Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/196/02. The contractual start date was in January 2016. The final report began editorial review in November 2017 and was accepted for publication in June 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Rob Anderson is a current member of the National Institute for Health Research Health Services and Delivery Research Researcher-led Prioritisation Committee. However, in this role he would not be involved in any discussions or decisions about grant proposals in which he has any personal, institutional or financial connections to any of the applicants. Alex Aylward declares personal fees outside the submitted work from the Northern, Eastern and Western Devon Clinical Commissioning Group, the Devon Local Medical Committee, the British Medical Association, the Collaboration for Leadership in Applied Health Research and Care (South West Peninsula) and the NHS England Medical Directorate (South).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Campbell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Understanding the general practitioner workforce crisis
Ninety per cent of NHS patient contact takes place within the context of primary care; this equates to 1.3 million consultations every working day and 340 million consultations per year, with a projected primary care workload of 430 million consultations per year by 2018. 1,2 Some patient groups disproportionately contribute to this demand for NHS services; for example, patients aged > 75 years – a population that is increasing – currently have an average of 15 contacts per year in primary care. 2 Such groups, who often have complex comorbidities, may therefore be particularly vulnerable to changes in the availability and accessibility of primary care services caused by workforce problems. In particular, around 66% of primary care contacts take place with a general practitioner (GP). GPs are trained in handling complex disease presentations and have unique abilities in respect of the diagnosis and management of this complex multimorbidity.
General practice has been described as ‘the jewel in the crown’ of the NHS. 3 International evidence has identified that, without strong primary-care-based health care, adverse consequences are likely to be reflected in increased costs of care, reduced satisfaction with care, increased health inequalities and adverse health outcomes for the population. 4 Authoritative reports have identified the need for both local and national approaches to workforce planning and for an acknowledgement of the inherent uncertainties of the process. 5
UK general practice is facing a workforce crisis, with imminent GP shortages and a clear resulting risk to patient health and well-being. More than 50% of GPs aged > 50 years (who account for 32% of all practitioners6) anticipate quitting direct patient care within 5 years. Research from the British Medical Association (BMA) has highlighted the continuing problem. In the study of 431 doctors from the 2006 cohort of medical graduates, those in general practice reported the lowest morale of all cohort doctors, with higher than expected workload being identified as a key problem. 7 In addition, the shifting demographic profile of GPs is likely to contribute to full-time equivalent (FTE) shortages. Ninety per cent of male doctors plan to work full time, compared with just 40% of female doctors. Among doctors who graduated 7 years previously, 35.1% were working in general practice; the figure for male doctors was just 25.6%, whereas for female doctors it was 42.5%. These figures thus set the scene for a potential problem in workforce capacity. A near quadrupling of unfilled GP posts was observed between 2010 and 2013 (from 2.1% to 7.9%). 8
Our research aimed to develop policies and strategies to support GPs returning to work after a career break or retaining the experienced GP workforce. We anticipated that the policies and strategies may have components relating to the clinical support of GPs and, thus, may build on the work of Drennan et al. 9,10 on the potential for physician assistants in supporting GPs, Sibbald et al. 11 in relation to the potential of diversifying the primary care workforce through the increased use of nurses in primary care and Avery and Pringle12 regarding the potential for the increased use of pharmacists in roles extending beyond medication management to include structured care for individuals with long-term conditions and in the provision of health-care advice for a range of individuals. 13 The role of the pharmacist has been identified as an area of particular interest and scrutiny in the context of GP workforce issues. 14
What policies and strategies might avert the crisis in the general practitioner workforce?
The future of NHS care15 is likely to involve new models of care, with innovations in respect of both horizontal and vertical integration, involving professional skill mix and health/social care, and in respect of new approaches to managing the service15,16 and in federations of previously independent practices. 15 As these models develop and emerge, it is vital that the GP workforce is sustained now; without strong general practice input, the ability to develop and implement these new models of care will be threatened. Our research therefore targets the critically important area of developing policy and strategy interventions that target the retention of experienced GPs in direct patient care, especially those GPs considering or likely to take early retirement and those GPs who have taken a career break (most often on account of family circumstances).
A preliminary scoping search suggested that there was a pre-existing body of literature involving a range of methods and settings that needed to be formally reviewed and that appeared, on initial inspection, potentially to offer useful background information. Furthermore, a limited pilot survey of GPs, and beta-testing of a novel mathematical model for assessing the 5-year risk at the individual practice level of supply–demand imbalance, appeared successful17 but also identified missingness in data sets and limitations on data availability as issues to consider in future research, such as we describe here.
Our earlier preliminary research also involved qualitative work with a small sample of experienced GPs in which we explored decision-making around quitting direct patient care. 18 In that preliminary work, we identified some factors that appeared to be of potential importance in influencing retirement/quitting decisions, including ‘push’ factors (e.g. health concerns, impact of personal ageing, workload concerns, changing work environment) and ‘pull’ factors (e.g. career opportunities, pension issues). However, although we succeeded in identifying potential retirees, we previously encountered difficulty identifying and accessing doctors on career breaks and implemented relevant strategies to take into our present research.
Evidence explaining why this research is needed now
Immediate challenges face the NHS in respect of GP workforce capacity. Recent years have seen falling recruitment to a GP career. In addition, 54.1% of GPs aged > 50 years anticipate quitting direct patient care within 5 years. 19 Thirty-two per cent of the UK GP workforce is aged > 50 years. 19 England has an ageing GP workforce, particularly in inner-city settings, where the problems of recruitment and retention are compounded by issues relating to the sociodemographic mix of the population and the increased demands for care. Retaining the GP workforce is, therefore, urgent. If unaddressed, some authorities have previously suggested that ‘meltdown’ in NHS care may follow within the foreseeable future. 1 The situation has been described as a ‘crisis’20 and there has been a call for policies and strategies to help retain GPs. 8,21
In England, at around the time this present research was commissioned (in August 2015), some major initiatives had been announced to support primary care and GPs. 22 NHS England announced (in January 2015) a £10M joint initiative administered via Health Education England (HEE), the Royal College of General Practitioners (RCGP) and the BMA, targeting enhanced training in difficult-to-recruit areas, offering part-time working arrangements for GPs considering retirement, actively promoting GP careers, examining the potential for non-medics to support GPs and providing enhanced induction and support for GPs considering returning to patient care after a career break. 23,24 Although the RCGP’s key policy statement on ‘The 2022 GP’ anticipated important changes in the organisation and delivery of care and the training and support of GPs, and suggested that by 2022 ‘the general practice workforce will have grown to reflect need, with more doctors and nurses working in practices and community-based settings, more GPs entering and remaining in the profession, and better support for GPs wishing to return to practice’, the challenges of attaining that vision were also recognised with a developing body of evidence and concern in respect of difficulties encountered in recruitment and increasing loss of GPs from direct patient care. 25 The Care Quality Commission (CQC) had also recently developed relevant policy and practice taking account of workforce considerations. 26 Despite these initiatives, little firm evidence existed at the time at which this research was commissioned to inform the development of policies and strategies targeting the recruitment and retention of the GP workforce. 27–34
Against this changing policy and practice background, there was also an evident need for detailed information at a practice level to facilitate and support the planning of services; use of GP workforce information has historically been at regional and national levels to understand current and future capacity. It appeared clear that greater granularity was urgently required to identify practices at imminent and foreseeable risk – the research specifically addresses this area of need for the NHS.
Elsewhere, the American Academy of Family Physicians (AAFP) and the US Institute of Medicine have recognised increasing pressures on, and opportunities for, the primary care workforce on account of changing demographics, and in fiscal and domestic health policy, and have suggested that there is a need for new models of integration in primary care. 35,36 In its study, the AAFP suggested that a predicted deficit of 44,000 US family doctors by 2025 may be an underestimate of the anticipated reality, with concerns being expressed regarding the recruitment and retention of family doctors. 35 Similar pressures, with an associated need for GP workforce planning, have also been recognised in Canada, Australia and New Zealand. 37–39
Targeting the recruitment and retention of the GP workforce is thus timely and urgent. Although provision of a primary care workforce benefits from skill mix (e.g. the use of nurses, pharmacists and physician assistants), unless the GP workforce issue is addressed urgently, an imminent crisis looms in respect of both leadership in primary care and inequalities in provision of care, especially for patients with complex multimorbidity. Failure to address these challenges runs the risk of failure in NHS care provision. Given the 10-year (minimum) trajectory for training a new medical student to become a qualified GP, and the falling recruitment to general practice, the research we report here will remain relevant and important to the needs of the NHS for at least the next 20 years.
Aims and objectives
Our research addressed two research questions. First, what are the key policies and strategies that might (1) facilitate the retention of experienced GPs in direct patient care and (2) support the return of GPs to direct patient care following a career break? Second, how feasible is the implementation of these policies and strategies? To address these questions, we outlined four aims, each of which is described below, along with its associated objectives.
Aim 1
To develop a conceptual framework and comprehensive assessment of factors associated with GPs’ decisions to (1) quit direct patient care, (2) take career breaks from general practice and (3) return to general practice after a career break. There are two objectives:
-
to conduct a systematic review of existing literature to describe factors affecting these decisions in the UK and other high-income countries
-
to conduct a census survey of GPs in south-west England to provide a sampling frame to provide qualitative evidence from GPs intending to quit direct patient care and those who are currently taking or who are considering taking a career break with a view to identifying factors affecting quitting intentions, and to identify potentially modifiable factors relevant to these groups of GPs.
Aim 2
To identify the potential content and assess the evidence supporting key potential components of policies and strategies aimed at retaining experienced GPs and/or supporting the return of GPs to direct patient care following a career break. There are two objectives:
-
to outline the content of policies and strategies that will support the retention of these groups of GPs in direct patient care
-
to prioritise, using an expert panel and validated methodology [RAND/UCLA Appropriateness Method (RAM)], the proposed policies and strategies in respect of their feasibility and effectiveness.
Aim 3
To identify practices that may face supply–demand workforce imbalances at the macro (regional) and micro (general practice/GP) level within the next 5 years, with a view to strategically targeting relevant policies and strategies. There are two objectives:
-
drawing on a range of data, including the previously mentioned survey, to specify, develop and test the approach necessary to identify supply–demand imbalance at the level of individual practices
-
to use the approach developed in aim 3, objective 1, to identify general practices in south-west England (an area with broad representation of practice settings) at risk of workforce shortages owing to early retirement from direct patient care among experienced GPs and owing to GPs planning, or currently taking, a career break.
Aim 4
To assess the acceptability and feasibility of implementing the policies and strategies. The objective is:
-
to gather feedback from key stakeholders on the acceptability and likelihood of implementing the policies and strategies at a local level.
Research plan and methods
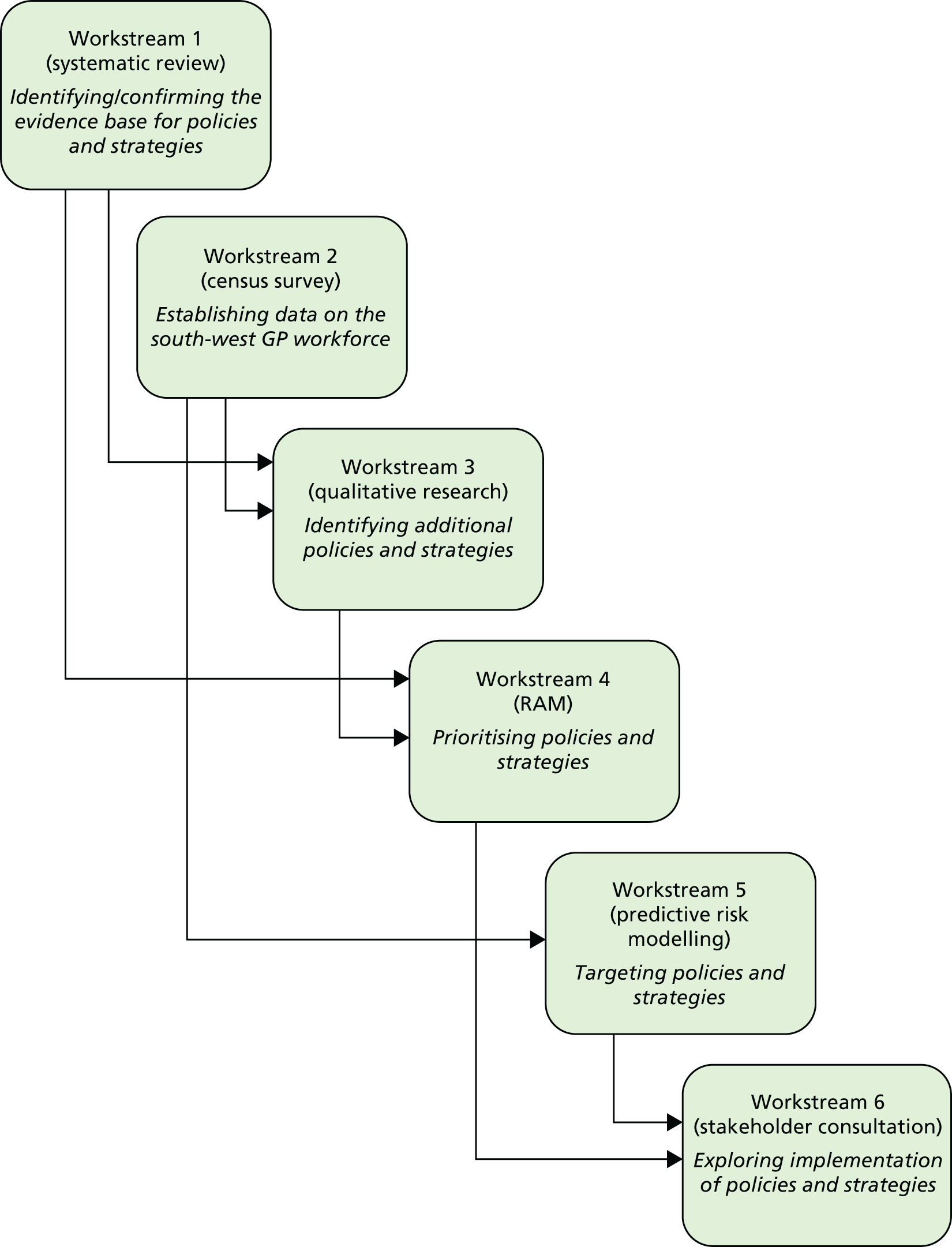
We conducted a mixed-methods project, consisting of six inter-related workstreams (Figure 1) to address our study aims and objectives. Patient and public involvement (PPI) was woven throughout the programme of work, including input to the development of the funding application, obtaining ethics approval, project management and contributions to individual workstreams (reported in full in Appendix 1). Each workstream is described in detail within the chapters following this section, with a list of abstracts for each piece of work available in Appendix 2.
FIGURE 1.
The ReGROUP project workstreams. ReGROUP, retaining experienced GPs and those taking a career break in direct patient care.
Chapter 2 Workstream 1: systematic review
Introduction
Current problems in the general practitioner workforce
There is said to be a ‘crisis’ in general practice in the UK on account of GPs leaving direct patient care or reducing their hours, and many others intending to do so. 40 A survey of UK GPs by the Commonwealth Fund in 2015 found that, at that time, nearly 30% of GPs planned to leave general practice within 5 years. 41 As well as those planning to retire, this included a substantial minority intending to switch medical specialty and others aiming to completely change career. Table 1 summarises the proportion of UK GPs who were aiming to leave general practice or direct patient care within the next 5 years from various studies.
| Study (year of publication) | Year surveyed | Percentage aiming to quit | Specific quitting question asked | Country (region) |
|---|---|---|---|---|
| Sibbald et al. (2004)11 | 1998 | 14.0 | Likelihood of leaving direct patient care within 5 years, on a 5-point scale (1 = none, 5 = high); score of 4 or 5 classified as intending to quit | England |
| Sibbald et al. (2004)11 | 2001 | 22.0 | England | |
| Simoens et al. (2002)42 | 2001 | 19.9 | Leave general practice within 5 years | England and Scotland |
| Gibson et al. (2015)43 | 2015 | 35.3 | A ‘considerable likelihood’ that GPs would quit patient care in next 5 years | UK |
| Davis et al. (Health Foundation/Commonwealth Fund; 2016)41 | 2015 | 29.0 | Wish to leave general practice within the next 5 years (an additional 17% were not sure) | UK |
| Campbell et al. (2015)17 | 2014/15 | 35.0 | At high risk of quitting direct patient care within 5 years | England (south-west) |
| Dale et al. (2015)44 | 2014/15 | 41.9 | Saying ‘no’ to intention to remain in general practice beyond the next 5 years | England (West Midlands) |
In the three earlier surveys, conducted in England and Scotland between 1998 and 2001, between 14% and 22% of GPs said that they were likely to leave direct patient care within 5 years. By 2014 and 2015, the proportion of GPs in the UK saying that they would leave general practice in the next 5 years varied from 29% to 42% in different regions of England, with proportions of 29% and 35.3% in two surveys that randomly sampled from all UK GPs.
General practitioners appear to be more stressed and more dissatisfied than ever before, and more so than GPs and primary care physicians (PCPs) in all other countries surveyed. 41,43 This is happening at a time of increasing demand for primary care services, owing to demographic changes, such as the ageing population, and to more health care shifting away from hospital settings and disease specialists. There is, therefore, an urgent need to understand what factors are driving GPs to leave patient care, and which GPs may be targeted by interventions that aim to improve the retention of GPs in patient care.
Justification and review question
Although there have been recent systematic reviews of the effectiveness of strategies to retain primary care doctors in the workforce, or of strategies to reduce specific determinants of quitting (such as ‘burnout’), this is the first comprehensive systematic review to identify and describe the factors that underlie GPs’ decisions and intentions about quitting, taking career breaks or reducing their work hours. Our review question was ‘what are the factors which affect GPs’ decisions to quit direct patient care (including reducing their time commitment to it), take career breaks from general practice or return to general practice after a career break?’.
The review protocol was registered on the PROSPERO prospective register as PROSPERO CRD42016033876.
Review methods
Searches
We sought published articles and ‘grey’ literature published in English from 1990 onwards. The first search identified published, unpublished and grey literature studies and was run in a variety of relevant databases. The second search drew on supplementary search methods (e.g. forward and backward citation chasing, web searches of relevant organisations) to locate unpublished studies and grey literature. The grey literature searches are fully described in Appendix 3.
The following databases were searched in January 2016 with update searches in April 2016: MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, PsycINFO, Healthcare Management Information Consortium (HMIC), The Cochrane Library, Applied Social Sciences Index of Abstracts (ASSIA) and Web of Science.
Inclusion criteria and processes
Condition or domain being studied
This was leaving or returning to direct patient primary care for any reason (e.g. through early retirement or taking a career break). Early retirement is defined as retirement before the statutory age of retirement for medical professionals in a given country.
Participants/population
The participants were GPs and other primary-care-based generalist doctors practising in high-income Organisation for Economic Co-operation and Development (OECD) countries (see Appendix 4), regardless of age or number of years since qualification.
Types of study included
Any empirical research studies (qualitative, quantitative or mixed methods) that either aimed to assess factors that are associated with GP retention/return to patient care decision-making or are likely to have generated research data about such factors were included. We therefore excluded opinion or discussion papers and highly summarised sources (such as conference abstracts).
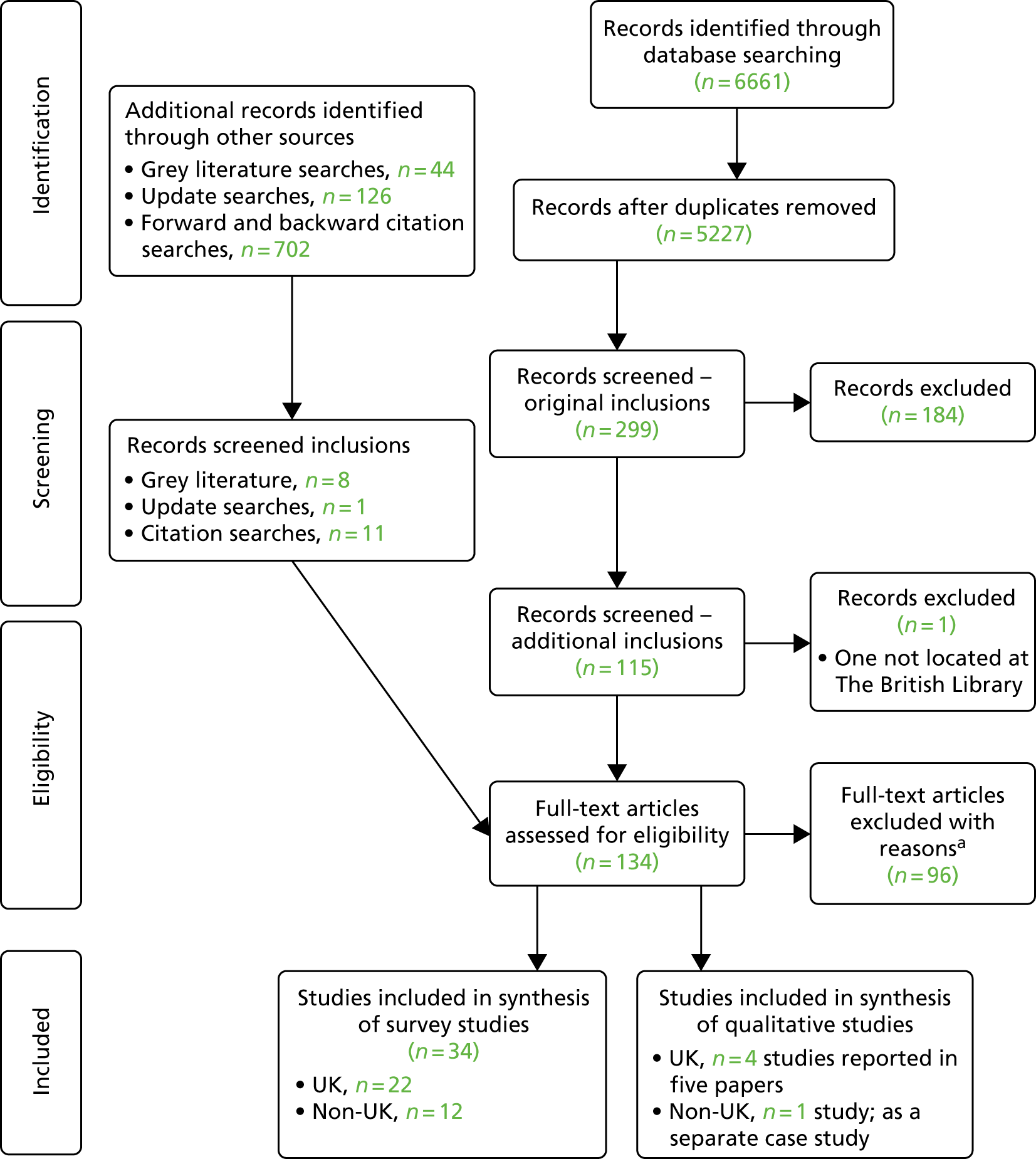
Process of identification and selection of studies
The titles and abstracts of search results were screened against these criteria (an initial sample was independently screened by two reviewers to establish consistency in exclusion decisions). Titles and abstracts that could not be excluded were sought as full-text articles, and the inclusion criteria were applied to these. The process and resulting search hits are shown in Figure 2.
FIGURE 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram showing the process of study selection. a, See Appendix 5 for a list of full-text exclusions with reasons.
Data extraction and quality assessment
Data extraction
Data to capture study aims, setting, methods and findings data were entered in a Microsoft Excel® spreadsheet (Microsoft Corporation, Redmond, WA, USA) (see Protocol47). If included studies involved evaluation of or information about a specific strategy or policy affecting early retirement or career break flexibility, any available information about the components and implementation of the strategy was captured (including, if necessary, through contacting study authors).
Main variables or issues of interest in studies
These were factors, either positive (enablers) or negative (barriers), that affect the retention of GPs in primary care or their return to work following a career break. The review aimed to gather evidence on GPs’ actual quitting (behaviour) or intention to quit (attitudes) direct patient care, and any factors associated with these behaviours and attitudes. We also focused on how these factors relate to the individual characteristics of GPs, or to practice and country- or system-level characteristics (e.g. pension options, service changes).
Study quality assessment
For studies reporting surveys of GP attitudes and experiences, we adapted the Center for Evidence-Based Management (CEBM)’s quality-assessment tool for critically appraising survey studies. 48 The tool includes questions covering both the conduct and the reporting of studies. Our adaptations to the tool comprised the inclusion of a supplementary question (to the original selection bias question item) on the adequacy of the sample size, reframing three questions about representativeness of the sample and applicability of the findings to all GPs or PCPs in the source region or country of the study, and an additional generalisability question to assess whether or not the survey’s findings can be confidently applied to all GPs in the current UK NHS (see Appendix 7). For assessing the quality of qualitative research studies, we used an adapted version of the Wallace checklist (see Appendix 8). 49
Strategy for data synthesis
Methods for synthesis of quantitative survey studies
A narrative description, grouped by included studies assessing similar types of quitting and similar study design, was undertaken, supported by summary tables. Fuller and separate consideration was given to studies from the UK, both because they comprised the majority of included studies and because of the wide diversity and lower generalisability of the studies in non-UK countries (see Report Supplementary Material 1). The classification of the different types of quitting behaviour, plus whether it was intended or actual quitting, was developed from the types of such outcomes that were reported in included papers/reports. Similarly, the different broad types of factors (determinants or correlates) of quitting were based on an initial appraisal and grouping of the detailed factors that were analysed and reported in included studies.
Methods for synthesis of qualitative studies and evidence
Synthesis of qualitative study data broadly followed the principles of thematic synthesis of textual data and was conducted in three stages, which overlapped to some degree: the coding of text ‘line by line’, the organisation of these ‘free codes’ into related areas to construct data-driven ‘descriptive themes’ and the development of theory-driven ‘analytical’ themes through the application of a higher-level theoretical framework. 50 The textual data were both study authors’ descriptions and primary quotations from GPs.
Two key data-rich UK papers were coded by one reviewer (LL), and the descriptive themes were used to create an overall analytical framework consisting of five main themes. 17,51 The same two key papers were independently coded by a second reviewer (Dr Darren Moore) and the analytical framework was agreed through discussion. This framework was used to code the remaining four semistructured interview papers/reports (three of UK GPs and one of Australian GPs) by one reviewer, with modification or additional themes when necessary. Data, in the form of quotations from the GPs themselves, key concepts or succinct summaries of findings, were entered into QSR’s NVivo software (version 11) (QSR International, Warrington, UK) for qualitative data analysis.
The identified themes, specific factors and the links between them were also represented in a pictorial ‘explanatory model’, presented in the form of a flow diagram (see Figure 5). This model was also independently checked by a second qualitative reviewer (DM) and any suggested modifications were incorporated.
Results
Overview
Table 2 shows the key characteristics of the 22 survey studies of UK GPs published since 1990. Most of the studies were cross-sectional surveys and surveyed the actual quitting or quitting intentions of GPs in a particular year or month. The earliest survey gathered data from UK GPs in 1991–4,64 whereas five of the most recent surveys were conducted in 2014–15. 17,41,43,44,55 The sample sizes of the surveys of UK GPs ranged from 40 to 4421.
| Study (year of publication) | Year of survey(s) | Country or region | Types of GPs surveyed | Number of respondents (response rate, %) | Age of GPs (years), mean (SD if reported) | Percentage female |
|---|---|---|---|---|---|---|
| Baker et al. (1995)52 | NR | England (Trent) | Vocationally trained GPs not currently practising as GP principals | 166 (47.3) | Men: 37 | 60 |
| Women: 34.5 | ||||||
| Baker (2000)53 | 1998 | UK | GP principals and non-principals | 3969 (66.5) |
|
49.20 |
| Campbell et al. (2015)17 | 2014–15 | England (south-west) | All GPs | 529 (56.0) | NR | 66.5 |
| Chambers et al. (2004)54 | NR | Scotland | Unrestricted principals, aged > 55 years | 348 (72) | NR (all > 55 years) | NR |
| Dale et al. (2015)44 | 2014–15 | England (West Midlands) | All GPs | 1192 (NR) | NR | 44.30 |
| Doran et al. (2015)55 | 2014 | England | Early leavers aged < 50 years | 143 (35.0) | Median 40–44 | 50.3 |
| Evans et al. (2002)56 | 1994, 1995, 1998 and 1999 | UK | All GPs: 24, 11, 7 and 6 years since qualification | NR | NR | 38.5 (1974 graduates) |
| 51.2 (1983 graduates) | ||||||
| 55.5 (1988 graduates) | ||||||
| 67.6 (1993 graduates) | ||||||
| Total: 53 | ||||||
| French et al. (2005)57 | 2002 | Scotland | GP principals | 390 (55.0) | 39 (9) | 75 |
| French et al. (2006)58 | 2002 | Scotland | All GPs | 924 (50.0) | Male: 45 | 39 |
| Female: 42 | ||||||
| Gibson et al. (2015)43 | 2015 | UK | All GPs |
1172 (cross-sectional, 34.27) 1576 (longitudinal, 63.75) |
|
Cross-sectional sample: 50.35 |
| Hann et al. (2011)59 | 2001–6 | England | GPs aged < 50 years | 1174 (67) | NR | NR |
| Hutchins (2005)60 | 2002 | England (London) | All GPs in sampled general practices | 62 (84) | 53% between 40 and 49 years | 35 |
| Luce et al. (2002)61 | 2000 | England (northern) | GPs aged > 45 years | 518 (72.5) | 51.8 | 21 |
| Davis et al. (2016)41 | 2015 | UK | All GPs | 1001 (39.4) | NR | NR |
| McKinstry et al. (2006)46 | 2004 | Scotland | GP principals and non-principals | 2541 (67.2) and 749 (65.2) | NR | NR |
| Scott et al. (2006)45 | 2001 | England and Scotland | GP principals, salaried GPs and GP locums (GP principals, non-principals and PMS: GPs in Scotland) | 1968 (44.0) |
|
32 |
| Sibbald et al. (2003)62 | 1998 and 2001 | England | GP principals | 790 from 1998 and 1159 from 2001 (67) | In 1998: 43.75 | 31.3 in 1998 |
| In 2001: 44.35 | 29.4 in 2001 | |||||
| Simoens et al. (2002)42 | 2001 | Scotland | GP principals and non-principals | 802 (56.0) | GP principals: 45 | GP principals: 38 |
| Non-principals: 30 | Non-principals: 57 | |||||
| PMS GPs: 43 | PMS GPs: 60 | |||||
| Simoens et al. (2002)63 | 2001 | England and Scotland | GP principals and non-principals | 4421 (45.0) | English: 44 | 32 in England |
| Scottish: 43 | 37 in Scotland | |||||
| Taylor et al. (1999)64 | 1991–4 | UK | New-entrant GPs ≤ 35 years old (including the 252 who left within 2 years) | 1933 including 252 leavers (NA) | 30.4 (2.04) | 42.6 |
| Taylor et al. (2008)65 | 2004 | UK | All doctors who qualified in 1977 (GP results reported separately) | 864 (72.0) | 51 | 36.50 |
| Young et al. (2001)66 | 1998 | UK | GPs who were on GP census in 1996 but not 1997 | 613 (57.3) |
|
35.40 |
| Survey studies of non-UK GPs | ||||||
| Brett et al. (2009)27 | 2007–8 | Australia (Western Australia) | Aged 45–65 years | 178 | 52.4 (SD 5.2); median 51 (range 48–56) | 27 |
| Dewa et al. (2014)67 | 2007–8 | Canada | All | 32,026 | Mean: approximately 48.4
|
NR |
| McComb (2008)68 | 2006 | New Zealand | All | 566 |
|
38.3 |
| Norman and Hall (2014)69 | 2010/11 | Australia | All | 3377/2720 | 49.54 (11.31) | 49 |
| Nugent et al. (2003)70 | 1999 | Ireland | GP trainees who have left GP work | 209/36 | Women: 34 | 61 |
| Men: 35 | ||||||
| O’Kelly et al. (2008)71 | 2007 | Ireland | GP graduates 1997–2003 | 245 | NR | 70 |
| Pit and Hansen (2014)72 | 2011 | Australia (NSW) | All | 92 | 51 | 40 |
| RNZCGP (2014)39 | 2015 | New Zealand | All | 2486 | Mean: 50 (men, 53; women, 47) | 53 |
| Shrestha and (2011)73 | 2008 | Australia | All | 3906 | 49.5 | 45.6 |
| Sumanen et al. (2012)74 | 2008 | Finland | GPs and GP trainees | 559 | NR | 68 |
| Van Greuningen et al. (2012)34 | 2002 and 2007 | The Netherlands | Already retired | 405 | Mean retirement age: women, 54; men, 58 | 40 |
| Woodward et al. (2001)75 | 1993 and 1999 | Canada | All | 293 | NR | 57.3 |
The bottom third of Table 2 shows the key characteristics of the 12 survey studies of non-UK GPs, all but two of which report surveys conducted since 2006. The results and synthesis of these 12 non-UK studies are not reported further in this chapter (see Report Supplementary Material 1).
Geographical coverage of the surveys
Of the 22 surveys of UK GPs, seven surveyed GPs from the whole of the UK,41,43,53,56,64–66 two surveyed GPs from England and Scotland combined,45,63 two surveyed GPs from the whole of England,59,62 five surveyed GPs in a particular region or city of England17,44,52,61,76 and five surveyed GPs in Scotland. 42,46,54,57,58
Characteristics of general practitioners surveyed
Most of the surveys of UK GPs were of all practising GPs in the country or a region, regardless of age, year of qualification or contract type/mode of employment (Table 2). However, some surveyed only GP principals (i.e. practice partners)54,58,62 or recruited only GP principals and non-principals (not locums). 42,46,63 Only four studies surveyed GPs who had already quit patient care. 52,59,64,66
Most UK studies reported a mean age (or median age band) of between 40 and 55 years. However, one study had much younger respondents, because it set out to survey recently qualified GPs. 64 Two surveys specifically targeted older GPs: Chambers et al. 54 surveyed only unrestricted principals aged > 55 years (mean age not reported), whereas Luce et al. 61 surveyed GPs aged ≥ 45 years (mean age 52 years). Across the UK studies, female GPs accounted for between 29% and 75% of the GPs surveyed and tended to account for a higher proportion of GPs in the later surveys.
Overview of the UK questionnaire surveys
Coverage of different types of quitting direct patient care
Table 3 summarises the broad quitting construct investigated, together with the personal, job and other GP or practice characteristics assessed as potential factors associated with quitting. Appendix 9 shows the specific quitting constructs (and verbatim questions) in each study and the potential determinants of quitting for which data were collected.
| Study (year of publication) | Quitting construct investigated | Personal | Job characteristics | Household | Area | Policy/organisational changes | Other | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Actual quitting/retention | Intention to quit within 5 years | Planned age of retirement | PT/flexible working | Taking career break | Other | Age | Gender | Ethnicity | Contract type/partner/locum, etc. | Practice/list size | Working hours PT/FT | Job satisfaction | Job stressors | On call/out of hours | Income | Marital/family status | Social deprivation | Region/country | Urban/rural | |||
| Hann et al. (2011)59 | ✓ | ✓a | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||
| Taylor et al. (1999)64 | ✓ | b | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||
| Young et al. (2001)66 | ✓ | ✓ | ✓ | |||||||||||||||||||
| Doran et al. (2015)55 | ✓ | ✓c | ||||||||||||||||||||
| ✓d | ||||||||||||||||||||||
| Martin et al. (2015)41 (Health Foundation) | ✓e | ✓ | ||||||||||||||||||||
| Dale et al. (2015)44 | ✓f | ✓f | ✓f | ✓g | ||||||||||||||||||
| Gibson et al. (2015)43 | ✓ | ✓ | ✓ | |||||||||||||||||||
| Scott et al. (2006)45 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓h | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||
| Simoens et al. (2002)63 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Sibbald et al. (2003)62 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||
| Simoens et al. (2002)42 | ✓i | ✓i | ✓ | ✓ | ✓ | ✓ | ✓j | ✓ | ✓ | ✓ | ✓ | |||||||||||
| Campbell et al. (2015)17 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓k | ||||||||||||
| Baker et al. (2000)77 | ✓l | ✓l | ✓m | ✓ | ✓ | ✓ | ||||||||||||||||
| Evans et al. (2002)56 | ✓ | ✓ | ✓ | Free-text reasons for reduced time commitment to being a GP | ||||||||||||||||||
| Chambers et al. (2004)54 | ✓ | ✓n | ||||||||||||||||||||
| French et al. (2005)57 | ✓ | ✓o | ✓p | |||||||||||||||||||
| McKinstry et al. (2006)46 | ✓ | ✓ | ✓ | ✓q | ||||||||||||||||||
| French et al. (2006)58 | ✓ | ✓ | ✓ | |||||||||||||||||||
| Luce et al. (2002)61 | ✓r | ✓ | ✓ | ✓ | ✓ | ✓s | ||||||||||||||||
| Taylor et al. (2008)65 | ✓ | ✓ | ||||||||||||||||||||
| Hutchins 200560 | ✓t | ✓u | ||||||||||||||||||||
| Baker et al. (1995)52 | ✓ | ✓ | ✓ | ✓v | ||||||||||||||||||
Among these studies, 13 explicitly focused on retirement/quitting intentions (either within a certain number of years or at the intended retirement age) and four included GPs who had already retired or quit general practice. A longitudinal cohort study by Hann et al. 59 was the only study that included both actual quitting status and previous intention-to-quit data for the same group of GPs. Nine surveys investigated factors associated with intentions to reduce hours or take up part-time working, and four surveys included a focus on taking career breaks.
The quality of included survey studies of UK general practitioners
Table 30, in Appendix 7, shows how each of the studies was assessed against each of the items in our adapted CEBM critical appraisal tool. Most of the studies were of good quality in relation to key question items, such as the appropriateness of the research survey methods for answering the stated question. However, many had limitations in relation to the pre-study determination of the sample size and the assessment of the statistical significance of relevant associations [and presentation of confidence intervals (CIs) when relevant]. Most analyses were restricted to presenting the associations between two or three variables, typically in a contingency table, and were, therefore, deemed not to have accounted for all possible confounding variables.
In terms of reporting quality, a substantial minority of studies did not clearly report how the sample was obtained (and, therefore, are at risk of potential selection bias) or whether or not the sample obtained was representative of all GPs in that region or country. In relation to this, response rates were generally poor, with only five studies having a satisfactory response rate (of > 70%), five having unsatisfactory response rates (< 50%) and two studies not reporting the response rate.
Study generalisability was assessed in two stages (items): first, in terms of whether or not the results could be confidently applied to the GPs in the source region or country, in the year the survey was conducted; and, second, whether or not the results could be confidently applied to all GPs in the UK NHS in 2016 (which is the policy context of this systematic review).
Synthesis of findings: questionnaire survey studies
The 22 UK survey studies that focused on GPs’ intentions to quit fully from general practice (e.g. early retirement), their reasons for actually quitting general practice/patient care or intending to reduce hours/working part-time all revealed a recurrent and linked set of key job-related factors that are associated with leaving, intending to leave or reducing their hours devoted to patient care. They are workload, job (dis)satisfaction, work-related stress and work–life balance. These high-level factors associated with quitting are all inherently related to the nature of being a GP and working in NHS general practice, although they may also be related to lifestyle/personal expectations and family circumstances.
Although most of the included studies examined the bivariate associations of intention to quit or planned retirement age with some other factors (notably age, gender or contract status), four studies evaluated intention-to-quit decisions using multivariable analyses and incorporating a larger range of potential explanatory variables. These studies showed that the consistent determinants of GPs wishing to retire earlier were older age, having low job satisfaction (or job dissatisfaction) and high or intense workload. When measures of work–life balance or flexibility/choice in relation to job demands were included in the analysis, these were also often statistically significant. There seems to be a complex interplay between these three key broad factors – satisfaction, workload and work–life balance/flexibility – with the third factor possibly mediating the effects of workload on job satisfaction. Although gender was not found to be an important determinant after adjusting for age and other factors, this does not preclude that the balance of these other main determinants might be different for men and women. Social deprivation of area or practice population was not associated with intention to quit in any of the three multivariable analyses that included it as a potential factor. The finding (in one study) that either small practices or larger than average practices are associated with a more common intention to quit is intriguing and worth exploring with GP stakeholders to understand why this might be.
The UK studies that reported the stated reasons of GPs for intending to quit patient care or retire early also underlined the importance of the main factors already revealed to be associated with assessed variations in intention to quit, namely job satisfaction, workload, work-related stress and work–life balance. However, the studies of the self-reported reasons for quitting general practice reveal much more detail within and beyond these reasons; for example, underlying problems of high workload appear to be issues relating to high clinical work hours, more demanding patients and perceptions of excessive paperwork/administration. In addition, job dissatisfaction (and perhaps also work-related stress) is now reported alongside undesirable changes in the NHS, excessive managerial duties and fear of making mistakes.
These observations highlight the danger of interpreting survey findings in terms of just the most frequently cited reasons or the statistically significant associations. These studies clearly show that there are many other, more specific, reasons operating at levels other than the top-level work-related factors. These more specific and diverse reasons may be important to a substantial minority of GPs in their decisions to quit patient care or to go part-time. The survey evidence considered here suggests that there will be many GPs who have good job satisfaction and low levels of work-related stress but who nevertheless still want to quit direct patient care or retire early for one or several of the many other reasons reported. These are ultimately individual (or at least family/couple) decisions, and focusing exclusively on ‘averages’ or overemphasising the most frequently cited reasons may overlook other reasons (e.g. mental health problems or fear of litigation) that may be amenable to intervention.
As expected, age was an important determinant of intending to quit or reduce direct patient care, with the most dominant association being that older GPs of both genders were more likely to quit fully or retire early. However, gender was more likely to be a factor determining preferences related to working reduced hours and taking a career break. Although surprisingly few studies examined associations of quitting with both age and gender together, there are clues in many of the studies that there are substantial differences in the main determinants of quitting or part-time working for, for example, younger female GPs and older male GPs. Although age is clearly an important direct determinant of intentions to quit, it is also a proxy for various other potentially important factors, such as position/contract type within a practice, and there may also be cohort effects associated with differences in expectations and administrative burdens when becoming a GP, and altered patient and other demands over time. In relation to preferences for part-time working, studies showed relatively high proportions of UK GPs of all ages, both male and female, and with most contract or employment types, saying that they wish to reduce their work hours or weekly number of clinical sessions. There was some evidence that female GPs, ‘non-principals’ and ‘assistants’ were more likely to want to increase their work hours in coming years, but this may merely reflect the current lower number of working hours of these subgroups. Finally, one study highlighted the potential trade-off between part-time working and intended later retirement. Overall, although no clear picture emerges of what the main determinants of preferences to work part-time are, there are clear indicators that the motivations may be based on the age, gender and the contractual status/practice role of GPs.
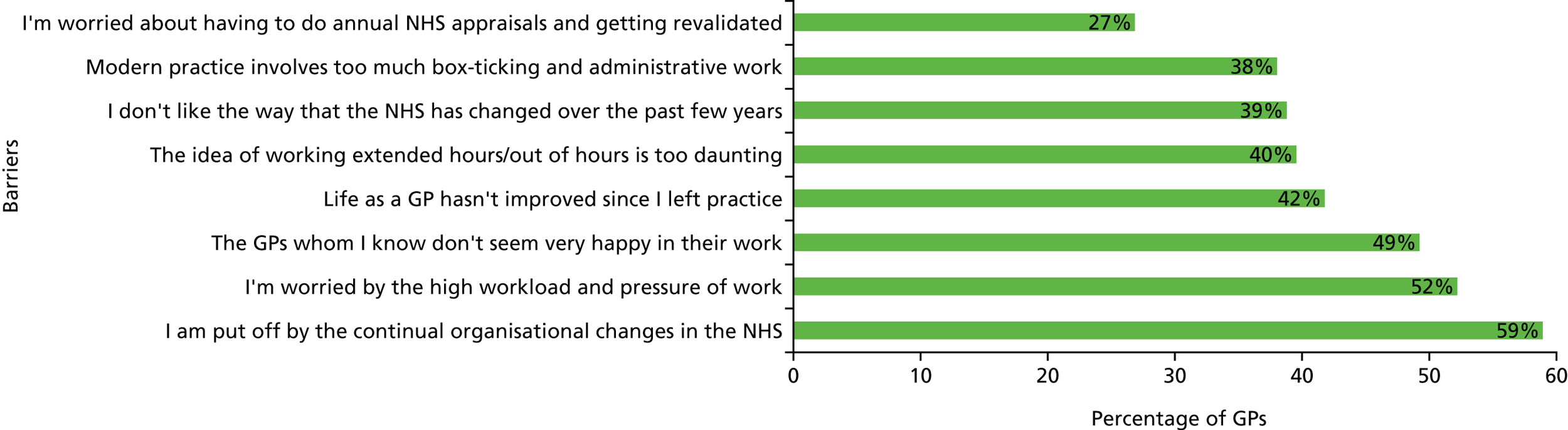
Unlike the other ways in which GPs may quit practice, intentions to take a (temporary) ‘career break’ appear to be influenced more by a specific range of ‘pull’ factors than by negative ‘push’ factors to do with the job or workload. The main reasons GPs say they will be taking a career break are to work abroad, to have or look after children, or to engage in research or further study. Although the stated reasons for intending to take a career break seem fairly different from those relating to intending to permanently quit patient care (e.g. reasons for early retirement) or intentions to reduce working hours, many of the barriers that they say would prevent them from returning to work as a GP relate to negative perceptions about the changing job of being a GP, high workload, low job satisfaction, unsociable hours, excessive administrative work, and recurrent and unwanted changes in the way the NHS and primary care is organised, which now includes revalidation (Figure 3).
FIGURE 3.
Common barriers to returning to work as a GP percentage citing each barrier in England (2014). Data from Doran et al. 55 (From the 134 GP leavers who gave reasons relating to changes in GP work, loss of skills and concerns about life as a GP.)
Finally, the UK studies of the more detailed self-reported reasons for intending to quit or actual quitting also showed that intentions to quit general practice are not exclusively about the main job-related ‘push’ factors (workload, work-related stress, job satisfaction and work–life balance). For example, in a 2002 study, among the factors cited more than one-third of older GP principals as having a ‘great influence’ on the early retirement intentions of these GPs were the ‘pursuit of other interests’ and the ‘financial ability to retire’. 61
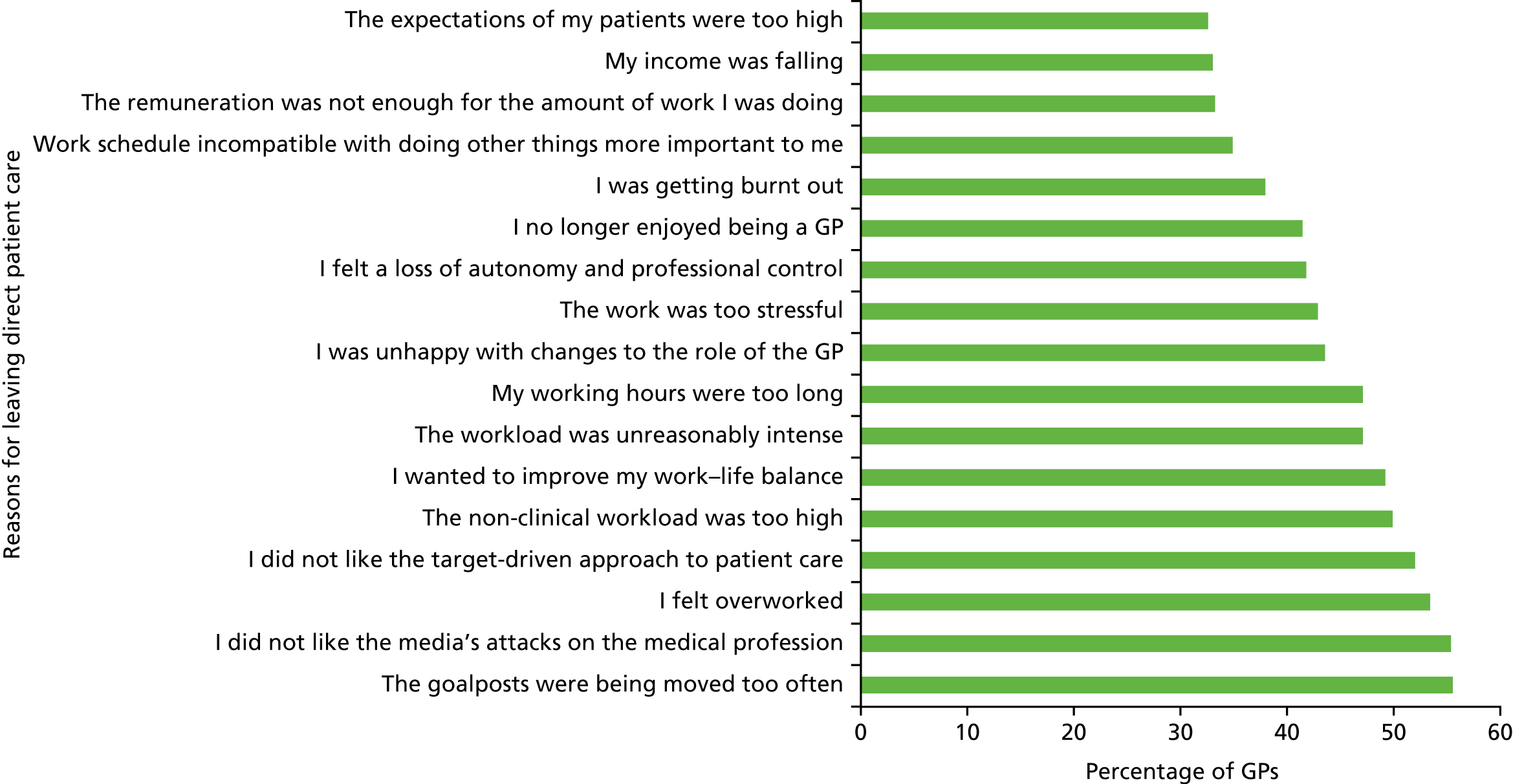
General practitioners’ stated reasons for having actually left general practice show a larger range and mix of both job-related ‘push’ factors and some family- and leisure-related ‘pull’ factors than shown by the survey studies examining associations between variables. The most common specific reasons given by GP leavers in a 2014 study by Doran et al. 55 are shown in Figure 4.
FIGURE 4.
General practitioner leavers’ most common specific reasons for leaving direct patient care (those cited by over one-third of GP leavers) (2014). Data from Doran et al. 55
Synthesis of qualitative studies
Overview of the qualitative research studies and data
Five papers based on qualitative semistructured interviews with practising or retired British GPs were retrieved; all studies had been conducted in England. A further qualitative semistructured interview study, with practising GPs who were working part-time in clinical practice in Australia, was found but is not reported in this chapter (see www.journalslibrary.nihr.ac.uk/programmes/hsdr/1419602/#/). The main characteristics of these studies, and the GPs interviewed within them, are shown in Table 4.
| Study (year of publication) | Characteristic | ||||||
|---|---|---|---|---|---|---|---|
| Year of survey(s) | Country or region | Types of GPs surveyed | Aim of study | Number of GPs (interview type) | Age of GPs (years) | Percentage female | |
| Doran et al. (2016)51 | NS | England | Early leavers aged < 50 years | To explore the reasons why GPs leave general practice early | 21 (by telephone) | Median age band: 40–44 | 50.3 |
| Hutchins (2005)76 | NS | England (London) | GP principals near retirement age | Considers the reasons many GPs are wishing to take early retirement, and measures to help retain them | 20 (at surgery) | NS | 55 |
| Newton et al. (2004)78 | 2001 (implied) | England (northern) | Aged > 45 years, subgroup from Luce et al. (2002)61 | To describe ‘Plans, reasons for, and feelings about retirement’ | 21 (at surgery or GP home, except 2 by telephone) | All aged > 45 | 38 |
| aSansom et al. (2016)18 | 2015 | England (south-west) | Experienced GPs aged 50–60 years (20 still working and three retired) | To investigate the reasons behind intentions to quit direct patient care among experienced GPs aged 50–60 years | 23 (by telephone) | Age range: 51–60 | 39 |
| aCampbell et al. (2015)17 | 2014–15 | England (south-west) | Experienced GPs aged 50–60 years intending to retire in the next 5 years (n = 14) | To explore reasons behind GPs’ intentions to quit direct patient care | 17 (by telephone) | Aged 51–60 | 23.5 |
| GPs who took early retirement in the previous 5 years (n = 3) | |||||||
| 15 partners and two locums | |||||||
| Dwan et al. (2014)79 | 2008–9 | Australia | GPs working six or fewer clinical sessions per week | To explore the nature and extent of GPs’ paid and unpaid work, why some choose to work less than full-time, and whether or not sessional work reflects a lack of commitment to patients and the profession | 26 (at a location determined by GP participant) | Average age: 47 (females); 58 (males) | 66 |
Two of the papers reporting studies from England were based on almost the same set of interviews. 17,18 The 2016 study by Doran et al. 51 focused on why GPs had left medical practice, whereas the other four studies were wholly or dominantly with practising GPs. All of the semistructured interviews were quality appraised using an adapted Wallace checklist and found to be of reasonable76,80 to good17,18,51,79 quality.
The synthesis is presented as a series of linked themes, each of which belongs to one of five categories. The five main categories of explanatory theme were undoable/unmanageable (including workload and related pressures), morale, impact of organisational changes, projected future and multiple options and strategies. This analytical framework is summarised in Table 5.
| Undoable/unmanageable | Morale | Impact of organisational changes | Projected future | Multiple options and strategies |
|---|---|---|---|---|
|
|
What then follows is a heavily abridged version of the qualitative synthesis; some subthemes are mentioned very briefly and there are no illustrative quotations. The full write-up of the synthesis of qualitative studies, with direct GP quotations, is available in our separate full report of the systematic review (see Report Supplementary Material 1).
Undoable and unmanageable
Many GPs are experiencing working as a GP as undoable and unmanageable owing to, among other things, high/increasing administrative workloads, high/increasing patient demand (both number of patients and their complexity and higher expectations), and a perceived lack of training and resources to cope with these pressures.
Low levels of morale
Low levels of morale were attributed by GPs to reductions in the perceived value of GP work (with loss of identity), and changes in professional culture in relation to a range of aspects of work such as a more target- and standards-driven reward system, multidisciplinary team (MDT)-based working (yet, for some, paradoxically, also lone working/isolating culture), a more aggressive top-down managerial culture within the NHS, and more widespread norms and expectations for early retirement. Low levels of morale were also seen to be associated with a perceived lack of support from both government and political parties, and negative portrayals of GPs by news media. Morale was also closely linked with job satisfaction (or dissatisfaction), neglect of personal well-being/health and feelings about work–life balance.
Impact of organisational changes
The perceived key changes or factors under this theme were changes in referrals (both restricted opportunities to refer to secondary care and higher numbers of, and more complex, referrals from secondary care), a greater focus on targets and assessments, and fears about reaccreditation (including evidence that some GPs might retire early in order to avoid reaccreditation). Some of the organisational changes had imposed increased clinical and non-clinical responsibilities and work on GPs. Together, such changes were believed to have undermined some of the basic tenets and traditional expectations of being a GP, such as the doctor–patient relationship and having autonomy and control over one’s clinical work.
Projected future
The fourth theme was how GPs projected or envisaged their future, which related to ageing, the financial viability of reducing hours or retiring early, and the extent to which GPs were personally committed and financially invested in their practices. This included problems linked to whether or not younger GPs wanted to take on the responsibility of becoming practice partners, as well as possible tensions between older and younger GP partners (in the way practices are run, in major investment/refurbishment decisions or in relation to planning for partners retiring and needing new partners to buy out their share of a practice).
Multiple options and strategies
Finally, the fifth theme and group of factors referred to the various ways in which GPs of different personalities either continue and cope or – perhaps if less committed or less resilient, or if they can simply afford to financially – decide to leave or go part-time. This theme also highlighted the major importance of flexible working or working reduced hours (e.g. by becoming a locum) as a method of coping and regaining work–life balance and job satisfaction. For others, the adoption of alternative work roles outside general practice, often part-time, allowed use of and learning of other skills – either as relief and variety from working as a GP or, for some, as a potential alternative career option. The kinds of alternative roles and options GP interviewees mentioned included becoming complementary therapists, Clinical Commissioning Group (CCG) leads or advisory committee members, working for pharmaceutical consultancies or teaching in medical schools. Like part-time working, for some these might be clear routes for quitting general practice, but, for others, such variety of roles and opportunities for job satisfaction may keep them in general practice.
Explanatory model and narrative
The themes and detailed factors emerging from the qualitative synthesis of semistructured interview studies conducted in the UK were also used to construct a pictorial explanatory model (Figure 5). It provides an overview of the key contexts and factors that were found to relate to GPs quitting or intending to quit patient care. The applicability of the explanatory model was confirmed following feedback on the model during meetings with PPI representatives and co-investigators.
FIGURE 5.
Flow diagram of factors contributing to GPs leaving general practice. Admin, administrative; IT, information technology.
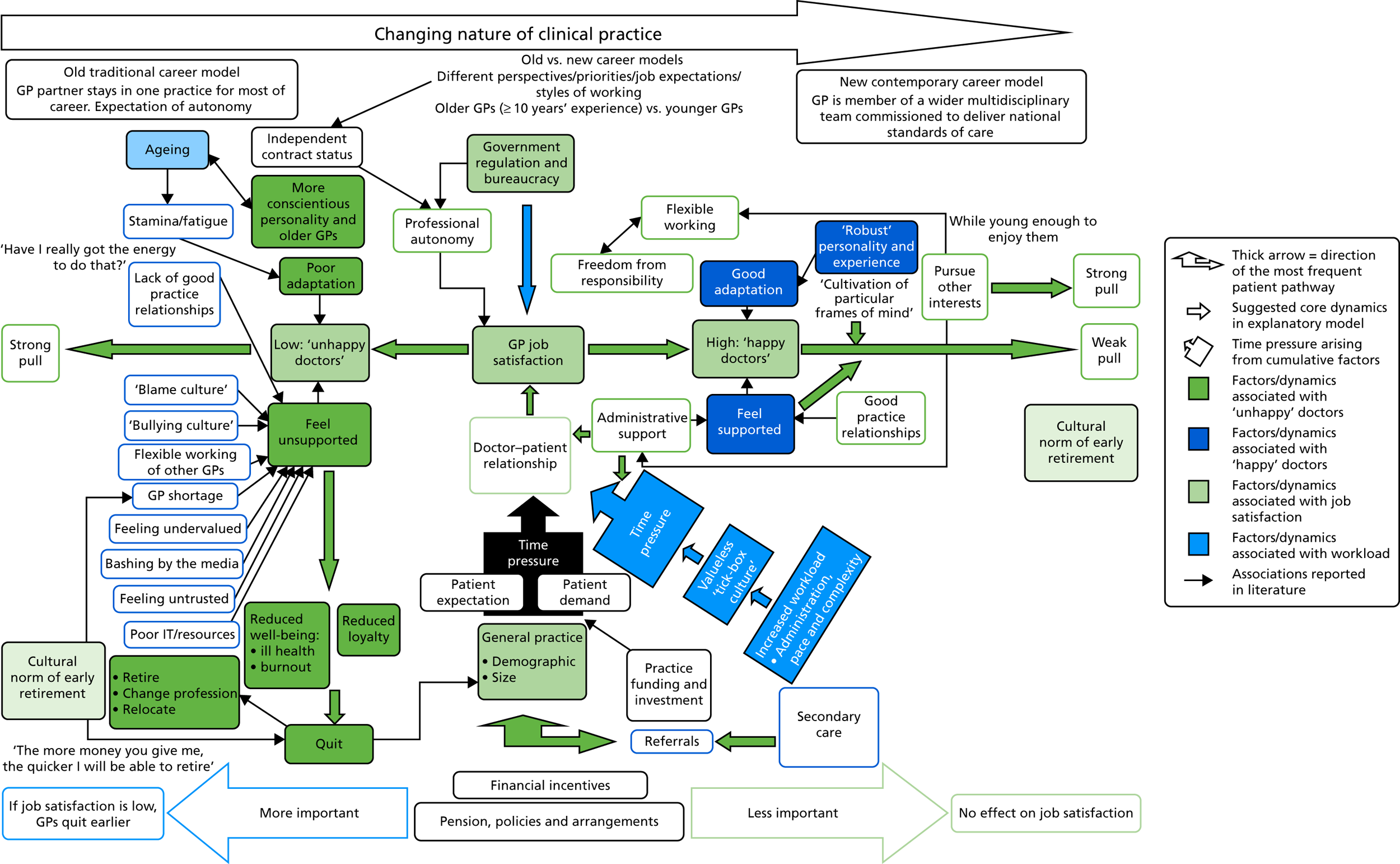
There are three main ‘domains’ in the flow diagram: (1) factors associated with low levels of job satisfaction, (2) factors associated with high levels of job satisfaction and (3) factors associated with linked to the doctor–patient relationship. In addition, the overarching historical context to these factors is that the career path, pressures and expectations of GPs in the UK have changed considerably since the 1990s. Today’s GP is expected to be a member of a wider MDT commissioned to deliver national standards of care and has a role barely recognisable to the one many older GPs remember (e.g. GP partners typically staying in one practice for most of their career, with less regulation and an expectation of autonomy).
Discussion
For many UK GPs, four closely related job-related factors seemed to play a major part in decision-making about both early retirement and part-time working: workload, job (dis)satisfaction, work-related stress and work–life balance. These factors were prominent in studies of both intention to quit or to reduce hours and actual decisions to quit or to go part-time. However, there were clearly many other detailed factors involved for some GPs that either underlie these higher-level factors (e.g. health service reform fatigue or unsupportive practice partner relationships) or may combine to influence an individual GP’s decision to quit general practice or reduce their hours devoted to it. Although many of the drivers of GP dissatisfaction, high workload and work-related stress seem to be at the level of the health system, medical profession or within a GP’s own general practice and the population it serves, how GPs cope with these problems may be amenable to interventions at the individual GP level.
Moreover, both the questionnaire survey and qualitative interview evidence indicate that it is not just ‘unhappy GPs’ (e.g. those with poor job satisfaction and high workload) who wish to reduce their hours or retire early. Early retirement is now a cultural norm and lifestyle choice for many in the medical profession, for example to spend more time pursuing their own interests or caring for loved ones. The five main themes and the subthemes that emerged from the synthesis of qualitative evidence include all four of the main recurrent factors that were evident in questionnaire surveys of GPs. For example, the broad factors of workload and work-related stress from the survey studies seem to map closely to the subthemes from qualitative research under the ‘undoable/unmanageable’ theme. However, the broad factors of work–life balance and job dissatisfaction (from the survey studies) appear alongside a wider range of other subthemes – identity/perceived value, lack of support, well-being and negative ‘bashing’ by the media – within the qualitative synthesis, under the major theme of ‘morale’. Understandably, the more open-ended data collection approach of interviews seems to capture a more diverse range of potential determinants of GP satisfaction and quitting, and how they appear to be conceptually or causally related. But the main factors emerging from the synthesis of quantitative studies reflect a narrower range of the more recurrent factors.
Although there were differences between male and female GPs in their intentions or preferences for part-time working, such differences were inconsistent between studies and did not adjust for current hours worked, so it is difficult to draw clear conclusions. However, overall, younger female GPs and older male GPs were generally more likely to want to work part-time. Only groups already working reduced hours wished to increase their hours. One of the survey studies and the qualitative evidence synthesis suggested an association between opportunities for part-time working and delaying retirement. That is, for some GPs, being able to work part-time (and more flexibly) may incentivise them to retire later. In contrast, there is no evidence that financial incentives would discourage early retirement; this would possibly have the opposite effect.
General practitioners’ intentions to take a ‘career break’ appear to be more influenced by a specific range of ‘pull’ factors than by negative ‘push’ factors to do with the job or workload. The main reasons GPs say they will be taking a career break are to work abroad, to have or look after children or to engage in research or further study. Although the stated reasons for intending to take a career break seem fairly different from those related to intending to permanently quit patient care, many of the barriers that GPs say would prevent them from returning to work as a GP relate to negative perceptions about the current job of being a GP (e.g. high workload, low job satisfaction, unsociable hours, excessive administrative work).
There were 12 survey studies of GPs outside the UK, from six countries (including four surveys from Australia) and covering areas such as early retirement, quitting general practice soon after qualification and working part-time. Despite the substantial differences in the way general practice is organised in these countries, among the leading reasons for intending to retire early in Australia, New Zealand and Canada were low job satisfaction and the pressure of work. One of the Australian studies assessed the factors that GPs said might encourage them to retire later than currently planned; more than one-third stated better remuneration, higher staffing levels, more general support, more flexible working hours, part-time work and reduced workload – similar to the reasons emerging from UK studies that asked an equivalent question. The main stated determinants of part-time working in Australia and New Zealand were age, poor work–life balance and having family or child-care responsibilities.
Strengths of the review methods
This systematic review was conducted by an experienced and collaborative review team, addressing clear review questions and using a prespecified and published systematic review protocol (CRD42016033876) and search strategy. 47 We worked closely with experienced information specialists to design the most effective possible searches for obtaining bibliographic and web sources. We found substantially more includable studies than a recent literature review that had a similar review question. 17
In terms of involving relevant stakeholders in the review, several GPs were involved in the development of the review protocol, and two GPs were closely involved in the conduct of the review (a GP trainee, and an experienced GP and Professor of Primary Care). Patients were also involved, both as co-investigators in the wider mixed-methods project and through contributing to a PPI workshop, which presented and discussed emerging findings from the qualitative and quantitative evidence syntheses. Reassuringly, the PPI workshop both endorsed and expanded our understanding of our emerging interpretations (see Appendix 10 for a fuller description of that discussion).
In terms of quality assurance, we used either two reviewers making independent inclusion/exclusion decisions or checking by a second reviewer with an independent assessment of a sample of included studies (for data extraction and quality assessment) and used established study quality assessment tools.
Limitations of the review methods
Although this review captured information about specific retention strategies, where they provided the background to a particular survey, or if the strategy was suggested on the basis of an included survey’s findings, it should be noted that identifying and evaluating GP retention strategies was not the primary aim of this systematic review and, therefore, we did not explicitly search for studies that either evaluated or described different approaches to GP retention. Although we used the most appropriate and established quality assessment tools available, the tool we adapted and used for the quantitative survey studies had a few limitations. First, there was no separate score/assessment of study design and reporting quality. Second, our judgements about the applicability of findings to GPs in the UK NHS in 2016 were based on subjectively weighing up information such as the age of the study data, the geographical scope of the study, whether or not it was limited to certain types of GP (e.g. older/younger, practice principals/non-principals) and whether or not there were differences between respondent characteristics and target GP population characteristics.
The study pragmatically focused on either survey-based (mainly quantitative) studies or qualitative interview studies. However, some of the survey studies also collected and reported some qualitative data, in the form of free-text answers to open questions (one survey study was purely a collation of such data56). We did not incorporate or separately content analyse these disparate data.
In December 2016, another qualitative research study that should have been included – unfortunately missed by our grey literature searches – came to our attention. 81 The detailed findings and four groups of ‘deeper frustrations’ identified in this study largely corroborated the insights from our synthesis of qualitative studies, including the finding that workload was the overarching factor causing GPs to leave.
Limitations of the current evidence base
Most studies examined only the association of a single quitting construct (e.g. intention to reduce work hours) with a few variables, one variable at a time. There were only four comprehensive survey studies that used multivariable analyses. The most commonly used quitting construct/question was GP intention to retire/quit direct patient care within 5 years, which was used in eight studies. But even this apparently standard question was asked in a number of slightly different ways, and questions relating to actual or preferred part-time working varied even more. Only three UK studies and no non-UK studies had any focus on why GPs take career breaks, and no studies explicitly examined the benefits and determinants of flexible working arrangements. Few studies explicitly assessed the role of GP health or ageing, or potential mediating factors, such as ‘commitment’ or ‘emotional exhaustion’ (a key component of instruments for assessing ‘burnout’), which may attenuate or accelerate the effects of job satisfaction on intentions to quit.
Most questionnaire surveys of GPs provide a snapshot of factors in a particular year and region. They therefore capture the absolute levels of perceived factors, but do not capture prior levels or prior expectations. What is clear from both the quantitative and qualitative studies is that many of the causes of quitting or deciding to work part-time have a temporal element (i.e. they relate to widening gaps between initial expectations of being a GP and current reality, or the cumulative effect of recurrent organisational changes over many years).
There were only five qualitative studies of GPs (four based on interviews with UK GPs). 17,18,51,76,77 Two of them, by Hutchins76 and Newton,80 pre-date a number of substantial changes in the organisation of general practice and the remuneration of GPs and general practices, which may limit their generalisability to UK general practice in 2016.
Conclusions
General practitioners in the UK leave general practice for a very wide range of factors, both negative, job-related, ‘push’ factors and positive, leisure-, retirement- and home-life-related, ‘pull’ factors. Although some factors clearly operate at an individual, personal level, such as the financial ability to retire, health, family/marital circumstances, or good/poor relationships with practice partners, other factors operate at the level of the general practice, local area, the whole profession or the national health system (e.g. the media portrayal of GPs, service reform and performance targets, CQC inspections and professional revalidation).
We found that four overlapping job-related factors seemed to play a major part in decision-making about both early retirement and part-time working: workload, job (dis)satisfaction, work-related stress and work–life balance. However, many other detailed factors either underlie these higher-level factors or may combine to influence a particular GP’s decision to quit general practice or reduce the hours they devote to it. In contrast, GPs’ intentions to take a ‘career break’ appear to be more often influenced by a specific range of ‘pull’ factors (e.g. working abroad, looking after children, further study) than by negative ‘push’ factors to do with the job or workload. However, many of the barriers that deter them from returning to work as a GP relate to negative perceptions about being a GP (e.g. high workload, low job satisfaction, unsociable hours and excessive administrative work). This review therefore provides a comprehensive and rich description of the wide range of possible factors on which GP retention and return initiatives could focus.
Chapter 3 Workstream 2: census survey
Introduction
This chapter presents the methods and results of the census survey undertaken with all GPs in south-west England registered on the National Performers List. 82 The principal aim of the survey was to canvass the perspectives of GPs in the region to establish the proportion of GPs planning to leave direct patient care through early retirement or career breaks, and also to provide a sampling frame to support recruitment of GPs to participate in qualitative interviews (workstream 3).
Methods
Under a data-sharing agreement between NHS England and the University of Exeter Medical School (UEMS), the National Performers List of 3523 GPs registered to practise in south-west England was provided to us by two NHS organisations responsible for maintaining the list over the region: Capita/Primary Care Services (the ‘north patch’, covering Bristol, North Somerset, Somerset, South Gloucestershire and Bath and North East Somerset CCGs) and NHS Shared Business Services (the ‘south patch’, covering Devon and Cornwall and Isles of Scilly CCGs). All GPs on the list were assigned a unique study identification (ID) number, reflecting the CCG and general practice in which the GP was located.
The survey was piloted in February 2016, using a random sample of 60 GPs from the list, stratified to ensure a 50/50 split by gender (30 male, 30 female) and, within each gender, there was a selection of 15 GPs aged < 50 years and 15 GPs aged > 50 years. Following piloting, the main survey was administered to 3453 GPs in April 2016 and closed at the end of June 2016.
The ‘Removals Log’
The list of GPs provided by the National Performers List was also supplemented by a small additional list maintained by NHS England local area teams, containing the names of all GPs who are due to be removed from the List, through notification of their intention to resign, retire, relinquish their licence to practise or cease to practise in their current region (the ‘Removals Log’).
NHS England permitted the research team access to this list of 152 GPs who had been removed (or were shortly to be removed) from the National Performers List between April 2015 and March 2016. Of these 152 GPs, 77 were still on the List (i.e. they had not yet been removed and we already had their contact details), six were not to be contacted [one was deceased, four were mandatory removals from the List, one had been suspended by the General Medical Council (GMC)] and two had moved onto the Welsh Performers List. We requested postal and/or e-mail addresses from NHS England for the remaining 97 GPs, eight of which were not supplied (one was a mandatory removal from the List, two had no contact details available, four had retired owing to ill health and one had retired owing to personal circumstances).
We therefore received additional contact details for a total of 89 of the 152 Removals Log GPs. Sixty-five of the 89 had a postal address, all of which were home addresses, and 51 of these 65 also had an e-mail address. The remaining 24 had an e-mail address only.
Questionnaire
The questionnaire was based on that used within earlier work, modified to increase the number of questions from 11 to 24, including rewording of four questions to reflect alignment of wording with other questionnaires of broadly similar intent, and by providing clear definitions for key concepts in the questionnaire, including a career break, taking steps towards changing work–life balance and defining a clinical session. 17 The questionnaire (see Appendix 11) comprised items that asked GPs about their career intentions, reporting on the likelihood that they would permanently leave direct patient care within the next 2 years or within the next 5 years. 82 GPs were also asked to report the likelihood that they would take a career break within the next 5 years, or that they would reduce their weekly average hours spent in direct patient care during this time period. GPs rated the likelihood of these events from ‘very likely’ to ‘very unlikely’ using a four-point scale. The questionnaire also included a question about current level of morale and captured general demographic data: gender, age, ethnicity, region and year of graduation, current GP employment status (e.g. partner, salaried), number and pattern of sessions worked in a typical week and involvement in delivering out-of-hours care.
Data collection
General practitioners were sent study materials through the post to either their practice or their home address, and also by e-mail, if available. 82 The questionnaire was available for completion by post or online. The survey was supported by a comprehensive strategy of publicising the research through routine newsletters and circulars of relevant organisations and networks, including Local Medical Committees (LMCs), Clinical Research Networks (CRNs), HEE South West, the RCGP, UEMS and the South-West Academic Health Sciences Network (AHSN).
If a GP returned multiple online or postal surveys, only the first response received by the research team was analysed. Postal response data were double entered and discrepancy checking was undertaken. Response data were stored securely and without participant names or addresses.
Patient involvement
Although the study participants were GPs rather than patients, patient representatives contributed to the design of the survey. 82 The planned work was presented to the wider project’s PPI group, by way of sharing the process and to check the integrity of the work, and the group provided supportive feedback. 83 The survey results were presented at a project management group meeting, which included PPI representatives who directly contributed to interpreting and contextualising the results.
Statistical analysis
Differential response rates between different groups of GPs would potentially introduce bias into crude survey findings. To counter this, we employed non-response weights. 82 Inverse probability weights were calculated based on three factors: age (< 40, 40–49, 50–54, 55–59 and ≥ 60 years), gender (male and female) and role (partner, salaried and locum/other). These factors were used as they were the only ones consistently recorded for both responders and non-responders. By employing these weights, it was estimated what responses would have been received with a 100% response rate under the assumption that non-responders would have responded similarly to GPs of the same age, gender and role. Logistic regression was used to investigate the association between responses to questions regarding future career intentions (permanently leaving direct patient care within the next 2 and 5 years, taking a career break within the next 5 years and reducing average hours spent in direct patient care within the next 5 years). Each of the four sets of responses was dichotomised into ‘very likely’ and ‘likely’ versus other responses. Initially, unadjusted associations were examined for effects attributable to the explanatory factors of gender, age, country of qualification, ethnicity, role/position and rating of current morale. Subsequently, regression models adjusting simultaneously for all explanatory factors were used to examine adjusted associations. Similar models were used with reported morale as the outcome (but not including morale as an explanatory factor). Regression analyses were restricted to those respondents with complete data on gender, age, country of qualification, ethnicity, role/position and rating of current morale.
Supplementary analysis
Interactions were explored between various factors in the models. 82 Although some of these were found to be statistically significant, the magnitude of the interaction terms was generally small and did not alter the interpretation of the data, with one exception commented on in the results. For this reason, the more complex interaction models have not been reported here.
In addition, the possibility was considered that some groups of GPs, for example female GPs, may not report the intention to reduce hours spent in direct patient care because they already work fewer hours, on average, than other groups. Therefore, two supplementary analyses were conducted, including either a binary variable indicating part-time working (defined as working fewer than eight sessions per week) or a continuous variable detailing the reported number of sessions worked per week.
All analyses were conducted in Stata® version 14.2 (StataCorp LP, College Station, TX, USA).
Results
Questionnaires were distributed by post to 3370 GPs, with 1841 GPs (55%) also sent the questionnaire by e-mail (see Appendix 12, Table 36). Completed questionnaires were received from 2248 of the GPs who were surveyed (response rate 67%). 82 Of the 2248 GP respondents, 673 (30%) used the online survey. Response rates were as high for both men and women (67% and 66%, respectively). Participation was lower among GPs aged < 40 years (54%) than among GPs aged ≥ 50 years (in excess of 68% in each age group), and was lower for salaried GPs (57%) than for GP partners (71%) and non-principal/locum GPs (64%).
The median age of respondents was 48 years [interquartile range (IQR) 40–55 years, range 28–84 years] (Table 6). Eighty-five per cent of respondents reported having a practice with which they were primarily affiliated; 25% of respondents reported that they were involved in the delivery of out-of-hours primary medical care. The majority (62%) of respondents were partners in their practices.
| Characteristic | Proportion, n (%) |
|---|---|
| Gender | |
| Male | 1053 (46.8) |
| Female | 1190 (52.9) |
| Prefer not to say | 3 (0.1) |
| Missing | 2 (0.1) |
| Age (years) | |
| < 40 | 497 (22.1) |
| 40–49 | 735 (32.7) |
| 50–54 | 394 (17.5) |
| 55–59 | 408 (18.2) |
| ≥ 60 | 209 (9.3) |
| Missing | 4 (0.2) |
| Spoiled | 1 (0.0) |
| Ethnic group | |
| White | 2100 (93.4) |
| Mixed/multiple ethnic groups | 29 (1.3) |
| Asian/Asian British | 78 (3.5) |
| Black/African/Caribbean/black British | 9 (0.4) |
| Other ethnic group | 19 (0.9) |
| Missing | 13 (0.6) |
| Region of qualification | |
| UK/Ireland | 2107 (93.7) |
| Europe (non-UK/Ireland) | 70 (3.1) |
| South Asia | 21 (0.9) |
| Other | 42 (1.9) |
| Missing | 7 (0.3) |
| Spoiled | 1 (0.0) |
| Role/position | |
| GP partner | 1403 (62.4) |
| Salaried GP | 454 (20.2) |
| Locum GP | 287 (12.8) |
| Other | 68 (3.0) |
| Missing | 7 (0.3) |
| Spoiled | 29 (1.3) |
| Current work status | |
| Currently working in patient care | 2113 (944) |
| Currently on a career break | 58 (2.6) |
| Permanently left patient care within past 5 years | 55 (2.4) |
| None of the above | 16 (0.7) |
| Missing | 6 (0.3) |
| Total | 2248 (100.0) |
Career intentions
Of the 2248 responding GPs, 55 had already permanently left direct patient care (Table 7); 16 had selected ‘none of the above’ to reflect their working status in direct patient care (i.e. they were not currently working in direct patient care, nor were they on a career break, but they had not permanently quit) and were removed from further analysis. A further 58 GPs reported being currently on a career break. Differential response by age and role meant that GP groups reporting an intention to quit direct patient care were somewhat over-represented, introducing a small bias into the crude results, which is accounted for in the weighted percentages.
| Response | How likely is it that you will permanently leave direct patient care within the next 2 years? | How likely is it that you will permanently leave direct patient care within the next 5 years? | How likely is it that you will reduce your weekly average hours spent in direct patient care within the next 5 years? | How likely is it that you will take a career break (or another career break) within the next 5 years? | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % crude | % weighted (95% CI) | n | % crude | % weighted (95% CI) | n | % crude | % weighted (95% CI) | n | % crude | % weighted (95% CI) | |
| Very likely | 255 | 11.7 | 10.8 (9.6 to 12.1) | 607 | 27.9 | 25.4 (23.6 to 27.2) | 773 | 35.5 | 34.0 (32.0 to 36.0) | 453 | 20.8 | 20.7 (19.0 to 22.5) |
| Likely | 218 | 10.0 | 9.5 (8.4 to 10.8) | 256 | 11.7 | 11.4 (10.1 to 12.8) | 479 | 22.0 | 22.7 (20.9 to 24.5) | 317 | 14.5 | 15.6 (14.0 to 17.2) |
| Unlikely | 795 | 36.5 | 36.6 (34.6 to 38.7) | 675 | 31.0 | 32.3 (30.3 to 34.3) | 585 | 26.8 | 27.5 (25.7 to 29.5) | 756 | 34.7 | 34.9 (32.9 to 36.9) |
| Very unlikely | 899 | 41.3 | 42.6 (40.5 to 44.7) | 622 | 28.5 | 30.1 (28.2 to 32.1) | 326 | 15.0 | 15.2 (13.7 to 16.8) | 614 | 28.2 | 27.3 (25.4 to 29.2) |
| Missing | 12 | 0.6 | 0.5 (0.3 to 1.0) | 17 | 0.8 | 0.8 (0.0 to 0.4) | 15 | 0.7 | 0.6 (0.0 to 0.2) | 36 | 1.7 | 1.5 (1.1 to 2.1) |
| Spoiled | 0 | 0.0 | 0.0 | 2 | 0.1 | 0.1 (0.5 to 1.2) | 1 | 0.0 | 0.0 (0.4 to 1.0) | 3 | 0.1 | 0.1 (0.0 to 0.4) |
| How would you describe your current level of morale? | ||||||||||||
| n | % crude | % weighted (95% CI) | ||||||||||
| Very low | 352 | 16.2 | 15.6 (14.1 to 17.2) | |||||||||
| Low | 843 | 38.7 | 38.8 (36.7 to 40.9) | |||||||||
| Neither low nor high | 664 | 30.5 | 30.8 (28.8 to 32.8) | |||||||||
| High | 276 | 12.7 | 12.9 (11.6 to 14.4) | |||||||||
| Very high | 29 | 1.3 | 1.3 (0.9 to 1.8) | |||||||||
| Missing | 11 | 0.5 | 0.5 (0.1 to 0.5) | |||||||||
| Spoiled | 4 | 0.2 | 0.2 (0.3 to 0.9) | |||||||||
Of the 2179 GP participants included in the analysis,82 473 (weighted percentage 20.3%, 95% CI 18.7% to 22.0%) reported a high likelihood of quitting direct patient care (‘likely’ or ‘very likely’) within the next 2 years, and 863 (weighted percentage 36.7%, 95% CI 34.7% to 38.8%) within the next 5 years (see Table 7). There were 1252 participants (weighted percentage 56.7%, 95% CI 54.5% to 58.8%) who reported being likely or very likely to reduce their working hours, and 770 (weighted percentage 36.3%, 95% CI 34.3% to 38.4%) who reported the intention to take a career break within the next 5 years. Considered together, 1535 participants (weighted percentage 69.9%, 95% CI 67.9% to 71.8%) reported that they were likely/very likely to pursue a career intention (one or more of the four presented) that would potentially adversely affect the workforce available in south-west England within the next 5 years. The majority of participants also had low levels of morale, with a substantially greater proportion of participants (1195; weighted percentage 54.4%, 95% CI 52.2% to 56.5%) reporting ‘low’ or ‘very low’ levels of morale than of those reporting ‘high’ or ‘very high’ levels of morale (305 participants; weighted percentage 14.2%, 95% CI 12.7% to 15.7%).
Associations between general practitioner characteristics and career intentions/morale
Figure 6 illustrates the reported intention to quit direct patient care of responding GPs broken down by gender and each year of GP age, aggregating likely and very likely responses together. Reported quit intentions are strongly related to age, remaining low (< 20%) among younger GPs (≤ 45 years) for quitting direct patient care in both of the next 2 and 5 years. Both of these outcomes show a sharp rise from the age of 52 years, with the proportion stating they were likely to quit in 5 years rising to almost 90% by the age of 56 years. The proportion anticipating taking a career break as ‘likely’ was highest for the youngest GPs, especially among younger women; nearly 9 out of 10 female GPs aged 30 years reported the intention to take a career break, presumably on account of anticipated maternity leave.
FIGURE 6.
Career intentions to quit direct patient care by gender and age. (a) Male; and (b) female. Reproduced with permission from Fletcher et al. 82 Quitting patient care and career break intentions among general practitioners in south-west England: findings of a census survey of general practitioners. BMJ Open 2017;7:e015853. https://doi.org/10.1136/bmjopen-2017-015853. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
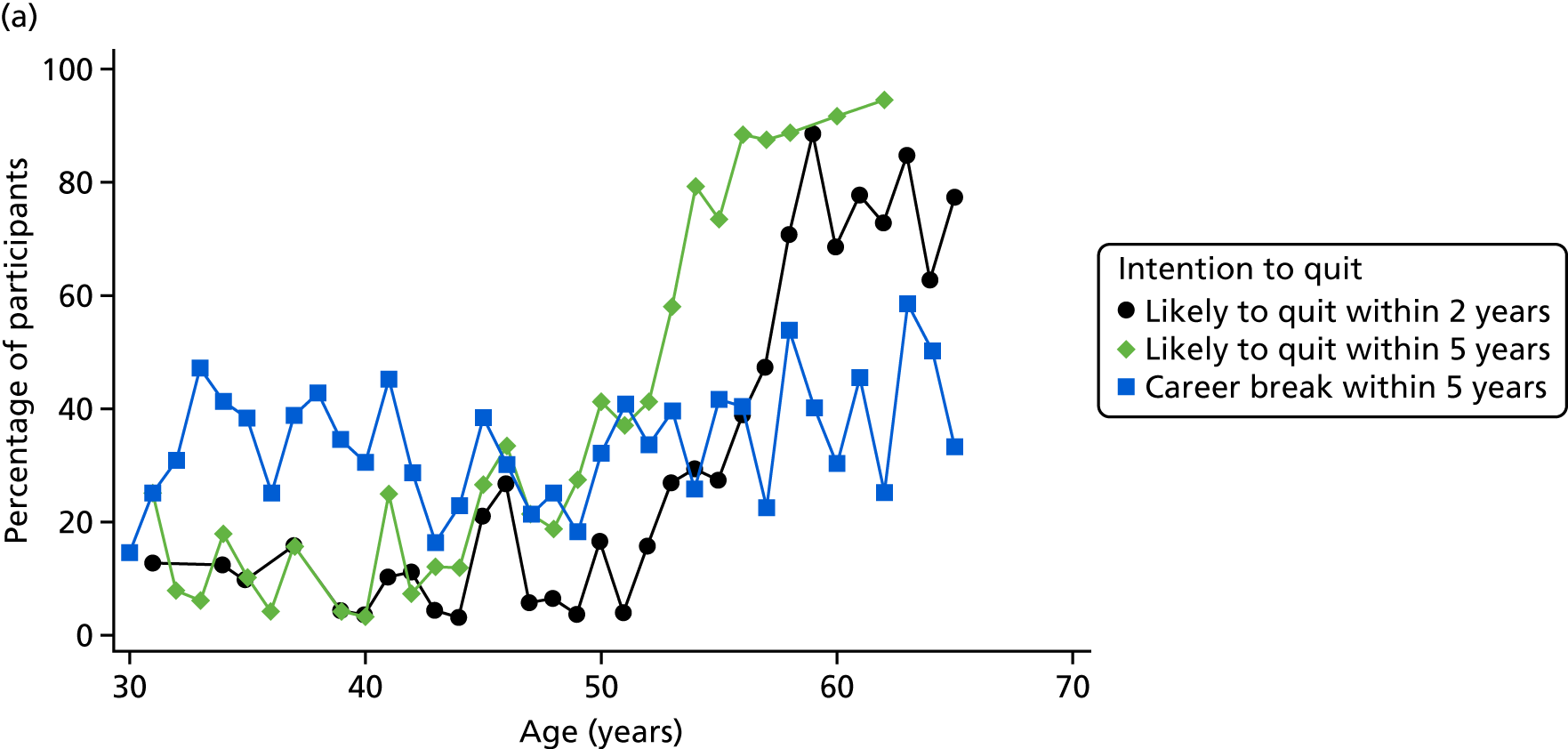
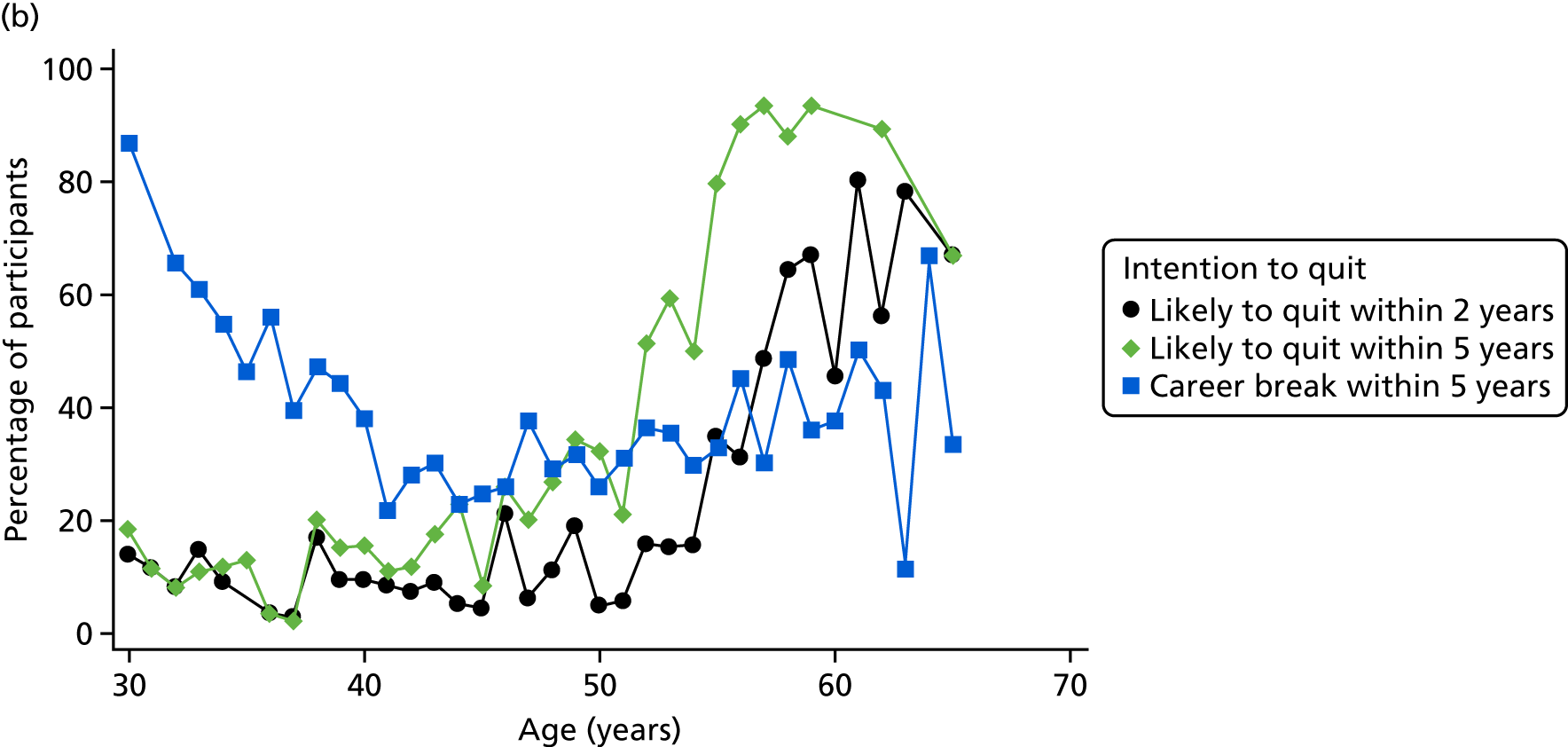
Of the 2179 respondents reporting that their current role involved direct patient care, 2119 (97%) provided complete information on gender, age, region of qualification, ethnicity, role/position and rating of current morale and were included in the regression analyses. Tables 8 and 9 show the results of the unadjusted and adjusted logistic regression analyses, respectively, for career intentions. In unadjusted analyses, there is strong evidence (p < 0.001 for all) that gender and role are associated with being likely to report the intention to leave patient care within both 2 and 5 years, with female GPs being less likely to quit patient care than male GPs [odds ratio (OR) 0.55, 95% CI 0.46 to 0.66, for leaving patient care in 5 years], and with locum GPs being the most likely to quit patient care and salaried GPs least likely. However, these associations are likely to be confounded, for example by the fact that younger doctors were more likely than older doctors to be female. Once adjustment is made for all other factors, the effects of these characteristics on intentions to quit are no longer significant. However, after adjustment for other variables, women were still substantially less likely to report intending to reduce hours spent in direct patient care (OR 0.58, 95% CI 0.47 to 0.71), and locum GPs remained more likely to report intending to take a career break than GPs in other roles.
| Characteristic | How likely is it that you will permanently leave direct patient care within the next 2 years? | How likely is it that you will permanently leave direct patient care within the next 5 years? | How likely is it that you will reduce your weekly average hours spent in direct patient care within the next 5 years? | How likely is it that you will take a career break (or another career break) within the next 5 years? | ||||
|---|---|---|---|---|---|---|---|---|
| ORa (95% CI) | p-value | ORa (95% CI) | p-value | ORa (95% CI) | p-value | ORa (95% CI) | p-value | |
| Gender | ||||||||
| Male | Reference | < 0.001 | Reference | < 0.001 | Reference | < 0.001 | Reference | 0.046 |
| Female | 0.51 (0.41 to 0.63) | 0.55 (0.46 to 0.66) | 0.48 (0.41 to 0.58) | 1.20 (1.00 to 1.44) | ||||
| Age (years) | ||||||||
| < 40 | 0.75 (0.48 to 1.16) | < 0.001 | 0.49 (0.34 to 0.70) | < 0.001 | 1.24 (0.98 to 1.56) | < 0.001 | 2.34 (1.83 to 2.98) | < 0.001 |
| 40–49 | Reference | Reference | Reference | Reference | ||||
| 50–54 | 1.65 (1.12 to 2.43) | 4.00 (3.02 to 5.28) | 2.04 (1.58 to 2.63) | 1.24 (0.95 to 1.63) | ||||
| 55–59 | 9.32 (6.72 to 12.92) | 30.04 (21.04 to 42.90) | 5.00 (3.74 to 6.69) | 1.59 (1.22 to 2.08) | ||||
| 60–69 | 22.22 (14.43 to 34.22) | 91.60 (41.88 to 200.36) | 7.38 (4.58 to 11.88) | 1.61 (1.11 to 2.35) | ||||
| ≥ 70 | 45.86 (12.84 to 163.84) | b | 3.86 (1.23 to 12.10) | 1.55 (0.56 to 4.32) | ||||
| Country of qualification | ||||||||
| UK/Ireland | Reference | 0.450 | Reference | 0.132 | Reference | 0.921 | Reference | 0.470 |
| Europe | 0.56 (0.27 to 1.14) | 0.60 (0.35 to 1.02) | 0.85 (0.52 to 1.39) | 0.65 (0.37 to 1.12) | ||||
| South Asia | 0.88 (0.29 to 2.66) | 0.43 (0.14 to 1.32) | 1.10 (0.45 to 2.70) | 0.95 (0.38 to 2.39) | ||||
| Other | 1.05 (0.47 to 2.32) | 0.98 (0.51 to 1.90) | 0.95 (0.50 to 1.80) | 0.88 (0.45 to 1.73) | ||||
| Ethnic group | ||||||||
| White | Reference | 0.300 | Reference | 0.032 | Reference | 0.581 | Reference | 0.610 |
| Mixed | b | 0.60 (0.26 to 1.36) | 0.74 (0.35 to 1.57) | 1.57 (0.74 to 3.31) | ||||
| Asian | 0.87 (0.48 to 1.57) | 0.43 (0.25 to 0.76) | 1.27 (0.78 to 2.05) | 1.00 (0.61 to 1.63) | ||||
| Black | 3.59 (0.89 to 14.41) | 1.49 (0.37 to 5.99) | 2.23 (0.45 to 11.07) | 0.60 (0.12 to 2.99) | ||||
| Other | 0.77 (0.22 to 2.69) | 0.68 (0.24 to 1.96) | 1.36 (0.50 to 3.70) | 1.61 (0.62 to 4.18) | ||||
| Role/position | ||||||||
| GP partner | Reference | < 0.001 | Reference | < 0.001 | Reference | < 0.001 | Reference | < 0.001 |
| Salaried GP | 0.61 (0.46 to 0.83) | 0.43 (0.34 to 0.55) | 0.63 (0.51 to 0.78) | 1.25 (1.00 to 1.56) | ||||
| Locum GP | 1.58 (1.18 to 2.11) | 1.08 (0.82 to 1.41) | 1.34 (1.02 to 1.76) | 1.72 (1.32 to 2.24) | ||||
| Other | 1.12 (0.61 to 2.08) | 0.72 (0.40 to 1.26) | 0.79 (0.47 to 1.34) | 0.85 (0.48 to 1.52) | ||||
| Reported morale | ||||||||
| Very low | 0.99 (0.45 to 2.17) | < 0.001 | 1.85 (0.81 to 4.19) | < 0.001 | 2.58 (1.19 to 5.59) | < 0.001 | 2.24 (1.01 to 4.95) | < 0.001 |
| Low | 0.42 (0.19 to 0.91) | 0.78 (0.35 to 1.75) | 1.31 (0.62 to 2.77) | 1.14 (0.52 to 2.49) | ||||
| Neither low or high | 0.30 (0.14 to 0.65) | 0.62 (0.28 to 1.40) | 0.82 (0.39 to 1.73) | 0.81 (0.37 to 1.78) | ||||
| High | 0.40 (0.18 to 0.90) | 0.62 (0.27 to 1.42) | 0.54 (0.25 to 1.16) | 0.55 (0.24 to 1.24) | ||||
| Very high | Reference | Reference | Reference | Reference | ||||
| Characteristic | How likely is it that you will permanently leave direct patient care within the next 2 years? | How likely is it that you will permanently leave direct patient care within the next 5 years? | How likely is it that you will reduce your weekly average hours spent in direct patient care within the next 5 years? | How likely is it that you will take a career break (or another career break) within the next 5 years? | ||||
|---|---|---|---|---|---|---|---|---|
| ORa (95% CI) | p-value | ORa (95% CI) | p-value | ORa (95% CI) | p-value | ORa (95% CI) | p-value | |
| Gender | ||||||||
| Male | Reference | 0.181 | Reference | 0.810 | Reference | < 0.001 | Reference | 0.019 |
| Female | 0.83 (0.64 to 1.09) | 1.03 (0.80 to 1.33) | 0.58 (0.47 to 0.71) | 1.27 (1.04 to 1.55) | ||||
| Age (years) | ||||||||
| < 40 | 0.89 (0.56 to 1.41) | < 0.001 | 0.58 (0.40 to 0.85) | < 0.001 | 1.47 (1.14 to 1.90) | < 0.001 | 2.63 (2.02 to 3.42) | < 0.001 |
| 40–49 | Reference | Reference | Reference | Reference | ||||
| 50–54 | 1.70 (1.14 to 2.55) | 4.73 (3.49 to 6.41) | 2.11 (1.61 to 2.77) | 1.31 (0.98 to 1.73) | ||||
| 55–59 | 11.69 (8.18 to 16.72) | 44.15 (29.77 to 65.48) | 5.62 (4.12 to 7.66) | 1.79 (1.35 to 2.38) | ||||
| 60–69 | 36.87 (22.53 to 60.34) | 194.43 (84.32 to 448.34) | 9.58 (5.76 to 15.95) | 2.03 (1.35 to 3.04) | ||||
| ≥ 70 | 110.61 (25.85 to 473.26) | b | 4.93 (1.47 to 16.55) | 1.83 (0.61 to 5.48) | ||||
| Country of qualification | ||||||||
| UK/Ireland | Reference | 0.193 | Reference | 0.048 | Reference | 0.829 | Reference | 0.738 |
| Europe | 0.60 (0.27 to 1.37) | 0.48 (0.23 to 0.99) | 0.98 (0.57 to 1.70) | 0.73 (0.41 to 1.29) | ||||
| South Asia | 0.21 (0.04 to 1.15) | 0.13 (0.02 to 0.97) | 0.61 (0.19 to 1.96) | 0.98 (0.31 to 3.05) | ||||
| Other | 0.83 (0.30 to 2.31) | 0.94 (0.39 to 2.25) | 0.83 (0.40 to 1.71) | 1.08 (0.53 to 2.22) | ||||
| Ethnic group | ||||||||
| White | Reference | 0.109 | Reference | 0.142 | Reference | 0.209 | Reference | 0.483 |
| Mixed | b | 2.84 (1.15 to 7.04) | 1.32 (0.60 to 2.92) | 1.74 (0.79 to 3.81) | ||||
| Asian | 1.58 (0.70 to 3.54) | 0.84 (0.38 to 1.86) | 1.89 (1.04 to 3.46) | 0.87 (0.48 to 1.57) | ||||
| Black | 6.07 (1.00 to 36.99) | 2.26 (0.29 to 17.71) | 2.89 (0.48 to 17.28) | 0.54 (0.10 to 2.87) | ||||
| Other | 0.45 (0.10 to 2.16) | 0.45 (0.08 to 2.43) | 1.17 (0.39 to 3.45) | 1.57 (0.56 to 4.41) | ||||
| Role/position | ||||||||
| GP partner | Reference | 0.177 | Reference | 0.153 | Reference | 0.005 | Reference | < 0.001 |
| Salaried GP | 1.10 (0.76 to 1.59) | 0.81 (0.58 to 1.14) | 0.97 (0.75 to 1.24) | 1.15 (0.89 to 1.47) | ||||
| Locum GP | 1.55 (1.04 to 2.30) | 1.37 (0.91 to 2.07) | 1.74 (1.26 to 2.39) | 2.09 (1.55 to 2.81) | ||||
| Other | 0.91 (0.39 to 2.15) | 0.73 (0.29 to 1.86) | 1.19 (0.64 to 2.20) | 1.15 (0.62 to 2.13) | ||||
| Reported morale | ||||||||
| Very low | 5.77 (1.96 to 17.00) | < 0.001 | 13.07 (3.72 to 45.88) | < 0.001 | 6.74 (2.76 to 16.47) | < 0.001 | 3.49 (1.49 to 8.14) | < 0.001 |
| Low | 1.87 (0.65 to 5.38) | 3.89 (1.13 to 13.34) | 3.27 (1.38 to 7.74) | 1.50 (0.66 to 3.45) | ||||
| Neither low nor high | 0.86 (0.30 to 2.47) | 2.15 (0.63 to 7.39) | 1.75 (0.74 to 4.14) | 0.93 (0.40 to 2.12) | ||||
| High | 0.80 (0.27 to 2.39) | 1.29 (0.36 to 4.60) | 0.86 (0.36 to 2.08) | 0.59 (0.25 to 1.40) | ||||
| Very high | Reference | Reference | Reference | Reference | ||||
Age was a very strong predictor of reported intention to leave direct patient care, a finding that persisted after adjustment (e.g. 60- to 69-year-olds vs. 40- to 49-year-olds: OR 194.4, 95% CI 84.3 to 448.3 for leaving patient care in 5 years). Age was also a strong predictor of the intention to reduce hours in the adjusted model, with older GPs more likely to report this intention than younger GPs. Female GPs, GPs aged < 40 years and locum GPs were most likely to report the intention to take a career break after adjustment for other factors. A model including an interaction between age and gender showed that the effect of GPs aged < 40 years, being more likely to report intentions to take a career break was strongest in female GPs, consistent with the pattern shown in Figure 6 (results not shown).
Self-reported morale was a strong predictor of all four outcomes shown in Tables 8 and 9. In the unadjusted analysis, a ‘U-shaped’ relationship is seen for all four quitting outcomes, with those with ‘very high’ levels of morale being more likely to report intentions to leave direct patient care/reduce hours/take a career break than those with ‘high’ or ‘neither low nor high’ levels of morale (and in the case of leaving patient care within 2 years, more likely than any other morale category), but less likely to intend to leave/reduce hours/take a career break than those with ‘very low’ levels of morale. This U-shaped relationship largely disappears after adjustment, however, and it is those GPs with ‘very low’ levels of morale who are most likely to report intending to leave direct patient care, reduce hours in patient care or to take a career break. Moreover, the change in odds between ‘low’ and ‘very low’ levels of morale is particularly strong. Table 10 shows the results of the logistic regression analysis modelling of factors associated with low or very low levels of morale. Only age and practice role show any evidence of being associated with reported morale (p < 0.001 for both). Those aged 50–54 years are most likely to report low levels of morale. In respect of role, GP partners are the most likely to report low levels of morale, followed by salaried GPs, and locums and other GPs are the least likely groups to report low levels of morale.
| Characteristic | Association | |||
|---|---|---|---|---|
| Unadjusted | Adjusted | |||
| ORa (95% CI) | p-value | ORa (95% CI) | p-value | |
| Gender | ||||
| Male | Reference | 0.134 | Reference | 0.231 |
| Female | 0.87 (0.72 to 0.72) | 0.90 (0.76 to 0.76) | ||
| Age (years) | ||||
| < 40 | 0.73 (0.57 to 0.57) | < 0.001 | 0.69 (0.55 to 0.55) | < 0.001 |
| 40–49 | Reference | Reference | ||
| 50–54 | 1.06 (0.81 to 0.81) | 1.10 (0.85 to 0.85) | ||
| 55–59 | 0.85 (0.66 to 0.66) | 0.92 (0.71 to 0.71) | ||
| 60–69 | 0.38 (0.26 to 0.26) | 0.33 (0.23 to 0.23) | ||
| ≥ 70 | 0.07 (0.01 to 0.01) | 0.04 (0.01 to 0.01) | ||
| Country of qualification | ||||
| UK/Ireland | Reference | 0.157 | Reference | 0.194 |
| Europe | 0.74 (0.45 to 0.45) | 0.73 (0.45 to 0.45) | ||
| South Asia | 0.97 (0.32 to 0.32) | 0.97 (0.40 to 0.40) | ||
| Other | 0.50 (0.25 to 0.25) | 0.55 (0.29 to 0.29) | ||
| Ethnic group | ||||
| White | Reference | 0.534 | Reference | 0.721 |
| Mixed | 0.82 (0.38 to 0.38) | 0.82 (0.39 to 0.39) | ||
| Asian | 1.59 (0.89 to 0.89) | 1.31 (0.81 to 0.81) | ||
| Black | 1.64 (0.37 to 0.37) | 0.82 (0.20 to 0.20) | ||
| Other | 1.01 (0.36 to 0.36) | 0.73 (0.28 to 0.28) | ||
| Role/position | ||||
| GP partner | Reference | < 0.001 | Reference | < 0.001 |
| Salaried GP | 0.75 (0.59 to 0.59) | 0.67 (0.54 to 0.54) | ||
| Locum GP | 0.40 (0.30 to 0.30) | 0.33 (0.25 to 0.25) | ||
| Other | 0.22 (0.12 to 0.12) | 0.20 (0.11 to 0.11) | ||
Supplementary analyses exploring the contribution of current working patterns to any association with intentions to reduce hours spent in direct patient care did explain some of the difference between genders. However, even after adjustment for current working patterns, female GPs were still substantially less likely to report intentions to reduce hours spent in direct patient care than their male counterparts (results not reported).
Discussion
Main findings
A high proportion of GPs – around two in every five – currently working within direct patient care in south-west England reported an intention to permanently quit direct patient care within the next 5 years, this being one in five within the next 2 years. Further depletion of the GP workforce in this region of England through the reduction of weekly average hours or through taking a career break within the next 5 years also emerged as an impending risk. Overall, 7 out of every 10 GPs in this region reported a career intention that, if implemented, would adversely affect the GP workforce capacity in south-west England through GPs leaving direct patient care, reducing hours spent in direct patient care or by taking a career break within the next 5 years.
Older age is highly predictive of a GP’s intentions to permanently quit direct patient care and to reduce hours. The intention to quit was independent of the GP’s role (partner, salaried or locum) and gender. The gender differences observed among younger GPs in respect of intended career breaks is a particular issue because, currently, 69% of the GP trainee workforce is female,84 because a substantial proportion of younger women returning to clinical care do so on the basis of reduced hours,1 and because doctors who wish to return to clinical practice may face significant bureaucratic obstacles in doing so. 85 The decision to reduce hours or to take a career break varied with employment status, with locum GPs being most likely to report intentions to reduce hours or to take a career break. In a situation in which GPs who are not partners in a practice do in fact leave direct patient care, the system of care appears vulnerable, with added strain likely to be placed on GPs who are partners in their practice.
A key issue is whether or not the intention to leave is translated into reality, and few studies have explored this important question. However, Hann et al. 59 explored this question with nearly 1200 UK GPs who were followed up over 5 years and identified a strong relationship between a stated intention to leave patient care and actually doing so, reflected in a 4.5-fold difference in odds of leaving between those with no stated intention to leave patient care and those reporting a high intention to do so.
The majority of responding GPs in our study reported low levels of morale, with < 15% reporting high levels of morale. GP morale was identified as an important predictor of future career intentions, particularly when morale was very low.
Strengths and limitations
Ensuring the alignment of wording with other surveys of similar intent allows the opportunity to compare and contrast results. Recent high-quality surveys support our estimate of the proportion of GPs intending to leave general practice within the next 5 years. 17,41,43,44 Unlike most other similar surveys, which tend to survey samples of GPs,19,86 we undertook a census survey of all GPs currently eligible to provide patient care across a large area, providing a cross-sectional overview of the quit intentions of all GPs in south-west England. The response rate was high (67%), reflecting both rigorous planning and implementation of the survey and interest among GPs in the subject matter of workforce challenges. Furthermore, we have reduced the potential for non-response bias by weighting our estimates to account for differential response rates by age, gender and practice role. The overall programme of work, of which this survey is one element, includes the planned development of a predictive risk modelling tool to enumerate risk of future workforce undersupply at local levels, thus offering the potential of providing data that will be of value to health-care planners and policy-makers. In addition, our study relates to a key current area of national interest and concern.
The study has a number of limitations. The survey was conducted among GPs in a single region of England, which may not be entirely typical of England as a whole. For example, a higher proportion of GPs in the region are trained in the UK and a lower proportion are partners (see Appendix 13, Table 37). Furthermore, differences may exist in respect of population mix and practice setting. 87 The region is often informally regarded as having desirable living and working conditions. 88 It seems likely that other regions of England, with more inner-city areas with higher levels of deprivation, are likely to face even greater challenges in respect of the GP workforce than in the findings we have presented here. A further limitation is that the research was undertaken within a rapidly changing GP workforce policy environment, for example the implementation in 2015–16 of a 10-point plan agreed between authoritative UK health, governmental and professional bodies concerned about GP workforce issues. 89 Finally, this survey was cross-sectional, rather than longitudinal in design, and so we are unable to report on the actual translation of GPs’ reported career intentions into actual career decisions, although previous work has demonstrated intention to quit to be a strong predictor of actually leaving. 59
Implications for research
Our survey is part of a multimethod suite of work commissioned by the NHS, seeking to inform evidence-based policies and strategies in a key area of national concern, which will involve stakeholder consultations with policy-makers who have oversight of GP workforce planning. 83 Future research should include an assessment of the predictive validity of GPs’ reported career intentions by longitudinal follow-up of GPs, an investigation of how reducing hours or better flexible working arrangements may influence GP retention, and research exploring the potential for extended clinical roles among important allied health-care professionals in the clinical workforce. Such groups might include nurses, physiotherapists and pharmacists, and developing such extended roles for these professionals within the primary care team may offer a rapid and potentially effective contribution to the alleviation of current GP workforce pressures. Research into the determinants and impact of working reduced hours should also encompass other aspects of flexible working arrangements in general practice, and how such arrangements may improve job satisfaction and work–life balance and thereby potentially increase GP retention in the longer term. This work also provides insight into those groups of GPs that might best be targeted with interventions aiming to improve workforce retention.
Implications for policy and practice
Concerns regarding the GP workforce are now recognised widely by authoritative bodies in the UK, leading to recent policy statements and initiatives89 and to the establishment of a Primary Care Workforce Commission by HEE8. Our research can inform this policy agenda by providing an estimate of the likely proportion of south-west GPs intending to leave direct patient care within the next 5 years through permanently quitting patient care or by taking a career break. Our findings are likely to be of relevance in other areas of England that may face even greater challenges in respect of the GP workforce. Retaining the direct patient care capacity of established GPs represents an immediate challenge for health-care planners. Recognising and addressing issues of low GP morale is an area of importance, and addressing the issue may not only improve how GPs feel about their work but also potentially be associated with improvements in patients’ experience of the care received. 90 In the light of problems of recruiting to general practice91 and the wider workforce problems, the UK government recently announced an increase in the number of training places for GPs89 and an increase in the number of medical training places in the UK. 92 However, these medium- to long-term solutions do not address the immediate workforce crisis. In contrast, policy initiatives to support the retention of the existing GP workforce, the rapid development of and support for new models of care, and the implementation of policies aimed at alleviating workload pressures for GPs are potential short- to medium-term solutions that need to be urgently considered. Developing and implementing relevant policies and strategies to achieve those ambitions will be important for the alleviation of the immediate pressures faced by the GP workforce and the populations of patients they serve.
Conclusions
Health care in England faces imminent challenges in respect of GP workforce capacity. This survey identifies the magnitude of the problem in south-west England and highlights the important role of GP morale as one important factor contributing to that challenge. Acknowledgement of the magnitude of the problems is urgently required, along with implementation and monitoring of relevant policy and strategy. Failure to do so will risk serious adverse effects on the capacity and ability of the NHS to provide effective primary care to the UK population.
Chapter 4 Workstream 3: qualitative research
Introduction
An increasing number of GPs are leaving direct patient care, significantly reducing their hours or retiring early, and recruiting new GPs has been difficult. 93,94 The results from the ReGROUP (retaining experienced GPs and those taking a career break in direct patient care) GP Workforce Survey suggest that around two in every five GPs currently working in direct patient care intend to leave within 5 years. 82 The systematic review of the literature describes factors that are involved in decisions to leave primary care, operating on an individual, practice and national level. The review of UK literature suggests that issues around workload, job dissatisfaction, work-related stress and work–life balance play a major part in decisions related to leaving, taking early retirement and moving to part-time working. In addition, change fatigue, deteriorating or unsupportive practice partner relationships and the cultural norm of early retirement may combine to influence GPs’ quit decisions.
It is widely acknowledged that GPs experience high levels of stress, burnout and emotional exhaustion,95,96 and previous research has found that burnout levels were higher among GPs than among other medical doctors. 97 A substantial body of literature focusing on GP well-being, morale and job satisfaction already exists (e.g. Murray et al. 98). A number of strategies and policies are in place – or are being introduced – to address some of these issues. 99
Sansom et al. 18 explored the quitting decisions of GPs who had either retired or reported being likely to leave or retire from the profession in the next 5 years. They found that, although participants faced numerous difficulties and cited negative experiences of working as a GP, those who left did so because they were in a position to or because other options became more attractive. To help retain the current GP workforce, it is important to understand GPs’ views of the options they have to manage and mitigate any negative experiences of working in primary care. This workstream sought to understand the lived experiences of GPs currently working within the profession, those returning after a break from direct patient care and those who had left or taken early retirement.
Aim
The aim of the qualitative workstream was to identify the potential content of policies and strategies aimed at retaining experienced GPs and/or supporting the return of GPs following a career break. To do this, an exploration of the lived experience of GPs was required, including the investigation of remaining/leaving decision-making processes among GPs.
Approach
We incorporated a thematic analysis of CQC practice report data to explore examples of potentially good and poor practice in south-west England in respect of the quality of care delivered, followed by semistructured interviews with GPs and key stakeholders. The CQC strand aimed to inform the content of interview questions and to provide contextual information to inform the RAM expert panel workstream. Interviews were undertaken to explore the lived experiences and perspectives of GPs and the impact of GP quitting decisions on practice management and organisation, and to further inform the content of policies and strategies.
Methods
Care Quality Commission inspection reports
The aim was to use CQC report data to produce a briefing document that could:
-
inform the content of interviews with GPs
-
provide contextual information and case examples to inform workstream 4.
Full details of the methodology are provided in Appendix 14. There were five key stages to working with the CQC report data:
-
identification of general practices in south-west England that had been rated by the CQC, and their overall rating category
-
familiarisation with the approach, content and report layout
-
use of an iterative approach to determine the best method for extracting information and examples from the reports
-
identification of a maximum variation sample consisting of CQC reports of general practices in south-west England
-
extraction and summarising of report data.
Identifying the number of general practices in south-west England that had been reported on by the Care Quality Commission
Care Quality Commission report data are publicly accessible (see www.cqc.org.uk/content/how-get-and-re-use-cqc-information-and-data#directory; accessed 30 November 2017).
Sampling took place in January 2016 using the CQC data set that had been completed up to 1 December 2015. There were 442 active location practices in the ReGROUP catchment area, of which 227 (51.4%) had been inspected, rated and had their inspection results made publicly available (Table 11).
| CQC rating category | Number of practices | Percentage |
|---|---|---|
| Outstanding | 16 | 7 |
| Good | 203 | 89 |
| Requires improvement | 4 | 2 |
| Inadequate | 4 | 2 |
Sampling Care Quality Commission reports for analysis
A maximum variation sample was taken based on practice list size and urban or non-urban locality. The sample included 8 out of 16 (50%) ‘outstanding’ reports and 6 out of 8 (75%) ‘requires improvement’ and ‘inadequate’ reports (see Appendix 14, Tables 38 and 39, for full details). Practices rated ‘good’ were not included as it was agreed by the workstream 3 team that a sufficient number and range of examples could be drawn from those reports at the extremes of good and poor practice. Pragmatic considerations guided the number of sampled reports (Table 12).
| CQC report rating | Practice | |||||
|---|---|---|---|---|---|---|
| List size | Settinga | Deprivationb | ||||
| Small–medium: < 8000 | Large: ≥ 8000 | Urban | Non-urban | More deprived | Less deprived | |
| Outstanding (n = 8) | 3 | 5 | 2 | 6 | 2 | 6 |
| Requires improvement or inadequate (n = 6) | 4 | 2 | 3 | 3 | 3 | 3 |
| Total | 7 | 7 | 5 | 9 | 5 | 9 |
Determining the best method for extracting information and examples from the Care Quality Commission reports
An iterative approach was used to determine the best method for extracting information and examples from the CQC report secondary data. All approaches were discussed and reflected on by the workstream 3 team until a final decision about the methodology was reached.
The final approach was to categorise themes from the CQC’s own identified examples of good practice along with examples extracted from the sampled reports. 100 These themes and examples were used to identify prompts and questions for GP interviews and to provide illustrated examples from practice. Full details of this approach are provided in Appendix 14.
This approach was used for four of the CQC’s five key lines of enquiry (KLOEs), namely whether or not services were ‘effective’, ‘responsive’, ‘caring’ and ‘well-led’. A modified approach was used for the fifth KLOE, ‘safe’, as the data for this question from the ‘outstanding’ rated south-west England reports were mainly merely confirmatory of the CQC’s inspection questioning. In order to explore items within ‘safe’ for examples that could be used in GP interviews, the extraction process was repeated using the sample of reports rated as ‘inadequate’ and as ‘requires improvement’.
Interviews
Eligible general practitioners
General practitioners were identified from responses to the GP Workforce Survey. 82 The sample population was drawn from those who indicated a willingness to be interviewed and who met the eligibility criteria for one of five participant categories:
-
GPs who had retired or taken early retirement (before the age of 60 years)
-
GPs aged 50–59 years who reported being likely or very likely to take early retirement within 5 years
-
GPs of any age who were currently on a career break or who reported being very likely to take a career break within 2 years
-
GPs aged 35–49 years who had left direct patient care or who reported that they were very likely to leave within 2 years
-
GPs who reported intending to remain in direct patient care for the next 5 years and reported their morale as high or very high.
Eligible stakeholders
Key stakeholder groups were identified by the research team: practice-level roles (practice managers, GPs interested in workforce issues, nurses, pharmacists and other allied health professionals) and area-level roles (representatives of LMCs, CCGs, the CQC and other regional bodies). Convenience sampling (based on local knowledge, information from the internet and snowballing) was used to identify people from different organisations, roles and areas within the south-west England region.
Recruitment
The details of eligible GPs in each of the participant categories were entered into a sampling frame (n = 694). A maximum variation approach was employed to identify a purposive subsample of potential participants from practices of varying size (small, medium and large) and deprivation (less deprived/more deprived), GP demographic profiles (age, gender, ethnicity) and GP role (partner, salaried or locum). A second sampling frame of practice-level (n = 10) and area-level (n = 10) potential stakeholder participants was also created.
All potential participants identified in the sampling frames received an invitation letter, the participant information sheet and a consent form (see Appendix 17). GPs were initially contacted by e-mail by the qualitative researchers (AS and RT), with subsequent approaches by e-mail or telephone. Stakeholders were contacted by the study lead (JLC) by e-mail (when publicly available) or post (details from the practice/organisation’s website). All approaches were followed up by the qualitative researchers. Potential participants were invited to respond (by e-mail or telephone) with their willingness and availability for interview. A maximum of three attempts were made to contact and schedule an interview with each potential participant before moving on to the next one on the list.
There was a pause halfway through recruitment to review the sample and to determine whether or not any adjustments were needed; these discussions were held by the workstream 3 researchers with the systematic review team, PPI members and the GP representative. There were three outcomes of these discussions: (1) the number of participants in each GP category was adjusted, (2) the fifth GP category of ‘staying GPs’ was introduced to capture a broader range of experiences and (3) additional stakeholders were identified using opportunistic and snowballing methods. Recruitment stopped when the workstream 3 team agreed that code and meaning saturation had been reached. 101
Interview process
Semistructured interview schedules (see Appendix 17) were developed using themes identified from the literature and the CQC analysis and in discussion with the PPI group and GP representative. Interviews were conducted by telephone, face to face or via Skype™ (Microsoft Corporation, Redmond, WA, USA) depending on the participant’s preference. Participants provided verbal and written consent and were offered a gift voucher in acknowledgement of their time. Each interview was transcribed verbatim and anonymised. Interviews were conducted by Anna Sansom and Rohini Terry from May to November 2016.
Qualitative analysis
Transcripts from GP and stakeholder interviews were analysed together. The transcribed interviews were entered into data management software QSR NVivo version 11 and analysed using thematic analysis. An initial coding frame was independently constructed by Anna Sansom and Rohini Terry, based on the first five interviews. Following discussions, a consensus about the coding frame was reached and it was refined to reflect this. The new coding frame was then independently tested by Anna Sansom and Rohini Terry with two further interview transcripts, and final modifications were made. All transcripts were coded using this agreed coding frame. Detailed project notes were kept regarding the further refinement of any existing, or the addition of new, codes.
Key themes were identified from the codes, and cases and themes compared within and between one another using constant comparison techniques. 102 Discussions about the emerging themes were held with the PPI group and GP representative. Descriptive accounts were prepared to identify key dimensions and to map the range and diversity of each phenomenon, followed by explanatory accounts to inform the findings and recommendations.
A protocol for assessing, reporting and monitoring risk was developed by the qualitative team to provide an agreed and documented route for the research team to discuss and report any issues that may potentially have an impact on the GP participant’s own health and safety, and/or that of their patients (see Appendix 18).
Results
Key findings from Care Quality Commission inspection reports
See Appendix 14 for detailed findings.
Examples of good practice: Care Quality Commission all-England
Twenty-one (45%) of the CQC’s all-England examples of good practice were used to identify categories related to:
-
sharing safety lessons
-
open safety culture
-
supporting patients’ emotional and social well-being
-
health promotion for patients
-
shifting care from secondary to primary care services
-
working with external or other community organisations
-
improving access to general practices for hard-to-reach groups
-
expanding the skill mix and roles within the general practice team
-
providing direct support to GPs (e.g. GP mentoring).
Examples of good practice: south-west
The categories identified from the CQC all-England examples were compared with the examples extracted from the subsample of the south-west ‘outstanding’-rated reports (n = 8). The workstream 3 team agreed that this sample was sufficient: no new factors were emerging and theoretical saturation was determined to have been reached in respect of each of the KLOEs: ‘effective’, ‘responsive’, ‘caring’ and ‘well-led’. The subsample of six ‘inadequate’/’requires improvement’ reports was determined to be sufficient for the additional exploration of the KLOE ‘safe’.
Sixty-five examples from the south-west reports were extracted. These examples provided the following additional thematic categories:
-
structuring and organising practice
-
forward planning
-
sharing with other practices
-
role of other practice staff in patient care
-
training opportunities
-
morale
-
use of technology.
Twenty-three of the extracted south-west examples were identified for use as prompts or suggestions for discussion within the GP interviews. In addition to their use as examples within the GP interviews, the categorised examples also suggested additional potential interview question areas for GPs concerning potential policy/strategy directions, namely:
-
additional members of staff for the practice
-
additional services or resources offered by the practice
-
working with other organisations
-
providing support for GPs
-
restructuring or reorganising practice
-
developing or better utilising GPs with specialisms.
Findings were shared and discussions were held with the research team members undertaking the RAM workstream to contribute to development of their statements and subgroups.
Recruitment and interviews
General practitioners
The GP Workforce Survey resulted in 2248 returned surveys (out of a possible 3370; 67% response rate). Of these, 1410 individuals (63%) had indicated their agreement to be contacted for interview. Nearly half (49%, n = 694) met the criteria for interview. Table 13 shows the number of GPs eligible for interview in each respondent category, the target number of interviews for each group and the final number interviewed.
| GP interview category | Number of interviewees | |||||
|---|---|---|---|---|---|---|
| Eligible for interview | Initial aim | Revised aim | Approached for interview | Agreed to interview | Interviewed | |
| Retired GPs | 22 | 10 | 8 | 16 | 8 | 7 (3 aged ≥ 60 years; 4 aged 50–59 years) |
| GPs intending early retirement (aged 50–59 years) | 299 | 10 | 8 | 20 | 9 | 8 (1 aged 60 years; 7 aged 50–59 years) |
| GPs on (n = 40) or intending (n = 314) a career break (any age) | 354 | 15 | 13 | 32 | 11 | 11 (7 on break; 4 intending break) |
| GPs who had quit (n = 5) or were intending to quit (n = 14) (aged 35–49 years) | 19 | 10 | 10 | 17 | 9 | 9 (4 quit; 5 intending to quit) |
| Staying GPs | 119 | N/A | 6 | 13 | 7 | 6 (aged 40–56 years) |
| Total | 694 | 45 | 45 | 98 | 44 | 41 |
Forty-one GP interviews took place: eight face to face, 31 by telephone and two by Skype. Interviews lasted 15–71 minutes (mean = 38 minutes). Interviewees were distributed across the south-west and comprised partner, salaried and locum GPs. Tables 43 and 44 in Appendix 19 illustrate participants’ demographic and practice characteristics (when known). Scheduling difficulties resulted in three GPs who had agreed to interview not being interviewed.
Stakeholders
Invitations were sent to 41 stakeholders and 19 agreed to be interviewed. Table 14 shows the stakeholders’ roles and the organisations they represented. Participants were distributed across the south-west.
| Role/organisations represented | Number of stakeholders | |||
|---|---|---|---|---|
| Aim | Approached for interview | Agreed to interview | Interviewed | |
| CCG | 2 | 10 | 4 | 4 |
| LMC | 2 | 9 | 3 | 3 |
| CQC | 2 | 2 | 2 | 2 |
| Regional organisation | 2 | 4 | 1 | 1 |
| GP with interest in workforce issues | 2 | 6 | 4 | 4 |
| Practice manager | 2 | 4 | 1 | 1 |
| Nurse practitioner | 2 | 1 | 1 | 1 |
| Other allied health professional | 2 | 1 | 1 | 1 |
| Pharmacist | 2 | 2 | 2 | 2 |
| Federation practice | 2 | 2 | 0 | 0 |
| Total | 20 | 41 | 19 | 19 |
Four stakeholder interviews were conducted face to face and 15 were conducted by telephone. Interviews lasted 17–73 minutes (mean = 43 minutes). Eleven of the stakeholders were, or had been, GPs in addition to any other role.
Key findings from interviews
To contextualise the findings, interview questions included an exploration and reiteration of the problems faced by GPs. It was clear that these were not ‘standalone’ issues but complex interactions of GP experiences. The problems/issues were divided into five main topics:
-
workload
-
GP health and well-being
-
support and relationships
-
finances, investment and fiscal reward
-
change, uncertainty and the future.
Three underlying themes were identified concerning the GPs’ experiences and perceptions of their working lives and environment:
-
identity and value
-
fear and risk
-
choice and volition.
General practitioners described a range of ‘push’ and ‘pull’ factors and how these influenced their own staying/quitting intentions and behaviours. Comments were also provided by stakeholders regarding GP experiences.
The following sections provide further details of the topics and themes related to the issues or problems identified by the participants and quitting decisions. These are followed by participants’ suggested ‘solutions’ to these issues, and the inherent tensions and contradictions that they identified within these.
Context and reiteration of issues faced by general practitioners working in direct patient care
Appendix 20 summarises the issues faced by GPs and concurs largely with what is already known from the literature (see Doran et al. 51 and Sansom et al. ;18 see also Chapter 2, Synthesis of qualitative studies). As this is broadly a reiteration of what is already known, and for brevity within this report, the findings are tabulated and summarised in Appendix 20.
Underlying themes that affect decisions to remain in or leave direct patient care
The analysis also identified three underlying themes that gave more in-depth understanding of the lived experiences of the GPs and helped to contextualise decision-making about remaining in or leaving direct patient care. The underlying themes were:
-
identity and value
-
fear and risk
-
choice and volition.
Figure 7 illustrates the multidirectional relationships between the problems and solutions, the underlying themes, and also the influence of tensions and contradictions (see Tensions and contradictions). The underlying themes are presented in detail with illustrative quotations (with supplementary quotations in Appendix 21).
FIGURE 7.
Illustrative model of the complexity and multilayered relationships between problems, solutions, GP perspectives and experiences.
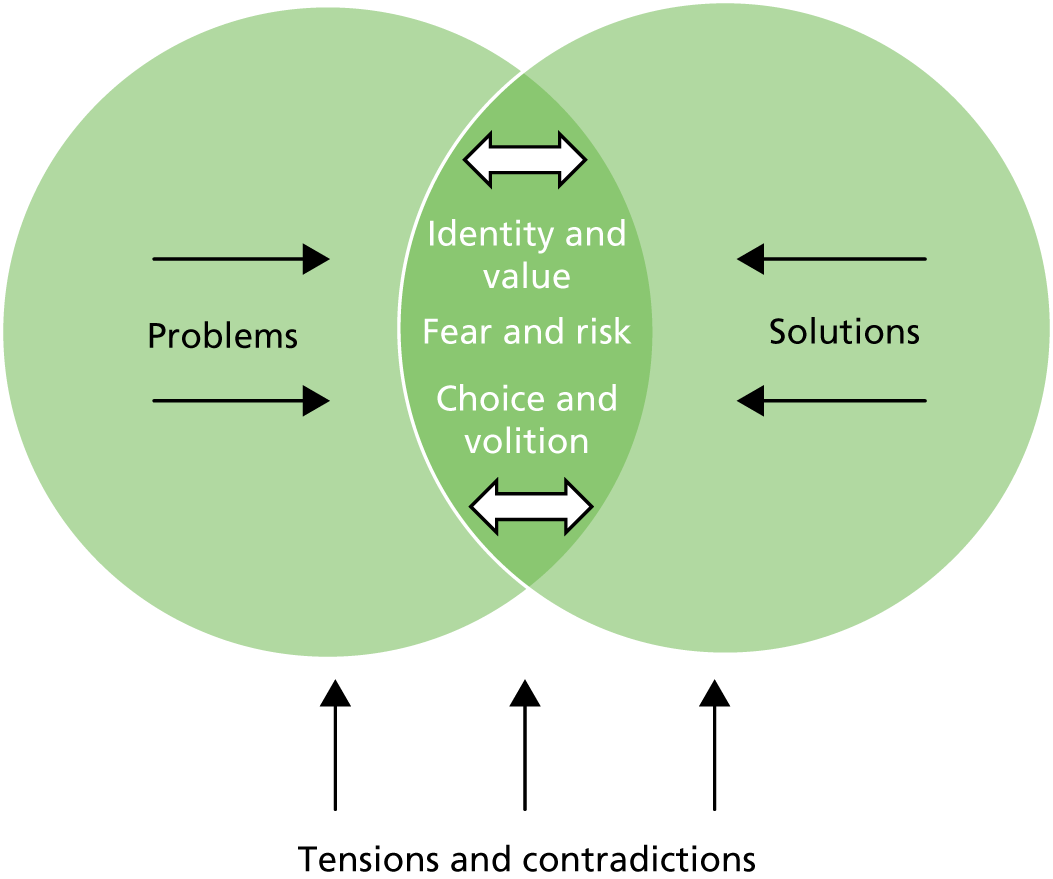
Identity and value
Participants described three key subthemes related to identity and value:
-
the identity of general practice as a profession lacks clarity and boundaries
-
GP identity, professionalism and morale
-
being listened to and being valued.
Participants discussed how changes within general practice had led to a lack of clarity of professional boundaries and realistic expectations of what general practice could (and should) deliver. They identified unrealistic expectations from patients, government and secondary care, and voiced their own uncertainty about the future of general practice, along with personal experience of changing roles and organisational structures and systems.
Tensions were noted between the interface of primary and secondary care, and it was felt that general practice tended to ‘pick up’ and manage aspects of care that should be delivered by other services. A common experience was that ‘the buck stops’ with general practice:
GPs being the out-of-hospital doctors have had to pick up everything. We have an artificial divide in hospital that if you are within the walls of the hospital you come under a specialist; if you’re outside it you come under primary care . . . And eventually the buck stops with the GP.
SH1006 – GP stakeholder
General practitioner identity, professionalism and morale
Many GPs felt that their professional identity and ability to practise in their preferred ways were being compromised. This was considered to be partly due to unrealistic demands, concerns about complaints, targets and guidelines, the complexity of cases and lack of time to address them, a lack of continuity and loss of autonomy.
General practitioners felt compromised when trying to deliver high-quality care within the constraints and burdens they experienced. Compromising could lead to cutting corners and/or a negative impact on the GPs’ own well-being:
GPs tend to go down one of two routes: they either – to cope with demand – start to cut corners . . . Or . . . you overburden yourself and you won’t cut corners . . . and that has its consequences at the end of the day.
GP322 – male, aged 40–49 years, locum GP, intending career break
‘Sacrifices’ were made in order to practise the kind of medicine they valued and to be a ‘good GP’:
. . . my practice is a high-earning practice, it’s a very efficient practice, but actually we spend a lot of money on our staff, so I don’t take home lots of money . . . we believe in providing personal care for our patients and that’s the sacrifice we decided to make to make sure we continue to do that.
SH1045 – CCG stakeholder
Morale and job satisfaction were influenced by enjoyment; however, general practice had become less enjoyable over recent years:
I stopped enjoying the job. I think that’s when I realised it was time to have a break.
GP412 – female, aged 30–39 years, GP partner, early leaver
The enjoyable aspects of the job included GP–patient interactions. However, it could be increasingly difficult to maintain continuity and doctor–patient relationships owing to part-time working and patient attitudes. Seeing only the complex patients [not the ‘people with things you can make better quickly’ (GP324 – female, aged 30–39 years, locum GP, intending career break)] made the role less enjoyable. Enjoyment also came from ‘being part of trying to figure out how the practice can deliver the best-quality care’ (GP509 – male, aged 40–49 years, GP partner, staying). Being part of a team and having supportive relationships with colleagues added to this.
Being listened to and being valued
General practitioners expressed their frustration over feelings of not being listened to or valued. They felt strongly that the government had failed to listen to them, to general practice as a profession, and to the BMA, about the impending workforce crisis. This was mirrored in matters relating to organisational change and demands on the service. When GPs did voice concerns or complain, the outcomes were generally unsatisfactory:
I don’t think politicians and managers necessarily manage professionals who complain, very well.
SH1006 – GP stakeholder
Participants highlighted the importance of feeling valued for one’s work, and the perceived lack of valuing of GPs by the general public, the NHS, the media and the government:
I think most people, if you ask them why they do jobs, it’s a complex mixture and a lot of it comes about being valued and appreciated. I mean, people always focus on incomes and things but, the more detailed the analysis is, it always comes back to things like being appreciated, feeling valued.
GP202 – male, aged ≥ 60 years, GP partner, intending retirement
Fear and risk
Participants described feelings of fear and anxiety that focused on different aspects of risk that had to be managed within the GP role. There was a general perception that risks had increased in recent years, practice had changed to accommodate those risks and the risks were ‘not proportional to the rewards’ (GP311 – male, aged 30–39 years, GP partner, intending career break). There were six subthemes:
-
risk to patient care and safety
-
fear of complaints and being sued
-
risk to professional status and identity
-
risk to own health and well-being
-
uncertainty about the future of general practice
-
financial risk.
Risk to patient care and safety
Participants described concerns about the safety of practice and the quality of care being delivered to patients. This arose from having to manage imposed ‘unmanageable’ workloads, and focused primarily on the large number of decisions that had to be made, the complexity of cases and the impact of accumulative decision-making throughout the day:
. . . you have to balance priorities and triage things and I think . . . the busier you get the more dangerous your decision-making becomes on that front, and the riskier it can get.
GP510 – female, aged 40-49 years, GP partner, staying
Fear of complaints and being sued
There was an acknowledgement that general practice has an inherent level of risk that may be different from other aspects of medicine:
I’m the paid risk-taker for the NHS . . . with specialists, everything will be excluded but it will cost a fortune. If you see a GP, it will be cheap, but occasionally things will go wrong. And that’s the nature of the risk.
SH1045 – CCG stakeholder
Owing to the nature and pace of work, ‘there was potential for error’ (GP101 – female, aged ≥ 60 years, GP partner, retired) and GPs who had not made a mistake were regarded as ‘fortunate’ or ‘lucky’ (SH1001 – GP stakeholder; SH1040 – CCG stakeholder).
Risk was exacerbated by the perceived culture of patients being encouraged, and having easy routes, to complain, contrasted with a lack of support and little recourse for GPs:
. . . there’s no recourse . . . patients can complain about you and you’re the one that gets penalised repeatedly.
GP322 – male, aged 40–49 years, locum GP, intending career break
The fear of making mistakes led to some GPs practising more defensively (e.g. spending more time writing notes, and choosing face-to-face rather than telephone consultations), thus adding further to their workload. This was directly linked to fear of litigation. One stakeholder termed this ‘legal-based medicine’:
We don’t really practise evidence-based medicine; we practise a sort of legal-based medicine.
SH1001 – GP stakeholder
Defensive practice was also seen as a response to patient expectations, with one GP describing the feeling of ‘I’d better give this person what they want or they will complain!’ (GP417 – male, aged 40–49 years, salaried GP, intended early leaver).
When complaints had been made, or GPs had been sued, the process had been drawn out and stressful for GPs. As well as fear about the outcome of any complaint, it was noted that complaints ‘wound the doctor severely . . . When you’re kicked in the teeth like that, either by the government or the patient, it really hurts’ (SH1006 – GP stakeholder).
Risk to professional status and identity
There was general agreement that ‘to survive in today’s NHS you have to be comfortable taking risks and cutting corners’ (SH1040 – CCG stakeholder). However, GPs reported tension between ‘cutting corners’ and being thorough and conscientious in their practice:
. . . that’s a very uncomfortable position for GPs in particular to be, and I think that then can cause them some problems as to quite what to do and there was a lot of feeling a bit trapped, I think.
SH1027 – LMC stakeholder
Risk to own health and well-being
The consequences of experiencing fear and anxiety, and of having to manage risks, were noted as potentially affecting the GP’s own health and well-being. Participants described seeing GP colleagues going off sick as a result of the pressures of work. Some GP participants also had direct experience of work negatively affecting their own health:
I was just working at such a pace and I knew I was making myself ill.
GP201 – female, aged 50–59 years, locum GP, intending retirement
One GP described how the fear of becoming ill compounds the fear of making mistakes:
You can’t make yourself ill. If you make yourself ill, you’re going to make mistakes anyway and no one wants that.
GP311 – male, aged 30–39 years, GP partner, intending career break
Uncertainty about the future of general practice
Some participants had a pessimistic view of the future:
There seems to be a lack of belief that the NHS will survive, let alone GPs [as] part of it.
SH1042 – CQC stakeholder
They described how this directly affected decisions about staying in or returning to direct patient care. One GP described a colleague’s decision to leave:
I prefer to get out of this before it gets worse, which is sort of the sense that it’s only going to get harder.
GP510 – female, aged 40–49 years, GP partner, staying
A GP on a career break described uncertainty about the situation improving as a barrier to returning to practice:
. . . it feels like something in crisis and who wants to jump into that?
GP307 – male, aged 50–59 years, GP partner, on career break
Within this uncertainty was also frustration at a lack of ability to determine the future of general practice, and the lack of a unified model that could be implemented:
There is so much uncertainty and the biggest frustration of being a GP is that you’re beholden to whatever the NHS England decision is, or whatever the Department of Health’s decision is . . .
GP501 – male, aged 40–49 years, GP partner, staying
Financial risk
Participants described how the risk of financial investment in a practice was perceived to be greater than in previous times and how this was both a burden and a barrier to investment. GPs felt that they were exposing themselves to the risk of personal debt if they bought into a practice, and also to increased stress. Whereas, traditionally, GPs may have been willing to make a long-term financial investment, other pressures on personal finances, uncertainty about the viability of long-term commitment and concerns about the future of general practice meant that younger GPs were reluctant to invest:
. . . if I had been willing to take on the whole practice and just tough it out, there’s a chance that in 20 years I would have £800,000 of equity in a building, but there is an equal chance I would burn out, be reported to the GMC, gone crazy . . .
GP311 – male, aged 30–39 years, GP partner, intending career break
Older GPs who had previously invested were also experiencing stress and anxiety owing to concerns about changes to practice mortgages, the threat of having to make staff redundant or practice closure, and responsibilities arising from joint civil liability for a practice.
Choice and volition
The theme choice and volition concerns the feelings that participants had about making their decisions to leave or to remain and the degree of choice they felt they had.
Four subthemes were identified:
-
accumulation, compounding and combinations of factors
-
GP resilience
-
decisions do not happen in isolation
-
the only route left.
Accumulation, compounding and combination of factors
Many GPs described a range of inter-related factors that had contributed to their decision-making: factors relating to workload, their practice, their personal circumstances and the wider social context (e.g. ‘GP bashing’). GPs described how these factors accumulated and how each had a compounding effect, to create a ‘perfect storm’ situation over time that ultimately could lead to decisions to leave or to reduce their hours. Most GPs described this process as happening over a period of time:
It’s really like an insidious, drip drip drip thing really that’s been happening for 10 plus years, really. There’s more and more and more things coming our way.
GP207 – male, aged 50–59 years, GP locum, intending retirement
For some GPs, there had been a key point at which a range of factors came together in a much shorter space of time and led to a quicker decision-making process:
. . . everything happened at once: the menopause, the awful complaint, my in-laws being ill, the locum work that I wasn’t particularly enjoying . . . and I got to the stage of thinking, ‘I don’t have to do this. I’m not enjoying it. Why am I doing it? Let’s just stop and see if I miss it’.
GP108 – female, aged 50–59 years, GP locum, retired
General practitioner resilience
Participants noted that GPs’ resilience had been eroded over recent years; however, there was strong agreement from a number of GPs that the solution to the current workforce crisis was not simply to make GPs more resilient:
I teach people stress relief, self-care, time-management if you like. But that is the wrong approach from my point of view because, if you look at doctors, these are people who are highly resilient already . . . ultimately if you are teaching burnt out, stressed people about . . . self-care, self-worth, the only consequence would have to be to leave that system . . . the system is so cruel . . . You’ve got to make changes to the system. Just supporting people is the wrong approach.
GP404 – female, aged 40–49 years, GP locum, early leaver
Erosion of resilience was linked to a loss of control:
. . . not feeling in control of where the money’s coming from, not feeling in control of your future because if you’re going to have contracts imposed on you by the government, you’re not in control. So that’s where I feel the loss of resilience is coming from, primarily.
GP505 – female, aged 40–49 years, salaried GP, staying
Those participants who had personal experience of GP burnout, as well as those who had observed the impact of work-related stress on colleagues and peers, all agreed that the system had to be addressed rather than there being a focus solely on increasing GP resilience:
If the purpose of resilience is to enable the same workforce to cope with every increasing demand, that’s not on, we actually have to make the job doable.
SH1006 – GP stakeholder
Decisions do not happen in isolation
Participants identified different routes to decision-making about whether to remain in, take a break from/return to or permanently leave direct patient care. For some, there was a stepped approach that involved reducing hours or taking a career break before deciding to permanently leave. Many of the GPs described this stepped process as coping strategies adopted at different stages in their careers.
Four key coping strategies were identified:
-
reducing hours/number of sessions worked
-
change in role (e.g. from partner or salaried GP to locum)
-
taking a career break
-
portfolio working.
These strategies generally illustrated attempts by the GPs to make their working lives more sustainable:
I have got friends in their late 40s who’ve just actually had enough . . . They’ve given up on being partners, they might be doing some locum sessions, but actually, they’re back in control . . . I’ve still maintained working half-time in the practice but I have other stuff happening on other days to keep things in perspective . . . I admire anybody who does the job full-time now, because I don’t think I would be able to sustain that myself, personally.
SH1011 – LMC stakeholder
However, there was also awareness that individual decisions often had an impact on colleagues, peers, patients and the profession in general, for example in terms of the decision to retire early from a partner position when the practice was experiencing recruitment difficulties, or the decision to work part-time knowing that others would need to provide cover:
And if individual partners jumped ship, it was incredibly disruptive . . . Certainly, that had a knock-on effect, not just within the doctors who are the partners, but the wider staff, the nurses, the receptionists, everybody. And it was a less good place to come to work.
GP107 – male, aged 50–59 years, GP partner, retired
For some, the decision to leave or stay was interpreted as being for their own best self-interest; however, for others, there was also an altruistic element:
The worry is about being miserable around people who don’t need misery . . . Like I say, sever the gangrenous limb and you save the patient! And it’s funny feeling like that, I’ve never thought of myself as a gangrenous limb, but actually perhaps that’s what happens when you get older in a practice. That is coming to terms with the fact that the best thing you could do is leave so that actually you’re not polluting in any way.
GP212 – male, aged 50–59 years, GP partner, intending retirement
The only route left
The range and combination of push and pull factors were individualised, as were the decisions the GP participants made about their role, number of sessions and when to leave or return to direct patient care. Concern was expressed about GPs reaching a point at which the only route left was to ‘vote with their feet’:
I’ve just become more and more desperate . . . in past years I have just felt terribly angry with the way things are going and now I think, ‘I can’t actually do anything more about it’. And if I could do anything but vote with my feet, but ultimately it’s the only vote which they’re going to listen to. And one does definitely feel guilty about leaving one’s partners trying to . . . keep the boat afloat as it were. But, I can’t . . . there just comes a point, you’ve got one life and one can’t sacrifice oneself totally, so, yeah, I’m gonna go.
GP208 – male, aged 50–59 years, GP partner, intending retirement
Reasons for retiring, leaving or taking a career break
Participants recognised that an accumulation of factors generally led to decisions to leave direct patient care. Different combinations of factors could feature, and there was often a compounding effect. For some, depending on the combination of push and pull factors they experienced, leaving general practice, retiring (often earlier than planned), taking a career break or substantially reducing the number of hours worked was the only solution they saw as being available to them.
Appendix 22 details the variety of stated factors for each GP interview category that contributed to leaving, taking a break from or remaining in direct patient care, and (when known) the intentions of GPs at the time of the interview.
Possible solutions/participant suggestions and experiences about what might help to retain experienced general practitioners
Participants suggested a multilayered and multifactored approach to retaining GPs:
. . . the answer is multilayered. The issues – from a top-down perspective – there are issues around the NHS valuing what we’re doing, giving us enough money to deliver high-quality patient care, at scale. There are issues around the morale and how the media portrays what we’re doing, and how other elements of the profession perceives what we’re doing. And then at a local level, it’s about making sure that we’ve got space for GPs to figure out how to run the system better and more effectively with less money and with all the other pressures that we’ve got to factor in. And it’s also about making sure that the job is enjoyable on the ground. For people to be able to want to stick in the practices. Because, if everybody’s just going to locum, it’s going to fall apart quite quickly. And so, there’s no one thing that’s going to make a big difference. It’s got to be all of those factors, all put together.
GP509 – male, aged 40–49 years, GP partner, staying
Three key topics were discussed:
-
changes to the way primary health care is financed, organised and delivered
-
showing that the GP role is valued through support, flexible working, streamlined return-to-work processes and changes to the complaints system
-
creating a new culture and systems to help GPs meet the demands of their job, including supporting GP well-being, changing the appraisals and revalidation system, improving the primary–secondary care interface, branding and defining general practice and managing patient expectations.
Further details are provided in Appendix 23.
Tensions and contradictions
Participants described inherent tensions and contradictions within the current structure and delivery of general practice. Solutions that could potentially benefit some GPs could simultaneously disadvantage others. Thus, participants noted that there was no one ‘ideal’ solution to address the workforce crisis.
Six topics were identified:
-
GP roles – individual GP choices versus impact on practice and colleagues
-
GP health and well-being – the need to maintain good health versus stresses and barriers to this
-
expanding the practice team – optimum team size, composition and funding versus availability, confidence and trust
-
practice size and federations – need to be responsive to local population versus optimum business models
-
access to GP services – managing workload versus availability of resources and impact on GPs and patients
-
how practices cope – being proactive versus being reactive.
These topics are discussed in Appendix 24.
Discussion
This study identified three underlying themes that may influence GPs’ experiences and decisions about remaining in or leaving direct patient care, namely (1) identity and value, (2) fear and risk and (3) choice and volition. The findings also provided insight into some of the tensions and contradictions that exist within the problems and potential solutions in the GP workforce crisis, suggesting the need for detailed consideration of the pros and cons of any proposed policy or strategy.
Le Floch et al. 103 found general profession-related themes and specific GP factors related to GPs’ job satisfaction (a key aspect of retention identified in the systematic review). Also common to other professions, they found that workload, income and the balance between them, and having responsibility and recognition for work were key factors in satisfaction. Specific GP factors included feeling competent; being able to be the kind of GP they wanted to be; the GP’s own good health; opportunities for intellectual stimulation, variety, professional challenges and continuing professional development; and relationships with patients and with other professionals. The current study identified similar factors and, because a number of these could be generalisable to other professions, there is an opportunity to explore how generic workplace theories and models could inform strategies and policies aimed at GPs. There is a paucity of applied theories in the GP workforce literature. Drawing on the wider literature (including from occupational psychology and occupational health) has the potential to add to current understanding of GP workforce issues. Such theories include those related to organisational justice/fairness, psychosocial safety climate (PSC)/psychological health and safety, burnout and positive mental well-being. These may help to better understand the impact of the different factors and underlying themes (and therefore how to mitigate them). For example, theories of organisational justice could help to inform the theme identity and value, psychological safety climate could inform fear and risk and positive mental well-being could inform choice and volition. The following discussion provides further details and illustrates why a climate that is perceived as fair and safe and that promotes GP well-being could help to retain GPs, and how the study findings suggest that this climate is currently lacking for many GPs.
Many of the GPs described their role as a ‘vocation’, emphasising that ‘it’s not about the money’. However, the large majority of those interviewed felt let down by what they perceived as a lack of fairness within the primary care system. Organisational justice theory posits that judgements of fairness stem from the perception of input or contribution to a role or job (e.g. knowledge and effort) in relation to outcomes (e.g. pay or recognition). 104 Heponiemi et al. 105 found a decrease in job satisfaction and job involvement when GPs perceived some degree of unfairness. Participants in the current study repeatedly described a perception of unfairness and feeling undervalued, sometimes using colloquialisms such as ‘GP bashing’. Miller106 suggests that individuals experience injustice when they perceive that they are treated in a way that they do not deserve, or that they are not treated as they deserve to be. In the current study, unfairness and undervaluing were described by participants as stemming from within individual practices (e.g. descriptions of bullying or allocation of responsibility), or from perceived constant demands being placed on GPs (e.g. by government guidelines, and unrealistic expectations held by the government, patients and the media).
A study of Finnish physicians found that problems with their health could push older physicians towards retirement. 31 Organisational injustice and low job control added to retirement intentions. Therefore, it seems reasonable to suggest that supporting GP health, and promoting control opportunities and organisational justice, could reduce early retirement and potentially assist GPs to remain in direct patient care.
Sutinen et al. 107 explored organisational fairness among hospital physicians. They found an association (for male doctors) between low organisational fairness and the risk of psychological distress (mediated by decreased job control and increased workload). Dollard and Bakker108 offer a theoretical model of PSC that relates to policies, practices and procedures to protect workers’ psychological health and safety. PSC affects a range of psychosocial factors, including work pressure and job control. They conclude that PSC is a logical focus for workplace stress intervention, through its relationships with psychological health and job demands. GPs in the current study suggested that the current climate of general practice was one of high risk, and they identified elements that could cause them fear and anxiety. Thus, creating a ‘fairer’ and ‘safer’ work environment for GPs could be key to helping decrease the fear and risk they currently experience, and the negative outcomes associated with this.
There also needs to be a focus on GPs’ well-being. Orton et al. 109 found that 46% of UK GPs reported high levels of emotional exhaustion, 42% reported depersonalisation and only 34% reported personal accomplishment [the three components of burnout as measured by the validated Maslach Burnout Inventory (MBI)110]. The MBI defines burnout as an imbalance between the demands and the resources available to the individual. GPs in the current study talked about different coping strategies they had adopted (e.g. part-time working) to try and balance their personal resources (e.g. time, stamina) with the demands of their role (e.g. high workload, complex cases, long working days). Torppa et al. 96 found that emotional exhaustion (a signal of the development of burnout) was common among Finnish GPs. It was associated with older age, high workload, fear of medical errors and feelings of isolation at work (all factors described by GPs in this current study). Torppa et al. 96 concluded that GPs should receive more support throughout their careers, including clinical supervision and peer support.
Murray et al. 98 discuss rising levels of job-related stress and falling job satisfaction for GPs and the need to protect GPs’ mental health and to promote positive mental well-being. However, their systematic review found only four studies detailing successful interventions for GPs’ self-reported mental health, revealing a research and knowledge gap about interventions to support GP positive mental health and well-being. GPs in the current study felt strongly that the ‘answer’ was not simply to make GPs more resilient (changes were required at a systems level). However, supporting GPs’ positive mental well-being could also be important.
The findings from this qualitative study suggest that addressing GPs’ well-being, psychological health and safety, and organisational fairness (including job control) could all be important elements of policies and strategies to help retain the experienced GP workforce. Appendix 25 offers recommendations for the content of policies and strategies based on the findings of this qualitative workstream.
Strengths and limitations
Strengths
A key strength of this study was the number of in-depth interviews conducted with a range of GPs and with stakeholders. These provided rich data and the opportunity to explore similar and divergent opinions and experiences. Sampling GPs from the survey returns gave a large pool to draw from and also provided the opportunity to ensure a maximum variation sample. Given the expressed time pressures and constraints of many of the respondents, it is gratifying that so many GPs were willing to engage beyond the brief survey stage of this programme of research. It is also notable that the GPs who were interviewed were all forthcoming with their views and experiences and were willing to answer the questions from a personal perspective and to consider the wider context of the experiences of their colleagues and peers. The identification of stakeholders enabled us to approach participants across the south-west of England, who had a range of roles within key organisations. Researchers were able to offer flexibility in the mode and timing of the interviews.
Patient and public involvement and project team discussion enabled modification of the original sample targets to ensure that the views and experiences of ‘staying’ GPs were also captured. The PPI group and the GP representative supported the analysis process and reflective practice.
Finally, the conduct of a previous, preliminary study by one of the qualitative researchers (AS) contributed further to the analysis and understanding of the findings and implications of the current study. Having a team of qualitative researchers (AS, RT and SGD) engaged in this workstream added to the rigour and trustworthiness of the analysis process and the findings presented.
Limitations
The main limitation was that the GPs were self-selecting: they responded to the original survey and agreed to be contacted about possible interview, and they also consented to interview. It is possible that those GPs who were not available for interview may have had different experiences to report. Although self-selection is a limitation of the current study, given the similarities between the findings of this study and those identified within the literature review, it seems likely that the interview sample was not particularly unusual in their views or experiences.
Of the survey returns (workstream 1), 93% of respondents were white and 96% of those eligible for interview were white. GPs from other ethnic groups were approached but none agreed to be interviewed.
It is also of note that all of those GPs interviewed and who were attached to one practice were from practices rated as ‘good’ or ‘outstanding’ by the CQC. Data were not collected to determine whether or not any of the locum or retired GPs were attached to practices rated as ‘inadequate’ or ‘requires improvement’. However, the interview sample reflects the regional CQC reporting data: only 4% of practices in the ReGROUP south-west catchment area (see Table 1, based on 1 December 2015 data) were rated as ‘requires improvement’ or ‘inadequate’, and the majority (89%) were rated as ‘good’ [also confirmed for the data collection period using data from the archived CQC Directory with Ratings, May 2016; see https://drive.google.com/drive/folders/0B1jvn_rdpdEzX3RxZ21kZHdkYTA (accessed 26 April 2017)].
Finally, a proportion of time was initially spent analysing CQC reports. One output of this part of the study was questions and case examples that could be used as prompts during interviews. However, these were not necessary for the majority of the interviews as participants (in general) required little prompting to elicit their responses.
Patient and public involvement group comments
A meeting with five members of the PPI group was held (May 2017) to discuss the findings of the qualitative workstream and to gain their perspectives on the underlying themes.
The group expressed general sympathy towards, and understanding of, the pressures that GPs can experience, and noted the potential negative impact on patients of GPs being under pressure. The PPI members noted that there is an opportunity, and desire, for patients to be more involved in supporting GPs and the organisation and delivery of primary care. There was agreement that more involvement and inclusion of patient participation groups (PPGs) could benefit GPs: positive interactions with patient representatives could help to reduce GP anxiety (e.g. about complaints). However, it was also noted that, for PPGs to be of value to GPs, there was a need for practice staff and patient representatives to be perceived as ‘all being on the same side’, and for GPs and non-clinical staff to trust patients as part of the practice team. The PPI members felt that there was a role for PPGs to be supportive of GPs, namely helping GPs to feel more valued. They identified a ‘positive feedback loop of fear’: when doctors change their working practices, patients change their habits in response, but without clear communication this leads to anxiety, fear and irritation in both groups. The PPI members noted that more involvement and inclusion of patients, along with good communication, could aid the relationship between patients and practice staff and, thus, help to address patient demands and expectations. The PPI members suggested that involving PPGs as part of the practice team could help the identification of models and examples of good practice that could then be shared by PPGs with other practices.
The discussion also highlighted some of the limitations or disadvantages of PPGs: they can be used as platforms for disgruntled patients, they may not be very representative of the local population and they can feel unwanted by the practice staff (clinical and/or non-clinical). Thus, the PPI group identified an opportunity for proactive recruitment of PPG members and promotion of a culture of mutual support and trust.
How workstream 3 adds to ReGROUP
The findings from the qualitative workstream informed the qualitative modelling and verification of findings from the evidence synthesis of qualitative studies, the background contextual information and the development of statements and subgroups used for the RAM workstream. They also helped to inform the content and direction of the stakeholder consultations.
Recommendations directly arising from workstream 3 are provided in Appendix 25.
Conclusion
The breadth of issues influencing GPs’ decisions to leave direct patient care has been extensively reported. This current research found that the same issues are still identified by GPs, at a time of rapid introductions of policy and strategy aimed at ameliorating the workforce crisis. This study indicated that, in order to address the issues, each issue should not be taken in isolation. Rather, the findings from this study showed that (1) factors and issues need to be addressed collectively, (2) there are inherent tensions and contradictions within potential solutions that need to be considered and (3) there is also a need to address GPs’ lived experiences of their work and role in the current health-care climate. The lived experience was illustrated through three underlying themes that emerged from the data: (1) identity and value, (2) fear and risk and (3) choice and volition.
The application of theories and models may help to further an understanding of the implications of GPs’ feelings and experiences (the underlying themes) on GP retention. Use of evidence from occupational and workplace literature adds weight to the argument that solutions should not be ‘sticking plasters’ but rather implementable policies and strategies that will help to (1) increase the perceived value and clarify the identity and future of general practice, (2) reduce the levels of fear and risk that GPs are experiencing (to acceptable and manageable levels) and (3) provide GPs with feasible, acceptable and sustainable routes to remaining in direct patient care.
The findings from this workstream add to the ReGROUP study, providing further insight into ways to help retain the experienced GP workforce and giving a ‘voice’ to GPs at this pivotal time of change and initiative.
Chapter 5 Workstream 4: the RAND/UCLA Appropriateness Method
Introduction
The RAM is an internationally recognised technique using a panel of experts to classify procedures or items relating to practice and policies on ‘appropriateness’. 111 The consensus between panellists is used to inform the content of policies or practices under development. The RAM panel method is commonly used when the evidence base underlying policies or practices may need to be tailored for a particular context or group before being applied, or when there is limited evidence to support decision-making. This modified Delphi technique specifically seeks panellists’ own experiences and observations as part of informing the appropriateness of different policies or practices.
The RAM methodology is typically applied to clinical practice, such as in the development of clinical guidelines and recommendations;112–114 however, there are examples of its use in developing policy and organisational interventions. Wright et al. 115 applied the approach to the development of interventions to support patients on sickness absence from work; Bell et al. 116 used the RAM approach for identifying ‘necessary’ items for assessing patient safety in general practice. These studies illustrate the potential for the RAM methodology to be used in health policy at a local and national level.
Two research questions were addressed in this workstream:
-
What are the potential policies and strategies that might facilitate the retention of experienced GPs in direct patient care and support the return of GPs to direct patient care following a career break?
-
How appropriate are these policies and strategies and how feasible are they to implement from the perspective of GPs?
The RAM approach was used to assess the appropriateness and feasibility of policies and strategies aimed at improving the retention of GPs. The policies and strategies selected for assessment were informed by the systematic review, census survey and qualitative interviews with GPs.
Methods
Study design
A RAM panel was used to assess the appropriateness and feasibility of candidate policies and strategies and involved two rounds of data collection via an online survey. RAM panels typically consist of between 7 and 15 members, selected on the basis of their expertise in the topic under consideration. 111
We aimed to recruit 15 panel members to allow for attrition and to secure responses from at least seven respondents completing both rounds of data collection.
Eligibility criteria
The composition of our panel was limited to GP partners and GPs working in national stakeholder organisations with a role in workforce planning, as they represent an influential group in primary care who are directly responsible for managing GP recruitment/retention. These participants are also the intended recipients of the policy and strategies, and are employers of other GPs and primary care teams with responsibility for direct patient care within their general practices. By maintaining homogeneity in the composition of panel membership, there is a higher likelihood that the panel would reach consensus and the findings would be of wider applicability to GPs with managerial and operational responsibilities in primary care.
As challenges to GP recruitment and retention might plausibly vary by geographical setting,117 we planned to recruit GP participants from general practices located in south-west England (urban and rural areas) and London (high population density urban areas), as well as GPs working in relevant national stakeholder organisations including the RCGP and the BMA.
Sampling procedures
Potential participants were identified through different mechanisms for the south-west of England, for London and for the national stakeholder organisations.
In the south-west of England, the National Performers List of all GPs registered to practise in south-west England was used (see Chapter 3). Participants in the qualitative research were excluded to avoid individuals being invited to give substantial time in the same research project. We then purposively sampled 34 GP partners from the south-west, ensuring that an equal number of GPs were identified from urban and rural settings.
As the National Performers List was not available for London, we constructed a sampling frame from publicly available information. The process included collating information on all CCGs in London and then restricting the sample to 12 CCGs with the highest population densities. A list of all practices, including the number of GP partners at each practice, was then collated using information published by 12 CCGs. The sample of 16 practices on the list was then selected at random and the names of individual GPs were extracted from the websites for the selected general practices. In each practice, one of the partners was picked by the researcher to be contacted.
The south-west of England and London samples were then combined into one list (50 GPs) and 25 individuals were selected at random (16 from the south-west and 9 from London) and invited to participate.
Representatives from national stakeholder organisations were identified using expert knowledge and snowballing techniques. We identified key organisations and individuals involved in recruitment and retention issues for GPs such as the Deaneries, BMA, RCGP and the Nuffield Institute. A total of seven individuals were identified and approached to take part, with individuals asked to nominate another person from their organisation to take part if they were unable to do so themselves.
Participant recruitment
Potential participants were sent a recruitment pack consisting of a covering letter from the research team and a participant information sheet. Invitations were sent electronically when possible and by post for all other potential participants. A reminder invitation pack was sent within 2 weeks. Interested participants were provided with a link to an online form and asked to complete it to indicate their willingness to participate. Following agreement to participate, members were provided with further information via e-mail and informed of the dates of the two rounds of data collection (see Appendix 26).
Data collection
Developing survey materials
Evidence summary
Potential policies and strategies were developed into summarising statements (hereafter ‘statements’) for the RAM panel to consider. These statements were informed by (1) the best available research evidence from the systematic reviews and key reports with research literature reviews, (2) pre-existing UK policy documents and recommended areas for future development linked to GP retention (as of 17 January 2017) using online government publications89,118 and direct communications, when required, with lead contributors, and (3) the developing evidence-base derived from ongoing research undertaken as part of the ReGROUP project.
Evidence from two systematic reviews [Anderson et al. 119 (unpublished ReGROUP workstream) and Verma et al. 120) and two main reports (Barriball et al. 121 and Peckham et al. 122) provide the evidence base for this study.
Owing to the wealth of evidence from reviews, data were not routinely sought from individual studies, with the notable exception of two recent studies testing the development of interventions for retention of GPs in England: Doran et al. 51 and the Ipsos MORI 2015 report. 81
We drew on the plethora of current/forthcoming policies and strategies being proposed/implemented relating to the General Practice Forward View for England,89 which builds on some of the jointly agreed actions through the Building the Workforce 10-point plan. 118
The same key sources of evidence were also used to populate the evidence summary provided to panel members to support their completion of the online survey (see Report Supplementary Material 2). The summary of the key research evidence sources and the individual government policies were included as the appendices within the evidence summary document. This summary included three short sections: (1) introducing the RAM process and the definitions for the ratings, (2) a brief overview of the key sources of research and published sources and (3) an overview of the current policy context.
Statement generation
The statements were based on potential policies or strategies that may provide support and incentives to retain GPs in direct patient care (i.e. prevent them reaching the point of deciding to leave or to change their mind about leaving), slow down the pace of exit when it is inevitable or enable faster and smoother entry/re-entry after a period of absence. In developing and organising the potential policies and strategies, we focused on areas linked to GP job satisfaction as well as workforce-related topics, such as professional development, and incentive and support schemes for retention. The following inclusion and exclusion criteria were applied.
Inclusion and exclusion criteria
Inclusion criteria:
-
Policies and strategies extracted from key sources that have already been identified by research, national policy or equivalent publications in our selected areas of investigation.
-
Novel policies and strategies that addressed known barriers to and facilitators of increasing retention, reducing intention to leave or encouraging re-entry into direct patient care (as identified from the key sources and internal contributions from the ReGROUP workstreams).
-
Policies and strategies that build on known and existing schemes or approaches in order to increase the potential impact on increasing retention, reducing intention to leave or encouraging re-entry into direct patient care. The intervention(s) proposed or tested may also be within the context of increasing job satisfaction, which was considered to be an influential factor for GP retention.
Exclusion criteria:
-
The policies and strategies that did not fit the UK general practice context in terms of how GPs, practices and commissioning are managed.
-
Policies and strategies for which it is estimated that it would take > 5 years to implement (e.g. increasing medical student numbers), and/or for which a direct impact on retention rates is unlikely to take place regardless of the time frame.
-
Policies and strategies that are not described in current research and policy documents. Policy documents include innovations that might plausibly be used to facilitate GP retention but that were untested or not specified within the literature.
One area that met the inclusion criteria, but was subsequently excluded after discussion with the research team, related to interventions of extended roles for non-GP health-care practitioners (e.g. extended roles for practice nurses). Although such strategies might clearly plausibly influence GP retention by having an impact on job satisfaction and working conditions (e.g. by reducing workload), incorporating this within this present research would have required generating a very substantial number of statements given the plethora of new roles currently emerging in primary care (e.g. extended nursing roles/clinics, or embedding physician assistants or pharmacists in general practices). The simple number of data would, it was judged, have the potential to distract and undermine the main focus of the research. To minimise the burden on panel members and to facilitate the research focus and process, this area was therefore omitted.
The policy and strategy areas were developed through two facilitated sessions with the ReGROUP researchers (including the leads from all the workstreams) and the PPI leads. The discussions were focused on prioritising important concepts and their definitions, and the potential subgroups of GPs (e.g. based on age, or geographical differences) identified through the research and policy literature as potentially requiring different policies or strategies to facilitate GP retention. One patient representative workshop was held in October 2016 to gather feedback on the scope of the policy and strategy areas and the panel membership.
Following this exercise, statements were generated relating to 54 policies and strategies presented under three different ‘levels’ for implementation (i.e. national/regional initiative, general practice or individual GPs). For the purposes of the online survey, these were presented as 11 section headings, and each policy and strategy was converted into a statement. Some policies and strategies could be applied differentially to different settings or groups, referred to here as subgroups (i.e. all general practices/employers or just for general practices/employers operating in traditionally ‘hard-to-recruit’ settings), as compulsory or optional for implementation, or other GP subgroups (by eligibility to retire). Therefore, there were multiple statements for some policies and strategies based on the applicable subgroups, resulting in a total of 100 statements to be rated in the online survey. Table 15 provides an overview of the number of policies and strategies by levels and subgroups. A full list of the statements is provided in Appendix 27.
| Level | Number of policies and strategies | Number of subgroups | Use of subgroups in the statements | Number of statements |
|---|---|---|---|---|
| National/regional level | ||||
| Section 1. Supporting areas based on risk | 10 | 2 | Compulsory/optional implementation | 12 |
| Section 2. Encouraging growth of new general practices and systems | 5 | 2 | All practices/only those in traditionally ‘hard-to-recruit’ settings | 6 |
| Section 3. Marketing-based interventions | 3 | 0 | 3 | |
| General practice level | ||||
| Section 4. Focusing on GP returners | 3 | 2 | Compulsory/optional implementation | 4 |
| Section 5. Flexible working and managed exits | 6 | 0 | 6 | |
| Section 6. HR management for GPs | 5 | 2 | All practices/only those in traditionally ‘hard-to-recruit’ settings | 10 |
| GP level | ||||
| Section 7. Health and well-being | 3 | 3 | For all GPs/those nearing retirement age and who could take their pension/those not nearing retirement age and who could not take their pension | 9 |
| Section 8. Professional support | 3 | Three of one subgroup and two of another subgroup | Subgroup 1. For all GPs/those nearing retirement age and who could take their pension/those not nearing retirement age and who could not take their pension | 8 |
| Section 9. Support for portfolio working | 4 | Subgroup 2. Compulsory/optional implementation | 15 | |
| Section 10. Employment, contracts and transition | 6 | 3 | For all GPs/those nearing retirement age and who could take their pension/those not nearing retirement age and who could not take their pension | 18 |
| Section 11. Additional support for GPs nearing retirement age and who could take their pension | 6 | 2 | GPs who have not encountered any concerns in the previous revalidation or appraisal processes/for such GPs who would like to work with a specified and limited scope of practice | 9 |
| Totals | 54 | 100 | ||
Survey procedures
Panel members were invited to complete the two rounds of data collection via an online survey, with paper completion available on request (requested by one participant). The first round of the online survey took place in February 2017 and the second round took place in April 2017.
In round 1, 1 week before the online survey was activated, participants were e-mailed with instructions on how to complete the online survey, with a username and password unique to that individual, and an electronic copy of the evidence summary (see Report Supplementary Material 2). The potential policies and strategies were presented as statements in the online survey link for rating and also sent as an electronic copy in the e-mail. Participants were asked to use their professional judgement and the best available evidence to rate the statements on ‘appropriateness’ of the policies and strategies. Free-text comments were invited at the end of the questionnaire. The panel was given 4 weeks to complete the online survey, with a reminder e-mail sent within 10 days to those who had yet to respond. An interim analysis was then undertaken, with a panel median score calculated for each statement and degree of consensus between panel members noted. The subset of statements identified as ‘appropriate’ based on first-round ratings was then included for ‘feasibility’ ratings in the second round.
In round 2, each participant was sent an e-mail for the online survey with a username and password unique to that individual. Participants were shown their own ratings for each statement from the first round, alongside the group’s ratings shown as frequency data on the rating scale for that item. Participants were then asked to review their original rating and had the opportunity to change their rating in the light of the group ratings if they so wished. In addition, for the subset of statements rated as ‘appropriate’ in the first round (see Data analysis), participants were asked to provide a ‘feasibility’ rating. Participants were given 3 weeks to complete the second round, with a first reminder sent to non-responders after 10 days and a second reminder sent after 3 weeks.
Rating scales
In round 1, participants were asked to rate the ‘appropriateness’ of each policy or strategy statement using a 9-point scale ranging from 1 (extremely inappropriate) to 9 (extremely appropriate). Participants were advised to rate a statement as ‘appropriate’ when the expected benefits exceeded the expected risks. Here, the expected benefit is assumed to occur when, after applying the potential policy or strategy approach, GPs would be more likely to continue to provide clinical care without quitting or without substantially reducing their commitment. This may happen directly through the use of targeted incentives or indirectly by increasing an individual’s confidence and/or competence or morale. The expected risk is that the potential policy or strategy approach will have no impact on GPs’ intentions to quit or substantially reduce their commitment and/or that it might have unintended consequences that might exacerbate the problem. When making this judgement, participants were specifically advised not to consider the cost implications when making their rating. Thus, a consideration of benefits and risks should take into account issues relating to access, equity and the safety of the health-care service being provided combined with patient experience. At the very least, the activity associated with the statement would be expected to maintain the current levels of service and patient experience, and, at best, it might actually contribute to improvements in workforce availability and service provision.
In round 2, in addition to reviewing their round 1 appropriateness ratings, participants were asked to rate the ‘feasibility’ of the subset of statements deemed by the panel to be ‘appropriate’ after the first round. Here, feasibility is said to occur when implementation can take place at least at one level (national, regional or local) within 5 years and is deemed to be of reasonable cost or judged as not imposing an inappropriate burden on the health-care system. Participants were asked to complete a 9-point rating scale from 1 (definitely not feasible) to 9 (definitely feasible).
Data analysis
In line with the RAM approach, a descriptive analysis of data emanating from round 1 for all panel members was undertaken. 111 For each statement, the panel median score was calculated and categorised into a median band classification with the following classifications applied: 1–3 (inappropriate or unfeasible), 4–6 (uncertain) and 7–9 (appropriate or feasible). As an even number of panel members could yield panel median ratings in decimal places, this was taken into account in the analysis by adjusting the median band classifications. As our statements were about informing policy directions as opposed to clinical decisions, the ‘relaxed’ and simpler approach was used (see Fitch et al. 111). We applied classification boundaries that would make a statement less likely to be included in the uncertain/unequivocal classification (appropriate as 1.0–3.5; inappropriate as 6.5–9.0).
For interpretation, the final outcomes were then determined based on the level of agreement between panel members. Here, consensus was defined as no more than two panel members rating the statement outside the classification in which the group median score was located. Thus, to be considered ‘inappropriate’/’unfeasible’ or ‘appropriate’/’feasible’ the group median score was required to fall within the defined range. Irrespective of the group median score, if the panel did not reach consensus then the statement was deemed to be of uncertain or equivocal value.
Although an interim analysis of appropriateness was undertaken after the first round, this was used only to identify a subset of statements rated (with consensus) as ‘appropriate’ in order to inform the feasibility ratings in round 2. The primary analysis is based on the analysis of round 2 panel ratings. As the statements were repeated for different subgroups, in some cases there were different ratings for a given statement based on the subgroup (e.g. a rating of appropriateness or feasibility when applied to GPs not nearing retirement age and uncertain when applied to GPs nearing retirement age). In these cases, the policy and strategy relating to the statement was included in the category for appropriateness (biased towards showing that consensus was reached), and the differences in ratings for the subgroups were presented in the findings. This resulted in policies and strategies being included in the results as having reached consensus even if this did not take place for all the subgroups included in the statements. These are referred to in Results as differential outcomes.
Results
A total of 12 out of 28 (43%) of the GP partners approached agreed to take part in the panel, with 10 out of 28 (38%) completing the first round of data collection. Participants included five GP partners from the south-west of England, three from London and two from national organisations. Eight GPs completed the second round of data collection, with the non-respondents including two GPs from the south-west of England. One of these GPs (south-west) completed round 2 by reviewing the appropriateness ratings, but did not complete the feasibility ratings. The results are presented initially for the analysis at the level of the 100 statements rated in rounds 1 and 2, then for subsequent analysis if round 2 data are aggregated at the level of the 54 policies and strategies.
Analysis of policies and strategies for appropriateness and feasibility
Statement ratings in rounds 1 and 2
In round 1, 30 statements were rated as appropriate, three as inappropriate and 67 as uncertain (Figure 8). Included within the ‘uncertain’ statements were 25 for which the median panel score was within the ‘potentially appropriate’ band and eight in the ‘potentially inappropriate’ band, but with lack of consensus; therefore, they remained as ‘uncertain’ in the round 2 results. As panel members were requested to rate feasibility for the statements that have been rated as appropriate (with agreement) in round 1, 30 statements were identified for feasibility rating in the second round.
FIGURE 8.
Summary of rounds 1 and 2 ratings for appropriateness and feasibility of the 100 statements. a, The 30 statements rated as ‘appropriate’ and with consensus were the same 30 statements put forward for feasibility rating in round 2. Light blue shading indicates the numbers of statements for which the panel reached consensus (whether ‘appropriate’/‘inappropriate’ or ‘feasible’/‘not feasible’). Light green shading indicates the numbers of statements for which consensus was not reached regarding appropriateness/feasibility, or for which consensus was reached that statements were ‘uncertain’ regarding appropriateness/feasibility. Dark blue shading indicates the numbers of statements for which the panel reached consensus that a statement was either ‘inappropriate’ or ‘not feasible’.
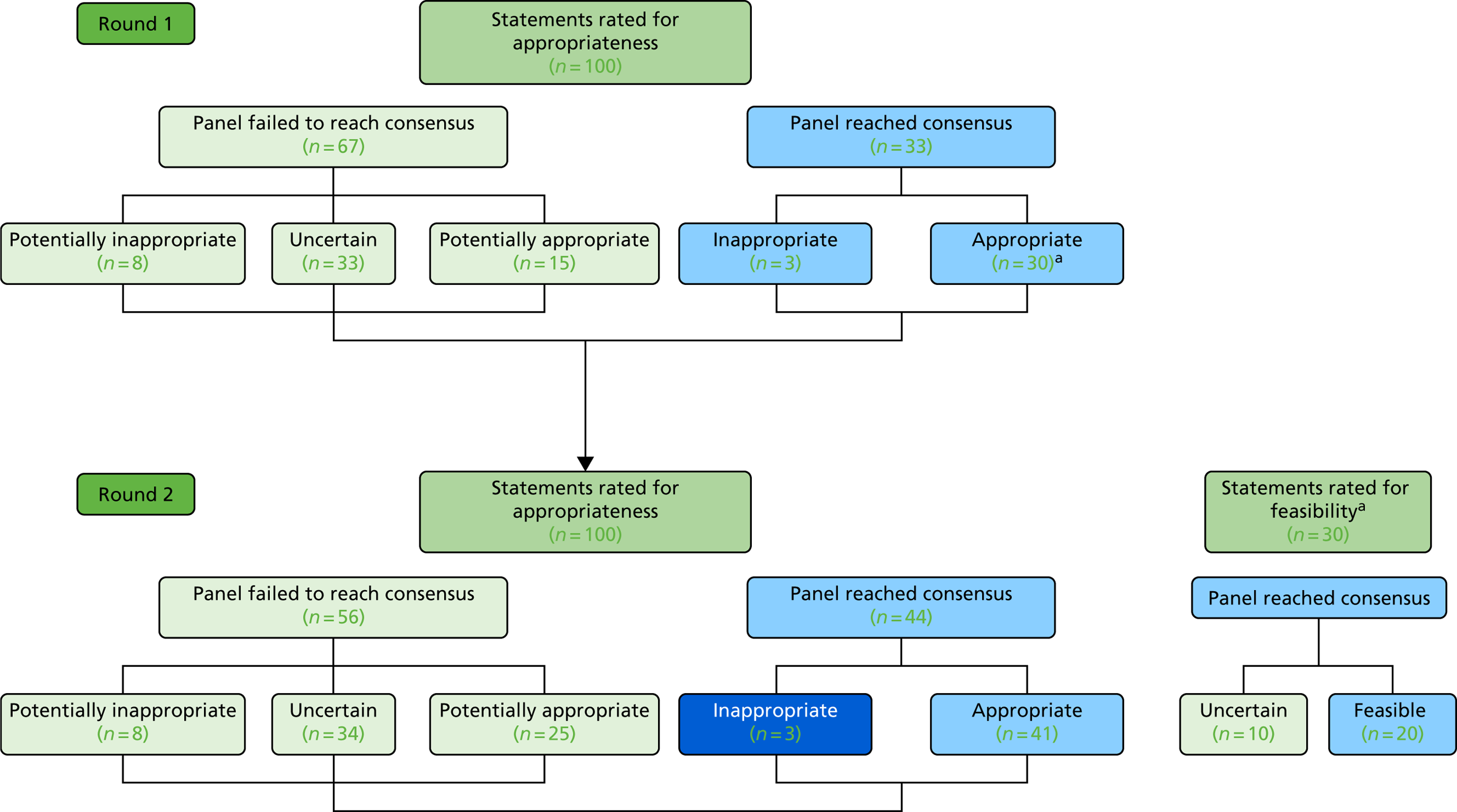
From rounds 1 to 2 (when panel members were invited to review and change their previous ratings if they wished), consensus was reached for an additional 11 (out of 67) statements that had previously been classified as ‘uncertain’ in the first round. All these statements had a median panel score within the ‘potentially appropriate’ median score band in round 1 and reached consensus in round 2, resulting in all of these statements being judged as ‘appropriate’. The average change in the median appropriateness score was small (increase of 0.13 points, minimum of –1 point, maximum of 1.5 points). The classifications changed for only 3 out of 100 statements, with two statements reclassified from ‘uncertain’ to ‘potentially appropriate’ and one statement from ‘potentially appropriate’ to ‘uncertain’ in round 2. Owing to a lack of consensus for all three statements in both rounds, the ratings for these remained ‘uncertain’ in the final analysis.
Each policy or strategy may have multiple ratings if statements were generated for different subgroups (e.g. GP ages in relation to retirement, or optional vs. compulsory implementation). The results in the next section are presented at the level of policies and strategies, rather than individual statements.
Identifying appropriate policies and strategies
Based on the analysis of the round 2 ratings for appropriateness and feasibility, a total of 24 out of 54 policies and strategies were deemed by consensus as ‘appropriate’ (Table 16). Out of the 24 policies and strategies (arising from 41 statements), six were deemed appropriate for national-/regional-level implementation, four were deemed appropriate at a general practice level and 14 were deemed appropriate at a GP level. It is important to note that five of the policies and strategies classified as ‘appropriate’ in round 2 were not assessed for feasibility as they were not classified as ‘appropriate’ in round 1.
| Appropriateness | Feasibility | Levels | Total | ||
|---|---|---|---|---|---|
| National/regional | General practice | GP | |||
| Appropriate | Feasible | 4 | 3 | 9 | 16 |
| Uncertain | 0 | 0 | 3 | 3 | |
| Not feasible | 0 | 0 | 0 | 0 | |
| Not rated | 2 | 1 | 2 | 5 | |
| Total | 6 | 4 | 14 | 24 | |
| Uncertain | Not rated | 12 | 10 | 8 | 30 |
| Inappropriate | Not rated | 0 | 0 | 0 | 0 |
| Total | 18 | 14 | 22 | 54 | |
Of the 19 policies and strategies rated for feasibility (arising from 30 statements) in round 2, 16 were deemed by consensus to be ‘feasible’ and three were deemed ‘uncertain’. All the policies and strategies presented for feasibility rating at a national/regional level (4/4) and a general practice level (3/3) were classified as feasible, compared with 9 out of 12 at the GP level. This resulted in 16 policies and strategy areas deemed by consensus as both appropriate and feasible, which are presented in Table 17. Those rated as uncertain regarding appropriateness are presented in Appendix 28. Table 18 shows the policies and strategies that were rated as appropriate but as uncertain regarding feasibility. Table 19 shows those that were rated as appropriate but that were not rated for feasibility.
| Number | Policy and strategy |
|---|---|
| For implementation at national/regional level | |
| 1 | General practices identified as being ‘at risk’ should be managed with an appropriate and sensitive supportive arrangement and this should be optional (uncertain for compulsory) |
| 2 | General practices identified as being ‘at risk’ should be allocated a specialist team for managing recruitment and retention, and this should be optional (uncertain for compulsory) |
| 3 | New incentive and support packages should be available to GPs and other organisations setting up new practices or new ways of working in under-doctored areas |
| 4 | There should be a publicity campaign focusing on managing expectations of patients in line with the resources and constraints of GP-based primary care services |
| For implementation at general practice level | |
| 5 | GPs who are returning to work after a period of absence or after a career break should have access to ‘health and well-being programmes’ to help them manage their re-entry into the workforce. Engagement with such a course should be optional |
| 6 | GPs who are returning to work after a period of absence or after a career break should have access to schemes that have a range of routes and options that can be combined in a personal package for re-entry |
| 7 | GPs who are returning to work after a period of absence or after a career break should have access to schemes that use a mix of online education and face-to-face meetings to ensure timely access to induction and refresher courses |
| For implementation at GP level | |
| 8 | Peer support initiatives should be made available to GPs aimed specifically at health and well-being. Shown as appropriate specifically for those not near retirement age |
| 9 | GPs should have access to their own specialised health-care service to ensure a quick and confidential occupational health-care service |
| 10 | A structured programme of training and support should be made available to all GPs in their first 5 years following qualification as an independent GP to help them establish healthy, productive careers. Engagement with such a course should be optional (uncertain for compulsory) |
| 11 | GPs should consider portfolio working as part of their career pathway and this should be optional (inappropriate for compulsory) |
| 12 | Incentives and support packages should be available for those GPs developing portfolio careers who are linking their portfolio activities to specialisms/areas that are directly beneficial to local clinical priorities |
| 13 | For GPs who are reaching retirement age and could take their pensions on exit, a comprehensive flexible careers scheme should be introduced with a view to supporting annualised hours, part-time working and/or ad hoc contributions to direct patient care |
| 14 | For GPs who are reaching retirement age and could take their pensions on exit, the annual appraisal and revalidation process for such GPs should be reviewed with a view to streamlining and simplifying the process for such GPs who have not encountered any concerns in the previous revalidation/appraisal processes/for such GPs who would like to work with a specified and limited scope of practice |
| 15 | For GPs who are reaching retirement age and could take their pensions on exit, the working hours of GPs should routinely include fully funded, dedicated time to accommodate the full range of roles (administrative, clinical, training, management, CPD, business) undertaken as part of care professional activity |
| 16 | For GPs who are reaching retirement age and could take their pensions on exit, contracts based on specified programmed activities should be available to GPs to work across several general practices and on other health-related activities |
| Number | Policy and strategy |
|---|---|
| For implementation at GP level | |
| 17 | Where a strong case can be made that there is a financial risk directly relating to the work of the practice (e.g. ownership of premises), GPs should have access to schemes to reduce financial burden (e.g. buy-back schemes for premises) (uncertain when applied to all GPs) |
| 18 | There should be an agreed maximum in the number of consultations that a GP should be allowed to conduct in a working day in order to protect patient safety as well as the health of the GP |
| 19 | There should be contractual changes to encourage longer consultations when appropriate |
| Number | Policy and strategy |
|---|---|
| For implementation at national/regional level | |
| 20 | General practices should be able to self-register their organisation’s ‘at-risk’ status (ID 4) |
| 21 | General practices identified as being ‘at risk’ should be provided with a toolkit to manage recruitment and retention |
| For implementation at general practice level | |
| 22 | To support flexible working and managed exits, general practices should implement strategically planned exits for retiring GPs |
| 23 | Career support should be available to GPs to enable portfolio opportunities to be identified and taken up in a strategic way to inform their future ambitions for all GPs or specifically those who are not reaching retirement age and cannot take their pension on exit |
| 24 | For GPs who are reaching retirement age and could take their pensions on exit, there should be financial incentives for such GPs who have maintained a prolonged/sustained period of direct patient care |
As some of the policies and strategies included subgroups, the panel was given the opportunity to identify particular circumstances or groups in which the policy and strategy may be considered as appropriate/feasible compared with a generic ‘one-size-fits-all’ approach. For example, panel members deemed the strategy ‘GPs should consider portfolio working as part of their career pathway’ (policy and strategy 11 in Table 17) as appropriate when applied as an optional strategy and inappropriate when applied as a compulsory requirement. Differential outcomes were also observed and were also found in four other policy and strategy areas in which compulsory application was deemed uncertain regarding appropriateness but optional implementation was deemed appropriate (policy and strategy 1, 2, 9 and 11 in Table 17).
For nearly all of the GP-level policies and strategies, the panel considered appropriateness based on application ‘for all GPs’ (subgroup A), ‘for GPs who are nearing retirement age and eligible for taking their pensions’ (subgroup B) and ‘for GPs who are not near retirement age and not eligible for retirement’ (subgroup C). There were differences in the ratings for the subgroups as follows:
-
Peer support initiatives for GPs aimed specifically at health and well-being (see Table 17, policy and strategy 8) were deemed appropriate for subgroup C, but the panel was uncertain for those who are in subgroups A and B.
-
Career support being available to GPs to enable portfolio opportunities to be identified and taken up (see Table 19, policy and strategy 23) was endorsed for subgroup A or C, but the panel was uncertain for those in subgroup B.
-
GPs being given access to schemes to reduce financial burden ‘where a strong case can be made that there is a financial risk directly relating to the work of the general practice’ (see Table 18, policy and strategy 17) was rated as appropriate for subgroups A and B and uncertain for subgroup C.
In considering the possibility of developing policy to simplify appraisal and revalidation (see Table 17, policy and strategy 14) for GPs who are nearing retirement age and eligible for taking their pensions, participants expressed uncertainty that this might apply to all GPs in this group. However, panellists found it appropriate to be applied to ‘those who have not encountered any concerns in the previous revalidation/appraisal processes’ and for GPs ‘who would like to work with a specified and limited scope of practice’.
One set of policies and strategies that was uniformly identified as ‘uncertain’ was the introduction of external human resources (HR) management systems to support general practices. This was assessed using a wide range of potential interventions, such as monitoring and supporting the implementation of flexible working arrangements, all activities associated with retention of GPs, professional development and training, and implementing standards for working hours and conditions. The panel median for most of the statements presented relating to these five policies and strategies was judged as ‘potentially inappropriate’ when considered in relation to ‘all general practices’ and ‘uncertain’ when applied to ‘general practices/employers operating in traditionally ‘hard-to-recruit’ settings’. However, overall, there was a lack of consensus in respect of this area of consideration.
Two policies and strategies included in feasibility ratings included subgroups and they were both at the GP level and targeted: (1) the inclusion of funded and dedicated time to accommodate the full range of roles and (2) contracts for specified programmed activities to be worked across several general practices. In both cases, the panel rated the statement as feasible only when it applied to GPs ‘reaching retirement age and [who] could take their pension on exit’.
Discussion
Main findings
This study rated appropriateness and feasibility for a set of potential policies and strategies that might be expected to facilitate the retention of GPs in providing direct patient care through prevention of quitting or through substantially reducing their commitment. The final set of these potential policies and strategies was selected following review of the research literature and current and planned government policies, and consensus from the ratings of panel members. Overall, most of the policies and strategies rated as ‘appropriate’ were also rated as ‘feasible’. Many of these policies and strategies related to the provision of personal or professional support, such as ‘health and well-being programmes’ to support GPs who were returning to work, which aim to manage their re-entry into the workforce; flexible working; and targeting career stages in the first 5 years or when nearing retirement. When considered at a national level, there was recognition that early self-reporting of practice at-risk status in respect of retention issues was appropriate and feasible. Such interventions may offer potential for enhanced systematic identification of vulnerable practices, drawing on information from routinely available data sets and local intelligence and may facilitate recognition of practice progression to ‘vulnerable’ or ‘at-risk’ status.
Taking into consideration the possibility that policies and strategies might be implemented on a ‘compulsory’ or ‘optional’ basis, panellists were more likely to rate those involving optional implementation as appropriate. This was particularly noted for the compulsory introduction of portfolio working as part of the GP career pathway: implementation was determined to be both appropriate and feasible when introduced as an optional part of the career pathway (as is the case in the current system) but inappropriate when presented as a ‘compulsory’ measure.
Some of the policies and strategies considered to be both appropriate and feasible and already presented above relate to HR management, which is currently managed by each general practice or by a federation. However, when the panellists were presented with policies and strategies relating to the introduction of external HR management to support the implementation of areas such as flexible working and professional development (policies and strategies 42 to 46 in Appendix 27), the panel median scores were in the ‘inappropriate’ band but without consensus, and therefore, following our methodology, these were rated as ‘uncertain’. This may be indicative of a reluctance for panellists (many of whom were recruited in their capacity as GP partners) to support a loss of direct control over the implementation of policies and strategies or management of staff.
When the policies and strategies related to operational functions and day-to-day management of the general practice, they could be considered as protective measures to reduce work-related stressors. These include incentivising and supporting the set-up and operationalisation of new approaches in under-doctored areas, managing high or intense workload by limiting the number of consultations that GPs carry out in a given day or in increasing consultation lengths (all identified as appropriate). Others related to ways in which contracts may be used, for example in terms of reducing the financial risk of general practice ownership, establishing contracts based on programmed activities across several general practices to increase flexibility or in using a national campaign to manage patients’ expectations of general practice. However, although panellists deemed these policies and strategies to be appropriate, there was uncertainty for some of these in terms of feasibility. This is not a surprising finding given that previous research and policy literature have highlighted these issues as affecting patient experience123 and there is still little in terms of tangible progress in addressing these concerns. Nevertheless, the importance of these protective measures to retain experienced GPs in direct patient care has been highlighted throughout this research study and the issue of feasibility requires further exploration.
Research in context
In considering relevant research, it is important to consider some of the limited viewpoints relating to health-care workforce recruitment and retention literature to date. For example, Barriball et al. 121 reviewed the primary research and policy practices for all health-care workforce recruitment and retention in Europe, focusing on educational interventions, financial incentives, professional and personal support, and regulation interventions, as would be expected using the usual recruitment and retention categorisations. Their research and policy is aligned with the international guidelines for improving access to health workers in remote and rural areas,124 often used in health workforce research125,126 and also influential in the UK at a national level. 127 However, this study addresses the recognised gap between consideration and incorporation of these wider contexts in the day-to-day running of general practices and workloads in informing the development of policies and strategies targeting retention among the experienced GP workforce in UK primary care. 120,122 These contexts are particularly important in primary care where GPs in their role as GP partners are responsible for managing workforce issues, as well as for having an interest in and at least shared responsibility for the contractual implications associated with service delivery as part of owning general practices.
There are indications in the General Practice Workforce Action Plan (focusing on England) that a system-wide approach is required. 99 However, the nature and magnitude of any interdependencies of the key areas of workload, practice infrastructure and care (re)design to GP workforce and retention are not yet defined or quantified. At the policy level, the focus is on levers such as skill mix and technology to reduce the workload pressures on GPs. 128 These could result in GPs spending more time on direct patient care and potentially focusing their care on a subset of patients with complex conditions. Implementing these operational-level changes without protective measures on managing the cognitive workload associated with patient consultations may result in increased stressors129,130 and may contribute to ‘push’ factors, with a resultant negative effect on retention. The polices and strategies related to operational functions and the day-to-day management of general practices rated as appropriate (but not necessarily feasible) in this study take into account some of these protective measures and can be used to widen the scope of the current policies when considering the reduction of work pressures on GPs to support retention in direct patient care.
Strengths and limitations
This study used the RAM, widely adopted as a formal group consensus method,131 to undertake a systematic consensus exercise as part of health workforce policy development. Applied for the first time in health workforce policy research, the RAM has been shown to represent a viable approach within this context. The opportunities afforded by this methodology include the ability to present a large number of statements with multiple layers (in this case subgroups) to establish a more refined set of policies and strategies for consideration at national and local levels. There are nuances with the use of this methodology, for example in terms of the tight criteria for reaching consensus, which leads to classifications of uncertainty when a different RAM panel or a larger group may tip the balance into a consensus. In addition, the inability to tease out why some policies and strategies were appropriate or feasible over and above others with subtle differences creates challenges for interpreting the findings. It has already been argued in earlier workstreams that retaining GPs in direct patient care requires a multilayered and multifactored approach. This study builds on these findings and provides a set of policies and strategies with consensus that they are appropriate (and mostly feasible) for implementation as part of interventions to retain GPs in direct patient care.
The main limitations include the selection of just one professional group for the panel, the paucity of evidence regarding the effectiveness of policies and strategies aimed at retaining GPs within the workforce, the exclusion of skill mix/multidisciplinary working policies and strategies in the statements, and the use of appropriateness and feasibility as the rating scales. Each of these is discussed in turn.
It might be argued that, because the panellists were GP partners, the ratings could be biased given their dual role as both beneficiaries of the policies and strategies and as employers who may have to manage the potential burden of implementation as employers. A panel specifically chosen because of their in-depth knowledge about GPs who have left the profession or have transferred from or avoided GP partnership to provide care as locums, salaried doctors or who are just working in the out-of-hours teams may have yielded different results. By targeting GP partners, we had an opportunity to understand and meet the needs of a group of health-care professionals who are influential in facilitating or undermining the implementation of any such policies or strategies. Future studies might consider using panels of individuals from a wider variety of backgrounds working in primary care, including commissioners/workforce planners or other GPs (such as locums or associates, or GPs employed under ‘retainer’ arrangements). To balance the size of the panel (recommended as between 7 and 15 panel members for RAM111), multiple panels may be required to accommodate heterogeneity without distilling the representation from any given group to an individual member.
Similarly, panels drawn from different geographical areas and/or GPs drawn from different types of practice may also be beneficial in relation to the transferability of our findings to more varied general practice configurations.
This panel method required GPs to rate the appropriateness of policies based on the best available evidence combined with their professional judgement. As this study developed, it became apparent that there was a paucity of evidence across a number of policy areas regarding the effectiveness of strategies aimed at maximising GP retention, particularly for those targeting management and HR functions. GPs were provided with the best available evidence, but it is acknowledged that, in some areas, the panellists may have had to rely mostly on their professional judgement. Although less than ideal, as it is assumed that panellists will weight their judgements based on the strength of evidence available, we believe this approach to be defensible. Indeed, it could be argued that many of the emergent policies and strategies currently being introduced in the UK to aid GP retention are based on limited evidence.
Another limitation related to the decision taken by the research team to exclude policies and strategies regarding multidisciplinary working and role substitution and skill mix from the statements presented to the panel. This decision was partly because of the ongoing implementation of new roles (e.g. introduction of clinical pharmacists), but was also influenced by a desire to reduce participant burden by constraining the number of statements presented. Even though there is recognition that skill mix is likely to be of importance in addressing recruitment and retention issues from the perspective of increasing supply to meet demand,128 detailed research that takes into account the impact of such policies and strategies on job satisfaction and GP retention is required. Thus, the detail was judged to be beyond the scope of this immediate piece of work.
Finally, we acknowledge that the use of ‘appropriateness’ and ‘feasibility’ as the rating scales could be called into question compared with ratings on ‘acceptability’. In developing this workstream, we recognised that multiple alternatives may be used. To reduce the potential variation in the interpretation of the rating scales, we provided panellists with clear definitions on how to apply the ratings of appropriateness and feasibility. Such ratings might also be limited by the complex context in which interventions are likely to be implemented; in Chapter 2, it was shown that GP decision-making to stay in direct patient care is influenced by a range of competing ‘push’ and ‘pull’ factors. Similarly, feasibility may be viewed differently based on the panellist’s experience of working in or managing particular types of practices, although this should be ameliorated by the requirement for panels to reach consensus for statements to be deemed appropriate or feasible.
Conclusion
Understanding the views of the GP partners and involving them as those who work on implementation in their role as employers is rarely acknowledged in UK policy research and development. In the absence of a wealth of contextually relevant effectiveness research to directly inform policy decisions on retaining GPs in direct patient care in the UK, the systematic and panel approach provides important focus on 16 potentially appropriate and feasible policies and strategies for implementation at the national/regional level, general practice level and GP level. These 16 areas of policy and strategy formed the basis of the material that was presented for consideration by key stakeholder organisations within the stakeholder consultations workstream.
Chapter 6 Workstream 5: workforce predictive risk modelling
Introduction
The aim of this workstream was to develop a method to identify NHS general practices in south-west England that may face supply–demand workforce imbalances within the next 5 years. The output of the model also seeks to inform relevant policies and strategies that can be deployed to address any imbalances that are identified. Previous workforce modelling has focused on determining insights that are derived from analyses at the regional or national (macro) level. In contrast, this research focuses on undertaking predictive risk modelling at a practice (micro) level. These predictions are, in part, informed by the primary data collected as part of the ReGROUP survey regarding GPs’ reported intentions to leave their employment providing patient care, or to take a career break. By surveying GPs in this way, we address the question of whether or not undertaking a survey of quitting intentions adds value beyond the incorporation of routinely available data on doctors’ ages and genders.
Conceptual model of supply–demand imbalance
To identify practices at risk of supply–demand imbalance, we first sought to define the concept (Figure 9). The model incorporates two domains and provides a potential framework for evaluating risk of imbalance. The first domain is the ratio of workload (demand) to GP workforce availability (supply); this ratio is shown on the x-axis of Figure 9. Neither workload nor workforce should be considered in isolation, as a large practice may have a large workload but may also a have large workforce. For this reason, we considered the ratio of the two quantities, which can be considered as standardised across different practice sizes. It was also judged that the consideration of this ratio in isolation might produce erroneous inferences. For example, practices with a high workload may be meeting patient demand through innovative and efficient service delivery systems. This discussion was reflected through the incorporation of a marker of a practice’s ability to meet patient demand (y-axis). It was considered that the ability of a practice to meet patient demand under conditions of high workload would not necessarily reflect supply–demand imbalance. On the contrary, such a scenario may be judged by some to imply a desirable efficiency in service delivery (although this may not necessarily reflect desirable working conditions from the GP’s perspective).
FIGURE 9.
Conceptual model of supply–demand imbalance. The gradient in colour indicates efficiency in service delivery.
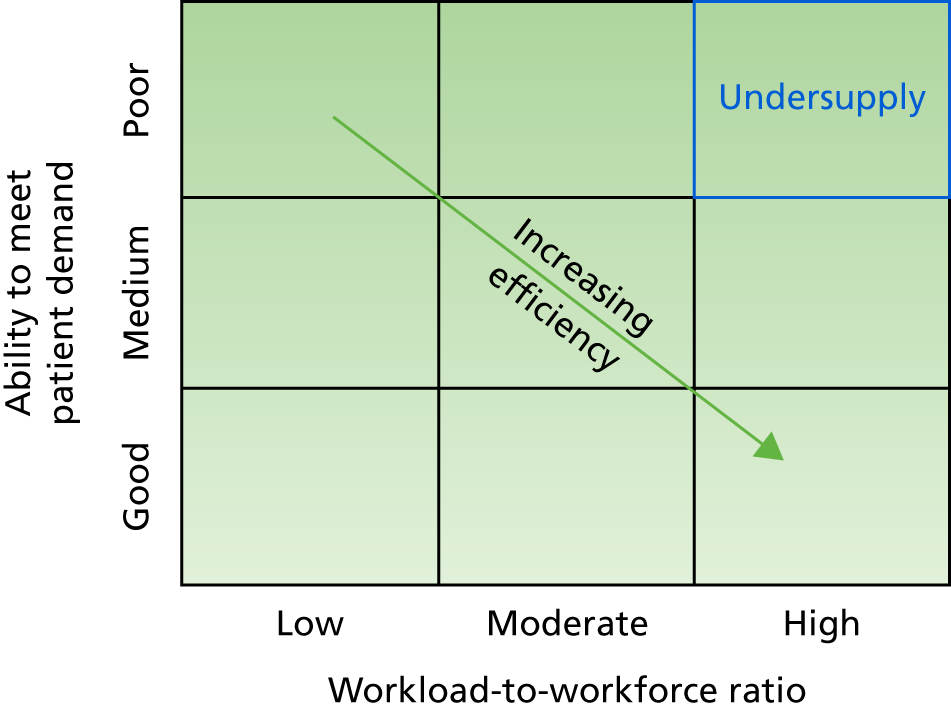
Considering GP workload-to-workforce ratio and the ability to meet patient demand at the practice level, Figure 9 shows the potential to identify several ‘types’ of practice reflected in the nine internal cells. The following descriptions should be seen only within the context of this model and we recognise that other factors exist that cover the wider concept of service delivery and quality.
Practices with a high workload-to-workforce ratio and good ability to meet patient demand (see Figure 9, bottom right) might be considered as delivering the most efficient practice.
When the ability to meet patient demand is good but the workload-to-workforce ratio is low (see Figure 9, bottom left), this may be considered to reflect a situation whereby supply and demand is imbalanced but not on account of a shortage of workforce. Although identification of these practice types may highlight practices that may benefit from operations improvement focused on increasing efficiency, these do not represent a direct detriment to patient care and are therefore considered to be outside the scope of this work.
When workload-to-workforce ratio is moderate and the ability to meet patient demand is identified as ‘medium’ (see Figure 9, centre cell), we considered this to reflect a ‘stable’ or ‘sustainable’ practice. We note, however, that this classification assumes that the overall situation is itself sustainable, which may not be the case in times of national GP workforce difficulties.
When the ability to meet patient demand is ‘poor’ and the workload-to-workforce ratio is ‘low’ (see Figure 9, top left), this may be considered to reflect less efficient practice rather than to reflect an imbalance between supply and demand.
Within this framework, it is those practices that have a poor ability to meet patient demand in association with a high workload-to-workforce ratio (see Figure 9, top right) that may be considered to represent an adverse imbalance of supply and demand (‘undersupply’). Within our model there are two routes for a practice to move away from the ‘undersupply’ category: either by increasing the workforce while maintaining efficiency (moving to the centre cell) or by increasing the efficiency within the existing workforce (moving towards the bottom right). We assumed that continuing to evidence a poor ability to meet patient demand was judged not to be a viable option.
We focused only on the GP workforce and neither nurses nor other allied health-care professionals were included in our consideration. This was for two main reasons. First, on a conceptual level, the primary focus of the ReGROUP study was the GP workforce. Second, a practical reason relating to operationalising the model meant that some estimate of nurse and GP equivalence (i.e. each nurse is ‘worth’ X% of a GP) would be necessary. Such a metric would be difficult to justify on the basis of published literature, and for this reason we did not attempt to do so. Rather, our approach was based on the idea that the use of nurses and other health-care professionals may be considered a way to achieve practice-level efficiencies and permit effective use of the GP workforce consistent with service delivery system design. 132 Practice-level efficiencies are likely to have an impact on the ability to meet patient demand even in the presence of a high workload-to-workforce ratio.
Operationalisation of the conceptual model
To operationalise the conceptual model summarised in Figure 9, we needed to identify measurable quantities relating to the two domains (when the workload-to-workforce ratio domain comprises two measurable quantities). Estimates of workload were based on the practice registered population on the basis that this represents a proxy for demand placed on the practices. To account for the fact that the needs of patients vary by age, with older patients and children having the highest expressed need, we incorporated weights based on the age and gender composition of the practice population. 2,133 A further adjustment was incorporated to account for additional needs associated with deprived populations. 134,135 Estimates of workforce were based on the FTE GP workforce of the practice. Finally, the ability to meet patient demand was quantified using a measure of patient access, based on the widely adopted national GP Patient Survey (GPPS) in the belief that access is an important measure, reflecting the ease with which patients might engage with the primary health-care system. 136
Methods
Overview
The investigation of supply–demand imbalance at a general practice level requires the synthesis of data from a number of sources, and the explicit consideration of a number of factors (Figure 10). A detailed description of how we operationalised these factors is provided below. A predictive risk model (to predict the risk of a practice being in a state of ‘undersupply’ within 5 years) was developed by assessing the associations between current (2016) ‘undersupply’ status and data (when available) from 2012 on the factors included in the model. The rationale for this approach was to obtain factor weightings informed by evidence developed on past data. This model was then used to identify practices and areas in south-west England that are likely to experience a supply–demand imbalance (‘undersupply’) in the future.
FIGURE 10.
Factors used in the construction of the risk prediction model. ONS, Office for National Statistics.
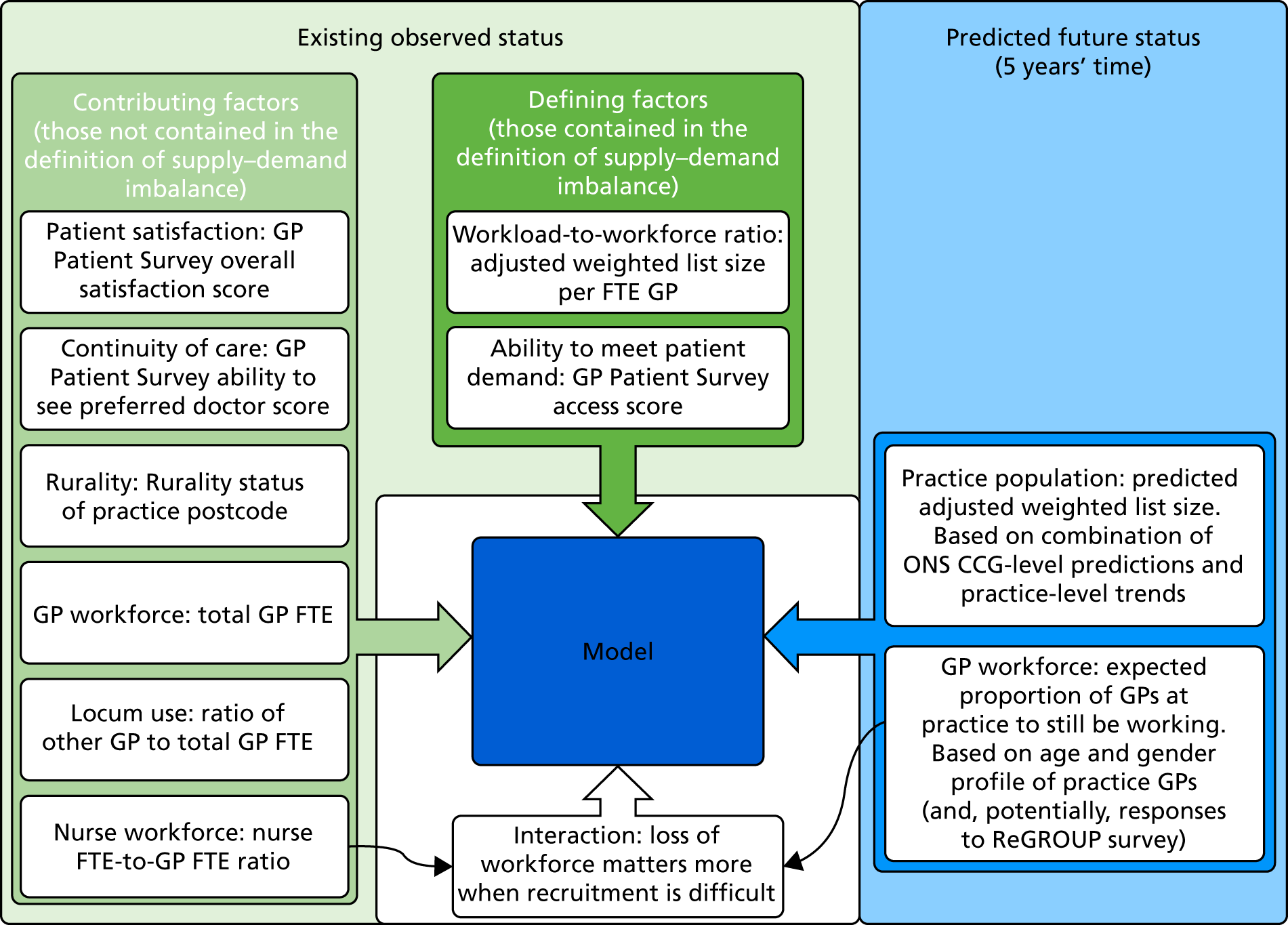
Data sources and preparation
Except where specified, national data for England were obtained and processed. For a summary of data sources and data flow used in the modelling process, see Figure 14.
GP Patient Survey
The GPPS is a national postal survey of patients’ experiences of primary care in England. Patients from practices that are known from prior surveys to have low response rates are oversampled. Full details of the sampling strategy are published elsewhere. 137 We used data from the 2011/12 and 2015/16 surveys. The contents of the survey have remained largely consistent over this time period. Response rates were 38% in 2011/12 (1,037,946 responses) and 39% in 2015/16 (836,312 responses).
We made use of three items from the GPPS: reflecting access, continuity of care and overall experience. For each of these items, Likert response scales were dichotomised into positive or neutral/negative responses, treating uninformative responses (e.g. ‘cannot remember’) as missing (see Appendix 30 for details). Owing to certain patient groups tending to give more positive responses in patient surveys, case-mix-adjusted practice scores were created. This was achieved using mixed-effects logistic regression, adjusting for patient age, gender and ethnicity, presence of a long-term condition, deprivation [using the Index of Multiple Deprivation (IMD), an area-based measure assigned in accordance with the patient’s residential postcode138,139] and a random intercept for practice. The case-mix adjustment provides scores for individual practices based on a standardised mix of patients. The case-mix-adjusted scores were used in the form of log-odds ratios relative to the average practice nationally.
Workforce
Workforce data were obtained from NHS Digital and related to the GP census data taken on 30 September 2012, 2013 and 2016. 140–142 Each data set gave the headcount of GPs in 5-year age bands for each practice. The 2012 data set contained total GP headcount by gender, as did the 2016 data set. In the 2016 data set, additional detail of GP FTE by gender was provided. Both data sets contained total GP FTE as well as GP FTE broken down by GP role. We also extracted the total nurse FTE from the 2016 data set. As nurse FTE data were not available in 2012, the relevant data were extracted from the 2013 data set in their place. From these data, two additional variables were derived: the ratio of nurse FTE to GP FTE and the ratio of ‘other’ category FTE to total GP FTE (when ‘other’ is assumed to mostly be locum GPs given that GP registrars, salaried GPs and those on the GP Retention Scheme are captured in other categories). These data were also used in the derivation of workload and the predicted remaining future workforce (see Appendices 31 and 32).
Practices with less than a 0.5-FTE GP (38 out of 7484 practices in 2012 data and 41 out of 6709 practices in 2016 data) were excluded from all analyses on the basis that such a low staff record indicated either that these were unusual practices or that the workforce data were in error. In the former case such unusual practices are not the focus of this work and in the latter case erroneous inferences may have been made if they had been included.
General practitioner quitting intentions
To predict remaining future workforce (see Appendix 32), we utilised self-reported GP intentions to cease practice collected through the census survey. A brief questionnaire was administered to all active GPs in south-west England enquiring about their intentions to cease/interrupt practice in the next 2 and 5 years. We combined responses to two questions:
-
‘How likely is it that you will permanently leave direct patient care within the next 5 years?’
-
‘How likely is it that you will take a career break (or another career break) within the next 5 years?’
Each question had response options of ‘very likely’, ‘likely’, ‘unlikely’ and ‘very unlikely’. When GPs gave different response options for these two questions, the response with the highest likelihood of cessation or interruption was taken. This reflects the most likely chance of impact to future GP workforce in the next 5 years. We also used respondents’ answers to the question:
-
‘In your current/most recent direct patient role, how many sessions do/did you work in a typical week?’
Survey responses provided data from which an estimate of each responder’s current FTE work commitment could be calculated. Working eight sessions per week was taken as 1 FTE, consistent with the approach used in the GP census. 142 When more than eight sessions was given as a response, the FTE was capped at 1. If more than 24 sessions was given as a response, it was assumed that the question had been answered incorrectly and the data were treated as missing. Data for all GPs surveyed on age, gender and affiliated practice were obtained from the National Performers List.
Practice rurality and deprivation
Practice rurality was contained within the GPPS 2016 data set and was based on an Office for National Statistics (ONS) categorisation of the postcode of the practice. We used a rural/urban version of this categorisation. Practice deprivation score was obtained from Public Health England and was based on the 2015 IMD. Individual patient IMD is based on each patient’s residential postcode, and the practice score is the mean of individual patient scores using all patients registered at the practice. 143
Practice registered population
Data on the registered populations for each general practice were obtained from NHS Digital for each quarter from April 2014 to April 2016 (nine data sets), as well as April 2012. These data sets provided the count of patients in each gender by 5-year age band (with the highest age band being ≥ 95 years). We aggregated the top three age bands, resulting in a top age band category of ≥ 80 years. The list sizes for 2012 and 2016 were adjusted for the age and gender composition of the practice population, accounting for the fact that GPs spend longer consulting with patients who are very young, are older or are female. 133 Further adjustment was made for the deprivation of the practice population to reflect higher health needs (see Appendix 33 for details). The data from April 2014 to April 2016 were used in the prediction of future practice populations (see Appendix 31).
The adjusted weighted list sizes were divided by the total GP FTE to obtain a measure of workload per GP. Initial inspection of the workload figures showed that the distribution contained some infeasibly large and small values. These may have arisen from errors in either the workforce or practice population data. Unfortunately, there was no clear separation between typical values and those that were infeasible. A pragmatic approach was taken whereby practices in the top and bottom 2.5% of the distribution were excluded from all further analysis. This exclusion took place following the removal of practices with less than 0.5 GP FTE.
Subnational population projections
We made use of ONS subnational population projections at the level of CCGs (used to inform local planning of health care and other public services144) in the prediction of future practice populations (see the following section). The subnational ONS projections are demographic, trend-based projections that indicate the ‘likely levels of future population’ and are currently produced every 2 years; they present projections for every year for the next 25 years from the base year. 145 The underlying data sources that inform the calculations include national population projections, registration of births and deaths (General Register Office), armed forces data (Ministry of Defence), data extracts from the Patient Register Data System (NHS), student location data (Higher Education Statistics Agency) and data on asylum seekers (Home Office). Adjustments were then made to the data sets for factors such as assumed fertility and mortality rates, internal and international migration. However, the projections do not account for local development aims and policies, economic factors and, indeed, any international factors that are likely to affect the UK population. 145 We extracted projected populations for 2021 for the eight CCGs within the scope of the ReGROUP project: NHS Bath and North East Somerset CCG; NHS Kernow CCG; NHS Northern, Eastern and Western Devon CCG; NHS South Devon and Torbay CCG; NHS Bristol CCG; NHS North Somerset CCG; NHS Somerset CCG; NHS South Gloucestershire CCG. Projections are made in 5-year age bands for each gender. As with practice population data, the upper age groups were combined to form an ≥ 80-year age band.
Predicting remaining future workforce
When predicting future workforce (supply), we concentrated on predicting what fraction of the existing workforce will remain available to the practice in 5 years’ time. We did this in two principal ways: (1) based on the age and gender of GPs at the practice and (2) based on responses to the ReGROUP survey. Predictions are made based on 2012 data and 2016 data (with the survey being available only for the 2016 data). We used predictions of future workforce made on 2012 data to build the model and then predictions made on 2016 data to further predict the supply imbalance status of practices in 2021. The approaches are detailed in full in Appendix 33. The predictions took the form of the proportion of GP FTEs that would be expected, on average, to remain at the practice in 5 years’ time.
Mapping the current situation
Before producing a predictive risk model (to predict risk of practice undersupply of GP workforce), we first operationalised our conceptual model and then mapped the current situation. Owing to a lack of any clear shoulders/inflections in the distribution of GPPS case-mix-adjusted access scores (our operational definition of the ability to meet patient demand), we simply divided the national distribution into three groups based on tertiles. Similarly, we divided adjusted weighted list size per FTE (our operational definition of workload-to-workforce ratio) into three equally sized groups nationally. We then described how practices in south-west England are currently distributed among the nine cells shown in Figure 9. We also described how those practices defined as being in a state of undersupply differ from other practices in south-west England based on adjusted weighted list size, list size, GP FTE, the ratio of nurse FTE to GP FTE, the three GPPS scores considered, the percentage of the population aged ≥ 65 years, practice setting (deprivation and rurality) and CCG. For continuous variables, differences were tested using a Mann–Whitney U-test, and for categorical variables, a Fisher’s exact chi-squared test was used.
Development of a predictive risk model
To develop a risk prediction model, modelling the risk of a practice being in a state of supply–demand imbalance within 5 years, we used historical data to produce model coefficients that could then be applied to current data. The model development was based on national data in order to maximise power. The factors used in the model are shown in Figure 10. Data from 2012 were used to quantify independent associations between the considered factors and supply–demand imbalance (undersupply) in 2016. We used 2012, rather than 2011, data (which would have provided a 5-year period) owing to a lack of comparable data. Further complicating this data set, 2013 data on nurse capacity were used to supplement the 2012 data as nurse data were not available in 2012. As described in Predicting remaining future workforce, the expected proportion of the GP workforce remaining in patient care was estimated from 2012 data. We did not attempt to predict the 2016 practice populations using only data available in 2012 and instead used the observed 2016 practice populations in our model development (based on 2012 data). This was because historical data on practice populations were not routinely available for all of the 3 years prior to 2012. Furthermore, the available data were of lower fidelity and for fewer time points, making comparable predictions difficult.
A logistic regression model was used with a binary outcome of a practice being in a state of relative undersupply based on our conceptual model (see Figure 9) and using the definition described earlier in this section. Practices were the unit of analysis. All items shown in Figure 10 were included and retained regardless of statistical significance. We recognised the need to account for the fact that GPs leaving patient care would be most likely to affect the supply–demand balance when recruitment of GPs is difficult. This need was accounted for by including an interaction between the expected proportion of the GP workforce remaining in patient care after 5 years and the ratio of total nurse FTE to total GP FTE based on NHS workforce data. The rationale for this decision is outlined in Appendix 34.
The predictive value of our model was assessed using a receiver operating characteristic (ROC) curve analysis of predicted probabilities for all practices in England based on the data used to build the model (i.e. 2012 data and 2016 supply–demand imbalance classifications). The area under a ROC curve provides a measure of the predictive ability of a model, with an area under the curve of 1 indicating perfect prediction and an area under the curve of 0.5 indicating a performance equivalent to pure chance. These were compared with a simpler model developed using only defining factors (GPPS access scores and adjusted weighted list size per FTE).
Future risk prediction
The coefficients from the historical model (see Development of a predictive risk model) were applied to 2016 data to form our baseline risk predictions with a 5-year forward view. To calculate a predicted probability of future workforce undersupply for a practice, each of the variables for the practice was multiplied by the corresponding regression coefficient. These products were then summed together with the constant term and, finally, the inverse logit transform was applied. Predictions were made only for practices in south-west England, as these are the only practices for which we had survey responses on future career intentions. In the case of the expected proportion of the GP workforce remaining in patient care in 5 years’ time, we used the predictions based on the ReGROUP survey. After applying the model, we categorised practices into three risk groups. Those in the highest 25% of the predicted risk profile were flagged as being at ‘high risk’ of future undersupply of GP workforce, those in the lowest 25% were flagged as being at ‘low risk’ and those in between were flagged as being at ‘moderate risk’.
To examine the usefulness of the additional information regarding future career intentions gained from the ReGROUP survey, we compared the above prediction with an alternative prediction using the expected proportion of the GP workforce remaining in patient care in 5 years’ time based only on the routinely available age and gender profile of GPs in the practice.
In addition to baseline predictions, we explored a number of scenarios. These scenarios can be considered as stress tests of the model to identify practices that might be more (or less) vulnerable to particular challenges. First, we explored the effect of increased difficulty in recruiting GPs. The difficulty of recruiting staff is a particular issue when GPs are leaving practices and/or patient care. Thus, we modelled this difficulty as an increase in the coefficient for the expected proportion of GPs remaining in patient care (in which an increased coefficient implies a greater impact for the GP workforce leaving patient care). Second, we explored those practices that might be at particular risk of a marked increase in local population, such as an increase resulting from a new housing development in the catchment area. This was done by inflating the predicted adjusted weighted list size. The following scenarios were explored:
-
The coefficient for the expected proportion of GPs remaining in patient care increased by 2 (equivalent to a 22% increase in the odds of being in supply–demand imbalance when 10% of GPs are expected to leave, representing a modest increase in the difficulty of recruiting GPs).
-
The coefficient for the expected proportion of GPs remaining in patient care increased by 4 (equivalent to a 49% increase in the odds of being in supply–demand imbalance when 10% of GPs are expected to leave, representing a substantial increase in the difficulty of recruiting GPs).
-
The predicted adjusted weighted list size increased by 20%.
-
The predicted adjusted weighted list size increased by 40%.
-
There was a modest increase in difficulty recruiting GPs combined with a 20% increase in list size [(a) and (c) combined].
-
There was a substantial increase in difficulty recruiting GPs combined with a 40% increase in list size [(b) and (d) combined].
The last two scenarios [(e) and (f)] helped to identify those practices that might be at risk from the combined effect of substantially increased populations and shortage of supply of the GP workforce.
Results
Mapping the current situation
Figure 11 summarises the distribution of practices in England and in south-west England across the nine categories defined within our conceptual model on the basis of their 2016 data. Practices with access scores in the top third nationally were over-represented in south-west England, with 57% of practices in this region falling in that category. There was also an under-representation of south-west England among practices with the highest workload (only 22% of practices in the region were classified as in the top third of practices nationally). As a result, the percentage of practices defined as being in undersupply was considerably lower in south-west England (5.1%) than in England as a whole (13.5%). We also note that the percentage of practices with good patient access and a low workload per GP was much higher in south-west England (24.5%) than in England overall (13.2%).
FIGURE 11.
Distribution of practices in England and in south-west England across categories defined by our conceptual model of supply–demand imbalance. SW, south-west.
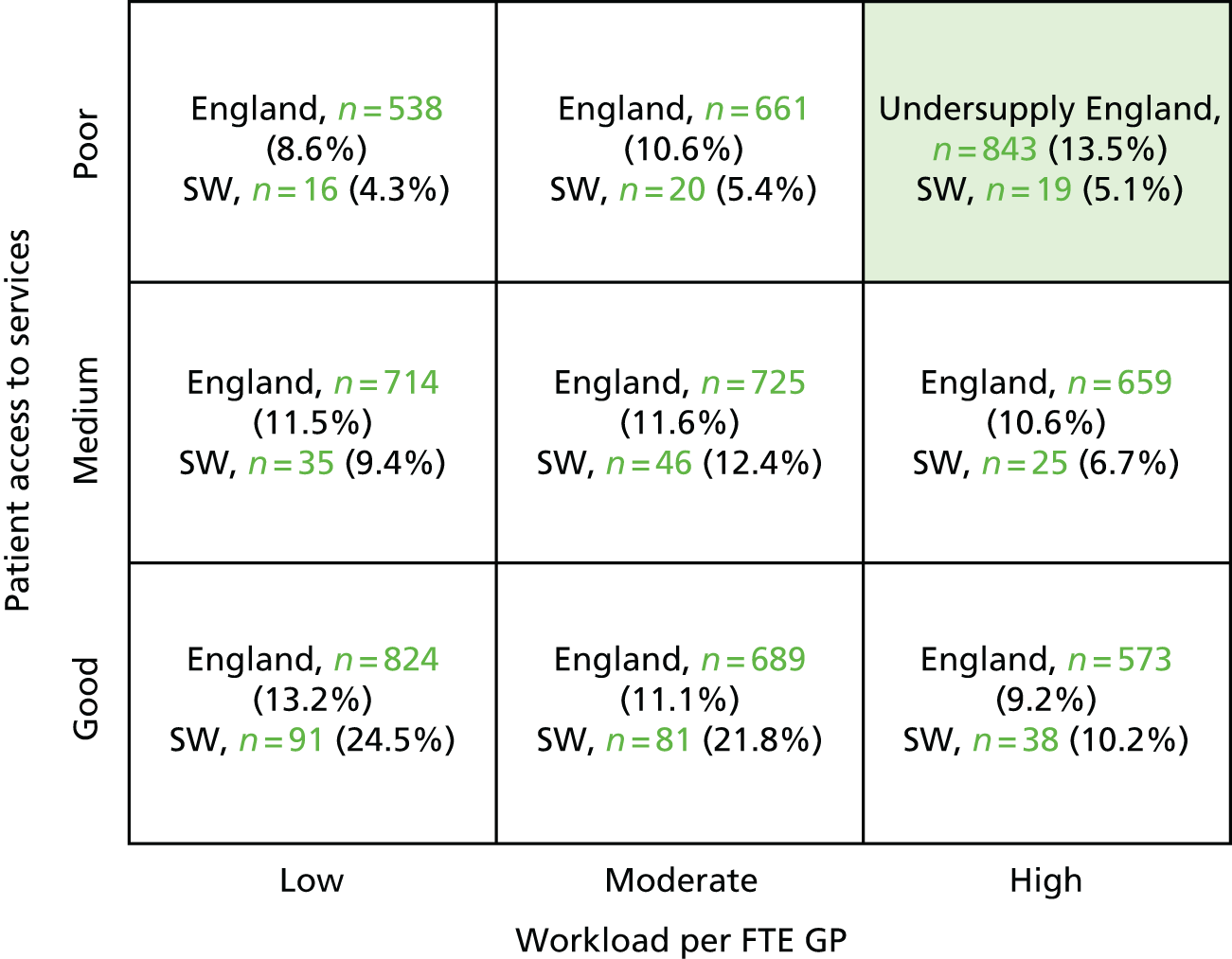
Table 20 provides a description of practices in south-west England, comparing those defined as currently in undersupply and those not currently in undersupply in accordance with our conceptual model. There was no evidence that either list size or list size adjusted for deprivation and weighted for population varied between the two groups. However, there was evidence that practices in undersupply had fewer FTE GPs, indicating that the differences in workload are driven more by the supply of GP workforce than the demand of the registered patient population. Practices in undersupply also had lower patient experience scores, not only for access (which forms part of our definition of undersupply) but also for continuity of care and overall satisfaction. Practices currently in undersupply also tended to have a higher ratio of nurse FTE to GP FTE, had fewer patients over the age of 65 years, served more deprived populations and were more likely to be in urban areas. There was no evidence (p = 0.34) that the distribution of practices currently in undersupply varied by CCG.
| Practice characteristics | Undersupply (n = 19) | Other (n = 352) | p-value | ||||
|---|---|---|---|---|---|---|---|
| Median | 25%a | 75%b | Median | 25%a | 75%b | ||
| List size | 9264 | 5361 | 11,576 | 7598 | 5270 | 11,077 | 0.448 |
| Adjusted weighted list size | 8959 | 5212 | 12,287 | 8099 | 5638 | 11,570 | 0.550 |
| GP FTE | 3.1 | 2 | 5.1 | 4.7 | 3.2 | 6.6 | 0.012 |
| Nurse-to-GP FTE ratio | 0.8 | 0.7 | 1 | 0.5 | 0.4 | 0.7 | < 0.001 |
| IMDc | 25.7 | 20.2 | 30.9 | 18.7 | 13.5 | 24.4 | 0.003 |
| GPPS accessd | 0.2 | 0.1 | 0.2 | 0.7 | 0.5 | 0.9 | < 0.001 |
| GPPS continuityd | 0.2 | 0.2 | 0.3 | 0.6 | 0.4 | 0.8 | < 0.001 |
| GPPS satisfactiond | 0.2 | 0.1 | 0.4 | 0.7 | 0.5 | 0.9 | < 0.001 |
| Percentage of patients aged ≥ 65 years | 16.8 | 13.3 | 21 | 22.6 | 17.6 | 26 | 0.004 |
| CCG areas | n (%) | n (%) | p-valuee | ||||
| Bath and North East Somerset | 1 (4) | 24 (96) | 0.337 | ||||
| Bristol | 3 (6.8) | 41 (93.2) | |||||
| Kernow | 4 (7.4) | 50 (92.6) | |||||
| North Somerset | 3 (15) | 17 (85) | |||||
| Somerset | 2 (3) | 65 (97) | |||||
| South Gloucestershire | 0 (0) | 23 (100) | |||||
| Northern, Eastern and Western Devon | 6 (5.6) | 102 (94.4) | |||||
| South Devon and Torbay | 0 (0) | 30 (100) | |||||
| Urban practices | 17 (6.8) | 232 (93.2) | 0.042 | ||||
| Rural practices | 2 (1.6) | 120 (98.4) | |||||
Predictive risk model
The predictive risk model was developed using 2012 data from 6398 practices across England (where possible) to predict current (2016) undersupply status. The regression coefficients for the logistic model used are shown in Table 21. Predictive risk model coefficients were estimated using 2012 data when possible to estimate the independent association with 2016 undersupply status. A negative coefficient in the model implies a reduced risk of future undersupply as the value of the variable increases. Because our model was designed to be predictive rather than explanatory, it is difficult to directly interpret coefficients as they may well share predictive power with other variables with which they have a high degree of collinearity. In particular, we note that continuity of care (as measured by GPPS) and rurality of practices were not statistically significant predictors of future undersupply status, although we did retain these variables in the model. This is not to say that they are not themselves associated with undersupply status, but that other variables in the model already account for their predictive contribution. Furthermore, we note that the interaction between the expected proportion of GP FTEs still working in patient care and the ratio of nurse FTE to GP FTE had a relatively large p-value (0.177). In initial modelling (before excluding practices on the basis of data quality; see Practice registered population), this variable had a smaller p-value (0.06), indicating that there was some evidence that it was worth including. When exclusions were applied, the coefficient did not change meaningfully. This fact, combined with the a priori expectation that the effect of expected future GP workforce would be dependent on recruitment, provided sufficient support to maintain the interaction term.
| Data type and variable | Note on units | Logistic regression coefficient (95% CI) | p-value |
|---|---|---|---|
| GPPS scoresa | |||
| Access | Random effect (log-odds ratio) from logistic case-mix adjustment model | –0.96 (–1.21 to –0.70) | < 0.001 |
| Continuity of care | –0.09 (–0.25 to 0.07) | 0.274 | |
| Overall satisfaction | –0.48 (–0.70 to –0.27) | < 0.001 | |
| Baseline workforceb | |||
| Ratio of nurse FTE to GP FTE | 1.02 (–0.05 to 2.09) | 0.062 | |
| Adjusted weighted list size per GP FTE | Per 1000 patients per GP FTE | 0.40 (0.18 to 0.62) | < 0.001 |
| Total GP FTE | –0.17 (–0.25 to –0.10) | < 0.001 | |
| Ratio of ‘other’ GP FTE to total GP FTE | 0.65 (0.32 to 0.98) | < 0.001 | |
| Rurality settingc | |||
| Urban practice | Reference | 0.404 | |
| Rural practice | –0.13 (–0.43 to 0.17) | ||
| IMD – practice in quintilec | |||
| 1 – least deprived | Reference | < 0.001 | |
| 2 | 0.02 (–0.29 to 0.32) | ||
| 3 | 0.13 (–0.16 to 0.42) | ||
| 4 | 0.57 (0.29 to 0.85) | ||
| 5 – most deprived | 0.36 (0.06 to 0.66) | ||
| Projected quantities | |||
| Adjusted weighted list sized | Per 1000 patients | 0.14 (0.10 to 0.18) | < 0.001 |
| Proportion of GP FTEs still in patient carea | Varies from 0 to 1 | 0.38 (–0.78 to 1.54) | 0.520 |
| Proportion of GP FTEs still in patient care × ratio of nurse FTE to GP FTEa | –1.01 (–2.48 to 0.46) | 0.177 | |
| Constant | –4.15 (–5.10 to –3.21) | < 0.001 | |
We applied the predictive risk model to the 2012 data on which it was developed to estimate historical predictive risk scores for each practice in England with available data. A comparison of these predictive risk scores to the 2016 supply–demand categorisation was used to assess the predictive value of the model. Figure 12 shows the ROC curve from this comparison. The area under the curve is 0.759. The ROC curve from a model including only the defining factors (GPPS access scores and adjusted weighted list size per FTE) was 0.718, suggesting that the full model provided a modest, but meaningful, improvement in predictive value.
FIGURE 12.
Receiver operating characteristic curve for the predictive risk model based on the national data used to build the model. Area under ROC curve = 0.7586.
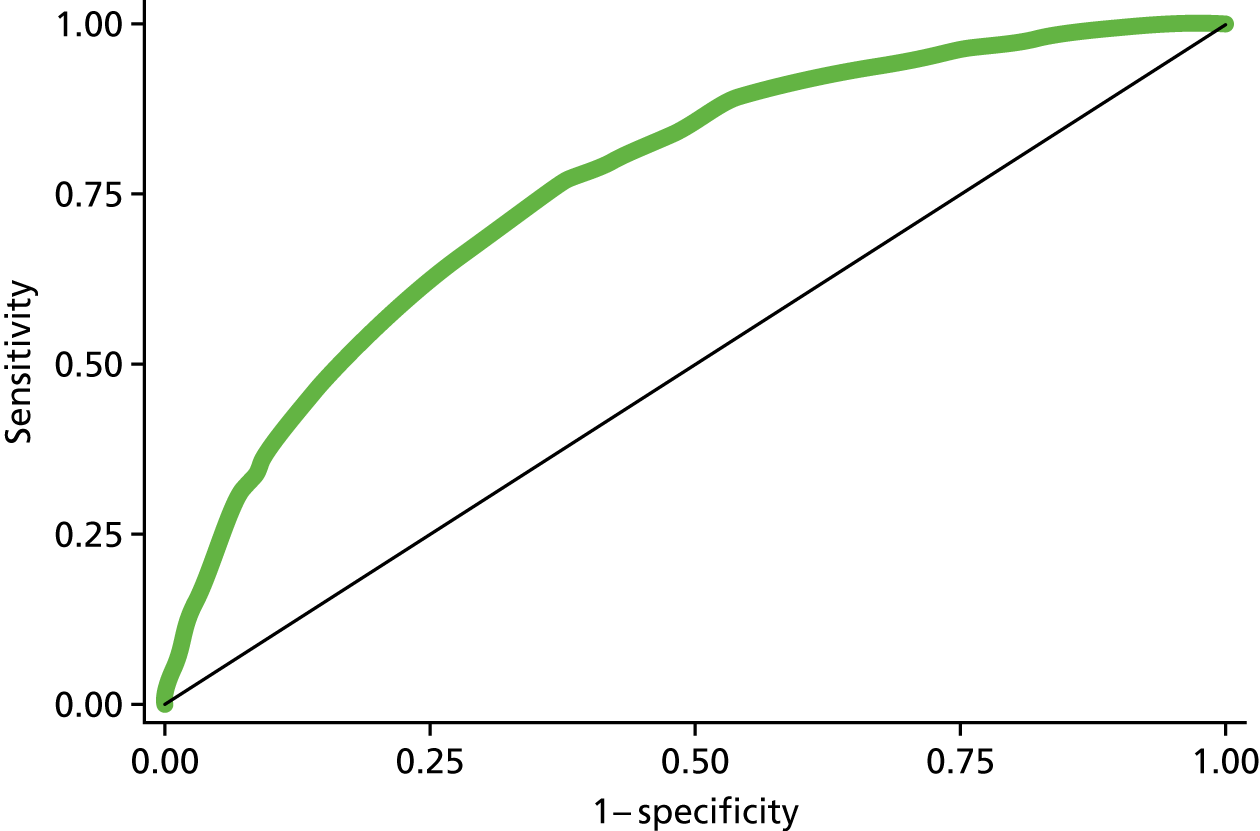
Future risk predictions
Applying the risk prediction model to data from 2016, seeking to predict the risk of future supply–demand imbalance for individual practices in south-west England, we obtained risk scores for 368 practices with available data remaining after applying exclusions. This risk prediction was based on the projected future workforce from responses to the ReGROUP survey. The median probability of future supply–demand imbalance across practices was 5.4% (IQR 2.8–10.0%). In total, 40 (10.9%) practices had a risk of > 20% and 12 (3.3%) had a risk of > 50%. In the absence of any clear separation in the distribution, we defined the highest 25% of practices as being at ‘high risk’ (> 10% risk) and the lowest 25% of practices as being at ‘low risk’ (< 2.8% risk). Using these cut-off points we rated the practices in south-west England. Table 22 shows the characteristics of those practices in south-west England classified as being at high risk of future supply–demand imbalance compared with other practices. In contrast to the current situation shown in Table 21, there was no evidence (p = 0.445) that the total GP FTE varies between high/other risk classification. There was evidence, however, that all other descriptive factors varied between those practices classified as being at ‘high risk’ when compared with other practices. The practices at ‘high risk’ of supply–demand imbalance over the next 5 years tend, currently, to have larger list sizes, to have a higher nurse workforce (relative to GP workforce), to serve more deprived and younger populations, to be in urban areas and to have considerably worse GPPS scores. There was also variation between CCGs, with over half of practices in North Somerset being classified as ‘high risk’ compared with only 15% in Northern, Eastern and Western Devon.
| Practice characteristics | High risk (n = 92) | Other (n = 276) | p-value | ||||
|---|---|---|---|---|---|---|---|
| Median | 25%a | 75%b | Median | 25%a | 75%b | ||
| List size | 10,625 | 7732 | 13,195 | 6915 | 4941 | 10,206 | < 0.001 |
| Adjusted weighted list size | 11,133 | 7369 | 13,252 | 7398 | 5251 | 10,615 | < 0.001 |
| GP FTE | 5 | 3.1 | 6.6 | 4.5 | 3.1 | 6.6 | 0.445 |
| Ratio of nurse FTE to GP FTE | 0.7 | 0.5 | 1 | 0.4 | 0.4 | 0.6 | < 0.001 |
| IMD | 25.6 | 18.7 | 31.7 | 17.6 | 13.1 | 22.2 | < 0.001 |
| GPPS accessc | 0.4 | 0.2 | 0.6 | 0.8 | 0.6 | 0.9 | < 0.001 |
| GPPS continuityc | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| GPPS satisfactionc | 0.4 | 0.2 | 0.6 | 0.7 | 0.5 | 0.9 | < 0.001 |
| Percentage of patients aged ≥ 65 years | 18.3 | 14.1 | 23.4 | 23.2 | 18.5 | 26.5 | < 0.001 |
| CCG areas | n (%) | n (%) | p-valued | ||||
| Bath and North East Somerset | 3 (12) | 22 (88) | < 0.001 | ||||
| Bristol | 18 (41.9) | 25 (58.1) | |||||
| Kernow | 11 (20.4) | 43 (79.6) | |||||
| North Somerset | 10 (52.6) | 9 (47.4) | |||||
| Somerset | 16 (23.9) | 51 (76.1) | |||||
| South Gloucestershire | 8 (34.8) | 15 (65.2) | |||||
| Northern, Eastern and Western Devon | 16 (14.8) | 92 (85.2) | |||||
| South Devon and Torbay | 10 (34.5) | 19 (65.5) | |||||
| Urban practices | 77 (31.3) | 169 (68.7) | < 0.001 | ||||
| Rural practices | 15 (12.3) | 107 (87.7) | |||||
Stress-testing scenarios
Further risk predictions were calculated using the expected future workforce based on GP age and gender alone and through exploring a number of hypothetical scenarios building on the baseline scenario described immediately above. For each of these scenarios, we classified each practice in terms of relative risk and absolute risk. Relative risk classifications are defined in accordance with the position of each practice in the distribution of risk scores for all practices for a given scenario. Relative risk classifications are used to illustrate how the ordering of practices, in terms of risk, changes under different scenarios. We classify the 25% of practices with the highest risk scores (under a given scenario) as ‘high relative risk’ and the 25% of lowest practices with the lowest risk scores as ‘low relative risk’. Absolute risk classifications are used to illustrate how the actual risk of supply–demand imbalance increases with increased stresses on the system. We classify practices in terms of absolute risk using the cut-off points used in the baseline predictions (i.e. a risk of being in a state of supply–demand imbalance in 5 years’ time of 10% and 2.8%). Figure 13 illustrates the changes to relative risk (see Figure 13a) and absolute risk (see Figure 13b) using these classifications. In this figure, each practice is represented by a horizontal bar. The ordering of each practice (vertical position) is the same for each scenario based on the rank ordering of each practice in accordance with the baseline risk prediction. For each scenario, the colouring of each practice illustrates the relative or absolute risk classification (see Figure 13a and Figure 13b, respectively) such that changes in colour indicate changes in risk classification.
FIGURE 13.
Rating of practices in south-west England from different risk prediction scenarios a–d using cut-off points defined by (a) the quartiles of each prediction (relative risk); and (b) the quartiles of the baseline prediction (absolute risk). a, Risk prediction as for baseline, but using ages and genders of GPs alone rather than including responses to ReGROUP survey. In each case the practices are ordered by the baseline scenario.
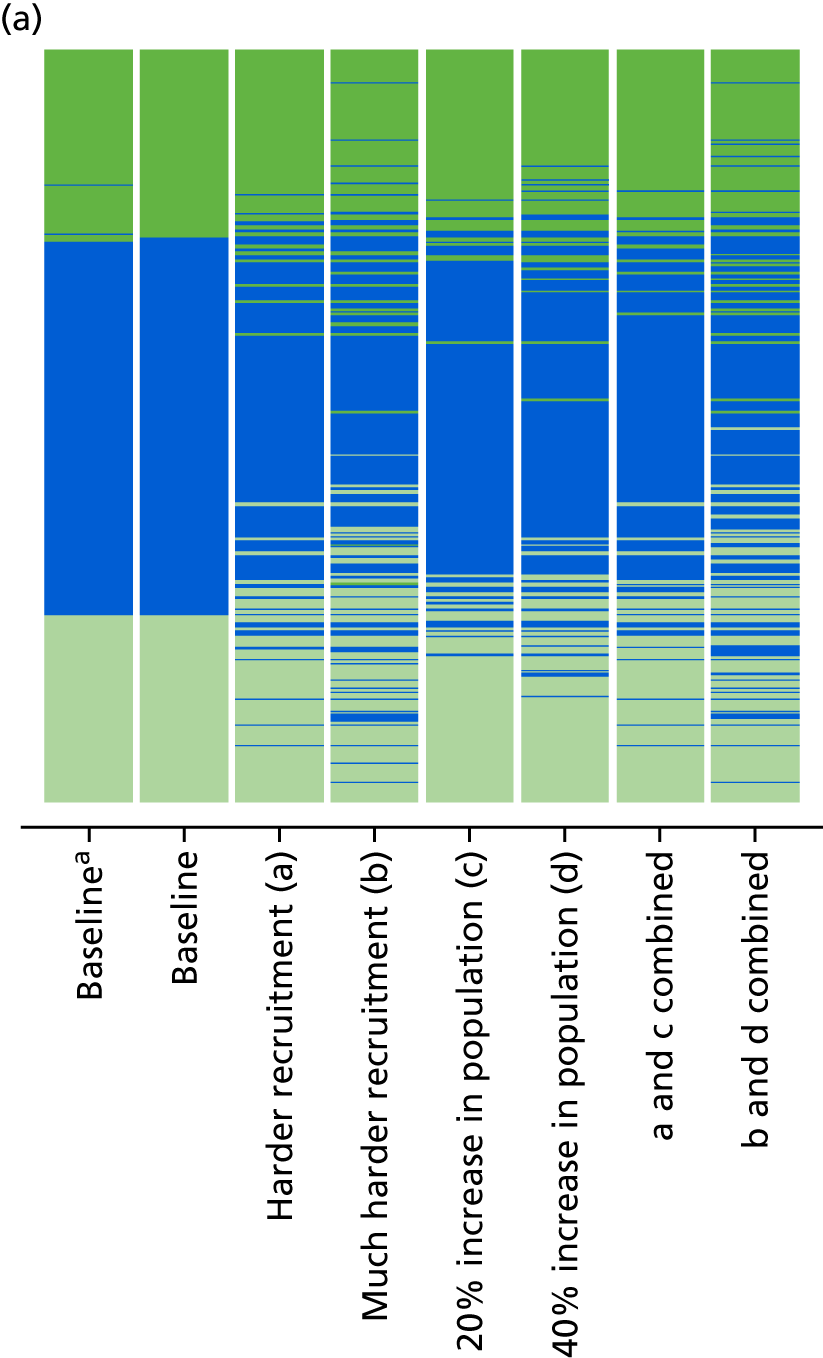
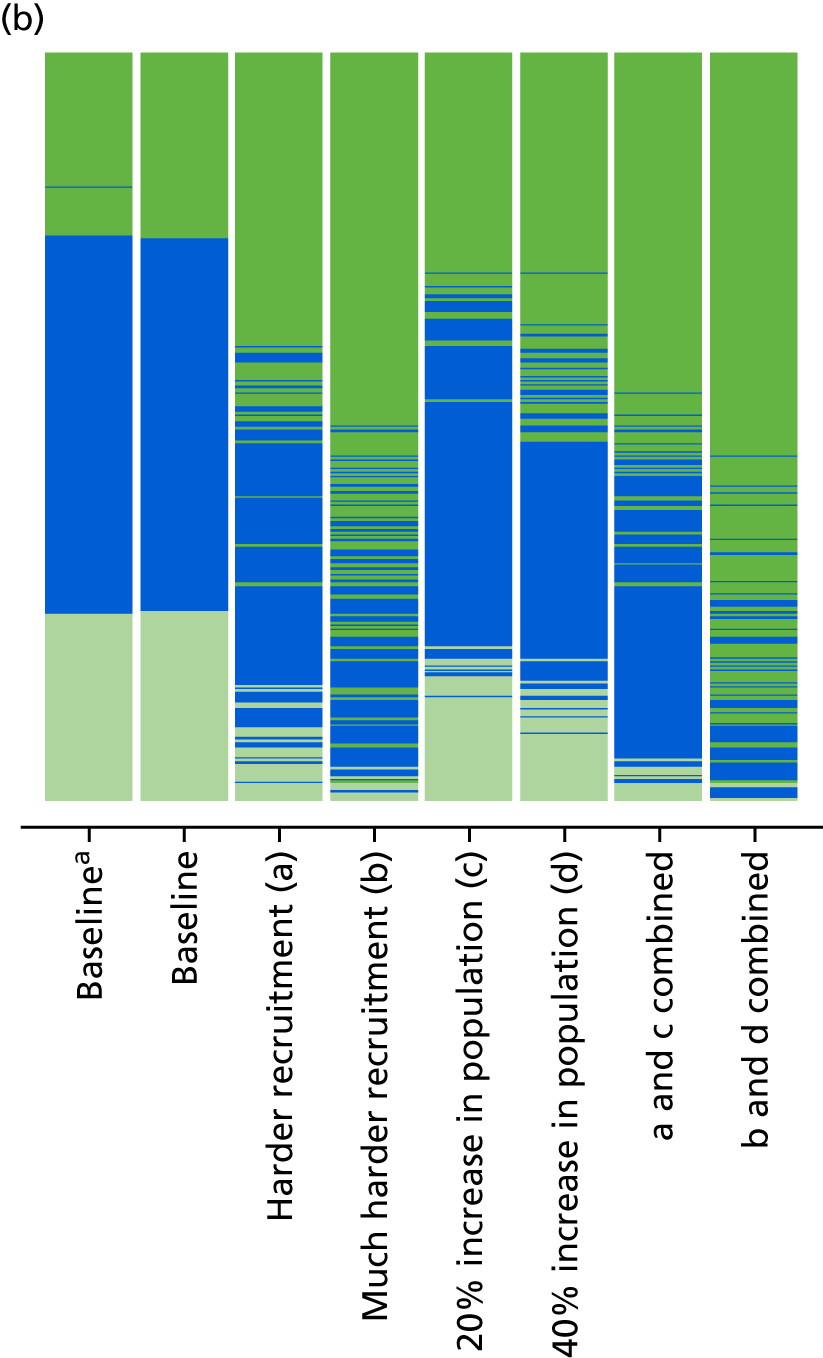
Comparing the baseline prediction in which responses to the ReGROUP survey were used to predict the future GP workforce remaining in patient care with a prediction in which GP age and gender alone was used, very little difference was observed in practices categorised as being either at ‘high relative risk’ or ‘high absolute risk’ of undersupply (seen in Figure 13 as limited reclassification of practices, correlation of ranks = 0.999).
‘Scenario a’ was intended to illustrate the effect of a modest increase in the difficulty in recruitment of GPs to replace those leaving (where the model coefficient for the expected proportion of GP FTEs remaining in patient care is increased by 2). For the most part, those practices classified as being at ‘high relative risk’ in the baseline scenario remained so under this scenario, as can be seen by the limited changes in Figure 13a (correlation in ranks between scenario a and baseline = 0.97). However, there was a dramatic increase in the number of practices with a predicted absolute risk of future undersupply of > 10%, illustrated in Figure 13b (scenario a), in which there is an increase in the number of practices coloured dark green. Increasing the model coefficient for the expected proportion of GP FTEs remaining in patient care further (by four from baseline) illustrates the potential effect if the recruitment of GPs was to become much harder (scenario b). Although a greater disturbance in the classification of practices was observed, the reclassification in terms of relative risk was still relatively modest (see Figure 13a, scenario b, correlation in ranks between scenario b and baseline = 0.90). Conversely, the reclassification in terms of absolute risk (see Figure 13b, scenario b) was significantly greater; the majority of practices had a predicted risk above 10% (see Figure 13a, scenario b). Practices at increased risk of undersupply from difficulty in recruiting GPs were likely to be those where current doctors are older. However, little difference was seen in the type of practice affected under these scenarios (see Appendix 35).
As with scenarios a and b, increasing the projected practice population resulted in only modest changes in respect of which practices are classified as being at ‘high relative risk’. Only a small relative increase was seen when comparing scenarios c and d (see Figure 13a, correlation in ranks between scenario c and baseline = 0.99 and scenario d and baseline = 0.98). However, substantial changes were seen in the number of practices with an absolute risk of undersupply of > 10% (see Figure 13b, scenarios c and d). Appendix 35 shows the descriptive features of practices classified as ‘high relative risk’ under these two scenarios of increased practice populations. In general, the type of practice classified as being at ‘high relative risk’ was similar to that seen under other scenarios (baseline, a and b), but under the scenarios of increased projected populations, those with more GP FTEs were also more likely to be at high risk. Combining the effect of scenarios a and c resulted in relative risk classifications closer to the baseline predictions than that for scenario a alone. However, in terms of absolute risk, more practices had a risk of > 10% (see Figure 13b, scenarios a and c). When scenarios b and d were combined (illustrating a situation in which it was much harder to recruit GPs combined with an increased practice population of 40%), it was evident that nearly all practices (88%) exceeded a 10% absolute risk of supply–demand imbalance within 5 years, with only nine practices (2.4%) classified as being at ‘low absolute risk’ using the cut-off points derived from the baseline predictions. Descriptive statistics for those practices at ‘high relative risk’ under these scenarios are shown in Appendix 35. It should be noted that we would not expect these substantial increases in practice populations to apply to all practices, but this illustrates those that would be at high risk if such an increase did occur.
Discussion
Summary of main findings
The aim of this research was to identify NHS general practices that may face an undersupply in GP workforce within the next 5 years. To illustrate this, we developed and evaluated a conceptual model of workforce supply–demand imbalance and, based on this, produced a risk prediction model informed by historical data that could be used to predict an individual practice’s risk of being in a state of undersupply in 5 years’ time. The risk prediction model produced a range of risk scores across south-west England and might be considered to have a fair to good discriminatory ability in this context (based on the ROC curve analysis). Applying this to current data suggests that the practices at highest risk of an undersupply of GP workforce in the future have, on average, larger patient lists, employ more nurses relative to GPs, serve more deprived and younger populations and have considerably worse patient experience ratings. Furthermore, we found that there was geographical variation in those practices being classified as at ‘high risk’, with the majority of practices in North Somerset being classified as being at ‘high risk’.
We then modelled scenarios in which the recruitment of GPs becomes harder and/or practice populations increase dramatically beyond what would be expected from historical trends (such as might be expected with a new housing development). These scenarios do increase absolute risk dramatically, but by and large it is the same practices in all scenarios that are at highest risk of future undersupply of GP workforce. This almost certainly reflects the fact that those practices most likely to have problems in the future are those currently experiencing difficulties. This can be seen in the relatively good predictions from a simple model including only defining factors based on routinely available data (i.e. workload-to-workforce ratio and access scores), which had an area under the ROC curve that was not dramatically less than in the full model. In particular, we found that the inclusion of findings from our survey of GPs’ career intentions had very little impact on the predictions, compared with using expected future workforce projections based only on data regarding GPs’ genders and ages.
During the course of our research, a serious situation emerged in respect of the GP workforce in Plymouth,146 a city within the geographical area of our research interest. An opportunistic secondary analysis of our data (Box 1), identified findings that, although preliminary, tended to support the validity of the model we described.
During the period of the risk prediction modelling work, major problems became evident in GP recruitment and retention within the city of Plymouth. Using our model to examine general practices in Plymouth (defined as practices with postcodes starting PL1, PL2, PL3, PL4, PL5 or PL6), we found that of the 28 practices with available data, just under half (43%) were at a > 10% risk of being in a state of undersupply within 5 years. This compares with 13% of practices with a risk of undersupply of > 10% in the rest of Devon (Northern, Eastern and Western Devon, and South Devon and Torbay). This provides some preliminary evidence of the validity and utility of our model.
Strengths and weaknesses
The strengths of this work include the comprehensive use of freely available data as well as the exploratory use of a census survey of career intentions of GPs in the region. However, the main strength is the development of factor weightings based on routinely available historical data. This allows confidence to be placed in these weightings because they are based on observed practice changes over time. However, we recognise that this assumes that factors driving changes are constant from the historical time period of model development to the future time period of prediction. This is unlikely to be the case given the observed increasing problems in GP workforce recruitment. To this end, we have modelled what might be expected if recruitment was harder than it has been historically, and we also modelled scenarios that account for substantive increases in the practice population, and perhaps we should consider these scenarios to be more reflective of what we might expect going forwards.
The main weakness of this work concerns our ability to distinguish in what situations, and in which practices, the future GP workforce leaving patient care will affect the level of continuing GP workforce and its ability to meet patient requirements. For practices that do not encounter problems in recruiting GPs, retiring GPs pose much less of an issue than in practices where recruitment is difficult. Here, we relied on the level of nurse staffing by a practice as a proxy for recruitment issues; importantly, this means that the association of greater numbers of nurses relative to GPs with at-risk practice status is likely to be attributable to practices not being able to fill GP vacancies, and not because more nurses per se puts a practice at risk. Owing to our focus on GP workforce, we have not explicitly examined here how the supply of nurse and other allied health professional workforce may have an impact on a practice’s ability to meet patient demand. This may be increasingly important as English general practice moves to new models of care. A more direct measure of recruitment problems, which was consistently and widely collected (such as duration of advertising for vacant posts, using a consistent methodology to track this), would be expected to provide a better model. Unfortunately, no robust freely available measure exists. The NHS GP census does collect data on time to fill vacancies142 and existing unfilled vacancies. However, these data are not freely available and, furthermore, are not mandatory for completion by practices.
Another weakness was that historical workforce data were not available with the same detail as current data. This meant that future workforce predictions using historical data would not be as accurate as those made using current data. These inaccuracies would lead to a loss of power and, potentially, to an attenuation of the associated regression coefficients. This may explain the low statistical significance of associated coefficients in the model. Even the more detailed current workforce data have concerns regarding data quality (see Workforce).
When considering practice workforce and practice patient populations together, we found both infeasibly high and infeasibly low workloads per FTE. This implied that either the workforce or population data were in error (or both). Unfortunately, it is not generally clear when such errors take place and so we could only exclude practices with a high likelihood of having incorrect data. The result is that our risk predictions almost certainly include practices with erroneous, but plausible, workforce or patient population data. We note that the current Workforce Minimum Data Set collection method is experimental and noted to have poor response compliance by some practices. 147 As these data collection methods mature, we might expect the quality of data to increase. Furthermore, exclusions made on the basis of erroneous and missing data mean that risk predictions were not available for a substantial number of practices. Finally, we note that our assessment of the performance of our model was made on the same data on which the model was developed, thus it is likely to overestimate the performance of the model. A validation of the future risk predictions would be welcome, but can be undertaken only in 5 years’ time.
Implications
We have demonstrated that it is possible to make reasonable predictions of an individual general practice’s future risk of undersupply of GP workforce with respect to its patient population. With ongoing GP workforce issues in south-west England and nationally, many local models are being developed to identify potentially ‘at-risk’ practices. However, unlike the model we present here, it is not clear to what extent these models are evidence based or to what extent their limitations are recognised by the users of the models. The predictions are inherently limited by the data that are available. Improvements in data going forwards will help the situation, particularly if data on practice recruitment are released. However, it will be some time before robust historical data exist that can be used for the model development process outlined here. If models such as the one outlined here are to be produced and used, it is important that high-quality data continue to be collected. The predictions produced by our model may allow targeting of interventions to retain and attract GPs either in specific practices or in specific regions currently at high risk of problems driven by workforce supply. Although the model we present here provides fair discrimination, much could be achieved by focusing efforts on those practices currently experiencing difficulties.
Although a policy of targeted interventions may have a place, most practices are likely to be at a high risk of workforce undersupply when faced with a substantial increase in demand from an increased patient population combined with major difficulties in recruiting GPs. For this reason, local knowledge of drivers of increased practice populations, such as housing developments, will be key to being able to suitably apply targeted interventions. Even in south-west England where workload and ability to meet patient demand are better than in England overall, most practices are vulnerable to recruitment challenges. Given this, overarching policies and strategies may be more effective than targeted ones, especially if areas of population growth are not known.
Chapter 7 Workstream 6: stakeholder consultation
Introduction
Whereas other workstreams sought to inform the identification of potential policies and strategies that may be of relevance to GP workforce retention, the aim of this workstream was to provide preliminary evidence on the feasibility and acceptability of implementing these prioritised policies and strategies. Building on the findings from the other workstreams, particularly the RAM expert panel, and drawing from experience of other research involving similar consultations with stakeholders,148 we aimed to gather feedback from a wide range of organisations. In particular, we aimed for stakeholders to explore factors that might affect the implementation of these strategies. We drew from experience of previous research involving similar consultation with stakeholders to inform our approach. This last step is critical if the NHS is to benefit from this research. This chapter presents the methods, and documents the views gathered during the consultation meetings undertaken with representatives from key national, regional and local stakeholder groups.
Methods
To explore issues of implementation regarding the emergent policy and practice proposals, we conducted facilitated stakeholder group consultation meetings in two locations in England: one in London and one in Leeds.
Recruitment
Target stakeholder groups included representatives of CCGs, LMCs, NHS England Local Area Teams, AHSNs and PPI groups, as well as representatives from national medical and government organisations including the Department of Health and Social Care (DHSC), the BMA, the RCGP, HEE, NHS Employers and the GMC. Members of our project advisory board provided key stakeholders from within HEE, NHS England, the BMA and the RCGP, and these were supplemented by extensive web searches for names and contact details of CCG/LMC chairpersons and others in workforce planning roles within national organisations or who had published on the subject of GP workforce in recent years.
The project management group reviewed the list of potential participants to ensure that no key groups or individuals had been omitted. All participants were e-mailed a formal invitation containing web-page links to register attendance at a meeting in June 2017 in either London or Leeds. Non-respondents were followed up by e-mail at regular intervals, and a new invitation was sent to any new individuals suggested by those unable to attend. Of 121 individuals approached, 48 registered to attend one of the meetings, of whom 44 (36% of those approached) attended on the day (22 at each meeting) (see Appendix 36).
Formulating the discussion topics
Both meetings involved discussion of the same topics to facilitate comparisons and identify differences between regions on emergent ideas. We identified 11 policy/strategy topics for discussion.
The discussion topics were derived mainly from the key policies and strategies prioritised by the RAM workstream (see Chapter 5) where the RAM panel had reached overall agreement that these policies and strategies were ‘appropriate’ and some where there was also consensus on them being ‘feasible’.
Topics 1–10 encompass the 16 policies and strategies that had been rated by the RAM panel (with consensus) as ‘appropriate’ and ‘feasible’ (Table 23).
| Number | Policy and strategy | Draft discussion topic title | Topic number |
|---|---|---|---|
| For implementation at national/regional level | |||
| 1 | General practices identified as being ‘at risk’ should be managed with an appropriate and sensitive supportive arrangement and this should be optional (uncertain for compulsory) (ID 9) | Identifying ‘at-risk’ (over workforce undersupply) status of general practices and providing support | 1 |
| 2 | General practices identified as being ‘at risk’ should be allocated a specialist team for managing recruitment and retention, and this should be optional (uncertain for compulsory) (ID 10) | ||
| 3 | New incentive and support packages should be available to GPs and organisations setting up new practices or new ways of working in under-doctored areas (ID 11) | A new focus on under-doctored areas and rethinking definitions | 2 |
| 4 | There should be a publicity campaign focusing on managing expectations of patients in line with the resources and constraints of GP-based primary care services (ID 18) | Using marketing strategies to influence demand | 3 |
| For implementation at general practice level | |||
| 5 | GPs who are returning to work after a period of absence or after a career break should have access to ‘health and well-being programmes’ to help them manage their re-entry into the workforce. Engagement with such a course should be optional (ID 19) | Supporting successful implementation and uptake of health and well-being interventions for GPs | 4 |
| 6 | GPs who are returning to work after a period of absence or after a career break should have access to schemes that have a range of routes and options that can be combined in a personal package for re-entry (ID 20) | Developing incentives and support packages within the current context | 5 |
| 7 | GPs who are returning to work after a period of absence or after a career break should have access to schemes that use a mix of online education and face-to-face meetings to ensure timely access to induction and refresher courses (ID 21) | ||
| For implementation at GP level | |||
| 8 | Peer support initiatives aimed specifically at health and well-being should be made available to GPs. Shown as appropriate specifically for those not near retirement age (ID 33) | Supporting successful implementation and uptake of health and well-being interventions for GPs | 4 |
| 9 | GPs should have access to their own specialised health-care service to ensure a quick and confidential occupational health-care service (ID 34) | ||
| 10 | A structured programme of training and support should be made available to all GPs in their first 5 years following qualification as an independent GP to help them establish healthy, productive careers. Engagement with such a course should be optional (uncertain for compulsory) (ID 36) | Professional support in the first 5 years of career | 6 |
| 11 | GPs should consider portfolio working as part of their career pathway and this should be optional (inappropriate for compulsory) (ID 39) | Portfolio working while retaining the core role of the GP | 7 |
| 12 | Incentives and support packages should be available for those GPs developing portfolio careers who are linking their portfolio activities to specialisms/areas that are directly beneficial to local clinical priorities (ID 42) | Linking portfolio activities to local population priorities and benefits | 8 |
| 13 | For GPs who are reaching retirement age and could take their pensions on exit, a comprehensive flexible careers scheme should be introduced with a view to supporting annualised hours, part-time working and/or ad hoc contributions to direct patient care (ID 49) | Support and planned exits for GPs nearing retirement age | 9 |
| 14 | For GPs who are reaching retirement age and could take their pensions on exit, the annual appraisal and revalidation process for such GPs should be reviewed with a view to streamlining and simplifying the process for such GPs who have not encountered any concerns in the previous revalidation/appraisal processes/for such GPs who would like to work with a specified and limited scope of practice (ID 51) | ||
| 15 | For GPs who are reaching retirement age and could take their pensions on exit, the working hours of GPs should routinely include fully funded, dedicated time to accommodate the full range of roles (administrative, clinical, training, management, CPD, business) undertaken as part of care professional activity (ID 47) | ||
| 16 | For GPs who are reaching retirement age and could take their pensions on exit, contracts based on specified programmed activities should be available to GPs to work across several general practices and on other health-related activities (ID 48) | Contractual arrangements for working across general practices | 10 |
A further six topics were then added for consideration within the stakeholder consultations. Topics 11–13 had been rated (in the form of statements) by the RAM panel as being ‘uncertain’ or with no consensus regarding appropriateness (‘external HR interventions and monitoring/support’) or as being ‘appropriate’ but ‘uncertain’ regarding feasibility (‘maximum number of consultations for GPs’ and ‘making consultations longer’). Topics 14 and 15 had been suggested as areas for potential inclusion in the RAM during the initial statement development work, but had not been taken forward for rating by the RAM panel. Topic 16 was added as an area of methodology for supporting implementation of policies and strategies, or for future research.
From the 16 topics in Table 24, we formed three broad categories (Box 2). Eleven discussion topics were formed from the 16 draft topic titles by combining the two topics concerning identifying the ‘at-risk’ (of workforce undersupply) status of general practices and a new focus on under-doctored areas (1 and 2); the two topics concerning portfolio working (7 and 8); the two topics concerning incentives and support packages for GPs (4 and 5); and also the three topics covering support and planned exits for GPs nearing retirement and the implications of losing previous pension incentives (9, 15 and 16).
| Number | Topics |
|---|---|
| Topics covering the policies/strategies rated in the RAM as ‘appropriate’ and ‘feasible’ | |
| 1 | Identification of at-risk status of general practices and providing support |
| 2 | A new focus on under-doctored areas and rethinking definitions |
| 3 | Using marketing strategies to influence demand |
| 4 | Supporting successful implementation and uptake of health and well-being interventions for GPs |
| 5 | Developing incentives and support packages within the current context |
| 6 | Professional support in the first 5 years of career |
| 7 | Portfolio working while retaining the core role of the GP |
| 8 | Linking portfolio activities to local population priorities and benefits |
| 9 | Support and planned exits for GPs nearing retirement age |
| 10 | Contractual arrangements for working across general practices |
| Additional topics for consideration within the stakeholder consultations | |
| 11 | External HR interventions and monitoring/support (rated as uncertain in the RAM for appropriateness) |
| 12 | Maximum number of consultations for GPs (rated as appropriate in the RAM, but as uncertain for feasibility) |
| 13 | Making consultations longer (rated as appropriate in the RAM, but uncertain for feasibility) |
| 14 | Widening MDTs and role substitutions (not rated in the RAM) |
| 15 | Implications of losing previous pension incentives to stay in practice (not rated in the RAM) |
| 16 | Definitions and criteria for GPs nearing retirement age who are accessing support (not rated in the RAM) |
-
Using marketing strategies to influence demand (topic 3).
-
Maximum number of consultations for GPs (topic 12).
-
Making consultations longer (topic 13).
-
Identification of at-risk status of general practices and providing support (topics 1 and 2).
-
External HR interventions and monitoring/support (topic 11).
-
Supporting successful implementation and uptake of health and well-being interventions for GPs (topics 4 and 5).
-
Professional support in the first 5 years of career (topic 6).
-
Support and planned exits for GPs nearing retirement age/implications of losing previous pension incentives to stay in practice (topics 9, 15 and 16).
-
Portfolio working while retaining the core role of the GP/linking portfolio activities to local population priorities and benefits (topics 7 and 8).
-
Contractual arrangements for working across general practices (topic 10).
-
Widening MDTs and role substitutions (topic 16).
Definitions of each policy and strategy referred to by the discussion topics are given in full alongside the findings from the consultation.
In addition, graphic facilitation was seen as an innovative and potentially useful means of capturing some of the process and key discussion points from the stakeholder events and so was undertaken at each meeting with the aim of capturing the key themes generated by the group discussions.
Data collection and analysis
We adopted a consistent structure for the two meetings (see Appendix 37). Following presentation of our research findings, stakeholders were asked to work in their allocated round-table groups, seated at tables of seven or eight people. During round-table discussions, each group covered between one and three policy and strategy areas in each 45-minute discussion session.
We anticipated that stakeholders would take a broad view of the feasibility of policy and strategy implementation, noting barriers and facilitators that might impede or enhance the utility of our research to the front-line NHS. Discussions were facilitated by two project team members at each of the table groups and were structured as follows:
-
What factors could have an impact – positively or negatively – on the implementation of the emergent recommendation?
-
Please comment on feasibility and acceptability of the emergent recommendation.
-
What are the structures or groups that would need to be involved in introducing change to this area?
-
What are the three key next steps to move this agenda forward?
Facilitators recorded stakeholders’ comments on sticky notes (and/or stakeholders did this themselves) and added them to flip charts during the discussion, which were referred back to during the closing summary session. In addition, stakeholders were provided with a poster summarising the findings of the systematic review, and facilitated whole-group discussion throughout the event and at the end of the day’s proceedings.
Post-event processing of collected information
Following discussion among the research team, Emily Fletcher summarised the key messages that had been collected on the sticky notes on flip charts by examining those comments that fell within the following broad categories: (1) positive and negative factors for implementation; (2) comments regarding feasibility and acceptability; (3) region-specific (i.e. ‘north’ or ‘south’) issues raised; and (4) key actions required, including those organisations that needed to be involved to make changes to the policy area. This summary was initially produced by Emily Fletcher and was cross-checked with members of the project team who had acted as table group facilitators (JLC, RA, CS, SD, SR, RC and AA).
Stakeholder views captured
To summarise the discussions that took place at each of the London and Leeds meetings, each of the policy/strategy discussion topics outlined positive enablers and negative barriers regarding implementation identified by stakeholders. Specific actions recommended by stakeholders to be taken relating to the policy areas, and by whom (when it was possible to identify a relevant group or network), are summarised in Box 3.
The large-format cartoon graphics produced from each meeting are reproduced in Appendix 38. Given the nature of the initiative, bullet points and notes rather than extended narrative are used here to report the content of discussions that took place; discussion points specific to either the London or the Leeds stakeholder event only are noted.
A strategy to introduce a publicity campaign focusing on managing the expectations of patients in line with the resources and constraints of GP-based primary care services.
Positive factors
-
Co-ordination of existing publicity campaigns regarding use of general practice and primary care services is needed.
-
Supportive PPGs in general practices and in CCGs could have a potential role in any campaign that is aimed at educating patients or changing their help-seeking behaviour.
-
There is a need for such publicity campaigns to target ‘high-user’ patient groups.
Barriers
-
There is currently no overall media strategy that allows for consistent, multichannelled sustainable messages that can be delivered both at national and local levels, without misinterpretation, which has been informed by and has buy-in of clinicians and staff at practice level.
-
Small campaigns may work, but are likely to be unsustainable.
-
GPs can inform/educate patients, but often patients cannot readily change their consulting behaviour owing to broader environmental factors and/or social constraints.
A policy to reconsider the limitations imposed by rigid structures on consultation and appointment times, with an anticipated inevitable impact on meeting contractual obligations, finances and patient demand.
Positive factors
-
Setting a maximum number of consultations could be achieved (e.g. as per hospital outpatient clinics), potentially positioned as a quality and safety issue.
-
Capping the number of consultations may negate ‘supply-induced demand’ [sic] (i.e. additional use of primary care services by patients as a result of increasing access). 149
-
Not all consultations are necessarily for a GP – other health professionals can be used differently such that the overall number of appointments could be increased, which would allow a limit to be set per GP.
-
Both the number and length of appointments need to be calibrated to individual patients’ needs.
-
It is a GP’s duty to decide when/if he or she is unsafe to see patients.
Barriers
-
Individual GPs have different consulting styles (longer vs. shorter consulters); achieving consistency of individual ways of working is challenging.
-
Setting a maximum number of consultations per day may be less acceptable to patients.
-
There will inevitably be a need for a ‘pressure valve’ service for occasions when demand exceeds the maximum number of consultations available. The nature, cost, capacity and quality of such services are of key importance to the success of setting a limit on the number of GP consultations.
-
GPs may fear increased complaints from patients.
-
There is uncertainty over whether or not patient safety is affected by the number or length of consultations, and the point at which care delivery becomes ‘unsafe’.
-
The content of consultations is key and can make a consultation more or less stressful for a GP.
-
What would be the reaction of CCGs to setting a maximum number of consultations?
-
It would be challenging to square the aims of setting a maximum number of consultations with the fact that Sustainability and Transformation Partnerships involve shifting work to primary care.
A policy that might place limitations on the number of consultations a GP might be expected to undertake in a working day in order to protect both patient safety and the health of the GP.
Positive factors
-
Containing a consultation within 10 minutes is a challenge, but longer consultations are likely to increase patient and GP satisfaction.
-
One 15-minute appointment may comprise higher-quality care than two 10-minute appointments, and may prevent the need for follow-up.
-
Certain patient groups need longer than the traditional 10-minute appointment than other patient groups.
-
GPs need to be able to work in different ways to suit individual consulting styles – use of the wider health professional skill mix can help meet overall demand.
-
Research evidence suggests that patients are fairly accurate in assessing how long they require if allowed choice of appointment length.
-
Combining longer consultations with telephone triage and patient education may be the most effective strategy.
-
Introducing longer consultations will inevitably have an impact on access and GPs’ stress initially, but over time the length of a GP’s overall working day is likely to be the same.
Barriers
-
Offering many longer appointments would potentially affect access and patients’ expectations.
-
GPs fear that workload will increase within a longer consultation (supply-induced demand).
A strategy for practices to have the option to self-register their ‘at-risk’ status (in relation to workforce undersupply within the next 5 years), and those identified as being ‘at-risk’, to have the option of having appropriate and sensitive supportive arrangements, a specialist team and/or a toolkit to support their management of recruitment and retention.
The nature of a practice being ‘at risk’ and the process of identifying ‘at-risk’ practicesPositive factors
-
A practice’s ‘at-risk’ status should be on a sliding scale (recognising that particular practices may become ‘at risk’ unpredictably and at short notice), rather than a binary, objective, stable state.
-
Definition of ‘at-risk’ status could be considered at the town/regional level (i.e. a shared problem in an area), rather than individual practice level.
Barriers
-
There were concerns/uncertainty over the implications of being ‘at risk’ regarding whether this status would be public or anonymous, and how long the status would last (i.e. when would it be reviewed).
-
What data would be used to define ‘at-risk’ status (i.e. what balance of routine indicators vs. local knowledge/intelligence)?
-
Who would define ‘at-risk’ status (and is it most appropriate for a CCG to make the assessment)? Self-identification by a practice was not seen as viable/practical – if a practice would receive greater resources, assessment of ‘at-risk’ status would need to be backed up by external judgements and/or data.
Positive factors
-
Support arrangements should tackle the root causes of organisational problems that are beyond issues relating to GP recruitment and retention, to include organisational development, training (e.g. team coaching), recruitment and retention of all practice team staff groups (Leeds) and assessment of clinical resources and the causes of vulnerability (London).
-
Support would need to be tailored, locally delivered and flexible.
-
It would be preferable if support was led by peers (possibly local or regional peers), rather than external parties – it needs people who are knowledgeable about the nature and business of being a GP, including experienced practice managers.
-
The processes and networks involved in identifying ‘at-risk’ practices should be linked to the provision of support.
Barriers
-
What would be the scope of support for ‘at-risk’ practices?
-
There were concerns regarding whether information about practices receiving support ‘stays local’ (e.g. within CCG) or if it is shared nationally.
A strategy for the use of HR arrangements that are managed externally to the practice and that would oversee the consideration and implementation of flexible working arrangements, retention, professional development and standards for working hours and conditions.
Positive factors
-
Careful management of a transition to using external HR would be needed for it to be accepted and helpful.
-
External HR arrangements would need to be sustainable, to fit in with current and future service reforms and to be supportive and not proscriptive.
-
Use of external HR systems may be better suited to vulnerable practices.
Barriers
-
There was hesitancy/reluctance among stakeholders regarding the use of external HR support.
-
Practices (particularly GPs and practice managers) need to be involved and in control of HR processes; GPs and practice staff could be better supported to manage HR processes internally.
-
There was no overall consensus on whether or not the use of external HR is a ‘good idea’.
A strategy to support the successful implementation/uptake of a number of initiatives, including GPs being given access to their own specialised occupational health-care service and to peer support initiatives being made available to GPs who are not nearing retirement.
Positive factors
-
Priorities in this area are to raise awareness of health and well-being interventions and to ensure their confidentiality.
-
Wider support structures can affect GPs’ health (e.g. career advice, RCGP roles).
Barriers
-
Occupational health can be seen as a ‘sticking plaster’ solution that does not deal with underlying causes of problems.
-
Bureaucracy around new schemes and initiatives acts as a disincentive; new schemes and initiatives are seen as ‘bombs’ that are created by one group and that are swiftly passed to GPs to defuse/manage.
-
Informal support networks (such as practice teams/GP colleagues) are being eroded under current working conditions.
A policy for a structured programme of training and support being made available to all GPs in their first 5 years following qualification as a GP to help them establish healthy, productive careers.
Positive factors
-
Professional support (peer to peer) can help with recruitment and reduce isolation.
-
Examples of a model for support include the Practice Based Small Group Learning approach, led by a trained mentor, and the HEE Yorkshire & Humber Nurse Preceptorship Programme.
-
Objectives for professional support need to be set but kept informal; such approaches should not be mandatory but kept as an ‘offer’.
-
Use of virtual meetings/communication to deliver professional support could be explored in cases in which participation rates among GPs might be lower.
Barriers
-
Consideration needs to be given to who could deliver various components of professional support and the practicalities of fitting this in with other commitments (e.g. pastoral care does not necessarily require delivery by doctors).
A policy specifically focusing on those nearing retirement, with structured and targeted support for flexible career schemes, simplifying the annual appraisal/revalidation process, acknowledging the potential impact of changes to pensions.
Positive factors
-
To enable GPs nearing retirement to want to continue working, job satisfaction needs to be increased and end-career role options need to be professionally fulfilling.
-
There may be particular role(s) that would persuade a GP to remain in direct patient care and certain elements of work (such as some elements of routine practice administration) from which these experienced GPs might be excused. Alternatively, other support mechanisms might be put in place (such as extended administrative/secretarial support) in order to keep GPs within the workforce.
-
Simplifying the appraisal/revalidation process for this group of GPs is essential; its benefits are far outweighed by the bureaucracy involved.
Barriers
-
Retaining these GPs through financial incentives was felt to be controversial.
A policy for portfolio careers to be used to support GPs at different stages of their career and to formally provide portfolio options incorporating the ongoing provision of direct patient care.
Positive factors
-
Portfolio careers are now widely accepted as a legitimate career option.
-
Such an approach may help GPs achieve vital ‘headspace’ and reflection time.
-
Portfolio working should be seen as a positive mid-career option/reward for experienced GPs, rather than for early-career GPs who were thought to lack the core clinical experience needed for portfolio roles.
Barriers
-
Conflicting opinions were expressed regarding the definition/scope of portfolio working.
-
Is portfolio working just part of what a GP is/does, or does ‘being a GP’ fundamentally involve adopting a range of roles?
-
It is currently hard to define and monitor the scope of portfolio working.
-
Organisational issues arise from the unintended ‘knock-on’ effects of GPs taking time away from direct patient care for portfolio roles.
-
Overall, there was no clear shared view on how to provide a ‘career structure’ for portfolio roles.
A policy to increase the positive impact of portfolio working in the local area by introducing contracts based on specified programmed activities for GPs to enable them to work across several different practices and on other health-related activities.
Positive factors
-
Introducing contracts for GPs working across practices would be feasible and acceptable to some, but may not be universally acceptable to GPs.
-
Positive examples already exist of this type of arrangement working well (e.g. GP Retention Scheme).
-
Introducing contractual arrangements for this approach reflects the importance of job satisfaction to GPs over simply being paid more to undertake more work (and thus potentially increase workload and concomitant work-related stress).
-
‘Super practices’ may be in a good position to offer such approaches to new GPs.
Barriers
-
Uncertainties and potential problems were identified regarding who should manage the employment of GPs working across practices and also deal with related legal/liability matters.
-
An associated potential negative impact on continuity of care, team working and long-term commitment to a practice was identified.
-
This style of working may be daunting to older GPs used to a more traditional model.
-
Cross-practice working seems not to last; GPs tend to end up in one practice.
-
Lack of clear career path for a GP working across practices in this way.
A policy to address the impact of increased uptake of portfolio working through the appropriate allocation of workload to other health-care professionals with clarity on the levels of responsibility and without diminishing or substantially changing their role as a GP.
Positive factors
-
Widening the skill base and professional mix of practice teams is seen as an essential way to cope with workload.
-
Patients like having access to a range of health professionals.
-
Other health professionals can indeed help to provide care; GPs are skilled at – and essential for – conducting core elements of diagnosis and care.
-
Practice managers are a crucial conduit for multidisciplinary working.
Barriers
-
There are limited numbers of health professionals available. Bringing such individuals into primary care may denude other areas; groups recognised a crisis in the nursing workforce of similar magnitude to that being experienced among GPs.
-
Effective multidisciplinary working requires time, capacity and resources.
-
Uncertainty was evident over the governance of extended primary care teams (training, support and ‘checking up on’ is also needed).
-
There is a need for career planning for other health professionals (their career paths in primary care are largely unknown territory).
-
Costs of employing other health professionals may be almost equivalent to hiring another GP.
-
GPs retain key diagnostic skills and are ‘better value for money’.
-
GPs may end up dealing with a highly complex workload, with little respite in intensity of workload.
-
Widening/extending roles across the MDT is affecting GP identity, role and skills.
-
GP trainees are becoming ‘de-skilled’ in respect of chronic disease management and complex comorbidity, through becoming ‘specialist’ too soon in their careers and opting to undertake specific activities and not others.
The main considerations regarding emergent policy and strategy arising from the stakeholder consultation are summarised in Table 25.
| ‘Protection’ of GPs and managing patient expectations | Incentives and support mechanisms for GPs | Portfolio and wider working arrangements |
|---|---|---|
| Maximum number of consultations | Identification of ‘at-risk’ status of general practices and providing support | Portfolio working |
NHS England/CQC/RCGP, CCGs:
|
NHS England:
|
GMC/RCGP – collect/provide data on scope of portfolio working and on current GP activity CCGs/federations/STPs – establish a co-ordinating role for the management of portfolio working RCGP/HEE – revisit the current training structure with a view to increasing flexibility in training and supporting development of portfolio careers GMC – include recognition/management of portfolio roles within the appraisal/revalidation process |
| Making consultations longer | External HR interventions and monitoring/support | Contractual arrangements for GPs working across several practices |
|
Practices:HEE – consider amending the Clinical Skills Assessment to reflect the need for GPs to develop skills to consult within a longer consultation time Academic partners – participants suggested undertaking a UK study to provide evidence on offering longer appointments/choice of appointment length, including qualitative interviews with GPs about introducing such a system NICE – guidelines could be a mechanism for bringing about change to the traditional length of consultations |
If HR processes are managed externally, a centralised, consistent, sustainable model would need to be available If HR processes are managed internally, training and support should be available to GPs and practice managers |
Practice groups/federations, super practices and locum banks should be involved in formalising contractual arrangementsBMA/NHS England – clarify guidance on legal/liability issues and the best arrangement(s) for employment and management by one practice of GPs working across practices BMA/RCGP/GMC/NHS Digital – agree a definition of FTE for a GP (current definitions differ across NHS Digital, HEE and the BMA differ) RCGP/HEE – long-term commitment to defining a path for this type of career |
| Using marketing strategies to manage patients’ expectations | Supporting uptake of health and well-being interventions for GPs | Widening skill base across MDTs and role substitution |
NHS England:
|
Those introducing new schemes and initiatives:Practice teams – should create clear space during the working day for ‘headspace’ and support (e.g. regular morning coffee gathering) National and professional groups (e.g. the RCGP and RCN) – health and well-being schemes should consider support for other clinicians who are part of the MDT |
Practice groups/federations – share resources and experiences (e.g. a specialist GP to support multidisciplinary working across practices) Practice teams – structure time for multidisciplinary working and related discussions during the working day RCGP/HEE – define the required competencies, skills and experience to be a ‘consultant GP’ and to ensure ‘learning on the job’ for GP trainees that includes observing other health professionals working in practice DHSC/NHS England – revive the previous financial incentive to employ a range of health professionals; establish arrangements to anchor such individuals to a practice by passing this money directly to practices, rather than to CCGs/trusts RCGP – define formal training and career progression for practice managers |
| Professional support in the first 5 years of career | ||
|
CEPNs/HEE training hubs – should co-ordinate and link with current RCGP First5 activities and responsibilities151 RCGP – should embed professional support in the first 5 years and make pastoral/peer-to-peer care an important part of training |
||
| Supporting planned exits for GPs nearing retirement age/implications of losing pension incentives | ||
|
The NHS regional offices were highlighted as the organisations that could take action The National Performers List could be used to limit the scope of a GP’s practice in a positive way (i.e. rather than for disciplinary processes) Fresh approaches to the appraisal/revalidation process are urgently needed (for GPs of all ages) to reduce burden and make appropriate to a GP’s existing role Introduce (to appraisal/revalidation) a compulsory interview with a trained GP career advisor, with special appraisal at age 50/55 years to give an informed career review of role options |
Discussion
Members of key stakeholder organisations with involvement and expertise in NHS and primary care workforce planning worked in small round-table groups to consider 11 policy and strategy areas focused on retention of the existing GP workforce in three broad categories (‘protection’ of GPs and managing patient expectations; incentives and support mechanism for GPs; and portfolio and wider working arrangements). Discussions were structured to record key comments and views and beliefs relating to feasibility, acceptability, positive and negative factors that might affect implementation, and key actions to be taken forward by particular workforce partner groups or stakeholder organisations.
A number of policy and strategy areas generated clear actions, with potential responsibility for implementation and response being attributable to specific organisations.
In addressing issues regarding protection of GPs in their current roles and in seeking to manage patients’ expectations of primary care, emergent policies and strategies from this project highlighted the importance of routine practice operation and management. Discussions about setting a maximum number of GP consultations per working day and also on increasing the traditional length of consultations concluded that these were potentially both helpful policies that were also considered to be potentially feasible. However, the inherent contradiction of attempting to constrain individual workload in the face of recruitment challenges that are likely to represent countervailing forces was fully recognised.
Actions were identified for organisations at a range of levels: practice teams being responsible for analysing their workload and improving consultation planning. Nationally (NHS England, HEE, RCGP), proposing a maximum limit on consultation number and making a change to the traditional 10-minute consultation length could be introduced via the use of National Institute for Health and Care Excellence (NICE)-supported guidelines providing evidence-based summaries of relevant evidence, and GP training (i.e. the RCGP postgraduate training curricula and the summative clinical skills assessment of trainee GPs) might also be a vehicle to influence GPs’ consulting style. Discussion on the use of marketing strategies to manage patients’ expectations of GP services (national/regional-level policy) led stakeholders to conclude that a national, consistent strategy developed, and with implementation overseen, by NHS England (co-ordinated and with national branding) was needed in order for such interventions to be effective.
In discussing incentives and support mechanisms, emergent policies and strategies related to both overarching HR management systems and actual HR practices, potentially implementable at all three levels considered (national/regional, practice and GP level). Discussion of practices being able to self-register their ‘at-risk’ status regarding workforce undersupply highlighted considerable uncertainty among expert stakeholders over both the method of defining at-risk status and the practical implications of being identified as being ‘at risk’. Informal/local knowledge on ‘struggling’ practices was identified as being key, and, for this reason, CCGs (overseeing the process of definition and assessment of ‘at-risk’ status) and practice groups or federations were suggested as possible organisations that might lead action around providing support to ‘at-risk’ practices. Our predictive risk modelling work within ReGROUP provides a potential model to apply in practice.
Discussions on practices’ HR systems being managed via arrangements that were external to practice administration and organisation reflected the uncertainty expressed by participants in the RAM panel (see Chapter 5). Stakeholders concluded that GPs and practice managers are central to the success of practice HR processes but could be better supported with training (perhaps within the responsibility of HEE or NHS England) to oversee this element of general practice.
Discussions on both supporting the uptake of GP health and well-being interventions, and also on professional support for GPs in their first 5 years post GP qualification acknowledged the importance of policies/strategies to ensure and promote the success of these recently established initiatives (such as the NHS-supported GP Health Service152). National organisations with an interest in GP health and well-being [RCGP, Community Education Provider Networks (CEPNs), HEE], along with any group that might develop and implement a new scheme or initiative, should be encouraged to develop schemes and services that have limited bureaucracy and good ease of access and clarity of purpose. Professional groups, including the RCGP and the Royal College of Nursing, were called on to consider health and well-being support for all health professionals, in addition to GPs, who are working in general practice; stakeholders suggested that CEPNs/HEE should ensure that efforts to support newly qualified GPs are linked with current RCGP First5 activities, thus providing a co-ordinated approach across organisations. Practice teams also have responsibility for planning time during the working day in order that the practice team create ‘headspace’ for thinking, planning and reflection, and act as a focus for internal mutual support between colleagues.
Finally, discussions on supporting ‘planned exits’ for GPs nearing retirement (and the implications of losing previous pension incentives) were a key addition to the RAM workstream, which had not included this area within those presented to the RAM panel. NHS regional offices were identified as being in a position to support the identification of this target GP group and proactively offer support in making changes to the scope of practice of these individuals in a positive and supportive way. Review of the appraisal/revalidation process, particularly for these GPs, was seen as a key priority and was identified by stakeholders as an important area of concern, which warranted reducing the bureaucratic burden for GPs. Such approaches were seen as being within the remit of the GMC and appraisal infrastructure and were seen as possible successful targets for innovative thinking and service redesign.
In supporting GPs to develop portfolio working and in supporting their wider working arrangements, emergent policies and strategies related to both HR practices and operational functions/practice management, implementable at practice level. Discussions on portfolio careers, contracts for GPs to work across several practices and allocation of workload to other health-care professionals were all viewed as ways to formalise and support various styles of managing workload/work–life balance that are already widely in use. In almost all areas, national organisations were identified as having a part to play: the GMC to provide data on the scope of GPs’ portfolio roles and to reflect these roles within the appraisal/revalidation process; and the RCGP/HEE to increase flexibility within GPs’ training to promote and support the development of portfolio careers, clarify the career path for GPs working across practices, and define the required competencies, skills and training needed to be a ‘consultant GP’. The BMA and NHS England nationally, as well as regional CCGs and practice federations, were called on to clarify the often complex statutory and governance issues and employment arrangements for GPs with portfolio careers or who work across multiple practices. Successful employment of other health professionals in general practice would be supported by practice teams planning time for MDT discussions during the working day, by the DHSC/NHS England providing financial incentives (directly to practices) for employing a wider range of health professionals, and by other key groups (RCGP, GMC) identifying a regulatory body to manage indemnity arrangements associated with the work of all health professionals in the primary care team.
Strengths and limitations
A strength of this work was the successful recruitment and involvement of representatives from key stakeholder organisations, including some in very senior and influential roles within medicine and in health more widely, and within major professional, government, policy and related organisations. Importantly, we incorporated the participation of PPI representatives at both meetings. A core member of the project’s PPI group acted as a facilitator for the round-table discussions in London, and two members of the public in Leeds representing a local practice PPG and the University of Manchester PPI network actively participated as stakeholders. This directly supported the view of the project’s PPI group that patients and members of the public should take part in the conversations and could bring their experience as patients or from other fields of work or industry.
The meetings followed an identical structure and used focused discussions on answering specific questions, and yielded clear statements on both the perceived feasibility of the strategies and potential specific actions to be taken by particular organisations or groups.
Although the RAM workstream excluded the consideration of policies and strategies regarding MDT working, role substitution and skill mix, and also the implications of recent changes in pension policies, this stakeholder consultation workstream did seek views on these areas. These were felt to be important areas for consideration by stakeholder participants, owing to the ongoing implementation of new roles and the likely impact of changes to pension arrangements on the number of older GPs considering early retirement.
Limitations include the fact that our findings comprise a summary list of the views captured across both meetings; the finer detail of individual comments are not reported. Nor have we systematically attempted to draw out the potential complementarity or inevitable tensions between some of the proposed retention strategies (e.g. between having a daily maximum limit on the number of consultations and increasing the typical length of GP consultations). In addition, in order to make good use of stakeholders’ time at the meetings and to present sufficient background material on the findings of the whole of the ReGROUP project, we needed to restrict the number of discussion topics that were possible to cover in detail. Furthermore, each of the 11 potential strategies was discussed in detail by only one table group of stakeholders at each meeting. Nevertheless, an attempt to implement change in 11 policy and strategy areas at the same time would cause disruption; further consideration of prioritising these areas to avoid creating additional pressure on the existing GP workforce is needed.
Conclusions
Following identification of policies and strategies that are likely to support the retention of GPs in direct patient care through the work described in the preceding chapters, we organised two successful stakeholder engagement events, which proved dynamic, supporting wide-ranging but focused discussion. The consultation has identified potentially important areas for policy and strategy development and has crystallised which workforce partner groups and stakeholder organisations might be best placed to lead on innovation and change. However, most of these areas will require some form of evaluation and so this work is a first step towards testing potentially important areas and gaining preliminary evidence on feasibility and acceptability.
Chapter 8 Conclusion
Summary
This research adopted a mix of methods to address two research questions relevant to the current major difficulties being experienced in the UK in respect of GP workforce capacity. We aimed to inform effective policies and strategies aimed at retaining experienced GPs in direct patient care, and at supporting the return of GPs to direct patient care following a career break.
A systematic review synthesised relevant literature originating from the UK and elsewhere, including studies that had adopted qualitative and/or quantitative methods. Early retirement among GPs, or a move to part-time working, were associated with negative ‘push’ factors, including concerns regarding workload, job dissatisfaction, work-related stress and work–life balance. These concerns covered health-system, professional and individual levels of operation; early retirement and part-time working were sometimes seen as a cultural norm among older GPs. Some gender differences were observed in the literature, with our observations supporting published evidence that younger women and older men may aspire to part-time working, and that such arrangements may be seen as personally and professionally important in terms of career longevity. There was very little evidence that financial incentives might discourage early retirement. In contrast, a move to take a career break was more often associated with positive ‘pull’ factors, concerning family and child-related issues, a desire to work abroad or to undertake professional development, such as research or further study.
Our census survey sampled the entire potential GP workforce of the south-west health region and achieved a high response rate. Our findings revealed that around two in five GPs reported intending to permanently leave patient care within 5 years, and one in five reported intending to permanently leave within 2 years. Overall, around 7 out of 10 GPs reported planning a career change that would involve leaving or reducing commitment to direct patient care within 5 years. The age of the GP was identified as a strong predictor of intention to quit patient care, in contrast with GP role or gender, which were not such strong predictors. In regression modelling, it was younger women who were most highly ‘at risk’ of planned career breaks. An intention to reduce working hours or to take a career break was predicted by employment status, with locum status, rather than status as GP partners or employed GPs, being predictive. These findings raise concerns about system sustainability through GP partners facing increasing work-related pressure compared with other GPs.
Our qualitative research adds further depth of understanding of these findings and informed later stages of the research. Participants highlighted the need for a co-ordinated, collective approach to addressing concerns about the GP workforce. The underlying issues were seen as complex, with inevitable inherent contradictions and tensions in the key issues to be considered. In particular, participants emphasised the need to address the lived reality of the present situation, focusing on the actual lived experience of GPs, and seeing the central role of the GP in health-care delivery within the context of the whole system of health care in the UK. Specific concerns were expressed about current perceptions in respect of GPs’ professional identity, and the perceived value of the GP role. Concerns were expressed about a prevailing sense of fear and professional risk – especially because GPs were involved in delivering care to patient populations with increasingly complex needs. Anxiety was expressed regarding the potential for patient complaints and litigation. GPs were seen as having a range of high-quality skills extending beyond direct patient care, and, in this context, the decision to continue delivering care was seen as a matter of choice and volition rather than a career default. Participants wanted to see implementable, sustained policies and strategies, not short-term, ‘sticking-plaster’ solutions. Such approaches should focus on providing evidence in respect of the role and contribution of GPs and of general practice, addressing issues relating to fear and risk in the context of professional practice.
Modelling approaches, drawing on our research data set as well as on routinely available data from NHS Digital, led to the successful development of a computer model of current GP workforce supply–demand imbalance, and the development of a risk-prediction model using a window of 5 years. Although the survey workstream reported important contextual information, GPs’ reports of their career intentions from that survey added little to a model of risk that drew only on routinely available data. Practices that were judged to be at potential risk of supply–demand imbalance (exceeding 10% risk over 5 years) were characterised as having larger list sizes, employing more nurses than other practices with the same number of GPs, serving younger and/or more deprived populations; as far as this geography is concerned, important observations were observed across CCG areas.
Our findings were discussed at two major stakeholder events at which a wide variety of patients, senior personnel, and key organisations were represented. The events were geographically disparate (London and Leeds) and addressed the potential feasibility of implementing those emergent policies and strategies that had been identified through the other workstreams. Discussion was wide-ranging but focused on three broad areas of consideration: (1) the need to protect GPs and to manage expectations in terms of the GP role within the current health-care system, (2) the potential of incentives and support mechanisms for GPs and practices and (3) the potential for new approaches to managing GP careers and wider working arrangements, most notably in relation to portfolio working. Each of these areas was associated with considerable underlying and often very practical detail, which allowed the research team to build on stakeholders’ suggestions and develop a provisional allocation of lead-organisational responsibility should any/all of these emergent policies and strategies be taken forward to implementation. These findings were summarised in Table 25 and are presented in a separate output document in Appendix 39.
Research in context
This research was commissioned in August 2015, following completion of locally funded pilot research undertaken in conjunction with the South West AHSN. 17,18 The research addresses a key area of national concern, which has led to widely publicised national statements from the key leading bodies engaged in GP workforce and health-care planning, including the UK government. Publication of findings is ongoing82 and having an impact. 153
The Health Services and Delivery Research (HSDR) workstream of the National Institute for Health Research (NIHR) has already commissioned many studies of relevance in informing GP workforce capacity. 154,155 In addition, the HSDR programme has recently also initiated a specific call for research targeting GP workforce issues,156 resulting in several shortlisted submissions for further consideration. 157 The NIHR-funded National School for Primary Care Research has also funded one project of direct relevance to the GP workforce agenda. 158
Under present arrangements,159 the responsibility for GP workforce planning falls within the remit of NHS England, working closely with HEE, the RCGP and the GP Committee of the BMA. Building on some recent key initiatives, a ‘10 point plan’160 has been developed to target key areas of concern regarding the GP workforce. Important antecedents to the plan included the reporting of a GP taskforce, established jointly between Medical Education England and the DHSC in response to persistently ‘stubbornly low’ GP recruitment and seeking to recommend how the system could achieve the longstanding workforce target for 3250 trainees to enter GP training in England each year by 2015. 161 In addition, a Primary Care Workforce Commission reported on the future of primary care in July 2015. 128 Recent announcements indicate that these targets are being met in 2018. 162,163
Finally, and more recently, the Wass report (By Choice – Not By Chance) commissioned by HEE made recommendations following an investigation of the role of medical schools in promoting primary care as a career. 164
Strengths and limitations
This research adopted a mixed-methods, multidisciplinary approach to investigate an area of national concern and importance. The literature-based research drew on the expertise of a team with extensive experience of conducting systematic reviews. The survey of GPs was conducted in partnership with and supported by NHS England. The survey sample drew, unusually, on the National Performers List held by NHS England – a statutory regional database and the only authoritative list of GPs in south-west England eligible to potentially engage in direct patient care in primary care settings. We know of no other academic surveys that have used the Performers List as the sampling frame; achieving this required careful, respectful partnership working. The sampling frame was as up-to-date as possible at the time our survey was conducted. Approaches to GPs were made jointly with the NHS and this collaborative approach contributed to the very high response rate we observed.
Potential participants were offered two modes of survey response. Qualitative work adopted a range of research approaches and informed the delivery of subsequent components of the research. The RAM process was delivered by a team that was experienced with the approach. The modelling work drew on established, routine data sets, and the findings highlighted that additional information, such as may be derived from conducting a survey of GPs, was likely to provide only limited additional benefit in model development and refinement. The modelling involved the use of routine historical data to develop the model, and the use of the developed model to forecast likely risk of supply–demand imbalance within a reasonable time frame. The model was seen to have predictive validity, when compared with publicly recognised concerns regarding GP recruitment and workforce viability that developed in one area of the south-west of England (Plymouth) during the course of our research.
The two stakeholder events held as part of the research grounded the work in the reality of NHS service planning and delivery as seen by and reported on by the excellent range of stakeholders attending the two events. The events themselves were carefully planned and executed. Careful training and briefing of the research team was carried out prior to the stakeholder events, and creative approaches were taken to ensure that the events lived up to their potential.
The research findings are subject to some limitations. The survey, modelling and qualitative research was conducted in only one region of England – an area that, despite having a diverse geography and population base, is often seen as a ‘desirable’ place to live compared with other regions that may, for example, have a less diverse sociodemographic mix than the UK generally, and be more dominantly rural than urban. Appropriate consideration should be given to this observation when considering the generalisability of the findings reported here. Our research has highlighted current problems and substantial concerns regarding the GP workforce in this region, an area that currently displays the age demographic expected for the rest of the UK in 20 years’ time. 165 Given the earlier observations, it seems probable that other regions are likely to be facing GP workforce issues that are worse rather than better. The research was conducted in the context of a rapidly changing policy environment, highlighting the possibility that informing emergent potential policy and practice, a key ambition of the research, might deliver findings that were already of restricted value. This observation highlights the need for highly streamlined research commissioning, procurement and delivery processes to ensure that research findings remain of immediate and direct relevance to NHS circumstances. Surveys run the risk of bias in respect of survey sampling and by the use of a survey instrument that was kept short (two pages) with a view to maximising participation rates but that, therefore, inevitably, drew on only a limited range of potential explanatory variables. More might have been done, for example, to consider the granularity of possible responses in respect of working arrangements (morning/afternoon/evening working, range of clinical interests represented, etc.).
The modelling of the data involved forecasting, but it is not possible for us to definitively test this model until the relevant time horizon (in our case, 5 years) has elapsed and relevant accurate data become available. Despite this, we believe that we have provided preliminary evidence that the developed model may be of some potential use and value to the health service.
Future research
Researching issues relating to the capacity and service delivery of the GP workforce requires adopting a range of research methods to deliver a meaningful agenda – from secondary, literature-based studies through to case studies, modelling studies and large-scale, likely complex studies probably involving experimental designs, such as randomised trials, cohort studies or stepped wedge. This agenda is likely to extend well beyond the skills represented in one research group, and is likely to involve novel collaborations – for example between health and health services researchers (themselves with a range of quantitative, qualitative and clinical training and skills) working with occupational psychologists, geographers and business schools or other centres with academic HR expertise.
Specific areas that future research might target:
-
developing and evaluating interventions investigating optimal professional skill mix, and extended/new clinical roles as a means of providing additional support to GPs
-
examining support for GPs through new working patterns, including interventions supporting the development of portfolio careers
-
developing a robust evidence base around GP return-to-work schemes
-
developing clear and robust measures of ‘effectiveness’ and ‘efficiency’ in studies examining the organisation and delivery of primary care – for example, adopting measures that might usefully inform what is the ‘optimal’ configuration of a primary care team
-
undertaking research that sees GPs operating as members of practice teams
-
undertaking research targeting GP stress and burnout, with a view to developing suitable interventions to anticipate and effectively address these GP health-related issues
-
undertaking secondary research that uses learning from other sectors, which may be of relevance to the GP workforce (e.g. considering evidence relating to nurse or social-worker recruitment)
-
developing robust models of GP workforce capacity and risk at meso (CCG, regional) or micro (practice) levels with a view to establishing robust risk profiles that might act as early-warning systems
-
evaluating alternatives to the current system of appraisal and revalidation that might encourage and support GPs to remain in the workforce after a career break or change in working pattern.
Summary
The status of the GP workforce in the UK represents an ongoing issue of concern to patients, government and the health profession. Specific issues relate to the recruitment and retention of GPs in direct patient care. This research has documented the magnitude of the issue in south-west England and has identified some potential policies and strategies for retaining more GPs in the NHS workforce, which may be helpful for the NHS to consider. GPs and their practice teams remain at the very heart of health-care provision in the UK. Opportunities remain, and must be grasped, for urgent action to be taken to address the issues highlighted in this research report if the future well-being of NHS care in the UK is to be assured.
Acknowledgements
We would like to thank the GPs, primary care stakeholders and the regional- and national-level stakeholders who gave generously of their time to support the study.
Our thanks also go to our PPI group for their input throughout the project and across all workstreams, including Alex Aylward, Diana Frost, Nigel Reed, Lynn Tatnell and Heather Boult. We wish also to thank the external members of the Project Advisory Board for their advice and support for the project: Dr Jo Roberts (NHS South Devon and Torbay CCG), Dr Nigel Starey (CQC), Dr Liz Thomas (NHS England), Dr Paul Thomas (HEE South West), Dr Krishna Kasaraneni (BMA) and Ms Danielle Fisher (RCGP).
In addition, we thank Dr Nigel Acheson, Dr Liz Thomas, Mrs Nicolette Williams and Mr Andrew Postgate-Cronbach (NHS England) for providing access to the National Performers List, for their covering letter and e-mail to accompany the census survey and for their assistance with administering the survey.
We thank also Dr Arvind Madan and Mr Ian Biggs (NHS England) and Dr Krishna Kasaraneni (BMA) for their keynote speeches at the consultation meetings. Likewise, we thank staff within UEMS ethics committee and CRN South West Peninsula.
Contributions of authors
Professor John L Campbell (Professor of General Practice and Primary Care, Chief Investigator) took overall responsibility for the project, supervised the project conduct, was involved in all stages of the project, including conception, design, analysis and interpretation of data, drafted and critically revised the report for important intellectual content and approval of the final version.
Mrs Emily Fletcher (Research Fellow, Project Manager; researcher for the Census Survey and Stakeholder Consultations) was responsible for the day-to-day management of the project and acquisition of data. She co-ordinated research staff across workstreams, contributed to the analysis and interpretation of data, drafted and critically revised the report for important intellectual content and was responsible for approval of the final version.
Dr Gary Abel (Senior Lecturer, Predictive Risk Modelling Lead) took overall responsibility for the predictive risk modelling workstream, including design, data acquisition, analysis, data interpretation and co-ordination of research staff and, for the overall project, was involved in the analysis and interpretation of data and contributed to drafting and critically revising the report for important intellectual content and approval of the final version.
Professor Rob Anderson (Associated Professor of Health Economics and Evaluation, Systematic Review Lead) took overall responsibility for the systematic review workstream and was involved in all stages of the project, including conception, design, analysis, interpretation of data and drafting and critically revising the report for important intellectual content and approval of the final version.
Dr Rupatharshini Chilvers (Tangerine Bee Ltd, RAM Researcher) operationalised the RAM protocol, was involved in acquisition of data, analysis and interpretation of data and contributed to drafting and critically revising the report for important intellectual content and approval of the final version.
Dr Sarah G Dean (Associated Professor of Psychology Applied to Rehabilitation and Health, Qualitative Research Lead) took overall responsibility for the qualitative research workstream and was involved in all stages of the project, including conception, design and interpretation of data, and critically revising the report for important intellectual content and approval of the final version.
Professor Suzanne H Richards (Professor of Primary Care Research, RAM Lead) took overall responsibility for the RAM workstream and was involved in all stages of the project, including the conception, design, interpretation of data and drafting and critically revising the report for important intellectual content and approval of the final version.
Dr Anna Sansom (Research Fellow, Qualitative Researcher) operationalised the qualitative research protocol, was involved in acquisition of qualitative data, analysis and interpretation of data, and contributed to drafting and critically revising the report for important intellectual content and approval of the final version.
Dr Rohini Terry (Research Associate, Bristol Qualitative Researcher) operationalised the qualitative research protocol in the Bristol region, was involved in the acquisition of qualitative data, analysis and interpretation of data, and contributed to drafting and critically revising the report for important intellectual content and approval of the final version.
Mr Alex Aylward (PPI Group Member, PPI Representative) participated in the PPI group across the various workstreams, attended regular project management meetings and joined the project team as a facilitator for the round-table discussions in the stakeholder consultations workstream. In the overall project, he has been involved in drafting and critically revising the report for important intellectual content and approval of the final version.
Mr Grant Fitzner (Chief Executive Officer at Kantar Public UK, Predictive Risk Modelling Co-applicant) contributed to the development of the predictive risk modelling protocol, and, for the overall project, contributed to approval of the final version of the report.
Dr Mayam Gomez-Cano (Research Fellow, Predictive Risk Modelling Researcher) operationalised the predictive risk modelling protocol, was involved in acquisition of data, analysis and interpretation of data, and contributed to approval of the final version of the report.
Dr Linda Long (Research Fellow, Systematic Review Researcher) operationalised the systematic review protocol, was involved in acquisition of data, analysis and interpretation of data, and contributed to drafting and critically revising the report for important intellectual content and approval of the final version.
Dr Navonil Mustafee (Senior Lecturer, Predictive Risk Modelling Researcher) contributed to the development and operationalisation of the predictive risk modelling protocol, data acquisition, analysis and interpretation of data, and contributed to critically revising the report for important intellectual content and approval of the final version.
Dr Sophie Robinson (Research Fellow, Information Specialist on the Systematic Review) developed the literature search strategy and carried out the bibliographic searches. She developed and implemented a strategy for grey literature searching and carried out the grey literature searches, title and abstract screening and full-text screening and paper selection. She undertook first reviewer data extraction and critical appraisal for included quantitative survey papers and wrote the literature searching methods and results, the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart and appendices. She contributed to the drafting and editing of the final report.
Professor Philip A Smart (Professor of Operations and Process Management, Predictive Risk Modelling Co-applicant) contributed to the development of the predictive risk modelling protocol and interpretation of data, and, for the overall project, contributed to approval of the final version of the report.
Dr Fiona C Warren (Senior Lecturer, Statistician) contributed to the development of the statistical analysis plans, contributed to critically revising the report for important intellectual content and approval of the final version.
Dr Jo Welsman (Research Fellow, PPI Lead) took overall responsibility for the PPI activities across the various workstreams and was involved in the overall project, including conception, design, and interpretation of data, and drafting and critically revising the report for important intellectual content and approval of the final version.
Professor Chris Salisbury (Professor of Primary Health Care, Bristol Principal Investigator) co-ordinated qualitative research staff in the Bristol region and was involved in all stages of the project, including conception, design and interpretation of data, and critically revising the report for important intellectual content and approval of the final version.
Contributions of others
Dr Felix Gradinger (Research Fellow) contributed to the systematic review and draft report chapter.
Dr Judit Konya (Research Fellow) contributed to the systematic review and draft report chapter.
Ms Sarah Dawkins (Research Administrator) provided project administration support across all workstreams.
Mrs Ellie Kingsland (Research Administrator) provided project administration support for the stakeholder consultations workstream and the end of the project.
Dr Laura Sims (Research Fellow) was a GP advisor alongside the PPI group, providing input across workstreams.
Mr Neil French (University of Exeter Marketing Research and Data Manager) was involved in census survey data management and the hosting of the online version of the survey.
Mr Pete Hodges (University of Exeter Events Manager) supported the administration of invitations to the stakeholder consultation meetings and advised on the use of Eventbrite (San Francisco, CA, USA) to advertise the meetings.
Mr Clive Betts (University of Exeter Head of People Development) delivered training to the project team on facilitating round-table discussions for the stakeholder consultations.
Publications
Anderson R, Long L, Robinson SR, Gradingner F, Konya J, Fletcher E, et al. Why do Primary Care Doctors Quit Direct Patient Care? A Systematic Review of Empirical Research. Exeter: University of Exeter Medical School; 2016.
Fletcher E, Abel GA, Anderson R, Richards SH, Salisbury C, Dean SG, et al. Quitting patient care and career break intentions among general practitioners in South West England: findings of a census survey of GPs. BMJ Open 2017;7:e015853.
Sansom A, Terry R, Fletcher E, Salisbury C, Lond L, Richards SH, et al. Why do GPs leave direct patient care and what might help to retain them? A qualitative study of GPs in South West England. BMJ Open 2018;8:e019849.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- In-depth Review of the General Practitioner Workforce. Final Report. London: UK Government; 2014.
- Hippisley-Cox J, Vinogradova Y. Trends in Consultation Rates in General Practice 1995/1996 to 2008/2009: Analysis of the Qresearch® Database. Leeds: NHS Digital; 2009.
- Berwick DM. A transatlantic review of the NHS at 60. BMJ 2008;337:212-4. https://doi.org/10.1136/bmj.a838.
- Davis K, Stremikis K, Squires D, Schoen C. Mirror, Mirror on the Wall: How the Performance of the U.S. Healthcare System Compares Internationally. New York, NY: The Commonwealth Fund; 2014.
- Imison C, Buchan J, Xavier S. NHS Workforce Planning: Limitations and Possibilities. London: The King’s Fund; 2009.
- General and Personal Medical Services, England as at 30 June 2017, Provisional Experimental Statistics. Leeds: NHS Digital; 2017.
- The Cohort Study of 2006 Medical Graduates. Eighth Report. London: BMA; 2014.
- Securing the Future GP Workforce – Delivering the Mandate on GP Expansion. Leeds: HEE; 2014.
- Drennan VM, Halter M, Joly L, Gage H, Grant RL, Gabe J, et al. Physician associates and GPs in primary care: a comparison. Br J Gen Pract 2015;65:e344-50. https://doi.org/10.3399/bjgp15X684877.
- Drennan V. Investigating the Contribution of Physician Assistants to Primary Care in England 2014. www.nets.nihr.ac.uk/projects/hsdr/0918011066 (accessed December 2014).
- Sibbald B, Shen J, McBride A. Changing the skill-mix of the health care workforce. J Health Serv Res Policy 2004;9:28-3. https://doi.org/10.1258/135581904322724112.
- Avery AJ, Pringle M. Extended prescribing by UK nurses and pharmacists. BMJ 2005;331:1154-5. https://doi.org/10.1136/bmj.331.7526.1154.
- Roland M. So Will Pharmacists Save the NHS?. Cambridge: Cambridge Centre for Health Services Research; 2015.
- Royal College of General Practitioners and Royal Pharmaceutical Society . Breaking Down the Barriers – How Community Pharmacists and GPs Can Work Together to Improve Patient Care n.d. www.pharmaceutical-journal.com/news-and-analysis/news/pharmacists-and-gps-join-forces-to-improve-patient-care/11081380.article (accessed 1 October 2017).
- Five Year Forward View. London: NHS England; 2014.
- Securing the Future of General Practice: New Models of Primary Care. London: The King’s Fund and Nuffield Trust; 2013.
- Campbell J, Calitri R, Sansom A. Retaining the Experienced GP Workforce in Direct Patient Care (ReGROUP): Final Report. Exeter: University of Exeter; 2015.
- Sansom A, Calitri R, Carter M, Campbell J. Understanding quit decisions in primary care: a qualitative study of older GPs. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010592.
- Hann M, McDonald J, Checkland K, Coleman A, Gravelle H, Sibbald B, et al. Seventh National GP Worklife Survey. Manchester: University of Manchester; 2013.
- Dayan M, Arora S, Rosen R, Curry N. Is General Practice in Crisis?. London: Nuffield Trust; 2014.
- Pulse . RCGP Petitions Government to Create New ‘Medical Assistant’ Role to Relieve Admin Pressures on GPs 2014. www.pulsetoday.co.uk/20008118.article#.VD_Iv01wbcs (accessed October 2014).
- Outcome of 2017/18 GMS Contract Negotiations: Letter to Commissioners, Regional Heads of Primary Care, Heads of Primary Care, CCG Clinical Leads and Accountable Officers. Leeds: NHS England; 2017.
- Rimmer A. NHS England to Invest £10m in GP Workforce Expansion n.d. http://careers.bmj.com/careers/advice/view-article.html?id=20020843 (accessed April 2015).
- Rimmer A. GP Workforce Planning Needs New Approach, Say NHS Confederation and National Association of Primary Care n.d. http://careers.bmj.com/careers/advice/view-article.html?id=20021323 (accessed April 2015).
- The 2022 GP. A Vision for General Practice in the Future NHS. London: RCGP; 2013.
- Framework for Responding to CQC Inspections of GP Practices. London: NHS England; 2014.
- Brett TD, Arnold-Reed DE, Hince DA, Wood IK, Moorhead RG. Retirement intentions of general practitioners aged 45–65 years. Med J Aust 2009;191:75-7.
- Davidson JM, Lambert TW, Goldacre MJ, Parkhouse J. UK senior doctors’ career destinations, job satisfaction, and future intentions: questionnaire survey. BMJ 2002;325:685-6. https://doi.org/10.1136/bmj.325.7366.685.
- Gardiner M, Sexton R, Kearns H, Marshall K. Impact of support initiatives on retaining rural general practitioners. Aust J Rural Health 2006;14:196-201. https://doi.org/10.1111/j.1440-1584.2006.00808.x.
- Hansen V, Pit SW, Honeyman P, Barclay L. Prolonging a sustainable working life among older rural GPs: solutions from the horse’s mouth. Rural Remote Health 2013;13.
- Heponiemi T, Kouvonen A, Vänskä J, Halila H, Sinervo T, Kivimäki M, et al. Health, psychosocial factors and retirement intentions among Finnish physicians. Occup Med 2008;58:406-12. https://doi.org/10.1093/occmed/kqn064.
- Jones JA, Humphreys JS, Adena MA. Rural GPs’ ratings of initiatives designed to improve rural medical workforce recruitment and retention. Rural Remote Health 2004;4.
- Lorant V, Geerts C, Duchesnes C, Goedhuys J, Ryssaert L, Remmen R, et al. KCE study group . Attracting and retaining GPs: a stakeholder survey of priorities. Br J Gen Pract 2011;61:e411-8. https://doi.org/10.3399/bjgp11X583191.
- Van Greuningen M, Heiligers PJ, Van der Velden LF. Motives for early retirement of self-employed GPs in the Netherlands: a comparison of two time periods. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-467.
- American Academy of Family Physicians (AAFP) . Family Physician Workforce Reform: Recommendations of the American Academy of Family Physicians n.d. www.aafp.org/about/policies/all/workforce-reform.html (accessed April 2015).
- Institute of Medicine (IOM) . Primary Care and Public Health: Exploring Integration to Improve Population Health 2012. www.iom.edu/~/media/Files/Report%20Files/2012/Primary-Care-and-Public-Health/Primary%20Care%20and%20Public%20Health_Revised%20RB_FINAL.pdf (accessed October 2017).
- Canada’s Largest Physician Survey Flags a Lack of Patient Care Resources and Workforce Planning. Mississauga, ON: CFPC; 2013.
- Review of Australian Government Health Workforce Programs. Canberra, ACT: Australian Government Department of Health; 2013.
- Forecasting GP Workforce Capacity. Wellington: Royal New Zealand College of General Practitioners; 2014.
- Roland M, Everington S. Tackling the crisis in general practice. BMJ 2016;352. https://doi.org/10.1136/bmj.i942.
- Davis E, Martin S, Gershlick B. Under Pressure: What The Commonwealth Fund’s 2015 International Survey of General Practitioners Means for the UK. London: The Health Foundation; 2016.
- Simoens S, Scott A, Sibbald B. Job satisfaction, work-related stress and intentions to quit of Scottish GPS. Scott Med J 2002;47:80-6. https://doi.org/10.1177/003693300204700403.
- Gibson J, Checkland K, Coleman A, Hann M, McCall R, Spooner S, et al. Eighth National GP Worklife Survey. Manchester: Policy Research Unit in Commissioning and the Healthcare System, Manchester Centre for Health Economics, University of Manchester; 2015.
- Dale J, Potter R, Owen K, Parsons N, Realpe A, Leach J. Retaining the general practitioner workforce in England: what matters to GPs? A cross-sectional study. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0363-1.
- Scott A, Gravelle H, Simoens S, Bojke C, Sibbald B. Job satisfaction and quitting intentions: a structural model of British general practitioners. Br J Indust Relations 2006;44:519-40. https://doi.org/10.1111/j.1467-8543.2006.00511.x.
- McKinstry B, Colthart I, Elliott K, Hunter C. The feminization of the medical work force, implications for Scottish primary care: a survey of Scottish general practitioners. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-56.
- Anderson R, Gradinger S, Robinson S, Campbell J, Fletcher E. Why do General Practitioners (GPs)/Primary Care Doctors Quit Direct Patient Care? A Systematic Review of Empirical Research in High-income Countries. York: University of York; 2016.
- Critical Appraisal of a Survey. Leiden: Center for Evidence-Based Management; 2016.
- Wallace A, Croucher K, Quilgars D, Baldwin S. Meeting the challenge: developing systematic reviewing in social policy. Policy &Amp; Politics 2004;32:455-70. https://doi.org/10.1332/0305573042009444.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-45.
- Doran N, Fox F, Rodham K, Taylor G, Harris M. Lost to the NHS: a mixed methods study of why GPs leave practice early in England. Br J Gen Pract 2016;66:e128-35. https://doi.org/10.3399/bjgp16X683425.
- Baker M, Williams J, Petchey R. GPs in principle but not in practice – a study of vocationally trained doctors not currently working as principals. BMJ 1995;310:1301-4. https://doi.org/10.1136/bmj.310.6990.1301.
- Baker M. The Work Commitments of General Practitioners: A Study of 1986, 1991 and 1996 Cohort JCPTGP Qualifiers. Nottingham: University of Nottingham Division of General Practice; 2000.
- Chambers M, Colthart I, McKinstry B. Scottish general practitioners’ willingness to take part in a post-retirement retention scheme: questionnaire survey. BMJ 2004;328. https://doi.org/10.1136/bmj.328.7435.329.
- Doran N, Fox F, Taylor G, Harris M. Early GP Leavers Interim Report: Report to HEE & NHS England. Bath: University of Bath; 2015.
- Evans J, Lambert T, Goldacre M. GP recruitment and retention: a qualitative analysis of doctors’ comments about training for and working in general practice. Occas Pap R Coll Gen Pract 2002;83:iii-vi.
- French F, Andrew J, Awramenko M, Coutts H, Leighton-Beck L, Mollison J, et al. General practitioner non-principals benefit from flexible working. J Health Organ Manag 2005;19:5-15. https://doi.org/10.1108/14777260510592103.
- French F, Andrew J, Awramenko M, Coutts H, Leighton-Beck L, Mollison J, et al. Why do work patterns differ between men and women GPs?. J Health Organ Manag 2006;20:163-72. https://doi.org/10.1108/14777260610661556.
- Hann M, Reeves D, Sibbald B. Relationships between job satisfaction, intentions to leave family practice and actually leaving among family physicians in England. Eur J Public Health 2011;21:499-503. https://doi.org/10.1093/eurpub/ckq005.
- Hutchins A. An investigation into the benefits of prolonged study leave undertaken by general practitioners. Educ Primary Care 2005;16:57-65. https://doi.org/10.1080/14739879.2005.11493483.
- Luce A, van Zwanenberg T, Firth-Cozens J, Tinwell C. What might encourage later retirement among general practitioners?. J Manag Med 2002;16:303-10. https://doi.org/10.1108/02689230210445112.
- Sibbald B, Bojke C, Gravelle H. National survey of job satisfaction and retirement intentions among general practitioners in England. BMJ 2003;326. https://doi.org/10.1136/bmj.326.7379.22.
- Simoens S, Scott A, Sibbal B, Bojke C, Gravelle H. Job satisfaction, Intentions to Quit, and the Retention of GPs in England and Scotland. Aberdeen: Health Economics Research Unit, University of Aberdeen; 2002.
- Taylor DH, Quayle JA, Roberts C. Retention of young general practitioners entering the NHS from 1991–1992. Br J Gen Pract 1999;49:277-80.
- Taylor K, Lambert T, Goldacre M. Future career plans of a cohort of senior doctors working in the National Health Service. J R Soc Med 2008;101:182-90. https://doi.org/10.1258/jrsm.2007.070276.
- Young R, Leese B, Sibbald B. Imbalances in the GP labour market in the UK: evidence from a postal survey and interviews with GP leavers. Work Employment Soc 2001;15:699-71. https://doi.org/10.1177/095001701400438161.
- Dewa CS, Jacobs P, Thanh NX, Loong D. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-254.
- McComb ED. Which psycho-demographic factors predict a doctor’s intention to leave New Zealand general practice?. N Z Med J 2008;121:25-36.
- Norman R, Hall JP. The desire and capability of Australian general practitioners to change their working hours. Med J Aust 2014;200:399-402. https://doi.org/10.5694/mja13.10776.
- Nugent A, Black N, Parsons B, Smith S, Murphy AW. A national census of Irish general practice training programme graduates 1990–1996. Ir Med J 2003;96:10-2.
- O’Kelly F, O’Kelly M, Ni Shuilleabhain A, O’Dowd T. A National Census of Irish General Practice Training Programme Graduates 1997–2003. Dublin: Department of Public Health and Primary Care, Trinity College Dublin; 2008.
- Pit SW, Hansen V. Factors influencing early retirement intentions in Australian rural general practitioners. Occup Med 2014;64:297-304. https://doi.org/10.1093/occmed/kqu028.
- Shrestha D, Joyce CM. Aspects of work-life balance of Australian general practitioners: determinants and possible consequences. Aust J Prim Health 2011;17:40-7. https://doi.org/10.1071/PY10056.
- Sumanen M, Aine T, Halila H, Heikkilä T, Hyppölä H, Kujala S, et al. Where have all the GPs gone – where will they go? Study of Finnish GPs. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-121.
- Woodward CA, Ferrier B, Cohen M, Brown J. Professional activity. How is family physicians’ work time changing?. Can Fam Physician 2001;47:1414-21.
- Hutchins A. Influences on GPs’ early retirement, and how to keep them. Br J Health Care Manag 2005;11:367-71.
- Baker M, Flett A, Williams J. The work commitments of British general practitioners: A national survey. Br J Gen Pract 2000;50:730-1.
- Newton J, Luce A, van Zwanenberg T, Firth-Cozens J. Job Dissatisfaction and early retirement: a qualitative study of general practitioners in the Northern Deanery. Prim Health Care Res Devel 2004;5:68-76. https://doi.org/10.1191/1463423604pc191oa.
- Dwan KM, Douglas KA, Forrest LE. Are ‘part-time’ general practitioners workforce idlers or committed professionals?. BMC Fam Pract 2014;15. https://doi.org/10.1186/1471-2296-15-154.
- Newton J. Job Dissatisfaction and Early Retirement: A Qualitative Study of General Practitioners in the Northern Deanery. Newcastle upon Tyne: Health Education England; 2004.
- Looking to the Future: the Recruitment, Retention and Return of GPs (Summary and Next Steps Report for NHS England). London: Ipsos MORI Social Research Institute; 2015.
- Fletcher E, Abel GA, Anderson R, Richards SH, Salisbury C, Dean SG, et al. Quitting patient care and career break intentions among general practitioners in South West England: findings of a census survey of general practitioners. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-015853.
- The Changing General Practitioner Workforce: the Development of Policies and Strategies Aimed at Retaining Experienced GPs and Those Taking a Career Break in Direct Patient Care: ReGROUP Project. Exeter: University of Exeter Medical School; 2016.
- The State of Medical Education and Practice in the UK. London: General Medical Council; 2015.
- Thousands of Doctors Prevented from Returning to GP Workforce by Red Tape. London: RCGP; 2014.
- BMA Quarterly Tracker Survey: Current Views from Across the Medical Profession. Quarter 3: JulyAugust 2014. London: BMA; 2014.
- UK Government . English Indices of Deprivation 2015 n.d. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed November 2016).
- South West England. San Francisco, CA: Wikipedia; 2016.
- General Practice Forward View. London: DHSC; 2016.
- Does NHS Staff Wellbeing Affect Patient Experience of Care? Policy Plus Evidence, Issues and Opinions in Healthcare, Issue 39. London: King’s College London; 2013.
- Rimmer A. A Third of GP Training Posts Are Vacant After First Recruitment Round 2015. http://careers.bmj.com/careers/advice/A_third_of_GP_training_posts_are_vacant_after_first_recruitment_round (accessed November 2016).
- Hunt J. Up to 1,500 Extra Medical Training Places Announced. London: Department of Health and Social Care; 2016.
- National Survey of GPs: the Future of General Practice. London: ICM Research Ltd; 2015.
- Rimmer A. One in eight GP training posts vacant, despite unprecedented third round of recruitment. BMJ 2014;349. https://doi.org/10.1136/bmj.g6478.
- Appleton K, House A, Dowell A. A survey of job satisfaction, sources of stress and psychological symptoms among general practitioners in Leeds. Br J Gen Pract 1998;48:1059-63.
- Torppa MA, Kuikka L, Nevalainen M, Pitkälä KH. Emotionally exhausting factors in general practitioners’ work. Scand J Prim Health Care 2015;33:178-83. https://doi.org/10.3109/02813432.2015.1067514.
- Halliday L, Walker A, Vig S, Hines J, Brecknell J. Grit and burnout in UK doctors: a cross-sectional study across specialties and stages of training. Postgrad Med J 2017;93:389-94. https://doi.org/10.1136/postgradmedj-2015-133919.
- Murray M, Murray L, Donnelly M. Systematic review of interventions to improve the psychological well-being of general practitioners. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0431-1.
- General Practice Workforce Action Plan. Leeds: NHS England; 2016.
- Examples of Outstanding Practice for GPs. Newcastle upon Tyne: Care Quality Commission; 2017.
- Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough?. Qualitative Health Research 2017;27:591-608. https://doi.org/10.1177/1049732316665344.
- Glaser BG. The constant comparative method of qualitative analysis. Soc Prob 1965;12:436-45. https://doi.org/10.2307/798843.
- Le Floch B, Bastiaens H, Le Reste JY, Lingner H, Hoffman RD, Czachowski S, et al. Which positive factors determine the GP satisfaction in clinical practice? A systematic literature review. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0524-x.
- Greenberg J. A taxonomy of organizational justice theories. Acad Manag Rev 1987;12:9-22. https://doi.org/10.2307/257990.
- Heponiemi T, Manderbacka K, Vänskä J, Elovainio M. Can organizational justice help the retention of general practitioners?. Health Policy 2013;110:22-8. https://doi.org/10.1016/j.healthpol.2013.02.001.
- Miller DT. Disrespect and the experience of injustice. Annu Rev Psychol 2001;52:527-53. https://doi.org/10.1146/annurev.psych.52.1.527.
- Sutinen R, Kivimäki M, Elovainio M, Virtanen M. Organizational fairness and psychological distress in hospital physicians. Scand J Public Health 2002;30:209-15. https://doi.org/10.1080/14034940210133843.
- Dollard MF, Bakker AB. Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement. J Occupat Organiz Psychol 2010;83:579-99. https://doi.org/10.1348/096317909x470690.
- Orton P, Orton C, Pereira Gray D. Depersonalised doctors: a cross-sectional study of 564 doctors, 760 consultations and 1876 patient reports in UK general practice. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2011-000274.
- Maslach C, Jackson SE. The measurement of experienced burnout. J Occupat Behav 1981;2:99-113. https://doi.org/DOI 10.1002/job.4030020205.
- Fitch K, Bernstein S, Aguilar M, Burnand B, LaCalle J, Lazaro P, et al. The RAND/UCLA Appropriateness Method User’s Manual. Santa Monica, CA: RAND Corporation; 2001.
- Chopra V, Flanders SA, Saint S, Woller SC, O’Grady NP, Safdar N, et al. The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC): results from a multispecialty panel using the RAND/UCLA appropriateness method. Ann Intern Med 2015;163:1-40. https://doi.org/10.7326/M15-0744.
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 2015;1:40-3. https://doi.org/10.1016/j.sleh.2014.12.010.
- Basger BJ, Chen TF, Moles RJ. Validation of prescribing appropriateness criteria for older Australians using the RAND/UCLA appropriateness method. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2012-001431.
- Wright C, Moseley A, Chilvers R, Stabb L, Campbell JL, Richards SH. Development of an early intervention to prevent long-term incapacity for work: using an online RAND/UCLA appropriateness method to obtain the views of general practitioners. Prim Health Care Res Dev 2009;10:65-78. https://doi.org/doi:10.1017/S1463423608000947.
- Bell BG, Spencer R, Avery AJ, Campbell SM. Tools for measuring patient safety in primary care settings using the RAND/UCLA appropriateness method. BMC Fam Pract 2014;15. https://doi.org/10.1186/1471-2296-15-110.
- Health Workforce Policies in OECD Countries: Right Jobs, Right Skills, Right Places. Paris: OECD Health Policy Studies, OECD Publishing; 2016.
- Waqar S, Snow-Miller R, Weaver R. Building the Workforce – the New Deal for General Practice. Leeds: NHS England; 2015.
- Anderson R, Long L, Robinson SR, Gradingner F, Konya J, Fletcher E. Why do Primary Care Doctors Quit Direct Patient Care? A Systematic Review of Empirical Research. Exeter: University of Exeter Medical School; 2016.
- Verma P, Ford JA, Stuart A, Howe A, Everington S, Steel N. A systematic review of strategies to recruit and retain primary care doctors. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1370-1.
- Barriball L, Bremner J, Buchan J, Craveiro I, Dieleman M, Dix O, et al. Recruitment and Retention of the Health Workforce in Europe: Final Report. Brussels: European Commission; 2014.
- Peckham S, Marchand C, Peckham A. General Practitioner Recruitment and Retention: An Evidence Synthesis: Final Report. London: Policy Research Unit in Commissioning and the Healthcare System; 2016.
- Elmore N, Burt J, Abel G, Maratos FA, Montague J, Campbell J, et al. Investigating the relationship between consultation length and patient experience: a cross-sectional study in primary care. Br J Gen Pract 2016;66:e896-e903. https://doi.org/10.3399/bjgp16X687733.
- Increasing Access to Health Workers in Remote and Rural Areas Through Improved Retention: Global Policy Recommendations. Geneva: World Health Organization; 2010.
- Chopra M, Munro S, Lavis JN, Vist G, Bennett S. Effects of policy options for human resources for health: an analysis of systematic reviews. Lancet 2008;371:668-74. https://doi.org/10.1016/S0140-6736(08)60305-0.
- Lopes MA, Almeida AS, Almada-Lobo B. Handling healthcare workforce planning with care: where do we stand?. Hum Resour Health 2015;13. https://doi.org/10.1186/s12960-015-0028-0.
- Workforce Risks and Opportunities: Technical Report. London: CFWI; 2012.
- The Future of Primary Care: Creating Teams for Tomorrow. Leeds: Health Education England; 2015.
- Patient Safety Implications of General Practice Workload. London: RCGP; 2015.
- Croxson CH, Ashdown HF, Hobbs FR. GPs’ perceptions of workload in England: a qualitative interview study. Br J Gen Pract 2017;67:e138-e147. https://doi.org/10.3399/bjgp17X688849.
- Nair R, Aggarwal R, Khanna D. Methods of formal consensus in classification/diagnostic criteria and guideline development. Semin Arthritis Rheum 2011;41:95-105. https://doi.org/10.1016/j.semarthrit.2010.12.001.
- Ponsignon F, Smart PA, Maull RS. Service delivery system design: characteristics and contingencies. Int J Oper Prod Manag 2011;31:324-49. https://doi.org/10.1108/01443571111111946.
- Hobbs FDR, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. National Institute for Health Research School for Primary Care Research . Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet 2016;387:2323-30. https://doi.org/10.1016/S0140-6736(16)00620-6.
- Watt G, Brown G, Budd J, Cawston P, Craig M, Jamieson R, et al. General practitioners at the deep end: the experience and views of general practitioners working in the most severely deprived areas of Scotland. Occas Pap R Coll Gen Pract 2012;89:i-40.
- Hart JT. The inverse care law. Lancet 1971;1:405-12. https://doi.org/10.1016/S0140-6736(71)92410-X.
- Campbell J, Smith P, Nissen S, Bower P, Elliott M, Roland M. The GP Patient Survey for use in primary care in the National Health Service in the UK – development and psychometric characteristics. BMC Fam Pract 2009;10. https://doi.org/10.1186/1471-2296-10-57.
- GP Patient Survey. Leeds: NHS England; 2018.
- Paddison C, Elliott M, Parker R, Staetsky L, Lyratzopoulos G, Campbell JL, et al. Should measures of patient experience in primary care be adjusted for case mix? Evidence from the English General Practice Patient Survey. BMJ Qual Saf 2012;21:634-40. https://doi.org/10.1136/bmjqs-2011-000737.
- Abel GA, Saunders CL, Lyratzopoulos G. Cancer patient experience, hospital performance and case mix: evidence from England. Future Oncol 2014;10:1589-98. https://doi.org/10.2217/fon.13.266.
- NHS Digital . General and Personal Medical Services, England 2002–2012 2013. http://content.digital.nhs.uk/searchcatalogue?productid=10382&topics=1%2fWorkforce%2fStaff+numbers&kwd=GP+staff&geo=England&sort=Relevance&size=10&page=2#top (accessed 31 July 2017).
- General and Personal Medical Services, England 2003 – 2013, As at 30 September. Leeds: NHS Digital; 2014.
- General and Personal Medical Services, England September 2015–March 2016, Provisional Experimental Statistics. Leeds: NHS Digital; 2016.
- National General Practice Profile. London: Public Health England; 2013.
- Subnational Population Projections for England: 2014-Based. Newport: ONS; 2014.
- Quality and Methodology Information – Subnational Population Projection. Newport: ONS; 2015.
- Practice Business . Three Plymouth GP Surgeries Have Been Left Without a Permanent Provider 2017. http://practicebusiness.co.uk/three-plymouth-gp-surgeries-have-been-left-without-a-permanent-provider/ (accessed 14 September 2017).
- Workforce Minimum Data Set (wMDS). Leeds: NHS Digital; n.d.
- Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CF, Askham J, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess 1998;2.
- Mulley AG. Inconvenient truths about supplier induced demand and unwarranted variation in medical practice. BMJ 2009;339. https://doi.org/10.1136/bmj.b4073.
- Safe Staffing for Nursing in Adult Inpatient Wards in Acute Hospitals. London: NICE; 2014.
- Newly Qualified GPs. London: RCGP; 2017.
- NHS GP Health Service . What Is the NHS GP Health Service 2017. http://gphealth.nhs.uk/welcome-to-gp-health/ (accessed 13 September 2017).
- GP Leaders Warn Study Shows GP Workforce Crisis Continues to Worsen. London: BMA; 2017.
- Drennan VM, Chattopadhyay K, Halter M, Brearley S, de Lusignan S, Gabe J, et al. Physician assistants in English primary care teams: a survey. J Interprof Care 2012;26:416-18. https://doi.org/10.3109/13561820.2012.686538.
- Salisbury C, Montgomery AA, Hollinghurst S, Hopper C, Bishop A, Franchini A, et al. Effectiveness of PhysioDirect telephone assessment and advice services for patients with musculoskeletal problems: pragmatic randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.f43.
- Commissioned Research Brief 17/08 – Work Force and Skill Mix in GP Primary Care Services. Southampton: NIHR; 2017.
- HS&DR Prioritisation Panel (Commissioned Work Stream). Decisions from 14–15 June 2017 Meeting. Southampton: NIHR; 2017.
- Division of Population Health, Health Services Research & Primary Care . NIHR SPCR Grant Ref: 354. An Investigation of the Factors Which Are Associated With Successful Transitions from GP Speciality Training Programmes to Long-Term Careers in NHS General Practice (PROJECT) 2017. www.research.manchester.ac.uk/portal/en/projects/nihr-spcr-grant-ref-354-an-investigation-of-the-factors-which-are-associated-with-successful-transitions-from-gp-speciality-training-programmes-to-longterm-careers-in-nhs-general-practice-project(e8ff560c-568b-4df2-b399-69a00a77d57d).html (accessed 11 October 2017).
- Investing in People for Health and Healthcare: Workforce Plan for England-Proposed Education and Training Commissions for 2016/17. Leeds: HEE; 2016.
- GP Workforce ‘10 Point’ Plan. London: BMA; 2017.
- Securing the Future GP Workforce: Delivering the Mandate on GP Expansion. GP Taskforce Final Report. London: NHS; 2014.
- General Practice Forward View: Progress Update at End of Year Two (April 2018). Leeds: NHS England; 2018.
- Record breaking Round 1 GP fill rate figure announced. Leeds: HEE; 2018.
- By Choice – Not By Chance. Supporting Medical Students Towards Future Careers in General Practice. Leeds: HEE; 2016.
- Population Estimates for UK, England and Wales, Scotland and Northern Ireland: mid-2016. Newport: ONS; 2016.
- RNZCGP Workforce Survey. Wellington: Royal New Zealand College of General Practitioners; 2015.
- Warr P, Cook J, Wall T. Scales for the measurement of some work attitudes and aspects of psychological well-being. J Occup Psychol 1979;52:129-48. https://doi.org/ 10.1111/j.2044-8325.1979.tb00448.x.
- Davis E, Martin S, Gershlick B. Under Pressure: What the Commonwealth Fund’s 2015 International Survey of General Practitioners Means for the UK. London: The Health Foundation; 2016.
- Taylor K, Lambert T, Goldacre M. Career destinations, job satisfaction and views of the UK medical qualifiers of 1977. J R Soc Med 2008;101:191-200. https://doi.org/10.1258/jrsm.2007.070277.
- Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-325.
- General and Personal Medical Services, England September 2015–March 2016, Provisional Experimental Statistics. Leeds: NHS Digital; 2016.
- Mental Health Act 2005. London: The Stationery Office; 2005.
- General Practice Trends in the UK to 2014. Version 1. Leeds: NHS Digital; 2015.
Appendix 1 Patient and public involvement report
This report provides a record of the role of the PPI group within the ReGROUP study, including the development of the initial application, obtaining ethics approval, project management and contributions to individual workstreams.
Application development
An initial half-day workshop was attended by seven patients with experience of long-term conditions and accessing primary care. The project manager outlined the project and invited an open discussion about the project in general, and specifically where and how the group felt the project might benefit from PPI. Members of the group were also asked to discuss what they thought a support package for GPs might look like (see Table 25).
Overall, members of the group were supportive of the scope and content of the project and shared the project team’s concerns regarding the retention of experienced GPs.
There was an initial query from project academics about whether or not GPs, as the subject of the project, should constitute the participants of the PPI group. However, the workshop attendees were emphatic that a patient voice was essential throughout this project for two reasons. First, any strategies designed to influence GPs’ working patterns are likely to affect patients, particularly those with multimorbidities or long-term conditions. Second, participants felt that the public would be able to contribute to the development of policies or strategies through their awareness of issues in primary care that might lead to wasted GP time, and of which neither researchers nor health professionals were aware. Participants thus felt that they would be able to contribute a unique perspective to inform the project’s outcomes.
Outcomes
The points raised by the PPI group were well received by the project team and their recommendations significantly informed the final application, which saw PPI activities embedded throughout the project (Box 4). The full bid was also reviewed by lay representatives, and workshop attendees also commented on and amended the lay summary.
-
Pressure from CCGs.
-
Could routine care be moved (e.g. flu jabs)?
-
Very long working days.
-
Non-medical duties (e.g. CPD safety/quality, etc., burdensome).
-
Burdens on partners.
-
Short-term vs. long-term solution – urgent need to keep GPs for 1–2 years.
-
Incentives for trainees.
-
Alternative ways of seeing a GP.
-
‘Waiting room’ (as in Penzance surgery).
-
‘Under GP’ physician assistant.
-
Increase job satisfaction earlier in career.
-
Distribution of care (e.g. dedicated GPs for older people vs. families).
-
Better communication between professionals.
-
What about increasing personal support?
-
Reduction in workload over time but without a reduction in status.
-
Threatening behaviour of patients.
-
Involve PPGs.
-
Increase community hospitals.
CPD, continuous professional development.
| Pre-application PPI group suggestions | PPI activities stated in final bid | PPI activities completed |
|---|---|---|
| Patients should be on the management group | Setting up a PPI group | Group of 7 people with relevant experience established (January 2016) |
| Representation on Project Management Group | PPI representation and contribution to monthly project meetings (January 2016 onwards) | |
| Systematic review | Lay contribution to the systematic review | Workshop held (June 2016) |
| Qualitative interviews | Review of qualitative interview schedule and contribution to the analysis of the qualitative data | Two workshops held (October 2016, May 2017) |
| RAM expert panel – there should be patient representation on this. Possibly have independent PPI group meeting first | Contribution to the RAM ‘expert panel’ prioritising proposed policies and strategies | PPI attendance at 3 planning meetings. Workshop held (October 2016) |
| Participation in the stakeholder consultations | Two PPI representatives at both consultation meetings. PPI representative acted as facilitator at one meeting | |
| Contributing to dissemination (e.g. preparing lay summaries of project outcomes) | Workshop held to brief PPI group on key results | |
| PPI representative at project team results sharing meeting | ||
| Be more explicit about patients’ voices to ensure that intervention does not negatively affect patients. Patients know where time may be wasted so need to ask them – GPs may not be aware of them | These two suggestions did not map directly into the scope of the project | However, these comments were noted and patient concerns were discussed in all workshops and formed an explicit discussion topic in the RAM workshop |
| Can patients be interviewed about what impact any potential intervention will have on patients? |
Ethics application
The ethics application was submitted before the start date of the project and the final PPI group was formed. However, three members of the initial workshop reviewed the documentation for the ethics application and their written comments were incorporated into the final versions of these.
Post award
Patient and public involvement group recruitment and composition
The project PPI group was recruited from local PPI networks. People who had attended the initial workshop were invited to continue participating. The final group consisted of two men and five women, representing individuals with experience of a range of long-term physical and mental health conditions and experience of regular contact with GP/primary care services. Some of the group also had experience as carers for elderly relatives or for children with life-altering health conditions. One member had extensive experience as a lay representative within CCGs, and with the Quality Outcome Framework as a lay assessor of general practices.
Initial patient and public involvement meeting
At the outset of the project (January 2016), the PPI group was invited to a half-day workshop facilitated by the PPI lead (JW), the project manager (EF), a qualitative researcher (AS) and a systematic review researcher.
Aims
Following introductions, members of the project team presented an overview of the project workstreams and PPI members were encouraged to ask questions and to participate in active discussion. There was a particular focus on the systematic review and qualitative workstreams and how PPI might be incorporated.
Outcomes
The PPI group discussed, agreed and documented ways of working, including contact preferences, times/days for meetings, meeting venues, payments and confidentiality. Throughout the project, PPI representatives were paid £25 per half day plus travel expenses at UEMS rates.
In addition, the PPI members were given access to training in systematic reviewing and qualitative research methodologies provided through the NIHR Collaboration for Leadership in Applied Health Research and Care, South West Peninsula (PenCLAHRC) early in the project.
Patient and public involvement in project management
Two PPI representatives were initially selected by the broader group to attend the monthly project management group meetings. Unfortunately, one member had to step down after the first meeting owing to illness. However, as the other member (AA) had considerable experience of lay representation around primary care, it was not considered necessary to replace the other member. Alex Aylward attended almost all of the meetings and proved to be an exceptionally valuable and supportive member of the project team. In addition to contributing to discussions, Alex Aylward reviewed and provided feedback on all draft papers and conference abstracts and assisted with the flow and running of the PPI group meetings.
Involvement in workstreams
Workstream 1: systematic review
A meeting was held between the PPI lead (JW), the systematic review lead (RA) and one of the systematic review researchers to consider how best to involve the PPI group in the review. Given the time constraints of the project and the need to produce findings promptly, the review process was under way before the PPI group was in place. It was decided that the PPI group could have the most impact by being involved in sharing and discussing emerging findings from the review with the systematic review team.
A half-day workshop was held in June 2016, attended by Rob Anderson, the project information specialist, one of the systematic review researchers and the PPI group.
Aims
The aims of this workshop were to provide an overview of the project (by way of reminder), to overview the systematic review process, and preview and discuss emerging UK findings, specifically regarding:
-
the different ways GPs leave practice/reduce hours
-
results from quantitative surveys of GPs
-
indications from qualitative interview studies.
Findings were presented visually with Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) (quantitative results) and a colourful paper-based ‘mind map’ (see Figure 5) of the initial findings of the qualitative synthesis. The materials were circulated to the group for future reference.
Outcomes
As a result of this workshop, the systematic review researcher reflected that the PPI comments ‘may add to our understanding of particular themes that have emerged in the qualitative synthesis’.
A detailed reflection on the PPI discussions is provided in Appendix 10. This summarises how the discussion ‘broadened our understanding of the above literature-derived themes (especially in response to the initial synthesis of qualitative interview-based studies)’. The themes identified were flexible working, continue and cope, viability of early retirement, ageing, partnership issues, and commitment and investment. Themes around organisational changes identified were referrals, doctor–patient relationship, patients’ demands and practice demands. In terms of professional culture, the theme of acceptability of early retirement was discussed.
An additional important benefit of this workshop for the PPI group was that it enabled the members to discover and discuss the broader context of the project and thus be better prepared for future PPI input.
The review of survey studies is now in press (i.e. Anderson et al. 119), but the paper reporting the qualitative synthesis of the systematic review is still in preparation. Write-up of both of these papers also generated associated conference abstracts.
Workstream 2: census survey of south-west general practitioners
The survey instrument used in this project was based on that used in preliminary work, the design of which had been informed by that study’s PPI group. 17 The current PPI group were, however, sent the survey via e-mail for additional comments.
Outcomes
The phrase ‘quit’ was replaced by ‘permanently leave’ in the final survey draft.
Workstream 3: qualitative research
An initial planning meeting was held between the PPI lead (JW) and the two qualitative researchers (AS and RT). As a result of this, the qualitative researchers decided to produce a briefing document for the PPI group with key areas on which they wished to receive PPI feedback.
The PPI group were offered the opportunity to attend a half-day qualitative research training course: ‘An Introduction to Qualitative Research’ delivered by the PenCLARHC (http://clahrc-peninsula.nihr.ac.uk/event/making-sense-of-evidence-an-introduction-to-qualitative-research1; accessed 4 December 2018). Several members attended. Others had either previously attended this course or contributed to PPI in qualitative research in other studies.
Workshop 1
This was held in October 2016 and was attended by PPI representatives and the two qualitative researchers. A short, plain English briefing document was circulated via e-mail with paper copies available at the workshop.
Aims
The aims of this workshop were to:
-
update the PPI group on the progress to date of the qualitative workstream
-
share and discuss early thoughts arising from the qualitative interviews with GPs
-
discuss possible solutions to the issues raised by the GPs in the interviews.
Outcomes
Notes from the PPI workshop were taken by the researchers and considered in their analyses. In particular, the need to consider the views of ‘staying’ GPs as well as those considering leaving direct patient care were highlighted.
Three key issues arising from the data were discussed by the group:
-
GPs are finding ways to cope with the demands of general practice. These include working part-time, taking career breaks and becoming a locum. How is this affecting patent care? What work patterns would be best for the patient (out-of-hours care, access to appointments, etc.).
-
GPs experience fear and (fear of) the risk of making mistakes or being complained about. This fear may affect their own health and well-being, anxiety and pessimism about the future of general practice and whether or not the current conditions will inevitably get worse. How is this affecting patient care and what might be done about it?
-
GPs feel that their role has changed. They feel that more demands are made from secondary care, that the amount and complexity of work have increased, that paperwork and administration have increased and that ‘the buck always stops with the GP’. What could help to reduce GPs’ workload and/or help them to manage it better? Can you give examples from your practice, what works and does not work from a patient’s perspective?
Workshop 2
A second workshop was held by Anna Sansom and Emily Fletcher in May 2017, attended by five PPI members. Anna Sansom produced the qualitative workstream findings in a briefing document for the group. The presentation and discussion followed the following format:
-
overview of approach and who was interviewed (AS)
-
each theme described (by AS) and discussed (by PPI, facilitated by AS) individually before moving on to the next theme
-
invitation to the group members to raise and discuss any other issues that they felt were important to the interpretation, understanding and implications of the findings.
The group was invited to discuss the following key points:
-
What are your reactions to the overarching themes of identity and value, fear and risk, and choice and volition? What are the impacts of these on patients?
-
What could be done to help GPs with these issues? How might this affect patient care?
-
What role (if any) do patients have in helping to retain GPs?
-
Anything else you want to add?
The meeting was audio-recorded (with consent from the group) and Anna Sansom typed up summary notes after the meeting. Researcher reflections were included to identify any potential researcher bias.
These notes helped to provide content for both the qualitative report chapter, and also a PPI section for a paper written for an academic journal.
The write-up of the qualitative workstream reflects the PPI input, summarised below:
-
The group were sympathetic to the pressures GPs experience. They noted the negative impact this pressure might have on patients.
-
The PPI members suggested that there was opportunity and desire for patient involvement in supporting GPs and in the organisation and delivery of primary care.
-
Greater involvement and inclusion of PPGs could benefit GPs, in helping them to feel more valued and working to reduce GP fear around patient complaints.
-
A need for practice staff and patient representatives to be seen as ‘all being on the same side’, and for GPs and other non-clinical staff to trust patients as part of the practice team.
-
More involvement and inclusion of patients could support the relationship between patients and practice staff, thus helping to manage patient demands and expectations.
-
Involving PPGs as part of the practice team could help the identification of models and examples of good practice that could then be shared by PPGs with other practices.
Workstream 4: RAND/UCLA Appropriateness Method
In the early stages of the RAM workstream, the RAM researcher (RC) circulated explanatory documents to the PPI group. These included a plain English ‘Introduction to the RAM Process’ and a completed example from a previous research study.
Two planning meetings were held before the PPI workshop, attended by the RAM researcher (RC) and PPI lead (JW), and with a member of the PPI group (AA). Given the novelty and complexity of the process, it proved useful for Alex Aylward (with background experience of working as a lay representative with CCGs and general practices) to inform the development of the PPI process.
In October 2016, a half-day workshop was led by Rupatharshini Chilvers and Jo Welsman and attended by members of the PPI group. At this stage, the RAM categories and policy statements were in development, and thus there was scope to incorporate PPI into both the contextual information around the statements and the statements themselves that would be provided to RAM panel members. PPI was considered less relevant in the formal RAM panel process and analysis owing to its prescriptive and quantitative nature.
Aims
The aims of this workshop were to:
-
review the RAM process and give the PPI group the opportunity to ask questions and familiarise themselves with the aims and objectives of the RAM in the project
-
outline the boundaries for the policies and strategies for the RAM, in order to manage the group’s expectations around what PPI could and could not be included within the RAM process
-
obtain feedback from the group specifically around the consequences and impact of suggested RAM themes/categories for local communities or specific groups of patients.
Outcomes
Detailed notes of the discussions were taken by Rupatharshini Chilvers and fed back to the project team at the RAM development meetings. Discussion and action points raised for Rupatharshini Chilvers were documented. Although not all points were directly relevant to, or easily incorporated into, the RAM, these were noted for future consideration. Specific comments that were considered for incorporation into the RAM process are summarised in Table 27. Although some of this discussion did not feed directly into the RAM process, the concerns and issues raised were also discussed and incorporated into other workstreams, notably the qualitative research.
| Discussion point (PPI group) | Action point (RAM lead) |
|---|---|
| The setting is changing for GPs and some are moving to very large practices, and one GP is leaving because they do not want to move to the amalgamated general practice | The size is a consideration, and the panel will be asked to think about this as part of their consideration of the practice setting |
| There is a potential conflict of interest in the panel and the statements could be used for a political stand and it is important to show that this is not the perspective that the panel brings to the discussion | Develop a code of conduct for the panel and ask them not to consider the political implications of this |
| Include junior doctors in the panel as they will be able to say what type of incentives will be suitable as they enter the profession | The time range is the next 5 years and for the experienced group of GPs, and the junior doctors will not be directly affected by this set of policies and strategies in the next 5 years. It would be good for another project to review this side of it |
| GPs are under strain (e.g. with shorter lengths of surgery time, patient anxiety in the system is increasing). Therefore, this should be included in some way in the panel information/rating. The strategies and policies should not make patient experience any worse and should not be at the cost of the patient’s experience and care. Set the rules that the policies and strategies result in patient care at least the same as now and see the same number of patients (throughput) | Consider the addition of a section on expected impact on patient experience scores or equivalent. The assumption could be that if there is no change, patient experience may not be improved |
| Educate the patients not to overload the practices | Need to consider how it could be related to retention statements |
| Patient groups helping with the running of practices could be good for making the type of improvements discussed, such as explaining the reasons for the policies | This is not directly related to the project and has been noted as part of involving patient groups in the discussion on policies and strategies that require explanation because of either absence or other reasons |
| The paperwork and computer systems could be improved | This is not directly related, but is in line with other discussions on organisational factors |
The contribution of the PPI group to the development of the RAM statements is acknowledged in the RAM chapter.
Workstream 5: workforce predictive risk modelling
Given the nature of the work involved in this workstream, no formal input from the whole PPI group was sought. However, Alex Aylward was involved in project management meetings and participated in discussions regarding results and interpretation, and commented on drafts of the write-up.
Workstream 6: stakeholder consultations
Alex Aylward received facilitator training and facilitated round-table discussions at the London stakeholder consultation meeting. In addition, two experienced PPI representatives from Leeds were recruited to attend the Leeds stakeholder consultation meeting as stakeholders in their own right to participate in the round-table discussions of emergent policies and strategies for retention, as described in Chapter 7. Both PPI representatives provided positive feedback via e-mail on the success of the meeting and on their experience of being involved in the conversations.
Additional patient and public involvement activities
Results meeting
In preparation for the stakeholder consultation meetings, the research team rehearsed presentations of the project’s results at a meeting attended by two PPI members, who fed back to help finalise presentation content.
Dissemination
Three PPI members attended an informal workshop to review their participation and input throughout the project, and also to hear the whole project’s conclusions. They were asked for their ideas regarding dissemination to non-academic/clinical groups. Following discussion, it was suggested that a short film or infographic could be produced, highlighting the issues of GP retention and the ways in which the public might support their GPs, based on the main findings of the project. In terms of routes for dissemination, PPI members suggested that these may include practice waiting room screens/websites, circulation to PPGs, CCGs and various patient care forums and condition-specific charities.
Report writing
Alex Aylward co-authored this PPI report. The report was circulated to the wider PPI group for comments and amendments.
In addition, the Plain English summary for this final HSDR report was circulated to all members of the PPI group for comments and amendments. The following key points were changed/incorporated/recommended:
-
‘quit’ was replaced by ‘leave’ in order to avoid negative connotations associated with GPs leaving the profession
-
‘stakeholder’ was replaced by ‘interested parties’ and ‘people with a specific interest in the subject’
-
‘workstreams’ was replaced by ‘activities’.
Conclusion
Patient and public involvement was woven throughout this programme, including input to the funding application, obtaining ethics approval, project management and contributions to the workstreams. Input was supportive and added the important element of the patient voice to the issue of the GP workforce crisis.
Appendix 2 Workstream abstracts
Systematic review
Objective
This systematic review aimed to answer the following question: what are the factors in the UK and other high-income countries that affect GPs’ decisions to (1) quit direct patient care (including reducing their time commitment to it), (2) take career breaks from general practice and (3) return to general practice after a career break?
General practitioner is used here to denote any medically qualified clinical professional (doctor) whose main clinical role is community based, outside hospital, and who is a primary care specialist rather than a clinical specialist focusing on a disease or disease process.
Methods
Searches identified both published articles and ‘grey’ literature in English and from 1990 onwards, using both conventional bibliographic searches of relevant databases (MEDLINE, MEDLINE in Process, PsycInfo, HMIC, Cochrane, ASSIA, Web of Science) and complementary methods (web searching, forwards and backwards citation chasing). Searches were conducted in January 2016 and updated in April 2016 and yielded 5227 records after deduplication. The review used prespecified inclusion and exclusion criteria and was registered on PROSPERO.
Included studies
We included 34 survey-based (mostly quantitative; 22 studies from the UK) and five qualitative interview-based (four from the UK) studies.
Results
General practitioners in the UK leave general practice for a very wide range of factors: both negative job-related ‘push’ factors and positive, leisure-, retirement- and home-life related ‘pull’ factors. Although some factors clearly operate at an individual, personal level (such as the financial ability to retire, health, family and marital circumstances, or good/poor relationships with practice partners), other factors operate at the level of the general practice, local area, the whole profession or the national health system (e.g. media portrayal of GPs, service reform and performance targets, CQC inspections and professional revalidation).
Conclusions
Four closely related, job-related factors play a major part in decision-making about both early retirement and part-time working: workload, job (dis)satisfaction, work-related stress and work–life balance. However, many other detailed factors either underlie these higher-level factors or are more important for a significant minority of GPs. These factors could provide a focus for developing a variety of GP retention initiatives.
Census survey
Reproduced with permission from Fletcher et al. 82 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Objectives
Given recent concerns regarding general practice workforce capacity, we aimed to describe GPs’ career intentions, especially those that might have an impact on GP workforce availability over the next 5 years.
Design
Census survey, conducted between April and May 2016 using postal and online responses, of all GPs on the NHS National Performers List and eligible to practise in primary care. Two reminders were used as necessary.
Setting
South-west England (population 3.5 million), a region with low overall socioeconomic deprivation.
Participants
A total of 2248 out of 3370 eligible GPs (67% response rate).
Outcomes
Reported likelihood of permanently leaving or reducing hours spent in direct patient care or of taking a career break within the next 5 years, and present morale weighted for non-response.
Results
Responders included 2179 GPs engaged in patient care. Of these, 863 (37% weighted, 95% CI 35% to 39%) reported a high likelihood of quitting direct patient care within the next 5 years. Overall, 1535 (70% weighted, 95% CI 68% to 72%) respondents reported a career intention that would negatively affect GP workforce capacity over the next 5 years, through permanently leaving or reducing hours spent in direct patient care, or through taking a career break. GP age was an important predictor of career intentions; sharp increases in the proportion of GPs intending to quit patient care were evident from the age of 52 years. Only 305 (14% weighted, 95% CI 13% to 16%) GPs reported high levels of morale, whereas 54% (weighted, 95% CI 52% to 56%) reported low levels of morale. Low levels of morale was particularly common among GP partners. Current morale strongly predicted GPs’ career intentions; those with very low levels of morale were particularly likely to report intentions to quit patient care or to take a career break.
Conclusions
A substantial majority of GPs in south-west England report low levels of morale. Many are considering career intentions that, if implemented, would adversely affect GP workforce capacity within a short time period.
Qualitative research
Objective
To help identify the potential content of policies and strategies aimed at retaining experienced GPs and/or supporting the return of GPs following a career break, through an exploration of the lived experience of GPs, including their remaining/leaving decision-making.
Design and setting
Thematic analysis of CQC practice report data to explore examples of good and poor practice in south-west England, followed by semistructured interviews with GPs and other primary care stakeholders in south-west England. Transcribed interviews were analysed thematically.
Participants
Forty-one GPs identified from GP workforce census survey returns: seven retired GPs; eight GPs aged 50–59 years who were intending to retire; 11 GPs on a career break or intending to take one; nine GPs aged 35–49 years who had quit or were intending to quit direct patient care; and six GPs who did not intend to quit and had good morale. In addition, 19 stakeholders were opportunistically sampled from primary-care-related settings (local and regional) in the south-west.
Results
Examples of good practice were extracted from the CQC report data and these were used to develop interview prompts and questions, and to inform workstream 4. The interview findings showed that (1) factors and issues need to be addressed collectively, (2) there are inherent tensions and contradictions within potential solutions that need to be considered and (3) there is also a need to address GPs’ lived experiences of their work and role in the current health-care climate. The lived experience was illustrated through three underlying themes that emerged from the data: identity and value, fear and risk, and choice and volition.
Conclusions
Use of evidence from occupational and workplace literature adds weight to the argument that solutions should not be ‘sticking plasters’ but rather implementable policies and strategies that will help to (1) increase the perceived value of GPs and clarify the identity and future of general practice, (2) reduce the levels of fear and risk that GPs are experiencing (to acceptable and manageable levels) and (3) provide GPs with feasible, acceptable and sustainable routes to remaining in direct patient care.
RAND/UCLA Appropriateness Method
Background
The development of policies and strategies to retain experienced GPs in direct patient care in the UK must acknowledge the current policy and practice contexts within which GPs are working. Using this contextual information and research evidence, we generated a set of potential policies and strategies aimed at maximising GP retention and tested their appropriateness and feasibility for implementation.
Methods
Using the RAM, a panel of GP partners and GPs working in national stakeholder organisations assessed the appropriateness of potential policies and strategies in two rounds of an online survey. The policies and strategies were those that could plausibly maximise GP retention within a 5-year window. Supported by an evidence briefing paper, panellists evaluated 54 potential policies and strategies that could be targeted at either national/regional, general practice or individual GP levels. Ratings were analysed for consensus and categorised based on appropriateness (appropriate, uncertain, inappropriate). A subset of statements rated as ‘appropriate’ after the first round of the online survey was also assessed for feasibility (feasible, uncertain, unfeasible) in the second round.
Results
The panel deemed 24 out of 54 policies and strategies as appropriate and 16 out of 19 as feasible. Policies and strategies were endorsed from a number of areas and considered suitable for implementation at national/regional, general practice or GP levels.
Conclusion
This systematic approach identified 24 potential policies and strategies deemed to be appropriate for improving retention of GPs in the workforce, the majority of which were deemed feasible. Of these, six were for implementation at national/regional level, four at general practice level and 14 at GP level. Future research evaluating the appropriateness and feasibility of other policies and strategies falling outside the scope of our research (e.g. primary care skills mix) is warranted.
Predictive risk modelling
Objectives
Through other workstreams, the wider ReGROUP project has identified and proposed some potential policies and strategies targeting the retention of the experienced GP workforce. To most effectively apply these it would be beneficial to identify those practices at highest risk of facing a supply–demand imbalance. We therefore aimed to develop a modelling framework to identify such practices.
Design
A hybrid modelling approach was used to predict imbalance based on practice factors including current workload, current GPPS scores, nurse workforce, projected populations and the projected fraction of existing GP workforce remaining in direct patient care. A predictive model was developed using historical data (2012–16), and current data (2016), which were used to predict future risk. The utility of surveying GP quitting intentions was explored.
Setting/participants
Predictive model development used data for all general practices in England, whereas predictions of future supply–demand risk status were restricted to south-west England.
Results
Based on historical data, the predictive model had fair to good discriminatory ability to predict which practices faced supply–demand imbalance (area under the ROC curve of 0.759). Predictions using current data suggested that practices at highest risk of future supply–demand imbalance on average have larger patient lists, employ more nurses, serve more deprived and younger populations, and have considerably worse patient experience ratings. Findings from a survey of GPs’ career intentions had very little impact on the predictions of future supply–demand risk status, when compared with using expected future workforce projections based only on routinely available data on GPs’ genders and ages.
Conclusions
It is possible to make reasonable predictions of an individual general practice’s future risk of undersupply of GP workforce with respect to its patient population. However, the predictions are inherently limited by the data available. Although targeted interventions may have a place, blanket policies may be more effective, given that most practices in south-west England are likely to be ‘at risk’ if faced with substantial increases in demand combined with major difficulties in recruiting GPs.
Stakeholder consultations
Objectives
Other ReGROUP project workstreams have identified potential policies and strategies to support the retention of GPs. From the stakeholder consultations we aimed to gather preliminary evidence from workforce partners and key stakeholder organisations on the feasibility and acceptability of implementing the policy changes and initiatives proposed.
Design
Two consultation meetings were organised at which stakeholders were invited to listen to the research evidence produced by the ReGROUP project. Discussions on 11 policy and strategy areas took place in small round-table groups, facilitated by project team members, and comments were captured using sticky notes and flip charts.
Setting
London and Leeds, UK.
Participants
Stakeholders comprised regional representatives of CCGs, LMCs, NHS England Local Area Teams, AHSNs and PPI groups, and also included representatives from national bodies such as the BMA, RCGP, HEE, NHS Employers and GMC.
Outcomes
Stakeholders explored the practicalities of implementing change to the proposed areas of policy and strategy to support retention, specifically focusing on barriers to and facilitators of change, feasibility and acceptability, and key actions that could be undertaken by particular organisations to introduce change.
Results
Stakeholder feedback was obtained for three broad areas of policy and strategy: (1) ‘protecting’ GPs and managing expectations of patients, (2) incentives and support mechanisms for GPs and (3) portfolio and wider working arrangements. Tangible actions were identified for national organisations including NHS England, the RCGP, HEE and CEPNs, as well as for CCGs and individual practices, or federations/groups of practices.
Conclusions
A broad range of stakeholders involved in workforce planning had the opportunity to contribute to discussions on emergent policies and strategies to support retention of GPs from our research. Although this work has successfully highlighted specific actions that could be taken by workforce partner groups and stakeholder organisations, it is a first step towards formal evaluation of the feasibility and acceptability of the potential policies and strategies to support retention.
Appendix 3 Literature search strategies
Detailed approach
Published articles and grey literature were considered with articles restricted to those published in English from 1990 onwards. Two searches were carried out. The first search identified published, unpublished and grey literature studies and was run in a variety of relevant databases. The second search drew on supplementary search methods to locate unpublished studies and grey literature. This search built on articles included as full text in the first search, using forward and backward citation chasing. Other sources (e.g. relevant organisation websites) were also searched for grey literature. The first search was based on combining population and care setting terms (e.g. GPs and primary care) and exposure terms (e.g. part-time working, medical retirement), and no study design filters were used.
Searching the databases
The following databases were searched on 28/29 January 2016: MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, PsycInfo, HMIC, The Cochrane Library, ASSIA and Web of Science. We tested searching Cumulative Index to Nursing and Allied Health Literature (CINAHL) but the records found were largely concerned with nursing practice rather than with medical practice so we decided to exclude this database.
Searching these databases yielded 6661 abstracts. After deduplication, the number of results was reduced to 5227. Updates to these searches were carried out on 22 April 2016. Forward and backward citation searches were carried out for the final full text included on 29 April 2016 using Scopus, Web of Science and Google Scholar.
Grey literature search methods
The individual websites of the GP representative organisations of all OECD countries were searched for any relevant policy documents or GP surveys in English on 24/25 February 2016. For each OECD country’s department of health or equivalent, we searched on their website for government policy documents on GP working conditions in English on 7 March 2016. We also carried out a broad Google search (Google Inc., Mountain View, CA, USA) on 24/25 February 2016 for surveys, reports and policy documents from OECD countries on GP burnout, retention, early retirement and part-time working.
Grey literature sources, including GreyNet, OpenGrey, Trip database, NHS Evidence, Public Health England and NHS networks sources, were searched on 7 March 2016. A Google search for newspaper articles reporting on relevant studies was also carried out on the same date. Forward and backward citation searches were carried out for the final full text included on 29 April 2016 using Scopus, Web of Science and Google Scholar.
Search strategies
MEDLINE (via OvidSP)
Date range searched: 1946 to January week 3 2016.
Date searched: 29 January 2016.
Searcher: SR.
Hits: 3655.
Search strategy
-
Family Practice/ or General Practice/
-
physicians, family/ or physicians, primary care/
-
General Practitioners/
-
Primary Health Care/
-
“primary care”.tw.
-
“general practi$”.tw.
-
“family doctor$”.tw.
-
“family physician$”.tw.
-
“family medic$”.tw.
-
(GP or GPs).tw.
-
or/1-10
-
(career$ adj3 (interrupt$ or chang$ or pattern$ or decision$ or leav$ or break$)).tw.
-
(retire$ adj3 (decision$ or medical$ or option$ or choice$ or pattern$ or determin$)).tw.
-
(job$ adj3 (chang$ or leav$)).tw.
-
(work$ adj3 (retention or retain$)).tw.
-
(long adj3 (sick$ or absen$ or ill$)).tw.
-
(burnout or “burn out”).tw.
-
Job Satisfaction/
-
Personnel Turnover/
-
Career Choice/
-
Retirement/
-
or/12-21
-
11 and 22
-
limit 23 to yr=“1990 -Current”
MEDLINE(R) In-Process & Other Non-Indexed Citations (via OvidSP)
Date range searched: 28 January 2016.
Date searched: 28 January 2016.
Searcher: SR.
Hits: 87.
Search strategy
-
“primary care”.tw.
-
“general practi$”.tw.
-
“family doctor$”.tw.
-
“family physician$”.tw.
-
“family medic$”.tw.
-
(GP or GPs).tw.
-
or/1-6
-
(career$ adj3 (interrupt$ or chang$ or pattern$ or decision$ or leav$ or break$)).tw.
-
(retire$ adj3 (decision$ or medical$ or option$ or choice$ or pattern$ or determin$)).tw.
-
(job$ adj3 (chang$ or leav$)).tw.
-
(work$ adj3 (retention or retain$)).tw.
-
(long adj3 (sick$ or absen$ or ill$)).tw.
-
(burnout or “burn out”).tw.
-
or/8-13
-
7 and 14
PsycINFO (via OvidSP)
Date range searched: 1806 to January week 4 2016.
Date searched: 29 January 2016.
Searcher: SR.
Hits: 511.
Search strategy
-
family medicine/
-
family physicians/
-
general practitioners/
-
primary health care/
-
“primary care”.tw.
-
“general practi$”.tw.
-
“family doctor$”.tw.
-
“family physician$”.tw.
-
“family medic$”.tw.
-
(GP or GPs).tw.
-
or/1-10
-
(career$ adj3 (interrupt$ or chang$ or pattern$ or decision$ or leav$ or break$)).tw.
-
(retire$ adj3 (decision$ or medical$ or option$ or choice$ or pattern$ or determin$)).tw.
-
(job$ adj3 (chang$ or leav$)).tw.
-
(work$ adj3 (retention or retain$)).tw.
-
(long adj3 (sick$ or absen$ or ill$)).tw.
-
(burnout or “burn out”).tw.
-
job satisfaction/
-
employee turnover/
-
occupational choice/
-
retirement/
-
or/12-21
-
11 and 22
-
limit 23 to yr=“1990 -Current”
Health Management Information Consortium (via OvidSP)
Date range searched: 1979 to November 2015.
Date searched: 29 January 2016.
Searcher: SR.
Hits: 417.
Search strategy
-
exp general practice/
-
exp general practitioners/
-
primary care/
-
“primary care”.tw.
-
“general practi$”.tw.
-
“family doctor$”.tw.
-
“family physician$”.tw.
-
“family medic$”.tw.
-
(GP or GPs).tw.
-
or/1-9
-
(career$ adj3 (interrupt$ or chang$ or pattern$ or decision$ or leav$ or break$)).tw.
-
(retire$ adj3 (decision$ or medical$ or option$ or choice$ or pattern$ or determin$)).tw.
-
(job$ adj3 (chang$ or leav$)).tw.
-
(work$ adj3 (retention or retain$)).tw.
-
(long adj3 (sick$ or absen$ or ill$)).tw.
-
(burnout or “burn out”).tw.
-
job satisfaction/
-
occupational choice/
-
exp retirement/
-
or/11-19
-
10 and 20
-
limit 21 to yr=“1990 -Current”
Applied Social Sciences Index of Abstracts (via ProQuest)
Data parameters: not applicable.
Date searched: 29 January 2016.
Searcher: SR.
Hits: 214.
Search strategy
-
TI,AB(“primary care” OR “general practi*” OR “family doctor*” OR “family physician*” OR “family medic*” OR GP OR GPs) OR SU.EXACT(“General practice” OR “General practitioners” OR “Primary health care”)
-
TI,AB((career* NEAR/2 (interrupt* OR chang* OR pattern* OR decision* OR leav* OR break*)) OR (retire* NEAR/2 (decision* OR medical* OR option* OR choice* OR pattern* OR determin*)) OR (job* NEAR/2 (chang* OR leav*)) OR (work* NEAR/2 (retention OR retain*)) OR (long NEAR/2 (sick* OR absen* OR ill*) OR (burnout OR “burn out”))) OR SU.EXACT((“Job satisfaction”) OR (“Career choice”)) OR SU.EXACT.EXPLODE(“Early retirement” OR “Mandatory retirement” OR “Retirement”)
-
1 AND 2
Cochrane (Cochrane Collaboration)
Data parameters: CENTRAL – Issue 12 of 12, December 2015; CDSR – Issue 1 of 12, January 2016.
Date searched: 29 January 2016.
Searcher: SR.
Hits: 75.
Search strategy
-
Medical Subject Heading (MeSH) descriptor: [General Practice] this term only
-
MeSH descriptor: [Family Practice] this term only
-
MeSH descriptor: [Physicians, Family] this term only
-
MeSH descriptor: [Physicians, Primary Care] this term only
-
MeSH descriptor: [General Practitioners] this term only
-
MeSH descriptor: [Primary Health Care] this term only
-
“primary care”:ti or “primary care”:ab
-
“general practi*”:ti or “general practi*”:ab
-
“family doctor*”:ti or “family doctor*”:ab
-
1“family physician*”:ti or “family physician*”:ab
-
“family medic*”:ti or “family medic*”:ab
-
(GP or GPs):ti or (GP or GPs):ab
-
or #1-#12
-
(career* near/3 (interrupt* or chang* or pattern* or decision* or leav* or break*)):ti
-
(career* near/3 (interrupt* or chang* or pattern* or decision* or leav* or break*)):ab
-
(retire* near/3 (decision* or medical* or option* or choice* or pattern* or determin*)):ti
-
(retire* near/3 (decision* or medical* or option* or choice* or pattern* or determin*)):ab
-
(job* near/3 (chang* or leav*)):ti
-
(job* near/3 (chang* or leav*)):ab
-
work* near/3 (retention or retain*):ti
-
work* near/3 (retention or retain*):ab
-
long near/3 (sick* or absen* or ill*):ti
-
long near/3 (sick* or absen* or ill*):ab
-
(burnout or “burn out”):ti
-
(burnout or “burn out”):ab
-
MeSH descriptor: [Job Satisfaction] this term only
-
MeSH descriptor: [Personnel Turnover] this term only
-
MeSH descriptor: [Career Choice] this term only
-
MeSH descriptor: [Retirement] this term only
-
or #14-#29
-
#13 and #30
Web of Science (via Thomson Reuters)
Data parameters: SCI-EXPANDED and SSCI.
Date searched: 29 January 2016.
Searcher: SR.
Hits: 1702.
Search strategy
-
TOPIC: (family (practic* or doctor* or physician* or medic*))
-
TOPIC: (“general practi*”)
-
TOPIC: (“primary care”)
-
TOPIC: (GP or GPs)
-
1 OR 2 OR 3 OR 4
-
TOPIC: (career near/2 (interrupt* or chang* or pattern* or decision* or leav* or break*))
-
TOPIC: (retire* near/2 (decision* or medical* or option* or choice* or pattern* or determin*))
-
TOPIC: (job* near/2 (chang* or leav*))
-
TOPIC: (work* near/2 (retention or retain*))
-
TOPIC: (long near/2 (sick* or absen* or ill*))
-
TOPIC: ((burnout or “burn out”))
-
6 OR 7 OR 8 OR 9 OR 10 OR 11
-
5 AND 12
-
Limit to 1990-
Number of hits
| Database | Number of hits |
|---|---|
| MEDLINE | 3655 |
| MEDLINE In-Process & Other Non-Indexed Citations | 87 |
| ASSIA | 214 |
| PsycINFO | 511 |
| HMIC | 417 |
| Cochrane | 75 |
| Web of Science | 1702 |
| Total | 6661 |
| Duplicates | 1434 |
| Total unique references | 5227 |
Appendix 4 List of high-income Organisation for Economic Co-operation and Development countries
-
Australia.
-
Austria.
-
Belgium.
-
Canada.
-
Chile.
-
Czech Republic.
-
Denmark.
-
Estonia.
-
Finland.
-
France.
-
Germany.
-
Greece.
-
Hungary.
-
Iceland.
-
Ireland.
-
Israel.
-
Italy.
-
Japan.
-
Luxembourg.
-
The Netherlands.
-
New Zealand.
-
Norway.
-
Poland.
-
Portugal.
-
Republic of Korea.
-
Slovak Republic.
-
Slovenia.
-
Spain.
-
Sweden.
-
Switzerland.
-
UK.
-
USA.
Appendix 5 List of full-text exclusions, with reasons
| Number | Paper | Reason for exclusion |
|---|---|---|
| 1 | Aseltine RH Jr., Katz MC. Connecticut physician workforce survey 2008: initial findings on physician perceptions and potential impact on access to medical care. Conn Med 2008;72:539–46 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 2 | Aseltine RH Jr., Katz MC, Geragosian AH. Connecticut physician workforce survey 2009: physician satisfaction, physician supply and patient access to medical care. Conn Med 2010;74:281–91 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 3 | Ashworth M, Armstrong D. Sources and implications of dissatisfaction among new GPs in the inner city. Fam Pract 1999;16:18–22 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Career decisions and progression | ||
| 4 | Barnett RC, Gareis KC, Carr PL. Career satisfaction and retention of a sample of women physicians who work reduced hours. J Womens Health 2005;14:146–53 | Not clear whether GPs/PCPs |
| 5 | Beasley JW, Karsh BT, Sainfort F, Hagenauer ME, Marchand L. Quality of work life of family physicians in Wisconsin’s health care organizations: a WReN study. Wisconsin Med J 2004;103:51–5 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 6 | Beasley JW, Karsh BT, Hagenauer ME, Marchand L, Sainfort F. Quality of work life of independent vs. employed family physicians in Wisconsin: a WreN study. Ann Fam Med 2005;3:500–6 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 7 | British Medical Association (BMA). National Survey of GPs: the Future of General Practice Full Report December – February 2015 (a report by ICM on behalf of the BMA). London: BMA; 2015. URL: www.bma.org.uk/collective-voice/committees/general-practitioners-committee/gpc-surveys/future-of-general-practice (accessed 4 December 2018) | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 8 | Buchbinder SB, Wilson M, Melick CF, Powe NR. Primary care physician job satisfaction and turnover. Am J Manag Care 2001;7:701–13 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Turnover between different employers | ||
| 9 | Buddeberg-Fischer B, Stamm M, Buddeberg C, Bauer G, Haemmig O, Knecht M, et al. The impact of gender and parenthood on physicians’ careers – professional and personal situation seven years after graduation. BMC Health Serv Res 2010;10:10 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 10 | Calitri R, Adams A, Atherton H, Reeve J, Hill NR. Investigating the sustainability of careers in academic primary care: a UK survey. BMC Fam Pract 2014;15:205 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 11 | Cameron R, Redman S, Burrow S, Young B. Comparison of career patterns of male and female graduates of one Australian medical school. Teach Learn Med 1995;7:218–24 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Career decisions and progression | ||
| 12 | Carr PL, Gareis KC, Barnett RC. Characteristics and outcomes for women physicians who work reduced hours. J Women Health Gender Med 2003;12:399–405 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 13 | Cheraghi-Sohi S, McDonald R, Harrison S, Sanders C. Experience of contractual change in UK general practice: a qualitative study of salaried GPs. Br J Gen Pract 2012;62:e282–7 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 14 | The Commonwealth Fund. Primary care providers’ views of recent trends in health care delivery and payment: findings from The Commonwealth Fund/Kaiser Family Foundation 2015 national survey of primary care providers. Issue Brief 2015;24 | < 90% are GPs/PCPs and results for GPs not reported separately |
| 15 | Cossman JS. Mississippi’s physician labour force: current status and future challenges. J Miss State Med Assoc 2004;45:8–31 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 16 | Crouse BJ. Recruitment and retention of family physicians. Minn Med 1995;78:29–32 | Uses pre-1990 data (from 1982 and 1984) |
| 17 | Davidson JM, Lambert TW, Parkhouse J, Evans J, Goldacre MJ. Retirement intentions of doctors who qualified in the United Kingdom in 1974: Postal questionnaire survey. J Pub Health Med 2001;23:323–8 | Not clear whether GPs/PCPs |
| 18 | Degen C, Li J, Angerer P. Physicians’ intention to leave direct patient care: an integrative review. Hum Res Health 2015;13 | Not clear whether GPs/PCPs |
| 19 | DesRoches CM, Buerhaus P, Dittus RS, Donelan K. Primary care workforce shortages and career recommendations from practising clinicians. Acad Med 2015;90:671–7 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Career decisions | ||
| 20 | Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res 2014;14 | Not clear whether GPs/PCPs |
| Burnout but not associated with absence from work | ||
| 21 | Dowell AC, Hamilton S, McLeod DK. Job satisfaction, psychological morbidity and job stress among New Zealand general practitioners. N Z Med J 2000;113:269–72 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 23 | Gregory ST, Menser T. Burnout among primary care physicians: a test of the areas of worklife model. J Healthc Manag 2015;60:133–48 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Burnout but not associated with absence from work | ||
| 24 | Hall CB, Brazil K, Wakefield D, Lerer T, Tennen H. Organizational culture, job satisfaction, and clinician turnover in primary care. J Prim Care Commun Health 2010;1:29–36 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 25 | Heponiemi T, Kouvonen A, Vänskä J, Halila H, Sinervo T, Kivimäki M, et al. Health, psychosocial factors and retirement intentions among Finnish physicians. Occup Med 2008;58:406–12 | Not clear whether GPs/PCPs |
| 26 | Heponiemi T, Kouvonen A, Vanska J, Halila H, Sinervo T, Kivimaki M, et al. Effects of active on-call hours on physicians’ turnover intentions and well-being. Scand J Work Environ Health 2008;34:356–63 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Turnover between different employers | ||
| 27 | Heponiemi T, Kouvonen A, Vänskä J, Halila H, Sinervo T, Kivimäki M, et al. The association of distress and sleeping problems with physicians’ intentions to change profession: the moderating effect of job control. J Occup Health Psychol 2009;14:365–73 | Not clear whether GPs/PCPs |
| 28 | Heponiemi T, Kouvonen A, Aalto AM, Elovainio M. Psychosocial factors in GP work: the effects of taking a GP position or leaving GP work. Eur J Public Health 2013;23:361–6 | Employment change either from or to general practice |
| Turnover between different employers | ||
| 29 | Heponiemi T, Manderbacka K, Vanska J, Elovainio M. Can organizational justice help the retention of general practitioners? Health Policy 2013;110:22–8 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 30 | Heponiemi T, Elovainio M, Presseau J, Eccles MP. General practitioners’ psychosocial resources, distress, and sickness absence: a study comparing the UK and Finland. Fam Pract 2014;31:319–24 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| All sickness absence included, not necessarily long-term sickness absence | ||
| 31 | Hockly A. Could health service reforms make general practitioners ill? J Pub Mental Health 2012;11:50–3 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 32 | Hojat M, Gonnella JS, Erdmann JB, Veloski JJ, Xu G. Primary care and non-primary care physicians: a longitudinal study of their similarities, differences, and correlates before, during, and after medical school. Acad Med 1995;70(Suppl. 1):17–28 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Career decisions | ||
| 33 | Hung DY, Rundall TG, Cohen DJ, Tallia AF, Crabtree BF. Productivity and turnover in PCPs: the role of staff participation in decision-making. Med Care 2006;44:946–51 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Turnover between different employers | ||
| 34 | Jamieson JL, Webber EM, Sivertz KS. Re-entry residency training: opportunities and obstacles. Can Fam Phys 2010;56:e226–32 | Career decisions and progression |
| Retraining programmes to change specialty and/or retraining as a GP. Balance of focus unclear | ||
| 35 | Jewett EA, Brotherton SE, Ruch-Ross H. A national survey of ‘inactive’ physicians in the United States of America: enticements to reentry. Hum Resour Health 2011;9:7 | < 90% are GPs/PCPs and results for GPs not reported separately |
| 36 | Johnson N. General practice careers: changing experience of men and women vocational trainees between 1974 and 1989. Br J Gen Pract 1993;43(369):141–5 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 37 | Jones L, Fisher T. Workforce trends in general practice in the UK: results from a longitudinal study of doctors’ careers. Br J Gen Pract 2006;56:134–6 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Career decisions and progression | ||
| 38 | Joyce CM, Scott A, Jeon SH, Humphreys J, Kalb G, Witt J, et al. The ‘medicine in Australia: balancing employment and life (MABEL)’ longitudinal survey--protocol and baseline data for a prospective cohort study of Australian doctors’ workforce participation. BMC Health Serv Res 2010;10:50 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 39 | Joyce CM, Wang WC, McDonald HM. Retirement patterns of Australian doctors aged 65 years and older. Aus Health Rev 2015;39:582–7 | < 90% are GPs/PCPs and results for GPs not reported separately |
| 40 | Karsh BT, Beasley JW, Brown RL. Employed family physician satisfaction and commitment to their practice, work group, and health care organization. Health Serv Res 2010;45:457–75 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 41 | Kelley ML, Kuluski K, Brownlee K, Snow S. Physician satisfaction and practice intentions in Northwestern Ontario. Can J Rural Med 2008;13:129–35 | Not clear whether GPs/PCPs |
| Focus on remote rural retention | ||
| 42 | Kerstein J, Pauly MV, Hillman A. Primary care physician turnover in HMOs. Health Serv Res 1994;29:17–37 |
No examination of factors/associations with/determinants of quitting/intention to quit profession Turnover between different employers |
| 43 | Kilmartin MR, Newell CJ, Line MA. The balancing act: key issues in the lives of women general practitioners in Australia. Med J Aust 2002;177:87–9 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 44 | Kirwan M, Armstrong D. Investigation of burnout in a sample of British general practitioners. Br J Gen Pract 1995;45:259–60 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Burnout but not associated with absence from work | ||
| 45 | Kuusio H, Heponiemi T, Sinervo T, Elovainio M. Organisational commitment among general practitioners: a cross-sectional study of the role of psychosocial factors. Scand J Prim Health Care 2010;28:108–14 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 46 | Kuusio H, Heponiemi T, Vanska J, Aalto AM, Ruskoaho J, Elovainio M. Psychosocial stress factors and intention to leave job: differences between foreign-born and Finnish-born general practitioners. Scand J Public Health 2013;41:405–11 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 47 | Langballe EM, Innstrand ST, Aasland OG, Falkum E. The predictive value of individual factors, work-related factors, and work-home interaction on burnout in female and male physicians: A longitudinal study. Stress Health 2011;27:73–87 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Burnout but not associated with absence from work | ||
| 48 | Lawrence J, Poole P. Career and life experiences of New Zealand women medical graduates. N Z Med J 2001;114:537–40 | < 90% are GPs/PCPs and results for GPs not reported separately |
| Career decisions and progression | ||
| 49 | Leese B, Young R, Sibbald B. GP principals leaving practice in the UK. Eur J Gen Pract 2002;8:62–8 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Examines leaving GP principal job for another GP job, factors for returning | ||
| 50 | Linzer M, Manwell LB, Williams ES, Bobula JA, Brown RL, Varkey AB, et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med 2009;151:28–36 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 51 | Lloyd JR, Leese B. Career intentions and preferences of GP registrars in Yorkshire. Br J GP 2006;56:280–2 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Career decisions and progression | ||
| 52 | Landon BE, Reschovsky JD, Pham HH, Blumenthal D. Leaving medicine: the consequences of physician dissatisfaction. Med Care 2006;44:234–42 | < 90% are GPs/PCPs and results for GPs not reported separately |
| 53 | Lorant V, Geerts C, Duchesnes C, Goedhuys J, Ryssaert L, Remmen R, et al. Attracting and retaining GPs: a stakeholder survey of priorities. Br J Gen Pract 2011;61:e411–8 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Retention and recruitment | ||
| 54 | Mayorova T, Stevens F, Scherpbier A, van der Velden L, van der Zee J. Gender-related differences in general practice preferences: longitudinal evidence from the Netherlands 1982–2001. Health Policy 2005;72:73–80 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Career decisions | ||
| 55 | Misra-Hebert AD, Kay R, Stoller JK. A review of physician turnover: Rates, causes, and consequences. Am J Med Qual 2004;19:56–66 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Turnover between different employers | ||
| 56 | Miedema B, Easley J, Fortin P, Hamilton R, Tatemichi S. Crossing boundaries: family physicians’ struggles to protect their private lives. Can Fam Phys 2009;55:286–7.e5 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 57 | Miedema B, Hamilton R, Fortin P, Easley J, Tatemichi S. The challenges and rewards of rural family practice in New Brunswick, Canada: lessons for retention. Rural Remote Health 2009;9:1141 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Focus on remote rural retention | ||
| 58 | Moreno-Jiménez B, Gálvez-Herrer M, Rodríguez-Carvajal R, Vergel AIS. A study of physicians’ intention to quit: the role of burnout, commitment and difficult doctor–patient interactions. Psicothema 2012;24:263–70 | Not clear whether GPs/PCPs |
| 59 | Myhre DL, Konkin J, Woloschuk W, Szafran O, Hansen C, Crutcher R. Locum practice by recent family medicine graduates. Can Fam Phys 2010;56:e183–90 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 60 | Odom Walker K, Ryan G, Ramey R, Nunez FL, Beltran R, Splawn RG, et al. Recruiting and retaining primary care physicians in urban underserved communities: the importance of having a mission to serve. Am J Public Health 2010;100:2168–75 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Career decisions and progression | ||
| 61 | Pathman DE, Konrad TR, Williams ES, Scheckler WE, Linzer M, Douglas J, et al. Physician job satisfaction, dissatisfaction, and turnover. J Fam Pract 2002;51:593 | Not clear whether GPs/PCPs |
| Turnover between different employers | ||
| 62 | Pedersen AF, Andersen CM, Olesen F, Vedsted P. Risk of burnout in Danish GPs and exploration of factors associated with development of burnout: a two-wave panel study. Int J Fam Med 2013;2013:603713 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Burnout but not associated with absence from work | ||
| 63 | Plomondon ME, Magid DJ, Steiner JF, MaWhinney S, Gifford BD, Shih SC, et al. Primary care provider turnover and quality in managed care organizations. Am J Manag Care 2007;13:465–72 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Turnover between different employers | ||
| 64 | Presseau J, Johnston M, Johnston DW, Elovainio M, Hrisos S, Steen N, et al. Environmental and individual correlates of distress: testing Karasek’s demand-control model in 99 primary care clinical environments. Br J Health Psychol 2014;19:292–310 | < 90% are GPs/PCPs and results for GPs not reported separately |
| 65 | Putnik K, Houkes I. Work related characteristics, work-home and home-work interference and burnout among primary healthcare physicians: a gender perspective in a Serbian context. BMC Public Health 2011;11:716 | No examination of factors/associations with/determinants of quitting/intention to quit |
| Burnout but not associated with absence from work | ||
| 66 | Qidwai W, Beasley JW, Gomez-Clavelina FJ. The present status and future role of family doctors: a perspective from the International Federation of Primary Care Research Networks. Prim Health Care Res Dev 2008;9:172–182 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 67 | Rabatin J, Williams E, Baier Manwell L, Schwartz MD, Brown RL, Linzer M. Predictors and outcomes of burnout in primary care physicians. J Primary Care Commun Health 2016;7:41–3 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Burnout but not associated with absence from work | ||
| 68 | Rittenhouse DR, Mertz E, Keane D, Grumbach K. No exit: an evaluation of measures of physician attrition. Health Serv Res 2004;39:1571–88 | Not clear whether GPs/PCPs |
| 69 | Ruhe M, Gotler RS, Goodwin MA, Stange KC. Physician and staff turnover in community primary care practice. J Ambul Care Manage 2004;27:242–8 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 70 | Savageau JA, Ferguson WJ, Bohlke JL, Cragin LJ, O’Connell E. Recruitment and retention of primary care physicians at community health centres: a survey of Massachusetts physicians. J Health Care Poor Underserved 2011;22:817–35 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Turnover between different employers | ||
| 71 | Schattner PL, Coman GJ. The stress of metropolitan general practice. Med J Aust 1998;169:133–7 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 72 | Schofield DJ, Beard JR. Baby boomer doctors and nurses: demographic change and transitions to retirement. Med J Aust 2005;183:80–3 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 73 | Schofield DJ, Fletcher SL, Callander EJ. Ageing medical workforce in Australia -- where will the medical educators come from? Hum Resour Health 2009;7:82 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Workforce planning data | ||
| 74 | Shaw S, Goplen G, Houston DS. Career changes among Saskatchewan physicians. Can Med Assoc J 1996;154:1035–8 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Career decisions and progression | ||
| 75 | Shorer Y, Biderman A, Rabin S, Karni A, Levi A, Matalon A. Voluntary departure of family physicians from their workplace: A reflective outlook. Isr J Psych Rel Sci 2015;52:137–44 | Not clear whether or not each of four cases described involved leaving general practice. One is about returning to direct patient care. GP emotions around leaving examined, not determinants for quitting |
| 76 | Simon AB, Alonzo AA. The demography, career pattern, and motivation of locum tenens physicians in the United States. J Healthc Manag 2004;49:363–75; discussion 75–6 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Career decisions and progression | ||
| 77 | Solberg IB, Ro KI, Aasland O, Gude T, Moum T, Vaglum P, et al. The impact of change in a doctor’s job position: a five-year cohort study of job satisfaction among Norwegian doctors. BMC Health Serv Res 2012;12:41 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Career decisions and progression | ||
| 78 | Solberg IB, Tómasson K, Aasland O, Tyssen R. The impact of economic factors on migration considerations among Icelandic specialist doctors: A cross-sectional study. BMC Health Serv Res 2013;13 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 79 | Soler JK, Yaman H, Esteva M, Dobbs F, Asenova RS, Katic M, et al. Burnout in European family doctors: the EGPRN study. Fam Pract 2008;25:245–65 |
No examination of factors/associations with/determinants of quitting/intention to quit profession Burnout but not associated with absence from work |
| 80 | Department of Health and Social Care. Statistics for General Medical Practitioners in England: 1994–2004. Statistical Bulletin. No. 2005/02. London: Department of Health and Social Care; 2005. URL: https://webarchive.nationalarchives.gov.uk/20070306013912/http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsStatistics/PublicationsStatisticsArticle/fs/en?CONTENT_ID=4106726&chk=nKjsm8 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 81 | Stearns J, Everard KM, Gjerde CL, Stearns M, Shore W. Understanding the needs and concerns of senior faculty in academic medicine: building strategies to maintain this critical resource. Acad Med 2013;88:1927–33 | Not clear whether GPs/PCPs |
| Academic medicine | ||
| 82 | Stevenson AD, Phillips CB, Anderson KJ. Resilience among doctors who work in challenging areas: A qualitative study. Br J Gen Pract 2011;61:e404–10 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 83 | Taylor DH Jr, Leese B. Recruitment, retention, and time commitment change of general practitioners in England and Wales, 1990–4: A retrospective study. BMJ 1997;314:1806–10 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 84 | Taylor DH Jr, Leese B. General practitioner turnover and migration in England 1990–94. Br J Gen Pract 1998;48:1070–2 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Turnover between different employers | ||
| 85 | Taylor DH, Esmail A. Retrospective analysis of census data on general practitioners who qualified in South Asia: who will replace them as they retire? BMJ 1999;318:306–10 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Workforce planning | ||
| 86 | Taylor K, Lambert T, Goldacre M. Future career plans of a cohort of senior doctors working in the National Health Service. J Roy Soc Med 2008;101:182–90 | Not clear whether GPs/PCPs |
| Career decisions and progression | ||
| 87 | Taylor KS, Lambert TW, Goldacre MJ. Career progression and destinations, comparing men and women in the NHS: postal questionnaire surveys. BMJ 2009;338:b1735 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Career decisions and progression | ||
| 88 | Taylor K, Lambert T, Goldacre M. Career destinations, views and future plans of the UK medical qualifiers of 1988. J Roy Soc Med 2010;103:21–30 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| Career decisions and progression | ||
| 89 | Thommasen HV, Lavanchy M, Connelly I, Berkowitz J, Grzybowski S. Mental health, job satisfaction, and intention to relocate. Opinions of physicians in rural British Columbia. Can Fam Phys 2001;47:737–44 | Not clear whether GPs/PCPs |
| Focus on remote rural retention | ||
| Burnout but not associated with absence from work | ||
| 90 | Thornett A, Cobb S, Chambers R, Mohanna K. Accessing careers support in primary care. Educ Prim Care 2005;16;66–73 | Not clear whether GPs/PCPs |
| Career decisions and progression | ||
| 91 | Toyry S, Kalimo R, Aarimaa M, Juntunen J, Seuril M, Rasanen K. Children and work-related stress among physicians. Stress Health 2004;20:213–21 | Not clear whether GPs/PCPs |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 92 | Virtanen P, Oksanen T, Kivimaki M, Virtanen M, Pentti J, Vahtera J. Work stress and health in primary health care physicians and hospital physicians. Occup Environ Med 2008;65:364–6 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Examines differences between GPs and consultants not factors leading to long term sickness | ||
| 93 | Wainer J. Work of female rural doctors. Aust J Rural Health 2004;12:49–53 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| 94 | Wordsworth S, Skatun D, Scott A, French F. Preferences for general practice jobs: A survey of principals and sessional GPs. Br J Gen Pract 2004;54:740–6 | No examination of factors/associations with/determinants of quitting/intention to quit profession |
| Career decisions and progression | ||
| 95 | Xu G, Veloski JJ, Hojat M, Fields SK. Physicians’ intention to stay in or leave primary care specialties and variables associated with such intention. Eval Health Prof 1995;18:92–102 | < 90% are GPs/PCPs and results for GPs not reported separately |
| No examination of factors/associations with/determinants of quitting/intention to quit profession | ||
| 96 | Croft M. ‘First 5’s in Cornwall – what are their intentions and what influences their career choices?’ (Peninsula Deanery, Health Education England (South West), 2015–16; unpublished survey) | Unpublished (survey conducted for a GP academic trainee research project) |
Appendix 6 Overview of non-UK questionnaire studies
Coverage of different types of quitting direct patient care
Of the 12 non-UK survey studies, most of the studies (n = 11) were cross-sectional surveys and surveyed the quitting intentions of GPs at a particular point in time. One was based on panel survey data from the Australian MABEL (Medicine in Australia: Balancing Employment and Life) study. Of the non-UK studies, five explicitly focused on retirement intentions, three focused on actual quitting and five focused on preferences or intentions to reduce hours or work part-time.
Table 28 shows the types of quitting from direct patient care that were assessed in the included studies, and the types of variable or factor with which associations with quitting were explored.
Owing to space limitations, the synthesised findings of the non-UK survey studies are not described in this report. For this information, please see our full report of the systematic review (see Report Supplementary Material 1).
| Study first author, year and country | Quitting construct investigated | Personal characteristics | Job characteristics | Household characteristics | Area characteristics | Policy/organisational changes | Other | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Actual quitting/retention | Intention to quit within 5 years | Planned age of retirement | PT/flexible working | Taking career break | Other | Age | Gender | Ethnicity | Contract type/partner/locum, etc. | Practice/list size | Working hours/PT/FT | Job satisfaction | Job stressors | On call/out of hours | Income | Marital/family status | Social deprivation | Region/country | Urban/rural | |||
| Van Greuningen 2012,34 the Netherlands | ✓ | ✓a | ✓ | ✓b | ✓ | ✓c | ||||||||||||||||
| O’Kelly 2008,71 Ireland | ✓ | Self-reported reasons for leaving general practice | ||||||||||||||||||||
| Self-reported factors that would have kept them in practice | ||||||||||||||||||||||
| Nugent 2003,70 Ireland | ✓ | Self-reported reasons for leaving general practice | ||||||||||||||||||||
| McComb 2008,68 New Zealand | ✓ | ✓ | ✓d | |||||||||||||||||||
| Dewa 2014,67 Canada | ✓e | ✓e | ✓ | ✓ | ✓f | ✓ | ||||||||||||||||
| Brett 2009,27 Australia | ✓g | ✓ | ✓ | ✓ | ✓ | ✓ |
✓h ✓i |
|||||||||||||||
| Pit 2014,72 Australia | ✓ | ✓ | ✓ | ✓ | ✓j | ✓k | ✓l | |||||||||||||||
| Norman 2014,69 Australia | ✓m | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||
| Shrestha 2011,73 Australia | ✓ | ✓ | ✓n | |||||||||||||||||||
| RNZCGP 2015,166 New Zealand | ✓ | Stated reasons for working part-time (five prespecified options) | ||||||||||||||||||||
| Woodward 2001,75 Canada | ✓ | ✓ | ✓ | ✓ | ✓o,p | |||||||||||||||||
| Sumanen 2012,74 Finland | ✓q | ✓ | ✓ | ✓ | ✓r,s | |||||||||||||||||
Appendix 7 Quality-assessment tools used
| Question | Study first author, year of publication | |||||
|---|---|---|---|---|---|---|
| Newton, 200478 | Hutchins, 200560 | Campbell, 201517 | Sansom, 201618 | Doran, 201651 | Dwan, 201479 | |
| 1. Is the research question clear? | Y | Y | Y | Y | Y | Y |
| 2. Is the theoretical or ideological perspective of the author (or funder) explicit? | N | N | N | N | N | Y |
| 2b. Has this influenced the study design, methods or research findings? | CT | CT | CT | CT | CT | N |
| 3. Is the study design appropriate to answer the question? | Y | Y | Y | Y | Y | Y |
| 4. Is the context or setting adequately described? | N | N | Y | Y | Y | Y |
| 5. Is the sample adequate to explore the range of subjects and settings, and has it been drawn from an appropriate population? | CT | Y | Y | Y | Y | Y |
| 6. Was the data collection adequately described? | Y | N | Y | Y | Y | N |
| 7. Was data collection rigorously conducted to ensure confidence in the findings? | CT | CT | Y | Y | Y | Y |
| 8. Was there evidence that the data analysis was rigorously conducted to ensure confidence in the findings? | Y | Y | Y | Y | Y | Y |
| 9. Are the findings substantiated by the data? | Y | Y | Y | Y | Y | Y |
| 10. Has consideration been given to any limitations of the methods or data that may have affected the results? | N | Y | Y | Y | Y | Y |
| 11. Do any claims to generalisability follow logically and theoretically from the data? | Y | N | Y | Y | Y | Y |
| 12. Have ethical issues been addressed and confidentiality respected? | CT | Y | Y | Y | Y | Y |
| 13. Is/are the author/s reflexive? | N | N | N | N | N | N |
| Question | Yes | Partly | No | Cannot tell | Notes and caveats |
|---|---|---|---|---|---|
| 1. Did the study address a clearly focused question/study aims? | |||||
| 2a. Is the research method (study design) appropriate for answering the research question/aims? | |||||
| 2b. Was the questionnaire piloted prior to the main survey? (or previously validated/used) | |||||
| 3. Is the method of selection/eligibility criteria of the subjects (GPs/Physicians) clearly described? | |||||
| 4a. Could the way the sample was obtained introduce (selection) bias? | |||||
| 4b. Was the sample size adequate for generalisability? (> 500 = Yes, < 50 = No) | |||||
| 5. Was the sample of subjects representative with regard to the all GPs/PCPs in that region or country? (or specific subtypes of GP, or age, etc.?) | |||||
| 6. Was the sample size based on pre-study considerations of statistical power? | |||||
| 7. Was a satisfactory response rate achieved? (> 70% = Yes, < 50% = No) | |||||
| 8a. Were the variables (e.g. question(s)) for capturing quitting/intention to quit clearly described and likely to be valid and reliable? | |||||
| 8b. Were the variables [e.g. question(s)] for capturing potential determinants/factors clearly described, comprehensive, valid and reliable? | |||||
| 9. Was the statistical significance (of relevant associations) assessed? | |||||
| 10. Are CIs given for the main results? | |||||
| 11. Could there be confounding factors that have not been accounted for? | |||||
| 12a. Generalisability: Can the results be confidently applied to all GPs/PCPs in the source region and country? (Combined judgement on Q5, Q7 and country/geography) | |||||
| 12b. Generalisability: Can the results be confidently applied to all GPs in the UK NHS? (12a + Sample size Q4b and time – how old is paper?) |
Appendix 8 Tables showing study quality assessment
Tables 31 and 32 show the assessed quality of each included survey study.
| Question | Study first author, year of publication | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baker, 199552 | Baker, 200077 | Campbell, 201517 | Chambers, 200454 | Dale, 201544 | Doran, 201555 | Evans, 200056 | French, 200557 | French, 200658 | Gibson, 201543 | Hann, 201059 | Hutchins, 200576 | Luce, 200261 | Martin, 201541 | McKinstry, 200646 | Scott, 200645 | Simoens, 200263 | Simoens, 200242 | Sibbald, 200362 | Taylor, 199964 | Taylor, 200865 | Young, 200166 | |
| Did the study address a clearly focused question/study aims? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | P | Y | Y | Y | Y | Y | Y | Y |
| Is the research method appropriate for answering the research question/aims? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the questionnaire piloted prior to the main survey (or previously validated/used)? | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | CT | Y | Y | Y | Y | CT | N | CT | Y | N | P | Y |
| Is the method of selection criteria of the subjects clearly described? | Y | Y | Y | Y | Y | Y | Y | Y | P | Y | N | Y | Y | CT | Y | Y | P | Y | Y | Y | Y | P |
| Could the way the sample was obtained introduce (selection) bias?a | P | N | P | N | CT | P | N | CT | P | CT | CT | N | N | CT | P | N | CT | N | P | N | N | CT |
| Was the sample size adequate for generalisability? | P | Y | Y | P | Y | Y | Y | P | Y | Y | Y | P | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the sample of subjects representative with regard to the all GPs/PCPs in that region or country? | N | Y | CT | CT | P | Y | Y | CT | Y | P | P | CT | P | CT | P | Y | CT | Y | Y | Y | Y | P |
| Was the sample size based on pre-study considerations of statistical power? | N | N | N | N | N | N | N | N | N | CT | CT | N | N | CT | N | CT | N | N | N | N | N | N |
| Was a satisfactory response rate achieved? | N | P | P | Y | CT | N | Y | P | P | P | P | Y | Y | N | P | N | N | P | P | CT | Y | P |
| Were the variables for capturing quitting/intention to quit clearly described and likely to be valid and reliable? | Y | Y | Y | P | Y | Y | P | Y | P | Y | P | P | P | Y | P | Y | Y | Y | P | Y | Y | Y |
| Were the variables for capturing potential factors clearly described, comprehensive, valid and reliable? | Y | Y | Y | P | Y | Y | N | Y | P | Y | Y | P | Y | Y | P | Y | Y | Y | Y | Y | Y | Y |
| Was the statistical significance (of relevant associations) assessed? | Y | Y | Y | N | Y | N | N | Y | Y | N | Y | N | Y | N | Y | Y | Y | Y | Y | Y | Y | Y |
| Are CIs given for the main results? | N | N | Y | N | Y | N | N | Y | Y | N | Y | N | N | N | N | N | P | N | N | Y | Y | N |
| Could there be confounding factors that have not been accounted for?a | Y | P | P | Y | P | Y | Y | Y | P | Y | CT | Y | Y | P | Y | Y | N | N | N | N | Y | P |
| Can the results be confidently applied to all GPs in the source region and country? | N | P | P | Y | CT | P | Y | P | P | P | P | CT | P | CT | P | P | N | P | P | Y | P | P |
| Can the results be confidently applied to all GPs in the UK NHS in 2016? | N | P | P | P | P | P | P | P | P | P | P | P | P | CT | P | P | N | P | P | P | P | P |
| Question | Study first author, year of publication | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brett, 200927 | Dewa, 201467 | McComb, 200868 | Norman, 201469 | Nugent, 200370 | O’Kelly, 200871 | Pit, 201472 | RNZCGP, 2015166 | Shrestha, 201173 | Sumanen, 201274 | Van Greuningen, 201234 | Woodward, 200175 | |
| Did the study address a clearly focused question/study aims? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Is the research method appropriate for answering the research question/aims? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the questionnaire piloted prior to the main survey (or previously validated/used)? | P | Y | N | Y | Y | N | N | Y | N | N | N | N |
| Is the method of selection criteria of the subjects clearly described? | Y | Y | P | Y | Y | Y | P | Y | Y | Y | Y | Y |
| Could the way the sample was obtained introduce (selection) bias?a | N | CT | CT | N | N | N | CT | N | N | N | N | N |
| Was the sample size adequate for generalisability? | P | Y | Y | Y | P | P | P | Y | Y | Y | P | P |
| Was the sample of subjects representative with regard to the all GPs/PCPs in that region or country? | CT | P | P | Y | Y | Y | CT | Y | Y | Y | CT | CT |
| Was the sample size based on pre-study considerations of statistical power? | N | N | N | N | N | N | N | N | N | N | N | N |
| Was a satisfactory response rate achieved? | P | N | P | Y | Y | Y | P | P | N | P | P | P |
| Were the variables for capturing intention to quit clearly described and likely to be valid and reliable? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | P |
| Were the variables for capturing potential factors clearly described, comprehensive, valid and reliable? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the statistical significance (of relevant associations) assessed? | N | Y | Y | Y | N | N | Y | N | Y | Y | Y | Y |
| Are CIs given for the main results? | Y | Y | Y | Y | P | N | Y | N | Y | Y | Y | Y |
| Could there be confounding factors that have not been accounted for?a | Y | Y | N | N | Y | Y | N | Y | N | N | CT | N |
| Can the results be confidently applied to all GPs in the source region and country? | P | N | P | Y | Y | P | CT | P | N | P | CT | CT |
| Can the results be confidently applied to GPs in the UK NHS in 2016? | CT | P | P | Y | P | P | CT | P | N | P | CT | CT |
Appendix 9 Tables showing level of quitting and the main results/associations in each study
For each study, Tables 33–35 show (1) the overall level of intention to quit direct patient care (e.g. early retirement intention or intention to reduce hours) and (2) the potential factors explored in relation to that quitting construct.
| Study first author | Year of publication | Determinants/associations assessed (verbatim) | Level of retirement intention/hours reduction planned in all respondents | Text describing the relevant results/associations (or retirement intentions, etc., in subgroups) |
|---|---|---|---|---|
| Baker77 | 2000 | Gender, age (10-year age bands), principal/non-principal status, GP qualification cohort (1986, 1991, 1996) | 64.1% would prefer to work fewer hours per week | 50.7% wanted to retire aged 56–60 years |
| 23.8% of women would like to retire aged 51–55 years and 26.9% of men would like to retire aged 61–65 years | ||||
| Intended retirement age: see Table 24 | ||||
| Campbell17 | 2015 | Age, gender, ethnic group, region graduated, position, practice deprivation, practice size, practice location | 35% of GPs reported high risk of quitting direct patient care in next 5 years. 22% reported intention to take a career break in next 5 years | Intention to quit increased with age; significantly more men than women were intending to quit and more GP partners intending to quit |
| Chambers54 | 2004 | NS (probably only open question about reasons for intention to retire early) | 54 (81%) intended to retire before the age of 60 years and 170 (51%) intended to retire at 60 years old | Of those intending to retire before 60 years of age, 55 (81%) ‘cited excessive workload as the reason’ |
| Dale44 | 2015 | List of factors that might influence/reverse decision taken from recent media coverage and policy documents, plus free-text comments. Workplace influences and individual motivators | 82% intend to leave GP work, take career break, reduce hours of work in next 5 years (41.9% intend to leave, 23.3% intend to take career break) 5.6% intend to increase hours | 65.6% of men intend to leave within next 5 years; 64.3% of those aged 50–59 years intend to leave within 5 years, 84% of GP principals intend to leave within 5 years |
| Greatest work influence: intensity of workload, volume of workload, time on unimportant tasks, 7-day working week, job satisfaction. Greatest individual motivators: changes to pension taxes and age | ||||
| Overall workload more important for GPs aged < 50 years and for GP principals. Working conditions more important to men than women and less important with increasing age. Work–life flexibility less important with increasing age and more important for women, personal development more important for women, GPs with > 10 years’ service and GP principals (see Table 2). Table 3 has summary of GP attributes associated with principal components linked to intention to leave within 5 years | ||||
| French57 | 2005 | Inducement factors (implicitly, that would induce GPs ‘to consider working longer’ – that is, beyond their planned retirement age | Mean planned retirement age = 59 years (SD 5 years) | 70% (49) of male GPs and 55% (121) of female GPs would consider working longer if they could do so on a part-time basis. From free-text comments: other possible inducements to work longer were financial need (30%), sufficient job satisfaction (19%), financial incentives (13%) and reduced/no on-call work (4%) |
| French58 | 2006 | Warr–Cook–Wall job satisfaction scale167 (10 items) gender, whether or not spouse is doctor | Planned to retire at average ages of 59 years. Where women and men worked comparable hours, differences in job satisfaction disappeared | Women with greater job satisfaction = worked fewer hours. Males would delay retirement (57% compared with 44% of women) if they could work part-time with protected pension rights |
| Men worked mean of 55 hours per week; women worked 42 hours per week (mean). Mean sessions per week: 10 for men and 7 for women. Mean number of hours in clinical work: 33 for men and 26 for women. 92% of men participate in out-of-hours work but 74% of women. Of those who wish to change sessions, 96% of men wished to reduce their hours compared with 80% of women | ||||
| Gibson43 | 2015 | Age, gender, hours of work, contract type, practice size; job stressors on 14-item scale; job attributes on 15-item list; likelihood of retiring, increasing or reducing work hours, leaving in next 5 years; job satisfaction on 9-item Warr–Cook–Wall scale | 35.34% of respondents indicated a considerable likelihood that they would quit patient care in next 5 years | Proportion expecting to quit increased from 8.9% in 2012 to 13.1% in 2015 among GPs aged < 50 years. Increased from 54.1% in 2012 to 60.9% in 2015 among GPs aged ≥ 50 years. Planned age of retirement for those aged ≥ 50 years is average 61 years, range of 51–75 years |
| 50.96% intending to reduce work hours in next 5 years | Table 15 shows the likelihood of intention to quit by gender and age | |||
| 41% have considerable/high intention to leave UK/leave patient care/leave medical work in next 5 years. 35.29% high likelihood of reducing work hours in next 5 years vs. 4.50% high likelihood of increasing work hours. (See Table 19.) Likelihood of changing working hours in next 5 years | Table 18 shows the likelihood of leaving patient care within 5 years by age group. 21% of GPs aged < 50 years and 63% of those aged ≥ 50 years have high intention to leave UK/leave patient care/leave medical work in next 5 years. GPs aged < 50 years – 25% who did not intend to leave did intend to reduce work hours in next 5 years. 44% of GPs aged ≥ 50 years did not intend to leave but did intend to reduce hours in next 5 years | |||
| Hutchins76 | 2005 | Whether or not plan to continue as principal after study leave; perceived benefits of study leave | Only one respondent planned not to continue as principal after study leave | Positive reassessment of work and career 23%; renewed enthusiasm for primary care 21%; enjoyment of learning and working 10%. 68% achieved new appointment as a result, with 60% undertaking committee or advisory roles in addition to clinical work. 17% developed medical specialist role, 11% academic training role while continuing as GP. 10% said that it had not been altogether positive taking study leave |
| Luce61 | 2002 | 12 factors influencing retirement decision (great, moderate or no influence); 14 factors influencing later retirement (before, at or after 60 years of age) | 68.7% had made plans to retire, average planned age 59.2%; 34.6% planned early retirement (before 60 years); 49% planned to retire at 60 years; 15% between 61 and 65 years and 1.5% at 66 years or older. Ideally would retire almost 2 years before planned but 12.9% would ideally retire later than planned. 78.3% planned to undertake some work after retirement, 34.5% planned complete retirement | Women more likely to plan early retirement (46.2%) than men (32.1%); 23.7% of those over 55 years wanted to retire later than planned ideally (and 8.2% of those under 55 years). Higher psychological distress on General Health Questionnaire = planned to retire earlier |
| Men more influenced to delay retirement by change in work role (62.8%), decreased clinical role (58.9%), opportunity to work peripatetically (24.4%), during term time only (22.4%). No specific factors for women | ||||
| Reducing clinical work seen as reason to delay retirement for GPs planning retirement before or at 60 years; increased pensions for later retirement and being encouraged to stay by partners more important for older GPs planning late retirement | ||||
| Martin41 (The Health Foundation) | 2015 | Job satisfaction and stressors | 30% plan to leave GP work in next 5 years | 67% of UK GPs very satisfied or satisfied with practising medicine, compared with 79% average for GPs in other countries (was 84% of UK GPs in 2012 survey) |
| 59% of UK responders found practising ‘very stressful’ or ‘extremely stressful’, higher than any other country surveyed | ||||
| Of the 12% of GPs planning to switch careers or specialisms, 77% are under 55 years old. Of the 29% of GPs who intend to leave within 5 years, a third are under 55 and not planning to retire | ||||
| Figure 9 in Davis et al.168 shows correlation between stress level and intention to leave | ||||
| McKinstry46 | 2006 | Expectation of change in workload and number of sessions in next 2 years, retirement intentions | Overall doctors provide 7.4 clinical sessions a week and an additional 0.9 hours of NHS work, educational or research | ‘Doctors over the age of 35 infrequently worked more than 5 sessions.’ Mean of 5.15 sessions per week of clinical work. Men 5.8 sessions, women 4.9 sessions per week |
| 22 respondents intended to retire in next 5 years (mainly men). 12 intended to leave owing to stress of job | ||||
| Women more likely to think commitment to GP work would increase in next 5 years (28.5% women, 19.2% men) | ||||
| Simoens42 | 2002 | Job satisfaction with nine aspects of work (Warr–Cook–Wall scale); job stressors on 31-item scale; gender, age, ethnicity, hours worked per week, type of GP, household income, number of GPs in practice, practice location, level of deprivation | ‘Around one-third’ intend to reduce working hours within 5 years | Intend to leave within 2 years – 11% GP principals, 38% non-principals, 14% PMS GPs |
| Household income not associated with intention to quit | ||||
| PMS GPs = greater job satisfaction and lower intention to quit | ||||
| GP principals most likely to intend to leave within 5 years and PMS GPs least likely to intend to quit | ||||
| Male GPs more likely to intend to quit than female GPs. White GPs more likely to intend to quit than those from other ethnicity. GP principals who worked > 50 hours per week more likely to intend to quit than GPs who worked < 50 hours per week. GP non-principals in rural areas had higher intention to quit than those in urban areas | ||||
| Taylor64 | 1999 | Practice size, gender, deprived areas, inner/outer London | 13% left practice in their health authority within 2 years | Inner London, new entrant GPs retention rate was 82% compared with 89% outside London; 84% of women were retained compared with 90% of men |
| Taylor169 | 2008 | Job satisfaction | 11.1% of male GPs work part-time compared with 53.8% of female GPs. 26.7% of GPs overall work part-time | Part-time doctors much more satisfied with their leisure time (see table 5) leisure satisfaction score 4.4 for full time and 6.7 for part-time (scale of 1–10) |
| French58 | 2006 | Warr–Cook–Wall job satisfaction scale,167 (10 items) gender, whether or not spouse is doctor | Where women and men worked comparable hours, differences in job satisfaction disappeared | Women had greater job satisfaction if they worked fewer hours |
| Men worked mean of 55 hours per week, women worked a mean 42 hours per week. Mean sessions per week: 10 for men and 7 for women. Mean hours in clinical work: 33 for men and 26 for women. 92% of men participate in out-of-hours work but 74% of women. Of those who wish to change sessions, 96% of men wished to reduce their hours compared with 80% of women | ||||
| Young66 | 2001 | Importance of 12 job-related and 9 personal factors in prompting them to leave |
Table 2 has detailed findings – job and personal factors by age and gender Overall, most important factors were workload, NHS changes, high patient expectations, retirement |
Table 2 |
| Dissatisfaction with NHS changes was more important among older age groups as a trigger to early retirement | ||||
| Job related factors – partnership problems, lack of career development, lack of flexible working hours, more important for younger leavers | ||||
| Personal factors: family–work balance, geographical mobility, more important for younger leavers | ||||
| Gender differences – older women rated partnership problems as more important | ||||
| Age, gender | Younger women rated childcare responsibilities and partner moving jobs | |||
| Younger men: job-related factors, NHS changes | ||||
| Only 7% said increased remuneration would make them return | ||||
| 17% said needed greater flexibility and 11% change of family circumstances | ||||
| 40% of younger leavers had not returned |
| Study First author (country) | Year | Determinants/associations assessed (verbatim) | Level of retirement intention/hours reduction planned in all respondents | Text describing the relevant results/associations (or retirement intentions, etc., in subgroups) |
|---|---|---|---|---|
| McComb68 (New Zealand) | 2006 | Demographic (gender, age, life status, number of children, number of family members who are also GPs, practice ownership, income, hours worked) | 12.2% intended to leave within 6 months | Self-employed GPs: 10% intended to leave within 6 months, 25% within 5 years |
| Locums: 18% within 6 months, 36% within 5 years | ||||
| Psychological (satisfaction with general practice and commitment to general practice) – scored with five-point Likert scale. Commitment scale had 18 questions, satisfaction scale had one item only | 28.8% intended to leave within 5 years | Other: 17% within 6 months, 34% within 5 years | ||
| Dewa67 (Canada) | 2007 | Professional dissatisfaction using five-point scale (Likert?); Burnout using nine items from MBI; age | Intention to retire within next 2 years (not reported for whole group) | Of those who were professionally dissatisfied:
|
| Brett27 (Australia) | 2007–8 | Age, gender, nine options why leaving early, seven options that might encourage to stay | 63% intend to work as GP until at least 65 years, 6% unsure when they will retire | 75% of women GPs plan to work to age 65 years but only 59% of men; men more likely to intend to retire early. (NB women more satisfied with their work and working fewer hours but carry on working for longer) |
| (i.e. 31% intending to retire before age 65 years) | ||||
| Pit72 (Australia) | 2011 | Burnout and occupational health measures: MBI (9-item Emotional Exhaustion subscale only); single-item job satisfaction measure; 5-item version of Effort–Reward Imbalance Questionnaire; 3-item version of Work Ability Index; 6-item Kessler Psychological Distress Scale; global health question from SF-36 | Mean age of intended retirement from direct patient care was 63.5 years (SD = 6.9 years); 47% intending to retire before 65 years | GPs with early retirement intentions = younger, worked average 8 hours more per week, more sleep problems, feel they do not get respect deserved at work, higher levels of burnout and distress, lower job satisfaction and perceived lifetime best work ability |
| GPs with medium or high burnout scores had four times the odds of wanting to retire early (see table 2, p. 302) | ||||
| GPs reporting work-related sleep problems = 3 × increase in odds of early retirement intentions. Early retirement intentions increased with higher psychological distress scores and in those in fair/poor general health | ||||
| Presenteeism = 74% among those planning early retirement |
| Study first author (country) | Year of publication | Determinants/associations assessed (verbatim) | Level of actual part-time working or hours reduction planned, in all respondents | Text describing the relevant results/associations (or reduction/part-time intentions in subgroups) |
|---|---|---|---|---|
| Woodward75 (Canada) | 1993 and 1999 | Gender, spouse working full-time, child younger than 6 years, no children, spouse is physician, rural practice | In 1993 physicians would prefer to work 37 hours a week; in 1999 would prefer to work 34 hours per week. Actual hours worked did not change significantly | Of those who were professionally dissatisfied:
|
| Dewa170 (Canada) | 2007 | Professional dissatisfaction using five-point scale (Likert?); burnout using nine items from MBI; age | Not specified | |
| Shrestha73 (Australia) | 2008 | WLB satisfaction (Likert scale) | 52.9% reported good WLB | GPs reporting poor WLB intend to reduce hours (OR 0.10, 95% CI 0.09 to 0.12; p < 0.001). However, this association not explained by lower job satisfaction. WLB alone explained 20% of the variation in intention to reduce hours |
| Norman69 (Australia) | 2010 and 2011 | Age, gender, health, family circumstances, work satisfaction, work hours, whether or not they do on-call work, business relationship with practice, practice location, income, density of GPs, patient population | 43% of 3377 GPs stated a desire to reduce hours in 2010 (wave 3 of MABEL survey). Of 1177 of those GPs who also had data in 2011 survey, 26.8% had successfully reduced their working hours by more than 5 hours. Of the 861 GPs unable to reduce their hours, 75.1% still had desire to reduce hours in 2011 | Older GPs, females, those in less good health, less satisfied were more likely to want to reduce hours. GPs working > 60 hours per week more likely to want to reduce hours (six times more likely). GP partners more likely to want to reduce hours. Middle-aged male GPs had very strong desire to reduce hours |
| Ability to actually reduce hours was predicted by age, gender and number of hours currently worked. Middle-aged GPs around 50 years least likely to achieve desired reduction in hours. Female GPs more likely to reduce hours. GPs working longer hours more likely to successfully reduce hours | ||||
| RNZCGP39 (New Zealand) | 2015 | Gender, age, reasons for working part-time, urban and rural | Figure 12 has hours worked per week as GP: largest group works 31–40 hours per week (32.1%) | Gender: mean hours per week worked: men 38.7, women 30.1 (see figure 13). 65% of women worked part-time as GP and 31% of men. 70% of part-time GPs were female and 30% were male (see table 7) |
| Age: longest hours worked by 25–29 years age band and 55–65 years age band (see figure 14). Females in all age bands worked fewer hours than males, especially in 35–44 years age band (see figure 15) | ||||
| Figure 16 has age profile by gender of responders working 20 hours or fewer per week – average age for women 46 years and for men 59 years | ||||
| 53% cited family responsibilities as reason for working part-time – and 89% of these were female. Figure 19: 45% of females cited family as reason for part-time work; 46% of males cited personal choice | ||||
| Figure 20 shows family responsibilities of those working part-time for family reasons | ||||
| Figure 21: female respondents intended working hours in 5 years – those aged 35–39 years intend to increase hours (38%) | ||||
| Table 9: 25% of men have weekly after-hours work |
Appendix 10 Summary of patient and public involvement discussion of emerging review findings
The following PPI discussion points broadened our understanding of the literature-derived themes (especially in response to the initial synthesis of qualitative interview-based studies).
Flexible working
Although flexible working can bring benefits to individual GPs (young and old), such as freedom from paper work and freedom to pursue other interests, it can increase workload for other practice GPs if they have difficulty recruiting other partner GPs or locums. Discussion with our PPI group suggested that flexible working can have a potentially negative effect on patients who seek appointments with the same GP who they know and have built history and rapport with. If they are consistently inaccessible to them because of their flexible working patterns, patients may experience grief at the loss of the relationship. This could have implications for the NHS, as there may be more referrals to secondary care as a consequence. In such circumstances, it is often more acceptable to the patient if the GP retires as this is a predictable and understandable reason for the end of the doctor–patient relationship.
Although increasing the availability of locums may relieve pressure on full-time GPs and aid retention of salaried GPs/partners, there was concern from the PPI group that GPs who preferred to travel between general practices working as locums may choose to do so because it means that they avoid building doctor–patient relationships. Different personalities may suit different working styles, with permanent salaried GPs/partners having different values and personalities from locums and perhaps valuing the doctor–patient relationship more highly.
Continue and cope
Although GPs talked in the semistructured interviews about strategies that help them to cope with increasing workload and pressures, members of the PPI group note that there is no mention of destructive ‘coping strategies’, such as misusing alcohol or drugs, and no mention of GP use of antidepressants. There is also no reporting of GPs accessing counselling services in the interviews.
Viability of early retirement
The PPI group expressed the view that the cultural norm of acceptability of GP early retirement may be compounded further by GPs’ expert knowledge about the human body. Because GPs are more able to predict expected deterioration with age, they may be more likely to plan for early retirement so that they can physically do the things they enjoy.
Ageing
The PPI group noted that holiday entitlement is not mentioned in any of the GP interviews and suggested that increased holiday entitlement for ageing GPs may help GPs manage their natural fatigue and ultimately improve retention.
Partnership issues
The qualitative synthesis and explanatory model in this review highlights the importance of good practice relationships for GP retention. When these are not in place, GPs can experience a lack of support, which may lead to quitting. The PPI group note that different GPs with different personalities/values/working styles may experience conflict when working together in the same practice. PPI members consider GPs to be naturally competitive and prone to compare themselves with each other. A more sociable patient-focused GP may have a different working style to a more ‘efficient’ target-focused GP and the target-focused GP may comment negatively on such differences.
Commitment and investment
The qualitative synthesis highlights the uncertainty around future commitment to investing in future general practice. The PPI group notes that GPs are a risk-averse group who are driven by financial security. They suggest that younger GPs coming out of medical school with financial debts may be less inclined to take on the financial risk of becoming a partner, especially with the negative media portrayal and general uncertainty. The PPI group note that salaried GPs are better off than partners as they do not have the financial risks associated with being a partner, and the PPI group posed the questions ‘Would all GPs prefer to be salaried? Could this be a way forward?’.
The qualitative synthesis highlights concerns about the difficulties of recruiting new partners to a general practice to replace a retired GP partner. Because general practices are independent businesses, GP partners are needed. However, younger GPs may be reluctant to take on partnerships because of the added responsibilities involved. The PPI group note that practice environment/demographic may affect GP recruitment, with smaller practices suffering most. The PPI group also expressed the view that many GPs may not have good business skills or be trained in HR, and, consequently, may not be skilled in interviewing and recruitment. They may be less likely to take a professional approach to legal matters (e.g. signing contracts, with some preferring to do things ‘on trust’ and hence deny/hide/ignore commitment issues).
Impact of organisational changes
Referrals
Complex referral systems, more specialised hospitals and delays in communication contribute to GPs’ experiences of fragmentation and a depersonalised health-care system. The PPI group confirmed that in their experiences there is poor linking of secondary and primary care. They observed that decisions to change medications/dose are made in secondary care by nurses and pharmacists and that there is much more choice available in secondary care. When patients then come back under the responsibility of the GP, the GP may not be familiar with the drug(s) prescribed. This responsibility, coupled with a lack of knowledge, may cause stress. It was noted by the PPI group that GPs were naturally proud and so less able to admit if they do not know something, and this may compound the issue.
Doctor–patient relationship
The qualitative synthesis indicates that lack of time with patients means the ability to practise patient-centred continuity of care is compromised. This affects the GPs’ professional autonomy and values, resulting in diminished job satisfaction for GPs and diminished satisfaction for patients. The PPI group noted how important and valued by patients the doctor–patient rapport and personalised knowledge was, and how this could sometimes result in increased efficiency with respect to referrals. Members of the group explained how a GP who knows a patient’s history and who has a good rapport may be more likely to prescribe a drug/therapy already prescribed that might reduce the need for secondary care. Such GPs may also make appropriate and timely referrals to secondary care based on a patient’s request and their knowledge of the patient’s history.
Patient demand
The qualitative synthesis indicates that patient demand (increased number and increased expectations), coupled with a shortage of GPs and available appointments, is adding to a feeling of increased pressure, which is making some GPs consider retiring. Patient demands may be higher if general practices are situated in areas of higher deprivation with populations with multiple health and social problems and working with elderly populations with multiple comorbidities and social care needs.
The PPI group noted that patient demands may also be higher in multicultural communities as they may require more skilled communication from the GPs. In response to the discussion, the PPI facilitator also noted that patients are often ill-informed about how a practice works and so may be unknowingly wasting time and adding to GP pressure. It was suggested that this could be avoided if patients were provided with information about the structure and function of the practice and were guided in how to most efficiently engage with the practice.
Practice demands
The qualitative synthesis indicates that GPs in smaller practices were more likely to feel trapped between continuing to work full time under extreme pressure in order to support colleagues, or to retire completely. Difficulty in recruiting locums precluded many from working part-time. In an unsupportive environment, having to take on the responsibility for a partner’s absence, ill health or early retirement can add to feelings of burden and stress. However, in the more supportive practice, such scenarios are better managed by the team.
The PPI group commented on the finding (from the review of survey studies) that GPs working in very small and in large practices (> 10 partners) are more likely to quit, with medium-sized practices more likely to retain GPs. They suggest that this could be down to smaller practices being less able to adapt and being more reactive, and larger practices not having the strong relationships in place to support the GPs as they may be less able to get everyone together at the same time and there may be less opportunity for communication and relationship building. Consequently, GPs in large practices may feel ‘invisible’, not ‘part of something’ and, therefore, less loyal.
Acceptability of early retirement
In the qualitative synthesis, GPs describe a permeating ‘bullying culture’ form the top down and the PPI group acknowledged this and confirmed a culture of government bullying via NHS England to salaried GPs. The PPI group think that this is one of the reasons why autonomy is so important to GPs. They also noted a historical precedence for GPs to be independent and autonomous owing to GP clinics traditionally being operated from a GP’s living room. The PPI group describe how sometimes practice managers may be strong characters with too much influence over the practice GPs. They suggest that better training in HR and interviewing for GPs may aid recruiting and could potentially avoid such circumstances.
Appendix 11 ReGROUP GP Workforce Survey
Appendix 12 GP Workforce Survey sample characteristics
| Characteristic | Responded, n (%) |
|---|---|
| Gender | |
| Male | 1051 (67) |
| Female | 1197 (66) |
| Age (years) | |
| < 40 | 500 (54) |
| 40–49 | 738 (68) |
| 50–54 | 391 (72) |
| 55–59 | 409 (76) |
| 60–69 | 192 (74) |
| ≥ 70 | 18 (75) |
| Employment status | |
| GP provider | 1335 (71) |
| GP salaried | 394 (57) |
| Non-principal/locum | 519 (64) |
| Survey sent by e-mail | |
| Yes | 1304 (71) |
| No | 944 (62) |
| Postal address used | |
| Practice address | 1744 (67) |
| Home address | 504 (64) |
Appendix 13 Comparison of general practitioners in south-west England and those in the rest of England
| Characteristic | Region | |
|---|---|---|
| South-west England | Rest of England | |
| Gender, n (%) | ||
| Male | 1157 (45.4) | 15,922 (47.5) |
| Female | 1390 (54.6) | 17,568 (52.5) |
| Unknowna | 4 | 0 |
| Country of qualification, n (%) | ||
| UK | 2288 (92.5) | 24,062 (76.9) |
| EEA | 98 (4.0) | 1335 (4.3) |
| Elsewhere | 88 (3.6) | 5906 (18.9) |
| Unknowna | 73 | 2191 |
| Role, n (%) | ||
| Partner | 321 (12.6) | 4453 (15.5) |
| Salaried | 681 (26.7) | 8083 (28.2) |
| Other | 1545 (60.7) | 16,175 (56.3) |
| Unknowna | 0 | 4783 |
| Age (years), mean (SD) | 45.6 (9.0) | 45.3 (10.3) |
| FTE, mean (SD) | 0.80 (0.29) | 0.77 (0.27) |
Appendix 14 Findings from Care Quality Commission reports of general practices in the south-west of England
Abstract
Background
This document describes the use of secondary data (CQC reports of general practices) to explore current examples of good and poor practice in the south-west of England. CQC reports are publicly available on its website. This work constitutes one strand of the qualitative work (workstream 3) of the ReGROUP study. Subsequent strands include semistructured, in-depth interviews with GPs and stakeholders about reasons why GPs leave direct patient care and the impact of GPs leaving direct patient care, and possible policies and strategies that may help to retain GPs.
Aim
The aim of this strand of workstream 3 was to produce a briefing document that could:
-
inform the content of interviews with GPs
-
provide contextual information and case examples to inform the RAM expert panel work (workstream 4) of ReGROUP.
Method
A maximum variation sample was taken, consisting of CQC reports of general practices in the south-west of England. The sample included eight reports of practices that CQC had rated as overall ‘outstanding’, and six that had been rated overall as either ‘requires improvement’ or ‘inadequate’. In addition, 21 CQC-identified and summarised (all-England) examples of good practice were sampled. Thematic categories were identified from the full reports and the good practice examples were summarised.
Findings
Sixteen thematic categories were identified from the combined CQC all-England examples of good practice and the sampled south-west of England reports. Good practice examples were drawn from four of the five KLOEs detailed in CQC reports, namely whether or not the practice is ‘effective’, ‘responsive’, ‘caring’ and ‘well-led’. Twenty-three extracted south-west examples were identified for use as prompts or suggestions for discussion within the GP interviews. Six additional potential interview questions were also identified. These questions concerned potential policy/strategy directions, namely:
-
additional members of staff for the practice
-
additional services or resources offered by the practice
-
working with other organisations
-
support for GPs
-
restructuring or reorganising practice
-
developing or better utilising GPs with specialisms.
Conclusion
The use of CQC reports enabled six key questions to be developed with actual practice examples of good practice that could be explored in the interviews with GPs. The relevance and implications of these good-practice examples to GP work–life balance (including job satisfaction, workload, stress and team working) could also be explored. The range of examples may also help to provide contextual information for the RAM expert panel of workstream 4.
Introduction
The CQC is an executive non-departmental public body of the DHSC. It was established in 2009 to regulate, inspect and monitor the following aspects of health and social care services in England:
-
treatment, care and support provided by hospitals, GPs, dentists, ambulances and mental health services
-
treatment, care and support services for adults in care homes and in people’s own homes (both personal and nursing care)
-
services for people whose rights are restricted under the Mental Health Act 2005. 172
For the ReGROUP study, we were interested in the findings from CQC reports of general practices in the south-west of England.
The CQC asks five key questions (known as KLOEs) of all the services that it inspects. The five key questions are:
-
Are they safe?
-
Are they effective?
-
Are they caring?
-
Are they responsive to people’s needs?
-
Are they well-led?
Inspected services are rated in response to each KLOE and also given an overall rating. Services can be rated as ‘outstanding’, ‘good’, ‘requires improvement’ or ‘inadequate’.
The reports from inspections are publicly available on the CQC website (see www.cqc.org.uk; accessed 31 November 2017).
Aim and rationale
The aim of this strand of ReGROUP workstream 3 was to use CQC report data to produce a briefing document that could:
-
inform the content of interviews with GPs
-
provide contextual information and case examples to inform workstream 4.
In the original, main ReGROUP protocol, we stated:
The analysis of CQC report data will seek to identify key practice issues related to staffing levels and related factors (e.g. succession planning, business management, indicators of staff stress, and how well the practice is led). We wish to explore examples from practices that are failing as well as those that are thriving.
The aim was to use this detailed and collated secondary data source to examine what is currently happening within practices, specifically with regard to the working environment for GPs and how this might affect their decisions about remaining in or quitting direct patient care. We wanted to identify examples of good practice that could be used as discussion prompts with the GP interviewees.
Our preliminary study focused mainly on the factors contributing to decision-making about when to quit direct patient care, and we asked the GPs to discuss strategies from their own practice that they saw as helping GPs to remain in direct patient care (actual examples), and to describe any other strategies that they thought might further help (hypothetical examples). 18
In this current study, we wanted to build on the foundations of the preliminary study by further exploring with interviewee GPs actual examples of good practice, that is examples taken from other practices (identified in the CQC reports) and from current policy and practice initiatives and strategy documentation (such as the General Practice Forward View89).
Care Quality Commission data offer the advantage of having been collected and reported on independently of our study. The range of factors they investigate within each KLOE is broad, and the examples offered within reports have been rigorously chosen by CQC. Such comprehensive data would not be available from practices’ own websites. Thus, use of CQC data was chosen in this study to enable us to quickly and easily access independently collated examples of good practice, and of poor practice, and to relate these to the types (size, location and staffing) of general practices included in the south-west of England region.
Method
The method for working with the CQC report data consisted of six key stages:
-
identify the numbers of general practices in the south-west of England that had been reported on by the CQC, and the number in each overall rating category
-
read a random selection of the south-west reports to become familiar with the approach, content and report layout
-
determine the best method for extracting useful information and examples from the reports
-
sample a number of reports for analysis
-
extract and summarise report data
-
format and discuss the extracted data for use within workstream 3 (qualitative interviews) and workstream 4 (RAM expert panel work).
Identifying the number of general practices in the south-west that had been reported on by the Care Quality Commission
The CQC has publicly accessible data on its website (see www.cqc.org.uk/content/how-get-and-re-use-cqc-information-and-data#directory).
The steps followed to identify general practices are detailed in Appendix 15. This process produced a list of all the general practices within the ReGROUP catchment area that had been reported on by the CQC (see Table 38). The ReGROUP catchment area includes the City of Bristol, Cornwall, Devon, the Isles of Scilly, North Somerset, Plymouth, Somerset, South Gloucestershire and Torbay.
Sampling took place in January 2016 using the CQC data set that had been completed up to 1 December 2015. There were 442 active location practices in the ReGROUP catchment area, of which 227 (51.4%) had been inspected and rated and had had their inspection results made publicly available (see Table 11).
Sampling Care Quality Commission reports for analysis
A number of reports were selected for a maximum variation sample. Practices were sampled based on practice list size [small (< 3500 patients), medium (3500–8000 patients) or large (> 8000 patients)] and urban or non-urban locality (based on practice postcode). We did not aim to sample across all geographical locations in the catchment area as (1) available reports were not distributed across all of the geographical areas and (2) it was agreed that the issue of interest was whether a practice was in an urban or non-urban area (rather than the county it was based in).
We initially sampled 8 out of 16 (50%) of the available ‘outstanding’ reports, and 6 out of 8 (75%) of the available ‘requires improvement’ and ‘inadequate’ reports (Tables 38 and 39). No practices rated ‘good’ were included. The rationale was that a sufficient number and range of examples could be drawn from those reports at the extremes of good and poor practice. Pragmatic decisions (taking account of researcher time and resources available, and the aim of this part of workstream 3) were made about the number of reports initially sampled, with the understanding that additional reports could be included if required.
| ReGROUP identifier | Location local authority | Number of GPsa | Deprivation decileb | Practice sizec | Settingd | Sampled? |
|---|---|---|---|---|---|---|
| 3 | Bristol, City of | 7 | 3 | Large | Non-urban | Yes |
| 32 | Cornwall | 2 | 5 | Medium | Non-urban | Yes |
| 69 | Devon | 11 | 6 | Large | Non-urban | Yes |
| 83 | Devon | 9 | 8 | Large | Non-urban | Yes |
| 89 | Devon | 12 | 8 | Large | Non-urban | No |
| 110 | Devon | 13 | 7 | Large | Urban | Yes |
| 113 | Devon | 5 | 8 | Medium | Non-urban | No |
| 114 | Devon | 7 | 4 | Large | Non-urban | No |
| 118 | Devon | 2 | 6 | Medium | Urban | Yes |
| 119 | Isles of Scilly | 3 | 9 | Small | Non-urban | No |
| 121 | North Somerset | 3 | 1 | Medium | Non-urban | No |
| 145 | Somerset | 18 | 6 | Large | Non-urban | No |
| 156 | Somerset | 3 | 6 | Small | Non-urban | Yes |
| 167 | Somerset | 3 | 6 | Small | Non-urban | No |
| 198 | South Gloucestershire | 13 | 9 | Large | Non-urban | Yes |
| 199 | South Gloucestershire | 9 | 10 | Large | Non-urban | No |
In summary, the ‘outstanding’ subsample (n = 8) consisted of the following characteristics: practice size [large (n = 5), small/medium (n = 3)], setting [urban (n = 2), non-urban (n = 6)] and deprivation rating [1–5 (more deprived) (n = 2), 6–10 (less deprived) (n = 6)].
| ReGROUP (workstream 3) identifier | Location local authority | Number of GPsa | Deprivation decileb | Practice sizec | Settingd | Sampled? |
|---|---|---|---|---|---|---|
| (RI) 122 | North Somerset | 9 | 4 | Large | Rural | No |
| (RI) 135 | Devon | 4 | 2 | Medium | Urban | Yes |
| (RI) 162 | Somerset | 5 | 8 | Medium | Urban | No |
| (RI) 172 | Somerset | 8 | 9 | Large | Rural | Yes |
| (I) 5 | Bristol, City of | 1 | 8 | Small | Urban | Yes |
| (I) 28 | Devon | 2 | 4 | Medium | Rural | Yes |
| (I) 132 | Devon | 2 | 9 | Small | Rural | Yes |
| (I) 136 | Devon | 8 | 3 | Large | Urban | Yes |
In summary, the ‘requires improvement’/’inadequate’ subsample (n = 6) consisted of the following characteristics: practice size [large (n = 2), small/medium (n = 4)], setting [urban (n = 3), non-urban (n = 3)] and deprivation rating [1–5 (more deprived) (n = 3), 6–10 (less deprived) (n = 3)].
Obtaining Care Quality Commission report data
Each rated practice has a dedicated web page on the CQC website (e.g. see www.cqc.org.uk/location/1-550789003) with the following data publicly available:
-
an Overview tab that contains:
-
inspector’s description of the practice
-
overall rating
-
rating for each of the five key questions
-
rating for each of the key services/population groups
-
link to a portable document format (PDF) of the CQC inspection report.
-
-
an Inspection Summary tab
-
a Reports tab
-
a Registration Info tab
-
a Contact tab.
For each practice included in this analysis, we extracted:
-
overall rating
-
location ID
-
location name
-
postcode
-
publication date
-
copy of the inspector’s description text pasted onto the template.
A copy of the full CQC inspection report PDF was also downloaded, saved, and printed.
Determining the best method for extracting useful information and examples from the Care Quality Commission reports
An iterative approach was used to determine the best method for extracting useful information and examples from the CQC report secondary data. All approaches were discussed and reflected on by the workstream 3 team, until a final decision about the methodology was reached.
Initially a standard thematic analysis was attempted: all report data were uploaded to NVivo version 10, a coding frame was jointly agreed by the workstream 3 team, and three complete reports were individually coded. However, it quickly became apparent that the amount of detail and repetition within the CQC reports meant that a content analysis approach was time-consuming and resulted in extraneous coding that did not meet with the aims and time frame of this aspect of the qualitative work.
The second approach was to apply a typology analysis to the report data, this time reviewing the responses to each of the five key questions across the reports, sampled from all of the four rating categories. This was completed for one question using a sample of 10 reports. However, it was recognised that this output did not provide any useful findings over and above the question prompt list provided by CQC for each of the KLOEs.
The final approach was to categorise themes from the CQC’s own identified examples of good practice (see www.cqc.org.uk/content/examples-outstanding-practice-gps; accessed 25 April 2016) along with examples extracted from the sampled reports. These themes and examples were used to identify key interview prompts for GP interviews, and to provide illustrated examples from practice. This approach is detailed below.
Identifying themes and extracting examples of good practice
The following steps were taken:
-
A selection of CQC reports was read to become familiar with KLOEs, reporting style, etc.
-
All of the CQC’s own all-England case study examples were read.
-
From the CQC’s all-England examples, a selection was identified that was deemed to have relevance to ReGROUP’s aims and objectives (i.e. where examples of good practice may have an impact on the working environment and workload of GPs).
-
Key themes and categories were identified from the CQC all-England selected examples.
-
The eight sampled south-west reports from the CQC overall rating category ‘outstanding’ were read and examples of good practice were extracted for the KLOEs ‘effective’, ‘responsive’, ‘caring’ and ‘well-led’. (For KLOE ‘safe’, see below.) To determine which examples were extracted, we asked the following questions:
-
Does this example highlight an element of good practice that could be transferable to other practices?
-
Who does this example affect: patients, carers, GPs, other practice staff, external agencies?
-
Is there evidence to show that this has an impact on GP workload and, if so, is that impact positive or negative?
-
Has this been identified in the literature and/or the ReGROUP preliminary research as having a bearing on GPs’ decisions about whether or not to quit direct patient care/their experiences of work-related pressures?
-
Could this example prompt GPs to discuss it in relation to their own practice and/or locality?
-
-
These extracted examples were categorised using the themes from the all-England examples. Emerging themes from the south-west examples were added.
-
Themes were grouped to form overarching themes and these were developed into key questions for the GP interviews. Examples for each question were collated.
-
For each key interview question, a table of examples was produced that included practice size and whether or not it was urban.
This approach was taken for four of the five KLOEs, namely effective, responsive, caring and well-led. A modified approach was used for the KLOE ‘safe’ owing to the nature of the data provided in the CQC reports. Use of the ‘outstanding’-rated south-west reports did not provide sufficiently detailed examples for use in our interviews as the data from ‘outstanding’ practices were mainly merely confirmatory of the CQC’s inspection questioning. In order to explore items within ‘safe’ for examples that could be used in GP interviews, we repeated the process above using four reports rated as ‘inadequate’ and two rated as ‘requires improvement’.
Findings
Examples of good practice: Care Quality Commission all-England
From the 47 examples provided by the CQC, 21 (45%) were selected to help produce the thematic categories (Table 40).
| KLOE | Number of examples provided by CQC | Number included in ReGROUP categorising process |
|---|---|---|
| Are they safe? | 5 | 2 |
| Are they effective? | 11 | 6 |
| Are they caring? | 10 | 5 |
| Are they responsive? | 13 | 5 |
| Are they well-led? | 7 | 3 |
| Total | 47 | 21 |
The broad categories identified from CQC all-England examples were related to:
-
sharing safety lessons
-
open safety culture
-
supporting patients’ emotional and social well-being
-
health promotion for patients
-
shifting care from secondary to primary care services
-
working with external or other community organisations
-
improving access to general practice for hard-to-reach groups
-
expanding the skill mix and roles within the general practice team
-
direct support to GPs (e.g. GP mentoring).
Examples of good practice: south-west
The categories identified from the CQC all-England examples of outstanding practice were applied to the examples extracted from the subsample of south-west reports rated as ‘outstanding’ (n = 8). It was agreed within the research team that this sample was sufficient: no new factors were emerging and theoretical saturation was determined to have been reached in respect of each of the KLOEs ‘effective’, ‘responsive’, ‘caring’ and ‘well-led’. The subsample of six ‘inadequate’/’requires improvement’ reports was determined to be sufficient for the additional exploration of the KLOE ‘safe’.
Sixty-five examples from the south-west ‘outstanding’ reports were extracted. These examples related to four of the five KLOEs, namely effective, caring, responsive and well-led.
The south-west examples provided the following additional thematic categories:
-
structuring and organising practice
-
forward planning
-
sharing with other practices
-
role of other practice staff in patient care
-
training opportunities
-
morale
-
use of technology.
Twenty-three of the extracted south-west examples were identified for use as prompts or suggestions for discussion within the GP interviews.
In addition to being used as examples within the GP interviews, the categorised examples also suggested additional potential interview questions for GPs, namely:
-
If you could have additional member(s) of staff who might help relieve some of the pressures on the GPs, who would that be and why that role (e.g. mental health nurse consultant)?
-
If you could offer additional service(s) or resource(s) within your practice to help relieve some of the pressures on the GPs, what would that be and why (e.g. patient self-assessment health pod; befriending service – Includes technology, plus patient and carer emotional and social well-being support)?
-
If you could work with another organisation(s) – another practice or an external organisation – in such a way that your joint working would relieve some of the pressures on GPs, who would you work with and why (e.g. Age UK, drug rehabilitation team)?
-
If you could provide support directly to GPs to help them personally manage their work–life balance, what would this support look like and why (e.g. mentoring)?
-
If you could restructure or organise your practice differently in order to relieve the pressure on GPs, what would you do and why (e.g. telephone triage, longer appointments)?
-
If you could develop or better utilise GPs in your practice with specialisms in order to relieve the pressure on GPs, what would you do and why?
Appendix 16 details the specific good-practice examples that relate to each of these key questions.
The above questions can be used as prompts to elicit GP’s actual examples from their own practice and as prompts to elicit discussion of what could hypothetically improve their current working environment/facilitate GP retention.
Discussion
Prior to beginning to work with the CQC reports, we had anticipated being able to use such reports to ‘identify key practice issues related to staffing levels and related factors (e.g. succession planning, business management, indicators of staff stress, and how well the practice is led)’. In addition, we originally stated that we would ‘explore examples from practices that are failing as well as those that are thriving’.
It should be noted that the CQC KLOEs (‘safe’, ‘effective’, ‘responsive’, ‘caring’ and ‘well-led’) have a primary focus on the implication of meeting these requirements for the delivery of services to patients. The direct impact on GPs and other members of the practice team are featured far less prominently. CQC reports directly on feedback received from patients and patient representatives, and also from discussion with some staff members (e.g. related to whether or not the practice has an open culture such that they feel able to report on safety issues); however, the specific views and experiences of GPs working within the practices are not reported on. Consequently, although it is possible to speculate that an example of good practice may enhance the working environment for a GP and encourage them to remain in direct patient care, it cannot be assumed (from the CQC data available) that this is the case.
In addition, the CQC reports are written in response to a checklist of questions. Much of the reporting consists of statements confirming whether or not the practice meets the CQC checklist requirements. Only some of these statements are supported with illustrative examples, and the level of detail contained within these examples varies.
Owing to these issues encountered when working with the CQC data, the research team agreed to shift approach: rather than attempt to draw conclusions from the data and to focus on examples from ‘failing’ practices as well as those that were ‘thriving’, we agreed to extract key issues from the data with a focus on achieving examples of good practice. This resulted in drawing examples only from reports that had been rated overall as ‘outstanding’. Although it is acknowledged that useful examples may have also been drawn from the rated ‘good’ reports (and conversely examples of poor practice from the rated ‘inadequate’ and ‘requires improvement’ reports), it was agreed that use of the ‘outstanding’ examples would enable us to explore with the interviewee GPs the potential usefulness and impact of examples proposed as the way that general practice ‘should’ be structured and delivered to provide the best-quality care and services. We were keen to explore the impact of practice management and organisation on GP decision-making about remaining in direct patient care. For example, a GP at a practice that the CQC rated as ‘inadequate’ may actually relish the challenge of improving practice and so be committed to remaining in direct patient care, whereas a GP at a highly innovative and rated ‘outstanding’ practice, with lots of examples of ‘good practice’, may actually find the expectations of innovation add to their work pressure and stress, and, consequently, they may wish to leave direct patient care.
It was agreed by the research team that exploring GPs’ responses to proposed strategies and initiatives drawn from the CQC reports (and other key documents, such as General Practice Forward View89) would help to increase our understanding of what might help to retain existing GPs, and to inform and contextualise the workstream 4 statements for the RAM expert panel – offering real-life examples of policy and strategy and GPs’ responses to these.
Our preliminary study identified four key themes that related to GPs’ decisions about remaining in or quitting direct patient care: (1) early retirement is a viable option for many GPs, (2) GPs have employment options other than undertaking direct patient care, (3) GPs report feeling they are doing an (almost) undoable job and (4) GPs may have other aspirations that pull them away from practice. 17 The CQC report data can be related primarily to the individual factors contained within the theme of the ‘almost undoable job’, specifically workload, structures and systems. However, the CQC data do not sufficiently illuminate the other factors that we identified, namely politics, partnership issues, GP concerns about the future of general practice, GP ageing and ill health, and reduced GP morale and emotional resilience.
A recent paper from Doran et al. 51 identified six key factors that can influence GPs’ decisions to stay in direct patient care or to leave:
-
organisational changes (fragmented care, methods of referral, communication across services)
-
clash of values (less patient centred, unrealistic appointment times, impossible targets)
-
increased workload (patient demand, time pressures, work shifting from hospital to primary care, more bureaucracy)
-
negative media portrayal
-
workplace issues and lack of support (partnership issues, flexible hours, funding, career progression, lack of informal support, feeling more isolated in practice, bullying culture, occupational health, government expectations)
-
impact on GP well-being and low job satisfaction.
The examples we have chosen from the CQC-rated ‘outstanding’ reports attempt to encapsulate factors 1–3. However, the CQC report data are limited when it comes to better understanding factors 4–6 and what is needed for ‘best practice’. Our interviews with individual GPs shall, we anticipate, help to expand on these while also allowing us to ‘test out’ any assumptions about practice examples from factors 1–3. In addition, we shall be able to further identify any other key factors that are currently contributing to GPs’ decision-making about remaining in or quitting direct patient care.
Strengths and limitations
The key strength of using the CQC reports was that they provided us with immediate access to existing data (i.e. before we had begun to collect our own data). Given the timeliness of the research topic, and the time constraints within the ReGROUP project time scale, being able to access and use a large number of published secondary data was advantageous.
The CQC has made its list KLOEs, the subsections and the prompts within each of these publicly available. The reports all follow the same template, making extraction of data simplified as we were able to focus on the specific, relevant sections of each report. In addition, the CQC’s provision of the Inspectors’ Summaries helped to contextualise each practice in terms of number of GPs, population served and type of area.
The limitations of working with the secondary data obtained from CQC reports include working with an incomplete data set: only 51.4% of practices in the south-west had been inspected and reported on by the CQC at the time of our data extraction. Given the time constraints of our project, working with half of the data set was a pragmatic decision. In addition, as we were confident in having reached sufficient saturation with a subsample of these data, delaying this work was not necessary.
The main limitation of the data was evident from our attempt at content analysis: the data presented had been collected and reported to meet the CQC’s own requirements (the quality of care being delivered) and, consequently, did not focus sufficiently on our line of enquiry (the impact of care organisation and delivery on GPs). It is also important to note that CQC is a DHSC-funded regulatory and inspection body, and, thus, the GPs may have been reluctant to share data relating to their own morale, resilience, etc.
It is notable that, although the KLOEs ‘effective’, ‘responsive’, ‘caring’ and ‘well-led’ tended to outline issues and examples that could be viewed on a spectrum (from good practice to poor practice), the items in the ‘safe’ section of the CQC reports were generally more binary in nature. For example, medicines stored at the surgery were either stored correctly (safe) or stored incorrectly (unsafe). Much of the ‘safe’ category concerned reliable systems, processes and practices to keep people safe and safeguarded from abuse. Other items included in this KLOE were staffing and recruitment, lessons learned and improvements made, and potential risks anticipated and planned.
In general, the examples related to safety provided by the CQC reports did not provide sufficient detail for our use and were considered to describe standard good practice rather than describing exceptional or innovative practice (i.e. examples that could be presented to interviewees for discussion). Although our original aim was to explore examples related to practice staffing levels, the specific details of this were not provided by the CQC reports. For example, the CQC reports on whether or not recruitment checks and training (e.g. safeguarding) have been completed and are up to date; however, they do not provide details of how GPs could access (or are unable to access) training, or provide detailed breakdown of the actual and required staffing levels and mix (e.g. the number of FTE GPs or nurses related to practice list size and whether or not this is sufficient). Instead, reports frequently contain a broad statement about whether or not the practice staff report that staffing levels and skill mix are adequate. Consequently, we were unable to draw on the ‘safe’ KLOE for our practice examples.
Finally, the aim of this piece of work was to produce an internal briefing report to inform workstreams 3 and 4 of the ReGROUP study. In order to deliver this briefing report within the time scales available, several pragmatic decisions had to be made, most notably around sampling and the selection of examples of good practice from all those available in the CQC reports. The use of researcher judgement may have affected the rigour and credibility of this process; however, it is hoped that the methodological description provided above, and the detailing of the decision processes, offer a transparency that aids interpretation and application of these findings.
Conclusion
Familiarisation with the content of CQC reports has been a useful exercise to help provide this briefing document for the start of workstream 3. Use of CQC reports enabled six key questions to be developed with actual practice examples of good practice that can be explored with interviewed GPs. We focused mainly on the use of reports rated by the CQC as ‘outstanding’ to extract these examples of innovative and good practice, and on four of the CQC’s KLOEs, namely ‘effective’, ‘responsive’, ‘caring’ and ‘well-led’. The fifth KLOE – ‘safe’ – was also explored; however, the nature of the data presented meant that specific practice examples were not extracted for this category. However, it is notable that good practice examples will generally have an impact across the practice, such that the distinction between the categories/KLOEs may be arbitrary.
The opportunity to explore these good-practice examples with GPs was welcomed as the interview stage of workstream 3 began. We were able to add to the ‘bank’ of good-practice examples using GPs’ own examples from their practices (where available), and to consider the implications of these on issues such as GP job satisfaction, workload, team working and stress. In this way, we aimed to collate a range of suggestions and strategies that can feed into the next stages of the ReGROUP project overall and help identify strategies and policies that could help to retain GPs in direct patient care.
Appendix 15 Care Quality Commission report analysis: identifying the number of general practices in the south-west of England that had been reported on by the Care Quality Commission
We drew from two key data sets:
-
a spreadsheet (Microsoft Excel file) of all the active locations (dated 1 December 2015): see www.cqc.org.uk/sites/default/files/HSCA%20Active%20Locations.xlsx
-
a spreadsheet (Microsoft Excel file) of all the rated locations (dated 1 December 2015): see www.cqc.org.uk/sites/default/files/Latest%20ratings.xlsx.
Each data file was filtered to identify the number and name of general practices in the ReGROUP catchment area. Each practice retained after filtering was given a sequential number: ReGROUP workstream 3 ID number.
Appendix 16 Care Quality Commission report analysis: south-west England good practice examples related to each of the key interview questions
| Question | Details |
|---|---|
| Question 1 | If you could have additional member(s) of staff who might help relieve some of the pressures on the GPs, who would that be and why that role? (E.g. mental health nurse consultant) |
| Example 1 | Practice involved in co-commissioning for specialist services with other practices (e.g. had co-commissioned a nurse for > 75-years-olds specifically to visit patients at home to carry out routine health-care checks and care planning) |
| ID: 23 | |
| Large, urban, inner city | |
| Example 2 | Patients with long-term conditions and chronic diseases attended clinics led mostly by the practice nurses. All of the nurses held specialist qualifications and had expertise and were delivering these effectively (e.g. a nurse prescriber with advanced qualifications and experience as a hospital specialist took the lead for diabetic care; data for 2014/15 showed that the practice achieved the maximum points available for monitoring and treating patients with diabetes mellitus) |
| ID: 69 | All of the GPs had specialist interests and provided leadership and clinical governance for clinics for patients with long-term conditions and chronic diseases |
| Large, urban and rural | |
| Example 3 | The nurse partner and a practice nurse were qualified prescribers, which meant that they could diagnose and prescribe some types of medicines for patients. The nurses had been assessed as competent to see patients with long-term diseases such as asthma, COPD, diabetes mellitus and coronary heart disease, and help them manage their care. A MDT approach was taken with patients with complex needs, which involved joint discussions with the GPs and other specialists |
| ID: 118 | |
| Medium, city centre and villages | |
| Example 4 | The practice reviewed attendance for specific patient groups and found that mental health had high attendance. GPs were concerned that they could not give these patients the time in their 10-minute slot and, after retirement of a GP, they decided to recruit a mental health nurse consultant. This had proved to be successful and the mental health nurse consultant had improved faster patient access for mental health treatment and reduced patient referrals to secondary care by 85%. They had reduced GP workload as they saw 40 patients and produced 20 prescriptions per week. This would otherwise have been part of the GPs’ workload and GPs now reported less pressurised surgeries. The mental health nurse consultant also had an important role in working closely with health visitors and GPs to help prevent families from reaching crisis point and needing intervention. Patient feedback was positive and had attracted more patients to register at the practice |
| ID: 198 | |
| Large | |
| Question 2 | If you could offer additional service(s) or resource(s) within your practice to help relieve some of the pressures on the GPs, what would that be and why? (E.g. patient self-assessment health pod; befriending service – includes technology, plus patient and carer emotional and social well-being support) |
| Example 1 | Innovative technology had been purchased to promote greater involvement for patients in monitoring their own health, and helped them to focus their appointments with the GP (e.g. a health pod had been installed in the waiting room, which enabled patients to do blood pressure, weight, height and lifestyle checks. Patients could then choose whether or not to consent to these data being uploaded to their records held by the practice. GPs received automatic alerts for any abnormal results, which they were then able to follow up with the patient) |
| ID: 83 | |
| Large | |
| Example 2 | The practice worked with a small number of other practices to provide a walking group for patients who did not feel confident to join the city walking group |
| ID: 110 | |
| Large, city centre | |
| Example 3 | The practice worked closely with the local community. Patients at the practice had set up an allotment club, which provided network opportunities in the community to help reduce the risk of isolation. Patients were signposted to other activities in the community such as singing groups, lunch clubs and well-being services. Staff reported that patients who had attended healthy living centres had reduced weight and made new friends, thus reducing their social isolation. A patient who had joined the singing group had made new friends and had lifted her mood and self-esteem, and the number of appointments with the nurse practitioner had reduced |
| ID: 118 | |
| Medium, city centre and villages | |
| Question 3 | If you could work with another organisation(s) – another practice or an external organisation – in such a way that your joint working would relieve some of the pressures on GPs, who would you work with and why? (E.g. Age UK, drug rehabilitation team) |
| Example 1 | Practice involved in co-commissioning for specialist services with other practices (e.g. had co-commissioned an over-75-year-olds nurse specifically to visit patients at home to carry out routine health-care checks and care planning) |
| ID:23 | |
| Large, urban, inner city | |
| Example 2 | The practice collaborated with other practices in the area, and the practice manager is currently seconded to neighbouring practice in order to share different ways of working and expertise. An outcome of this had been shared training. This was a benefit to both practices as they learned from each other and developed a joint understanding of the patient need in this area |
| ID: 23 | |
| Large, urban, inner city | |
| Example 3 | The practice worked with a small number of other practices to provide a walking group for patients who did not feel confident to join the city walking group |
| ID: 110 | |
| Large, city centre | |
| Example 4 | The practice had started a pilot project with Age UK whereby volunteers would visit patients with two or more long-term conditions to offer a befriending service and build a life plan. The practice had also involved a practice nurse from another surgery who would provide assistance with creating personalised care plans for these patients. All patients with long-term conditions had a personal management plan |
| ID: 156 | |
| Small, rural | |
| Question 4 | If you could provide support directly to GPs to help them personally manage their work–life balance, what would this support look like and why? (E.g. mentoring) |
| Example 1 | There was a stable staff group. Many staff had worked at the practice for many years and were positive about the open culture within the practice. Nursing and administration staff spoke positively about the communication, team-work and their employment at the practice. They were actively supported in their employment and described the practice as having an open, supportive culture and being a good place to work. GPs said that there was support for each other when it was identified as being needed. However, the CQC did not see the same level of proactive support or risk assessment given by GPs to themselves as a staff group (e.g. risk assessments were in place to identify stress in the nursing team and administrative team, but this assessment had not been routinely conducted on GPs) |
| ID: 110 | |
| Large, city centre | |
| Question 5 | If you could restructure or organise your practice differently in order to relieve the pressure on GPs, what would you do and why? (E.g. telephone triage, longer appointments) |
| Example 1 | Practice involved in co-commissioning for specialist services with other practices (e.g. had co-commissioned an over-75-year-olds nurse specifically to visit patients at home to carry out routine health-care checks and care planning) |
| ID: 23 | |
| Large, urban | |
| Example 2 | GPs aimed to promote patient dignity and respect in the way they approached requests for a home visit or repeat prescriptions (e.g. elderly and frail patient called the practice to request a repeat prescription. Currently unwell and worried about being unable to get to the pharmacy. Reception staff reassured the patient that they would arrange for their repeat medication request to be dealt with quickly, passed on to the chemist, and arrangements would be made for it to be delivered to them at home. The staff immediately asked the GP to review and approve the request, then liaised with the chemist to dispense and deliver the medicines to the patient at home) |
| ID: 32 | |
| Medium, town and villages | |
| Example 3 | Practice based in a popular holiday resort and patient list could increase by up to one-third at the height of summer, with > 500 temporary patients. The practice increased the number of appointments available in these summer months and regular patients remained unaffected |
| ID:32 | |
| Medium, town and villages | |
| Example 4 | Every patient registered with the practice had a named GP who was supported by their own administration team. Staff knew patients well and co-ordinated follow-up care and support to meet each person’s needs. National resources had been used to develop a person-centred approach (e.g. dementia care plans were used and followed current recommended practice by the Alzheimer’s Society) |
| ID: 69 | All patients had a named GP who specialised in particular chronic health diseases and long-term conditions. Patients were linked with the most appropriate GP and had a named secretary to handle correspondence about pathology results and hospital appointments. Patients knew the name of the secretary dealing with this flow of information and were able to liaise directly with that person to follow up when letters were sent and received. Thus, staff were able to complete a task from start to finish, ensuring that results were handled quickly for patients (e.g. a personal care plan for a patient diagnosed with dementia whose kidney function was poor. Regular telephone calls to the patient were followed up in writing. This provided the patient with reminders to attend for blood tests so that their kidney function could be monitored. The team worked closely with the patient’s care support team, mental health worker and consultant psychiatrist to reduce the risk of unplanned hospital admissions) |
| Large, urban and rural | |
| Example 5 | An effective process was in place for managing blood and test results from investigations. When GPs were on holiday the other GPs covered for each other. Results were reviewed within 24 hours, or 48 hours if test results were routine. Patients said they had not experienced any delays receiving test results |
| ID: 110 | The GPs provided a personal patient list system. These lists were covered by colleagues when the GPs were absent. Patients appreciated this continuity and GPs stated that it helped with communication |
| Large, city centre | |
| Example 6 | Patients with long-term conditions were given longer appointments of 40 minutes owing to the complexity of their conditions, which included routine questions around anxiety and depression. Housebound patients were visited by the nurses who undertook 6-monthly reviews |
| ID: 156 | The practice also employed a home support nurse to support older people in their own homes (with an emphasis on the top 2% at risk of admission to hospital or those in greatest need, e.g. for end-of-life care). A large number of the patients visited were isolated and the nurse was able to provide them with additional support to cope with physical and emotional needs. The nurse worked within the MDT, attending meetings to discuss patients’ needs and visiting them at home to provide support and assessments. Her role had reduced isolation and anxiety, which in turn had reduced telephone calls to the practice and NHS 111; however, the GPs were always responsive to need and would visit a patient within 1 hour if needed |
| Small, rural | |
| Example 7 | Following patient feedback, the practice had identified that telephone access needed improving. The main problem was for patients getting through to the practice in the morning. They now had all administration staff answering telephones in the morning during busy periods and then reduced staffing levels as the telephone calls reduced. This was monitored continuously by the patient co-ordinator and other trained staff who would increase or decrease the number of staff answering calls depending on the need |
| ID: 198 | All call handlers and patient-facing staff had knowledge of all the GPs and their specific skills (e.g. dermatology, family planning, steroid injections). This awareness enabled them to allocate appointments or queries to the most appropriate GP. They had the same system for nursing staff (e.g. the chart informed staff who could see patients for annual diabetes mellitus or asthma checks or immunisations) |
| Large | There was also a duty GP within the call-handling area to speak with patients and to answer any direct queries form staff |
| Question 6 | If you could develop or better utilise GPs in your practice with specialisms in order to relieve the pressure on GPs, what would you do and why? |
| Example 1 | All of the GPs had specialist interests and provided leadership and clinical governance for clinics for patients with long-term conditions and chronic diseases |
| ID: 69 | |
| Large, urban and rural | |
| Example 2 | All of the GPs had specialist interests and provided leadership and clinical governance for clinics for patients with long-term conditions and chronic diseases (e.g. one GP held a master’s degree in management of respiratory conditions and patients benefited from their expertise with this. Data for hospital referrals for patients with respiratory diseases was nearly 50% lower than the CCG and national averages. This showed that the practice was effective in managing long-term and chronic conditions) |
| ID: 83 | |
| Large | |
| Example 3 | GPs had lead roles aligned with post-qualification qualifications and experience (e.g. a GP partner was the lead for patient cancer care. The role covered dissemination of educational information to the team, regular review of referrals so that shared learning took place, and monitoring referral rates for patients with suspected cancer. The practice demonstrated that screening for bowel, breast and cervical cancer was higher than the national average) |
| ID: 83 | |
| Large | |
| Example 4 | There was a high incidence of patients registered at the practice with substance misuse problems who wished to change their lifestyle. The GP partner had completed additional training and was a qualified pharmacist so had the skills and experience to safely manage the detoxification process for suitable patients living in the community. He did this in conjunction with specialist agencies who provided further support for the patients. This facilitated continuity of care for patients in such situations |
| ID: 118 | |
| Medium, city centre and villages |
Appendix 17 Interview schedules, participant information sheet and consent form
Interview schedules
There were five versions of the GP interview schedule, one for each GP interview category. The general questions and topic areas were the same, but they were modified to accommodate each category. An example of the interview questions and topics is given here using the ‘Intending to Retire’ interview schedule. The topic guide for stakeholders is also provided.
| Key questions for GPs | Prompts |
|---|---|
| Can you tell me about your current working situation? | How many hours do you currently work per week? |
| What is your role in the practice? | |
| What type of area do you work in: rural, semirural, suburban, town/city, inner city? | |
| What type of population does your practice cover: deprived, mixed poor, average, mixed well off, affluent? | |
| How is your practice staffed with GPs (partner, salaried, locum, part-time/full-time) | |
| Have you reduced your hours or made any other changes to your working pattern? | In recent years (past 5 years) |
| Do you know when you are likely to retire? | During the next 12 months |
| How old will you be then? | Within the next 5 years |
| Within the next 10 years | |
| Has it always been your intention to retire at this age? | Yes – how did you decide on that age? |
| No – what made you change your mind? | |
| What factors have an influence on your decisions about when to retire? These might be work-related things or things outside work | Job satisfaction/dissatisfaction |
| Have there been any ‘critical’ or key events that have influenced your decisions or plans? If so, can you tell me a bit about this/these? | Stress |
| Workload | |
| Length of working day | |
| Pace of working day | |
| Bureaucracy/paperwork/over-regulation | |
| Financial security – including pension issues | |
| Change | |
| Ageing | |
| Unmet clinical/patient needs – say what these are | |
| Managing the business (staffing, buildings, etc.) | |
| Work-related sleep issues | |
| Health and well-being (physical and psychological) | |
| Outside interests, such as wanting to spend more time with family or leisure pursuits | |
| Wanting to enjoy good health while they can | |
| Appraisals and/or revalidation | |
| IT systems | |
| Referral systems and pathways | |
| Concerns about the future of general practice | |
| Low levels of morale/reduced emotional resilience | |
| Struggling to stay up to date | |
| Other | |
| What, if anything, might persuade you to change your plans? | Reduced workload |
| Reduced working hours | |
| Increased financial reward | |
| Change of role (e.g. from partner to locum or salaried GP) | |
| Support with managing your own physical and emotional health status and well-being (e.g. mindfulness course, counselling) | |
| A flexible model of employment to help retain doctors at the end of their careers | |
| Additional paraclinical support (e.g. senior nurses or pharmacists supporting the management and co-ordination of structured care for patients with long-standing health conditions) | |
| Additional administrative support (e.g. a ‘medical assistant’ to relieve admin pressures) | |
| GP mentoring | |
| Other | |
| Is there anything else you would like to tell me about your retirement intentions or any specific issues that we have not discussed yet? | What would you say to someone thinking about coming to work in a primary care practice/this practice (if they were asking about the shortage of GPs)? |
| Do you have any other questions? | |
| Would you like to receive a summary of the research findings when the study is finished? | Would you prefer this by post or electronically? |
| Thank participant |
| Key questions for stakeholders | Prompts |
|---|---|
| Can you tell me about your current role? | What are the key aspects of your role in relation to patient care, planning, organisation, management |
| What type of area do you work in: rural, semirural, suburban, town/city, inner city? | |
| What type of population does your practice/area cover: deprived, mixed poor, average, mixed well off, affluent? | |
| If applicable – how is your practice staffed with GPs (partner, salaried, locum, part-time/full-time) | |
| From your perspective, why do you think that GPs choose to quit direct patient care (i.e. take a career break or early retirement)? | Maternity/paternity |
| Other family dependents | |
| Professional development | |
| Personal development | |
| Working abroad | |
| Health issues | |
| These might be work-related things or things outside work | Workload |
| Pension availability | |
| Low levels of morale | |
| Poor job satisfaction | |
| Paperwork/bureaucracy/over-regulation | |
| Other | |
| What do you think is the impact of GPs quitting direct patient care? | Can you give some specific examples (e.g. impact on your workload/role, other staff, patients, finance of the practice, leadership of practice/succession planning concerns about unmet clinical/patient needs) |
| This could be things related to a specific practice or locality | |
| Can you give me any examples from your own practice/role (or other) of how the impact has been managed? | Recruitment |
| Team composition/team working | |
| Phased return | |
| Rotas | |
| Mentoring | |
| Leadership | |
| Other | |
| What do you think might help GPs to remain in direct patient care (i.e. to wait until 60 years of age to retire or to return after a career break)? | What are the barriers that career-break GPs may face when it comes to returning to direct patient care/what makes it more difficult or less desirable? |
| What might help to overcome these barriers? | |
| What might influence GPs to wait until they are 60 years old to retire (rather than retire before 60 years)? | |
| Anything else you want to tell me about your experiences or opinions of GPs leaving direct patient care and the impact of this on practice management and organisation? | What would you say to someone thinking about coming to work in a primary care practice/this practice (if they were asking about the shortage of GPs)? |
| Do you have any other questions? | |
| Would you like to receive a summary of the research findings when the study is finished? | Would you prefer this by post or electronically? |
| Thank participant |
Participant information sheet: general practitioners
Participant information sheet: stakeholders
Consent form: general practitioners
Consent form: stakeholders
Appendix 18 Protocol for assessing, reporting and monitoring risk
Purpose
To provide an agreed and documented route for the research team to discuss and report any issues that may potentially have an impact on the GP participant’s own health and safety and/or that of their patients.
Principles
The following principles and procedures govern risk assessment, reporting and monitoring for ReGROUP.
The chief investigator has overall responsibility for risk assessment and management and must ensure that any research personnel are adequately qualified and trained on risk assessment prior to any participant contact in which risk could be disclosed, and that these personnel receive support and supervision around risk issues.
All cases in which significant risk is identified by researchers will be managed in accordance with the ReGROUP risk protocol and discussed with the chief investigator and the project manager. All reports and correspondence relating to risk sent by research staff will be checked by the chief investigator or project manager before they are reported on.
The chief investigator and project manager are responsible for ensuring that appropriate cover is arranged for any risk issues that might arise in their absence. This will entail a person being named as responsible for overseeing risk assessments in their absence and contact details being shared with the project manager.
Definition of risk
Research team members are expected to use their own professional judgement regarding any situation or issue in which harm to the participating GP and/or their patient/s may be reported or inferred. Examples include:
-
obvious distress during the interview (e.g. crying, aggression, withdrawal)
-
disclosure of poor health status that significantly impairs their functioning at work
-
disclosure of depression or suicidal thoughts
-
disclosure of alcohol or drug dependence/use
-
disclosure of serious errors in clinical practice or serious concerns about adverse consequences for a patient’s health following their treatment decisions.
Procedures for research personnel
Researchers must initiate the risk protocol each time a participant discloses information during an interview that leads the researcher to believe that there are thoughts of suicide or harm to self or others. The researcher should initiate the risk protocol and notify the chief investigator (or nominated deputy).
Risk protocol
Step 1: debrief with workstream 3 lead
Researchers (AS and RT) should seek debriefing opportunities with workstream 3 lead (SD) following any interview that they have concerns about, or that has left them with a sense of unease or burden. Ideally, an opportunity to debrief should be made available on the same day or within 24–48 hours. The responsibility to request a debrief lies with the researcher.
Following the debrief, the workstream 3 lead and the researcher will jointly decide if:
-
escalation to risk protocol is not required, debrief noted on risk form and filed, and no further action is needed
-
escalation to risk protocol is not required, but other further action is needed (e.g. further support to the researcher; a reminder to the GP of the support resources detailed on the participant information sheet); this is noted on risk form and filed
-
escalation to risk protocol is required (see step 2 below).
Step 2: inform research clinician/chief investigator
Should an urgent/high-risk issue arise, the interviewer should inform the chief investigator (JLC) or research clinician (JLC or CS). They may wish to speak first with the workstream 3 lead to clarify the issues and receive support. If at all possible, the chief investigator/research clinician should be informed of the risk situation on the day of the interview, or as soon afterwards as possible. Researchers should ensure that management of the information has been handed over correctly.
Step 3: research clinician/chief investigator action
Once the chief investigator/research clinician has been made aware of a risk issue, they are responsible for the next action step. Depending on the risk assessment they make, possible action routes include:
-
No further action. Risk information form completed and filed.
-
Chief investigator/research clinician makes direct contact with the participating GP by telephone or e-mail. This is also documented on the risk assessment form.
-
If a participant discloses an issue that indicates the potential for a significant risk to a participant’s patients, the chief investigator/research clinician will contact the participant and agree with them what steps they will take to protect patient safety. They will also report the matter to the appropriate responsible person in line with the GMC guidance on reporting concerns. This would be the senior partner in the case of a salaried GP or the medical director of the local NHS England site for GP partners.
All cases
Any instance of debrief or escalated research clinician/chief investigator involvement should be documented using the risk information form. All involved personnel are responsible for completing their identified section of the form. Completed forms should be (counter-) signed by the chief investigator and retained by the project manager (EF) in a locked filing cabinet.
Where the participating GP is at immediate high risk and/or the researcher is concerned for their own safety, appropriate action must be taken by the researcher. This may require emergency services (ambulance, police) to be called, or the researcher to take the participant to accident and emergency. In any such instance, the researcher must inform the workstream 3 lead and/or the chief investigator of the situation as soon as possible.
(Note: please refer to lone worker policy for procedures to ensure interviewer safety.)
ReGROUP risk information form
Research supervisors and emergency contact numbers
If you are unable to reach staff by mobile phone, then please text ‘URGENT please contact regarding ReGROUP risk protocol’.
Research supervisors
Sam Scott holds John Campbell’s diary and can help locate him during working hours if he does not answer his telephone.
Nancy Horlick (working hours: Monday and Tuesday, 08.30–17.00; Thursday, 09.30 to 14.30) holds Chris Salisbury’s diary.
-
Chief investigator
-
Co-investigators
-
Project manager.
For use by research supervisors only
Emergency contact numbers
-
The Mental Wellbeing and Access Networks are the first points of contact for crisis intervention during normal working hours:
-
Exeter: Exeter team: 08.00–18.00
-
Newton Abbot: Teignbridge team: 08.00–18.00
-
Barnstaple: Tawside team – 08.00–18.00
-
Bristol: 08.00–20.00
-
Plymouth:
-
-
Out of hours or in an emergency when you cannot get hold of the Mental Wellbeing and Access Network team, contact the Crisis Resolution Home Treatment Team:
-
Exeter: Exeter, East and Mid Devon team
-
Newton Abbot: Teignbridge team
-
Barnstaple: North Devon team
-
Bristol: Central Bristol Mental Health team
-
Plymouth: South Hams and West Devon team.
-
Please note that these numbers are to make an urgent referral to the crisis team and should not be given out to participant/members of the public under any circumstances. The participant’s GP can also make an urgent referral to the crisis team and should be the first port of call.
-
Accident and emergency department:
-
Exeter: Royal Devon & Exeter Hospital, Barrack Road, Exeter EX2 5DW
-
Newton Abbot: Torbay Hospital, Newton Road, Torquay, Devon TQ2 7AA
-
Barnstaple: North Devon District Hospital, Raleigh Park, Barnstaple, Devon EX31 4JB
-
Bristol (north): Southmead Hospital, Southmead Road, Westbury-on-Trym, Bristol BS10 5NB Emergency Department Main Reception Gate 35: 0117 4145100 or 0117 4145101
-
Bristol (central): Bristol Royal Infirmary, Upper Maudlin Street, Bristol BS2 8HW
-
Plymouth: Derriford Road, Crownhill, Plymouth, Devon PL6 8DH
-
Somerset: Musgrove Park Hospital, Taunton, TA1 5DA.
-
Appendix 19 Demographic distribution of general practitioner interview sample
| Characteristic | Number of interviewees |
|---|---|
| Role (current or most recent) | |
| Partner | 22 |
| Salary | 5 |
| Locum | 14 |
| Gender | |
| Male | 20 |
| Female | 21 |
| Ethnicity | |
| White | 41 |
| Other | 0 |
| Age (years) | |
| < 40 | 7 |
| 40–49 | 16 |
| ≥ 50 | 18 |
| Practice list size | |
| Small/medium (< 3500–8000) | 8 |
| Large (> 8000) | 21 |
| Not knowna | 12 |
| CQC practice rating | |
| Inadequate | 0 |
| Requires improvement | 0 |
| Good | 24 |
| Outstanding | 1 |
| Not knowna,b | 16 |
| Deprivation rating of practice | |
| 1–5 (more deprived) | 10 |
| 6–10 (less deprived) | 19 |
| Not knowna | 12 |
| Area | Number of GPs |
|---|---|
| Bath and North East Somerset | 2 |
| Bristol | 11 |
| Devon (locum) | 7 |
| Kernow/Cornwall | 6 |
| Northern, Eastern and Western Devon | 4 |
| North Somerset | 4 |
| Somerset | 4 |
| South Devon and Torbay | 0 |
| South Gloucestershire | 3 |
Appendix 20 Problems/issues identified by participants that affect decisions to remain in or leave direct patient care
| Topic | Issues | Summary |
|---|---|---|
| Workload | Bureaucracy, paperwork, targets and assessments | Although the potential value and benefits of targets, guidance and CQC inspection were recognised, the additional work created by these was burdensome. There was concern that regulations can devalue GP knowledge and experience, and deskill GPs – especially regarding problem-solving, creating and testing hypotheses. This could lead to clinical over-investigation |
| Many GPs strongly disliked CQC inspections (which they felt had a negative, punitive slant) and other aspects of their work that they considered to be ‘pointless’ or ‘tick box exercises’ | ||
| Pace, intensity and length of day, fewer support services available | There was almost unanimous agreement regarding workload increase, and increased length of working day, in combination with diminishing support services (e.g. mental health and social care for an ageing population). The wider practice team helping with ‘quick win’ consultations led to an increasing proportion of complex cases being seen by the GP, further exacerbating workload intensity. Specific patient groups (such as those being managed at home, people with mental health issues, and people living in areas of high deprivation) also added to workload | |
| Complex patient care | A high number of patients combined with increasingly complex health needs were reported by almost all participants. The issue of a steep rise in costs, time and complexity associated with an ageing population and multimorbidity was discussed. Increased polypharmacy increased monitoring requirements. Clinical decision-making was more complex | |
| Appointment structure | There was general agreement that 10-minute appointment times were too short and based on outdated calculations. Complex patients and increased additional workload (targets, administration, etc.) meant that many consultations required more than 10 minutes. Reallocation of the ‘easy’ appointments to other team members also meant less opportunity for the GPs to use minutes saved from easier/shorter appointments as ‘catch up’ time. Some GPs noted that 10-minute appointments were adequate if the practice was suitably staffed and a personal list system employed. Some practices already worked to different (longer) appointment structures | |
| There was some concern that patients may ‘fill up’ longer appointment times if they were made available, irrespective of clinical need | ||
| Shift in workload from primary to secondary care | Many GPs had struggled with maintaining good communication between primary and secondary care and recognised issues relating to the distribution of funding. Communication pathways were seen as complicated and created opportunities for misunderstanding | |
| Some activities that traditionally would have come under the secondary care remit had been passed to primary care. Some GPs felt that there was a lack of understanding from secondary care on the consequences of their actions/requests. Transfer of care was not adequately recognised or resourced | ||
| Participants felt that existing systems and processes could waste time and be unduly convoluted; the system was not joined up and there were gaps. Participants noted that the ‘buck [often] stops’ with the GP | ||
| GP health and well-being | Appraisal and revalidation | Participants recognised that the appraisal system was designed to help, but the majority of participants found it to be an unhelpful or time-wasting process; only a minority reported positive experiences. Most felt that appraisal and revalidation were a ‘missed opportunity’ to provide support and could be more beneficial to the GP |
| GP health | GPs noted the implications of the current working situation on their own and other GP colleagues’ mental and physical health and well-being. Some recognised that they did not have a good work–life balance; stress had affected sleep and their health was being jeopardised. GPs described colleagues having periods of sick leave, some not returning to work, and being visibly exhausted. Participants recognised that there was then an increased risk of making a mistake | |
| The impact of ageing was also discussed (including the effects of menopause); some GPs felt less able to carry out the demands of their role with increasing age, or expressed a desire to ‘quit while ahead’, and had noticed a reduction in their stamina | ||
| The need for opportunities to debrief or have supervision-style support (similar to the support that counsellors receive) was identified, to help GPs ‘carry the burden’ of their role. However, it was noted that many GPs have concerns about confidentiality and stigma attached to accessing mental health support | ||
| Support and relationships | Peer support | Participants described fewer opportunities for peer support activities (e.g. meeting for coffee during the working day). Colleague support was deemed important by most and vital for some. However, the pressured environment led to instances of bullying, conflict over work patterns and lack of understanding between colleagues (e.g. older and younger GPs) |
| Organisational issues, primary and secondary care interface | Many GPs had struggled with maintaining good communication with secondary care. Relationships had changed to become less supportive and less accessible. Participants recognised issues relating to the distribution of funding contributing to an ‘us and them’ mentality | |
| Employer relationships: GP contract/government/organisational-level support | There was a perception of unfairness and a consistent reduction in rewards and rights. This affected morale deeply | |
| Relationships with patients; demand and expectations | Expectations and demands of patients were identified as a considerable burden and source of stress for many GPs. This was complicated by feelings of diminished GP–patient relationships owing to lack of continuity of care, unrealistic patient demands and fear of litigation | |
| The media | Participants talked about ‘GP bashing’ and the feeling that the media wanted only to report negatively about GPs rather than acknowledge the positive contribution that GPs can make. The media was also identified as having a role in encouraging unrealistic expectations from patients | |
| GP role and pattern (partner/salaried/locum; part-time/full-time/portfolio) | Many GPs perceived their role as being less clear than, or as being different from, the one they had envisaged at the start of their career. Several GPs described part-time and/or portfolio working as ‘coping strategies’ adopted to help them sustain working in direct patient care. There was a view that fewer GPs are now able and/or willing to work full-time in a direct patient care role owing to the high demands and personal costs to GP well-being. Tensions existed between partner, salaried and locum GPs, and pros and cons of the different roles were perceived for both the GP in that role and their impact on other GPs in the practice. There was an acknowledgement that many GPs are increasingly wary about taking on partnerships | |
| The practice team composition | Some participants felt that widening the practice team was a reactive rather than proactive change: through necessity, GPs had recruited a wider clinical practice team in response to workload, recruitment and financial pressures. Although a diverse workforce sometimes reduced the workload of the GP, and was considered to be a positive adaptation or response to the changing workload and demands, this was not always the case. Other health professionals were sometimes considered to be an alternative solution to the ‘ideal’ of recruiting another GP. Some participants felt that additional non-GP staff could be expensive/not cost-efficient | |
| Feelings of isolation for GPs, and reduced opportunities to build rapport with patients, were compounded by a changing pattern of workload management, whereby GPs took on only the most complex patients and ‘outsourced’ the more straightforward ‘quick wins’ to other health professionals, such as nurse practitioners | ||
| IT and systems | Several participants noted that some IT and systems that had been introduced to help manage workload or reduce GP tasks had, conversely, created additional work. They described how IT facilitated counting, measuring and ‘double-checking’ but that this, in turn, could lead to additional (unnecessary) work | |
| Finances, investment and fiscal reward | Practice finances | There were divergent views regarding primary care funding models: some participants preferred and highly valued the partnership model, others suggested that salaried GPs were a more viable option for the future delivery of general practice. Some participants noted that practice funding formulas did not always work and could disadvantage practices in certain areas or that provided care for specific populations. There was consensus about a lack of financial support for general practice |
| Indemnity | It was noted that the cost of indemnity is increasing and becoming prohibitive, especially for part-time workers. Comparisons were made with other parts of the world (e.g. New Zealand where Crown Indemnity exists) | |
| Investment and reward (including pay) | Several GPs noted a relative decrease in their salary in recent years. GPs felt that they were asked to take on more and more responsibilities but their pay was relatively less. This contributed to feelings of not being valued | |
| Pensions | Changes to pensions had a varied effect on GPs. There was a cohort effect with this, such that those on the older pension schemes were in more favourable circumstances to retire relative to their younger counterparts (who were on different schemes) | |
| Change, uncertainty and the future | The crisis rhetoric, future investment | There was a perception that the current situation in primary care is unsustainable and ‘in crisis’. This rhetoric was perceived to be unhelpful and demoralising for GPs |
| Recruitment and retention | Participants recognised the problems of fewer GP partners and increasing numbers of salaried or locum GPs. Recruitment was increasingly difficult and many GPs did not want/did not feel able to work full-time. There was a widespread unwillingness to take on partnerships | |
| Models of primary care: past, present and future | There was an emotive split between GPs: although some were very saddened and upset at the loss of the ‘traditional’ model of general practice, others saw new models as being the only way forward. GPs were also divided in their opinions regarding new models of care, with some feeling that it was another unwanted result of a lack of government support for the current model of general practice. Regardless of their standpoint, GPs recognised the widespread unwillingness to take on partnerships as having an effect on leadership and on the sustainability of current general practice | |
| Returning to work after a career break | Those who considered or who had returned after a maternity break noted difficulties relating to childcare flexibility (especially for partners and locums). Those who were considering returning or had returned after a period working abroad noted difficulties with accessing reliable information and support for return, and also issues related to staying up to date and meeting the requirements to practise in the UK. Some GPs were reluctant to return ‘in the middle of a workforce crisis’, and comparisons of their working conditions overseas with returning to the UK were often unfavourable |
Appendix 21 Additional quotations from participants to support qualitative interview findings
General practitioner identity, professionalism and morale
I like to listen to people, I like to give people time, so I’m a very popular GP, but I’m quite a stressed GP in the NHS setting.
GP324 – female, age 30–39 years, locum GP, intending career break
The fun’s going and it’s becoming increasingly hard work . . .
GP212 – male, age 50–59 years, GP partner, intending retirement
Risk to patient care and safety
About 7.30 in the evening, having been there for 12 hours, I’ve just had enough and I think it’s unsafe, so I go home.
GP208 – male, age 50–59 years, GP partner, intending retirement
Fear of complaints and being sued
Nobody cuts you any slack, so if I make a mistake, I will be held responsible, and nobody will ask you ‘how busy were you that day? Were you being supported?’. Nobody’s interested.
GP417 – male, age 40–49 years, salaried GP, intending early leaver
Risk to own health and well-being
I began to feel that it was probably not so good for my health in terms of the amount of stress that I was having to cope with.
GP208 – male, age 50–59 years, partner GP, intending retirement
Uncertainty about the future of general practice
If I ask the question ‘tell me which model of care is going to stop the problem now that we can see it coming?’. There’s isn’t an answer. We don’t know. There are lots of ideas and there’s lots of issues around those ideas, but there’s no unified model.
GP509 – male, age 40–49 years, GP partner, staying
Accumulation, compounding and combination of factors
I think that I have probably been in survival mode, for the last 5 or 6 years.
GP212 – male, age 50–59 years, GP partner, intending retirement
General practitioner resilience
The conclusion I came to was, unless the workload changed, which it wasn’t going to, I couldn’t carry on. I could’ve had counselling until the cows came home. But whilst I was working at such a frantic pace every single day, nothing was going to change. Which is why I made the decision that really I just had to leave and have a break.
GP412 – female, age 30–39 years, GP partner, early leaver
The only route left
So the impact and the worry is around, that people will start to vote with their feet, will start to move out. They can see this new model coming and if they can’t see where their own individual role fits with that (. . .) will feel quite threatened and uncomfortable about working outside their own practice or in a different way (. . .) People will start to vote with their feet and will start to retire earlier than they may have done.
SH1041 – CCG stakeholder
Appendix 22 Reasons for retiring, taking a career break and leaving or remaining in direct patient care
| Interview category | Stated ‘pull’ factors | Stated ‘push’ factors | Stated intentions |
|---|---|---|---|
| Retired GP (any age)/GP intending early retirement (age 50–59 years) | Enjoying other work roles/wanting to do something different | The ‘final straw’ following an accumulation of factors. Feeling ‘what’s the point’/ran out of drive/no longer enjoyable/rewards no longer so great | Had intended to retire later |
| Good time to go in personal life | Financial reasons | Had always been the intention to leave at that age | |
| Health problems | Had intended to retire earlier | ||
| Tired of targets/paperwork/’hoops’ to jump through | |||
| Workload-related stress (e.g. no longer had any control over workload; no longer had lunch breaks; no time to reflect) | |||
| Constraints of work (difficulties booking holidays/time away from practice) | |||
| Family circumstances | |||
| Quitting while ahead/not wanting to ‘outstay welcome’ | |||
| Unsupportive government/press/patient relationship | |||
| Unwilling to ‘sacrifice oneself’ | |||
| Staffing/recruitment issues | |||
| Resents being told to be more resilient/being the whipping boy | |||
| GP early leavers (age < 50 years) | Other interests have superseded desire to practise medicine | Workload too great/uncontrollable | Does not intend to return |
| Childcare/family life | |||
| Job has changed/getting worse | |||
| Job is not sustainable | Has thought about leaving but currently has no plans | ||
| Underfunded system | |||
| Felt forced to resign following a range of negative experiences | |||
| Felt triage systems unsafe | Unsure whether to return or permanently leave direct patient care | ||
| Pressure from government/undermining from government and/or media | |||
| Could no longer offer patients the best | |||
| Appraisal and revalidation | Still working because there are no other options but can only tolerate part time | ||
| Pay and remuneration | |||
| Bullying/distrust/siege mentality | |||
| Health could be affected | |||
| Stopped enjoying the job | |||
| Feels burnt out | |||
| Pressure to merge | |||
| Pessimism about the future | |||
| Increase in litigation | |||
| Patient expectations | |||
| Appointment times | |||
| CQC inspection | |||
| GP career breakers (any age) | Maternity leave | Reluctant/unable to work long days with baby | Intends to return to part-time salaried or partner post |
| Left the country for better working conditions | Risks not proportionate to rewards | Does not envisage returning | |
| Good time in personal life/good opportunity | Number of patients, complexity, unrealistic patient demands | May return after 2 years | |
| Increasing indemnity/clinical risk | May return at some point | ||
| Primary and secondary care difficulties | Would find it difficult to return as a locum owing to lack of support | ||
| Guidelines | |||
| Lack of resources | |||
| Personal financial risks to GP too high | |||
| Low levels of morale | |||
| Staying GPs (any age) | Working full-time allows patient list to be managed better | Increasingly hard to manage workload | No intention to leave |
| Pleasant working environment | Increasingly hard to manage patient demand | Not sure of future plans, previously had time off with burnout, now working as a locum | |
| Peer support | Increasingly hard to manage primary–secondary care interface | ||
| Has high morale | Working full-time in same role exhausting and not sustainable | ||
| Stays for family/home reasons | Managing uncertainty and lack of success can be tiring | ||
| Teaching helps to improve morale and optimism | |||
| Good work–life balance | |||
| Stakeholders: reasons cited that may apply to GPs in general | GPs get exhausted by the pace and responsibility | ||
| Pressures caused by social changes (e.g. less family support, more geographical mobility) | |||
| IT makes the job easier but increases the pace | |||
| The crisis rhetoric (the media circus) makes GPs feel unable to do their job or feel unable to cope | |||
| GPs struggle to define their role | |||
| Clinical responsibility for wider GP team |
Appendix 23 Suggested policy and strategy topics and content
| Topics | Elements | Content and complexities |
|---|---|---|
| Changing the system | Financial investment in primary care | Long-term commitment and follow-through from the government and NHS to appropriately finance primary care |
| Changes to GP business model/primary care infrastructure/the way health care is organised and delivered | Practice size | Support to determine optimum practice size so that practices can benefit from economies of scale while retaining a supporting culture. GP support may be compromised above a certain practice size and personal lists (important factor in job satisfaction for some) difficult to maintain |
| A move from partnerships to salaried federations, etc. | Clarification of new models of care, including whether or not the partnership model will be viable in the future. Buy-in from GPs will be needed; however, currently GPs have different views about ‘losing’ traditional general practice and the evidence for other practice models (e.g. federations) | |
| Widening the team | There were mixed experiences and views regarding widening the practice team. Some had found practice nurses, pharmacists, paramedics, etc., useful additions to help manage the workload. Others were concerned that widening the team would cause extra work, as the ultimate responsibilities would still lie with the GP and there would still be a need for GP leadership | |
| Evidence about how this works in practice in the longer term, including the cost implications, and patient satisfaction with seeing non-GPs, could be helpful | ||
| Triage | Many GPs had adopted a triaging system to help manage workload but the effectiveness of this was variable (e.g. the amount of decision-making could be exhausting and there was a perceived increase in the risk of making the wrong decision) | |
| Support and evidence to practices about the costs and benefits of different workload management methods, including shared learning from ‘success stories’ and good practice, could be helpful | ||
| Support | Administration and training | Administrative support would be widely welcomed but with the recognition that there may be additional training requirements, and funding implications. Additional training for GPs could be helpful (e.g. managing telephone triage, business and HR issues). Support with keeping up to date would be useful |
| Adding value to the GP role | Time | A cap on the number of hours worked each day could help make direct patient care more sustainable. Longer appointment times are required owing to increasing complexity – especially if the more ‘straightforward’ care is dealt with by a wider workforce |
| Retainer schemes and decision-making support | Support for those who might otherwise leave could encourage experienced GPs to continue to contribute to the workforce, including supporting trainee/less experienced colleagues. Options need to be clearly signposted, making it ‘easy’ to stay. Additional support could be helpful for those who have indicated an intention/taken action to leave. Provide GPs with a supportive review of options including a ‘cooling-off’ period before any decision is final | |
| Career development, portfolio careers and flexible working | Actively and formally support GPs to have flexible working, including having portfolio careers. Organise portfolio working in ways that minimise any negative impact on other colleagues and the wider workforce. Offer and facilitate choice and career development in the workplace | |
| Support for GPs after career break | Simplify and streamline return-to-work processes. One clear source of reliable and up-to-date information, and individual support and advice (if required) would be helpful. Additional peer support, banks or chambers, along with practical support such as longer appointment times, could also be helpful | |
| Indemnity and changes to complaints system and culture | Demonstrate support for primary care (e.g. Crown Indemnity), change in press/media culture towards reporting mistakes, etc. Provide a quick and supportive process for minor complaints. Help GPs to feel that they are valued, their opinions are respected, their views are taken into consideration and that the public, media and government support general practice | |
| Taking the pressure off | Improved primary–secondary care interface | Address funding of primary–secondary care workload. Develop effective and closer communication between GPs and hospitals/consultants, and clarify the boundaries of responsibility. Address the ‘us and them’ feelings |
| Creating a new culture and systems to help GPs meet the demands of the job | Changing the appraisal and revalidation system | Reduce the amount of work required by the appraisal and revalidation processes. Make appraisals and revalidation more supportive and less onerous |
| Addressing GP well-being | Provide occupational health resources, particularly related to mental health. These need to be accessible, confidential, anonymous and available proactively or in the early stages of a problem or crisis | |
Supporting GP well-being could include:
|
||
| Authentic government support | Ensure government support and commitment to the future of primary care | |
| Relationship with patients, patient responsibility | Enable GPs to offer longer appointment times when necessary. Help manage patient demand and expectations | |
Support provision of continuity of care as this:
|
||
|
Support patients to take more ownership of their own health Improve patients’ knowledge and awareness about when to see a GP and when to see another health professional. Patient education could be formal and irrespective of demand (e.g. teaching children before school leaving age, antenatal education, public health and education programme) |
||
| Introducing a fee system may increase patients’ perception of service value | ||
| Support to patients and appropriate signposting to help them access non-medical services (when appropriate) and to address lifestyle and social circumstances [which currently lead to (inappropriate) consultations with GPs] | ||
| Branding and defining general practice | Create a shared future strategic vision of general practice. This could help to reduce GP uncertainties and anxieties about the future, help manage patient demand and help GPs to feel more in control. Consultants’ expectations of primary care also need to be managed and the GP role clarified | |
| GP pay/remuneration and reward | Short-term incentives are unlikely to be effective in longer term. GPs need to feel ‘fairness’ in their remuneration | |
| Peer support systems and infrastructure | Ensure more support from GP colleagues within the workforce (e.g. between younger and older GPs; part-time and full-time GPs) |
Appendix 24 Tensions and contradictions
General practitioner roles: locum, salaried or partner general practitioner; portfolio careers; part-time versus full-time
It was acknowledged that, within traditional practice models, the requirement for GP partners is essential (especially regarding financial investment and leadership). Existing partners expressed differing feelings about their responsibility to the practice: some enjoyed the remaining autonomy of running a small business, whereas others were frustrated and concerned about the negative impact on their well-being and income from ‘shouldering’ so much responsibility in increasingly difficult times. Being a locum was one route that some GPs took to sustain their role in direct patient care. Tensions between partners and locums were identified, with each feeling that the other sometimes had the ‘better deal’. Partners saw locums as being in a ‘seller’s market’ with the advantages of being able to dictate their own working terms, including payment. They often perceived them as avoiding responsibility and commitment, and shifting the burden on to existing partners. Conversely, locum GPs described the difficulty of their role especially when it came to continuity, in terms of having to learn different systems and how different practices work, a lack of continuity with patients and lack of support from colleagues. The pros and cons of salaried posts were least spoken about.
There were also differences between different age cohorts. Older GPs tended to perceive the younger GPs as choosing to avoid the responsibility of buying into partnerships. This put additional pressure on the current partners, particularly those who were approaching retirement age and had concerns about succession for the practice and patients and receiving return on their long-term investment in the practice. Younger GPs tended to perceive the older GPs as having more control over their workload and a better deal financially (younger GPs described feeling more financially constricted than their older counterparts regarding the costs of personal as well as practice mortgages, and uncertainty about future financial returns). GPs had to navigate working together despite generational differences in career path and preferences for different models of practice.
Participants recognised that working full-time was not sustainable for many GPs; however, part-time working had disadvantages: GPs could not necessarily leave a task to be finished the next day and/or had to delegate to have it completed. Although not considered sustainable for many, participants recognised some benefits of working full-time: particularly related to being able to provide continuity of care for patients and keeping up to date with guidelines. One strategy adopted by several of the GPs was to work full-time but to have a portfolio career (i.e. they did not deliver full-time direct patient care and filled non-direct patient care sessions with other activities that were felt to increase their resilience and overall capacity to remain in direct patient care). Thus, part-time and portfolio GPs may increase their longevity in direct patient care; however, in the short term ‘there are less people to do more work’ (SH1006).
General practitioner health and well-being
Participants recognised, and several had personal experience of, the potential negative impact of the GP role on a GP’s own health and well-being. Support for GPs was required; however, they noted the stigma that exists around GPs accessing help – particularly mental health support – and concerns about confidentiality. Those feeling the most pressure could also be those who would find it the most difficult to take the time to look after their own health/access support.
Expanding the practice team
Participants recognised that a shortage of GPs, and existing GPs already working to full capacity, meant that expanding the practice team was necessary. They also recognised that providing a greater skill mix in primary care was advantageous. However, there were concerns about shortages of other health professionals too (e.g. paramedics, nurses), the implications of diverting these roles into primary care and away from other areas of need, and meeting demand in the long term. Difficult decisions had been made about whether to allocate practice funding to a GP or other health practitioner roles. Some questioned the economy, efficiency and effectiveness of non-GP roles. In some instances, GPs felt more confident with ‘doing it myself’ rather than delegating. Where patients/tasks were allocated to other team members, GPs noted that this could detract from the quality of the GP–patient relationship, there were fewer opportunities for GPs to address and educate patients about (unrealistic) expectations and GPs did not receive the ‘respite’ of having simpler/’easy win’ cases throughout their day. One participant also questioned how the other health professionals felt about being given ‘GPs’ tasks’, especially in relation to salary expectations. Finally, it was noted that expanding the team resulted in GPs becoming ‘primary care consultants’: this could suit some GPs, but not others. Participants identified a need for funding for other team members, and evidence to help them create optimum team roles and structures.
Large versus small practice sizes
Participants noted that size of practice should be driven by local population needs and that ‘one size’ does not fit all. They recognised that practices that were too large could find it difficult to effectively commission services and develop relationships with patients. It was suggested that rural areas (in particular) may need smaller practices. There was a perceived lack of evidence about the benefits of federating practices.
Access to general practitioner services: routes and appointments
Access to GP services and time spent waiting for appointments were noted as being important to patient satisfaction and good-quality care. However, one GP noted that ‘the more accessible you become, the busier you become’ (GP210). Telephone access and triage were extensively discussed. Telephone triage (along with e-mail and other technologies) was recognised as potentially helping to manage/reduce the demand for face-to-face appointments. However, participants described experiences of increased workload and stress resulting from telephone triage, with some questioning the safety of such a high workload and non-face-to-face decisions that had to be made.
Although there was a general call from GPs for longer appointment times, it was recognised that longer appointments would require more GPs (i.e. doubling appointment length would require a doubling of the GP workforce) and more consulting rooms. There were concerns that patients would take up longer appointments, regardless of need.
How practices cope
Although there was a general wish to be proactive, innovative and forward-thinking, participants also recognised the difficulty of this in a ‘crisis’ environment where many GPs feel they are ‘fire-fighting’. Where previously a practice could try out new things, evaluate them and share good practice, this was made difficult by current limitations on time and resources. Some participants noted that any direction and guidance provided to them [e.g. the General Practice Forward View,89 tended to be met with distrust (especially in relation to funding of new initiatives and evidence to support them)].
Appendix 25 Recommendations arising from interviews for policy and strategy content
The findings of this research suggest that initiatives are more likely to be successful if they aim to:
-
clarify the identity of general practice and the role of GPs, and increase perceived fairness, value and job control
-
reduce the levels of fear and risk that GPs are exposed to and called on to manage
-
promote working environments where GPs’ health is fostered and they are empowered to make decisions that are favourable and acceptable to the individual GPs as well as to the profession.
The content of policies should be based on evidence and a clear, honest rationale for their implementation. Long-term commitment to strategies is required, rather than strategies that can be withdrawn or modified as a result of new political environments. A historical perception of funding cuts is seen as ‘the elephant in the room’ and GPs need to be convinced that the widely cited commitment to higher levels of funding will be fulfilled. Mechanisms are needed to ensure that resources that are available to GPs and practices are being utilised and that appropriate recommendations can be acted on.
A multilayered and joined-up approach is required, with consideration of the pros and cons of any policies and strategies to be implemented. Specific ideas that could be considered include those listed below.
Individual level:
-
support GPs to have flexible working and career development choices
-
provide access to personalised support and advice for those considering leaving/not returning
-
provide and actively encourage access to supportive mechanisms and resources to help GPs maintain their own good health and well-being.
Practice level:
-
provide support and evidence – to determine optimum practice size and on widening of the practice team, and about different workload management approaches (including telephone triage and new technologies)
-
enable practices to have appropriate administrative support
-
provide training and support for GPs in business and HR issues
-
provide (formal and informal) peer support initiatives and opportunities within the workplace.
Organisational level:
-
increase funding and commitment to primary care
-
create a shared future strategic vision of general practice
-
provide clarification of, and evidence for, new models of care
-
improve relationships between, and clarify responsibilities of, primary and secondary care
-
review GP indemnity and consider introduction of Crown Indemnity
-
simplify and streamline return-to-work processes
-
redesign the appraisals and revalidation processes to make them more supportive and less onerous
-
provide occupational health resources to GPs, including support for physical and mental well-being
-
provide initiatives to help address patient expectations and educate patients around self-management.
Recommendations for future research
Further review of occupational and workplace literature is recommended (considered in the specific context of general-practice-based primary care), alongside knowledge obtained from GP workforce studies, to ensure that policies and strategies are informed by relevant theories and understanding. Further research into interventions that support GPs’ positive mental well-being would also be of value. In addition, reviewing and sharing evidence and good-practice examples of how general practices organise and deliver care would be beneficial.
Appendix 26 The RAM panel information sheet
Appendix 27 Breakdown of potential policies and strategies as presented to the RAM panel
| Policies and strategies presented as statements | Feasibility ratings? |
|---|---|
| Risk status assessment using different approaches (assess ‘at-risk’ status in a commissioning/planning area while taking into account confidentiality) | |
| Section 1. Set 1. Assessment at GP level | |
|
1. GPs should be required to provide ‘intention-to-quit’ information regularly to assess areas ‘at risk’ |
N |
|
2. GPs should be required to complete job satisfaction surveys (or equivalents) regularly to assess areas ‘at risk’ |
N |
|
3. General practices should be required to register their organisation’s at-risk status |
N |
|
4. General practices should be able to self-register their organisation’s ‘at-risk’ status |
N (but met criteria in R2) |
|
5. There should be regular audits to identify general practices ‘at risk’ |
N |
| Section 1. Set 2. Supporting those identified as at risk at practice | |
|
1. Targeted with additional support and incentives |
N |
|
2. Provided with a toolkit to manage recruitment and retention |
N (but met criteria in R2) |
|
3. Prioritised for new/innovative national schemes to support GP retention and/or return to work |
N |
|
4. Managed with an appropriate and sensitive supportive arrangement (subgroup: compulsory/optional) |
Y |
|
5. Allocated a specialist team for managing recruitment and retention (subgroup: compulsory/optional) |
Y |
| Section 2. Set 1. Encouraging growth of new general practices and systems | |
|
1. New incentive and support packages should be available to GPs and other organisations setting up new practices or new ways of working in under-doctored areas |
Y |
|
2. New arrangements should be developed so that GPs can become more involved in general practice management without being partners |
N |
|
3. New business models should be developed for GPs who wish to provide care within the NHS but prefer not to own a general practice |
N |
| Section 2. Set 2. Encouraging growth of new general practices and systems | |
|
1. There should be incentive and support packages for not-for-profit organisations employing GPs to work across general practices |
N |
|
2. Hospitals should be permitted to open general practices with registered lists (subgroup: all areas/in traditionally ‘hard-to-recruit’ settings) |
N |
| Section 3. Set 1. Marketing-based interventions | |
|
1. There should be a publicity campaign highlighting the experiences of GPs who have successfully been retained in direct patient care as part of a marketing-based intervention aimed at GPs |
N |
|
2. The positive experiences of GPs who are providing direct patient care should be consistently shared in a number of ways such as blogs and articles as part of a marketing-based intervention aimed at GPs |
N |
| Section 3. Set 2. Marketing-based interventions | |
|
1. There should be a publicity campaign focusing on managing expectations of patients in line with the resources and constraints of GP-based primary care services |
Y |
| Policies and strategies presented as statements | Feasibility ratings? |
|---|---|
| Section 4. Set 1. Making it easier for GP returners | |
|
1. GPs who are returning to work after a period of absence or after a career break should have access to ‘health and well-being programmes’ to help them manage their re-entry into the workforce (subgroup: compulsory/optional) |
Y |
|
2. Access to a range of routes and options that can be combined in a personal package for re-entry |
Y |
|
3. Access to a mix of online education and face-to-face meetings to ensure timely access to induction and refresher courses |
Y |
| Section 5. Set 1. Flexible working and managed exits | |
|
1. General practices should have systems in place to accommodate flexible ways of working |
N |
|
2. General practices should be able to demonstrate commitment to flexible ways of working through written HR policies, guidelines or equivalents |
N |
|
3. HR management support should be available to general practices who are actively supporting GPs in combining other career interests with direct patient care |
N |
| Section 5. Set 2. Flexible working and managed exits | |
|
1. General practices should receive guidance on recommended approaches to supporting the staged exit of GPs who are looking to leave direct patient care |
N |
|
2. General practices should receive a toolkit on recommended approaches to supporting the staged exit of GPs who are looking to leave direct patient care |
N |
|
3. General practices should implement strategically planned exits for retiring GPs |
N (but met criteria in R2) |
| Section 6. Set 1. HR management for GPs | |
|
1. HR responsibilities should be carried out externally to the employer/practice with responsibility and applied for different subgroups and situations (subgroup: all areas/in traditionally ‘hard-to-recruit’ settings) |
|
|
2. Ongoing monitoring of how many GPs within an area have requested and successfully implemented flexible working arrangements |
N |
|
3. Managing flexible working arrangements for GPs |
N |
|
4. All activities associated with retention of GPs |
N |
|
5. All activities associated with professional development and training |
N |
|
6. Implementing standards for working hours and conditions |
N |
| Policies and strategies presented as statements | Feasibility ratings? |
|---|---|
| Section 7. Set 1. Health and well-being (subgroup: all GPs/reaching retirement age and could take their pensions on exit/who are not reaching retirement age and cannot take their pension on exit) | |
|
1. Peer support initiatives should be made available to GPs aimed specifically at health and well-being |
Y |
| Section 7. Set 2. Health and well-being (subgroup: all GPs/reaching retirement age and could take their pensions on exit/who are not reaching retirement age and cannot take their pension on exit) | |
|
1. GPs should have access to their own specialised health-care service to ensure a quick and confidential occupational health-care service |
Y |
|
2. GPs should have access to their own specialised health-care service to ensure a quick and confidential general health service |
N |
| Section 8. Set 1. Professional support (applied to all GPs and subgroup: compulsory/optional) | |
|
1. A structured programme of training and support should be made available to all GPs in their first 5 years following qualification as an independent GP to help them establish healthy, productive careers |
Y |
| Section 8. Set 2. professional support (subgroup: all GPs/reaching retirement age and could take their pensions on exit/who are not reaching retirement age and cannot take their pension on exit) | |
|
1. GPs should receive business management training and opportunities as a component of updating their skill sets |
N |
|
2. Clinical mentorship should be available to GPs as part of a nationally managed scheme |
N |
|
Section 9. Set 1. Support for portfolio working Portfolio working includes activities such as medical/NHS management, medical education, research/academia, charitable medical work, commissioning, private sector, clinical informatics, and following additional training routes (subgroup: all GPs (A)/reaching retirement age and could take their pensions on exit (B)/who are not reaching retirement age and cannot take their pension on exit) (C) |
|
|
1. GPs should consider portfolio working as part of their career pathway (subgroup: compulsory/optional) |
Y (only for subgroup C) |
|
2. Career support should be available to GPs to enable portfolio opportunities to be identified and taken up in a strategic way to inform their future ambitions |
N (but met criteria in R2) |
|
3. Incentives and support packages should be available for those GPs developing portfolio careers who are making a substantial contribution to direct patient care |
N |
|
4. Incentives and support packages should be available for those GPs developing portfolio careers who are linking their portfolio activities to specialisms/areas that are directly beneficial to local clinical priorities |
Y |
| Section 10. Set 1. Employment, contracts and transition (subgroup: all GPs (A)/reaching retirement age and could take their pensions on exit (B)/who are not reaching retirement age and cannot take their pension on exit) (C) | |
|
1. Where a strong case can be made that there is a financial risk directly relating to the work of the practice (e.g. ownership of premises), GPs should have access to schemes to reduce financial burden (e.g. buy-back schemes for premises) |
Y (only for subgroup A) |
| Section 10. Set 2. Employment, contracts and transition (subgroup: all GPs/reaching retirement age and could take their pensions on exit/who are not reaching retirement age and cannot take their pension on exit) | |
|
1. GPs should be expected to include regular supervision/mentoring sessions as part of their normal professional activity |
N |
| Section 10. Set 3. Employment, contracts and transition (subgroup: all GPs/reaching retirement age and could take their pensions on exit/who are not reaching retirement age and cannot take their pension on exit) | |
|
1. There should be an agreed maximum in the number of consultations that a GP should be allowed to conduct in a working day in order to protect patient safety as well as the health of the GP |
Y |
|
2. There should be contractual changes to encourage longer consultations where appropriate |
Y |
|
3. The working hours of GPs should routinely include fully-funded, dedicated time to accommodate the full range of roles (administrative, clinical, training, management, CPD, business) undertaken as part of care professional activity |
Y |
|
4. Contracts based on specified programmed activities should be available to GPs to work across several general practices and on other health-related activities |
Y (for subgroups A and B only) |
| Section 11. Set 1. Additional support for GPs who are reaching retirement age and could take their pensions on exit | |
|
1. A comprehensive flexible careers scheme should be introduced with a view to supporting annualised hours, part-time working, and/or ad-hoc contributions to direct patient care |
Y |
|
2. There should be financial incentives for such GPs who have maintained a prolonged/sustained period of direct patient care |
N (but met criteria in R2) |
| Section 11. Set 2. Additional support for GPs who are reaching retirement age and could take their pensions on exit | |
|
1. The annual appraisal and revalidation process for such GPs should be reviewed with a view to streamlining and simplifying the process (all GPs/GPs who have not encountered any concerns in the previous revalidation/appraisal processes/for such GPs who would like to work with a specified and limited scope of practice) |
Y |
| Section 11. Set 3. Additional support for GPs who are reaching retirement age and could take their pensions on exit | |
|
1. Such GPs should be eligible for and offered support to facilitate direct patient care including additional dedicated administrative support |
N |
|
2. Such GPs should be eligible for and offered support to facilitate direct patient care including medical assistants and other equivalent roles |
N |
|
3. Where appropriate, planned exits for such GPs should include pairing them in job share schemes (GPs returning to practice/with newly qualified GPs) |
N |
Appendix 28 Potential policies and strategies rated as uncertain or without consensus for any statement within a specified area
Policy and strategy 25
In order to assess ‘at-risk’ status in a commissioning/planning area and taking into account confidentiality, GPs should be required to provide ‘intention-to-quit’ information regularly to assess areas ‘at-risk’.
Policy and strategy 26
In order to assess ‘at-risk’ status in a commissioning/planning area and taking into account confidentiality, GPs should be required to complete job satisfaction surveys (or equivalents) regularly to assess areas ‘at-risk’.
Policy and strategy 27
In order to assess ‘at-risk’ status in a commissioning/planning area and taking into account confidentiality, general practices should be required to register their organisation’s at-risk status.
Policy and strategy 28
In order to assess ‘at-risk’ status in a commissioning/planning area and taking into account confidentiality, there should be regular audits to identify general practices ‘at-risk’.
Policy and strategy 29
General practices identified as being ‘at-risk’ should be targeted with additional support and incentives.
Policy and strategy 30
General practices identified as being ‘at-risk’ should be prioritised for new/innovative national schemes to support GP retention and/or return to work.
Policy and strategy 31
New arrangements should be developed so that GPs can become more involved in general practice management without being partners.
Policy and strategy 32
New business models should be developed for GPs who wish to provide care within the NHS but prefer not to own a general practice.
Policy and strategy 33
There should be incentive and support packages for not-for-profit organisations employing GPs to work across general practices.
Policy and strategy 34
Hospitals should be permitted to open general practices with registered lists (all areas or specifically in traditionally ‘hard-to-recruit’ areas).
Policy and strategy 35
There should be a publicity campaign highlighting the experiences of GPs who have successfully been retained in direct patient care as part of a marketing-based intervention aimed at GPs.
Policy and strategy 36
The positive experiences of GPs who are providing direct patient care should be consistently shared in a number of ways such as blogs and articles as part of a marketing-based intervention aimed at GPs.
General practice level
Policy and strategy 37
General practices should have systems in place to accommodate flexible ways of working.
Policy and strategy 38
General practices should be able to demonstrate commitment to flexible ways of working through written HR policies, guidelines or equivalents.
Policy and strategy 39
Human resources management support should be available to general practices who are actively supporting GPs in combining other career interests with direct patient care.
Policy and strategy 40
General practices should receive guidance on recommended approaches to supporting the staged exit of GPs who are looking to leave direct patient care.
Policy and strategy 41
General practices should receive a toolkit on recommended approaches to supporting the staged exit of GPs who are looking to leave direct patient care.
Policy and strategy 42
Human resources responsibilities should be carried out externally to the employer/practice with responsibility for ongoing monitoring of how many GPs within an area have requested and successfully implemented flexible working arrangements.
Policy and strategy 43
Human resources responsibilities should be carried out externally to the employer/practice with responsibility for managing flexible working arrangements for GPs.
Policy and strategy 44
Human resources responsibilities should be carried out externally to the employer/practice with responsibility for all activities associated with retention of GPs.
Policy and strategy 45
Human resources responsibilities should be carried out externally to the employer/practice with responsibility for all activities associated with professional development and training.
Policy and strategy 46
Human resources responsibilities should be carried out externally to the employer/practice with responsibility for implementing standards for working hours and conditions.
General practitioner level
Policy and strategy 47
General practitioners should have access to their own specialised health-care service to ensure a quick and confidential general health service.
Policy and strategy 48
General practitioners should receive business management training and opportunities as a component of updating their skill sets.
Policy and strategy 49
Clinical mentorship should be available to GPs as part of a nationally managed scheme.
Policy and strategy 50
Incentives and support packages should be available for those GPs developing portfolio careers who are making a substantial contribution to direct patient care.
Policy and strategy 51
General practitioners should be expected to include regular supervision/mentoring sessions as part of their normal professional activity.
Policy and strategy 52
General practitioners who are reaching retirement age and could take their pensions on exit should be eligible for and offered support to facilitate direct patient care including additional dedicated administrative support.
Policy and strategy 53
General practitioners who are reaching retirement age and could take their pensions on exit should be eligible for and offered support to facilitate direct patient care including medical assistants and other equivalent roles.
Policy and strategy 54
General practitioners who are reaching retirement age and could take their pensions on exit and where appropriate, planned exits for such GPs should include pairing them in job share scheme with GPs returning to practice or with newly qualified GPs.
Appendix 29 Data flow for predictive risk modelling work
FIGURE 14.
Data flow for predictive risk modelling work.
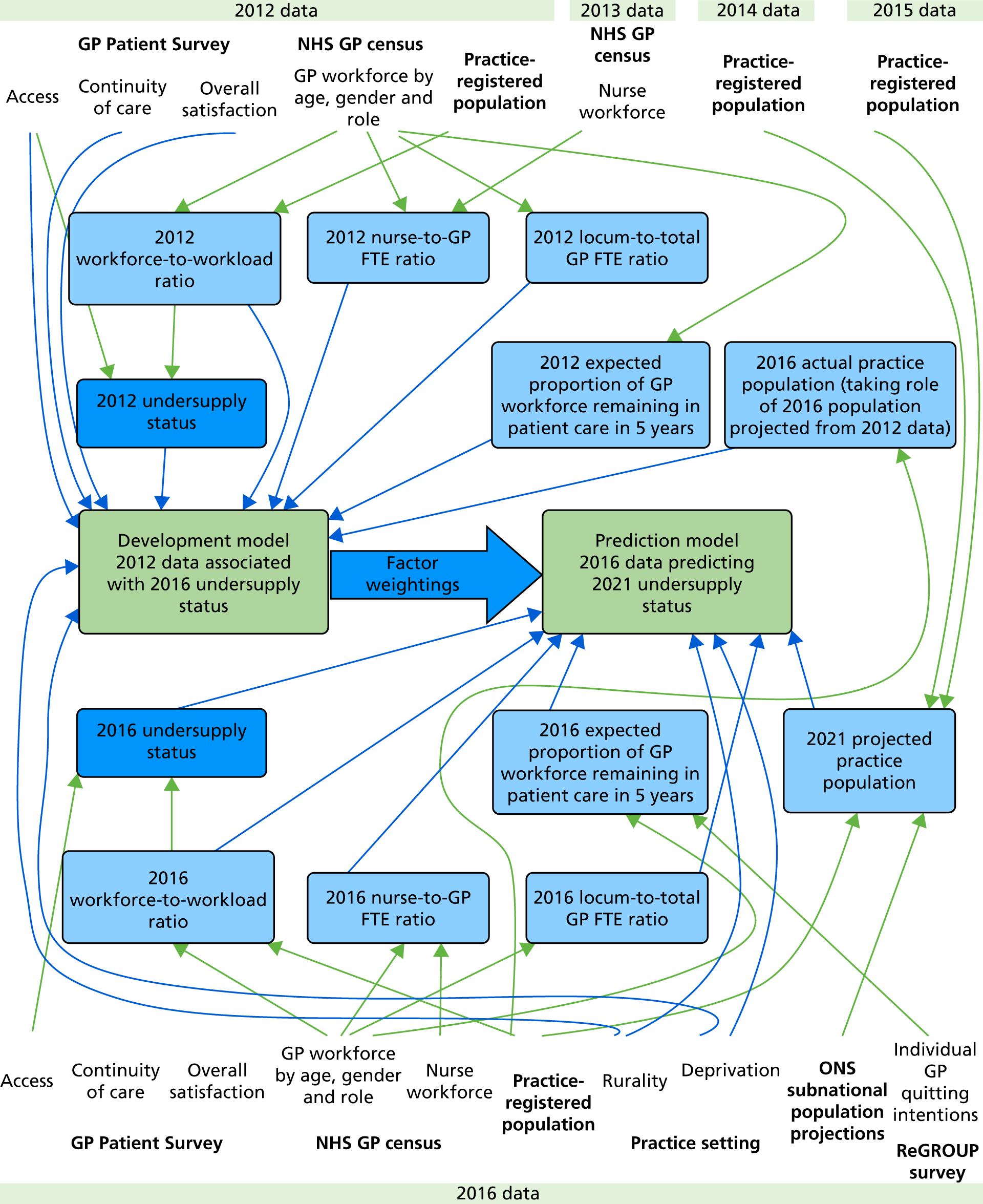
Appendix 30 GP Patient Survey questions and response options
For patients’ experiences of access, the following question was used:
Last time you wanted to see or speak to a GP or nurse from your GP surgery: were you able to get an appointment to see or speak to someone?
Responses of ‘yes’ and ‘yes, but I had to call back closer to or on the day I wanted the appointment’ were coded as a positive response and responses of ‘no’ were coded as a negative response. Responses of ‘can’t remember’ were treated as uninformative and excluded from the analysis.
The item on ability to see a preferred doctor is taken as a proxy measure for continuity of care:
How often do you see or speak to the GP you prefer?
Responses of ‘always or almost always’ and ‘a lot of the time’ were coded as a positive response and responses of ‘some of the time’ and ‘never or almost never’ were coded as a negative response. Responses of ‘not tried at this GP surgery’ were treated as uninformative and excluded from the analysis.
Finally, an item capturing data on the patient’s overall experience of care was included:
Overall, how would you describe your experience of your GP surgery?
Responses of ‘very good’ and ‘fairly good’ were coded as a positive response and responses of ‘neither good nor poor’, ‘fairly poor’ and ‘very poor’ were coded as a negative response. There were no uninformative options for this question.
Appendix 31 Projecting future workload
Our projections of future practice workloads were based on the number of patients registered at each of the 423 general practices in south-west England, in 5-year age bands, split by gender combined with subnational population projections from the ONS as described in Chapter 6. The approach comprises the following five steps.
-
Assess congruency of ONS predictions with list size (Figure 15). ONS subnational population projections were compared with GP list size data aggregated to CCG level for 2014, 2015 and 2016. This provided an assessment of the degree to which ONS predications reflect the actual GP list size data in those years. An example comparison is shown below, where it can be seen that although the practice population data indicates a higher population than the ONS projections, variably by age group, the difference between practice population data and ONS projections is stable over time. This difference between the two data sources is most likely to be attributable to ‘list inflation’, caused by patients who have not been removed from the list following death, dual registrations for patients when moving homes or by a registered patient’s failure to complete the national census. 173 Given that the average consultation times used to weight the populations are based on registered patients, we did not consider it appropriate to resize practice list sizes to reflect the identified difference.
-
Calculate the proportion of the CCG population registered at each general practice. For each practice, and for each age-band-by-gender stratum, we identified the number of patients registered with the practice and the expected number of patients within a CCG for nine time points between April 2014 and April 2016. This allowed us to derive the proportion of the total CCG population by gender/age interval registered at each practice. If the number of practices in a CCG is declining over time, we might expect the proportion of the CCG to be rising at the remaining practices.
-
Quantify trends in the proportion of the CCG population registered at each general practice. The data from step 2 were used as the outcome variable in a logistic regression model that included a linear term for time as well as a categorical variable for quarter to quantify trends. A separate regression model was used for each practice-by-age-band by gender stratum.
-
Determine the projected count of patients. We used the resultant regression equation to predict the proportion of CCG patients by practice/gender/age-interval for 5 years beyond the final data point. Multiplying this proportion by the ONS predicted population for the same time point gives a projected count of patients.
-
Project adjusted list size. The projected populations were used to create a projected adjusted weighted list size using the same algorithm used above for observed populations.
Appendix 32 Predicting remaining future workforce
When predicting future workforce (supply), we concentrated on predicting what fraction of the existing workforce will remain available to the practice in 5 years’ time. We did this in two principal ways: (1) based on the age and gender of GPs at the practice and (2) based on responses to the ReGROUP survey. Predictions are made based on 2012 data and 2016 data (with the survey being available only for the 2016 data).
Approach 1: using the age and gender profile of general practitioners at each practice
Previous work has identified the probability that GPs of a given single year of age and gender will remain in the workforce 12 months later. 1 By multiplying these probabilities over five consecutive single-year age bands, we obtain the probability that GPs of a given single year of age and gender will remain in the workforce in 5 years’ time. As the routinely available GP census data is available only in five-year age bands, we take the mean of these 5-year probabilities over the 5-year age bands used in the GP census data. Unfortunately, the GP census data published at practice level give data by either age or gender, but not both. Furthermore, data by age are given only in terms of headcount, as are data by gender in 2012 (data by gender are given in terms of headcount and FTE in 2016). Thus, we adopted the following procedure to estimate remaining workforce:
-
Using the probabilities described above, identify the probability that each GP in the practice will remain in patient care in 5 years’ time based on their age band, assuming that they are male.
-
Calculate the mean of these probabilities over all GPs in the practice.
-
Repeat steps 1 and 2, assuming that GPs are female.
-
Take a weighted average of the probabilities obtained in steps 2 and 3 weighted by the FTE of male and female GPs in the practice (in 2012 data headcount by gender is used instead).
The resulting probabilities can then be interpreted as the proportion of FTE GPs who are expected, on average, to remain at the practice in 5 years’ time.
Approach 2: using the ReGROUP survey responses.
An alternative approach used in the forecasting utilised the results of the ReGROUP survey where all GPs in south-west England were asked about their future career intentions. For GPs who responded to the survey (67%), we used both stated career intentions, stated FTE (as described above), and information on age and gender. For non-responders, we simply used age and gender information (provided within the National Performers List). To incorporate the survey responses, we made use of ORs estimated from a previous study, which linked stated quit intentions to working status 5 years later and adjusted for age and gender. 59 ORs for their 5-point scale are mapped to our 4-point scale by ignoring the middle (neutral) option.
-
It proved difficult to map the ReGROUP survey responses to the NHS GP census data (owing to inconsistent age, gender and FTE information between the two data sources). Therefore, in this methodology, the GP census data are used only in the estimation of FTE of survey non-responders based on difference between the total GP FTE (GP census data) and the total FTE stated by responders linked to each practice within the National Performers List. This was done using the following method. We calculated the difference between the total GP FTE given in the GP census data and the stated total GP FTE of responders to the survey linked through the National Performers List to each practice in the study. The assumed that the FTE of non-responders was this difference divided by the number of non-responders linked to the practice. Where this difference was greater than the number of FTEs, the non-responders were assigned a FTE of 1. Where this difference was negative non-responders were assigned an FTE of 0.
-
We then calculated the probabilities of remaining in patient care for the forthcoming 5 years. For the survey non-responders, we assigned a probability of remaining in patient care using the same method as in approach 1 but based on the individual GP’s gender and current year of age taken from the National Performers List (rather than the GP census). For responders, we similarly assigned a probability of remaining in patient care based on the individual GP’s age and gender and then adjusted that probability using the following ORs (calculated from Hann et al. 59 but changing the baseline to the neutral category): ‘Very likely’ 1.94, ‘Likely’ 1.3, ‘Unlikely’ 0.70 and ‘Very unlikely’ 0.43.
-
For each practice, we then took the weighted average of the probabilities obtained in step 2 (over GPs associated with a practice, weighted in accordance with their FTE).
The resulting probabilities can then be interpreted as the proportion of FTE GPs who would be expected, on average, to remain at the practice in 5 years’ time.
Appendix 33 Calculating adjusted weighted list sizes
The April 2012 and April 2016 data sets were used to calculate list sizes weighted for the demographics of the populations and adjusted for deprivation. The reason for weighting for patient demographics is that certain types of patients (older, female and very young) place a higher demand on practices than others. The adjustment for deprivation acknowledges that deprived populations have higher health needs than less deprived populations with a similar demographic profile. To calculate weighted list sizes, the practice populations were weighted in accordance with the average time spent consulting with patients in 14 age-by-gender groups in 2013/14, in accordance with a recent study based on routine patient records from 674 practices. 133 Weighted lists sizes (PW) were then normalised so that the total population across the country remained unchanged. These weighted list sizes are taken as a measure of workload on the basis that they represent a measure of the expected time spent consulting. This assumes that, on average, patients in the same demographic group require the same amount of consultation time. Because age and gender do not capture the health status of the population, the weighted list sizes were then adjusted for deprivation (IMD decile, IMDi, taking a value between 1 and 10, based on all practices in England) assigning a 10% weighting to a deprived population. The adjusted weighted population will thus be given by:
This approach is intended to mirror that used in the current resource allocation to CCGs. However, the CCG allocations do not use deprivation, but rather make use of a measure of premature mortality (the < 75 standardised mortality ratio, which is the ratio of mortality in under 75-year-olds to that expected given the age and gender composition of the CCG population). We chose to use deprivation here as standardised mortality ratios are not published for individual practices.
Appendix 34 Rationale for the use of the interaction between the ratio of total nurse full-time equivalent to total general practitioner full-time equivalent and the expected proportion of general practitioner full-time equivalents remaining in patient care in the predictive risk model
We recognised the need to account for the fact that GPs leaving patient care would be most likely to affect the supply–demand balance when recruitment of staff is difficult. We were unable to obtain any direct measure of the difficulty any one practice has in recruitment and so instead we explored the use of three proxy measures:
-
the use of locums (operationalised as the proportion of total GP FTE falling in the ‘other’ category using NHS workforce data) on the basis that practices are likely to make greater use of locums when they are struggling to recruit partners or salaried GPs
-
patient access (using GPPS scores) on the basis that when there is a prolonged period in which a practice is understaffed access may be compromised
-
the use of nurses (operationalised as the ratio of total nurse FTE to total GP FTE using NHS workforce data) on the basis that practices who struggle long term to recruit GPs may pass greater amounts of patient care on to nurses to maximise use of GP resource.
In an exploratory analysis, an interaction between the expected proportion of the GP workforce remaining in patient care after 5 years and each of the identified proxy measures (use of locums, access, use of nurses) individually were included in the predictive model in turn. There was no evidence that either locum use or access modified the effect, in the model, of the expected proportion of the GP workforce remaining in patient care. However, there was weak evidence that the use of nurses did modify the effect of the expected proportion of the GP workforce remaining in patient care. This interaction was, therefore, retained in the final model.
Appendix 35 Stress test scenario results
| Practice characteristic | Undersupply (N = 96) | Other (N = 288) | p-valuea | ||||
|---|---|---|---|---|---|---|---|
| Median | 25% | 75% | Median | 25% | 75% | ||
| List size | 10,158 | 7561 | 12,959 | 6873 | 4880 | 10,116 | < 0.001 |
| Adjusted weighted list size | 10,597 | 7545 | 13,041 | 7349 | 5145 | 10,601 | < 0.001 |
| GP FTE | 5 | 3 | 6.5 | 4.4 | 3.1 | 6.6 | 0.942 |
| Ratio nurse/GP FTE | 0.8 | 0.6 | 1 | 0.4 | 0.4 | 0.6 | < 0.001 |
| IMD | 26.1 | 18.7 | 32.3 | 17.6 | 13.1 | 22.3 | < 0.001 |
| GPPS accessb | 0.3 | 0.2 | 0.5 | 0.8 | 0.6 | 0.9 | < 0.001 |
| GPPS continuityb | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| GPPS satisfactionb | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| % aged > 65 years | 19.1 | 14.4 | 23.4 | 23.3 | 18.5 | 26.5 | < 0.001 |
| CCG areas | n (%) | n (%) | p-valuec | ||||
| Bath and North East Somerset | 4 (14.8) | 23 (85.2) | 0.002 | ||||
| Bristol | 20 (44.4) | 25 (55.6) | |||||
| Kernow | 13 (22) | 46 (78) | |||||
| North Somerset | 10 (50) | 10 (50) | |||||
| Somerset | 17 (23.9) | 54 (76.1) | |||||
| South Gloucestershire | 7 (30.4) | 16 (69.6) | |||||
| Northern, Eastern and Western Devon | 15 (13.8) | 94 (86.2) | |||||
| South Devon and Torbay | 10 (33.3) | 20 (66.7) | |||||
| Urban practices | 81 (31.5) | 176 (68.5) | < 0.001 | ||||
| Rural practices | 15 (11.8) | 112 (88.2) | |||||
| Practice characteristic | Undersupply (N = 96) | Other (N = 288) | p-valueb | ||||
|---|---|---|---|---|---|---|---|
| Median | 25% | 75% | Median | 25% | 75% | ||
| List size | 9648 | 6996 | 12,688 | 6957 | 4941 | 10,327 | < 0.001 |
| Adjusted weighted list size | 10,355 | 7285 | 13,041 | 7424 | 5251 | 10,659 | < 0.001 |
| GP FTE | 4.8 | 3 | 6.1 | 4.6 | 3.1 | 6.7 | 0.662 |
| Ratio nurse/GP FTE | 0.8 | 0.5 | 1.1 | 0.4 | 0.3 | 0.6 | < 0.001 |
| IMD | 25.7 | 18.7 | 31.9 | 17.7 | 13.1 | 22.3 | < 0.001 |
| GPPS accessc | 0.4 | 0.2 | 0.6 | 0.8 | 0.6 | 0.9 | < 0.001 |
| GPPS continuityc | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| GPPS satisfactionc | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| % aged > 65 years | 18.9 | 14.7 | 24 | 23.1 | 18.5 | 26.2 | < 0.001 |
| CCG areas | n (%) | n (%) | p-valued | ||||
| Bath and North East Somerset | 4 (14.8) | 23 (85.2) | 0.003 | ||||
| Bristol | 19 (42.2) | 26 (57.8) | |||||
| Kernow | 13 (22) | 46 (78) | |||||
| North Somerset | 10 (50) | 10 (50) | |||||
| Somerset | 16 (22.5) | 55 (77.5) | |||||
| South Gloucestershire | 7 (30.4) | 16 (69.6) | |||||
| Northern, Eastern and Western Devon | 17 (15.6) | 92 (84.4) | |||||
| South Devon and Torbay | 10 (33.3) | 20 (66.7) | |||||
| Urban practices | 78 (30.4) | 179 (69.6) | < 0.001 | ||||
| Rural practices | 18 (14.2) | 109 (85.8) | |||||
| Practice characteristic | Undersupply (N = 96) | Other (N = 288) | p-valueb | ||||
|---|---|---|---|---|---|---|---|
| Median | 25% | 75% | Median | 25% | 75% | ||
| List size | 9449 | 6651 | 12,768 | 6976 | 4985 | 10,375 | < 0.001 |
| Adjusted weighted list size | 10,061 | 6824 | 13,088 | 7437 | 5468 | 10,717 | < 0.001 |
| GP FTE | 4.8 | 2.8 | 6.1 | 4.6 | 3.1 | 6.6 | 0.464 |
| Ratio nurse/GP FTE | 0.7 | 0.5 | 1.1 | 0.4 | 0.3 | 0.6 | < 0.001 |
| IMD | 25.7 | 18.9 | 31.7 | 17.7 | 13.1 | 22.3 | < 0.001 |
| GPPS accessc | 0.4 | 0.2 | 0.7 | 0.8 | 0.6 | 0.9 | < 0.001 |
| GPPS continuityc | 0.3 | 0.2 | 0.6 | 0.7 | 0.5 | 0.8 | < 0.001 |
| GPPS satisfactionc | 0.3 | 0.2 | 0.6 | 0.7 | 0.5 | 0.8 | < 0.001 |
| % aged > 65 years | 18.9 | 14.4 | 24.3 | 23.1 | 18.5 | 26.2 | < 0.001 |
| CCG areas | n (%) | n (%) | p-valued | ||||
| Bath and North East Somerset | 3 (11.1) | 24 (88.9) | 0.001 | ||||
| Bristol | 19 (42.2) | 26 (57.8) | |||||
| Kernow | 13 (22) | 46 (78) | |||||
| North Somerset | 10 (50) | 10 (50) | |||||
| Somerset | 15 (21.1) | 56 (78.9) | |||||
| South Gloucestershire | 7 (30.4) | 16 (69.6) | |||||
| Northern, Eastern and Western Devon | 18 (16.5) | 91 (83.5) | |||||
| South Devon and Torbay | 11 (36.7) | 19 (63.3) | |||||
| Urban practices | 79 (30.7) | 178 (69.3) | < 0.001 | ||||
| Rural practices | 17 (13.4) | 110 (86.6) | |||||
| Practice characteristic | Undersupply (N = 96) | Other (N = 288) | p-valueb | ||||
|---|---|---|---|---|---|---|---|
| Median | 25% | 75% | Median | 25% | 75% | ||
| Adjusted weighted list size | 10,586 | 7856 | 12,959 | 6862 | 4880 | 10,061 | < 0.001 |
| GP FTE | 10,987 | 7799 | 13,088 | 7316 | 5145 | 10,519 | < 0.001 |
| Ratio nurse/GP FTE | 5.1 | 3.1 | 6.6 | 4.4 | 3 | 6.6 | 0.318 |
| IMD | 0.8 | 0.5 | 1 | 0.4 | 0.3 | 0.6 | < 0.001 |
| GPPS accessc | 25.7 | 18.9 | 31.9 | 17.6 | 13.1 | 22.2 | < 0.001 |
| GPPS continuityc | 0.3 | 0.2 | 0.6 | 0.8 | 0.6 | 0.9 | < 0.001 |
| GPPS satisfactionc | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| % aged > 65 years | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| CCG areas | n (%) | n (%) | p-valued | ||||
| Bath and North East Somerset | 4 (14.8) | 23 (85.2) | < 0.001 | ||||
| Bristol | 20 (44.4) | 25 (55.6) | |||||
| Kernow | 13 (22) | 46 (78) | |||||
| North Somerset | 10 (50) | 10 (50) | |||||
| Somerset | 18 (25.4) | 53 (74.6) | |||||
| South Gloucestershire | 7 (30.4) | 16 (69.6) | |||||
| Northern, Eastern and Western Devon | 15 (13.8) | 94 (86.2) | |||||
| South Devon and Torbay | 9 (30) | 21 (70) | |||||
| Urban practices | 80 (31.1) | 177 (68.9) | < 0.001 | ||||
| Rural practices | 16 (12.6) | 111 (87.4) | |||||
| Practice characteristic | Undersupply (N = 96) | Other (N = 288) | p-valueb | ||||
|---|---|---|---|---|---|---|---|
| Median | 25% | 75% | Median | 25% | 75% | ||
| Adjusted weighted list size | 11,064 | 8178 | 13,547 | 6731 | 4802 | 9755 | < 0.001 |
| GP FTE | 11,544 | 8462 | 14,319 | 7234 | 4992 | 10,113 | < 0.001 |
| Ratio nurse/GP FTE | 5.3 | 3.6 | 7 | 4.3 | 3 | 6.4 | 0.014 |
| IMD | 0.7 | 0.5 | 1 | 0.4 | 0.3 | 0.6 | < 0.001 |
| GPPS accessc | 25 | 18.1 | 31.3 | 17.7 | 13.1 | 22.8 | < 0.001 |
| GPPS continuityc | 0.3 | 0.2 | 0.6 | 0.8 | 0.6 | 0.9 | < 0.001 |
| GPPS satisfactionc | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| % aged > 65 years | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| CCG areas | n (%) | n (%) | p-valued | ||||
| Bath and North East Somerset | 4 (14.8) | 23 (85.2) | < 0.001 | ||||
| Bristol | 19 (42.2) | 26 (57.8) | |||||
| Kernow | 14 (23.7) | 45 (76.3) | |||||
| North Somerset | 10 (50) | 10 (50) | |||||
| Somerset | 18 (25.4) | 53 (74.6) | |||||
| South Gloucestershire | 8 (34.8) | 15 (65.2) | |||||
| Northern, Eastern and Western Devon | 14 (12.8) | 95 (87.2) | |||||
| South Devon and Torbay | 9 (30) | 21 (70) | |||||
| Urban practices | 80 (31.1) | 177 (68.9) | < 0.001 | ||||
| Rural practices | 16 (12.6) | 111 (87.4) | |||||
| Practice characteristic | Undersupply (N = 96) | Other (N = 288) | p-valueb | ||||
|---|---|---|---|---|---|---|---|
| Median | 25% | 75% | Median | 25% | 75% | ||
| Adjusted weighted list size | 10,586 | 7595 | 13,195 | 6862 | 4880 | 10,061 | < 0.001 |
| GP FTE | 10,987 | 7799 | 13,698 | 7316 | 5145 | 10,519 | < 0.001 |
| Ratio nurse/GP FTE | 5 | 3.2 | 6.6 | 4.4 | 3 | 6.6 | 0.339 |
| IMD | 0.8 | 0.6 | 1.1 | 0.4 | 0.3 | 0.6 | < 0.001 |
| GPPS accessc | 25.7 | 19.2 | 31.8 | 17.6 | 13.1 | 22.4 | < 0.001 |
| GPPS continuityc | 0.4 | 0.2 | 0.6 | 0.8 | 0.6 | 0.9 | < 0.001 |
| GPPS satisfactionc | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.001 |
| % aged > 65 years | 0.3 | 0.2 | 0.5 | 0.7 | 0.5 | 0.9 | < 0.01 |
| CCG areas | n (%) | n (%) | p-valued | ||||
| Bath and North East Somerset | 4 (14.8) | 23 (85.2) | 0.002 | ||||
| Bristol | 18 (40) | 27 (60) | |||||
| Kernow | 15 (25.4) | 44 (74.6) | |||||
| North Somerset | 10 (50) | 10 (50) | |||||
| Somerset | 17 (23.9) | 54 (76.1) | |||||
| South Gloucestershire | 7 (30.4) | 16 (69.6) | |||||
| Northern, Eastern and Western Devon | 15 (13.8) | 94 (86.2) | |||||
| South Devon and Torbay | 10 (33.3) | 20 (66.7) | |||||
| Urban practices | 77 (30) | 180 (70) | 0.002 | ||||
| Rural practices | 19 (15) | 108 (85) | |||||
| Practice characteristic | Undersupply (N = 96) | Other (N = 288) | p-valueb | ||||
|---|---|---|---|---|---|---|---|
| Median | 25% | 75% | Median | 25% | 75% | ||
| Adjusted weighted list size | 10,608 | 7926 | 13,428 | 6766 | 4879 | 9990 | < 0.001 |
| GP FTE | 11,138 | 8312 | 13,807 | 7301 | 5172 | 10,458 | < 0.001 |
| Ratio nurse/GP FTE | 5.1 | 3.2 | 6.6 | 4.3 | 3 | 6.6 | 0.201 |
| IMD | 0.7 | 0.5 | 1.1 | 0.4 | 0.3 | 0.6 | < 0.001 |
| GPPS accessc | 25.5 | 18.8 | 31.7 | 17.7 | 13 | 22.6 | < 0.001 |
| GPPS continuityc | 0.4 | 0.2 | 0.7 | 0.8 | 0.6 | 0.9 | < 0.001 |
| GPPS satisfactionc | 0.3 | 0.2 | 0.6 | 0.7 | 0.4 | 0.8 | < 0.001 |
| % aged > 65 years | 0.3 | 0.2 | 0.6 | 0.7 | 0.4 | 0.8 | < 0.01 |
| CCG areas | n (%) | n (%) | p-valued | ||||
| Bath and North East Somerset | 3 (11.1) | 24 (88.9) | < 0.001 | ||||
| Bristol | 21 (46.7) | 24 (53.3) | |||||
| Kernow | 14 (23.7) | 45 (76.3) | |||||
| North Somerset | 10 (50) | 10 (50) | |||||
| Somerset | 15 (21.1) | 56 (78.9) | |||||
| South Gloucestershire | 7 (30.4) | 16 (69.6) | |||||
| Northern, Eastern and Western Devon | 17 (15.6) | 92 (84.4) | |||||
| South Devon and Torbay | 10 (33.3) | 20 (66.7) | |||||
| Urban practices | 79 (30.7) | 178 (69.3) | < 0.001 | ||||
| Rural practices | 18 (14.2) | 109 (85.8) | |||||
Appendix 36 List of stakeholder participants
| Job role | Employer |
|---|---|
| London | |
| Director of Primary Care | NHS England |
| Director for Workforce & Infrastructure programme | NHS England |
| Medical Director | NHS Practitioner Health Programme |
| Chief Executive Officer | NHS Practitioner Health Programme |
| GP Director and Head of School | HEE – Wessex |
| Programme Manager Sustainability and Transformation Partnership | HEE – South London |
| Postgraduate GP Dean | HEE – East of England |
| Primary Care Lead Nurse – Workforce | HEE – West Midlands |
| Interim Deputy Head of Workforce Planning | HEE |
| Deputy Head of Workforce Planning | HEE |
| Deputy Chairperson of GPC | BMA |
| Assistant Director: Policy | RCGP |
| Senior Programme Manager | NHS Employers |
| Regional Project Manager | South-west AHSN |
| Senior Fellow | The Nuffield Trust |
| Director | Primary Care Foundation |
| Assistant Director | GMC |
| Education Quality Analyst | GMC |
| Clinical Lead for Medicines Optimisation and Innovation | South Devon and Torbay CCG |
| GP and LMC Chairperson | North Staffs LMC |
| Vice Chairperson | Kent LMC |
| Chairperson | Cheshire LMC |
| Leeds | |
| Medical Director | NHS England (North) |
| Acting Director Postgraduate GP Education | HEE – North West |
| Associate Postgraduate Dean Post-Certificates of Completion of Training GP Education | HEE – South West |
| Head of School of Primary Care | HEE – East Midlands |
| Programme Lead | NHS Employers |
| Education, Training & Workforce Policy Lead | BMA |
| Regional Liaison Adviser | GMC |
| Public contributor | University of Manchester |
| PPG member | General Practice PPG |
| GP Health Yorkshire/Humber Clinical Lead | GP Health and Leeds North CCG |
| GP Mentor | Mentoring Matters |
| Locum GP | Co-Chairperson Leeds Sessional GPs |
| GP | Retired |
| Strategic Lead for Workforce | Wakefield GP Workforce Development Academy |
| Clinical Director | NEMS Community Benefit Services |
| Head of Portfolio and Partnerships | Sheffield Hallam University |
| Chairperson | NHS Sheffield CCG |
| Workforce Transformation Programme Manager | Mid Nottinghamshire CCGs |
| GP | Rawdon Surgery/NHS Leeds West CCG |
| Associate Medical Director | Leeds West CCG |
| Clinical Chairperson | Durham Dales Easington and Sedgefield CCG |
| Chairperson | Leeds LMC |
Appendix 37 Structure of the stakeholder consultation meetings
10.00 – Arrival and tea/coffee.
10.30 – Welcome and introductions.
10.40 – Project presentation 1 (systematic review, survey, qualitative, modelling).
11.10 – Questions and discussion.
11.20 – Project presentation 2 (RAM panel).
11.30 – Questions and discussion.
11.40 – Speaker.
11.55 – Questions/discussion.
12.15 – Lunch.
13.00 – Reconvene.
13.05 – Round-table discussion 1.
Maximum number of consultations, making consultations longer.
Identification of at-risk status of general practices and providing support, external HR interventions.
Portfolio working while retaining the core GP role, linking portfolio activities to local priorities.
13.50 – Round-table discussion 2.
Using marketing strategies to influence demand.
Supporting implementation/uptake of health and well-being interventions for GPs, professional support in the first 5 years of career, supporting planned exits for GPs nearing retirement.
Contractual arrangements for working across general practices, widening MDTs and role substitutions.
14.35 – Tea/coffee.
14.50 – Summary.
15.30 – Close.
Appendix 38 Graphic illustrations of the stakeholder consultation meetings
FIGURE 16.
Graphic illustration of the London stakeholder consultation meeting.
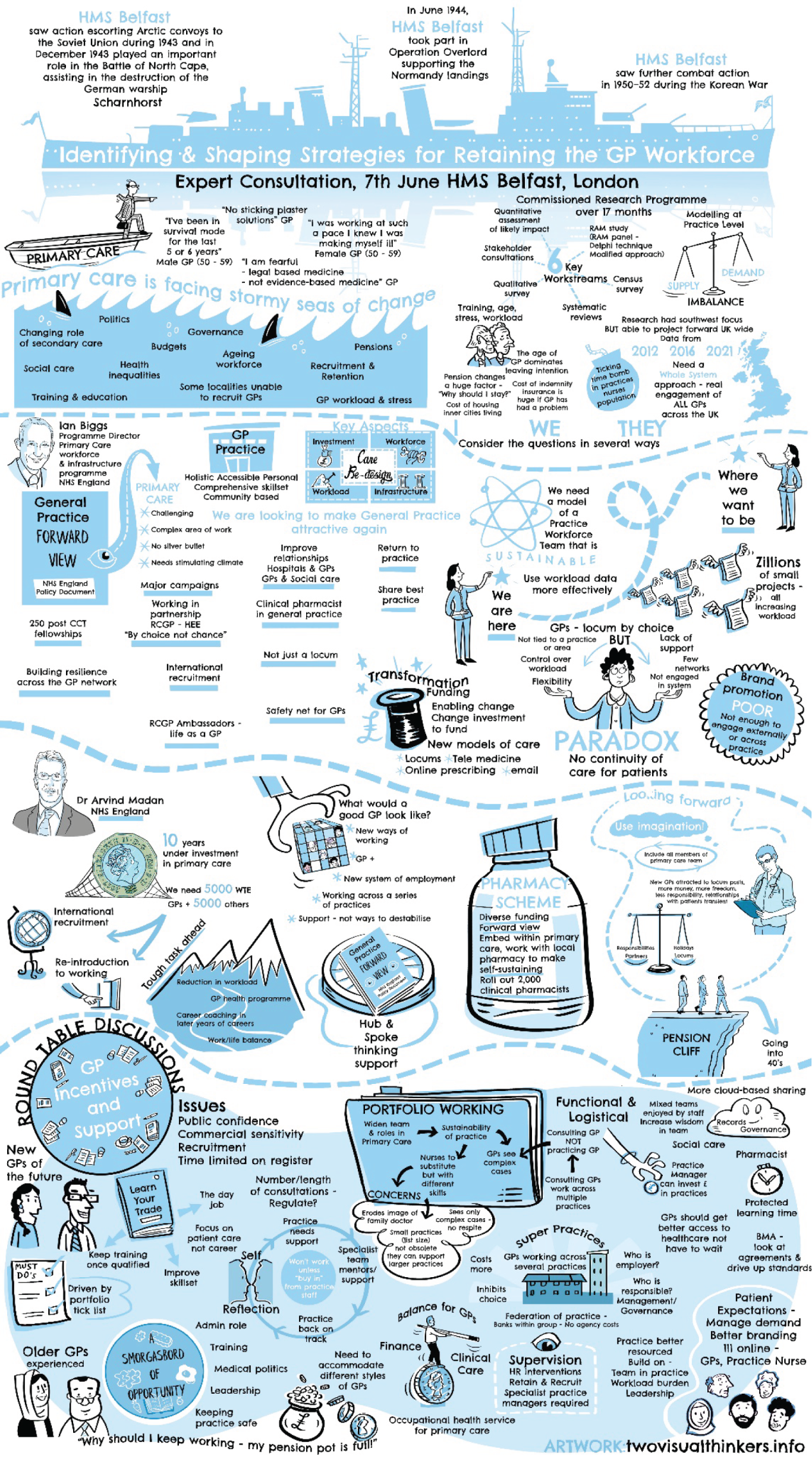
FIGURE 17.
Graphic illustration of the Leeds stakeholder consultation meeting.
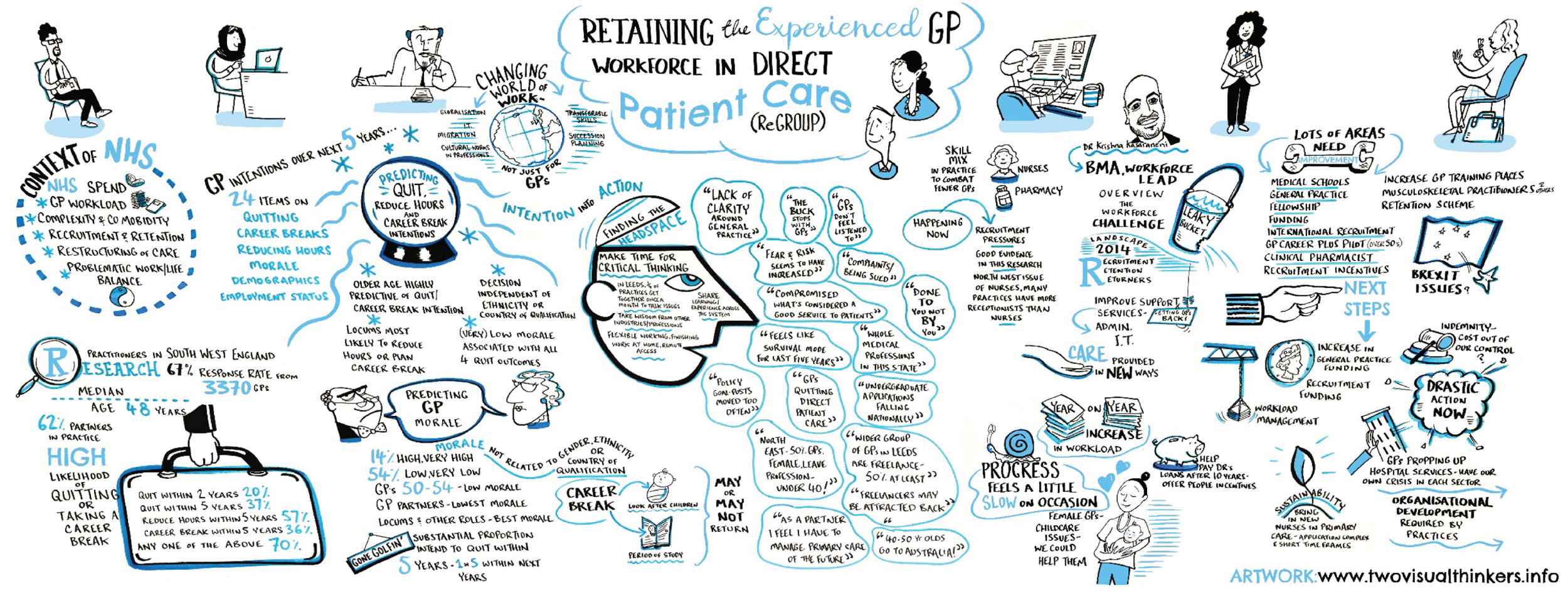
Appendix 39 Summary of findings for the ReGROUP general practitioner workforce project
Glossary
- Certificates of Completion of Training
- Confirmation that a doctor has completed an approved UK training programme and is eligible for entry onto the General Practitioner Register or the Specialist Register.
- Federation
- A group of general practices or surgeries forming an organisational entity and working together within the local health economy.
- First5
- An initiative by the Royal College of General Practitioners whereby newly qualified general practitioners are given extra support for the first 5 crucial years between qualification and the first point of revalidation.
- NVivo (QSR International, Warrington, UK)
- A qualitative data analysis computer software package.
- Policy and strategy
- Policy refers to a set of rules or principles that are made for rational decision-making; strategy refers to the approaches that different individuals or organisations deploy to achieve certain goals.
- PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)
- An evidence-based minimum set of items for reporting in systematic reviews and meta-analyses.
- PROSPERO
- An international database of prospectively registered systematic reviews of health and social care, welfare, public health, education, crime, justice and international development, for which there is a health-related outcome.
- Receiver operating characteristic
- A graphical plot that illustrates the diagnostic ability of a binary classifier system as its discrimination threshold is varied.
- Stakeholder
- A person or an organisation with a specific interest in general practitioner workforce planning.
- Super practice
- A number of individual practices merging into a single businesses unit, covering multiple sites across a large geographical area.
List of abbreviations
- AAFP
- American Academy of Family Physicians
- AHSN
- Academic Health Sciences Network
- ASSIA
- Applied Social Sciences Index of Abstracts
- BMA
- British Medical Association
- CCG
- Clinical Commissioning Group
- CCT
- Certificates of Completion of Training
- CEBM
- Center for Evidence-Based Management
- CEPN
- Community Education Provider Network
- CI
- confidence interval
- CQC
- Care Quality Commission
- CRN
- Clinical Research Network
- DHSC
- Department of Health and Social Care
- FTE
- full-time equivalent
- GMC
- General Medical Council
- GP
- general practitioner
- GPPS
- GP Patient Survey
- HEE
- Health Education England
- HMIC
- Healthcare Management Information Consortium
- HR
- human resources
- HSDR
- Health Services and Delivery Research
- ID
- identification
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- KLOE
- key line of enquiry
- LMC
- Local Medical Committee
- MBI
- Maslach Burnout Inventory
- MDT
- multidisciplinary team
- MeSH
- Medical Subject Heading
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OECD
- Organisation for Economic Co-operation and Development
- ONS
- Office for National Statistics
- OR
- odds ratio
- PCP
- primary care physician
- portable document format
- PPG
- patient participation group
- PPI
- patient and public involvement
- PSC
- psychosocial safety climate
- RAM
- RAND/UCLA Appropriateness Method
- RCGP
- Royal College of General Practitioners
- ReGROUP
- retaining experienced GPs and those taking a career break in direct patient care
- ROC
- receiver operating characteristic
- UEMS
- University of Exeter Medical School
