of the development of a decision support tool | Used production theory to provide the framework for the development of decision support objects: graphic displays of nursing hours, budgeted, scheduled and worked within institution-specific control limits | Commentary by the tool developers, but some information on barriers to organisational support for implementation and an emphasis on flexibility in the system |
| Douglas199 | What every nurse executive should know about staffing and scheduling technology initiatives. Nurs Econ 2011;29:273–5 | USA | Commentary by a nurse executive | Discusses the role of managers related to safe staffing and how leadership is key to the use of tools and technology. Discusses the leadership role during selection, development, implementation and evaluation | Offers practical advice based on personal experience about the implementation of technology and the role of leadership; no supportive evidence |
| Drake162 | The ‘Robust’ roster: exploring the nurse rostering process. J Adv Nurs 2014;70:2095–106 | Malaysia | Regression analysis to compare the published roster with an actual roster | Comparison between the rostering process and the robustness of the worked roster, following the introduction of an electronic roster for 42 roster periods from 15 wards. Shift assignment before approval and the number of changes post approval affect the robustness of the roster | Considers how an electronic roster or a manual roster was used and how ‘rules within the system’ were broken or not, offers a discussion on barriers and preferences |
| Drake143 | The nurse rostering problem: from operational research to organizational reality? J Adv Nurs 2014;70:800–10 | Malaysia | Mixed methods: interviews and quantitative analysis | Interviewed senior nursing staff and ward managers regarding rules defining the roster, also analysed actual roster data to establish unfilled shifts and rule breakages. Findings indicate how informal rules have an impact on the roster and how formal policies need to be adhered to by the manager | This contrasts the perceptions of roster ‘constraints’ with the subjective, often political, rules governing practical rosters. Some comparison of manual and electronic roster preferences and key influencing factors on decisions |
| Dubois et al.123 | Associations of patient safety outcomes with models of nursing care organization at unit level in hospitals. Int J Qual Health Care 2013;25:110–17 | Canada | Cross-sectional, correlational | Compared four models of nursing care against nurse sensitive outcomes. Findings suggest that a professional model of care, particularly when innovative, was associated with positive patient outcomes in four indicators | Does not consider tools/technology or management decision-making, but indicates the importance of the nurse model of organisation, context and professional values for patient outcomes |
| Eduardo et al.148 | Analysis of the decision-making process of nurse managers: a collective reflection. Rev Bras Enferm 2015;68:582–8, 668–75 | Brazil | Qualitative. Uses action research and logical framework for analysis | Reviews important influences on decision-making, such as organisational preparation, powerful others and experience. Relates to rational decision-making | Looks at reactive and collective decision-making. Does not relate to staffing. Mainly interviewed young, inexperienced managers |
| Effken211 | Informational basis for expert intuition. J Adv Nurs 2001;34:246–55 | USA | Literature review on the use of intuition in decision-making | Looks at definitions of intuition and perception. Looks at expertise and skills acquisition in relation to knowledge, control and flexibility. Proposes that it is direct perception that can be measured and taught. Suggests the use of simulation for support | Considers computerised data for capturing information and decision- making briefly, and how this may clarify and simplify intuition. However, the focus is on intuition and decision-making and not staffing or nurse managers |
| Effken209 | Different lenses, improved outcomes: a new approach to the analysis and design of healthcare information systems. Int J Med Inform 2002;65:59–74 | USA | Case study | Uses a case study in intensive care to examine the implementation of patient information systems. Integrates Carper’s four ways of knowing and cognitive work analysis to demonstrate the achievement of successful designs for health-care systems | Examines technology complexity/human interface in health. Goal achievement uncertainty and environmental constraints reviewed. Focuses on collaboration in design and clinical decisions, not staffing |
| Effken et al.212 | Nurse managers’ decisions: fast and favoring remediation. J Nurs Adm 2010;40:188–95 | USA | Qualitative interviews with 10 nurse managers | Managers tended to use a linear strategy in decisions on quality issues, but often jumped from problem to solution without a clear goal, selecting solutions biased towards remedial education. Authors suggest that decision support tools should help managers to think more systematically and efficiently | Focus on how decisions are made related to a decision tree. Linked to the development of DyNADS. Lacks detail on the use of tools or staffing |
| Effken et al.145 | Using Cognitive Work Analysis to fit decision support tools to nurse managers’ work flow. Int J Med Inform 2011;80:698–707 | USA | Qualitative interviews with 20 nurse managers from three Magnet hospitals | A cognitive work analysis was conducted to understand environmental constraints on nurse managers that affect their need for, and use of, decision support tools, such as competing priorities. Explores managers’ role in relation to the development of a decision support tool | Detailed exploration of the contextual influences on the manager’s role and decision-making. Considers skills and goals and how data, dashboards and decision support tools may help. Emphasises the need for the integration of data |
| Fagerström and Rauhala210 | Benchmarking in nursing care by the RAFAELA patient classification system – a possibility for nurse managers. J Nurs Manag 2007;15:683–92 | Finland | Quantitative survey of 86 wards from 14 different hospitals | The aim of the study was to explore the possibilities of benchmarking with the RAFAELA nurse workforce planning system. Benchmarking with the system provided many opportunities for the nurse managers’ resource allocation and their personnel administration and data for decision-making | Highlights the importance of standard approaches for effective benchmarking, but is weak on subsequent decision-making. Notes that imbalances between nursing care interventions and staffing affect quality |
| Fairbrother et al.121 | Changing model of nursing care from individual patient allocation to team nursing in the acute inpatient environment. Contemp Nurse 2010;35:202–20 | Australia | Non-randomised experimental design and action research | Evaluation of team nursing in comparison with individual patient allocation. Team nursing was associated with increased nurse satisfaction and retention | Not related to decisions about staffing, but more so about staff well-being related to organising care |
| Fasoli et al.146 | Going beyond patient classification systems to create an evidence-based staffing methodology. J Nurs Adm 2011;41:434–9 | USA | Literature review, expert panel, operational assessment, manager interviews and survey | Considered the evidence for the Department of Veterans Affairs’ development of a nationally standardised nurse staffing methodology. This resulted in seven candidate indicators for inclusion in unit-specific staffing models | The focus is on the development of patient classification systems with the implementation of the staffing model yet to be evaluated, other than a pilot implementation. Does consider influences on staffing decisions; some mention of tools, but lacks detail |
| Fenton and Casey147 | A tool to calculate safe nurse staffing levels. Nurs Times 2015;111:12–14 | England | Commentary | Explains how the tool works and how individual patient requirement is the main factor for calculation. Highlights how a standard approach facilitates benchmarking. Offers examples from practice | Commentary by practitioners involved in the development of the NICE-recommended tool. Case study examples offer details on its implementation |
| Finn206 | Does staff eRostering boost patient outcomes? Nurs Times 2013;109:20–1 | England | Commentary on the impact of an electronic roster system by a NHS manager | Outlines how a range of tools and technology have been implemented in an NHS trust with e-roster (e.g. a dashboard). Offers some evidence of improved patient outcomes | Indicates how technology can facilitate transparency and data analysis, which positively affects ward managers’ role. Implementation processes not described. Author had responsibility for technology |
| Flynn et al.203 | Workload and workforce planning: tools, education and training. Nurs Manag 2010;16:32–5 | Scotland | Commentary on the Scottish workforce planning programme | Explains the tools, education and training processes. There is some description of leadership and education support. Highlights the integration of data | Outlines some basic criteria for tool requirements. Indicates some process for gaining consensus on tools. Authors contribute to the programme |
| Flynn et al.165 | Nurse staffing levels revisited: a consideration of key issues in nurse staffing levels and skill mix research. J Nurs Manag 2009;17:759–66 | UK | Literature review | Considers the evidence of the effects of safe staffing, staffing ratios and models of care on quality and safety outcomes. Finds that there is a lack of standardisation for measurement and no clear evidence of staffing levels, skill mix or ratios | Offers an analysis of the UK context and the impact of tools on managers. Highlights deficits and confounders in evidence on measurement and barriers to the use of tools (e.g. impact on managers’ time) |
| Frith et al.183 | Assessing and selecting data for a nursing services dashboard. J Nurs Adm 2010;40:10–16 | USA | Commentary academics | Considers the evidence on the standard approach to measurement and examines how real-time data are vital using standard measurement. Highlights how nursing dashboards are useful for decision-making | Useful consideration of how nurse managers should collaborate to have real-time and predictive data that are integrated effectively to support decision-making. No consideration of implementation |
| Fram and Morgan174 | Ontario: linking nursing outcomes, workload and staffing decisions in the workplace: the Dashboard Project. Nurs Leadersh 2012;25:114–25 | Canada | Evaluation of the development and application of an electronic monitoring tool | Looks at staff perceptions on the use of the system and how they misunderstood the goals. Emphasis on the need for accurate real-time data. The original indicators in the dashboard were refined and revised based on suggestions from the project participants | Useful for information on implementation. Indicates the need for collaboration to develop bespoke requirements for the tool. Authors are the chief nursing executive and the project co-ordinator. Acknowledges ongoing development |
| Harris and McGillis Hall133 | Evidence to Inform Staff Mix Decision-Making: A Focused Literature Review. Ottawa, ON: Canadian Nurses Association; 2012 | Canada | Literature synthesis to support an evaluation framework | Offers a review of the literature on the evidence and information that affects decisions about staffing, with a brief section on the use of tools | Does not focus on how decision-making can be supported using tools, but does offer some influence for nurse staffing decisions |
| Hockley and Boyle166 | NHS Safe Staffing: Not Just a Number. London: London School of Economics and Political Science; 2014 | England | Discussion paper. Interviews and observation inform the paper | Reviews potential weaknesses and opportunities in the implementation of safe staffing policies in NHS hospitals following the introduction of e-rosters. Highlights the strengths of e-rostering with regard to payroll and budget and the importance of strong leadership | Does not propose strategies for implementation, but looks at the need for transparency of staff levels and the role of leadership and culture for the use of e-rosters |
| Hyun et al.180 | Evidence-based staffing: potential roles for informatics. Nurs Econ 2008;26:151–8, 173 | USA | Evidence review | Reviews nurse staffing and patient outcomes. Provides an overview of the current methods used to inform nurse staffing and discusses potential informatics solutions that could support evidence-based nurse staffing decisions | Critiques the evidence for informatics solutions and how this can inform nurse staffing decisions. Focuses on measuring nurse staffing activity |
| Junttila et al.192 | Data warehouse approach to nursing management. J Nurs Manag 2007;15:155–61 | Finland | Evaluation of a nursing MIS pilot, using a survey and interviews | Uses the RAFAELA system (patient classification and assessment of nursing care intensity level) in combination with payroll, rostering and patient information data. Examined clinical processes and use of the data system. Found that quality checks and IT support were vital | Offers feedback of users’ perceptions of the system. Interviews small numbers of managers but compares managers’ needs to data capture development |
| Kalisch et al.120 | Train-the-trainer intervention to increase nursing teamwork and decrease missed nursing care in acute care patient units. Nurs Res 2013;62:405–13 | USA | Quasi-experimental design | Reviewed from the train-the-trainer perspective. The intervention increased teamwork and reduced missed nursing care | Some insight into teamwork and staff satisfaction and perceptions on the level of staffing; however, is not linked to managers’ decision-making |
| Kane179 | Capturing district nursing through a knowledge-based electronic caseload analysis tool (eCAT). Br J Community Nurs 2014;19:116, 118–24 | Ireland | Evaluation of the impact of the e-CAT tool using focus groups and scrutiny of data from the tool | Reports on the implementation process and the impact of IT support, staff worries and inaccuracies in compiling data. Found that organisational support and a standard approach were important; also indicates how the tool has been adapted and assessed | Little detail on focus group findings, but highlights the need for stakeholder engagement and transparency for user acceptance. Those with better IT skills used the tool more effectively; training improved skills in those who were anxious |
| Kellagher et al.202 | Workload and workforce planning: developing a learning toolkit. Nurs Manag 2010;17:32–4 | Scotland | Review of tools | Brief description of evidence-based tools used in Scotland for workforce planning and deployment | Minimal detail on the toolkit and its expected outcomes from use, some commentary on users’ perceptions and the format for education and engagement of staff |
| Kerr and Timony167 | Review of an automated rostering system from a nurse manager’s perspective. Stud Health Technol Inform 2009;146:96–102 | Ireland | Audit of a manager’s use of a computerised rostering system | Reviewed staff computer skills, preparation for use, time to use the system, preferences and effect of the system and the user’s rostering experience. Emphasis on the importance of education for managers | Considers manager’s perceptions, the use and non-use of the system and strategies to support them. Clerical staff were involved |
| Kivinen and Lammintakanen182 | The success of a management information system in health care – a case study from Finland. Int J Med Inform 2013;82:90–7 | Finland | Case study approach with interviews in one specialised health-care organisation | Describes information availability and use among users of a MIS. Found that planning, organisational and cultural aspects were important for implementation | Useful for user perception and suggestions for embedding the tool as part of strategic information management. Only one organisation |
| Kontio et al.151 | Information utilization in tactical decision making of middle management health managers. Comput Inform Nurs 2013;31:9–16 | Finland | Qualitative interviews with 14 cardiac care managers | The study identified the tactical decisions that middle management health managers make based on available and missing information. The collation of information was difficult because of the multitude of sources | Explores the impact of missing information on the decision-making process. Looks at tacit knowledge. All informants worked at the same department in one hospital |
| Kooker and Kamikawa118 | Successful strategies to improve RN retention and patient outcomes in a large medical centre in Hawaii. J Clin Nurs 2011;20:34–9 | USA | Commentary by managers | Describes an initiative to improve the retention of staff utilising Magnet principles, training and coaching. Retention and patient outcomes improved | Gives information on the context and support required to improve retention. No depth of detail given on the processes related to decision-making on staffing |
| Lacey et al.119 | Nursing support, workload, and intent to stay in Magnet, Magnet-aspiring, and non-Magnet hospitals. J Nurs Adm 2007;37:199–205 | USA | Survey – comparison of Magnet, Magnet-aspiring, and non-Magnet hospitals in relation to nursing factors | Examined the differences between scores on organisational support, workload, satisfaction and intent to stay. Found that nurses in Magnet settings generally had more positive scores as a result of support for professional practice | Large data set (n = 3337). Highlights the importance of professional practice for staff satisfaction and retention. However, does not relate to tools/technology or management decisions |
| Lammintakanen et al.197 | Use of electronic information systems in nursing management. Int J Med Inform 2010;79:324–31 | Finland | Qualitative – 8 focus groups with 48 managers | Describes nurse managers’ perceptions of electronic information systems. Barriers to IT use highlighted, such as immature systems, lack of time or lack of strategic planning and co-ordination | Useful for barriers to, and facilitators of, effective use of IT and how data are used; some information on how to facilitate managers’ skills, but lacks details |
| Maenhout and Vanhoucke184 | Analyzing the nursing organizational structure and process from a scheduling perspective. Health Care Manag Sci 2013;16:177–96 | Belgium | Literature review and development of a staffing simulation tool | Explores the components of nurse staffing and decision-making through a literature review to develop a nurse staffing and shift-scheduling methodology; proposes a conceptual model of organisational factors | The focus is on the design of a decision support simulation tool, but does consider important influencing factor on scheduling and rescheduling: nurse satisfaction and unit effectiveness |
| Hall et al.144 | Decision making for nurse staffing: Canadian perspectives. Policy Polit Nurs Pract 2006;7:261–9 | Canada | Qualitative – uses interviews with nurse managers and nurses at all levels | Examines the influences on decision-making on staffing and deployments. Critiques the use of tools, frameworks, ratios and nursing workload measurement. Makes suggestions for moving forward so that decision-making may be supported | Useful on managers’ perceptions of systems, but these were paper-based systems. Minimal review of intuition. Focuses on the reliability and the validity of tools from the manager’s perspective. Some information on implementation challenges |
| McIntyre129 | Good Practice Guide: Rostering. NHS Improvement guidance; 2016 | England | Guidance | Indicates requirements for safe staffing with links to e-rostering. Emphasises the need for policies and the formalisation of staffing requests. Indicates how the mastery of e-rostering should be part of managers’ personal learning plan | Offers information on political and strategic requirements, with a focus on policies and practical issues related to collation and action on real-time data in response to patient needs |
| Murtola et al.186 | Information systems in hospitals: a review article from a nursing management perspective. Int J Networking and Virtual Organisations 2013;13:81–100 | Finland | Literature review | Describes the information systems available for nurse managers in hospitals to support decision-making. Found that the systems developed mostly focus on strategic and tactical decision-making levels without real-time information support; operational decision-making is weakly supported | Considers the impact of a lack of data integration and nurse manager dissatisfaction with usability. Strong focus on decision-making and types of decisions. Proposes a decision-making framework |
| Nagy and Nathan181 | Scheduling out of control? Consider workforce management options. Nurs Manage 2010;41:52–3 | USA | Commentary by CNO and scheduling analyst | Discusses the process of developing and embedding nurse staffing technology and its impact. Considers key factors (e.g. staff mix, regulation, retention, agency, finance and equity, plus quality indicators) | Written by managers’ responsible for the tool, lacks supportive evidence. However, offers an insight into organisational implementation |
| NHS Education for Scotland131 | Nursing and Midwifery Workload and Workforce Planning Learning Toolkit. 2nd edition. Edinburgh: NHS Education for Scotland; 2013 | Scotland | Guidance | Sets the context for staffing decisions and indicates the complexity of the decision-making process. Refers to the triangulated approach. Offers guidance for managers and explains different processes | Useful for work-based learning guidance, and has an emphasis on mentorship and collaboration |
| Pappas et al.176 | Risk-adjusted staffing to improve patient value. Nurs Econ 2015;33:73–8, 87 | USA | Interviews and review of four nurse-sensitive indicators on a surgical unit | Using the Patient Risk Assessment Profile, nurses assessed patient risk in order to guide nurse–patient assignment to improve patient outcomes. Findings showed decreased adverse events and a positive impact on hospital finances | Useful for decision-making of nurse managers in the light of patients’ presentation, but lacks detail. Focus of risk adjustment. Charts how the local tool was developed |
| Perroca and Ek208 | Utilization of patient classification systems in Swedish hospitals and the degree of satisfaction among nursing staff. J Nurs Manag 2007;15:472–80 | Sweden | Postal survey to 18 Swedish hospitals (n = 128) | This paper investigates the patient classification systems implemented in hospitals in Sweden and nurse satisfaction with the instrument. Nurse managers were satisfied with the tools, except for their inability to measure quality | Offers an insight into managers’ use and perception of patient classification tools related to workload; some suggestions on how improvements can be made. Brazilian academics investigated Swedish hospitals |
| Pruinelli et al.175 | Nursing management minimum data set: cost-effective tool to demonstrate the value of nurse staffing in the big data science era. Nurs Econ 2016;34:66–71, 89 | USA | Discussion on the NMMDS | Discusses the use of, and evidence for, big data and how this can influence and enhance patient and nurse outcomes in the light of facilitation of staffing decisions. Indicates the challenges for nurse managers and the need for standardisation | Considers collaboration for technology development and factors related to implementation. Authors are academics and nurse managers. Has a focus on Clairvia technology, which is capacity management technology used with NMMDs |
| Rapala198 | Staffing excellence: moving from retrospective to prospective management of risk. Nurs Econ 2011;29:211–14 | USA | Commentary by a clinical risk manager | Focus on risk management with consideration of how staffing data should be scrutinised for root-cause analysis (e.g. staff mix, experience). Explores staff fatigue with excess shift work and tracking of shifts in own organisation (and possibly others) | Useful for consideration of staff fatigue, clinical risk and patient outcomes in relation to tracking and management by technology. Also explores the influence of patient acuity. Generally uses a personal perspective, with some links to evidence |
| Robinson et al.126 | Factors that affect implementation of a nurse staffing directive: results from a qualitative multi-case evaluation. J Adv Nurs 2016;72:1886–98 | USA | Evaluation of the implementation of a mandated staffing methodology with case study interviews | Classified sites as having ‘high’, ‘low’ and ‘medium’ levels of implementation and conducted interviews in exemplars. Found a lack of management buy-in and confidence in the data in sites with a low level of implementation | Offers a depth of commentary on managers’ perceptions in relation to the organisational implementation of the methodology. Gives an insight into the barriers to, and the facilitators and importance of, organisational commitment |
| Rischbieth160 | Matching nurse skill with patient acuity in the intensive care units: a risk management mandate. J Nurs Manag 2006;14:397–404 | Australia | Commentary by ITU nurse manager on agency use and risk | Reviews the evidence for agency use and safe staffing. Looks at the knowledge required to make nurse–patient allocations and the risk related to the lack of knowledge on agency staff competence and capability | Examines nurse experience, capacity and capability in relation to patient safety and risk; the focus is intensive care. An experienced manager but commentary |
| Ruland171 | Developing a decision support system to meet nurse managers’ information needs for effective resource management. Comput Nurs 2001;19:187–93 | Norway | Describes the development of a decision support system: CLASSICA | The makers of CLASSICA claim that it assists managers in resource allocation and quality control. It integrates information about patient flow and activity, staffing and the cost of nursing care at the nursing-unit level | Charts the process of development, but not the tool’s effectiveness. Useful for organisational implementation, but no manager feedback explored |
| Ruland and Ravn172 | Usefulness and effects on costs and staff management of a nursing resource management information system. J Nurs Manag 2003;11:208–15 | Norway | Evaluation of CLASSICA using a survey, interviews and a financial review | The evaluation focused on costs and found a 41% reduction in costs for overtime and a high level of nurse manager satisfaction with the system | Only brief statements given from interviews. Evaluation undertaken four months after implementation. Discusses users’ perceptions of ease of use and usefulness |
| Scott and Van Norman200 | Managing the complexity of a system wide electronic medical record design and implementation: lessons for nurse leaders. Nurs Adm Q 2009;33:109–15 | USA | Commentary by nurse managers on the implementation experience of an organisation | Relates the complexity theory to nurse executives’ role in the implementation of technology to support the patient record; has a focus on the structure of the organisation’s leadership and support for the project | Some detail on the organisation’s promotion of the implementation. Not linked to how managers can be supported, but does discuss education. Technology but not a staffing tool |
| Shirey et al.187 | Nurse manager cognitive decision-making amidst stress and work complexity. J Nurs Manag 2013;21:17–30 | USA | Qualitative study using 21 interviews with nurse managers | Found that experience in the role, the organisational context and situational factors influenced nurse manager decision-making, and this has coaching and mentoring implications. Produces a cognitive model to guide decision-making related to stressful situations | Decision-making varies based on nurse manager experience. Some review of data and technology and how this may enhance decision-making. Reviews the impact of organisational influences and the need for support |
| Siirala et al.159 | Nurse managers’ decision-making in daily unit operation in peri-operative settings: a cross-sectional descriptive study. J Nurs Manag 2016;24:806–15 | Finland | Qualitative cross-sectional design using a think-aloud interview technique | Describes decisions made by 20 nurse managers from two sites. Looks at ad hoc, near-future and long-term decisions related to staffing. Decisions were often made simultaneously, with many interruptions | Describes the complexity of the decision-making process in relation to staffing and links to the knowledge needed to make decisions. One setting only; does not compare sites |
| Silvestro and Silvestro201 | An evaluation of nurse rostering practices in the National Health Service. J Adv Nurs 2000;32:525–35 | UK | An evaluation of rostering in 50 NHS wards using a survey and case study on seven wards | Reviews different forms of rostering: manager led, team and self-rostering. Determined the strengths and limitations of each approach and recommended when they are appropriate to use | Although it does not review technology, it links rostering to staff satisfaction and the potential for inconsistencies and unfairness in roster allocation |
| Silvestro and Silvestro185 | Towards a model of Strategic Roster Planning and Control: an empirical study of nurse rostering practices in the UK National Health Service. Health Serv Manage Res 2008;21:93–105 | UK | An evaluation of rostering in 50 NHS wards using a survey and case study on seven wards | Longitudinal findings related to the previous study.201 Reports the challenges to rostering, the need for multiple considerations and the potential negative outcomes linked to the impact of local practice with a manual approach | Does not refer to tools, but highlights areas in which inaccuracies occur when rostering is ad hoc and lacks standardisation and collaboration between clinical areas |
| Subirana et al.128 | A realist logic model of the links between nurse staffing and the outcomes of nursing. J Res Nurs 2014;19:8–23 | UK | Used a realist approach to literature review and the development of a logic model | Has a focus on the underlying mechanisms that influence patient and nursing outcomes related to staffing. Explores how experience and clinical judgement relate to contextual issues | The logic model is useful and considers staff education and experience. Emphasises the importance of supportive management, but does not consider how this can be implemented |
| Szumlas204 | Leveraging staff nurse engagement to design effective patient care assignments. Nurse Leader 2013;11:46–49 | USA | Commentary by the director of quality | Briefly reviews the evidence and considers the manager’s role in decision-making and how the use of tools indicates the importance of collaboration. Considers measurement of nursing care | A different perspective on staffing to account for nursing work that is non-value added and therefore does not contribute to quality outcomes. Relates to the literature, but the focus is a commentary on performance metrics for staffing |
| Taylor et al.127 | Evaluating the Veterans Health Administration’s staffing methodology model: a reliable approach. Nurs Econ 2015;33:36–40, 66 | USA | Evaluation using interviews and a database review of nursing hours per patient-day using interrupted time series analyses | Linked to Robinson et al.126 Charts the process of evaluation (e.g. organisational documentation review, full-time equivalent staff information and recommendations from the unit and facility-based expert panels). Reports preliminary findings on implementation and development of the methodology | Useful information around implementation, comparison of data on leadership factors and how staffing methodology was supported by the organisation |
| Tran et al.122 | A shared care model vs. a patient allocation model of nursing care delivery: comparing nursing staff satisfaction and stress outcomes. Int J Nurs Pract 2010;16:148–58 | Australia | Quasi-experimental design to compare nurse outcomes with different models of care | Compared nurse outcomes between the SCN and patient allocation models. No difference found between the models on nurse satisfaction, but the role was stressful for some team leaders in SCN | The challenges for team leaders in supervising and negotiation with staff; this can improve confidence and facilitate communication skills. No focus on tools or decision-making. Some difficulties with follow-up data collection in the study |
| Valentine et al.190 | Achieving effective staffing through a shared decision-making approach to open-shift management. J Nurs Adm 2008;38:331–5 | USA | Commentary by nurse managers on the introduction of a self-rostering tool | Implementation of the tool across three hospitals. Reviews challenges the role of: leadership, education, communication, mandate and feedback. Demonstrated cost-savings and staff satisfaction | Insight into how a new technology was embedded through organisational commitment and incentives for staff. Commentary by those responsible for the tool in one organisation |
| van Oostveen et al.178 | Developing and testing a computerized decision support system for nurse-to-patient assignment: a multimethod study. Comput Inform Nurs 2014;32:276–85 | The Netherlands | Mixed methods for tool development and before-and-after studies | Development and evaluation of a decision support tool for nurse–patient assignment. Used focus groups and a survey. Found a 30% reduction in nurse-to-patient assignments; therefore, the workload was reduced | Main focus is the efficacy of the tool, but considers influences on clinical decision-making (e.g. patient acuity and broad view of nurse characteristics and experience, including physical and mental state) |
| van Oostveen et al.132 | Nurse staffing issues are just the tip of the iceberg: a qualitative study about nurses’ perceptions of nurse staffing. Int J Nurs Stud 2015;52:1300–9 | The Netherlands | Qualitative – interviews (n = 27) and four focus groups (n = 44 participants) | Considered nurse staffing levels and the use of nurse-to-patient ratios and PCSs. Found a lack of confidence in PCSs in quantifying nursing work plus powerful others (e.g. doctors impact adversely on decision-making) | Highlights the importance of professional confidence and organisational culture in decision-making and how leadership can have a positive role |
| van Oostveen et al.124 | Pre-implementation studies of a workforce planning tool for nurse staffing and human resource management in university hospitals. J Nurs Manag 2016;24:184–91 | The Netherlands | Quantitative – regression analysis and survey following the introduction of the RAFAELA tool | Tested the validity, reliability and feasibility of a workforce planning system through comparison of nurse calculations. Found variable agreements in comparing tool use; only in 1 in 12 wards was the calculation of the nursing care index valid | Nursing staff, although positive about the tool, did not implement it. The study offers an insight into barriers to accepting the tool, despite training and organisational factors, as these both facilitated and impeded implementation |
| Wadsworth and Kurilla194 | An automated solution for managing your workforce. Nurs Manage 2009;40:49–51 | USA | Commentary by CNO and nurse manager | Charts the impact of an automated workforce management solution for time, attendance and staff scheduling | Limited detail on managers’ use of the system, but looks at the transparency of staff numbers and the effective use of the staffing budget. Considers rule-setting and breaches |
| Wallace and Pierson195 | A case study: the initiative to improve RN scheduling at Hamilton Health Sciences. Nurs Leadersh 2008;21:33–41 | USA | Commentary by the project lead and an external consultant | Reviews the experience of an organisation in developing and implementing a new scheduling system. Describes the implementation and evaluation process in detail | Written by those who led the development, but offers an insight into the need for policy and rules on allocation, in order to ensure parity |
| Wyatt and Healey161 | Managing capacity and workload in children’s services. Paediatr Nurs 2005;17:31–4 | Wales | Commentary by managers on an acuity tool for neonates: STEAM | Describes the development of the tool. Explains the policy and procedures that accompany it, with regard to escalating the need for staffing or stopping procedures and closing beds. Reports staff satisfaction. Paper-based tool | Offers some insight into how the integration of data can affect managers’ staffing decisions and strategies |
| Wilson et al.150 | Mindful staffing: a qualitative description of charge nurses’ decision-making behaviors. West J Nurs Res 2011;33:805–24 | USA | Qualitative – interviewed 24 charge nurses, nurse managers and staff nurses | Staffing the unit was the most important role for charge nurses. Five decision-making behaviours emerged: resourcefulness, tactful communication, flexibility, decisiveness and awareness of the big picture. Considers changes to nurses’ education | Focuses on the process of decision-making and its influences in relation to safe staffing. Does not relate to tools or technology. Offers key insights into the qualities of a good nurse manager in decision-making. Indicates the importance of resilience |
| Wilson and Weiss153 | Police staffing allocation and managing workload demand: a critical assessment of existing practices. Policing 2014;8:96–108 | USA | Literature review and focus groups | Assesses current trends and experiences in staffing allocation. Reviews staffing tools and examines the strengths and weaknesses of alternative approaches to determining staffing need and managing workloads | Highlights some similarities in nursing with regard to budget constraints, complexity, environment/geography and reactive decision-making, plus skill mix with non-trained staff |
| Zori et al.188 | Critical thinking of nurse managers related to staff RNs’ perceptions of the practice environment. J Nurs Scholarsh 2010;42:305–13 | USA | Randomised survey, 12 nurse managers and a random sample of 132 RNs | Compares the skills and attributes of critical thinking in nurse managers with staff perceptions. Found a positive relationship between the critical-thinking dispositions of nurse managers and staff perceptions of practice | Considers emotional and social intelligence to improve leadership effectiveness in nurse managers. Also reviews the experience of, and impact of culture and organisation on, decision-making and decision-making support |
Appendix 10 Theory areas: codes (sub-elements) and themes
Theory area 1: the world view on staffing (meta-explanations, legislation and guidance)
Budget restrictions – effective management of finance: the important influence of finance on staffing; the manager’s role; budget, tools and technology.
Corporate reputation, patient and public confidence.
Legislation, mandates, guidance: legislation to protect the workforce; legislation for staffing ratios or levels; regulatory processes for professionals; strategy and policy leading to mandates; guidance; policy and guidance for the use of technology.
Patient safety and quality outcomes: policies for patient safety; manager’s role and responsibilities; evidence for the impact of staffing on quality.
Professional obligations for achievement of quality and safe patient care: responsibility and accountability; models of care associated with professionalism; professionalism, skill mix and patient safety; safe staffing, risk and professional obligations.
Risk management – reduced risk of litigation: staffing and risk management; the nurse managers’ decision-making; tools and technology and their impact on risk management.
Workforce well-being – staff recruitment and retention: the impact of inadequate staffing; the importance of recruitment and retention; balance between patient and staff outcomes; the impact of technology and tools on workforce well-being.
Theory area 2: organisational influences, context and responses to staffing deployment and evaluation
Leadership and powerful others: the importance of leadership for the implementation of tools and technology for safe staffing deployment; the importance of leadership for the development of tools and technology; engagement; the importance of the nurse executive role (and other corporate-level roles); leadership, collaboration, teamwork and delegation; leadership at different levels of the organisation and shared leadership; accountability and responsibility; setting expectations, monitoring and evaluating; important and powerful others; leadership qualities; areas in which leadership may impede.
Organisational culture and attitude to risk management: the importance of the consideration of culture when technology or tools are implemented; professional model of care; the influence of culture on decision-making; attitude to risk; cultural change; negative aspects of culture.
Organisational feedback and evaluation: the importance of evaluating the use of tools and technology; evaluation/staff feedback to assist with tool/technology selection or development; evaluation to determine errors and the links to finance and poor patient outcomes; formulation of action plans as a result of evaluation.
Organisational investment in the system and support for users: the importance of the investment of time and resources; the importance of perceptions of support by managers; the importance of a dedicated support team; the need for IT expertise; training; peer support; barriers.
Organisational trial, adaptation and innovation of technologies and tools: trial; stakeholder engagement and feedback in trials and pilots; acting on results; adaption and tailoring to needs; innovation.
Theory area 3: the influences of clinical need
Patient dependency and acuity: the use of patient dependency and/or acuity classification for determining staffing levels linked to workload; lack of credibility of the tool; failure to use the tool.
Patient feedback and experience: the impact of staffing on patient satisfaction; the impact of the use of tools and technology on the patient experience.
Public perceptions: (no themes).
Good-quality care, patient safety: the influence of quality care and patient safety; the influence of rostering and patient–nurse allocation; the impact of tools and technology for quality.
Impact on carers: (no data were coded).
Theory area 4: technologies and tools for articulating predictive and real-time data on patient need
Data for risk management (red flags and staffing): the impact of risk identification management on staffing; tools and technology.
Standard approach to compilation of patient dependency and acuity data: evidence for standard approaches to measurement of the nursing workload; the importance of a standard approach to nurse-to-patient allocation; barriers to a standard approach; problems with accuracy and consistency of standard approaches; lack of acceptance; need for training; effects of a lack of standardisation.
Visibility of good-quality care and safety outcome data for evaluation and comparison: visibility of the nurse’s role in relation to patient outcomes and safety; technology and tools; data for prediction via technology.
Theory area 5: resource availability
Bank/agency availability and costs: the impact of agency use; the importance of reduction in agency and bank costs; clear policies for agency use recommended; need for a flexible workforce; the nurse manager’s role.
Bed state, caseload, admissions and discharges: the impact of patient flow on staffing requirements; tools to assess ward processes; the need for real-time data on patient flow for decision-making.
Clinical environment and geography: the impact of environment/geography on outcomes; the impact of environment/geography on decision-making; how the clinical environment affects staffing allocation objectives; the impact of environment on the usability of tools and technology.
Staff experience, capacity, capability: education and skills; experience; competence; matching nurse characteristics with patient need; use of tools/technology to identify levels of skills and education.
Staff roles, skill mix, staff numbers: establishment; numbers and patient outcomes; numbers and staffing ratios; numbers and patient acuity; numbers and organisational factors; skill mix; role development/role shifts; making do; tools to identify and manage establishments – numbers and skill mix; visibility of staff numbers and skill mix for decision-making.
Staff requirements (shift requests): the importance of staff preferences for shift patterns; the need for flexibility; fairness and the equitable assignment; challenges with accommodation of staff preferences.
Theory area 6: day-to-day management of resources (with/without technology)
Data for evaluation: comparison of clinical areas’ actual staffing needs compared with predicted needs – transparency and visibility of data; retrospective data for measurement and comparison; multiple sources of data; data to support managers’ decision-making; data to influence change; data to empower managers; data for prediction; data to identify variances, inconsistencies or inaccuracies; data may be inaccurate; impact on workload.
Comparison between clinical areas: data for benchmarking intraorganisation; determining examples of good practice; data for benchmarking intraorganisation; data for benchmarking interorganisation (with similar organisations); comparison data to calculate staffing; comparison data for quality improvement; difficulties with comparative data; need for consistencies with data collection; need to understand context; data for service development.
Integration and visibility of complex data for comparison of patient needs and staffing requirements in the light of real-time resources: nurse managers’ data requirements for decision-making to ensure patient safety and quality outcomes; integration of data from tools and multiple sources; how IT can help to integrate data; integration for evidence-based staffing – examples of tools/technology, visibility; integration of data for decision support systems; integration of data for prediction – forecasting/modelling, need for real-time data, need for integration of information that is useful for managers for specific clinical areas and strategic levels, need for integration that can be interpreted and understood, need for expert support; lack of integration; complexity – multiple sources and different technology can prevent integration; inconsistencies in measurement or non-use of tools; lack of real-time data; systems that require additional data collection (time-consuming).
Rule-setting system (e.g. skill mix, staffing requests and adaptation for patient needs): parameter/constrained (numbers, skill mix, annual leave, hours, legislation – e.g. working time directive – headroom); rules linked to budget; policies, protocol and guidance; rules embedded in technical systems (e-rostering); triggers and escalation when rules are breached; rules for agency and bank; rules for equity and fairness; local interpretation of constraints and rule breakages; post-approval changes.
Standardised approach for establishment setting in accordance with budget: the importance of a standard approach (owing to the ease of measurement, comparison with regard to mandates, legislation and guidance); benefits of standardisation; strategies for standardisation (tools, frameworks, technology, expert panels); examples of a lack of standardisation; barriers to standardisation – unique settings, tools to capture data, lack of resources.
Theory area 7: nurse managers’ use of professional judgement for staffing deployment
Clinical understanding of patient acuity/dependency: the role of managers; importance for rostering and allocation; use of tools and technology.
Confidence: confidence for negotiation; confidence associated with decision-making; confidence with tools and technology.
Experience: nurse managers’ experience and decision-making; nurse managers’ experience and action; experience as an important factor for managing nurse staffing related to patient and nurse assessment; use of tools and technology to align with experience.
Fairness: nurse managers should be fair and promote equity in nurse staffing; equity, fairness and the roster; support to achieve an equitable and fair assignment through tools/technology.
Flexibility and adaptability: managers need to be flexible; the system needs a flexible approach; planning ahead; how tools and technology may help.
Leadership skills: leadership skills and qualities; leadership for rostering and allocation; leadership skills for implementation of tools/technology.
Local knowledge: staff capabilities and environment of care – local knowledge of staff capabilities and capacities; local knowledge of the environment of care; local knowledge for tool/technology implementation; the need for access to data on staffing competencies.
User perceptions of technologies and tools (complexity/simplicity/trustworthiness): perceptions of tools and technology; data credibility; acting on findings; time; ease of use of tools or technology.
Professional values: models of care; values and decision-making; value conflict.
Theory area 8: effects of managers’ day-to-day work in balancing resources and demand
Cost reduction: the importance of the manager’s role for cost-effectiveness; the effects of poor resource management leading to escalating costs; the positive impact of tool/technologies on cost-savings as a result of data integration resources and alignment with budget.
Improved organisational reputation: rostering and nurse assignment/allocation effects on staff satisfaction; organisation; self-rostering improves nurse satisfaction.
Improved patient safety and quality outcomes: nurse managers’ decision-making affects safety and quality outcomes; nurse managers’ influence on the work environment and the impact on quality; good rostering practices for safety and quality outcomes; nurse–patient allocation for patient safety and quality outcomes.
Staff satisfaction, recruitment and retention: impact of the manager’s role on staff satisfaction; impact of organisational factors on staff satisfaction; impact of rostering and scheduling; impact of the tools/technology.
Additional codes
Communication: communication and collaboration for decision-making on nurse staffing; barriers to communication and collaboration for staffing; communication for staff well-being and engagement; collaboration to select and develop a tool; communication and collaboration to implement a tool; tools can enhance communication.
Gaming.
Data real-time availability: the importance of access to real-time data for decision-making; a lack of real-time data adversely affects decision-making; lack of credibility for real-time data; barriers to real-time data; tools/technology and real-time data; the importance of updating data.
Decision-making: types of decisions; components and complexity for decisions on safe staffing allocation; balancing demands in decision-making; technology and tools for decision-making.
Flexibility in the system: flexibility in the technological system or tool.
Affects of managers’ work around nurse staffing.
Negotiation: the manager’s role; negotiation for the roster.
Organisational factors: a supportive environment; assigning responsibility; nursing attitudes.
Reactive decision-making versus planned decisions: planned versus reactive decision-making by managers; the consequences of reactive decision-making; how tools/technology may help planned decision-making.
Seeing the bigger picture: the use of tools or technology.
Need for policies.
The need for a whole-systems approach.
System complexity.
Appendix 11 Example of evidence analysis
Theory area 6: day-to-day management with or without tools and technology
Code 1: data for evaluation – comparison of clinical areas’ actual staffing with predicted staffing
Transparency and visibility of data
Hockley and Boyle166 highlight the paucity of robust data:
NHS ill-equipped to manage the workforce or measure its productivity
p. 7, Hockley and Boyle166
There is a need for leadership for a transparent and robust system. Tools and technology enable access to ‘contemporaneous collated data’,179 such as an e-roster. 162 Wyatt and Healey161 comment on the need for visibility and transparency of data.
Retrospective data for measurement and comparison
The technology is available to equip nurse managers with powerful tools for retrospective analysis of process management.
Diers et al. 154
E-rostering facilitates measurement and understanding. 206 Retrospective review enables the evaluation of staffing levels124,170,175 to identify the need for further resources. 168
This enables monitoring for cost, efficiency and quality purposes129,175,194,210 on finance, for actual compared with predicted206 and the impact of bank/agency spend. 129,206
Multiple sources of data
Nurse managers need data for multiple purposes180 (e.g. strategic, financial – there are different information needs at different levels of the organisation in which nurse managers work131,186,197). eCAT can collate information across the full range of organisational levels (practice, operational, strategic and commissioning). 179 This facilitates user choice in data selection for evaluation. 171
Data to support managers’ decision–making
Data are needed to rationalise and justify the utilisation of resources131,144 and the reality of managing the service and resource issues. 161
Data to influence change
Used in the right way rostering (both electronic and paper based) can influence culture change and give staff the evidence they need to make change happen at the front line. It gives an overview across the organisation, not only month by month but also day to day, highlighting hotspots where intervention is required to ensure safe staffing levels and efficient deployment of staff.
p. 5, McIntyre129
Nurse leaders can collect, track and analyse assignment and outcome data and then modify hospital-, division- and unit-level practice based on specific evidence.
Allen164
For the reallocation of resources:169,192
This information was found to be useful in redefining care profile of ward units and reallocation of nursing resources.
Junttila et al. 192
Data to empower managers
An effective roster empowers ward managers to make informed decisions and make changes.
p. 5, McIntyre129
Nurse managers were hungry for data, and when they saw how the information generated by the system could help them improve staffing, they became enthusiastic supporters.
Barton168
Nurse leaders need to determine what data they will generate from the system and what will be done with that data. Information is power, but only if there’s a process in place to interpret the data and then make policy and procedure decisions based on the evidence the system provides.
Crist-Grundman and Mulrooney169
Data for prediction
For the development of ‘what-if staffing scenarios’ to determine potential financial and patient outcome feedback. 134
For long-term planning. 168,182
For forecasting need. 170
For prognostic data. 171
Data to identify variances, inconsistencies or inaccuracies
Dent,130 Silvestro and Silvestro185 and Diers et al. 154
However, deficits in staffing may be highlighted in comparison with establishment, but no response is given:
. . . if the measurement system calls for additional staff when there are none available. In this situation the organization may be unable to respond to the immediate needs highlighted by the WMS, yet they use the data to retrospectively justify their staffing model.
Hall et al. 144
Crist-Grundman and Mulrooney169 – data review may expose flaws in scheduling measures and provoke change.
Data may be inaccurate
May not capture intrashift adjustments. 150
Difficulties in obtaining real-time information – not input in the system or available because of slow response times or systems being too fragmented. 151
Discrepancies between staff rosters and ward reality; on unannounced NHS hospital inspections. A roster is merely a forecast:
Safe staffing is more than just a number on a roster.
p. 4, Hockley and Boyle166
Post-approval changes of rosters without compromising the original constraints – e-rostering may provide transparency:143
Published rosters were approved as safe and fair, but the actual safety, fairness and cost-effectiveness of the worked roster were unknown. Consequently, one worked roster examined showed a nurse working 39 shifts in 28 days, 17 of which broke rules. Another showed a nurse working 62 shifts in 56 days, including 22 days without a rest day.
Drake143
It is debatable whether staffing models can be effective tools for nurse managers or if they have merely gained credibility and assumed utility through custom and practice.
Flynn and McKeown165
Data may lack detail or be integrated to provide effective information comparing patient requirements with staffing levels. 172
Appendix 12 WeChat#WeNurses summary
27 July 2017: helping managers to deploy the nursing workforce effectively
The chat was begun by discussing what approaches are used to indicate staffing availability and capability. There use of computer printouts, and managers visiting wards, to determine staffing had been observed. Others talked about templates, spreadsheets and boards displaying the number of staff on duty. The chat then moved to people’s experience of staffing tools or technologies, which included apps, web-based rotas and live acuity reporting. Many had experience of e-rosters. One commenter highlighted that a web-based rota can be logged into by staff to view and book shifts. However, others had no remote access to a rota and used written templates, which are constantly adjusted and can become difficult to read.
The dynamic nature of staffing in the light of patient need was emphasised and related to acuity assessments:
Some day optimal staffing isn’t enough, some days it is.
In some areas, the Safer Nursing Care tool or other assessment measures are ‘bolted on’ to e-rostering. The flexibility of tools and technology was important. The chat host wondered if e-rosters are referred to when changes occur. Participants suggested that there is a need for technology to be flexible to real-time demand, particularly when patient needs are rapidly changing. Community caseload tools should capture routine and unscheduled work, plus travel time.
The chat audience emphasised using technology alongside professional judgement, noting the challenges of balancing real-time needs with expertise and system advice. Determining skill mix in accordance with patient need is vital, but it is difficult with low staffing levels. Managers must account for staff sickness and student needs, and they must know the escalation policy. The costs of agency and bank staff were also a focus. Professional judgement can be developed through reflection within a supportive environment. Managing staffing is stressful, particularly moving staff. Knowing staff preferences to achieve a work–life balance is important.
The discussion moved to the pros and cons of tools/technology. A strong theme was standardisation versus flexibility. Staffing levels can be instantly available and this can save time. Tools were quick and straightforward for booking agency staff. However, solutions were not always provided, and tools and technology are not always staff-friendly or do not always connect demand to capacity well. In some instances, tools may not account for patient complexity. As one commentator summarised:
Always helpful to have tools but only as good as the info that is input and don’t replace the expertise of a qualified nurse.
There were examples of local use. Texts, WhatsApp Messenger (WhatsApp Inc., Mountain View, CA, USA) or Facebook were used to connect staff looking for shifts. A live mobile phone app enabled real-time recorded shift swap. The development of an in-house designed app was shared. On discussing education, concerns were raised that some people are not technologically savvy. Nurse involvement in the creation of technology is therefore vital for effectiveness in supporting practice. Tools and technology should be developed for intuitive use and balanced with training and support. E-rostering helps to ensure that education updates are built into the off-duty:
. . . a little bit of training unlocked so much power and saved me time.
Further information on this discussion can be found via the following link: www.wecommunities.org/tweet-chats/chat-details/3029
Appendix 13 Theory compendium
Professional judgement
| Theory | Key citation(s) | Description of theory | Application to workforce planning |
|---|---|---|---|
| Intuition |
Dreyfus H, Dreyfus S. Mind Over Machine. New York, NY: Free Press; 1982229 Benner P. From Novice to Expert. Excellence and Power in Clinical Nursing Practice. Menlo Park, CA: Addison-Wesley; 1984230 |
Intuitive judgements are a manifestation of expertise – based on pattern recognition, salience, common-sense understanding, skills and knowledge | Professional judgement as part of the triangulation process – based on an understanding of the right skills and staff to meet the patients’ needs |
| Bayes’ theorem/rationality |
Bayes T. An Essay Towards Solving a Problem in the Doctrine of Chances. 1763231 Laplace PS. The Bayesian Interpretation of Probability. 1812232 |
Normative approach based on probability | Utilised in regression modelling for nurse staffing requirements; enables simulation of decision-making outcomes |
| Social judgement theory | Brunswick’s lens model (Brunswick E. Organismic achievement and the environment probability. Psych Rev 1943;50:255–272233) | Judgements are based on environmental cues and on the reality of an environment, which offers information but can also be biased | Potential to inform on the influences behind professional judgement and decision-making |
| Cognitive continuum | Hammond KR, Hamm RM, Grassia J, Pearson T. Direct comparison of the efficacy of intuitive and analytical cognition in expert judgement. IEEE Trans Cybern 1987;17:754–70234 | Types of cognitions on judgement move along a continuum, from analytical to intuitive, based on the task and time available | Potential to unpick when metrics and hard data can be triangulated with professional judgement, based on tacit and craft knowledge |
Decision-making
| Theory | Key citation(s) | Description of theory | Application to workforce planning |
|---|---|---|---|
| Bounded rationality | Simon H. Designing Organizations for an Information-Rich World. In Greenberger M, editor. Computers, Communication and the Public Interest. Stanford, CA: Stanford University Press; 1971. pp. 40–1235 | Judgements are bounded by attention, memory and communication – hence, decisions are satisficing (good enough dependent on a given set of circumstances) | How decisions on staffing may be made to fit with resources and circumstances within clinical practice |
| Theory of planned behaviour | Ajzen I. The theory of planned behaviour. Organ Behav Hum Decis Process 1991;50:179–211236 | Proposes that behaviour is influenced by behavioural intention, perceived behavioural control, attitudes and subjective norms | Offers an explanation of influences on the decision-making process and the effect of self-efficacy |
| Behavioural theories of the firm | Cyert R, March J. Behavioural Theory of the Firm. Oxford: Blackwell; 1963237 | Economic theory. Goals are negotiated and compromised dependent on group decisions. Behaviour based on profit. Links to satisficing and bounded rationality | Socioeconomic influences on decision-making within safe staffing and the use of WPTs |
| Game theory | Von Neumann J, Morgenstern O. Theory of Games and Economic Behaviour. Princeton, NJ: Princeton University Press; 1944238 | Originally a mathematical study of conflict and decision-making based on the rational responses to decisions of others | There is some implication that the assessment of patient dependency and acuity and bed state is prone to gaming, thus affecting the accuracy of technology |
Capability
| Theory | Key citation(s) | Description of theory | Application to workforce planning |
|---|---|---|---|
| Self-efficacy | Bandura A. Self-efficacy mechanism in human agency. Am Psychol 1982;37:122–47225 | Confidence in capability is linked to outcome expectancy, social influence, vicarious experience and mastery | Managers’ confidence in workforce deployment using WPTs, and how this is influenced in the workplace |
| Emotional intelligence | Goleman D. Leadership that gets results. Harv Bus Rev March–April 2000; R00204226 | The ability to use emotions, to facilitate thinking, to understand and reason with emotions and to effectively manage emotions within oneself and in relationships with others | Managers may use emotional intelligence to make decisions on staffing in complex, dynamic environments, linked to understanding and knowing staff |
| Transformational leadership | Bass BM. Leadership and Performance Beyond Expectations. New York, NY: Free Press; 1985227 | Transforming leaders raise the consciousness of followers for what is important, especially with regard to moral and ethical implications; self-interest is subsumed for that of the greater good | Managers’ ability to inspire and lead staff; important for flexible deployment of staffing, but also for staff well-being |
| Authentic leadership | Avolio B, Luthans F, Walumbwa, FO. Authentic Leadership: Theory-building for Veritable Sustained Performance. Working Paper. Lincoln, NE: Gallup Leadership Institute, University of Nebraska; 2004228 | Individuals who understand how they think and behave, and who are seen by others as being aware of the environment and of people’s value. These leaders are confident, hopeful, optimistic and resilient | Managers who are trusted by staff so that staff feel that their views will be positively regarded. This links to valuing staff as part of planning and deployment processes to facilitate staff well-being |
Complexity
| Theory | Key citation(s) | Description of theory | Application to workforce planning |
|---|---|---|---|
| Chaos theories | Applied to health care in Rickles D, Hawe P, Shiell A. A simple guide to chaos and complexity. J Epidemiol Community Health 2007;61:933–7215 | From mathematical perspectives, small changes in initial conditions offer diverse outcomes in an open, dynamic system. Used for modelling group behaviour | Potentially initial establishment figures may not capture day-to-day staffing requirements and skill mix in dynamic, uncertain environments |
| Systems theory | von Bertalanffy L. General System Theory: Foundations, Development, Applications. New York, NY: George Braziller; 1968216 | Interdisciplinary study of systems aims to discover patterns or principles that can be applied to a range of systems. Reviews self-regulation to feedback and adaptive processes | Predictability of WPTs and adaptability to feedback. Can also be applied to social systems. Relates to system alignment for the effective implementation of WPTs |
| Complexity theory | Zimmerman B, Lindberg C, Plsek P. Edgeware: Insights From Complexity Science for Health Care Leaders. Irving, TX: VHA, Inc.; 1998217 | Compares the management of organisational processes in a rational, planned, standardised, repeatable, controlled and measured way with the management of processes that explore new possibilities through trial and error, freedom, intuition and working at the edge of knowledge and experience | The predictive structures within the WPTs for planning and rule-setting compared with the complexity of the real world and the need for dynamic decision-making |
| Contingency theory | Fielder F. Contingency model of leadership effectiveness. Adv Exp Soc Psychol 1964;1:149–90218 | Optimal course of action is dependent on circumstances, including available resources and context | The decision-making process and leadership style are dependent on context and resources for safe staffing |
| Actor–network theory | Latour, B. Reassembling the Social: An Introduction to Actor-Network-Theory. Oxford: Oxford University Press; 2005219 | Concerned with how multiple networks come together to make a whole. Focuses on human and non-human actors and causality; constructionist perspective | The network may consist of WPTs, nurses and managers, and the influences on their interaction |
Knowledge transfer/implementation/change
| Theory | Key citation(s) | Description of theory | Application to workforce planning |
|---|---|---|---|
| Social learning theory | Bandura A. Social Learning Theory. New York, NY: General Learning Press; 1977221 | Learning is a social process, developed through observation, mimicry and reinforcement | How social cognitions and support for skills development can affect managers’ use of WPTs |
| Diffusion of innovations | Rogers EM. Diffusion of Innovations. New York, NY: Free Press; 2003109 | Explains how new innovations spread through reviewing individual and social interaction | Related to the implementation and acceptance of WPTs by the organisation and individuals |
| Organisational readiness | Weiner BJ. A theory of organizational readiness for change. Implement Sci 2009;4:67222 | Organisation viewed as multifaceted, with organisational readiness being a shared resolve and belief in the capability needed for the adoption of interventions | How managers and organisations are prepared to adapt to WPTs; considers the influence of context |
| Organisational knowledge creation theory | Nonaka I, Von Krogh G. Perspective – tacit knowledge and knowledge conversion: controversy and advancement in organizational knowledge creation theory. Organ Sci 2009;20:635–52223 | The conversion of tacit knowledge into explicit knowledge for shared use. Knowledge is contained in individuals but needed by the organisation | How knowledge may be privileged in certain people but required throughout the organisation. How data from WPTs are created and used |
| Organisational learning | Argyris C, Schon DA. Organisational Learning. A Theory of Action Perspective. Boston, MA: Addison-Wesley; 1978224 | Considers the interaction of people and organisational learning. Proposes double-loop learning based on reflective processes | How the evaluation of, and reflection on, the implementation of WPTs and the individual application of them to staffing decisions can promote learning |
Information systems
| Theory | Key citation(s) | Description of theory | Application to workforce planning |
|---|---|---|---|
| Human–computer interaction | Jacko J, Stephanidis C. Human-Computer Interaction: Theory and Practice (Part 2), Volume 2. HCI International Conference Proceedings. Boca Raton, FL: CRC Press; 2003239 | Focuses on the interface and the interaction between technology and users, and how this influences design | The design of WPTs in the light of managers’ use and requirements. Links to the importance of co-design |
| Safety-critical systems | Perrow C. Normal Accidents, Living with High Risk Technologies. New York, NY: Basic Books; 1984220 | Failure in one aspect of a system can result in catastrophic outcomes. Safety is influenced by the interaction of human factors with systems and culture | The impact and influence of safety on the deployment of workforce staffing through WPTs and decision-making influences |
| Social construction of technology | Bijker WE, Hughes TP, Pinch T. The Social Construction of Technological Systems: New Directions in the Sociology and History of Technology. Cambridge, MA: Massachusetts Institute of Technology (MIT); 1987240 | Human actions shape technology – the use of technology and problems with technology are constructed socially and adapted socially | How managers’ use of WPTs may shape their development to be flexible for local requirements and have an impact on implementation |
| Computer-supported co-operative work | Ackerman MS. The intellectual challenge of CSCW: the gap between social factors and technical feasibility. Hum Comput Interact 2000;15:179–203241 | Developed from human–computer interaction; the article considers the collaborative use of computers in the workplace | Looks at real-time processing of local information and how this relates to tacit knowledge. Highlights that technology may miss important aspects of knowledge and offer a poor fit to the situation |
Glossary
- Care hours per patient day
- Care hours are related to patient requirement by dividing the numbers of registered and non-registered staffing hours by the number of patients.
- Context
- The features and resources that have an impact on the success or failure of an intervention.
- Cumulation
- Increasing understanding, through ongoing inquiry, of programme mechanisms, context and outcomes to increase the transferability of knowledge.
- Dashboard
- A technology or tool that visually combines data relevant to nurse staffing to facilitate meaningful understanding on needs and resources.
- Data warehouse approach
- The amalgamation of data relevant to nurse staffing from multiple sources within one information system.
- Establishment
- The number and skill mix of staff allocated to each shift within a 24-hour period within a clinical area. This is related to the evaluation of patient requirements.
- Headroom
- A staffing allowance of typically 22–25% that accounts for annual leave, sickness and other reasons for using staffing hours, such as study leave.
- LEGO® SERIOUS PLAY® methodology [© (2017) The LEGO Group, Billund, Denmark]
- Within this evidence synthesis this approach was integrated within a soft systems methodology to produce models of the system of nurse workforce planning and deployment.
- Magnet organisation
- An organisation characterised by a collaborative approach that seeks to promote professional development and innovation, and which places emphasis on valuing staff.
- Mechanism
- How the programme resources impinge on stakeholders’ reasoning, decision-making and responses.
- Mid-range theories
- Theories, located between grand theories and the day-to-day working in research, that explain phenomena.
- Outcome
- The impact of the influence of context on mechanisms.
- Professional judgement
- A process of reflection, integration and analysis of observable data to arrive at a decision.
- Programme theory
- The hypothesis of how an intervention may work.
- RAFAELA
- RAFAELA® System (Finnish Consulting Group, 20020) is the name given to a nursing intensity and staffing system. The RAFAELA system comprises the OPCq (Oulu Patient Classification Qualisan) instrument for measuring the nursing intensity, registration of the daily nursing resources and the PAONCIL (Professional Assessment of Optimal Nursing Care Intensity Level) method.
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES)
- Publication standards for realist synthesis.
- Realist synthesis
- A theory-driven evidence review that follows a realist approach.
- Self-rostering technology
- Technology to help staff to identify when shifts are available and reserve them to work.
- Skill mix
- The blend of registered and non-registered nursing staff to patient ratios. Also relates to the individual skills of nursing staff.
- Soft systems methodology
- An approach to understanding different perspectives and requirements from a real-world situation.
- Technology
- An electronic or web-based resource that communicates, collates or integrates data for staffing decisions.
- Tool
- A resource, generally paper based, that collates or integrates data for staffing decisions. Tools may be adapted to electronic or web-based format.
- Triangulated approach
- An approach to safe staffing decisions that combines evidence-based staffing tools and technology, professional judgement and comparison of data.
- UNIFY
- UNIFY is the name given to a NHS England database for statistical information. A staffing data collection database that facilitates benchmarking and comparison of the staffing data of health-care organisations in England.
- @WeNurses Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) chat for nurses
- An online discussion forum for nurses.
- Workforce planning and deployment tools and technologies
- These are used directly or indirectly to determine staffing numbers and skill mix based on patient need. They range from sophisticated technology to paper-based tools.
List of abbreviations
- A&E
- accident and emergency
- app
- application
- CHPPD
- care hours per patient day
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMO
- context–mechanism–outcome
- CNO
- Chief Nursing Officer
- DyNADS
- Dynamic Network Analysis Decision Support tool
- eCAT
- Electronic Caseload Analysis Tool
- e-roster
- electronic rostering system
- HCSW
- health-care support worker
- HSDR
- Health Services and Delivery Research
- ICU
- intensive care unit
- IT
- information technology
- MeSH
- medical subject heading
- MIS
- management information system
- NHSI
- NHS Improvement
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NMMDS
- Nursing Management Minimum Data Set
- NQB
- National Quality Board
- OR
- odds ratio
- PPI
- patient and public involvement
- RN
- registered nurse
- SEN
- state enrolled nurse
- STEAM
- system to escalate and monitor clinical capacity
- WPT
- workforce planning and deployment tools and technology
