Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal. The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/182/13. The contractual start date was in February 2018. The final report began editorial review in April 2018 and was accepted for publication in July 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Rob Anderson is a current member of the National Institute for Health Research Health Services and Delivery Research (HSDR) (researcher-led) Prioritisation Panel. However, this panel has no role in the allocation of review and research topics to the Exeter HSDR Evidence Synthesis Centre.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Shaw et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
This report is concerned with the ‘Nearest Relative’ (NR) provisions of the Mental Health Act 1983 (MHA 1983). 1 The work was commissioned by the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme. The following sections provide a brief overview of the key features of the MHA 19831 and the NR provisions contained within it, or as amended since 1983. Perceived problems regarding the use of the NR provisions are briefly discussed, and the relevant legislative changes that apply to Scotland and Northern Ireland are also described. Finally, justification for the methodological approach and the aims and objectives of the review are set out.
The Nearest Relative provisions of the Mental Health Act 1983
The Mental Health Act 1983
The MHA 19831 is a piece of UK legislation that governs the assessment, care, treatment and related matters pertaining to individuals with a ‘diagnosed mental health disorder’ who are detained in hospital via civil or criminal pathways. The MHA 19831 outlines the process by which individuals may be detained and treated, their rights to appeal and the rights of those receiving aftercare. The MHA 19831 also outlines the rights of the family and carers of the person being detained. The MHA 19831 fully applies to England and Wales, and partly applies in Scotland and Northern Ireland.
‘Sectioning’ under the Mental Health Act 1983: civil pathway
Section 2 of the MHA 19831 states that a person may be involuntarily admitted to hospital for a period of assessment of no longer than 28 days if they are suffering from a mental disorder ‘of a nature or degree which warrants the detention of the service user in a hospital’ (contains public sector information licensed under the Open Government Licence v3.0.) and it is in the interests of the health or safety of the service user or for the protection of the public. 1
A person can be involuntarily admitted to hospital under section 3 of the MHA 19831 for treatment for a period of up to 6 months initially if they are deemed to be suffering from a ‘mental disorder’ requiring treatment in hospital, and it is necessary for the safety of the service user or anyone else that treatment is given under detention. 1
The MHA 19831 has a series of safeguards to ensure that the powers to detain individuals in hospital involuntarily for a period of assessment and/or treatment are used appropriately. Before an individual can be detained under section 2 or 3 of the MHA 1983,1 two medical practitioners should independently assess the service user. The two practitioners should discuss the results of their assessments together, before reporting to an approved mental health professional (AMHP), who then decides whether or not to apply to a hospital to detain the service user. 1 An emergency detention can be sought under section 4 or 5 of the MHA 19831 when seeking an assessment by a second medical professional may ‘involve undesirable delay’. A section 4 detention can be converted to a section 2 or 3 detention if a second assessment, by a different medical professional, is conducted within 72 hours.
A service user sectioned under section 2 or 3 of the MHA 19831 has the right to appeal against the decision via a mental health tribunal. The decision to detain a service user also has to be reviewed regularly, although the time frame for this varies in accordance with which section has been used to detain the service user in hospital. 1
The Nearest Relative provision
The NR provision of the MHA 19831 was intended as another safeguard to protect the rights of a service user who is being involuntary detained. The NR is an individual assigned to the service user who has several rights and responsibilities relating to the care the service user receives. The NR:
-
can make a direct application to a hospital for the detention of the service user
-
can object to the detention of the service user under section 3 and, if this occurs, the service user cannot be compulsorily admitted
-
receives confidential information about the detained person
-
can request that the service user be discharged from sections 2 and 3 and a section 7 guardianship order.
Although a NR can also request the discharge of a service user from a community treatment order (CTO), they are unable to object to the initial imposition of the CTO or the recall of a service user to hospital should they not meet the criteria set by a CTO. 1 For ‘unrestricted’ service users admitted via the criminal pathway on section 37, their NR can apply to the tribunal to request a discharge from their section. 1
Identification of the Nearest Relative
Section 26 of the MHA 19831 defines and differentiates ‘Relatives’ and ‘Nearest Relatives’. ‘Relative’ means anyone in the following hierarchical list:
-
husband, wife or civil partner
-
son or daughter
-
father or mother
-
brother or sister
-
grandparent
-
grandchild
-
uncle or aunt
-
niece or nephew.
Under the MHA 1983,1 the AMHP will proceed through this list from top to bottom until an eligible NR, who meets the criteria required to take up the position, has been identified. To be considered eligible for the NR role a person must be > 18 years of age, living in the UK if this is the service user’s country of residence and, in the case of partnerships, in a relationship with the service user for > 6 months. 1 Ex-partners who have permanently separated from the service user cannot be considered for the role. In circumstances in which two individuals are eligible to fulfil the role (e.g. two siblings), the eldest and/or whole-blood relatives are selected.
Displacement and delegation of the Nearest Relative role
The NR may be ‘displaced’ (i.e. a different person appointed to the role) through application by an AMHP to the County Court. Possible reasons for displacement include when the NR cannot take up their duties because of illness, objects to an admission for treatment (or guardianship application) without good reason, has not considered the service user’s welfare or protection of the public in their application to discharge the service user or is considered unsuitable to act for any other reason. 1 Displacement of the NR is the only way to detain a service user under section 3 of the MHA 19831 if their NR has objected to the detention.
The NR can choose to nominate someone else if they do not wish to take up the responsibilities associated with the role, and may delegate responsibilities to the next eligible NR. 2
Legislative amendments influencing the Nearest Relative provisions
The NR role emerged in the Mental Health Act 19593 and was largely unchanged in the 1983 Act. 4 However, since 1983 elements of the MHA 19831 have been amended or influenced by the development of other legislation and codes of practice, which has influenced how the NR provisions are implemented. The key legislative changes are summarised below.
The Mental Health (Northern Ireland) Order, 1986
This legislation is broadly similar to the MHA 1983. 1 It specifies that compulsory admission will normally be on the basis of a recommendation by a general practitioner and application by an approved social worker (ASW). 5 The role of the NR is similar to that detailed by the MHA 1983. 1
The Human Rights Act 1998
The Human Rights Act 19986 outlines the rights and freedoms that everyone in the UK is entitled to. 6 These rights are set out in a series of 12 articles, each of which details a different right. Such rights include the right to life, the right to privacy, freedom from torture and inhumane or degrading treatment, and the right to a fair trial. 6 The Act means that people in the UK can seek justice in court if they feel that their rights have been violated and that public bodies, such as hospitals, courts and the police, must respect people’s rights. 7 The Human Rights Act was implemented in the UK in October 2000.
The implementation of the Human Rights Act provides a context for issues relating to information-sharing, and confidentiality in particular, given that the assigned NR is entitled to receive confidential information about the service user. 6 Because all health legislation post 1998 must be compliant with the Human Rights Act,6 we believe that it is of central importance for interpreting and implementing the MHA 1983. 1
The National Service Framework for Mental Health 1999
The National Service Framework for Mental Health8 section 6 outlines the support that carers of individuals with mental ill health should expect. This includes a yearly assessment of their needs and an implementation of a care plan based on this. The framework also advises that carers are provided with information regarding the mental health needs of the person they care for, including an explanation of the person’s care plan.
The Mental Capacity Act 2005
The Mental Capacity Act (MCA)9 is intended to protect individuals aged ≥ 16 years who do not have the capacity to make certain decisions for themselves. The MCA is intended to support professionals to assess the capacity of an individual regarding a specific choice and, if capacity is lacking, make a decision that is in the best interests of that person. 10
The Mental Health (Care and Treatment) (Scotland) Act 2003
The Mental Health (Care and Treatment) (Scotland) Act 2003 (MHCT)11 introduced key changes to the processes involved in the detention of people with ‘mental disorders’ in Scotland. The change of greatest relevance to the present review was the introduction of the ‘Named Person’ (NP) role, in place of NR provision. The Millan Committee was established to review the Mental Health (Scotland) Act 1984, which included NR provision as set out in the MHA 1983. 1,12 The NP was recommended in response to a number of concerns over the suitability of the NR, namely that the appointed NR may not be appropriate for reasons of practicality, lack of genuine interest in the service user or the potential for abuse of powers. 13
Under the MHCT, the powers of the NP are reduced, and the service user has choice over who is appointed and can revoke the NP in writing. 11 If the service user does not nominate a NP, an individual can be appointed by default, turning first to the primary carer, and then to the NR hierarchy set out in the MHA 1983 [with the addition of civil partners as set out in the Mental Health Act 2007 (MHA 2007)]. 1,14 Key differences between the NR and NP are shown in Table 1.
| Application of act | NR (MHA 2007)1,14 | NP (MHCT)11 |
|---|---|---|
| Region | England and Wales | Scotland |
| Appointment | By default, in accordance with hierarchy of ‘nearness’ of relatives set out in MHA 19831 | Nominated by service user. In absence of nomination, defaults to primary carer, then in accordance with the hierarchy of ‘nearness’ of relatives set out in MHA 19831 |
| Displacement | Via application to a County Court | Can be revoked in writing by the service user. Can be challenged by a mental health professional if deemed inappropriate |
| Option to decline | Powers can be delegated by the NR to another eligible relative | Can be declined by the NP |
| Rights to information |
|
To:
|
| Discretionary powers | To:
|
To:
|
The Mental Health Act 2007
The MHA 19831 was revised in 2007,14 leading to a number of significant changes to the Act. These include changes to professional roles, such as introducing the AMHP to replace the ASW, introducing CTOs to replace supervised discharge, certain definitions, interaction with the Mental Capacity Act 2005 and the structure of mental health tribunals. 14 Of direct relevance to the NR provisions were the following amendments:
-
When identifying the NR, those in civil partnerships were considered as being of equal status to people who were married.
-
Service users were given the power to displace the NR on grounds of unsuitability. Applications were to be made to a County Court.
Information Sharing and Mental Health: Guidance to Support Information Sharing by Mental Health Services 2009
This Department of Health and Social Care (DHSC) publication15 discusses the rights of service users to know about the information that is held about them by public bodies, and the right of carers and other members of the public to receive enough information to enable them to support the service user and protect themselves. 15 The document also acknowledges the role that carers may play in providing information to services. It recommends criteria that should be fulfilled when sharing information regarding a service user between different parties.
The Mental Health (Wales) Measure 2010 and associated Code of Practice to Parts 2 and 3
The Mental Health (Wales) Measure (MHWM) 201016 details the support people living with a mental health problem should receive in both primary and secondary care. With regard to the NR role, the MHWM 2010 aims to ensure that people receiving secondary mental health services in Wales all have a care and treatment plan. The associated Code of Conduct for parts 2 and 3 of the MHWM 2010 stipulates that the service user should be involved as much as possible with the assessment to inform their care and treatment plan, and their carers and ‘significant others’ should be involved when appropriate. 17
The NHS Five Year Forward View 2014
This policy document18 outlines government proposals regarding new models of care within the NHS. Of particular relevance to the NR role, this document outlines a commitment to improve the support that carers of individuals with long-term conditions receive. The document outlines the goal to improve access to information regarding the service user’s condition, history and care, not only for the service user themselves, but also for any other individuals whom the patient wishes to share this information with.
The Mental Health Act Code of Practice 2015
The Code of Practice provides guidelines for professionals on their roles and responsibilities under the MHA 1983. 1,2 Revisions to the Code were made in 2015, in the light of changes in law and policy since it was first published, and aims to improve protection of the rights of service users, families and carers. It also outlines how to determine when the MHA 19831 should be used instead of the MCA and vice versa. 2
Issues regarding the Nearest Relative provisions
Despite amendments to the MHA 19831 (in 2007)14 and the introduction of a revised Code of Practice (2015)2 to give guidance in applying the MHA 1983,1 there are still concerns about the use of NR provisions. The Care Quality Commission has raised concerns that detained service users are not given enough say in their care. 19 Others have highlighted how the system for involving partners, carers and family members in the care service users receive under the NR provision of the MHA 19831 is inflexible, and does not always represent either the wishes of the service user or the person identified as their NR. 20 This is despite the amendments to the MHA 19831 in 2007, which recognised same-sex relationships within the NR hierarchy and enabled detained service users to displace people who they felt were inappropriate to act for them within the NR role. 14
In 2017, the government commissioned an independent review of the MHA 1983,1 to focus on how the legislation is being used in practice and examine its impact on service users, families and carers. 21
Overall aims and objectives of the systematic review
The aim of this systematic review is to summarise and synthesise experiences of the NR provisions of the MHA 19831 from the perspectives of service users, family members, carers and relevant professionals. More specifically, it aims to gather research evidence to answer the following question: what are the experiences of services users, family members, carers and relevant professionals of the use of the NR provisions in the compulsory detention and ongoing care of people under the MHA 1983?1
This included objectives, from the perspective of service users, family members, carers and relevant professionals. These were to explore:
-
experiences relating to the identification of the NR in the care of an individual who has been compulsorily detained under the MHA 19831
-
experiences of requesting displacement of the assigned NR, including the process of going through a tribunal and issues associated with this, such as influences on ongoing care
-
issues relating to service user confidentiality and information-sharing, relating to all aspects of compulsory detention
-
issues relating to decisions about care during detention and after discharge, including discharge to a CTO
-
issues relating to service users having access to support from individuals who they want to be involved with or informed about their care.
Chapter 2 Methods
This systematic review was conducted in 6 weeks. The methods used to identify and select evidence followed the best practice approach recommended by the University of York’s Centre for Reviews and Dissemination. 22 Reporting of the methods and results was consistent with Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) reporting guidelines23 and Enhancing Transparency in Reporting the synthesis of Qualitative Research (ENTREQ) checklist guidelines. 24 A protocol was registered on the PROSPERO database (PROSPERO CRD42018088237).
Search strategy
Background scoping searches were carried out to help develop a bibliographic database search strategy for the identification of evidence. This predominantly consisted of basic keyword searching in Google (Google Inc., Mountain View, CA, USA) and Google Scholar. Whenever possible, we ensured that relevant papers identified in the background scoping process would be retrieved by our bibliographic database searches by deriving search terms from the titles and abstracts.
An information specialist (SB) developed the bibliographic database search in consultation with the review team. The search strategy made use of both controlled indexing (e.g. medical subject headings in MEDLINE) and free-text (i.e. title and abstract) searching. A qualitative study search filter was used with adaptations to limit the results to qualitative studies. 25 We also included search terms for ‘questionnaires’ and ‘surveys’ in order to complement the limited qualitative evidence that our background scoping indicated would be available to us. The search results were limited to English-language publications in view of the UK focus of our review, and to publications from 1998 onwards in view of the central importance of the Human Rights Act 19986 for interpreting and implementing the MHA 1983. 1 The final search strategy was translated for use in seven bibliographic databases, which were selected based on their relevance to the topic area: MEDLINE (via Ovid), MEDLINE In-Process & Other Non-Indexed Citations (via Ovid), PsycINFO (via Ovid), Social Policy and Practice (via Ovid), HMIC (via Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (via EBSCOhost) and Applied Social Sciences Index and Abstracts (ASSIA) (via ProQuest). The bibliographic database search strategies are reproduced in Appendix 1, Bibliographic databases.
Forward citation-chasing (identifying papers that cite our included studies) was conducted using Web of Science, Scopus and Google Scholar. Backward citation-chasing (inspecting the reference lists of included studies) was carried out manually by reviewers. The reference lists of previously conducted systematic reviews on topics related to the NR provision of the MHA 19831 were also inspected.
The websites of several relevant organisations that were identified through our background scoping were searched using basic keyword searching, as permitted by the search interfaces of the websites. The website search strategies and list of websites searched are reproduced in Appendix 1, Website searches. Finally, authors of relevant studies were contacted with regard to unpublished or unobtainable studies.
Inclusion and exclusion criteria
The following inclusion criteria and exclusion criteria, in accordance with the Population, phenomenon of Interest and Context (PICo)26 categories were applied to the studies identified through the search strategy.
Population
This was defined as people detained under section 2 or 3 of the MHA 1983,1 their family and carers and the individuals involved with their care who work within the remit of the MHA 1983. 1
More specifically, the population may include:
-
current service users
-
former service users
-
service users’ family members and carers
-
health and social care professionals
-
approved mental health professionals (community nurses, psychologists, occupational therapists, social workers)
-
advocates
-
police officers.
Studies were included if the individuals were:
-
a service user who has experience of being compulsorily detained under section 2 or 3 of the MHA 19831
-
carers, relatives related professionals (listed above).
Studies were excluded if the individuals were:
-
people who have agreed to a voluntary admission and carers, relatives and relevant professionals involved in their care
-
people with mental health difficulties not leading to compulsory detention under the MHA 1983. 1
Phenomenon of interest
This was defined as experiences of, or attitudes towards, the application of the NR provisions of the MHA 1983. 1 This includes any experiences in relation to the involvement of relatives, carers or professionals in the care of or decisions about a compulsorily detained person.
Studies were included if data about experiences were obtained through:
-
qualitative means (e.g. interview, focus group)
-
a survey or questionnaire.
Context
This was defined as the use of the NR provisions of the MHA 19831 within the UK only.
Studies were included if:
-
detention took place under the jurisdiction of England, Wales, Scotland or Northern Ireland
-
data were from any time since the publication of the Human Rights Act 1998.
Studies were excluded if:
-
detention was not under the jurisdiction of England, Wales, Scotland or Northern Ireland
-
detention of an individual was undertaken by forensic services.
Study design
Studies were included if data came from:
-
studies using stand-alone qualitative studies and from mixed-methods studies using several
-
different methods.
Studies were excluded if data came from:
-
blogs or social media posts
-
commentaries, opinion pieces and editorials
-
case studies
-
conference abstracts
-
case law.
Study selection
Searches were undertaken and all results were downloaded into EndNote [EndNote X8; Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] for removal of duplicate records. A pilot screening exercise was carried out on a sample (n = 100) of bibliographic database search results in order to calibrate inclusion/exclusion judgments for all reviewers (MN, LS and SB) and refine the clarity of inclusion criteria. Decisions were discussed in a face-to-face meeting to ensure consistent application of criteria. When necessary, inclusion and exclusion criteria were revised to reflect reviewer interpretation and judgment.
The revised inclusion and exclusion criteria were then applied to the title and abstract of each identified citation independently by two reviewers (MN and LS). Disagreements were resolved through discussion, with unresolved disagreements resulting in inclusion for full-text screening. Sources excluded on the basis of relating to forensic detention were labelled on exclusion.
The full text of each source taken forward from title and abstract screening was assessed independently for inclusion by two reviewers (LS, MN or SB). Disagreements were settled by discussion with a third reviewer when necessary.
References were managed in EndNote software. Reasons for exclusion were recorded at full-text screening and documented in a PRISMA flow chart (see Figure 2). 23
Data extraction
A data extraction form was developed using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA), piloted by Michael Nunns, Liz Shaw and Simon Briscoe and refined accordingly. Summary data were extracted for each study included after full-text screening (both ‘tiers’ of studies) by one reviewer (MN, LS or SB) and checked by a second reviewer (SB, LS or MN). Extracted data included first author, date of source, title of source, focus/aim of source, sample size, sample demographics, stakeholder groups represented, data collection technique (e.g. survey, interviews, focus group), type of analysis done and themes or ideas presented relevant to the research question.
Critical appraisal strategy
Critical appraisal was carried out on studies prioritised for synthesis only (‘top tier’). Critical appraisal was done by one reviewer (LS or MN) during data extraction using the Wallace checklist27 and checked by a second reviewer (MN or LS). Disagreements were resolved through discussion. Critical appraisal did not influence eligibility for inclusion or synthesis, but was intended to provide context to findings.
Methods of data synthesis
Owing to the time restrictions imposed on the review process, after full-text screening decisions had been completed, a purposive sampling approach was applied to prioritise the best available evidence for inclusion. This was a pragmatic step that considered both the quality and the quantity of relevant evidence available in each record. All included studies were rated by two reviewers (MN and LS) based on the number of relevant primary data collected. Studies that contained at least half a page of qualitative data directly relating to the research objectives were prioritised into the ‘top tier’ of included studies, ready for inclusion in the framework synthesis. Data from surveys and questionnaires were not prioritised as there were no free-text responses to open questions presented. Disagreements on the classification of studies were resolved with discussion. Studies that did not meet this rating were retained in the ‘second tier’ of studies. Key details (country, aim of paper, data collection methods and sample characteristics) of studies sorted into the second tier were described and tabulated.
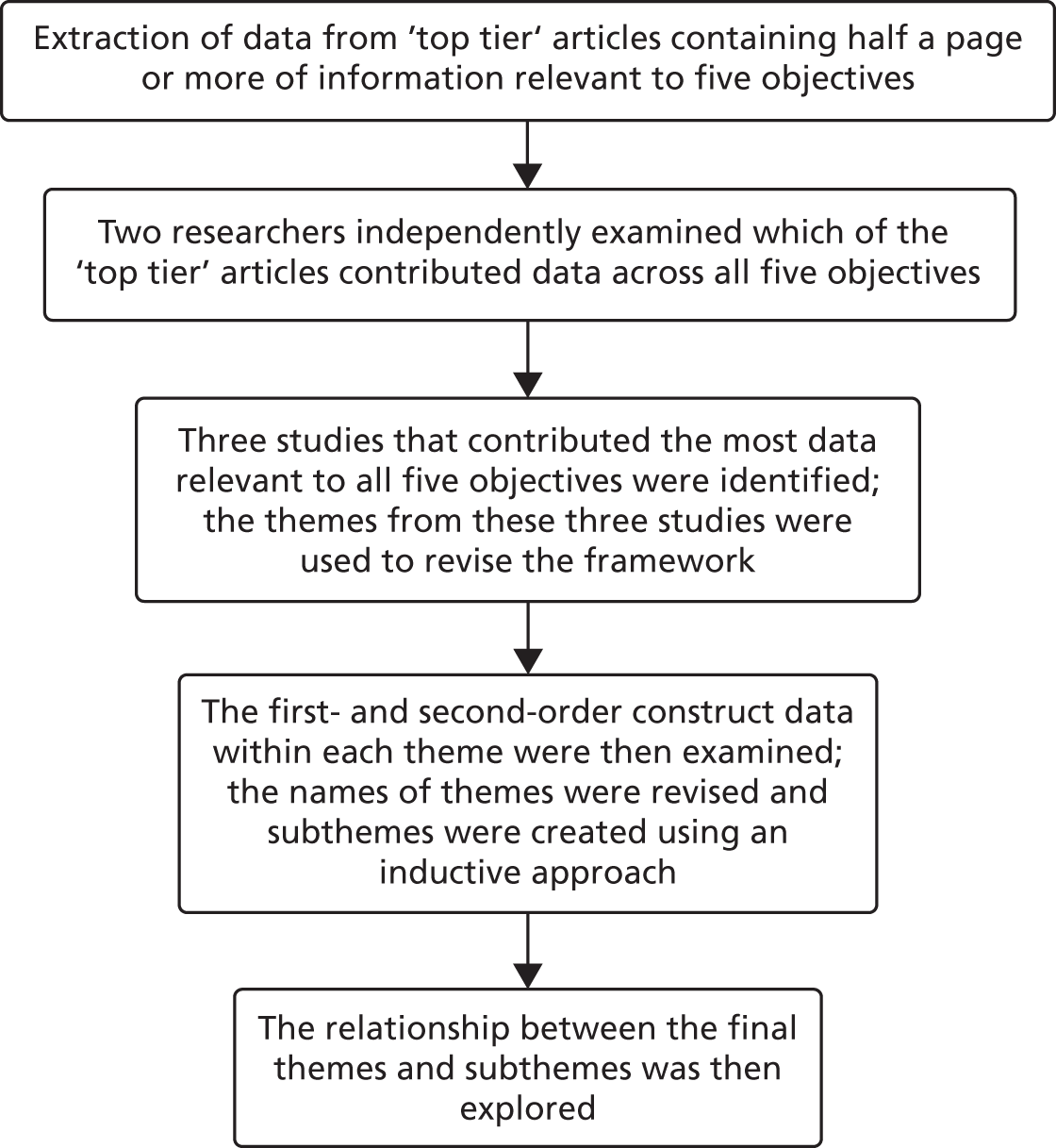
We made a pragmatic decision to use a framework synthesis approach, because a thematic analysis utilising an inductive interpretative approach would not have been possible within the limited period of time available to complete this review. Framework syntheses have been recognised for their utility in making sense of qualitative evidence within the short time frame associated with rapid reviews of health research. 28
Typically, the initial framework used within a framework synthesis would be selected from an existing theory or model relevant to the field or constructed by drawing on a thorough understanding of relevant background literature and related theory (e.g. see Dixon-Woods29). However, our background scoping and preliminary searches did not identify any accessible theory or framework that was relevant to all of our research objectives. Hence, the process used for the framework synthesis differed from that stated in our protocol. The synthesis process used in this review was as follows.
Extraction of data relevant to the research question(s)
Participant quotations illustrating the views of service users, carers and NRs and the author interpretation of these views (known as first- and second-order construct data, respectively30) were extracted from the results section of each ‘top tier’ article. The information was placed within a framework based on our five research objectives by one reviewer (LS or MN), and checked by a second reviewer (MN or LS) using Microsoft Excel®. This information was used to identify which papers contributed towards a range of different research objectives and represented a variety of participant perspectives.
Identification of initial themes
This process was carried out independently by two reviewers (LS and MN) identifying eight ‘top tier’ papers from three studies with the most data relevant to multiple research objectives, accounting for a range of participant perspectives. One of these studies was conducted in England31 and two were conducted in Scotland. 32,33 One reviewer (LS) selected the themes presented in each article that were most relevant to the research objectives. A second reviewer (MN) checked the selection of themes (see Appendix 2), which were then used to revise the stage 1 framework. Studies in the ‘second tier’ of included studies did not influence the identification or development of themes.
Final framework revisions using thematic analysis
The content of each of the themes generated through stage 2 of the synthesis was then re-examined. Within each broad theme, first- and second-order data that appeared to be discussing similar or related concepts were grouped together. This formed the beginnings of descriptive subthemes. The data contained under these subthemes were moved both within and across existing subthemes to reflect changes in their content. Preliminary subthemes were divided and merged and content changed in an inductive, iterative process, in order to capture current or relevant ideas within the included studies that were not represented by the initial framework. As this process evolved and additional interpretation occurred, the names of subheadings and their placement under certain themes were changed in order to reflect the data within them. Towards the end of the process, some theme names were also changed in order to better represent the content of the framework and the reviewer’s understanding of the data.
The synthesis was conducted by one reviewer (LS) within Microsoft Excel®. The names of emerging subthemes and themes were checked with other members of the review team (MN, SB, JTC and RA), whose feedback was incorporated into the developing themes and subthemes to ensure that their names accurately reflected their content.
Relationship between the themes
A figure representing the relationship between the themes identified through the framework synthesis of the ‘top tier’ papers was then developed through discussion (LS, SB, MN, RA and JTC). The data synthesis process is summarised in Figure 1.
FIGURE 1.
Framework synthesis process for prioritised studies.
End-user involvement
One carer with experience of the NR provisions provided feedback on the themes and subthemes identified by the synthesis and commented on the write-up of the results within this report.
Reflexive statement
The methods utilised within this review were reflective of the expertise and experience within the review team. The team consisted of three systematic reviewers (JTC, MN and LS), an information specialist (SB) and a health economist (RA) with prior experience of conducting systematic reviews for the National Institute for Health Research. This prior experience meant that the team aimed to maintain a rigorous methodology throughout the review, despite the limited time frame available. This is reflected in the decision to retain searching across multiple databases, double screening of references at both title/abstract and full-text level, searches within the grey literature and citation-chasing. The team’s prior experience of managing large numbers of retrieved studies within a set time frame meant that we were able to quickly identify a method to prioritise the studies for inclusion in the main synthesis.
The focus of the review was novel for most members of the team. This meant that the background reading and identification of search terms was informed by objective appraisal of existing literature, albeit restrained by the time available. The team knew of some relevant policy because of previous projects and the experience of one reviewer (LS) of working alongside individuals detained under the MHA 19831 and working in accordance with the MCA. This reviewer utilised her prior experience and knowledge gained through her training as a clinical psychologist and of conducting qualitative synthesis within this review. Her experience provided a lens through which the information included in this review was selected, placed within themes and interpreted. This was balanced by the checking of extracted data by a second reviewer (MN) and incorporation of views from other members of the team and a carer with experience of the MHA 1983. 1 The limited time frame necessitated the use of a framework methodology and a more descriptive analysis, which also limited the potential bias during the synthesis process.
Chapter 3 Results
Study selection
The PRISMA flow diagram in Figure 2 summarises the study selection process. Bibliographic database searches identified 2439 records and supplementary search methods identified 126 records. Following the removal of duplicates there were a total of 1851 unique records that were screened against our inclusion and exclusion criteria. The full texts of 173 papers were sought for further consideration. Of these, 159 full texts were successfully retrieved (92%). Following full-text screening, 124 papers were excluded for the reasons specified in Figure 2. Half of the excluded papers (n = 62) were excluded because they did not report relevant data. Other common reasons for exclusion included being a non-UK study (n = 22) and having no primary study data (n = 21). A smaller number of papers were not about compulsory detention (n = 12), were not about the MHA 19831 or a relevant section of the MHA 19831 (n = 1 and 3, respectively) and there was one conference abstract for which no follow-up journal article could be identified. Thirty-eight papers identified at the title and abstract screening stage focused on involuntary hospital admissions through the criminal pathway of the MHA 1983. 1 The citations of these records are listed in Appendix 3. These were not full-text screened and are not included in any further analysis.
FIGURE 2.
The PRISMA flow chart.
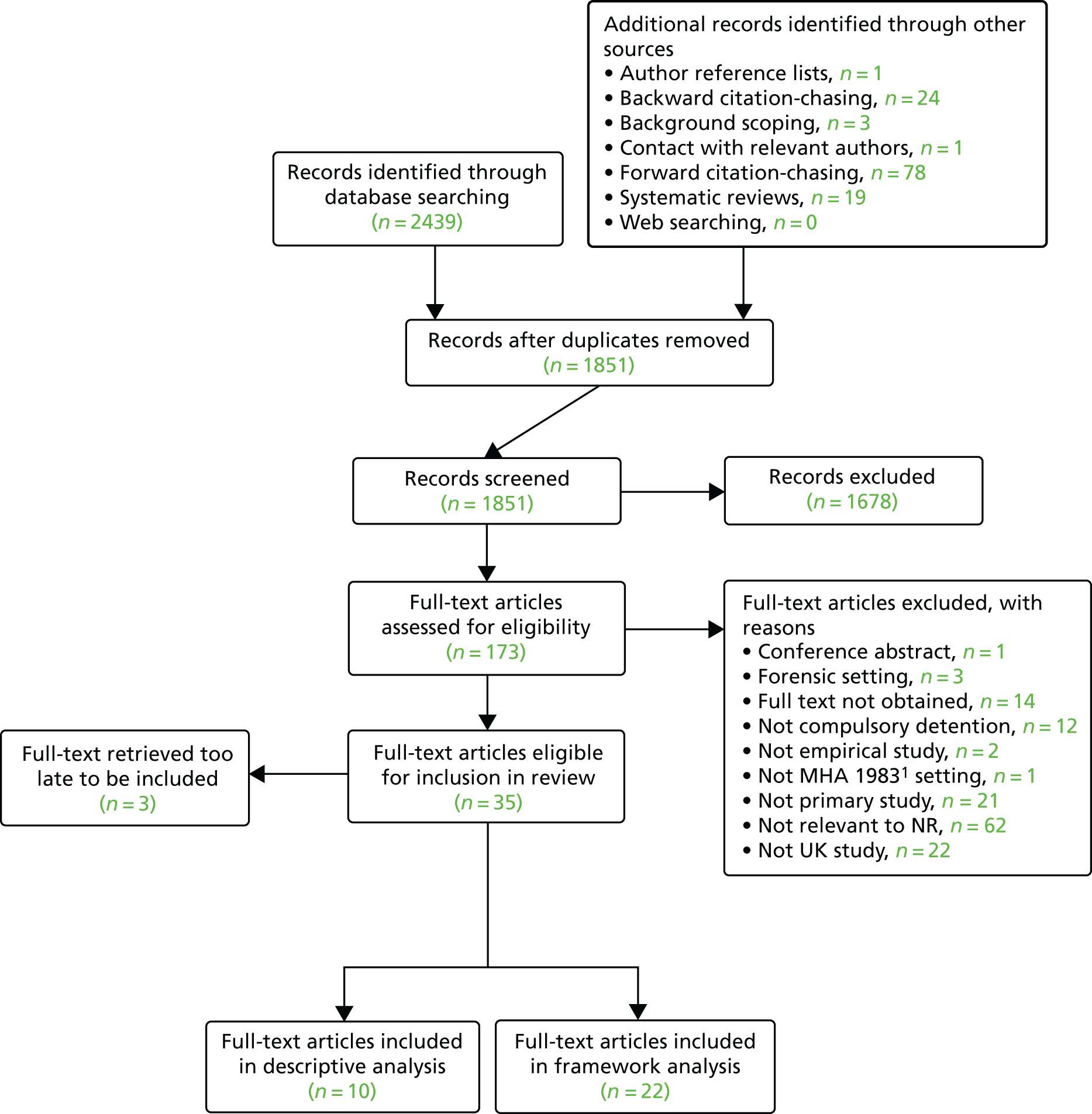
In total, 35 papers4,20,31–63 were identified that met our inclusion criteria: 22 papers via searching bibliographic databases and 13 papers via supplementary search methods.
As described in Chapter 2, Inclusion and exclusion criteria, papers that met our inclusion criteria were categorised in accordance with the number of relevant primary data presented. Papers with several paragraphs or more of data were prioritised into the ‘top tier’ of included studies for synthesis, and studies that did not meet this rating were retained in the ‘second tier’ of studies for narrative description.
Description of included studies
Included sources: prioritised studies
Of the 20 studies that met criteria for inclusion in the review, there were 12 studies, reported across 22 papers,4,31–33,36–38,40,45,46,48,49,51–60 that contained enough relevant and usable data for inclusion in the framework synthesis. Table 2 contains a summary of the foci, sample characteristics and qualitative data collection and analytic methods employed in these studies.
| First author, year of publication | Country | Publication type | Study focus | Qualitative data collection method (date of data collection) | Participants providing qualitative data | Study context and sampling | Type of qualitative data analysis |
|---|---|---|---|---|---|---|---|
| Berzins, 2009;32 2009;37 and 201036 | Scotland | D; JP; JP | Perceptions of NP provisions | Semistructured telephone (carers) and face-to-face (service users) interviews (data collected 2005–7) | Total, N = 46: service users, n = 20; carers, n = 10 (as potential NPs, n = 3; already NPs, n = 4; considering, n = 3; not considering, n = 0); MHOs, n = 7 (social workers); professionals with influence on government policy, n = 9 | MHOs from local authorities, service users and carers recruited from voluntary organisations, policy influencers recruited at national level. Direct contact/newsletter | Thematic analysis |
| Campbell, 200838 | Northern Ireland | JP | Nature of legal advocacy services available after compulsory admission | Focus group interviews and questionnaires (date of collection NR) | Total, N = 44 respondents from five mental health service user groups: carer group, lawyers, mental health review tribunal member, professional advocacy service managers, hospital administrators | Questionnaires posted to solicitors and hospital administrators in Northern Ireland. Focus group recruitment NR | Thematic analysis |
| Dawson, 200933 | Scotland | R | Perceptions of NP provisions | Face-to-face interviews, telephone interviews and focus groups (data collected 2007–8) | Total, N = 44: service users, n = 2; NPs, n = 4; tribunal members, n = 13; MHOs, n = 14; nurse, n = 1; legal reps, n = 3; independent advocates, n = 5; tribunal clerks, n = 2 | Four local authority areas and their associated health board across Scotland. Contact with voluntary sectors, written invitations, bespoke events with stakeholder groups | Framework analysis |
| Henderson, 200245 | England | JP | Service users’ experiences of mental health care after compulsory admission | Semistructured interviews and observation of group discussions (data collected 2001) | Total, N = 21: carers, n = 11; service users, n = 10 | Participants had to be or have been in a relationship in which one partner has a diagnosis of bipolar disorder | Phenomenological framework analysis |
| Jankovic, 201146 | England | JP | Experiences of family caregivers of relatives involuntarily admitted to psychiatric hospital | In-depth, semistructured interviews (date of collection NR) | Total, N = 31 family caregivers | Contact by letter or telephone. Service users recruited in larger national multicentre study on Outcomes of Involuntary Hospital Admission in England provided informed written consent to approach their family caregivers | Thematic analysis |
| Marriott, 200148 | England | JP | Opinions about the MHA 19831 from those subjected to or affected by it | Focus group, telephone interviews, consensus meeting or written responses (date of collection NR) | Total N = 85a in three groups. Group 1, n = 40: mental health nurses, n = 9; ASWs, n = 10; general psychiatrists, n = 4; MHA 19831 administrators, n = 5; service users, n = 5; carers, n = 7. Group 2, n = 19: hospital managers, n = 2; solicitors, n = 2; general practitioners, n = 3; policy-makers, n = 4; police surgeons, n = 2; police liaison officers, n = 3; specialist psychiatrists (one from each of learning disability, forensic, and child and adolescent services), n = 3. Group 3, n = 26, consisting of people leading organisations representing groups 1 and 2: including a number of national organisations representing users and carers and professional groups affected by or using the Act | Initial nominations made by national experts or representative organisations. Contacted by telephone or in writing | Thematic analysis |
| Pinfold, 200449 | England | R | Identify examples of good practice, or issues with information-sharing between mental health practitioners and carers | Telephone interviews, face-to-face group discussions, multidisciplinary workshop events, open-ended survey questions (date of collection NR) | Survey, N = 998: service users, n = 168; professionals, n = 212; carers, n = 496; carer support workers, n = 93; young carers; n = 29. Interviewed, n = 34: service users, n = 5; professionals working in mental health and ageing, n = 5; professionals working in adult mental health services, n = 9; carers for people with severe mental illness, n = 7; carers supporting people with dementia, n = 5; carer support workers n = 3 | National advertising. Convenience, purposive and snowball sampling techniques. Purposive sample recruited via services in mental health charities Rethink Mental Illness and Mind | Thematic analysis of interview data and content analysis of open responses |
| Rapaport, 1999;51 2002;31 2003;52 2004;4 and 201253 | England | JANP; D; JP; JP; JP | Investigate conceptual and ethical issues and carers’ and service users’ perspectives of NR provisions | Focus group interviews, role information, vignettes and group exercises, questionnaires (data collected 1997–9) | Total, N = 79: carers, n = 34; service users, n = 19; ASWs, n = 26 | Recruited through local groups. Invited by letter, followed up by telephone and visit. All had to have experience of NR provisions | Comparative content analysis of historical data. Grounded theory and multiple case design analysis of contemporary data |
| Ridley 2009;56 2010;55 and 201354 | Scotland | R; JP; JP | Experiences and views of the early implementation of MHCT | Focus group and telephone interviews (data collected 2007–9) | Total, N = 120: service users, n = 49; carers, n = 33; professionals, n = 38, of which n = 15 representatives of organisations and n = 23 individual practitioners (general practitioners, psychiatrists, community psychiatric nurses, nurses, psychologists, MHOs, lawyers and advocacy workers) | Purposive sampling from four health board areas in Scotland, chosen to reflect rural, urban and mixed geographical areas (Dumfries and Galloway, Fife, Greater Glasgow and Clyde) and the state hospital | Grounded theory |
| Rugkåsa, 2017;57 and Canvin, 201440 | England | JP; JP | Experiences of carers and involvement of family in CTOs | Interviews (data collected 2012) | Total, n = 24 family carers | Family carers of service users with experience of CTOs | Thematic analysis |
| Smith, 201558 | England | JP | NR’s experiences of mental health crises, identifying improvements that could be made to AMHP practice | Telephone interviews (data collected 2014) | Total, n = 32 NRs | NRs in contact with ASWs in the south of England | Inductive thematic analysis |
| Stroud, 2013;60 and 201559 | England | R; JP | Service user and practitioner experiences of the use of CTOs | In-depth semistructured interviews (data collected 2011–12) | Total, N = 72: service users, n = 21; NRs, n = 7; care co-ordinators, n = 16; responsible clinicians, n = 10; AMHPs, n = 9; service providers, n = 9 | Consulted CTO records from Sussex Partnership NHS Trust, approached by letter of invitation | Thematic analysis |
Among the ‘top tier’ studies, there were two PhD theses31,32 and four reports. 33,49,56,60 The three studies from Scotland32,33,56 consisted solely of government reports and subsequent publications in peer-reviewed journals, all focusing on the implementation of the MHCT, with specific regard to the NPs provisions. One study38 was conducted in Northern Ireland and focused on the views of various stakeholders on advocacy services available after compulsory detention. The remaining eight studies, conducted in England, could broadly be grouped as focusing on experiences of CTOs,57,60 interactions with various mental health professionals49,58 or perceptions of the MHA 19831 and the NR provisions and their implications for care. 31,45,46,48
All of the ‘top tier’ studies collected data using interviews. Other data collection methods used included administering questionnaires with space for open responses,31,38,49 observation of group discussions,45,49 and workshop events or group exercises. 31,48,49 There was a mixture of national and local sampling approaches, resulting in sample sizes ranging from 21 carers45 to 998 survey respondents. 49 Interviews were conducted with samples ranging from 2145 to 11556 individuals, from a range of perspectives. Analysis was described as ‘thematic analysis’ (eight studies),32,36–38,46,48,49,57–60 ‘grounded theory’ (two studies)33,45 or ‘framework analysis’ (two studies). 4,31,51–56
Included sources: ‘second tier’ studies
Ten papers, reporting eight studies, met the inclusion criteria for the review but did not contain enough relevant data for synthesis. 20,34,39,41–44,47,50,61 Table 3 contains a summary of the aims, sample characteristics and methods for these 10 papers.
| First author, year of publications | Country | Aim or focus of paper (from paper) | Sample | Data collection and analytic approach |
|---|---|---|---|---|
| Banks, 201634 | England | Understand experiences of CTO practice within the context of the personalisation agenda, in particular, aspects of person-centred support | Total, N = 72: service users, n = 21; practitioners (n = 35, of whom, care coordinators, n = 16; responsible clinicians, n = 10; AMHPs, n = 9); NRs, n = 7; service (supported housing) providers, n = 9 | Thematic analysis of semistructured interviews |
| Campbell, 2001;39 and Manktelow, 200247 | Northern Ireland | Reports on the first extensive survey of ASW activity in Northern Ireland. The research aimed to explore the training, practice and management of ASWs | Total, N = 282: service users/carers, n = 28; ASW managers, n = 11; ASWs, n = 243 survey respondents | Thematic analysis of semistructured interviews conducted via telephone, face to face or in focus groups. Additional postal survey of ASWs |
| De Maynard, 200741 | England | Seeks to examine the experiences of black men detained under the MHA 19831 | Total, n = 8: BME men (specifically of African or African Caribbean descent) living with severe mental illness | Grounded theory approach to analysis of qualitative interviews |
| Department of Health and Social Care, 201542 | England | The Department of Health and Social Care consulted people and organisations about strengthening the rights and choices of people to live in the community, especially people with learning disabilities, autism or mental health conditions. This document summarises the main trends in responses to the consultation | Total, N = 468. Responses from individuals, n = 219: service users (48%); carers, family or friends of service users (25%);a health and social care professionals, support workers and advocates and others (27%). Responses from various organisations, n = 221; other groups, n = 28 | 50-item ‘agree/disagree’ questionnaire, with space for open comments. Content analysis of open responses |
| Gault, 2009;43 and Gault, 201344 | England | Describes people’s experience of being compliant or non-compliant with treatment, their experience of compulsory treatment and how they feel that they should be encouraged to comply | Total, N = 19: service users, n = 11; carers, n = 8 | Two largely unstructured focus groups 10 or 12 months apart, coded with a grounded theory approach |
| Mental Health Alliance, 201720 | England | The survey focuses on the underlying principles of the MHA 19831 and how people’s rights are currently protected, where it is working well and what could be changed and improved | Total, n = 8631: survey responses from service users, carers and mental health professionals | Questionnaire with opportunity for free-text responses |
| Rabiee, 201350 | England | This paper examines the views and experiences of using and providing mental health services from the perspectives of black African and black African Caribbean mental health service users, their carers, voluntary services and a range of statutory mental health professionals and commissioners in Birmingham, UK | Total, N = 65: BME service users, n = 25; carers, n = 24; a range of statutory mental health professionals, n = 16 | Grounded theory approach to analysis of telephone interviews, face-to-face interviews and focus groups |
| Taylor, 201361 | England | Sets out the views of AMHPs on the impact of SCT on their work and their service users’ lives in the community | Total, n = 14 AMHPs | 50-item questionnaire, with opportunity for open comments |
There were eight peer-reviewed journal articles reporting six primary studies34,39,41,43,44,47,50,61 and two survey-based reports. 20,42 Eight papers reported research conducted in England and/or Wales,20,34,41–44,50,61 and two reported research conducted in Northern Ireland. 39,47 The papers by Campbell et al. 39 and Manktelow et al. 47 were based on survey data collected in 1998–9, in the context of the Mental Health (Northern Ireland) Order (1986). 5 Of the studies conducted in England and Wales, only the study by De Maynard41 may have been conducted prior to the 2007 amendments to the MHA 1983,1,14 although the date of data collection was not reported.
Telephone and face-to-face interview and focus groups were used in five studies to capture experiences. 34,39,41,43,50 Survey methods with opportunities for free-text or open responses were used on their own in three studies20,42,61 and used in conjunction with interviews by Campbell et al. 39
The views of service users were captured in seven studies,20,34,39,41–44,47,50 including two focusing on the experiences of black and minority ethnic service users. 41,50 Appointed NR or NPs were specifically sampled only in the study by Banks et al. 34 Other family members or carers (i.e. not necessarily in any formal statutory role) contributed views in five studies. 20,39,42,43,50 Mental health professionals, including AMHPs and ASWs, were sampled in six studies. 20,34,39,42,50,61
Eligible sources retrieved late
Three additional records were identified at title and abstract screening as being eligible for inclusion in the review, but could not be retrieved in time to be considered for data extraction or synthesis because of the rapid review timeline. These consisted of (1) a PhD thesis,62 acquired via expert recommendation, about approved mental health practice in England and Wales; (2) a journal article,35 identified through database searches and retrieved via The British Library, about service users’ experiences of compulsion under the MHA 1983;1 and (3) a report by the Social Services Inspectorate,63 part of the Social Care Group in the Department of Health and Social Care (DHSC), that provided relevant data about the involvement of social workers in the care and treatment of involuntarily detained service users. Of the three additional records, only the PhD thesis62 would have been eligible for inclusion in the framework synthesis, based on the quantity of relevant data presented.
Critical appraisal
The quality of the 12 studies included in the framework synthesis is shown in Table 4. Overall, studies scored well in several domains. All studies provided a clear question and subsequently used appropriate study designs to answer them. Findings were always substantiated by data and largely generalised to an appropriate degree. Reflexivity was explicitly considered only in two studies,31,32 and for this reason they were the only studies in which it was possible to determine the effect of the authors’ ideological or theoretical perspectives on their findings. In terms of the reporting of methods, the context or setting was described well in only 5 out of 12 studies. 31,32,46,49,56 Samples were usually appropriate, or their limitations acknowledged. For the description of data collection, three studies did not provide enough information to be able to reproduce the data collection setting,33,45,60 and there was insufficient evidence of rigorous data collection in two studies that described only the use of an interview schedule. 38,46 Other studies described the use of additional markers of rigorous methods, such as the use of audio-recordings, checking transcripts and supplementary note-taking. Four studies were judged to have lacked evidence of rigorously conducted data analysis. 38,45,58,60 In order to score positively for this outcome, studies needed to have included an explicit description of the process of qualitative data analysis, for example the pathway from initial coding of transcripts to the development of final themes. Finally, there was no explicit reference to ethical issues, ethics approval or confidentiality issues in three studies. 45,48,58
| First author, year of publication | Is the research question clear? | Is the theoretical or ideological perspective of the author (or funder) explicit? | Has this perspective influenced the study design, methods or research findings? | Is the study design appropriate to answer the question? | Is the context or setting adequately described? | Is the sample adequate to explore the range of subjects and settings, and has it been drawn from an appropriate population? | Was the data collection adequately described? | Was data collection rigorously conducted to ensure confidence in the findings? | Was there evidence that the data analysis was rigorously conducted to ensure confidence in the findings? | Are the findings substantiated by the data? | Has consideration been given to any limitations of the methods or data that may have affected the results? | Do any claims to generalisability follow logically and theoretically from the data? | Have ethical issues been addressed and confidentiality respected? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Berzins, 200932 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Campbell, 200838 | Yes | No | CT | Yes | No | Yes | Yes | No | No | Yes | Yes | Yes | Yes |
| Dawson, 200933 | Yes | No | CT | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Henderson, 200245 | Yes | No | CT | Yes | No | No | No | Yes | No | Yes | Yes | Yes | No |
| Jankovic, 201146 | Yes | No | CT | Yes | Yes | CT | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Marriott, 200148 | Yes | No | CT | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Pinfold, 200449 | Yes | No | CT | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Rapaport, 200231 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ridley, 200956 | Yes | No | CT | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Rugkåsa, 201757 | Yes | No | CT | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Smith, 201558 | Yes | No | CT | Yes | No | Yes | Yes | Yes | No | Yes | No | No | No |
| Stroud, 201360 | Yes | No | CT | Yes | No | Yes | No | Yes | No | Yes | No | Yes | Yes |
Framework synthesis
Four themes were identified. These were (1) issues regarding the identification of the NR/NP, (2) confidentiality and information-sharing, (3) enabling the use of the NR/NP role and (4) the importance of maintaining relationships.
The first two of these themes are descriptive in nature and closely reflect our research objectives. Themes 3 and 4 are more interpretative and arose from the thematic analysis. This is because it was felt that themes directly based on our remaining research objectives (‘Exploring issues related to care during detention and after discharge’ and ‘Exploring issues related to service users having access to support from carers’) would not be very meaningful and thus further interpretation by the reviewers was required. Within this synthesis, ‘importance of maintaining relationships’ is considered to be a theme underpinning the other three themes. When there is overlap in the concepts between themes, this has been acknowledged.
The relationship between the four themes identified and our research objectives is detailed in Table 5, which also provides an overview of the studies that contributed towards the development of each theme. Table 5 also highlights which population groups provided data for each theme.
| Participant group | Themes (research objectives)a | |||
|---|---|---|---|---|
| Identification of NR/NP (1 and 2) | Confidentiality and information-sharing (3) | Enabling use of the NR/NP role (4 and 5) | Importance of maintaining relationships (4 and 5) | |
| Service users | Berzins (2009)32 [2005–7] [20] | Berzins (2009)32 [2005–7] [20] | Berzins (2009)32 [2005–7] [20] | Berzins (2009)32 [2005–7] [20] |
| Henderson (2002)45 [2001] [11] | Henderson (2002)45 [2001] [11] | Dawson (2009)33 [2007–8] [2] | Campbell (2008)38 [NS] [NS] | |
| Rapaport (2002)31 [1997–9] [19] | Pinfold (2004)49 [NS] [5] | Rapaport (2002)31 [1997–9] [19] | Dawson (2009)33 [2007–8] [2] | |
| Ridley (2009)56 [2007–8] [49] | Rapaport (2002)31 [1997–9] [19] | Ridley (2009)56 [2007–8] [49] | Henderson (2002)45 [2001] [11] | |
| Stroud (2013)60 [2011–12] [21] | Ridley (2009)56 [2007–8] [49] | Rapaport (2002)31 [1997–9] [19] | ||
| Ridley (2009)56 [2007–8] [49] | ||||
| Stroud (2013)60 [2011–12] [21] | ||||
| NRs | Rapaport (2002)31 [1997–9] [NS] | Rapaport (2002)31 [1997–9] [NS] | Henderson (2002)45 [2001] [NS] | Rapaport (2002)31 [1997–9] [NS] |
| Smith (2015)58 [2014] [32] | Smith (2015)58 [2014] [32] | Rapaport (2002)31 [1997–9] [NS] | Smith (2015)58 [2014] [32] | |
| Stroud (2013)60 [2011–12] [7] | Smith (2015)58 [2014] [32] | Stroud (2013)60 [2011–12] [7] | ||
| Stroud (2013)60 [2011–12] [7] | ||||
| NPs | Berzins (2005–7; 2009)32 [3] | Berzins (2009)32 [2005–7] [7] | Berzins (2005–7; 2009)32 [3] | Berzins (2009)32 [2005–7] [3] |
| Campbell (2008)38 [NS] [NS] | Dawson (2009)33 [2007–8] [4] | Dawson (2009)33 [2007–8] [4] | Campbell (2008)38 [NS] [NS] | |
| Dawson (2009)33 [2007–8] [4] | Ridley (2009)56 [2007–8] [NS] | Campbell (2008)38 [NS] [NS] | Dawson (2009)33 [2007–8] [4] | |
| Ridley (2009)56 [2007–8] [NS] | Ridley (2009)56 [2007–8] [NS] | |||
| Carers other than statutory NPs or NRs | Berzins (2009)32 [2005–7] [7] | Berzins (2009)32 [2005–7] [7] | Berzins (2009)32 [2005–7] [7] | Berzins (2009)32 [2005–7] [7] |
| Henderson (2002)45 [2001] [11] | Jankovic (2011)46 [NS] [31] | Campbell (2008)38 [NS] [NS] | Henderson (2002)45 [2001] [11] | |
| Rapaport (2002)31 [1997–9] [34] | Pinfold (2004)49 [12] | Pinfold (2004)49 [NS] [12] | Jankovic (2011)46 [NS] [31] | |
| Rapaport (2002)31 [1997–9] [34] | Rapaport (2002)31 [1997–9] [34] | Pinfold (2004)49 [NS] [12] | ||
| Ridley (2009)56 [2007–8] [33] | Ridley (2009)56 [2007–8] [33] | Rapaport (2002)31 [1997–9] [34] | ||
| Rugkåsa (2017)57 [2012] [24] | Rugkåsa (2017)57 [2012] [24] | Ridley (2009)56 [2007–8] [33] | ||
| Rugkåsa (2017)57 [2012] [24] | ||||
| AMHPs, ASWs and MHOs | Berzins (2009)32 [7] | Berzins (2009)32 [7] | Berzins (2009)32 [7] | Berzins (2009)32 [7] |
| Dawson (2009)33 [2007–8] [14] | Pinfold (2004)49 [NS] [NS] | Rapaport (2002)31 [1997–9] [26] | Dawson (2009)33 [2007–8] [14] | |
| Rapaport (2002)31 [1997–9] [26] | Rapaport (2002)31 [1997–9] [26] | Rapaport (2002)31 [1997–9] [26] | ||
| Ridley (2009)56 [2007–8] [NS] | ||||
| Legal professionals | Dawson (2009)33 [2007–8] [solicitor, 3] | Dawson (2009)33 [2007–8] [solicitor, 3] | Campbell (2008)38 [lawyers, NS] | Dawson (2009)33 [2007–8] [solicitor, 3] |
| Dawson (2009)33 [2007–8] [solicitor, 3] | ||||
| Tribunal members | Dawson (2009)33 [2007–8] [tribunal member, 15] | Dawson (2009)33 [2007–8] [tribunal member, 15] | Campbell (2008)38 [NS] [1] | Campbell (2008)38 [NS] [1] |
| Dawson (2009)33 [2007–8] [tribunal member, 15] | ||||
| Health professionals (e.g. general practitioners, nurses) | Stroud (2013)60 [2011–12] [responsible clinician, 10] | Pinfold (2004)49 [NS] [psychiatrist, NS, GP, NS] | Dawson (2009)33 [2007–8] [5] | Ridley (2009)56 [2007–8] [psychiatrist] |
| Mental health advocates | Dawson (2009)33 [2007–8] [5] | |||
| Other | Berzins (2009)32 [policy influencer, 9] | Berzins (2009)32 [policy influencer, 9] | Berzins (2009)37 [policy influencer, 9] | Berzins (2009)37 [policy influencer, 9] |
| Marriott (2001)48 [NS] [mix, NS] | Campbell (2008)38 [NS] [author views] | Campbell (2008)38 [NS] [NS] | Marriott (2001)48 [NS] [mix, NS] | |
| Marriott (2001)48 [NS] [mix, NS] | ||||
The second-order construct data that contributed towards each theme, along with reviewer interpretation of these data, are discussed within each section and are supported by quotations from the study participants. Each quotation is accompanied by a label to acknowledge the type of participant providing the quotation and, when possible, their relationship to the service user (e.g. carer and mother). When it is clear that the participant is a NR, this has been indicated. When the status of a carer or relative as a NR is unclear, the participant is referred to as a carer. For a breakdown of the quotations and author ideas that contributed to each theme, please contact the corresponding author of this report.
Theme 1: issues with the identification of the Nearest Relative/Named Person
Four subthemes were identified. Subtheme 1.1, ‘service user vulnerability’, explores how the hierarchical nature of the NR provision in England can leave service users vulnerable to abuse and biased care. Subtheme 1.2, ‘not representative of real relationships’, reflects on how the NR provision in England is not always representative of the family circumstances of service users and those involved with supporting them. Subtheme 1.3, ‘displacement’ details service users’, experiences of changing their NR/NP. Subtheme 1.4, ‘service user isolation’, discusses how both the NR provision in England and the NP provision in Scotland do not fully support the needs of individuals who do not have and/or do not wish to have an identified NR/NP. Author and participant views from eight studies support this theme (see Table 5).
Subtheme 1.1: service user vulnerability
This subtheme discusses how the hierarchical nature of the selection process of the NR may leave service users vulnerable to abuse and violation of their privacy. The impact of unconscious carer bias on the process of involuntary detention is also explored, with comparisons made with the NP provision in Scotland.
Vulnerability to abuse
Authors of five studies31–33,45,49 acknowledged the potential of the NR/NP provisions to allow for the disclosure of information to a person who has abused, or is at risk of abusing, the service user. Three of these studies31,45,49 were conducted before the 2007 amendment of the Act that allowed service users to displace people they did not want to act as their NR. Rapaport31 provided several examples that illustrate how the disclosure of sensitive personal information to the NR can be harmful to service users, as illustrated by one ASW:
It’s something so antitherapeutic to be giving the power to the historical abuser, power of information, power to determine whether the patient receives treatment . . . Particularly if one’s feeling that there is a link between that experience in childhood and the illness that they throw out really.
ASW. 31
Pinfold et al. 49 advise caution with respect to sharing information with carers and relatives, suggesting that the quality of the service user’s relationship with the person with whom the intervention was being shared needs to be considered prior to disclosure. They suggest an approach to appropriate and timely information-sharing based upon a series of decisions balancing the needs of carers and service users. However, the acquisition of knowledge regarding the service user’s current and historical social context takes time and may not be available to social workers, or other professionals, when required. 31 Other issues that may influence information-sharing between service users, carers and professionals are discussed within Theme 2: confidentiality and information-sharing.
Berzins32 acknowledges that the NP provision in Scotland permits the service user to choose a person they feel is best suited to the role, whether that is a friend who they feel is familiar with their wishes or a close relative whom they perceive could withstand the pressure/stress associated with the role. One service user talking about the prospect of nominating a NP stated that they would not worry about their prospective NP receiving personal information about them, as they felt that their NP would know it all anyway:
Any friend that I would have nominated I’ve probably told them everything anyway. It’s probably something that I’ve talked about.
Service user32 (p. 162).
Here the service user highlights how they would choose someone to support them who was already familiar with their personal information, whom they knew they could trust. However, the NP provision does not prevent the service user from appointing a person whom other people may view as unsuitable to the role, and this may leave them vulnerable to abuse or manipulation. This was illustrated by Dawson et al.,33 who provided an example of a service user appointing their drug dealer as their NP.
When a NP has not been appointed, the system defaults to a primary carer, and then to the hierarchical system currently still used in England. In first instances of acute mental illness, it is unlikely that a service user will have nominated a NP as they may not be well enough33 or have the time available32 to choose one immediately following an emergency admission. There are a number of additional issues influencing whether or not people identify their NP in advance of them being needed, as well as the potential implications of their choice for the relationship between service users and their carers. These are discussed further in Theme 4: importance of maintaining relationships.
Caregiver bias
The potential for abuse is not the only risk associated with the prescriptive nature of the NR selection process and the use of this hierarchy when identifying a NP when none has been nominated in advance. The pressures associated with caring for someone prior to an involuntary admission (as discussed within Theme 4: importance of maintaining relationships) may affect the ability of the carer to act in accordance with the best interests of the service user within their role as the NR/NP. Author views from three studies31,49,60 highlight how the carer’s own needs may affect their decision-making in relation to the NR role. Pinfold et al. 49 indicate how carers may be deterred from seeking help for themselves, and by extension the patient, because they rely on the patient to meet their own needs. In another study, one clinician describes how a patient’s daughter did not enlighten her mother around the rules associated with a CTO:
The daughter of the [patient] did get it but she knew that what the system was effectively doing was tricking her mother into thinking that we could compel her to have medication.
Responsible clinician60 (p. 48).
Amendments to the MHA 19831 in 2007 mean that family members and carers in England and Wales who have been assigned to the role of NR can now delegate the position to someone else if they do not want the responsibility of the role. 14 In Scotland, revisions to the MHCT11 in 2015 mean that carers can choose to apply through the tribunal process to represent adults who lack the capacity to make decisions about their care. 64 We suggest that these changes may go some way towards alleviating the influence of carer stress on their decision-making. The 2007 amendments to the MHA 19831,14 represent a partial response to this issue, by allowing service users and/or the professionals involved in their care to apply to the County Court to displace their allocated NR on grounds of unsuitability. The issues surrounding the process of the displacement of the NR are discussed in Subtheme 1.3: displacement.
Subtheme 1.2: not representative of real relationships
This subtheme discusses how selection of the person to fulfil the NR role in England may not be representative of a service user’s family circumstances and may inhibit information-sharing with individuals closest to them or with those who support them.
Author views from three studies conducted in England suggest that service users,31 their carers48,58 and the professionals31 involved with supporting them during involuntary admissions did not find the predetermined hierarchy a convenient or useful method of identifying the most appropriate NR. One service user gave her views on how the NR provision distinguishes between the rights of full and half siblings:
I mean what is a half-sister, half-brother? Because sometimes in our family, my mum’s got six kids. All of them are my mother’s kids and as far as I am concerned they’re all my brothers and sisters.
Service user. 31
The above quotation provides an example of how the hierarchy used to identify the NR in England may not always represent the service user’s family circumstances. This is further illustrated by a quotation from an ASW interviewed in the same study:
. . . her father only lived 200 yards away and he was the Nearest Relative as defined by the Act. But the social worker used the mother as the nearest relative on the basis that she was actually offering the care and because it was her mother and so on . . .
ASW. 31
The above quotation illustrates how the concept of NR may not always equate to the person who is usually involved with the service user’s care. 58 As well as causing difficulty in the identification of the NR, the use of the strict NR hierarchy can also create difficulties with the sharing of information. 49,58 One woman expresses her frustration with the way information-sharing was restricted to her alone:
After the assessment another social worker contacted us for an update but would not speak with my husband because I am legally the Nearest Relative, it was upsetting at such a difficult time.
NR58
Restricting information-sharing to only one carer/NR has important implications for the level of expectation and responsibility placed on carers by professionals. This may have an impact on the support they feel able to offer the service user and undermine their relationship with professionals, as discussed further in Theme 2: confidentiality and information-sharing and Theme 4: importance of maintaining relationships.
In summary, family structures in the UK in the 21st century are highly diverse and often quite removed from either the simple or the reliably harmonious and caring relationships between close blood relatives that the NR provisions presume. Furthermore, as well as the presumption of the importance of blood relatives in the service user’s life, the NR provisions imply that there is one person who is at the same time (1) their primary or sole carer/usual support, (2) the person the service user would trust to act in their best interests and (3) the person whom they would trust with personal or sensitive information about them.
Subtheme 1.3: displacement
The 2007 amendments to the MHA 19831,14 mean that the service user, a relative, anyone living with the service user or an AMHP can apply to the County Court to displace a person who is unsuitable for the role and nominate someone whom they feel would be more appropriate. Issues discussed within this subtheme include how the displacement process can be exploited by both NRs and professionals and how the displacement process in Scotland can provide service users with an opportunity for choice and autonomy over the care that they receive. Four studies contributed towards the development of this subtheme. 31,32,56,57
Of the studies relevant to the NR provision in England, only Rapaport31 contributed significantly to this subtheme. This paper was published prior to the 2007 amendments of the MHA 1983,1,14 which means that at this time service users could not apply to the County Court for the displacement of their NR. This study highlights how some professionals viewed the process of displacing an unsuitable person from the role of the NR as time-consuming, expensive and having the potential to jeopardise their working relationships with carers. The author also indicates how the tribunal system could be misused by individuals who did not want to be displaced. One ASW illustrated this by discussing how her team had struggled to displace one woman who had inherited the NR role from another person:
She [NR] got the original Nearest Relative to sign them over to her brother, so she was out of the legal loop . . . He continued to object although he was really doing it by proxy for her. She was still pulling all the strings.
ASW. 31
In this example, the NR managed to use the tribunal system and use their influence within the wider family to retain influence over the service user’s care. Overall, the lack of available evidence regarding experiences of displacing the NR in England, particularly after the 2007 amendments of the MHA 1983,1,14 limits the conclusions that can be drawn.
In Scotland, service users can make a written application to displace (i.e. change) their NP under the MHCT. 11 This seems to be viewed positively by service users:
You might nominate a friend who you’re very friendly with but they might turn out to be totally unsuitable . . . At least you’re not stuck with someone who’s against you and they can always be revoked.
Service user32 (p. 130).
This quotation illustrates how the process for displacing a NP in Scotland can avoid the involvement both of someone the service user does not have a good relationship with, or who they feel would not support them in a way that is consistent with their wishes. The displacement process was also viewed positively by the individuals involved with creating government policy interviewed in the same study:
. . . revisiting of it is important and we stress that . . . just because someone ends up with someone who’s down as the default Named Person that should be reviewed and discussed with the person as soon as they’re in a position to do that and not just set in stone.
Policy influencer32 (p. 120).
This quotation acknowledges that under some circumstances (e.g. an emergency admission), a service user may need to be allocated a NP using the default process. The ability to revisit the decision when they are able provides an important opportunity for the service user to exercise choice and autonomy.
Ridley et al. 56 reflect that by the time participants in their study were interviewed for a second time 1 year later almost one-quarter of the service users had changed their NP. Among the reasons given was that the NP had disagreed with the service user’s wishes. The authors report that carers found the process of being displaced unsettling and that it made them uncertain of their rights and responsibilities. 56 We suggest that this may have important implications for the provision of consistent care and/or maintaining working relationships with professionals in the longer term.
Subtheme 1.4: service user isolation
This subtheme aims to highlight the issues encountered by service users who may not be able, or may not wish to, have someone appointed as a NR in relation to their care/detention.
Author31–33,56,60 and participant31–33,56 views from five studies indicated that the NR provision of the MHA 19831 did not account for the fact that some service users may not have a person to act as their NR. Issues with this situation may arise because of family estrangement60 and relatives living outside the country. 31 A quotation from one service user illustrates how the process of identifying the NR does not account for poor family relationships:
. . . this seems to be geared for, you know, nice families as it were [laughing] you know . . . families where the mother comes round and comes into hospital and says ‘how are you son?’.
Service user. 31
Here, the advantages of the NP provision used in Scotland are easily identifiable, in that service users without a partner or family member to act as their NR can choose to nominate a friend instead. Following the introduction of the MHCT, some service users32,56 and professionals6,32,33 disliked the necessity of a service user having to identify a NP. This is illustrated by two quotations, one from a service user and one from the perspective of a person involved in influencing government, or ‘policy influencer’,32 in this area:
If it’s the patient’s right to name a Named Person than that’s their right. If they say: ‘I don’t want anything to do with that,’ then that’s it. End of story.
Service user32 (p. 157).
. . . Because otherwise it just gets very silly and stops being about the person’s best interests and starts being about obeying the letter of the law . . . and at the end of the day is that going to help the individual?
Policy influencer32 (p. 135).
In 2015, amendments were made to the MHCT that meant that service users would no longer have to nominate a NP and that one would no longer be allocated to them by default. 64 These changes started to be phased in during June 2017 and, although they have the potential of resolving some of the issues discussed in this subtheme, this review did not identify any evidence evaluating these changes.
Summary
In England, Wales and Northern Ireland, the NR is allocated by default, based on a defined hierarchy. Several issues with this process were identified:
-
There were occasions when the assigned NR was a person with a history of an abusive relationship with the service user.
-
The arbitrary allocation of a NR may lead to the identification of someone who, in the context of individual family situation and relationships, is not best placed to fulfil the role.
-
The role of NR may be allocated to someone who is not involved with the care of the service user.
Introduction of the NP provisions in Scotland11 has given service users the option to identify a NP of their choice. Experience of the NP provision in Scotland has revealed the following issues:
-
It is beneficial to be able to allocate a friend or carer of a service user’s choice, and to easily displace a default nomination.
-
The choice to opt for no NP or NR was considered favourably. Amendments to the MHCT64 now allow for this, but no evidence was identified to allow discussion of the relative merits and drawbacks of this approach.
Theme 2: confidentiality and information-sharing
This theme relates to the third objective of this review, which was to ‘explore issues relating to patient confidentiality and information-sharing, relating to all aspects of compulsory detention’. This encompasses the value of confidentiality to both service users and carers, alongside the tension this can create with the need for professionals and carers to share information with each other about the service user and their care. Examples are provided of how professionals work flexibly within the legal framework of the MHA 19831 to provide carers with the support they need while also respecting the service user’s right to privacy. The section ends by highlighting the need for professionals working with service users and their families to consider the wider family and historical context of the service user when considering issues of confidentiality and information-sharing. Nine studies contributed evidence within this theme (see Table 5).
Under the MHA 19831 and MHCT,11 both the NR and the NP are privy to confidential information about the service user. This can potentially lead to unwanted sharing of information and, in some cases, cause harm or distress to the service user (as discussed within Theme 1: issues regarding the identification of Nearest Relatives/Named Persons).
Six studies31–33,45,49,56 highlighted how much service users valued being able to choose who received information about them and the health care that they were receiving. Mental health service users interviewed as part of an English nationwide study49 and service users with experience of involuntary inpatient admission31 felt that consent should be sought from service users before any information regarding their care was shared with carers. Service users felt that this helped preserve their sense of autonomy and identity,49 factors that could be perceived as contributing towards service users’ empowerment within their relationship with professionals and carers and within the wider mental health system. One woman with bipolar disorder who had experienced involuntary admission under the MHA 19831 explained why she did not wish for her husband to know about the care she was receiving:
He often says ‘just let me get involved, I don’t understand what’s going on’. I don’t want him to understand what’s going on, I don’t want it taken away from me. It’s my life, my illness, if you like . . .
Service user45
The above quotation illustrates how for this service user, limiting the amount her partner knew about the care she was receiving enabled her to take ownership of her own mental health and provided her with a sense of control. The sense of control may be especially important for people undergoing the process of an involuntary admission. Service users in Scotland, giving their views on the NP,11 indicated that it gave them the control to ensure that their information was not shared with people who did not know them or with whom they did not get on. 33 This clearly has the potential to act as a protective factor against service users’ vulnerability to abuse, or the sharing of information with people who may not act in their best interest, in the context of the hierarchical allocation of the NR utilised in England and Wales, as discussed in Subtheme 1.1: service user vulnerability. As one service user points out, once information is shared, there ‘is no going back’. 49 The perceived impact of confidentiality on the relationship between carers/NRs and professionals is discussed in Theme 4: importance of maintaining relationships.
Five studies highlighted that carers also had a need for confidentiality. 31,46,56,57 Carers stated that they would value having time alone with a professional in which they could talk about any concerns, without the worry that the person they support would feel criticised or undermined. 46,57,58 One carer highlights how talking with professionals about their concerns may put their relationship with the service user at risk:
I don’t want to know what [name of the patient] is telling them . . . I just want them to listen to what I’ve got to say about how I think he is without telling him, because he says, ‘oh you’ve been talking to the nurses’.
Carer46
Carers appreciated being able to talk confidentially with professionals about the service user they were supporting. 46,57,58 They were also concerned about personal family information, shared in confidence with members of the professional team, being passed on to their relative when they did not want it to be4,31 and the implications of providing information within a tribunal setting that disagreed with a service user’s wishes on their relationship with their friend or relative. 32,57 This is discussed further within Theme 4: importance of maintaining relationships.
Five studies discussed the importance of professionals sharing information with their carers. 31,46,49,56,57 Carers appeared to appreciate the need for the people they support to maintain a degree of confidentiality, but highlighted how they still required some information if they were expected to continue supporting a person31,46,49 or if the service user’s behaviour may put themselves as a carer at risk. 46 In the study conducted before the 2007 review of the MHA 1983,1 Rapaport31 highlights that information-sharing between professionals and carers/NRs did not always take place because of concerns about confidentiality. In a later study evaluating the implementation of the MHCT in Scotland,56 one NP observed that despite the additional rights conveyed by the 2003 Act, information-sharing was still dependent on a decision being made by a professional:
It’s up to them if they want to change it but you can be totally discarded . . . you’re still the carer, but you’re not going to find anything out unless they tell you themselves. I don’t know how you can fix that.
Carer/NP56
This indicates that even when there are laws and guidelines in place to support information-sharing, the implementation of these may be variable and carers/NRs/NPs may not always receive the information they are entitled to.
Although some carers wanted to receive more information in certain circumstances, data from five studies31–33,56,60 indicate that it was possible for carers and NRs/NPs to feel overwhelmed by too much information, especially when it was in a format they found inaccessible31,60 or contained distressing personal information pertaining to the service users that they may not wish to know about. 32,33 Relatives also acknowledged that at times of distress they may not be able to take on board information that was offered to them. 58
Professionals supporting service users appear to experience a dilemma between preserving service user confidentiality and autonomy and providing carers/NRs with enough information so that they are able to support the person. This is illustrated by a quotation from a carer:
. . . the rights of the Nearest Relative versus the fact that he’s an adult in his own right . . . in the end we kind of found out what we wanted to know . . . But it was quite a shock to find out we were . . . not being told anything.
Carer. 31
Here, the carer talks about their experience of trying to obtain information from a professional care team about their son who had been involuntarily admitted to hospital. A need for additional explanation for service users32 and carers49 and training for professionals56 has been proposed to ensure that all parties understand the rights of carers to receive certain information, which may facilitate the information-sharing process. Although the MHA 19831 Code of Practice dictates that informal patients should have their legal positions and rights explained to them,2 this may not be consistently applied and may be impractical in certain situations. In addition, the complexity of the NR provisions may not be retained by service users, carers or professionals, particularly in distressing circumstances.
Three studies provide examples of the professionals who support individuals involuntarily detained in hospital or on CTOs working flexibly to allow carers to discuss their concerns freely, but also ensuring that the privacy of service users is protected. 32,46,57 Some professionals deliberately tempered information they knew would be copied to a NP/NR32,33 or provided carers with a confidential space to share concerns. 57 This is illustrated by a carer describing a psychologist’s willingness to talk with her confidentially regarding her concerns about her son, who is on a CTO:
. . . it means that the psychologist may phone him or drop a note through the door. Yes it does make it easier. But it’s also made easier by the psychologist agreeing not to say ‘hello [patient], your mother rang me, I hear you’re not too well’.
Carer57
Pinfold et al. 49 and Henderson45 highlight the importance of professionals working with service users to consider the wider and historical family context and the quality of the relationship between the service user and their NR/NP before sharing information with carers/NRs. Although historical abuse is an important issue to consider, there are also other factors that may influence the quality of this relationship and thus the decision to share sensitive information with a NR/NP. These are discussed in more detail within Theme 3: enabling use of the Nearest Relative/Named Person role and Theme 4: Maintaining relationships.
Summary
This theme is concerned with issues of confidentiality and the sharing of information about compulsorily detained patients. The NR is entitled to receive certain information about the care of the patient, whereas other individuals, who may in reality be the main carer or the closest family member, are not. As discussed in Theme 1: issues with the identification of the Nearest Relative, there is the potential through the default identification of the NR to lead to information being shared with a recipient who is undesirable in the eyes of the service user. However, even when the NR or NP is identified in line with the wishes of the patient, the following issues were identified:
-
Service users valued the opportunity to exercise their right to withhold certain information from their NR, as this gave some sense of control.
-
Information shared can be complicated, sensitive and unpleasant. There is a certain level of information that some carers felt was necessary to receive in order to be able to carry out their duties, but it was felt by service users, carers and professionals alike that it might not be beneficial to share too much information.
-
There was a desire to improve processes by which carers are involved in discussing information about a patient with professionals. Carers wanted to be able to provide what they felt was useful information about the service user. However, they did not always want the patient to know about such conversations, as this could damage their relationship.
-
It was considered useful when professionals took a flexible approach to information-sharing with carers, in particular when this considered the wider context of family dynamics.
-
It was also noted that the rights of carers, service users and professionals are complicated and not easily explained.
Theme 3: enabling use of the Nearest Relative/Named Person role
This theme encompasses three subthemes: (3.1) being heard, (3.2) need for information and (3.3) proactive support and engagement. The theme relates to the research objective of exploring issues relating to decisions about care during detention and discharge and issues relating to service users having access to support from carers. The first subtheme, ‘being heard’, describes how the NR provision supports carers and service users to have their say during an involuntary admission, and factors that may prevent them from expressing their views. The second subtheme, ‘need for information’, describes the type of information service users, carers, NRs and professionals need to fulfil their roles in the patient’s care. The final subtheme, ‘proactive support and engagement’, illustrates the type of support required from professionals to ensure that carers and service users are able to make use of the information they are given about the NR role. Together, the concepts explored within these subthemes can empower all stakeholders to make full use of the NR provisions of the MHA 1983. 1 Eleven studies contributed towards the development of this theme (see Table 5).
Subtheme 3.1: being heard
Evidence under this subtheme conveys how carers and NRs value the NR provision of the MHA 19831 as something that empowers them to ask for information and challenge the views of the professionals regarding the care that they provide. NRs also perceive their opinions to carry more weight with professionals than those of a regular carer.
Five studies31,32,45,56,60 highlighted several ways in which the NR/NP provisions enhanced carers’ involvement in planning the care of service users. First, authors of three studies31,32,56 noted how the NR/NP provisions improved carers’ access to information about service users’ current or past care and treatment. This is illustrated by a NP, discussing how their relative’s detention under the MHCT meant that they received more information from services within their role as NP:
Until we had the compulsory order you really were largely on your own and the information didn’t come to you, you had to seek it out and it was hard to come by . . .
NP56
Participants from three studies31,45,60 highlighted how their NR/NP status increased their say in the care their relatives received. One example of this was provided by a man discussing how he managed to prevent the involuntary admission of his partner:
They seemed to need my word, I can never remember exact details, but they seemed to need a yes from me before they could go ahead. The last time it was actually me who refused to give it and made a determined effort to keep Elaine at home . . .
Partner and carer45
A NR from another study perceived that professionals appeared to be more responsive to her requests:
I’ve dealt with something . . . I’ve got the right . . . what I felt about a situation that they were in. And it was responded to, it was wonderful . . . I also had the right then to say that I’ve got the right not to have to keep chasing . . .
NR. 31
This quotation suggests that the legislation outlined by the NR provision of the MHA 19831 can enhance the confidence of those within the NR role to give their views on the care of the person they support. However, other individuals did not always make use of the opportunity to discuss, endorse or object that the NR/NP is intended to provide them with. Berzins37 suggested that the class, race and gender of people nominated as NPs may influence their ability to carry out their role. One mental health officer (MHO) illustrates this by talking about the development of a DVD (digital versatile disc), presumably to support individuals detained under the MHCT and their carers:
Those tensions again around disadvantage, around class, race and gender come up and bite you. Have you seen the HUG DVD which is a group of fantastically articulate middle-class people . . . but there is a bit where the middle-class are incredibly adept at appropriating things for themselves.
MHO32 (p. 143).
The above quotation suggests that the class and/or education level of service users and their carers may affect their ability to first understand the information that is given to them and then make use of this information in order to make their voices heard.
Subtheme 3.2: need for information
This subtheme discusses the information that service users, carers, NRs/NPs and professionals require in order for the service user to benefit from the intended function of the NR/NP provision. The section discusses how carers need some knowledge regarding the different section of the MHA 19831 as well as more specific information regarding the NR/NP role. Authors of three studies32,56,57 indicated the need for service users and carers to be more informed about the MHA 19831 in both England and Wales or the MHCT11 in Scotland. The quotation below highlights one carer’s lack of knowledge regarding the implementation of a CTO:
. . . I couldn’t get a clear grip on that ‘if you don’t do A then B will happen’, what B was. That they would within 24 hours come and chase him? Or that they would call him on the phone . . .
Mother and carer57
Here, the carer wishes to know more about the consequences of a service user not adhering to the conditions associated with their CTO. This viewpoint is contradicted by one example presented by Stroud et al. ,60 who interviewed a service user who felt that they did not need to know the finer details associated with the use of a CTO. This stance may reflect the more limited role of the NR in the implementation of CTOs and also suggests that the level of information provided may need to be tailored to the individual circumstances of the carer/service user.
In addition to improving knowledge about the different sections of the MHA 1983,1 and the different levels of care they define, the authors of five studies31–33,38,56 highlight that service users and/or carers needed more information about the role of the NR/NP:
Are they new may I ask? Or is it that they’ve always been there but hardly anyone knows about it? Because I’m only recently hearing about it as though it’s a new piece of legislation?
Carer. 31
The above two quotations suggest that service users and carers need a working knowledge of the parts of the MHA 19831 that are relevant to their circumstances, and may need to be informed of how the NR role can support them in this context. Authors from two studies32,33 highlight how knowledge of the NP role among service users and carers may be particularly limited if the service user has not had a previous involuntary hospital admission. The need for accessible information about the NR/NP role was noted by participants and authors of five studies,31,33,38,56,60 although NRs/NPs may not always understand the information that they are given regarding their responsibilities, as illustrated by one policy influencer commenting on the nomination of a NP following an emergency admission:
. . . you appear at some sort of meeting and somebody says, ‘do you want to be your son’s Named Person?’ but you’re not really listening as you’re far too distressed. You realise it’s something quite important and you care about your son so you say yes . . .
Policy influencer32 (p. 119)
This relates to information presented within Theme 2: confidentiality and information-sharing, which cautions against overburdening carers and NRs/NPs with information about the care the service user is receiving.
Finally, authors of two studies48,56 indicate that in some cases, the professionals involved with supporting service users and carers may benefit from more knowledge regarding the NR/NP role and how to incorporate it into the care that they provide. This is illustrated by one woman talking about her involvement as a NP:
It’s made the professionals feel they don’t really know what to do with us as Named Persons . . . now they’ve got to find a place for us, but they’re still not sure about what that is.
NP, friend55
This suggests that professionals involved with supporting service users and their NR during an involuntary admission process could benefit from training and support on what the NR/NP role is, how to inform the NR/NP of their rights and involving them, when appropriate, in the care of the service user they support.
Subtheme 3.3: proactive support and engagement
This subtheme discusses the need for professionals to be proactive in identifying the needs of carers that may affect their ability to provide support to the service user within their NR role. The advantages and disadvantages of the approach by professionals used in Scotland to encourage individuals to identify a NP in advance are also explored.
Authors of three studies31,32,49 acknowledged the importance of identifying the needs of the carers and NR involved with providing support to service users. In addition to the need for information (highlighted above in the previous subtheme), Pinfold et al. 49 reflect on the important role professionals have in providing emotional support and comfort to carers during times of distress, although the demands placed on professionals’ time may not always allow for this. 31 Carers also welcomed practical support, such as guidance with filling in forms and referral to services for their own needs. 49
Authors of two studies in Scotland32,33 highlighted the proactive approach used by some professionals to encourage service users, carers and other professionals to think about nominating a NP in advance. This is illustrated by a member of one tribunal panel discussing how MHOs play an important role in advertising the NP role in Scotland:
. . . my experience of mental health officers is that they’re very actively out there in the community talking to the people who are concerned with the care of people.
Tribunal member33 (p. 53).
Although this approach was seen as positive by some professionals, others felt that it represented a potential conflict of interest, and felt that professionals should not become involved in what they regarded as a private agreement between the service user and their nominated NP. 32 One MHO reflects on the potential impact of any reluctance from professionals to support the process of a NP:
If that’s the message then you’re not going to get a high take up. You’ve got to be quite proactive to get people thinking about it.
MHO32 (p. 147).
Although this quotation illustrates the perception that a proactive approach used by professionals may encourage people to nominate a NP, it conflicts with information presented in Theme 4: importance of maintaining relationships that indicates that some service users may not wish to think about the possibility of being ill in the future. Professionals appear to play an important role in recognising when it may be an appropriate time to discuss the nomination of a NP with a service user. We would suggest that factors that may influence this decision include the length of time they have supported them, the quality of the relationship and the service user’s mental health at the time.
Finally, three studies also indicated that carers and NPs may require additional support during the tribunal process to enable them to fulfil their role, including the provision of accessible information,38,56 as indicated within Subtheme 3.2: need for information, and explicit encouragement to share their views. 33,56 Two studies noted that the scheduling of tribunals during the working day could sometimes exclude carers from taking part (Dawson et al. ,33 Ridley et al. 56). One NP stated:
It’ll go ahead regardless of whether me as Named Person can go.
NP56
We suggest that the above statement indicates that the lack of flexibility in scheduling tribunals according to NPs could lead to the views of carers and NRs/NPs being overlooked within the tribunal process and contribute to NRs/NPs feeling unheard and undervalued, as discussed within Subtheme 4.3: carer/professional relationships. This highlights the need for organisers of the tribunal process to be proactive in ensuring that family members, carers and NRs/NPs are supported to attend when appropriate.
Summary
This theme discusses the ways in which support is needed and can be provided with respect to the compulsory detention of a service user and the role of the NR in their care. The following key points emerged from the evidence:
-
The role of the NR or NP is complex and may be poorly understood by service users, carers and professionals alike.
-
It should be recognised that the NR or NP, as well as other relatives and carers without statutory roles in the admission or ongoing care, may require emotional and informational support at various stages throughout the process of detention and treatment, and that professionals involved in these processes are well placed to deliver them.
-
Carers reflected that being recognised as a NR or NP enabled them to offer better support to the service user throughout the processes of detention/treatment under the MHA 19831 through their improved awareness of their rights under the NR/NP provision and the recognition of these by professionals.
Theme 4: importance of maintaining relationships
Three subthemes contributed towards this theme: (4.1) service user/carer relationships, (4.2) service user/professional relationships and (4.3) carer/professional relationships. This theme explores the issues that can influence the development and maintenance of good relationships between each of the three main stakeholder groups involved in the process of involuntary hospital admission. These relationships may influence the balance between protecting the service user’s confidentiality and information-sharing as discussed within Theme 2: confidentiality and information-sharing, and also empower service users and carers and thus act as a protective factor against abuse and carer burnout. Data from 12 studies contributed towards the evidence within this theme (see Table 5).
Subtheme 4.1: service user/carer relationships
This subtheme discusses issues that may affect the relationship between service users and their carers and NRs/NPs. The issues include the impact on the carer of the responsibility of taking on the NR/NP role, the ability of the NR/NP to act in the best interests of the service user and how the duties associated with the NR/NP role may be a source of conflict between service users and their carers.
The responsibility of caring for someone with mental health difficulties can be very physically and emotionally challenging for the carer at times, as evidenced by author and participant views included within this review. 31,45,46,56,57 The additional responsibility associated with the NR/NP role can contribute towards the stress of responsibility experienced by carers. Authors from five studies31–33,38,56 indicate that carers and NRs/NPs can feel daunted by the responsibility of their role. This is illustrated by a MHO discussing how some carers experience the process of contributing within a tribunal:
People generally appreciate that sense of, kind of empowerment [. . .]. Again because I’m mainly involved with older people sometimes people feel a bit frightened by the process . . . I think for those people who would actually feel frightened rather than empowered by an involvement.
MHO33 (p. 47)
One service user discussed how they would use the flexibility associated with the NP provision in Scotland (MHCT) to choose a friend as their NP in order to relieve the responsibility from family members:
You know, it’s about taking the pressure off them and that could be beneficial for the family member as well, as they can be so busy caring.
Service user32 (p. 138).
Under the NR provisions of the MHA 1983,1 the service user cannot choose who is involved in decision-making. This means that service users may feel that they have to place extra responsibility on carers without wanting to, or discuss issues with people they find it hard to communicate with. This has clear implications for service users, who may have to accept care or treatment conditions if their NR/NP perceives them to be in their best interests.
Authors of three studies conducted in Scotland32,33,56 highlight the importance of the NP being able to understand, respect and carry out the wishes of the service user, which is clearly related to the quality of their personal relationship. In Scotland, some service users selected friends to be their NP because they perceived them to be more ‘equal’ in terms of their relationship56 and trusted that they would be more aware and supportive of their wishes when it came to being offered certain treatments. 32 However, some service users were concerned with the possible impact the NP role would have on their relationships with friends, and felt that the closeness associated with good family relationships was necessary to undertake the NP role. 56
Authors of two studies highlighted concerns that both service users and NPs did not fully understand the level of information that would be shared with the NP. 33,37 We suggest that this has the potential to place strain on the services user’s relationship with their NP. The need for adequate information about the NR/NP role is discussed further in Theme 2: enabling use of the Nearest Relative/Named Person role. Participant and author views from seven studies31,33,37,45,46,56,57 indicate that another factor that may affect the quality of the service user–NR relationship was when the NR felt that they needed to express views that conflicted with the service user’s, during a tribunal,32,33,57 prior to admission45,46 or while on a CTO. 57 This is illustrated by the observation of two people involved with influencing government policy:
Their care and friendship is with the person [service user] but they are certainly allowed to have an independent view and that is exactly why they don’t want to go to the tribunal and say it to the person, for fear of the reaction.
Policy influencer32 (p. 154).
It’s most awkward at the tribunal stage where there’s tension between the user and the apparent Named Person, where the MHO has imposed one and, where that happens, there’s still a great deal of bad feeling, I think, and it really doesn’t seem to suit either party.
Policy influencer32 (p. 159).
Subtheme 4.2: service user/professional relationships
This subtheme discusses how the disclosure of information to NRs against the service user’s wishes can challenge their relationship with the ASWs, psychiatrists and other service staff who support them. Other issues that may affect the service user’s relationship with services, such as the identification of a NP and preparation of an advance statement (‘. . . a document ‘‘completed by a service user when they are well and judged to be able to make decisions for themselves’’. The documents state how the service user would like to be treated in the future if they later did not have the capacity to decide this for themselves‘65) are also explored.
Along with some of the information presented earlier within Theme 2: confidentiality and information-sharing, author views from two studies indicate how the sharing of information without the consent of the service user has resulted in feelings of anger or distress. 31,49 One service user felt that a request by the service user to not share information with their NR should be respected, even at times when they lacked the capacity to make a fully informed decision:
If a service user thinks the carer is the devil, even if this is false, it is clear it will distress the service user to inform the carer. The approach here is to wait until the paranoia has passed. My view here is to follow the service user wishes . . .
Service user49 (p. 110).
This contrasts with the view of a psychiatrist interviewed in the same study:
. . . I think there are times when you really want to tell relatives about the patient’s behaviour. Sometimes you have to say ‘I can’t let you go home unless I tell them this’.
Psychiatrist49 (p. 115).
This conflict between the desire of the service user to retain their autonomy and the professional obligation of those who support them to protect both the service user and members of the public from harm could have an undesirable impact on the service user’s future willingness to share information with care professionals or to access services. This interpretation is supported by four service users interviewed by Berzins,32 who said that they provided their psychiatrist with the minimum level of information necessary:
I haven’t told the psychiatrist a lot of things. I don’t really tell them very much at all, just a quick how it’s going and how’s the medication, and this is why I think they‘re not always the best person to make a judgement about your situation.
Service user32 (p. 163).
Service user and author views from two studies indicate that some professionals were reluctant to discuss issues relating to the possibility of a future hospital admission, including the nomination of a NP, for fear of damaging their relationship with the service user. 31,32 Author views from two studies also indicate that there may be issues around staff knowledge on how to implement or access advance statements. 49,56 This is discussed further in Theme 1: enabling use of the Nearest Relative/Named Person role.
Subtheme 4.3: carer/professional relationships
This subtheme explores how the relationship between carers and the professionals who support service users can be influenced by the degree that carers feel listened to, valued and involved in the care of the service users.
Four studies33,45,46,57 present the views of participants and authors that indicate that carers and NRs/NPs do not always feel that professionals consider their needs or views when supporting service users. This appears to be an issue at different stages of the service user’s involuntary hospital admission, including pre-admission and discharge, as illustrated by two carers and a NR below:
When I’ve known he’s going downhill and I have felt that I wasn’t really being listened to enough then and I had tried to speak to the doctor but I’ve never been able to.
NR60 (p. 57).
We were shattered . . . I didn’t really want him to come and spend the night at home already, and one day I went in and it took me completely by surprise Dr X wanted him released that day . . .
Mother and carer46
[The psychiatrist] said at the last meeting was ‘I am going to keep you on your CTO’. And I asked why because I said ‘to be honest with you I don’t want him to go back into hospital [through recalls].’ . . . And she wasn’t taking him off it.
Mother and carer57
Author views from four studies31,45,48,56 indicate that carers can feel excluded from the decisions being made about the care of service users during an involuntary admission. This is illustrated by one carer talking about the admission of their partner to hospital:
You don’t always know at the hospital that this is going to happen. I’ve had times when yes, they’re talking about sectioning and then the next thing I know I get a letter in the post saying it’s happened . . . They’ve decided after I’ve gone home . . .
Partner and carer45
Author and participant views from five studies31,49,56–58 indicate that carers may experience the need to protect service users’ right to privacy as a barrier to their own working relationship with professionals. Although carers perceived that information may not be passed on to them because of the automatic assumption by professionals that service users would not want their information to be shared,58 some carers perceived that confidentiality was used by professionals to deliberately exclude them from discussions about a service user’s care. 49,57 One ASW discusses how the potential for conflict between the views of the NR and ASW limited the information NRs were given about their role:
. . . we have a competing element which may not in our view, be the best interests of the particular client . . . I think that’s the real issue . . . I wonder sometimes whether we fully inform Nearest Relatives about their, about their powers, given the kind of practical conflict.
ASW. 31
The perceived power imbalance between carers and professionals was also discussed in relation to carers’ experiences of taking part in tribunals in Scotland. 32,33,56 In addition to the intimidating tribunal setting,32,56 carers noted that, although the tribunal system provided the opportunity for them to air their views and feel listened to, they also perceived that professional voices carried more weight. 32,33,56 One solicitor observed:
I think Named Persons feel as though, in relation to the tribunal process, they’ve got a powerful voice but when it comes with wanting to meet with doctors and to speak to other professionals, sometimes they feel as though that voice isn’t quite as powerful in relation to that.
Solicitor33 (p. 44)
Author views from two studies indicate that carers may refrain from complaining about any treatment to themselves or actions on behalf of the service user they perceive to be unfair because they fear damaging their relationships with professionals. 31,57 However, the same studies provide examples of where, when a mutually respectful and open relationship is cultivated between carers/NRs and professionals, they can work together to have a meaningful impact on the care that service users receive. 31,57,60 Some examples of the benefits of carers/NRs and professionals working together include preventing the inappropriate recall from a CTO of a service user back to hospital57 and the delivery of a person-centred care package to prevent an involuntary hospital admission. 31
This subtheme brings together evidence about perceived power imbalances between professionals and carers, including issues regarding maintaining service user confidentiality, and how these imbalances may have an impact on the ability for professionals and carers to work together to support the service user leading up to and during a hospital admission. However, opportunities for professionals to listen to the views of carers and NRs, either through creating opportunities to meet with them privately (as discussed within Theme 2: confidentiality and information-sharing) or through the tribunal system, may help create a mutually respectful working relationship.
Summary
This theme is concerned with the relationships between professionals, carers (NRs or otherwise) and service users during the treatment of individuals subjected to compulsory detention and treatment. Relationships with professionals can have a significant bearing on the experiences of care, whereas the relationships between service users and carers may last a lifetime. The experience of being compulsorily detained places strain on these relationships. There was evidence of experience of a heavy responsibility on carers and a NR or NP alike, and data from this theme highlighted some of the circumstances in which vital relationships can become strained. The following issues emerged:
-
The role of NR confers a lot of responsibility and, in some cases in which the NR is the primary carer, this can be overwhelming.
-
Disagreements over treatment decisions, carers feeling ignored or cut out and conflicts with mental health professionals are some of the ways in which relationships can be placed under significant strain.
-
Another perceived benefit of the NP provision over the NR provision was the flexibility to choose a friend as a NP because the service user felt that they would be more aware of, and more likely to implement, their wishes than certain family members.
-
There were positive reflections on instances when professionals worked closely with carers to optimise care outcomes.
The different factors that may support the development of a constructive working relationship between service users, carers and professionals are discussed in Theme 1: enabling use of the Nearest Relative/Named Person role.
Overall synthesis summary: how do the themes relate to one another?
This section presents how we believe the four themes identified through the framework synthesis may influence one another. The proposed links should be interpreted in the context of the limited number of studies contributing towards the overall synthesis. The proposed relationship between the themes is suggested in Figure 3.
FIGURE 3.
Proposed relationship between the four themes identified by the framework synthesis.
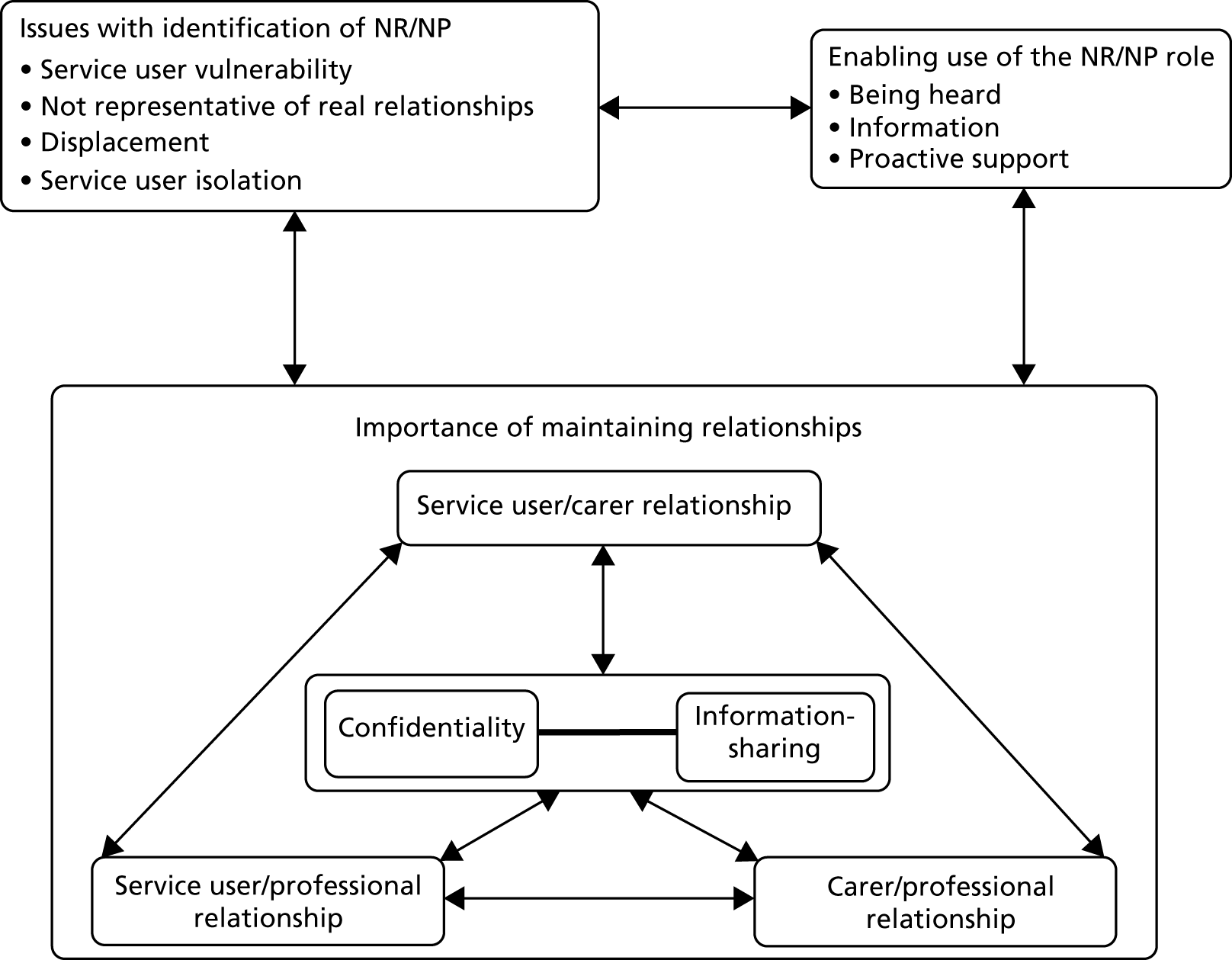
Although not directly relating to the NR provision of the MHA 1983,1 we view the interaction between the three types of relationship identified within the theme ‘importance of maintaining relationships’ as underpinning each of the other three themes. First, the tension between maintaining service user confidentiality and the need to share certain information with the carers/NRs who support them, as discussed in Theme 2: confidentiality and information-sharing, may be mediated by the quality of the relationships between service users, carers/NRs and professionals. For example, service user confidentiality may be prioritised in situations in which the relationship between the service user and their carer/NR is strained. Alternatively, in situations in which the working relationship between carers/NRs and professionals is not cultivated, appropriate information-sharing may not take place. The balance between maintaining service user confidentiality and information-sharing may also affect these relationships. The relationship between carers/NRs and professionals may be adversely affected when carers perceive that they are being excluded from decision-making. A lack of appropriate information may also add to carer/NR stress, which may reduce their ability to support the service user and fulfil the role of NR. Finally, any miscalculation between information-sharing and respecting the privacy of service users by professionals, such as disclosing information to a NR the service user does not get on with, may distress the service user. This may have a negative influence on their relationship with the professionals who support them. In short, the quality of the relationships between service users, carers/NRs and professionals can influence the balance between the need to respect service user privacy and the need to share information with the carers/NRs who support them. How this balance is achieved (or not) may in turn influence the quality of these relationships.
It seems likely that this interaction between the themes ‘confidentiality and information-sharing’ and ‘importance of maintaining working relationships’ described above may influence the issues described within Theme 3: issues regarding the identification of the Nearest Relative. Inadequate information-sharing and involvement with decision-making from the point of view of carers/NRs may increase feelings of carer stress, which may introduce bias into how they fulfil the role of NR. This, along with any perceived violation of the service user’s privacy, may influence the desire to apply to displace the NR through the County Court. Any efforts to displace the NR have the potential to negatively affect the relationship between them and the service user they support and/or the professionals who support them.
Information-sharing, a good relationship between carers/NRs and professionals and reduced carer stress may in turn help carers and NRs to feel more confident within their role, as described within Theme 1:enabling use of the Nearest Relative/Named Person role. NRs and NPs who feel more able to fulfil their role in supporting the service user may have a positive influence on the relationships described within Theme 4: importance of maintaining relationships. Increased carer empowerment through receipt of adequate information about their role and rights conveyed by the NR/NP role may also reduce the impact of carer bias on decision-making, as described within Theme 3: issues regarding the identification of the Nearest Relative and reduce the desire of service users to displace their NR/NP. Finally, the right of service users to displace their NR/NP who they view as ‘unsuitable’ can be viewed as one way in which service users can make their voices heard and thus contribute towards the theme ‘enabling use of the NR/NP role’.
Chapter 4 Discussion
Summary of findings
This rapid systematic review of qualitative evidence seeks to answer the overarching review question: what are the experiences of services users, family members, carers and relevant professionals of the use of the NR provisions in the compulsory detention and ongoing care of people under the MHA 1983?1
In addition, we sought to fulfil the following specific research objectives, from the perspective of service users, family members, carers or relevant professionals:
-
Explore experiences relating to the identification of the NR in relation to the care of an individual who has been compulsorily detained under the MHA 1983. 1
-
Explore the experiences of requesting displacement of the assigned NR, including the process of going through a tribunal and issues associated with this, such as influences on ongoing care.
-
Explore issues relating to patient confidentiality and information-sharing, relating to all aspects of compulsory detention.
-
Explore issues relating to decisions about care during detention and after discharge, including to a CTO.
-
Explore issues relating to service users having access to support from those carers who they want to be involved with or informed about their care.
We identified 32 sources4,20,31–34,36–61 reporting on 20 studies, before prioritising 12 studies from 22 sources4,31–33,36–38,40,45,46,48,49,51–60 that contained the richest and most relevant evidence reflecting a range of perspectives, for analysis in a framework synthesis. Within these 12 studies was evidence from across the UK, allowing comparisons to be drawn between experiences of the NR provisions (MHA 1983,1 England, Wales and Northern Ireland) and the NP provisions (MHCT, Scotland). Some of the studies conducted in England reflected experiences of the NR provisions from before the 2007 amendments to the MHA 1983. 1 Only one study was identified from Northern Ireland38 and none was conducted in Wales, so our findings generally reflect the experience of legislation as it applies in England and Scotland. The views of service users, the NR or NP, carers, professionals, lawyers and policy influencers were represented in the synthesis.
Evidence was initially mapped using a framework based on the five research objectives before being refined into themes. Four themes emerged from the framework synthesis: (1) issues with identification of the NR, (2) confidentiality and information-sharing, (3) enabling the use of the NR/NP role and (4) importance of maintaining relationships.
The theme ‘issues with the identification of the Nearest Relative’ highlighted various problems with the prescriptive appointment of the NR under the MHA 1983,1 including situations in which someone with a history of an abusive relationship with the service user is appointed, and the appointment of someone not involved with care of the service user. In contrast, under the MHCT in Scotland, service users can nominate a NP or, since 2017, can opt to have no NP. 64 Although we found no evidence pertaining to experiences of the option to forgo having a NP, the MHCT legislation was discussed in three sources. 32,33,56 Under the first theme of the synthesis, service users and professionals considered the option to nominate a NP as a positive development, as it allowed the flexibility to take pressure away from primary caregivers, or nominate individuals, such as trusted friends.
Another benefit of the MHCT in Scotland is the relative ease with which service users can displace (i.e. change) their nominated or, in the absence of a nomination, their allocated NP. This was summarised in the subtheme ‘displacement’. Since the 2007 amendments to the MHA 1983,1 service users can apply to County Courts to have their NR displaced on grounds that they were an inappropriate choice. 14 The equivalent process in the Scottish system is simpler, requiring the service user to make a (witnessed) written declaration to revoke their chosen NP, or apply in writing to request displacement of a tribunal-appointed NP. There was no evidence from England about the experiences of applications to displace the NR since 2007, with only one study contributing evidence under this theme from England since 1998. 31 Service users reported negative experiences of the system, reporting the threat of a tribunal as a deterrent, or reflecting that ways to circumvent a court order could be more easily achieved than going through the tribunal system.
Although we found no evidence relating to the displacement of a NR since the MHA 19831 amendments in 2007,14 the evidence from Scotland revealed that service users welcomed the ease with which they could displace their NP, and professionals considered this a positive move when the NP was considered inappropriate. Carers, however, found it unsettling that they could be easily displaced if they disagreed with the service user, and subsequently be omitted from important decisions about care. The right to be involved in decisions about care was both valued and considered a heavy responsibility by NRs and NPs, these contrasting sentiments often mentioned across themes.
Issues regarding access to information about the patient and involvement in decisions about care were identified in Theme 2: confidentiality and information-sharing. The sort of information that is shared about a service user’s compulsory detention and treatment can be highly sensitive and distressing for both service users and their carers. In some instances, service users saw the option to withhold information from their NR or NP as a means of gaining some control over their situation, and carers and professionals commented that it was not in the best interests of all parties to share all sensitive information. However, it was agreed that a certain level of information must be shared in order for NRs/NPs to fulfil their roles as carers. NRs/NPs also felt wary of sharing information about the service user with professionals, for fear of that information being disclosed to the service user. Failure to adequately inform service users and carers about the powers and potential benefits of the NR role, as well as evidence of poor understanding by some professionals, may hinder its application.
In general, issues about confidentiality and information-sharing were seen as complex, and there was confusion about the rights of carers and NRs/NPs to be given certain information. This sentiment was echoed in theme 3, ‘enabling the use of the NR/NP role’, in which it was clear that the complexities of the NR or NP provisions were not well explained to service users and carers, to the extent that it prevented the exercise of important rights and powers. The need for professionals to be better trained in communication was noted in themes 2 and 4.
The quality of the relationships between the carer or NR/NP and the service user, the professionals involved in care and the service user, and the professionals and carer or NR/NP were fundamental considerations throughout and were described in Theme 4: importance of maintaining relationships. The relationships between professionals involved in the care of service users and both the service user and their NR/NP were strengthened when professionals took a flexible approach to information-sharing (theme 2, ‘confidentiality and information-sharing’) or worked closely to optimise patient outcomes (theme 4, ‘importance of maintaining relationships’). However, there were instances when professionals were perceived as difficult to communicate with, and did not listen to the opinions of the NR/NP. Professionals also noted the challenge of knowing which information to share with carers about the service user, for fear of disrupting relationships.
Evidence from Theme 4: importance of maintaining relationships again emphasised that the role of NR or NP confers a heavy responsibility, particularly when the appointed individual is already the primary carer. The option in Scotland to appoint a different person (e.g. a friend or family member) as the NP was seen as a way of reducing the burden on the primary carer. This contrasts with some statements in Theme 3: enabling use of the Nearest Relative/Named Person role, in which some carers appreciated the status of NR/NP. They felt that the role conferred a number of positive benefits, such as feeling empowered and involved in treatment decisions, being recognised as an important person and getting proper access to information. It was noted in theme 4, however, that it would be useful for carers’ needs to be considered by professionals involved in the service user’s treatment. This included both informational needs, such as help with understanding reports and filling in forms, and emotional support throughout the process. These supportive actions by professionals may go some way towards easing the responsibility associated with the NP/NR role and, therefore, enabling people to fulfil the roles confidently and effectively.
Limitations of the review
Limitations of the evidence
This review identified and summarised a body of qualitative evidence about the experiences of those involved with the compulsory detention of people with mental health problems in the UK. After initially determining included studies, we prioritised and synthesised those studies that offered the most abundant and the most relevant primary data. We identified 12 such studies; however, when developing the framework, only six or seven contributed significantly (see Table 5). 31–33,45,46,56,57 Although experiences of the use of NP provisions in Scotland were represented by only three studies, these were arguably the richest, coming from a PhD thesis32 and two government reports commissioned to examine the implementation of the MHCT. 33,56 Lengthier reports inevitably have scope to include richer accounts of interview participants, for example, than journal articles. Service users’, carers’, NPs’ and professionals’ experiences of the NP provisions were all well represented by the evidence from Scotland. However, there were no studies offering comparisons with the NR provisions of the MHA 19831 in England and Wales. Although the 2015 amendments to the MHCT allow the service user to opt to not have a NP, there was no evidence relating to this. The amended Act was only implemented in 2017, so published studies of its implementation would not be expected at the time of this report.
The evidence of experiences of the MHA 19831 in England and Wales came from eight studies;31,45,46,48,49,57,58,60 however, only four46,57,58,60 collected data after the implementation of the 2007 MHA 19831 amendments. 14 These amendments were notable in that they introduced the option to withhold information from the NR or to displace the NR through application to County Courts, and gave civil partners equal status to married partners in the hierarchy of relatives. Those four studies represented the views of 55 family caregivers,46,57 21 service users and 19 mental health professionals. 60 Thirty-two NRs were interviewed by Smith,58 but few rich and relevant data from this study featured in our synthesis (see Table 5), and seven NRs were interviewed by Stroud et al. 60 Perspectives on current aspects (since 2007) of the NR provisions of the MHA 19831 in England and Wales are therefore represented by a very small number of participants and may not reflect wider experiences of the current legislation and related practices. The data pertaining to the MHA 19831 in England and Wales prior to the 2007 amendments14 were mainly from three studies offering rich data that featured heavily in the synthesis. 31,45,49 These studies represented the views of 57 carers, 34 service users and 43 mental health professionals through the analysis of interview data (Pinfold et al. 49 also conducted a questionnaire survey of 998 stakeholders).
In summary, the limitations of the available evidence should be considered when drawing conclusions from this review. In particular, although a number of the included qualitative studies provided rich data about the experiences of a variety of stakeholders involved in compulsory detention under the MHA 19831 and MHCT, the samples drawn on were predominantly from England and Scotland, and most evidence predated the 2007 MHA amendments;14 therefore, they may not be completely representative of the wider population experiencing or providing such care in the UK in 2018. Nevertheless, although we cannot claim to have conducted an in-depth analysis that has reached conceptual ‘saturation’, there is reasonable analytical generalisability over time and between localities in terms of the recurrence of a considerable number of common plausible issues.
Experiences of the MHA 19831 in Northern Ireland were investigated in just one study38 included in the synthesis. The evidence from Scotland focused on experiences of implementation of the MHCT, without direct comparison with older legislation or legislation in England and Wales. The evidence from England was again drawn from a handful of small studies, and in particular there was a dearth of evidence attempting to examine experiences of the NR provisions since the MHA 19831 was amended in 2007. 14 At best, the evidence can be considered indicative of issues with the MHA 19831 and MHCT11 legislation that may be experienced by service users and carers in particular, rather than representative of the majority of experiences.
Methodological limitations of the review
This systematic review was conducted within a rapid time frame (6 weeks) and the following limitations resulting directly from this approach should be acknowledged:
-
A pragmatic decision was made to prioritise studies that contained more than a few paragraphs of relevant primary qualitative data for inclusion in the framework synthesis. With more time, all included studies would have been considered for inclusion in the synthesis.
-
A framework approach was used for the synthesis of included studies. The period available for synthesis of the prioritised studies (1–2 weeks) did not lend itself to the preferred method of synthesis, which would have used an iterative, inductive approach. For this reason, the findings of this review are largely descriptive in nature, and are not able to reflect on the nuance and underlying issues identified by the included studies. In addition, it was not possible to include all coded data in the write-up of the synthesis.
-
Citation-chasing was undertaken only on those studies prioritised for inclusion in the synthesis. With more time, all eligible studies would have been searched.
-
Critical appraisal was undertaken in full, but only for those studies included in the framework synthesis. This was deemed as an appropriate time-saving approach, as findings from the non-prioritised batch of studies were not synthesised and did not influence the conclusions of the review.
-
Three studies, which may have contributed useful information to the synthesis, were retrieved too late for inclusion in the review.
Despite these limitations, the processes of searching, study selection and critical appraisal (for prioritised studies) were conducted rigorously and in line with published international standards. 22 The findings of our synthesis should be considered in the light of these restrictions, and the stated limitations of the evidence base.
Chapter 5 Conclusions
This rapid review synthesised qualitative evidence regarding experiences of service users, carers and other stakeholders regarding the NR provisions of the MHA 19831 in England and the NP provisions of the MHCT in Scotland. A number of common themes were identified across a small number of included studies. Given the paucity of evidence available, the outcomes that emerged from the synthesis must be considered as examples or indicators of experiences, rather than representative of the experiences and impact of current legislation across the UK.
The research included in this review indicates that:
-
The role of the NR under the MHA 19831 is important and can carry a heavy responsibility. It is important that the most suitable person is identified for the role, whenever possible. Possible issues to consider when trying to identify a suitable person to fulfil the NR role may include, but are not limited to –
-
considering with the service user who they feel would be a suitable person to fulfil the NR role
-
confirming with the service user that they have a good relationship with the potential NR, with no past or ongoing abuse
-
confirming that the potential NR is both willing and able to support the service user within the NR role
-
ensuring that the potential NR is aware of the service user’s wishes regarding future treatment and is willing to act on them when appropriate
-
ensuring that the potential NR has an adequate understanding of both the parts of the MHA 19831 relevant to the circumstances of the service user and their role as the NR
-
confirming that the potential NR is in receipt of appropriate support from services, both in terms of their own needs as a carer and in order to fulfil their role as NR.
-
-
Under the MHCT in Scotland, service users welcome the opportunity to choose their NP.
-
The power to easily displace the NR or NP is perceived as beneficial, but may be used in a manner that may be harmful to important long-term relationships between the service user and their relatives or carers.
-
The rights, powers and responsibilities of the NR or NP appear poorly understood by some professionals, and are sometimes poorly communicated to service users and carers.
-
When possible, a flexible and positive approach to communication between professionals involved with care, service users and NRs/NPs may help to achieve agreed suitable levels of information-sharing.
-
Although some carers value the opportunity to be involved with decisions about the care of the service user that the role of NR or NP confers, it should be understood that there are significant responsibilities that come with the role. The emotional and informational needs of carers in this situation should be considered and appropriate support provided.
Implications and recommendations for research
Implications
Evidence was scarce and much of it was over 10 years old and comprised samples of individuals from a limited range of localities and services. Studies also suffered from a lack of evidence of rigour when collecting or analysing qualitative data. Despite the general consistency of experiences that contributed to themes across studies, only 12 studies contributed to the synthesis. The timeline of this rapid review prevented further exploration of the evidence; however, drawing further conclusions from the limited evidence pool may have exacerbated the potential for biased, unrepresentative experiences to be captured.
For this reason, the main implications of this review are that the topic of the NR provisions of the MHA 19831 is complex, of significant importance to individuals detained under the MHA 19831 and insufficiently studied to date.
Recommendations for research
It is imperative that high-quality primary research is undertaken to explore the current issues around the NR provisions of the MHA 19831 in England and Wales. There is no population group that has been recently and rigorously sampled to inquire about their experiences of the NR provisions, particularly since the introduction of the 2007 amendments to the MHA 1983. 1 Although all areas and topics related to the NR provisions of the MHA 19831 warrant further investigation, some of the specific directions for primary research include:
-
Examination of experiences of the NR/NP in the light of the most recent legislative changes throughout the UK, for example the option to opt for no NP in Scotland.
-
Further research is warranted in all areas of the UK. There was very little evidence from Northern Ireland and none from Wales and, although the studies based in Scotland were of good quality, they were few in number and all commissioned by the government. Despite the greater number of studies conducted in England, most of the useful evidence arose from a very small number of studies, and none of these had been conducted since key legislative amendments were made in 2007. 14
-
There has been a lack of consideration of the experiences of those who are not married or in a civil partnership.
-
The views of mental health professionals and mental health advocates were not well represented.
-
A dearth of evidence was uncovered relating to the specific experiences of the NR/NP provisions from the perspective of ethnic minorities.
Qualitative methods may be the most appropriate means of eliciting data about experiences of the NR/NP provisions of the MHA 1983. 1 However, reporting of methodological considerations could be improved.
Acknowledgements
We are grateful for insightful feedback on the draft report from an individual with experience of the NR provision.
We would like to thank Sue Whiffin and Jenny Lowe for administrative support and Hannah Jones for proofreading.
Contributions of authors
Liz Shaw was involved in all stages of the review, including direction/conception, planning searches, screening, data extraction, critical appraisal, synthesis and write-up. She led and directed the framework synthesis and subsequent write-up.
Michael Nunns was involved in all stages of the review, including direction/conception, planning searches, screening, data extraction, critical appraisal, synthesis and write-up. He was involved in the synthesis and validation of the findings. He led the write-up of the remaining sections of the report.
Simon Briscoe was involved in direction/conception, designing and conducting the database and supplementary searches, screening, data extraction, critical appraisal and write-up. He managed the reference library and commented on and edited draft sections of the report.
Rob Anderson was involved in guiding the direction of the review, advised on all stages of conducting the review and critically read and edited all sections of the report.
Jo Thompson Coon was involved in guiding the direction of the review, advised on all stages of conducting the review and critically read and edited all sections of the report. She is also the guarantor of the report.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Mental Health Act 1983. London: The Stationery Office; 1983.
- Code of Practice: Mental Health Act 1983. London: DHSC; 2015.
- Mental Health Act 1959. London: The Stationery Office; 1959.
- Rapaport J. A matter of principle: the Nearest Relative under the Mental Health Act 1983 and proposals for legislative reform. J Soc Welf Fam Law 2004;26:377-96. https://doi.org/10.1080/0964906042000323471.
- Mental Health (Northern Ireland) Order 1986. London: The Stationery Office; 1986.
- Human Rights Act 1998. London: The Stationery Office; 1998.
- The Human Rights Act. Equality and Human Rights Commission; 1998.
- National Service Framework for Mental Health: Modern Standards and Service Models. London: DHSC; 1999.
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Mental Capacity Act 2005 at a Glance. Social Care Institute for Excellence; 2009.
- Mental Health (Care and Treatment) (Scotland) Act 2003. London: The Stationery Office; 2003.
- Mental Health Act (Scotland) 1984. London: The Stationery Office; 1984.
- New Directions: Report on the Review of the Mental Health (Scotland) Act 1984. Edinburgh: Scottish Government; 2001.
- Mental Health Act. London: The Stationery Office; 2007.
- McDonald B. Information Sharing and Mental Health: Guidance to Support Information Sharing by Mental Health Services. London: Department of Health and Social Care; 2009.
- Mental Health (Wales) Measure 2010. London: The Stationery Office; 2010.
- Code of Practice to Parts 2 and 3 of the Mental Health (Wales) Measure 2010. Cardiff: Welsh Government; 2012.
- Five Year Forward View. Leeds: NHS England; 2014.
- Monitoring the Mental Health Act in 2015/16. Newcastle upon Tyne: CQC; 2016.
- Mental Health Act Fit for Tomorrow: an Agenda for Reform. London: Mental Health Alliance; 2017.
- Wessely S. Independent Review of the Mental Health Act 2017. www.gov.uk/government/groups/independent-review-of-the-mental-health-act (accessed 30 April 2018).
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York: CRD, University of York; 2009.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339. https://doi.org/10.1136/bmj.b2535.
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12. https://doi.org/10.1186/1471-2288-12-181.
- Wong SS, Wilczynski NL, Haynes RB. Developing optimal search strategies for detecting clinically relevant qualitative studies in MEDLINE. Stud Health Technol Inform 2004;107:311-16.
- Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. Am J Nurs 2014;114:53-6. https://doi.org/10.1097/01.NAJ.0000445689.67800.86.
- Wallace A, Croucher K, Quilgars D, Baldwin S. Meeting the challenge: developing systematic reviewing in social policy. Policy Polit 2004;32:455-70. https://doi.org/10.1332/0305573042009444.
- Booth A, Carroll C. How to build up the actionable knowledge base: the role of ‘best fit’ framework synthesis for studies of improvement in healthcare. BMJ Qual Saf 2015;24:700-8. https://doi.org/10.1136/bmjqs-2014-003642.
- Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-39.
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-21.
- Rapaport J. The Nearest Relative Under the Mental Health Act 1983: A Relative Affair 2002.
- Berzins KM. Mental Health Service Users’, Carers’ and Professionals’ Perceptions of the Named Person Provisions of the Mental Health (Care and Treatment) (Scotland) Act 2003 2009.
- Dawson A, Ferguson I, Mackay K, Maxwell M. An Assessment of the Operation of the Named Person Role and its Interaction with Other Forms of Patient Representation. Edinburgh: QPS; 2009.
- Banks LC, Stroud J, Doughty K. Community treatment orders: exploring the paradox of personalisation under compulsion. Health Soc Care Community 2016;24:e181-90. https://doi.org/10.1111/hsc.12268.
- Barnes M, Davis A, Tew J. Valuing experience: users’ experiences of compulsion under the Mental Health Act 1983. Ment Health Rev 2000;5:11-4. https://doi.org/10.1108/13619322200000024.
- Berzins KM, Atkinson JM. The views of policy influencers and mental health officers concerning the Named Person provisions of the Mental Health (Care and Treatment) (Scotland) Act 2003. J Ment Health 2010;19:452-60. https://doi.org/10.3109/09638231003728117.
- Berzins KM, Atkinson JM. Service users’ and carers’ views of the Named Person provisions under the Mental Health (Care and Treatment) (Scotland) Act 2003. J Ment Health 2009;18:207-15. https://doi.org/10.1080/09638230802523021.
- Campbell J. Stakeholders’ views of legal and advice services for people admitted to psychiatric hospital. J Soc Welf Fam Law 2008;30:219-32. https://doi.org/10.1080/09649060802550659.
- Campbell J, Wilson G, Britton F, Hamilton B, Hughes P, Manktelow R. The management and supervision of approved social workers: aspects of law, policy and practice. J Soc Welf Fam Law 2001;23:155-72. https://doi.org/10.1080/01418030122030.
- Canvin K, Rugkåsa J, Sinclair J, Burns T. Patient, psychiatrist and family carer experiences of community treatment orders: qualitative study. Soc Psychiatry Psychiatr Epidemiol 2014;49:1873-82. https://doi.org/10.1007/s00127-014-0906-0.
- De Maynard V. An ethnographic study of black men within an inner London area to elicit relatedness between black human condition and the onset of severe mental illness: what about the black human condition?. Int J Ment Health 2007;36:26-45. https://doi.org/10.2753/IMH0020-7411360403.
- No Voice Unheard, No Right Ignored: Key Themes from the Consultation Responses. London: Department of Health and Social Care; 2015.
- Gault I. Service-user and carer perspectives on compliance and compulsory treatment in community mental health services. Health Soc Care Community 2009;17:504-13. https://doi.org/10.1111/j.1365-2524.2009.00847.x.
- Gault I, Gallagher A, Chambers M. Perspectives on medicine adherence in service users and carers with experience of legally sanctioned detention and medication: a qualitative study. Patient Prefer Adher 2013;7:787-99. https://doi.org/10.2147/PPA.S44894.
- Henderson J. Experiences of ‘care’ in mental health. J Adult Prot 2002;4:34-45. https://doi.org/10.1108/14668203200200020.
- Jankovic J, Yeeles K, Katsakou C, Amos T, Morriss R, Rose D, et al. Family caregivers’ experiences of involuntary psychiatric hospital admissions of their relatives – a qualitative study. PLOS ONE 2011;6. https://doi.org/10.1371/journal.pone.0025425.
- Manktelow R, Hughes P, Britton F, Campbell J, Hamilton B, Wilson G. The experience and practice of approved social workers in Northern Ireland. Br J Soc Work 2002;32:443-61. https://doi.org/10.1093/bjsw/32.4.443.
- Marriott S. Research into the Mental Health Act: a qualitative study of the views of those using or affected by it. J Ment Health 2001;10:33-9. https://doi.org/10.1080/09638230124934.
- Pinfold V, Farmer P, Rapaport J, Bellringer S, Huxley P, Murray J, et al. Positive and Inclusive? Effective Ways for Professionals to Involve Carers in Information Sharing. London: National Coordinating Centre for the Service Delivery and Organisation; 2004.
- Rabiee F, Smith P. Being understood, being respected: an evaluation of the statutory and voluntary mental health service provision in Birmingham, UK. Int J Ment Health Prom 2013;15:162-77. https://doi.org/10.1080/14623730.2013.824163.
- Rapaport J. Rise and demise of the nearest relative. Professional Social Work 1999:14-5.
- Rapaport J. The ghost of the Nearest Relative under the Mental Health Act 1983 – past, present and future. J Ment Health Law 2003;9:51-65.
- Rapaport J. Reflections on ‘A Relative Affair’: the Nearest Relative Under the Mental Health Act 1983. London: Social Care Workforce Research Unit, King’s College London; 2012.
- Ridley J, Hunter S. Subjective experiences of compulsory treatment from a qualitative study of early implementation of the Mental Health (Care & Treatment) (Scotland) Act 2003. Health Soc Care Community 2013;21:509-18. https://doi.org/10.1111/hsc.12041.
- Ridley J, Hunter S, Rosengard A. Partners in care?: views and experiences of carers from a cohort study of the early implementation of the Mental Health (Care & Treatment) (Scotland) Act 2003. Health Soc Care Community 2010;18:474-82. https://doi.org/10.1111/j.1365-2524.2010.00920.x.
- Ridley J, Rosengard A, Hunter S. Experiences of the early implementation of the Mental Health (Care and Treatment) (Scotland) Act, 2003. Health Community Care Res Find 2009;80.
- Rugkåsa J, Canvin K. Carer involvement in compulsory out-patient psychiatric care in England. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2716-z.
- Smith MS. ‘Only connect’ ‘Nearest Relative’s’ experiences of mental health act assessments. J Soc Work Pract 2015;29:339-53. https://doi.org/10.1080/02650533.2015.1057802.
- Stroud J, Banks L, Doughty K. Community treatment orders: learning from experiences of service users, practitioners and Nearest Relatives. J Ment Health 2015;24:88-92. https://doi.org/10.3109/09638237.2014.998809.
- Stroud J, Doughty K, Banks L, Hayward M, Ashdown H, Sherlock M, et al. An Exploration of Service User and Practitioner Experiences of Community Treatment Orders. Brighton: University of Brighton; 2013.
- Taylor AJ, Lawton-Smith S, Bullmore H. Supervised community treatment: does it facilitate social inclusion? A perspective from approved mental health professionals (AMHPs). Ment Health Soc Inclus 2013;17:43-8. https://doi.org/10.1108/20428301311305304.
- Vicary S. An Interpretative Phenomenological Analysis of the Impact of Professional Background on Role Fulfilment: A Study of Approved Mental Health Practice. Manchester: University of Manchester; 2016.
- Detained. SSI Inspection of Compulsory Mental Health Admissions. Manchester: Department of Health and Social Care; 2001.
- Scotland Mental Health (Care and Treatment) (Scotland) Act 2015. Edinburgh: The Stationery Office; 2015.
- Planning Your Care: Advanced Statements. Rethink Mental Illness; 2018.
Appendix 1 Literature search strategies
Bibliographic databases
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations
Host: Ovid.
Data parameters: 1946 to January week 2 2018 and 22 January 2018.
Date searched: 23 January 2018.
Searcher: Simon Briscoe.
Hits: 596.
Search strategy
-
(famil* or relative or relatives or relation*).tw.
-
(husband* or wife or wives or ”civil partner*” or son* or daughter* or father* or mother* or grandparent*).tw.
-
(”named person*” or carer* or caregiver*).tw.
-
(”approved mental health professional*” or AMHP*).tw.
-
(”social worker*” or ”occupational therapist*” or psychologist* or psychiatrist* or police).tw.
-
(nurse* adj3 (”mental health” or psychiatric or ”learning disabilit*” or ”occupational health”)).tw.
-
exp Family/
-
Caregivers/
-
psychiatric nursing/
-
Social Workers/
-
occupational health nursing/
-
*Psychiatry/
-
or/1-12
-
((involuntary or forced or compulsory) adj3 (admission* or hospitali?ation* or care)).tw.
-
((sectioned or sectioning or detain* or detention) adj14 (mental* or psychiatr* or hosptial*)).tw.
-
”Commitment of Mentally Ill”/
-
”mental health act”.tw.
-
(”community treatment order*” or ”supervised community treatment*”).tw.
-
”mental health tribunal*”.tw.
-
or/14-19
-
((mental* or psychiatr*) adj3 (health* or care or ill or illness or disorder* or service*)).tw.
-
Mental Health/
-
exp Mental Disorders/
-
or/21-23
-
qualitative*.tw.
-
(interview* or experience* or view*).mp.
-
Qualitative Research/
-
(”focus group” or survey* or questionnaire*).tw.
-
Focus Groups/
-
”Surveys and Questionnaires”/
-
or/25-30
-
13 and 20 and 24 and 31
-
limit 32 to english language
PsycINFO
Host: Ovid.
Data parameters: 1806 to January week 3 2018.
Date searched: 23 January 2018.
Searcher: Simon Briscoe.
Hits: 578.
Search strategy
-
(famil* or relative or relatives or relation*).tw.
-
(husband* or wife or wives or ”civil partner*” or son* or daughter* or father* or mother* or grandparent*).tw.
-
(”named person*” or carer* or caregiver*).tw.
-
(”approved mental health professional*” or AMHP*).tw.
-
(”social worker*” or ”occupational therapist*” or psychologist* or psychiatrist* or police).tw.
-
(nurse* adj3 (”mental health” or psychiatric or ”learning disabilit*” or ”occupational health”)).tw.
-
exp family members/
-
Caregivers/
-
psychiatric nurses/
-
social workers/
-
occupational therapy/
-
*psychiatry/
-
or/1-12
-
((involuntary or forced or compulsory) adj3 (admission or hospitali?ation or care)).tw.
-
((sectioned or sectioning or detain* or detention) adj14 (mental* or psychiatr* or hosptial*)).tw.
-
”commitment (psychiatric)”/
-
”mental health act”.tw.
-
(”community treatment order*” or ”supervised community treatment*”).tw.
-
”mental health tribunal*”.tw.
-
or/14-19
-
((mental* or psychiatr*) adj3 (health* or care or ill or illness or disorder*)).tw.
-
Mental Health/
-
exp Mental Disorders/
-
or/21-23
-
qualitative*.tw.
-
(interview* or experience* or view*).mp.
-
Qualitative Research/
-
(”focus group” or survey* or questionnaire*).tw.
-
questionnaires/
-
or/25-29
-
13 and 20 and 24 and 30
-
limit 31 to english language
Social Policy and Practice
Host: Ovid.
Data parameters: 201710
Date searched: 23 January 2018.
Searcher: Simon Briscoe.
Hits: 179.
Search strategy
-
(famil* or relative or relatives or relation*).tw.
-
(husband* or wife or wives or ”civil partner*” or son* or daughter* or father* or mother* or grandparent*).tw.
-
(”named person*” or carer* or caregiver*).tw.
-
(”approved mental health professional*” or AMHP*).tw.
-
(”social worker*” or ”occupational therapist*” or psychologist* or psychiatrist* or police).tw.
-
(nurse* adj3 (”mental health” or psychiatric or ”learning disabilit*” or ”occupational health”)).tw.
-
or/1-6
-
((involuntary or forced or compulsory) adj3 (admission* or hospitali?ation* or care)).tw.
-
((sectioned or sectioning or detain* or detention) adj14 (mental* or psychiatr* or hosptial*)).tw.
-
”mental health act”.tw.
-
(”community treatment order*” or ”supervised community treatment*”).tw.
-
”mental health tribunal”.tw.
-
or/8-12
-
((mental* or psychiatr*) adj3 (health* or care or ill or illness or disorder* or service*)).tw.
-
qualitative*.tw.
-
(interview* or experience* or view*).mp.
-
(”focus group” or survey* or questionnaire*).tw.
-
or/15-17
-
7 and 13 and 14 and 18
Database: Health Management Information Consortium
Host: Ovid.
Data parameters: 1979 to November 2017.
Date searched: 23 January 2018.
Searcher: Simon Briscoe.
Hits: 139.
Search strategy
See Social Policy and Practice search strategy above.
Cumulative Index to Nursing and Allied Health Literature
Host: EBSCOhost.
Data parameters: not applicable.
Date searched: 23 January 2018.
Searcher: Simon Briscoe.
Hits: 362.
Search strategy
-
TI ( famil* or relative or relatives or relation* ) OR AB ( famil* or relative or relatives or relation* )
-
TI ( husband* or wife or wives or ”civil partner*” or son* or daughter* or father* or mother* or grandparent* ) OR AB ( husband* or wife or wives or ”civil partner*” or son* or daughter* or father* or mother* or grandparent* )
-
TI ( ”named person*” or carer* or caregiver* ) OR AB ( ”named person*” or carer* or caregiver* )
-
TI ( ”approved mental health professional*” or AMHP* ) OR AB ( ”approved mental health professional*” or AMHP* )
-
TI ( ”social worker*” or ”occupational therapist*” or psychologist* or psychiatrist* or police ) OR AB ( ”social worker*” or ”occupational therapist*” or psychologist* or psychiatrist* or police )
-
TI ( nurse* N2 (”mental health” or psychiatric or ”learning disabilit*” or ”occupational health”) ) OR AB ( nurse* N2 (”mental health” or psychiatric or ”learning disabilit*” or ”occupational health”) )
-
(MH ”Family+”)
-
(MH ”Caregivers”)
-
(MH ”Psychiatric Nursing”)
-
(MH ”Social Workers”+)
-
(MH ”Occupational Health Nursing”)
-
(MM ”Psychiatry”)
-
S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12
-
TI ( (involuntary or forced or compulsory) N2 (admission* or hospitali?ation* or care) ) OR AB ( (involuntary or forced or compulsory) N2 (admission* or hospitali?ation* or care) )
-
TI ( (sectioned or sectioning or detain* or detention) N13 (mental* or psychiatr* or hospital*) ) OR AB ( (sectioned or sectioning or detain* or detention) N13 (mental* or psychiatr* or hospital*) )
-
(MH ”Involuntary Commitment”)
-
TI ”mental health act” OR AB ”mental health act”
-
TI ( ”community treatment order*” or ”supervised community treatment*” ) OR AB ( ”community treatment order*” or ”supervised community treatment*” )
-
TI ”mental health tribunal*” OR AB ”mental health tribunal*”
-
S14 OR S15 OR S16 OR S17 OR S18 OR S19
-
TI ( (mental* or psychiatr*) N2 (health* or care or ill or illness or disorder* or service*) ) OR AB ( (mental* or psychiatr*) N2 (health* or care or ill or illness or disorder* or service*) )
-
(MH ”Mental Health”)
-
(MH ”Mental Disorders+”)
-
S21 OR S22 OR S23
-
TI qualitative* OR AB qualitative*
-
TX ( interview* or experience* or view* ) OR TX ( interview* or experience* or view* )
-
(MH ”Qualitative Studies+”)
-
TI ( ”focus group” or survey* or questionnaire* ) OR AB ( ”focus group” or survey* or questionnaire* )
-
(MH ”Focus Groups”)
-
(MH ”Surveys”)
-
S25 OR S26 OR S27 OR S28 OR S29 OR S30
-
S13 AND S20 AND S24 AND S31
Note: limited to English-language studies.
Applied Social Sciences Index and Abstracts
Host: ProQuest.
Data parameters: not applicable.
Date searched: 23 January 2018.
Searcher: SB.
Hits: 585.
Search strategy
-
((TI,AB(famil* OR relative OR relatives OR relation* OR husband* OR wife OR wives OR ”civil partner*” OR son* OR daughter* OR father* OR mother* OR grandparent* OR ”named person*” OR carer* OR caregiver* OR ”approved mental health professional*” OR AMHP* OR ”social worker*” OR ”occupational therapist*” OR psychologist* OR psychiatrist* OR police)) OR (nurse* NEAR/2 (”mental health” OR psychiatric OR ”learning disabilit*” OR ”occupational health”))) OR MAINSUBJECT.EXACT.EXPLODE(”Families”) OR MAINSUBJECT.EXACT(”Carers”) OR MAINSUBJECT.EXACT(”Psychiatric nursing”) OR MAINSUBJECT.EXACT.EXPLODE(”Social workers”) OR MAINSUBJECT.EXACT(”Occupational health nursing”) OR MAINSUBJECT.EXACT(”Psychiatry”)
-
(TI,AB((involuntary OR forced OR compulsory) NEAR/2 (admission* OR hospitali?ation* OR care)) OR ((sectioned OR sectioning OR detain* OR detention) N13 (mental* OR psychiatr* OR hosptial*)) OR ”mental health act” OR ”mental health tribunal*” OR ”community treatment order*” OR ”supervised community treatment*”) OR MAINSUBJECT.EXACT(”Sectioning”)
-
((mental* OR psychiatr*) NEAR/2 (health* OR care OR ill OR illness OR disorder* OR service*)) OR MAINSUBJECT.EXACT(”Mental health”) OR MAINSUBJECT.EXACT.EXPLODE(”Psychiatric disorders”)
-
(interview* or experience* or view*) OR TI,AB(qualitative* OR ”focus group” OR survey* OR questionnaire*) OR MAINSUBJECT.EXACT(”Qualitative methods”) OR MAINSUBJECT.EXACT(”Qualitative research”) OR MAINSUBJECT.EXACT(”Focus groups”)
-
1 AND 2 AND 3 AND 4
Note: limited to English-language studies.
| Database | Number of hits |
|---|---|
| MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations | 596 |
| PsycINFO | 578 |
| Social Policy and Practice | 179 |
| Health Management Information Consortium | 139 |
| CINAHL | 362 |
| ASSIA | 585 |
| Total number of hits | 2439 |
| Duplicate number of hits | 696 |
| Total number of unique hits | 1743 |
Website searches
| Website | URL | Search strategy | Limits | Date | Number of hits |
|---|---|---|---|---|---|
| Centre for Mental Health | www.centreformentalhealth.org.uk/ | Searched for ‘Nearest Relative’ using website search function | None | 24 January 2018 | 16 |
| Mental Health Alliance | www.mentalhealthalliance.org.uk/news/index.html | Scanned the News and Publications pages | None | 24 January 2018 | N/A |
| Mental Health Foundation | www.mentalhealth.org.uk/publications/listing | Searched for (1) ‘Nearest Relative’ and (2) ‘mental health act’ using Publications page search function | None | 24 January 2018 | 8 |
| Mind | www.mind.org.uk/ | Searched for ‘Nearest Relative’ in website search box | None | 24 January 2018 | 54 |
| Rethink Mental Illness | www.rethink.org/resources/a | Browsed the website library for relevant studies | None | 24 January 2018 | N/A |
| Royal College of Psychiatrists | www.rcpsych.ac.uk/usefulresources/publications.aspx | Searched for ‘Nearest Relative’ using website search function and browsed the Publications page for relevant studies | None | 24 January 2018 | 86 |
| SANE | www.sane.org.uk/resources/publications/ | Scanned the Publications page for relevant studies | None | 31 January 2018 | N/A |
| Time to Change | www.time-to-change.org.uk/resources/research-reports-publications | Scanned the Research and Reports page for relevant studies | None | 1 February 2018 | N/A |
| Young Minds | https://youngminds.org.uk/ | Searched for (1) ‘Nearest Relative’ and (2) ‘mental health act’ using search function | Search limited to publications | 1 February 2018 | 15 |
Forward citation-chasing
Date searched: 2 February 2018.
Databases: Web of Science Core Collection, Scopus, Google Scholar.
Hosts: Clarivate Analytics (Web of Science) and Elsevier (Scopus).
Searcher: Simon Briscoe.
Search strategy
Citations of each study were searched for using Web of Science. If a study was not indexed in Web of Science then we searched using Scopus, and if study was not indexed in Scopus then we searched using Google Scholar.
| First author and year of publication | Number of citations | Database |
|---|---|---|
| Banks 201634 | 2 | WoS |
| Berzins 200932 | 0 | GS |
| Berzins 200937 | 7 | GS |
| Campbell 200838 | 4 | Scopus |
| Jankovic 201146 | 17 | WoS |
| Marriott 200148 | 9 | Scopus |
| Rapaport 20044 | 13 | GS |
| Rapaport 201253 | 3 | GS |
| Ridley 201055 | 10 | WoS |
| Ridley 200956 | NKa | WoS/Scopus/GS |
| Rugkåsa 201757 | 0 | Scopus |
| Smith 201558 | 0 | WoS/Scopus |
| Stroud 201360 | 6 | GS |
| Stroud 201559 | 7 | WoS |
| Total number of citations | 78 | |
| Duplicate number of citations | 18 | |
| Unique number of results | 60 |
Appendix 2 Identification of initial themes for framework synthesis
| Study | Themes (and subthemes) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Research objective 1 | Research objective 2 | Research objective 3 | Research objective 4 | Research objective 5 | |||||
| Berzins 200932 | Perceptions of the introduction of the NP | Autonomy and choice | Reasons for nominating someone as a NP:
|
Advantage for service users and carers | Autonomy: understanding and information:
|
Low uptake | Power imbalances:
|
The NP provisions and human rights:
|
|
| Dawson 200933 | The appointment of the NP:
|
Interaction and overlap, NP and other forms of representation:
|
Definitions of the role of the NP and its perceived impact:
|
Definitions of the role of the NP and its perceived impact:
|
|||||
| Rapaport 200231 | Bias and abuse | Recognition of patients without relatives:
|
Inflexible identification:
|
NR and ASW:
|
Safeguards and relative relevance | Under statute:
|
Build-up to crisis and assessment: relatives’ perspectives:
|
NR recognition | |
Appendix 3 List of excluded studies coded as ‘forensic’ during title and abstract and full-text screening
Aalsma MC, Brown JR, Holloway ED, Ott MA. Connection to mental health care upon community reentry for detained youth: a qualitative study. BMC Public Health 2014;14:117. https://doi.org/10.1186/1471-2458-14-117
Bamford K, Benton C. Gathering meaningful service user feedback regarding a community forensic service. J Intellect Disabil Offending Behav 2015;6:81–93.
Buchanan A, Gunn J. What psychiatrists think about Part III of the Mental Health Act 1983. Psychiatr Bull 1999;23:721–5.
Chandley M, Cromar-Hayes M, Mercer D, Clancy B, Wilkie I, Thorpe G. The development of recovery based nursing in a high-security hospital: nurturance and safe spaces in a dangerous world? Ment Health Soc Inclus 2014;18:203–14.
Cooke K, Bailey D. Women’s experience of forensic mental health services: implications for practice. J Ment Health Train, Educ Pract 2011;6:186–94.
Cummins I. Mental health and custody: a follow on study. J Adult Prot 2012;14:73–81.
Department of Health and Social Care (DHSC), Home Office, Green D, Lamb N. Review of the Operation of Sections 135 and 136 of the Mental Health Act 1983: Review Report and Recommendations. London: DHSC; 2014.
Department of Health and Social Care (DHSC), Home Office. Review of the Operation of Sections 135 and 136 of the Mental Health Act 1983 in England and Wales: A Survey. London: DHSC; 2014.
Docking M. Safe haven (custody for people with mental illness). Police Rev 2008;116:36–7.
Douglas N, Plugge E. The health needs of imprisoned female juvenile offenders: the views of the young women prisoners and youth justice professionals. Int J Prison Health 2008;4:66–76. https://doi.org/10.1080/17449200802038256
Ford K, Sweeney J, Farrington A. User views of a regional secure unit – findings from a patient satisfaction survey. Int J Psychiatr Nurs Res 1999;5:526–41.
Gorsuch N. Disturbed female offenders: helping the ‘untreatable’. J Forensic Psychiatry 1999;10:98–118.
Haddock A, Snowden P, Dolan M, Parker J, Rees H. Managing dangerous people with severe personality disorder: a survey of forensic psychiatrists’ opinions. Psychiatr Bull 2001;25:293–6.
Hartford K, Carey R, Mendonca J. Pre-arrest diversion of people with mental illness: Literature review and international survey. Behav Sci Law 2006;24:845–56. https://doi.org/10.1002/bsl.738
Hewitt D. The Nearest Relative: losing the right to concur? J Adult Prot 2010;12:35–9. https://doi.org/10.5042/jap.2010.0413
HM Inspectorate of Constabulary, HM Inspectorate of Prisons, Care Quality Commission, Health Care Inspectorate Wales. A Criminal Use of Police Cells? The Use of Police Custody as a Place of Safety for People with Mental Health Needs. London: HM Inspectorate of Constabulary; 2013.
Hörberg U, Sjögren R, Dahlberg K. To be strategically struggling against resignation: the lived experience of being cared for in forensic psychiatric care. Issues Ment Health Nurs 2012;33:743–51. https://doi.org/10.3109/01612840.2012.704623
Irvine A, Allen L, Webber M. Evaluation of the Scarborough, Whitby and Ryedale Street Triage Service. York: Department for Social Policy and Social Work, University of York; 2016.
Jones SL, Mason T. Quality of treatment following police detention of mentally disordered offenders. J Psychiatr Ment Health Nurs 2002;9:73–80.
Kravitz HM, Cavanaugh JL, Rigsbee SS. A cross-sectional study of psychosocial and criminal factors associated with arrest in mentally ill female detainees. J Am Acad Psychiatry Law 2002;30:380–90.
Lea S, Callaghan L, Eick S, Heslin M, Morgan J, Bolt M, et al. The management of individuals with enduring moderate to severe mental health needs: a participatory evaluation of client journeys and the interface of mental health services with the criminal justice system in Cornwall. Health Serv Deliv Res 2015;3(15).
Leese M, Russell S. Mental health, vulnerability and risk in police custody. J Adult Prot 2017;19:274–83.
MacInnes D. Interventions in forensic psychiatry: the caregiver’s perspective. Br J Nurs 2000;9:992–8. https://doi.org/10.12968/bjon.2000.9.15.5494
Marks L, Grey A, Pearce S. General practice in prisons in England: views from the field. Int J Prison Health 2006;2:49–62.
McGilloway S, Donnelly M. Mental illness in the UK criminal justice system: a police liaison scheme for mentally disordered offenders in Belfast. J Ment Health 2004;13:263–75.
McKinnon IG, Thomas SD, Noga HL, Senior J. Police custody health care: a review of health morbidity, models of care and innovations within police custody in the UK, with international comparisons. Risk Manag Healthc Policy 2016;9:213–26.
Menkes DB, Bendelow G. Diagnosing vulnerability and ‘dangerousness’: police use of Section 136 in England and Wales. J Public Ment Health 2014;13:70–82.
Mental Welfare Commission for Scotland. Mental Health of Women Detained by the Criminal Courts: Visit and Monitoring Report. Mental Welfare Commission for Scottland. 2014. URL: www.mwcscot.org.uk/media/190441/women_offenders_final_report.pdf (accessed 4 March 2018).
Mezey GC, Kavuma M, Turton P, Demetriou A, Wright C. Perceptions, experiences and meanings of recovery in forensic psychiatric service users. J Forens Psychiatry Psychol 2010;21:683–96.
Ogloff J, Warren L, Tye C, Blaher F, Thomas S. Psychiatric symptoms and histories among people detained in police cells. Soc Psychiatry Psychiatr Epidemiol 2011;46:871–80. https://doi.org/10.1007/s00127-010-0256-5
Palmer D, Nixon J, Reynolds S, Panayiotou A, Palmer A, Meyerowitz R. Getting to know you: reflections on a specialist independent mental health advocacy service for Bexley and Bromley residents in forensic settings. Ment Health Rev 2012;17:5–13.
Riley G, Freeman E, Laidlaw J, Pugh D. ‘A frightening experience’: detainees’ and carers’ experiences of being detained under Section 136 of the Mental Health Act. Med Sci Law 2011;51:164–9. https://doi.org/10.1258/msl.2011.010074
Riley G, Laidlaw J, Pugh D, Freeman E. The responses of professional groups to the use of Section 136 of the Mental Health Act (1983, as amended by the 2007 Act) in Gloucestershire. Med Sci Law 2011;51:36–42. https://doi.org/10.1258/msl.2010.010072
Royal College of Psychiatrists (RCPsych). CR159. Standards on the Use of Section 136 of the Mental Health Act 1983 (England and Wales). London: RCPsych; 2008.
Sadiq KT, Moghal A, Mahadun P. Section 136 assessments in Trafford Borough of Manchester. Clin Govern 2011;16:29–34.
Völlm B, Edworthy R, Holley J, Talbot E, Majid S, Duggan C, et al. A mixed-methods study exploring the characteristics and needs of long stay service users in high and medium secure settings in England: implications for service organisation. Health Serv Deliv Res 2017;5(11).
Walker J, Gudjonsson G. The Lancashire Quality of Life Profile: data and experiences with 58 detained mentally disordered offenders. Crim Behav Ment Healt 2000;10:123–35.
Watson J, Daley S. The use of section 135(1) of the Mental Health Act in a London borough. Ment Health Rev 2015;20:133–43.
Glossary
- Approved mental health professional
- An individual responsible for the assessment and hospital admission of people who have been detained under the Mental Health Act 1983 (Great Britain. Mental Health Act 1983. London: The Stationery Office; 1983). Approved mental health professionals were introduced in the 2007 amendment to the Mental Health Act 1983 and replaced the role of approved social workers. They include social workers, nurses, occupational therapists and psychologists.
- Community treatment order
- An order allowing people who have been detained under the Mental Health Act 1983 to be discharged from hospital on the condition of meeting certain requirements. If the requirements are not met, then a person can be involuntarily readmitted to hospital.
- Forensic detention
- The detention of an individual under the Mental Health Act 1983 by any of the forensic services, for example police or a court of law.
- Mental Health Act 1983
- A UK Act of Parliament that applies in England and Wales and gives approved mental health professionals the power to detain people who have a mental health disorder in hospital. The Act was amended in 2007.
- Mental Health (Care and Treatment) (Scotland) Act 2003
- An Act that replaced the Mental Health (Scotland) Act 1984. As per the 1984 Mental Health Act, it is primarily concerned with the detention of people with mental health disorders.
- Mental health officer
- An individual responsible for the assessment and hospital admission of people who have been sectioned under the Mental Health (Scotland) Act 1984. The role is broadly similar to that of approved mental health professionals in England and Wales.
- Mental Health (Scotland) Act 1984
- The Act that replaced the Mental Health (Scotland) Act 1960 and is primarily concerned with the detention of people with mental health disorders. It is comparable to the Mental Health Act 1983 for England and Wales.
- Mental health tribunal
- A legal proceeding that people who are sectioned under the Mental Health Act 1983 can apply for in order to be discharged. It involves a panel of experts including a judge, a psychiatrist and a lay person with specialist knowledge of the Mental Health Act, and usually takes place in a hospital.
- Named Person
- An individual who is chosen by a person who is detained under the Mental Health (Scotland) Act 1984 to represent their interests. The Named Person role is similar to the Nearest Relative role in England and Wales, under the Mental Health Act 1983.
- Nearest Relative
- A family member allocated to represent the interests of a person who is, or may be, detained under the Mental Health Act 1983. The Nearest Relative is a safeguard to protect the rights of a service user, with particular importance when the service user lacks mental capacity.
- Reflexivity
- This refers to the reflections of an author conducting qualitative research on how their knowledge, views and experiences may influence the research process.
- Restricted service user
- A service user who is involuntarily admitted to hospital under the criminal pathway of the Mental Health Act 1983 and who is subject to a ‘restriction order’. Among other things, approval of leave, transfer and discharge needs to be granted by the Ministry of Justice for these individuals.
- Sectioned
- A person who is detained under the Mental Health Act 1983 under sections 2 or 3 is sometimes described as ‘sectioned’.
- Supervised community treatment
- Takes place under a community treatment order.
List of abbreviations
- AMHP
- approved mental health professional
- ASSIA
- Applied Social Sciences Index and Abstracts
- ASW
- approved social worker
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CTO
- community treatment order
- DHSC
- Department of Health and Social Care
- HSDR
- Health Services and Delivery Research
- MCA
- Mental Capacity Act
- MHA 1983
- Mental Health Act 1983
- MHA 2007
- Mental Health Act 2007
- MHCT
- Mental Health (Care and Treatment) (Scotland) Act 2003
- MHO
- mental health officer
- MHWM
- Mental Health (Wales) Measure 2010
- NIHR
- National Institute for Health Research
- NP
- Named Person
- NR
- Nearest Relative
- PRISMA
- Preferred Reporting Items for Systematic reviews and Meta-Analyses
- SCT
- supervised community treatment
