Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/07/49. The contractual start date was in September 2014. The final report began editorial review in March 2017 and was accepted for publication in July 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Jill Maben reports that she was a member of an advisory group from 2006 to 2009, advising on the development of the Point of Care project at The King’s Fund, and a member of the Point of Care Foundation (PoCF) Board 2013–14; she stepped down as board member at the start of the evaluation. Jeremy Dawson reports that he is a board member of the National Institute for Health Research Health Services and Delivery Research programme. Shilpa Ross and Laura Bennett report that they are currently employed by The King’s Fund, and Catherine Foot reports that she was previously employed by The King’s Fund. The PoCF, which supports the implementation of Schwartz Center Rounds® in the UK, was set up in 2013 by colleagues who were previously also employed by The King’s Fund between 2007 and 2013.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Maben et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction and background
Introduction
Our mixed methods, realist-informed, two-phase study aimed to evaluate Schwartz Center Rounds® (Rounds), an intervention to support health-care staff to deliver compassionate care. This chapter describes the background to Rounds in the UK and the structure of the report.
Schwartz Center Rounds®
Rounds were developed over 20 years ago and implemented in North America via the Schwartz Center for Compassionate Healthcare (SCCH), which is based in Boston, MA, USA, and is an autonomous, non-profit organisation (www.theschwartzcenter.org). Rounds were implemented in the UK via the Point of Care Foundation (PoCF), which was established in 2013 as an independent charity and has held the licence with SCCH to run Rounds in the UK since 2009. 1 Originally, the Point of Care programme was hosted at The King’s Fund, where the work commenced in 2007. Rounds were inspired by the experiences of a health-care lawyer, Kenneth Schwartz, who became terminally ill with lung cancer and wrote about his experiences of health care in the Boston Globe in 1995. 2 Kenneth noticed that ‘small acts of kindness made the unbearable bearable’2 and reminded caregivers to stay in the moment with their patients. He noted how some health-care staff were able to be compassionate while others were not, and how the same staff member could be compassionate one day and not the next. Before his death, he set up SCCH as a non-profit organisation designed to nurture compassion in health-care workers.
Rounds provide a regular (usually monthly) structured time and a safe, confidential setting for all staff employed in all organisational roles to get together to share the emotional, psychological and social impacts of working in health care. The purpose of Rounds is to support staff and enhance their ability to provide compassionate care. Unlike other types of reflective practice interventions, Rounds are a place not for solving problems or focusing on the clinical aspects of patient care, but for sharing the emotional, social and ethical challenges of providing care. Each Round lasts for 1 hour and begins with a multidisciplinary panel presentation of a patient case by the team who cared for the patient, or a set of different patient stories based around a common theme. The panellists each describe the emotional impact that the experience of looking after the patient has had on them. A trained facilitator then guides a discussion of emerging themes and issues, allowing time and space for the audience to reflect with the panel on similar experiences that they have had. Attendance is voluntary and staff attend as many or as few Rounds as they are able. When we began this work in 2013 (initial proposal), Rounds were running in 300 health-care organisations in the USA and 31 in the UK. At the time of writing, 425 health-care organisations are running Rounds in the USA and over 150 are running them in the UK.
The changing context of Schwartz Rounds development in the UK
Between the submission of the grant application for this study in May 2013 and the end of the study period in December 2016, the uptake of Rounds in the UK developed substantially. In May 2013, there were 30 organisations running Rounds, and on past uptake we anticipated that, if funded, there would be approximately 40 organisations running Rounds. By the time we started the project in September 2014, there were 77 organisations running Rounds in England, and we absorbed this additional sample into our mapping study without further resource. By the time we completed data collection in June 2016, there were over 150 organisations running Rounds. Our study needs to be understood in the light of certain events, and the reactions to those events, that occurred during this period (Figure 1).
FIGURE 1.
The context of implementation of Schwartz Rounds in the UK in relation to this study. DHSC, Department of Health and Social Care; LETB, Local Education and Training Board.
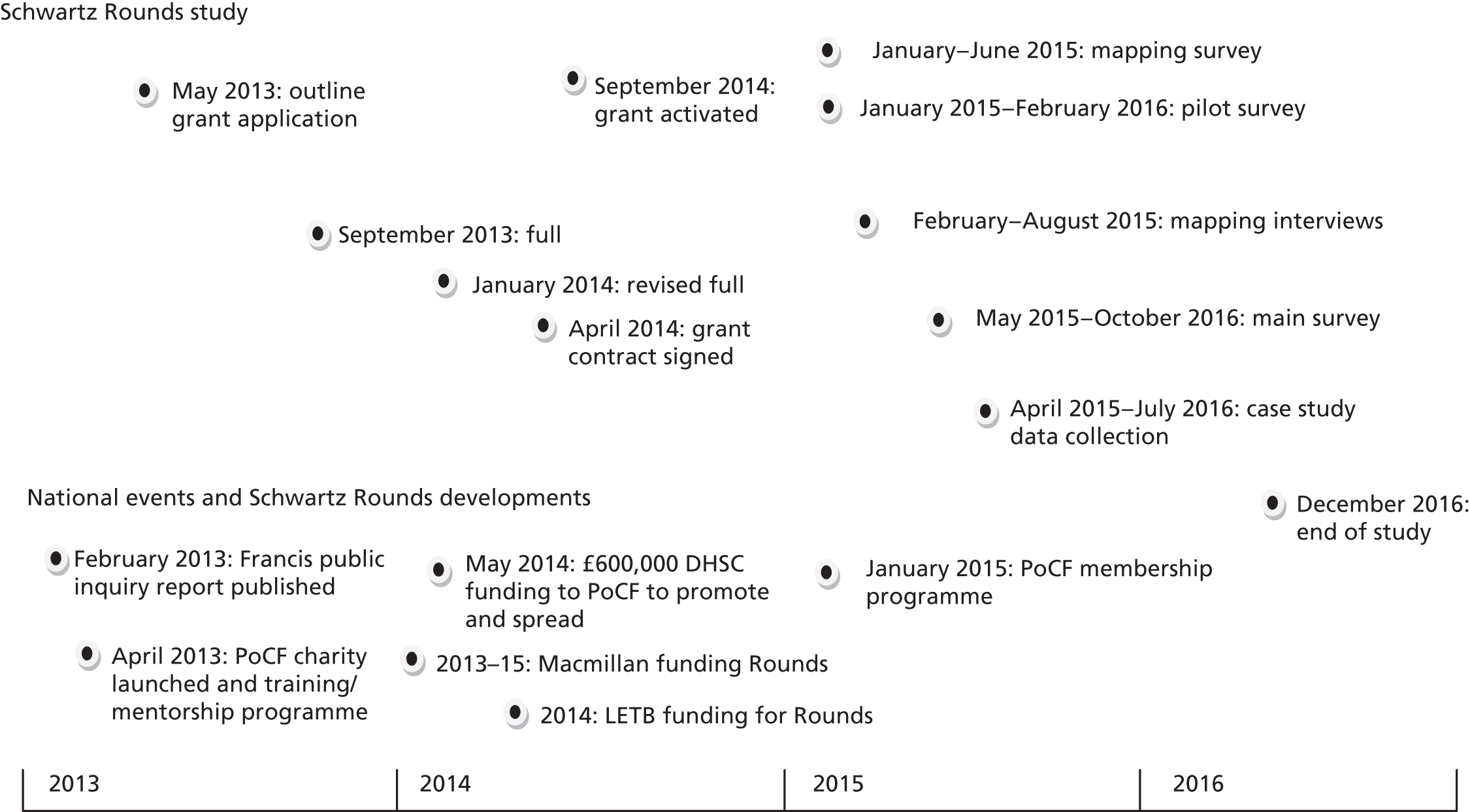
In February 2013, the Francis report3 into the failings in care at Mid Staffordshire NHS Foundation Trust was published. Francis recommended that:
A sense of there being one team for the patient should be fostered where possible. One way to help in this might be to involve staff of all backgrounds in case reviews, clinical audit, and in overall team meetings [. . .] One method whereby this has been achieved has been by Schwartz rounds [sic].
Volume 3, p. 1394. 3
As part of the UK government’s response to Francis in May 2013, funding of £600,000 was granted to the PoCF over 2 years to promote and spread Rounds across the NHS through training and mentorship. Local Education and Training Boards (LETBs) and Macmillan Cancer Support (Macmillan) invited organisations to apply for funding to support the costs of running Rounds, which may have increased uptake. 1
In April 2013, the Point of Care moved from The King’s Fund, where it had been since 2007, and became the PoCF. It subsequently developed its own training and support for Rounds organisations in the UK, as well as a membership programme (see Figure 1). (See Chapter 7 for further exploration of this.)
Report structure
In Chapter 2, we detail our aims and objectives and present the methods we have used to answer these, and describe how the wider context of our study has changed over the evaluation period in relation to the publication of the Francis report3 and the adoption of Rounds in the UK. Chapter 3 presents our scoping reviews of the literature and provides a composite definition of Rounds to enable us to compare Rounds with other similar interventions. The results of the survey, interviews and secondary data collation we undertook to map Rounds provider profiles in England are presented in Chapter 4. To determine if Rounds have an impact on staff well-being, we report survey findings comparing new Rounds attenders with staff who had never attended Rounds, from 10 Rounds providers, in Chapter 5. Staff experiences of attending, facilitating, presenting and supporting Rounds as steering group members, together with the experiences of non-attenders and board members, are in Chapter 6. Chapters 7 and 8 support our realist evaluation of Rounds reporting data analysis to support our question: what works, for whom, in what respects, to what extent, in what contexts, and how? Finally, we summarise and discuss our findings and present our conclusions in Chapter 9.
Chapter 2 Methods
Introduction
This report is based on data collected in a two-phase mixed-methods evaluation of Rounds. This chapter provides an overview of the research approach and questions. Further specific details are presented in Chapters 4–7.
Our approach has been broadly informed by ‘realist’ principles, and our aim is to understand how, in which contexts and for whom does participation in Rounds affect staff well-being at work, social support for staff, changes in relationships between staff and patients, ‘ripple’ effects in the wider teams and organisation in terms of compassionate care and patient care improvements; and to make recommendations regarding the role of Rounds in health-care provider staff support in order to inform future practice. 4–6
Overview of study
A mixed-methods evaluation of Rounds was conducted in two sequential phases.
-
Phase 1 (scoping reviews, review of relevant theories, interviews with Rounds architects, and national mapping study):
-
scoping reviews of Schwartz Rounds literature and alternative interventions to define Rounds, compare Rounds with alternatives and summarise the evidence base
-
exploring relevant theories and conducting interviews with original Rounds architects to identify programme theory and understand how Rounds might work.
-
-
Phase 2 (survey and nine organisational case studies):
-
a survey of health-care staff who attend Rounds and those who do not (within case controls) in 10 sites to determine if Rounds have an impact on staff engagement and well-being
-
realist informed in-depth organisational case studies to understand how Rounds ‘work’ (context and outcomes), the mechanisms by which well-being and social support might be influenced, and staff experiences of attending, presenting and facilitating Rounds. 4
-
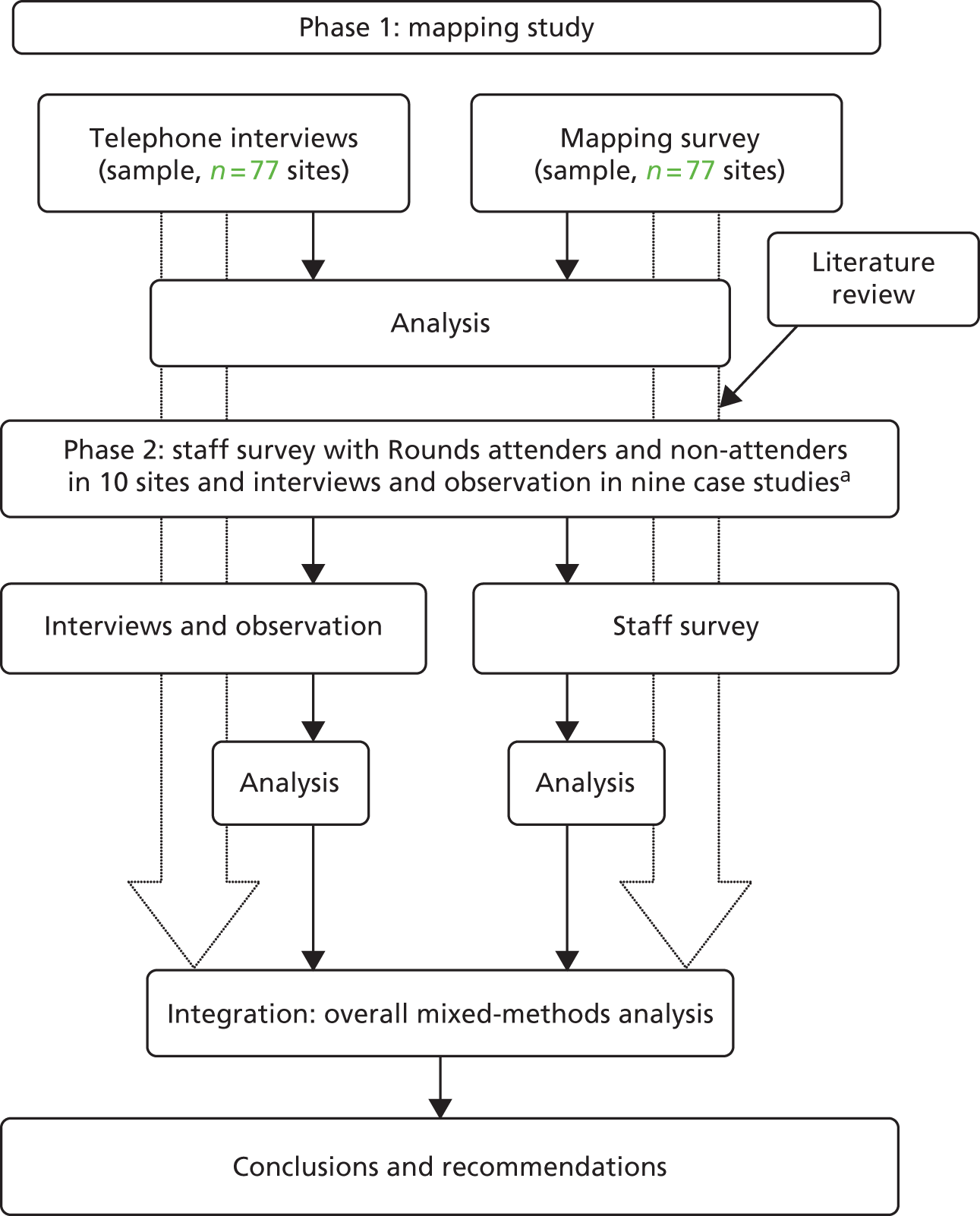
Our mixed-methods approach enabled us to address our varied aims and objectives (Table 1), and to seek elaboration, enhancement and clarification of results from one method with results from another, providing more than the sum of their parts. Some methods were sequential (e.g. mapping interviews were used to further understand data provided in mapping survey) and others were concurrent (phase 2 surveys and case studies). Data were mixed at numerous points (e.g. the mapping survey informed our sampling for phase 2). The quantitative and qualitative phases were equally weighted, and the findings were integrated and discussed after first being analysed and discussed separately. The overall study design is illustrated in Figure 2 and the relationship to the study objectives and data collected is detailed in Table 1.
| Study phase | Key aims and objectives | Research methods |
|---|---|---|
| Phase 1: literature review |
1. Identify literature providing a definition of Rounds to identify key features of Rounds and create a composite definition 2. Identify and critically appraise all empirical evaluations of Rounds 3. Identify alternative interventions, describe their key features and scope their evidence base 4. Compare each intervention in relation to the core features of Rounds 5. Identify how Rounds might work by: |
Scoping reviews of the following literature:
|
| Phase 1: mapping study |
6. Map the profiles of current UK Rounds provider organisations to inform sampling of case study sites for maximum variation: |
Primary data:
|
| Phase 2a: staff survey |
7. Evaluate whether or not regular Rounds attendance has an impact on health-care staff engagement and well-being, social support for staff, behavioural change towards patient and colleagues compared with non-attenders 8. Investigate whether or not frequency of Rounds attendance was associated with greater improvements in health-care staff work engagement, well-being, social support for staff and behavioural change towards patients and colleagues 9. Determine factors associated with Rounds being perceived as useful, or barriers, to attending Rounds |
Two-wave survey in 10 Rounds providers:
|
| Phase 2b: organisational case studies |
10. Examine staff experiences of attending, presenting, facilitating and leading Rounds and reported outcomes 11. Examine how Rounds are operationalised and the mechanisms by which well-being and social support might be influenced (or not), including: 12. Understand how Rounds ‘work’ in the UK, for whom and in what contexts; to suggest ways to improve their effectiveness; to inform decisions about their implementation in other contexts, and to understand what is causing variations in implementation or outcomes |
Case study in nine Rounds providers (realist evaluation):
|
| Overall analysis and cross-case analysis |
13. Establish contexts and mechanisms whereby Rounds influence staff well-being at work and social support 14. Identify and evaluate any changes (outcomes) that take place in relationships between staff who attend Rounds and their patients and colleagues 15. Identify and consider any wider changes that may be felt in teams or across the wider organisation regarding the quality of patient care and staff experience and, if so, how these may be linked 16. Make recommendations regarding the role of Rounds in health-care provider staff support |
Integration of all data:
|
FIGURE 2.
Overview of Schwartz evaluation components and processes. a, Six out of nine case studies (interviews and observation) and six out of 10 sites (survey) were the same.
Phase 1
We undertook two scoping reviews of the literature on Rounds to define Rounds and determine the evidence base, and of other interventions similar to Rounds in order to compare them. 7 We also explored the theoretical literature on reflection, group work and disclosure/discussion of emotional/challenging events to try to identify the mechanisms by which Rounds may work, which helped develop our survey for phase 2 (see Chapter 3), and, together with our interviews with the original architects of Rounds, informed our initial programme theory (see Chapter 8). The methods and findings from the scoping review are reported in detail in Chapter 3 and Taylor et al. 7
We conducted an online cross-sectional survey of all Rounds providers in England that had signed a contract with the PoCF by the start of the project in September 2014 when the mapping phase began (n = 77). We then undertook telephone interviews with Rounds champions (usually facilitators or clinical leads) in the same sample to explore their reasons for adoption and experiences of implementation further. For the collation and analysis of secondary data to map and profile providers running Rounds, the sample comprised all organisations implementing Rounds in the UK by July 2015 (n = 115). We wanted to map the profiles of current UK Rounds provider organisations to determine the reasons for implementation of and, when adopted, attendance at Rounds, and estimate the resource implications of establishing and sustaining Rounds. These data also informed sampling of the case study sites in phase 2. The methods and findings of the survey and telephone interviews are reported in detail in Chapter 4.
Phase 2
Thirteen providers were purposively sampled from phase 1 [to maximise the variation of organisations in terms of size, location and type of provider (acute trusts, hospice, community/mental health care providers)] and length of time running Rounds to provide 10 sites for the longitudinal survey, and nine organisations for the organisational case studies. Six sites participated in both survey and organisational case study components (Table 2). A long list of potential case study sites was drawn up against the sample quota in our protocol while phase 1 mapping data (survey and interviews) were being gathered. Approximately 20 providers were on this list, and in-depth discussions (including presenting to steering groups) in 16 providers ensued; one declined to take part, one was not suitable as Rounds rotated in four sites, and we decided that one was not suitable for a variety of reasons. Rounds were not sampled as a result of phase 2 survey responses, as survey and in-depth field work were often concurrent.
| Sitea | Survey, case study or both | Sizeb | Type | Location | Date startedc |
|---|---|---|---|---|---|
| Mulberry | Both | Large | Acute | Southern England | During study (after 1 September 2014) |
| Juniper | Both | Medium | Acute | Southern England | During study (after 1 September 2014) |
| Cedar | Both | Large | Acute | Southern England | Before 31 December 2012 |
| Cherry | Both | Medium | Mental health | Southern England | During study (after 1 September 2014) |
| Sycamore | Both | Medium | Acute | Southern England | 1 January 2013–1 September 2014 |
| Willow | Both | Large | Acute and mental health | Southern England | 1 January 2013–1 September 2014 |
| Oak | Survey only | Medium | Acute | Southern England | During study (after 1 September 2014) |
| Beech | Survey only | Medium | Acute | Northern England | During study (after 1 September 2014) |
| Elm | Survey only | Small | Hospice | Northern England | During study (after 1 September 2014) |
| Larch | Survey only | Medium | Acute | Northern England | During study (after 1 September 2014) |
| Ash | Case study only | Large | Acute | Southern England | Before 31 December 2012 |
| Elderberry | Case study only | Small | Hospice | Southern England | Before 31 December 2012 |
| Horse-chestnut | Case study only | Medium | Mental health | Northern England | Before 31 December 2012 |
Following a pilot survey, we conducted a two-wave survey with 833 Rounds attenders at baseline (follow-up, n = 484) and 2680 Rounds non-attenders at baseline (follow-up, n = 578), to provide within-case controls. To maximise new attenders, seven sites were selected in which Rounds began during the study (see Chapter 5). Surveys comprised eight validated measures and additional demographic and Rounds-specific information, with a total of 47 items (see Report Supplementary Material 1 for details of the survey items). These items were selected to measure hypothesised mechanisms by which Rounds might be expected to work (see Appendix 1). Surveys were longitudinal and were administered before Rounds attendance (for attenders) and after 8 months (see Appendix 2 for the baseline and follow-up surveys). They were designed to evaluate whether or not regular attendance at Rounds has an impact on health-care staff well-being, social support for staff and behavioural change towards patients and colleagues, compared with staff who do not attend Rounds. The detailed methods and findings of the survey are reported in Chapter 5.
Realist evaluation methods were used in nine case study sites. 4–6,8 These sites were identified, using purposive sampling, to allow more in-depth work to be undertaken through interviews with Rounds attenders, panellists, facilitators, clinical leads, steering group members, board members and non-attenders, and non-participant observation of Rounds, steering group meetings and panel preparation. The case study sites were sampled to provide maximum variation of information-rich cases9,10 that included aspects of Rounds implementation theorised to have an important effect on implementation and Rounds impact (size of institution and percentage of total staff who attend; established and new Rounds providers11,12 and early and late adopters),13 and also a range of providers (see Table 2). Data from case study sites were collected to examine staff experiences of attending, presenting and facilitating Rounds and how Rounds are conceptualised and implemented, and the mechanisms by which well-being and social support might be influenced (or not). This included, for example, reasons for variance in attendance and attendees’ experiences, any influence on team hierarchy/teamwork and on coping with stress, and any reported behaviour change towards patients and colleagues, including wider ‘ripple’ effects felt in day-to-day practice. It had been our intention (as per protocol) to shadow staff in practice to observe ‘ripple’ effects, and we developed observation protocols to observe staff with patients with support from our patient and public involvement (PPI) group members. However, practically, it was very difficult to identify specific ‘ripple’ effects and follow staff in practice at the right times to observe these effects. We therefore omitted this aspect of data collection and informed the National Institute for Health Research of this change to the protocol. ‘Ripple’ effects were gathered through reporting in interviews.
Case study interviewees were identified through purposive and snowball sampling and then invited to take part. Informed written consent was taken and participants were given a unique identification (ID) number to ensure anonymity and confidentiality. The selection of panel preparation, steering groups and Rounds for observation was negotiated with the facilitator/lead site contact with the steering group and with individuals involved (panellists in panel preparation). In practice, researchers tried to observe every Round during their fieldwork period in each case study (5–6 months) and as many steering groups and panel preparation meetings as possible. Consent and confidentiality procedures were more challenging in Rounds. However, every effort was made to inform potential attenders about the presence of the researchers before the Round took place (e.g. on posters and in e-mails), thus giving attenders sufficient time to make a decision about attendance based on their knowledge of our presence. On arrival, attenders were asked to tick a box on a modified sign-in sheet, saying that they were happy for the King’s College London research team to observe the Round. As there was a possibility that attenders would not be aware of our presence prior to the Round, at the start of each Round either the researchers or the facilitators announced that researchers were present and were taking field notes, and explained that any participant could approach the researcher (who was identified to attenders) and ask for any information they may have provided during the Round to be withdrawn and not used in the research. We also undertook two focus group interviews in November 2016 with Rounds experts (mentors from within and outside our case study sites) to test our realist findings. Further details of the methods and findings from the in-depth qualitative case studies are reported in Chapters 6–8.
Mixed-methods analysis
Following the completion of all data analyses, we carefully examined the data from our separate phases/methods;14 for example, three members of the team (JM, CT and JD) interrogated our phase 2 survey data for the six case studies for which we also had qualitative data, and vice versa, and cross-referenced these in our findings where applicable. We reviewed the survey data by case study site and examined the descriptive statistics. Although the small numbers of regular attenders in each case study site prevented us from analysing these data any further, we have explored our divergent and similar results (see Table 28) and present the limitations of each method in Chapter 9. Our phase 1 mapping interviews were also analysed to inform our realist questions in phase 2.
Methodological frameworks
This mixed-methods study is significantly informed by realist evaluation as follows:4,6
-
phase 1: literature review – although we did not undertake a realist synthesis, we did use the literature to identify our initial programme theory and identify proposed mechanisms by which Rounds might work
-
phase 1: mapping survey – not realist informed
-
phase 1: mapping interviews – realist informed regarding identifying mechanisms of action
-
phase 1: visit to SCCH in Boston – informed initial realist programme theory
-
phase 2: survey – measures informed by mechanisms identified in literature
-
phase 2: case study data collection and analysis – realist evaluation.
The realist evaluation approach acknowledges that intervention programmes do not necessarily work for everyone, as people are different and are embedded in different contexts,4 and so it helps researchers to go beyond the simple question ‘do Schwartz Rounds work?’ It seeks to understand better what works, and for whom: which staff, which organisations, in what circumstances. Realist evaluation is concerned with understanding causal mechanisms and the conditions under which they are activated to produce specific outcomes, which is highly relevant for this study. It recognises the interwoven variables that operate at different levels in organisations and thus suits complex social interventions. The realist approach to data collection and analysis is driven by retroduction, which starts with the empirical and explains outcomes and events through identifying the underlying mechanisms that are capable of producing them. 15 (See Chapters 7 and 8 for more details of realist evaluation methodology and analysis, and see Chapters 4–6 for the mixed methods and analysis used in the mapping survey and experience interviews.)
Research ethics
Three different ethics approvals were necessary for this study. The pilot survey and mapping study were not subject to NHS ethics or other NHS research governance processes as they involved only NHS staff, not patients.
-
Ethics approval for the mapping study in phase 1 was granted by the ethics committee at King’s College London (King’s College Psychiatry, Nursing and Midwifery Research Ethics Review Sub-Committee reference PNM/13/14–159). Research and development (R&D) approval and letters of access [CSP (Coordinated System for gaining NHS Permissions) number 148528] were also required for all sites before invitations to participate could be sent. These were issued by individual trusts/hospices (see Data collection access and Figure 3).
-
Ethics approval for the phase 2a pilot survey was obtained from University of Sheffield Research Ethics Committee (REC) (application number 001869).
-
Ethics approval for phase 2 survey and case study interviews and observation was granted by the National Research Ethics Service Committee London-South East (REC reference 15/LO/0053).
Following receipt of the favourable opinion from the REC, we obtained R&D permissions from our study sponsors and then local R&D permissions from each trust with a view to starting data collection. Research passports were obtained for the study researchers who conducted on-site data collection. Once each study site checked and approved the application, letters of access were issued.
Patient and public involvement in the study
Our approach to PPI was based on the principles that such involvement should be meaningful, respectful, relevant and collaborative. Patient representatives were involved from the project’s inception. Patients understood the challenges staff faced and believed, post Francis, that interventions to support staff, which had the potential to have an impact on patients, were very important and required studying. We took the view at the grant application stage, and thereafter, that those whom this study would benefit were both staff (the proximal outcome target group for our intervention) and patients (the distal outcome target group). We therefore involved both throughout the study. We actively involved patients through membership of the Project Steering Group (PSG) in order to improve the quality of the research and relevance of the study to NHS users and to support our dissemination activities. Members of the PSG included two PPI representatives who had previously provided input at the proposal stage, as well as a Schwartz Rounds staff representative. The PSG provided oversight of all aspects of the study, and, alongside other group members, our PPI representatives and Rounds staff members advised on data collection, commented on the findings emerging from the research and supported dissemination through links with their local networks. In phase 2, the PPI representatives were closely involved in drafting the staff and patient information leaflets explaining how we intended to observe and shadow staff in their everyday practice to observe the ‘ripple’ effects of attending Rounds (see above regarding the non-completion of this aspect of data collection). Collectively, their contribution has been highly valued in relation to highlighting the benefits to patients of Rounds. Details of the advisory and steering groups are provided in Acknowledgements.
Study management
The project was led and managed by the principal investigator (PI) at King’s College London. At the University of Sheffield and The King’s Fund there was a lead investigator. To co-ordinate work across the centres, weekly or fortnightly teleconferences were held involving the PI, all of the co-applicants and the staff employed on the grant. During the study period, three project advisory group meetings and five steering group meetings were held (see Acknowledgements for details of the steering group and advisory group membership).
Summary
This chapter reports the methods used in our mixed-methods study, which were significantly informed by realist methods. The study was undertaken in two phases: (1) scoping the literature and mapping of Rounds in the UK and (2) a survey for Rounds attenders and non-attenders in 10 sites and interviews and observation of Rounds in nine case studies. PPI was included throughout the study. Governance arrangements included advisory and steering group meetings. The backdrop to the study was a rapidly changing landscape in terms of uptake of Rounds in the UK following the publication of the Francis report3 and financial support from the Department of Health and Social Care, LETBs and Macmillan.
Chapter 3 Literature reviews
Introduction
This chapter addresses objective 1 to meet the following aims:
-
Part A: (1) to identify literature providing a definition of Rounds to identify the key features of Rounds and create a composite definition; (2) to identify and critically appraise all empirical evaluations of Rounds; (3) to identify alternative interventions, describe their key features and scope their evidence base; and (4) to compare each intervention in relation to the core features of Rounds. 7
-
Part B: (5) to identify how Rounds might work by (a) exploring the theoretical literature on reflection, group work, disclosure and safe environment; and (b) speaking to the original architects of Rounds to determine the underlying ‘programme theory’.
The reviews of literature pertaining to Schwartz Rounds and alternative interventions (part A) are scoping reviews, aimed at summarising the literature in relation to the volume, nature and characteristics of primary research. 16 The exploration of the theoretical literature and the interviews with Rounds architects (part B) were informed by realist evaluation principles in that they aimed to search for explanations regarding the mechanisms by which Rounds work, the processes that might trigger these mechanisms (contexts) and the possible outcomes associated with Rounds.
Part A: defining Rounds, reviewing their evidence base (scoping review 1) and reviewing the evidence base for alternative interventions (scoping review 2) and comparing them with Rounds
Defining Rounds and reviewing their evidence base: methods
Searches for relevant material were made using (1) the databases PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL), MEDLINE and EMBASE, giving comprehensive coverage of medical, psychological, nursing and social sciences literature (see Appendix 3); (2) contact with experts/Rounds leaders; and (3) internet searches. Searches were from inception to 2015; all searches were conducted between 14 October 2014 and 5 February 2015, except empirical studies evaluating Rounds, which we continued to search for over the duration of the project, resulting in two further papers included for this component.
For the composite definition of Rounds, we included all literature (including non-empirical literature, e.g. letters and editorials), providing that it included a definition of Rounds. Literature contributing to the evidence base for Rounds had to apply explicit research methodology.
Creating a composite definition of Rounds
Literature was screened to remove duplicate definitions (e.g. the same definition in multiple publications) to avoid ‘double counting’. Text describing Rounds (what they were and their aims, e.g. structure and purpose, as well as any text describing what they were ‘not’) was extracted. The text was analysed thematically by four team members independently (Michelle Hope, CT, JM and ML), core concepts were discussed and agreed, and a single definition was produced. The face validity of the definition was confirmed after review by members of the study advisory and steering groups (with expertise in Rounds/well-being interventions in health care).
Evidence base for Rounds
For empirical papers, data were extracted on standard features (authors, setting, aims, design/methodology, measures and findings). Quality assessment of qualitative and quantitative primary studies was undertaken using the tools developed by Jones et al. ,17 which include an assessment of the key criteria and then an overall rating (high, no or few flaws; moderate, some flaws; low, significant flaws). Mixed-methods studies were, in addition, assessed against the six criteria for good reporting of mixed-methods studies developed by O’Cathain et al. 14 Their quality was rated as low (< 3 criteria were met), moderate (3 or 4 criteria were met) or high (≥ 5 criteria were met).
Results
A total of 41 documents/sources were included in the review of definitions for Rounds (see Appendix 4 for the included references). The majority (n = 28) were non-empirical publications (e.g. commentaries, descriptive reports of a single Round, service evaluations of implementation). Thirteen research evaluations were identified (11 via the electronic/internet/expert searches, and two subsequent to this as published in 2016);18,19 however, for three of these20–22 only conference abstracts were available, and thus 10 publications were included in the review of evidence base for Rounds.
Composite definition of Rounds
The definition arising from thematic synthesis is:
Schwartz Rounds are the signature programme of the Schwartz Center for Compassionate Care. They provide a regular (usually monthly) open forum (drop-in rather than by invitation) for multidisciplinary clinical and non-clinical staff at all positions within the health-care organisation to come together in an environment that is safe and confidential. They provide staff with a level playing field to reflect on, explore and tell stories about the difficult, challenging and rewarding experiences they face when delivering patient care, and receive the support of their colleagues. Rounds are typically organised and managed by a steering group, championed by a senior doctor/clinician. They last for 1 hour and are often held during lunch periods (with food provided). They are a group intervention within which multiple perspectives on a theme, scenario or patient case (i.e. their stories) are briefly presented by a pre-arranged and pre-prepared panel and then opened to the audience for group reflection and discussion, usually facilitated by a senior doctor and psychosocial practitioner. The focus is on the non-clinical aspects (e.g. psychosocial, ethical and emotional issues) surrounding the patient–caregiver relationship – thereby addressing a wide range of important topics rarely discussed elsewhere – and the attendees are encouraged to be open and honest, and reflect, discuss and explore their experiences thoughts and feelings. The interaction between the panellists and audience is felt to foster insight and support from colleagues, create a sense of working in a supportive environment and lead to improved relationships and communication within the hospital hierarchy, improved communication and teamwork between staff and patients and among staff, improved well-being of staff including enhanced resilience, improved compassionate care and ultimately impact on organisational culture.
Some sources explicitly articulated what Rounds were not. This included that aims were distinct from traditional clinical/grand rounds; that stories and discussions should not focus on the patient, their diagnosis or plan of care; that Rounds should not be used for problem-solving or to determine what could be learned clinically; and that they were not intended to produce actionable outputs.
The evidence base for Rounds
We included 10 publications18,19,23–30 that reported findings from eight separate studies (four in the USA,24–28 comprising five publications; and four in the UK,18,19,23,29,30 also comprising five publications) (see Report Supplementary Material 2). The majority were mixed-methods evaluations (n = 5 studies,18,19,23,27–30 seven publications), with two quantitative studies25,26 and one qualitative study. 24 Mixed-methods studies typically comprised attenders completing evaluation forms post Round attendance, together with either interviews or focus groups. Only one study23 included non-attenders. No studies reported the characteristics of the audience samples they recruited from (e.g. in relation to professional groups), although one study reported a higher proportion of doctors in one site that they hypothesised was related to Rounds being held in a medical education building and championed by the medical director. 29 Participants in three of the studies18,25,26 were students, and for the qualitative studies were typically purposively selected to represent a range of professional groups and/or roles within Rounds, but findings were not presented according to these characteristics. In two studies19,27 that did report the characteristics of their quantitative sample, most were female and of white ethnicity, and nurses predominated (but neither study reported the seniority of the nurses). In one paper,24 the authors mentioned, when justifying their planned focus group with nurses, that many nurses could not attend Rounds, but did not provide any data to support this. The overall quality of the evidence base is low to moderate: the majority of studies have weak study designs (cross-sectional), use non-validated questionnaires (typically self-report views/satisfaction with Rounds and impact of attendance, most using the same questions as, or similar questions to, the US evaluation),27 and none of the quantitative evaluations had control group (non-attender) comparisons.
The findings show that Rounds are highly valued by attenders. In relation to impact, most studies reported positive impacts on ‘self’ (e.g. improved well-being, improved ability to cope with emotional difficulties at work, self-reflection/validation of experiences),18,19,23,24,26–30 on patients (increased compassion, empathy),23,26–30 and on colleagues (improved teamwork, compassion/empathy). 18,19,23,24,27–30 Four studies (five publications) provide evidence of wider institutional impacts from interviews with attenders, such as improving patient-centredness of care, and access to specific services (e.g. palliative care), and culture change through having dialogue that did not happen elsewhere, helping to build shared values and support a strategic vision. 23,24,27,29,30 Three of the included studies18,25,26 are evaluations of Rounds adapted for educational purposes, all reporting that Rounds were felt to be useful and that students gained knowledge/understanding about the emotional side of providing patient care.
Critical review of the alternatives to Rounds and their evidence base
Methods
Identification of alternative interventions to include in the review
Our prime aim was to identify interventions that aim to help support health professionals with the emotional challenges of delivering patient care. At the outset we identified some aspects of Rounds that we felt were fundamental to the intervention (i.e. hypothesised programme resources offered by the intervention) and that our informed choices regarding ‘alternative’ interventions. This included providing an opportunity for reflection and disclosure, and offering psychological safety. Other inclusion criteria included that interventions needed to focus on the psychological (as opposed to the physical) well-being of staff; be person directed (vs. work directed); and provide primarily emotional rather than cognitive/clinical support (thus, for example, excluding mortality/morbidity meetings that aim to provide lessons in terms of cognitive errors or systems issues). Although Schwartz Rounds are a ‘group’ (rather than an individual) intervention, we chose not to limit alternative interventions by this characteristic because of the importance of reflection and/or disclosure as a key potential mechanism in Rounds that is shared by other, non-group-based interventions. Existing reviews of psychological/emotional support interventions for clinical staff were used to identify alternative interventions. 31–34 Consultation with the PSG and advisory group led to the inclusion of other interventions (including action learning sets, restorative supervision, reflective practice groups, Balint groups and critical incident stress debriefing). A total of 11 alternative interventions were included (see Table 3).
Search strategy
Following the scoping literature review methodology outlined by Arksey and O’Malley,16 the search strategy involved three components: (1) a database search, (2) internet searches and (3) consultation with experts. To be included, evaluations of interventions had to (1) have a health professional sample (either qualified or trainee) and (2) evaluate the intervention using qualitative and/or quantitative methods. The review excluded non-English-language sources, unpublished dissertations or theses and any records not accessible via the methods stated below. Searches were from inception to 2015; all searches were conducted between 14 October 2014 and 5 February 2015, using the same databases as for the Schwartz review (see Appendix 3).
All records were pooled in a bibliographic database. First, records were screened to exclude duplicate entries. Second, the title and abstract of remaining records were reviewed for eligibility. Three attempts were made to access the full texts of papers: (1) university online library, (2) Google Scholar™ (Google, Inc., Mountain View, CA, USA) and (3) journal website. If the full texts were unavailable through these sources, then the papers were excluded.
Charting the data
The data from the included papers were extracted into a spreadsheet that included standard items to describe the paper (e.g. citation, country, setting, population/sample and overall design) and the evaluation [e.g. length of evaluation, data collection method(s), outcome measures and key findings]. In addition, items were developed that were specific to each intervention, for example whether the intervention was group or individual focused, the size of group, the length/number of sessions, the content of sessions, whether or not the intervention was facilitated and whether or not training was provided for facilitation/supervision. The key findings were examined across all of the included literature and analysed thematically to enable synthesis within, and comparison across, each intervention. This resulted in the identification of three categories regarding outcomes relating to (1) self, (2) others (e.g. patients and colleagues) or (3) organisational level (see Report Supplementary Material 3).
Quality appraisal
A quality assessment of each paper was conducted as described in Evidence base for Rounds.
Synthesis
A detailed descriptive summary of each intervention was produced, which included a narrative description of the intervention [including the number of participants, the original setting and health-care setting(s), and the intended aims/outcomes], the number and type of included papers, the variability in intervention (fidelity to original format), a synthesis of the main findings across papers, and the overall quality of the evidence base. See Table 3 for a summary description of each intervention and see Report Supplementary Material 3 for other information.
Comparing alternative interventions with Rounds
To compare each intervention with Rounds, it was necessary first to define the key features of Rounds. The composite definition of Rounds, and features that were explicitly ‘not’ part of Rounds, underpinned this. Each descriptive feature in the definition was extracted into a table, together with the features that were ‘not’ part of Rounds. Further clarification was added for some descriptive features to ensure clarity of meaning (e.g. ‘reflection’ became ‘provides an explicit opportunity for reflection’), which became the basis for comparison with other interventions (see Tables 4 and 5). The intended outcomes within the composite definition were not included in the comparisons owing to their broad nature and, therefore, lack of discriminatory power. The completed table was shared with the study advisory and steering groups to test the face validity of the ratings.
Results
A total of 11 alternative interventions were identified (Table 3). Electronic searches yielded a total of 1725 papers, of which 146 were included (ranging between 1 and 64 across interventions) (see Appendix 5 for a list of the included references). Of these, 74 were quantitative (randomised controlled trial, observational, quasi-experimental), 41 were qualitative (mixed designs, interviews, focus groups), 22 were mixed methods and nine were secondary studies (literature reviews). The literature was international, with the majority of studies from the USA and the UK; other countries represented included Canada, Australia, Finland, Norway, Sweden, Croatia, Spain, Italy, Israel and South Africa. There was a distinct lack of studies from Asia, although that may have been a result of the requirement that studies had to be in the English language.
| Intervention | Description of intervention | Database search result | Total excluded (duplicates; not eligible; full paper not available) | Papers from experts/internet search | Total number included for review |
|---|---|---|---|---|---|
| ALS | Based on the concept of learning by reflection on (or reviewing) an experience, an ALS usually contains 4–6 members (peers), with (or without) a ‘set advisor’ to facilitate the process. ALSs tend to be held intermittently, over a fixed programme cycle, and most participants contract with the facilitator for an agreed length of time. They are often closed groups. The set is not a team, as the focus is on actions of individuals, rather than shared work objectives | 83 | 70 (8; 36; 26) | 1 | 14 |
| AAR | AARs are facilitated meetings, led by a senior member of staff, that aim to encourage active reflection on performance following a specific event. An AAR is a one-off meeting post event and includes those who were involved with the event. The focus is on gaps in performance, and what could be done differently to enhance the outcome. AARs generally last about 30 minutes | 76 | 74 (9; 64; 1) | 0 | 2 |
| Balint groups | Balint groups meet every 1–4 weeks for 1–3 years. In the group, typically a doctor presents a troubling patient incident while the group listens. The goal of the presentation is to understand the issue from both the patient’s and doctor’s perspectives. The presentation can last about 10 minutes, after which group members can ask clarifying questions. When all questions are exhausted, the group is invited to imagine themselves in the roles of the doctor and the patient | 384 | 358 (170; 151; 37) | 0 | 26 |
| CSP | Originally developed for mental health/learning disability care homes, CSP is described as a theory-based social support intervention aimed at increasing exchanges of social support and decreasing negative social interaction. It consists of six 4- to 5-hour group training sessions (10 managers, 10 direct-care staff and two facilitators) conducted over a 9-week period. Strategies for improvement are drawn from the participants, based on their own experiences | 84 | 83 (10, 71, 2) | 2 | 3 |
| Clinical and restorative supervision | Clinical supervision originally arose out of psychotherapy but has been adopted by other disciplines, such as psychology and nursing. The process has been described as identifying a key issue, describing and defining it, undertaking a critical analysis, examining solutions, formulating an action plan, implementation and evaluation. It can take five different forms: one-to-one with expert from same discipline; one-to-one with supervisor from different discipline; one-to-one with colleague of similar expertise; supervision between groups of colleagues working together, and network supervision between people who do not usually work together | 307 | 252 (42, 160, 50) | 9 | 64 |
| Resilience training | Resilience training is in part based on CBT theories and in its original form is a manualised intervention comprising 18 hours of workshops. The key characteristics are that it is delivered to groups of practitioners who support one another, and is facilitated by an expert in personal and professional transition supervision. One of the better known Resilience training programmes was developed at the University of Pennsylvania and consists of: learning ways to challenge unrealistic negative beliefs, strengthening problem-solving, adopting assertiveness and negotiation skills, improving ability to deal with strong feelings, and learning how to tackle procrastination through use of decision-making and action-planning tools | 144 | 138 (36, 72, 30) | 0 | 6 |
| CISD | In its original form, CISD is a single-issue debriefing session in a group context, led by an external team, following a traumatic event. CISD has seven phases: introduction, fact, thought, reaction, symptom, teaching and re-entry. The debriefing session lasts for approximately 1.5–3 hours and takes place 24–72 hours after the traumatic event. The debriefing team is made up of a leader, a co-leader and a support, who work in conjunction to support the participants and to allow them to feel safe | 388 | 386 (62; 248; 76) | 0 | 2 |
| Peer-supported storytelling | Narrative storytelling is the act of an individual recounting verbally to one or more people a plausible account of an event, or series of events, possessing narrative truth for the teller. The story is arranged in a time sequence with plot, characters, context, intentionality and perspective taking, possibly including the teller’s actions, thoughts and feelings | 4 | 3 (3; 0; 0) | 0 | 1 |
| RPG | RPGs are facilitated groups of about 10 health-care professionals or students in which participants share and explore professional, clinical, ethical, and personal insights arising from their clinical work or training. RPGs are ongoing and convene regularly, with each group lasting for about 1 hour. Discussion topics can be raised by either the facilitator or the participants. The discussion is meant to be supportive as well as challenging, encouraging consideration of alternative viewpoints | 91 | 83 (8; 73; 2) | 0 | 8 |
| Psychosocial intervention training | Psychosocial intervention training involves cognitive behavioural approaches for managing symptoms, understanding symptom-related behaviour, relationship formation and helping service users to cope with symptoms. Teaching sessions are supplemented by small group supervision. Students are required to provide brief case study presentations about service users they are working with and receive feedback. Early courses were developed for nurses but quickly became multidisciplinary | 37 | 35 (6; 25; 4) | 1 | 3 |
| MBSR | The central principle of MBSR is mindfulness: being focused on and aware of the present moment with a non-judging attitude of acceptance. The original training module is 8 weeks long with weekly sessions of 2.5 hours each. There is a 7-hour session, which takes place between weeks 6 and 7, and participants are asked to complete 45 minutes of daily formal mindful practice. They are taught a variety of mindful meditative practices, and there are group discussions about the application of these practices | 127 | 110 (13; 72; 25) | 0 | 17 |
| Total | 1725 | 1592 (367; 972; 253) | 13 | 146 |
A summary of the evidence base for each intervention is provided in Report Supplementary Material 3. For most interventions the evidence was sparse. Populations for many of the interventions lacked diversity across health professions and settings, with many mostly nursing-focused. The aims of studies varied widely, with a few aimed at assessing efficacy/effectiveness, but most were small-scale exploratory descriptive studies. The content/format of interventions (fidelity) was, in most cases, widely heterogeneous (and/or lacked detail), and, consequently, a synthesis of findings is problematic. Most of the quantitative evaluations across all interventions relied on weak study designs (e.g. they were cross-sectional studies or post-intervention evaluations, or were lacking control comparisons), used non-probability sampling and had small samples likely to be underpowered, and used non-validated outcome measures. Many qualitative studies also lacked rigour (e.g. limited reporting of member checking, deviant cases, reflexivity or evidence of data saturation).
Most interventions had been evaluated in relation to impact on all three layers of outcomes (self, others and organisation). Evidence for resilience training, mindfulness-based stress reduction and reflective practice groups lacked inclusion of organisational outcomes.
The findings suggest that all of the interventions had evidence of positive benefits to self (e.g. raised self-awareness, resilience, job satisfaction, empowerment, or overall well-being), and most provided some evidence of positive benefits to ‘others’ (albeit that interpretation is constrained by the methodological limitations highlighted above). For patients, this included a fostering of better relationships, communication with and/or attitudes towards patients; and improved patient-centredness, knowledge of patients’ suffering and empathy. For colleagues, this included associations with better teamwork, peer support and knowledge/understanding of colleagues.
At organisational level, there was evidence from some interventions of association with improved practice, for example reductions in unnecessary prescriptions, an increased uptake of psychosocial support (Balint groups), a reduction in task and co-ordination errors, and an increased uptake of post-fall huddles (after-action reviews). Two interventions provided evidence of a positive impact on the workforce, including providing opportunities for mentoring and advice (action learning sets) and improved staff retention (clinical supervision).
Rounds versus alternative interventions: comparative features
In comparison with the alternative interventions, Rounds offer a unique organisation-wide ‘all-staff’ open forum to share stories about the emotional impact of providing patient care (Tables 4 and 5). Although many of the other interventions expect ‘open, honest communication’ as a key feature, and provide an explicit opportunity for reflection, none is open to all staff (e.g. clinical and non-clinical, voluntary attendance), and many are not ongoing programmes but are instead one-off training courses or events. Some of the training interventions (e.g. mindfulness-based stress reduction or resilience training) are multidisciplinary, but the intended outcome is practice of the skills learned, and so is individual based rather than group based.
| Number | Feature of Rounds | Intervention | |||||
|---|---|---|---|---|---|---|---|
| Balint groups | Clinical and restorative supervision | AARs | ALS | RPGs | CISD | ||
| 1 | Share challenging/rewarding experiences about delivering patient care | Yes | Yes | No | Not necessarily | Yes | Yes |
| 2 | Focus on psychosocial and emotional issues of patient–caregiver relationships | Yes | Not necessarily | No | Not necessarily | Not necessarily | Not necessarily |
| 3 | Provides an explicit opportunity for reflection | Yes | Yes | Yes | Yes | Yes | Yes |
| 4 | Open, honest communication | Yes | Yes | Yes | Yes | Yes | Yes |
| 5 | Provides an opportunity to give and/or receive peer support | Yes | Yes, if group supervision | Not necessarily | Yes | Yes | Yes |
| 6 | Telling and hearing stories related by theme, scenario or patient case | No | No | Yes | No | No | No |
| 7 | Ongoing programme (vs. one-off) | Yes | Yes | No | No | Yes | No |
| 8 | Time-fixed session (vs. flexible length/unspecified) | Yes | Yes | No | No | No | No |
| 9 | Planned provision of food/refreshments | No | No | No | No | No | No |
| 10 | Open to all/any clinical and non-clinical staff | No | No | Yes | No | No | No |
| 11 | All levels of staff/no hierarchy | No | No | Yes | Yes | No | No |
| 12 | Open group membership (vs. closed/invited members only) | No | No | No | No | No | No |
| 13 | Multidisciplinary | Not necessarily | No | Yes | Yes (can be uni or multi) | No | Yes (can be uni or multi) |
| 14 | Pre-prepared/rehearsed stories or focus | No | No | No | Yes | No | No |
| 15 | Facilitated discussions | Yes | Yes | Yes | Not necessarily | Yes | Yes |
| 16 | Panel presenters tell stories giving their perspectives on a theme, scenario or patient case | No | No | No | No | No | No |
| 17 | Group intervention | Yes | Yes (can be) | Yes | Yes | Yes | Yes |
| 18 | Organisational support: senior doctor/clinician champions | Yes | Yes | Yes | Not necessarily | No | Not necessarily |
| 19 | Safe and confidential environment | Yes | Yes | Yes | Yes | Yes | Yes |
| Features that define what Rounds are ‘not’ | |||||||
| 1 | Problem-solving | Yes | Yes | Yes | Yes | No | Not necessarily |
| 2 | Production of actionable outputs | No | Not necessarily | Yes | Yes | No | No |
| 3 | Flexibility in format (vs. licensed/contracta) | Yes (though facilitators should be accredited) | Yes | Yes | Yes | Yes, lack a standardised consistent approach | Yes |
| 4 | Focus on clinical aspects of patient care, their diagnosis or plan of care | No | Not necessarily | Not necessarily | Not necessarily | Not necessarily | Not necessarily |
| Number | Feature of Rounds | Intervention | ||||
|---|---|---|---|---|---|---|
| MBSR programmes | Peer-supported storytelling | Psychosocial intervention training | CSP | Resilience training | ||
| Features that are part of Rounds | ||||||
| 1 | Share challenging/rewarding experiences about delivering patient care | No | Not necessarily | Yes | Not necessarily | Not necessarily |
| 2 | Focus on psychosocial and emotional issues of patient–caregiver relationships | No | Not necessarily | Not necessarily | Not necessarily | Not necessarily |
| 3 | Provides an explicit opportunity for reflection | Yes | Yes | Yes | Not necessarily | Not necessarily |
| 4 | Open, honest communication | Yes | Yes | Yes | Yes | Not necessarily |
| 5 | Provides an opportunity to give and/or receive peer support | Yes | Yes | No | Yes | Yes |
| 6 | Telling and hearing stories related by theme, scenario or patient case | No | Yes | No | Not necessarily | No |
| 7 | Ongoing programme (vs. one-off) | No | No | No | No | No |
| 8 | Time-fixed session (vs. flexible length/unspecified) | Yes | No | Yes | Yes | Yes |
| 9 | Planned provision of food/refreshments | No | No | No | No | No |
| 10 | Open to all/any clinical and non-clinical staff | No | No | No | No (only direct care and managers) | Not necessarily |
| 11 | All levels of staff/no hierarchy | Yes | Yes (probably) | Yes | Yes | Yes |
| 12 | Open group membership (vs. closed/invited members only) | No | No | No | No | No |
| 13 | Multidisciplinary | Yes | Not necessarily | Yes | Yes | Not necessarily |
| 14 | Pre-prepared stories/focus; steering group | No | Yes | No | No | No |
| 15 | Facilitated discussions | Yes | No | Yes | Yes | Yes |
| 16 | Panel presenters tell stories giving their perspectives on a theme, scenario of patient case | No | No | No | No | No |
| 17 | Group intervention | Yes | No | Yes | Yes | Yes |
| 18 | Organisational support: senior doctor/clinical champions | No | No | No | Yes | No |
| 19 | Safe and confidential environment | Yes | Yes | Yes | Yes | Yes |
| Features that define what Rounds are ‘not’ | ||||||
| 1 | Problem-solving | No | No | Yes | Yes | Yes |
| 2 | Production of actionable outputs | No | No | No | No | No |
| 3 | Flexibility in format (vs. licensed/contracta) | Yes | Yes | No | Manualised but adapted to experiences of group | Manualised but adapted to experiences of group |
| 4 | Focus on clinical aspects of patient care, their diagnosis or plan of care | No | Not necessarily | Yes | Not necessarily | Not necessarily |
Other key aspects in which Rounds are distinct from the alternative interventions relate to what Rounds are intentionally ‘not’ meant to be. In particular, discussions within Rounds should not ‘problem solve’, whereas problem-solving/action-planning are key features of many of the other interventions (e.g. action learning sets, after-action reviews, critical incident stress debriefing). Most of the alternative interventions also offered flexibility in format, compared with the contractual licence (with stipulated conditions) required for running Rounds.
Arguably the closest types of interventions to Rounds are Balint groups (albeit rooted in unidisciplinary primary care with closed membership) and reflective practice groups (again generally closed membership and can be unidisciplinary). In particular, both are ongoing group programmes in which challenging/rewarding experiences about delivering patient care are shared and discussions are facilitated, and both provide the opportunity to give and/or receive peer support in safe and confidential environments. However, neither offers an organisation-wide opportunity for staff to attend, and both would have an expectation that members/attenders would contribute, whereas in Rounds, attenders can choose to be silent listeners.
Part B: developing an understanding about how Schwartz Rounds may work
To develop an initial understanding about how Rounds may work (to inform the initial programme theory, see Chapter 8, and to inform phase 2 work) we undertook two activities: (1) we explored theories about how rounds may work and (2) we interviewed the original architects of Rounds in Boston, MA, USA.
Exploration of theories about how Rounds may work (e.g. the context, mechanisms and outcomes related to Rounds)
This section aims to answer aim 5 above: to explore the theoretical literature on reflection, group work, disclosure and safe environment. In theorising about how Rounds might work, we needed to try to unpack the ‘black box’ of what happens in the monthly 1 hour of Rounds. To do this we drew on realist terminology, which uses the term ‘mechanisms’ to describe how interventions work, ‘context’ to describe the factors that trigger (or not) the mechanisms and ‘outcomes’ to describe the resulting effects. This initial theorising informed the development of our survey (see Chapter 5) and initial programme theory and interpretation of our study findings (see Chapter 8) (see Appendix 6 for a fuller review).
Methods
Theoretical literature was obtained using multiple strategies, including conducting searches on the internet and using databases such as Google Scholar; using key textbooks;35–38 consulting with our advisory and steering group members; and hand-searching references of key literature. Our approach to inclusion was broad at the outset – we did not restrict to theories that had a health-professional focus – but was focused by our understanding at that time about how Rounds worked and the key components of Rounds (e.g. from our composite definition reported earlier). For example, we initially explored all theories that had ‘reflection’ as a key component, but found that many early theories separated learning and emotion, and as emotion is central to Rounds we instead searched for theories of reflection that included emotion as a key element. We searched for theories describing reflection, group work, disclosure and/or safe environments either as outcomes (enabling us to examine mechanisms/antecedents to them) or as processes/mechanisms in themselves, leading to other outcomes. Theories were examined and included based on (1) their relevance to Rounds (e.g. group setting and emotion central to reflection) and (2) their relationship to context, mechanisms and outcomes based on our developing programme theory.
Disclosure
Disclosure is the action of making new information known. In psychological terms, it is the ‘social sharing of emotion’. 39 Two main theorists on the psychological aspects of disclosure are Rimé and Pennebaker. Rimé and colleagues39–41 have focused on how individuals socially share emotions with others following an emotional event, and the effects of this on emotional recovery. Pennebaker and colleagues35,42–44 have focused on the effects of disclosure of emotional events on physical and psychological health.
Emotion is an essential aspect of describing trauma. People experience greater health benefits if they share emotions and thoughts surrounding trauma than if they share facts;42,45 using language to label an emotion/experience creates a structure, which facilitates understanding of the event. 43 Similarly, Lepore et al. ’s46 ‘completion hypothesis’ states that putting one’s experiences into language allows individuals to impose a narrative around it, making it comprehensible to themselves and others. Conversely, actively inhibiting thoughts and feelings ‘gradually undermines the body’s defences’ (p. 2),35 which leads to reduced physical well-being. Confronting significant events helps us understand and assimilate the event, which improves physical and emotional well-being. 35
Of all emotions, people are least likely to share feelings of guilt or shame. 39 Non-disclosure is associated with the anticipation of negative interpersonal responses to disclosure (e.g. labelling or judging). 47 The benefits of disclosure vary according to the listener’s response to it. 45,48 Nils and Rimé48 identified two responses: the empathic mode buffers emotional distress temporarily (the individual feels better) and the reframing mode leads to emotional recovery (the individual’s basic assumptions are positively modified). However, when disclosure of events is invalidated, any benefits may be diluted. 46
Application of disclosure theories to Rounds
Drawing on the disclosure theories above, Rounds focus on non-clinical aspects of the patient–caregiver relationship, not problem-solving, and allow individuals to share difficult, challenging and rewarding experiences. Rounds allow individuals to disclose emotional experiences; greater health benefits ensue following the sharing of emotions and thoughts rather than the sharing of facts. Round attendees and panellists are encouraged to be open and honest and to discuss their experiences, thoughts and feelings: using language to help understand their emotional response to an event/experience. Effective facilitation by the facilitator/clinical lead can help individuals reframe and label their emotions, and thus begin to process and understand them. The benefits of disclosure vary according to the listener’s response. Group interventions mean that it is difficult to control others’ reactions to what has been disclosed. However, Rounds are designed to be a safe, confidential space where staff can share their experiences without fear of blame or judgement.
Safe environment
A safe emotional environment is important for group work, reflection and disclosure. Emotional safety is achieved in attached relationships where there is openness, vulnerability and trust. Emotional safety at work derives primarily from the experience of feeling valued, accepted, recognised and respected. 49
Emotional safety is one element that generates a sense of community,50 where it is safe to tell the ‘truth’, requiring community empathy, understanding and caring. Boundaries – or containment – ensure that the group is ‘purposeful, bounded and safe’. 51 Effective leaders (in Rounds this means clinical leads and facilitators) are necessary to construct these conditions. Another element necessary to develop a community is a sense of belonging.
Psychological safety ‘is a shared belief that the team is safe for interpersonal risk taking’. 52 In psychologically safe teams, members feel accepted and respected and think less about the potential negative consequences of expressing themselves. Leaders increase psychological safety by empowering members of the group to participate, and in collaboratively addressing concerns. With psychological safety there is a ‘sense of confidence that the team will not embarrass, reject or punish someone for speaking up’. 52
Application of the ‘safe environment’ theories to Rounds
Drawing on the safe environment theories above, the panellists and audience need to feel emotionally safe in Rounds to share their story or experience without fear of reprisal or blame. Facilitators foster a sense of psychological safety in the Round through their skills in facilitation, group work and psychological insights. Ground rules and the use of an established protocol for Rounds helps create a confidential and safe environment that, together with a sense of community, is necessary for Rounds to work (see Chapter 7, Fidelity to the Schwartz Rounds model). The experiences shared are contained as a result of the clear boundaries established, which creates a safe, confidential space for reflection.
Reflection
Reflection is a ‘generic term for those intellectual and affective activities in which individuals engage to explore their experiences in order to lead to new understandings and appreciation’ (p. 3). 53 Theories of reflection suggest that it is a structured learning activity in which questions are answered and knowledge is created36,54,55 and argue that reflection is a rational act, and although emotion is a trigger or catalyst for reflection, its role is limited.
More recently, psychologists and sociologists including Lazarus,56 Mezirow57 and Goleman58 have argued that emotion plays a central role throughout the reflective process and that emotion cannot be separated from learning. Emotional intelligence is said to be highly complementary to reflective practice;58 individuals need to understand not only themselves, but also others, and their feelings and empathy are key to emotional intelligence and important to reflective practice. 59 For a person to ‘grow’, an environment is required that provides genuineness (openness and self-disclosure), acceptance (being seen with unconditional positive regard) and empathy (being listened to and understood). 60
Barriers to reflection can be practical (e.g. finding the time,55 location) and/or psychological (e.g. fear of judgement, criticism). The timing of reflective practice is crucial, especially in relation to stressful/tense experiences. A review soon after an incident is deemed ‘hot’ (emotive): it is subjective and influenced by emotions. Reviews held later are ‘cold’: emotions have cooled and the reflective practice is clearer, more balanced and objective, which leads to improved reflections. 61 Ixer62 suggests that individuals need non-judgemental support; they need to feel ‘safe’; they need a role model (e.g. a mentor who reflects on their own practice); they need opportunities for reflection; and they need time and energy. 63
Application of reflection theories to Rounds
Drawing on the reflection theories above, Rounds are not designed for problem-solving or to determine what can be learned clinically, although learning may occur. Nor are they intended to produce actionable outputs. Theories of experiential learning – where emotion plays a central role in reflection – therefore appear more relevant.
Consideration of the timing of a Round is important and it is, therefore, important that those preparing Rounds carefully consider who they ask to present and when: not too soon, or when the subject matter is too ‘hot’.
Reflective rational enquiry64 seems particularly relevant to the workings of a Round. Rounds are a combination of self-reflection and collective reflective work, which create shared knowledge at the individual and institutional levels. This may include personal outcomes such as improved well-being, dyadic and team-based outcomes such as better communication and teamwork, and institutional outcomes such as changes to hospital culture. 27,29,30 Finally, empathy is key to reflective practice. Increased compassion and empathy is the main intended outcome of Rounds: for the individuals attending but also in their interactions with patients and their families.
Social support and group work
Social support is the perception and actuality that you are cared for, that you have assistance available from other people and that you are part of a supportive social network; ‘group work provides a context in which individuals help each other and can enable individuals and groups to influence and change personal, group, organisation and community problems’ (p. 8). 38
Social support is associated with psychological well-being in the workplace and is hypothesised to work by having either a buffering effect (where it moderates an outcome) or a direct effect (leading directly to something). 65,66 Karasek’s65 job–demands–control model is a ‘buffering model’, as work social support (such as support from colleagues and supervisors) is said to buffer against job demands/lack of control, thereby protecting mental and physical health. 67,68
Social exchange theory details the negotiated exchanges between people (tangible and intangible) as more or less rewarding or costly. 69 Cost could be the effort put into a relationship (e.g. time). Rewards include elements of the relationship that have positive value (e.g. acceptance, support and companionship). Social exchange involves a connection and trust with another and brings satisfaction when people receive fair returns for their expenditures. The effort–reward imbalance is associated with poor health functioning.
Group work is the opportunity to reflect on, and learn from, the nature of the group interaction itself. The group context and group process is explicitly utilised as a mechanism of change by developing, exploring and examining interactions within the group. A number of therapeutic factors that facilitate group work include universality, altruism, instillation of hope, cohesiveness, catharsis, interpersonal learning and self-understanding. 37
Application of social support and group work theories to Rounds
Drawing on the social support and group work theories above, Rounds are a group intervention, with social support provided through group reflection. Social identification as a member of a Round may serve to boost self-esteem as individuals have a sense of belonging to an organisation-wide forum. The cost–benefit analysis of social exchange theory appears pertinent to how a Round works. Costs might include the courage, emotional effort and time put into sharing one’s story publicly (panel preparation, sharing the story during the Round). Rewards may include increased compassion and empathy for others, improved well-being (e.g. reduced stress) and camaraderie (better work engagement and teamwork).
When members tell their story to a supportive audience, they can obtain relief from feelings of shame and guilt. Yalom and Leszcz’s37 therapeutic factors appear relevant to how Rounds work, and these are explored further in Chapter 8.
In addition to work reviewing theories in the literature, which informed our initial programme theory (see Chapter 8) and the selection of items for our survey (see Appendices 1 and 6), we thought it important to understand more about the development and origins of Rounds in Boston, MA, USA, and any programme logic behind their development.
The initial development of Rounds in Boston, MA, USA, and underlying principles
Two members of the research team (ER and ML) visited the SCCH in Boston, MA, USA (8–12 June 2015). The purpose of the trip was to help develop our initial realist evaluation programme theory and identify the underpinning programme logic behind how Rounds are intended to work (see Box 3). This was based on information from those involved in developing and running Rounds, including the ‘programme architects’, Kenneth Schwartz’s family members, facilitators and members of the SCCH, and others currently running Rounds in the USA. We conducted two group interviews and three individual interviews, and observed two Rounds and one debriefing meeting between facilitators and a regional advisor from the SCCH.
Analysis
The interviews with key stakeholders and observations of Rounds were analysed separately, before the main data collection and analysis of case studies in phase 2. A semistructured interview schedule (see Appendix 7) was developed to describe and explore participants’ experience of developing and/or running Schwartz Rounds in the USA. Each interview was transcribed by a professional transcription service and analysed using a thematic analysis approach, following the key stages of data familiarisation, data reduction and interpretation.
Key findings
From the visit, we identified some guiding principles underlying Rounds:
-
they were a way of teaching caregivers to be compassionate and that compassion could be taught
-
they needed to be inclusive and multidisciplinary
-
they needed to be structured in a way that would encourage doctors to attend
-
they needed to be structured and have a format with a topic and a panel, to focus on the non-medical aspects of care and to not be a forum for problem-solving
-
they needed to have support from organisation’s leadership (including attendance) to make visible the organisation’s values that connecting with patients and supporting staff is important
-
the space created needed to be non-judgemental and safe to encourage people to speak and share their experiences and to protect panel members and participants from any bullying behaviour that could arise from sharing their experiences
-
the role of the moderator was important and they needed to create a safe space and show vulnerability.
These principles informed our initial programme theory (see Chapter 8) and led to the research team reflecting and theorising about fidelity and adaptation issues, and identifying and testing which aspects of Rounds could be considered (i.e. core and adaptable periphery components in phase 2 case studies). 70
Chapter summary
There is an emerging literature regarding Rounds, although much of this is non-empirical in nature. Few research evaluations have been published, and those that have are generally limited in relation to their quality. Particular problems in quantitative studies include the lack of control/comparison groups and the use of unvalidated measures. However, findings are consistent across studies about the value of Rounds to attenders, and the self-reported positive impact on individuals, their relationships with colleagues and patients, and wider cultural changes. Key mechanisms by which Rounds are hypothesised to work are through reflection, group work, disclosure and a safe environment (see Chapter 8).
The evidence base for other interventions that may be comparable with Rounds is sparse and lacking in quality. Major challenges include fidelity across different studies and lack of robust methodology. The process of implementation is rarely described in adequate depth to understand the extent to which results are a direct result of an intervention or the way in which an intervention is implemented. Compared with these alternative interventions, Rounds offer a unique organisation-wide ‘all-staff’ forum to reflect on the emotional impact of providing patient care, offering opportunities for staff to reflect, whether or not they choose to disclose or contribute to discussions.
Chapter 4 Mapping Schwartz Rounds
Introduction
The aims and objectives of the mapping element of phase 1 were to map the profiles of current UK Rounds providers including the reasons for (and time since) implementation, how organisations had implemented Rounds, and attendance at Rounds; and to determine the cost and resource implications required to establish and sustain Rounds (objective 6). These profiles also informed sampling of phase 2 case study sites for maximum variation.
This chapter includes reference to findings reported in Robert et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Methods
Overall design
A mixed-methods approach comprising:
-
the collation and analysis of secondary data to map and profile Rounds providers
-
an online cross-sectional survey and telephone interviews completed by the clinical lead or facilitator in Rounds providers.
Sampling frames and samples
In our study protocol we estimated that there would be 40 Rounds providers by the start date of the evaluation (see Chapter 2). By September 2014, when the mapping phase began, there were 81 Rounds providers, and by the end of 2016 there were 154 providers. Given the challenge of evaluating a ‘live’ intervention (with Rounds adoption spreading rapidly during the life of the evaluation) and to provide as many current data as possible, the sampling frames differed for primary and secondary data sources.
The sampling frame for primary data collection (survey and interviews) was all providers in England that were running Rounds (defined as having been sent a contract by PoCF) at 1 September 2014 (evaluation start date) (n = 77). For secondary data, the sampling frame comprised all Rounds providers in England at 15 July 2015 (n = 115; see also Robert et al. 1). Providers in Scotland and Wales (n = 8) were excluded as (1) contracts were with health boards rather than individual providers and (2) comparable secondary data were unavailable. Provider details were obtained from the PoCF, as a licence was required from PoCF before Rounds were implemented, and so this was a reliable data source.
Data collection access
The PoCF requested permission from providers to share their details with the research team, giving 2 weeks to opt out: no provider refused permission. Local R&D approval was required for 66 of the 77 providers before invitations to participants could be sent. This was received from only 53 of the 66 that required approval (Figure 3). The clinical lead or facilitator for each provider that we had permission to contact was e-mailed the study information and invited to participate in the survey and interview.
FIGURE 3.
Recruitment and data completion for survey and interviews.
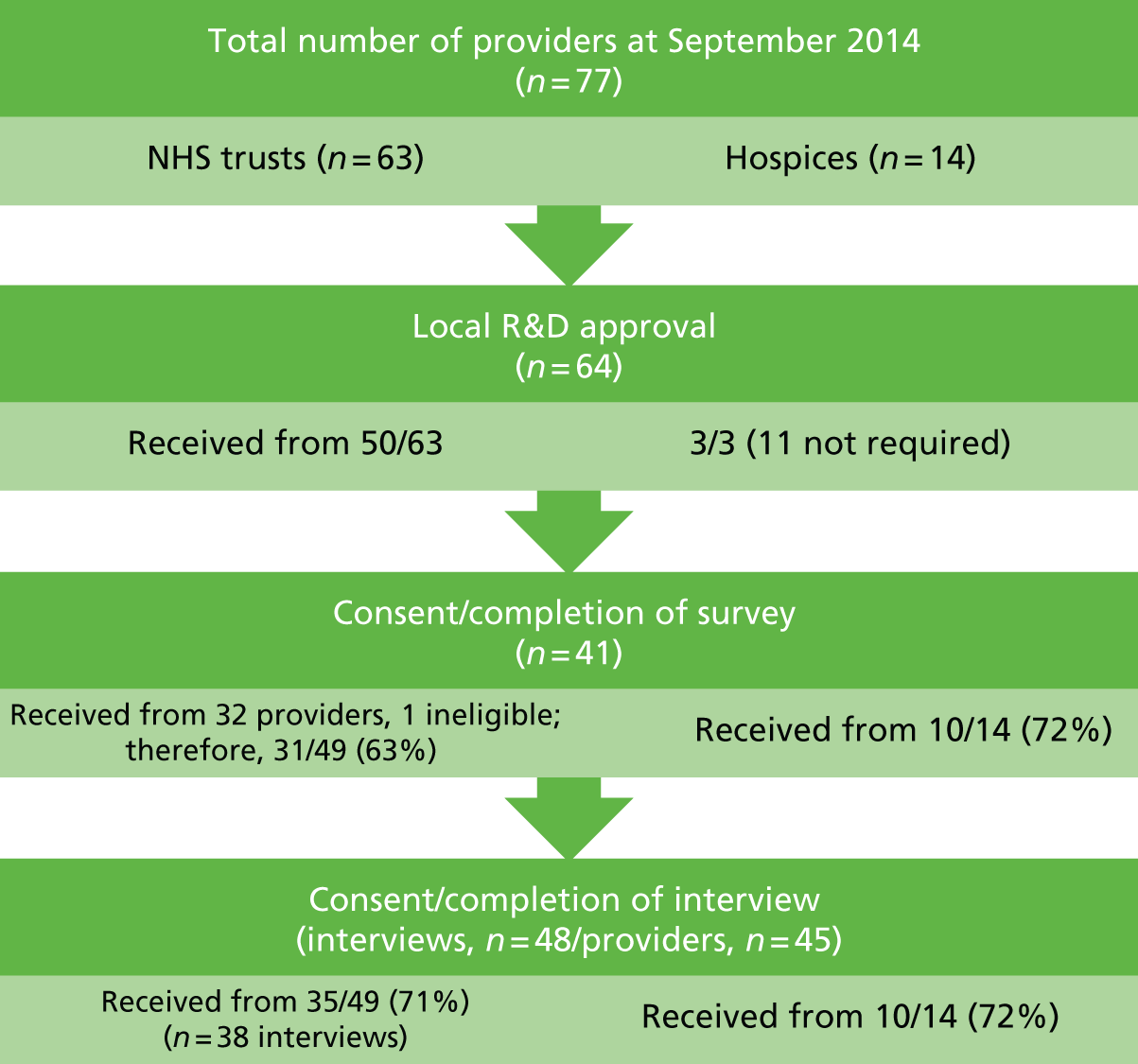
Surveys were received from 42 providers, although one was ineligible as it had not started running Rounds. Interviews were conducted with 48 individuals from 45 providers (three were interviews involving two participants together). Of the eligible providers (n = 76), the survey response rate was 41 out of 76 (54%) and for interviews the rate was 45 out of 76 (59%; see Figure 3). Among the providers that granted local governance approval (or did not require this), response rates were 41 out of 64 (64%) for the survey and 45 out of 64 (70%) for interviews. All sites were given pseudonyms to protect their anonymity. For site IDs we have used pseudonyms (rivers for mapping sites and trees for case study sites) (see Appendix 8 for provider profiles).
Most providers completed both the survey and the interview (n = 39; the same participant completed both in 35 providers). Six providers participated in the interview only, and three completed the survey only.
Data collection
Secondary data
Secondary data for the 115 providers in England (at 15 July 2015) were collated from the PoCF, NHS Digital (www.hscic.gov.uk), Hospice UK (www.hospiceuk.org) and provider websites. These included the date of adoption of Rounds, their location, and the size and type of provider. When available, data were extracted for each provider from the NHS staff and patient surveys, and from the Care Quality Commission (CQC) (see Appendix 9 for further details).
Online survey
Questions were developed by the project team (with input from advisory and steering group members) to capture details of implementation of Rounds. The survey comprised seven sections with between 45 and 84 questions, covering preparation for implementation, how Rounds had been implemented (e.g. frequency of Rounds, typical attendance numbers and staff groups, how Rounds are publicised) and the resources/costs (staff and non-staff) incurred (see Appendix 10 for the survey). The survey was managed via Qualtrics (an online survey program; Provo, UT, USA; www.qualtrics.com). A survey link was e-mailed to all consenting participants (with reminders 10 and 20 days after the initial invitation).
Telephone interviews
Semistructured telephone interviews, lasting between 30 and 60 minutes, covered how Rounds were introduced, organised and run; and respondents’ views on their impact, and sustainability (see Appendix 11 for the interview schedule). Interviews were digitally recorded, saved to a password-protected network drive and transcribed for analysis (except one for which notes were recorded by hand). Interview data were also used in staff experiences and realist evaluation chapters (see Chapters 6 and 8).
Survey and interview data were collected between January and August 2015.
Pilot testing
The survey and interview schedule were piloted with project advisory and steering group members, and three ‘critical friends’ who facilitated or led Rounds. Minor changes to the survey resulted (e.g. ensuring that staff groups also reflected non-NHS categories). Following discussion of interview questions in the first 3 months of data collection, a question asking how respondents felt Rounds ‘worked’ was removed (as interviewees found this difficult to understand and answer). This was replaced with ‘Do you think Rounds have an impact on staff? If so in what way(s)’ (respondents were encouraged to consider short-, medium- and longer-term impacts).
Data analysis
Secondary data
Descriptive statistics were used to describe the profiles of the Rounds organisations (including the type of service provider and location). We examined the timing of adoption of Rounds and categorised each site according to the categories of adopters described by Rogers71 in his ‘diffusion of innovation’ theory: innovators (first 2.5%), early adopters (next 13.5%), early majority (next 34%), late majority (next 34%) and laggards (final 16%) (see also Robert et al. 1). Inferential statistics were applied to compare adopters and non-adopters, and Rounds sites in different adoption categories, in relation to the three quality of care indicators, for all providers for which such data were available (see Appendix 9). Statistical significance was set at a p-value of < 0.05.
Survey
Data were examined for completeness and anomalies, and free-text responses were recategorised into existing or new categories when appropriate. It was necessary to exclude some providers from certain analyses, either because they were very early adopters (e.g. thereby preceding the PoCF licence/support package) or because they were very recent adopters (and thereby not able to provide reliable data about, for example, the frequency of Rounds). All quantitative data were analysed descriptively, initially as a total sample and then according to type of provider (e.g. NHS trust vs. hospice) and size of provider (small, < 2000 staff; medium, 2000–4999 staff; large, ≥ 5000 staff) using cross-tabulations. Cases were removed listwise if responses were missing. Free-text responses that could not be categorised were analysed thematically. Costs data were analysed as follows: average catering costs were divided by the mode attendance figure to give an average cost per person. Staff costs were calculated from the Agenda for Change (AfC) bands/staff grades provided and based on the hourly rates for hospital-based health-care staff provided by the Personal Social Services Research Unit. 72 Staff costs are based on 21 providers (seven small, seven medium and seven large) that gave complete data for their administrator(s), facilitator(s) and clinical lead(s), unless otherwise stated.
All quantitative analyses (secondary and survey) were conducted using SPSS (Statistical Product and Service Solutions) (version 22.0, 2013; IBM SPSS Statistics, Armonk, NY, USA).
Interviews
The interviews were analysed using a framework approach to organise the data around key topics addressed in the interview and themes that emerged from respondents’ accounts of their experiences of Rounds73,74 both inductively and deductively (e.g. reasons for adoption were analysed according to the six attributes of an innovation argued to predict adoption from Rogers’71 diffusion of innovation model). Four research team members familiarised themselves with the interview transcripts and contributed to the iterative process of clarifying, refining and elaborating themes. Our aim was to provide a rich picture of the diversity of practice, experiences and views in relation to running Rounds; to highlight the challenges faced and adaptations made by organisations; and to identify possible patterns and associations in the data. Matrices were developed to summarise and enable review of the data for each theme (akin to Gale et al. 75).
Results
How many and what types of organisations were running Rounds?
At 15 July 2015, 115 organisations in England had ‘adopted’ Rounds (Table 6). Over half (n = 71, 62%) were based in the south of England, with over one-quarter of all providers located in London (28%). Figure 4 shows the location of current Rounds providers (up to the end of 2016) (n = 154).
| Region | Frequency | Percentage of adopters (n = 115) |
|---|---|---|
| London | 32 | 27.8 |
| South East | 28 | 24.3 |
| South West | 11 | 9.6 |
| East of England | 8 | 7.0 |
| West Midlands | 8 | 7.0 |
| East Midlands | 3 | 2.6 |
| Yorkshire and the Humber | 7 | 6.1 |
| North East | 5 | 4.3 |
| North West | 13 | 11.3 |
| Total | 115 | 100 |
FIGURE 4.
Location of Schwartz Rounds sites in England (n = 154) up to the end of 2016. © OpenStreetMap contributors. These data are made available under the Open Database Licence http://opendatacommons.org/licenses/odbl/1.0/. Any rights in individual contents of the database are licensed under the Database Contents License: http://opendatacommons.org/licenses/dbcl/1.0/.
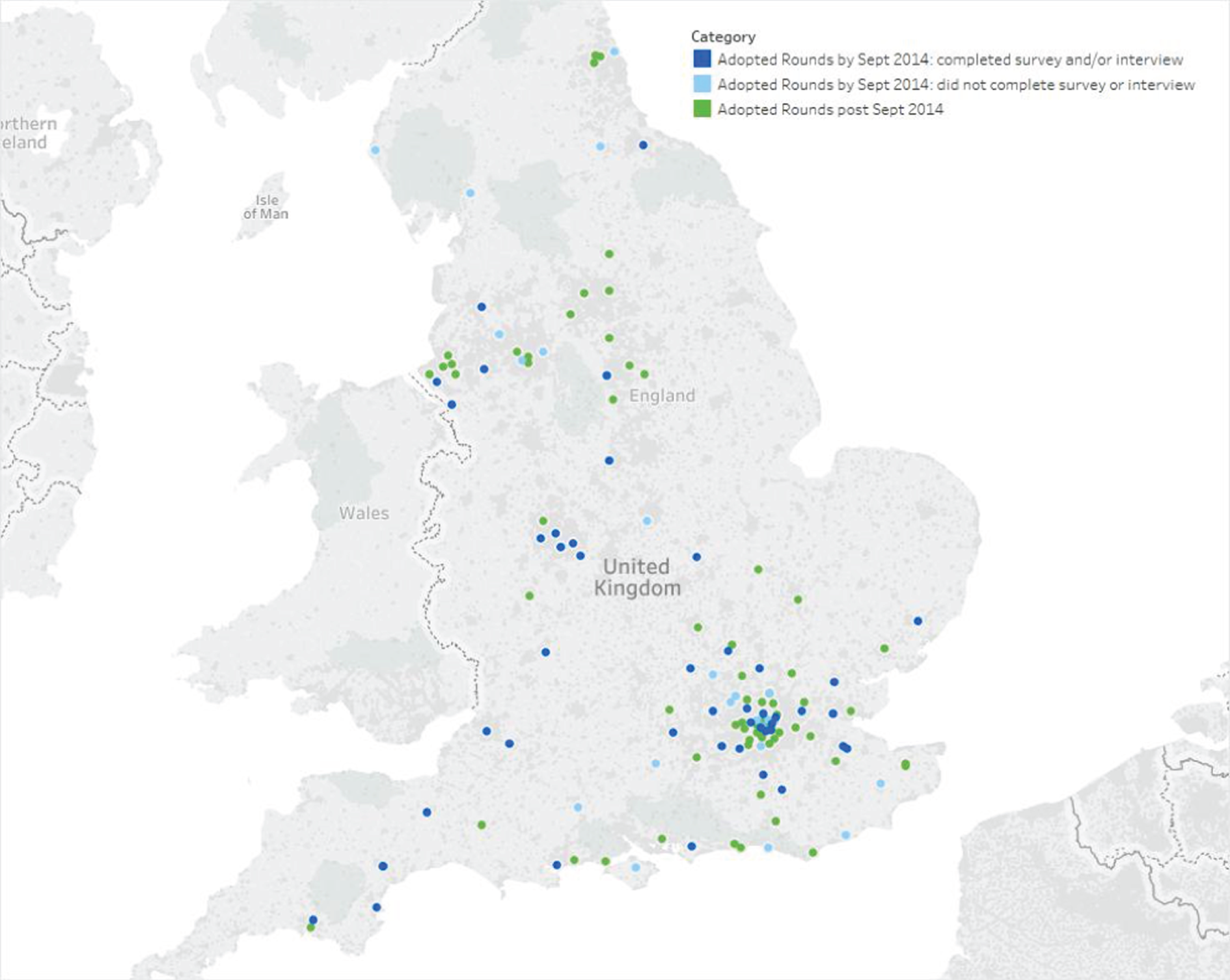
Types of organisations
The majority of sites in England were acute, community or mental health trusts (n = 86, 75%), followed by hospices (n = 25, 22%), with the remaining sites a prison, a university medical school, a private hospital and an ambulance trust. The adoption of Rounds varied by type of organisation, with, by July 2015, nearly half of all acute trusts in England adopting Rounds (68/155, 44%); 26% of mental health/learning disability trusts adopting Rounds (15/57) and 18% of community trusts adopting Rounds (3/17). An estimated 13% (25/197) of organisations offering hospice care had adopted Rounds.
Year of implementation
There was a sharp increase in the implementation of Rounds in England between 2013 and 2015, coinciding with the publication of report of the Mid Staffordshire inquiry (Francis report)3 in February 2013, which mentioned Schwartz Rounds (Figure 5). This rate appeared to have slowed in 2016.
FIGURE 5.
Implementation of Rounds: number of new providers running their first Round per year (to December 2016; n = 154). Figure excludes providers outside England (n = 10) and ‘other’ providers (n = 5) including an ambulance trust, three medical schools and a private hospital. LD, learning disability.
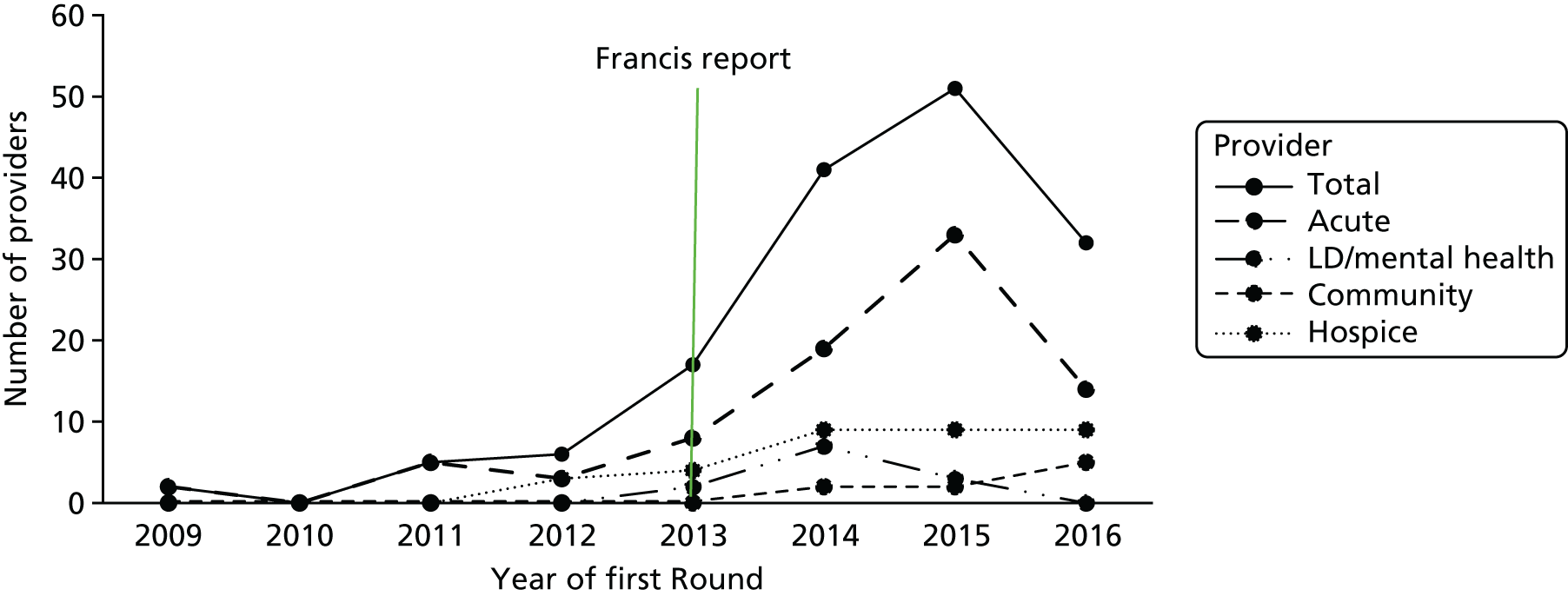
Why were Rounds implemented?
A combination of secondary data, survey and interview data was used to explore this.
How did staff first hear about Rounds?
Respondents were most likely to have heard about Rounds through recommendation from an internal colleague or peer (n = 25, 60%), followed by an external colleague/peer (n = 8, 19%), via research about support mechanisms for staff, and by attending a Round elsewhere (both n = 7, 17%). Other sources included other training courses or programmes (e.g. at The King’s Fund or NHS Leadership Academy), newspaper reports and Hospice UK.
Are Rounds adopters different from non-adopters, or earlier adopters different from later adopters?
Adopters were not significantly different from non-adopters in relation to the NHS Patient Survey scores or CQC risk bandings, but adopters had higher scores on NHS Staff Survey ‘engagement’ in 2013 (Tables 7 and 8, and see Robert et al. 1).
| Status | Band, n (%) | Total, n (%) | Chi-squared test results | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |||
| Adopter | 9 (14) | 12 (19) | 8 (13) | 8 (13) | 8 (13) | 18 (28) | 63 (100) | χ2 = 6.84; 5 df; p = 0.23 |
| Non-adopter | 13 (14) | 8 (9) | 20 (22) | 16 (17) | 16 (17) | 19 (21) | 92 (100) | |
| Total | 22 (14) | 20 (13) | 28 (18) | 24 (15.5) | 24 (15.5) | 37 (24) | 155 (100) | |
| Status | Year, mean (SD) (n; range) | |||||
|---|---|---|---|---|---|---|
| Staff overall engagement scorea (maximum score of 5) | Inpatient survey overall experience scoreb (maximum score of 100) | |||||
| 2015 | 2014 | 2013 | 2015 | 2014 | 2013 | |
| Adopter |
3.79 (±0.11) (82; 3.47–4.04) |
3.72 (±0.12) (82; 3.43–4.03) |
3.74 (±0.13) (82; 3.38–4.09) |
76 (±3.7) (76; 67–87) |
75 (±4.2) (76; 65–87) |
76 (±3.8) (76; 68–88) |
| Non-adopter |
3.77 (±0.15) (159; 3.11–4.03) |
3.70 (±0.18) (159; 2.77–4.02) |
3.69 (±0.16) (159; 2.92–4.06) |
76 (±3.1) (129; 71–87) |
75 (±4) (128; 68–87) |
76 (±2.8) (129; 70–87) |
| National mean | 3.78 | 3.75 | 3.75 | 77 | 76 | 75 |
| U | U = 6517.5; p = 0.99; r = –0.19 | U = 6476.5; p = 0.93; r = –0.5 | U = 5464.5; p = 0.04*; r = –0.13 | U = 4710.5; p = 0.64; r = –0.03 | U = 4846.5; p = 0.96; r = –0.003 | U = 4893.5; p = 0.98; r = –0.001 |
In relation to the timing of adoption, analyses of data for the 3 years before adoption according to whether adopters were early or later adopters resulted in two weak positive correlations: earlier adopters had better NHS patient experience results in 2013 and 2015 (r = 0.25, p = 0.02, and r = 0.24, p = 0.03, respectively). Additionally, providers that adopted Rounds earlier (i.e. innovators and early adopters) tended to have better NHS staff and NHS patient survey results than non-adopting providers or providers that adopted later (late majority, laggards). However, we found little evidence in our interviews that the adoption of Rounds was driven by such performance indicators. 1
Reasons for adopting Rounds
Explanations for adopting Rounds often referred to the need to focus on staff well-being and support as the key to improving patient care, slightly different from the stated intention of Rounds developers, that Rounds were an innovation to teach compassion and strengthen patient–caregiver relationships (see Chapters 2 and 7):
We identified [. . .] there was a gap around if you like the emotional side of support for staff [. . .] filling that gap in a way that we thought would be both beneficial and supportive [. . .] the format is that it gives a safe environment for people to raise, discuss, reflect on the emotions and pressures of caring.
Tyne-172-Clinical-Lead
Most interviewees cited the emotional well-being of staff as an important motive for adopting Rounds, but some participants mentioned organisational reasons, with Rounds as a vehicle for culture change being important:
We did a specific piece of work looking at the (organisational) culture and the attitude of staff towards each other and so this [Schwartz] kind of came as a change-management-type intervention following a specific piece of work. [. . .] it came off the back of an investigation into kind of a bullying culture [. . .] and we had a steering group and from that came this idea of introducing Schwartz regularly.
Esk-123-Clinical-Lead
I think when you want to have cultural change in any organisation you’re looking at a drip effect. And so if you want to eradicate some of the harsher and more judgemental ways of dealing with people [. . .] and the subscript of Schwartz is, don’t punish people, support them [. . .] and changing the culture or improving the culture making us a place that people want to work, despite the hard work and despite, you know, the resource issues.
Axe-389-Facilitator
Although the increase in the uptake of Rounds in 2013/14 might suggest that providers were responding to the Francis report,3 we found little evidence of this, although the report may have proved a catalyst. Our analysis using Rogers’ Diffusion of Innovation model71 suggests that, initially (2009–13), adoption was driven by ‘passive spread’ through informal communication, whereas following the Francis report, more active processes – led by the PoCF with planned, targeted dissemination, advocacy from opinion leaders and a perceived need to be seen to be addressing staff well-being – led to more active adoption. More recent adopters were also influenced by the provision of funding (e.g. from charities such as Macmillan, Hospice UK, and LETBs). 1 Report Supplementary Material 4 summarises the data according to the attributes argued to predict adoption: relative advantage, compatibility, complexity, trialability, observability and reinvention.
How are Rounds being implemented?
Preparation for implementing Rounds
As per PoCF guidance (see Report Supplementary Material 5), nearly all providers had attended Rounds in other sites (n = 35/41), with early pilot sites visiting Boston. Most had utilised facilitator training (after April 2013; n = 31) and/or accessed mentorship (n = 31). One respondent recommended attending Rounds in other sites as preparation:
Visit Rounds, go see them, get your key people in to come and see them. They are hard to describe. You need to go witness [. . .] be there and feel the hairs rise on the back of your neck when you hear the stories.
Ash-400-Facilitator
Attending a steering group meeting or speaking to a facilitator or clinical lead in another organisation was reported by half (n = 21), and a similar number had attended an introductory talk at the PoCF (n = 18). Other preparatory activities included having planning and preparation meetings (n = 38), and marketing activities such as articles in staff newsletters (n = 31) or launch events (n = 7). A few organisations (n = 12) organised additional training for facilitators. Having organisational board support is a contractual condition for running Rounds; in addition, one provider reported giving presentations to ‘lots of senior management groups’ to inform them about Rounds. A facilitator at one acute trust reflected on the importance of board support:
You’ve got to have the board in on this. [. . .] I don’t expect the chief executive to come; he’s very busy but we need someone at that level of seniority [. . .] to advertise the fact that they give this activity their approval and blessing [. . .]. I think without that you can’t get going.
Thames-199-Clinical-Lead
Organisational structure for Rounds
Rounds require a clinical lead, at least one facilitator and an administrator, together with a steering group (recommended to be 8–12 members from across the organisation for larger organisations; see Report Supplementary Material 5). All organisations had at least one clinical lead and facilitator, but some (n = 4) did not have dedicated administrative support. Interview respondents reinforced the importance of having adequate administrative support:
Make sure that you’ve got adequate resources and support [. . .] it needs to have some finances attached to it so that you’ve got some admin[istrative] support [. . .] so that somebody can develop your posters and your flyers to get out there advertising the event. Somebody who can co-ordinate organising the lunch for the day [. . .] checking out that the room’s ready and prepared for people coming and then collecting in the paperwork and getting it sent back to the Point of Care.
Clyde-361-Facilitator
The PoCF states that it helps if facilitators have experience of group work and managing difficult emotions, and that often facilitators have psychological or social work backgrounds. Of the 37 Rounds providers that gave details, 20 (54%) had at least one psychologist/counsellor/psychotherapist as a facilitator, and 8 out of 37 (22%) had social workers or allied health professionals (AHPs) (mostly art therapists). Others included doctors, nurses, chaplains/spiritual leads and managers. Of the 35 Rounds providers that provided data about their clinical lead, 30 (86%) had a senior doctor (medical director/consultant); others included nurses, psychologists and psychotherapists.
A key theme from the interviews was the importance of finding the ‘right’ people for the clinical lead and facilitator roles, who had sufficient commitment and enthusiasm for Rounds, the appropriate skills and the time to plan and prepare Rounds thoroughly: ‘I think the passion has got to show, you have to be passionate about it for it to succeed’ (Tay-127-Clinical Lead). Several respondents specified that facilitation skills were preferable to psychological training, and others recommended establishing a group of facilitators:
Get a team of facilitators together so it doesn’t rely on just one or two members of staff. Because if you get illness or somebody moves on to another position then the entire safety of the Rounds hinges on maybe just one or two people and that just doesn’t feel safe really.
Looe-381-Facilitator
One-third of providers reported that their steering group met monthly as recommended by PoCF (n = 14), but a number reported meeting less frequently, for example quarterly (n = 6) or every 6–8 weeks (n = 5). In two providers, the steering group met twice per month (both before and after each Round). In 40% of organisations (n = 19), the steering group reported directly to its board. Many interview respondents spoke about the importance of the steering group composition, suggesting that this was less about size and more about ensuring that there were sufficient ‘champions’ to spread the word about Rounds and supporting the ‘core team’ to plan Rounds and, in particular, to identify panellists (see also Chapter 6). Diverse steering groups were generally favoured and enthusiastic self-selected members were preferred. Including senior members of the organisation was felt to be important as they could use their authority, visibility, ‘reach’ and ‘clout’ to support clinical leads and facilitators to establish and sustain Rounds:
It does help to have somebody higher up in the organisation, like [senior nurse] [. . .] It’s a bit difficult sometimes [. . .] for the clinical lead and the facilitator to go out there and recruit people [. . .] Somebody a bit further up, in some ways has a bit more clout [. . .] [to] open doors a bit more [. . .] So she can go in and say to people, ‘Look, could your area look at providing somebody for the Schwartz Rounds?’ and I think that’s worked.
Tiber-151-Clinical-Lead
The frequency, timing and scheduling of Rounds
Organisations are contractually obliged to run a minimum of six Rounds per year in hospices and nine in ‘larger’ organisations (e.g. NHS trusts). Of the 20 providers that had run Rounds for ≥ 1 year at the time of survey completion, two of the 16 NHS trusts did not meet this criterion (running them every second or third month, with one site explaining in the interview that running them monthly had been too onerous); all four hospices were running Rounds at least six times per year. Most NHS trust providers that had been running Rounds for < 1 year at survey completion (2013/14) intended to run at least nine, with most aiming for 10; and all six hospices intended to run at least six (with half intending to hold 10–12 per year).
From the interviews it became apparent that 10 Rounds per year was felt to be feasible as it enabled ‘monthly’ Rounds while avoiding holiday periods (e.g. summer or Christmas). One outlier was a mental health/learning disabilities trust that reported running 26 Rounds per year. Here Rounds were run monthly simultaneously across multiple sites owing to the trust being geographically spread. One-third of organisations (n = 14) reported rotating the location of Rounds across multiple (up to five) sites in their organisation. This was more common in NHS trusts (n = 12, 39%) than in hospices (n = 2, 20%), the latter tending to have only one site. Apart from the core Rounds team, it was rare for staff to travel between sites to attend Rounds, and therefore in these providers most staff could attend Rounds only every 2–3 months when one was held where they worked.
Interviews revealed that most organisations spent time trialling different days and times before determining what ‘worked’ best, acknowledging that whenever Rounds were held, some groups of staff would be excluded (see also Chapter 6). Most organisations ran Rounds at lunchtime (n = 30), although some ran Rounds in the afternoon (n = 5) and six providers varied the time of Rounds rather than having a typical time in order to enable wider accessibility across staff groups. Nineteen providers varied the day of the week for Rounds, although one provider reported that it had tried this but decided that having a fixed day and time was preferable.
Publicising Rounds
Regardless of trends in attendance or the length of time running Rounds, interview respondents saw promoting Rounds as key to drawing in an audience, and interview and survey data showed that significant time was dedicated to this, as it was felt to be fundamental to Rounds’ sustainability:
Well you have to [spend lots of time on publicity]. If you don’t do that it goes away.
Chess-388-Facilitator
Most organisations followed PoCF guidance on using multiple approaches to publicise Rounds, and some had access to communications expertise/resources. Most commonly this included posters (93%, n = 38) and e-mails (90%, n = 37). Two-thirds of sites publicised Rounds in staff communications such as newsletters (n = 29) or discussed them at internal meetings (n = 29). In one organisation, the chief executive included Rounds in his weekly blog. Others reported using the intranet (n = 5) and word of mouth (n = 4). Most organisations showed ingenuity in finding ways of drawing attention to Rounds, for example using colourful posters, using the public address system and advertising on screensavers or television screens in staff/reception areas.
Attendance at Rounds
There was considerable variation in the typical attendance figures for Rounds, with the estimated average attendance ranging from 17 to 150 people at NHS trusts, and from 18 to 45 people in hospices (Table 9).
| Type of provider | Attendance | ||
|---|---|---|---|
| Mode (range) | Lowest (range) | Highest (range) | |
| NHS trusts (all) | 17–150 | 2 (2–140) | 190 (30–190) |
| Small | 20–40 | 9 (9–28) | 80 (30–80) |
| Medium | 17–130 | 2 (2–12) | 147 (32–147) |
| Large | 22–150 | 11 (11–140) | 190 (31–190) |
| Hospices | 18–45 | 9 (9–30) | 78 (24–78) |
Maintaining or increasing attendance was perceived as crucial to sustaining Rounds and was a concern for most interviewees, who considered achieving ‘good attendance’ (however this was defined) as a key challenge that they faced (see Chapter 6). Survey respondents were asked about trends in attendance over the previous six Rounds. No clear patterns emerged according to the type of organisation or length of time running Rounds: similar proportions of organisations reported that attendance had been ‘about the same’ (41%, n = 16) as those that had reported that it ‘varies each time’ (39%, n = 15). Four organisations reported that attendance had increased over the previous six Rounds, and four reported that it had declined. Concern about attendance was expressed by many, particularly when attendance had declined:
So what we’ve noticed is that the number of attendees is dwindling. In the early days I would say we started with approximately 100 people attending and we’re routinely down to about maybe 30 or 40 now [. . .] So that’s a challenge in itself, the number of attendees.
Looe-381-Facilitator
Another key aspect was the attendance (or not) of specific staff groups. Survey respondents reported that doctors and nurses were represented at Rounds in all providers. However, interviewees reported that this masked the most commonly mentioned under-represented groups: front-line clinical staff, particularly ward nurses and doctors. Other under-represented groups included porters, maintenance and domestic staff, AHPs and board members (see Chapter 6). Most respondents were alert to the structural barriers preventing ward staff attending Rounds but found these difficult to address because of the nature of clinical work and staffing levels:
The biggest challenge really has been getting people from the wards to come because they are so busy. [. . .] I think that’s because we run on quite a thin line of staffing and it’s difficult to release staff.
Neath-327-Facilitator
The importance of senior clinical members of staff and board members attending Rounds was often mentioned in interviews, both to experience Rounds themselves and to demonstrate endorsement of them. Respondents in some organisations claimed good attendance by executive team members but others expressed disappointment that such staff were rarely present (see also Chapter 6).
Measuring/evaluating the impact of Rounds
The PoCF require organisations to use a bespoke evaluation form, and to provide a review of findings after the first nine Rounds. Most sites (n = 35) reported collating summaries of Rounds, and having systems for collating and summarising feedback. Three-quarters of sites reported that they analysed sign-in sheets, and all analysed the evaluation forms. These analyses were most commonly used to report to the steering committee (n = 38) and to the board (n = 27). Some used the analyses for promotional material (n = 9) or quality accounts (n = 7).
Determining the impact of Rounds was a topic that elicited a variety of responses in interviews. Some interviewees said that they found the questions about impact difficult, were hesitant, or prefaced their answers with comments about the lack of ‘hard evidence’ for the effects of Rounds or the difficulties of measurement and attributing causality. Most respondents referred to overwhelmingly positive attender feedback on Rounds, but clearly felt that they needed to give circumspect answers in the absence of ‘direct evidence’ of impact:
It’s very hard to give you tangible [. . .] hard quantitative type of evidence, but what is clear is that when staff attend, the evaluations after the event are incredibly positive.
Severn-395-Facilitator
Respondents were often reluctant to answer questions about the impacts of Rounds, such as on staff well-being or delivery of patient care, saying that it was too early to tell, or that they were not in a position to observe (or measure) effects or make judgements about them. In relation to the impact on themselves, respondents who had been panellists spoke about this [e.g. ‘helped me process some, perhaps difficult, emotions that I hadn’t been able to do before’ (Horse-chestnut-194-Clinical Lead)]. Others highlighted the benefits of taking the role of the clinical lead or facilitator, giving examples of Rounds influencing their behaviour towards patients or colleagues:
It certainly makes me a bit more aware of colleagues and pressures and things like that, so yes, I’d have to say yes, a slightly different approach. Probably don’t send off as many angry e-mails as I used to.
Tiber-151-Clinical-Lead
Although interviewers asked respondents to consider negative impacts as well, respondents mostly gave examples of positive effects and few discussed the possibility of harm. One exception was a facilitator who spoke of an audience member who had been adversely affected by a Round:
So we’ve had an allied health professional who wasn’t able to sleep the night after the Round, it churned things up for them, resonated with them, some case that they hadn’t resolved in their mind.
Chess-388-Facilitator
Challenges in running/sustaining Rounds
The main challenges to running and/or sustaining Rounds were subsumed under two themes: (1) issues to do with attendance and in particular widening accessibility, and (2) issues to do with the workload and resources required to run Rounds (Table 10; see also Appendix 12 and Chapter 7).
| Theme | Subtheme | Illustrative quotations |
|---|---|---|
| Attendance |
|
The biggest challenge has been to actually get the audience to the meetings. [. . .] We’re an organisation of 10,000 people across three sites and the average attendance [. . .] is about 35, and that’s despite putting up posters, putting out e-mail invitations to everybody, word of mouth, and pushing them alongRibble-161-Clinical-LeadThere’s a recognition that [Schwartz] is a whole hospital thing but it’s difficult to get nurses in any numbers because of their shift patterns, so we’ve explored it with the nursing director [. . .] and the time we’ve come up with is towards the end of the afternoon, so instead of having lunch we’ll have afternoon teaCarmel-385-FacilitatorThe other tricky thing for us has been getting the hard-to-reach groups to actually attend, so we’ve found people like maintenance guys, the kitchen staff, the housekeeping staff, they’ve been very, very hard to get to come [. . .] [The manager] of the maintenance, housekeeping and kitchen, etc., he’s only been once and that’s when he was pressganged into it. Nobody from those groups has ever sat on the panel because we just can’t get them toEsk-123-Clinical-Lead |
| Workload and resources |
|
Preparing for [Rounds] probably takes up much more time than I anticipated and particularly because the other co-facilitator is part time, so I often feel I’m doing a lot of the [. . .] identifying and preparing panel members and organising steering groups and that sort of thing. And the reports and presentationsStour-358-FacilitatorThere has been no admin[istrative] support at all, so it falls to [one of the rest of us] [. . .] it takes about 2 whole days a month to prepare for a Round and do all the administration [. . .] So that’s been the biggest challengeLooe-381-FacilitatorAfter 2 years [. . .] we were a bit exhausted [. . .] and it’s not lack of enthusiasm but it’s just hard because you’re all putting in the time in general over and above your day job [. . .] you may have some nominal time for it in your job plan, but it would generally be nominal rather than actualOtter-190-Clinical-Lead |
What were the resource implications of running Rounds in organisations?
Non-staff costs
Fees to the Point of Care Foundation
The cost of the licence to implement Rounds, including 2 years of operational support (comprising facilitator training, mentorship, webinars and web resources access) and two places at its annual conference for Schwartz Community members, is £15,960 for NHS trusts (in 2009 this was £2500). Hospices and similar small providers are provided with the support in group cohorts at a cost of £4500 for 2 years.
After the first 2 years, providers can enter into ‘membership’, which renews the licence (enabling Rounds to continue) and provides ongoing support. The current 2-year membership rate is £3780 for large organisations and £1680 for small organisations. (All figures include value-added tax and were correct on 13 February 2017.)
Various providers have benefited from subsidised rates, with grants variously from the Department of Health and Social Care, LETBs and Macmillan (see Figure 1).
Other non-staff costs
-
Eight organisations reported having one-off costs associated with a launch event, ranging from £35 to £1500.
-
Most (34/42) organisations were not charged any room hire fee. Four (three NHS trusts and one hospice) paid a fee of between £100 and £310 for each Round.
-
Most organisations (30/42) either minimised printing/advertising costs by only using online forms of communication, or stated that such costs were met by provider communications teams and not charged directly to Rounds. Seven organisations incurred small sums (£10–25) for printing or other costs associated with promoting Rounds. One organisation had purchased a public address system for Rounds at £400.
-
All provided catering (although two stated that this was provided ‘in house’ and could not provide costs). Most frequently this was a sandwich buffet (57%). Cost varied from £10 to £700 a Round, with a median of £225 (Table 11). The average cost for a sandwich buffet was around £5 per head.
| Size of organisation | Range in mode attendance (n) | Range in cost per Round (£) | Range in cost per head based on mode (£) | Median cost per Round (£) |
|---|---|---|---|---|
| All | 17–150 | 10–700 | 0.29–4.66 | 225 |
| Small | 18–45 | 25–250 | 1.39–8.33 | 124.50 |
| Medium | 17–130 | 50–550 | 2.94–4.23 | 181.50 |
| Large | 22–150 | 10–700 | 0.29–4.66 | 250 |
Staff costs
The main staff time associated with Rounds is for administration, facilitation and clinical leadership. There are also costs associated with steering group membership. Steering group sizes ranged from two or three members, plus the core team, to 35 members, but their role, and the regularity and amount of contribution, was highly variable. Costs and time here are therefore presented in relation to the core roles: administration, facilitation and clinical lead (see also Report Supplementary Material 6 for extended version with data tables).
There was wide variability in the total number of hours dedicated to administration, facilitation and clinical lead tasks in Rounds, even taking into account the size of the organisation. Time spent on all roles taken together ranged from 7 hours to 82.15 hours per month, with an average of 24/28 hours (median/mean). Whereas all sites had at least one facilitator and clinical lead, four sites did not have any administrative support (all were NHS trusts).
Owing to the fact that organisations chose to resource Rounds in such variable ways, with blurred boundaries between facilitator and administrator, or between facilitator and clinical lead roles in some organisations, we present the total costs for these three staff roles together. There was a wide range in band/time spent for all three roles, and consequently costs were highly variable (Table 12). However, this indicated that median monthly cost for these roles was approximately £650 (small provider) or £2000 (medium/large providers) (see Report Supplementary Material 6 for details of each role separately).
| Size of organisation (definition, number of sites providing information) | Range in staff costs per month (for administrator, facilitator and clinical lead) (£) | Median cost per month (£) |
|---|---|---|
| Small (< 2000 employees, seven sites) | 380–4477.50 | 666 |
| Medium (2000–4999 employees, seven sites) | 767.50–2199 | 2000 |
| Large (≥ 5000 employees, seven sites) | 980–4420 | 1964 |
Chapter summary
There has been a rapid uptake of Rounds in the UK, particularly during 2013–15, although uptake has been variable across different types of organisations and geographically – and now appears to be slowing. Although the peak of uptake coincided with the publication of the Francis report in 2013,3 we found little evidence of a direct causal relationship, although it may have been a catalyst. Explanations for adoption were most likely to concern a felt need to provide staff support/well-being, perhaps in recognition of the established link between staff well-being and patient experience. 68,76,77 Earlier adopters appear to have been influenced by a combination of factors, including that Rounds have many favourable attributes to support uptake, together with the active dissemination by organisations such as the PoCF, and the felt need to be addressing staff well-being. More recent adopters have also been influenced by the provision of funding to support Rounds. We found little evidence of performance driving adoption, although there were several weak correlations: adopting providers had higher levels of staff engagement (compared with non-adopters) and earlier adopters had better staff and patient survey results than later adopters and non-adopters.
There is wide variability in relation to how Rounds have been implemented. Challenges to implementing and sustaining Rounds include issues regarding attendance (particularly widening accessibility to groups of staff tied to wards, those with less autonomy), and the workload and resources required for planning and running Rounds. The resources for running Rounds are highly variable – both staff and non-staff costs – across and within types of providers. The majority of time spent on Rounds activities was non-contracted/job planned, and often a considerable number of hours per month.
Chapter 5 Schwartz Center Rounds evaluation: survey
Overview
This chapter describes the survey element of the evaluation that was conducted concurrently with the case studies and represented the primary quantitative component.
Objectives
The primary objectives were to:
-
evaluate whether or not regular attendance at Rounds has an impact on health-care staff work engagement, well-being, social support for staff and behavioural change towards patients and colleagues compared with non-attenders (objective 7)
-
investigate whether or not frequency of Rounds attendance was associated with greater improvements in health-care staff work engagement, well-being, social support for staff and behavioural change towards patients and colleagues (objective 8)
-
determine factors associated with Rounds being perceived as useful, or barriers, to attending Rounds (objective 9).
Objective 1 was achieved by comparing changes over time in outcomes (0–8 months) between regular Rounds attenders and non-attenders from 10 providers. Objective 2 was achieved by examining relationships between the number of Rounds attended and level of change. Objective 3 was achieved by summarising responses to relevant survey questions (see also Chapter 6).
Methods
Design and setting
A two-wave survey of new Rounds attenders and non-attenders was conducted in 10 case study sites from 29 May 2015 to 8 October 2016. New attenders (i.e. those who had not attended a Round previously) were chosen for the intervention group so that it would be possible to detect the effect of starting to attend Rounds.
The 10 case study sites were identified, using purposive sampling, in order to maximise the variation of organisations in terms of size, location and type of provider. Four of the sites had been running Rounds for a number of years; at the other six, Rounds began during the study, meaning that we could recruit participants at their first ever Round (and most attenders would be attending their first Round). Six of the sites (including two ‘new’ Rounds providers) were also main case study sites (see Table 2). Originally we planned that the same 10 sites would fulfil both purposes, but following the pilot study it was determined that this may not yield enough new attenders, and therefore four established Rounds sites were replaced by four new Rounds sites.
Seven of the sites were acute trusts. One site ran Rounds jointly between an acute trust and a nearby mental health trust. One site was a mental health trust alone, and the final site was an independent (non-NHS) hospice. Negotiation for access to each was sensitive throughout to issues of data anonymity, confidentiality, informed consent and burden placed on staff.
The sample size for the survey was based on a power calculation involving the primary outcome, work engagement (see Appendix 13 for details). 78 An increase of 0.33 in work engagement is associated with a 0.5% drop in staff absence (per staff member, this translates to more than 1 day fewer absences annually); we considered this an important difference. Based on the variance in work engagement from the national NHS staff survey, the total sample size required to detect this effect, with 80% power and allowing for clustering, was 228 (114 in each group). Allowing for a 50% response rate, a dropout between baseline and follow-up of 40–50%, and assuming that 50% of new attenders would become regular attenders (see definition below), a sample of 800 new attenders was needed. Following the pilot study, it was acknowledged that an average of 80–100 attenders in new Rounds sites, and 30–50 in established sites, could be achieved by recruiting up to four Rounds in each site, yielding a probable total sample of between 650 and 850 attenders.
For non-attenders, we assumed that the initial response rate would be lower, and the dropout rate between baseline and follow-up would be higher (as some respondents may become Rounds attenders). In addition, it was not possible to know in advance who had attended Rounds previously. Therefore, an initial random sample of 250 staff per site was chosen at eight sites. At the hospice, however, the size of the whole organisation was smaller than this, and at the joint acute/mental health site a sample of 250 staff across each organisation was used, meaning that the total initial sample size for the non-attender arm was 2680.
Recruitment and administration
Inclusion and exclusion criteria for participation were as follows. Note that categorisation into different groups could not happen until after the follow-up survey.
-
Inclusion criteria:
-
(all groups) staff who have the opportunity to attend Rounds, and have not attended Rounds before the baseline survey
-
(regular attenders) staff who attended ≥ 50% of available Rounds between the two surveys
-
(irregular attenders) staff who attended at least one Round but < 50% of available Rounds between the two surveys
-
(non-attenders) staff who had not attended a Round previously, and did not attend one during the study period.
-
-
Exclusion criteria:
-
people not employed by the provider
-
staff who had attended Rounds previously, including with a previous employer.
-
Recruitment and survey administration differed for attender and non-attender arms. In both cases, potential participants were first asked whether or not they had previously attended any Rounds: if they had, their participation ceased. See Appendix 13 for details of recruitment.
Measures
The 47-item questionnaire included the following measures, selected based on our literature review and initial theorising regarding how Rounds were expected to work (see Chapter 3). Unless stated, questions were asked in both the baseline and follow-up surveys in the attender and non-attender arms (see Report Supplementary Material 1 for full details of the measures and their reliability and validity):
-
work engagement
-
psychological well-being 12-item General Health Questionnaire (GHQ-12)
-
self-reflection
-
empathy
-
communication with patients
-
compassion
-
peer support
-
organisational climate for support
-
absenteeism
-
age, gender, occupational group, tenure with the organisation, grade, working hours
-
extent of contact with patients
-
(follow-up survey only) number of Rounds attended in the previous 8 months
-
(attenders only) reasons for attending Rounds; whether or not they had attended in their own time; whether or not they had attended with immediate colleagues; whether or not they had ever presented at a Round; whether or not they contributed to Round discussions; and perceived usefulness of Rounds
-
(non-attenders only) reasons for not attending Rounds.
Analysis strategy
The primary hypothesis was that there was a greater improvement in work engagement for regular Rounds attenders than for non-attenders. This was tested via a multilevel (to adjust for clustering within sites) analysis of covariance (ANCOVA), with work engagement at follow-up as the dependent variable, and work engagement at baseline as a covariate (this is mathematically equivalent to examining the change in work engagement with the baseline value as a covariate, but reduces non-essential covariance and other problems associated with difference scores). 79 The analysis also included occupational group, grade, gender, age, length of service, working hours and extent of contact with patients as covariates.
The secondary outcomes were psychological well-being (Likert and ‘caseness’), self-reflection, empathy, communication with patients, compassion, peer support, organisational climate for support, and absenteeism. Most were examined using the same model as for the primary outcome (with checks to ensure that key assumptions of the model were not violated). The ‘caseness’ score of the GHQ-12 was analysed with a multilevel logistic regression model, and absenteeism with a multilevel negative binomial model.
Three further analyses were completed:
-
We used alternative definitions of regular attenders. It became clear during the fieldwork that using a strict 50% definition might mean that an irregular attender at one site had actually attended more Rounds than a regular attender at a different site, owing to imbalances in the frequency of Rounds at different sites. We adhered to this definition in our main analysis, but also tested alternative definitions of regular attenders in which two, three or four Rounds, respectively, were attended to meet the definition.
-
We tested the difference between anyone who had attended Rounds and those who had not, and used the number of Rounds attended as a numerical predictor of outcomes (with both linear and quadratic models): this is a direct test of whether or not the dose of Rounds has an association with changes observed.
-
To account for imperfections in the design and data collection, we also conducted three sensitivity analyses and examined potential moderators of the effects.
Pilot study
Before the survey methods were finalised, a two-wave pilot survey was conducted in two sites from 27 January 2015 to 1 January 2016 to test (1) the administration method for attenders, (2) the administration method for non-attenders and (3) the usefulness of measures (for both attenders and non-attenders). The pilot study comprised 52 questionnaires administered to attenders, 500 questionnaires sent to non-attenders, and 12 cognitive interviews.
In general, the pilot study confirmed that the methods used were appropriate, although a few small but important changes were made as a result. The full details of the methods and findings of the pilot study can be found in Appendix 14. Because most of the survey details remained unchanged, respondents to the pilot study in two organisations were also included in the main analysis.
Results
Descriptive statistics: sample
Including respondents from our pilot study, there were 1140 responses at baseline and 500 at follow-up, excluding 18 blank responses (15 in the main study and three in the pilot study) (Table 13).
| Attendance | Responses, n/N (%) | |||||
|---|---|---|---|---|---|---|
| Total | Main study | Pilot study | ||||
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Attenders | 512/885 (58) | 207/512 (40) | 484/833 (58) | 194/484 (41) | 28/52 (54) | 13/28 (46) |
| Non-attenders | 628/2930 (21) | 293/628 (47) | 578/2680 (22) | 274/578 (47) | 50/250 (20) | 19/50 (38) |
| Total | 1140/3815 (30) | 500/1140 (44) | 1062/3513 (30) | 468/1062 (44) | 78/302 (26) | 32/78 (41) |
There were 500 responses from participants at both time points: 207 of these were originally recruited as attenders, and 293 as non-attenders. However, 54 of the non-attender group subsequently attended at least one Round. A further six did not indicate (on the follow-up survey) whether or not they had attended any. Five of the attender group also did not indicate (on the follow-up survey) how many Rounds they had attended. Therefore, these 11 respondents could not be categorised. The total number in the final sample (293 + 207 = 500; 468 from the main study) (see Table 13) is larger than the 489 classified into the three groups (see below) because of the 11 who could not be categorised.
The numbers in each group, as defined in the protocol, were as follows:
-
regular attenders – 51
-
irregular attenders – 205
-
non-attenders – 233.
Of the combined attender groups, 140 had attended at least two Rounds, 77 had attended at least three Rounds and 40 had attended at least four Rounds. The number of regular attenders was smaller than anticipated. This was because of a lower conversion rate to regular attendance than had been anticipated in the study design.
A breakdown of attendance, other background characteristics and survey completion details is given in Appendix 15. In many aspects, the profile of attenders and non-attenders is fairly similar. However, there is a bias towards clinical staff (particularly AHPs/scientific and technical staff) among attenders, and also towards more senior staff (particularly bands 7 and 8a). These differences are controlled for by including background variables (site of study, occupational group, grade, gender, age, length of service, working hours and extent of contact with patients) as covariates. Unless otherwise stated, all subsequent analysis includes these covariates and accounts for clustering by site using multilevel analysis.
Comparison of regular attenders and non-attenders on outcomes (primary method)
Table 14 shows the raw (unadjusted) means and standard deviations for each survey measure at baseline and follow-up in each of the groups. Of note is the high levels of poor staff well-being in our sample, as measured by the GHQ-12 caseness, suggesting that, at baseline, between one-quarter and one-third of the staff in our sample had sufficiently poor psychological health that they would benefit from professional intervention. This was a slightly higher than the 27% prevalence reported in a large previous study of NHS staff. 80
| Survey scales | Time point, mean (SD) | |||||||
|---|---|---|---|---|---|---|---|---|
| Total | Regular attenders | Irregular attenders | Non-attenders | |||||
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Engagement | 3.80 (0.73) | 3.76 (0.79) | 4.01 (0.56) | 4.07 (0.57) | 3.93 (0.69) | 3.87 (0.73) | 3.64 (0.76) | 3.61 (0.84) |
| GHQ-12 (caseness) (%) | 32 | 29 | 25 | 12 | 28 | 26 | 37 | 34 |
| GHQ-12 (Likert score) | 2.08 (0.48) | 2.04 (0.49) | 2.03 (0.38) | 1.84 (0.31) | 2.04 (0.43) | 2.00 (0.42) | 2.13 (0.54) | 2.10 (0.57) |
| Self-reflection | 4.31 (0.99) | 4.33 (0.99) | 4.42 (1.10) | 4.45 (0.98) | 4.45 (0.94) | 4.50 (0.90) | 4.17 (1.00) | 4.16 (1.05) |
| Empathy | 3.36 (0.46) | 3.39 (0.52) | 3.38 (0.43) | 3.45 (0.51) | 3.35 (0.46) | 3.38 (0.53) | 3.37 (0.46) | 3.39 (0.51) |
| Communication with patients | 7.39 (1.74) | 7.44 (1.90) | 7.64 (1.80) | 7.94 (1.86) | 7.50 (1.59) | 7.58 (1.72) | 7.21 (1.86) | 7.20 (2.02) |
| Compassion | 6.01 (0.94) | 6.03 (0.95) | 6.08 (0.90) | 6.11 (0.95) | 6.03 (0.84) | 6.01 (0.93) | 5.96 (1.05) | 6.02 (0.97) |
| Peer support | 3.71 (0.92) | 3.67 (0.96) | 3.91 (0.66) | 3.98 (0.86) | 3.84 (0.83) | 3.79 (0.83) | 3.55 (1.02) | 3.50 (1.04) |
| Organisational climate for support | 2.62 (0.66) | 2.63 (0.63) | 2.69 (0.58) | 2.58 (0.60) | 2.73 (0.58) | 2.68 (0.58) | 2.52 (0.72) | 2.60 (0.68) |
| Days absent in previous 6 months | 3.41 (11.17) | 3.23 (11.21) | 2.36 (7.20) | 1.86 (4.93) | 2.84 (9.59) | 3.44 (14.20) | 4.13 (13.00) | 3.34 (9.00) |
There are some baseline differences between the groups, in particular between attenders and non-attenders. To examine the extent to which these reflect genuine systematic differences, as opposed to random fluctuations or differences in the background profile of the groups, we ran multilevel ANCOVAs (or equivalent multilevel generalised linear models) in which baseline values were predicted by group membership, controlling for background variables.
Most of the differences were not significant, with one important exception. Engagement was significantly lower among non-attenders than among regular attenders [adjusted difference 0.33; 95% confidence interval (CI) 0.05 to 0.62; p = 0.022]. This has implications for how subsequent results are interpreted, not least because engagement was specified as the primary outcome measure. It may be that findings could be affected by the baseline imbalance, which would justify using baseline measures as covariates in the main analysis.
There appear to be differences between the groups for self-reflection [F(2,320.8) = 4.886; p = 0.008]; however, post hoc tests of the specific group differences do not yield significant results. In particular, the difference between regular attenders and non-attenders is not quite significant (difference 0.36; 95% CI –0.02 to 0.75; p = 0.064). Nevertheless, this difference could have an impact on findings. Likewise for peer support, the overall group difference was just significant [F(2,324.2) = 3.048; p = 0.049], but the pairwise group differences were not, with the difference between regular attenders and non-attenders being 0.33 (95% CI –0.04 to 0.70; p = 0.076). For no other variables did the differences come close to significance. Correlations between survey variables are shown in Appendix 16. One aspect of the correlation between all the survey scores and the number of Rounds attended (see Appendix 16, Table 44) is that there do not appear to be any substantial correlations between psychological well-being and the expected intermediate mechanisms of self-reflection, empathy, communication with patients and compassion, suggesting that levels of psychological well-being are not related to these mechanisms in the way that had been anticipated. Table 15 shows the change from baseline to follow-up surveys in these scores for the two principal study groups, together with the adjusted difference between these groups.
| Survey scales | Attenders | Adjusted difference (95% CI) | |
|---|---|---|---|
| Regular attenders | Non-attenders | ||
| Engagement | 0.05 | –0.03 | 0.09 (–0.16 to 0.35) |
| GHQ-12 (caseness) | –13% | –3% | –19% (–37% to –1%)a |
| GHQ-12 (Likert score) | –0.19 | –0.03 | –0.13 (–0.31 to 0.05) |
| Self-reflection | 0.10 | –0.01 | 0.05 (–0.32 to 0.42) |
| Empathy | 0.07 | 0.05 | –0.06 (–0.23 to 0.12) |
| Communication with patients | 0.23 | 0.13 | 0.16 (–0.33 to 0.65) |
| Compassion | 0.02 | 0.06 | 0.00 (–0.29 to 0.30) |
| Peer support | 0.08 | –0.03 | 0.04 (–0.30 to 0.37) |
| Organisational climate for support | –0.12 | 0.09 | –0.11 (–0.34 to 0.12) |
| Days absent in previous 6 months | –0.44 | –0.59 | –0.26 (–4.29 to 3.77) |
It can be seen that most of the differences are small and non-significant. In particular, there is no effect found with the primary outcome (engagement).
The only significant effect is on the caseness score of GHQ-12: the binary categorisation of whether or not the respondent is sufficiently stressed as to warrant intervention. This decreased significantly more in the regular attenders than in the non-attenders group (a 13% decrease, compared with a 3% decrease in unadjusted scores). The odds ratio for this effect was 0.28 (95% CI 0.08 to 0.98); that is, the odds of being identified a case by the GHQ-12 were approximately 72% lower for regular attenders than for non-attenders.
The full results from the models reported in this section are available in Appendix 16.
Comparison of regular attenders and non-attenders on outcomes (alternative definitions)
As reported earlier, owing to inconsistency in the number of available Rounds at different sites, we also tested different thresholds for ‘regular’ attendance. We tried this with the requirement that either two, three or four Rounds should have been attended. In addition, we examined effects of any attendance.
In most cases the same conclusion was reached: there was no overall difference between regular attenders and non-attenders for most of the variables. Table 16 shows the regression coefficients for the primary outcome (engagement) and odds ratios for GHQ-12 (caseness) that had the significant result in the main test.
| Survey scales | Number of Rounds | |||
|---|---|---|---|---|
| ≥ 4 | ≥ 3 | ≥ 2 | ≥ 1 | |
| Engagement (95% CI) | 0.16 (–0.13 to 0.45) | –0.02 (–0.23 to 0.19) | 0.04 (–0.12 to 0.20) | 0.06 (–0.07 to 0.19) |
| GHQ-12 (caseness) (95% CI) | 0.19 (0.04 to 1.03) | 0.46 (0.18 to 1.17) | 0.40 (0.19 to 0.86) | 0.57 (0.33 to 0.97) |
There was no difference between the groups in engagement regardless of the definition. For GHQ-12 caseness, measuring psychological well-being, there is a significant effect for attendance at two or more Rounds. The odds ratio of 0.40 suggests that the odds of being severely stressed are nearly two and a half times smaller for people who attend (at least two) Rounds than for people who do not attend, controlling for their psychological well-being before attendance. The effects for attending at least three or four Rounds are not statistically significant, even though the odds ratios are of a similar magnitude (for at least three Rounds) or greater (at least four Rounds). This is probably because of the smaller numbers attending at least three Rounds (n = 77) or at least four Rounds (n = 40). Even if a single Round is attended, there appears to be a significant effect: the odds of caseness are reduced by 43% compared with non-attenders.
We also examined whether or not there was any evidence that attending a greater number of Rounds was associated with a greater degree of change in outcomes. Full details are given in Appendix 16, but the analysis backed up the previous results: there was a significant effect for psychological well-being only (in both caseness and Likert form this time), with more Rounds attended associated with better well-being at follow-up.
Sensitivity analyses
As with most studies, the administration of the survey and integrity of the sample were not perfect, with three areas of concern:
-
incomplete data (< 10% on most variables, although slightly higher for some demographic variables; see Appendix 15)
-
some areas of the survey applying only to staff who had regular contact with patients
-
changes in respondents’ work between baseline and follow-up surveys.
As such, the principal analyses [those reported in Comparison of regular attenders and non-attenders on outcomes (primary method)] were repeated under different conditions.
-
A full information maximum likelihood analysis was conducted (using Mplus; Muthén & Muthén, Los Angeles, CA, USA81) with all data to examine whether or not the results were affected by incomplete data.
-
Analyses were repeated with only those respondents indicating that they had regular contact with patients.
-
Analyses were repeated excluding any respondents who indicated in their follow-up questionnaire that their role had changed in any significant way, or (in a separate set of analyses) that they had moved organisation since the baseline survey.
In all cases, the conclusions reached were the same as those from the main analyses (i.e. that there was a significant effect on the GHQ-12 caseness score of psychological well-being, but not on the other outcomes). Therefore, we can conclude that the findings we reach (including the lack of significant results in most cases) are unlikely to be because of these areas of concern.
Moderator analysis
We examined a variety of other factors that might have had an impact on any effects of attendance at Rounds. The full results are in Appendix 16, but there were only three significant findings, which did not fit with prior expectations and are not easily explainable, and therefore are likely to have been type I errors.
Usefulness of Rounds
Respondents who had attended Rounds (whether or not regularly) were asked (in the follow-up survey) how useful they considered Rounds to be, on a scale from 1 (not at all useful) to 5 (very useful) (Table 17).
| How useful would you say Schwartz Center Rounds are? | Attenders (%) | |
|---|---|---|
| Regular | Irregular | |
| Not at all useful | 0 | 2 |
| Not very useful | 0 | 3 |
| Neutral | 6 | 16 |
| Somewhat useful | 27 | 39 |
| Very useful | 67 | 40 |
The majority of respondents in both groups found them more useful than not, but a higher proportion of regular attenders than irregular attenders described them as very useful, with a more even balance between somewhat useful and very useful. Among the irregular attenders, 5% found them not to be useful, and 16% felt neutral about their usefulness. This may give some clue as to why these respondents did not become regular attenders, although as the following section will show, there are other reasons.
We examined whether or not the perceived usefulness of Rounds (among attenders only) was associated with changes in the outcome variables. These models were based on the same types as previous models [multilevel ANCOVA for most outcomes, but multilevel logistic regression for GHQ-12 (caseness) and multilevel negative binomial regression for absence], controlling for the same covariates as the previous analysis.
Most models did not produce significant results, with no reason to suggest that the more useful an attender found Rounds, the more likely outcomes were to improve. However, the exception again was psychological well-being. For both versions of this outcome, relationships were found. In particular:
-
For the caseness version of GHQ-12, there was an odds ratio of 0.56 (95% CI 0.36 to 0.86; p = 0.009); that is, for each extra degree of usefulness perceived (e.g. moving from neutral to somewhat useful), the odds of being classed as a case would diminish by about 44%.
-
For the Likert version of GHQ-12, there was a regression coefficient of –0.11 (95% CI –0.16 to –0.05; p < 0.001); that is, for each extra degree of usefulness perceived (e.g. moving from neutral to somewhat useful), the GHQ-12 Likert score would move down on average by 0.11 points.
The two versions here give somewhat differing estimates of the importance of the effect; however, the conclusion from both is similar. The more useful attenders perceive Rounds to be, the higher their levels of psychological well-being after 8 months (when compared with their levels at baseline).
Other survey results
The survey included a variety of questions about perceptions of the Rounds and availability to attend (for attenders), or reasons for not attending (for non-attenders). These are summarised in the following tables.
Table 18 shows the reasons that regular and irregular attenders started attending Rounds. Being prompted to attend by managers or colleagues was an important reason for attending; however, interest in a topic was also regularly cited, and publicity had an effect.
| Reason | Attenders (%) | |
|---|---|---|
| Regular | Irregular | |
| A manager/colleague suggested I attend | 50 | 30 |
| I was interested in a topic | 36 | 35 |
| I saw publicity about it and wanted to find out more | 32 | 34 |
| A friend/team member was presenting | 18 | 14 |
| I was asked to present | 16 | 10 |
| I heard about it because of the research project | 8 | 5 |
| Other | 4 | 11 |
Under the ‘other’ option, respondents were invited to write why they had begun to attend. Most responses here were variations on the above options, including combinations of them, but others included ‘I’m interested in finding out if the Trust will be improving how staff deal with their emotions regarding stress’; ‘It was offered at work and I had emotional admissions at work this last few weeks so came for support and to see if it helps’; ‘I think it has been a time of many changes and an opportunity to stop, reflect and take stock is important’; ‘I am very interested in the reflective process and encouraging staff to discuss and explore their feelings’; and ‘To see if it would add anything to what we already do in our team’. Clearly, the role of stress and emotions at work was important for some people, and also some people saw Rounds as an opportunity to take time out, reflect, and determine whether or not things could be improved.
Thirty per cent of regular attenders and 27% of irregular attenders said that they always managed to attend Rounds when they wanted to. Barriers preventing attendance are shown in Table 19 (respondents could choose as many options as they wanted).
| Barrier | Attenders (%) | |
|---|---|---|
| Regular | Irregular | |
| I am too busy and not able to find the time | 41 | 40 |
| They conflict with other clinical priorities | 34 | 30 |
| There is no one to cover my work | 20 | 23 |
| They occur when I am not working | 16 | 17 |
| They conflict with other non-clinical priorities | 10 | 16 |
| The time is not convenient | 10 | 7 |
| I do not have autonomy over my work schedule | 4 | 5 |
| They occur in a different location from the site in which I am based | 4 | 11 |
| My break is too short | 4 | 9 |
| I have to wait to attend as we rotate attendance among the team | 4 | 4 |
| The topics do not seem relevant to me | 2 | 4 |
| I am not supported by my line manager to attend | 2 | 3 |
| Announcement of Rounds is at too short notice | 2 | 4 |
| The location is not convenient for me | 0 | 4 |
| I have moved to an organisation that does not run Rounds | 0 | 1 |
The main reasons for not attending Rounds more regularly were practical: most of all, the pressure of time, and either not physically being able to get to Rounds (because of schedules or locations) or other things being seen as priorities. The role of seniority and autonomy in being able to attend was clear from a couple of the comments (e.g. ‘I had time, when I was on an office day. These are unrealistic for clinical floor staff like nurses who have a job to do on the shop floor’). When asked why Rounds were useful or not, one respondent said:
For most of the floor caregivers they have no idea of the existence of these Rounds let alone what happens at them. They seem to cater for middle managers, and doctors at a certain grade who can take an hour out of their day to go and attend. Mostly they are scheduled at a lunchtime. In a 40-bed ICU [intensive care unit] or A&E [accident and emergency] it seems a little unrealistic to send staff as each nurse always requires another nurse to relieve her to go anywhere.
Other questions about attending Rounds are summarised in Table 20.
| Question/response | Attenders (%) | |
|---|---|---|
| Regular | Irregular | |
| Have you attended Rounds in your own time? | ||
| Yes, always | 18 | 30 |
| Yes, sometimes | 31 | 16 |
| No | 51 | 54 |
| Have you attended Rounds with immediate colleagues? | ||
| Yes, always | 33 | 28 |
| Yes, sometimes | 57 | 39 |
| No, only by myself | 10 | 33 |
| % who have presented at a Round | 31 | 12 |
| % who have frequently contributed to discussions at Rounds | 29 | 9 |
| % who have occasionally contributed to discussions at Rounds | 51 | 39 |
| % who have never contributed to discussions at Rounds | 20 | 53 |
Clearly, attending Rounds in one’s own time was crucial for attendance, with nearly half of all respondents having done this at least some of the time. Attendance with colleagues was another important factor, with just 10% of regular attenders not having attended with immediate colleagues. Regular attenders appeared more likely to contribute to discussions (although this may be because more Rounds attendance increases opportunities for participation in discussions).
Non-attenders were asked why they had never attended Rounds (Table 21) (respondents could select multiple options).
| Reason | Response (%) |
|---|---|
| I am not able to attend at the time they occur | 37 |
| I was unaware of what they were | 34 |
| There is no one to cover my work | 20 |
| I am too busy and not able to find the time | 18 |
| I do not think they are relevant to my role | 17 |
| I did not think I was invited | 17 |
| They occur when I am not working | 13 |
| They conflict with other clinical priorities | 13 |
| The topics do not seem relevant to me | 9 |
| They occur in a different location from the site in which I am based | 9 |
| The location is not convenient for me | 8 |
| I have no interest in attending | 8 |
| They conflict with other non-clinical priorities | 7 |
| I am not supported by my line manager to attend | 6 |
| I do not have autonomy over my work schedule | 6 |
| My break is too short | 6 |
| Announcement of Rounds is at too short notice | 3 |
| I have to wait my turn to attend as we rotate attendance among the team | 0 |
| I have moved to an organisation that does not run Rounds | 0 |
Some of the key reasons for non-attendance were respondents being unaware of what Rounds were, not thinking that they were invited (publicity issues) or not thinking that Rounds were relevant to their role; however, other key reasons fitted with the attenders’ barriers regarding time and other priorities.
Conclusions
The survey aimed to test whether or not regular attendance of NHS staff at Rounds was associated with higher engagement, well-being and other perceptions, attitudes and emotions than in those who did not attend. In addition, it sought to determine whether or not the extent of attendance (i.e. number of Rounds attended, or dose) was linked to the level of change.
We found no support for the primary hypothesis, that work engagement was higher as a result of attending Rounds, in terms of either regular attendance or the dose received. There are several possible explanations for this result (and for most of the secondary outcomes for which there were also no significant effects), which we discuss below.
However, an important result is for psychological well-being, for which we did find evidence of several effects. This was measured using the GHQ-12,82 which measures minor incidence of psychiatric morbidity. This tool is clinically validated, is well used in health-care and other populations, and has been shown to have links with other key outcomes across a variety of settings. Indeed, it is likely to be the best quality measure (in terms of validity and importance) of all those included in the survey. Therefore, the effects can be treated as important, particularly given the scale of the effects for the ‘caseness’ version of the measure, which is a clinically-validated classification of whether or not an individual would benefit from treatment. Among regular attenders of Rounds, the incidence dropped from 25% to 12%, compared with a drop of 37% to 34% among non-attenders.
The differences between the two groups at baseline should be acknowledged, and are an important feature of the interpretation. However, this is mitigated by three factors:
-
First, the models controlled for baseline values, so the changes were the focus of the analysis.
-
Second, the higher level of ‘caseness’ was found in the non-attenders group, where there was less change over time: this rules out any regression to the mean effects.
-
Third, the effect with psychological well-being was not limited to this one effect but was consistent across a range of effects. In particular, there was an association with ‘caseness’ levels using different definitions of regular attendance, or comparing any attendance with non-attenders; there was an effect of the number of Rounds attended, and of the perceived usefulness of Rounds.
There were also significant effects when performing sensitivity analyses to account for incomplete data, and for several of these effects there were also associations with the other scoring method for the GHQ-12 (the Likert method). Therefore, the finding appears robust, and seems unlikely to be because of a type I error. This is despite a relatively small sample size for regular attenders (in particular, the 25% and 12% at baseline and follow-up represent just 13 and six respondents of the 51 who were defined as regular attenders according to our protocol).
Given the importance of this finding, therefore, it bears further examination of why no significant main effects were found with most of the other outcomes: not only engagement, but also self-reflection, empathy, communication with patients, compassion, peer support and organisational support. It is possible that, with the relatively small sample size, there is an effect that was not picked up, given some credence by the fact that in all five scores there was a move in the expected direction among regular attenders (the same was true for just two of the five scores in the non-attender group). It seems unlikely that it is entirely down to this, given the significant change in well-being, although it is worth noting that for empathy, communication with patients and compassion, the sample size was smaller still, as non-clinical staff generally did not respond to these questions, and therefore type II errors are more plausible for these.
It is also possible that the measures used were not sufficiently sensitive to change, or robust, to capture any differences that may have occurred. Although most had been used before in health-care settings, they are not as well-validated as the GHQ-12, and in some cases had response tendencies towards one end of the scale (particularly compassion, for which most respondents scored very highly even at baseline). It should also be considered that the intervention delivered, namely attending Rounds, was not consistent across the whole sample (even within sites); no two Rounds are the same, and in particular those sites starting Rounds (from which a substantial number of participants came) may take longer to develop a consistent approach.
Another possibility is that this is a limitation of the self-report nature of the questionnaires, combined with self-selection into the attender group. The very act of deciding to attend a Round may be an indication that the respondent is, for example, more ‘engaged’ in organisational life and has also begun to consider some of the key issues and how they might address them, meaning that scores are more positive even at baseline, giving less opportunity to improve. This is exacerbated by the fact that two-thirds of respondents did not manage to complete the questionnaire before the first Round had begun, but sometimes completed it during or after the Round. In these cases, there may have already been some effect of Rounds attendance: if not on outcomes, then on cognitive processes such as those measured. This would also explain why there might be substantial (although not always statistically significant) differences in baseline values between the groups.
The finding that psychological well-being is significant despite this actually gives further support to this hypothesis. The GHQ-12 asks about actual symptoms during the previous month; therefore, responses to this are not likely to be affected by having just attended a Round. However, the same cannot be said for many of the other measures.
Overall, the conclusion appears to be that attendance at Rounds might not have any particular impact on work engagement, or certain other attitudes and emotions, but there is good evidence to suggest that there could be a significant reduction in poor psychological well-being as a result of attending Rounds.
Chapter 6 Staff experiences of Rounds
Overview
This chapter provides an overview of findings from the case studies in relation to staff experiences of Rounds.
Objectives
The objectives are to identify:
-
staff experiences of attending, presenting at, facilitating and leading Rounds and reported Rounds outcomes (objective 10)
-
reasons for variance in attendance, including enablers of and barriers to attendance (objective 11a)
-
reasons for variation in facilitation (objective 11b).
Methods
Data are drawn from our nine case studies (Tables 22 and 23) and phase 1 mapping interviews (Table 24). Further details of methods and analysis are given in Chapters 2 and 4.
| Site ID | Interviews (n) | ||||||
|---|---|---|---|---|---|---|---|
| Facilitator/clinical lead | Steering group | Senior stakeholder | Panellist | Attender | Non-attender | Total | |
| Mulberry | 3 | 3 | 4 | 5 | 13 | 2 | 30 |
| Juniper | 2 | 2 | 2 | 5 | 7 | 2 | 20 |
| Cedar | 2 | 2 | 0 | 7 | 7 | 1 | 19 |
| Cherry | 2 | 2 | 1 | 4 | 4 | 2 | 15 |
| Willow | 5 | 4 | 3 | 4 | 12 | 1 | 29 |
| Sycamore | 4 | 2 | 1 | 4 | 3 | 3 | 17 |
| Horse-chestnuta | 4 | 1 | 0 | 1 | 2 | 0 | 8 |
| Elderberry | 3 | 1 | 2 | 3 | 4 | 2 | 15 |
| Ash | 2 | 4 | 2 | 6 | 7 | 3 | 24 |
| Total | 27 | 21 | 15 | 39 | 59 | 16 | 177 |
| Site ID | Observations (n) | |||
|---|---|---|---|---|
| Panel preparations | Schwartz Rounds | Steering group meetings | Total | |
| Mulberry | 4 | 6 | 6 | 16 |
| Juniper | 2 | 5 | 3 | 10 |
| Cedar | 6 | 6 | – | 12 |
| Cherry | 2 | 5 | 3 | 10 |
| Willow | 3 | 5 | 6 | 14 |
| Sycamore | 6 | 6 | 3 | 15 |
| Horse-chestnuta | – | – | – | – |
| Elderberry | 3 | 4 | 4 | 11 |
| Ash | 3 | 5 | 3 | 11 |
| Total | 29 | 42 | 28 | 99 |
| Type of site | Interviews (n) | ||
|---|---|---|---|
| Facilitators | Clinical lead | Total sites | |
| Hospice | 7 | 3 | 10 |
| Acute | 20 | 15 | 32 |
| Mental health/community | 1 | 3 | 4 |
| Total | 28 | 21 | 46 |
Case study participants were identified through purposive and snowball sampling. Participants who agreed to be contacted were sent a participant information sheet (see Appendix 17) and invited to take part in a 30- to 60-minute interview. These took place by telephone or in person between April 2015 and June 2016, at which time the interviewer explained the objectives of the study, answered questions and took informed written consent (see Appendix 18). The semistructured interview schedule (see Appendix 19) was developed to explore participants’ experiences of facilitating, leading, supporting, and attending and/or not attending Rounds. Each interview was transcribed by a professional transcription service and analysed using a thematic analysis approach, following key stages of data familiarisation, data reduction and interpretation. A two-stage thematic analysis process was conducted using (1) an inductive analysis of a sample of transcripts to generate initial codes and themes that fed into the development of (2) an a priori coding scheme, informed by the findings from the literature review (see Chapter 3) and early observations of Rounds. The themes were examined across participants for consistency and, when appropriate, constructs were categorised into smaller units. All data were coded in the qualitative data analysis software package NVivo (QSR International, Warrington, UK).
Results
Attendees’ experiences
In this section, we describe the enablers of and barriers to attendance at Rounds, factors influencing whether or not audience members speak, staff perceptions of Rounds, and Round attendance outcomes.
Reasons for attendance: enablers
Word of mouth was effective in encouraging people to attend Rounds:
I do try to encourage a number of my colleagues to go [. . .] I sometimes think when you see it [the round publicity] [. . .] I didn’t have a clue what that was about [. . .] and I passed it by for a bit. So a bit more explanation under it [the publicity] that you can easily see might capture people’s attention [so they might be persuaded] to go.
Willow-32-Attender
When a topic seemed relevant and resonated with potential audience members, they were more likely to go:
I went to the [name of hospital] one because the topic was relevant to me, which was ‘the hospital at night’. And I wanted to go because I often am here by myself working [. . .] it’s a very intimidating place to be at night for me by myself.
Cherry-71-Attender
The publicity for and titles of Rounds were important influences on whether or not staff attended:
I just saw a poster in the ward, and actually I was saying to someone ‘I can understand why patients feel angry’ and then I said, ‘Oh, maybe I should go to this’.
Juniper-14-Attender
In other examples, a lack of knowledge about Rounds meant that the publicity did not initially engage:
I used to see the Schwartz Round advertised and [. . .] delete the e-mail because it didn’t make sense. The title didn’t really mean very much to me. I get lots of e-mails. Then one day I read it a bit more and I thought ‘oh that sounds really interesting’.
Willow-32-Attender
For many staff, it was not enough to be told about Rounds, or to see publicity, to really understand what Rounds were: they needed to experience them.
Finally, non-clinicians told us that they thought that Rounds were a helpful way of finding out about the experience of clinicians and, as a consequence, they felt more connected to the organisation’s purpose of delivering excellent patient care. Some participants told us that they found witnessing colleagues’ distress in Rounds uncomfortable and that it felt voyeuristic.
Reasons for attendance: barriers
Reasons given for not attending included not understanding what Rounds were and practical difficulties such as location and timing.
A few Rounds attenders whom we spoke to decided that Rounds were not for them, and Rounds attendance was an issue for some staff. Certain groups were more likely to attend than others. Ward-based staff in acute care and community staff, who faced geographical challenges accessing Rounds, struggled to attend Rounds, despite initiatives to address the barriers. Ward nurses, on 12-hour shifts with only two half-hour breaks, lacked the autonomy to make the decision to attend or found it hard to find the time to attend, particularly at lunchtime when patients needed support with meals, unless someone else covered the ward or it was particularly quiet. Even those with autonomy over their work schedule experienced some difficulty, with work pressures being the biggest obstacle to attendance. Some organisations experimented with running Rounds at different times of the day to attract different staff groups. Other strategies included releasing staff to attend Rounds on a rotational basis and prioritising attendance among those who had a personal connection with the case being discussed:
It tends to be quite a lot of senior people that go [. . .] What’s up with one person feeding back at that senior level and getting the girls on the ward [to attend], giving them a little break to go to the Schwartz Round because it’s beneficial for them? It’s good for the health-care assistants, it’s good for the ward clerk, everybody makes a team [. . .] One senior member go, feedback, take it in turn every Schwartz Round, utilise that time to go and cover your member of staff on the ward to free them up, make them feel valued and let them go to the Schwartz Round and hear how good it is.
Sycamore-26-Attender
Staff perceptions of Rounds
Several interviewees were surprised by the extent of audience discussion and involvement, expecting the time to be occupied by formal presentations, or were surprised by their own emotional reaction and that of others.
In terms of Rounds’ structure, many appreciated the ritual and predictability, suggesting that this contributed to feeling safe; audience members valued hearing about the origins and history of Rounds, feeling that this contributed to Rounds’ legitimacy. It was recognised that Rounds needed time to evolve within organisations, especially as audience members became more accustomed to Rounds and the associated behaviours and etiquette.
Participants described Rounds as interesting, engaging and a source of support. Participants valued the opportunity to reflect and process work challenges. Many appreciated the opportunity to learn more about their colleagues, understand their perspectives and motivations, and engage in multidisciplinary interaction. This led to greater understanding, empathy and tolerance towards colleagues and patients. Key themes included:
-
contextualising patients and staff
-
seeing the person in the professional
-
feeling that their experiences are validated and they are not alone
-
levelling effect of Rounds
-
acknowledging vulnerability (see Chapter 8).
These findings link closely to Chapter 8; thus, here we briefly present these themes, with further data provided in Chapter 8.
Rounds stories provided greater context regarding patients and staff, and attendees described gaining insight into the daily reality of other staff, which helped them recognise that they were united in common efforts to deliver health care. Attendees voiced greater respect and appreciation for colleagues after learning more about their role and had a better understanding of patients’, carers’ and staff’s behaviour, as well as the uncertainty involved in health-care work:
I think it certainly has enabled me to put myself a little bit more in the situation of my patients and think ‘actually what are they going through?’ It enables you to stop and draw on the experience [. . .] and that’s where I think it makes you better because you perhaps get less angry at people’s responses to things and realise that actually there is a lot of emotion involved within these situations and that they’re not just robots that are dealing with a case and it’s never black and white, I think you realise more and more as you listen to these Schwartz Rounds, there’s never a true right or wrong.
Cedar-29-Panellist
Rounds stories allowed staff to see the person in the professional, and corrected misconceptions that they held about individuals, helping staff understand each other’s behaviour, promoting tolerance and greater empathy in times of adversity:
I think it helps me understand other people’s perspectives. [. . .] If I can understand people that means I can feel more empathetic. [. . .] I like to think there’s a lot of understanding and empathy being created within the audience, [which] I hope is undoing some negative psychological processes as well as creating some important ones.
Willow-20-Attender
The majority described how Rounds validated their actions and emotions, helping reduce feelings of isolation. Rounds had a levelling effect by highlighting the reality that all staff groups, regardless of seniority and experience, encountered difficulties:
I find it of huge benefit to know that we are all in this together, that we do not have our heads down in the dust and the dirt pretending everything is all right. That it is OK to speak and say it is a really shocking environment that we work in and that we are all pushed to our limits on many occasions, affecting all aspects of our work. It makes us feel very uncomfortable because you want to give good care [. . .] and also [. . .] the target-driven nature of things [. . .] that human interaction with the patients [and] relatives has a tendency to go. [. . .] I just find [. . .] every meeting is enriching and a nourishment to one’s soul and psyche that [. . .] we can talk about it.
Kennett-155-Clinical-Lead
Rounds attenders were impressed by their colleagues’ honesty, especially those who showed vulnerability. Many felt that this was countercultural to the NHS mentality of appearing resilient at all times and was all the more notable when recognised in a public forum. Hearing senior colleagues express vulnerability, emotion and regret was said to be powerful and connecting and to provide role models. Such knowledge supported participants in the realisation that no one is infallible, acquitting many of unrealistic expectations. Awareness that all staff encounter difficulties in the emotional, social and ethical aspects of their work contributed to feelings of relief. Interviewees told how Rounds had been educational in helping them understand situations more fully and not as ‘black and white’, and promoting coping strategies to help them manage difficult situations.
Factors influencing whether or not audience members speak at Rounds
Audience members spoke when they had experienced a similar situation, when they felt that panel members would benefit from their contribution, when they wanted to provide moral support, and when they wanted their story ‘heard’. Some contributed only when they had sufficient authority on the topic and deliberately held back to allow colleagues an opportunity:
I’m not a person who says a lot, but I’ve probably [spoken] once [or] twice [if] there’s a topic or an area [that] I have an opinion or an experience [in and] that I feel is probably good to share with the audience.
Cedar-9-Attender
Others spoke in support of colleagues on the panel or the facilitator to keep the Round safe; some were reluctant to show emotions publicly, and the presence of a line manager prevented some contributing. Other reasons why audience members did not speak in Rounds included a lack of confidence, not having a connection with the case, and a reluctance to engage with a contentious topic.
Round attendance outcomes
Individual-level outcomes
Individuals reported positive outcomes, for example increased reflection, self-efficacy, well-being, understanding of their own and others’ emotions, and a connection to others and to the organisation and its values. The free lunch made people feel cared for by the organisation. Rounds provided psychological relief through the open expression of strong emotions for those who shared their story:
It gives them that outlet [. . .] the gentleman that was upset about how that patient was treated a couple of days ago, it was still fresh in his mind you could clearly see he was quite distressed by what had happened and it was just allowing him just to talk about what had happened to other people [. . .] to get it off his chest and hopefully he will settle a little bit more after that.
Mulberry-20-Attender
Rounds helped remind staff to pay attention to their own well-being:
I’ve seen colleagues go off sick and [. . .] I think this is a reminder that we need to pay attention to those things. And although we help clients embrace change and cope with change, we need to make sure that we can do that with ourselves.
Willow-37-Attender
Group-level outcomes
Group-level outcomes included greater knowledge of colleagues’ roles and challenges; creating new connections between staff groups; better teamwork; improved communication; and feelings of greater compassion, empathy, cohesion and trust between colleagues:
What you can actually see is that cohesive team spirit being built [. . .] if you realise that other people are going through similar things. Or other people are going through things that you never even realised and they’re prepared to tell you and share that with you, it definitely builds up a level of trust which makes the team work better.
Severn-396-Facilitator
Rounds were reported by one facilitator to ‘change the nature of conversations’, and participants identified ways in which they had altered relationships between colleagues, including an increase in emotionally focused discussions and communication, resulting in less superficial dialogue between colleagues outside Rounds.
Patient-level outcomes
Rounds attendance contributed to patient care by allowing attenders to understand the wider context of patients’ and their families’ attitudes and/or behaviour, resulting in greater empathy and compassion towards them. This was especially important when staff had encountered hostile, aggressive, difficult or challenging individuals and situations. Some thought that Rounds had reminded them to see patients as people, helping them keep in touch with their own humanity while caring:
Under pressure to just keep doing more and more, it’s very easy to forget that your patients are people and just see them as tasks to be completed as quickly as possible. So I think a real reminder of the importance of a human element to care for the patients is huge and also a reminder to keep in touch with your own humanity as a health professional is important for [. . .] Self-preservation in this kind of environment.
Willow-34-Attender
Non-clinical staff and/or staff with limited patient contact told how Rounds provided them with a reminder of the clients they serve (the public):
I went because I sit in my office and a lot of times you forget that it’s actually patients you’re [helping]. I could be in a factory. It was nice for me to remember that when I’m doing my contracts and saying yes or no to a trial based on money.
Mulberry-13-Attender
Neutral or negative outcomes
Despite looking long and hard, we found very few participants who spoke negatively about Rounds, but those who did questioned the purpose of unearthing feelings of sadness, anger and frustration, and said that they found witnessing the agony of others uncomfortable:
If I switch my cynical head on it almost felt a bit like Alcoholics Anonymous[®] [. . .] I’m not sure about the format where you kind of make four people share an experience as a catalyst to try to get the audience to participate, I thought that was a bit harrowing really.
Mulberry-19-Attender
The story was about how a professional who got involved with a patient, in the broadest sense and [the panellist’s] reflection was on how he dealt with that and so on. I did think that he [the panellist] was basically spying on other people’s agony somewhat.
Mulberry-19-Attender
Some participants found it hard to isolate the impact of attending Rounds, saying that Rounds did not single-handedly trigger change but were part of a diverse body of experiences that, collectively, had an impact on behaviour:
No [nothing had changed] not as a result of that [Rounds] directly. I think it’s very tough to assign changes in practice to one particular set of conditions, all these things get internalised don’t they?
Cedar-22-Attender
I don’t think single-handedly they’ve changed anything for me, but they have reinforced other learning or teaching I’ve had from other sources. [. . .] They have confirmed aspects of what I now see I do as good practice, which is encouraging.
Cedar-20-Attender
Interviewees were asked if they had been to any Rounds that they felt were ‘unsuccessful’ and to explain what it was about the Round that contributed to that. Attendees suggested that poor attendance, prolonged silences, strained discussions and perhaps a lack of personal interest in the Round topic defined whether or not they felt that the Round was successful:
I think there has been a couple [. . .] I don’t know if they didn’t work, but weren’t as well attended, lots of silences and it was quite difficult to get the discussion going. I don’t know whether [that’s because it] has to touch you personally or whether you have to have some investment in the topic.
Horse-chestnut-12-Attender
Others, however, identified the importance of silence as a unique aspect of Rounds that supported contemplation, and provided a counterweight to their usual busy, noisy professional lives (see Chapter 8, Countercultural/third space for staff).
Panellists’ experiences
The panellists we interviewed came from diverse backgrounds, disciplines and roles. Most had attended Rounds as an audience member, and a few were, or had been, facilitators. We interviewed 39 panellists to gain their perspectives.
Motivations for presenting
Reasons given for agreeing to be panellists included professional development, increasing visibility and their own or team’s profile, seeking closure on a difficult situation, showing appreciation towards colleagues, sharing knowledge and helping others learn from their experiences. Panellists reported wanting to process a difficult clinical experience and said that they felt a sense of achievement after receiving positive audience feedback. Some respondents valued the opportunity to say thank you to colleagues publicly. In established Rounds sites, audience members were more likely to volunteer to be a panellist or suggest that their team might be willing, and learnt what makes a good Schwartz Round case or topic: ‘often people say “oh this is definitely going to be a Schwartz Round” ’ (Cedar-28-Panellist).
Panellists also described utilising Rounds to share experiences to enable learning, especially when the topic was associated with a misunderstanding or a lack of action:
I wanted to share that experience because I know that mental illness is quite stigmatised still in medical profession especially with colleagues in sort of A&E [accident and emergency] departments [. . .] I thought it would be a good opportunity to put it out there that if you’re frustrated, angry, scared and confused with our patients, we feel it as well sometimes.
Willow-29-Panellist
Panellists’ experiences of Rounds’ stages
Panellists described their experiences of Rounds’ stages: ‘sourcing stories and panellists’, ‘panel preparation’ and ‘telling stories to trigger reflection and resonance in Rounds’ (Figure 6; see Report Supplementary Material 7 for a summary of these stages).
FIGURE 6.
Stages of Rounds.
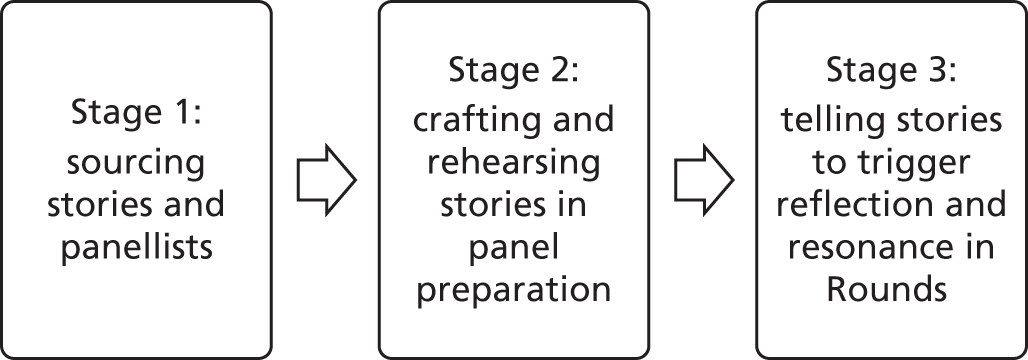
Experiences of panel preparation
Panel preparation played a significant role in shaping stories, giving panellists the confidence to tell their story publicly, and defused some of the raw emotion:
Well I burst into tears, I cried through the whole thing. [I felt] so much better that [I’d] done that. Yeah so we just had a quick run-through about how what we were going to talk about affected us and the wider kind of organisation.
Sycamore-09-Panellist
For many, this preparation helped panellists feel ‘safe’ to tell their story and provided emotional support, some ‘closure’, and catharsis:
Yeah. I think – [in the panel preparation] the planning, I think we certainly got – I think we were using the word ‘closure’ quite a lot, and I think that was really helpful.
Cedar-27-Panellist
It also helped panellists decide on the content (critical moments or an aspect of an experience), style and structure, and to think through the implications of what they chose to reveal, for both them and the audience, so that whatever they decided to share was done so with informed consent. Panellists varied considerably in the amount and type of preparation that they needed, and received. The panellist quoted below (who had presented several times before) explained how he felt that the preparation was more for the facilitator’s benefit:
It was more of a reality check for them because they [facilitator] didn’t really know what we would be coming up with [. . .] they didn’t necessarily know whether I would be able to present it in a way that was interesting to people coming to a Schwartz Round [. . .]. So it was much more of them listening to what we were going to talk about. Maybe one or two queries about ensuring that we were going to be able to discuss how we felt about it at the time.
Sycamore-12-Panellist
Panel preparation was not available to all, and when it was available it varied in frequency and quality. Some who received no or limited panel preparation felt that they had ‘survived’ the Round rather than fully engaged with it:
I did feel relieved that I survived it and I felt relieved that [my story] hadn’t been in one direction and everybody else has been in the other.
Ash-04-Panellist
Pre-Round expectations
It was not unusual for panellists to present at a Round without having attended one, and some had preconceived ideas of what it might be like:
I almost thought it was going to be like a circle [. . .] and everyone shares experiences within that. It wasn’t like that [. . .] it felt very safe.
Mulberry-25-Panellist
Participants explained that they had been worried about the relevance of their story or that having people they knew in the audience would make them more nervous, or that they would feel intimidated by the seniority of other panellists:
Yeah I was a little bit nervous at first when I realised who else was on the panel. And it seemed to be that everybody there was quite a lot higher up than me. But I think it went quite well.
Ash-02-Panellist
Experience of presenting
Facilitators were described as supportive and their role in keeping Rounds safe was recognised. Some panellists felt anxious because they had performance nerves, or they were worried about the audience’s reaction to their story or about being emotional in the Round. However, once panellists had presented, their concerns were generally replaced with feelings of fulfilment, benefit and privilege. Most spoke positively about the experience:
It was really good yeah. I was really surprised at the amount of people that turned up [. . .] I think I probably hadn’t really thought about what it would be like to do it. So I mean it was good really, I hadn’t really known what to expect, but the experience was really good.
Trent-29-Panellist
Several judged the success of the experience by the level of discussion following their presentation, and whether or not their story was referred to. Most found the audience receptive and supportive.
Many panellists reported that they felt honoured by the realisation that they had held the audience’s attention:
Yeah, I felt listened to, I felt – and I was scanning the room as much as I could to see people’s faces and they were all focused and whoever was talking they was all focused on that one person [. . .] that’s quite an honour to be in that position to have people’s attention for that length of time.
Mulberry-01-Panellist
I think it went well [. . .] the feedback when people took part, that was really interesting. So I felt that people were engaged and that must be deemed as a sign of success really.
Ash-01-Panellist
A minority told how they had witnessed direct negativity from members of the audience, which left them feeling upset. Although many panellists embraced the emotions associated with Rounds, some found the experience emotionally exhausting. In a Round, after the panellists share their stories, the facilitators hand over to the audience, and there is often silence before the first person speaks, which can be uncomfortable:
After the panel had spoken, the audience I find go into this terrible silence, you can almost hear people thinking shall I say something, I’d really like to say but I’m not brave enough, but then once someone gives their opinion or gives their thought then other people start to put their hand up and speak.
Elderberry-04-Panellist
Others, however, learned to appreciate the silence. The interviewee quoted below explained how she interpreted the silence:
I think for me it was the silences [. . .] that’s what’s so powerful about Schwartz is that it’s, there’s that pause, it’s you’ve been and you’ve shared [. . .] And sitting there for me having shared that, that sacred space if you like, that gap wasn’t suddenly filled unnecessarily. It was like it was all this is, and then people did come and chip in, but that was really powerful that gap [. . .] And it really makes it feel really, really sacred and puts the dignity into what’s being said, or it did for me that day.
Elderberry-11-Panellist
Panellists reported a number of positive outcomes associated with their experience on the panel, including a greater sense of affiliation with the wider organisation and feelings of fulfilment, energy, inspiration, motivation, catharsis, closure and validation. Several felt that the experience had brought a new perspective to their story, prompting them to share previously unspoken feelings. Others described how the experience had increased their resilience and self-awareness and had altered their interactions with others, for example increased dialogue between colleagues, feelings of greater approachability and trust between coworkers, and more acceptance of others’ behaviour.
Facilitators’ and clinical leads’ experiences
Rounds are usually co-facilitated by facilitators and clinical leads. A facilitator often takes the lead role (especially in audience discussion, holding responsibility for the Round) and the clinical lead takes a supportive role (explaining the purpose of Rounds and establishing the ground rules). We interviewed 27 participants from the nine case study sites. Facilitator style is presented in Chapter 7.
Overall experiences
Facilitators perceived Rounds facilitation as a great responsibility, wanting to ‘get it right’ and feeling quite daunted by the whole experience. Facilitators were keen to make it safe for staff to share experiences, and to gain the audience’s acceptance and participation while maintaining control. Facilitators spoke of the courage needed to stand at the front of the room and ‘carry the Round’: ‘initially it’s completely scary in case you put your foot in it and fall flat on your face’ (Ash-400-Facilitator).
There were also some apprehensions that the Round discussion might not ‘work’ or be appreciated by staff, especially when Rounds were new to an organisation:
I was hoping it went well. It felt good. The evaluations were positive. I was just nervous because I was prepared as much as I could be and then realised as soon as we got to the audience bit I had no control.
Willow-16-Facilitator
Over time, many concerns decreased as facilitators’ confidence and experience increased.
Some held the joint role of clinical lead and facilitator. Key responsibilities of the clinical lead included spreading the word about Rounds and supporting the facilitator and steering group in finding and developing stories, and encouraging their medical colleagues to attend, as identified in the PoCF handbook. Clinical lead involvement varied across sites (see Chapter 7).
A lack of capacity to offer support before the Round, owing to other work commitments, was a challenge that the majority of clinical leads acknowledged and that meant that they could not support or release the facilitator from the Rounds’ associated task of panel preparation. Another downside of having missed panel preparation was the potential for clinical leads to be emotionally affected by the panellists’ stories during the Round:
I have to say [the facilitator] does all the [laborious work], all the preparation. I have tried to be present to prepare a few of the panel members, but it’s only been a handful and fortunately they appreciate how busy I am and they just prepare the panels and I just pitch up often. Which sometimes means that I haven’t heard the panel stories before and I get a bit hijacked by the emotions sometimes, because I’m hearing the stories fresh for the first time.
Mulberry-168-Clinical-Lead
As with other key Rounds roles, clinical leads described giving over and above the formal resource allocation for Rounds. Despite their efforts, this still limited the amount of support they could offer, which contributed to feelings of guilt and/or a lack of preparedness for some. Clinical leads highlighted the impact that Rounds involvement had had on their practice:
It’s always a bit of time pressure fitting in the panel work and fitting in the Schwartz Rounds. There have been times where I’ve had to delay the start of my clinic because I’ve got a Schwartz Round steering group. But then that’s outweighed by the positive benefits of learning so much from attending the Schwartz Rounds and reflecting on your own practice and resonating with the case. So I think the positives outweigh the negatives.
Willow-178-Clinical-Lead
I don’t have the opportunity to particularly clear my desk, clear my morning either before or after the Round [. . .] One day I went from the Schwartz Round straight into my performance meeting [. . .] And it’s really interesting in my head to compare the hour or so in the Schwartz Round which is a very compassionate, kind, listening environment to the very aggressive, unforgiving environment of my performance meeting.
Mulberry-168-Clinical-Lead
(See Chapter 8, Countercultural/third space for staff for more about contrasting culture.)
Motivation and rewards
Facilitators and clinical leads were often important champions, motivating others to be involved and helping bring Rounds to their organisation. They were highly motivated and had a strong belief in Rounds and their importance in supporting staff in the difficulties they faced in their work. Facilitators described their personal reasons for being involved. These included a perceived alignment between the objectives of Rounds and the facilitator’s values, such as a professional interest in employee engagement and/or reflective practice. Interviewees reported that facilitating Rounds was a privilege, a pleasure and enjoyable, and gave them satisfaction:
As a facilitator, you have that wonderful, very privileged position of seeing both audience and panel, you can see everybody, and it’s just watching people’s reactions as they listen to stories, as they pluck up the courage to put their hand up and participate. It’s quite nice for you to see it flourish.
Tay-127-Clinical-Lead
Facilitators found it rewarding when staff engaged in the discussion. Some considered this an indication of success:
It gives me a buzz when you see that people have really engaged with an issue and that it had some kind of impact on them, whether that’s about them feeling much better supported or perhaps it’s about them feeling better equipped to deal with a similar situation.
Ash-05-Facilitator
Being a facilitator was described as a challenging, rewarding and career-enhancing experience that brought new skills and confidence, which was good for personal and professional development:
I think it’s been a fantastic experience for me. I hadn’t done anything like this before [. . .] I’ve got more confident in helping facilitate Rounds. Initially, I remember feeling absolutely petrified, thinking how are we going to keep going. I still do that to a certain extent because I’m not in my comfort zone, so actually I think doing something out of your comfort zone is actually incredibly rewarding, especially when people are positive about it.
Elderberry-324-Facilitator
Facilitators felt that Rounds had caused them to reconsider the wider implications of their actions and behaviours, especially when interacting with patients and relatives:
I think they [Rounds] make me more reflective as a clinical practitioner. So I’m much more tuned in to how the patient might be feeling, how their family might be feeling and [so I] don’t concentrate so much on the medicine but think about the bigger picture and probably practise more holistically.
Willow-178-Clinical-Lead
Facilitators also described how their involvement had made them more visible and created new connections:
You’re no longer invisible and it has been absolutely lovely forming connections with people who I’d have never got to meet otherwise and hearing about their work and hearing what they do and that has been wonderful.
Ash-400-Facilitator
Challenges
The challenges associated with facilitating Rounds included emotional and psychological concerns, a lack of time and support for Rounds, and pressure to make Rounds a success. For example, facilitators described concerns about keeping Rounds safe and their dilemmas about when and how far to intervene. Some deliberately held back in their facilitation, feeling that they did not always have the permission to step in, as Rounds, although having therapeutic benefits, were not a therapeutic intervention. Addressing the important issues while not taking the discussion ‘too far’ was a challenge. For example, a lack of expertise or experience concerning the content of the Round discussion was a factor that might prevent some facilitators from intervening when needed, yet a reluctance to engage in deeper emotional discussions regarding issues that happen in the workplace might prevent Rounds reaching their full potential:
If something was presented as a risk or issues of malpractice that would worry me because that’s where my clinical expertise is lacking and so I wouldn’t feel comfortable facilitating because I don’t deal with those situations routinely.
Willow-16-Facilitator
Facilitators were very mindful of not wanting to push panellists too far and cause distress, and they were alert to providing emotional safety and containment (see Chapter 8).
Lack of time and support for Rounds
A key challenge was having the motivation and resources to sustain Rounds. Many felt that the resources to deliver Rounds successfully were insufficient and diminished over time (e.g. steering group support) or had been underestimated. Many reported that there had been a surge of support for Rounds when first launched, which diminished with time. In some organisations facilitators were left to manage much of the planning and delivery, as those charged with the task of supporting Rounds (non-facilitating clinical leads, steering group members and Rounds administrators) became preoccupied by other priorities. Facilitators described how a lack of support made delivering Rounds difficult:
Preparing for them [Rounds] probably takes up much more time than I anticipated and particularly because the other co-facilitator is part time, so I often feel I’m doing a lot of the preparation – identifying and preparing panel members and organising steering groups.
Stour-355-Facilitator
Some facilitators were left to manage the weight of responsibility owing to their perceived expertise. However, there was widespread agreement that the responsibility of Rounds should not rest with one or two individuals given the enormity of the task and the issue of sustainability:
It’s important [Rounds are] not just for two people to run, especially given how huge it is and how difficult engaging people [can be] [. . .] [Rounds need] at least 10 different people and they pair up in fives and they do different ones, at least every other month, if not every month with different teams and in different settings.
Willow-177-Clinical-Lead
Good administrative support was key to the success of Rounds but was not available to all, and the task fell on the facilitator or clinical lead, which amplified the other challenges.
Many facilitators felt that the onus was on them to make Rounds a success. Given the challenges of measuring outcomes, ‘success’ was often measured by attendance numbers. Most facilitators we spoke to felt that having good monthly attendance figures was an important marker of success, but others felt that to reach a few people was sufficient:
So the numbers don’t necessarily mean all of it and if we change two or three people’s lives in 1 hour then that’s a Round. And that’s why I love it and that’s why I’d want to carry on doing it, because you can’t save a hundred people from emotional woe all in one go. I think it’s baby steps.
Willow-16-Facilitator
Facilitators also highlighted misunderstandings about the purpose of Rounds, as some employees were advised (by management) to attend Rounds to help address problems, grievances and personal issues. This meant that responsibility passed on to Round organisers to deal with issues that would have been better addressed elsewhere. Many suggested that Rounds were a ‘slow burn’ intervention that took time to develop and be effective, and part of the effectiveness was educating staff about how they worked, developing emotional literacy and creating a Schwartz-savvy audience (see Chapter 8). Some facilitators worried that staff would become bored with the repetitive nature of the Rounds format (whereas others suggested that the routine and ritual were important for emotional safety). Some facilitators felt that they would benefit from support and debriefing for their own emotional well-being.
Steering group members’ experiences
We interviewed 25 steering group members from the nine case study sites. An active steering group was reported as essential in supporting Rounds, for example in sourcing stories and panellists, debriefing and evaluating Rounds, advertising Rounds and booking venues. We noted the diversity of steering groups, in terms of how often they met, the types of contributions made by members, and the size of the core and extended steering groups (see Chapter 4 for more on steering groups).
Some facilitators valued the steering group presence with the Round audience, both as a source of observation (when considering ways to improve) and as an opportunity to role model (preferred audience behaviours) through their contribution to the discussion (see Chapter 7 for more on what makes a Schwartz-savvy audience): ‘I think it’s about having the steering group in the audience and alert and ready to pick things up and just giving support to the facilitators at the front’ (Cedar-05-Facilitator).
Some steering group members described how they had been part of the team that brought Rounds to their organisation, having led negotiations with senior stakeholders: ‘I was part of the original steering group that helped to get them [Rounds] going. My role involved helping to get a buy-in from the board’ (Mulberry-05-Steering-Group-Member).
Those whose involvement began once Rounds had been established described being invited to join the steering group as a representative for some (often under-represented) staff groups, with the intention of promoting attendance among such groups:
[The clinical lead] was keen that there would be a junior doctor representative because we’re quite an under-represented group in terms of the people who go to Schwartz Rounds at the moment [. . .] So I said that I would encourage my peers to go.
Willow-05-Steering-Group-Member
Steering group members described their contribution, most of which related to Rounds promotion: displaying posters, updating the staff intranet pages and telling people about Rounds. Some helped identify panellists and stories. Others saw their role as a reviewer, assessing the Round and making suggestions for change if necessary:
I think the role on the steering group is just to try and give honest feedback about the particular Round – about what could have been done differently. Not necessarily better, but just differently – whether a new idea or something worked or didn’t work.
Willow-06-Steering-Group-Member
We often heard from facilitators that the steering group had diminished in size, with enthusiasm and attendance dropping over time.
Stakeholder experiences
We explored how board members (e.g. executive and non-executive directors) viewed and contributed to Rounds.
Most spoke positively of Rounds, for example:
I think they’re [Rounds] a really important part of what we offer [. . .] the Schwartz Rounds brings people together from all walks of life, all jobs and it gives them permission to speak and it feels safe.
Elderberry-08-Stakeholder
In our case study interviews with facilitators, we detected an anxiety concerning the need to produce ‘results’ (i.e. that some measurable impact of Rounds was required to get continued support from stakeholders), but this was not reflected in stakeholders’ interviews.
Some board members had been panellists and had talked about their own emotional distress in the hope that others would benefit from their experience:
I spoke about my own personal experience of having suffered from depression [. . .] I just didn’t find it easy to talk about it, but I think it was fine. And I was really glad that I had done it [. . .] I had a feeling that there were people there who may have also suffered from depression or be suffering from depression and may have found it quite a hopeful story.
Cedar-24-Stakeholder
Despite being a regular attender, one board member explained her reluctance to contribute as a panellist or an audience member:
I mean my own philosophy is that I don’t really talk at that [Rounds] because I’m just wondering what, I don’t know, because of my position I’m not sure that it’s necessarily a great idea [. . .] not appropriate [. . .] I see myself very much as watching and listening rather than taking part.
Elderberry-20-Stakeholder
The opportunity to be an influential role model for junior staff was welcomed by one board member who, as a panellist, spoke about their (sometimes negative) feelings towards patients, in the hope that others would follow:
I believe you’ve got to lead by example really [. . .] [I spoke about] a patient from a personal point of view [and asked the audience] could you ever like this person? And they were all saying no. They were talking as human beings and I let them do that and I think that’s what Schwartz Rounds are about, they’re just, we are all human beings. So yes leading by example and let them know it’s OK to do it and if the boss is doing it then it’s OK for them.
Juniper-25-Stakeholder
Some described their involvement as that of a figurehead. Although board members might not always attend Rounds, a number kept informed through minutes and reports.
Stakeholders from new providers anticipated positive changes to employees’ experiences at work as a result of the introduction of Rounds:
I’d like to think in our snap surveys of staff that people will start to report that actually they feel that there’s a greater recognition of the demands for them in their work.
Mulberry-26-Stakeholder
It was predicted that such changes might be accompanied by improvements in organisational performance:
There will be evidence [of impact] I think there’ll be some hard outcomes and some soft outcomes [. . .] People feeling a bit of confidence and trust in the organisation which should then potentially lead to high levels of retention, because people feel as if all of their learning needs are being met. The soft outcomes, people will really feel safe and have that confidence and trust in the organisation.
Juniper-26-Stakeholder
Non-attenders’ experiences
We interviewed people who said that they had never been to a Round to find out why this was the case (see Chapter 5 for survey respondent reasons).
A few participants were well informed about what happens in Rounds and had deliberately decided to opt out:
I had the opportunity to attend, but when I realised it was as emotionally charged as it was I went, yeah, I’m not sure I’m really ready, to go there and be faced with that level of emotion [. . .] I thought it may be just a bit too much for me.
Elderberry-36-Non-Attender
The non-attender data suggested that many staff did not really understand what Rounds were. A few gave generic explanations, for example that it was an intervention intended to help staff deal with difficult issues. Others (from across all staff groups) felt that Rounds publicity did not always give enough information to make a decision about whether or not to attend, particularly in the new Rounds sites: ‘I read about Rounds quite a lot but I have no idea what they are or what they do or what they’re intended to do’ (Mulberry-29-Non-Attender). There were also other misunderstandings. For example, one non-attender’s response showed that they were unaware that Rounds were open to all:
I might ask the manager how can I go about inviting myself and take it from there, or I could speak to the person that sends out the e-mails, I’ll probably ask her as well how I could get myself invited, just as long as I could stay at the back and I could just listen as opposed to being somebody that has to talk.
Elderberry-36-Non-Attender
A few interviewees said that they had attended Rounds but went on to describe a different meeting, highlighting the misunderstanding that existed for some. Others did not feel that Rounds were for their staff group, suggesting that they were more for doctors than nurses, and that certain roles, such as non-clinical, did not warrant attendance.
Chapter summary
This chapter has explored staff experiences of attending, presenting and facilitating Rounds and has highlighted the importance of panel preparation in shaping the stories that were presented and in preparing the panellists for the Round itself. Participants reported that Rounds were interesting, engaging and a source of support, providing useful opportunities to reflect and process the challenges they faced at work. Audience members reported learning more about their colleagues and about patient situations, and this, together with engaging with multidisciplinary colleagues, created greater understanding, empathy and tolerance towards colleagues, and patients and their families. A few reported negative feelings and some were unprepared for the sadness, anger and frustration that they experienced or witnessed in Rounds. Having control over their day (which was less possible for ward-based staff) and a convenient location facilitated attendance, while conflicts with other work/clinical priorities and having no one to cover their work were identified as barriers. Panellists were motivated to present for a number of reasons including increasing visibility, providing learning for others and seeking to be heard or have closure on a difficult issue. Most panellists spoke positively about Rounds, attributing this to the reassurance provided by the facilitator and the friendly reaction of the audience. A few panellists reported being frustrated by the audience turnout or composition, and one person described how the facilitator’s attempts to protect had resulted in an uncomfortable silence.
The chapter also explored experiences of facilitating Rounds. Facilitators were often Rounds champions, having brought Rounds to the organisation, and some felt very responsible for the planning and execution of Rounds. The characteristics of facilitation were identified. Many of these paralleled facilitation in general, in addition to managing emotional disclosure, promoting reflection and discouraging problem-solving. Participants drew on many sources to support them in their facilitation, including former roles that had required similar skills. Experiential and peer learning also prevailed. An alignment with one’s professional values, an activation of positive feelings, professional development and an expansion of one’s professional network were cited as reasons why participants had become involved in Rounds facilitation. Challenges felt by facilitators included having sufficient time to undertake the role properly, or as they would wish, especially as it was often in addition to their usual work. Facilitators felt pressure to make Rounds a success, often with minimal resource. Clinical leads were important Rounds champions and most board interviewees spoke positively of Rounds. Steering groups provided support by sourcing stories and panellists, and debriefing, evaluating and promoting Rounds. Sufficient administrative support and an active steering group were key to Rounds sustainability, and these varied between sites.
Chapter 7 Contextual factors influencing variation in implementation and outcomes of Rounds
Chapter overview
Realist evaluation is a theory-driven evaluation that involves identifying causal explanations of how interventions work, for whom and under what circumstances. Causal mechanisms are always embedded within particular contexts and social processes, so that Rounds might work differently in different situations, and, as a result of different contexts, trigger mechanisms that generate outcomes. Pawson and Tilley4 sum this up as context (C) + mechanism (M) = outcome (O). In realist evaluation, therefore, one key aim is to understand the effect that context has on how an intervention works: how context can act as a ‘dimmer switch’ to turn up or down the effects of mechanisms. In this chapter and Chapter 8, we report the key findings from our realist evaluation. We build on some of the themes introduced in Chapter 6 and introduce layers of context that fire mechanisms and lead to outcomes, as described in Chapter 8.
We present our findings as follows:
-
contextual layers of Rounds – four layers of contextual factors that have an impact on the effectiveness of an intervention
-
fidelity to the Schwartz Rounds model – implementing the intervention as intended and comparing case study similarities and differences
-
characteristics of ‘successful’ and ‘unsuccessful’ Rounds.
Objectives
We aim to understand whether or not and how Rounds ‘work’ in the UK, for whom and in what contexts (objective 12) to inform decisions about their implementation in other contexts, and to understand what is causing variations in implementation or outcomes.
In this chapter, we examine how Rounds are operationalised, in particular:
-
the influence of variance in facilitation (objective 11b)
-
the topics presented and Rounds climates (objective 11c)
-
the factors influencing ‘success’, or otherwise, of Rounds in organisations (objective 11d).
Methods and analysis
This chapter draws on data from our case studies, two theory-testing focus groups, and our mapping interviews, as described in Chapters 3, 4, 6 and 8. A thematic analysis, informed by realist theory, was used to identify patterns in the data, which were used to undertake a cross-case analysis to identify the contextual layers. Chapter 8 has more details on realist methodology.
Contextual layers of Rounds
Pawson83 and Pawson et al. 84 identified four contextual layers that influence variation in outcomes:
-
the individual capabilities and characteristics of key actors taking Schwartz Rounds forward (e.g. values, roles, knowledge and purpose)
-
interpersonal relationships – behind-the-scenes support given by the core team and steering group (e.g. communication, collaboration and networks)
-
the organisational setting (e.g. the reasons for the adoption of Schwartz Rounds, organisational cultures, senior leadership support, audience characteristics, resource allocation, local priorities)
-
the intrastructural setting (e.g. prevailing NHS cultures and staff experiences at work).
We draw on these four layers to present our context findings.
Individual capabilities and characteristics of key actors
Rounds are usually run by a core group of key actors: one or more facilitators, a clinical lead, an administrator and steering group members. In this section, we focus on the roles of facilitators and clinical leads (see Chapters 4 and 6 for more on other roles, and Report Supplementary Material 5 for selected role guidance from PoCF). We identified differences between our case studies in the following:
-
facilitators’ background, experience, skills, knowledge and training
-
facilitators’ passion, understanding and belief in Rounds
-
facilitator and clinical lead style.
Facilitators’ background, experience, skills, knowledge and training
The national variation in facilitator backgrounds has been illustrated (see Chapter 4 and Report Supplementary Material 6). In our nine in-depth case study sites (see Table 2), we interviewed facilitators who were psychologists, chaplains, nurse specialists, social workers, therapists, counsellors and administrators.
Interviewees suggested that psychologists were well suited to the facilitation task and could be good role models:
I do think psychologists make brilliant facilitators. And I come away from the Rounds where I see particularly psychologist facilitators and think ‘oh wow you just knocked my socks off with how you’ve done that. I couldn’t even aspire to be as good as you’. So I wouldn’t necessarily include myself in that, but really, really impressed with psychologists as facilitators.
Why do psychologists make such good facilitators?
I don’t think they’re fazed by it. I think they’re really good at picking different people, they’re really good at modelling that it’s OK to sit with the discomfort, with things aren’t as we would like them to be, [. . .] with the silence, to not to rush in and try and fix it.
In our focus group with mentors, it was felt important for facilitators to have group work and facilitation skills, with their background seen as less important:
I don’t think that you have to be a psychologist or have done any formal psychotherapeutic training, but I do think you need those skills and how you develop them could be in a range of different ways.
Focus group-Participant 03-22.11.16
A facilitation style combining technical skills with a knowledge of group and psychotherapeutic processes informed this interviewee’s facilitation of Rounds:
I have been trained as an action learning facilitator so I know how to facilitate [. . .] the discipline of timing your introduction, timing your main discussions. I’m also trained as a systemic psychotherapist so I know that questions have different meanings and enlist different responses [. . .] and I suppose [I have] the technical skills of questioning and listening.
Sycamore-02-Facilitator
Facilitators from more established Rounds sites had expertise and insights gained from facilitating their own Rounds and sometimes from providing mentorship to facilitators in other organisations. In our case studies, seven facilitators acted as PoCF mentors to new sites. As part of the PoCF mentorship and training scheme, facilitators were encouraged to engage in peer observation, and being a mentor had other benefits:
I’ve had the advantage to being [able to see Rounds run in other sites], so seeing how it’s being done elsewhere and that works really well [. . .] So just being exposed to them, seeing lots and lots of Rounds has been my training.
Ash-400-Facilitator
Facilitators’ passion, understanding and belief in Rounds
As shown in Chapter 6, facilitators often take on responsibility for ensuring that Rounds run each month and for the bulk of time-consuming tasks. This requires facilitators who are highly motivated and passionate advocates for Rounds, and for the majority of facilitators their deep-rooted commitment and belief in the benefits of Rounds was evident. Many had championed Rounds and been instrumental in getting them introduced into their organisation. On most occasions, facilitators volunteered for the role and were often asked because they were already frequent attenders or were Rounds champions (see Chapter 6); however, we found one exception:
When I started my post they said ‘oh, you’ll be involved in the Rounds’, so I didn’t feel like I had very much choice in it.
Horse-chestnut-10-Facilitator
Facilitators’ passion for Rounds was hard to sustain when facilitators felt unsupported and overburdened. We noted a degree of burnout in a few for whom the high initial enthusiasm and drive had been unsustainable, as this quotation illustrates:
So I think what’s wrong in my view is that we are prioritising doing so many things, let’s do this, let’s do this target, this to be met and everyone is running around, and there’s lots of urgent and important stuff to do all the time [. . .] And then no wonder then your own enthusiasm dies after some time and I have to say my enthusiasm has gone down and I’m not going to blame anyone else, but it’s just like ‘what’s the point, we don’t have a venue, we tried doing this, we haven’t got enough support’ [. . .] after 2 years I really didn’t want to continue it.
Willow-177-Facilitator
(See Chapters 4 and 6 for more exploration of facilitator burden and sustainability issues.)
Facilitator and clinical lead style
Good facilitation involves ensuring fidelity to the Schwartz Rounds model (see Fidelity to the Schwartz Rounds model). The core component of fidelity, ‘focusing on emotional impact on staff, the non-medical aspects of work’, was mentioned by all facilitator interviewees, particularly the issue of discouraging ‘problem-solving’. Taking action to address this was said to require a level of tact and discretion, as facilitators attempted to carefully move the discussion away from problem-solving and towards reflection, without appearing to reprimand and discourage participants from participating again:
[After telling his/her story the panellist said] ‘I really want your help now with how I sort out this problem’. So [the panellist] made an invitation to problem solve and [the facilitator] beautifully turned it around [. . .] she turned it into an invitation to reflect.
Ash-400-Facilitator
Another interviewee shared their opinion on what style of facilitation did not work and thereby created a less safe environment:
It was far too much putting people on the spot, too controlling, too much trying to pull out information. [. . .] They weren’t relaxed enough to let it flow and the discussion to evolve [. . .] they jumped in too quickly, is what people were saying, shut us down [. . .] it felt like people who were often moving into problem solving were jumped on and it felt like, they may have felt very slapped, slapped down in terms of their contribution. And again that just makes it feel unsafe if that happens.
No ID (anonymised to fully protect identity)
Co-facilitation was usual, and part of the ‘facilitation’ core component of fidelity to the Schwartz Rounds model (see below). All of the facilitators we interviewed saw it as desirable to have two facilitators, because facilitating Rounds successfully and maintaining safety in the group was deemed onerous and difficult for one facilitator to do alone. Those who had attempted it (in an emergency) told of how scary and difficult it was and how they would seek to avoid repeating the experience (see Chapter 8, Trust, safety and containment). Interviewees acknowledged that this working relationship was most successful when both parties had complementary skills, offsetting mutual limitations and enhancing mutual strengths, explaining that successful co-facilitation was promoted by:
Being explicitly interactional with my co-facilitator. So doing the reflecting about how we use our roles and how we use our different characteristics to play to our strengths.
Willow-01-Facilitator
The distinction between the role and the style of the facilitator and clinical lead is further explored in Chapter 6, Facilitators’ and clinical leads’ experiences.
Interpersonal relationships: behind-the-scenes support given by core team and steering group
The majority of Rounds attenders only see what happens during the 1 hour of a Round; however, the core team and steering group provide behind-the-scenes help to put on a Round, including using their networks to gather organisational intelligence.
Facilitators’ and clinical leads’ reputation, credibility, seniority and networks
One of the core components of fidelity is having a senior clinical lead (see Fidelity to the Schwartz Rounds model). We found that clinical leads varied in their level of seniority and their ability to provide organisational intelligence on the most complex, challenging, topical and interesting cases, incidents or issues facing the whole organisation. For instance, the clinical lead in some sites was a medical director (Cedar, Sycamore and Cherry) or a nursing director (Elderberry and Sycamore), whereas in the remaining four out of nine sites the clinical lead was a medical consultant. Clinical leads whose seniority resulted in them working across the whole organisation and with staff on the front line, as well as those in middle, senior and executive-level management positions, heard about suitable cases and topics more readily than consultants whose everyday work was limited to a particular specialty. For instance:
Being a [divisional director] certainly keeps me in touch with many colleagues. We’ve just been talking a few minutes ago about a serious incident that occurred 18 months ago in the hospital. So I’ve become aware of issues like that which may cause an emotional reaction in the staff looking after their patients. So there are times when I think well perhaps that’s a topic we could discuss in the Schwartz Round, if the team are comfortable with that. So I think that role helps me communicate and hear in a formal and informal way what’s going on.
Sycamore-03-Clinical-Lead
Some facilitators and clinical leads had worked in a staff support and well-being capacity, so they brought that source of personal credibility and trustworthiness (Cedar and Ash). When facilitators were new to their organisations, they had to work harder to establish this personal credibility and trustworthiness, and found it harder to source stories because they had little organisational intelligence, they knew fewer people and fewer people knew them, so stories were not brought to their attention in the same way as in more established sites with well-known facilitators. Others felt disadvantaged by not having such access to these sources because their role did not involve working across departments and wards:
So I often couldn’t come up with, there’s the stand-out patient or family that everyone’s talking about and they will notice on the ward and someone will usually say, ‘I think that would be really good for a Schwartz Round’? Well, I wouldn’t come across those stories, so that hampers me.
Elderberry-02-Facilitator
Organisational setting
In this section, we compare across organisational settings in relation to:
-
organisational factors
-
time running Rounds
-
audience characteristics
-
Rounds’ characteristics.
Organisational factors
The sampling criteria for our case study sample are outlined in Chapter 2.
Motivations for adoption
In our case study sites, three reasons were given for adopting Rounds: (1) they fitted with existing organisational vision and activities; (2) they were seen as a useful vehicle for promoting desired organisational change and (3) they offered a means of addressing an unmet need for staff support (see Chapter 4 and Table 25). Two sites introduced Rounds because of the clear alignment with their existing organisational vision and activities:
The director of workforce and organisational development e-mailed back and said ‘the trust is trying to do some wider scale work around compassionate employer and this dovetails with it really nicely’, she said ‘yeah, I’d like to take this to the board and champion it’ and then went to the chief executive, they supported it and that’s how it got picked up really.
Horse-chestnut-01-Facilitator
| Site | Reason | ||
|---|---|---|---|
| Fit with existing organisational vision and activities | Vehicle for organisational change | Unmet need for staff support | |
| Mulberry | ✓ | ✓ | |
| Juniper | ✓ | ||
| Cherry | ✓ | ||
| Sycamore | ✓ | ✓ | ✓ |
| Ash | ✓ | ✓ | |
| Cedar | ✓ | ✓ | ✓ |
| Willow | ✓ | ||
| Horse-chestnut | ✓ | ✓ | ✓ |
| Elderberry | ✓ | ||
In contrast, two others had seen Rounds as a vehicle for organisational change:
I’d joined that team [. . .] there were still a lot of problems, culturally, [. . .] it felt like people were disconnected from the emotion of what they were doing a bit and I think that was pressure as well, it was a way of managing people’s feelings, [. . .] people often close themselves down, that’s a way to get through every day isn’t it, and I would say that would be an observation I’d have made.
Sycamore-14-Senior stakeholder
Perceptions about organisational culture
Organisational readiness for Rounds differed. One facilitator felt that her organisation had decided ‘to take a leap of faith’ in adopting Rounds, and described the right conditions for adoption:
Right at the beginning, we were all finding our way there was a lot of freedom but the organisation was ready [. . .] there was a right mixture of authority and legitimising it and freedom I think.
Cedar-01-Facilitator
In a few sites, participants specifically commented on their perceptions of the (lack of) fit between their organisation’s culture and Rounds, suggesting that they were perhaps less ready to adopt Rounds (e.g. Cherry, Horse-chestnut and Juniper). In one of our new case studies, steering group members reflected on a particularly difficult Round:
Rounds don’t fit with [trust’s name] macho culture, where the focus is on ‘we’ve got to get things done’ versus the Schwartz Round ethos of being designed to help people access their emotions, providing a reflective space.
Crying does give people relief, when there is no clinical supervision within an organisation it gives people a chance to open up, but it’s messaging that there is nowhere to take these feelings outside of Rounds, they are showing up the problem of lack of clinical supervision.
If Round is a forum for discussions, and you get consistently the same themes coming up and they are not dealt with, if nothing happens, then Round participants will become disillusioned. We need to get data out about the evidence base of Rounds that it’s not meant to give solutions, Rounds5 purpose is to have a reflective space, it’s experimental at the moment. When we publicise the next Round we need to be clearer about the purpose.
Juniper-Steering-group-meeting-fieldnotes
Senior leadership support
In our case study sites, senior leadership support was broadly provided in four ways: by board-level senior managers (1) pledging their support for Rounds, (2) visibly demonstrating their support by attending and presenting at Rounds, (3) financially, by agreeing to fund adoption and implementation, and (4) practically, by telling managers to put in place measures to encourage and support their staff’s attendance (Table 26).
| Site | Board-level senior managers pledged support | Attending and presenting at Rounds | Encouraging measures to support attendance | Funding source |
|---|---|---|---|---|
| Mulberry | ✓ | ✓ | Charity | |
| Juniper | ✓ | Charity | ||
| Cherry | ✓ | ✓ | Charity | |
| Sycamore | ✓ | ✓ | ✓ | Internal |
| Ash | ✓ | Internal | ||
| Cedar | ✓ | ✓ | Internal | |
| Willow | ✓ | Internal | ||
| Horse-chestnut | ✓ | ✓ | Internal | |
| Elderberry | ✓ | ✓ | Internal |
Round organisers considered the extent to which they were held accountable by their senior management in justifying the existence of Rounds within their organisation. Overall, accountability was fairly light touch. Some senior stakeholders explained that they might begin to ask questions about the feasibility of running Rounds if attendance numbers became a problem:
If the attendance fell off (below 20, on consecutive occasions), I wouldn’t stop them, but I’d ask the question ‘what are we doing wrong?’.
Ash-24-Senior stakeholder
The chief exec[utive] has said that you can have an hour of your working time to spend once a month, to come together to share your stories. And if we don’t use that then it will disappear.
Mulberry-367-Facilitator
In some sites, the clinical lead sat on the trust board, which had advantages:
I think in principle it has been useful and it has actually allowed me to be an advocate for Schwartz on the board [. . .] and I think it would be quite useful when it comes to arguing for continued funds.
Cherry-65-Senior stakeholder
In the majority of case study sites, attendance among senior staff was sparse, although there were exceptions. In Sycamore, we found an exceptionally high level of senior management support, with senior staff attending and contributing regularly, and using Rounds strategically:
I remember our first Round all the executive directors attended [. . .] and other things happened in that it coincided with us as an organisation going through some very difficult times operationally [. . .] We spoke to our chief exec[utive] about it, our deputy chief exec who was in charge of operations was also on the Round, together with lead nurse and senior clinicians in the organisation, so we used the Rounds to have conversations about big problems and we saw the impact of that. I think word of mouth spread and non-executive directors were encouraged to be part of the conversations.
Sycamore-02-Facilitator
Often senior staff attended Rounds only if they were presenting on the panel. Such occurrences were considered a success [‘We asked the chief exec to be on the panel. I think that really boosted numbers’ (Willow-178-Clinical-Lead)], as when senior trust people are present staff feel that their concerns are being heard.
Participants suggested that the value of the intervention is undermined when senior staff do not attend Rounds, inadvertently giving staff licence to do the same:
If you show a commitment and you want to show to everyone that this is how important this is, that tells me volumes. If the chief exec[utive] is saying I’m so busy I can’t go there, that’s the message we are giving the people, if you are busy don’t go.
No ID anonymised to fully protect identity
We did hear examples of senior managers supporting attendance by, for example, putting measures in place to encourage and enable ward-based staff to attend Rounds:
So what happens now is if it’s a nurse-related Round the matrons will make sure the nurses are attending because the ‘frequent flyers’ tend to be the corporate staff and people who have the times in their diaries to manoeuvre around and one particular Round [. . .] corporate teams [were] going to relieve the nurses for an hour so they could come.
Sycamore-02-Facilitator
Reasons for pausing Rounds
We noted the challenges of sustaining Rounds in many case studies, and how a number of factors contributed towards making Rounds unsustainable (see also Chapters 4 and 6). In the words of one case study facilitator (Ash), which was struggling to run Rounds, the core Rounds team faced a ‘perfect storm’ of simultaneous contextual factors, which contributed to the decision to temporarily pause Rounds. These included individual and interpersonal factors (facilitators and clinical leads taking on more roles and duties outside Rounds, reducing capacity; difficulties accessing clinical cases and panellists; loss of administrative support; and newly trained facilitators leaving); organisational and intrastructural factors (the need to cancel Rounds owing to NHS pressures such as junior doctors’ strike or a lack of beds); and changes to the e-mail system meaning that it was not possible to publicise Rounds via organisation-wide e-mails.
Similarly, another of our case studies (Horse-chestnut) attempted to restart Rounds, but this was unsuccessful because of a combination of factors.
-
Individual factors: facilitator burden, turnover – loss of the passionate original facilitator who had established Rounds, another facilitator leaving post, facilitator burnout and associated disillusionment with Rounds.
-
Interpersonal factors: facilitators and clinical leads in roles that limited their capacity and ability to find suitable stories and panellists.
-
Organisational factors: reduced senior management support, increased workloads and pressures leading to less attenders/less diverse audiences, loss of suitable Rounds venue owing to resources being cut, difficulties of sustaining Rounds in two locations because of wide geographical location/scattered teams and a perception that the organisation had a ‘blame culture’, which led at least one attender to report an unwillingness to volunteer as a panellist.
Time running Rounds
One criterion on which we purposively sampled case study sites was the length of time running Rounds. Of our nine in-depth case studies:
-
four commenced Rounds before the end of 2012 (Ash, Cedar, Elderberry and Horse-chestnut)
-
two commenced rounds between January 2013 and the start of our study (1 September 2014) (Willow and Sycamore)
-
three commenced Rounds during our study (after 1 September 2014) (Mulberry, Juniper and Cherry).
Over time, we expected facilitators to become more skilled with experience, and Rounds would take time to become known and embedded. We had not anticipated the cumulative impact of multiple Rounds in other ways.
An analysis of our case study data suggested that, over time, each Round has a cumulative impact on the next, building capacity and developing and deepening the community resource that Rounds provide and enable to have effects. We previously presented a linear ‘three-stage’ diagram (see Figure 6 and Chapter 6). A further analysis of our case study data revealed this cycle to have an additional stage alluded to in terms of outcomes in Chapter 6 (stage 4: a range of post-Round after-effects), and also revealed the cyclical nature of the four stages (Figure 7). Stages 3 and 4 of one Round, or a series of Rounds, have an impact on the early stages of the next Round/Rounds.
FIGURE 7.
Cumulative impact of stages of Rounds.
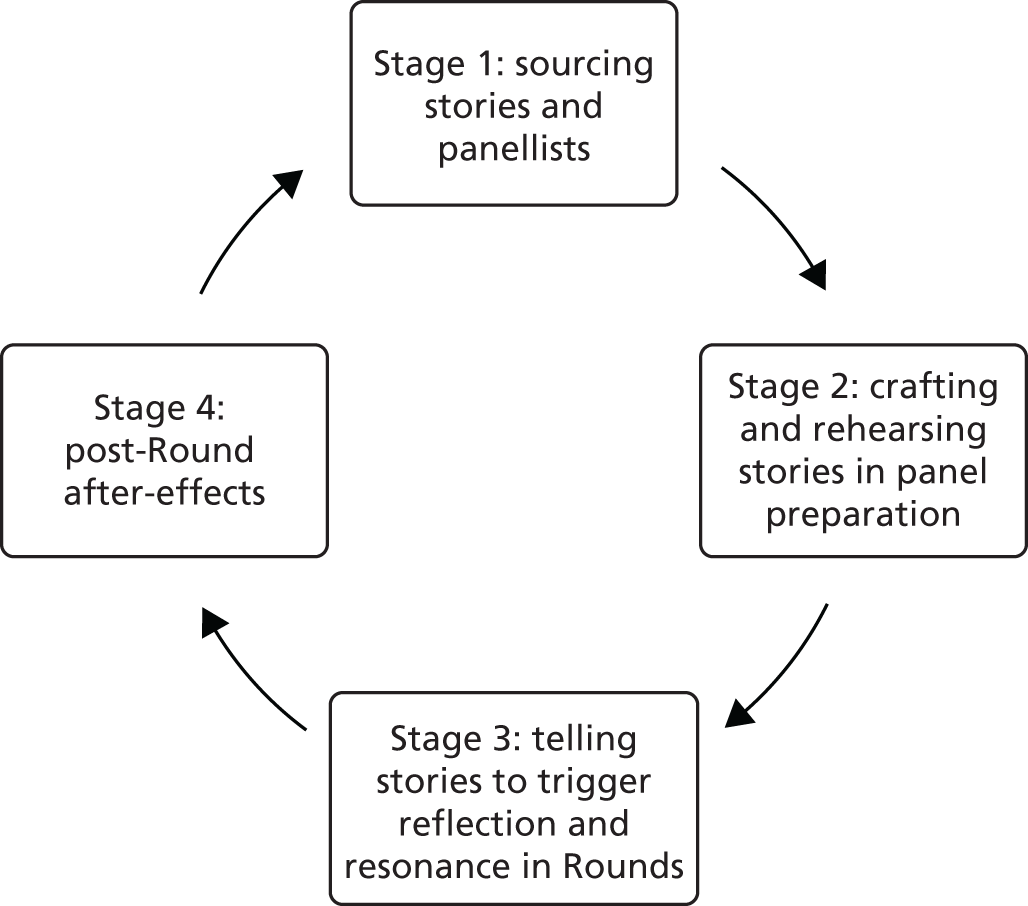
When further comparing sites new to running Rounds with more established sites, we have noticed differences in (1) audience ‘Schwartz savviness’, (2) audience trust and confidence and (3) facilitator confidence.
Audience ‘Schwartz savviness’
Over time, Rounds participants become ‘Schwartz-savvy’, by which we mean that they really understand the purpose of Rounds, know and follow the explicit and implicit rules of how to contribute appropriately and support each other in a non-judgemental way. In some sites, we observed that facilitators, clinical leads and steering group members in the audience role model appropriated contributions and support, sometimes intentionally and other times unintentionally. In one sense, having a ‘Schwartz-savvy audience’ is a sign that Rounds are becoming embedded within the organisation.
Some interviewees suggested that Rounds were a ‘slow-burn intervention’, that they took time to develop successfully and that there was an important longitudinal element to participation, which over time created a staff community intervention in organisations. Our data in longer-established Rounds sites suggest that, over time, if the Rounds have fidelity to the core Rounds components, this creates a ‘Schwartz-savvy audience’, which provides a further resource in terms of a support community that newly set-up Rounds organisations do not have. Two mentors discussed this in our theory testing focus group:
I think it’s what you call [a Schwartz-savvy audience] a massive resource for the facilitators because I think [. . .] when you start initially, you are on your own, a few of you taking a massive risk and being very publicly exposed. And if it becomes embedded, you start to not be on your own anymore. The Schwartz-savvy people carry it with you [. . .] And there are more of them and initially even the first year, possibly the second year [. . .]
. . . Yeah, it’s into the second year and I remember we did a really risky one I think on organisations and we got about 150 people and I thought this is going to be impossible to facilitate, we’ll never be able to do it, and then I realised that there was a community – what you’re calling the ‘Schwartz-savvy people’ – that held it with us. So they started speaking – most people wouldn’t speak in front of 150 people [. . .], and that’s why I think it’s a slow intervention because you have to create that organically over time.
Focus group-14.11.16
Panellist, audience and facilitator trust and confidence
Facilitators spoke of needing to gain confidence in their facilitation style (see Chapter 6) to take more calculated risks in Rounds when they felt that the organisation and audience was ready, for example, to run Rounds on staff bullying and harassment, receiving a poor CQC report or making mistakes. There were also differences in facilitators’ confidence levels about being creative with Rounds:
I think because we started doing them [. . .] the format was evolving that I’ve always felt that we had the sense of it’s OK to play with this, right from the beginning.
Ash-400-Facilitator
It often took time for Rounds to feel safe for staff. A facilitator highlighted a doctor who had been in Rounds’ audiences for 6 months before volunteering to be a panellist and share an experience. The story they then told was one of sharing their vulnerability about feeling that they had made a mistake:
I’ve got a doctor watching and then 6 months later offering a Round which was one of our most powerful Rounds because they watched to see how safe it was.
Focus group-Participant 01-14.11.16
Similarly, audience members spoke about how they often attended Rounds several times before building up the confidence to contribute:
It might be that it takes people a few Rounds. They’ve heard something and they’re formulating a thought but they don’t feel confident to be able to say it and then they go to another Round a few months later and by then they go, ‘This is how I feel about it’ and they say it.
Elderberry-06-Panellist
As I went to a few I felt more and more comfortable about sharing some quite personal stuff [. . .] I shared something that was really personal and it felt OK [. . .] you’re not judged there [. . .] when, you get such a wide spectrum of people there [. . .] when some of the doctors and people that I suppose traditionally tend to think they keep it all together [. . .] when they were there making a commitment to it, actually sharing their vulnerability [. . .] ward sisters [. . .] didn’t seem scared to say ‘I found that really difficult’. Or ‘I didn’t think I did that very well’. I think that gives you confidence to think ‘oh it’s OK’.
Willow-37-Attender
These suggest that, for some people, regular attendance at Rounds is a necessary step towards building confidence and trust in facilitators, and in the Rounds structure and process, so that they can follow the examples set by panellists and other contributors and publicly disclose their own similar experiences. The greater the depth of the discussions, the more likely the person is to feel vulnerable. Therefore, the trust built over time among the disclosers (and often among panellists or audience members) and the facilitator/audience is essential to reach deep discussion, which theory suggests produces outcomes (see Chapter 8). In new Rounds sites, or in established sites where the audience is relatively inexperienced or unfamiliar with Rounds, there are differences in levels of audience confidence and trust, so discussions may be relatively superficial.
Audience characteristics
Size
The size of Rounds audiences varied considerably between and within sites (see Chapter 4). They varied from 150 (Cedar) and occasionally dropped to single figures, with sites reporting audiences of fewer than 10 (Ash, Horse-chestnut). Attitudes to a viable number also varied. Rounds were sometimes cancelled because panellists were not available; for example, in Elderberry the Round was cancelled 5 minutes after it had been due to start because the numbers were considered too low for it to be viable (n = 15). The facilitator explained that running the Round would have put too much pressure on audience members to contribute and that it would have been an uncomfortable experience for everyone involved. At other sites, however, we observed Rounds running with a number smaller than this, and working well for the audience and panellists (see Appendix 20).
Composition and diversity
A diverse audience was felt to be important for a number of reasons, most notably because it is associated with firing mechanisms on ‘contextualising patients and staff’ and ‘shining a spotlight on hidden stories and roles’ (see Chapter 8). Many sites found it hard to achieve audience diversity consistently, despite valiant attempts, with some staff groups (such as ward-based staff; see Chapters 4 and 6) being continually under-represented.
Having a visible senior management presence at Rounds was viewed by some participants as a ‘double-edged sword’. As outlined above, their presence was considered helpful in demonstrating the value the organisation placed on Rounds, and in some new case study sites chief executives/board directors were panellists at their early Rounds, which was well received by audience members. It provided powerful, memorable examples of ‘role modelling of vulnerability’, and opportunities for ‘shining a spotlight on hidden stories and roles’ (see Chapter 8). However, a few facilitators noted that there were benefits from having an intervention that was ‘under the radar’ and there were dangers in managers wanting to influence how Rounds were run. Rounds becoming ‘corporate’ needed to be firmly resisted, as this would be the antithesis of Rounds:
Why Rounds have value is they sit right at the section between the organisation and clinical work and that’s where the culture of change can happen because they’re not corporate even though they actually are because the organisation has to endorse them.
Cedar-01-Facilitator
Others suggested that audience members also had to feel very ‘safe’ in Rounds to disclose challenging views on their organisation in front of senior board members.
Rounds characteristics
The stories presented could be either theme or case based (see Chapter 8). Facilitators stated that often when they set up Rounds these tended to be more theme based, rather than case based, as theme-based Rounds were easier to prepare for, and cases were often more difficult to find (see Appendix 21):
It has tended to be that most people have been prepped individually and then put together around themes. So we’ve had one clinical case [. . .] come forward, which is quite interesting in a trust that’s full of clinical cases, people feel a bit more comfortable talking about themes at the moment.
Cherry-01-Facilitator
A few facilitators talked about case-based Rounds being more powerful than theme-based Rounds:
So, although we could get issues, they [. . .] weren’t the ones that made your hair stand up on the back of your neck. So they were more of the thematic ones which I think start to lose a bit of their power if they’re just those. So we were struggling to get more of the case-related issues because it was falling more to me to do them.
Can you say a little bit more about the thematic Rounds not being so powerful?
Well sometimes they work, sometimes they don’t, [. . .] but we were getting health-care [scientists], somebody from pathology sharing their story and whilst that may be very powerful, it probably has less immediacy, less of a life-and-death issue.
Observing multiple Rounds across different settings, we noticed familiar themes being discussed in our case study sites: ‘compassionate care’, ‘population specific’, ‘challenging topics and themes’, ‘challenging families and patients’, ‘staff-focused’, ‘organisation focused’, ‘safety’ and ‘upbeat and general’ Rounds. The topics that staff brought to Rounds reflected the increasingly complex and challenging health-care environment in which they work, and we were struck by the universality of some of the topics (see Appendix 21).
Intrastructural system
An example of the wider and intrastructural system context that had an impact on Rounds was our participants identifying the felt need for Rounds to support staff (see Chapter 4) in a service with complex emotional work with patients/colleagues and high levels of psychological distress. Interviewees also reported increasing levels of scrutiny, regulation and demand, which, coupled with more limited resources, resulted in staff experiencing higher work intensity and increased levels of stress.
Some case study interviewees identified that in the prevailing culture of health-care organisations – with protocol-driven outcome-orientated care, rigid hierarchies and emotional stoicism – it takes time for staff to adjust to and accept the culture of Rounds as support spaces where emotions are shared (vs. stoicism), where hierarchies are flattened and where there are no explicit outcomes (see Chapter 8, Countercultural/third space for staff).
In terms of the outer context influencing the adoption of Rounds, interviewees in our mapping study suggested that a reason for the adoption of Rounds was to improve patient care by attending to staff well-being through a form of emotional support. This is slightly different from the original aim of Rounds – as developed in the USA – (see Chapters 2 and 4) as an innovation to teach compassion and strengthen the patient–caregiver relationship (see Boxes 3 and 4). Our interview with the PoCF director suggested that, initially, Rounds had been brought to the UK with the same intention, but the increased evidence of a link between staff well-being and patient experiences of care in the UK32,68,77,85 shifted the focus a little, so that attending to staff well-being became more central as an interim outcome: also important in its own right, but also with the ultimate goal of improving patient experiences of care. Interviewees in our mapping study and case studies also cited the Francis report, the dissemination activities of the PoCF and the availability of funding from recognised national charities1 as influences on the adoption of Rounds (see Chapter 4).
Fidelity to the Schwartz Rounds model
Fidelity is the idea that intended results can accrue if there is adherence to well-evidenced and successfully developed intervention components. Put simply, fidelity means that Rounds are conducted as intended, in this case using the UK ‘Schwartz Rounds model’ taught in training, using the PoCF handbook and via mentors.
The Consolidated Framework for Implementation Research offers an overarching typology for implementation science,70 and suggests that interventions can be conceptualised as having ‘core components’ (the essential and indispensable elements of the intervention) and an ‘adaptable periphery’ (adaptable elements, structures and systems related to the intervention and the organisation into which it is being implemented). Rounds are a complex and multifaceted intervention, with many interacting components. Using the Damschroder et al. 70 typology, we analysed our data to identify and determine the ‘core’ (Box 1) and ‘adaptable peripheral’ components (Box 2) of Rounds to make these visible (they were hitherto implicit and unidentified). We tested them with experienced mentors and key PoCF stakeholders in focus groups to check for comprehensiveness and agreement.
Leadership: senior clinician leadership.
Facilitation: facilitator led, neutral, group work, psychology and/or psychotherapeutic skills. Two facilitators/co-facilitation.
Regularity: series of events over time (i.e. not one-off events).
Integrity: Rounds not combined with other interventions or used for other organisational purposes.
Food: available for Rounds attenders.
Group setting: Rounds is a group intervention with group participation.
Participants: (panellists and audience) – staff only (no patients).
Audience discussion: stories to trigger reflection and sufficient time for audience discussion.
Trust, safety and containment: pre-Round safety checks, ground rules on confidentiality.
Pre-prepared staff stories: guidance on crafting story and identifying what will resonate with audience in panel preparation.
Focus on emotional impact on staff, the non-medical aspects of work: rather than clinical details, problem-solving, outcomes-oriented.
Diversity: open to all vs. targeted, multidisciplinary vs. unidisciplinary groups.
Duration: 1 hour vs. < 1 hour.
Panellists: minimum of two, maximum of four.
Staff stories: live vs. filmed stories.
Rounds format: (a) live vs. teleconferencing/videoconferencing, (b) panellists’ stories first vs. staff stories and audience discussion integrated.
Scale: single organisation vs. multiorganisation.
Regularity: more than vs. less than monthly.
Built environment: differing room layouts can be used [panellists at front (usual), some circular, some theatre style].
Focus of story: the style and structure of the stories – theme vs. case-based stories.
The principles of realist evaluation challenge the idea that context is always changing and that adaptability to context, as opposed to fidelity to implementation, holds the key to intervention success. It is possible that there are settings and cultures in which Rounds do not hold or produce intended positive outcomes when adherence to the core components is maintained. However, in the context of a high-income health-care setting, we have found that maintaining fidelity to core components, while being willing to tailor an intervention to particular local contexts if required (i.e. changing the adaptable periphery components), is consistent with a realist evaluation approach.
We report and discuss three of the core components in the following sections, as we have not presented data on these three elsewhere and all others have been summarised earlier in the report.
Participants
In the UK, Rounds are open only to staff. In a small number of Rounds a patient has been invited to present a story, and the ‘exclusion of patients’, as some people see it, is often controversial. Our interviewees suggested that it was not so much an excluding frame of reference; rather it was about making Rounds a safe place for staff to speak openly without feeling the need to protect or care for patients, as is the norm outside Rounds. This is a key element supporting the concept of a ‘countercultural space for staff’ (see Chapter 8), where Rounds provide opportunities and space outside the realms and demands of their normal role:
So often we put patients at the forefront of everything and that has its place, but we tend to forget the staff. So for me it’s about staff are hugely important too. They’re our biggest asset in the organisation. And Rounds is [. . .] about supporting staff and helping them to think about the impact of situations on themselves to enable them to be better carers.
Ash-05-Facilitator
It really worries me, it sounds extreme, but for me I think places where staff and patients talk together would be incredibly valuable but it wouldn’t be Schwartz Rounds, because I think it’s fundamentally about safety [. . .]. For me that’s [patients in audience/on panel] a major line you just wouldn’t dream of crossing and yet it has been asked of us often and [. . . I] say no quite confidently.
Focus group-22.11.16-Participant-01-Facilitator
Trust, safety and containment
The Rounds model, with ground rules and an emphasis on purpose and what Rounds were not (problem-solving or outcome orientated), was important for creating a safe emotional space for the sharing of stories and reflection:
I think between us, the clinical lead facilitator reminding everybody of the ground rules explicitly, reminding everybody of the purpose, being really rigid about the boundaries, sticking to time, so all the ritual and the content. Being careful to look for everyone to speak, monitoring emotion in the room, protecting the panel members if it feels like it’s moving in a problem [solving] direction, actively intervening to say ‘that’s not our job here’, reminding people of the time as we get towards the end [and of confidentiality], saying things like ‘there may well be emotions and stories that have been stirred up here that you will want to carry on talking about afterwards’, it’s great to do that without mentioning names.
Willow-01-Facilitator
The model and [. . .] how we do train people in the model [. . .] is a huge part of what creates the safety.
Focus group-Participant-04-22.11.16
I think the magic is made in part by the process, by following the process carefully and by always saying the same things always having the same timing always having the same format, I think that gives it a therapeutic sort of holding, but I think the magic happens when [. . .] the audience really engage in the process and are willing to share their own vulnerability and then just amazing things happen.
Mulberry-367-Facilitator
Pre-prepared staff stories
Our data suggest that having the opportunity to pre-prepare stories with the assistance of a facilitator or clinical lead is a core component (although we noted that, in practice, such preparation varied considerably), because all of the facilitators we spoke to felt that it was highly desirable to ensure emotional safety in the Round by pre-preparing panellists and stories and checking that individual panellists were ready to tell their story:
I think we’ve really followed the model here, we’ve done all the preparation which does pay off, [. . .] you don’t want to put the person in the position where they feel very vulnerable, raw and totally exposed.
Elderberry-08-Stakeholder–speaking as a panellist
It seems obvious to me because I follow the Schwartz Rounds model very closely but I am aware [. . .] there are some people who are feeling that it’s a very curious model and that it needs to be much more flexible and so I’ve heard people saying [. . .] ‘I don’t think it’s necessary to practise and we could just do it’, which I find quite alarming [. . .] and I feel [the Round is] safer when [. . .] I know the gist of what people are going to say and I think the other panellists need to know that as well and I do [all the things I was taught by the lead mentor] because I’ve seen that they work.
Focus group-Participant-ID:02-22.11.16
With regard to the adaptable periphery components70 of Rounds, we suggest these in Box 2.
Our data suggest that many of these aspects have been, or are about to be, implemented as adaptations (diversity, duration, number of panellists, scale, regularity, built environment and focus of the story, and live vs. filmed stories). For example, the Rounds we observed were all 1 hour in duration, but we heard of sites that were experimenting with shorter, 30-minute ‘pop-up’ Rounds to ‘take Rounds to those who found it hard to attend’ (ward-based staff). These pop-up Rounds also had fewer panellists and only one facilitator.
We discuss some ‘adaptable periphery’ components (diversity, duration and number of panellists) in the following sections; others are covered in our organisational guide. 86 Other adaptations were suggested and were being trialled at the time of writing as solutions to particular issues [e.g. live vs. filmed (digital) staff stories and Rounds format and scale].
Diversity and duration
The Schwartz Rounds model suggests that Rounds should be open to all staff, and this was true of the majority of the 43 Rounds we observed. Being ‘open to all’ might, therefore, be considered a core component by many, although we observed one unidisciplinary Round, which, on reflection, seemed less powerful, but may have allowed those staff to speak about issues that concerned them, and that might not have resonated with a wider group. Two mentors debated the advantages and disadvantages of running unidisciplinary Rounds in our theory testing group:
I would feel that the multidisciplinary aspect is core just because I think that is one of the things that makes a Schwartz Round different to other spaces because people listen differently when it’s a case that they weren’t involved in or when it’s a profession who they’re different to, it does something to the reflection which allows you to sit back and listen in a slightly different way. I think when you’re in a unidisciplinary space [. . .] they feel different to Schwartz [. . .] and I wouldn’t call it a Round.
Focus-group-Participant-03-22.11.16
I would say differently to you because I have facilitated unidisciplinary Rounds [. . .] and because we kept to the model very clearly with the panel preparation and all the timing, time was shorter, but the model itself was maintained and I think they have a place to play. I would have agreed with you before I did it.
Focus-group-Participant-02-22.11.16
The benefits of ‘unidisciplinary’ and ‘pop-up’ Rounds are that more staff are exposed to Rounds and have an opportunity to speak and hear about the human dimensions of care. The potential disadvantages are that some benefits may be reduced (such as the wider multidisciplinary reflection; shining a light on hidden stories and roles/people in the organisation; and the multiple perspectives of staff) (see Chapter 8).
In one of our case studies (hospice), we learnt how there had been an incident that had led to more specific criteria on whom Rounds are for, to protect and ensure the safety of staff, although we heard that this is not widespread practice among hospices:
The Rounds are for any employee, but we say no to volunteers [. . .] I think we’ve had a number of issues where volunteers have misunderstood what they’ve seen or heard. My feeling is it wouldn’t be a safe environment if you had people who often don’t understand the context. And what we want is staff to be able to feel safe to say anything like, ‘I’m so glad that person died’, or – but if you have people who might misunderstand you and have done in the past, then you wouldn’t feel safe.
Elderberry-01-Clinical Lead
Similarly, we observed one Round where audience members and panellists were invited from an organisation that worked closely with the trust, and this site was considering running Rounds occasionally as a way of increasing communication between partner organisations within their locality. In this Round, we noticed that the increased number of new attenders had an impact on the overall ‘Schwartz savviness’ of the audience, making the Round more difficult to facilitate.
We suggest, therefore, that although adapting Rounds so that they are no longer open to all (e.g. pop-up Rounds or unidisciplinary Rounds) or are opened up to staff outside the host organisation (e.g. who worked in partner organisations) has a purpose, namely to enable more staff to experience Rounds and increase communication and working relationships, this adaptation of one of the ‘core components’ may come at a cost, and requires further evaluation.
Number of panellists
Although the usual number of panellists was three or four, we observed Rounds with one panellist (in the UK) and with six (in the USA). We would suggest that, although the number of panellists is an adaptable periphery component, Rounds should, when possible, have no more than four panellists in order to reduce facilitator workload and allow sufficient time for audience reflection and discussion.
A further comparison of the Rounds case study sites in terms of fidelity to core components of Rounds sites was undertaken (see Appendix 22).
Characteristics of ‘successful’ and ‘unsuccessful’ Rounds
During our analysis phase, two of the team (ER and ML) each identified a Round that they considered was ‘successful’ and ‘unsuccessful’ in each of their case study sites, and for which they had observation field-notes from a panel preparation meeting and from the Round itself. One example came from a new Rounds site and the other came from a more established Rounds site. From these observations, we compiled a joint list of characteristics of successful and unsuccessful panel preparation meetings and Rounds (see Report Supplementary Material 8).
Summary
In summary, we have identified multiple, interconnected contextual layers that affect and explain variation in Rounds implementation (see Chapter 8). In realist evaluation terminology, these contextual factors operate together to ‘fire’ or turn up a ‘dimmer switch’ underlying ‘mechanisms of action’, so they are perhaps best viewed as operating in bundles of factors. We have further identified core and periphery elements of fidelity to the Schwartz Rounds UK model. The case study Rounds we observed were run regularly and were not combined with other interventions, and food was always provided. Panellists and an audience were present, stories were pre-prepared and there was time (usually 30 minutes) for audience involvement and group discussion. All Rounds providers had a senior clinician as leader and usually the Rounds we observed had two facilitators. We have identified key differences between new and established rounds and have suggested that Rounds are a ‘slow burn’ intervention that have a cumulative effect over time, such as audience ‘Schwartz savviness’, audience trust and confidence, and facilitator confidence. These are explored in more detail in Chapter 8.
Chapter 8 Realist evaluation
Chapter overview
This chapter, as well as Chapter 7, reports the key findings from the realist evaluation. The data reported here include the interview and observation data from the nine case study sites (see also Chapters 3 and 6) and data from the telephone mapping interviews (see Chapter 4).
Aims and objectives
We aim to understand how Rounds ‘work’ in the UK, for whom and in what contexts; to suggest ways to improve their effectiveness; to inform decisions about their implementation in other contexts; and to understand what is causing variations in implementation or outcomes (objective 12).
There were four further objectives:
-
to identify and evaluate changes that take place in relationships between staff who attend Rounds and their patients and colleagues, including any reported behaviour change towards patients and colleagues (objective 11f)
-
to identify the programme theory and mechanisms by which well-being and social support might be influenced (or not) by:
-
variance in facilitation (objective 11b)
-
team hierarchy and teamwork and on coping with stress (objective 11e)
-
wider ‘ripple’ effects felt in day-to-day practice (objective 11g).
-
Methods
Realist evaluation
Realist evaluation is concerned with the identification of underlying causal mechanisms that explain how an intervention such as Rounds works, for whom it works and under what conditions. Causal mechanisms are always embedded within particular contexts and social processes, meaning that Rounds might work differently in different situations and circumstances. The overarching aim in a realist evaluation is to understand the complex relationship between these mechanisms and the effect that context has on their operationalisation and outcome. This is summed up as context + mechanism = outcome. 4 This is subsequently represented as context–mechanism–outcome (CMO) configuration. The CMO configuration is used as the main structure for realist analysis. 4 It is a heuristic device/proposition detailing what it is about an initiative that works, for whom and in what circumstances, and is used to generate causative explanations. 87 From an iterative analysis process of scrutinising mechanisms, context and outcomes, we propose some theoretically generalisable features about Rounds (i.e. refined CMO configurations)88 (see Report Supplementary Material 9).
Setting and participants
Four members of the research team undertook 177 semistructured interviews with Rounds attendees, facilitators, steering group members and panellists in nine case study sites (see Chapter 6) and observed 42 Rounds in eight case study sites (see Chapter 7; it should be noted that we could not observe Rounds in Horse-chestnut).
Data collection
One of two researchers (ML and ER) led data collection in four or five case study sites from September 2015 to June 2016, supported and supervised by the PI (JM).
Interview and observations
The interviews were initially quite open, with interviewees asked how they understood Rounds to ‘work’, how they identified and explained any changes that generated outcomes, and which aspects of the Rounds process were key mechanisms in this (see Appendix 19). Some interviewees found this easier than others. Subsequent interviews built on mechanisms identified in findings from phase 1 interviews and initial phase 2 interviews (see below). In such a complex intervention, where mechanisms and outcomes are not easily visible (taking place in the minds and later behaviour of participants), interviews with key informants (i.e. experienced audience members, panellists and facilitators, who had thought about how Rounds ‘worked’ and changed behaviour) were most beneficial. Our interviews developed over the data collection period, focusing on one or more key mechanism and testing ideas and theory with new, and at times the same, participants, to explore and test our emerging CMO configurations.
In each case study site, we observed a minimum of four Rounds (43 in total) (apart from Horse-chestnut). Observations were usually undertaken by one member of the team, but two members observed at least one Round in each site to enable them to compare notes and generate discussion. The focus of our observations shifted as data collection progressed and we identified new candidate programme theories to ‘test’. All field-notes captured the number of attendees, the room layout, the number of facilitators, the topic, and the number and role of panellists, and captured the key moments and elements of the Round. As data collection progressed, the team focused on some aspects of Rounds more specifically, for example the facilitator role and how emotional safety was supported or compromised; the use of silence; the use of Rounds ‘rituals’ and rules; and how the audience responded and supported safety in Rounds (or not). We also sought to identify the contexts and specific conditions in different sites that influenced Rounds mechanisms (see Chapter 7).
Data analysis
Realist data analysis is driven by explaining change brought about by an intervention and suggests that programmes offer resources or opportunities, but the decision-making of participants causes the outcomes (it is still necessary for the programme to be implemented as intended for it to be effective; see Chapter 7). 5 Data analysis and data collection were undertaken concurrently and we focused our initial realist analysis on interview data with Rounds key experts to search for CMO configurations to find support for causal explanations.
Interviews were multistaged and served different purposes at different phases: theory gleaning, theory refining, theory testing and consolidating interviews. 8 We drew on our own expertise gained through observing key Rounds stages, such as panellist preparation, Rounds and steering group meetings, to develop, test and refine our candidate programme theories (CMO configurations) (Figure 8).
FIGURE 8.
Data analysis process.
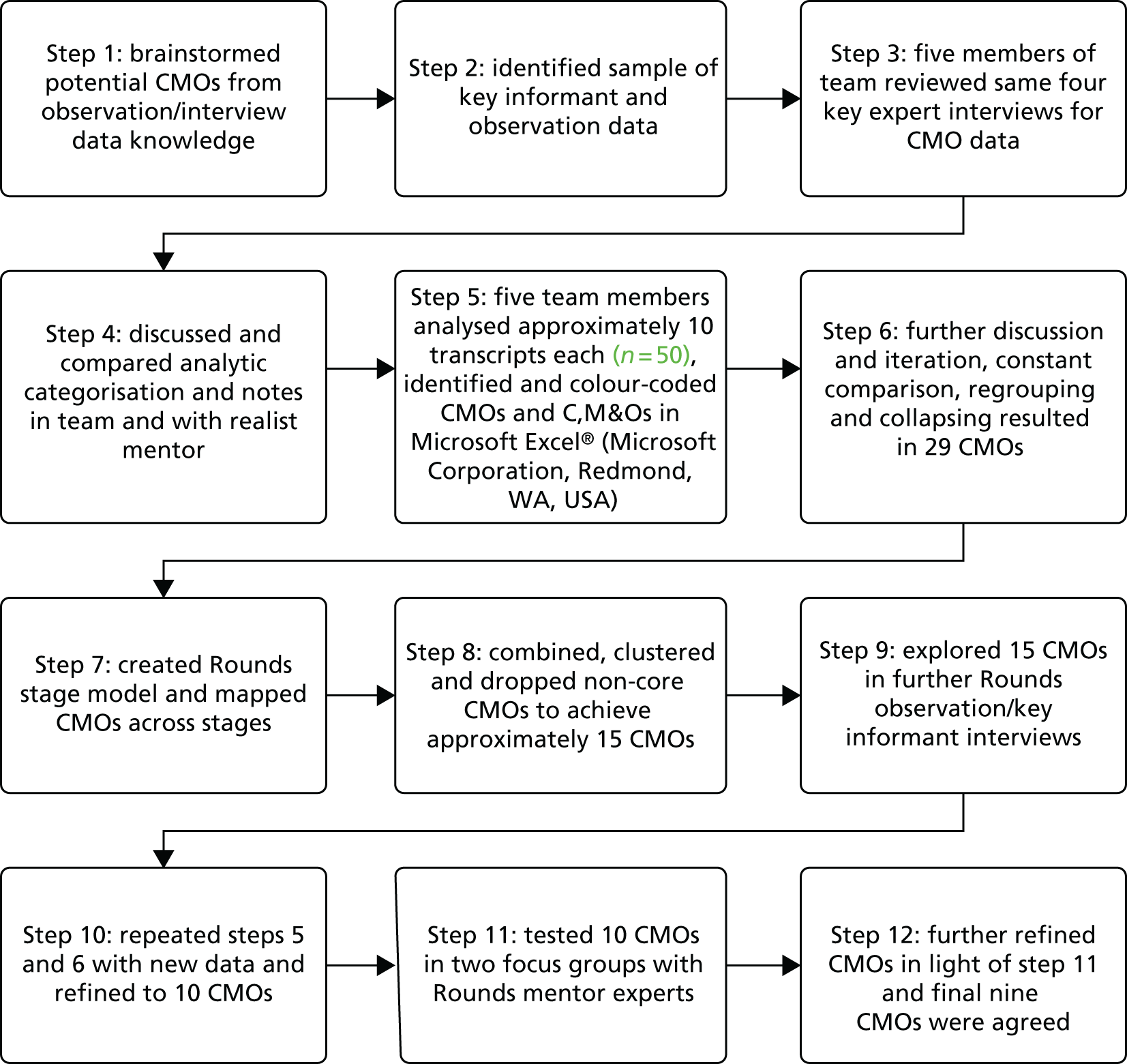
We systematically analysed a selection of key experts’ (facilitators and clinical leads) interviews for CMO configurations and causal explanation (across all case studies), and labelled the CMO components in author comments in Microsoft Word (Microsoft Corporation, Redmond, WA, USA) to enable us to review each other’s CMOs and discuss. Five members of the research team (JM, ML, ER, CT and IM) read and analysed the same four transcripts, and discussed and compared analytic categorisation and notes. The team then analysed up to 10 transcripts each, identified overlap and colour-coded data sections relating to context, mechanism and/or outcome (see Figure 8), and discussed these in 10 half-day meetings, with and without support from Justin Jagosh, our realist methodology expert and mentor. We initially generated 29 CMOs and organised them across the four stages of our Rounds model (see Figure 7), and by key player (audience, facilitator, clinical lead or panellist). Further analysis cycles and testing causative configurations in repeat interviews with our well-informed ‘experts’ and two focus groups with Rounds mentors allowing us to refine and collapse our 29 CMO configurations to the nine presented below. Finally, in meetings with Justin Jagosh, we grouped and causally linked our nine CMO configurations together (see Figure 10).
We revisited our initial programme theory and refined this in the light of our CMO data to develop our evidence-informed programme theory (see below). Report Supplementary Material 10 provides a summary of nine data themes that informed our revised CMOs and their inter-relationships.
Our field notes of observations of Rounds, steering groups and panel preparation were managed and analysed as textual qualitative data. 89 We followed steps 3–6 above for our field notes on Rounds to examine data to confirm or disconfirm our CMO configurations. We organised our data in Microsoft Word files and using some aspects of framework analysis to determine key descriptive elements across panel preparation and Rounds observation field notes, for example the timing and stages of Rounds; where and how facilitators intervened to support panellists or audience members and maintain safety (or not); and, in panel preparation, how facilitators gathered information and supported panellists to craft stories (including safety and trust aspects). We have not been able to include many fieldwork data from Rounds owing to the sensitivity of the material and the challenges of maintaining anonymity and confidentiality.
Findings
Here we present our initial and evidence-informed programme theory to give a broad overview of how Rounds work. We then present our detailed CMO configurations, explain their inter-relationships and provide supporting data.
Programme theory
All programmes or initiatives will (implicitly or explicitly) have a programme theory, or theories,6 about how the programme is expected to cause its intended outcomes.
Specific data used to develop our initial programme theory included our:
-
initial review of the literature to identify mechanisms of Rounds to enable us to design our survey (see Chapter 3)
-
composite definition of Rounds in our literature review (see Chapter 3)
-
interviews with programme architects in the USA (see Chapter 3)
-
initial observations of Rounds and discussions with key players in UK implementation
-
review of programme documentation including SCCH in Boston and PoCF websites and contracts.
These approaches enabled us to develop initial programme theories about how, for whom, and under what circumstances the Rounds help health-care staff with the human dimensions of their work (Box 3).
Our initial programme theories (highlighting the underlying psychosocial mechanisms providing the active ingredients to facilitate change), suggested that Rounds ‘work’ by:
-
providing an inclusive multidisciplinary group with a level playing field for reflection and discussion in a safe, non-judgemental space to encourage communication between staff who support and teach each other how to better connect with patients and provide compassionate care
-
providing social support for staff where disclosure makes events comprehensible and buffers distress and a supportive environment to encourage people to share and learn from the non-medical aspects of their work (not problem-solving), which strengthens the patient–caregiver relationship through empathy
-
having a range of attendees, including doctors; the programme provides a forum for all staff (because all staff can influence patient experience and connect with patients) and creates an opportunity for (senior) staff and facilitators to role model vulnerability, which encourages participation and gives permission for others to speak freely and honestly
-
having visible organisational support to make evident the organisation’s values on the importance of connecting with patients and supporting staff and role modelling that this matters to leaders to show what works with patients (see Chapter 7 for details).
When a programme like Schwartz Rounds is implemented, it is testing a theory about what ‘might cause change’ (p. 1), even though that theory may not be explicit. 5 When we started, we found that the theories or mechanisms by which change might occur were not very explicit (see Box 3). Thus, a key task in our realist evaluation was to make the theories within the programme explicit, by developing clear hypotheses about how, and for whom, programmes might ’work’ (see Chapter 3).
Revised evidence-informed programme theory
Box 4 details our refined programme theory, informed by the evidence from our study, through an iterative CMO configuration process, distilling from the configurations how the Rounds (the programme) cause their intended outcomes based on an analysis of our data.
Adherence to the core components of the Schwartz Rounds model (e.g. group intervention with good facilitation and the creation of a safe space) (see Chapter 7) provides support for staff with their work in health care. It ensures an opportunity for staff to feel safe enough to reveal themselves as human and vulnerable, and for those emotions to be contained in Rounds. This reduces shame, stress and anxiety and improves coping, allowing staff to process difficult emotions and experiences, making themselves more emotionally open and available to patients and colleagues (and self), fostering empathy, compassion and an acceptance of the grey areas and messy realities of emotional work in health care.
When staff are given an opportunity to share experiences and disclose previously hidden experiences, peers get to know each other better, creating greater trust and empathy for each other and improved connections and teamwork.
Stories that reveal the difficult, demanding and satisfying aspects of health-care work, and that provide multiple perspectives on staff and patient experiences, help staff to make sense of their experiences and communicate these to others, creating empathy and compassion for actors in the story (patients, family members and staff) and enable staff, patient and carer behaviours to be seen in context rather than in a one-dimensional way, reducing stereotyping.
Staff group reflection on stories/experiences (that resonate and trigger reflection) create a recognition of shared experiences and feelings, reducing isolation and creating a cohesive community in which staff offer and receive help and encourage and inspire each other, creating support, adaptive coping and motivation for future health-care work.
By putting staff experience at the centre of Rounds, creating a countercultural space that is not outcome orientated, Rounds create an important time when staff are present with each other. This creates openness and honesty, validating conversations about the difficult emotions associated with health-care work and making them culturally acceptable, and shifting conversations in the organisation towards more openness, honesty and compassion for each other.
Rounds, by being open to all and multidisciplinary, enable staff to recognise they are not alone, that others feel the same and that all roles and stories (highly visible or invisible) are valued and important for patient care, which strengthens teamwork and creates a more unified community and stronger ethic of working together.
Witnessing peers and senior colleagues being courageous and role-modelling vulnerability is contagious, inspires others to be honest and allows staff to see colleagues as human, breaking down barriers and creating a level playing field, which can facilitate support and increase challenge and patient safety.
Rounds work by having a cumulative effect over time, with the intermediate outcomes of one Round (increased trust and empathy) becoming a resource for the next Round by creating a Schwartz-savvy audience who support the facilitator in ensuring safety and containment, building trust and a supportive community.
We found that there was less evidence of specific ‘teaching’ than our initial programme theory had implied, although participants spoke of providing learning for others, but we did identify that Rounds strengthen empathy, compassion and relationships between staff, as well as strengthening the patient–caregiver relationship. We also found that visible organisational support had pros and cons (see Chapter 7). Our revised programme theory provided greater insights into how Rounds generated their effects (see above) and we identified some additional mechanisms, including:
-
the importance of resonance as well as reflection
-
the importance of containment and trust as well as safe and non-judgemental space
-
the key mechanism of storytelling and the important role of panel preparation for crafting and telling powerful emotional stories of staff experiences
-
that the impact of Rounds develops over time and has a cumulative effect
-
the mechanism of contextualising patients and staff and shining a light on hidden roles and stories
-
that Rounds provide a countercultural third space (see below).
We now provide a detailed exploration of our refined CMO configurations, which informed the revised programme theory (see Box 4).
Cumulative and linked context–mechanism–outcome configurations
Our findings (CMO configurations) are cumulative and linked.
Cumulative impact of stages of Rounds
In Chapters 6 and 7 we presented our Rounds stages diagram (see Figures 6 and 7). Here we illustrate where our analysis suggests that the nine CMO configurations map across the four stages (Figure 9). It can be seen that not all CMO configurations work across all four stages, with self-disclosure, contextualising patients and staff, reflection and resonance, and group interaction occurring only in panel preparation and Rounds, and not in stage 1.
FIGURE 9.
The CMO configurations mapped to the stages of Rounds.
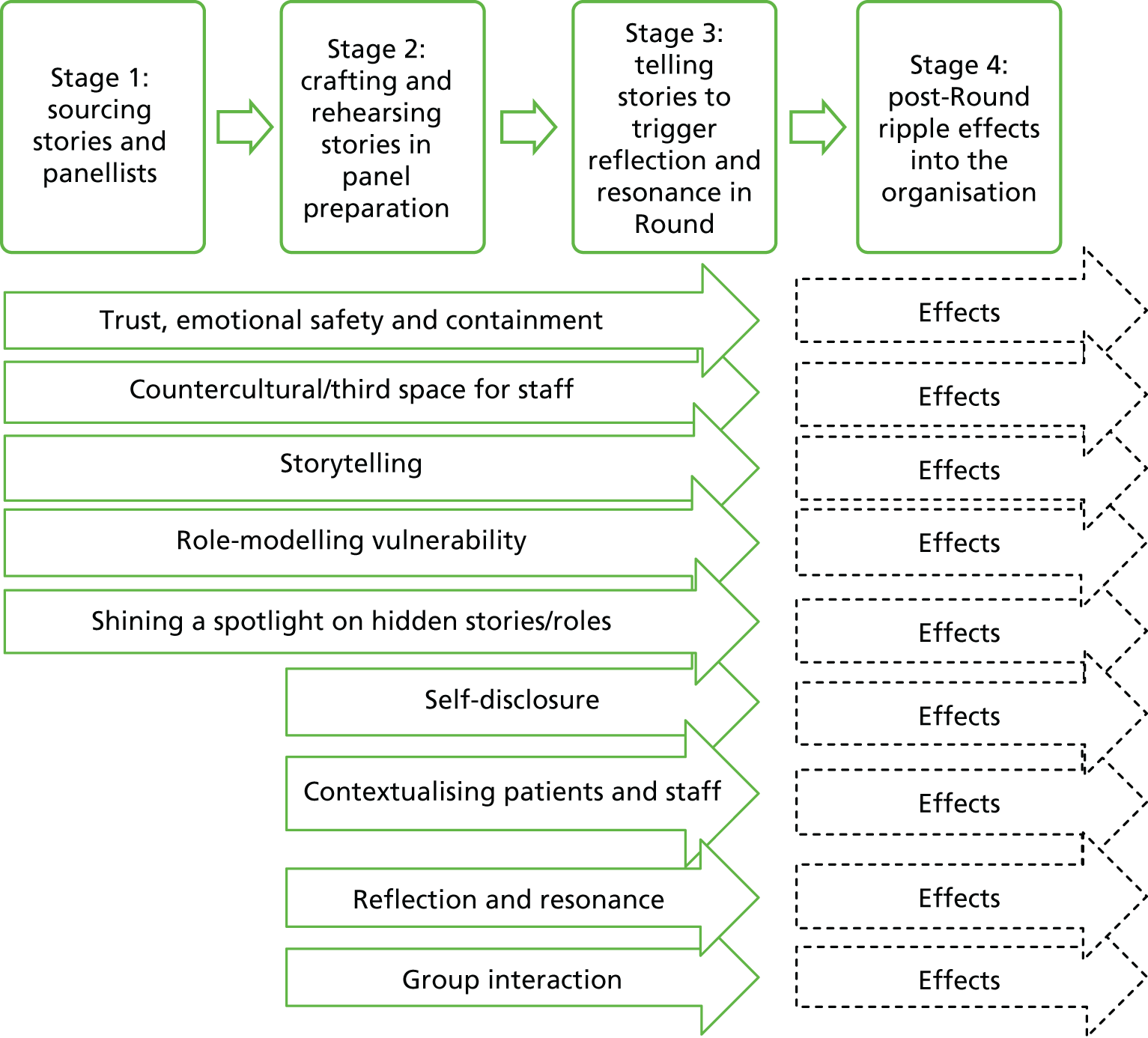
As well as being a four-stage cycle for each Round, our findings suggest that each stage has a cumulative impact on the next. Thus, temporally, stage 4 of one Round or a series of Rounds has an impact on the early stages of the next Round or Rounds. This is important, as it takes time to establish Rounds and create resources, for example experienced facilitators, trust and psychological safety, and a ‘Schwartz-savvy’ audience.
Linked cumulative context–mechanism–outcome configurations
To illustrate the cumulative impact of Rounds another way, we present how our nine refined CMO configurations are interlinked (Figure 10). Group interaction, and trust safety and containment, which are both core components of the Schwartz Round model, are prerequisites for all other CMO configurations. Storytelling and self-disclosure share similar theoretical processes (e.g. cognitive integration, making sense of experiences), so they have been grouped together, whereas ‘role-modelling vulnerability’, ‘contextualising patients and staff’ and ‘shining a spotlight on hidden roles’ are all examples of what is being offered and revealed as part of the process of self-disclosure and storytelling. Reflection and resonance is triggered by hearing stories and witnessing the self-disclosure of panellists, and, as audience members also share their stories and self-disclose, this creates cumulative effects for future Rounds.
FIGURE 10.
Visual representation of evidence to illustrate how CMO configurations link together to explain how Rounds ‘work’.
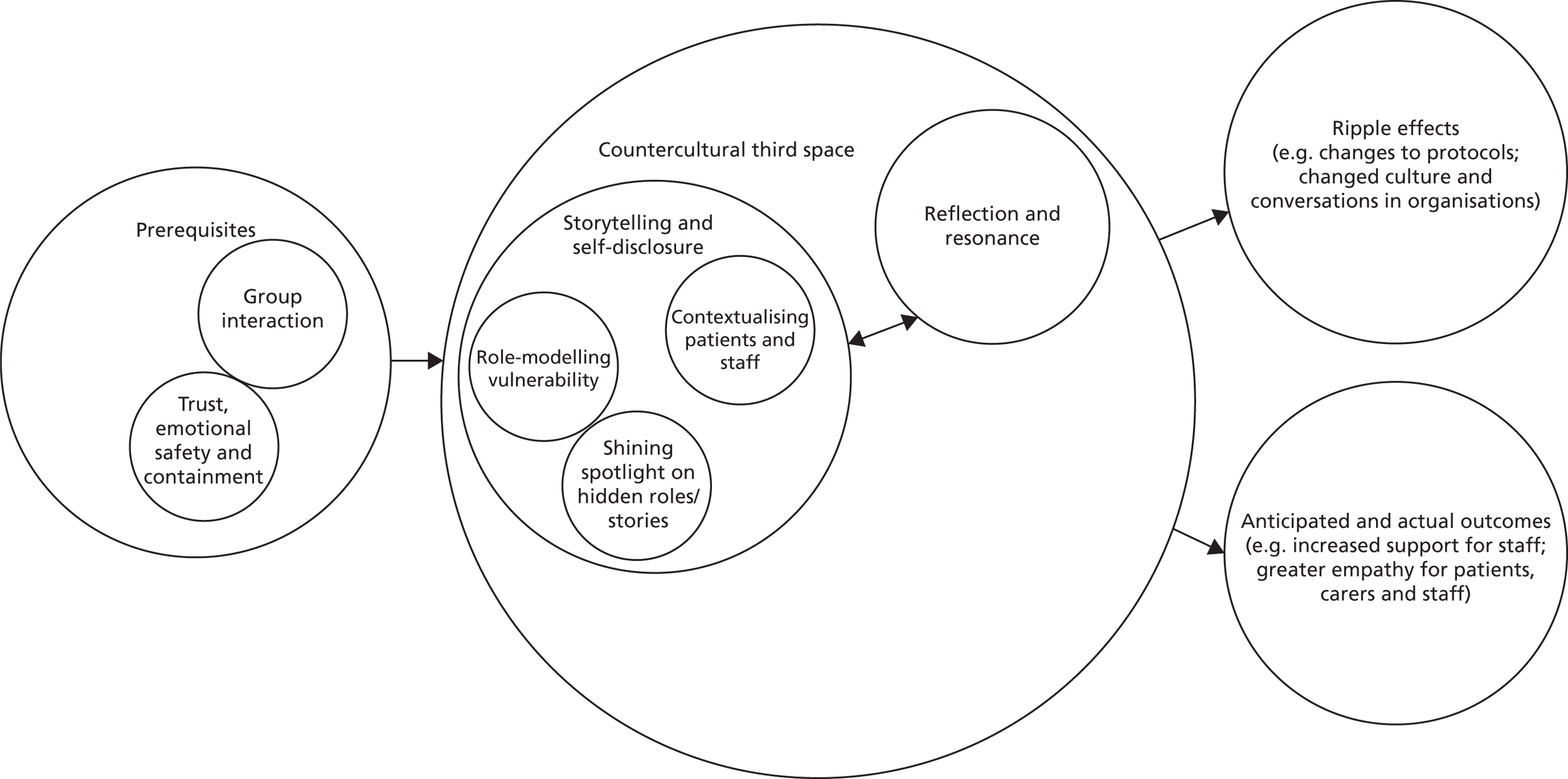
Ripple effects may occur as ‘unanticipated outcomes’ or ‘side effects’ of Rounds, because part of the countercultural nature of Rounds is that they are explicitly free from the usual expectations around the identification and allocation of tasks, responsibilities, actions and changes that would normally be part of team meetings or similar interventions such as reflective practice or clinical supervision. Ripple effects occur because individuals, or groups of individuals, decide to act on or take forward initiatives outside Rounds as a result of what they have heard. This can be difficult for new attendees to grasp and, because of the prevailing NHS culture, some attendees felt some frustration that there were no action plans or outcomes. Over time participants reported that they came to appreciate the different space provided by Rounds and realised they could take action: just that it was not a requirement. In terms of the countercultural/third space, we suggest that this is driven by fidelity to the model (not problem-solving; safe and confidential space) also outlined in Chapter 7 and is an accumulation of all of the other CMO configurations, thus making the whole Schwartz Round a countercultural and a ‘third space’ (see below for further explanation). Outcomes are either predicted on the basis of theory (i.e. programme or existing relevant theory) (anticipated) or evidenced by data.
Detailed context–mechanism–outcome configurations
We now present each of the nine CMO configurations in detail. We have separated the resource and response in the mechanisms where applicable. Further supporting data for each CMO configuration are presented in Report Supplementary Material 11.
Trust, safety and containment
Our data suggest that key to the successful implementation of Rounds is the concept of trust and safety (Box 5). This is important in all three initial Rounds stages: selecting the story or theme, the panel preparation and the Round itself (see Figure 10). Participants’ feelings of trust, safety and containment develop throughout the stages of a Round and intensify and are reinforced over time, through constant repetition and reinforcement for subsequent Rounds. Safety in Rounds means a space where panellists and audience members feel accepted, respected and valued. Facilitators ensure psychological safety through the use of ground rules including confidentiality and anonymity, through providing non-judgemental support, through the use of the Schwartz model to provide a bounded and established time and through the use of the routine and rituals of Rounds. Conversely, an ‘unsafe’ Round would include panellists and audience members experiencing embarrassment, rejection, reprisal or blame, or experiencing bullying and punishment for speaking out. Thus, in Rounds where safety may have been compromised, this can have a damaging impact on participants’ feelings of trust, safety and containment and, thus, on their willingness to attend, participate and disclose.
Readiness in terms of emotional literacy, willingness to take risks, encouraging openness and transparency, avoiding blame.
IndividualReadiness in terms of ability and willingness to tell story and trust the process that might make them feel vulnerable.
Rounds processThe extent to which facilitators/clinical leads ensure fidelity to the ‘Schwartz Rounds model’, have experience in group work and training in Rounds facilitation. The ‘facilitation style’ that they bring varies between facilitators, between clinical leads and between Rounds.
MechanismsGood facilitation involves conducting a number of ‘safety checks’ during the selection and preparation of stories, cases and panellists to reassure would-be panellists and build a trusting panellist–facilitator relationship and using therapeutic processes of ‘maintaining boundaries’, ‘ensuring confidentiality’ and ‘intervening when necessary to protect panellists’ to hold and contain a safe space (Resources). By demonstrating their ability to keep Rounds safe, this maximises the panellists’ and audience’s trust and confidence in the facilitator and clinical lead (response/reaction).
Which then leads to willingness to ‘self-disclose’, ‘role-model vulnerability’, ‘tell stories’ that ‘contextualise patients and staff’ and ‘shine spotlight on hidden roles and stories’.
OutcomesLess stress in staff, less psychological morbidity, better coping and greater understanding and empathy for patients and staff.
We had not fully appreciated the importance of trust and containment as a mechanism in the implementation of Rounds at the beginning of our study, despite ‘safe and non-judgmental space’ being in our original programme theory. However, through our interviews and observation it became clear that in order for people to feel confident to speak, to allow themselves to be vulnerable and to share their stories, emotional safety (held and supported largely by the facilitator/clinical lead), which includes the concept of ‘containment’, allows trust to develop in audience and panel members, thereby facilitating open and honest dialogue. The aim is to allow panellists and attenders to express and explore feelings that may feel too shameful or painful to be shared with others; theory suggests that it is through this process that attenders learn to cope with those damaging, overwhelming or potentially explosive emotions. 90
Aspects of safety noted by our panellists, audience members and facilitator interviewees included pre-Round safety checks, such as checking that panellists understand the potential consequences of publicly telling their story and countering the ‘urge to confess’, ground rules on confidentiality stated at the start of every Round, and a signed agreement regarding confidentiality when attenders sign in.
Intermediate outcomes
Our survey data support the outcomes from this CMO configuration, identifying stress reduction (GHQ-12 ‘caseness’) in Rounds attenders versus non-attenders (see Chapter 5). In interviews, staff reported that the safe, confidential space provided by Rounds enabled them to be better practitioners, to think about their behaviour, to make different future choices and to be more empathic with patients, for example:
[Rounds are] a safe space to discuss things that are challenging [. . .] this enables practitioners to be better practitioners and be more empathic, have a moment to stop and think about themselves and their behaviours and others’ behaviours, and that reflection may help [. . .] in the future.
Juniper-11-Panellist
Our data support other work that suggests that some mechanisms operate on a continuum, like a ‘dimmer switch’, rather than simply the mechanism ‘firing’ or ‘not firing’. 91 Contextual factors that turn up this mechanism’s dimmer switch include the extent of panel preparation, the facilitator’s skill and/or experience, and the audience’s Schwartz savviness (see Chapter 7).
Theory suggests that containment provides a sense of safety for the panellist and audience members to explore feelings that may otherwise be experienced as overwhelming and confusing. It is often about ‘holding’ the alarm, confusion and pain of unfamiliar or overwhelming feelings, and can be described as the capacity of one person to stay with, and psychologically and emotionally hold, the distress of another person in such a way as to allow it to be coped with. 92 It requires the facilitator to manage their own sense of uncertainty and confusion in order to be effective in helping those in Rounds to manage their own feelings. The facilitator needs to provide the confidence and presence to enable panellists and Rounds attenders to believe that their difficult feelings can be managed, explored and understood to avoid unsatisfactory coping mechanisms. 93 Confidentiality is crucial if members are to take risks necessary for real growth;37 our data provided evidence to support these theories:
It’s set up to be a safe, confidential forum [. . .] I mean often it’s come to my mind about using a psychotherapy term of ‘containment’ but a place for people to express their feelings, some containment both from the panel and other people in the audience, to understand the emotional reaction to it, for it to be OK to express feelings that might seem strange, unacceptable, awful. [. . .] some understanding about why people are feeling that way
Anonymised-site-17-Panellist-speaking-from perspective-of-facilitator/psychiatrist
Group interaction
This CMO configuration (Box 6) primarily relates to the Round itself (i.e. stage 3) and only relates to some panel preparation meetings (stage 2), as some are conducted one to one and not in a group. Our initial programme theory identified that it was important to have a range of attendees in a multidisciplinary group of health-care staff but did not identify which aspects of this would be an important mechanism.
The characteristics of the audience in terms of size, composition and Schwartz Round savviness vary between sites and between Rounds.
MechanismsThe group setting provides an opportunity for panellists and audience members to tell their story to a group of colleagues (resource) and reflect on and learn from the nature of the group interaction itself (resource), which sparks recognition of shared experiences and feelings (reaction) and giving and receiving help, encouragement and inspiration to each other (response). This leads to the removal of a group member’s sense of isolation, validates their experiences, raises their self-esteem, and helps them to develop more adaptive coping styles and more self-awareness of their own behaviour/motivations through receiving feedback on their own behaviour and its impact on others. Participants gain a sense of belonging, acceptance and validation through group membership. They can experience relief from emotional distress (e.g. chronic feelings of shame and guilt).
OutcomesIncreased staff support, cohesiveness and better teamwork supporting improvements in patient care.
Our data analysis has unpacked this mechanism further, highlighting the importance of sharing stories and reflecting as a group activity. Reflection can often be an individual introspective process with little insight into the similar experiences of others. Rounds as a group process of interaction provide an opportunity to trigger reflection in others through hearing stories and hearing others ‘reflect on action’, triggering resonance and reflection in individuals. Individuals are able to achieve higher levels of learning and retain more information when they work in a group rather than individually. 94
The experience of listening to the stories of others and sharing stories underpins Rounds, creating a group intervention in which staff can feel heard and supported, and are exposed to the experiences of others. This gives the potential for Rounds to be a ‘richer’ intervention than one-to-one reflective sessions or supervision, and we suggest that the group interaction element of Rounds is an important prerequisite for other CMO configurations. Drawing on theory, we identified six factors that add to the experiences of Rounds participants because it is a group intervention: (1) cohesiveness, (2) universality, (3) shared values and motivation, (4) catharsis, (5) interpersonal learning and (6) self-understanding. 37 Being in a group can help participants learn factual information from others and how to share personal feelings, show concern, and support others through a modelling process, observing and imitating the facilitator, clinical lead, panellist and audience. 37
The resources offered by Rounds being a group intervention included the recognition of shared experiences and feelings (reaction); insights into others’ experiences and how they connect everyone; and the acknowledgement of the contribution and work of less visible, non-clinical staff. Interviewees identified the importance of the multidisciplinarity of the group, the flattened hierarchy and the opportunity to think and learn from each other (see Report Supplementary Material 11 for more supporting data):
I think the very big difference [between Rounds and one-to-one supervision] is, particularly in a big organisation like this, is that there is no other forum that’s multidisciplinary and there is no other forum where no matter where you are in the staff hierarchy you are empowered, if you wish to take it, to have a voice, I think that’s the hugest difference.
Mulberry-367-Facilitator
All in it together and it’s kind of ‘oh I didn’t know it was like that for you’. I think it strengthens the connections and the relationships with other people [. . .] it’s this kind of shared experience around challenges, making change or dealing with loss or feeling stressed by your work, whatever it might be.
Ash-400-Facilitator
Countercultural/third space for staff
The countercultural and third-space mechanism of Rounds was not explicitly in our original programme theory, but our data and recent literature shifted our thinking. In late 2016, a book by the former lead mentor for Rounds in the UK, Barbara Wren, was published in which she wrote: ‘the process of Schwartz Round implementation is in many ways counter-cultural. Good Rounds shift an organisation and its workers away from their default position of urgent action, reaction and problem solving to an hour of stillness and slowness’ (p. 41). 95 Our data supported this and helped us to identify the countercultural nature of Rounds as a key mechanism: albeit as a group-level mechanism. The countercultural/third-space environment is a mechanism but also over time becomes the resource and context for the other CMO configurations, as outlined above: storytelling and self-disclosure and reflection and resonance sit within this third space (see Figure 10). The third space is a resource provided/offered and co-created by participants to enable other mechanisms to ‘fire’ (Box 7).
In the busy, hierarchical, outcome-oriented environment of the NHS, where stoicism is valued and where staff are exhorted to put patients first, if there is good facilitation in Rounds that put staff experience centre stage and supports ‘no problem-solving’, safety and confidentiality . . .
Mechanisms. . . then Rounds are able to offer a unique countercultural physical and psychological third space and time (resource) that sparks a shift in what is valued/privileged and spoken about [e.g. emotion, silence, stillness (co-created by the audience)] (response), which . . .
. . . leads to reflection, openness, honesty; different types of conversations; and staff being revealed as human, which can make talking about emotions more culturally accepted . . . and can reveal the person in the professional.
OutcomesThese included improved compassion and understanding for others (including patients and staff) and self, creating greater resilience, via the mechanism of reflection (see Reflection and resonance CMO).
We drew on and tested our findings regarding Rounds being a countercultural space in relation to third-space theory. First and second spaces are two different spatial groupings where people interact physically and socially, such as home (everyday knowledge) and school (academic knowledge). Third spaces are the in-between, or hybrid, spaces, where the first and second spaces work together to generate a new third space96,97 to create a hybrid culture and identity because respite is needed from any challenges to functioning in the second space. 96,98
We identified nine aspects of ‘third space’ in the literature98 and tested if these ‘fitted’ well with Schwartz Rounds in focus group interviews with mentors. Participants agreed with items 1–6, and less so with items 7–9:
-
free – third spaces also generally offer food and drink, the staples of socialising
-
neutral ground
-
leveller
-
conversation is the main activity
-
easy to access and accommodating
-
cadre of regulars
-
low profile*
-
playful*
-
home away from home.*
Items marked by asterisks were felt by some not to fit so well with Rounds, but one facilitator felt that Rounds were low profile in that by their countercultural nature they could be ‘under the radar’ of the organisation’; and that they could at times be fun and playful, and certainly that a ‘home away from home’ atmosphere was strived for, although it was recognised that this was different from the examples in the literature, such as coffee shops.
One aspect that does relate to other third spaces such as coffee shops is the provision of food (which is in the PoCF contract, is symbolic of community and ‘breaking bread together’, and is also somewhat countercultural). Our data suggest that Rounds are third spaces where staff can connect with their values and humanity, with the first and second spaces being (1) professional/role identification and values (everyday work) and (2) NHS/organisation (imposed work practices) spaces. 99 Third space offered four applications for our work on Rounds:
-
recognised space, in which professionals could ‘hang the confusion and chaos’99 of the workplace for a time while they thought through their practice100
-
community space, creating a community of commitment101 and a community of creation102 not centred around targets, objectives and rational negotiations about how goals can be achieved, but on ‘what people care about and want’ to create together103
-
conversational space, for dialogue between participants that is safe, secure and supportive, space that ‘stands in between’ the formal areas of practice104
-
learning space –
places of transition, and sometimes transformation, where the individual experiences some kind of shift or reorientation in their life world [. . .] [where] a shift in identity or role perception [occurs] so that issues and concerns are seen and heard in new and different ways.
Savin-Baden, pp. 8–9105
Wren95 suggests that:
by keeping connected to the three overlapping contexts of the patient, the staff member and the organisation, without a requirement to produce an outcome for any of them, Rounds can create a space within which the triangulation of healthcare experience can be both noticed and resisted.
Wren, pp. 44–595
For example:
It would be the factors from the reflections on the Rounds for me [. . .], the reflection that we do as a team on our practice [. . .] just helping me to be better at being compassionate and understanding and open to people recognising the impact on ourselves emotionally. And just that greater resilience.
Ash-05-Facilitator
Others suggested that there had been wider cultural changes (‘ripple’ effects) through changed conversations in organisations, which had been facilitated by the countercultural third space offered by Rounds:
It’s sort of softened the ground for things to grow, the kind of conversations that [a colleague] has with the medics and the different clinicians that are very different to the ones that she was having about a year ago [. . .]. The actual human effect, the empathetic affect of what happens when you’re caring for staff.
Carmel-385-Facilitator
Staff spoke about ‘leaving things at the door’ and being in a different ‘zone’ that provided a headspace to reflect. This creates behaviour change by providing an opportunity to do things differently; the honesty, without judgement or fear of any backlash, that was provided in this space was the power of Rounds:
To hear doctors being very honest about a difficult patient and how they handled it. I’d never heard this in this building and I’ve been around 49 years and it was the honesty of it without judgement and I think that was the powerful thing that got to me.
Cedar-04-Panellist-frequent attender
Uncluttered headspace to a certain extent, communal headspace as well, where people can take that hour where you can put the brakes on, you can stop, you can leave that constant drive for performance targets at the door and have that clarity where you can just breathe and start thinking with like-minded colleagues who experience the same pressures where we’re at, where the difficulties are and, kind of, reflect on those [. . .] being able to sit with the emotion, be with the emotion, that you normally just press, push it down, push it down, push it down, move to the next task, [. . .] so, that ability to reflect on your practice and have that headspace I guess when you walking out of the Round and you go back to your clinical practice, that’s where that opportunity to do things differently comes from.
Horse-chestnut-07-Clinical-Lead
Rounds provided a confidential space that was counter to the prevailing culture in health-care organisations in the following ways:
-
flattened hierarchy
-
staff experience valued
-
emotional disclosure encouraged
-
stillness
-
resisting outcomes
-
revealing and discussing own emotional needs and vulnerability (vs. the myth that this is undesirable for health-care professionals or a sign of weakness)
-
support and listen to each other without judgement
-
attending to own emotional needs rather than those of patients
-
slow reflective space with some silence (see Report Supplementary Material 11 for supporting data).
This resulted in staff being able to be honest, and in revealing emotions being more culturally acceptable.
Self-disclosure
Self-disclosure is the process of sharing information about yourself with another person (or people). Disclosing the human aspects of staff’s work – the social, emotional and ethical issues that they face in their professional lives – is a key element of Rounds. Self-disclosure was part of our original programme theory, but our data shed light on the ways in which it is a key Schwartz mechanism: as part of sharing stories and prompting others to reflect and self-disclose, allowing stronger relationships and trust to develop (Box 8).
An environment that supports trust, safety and containment through good facilitation, and where there is good-quality listening and reciprocity this creates an environment in which staff are willing to self-disclose.
MechanismsWhen facilitators are trusted by panellists and audience members to keep a safe space (resource), this sparks a willingness to be a panellist and to disclose deeper thoughts and feelings, including distressing stress-related thoughts and experiences (panellist response); and when the audience is Schwartz savvy (i.e. listens well, understands the purpose of Rounds, is supportive and non-judgemental) (resource) this emboldens others to do the same (audience response), thus creating reciprocity in self-disclosure.
Self–disclosure allows transparency and some catharsis, and supports participants to make sense of distressing emotional experiences. Staff make themselves vulnerable and ‘human’ to each other, which increases trust in relationships. The audience may also support through self-disclosure and suggest ways to cope with, validate or reframe the experience more positively. The process of self-disclosure supports staff well-being, enabling participants to form new associations with trauma-related stimuli.
OutcomesBetter staff well-being with improved relationships with previous trauma and new associations with trauma-related stimuli; staff feel better supported and more resilient.
Psychological theory suggests that emotional self-disclosure makes individuals ‘transparent’ and vulnerable to others. 106 The greater the depth of the discussions, the more likely the person is to feel vulnerable. Therefore, trust built over time among the disclosers (often a panellist or an audience member) and the facilitator/audience is essential to reach deep discussion.
Social penetration theory proposes that, as relationships develop, interpersonal communication moves from relatively shallow, superficial levels to deeper, more familiar ones. 107 Disclosure reciprocity is when a panellist reveals personal information of a certain intimacy level, and another panellist or audience member will in turn disclose information of the same intimacy level, creating a sense of emotional equity. 108 Disclosure is particularly beneficial in helping people come to terms with chaotic and unexplained events. Empirical evidence suggests that ‘opening up’ and expressing stress-related thoughts and feelings is associated with improved physical and mental health. 44 Theory also suggests that sharing fears and problems (as well as good news) with others who are trustworthy and supportive plays a key role in mental health109 and can reduce stress. 110 After mutual self-disclosures (as in Rounds) people can feel a boost in positive feelings111 and build relationships with friends and coworkers,112 and emotional, not factual self-disclosures can lead to closeness as long as disclosers feel that listeners are understanding and accepting,113 which links to the importance of good preparation and to the CMO of trust, emotional safety and containment, described earlier in the report.
In sharing information about themselves, people make choices about what to share and with whom to share it. Our data suggest that coming to a different ‘third space’ (see Countercultural/third space for staff) allows people to share and self-disclose in ways that they would not elsewhere, so that they come into the room as a person and not only as a professional. Some suggest that this enables barriers to come down and allows them to ‘share from the heart’:
Outside of Schwartz Rounds people tend not to share as much, for whatever reason [. . .] it’s often the most junior members of staff that set the ball rolling with deep sharing, such as the health-care assistants for example. They share from the heart and I just wonder whether it’s the actual humanity where you’ve taken your professional badge or hat off, metaphorically speaking obviously, that you come in as a person and I think the subject themes guide that in many ways because it allows you just to be vulnerable, to share about a time or an experience in your life and I just think that really just maybe energises others to feel safe [. . .] I think we just connect with that human sense of caring [. . .] and I think it’s maybe that it just pulls down so many barriers that people and I think [. . .] there’s some connection or some energy I think that it generates in the room.
Elderberry-11-Panellist-and-Steering-Group-Member
An outcome of this is connecting staff back to their own humanity and the ‘human sense of caring’, connecting staff together by ‘pulling down so many barriers’, revealing the person in the professional and connecting staff to their empathy and compassion for self and others (staff, patients and carers). Emotional self-disclosure makes individuals ‘transparent’ and vulnerable to others. The greater the depth of the discussions, the more likely participants are to feel vulnerable. Trust built over time is essential to reach the deep discussion and to provide some catharsis:
And I think it’s often that cascade where people just feel safe. I suppose going to a lovely gathering with people that you feel really comfortable with and you have a good old laugh. That cathartic sense of being together or a cry or a row or whatever it is, but it feels safe to do that and you can recollect and it, the connection and the bond are still there.
Elderberry-11-Panellist-and-Steering-Group-Member
Participants reported that the audience response and acceptance is validating, with a supportive audience helping panellists reframe and see an experience they have ‘held’ for a long time more positively and so make it less stressful and emotionally challenging for them (see Report Supplementary Material 11). A panellist who had been assaulted by a patient reflected:
We started talking about how the patient must have felt, how frightened he must have been [. . .] and I’ve never really had that kind of thoughts about what it would have been like for him [. . .] and [now] that anger has largely gone actually and I felt much more connected to his distress and I was able to get through that anger and, to a certain extent, that hatred for him [. . .] hate is a very, very strong word but if you are insulted or hit or assaulted by a patient sometimes hate is an emotion that it can instil within.
Horse-chestnut-01-Clinical-Lead-speaking-as-a-panellist
Storytelling
Telling a powerful Round story starts with an initial idea for a generic theme (e.g. ‘a patient I’ll never forget’), or a wider organisational incident, event or issue (e.g. ‘the junior doctors’ strike’), or a particular case, team or individual (e.g. ‘making a conscious decision to die’). The mechanism of crafting and telling a powerful story that resonates with others was not initially in our programme theory, yet as we began our interviews and observations we were struck again and again by how moved we were by the stories we heard, how they resonated with us and how so many people spoke of the ‘power of the story’. Storytelling and stories as a trigger for reflection are central to Rounds and therefore emerged as a key element of our revised programme theory (Box 9). Wren95 writes that ‘the story is the engine’ (p. 43) and highlights the importance of the ‘use of story to reveal experience in a prepared and crafted way, which allows the audience to move closer to a positive experience of managed exposure and a gradual acceptance of incompleteness and unfinished business’ (p. 43).
Key players with high levels of ‘organisational intelligence’ who can source cases, themes and panellists, and facilitators/clinical leads who are skilled at helping panellists to craft a story.
MechanismHaving the opportunity to put one’s experiences into language (resource) allows individuals to impose a coherent structure or narrative around it (response).
Rounds stories are well digested, are full of ‘Schwartz gold’ and have a clear narrative order and structure (i.e. effective story-resource). Panellists review situations (take ‘armour off’); they make sense of and emotionally process difficult experiences and feel heard (response). Audiences’ attention is captured and held; they are emotionally moved, mentally engaged, and able to learn from and identify with panellists’ experiences (response).
Outcomes For panellistsTelling stories can lead to closure and affirmation through being heard and the creation of alternative narratives, and, in the longer term, build resilience and improved psychological well-being.
For audience and panellistsHearing stories can lead to increased empathy and compassion for colleagues and patients, increased connection with own values and work motivation, wider knowledge of colleagues and organisation, increased sense of organisational cohesion and feelings of pride in belonging to organisation.
Stories are vehicles for behaviour change and can have longer-term outcomes/ripple effects, such as changes in practice, including changes to resuscitation protocols, and long-term benefits for staff well-being:
It has led to some additional work being done [. . .] In one case it led to the review of a particular protocol. [. . .] We had one particular Round, which was around ‘do not resuscitate’, and I know that that fed into more work being done around procedures and protocols around resuscitation. So, very often, it will feed into the current debates in the trust around whether it’s resuscitation or end-of-life care or, drug safety or whatever.
Axe-389-Facilitator
A colleague e-mailed her boss to say, ‘I have attended a Schwartz Round, don’t you think it’s a good idea if we reintroduce clinical supervision in our practice?’ And, indeed, they reintroduced it, purely because they heard the stories of people going through something, and perhaps they should change. She said, ‘Just to let you know, we’re back to doing this in nursing because of hearing the Schwartz Round,’ so you know, I have a direct example of people actually proactively changing something.
Tay-127-Clinical lead
Other data, detailing outcomes such as support and affirmation, a sense of closure for staff, an opportunity to discuss previously unsaid things leading to some resolution and (positive) impact on teamwork, can be found in Report Supplementary Material 11.
Stories are an effective way to transmit important information and values from one individual or community to the next. Personal and emotionally compelling stories engage more of the brain and are better remembered than simply stating a set of facts, and theory suggests that stories are ‘empathy workhorses’. 114 An effective story captures and holds attention and transports us into the character’s world. ‘Transporting’ is the ‘magic’ that happens when a story holds full emotional and mental attention; we experienced this often in Rounds observation when it felt like everyone in the room was holding their breath and it would have been possible to ‘hear a pin drop’. An example was an organisation’s first Round that was called ‘too young to die’:
We had a really good attendance, we had four panellists who were all really good and had a massive impact. I’m sure you have, but have you ever been in a room where it just goes totally silent? [. . .] And you can feel it? [. . .] We had that [. . .] people talked about it for months after [. . .] we had a wide range of panellists [. . .] and they all told a different story, but really, really, really strong stories, it was brilliant.
Beck-336-Facilitator
Good stories (‘Schwartz gold’) spark and engage through emotions and connect people. Stories were crafted in panel preparation to resonate, ‘paint pictures’ and transport listeners to a scene:
I relived it in my head so I could still remember the person’s room as I was sharing it and although I was picking up eye contact with the audience and kind of, I was kind of back in that person’s room. And even I could hear the clock ticking that he had on his sideboard. I could still hear that when I was passing that onto the audience. Yeah it took me back there and it brought it alive again.
Elderberry-11-Panellist-and-Steering-Group-Member
Our data suggested that the trigger stories were key to Rounds’ success. Respondents seemed to locate the essence of the Round in the emotional experience of the creation of a powerful, positive or rewarding embodied experience for them:
Powerful to be honest, very different stories and I think I don’t know that I was prepared for the outward emotion from the storytellers [. . .] actually witnessing that for real and it’s reliving it even though it was some time ago, you know, that whole outpouring of emotion was quite powerful. And [. . .] it’s the variation in the stories were massive actually. You’ve got clinical director right through to a health-care assistant that’s holding someone’s hand.
Juniper-27-Panellist
When stories ‘transport’, they generate empathy and the brain produces oxytocin, which, when synthesised, makes people more trustworthy, generous, charitable and compassionate, and more sensitive to social cues around them. 114 Stories were important vehicles for reflection:
It was very powerful hearing other people’s stories [it] makes you think about your own practice and how you deliver the care that you deliver [. . .] as well as the bigger picture.
Juniper-27-Panellist
Role-modelling vulnerability
As outlined in Figure 10, ‘role-modelling vulnerability’ is an important aspect of ‘self-disclosure’ and of the countercultural/third space. Revealing, and specifically role modelling, vulnerability is unusual for health-care staff, who rarely show vulnerability in their daily work, and instead display confidence, certainty and invincibility so that they reassure patients and facilitate patients’ confidence in them. Role-modelling vulnerability was identified in our original programme theory, and our data reveal why this aspect is important in how Rounds may ‘work’ (Box 10).
Where there is fidelity to Rounds’ purpose and core components, and when trust, safety and containment are ensured, panellists and audience members have the confidence and courage to speak authentically, from the heart, and to participate in self-disclosure by providing examples of their vulnerability.
MechanismsFellow panellists and audience members witness their peers role modelling courage and bravery as they share examples of vulnerability and reveal their humanity (resource); this sparks an insight to ‘see the person in the professional’ (response/reaction) as well as feelings of empathy and compassion (response/reaction), and because their courage is contagious audience members (particularly junior staff) feel able to do the same (reaction/response) . . .
. . . which connects audience and panellists as human beings, creates a ‘level playing field’, reduces feelings of isolation and engenders a commitment to show more understanding and empathy towards colleagues.
OutcomesAllows staff to be more comfortable with their feelings and that it is all right not to always feel OK. A ‘level playing field’ is a healthy counter to the traditional organisational hierarchy, and, through increased approachability and understanding, junior staff can feel more able to challenge senior staff, which can increase patients’ safety.
Vulnerability facilitates human connection through the willingness to be present and let ourselves be seen, yet shame gets in the way of authenticity as people become paralysed with fear about what others might see. 115 In health care, Tomlinson116 suggests that public shame and humiliation on ward rounds in medical education gets in the way of honesty or openness for fear of making a mistake or being ridiculed. Brown115 suggests that vulnerability is not a weakness, but it is an emotional risk, and it is the most accurate measurement of courage; shame inhibits connection with others, with people fearful that they are not worthy of it. Being vulnerable allows Rounds participants to connect at the level of their humanity with each other, not as professionals but as fellow human beings. It also demonstrates courage and empowers others to be authentic and vulnerable, creating a circle of connection and allowing staff to be more honest, open and empathetic with each other. Brown117 suggests that shame cannot survive empathy or being spoken about, and that talking about shame ’cuts it off at the knees’ (p. 58117). Our data suggest that good facilitation (supporting emotional safety) can prevent vulnerability turning to shame.
Witnessing peers role modelling courage and bravery creates a level playing field, which breaks down barriers between staff groups and is empowering for others. The language of vulnerability revealed much about how health-care professionals cope in their daily work. Our interviewees spoke of ‘masks’, ‘armour’ and ‘protective shells’ being removed:
It’s interesting to break down some of those barriers of the façade of the consultant, the façade of the surgeon, the façade of the bed manager and actually get to the human being behind the role, because I think that that really puts us on a level which I think is a very healthy place to be [. . .] think that that’s a real leveler within a working environment in a very healthy way [. . .] it’s also a very helpful thing to see the human being behind the mask, so to speak.
Ash-14-Clinical Lead
You are allowed to be a human being and to be vulnerable, and I guess that’s what we were all doing at Schwartz. We were all showing our vulnerability in different ways and . . . being honest about that and not trying to pretend that this stuff doesn’t have an impact, ‘cause it does.
Willow-03-Panellist
The revealing of vulnerability by senior staff in particular was felt to reduce feelings of isolation, and to be empowering, encouraging and supportive to other staff (see Report Supplementary Material 11 for more supporting data).
Contextualising patients and staff
‘Contextualising patients and staff’ is an important aspect of ‘storytelling’ and ‘self-disclosure’ (see Figure 10); it was not in our original programme theory, but we suggest that this CMO illuminates how staff ‘support and teach each other how to better connect with patients (and each other)’ (Boxes 11 and 12). As a result of panellists’ willingness to self-disclose, show their vulnerability and tell their story publicly, audience members and fellow panellists gain an expanded knowledge of patients and staff. They hear multiple perspectives about the same patient from different colleagues, and hear more about the external and contextual factors that impinge on individual patients’ and staff’s decision-making and behaviour. This also gives staff a longitudinal, rather than cross-sectional, perspective of what happened to a patient, which can be particularly important for junior staff/students and colleagues who were involved in one part of a particular patient’s care. In short, they are able ‘to put themselves in the patient’s shoes’ or get a ‘glimpse into the everyday world of that individual staff member’.
If there is careful choice and effort in sourcing, preparing and telling patient-related stories in Rounds, good facilitation that supports self-disclosure, and safety and containment . . .
Mechanisms (for patients). . . then personal stories are shared, which provide context to the patient’s experience (resource), sparking a broader view of patients and their families, which leads to feelings of increased insight and understanding, resulting in empathy by panellists and audience members (response).
This leads to a sense of closure on a difficult experience, and compassion and empathy for actors in the story.
Outcomes (for patients)Greater insights and understanding of the context of patients’ and carers’ lives, resulting in increased empathy and compassion for patients and improved care through enhanced teamwork.
If there is careful choice and effort in sourcing, preparing and telling patient-related stories in Rounds, good facilitation that supports self-disclosure, and safety and containment . . .
Mechanisms (for staff). . . then stories provide context to the staff experience through stories about the everyday reality of colleagues, their roles, and the difficult decisions that they have had to make (resource) . . . it can help them to ‘put themselves in their shoes’, see the person in the professional, resulting in staff being humanised, and staff understand the reasons for their colleagues’ attitudes and behaviour (response).
Outcomes (for staff)This led to closer professional relationships; improved teamwork, improved communication, improved working relationships, increased empathy for each other and improved care for patients.
Our observation of Rounds provided data to support these insights. For example, after hearing experienced and expert panellist colleagues’ insights into why a patient infected with HIV (human immunodeficiency virus) had not disclosed this to her partner, the initial judgments from a junior colleague changed to a compassionate understanding of the woman’s circumstances and situation, and awe at colleagues’ ability to support the woman to subsequently disclose in a safe way.
Theoretically, the fundamental attribution error supports our understanding of this CMO. Fundamental attribution error is the tendency to explain someone’s behaviour based on internal factors (personality or disposition) while underestimating the influence that external and situational factors and influences have. 118,119 Rounds remind people that others’ behaviour is constrained by situational factors and present an opportunity to take into account behavioural and situational information simultaneously to characterise the actors (patients, carers and staff). Our data suggest that fundamental attribution error applies to contextualising both patients and staff, and we provide separate CMOs for (1) patients and (2) staff.
Interviewees spoke of Rounds providing greater context for their patients’ lives and facilitated greater insight into people’s behaviour, changing perspectives:
I think it’s enabled ‘difficult patients’ or difficult cases to be understood and digested in a more constructive way, in a less defensive way, in a more reflective way. [. . .] but I do think [. . .] that it’s helped people understand the more complex and more challenging cases and why people behave like they do.
Esk-123-Facilitator
Well it’s certainly changed the way I view patients [. . .] I think I’m much more aware of their back story, if that makes sense.
Looe-381-Facilitator)
This allowed staff to step back from challenging and distressing incidents and to ‘walk’ in their patients’ shoes, thereby fostering empathy and changing behaviour:
It makes us think about what we’re doing and we’re walking in their shoes a bit more. I think also you reflect on and you internalise what you’ve heard so even subconsciously you think ‘I might try or do that a bit differently’.
Ash-02-Facilitator
Interviewees spoke movingly of the insights Rounds gave them into colleagues’ worlds and behaviours through the telling of honest, open and powerful stories in which staff revealed their vulnerability; this resulted in attendees feeling more generous towards colleagues and themselves, and having greater tolerance and empathy, resulting in compassion and greater trust (see Report Supplementary Material 11 for further data):
You’re much more sympathetic and tolerant of the decisions other people make [. . .] Rounds are really helpful in reminding [us] that everybody is trying to do their best. [. . .] a more generous understanding of other peoples’ difficulties and how hard everybody is trying [. . .] which makes it easier to be generous to ourselves then as well, in the sense of acknowledging that we do a really hard job.
Taff-138-Clinical-Lead
Hearing more about what the challenges are for us all in our different professions, I think is a useful [. . .] it does make us more tolerant towards each other.
Seine-378-Facilitator
Shining a spotlight on hidden stories and roles
‘Shining a spotlight on hidden stories and roles’ is an important aspect of ‘storytelling’ (see Figure 10), but was not in our original programme theory. We suggest that it illuminates how staff ‘support and teach each other how to better connect with patients (and each other)’ through providing staff with greater insight and understanding of what people’s roles involve, enabling them to learn from each other, foster mutual respect and value a wider range of staff/colleagues, strengthening relationships with other staff, team relationships and spirit (Box 13).
If there is careful choice in selecting stories and panellists from all parts of an organisation and stories are prepared from less visible roles/people . . .
MechanismsThen hearing stories from diverse range of panellists with audience members from multidisciplinary backgrounds and different parts of organisation (resource) sparks greater insight into and understanding of what people’s roles involves (response); less isolation (response); staff realise that many others have the same experiences/feelings despite their role (response) . . .
. . . which leads them to see the bigger picture of how the organisation functions, which helps develop organisational cohesiveness/connectedness, know where their role fits in with those of others and feel part of something bigger than they are, which connects them to values, learn from each other, foster mutual respect and value a wider range of staff/colleagues, strengthen and improve relationships with other staff, feeling a cohesive team spirit and trust being built and storytellers feel valued and appreciated.
OutcomesLess isolation; improved working relationships and improved care for patients.
Our data supported the theory that suggests that Rounds enable less visible roles to be made visible, enabling work perceived as routine to be reframed so that what might be seen as background work with low status can potentially be elevated in care work terms. 120 Our data suggested that attendees gained powerful insights into the roles of others, realising that all staff are affected by the challenges of patient care and experience difficult emotional responses. This enables attendees to create and sustain different notions of what the work is and of the person doing the work, because part of the identity-shaping process in ‘job crafting’ is relational. 121 This also enables some staff to connect with the ‘bigger project’ and the purpose of the organisation (caring for and helping patients recover or die well) to others and their values, and reinforces their own values.
By ‘shining a light on hidden roles’, staff reported connecting with each other and feeling less isolated, and we were provided with a concrete ripple effect of staff meeting up who had not done so before (connecting people and reducing isolation):
But in our last Round, we brought a person from A&E [accident and emergency] and a person from the hospital co-ordinator side, and a person from mortuary [. . .] They were talking as if they were on separate planets, not one person knew what the other person was going through, at the very same time, but it was the exact same event [. . .] afterwards, [. . .] I saw them in the corridor and they said, they’ve invited each other for cups of tea, if they’re in in the evening, because they’re all there in the hospital, feeling very isolated [. . .] so these departments are now meeting up for cups of tea every now and then in evening, on the power of realising that, [they felt] isolated that day [. . .] just people realising that they’re not alone, which to me, is a very good impact.
Tay-127-Clinical-Lead
Interviewees spoke of Rounds stories presented by staff they rarely encountered providing new ‘windows into other people’s worlds’, making visible invisible work/workers and giving greater insights into the organisation, allowing staff to feel part of a bigger ‘jigsaw’:
I’ve learnt a great deal about what other colleagues do, but also [. . .] how they see their working worlds [. . .] it’s those windows into other people’s worlds [. . .] for example there’ve been some amazing things that some housekeeping people and facilities have talked about that certainly other people didn’t realise and I didn’t realise [. . .] And then at the other end of the professional spectrum [. . .] the experience of more senior doctors, the consultants, having that ultimate clinical responsibility, and having to give the impression of being sure and confident when actually they feel anything else but that, the weight of that responsibility.
Avon-391-Facilitator
Those whose roles and hidden stories were ‘spotlighted’ spoke of feeling appreciated, supported and valued for their work. Interviewees also spoke of the link between personal stories of health care and organisational life: linking these; making staff visible; shining a spotlight being an exercise in enhancing teamwork; having the opportunity to meet new people at Rounds and put names to faces; and helping staff appreciate and know about each other’s roles much more, resulting in greater understanding and appreciation of their work (see Report Supplementary Material 11 for more supporting data).
Reflection and resonance
Reflection and resonance (situated within the third space CMO; see Figure 10) is triggered as the result of hearing stories and witnessing the self-disclosure of panellists, and as audience members also share their stories and self-disclose, this creates a resource for others (Box 14).
If there is careful choice and effort in sourcing, preparing and telling stories that resonate in the Rounds and if Round facilitation creates a trusting and safe space for reflection . . .
Mechanisms. . . then Rounds provide time, a safe and countercultural space, panellists trigger stories and audience reflections (resource) which facilitates audience members to remember and connect with the feeling evoked by similar experiences and reflect upon these, offload and share and make sense of their experiences. It helps staff process their emotions and reframe their experiences to be more compassionate to patients and self, reduce staff isolation (staff realise they are not the only ones feeling a certain way), improving connectedness with colleagues, teamwork and allows staff to be self-compassionate, less reactive and more holistic with patients, may increase individual preparedness for dealing with emotions in the future and increase self-awareness (response).
OutcomesChanges culture through supporting and enhancing staff well-being, which improves relationships with patients and colleagues, and improves empathy and compassion for patients.
Reflection was in our original programme theory and is the vehicle through which staff make sense of their own and others’ experiences. Resonance was not identified in the original programme theory; however, our data suggest that when the story or experience resonates, reflection is triggered, which can ‘strengthen the carer/patient relationship by providing space to reflect on the cost and impact of caring’ (p. 39). 95 Reflective practice is the process of learning through and from experience to gain new insights of self and/or practice through examining assumptions of everyday practice, being self-aware and critically evaluating their own responses to practice situations. 53,122–124 ‘Reflective practices offer us a way of trying to make sense of the uncertainty in our workplaces and the courage to work competently and ethically at the edge of order and chaos’ (p. 7),125 which resonated with our Rounds data.
Longer-term outcomes and ripple effects included improvements in patient care through recognising the importance of staff well-being and its direct connection to patient care. By sharing and learning from one’s own and others’ mistakes, care can be improved in the future, by embedding a culture of reflection and Rounds that results in recognition of nurses needing more support, leading to a reintroduction of clinical supervision:
Sometimes people do talk about their mistakes and [. . .] that by talking about these things we improve care. [. . .] ultimately one of the cases we can make for why you must continue to fund them is actually well-being for staff, if we’re going to directly impact on helping the patients [. . .] via self-well-being it would improve patient care [. . .] are we well enough to do good patient work?
Focus group-22.11.17-Participant05
Rounds were identified as an important, safe space to offload, think creatively and be challenged, and through this process staff learnt to think back on previous experiences, learn from each other and apply that learning in future encounters with patients:
In terms of my relationships with patients it’s been very helpful to have some time for reflection and I think maybe I would like to think [. . .] that I might try and react differently and try a different approach, whether it be just standing up, leaving the room and shutting the door which I think might be what I try next time and seeing what effect that has.
Juniper-11-Panellist
Many staff suggested that this was the only opportunity for them to have a safe space to reflect and think about ‘tacit knowledge’ in a safe space, which provides a resource to share knowledge and, through that process, has an impact on the practitioner and improves patient care:
I think one of the biggest impacts is [. . .] on the quality of people, patient’s experience [. . .] that space to kind of reflect in a safe space away from the coalface of what is happening, surely has an impact on how good a practitioner someone is [. . .] it gives them a little bit of space to kind of have their reflection in a way which is well structured. Whereas many of us, you know, don’t have any of those things and [. . .] it’s one of the very few learning interventions which has that kind of effect of helping people really gather up and pause and think about actually that tacit knowledge which you don’t get from anywhere else other than those conversations.
Juniper-26-Steering-Group-Member
Interviewees suggested several ways in which this happened: (1) through validating the work they do (we repeatedly heard staff suggesting that what they did ‘was just part of the job’ and ‘not extraordinary’, whereas their colleagues were often humbled and in awe of their practice, validating and supporting through their feedback); (2) through recognising that their experiences and feelings were not unique, and that by talking about their experiences, rather than internalising them, realising that their experiences are shared and are a normal part of the job, which reduces feelings of isolation; and (3) through reflection, allowing them a pause from the busy environment of care work (in a countercultural space), which enables them to be less reactive (see Report Supplementary Material 11 for supporting data).
Summary
We have identified nine CMOs, which are cumulative and interconnected. Together with Chapter 7, this provides insights into what works, for whom and in what circumstances. We have used these data to refine our initial programme theory and to develop our evidence-informed programme theory.
Chapter 9 Discussion and conclusions
Introduction
This chapter discusses our findings in relation to the aims and objectives of the study, as outlined in the protocol and in Chapter 2. We examine our findings in the context of existing evidence, consider the strengths and limitations, and draw conclusions.
Overview of findings
Below we present a narrative summary of our findings; we also summarise our findings and reported outcomes alongside our aims and objectives in Table 27.
Literature review
We reviewed the Schwartz Rounds literature to identify the key features of Rounds and created a composite definition to aid comparison with alternative interventions. Eleven alternatives were identified, each of low to moderate quality and limited evidence base. By comparison, Rounds offer a unique organisation-wide open staff forum to reflect on the emotional impact of providing patient care that no other alternatives provide. We found that the few published research evaluations of Schwartz Rounds were also of low to moderate quality (weak study designs without control groups), but the findings indicate self-reported positive impact on individuals, their relationships with colleagues and patients, and wider culture changes. We identified key mechanisms by which Rounds may have an impact (reflection, group work, disclosure and safe environment), which we tested in our realist evaluation. We identified seven guiding principles underlying Schwartz Rounds from interviews with programme architects in Boston, MA, which contributed to the initial programme theory of how Rounds work.
Mapping Rounds providers
Our mapping data (interviews, online survey and secondary analysis) found that most providers were NHS trusts (n = 86, 75%) and hospices (n = 25, 22%). Almost half of all acute trusts in England had adopted Rounds by July 2015 (44%), which is greater than Rounds adoption by mental health/learning disability trusts (26%), community trusts (18%) or hospices (13%). Of the 115 organisations running Rounds in England at 15 July 2015, over half were based in the south of England, with over one-quarter of all providers in London. We found considerable variability in the resourcing of Rounds; the median staff cost for a small organisation was £650 per month, whereas for a medium or large organisation the cost was £2000 per month. There was variability in how Rounds were implemented, and challenges to implementation and sustainability were attendance (particularly ward staff, those with less autonomy), and the workload and resources required for planning and running Rounds.
Staff survey
A two-wave survey (8 months apart) of new Rounds attenders and non-attenders was undertaken in 10 sites. Five hundred staff responded at both time points: 51 were regular attenders, 205 were irregular attenders and 233 were non-attenders (11 could not be categorised).
Our primary hypothesis (that work engagement is positively associated with attendance at Rounds) was not supported. However, the incidence of GHQ-12 ‘caseness’ (minor psychiatric disorders) dropped significantly for regular attenders compared with non-attenders, with evidence to suggest that attending more Rounds led to greater improvement.
Realist evaluation
We identified multiple, interconnected contextual layers that have an impact on and explain variation in Rounds implementation. These included the individual capabilities and characteristics of key actors (e.g. facilitators); support given by the core team and steering group; length of time running Rounds; audience characteristics (size, composition and diversity); Rounds characteristics (theme or case based); and the wider health-care and policy context for Rounds. Our data support other work that suggests that some mechanisms operate on a continuum, like a dimmer switch. 91 Favourable contextual conditions that activated the ‘trust, emotional safety and containment’ mechanism, for example, included the presence of safety checks in panel preparation; the level of facilitator skill, confidence and/or experience (knowing how to intervene when required, not reprimanding the audience and/or no repercussions); and the extent to which the audience had developed a Schwartz-Rounds savviness (knowing how to contribute in a way that supports facilitators in keeping Rounds safe).
We identified four stages of a Round with different stages having a cumulative impact on subsequent Rounds (e.g. organisational longevity of providing rounds, a ‘Schwartz-savvy audience’; audience trust and confidence, facilitator experience and confidence). We identified which components were ‘core’ in terms of fidelity (e.g. senior clinical leadership, facilitation, regularity, food available, focus on emotional impact, and only staff participants) and which were ‘adaptable’ (e.g. duration, number of panellists and Rounds format).
We also identified nine cross-cutting and interlinking themes represented as CMO configurations, namely (1) trust, emotional safety and containment; (2) group interaction; (3) a countercultural third space for staff; (4) self-disclosure; (5) storytelling; (6) role-modelling vulnerability; (7) contextualising patient, carer and staff behaviours; (8) shining a spotlight on hidden organisational stories and roles; and (9) providing an opportunity for reflection and resonance. Rounds offer an opportunity for organisations to have a community conversation and for staff to speak honestly and openly about their experiences of delivering health care. Our realist analysis suggests that the Rounds impact develops over time and has a cumulative effect resulting in ripple effects and outcomes (e.g. greater insights and increased empathy and compassion for colleagues and patients; support for staff; reduced isolation; improved teamwork and communication; and reported changes in practice). We identified some examples of ripple effects felt in day-to-day practice across the organisation (e.g. changes to protocols, changes to culture and conversations, and the set-up of support groups for specific staff), but we did not shadow staff to observe these.
Staff experiences
Our interview participants (n = 177) largely described Rounds as interesting, engaging and a source of support. Participants valued the opportunity to reflect and mentally process work challenges and learn more about colleagues and their management of challenging patient cases. This led to greater understanding, empathy and tolerance towards colleagues and patients. A few questioned the purpose of unearthing feelings of sadness, anger and frustration, and felt that the outcomes of Rounds were neutral or negative. We identified enablers of (e.g. convenient location and freedom over schedule) and barriers to attendance (e.g. conflict with other clinical priorities). Sufficient administrative support and an active steering group were key to supporting and sustaining Rounds, but these varied between sites. Key challenges were maintaining motivation and enough resources to sustain Rounds.
Overall outcomes
We have noted above, and in the preceding chapters, some of the reported outcomes identified by Rounds participants and others in this study. We have also noted that it was not possible to observe ‘outcomes’ by shadowing staff and that Rounds themselves are not outcome orientated, nor do they encourage problem-solving. However, we did identify a number of organisational ‘ripple effects’ (changes in protocols and conversations were reported, as were the setting up of new support groups), and our participants noted a number of changes to self (greater self-compassion, more reflective, more open to emotional aspects of their work and to learning from others) and to their own and others’ behaviours (changing how they work with patients, trying something new, being open to challenge from others and being prepared to challenge colleagues). It is worth noting that ‘O’ in CMO is ‘altered state of attendee’, which is the outcome of focus of the report, and we have noted throughout the report, and summarise in Table 27, these altered states and related reported outcomes, such as improved psychological well-being (attendee survey). Through our realist evaluation interviews we have noted the increased empathy; compassion for self and other staff, patients and carers; increased openness and honesty; increased resilience; improving teamwork; and changing the culture of the organisation. It is also important to note that Rounds did not ‘work’ for everyone, and that some attendees questioned the purpose of Rounds and noted no or negative outcomes for them personally.
| Study phase | Key aims and objectives | Summary findings/outcomes |
|---|---|---|
| Phase 1: literature review |
1. Identify literature providing a definition of Rounds to identify key features of Rounds and create a composite definition 2. Identify and critically appraise all empirical evaluations of Rounds 3. Identify alternative interventions, describe their key features and scope their evidence base 4. Compare each intervention in relation to the core features of Rounds 5. Identify how Rounds might work by (a) exploring the theoretical literature on reflection, group work, disclosure and safe environment; and (b) speaking to the original architects of Rounds to determine the underlying ‘programme theory’ |
|
| Phase 1: mapping study |
6. Map the profiles of current UK Rounds provider organisations to inform sampling of case study sites for maximum variation: |
|
| Phase 2a: staff survey |
7. Evaluate whether or not regular Rounds attendance has an impact on health-care staff engagement and well-being, social support for staff and behavioural change towards patients and colleagues, compared with non-attenders 8. Investigate whether or not frequency of Rounds attendance was associated with greater improvements in health-care staff work engagement, well-being, social support for staff and behavioural change towards patients and colleagues 9. Determine factors associated with Rounds being perceived as useful, or barriers to attending Rounds |
|
| Phase 2b: organisational case studies |
10. Examine staff experiences of attending, presenting at, facilitating and leading Rounds and reported outcomes 11. Examine how Rounds are operationalised and the mechanisms by which well-being and social support might be influenced (or not), including: 12. Understand how Rounds ‘work’ in the UK, for whom and in what contexts; to suggest ways to improve their effectiveness; to inform decisions about their implementation in other contexts; and to understand what is causing variations in implementation or outcomes |
|
| Overall analysis and cross-case analysis |
13. Establish contexts and mechanisms whereby Rounds influence staff well-being at work and social support 14. Identify and evaluate any changes (outcomes) that take place in relationships between staff who attend Rounds and their patients and colleagues 15. Identify and consider any wider changes that may be felt in teams or across the wider organisation regarding quality of patient care and staff experience and, if so, how these may be linked 16. Make recommendations regarding the role of Rounds in health-care provider staff support |
|
Mixed-methods integration of findings
We have described in Chapter 2 the extent to which we have used mixed methods and integrated findings to incrementally build our understanding of how Rounds work. In relation to the qualitative and quantitative approaches in phase 2, there were some key similarities and differences in findings that warrant attention. Both data sets provided evidence that attendance/contributing to Rounds is associated with improved well-being. The qualitative data reported increases in empathy, compassion, peer support, reflection, work engagement and communication with patients (in addition to other outcomes not measured in the survey). However, although the survey reported small increases in all of these measures for regular attenders, none was statistically significant. We have explored the potential reasons for these differences (Table 28). Overall, we suggest that the complementary and contradictory findings of the qualitative and quantitative methods have provided richer insights and a more comprehensive evaluation of Rounds.
| Approaches to explore data disparities (Moffat et al.126) | Application to our evaluation [quantitative = survey; qualitative = case study (interviews/observations)] |
|---|---|
| Treating methods as fundamentally different | Quantitative and qualitative components had different (although related) research questions, and approaches to data collection/analyses are based on fundamentally different theoretical paradigms. While this may partially explain the disparities, the selection of survey measures was realist-informed (by our initial programme theory) |
| Exploring the methodological rigour of each component |
Both quantitative and qualitative were conducted rigorously Quantitative: power calculation was based on whole sample of attenders vs. non-attenders across all 10 sites (thereby not sufficient for individual case analysis) Qualitative: our interview sample was diverse, large and included non-attenders. We actively sought disconfirming cases |
| Exploring data set comparability |
Quantitative: most sites (and all participants) were new attenders at baseline and remained relatively ‘new’ even if classified as regular attenders Qualitative: most sites were established Rounds sites (and participants were mostly experienced Rounds attenders and/or panellists) We cannot know the GHQ-12 status of our qualitative sample |
| Collection of additional data and making further comparisons | The research timetable (survey completed October 2016) did not allow for analysis to inform further data collection in the qualitative component |
| Exploring whether or not the intervention under study worked as expected |
Quantitative: each ‘dose’ of a Round is treated as identical. Few regular attenders came from established Rounds sites Qualitative: Rounds type and intensity varied within and between case study sites (impacts on mechanisms and outcomes). In addition, fidelity across sites was variable |
| Exploring whether or not the outcomes of the quantitative and qualitative components match |
Quantitative: most of the survey measures were not validated for this population; survey measures were selected at the study start, before the complexity of Rounds was fully appreciated. All measures did move in expected direction, although not statistically significant Qualitative: some findings were not captured in survey (e.g. vulnerability, contextualisation of patients and staff); the complexity of participants’ accounts (e.g. emotion in reflection) were not encapsulated in the measures |
Strengths and limitations of the study
This was a very challenging intervention to evaluate and we note the complexity of the study, in particular (as outlined above) the challenges of synthesising the methods and the diverse findings. One of the main strengths of our study is the use of mixed methods and their integration to support a more comprehensive interpretation of our findings. Our study focused only on staff experiences. We initially considered including the impact of Rounds on patient experience, given that Rounds are predicted to have an impact on patient care. However, the difficulties of attribution of effects of Rounds on patients, given the complexity of health-care provision (confounders), meant that this was not possible. Furthermore, substantial evidence now links staff well-being with patient experiences of care,68,76,77 justifying the focus on staff well-being. Other strengths and limitations are detailed below.
Literature review
The strengths of this review are the inclusion of all literature regarding Schwartz Rounds (including non-empirical literature), enabling our composite definition and features for comparison with other interventions to be based on a hybrid UK/USA literature base. The comparison of Rounds with alternative interventions provides a framework for managers/providers to examine and compare the different staff support/well-being interventions they may offer or be considering implementing. However, the breadth of the review of alternative interventions was considerable. As we developed our understanding of which mechanisms have an impact on Rounds, through our realist analysis, we realised that we could have restricted the number of alternatives to Schwartz Rounds to those that shared the most similarities. Conducting a realist synthesis of Schwartz Rounds and their alternatives, rather than a scoping review would have been a beneficial precursor to the realist evaluation to further help us develop our candidate programme theories. It is also possible that our review did not capture some of the literature, although our use of multiple search strategies aimed to minimise this.
Despite a major review of the well-being of the UK NHS workforce in 2009,32 we continue to lack evidence regarding the most effective intervention strategies owing to the poor quality of the evidence base as highlighted by previous reviews127–130 and confirmed in our scoping review.
Maintaining staff well-being requires strategies and interventions aimed at individuals and organisations. Organisational-level interventions for staff well-being are scarce, with attention primarily focused on prevention or treatment at an individual level (e.g. stress management or counselling interventions). 129 Evidence shows that interventions aimed at behaviour change – a critical feature of many staff support interventions – are more likely to be effective if tackled from multiple levels (individual, organisational and wider society). 131,132 We have shown that Rounds are unique in providing an intervention that straddles the individual and organisational levels.
Mapping survey and telephone interviews
To our knowledge, this is the first attempt to describe variation in implementation of Rounds and has highlighted differences in how Rounds are run and resourced, but also consistency across providers in relation to key challenges despite these contextual differences. The variability in implementation is unsurprising given the evidence of the ‘implementation gap’ and variation in adherence to guidance across health care generally, highlighting the complex interplay of factors affecting ‘supply’ and ‘demand’ – and thereby the importance of contextual factors. 133
The use of a range of data sources enabled an up-to-date report of the implementation of Rounds in England, although our detailed profiles (based on survey and interview data) were necessarily based on the subsample of providers running Rounds when we commenced our evaluation. The main limitations here concerned difficulties obtaining R&D approvals. This was an onerous task and we faced considerable delays in getting permission, which limited our sample size. Furthermore, some mapping survey data were poorly completed, inaccurate or difficult to interpret, especially the cost/resource data. We addressed this by requesting clarification from a subsample – purposively selected to represent different size/types of organisations – to help complete, correct and interpret data.
Staff survey
This study is the first to use a longitudinal design with a control group to evaluate Rounds. The sample of 500 participants providing data at both time points enabled an examination of relationships with engagement, psychological well-being and intervening mechanisms, using a clinically well-validated measure of psychological wellbeing (GHQ-12). In contrast to previous studies, we were able to demonstrate a clear association between Rounds attendance and subsequent psychological well-being.
One key limitation was that we had a smaller than desired sample of regular attenders (and for some outcomes, data excluded staff without regular patient contact, resulting in smaller samples still). The resultant lower power may explain, at least partially, why more significant differences between attenders and non-attenders were not detected. In addition, some of the measures may not have been sufficiently sensitive to change, or robust enough to capture any differences that may have occurred. For example, any changes that may have occurred outside the direct influence of the attender (e.g. peer support) may see very little change. The self-report nature of the questionnaires, combined with self-selection into the attender group, may have led to positive evaluations and ‘ceiling effects’ in the baseline survey, giving less opportunity to improve at follow-up. In addition, there were clear baseline differences between the groups of regular attenders and non-attenders, with regular attenders typically being more senior and more likely to come from medical professions. Although we control for this as far as possible in the analysis, it is impossible to remove the confounding completely. Furthermore, this analysis necessarily treated all Rounds as equal, whereas no two Rounds are the same (see Table 28).
Realist evaluation
The strengths of our work include the variation in case study sites (purposively sampled to reflect issues that affected context), the number of Rounds we observed, the number of interviews and their depth and breadth. Finding staff to interview who stopped attending Rounds was challenging, and despite using a number of methods to source participants who were negative about Rounds, we found only a few. Our data suggested practical reasons people stopped attending or found it hard to attend. In terms of limitations, our case study observations did not include an observation of mentor–facilitator/clinical lead debriefing and support meetings, providing an opportunity for facilitators/clinical leads to reflect on where Rounds sit within the wider organisational context, which could have provided further data on contextual variations between sites.
It was not possible to observe ripple effects of Rounds (actual changes that occurred as the result of attending Rounds) because interviewees found it very hard to identify concrete examples of changes in practice that could be observed.
Recommendations for future research
This study has identified the need for research in the following areas.
-
Evaluation of Rounds implementation: (1) in new settings (e.g. primary care, prisons, medical schools), (2) to extend reach (e.g. ward-based staff) and (3) adaptations (e.g. filmed stories).
-
Storytelling: telling stories as a way of sharing personal experiences is increasingly being used in the field of mental health, well-being and recovery. The potential benefits for health-care staff in gathering and sharing stories in other formats, settings and audiences should be explored and evaluated.
-
Development of outcome measures that are fit for purpose (e.g. compassion, quality of communication with patients, staff empathy as experienced by patients and staff).
-
Evaluating the impact of Rounds on organisational culture, although, given the challenges we experienced observing ripple effects, this is difficult.
-
Rounds legacy, spread and sustainability over time, and where and how adopted and adapted, for example in settings outside acute care – nursing homes, ambulance staff and primary care – and also possibly outside health care – police, teaching, armed forces.
-
Methodologically: our experience highlights the importance of using mixed-methods designs for evaluating such complex interventions, which, together with the use of realist evaluation, provides much greater insights – moving the analysis beyond description – and allowing the team to draw on a wide range of theories to support understanding of the mechanisms at play.
Implications for policy and practice (objective 16)
Our study suggests that there are some core components [senior clinician leadership; two facilitators with group work skills; that Rounds are not one-off events but a series; that they are not combined with other interventions (integrity); that food is available; that a Round is a group intervention with group participation; that Rounds are staff-only events (not patients); that stories are told to trigger audience discussion; that trust safety and containment is maintained; that staff stories are pre-prepared; and that Rounds focus on the emotional impact of work on staff, rather than on problem-solving or clinical detail]. These components and others are expanded on to provide more detailed recommendations for policy and practice in our accompanying organisation guide86 to implementing and sustaining Rounds.
Higher-level implications for policy and practice that arise from this study are as follows.
-
Our data suggest that Rounds support staff and improve staff psychological well-being, enabling them to provide better patient care. Rounds may help organisations meet the National Institute for Health and Care Excellence (NICE) guidance129,134 and the Commissioning for Quality and Innovation (CQUIN)135 framework for ensuring well-being of staff. They may also support organisations to improve quality of care and change organisational culture. Rounds were not suitable for or accessible by everyone, and should be offered in addition to other forms of psychological support for staff, such as clinical supervision, and not instead of these interventions. Organisations yet to implement Rounds may want to consider this evidence when making their decisions.
-
Organisations may want to consider implementing Rounds alongside other interventions as part of their quality improvement and staff support strategies because our evidence has highlighted the unique resources offered by Rounds – in particular that they are open to all in the organisation.
-
Our findings suggest that the countercultural space that Rounds provide is an important aspect of organisational culture change, and may help organisations meet recommendations arising from the Francis inquiry. 3
-
Our findings suggest that it is important to ensure board clarity about the ‘slow’ nature of the intervention, the difference of the space and the ways in which the Round is likely to have an impact on staff experience and organisational culture over time. Furthermore, the felt need to demonstrate outcomes by facilitators (and some board members) in our study – in line with the prevailing health-care culture – is in stark contrast to this counterculture space, and should be treated with caution.
-
Although Rounds are intended to be open to all, in practice we found that this was not the case. Senior management support is needed to put in place initiatives that enable all staff groups to attend.
-
The evidence in this report suggests that there are challenges to the sustainability of Rounds, and organisations may want to consider how Rounds are resourced given the time and workload required. Organisational support, particularly in the form of administrative support, is needed to sustain Rounds.
-
Our findings revealed that running Rounds places considerable strain and burden on facilitators, and suggests that the long-term sustainability of Rounds depends on shared ownership of Rounds. Organisations (rather than the facilitators) might consider taking responsibility for ensuring sustainable success.
-
In terms of sustainability, our findings suggest that steering group members attend Rounds regularly and refresh/renew their membership on a rolling basis, for example 6 to 12 months. This is anticipated to reduce the burden on individual members and better support facilitators and clinical leads by finding stories and panellists, reviewing what worked and what could be improved and, when necessary, help support facilitators to maintain and improve psychological safety in Rounds.
Full details of our implications and recommendations for policy and practice can be found in our Organisational Guide to Implementation. 86
How has this study contributed to strengthening the evidence base on Schwartz Rounds?
Previous evaluations of Rounds have been limited quantitatively by their use of non-validated outcome measures, and lack of control group comparisons (see Chapter 3). Our evaluation addressed these limitations by using the most robust validated measures of outcomes available, and by including a non-attender control group in the survey. Furthermore, previous evaluations had focused solely on the impact of Rounds on attenders, whereas the realist-informed evaluation we undertook examined how, why and for whom Rounds had an impact. This required determining an initial programme theory about how we felt Rounds worked, based on evidence and theory, which we then used to explicitly underpin our mixed-methods evaluation. The causal explanations and evidence-informed programme theory provide a rich, in-depth explanation about how Rounds work, for whom and why, providing an important framework for future evaluations of Rounds, and their implementation.
Conclusions
This is the first longitudinal realist-informed mixed-methods, large scale evaluation of Schwartz Center Rounds® in the UK. Rounds have been shown to offer unique support compared with other interventions, and attending Rounds is associated with improved staff psychological well-being. Providing high-quality health care has an emotional impact on staff. They experience high levels of psychological distress, face increasing levels of scrutiny, regulation and demand, and have increasingly limited resources. Within this context, Rounds offer a safe, reflective space for staff to share stories with their peers about their work and its impact on them. Staff report increased empathy and compassion for patients and colleagues and report positive changes in practice as a result of attending Rounds. Some staff reported that attendance was an issue for some groups (especially ward-based staff) and that organisational support is needed to sustain the initiative. It is feasible for Rounds to be implemented across a range of health-care organisations, and, although costs varied, these should be considered acceptable for achieving such outcomes for staff and patients.
Acknowledgements
Our thanks go to all of the staff who participated in this research through completing a survey and/or being interviewed or observed as part of our fieldwork. Without them, this study would not have been possible. We are also grateful to our colleagues at the PoCF – Joanna Goodrich, Bex Wickens, Esther Flanagan, Jocelyn Cornwell and Aggie Rice – for their help and support throughout the study. Grateful thanks to Jo Maybin, Alex Baylis and David Maguire at The King’s Fund. We would also like to thank the staff at the SCCH in Boston, MA, for their support and encouragement, particularly Marjorie Stanzler and Beth Lown. Thank you also to Stephanie Waller, Project Administrator, for her excellent administrative support throughout the study; Jane Hughes, Research Fellow, who supported the mapping qualitative interview data analysis; Emma Scott, Research Fellow, who supported literature reviewing of Rounds mechanisms; Andreas Xyrichis, Lecturer, who supported the scoping review of alternatives to Schwartz Rounds; Michelle Hope, master’s student, who supported the development of the composite definition; and Julia Philippou, lecturer, who supported mapping survey data analysis and secondary analysis. Many thanks also to Justin Jagosh, Centre for Realist Evaluation, who was a source of support, inspiration and wisdom on our realist evaluation journey. Finally, we are grateful to the following members of the Advisory Group and Steering Group for their advice on the study design and support along the way.
Advisory Group
Joanna Goodrich, Head of Evidence, PoCF.
Barbara Wren, Consultant Psychologist and Schwartz Round Lead, Royal Free London NHS Foundation Trust.
Jenny Firth Cozens, Consultant Psychologist.
Michael West, Head of Thought Leadership, The King’s Fund.
John Pepper, Professor of Cardiothoracic Surgery, Royal Brompton and Harefield NHS Foundation Trust.
Glenn Robert, Professor of Health Care Quality and Innovation, King’s College London.
Steering Group
Dean Fathers, Chairperson, United Lincoln Hospitals NHS Trust.
Sharon Fleming, Head of Nursing Research, Royal Brompton and Harefield NHS Foundation Trust.
Nicola Mackintosh, Research Fellow, King’s College London.
Rachel Massey-Chase, Clinical Psychologist, King’s College Hospital.
Katherine Hopkins, Nurse Consultant, Royal Free London NHS Foundation Trust.
Jude Bayly, Midwife, Royal Free London NHS Foundation Trust.
Havi Carel, patient representative.
Christine Chapman, patient representative.
Elisabeth Buggins, Chairperson, Birmingham Women’s and Children’s NHS Foundation Trust.
Jennifer Gardner, Programme Lead, Health and Well-being, NHS Employers.
Ruth Harris, Professor of Nursing Practice and Innovation, King’s College London.
The late Lisl Klein (died 11 December 2015), Director, the Bayswater Institute (September 2014–December 2015).
Patient and public involvement in research
The study owes great thanks to patients and the public who commented on our research design and who supported us as part of the advisory group, notably Christine Chapman and Havi Carel; their insights and understanding helped improve our understanding of Rounds and our interpretation of some of our data.
Contributions of authors
Jill Maben (Professor of Nursing Research; Social and Health Sciences) was the PI. She led the overall study design; led and managed the study team, including the research fellow and research associate; and undertook data collection, analysis and the final writing of the report.
Cath Taylor (Senior Lecturer; Psychology) contributed to the overall study design; led the literature review design, analysis and write-up; contributed to the mapping design; led the analysis and write-up of mapping and costs data; contributed to the case study analysis; and was involved in the overall writing of the report.
Jeremy Dawson (Professor of Health Management; Statistics and Work Psychology) contributed to the overall study design; led the survey study design, analysis and write-up; and was involved in the overall writing of the report.
Mary Leamy (Research Fellow, Psychology) led and conducted the data collection analysis and the write-up of case study qualitative data; undertook the collection of mapping data; undertook literature reviewing; and was involved in the overall writing of the report.
Imelda McCarthy (Research Associate, Psychology) led and conducted the collection and analysis of survey data; led the analysis and write-up of key players’ experiences interview data; and was involved in the overall writing of the report.
Ellie Reynolds (Research Associate, Anthropology and Nursing) led and conducted the collection and analysis of case study qualitative data; undertook the collection of mapping data; undertook literature reviewing; and was involved in the overall writing of the report.
Shilpa Ross (Senior Researcher, Health and Social Care Policy) led and conducted the collection of mapping survey and interview data, and contributed to analysis and to the writing of the report.
Caroline Shuldham (Independent Consultant and Visiting Professor, Buckinghamshire New University, formerly Director of Nursing and Clinical Governance Royal Brompton and Harefield NHS Foundation Trust: Health Sciences) contributed to the overall study design, contributed to the survey data collection and analysis and the costs data analysis, and was involved in the overall writing of the report.
Laura Bennett (Researcher, Health and Social Care Policy) contributed to the collection and analysis of mapping survey and interview data, and contributed to the writing of the report.
Catherine Foot (Director, Centre for Ageing Better, formerly Assistant Director of Policy, The King’s Fund: Health Policy) led the collection of mapping survey and interview data, contributed to analysis and contributed to the writing of the report.
Publications
Journal publications
Taylor C, Xyrichis A, Leamy MC, Reynolds E, Maben J. Can Schwartz Center Rounds support healthcare staff with emotional challenges at work, and how do they compare with other interventions aimed at providing similar support? A systematic review and scoping reviews. BMJ Open 2018;8:e024254.
Robert G, Philippou J, Leamy M, Reynolds E, Ross S, Bennett L, et al. Exploring the adoption of Schwartz Center Rounds as an organisational innovation in England to improve staff wellbeing in England 2009–2015. BMJ Open 2017;7:e014326.
Oral conference presentations
Leamy M, Maben J, Taylor C, Reynolds E. Supporting NHS Staff at Work: What are Schwartz Rounds and How do They Work? Early Findings from a National Research Study, The Caring Organisation: Enabling Compassion to Flourish. Point of Care Conference, Royal Society of Medicine, London, 16 December 2015.
Robert G, Philippou J, Ross S, Bennett L, Taylor C, Reynolds E, et al. Supporting the Wellbeing of Staff and Improving Compassionate Care: Exploring the Adoption of Schwartz Centre Rounds in the United Kingdom, 2009–2015. National Institute for Health Research Health Services and Delivery Research Conference, Nottingham, 13–14 July 2016.
Maben J. The Links Between Staff and Patient Experience of Hospital Care: A UK Perspective. Invited presentation. Presentation to Faculty of Health Sciences, Murdoch University, Perth, WA, 25 August 2016.
Maben J. Schwartz Rounds. Presentation to Sir Charles Gairdner Hospital. Invited presentation. Perth, WA, 31 August 2016.
Leamy M, Reynolds E, Taylor C, Maben J. Ongoing Learning and Reflections from Undertaking a Realist Evaluation of Schwartz Rounds: A Health-Care Intervention to Promote Compassionate Care. Invited presentation. Second International conference on Realist Evaluation and Synthesis: Advancing Principles, Strengthening Practice, London, 2–6 October 2016.
Leamy M, Maben J. Schwartz Rounds: Origins, Early Development and Implementation in the USA and UK. Point of Care Foundation Conference, Senate House, London, 27 October 2016.
Maben J, Leamy M. Schwartz Rounds: Realist Evaluation Draft Findings from National Research Study. Point of Care Foundation Conference, Science Museum, Manchester, 24 November 2016.
Taylor C, Maben J. Schwartz Center Rounds to Enhance Compassionate Care: Results from a UK Mapping Survey. European Oncology Nursing Society conference, European Cancer Congress, Amsterdam, 27–30 January 2017.
McCarthy I, Dawson J, Maben J, Taylor C, Leamy M, Reynolds E, Shulham C. Schwartz Center Rounds®: An Intervention to Support Employee Well-being. British Psychological Society Division of Occupational Psychology Annual Conference, Stratford-upon-Avon, 10–12 January 2018.
Maben J, Taylor C. (On behalf of the project team.) UK National Evaluation of Schwartz Rounds: Launch of Film and Organisational Guide. Invited presentation. Point of Care Schwartz Conference, London, 23 January 2018.
Maben J, Taylor C. (On behalf of the project team.) UK National Evaluation of Schwartz Rounds: Launch of Film and Organisational Guide. Invited presentation. Point of Care Schwartz Conference, Manchester, 6 February 2018.
Maben J (Keynote.) Enhancing Compassion in Relationships Between Staff and Patients: A National Evaluation of Schwartz Rounds in the UK 2014–2017. National Schwartz Rounds Conference, Dublin, 28 February 2018.
Maben J. (Keynote) Enabling and Supporting Staff to Care Well. Humanising HealthCare conference, Point of Care Foundation, London, 28 March 2018.
Maben J, Dawson J, Leamy M, Taylor C, Reynolds E, Shuldham C, et al. Schwartz Center Rounds®: A UK Evaluation of a Complex Intervention to Support Health-care Staff Deliver Compassionate Care. Royal College of Nursing International Research Society conference, Birmingham, 16–18 April 2018.
Maben J, Leamy M, Taylor C, Reynolds E, Shuldham C, McCarthy I. Learning and Reflections From a Realist Evaluation of Schwartz Rounds® – An Intervention to Promote Compassionate Care. Royal College of Nursing International Research Society conference, Birmingham, 16–18 April 2018.
Maben J, Dawson J, Leamy M, Taylor C, Reynolds E, Shuldham C. A Realist Evaluation of Schwartz Center Rounds®: An Intervention To Support Compassionate Care in Health-care Staff. WELL-Med 3 Conference, Thessaloniki, 9–13 May 2018.
Taylor C, Ross S, Phillipou J, Robert G, Leamy M, Reynolds E, et al. The UK Implementation of Schwartz Rounds: An Intervention to Improve Care Through Enhancing Staff Well-being. WELL-Med 3 Conference, Thessaloniki, 9–13 May 2018.
McCarthy I, Dawson J, Maben J, Taylor C, Shuldham C, Leamy M, Reynolds E. The Impact of a Social and Emotional Workplace Intervention on Employee Psychological Well-being. Institute of Work Psychology Conference, University of Sheffield, Sheffield, 19–21 June 2018.
Maben J, Dawson J, Leamy M, Taylor C, Reynolds E, Shuldham C, et al. (Keynote.) Schwartz Rounds as Response to Moral Distress. What is Moral Distress in Nursing? How, Can and Should we respond to it? Public engagement event, Wellcome Trust, 21 June 2018.
Taylor C, Maben J, Dawson J, Shuldham C, Foot C, et al. The Emotional Impact of Care. ‘Time to Talk’ conference, Hampshire Hospitals NHS Foundation Trust, 25 June 2018.
Poster conference presentation
Leamy M, Reynolds E, Taylor C, Maben J. Ongoing Learning and Reflections from Undertaking a Realist Evaluation of Schwartz Rounds: A Healthcare Intervention to Promote Compassionate Care. Poster presentation. 2nd International Conference on Realist Evaluation and Synthesis: Advancing Principles, Strengthening Practice, London, October 2016.
Blogs
Maben J. How Can we Support Healthcare Staff to Care Well? A National Evaluation of Schwartz Center Rounds®. National Institute for Health Research; 23 January 2018. URL: www.nihr.ac.uk/blogs/how-can-we-support-healthcare-staff-to-care-well-a-national-evaluation-of-schwartz-center-rounds/7765
Maben J. Enabling and Supporting Staff to Care Well. The Point of Care Foundation; 30 April 2018. URL: www.pointofcarefoundation.org.uk/blog/enabling-and-supporting-staff-to-care-well/
Organisational guide
Maben J, Leamy M, Taylor C, Reynolds E, Shuldham C, Dawson J. Understanding, Implementing and Sustaining Schwartz Rounds: An Organisational Guide to Implementation. London: King’s College London; 2018. URL: www.surrey.ac.uk/content/schwartz-organisational-guide-questionnaire
Media output: 9-minute research film
Maben J, Taylor C, Leamy M, Shuldham C. (On behalf of the project team.) Understanding Schwartz Rounds: Findings from a National Evaluation. © 2018 King’s College London. URL: https://youtu.be/C34ygCIdjCo
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. Exclusive use will be retained until the publication of major outputs.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Robert G, Philippou J, Leamy M, Reynolds E, Ross S, Bennett L, et al. Exploring the adoption of Schwartz Center Rounds as an organisational innovation in England, 2009–2015. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014326.
- Schwartz K. A Patient’s Story. Boston Globe Magazine 1995.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Westhorp G, Prins E, Kusters C, Hultink M, Guijt I, Brouwers J. Realist Evaluation: An Overview Report from an Expert Seminar with Dr Gill Westhorp. Wageningen: Wageningen UR Centre for Development Innovation; 2011.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0643-1.
- Taylor C, Xyrichis A, Leamy MC, Reynolds E, Maben J. Can Schwartz Center Rounds support healthcare staff with emotional challenges at work, and how do they compare with other interventions aimed at providing similar support? A systematic review and scoping reviews. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-024254.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60. https://doi.org/10.1177/1356389016638615.
- Patton MQ. Qualitative Evaluation and Research Methods. Newbury Park, CA: Sage; 1990.
- Mason J. Qualitative Researching. London: Sage; 2002.
- Klein L. Some implications of rationalised production. Occupational Psychology 1962;36.
- Klein L. Multiproducts Ltd. A Case Study in the Social Effects of Rationalised Production. London: HMSO; 1964.
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 2005;331:1064-5. https://doi.org/10.1136/bmj.38636.593461.68.
- O’Cathain A, Murphy E, Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy 2008;13:92-8. https://doi.org/10.1258/jhsrp.2007.007074.
- Sayer A. Method in Social Science: A Realist Approach. London: Routledge; 1992.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Jones CE, Maben J, Jack RH, Davies EA, Forbes LJ, Lucas G, et al. A systematic review of barriers to early presentation and diagnosis with breast cancer among black women. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-004076.
- Gishen F, Whitman S, Gill D, Barker R, Walker S. Schwartz Centre Rounds: a new initiative in the undergraduate curriculum–what do medical students think?. BMC Med Educ 2016;16. https://doi.org/10.1186/s12909-016-0762-6.
- George M. Stress in NHS staff triggers defensive inward-focussing and an associated loss of connection with colleagues: this is reversed by Schwartz Rounds. J Compassionate Health Care 2016;3. https://doi.org/10.1186/s40639-016-0025-8.
- Berry M, Chaggar R. Introducing Schwartz centre rounds® to Watford General Hospital–challenging the status quo. Abstracts of the Association of Anaesthetists of Great Britain and Ireland Annual Congress 17–19 September 2014, Harrogate, UK. Anaesthesia 2014;69. https://doi.org/10.1111/anae.12866.
- Gishen F, Wood M. Using Schwartz Centre Rounds to change hospice culture: does it work?. BMJ Support Palliat Care 2015;5. https://doi.org/10.1136/bmjspcare-2014-000838.17.
- Whitehead P. The impact of Schwartz Center Rounds on moral distress in a large healthcare system. J Pain Symptom Manage 2015;49. https://doi.org/10.1016/j.jpainsymman.2014.11.281.
- Reed E, Cullen A, Gannon C, Knight A, Todd J. Use of Schwartz Centre Rounds in a UK hospice: Findings from a longitudinal evaluation. J Interprof Care 2015;29:365-6. https://doi.org/10.3109/13561820.2014.983594.
- Deppoliti DI, Côté-Arsenault D, Myers G, Barry J, Randolph C, Tanner B. Evaluating Schwartz Center Rounds® in an urban hospital center. J Health Organ Manag 2015;29:973-87. https://doi.org/10.1108/JHOM-09-2013-0189.
- Corless IB, Michel TH, Nicholas M, Jameson D, Purtilo R, Dirkes AM. Educating health professions students about the issues involved in communicating effectively: a novel approach. J Nurs Educ 2009;48:367-73. https://doi.org/10.3928/01484834-20090615-03.
- Shield RR, Tong I, Tomas M, Besdine RW. Teaching communication and compassionate care skills: an innovative curriculum for pre-clerkship medical students. Med Teach 2011;33:e408-16. https://doi.org/10.3109/0142159X.2011.586748.
- Lown BA, Manning CF. The Schwartz Center Rounds: evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med 2010;85:1073-81. https://doi.org/10.1097/ACM.0b013e3181dbf741.
- Manning CF, Acker M, Houseman L, Pressman E, Goodman IF. Schwartz Center Rounds®: Evaluation Report Executive Summary. Boston, MA: Goodman Research Group, Inc; 2008.
- Goodrich J. Supporting hospital staff to provide compassionate care: do Schwartz Center Rounds work in English hospitals?. J R Soc Med 2012;105:117-22. https://doi.org/10.1258/jrsm.2011.110183.
- Goodrich J. Schwartz Center Rounds®: Evaluation of the UK Pilots. London: The King’s Fund; 2011.
- Ruotsalainen J, Serra C, Marine A, Verbeek J. Systematic review of interventions for reducing occupational stress in health care workers. Scand J Work Environ Health 2008;34:169-78. https://doi.org/10.5271/sjweh.1240.
- Boorman S. NHS Health and Wellbeing Review. London: Department of Health and Social Care; 2009.
- Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev 2015;4. https://doi.org/10.1002/14651858.CD002892.pub5.
- Harvey SB, Laird B, Henderson M, Hotopf M. The Mental Health of Health Care Professionals: A Review for the Department of Health. London: King’s College London; 2009.
- Pennebaker JW. Opening Up: The Healing Power of Expressing Emotions. New York, NY: Guilford Press; 1997.
- Schon D. The Reflective Practitioner. London: Temple Smith; 1983.
- Yalom ID, Leszcz M. The Theory and Practice of Group Psychotherapy. New York, NY: Basic Books; 2005.
- Brown A. Groupwork. London: Heinemann; 1992.
- Rimé B. Emotion elicits the social sharing of emotion: theory and empirical review. Emotion Review 2009;1:60-85. https://doi.org/10.1177/1754073908097189.
- Rimé B, Philippot P, Boca S, Mesquita B, Stroebe W, Hewstone M. European Review of Social Psychology. Chichester: John Wiley & Sons Ltd; 1992.
- Rimé B, Finkenauer C, Luminet O, Zech E, Philippot P. European Review of Social Psychology. Chichester: John Wiley & Sons Ltd; 1998.
- Pennebaker JW, Beall SK. Confronting a traumatic event: toward an understanding of inhibition and disease. J Abnorm Psychol 1986;95:274-81. https://doi.org/10.1037/0021-843X.95.3.274.
- Pennebaker JW. Emotion, Disclosure and Health. Washington, DC: American Psychological Association; 1995.
- Pennebaker JW, Zech E, Rime B, Stroebe MS, Stroebe W, Hansson RO, et al. Handbook of Bereavement Research: Consequences, Coping, and Care. Washington, DC: American Psychological Association; 2001.
- Chaudoir SR, Fisher JD. The disclosure processes model: understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity. Psychol Bull 2010;136:236-56. https://doi.org/10.1037/a0018193.
- Lepore SJ, Ragan JD, Jones S. Talking facilitates cognitive–emotional processes of adaptation to an acute stressor. J Pers Soc Psychol 2000;78:499-508. https://doi.org/10.1037/0022-3514.78.3.499.
- MacDonald J, Morley I. Shame and non-disclosure: a study of the emotional isolation of people referred for psychotherapy. Br J Med Psychol 2001;74:1-21. https://doi.org/10.1348/000711201160731.
- Nils F, Rimé B. Beyond the myth of venting: social sharing modes determine the benefits of emotional disclosure. Eur J Soc Psychol 2012;42:672-81. https://doi.org/10.1002/ejsp.1880.
- Schwartz T. The magic of feeling safe at work. The New York Times 2014. https://dealbook.nytimes.com/2014/08/01/the-magic-of-feeling-safe/ (accessed 1 August 2018).
- McMillan DW. Sense of community. J Comm Psychol 1996;24:315-25. https://doi.org/10.1002/(SICI)1520-6629(199610)24:4<315::AID-JCOP2>3.0.CO;2-T.
- Ringer M. Two vital aspects in the facilitation of groups: connections and containment. Aus J Outdoor Education 1999;4.
- Edmondson A. Psychological safety and learning behavior in work teams. Adm Sci Q 1999;44:350-83. https://doi.org/10.2307/2666999.
- Boud D, Keogh R, Walker D. Reflection: Turning Experience into Learning. London: Kogan Page; 1985.
- Dewey J. Logic: The Theory of Inquiry. New York, NY: Rinehart & Winston; 1938.
- Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Englewood Cliffs, NJ: Prentice Hall; 1984.
- Lazarus RS, Scherer K, Schorr A, Johnstone T. Appraisal Processes in Emotion: Theory, Methods, Research. New York, NY: Oxford University Press; 2001.
- Learning as Transformation – Critical Perspectives on a Theory in Progress. San Francisco, CA: Jossey-Bass; 2000.
- Goleman D. Emotional Intelligence. London: Bloomsbury; 1996.
- Rogers C. On Becoming a Person: A Therapist’s View of Psychotherapy. London: Constable; 1961.
- McLeod SA. Carl Rogers 2014. www.simplypsychology.org/carl-rogers.html (accessed 17 February 2017).
- Lawrence-Wilkes L, Chapman A. Reflective Practice Theory, History, Definitions, Methods, Process Models, and Self-Assessment Tools, for Self-Improvement, Training, and Organizational Development 2015. www.businessballs.com/reflective-practice.htm (accessed 27 February 2017).
- Ixer G. Developing the relationship between reflective practice and social work values. J Practice Teaching 2003;5:7-22. https://doi.org/10.1921/17466105.5.1.7.
- Manthorpe J, Baginsky M. Reflective Practice. London: King’s College London, Social Care Workforce Research Unit; 2015.
- Lawrence-Wilkes L, Ashmore L. The Reflective Practitioner in Professional Education. Basingstoke: Palgrave Macmillan; 2014.
- Karasek RA. Job demands, job decision latitude, and mental strain: implications for job design. Adm Sci Q 1979;24:285-308. https://doi.org/10.2307/2392498.
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull 1985;98:310-57. https://doi.org/10.1037/0033-2909.98.2.310.
- Stansfield S, Head J, Marmot M. Work Related Factors and Ill Health. The Whitehall II Study 2000.
- Maben J, Peccei R, Adams M, Robert G, Richardson A, Murrells T, et al. Patients’ Experiences of Care and the Influence of Staff Motivation, Affect and Well-being. Final report. Southampton: NIHR Service Delivery and Organisation programme; 2012.
- Homans GC. Social behavior as exchange. Am J Sociol 1958;63:597-606. https://doi.org/10.1086/222355.
- Damschroder L, Aron D, Keith R, Kirsh S, Jeff A, Alexander J, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Rogers E. Diffusion of Innovations First. New York, NY: Free Press of Glencoe; 1995.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: Personal Social Services Research Unit, University of Kent; 2016.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Taylor C, Graham J, Potts H, Candy J, Richards M, Ramirez A. Impact of hospital consultants’ poor mental health on patient care. Br J Psychiatry 2007;190:268-9. https://doi.org/10.1192/bjp.bp.106.023234.
- Raleigh VS, Hussey D, Seccombe I, Qi R. Do associations between staff and inpatient feedback have the potential for improving patient experience? An analysis of surveys in NHS acute trusts in England. Qual Saf Health Care 2009;18:347-54. https://doi.org/10.1136/qshc.2008.028910.
- West MA, Dawson JF, Admasachew L, Topakas A. NHS Staff Management and Health Service Quality: Results from the NHS Staff Survey and Related Data. London: Department of Health and Social Care; 2011.
- Edwards JR. Ten difference score myths. Org Res Methods 2001;4:265-87. https://doi.org/10.1177/109442810143005.
- Wall TD, Bolden RI, Borrill CS, Carter AJ, Golya DA, Hardy CE, et al. Minor psychiatric disorder in NHS trust staff: occupational and gender differences. Br J Psychiatry 1997;171:519-23. https://doi.org/10.1192/bjp.171.6.519.
- Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; 2011.
- Goldberg D. Manual of the General Health Questionnaire 1978.
- Pawson R. Evidence-Based Policy: A Realist Perspective. Thousand Oaks, CA: Sage; 2006.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Maben J, Adams M, Peccei R, Murrells T, Robert G. ‘Poppets and parcels’: the links between staff experience of work and acutely ill older peoples’ experience of hospital care. Int J Older People Nurs 2012;7:83-94. https://doi.org/10.1111/j.1748-3743.2012.00326.x.
- Maben J, Leamy M, Taylor C, Reynolds E, Shuldham C, Dawson J, et al. Understanding, Implementing and Sustaining Schwartz Rounds: An Organisational Guide to Implementation. London: King’s College London; 2018.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46. https://doi.org/10.1111/j.1468-0009.2012.00665.x.
- Rycroft-Malone J, Fontenla M, Bick D, Seers K. A realistic evaluation: the case of protocol-based care. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-38.
- Bernard HR. Research Methods in Anthropology: Qualitative and Quantitative. Oxford: AltaMira Press; 2006.
- Finlay L. Relational Integrative Psychotherapy: Processes and Theory in Practice. Chichester: Wiley; 2016.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Casement P. On Learning from the Patient. Abingdon: Routledge; 1985.
- Ruch G. Identifying ‘the critical’ in a relationship-based model of reflection. Eur J Soc Work 2009;12:349-62. https://doi.org/10.1080/13691450902930761.
- Gokhale AA. Collaborative learning enhances critical thinking. J Tech Educ 1995;7.
- Wren B. True Tales of Organisational Life: Using Psychology to Create New Spaces and Have New Conversations at Work. London: Routledge; 2016.
- Bhabha HK. The Location of Culture. Abingdon: Routledge; 2004.
- Soja WT. Third Space: Journeys to Los Angeles and Other Real-and-imagined Places. Oxford: Blackwell; 1996.
- Oldenburg R. The Great Good Place: Cafes, Coffee Shops, Bookstores, Bars, Hair Salons, and Other Hangouts at the Heart of a Community. New York, NY: Marlowe & Company; 1999.
- Hulme R, Cracknell D, Owens A. Learning in third spaces: developing trans-professional understanding through practitioner enquiry. Educ Act Res 2009;17:537-50. https://doi.org/10.1080/09650790903309391.
- Britzman D. Practice Makes Practice: A Critical Study of Learning to Teach. New York, NY: State University of New York Press; 2003.
- Kofman F, Senge P. Communities of commitment: the heart of learning organizations. Organ Dyn 1993;22:5-23. https://doi.org/10.1016/0090-2616(93)90050-B.
- Sawhney M, Prandelli E. Communities of creation: managing distributed innovation in turbulent markets. Calif Manage Rev 2000;42:24-5. https://doi.org/10.2307/41166052.
- Scharmer O. Self-transcending knowledge: sensing and organizing around emerging opportunities. J Knowl Manag 2001;5:137-51. https://doi.org/10.1108/13673270110393185.
- Moje EB, Ciechanowski KM, Kramer K, Ellis L, Carrillo R, Collazo T. Working toward third space in content area literacy: an examination of every day funds of knowledge and discourse. Read Res Quart 2004;39:38-70. https://doi.org/10.1598/RRQ.39.1.4.
- Savin-Baden M. Learning Spaces : Creating Opportunities for Knowledge Creation in Academic Life. Buckingham: McGraw-Hill Education; 2008.
- Howard S. A Primer on Communication and Communicative Disorders. London: Pearson Education Inc.; 2011.
- Altman I, Vinsel A, Brown B. Dialectic conceptions in social psychology: an application to social penetration and privacy regulation. Adv Exp Soc Psychol 1981;14:107-60. https://doi.org/10.1016/S0065-2601(08)60371-8.
- West R. Introducing Communication Theory-Analysis and Application. McGraw-Hill; 2013.
- Greene K, Derlega VJ, Mathews A, Vangelisti AL, Perlman D. The Cambridge Handbook of Personal Relationships. Cambridge: Cambridge University Press; 2006.
- Weiten W, Dunn DS, Hammer EY. Psychology Applied to Modern Life: Adjustment in the 21st Century. Belmont, CA: Wadsworth Publishing Co Inc; 2014.
- Vittengl JR, Holt CS. Getting acquainted: the relationship of self-disclosure and social attraction to positive affect. J Soc Pers Relat 2000;17:53-66. https://doi.org/10.1177/0265407500171003.
- Tardy C, Dindia K, Hargie O. The Handbook of Communication Skills. East Sussex: Routledge; 2006.
- Laurenceau J-P, Kleinman BM, Perlmad D. The Cambridge Handbook of Personal Relationships. New York, NY: Cambridge University Press; 2006.
- Zak PJ, Kurzban R, Matzner WT. Oxytocin is associated with human trustworthiness. Horm Behav 2005;48:522-7. https://doi.org/10.1016/j.yhbeh.2005.07.009.
- Brown B. TEDxHouston 2010: The Power of Vulnerability 2010. www.ted.com/talks/brene_brown_on_vulnerability (accessed 24 May 2018).
- Tomlinson J. Blog: Shame 2012. https://abetternhs.net/2012/11/16/shame/ (accessed 23 January 17).
- Brown B. Daring Greatly: How the Courage to Be Vulnerable Transforms the Way We Live, Love, Parent, and Lead. London: Penguin; 2015.
- Ross L. The intuitive psychologist and his shortcomings: distortions in the attribution process. Adv Exp Soc Psychol 1977;10:173-220. https://doi.org/10.1016/S0065-2601(08)60357-3.
- Jones EE, Harris VA. The attribution of attitudes. J Exp Soc Psychol 1967;3:1-24. https://doi.org/10.1016/0022-1031(67)90034-0.
- Star SL, Strauss A. Layers of silence, arenas of voice: the ecology of visible and invisible work. Comp Support Comp W 1999;8.
- Wrzesniewski A, Dutton JE. Crafting a job: revisioning employees as active crafters of their work. Acad Manage Rev 2001;26:179-201.
- Boyd EM, Fayles AW. Reflective learning: key to learning from experience. J Humanist Psychol 1983;23:99-117. https://doi.org/10.1177/0022167883232011.
- Mezirow J. A criticial theory of adult learning and education. Adult Educ 1981;32:3-24. https://doi.org/10.1177/074171368103200101.
- Jarvis P. Reflective practice and nursing. Nurse Educ Today 1992;12:174-81. https://doi.org/10.1016/0260-6917(92)90059-W.
- Ghaye T. Into the reflective mode: bridging the stagnant moat. Reflectice Practice 2000;1:5-9.
- Moffatt S, White M, Mackintosh J, Howel D. Using quantitative and qualitative data in health services research – what happens when mixed method findings conflict?. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-28.
- Graveling RA, Crawford JO, Cowie H, Amati C, Vohra S. A Review of Workplace Interventions that Promote Mental Wellbeing in the Workplace. Edinburgh: Institute of Occupational Medicine; 2008.
- Marine A, Ruotsalainen JH, Serra C, Verbeek JH. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev 2006;4. https://doi.org/10.1002/14651858.CD002892.pub2.
- Promoting Mental Wellbeing Through Productive And Healthy Working Conditions: Guidance For Employers. London: NICE; 2009.
- Seymour L, Grove B. Workplace Interventions for People with Common Mental Health Problems. London: British Occupational Health Research Foundation; 2005.
- Behaviour Change at Population and Community Levels. London: NICE; 2007.
- Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med 2003;60:3-9. https://doi.org/10.1136/oem.60.1.3.
- Appleby J, Raleigh V. Variations in Health Care – The Good, the Bad and the Inexplicable. London: The King’s Fund; 2011.
- Workplace Health: Management Practices. London: NICE, Department of Health; 2015.
- NHS England . NHS Staff Health and Wellbeing: CQUIN Guidance 2016. www.england.nhs.uk/wp-content/uploads/2016/03/HWB-CQUIN-Guidance.pdf (accessed 24 May 2018).
- Schaufeli WB, Bakker A, Salanova M. The measurement of work engagement with a short questionnaire: a cross-national study. Educ Psychol Meas 2006;66:701-16. https://doi.org/10.1177/0013164405282471.
- Maslach C, Jackson SE, Leiter MP, Zalaquett CP, Wood RJ. Evaluating Stress: A Book of Resources. Lanham, MD: Scarecrow Education; 1997.
- Deci EL, Ryan RM. The’ what’ and’ why’ of goal pursuits: human needs and the self-determination of behavior. Psychol Inq 2000;11:227-68. https://doi.org/10.1207/S15327965PLI1104_01.
- Gilbert P. The Compassionate Mind. London: Constable; 2010.
- Grant AM, Franklin J, Langford P. The self-reflection and insight scale: a new measure of private self-consciousness. Soc Behav Personality 2002;30:821-35. https://doi.org/10.2224/sbp.2002.30.8.821.
- Kember D, McKay J, Sinclair K, Wong FK. A four-category scheme for coding and assessing the level of reflection in written work. Assess Eval High Edu 2008;33:369-79. https://doi.org/10.1080/02602930701293355.
- Baron-Cohen S, Wheelwright S. The empathy quotient: an investigation of adults with Asperger syndrome or high functioning autism, and normal sex differences. J Autism Dev Disord 2004;34:163-75. https://doi.org/10.1023/B:JADD.0000022607.19833.00.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. https://doi.org/10.1037/0033-295X.84.2.191.
- Parle M, Maguire P, Heaven C. The development of a training model to improve health professionals’ skills, self-efficacy and outcome expectancies when communicating with cancer patients. Soc Sci Med 1997;44:231-40. https://doi.org/10.1016/S0277-9536(96)00148-7.
- Chochinov HM. Dignity and the essence of medicine: the A, B, C, and D of dignity conserving care. BMJ 2007;335:184-7. https://doi.org/10.1136/bmj.39244.650926.47.
- Neff KD, Dahm KA, Ostafin B, Robinson M, Meier B. Handbook of Mindfulness and Self-Regulation. New York, NY: Springer; 2015.
- Sprecher S, Fehr B. Compassionate love for close others and humanity. J Soc Pers Relat 2005;22:629-51. https://doi.org/10.1177/0265407505056439.
- Hwang J, Plante T, Lackey K. The development of the Santa Clara Brief Compassion Scale: an abbreviation of Sprecher and Fehr’s Compassionate Love Scale. Pastoral Psychol 2008;56:421-8. https://doi.org/10.1007/s11089-008-0117-2.
- Haynes CE, Wall TD, Bolden RI, Stride C, Rick JE. Measures of perceived work characteristics for health services research: test of a measurement model and normative data. Br J Health Psychol 1999;4:257-75. https://doi.org/10.1348/135910799168614.
- Robinson SL, Rousseau DM. Violating the psychological contract: not the exception but the norm. J Organiz Behav 1994;15:245-59. https://doi.org/10.1002/job.4030150306.
- Guest D. Is the psychological contract worth taking seriously?. J Organiz Behav 1998;19:649-64. https://doi.org/10.1002/(SICI)1099-1379(1998)19:1+<649::AID-JOB970>3.0.CO;2-T.
- Patterson MG, West MA, Shackleton VJ, Dawson JF, Lawthom R, Maitlis S, et al. Validating the organizational climate measure: links to managerial practices, productivity and innovation. J Organiz Behav 2005;26:379-408. https://doi.org/10.1002/job.312.
- Anon . A Place to Heal 2008. www.nurse.com/blog/2008/09/08/a-place-to-heal/ (accessed 1 March 2017).
- Barnard P. Schwartz Rounds: librarian roles and opportunities. J Hosp Librarianship 2013;13:71-8. https://doi.org/10.1080/15323269.2013.743368.
- Baverstock AC, Finlay FO. Maintaining compassion and preventing compassion fatigue: a practical guide. Arch Dis Child Educ Pract Ed 2016;101:170-4. https://doi.org/10.1136/archdischild-2015-308582.
- Booth M. Schwartz Center Rounds – A Moment to Reflect at St Wilfrid’s Hospice 2014. www.ehospice.com/uk/Default/tabid/10697/ArticleId/11798 (accessed 1 March 2017).
- Cornwell J, Goodrich J. Supporting staff to deliver compassionate care using Schwartz Center rounds – a UK pilot. Nurs Times 2010;106:10-2.
- Davis C. Forum to help staff deal with day-to-day stress. Nurs Manag 2011;18:18-21. https://doi.org/10.7748/nm2011.07.18.4.18.c8589.
- Dean E. Time for reflection. Nurs Stand 2013;27. https://doi.org/10.7748/ns2013.07.27.48.61.s52.
- Dedier J, Penson R, Williams W, Lynch T. Race, ethnicity, and the patient–caregiver relationship. Oncologist 1999;4:325-31.
- Foster S. Schwartz Rounds: our experience. Br J Nurs 2015;24. https://doi.org/10.12968/bjon.2015.24.5.309.
- Gannon C, Cullen A, Knight A. Contrasting Schwartz Rounds with clinical ethics: three perspectives on their potential to impact on end-of-life care. Nurs Ethics 2014;21:621-6. https://doi.org/10.1177/0969733014526965.
- Gibson S. Schwartz Center Rounds: focusing on the patient-caregiver relationship. This national model offers emotional support to doctors and other medical professionals. Health Prog 2008;89:40-3.
- Goodrich J. Compassionate care and Schwartz Rounds: the nature of the work – acknowledging it is hard. Nurse Educ Today 2014;34:1185-7. https://doi.org/10.1016/j.nedt.2014.06.002.
- Hargreaves R. The value of Schwartz Rounds should not be underestimated. Nurs Times 2015;111.
- Johal J. Kindling Kindness for Compassionate Disaster Management 2015. http://currents.plos.org/disasters/article/kindling-kindness-for-compassionate-disaster-management/ (accessed 1 March 2017).
- Justice S, Rawles J, Brown J, Szczepanska S. Will introducing ‘Schwartz rounds’ help foster a culture of compassionate care in the NHS?. Nurs Stand 2013;27:26-7. https://doi.org/10.7748/ns2013.08.27.52.26.s32.
- Kaplan K. Leading Important Conversations in Healthcare: The Schwartz Center Rounds n.d. https://cdn.ymaws.com/www.odnetwork.org/resource/resmgr/2011_conf_ppts/g3_-_leading_important_conve.pdf (accessed 3 January 2017).
- Lee KJ, Forbes ML, Lukasiewicz GJ, Williams T, Sheets A, Fischer K, et al. Promoting staff resilience in the pediatric intensive care unit. Am J Crit Care 2015;24:422-30. https://doi.org/10.4037/ajcc2015720.
- Lima J, Cavaliere R, Porensky E. Closing the gap: bereavement support for families, caregivers and medical staff. Neuro-Oncology 2014;16:178-83. https://doi.org/10.1093/neuonc/nou269.17.
- Moore CD, McCole Phillips J. In these rounds, health-care professionals heal themselves. J Soc Work End-of-Life Palliative Care 2009;5:116-25. https://doi.org/10.1080/15524250903555064.
- Mudge B, Stanzler M. Schwartz Center Rounds® and Magnet®: enhancing patient- and family-centered care. American Nurse Today 2012;7. www.americannursetoday.com/schwartz-center-rounds-and-magnet-enhancing-patient-and-family-centered-care/ (accessed 20 July 2018).
- Mullick A, Wright A, Watmore-Eve J, Flatley M. Supporting hospice staff: the introduction of Schwartz Center Rounds to a UK hospice setting. Eur J Palliat Care 2013;20:62-5.
- Pepper JR, Jaggar SI, Mason MJ, Finney SJ, Dusmet M. Schwartz Rounds: reviving compassion in modern healthcare. J R Soc Med 2012;105:94-5. https://doi.org/10.1258/jrsm.2011.110231.
- Raphael-Grimm T. Fostering compassionate patient care as an integrated, multidisciplinary outcome: lessons learned from facilitating Schwartz Rounds. Int J Hum Caring 2008;12.
- Raso R. Improving practice with Schwartz rounds; the DNP degree. Nurs Manage 2009;40. https://doi.org/10.1097/01.NUMA.0000359212.26779.15.
- Rees-Adams D, Hughes L. Introducing Schwartz Center Rounds into a Welsh NHS Health Board: six months in – a reflection on the process and experience to date. Clin Psychol Forum 2014;263.
- Ryan B. Schwartz Center Rounds are one way to boost compassion. Nurs Stand 2013;27:30-1. https://doi.org/10.7748/ns2013.08.27.50.30.s42.
- Sanghavi DM. What makes for a compassionate patient-caregiver relationship?. Jt Comm J Qual Patient Saf 2006;32:283-92. https://doi.org/10.1016/S1553-7250(06)32037-5.
- Smyth M. End of shift: Goodbye to baby?. Nursecom Nursing Spectrum (Greater Chicago) 2011;24. www.nurse.com/blog/2011/07/11/end-of-shift-goodbye-to-baby-2/ (accessed 20 July 2018).
- Thompson A. How Schwartz rounds can be used to combat compassion fatigue. Nurs Manag 2013;20:16-20. https://doi.org/10.7748/nm2013.07.20.4.16.e1102.
- Baillie L, Bromley B, Walker M, Jones R, Mhlanga F. Implementing service improvement projects within pre-registration nursing education: a multi-method case study evaluation. Nurse Educ Pract 2014;14:62-8. https://doi.org/10.1016/j.nepr.2013.06.006.
- Booth A, Sutton A, Falzon L. Working together: supporting projects through action learning. Health Info Libraries J 2003;20:225-31. https://doi.org/10.1111/j.1471-1842.2003.00461.x.
- Bourner T, Frost P. Experiencing action learning. J Workplace Learning 1996;8:11-8. https://doi.org/10.1108/13665629610150135.
- Burgess H, Carpenter J. Building capacity and capability for evaluating the outcomes of social work education (the OSWE project): creating a culture change. Soc Work Edu 2008;27:898-912. https://doi.org/10.1080/02615470701844308.
- Currie K, Biggam J, Palmer J, Corcoran T. Participants’ engagement with and reactions to the use of on-line action learning sets to support advanced nursing role development. Nurse Educ Today 2012;32:267-72. https://doi.org/10.1016/j.nedt.2011.03.012.
- Douglas S, Machin T. A model for setting up interdisciplinary collaborative working in groups: lessons from an experience of action learning. J Psychiatr Ment Health Nurs 2004;11:189-93. https://doi.org/10.1111/j.1365-2850.2003.00707.x.
- Eisen S, Sukhani S, Brightwell A, Stoneham S, Long A. Peer mentoring: evaluation of a novel programme in paediatrics. Arch Dis Child 2014;99:142-6. https://doi.org/10.1136/archdischild-2013-304277.
- Lamont S, Brunero S, Russell R. An exploratory evaluation of an action learning set within a mental health service. Nurse Educ Pract 2010;10:298-302. https://doi.org/10.1016/j.nepr.2010.01.002.
- Leggat SG, Balding C, Anderson J. Empowering health-care managers in Australia: an action learning approach. Health Serv Manage Res 2011;24:196-202. https://doi.org/10.1258/hsmr.2011.011012.
- Machin AI, Pearson P. Action learning sets in a nursing and midwifery practice learning context: a realistic evaluation. Nurse Educ Pract 2014;14:410-16. https://doi.org/10.1016/j.nepr.2014.01.007.
- Mann R, Ball K, Watson G. Mentoring for NHS general practitioners: a prospective pilot study of an action learning approach. Educ Prim Care 2011;22:235-40. https://doi.org/10.1080/14739879.2011.11494006.
- Moore LJ. Partnerships and work-based learning: an evaluation of an opportunity to pioneer new ways to care for the older people in the community. Assess Eval High Edu 2007;32:61-77. https://doi.org/10.1080/02602930600848283.
- Phillips S, Tapping J, Ooms A, Marks-Maran D, Godden R. A preceptorship programme for health visitors and school nurses: a pilot study. Community Pract 2013;86:18-22.
- Rivas K, Murray S. Our shared experience of implementing action learning sets in an acute clinical nursing setting: approach taken and lessons learned. Contemp Nurse 2010;35:182-7. https://doi.org/10.5172/conu.2010.35.2.182.
- Reiter-Palmon R, Kennel V, Allen JA, Jones KJ, Skinner AM. Naturalistic decision making in after-action review meetings: the implementation of and learning from post-fall huddles. J Occupat Psychol 2015;88:322-40. https://doi.org/10.1111/joop.12084.
- Walker J, Andrews S, Grewcock D, Halligan A. Life in the slow lane: making hospitals safer, slowly but surely. J R Soc Med 2012;105:283-7. https://doi.org/10.1258/jrsm.2012.120093.
- Abeni MS, Magni M, Conte M, Mangiacavalli S, Pochintesta L, Vicenzi G, et al. Psychological care of caregivers, nurses and physicians: a study of a new approach. Cancer Med 2014;3:101-10. https://doi.org/10.1002/cam4.163.
- Adams KE, O’Reilly M, Romm J, James K. Effect of Balint training on resident professionalism. Am J Obstet Gynecol 2006;195:1431-7. https://doi.org/10.1016/j.ajog.2006.07.042.
- Airagnes G, Consoli SM, De Morlhon O, Galliot AM, Lemogne C, Jaury P. Appropriate training based on Balint groups can improve the empathic abilities of medical students: a preliminary study. J Psychosom Res 2014;76:426-9. https://doi.org/10.1016/j.jpsychores.2014.03.005.
- Dahlgren MA, Almquist A, Krook J. Physiotherapists in Balint group training. Physiother Res Int 2000;5:85-9. https://doi.org/10.1002/pri.188.
- Dokter HJ, Duivenvoorden HJ, Verhage F. Changes in the attitude of general practitioners as a result of participation in a Balint group. Fam Pract 1986;3:155-63. https://doi.org/10.1093/fampra/3.3.155.
- Fitzgerald G, Hunter MD. Organising and evaluating a Balint group for trainees in psychiatry. Psychiatric Bulletin 2003;27:434-6. https://doi.org/10.1192/pb.27.11.434.
- Johnson AH, Brock CD, Hamadeh G, Stock R. The current status of Balint groups in US family practice residencies: a 10-year follow-up study, 1990–2000. Fam Med 2001;33:672-7.
- Johnson AH, Brock CD, Hueston WJ. Resident physicians who continue Balint training: a longitudinal study 1982–1999. Fam Med 2003;35:428-33.
- Johnson AH, Nease DE, Milberg LC, Addison RB. Essential characteristics of effective Balint group leadership. Fam Med 2004;36:253-9.
- Kjeldmand D, Holmström I. Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Ann Fam Med 2008;6:138-45. https://doi.org/10.1370/afm.813.
- Kjeldmand D, Holmström I. Difficulties in Balint groups: a qualitative study of leaders’ experiences. Br J Gen Pract 2010;60:808-14. https://doi.org/10.3399/bjgp10X532585.
- Kjeldmand D, Holmström I, Rosenqvist U. Balint training makes GPs thrive better in their job. Patient Educ Couns 2004;55:230-5. https://doi.org/10.1016/j.pec.2003.09.009.
- Kjeldmand D, Holmström I, Rosenqvist U. How patient-centred am I? A new method to measure physicians’ patient-centredness. Patient Educ Couns 2006;62:31-7. https://doi.org/10.1016/j.pec.2005.05.017.
- Lee E, Kealy D. Revisiting Balint’s innovation: enhancing capacity in collaborative mental health care. J Interprof Care 2014;28:466-70. https://doi.org/10.3109/13561820.2014.902369.
- Leggett A. Transcultural issues in the dynamics of a Balint clinical reflection group for community mental health workers. Transcult Psychiat 2012;49:366-76. https://doi.org/10.1177/1363461511432494.
- Levenstein S. A report of three years’ experience of a Balint group in Cape Town. S Afr Med J 1978;54:121-3.
- Levenstein S. An undergraduate Balint group in Cape Town. S Afr Med J 1981;59:642-3.
- Levenstein S. An undergraduate Balint group in Cape Town – a follow-up report. S Afr Med J 1982;62:89-90.
- Margalit AP, Glick SM, Benbassat J, Cohen A. Effect of a biopsychosocial approach on patient satisfaction and patterns of care. J Gen Intern Med 2004;19:485-91. https://doi.org/10.1111/j.1525-1497.2004.30059.x.
- Nielsen HG, Tulinius C. Preventing burnout among general practitioners: is there a possible route?. Educ Prim Care 2009;20:353-9. https://doi.org/10.1080/14739879.2009.11493817.
- Salander P, Sandström M. A Balint-inspired reflective forum in oncology for medical residents: main themes during seven years. Patient Educ Couns 2014;97:47-51. https://doi.org/10.1016/j.pec.2014.06.008.
- Samuel O. How doctors learn in a Balint group. Fam Pract 1989;6:108-13. https://doi.org/10.1093/fampra/6.2.108.
- Sekeres MA, Chernoff M, Lynch TJ, Kasendorf EI, Lasser DH, Greenberg DB. The impact of a physician awareness group and the first year of training on hematology-oncology fellows. J Clin Oncol 2003;21:3676-82. https://doi.org/10.1200/JCO.2003.12.014.
- Smith M, Anandarajah G. Mutiny on the balint: balancing resident developmental needs with the balint process. Fam Med 2007;39:495-7.
- Stojanović-Spehar S, Blazeković-Milaković S, Matanić D. Education about pharmacotherapy and psychotherapy of anxiety among primary care physicians in Croatia: Balint group approach. Croat Med J 2004;45:625-9.
- Torppa MA, Makkonen E, Mårtenson C, Pitkälä KH. A qualitative analysis of student Balint groups in medical education: contexts and triggers of case presentations and discussion themes. Patient Educ Couns 2008;72:5-11. https://doi.org/10.1016/j.pec.2008.01.012.
- Yakeley J, Shoenberg P, Morris R, Sturgeon D, Majid S. Psychodynamic approaches to teaching medical students about the doctor-patient relationship: randomised controlled trial. Psychiatrist 2011;35:308-13. https://doi.org/10.1192/pb.bp.110.033704.
- Heaney CA. Enhancing social support at the workplace: assessing the effects of the caregiver support program. Health Educ Q 1991;18:477-94. https://doi.org/10.1177/109019819101800406.
- Heaney CA, Price RH, Rafferty J, Murphy LR, Hurrell JJ, Sauter SL, et al. Job Stress Interventions. Washington, DC: American Psychological Association; 1995.
- Arvidsson B, Löfgren H, Fridlund B. Psychiatric nurses’ conceptions of how a group supervision programme in nursing care influences their professional competence: a 4-year follow-up study. J Nurs Manag 2001;9:161-71. https://doi.org/10.1046/j.1365-2834.2001.00220.x.
- Arvidsson B, Skärsäter I, Öijervall J, Fridlund B. Process-oriented group supervision implemented during nursing education: nurses’ conceptions 1 year after their nursing degree. J Nurs Manag 2008;16:868-75. https://doi.org/10.1111/j.1365-2834.2008.00925.x.
- Ashmore R, Carver N, Clibbens N, Sheldon J. Lecturers’ accounts of facilitating clinical supervision groups within a pre-registration mental health nursing curriculum. Nurse Educ Today 2012;32:224-8. https://doi.org/10.1016/j.nedt.2011.04.010.
- Bégat IBE, Severinsson EI. Nurses’ reflections on episodes occurring during their provision of care – an interview study. Int J Nurs Stud 2001;38:71-7. https://doi.org/10.1016/S0020-7489(00)00060-2.
- Bogo M, Paterson J, Tufford L, King R. Interprofessional clinical supervision in mental health and addiction: toward identifying common elements. The Clinical Supervisor 2011;30:124-40. https://doi.org/10.1080/07325223.2011.564961.
- Bondas T. Nursing leadership from the perspective of clinical group supervision: a paradoxical practice. J Nurs Manag 2010;18:477-86. https://doi.org/10.1111/j.1365-2834.2010.01085.x.
- Bradshaw T, Butterworth A, Mairs H. Does structured clinical supervision during psychosocial intervention education enhance outcome for mental health nurses and the service users they work with?. J Psychiatr Ment Health Nurs 2007;14:4-12. https://doi.org/10.1111/j.1365-2850.2007.01021.x.
- Brunero S, Lamont S. The process, logistics and challenges of implementing clinical supervision in a generalist tertiary referral hospital. Scand J Caring Sci 2012;26:186-93. https://doi.org/10.1111/j.1471-6712.2011.00913.x.
- Buus N, Angel S, Traynor M, Gonge H. Psychiatric hospital nursing staff’s experiences of participating in group-based clinical supervision: an interview study. Issues Ment Health Nurs 2010;31:654-61. https://doi.org/10.3109/01612840.2010.489991.
- Danielsson A, Sundin-Andersson C, Hov R, Athlin E. Norwegian and Swedish preceptors’ views of their role before and after taking part in a group supervision program. Nurs Health Sci 2009;11:107-13. https://doi.org/10.1111/j.1442-2018.2009.00455.x.
- Davey B, Desousa C, Robinson S, Murrells T. The policy–practice divide: who has clinical supervision in nursing?. NT Research 2006;11:237-48. https://doi.org/10.1177/1744987106060036.
- Davys AM, Beddoe L. Interprofessional learning for supervision: ‘taking the blinkers off’. Learn Health Soc Care 2009;8:58-69.
- Edwards D, Burnard P, Hannigan B, Cooper L, Adams J, Juggessur T, et al. Clinical supervision and burnout: the influence of clinical supervision for community mental health nurses. J Clin Nurs 2006;15:1007-15. https://doi.org/10.1111/j.1365-2702.2006.01370.x.
- Edwards D, Cooper L, Burnard P, Hannigan B, Hanningan B, Juggesur T, et al. Factors influencing the effectiveness of clinical supervision. J Psychiatr Ment Health Nurs 2005;12:405-14. https://doi.org/10.1111/j.1365-2850.2005.00851.x.
- Fläckman B, Fagerberg I, Häggström E, Kihlgren A, Kihlgren M. Despite shattered expectations a willingness to care for elders remains with education and clinical supervision. Scand J Caring Sci 2007;21:379-89. https://doi.org/10.1111/j.1471-6712.2007.00478.x.
- Gonge H, Buus N. Model for investigating the benefits of clinical supervision in psychiatric nursing: a survey study. Int Ment Health Nurs 2011;20:102-11. https://doi.org/10.1111/j.1447-0349.2010.00717.x.
- Gonge H, Buus N. Individual and workplace factors that influence psychiatric nursing staff’s participation in clinical supervision: a survey study and prospective longitudinal registration. Issues Ment Health Nurs 2010;31:345-54. https://doi.org/10.3109/01612840903427849.
- Hallberg IR. Clinical group supervision and supervised implementation of planned individualized care of severely demented people: effects on nurses, provision of the care, and patients. J Psychiatr Ment Health Nurs 1995;2:113-4. https://doi.org/10.1111/j.1365-2850.1995.tb00153.x.
- Hallberg IR. Systematic clinical supervision in a child psychiatric ward: satisfaction with nursing care, tedium, burnout, and the nurses’ own report on the effects of it. Arch Psychiatr Nurs 1994;8:44-52. https://doi.org/10.1016/0883-9417(94)90020-5.
- Hall-Lord M, Theander K, Athlin E. A clinical supervision model in bachelor nursing education – purpose, content and evaluation. Nurse Edu Pract 2013;13:506-11. https://doi.org/10.1016/j.nepr.2013.02.006.
- Hansebo G, Kihlgren M. Nursing home care: changes after supervision. J Adv Nurs 2004;45:269-79. https://doi.org/10.1046/j.1365-2648.2003.02888.x.
- Heaven C, Clegg J, Maguire P. Transfer of communication skills training from workshop to workplace: the impact of clinical supervision. Patient Educ Couns 2006;60:313-25. https://doi.org/10.1016/j.pec.2005.08.008.
- Holmlund K, Lindgren B, Athlin E. Group supervision for nursing students during their clinical placements: its content and meaning. J Nurs Manag 2010;18:678-88. https://doi.org/10.1111/j.1365-2834.2010.01157.x.
- Hyrkäs K. Clinical supervision, burnout, and job satisfaction among mental health and psychiatric nurses in Finland. Issues Ment Health Nurs 2005;26:531-56. https://doi.org/10.1080/01612840590931975.
- Hyrkäs K, Appelqvist-Schmidlechner K, Haataja R. Efficacy of clinical supervision: influence on job satisfaction, burnout and quality of care. J Adv Nurs 2006;55:521-35. https://doi.org/10.1111/j.1365-2648.2006.03936.x.
- Jones A. Some benefits experienced by hospice nurses from group clinical supervision. Eur J Cancer Care 2003;12:224-32. https://doi.org/10.1046/j.1365-2354.2003.00405.x.
- Jones A. Some experiences of professional practice and beneficial changes derived from clinical supervision by community Macmillan nurses. Eur J Cancer Care 2001;10:21-30. https://doi.org/10.1046/j.1365-2354.2001.00209.x.
- Kelly B, Long A, McKenna H. A survey of community mental health nurses’ perceptions of clinical supervision in Northern Ireland. J Psychiatr Ment Health Nurs 2001;8:33-44. https://doi.org/10.1046/j.1365-2850.2001.00341.x.
- Kennedy TJT, Lingard L, Baker GR, Kitchen L, Regehr G. Clinical oversight: conceptualizing the relationship between supervision and safety. J Gen Intern Med 2007;22:1080-5. https://doi.org/10.1007/s11606-007-0179-3.
- Kenny A, Allenby A. Implementing clinical supervision for Australian rural nurses. Nurse Educ Pract 2013;13:165-9. https://doi.org/10.1016/j.nepr.2012.08.009.
- Kilcullen N. An analysis of the experiences of clinical supervision on Registered Nurses undertaking MSc/graduate diploma in renal and urological nursing and on their clinical supervisors. J Clin Nurs 2007;16:1029-38. https://doi.org/10.1111/j.1365-2702.2007.01661.x.
- Knox S, Caperton W, Phelps D, Pruitt N. A qualitative study of supervisees’ internal representations of supervisors. Counselling Psychol Q 2014;27:334-52. https://doi.org/10.1080/09515070.2014.886999.
- Koivu A, Saarinen PI, Hyrkas K. Who benefits from clinical supervision and how? The association between clinical supervision and the work-related well-being of female hospital nurses. J Clin Nurs 2012;21:2567-78. https://doi.org/10.1111/j.1365-2702.2011.04041.x.
- Koivu A, Hyrkäs K, Saarinen PI. Who attends clinical supervision? The uptake of clinical supervision by hospital nurses. J Nurs Manag 2011;19:69-7. https://doi.org/10.1111/j.1365-2834.2010.01185.x.
- Koivu A, Saarinen PI, Hyrkas K. Does clinical supervision promote medical-surgical nurses’ well-being at work? A quasi-experimental 4-year follow-up study. J Nurs Manag 2012;20:401-13. https://doi.org/10.1111/j.1365-2834.2012.01388.x.
- Lakeman R, Glasgow C. Introducing peer-group clinical supervision: an action research project. Int J Ment Health Nurs 2009;18:204-10. https://doi.org/10.1111/j.1447-0349.2009.00602.x.
- Lantz I, Severinsson E. The influence of focus group-oriented supervision on intensive care nurses’ reflections on family members’ needs. Intensive Crit Care Nurs 2001;17:128-37. https://doi.org/10.1054/iccn.2000.1548.
- Lindgren B, Athlin E. Nurse lecturers’ perceptions of what baccalaureate nursing students could gain from clinical group supervision. Nurse Educ Today 2010;30:360-4. https://doi.org/10.1016/j.nedt.2009.09.008.
- Lindgren B, Brulin C, Holmlund K, Athlin E. Nursing students’ perception of group supervision during clinical training. J Clin Nurs 2005;14:822-9. https://doi.org/10.1111/j.1365-2702.2005.01245.x.
- Magnusson A, Lützén K, Severinsson E. The influence of clinical supervision on ethical issues in home care of people with mental illness in Sweden. J Nurs Manag 2002;10:37-45. https://doi.org/10.1046/j.0966-0429.2001.00292.x.
- Malin NA. Evaluating clinical supervision in community homes and teams serving adults with learning disabilities. J Adv Nurs 2000;31:548-57. https://doi.org/10.1046/j.1365-2648.2000.01309.x.
- O’Connell B, Ockerby CM, Johnson S, Smenda H, Bucknall TK. Team clinical supervision in acute hospital wards: a feasibility study. West J Nurs Res 2011;35:330-47. https://doi.org/10.1177/0193945911406908.
- Ödling G, Danielson E, Jansson L. Caregivers’ descriptions of patients with advanced breast cancer in connection with supervision sessions in a surgical ward. Cancer Nurs 2001;24:28-34. https://doi.org/10.1097/00002820-200102000-00005.
- Olofsson B. Opening up: psychiatric nurses’ experiences of participating in reflection groups focusing on the use of coercion. J Psychiatr Ment Health Nurs 2005;12:259-67. https://doi.org/10.1111/j.1365-2850.2005.00827.x.
- Olsson A, Björkhem K, Hallberg IR. Systematic clinical supervision of home carers working in the care of demented people who are at home: structure, content and effect as experienced by participants. J Nurs Manag 1998;6:239-46. https://doi.org/10.1046/j.1365-2834.1998.00068.x.
- Palsson MB, Hallberg IR, Norberg A, Isovaara S. Systematic clinical supervision and its effects for nurses handling demanding care situations. Interviews with Swedish district nurses and hospital nurses in cancer care. Cancer Nurs 1994;17:385-94.
- Pesut DJ, Williams CA. The nature of clinical supervision in psychiatric nursing: a survey of clinical specialists. Arch Psychiatr Nurs 1990;4:188-94. https://doi.org/10.1016/0883-9417(90)90008-9.
- Saarikoski M, Marrow C, Abreu W, Riklikiene O, Ozbicakçi S. Student nurses’ experience of supervision and Mentorship in clinical practice: a cross cultural perspective. Nurse Educa Pract 2007;7:407-15. https://doi.org/10.1016/j.nepr.2007.02.006.
- Severinsson EI, Hallberg IR. Systematic clinical supervision, working milieu and influence over duties: the psychiatric nurse’s viewpoint – a pilot study. Int J Nurs Stud 1996;33:394-406. https://doi.org/10.1016/0020-7489(95)00070-4.
- Sirola-Karvinen P, Hyrkäs K. Administrative clinical supervision as evaluated by the first-line managers in one health care organization district. J Nurs Manag 2008;16:588-600. https://doi.org/10.1111/j.1365-2834.2008.00903.x.
- Sloan G. Good characteristics of a clinical supervisor: a community mental health nurse perspective. J Adv Nurs 1999;30:713-22. https://doi.org/10.1046/j.1365-2648.1999.01121.x.
- Walsh K, Nicholson J, Keough C, Pridham R, Kramer M, Jeffrey J. Development of a group model of clinical supervision to meet the needs of a community mental health nursing team. Int J Nurs Pract 2003;9:33-9. https://doi.org/10.1046/j.1440-172X.2003.00400.x.
- White E, Butterworth T, Bishop V, Carson J, Jeacock J, Clements A. Clinical supervision: insider reports of a private world. J Adv Nurs 1998;28:185-92. https://doi.org/10.1046/j.1365-2648.1998.00743.x.
- White E, Winstanley J. A randomised controlled trial of clinical supervision: selected findings from a novel Australian attempt to establish the evidence base for causal relationships with quality of care and patient outcomes, as an informed contribution to mental health nursing practice development. J Res Nursing 2010;15:151-67. https://doi.org/10.1177/1744987109357816.
- Williams L, Irvine F. How can the clinical supervisor role be facilitated in nursing: a phenomenological exploration. J Nurs Manag 2009;17:474-83. https://doi.org/10.1111/j.1365-2834.2009.00973.x.
- Brunero S, Stein-Parbury J. The effectiveness of clinical supervision in nursing: an evidenced based literature review. Aust J Adv Nurs 2008;25:86-94.
- Butterworth T, Bell L, Jackson C, Majda P. Wicked spell or magic bullet? A review of the clinical supervision literature 2001–2007. Nurse Educ Today 2008;28:264-72. https://doi.org/10.1016/j.nedt.2007.05.004.
- Dawson M, Phillips B, Leggat S. Clinical supervision for allied health professionals: a systematic review. J Allied Health 2013;42:65-73.
- Ducat WH, Kumar S. A systematic review of professional supervision experiences and effects for allied health practitioners working in non-metropolitan health care settings. J Multidiscip Healthc 2015;8:397-40. https://doi.org/10.2147/JMDH.S84557.
- Farnan JM, Petty LA, Georgitis E, Martin S, Chiu E, Prochaska M, et al. A systematic review: the effect of clinical supervision on patient and residency education outcomes. Acad Med 2012;87:428-42. https://doi.org/10.1097/ACM.0b013e31824822cc.
- Henshaw AM, Clarke D, Long AF. Midwives and supervisors of midwives’ perceptions of the statutory supervision of midwifery within the United Kingdom: a systematic review. Midwifery 2013;29:75-8. https://doi.org/10.1016/j.midw.2011.11.004.
- Kilminster SM, Jolly BC. Effective supervision in clinical practice settings: a literature review. Med Educ 2000;34:827-40. https://doi.org/10.1046/j.1365-2923.2000.00758.x.
- Pearce P, Phillips B, Dawson M, Leggat SG. Content of clinical supervision sessions for nurses and allied health professionals: a systematic review. Clin Govern 2013;18:139-54. https://doi.org/10.1108/14777271311317927.
- Wheeler S, Richards K. The Impact of Clinical Supervision on Counsellors and Therapists, Their Practice and Their Clients: A Systematic Review of the Literature (BACP). Lutterworth: British Association for Counselling and Psychotherapy; 2007.
- Mealer M, Conrad D, Evans J, Jooste K, Solyntjes J, Rothbaum B, et al. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am J Crit Care 2014;23:e97-105. https://doi.org/10.4037/ajcc2014747.
- Peng L, Li M, Zuo X, Miao Y, Chen L, Yu Y, et al. Application of the Pennsylvania resilience training program on medical students. Pers Indiv Differ 2014;61–62:47-51. https://doi.org/10.1016/j.paid.2014.01.006.
- Sharma V, Bauer B, Prasad K, Sood A, Schroeder D. Self help intervention to decrease stress and increase mindfulness: a pilot trial. BMC Complement Altern Med 2012;12. https://doi.org/10.1186/1472-6882-12-S1-P253.
- Sharma V, Sood A, Prasad K, Loehrer L, Schroeder D, Brent B. Bibliotherapy to decrease stress and anxiety and increase resilience and mindfulness: a pilot trial. Explore 2014;10:248-52. https://doi.org/10.1016/j.explore.2014.04.002.
- Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among department of medicine faculty: A pilot randomized clinical trial. J Gen Intern Med 2011;26:858-61.
- Varker T, Devilly GJ. An analogue trial of inoculation/resilience training for emergency services personnel: proof of concept. J Anxiety Disord 2012;26:696-701. https://doi.org/10.1016/j.janxdis.2012.01.009.
- Matthews LR. Effect of staff debriefing on posttraumatic stress symptoms after assaults by community housing residents. Psychiatr Serv 1998;49:207-12. https://doi.org/10.1176/ps.49.2.207.
- O’Connor J, Jeavons S. Perceived effectiveness of critical incident stress debriefing by Australian nurses. Aust J Adv Nurs 2003;20:22-9.
- Macpherson CF. Peer-supported storytelling for grieving pediatric oncology nurses. J Pediatr Oncol Nurs 2008;25:148-63. https://doi.org/10.1177/1043454208317236.
- Abbas K, Pierce CM. Time to reflect: reflective practice groups for consultants and registrars on a neonatal and paediatric intensive care unit (N/PICU). 24th Annual Meeting of the European Society of Paediatric and Neonatal Intensive Care, ESPNIC 2013, Rotterdam, the Netherlands. Intens Care Med 2013;39:S51-S2.
- Binks C, Jones FW, Knight K. Facilitating reflective practice groups in clinical psychology training: a phenomenological study. Reflect Pract 2013;14:305-18. https://doi.org/10.1080/14623943.2013.767228.
- Dawber C. Reflective practice groups for nurses: a consultation liaison psychiatry nursing initiative: Part 2 – the evaluation. Int J Ment Health Nurs 2013;22:241-8. https://doi.org/10.1111/j.1447-0349.2012.00841.x.
- Gould B, Masters H. Learning to make sense: the use of critical incident analysis in facilitated reflective groups of mental health student nurses. Learning Health Soc Care 2004;3:53-6. https://doi.org/10.1111/j.1473-6861.2004.00063.x.
- Hansom J, Butler M. Sharing reflections in midwifery practice. Br J Midwifery 2003;11:34-7. https://doi.org/10.12968/bjom.2003.11.1.11010.
- Hayes J. Learning from practice: developing the reflective skills of forensic psychiatric nurses. Psychiatric Care 1998;5:30-3.
- Heneghan C, Wright J, Watson G. Clinical psychologists’ experiences of reflective staff groups in inpatient psychiatric settings: a mixed methods study. Clin Psychol Psychother 2014;21:324-40. https://doi.org/10.1002/cpp.1834.
- Hong LP, Chew L. Reflective practice from the perspectives of the bachelor of nursing students in International Medical University (IMU). Singapore Nurs J 2008;35.
- Johnston J, Paley G. Mirror mirror on the ward: who is the unfairest of them all? Reflections on reflective practice groups in acute psychiatric settings. Psychoanal Psychother 2013;27:170-86. https://doi.org/10.1080/02668734.2013.772535.
- Kiff J, Holmes G, Cushway D. Personal awareness / development groups and clinical training. Clin Psychol Forum 2010:30-4.
- Knight K, Sperlinger D, Maltby M. Exploring the personal and professional impact of reflective practice groups: a survey of 18 cohorts from a UK clinical psychology training course. Clin Psychol Psychother 2010;17:427-37. https://doi.org/10.1002/cpp.660.
- Kung JW, Eisenberg RL, Slanetz PJ. Reflective practice as a tool to teach digital professionalism. Acad Radiol 2012;19:1408-14. https://doi.org/10.1016/j.acra.2012.08.008.
- Manning A, Cronin P, Monaghan A, Rawlings-Anderson K. Supporting students in practice: an exploration of reflective groups as a means of support. Nurse Educ Pract 2009;9:176-83. https://doi.org/10.1016/j.nepr.2008.07.001.
- Parish C, Bradley L, Franks V. Managing the stress of caring in ITU: a reflective practice group. Br J Nurs 1997;6:1192-6. https://doi.org/10.12968/bjon.1997.6.20.1192.
- Platzer H, Blake D, Ashford D. An evaluation of process and outcomes from learning through reflective practice groups on a post-registration nursing course. J Adv Nurs 2000;31:689-95. https://doi.org/10.1046/j.1365-2648.2000.01337.x.
- Redhead K, Bradshaw T, Braynion P, Doyle M. An evaluation of the outcomes of psychosocial intervention training for qualified and unqualified nursing staff working in a low-secure mental health unit. J Psychiatr Ment Health Nurs 2011;18:59-66. https://doi.org/10.1111/j.1365-2850.2010.01629.x.
- Ewers P, Bradshaw T, McGovern J, Ewers B. Does training in psychosocial interventions reduce burnout rates in forensic nurses?. J Adv Nurs 2002;37:470-6. https://doi.org/10.1046/j.1365-2648.2002.02115.x.
- Doyle M, Kelly D, Clarke S, Braynion P. Burnout: the impact of psychosocial interventions training. Ment Health Pract 2007;10:16-9. https://doi.org/10.7748/mhp2007.04.10.7.16.c4298.
- Bazarko D, Cate RA, Azocar F, Kreitzer MJ. The impact of an innovative mindfulness-based stress reduction program on the health and well-being of nurses employed in a corporate setting. Employee Assist Q 2013;28:107-33. https://doi.org/10.1080/15555240.2013.779518.
- Beddoe AE, Murphy SO. Does mindfulness decrease stress and foster empathy among nursing students?. J Nurs Educ 2004;43:305-12.
- Brady S, O’Connor N, Burgermeister D, Hanson P. The impact of mindfulness meditation in promoting a culture of safety on an acute psychiatric unit. Perspect Psychiatr Care 2012;48:129-37. https://doi.org/10.1111/j.1744-6163.2011.00315.x.
- Cohen-Katz J, Wiley S, Capuano T, Baker DM, Deitrick L, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout: a qualitative and quantitative study, part III. Holist Nurs Pract 2005;19:78-86. https://doi.org/10.1097/00004650-200503000-00009.
- de Vibe M, Solhaug I, Tyssen R, Friborg O, Rosenvinge JH, Sorlie T, et al. Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Med Educ 2013;13. https://doi.org/10.1186/1472-6920-13-107.
- Foureur M, Besley K, Burton G, Yu N, Crisp J. Enhancing the resilience of nurses and midwives: pilot of a mindfulness-based program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemp Nurse 2013;45:114-25. https://doi.org/10.5172/conu.2013.45.1.114.
- Geary C, Rosenthal SL. Sustained impact of MBSR on stress, well-being, and daily spiritual experiences for 1 year in academic health care employees. J Altern Complement Med 2011;17:939-44. https://doi.org/10.1089/acm.2010.0335.
- Goodman MJ, Schorling JB. A mindfulness course decreases burnout and improves well-being among healthcare providers. Int J Psychiatry Med 2012;43:119-28. https://doi.org/10.2190/PM.43.2.b.
- Hallman IS, O’Connor N, Hasenau S, Brady S. Improving the culture of safety on a high-acuity inpatient child/adolescent psychiatric unit by mindfulness-based stress reduction training of staff. J Child Adolesc Psychiatr Nurs 2014;27:183-9. https://doi.org/10.1111/jcap.12091.
- Irving JA, ParkSaltzman J, Fitzpatrick M, Dobkin PL, Chen A, Hutchinson T. Experiences of health care professionals enrolled in mindfulness-based medical practice: a grounded theory model. Mindfulness 2014;5:60-71. https://doi.org/10.1007/s12671-012-0147-9.
- Mackenzie CS, Poulin PA, Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl Nurs Res 2006;19:105-9. https://doi.org/10.1016/j.apnr.2005.08.002.
- Martin-Asuero A, García-Banda G. The mindfulness-based stress reduction program (MBSR) reduces stress-related psychological distress in healthcare professionals. Span J Psychol 2010;13:897-905. https://doi.org/10.1017/S1138741600002547.
- Marx R, Strauss C, Williamson C, Karunavira T. The eye of the storm: a feasibility study of an adapted mindfulness-based cognitive therapy (MBCT) group intervention to manage NHS staff stress. Cog Behav Ther 2014;7. https://doi.org/10.1017/S1754470X14000300.
- Moody K, Kramer D, Santizo RO, Magro L, Wyshogrod D, Ambrosio J, et al. Helping the helpers: mindfulness training for burnout in pediatric oncology – a pilot program. J Pediatr Oncol Nurs 2013;30:275-84. https://doi.org/10.1177/1043454213504497.
- Poulin PA, Mackenzie CS, Soloway G, Karayolas E. Mindfulness training as an evidenced-based approach to reducing stress and promoting well-being among human services professionals. Int J Health Promot Edu 2008;46:72-80. https://doi.org/10.1080/14635240.2008.10708132.
- Rosenzweig S, Reibel DK, Greeson JM, Brainard GC, Hojat M. Mindfulness-based stress reduction lowers psychological distress in medical students. Teach Learn Med 2003;15:88-92. https://doi.org/10.1207/S15328015TLM1502_03.
- Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag 2005;12:164-76. https://doi.org/10.1037/1072-5245.12.2.164.
- Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med 1998;21:581-99. https://doi.org/10.1023/A:1018700829825.
- Jourard SM. The Transparent Self. New York, NY: Van Nostrand Reinhold; 1971.
- Buggins E. Create a Culture of ‘Psychological Safety’ 2013. www.hsj.co.uk/create-a-culture-of-psychological-safety/5052550.article (accessed 21 February 2017).
- Dewey J. How We Think. Boston, MA: Heath; 1933.
- Giles DE, Eyler J. The theoretical roots of service-learning in John Dewey: toward a theory of service-learning. J Commun Serv Learn 1994;1:77-85.
- Scherer KS, Schorr A, Johnstone T. Appraisal Processes in Emotion: Theory, Methods, Research. New York, NY: Oxford University Press; 2001.
- Lakey B, Cohen S, Cohen S, Underwood L, Gottlieb B. Measuring and Intervening in Social Support. New York, NY: Oxford University Press; 2000.
- Smith MK. ‘What Is Group Work?’, The Encyclopaedia of Informal Education 2008. http://infed.org/mobi/group-work/ (accessed 17 February 2017).
- Papell CP, Rothman B. Social group work models: possession and heritage. J Educ Soc Work 1966;2:66-77. https://doi.org/10.1080/00220612.1966.10778680.
- Picker Institute Europe . Focused on Staff Experience 2015. www.nhsstaffsurveys.com/Page/1010/Home/NHS-Staff-Survey-2015/ (accessed 8 June 2016).
- Admasachew L, Dawson J. Staff Engagement in the NHS – A Multilevel Analysis. Birmingham: Aston University; 2010.
- Care Quality Commission . Adult Inpatient Survey, 2015 2016. www.cqc.org.uk/content/adult-inpatient-survey-2015 (accessed 8 June 2016).
- Care Quality Commission . Hospital Intelligent Monitoring: October 2013 2013. www.cqc.org.uk/download/a-to-z/hospital-imonitoring-october-2013 (accessed 2 March 2016).
- Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997;27:191-7. https://doi.org/10.1017/S0033291796004242.
- Hardy GE, Shapiro DA, Haynes CE, Rick JE. Validation of the general health questionnaire-12 using a sample of employees from England’s health care services. Psycholog Assess 1999;11:159-65. https://doi.org/10.1037/1040-3590.11.2.159.
- Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Market Res 1981;18:39-50. https://doi.org/10.2307/3151312.
- Willis G. Cognitive interviewing as a tool for improving the informed consent process. J Emp Res Hum Res Ethics 2006;1:9-23. https://doi.org/10.1525/jer.2006.1.1.9.
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol 2001;52:397-422. https://doi.org/10.1146/annurev.psych.52.1.397.
Appendix 1 Theoretical rationale for survey measures
Staff well-being
There is a clear relationship between well-being of staff and patient experience. 68,76,77 As the goal of Rounds is to improve relationships with patients, improving the well-being of staff is key.
Rounds allow individuals to disclose and reflect on emotional experiences, both in written form and verbally. It has been argued that using language to label an emotion/experience creates a structure, which facilitates understanding of the event. 43 People experience greater emotional and physical health benefits if they share emotions than if they share facts. Rounds are about sharing difficult and challenging experiences, rather than problem-solving; therefore, it would be useful to measure the impact of Rounds on well-being.
Based on a review of literature on Schwartz Rounds, one of the anticipated outcomes for individuals is improved well-being. Previous evaluations of Rounds have shown that they benefit individuals through reducing levels of stress and isolation in their work with patients. 27,29 The US evaluation also found that individuals reported improvements in their ability to cope with the psychosocial demands of their job. 27
-
Reflection → coping with change/trauma → improved well-being.
-
Reflection → stress-reduction → improved well-being.
-
Disclosure → translating emotional/traumatic events into language → improved well-being.
The GHQ-1282 is a well-validated measure against the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for depression and anxiety. We decided to use this tool so that we could measure changes in staff well-being secondary to attending Rounds.
Work engagement
Work engagement is commonly defined as a positive work-related state of mind, characterised by vigour, dedication and absorption in one’s work tasks. 136 It has also often been defined as the opposite of burnout. 137 According to self-determination theory,138 the actualisation of the need for autonomy, competence and relatedness should lead to increased engagement. Given that one purpose of Rounds is to enable more understanding of how difficult situations at work and with patients may arise and be avoided (competence), and to an even greater extent enable social support between colleagues (relatedness), we would expect the attendance at Rounds to be associated with an increase in work engagement:
-
Reflection/disclosure → social support/relatedness → better work engagement.
-
Disclosure → hear about difficult situations at work and how to avoid (competence) → better work engagement.
The short (three-item) version of the Utrecht Work Engagement Scale (UWES-9)136 has good face validity and has been adapted for use among NHS staff through cognitive interviews. The measure has three underlying dimensions of work engagement: (1) vigour, (2) dedication and (3) absorption (see Report Supplementary Material 1).
Reflection
We believe reflection to be a core mechanism by which Rounds work. Therefore, to test this assumption it was deemed important to measure reflection explicitly.
Mezirow57 argued that emotion plays a central role throughout the reflective process and cannot be separated from learning. He proposed a theory of transformative learning: a process of individual critical reflection followed by the sharing of ideas with others to validate insights, culminating in action taken on the individual and collective reflection. Linking Rounds to this theory, Rounds are a combination of self and collective reflection. By selecting and sharing stories that resonate with the audience, this provides opportunities for reflection and disclosure by the individuals involved (panellists) as well as sparking reflection in the audience. This self and collective reflection creates shared knowledge at the individual and institutional levels. This may include personal outcomes such as improved well-being; dyadic and team-based outcomes such as better communication, work engagement and teamwork; and institutional outcomes such as changes to hospital culture.
Rounds may produce benefit through the mechanism of self-disclosure and group reflection, which Gilbert139 suggests is an important aspect of developing positive affect and compassion in others:
-
Individual critical reflection → sharing of ideas with others (self-disclosure) → collective reflection.
The measure of reflection developed by Grant et al. 140 was selected following piloting (see Report Supplementary Material 1) as it had better psychometric properties than that by Kember et al. 141
Empathy
Empathy is key to reflective practice, a mechanism through which Rounds are anticipated to work. Increased compassion and empathy are also the main intended outcomes of Rounds, both for the individuals attending Rounds and also in their interactions with patients and their families.
Rogers59 underscores the importance of empathy in reflective practice. For a person to ‘grow’, they need an environment that provides them with genuineness (openness and self-disclosure), acceptance (being seen with unconditional positive regard) and empathy (being listened to and understood). 60
Staff with high levels of empathy are less likely to suffer burnout and stress. 30 If staff are less stressed and burnt out, they may find it easier to be compassionate. As the goal of Rounds is to improve relationships with patients, high levels of empathy in staff are key. Anticipated outcomes of Rounds include beliefs in the importance of, and actual, empathy with patients. A US evaluation of Rounds showed that they benefited individuals through enhancing beliefs in the importance of empathy. 27
Sharing and reflecting on (examining) challenging and difficult experiences and emotions, including guilt and anger (experiences/emotions that are perceived as inconsistent with the caregiver role), in a safe, confidential environment (absence of threat) → can lead to acceptance and integration of those feelings → which could lead to greater empathy and compassion (more understanding of others).
The Empathy Quotient measure142 was originally developed for adults with high functioning autism but has been used in other populations including health-care professionals. We decided to use the subscale as it has been moderately used, including with health-care staff. It has good face validity and was a good fit with our understanding of empathy, as it relates to the practice of health-care professionals.
Self-efficacy in relation to communication with patients
Bandura143 defined self-efficacy as a person’s belief in their ability to succeed in specific situations or accomplish a task. An individual’s sense of self-efficacy can play a major role in how they approach goals, tasks and challenges. Mezirow57 suggests that self-reflection can empower us to be more open and emotionally capable of change.
One anticipated outcome of Rounds is enhanced confidence in handling non-clinical care, for example discussing sensitive topics, attending to non-verbal cues and communicating well with patients. Caregivers report greater feelings of adequacy responding to patients’ social and emotional issues after attending Rounds. 28,30
We felt that this was important to measure, as we wanted to examine the possibility of behaviour change as a result of attending Rounds, and improving skills in communicating with patients is one arena in which this change could be measured.
Reflection → fosters openness and emotional capability for change → enhanced confidence in communicating with patients → improved communication with patients.
Communication with patients was measured via the ‘communication skills with patients’ subscale of the self-efficacy scale,144 as this was designed for use with health-care staff and has good face validity.
Compassion
Compassion is defined as a deep awareness of the suffering of another coupled with the wish to relieve it. 145
According to Neff and Dahm:
In order to experience compassion, you must first acknowledge the presence of pain [. . .] This involves pausing, stepping out of your usual frame of reference, and viewing the world from the vantage point of another.
p. 3146
This can be achieved through disclosure and reflection.
Rounds were designed to strengthen caregiver/patient relationships through empathy and compassion. Rounds allow individuals to express emotions and feelings that they may not be able to express in other contexts, without fear of recrimination or judgement. Translating emotional/traumatic events into language facilitates acceptance and integration of those emotions, leading to better physical and emotional well-being, including (potentially) greater warmth and understanding for themselves (self-compassion). Staff who have self-compassion are reportedly less likely to experience personal distress, and are more able to confront others’ suffering without being overwhelmed (compassion for others). This is particularly relevant for caregivers who interact daily with patients and their families, many of whom have complex, sensitive and often distressing needs, in highly pressurised work environments.
A US evaluation of Rounds showed that they benefited individuals through improved ability to provide compassionate care. 27
Disclosure and reflection → self-compassion → compassion for others (patients).
Compassion was measured using the Santa Clara Brief Compassion Scale147 in a version adapted to five items. 148
Peer support
In Karasek’s65 Job Demand–Control–Support model, social support is associated with psychological well-being in the workplace. Karasek’s model is a ‘buffering model’ as work social support (such as support from colleagues and supervisors) is said to buffer against a high level of job demands/lack of control and thereby protects mental and physical health. 67 Rounds are a group intervention and social support is provided through group reflection. Individuals have a sense of belonging to a multidisciplinary forum that allows them a safe space to reflect on challenging and emotional experiences.
A sense of community is necessary for Rounds to work. Community is created in a Round when it is psychologically safe (a safe, confidential forum) and attendees feel that they belong (Rounds are multidisciplinary in nature; individuals are accepted and respected; there is a suspension of hierarchy).
A US evaluation of Rounds showed that they benefited individuals and teams through better appreciation of roles and responsibilities of colleagues. 27
Psychological safety → sense of community/belonging → better communication, social support, teamwork → better peer support.
Peer support was measured using a subscale from Haynes et al. 149 This subscale is taken from a wider tool made up of a variety of well-validated measures that examine the job-related factors affecting attitudes and mental health, and explores relationships among work colleagues. We decided to use this subscale as it has been used in a survey of 20,000 NHS staff. It is short and has good face validity.
Organisational climate for support
One aspect of organisational support is concern for employee welfare: the extent to which the organisation values and cares for its employees. 150,151
We felt that this was an important measure to use, as changes in perceived organisational concern for employee welfare was a factor that emerged from a survey of Rounds at two sites in the UK. The provision of Rounds led to attendees feeling valued by the organisation. 30
By setting up Rounds, organisations are demonstrating that they want employees to reflect on challenging psychosocial and emotional aspects of caring for patients in a psychologically safe environment, where members feel accepted and respected and think less about the potential negative consequences of expressing themselves. Employees feel part of a community or family.
Organisational support for Rounds → support for focus on impact of patient care on staff → staff perceived that management care about staff well-being.
Organisational climate for support was measured with the four-item support subscale of the Organisational Climate Measure. 152 This subscale measures perceived organisational concern for employee welfare.
Appendix 2 Survey of staff experiences, assessed at baseline and follow-up
The GHQ-12 was used with permission and in payment of the correct fee to GL Assessment; see www.gl-assessments.co.uk.
Appendix 3 Literature review: MEDLINE database search strategies
Action-learning sets
Last search run: 5 February 2015.
-
action learn$ set$.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
After-action reviews
Last search run: 3 December 2014.
-
(after adj2 action adj2 review*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
Balint Groups
Last search run: 14 October 2014.
-
exp Balint group/
-
balint group*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
or/1-2
-
limit 3 to English language
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; limit applied as there is literature in different languages.]
Caregiver support programme
Last search run: 15 December 2014.
-
care$ support program$.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
Clinical supervision
Last search run: 15 December 2014.
-
exp Clinical Supervision/
-
(clinical adj2 supervision).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(restorative adj2 supervision).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
or/1-3
-
(health* adj2 personel).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(health* adj2 staff).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
doctor*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
nurse*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
exp Health Personnel/
-
or/5-9
-
4 and 10
-
limit 11 to English language
Critical incident stress debriefing
Last search run: 15 December 2014.
-
(critical incident adj2 stress debriefing).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
Mindfulness-based stress reduction
Last search run: 5 December 2015.
-
Mindfulness-based stress reduction.mp.
-
(health* adj2 personel).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
(health* adj2 staff).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
doctor*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
nurse*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
-
exp Health Personnel/
-
or/2-6
-
1 and 7
[Note: search brought up a manageable number of results so no limit necessary.]
Psychosocial intervention training
Last search run: 5 February 2015.
-
(psychosocial adj2 intervention adj2 training).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
Peer-supported storytelling
Last search run: 5 February 2015.
-
(Peer adj2 Supported adj2 Storytelling).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
Reflective practice groups
Last search run: 17 September 2015.
-
reflect$ practice group$.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
Resilience training
Last search run: 5 February 2015.
-
(resilience adj2 training).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
Schwartz Rounds
Last search run: 15 January 2016.
-
(Schwartz adj2 Round*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
[Note: search brought up a manageable number of results so did not focus this further to health-care staff; no limit necessary either.]
Appendix 4 Literature sources for Schwartz Rounds composite definition and evidence base
References marked with * were also included in the review of the evidence base.
References marked with ** were only included in the review of the evidence base (as they were published after searches were run/composite definition was developed).
-
Anon. 153
-
Barnard. 154
-
Baverstock and Finlay. 155
-
Berry and Chaggar. 20
-
Booth. 156
-
*Corless et al. 25
-
Cornwell and Goodrich. 157
-
Davis. 158
-
Dean. 159
-
Dedier et al. 160
-
*Deppoliti et al. 24
-
Foster. 161
-
Gannon. 162
-
**George. 19
-
Gibson. 163
-
Gishen and Wood. 21
-
**Gishen et al. 18
-
Hargreaves. 165
-
Johal. 166
-
Justice et al. 167
-
Kaplan. 168
-
Lee et al. 169
-
Lima et al. 170
-
*Lown and Manning. 27
-
* Manning et al. . 28
-
Moore and McCole Phillips. 171
-
Mudge and Stanzler. 172
-
Mullick et al. 173
-
Pepper et al. 174
-
Raphael-Grimm. 175
-
Raso. 176
-
*Reed et al. 23
-
Rees-Adams and Hughes. 177
-
Ryan. 178
-
Sanghavi. 179
-
*Shield et al. 26
-
Smyth. 180
-
Thompson. 181
-
Whitehead. 22
-
Wren. 95
Appendix 5 References for included papers: alternatives to Rounds
List based on that in Taylor et al. 7 This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/
Action learning sets
Balint groups
-
Abeni et al. 198
-
Adams et al. 199
-
Airagnes et al. 200
-
Dahlgren et al. 201
-
Dokter et al. 202
-
Fitzgerald and Hunter. 203
-
Lee and Kealy. 211
-
Leggett. 212
-
Margalit et al. 216
-
Nielsen and Tulinius. 217
-
Salander and Sandström. 218
-
Samuel. 219
-
Sekeres et al. 220
-
Smith and Anandarajah. 221
-
Stojanovic-Spehar et al. 222
-
Torppa et al. 223
-
Yakeley et al. 224
Clinical and restorative supervision
Primary studies
-
Arvidsson et al. 227
-
Ardvidsson et al. 228
-
Ashmore et al. 229
-
Begat and Severinsson. 230
-
Bogo et al. 231
-
Bondas. 232
-
Bradshaw et al. 233
-
Brunero and Lamont. 234
-
Buus et al. 235
-
Danielsson et al. 236
-
Davey et al. 237
-
Davys and Beddoe. 238
-
Edwards et al. 239
-
Edwards et al. 240
-
Flackman et al. 241
-
Gonge and Buus. 242
-
Gonge and Buus. 243
-
Hallberg. 244
-
Hallberg. 245
-
Hall-Lord et al. 246
-
Hansebo and Kihlgren. 247
-
Heaven et al. 248
-
Holmlund et al. 249
-
Hyrkas. 250
-
Hyrkas. 251
-
Jones. 252
-
Jones. 253
-
Kelly et al. 254
-
Kennedy et al. 255
-
Kenny and Allenby. 256
-
Kilcullen. 257
-
Knox et al. 258
-
Koivu et al. 259
-
Koivu et al. 260
-
Koivu et al. 261
-
Lakeman and Glasgow. 262
-
Lantz and Severinsson. 263
-
Lindgren and Athlin. 264
-
Lindgren et al. 265
-
Magnusson et al. 266
-
Malin. 267
-
O’Connell et al. 268
-
Odling et al. 269
-
Olofsson. 270
-
Olsson. 271
-
Palsson et al. 272
-
Pesut and Williams. 273
-
Saarikoski et al. 274
-
Severinsson and Hallberg. 275
-
Sirola-Karvinen and Hyrkas. 276
-
Sloan. 277
-
Walsh et al. 278
-
White et al. 279
-
White and Winstanley. 280
-
Williams and Irvine. 281
Resilience training
Peer-supported storytelling
-
Macpherson. 299
Reflective practice groups
-
Abbas and Pierce. 300
-
Binks et al. 301
-
Boyd and Fayles. 122
-
Dawber. 302
-
Gould and Masters. 303
-
Hansom and Butler. 304
-
Hayes. 305
-
Heneghan et al. 306
-
Hong and Chew. 307
-
Johnston and Paley. 308
-
Kiff et al. 309
-
Knight et al. 310
-
Kung et al. 311
-
Manning et al. 312
-
Parish et al. 313
-
Platzer et al. 314
-
Schon. 36
Mindfulness-based stress reduction
-
Bazarko et al. 318
-
Beddoe and Murphy. 319
-
Brady et al. 320
-
Cohen-Katz et al. 321
-
de Vibe et al. 322
-
Foureur et al. 323
-
Geary and Rosenthal. 324
-
Goodman and Schorling. 325
-
Hallman et al. 326
-
Irving et al. 327
-
Mackenzie et al. 328
-
Martin-Asuero and Garcia-Banda. 329
-
Marx et al. 330
-
Moody et al. 331
-
Poulin et al. 332
-
Rosenzweig et al. 333
-
Shapiro et al. 334
-
Shapiro et al. 335
Appendix 6 Extended review of theories regarding mechanisms by which Schwartz Rounds may work
This appendix is a fuller version of the discussion of relevant theories and their link to Schwartz Rounds presented in Chapter 3 (literature review). The appendix aims to meet the following objective:
-
review the evidence base regarding reflection, group work and disclosure/discussion of emotional/challenging events for the mechanisms by which Rounds may work and scope the reflective learning literature.
In theorising about how Rounds might work, we needed to try to unpack the ‘black box’ of what happens in the monthly 1 hour of Schwartz Rounds. To do this, we drew on realist methodology, which uses the term ‘mechanisms’ to describe how interventions work. This initial theorising informed the development of our survey (see Chapter 2), our initial programme theory and the interpretation of our study findings (see Chapter 8).
Disclosure
Definition
Disclosure is the action of making new, or secret, information known. In psychological terms, it is the ‘social sharing of emotion’. 39
Sidney Jourard was a pioneer in the field of self-disclosure. He hypothesised that human beings can achieve health and the fullest personal development only when they take the risk of being themselves with others:
You cannot collaborate with another person toward some common end unless you know him. How can you know him, and he you, unless you have engaged in enough mutual disclosure of self to be able anticipate how he will react and what part he will play?
p. 3336
Theories regarding how disclosure works: conditions that allow disclosure to happen and responses to it
Two main theorists on the psychological aspects of disclosure are Rimé and Pennebaker. Rimé and colleagues39–41 have focused on how individuals socially share emotions with others following an emotional event, and the effects of this on emotional recovery. Pennebaker and colleagues35,42–44 have focused on the effects of disclosure of emotional events on physical and psychological health.
Stressors can cause emotional disturbance by challenging people’s basic and often optimistic beliefs about self and the world, such as sense of control, self-worth and coherence. 46 There are two important processes in the writing or talking about a traumatic event:
-
the need to construct a story or explanation of an event
-
the importance of labelling emotions. 35
Emotion is an essential aspect of describing trauma. People experience greater health benefits if they share emotions and thoughts surrounding trauma than if they share facts. 42,45 Pennebaker43 argues that using language to label an emotion/experience creates a structure, which facilitates understanding of the event. Similarly, Lepore et al. 46 examined the effect of disclosure on adjustment to emotional stressors and, specifically, the mechanisms by which the disclosure supports emotional adjustment. Lepore et al. 46 put forward two hypotheses. The completion hypothesis postulates that putting one’s experiences into language allows individuals to impose a narrative around it, making it comprehensible to themselves and others. Responses from a supportive audience may suggest ways of coping, or reframe the experience more positively. This should allow the individual to adjust to the experience. The desensitisation hypothesis argues that expressive acts allow people to form new associations with trauma-related stimuli. The results of Lepore et al. ’s46 study most strongly supported the completion hypothesis. Conversely, actively inhibiting our thoughts and feelings ‘gradually undermines the body’s defences’,35 which leads to reduced physical well-being (p. 13). Confronting significant events helps us understand and assimilate the event, which improves physical and emotional well-being. 35
Of all emotions, people are least likely to share feelings of guilt or shame. 39 Non-disclosure is associated with anticipation of negative interpersonal responses to disclosure (e.g. labelling, judging). 47 Following on from this, the benefits of disclosure vary according to the listener’s response. 45,46,48 Chaudoir and Fisher45 developed the disclosure processes model to assist individuals in maximising the likelihood of benefit from disclosure. 45 A framework with which to examine when and why interpersonal disclosure was put forward. The five main components of the process are:
-
antecedent goals:
-
approach-focused goals (e.g. to pursue positive outcomes such as educating others, understanding, and stronger relationships)
-
avoidance-focused goals (e.g. prevent negative outcomes such as social rejection and conflict)
-
-
the disclosure event itself:
-
content (e.g. emotional; depth)
-
reaction from confidant (e.g. supportive vs. unsupportive)
-
-
mediating processes: alleviation of inhibition, social support, changes in social information
-
outcomes:
-
individual (psychological, behavioural, health)
-
dyadic (trust)
-
social/contextual
-
-
feedback loop.
Nils and Rimé48 also tested a model of when and how sharing emotions is beneficial. They identified two responses to disclosure:
-
empathic mode – expected to buffer emotional distress temporarily (feel better)
-
reframing mode – anticipated to grant emotional recovery (basic assumptions positively modified).
However, when the disclosure of events is invalidated, any benefits may be diluted. 46
Application of disclosure theories to Rounds
Drawing on the disclosure theories above, Rounds focus on non-clinical aspects of the patient–caregiver relationship, not problem-solving, and allow individuals to share difficult, challenging and rewarding experiences. Rounds allow individuals to disclose emotional experiences; greater health benefits ensue following sharing of emotions and thoughts rather than sharing facts. Round attendees and panellists are encouraged to be open and honest and discuss their experiences, thoughts and feelings – using language to help understand their emotional response to an event/experience. Effective facilitation by the facilitator/clinical lead can help individuals (re)frame and label their emotions, and thus begin to process and understand them.
The benefits of disclosure vary according to the listener’s response to it. Group interventions mean it is difficult to control others’ reactions to what has been disclosed. However, Rounds are designed to be a safe, confidential space where staff can share their experiences without fear of blame or judgement.
Safe environment
Definition
For effective reflection, group work and disclosure, a safe environment is a prerequisite. Buggins337 argues that space to think, review and learn from experiences should be provided in care settings. It should be a place to unburden and to think about the ‘unconscious processes at work in oneself, the team and the patient population’. 337 This space needs to be regular, dedicated to the task of reflection and properly facilitated.
Theories regarding how a safe environment works: conditions that allow a safe environment to develop and responses to it
Emotional safety
Emotional safety is a state achieved in attachment relationships where individuals are open and vulnerable and trust each other. Emotional safety at work derives primarily from the experience of feeling valued: accepted, recognised and respected.
Emotional safety is one element that generates a sense of community. 50 The first task of the community is to make it safe to tell the ‘truth’, which requires community empathy, understanding and caring. Emotional safety cannot be maintained without an ‘authority structure’ to sustain the community: people need to know what to expect from each other in the community. Boundaries make emotional safety possible in terms of logistics (time, place of group, etc.). Boundaries – or containment – ensure that the group is ‘purposeful, bounded and safe’. 51 Effective leaders (in Rounds this means clinical leads and facilitators) are necessary to construct these conditions. Another element necessary to develop a community is a sense of belonging, which includes ‘faith that I will belong’, ‘acceptance’ by the wider community and ‘paying dues’: a sense of belonging, emotional safety, etc., are not achieved without sacrifice or challenge. 50
Psychological safety
Psychological safety ‘is a shared belief that the team is safe for interpersonal risk taking’. 52 In psychologically safe teams, members feel accepted and respected and think less about the potential negative consequences of expressing themselves. Leaders increase psychological safety through participatory management (empowering members of the group to participate) and inclusive management (inclusion of members in collaboratively addressing concerns). 52
Psychological safety is different from ‘group cohesiveness’, as cohesiveness can reduce willingness to disagree and challenge others’ views (i.e. participants are less likely to take risks). With psychological safety there is a ‘sense of confidence that the team will not embarrass, reject or punish someone for speaking up’. 52 This confidence stems from mutual respect and trust among members. Psychological safety goes beyond interpersonal trust: ‘it describes a team climate characterised by interpersonal trust and mutual respect in which people are comfortable being themselves’. 52
Application of emotional safety theories to Rounds
Drawing on the emotional safety theories above, in Rounds the panellist and audience need to feels emotionally safe to share their story/experience without fear of reprisal or blame. Facilitators foster a sense of psychological safety in the Round through their skills in facilitation, group work and psychological insights. Ground rules and the use of an established protocol for Rounds help to create a confidential and safe environment that, together with a sense of community, is necessary for Rounds to work. The experiences shared are contained as a result of the clear boundaries established. Psychological barriers to reflection in a Round, such as fear of judgement and criticism, may be overcome if the Round is set up as per the established protocol (see Fidelity to the Schwartz Rounds model in Chapter 7). This creates a safe, confidential space for sharing experiences and for reflection.
Reflection
Definition
Reflection is a ‘generic term for those intellectual and affective activities in which individuals engage to explore their experiences in order to lead to new understandings and appreciation’ (p. 3). 53
Theories regarding how reflection works: conditions that allow reflection to happen and responses to it
Theories of reflection as a structured learning activity have been put forward by Dewey54,338 (the founder of experiential learning), Kolb55 (cycle of experiential learning) and Schon36 (the ‘reflective practitioner’). They argue that reflection is a rational act and although emotion is a trigger or catalyst for reflection, its role is limited. In their theories, questions are answered and knowledge is created.
Dewey338 linked reflection and action to create new knowledge. He posited five phases/aspects of reflective thought (cited in Giles and Eyler pp. 79–80):339
-
suggestions
-
intellectualisation
-
the hypothesis
-
reasoning
-
testing the hypothesis in action.
According to Dewey,338 ‘the function of reflection is to bring about a new situation in which the difficulty is resolved, the confusion cleared away, the trouble smoothed out, and the question it puts is answered’ (p. 100).
Kolb’s55 cycle of experiential learning defined learning as ‘the process whereby knowledge is created through the transformation of experience’ (p. 38). In his model, learners move through a cyclic experience from feeling (experience) to watching (reflection) to thinking (learning/concluding) to doing (planning/trying out what you have learned). (Concrete experience → reflective observation → abstract conceptualism → active experimentation.)55
Schon36 explored ‘reflective practice’ and wrote about the ‘reflective practitioner’, that is, ‘the capacity to reflect on action so as to engage in a process of continuous learning’ (pp. 102–4). He distinguished between ‘reflection-in-action’ and ‘reflection-on-action’. Reflection-in-action refers to thinking about something while engaged in doing it (concerned with practising critically). Reflection-on-action occurs after the activity has taken place when you are thinking about what you (and others) did, judging how successful you were and whether or not any changes to what you did could have resulted in different outcomes. Together, these form a reflective process for decision-making and professional growth.
More recently, psychologists and sociologists, including Lazarus,56 Mezirow57 and Goleman,58 have argued that emotion plays a central role throughout the reflective process and that emotion cannot be separated from learning. Linking to the disclosure literature already discussed, through reflective practice we can label the emotions involved in an experience and learn from them.
Lazarus56 argues that emotions cannot occur without ‘cognitive appraisals’. The term ‘cognitive appraisal’ highlights the complex, judgemental and conscious process that must often be involved in appraising an event. In this process, individuals respond to an experience by asking, implicitly or explicitly, the following questions:
How relevant is this event for me? Does it directly affect me or my social reference group? (relevance)
What are the implications or consequences of this event and how do these affect my wellbeing and my immediate or long-term goals? (implications)
How well can I cope with or adjust to the consequences [of this event]? (coping potential)
What is the significance of this event with respect to my self-concept and to social norms and values? (normative significance)
Scherer et al. (p. 94)340
Individual responses to these questions dictate the labelling of the emotion involved in the experience.
For example, Mezirow57 defines transformative learning as the process of individual critical reflection followed by the sharing of ideas with others to validate insights and culminates in action taken on the individual and collective reflection. Mezirow asserts that examining our outlook on the world, and challenging the assumptions and preconceptions underlying our values and beliefs, can be emotionally threatening. Conversely, he suggests that self-reflection can empower us to be more open and emotionally capable of change.
Emotional intelligence is said to be a highly complementary theory to reflective practice. 58 Self-awareness and emotional growth increase through the development of interpersonal and intrapersonal skills and social relationships. For emotional intelligence, individuals need to understand not only themselves, but also others and their feelings. As such, empathy is key to emotional intelligence. 59 For a person to ‘grow’, they need an environment that provides them with genuineness (openness and self-disclosure), acceptance (being seen with unconditional positive regard) and empathy (being listened to and understood). 60
Lawrence-Wilkes and Ashmore64 developed a model of critical reflection that acknowledges social context. Reflective rational enquiry is a combination of self-reflection (self) and collective reflective communications (self plus others). This leads to a wider reflective approach and creates shared knowledge at the micro and macro levels.
Barriers to reflection can be practical (e.g. finding the time,55 location) and/or psychological (e.g. fear of judgement, criticism). The timing of reflective practice is crucial, especially in relation to stressful/tense experiences. A review held soon after an incident is deemed ‘hot’ (emotive): it is subjective and influenced by emotions. Reviews held later on are ‘cold’: emotions have cooled and the reflective practice is clearer, more balanced and objective. This can lead to improved reflections. 61 The place in which an individual reflects can also be significant, as it can have an effect on their thinking (e.g. stimulate/unlock or inhibit feelings).
Ixer62 created guidelines for engaging in reflective practice. He suggests that individuals need non-judgemental support, to feel ‘safe’, a role model (e.g. a mentor who reflects on their own practice), opportunities for reflection, and time and energy. 63
Application of reflection theories to Rounds
Drawing on the reflection theories above, Rounds are not designed for problem-solving or to determine what can be learned clinically, although learning may occur. Nor are they intended to produce actionable outputs. Theories of experiential learning – where emotion plays a central role in reflection – therefore appear more relevant.
Consideration of the timing of a Round is important and it is, therefore, important that those preparing Rounds carefully consider who they ask to present and when: not too soon, or when the subject matter is too ‘hot’.
Reflective rational enquiry seems particularly relevant to the workings of a Round. Rounds are a combination of self-reflection and collective reflective work, which create shared knowledge at the individual and institutional levels. This may include personal outcomes such as improved well-being, dyadic and team-based outcomes such as better communication and teamwork, and institutional outcomes such as changes to hospital culture. 27,29,30 Finally, empathy is key to reflective practice. Increased compassion and empathy is the main intended outcome of Rounds, both for the individuals attending and also in their interactions with patients and patients’ families.
Social support and group work
Definition
Social support is the perception and actuality that you are cared for, have assistance available from other people and are part of a supportive social network:
[G]roup work provides a context in which individuals help each other, it is a method of helping groups as well as helping individuals; and it can enable individuals and groups to influence and change personal, group, organisation and community problems.
Brown, p. 838
Theories regarding how social support/group work works: conditions that allow social support/group work to develop and responses to it
In Karasek’s65 Job Demand–Control–Support model, when the psychological demands of a job are high and control over the job is low, health status and well-being are reduced. Social support is associated with psychological well-being in the workplace. It can be a problem-focused (e.g. receive tangible information that helps to resolve an issue) or an emotion-focused coping strategy (e.g. used to regulate emotional responses that arise from a stressful event). Social support is hypothesised to work by having either a buffering effect (where it moderates an outcome) or a direct effect (leading directly to something). 65,66,341 Karasek’s model is a ‘buffering model’, as work social support (such as support from colleagues and supervisors) is said to buffer against a high level of job demands/lack of control and thereby protects mental and physical health. 67
Lakey and Cohen’s341 social support theory offers three theoretical perspectives on how social relationships influence health and well-being: (1) the stress and coping perspective – support contributes to health by protecting people from the adverse effects of stress (buffering hypothesis, as per Karasek65); (2) the social constructionist perspective – support directly influences health by promoting self-esteem and self-regulation, regardless of the presence of stress (direct effect); and (3) the relationship perspective – health effects of social support cannot be separated from relationship processes that often occur with support, such as companionship, intimacy and low social conflict (direct effect).
Social exchange theory69 suggests that social change is a process of negotiated exchanges between parties. Human relationships are formed by the use of a subjective cost–benefit analysis and comparison of alternatives. It is the exchange of activities (tangible and intangible), more or less rewarding or costly, between people. Social exchange brings satisfaction when people receive fair returns for their expenditures. It involves a connection and trust with another. Cost could be the effort put into a relationship (e.g. time). Rewards include elements of the relationship that have positive value (e.g. acceptance, support, companionship). The cost–reward imbalance is associated with poor health functioning.
Group work is the opportunity to reflect on, and learn from, the nature of the group interaction itself. The group context and group process is explicitly utilised as a mechanism of change by developing, exploring and examining interactions within the group. Yalom37 proposed a number of therapeutic factors that facilitate this group work. These include universality, altruism, instillation of hope, cohesiveness, catharsis, interpersonal learning and self-understanding.
Smith’s342 group work principles outline three foci for group workers: (1) think group, (2) attend to purpose and (3) stay in touch with self. ‘Thinking group’ refers to focusing on the group as a whole (group context). Individual growth and development is seen as something that emerges out of group interaction. ‘Attending to purpose’ refers to the individual and collective goals of the group. Individuals need to bear in mind the nature of the group and the context within which they are working. Papell and Rothman343 refer to three models regarding the nature of groups: (1) remedial (the aim of the group is individual social adaption, (2) reciprocal (where the aim is to strengthen mutual aid and to mediate between individual and society and (3) social goals (to further social justice through collective social action).
Application of social support and group work theories to Rounds
Drawing on the social and group work theories above, Rounds are a group intervention with social support provided through group reflection. Social identification as a member of a Round may serve to boost self-esteem as individuals have a sense of belonging to an organisation-wide forum that allows them a safe space to reflect on challenging and emotional experiences. The cost–benefit analysis of social exchange theory appears pertinent to how a Round works. Costs might include the courage, emotional effort and time put into sharing one’s story publicly (panel preparation, sharing the story during the Round). Rewards may include increased compassion and empathy for others, improved well-being (e.g. reduced stress) and camaraderie (better work engagement and teamwork).
When members tell their story to a supportive audience, they can obtain relief from feelings of shame and guilt. Yalom’s37 therapeutic factors appear relevant to how Rounds work and are explored further in Chapter 8.
In addition to work reviewing theories in the literature which informed our initial programme theory (see Chapter 8) and the selection of items for our survey (see Appendix 1), we also thought it important to understand more about the development and origins of Rounds in Boston, MA, USA, and any programme logic behind their development (see Chapter 3).
Appendix 7 Boston interview schedule
Origins of Schwartz Rounds
-
Can you tell me more about the history and thinking behind Schwartz Rounds?
Prompts:
-
Were the Schwartz Rounds modelled on an existing intervention? If so, what?
-
What was the underlying thinking behind Schwartz Rounds?
-
What were the initial thoughts and underlying assumptions behind Schwartz Rounds?
-
Why were Rounds needed?
-
How did you anticipate they would work? Has this view changed?
-
How did you think Rounds might affect staff, and patient care?
-
Who would benefit? Which health-care settings did you think Rounds might be most useful for?
Current thinking behind Schwartz Rounds/US experiences (context–mechanism–outcome configurations)
-
What elements did you consider important when designing Rounds to make them work?
Prompts:
-
What ideas can you think of that explain how Schwartz Rounds work?
What impact do you think Rounds have on presenters and audience, wider organisation?
Prompts:
-
Intended, unintended consequences? Any surprises?
What US contexts/settings have they been tried in? (Contexts.)
Prompts:
-
Geographical areas/states? Types of organisation? Groups of participants?
-
Have you noticed differences in how Rounds work in different areas, settings, groups of people? If so, what are these differences?
-
What lessons have been learnt from US Schwartz Rounds?
-
How have they been adapted to suit different settings/professional groups/types of organisation? Which contexts do they work best in and why? What settings are Schwartz Rounds best/least suited to and why? What groups of professionals are Schwartz Rounds best/least suited to, and why?
-
What communication networks, both formal and informal, have developed between Rounds providers in the USA, if any?
-
Have you made any changes to the way Rounds are run following their implementation in the UK?
Fidelity and quality assurance
-
How do you manage fidelity and quality assurance issues with the USA and beyond?
Spread of Rounds
-
How and where have you publicised Rounds more widely?
-
What other countries have adopted/will be adopting them?
-
Do you have any data on the uptake of Rounds and is it related to any specific incidents?
-
Do you have a strategy for spreading Rounds? If so, what?
How are you monitoring and evaluating Schwartz Rounds? (Evaluation.)
Own experience of Rounds
-
Can you describe the most memorable/most successful Round you’ve been to?
Prompts:
-
Why was it memorable/successful?
-
How do you manage to keep coming up with ideas for presentation?
Have there been any Rounds which you’ve thought did not really work?
Prompts:
-
Tell me about that/those Rounds? If what way/s did they not work?
-
How and why did they differ from other Rounds you’ve attended?
General observations
-
What did you see as the advantages and disadvantages of Schwartz Rounds?
-
What lessons have you learnt about Schwartz Rounds?
-
From your experience, what would be the three top tips you would give someone wishing to start Schwartz Rounds in their organisation?
Future plans
-
What are your future plans for Schwartz Rounds?
And finally
-
Is there anything else you would like to say?
Appendix 8 Mapping provider profiles
| Type of site | Sizea | Location | Survey and/or interview completed? | Pseudonym | Year commenced first Round |
|---|---|---|---|---|---|
| Acute | Large | Southern England | Both | Ashb | Before 31 December 2012 |
| Acute | Small | Southern England | Both | Thames | 2011 |
| Acute | Large | Northern England | Both | Helford | 2012 |
| Acute | Small | Northern England | Both | Severn | 2012 |
| Mental health | Medium | Northern England | Both | Horse-chestnutb | Before 31 December 2012 |
| Acute | Medium | Southern England | Both | Hayle | 2011 |
| Hospice | Small | Southern England | Both | Avon | 2012 |
| Acute | Medium | Southern England | Both | Otter | 2012 |
| Acute | Medium | Southern England | Both | Axe | 2012 |
| Hospice | Small | Southern England | Both | Chess | 2013 |
| Hospice | Small | Southern England | Both | Elbe | 2013 |
| Acute | Medium | Southern England | Both | Misbourne | 2013 |
| Acute | Medium | Northern England | Both | Carmel | 2013 |
| Acute | Medium | Southern England | Both | Looe | 2013 |
| Acute | Large | Southern England | Both | Seine | 2013 |
| Acute | Large | Southern England | Both | Willowb | After 31 December 2012 |
| Mental health | Small | Southern England | Interview | Willowb | After 31 December 2012 |
| Hospice | Small | Southern England | Both | Trent | 2014 |
| Acute | Large | Southern England | Both | Tyne | 2014 |
| Acute | Large | Southern England | Both | Mulberryb | After 31 December 2012 |
| Hospice | Small | Northern England | Both | Exe | 2014 |
| Acute | Medium | Southern England | Both | Ouse | 2014 |
| Mental health | Medium | Southern England | Interview | Clyde | 2014 |
| Mental health | Medium | Northern England | Both | Dart | 2014 |
| Acute | Medium | Southern England | Both | Fal | 2014 |
| Acute | Large | Northern England | Both | Ribble | 2014 |
| Hospice | Small | Northern England | Both | Stour | 2014 |
| Acute | Large | Southern England | Both | Wye | 2015 |
| Acute | Large | Southern England | Both | Kennett | 2014 |
| Acute | Medium | Northern England | Interview | Tiber | 2015 |
| Acute | Small | Northern England | Interview | Douro | 2014 |
| Acute | Medium | Southern England | Both | Rhine | 2014 |
| Acute | Large | Southern England | Both | Mississippi | 2014 |
| Acute | Large | Northern England | Both | Mackenzie | 2014 |
| Mental health | Medium | Northern England | Interview | Taff | 2014 |
| Acute | Large | Northern England | Both | Beck | 2014 |
| Acute | Medium | Southern England | Both | Congo | 2015 |
| Community | Small | Southern England | Both | Nile | 2014 |
| Acute | Medium | Southern England | Interview | Neath | 2014 |
| Acute | Medium | Southern England | Both | Tay | 2015 |
| Hospice | Small | Southern England | Both | Elderberry | Before 31 December 2012 |
| Hospice | Small | Southern England | Both | Wharfe | 2014 |
| Hospice | Small | Southern England | Both | Esk | 2014 |
| Hospice | Small | Southern England | Both | Eden | 2012 |
| Acute | Large | Southern England | Survey | Cedarb | 2009 |
| Acute | Large | Southern England | Survey | Fowey | 2011 |
| Acute | Medium | Southern England | Interview | Moselle | 2014 |
| Acute | Small | Southern England | Survey | Conway | 2015 |
Appendix 9 Phase 1 mapping: secondary data sources and analysis
Secondary data
Secondary data, available publicly, were collected for the 115 provider organisations in England identified as running Rounds by the most up-to-date PoCF database for Schwartz Center Rounds providers. Any organisation implementing Rounds had to obtain a licence from the PoCF; therefore, these databases are a reliable data source. Providers’ details were held by the Point of Care programme at The King’s Fund (up to March 2013) and the PoCF (from April 2013 onwards). By mid-July 2015, there were a total of 115 organisations in England running Rounds. These organisations were categorised as adopters. Secondary data were also collected from non-adopters in order to be able to contextualise and compare the characteristics of organisations running Rounds and meet the study’s objectives for phase 1: to map and profile providers running Rounds. Not all data types were available for all adopters or non-adopters; comparable data were often not available for non-NHS providers. The type and availability of secondary data collected for adopters and non-adopters and the sources of these data are presented below and summarised in Table 30.
| Data | Source | Variable characteristics |
|---|---|---|
| Date of adoption | PoCF database | Interval: calculated based on number of days from contract sent to 15 July 2015 (end of phase of mapping) |
| Location |
NHS Digital Hospital Estates and Facilities Statistics Report 2013/14 Provider’s own website |
Nominal: London South East South West East of England West Midlands East Midlands Yorkshire and the Humber North East North West |
| Size |
NHS Digital NHS Workforce Statistics Hospice UK Provider’s own website |
Ordinal: small, < 2000 staff; medium, 2000–4999 staff; large, ≥ 5000 staff |
| Type |
NHS Digital Hospital Estates and Facilities Statistics Report 2013/14 Hospice UK Provider’s own website |
Nominal: Acute trust Mental health/learning disability trust Community trust Ambulance trust Hospice Other |
| Quality of care | ||
| Staff overall engagement score | Picker Institute Europe – NHS [www.nhsstaffsurveys.com/Page/1021/Past-Results/Historical-Staff-Survey-Results/ (accessed 17 July 2018)] | Interval: maximum score of 5 |
| Overall patient experience score | NHS England [www.england.nhs.uk/statistics/statistical-work-areas/pat-exp/ (accessed 17 July 2018)] | Interval: maximum score of 10 |
| Priority bands for inspection | CQC [www.cqc.org.uk/download/a-to-z/hospital-imonitoring-october-2013 (accessed 17 July 2018)] | Nominal: band 1 (highest priority for inspection) and band 6 (lowest priority) |
The type and availability of secondary data collected were as follows.
-
The date when Rounds were adopted by each provider. The time of adoption was defined as the date on which an organisation – known to be running Rounds – was sent a contract by the PoCF to implement Rounds, as this data set was the most complete. Data were available for all providers in the adopters category.
-
Information on the location of providers adopting rounds based on the postcode (of main/headquarters site). Data were available for all providers. Information was collected through NHS Digital and through organisations’ own websites.
-
Information on the size of providers by number of staff in each organisation (small, < 2000 staff; medium, 2000–4999 staff; large, ≥ 5000 staff). For NHS providers this information was collected through NHS Digital. For non-NHS providers the information was sourced from the organisations’ own websites where available. It was not available for some non-NHS organisations.
-
Information on provider type, categorised as acute trust, mental health/learning disability trust, community trust, ambulance trust and hospice. An additional ‘other’ category was used for providers that did not fit into these categories, including a prison, a university medical school provider and a private hospital. An estimated total number of each provider type was also collected (to calculate an approximate rate of adoption) from NHS Digital for NHS trust provider types and from Hospice UK for hospices. Data were not available for organisations in the ‘other’ category (e.g. private hospitals, prisons and university medical schools).
-
Publicly available data on quality of care for the NHS provider organisations included:
-
NHS staff survey ‘overall engagement score key finding’344 (introduced in 2010) where possible 3 years prior to the adoption of Rounds. This overall score combines the scores of three dimensions of engagement (staff advocacy, motivation and involvement), converting them into an overall index of staff engagement. This score was selected as the overall engagement score and has the strongest relationship with the general health and well-being of NHS staff. 345 Data are available for NHS providers only.
-
NHS patient survey ‘overall experience score’ for each trust 3 years before they adopted Rounds from a national inpatient survey: this score is derived by calculating the average of five domain scores. 346 Data were available for only some NHS providers.
-
Risk bandings: the 2013 ‘priority bands for inspection’ from the CQC for acute, mental health and learning disability trusts. 347 Data are available for only some NHS providers and are not available for non-NHS organisations. Band 1 denotes organisations that are the highest priority for inspection, and band 6 denotes those that are the lowest priority.
-
Analysis of secondary data
All secondary data were prepared, examined for completeness and anomalies, and analysed quantitatively through SPSS version 22. The sample denominator differed by type of data indicated above, as data were not available for all organisations. The analysis results are based on the data available and this is noted in Tables 6–8 presenting different data. The first level of data analysis utilised descriptive statistics using frequency and percentages (based on the non-missing sample size) for all categorical variables (e.g. type of provider and location) and mean, SD, median, maximum and minimum numbers for continuous variables (e.g. date of Round adoption and quality-of-care indicators) accordingly. This first level of analysis aims to provide a broad picture of the characteristics of organisations providing Schwartz Rounds in England and to explore how many and what types of organisations were running Rounds.
We also used Rogers’71 diffusion of innovation theory to identify which organisations fit into the five categories of adopters. The categories of adopters are innovators (2.5%), early adopters (13.5%), early majority (34%), late majority (34%) and laggards (16%). The date the contact was sent to the organisation by the PoCF was used as the date of adoption and, based on this, organisations were mapped onto the categories of adopters outlined by Rogers. 71
Data were then tested for possible relationships, associations and significant differences based on variables identified above. The chi-squared test (χ2) was used to examine relationships between categorical variables (e.g. diffusion of innovation category – innovators, early adopters, early majority, late majority and laggards by type, size and location of organisations). Owing to the small sample size of adopters in each diffusion of innovation category, basic assumptions of the test were not met (e.g. minimum expected frequency > 5) and no meaningful statistical relationships were identified through this analysis. In addition, when variables included ordinal or interval data (e.g. examining relationships between diffusion of innovation categories and quality-of-care indicators’ data) the Spearman’s correlation coefficient (rs) test was used. Some correlations between these variables were identified and presented in the main report. Finally, the Mann–Whitney U-test (U) was used to identify differences between adopters and non-adopters and quality-of-care indicators. The level of significance is set at a p-value of < 0.05.
Appendix 10 Mapping survey
Appendix 11 Interview schedule used in telephone interviews in phase 1 (mapping)
Appendix 12 Sustaining Rounds
| Theme | Illustrative quotations from interviews |
|---|---|
| Attendance at Rounds: ‘getting people to come to the meetings’ | |
|
Maintaining or increasing attendance was perceived to be crucial to securing the future of Rounds and was a concern for most respondents, who considered achieving good attendance, however this was defined, as one of the main challenges they faced. Some respondents reported trends in Rounds’ attendance that they found worrying, for example attendance that was declining, erratic, generally low or not increasing as anticipated Attendance was one of the criteria used by respondents to judge the success of a Round, although a few respondents argued that the number of people attending per se did not determine the quality of a Round Regardless of trends in attendance or the length of time Rounds had been running in an organisation, respondents saw promoting and publicising Rounds as key to drawing in an audience. Most respondents reported following PoCF guidance on using multiple approaches to publicising Rounds, with the aim of informing everyone in the organisation. Some respondents who described multidimensional strategies for publicising Rounds also indicated that they had access to communications expertise and resources, through steering group membership or other organisational networks. Despite their efforts to promote and publicise Rounds in a multiplicity of ways, some respondents were daunted by the task and felt that the message about Schwartz Rounds was still not reaching everyone in the organisation Respondents wanted to give all groups of staff in the organisation the chance to experience a Round. Rounds’ teams in most organisations had experimented, or were planning to experiment, with holding Rounds on different days and at different times to give part-time staff, those working shifts and those with particular work patterns or fixed weekly commitments the opportunity to attend. Fewer respondents had altered where Rounds were held, often because organisations on a single site had only one venue with sufficient capacity for the meeting. Many hospital Rounds’ teams had concluded that lunchtime brought the best level of attendance, and varied the day to enable different people to attend. However, they recognised that lunchtime Rounds were excluding particular groups of staff, most notably ward nurses Respondents identified a range of different groups that they felt were under-represented among Rounds attenders in their organisation. The groups mentioned varied and were specific to each organisation, including board members, senior managers, doctors, ward staff, nurses, CNSs, porters, maintenance staff, domestics and AHPs. However, front-line clinical staff, particularly ward nurses and doctors (of all stripes), were most frequently said to be under-represented among Rounds attenders. Top managers and board members were another group whom respondents particularly wanted to attend, not only to experience Rounds but also to demonstrate their endorsement of them. Respondents in some organisations claimed good attendance by members of the executive team, but others expressed disappointment that authoritative figures were very rarely present at Rounds Introducing Rounds to people who had never experienced one was seen as particularly important by respondents, who argued that only by experiencing a Round would individuals understand what they could offer and make an informed choice about whether or not to attend in future The other important challenge in maintaining attendance at Rounds discussed by respondents was to continue to find topics and panellists that would provoke curiosity and attract people to Rounds. This was a concern for respondents in organisations where Rounds had been running for several years that the ‘novelty’ had worn off and other new initiatives made competing claims on people’s time. Respondents also emphasised using a wide range of networks, by involving steering group members, departments and senior managers, to identify topics and panellists (see sustaining Rounds theme on planning and producing Rounds) |
How do we get the news out there to people, [get them to] realise how important this is? I know this does not suit everybody [. . .] we do not expect people to be forced to come along but [. . .] I am sure that there are many, many, people out there who would benefit from the Schwartz Rounds who have not heard about them or who have not got the time to come, which is a real shameKennett-155-Clinical-LeadThere are people that are still unaware. [. . .] Even though we have advertised it quite widelyMackenzie-338-FacilitatorIt’s incredibly difficult to know how to get messages out to people, so we’ve done a number of things. We’ve had our comm[unication]s team involved, so it has been in [. . .] the weekly trust e-newsletter. Flyers have gone out to all the ward areas and posters put up within the hospital and [. . .] our administrator e-mails out a week before. Still we’ve got a problem, which is not about Schwartz Rounds, it’s about communication in general. E-mails become a not very effective method of communication because you get about 100 a day and, if you don’t happen to work at a desk, that’s not manageable. [. . .] So quite a lot of it ends up being on word of mouthWye-156-Clinical LeadWe’ve kept them at lunchtime [. . .] because we’ve had a good attendance, we haven’t changed times or venuesBeck-336-FacilitatorWe do now vary the time and the day of the week. Now that was because there were groups of staff that were excluded otherwise. So for example the community team and [. . .] social workers, therapists, others. [. . .] the best time for them is really first thing in the morning which is why we introduced a breakfast round, before they go out, so they’ll tend to come in here first. And lunchtime is particularly difficult for the ward, so actually we introduced the [. . .] half past two to half past three early teatime round, particularly because [. . .] that’s usually when they have extra staff on to allow time for training and handoverAvon-391-FacilitatorIt’s very difficult to get a time that works for everybody [. . .] we alternate [lunchtime and afternoon] [. . .] we’ve thought quite carefully about timings and [. . .] you feel like you’re going round in circles because whenever you suggest a time it’s not right for somebodyEden-122-Clinical LeadThe biggest challenge really has been getting people from the wards to come because they are so busy. [. . .] I think that’s because we run on quite a thin line of staffing and it’s difficult to release staffNeath-327-FacilitatorThere’s always a lot of scepticism when you bring in something new. [. . .] I haven’t really won over the medical staff [. . .] I’m not trying to force it down anyone’s throat, I think we’re trying to do it by word of mouth, we’re just putting it out there and, hopefully, people’s curiosity will bring them along. But, I guess, that’s been a bit frustrating, it’s a bit noticeable that a lot of the medical staff aren’t coming along, but again, with clinics and stuff it’s not always easyTiber-151-Clinical LeadThe ongoing challenge is around releasing staff from pressurised clinical areas to attend. It is an ongoing challenge and it always will be. That’s the way you work in health care I guessHorse-chestnut-194-Clinical LeadWe’ve had some non-clinical Rounds where we hoped we’d get better attendance from the non-clinicians, but actually that’s not really what happenedEsk-123-Clinical LeadYeah, so more people know about Schwartz Rounds, so if they’ve been to one, they’re more likely to come to anotherWillow-178-Clinical LeadEach of the directorates pick the topic [for the Round] and advertise it and round up support. [. . .] The really good directorates almost set the topic by talking about it at their team meetings, at their daily huddles, and picked out the topics that were relevant to people. Then kept talking about it when they were forming it and [. . .] [it’s] common sense, isn’t it, that the most engagement gets you the most attendance at the actual eventSevern-395-FaciliatorYeah, if people find that it’s the same old, same old, you know, they’re not going to want to keep comingWharfe-323-Facilitator |
| Rounds teams’ workload, responsibilities and resources | |
|
One of the main themes in the interviews was that respondents found producing Rounds on a regular basis more demanding and time-consuming than they had anticipated. This was particularly an issue for clinical leads and facilitators who had been organising and facilitating Rounds for some years, on a voluntary basis, in addition to busy and demanding jobs, and often without dedicated time identified for producing Rounds. Despite their evident commitment to and enthusiasm for Rounds, some were finding it difficult to maintain the momentum with limited resources. Similar issues were also raised by respondents who had started producing Rounds much more recently. Respondents drew attention to the amount of time they spent promoting, planning, preparing and facilitating Rounds; the need to take responsibility for driving all stages of the process, which meant that Rounds were constantly on their minds; difficulties finding panellists; the time required for panellist preparation; and the unremitting nature of the work involved in producing a Round every month The pressures were felt most acutely in organisations in which a few individuals were perceived to be shouldering most of the workload and responsibility for producing Rounds. Resources considered essential for sustaining Rounds and identified as lacking by some respondents were administrative assistance; clinical lead input; sufficient trained and experienced facilitators; active and consistent involvement of steering group members; and support from senior management. The ‘top tips’ respondents gave in the interviews highlight the importance of these resources, without which some Rounds teams struggled to continue to produce Rounds. Respondents were also concerned about maintaining the quality of the Rounds that they produced and about remaining faithful to key features of the Schwartz model Rounds steering groups in particular were seen by respondents as having the potential to increase the resources available to Rounds teams, by contributing ideas, access to personal and organisational networks, skills, authority, time and practical help. However, in some organisations, steering group attendance was said to have declined and few steering group members were actively involved in producing Rounds Some respondents referred to the impact of the pressures on themselves and others producing Rounds as ‘Schwartz fatigue’, which they recognised needed to be addressed to sustain Rounds Thus, Rounds teams were looking for ways to increase their resources and share or reduce the workload of producing Rounds; to bring in new blood and ideas; to change how they planned and produced Rounds; and to maintain their energy and enthusiasm. In general terms, the actions respondents described to increase sustainability of Rounds included: |
Respondent:I’d quite like to share the workload out a bit. It’s not just an hour a monthInterviewer:How much time do you think that it takes?Respondent:I would say probably at least 2 days a month. [. . .] the Round plus steering group is probably half a day. There’s [. . .] meeting and doing the panel prep beforehand and quite a bit of that is just finding times to meet with the panel [. . .] one or two or several meetings depending on the type of Round it is. I am now much more involved in finding cases and panellists. There’s lot of trying to find panellists. [. . .] There is a feeling of holding more of the responsibility [. . .] than I anticipated I would. [. . .] I get involved in doing some of the debriefing afterwards, some of the writing up afterwards and using that in the advertising, making sure that the admin team have the information that they need, they tend to come to me. [. . .] it takes up a chunk of time [. . .] keeping them alive and [. . .] fresh in the organisation. So I reckon it averages out probably about 2 days a month. [. . .] So, it just feels like a constant, there’s work to be done on Rounds all the time, it doesn’t fit neatly into 2 days. It’s a constant, just interweaved into everything elseAsh-400-FacilitatorPreparing for [Rounds] probably takes up much more time than I anticipated and particularly because the other co-facilitator is part time, so I often feel I’m doing a lot of the [. . .] identifying and preparing panel members and organising steering groups and that sort of thing. And the reports and presentationsStour-355-FacilitatorI find the whole of making it work rests on a handful of people in this organisation. [. . .] it’s not self-sustaining, it needs to be driven all the time. And I think that’s a big challenge for those who are the drivers and have other things to do as well. So if we all left the organisation I’m not sure it would continue and I don’t know what that means reallyOuse-363-FacilitatorSustaining the Rounds, I mean, I think if we weren’t prepared to work so hard, we would have a problem. But we’re both [clinical lead and facilitator] very committed to them [. . .] I think that’s really important. [. . .] I do have to be prepared to put as much time in as it will take, and some months that’s really quite difficultExe-135-Facilitator[Producing Rounds] occupies a lot of our thinking and it takes up quite a lot of time and there’s a responsibility to delivering [. . .] it’s something that you have to take on as a positive thing [. . .] it’s not something that you could do unless you were enthusiastic about the process and thought it was worthwhileRibble-161-Clinical LeadIt’s quite a big thing to get organised month after month after month, it takes more time than we thought it was going toSeine-378-FacilitatorWe’ve got a very focused and tight-knit steering group that work really well together. So the main challenge of Rounds is the actual time everything takes. [. . .] how time-consuming it is for [. . .] the three of us, the clinical lead and the two facilitators, to get together to keep the momentum going, because once you’ve done one Round you need to start preparing the next Round and that’s quite hardOuse-164-Clinical LeadThere has been no admin support at all, so it falls to [one of the rest of us] [. . .] it takes about 2 whole days a month to prepare for a Round and do all the administration [. . .] So it’s quite an addition really to somebody’s role. [. . .] So that’s been the biggest challengeLooe-381-FacilitatorWe’ve [held Rounds] now for [. . .] maybe 4 years in January, and I would say it’s fairly firmly embedded, although it takes a huge amount of work and effortElderberry-324-FacilitatorI’m the clinical lead and we have one other trained facilitator. [. . .] We need to swell our numbers because we’re getting a bit of Schwartz fatigue. [. . .] Because we are both part-time, we only overlap 1 day a week, if that, so actually the sustainability issue is quite key for usEsk-123-Clinical LeadAfter 2 years [. . .] we were a bit exhausted [. . .] and it’s not lack of enthusiasm but it’s just hard because you’re all putting in the time in general over and above your day job [. . .] you may have some nominal time for it in your job plan, but it would generally be nominal rather than actualOtter-190-Clinical Lead |
Appendix 13 Further details of survey
Recruitment of participants
The inclusion and exclusion criteria for participation were as follows. Note that the categorisation into different groups could not happen until after the follow-up survey.
Inclusion criteria:
-
(all groups) staff employed by the provider who had the opportunity to attend Rounds, and who had not attended Rounds before the baseline study
-
(regular attenders) staff who had attended at least 50% of available Rounds between the two surveys
-
(irregular attenders) staff who had attended at least one Round but fewer than 50% of available Rounds between the two surveys
-
(non-attenders) staff who had not attended a Round previously, and did not attend one during the study period.
Exclusion criteria:
-
people not employed by the provider
-
staff who did not have the opportunity to attend Rounds (e.g. in providers where Rounds are limited to one part of the organisation, or staff who do not work at times that Rounds operate)
-
staff who had attended Rounds previously, including with a previous employer.
The method of participant recruitment and questionnaire administration was substantially different for the attender and non-attender arms. In both cases, potential participants were first asked whether they had previously attended any Rounds: if they had, then their participation would not continue.
Attenders
Between one and four members of the research team attended up to four successive Rounds (usually monthly) at each site, sometimes supplemented by up to two research nurses based there. A buffet lunch was usually served in the 30 minutes before the start of the Round, so the researchers would be in place by the start of this period; as attenders signed in, a researcher approached them.
If someone was attending a Round for the first time, the researcher would give a summary (< 30 seconds) of the study, and invite them to take a questionnaire and information sheet and a yellow cover sheet, which asked for their preferred contact information and consent to contact them in the future. The questionnaire and cover sheet would include a unique ID number that would allow the two to be linked, and so that the follow-up survey could be linked to the respondent.
The questionnaire was short enough that people who arrived at least 10 minutes early could complete it before the start of the Round. They would be encouraged to do this if they agreed to take part in the study. If there was not enough time to complete the questionnaire before the Round, they would be encouraged to complete and return their yellow cover sheet for contact information and consent immediately, and return the questionnaire either in person after the Round or by post later (a return-paid envelope was included).
If the cover sheet was returned but the questionnaire was not, a reminder would be sent after 2 weeks, and then others after 4 and 6 weeks. This would be either by e-mail or by post depending on the communication preference stated (in the vast majority of cases this was e-mail).
The information sheet and consent form stated that a follow-up questionnaire would be sent after 8 months if the original questionnaire was returned. Therefore, for everyone who returned a questionnaire at or after their first Round, another questionnaire was sent 8 months later: a paper copy if post was preferred, or a link to an electronic (Qualtrics) version of the survey in an e-mail. Reminder letters for the follow-up questionnaire were sent (via the same method) to non-responders after 2, 4 and 6 weeks.
Participation was incentivised by offering a prize draw of four £50 shopping vouchers at each site to attenders who completed both questionnaires.
Non-attenders
Detailed instructions were given to a relevant person within each site (either a research nurse, a human resources employee, or another individual with the relevant permissions) about how to select a random sample of 250 employees from a list of all staff in the organisation using Microsoft Excel. This would normally be done around 1 month before researchers attended their first Round in that site. An e-mail was sent to all selected individuals to inform them about the study, and to give them an opportunity to opt out at that stage.
Names and e-mail addresses were entered into a sample file in the online survey software Qualtrics, which sent an e-mail to each person with a link to the online version of the survey, as well as including all relevant information (including that participation was voluntary). Participants were offered to be sent a paper version of the questionnaire if that was their preference.
Reminder e-mails to non-respondents were sent after 2, 4 and 6 weeks. The questionnaire also included a box for respondents to indicate that they gave consent for their data to be used, and also to be contacted again after 8 months. The follow-up survey was sent to all respondents 8 months later, with reminder e-mails to non-respondents sent after 2, 4 and 6 weeks.
In the same way as for the attenders, participation was incentivised by offering a prize draw of four £50 shopping vouchers at each site to people who completed both questionnaires (they were eligible for this draw even if they had attended one or more Rounds before the follow-up survey).
Questionnaire items
Work engagement
This was measured using the three-item ‘motivation’ section of the NHS Staff Survey [www.nhsstaffsurveys.com (accessed 17 July 2018)], which is itself a brief version of the UWES-9. 136 Responses were given on a five-option frequency scale, scored from 1 (‘never’) to 5 (‘always’). An example item is ‘I am enthusiastic about my job’.
Psychological well-being
This was measured via the 12-item version of the GHQ-12. 348 The GHQ-12 is a widely used and well-validated measure against the DSM-IV criteria for depression and anxiety. Each item has four possible response options; for example, the item ‘Have you recently (over the past month) been able to concentrate on whatever you’re doing?’ has the response options ‘better than usual’, ‘same as usual’, ‘less than usual’ and ‘much less than usual’. There are two scoring methods for the GHQ-12. In the ‘Likert’ version, each item is scored between 1 and 4 (4 representing the most negative scenario), and an average score across all 12 items is calculated. In the binary ‘caseness’ version, the number of items where the response was among the two worst categories was calculated. If there were four or more items where this was true, then the respondent was said to be a ‘case’ – that is, they were considered to be in sufficiently poor psychological health that they would benefit from professional intervention (a measure that was validated by Hardy et al. 349).
Self-reflection
This was measured via a six-item subscale of Grant et al. ’s140 scale on self-reflection and insight. The subscale name was ‘self-reflection’, and responses were made on a seven-point Likert-type scale ranging from 1 (‘strongly disagree’) to 7 (‘strongly agree’). An example item is ‘I frequently take time to reflect on my thoughts’.
Empathy
This was measured via the Empathy Quotient measure. 142 This is a five-item scale, with four response options ranging from 1 (‘strongly disagree’) to 4 (‘strongly agree’). An example item is ‘I am good at predicting how a patient will feel’.
Communication with patients
This was measured via the communication skills with patients subscale of the Self Efficacy scale,144 designed for use by health-care staff. This comprised eight items, scored from 1 (‘not certain at all’) to 10 (‘quite certain’). An example item is ‘How certain are you that you can successfully encourage patients to talk about their feelings?’.
Compassion
This was measured with the Santa Clara Brief Compassion Scale,147 in a version adapted to five items. 148 Measuring compassionate love for others and humanity, each item has seven response options ranging from 1 (‘not at all true of me’) to 7 (‘very true of me’). An example item is ‘I tend to feel compassion for patients, even when I do not know them well’.
Peer support
This was measured with a four-item subscale from a wider tool on job factors. 149 Responses ranged from 1 (‘not at all’) to 5 (‘completely’). An example item is ‘To what extent can you count on your colleagues to back you up at work?’.
Organisational climate for support
This was measured with the four-item support subscale of the Organizational Climate Measure,152 measuring the perceived organisational concern for employee welfare. Responses to each item ranged from 1 (‘definitely false’) to 4 (‘definitely true’). An example item is ‘This organisation tries to look after its employees’.
Absenteeism
This was measured by asking ‘In total, on how many working days during the last six months have you been absent due to sickness?’.
Demographic and other background data measured included age, gender, occupational group, tenure with the organisation, grade and working hours. In the follow-up questionnaire, rather than being asked all of these again, respondents were asked whether there had been any significant changes to their job role in the last 8 months, and, if so, what these had been.
Respondents were also asked whether they had regular contact, occasional contact or no contact with patients as part of their job. If they did not have regular contact with patients, they were invited to skip the questions on empathy, communication with patients and compassion.
Follow-up survey only
Respondents were asked to indicate how many Schwartz Center Rounds they had attended in the previous 8 months. Records were kept of how many Rounds had been held at their site in this time, and from this information the respondent was classified as a regular attender (≥ 50% of Rounds attended), an irregular attender (at least one Round attended, but < 50%) or a non-attender (no Rounds attended).
Attenders only, baseline survey
Respondents were asked why they attended Rounds (open text response).
Attenders only, follow-up survey only
Respondents were asked why they began attending Schwartz Center Rounds (options: ‘A manager/colleague suggested I attend’, ‘I was interested in a topic’, ‘A friend/team member was presenting’, ‘I saw publicity about it and wanted to find out more’, ‘I heard about it because of the research project’, ‘I was asked to present’ or ‘Other’, with open text response accompanying; respondents could tick as many as applied). They were also asked whether or not they always managed to attend Schwartz Center Rounds when they would like to, and if not, what barriers prevented them attending (options: ‘I do not have autonomy over my work schedule’, ‘They occur in a different location from the site in which I am based’, ‘I have moved to an organisation that does not run Rounds’, ‘Announcement of Rounds is at too short notice’, ‘The topics do not seem relevant to me’, ‘The location is not convenient for me’, ‘There is no one to cover my work’, ‘They occur when I am not working’, ‘I am too busy and not able to find the time’, ‘My break is too short’, ‘The time is not convenient’, ‘They conflict with other clinical priorities’, ‘They conflict with other non-clinical priorities’, ‘I am not supported by my line manager to attend’, ‘I have to wait my turn to attend as we rotate attendance amongst the team’ or ‘Other’, with open text response accompanying; respondents could tick as many as applied).
Attenders only, follow-up survey only
Respondents were also asked to say whether or not, when they had attended Rounds, they had done so in their own time; whether they had done so with immediate colleagues; whether they had ever presented at a Round; and whether they had contributed to Rounds discussions. They were also asked to rate the usefulness of Rounds on a scale from 1 (‘not at all useful’) to 5 (‘very useful’). An open text box was given for them to indicate why they thought Rounds were useful/not useful.
Non-attenders only
Respondents were asked for the reason they did not attend Rounds. In the baseline survey, possible answers were ‘I have no interest in attending’, ‘I do not think they would be useful’, ‘I was unaware of what they were’, ‘I am not able to attend at the time they occur’ or ‘Other’ (with an option to write in what the reason was). In the follow-up survey these options were expanded to include ‘They occur when I am not working’, ‘Announcement of Rounds is at too short notice’, ‘I am too busy and not able to find the time’, ‘There is no one to cover my work’, ‘My break is too short’, ‘They conflict with other clinical priorities’, ‘They conflict with other non-clinical priorities’, ‘I am not supported by my line manager to attend’, ‘I have to wait my turn to attend as we rotate attendance amongst the team’, ‘I do not have autonomy over my work schedule’, ‘I have no interest in attending’, ‘I do not think they are relevant to my role’, ‘I was unaware of what they were’, ‘I am not able to attend at the time they occur’, ‘I did not think I was invited’, ‘The topics do not seem relevant to me’, ‘They occur in a different location from the site in which I am based’, ‘The location is not convenient for me’, ‘I have moved to an organisation that does not run Rounds’ and ‘Other’, with open text response accompanying; respondents could tick as many as applied.
Validity and reliability of measures
The validity of all scale measures described in the previous section was checked using a confirmatory factor analysis on all data returned from the baseline survey, representing 1131 cases. An eight-factor model, representing the eight scales separately, revealed a good fit: comparative fit index = 0.943; Tucker–Lewis Index = 0.939; root mean squared error of approximation = 0.064; standardised root mean residual = 0.027; χ2 =5634.1 (1006 degrees of freedom). These fit indices all fall within the range considered acceptable or good. Although there were some high correlations between factors (e.g. self-efficacy with empathy: 0.895; self-efficacy with compassion: 0.891; empathy with compassion: 0.926; and peer support with organisational climate for support: 0.878), in all cases the criteria350 for discriminant validity were reached, and therefore it was sensible to treat the scales as separate variables.
Average variance extracted scores for the baseline survey data, together with reliability scores (Cronbach’s alpha) for the two surveys, are shown for each scale in Table 32. Each exceeds the 0.80 level representing good reliability.
| Scale | Average variance extracted score (baseline) | α (baseline) | α (follow-up) |
|---|---|---|---|
| GHQ-12 | 0.247 | 0.894 | 0.907 |
| Engagement | 0.664 | 0.783 | 0.809 |
| Self-reflection | 0.797 | 0.844 | 0.868 |
| Empathy | 0.953 | 0.854 | 0.877 |
| Communication with patients | 0.921 | 0.935 | 0.953 |
| Compassion | 0.945 | 0.884 | 0.882 |
| Peer support | 0.934 | 0.920 | 0.931 |
| Organisational climate for support | 0.906 | 0.898 | 0.896 |
Appendix 14 Details of pilot study
Pilot study methods
Before the precise methods (including administration and survey content) were finalised, a pilot survey was conducted to test (1) the administration method for attenders, (2) the administration method for non-attenders and (3) the usefulness of measures selected for the survey (for both attenders and non-attenders). The majority of the methods were kept for the main study, so the details of those that differed are noted here.
Two sites were used (sites P1 and P2) for the pilot study. Site P1 was an urban acute trust, split across two hospital sites, which had been running Rounds for several years. Site P2 was an acute trust in a largely rural area, which was running Rounds for the first time.
Researchers attended two Rounds in site P1 (one at each hospital), and the first Round in site P2. It was important to test the procedure in both sites, because the main study would include a mixture of ‘established’ Rounds sites and ‘new’ Rounds sites; however, at both the survey would only include people attending a Round for the first time. In site P1 there were far fewer of these, but the challenge was identifying them, while in site P2 almost everyone was a new attender, so the challenge was recruiting virtually all attenders in a short time scale.
In total, 22 questionnaires were distributed to new attenders at site P1, and 30 at site P2. Seventeen were returned from site P1 (a 77% response rate) and 11 from site P2 (37% response rate). As with the main study, responders were sent a follow-up survey after 8 months. Seven out of 17 were returned at site P1 (41%), and six out of 11 were returned at site P2 (55%).
The administration method for non-attenders was tested by sending a link to the online survey to a random sample of 250 staff from site P1 only. Fifty responses were received (20% response rate). For the follow-up survey sent to these 50 respondents after 8 months, 22 responses were received (44%) but three were blank; after these three were removed, the response rate was 19 out of 50 (38%).
The usefulness of questionnaire measures was tested in 12 cognitive interviews. 351 Ten were conducted with attenders at a Round from site P1 who had indicated to a researcher at the Round attended that they would be happy to participate in such an interview. The other two were non-attenders from site P1 who had indicated in their online questionnaire that they would be willing to participate in such an interview. Participants were selected from these volunteers purposively to ensure that a range of occupational groups were represented, and were offered a £25 shopping voucher in return.
Each interview covered a range of questions within the questionnaire, so that all questions were covered by at least two interviews, and those for which there was less prior evidence of validity (including those questions about Rounds that were developed specifically for this study) were covered by a larger number of interviews. Notes were made of all responses and details of any problems uncovered. These were then content analysed to enable a summary of all findings to be made.
Pilot study findings
In general, the administration methods tested proved successful, and most respondents could complete the questionnaire in < 10 minutes. However, a number of findings led us to change elements of the methods (Table 33).
| Finding | Change made |
|---|---|
| Attenders: there was sometimes insufficient time for respondents to complete the survey before leaving. Although they were able to post it back afterwards, there was no way of chasing them up | The consent to contact box was moved from the first page of the questionnaire to the separate cover sheet. This meant that we could ask for the cover sheet to be returned alone if time was short, and send reminder letters accordingly (an ethics committee amendment was approved). We added a question to ask whether questionnaires were completed before, during or after the Round |
| Attenders: at sites where Rounds were already established, there were relatively few new attenders. If the number in the pilot site was replicated across the whole study, we would be unlikely to achieve the sample size required | In the original design, all 10 survey sites were the same as the main case study sites. However, we changed the sample so six would have both and four sites would have the survey only (see Table 2). This way, 6 of the 10 were new providers, in which there would be more new attenders |
| Attenders: there is often a rush of attenders arriving shortly before the Round (or as it is beginning), making it difficult to approach everyone. This is exacerbated in sites running Rounds for the first time, where everyone is new and the approach takes longer. Any researchers present whose purpose was to observe the Round (case study) would be unable to help |
Survey packs prepared and numbered sequentially in advance Learn as much as possible in advance about the layout of the room, so that strategies could be formed for ensuring people are not missed Liaise with Rounds facilitators to give a short (30 seconds) message at the start of the Round for any new attenders not approached to seek out a researcher at the end of the Round Increase number of research team at Rounds and, where possible, enlist the help of research nurses or equivalent from the sites to help with survey administration |
| Non-attenders: NHS IT systems may not be compatible with Qualtrics automatic e-mails (some e-mails appeared to have been blocked) |
Liaison with site IT departments in advance An e-mail to be sent to the sample in advance, from a researcher’s e-mail account, to alert the sample to expect an e-mail from the Qualtrics system, and that this would not be spam |
| Measures: the full UWES-9136 included. Some items were seen as inappropriate | Only the three-item version of the scale from the NHS Staff Survey was retained |
| Measures: the ‘Depersonalisation’ Scale352 was seen as inappropriate for health-care employees | The Depersonalisation Scale was dropped (the GHQ-12 is similar enough for this not to matter) |
| Measures: the ‘Reflection’ subscale141 had low reliability and did not adequately discriminate between respondents. Almost all responses were at the highest end of the response scale | The Reflection Scale was replaced by a different reflection scale that appeared to have better psychometric properties140 |
Appendix 15 Background details of survey respondents
| Number of Rounds | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| 0 | 233 (47.6) | 0 (0.0) | 0 (0.0) | 233 (100.0) |
| 1 | 116 (23.7) | 0 (0.0) | 116 (56.6) | 0 (0.0) |
| 2 | 63 (12.9) | 6 (11.8) | 57 (27.8) | 0 (0.0) |
| 3 | 37 (7.6) | 12 (23.5) | 25 (12.2) | 0 (0.0) |
| 4 | 24 (4.9) | 17 (33.3) | 7 (3.4) | 0 (0.0) |
| 5 | 10 (2.0) | 10 (19.6) | 0 (0.0) | 0 (0.0) |
| 6 | 4 (0.8) | 4 (7.8) | 0 (0.0) | 0 (0.0) |
| 7 | 1 (0.2) | 1 (2.0) | 0 (0.0) | 0 (0.0) |
| 8 | 1 (0.2) | 1 (2.0) | 0 (0.0) | 0 (0.0) |
| Age group (years) | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| 21–30 | 59 (12.1) | 8 (15.7) | 21 (10.2) | 30 (12.9) |
| 31–40 | 97 (19.8) | 8 (15.7) | 50 (24.4) | 39 (16.7) |
| 41–50 | 150 (30.7) | 16 (31.4) | 62 (30.2) | 72 (30.9) |
| 51–65 | 164 (33.5) | 18 (35.3) | 66 (32.2) | 80 (34.3) |
| ≥ 66 | 3 (0.6) | 0 (0.0) | 1 (0.5) | 2 (0.9) |
| Did not respond | 16 (3.3) | 1 (2.0) | 5 (2.4) | 10 (4.3) |
| Gender | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| Male | 77 (15.7) | 6 (11.8) | 24 (11.7) | 47 (20.2) |
| Female | 395 (80.8) | 45 (88.2) | 175 (85.4) | 175 (75.1) |
| Prefer not to say | 2 (0.4) | 0 (0.0) | 1 (0.5) | 1 (0.4) |
| Did not respond | 15 (3.1) | 0 (0.0) | 5 (2.4) | 10 (4.3) |
| Occupation | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| Medical/dental | 45 (9.2) | 7 (13.7) | 26 (12.7) | 12 (5.2) |
| Nursing/midwifery | 192 (39.3) | 22 (43.1) | 87 (42.4) | 83 (35.6) |
| AHPs/S&T | 110 (22.5) | 16 (31.4) | 46 (22.4) | 48 (20.6) |
| General managers | 9 (1.8) | 1 (2.0) | 3 (1.5) | 5 (2.1) |
| Administrative, clerical and central functions | 105 (21.5) | 4 (7.8) | 32 (15.6) | 69 (29.6) |
| Other | 3 (0.6) | 0 (0.0) | 0 (0.0) | 3 (1.3) |
| Did not respond | 25 (5.1) | 1 (2.0) | 11 (5.4) | 13 (5.6) |
| Grade | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| Band 1 | 1 (0.2) | 0 (0.0) | 1 (0.5) | 0 (0.0) |
| Band 2 | 26 (5.3) | 2 (3.9) | 5 (2.4) | 19 (8.2) |
| Band 3 | 41 (8.4) | 0 (0.0) | 12 (5.9) | 29 (12.4) |
| Band 4 | 36 (7.4) | 0 (0.0) | 15 (7.3) | 21 (9.0) |
| Band 5 | 61 (12.5) | 6 (11.8) | 21 (10.2) | 34 (14.6) |
| Band 6 | 91 (18.6) | 7 (13.7) | 34 (16.6) | 50 (21.5) |
| Band 7 | 81 (16.6) | 13 (25.5) | 36 (17.6) | 32 (13.7) |
| Band 8a | 37 (7.6) | 1 (2.0) | 20 (9.8) | 16 (6.9) |
| Band 8b | 11 (2.2) | 2 (3.9) | 5 (2.4) | 4 (1.7) |
| Band 8c | 4 (0.8) | 2 (3.9) | 1 (0.5) | 1 (0.4) |
| Band 8d | 1 (0.2) | 0 (0.0) | 1 (0.5) | 0 (0.0) |
| Band 9 | 1 (0.2) | 0 (0.0) | 1 (0.5) | 0 (0.0) |
| Non AfC contracta | 23 (4.7) | 2 (3.9) | 15 (7.3) | 6 (2.6) |
| Did not respond | 75 (15.3) | 16 (31.4) | 38 (18.5) | 21 (9.0) |
| Working hours per week | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| < 30 | 83 (17.0) | 4 (7.8) | 36 (17.6) | 43 (18.5) |
| ≥ 30 | 371 (75.9) | 41 (80.4) | 153 (74.6) | 177 (76.0) |
| Did not respond | 35 (7.2) | 6 (11.8) | 16 (7.8) | 13 (5.6) |
| Tenure (years) | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| < 1 | 62 (12.7) | 8 (15.7) | 37 (18.0) | 17 (7.3) |
| 1–2 | 44 (9.0) | 5 (9.8) | 14 (6.8) | 25 (10.7) |
| 3–5 | 82 (16.8) | 8 (15.7) | 36 (17.6) | 38 (16.3) |
| 6–10 | 85 (17.4) | 4 (7.8) | 39 (19.0) | 42 (18.0) |
| 11–15 | 65 (13.3) | 6 (11.8) | 26 (12.7) | 33 (14.2) |
| > 15 | 120 (24.5) | 18 (35.3) | 40 (19.5) | 62 (26.6) |
| Did not respond | 31 (6.3) | 2 (3.9) | 13 (6.3) | 16 (6.9) |
| Patient contact | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| Baseline | ||||
| Regular | 324 (66.3) | 40 (78.4) | 139 (67.8) | 145 (62.2) |
| Occasional | 50 (10.2) | 6 (11.8) | 22 (10.7) | 22 (9.4) |
| Rare/never | 61 (12.5) | 3 (5.9) | 24 (11.7) | 34 (14.6) |
| Did not respond | 54 (11.0) | 2 (3.9) | 20 (9.8) | 32 (13.7) |
| Follow-up | ||||
| Regular | 336 (68.7) | 41 (80.4) | 143 (69.8) | 152 (65.2) |
| Occasional | 61 (12.5) | 5 (9.8) | 25 (12.2) | 31 (13.3) |
| Rare/never | 78 (16.0) | 4 (7.8) | 31 (15.1) | 43 (18.5) |
| Did not respond | 14 (2.9) | 1 (2.0) | 6 (2.9) | 7 (3.0) |
| Mode of completion | Total, N (%) | Group, n (%) | ||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| Baseline | ||||
| Electronic | 316 (64.6) | 13 (25.5) | 70 (34.1) | 233 (100.0) |
| Paper | 173 (35.4) | 38 (74.5) | 135 (65.9) | 0 (0.0) |
| Follow-up | ||||
| Electronic | 481 (98.4) | 49 (96.1) | 200 (97.6) | 232 (99.6) |
| Paper | 8 (1.6) | 2 (3.9) | 5 (2.4) | 1 (0.4) |
| Total, N (%) | Group, n (%) | |||
|---|---|---|---|---|
| Regular attender | Irregular attender | Non-attender | ||
| Before Round | 50 (10.2) | 13 (25.5) | 37 (18.0) | – |
| After Round | 108 (22.1) | 19 (37.3) | 89 (43.4) | – |
| Mixed/in Round | 24 (4.9) | 7 (13.7) | 17 (8.3) | – |
| Did not respond | 307 (62.8) | 12 (23.5) | 62 (30.2) | – |
Appendix 16 Details of analysis of survey data
Correlations between survey variables
Correlations between all the survey scores and the number of Rounds attended are shown in Table 44. Although these are largely presented without comment for the sake of completeness, a few aspects are noteworthy. There is a strong correlation between most variables at baseline and the same variables at follow-up. The exception is days absent, which may point to this being a less reliable score (either because it relies on participant recall or because there is relatively little consistency within people across time). Second, the two psychological well-being (GHQ-12) scores are highly correlated. Third, there do not appear to be any substantial correlations between psychological well-being and the expected intermediate mechanisms of self-reflection, empathy, communication with patients and compassion, suggesting that levels of psychological well-being are not related to these mechanisms in the way that had been anticipated.
| Survey scales | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Number of rounds attended | ||||||||||||||||||||
| 2. Engagement (t1) | 0.19** | |||||||||||||||||||
| 3. GHQ-12 (caseness) (t1) | –0.09* | –0.28** | ||||||||||||||||||
| 4. GHQ-12 (Likert score) (t1) | –0.08 | –0.38** | 0.79** | |||||||||||||||||
| 5. Self-reflection (t1) | 0.14** | 0.11* | 0.01 | –0.02 | ||||||||||||||||
| 6. Empathy (t1) | 0.01 | 0.13** | 0.03 | 0.00 | 0.11* | |||||||||||||||
| 7. Communication with patients (t1) | 0.10* | 0.13** | 0.08 | 0.07 | 0.26** | 0.46** | ||||||||||||||
| 8. Compassion (t1) | 0.06 | 0.20** | 0.09 | 0.07 | 0.10* | 0.35** | 0.32** | |||||||||||||
| 9. Peer support (t1) | 0.12* | 0.27** | –0.27** | –0.33** | 0.09 | 0.11* | 0.14** | 0.08 | ||||||||||||
| 10. Organisational climate for support (t1) | 0.16** | 0.32** | –0.25** | –0.30** | 0.03 | –0.01 | –0.03 | 0.09 | 0.38** | |||||||||||
| 11. Days absent (t1) | –0.04 | 0.01 | 0.11* | 0.13** | –0.07 | 0.06 | 0.00 | 0.05 | 0.00 | –0.02 | ||||||||||
| 12. Engagement (t2) | 0.20** | 0.65** | –0.21** | –0.29** | 0.07 | 0.12** | 0.15** | 0.18** | 0.23** | 0.29** | 0.02 | |||||||||
| 13. GHQ-12 (caseness) (t2) | –0.16** | –0.19** | 0.37** | 0.42** | –0.07 | –0.02 | 0.00 | –0.03 | –0.17** | –0.26** | 0.03 | –0.34** | ||||||||
| 14. GHQ-12 (Likert score) (t2) | –0.18** | –0.26** | 0.40** | 0.50** | –0.09* | –0.04 | 0.00 | 0.00 | –0.26** | –0.30** | 0.04 | –0.44** | 0.79** | |||||||
| 15. Self-reflection (t2) | 0.12* | 0.06 | 0.01 | 0.01 | 0.64** | 0.13** | 0.23** | 0.11* | 0.06 | 0.05 | –0.01 | 0.03 | –0.05 | –0.03 | ||||||
| 16. Empathy (t2) | 0.05 | 0.10* | 0.06 | 0.09 | 0.05 | 0.51** | 0.36** | 0.34** | 0.01 | –0.09 | 0.00 | 0.11 | 0.01 | 0.03 | 0.08 | |||||
| 17. Communication with patients (t2) | 0.15** | 0.14** | 0.05 | 0.06 | 0.21** | 0.37** | 0.70** | 0.22** | 0.11* | –0.02 | 0.02 | 0.22** | –0.03 | –0.05 | 0.24** | 0.50** | ||||
| 18. Compassion (t2) | 0.04 | 0.22** | 0.02 | 0.01 | 0.10* | 0.32** | 0.24** | 0.65** | 0.08 | 0.07 | 0.01 | 0.26** | –0.05 | –0.02 | 0.13* | 0.41** | 0.37** | |||
| 19. Peer support (t2) | 0.18** | 0.32** | –0.16** | –0.23** | –0.01 | 0.03 | 0.11* | 0.06 | 0.58** | 0.28** | 0.01 | 0.39** | –0.24** | –0.35** | –0.01 | 0.04 | 0.17** | 0.11* | ||
| 20. Organisational climate for support (t2) | 0.07 | 0.23** | –0.19** | –0.19** | 0.09 | 0.00 | 0.03 | 0.07 | 0.23** | 0.61** | –0.03 | 0.32** | –0.30** | –0.33** | 0.09 | –0.08 | 0.01 | 0.10* | 0.28** | |
| 21. Days absent (t2) | –0.05 | –0.02 | 0.14** | 0.14** | –0.03 | –0.02 | 0.00 | 0.01 | –0.15** | –0.14** | 0.04 | –0.01 | 0.13** | 0.19** | –0.04 | 0.01 | –0.06 | 0.03 | –0.08 | –0.10* |
Full model parameters for regular attendance predicting outcomes
| Predictor variable | Outcome | |||
|---|---|---|---|---|
| Engagement | GHQ-12 (caseness) | GHQ-12 (Likert score) | Self-reflection | |
| Intercept | 0.39 (–0.81 to 1.60) | 0.00 (0.00 to 0.00) | 1.21 (0.40 to 2.02) | 1.86 (0.17 to 3.54) |
| Regular attender | 0.09 (–0.16 to 0.35) | 0.20 (0.05 to 0.82) | –0.13 (–0.31 to 0.05) | 0.05 (–0.32 to 0.42) |
| Gender (female)a | 0.06 (–0.16 to 0.29) | 1.64 (0.70 to 3.88) | –0.18 (–0.33 to -0.02) | –0.13 (–0.44 to 0.18) |
| Medical/dentalb | 0.84 (–0.06 to 1.75) | –0.48 (–1.12 to 0.17) | –0.29 (–1.55 to 0.96) | |
| Nursing/midwiferyb | 0.34 (0.08 to 0.60) | 1.42 (0.51 to 3.96) | –0.03 (–0.21 to 0.16) | –0.14 (–0.51 to 0.22) |
| AHP/S&Tb | 0.24 (–0.04 to 0.53) | 1.69 (0.53 to 5.34) | –0.04 (–0.24 to 0.16) | 0.12 (–0.28 to 0.52) |
| Part-timec | –0.07 (–0.29 to 0.16) | 1.01 (0.40 to 2.57) | –0.02 (–0.18 to 0.14) | 0.04 (–0.28 to 0.37) |
| Bands 1–5d | 0.61 (–0.39 to 1.61) | –0.23 (–0.94 to 0.48) | –0.37 (–1.77 to 1.03) | |
| Band 6d | 0.61 (–0.36 to 1.58) | –0.19 (–0.88 to 0.49) | –0.31 (–1.67 to 1.05) | |
| Band 7d | 0.61 (–0.40 to 1.61) | –0.24 (–0.95 to 0.47) | –0.16 (–1.57 to 1.24) | |
| Bands 8–9d | 0.57 (–0.45 to 1.59) | –0.22 (–0.95 to 0.50) | –0.32 (–1.76 to 1.11) | |
| Regular patient contacte | –0.24 (–0.52 to 0.03) | 0.82 (0.28 to 2.44) | 0.03 (–0.17 to 0.23) | 0.16 (–0.23 to 0.54) |
| Occasional patient contacte | –0.01 (–0.36 to 0.34) | 0.65 (0.17 to 2.49) | 0.13 (–0.13 to 0.38) | 0.20 (–0.29 to 0.69) |
| Age | –0.01 (–0.10 to 0.09) | 1.10 (0.75 to 1.59) | 0.02 (–0.04 to 0.09) | 0.01 (–0.12 to 0.15) |
| Length of service | –0.01 (–0.06 to 0.05) | 1.13 (0.90 to 1.43) | –0.02 (–0.06 to 0.02) | –0.03 (–0.11 to 0.05) |
| Baseline value | 0.72 (0.60 to 0.83) | 6.98 (3.36 to 14.53) | 0.58 (0.46 to 0.69) | 0.65 (0.53 to 0.77) |
| Predictor variable | Outcome | ||
|---|---|---|---|
| Empathy | Communication with patients | Compassion | |
| Intercept | 1.28 (0.39 to 2.17) | –0.12 (–2.47 to 2.22) | 1.25 (–0.14 to 2.64) |
| Regular attender | –0.06 (–0.23 to 0.12) | 0.16 (–0.33 to 0.65) | 0.00 (–0.29 to 0.30) |
| Gender (female)a | –0.07 (–0.22 to 0.09) | –0.09 (–0.56 to 0.39) | –0.08 (–0.36 to 0.19) |
| Medical/dentalb | 0.14 (–0.46 to 0.74) | 1.02 (–0.73 to 2.78) | 0.26 (–0.79 to 1.31) |
| Nursing/midwiferyb | 0.22 (0.04 to 0.41) | 0.68 (0.10 to 1.26) | 0.32 (–0.01 to 0.64) |
| AHP/S&Tb | 0.19 (–0.02 to 0.39) | 0.93 (0.31 to 1.55) | 0.33 (–0.03 to 0.69) |
| Part-timec | 0.03 (–0.13 to 0.20) | 0.02 (–0.45 to 0.49) | 0.03 (–0.26 to 0.31) |
| Bands 1–5d | 0.05 (–0.60 to 0.71) | –0.25 (–2.15 to 1.66) | –0.23 (–1.38 to 0.92) |
| Band 6d | 0.12 (–0.52 to 0.76) | 0.12 (–1.72 to 1.96) | –0.05 (–1.17 to 1.07) |
| Band 7d | 0.22 (–0.44 to 0.88) | 0.08 (–1.82 to 1.99) | –0.11 (–1.27 to 1.04) |
| Bands 8–9d | 0.05 (–0.63 to 0.73) | 0.06 (–1.89 to 2.00) | 0.12 (–1.06 to 1.30) |
| Regular patient contacte | 0.16 (–0.08 to 0.39) | 1.19 (0.50 to 1.87) | 0.28 (–0.13 to 0.69) |
| Occasional patient contacte | 0.29 (–0.02 to 0.60) | 1.10 (0.12 to 2.07) | 0.56 (0.02 to 1.10) |
| Age | 0.03 (–0.03 to 0.10) | 0.12 (–0.08 to 0.32) | 0.14 (0.02 to 0.25) |
| Length of service | –0.05 (–0.09 to –0.01) | 0.02 (–0.11 to 0.14) | –0.02 (–0.09 to 0.05) |
| Baseline value | 0.55 (0.41 to 0.69) | 0.74 (0.62 to 0.85) | 0.67 (0.56 to 0.78) |
| Predictor variable | Outcome | ||
|---|---|---|---|
| Peer support | Organisational climate for support | Days absent in previous 6 months | |
| Intercept | 2.52 (1.03 to 4.00) | 0.65 (–0.35 to 1.66) | 26.30 (0.76 to 915.04) |
| Regular attender | 0.04 (–0.30 to 0.37) | –0.11 (–0.34 to 0.12) | 1.20 (0.52 to 2.73) |
| Gender (female)a | 0.18 (–0.11 to 0.47) | –0.10 (–0.29 to 0.10) | 0.99 (0.51 to 1.92) |
| Medical/dentalb | –0.23 (–1.41 to 0.95) | 0.19 (–0.60 to 0.97) | 0.62 (0.03 to 11.21) |
| Nursing/midwiferyb | 0.26 (–0.08 to 0.59) | 0.04 (–0.19 to 0.26) | 1.56 (0.72 to 3.42) |
| AHP/S&Tb | 0.13 (–0.24 to 0.50) | 0.03 (–0.21 to 0.28) | 1.63 (0.69 to 3.86) |
| Part-timec | –0.04 (–0.34 to 0.26) | –0.10 (–0.30 to 0.10) | 0.45 (0.21 to 0.96) |
| Bands 1–5d | –1.01 (–2.31 to 0.30) | 0.21 (–0.65 to 1.08) | 0.13 (0.01 to 3.08) |
| Band 6d | –0.87 (–2.14 to 0.40) | 0.28 (–0.56 to 1.12) | 0.08 (0.00 to 1.76) |
| Band 7d | –0.90 (–2.21 to 0.41) | 0.14 (–0.73 to 1.02) | 0.03 (0.00 to 0.82) |
| Bands 8–9d | –0.98 (–2.32 to 0.35) | 0.22 (–0.66 to 1.11) | 0.10 (0.00 to 2.63) |
| Regular patient contacte | –0.12 (–0.48 to 0.25) | 0.05 (–0.19 to 0.30) | 0.41 (0.18 to 0.92) |
| Occasional patient contacte | –0.10 (–0.56 to 0.37) | 0.02 (–0.29 to 0.33) | 0.66 (0.22 to 2.00) |
| Age | –0.01 (–0.13 to 0.12) | 0.07 (–0.01 to 0.16) | 1.19 (0.89 to 1.59) |
| Length of service | –0.05 (–0.13 to 0.02) | –0.01 (–0.06 to 0.04) | 0.96 (0.81 to 1.15) |
| Baseline value | 0.57 (0.45 to 0.69) | 0.58 (0.47 to 0.69) | 1.01 (0.99 to 1.04) |
Examination of dose effect
One hypothesis put forward by previous evaluations27 was that a higher number of Rounds attended would result in a better chance of improved outcomes. Therefore, we tested further models with the various outcomes, but this time using the number of Rounds attended as the predictor. To allow for the possibility that there may be a non-linear effect of attending more Rounds – for example, the effect may start only after a certain number were attended, or alternatively the effect may diminish after a certain number – after fitting models with a linear effect, quadratic terms for number of Rounds attended were added to the model to allow for these possible non-linear effects.
The results of the linear effect models are shown in Table 48. Consistent with the previous tests, there was no effect of number of Rounds attended on most of the outcomes. However, there was an effect on psychological well-being, this time on both versions of the GHQ-12. The caseness outcome showed an odds ratio of 0.75 (95% CI 0.59 to 0.94), indicating that for each extra Round attended, the odds of being classed as a case shrink by about one-quarter. The Likert version had a coefficient of –0.04 (95% CI –0.07 to –0.01), suggesting that for each extra Round attended, the score was about 0.04 points lower on average. As this represents < 10% of a standard deviation in the variable (see Table 48), this should be considered a relatively small effect: even attending five Rounds would result in a change of less than half of one standard deviation. Nevertheless, it adds further evidence to the other results relating to the caseness version, meaning that a relationship with psychological well-being is more credible still (even allowing for the fact that the two scores are not independent of each other).
| Outcome | Effecta (95% CI) |
|---|---|
| Engagement | 0.03 (–0.02 to 0.08) |
| GHQ-12 (caseness) | 0.75 (0.59 to 0.94) |
| GHQ-12 (Likert score) | –0.04 (–0.07 to –0.01) |
| Self-reflection | 0.02 (–0.04 to 0.09) |
| Empathy | 0.00 (–0.03 to 0.04) |
| Communication with patients | 0.07 (–0.04 to 0.17) |
| Compassion | 0.02 (–0.04 to 0.08) |
| Peer support | 0.04 (–0.02 to 0.10) |
| Organisational climate for support | –0.01 (–0.05 to 0.03) |
| Days absent in previous 6 months | 0.92 (0.78 to 1.09) |
None of the models with non-linear effects was significant, indicating that there is no evidence that a particular number of Rounds is necessary, or that there is a diminishing effect of attending a larger number of Rounds. However, this has to be considered in conjunction with two other factors. First, most of the linear models were not significant, so the non-linear models also not showing significant effects only means that neither is there a non-linear effect that was not apparent before. Second, relatively few of the sample attended more than four Rounds. Therefore, if there were to be a drop-off when attending more Rounds than this (or a higher number), it is unlikely that it would be seen clearly in this sample.
Moderator analysis
A number of variables were considered as possible moderators of the effects; that is, any effects may vary according to the level of these variables. Those considered as possible moderators were the following:
-
Whether or not the respondent had presented at a Round. It was hypothesised that having a greater involvement in Rounds may increase their positive impact, and therefore presenting (representing a large involvement) may strengthen effects.
-
Whether or not the respondent had contributed to discussions in Rounds. As previously, it was hypothesised that having a greater involvement in Rounds may increase their positive impact, and therefore those contributing to discussions may have slightly larger effects.
-
Whether or not the baseline questionnaire had been completed before the first Round attended began. It was thought that some of the effect of attending may have an immediate impact, and therefore effects might be diminished if the baseline scores were collected after attending the first Round.
-
Whether the site was a new provider of Rounds, or whether Rounds were more established there. It was hypothesised that Rounds that had more organisational experience behind them, and a more established group of attenders, may provide more potential for improvement in outcomes than a new provider.
-
What type of organisation the site was. It was thought that Rounds may have greater effects in some types of organisations than others. Ideally, it would be possible to examine the difference between all sorts of provider; however, in the final sample, only two sites were not acute trusts. Therefore, the analysis only looked at a contrast between acute trusts and non-acute sites.
In total, therefore, there were five potential moderating variables. The first three of these were variables that would only differ for attenders; therefore, these were tested by first forming three-category variables: attenders with the characteristic in question, attenders without the characteristic in question, and non-attenders. If there were a significant effect of this variable on outcomes, then a post hoc analysis would be used to examine where the differences lay.
The last two of these were moderating factors related to the site; therefore, a traditional cross-level interaction test was done.
Most of the tests yielded non-significant results, and those that were significant are reported below. There were no significant effects for presenting at Rounds or time of survey completion.
-
Contributing at Rounds. Absence in the previous 6 months was lowest among regular attenders who did not contribute to discussions; in particular, they had significantly lower absence than regular attenders who did contribute (p = 0.031). Further examination of this effect reveals that there was a substantial decrease in absence in the non-contributing group (mean at baseline = 8.2 days; mean at follow-up = 0.1 days), but this is because of a small sample in this group (10 participants) and two outliers at baseline (reporting 32 and 38 days’ absence, respectively, in the previous 6 months). Meanwhile, regular attenders who did contribute had a mean of 1.0 days’ absence at baseline and 2.3 days’ absence at follow up. Non-attenders had means of 4.1 and 3.4 days’ absence, respectively.
-
Acute versus other sites. In acute trusts there is very little difference between attenders and non-attenders in terms of empathy; however, for non-acute sites, empathy actually appears to be higher among non-attenders (controlling for baseline levels) (p = 0.017). This is demonstrated in Figure 11.
-
Established vs. new providers. Organisational climate for support was higher among regular attenders than among non-attenders in sites where Rounds had been established for longer. In sites newly running Rounds, however, the perceived support was slightly lower among regular attenders (p = 0.027). However, only seven regular attenders in established providers were included in this analysis, so the sample is more prone to outliers, demonstrated in Figure 12.
FIGURE 11.
Empathy for regular attenders and non-attenders in acute and non-acute sites.
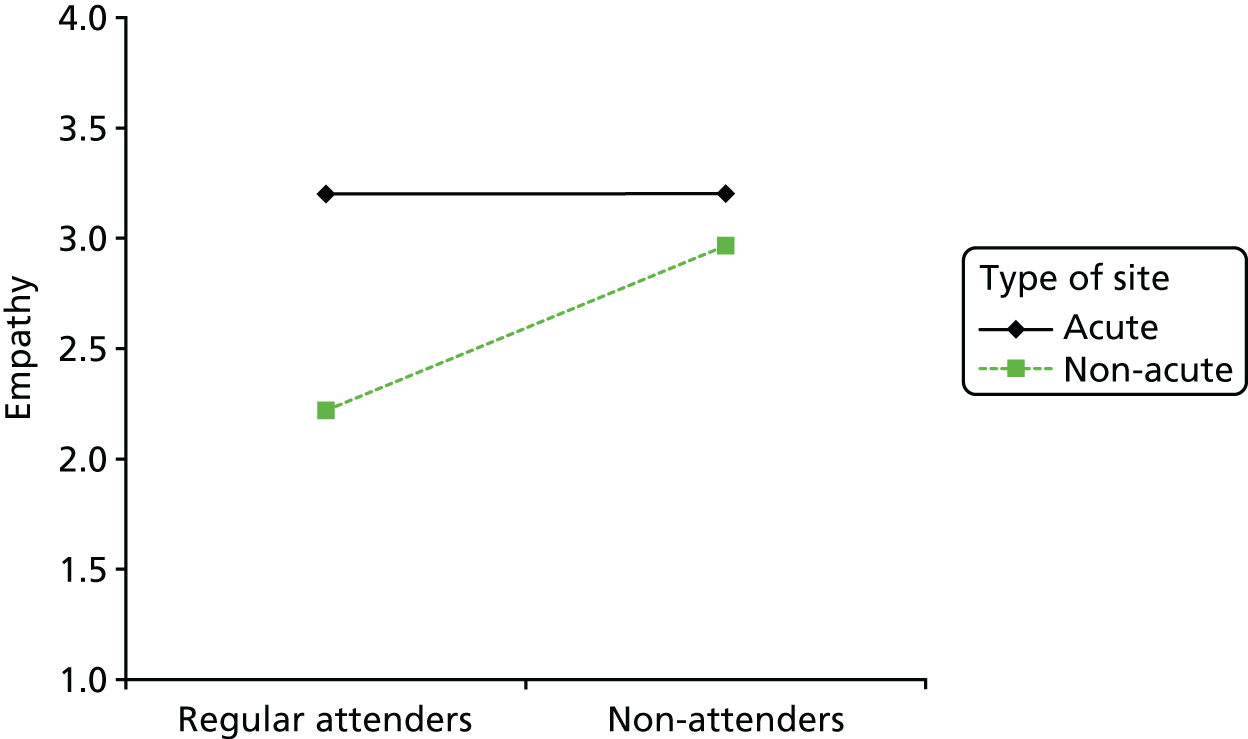
FIGURE 12.
Organisational climate for support for regular attenders and non-attenders in sites where Rounds were established or new during the study.
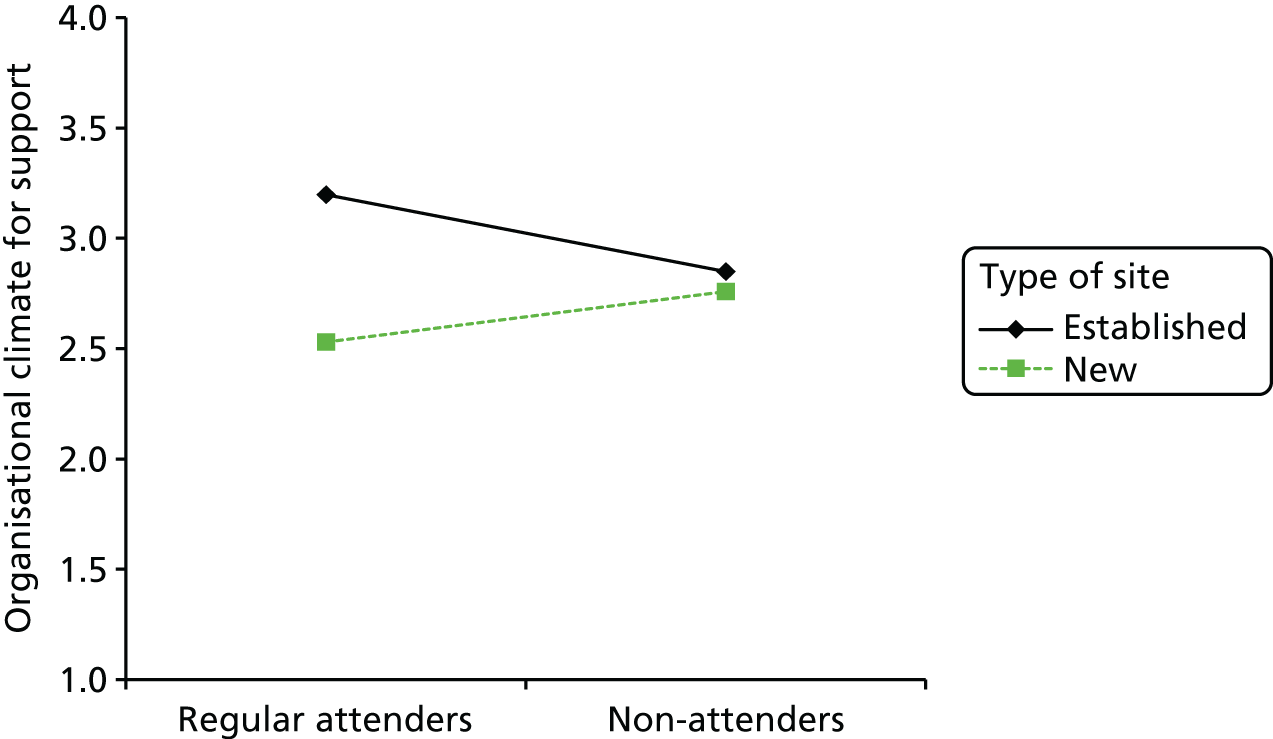
Only 3 out of 50 tests for moderators were statistically significant. This rate, 6%, is close to the 5% rate that would be expected by chance if there were no moderation effects at all. Therefore, it seems highly plausible that one, two or even all three of these effects are type I errors; that is, they are fluke results and do not represent the reality of differences between regular and non-attenders. This is particularly relevant as some aspects of the results are contrary to what might have been expected. For example, although it is possible that a good reason exists that regular attenders in non-acute sites would have lower empathy than non-attenders, it is more likely that this is a type I error. Therefore, although the significant results are described here for the sake of completeness, it is likely that nothing should be read into them.
Appendix 17 Participant information sheets (phase 2)
Appendix 18 Staff consent forms (phase 2)
Appendix 19 Interview schedule
Appendix 20 New sites and established sites: Rounds observed by date, type and number of attenders
| Number | Site | Date | Type of Round | Number of attenders |
|---|---|---|---|---|
| 1 | Mulberry | June 2015 | Theme | ≥ 40 |
| 2 | Mulberry | July 2015 | Theme | 22 |
| 3 | Mulberry | August 2015 | Case | 49 |
| 4 | Mulberry | September 2015 | Theme | 43 |
| 5 | Mulberry | October 2015 | Theme | 62 |
| 6 | Mulberry | November 2015 | Case | 18 |
| 7 | Juniper | August 2015 | Case | 31 |
| 8 | Juniper | September 2015 | Case | 23 |
| 9 | Juniper | October 2015 | Theme | 7 |
| 10 | Juniper | December 2015 | Theme | 20 |
| 11 | Juniper | June 2016 | Casea | 10 |
| 12 | Cherry | November 2015 | Theme | 23 |
| 13 | Cherry | December 2015 | Case | 67 |
| 14 | Cherry | January 2016 | Theme | 22 |
| 15 | Cherry | February 2016 | Theme | 50 |
| 16 | Cherry | March 2016 | Theme | 22 |
| Number | Site | Date | Type of Round | Number of attenders |
|---|---|---|---|---|
| 17 | Cedar | September 2015 | Case | 124 |
| 18 | Cedar | November 2015 | Case | 55 |
| 19 | Cedar | December 2015 | Theme | 16 |
| 20 | Cedar | January 2016 | Case | 28 |
| 21 | Cedar | February 2016 | Theme | 66 |
| 22 | Cedar | March 2016 | Case | 46 |
| 23 | Sycamore | October 2015 | Theme | 26 |
| 24 | Sycamore | November 2015 | Theme | 25 |
| 25 | Sycamore | January 2016 | Case | 40 |
| 26 | Sycamore | February 2016 | Case | 35 |
| 27 | Sycamore | March 2016 | Case | 40 |
| 28 | Sycamore | April 2016 | Case | 42 |
| 29 | Willow | October 2015 | Case | 46 |
| 30 | Willow | November 2015 | Theme | 48 |
| 31 | Willow | February 2015 | Theme | 55 |
| 32 | Willow | January 2016 | Theme | 70 |
| 33 | Willow | March 2016 | Case | 60 |
| 34 | Elderberry | September 2015 | Theme | 20 |
| 35 | Elderberry | January 2016 | Theme | 42 |
| 36 | Elderberry | November 2015 | Case | 15 |
| 37 | Elderberry | March 2016 | Theme | 24 |
| 38 | Ash | October 2015 | Theme | 19 |
| 39 | Ash | November 2015 | Case | 19 |
| 40 | Ash | December 2015 | Case | 27 |
| 41 | Ash | February 2016 | Case | 10 |
| 42 | Ash | March 2016 | Case | 40 |
Appendix 21 Examples of Rounds topics and titles
The topics that staff brought reflected the increased complexity and challenging health-care environment in which staff work, and we were struck by the universality of some of the topics. For example, the communication difficulties arising from an increased number of patients presenting with multiple diagnoses and the extensive communication required to co-ordinate health care between multiple disciplines, teams and individuals within the organisation and outside agencies, and associated cross-boundary challenges. There were also Rounds that presented ethical and moral dilemmas, such as whether to continue feeding a patient who had expressed a wish to die and differences in opinion between staff on how to deal with the situation. Challenging patients were frequently discussed, for example when they had made a complaint against staff, what that process felt like and the repercussions of it for staff well-being. Similarly, Rounds provided an opportunity for staff to talk about challenges presented by patients’ relatives, for example ‘when relatives obscure our view’ or ‘not the whole truth – working with secrets’. There were examples of Rounds in which limited NHS finances, political climate and organisational policies regarding allocation of resources were leading to hard decisions on the ground, for example ‘junior doctors’ strike’, ‘black alerts’, ‘winter pressures’ and ‘making cuts’, or of Rounds on organisational topics such as bullying and harassment. There were also Rounds that were deliberately upbeat and uplifting, and that provided an opportunity to celebrate examples of excellent patient care in which staff had gone above and beyond what is usually expected of them.
| Type of topic | Rounds title |
|---|---|
| Compassionate care | ‘What makes a compassionate caregiver/patient relationship?’ |
| Compassionate care | ‘Promoting compassionate care – context is everything’ |
| Moral dilemma | ‘“Homeless” (homeless person being discharged with nowhere to go)’ |
| Population specific | ‘Meeting the needs of patients with learning disabilities’ |
| Population specific | ‘HIV prevention, more costly than a condom’ |
| Challenging topics | ‘Managing anger’ |
| Challenging topics | ‘Pressure to make the right decisions about patient feeding’ |
| Challenging topics | ‘Let’s talk about sex’ |
| Challenging topics | ‘Not the whole truth – working with secrets’ |
| End of life | ‘Lost in translation: when communication difficulties prolong the inevitable’ |
| End of life | ‘Matters in life and death’ |
| End of life | ‘Making a conscious decision to die’ |
| End of life | ‘Difficult beginnings’ (end-of-life care for 16-year-olds) |
| Challenging families and patients | ‘Managing families’ expectations’ |
| Challenging families and patients | ‘Being in the dark, withstanding complaints while managing difficult risks posed by challenging patients’ |
| Challenging families and patients | ‘One patient, two health issues, many concerns’ |
| Challenging families and patients | ‘Fighting for a young person’s right to a healthy life; chronic pain, family dysfunction and litigation’ |
| Staff focused | ‘Why am I here? Meaning and purpose of today’s NHS’ |
| Staff focused | ‘We’re only human after all’ |
| Staff focused | ‘Holding onto hope across the lifespan’ |
| Staff focused | ‘Blinded by certainty: a team share their experience of secondary trauma’ |
| Staff focused | ‘Being on the receiving end’ |
| Staff focused | ‘On the front line’ |
| Organisation focused | ‘Hospital at night’ |
| Organisation focused | ‘Making cuts’ |
| Organisation focused | ‘Cross-boundaries challenges’ |
| Organisation focused | ‘When a young adult’s care pathway results in confusion and frustration for everyone involved’ |
| Safety | ‘Keeping Rounds safe’ |
| Safety | ‘Making it safe when innovating: understanding impact of past and making best use of team’ |
| Upbeat/general Rounds | ‘They’re getting married in the morning’ |
| Upbeat/general Rounds | ‘A Schwartz Round I’ll never forget’ |
| Upbeat/general Rounds | ‘Wow, getting recognition for doing a great job’ |
| Upbeat/general Rounds | ‘All in a day’s work’ |
Appendix 22 Comparison of core components of fidelity
| Site | Numbers of facilitatorsa | Regularity | Integrity | Food |
|---|---|---|---|---|
| Mulberry | 3 | Monthly (in two sites, alternating between sites each month) | ✓ | ✓ |
| Juniper | 3 | Monthly (in one site, but Rounds paused during fieldwork period) | ✓ | ✓ |
| Cedar | 3 | Monthly (one Round per month in two sites) | ✓ | ✓ |
| Cherry | 3 | Monthly (in two sites alternate between sites each month) | ✓ | ✓ |
| Willow | 4 | Monthly (in two sites, alternating between sites each month. Shared same location) | ✓ | ✓ |
| Sycamore | 4 | Monthly (in two sites; occasionally second site ran Rounds in addition to first site) | One Round observed during which integrity was compromised | ✓ |
| Horse-chestnut | 4 | Paused during fieldwork period | ✓ | ✓ |
| Elderberry | 4 | Monthly (in one site; not run in August) | ✓ | ✓ |
| Ash | 5 | Monthly (in two sites, alternating between sites each month; paused during fieldwork period) | ✓ | ✓ |
| Site | Group setting/built environment | Participants/audience (Schwartz savviness) | Audience discussion | Trust, safety and containment | Pre-prepared panel stories | Focus on emotional impact, vs. not problem-solving, clinical details |
|---|---|---|---|---|---|---|
| Mulberry |
Rooms: large lecture room, few windows, short rows (venue 1) and medium-sized room – large windows, long rows (venue 2) Within main building |
New Rounds site, ‘Schwartz savviness’ being learnt Good support from steering group members in supporting this |
Always well-controlled timing of Rounds’ stages to allow sufficient time for audience discussion and reflection |
Observed pre-Round safety checks Examples where panellists and audience members reported not feeling safe in Rounds |
Well-prepared stories, individual preparation; whole panel preparation when possible | Clear focus on emotional impact vs. problem-solving |
| Juniper |
Rooms: medium-sized room, windows In main building and sometimes on site, but not in main building |
New Rounds site, ‘Schwartz savviness’ not apparent during observation Evidence during observations that facilitating team recognise this and are addressing it |
Observed Rounds in which time for panellist stories and audience discussion not always tightly controlled, resulting in less time for audience discussion and reflection |
Less evidence of pre-Round safety checks during observed panel preparation meetings Evidence during observations and interviews that some Rounds felt unsafe |
Compared with other sites, panellists given less feedback/guidance on how to craft their stories | Examples observed of problem-solving, clinical focus rather than emotional impact |
| Cedar | Rooms: large room, light filled, long rows. Within main building |
Established Rounds site ‘Schwartz savviness’ is always evident and well developed |
Always well-controlled timing of Rounds’ stages to allow sufficient time for audience discussion and reflection |
Pre-Round safety checks observed Usually high levels of trust, safety and containment |
Well-prepared stories, individual preparation and part/whole panel preparation when possible Possible themes that resonate identified in advance |
Clear focus on emotional impact vs. problem-solving |
| Cherry |
Rooms: large room, used for training. On site, but not within main building (venue 1) Medium room, light filled, on site, but not within main building (venue 2) |
New Rounds site Level of ‘Schwartz savviness’ varies between two Rounds sites |
Always well-controlled timing of Rounds’ stages to allow sufficient time for audience discussion and reflection |
Pre-Rounds safety checks observed Usually high levels of trust, safety and containment |
Well-prepared stories, often individual preparation, rarely whole panel preparation Possible themes that resonate identified in advance |
Clear focus on emotional impact vs. problem-solving |
| Willow |
Rooms: often in medical education centre, not usually in main building Loss of venue affected attendance levels and audience composition |
Established Rounds site ‘Schwartz savviness’ is well developed Unusually high proportion of medical doctors present (compared with other sites) |
Always well-controlled timing of Rounds’ stages to allow sufficient time for audience discussion and reflection |
Pre-Rounds safety checks Usually high levels of trust, safety and containment |
Always well-prepared stories. Whole panel preparation for case based Rounds observed. Recalled one panellist being prepared by telephone to make a whole panel preparation (i.e. all panel presented and he telephoned in). But this is from interview, not observed | Clear focus on emotional impact vs. problem-solving |
| Sycamore |
Rooms: large room, long rows, on site, but not in main building (venue 1) Medium room, short rows, in main building (venue 2) |
Established Rounds site ‘Schwartz savviness’ noticeably varies between Rounds (compare with other sites) |
Always well-controlled timing of Rounds’ stages to allow sufficient time for audience discussion and reflection |
Less evidence of pre-Rounds safety checks Usually high levels of trust, safety and containment |
Panellists given less feedback/guidance on how to craft their stories Individual panel meetings and part or whole panel meetings when possible Fewer examples of themes that resonate pulled out in advance |
Examples observed of problem-solving, clinical focus rather than emotional impact |
| Horse-chestnut | Rooms: trust buildings were sold, and the loss of a large enough venue located on site affected attendance levels | Not observed | Not observed | Not observed | Not observed | Not observed |
| Elderberry | Rooms: large room, long rows, on site and within main building |
Established Rounds site ‘Schwartz savviness’ is always evident and well developed |
Always well-controlled timing of Rounds’ stages to allow sufficient time for audience discussion and reflection |
Pre-Rounds safety checks observed Usually high levels of trust, safety and containment |
Well-prepared stories; panellists presenting more than once; individual preparation; often whole panel rehearsal | Clear focus on emotional impact vs. problem-solving |
| Ash | Rooms: medium room, short rows, on site but not in main building |
Established Rounds site ‘Schwartz savviness’ is usually evident and well developed |
Creativity with format observed |
Pre-Rounds safety checks observed Usually high levels of trust, safety and containment, although facilitator and participants gave examples of Rounds that felt less safe |
Well-prepared stories; panellists given individual preparation Try to prepare in groups, but often not possible. Prepared in group when unsafe not to |
Clear focus on emotional impact vs. problem-solving |
Glossary
- Board (trust board)
- A body with overall responsibility for the activity, integrity and strategy of the trust (accountable to the NHS Trust Development Authority and the Secretary of State for Health and Social Care).
- Caseness
- A scoring mechanism for the 12-item General Health Questionnaire that categorises respondents into two groups based on scoring below or above the threshold of 4 out of 12 symptoms.
- Context–mechanism–outcome configuration
- A hypothesis that the programme outcome (O) emerges because of the action of some underlying mechanism (M), which comes into operation only in particular contexts (C).
- Cronbach’s alpha
- A measurement of the internal consistency (reliability) of measurement scales.
- F
- A test statistic that is compared with an ‘F’ distribution.
- Foundation trust
- A trust that has a greater degree of managerial and financial autonomy than a standard NHS trust (see also Trust).
- Francis report
- The report of the inquiry into the care provided by Mid Staffordshire NHS Foundation Trust between January 2005 and March 2009.
- Help the Hospices
- Now called Hospice UK, an organisation that supports the development of hospice care across the UK.
- Hospice
- An organisation providing care for people who have a long-term illness or are terminally ill.
- Intranet
- A private internet network accessible only to an organisation’s staff.
- Likert
- A scoring system applying scaled numbers to questionnaire responses.
- Listwise
- A method for handling missing data whereby an entire record is excluded from analysis if any single value required for the analysis is missing.
- Logistic regression
- A method for analysing binary outcome data (e.g. yes/no).
- Macmillan
- The abbreviated name of Macmillan Cancer Support (a national charity).
- Multilevel
- A method of analysis that accounts for clustering of data (e.g. within sites).
- Negative binomial
- A statistical distribution for modelling count data (e.g. the number of Rounds attended).
- NHS Leadership Academy
- An organisation that provides tools and training for individual NHS staff and providers.
- NVivo
- Qualitative data analysis software.
- Purposive sampling
- A non-probability sampling technique whereby the sample is selected for inclusion based on specific criteria (e.g. length of time running Rounds).
- Realist evaluation
- A type of theory-driven evaluation based on the epistemological foundations of critical realism that aims to refine understanding of how, why, when and for whom an intervention works.
- Ripple effects
- The continuing and spreading results of an event or action (used here to describe the impact that Rounds have beyond the immediate responses/actions, for example after participants return to clinical practice).
- Rounds administrator
- A staff member responsible for helping prepare and organise Rounds (including booking rooms, organising lunch, supporting promotions activities, co-ordinating steering group meetings and preparing for Rounds, for example paperwork and managing sign-in/feedback forms).
- Rounds clinical lead
- Typically a senior medic, an individual who works closely with the facilitator and undertakes a skilled co-facilitation role (responsibilities include helping to find cases/panellists, co-facilitation and championing Rounds).
- Rounds facilitator
- A person responsible for leading and co-ordinating the preparation and conduct of Rounds (responsibilities include panel preparation, ensuring safety and confidentiality, opening up reflective discussion, ensuring Rounds fidelity, and managing challenges and uncertainty).
- Rounds mentor
- A person experienced in Rounds (usually a facilitator) who supports new facilitators, clinical leads and steering groups in the development and consolidation of the skills required to run high-quality Rounds (e.g. by observing/debriefing, and providing off-site support via e-mail and telephone).
- Rounds steering group
- A group comprising staff from varied clinical and non-clinical disciplines and representing different levels of seniority (e.g. board members, junior nurses/doctors, porters, Human Resources managers, and marketing/communication professionals). Responsibilities include raising the profile of Rounds, sharing ownership, helping to find cases/panellists, supporting the clinical lead and facilitator, and debriefing Rounds).
- Schwartz Rounds
- Organisation-wide forums for health-care staff developed by the Schwartz Center for Compassionate Healthcare. They are named after Kenneth Schwartz, a patient in whose memory the Schwartz Center for Compassionate Healthcare (a non-profit organisation) was established in the USA in 1995. Frequently abbreviated to ‘Rounds’.
- Schwartz savvy
- A term referring to Rounds attenders who really understand the purpose of Rounds, know and follow the explicit and implicit rules of how to contribute appropriately, and support each other in a non-judgemental way.
- Snowball sampling
- A non-probability sampling technique whereby existing participants suggest/help to recruit future participants from their networks/knowledge.
- The King’s Fund
- An independent charity working to improve health and care in England.
- Trust
- A body that manages hospitals or community services. A NHS trust may be responsible for managing one or many hospitals or community services, and can manage both hospitals and community services.
List of abbreviations
- AfC
- Agenda for Change
- AHP
- allied health professional
- ANCOVA
- analysis of covariance
- CI
- confidence interval
- CMO
- context–mechanism–outcome
- CQC
- Care Quality Commission
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- GHQ-12
- 12-item General Health Questionnaire
- ID
- identification
- LETB
- Local Education and Training Board
- PI
- principal investigator
- PoCF
- Point of Care Foundation
- PPI
- patient and public involvement
- PSG
- Project Steering Group
- R&D
- research and development
- REC
- Research Ethics Committee
- SCCH
- Schwartz Center for Compassionate Healthcare
- SPSS
- Statistical Product and Service Solutions
- UWES-9
- Utrecht Work Engagement Scale
