Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/01/17. The contractual start date was in October 2014. The final report began editorial review in November 2017 and was accepted for publication in September 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimers
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Beresford et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
Increased life expectancy, brought about mainly by improvements in health care, presents a number of health and care policy challenges. Increased rates of hospital admissions due to long-term health problems or frailty, subsequent delays in discharge from hospital, and growing demands for social care caused by heightened rates and levels of dependency have placed significant demands on services.
The 1990s saw the development of models of care to address these challenges, which, collectively, came to be designated as ‘intermediate care’. 1,2 This concept became formally recognised and defined in the National Service Framework for Older People,3 published in 2001:
. . . a new layer of care, between primary and specialist services . . . to help prevent unnecessary hospital admission, support early discharge and reduce or delay the need for long-term residential care.
p. 13. 3
In response to the National Service Framework, and supported by £900M investment from the UK government, new models of care, or practices, emerged.
The health-care sector saw the development of admission avoidance and supported early discharge schemes, typically described, or defined, as intermediate care. Importantly, some – but not all – supported early discharge schemes specifically sought to restore an individual’s ability to look after themselves, perhaps independently, in their own homes.
Similarly, local authorities (LAs) began to develop interventions for individuals who presented concerns in terms of their ability to continue to stay well and live independently, or at least remain in their homes with low levels of support. 4 Importantly, these latter developments were informed by a challenge, issued by the Department of Health and Social Care and directed at LAs, to develop approaches to care that reduced dependency on services and supported individuals to ‘make most use of their own capacity and potential’. 5 These twin levers saw the emergence of services across the country that shared similar features: short-term and intensive support delivered in the home with a focus on regaining, or preventing the decline of, daily living skills and social participation. By the early 2000s this approach had gained considerable traction and government support. 5,6 The term ‘reablement’ was used to describe the approach and significant levels of investment made in the development of such provision. In some countries, a similar shift in, approach to providing social care support was also taking place; some also referred to this new approach as ‘reablement’. Others, for example the USA, Australia and New Zealand, used the term ‘restorative care’. 7
The challenge of defining reablement
The past 15 or so years have seen changing and inconsistent use of the terms ‘intermediate care’ and ‘reablement’, both within policy8 and as applied to specific health and social care provision. In terms of the latter, the criteria, or ‘labels’, applied to different government funding initiatives (typically directed via health to encourage integrated planning) go some way to accounting for this.
In the context of this study, it is not useful or necessary to recount these changes in great detail. However, this lack of a shared definition was something that had to be explicitly addressed when developing the bid for funding and the study protocol. Indeed, the lack of an agreed description of reablement using a standard intervention framework9 continues to present significant challenges to those seeking to review existing evidence and those conducting primary research. 10
Defining reablement for the purposes of the study
This study was commissioned in mid-2014, and arose from a commissioning call issued by the National Institute for Health Research (NIHR) in early 2013. From the outset, it was essential that a clear definition of reablement was established that was relevant and meaningful in terms of current policy and practice, and made reference to the concepts of intermediate care and rehabilitation. Therefore, an analysis of recent evaluative literature11,12 and current policy and practice guidance documents7,13 was carried out. It was clear from this exercise that two key characteristics distinguish intermediate care and reablement from other health and care services:
-
The objectives of intermediate care/reablement. These are – acute admission avoidance at the point of clinical need for acute care; early supported discharge after acute admission; longer-term avoidance of unplanned hospital admission; reduction in the use of home-care services; and avoidance of admission to long-term care.
-
The time-limited nature of the service offered (usually up to a maximum of 6 weeks). This is the key defining characteristic that distinguishes intermediate care or reablement from, for example, generic rehabilitation services.
A further characteristic emerged as distinguishing reablement from intermediate care, namely its restorative, self-care approach. In other words, a reablement service is about enabling people to regain or retain self-care function for themselves, rather than providing input that replaces that function (e.g. reablement teaches people how to cook for themselves again, rather than providing meals on wheels). Table 1 sets out these distinctions, and overlaps, between reablement and intermediate care.
| Intervention characteristics/objective | Type of intervention | ||
|---|---|---|---|
| Time-limited? | Restoring self-care abilities? | Intermediate care or reablement? | |
| Acute admission avoidance at the point of clinical need for acute care | Yes | Not usually | Intermediate care |
| Early supported discharge after acute admission | Yes | Sometimes | Reablement if it includes a restorative element, otherwise intermediate care |
| Longer-term avoidance of unplanned hospital admission | Yes | Yes | Reablement |
| Reduction in the use of home-care services | Yes | Yes | Reablement |
| Avoidance of admission to long-term care | Yes | Yes | Reablement |
The study’s definition of reablement
Drawing on the work referred to above, the following definition of reablement was used.
-
Intervention objective:
-
to support people to regain or maintain independence in their daily lives.
-
-
Intervention approach:
-
to restore previous self-care skills and abilities (or relearn them in new ways) that enable people to be as independent as possible in the everyday activities that make up their daily lives (e.g. cleaning the house, shopping, or bathing and dressing themselves) rather than having someone (e.g. an informal or formal carer) do things ‘to’ them or ‘for’ them. 7,8 The provision of equipment may be used to support this
-
individualised and goals-focused.
-
-
Population:
-
individuals returning home from hospital or other inpatient care setting following an acute episode
-
individuals in whom there is evidence of declining independence or ability to cope with everyday living.
-
-
Nature of intervention delivery:
-
intensive
-
time-limited (up to 6 weeks)
-
goals-focused
-
delivered in the usual place of residence.
-
This definition aligns with current policy and practice guidance. 14,15
Subsequent developments in policy and definitions of reablement
While the study was under way, the Care Act 201415 – heralded as the most significant reform to social care in over 60 years – became law. Full implementation of the Act is ongoing, but phase 1 implementation had significant implications in terms of the perceived role of reablement within the wider portfolio of social care provision.
First, reablement was presented as one of the core interventions that can delay, or reduce, demands for care services and keep individuals living independently in their own homes. To this end, LAs are now required to consider providing reablement before, or alongside, carrying out a needs assessment. Furthermore, this approach should now be considered both for individuals not previously known to adult social care and for existing users. Second, reablement was presented as an intervention falling under the umbrella term of ‘intermediate care’, and was specifically identified as having the function of helping individuals leave hospital in a timely way and regain their independence. The need for integrated working with health services to deliver this was made explicit.
Together, these elements of the Care Act 2014 – and the continued growing and significant concerns within the NHS about the delayed discharge of older patients16 – have seen the emergence and adoption of ‘discharge to assess’ pathways, with these pathways including discharge to social care for assessment and reablement. 17
The 2017 National Institute for Health and Care Excellence (NICE) guidance, Intermediate Care Including Reablement14 makes clear that, as an intervention, reablement is regarded as one of the four core elements of ‘intermediate care’, the other three being (health) crisis response and bed- and home-based intermediate (health) care. It is important to note that the guidance continues to represent reablement as being distinctive in its restorative approach and focus on supporting independence in self-care and everyday life skills, with social care leading on its delivery. The guidance also stresses the need for integrated working within the context of providing intermediate care.
These significant changes in health and social care policy and guidance had two important implications for this study. First, it meant that changes to services and service developments were happening during the study period (2014–17), and are ongoing. Second, it signals that, as an intervention, reablement is highly topical and likely to remain a core aspect of meeting the health and social care needs of older people. As a result, the findings from this study are highly relevant and timely.
Existing evidence on reablement
The 2017 NICE guideline14 offers a useful review of existing evidence. It concludes that the quality of existing evidence on the effectiveness of reablement is not as high as for other forms of intermediate care (e.g. home- or bed-based intermediate care). To date, there have been just three comparative evaluations, of variable quality, that have used randomisation,18 none of which is UK-based. Among another four non-randomised comparative evaluations,19–22 two were carried out in England, both of which reported in 2010. 19,20 On the basis of this set of evidence, the following conclusion was drawn:
There is a moderate amount of moderate quality evidence that reablement is more effective when compared with conventional home care.
It was noted that the evidence was most consistent and positive with respect to care needs or impact on service use. Similarly, overall, findings related to quality of life and ability to carry out activities of daily living (ADL) suggest that reablement is an effective intervention, although this was not found in a low-quality trial. 11,12 NICE also reports that it did not find any evidence on cost-effectiveness that was relevant to the UK.
A separate set of evidence concerns issues of the design of reablement services. Here, low- to moderate-quality evidence indicates that access to particular specialisms (e.g. physiotherapy, occupational therapy) may influence the effectiveness of reablement. 19,23,24 In addition, there is reasonable evidence to suggest that the skills of reablement workers may have an impact on outcomes,24,25 for example being able to judge the timing and degree of support to offer a service user when carrying out a task and increasing service users’ confidence and motivation. Two studies conclude that reablement services should include the ability to respond to users’ goals that concern their social or leisure lives, which, for some users, will be a high priority or have the greatest impact on their lives. 25,26 Finally, there is some indication that service models should incorporate the ability to be flexible and responsive to user needs and progress. 24 However, this may have implications for service users’ views and experiences of the service. 23,24
Some existing studies have investigated issues related to the characteristics of the service user. There is reasonable evidence that individual motivation may have an impact on the effectiveness of reablement. 24,25 More specifically, there is weak- to moderate-quality evidence, primarily based on practitioner views, that individuals with end-of-life care needs or complex needs should not be referred to reablement services. 19,20,27 No studies have investigated the effectiveness of reablement in people living with dementia.
Finally, in terms of service users’ and family members’ views and experiences, the key issue identified by existing research is the potential lack of understanding of the objectives of reablement, and the fundamental difference of approach compared with home care. 23,24,26,27
A number of other systematic reviews of reablement were published in 2016/17. 10,28–30 Their inclusion criteria (in terms of study design and quality) vary and, as a result, the conclusions drawn differ somewhat. However, all note the pressing need for further research as a result of the core place given to reablement within health and social care policy, particularly with respect to older people and the investment in services delivering this intervention.
Evidence gaps
Studies into the effectiveness of reablement per se are beginning to be reported, although, as noted above, more are required. A further gap in evidence concerns the way in which to deliver reablement. Since the early days of ‘reablement’ in the late 1990s, different localities and sectors have developed different service models by which to deliver this intervention. 7,14,31 Thus, in addition to evaluating the impact of reablement with a no-intervention comparator group, a complementary stream of research is required that looks at different approaches, or service models, to providing reablement. In addition, although there is some evidence on factors that may have an impact on intervention outcomes (e.g. service user characteristics such as motivation/engagement, reason for referral to reablement, comorbidities and living circumstances), clearly, further work in this area is required and particularly with respect to factors that are amenable to intervention. Finally, and also highlighted in the 2016 NICE guidance,32 increasing the evidence base on the costs and cost-effectiveness of reablement and providing reablement to people with dementia are both important priorities.
Study aims and objectives
This study was funded by NIHR in response to a commissioned call33 that sought research proposals addressing the following overarching questions: how effective are reablement services in enhancing self-care and independence in the population they are designed to cover; and how are they best delivered?
When responding to this call, we chose to focus on some of the specific evidence gaps discussed in the previous section. Table 2 presents the study aims and associated objectives as set out in the study protocol. 34
| Aim | Objective |
|---|---|
| To establish the characteristics of generic and specialist reablement services in England | Undertake a national (England) survey to map different models of reablement services that currently exist (WP1) |
| To establish the impact of different models of reablement on service-level and service user outcomes | Using an observational cohort study design, to carry out outcomes and economic evaluations of different generic reablement models. Follow-up time points are to be at discharge from reablement and 6 months later. In addition, to carry out a nested process evaluation to understand the views and experiences of all relevant stakeholder groups (WP2) |
| To establish the impact of different models of reablement on different groups of service users | |
| To establish the indicative costs to the health and social care system of different models of reablement | |
| To establish how local context influences the ability of reablement services to achieve their goals | |
| To establish how specialist practice/services have developed for individuals with complex needs or ‘atypical’ populations who would benefit from reablement | To carry out a qualitative study of specialist reablement practice and service models (WP3) |
Thus, the focus of the study was not the effectiveness per se of reablement. Rather, its aim was to evaluate and compare existing reablement service models and to also conduct a smaller, parallel piece of work focused on reablement for groups for whom adjustments to a generic model of provision may be required (e.g. young adults, people with dementia).
Structure of the report
The report comprises 10 chapters. Chapter 2 provides a high-level overview of the study and reports deviations from the original protocol. Chapter 3 reports on work package (WP) 1, the national survey of reablement services and the reablement service models derived from that work. Chapter 4 describes the selection and recruitment of research sites for WP2 and provides a description of the characteristics of each site. In Chapter 5 we report the outcomes evaluation (WP2a). Chapter 6 describes one element of the process evaluation (WP2b), namely the interviews with reablement staff. In Chapter 7 we report the second element of WP2b: the user perspective. The economic evaluation (WP2c) is reported in Chapter 8. Chapter 9 turns to WP3, the qualitative study of practitioner views and experiences regarding reabling people with dementia. Chapter 10 discusses the implications of the study findings for health and social care, and recommendations for future research.
Chapter 2 Overview of study design and methods
Introduction
This chapter provides a broad overview of the design of the study and any deviations from the protocol. A detailed description of objectives, design and methods are described in the chapters reporting the various aspects of the study. The original protocol for the study has been published. 35 However, deviations from this protocol were required, all of which were discussed with the project’s Study Steering Committee (SSC) and approved by NIHR.
Study design and structure
The study comprised three WPs:
-
WP1 – mapping reablement services and developing a typology of reablement service models.
-
WP2 – a mixed-methods comparative evaluation of up to four reablement service models, as identified in WP1, investigating outcomes, costs, cost-effectiveness, and service user and practitioner experiences.
-
WP3 – an investigation into specialist reablement services/practice approaches, and the rationale for adjustment made to generic provision.
A survey was used to map reablement services (WP1). An observational study design was used to generate quantitative and qualitative evidence regarding the outcomes, effectiveness and cost-effectiveness of different reablement service models and the factors affecting individual outcomes (WP2). Qualitative methods elucidated descriptions of practice and practitioners’ views regarding the provision of reablement to people with dementia. WP1 preceded WP2 and WP3. WP2 and WP3 ran concurrently. The study was conducted between October 2014 and November 2017.
Ethics considerations
Work package 1 was defined as a service audit by the Health Research Authority and did not require ethics approval. For WPs 2 and 3 ethics approval was obtained from the North East York Research Ethics Committee (REC), UK (REC reference 15/NE/0299). Substantial amendments arising from deviations from the original protocol were approved by this committee.
Public and service user involvement
We worked with public and service user representatives throughout the project. During the project design phase, we consulted our research unit’s longstanding Adults, Older People and Carers Consultation Group about the proposal we were developing. We also sought advice from professionals who represent voluntary sector organisations supporting people who use reablement services. These discussions highlighted several issues that informed our decision-making:
-
the need to track the use of health/community/social services and not just hospital services
-
the belief that in-house and outsourced services may be different, with in-house teams regarded as ‘care driven’ and contracted-out services perceived as ‘profit driven’
-
to compare, if possible, NHS and LA provision
-
the importance of exploring the ethos/philosophy used by service managers
-
the importance of examining the impact multiple impairments have on outcomes and how these are addressed by reablement services.
Throughout the project we updated, and sought feedback from, this group. This helped us to be certain that the aims of the project remained important to the public, as well as to service commissioners and providers, and that the outcome measures were relevant to service users.
The SSC included service users who had experience of reablement services and representatives of voluntary sector organisations supporting people who use reablement services. Throughout the project, the SSC provided advice on methods, research materials and project management. The service user and public representatives were contacted between meetings for feedback on recruitment and data collection materials. The SSC also provided a forum for the research team to discuss their initial research findings and consider their implications. Members were kept up to date between meetings with a quarterly newsletter.
Work package 1: mapping reablement services and developing a typology of reablement service models
The aims of WP1 were to generate ‘stand-alone’ evidence on reablement services in England and to develop a typology of reablement service models. This typology was then used to identify and select (up to) four service models for evaluation in WP2. It was also used to provide preliminary evidence and inform sampling decisions for WP3. Survey methodology, comprising a three-stage process, was used:
-
identification of all reablement services in England
-
identification of a key informant(s) in each reablement service
-
data collection from these key informants.
Deviations from the protocol
There were no deviations from the original protocol.
Work package 2: an evaluation of different models of providing a generic reablement service
The purpose of WP2 was to evaluate different reablement service models in terms of service user outcomes, the experiences of delivering and receiving reablement, and the relative costs and cost-effectiveness of the models. It comprised three elements:
-
WP2a – outcomes evaluation
-
WP2b – process evaluation
-
WP2c – economic evaluation.
Samples for WP2b were drawn from the WP2a sample (service users) and WP2a research sites (staff). Service user-reported data for WP2c were collected within WP2a data collection processes.
We encountered significant issues with WP2 with respect to:
-
recruitment of research sites
-
study set-up in research sites
-
in some research sites throughput was much lower than expected, which significantly affected recruitment.
The first two issues caused considerable slippage in the project timetable. Given this, and coupled with the very slow rates of recruitment in two research sites, the decision was made not to extend the study until sample size requirements had been achieved across all research sites. As a result, the study closed early in three sites and recruitment was not started in the final site. Deviations from the protocol are detailed later in this section.
Work package 2a: the outcomes evaluation
The original objectives of the outcomes evaluation were as follows:
-
to conduct a quantitative, comparative evaluation of the effectiveness of the four reablement service models identified by WP1 in terms of service user outcomes at discharge and 6 months post discharge
-
to explore and test the impact of service (e.g. in-house vs. contracted-out provider; skill mix on the team) and user characteristics (e.g. reason for referral, comorbidities, engagement with the intervention) on outcomes.
The evaluation design was an observational study of a cohort of service users receiving reablement from one of four reablement services across England, each identified as typical of one of the service models identified in WP1, in which outcomes were tracked from entry to the service (T0), at discharge (T1) and at 6 months post discharge (T2). Self- and practitioner-reported outcome measures were used. Data collection from service users was carried out via home visits.
Difficulties with under-recruitment within the study timeline required the following changes to the objectives and design of WP2:
-
significant under-recruitment in two sites meant that comparisons between service models were not possible
-
delays in the study and the decision not to extend the timeline to accommodate these delays meant that it was necessary to move the primary outcome time point from T2 (6 months post discharge) to T1 (discharge from intervention)
-
the small sample size meant that the exploration of the impact of user and service characteristics on intervention outcomes at T1 was only exploratory
-
only an initial and exploratory analysis of T2 data was possible.
The revised objectives, agreed with the SSC and NIHR, were as follows:
-
to provide a descriptive, exploratory description of changes in outcomes between entry into (T0) and discharge from (T1) a reablement intervention
-
to provide a descriptive, exploratory analysis of outcomes at 6 months post discharge (T2), compared with outcomes at entry into (T0) and discharge from the intervention (T1)
-
to explore whether or not outcomes at discharge from reablement are associated with –
-
individual characteristics
-
intervention delivery characteristics
-
service characteristics
-
-
to contribute to study design and methodological knowledge related to the evaluation of reablement interventions.
Deviations from the original protocol
Revised design and study objectives are reported above (see Work package 2a: the outcomes evaluation). Other deviations are reported here.
Number of service models represented in work package 2
Owing to significant delays in study set-up, one of the service models identified in WP1 was not represented in WP2.
Mode of data collection at 6-month follow-up in work package 2
Owing to the early closure of the study and the consequent loss of local study teams, some T2 data were collected via postal administration rather than home visits. Although this was a necessary deviation from the original protocol, it did allow us to collect some useful data on the impact of mode of administration on study retention.
The use of routinely collected service audit data
The original protocol included collecting 12 months’ service audit data from research sites (e.g. ‘destination’ after discharge). However, it became apparent in WP1, and confirmed when approaching services to act as research sites for WP2, that this information was not routinely recorded by services. Therefore, we did not attempt to collect these data.
Work package 2b: the process evaluation
The overall aim of the process evaluation was to generate rich data from the key stakeholders on the delivery of reablement, the impacts of reablement, and how and why these effects may vary between individuals and different service contexts. The objectives of this element of the evaluation were, therefore, to develop an understanding of:
-
the immediate and wider context in which reablement service models exist
-
the experiences of providing and delivering reablement, and what has an impact on the process of service delivery
-
the different effects reablement can have on service users
-
how and why these effects vary between recipients and different service models.
A qualitative, descriptive case study approach was used, with the unit of analysis being the delivery and receipt of reablement. We sought the perspectives of service users and family members, service leads, reablement assessors, reablement workers and commissioners. Individual interviews and focus groups were used to collect data.
Deviations from the protocol
There are two deviations to report. First, we had planned to identify and recruit reablement workers via service users participating in the process evaluation. The reason for this was to allow us to explore different perspectives with respect to the same delivery of reablement. However, the use of multiple reablement workers with a single case in some research sites meant that this was not appropriate. Second, we had planned to use individual interviews with reablement workers. We revised this to using focus groups, believing that this would generate a richer set of data as we were no longer seeking different perspectives with respect to specific instances of delivering/receiving reablement.
Work package 2c: the economic evaluation
The original objective of the economic evaluation was to evaluate the cost-effectiveness of four reablement service models. This objective was revised in response to under-recruitment and early closure of sites. The revised objectives were:
-
(as per the original protocol) to review the economic evaluation methods used to evaluate reablement and use this to inform data collection for WP2c; this has been published in Faria et al. 36
-
(as per the original protocol) to develop a new instrument to collect data on resource use and costs from service users [the Services and Care Pathway Questionnaire (SCPQ)] and to explore the feasibility of using the SCPQ in terms of data quality (e.g. number of missing data)
-
to describe the costs of providing reablement using data collected during WP1 and WP2
-
to describe and compare resource use and costs of reablement at T0, T1 and T2
-
to explore whether or not the costs during receipt of reablement and in the 6-month period following reablement can be predicted in terms of service user and service characteristics.
Deviations from the protocol
For WP2c, a site-specific questionnaire was developed collecting detailed information on caseload and costs of providing reablement. Unfortunately, research sites did not answer the questionnaire. As a result, we were only able to calculate an estimate of the cost of providing reablement based on the information collected in WP1.
Work package 3: an investigation into specialist reablement services/practice approaches
The aim of WP3 was to investigate the organisation and delivery of reablement services to people with specialist needs.
The findings from WP1 indicated that the majority of specialist provision or practice concerned people with dementia. Therefore, with support from the SSC, and with agreement from NIHR, WP3 focused exclusively on this population.
This WP comprised:
-
a case study of ‘adapted or extended practice’ within generic reablement services and of specialist provision across 10 case sites
-
an investigation into the costs of such provision in each site.
Qualitative interviews with service leads and reablement workers were used to investigate the approaches, service structures, practices and experiences of providing reablement to people with dementia. Data on service costs were collected via a structured questionnaire administered during the interview with service leads. Data were collected from January to July 2016.
Deviations from the protocol
There were no deviations from the original protocol.
Chapter 3 Work package 1: a national survey of reablement providers
Introduction
The main purpose of WP1 was to provide a current picture of reablement provision in England. This included describing the organisational, structural and skill mix features of reablement services and the scope of reablement being delivered, and then looking at how these features affect intervention objectives, operating practices, referral routes, assessment tools and processes, outcome measurement and destination following discharge. It also sought to establish the costs of reablement.
Findings informed a number of elements of the evaluation WP (WP2), including selection of sites, decisions regarding the selection of explanatory variables within the outcomes analyses and the topics covered in the process evaluation. WP1 data were also used to identify the focus of, and thereby potential services to approach for, WP3.
Methods
Identification of reablement services
All LAs (n = 152) in England were contacted for the details of individuals commissioning reablement in that locality. Thirteen LAs either declined to provide this information (n = 8) or did not respond (n = 5); therefore, Clinical Commissioning Groups (CCGs) in these localities were contacted, but this did not help identify any reablement services.
Introductory e-mails, followed up with telephone reminders, were used to contact the commissioners identified, inviting them to complete a brief screening survey, which was administered via a structured telephone interview (see Report Supplementary Material 1). This established whether or not the individual was commissioning any services that potentially fulfilled our definition of reablement (Box 1). When a service was identified, the commissioner was asked for the name of the service and its contact details.
-
Intervention objective: to support people to regain or maintain independence in their daily lives.
-
Intervention approach: to restore previous self-care skills and abilities (or relearn them in new ways) using a goals-focused approach.
-
Population: individuals returning home from hospital or other inpatient care setting following an acute episode; individuals in whom there is evidence of declining independence or ability to cope with everyday living.
-
Nature of intervention delivery: intensive, time-limited (up to 6 weeks) and delivered in the usual place of residence.
Confirmation that the service fulfils inclusion criteria and identification of ‘key informant’
Service managers/service leads of services identified by commissioners were contacted by the research team by telephone or e-mail to check that the service fulfilled the study inclusion criteria. In localities where commissioners had reported more than one service, we also clarified whether these were separate as opposed to being a locality team, or outsourced provider, within a wider service. The algorithm used to screen services into the survey sample was as follows:
Service helps people to leave hospital more quickly than they would otherwise
AND/OR
Service helps to prevent admission to long-term care when people are at risk of it
AND/OR
Service helps to reduce people’s need for home care (social care)
AND/OR
Service helps prevent longer-term avoidance of unplanned hospital admission
AND
Service helps people to regain everyday living skills
AND
Service is provided in person’s usual place of care
AND
Service is time limited (usually 6 weeks but may be some flexibility round this)
AND
Service users are not charged for the service
Service managers/service leads were then asked to confirm that they were the most appropriate individual to act as ‘key informant’ with respect to the service (i.e. the person most able to provide detailed information about the service).
Survey of key informants
Across the 139 LAs for which commissioners had provided information to the research team, 181 reablement services were identified. In the majority of LAs (n = 106; 76%) one reablement service was identified. In 28 LAs (20%) two separate services were identified, and a further five LAs (4%) reported three or more separate reablement services. Outside this process, the research team was notified about, or became aware of, additional services that potentially fulfilled the study inclusion criteria. The same process was used to screen these services: two were out of scope and one LA declined to provide the information required. In total, key informants of 201 reablement services were invited to take part in the survey.
The survey was administered by e-mail and completed electronically using Qualtrics© (Qualtrics, Provo, UT, USA) survey software. The survey questionnaire (see Appendix 1) collected information about service delivery and organisational characteristics previously identified as important in terms of process and intervention outcomes in these types of services. 20,37,38 It also collected information on service costs and funding.
E-mail reminders and telephone calls were used in cases of non-response. E-mails and telephone calls were also used as follow-up when responses were unclear. After excluding surveys that were minimally completed, a response rate of 71% was achieved (n = 143/201).
Plan of analysis
We used five variables to describe the core characteristics of the reablement services represented in the survey. Three were derived directly from survey questions: organisational base, organisational structure and contractual arrangements. Two were derived from cluster analysis of survey data with respect to staffing and reablement input provided. These core characteristics provided the framework for subsequent analyses that explored the way reablement was being implemented and delivered.
Findings
The survey findings are reported in three sections:
-
the core characteristics of reablement services
-
service provision and delivery
-
the costs of reablement.
Data not presented in the text are provided in Appendix 2.
The core characteristics of reablement services
Organisational base
Survey respondents were the individuals identified as the person able to provide the most information about individual services. The organisational base of over half (53%) of respondents was a local authority social services department (LASSD). Fifteen per cent were based in an integrated NHS and LA organisation and 4% were based in the NHS. Of the remainder, 14% were based in a private (for-profit) organisation or the voluntary (not-for-profit) sector (7%). A very small proportion were based in a social enterprise (n = 4) or LA trading company (n = 3).
Organisational structure
Just over half of the services (52%) were a separate, or stand-alone, service. The remainder were located within a wider organisation: 18% were reported to be part of intermediate care provision, 13% part of home care provision and 4% part of an early intervention/rapid response service. One service was described as part of ‘other intermediate community’ provision and two were described as part of an independent living service. Finally, three were described as part of a mental health service provision.
NHS-based services were more likely, and those based in LASSDs less likely, to be part of intermediate care provision within a locality. In addition, LASSDs were more likely, and NHS organisations less likely, to be providing a reablement service that was separate from other intermediate care provision in the locality [χ2 = 29.94, degrees of freedom (df) = 16; p = 0.018].
Contractual arrangements
Two-thirds of services (66%) were described as being wholly ‘in-house’ to their organisational base. A fifth had both ‘in-house’ and ‘contracted-out’ elements and 7% were wholly contracted out to another organisation. A small minority described other arrangements. Contractual arrangements were not related to a service’s organisational base or structure.
When some aspect of a service was ‘contracted out’ (38/143 services), this was most often the delivery of reablement support (n = 20/38), as opposed to the assessment of eligibility for the service (3/38) or the reablement assessment itself (4/38).
Staffing and skill mix
Cluster analysis was used to understand the different patterns of staffing and skill mix in the teams. There were sufficient data on 129 out of 143 services (90%) for them to be assigned to a cluster. Four distinct patterns of staffing were identified (see Appendix 2, Tables 20–22).
-
Cluster 1: reablement with occupational therapy (n = 24).
These services were very likely to have occupational therapy and social work involvement but, unlike the multidisciplinary teams in cluster 3, it was unusual for them to have a registered nurse or a health support worker.
-
Cluster 2: home-care reablement (n = 42).
All services in this cluster reported having home-care workers and were also likely to report having home-care organisers and reablement workers. They did not typically have an occupational therapist (OT).
-
Cluster 3: multidisciplinary reablement (n = 20).
All services in this cluster had OTs and physiotherapists. They were also highly likely to have registered nurses and more likely than any other type of team to include health support workers, although this was not typical.
-
Cluster 4: reablement workers (n = 43).
None of these services had home-care workers but they were highly likely to have reablement support workers and unlikely to have any of the other staff listed.
Bivariate analyses explored patterns of association between staffing and organisational characteristics. The key findings are reported below and further data are available in Appendix 2, Tables 22–27.
Staffing and organisational base
‘Reablement with OT’ teams were most likely to be found in LASSDs (28%, compared with 19% of all teams), while services based in the NHS or integrated health-social-care services were most likely to have ‘multidisciplinary’ teams (39% and 67% respectively, compared with 16% of all teams). Third-sector services were more likely to be ‘home care reablement’ teams (54%, compared with 32% of all services). These differences were statistically significant (χ2 = 44.97, df = 12; p < 0.001).
Staffing and organisational structure
Over two-thirds (68%) of reablement services being provided within wider home care provision had ‘home care reablement’ teams (68%, compared with 30% of all teams). By contrast, half of services that were part of wider intermediate care provision had ‘multidisciplinary reablement’ teams (50%, compared with 16% of all teams). These differences were statistically significant (χ2 = 51.40, df = 12; p < 0.001).
Type of reablement input
Respondents were asked about the scope of the reablement provided, that is, the domains of an individual’s life that they sought to ‘re-enable’ and which domain was the focus of the majority of the service’s input. (It was stressed that respondents should report only what they enabled service users, as opposed to what they did for them.) The domains were:
-
personal care
-
domestic tasks
-
safety (including preventing falls and providing aids and equipment)
-
information and signposting to other services or support
-
getting around in the home
-
getting out and about outside the home
-
re-engaging with social activities and friends
-
managing health-related needs
-
specific activities to help rebuild confidence and improve well-being.
Personal care re-enabling was the predominant activity, and the one that made up the majority of services’ work. Helping people to get out and about again outside the home and to re-engage with social activities were least commonly reported. Bivariate analysis suggested that patterns of reablement input varied systematically in terms of the organisational characteristics (e.g. organisational base, organisational structure, contractual arrangements) of the services (see Appendix 2, Tables 23–26).
Data reduction, again using cluster analysis, produced three stable and fairly distinct clusters of type of reablement input for 136 out of 143 of the services.
-
Cluster 1: ‘functional’ reablement (n = 40).
These services reported that they re-enabled personal care, domestic skills, safety, information, helping people to move about inside, health-related needs and confidence-building.
-
Cluster 2: comprehensive reablement (n = 87).
These services said that they re-enabled in all of the domains. Thus, they were similar to services delivering ‘functional’ reablement, but also helped people with getting out and about and with social activities.
-
Cluster 3: social reablement (n = 9).
These services reported that they re-enabled in the areas of safety, information, getting out and about, social activities and confidence-building.
Type of reablement input and staffing
Multidisciplinary teams were more likely than expected, and ‘reablement worker’ teams less likely, to be providing comprehensive reablement (see Appendix 2, Table 27). Indeed, ‘reablement worker’ teams were the only ones associated with providing social reablement.
Service provision and delivery
The final stage of analysis examined the way reablement was being provided and delivered in terms of the following:
-
service objectives
-
operating practices (e.g. referral pathways, eligibility criteria, reabling individuals with specialist needs, duration of reablement and charging policy, assessment and monitoring of outcomes)
-
destinations following discharge from reablement.
We also explored whether or not the core service characteristics described in the previous section (see The core characteristics of reablement services) were associated with the provision and delivery of reablement. Please note that the detail reported here is limited.
Service objectives
Respondents were presented with a list of service objectives and asked to select all that were part of the purpose of their service, and to identify the main objective. The objectives, drawn from policy and existing literature on reablement and/or intermediate care, were:
-
help people regain everyday living skills
-
reduce the need for ongoing (social) home care
-
prevent longer than necessary stays in hospital
-
prevent admission to long-term care when at risk
-
prevent hospital admission during acute illness.
The majority of respondents selected most of these objectives, but one (‘prevent hospital admission during acute illness’) divided the services almost equally (see Appendix 2, Table 28). NHS-based services were significantly more likely to report this as an objective than were other services (χ2 = 12.49, df = 4; p = 0.014). The most often reported main service objective was to ‘help people regain everyday living skills’ (58% of services), with LASSD-based services more likely to report this than others (χ2 = 56.38, df = 24; p < 0.001). Only two services reported ‘preventing hospital admission during acute illness’ as their main objective and, as might be expected, both of these were based in the NHS.
Services staffed by a multidisciplinary team were more likely to report ‘preventing hospital admission during acute illness’ as a service objective (40%, compared with 16% of all services). This was the only difference in objectives found across the different staffing models.
Operating practices
Referral pathways
Existing literature and our own preliminary work indicated that referrals to reablement services occurred in one of two main ways. Either everyone referred for home care or domiciliary support was first referred to the reablement service, or referral was selective (e.g. for those being discharged from hospital, those felt to be at risk of admission to long-term care, or those whom another professional felt might benefit from reablement). Survey respondents were asked to choose which of these two models best represented their service.
Just over half of respondents (52%) reported that access to their service was selective, 24% reported that it was non-selective, and 15% described other models, often incorporating some element of triaging. Over one-third of LASSD services (38%) reported that reablement was provided to all referrals for home care. Few services (27%) reported accepting self-referrals.
Not unexpectedly, a greater proportion of referrals to NHS-based services and/or those operating within wider intermediate care provision were from primary care than those to services with different organisational bases or relationships with wider intermediate care within their locality (see Appendix 2, Table 29).
Eligibility criteria
The majority of services (88%) represented in the survey accepted adults aged ≥ 18 years, imposing no upper age limit. However, social reablement was strongly associated with providing services to adults aged 18–65 years only (χ2 = 39.41, df = 6; p < 0.001).
The majority of services (86%) reported meeting the needs of a wide range of people; we defined these as ‘generic services’. We asked such services whether or not individuals who might have specialist needs [e.g. people with dementia, younger disabled adults (aged ≤ 65 years), people with learning disabilities, people with brain injury and people with sensory impairments] were eligible for their service. A great majority reported that they accepted referrals of individuals with these needs (Table 3).
| Specialist group | Type of service (%) | |
|---|---|---|
| Accepts individuals with specialist needs | Accepts and has specialist pathway or protocols | |
| People with dementia | 87 | 24 |
| Younger disabled adults (aged < 65 years) | 89 | 8 |
| People with learning disabilities | 81 | 20 |
| People with brain injury | 80 | 12 |
| People with sensory impairments | 89 | 20 |
| Total (n) | 123 | 123 |
| Missing (n) | 20 | 20 |
Half of the respondents stated that their service applied other exclusion criteria, assessed either at referral or following assessment, and some provided information about these. The most frequently reported criterion was whether the person was at the end of life and/or needed palliative care. This was followed by the person not having reablement ‘potential’ (29%), the presence of cognitive impairment or dementia (28%), identified risks to care staff (19%), the client having longer-term care needs (17%), and evidence of a lack of engagement with the reablement process (13%). Over one-third reported other exclusion criteria.
Reabling individuals with specialist needs by generic reablement services
Services reporting that they provided reablement to individuals who, potentially, might have specialist needs were asked whether the service had specialist pathways and/or protocols for such individuals. Few reported having specific pathways or protocols in place (see Table 3).
Duration of reablement and charging policy after 6 weeks
An intervention period of a maximum of 6 weeks has been a key feature of reablement in the UK since its inception in the early 1990s. In England it remains as the period of time during which service users cannot be charged. After this, LA and integrated NHS/LA providers have the option to charge for the service, in the same means-tested way that home care services are charged for.
Respondents were asked about the typical duration of reablement. Four out of five respondents reported that it was between 4 and 6 weeks, and 13% reported it as < 4 weeks (see Appendix 2, Table 30). An intervention period of < 4 weeks was significantly associated with services defined as providing ‘functional reablement’, as opposed to ‘comprehensive reablement’ (χ2 = 27.21, df = 6; p < 0.001).
The majority of services (85%) reported that the intervention period could be extended beyond 6 weeks in certain circumstances. The reason for extension was typically difficulties with onward referrals or finalising care packages (83%), rather than there being an expectation that extending the intervention would result in further improvement (22%). Of the services reporting that the duration of intervention could extend for more than 6 weeks, almost two-thirds (61%) said that there was no limit on this time period. In the remaining services, the duration of extension ranged from 7 to 21 days.
Fewer than one-third of respondents (28%) reported that service users were charged after the first 6 weeks. However, charging policies varied in terms of the organisational characteristics of services. LASSD-based services were much more likely than those based in the NHS or in integrated NHS and LA organisations to report charging after 6 weeks (χ2 = 19.47, df = 8, p = 0.013). Similarly, services that were part of wider home care provision were also more likely to report charging after 6 weeks (χ2 = 16.75, df = 8; p = 0.033) than those with other organisational structures. Wholly contracted-out services were more likely (75%), and those comprising both in-house and contracted-out elements less likely (14%), to report charging after 6 weeks (χ2 = 12.84, df = 6; p = 0.046).
Approaches to assessing and monitoring outcomes
Respondents were asked about the types of assessment carried out once an individual had been accepted by their service. Assessment, and tracking progress, may be informed by setting and reviewing personalised goals, using standardised measures, or other methods.
Most (73%) reported that assessment processes were multifaceted, covering planning how reablement could meet the person’s needs (85%), setting specific goals for reablement (79%), conducting a wider, full needs assessment (70%), and assessing any other needs (64%). Four respondents reported that their service followed a reablement programme set by another service. Only one respondent referred to carrying out ‘baseline’ assessments for outcome measurement purposes.
Goal-setting
Of the services using personalised goals (n = 118), 92% said that they always set the goals in partnership with the user, and this was done before reablement started (49%) or soon after (42%). Most services (83%) said that they used staff’s professional judgement regarding the achievement of personalised goals to monitor service users’ progress.
Occupational therapists were the professionals most often involved in goal-setting (56% of services), followed by reablement care workers (42%), physiotherapists (36%), social workers (35%) and nurses (12%). Almost half (45%) referred to a wide range of other people involved in goal-setting, including ‘assessors’ (not otherwise described) care managers, reablement managers or co-ordinators, and care co-ordinators.
Staff involved in goal-setting varied according to some service characteristics (see Appendix 2, Table 31). OTs and nurses were more likely to be involved when the services were ‘multidisciplinary’ and/or when the service ran as part of or alongside an intermediate care service. They were less likely to be involved when the reablement service was ‘standalone’ as opposed to being situated within a wider service/provision. This was also the case for physiotherapists, but they were also more likely to be involved with NHS-run services. Nurses were also more likely to be involved when the service was based in the NHS, and less likely to be involved in LA-based services. In terms of the impact of type of reablement input on the staff involved with goal-setting, OTs were less likely to be involved in goal-setting in social reablement.
Use of standard approaches for assessment and review
Of the 33 services that said they used ‘standard measures’ to assess progress towards reablement goals, almost all assessed mobility, quality of life, physical health and ADL. Fewer, but still the majority, assessed mental health and social and personal outcomes.
However, very few services reported using standardised measures. Only five reported using a standardised measure to assess mobility and quality of life, three used them for physical health outcomes, four for mental health outcomes, three for ADL, and two for social and personal outcomes.
Multidisciplinary teams were more likely to use standardised measures of ADL (50%, compared with 10% of all services, χ2 = 16.98, df = 9; p = 0.049), and/or NHS teams (20%, compared with 10% of all services, χ2 = 16.91, df = 9; p = 0.05). Small sample and subsample sizes mean that interpretation must be cautious, but these patterns do suggest different approaches that echo other differences between services reported.
Use of assessment tools other than personalised goals to review progress
Just one-quarter of services recorded outcomes (using an assessment tool other than personalised goals) at entry to the service and at some point later on. Thus, 30% of respondents reported that assessment tools were used at only one point during reablement. Of those who reported that they assessed before the service started (33% of all services; n = 47), six then also assessed during the service, six towards the end of the service and 36 after the service episode was over. Some services indicated that follow-up extended well beyond discharge, with five mentioning reviews at 6 weeks and 3 months.
Multidisciplinary services were more likely than other services to record outcomes (using an assessment tool other than personalised goals) at entry into the service and later (55%, compared with 36%); this difference was not statistically significant. Services situated within wider home care provision were very unlikely to assess outcomes before and at some later stage (5%, compared with 33% of all services). No other service characteristics were related to whether services recorded outcomes (using an assessment tool other than personalised goals) on entry to the service or at some later time point.
Destination following discharge
Respondents were asked to indicate the most common ‘destination’ for service users at the end of reablement. Almost two-thirds (62%) reported that service users were most often discharged without an ongoing care package. Eight per cent said that people were usually referred on for assessment of their eligibility for other social care, and 5% said that service users most often moved into long-term care.
One in ten gave other answers, most suggesting that outcomes were split relatively evenly between independent living (albeit with the possibility of involving informal carers) and ongoing requirements for care. Some said that although service users required further care, this was at a lower level than had previously been the case. Fourteen per cent either said that they did not know the answer to this question or did not answer it.
Services run by LASSDs were more likely than others to say that the most common outcome for service users was discharge without any ongoing involvement of care services (71%, compared with 63% of all services). Services run jointly between health and social services were most likely not to know or not to provide an answer to this question (50%, compared with 12% of all services). Services in the ‘other’ organisational category were more likely to say that the most common outcome was transfer into long-term care (29%, compared with 5% of all services). These differences were statistically significant (χ2 = 26.39, df = 12; p = 0.009), although many cell sizes were small.
Services providing ‘functional’ reablement were least likely to report that users were discharged without ongoing support (53%, compared with 66% of all services), and were most likely to report transfer into long-term care (15%, compared with 5% of all services). By contrast, ‘comprehensive’ reablement services were more likely to report discharge without other services being in place (74%, compared with 66%), and least likely to report transfers into long-term care (1%, compared with 5%). These differences were statistically significant (χ2 = 14.79, df = 6; p = 0.022).
The costs of reablement
Questions on service budgets and caseload were used to gather data on the costs of providing reablement. It was outside the scope of the survey to collect information on regional variances in workforce costs, size of the population, their demographics and the local organisation of services. Therefore, the results presented here are descriptive. No inferences about reasons for differences in service costs, or the association between costs and effectiveness, can be drawn from these data.
Data collection and analysis took the perspective of the NHS and Personal Social Services. Therefore, the relevant costs were those falling on the budgets of the CCG (representing the NHS) and/or LA (representing Personal Social Services). Ideally, the costs reported by survey respondents represent the full economic cost to the commissioner of providing the service, including direct and indirect costs, and overheads. However, given that it was not possible to corroborate the data provided by respondents, we cannot be certain of this. Furthermore, the information provided may not necessarily reflect the full economic cost of providing the service. For example, if the provider is a private contractor, the cost of providing the service to the commissioner may be lower than the cost charged to the commissioner to allow for profit; conversely, it may be higher if the service is provided at a loss.
The data collected
Respondents were asked to report for the 2014–15 financial year. Different commissioning and contracting arrangements meant that data had to be collected in different forms. Thus, expenditure (or ‘spend’) on the reablement service was collected as:
-
total expenditure for wholly ‘in-house’ services
-
total expenditure for in-house and contracted-out services where the service included both elements
-
value of the reablement contract if the service was fully contracted out
-
where respondents did not know the answer to the question but the service was run from a LASSD, the NHS, or an integrated service, we asked for the cost of the service as a proportion of the budget for all older people’s services.
The survey also asked about the number of reablement ‘cases’. ‘Cases’ refers to the number of individuals who received the service, recognising that some individuals may use a service more than once.
The analytical approach
Data were summarised in terms of mean, standard deviation, minimum and maximum. Analyses were conducted only if the minimum cell count was > 10. Additional data are presented in Appendix 2 (see Table 32).
Where respondents reported the total budget for older people’s services and the percentage dedicated to reablement, expenditure on reablement was calculated by multiplying the two values. The typical number of cases to whom the service was provided was converted to cases per year. The average cost per case was calculated by dividing the total expenditure for reablement in 2014–15 by the number of cases per year. The average cost per type of reablement service was explored using the core service characteristics described earlier (see Service provision and delivery) and by commissioner.
Findings
Expenditure on reablement
Around one-third of respondents (42/143; 29%) provided information on expenditure. Most answers referred to direct expenditure on the reablement service (n = 31; 22%). On average, expenditure was £2.6M. Some respondents reported expenditure in terms of the expenditure on in-house (n = 8; 6%) and on contracted-out elements (n = 7; 5%). In these cases, expenditure, on average, was £1.5M and £0.9M, respectively. Seven services reported expenditure as the proportion of the budget for older people’s services devoted to reablement; their average expenditure was £1.7M. Two services reported the total value of the reablement contract (£1.2M and £0.2M). Overall, the average expenditure on reablement was £2.4M. However, there was wide variation (range £5000 to £8.5M).
Caseload
One hundred respondents (70%) provided information on their annual caseload (n = 81; 57%) or on the typical number of cases per month (n = 19; 13%). On average, the caseload was 1383 per year (range 10 to 9500).
Cost per case
It was possible to calculate the cost per case for 37 (26%) services. The average cost per case was £1445 (range £20 to £2235). Clearly, the value of £20 per case is implausible. [This value was derived from the respondent stating that their budget for older people’s services was £1.5M, the percentage spent on reablement was 1.33% (hence £19,950) and the reablement service saw 1015 cases per year.] Data provided by a further five respondents yielded costs per case of below £500. Again, these are highly atypical. Excluding these six respondents increased the average cost per case to £1728.
Cost per case per type of reablement input
Among the services providing ‘functional reablement’ that reported costs (n = 10), the average cost per case was £1577 (range £533 to £2235). Among the services providing ‘comprehensive reablement’ that reported costs (n = 24), the average cost was £1512 (range £20 to £3333). Only six services providing ‘social reablement’ reported costs; therefore, we did not carry out a calculation with respect to this type of reablement input.
Summary
Reablement services varied in terms of their organisational base (LA vs. NHS vs. integrated service); over half were LA services. Just over half were ‘standalone’ services, as opposed to integrated within wider intermediate care provision in the locality. The latter was more likely to be observed if the service was based in the NHS. Most services were delivered by in-house teams. Where aspects of the service were outsourced, this was most likely to be the hands-on delivery of the intervention, as opposed to the assessment processes.
Services could be grouped according to the types of staff working in the service. Not all services had OTs, and LA-based services were most likely to have them. NHS or integrated services presented the most multidisciplinary profile. It appeared that workers in some services had both home care and reablement clients. The scope of reablement input varied between services. Some did not work on aspects of functioning external to the home environment: we labelled this ‘functional reablement’. ‘Comprehensive reablement’, which included reabling with respect to getting out and about outside the home and re-engaging with social activities and friends, was, however, the more common approach. The primary objective of services, and particularly among LA services, was to restore everyday living skills. Multidisciplinary teams, which tend to be based in the NHS, were most likely to report ‘preventing hospital admission’ as an objective.
Services varied in terms of the clients they worked with. Over one-third offered reablement to all referrals for home care received by their LA. Just over one-quarter accepted self-referrals. The majority of services reported that they accepted a wide range of people. The most commonly reported exclusion criteria were individuals requiring end-of-life care and for whom there was no evidence of reablement potential. Over one-quarter of services reported that cognitive impairment and/or dementia could be a reason to refuse a referral.
The typical duration of reablement reported was 4–6 weeks. Services delivering comprehensive reablement were more likely to report a longer duration than those delivering functional reablement. Most services reported that they were able to extend the period an individual remained in the service, but this was predominantly attributed to delays in arrangements for longer-term care. Charging policies for extended involvement varied. LA-based services were most likely to charge.
A small minority of services used standardised outcome measures. Professional judgement with respect to achievement of reablement goals appeared to be the predominant approach to assessing progress. Almost two-thirds of services reported that, on discharge from reablement, only a minority were transferred to home-care services. Services providing functional reablement were least likely to report this as the typical outcome at discharge.
The section of the survey on costs was poorly completed. When sufficient data were available, the average cost of reablement per case was calculated at £1728 (excluding six highly atypical cases). There was relatively little difference in cost between services providing functional reablement and those providing comprehensive reablement.
Chapter 4 Work package 2: identification and description of research sites
Introduction
This chapter reports the selection and recruitment of services to WP2, each representing one of the service models identified by WP1. Each service is then described in comparison with the others. These descriptions are based on data collected during WP1, information gathered at meetings with services during site recruitment and study set-up, documentary material, and interviews with staff and commissioners within the process evaluation (WP2c).
Identification and recruitment of the case sites
Work package 2 was a mixed-methods evaluation of up to four reablement services, each representing a different model of delivering reablement, using an observational study design. Identification of these service models was a key output of the national survey of reablement services (WP1) as reported in the previous chapter. Two concepts emerged from our analysis of the survey data that best served to distinguish reablement services: the type of reablement input, and staffing (see Chapter 3, The core characteristics of reablement services).
In terms of the type of reablement input, the survey identified three types: ‘functional’, ‘comprehensive’ and ‘social’. (The last was very unusual and not relevant to WP2 as it is restricted to mental health settings.) The majority of services (60.8%) represented in our survey reported that they delivered ‘comprehensive reablement’. ‘Comprehensive reablement’ fully adhered to what, at the time of the study, was understood to properly constitute a reablement intervention,15,39 and this remains the case. 7 Thus, for the evaluation phase, we sought only to recruit services delivering ‘comprehensive reablement’.
The second concept that best differentiated services was staffing. Four ‘types’ emerged:
-
reablement with occupational therapy
-
home-care reablement
-
multidisciplinary reablement
-
reablement workers.
For the evaluation, therefore, we sought to represent services that were delivering comprehensive reablement but differed in terms of staffing.
Outputs of the WP1 cluster analysis of staffing typologies were used to identify services to approach regarding participation in WP2. Services closest to the centre of each cluster (in other words, best representing each staffing typology) were approached first regarding their participation in the evaluation. If the invitation was declined we moved on to the next ‘closest’ service. This continued until the involvement of a service was secured. Hereafter, we refer to these services as our research sites.
Unfortunately, significant delays experienced by the project led to the decision to close, rather than extend, the study. This meant that recruitment did not open in the research site that would have represented the ‘reablement worker’ typology.
Alignment of research sites with the designated service model
By the time recruitment of service users to WP2a commenced, the three research sites had undergone significant changes. Two key factors contributed to this. First, the continued implementation of the ‘Transforming Care’ agenda and the Care Act 201415 resulted in changes in relation to wider intermediate care provision, integrated working with the NHS, and LA social care intake and assessment processes. Second, resource constraints had an impact on commissioning decisions. Examples of observed changes include changes in private providers; the introduction of joint working arrangements with other services, the reorganisation of intermediate care provision within the locality, and the reversal of joint working arrangements between the LA and NHS.
However, as this chapter reports, the research sites did represent differences according to a wide range of service characteristics that are highly relevant to policy-makers, commissioners and service providers. It is also the case that different models of provision were operating within each research site. It is the impact of these factors and characteristics that our evaluation was able to explore and test in terms of service users’ outcomes and experiences, and the experiences of providing and delivering reablement.
The work package 2 research sites
The checklist of features for describing complex interventions developed by Dorling et al. 40 was used to determine the range of information reported on research sites. This information is presented in the following sections. We note that the level of detail is constrained by the need to ensure the anonymity of the research sites. The information presented is correct for the time when recruitment to WP2 was open and the intervention was being delivered to study participants.
Overview of research sites
Information about the overall setting and location, and a high-level description of the service and the wider service context, are set out in Table 4. Sites differed in terms of their organisational context and sociogeographical characteristics. The core function of all sites was the delivery of social care assessment and reablement. All delivered reablement to individuals returning home from hospital and those living in the community who were at risk of significant increased demands on social care. Sites varied in the extent to which they were colocated within the wider intermediate care offer in the locality. In two sites there was some degree of joint working/integration of NHS and LA-funded intermediate care provision. In the two sites that used private providers for at least part of their reablement provision, private provider involvement in the study was limited in some way.
| Characteristic | Site | ||
|---|---|---|---|
| A | B | C | |
| Service setting | LA | A social enterprise commissioned to provide a range of community health and social care services | LA |
| Commissioner | LA | LA | LA |
| Location |
A small metropolitan borough in the northern half of England Comprises rural, urban and industrial areas. Two main conurbations, occupying around one-third of the land and where around two-thirds of the population lives. The remainder is predominantly rural Population: > 300,000; higher than national average proportion of the population is aged ≥ 65 years Relatively deprived, with many areas of significant deprivation Over 95% of the population are white British |
A small London borough Population: < 200,000; lower than national average proportion of the population aged ≥ 65 years Overall deprivation rate is low, but a few areas of high levels of deprivation Almost two-thirds of the population are white British; no large representations of specific minority groups |
A large county in the southern half of England Predominantly rural, it also has several large towns with sizeable populations Population: > 1 million; higher than national average proportion of the population is aged ≥ 65 years Overall deprivation rate is low, but there are pockets of high levels of deprivation The majority of the population (> 90%) are white British |
| Service function |
Assessment and reablement of individuals being discharged from hospital and those living in the community Delivery achieved through an in-house assessment team and two private providers |
Assessment and reablement of individuals being discharged from hospital and those living in the community Delivery achieved through in-house teams, (separate assessment and reablement worker teams). Private providers used to deliver home care when service is operating a waiting list |
Assessment and reablement of individuals being discharged from hospital and those living in the community Delivery achieved through in-house teams comprising assessment and reablement workers, and five private providers |
| Essence of service’s ‘operational definition’ of reablement | Not all/many clients (this proportion varied between services) will achieve significant functional improvements/independence, but any gains are worth trying to achieve and, aside from end-of-life care, should be sought before moving to home care | ||
| Wider intermediate care context |
Separate referral routes into community and hospital ‘assessment and reablement’ services and a ‘rapid response’ service. Implementing a single referral point, with triage decisions taken by a reablement assessor, a social worker and a nurse. Telephone call with referrer used to inform triage process The joint-funded NHS/LA ‘rapid response’ service responds within 4 hours and provides 72-hour intensive case management. The service is for individuals at risk of being admitted or whose discharge requires intensive support |
An integrated community health and social care team receives referrals for ‘intermediate care’, ‘assessment and reablement’, ‘community nursing’ and ‘rapid response’ services Assessors working across ‘reablement and assessment’ and ‘intermediate care’ assess referrals and allocate to ‘intermediate care’ or ‘reablement’ care pathway. The ‘intermediate care’ service is funded by the CCG. It provides short-term bed- or home-based care and rehabilitation for individuals with temporary problems (e.g. falls, fractures), no functional concerns and few comorbidities |
All other intermediate care provision delivered by NHS services |
| Participation of private providers in WP2a? | Declined participation in terms of staff completing measure of service user engagement at discharge | n/a | Three private providers declined participation and this precluded service users allocated to them being included in the study |
Core service features
Table 5 presents the core service features of the research sites. Geographical size and population density determined whether there was a single, colocated assessment team or locality/regional teams. The user profile in site B was of greater functional impairment, with many already known to social care. In this site, the pathway for ‘non-complex’ referrals – typically recovery from falls or fractures – was to a NHS-funded intermediate care service for short-term input.
| Characteristics | Site | ||
|---|---|---|---|
| A | B | C | |
| Organisation of reablement assessment staff | Three locality teams and a single, hospital-based team | A single colocated team | Four regional teams |
| User profile | Wide range of severity of functional impairment. Around half are reabled to independence with the remainder moving on to package of care | Severe functional impairment. Many already known to social care | Wide range of severity of functional impairment |
| Integrated working | Joint working arrangements with NHS with respect to referral processes for those being discharged from hospital | Service is sited in an integrated health and social care organisation; however, no posts in the service are funded by the NHS | No integrated working with NHS |
| Service delivery |
Two models: In-house staff assess and review; private provider delivers ‘hands-on’ reablement and monitor In-house staff assess; private providers deliver hands-on reablement, monitor and also review |
One model: In-house team assess, monitor and review Separate in-house team delivers ‘hands-on’ reablement |
Three models: In-house staff assess, monitor, review and deliver ‘hands on’ In-house staff assess and review; private provider delivers ‘hands-on’ reablement and monitor Assessment and review also carried out by private provider |
| Occupational therapy within service? | No one within the service is OT qualified. OT input secured on a case-by-case basis | All assessors are OT qualified | No one within the service is OT qualified. OT input secured on a case-by-case basis |
| Access to community health services | Referral on a case-by-case basis | In the same organisation and colocated with dementia, continence and district nursing services. Easy to source advice and describe ‘close-working’ and ‘liaise’ with relevant services on a case-by-case basis | Referral on a case-by-case basis |
| Roles in assessment and review process |
Team lead: accepts referrals, allocates cases, reviews complex referrals and oversees work of assessors Assessors: carry out assessment and review processes |
Team lead: accepts referrals and allocates cases Assessors: carry out assessment, monitoring and review processes |
Team lead: accepts referrals, allocates cases, and signs off all assessments and reviews Assessors: support assessment and review processes, and monitor intervention delivery |
| Referral routes |
Hospital-based assessment team receive referrals from hospital discharge teams Community-based assessment teams receive referrals from LA’s ‘central advice and duty team’ (includes self-referrals) |
Hospital discharge teams and locality’s community health and social care provider’s ‘central advice and duty team’ (includes self-referrals) | Hospital discharge teams and LA’s ‘central advice and duty team’ (includes self-referrals) |
All sites used private providers for the ‘reablement worker’ workforce, although one site also had an in-house team of reablement workers. There were different models of working with private providers, and this occurred within and between sites, particularly in terms of whether or not assessment and review responsibilities were also outsourced. All of the services were LA commissioned and funded. Referral routes were similar, although in one site different teams handled hospital discharge and social care referrals. This involved a joint working arrangement with the local hospital.
The degree to which assessors worked autonomously varied between services, reflecting level of qualification. In one site, the assessment team comprised OTs. In the other sites, no OTs were core members of the team. However, in one of these sites, all referrals were jointly reviewed by the assessment and reablement team and the community OT team with, if appropriate, joint-working initiated. These two teams were colocated. For the services without an OT within the core team, access to an OT’s input was on a case-by-case basis. In terms of access to community health-care services, in all sites this was on a case-by-case basis, but it was expedited in site B, which was located within an integrated community health and social care organisation. Ad hoc advice from community health practitioners was also easier to access in this site than in sites A and C.
Service processes and practices
Finally, in Table 6 we present some additional, more specific, comparisons between the research sites in terms of the processes and practices of the service. We focus particularly on those characteristics that, drawing on existing evidence, guidance and findings from the study’s process evaluation, are viewed as potentially able to have an impact on reablement outcomes.
| Characteristic | Site | ||
|---|---|---|---|
| A | B | C | |
| Waiting list? | No | Yes. Referrals referred on to private provider to deliver care package as an interim measure | No |
| Assessment and reviewing process | Single tier | Single tier | In-house service only: team leads involved in assessment process; and decide regarding discharge |
| Return home clients: location of assessment | Hospital | Home | Home |
| Decision-making regarding discharge involves a home visit by an assessor/team lead | No | No | Yes (for both in-house and outsourced clients) |
| Policy regarding the number of reablement workers assigned per case | Two | Multiple | Multiple |
| Reablement workers have a mixed caseload: reablement and home care | Yes | No |
In-house: no Outsourced: yes |
The assessment and reviewing process in site C presents it as having a higher level of surveillance and involvement by senior staff on the team, with team leads signing off reablement assessments via a home visit and leading the decision on discharge. In one site, assessment of referrals being discharged from hospital was carried out while the individual was still an inpatient.
Reablement workers based in outsourced services had mixed caseloads of reablement and home-care clients. This was not the case for reablement workers based in in-house reablement worker teams. Finally, sites differed in terms of policy regarding the number of workers involved in delivering reablement to an individual. In one site (B), the practice was to assign two workers (with back-up sickness/holiday cover). In the other sites, multiple workers were used; in site C this was the case for their in-house and outsourced provision.
Summary
This chapter describes the services that acted as research sites for the evaluation WP (WP2). It demonstrates the range of service and practice characteristics about which services may differ, many of which were explored in the outcomes and economic evaluation (WP2a and 2c). It also reveals that different service models may operate within a single commissioning locality. These findings highlight the importance of understanding a wide range of service and practice characteristics when conducting evaluations of complex interventions. Finally, we note that all of these services had changed in some way between the national survey and WP2 commencing (a period of around < 1 year), reflecting, we believe, changes associated with the implementation of the Care Act 2014. 15
Chapter 5 Work package 2a: the outcomes evaluation
Introduction
This chapter reports the outcomes evaluation (WP2a). The difficulties encountered during the execution of WP2 (see Chapter 2, Work package 2: an evaluation of different models of providing a generic reablement service), and its impact on sample sizes achieved across research sites, mean that the findings should be considered as indicative. However, they are important given the dearth of existing evidence, particularly in terms of the exploration of the impact on service user, intervention and service characteristics on outcomes, and findings regarding the different outcomes assessed.
Objectives and study design
The objectives of WP2a, revised in response to lower than expected sample sizes in research sites, were:
-
to describe changes in outcomes between entry into and discharge from reablement
-
to describe outcomes at 6 months post discharge, compared with outcomes at discharge
-
to explore whether outcomes at discharge are associated with individual and/or service/intervention delivery characteristics.
Study design
An observational study of a cohort of individuals receiving reablement from one of three reablement services across England in which outcomes were tracked from entry into the service, at discharge and at 6 months post discharge.
Methods
Setting
The setting was three reablement services (referred to as ‘research sites’) located in different regions of England. All fulfilled the study criteria of delivering comprehensive reablement. Chapter 4 reports the selection and characteristics of research sites (see Identification and recruitment of the case sites and The work package 2 research sites).
The local study team
Research sites had a local study team comprising a local study administrator and a local study officer (LSO). These teams were responsible for liaising with sites to ensure that all new referrals were approached regarding study participation, recruitment and consent processes, administration of research questionnaires to service users and service staff, and facilitating recruitment to the process evaluation (WP2c). They were located in the same building as the research site. Site-specific systems and processes were jointly developed to ensure smooth and efficient communication of relevant information between the site and local study team. Teams were fully trained and closely supervised and supported by the York research team via telephone, e-mail and face-to-face meetings.
Study participants
Inclusion criteria were:
-
had been offered, and accepted, reablement delivered by one of the research sites
-
were able to give informed consent, as judged by the practitioner carrying out the reablement assessment.
Variables: outcomes
A suite of outcome measures were used (Table 7). Outcomes were captured within the first week of referral to the reablement service (T0), within a week of discharge from the reablement service (T1) and at 6 months post discharge (T2 = T1 + 6 months).
| Variable | Measure/data source | Respondent | Data collection time point | ||
|---|---|---|---|---|---|
| T0 | T1 | T2 | |||
| Health-related quality of life | EQ-5D-5L | Service user | ✓ | ✓ | ✓ |
| Social care-related quality of life | ASCOT-SCT4 | Service user | ✓ | ✓ | ✓ |
| Mental health | GHQ-12 | Service user | ✓ | ✓ | ✓ |
| Functional status | Barthel Index of Activities of Daily Living | Reablement practitioner | ✓ | ✓ | |
| NEADL scale | Service user | ✓ | ✓ | ✓ | |
EuroQol-5 Dimensions, five-level version
The EuroQol-5 Dimensions, five-level version (EQ-5D-5L),41,42 is a standardised measure of health status, providing a descriptive profile of health-related quality of life with respect to five domains (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) and a single index value of health status. It is a self-report measure comprising five items and a visual analogue scale. Respondents report difficulty with each domain in terms of one of five levels: no problems, some problems, moderate problems, severe problems and extreme problems (coded 1 to 5, respectively). The five-digit figure generated is then converted into a single weighted index score. The EuroQol visual analogue scale (EQ VAS) records self-rated health on a vertical scale (1–100) from ‘worst imaginable health state’ to ‘best imaginable health state’.
The Adult Social Care Outcomes Toolkit – self-completed
The Adult Social Care Outcomes Toolkit – self-completed (ASCOT-SCT4)43,44 was designed to measure outcomes that may be affected by using social care. It captures nine social care-related domains of quality of life: control over daily life, personal cleanliness and comfort, food and drink, personal safety, social participation and involvement, occupation, accommodation, cleanliness and comfort, and dignity. Four response levels are offered: ideal state, no needs, some needs and high needs. It provides a descriptive profile of social care-related quality of life with respect to these domains. The single index score is calculated from these responses. The Adult Social Care Outcomes Toolkit (ASCOT) tools are used routinely by LAs and the government, and were used in a previous national evaluation of reablement services in England. 20
12-item General Health Questionnaire
The 12-item General Health Questionnaire (GHQ-12)45 was used to measure mental health. It focuses on two major areas: the inability to carry out normal functions and the appearance of new and distressing experiences. It comprises 12 items, with each item rated on a four-point scale: less than usual, no more than usual, rather more than usual and much more than usual. T0 scores were also used as a predictor.
The measures of functional status
A measure of functional status was proposed in the original protocol but not specified, as it was, to some extent, dependent on whether or not the research sites were routinely using such a measure. This was not the case and two measures were selected: the practitioner-completed Barthel Index (available only for T0 and T1) and the user-completed Nottingham Extended Activities of Daily Living (NEADL) scale. T0 scores were also used as predictors.
Barthel Index of Activities of Daily Living
The Barthel Index of Activities of Daily Living46 measures patients’ functional status, as assessed by health professionals based on observation. It assesses functional status across 10 domains: presence/absence of faecal incontinence, presence/absence of urinary incontinence, personal care (e.g. cleaning teeth, shaving), using the toilet, feeding, transfers (e.g. from chair to bed), walking, dressing, climbing stairs and bathing (or showering). Scoring of individual domains ranges between 0 and 15 (at 5-point intervals); domains vary in the number of intervals offered. The total score is used, which ranges from 0 (no functioning) to 100 (independent functioning).
Nottingham Extended Activities of Daily Living scale
The NEADL scale47 is a self-report measure of functional ability, or independence, with respect to a wide range of ADL. It comprises 22 items that are grouped into four areas of ADL: ‘mobility’ (six items), ‘kitchen’ (five items), ‘domestic’ (five items) and ‘leisure’ (six items) activities. Each item is scored on the response to four options: no (0 points), with help (0 points), on my own with difficulty (1 point) and on my own (1 point). The maximum score is 22 points, with higher scores indicating greater independence.
Variables: predictors
Data were also collected on a number of predictors, meaning that variables that we hypothesised might be associated with outcomes. They included characteristics identified in the research commissioning brief, findings from existing studies and findings emerging from our own process evaluation (WP2b). They comprised characteristics of the service user (Table 8), the intervention received and service-level characteristics (Table 9).
| Variable | Data source and measurement |
|---|---|
| Age (years) | Sociodemographic and health status questionnaire completed by the service user |
| Sex | Sociodemographic and health status questionnaire completed by the service user |
| T0 assessor-rated functioning | Barthel Index of Activities of Daily Living: total score |
| T0 self-rated functioning | NEADL scale: total score |
| T0 mental health | GHQ-12: total score |
| Engagement with reablement | HRERS-RV (see below): total score |
| Reason for referral to reablement | Participant classified by reablement service as ‘remain at home’ or ‘return home’. Classification shared with research team |
| Key physical health comorbidities |
Derived from a question in the sociodemographic and health status questionnaire completed by the service user Question: Do you have any health problems in addition to any associated with the need for reablement? Responses were categorised as ‘none’, ‘one’ or ‘two or more’ comorbidities |
| Living situation |
Derived from sociodemographic and health status questionnaire Question: Who do you usually live with? Response options: ‘alone’, ‘with partner’, ‘with family’ or ‘other’ |
| Perceived financial situation |
Derived from sociodemographic and health status questionnaire Question: Do you feel you have enough money to live on? Response options: ‘yes’ or ‘no’ |
| Informal carer involvement |
Derived from sociodemographic and health status questionnaire: Question: Have you received help from friends and family in the past two weeks? Response options: ‘yes’ or ‘no’ |
| Variable | Data source and measurement |
|---|---|
| Duration of intervention (weeks) | Derived from the administrative data held by the service |
| Intervention fidelity |
ERPC (see Experiences of Reablement Practice Checklist) All five items reported to have been present = complete implementation Binary variable: ‘complete’ vs. ‘incomplete’ implementation created |
| Reablement received from in-house vs. outsourced reablement workers |
Information collected from service leads by the research team Binary variable: ‘in-house’ vs. ‘outsourced’ |
| Single vs. multiteam model (assessors and reablement workers in same team) | Binary variable: ‘single’ vs. ‘multiteam’ |
| OT integral to team, or not | WP1: process evaluation |
| Service located within an integrated health and social care organisation vs. a single agency | WP1: process evaluation |
| Policy regarding number of reablement workers allocated per case | WP1: process evaluation |
The measures of user engagement [Hopkins Rehabilitation Engagement Rating Scale – Reablement Version (HRERS-RV)] and intervention fidelity [Experiences of Reablement Practice Checklist (ERPC)] were created for the purposes of the study and are described below.
Hopkins Rehabilitation Engagement Rating Scale – Reablement Version
As no measure of user engagement in reablement existed, we adapted the Hopkins Rehabilitation Engagement Rating Scale (HRERS)48 (see Appendix 3).
The HRERS-RV comprises five statements that capture the following domains of engagement: prepared for intervention, attitude towards intervention, acceptance of need for intervention, participation in intervention and impairments affecting participation. A six-point rating scale is used by the practitioners to indicate the degree to which each statement was observed in the target individual during the intervention period: never, rarely, some of the time, most of the time, nearly always and always. It was completed by a reablement practitioner immediately post discharge.
It was not possible to administer this measure in one of the research sites (site A) because the outsourced provider did not agree to including completion of the HRERS-RV as part of reablement workers’ usual roles and responsibilities.
Experiences of Reablement Practice Checklist
In the absence of an existing measure of intervention fidelity, a five-item checklist comprising statements that describe the domains of reablement practice was developed for the purposes of the study (see Appendix 4). The checklist comprised statements with respect to the understanding of the reablement approach, experience of a goals-focused approach, user involvement identifying goals, working towards achieving independence potential and reviewing progress. Completed by the service user at T1, ERPC asks respondents to report on their overall experience of reablement by answering ‘yes’ or ‘no’ to each statement.
Piloting the research instrument
The suite of questionnaires administered to service users was piloted to test overall respondent burden, comprehension of items and response formats for the sociodemographic and health status questionnaire, and the data collection instrument developed for the economics evaluation (WP2c): the SCPQ. It also explored preferences with respect to the mode of administering study questionnaires: self-completion or via a structured interview.
The findings indicated the importance of offering choice in how participants completed the study questionnaires. Pilot respondents typically preferred completing the SCPQ via a structured interview. Items on all questionnaires that raised queries were noted, and particular instructions regarding how to respond to such queries were included in LSO training. In terms of respondent burden, mixed mode of administration, pacing, and the benefit of company seemed, together, to mean that pilot respondents did not find the battery of questionnaires too burdensome.
Data collection
The T0 and T1 measures completed by service users were administered during a home visit by the LSO. Study participants chose whether to complete questionnaires themselves or through a structured interview.
The T2 measures completed by service users were administered during a home visit or by post. Postal administration was used when the LSO was no longer in post due to the closure of the study (see Chapter 2, Work package 2a: the outcomes evaluation).
Administration of practitioner-completed questionnaires [i.e. Barthel Index (T0 and T1), HRERS-RV (T1)] was also carried out by the local study team. In addition, the local study team requested data from the service with respect to study participants’ reasons for referral and intervention duration.
Study recruitment and retention
Recruitment, taking place over a 6-month period (between autumn 2016 and late spring 2017), was a three-stage process.
-
Assessor seeks consent to contact: during the assessment of a new referral, carried out within 1–3 days of referral, the assessor briefly introduced the study, handed over the study information sheet and requested permission for the LSO to contact the service user by telephone to discuss participation (‘consent to contact’). Research sites were instructed that ‘consent to contact’ should be sought from all eligible referrals. The outcome of that discussion was recorded on a pro forma, and, for those not agreeing to ‘consent to contact’, the reason for this decision was recorded.
-
LSO contacts service user: service users agreeing to be contacted by the research team were contacted by telephone by the LSO. During the call, further explanation was given regarding study participation and, if agreed, arrangements were made for a home visit.
-
Home visit by the LSO: during the home visit, consent was taken and T0 data collection was undertaken.
Figure 1 provides an overview of the recruitment process and outcomes. Recruitment materials are available (see Report Supplementary Material 2). A discussion of our experiences of recruitment to and retention within the study, and their implications, can be found in Appendix 5.
FIGURE 1.
Recruitment process and retention: T0 to T1.
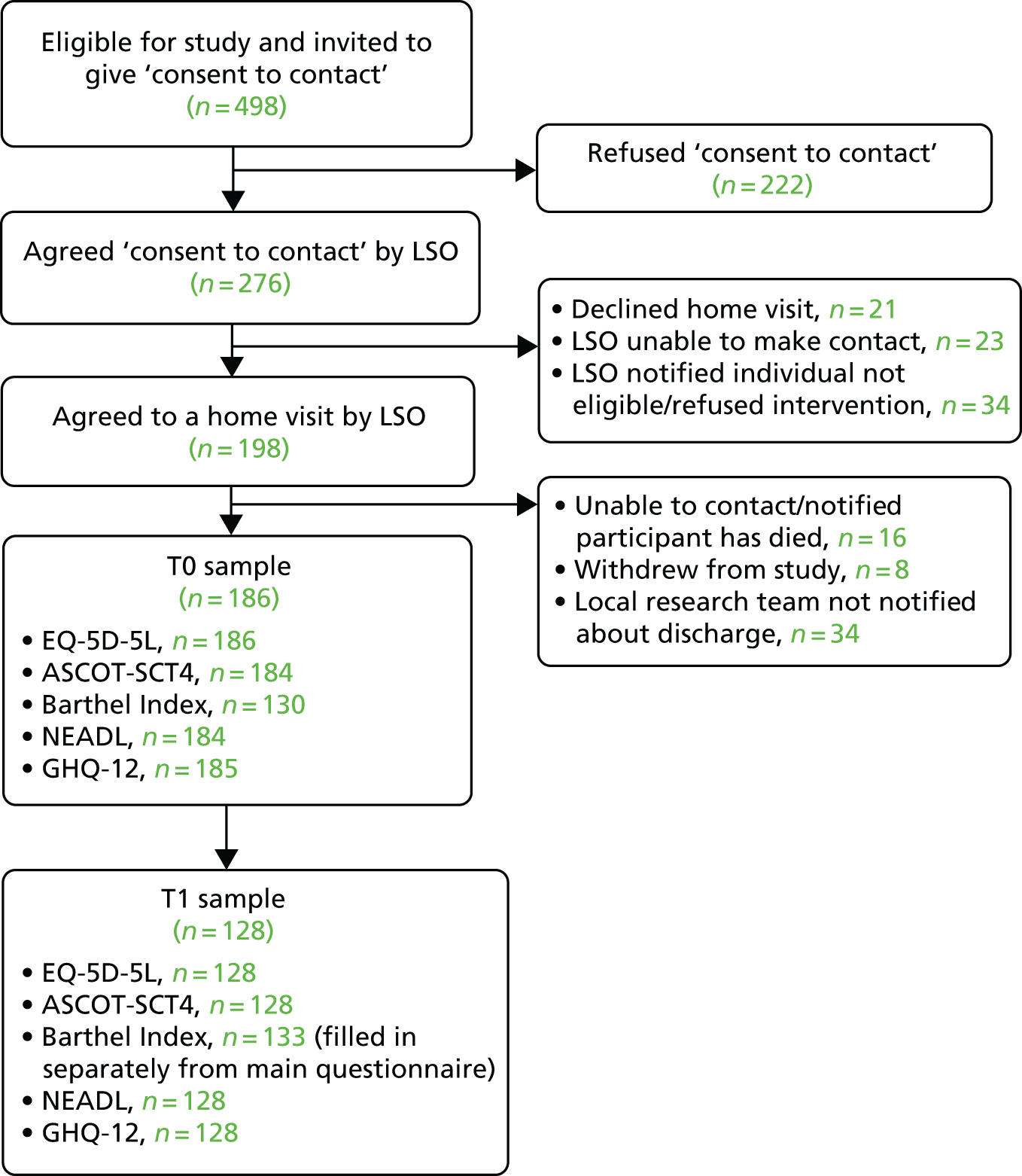
Recruitment
In total, 498 individuals across the three research sites were invited to give ‘consent to contact’. Over half (n = 276, 55.3%) agreed. Of these, 198 (71.7%) agreed to a home visit once they had been contacted by the LSO. A total of 186 individuals (representing 67.4% of those who gave ‘consent to contact’ and 37.3% of those invited to give ‘consent to contact’) were recruited to the study and had baseline data collection completed.
Retention at T1
The reablement service notified the local study team when a study participant was being discharged. This prompted the LSO to recontact the study participant to request a home visit to conduct T1 data collection. Unfortunately, in two research sites, on 34 occasions the service failed to notify the local study team about a discharge (18.3% of the T0 sample). These individuals were retained for T2. Among the remaining study participants, retention at T1 was good (84.2%). Thus, T1 data collection was achieved for 128 out of 186 study participants. Figure 2 provides an overview of attrition and retention between discharge and T2.
FIGURE 2.
Retention: T1 to T2.
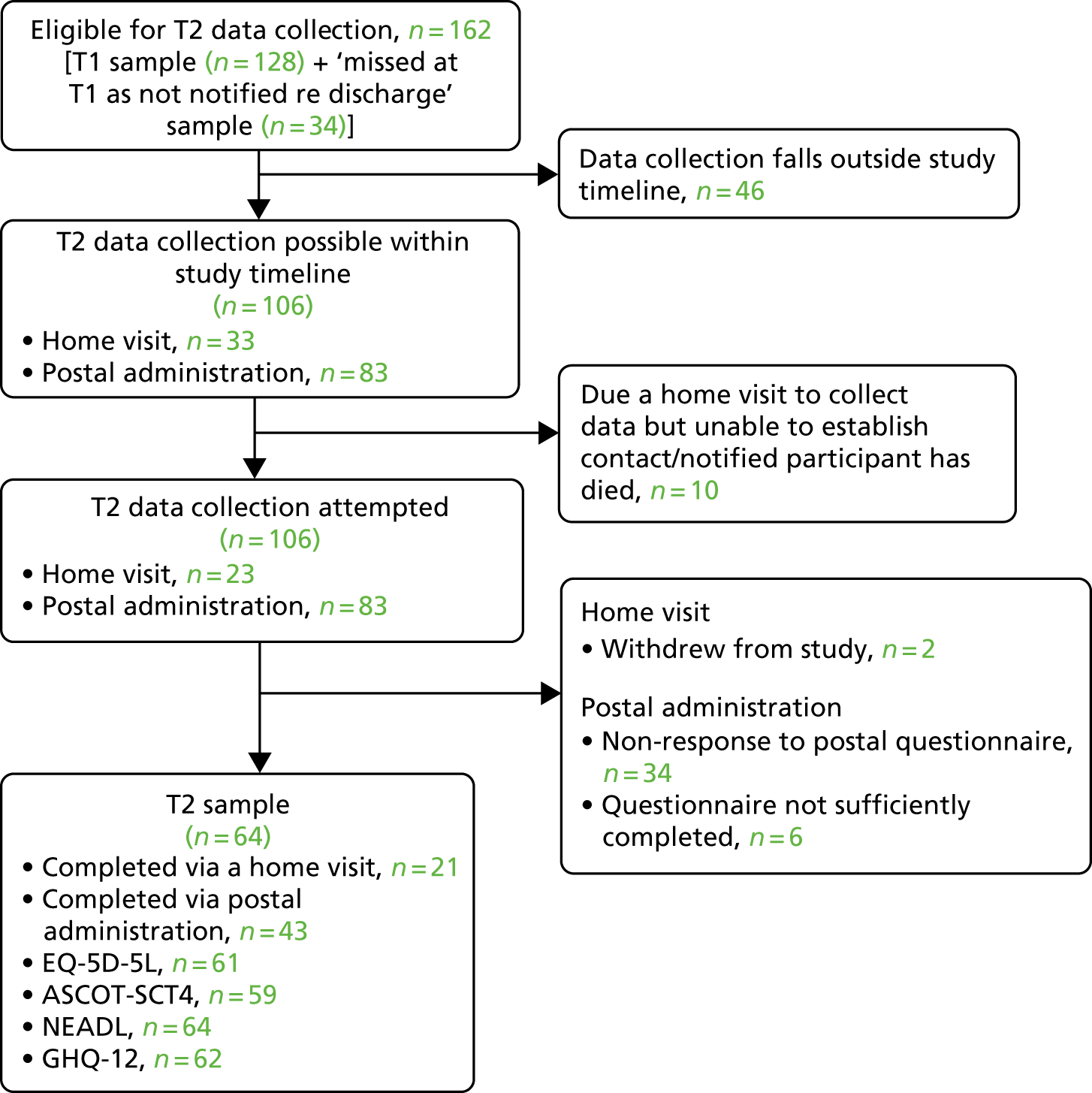
Retention at T2
In total, 162 individuals were retained for follow-up 6 months after discharge from the reablement service. Unfortunately, 46 individuals could not be followed up because of the closure of the study. However, we attempted T2 data collection with the remaining 116 study participants. In the original study protocol we had planned to use home visits again to collect T2 data. In two sites, owing to study closure, local study teams were no longer in place. As a result, we administered the research instruments by post. In the third site (site C), for those recruited early in the study timeline, it was possible for the LSO to attempt to collect T2 data via home visits (n = 21). A T2 sample size of 64 out of 116 was achieved (55.2%). Retention was higher when home visits were used to collect data than when postal administration was used (91% vs. 51.8%). In total, the number of study participants for whom we had complete T0, T1 and T2 data was 52 out of 186.
Loss to study through death or permanent move to residential care
According to the information available to us, very few participants were lost to the study because they had died (n = 10) or permanently moved to residential care (n = 1). We would note, however, that these may also be the reasons why we failed to re-establish contact with some study participants at T1 and T2.
Analytical plan
The statistical software Stata® 14.2 (StataCorp, College Station, TX, USA) was used.
Sample characteristics
Descriptive statistics explored the sociodemographic characteristics of study participants. For continuous variables means, standard deviations, minimum and maximum values, and medians were used. Categorical data were calculated as counts and percentages. The characteristics of study participants retained to the study and those lost to follow-up were compared. Comparisons between sites were also made.
Outcomes
Scores on outcome measures were explored by examining their mean, standard deviation, median, minimum and maximum values at T0, T1 and T2. We also examined changes in scores between time points (T0 to T1, T1 to T2). Overlaid histograms were used to visually present the score distributions. An analysis of EQ-5D-5L index scores used the 2017 tariff, with the 2016 tariff used for a sensitivity analysis. We also conducted an ancillary analysis of EQ-VAS scores. Finally, we examined the number and percentage of respondents reporting deteriorating, maintained and improved outcomes at each time point.
Associations between predictors and outcomes at discharge
Linear regression techniques were utilised to investigate associations between predictor variables and outcomes at T1, taking account of clustering of data. These analyses were then repeated controlling for site. Sample size limited our ability to control for explanatory variables simultaneously, and hence only baseline characteristics and one other single predictor were added to each regression model. In addition to estimates, we report associated 95% confidence intervals (CIs) and p-values.
Results
Sample characteristics
Sociodemographic characteristics
Characteristics of the sample, also stratified by site, are presented in Table 10.
| Variable | Site, n (%) | Total, n (%) | ||
|---|---|---|---|---|
| A | B | C | ||
| Total recruited | 33 | 14 | 139 | 186 |
| Age (years) | ||||
| Mean (SD) | 77.3 (9.13) | 83.0 (8.33) | 81.5 (9.06) | 80.8 (9.13) |
| Median (range) | 75 (51–89) | 83.5 (70–95) | 82 (52–102) | 82 (51–102) |
| Sex | ||||
| Female | 23 (70) | 12 (86) | 84 (60) | 119 (64) |
| Male | 10 (30) | 2 (14) | 55 (40) | 67 (36) |
| Living alone | ||||
| No | 16 (48) | 7 (50) | 56 (40) | 79 (42) |
| Yes | 17 (52) | 7 (50) | 83 (60) | 107 (58) |
| Sufficient money | ||||
| No | 4 (13) | 2 (18) | 25 (18) | 31 (17) |
| Yes | 28 (88) | 9 (82) | 112 (82) | 149 (83) |
| Referral reason | ||||
| Return home | 12 (36) | 9 (64) | 54 (61) | 75 (40) |
| Remain at home | 21 (64) | 5 (36) | 85 (61) | 111 (60) |
| Informal carer involved | ||||
| No | 9 (29) | 1 (7) | 10 (7) | 20 (11) |
| Yes | 22 (71) | 13 (93) | 129 (93) | 164 (90) |
| Number of health comorbidities | ||||
| None | 19 (58) | 8 (57) | 40 (29) | 67 (36) |
| 1 | 8 (24) | 4 (29) | 67 (48) | 79 (42) |
| ≥ 2 | 6 (18) | 2 (14) | 32 (23) | 40 (22) |
The mean age of study participants was 80.8 years (range 51–102 years). The median age (total sample, 82 years) varied between sites, with a lower median age in site A (75 years) than in sites B (83.5 years) and C (82 years).
The majority of participants were female (n = 119). The proportion who were male varied between sites. Over half the sample (58%) lived on their own, and this varied a little between sites. The majority of study participants (83%) reported having sufficient money to live on. In sites A and C, the majority of participants (60%) had been referred to the service because of concerns about their ability to continue living independently at home (classified as ‘remain at home’). This figure was much lower in site B 36% (n = 5), where the majority had been referred to the service following discharge from hospital (classified as ‘return home’). Around 90% of study participants in sites B and C reported receiving regular help from friends and family (classified as ‘informal carer involved’); this proportion was smaller in site A. One-third of the sample (36%) reported no key health comorbidities, 42% reported one key comorbidity, and nearly one in five reported two or more key comorbidities.
Engagement with reablement
The HRERS-RV scores were collected in sites B and C only. On average, study participants in site C scored higher than those in site B {average score for site C 26.2 [standard deviation (SD) 4.64] (maximum score 30) vs. site B 25.4 (SD 4.24)}.
Intervention- and service-level characteristics
The nature of the sample in terms of intervention- and service-level characteristics is set out in Table 11. (Note: more than one model of service delivery was represented in site C; see Chapter 4, Core service features.)
| Variable | Site, n (%) | Total, n (%) | ||
|---|---|---|---|---|
| A | B | C | ||
| Duration of reablement (weeks) | ||||
| Mean (SD) | 3.87 (1.55) | 3.52 (1.47) | 3.93 (1.62) | 3.89 (1.59) |
| Median | 4.0 | 3.71 | 4.07 | 4.0 |
| Multiteam vs. single team model | ||||
| Multiteam | 32 (100) | 14 (100) | 29 (21) | 75 (41) |
| Single team | n/a | n/a | 110 (79) | 110 (59) |
| In-house vs. outsourced reablement workers | ||||
| In-house | n/a | 14 (100) | 104 (75) | 118 (64) |
| Outsourced | 32 (100) | n/a | 35 (25) | 67 (36) |
| Intervention fidelity (ERPC) (T1 sample) | ||||
| Partial | 10 (53) | 8 (57) | 26 (27) | 44 (34) |
| Complete | 9 (47) | 6 (43) | 69 (73) | 84 (66) |
The mean duration of reablement was similar across the sites. The median duration was slightly lower in site B (3.71 weeks) than in sites A (4.0 weeks) and C (4.07 weeks). Across the whole sample, just over 40% of service users had received reablement via a multiteam service model (i.e. assessors and reablement workers based in separate teams). In terms of the organisational base of the workers who delivered the reablement, just under two-thirds of the service user sample received reablement via an in-house team of reablement workers. Finally, intervention fidelity, as reported by study participants using the ERPC, varied between sites. The majority (73%) of the site C sample reported complete intervention fidelity, compared with fewer than half in site A (47%) and site B (43%).
The sample retained at T1
There were no significant differences between T0 and T1 samples with respect to sociodemographic characteristics and scores on outcome measures at T0 (see Appendix 6, Tables 40–43).
Health-related quality of life (EuroQol-5 Dimensions, five-level version)
Index and visual analogue scale score descriptives: T0, T1 and T2
Scores derived using the 2016 and 2017 tariffs were highly correlated at T0 and T1 (see Appendix 7, Tables 44 and 45 and Figure 10). Therefore, only the 2017 tariff is reported.
A comparison of total samples found a mean increase (represents improvement) in EQ-5D-5L index score from T0 to T1 of 0.16, and a mean increase in EQ VAS score of 11.7 (Table 12). At T2, the mean EQ-5D-5L index score was slightly improved compared with at T1, and there was a mean 5-point increase in EQ VAS score at T2. At T1 the minimum EQ VAS score was 1, whereas at T2 the minimum score was 20. Histograms presenting changes in distributions of EQ-5D-5L scores are presented in Appendix 7 (see Figure 14).
| Time point | n | Mean (SD) | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| EQ-5D-5L index | |||||
| T0 | 186 | 0.51 (0.23) | 0.52 | –0.09 | 0.92 |
| T1 | 128 | 0.67 (0.24) | 0.75 | –0.09 | 1.00 |
| T2 | 61 | 0.69 (0.26) | 0.78 | –0.01 | 1.00 |
| EQ VAS | |||||
| T0 | 185 | 51.83 (20.23) | 50 | 5 | 95 |
| T1 | 128 | 63.52 (20.45) | 69 | 1 | 100 |
| T2 | 61 | 68.77 (20.55) | 75 | 20 | 100 |
Change in index and visual analogue scale scores: T0 to T1, T1 to T2
There was a statistically significant improvement in EQ-5D-5L index and EQ VAS scores between T0 and T1 among participants who completed the measure at both time points (n = 128). The mean improvement in index score was 0.15 (95% CI 0.11 to 0.18), and for the EQ VAS the mean improvement was 11 (95% CI 8.1 to 15.5). Scores at T1 were positively linearly correlated with those at baseline. For the great majority (84%), an improved health-related quality of life was observed at T1 (see Appendix 7, Table 46). However, a deterioration was observed in over 1 in 10 (13%) participants.
For study participants for whom we have T1 and T2 data (n = 49), the difference in mean EQ-5D-5L index scores between these two time points (difference 0.023, 95% CI –0.0386 to 0.085) was not statistically significant (p = 0.451). The majority of respondents (57%) had maintained or improved EQ-5D-5L index scores at T2 compared with at T1 (see Appendix 7, Table 46). For the EQ VAS, the mean difference in T1 and T2 scores was not statistically significant (difference 3.22, 95% CI –9.923 to 3.492; p = 0.34, n = 51). Over 60% of study participants had maintained or improved their T1 EQ-5D-5L scores at T2.
Domain scores: T0 to T1
The reported levels of impairment (five-point scale: extreme, severe, moderate, slight or no impairment) at T0 and T1 (total samples), with respect to the five domains of health-related quality of life (mobility, self-care, pain or discomfort, usual activities, and anxiety or depression), are available (see Report Supplementary Material 3).
The majority of participants who completed the EQ-5D-5L at T0 and T1 reported improved mobility (52%), self-care (71%) and performance of usual activities (55%) at T1 (see Appendix 7, Table 47). In the case of the pain or discomfort and anxiety or depression dimensions, the level of impairment remained the same for the majority of study participants (49% and 48%, respectively). However, for almost one-fifth (19%) of the sample, the level of impairment had deteriorated in one domain at T1 compared with at T0. A further 5% of participants reported deterioration in two domains and just under 2% reported it in more than two domains. The proportion of study participants experiencing deterioration was small for mobility (9%), self-care (2%) and usual activities (7%), but larger for pain or discomfort (14%) and anxiety or depression (17%).
Social care-related quality of life (Adult Social Care Outcomes Toolkit – self-completed)
Index score descriptives: T0, T1 and T2
The mean ASCOT-SCT4 index score at T1 had improved by 0.11 compared with at T0 (Table 13). At T2, the mean score had decreased slightly, by 0.02.
| Time point | n | Mean (SD) | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| T0 | 184 | 0.71 (0.17) | 0.73 | –0.04 | 1.00 |
| T1 | 128 | 0.82 (0.15) | 0.86 | 0.06 | 1.00 |
| T2 | 59 | 0.80 (0.17) | 0.84 | 0.05 | 1.00 |
Histograms presenting changes in the distributions of ASCOT-SCT4 index scores across time points are presented in Appendix 8 (see Figures 17 and 18).
Change in index scores: T0 to T1, T1 to T2
There was a statistically significant improvement in ASCOT-SCT4 index scores between T0 and T1 for the 128 participants who completed this measure at both time points. The mean improvement was 0.09 (95% CI 0.06 to 0.11). Scores between baseline and discharge were positively correlated (correlation coefficient = 0.62). Among study participants for whom data were available at T0 and T1 (n = 128), the great majority (73%) reported improved health-related quality of life at discharge (see Appendix 8, Table 48). However, nearly one-quarter (24%) reported a deterioration in health-related quality of life.
For study participants for whom we have T1 and T2 data (n = 46), the difference between the mean ASCOT-SCT4 index scores at T1 and those at T2 was not statistically significant (difference 0.0018; p = 0.928). Over half (55%) maintained or improved ASCOT-SCT4 scores (see Appendix 8, Table 48).
Domain scores: T0 to T1
The distribution of scores at T0 and T1 (total samples) for the nine social care-related quality-of-life domains captured by ASCOT-SCT4 are available (see Report Supplementary Material 3).
For participants who completed the ASCOT-SCT4 at T0 and T1 (n = 128) (see Appendix 8, Table 49), the domains where greatest proportions reported improvements were feeling clean and presentable (46%), control over daily life (43%), spending time doing things which they value or enjoy (42%), social contact (38%) and having food and drink when they want it (35%). Over one-quarter of study participants reported improved outcomes with respect to their home feeling clean and comfortable (accommodation) (29%) and feelings about having help (26%). The two domains sharing the smallest increases in the proportion of patients reporting improvements were feeling safe (17%) and how being helped made them feel about themselves (17%). Typically, the proportions of study participants reporting deteriorations were small, at ≤ 10%. However, at discharge, almost one in five participants reported a deterioration in social contact (19%), 15% felt less safe and 13% reported a deterioration in the way they spent their time.
Practitioner-rated functioning (Barthel Index of Activities of Daily Living)
Completion of the Barthel Index of Activities of Daily Living
Reablement assessors completed the Barthel Index at the referral assessment visit (T0) and on discharge from the service (T1). Unfortunately, not all assessors adhered to the instructions regarding its completion. The most common issues were that respondents had not used the (up to 4 points) categorical scoring system (i.e. 0, 5, 10, 15) but had instead inserted a ‘score’ such as 2 or 8, or that items were missed or noted as ‘not applicable’. This issue was observed across all sites, but appeared to be less of a problem in the site in which the reablement assessors were OTs.
Total score descriptives: T0 and T1
A comparison of Barthel Index scores between T0 and T1 samples revealed a mean increase of 9.2 (Table 14). It was not possible to administer the Barthel Index to staff at T2.
| Time point | n | Mean (SD) | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| T0 | 130 | 71.692 (17.022) | 75 | 10 | 100 |
| T1 | 133 | 80.451 (20.277) | 90 | 5 | 100 |
Histograms presenting changes in the distribution of Barthel Index scores at T0 and T1 are presented in Appendix 9 (see Figure 19).
Change in total score: T0 to T1
Among the study participants for whom a Barthel Index score was available at T0 and T1 (n = 105), there was a statistically significant improvement in score at T1 (mean score change 8.4, 95% CI 11.8 to 5.0). Barthel Index scores at T1 were positively linearly correlated with those at T0 with a correlation coefficient of 0.53. Over two-thirds of participants were assessed as having improved functioning at T1, while one in five was assessed as having deteriorated (see Appendix 9, Table 50).
Domain scores: T0 to T1
The distributions of item scores at T0 and T1 (total samples) for the 10 domains of ADL assessed by the Barthel Index are available (see Report Supplementary Material 3).
Among participants for whom these data were available at T0 and T1 (n = 96), domains in which the largest number of study participants improved functioning were dressing (53% improved functioning at T1), bathing (49%), personal grooming (35%), transfers (25%) and managing stairs (21%) (see Appendix 9, Table 51). The proportion of study participants assessed as having deteriorated in functioning with respect to an ADL was never greater than the proportion assessed as having improved. Domains in which the largest proportions of deterioration in functioning were observed at T1 compared with T0 were mobility (17%), managing stairs (15%), using the toilet (13%) and transfers (13%).
Self-rated functioning (Nottingham Extended Activities of Daily Living scale)
Total score descriptives: T0, T1 and T2
There was a small (0.75 point) increase in the mean NEADL score at T1 compared with T0 (Table 15). At T2, there was an almost 3-point increase in the mean NEADL score compared with the T1 mean score. Histograms presenting changes in the distribution of NEADL scores can be found in Appendix 10 (see Figure 20).
| Time point | n | Mean (SD) | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| T0 | 184 | 9.65 (5.48) | 8.5 | 0 | 22 |
| T1 | 128 | 10.40 (4.46) | 10.0 | 3 | 22 |
| T2 | 64 | 13.22 (6.27) | 13.5 | 0 | 22 |
Change in total score: T0 to T1, T1 to T2
The change in mean NEADL scores (0.73, 95% CI 1.51 to 0.06) between T0 and T1 among participants who completed the NEADL questionnaire at both time points (n = 128) was not significant (p = 0.07). NEADL scores at T0 and T1 were significantly correlated (r = 0.625; p < 0.001). For over half of study participants, NEADL scores had improved at T1 compared with at T0, and fewer than one-third reported a deterioration in functioning (see Appendix 10, Table 52).
Among participants for whom data were available at T1 and T2 (n = 52), the mean self-reported functional status score was 1.79 higher at T2 than at T1, which is a statistically significant difference (95% CI 3.03 to 0.55; p < 0.01). The majority (73%) of respondents had a maintained or improved NEADL score. Two-thirds of NEADL scores had improved between T1 and T2, whereas scores for just over one-quarter of the sample had deteriorated.
Domain scores: T0 to T1
The distributions of item scores at T0 and T1 (total samples) with respect to the four domains of (extended) ADL (i.e. mobility, kitchen, domestic and leisure) assessed by the NEADL scale are available (see Report Supplementary Material 3).
Among participants who completed the NEADL scale at T0 and T1, similar proportions had improved or deteriorated with respect to mobility (e.g. walking, climbing stars, getting in and out of a car, and walking on uneven surfaces) (see Appendix 10, Table 53). For the majority (67–83%), their level of functioning remained the same at T1 as at T0. However, greater proportions had deteriorated (as opposed to improved) in functioning with respect to crossing roads and managing public transport at T1 compared with T0. Again, for the majority (77–85%), their level of functioning was unchanged.
With respect to the items comprising the kitchen domain, a deterioration in the level of functioning was extremely rare. Over 1 in 10 study participants had improved in functioning with respect to making a hot drink (12%), carrying a hot drink (16%), washing up (15%) and making a snack (13%). As with the mobility domain, for the majority (80–94%), their level of functioning was unchanged.
For the domestic domain, around one in five study participants had improved in functioning with respect to laundry tasks (e.g. handwashing small items, 20%; full clothes wash, 17%), and a small minority had improved their functional ability to go shopping (9%). However, around 1 in 10 participants had deteriorated with respect to being able to go shopping (9%) and do a full clothes wash (13%).
Finally, in terms of the leisure domain, for the great majority, their level of functioning with respect to constituent items was the same at T0 and T1 (84–97%). However, greater proportions reported deteriorating abilities to socialise (9%), garden (7%) and drive (9%) than reported improved functioning in these areas (7%, 3% and 3%, respectively). The item for which the largest proportion of study participants reported improved functioning at T1 compared with T0 was writing letters (16%).
Mental health (12-item General Health Questionnaire)
Finally, we conducted a preliminary exploration of changes in scores on the GHQ-12 across the outcome time points.
Total score descriptives: T0, T1 and T2
The mean GHQ-12 score was lower (improved) at T1 than at T0, and had further decreased at T2 (Table 16). Histograms presenting changes in the distribution of the score can be found in Appendix 11 (see Figure 21).
| Time point | n | Mean (SD) | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| T0 | 185 | 4.14 (2.85) | 4 | ||
| T1 | 128 | 2.42 (2.60) | 2 | 0 | 12 |
| T2 | 62 | 2.10 (2.65) | 1 | 0 | 12 |
Change in total score: T0 to T1, T1 to T2
For study participants for whom GHQ-12 scores were available at T0 and T1 (n = 128), over two-thirds (69.5%) had improved scores at T1 compared with T0. For around one-fifth (18%), scores had deteriorated (see Appendix 11, Table 54).
In terms of change in GHQ-12 scores between T1 and T2 (n = 50), scores were on average 0.56 points higher at T2 than at T1 (95% CI –10.157 to 1.277). This difference was not statistically significant (p = 0.123). A deterioration in score was observed in just under one-quarter of study participants (24%). However, scores further improved half of participants and remained unchanged in the remainder (26%).
Association between predictors and T1 outcomes
Regression analysis was used to carry out an initial exploration of whether or not identified individual and service/intervention characteristics (see Variables: predictors) were associated with T1 outcomes. It was not possible to carry out this analysis with respect to three identified service-level characteristics because these features were all unique to the research site where only 14 service users were recruited to the study. These were whether or not an OT was integral to the team, location of the service within an integrated health and social care organisation versus single agency and the policy regarding the number of reablement workers allocated per case.
Sample sizes were small, and multiple regression was not possible. Scrutiny of outputs from both regression analyses (both accounted for clustering by site, one also used site as an explanatory variable) in terms of statistical significance, regression coefficients and 95% CIs were used to allocate characteristics to one of three categories:
-
strong evidence found of an association between the characteristic and the outcome measure (p < 0.01)
-
some evidence found of an association between the characteristic and the outcome measure (p < 0.05)
-
insufficient evidence found of an association between the characteristic and the outcome measure.
Full analytical outputs are provided in Appendix 12 (see Tables 55–58). These analyses should be regarded as preliminary, as insufficient total sample size and small sample sizes in two sites means that more complex analyses were not possible. Thus, it was not possible to control for other predictors when testing the association between a particular characteristic and an outcome. Equally, it was not possible to explore the relative contribution of different predictors on outcomes. Finally, it is important to stress that evidence of an association cannot be taken to imply that the impact of a particular individual or service/intervention characteristic on an outcome is ‘clinically significant’ (i.e. that it is meaningful or of practical relevance to service users or service providers). The findings reported in this section should, therefore, be regarded as preliminary evidence that can be used to inform future research.
Associations between predictors and T1 health-related quality of life (EuroQol-5 Dimensions, five-level version)
Service user characteristics
Strong evidence was found of a positive association between the following variables and improved health-related quality of life (EQ-5D-5L index score) at T1: having sufficient money (as opposed to reporting insufficient money), greater engagement with reablement, being male and living with partner/family (compared with living alone).
Some evidence was found of an association between better mental health at entry into reablement and self-reported functional ability and greater improvement in EQ-5D-5L score at T1.
Service/intervention characteristics
There were no service/intervention characteristics for which strong evidence of an association with T1 EQ-5D-5L scores was found. Some evidence was found that receiving reablement from a worker based in an outsourced provider was associated with more negative outcomes than when reablement was provided by an in-house team. In addition, there was some evidence of an association between being reabled by a service that comprises a single team (as opposed to separate assessor and reablement worker teams) and greater improvements in the EQ-5D-5L index score.
Associations between predictors and T1 social care-related quality of life (Adult Social Care Outcomes Toolkit – self-completed)
Service user characteristics
Strong evidence was found of a positive association between improved social care-related quality of life (ASCOT-SCT4 index score) at T1 and the following service user characteristics: having sufficient money (as opposed to reporting insufficient money), better mental health at T0 and greater engagement with reablement.
There was also some evidence that referral to reablement to remain at home (compared with those referred to support a return home from hospital) and being older were associated with greater improvements in social care-related quality of life at T1.
Service/intervention characteristics
There was strong evidence of an association between greater improvements in T1 ASCOT-SCT4 scores and longer duration of reablement. In addition, there was some evidence of a positive association between greater gains in ASCOT-SCT4 scores at T1 and intervention fidelity and receiving reablement from in-house (as opposed to outsourced) providers.
Associations between predictors and T1 practitioner-rated functioning (Barthel Index of Activities of Daily Living)
We note that the sample size for Barthel Index scores was smaller than that for other analyses (n = 105/128) as a result of inaccurate completion of the measure [see Health-related quality of life (EuroQol-5 Dimensions, five-level version)].
Service user characteristics
Strong evidence was found of an association between greater improvements in practitioner-reported functioning (Barthel Index score) at T1 and the majority of service user characteristics: having sufficient money (as opposed to reporting insufficient money), having better self-reported functional status at T0, having greater engagement with the reablement intervention, being older, having no physical health comorbidities, having better mental health at T0, having no informal carer involvement and being female.
Service/intervention characteristics
There were no service/intervention characteristics for which strong evidence was found of an association with practitioner-rated functioning scores at T1. There was some evidence that receiving reablement from a single team (compared with separate teams assessing and delivering reablement) was associated with greater improvements with practitioner-rated functioning at T1.
Associations between predictors and T1 self-rated functioning (Nottingham Extended Activities of Daily Living scale)
Service user characteristics
Strong evidence was found of an association between self-rated functioning at T1 and the following service user characteristics: greater engagement with the reablement and assessor-reported functioning at T0. Some evidence was found of a positive association between this outcome and the following service user characteristics: being younger, being referred to support remaining at home (compared with those referred to support a return home from hospital), and having sufficient money (compared with those reporting insufficient money).
Service/intervention characteristics
Some evidence of association was found between greater improvements in self-rated functioning at T1 and two service characteristics: receiving reablement from a single team (compared with separate teams assessing and delivering reablement) and receiving reablement from in-house (as opposed to outsourced) providers.
Summary
The smaller than expected sample size, particularly in two research sites, means that the data presented should be considered as exploratory.
Improvements on all outcomes – health-related quality of life (EQ-5D-5L), social care-related quality of life (ASCOT-SCT4), practitioner-reported functioning (Barthel Index) and self-reported functioning (NEADL scale) – were observed at discharge from reablement (T1) compared with entry into the service (T0). For the subsample for whom data were collected at both time points, improvements in health-related quality of life, social care-related quality of life and practitioner-reported functioning were statistically significant.
Outcomes had further improved at 6 months post discharge, but the improvements in health-related and social care-related quality of life were not statistically significant. However, the improvement in self-reported functioning was statistically significant, a contrast with the degree of improvement at discharge, which was not significant. Barthel Index scores were not available at this time point. Using the GHQ-12, we also looked at mental health outcomes at 6 months’ follow-up. A (non-significant) improvement in the mean GHQ-12 score was observed between T1 and T2.
A set of regression analyses explored, in a preliminary way, the association between service- and individual-level characteristics on outcomes at discharge from reablement. There was some evidence of a positive association between intervention engagement, better mental health and having sufficient money and health-related quality of life at discharge. There was weaker evidence of a positive association between this outcome and sharing the home with others and self-reported functioning at entry into reablement. There was also weak evidence of an association with two service characteristics: receiving reablement from a single team (vs. multiteam) and from in-house (vs. outsourced) reablement workers.
In terms of social care-related quality of life, there was some evidence of association between this outcome at discharge and a number of individual (e.g. sufficient money, referral reason, mental health at entry, engagement with reablement) and service characteristics (e.g. intervention fidelity, duration of reablement). A weak association between this outcome and informal carer involvement and in-house versus outsourced reablement workers was also found.
With respect to practitioner-reported functioning at discharge, there was some evidence that the following individual characteristics were associated with more positive outcomes: having sufficient money, being referred for reablement to support return home from hospital (as opposed to support remaining at home) and engagement with reablement. There was also some evidence of a positive association between self-reported functioning at discharge and health-related quality of life at entry into the service and practitioner-reported functioning. There was also some evidence that informal carer involvement was negatively associated with this outcome. In addition, there was weak evidence that living alone and better mental health at entry into the service were associated with better practitioner-reported functioning at discharge. In terms of service characteristics, there was some evidence that practitioner-reported functioning at discharge was positively associated with receiving reablement from a single team. There was also weak evidence that receiving reablement from in-house, as opposed to outsourced, reablement workers was positively associated with practitioner-reported functioning at discharge.
Finally, in terms of self-reported functioning at discharge, there was some evidence of a positive association with engagement with reablement. There were a number of other individual characteristics for which there was weak evidence of a positive association with self-functioning at discharge. These were health-related quality of life and practitioner-reported functioning at entry into the service, living alone, having sufficient money, being referred to support a return home from hospital and being younger. There was some evidence of an association between self-functioning at discharge and two service characteristics: the reablement service being formed of a single team and having in-house reablement workers.
Chapter 6 Work package 2b: delivering reablement – practitioner views
Introduction
This chapter concerns the experiences of staff directly involved with delivering reablement, both those in reablement assessment teams and those who do the hands-on reablement work with service users. Investigating staff views was one element of the process evaluation (WP2b), the other being research with service users and family members. The purpose of this aspect was both to understand the experience of providing and delivering reablement and to elicit views regarding the outcomes of reablement and the factors that have an impact on outcomes.
Methods
Focus groups were held with assessors in each site and with reablement workers in two sites (the third site, an outsourced service, declined to participate). Data collection took place between April and July 2017.
Recruitment
Local study teams facilitated recruitment and liaised with service/team leads regarding the time and venue of focus groups. They distributed an invitation and study information sheet (hard copy or via e-mail) to all staff in assessment and reablement worker teams based in the research site, including any outsourced services. Staff were invited to respond if they were interested in taking part. Consent to participate was secured at the start of the focus group. Recruitment materials are available (see Report Supplementary Material 4).
Data collection
Focus groups were held at the organisational base of each research site and explored the following topics:
-
views and experiences regarding the processes involved in delivering reablement by their service, including the factors that inhibit and facilitate that process and the outcomes achieved
-
views regarding the intervention itself, its appropriateness and perceived effectiveness
-
views regarding the active ingredients of reablement and mechanisms for change.
The topic guides and visual tools/activities used to facilitate discussions are available (see Report Supplementary Material 5).
Data analysis
Data were analysed thematically. 49 The framework approach50,51 was used to ensure systematic data management and audit trails of the data management process. Data from assessor and worker focus groups were analysed together. Participant group and research site were key variables used to test and explore similarities and differences in views and experiences. The data analysis particularly focused on issues that were not context specific, such as a particular local sticking-point in terms of service delivery. The description of the analytical process below is based on the one set out in the study protocol. 34
There are four stages to the analytical process. First, researchers familiarise themselves with the data and identify themes and key issues (both a priori and emergent). An index of themes is then constructed (the thematic framework). Data are then indexed according to the theme(s) in the analytical framework they relate to. Finally, the indexed data from each case (e.g. participant, focus group) are summarised onto a series of thematic matrices (or charts). Each chart is divided into columns, allowing relevant data to be organised according to subthemes/issues. A single row on each chart holds one participant’s data. Thus, reading along a row provides an overview of everything an individual spoke about in terms of a specific issue. Reading down the chart (or down a column) allows comparison between participants. The final stage of analysis involves ‘reading’ the charts, composing ‘analytical notes’ that describe the data, and developing interpretations and hypotheses that are then tested against the charts and raw data. The thematic framework can be found in Appendix 13.
Sample
Across the three research sites, four focus groups with assessment team staff and two focus groups with reablement workers were achieved. Both staff working in-house and those working for outsourced providers were represented. A total of 20 reablement assessors (in four focus groups) and 12 reablement workers (in two focus groups) were involved. A breakdown of the sample by site (including highlighting any missing staff groups) is as follows:
-
Site A –
-
Assessment team (in-house): five participants.
-
Reablement workers (outsourced providers): not achieved, providers declined to participate.
-
-
Site B –
-
Focus group with assessment team (in-house): six participants.
-
Focus group with reablement workers (outsourced provider): six participants.
-
-
Site C –
-
In-house assessment team: seven participants.
-
Outsourced provider’s assessment team (other outsourced providers in locality do not conduct assessments): two participants.
-
In-house reablement workers: six participants.
-
Outsourced providers’ reablement workers: not achieved. Failed to recruit via one provider. Other providers declined to participate in study.
-
Findings
We report the findings under five key themes:
-
the impact of the Care Act 201415 on reablement services and practice
-
the impact, and suitability, of reablement as an intervention
-
user and family understanding of reablement
-
individual and contextual factors having an impact on reablement outcomes
-
practice and delivery issues.
Impact of the Care Act 2014 on services and practice
Most interviewees regarded the shift in approach to offering reablement to all relevant referrals to adult social care, as introduced by the Care Act 201415, as sensible and appropriate. Interviewees expressed the value of assessing an individual’s capacity for independence within the setting of their own homes and while monitoring the extent to which systematic efforts to restore independence in ADL were having an impact:
When they’re in hospital you might think ‘Oh yeah, they’re going to need a lot of help’; and then when they get home they actually somehow just sort of slot into doing it naturally. Put them in front of their own bathroom sink, and they know and just get on with it . . .
At the same time, it was noted that expectations for reablement necessarily had to be broader, and working towards the achievement of full independence could no longer be the default position:
. . . then it was pure reablement; now it’s a lot different because we’re an assessment team now, so we have different things coming through . . .
At the beginning, we saw people really achieve their goals. They were coming, they were with us for 6 weeks, and all of a sudden they didn’t need it any longer. It was like that constantly. But now, I don’t see it.
In addition, across all services, there was a belief that the capacity of reablement services had been compromised by these changes. The fact that assessment and reablement services may be the only ‘in-house’ provision within a LA meant that services were required to accept referrals who had no, or very minimal, reablement potential but who had been turned down by external care providers or if the locality did not have sufficient external care providers. As a result, throughput and the capacity to accept new referrals had been affected:
Lately, we were getting a lot of long-term care packages handed back to us because of the agencies going down. So it’s not really, it wasn’t really reablement.
We seem to be spending less time with our clients that we can reable.
There is a lot of cases when it [reablement] does work, but it’s the odd few that we’ve been referred, but they’re not reablement. They’re the ones it doesn’t work with.
The impact and suitability of reablement
We asked staff if they believed that reablement ‘worked’, if it was effective and if it was the best approach to use for people experiencing a decline in independence or recovering from an acute medical event that threatened their independence. There was strong and consistent support for reablement:
It definitely helps people to become independent, without a doubt.
[A service user said to me] . . . ‘I’ve got my life back, dear.’ People often to say that they never dreamed they’d come on so far as when they first come as to when they finish with us. Sometimes they’re even further than when they went in in the first place.
Many had experience of traditional home care, which does not seek to restore the skills of independent living, and there was great confidence among interviewees about the far superior outcomes achieved by the reablement approach:
It’s much better than dishing out packages of care.
Thus, although suggestions were made as to how local service structures and processes could be changed or improved, support for reablement as an intervention was unwavering and no suggestions were made as to how the intervention per se could, or should, be improved. Perhaps as a consequence of this, staff generally reported finding their work very satisfying and, aside from staff working for a private provider, no reference was made to changing jobs:
It’s very rewarding watching someone get better and they stay at home where they want to be which is nice. I like that. Love my job. You actually get a sense of achievement because we’re helping people. We’re trying to do our best for them.
It’s a fantastic buzz for us because you’ve seen a vast improvement and they’re getting back to doing their own thing.
The ‘active ingredients’ of reablement
Within this discussion about its effectiveness as an intervention, we asked interviewees for their views on the ‘active ingredients’ of reablement. A number of distinct components were consistently identified.
Workers’ knowledge
Two distinct domains of worker knowledge were identified. The first was practical knowledge and expertise with respect to finding solutions, or alternative ways, to carrying out ADL:
So it’s giving them little skills and tips. Sometimes just showing them a different way of doing something. And working with them to do things. [For example] . . . if you can’t do buttons up, but you’ve got several tops that you can just pull over your head.
It’s making a way for someone to do it, instead of saying ‘You can’t’. So there’s always a way that you can do something.
These solutions may include identifying and securing appropriate aids and equipment, or recommending to families where they can readily purchase aids and equipment that do not require specialist assessment or fitting:
I tell them to go down to [national DIY chain].
The second area of knowledge is with respect to local services, and particularly voluntary sector organisations that offer social and daytime activities:
We signpost them . . . to charities, organisations providing companionship.
Workers’ skills
Overall, an understanding of the differences between reablement and home care and having the skills to work with individuals using a reabling approach were regarded as core to the achievement of positive outcomes. Perceived threats to this were either where reablement workers had previously worked in home care and had not received adequate retraining and ongoing supervision, or where workers had a mixed caseload of reablement and home-care clients.
Across all focus groups, staff clearly articulated the interpersonal skills required to develop an effective therapeutic relationship in which the service user trusts the worker(s), accepts their need for support, and feels confident and motivated to work on their reablement goals:
The [reablement workers] are really good because they have all sorts of ways from laughing and joking and being a little but firm and every bit of their experience to try and get these people to engage.
And the client has to really like you. There’s got to be a good relationship there.
. . . you need to coax them into being able to be a bit more independence.
It’s trying to get people’s trust and to accept your assistance, as one would say, without forcing them. You’re there trying to help them and [sometimes] they don’t think they need our help.
Staff also highlighted the importance of the somewhat intangible skill of knowing at what level to ‘pitch’ the demands they place on a service user and to observe and respond to progress, or deterioration:
There’s a little bit of divide and conquer! So they still feel supported but they’re given autonomy and control to take the lead with certain tasks until they feel able to take more on.
It’s understanding when to step back and when to move in.
Social contact and reconnecting
Finally, staff believed that the delivery of reablement via home visits provided a source of company and served to re-establish routines and reconnect with everyday life:
They don’t see anyone else all that day, just sitting down, or even if you work alongside them, just having a chat. If they’ve got concerns or something, you can put their minds at ease. Just like a conversation.
These outcomes in themselves were regarded as improving mental well-being and confidence, which, in turn, placed the individual in a better position to engage with achieving their reablement goals.
Service users’ and family members’ understanding of reablement
The lack of understanding of reablement as an intervention, on the part of both service users and family members, and the impact this had on the expectations of the reablement service was a dominant theme:
Some of them [service users] have their own concept of caring. So, they’re expecting a domestic to come and do everything for them.
They [service users] just can’t get round the whole reablement process, they’re still back with the old dom [domestic] care days.
They [family members] say, ‘Well aren’t you supposed to making their cup of tea?’!
Typically, family members were presented as an unhelpful influence, urging the service user to adopt a passive role and being risk averse. This could jeopardise the therapeutic relationship, and managing family members diverted staff’s time away from their work:
We’ve had things like, ‘Oh my daughter’s told me not to do anything ‘cos otherwise I won’t get any help’.
How many times have we heard family say: ‘Don’t go out [to] the kitchen because it’s dangerous!’?!
Inaccurate representation of reablement on the part of referring agencies was viewed as an important contributor to these misunderstandings:
I think they’ve got misunderstandings of what the service is. There is misinformation at the time when patients are initially having contact [with professional managing hospital discharge] . . . that leads to these unfounded expectations from the patient. We’ve tried to educate the referrers but it doesn’t seem to be sticking.
However, service users’ and families’ more general understanding about social care, particularly an awareness that statutory social care usually comes with charge, led to confrontation when family members perceived workers as ‘not doing what they should be doing’ and disgruntlement when the intervention finished ‘before the full 6 weeks’:
Families are often harder to deal with. Trying to get the relatives to understand what reablement and intermediate care is about.
‘We’ve been told we’ll get 6 weeks of this’ is the classic line!
Interestingly, this sense of entitlement to care was regarded as a generational issue, not observed among very old clients (i.e. mid/late 80s and older):
. . . the 70-year-olds, there is this expectation: ‘I’m entitled to this . . .’. I see it more now than I ever have before: this expectation . . . even if the need isn’t there.
Overall, reablement staff described overcoming and changing these perceptions as very challenging.
Individual and contextual factors that have an impact on reablement outcomes
The previous section (see Service users’ and family members’ understanding of reablement) reported staff’s views on the impact that an individual’s and family members’ understanding and expectations of reablement might have on engagement with reablement and reablement outcomes. In this section, we report on other individual and contextual factors that staff identified as having an impact on the effectiveness of reablement. There was a remarkable level of consistency in the issues raised across all focus groups.
Personality
First, staff spoke of service users’ inherent qualities, such as temperament or personality. Here their discussions referred to concepts such as motivation, positive attitude, realism, adaptability (i.e. a willingness to try different things), and a sense of self-responsibility for themselves and their health:
Yeah, willing to give it a go. It’s not just motivation, but it’s just being like: ‘I’ll give it go! It sounds like a really different way of doing things but I’ll give it a try’. It’s beyond motivation, not just the talk of motivation, it’s the physical action of putting into practice as well.
Problem-solving skills
Second, staff described how users varied in their problem-solving skills or willingness to actively seek to manage the difficulties they were facing. It was noted that, particularly for those whom an acute medical crisis had led to their referral to the service, a previous experience of overcoming a significant challenge or setback was often helpful. This was so for two reasons. First, the individual may have acquired relevant problem-solving skills during that previous episode. In addition, they had learnt, and experienced, that recovery is possible. Typically, staff believed that these qualities were more usually observed among older service users:
It’s the 100-year-olds, they literally just get on with it. They’re just like ‘Oh don’t worry dear, I’ll do it this way’ . . . and then they do it. They have a stoic nature, they’re good problem-solvers. They’ve lived so long that they naturally have to problem solve . . . they have a really good skill set already.
Mental health and cognitive impairment
Low mood and mental health difficulties, such as anxiety and depression, were regarded as negatively affecting reablement outcomes. Comorbidites such as alcoholism, hoarding and dementia were also flagged as challenging to manage:
The most challenging are the ones who have the drug and alcohol problems. When they get back home to their own environment [with] the factors that make them drink or make them use . . . they’re not interesting in helping themselves any more; they’re just interested in that . . .
It’s people with depressions and things like that. I would imagine if you’re suffering from depression, one thing and another, you don’t want to do anything. You might be able to, but you just don’t want to. And they have to get past that.
There was widespread support for better access by the reablement service to mental health and other specialist input and/or rapid referral pathways.
Housing
The issue of housing was raised a number of times:
[Housing] can have an impact on what sort of equipment there is or whether people get outside. You have to work with it.
In particular, staff described delays in securing agreement, or experiencing outright refusal, to install aids and equipment for users living in rented housing. Private landlords could be very difficult, even impossible, to contact, which meant that equipment to support, for example, mobility or personal or self-care could not be installed:
Private landlords . . . it’s just impossible. Say if you’ve got to put in a grab rail. You’ve got to have written consent, and trying to get through to a private landlord is nigh on impossible. I mean some aren’t even in the country. For anything permanent, I find it impossible to progress it forward.
Reabling within a relationship
The issue of managing reablement in the context of a marriage/partnership was also raised, with the belief that it could both support and hinder reablement. Changes in health or functioning may have upset the equilibrium of previously established roles, with partners being required, if only temporarily, to assign new roles, something that may need negotiation and management and that reablement workers can support:
Cos they‘re codependent, so the way they’re functioning when they’re both well works. But whatever reason, if one does off-balance, they both off-balance, and then it’s trying to rectify that.
Practice and delivery issues
In this final section, we briefly report opinions regarding other practice and delivery issues that previous research, or practice guidance, have identified as being associated with intervention effectiveness or service user experience.
Flexibility in timing and duration of visits
There was a consistent view that flexibility in timing and duration of visits, and a gradual reduction in intensity, was essential to the reablement approach and allowed staff to be responsive to the needs of individual users. Some noted that this approach may be more difficult to secure with outsourced providers, whose contractual arrangements require a specific number and duration of visits. There may also be disincentives to reduce intervention intensity:
They’ll sometimes see eight patients in a morning. Imagine the pressure: ‘I’ve got to let her do everything’, ‘I’ve got to get to my next visit’.
Staff also identified an additional positive impact of flexible visiting times, with service users sometimes choosing to manage a reablement task independently rather than waiting for when the reablement worker arrived. Successfully achieving this could boost confidence and progress.
Monitoring and supervision of reablement workers
Adequate monitoring and supervision of reablement workers was viewed by assessors as very important and our study included a range in terms of the extent to which this was possible. A separation of assessors and reablement worker teams inevitably created a barrier that, potentially, was more evident when reablement workers were outsourced:
Once it’s passed over to the agency, it’s out of our hands, we have no control over it. We visit if we can, but that depends on caseloads . . . I suppose really we just try and oversee it as best we can. They’re still our responsibility . . .
Number of workers assigned to cases
One research site had a policy of assigning just two reablement workers to each case (with holiday and sickness cover as required). In the other sites, each service user could be visited by several reablement workers. The benefits of both approaches were identified. Multiple worker involvement was regarded as positive in terms of allowing a range of different ideas or approaches to be brought to supporting the reablement of a particular individual. It was also regarded as increasing the likelihood of a service user finding a worker they liked and ‘connected with’, which, in turn, supported the development of a positive therapeutic relationship. On the other hand, workers from the service where cases were assigned to two principal reablement workers believed that this approach offered important benefits in terms of continuity of care.
Access to specialist expertise
Finally, across all three sites, additional core posts, or timely and easy access, to further professional expertise was flagged. Staff in all services highlighted the importance of physiotherapy, addictions and mental health input:
I find people are waiting on a physio . . . then they’re sitting around also losing body muscle and it delays us doing our job.
It can almost become disenablement, can’t it?
For services without occupational therapy, this was equally, if not more, important. However, no issues were reported with respect to timely and efficient access to community equipment provision.
Summary
This chapter has reported on findings from focus groups with staff working in the reablement services acting as research sites for the study’s evaluation WP (WP2). Interviewees included those with an assessment and review role and reablement workers. Staff based in-house and outsourced teams were represented. The interviews explored experiences of delivering reablement from a number of perspectives.
Both assessment staff and reablement workers discussed the impact of the Care Act 2014,15 and also NHS discharge-to-assess policies, on the characteristics of their caseloads, with reabling to full independence no longer the predominant outcome. At the same time, reablement was still regarded as a relevant and effective intervention for individuals with support needs associated with staying in their own homes, or returning home following an inpatient episode.
A key impact of merging assessment and reablement services was the significant increase in the number of referrals, which some services were struggling to manage. This appeared to be exacerbated by a lack of sufficient home-care provision (typically outsourced) or a refusal by providers to accept referrals for onward transfer of individuals needing ongoing support. This had the impact of slowing the service throughput.
There was a strong and consistent belief of the superiority of reablement over ‘traditional home care’. The skills and knowledge of staff to adopt a reabling approach were regarded as vital to the success of the intervention. In addition, staff believed that the frequent social contact resulting from home visits by reablement workers served to reconnect, and rekindle, service users’ interest in everyday life.
The issue of user and family understanding of reablement was raised across all focus groups. A lack of understanding of the difference between reablement and home care was regarded as a barrier to the effectiveness of reablement and distracted staff time away from delivering the intervention. Staff reported that they had been unsuccessful in finding ways to address this issue.
Aside from the issue of user, or family, understanding of the intervention, a number of other factors were identified as having an impact on reablement outcomes. These included service user characteristics (e.g. personality, problem-solving skills, mental health, cognitive impairment, the presence of a partner/spouse). Housing was also identified as a potential barrier to success, as installation of aids or minor modifications to the home could be difficult to achieve if the individual rented their home.
A number of aspects of service delivery and practice were also identified as having an impact on the effectiveness of reablement. Flexibility in the timing and duration of visits, and an expectation that this would reduce over the course of reablement, was noted. However, some staff believed that this was not sufficiently incentivised in contracts with outsourced providers. Adequate monitoring of an individual’s progress and supervision of reablement workers was regarded as critical and more difficult to achieve in services where assessors and workers were based in different teams. There were mixed views about the optimum number of workers who should be assigned to a case: advantages of having one or two or, alternatively, multiple workers were both articulated. Finally, access to specialist expertise, particularly physiotherapy and mental health, was regarded as important, but difficult, if not impossible, to achieve in a timely way.
Chapter 7 Work package 2b: users’ and family members’ views and experiences
Introduction
This chapter reports the second element of WP2b, the study’s process evaluation of reablement, which involved interviews with service users and family members.
Methods
Identification and recruitment: service user sample
Interviewees were recruited from the outcomes evaluation (WP2a) sample. At the time of joining, the study individuals indicated whether or not they would be willing to take part in an interview about their experiences of reablement. We aimed to recruit 10–12 service users from each research site, using a purposive sampling frame to represent a range of outcomes at T1, service user characteristics (e.g. age, sex and living situation, lives alone or with partner or family) and the reason for referral for reablement (i.e. ‘remain at home’ vs. ‘return home’). In site C, we also sought to recruit participants from across the three services delivering reablement in that locality and taking part in the study. Sampling information was drawn from the data collected for the outcomes evaluation (WP2a).
In each research site, the research team passed details of the target sample to the LSOs. The LSO contacted potential interviewees by telephone to ascertain their interest in taking part in the study and, if agreed, to make arrangements for an interview. An information sheet was sent along with a covering letter confirming the date and time of the interview. On the agreed date and time, a member of the research team visited the participant at their home and obtained their written informed consent to take part in the study before the start of the interview. Copies of the recruitment materials are available (see Report Supplementary Material 4).
Sample: service users
Thirty-one participants were recruited from across the three research sites. An overview of the characteristics of the service users who took part in interviews is in Table 17.
| Sample size | Weeks since discharge | Age (years) | Sex | Living situation | Reason for referral | ||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Alone | With spouse/partner | With other family member | Remain at home | Return from hospital | |||
| Site A | |||||||||
| 11 | Mean 12 (range 2–21) | Mean 79 (range 67–89) | 2 | 9 | 4 | 6 | 1 | 8 | 3 |
| Site B | |||||||||
| 6 | Mean 17 (range 7–22) | Mean 85 (range 75–95) | 2 | 4 | 2 | 2 | 2 | 0 | 6 |
| Site C: outsourced provider (n = 2) | |||||||||
| 8 | Mean 15 (range 11–18) | Mean 83 (range 68–96) | 3 | 5 | 5 | 2 | 1 | 6 | 2 |
| Site C: in-house service | |||||||||
| 6 | Mean 10 (range 3–17) | Mean 78 (range 55–90) | 2 | 4 | 6 | 0 | 0 | 2 | 4 |
| Whole sample | |||||||||
| 31 | Mean 13 (range 2–22) | Mean 81 (range 65–96) | 9 | 22 | 17 | 10 | 4 | 16 | 15 |
Recruitment: family members
At the end of the service user interviews, respondents were asked if they had a family member supporting them who might be willing to take part in a short telephone interview about their views of, and involvement in, the reablement process. If they did, the research team sent the service user a ‘relative’s information pack’ to pass on to this individual. The pack included a response form (and a reply pre-paid envelope) to return to the research team if they were interested in taking part. A researcher then contacted the family member to discuss participating in the study and, if the family member was agreeable, to arrange an interview. The family member’s informed consent was collected in writing in advance of the interview or audio-recorded at the beginning of the interview. Copies of the recruitment materials are available (see Report Supplementary Material 4).
Sample: family members
Just two family members responded to the invitation to take part in an interview. Both agreed to be interviewed over the telephone. One lived with the relative they cared for and provided care in excess of 50 hours a week. Another lived separately from their relative and provided up to 19 hours of care a week.
Data collection
Topic guides (see Report Supplementary Material 6) were informed by findings from previous research and through discussion with members of the SSC. The interviews with service users focused on their experience of receiving reablement, their understanding and expectations of the service, the perceived outcomes and their views on aspects of the intervention that supported the achievement of those outcomes, their feelings and reflections when the service ended, and the longer-term outcomes. The interviews with family members covered the same topics but also explored the family members’ relationship with the reablement team and their role or involvement in supporting reablement. Data collection was carried out by Susan Clarke and Rachel Mann; they and Bryony Beresford met regularly during the fieldwork period to review interviews and ensure that the topic guide was used consistently.
With permission, the interviews were audio-recorded. The duration of the interviews was very variable, ranging from around 20 to 60 minutes. Fieldwork with service users took place between April and June 2017. The interviews with family members took place in September 2017.
Data analysis
The service user and family member interviews were analysed separately. The overall approach to the data analysis was a thematic analysis. 49 The Framework approach50,51 was used to facilitate systematic data management and data interpretation and to ensure audit trails of the data management process. Susan Clarke led the data analysis and writing.
There are four stages to this process. First, the researchers (SC and BB) involved in data analysis familiarised themselves with the data independently, with a view to identifying topics and issues emerging from the interviews. They then met on a number of occasions to review their impressions and to identify themes, a priori and emergent, present in the data set. This led to an index of themes being constructed (the thematic framework) (see Appendix 13). The framework was then tested by attempting to use it to index a subsample of interviews. The outcome of this was reviewed by the research team and led to refinements in the thematic framework. Once the team was satisfied with the framework, all of the transcripts were indexed according to which theme(s) in the analytical framework they relate to. Next, the indexed data from interviews were summarised on to a series of matrices (or charts) that are organised and labelled according to the thematic framework. Each chart is divided into columns, allowing relevant data to be organised according to subthemes/issues or themes to be grouped analytically. A single row on each chart holds one participant’s data. Thus, reading along a row provides an overview of everything an individual spoke about in terms of a specific issue. Reading down the chart (or down a column) allows comparison between participants. The final stage of analysis involved a process ‘reading’ of the charts and composing analytical notes to describe observations and findings. These notes included verbatim quotations, each of which included a note of their specific location in a transcript. Analytical notes were shared and discussed among the research team, and interpretation and writing were developed and refined in an iterative process.
Findings
We present the findings from the interviews with service users using a ‘chronological’ framework: presenting views and experiences encountered during an individual’s journey through reablement and life since being discharged. Although we tested and looked for discernible differences in respondents’ accounts between services and sites, none were apparent. Thus, findings are presented generically and concern experiences of five different reablement services: one each from sites A and B, and three from site C. Findings from the interviews with family members are situated towards the end of this account.
Being referred to, and anticipating receipt of, reablement
There was a confused picture, both from those who received reablement following discharge from hospital and from those referred to the service to prevent (increased) reliance on home care, as to the history of their referral. This is not surprising, given that this would have occurred when they may have been recovering from an acute or ongoing health issue or had been struggling with everyday life.
Among those being discharged from hospital, several described themselves as keen to return home and saw their referral to the reablement service as a means of doing so. What was not apparent, however, was whether or not they had properly understood the objective of the intervention, something we return to in the following section:
. . . in the end I just had to agree, ‘cos I just wanted to get home, that’s all I wanted to do was to get home.
X1
Others reported that they had been unaware of their referral to the service until a reablement worker arrived at their home:
The carers just came of their own accord, as far as I know.
W1
So they didn’t tell me that they were going to put someone in so I was quite surprised when it all happened and I was pleased.
S1
Among those who recalled anticipating receiving reablement, most described being pleased and relieved. They recognised that they needed help to manage living at home, and they reported being pleasantly surprised that such support was available:
So I was relieved, yeah, ‘cos I knew they’d . . . somebody would arrive each day and that’s, that was enough.
D1
For some, this relief centred on the fact that it meant that they did not have to rely on family members:
It gave me, yeah, it, it gave me some confidence . . . well just knowing that somebody was coming in . . . every morning, that somebody would come in and I’d be able to talk to somebody rather than me picking up the phone, bothering my daughter or somebody.
A2
Although most interviewees recalled recognising that they needed support, some spoke of a tension between receiving help and having a desire to (continue to) manage by themselves. Independence was very important to many interviewees, and some perceived receiving support as relinquishing this. It is possible that a lack of understanding of the objectives of reablement contributed to these feelings:
I was absolutely shocked. And I laid there one night and I thought [to myself] what’s happening, why is all this happening, why have I gotta have carers, why can’t I do it? And it just frustrates you and that’s the only word I could use.
X1
I didn’t like it at first ‘cos it was losing my independence, but I knew it was necessary – and I knew I couldn’t cope by myself – until such times as I could cope by myself
N1
Finally, a few believed that they had been referred to the service unnecessarily. They felt that they had been managing on their own from the outset and did not want to deprive others, needier than them, of valuable resources:
I, I felt it was a waste of their time when other people are more needy than, than me, you know.
C1
Understanding of the reablement approach
We asked interviewees about their understanding of the ethos and objectives of reablement. Views and understandings were mixed. Some, particularly those who had received reablement support previously, were clear that the overall objective of the service was to enable individuals rather than to do things for them, as with conventional home care:
Well the reablement people . . . their aim is to make you do it yourself, you know, they’re, they’re not there to do it for you, they’re there to encourage you to . . . do everything yourself if you can.
T1
The responses of others implied, rather than explicitly demonstrated, an understanding of the reablement approach in that they referred to how their reablement workers had supported and encouraged them to do things for themselves. Among other interviewees, however, it seemed that they had not fully grasped the difference between reablement and home care. There was evidence that, sometimes, reablement workers perpetuated this understanding and allowed a service user to assume a very passive role:
Whatever I asked them to do, you know, they, they would do it for you, so. Nothing was any trouble to them, no.
E1
Thus, these interviewees talked about their understanding and expectations of the service in terms of someone coming in to do ‘whatever needs to be done’ (F1) or simply ‘to help’ (I1). Some explained that they had understood that reablement was free care for up to 6 weeks, after which time it would be charged, suggesting that they were expecting to require support after that period.
There was evidence that a lack of understanding of the reablement approach had caused confusion as to the role and remit of the reablement workers who visited them:
At first I didn’t understand it until, as time went on and I realised what they could do for me and what they couldn’t do for me.
N1
Indeed, a couple of interviewees reported feeling concerned that they were not taking full advantage of the reablement service. The fact that there was some variability in the help and support provided by different reablement workers did not help with this. This lack of clarity led to some instances of awkwardness and embarrassment when reablement workers refused to assist with a task which the user had felt was reasonable to request (e.g. to buy a morning newspaper, to wash their hair).
Experiences of reablement practice and service delivery
The goals-focused approach
Only a minority of interviewees recalled a visit, or a telephone call, at the beginning of reablement in which what they wanted and needed from the reablement service was discussed:
Well I suppose they did ask us what I wanted doing and, or rather suggested, what things that they could do and what did I want.
H1
There was also little evidence in interviewees’ accounts of an awareness of joint goal-setting between themselves and reablement staff, something that is meant to be a core characteristic of the intervention:
They may have had goals I don’t know, but I don’t remember talking to them about them.
D1
I think, to be honest, I was pretty much told what they were going to do.
Q1
A few reported that it had been decided in hospital which tasks and activities the reablement workers would support them with. It was not clear from their accounts, however, whether or not they were at the centre of this decision-making process. By contrast, some interviewees did describe ongoing discussions with the reablement workers about the tasks and activities they wanted support with as reablement proceeded and their health, confidence and/or mobility improved.
Aspects of everyday life with which support was provided
Unsurprisingly, the aspects of everyday life with which service users described receiving support and assistance varied according to individual needs and, on occasion, varied between workers. Interviewees commonly described input and assistance with regard to managing personal care and mobility linked to these activities, such as getting in and out of bed or the shower or bath, on and off the toilet, or up and down stairs. A few service users described being helped by workers to prepare basic meals by, for example, getting the foodstuffs out of the cupboards or demonstrating how to heat up a meal in a microwave, and around one-third of interviewees reported having hot drinks made for them (particularly in the early days of reablement), of which they were very appreciative. Similarly, there were reports from around half the interviewees of workers doing domestic tasks or health-related tasks for them. Examples given included washing dishes, making the bed, taking out the rubbish, prompting to take medication, applying creams and ointments and helping with putting on and taking off compression stockings. Although most people did not receive support outside the home (or ask for this type of assistance), two interviewees receiving reablement from the same service said that they had been supported by their reablement workers to go for a walk in their garden or immediate vicinity.
Some interviewees complained that reablement workers did not support them with aspects of everyday life that they prioritised or placed importance on, such as having a bath (although inadequate facilities often accounted for this). Some also expressed disappointment that they did not get more help with domestic tasks such as shopping, cooking a fresh meal and general housework. Again, this is evidence that some interviewees believed they were receiving home-care support and lacked an understanding of the objectives of reablement.
Timing and time-keeping
One of the most frequently expressed criticisms of the service concerned the unpredictability of visits by reablement workers. However, this was not a universal complaint and the majority of respondents were sympathetic towards workers in the light of their busy schedules. They also felt that they could not complain about what they regarded as a ‘free’ service:
Well yeah, they’ve gotta lot on their books and there’s a lotta people worse than me.
U1
Well it’s just, you know, it’s one of those things you have to cope with because the care was there and it was free and you, you, you, you’re grateful for anything really.
R1
Another key source of dissatisfaction was the timing of visits. First, for the visits to help with washing and dressing, interviewees disliked it when these took place late in the morning, feeling that this held up their day. When visits were scheduled for later in the morning, or when workers were running late, a few respondents described trying to get washed and dressed themselves or (if available to them) getting others in the household to help them. Although, in a sense, this may serendipitously support the achievement of the objectives of reablement, it was not seen this way by the service users we interviewed:
I mean when they, they used to come I, and I was up, washed, dressed . . . hair done and everything, had me breakfast, washed up, tidied up and sitting down.
C2
Interviewees also disliked it when visits to help them with getting ready for bed were too early. Indeed, some interviewees had asked for these visits to cease as they had not enjoyed going to bed at a time earlier than usual:
In fact I didn’t have them in the evening, purely because they wanted to get me ready for bed at 5 o’clock in the afternoon.
M1
A few respondents reported other difficulties associated with the timing of workers’ visits. For example, one woman was anxious that if workers arrived too early to help her to shower then the bathroom might be in use by others in the household getting ready for work. Finally, some interviewees found the reablement visits restrictive or disruptive in terms of not being able to make other arrangements or participate in activities in and outside the home. For these individuals, it was often a relief when reablement ended:
Sometimes it’s a bloody nuisance, excuse my language . . . especially if you’re doing something, you know.
L1
Duration of visits
The majority of interviewees said that they found they were given the time they needed by the reablement workers. However, there were some reports of hurried visits, with workers being described as rushing through their duties to get to their next client. In one interview, unpleasant experiences of brusque care were directly attributed to the workers’ lack of time.
Workers’ sex
Reflecting the wider care workforce, the majority of reablement workers who had visited our interviewees were women. Some, but not all, of the men we interviewed specifically noted that they particularly enjoyed sessions with a male reablement worker. They described feeling that they had more in common with someone of their own sex, which made for easy conversation:
And he was a, a male carer that came, . . . [we’d] have a good old chat about the good old days.
U1
Although some interviewees recalled feelings of discomfort around nudity in general, no interviewee specified this discomfort, or greater discomfort, in relation to workers of the opposite sex supporting them with personal care:
I felt comfortable with all of them. I mean I, I know that I needed them and they had a job to do and it didn’t worry me, me whether it was male or female, ‘cos I, you know, when I first came out, I mean . . . I feel as one would put it, felt very exhausted, etc., you know, and . . . this was helping me to get back to normal.
J1
I wasn’t really expecting a man [laughs]. But never mind. It all went well. It worked fine.
V1
We would note that these reflections were being made after having received support, rather than in anticipation of having help with personal care from workers of the opposite sex for the first time.
Perceived outcomes and views on ‘active ingredients’
Reported outcomes
The great majority of interviewees were satisfied with the help, care and support they received from the reablement service they had used. They reported positive outcomes in terms of the core objective of reablement, namely regained independence. Within this notion of regained independence was the relief and pleasure of not feeling (further) reliant on family members. This could relate to both an awareness of their families’ lack of capacity to support them, and/or maintaining valued boundaries within their relationships:
. . . you know, I was able to, to get dressed or undressed without their help . . . you know, it’s not easy for a daughter to see her dad naked [laughs].
R1
Well they help you to get back your independence . . . and I, I mean you can’t rely on your, your family all the time.
E1
A few reported no notable changes resulting from their time with a reablement service. These were all interviewees with chronic poor health who were unconvinced that a return to independent living had ever been a real possibility. Nevertheless, they still reported gains from reablement:
Yes, that was very helpful. Well when you compare that with having nothing, you know, I mean it’s like a little miracle [laughs].
T1
I was just glad they were there.
Y1
Typically, it was these interviewees who, by the time of the interview, had moved on to a package of home care once reablement came to an end, or were receiving extensive support from informal carers.
A second outcome – companionship – was frequently experienced while receiving the intervention but not sustained afterwards. In the next section (see Views on how reablement ‘works’), we report interviewees’ views about how reablement supports regaining, or maximising, independence. The following section (see Companionship) considers the issue of companionship.
Views on how reablement ‘works’
Interviewees identified three aspects of the presence or activities of reablement workers that supported, or enabled, positive progress towards regained/maximised independence:
-
personalised and enabling assistance
-
advice and information
-
emotional support.
Interviewees described that, through the visits and input from reablement workers, they had regained the confidence and practical skills that enabled them to manage everyday life independent of any formal support.
Personalised and enabling assistance
Interviewees described being assisted with personal care, transfers and moving around (for those whose movements were limited by fractures and other injuries, acute and chronic illness or general frailty). Importantly, the majority described how this assistance was gradually reduced, with responsibility for doing tasks, or managing independently, being passed to them. This was recognised by most as being an important element of the way the intervention was delivered:
. . . where previously they did it [dressing] all, I could then start tugging things, you know, pulling me pants up and me trousers up and things. Yes, it just, it was just a gradual process.
J1
It was clear from interviewees’ accounts that having workers ‘stand by’ and observe while they attempted tasks, and knowing that they would ‘step in’ if things went awry, was very important to regaining confidence. The sense of safety and security offered by the presence of a reablement worker was particularly mentioned in relation to a fear of falling. Interviewees reported that they were more inclined to try to do things for themselves knowing that workers were standing by to help them if they got into difficulties:
It, it made you feel more confident, shall I say, ‘cos you knew that if . . . as soon as they see you sort of wobble they would, they would come to you straightaway; well they’re only just a shake away sort of thing.
B1
Furthermore, this sense of safety extended beyond the times the reablement worker was present. Those who lived alone described being reassured that, were they to fall and be unable to summon help, their workers would soon be calling. This gave them the confidence to begin to reassume tasks and activities when they were on their own:
. . . it’s just the fact that another human being comes to see you that makes you feel better and gives you the bit of confidence, oh well I’ll do that myself.
D1
Advice and information
Interviewees also spoke about, and appreciated, the advice and information they had received from their reablement workers. This included hints and tips on, for instance, how to wash, shower or dress themselves when their mobility was limited, safe ways to get in and out of bed, and removing and replacing a catheter bag. Respondents valued the time workers took to explain what they were doing and why:
Yes, yeah, little things . . . like putting your socks on, doing up your laces, you know, it’s easier if you’ve got slip-on shoes and things like that, all, all practical useful tips.
R1
It’s just somebody to say do you think, do you think I should do this, do you think I should do that; it’s just that little bit of backup or support to say yes, go on, I think you should do that, yeah.
D1
Emotional support
It was clear from interviewees’ accounts that the encouragement, reassurance and acknowledgement of achievements received from reablement workers was an important aspect of the intervention, increasing interviewees’ motivation, self-confidence and satisfaction with reablement:
. . . and to know how much they’d help me get on and do things for myself, I think that made . . . quite a lot of difference to me, and to know that they could turn round and say to me ‘You’re really doing well [XXXX], just keep it up’.
X1
In addition, and a quite different aspect of emotional support, some interviewees referred to the consolation, or comfort, of knowing that someone was aware of them and would be visiting them in the near future. There was a sense in some interviewees’ accounts that this knowledge made them more settled and comfortable and, for those being discharged from hospital, helped them to adjust to being back home:
Yeah, it was, I felt safe, you know, I was just so, at the beginning, I was so scared of falling again.
E2
Knowing that somebody’s gonna come and, you know, if I pass out or anything, they’d come and they’d find me. Otherwise, who knows?
U1
The physical benefit of this, in terms of better sleep, was also noted:
. . . you just feel more secure in your bed for some reason [. . .] it’s just the fact that somebody comes in in the morning makes you feel so much better and you sleep better, yeah.
D1
Some interviewees also noted that their families had found the schedule of regular visits reassuring following their relatives’ discharge from hospital:
I think they were relieved to know that there was somebody coming in and that if any, if there was anything wrong . . . they could . . . obviously phone [my sons] to say this, this or whatever.
X1
Companionship
Overwhelmingly, people reported increased positive emotions and social connectedness from the companionship that reablement workers provided. Social isolation and loneliness were common and, for some, the daily visits from reablement workers had, temporarily, addressed a significant area of unmet need:
Well you, one of the things you need is, especially when you’re in this bloody condition, is you need people to talk to and you don’t get anybody to talk to ‘cos they haven’t got long enough to listen to you.
F1
Typically, interviewees reported that their reablement workers took a friendly interest in their lives. Unsurprisingly, therefore, some service users explained they had become quite attached to their workers. Some viewed the conversations and ‘laughs’ they had with their workers as both the most enjoyable and the most important aspect of reablement:
. . . because at the time . . . I wasn’t able to get out anyway and I know . . . yes I did have visitors, but, you know, you, you do feel, you feel very strange coming out of hospital even into your own home, you know. So it was nice to have someone to chat [with], you know.
B1
. . . it was just that little bit of contact, human contact. ‘Cos some days I can go, I don’t speak to anybody.
A2
Key factors affecting outcomes
Key factors perceived as having an impact on outcomes were:
-
the client–reablement worker relationship
-
workers’ reablement skills
-
users’ confidence in the worker
-
the duration of visits
-
a reluctance to accept the need for support
-
records of progress.
The client–reablement worker relationship
Two, connected, aspects of the client–reablement worker relationship emerged from users’ accounts that appeared to be associated with the extent to which they engaged with reablement, either generally or during a specific visit by a reablement worker: first, whether or not they liked a reablement worker and, second, whether or not they liked the way that worker worked with them. This related particularly to the way in which the worker instructed or encouraged the service user and how personal care was managed.
Overall, interviewees typically said that they liked their reablement workers and enjoyed their visits:
They were absolutely marvellous, I can’t tell you how, you know, they were always cheerful and helpful and wonderful.
.B2
Inevitably people had ‘favourites’ and got on better with some than others. Generally, but not always, interviewees said that they preferred workers who were friendly, and interested in them, but maintained professional boundaries in terms of what they shared about their own lives:
I prefer them to be friendly; I don’t, I don’t want them falling over me or anything like that, but to be able to turn round and say something to them and have a laugh.
K1
However, interviewees also occasionally reported that they had not liked, or got on with, one of their reablement workers. Sometimes this was simply attributed to a difference in personality or because they simply did not ‘connect’. At other times, it appeared that the interviewee had not liked the worker’s approach to instructing and encouraging them as they worked on their reablement goals, or had felt that they were being overstretched:
Well they, on the whole they, they were treating you as if you’d no intelligence and couldn’t do anything, to be honest.
C1
Trying to get me to do things on me own but I couldn’t do ‘em, which I didn’t like.
U1
With respect to this, a range of preferences were expressed. Some, for example, appreciated workers taking control and making decisions for them, whereas others preferred a softer, more gentle approach.
Another issue that could engender, or threaten, a positive relationship was how reablement workers managed issues of dignity and discretion in relation to personal care. Again, preferences varied: some clients liked it better when workers were discrete, while others said that they would rather it was dealt with in a matter-of-fact way:
. . . rather than sit on the bed and watch me and embarrass both of ourselves, they used to go out in the kitchen and find out what wanted doing.
D2
And . . . and then when they used to . . . do the lower part of me they said ‘Stop worrying about it, [XXXX], just relax’. That’s all the word I can use. They used to say to me: ‘Relax, you’ve got nothing to worry about the, we do this every day of our lives’.
X1
Workers’ reablement skills
Achieving the right balance between providing care and supporting reablement was identified as an important skill by several interviewees. It was felt that some workers were better than others at judging when to step in to provide assistance. This was the case for one woman in chronic pain with a progressive health condition who struggled to dress herself. She explained that some workers recognised when she needed help while others did not:
Some of them were more helpful to you than others [. . .]. Some, some knew when to step in and, and others were more intent on you doing it yourself [laughs].
T1
Users’ confidence in the worker
Experiencing competent care and support engendered users’ confidence and, as a consequence, their willingness and/or confidence to engage in reablement tasks and activities. Judgements about competence were made on the basis of the skills shown in the way that a worker managed the balance between care and enabling practice. For some, these judgements were made with particular respect to managing new medical devices or procedures (e.g. changing a catheter or putting on and taking off compression stockings):
. . . they were very good, I mean they, they knew exactly what they were doing, exactly.
P1
The duration of visits
It was clear from interviewees’ accounts that a key factor regarded as contributing to poor outcomes was reablement workers having insufficient time for a visit. This resulted in reablement principles being abandoned and workers adopting a home-care role. Thus, interviewees reported that when workers were in a rush, they were more likely to take over tasks rather than support the service user to do it for themselves. Some interviewees were content to go along with this:
[Some workers] well needed to get on with things; ‘cos they’ve such a tight schedule that they were quite happy to do most of it all the time and I’m afraid I was quite happy to sit back and accept it.
J1
A reluctance to accept the need for support
A few interviewees described the difficulties they experienced accepting help from and relying on other people. Although this feeling was more prevalent at the beginning of reablement, for some it remained with them throughout the reablement process and created a tension within themselves while they came around to the idea:
. . . but . . . especially at the beginning . . . I felt very . . . not difficult, I, I just felt . . . that they were, you know, that it was having someone wait on me was . . . much more embarrassing to me because I’m not used to it, obviously, and I’m used to doing everything and . . . it just felt odd to be sitting in this chair and not . . . [laughs] and not saying no; in the end I, I was very pleased to have it.
Q1
I didn’t like it at first ‘cos it was losing my independence. But I knew it was necessary – and I knew I couldn’t cope by myself – until such times as I could cope by myself.
N1
Records of progress
In all research sites, reablement workers recorded details of their visits, including accounts of their client’s progress, in a folder kept in each service user’s home. A couple of users described how reading these notes acted as a strong motivator in making further progress. It was not clear from the interviews whether notes were reviewed with a reablement worker or alone:
. . . each time I progressed they would note it down on their paperwork and it would give me the incentive to get to the next bit where I could do a bit more for myself.
N1
The usefulness of these folders as a communication aid, between families of service users and their relative’s workers, was also noted by a family carer as reported in a later section.
Service delivery and practice issues
Two service delivery and practice issues, although not attributed to having an impact on outcomes, were explored in interviews with service users.
Continuity of workers
Research sites varied as to whether users were typically allocated a couple of reablement workers (one site), or whether any worker within the team could be allocated to visit a service user. Thus, some interviewees described a core team of two or more reablement workers who worked on rotation. These interviewees described how they had got to know these regular workers over a period time and felt at ease with them:
Well it, it is, it is nice to have familiarity, I suppose, you know, with the same, same person rather than different, different people every day.
L1
Interviewees from our other two case sites, however, were supported by a number of workers, with a few reporting that a different worker visited most days. Perhaps unexpectedly, complaints about this lack of continuity were rare. Overall, compared with the case site above, interviewees were no less positive in their views about the service they had received:
I mean there was a lot of carers in, in the time I was, 6 weeks and . . . they were all good, I’ve got nothing but praise for them really.
R1
Family involvement
During our interviews we explored whether or not service users were aware of any work with family members being done by their reablement workers, for example instructing them as to how they could best support their relative’s reablement. Although, as reported earlier, interviewees spoke of the way the intervention removed a possible pressure or burden on families, almost no reference was made to instances when they had observed a worker upskilling a family member in terms of supporting reablement. The only exception was a situation where a husband had been carefully instructed by reablement workers on how to put on and remove splinting equipment.
Family members’ accounts of the reablement intervention
In this section we present two case studies of reablement from the perspectives of a family member: first, a daughter and, second, a husband.
Family member case study 1
Our first family interviewee was a daughter who cared for her father, who lived alone. He was receiving reablement following a fall and a broken hip.
The daughter described making sure that she attended the reablement workers’ first visit to ‘back up’ what her father said and make sure that he got the care and support she felt he needed. She noted that she, and the wider family, had been very reassured by the arrangements made for her father following his discharge from hospital, both the fact that he was receiving twice-daily visits and support and that they would be contacted if there were any problems. She valued being able to view the progress record kept in her father’s home and also used this record to communicate with the reablement workers herself. She found this ‘two-way thing’ very helpful and was satisfied with her overall involvement in the reablement process:
. . . Dad couldn’t remember everything that had happened. It was always good to read it from the people that were actually there. Each time they came in, the notes they left were very comprehensive, exactly what they’d done and exactly how Dad was, physically and also in his mental health as well, because obviously he had down days when he’s stuck in there not being able to see and being on his own.
This interviewee was very pleased with the outcomes of the reablement her father received. She believed that the combination of physical support and encouragement to move around and carry out basic personal care and domestic tasks at home had led to him regaining his confidence to live independently. In addition, she believed that his recovery was, in no short measure, a result of the company the reablement workers also provided, which, his daughter said, ‘kept his spirits up and gave him a purpose’ at a vulnerable time:
Yes, otherwise I think he would have just sat and festered in the chair and become a bit of a recluse.
Family member case study 2
Our second family member interviewee was a husband. Owing to his wife’s degenerative physical illness, he also identified himself as her carer. We interviewed this gentleman after his wife received reablement following a period in hospital due to a number of falls. His understanding of the purpose of reablement was that it would help his wife to become as independent as possible in terms of getting up, washed and dressed.
This interviewee did not believe that reablement had achieved the desired objectives and identified reasons for this. First and foremost, he felt that the duration of the visits was inadequate for the pace at which his wife could manage her own personal care. Consequently, workers, pushed for time, did things for her rather than helped her to do things for herself. That said, our interviewee was grateful for this support as his own physical strength and mobility were compromised:
. . . they had a slotted time of about half an hour and they couldn’t stand there and wait for [his wife] to do things herself otherwise it would have taken forever; so they had to make sure that they dressed her and washed her and did everything else. [. . .] It saved me having to do it and perhaps have an accident falling over where the leg wasn’t strong enough.
Another issue for this couple was that reablement visits usually took place between 8.00 and 9.30 in the morning, and sometimes workers were considerably delayed. This unpredictability meant that they were unable to plan their mornings. The husband also believed that it meant that workers often had ‘nothing to do’ when they did arrive because, by that time, his wife had managed to get washed and dressed. He did note, however, that one or two workers would, instead, spend time supporting her with her mobility and strengthening exercises, which again was helpful to them both.
The service ended a week earlier than expected but this carer was ‘quite glad’ when it did finish because it was no longer necessary to plan the day around visits by reablement workers. However, given the nature of his wife’s illness, our interviewee did not think that the reablement service had helped to restore his wife’s independent functioning or reduce her need for ongoing support:
I don’t think there was anything to do with [reablement], no. I think confidence comes from being able to do things on your own and unfortunately, with [my wife’s] condition, it’s not there.
The end of the intervention
The majority of interviewees described themselves as feeling ready for reablement to end; some even reported asking for it to stop as soon as they felt that they were managing independently. However, some were encouraged to remain in the service to take full advantage of the ‘free’ support being offered. In addition, a few interviewees reported that reablement had ended unexpectedly with little or no notice. Typically, this was bound up in their understanding that the intervention was of a fixed duration of 6 weeks, suggesting an incomplete understanding of reablement as an intervention that seeks to support recovery of skills, with discharge being linked to this.
Some interviewees had moved on to home-care packages following discharge from reablement. For those eligible for statutory support, this had been a seamless transfer with the same agency now providing home care. Others had had to source and fund their continuing care. Interviewees reported that the reablement service had provided them with information about local care agencies, but a few people had experienced difficulties finding an agency with the capacity to take on their care.
Feelings were mixed when reablement came to an end. Those who were able to function independently again were pleased that they no longer had to plan their day around workers’ visits:
It became more of a nuisance to me ‘cos I have things to do here.
S1
Oh thank goodness, to be honest, yeah, I can get on with me life now [laughs] because I was invited out and I thought I, I can’t go out ‘cos those carers are coming.
C1
Those who still needed help with washing and dressing or preparing a meal were thankful when ongoing care was found.
On the other hand, many of those who had enjoyed the company of the reablement workers and grown close to their workers described feelings of sadness and loss that they would not be seeing them again:
Oh well I was sorry to see them go, not because I didn’t feel better . . . you get to know people a little bit and I thought oh they won’t be coming in, you know.
A1
I looked forward to them coming and I missed them when they went because they’d been very . . . friendly . . . you know, they, they didn’t stay long, obviously, ‘cos they’ve got other people to go and see to, but they always did make 5 minutes’ time for chat.
N1
For some, their feelings were tempered by gratitude that reablement had been made available to them, and by a desire not to divert valuable resources away from those in greater need:
I didn’t want to be that person that was stopping someone else coming out of hospital, I wasn’t that bad.
M1
. . . I wanted them to go because I felt that there was other people needing it more than me [laughs] type of thing, you know.
P1
Interviewees’ current situations
At the time of interview (between 2 and 21 weeks post discharge) most interviewees were managing without home-care support. Specialist equipment (e.g. dressing aids, walking sticks/frames, wheeled trolleys and grab rails), most of which had been brought in during reablement, played an important role in this. As noted above, a few had moved on to long-term care packages.
Many, however, described relying on family, friends and neighbours for help with shopping, cooking and other household tasks and for providing regular social contact and emotional support. A few also paid privately for help with housework or gardening or for meals-on-wheels services.
Views about service improvements
Interviewees were generally very positive about the reablement service they had received. Not unexpectedly, therefore, there were few suggestions about ways to improve the service. The suggestions that were made can be organised into three themes:
-
workforce issues
-
information at the start of the intervention
-
scope of reablement.
The majority of suggestions centred on the number of workers within a service and the need to bolster the pool of reablement workers. More workers, it was felt, would help to address the issue of the unpredictable nature of the timing of visits and visits that were rushed because of pressures of work. In terms of the pool of workers, it was suggested that more should be done to recruit men into the workforce. Indeed, one-third of male interviewees said that they preferred the company and attention of male reablement workers to that of female ones.
In a few instances, there was some evidence of confusion about when the reablement service would start following discharge from hospital. For example, a few reported that they had expected a reablement worker to call the day they had been discharged from hospital and had felt let down that the worker did not arrive until the following day or later.
The final suggested area of service improvement centred on a desire for the intervention to be used with respect to activities outside the home, for example going for a walk or catching the bus to the local shops and services. Some interviewees believed that help with these activities was just as necessary in enabling people to remain living independently in their own homes. Interviewees expressing these opinions said that it would be helpful if reablement services could be tailored to their individual needs and priorities.
Summary
This chapter reported the experiences of individuals who had received reablement. The experiences of the two family members we were able to recruit to the project, a spouse and a daughter, were also described.
The majority of interviewees, at least at the start of reablement, did not fully understand the nature of this intervention, regarding it instead as home care. The exception to this was individuals who had received reablement in the past. Some aspects of dissatisfaction with the service they had received can be attributed to this misunderstanding. Aside from this, the main source of dissatisfaction concerned unpredictable visit times and ‘bedtime’ visits happening too early in the evening.
Overall, the great majority of interviews reported positive outcomes in terms of the core objective of reablement, namely independence. Those not reporting these gains all had chronically poor health. That said, they had valued the support they had received. Four (connected) aspects of practice were identified as having supported reablement outcomes: first, the provision of personalised and enabling assistance; second, advice on alternative ways to carry out tasks and activities; third, building confidence; and, finally, interviewees spoke of the comfort of knowing that someone was aware of them and their situation and would be visiting them. It is important to note that few could recall goal-setting and it was not clear from service users’ accounts whether or not they had been involved in identifying intervention objectives. An additional outcome experienced during the intervention was companionship, and some described this as the most valued outcome.
Six factors were identified as having an impact on outcomes: the service user–worker relationship, workers’ reablement skills, service user’s confidence in the worker, duration of home visits, willingness or reluctance to accept support, and being able to review records of progress. Continuity of workers was not identified by interviewees as important to the outcomes achieved. Furthermore, those being supported by a number of reablement staff did not usually report this as a problem or a source of dissatisfaction with the service.
Chapter 8 Work package 2c: providing reablement – costs and impacts on resource use
Overview
This chapter reports WP2c, which examined the resource use and costs associated with the package of care used by individuals receiving reablement. In addition to the reablement service, it considers the resource use and costs falling on the health care, social care and voluntary sectors, as well as users’ out-of-pocket costs and any use of informal care.
Perspective: costs falling on public and non-public budgets
We chose a broad perspective of costs falling on public and non-public budgets, consistent with the NICE methods guide on social care guidance. 32 We focused on costs falling on the health and social care sector because reablement is funded by the NHS and/or LAs through their social-care budgets. 14 We included costs falling on non-public sector budgets, namely the voluntary or charitable sector, private out-of-pocket costs, and the use of any informal unpaid care. The rationale was that the use of reablement may have an impact on service users’ use of voluntary services, their out-of-pocket expenditure and the level of informal care required. Out-of-pocket costs were included because service users may have to contribute towards the cost of social-care and voluntary services, and may privately fund additional services, house modifications or equipment. Informal care time was included because service users may be supported to live in the community with the help of family and friends.
Methods
The costs of providing reablement
An assessment of the direct cost of providing reablement was carried out in WP1 (see Chapter 3, The costs of reablement). For WP2c we intended to examine the cost to LAs and CCGs for each of the research sites. To do this, the sites were asked to complete a questionnaire, specific to their service, that asked for information on costs, resources, caseload and number of sessions (see Report Supplementary Material 7). However, the sites did not respond to our requests for information within the time frame of the study.
Resource use
We developed a new questionnaire, the SCPQ, to collect information from study participants on their resource use (see Appendix 14 for details). It involved five steps:
-
identifying the resource use items to be collected given the objectives of reablement and the perspective of the evaluation
-
reviewing other questionnaires published in the economic evaluation literature
-
drafting the initial version of the questionnaire
-
piloting the questionnaire
-
developing the final version.
The Services and Care Pathway Questionnaire
The SCPQ included questions on resource use as follows:
-
hospital overnight stays, including planned admissions, unplanned admissions, stays post transfers and other hospital overnight stays
-
hospital visits without an overnight stay, including outpatient appointments, day case visits, visits to the accident and emergency (A&E) and calls to emergency numbers
-
community health care, including general practitioner (GP), nurse, nurse specialist and therapist appointments
-
care services, including home care and day care
-
other social-care services, including meals on wheels, social services appointments, sitting services and transport services
-
voluntary services, such as befriending, shopping and advice services, or other services provided by voluntary organisations or charities
-
informal care, referring to unpaid help from family and friends
-
private out-of-pocket costs, referring to whether or not individuals had paid anything for each service and to report their expenditure.
Period of recall
The period of recall varied according to the type of service or resource. This was because pilot work indicated that people found it easier to recall attending hospital appointments, having house modifications and receiving equipment, but found it more difficult to remember their use of community services. Thus, a recall period of 2 months was used for hospital services, home adaptations and equipment at T0 and T2. For T1, this was specified as the period during which the individual was receiving reablement. At all time points, a 2-week recall period was used for community health-care services, social-care services and voluntary services. The recall period for informal care was 7 days, asked in terms of help from family and friends.
Duration and intensity of reablement
Information about the duration and intensity of reablement was obtained by the local study team from case notes. We used a descriptive analysis to summarise the duration of reablement as the number of weeks between assessment at entry and service discharge, and intensity of reablement as the total number of contact hours.
Costing resource use
We calculated costs by multiplying the number of times each resource was used by its unit cost (see Appendix 15, Table 59). 52,53 Informal care time was valued using the opportunity cost method54 as the average hourly wage rate in England in 2016 of £15.72 per hour. 55 All costs are expressed in Great British pounds for 2015–16. Report Supplementary Material 8 details the assumptions used to clean and prepare the SCPQ data to estimate resource use and costs. We did not annuitise the cost of home adaptations given that the objective was descriptive rather than comparing costs between services.
Description and comparison of resource use and costs
We described resource use and costs as the average service use per individual at entry to the service, at discharge and at 6 months after discharge. We described informal care as the average hours of care per individual. We grouped resource use into categories: hospital overnight stay, hospital visit without overnight stay, community health care, social-care services (including care services and other social-care services), voluntary services, major house modifications, minor house modifications, equipment and informal care time cost (as explained in Resource use).
We grouped costs in sectors according to the budget. We considered public sector costs, meaning those costs that fell on the public budget, and included hospital overnight stays, hospital visits without overnight stay, community health care, care services and other social-care services. Out-of-pocket costs comprised private costs to the individual, including community health care (namely therapists), care services, other social-care services, financial contributions towards voluntary services, major and minor house modifications, and equipment. Other costs were the costs of resources that may or may not be funded by the public sector, namely voluntary services, major and minor home adaptations, equipment and informal care time, which were costed as if these services were provided by the public sector (i.e. using unit costs based on national public sector average costs).
Resource use and costs were scaled to 1 week to allow for comparisons between follow-up points.
Determinants of costs
Regression analysis investigated the predictors of costs during reablement and 6 months after discharge given the information available at baseline. A detailed description of methods is available (see Report Supplementary Material 9). In summary, we used stepwise regression at a critical alpha of 20% to select characteristics of the study participants and services that were associated with costs. We rescaled the costs before reablement to correspond to the same time period as the costs during reablement, based on the actual duration of reablement. The analysis aimed to predict (1) hospital costs, (2) community health-care costs and (3) social-care costs at discharge. The analytic sample consisted of study participants with complete data. A sensitivity analysis was conducted by re-estimating the regression on data from site C. The rationale was to explore whether or not there were systematic differences between the participants in site C and sites A and B that were reflected in the predictors of costs, given site C’s greater recruitment and retention rates.
Results
Duration and intensity of reablement
Figure 3 shows the duration and intensity of reablement.
FIGURE 3.
Duration and intensity of reablement.
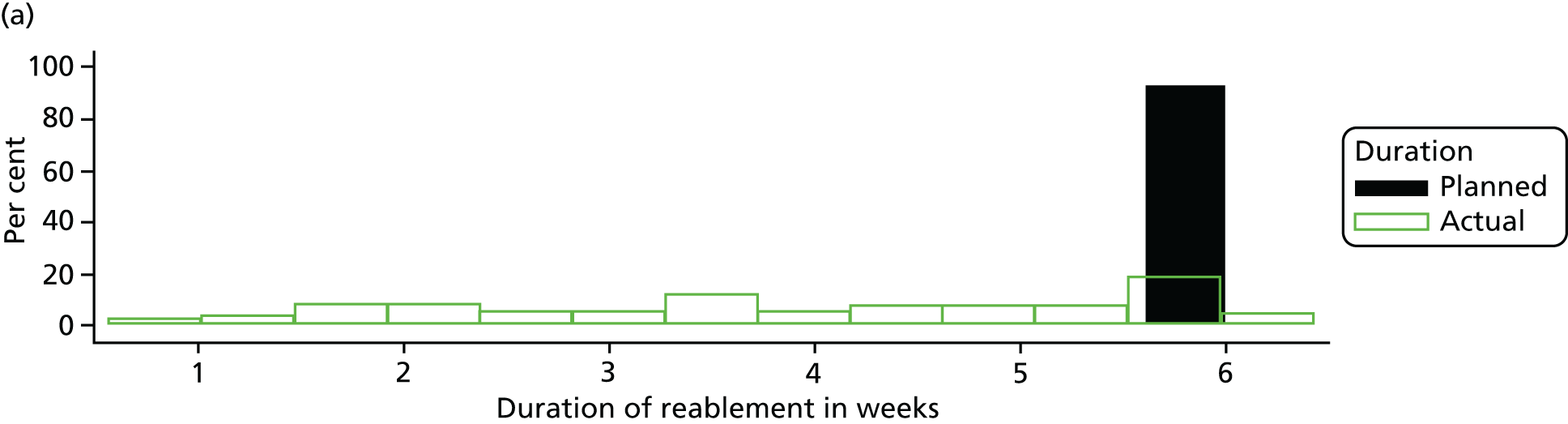
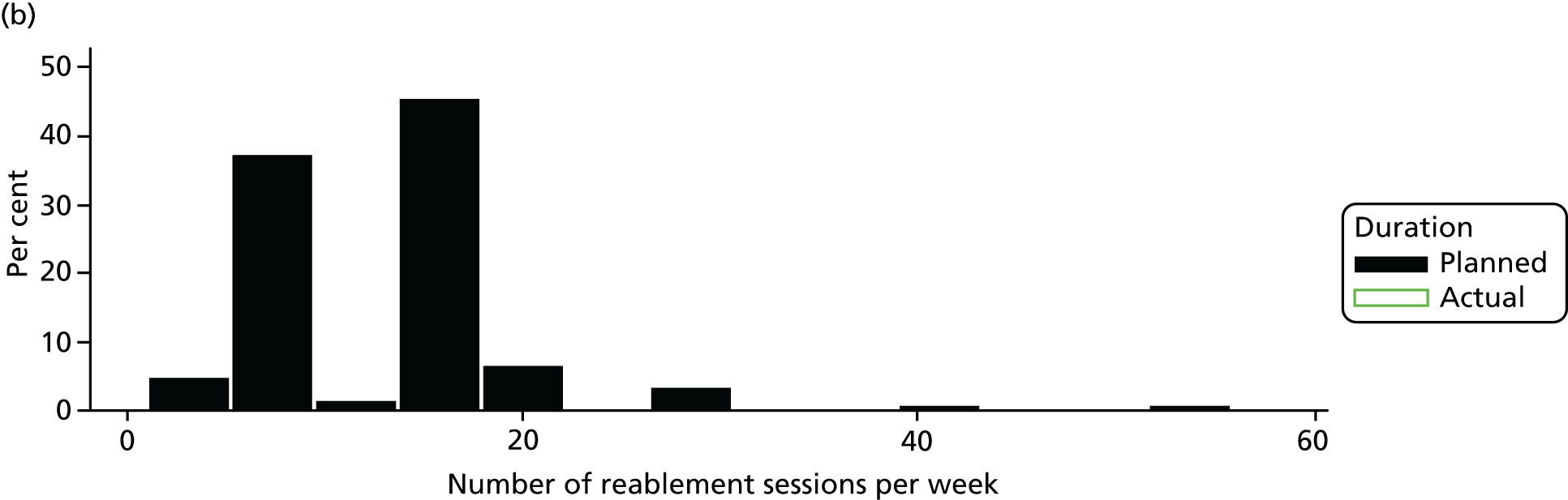
Planned duration and intensity of reablement
Information on the planned duration of reablement was available for 184 out of 186 (99%) study participants. For the majority of participants, reablement was planned to last 6 weeks (n = 170; 91%). The number of planned reablement sessions was recorded for all study participants but one. Most study participants had two sessions per day, which is equivalent to 14 sessions per week (n = 83; 45%). Over one-third had one session per day, equivalent to seven sessions per week (n = 66; 35%). Some study participants had a more irregular pattern, with 1–6 sessions per week (n = 12; 6%); a similar number of participants had three sessions per day (n = 12; 6%). Eight study participants (4%) had more than three sessions per day.
Actual duration of reablement
Information on the actual duration of reablement was available for 175 (94%) study participants, and was calculated as the time between baseline and discharge. The median duration of reablement was 4 weeks (mean 3.9 weeks; minimum 0.6 weeks, maximum 6.4 weeks). Information on the actual number of sessions was not recorded.
Resource use and costs
Responses and missing data
The proportion of missing data is shown in Appendix 15 (see Figure 22). At T0, all study participants apart from one completed the SCPQ. At T1 and T2, all study participants who remained in the study answered the SCPQ. The response rate for all questions was > 90%. The lowest response rate (91%) was for the question on whether or not any transfers had occurred to other hospitals from unplanned hospitalisations.
Resource use
Table 18 summarises the use of services, rescaled to use per week given the different recall periods for each follow-up questionnaire.
| Resource | Time point | |||||
|---|---|---|---|---|---|---|
| T0 | T1 | T2 | ||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Hospital length of stay (number of nights) | 158 | 2.32 (2.34) | 124 | 0.04 (0.27) | 50 | 0.16 (0.42) |
| Hospital visit without overnight stay (number of visits) | 174 | 0.31 (0.21) | 127 | 0.24 (0.34) | 65 | 0.18 (0.21) |
| Community health care (number of visits) | 180 | 2.08 (2.35) | 128 | 1.19 (1.61) | 62 | 0.90 (1.36) |
| Care services (number of hours) | 182 | 3.09 (2.51) | 127 | 2.10 (2.71) | 65 | 0.50 (1.65) |
| Other social-care services (number of times service was used) | 180 | 0.92 (1.29) | 123 | 1.00 (1.63) | 61 | 0.72 (2.77) |
| Voluntary or charity service (number of times service was used) | 183 | 0.04 (0.16) | 127 | 0.02 (0.12) | 64 | 0.07 (0.22) |
| Major home adaptations (number of adaptations) | 185 | 0.01 (0.03) | 128 | 0.01 (0.05) | 66 | 0.00 (0.01) |
| Minor home adaptations (number of adaptations) | 185 | 0.04 (0.09) | 128 | 0.09 (0.32) | 66 | 0.02 (0.04) |
| Equipment (number of equipment items) | 185 | 0.24 (0.23) | 128 | 0.21 (0.30) | 66 | 0.06 (0.09) |
| Informal care (hours) | 177 | 23.77 (35.76) | 123 | 20.03 (37.23) | 56 | 11.21 (27.68) |
Overnight hospital stays
In the 2 months prior to reablement, 72% (132/185) of study participants had unplanned hospitalisations. The average length of hospital stay per week was 2.32 nights (SD 2.34 nights). During the period of reablement, 6% (8/128) of study participants reported having unplanned hospitalisations. In the 6 months following discharge from reablement, hospitalisations slightly increased. This was driven by unplanned admissions with an overnight stay, which were reported by 23% (15/66) of study participants who returned a questionnaire.
Hospital visits without overnight stay
Hospital visits without an overnight stay were less frequent than nights in hospital at, on average, less than one per week. Most of the hospital visits without an overnight stay were visits to A&E and emergency calls in the period prior to reablement. In the 6 months following discharge from reablement, the average number of hospital visits was 0.18 per week; these were generally for outpatient appointments.
Community health services
On average, study participants used community health services twice per week before reablement, and around once per week during reablement and at the 6-month follow-up.
Care services
The use of care services was on average 3 hours per week before reablement, 2 hours per week during reablement and 30 minutes per week at the 6-month follow-up.
Other social-care services
Study participants reported using other social services once per week on average before and during reablement. The use of social services at the 6-month follow-up was slightly less frequent, at 0.7 times on average per week.
Voluntary services
Few study participants reported using voluntary services during the study period.
House adaptations
Few study participants had major or minor adaptions during the study period.
Equipment
The receipt of equipment was similar on a weekly basis before and during reablement, at 0.24 items per week. It was less frequent in the 6-month follow-up, at 0.06 items per week.
Informal care
On average, study participants received 24 hours of informal care in the week before entry into reablement, and 20 hours in the week prior to discharge. In the 7 days before the 6-month follow-up, service users had, on average, 11 hours of help from family and friends.
Costs
Table 19 summarises the package of service costs, rescaled to 1 week. Further results are available (see Report Supplementary Material 10).
| Sector | Time point | |||||
|---|---|---|---|---|---|---|
| T0 | T1 | T2 | ||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Costs falling on the public sector (£) | ||||||
| Hospital overnight stays | 158 | 719 (722) | 124 | 11 (81) | 50 | 52 (138) |
| Hospital visits | 174 | 31 (31) | 127 | 29 (46) | 65 | 26 (33) |
| Community health care | 180 | 27 (28) | 180 | 21 (22) | 62 | 16 (22) |
| Social care | 179 | 44 (33) | 126 | 32 (36) | 61 | 10 (27) |
| Out-of-pocket costs (£) | ||||||
| Community health care | 184 | 0 (1) | 128 | 0 (0) | 51 | 2 (6) |
| Social care | 182 | 2 (5) | 127 | 3 (8) | 59 | 2 (9) |
| Voluntary sector | 184 | 0 (1) | 127 | 0 (0) | 65 | 0 (0) |
| Major home adaptations | 181 | 13 (67) | 127 | 0 (0) | 62 | 3 (22) |
| Minor home adaptations | 180 | 0 (1) | 128 | 0 (1) | 53 | 0 (1) |
| Equipment | 172 | 1 (5) | 123 | 0 (2) | 58 | 0 (1) |
| Other costs (£) | ||||||
| Voluntary sector | 183 | 1 (4) | 127 | 0 (2) | 1 | 1 (3) |
| Major home adaptations | 182 | 32 (145) | 127 | 24 (268) | 228 | 9 (43) |
| Minor home adaptations | 182 | 1 (4) | 128 | 2 (9) | 13 | 1 (2) |
| Equipment | 180 | 23 (45) | 111 | 13 (39) | 139 | 6 (16) |
| Informal care | 177 | 374 (562) | 123 | 315 (585) | 176 | 176 (435) |
Public sector costs
Prior to reablement, hospital overnight stays were the main public sector cost driver. During reablement, the public sector costs consisted mostly of community health and social care, and hospital overnight stays were the smallest component. At the 6-month follow-up, hospital overnight stays were the main component of public sector costs.
Out-of-pocket costs
Out-of-pocket costs involved study participants’ privately paid costs. Out-of-pocket costs were small during the study. The exception were major home adaptations prior to reablement, which, although rare, involved large upfront costs of, on average, £13 per week per study participant. However, the costs would be considerably smaller had they been annuitised to reflect the useful life of the adaptation.
Other costs
Other costs are the costs of services, house adaptations and equipment costed according to the cost had they been provided by the public sector. It also includes informal care time costed using the average wage rate, which assumes that the cost of providing informal care corresponds to the average wage rate in the UK for all population in 2016. Informal care time is the major cost component, representing an input valued at £374 per week before reablement, £315 per week during reablement and £176 at the 6-month follow-up. The cost of house adaptations and equipment would be considerable to the public sector if funded by the public sector.
Determinants of costs
The analysis sample comprised data on study participants for whom there were complete data for T0 and T1 (n = 86). In total, 27 study participants had complete data for T0, T1 and T2 and 33 study participants had complete data for T0 and T2. The limited analysis sample for T0 and T2 precluded an analysis of the determinants of costs at 6 months post discharge. The reasons are twofold. First, it would be difficult to run regressions on such a small sample; and, second, any results would be unreliable and might not be generalisable to the full population of study participants.
Comparison analysis sample versus full sample
In general, participant and service characteristics were distributed similarly for the total sample recruited to the study and the analysis sample (see Report Supplementary Material 10). Note that the hospital costs in the period before reablement were adjusted to reflect the same time period as the questionnaire at discharge (i.e. the duration of reablement).
Predicting hospital costs during reablement
We summarised the statistically significant coefficients for the most comprehensive model as this was the model with the greatest explanatory power. We focused on those characteristics that seemed to affect costs in a meaningful way and did not report differences in magnitude smaller than £1. Data tables are available (see Report Supplementary Material 9).
Costs of hospital
Hospital costs during reablement were poorly predicted by any of the regression models examined. Given that hospital costs are typically highly variable and that the analysis sample was small, the performance of the prediction model was likely to be poor.
-
Significance level = 0.1: no predictors at this level.
-
Significance level = 1%: no predictors at this level.
-
Significance level = 5%: study participants who received reablement from outsourced providers were associated with higher hospital costs during reablement than those who received it from in-house services (£255.00, 95%CI £12.60 to £498.00).
Costs of community health care
The regression models explained less than half of the variation in community health-care costs in the 2 weeks before discharge from reablement.
-
Significance level = 0.1%: study participants who received reablement because of an infection had lower costs of community health care, controlling for other characteristics (£32.00, 95%CI –£34.95 to –£28.99, lower costs). Study participants with worse mental health had slightly higher community health-care costs (£2.00, 95% CI £2.19 to £2.58, increase during reablement per point increase in GHQ-12).
-
Significance level = 1%: study participants who had other comorbidities were associated with higher costs (£9.00, 95% CI £6.90 to £10.90, higher costs). Study participants who were referred for reablement to support return to home from hospital were associated with lower community-care costs of £9.00 (95% CI –£11.40 to –£7.20). This may reflect the recovery of individuals following a period of acute ill health that required hospitalisation.
-
Significance level = 5%: those who reported having enough money to live on and those who were older were associated with higher costs (£38.00, 95% CI £14.00 to £61.90, and £6.00, 95% CI £2.90 to £8.50, per additional year, respectively). Male study participants had £19.00 (95% CI –£34.50 to –£2.60) lower costs. Study participants for whom the problem leading to reablement was musculoskeletal or a fall were associated with £36.00 (95% CI –£59.80 to –£11.20) lower costs.
Costs of social care
The regression models predicting the costs of social care during reablement explain around 64% of the variation in the sample.
-
Significance level = 0.1%: study participants who received reablement from an outsourced provider had, on average, £42.00 (95% CI –£43.60 to £39.80) lower costs.
-
Significance level = 1%: no statistically significant predictors.
-
Significance level = 5%: study participants who rented privately had £28.00 (95% CI £5.10 to £50.00) higher costs than those owning their own home. Study participants who had a greater health-related quality of life had higher costs, but the association was small (£2.50, 95% CI £0.60 to £4.30, higher costs per 0.1 increase in EQ-5D-5L). Comorbidities showed an inconsistent association with social-care costs: there were higher costs for arthritis and chronic obstructive pulmonary disease/asthma and lower costs for cardiovascular disease.
Sensitivity analysis
We re-estimated the most comprehensive model using the data collected in site C (n = 61), and excluded sites A and B (see Report Supplementary Material 9). Consistent with the base-case results, outsourced providers were associated with higher hospital costs and lower costs of social care, and older age was associated with higher costs of community health care. These results should be interpreted not as causal effects, but instead as associations that warrant future research.
Summary
The analysis presented in this chapter is the first, to our knowledge, to explore the feasibility of collecting and using a broad set of costs and outcomes data in the context of reablement services in England. We undertook a comprehensive descriptive and exploratory analysis using regression analysis, to investigate the determinants of costs during reablement given the information available at baseline. This was informed by the first ever, to our knowledge, systematic review of the methods applied for the economic evaluation of reablement. 36
The tool developed to collect information on resource use and costs falling on health care, social care, voluntary services, private costs (out-of-pocket) and informal care time (SCPQ) appears to have performed well, with response rates (overall questionnaire and per question) generally high. We would note that study participants could choose to have the questionnaire administered by the LSO as a structured interview, or could self-complete it with support from the LSO. Thus, self-completion without support and/or no choice over mode of administration has not been tested.
The planned duration of reablement was, on average, 6 weeks and the actual duration of reablement was 4 weeks. Most study participants were planned to have one or two reablement sessions per day.
Services most used before receiving reablement and up to 6 months after discharge were hospital, community health care and social care. Few major house adaptations, mostly in the period before reablement, were reported. Some minor house adaptations and equipment items were reported. Most study participants received help from family and friends. A downwards trend in resource use from the period before reablement to 6 months post discharge was observed.
Public sector costs, falling on health and social care, constituted the largest cost category. Of the public sector costs, costs of hospitalisations with overnight stays were the largest cost item at all time points. Out-of-pocket costs were generally low, at a maximum of £3 per week on average. In the other costs category, the major cost item was informal care, followed by major house adaptations and equipment. From a public sector perspective, the key cost items were hospital overnight stays and social care.
Study participants who received reablement from outsourced providers were associated with higher hospital costs and lower social-care costs than those who received reablement from an in-house service.
Referrals to reablement because of a musculoskeletal problem or a fall, or because of an infection, were associated with lower costs of community health care during reablement. Furthermore, arthritis and chronic respiratory conditions were associated with higher costs, whereas cardiovascular conditions were associated with lower costs.
In terms of demographic characteristics, older study participants were associated with higher costs of community health care; by contrast, male participants were associated with lower costs. Study participants who rented their home were associated with higher costs of social care. Finally, study participants who reported having sufficient money to live on were associated with higher costs of community health care.
Finally, unit costs were sourced from national reference materials. 52,53 We were unable to find unit costs from some services, and had to generalise from similar services. We were explicit about the unit costs we used and our costing assumptions. Our extensive reporting of the use of services allows future studies, such as modelling studies, to use these data and apply other unit costs. However, the sample size limited the tests that could be undertaken, and the inferences that it is possible to draw. Specifically, we were unable to evaluate the cost-effectiveness of service models or to make robust inferences about which characteristics and factors are predictors of costs.
Chapter 9 Work package 3: reabling people with dementia
Introduction
There is a growing population of people who have need for reablement, which may challenge generic services and/or practice. In particular, the number of people in the UK living with dementia is expected to double in the next 30 years. 56 Evidence from previous UK studies indicates that people with complex needs (e.g. dementia, sight loss, learning disabilities) may be ineligible for support from generic reablement services, or may not experience the same level of benefit as ‘typical’ users. 20 Indeed, our own survey of services (WP1) (see Chapter 3, Service provision and delivery) found that over one-quarter of services (28%) reported specifically excluding people with dementia. Furthermore, people with dementia may also be more likely to be susceptible to commonly reported exclusion criteria, including not having reablement potential (29%), having longer-term care needs (17%) and a lack of engagement (see Chapter 3, Service provision and delivery).
However, there is growing interest in reablement for people with dementia. 7 The recent NICE guideline14 notes that people with dementia may be excluded from reablement services because they are perceived as unlikely to benefit from the intervention. NICE’s position, however, is that people with dementia should not be excluded from reablement on the basis of their diagnosis, stating:
Consider reablement for people living with dementia, to support them to maintain and improve their independence and wellbeing.
The guideline also draws attention to the virtual absence of any evidence on the effectiveness and cost-effectiveness of reablement for people with dementia, and the views and experiences of people with dementia, their families and professionals (e.g. managers and front-line practitioners) in terms of service delivery, practice and outcomes. Indeed, with respect to the topic of views and experience, no studies were identified by NICE in the evidence synthesis work carried out to support and inform the guideline’s development. Addressing these evidence gaps is presented as one of the research recommendations arising from the development of the guideline.
Our research questions, originally formulated in 2013, address some of these gaps in evidence and are as follows:
-
How are generic reablement services adapting their service model or practice to accommodate the needs of ‘specialist’ groups? What is the rationale for these adjustments?
-
What has been their learning experience as they have developed this provision?
-
What are the barriers to the delivery of reablement and achievement of positive outcomes for these groups in the context of generic reablement services?
-
How do specialist services approach and deliver reablement? How does it differ from generic provision?
-
What are the barriers to the delivery of reablement and achievement of positive outcomes for groups with specialist needs within specialist services? Do these differ from those for people with low-level needs using generic services?
-
What do specialist reablement approaches or services cost?
-
What specific ingredients of service and support arrangements might best support the quality of life and independence of people with specialist needs?
-
What outcomes might be appropriate to assess the success of these services in a future evaluation?
This workstream was led by Parveneh Rabiee. She conducted all data collection and led on the qualitative data analysis. All members of the research team were involved in the development of data collection tools, data analysis and interpretation. WP3 was conducted during January–July 2016.
Study design and methods
Work package 3 comprised a case study of adapted or extended practice within generic reablement services for people with dementia and dementia-specific provision. In terms of the generic services, we sought to include services reporting to have a ‘dementia protocol’ and those without such a protocol. Our assumption was that having a protocol might indicate more specialist or systematised approaches to providing reablement to service users with dementia. Data were gathered from service leads and reablement workers. We also sought to collect data on the costs of dementia-specific provision or practices. Qualitative and quantitative (costs only) methods were used.
The inclusion criteria were:
-
The service/practice had existed in their present form for at least 1 year, thereby ensuring that the sample would comprise practitioners who had some degree of experience of working with people with dementia and that the practice was reasonably well established.
-
The service had a relatively large proportion of people with dementia within their caseload; again, the rationale for this was that interviewees would have a depth of cumulative experience.
Identification and recruitment of case study sites
Case study sites were drawn from services that participated in WP1. Out of the 143 reablement services responding to the survey, 107 stated that they accepted referrals of people with dementia. Of these, three identified themselves as a specialist service, 30 (28%) as generic services with dementia-specialist protocol, and 74 (69%) as generic services with no specialist protocol.
We attempted contact on at least two occasions with service leads of all of these services (n = 107) by e-mail or telephone. The purpose was to confirm that the survey data remained correct, to secure an indication of the proportion of service users with a diagnosis of dementia, and to ascertain their willingness to be involved in the study. We sought to recruit 10 services, and efforts to establish contact with services were maintained until enough sites had been recruited.
No contact was achieved for 51 out of 107 services. Among those with which contact was established, 16 services had been in existence in their current form for < 12 months and were, therefore, excluded. None of the services with which contact was established was able to supply information on the proportion of their service users with dementia.
Agreement to participate in WP3 was secured from 9 out of the 40 remaining services, one specialist dementia service and eight generic reablement services. Of these, three reported using a dementia protocol. However, it emerged that these were restricted to generic and widely available guidance on working with people with dementia. Therefore, we treated all of the generic services as a single analytical entity. We had hoped to recruit 10 services but this did not prove possible within the WP3 timeline. In each service we sought to recruit the service lead and two reablement workers.
Recruitment of interviewees
Service leads were approached via e-mail and by telephone regarding their eligibility for inclusion in WP3 (see Study design and methods) and, if eligible, they were invited to participate in an interview. Service leads were also asked to nominate two reablement workers within their service who had good experience of working with people with dementia. Study recruitment packs were sent to these workers via the service leads. Workers willing to participate returned a consent form directly to the research team. A summary of the topics to be covered in the interview was sent in advance to all interviewees.
Data collection
Topic guides, one for service lead interviews and one for interviews with reablement workers, were developed by the research team, informed by existing literature and findings from WP1 (see Report Supplementary Material 11). The SSC commented on a draft version. Topic guides comprised structured and open questions. Each topic guide was piloted on one occasion, which highlighted the need for very minor revisions. No further pilot work was conducted.
The interviews with service leads covered the aims and objectives of the service; eligibility criteria; the professional skills within the team; the content and delivery of the reablement service to people with dementia; assessment, monitoring and discharge arrangements; and views on factors promoting and hindering successful outcomes of reablement for people with dementia.
The interviews with reablement workers covered the ways in which workers approached/adapted their practice to accommodate the needs of people with dementia; goal-setting, monitoring and discharge arrangements; views on what outcomes might be appropriate to assess the success of reablement for this group; and factors helping and constraining the benefit of reablement for people with dementia. These interviews also covered issues explored in the interviews with service leads.
Consent was secured before the start of the interview. The duration of interviews ranged from 60 to 75 minutes. All interviews were audio-recorded, with the participant’s consent, and subsequently transcribed.
Data on costs were collected during the interview with service leads (n = 9). When the service lead could not provide that information immediately, the interview was followed up by e-mail correspondence. Five out of nine service leads provided some data, although they were extremely limited and lacking in detail. After careful review of the data by the researchers leading on the economic work, the decision was taken not to analyse this material.
Sample
Service leads in eight out of the nine case study sites were interviewed. The manager in the remaining service was unavailable because of long-term sickness absence. With the individual’s consent, the pilot interview was also included as study data.
Sixteen out of the 18 reablement workers approached (two per service) agreed to participate in the study. The remainder did not respond to the invitation to participate despite e-mail and telephone reminders. All services were represented by at least one reablement worker.
Data analysis
Data were analysed thematically. 49 The Framework approach50,51 was used to support systematic data management, and to allow audit trails of the data management process and analysis and interpretation of the data. Service lead and reablement worker data were analysed together, but participant group and nature of service (specialist vs. generic) were key variables used to test and explore differences in experiences and beliefs. There are five stages to the analytical process. It was led by Parveneh Rabiee, with other members of the team involved in discussions at all stages.
First, researchers familiarise themselves with the data and identify themes and key issues. Based on identified themes (comprising a priori and emergent issues), an index of themes is constructed (the thematic framework; see Appendix 16). Data are then indexed according to which theme(s) in the analytical framework they relate to. Next, the indexed data from each case (e.g. participant, focus group) are summarised onto a series of thematic matrices (or charts). Each chart is divided into columns, allowing relevant data to be organised according to subthemes/issues. A single row on each chart holds one participant’s data. Thus, reading along a row provides an overview of everything an individual spoke about in terms of a specific issue. Reading down the chart (or down a column) allows comparison between participants. The final stage of analysis is examining the charts, composing analytical notes that describe the data, and developing interpretations and hypotheses that are then tested against the charts and raw data.
A dementia reablement service
One of the services recruited to this WP was a service describing itself as a ‘dementia reablement service’. During interviews with staff, it became clear that the service was outside the remit of this study. We do, however, offer a brief report on this service because it is an interesting example of implementing the reablement approach for a different purpose, as is also the case for reablement for people with mental health difficulties.
Client group and referral route
This service was described as being specifically for individuals who have been diagnosed with mild or moderate dementia within the past 12 months, and their families. The majority of referrals were from the local memory clinic.
Service objectives
The core objectives of this service were described as:
-
enabling and supporting the individual to access social activities
-
accepting and adjusting to the diagnosis of dementia
-
providing information relevant to future planning and empowering individuals, and family members, to (start to) plan for the future.
The area reported as that in which most work was typically done concerned supporting people to remain active or become engaged in social activities. The service did not address many of the domains covered by generic reablement provision. Indeed, if needs related to independent living were identified, this service either signposted to other services or made a referral for a social care assessment. Thus, it was clear that this service, although sharing the same overall objective with the generic services participating in this research (i.e. maximising independence), served a different population (those newly diagnosed) and had different functions.
Comment
This service clearly has some commonalities with post-diagnostic support services for people with dementia. However, the type and intensity of support provided appears to be different from that typically offered. Thus, in addition to offering information, advice and signposting, this service provided a degree of sustained and direct support, for example helping service users to access social groups by organising transport for them and accompanying them to a few sessions until they felt comfortable to attend independently.
It is certainly interesting to observe this model of care and support for people recently diagnosed with dementia and their families and, particularly, the services’ identification with the notion of reablement. Further work investigating this service would appear to be worthwhile. However, this service fell out of the scope of this study and we do not report any further data on this service.
Generic reablement services and people with dementia
The remainder of this chapter reports our findings with respect to the experiences and practices of generic reablement services in relation to working with service users with dementia, and how they have responded to any additional needs and challenges.
Overview of the case study sites
Within our eight case study sites, six services were based in adult social services and only delivered reablement. The other two services were independent providers of reablement and home care. Two were jointly commissioned by the NHS and LAs and were part of a wider initiative within their corresponding localities to improve both the integration of health and social care for older people and, more specifically, service provision for people living with dementia. All services accepted referrals of people with dementia for whom a potential benefit from receiving reablement was indicated, a criterion applied to all referrals.
We report our findings in terms of the following themes:
-
reablement objectives
-
the relevance of reablement for people with dementia
-
the opportunity for meaningful assessment
-
additional areas of reablement work
-
measuring success
-
commissioners’ and other services’ understanding of reablement for people with dementia
-
issues with referral information
-
adaptations to practice
-
staff training and access to dementia expertise
-
onward referral at discharge.
Reablement objectives
Interviewees regarded the overall objective of reablement for people with dementia, restoration of functioning with respect to everyday life, as no different from that for the wider population using the service. However, as we later report, the approaches taken to reach this outcome could differ, and the duration of that outcome may be more time-limited.
A second service objective, to carry out an in-depth assessment of the individual that would enable and support planning and decision-making with regard to longer-term support, was addressed simultaneously and the two objectives were regarded as interconnected and informing each other. Interviewees believed that this objective typically carried greater emphasis, and was of great value, for people with dementia than for service users without this diagnosis.
The relevance of reablement for people with dementia
All interviewees believed that reablement could have positive impacts on the lives of people with dementia. Staff believed that people with dementia could learn to do everyday living tasks differently, with the greatest successes likely to be seen in people in the earlier stages of dementia.
Although major improvements in the functional ability may be an unreasonable expectation for a person with dementia, most interviewees believed that reablement could lead to regained skills related to independent living. The positive impacts that these gains had on users’ sense of self-worth and quality of life were noted. Interviewees did, however, remark that such gains may be short-lived. Equally, there was a consensus that the severity of dementia affected the impact of reablement on functioning.
Reablement was also regarded as relevant and effective in terms of achieving positive social outcomes, such as connecting people into local sources of support and social networks. For example, some interviewees described successes in establishing regular use of day centres. Social outcomes are a core domain of comprehensive reablement but may receive less emphasis among other user groups. Typically, however, interviewees emphasised this aspect of reablement when discussing the relevance of this intervention for people with dementia:
. . . If they [family members] know that they can . . . respond to what they need . . . it can take the pressure off them so much and they can continue to support that person in the community, but if they don’t have any means to respite or additional support in the community, it’ll break down quickly.
Manager
The opportunity for meaningful assessment
Most interviewees reported that, compared with other service users, their expectations in terms of outcomes were centred less on regaining ‘full’ independence (although this may be possible, at least in the short term) and more on using the intervention period to achieve an in-depth assessment and knowledge of the individual. This enabled appropriate levels of care and support to be put in place that enabled the individuals to live at home safely and as independently and for as long as possible. One worker described her role as preparing ‘the stepping stone . . . [to] build up a better picture for the next agency that goes in’. This 6-week period of intense contact, and observation of the extent of an individual’s skills and abilities, was believed to be extremely valuable in decision-making about packages of care. Another outcome was that the individual was used to and/or accepted the involvement of external agencies in their lives.
A lack of complete information from referring agencies and/or there being no family members to contribute to a wider life story of the service user were reported as making the assessment process more challenging and could mean that the assessment took longer to complete.
Additional areas of reablement work
A number of additional areas of work were reported by interviewees as, potentially, needing to be incorporated into the process of reabling someone with dementia. We describe these in turn below.
Fostering engagement
An issue identified as particularly salient for people with dementia concerned the individual’s acceptance that they needed help and/or may need it in the future. This concerned both the reablement intervention and community and statutory services more generally. This issue was often spoken about as being bound up with an individual’s lack of insight into their dementia, believing themselves to be ‘just a bit forgetful’. Addressing this was regarded as essential to the individual’s engagement with reablement.
One of our case study sites, which was part of a wider integrated provision for people with dementia, had responded to this issue by offering a 2-week extended assessment period for those service users who were not accepting the involvement of statutory support. This was used, before making the referral to the reablement service, to assess whether an individual was ready, or able, to engage with this intervention. The two specialist outreach workers in the LA social work team had been appointed to this role. It was clear that this was a carefully paced process of initiating a relationship and establishing trust before moving on to assess whether or not reablement was an appropriate option for the individual. This is illustrated by one worker’s account, which is transcribed in Box 2.
. . . my first visit is just . . . showing my face and introducing myself; invariably I don’t get invited in and we just have a conversation on the doorstep; and that’s as far as it goes . . . sometimes you don’t even get that. But once . . . you do it time and time again and eventually it is the client that invites you in and once they invite you in then you can start slowly building up the trust between two of you and eventually you can work towards the goals . . . I’ll wait until the opportunity arises when I can see that I can . . . go forward . . . when the person asks me, would you like a drink or anything . . . cup of tea, coffee or, or water . . . that is a sign for me to, to feel that I’m beginning to break through, because we go into the kitchen together . . . and then I can start . . . seeing whether the client can actually make the tea herself . . . or whether just me being there and prompting her, she would be able to do it . . . invariably you get people putting the milk into the kettle instead of the water. So the first time I leave it in, just observe, but the second time I’m there then I, . . . just prompt a little bit; and it’s almost like a training for them again, what they have forgotten . . . it’s got to be coming from them . . . to be able to sort of move forward . . .
Reorientation to the home environment
For people with dementia being discharged from hospital, interviewees described the necessity of reorientating individuals back to their home environment before embarking on the usual work of reablement. Workers described giving additional levels of encouragement and reassurance and prompting service users to re-engage with tasks and activities around their home, and to return to old routines.
Re-establishing routines
Even among those who had not been hospitalised, the need to re-establish everyday routines was sometimes a prerequisite to starting reablement.
Connecting into local support services
Staff also reported that connecting individuals with local services – both voluntary-sector and statutory (commissioned) provision – during the period of reablement featured more strongly in the work they did than with other users who had greater potential to regain full independence.
Re-establishing relationships
As would be expected, workers reported that they often had to reintroduce themselves on each visit and, in a sense, re-establish an enabling relationship.
Corroborating accounts
Workers also reported that they could not necessarily rely on the individual’s accounts of whether they had, for example, had a shower or taken their medication. Thus, at each visit, it might have been necessary to establish what an individual had, and what they had not, done. Therefore, finding physical evidence of such activities (e.g. a wet bath towel) was sometimes part of the visit. Unsurprisingly, this was a particular issue when the individual lived alone and/or if family members were not in touch with the reablement service.
Work with family members
Several workers also highlighted the work they did with family members who had caring responsibilities. Again, it appeared that this work was more likely, or more intense, with families of people with dementia. The sorts of support included information and signposting to carer support networks and advice on how to manage and provide care to their loved one:
. . . when we’re going in with people with dementia . . . family members are, you know, sort of tearing their hair out . . . they don’t realise . . . that it’s them who needs, the family that needs the support to, you know, get through the day with their loved ones.
Manager
Thus, interviewees believed that reablement could have a positive impact on family members; removing the pressure from their caring responsibilities by connecting the service users into local support networks and activities, and enabling them in their role of informal carer.
Measuring success
Interviewees believed that it was incorrect to assume that outcome or performance indicators used to measure the success of reablement services for people without dementia could be used with people with this condition. Instead, an approach was required that took into account the ways in which the objectives, and the range of work done, may be different for a person with dementia. Thus, although regained independent living skills may be appropriate, the expectation, or indicator of success, should not be independent living per se. Furthermore, the long-term benefits (and savings) yielded by a meaningful and detailed assessment (in terms of appropriate levels and types of care, and how to best work with and support an individual) needed to be recognised. Thus, interviewees believed that requiring ongoing care after the period of reablement should not be considered as evidence that reablement does not ‘work’ for people with dementia, a stance reported to be taken by some commissioners. Other reablement outcomes – unique to, or certainly more typical of, people with dementia – were also identified. These included the willingness to engage with services and receive care and support; use of local (social) support networks and organisations; and the well-being, or quality of life, of informal carers.
Commissioners’ and other services’ understanding of reablement for people with dementia
Some service leads believed that, across both health and social care, incorrect assumptions were being made as to the appropriateness of referring a person with dementia to reablement. They spoke of two misperceptions that meant that people with dementia may not be offered this intervention: first, reablement should be provided only if an individual can be ‘fully’ reabled, and, second, if people have dementia they cannot learn new ways of doing things.
Issues with referral information
The amount of information that the reablement services received about new referrals was said to be largely dependent on where the referral had come from, and whether or not the person had a formal diagnosis of dementia. In general, it appeared that services received more detailed information from hospital referrals than from community referrals, and that dementia or other cognitive impairments were more reliably flagged up. When such information was not provided, reablement workers, who typically visit before the reablement assessment is carried out, felt unprepared. Interviewees also called for referrers to provide wider ‘life story’ information that may not be easy to access directly from the service user. Such information would, they believed, assist them when they were seeking to establish rapport and engage the individual in the intervention.
Adaptations to practice and service delivery by generic reablement services
In this section we report the adaptations to practice and service delivery that generic reablement services had implemented, or that they believed would be valuable if implementation was possible.
Dementia protocols
In sampling services for this study, we had sought to include services that identified themselves as having a ‘dementia protocol’. We had expected the content of such protocols to include permitted adaptations to usual service delivery, such as extended visits and a longer duration of reablement. However, this was not the case. Although, as we report below, some of those adaptations were being implemented for people with dementia, these were not presented as being a service’s protocol for delivering reablement to this population. The content of any dementia protocols was instead limited to non-specific information for workers about communicating with people living with dementia and guidance on safety and quality of care.
Adjusting instructions and the way they are delivered
All interviewees highlighted the importance of straightforward language to convey simple instructions, and the need for repetition of these instructions over, perhaps, a number of visits. Workers also spoke of the need to repeat tasks and processes, sometimes many times. Signs and labels were sometimes used to help people to remember where things were and the order in which tasks were expected to be carried out.
Duration of visits
There was a consensus that more time was required for reablement visits to people with dementia. As noted in the previous section, a worker may need to re-establish a rapport with an individual and identify what has been happening since the last visit. In addition, workers described how visits could include an extended period of encouragement or negotiation in order to support someone with dementia to, for example, eat, change clothes or take medication. Furthermore, there was the extra time required to allow the individual to repeat, perhaps a number of times, the steps in a process. Workers in two case study sites, both integrated services, reported that they were able to extend the duration of their visits when the individual had dementia. However, for most, and in particular for those working in contracted-out services, this was not the case. They either reported that people with dementia on their caseload could not or did not always receive a longer visit because they had a fixed number of visits to make and/or they understood that the duration of the visit was fixed, as determined by the service agreement between the agency and the LA.
Duration of the intervention
Interviewees also agreed that it took longer to reable a person with dementia. Three out of eight services (including the two services that were in partnership with the NHS) represented in this study had the facility to extend the duration of reablement support for people with dementia for up to 12 weeks.
Number of workers assigned to a case
All interviewees believed that there was benefit in having a small number of staff working with people with dementia. However, only two out of the eight services were represented, and both integrated provision, and operated a policy whereby a reduced number of staff, usually a couple of workers, worked with service users with dementia. Managers of the other services reported that their rota system did not allow them to specifically reduce the number of workers visiting service users with dementia. As a result, the number of workers involved was typically four to eight, and potentially greater.
The role of assistive technology
Workers across all services highlighted the use of assistive technology when working with people with dementia. Medication carousels or a dosette box to prompt people to take their medication and fire alarms and heat and door sensors to support safety within the home were the pieces of equipment most often mentioned by workers.
Onward referral at discharge
Several managers noted that identifying an agency to provide ongoing care for a person with dementia could be a protracted process, taking a few weeks or even months. This was particularly the case if a substantial package of care was required. For in-house providers, this could lead to slow throughput through the service and, potentially, to an inability to accept new referrals. In these instances, new referrals were assigned to a home-care agency to provide interim care.
Interviewees emphasised the importance of ensuring a smooth transition into ongoing care and support. In most services, the handover was a longer process for people with dementia, taking 1 or 2 days (sometimes longer) rather than the usual couple of hours.
Staff training and access to dementia expertise
A common feature of all services was that the same workers supported people with and people without dementia. As reported in previous sections (in particular Additional areas of reablement work and Adaptations to practice and service delivery by generic reablement services), they needed to and/or were expected to adapt the way they worked to accommodate the specific needs of people with dementia. Although all managers highlighted the value and importance of dementia training and for a service to have access to dementia expertise, there were differences between services in the extent to which this was realised, and the reach of this training across all staff in the service.
None of the reablement workers interviewed said that they had received training specific to reabling an individual with dementia. Although all of the workers reported that they had attended a basic dementia training session as part of a wider in-house training programme, this level of training was felt to be inadequate. It also appeared that it was not necessarily compulsory:
. . . they do have the basic video on dementia . . . but it’s not enough for, we need specific training on reablement with dementia . . . ‘cos if you don’t understand dementia then you’re not gonna know what to do . . . to reable them . . .
It’s a case of you go out there and . . . do it as best you can.
It should be noted that two services did report that they had recently accessed additional funding to provide advanced dementia training for all their staff.
Many of the workers we interviewed reported drawing on experiences of working with people with dementia from previous roles or their cumulative experiences to date within the reablement service. Concerns were expressed about the skills and competences of staff who do not have that experience to draw on. It appeared that staff working in ‘contracted-out’ services were particularly concerned about the inadequacy of dementia training within their agency:
Dementia can be a very complex . . . problem and to sort of try to squeeze it into a 2-hour session after lunch on a Friday type thing isn’t really enough, ‘cos there’s so much more to dementia than somebody being a little bit confused.
Access to more advanced levels of training on dementia were reported by managers of the two integrated reablement services, although this was not specific to delivering reablement to this population. In one service, all workers were reported as receiving advanced dementia training, whereas in the other this training had been made available to senior workers. These services also reported that accessing dementia-specific advice was relatively easy, given the expertise and remit of other services within their organisation, and reported liaising regularly with a community dementia nurse and specialist outreach workers.
Summary
Interviews with service leads and front-line practitioners drawn from eight generic reablement services and with extended experience of reabling people with dementia yielded rich data on reabling people with dementia.
Interviewees agreed that reablement is an appropriate intervention for people with dementia. However, the stage of the dementia will influence the focus of reabling work and intervention objectives. In addition, the expectation that reablement will eliminate the need for ongoing service involvement may not be appropriate, particularly in terms of expectations around long-term outcomes. Service leads did not always feel that commissioners understood the argument for this. Interviewees also believed that adopting a reablement approach within an extended assessment of social-care needs was an effective approach and supported service user acceptance of involvement of services should this be required.
Front-line practitioners offered detailed descriptions of the ways in which reabling people with dementia may involve additional areas of work, or increase the time and attention needed in these areas. These included fostering engagement, supporting reorientation to the home environment, re-establishing routines, connecting into local support services, working with family members and, at each visit, needing to re-establish the therapeutic relationship and finding a means to corroborate that self-care or other activities had been undertaken.
Interviews explored whether or not service policies and practices were adjusted to accommodate the additional or unique needs of people with dementia who are being reabled. None had formal processes or protocols related to the delivery of reablement to people with dementia. Although all interviewees agreed that longer home visits were typically required, only two services did this. Similarly, only a minority of services routinely provided reablement for longer than the usual 6-week period, or restricted the number of reablement workers assigned to a case.
Although access to generic training on working with people with dementia was reported, none of the reablement workers reported that they had received training on reabling people with dementia. Staff working in outsourced services were most concerned about the lack of training they had received.
Finally, in selecting case sites for this WP, a specialist dementia reablement service was identified that worked with people soon after their diagnosis. Its remit excluded it from our study, but a short description of the service was included in this chapter as an illustration of applying a reablement approach in a different context.
Chapter 10 Discussion
Introduction
This chapter considers the strength and limitations of this study before moving on to discuss the study findings, placing them in the context, where possible, of existing evidence.
Strengths and limitations
To our knowledge, the national survey of reablement services (WP1) generated the most comprehensive and detailed snapshot of reablement services ever conducted. It demonstrated that organisational and practice characteristics differentiate services and it also generated another source of evidence on the costs of providing reablement. The detailed descriptions of the organisation and practice of the services acting as research sites in WP2 are a rich case study of the variability of the way reablement services are organised and delivered.
The evaluation WP (WP2) encountered a number of challenges. The recruitment of research sites and study set-up took much longer than anticipated, and severely affected the progress of the study along the original timeline. A second key issue was that the rate of referrals and/or throughput of two research sites significantly affected the levels of recruitment to the study. As a result, the decision was taken to close the study rather than extend and/or add other research sites, which would have been required to achieve all of the study objectives. The implication of this was that our data set for the outcomes and economic evaluation was much reduced. Furthermore, it was not possible to collect T2 (6-month follow-up) data from all study participants. Thus, it is appropriate to conceive the outcomes and economic evaluations as both pilot and feasibility studies, rather than the full and robust study that was intended. Despite these difficulties, however, the recruitment rate (> 37%) was good, given the nature of the population and the study design. Retention to the study was good (> 80% at T1 and > 90% at T2, when, as per the protocol, home visits were used to collect data). In addition, for the first time, the association between a wide range of individual and service characteristics, some of which are amenable to change, have been subject to an initial exploration.
The process evaluation (WP2b) was less affected by these difficulties. Service users across all three research sites were recruited, although the recruitment of family members to interview about their experiences proved extremely difficult. Rich data were generated from interviews with service users and staff; both make a significant contribution to a rather limited existing evidence base.
Our investigation into staff’s views about reabling people with dementia (WP3) recruited one fewer service than was planned and we did not achieve total samples of service leads and front-line staff. However, again, the data generated were rich and, we believe, are an important addition to the very limited evidence base on this topic.
The limitations of the outcomes and economic evaluations places considerable restraint on the extent to which implications for policy and practice can be drawn. That said, we do believe that the study has strengths and makes an important and valuable contribution to the existing evidence base. They lie in the following areas: understanding of current service design, structures and practices with respect to the delivery of reablement; research design and research methods (including implementing research in non-NHS settings); and informing the future research agenda. Although it is not possible to draw firm implications for health and social care practice from our findings, some comments, based on both our qualitative and quantitative findings, are possible. Chapter 11 sets out these contributions and reflections regarding service organisation, delivery and practice.
The organisation and practice of reablement in England
The first WP of this project (WP1) (see Chapter 3) comprised a national survey of reablement services in England carried out in mid-2015. Surveys of services are, by definition, snapshots of provision at a particular moment. Findings, therefore, have to be read in that light.
Our findings also have to be understood in relation to the decisions we made while determining our sampling framework and selecting services to approach. Most important of these was the focus on services that aimed to help people regain everyday living skills, in their usual place of residence, for a defined period of around 6 weeks, and for which no charge was made. This definition is close to the original conception of ‘social’ reablement as envisaged by its originators in the Department of Health and Social Care. 4,57 It is also close to the definition of reablement used since 2013 in the annual National Audit of Intermediate Care (NAIC). The 2014/15 NAIC (which covers the period of our survey) received responses from only 44 reablement services. 5 To the best of our knowledge, then, our survey provides the first large-scale, detailed and comprehensive picture of reablement services in England.
At the time of the survey, the organisational base of over half of services was the LA. Such services were less likely to be part of any wider intermediate care provision within the locality and were typically presented as a separate, or standalone, service. A small minority of reablement services were based in the NHS, although there were others that were based in integrated NHS/LA organisations, or organisations jointly funded by the NHS and LA. In both cases, these services were more likely to be part of wider intermediate care provision.
The majority of reablement services did not contract out any aspect of the provision to another agency. If they did, it was most likely to be the delivery of reablement support: that is, the ‘hands-on’ work of delivering the intervention through home visits.
Overall, reablement services shared the common objectives of helping people regain everyday skills, reducing the need for ongoing home (social) care and preventing longer than necessary stays in hospital. Preventing admission to residential long-term care was less often reported (by around half) and was closely associated with certain types of organisational base and structure. In terms of services’ primary objectives, most identified this to be either help with regaining everyday skills or reducing the need for ongoing home (social) care. Two services, both of which were NHS based, identified preventing hospital admission during acute illness as the primary objective of their service.
Around two-thirds of reablement services reported that they worked to reable individuals across a wide range of domains of everyday living activities that allow people to live as independently as possible. We defined these types of service as ‘comprehensive reablement’. However, one-third of services were more restricted in the way they implemented the reablement approach and we labelled these types of service as ‘functional reablement’. An additional distinct cluster of reablement input was also identified, which we referred to as ‘social reablement’. It differed considerably from ‘functional’ and ‘comprehensive’ reablement in its service characteristics and aspects of service provision and delivery. Both our survey and other literature suggest that ‘social’ reablement is most likely to be delivered by mental health services. 58,59
How services assessed service users and measured progress towards reablement varied, with most apparently reliant on non-standardised measures or professional judgement to assess their effectiveness. A surprisingly high proportion of respondents were not able to report the usual outcome of service users after discharge. Nonetheless, where this information was provided, the usual outcome most often reported was discharge without involvement of care services. This is broadly in line with results from the 2015 NAIC. 5
Overall, therefore, this survey of reablement services revealed a common objective of restoring, as much as possible, an individual’s functioning and ability to live independently. There was, however, heterogeneity in terms of where services were located, the degree to which reablement was integrated into wider intermediate care provision, the staffing of services and the extent to which services were being outsourced. In addition, not all services reported delivering comprehensive reablement, focusing instead only on functioning with respect to ADL. Finally, it was clear that the routine use of standardised measures to assess and monitor outcomes was rare.
This broad understanding of reablement services is supplemented by the much more detailed picture of the three reablement services that constituted the research sites for the evaluation WP (WP2). Chapter 4 described and compared these services and it reinforced the notion of diversity that exists in reablement service models. Thus, even within just three services, varying approaches to, or models of, providing reablement are captured in terms of both organisational and service characteristics and practice. It also highlighted that, within a single site, a number of different delivery models may be operating. Importantly, no consistent patterns of association of service characteristics were observed, something sometimes also found in the analysis of the national survey. Indeed, it was a recognition of this variety in terms of service delivery and practice that stimulated NIHR’s commissioned research call on this topic, and the questions posed.
The costs of providing reablement
The national survey of reablement services (WP1) also collected data on the costs of reablement and service caseload. The average cost of reablement was £1455. However, 61% of services did not provide information on costs, and, among those that did, there was wide variation in the answers from £20 to £3333 per case. When services with a cost per case of under £500 were excluded, the average cost per case rose to £1728. Both of these figures are within the ranges reported in the literature. Using data from a previous evaluation of reablement,20 the 2015 Unit Costs of Health and Social Care52 reports a cost per case of £2096. The 2015 NAIC59 reported a cost per case of £1484. This provides some reassurance that most of survey respondents provided accurate information.
However, collecting provided information on costs did present issues, in terms of both non-response and apparently implausible answers. We can hypothesise that respondents found the questions difficult to understand or answer, or that they did not have access to the required information. Furthermore, some answers yielded such low costs being calculated (e.g. £20 per case) that errors in survey completion may have also occurred. Overall, our experiences suggest that future attempts to collect data on the costs of reablement services should consider targeting at least some questions to finance departments, which are more likely to understand the nature of the information required and have the relevant information to hand. Furthermore, to highlight errors to the respondent, electronic surveys could be designed so the implied cost per case is calculated automatically and made visible to the respondent.
The outcomes of reablement
The outcomes evaluation was reported in Chapter 5. Given issues with sample size, particularly in two research sites, it was not possible to compare outcomes between sites, and only descriptive analyses of the total sample were therefore reported.
Improvements on all outcomes [i.e. health-related quality of life (EQ-5D-5L), social care-related quality of life (ASCOT-SCT4), practitioner-reported functioning (Barthel Index) and self-reported functioning (NEADL scale)] were observed. For the subsample for whom data were collected at both time points, improvements in health-related quality of life (index score and VAS), social care-related quality of life and practitioner-reported functioning were statistically significant.
Outcomes (excluding the Barthel Index, which was not collected at this time point) had further improved at 6 months post discharge. Compared with the mean improvement in EQ-5D-5L and ASCOT-SCT4 index scores between T0 and T1, the difference between T1 and T2 scores was smaller and not statistically significant. However, for the NEADL scale, size of improvement in mean score was greater between T1 and T2 than between T0 and T1 and, unlike T0 to T1, it was statistically significant. Using the GHQ-12, we also looked at mental health outcomes at the 6-month follow-up. A (non-significant) improvement in mean GHQ-12 score was observed between T1 and T2.
One of the objectives of the study was to compare outcomes between the research sites, each site representing a different model of providing reablement. This was not possible because of inadequate sample sizes. However, our findings still make a useful and important contribution. First, they suggest that a number of outcome measures should be used to capture the impacts of reablement. Second, the inclusion of a measure of mental well-being, an outcome not usually included in evaluations of reablement, should be considered. This is particularly pertinent given concerns about mental well-being, social isolation and ageing. 60 Third, they indicate the validity and value of capturing longer-term outcomes. Fourth, and related to the previous point, they suggest that the chronology of the impact of reablement may vary between outcomes.
Factors associated with outcomes of reablement
Reablement is a complex intervention61 with no fixed protocol; rather, its core approach is to tailor the intervention to each individual while remaining within the overall paradigm of a restorative, intensive, time-limited intervention. 62 In addition, a number of external and person-centred factors are likely to moderate or mediate intervention effectiveness. 62 These issues were clearly reflected in NIHR’s commissioning brief for this study. 33 Emphasis was given to the need for evidence on service, intervention and individual characteristics that have an impact on intervention effectiveness.
A core objective of the study, therefore, was to explore the impact of a range of characteristics on reablement outcomes. We used regression analysis to conduct initial, exploratory analyses; the sample size limited the complexity of modelling work. However, we would argue that the findings are highly useful given that the existing evidence is extremely limited. 14 We now consider the findings (described in Chapter 5) with regard to each characteristic, placing it, where possible, in the context of existing evidence.
Overall, our findings support the notion that reablement should be offered to individuals regardless of age and sex. We have not identified any studies that offer counter-evidence. We used the question ‘Do you feel that you have enough money to live on?’ as a proxy indicator of perceived financial situation. The conclusion from our analysis is that having sufficient money may affect reablement outcomes. However, the nature of this association is likely to be complex, with a number of different issues at play, including, for example, housing quality and suitability63 and general physical health. An additional explanation that has begun to be explored within rehabilitation64 is the potential impact of service users’ socioeconomic status on therapist attitudes and decision-making.
We found evidence that not having family or friends as informal carers was associated with greater improvement in some outcomes (e.g. ASCOT-SCT4, Barthel Index). Similarly, there was weak evidence that living alone was associated with a greater improvement in professional and self-reported functioning (Barthel Index and NEADL scale, respectively). However, in terms of health-related quality of life, living alone was negatively associated with positive outcomes. Overall, these findings accord with a randomised controlled trial of reablement versus usual care11 in which having a carer was related to receiving ongoing care at 3 and 12 months post intervention in both arms of the study. The wider literature offers support for the notion that living alone may affect aspects of health status in a positive way. For example, a recently published systematic review65 of adherence to exercise programmes for older people found that living alone is associated with higher rates of adherence.
Our analysis indicated that the association between referral reason and outcomes may vary according to type of outcome. In terms of social care-related quality of life, there was some evidence that ‘return home’ referrals do better than ‘remain at home’ referrals. However, the opposite was observed with respect to self-reported functioning (NEADL scale). Findings such as these reiterate the importance of assessing a number of outcomes, as the concepts captured differ.
We found that functional ability at referral into the service may have an impact on quality-of-life outcomes and functional outcomes at discharge. This aligns with findings from a randomised controlled trial of reablement. 11 We note, however, that even small reductions in dependency can have an impact on levels of need for ongoing care. Related to this, and equally important, is the evidence that maintaining some degree of independence is highly valued by older people. 66 In terms of physical comorbidities, we found no evidence of an association between this variable and health and social care quality of life at discharge from reablement, and some evidence of possible association with functional outcomes. It is useful to refer to evidence from previous studies that ongoing health issues may affect reablement outcomes, as any gains in functioning and independence may be regarded as likely to be short-lived. 14
Two previous studies24,25 report practitioners’ and/or service users’ beliefs that service users’ motivation is an important factor in successful reablement. Another67 describes service users saying that they wanted to feel that they were ‘working with’ their reablement worker, which gives a sense of active, collaborative involvement. These studies, and practice guidance, identify motivating and increasing the confidence of service users to be key aspects of the reablement worker role. 7,14,24,25,67 We have not identified any previous evaluative research exploring this concept: the lack of a measure may account for this. This study has generated, in an initial and exploratory way, some evidence (and across all outcomes) of the association between engagement and outcomes. A 2015 conceptual review68 concluded that engagement is a multidimensional construct comprising both a co-constructed process and a patient state. The authors argue that this highlights the practitioner’s role in supporting engagement, and note that work to support engagement is likely to require an individualised approach by sufficiently skilled practitioners.
Our analyses also indicate that mental health at entry into reablement was associated with health and social care quality of life at discharge and also, although a weaker association was found, functioning. We have not identified any previous evaluative studies that have explored the association between mental health and reablement outcomes. The insufficient sample size means that we have not been able to run any multiple regression analyses; these would have allowed us to explore, for example, the relationship between mental health and intervention engagement. Intuitively, this would seem an important relationship to understand. Certainly, as reported in Chapter 6, practitioners believed that mental health has an impact on the effectiveness of reablement. For this reason, staff identified the need for access to mental health expertise and input within reablement provision.
We were also able to test, in a preliminary and exploratory way, the association between some service- or intervention-specific characteristics and reablement outcomes. Aside from some relevant qualitative evidence of user and practitioner views on the importance of access to physiotherapy and occupational therapy, and ‘joined-up’ provision with the service and between other services,19,23,24 to our knowledge this is the first time such work has been carried out.
The characteristics we tested were:
-
duration of the intervention
-
reablement workers’ adherence to reablement principles
-
whether the service comprised a single team or separate teams of assessment and reablement worker staff
-
whether reablement workers were located in-house or outsourced from a private provider.
In terms of functional outcomes, there was some evidence to indicate that being looked after by a single team was associated with better outcomes. There was also weak evidence that a single team model is associated with better health-related quality of life at discharge.
In addition, there was some evidence that intervention fidelity and duration of reablement are associated with outcomes, but only with respect to social care-related quality of life.
Finally, there was some or weak evidence from the regression analyses that in-house reablement workers, as opposed to workers from an outsourced team, are associated with more positive outcomes at discharge across all outcome measures.
The wider literature on outsourcing of adult social care has raised questions about the quality of care (e.g. Hudson69). Our interviews with staff offer some further reflections (see Chapter 6, Practice and delivery issues). They noted that outsourced providers may not be incentivised, and nor is it in their ‘business’ interests, to seek to reduce levels of input with a service user. This is contrary to practice within in-house teams, where this as a clear objective. Second are issues of training and skills; a number of interviewees believed that there is greater ‘churn’ within care agencies than among in-house workers, and thus the cumulative experience and skills of delivering reablement may be less evident. Third, outsourcing arrangements may place any ongoing monitoring and review by the assessment team, and supervision and support to reablement workers, at, at best, arm’s length. That said, this may also be the case where separate in-house services deliver assessment and ‘hands-on’ reablement.
Again, we note that we can only hypothesise about the possible mechanisms at play and the connections between some of these service characteristics, some of which may have become clearer had we been able to conduct multiple regression analyses.
Finally, we remind readers that the association between outcomes and other service characteristics could not be explored because the sample sizes were too small for some categories. These were as follows: whether or not an OT was integral to the team; location of the service within an integrated health and social care organisation versus a single agency; and the policy regarding the number of reablement workers allocated per case. Based on our interviews with service users and professionals working in reablement (reported in Chapters 6 and 7, respectively), and the wider literature on issues such as continuity of care and skill mix/access to skills within the reablement service,14,19,23,24 we would argue for the importance of including these characteristics in future research, as well as those for which we have been able to conduct some initial exploratory analyses.
The impact of reablement on resource use
An economic evaluation (WP2c), running in parallel with the outcomes evaluation (WP2a) and reported in Chapter 8, explored the impacts of reablement on resource use and costs. The findings from this aspect of the study are limited in a similar way to those of the outcomes evaluation, and, therefore, conclusions should be circumspect.
To support the economic evaluation, early in this project, a systematic review of the methods applied for the economic evaluation of reablement interventions was undertaken. 36 We identified five areas of methods uncertainty common to some, if not all, of the studies. There was a lack of clarity about which outcome measure(s) it was appropriate to use, as reported in four studies. 20,70–72 There was uncertainty in the cost savings achieved from reduced hospital stays. 72,73 Six studies20,29,71,74–78 discussed the uncertainty around the impact on carers. Six studies12,20,72,74,75,79 discussed the potential benefits of subgroup analysis to determine how the individual’s characteristics affect the costs and outcomes, and to tailor reablement to the individual’s needs. Two studies20,72 suggested that more research is required on the cost-effectiveness of different service models. The findings from this review supported the objectives and design of the economic evaluation. They also provided useful information regarding the methods and scope of data collection.
Overall, the findings from the economic evaluation suggest a downwards trend in resource use from the period before reablement to 6 months post discharge. This may reflect the study participants’ recovery after a period of ill health. However, it may be confounded by the losses to follow-up if the study participants who did not take part in the follow-up were those with the greater use of services. The frequent use of informal care suggests that this was an important source of support for study participants.
From a public sector perspective, the key cost items were hospital overnight stays and social care. Given the magnitude of the cost of hospital overnight stays, future studies should aim to collect this information in detail in order to cost it accurately. In addition, costs of major home adaptations and equipment should also be collected if this is funded by the NHS or the LA, given their magnitude. From a wider perspective, informal care time should be considered.
It is difficult to place our findings on the costs of reablement in context, given the paucity of previous research on reablement. Only one previous UK study reports this;20 in it, the health-care costs during reablement were mostly driven by hospitalisations. By contrast, in our study, hospitalisations during reablement were rare. The differences may be related to the different characteristics of the two study populations and the different study methodologies. Specifically, the study sample in Glendinning et al. 20 was much larger (n = 697), had a worse health-related quality of life at baseline, a greater proportion of study participants were categorised as ‘return home’ and a greater proportion were living alone. The duration of reablement was also longer at 8 weeks (vs. the 4 weeks in our study).
Factors affecting the costs of reablement
The type of provider, the reason for referral to the reablement service, comorbidities and the demographic and economic characteristics of service users were associated with higher costs.
Thus, study participants who received reablement from outsourced providers were associated with higher hospital costs and lower social-care costs than those who received reablement from an in-house service.
In addition, study participants who were referred to reablement because of a musculoskeletal problem or a fall, or because of an infection, were associated with lower costs of community health care during reablement. Furthermore, study participants with arthritis and chronic respiratory conditions were associated with higher costs, whereas cardiovascular conditions were associated with lower costs.
In terms of demographic characteristics, older study participants were associated with higher costs of community health care; by contrast, male participants were associated with lower costs. Study participants who rented their home were associated with higher costs of social care. Finally, study participants who reported having sufficient money to live on were associated with higher costs of community health care.
This analysis was conducted on a subset of the study sample (n = 86) for whom there were complete data on all variables of interest and, therefore, its predictive power should be interpreted with caution. Large sample sizes are usually required to predict health-care costs, given the high variability of costs. 80 We cannot exclude the possibility that these associations are spurious, given the limitations of the analysis, which we highlight below.
The results suggest that the type of provider (outsourced vs. in-house) may have an effect on costs associated with the use of health and social care services. Both in the main analysis and in the sensitivity analysis, outsourced providers were associated with higher hospital costs and lower social-care costs, controlling for other characteristics. This may reflect differences in the case mix that outsourced providers tend to receive that we were unable to control for, or differences in the way that reablement is delivered and its implications for service use.
The results also suggest that there may be some income inequality in the provision of hospital and community health-care services. These costs were higher for study participants who resided in more affluent areas or who perceived that they were in a better financial situation. Income inequality in the provision of health-care services in the UK has been reported in the literature. 81 By contrast, costs of social care were higher for those renting privately than for those who own their home. This is consistent with previous research. 20
At the individual level, we found that variation in costs was mostly related to the health of study participants, reflected in their EQ-5D-5L score, health problems leading to reablement or comorbidities. Therefore, we suggest that this information is collected, not only in future research but also as part of routine data collection by reablement services.
The experience of delivering reablement
To date there have been very few studies of practitioners’ views and experiences of delivering reablement, particularly in terms of intervention effectiveness and factors which support or act as barriers to this. Thus, some findings reported in Chapter 6 of this report [which form part of the project’s process evaluation (WP2b)] concern issues or topics not previously explored or identified.
Views on the importance of service user motivation – and the need, sometimes, for skilled workers to achieve this – was consistently expressed by staff taking part in WP2b (which have been previously described). 24 Staff participating in this study emphasised the importance of flexibility in the timing and duration of visits, and the difficulties and negative impacts of working with ‘resistant families’. Both this and another study27 also report views on the importance of access to specialist knowledge and expertise, with occupational therapy and physiotherapy, as well as community nursing teams, being variously mentioned. Finally, two previous studies24,27 also report reablement workers’ accounts of finding their work very satisfying.
The issue of a lack of awareness and understanding of the reablement approach, among service users and family members, was a dominant issue across interviews and something observed in previous research with staff. 24 It was perceived as affecting intervention effectiveness because of its impact on engagement with reablement and the therapeutic relationship.
The findings from our initial and exploratory modelling analyses of the impact of individual and service/intervention characteristics on outcomes [see Chapter 5, Social care related quality of life (Adult Social Care Outcomes Toolkit – self-completed)], and our tentative interpretations of them, certainly chime with the themes and issues that emerged from our interviews with reablement staff, which serve to offer further explanatory value.
The service user experience
Before this study, there was relatively little research on the perspectives of service users and family carers on reablement services. It was a topic area that was noted in the 2017 NICE guidance14 as needing to be incorporated into future research.
Some of the issues relating to the practicalities of service delivery that interviewees describe have been previously reported, for example dissatisfaction with unpredictable timings of reablement workers’ visits and experiences of rushed visits by reablement workers that may undermine reablement objectives. 23 Interestingly, previous studies23,67,82 have reported service users’ preferences for consistency in the reablement workers who visited them; this was something we did not find and, as reported in Chapter 6 (see Practice and delivery issues), it was not something that all staff agreed was helpful.
Despite some areas of dissatisfaction with the practicalities of service delivery, as have been reported in previous studies, our interviewees were typically extremely positive about their experience of receiving reablement and the outcomes it achieved. 20,26,27 Furthermore, the role of reablement workers in motivating service users, encouraging them to take responsibility and giving them confidence, and the impact on reablement outcomes, is something that other qualitative studies with service users have also reported. 25,83
Perhaps one of the most important issues emerging from these data is a lack of complete understanding about the approach and objectives of reablement. This resulted in individuals feeling dissatisfied or confused about the support they were receiving, and for a minority this remained their dominant view of the service. In addition, there was evidence that this misunderstanding of the role of the reablement worker, and their own role in the intervention, had an impact on the extent to which the service users engaged with the intervention. Another indicator of this issue is that there was inconsistency between interviewees as to whether or not they had understood, and co-developed, the objectives of their reablement. This issue has been reported in previous studies,23,26 although in another study27 service users were described as having a good understanding of reablement and its objectives. This is potentially significant in that it shows that it is possible for service users, and family members, to have a good understanding of the intervention.
Finally, we highlight the relational element to reablement that emerged from these data. Regular home visits by, typically, a positive and friendly workforce were often enjoyable, something that previous research has also reported. 67 For some service users, the visits addressed an issue of loneliness and social isolation. Importantly, our data reveal that the nature, or quality, of relationships with their reablement workers was identified as having an impact on service users’ engagement with the intervention. This accords with other work that argues that the worker/therapist–user/patient relationship plays a significant role in securing engagement with an intervention. 68
Reabling people with dementia
Existing research evidence on reabling people with dementia is extremely limited. At the same time, there is concern that people with dementia may be excluded from reablement. 7,14 Given the growing proportion of older people with dementia, and the implications, or associated risks, of the diagnosis in terms of need for support from health and social care services, it is not surprising that the NICE guidance includes, in its research recommendations, a call for evaluations of the effectiveness and cost-effectiveness of reablement for people with dementia and research to secure the views and experiences of key stakeholders. A standalone WP (WP3), reported in Chapter 9, comprising interviews with service leads and front-line staff explored their views and experiences of providing reablement to people with dementia.
Interviewees were in agreement that the dual objectives of ‘assessment and reablement’ services, which have formed the new ‘location’ for the delivery of reablement since the Care Act 2014,15 worked well for people with dementia. It was regarded as a positive and effective approach to needs assessment. People with dementia were also consistently viewed as having the potential to be reabled, particularly those with mild or moderate dementia. However, expectations about the extent to which everyday living skills/independence were restored, and the period of time over which these would be sustained, needed to differ from those for people without this diagnosis. There was strong consensus that a diagnosis of dementia should not, on its own, preclude offering reablement.
Another difference between reabling people with and reabling those without dementia identified by interviewees was that a greater emphasis was likely to be placed on working on, and supporting positive changes in, social outcomes (e.g. social networks, activities), both for the person with dementia and for family members.
For all of these reasons, interviewees were clear that adjustments should be made regarding the perceived objectives, and indicators of success, of reablement for people with dementia. This position accords with that set out in a 2017 ‘concept paper’ on reablement in dementia, which drew on both the existing evidence base and the views of strategic/service leads, practitioners and academics. 84
In terms of the practice of reablement, interviewees highlighted some distinctions and issues. Interviewees noted that greater investment had to be made in ‘pre-reablement’ work: getting the individual ‘ready’ for reablement. This included fostering engagement, re-establishing daily living routines and, for those returning home from hospital, settling into and reorienting to the home environment. In terms of ongoing adjustments to practice, practitioners spoke about, potentially, a need to re-establish their relationship with the user at each visit. When working with service users who lived alone, it was not always possible to reliably establish which tasks or activities had or had not been done (e.g. having meals, taking medication). Finally, work with family members was often presented as part of the intervention, although, as reported in Chapter 6, family members’ input was not always helpful or supportive of reablement objectives.
Interviewees also described the adaptations to their usual practice that may be needed. First, adjustments to communication were likely to be required, or helpful. This included simplifying language, repeating instructions and using visual cues. Second, there was agreement that it was likely that the duration and intensity (i.e. length of visits) of the intervention should, ideally, be extended, and that the number of reablement workers assigned to a case should be restricted. These adjustments were being formally implemented in only a minority of services represented in this study (although we would note that this gives no indication of a wider adoption of such approaches).
A final area of findings concerned staff training. Interviewees, and specifically those who were reablement workers, felt that the training they had received on dementia was inadequate.
Desiring to place these findings in some sort of context, and given the lack of existing evidence on staff’s views and experiences of reabling people with dementia, we have looked at existing evidence regarding the physical rehabilitation of people with dementia following hip fracture. There are certainly parallels in terms of findings. For example, a systematic review of the effectiveness of hip-fracture rehabilitation in people with dementia concluded that, for people with mild or moderate dementia, they may make similar gains in function and mobility to those of people without dementia. 85 A 2016 systematic review86 of ‘current best practice’ for rehabilitation interventions of older individuals with cognitive impairment post hip fracture concludes that implementing rehabilitation interventions with this population is feasible. It also notes that innovative approaches to support engagement with the intervention may be required. Finally, an Australian-based qualitative study of health professionals87 reported a strong consensus among interviewees that access to rehabilitation should be determined by an individual’s ability, or willingness, to engage with the intervention and not assessed solely on cognitive impairment. Linked to this, interviewees in this study reported that some professionals assumed that people with dementia have limited capability to benefit from rehabilitation.
Chapter 11 Conclusions
Contribution to understanding reablement services in England
The timing of this study within a changing policy landscape (in particular, the Care Act 201415 and its subsequent implementation) had both positive and negative impacts. It meant that the study was being carried out at a time of enormous change within social care for older people and intermediate care provision. Specifically, the notion that all (new) referrals for home care/support should undergo reablement alongside a comprehensive assessment process led to considerable changes in the organisation of services and the perceived role, or objectives, of reablement.
Although these changes, being implemented while we were seeking to recruit services to the study and during study set-up, created difficulties for us, they do mean that the study has generated early and detailed evidence in three localities on the ways in which LAs have responded to the Care Act and wider work on integrating intermediate care provision. Importantly, our research sites were quite diverse, with a range of differences in terms of their characteristics. We have been able, albeit sometimes only in a preliminary way, to explore the impacts of these characteristics on outcomes, user experience and practitioner experience.
In addition, this study makes a significant contribution to our understanding of the ways in which reablement services are responding to people with dementia. The findings from our national survey indicate that some reablement services may still exclude people with dementia. Our qualitative research with reablement staff has generated rich evidence on the way services are responding and, where possible, the development of practices and strategies to support engagement and positive outcomes. However, we also report concerns about the lack of training and a perceived lack of recognition on the part of commissioners to the value of reablement for this population and also, within commissioning arrangements, the adaptations that may be required to maximise its impact.
Contribution to research design and methods
In meeting the health and social care needs of the elderly population, specifically those at risk of (increased) use of social care or unsuccessful discharge from hospital following an acute episode, reablement continues to be key to the policy and practice response in England and elsewhere. Given the paucity of existing evidence, evaluative research on reablement is, and will continue to be, needed. The findings from this study are an important and useful resource for such research in terms of issues of both feasibility and study implementation.
First and foremost, the findings from this study, in terms of both the complexity of reablement provision and our (early) findings on the individual-, intervention- and service-level factors that may affect intervention effectiveness, point strongly to the value of observational studies within any body of work evaluating reablement.
Second, the findings offer insight into the individual-, service- and intervention-level characteristics that should be considered in future evaluative research.
Third, the study provides evidence, based on practitioner views, on the outcome dimensions that evaluations of the effectiveness of reablement for people with dementia should consider.
Fourth, when regarded as a feasibility study, it offers the following:
-
data on the performance of, and effect sizes for, four outcome measures – two quality-of-life measures and two measures of functional ability (at discharge and 6 months post discharge)
-
preliminary data on mental health outcomes
-
data on recruitment, retention and attrition rates
-
approaches to embedding research staff within LA services to support recruitment and timely data collection
-
information, of relevance to research teams and research funders, that may help to pre-empt the difficulties and challenges of implementing a complex study in LA settings
-
initial data on the effectiveness of alternative modes of administering research instruments.
Finally, the study has contributed in terms of the development of three new research instruments that we believe are highly relevant to future evaluations of reablement.
First, two new measures were created: the HRERS-RV and the ERPC. To our knowledge, no equivalent measures exist. We have noted that both would be improved by additional work; but, even in their current state, they offer a means by which user engagement in reablement and intervention adherence can be captured. Our initial findings suggest that these are, potentially, important variables in terms of their impact on user outcomes. Crucially, both are variables that are amenable to intervention by reablement services. Second, a questionnaire (the SCPQ) to assess resource use was developed and performed well.
Informing health and social care practice: some considerations
Although noting the time that has passed (and policy changes that have occurred) since the survey of reablement services (WP1) was carried out, it is valid and important to particularly highlight some findings. First, the evidence of ‘two tiers’ of reablement provision (comprehensive vs. functional) is of concern. Also concerning is that, based on evidence from our process evaluation, services that purport to provide comprehensive reablement are not necessarily doing so. Comprehensive reablement, which adheres to the original concept of reablement and pays attention to a holistic restoration of everyday living beyond simply basic functional skills, demands more from service providers, including having a knowledge of, for example, local social groups and daytime activities and being able to work with service users outside their home (should that be required). Our process evaluation suggests that this is an important issue. The lack of a more holistic approach was one of the few areas of improvement raised by service users we interviewed. Furthermore, a failure to do this meant that service users’ priorities were not necessarily attended to. From the interviews with professionals working in reablement services, workers’ knowledge of local social/activity provision was regarded as an active ingredient of reablement, and this was also stressed by staff who participated in WP3, during which we explored the issue of reabling people with dementia. These findings certainly align with wider evidence that attending to individuals’ social capital is a core aspect of preventing physical and mental health problems. 88 This is, perhaps, particularly pertinent for older people who are at an increased risk of social isolation and loneliness. 89
A second issue to particularly highlight from our survey of reablement services is that monitoring of outcomes through the use of a standardised measure is extremely unusual. Our experiences of using the Barthel Index is that, with training, it is feasible to integrate this into the assessment and review process. In addition, we encountered no difficulties using the NEADL scale, a self-report measure of (extended) ADL functioning.
The difficulties and challenges that this study encountered meant that an insufficient sample size was recruited for the evaluation WP. As a result, the findings from the outcomes and economic evaluation should be treated with caution. Indeed, with respect to these elements of the study, we would suggest regarding these as initial, exploratory evidence. It is, therefore, not appropriate to use these findings to draw implications for health and social care practice.
However, we do note that in our exploratory analyses of factors that may moderate or mediate the effectiveness of reablement, or explain differences in reablement outcomes between research sites, are user, service and intervention characteristics that are amenable to change in terms of service structure and practices.
In terms of individual characteristics, these include mental health and informal carer involvement. There are no indications that characteristics such as age or presence of comorbidities affect intervention outcomes. Engagement with reablement was the factor with the strongest and most consistent evidence regarding impact on outcomes. Although we have classified engagement as an individual characteristic, recent thinking stresses the role of the professional in engendering and maintaining engagement. Findings from our process evaluation fully align with that position. This also revealed that service user and family member (mis)understandings of reablement could be a barrier to engagement and that staff skills vary. We would suggest that these are two areas that service providers and commissioners may want to explore.
To our knowledge, this study is the first to explore the possible impact of organisation and delivery factors on outcomes. The findings are tentative and uncertain. However, intervention fidelity, duration of reablement, service structure (single vs. separate assessment and delivery teams), and in-house versus outsourced reablement worker teams were found to have some degree of (statistical) association with at least one outcome. The findings from the process evaluation, particularly the interviews with staff working in reablement services, both support and offer explanations for these findings. However, the significance of these associations in terms of practice or commissioning decisions could not be established.
Furthermore, this study incorporated collecting qualitative evidence from a range of stakeholders. Although this evidence is limited to three reablement services, and the data are incomplete in terms of full representation of all stakeholder groups across all research sites, our qualitative evidence consistently supports, and offers some degree of explanation for, our exploratory quantitative analyses.
Thus, although not able to draw practice implications from our study findings, we strongly advocate for the need for further research to ensure that commissioning, strategic and practice decision-making is evidence informed.
Finally, we draw attention to the findings from the final WP (WP3), which looked at reabling people with dementia. There was strong and consistent support from participants in this qualitative study that a diagnosis of dementia per se should not preclude someone from being offered reablement. However, interviewees consistently agreed that aspects of service delivery and practices may need to be adjusted or adapted. Within this, interviewees agreed that all staff working within the reablement pathway should be adequately trained in dementia. Although there is not necessarily yet the evidence to offer detailed guidance on practice, it should be possible to devise training that considers the implications of a dementia diagnosis on delivering reablement.
Recommendations for future research
The findings from this study indicate that securing robust evidence with regard to the following topic areas would be highly relevant and useful to commissioners, managers, front-line staff and policy-makers.
-
A large-scale, multisite, mixed-methods outcomes and economic evaluation of reablement. We would suggest an observational study design that allows a robust and thorough investigation of the impacts of service, intervention and individual characteristics on reablement outcomes, and includes people with dementia:
-
We recommend that such a study involves a larger number of services than were used for the current study.
-
We also note the importance of sufficient resources being made available to services acting as research sites.
-
Nesting a local study team within the service appears to work well. The success of the study in terms of retention and data quality indicates the value of using home visits for data collection.
-
-
Furthermore, to properly execute such a study, the following additional and preliminary pieces of work are recommended:
-
Identification of service and intervention characteristics deemed important and relevant to commissioners, strategic leads and service managers. These should then be represented in the research sites.
-
Further psychometric evaluation, and, if required, development, of the HRERS-RV and the ERPC is recommended.
-
Through consultation with stakeholders, via a systematic review and, if necessary, primary research, the identification and testing of a relevant set of reablement outcome indicators for people with dementia.
-
Exploration of using routinely collected data on service use (e.g. Hospital Episode Statistics) as part of the outcomes and resource use data set.
-
-
The development/identification and evaluation of feasible interventions, delivered prior to/on the point of entry into reablement, to improve understanding and expectations of reablement, both on the part of potential service users and family members.
-
The identification and evaluation of strategies and practices to support engagement with reablement. We would suggest a systematic review to start, which seeks to synthesise evidence across a wider scope of interventions including rehabilitation. Such a review, and any ongoing work, should include people with dementia.
-
A systematic review, again synthesising evidence from reablement and also other relevant interventions, of practices and technologies that support the understanding, assimilation and remembering of instructions, or stages, of executing tasks, routines and daily activities among people with dementia.
Acknowledgements
The research team would like to thank the SSC, chaired by Professor Carol Jagger, for their advice and support.
Gerald Pilkington acted as a consultant to the project.
We also thank Dawn Rowley-White for the administrative support she provided during the course of the project.
We acknowledge the work and contribution of Minzy (Min) Kang to the national survey of reablement services (WP1) in terms of the identification of services, data collection and preliminary data analysis.
We acknowledge the work of Noemi Kiss, who collaborated in the systematic review of economic evaluations of reablement; Melissa Harden, who conducted the searches for this review; and Professor Andrea Manca for his support to the work on the systematic review.
Finally, we would like to acknowledge the efforts of and thank our local study teams for their diligent work and enthusiasm for the project. They were as follows:
-
LSOs – Bronagh Hannon, Sabina Cargill and Anna Brown
-
local study administrators – Karen Astil, Ciara Galloway and Joanne Collins.
Contributions of authors
Bryony Beresford (Professor, Health and Care Services Research) was a co-applicant and principal investigator (May–November 2017). She oversaw the final stages of the project and the outcomes and process evaluations within WP2. She contributed to all WPs and led the writing of, or contributed to the chapters for, the final project report.
Rachel Mann (Research Fellow) was involved in the WP1 data collection and analysis. She supported/led study set-up and day-to-day management of research sites and data collection for WP2 and supported/led the supervision of local study teams. She contributed to the process evaluation (WP2b) data collection and analysis, the analysis of service characteristics and report writing. She supported the collection of costs data and contributed to all other aspects of the project.
Gillian Parker (Professor, Social Policy Research) was a co-applicant. She oversaw the WP1 data collection and the analysis and reporting of this element of the project. She contributed to all other elements of the project.
Mona Kanaan (Senior Research Fellow, Statistics) was a co-applicant. She provided statistical expertise to the project, led on the outcomes data analysis and reporting (WP2a) and supervised other staff involved.
Rita Faria (Senior Research Fellow, Health Economics) was a co-applicant. She worked on the costs aspects of the WP1 survey and the economics evaluation (WP2c), leading on data analysis, writing and the systematic review. She also led the analysis and reporting of ASCOT-SCT4 outcomes data (WP2a).
Parvaneh Rabiee (Senior Research Fellow, Health and Social Care Services Research) was a co-applicant. She led WP3, collected all data and conducted data analysis and report writing. She contributed to the data collection for WP2b (process evaluation) staff focus groups.
Helen Weatherly (Senior Research Fellow, Health Economics) was a co-applicant. She oversaw the health economics evaluation (WP2c) and supervised junior health economists working on the project.
Susan Clarke (Research Fellow) conducted the data collection for and data analysis of service user and family member interviews within WP2b, and also supported the focus groups with staff within this WP. She assisted and supported the production of the final report.
Emese Mayhew (Research Fellow) led on data management and cleaning of outcomes data (WP2a), conducted data analysis for the outcomes evaluation and report writing, and the psychometric testing of the HRERS-RV and the ERPC. She assisted and supported the production of the final report.
Ana Duarte (Research Fellow) contributed to the health economics evaluation (WP2c) in terms of data management and cleaning, analysis and writing.
Alison Laver-Fawcett (Senior Lecturer, Occupational Therapy) provided occupational therapy expertise and advice to all aspects of the project, and was directly involved in the development of the HRERS-RV and the ERPC used in WP2a.
Fiona Aspinal (Senior Research Fellow, Health and Social Care Services Research) was lead applicant and principal investigator (October 2014–May 2017). She oversaw the delivery of the project until May 2017 and contributed to all WPs. She supervised junior staff and local study teams and led on delivering WP1.
Publications
Faria R, Kiss N, Aspinal FJ, Harden M, Weatherly HLA. Economic evaluation of social care interventions: lessons drawn from a systematic review of the methods used to evaluate reablement. Health Econ Outcome Res Open Access 2015;1:1.
Faria R, Weatherly HLA, Kiss N, Manca A, Parker GM, Beresford BA, et al. The challenges in evaluating the cost-effectiveness of complex interventions. Value Health 2015;18:A727–8.
Mann R, Beresford B, Parker G, Rabiee P, Weatherly H, Faria R, et al. Models of reablement evaluation (MoRE): a study protocol of a quasi-experimental mixed methods evaluation of reablement services in England. BMC Health Serv Res 2016;15:375.
Mayhew E, Beresford B, Laver-Fawcett A, Aspinal F, Mann R, Bechtold K, Kanaan M. The Hopkins Rehabilitation Engagement Rating Scale – Reablement Version (HRERS-RV): development and psychometric properties [published online ahead of print December 12 2018]. Health Soc Care 2018.
Data-sharing statement
Available data have been included in appendices and supplementary material. Any queries or data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Steiner A. Intermediate Care: A Conceptual Framework and Review of the Literature. London: The King’s Fund; 1997.
- Parker G, Peet S. Position Paper on Intermediate Care for the Department of Health. Leicester: Nuffield Community Care Studies Unit, University of Leicester; 2001.
- National Service Framework for Older People. London: DHSC; 2001.
- Lovett C. Evaluation of the Intensive Community Independence Service. Leicester: Nuffield Community Care Studies Unit, University of Leicester; 1999.
- Homecare Re-ablement. Efficiency Delivery: Supporting Sustainable Transformation. London: DHSC; 2007.
- Homecare Re-ablement Workstream, Discussion Document HRA 002. London: Department of Health and Social Care; 2007.
- SCIE Guide 49: Maximising the Potential of Reablement. London: Social Care Institute for Excellence; 2013.
- Parker G. Intermediate Care, Reablement or Something Else? A Research Note About the Challenges of Defining Services. York: Social Policy Research Unit, University of York; 2014.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Legg L, Gladman J, Drummond A, Davidson A. A systematic review of the evidence on home care reablement services. Clin Rehabil 2016;30:741-9. https://doi.org/10.1177/0269215515603220.
- Lewin G, De San Miguel K, Knuiman M, Alan J, Boldy D, Hendrie D, et al. A randomised controlled trial of the Home Independence Program, an Australian restorative home-care programme for older adults. Health Soc Care Community 2013;21:69-78. https://doi.org/10.1111/j.1365-2524.2012.01088.x.
- Lewin G, Allan J, Patterson C, Knuiman M, Boldy D, Hendrie D. A comparison of the home-care and healthcare service use and costs of older Australians randomised to receive a restorative or a conventional home-care service. Health Soc Care Community 2014;22:328-36. https://doi.org/10.1111/hsc.12092.
- Department of Health and Social Care . Reablement: A Guide for Frontline Staff 2010. www.opm.co.uk/wp-content/uploads/2014/01/NEIEP-reablement-guide.pdf (accessed 4 October 2018).
- NICE Guideline NG74: Intermediate Care Including Reablement. London: NICE; 2017.
- Care Act 2014. London: The Stationery Office; 2014.
- Discharging Older Patients from Hospital. London: National Audit Office; 2016.
- Quick Guide: Discharge to Assess. London: NHS England; 2016.
- Tuntland H, Aaslund MK, Espehaug B, Førland O, Kjeken I. Reablement in community-dwelling older adults: a randomised controlled trial. BMC Geriatr 2015;15. https://doi.org/10.1186/s12877-015-0142-9.
- Home Care Enablement Service: Evaluation. Dundee: Dundee City Council; 2010.
- Glendinning C, Jones K, Baxter K, Rabiee P, Curtis L, Wilder A, et al. Home Care Re-ablement Services: Investigating the Longer-term Impacts (Prospective Longitudinal Study). York: University of York; 2010.
- Lewin G, Vandermeulen S. A non-randomised controlled trial of the Home Independence Program (HIP): an Australian restorative programme for older home-care clients. Health Soc Care Community 2010;18:91-9. https://doi.org/10.1111/j.1365-2524.2009.00878.x.
- Tinetti ME, Baker D, Gallo WT, Nanda A, Charpentier P, O’Leary J. Evaluation of restorative care vs usual care for older adults receiving an acute episode of home care. JAMA 2002;287:2098-105. https://doi.org/10.1001/jama.287.16.2098.
- Ariss S. National Audit of Intermediate Care: Patient Reported Experiences. Sheffield: University of Sheffield; 2014.
- Rabiee P, Glendinning C. Organisation and delivery of home care re-ablement: what makes a difference?. Health Soc Care Community 2011;19:495-503. https://doi.org/10.1111/j.1365-2524.2011.01010.x.
- Hjelle KM, Tuntland H, Førland O, Alvsvåg H. Driving forces for home-based reablement; a qualitative study of older adults’ experiences. Health Soc Care Community 2017;25:1581-9. https://doi.org/10.1111/hsc.12324.
- Wilde A, Glendinning C. ‘If they’re helping me then how can I be independent?’ The perceptions and experience of users of home-care re-ablement services. Health Soc Care Community 2012;20:583-90. https://doi.org/10.1111/j.1365-2524.2012.01072.x.
- Ghatorae H. Reablement in Glasgow: Quantitative and Qualitative Research. Glasgow: Glasgow City Council; 2013.
- Tessier A, Beaulieu MD, Mcginn CA, Latulippe R. Effectiveness of reablement: a systematic review. Healthc Policy 2016;11:49-5. https://doi.org/10.12927/hcpol.2016.24594.
- Cochrane A, Furlong M, McGilloway S, Molloy DW, Stevenson M, Donnelly M. Time-limited home-care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst Rev 2016;10. https://doi.org/10.1002/14651858.CD010825.pub2.
- Sims-Gould J, Tong CE, Wallis-Mayer L, Ashe MC. Reablement, reactivation, rehabilitation and restorative interventions with older adults in receipt of home care: a systematic review. J Am Med Dir Assoc 2017;18:653-63. https://doi.org/10.1016/j.jamda.2016.12.070.
- Peet S, Phelps K, Parker G, Turner D. An Evaluation of Admission Avoidance, Early Discharge and Community Reablement Schemes in Leicester City. Leicester: Nuffield Community Care Studies Unit, University of Leicester; 2002.
- The Social Care Guidance Manual. London: NICE; 2016.
- Commissioning Brief 13/01 – Self-care: A Focus on the Effectiveness of Re-ablement Interventions. Southampton: NIHR Evaluation, Trials and Studies Coordinating Centre, University of Southampton; 2013.
- Aspinal F, Beresford B, Faria R, Kanaan M, Laver-Fawcett A, Parker G, et al. Models of Reablement Evaluation: A Mixed Methods Evaluation of a Complex Intervention (The MoRE project). Southampton: NIHR; 2014.
- Mann R, Beresford B, Parker G, Rabiee P, Weatherly H, Faria R, et al. Models of reablement evaluation (MoRE): a study protocol of a quasi-experimental mixed methods evaluation of reablement services in England. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1600-6.
- Faria R, Kiss N, Aspinal F, Harden M, Weatherly H. Economic evaluation of social care intervention: lessons drawn from a systematic review of the methods used to evaluate reablement. Health Econ Outcome Res 2016;2.
- At a Glance 46: Reablement – A Key Role for Occupational Therapists. London: Social Care Institute for Excellence; 2011.
- Newbronner E, Baxter M, Chamberlain R, Maddison J, Arksey H, Glendinning C. Research into the Longer Term Effects of Re-ablement Services. York: Social Policy Research Unit, University of York; 2007.
- NICE Position Statement on the EQ-5D-5L. London: NICE; 2017.
- Dorling H, White D, Turner S, Campbell K, Lamont T. Developing a checklist for research proposals to help describe health service interventions in UK research programmes: a mixed methods study. Health Res Policy Syst 2014;12. https://doi.org/10.1186/1478-4505-12-12.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 2013;22:1717-27. https://doi.org/10.1007/s11136-012-0322-4.
- Netten A, Forder J, Malley J, Smith N, Towers A. ASCOT Adult Social Care Outcomes Toolkit: Additional Guidance Scoring ASCOT v2.1. Canterbury: Personal Social Services Research Unit; 2011.
- Malley JN, Towers AM, Netten AP, Brazier JE, Forder JE, Flynn T. An assessment of the construct validity of the ASCOT measure of social care-related quality of life with older people. Health Qual Life Outcomes 2012;10. https://doi.org/10.1186/1477-7525-10-21.
- Goldberg D. The Detection of Psychiatric Illness by Questionnaire: A Technique for the Identification and Assessment of Non-psychotic Psychiatric Illness. London: Oxford University Press; 1972.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965;14:61-5.
- Nouri F, Lincoln N. An extended ADL scale for use with stroke patients. Clin Rehabil 1987;1:301-5. https://doi.org/10.1177/026921558700100409.
- Kortte KB, Falk LD, Castillo RC, Johnson-Greene D, Wegener ST. The Hopkins Rehabilitation Engagement Rating Scale: development and psychometric properties. Arch Phys Med Rehabil 2007;88:877-84. https://doi.org/10.1016/j.apmr.2007.03.030.
- Miles M, Huberman A. Qualitative Data Analysis: An Expanded Sourcebook. London: Sage; 1994.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: University of Kent, Personal Social Services Research Unit; 2016.
- NHS Reference Costs 2015–2016. Leeds: Department of Health and Social Care; 2017.
- Weatherly H, Faria R, van den Berg B, Culyer A. Encyclopedia of Health Economics. San Diego, CA: Elsevier; 2014.
- All Data Related to Annual Survey of Hours and Earnings: 2016 Provisional Results. Newport: Office for National Statistics; 2017.
- Knapp M, Cornas-Herrera A, Somani A, Banerjee S. Dementia: International Comparisons. Summary Report for the National Audit Office 2007. http://eprints.lse.ac.uk/3353/1/dementia_international_comparison_%28published_version%29.pdf.
- Modernising Social Services: Promoting Independence, Improving Protection, Raising Standards. London: Department of Health and Social Care; 1998.
- Tew J, Nicholls V, Plumridge G, Clarke H. Family-inclusive approaches to reablement in mental health: models, mechanisms and outcomes. Br J Soc Work 2017;47:864-84.
- National Audit of Intermediate Care: Assessing Progress in Services for Older People Aimed at Maximising Independence and Reducing Use of Hospitals. Manchester: NHS Benchmarking Network; 2015.
- Growing Older in the UK. A Series of Expert-authored Briefing Papers on Ageing and Health. London: BMA; 2016.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2006.
- Hawe P, Shiell A, Riley T. Complex interventions: how ‘out of control’ can a randomised controlled trial be?. BMJ 2004;328:1561-63. https://doi.org/10.1136/bmj.328.7455.1561.
- Rugg J, Croucher K. Older People’s Experiences of Renting Privately. London: Age UK; 2010.
- Madsen EE, Morville AL, Larsen AE, Hansen T. Is therapeutic judgement influenced by the patient’s socio-economic status? A factorial vignette survey. Scand J Occup Ther 2016;23:245-52. https://doi.org/10.3109/11038128.2016.1154106.
- Picorelli AM, Pereira LS, Pereira DS, Felício D, Sherrington C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. J Physiother 2014;60:151-6. https://doi.org/10.1016/j.jphys.2014.06.012.
- Holm AL, Severinsson E. A qualitative systematic review of older persons’ perceptions of health, ill health, and their community health care needs. Nurs Res Pract 2013;2013. https://doi.org/10.1155/2013/672702.
- Gethin-Jones S. Focus on the micro-relationship in the delivery of care. BJHCA 2013;7:452-5. https://doi.org/10.12968/bjha.2013.7.9.452.
- Bright FA, Kayes NM, Worrall L, McPherson KM. A conceptual review of engagement in healthcare and rehabilitation. Disabil Rehabil 2015;37:643-54. https://doi.org/10.3109/09638288.2014.933899.
- Hudson A. Evaluation of Clinical Interventions Using the Goal Achievement Scale n.d.
- Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al. Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial. Health Technol Assess 2009;13. https://doi.org/10.3310/hta13390.
- Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N. A randomised controlled comparison of alternative strategies in stroke care. Health Technol Assess 2005;9. https://doi.org/10.3310/hta9180.
- Crotty M, Giles L, Halbert J, Stepien-Hulleman J, Eckermann S, Masters S, et al. National Evaluation of the Transition Care Program RFT 206/0506 – Final Evaluation Report. Adelaide, SA; 2008.
- Miller P, Gladman JR, Cunliffe AL, Husbands SL, Dewey ME, Harwood RH. Economic analysis of an early discharge rehabilitation service for older people. Age Ageing 2005;34:274-80. https://doi.org/10.1093/ageing/afi058.
- Anderson C, Mhurchu CN, Rubenach S, Clark M, Spencer C, Winsor A. Home or hospital for stroke rehabilitation? Results of a randomized controlled trial. Stroke 2000;31:1032-7. https://doi.org/10.1161/01.STR.31.5.1032.
- Donnelly M, Power M, Russell M, Fullerton K. Randomized controlled trial of an early discharge rehabilitation service: the Belfast Community Stroke Trial. Stroke 2004;35:127-33. https://doi.org/10.1161/01.STR.0000106911.96026.8F.
- Beech R, Rudd AG, Tilling K, Wolfe CD. Economic consequences of early inpatient discharge to community-based rehabilitation for stroke in an inner-London teaching hospital. Stroke 1999;30:729-35. https://doi.org/10.1161/01.STR.30.4.729.
- von Koch L, de Pedro-Cuesta J, Kostulas V, Almazán J, Widén Holmqvist L. Randomized controlled trial of rehabilitation at home after stroke: one-year follow-up of patient outcome, resource use and cost. Cerebrovasc Dis 2001;12:131-8. https://doi.org/10.1159/000047692.
- Rudd AG, Wolfe CD, Tilling K, Beech R. Randomised controlled trial to evaluate early discharge scheme for patients with stroke. BMJ 1997;315:1039-44. https://doi.org/10.1136/bmj.315.7115.1039.
- Parsons M, Anderson C, Senior H, Chen X, Kerse N, Jorgensen D, et al. ASPIRE: Assessment of Services Promoting Independence and Recovery in Elders. Auckland: University of Auckland; 2006.
- Polsky D, Glick H. Costing and cost analysis in randomized controlled trials: caveat emptor. PharmacoEconomics 2009;27:179-88. https://doi.org/10.2165/00019053-200927030-00001.
- Asaria M, Doran T, Cookson R. The costs of inequality: whole-population modelling study of lifetime inpatient hospital costs in the English National Health Service by level of neighbourhood deprivation. J Epidemiol Community Health 2016;70:990-6. https://doi.org/10.1136/jech-2016-207447.
- Trappes-Lomaz T, Hawton A. The user voice: older people’s experiences of reablement and rehabilitation. J Integr Care 2012;20:181-94. https://doi.org/10.1108/14769011211237528.
- Moe C, Brinchmann SB. Optimising capacity – a service user and caregiver perspective on reablement. Grounded Theory Rev 2016;15:25-40.
- Poulos C, Bayer A, Beaupre L, Clare L, Poulos R, Wang R, et al. A comprehensive approach to reablement in dementia. Alzheimers Dement (N Y) 2017;3:450-8. https://doi.org/10.1016/j.trci.2017.06.005.
- Allen J, Koziak A, Buddingh S, Liang J, Buckingham J, Beaupre LA. Rehabilitation in patients with dementia following hip fracture: a systematic review. Physiother Can 2012;64:190-201. https://doi.org/10.3138/ptc.2011-06BH.
- Resnick B, Wells C, Galik E, Holtzman L, Zhu S, Gamertsfelder E, et al. Feasibility and efficacy of function-focused care for orthopedic trauma patients. J Trauma Nurs 2016;23:144-55. https://doi.org/10.1097/JTN.0000000000000203.
- Isbel ST, Jamieson MI. Views from health professionals on accessing rehabilitation for people with dementia following a hip fracture. Dementia 2017;16:1020-31. https://doi.org/10.1177/1471301216631141.
- Coll-Planas L, Nyqvist F, Puig T, Urrútia G, Solà I, Monteserín R. Social capital interventions targeting older people and their impact on health: a systematic review. J Epidemiol Community Health 2017;71:663-72. https://doi.org/10.1136/jech-2016-208131.
- Victor C, Scambler S, Bowling A, Bond J. The prevalence of, and risk factors for, loneliness in later life: a survey of older people in Great Britain. Ageing Soc 2005;25:357-75. https://doi.org/10.1017/S0144686X04003332.
- Willis G. Cognitive Interviewing: A Tool for Improving Questionnaire Design. London: Sage; 2005.
- Tabachnick B, Fidell L. Using Multivariate Statistics. Harlow: Pearson; 2014.
- Brown T. Confirmatory Factor Analysis for Applied Research. New York, NY: Guildford Press; 2015.
- Hatcher L. A Step-by-step Approach to Using SAS for Factor Analysis and Structural Equation Modelling. Cary, NC: SAS Institute; 2006.
- Callery O, Kyle R, Weatherly H, Banks M, Ewing C, Powell P, et al. Substituting community children’s nursing services for inpatient care: a case study of costs and effects. Emerg Med J 2014;31:e55-9. https://doi.org/10.1136/emermed-2012-201926.
- Jolly K, Taylor R, Lip GY, Greenfield S, Raftery J, Mant J, et al. The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technol Assess 2007;11. https://doi.org/10.3310/hta11350.
- Waterhouse J, Walters S, Oluboyede Y, Lawson R. A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up. Health Technol Assess 2010;14. https://doi.org/10.3310/hta14060.
- Beecham J, Knapp M. Costing Psychiatric Interventions. Canterbury: Personal Social Services Research Unit, University of Kent; 1999.
- Clarke C, Patel S, Ives N, Rick C, Woolley R, Wheatley K, et al. Clinical effectiveness and cost-effectiveness of physiotherapy and occupational therapy versus no therapy in mild to moderate Parkinson’s disease: a large pragmatic randomised controlled trial (PD REHAB). Health Technol Assess 2016;20. https://doi.org/10.3310/hta20630.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- The Homecare Deficit 2016. A Report on the Funding of Older People’s Homecare Across the United Kingdom. Wallington: United Kingdom Home Care Association (UKHCA); 2016.
- Butcher L. This Short Briefing Provides an Overview of Community Transport Services. London: House of Commons Library; 2015.
- NHS Health Careers . Agenda for Change – Pay Rates 2017 2017. www.healthcareers.nhs.uk/about/careers-nhs/nhs-pay-and-benefits/agenda-change-pay-rates (accessed 26 July 2018).
- Pressure Ulcers: Prevention and Management. London: NICE; 2014.
- healthandcare.co.uk . Propad Profile Pressure Reduction Cushion 2017. www.healthandcare.co.uk/pressure-relief-cushions/propad-profile-pressure-reduction-cushion.html (accessed 26 July 2018).
Appendix 1 Work package 1: National Survey of Reablement Services in England
This survey was administered electronically using Qualtrics software. It is a complex instrument with considerable amounts of routing. For this reason, we offer a link to a copy of the questionnaire: https://york.qualtrics.com/jfe/form/SV_0cWUhIULIMocT0F.
This link will remain active until 31 December 2019. After that date, please contact the corresponding author.
Appendix 2 Work package 1: data tables
| Cluster number | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1 | – | 1.616 | 1.384 | 1.359 |
| 2 | 1.616 | – | 1.960 | 1.130 |
| 3 | 1.384 | 1.960 | – | 1.943 |
| 4 | 1.259 | 1.130 | 1.943 | – |
| Staff in core team | % of teams reporting type of staff as core member | Total | Significance | |||
|---|---|---|---|---|---|---|
| Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | |||
| Reablement worker | 54 | 57 | 85 | 81 | 69 | * |
| Social work assistants | 58 | 7 | 60 | 5 | 24 | *** |
| Senior social workers | 96 | 19 | 60 | 12 | 37 | *** |
| Care manager | 58 | 43 | 40 | 42 | 45 | NS |
| Home-care workers | 4 | 100 | 35 | 0 | 39 | *** |
| Home-care organiser | 21 | 69 | 40 | 26 | 41 | *** |
| Other social-care staff | 27 | 28 | 16 | 33 | 27 | NS |
| OT assistants | 50 | 7 | 70 | 7 | 25 | *** |
| OTs | 92 | 29 | 100 | 21 | 49 | *** |
| Physiotherapy assistants | 0 | 0 | 65 | 0 | 10 | *** |
| Physiotherapists | 29 | 12 | 100 | 0 | 25 | *** |
| Other therapists | 8 | 0 | 0 | 2 | 2 | NS |
| Health support workers | 8 | 5 | 30 | 12 | 12 | * |
| Registered nurses | 8 | 0 | 85 | 5 | 16 | *** |
| Other health-care staff | 4 | 0 | 0 | 0 | 1 | NS |
| OT access in team and/or from elsewhere | Type of service (%) | Total (%) | |||
|---|---|---|---|---|---|
| 1: reablement with OT | 2: home-care reablement | 3: multidisciplinary reablement | 4: reablement worker teams | ||
| Yes | 92 | 57 | 100 | 44 | 66 |
| No | 8 | 43 | 0 | 56 | 34 |
| Total (n) | 24 | 42 | 20 | 43 | 100 |
| Type of reablement input | Services reporting this type of reablement input (%) | Services reporting that this type of input makes up the majority of their work (%) |
|---|---|---|
| Personal care | 89 | 73 |
| Domestic tasks | 88 | 1 |
| Safety issues | 90 | 3 |
| Information and signposting | 87 | < 1 |
| Getting around inside the home | 90 | 2 |
| Getting out and about | 71 | 1 |
| Re-engaging with social activities | 68 | < 1 |
| Managing health-related needs | 83 | 2 |
| Confidence-building | 84 | 11 |
| Total (n) | 143 | 142 |
| Missing cases | – | 1 |
| Organisational base | Services reporting this type of reablement input (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Personal care | Domestic tasks | Safety issues | Information and signposting | Getting around inside | Getting out and about | Re-engaging with social activities | Managing health-related needs | Confidence-building | |
| LASSD | 97 | 97 | 92 | 96 | 99 | 78 | 77 | 89 | 93 |
| Health service | 100 | 100 | 100 | 100 | 100 | 67 | 67 | 100 | 100 |
| Joint health and SSD | 81 | 76 | 91 | 95 | 90 | 75 | 85 | 90 | 91 |
| Private provider | 100 | 90 | 100 | 74 | 100 | 90 | 61 | 100 | 80 |
| Voluntary provider | 57 | 86 | 100 | 100 | 71 | 86 | 100 | 71 | 100 |
| Social enterprise | 100 | 100 | 75 | 100 | 75 | 100 | 100 | 75 | 100 |
| Other | 100 | 100 | 100 | 86 | 100 | 86 | 50 | 86 | 83 |
| All | 93 | 93 | 93 | 92 | 96 | 81 | 77 | 89 | 91 |
| Missing cases | 9 | 9 | 8 | 11 | 10 | 19 | 19 | 12 | 13 |
| χ2 = 23.93, df = 6; p = 0.001 | χ2 = 12.21, df = 6; p = 0.057 | χ2 = 5.59, df = 6; p = 0.471 | χ2 = 12.53, df = 6; p = 0.051 | χ2 = 17.76, df = 6; p = 0.007 | χ2 = 3.184, df = 6; p = 0.785 | χ2 = 9.403, df = 6; p = 0.152 | χ2 = 6.102, df = 6; p = 0.412 | χ2 = 4.914, df = 6; p = 0.555 | |
| Contractual arrangement | Services reporting this type of reablement input (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Personal care | Domestic tasks | Safety issues | Information and signposting | Getting around inside | Getting out and about | Re-engaging with social activities | Managing health-related needs | Confidence-building | |
| Wholly in-house | 93 | 93 | 94 | 92 | 97 | 79 | 75 | 90 | 91 |
| In-house and contracted out | 92 | 92 | 92 | 92 | 92 | 83 | 88 | 87 | 96 |
| Wholly contracted out | 100 | 100 | 88 | 100 | 100 | 100 | 88 | 88 | 100 |
| Other | 93 | 86 | 93 | 92 | 93 | 75 | 58 | 93 | 77 |
| All | 93 | 93 | 93 | 93 | 96 | 81 | 77 | 89 | 91 |
| Missing cases | 8 | 8 | 7 | 10 | 9 | 18 | 18 | 11 | 12 |
| χ2 = 0.651, df = 3; p = 0.885 | χ2 = 1.66, df = 3; p = 0.645 | χ2 = 0.675, df = 3; p = 0.879 | χ2 = 0.694, df = 3; p = 0.875 | χ2 = 1.548, df = 3; p = 0.671 | χ2 = 2.147, df = 3; p = 0.542 | χ2 = 4.454, df = 3; p = 0.216 | χ2 = 0.358, df = 3; p = 0.949 | χ2 = 4.639, df = 3; p = 0.200 | |
| Organisational structure | Services reporting this type of reablement input (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Personal care | Domestic tasks | Safety issues | Information and signposting | Getting around inside | Getting out and about | Re-engaging with social activities | Managing health-related needs | Confidence-building | |
| Separate service | 97 | 97 | 93 | 86 | 96 | 76 | 68 | 85 | 93 |
| Part of intermediate-care service | 92 | 89 | 96 | 100 | 96 | 77 | 85 | 96 | 89 |
| Part of home-care service | 100 | 90 | 100 | 84 | 100 | 68 | 58 | 100 | 74 |
| Part of crisis/rapid response service | 100 | 100 | 100 | 100 | 100 | 80 | 80 | 60 | 100 |
| Other | 29 | 57 | 71 | 100 | 43 | 86 | 86 | 43 | 86 |
| All | 93 | 92 | 94 | 90 | 94 | 76 | 71 | 86 | 89 |
| Missing cases | 14 | 14 | 14 | 14 | 14 | 14 | 14 | 14 | 14 |
| χ2 = 48.48, df = 4; p < 0.001 | χ2 = 15.70, df = 4; p = 0.003 | χ2 = 7.93, df = 4; p = 0.094 | χ2 = 6.10, df = 4; p = 0.192 | χ2 = 33.55, df = 4; p < 0.001 | χ2 = 1.02, df = 4; p = 0.902 | χ2 = 5.19, df = 4; p = 0.268 | χ2 = 19.10, df = 4; p = 0.001 | χ2 = 6.54, df = 4; p = 0.162 | |
| Type of reablement input | Reablement input delivered by team (%) | Total (%) | |||
|---|---|---|---|---|---|
| Reablement with OT | Home-care reablement | Multidisciplinary reablement | Reablement only | ||
| Functional | 26 | 37 | 15 | 30 | 29 |
| Comprehensive | 74 | 63 | 85 | 51 | 65 |
| Social | 0 | 0 | 0 | 19 | 6 |
| N (100%) | 23 | 41 | 20 | 43 | 127 |
| Objective | Services reporting this as an objective of their service (%) | Services reporting this as the main objective of their service (%) |
|---|---|---|
| Help people regain everyday living skills | 95 | 58 |
| Reduce need for ongoing (social) home care | 90 | 24 |
| Prevent admission to long-term care when at risk | 80 | 1 |
| Prevent longer than necessary stay in hospital | 88 | 7 |
| Prevent hospital admission during acute illness | 49 | 1 |
| Other | 9 | 6 |
| N (100%) | 138 | 137 |
| Missing | 5 | 6 |
| Source of referral | Services taking referrals from this source (%) | Service delivery and organisational variables significantly associated with this source of referral | Statistical significance | Type of reablement input significantly associated with this source of referral | Statistical significance |
|---|---|---|---|---|---|
| Acute hospital | 60 | – | – | ||
| Early discharge team | 61 | – | – | ||
| Emergency department | 48 | – | – | ||
| Primary care | 45 | Services based in a health service are more likely to take referrals | χ2 = 9.88, df = 4; p = 0.043 | ‘Functional’ reablement less likely to take referrals | χ2 = 8.93, df = 2; p = 0.011 |
|
Services run as part of or alongside intermediate care are more likely to take referrals Services run as a separate reablement services are less likely to take referrals |
χ2 = 12.01, df = 4; p = 0.017 | – | |||
| Primary care out-of-hours service | 36 | Services run as separate reablement services are less likely to take referrals | χ2 = 9.09, df = 4; p = 0.059 | ‘Functional’ reablement less likely to take referrals | χ2 = 7.52, df = 2; p = 0.023 |
| Social services emergency duty team | 62 | – | – | ||
| Social services intake team | 75 | Services in ‘reablement only’ staffing cluster are more likely to take referrals | χ2 = 7.39, df = 3; p = 0.06 | – | |
| Intermediate care bed-based unit | 50 | Services run as part of or alongside intermediate care are more likely to take referrals | χ2 = 8.80, df = 4; p = 0.07 | – | |
| Intermediate care home-based service | 43 | – | – | ||
| Service user | 27 |
Services run as separate reablement services are less likely to take referrals Services run as part of crisis/rapid response services and ‘other’ services are more likely to take referrals |
χ2 = 15.32, df = 4; p = 0.004 |
‘Functional’ reablement less likely to take referrals ‘Social’ reablement more likely to take referrals |
χ2 = 18.57, df = 2; p < 0.001 |
| Voluntary sector | 27 | Services run as ‘other’ are more likely to take referrals | χ2 = 13.16, df = 4; p = 0.01 |
‘Functional’ reablement less likely to take referrals ‘Social’ reablement more likely to take referrals |
χ2 = 20.75, df = 2; p = 0.001 |
| Other | 13 | Services with ‘other’ contractual arrangements are more likely to take referrals | χ2 = 9.97, df = 3; p = 0.019 | – | |
| n (100%) | 143 |
| Typical duration (weeks) | % services |
|---|---|
| < 4 | 13 |
| 4–5 | 30 |
| 6 | 50 |
| ≥ 7 | 7 |
| n (100%) | 132 |
| Missing | 11 |
| Staff who usually set goals | Service delivery and organisational variables significantly associated with these staff setting goals | Statistical significance | Type of reablement significantly associated with this source of referrals | Statistical significance |
|---|---|---|---|---|
| OTs | Less likely to set goals in ‘social’ reablement | χ2 = 6.30, df = 2; p = 0.043 | ||
| More likely to set goals in multidisciplinary reablement services | χ2 = 13.41, df = 3; p = 0.004 | – | ||
|
Less likely to set goals when service is a separate reablement service More likely to set goals when service is part of or is run alongside an intermediate-care service |
χ2 = 12.99, df = 4; p = 0.011 | – | ||
| Physiotherapists | More likely to set goals in multidisciplinary reablement services | χ2 = 16.31, df = 3; p = 0.001 | – | |
| More likely to set goals in services run from a health service | χ2 = 10.06, df = 4; p = 0.039 | – | ||
|
Less likely to set goals when service is a separate reablement service More likely to set goals when service is part of or is run alongside an intermediate-care service |
χ2 = 14.36, df = 4; p = 0.006 | – | ||
| Nurses | More likely to set goals in multidisciplinary reablement services | χ2 = 18.23, df = 3; p = < 0.001 | – | |
|
Less likely to set goals in a service run from a LASSD More likely to set goals in services run from a health service |
χ2 = 23.29, df = 4; p < 0.001 | – | ||
|
Less likely to set goals when the service is a separate reablement service More likely to set goals when the service is part of or is run alongside an intermediate-care service |
χ2 = 24.36, df = 4; p < 0.001 | – |
| Answered, n (%) | Mean (SD) | Minimum | Maximum | |
|---|---|---|---|---|
| Expenditure on reablement service as reported by services (£) | ||||
| Total expenditure on reablement service | 31 (22) | 2,558,007 (2,196,177) | 5000 | 7,092,570 |
| Expenditure on in-house reablement | 8 (6) | 1,537,428 (2,083,990) | 300,000 | 6,500,000 |
| Expenditure on contracted-out elements | 7 (5) | 865,123 (642,622) | 269,678 | 2,000,000 |
| Total value of the reablement contract | 2 (1) | 200,000 (1,200,000) | ||
| Total budget for older people’s services | 10 (7) | 16,800,000 (16,700,000) | 1,013,000 | 50,400,000 |
| Percentage expenditure on reablement (%) | 8 (6) | 24 (34) | 0 | 100 |
| Total expenditure on reablement based on estimates provided by services (£) | ||||
| Total using expenditure, if expenditure and percentage of the budget were answered | 42 (29) | 2,366,626 (2,245,076) | 5000 | 8,500,000 |
| Total using percentage of older people’s budget, if expenditure and percentage of the budget were answered | 42 (29) | 2,359,779 (2,204,305) | 5000 | 8,500,000 |
| Number of cases | ||||
| Number of cases that the service provided reablement to in 2014–15 | 81 (57) | 1419 (1596) | 10 | 9500 |
| Typical number of cases per month | 19 (13) | 103 (91) | 8 | 275 |
| Calculated overall number of cases per year | 100 (70) | 1383 (1510) | 10 | 9500 |
| Cost per case | ||||
| Total using total expenditure, if total expenditure and percentage of the budget were answered | 37 (26) | 1445 (830) | 20 | 333 |
Appendix 3 Work package 2a: adaptation of the Hopkins Rehabilitation Engagement Rating Scale
Background
The HRERS48 was developed in the USA to measure engagement with physical/functional rehabilitation interventions. It is a five-item, practitioner-completed scale and has good psychometric properties. In developing the measure, and based on reviews of existing research into patients’ participation in rehabilitation interventions, the authors of the scale defined the construct of ‘engagement’ as comprising five dimensions: attendance, ability to participate affected by cognitive impairments or low mood, positive attitude, acknowledgement/acceptance of need, and active participation. The HRERS comprises five items, each representing a different dimension (Table 33).
| Item | Concept (Kortte et al.48) |
|---|---|
| The patient regularly attended my therapy/rehabilitation activity | Attendance |
| The patient required verbal or physical prompts to actively participate in my therapy/rehabilitation activity (reverse score) | Ability to participate/engage affected by cognitive impairments or low mood |
| The patient expressed a positive attitude towards my therapy/rehabilitation activity | Positive attitude |
| The patient acknowledged a need for rehabilitation services and the benefits of therapy exercises or rehabilitation activities | Acknowledgement/acceptance of need |
| The patient actively participated in his/her rehabilitation therapy/activity | Active participation |
A six-point response format (i.e. never, seldom, some of the time, most of the time, nearly always and always) is used by clinicians to report the frequency, or consistency, with which they observed each dimension.
The item adaptation process
Permission was sought from the authors of the scale [Dr Kathleen Bechtold (Kortte) (corresponding author), The Johns Hopkins School of Medicine, Baltimore, MD, USA, 2016, personal communication] to adapt the measure for use in reablement services. Permission was granted. The main adaptation requirement was changing references in the items from rehabilitation to reablement. Adaptation of item 2 was more challenging. Verbal/physical prompts/directions are used in rehabilitation when cognitive/memory impairments or low mood affect a patient’s engagement. By contrast, verbal/physical prompts are a core element of reablement, for example: providing instructions, or offering advice, about how to do a task; supporting mobility or a particular posture; and encouraging and building confidence through the spoken word. As a result, substantive changes to this item were required.
Two members of the research team (BB and AL-F), both of whom had previous experience of scale development and one of whom was also a qualified OT, examined the HRERS items and constructs. Each item was reviewed in turn as follows: does it need any adaptation with regard to its use in reablement services and in the UK. If an item was identified as needing adaptation, then an adapted version was created through discussion.
This first draft of the adapted version was then reconsidered on an individual basis by Bryony Beresford and Alison Laver-Fawcett and further adaptations were agreed. This second complete draft was shared with the remainder of the research team and the study’s SSC. Further revisions were made in the light of these comments. This yielded a first version of the HRERS-RV. In addition to the scale items, we inserted a separate, standalone questionnaire regarding changes in levels of engagement over time. This was included on the advice of the SSC to allow scope for a wider exploration of the concept of engagement in relation to receiving reablement (Box 3). These were then tested and evaluated using cognitive interviewing techniques.
The cognitive interviews and further adaptations
Cognitive interviews90 with reablement workers were used to evaluate their understanding or interpretation of the items and experiences of completing the questionnaire. Two approaches were used. First, the ‘think aloud’ technique, in which an individual verbalises their thoughts as they complete the draft questionnaire, was used to identify ambiguities or difficulties in the wording of items, instructions and/or the response format. Second, post completion, respondents were asked about their experiences of completing the draft tools and for their suggestions regarding modifications to the layout and response format.
Methods
Cognitive interviews were undertaken with 10 reablement workers based in two services. All except one completed this process with respect to two service users: this allowed us to explore whether or not the statements and response options were distinct enough to show differences between service users. A staged process was used, with revisions being made to the HRERS-RV during the process. Thus, a set of interviews were conducted, findings were shared and discussed within the research team and modifications were agreed. It was then subject to further cognitive interviews and so forth.
Issues raised during cognitive interviews and revisions of the Hopkins Rehabilitation Engagement Rating Scale – Reablement Version
Three practitioners were presented with the first adaptation of the HRERS-RV (see Box 3). They suggested including some additional statements:
-
Does the client accept their need for reablement?
-
Did the client have the potential (physically and cognitively) to be reabled?
-
To what degree were the client’s goals met?
We were surprised by the first of these comments, as this concept was already included in HRERS-RV (item 4). However, the practitioners’ response indicated that the wording of this statement was unclear. As a result, item 4 was reworded. We did not regard the other two suggested questions as relevant to the concept of ‘intervention engagement’. However, we decided to include two further supplementary questions that captured these two concepts, but not to treat them as part of the HRERS-RV. They were as follows:
-
Do you think that the client achieved their goals?
-
Did the client make the progress you expected with achieving their goals?
A second version of the HRERS-RV was then taken forward for further cognitive interviews. The findings and resulting adaptations to each item are reported below.
Item 1: when I made my visits, the person was ready for me
Five practitioners did not raise any issues about this item and interpreted it as we expected. However, the remaining five felt that this statement could be interpreted in several ways and they each gave at least two different interpretations. The range of interpretations is outlined below:
-
that the client is prepared to start the reablement session, for example they have chosen clothes to wear
-
that the client is aware of when the practitioner is due to arrive
-
that the client understands what reablement is about
-
that the client is ready to accept the reablement process.
In particular, they were concerned that the item might be interpreted as asking if the person was out of bed, washed and dressed; however, these activities could well be reablement objectives. In response, we revised the wording to clarify the meaning.
Item 2: learning or memory difficulties, or low mood, affected participation in reablement activities
As with the first statement, half of the respondents understood the statement and had no difficulty responding to it, but the other half identified some challenges with the statement. Two people felt that the wording was unclear and that this resulted in the purpose of the statement being unclear. Three people hesitated when responding to this statement. When asked about this, these practitioners said that they thought they understood the statement, but that summing up clients’ fluctuating mood and memory/cognitive difficulties over a 6-week period, into a single response option, took time. In response, we reordered the clauses in the statement to make it easier to understand and, after further cognitive interviews, revised the wording again. After these changes, practitioners taking part in the final phase of cognitive interviewing found it easier to complete this item.
Item 3: the person expressed a positive attitude towards the reablement activities we worked on together
All of the participants understood this item and were clear about how to choose appropriate response options.
Item 4: the person questioned their need to regain or improve their independence and/or ability to manage activities of daily living
In the early phase of cognitive interviewing, three people found the wording of this item too long and were uncertain of its meaning. In response, we simplified the item. Once this change had been made, no practitioners appeared to have, or reported, difficulties with this statement.
Item 5: the person actively participated in my reablement sessions/visits
All of the participants understood this item and were clear about how to choose appropriate response options.
Supplementary question 1: to what extent did the client’s engagement with reablement change across the period of time you worked with them?
All but one of the practitioners understood what this question was asking, but one thought that it was about the clients’ confidence. To minimise the risk of other practitioners misinterpreting the focus of the statement, we simplified it.
Supplementary question 2: do you think that the client achieved their goals? Supplementary question 3: did the client make the progress you expected with achieving their goals?
Practitioners had no difficulties with understanding and interpreting these questions.
Response format
Some practitioners did not know what ‘seldom’ meant. We discussed its meaning and practitioners suggested that ‘seldom’ should be replaced with ‘rarely’. This change was implemented.
Layout
Practitioners preferred the response option statements placed below the related tick figures. The scale was formatted accordingly. Overall, however, practitioners thought that the format was clear.
Instructions for completion
Some of the practitioners felt that the instructions could be written more clearly. Based on their comments, we identified key changes that could improve understanding and adapted the instructions accordingly.
Ability to distinguish between service users
Among those practitioners who completed the HRERS-RV with respect to two service users, there was good evidence that the scale was distinguishing between service users.
The final version of the Hopkins Rehabilitation Engagement Rating Scale – Reablement Version
The final version of the HRERS-RV administered as part of data collection for the outcomes evaluation (WP2) is set out in Box 4. Supplementary questions are presented in Box 5. The HRERS-RV was completed with respect to 126 study participants across two of our research sites. Psychometric evaluation of the scale was conducted using the data collected; this decided whether or not we would use the measure within our analyses. We present the findings of our psychometric evaluation in the following section.
Testing the psychometric properties of the Hopkins Rehabilitation Engagement Rating Scale – Reablement Version
Analytical methods
We examined the distributions of scores on each of the five items and that of the total score. Construct validity was tested using factor analysis using the principal factor method. The principal factor method uses the estimates of shared variance in the initial correlation matrix to calculate the communality and uniqueness value for each variable. Communality is the amount of variance that a variable has in common with all the other variables in the correlation matrix. Uniqueness is the amount of variance that is unique to the individual variable, and hence it is variance that is not captured by the factor. This approach was used because we wanted to estimate the degree of covariance across the five dimensions. 91 Scale reliability was measured using Cronbach’s alpha. Finally, given that the degree to which an individual engages with an intervention is thought to have an impact on intervention outcomes, we assessed predictive validity by testing the association between HRERS-RV summary score and scores on outcome measures at T1: EQ-5D-5L summary score, Barthel Index summary score and ASCOT-SCT4 index score.
Total scores and distribution of scores across items
A total score was calculated by summing the scores on each of the five items (maximum range 0–30). A higher score represents greater engagement with the intervention. Figure 4 presents HRERS-RV total scores for the sample. The distribution is skewed to the left, demonstrating a ceiling effect (see Figure 4). The majority of the participants (< 74%) scored highly on the instrument (total score of ≥ 25).
FIGURE 4.
The HRERS-RV: distribution of total scores.
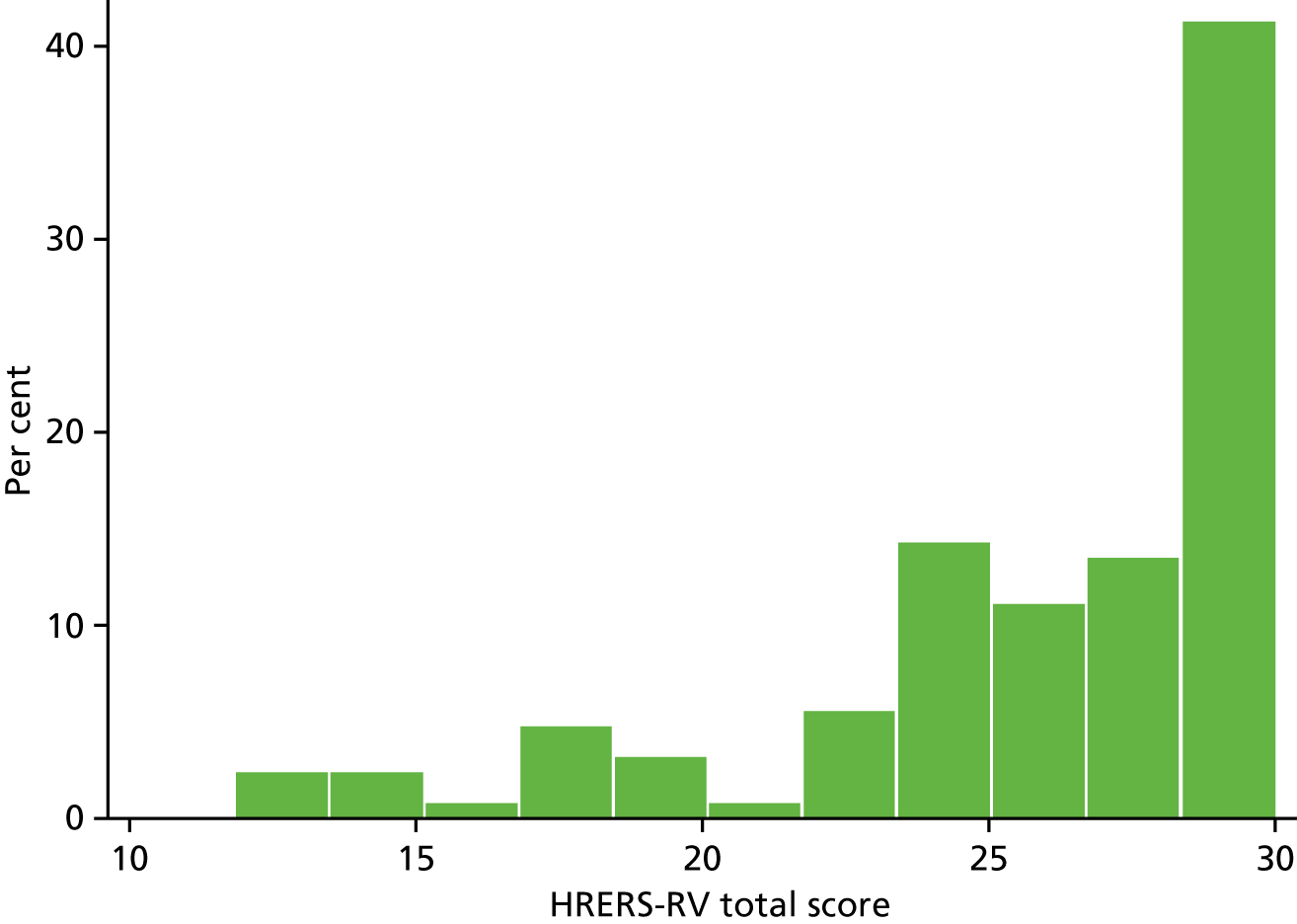
Looking at scores on an item by item basis, there was a pattern of high scores across all the dimensions regarded as contributing to the construct of engagement (Figure 5).
FIGURE 5.
Distribution of responses across the five dimensions of the HRERS-RV. (a) Readiness; (b) acceptance; (c) attitude; (d) active; and (e) cognitive.
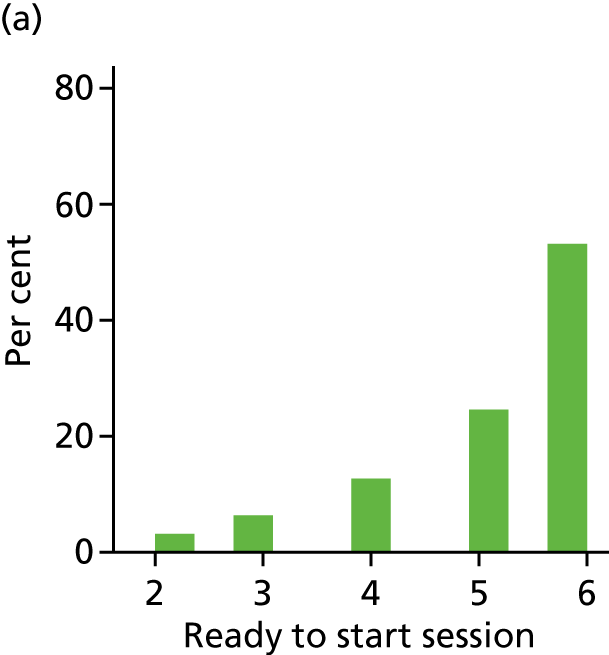
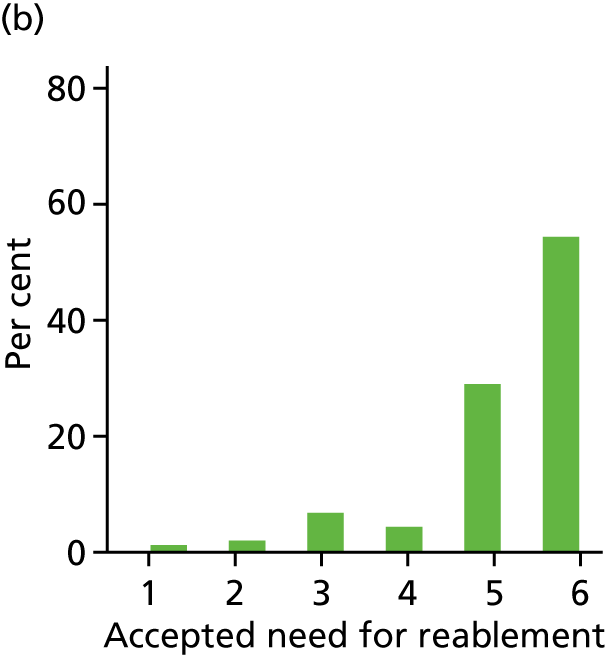
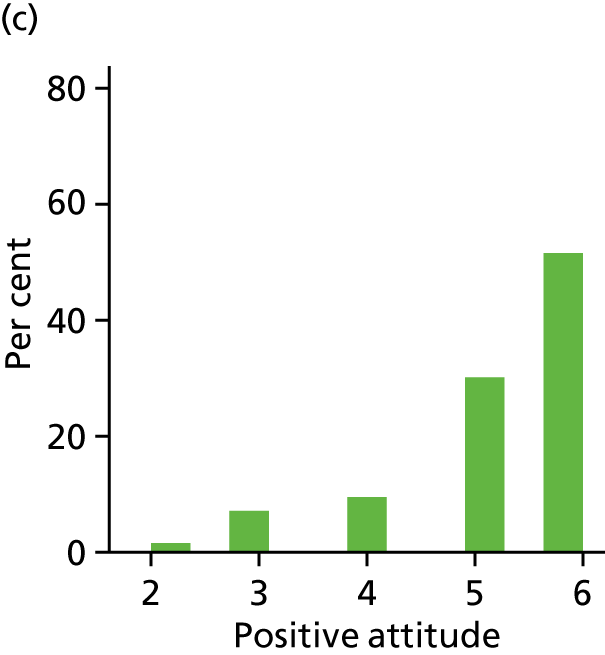
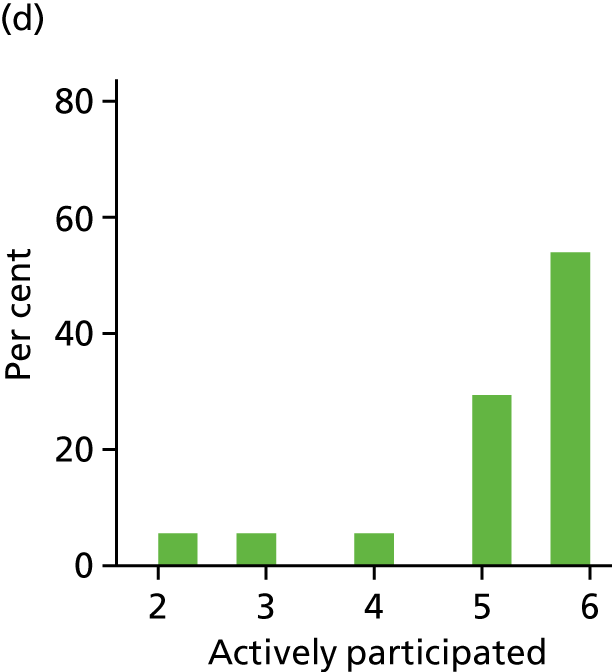
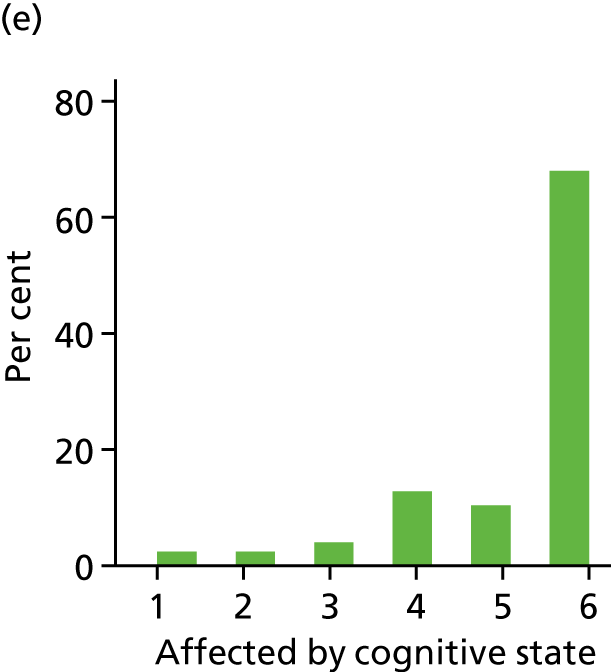
Construct validity
Factor analysis was performed to establish the construct validity of the HRERS-RV. An initial correlation matrix across the HRERS-RV variables confirmed that there was significant correlation between the five dimensions (Table 34).
| Readiness | Attitude | Acceptance | Active | Cognitive | |
|---|---|---|---|---|---|
| Readiness | 1.0000 | ||||
| Attitude | 0.7973* | 1.0000 | |||
| Acceptance | 0.7022* | 0.8098* | 1.0000 | ||
| Active | 0.7961* | 0.8988* | 0.7104* | 1.0000 | |
| Cognitive | 0.3430* | 0.3673* | 0.3158* | 0.3865* | 1.0000 |
Bartlett’s test showed that the correlations between the five components were, overall, significantly different from zero (p < 0.001; n = 126). The determinant of the correlation matrix (0.018) indicated that there was no extreme multicollinearity across the variables, although they were not completely unrelated either. [The determinant of the correlation matrix is a measure of collinearity. In case of perfect correlation (singularity) the determinant is 0, and if all variables are completely unrelated, the determinant is 1. To be able to perform factor analysis, the determinant of the correlation matrix needs to be > 0.00001.] Iterated principal factor method was conducted using orthogonal varimax rotation. The Kaiser–Meyer–Olkin (KMO) measure verified the sampling adequacy for the analysis (KMO 0.82).
There was only one factor with an eigenvalue > 1 (eigenvalue = 3.38, after rotation = 2.89), explaining over 80% of the total variance. The (rotated) factor loadings ranged from 0.36 to 0.94. The scree plot (Figure 6) showed a clear inflexion after the first factor, justifying keeping one single factor in the analysis.
FIGURE 6.
Scree plot: HRERS-RV.
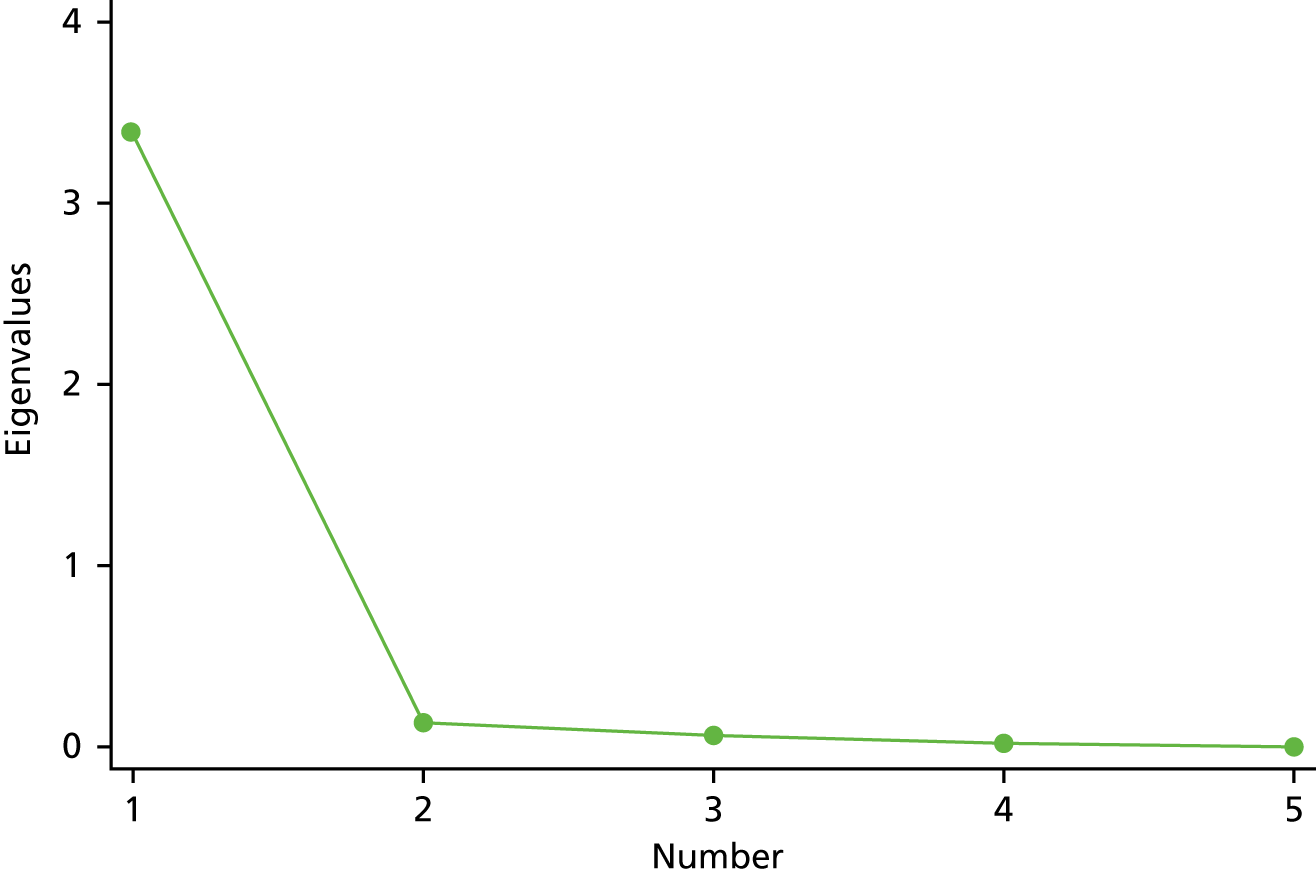
Table 35 shows the factor loadings for all five dimensions. Factor loadings show the degree to which a dimension is correlated to the underlying factor: ‘engagement with reablement practice’. Positive attitude and active participation in reablement have the highest factor loadings. Cognitive ability to take part in reablement has a factor loading of 0.36, which is below the threshold of 0.4 of significance. 92,93 Communalities represent the amount of variance in each variable that can be explained by the factor, whereas uniqueness shows the amount of variance that is not shared with other variables.
| HRERS-RV dimension | Rotated factor loading | Uniqueness | Communality |
|---|---|---|---|
| Ready to start session | 0.76a | 0.25 | 0.75 |
| Cognitive ability to take part | 0.36 | 0.81 | 0.18 |
| Positive attitude | 0.92a | 0.03 | 0.98 |
| Acceptance of the need for reablement | 0.67a | 0.25 | 0.75 |
| Active participation in reablement | 0.94a | 0.07 | 0.93 |
Reliability
We performed a Cronbach’s alpha reliability test, which indicated that this unidimensional scale had high reliability (α = 0.89, 95% CI 0.85 to 0.93).
Predictive validity
Finally, we explored associations between the HRERS-RV total score and the main outcome measures at T1: the EQ-5D-5L summary score, Barthel Index summary score and ASCOT-SCT4 index score (Figure 7).
FIGURE 7.
Associations between HRERS-RV score and main study outcomes. (a) ED-5D-5L; (b) Barthel Index; and (c) ASCOT-SCT4.
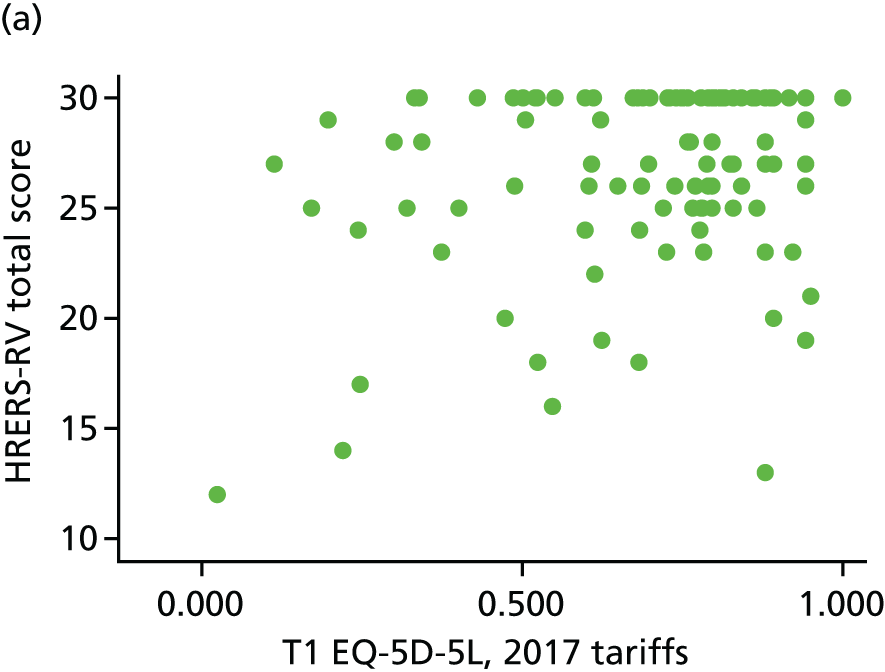
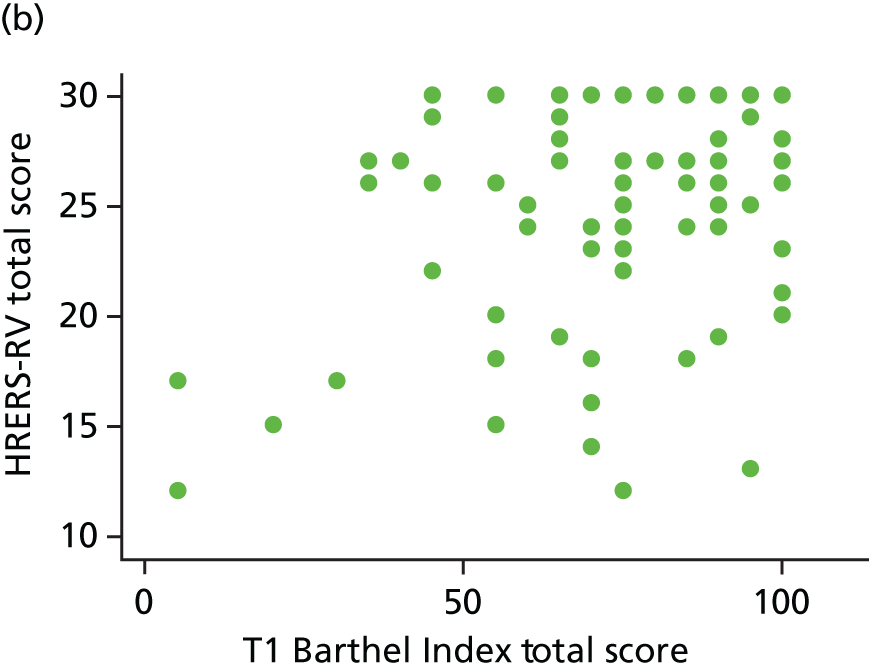
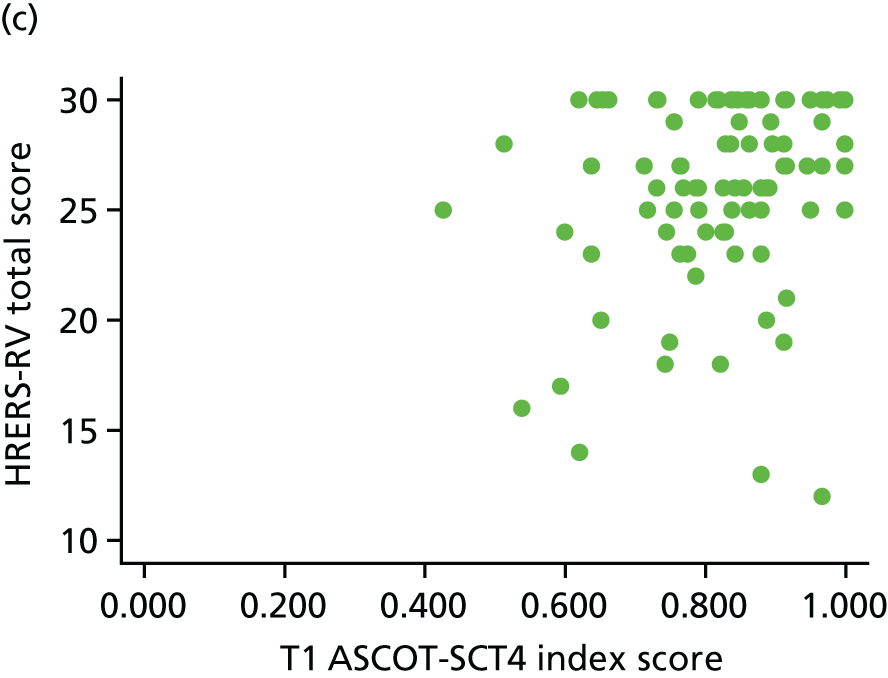
The HRERS-RV correlated weakly with the EQ-5D score (r = 0.263; p < 0.01) and the ASCOT score (r = 0.306; p < 0.01). It correlated more strongly with the Barthel Index measure of functional status (r = 0.454; p < 0.001).
Conclusions
The findings from our psychometric evaluation of the HRERS-RV raise some concerns but are, overall, positive. The relatively small sample size means that any interpretation should be cautious.
We would note the ceiling effect and question whether or not revisions to the response format may address this. Adding further items would mean a departure from the conceptual basis of this scale and its ‘parent version’ (HRERS). The tests of construct validity yielded good results, although we query whether item 2 should be retained or reworded. This was the most problematic item to adapt in terms of retaining a conceptual meaning true to the ‘parent version’. Finally, tests of predictive validity were in the direction expected, with strongest associations with functional ability outcomes at discharge from reablement.
On the basis of these results, we included the HRERS-RV within our suite of predictor variables. We refer the reader to Chapter 5, which reports that engagement in reablement, as measured by HRERS-RV, was found to be a significant predictor of health and functional outcomes. This supports the argument for including a measure of intervention engagement when evaluating reablement.
Further work to test, and perhaps to further refine, the HRERS-RV would appear to be worthwhile and important.
Appendix 4 Work package 2a: development of the Experience of Reablement Practice Checklist
The purpose of creating the ERPC was to allow us to assess, using a simple, user-completed tool, the extent to which reablement practitioners adhered to a reablement approach. That is, an intervention that seeks the regaining, or restoration, of daily living skills. This contrasts sharply with the traditional home-care approach, in which care is ‘done’ to the recipient. No equivalent measure already existed. The components of reablement practice that we sought to capture in this checklist were as follows:
-
the service user understands the objective of reablement
-
the service user understands that the intervention is working towards specific goals
-
the service user believes that they were involved in setting those goals
-
the reablement worker motivates the service user to work towards achieving those goals
-
during the intervention, the service user and reablement worker/assessor review progress towards those goals.
The intention was that the checklist would be administered at discharge from the service.
Development of the Experience of Reablement Practice Checklist
Two members of the research team (BB and A-LF), both of whom have experience of questionnaire development (one is also a senior OT with experience of delivering reablement), met to discuss and develop a set of five items that described the core components of the reablement approach. Each item was presented as a statement, with the respondent asked to report whether or not they agreed with a statement by answering ‘yes’ or ‘no’. After the meeting, the items were reviewed individually by the two researchers, after which a first full draft of the ERPC was agreed. This was then shared with the wider research team for comment. No further revisions were made at that stage. The draft version (Box 6) was then taken forward for testing via cognitive interview with 10 respondents, all of whom had recently used a reablement service and who were taking part in a wider pilot of the study’s research instruments.
Cognitive interviews with two respondents prompted some early revisions to the draft checklist. First, it was clear that they were struggling to know how to respond to the items that, at that stage, were presented as statements. They were heard reconstructing the statements into questions. It was also clear that they were not sure which ‘workers’ the checklist was referring to. It was also suggested that instructions about completion should be more detailed. Finally, in terms of layout, it was suggested that the checklist should be presented in portrait, rather than landscape, orientation, with response options given underneath.
Aside from retaining the items as statements, changes to the checklist were made in response to these observations and suggestions. Five further cognitive interviews indicated that we should reword the items into questions. We made this amendment and administered it, with a cognitive interview, to a further three respondents. We concluded from these cognitive interviews that respondents found it easy to complete; they had no suggestions about further improvements to the checklist. This version, therefore, became the final version of the ERPC (Box 7).
Psychometric properties
Methods
We ran descriptive statistics to summarise respondents’ experience of reablement across sites and across the sample as a whole. We explored the internal structure of the checklist by looking at response patterns across all five questions. We conducted exploratory factor analysis to determine whether or not the ERPC measured a single underlying construct. We performed chi-squared tests to explore associations between partial/complete adherence to the reablement approach and the site and type of service provision.
Results
Descriptives
Table 36 summarises the descriptive statistics for the five items constituting the ERPC. The majority of respondents were aware of the overall purpose of reablement (92–100% across sites). There were slight variations across sites regarding participants being aware of having specific goals (ranging from 71% in site B to 82% in site C) and being involved in goal-setting (ranging from 63% in site A to 80% in site C). There were relatively lower percentages of people who reported to be motivated to be independent in sites B (57%) and A (79%) than in site C (93%). Chi-squared and Fisher’s exact test statistics results suggest that this difference is mildly significant (χ2 = 14.51; p = 0.001, Fisher’s exact test = 0.001). Significantly smaller proportions of participants reported that they received feedback on progress in sites A (57%) and B (71%) than in site C (96%) (χ2 = 33.456; p < 0.001, Fisher’s exact test < 0.001). One must interpret these results with caution because of the small sample sizes, especially in site B.
| ERPC item | Site, n (%) | Total (N = 128) | ||
|---|---|---|---|---|
| A (N = 19) | B (N = 14) | C (N = 95) | ||
| Overall purpose | 17 (98.47) | 14 (100.00) | 88 (92.63) | 119 (92.97) |
| Specific goals | 14 (73.69) | 10 (71.43) | 78 (82.11) | 102 (79.69) |
| Own goal-setting | 12 (63.16) | 9 (64.29) | 76 (80.00) | 97 (75.78) |
| Motivation | 16 (78.95) | 8 (57.14) | 88 (92.63) | 111 (86.72) |
| Feedback | 9 (47.37) | 10 (71.43) | 91 (95.79) | 110 (85.94) |
Answer patterns across the five components of reablement practice
We explored the internal structure of the ERPC by looking at the frequency of specific types of response patterns across the sample (Table 37), where all the ‘yes’ answers were coded as 1 and all the ‘no’ answers were coded as 0 for each element of the reablement experience. The answer patterns of those reporting incomplete adherence to reablement practice seem to be evenly distributed across the sample; there were no items that were consistently under-reported or not reported. The most commonly occurring pattern (n = 8/129, 6.2%) is a negative response to the items ‘being aware of specific goals’ and ‘involved in all goal setting’, while affirming the remainder aspects of reablement practice. Because of the small cell numbers, it is hard to draw any conclusions from this finding. In addition, it was not possible to explore associations between patterns of response and sites because of the small sample sizes.
| Pattern | Frequency | Per cent | Cumulative |
|---|---|---|---|
| Missing | 1 | 0.78 | 0.78 |
| 00000 | 2 | 1.55 | 2.33 |
| 00001 | 2 | 1.55 | 3.88 |
| 00011 | 2 | 1.55 | 5.43 |
| 00110 | 1 | 0.78 | 6.20 |
| 01010 | 1 | 0.78 | 6.98 |
| 01111 | 1 | 0.78 | 7.75 |
| 10000 | 4 | 3.10 | 10.85 |
| 10001 | 2 | 1.55 | 12.40 |
| 10010 | 3 | 2.33 | 14.73 |
| 10011 | 8 | 6.20 | 20.93 |
| 10111 | 2 | 1.55 | 22.48 |
| 11001 | 1 | 0.78 | 23.26 |
| 11010 | 2 | 1.55 | 24.81 |
| 11011 | 4 | 3.10 | 27.91 |
| 11100 | 2 | 1.55 | 29.46 |
| 11101 | 4 | 3.10 | 32.56 |
| 11110 | 3 | 2.33 | 34.88 |
| 11111 | 84 | 65.12 | 100.00 |
| Total | 129 | 100.00 |
Factor analysis
The dichotomous nature of the response option meant that a polychoric correlation matrix was used to explore associations across the items constituting the checklist. We found significant associations across all five components. Effect sizes were largest between ‘aware of the overall purpose of reablement’ and ‘involved in setting goals’ (r = 0.943; p < 0.001; 95% CI 1.09 to 0.878), and between ‘aware of the overall purpose’ and ‘having specific goals to work towards’ (r = 0.726; p < 0.001; 95% CI 0.975 to 0.477). Exploratory factor analysis found one underlying factor with an eigenvalue of 2.549 (after orthogonal varimax rotation), explaining over 75% of the variance across the five components. The variables with the highest loadings on the factor are ‘being aware of overall purpose’ (0.92) and ‘being involved in own goal-setting’ (0.89) (Table 38).
| Experience of reablement component | Rotated factor loading | Uniqueness | Communality |
|---|---|---|---|
| Overall purpose | 0.65 | 0.45 | 0.55 |
| Specific goals | 0.92 | 0.06 | 0.94 |
| Own goal-setting | 0.89 | 0.08 | 0.92 |
| Motivation | 0.49 | 0.44 | 0.56 |
| Feedback | 0.48 | 0.41 | 0.59 |
A scree plot and factor loadings matrix (Figures 8 and 9) suggest that there is an additional underlying factor, albeit weaker, and with an eigenvalue of < 1.
FIGURE 8.
The EPRC factor analysis: scree plot.
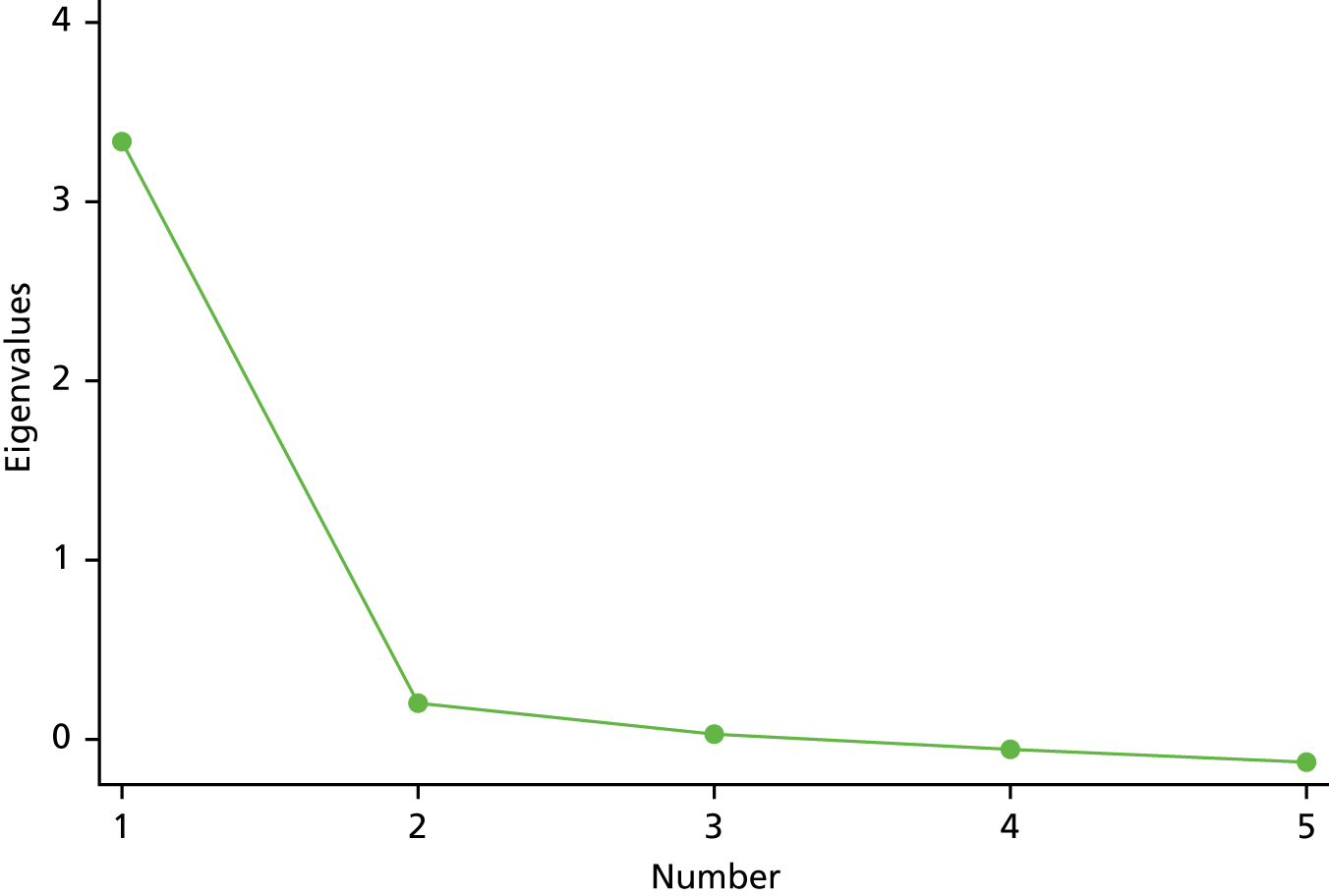
FIGURE 9.
The ERPC factor analysis: factor loadings plot. Rotation = orthogonal varimax, method = principal factors.
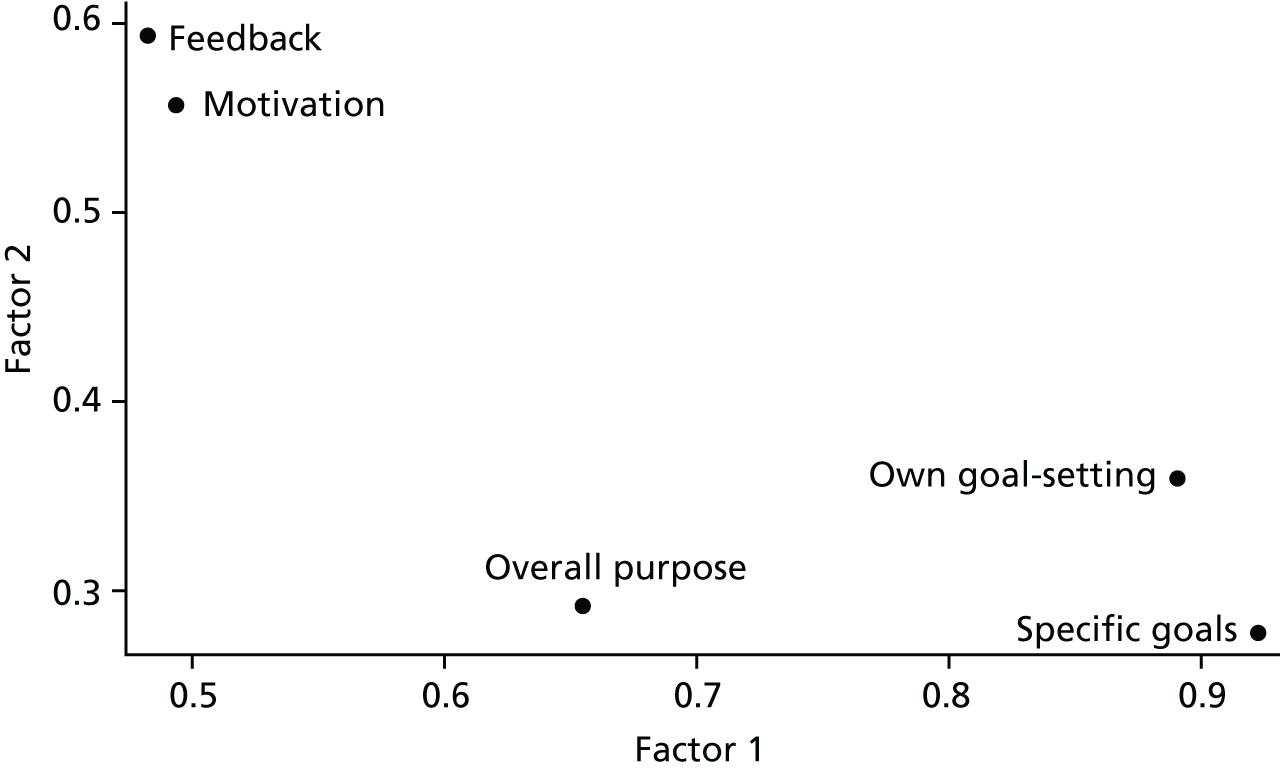
‘Being motivated to be independent’ and ‘receiving feedback’ load slightly higher on this second factor (0.56 and 0.59, respectively). On the basis of this exploratory analysis, we can conclude that there seems to be a dominant factor explaining most of the variance across five checklist items, and this seems to represent the ‘practical’ aspects of reablement: ‘being aware of the overall purpose’, ‘setting specific goals’ and ‘involvement in goal setting’. There is a secondary factor representing the ‘psychological’ component of reablement: encouraging independence by motivating the client and providing feedback on progress. However, these hypotheses need to be tested further with a larger sample.
For the purpose of this study, therefore, we chose to use the ERPC as a categorical variable, taking two values: (1) ‘complete intervention adherence’ and (0) ‘partial intervention adherence’.
Associations between Experience of Reablement Practice Checklist scores and service characteristics and user outcomes
Based on existing evidence about the delivery of reablement, we hypothesised that ERPC scores would be associated with service characteristics, particularly whether reablement workers were based in ‘in-house’ teams within the LAs or working for an outsourced provider.
The percentage of those receiving reablement from a single-team provider who reported ‘complete’ reablement experience (n = 58, 73.42%) was slightly higher than the percentage of those who received reablement from a mixed team (n = 25, 52.08%). Because of the skewness of the data and limited sample size, it is hard to establish whether or not this difference is significant (χ2 = 6.00; p = 0.014). These tentative results suggest that better outcomes may be expected from in-house providers than from outsourced providers.
Conclusions
We attempted to create a simple checklist, completed by service users at discharge from reablement, that would capture the extent to which the intervention they had received adhered to the ethos and approach of reablement. In other words, a user-report measure of intervention adherence. Our testing of the checklist’s psychometric properties suggests that additional items and/or revisions to the response format should be considered and tested. Specifically, based on ERPC scores, two-thirds of study participants received reablement that adhered to the five components of reablement practice represented in the checklist. In addition, it should be considered whether or not further items should be created and tested that further distinguish the so-called ‘practical’ and ‘psychological’ aspects of reablement detected in our analyses.
However, for the purposes of this study, we were comfortable taking the ERPC forward as a predicator in our outcomes evaluation, not using a score but treating the score as a categorical variable: complete versus partial adherence.
Appendix 5 Work package 2a: doing research in local authorities – experiences and implications
Introduction
The commissioners of this research (the NIHR Health Services and Delivery Research programme) requested that the research team record its experiences of delivering the study, and reflect on implications for future research. This appendix reports this and considers the following in turn:
-
research readiness and LAs
-
working in a fluid service landscape
-
the involvement of private providers in research
-
ambiguity regarding eligibility of NIHR Clinical Research Network support.
Research readiness and local authorities
The capacity of services to engage with the study
Four services were recruited as research sites. Securing the participation of these services involved approaching a total of 27 services. Often some initial discussions were held and, for a few, discussions had reached an advanced stage when the service withdrew. A lack of capacity was one of the reasons for declining participation. This was presented in two ways:
-
a lack of capacity within the service to accommodate the research within their usual processes; specifically, assessment staff having an initial conversation with new referrals about the study and seeking ‘consent to contact’
-
a lack of capacity in managers and senior management to oversee the research set-up.
Barriers to setting up the study in the research sites
In each research site, a significant period of time elapsed between informal confirmation of participation in the study and recruitment opening. Table 39 details this and the timings allocated in the original project timetable.
| Site | Duration (months) | Total (months) | |||
|---|---|---|---|---|---|
| Time elapsed approaching other servicesa | Initial contact with site to informal confirmation | Informal confirmation to contract signed | Contract signed to recruitment opening | ||
| A | 3 | 4 | 2 | 2 | 11 |
| B | 4 | 4 | 2 | 2 | 12 |
| C | 0 | 3 | 4 | 3 | 10 |
| D | 1 | 2 | 8 | 5 | 16 |
| Timings as per project timetable | 4 | 2 | 6 | ||
The delays encountered illustrate key issues in terms of the research capacity and research infrastructure within LAs. This, in turn, reflects the extent to which research is regarded as a core activity of an organisation and, as a result, the priority given to it.
A separate example of a lack of ‘research readiness’ within LAs was the withdrawal of a potential research site because they were unable to identify staff to second at the local study team posts. At that stage, they had to withdraw their involvement in the study as only people employed by the LA were allowed to work in or out of their premises. Although this is also a requirement for the NHS, the system of research passports addresses this.
Thus, a lack of capacity within the services (and organisational settings) recruited to the study affected the pace and progress of study set-up in terms of decision-making about the specifics of implementing study processes within the service. Service managers’ time and capacity to chase study set-up issues being dealt with at a higher level in the LA were highly constrained. Although they were very keen to be involved in the study, participating in or supporting research was not a specific role within their job descriptions. Similarly, dealings with more senior managers indicated a lack of existing processes, roles and responsibilities with regard to taking part in externally funded research. Research governance processes were highly variable and some of the issues raised suggested a certain degree of research naivety. The process of drawing up a research contract with a university was a new situation for all the sites.
Commentary
Before this study, the research team had extensive collective experience of carrying out research in non-NHS settings and were aware of the challenges. Some of the difficulties encountered were not unfamiliar. However, the scale and complexity of the project and the requirements it placed on LAs revealed the extent of the limitations of their research readiness. This can be observed at strategic and operational levels as follows:
-
There was a lack of an existing research infrastructure in terms of policies and procedures, and defined roles and responsibilities.
-
There was a lack of capacity among senior staff to engage with and work on setting up and implementing a complex study within their organisation.
-
Supporting or taking part in research was not within service leads’ and managers’ job descriptions and, therefore, they could not prioritise planning for and implementing the study.
-
The recruitment process necessarily required the service staff to have the capacity to seek ‘consent to contact’.
-
No pre-existing systems and practices were in place to facilitate arrangements regarding the local study teams being located within an organisation’s premises to fulfil recruitment and data collection duties.
Working in a fluid service landscape
This study commenced just after one of the most significant reforms in social care policy in recent times. As described in Chapter 1, this stimulated changes in the approach to managing individuals referred to adult social care who potentially may need long-term packages or care, at home or in a residential setting. Specifically, a parallel process of assessment and reablement was advocated. Furthermore, reablement was clearly positioned as part of a locality’s intermediate care provision, with the expectation of an integrated approach to delivery. NICE’s 2017 guidance Intermediate Care and Reablement14 reiterated and fleshed out policy guidance associated with the Care Act 201415 and also the move within the NHS to a model of ‘discharge to assess’. As a result, the service landscape at the time the study was seeking to recruit research sites was quite fluid. This had an impact on the study in two ways. First, services keen and interested to take part were not able to because they anticipated a period of service reorganisation. Second, the work carried out as part of the WP1 survey to assign each reablement service to a particular type of service model was not necessarily accurate, either at the time of approaching services to take part in the evaluation (WP2) or by the time recruitment began. This, indeed, was our experience.
Commentary
Generally speaking, within health services and care research it is important for researchers to have strategies in place with respect to responding to changes in the services they are investigating, and to incorporate this eventuality into the study design. Our experiences also point to the importance of having a clear understanding of the services in terms of their specific characteristics and ways of working, and particularly those thought to have an impact on service delivery and/or outcomes.
In terms of this study, we were careful to ensure that we were kept up to date with any changes or developments in services during study set-up and once recruitment was open. Good relationships with service leads in our research sites and the presence of local study staff proved useful in this regard. However, a naivety on the part of service staff in terms of the implications of service redesign for the research meant that such changes were not sufficiently communicated. However, the scope of the process evaluation included an exploration of any changes and a close examination of the features, or characteristics, of the service. In addition, the proposed design – in which service models would be compared and, also, through a within-group analysis, the impact of service characteristics on outcomes investigated – accommodated the fact that service models may not be as enduring or distinct as was conceived at the stage of designing the study.
Our experience also reiterates the importance of research teams being aware of the wider policy landscape in which their research is situated. In the case of this project, these changes, while substantially affecting one of our research sites, have reiterated the core role of reablement within intermediate care, thereby reconfirming the importance and timeliness of this commissioned study.
Participation of private providers in the study
All sites outsourced at least some of their reablement provision to private providers. In two sites we encountered difficulties securing their involvement in the research. As a result, in one site we were not able to collect, at discharge from reablement, reablement workers’ reports of user engagement in the intervention. In a second site, only two out of the five private providers agreed that the study could recruit individuals using their service. In all instances, non-involvement was attributed to the fact that involvement in research was not specified in the contract the provider had with the LA. We would note that this issue was also encountered at the survey stage (WP1), with some private providers declining to participate.
In addition, although they did not directly have an impact on the study, it is also useful to report that changes in private providers were observed during study set-up and recruitment, in terms of both providers losing or choosing to close contracts and new providers being commissioned.
Commentary
We encountered mixed attitudes to participating in research from private providers. Certainly, and not surprisingly, participating in or supporting research was not part of commissioning arrangements. As a result, private providers were not obliged to co-operate. This is an issue that may need to be considered when designing research and is also something that, potentially, needs to be considered as part of service commissioning arrangements.
Eligibility of National Institute for Health Research Clinical Research Network support
Finally, the study applied to be adopted by NIHR’s Clinical Research Network Portfolio but this was not successful. The reason was that none of the research sites was a NHS service; rather, they were LAs or a social enterprise funded by a CCG and LA.
Access to Clinical Research Network support may have eased some study set-up issues and, when the challenges with recruitment reported above began to emerge, may have also offered the potential of alternative recruitment pathways, certainly for individuals being discharged home and those referred to reablement by GPs or other NHS services.
Commentary
We have not been in a position to check if this decision, and the rationale behind it, would be the same today. If that were the case, it indicates that current NHS research support structures need to consider their ‘reach’ into social care. Furthermore, should investment be made in research infrastructure within LAs, it is important that any structures or resources do not, in themselves, create new barriers to research into integrated care and services and/or the care of, or services being used by, NHS patients.
Concluding comments
Integration, or joint working, between health and social care is regarded as an essential core feature of ensuring that older and disabled people live healthy lives and are as independent as possible. This means that research into these populations has, and will continue to, cut across the two sectors. This will, perhaps increasingly, require the active involvement of LAs in what might be regarded as health services research. The experiences of this study, and also reported by others, point to substantive differences in research awareness, capacity and infrastructure between LAs and the NHS. This has significant implications in terms of the efficiency of research and the ability to deliver, in a robust way, large and complex projects. It is for these reasons that the research team was encouraged by the funder to provide an account and commentary of the issues and challenges encountered in this study. The purpose of preparing this account is to support an awareness among the health and social care research community and research funders of the issues that may be encountered when engaging in social care research. It also raises the question of whether or not strategic investment in research capacity and infrastructure within LAs, as has been seen in the NHS, is required.
Appendix 6 Work package 2a: sample characteristics – T0, T1 and T2
| Variable | Time point, n (%) | ||
|---|---|---|---|
| T0 | T1 | T2 | |
| n | 186 (100) | 129 (100) | 64 (100) |
| Individual characteristics | |||
| Sex (reference: female) | |||
| Male | 67 (36.02) | 41 (31.78) | 20 (31.25) |
| Living alone (reference: no) | |||
| Yes | 107 (57.53) | 78 (60.47) | 37 (57.81) |
| Sufficient money (reference: no) | |||
| Yes | 149 (82.78) | 104 (83.20) | 48 (81.36) |
| Referral reason (reference: return to home) | |||
| Remain at home | 111 (59.68) | 76 (58.91) | 42 (65.63) |
| Help from friends and family (reference: no) | |||
| Yes | 164 (89.13) | 116 (89.92) | 57 (89.06) |
| Number of comorbidities | |||
| None | 67 (36.02) | 46 (35.66) | 28 (43.75) |
| 1 | 79 (42.47) | 56 (43.41) | 25 (39.06) |
| ≥ 2 | 40 (21.51) | 27 (20.93) | 11 (17.19) |
| Service/intervention characteristics | |||
| Provider type (reference: in-house) | |||
| Outsourced | 67 (36.22) | 39 (30.47) | 30 (47.62) |
| Practitioners’ adherence (reference: partial) at T1 | |||
| Complete | – | 84 (65.63) | – |
| Team model (reference: mixed team) | |||
| Single team | 110 (59.46) | 80 (62.50) | 29 (46.03) |
| Time point | n | Mean (SD) | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| Individual characteristics | |||||
| Age (years) | |||||
| T0 | 186 | 80.849 (9.127) | 82 | 51 | 102 |
| T1 | 129 | 80.822 (9.200) | 82 | 51 | 102 |
| T2 | 64 | 81.047 (8.806) | 83 | 51 | 98 |
| NEADL scale (T0) | |||||
| T0 | 184 | 9.652 (5.480) | 8.5 | 0 | 22 |
| T1 | 129 | 9.651 (5.633) | 8 | 0 | 22 |
| T2 | 64 | 11.578 (6.312) | 11 | 0 | 22 |
| GHQ-12 (T0) | |||||
| T0 | 185 | 4.135 (2.849) | 4 | 0 | 12 |
| T1 | 129 | 3.930 (2.878) | 3 | 0 | 12 |
| T2 | 64 | 3.844 (2.835) | 3 | 0 | 12 |
| HRERS-RV | |||||
| T1 | 126 | 26.103 (4.59) | 27 | 12 | 30 |
| Intervention characteristics | |||||
| Reablement duration (weeks) | |||||
| T1 | 175 | 3.889 (1.596) | 4 | 0.571 | 6.429 |
| Variable | Site A | Site B | Site C | ||||||
|---|---|---|---|---|---|---|---|---|---|
| T0, n (%) | T1, n (%) | T2, n (%) | T0, n (%) | T1, n (%) | T2, n (%) | T0, n (%) | T1, n (%) | T2, n (%) | |
| N | 33 | 19 | 14 | 14 | 14 | 9 | 139 | 96 | 41 |
| Individual characteristics | |||||||||
| Sex (reference: female) | |||||||||
| Male | 10 (30.3) | 5 (26.32) | 3 (21.43) | 2 (14.29) | 2 (14.29) | 1 (11.11) | 55 (39.57) | 34 (35.42) | 16 (39.02) |
| Living alone (reference: no) | |||||||||
| Yes | 17 (51.52) | 7 (36.84) | 7 (50.00) | 7 (50.00) | 7 (50.00) | 3 (33.33) | 83 (59.71) | 64 (66.67) | 27 (65.85) |
| Sufficient money (reference: no) | |||||||||
| Yes | 28 (87.5) | 17 (89.47) | 11 (84.62) | 9 (81.82) | 9 (81.82) | 6 (85.71) | 112 (81.75) | 78 (82.11) | 31 (79.49) |
| Referral reason (reference: return to home) | |||||||||
| Remain at home | 21 (63.64) | 14 (73.68) | 2 (14.29) | 5 (35.71) | 5 (35.71) | 5 (55.56) | 85 (61.15) | 57 (59.38) | 15 (36.59) |
| Help from friends and family (reference: no) | |||||||||
| Yes | 22 (70.97) | 15 (78.95) | 12 (85.71) | 13 (92.86) | 13 (92.86) | 9 (100.00) | 129 (92.81) | 88 (91.67) | 36 (87.80) |
| Number of comorbidities | |||||||||
| None | 19 (57.58) | 10 (52.63) | 9 (64.29) | 8 (57.14) | 8 (57.14) | 4 (44.44) | 40 (28.78) | 28 (29.17) | 15 (36.59) |
| 1 | 8 (24.24) | 5 (26.32) | 2 (14.29) | 4 (28.57) | 4 (28.57) | 3 (33.33) | 67 (48.2) | 47 (48.96) | 20 (48.78) |
| ≥ 2 | 6 (18.18) | 4 (21.05) | 3 (21.43) | 2 (14.29) | 2 (14.29) | 2 (22.22) | 32 (23.02) | 21 (21.88) | 6 (14.63) |
| Service/intervention characteristics | |||||||||
| Provider type (reference: in-house) | |||||||||
| Outsourced | 32 (100.00) | 18 (100.00) | 13 (100.00) | 14 (100.00) | 14 (100.00) | 9 (100.00) | 35 (25.18) | 21 (21.88) | 17 (41.46) |
| Practitioners’ adherence (reference: partial) (T1) | |||||||||
| Complete | – | 9 (47.37) | 6 (54.55) | – | 6 (42.86) | 5 (55.56) | – | 69 (72.63) | 23 (71.88) |
| Team model (T1) (reference: mixed team) | |||||||||
| Single team | 0 | 0 | 0 | 0 | 0 | 0 | 110 (79.14) | 80 (83.33) | 29 (70.73) |
| Site | n | Mean | SD | Median | Minimum | Maximum | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T0 | T1 | T2 | T0 | T1 | T2 | T0 | T1 | T2 | T0 | T1 | T2 | T0 | T1 | T2 | |
| Individual characteristics | ||||||||||||||||||
| Age (years) | ||||||||||||||||||
| A | 33 | 19 | 14 | 77.3 | 76 | 76.2 | 9.1 | 10 | 9.9 | 75 | 75 | 75 | 51 | 51 | 51 | 89 | 89 | 89 |
| B | 14 | 14 | 9 | 83 | 83 | 81.7 | 8.3 | 8.3 | 6.63 | 83.5 | 83.5 | 83 | 70 | 70 | 72 | 95 | 95 | 92 |
| C | 139 | 96 | 41 | 81.5 | 81.5 | 82.6 | 9.1 | 9.1 | 8.4 | 82 | 82 | 84 | 52 | 52 | 62 | 102 | 102 | 98 |
| NEADL scale (T0) | ||||||||||||||||||
| A | 31 | 19 | 14 | 10.9 | 9.9 | 9.9 | 5.8 | 4.1 | 4.7 | 11 | 8 | 9 | 1 | 1 | 2 | 22 | 22 | 18 |
| B | 14 | 14 | 9 | 7.6 | 7.6 | 9 | 3.4 | 3.4 | 3.2 | 8 | 8 | 10 | 3 | 3 | 3 | 13 | 13 | 13 |
| C | 139 | 96 | 41 | 9.6 | 9.9 | 12 | 5.5 | 5.7 | 6.5 | 8 | 8.5 | 12 | 0 | 0 | 0 | 22 | 22 | 22 |
| GHQ-12 (T0) | ||||||||||||||||||
| A | 32 | 19 | 14 | 4.8 | 5.4 | 4.5 | 3.5 | 3.7 | 3.7 | 4 | 5 | 3.5 | 0 | 0 | 0 | 12 | 12 | 12 |
| B | 14 | 14 | 9 | 4.9 | 4.9 | 4.3 | 2.9 | 2.9 | 3.0 | 4.5 | 4.5 | 4.0 | 0 | 0 | 0 | 10 | 10 | 8 |
| C | 139 | 96 | 41 | 3.9 | 3.5 | 3.5 | 2.7 | 2.6 | 2.5 | 3 | 3 | 3 | 0 | 0 | 0 | 11 | 11 | 9 |
| HRERS-RV | ||||||||||||||||||
| A | 0 | 0 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| B | 14 | 14 | 9 | 25.4 | 25.4 | 25.9 | 4.2 | 4.2 | 4.5 | 25.5 | 25.5 | 27 | 17 | 17 | 17 | 30 | 30 | 30 |
| C | 112 | 95 | 35 | 26.2 | 26.7 | 27.2 | 4.6 | 4.1 | 2.9 | 27 | 28 | 28 | 12 | 12 | 20 | 30 | 30 | 30 |
| Intervention/service characteristics | ||||||||||||||||||
| Duration (weeks) | ||||||||||||||||||
| A | 27 | 19 | 14 | 3.9 | 3.9 | 3.9 | 1.6 | 1.7 | 1.4 | 4 | 4.1 | 3.9 | 1.3 | 1.3 | 1.9 | 6.4 | 6.4 | 6.0 |
| B | 14 | 14 | 9 | 3.5 | 3.5 | 3.6 | 1.5 | 1.5 | 1.6 | 3.7 | 3.7 | 4.1 | 1.7 | 1.7 | 1.7 | 6.3 | 6.3 | 6.3 |
| C | 134 | 96 | 40 | 3.9 | 4.3 | 4.1 | 1.6 | 1.6 | 1.5 | 4.1 | 4.9 | 4.3 | 0.6 | 0.6 | 1.0 | 6.1 | 6.1 | 6.1 |
Appendix 7 Work package 2a: EuroQol-5 Dimensions, five-level version – additional data
2016 versus 2017 EuroQol-5 Dimensions, five-level version, tariffs: index and EuroQol visual analogue scale scores
| Tariff | Correlation coefficient |
|---|---|
| 2017 | 0.71 |
| 2016 | 0.70 |
| EQ VAS | 0.46 |
Scores for the two tariffs were highly correlated both at baseline and at discharge, with a correlation coefficient of 0.9988 and 0.9995, respectively. The mean difference between the two tariffs was approximately 0.014. The intraclass correlation coefficient estimate for the EQ-5D-5L 2017 tariff at discharge was 0.114 (standard error 0.116, 95% CI 0.0085 to 0.4898); using the 2016 tariff gave similar results (intraclass correlation coefficient estimate 0.116; standard error 0.117, 95% CI 0.0090 to 0.4914). Table 45 provides further summary statistics of the difference between the two tariffs at baseline and discharge.
| Difference | n | Mean (SD) | Minimum | Maximum |
|---|---|---|---|---|
| At T0 | 186 | –0.013 (0.012) | –0.035 | 0.017 |
| At T1 | 128 | –0.014 (0.008) | –0.032 | 0.008 |
FIGURE 10.
The T0 EQ-5D-5L index scores: 2016 and 2017 tariffs (site A).
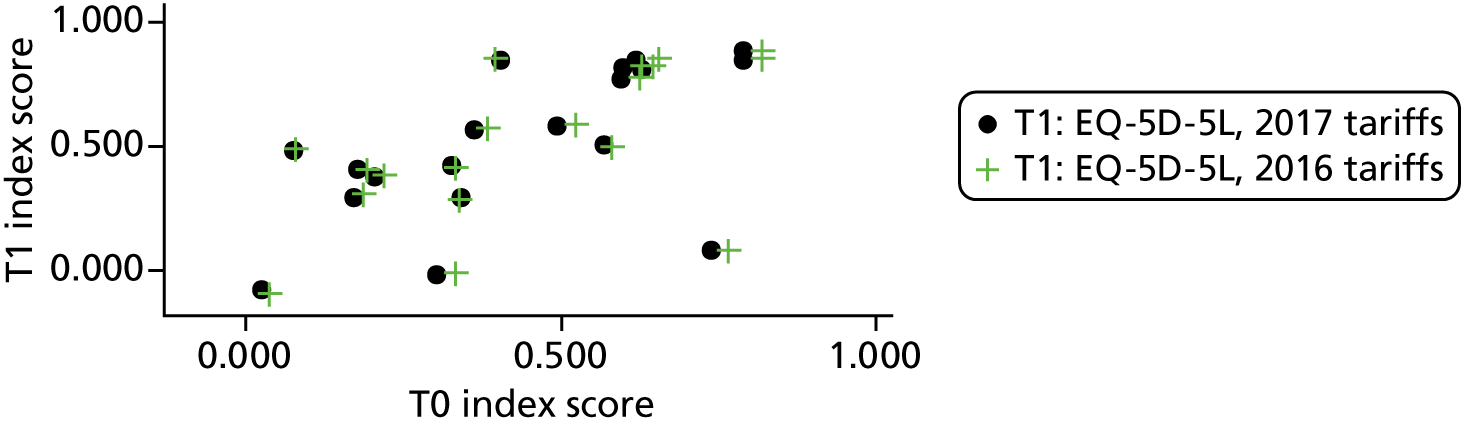
FIGURE 11.
The T0 EQ-5D-5L index scores: 2016 and 2017 tariffs (site B).
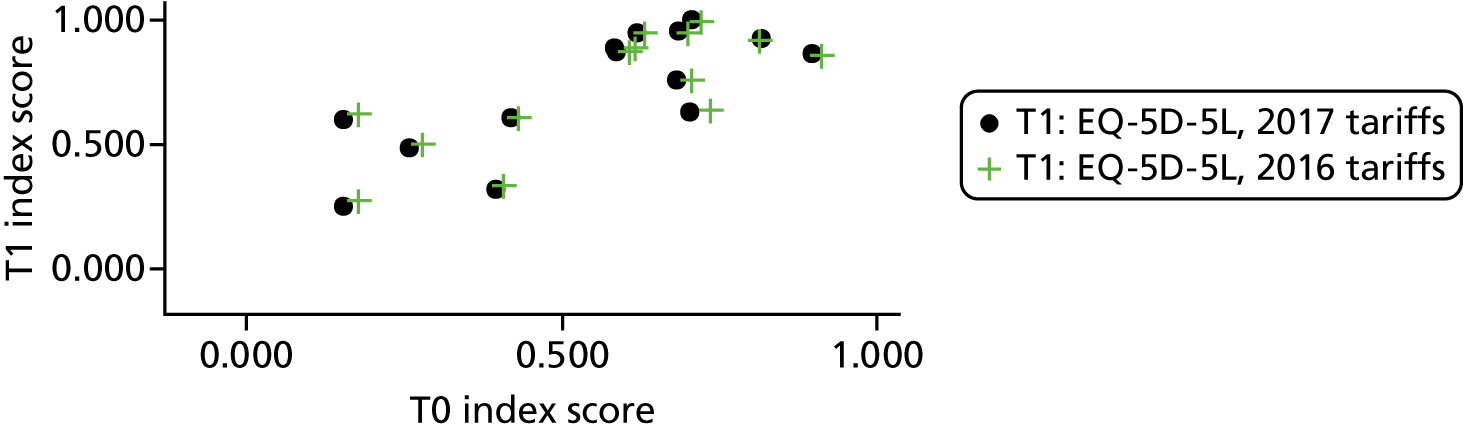
FIGURE 12.
The T0 EQ-5D-5L index scores: 2016 and 2017 tariffs (site C).
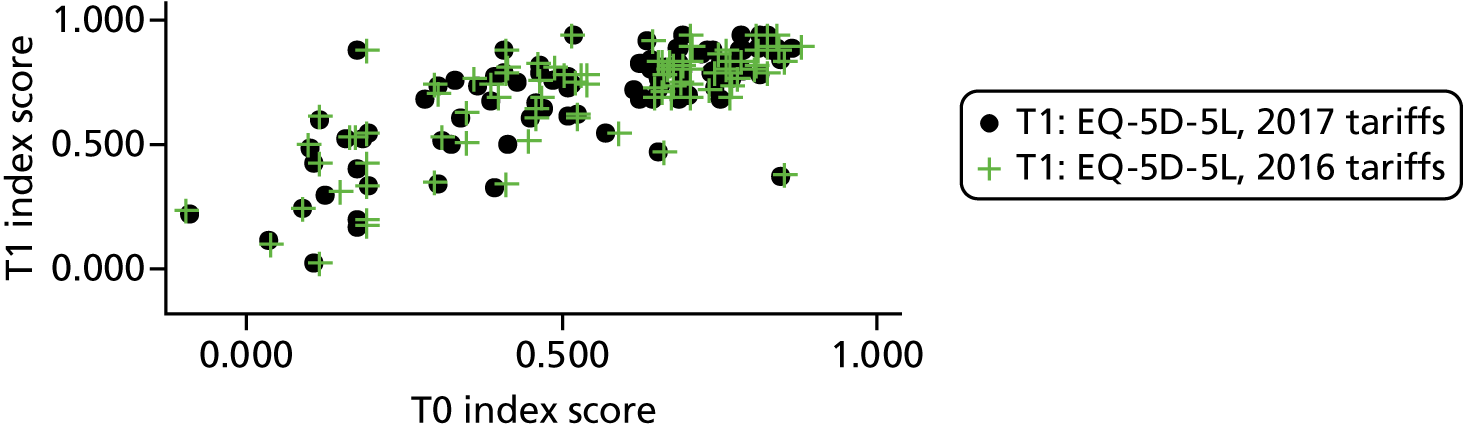
FIGURE 13.
The T0 EQ-5D-5L index scores: 2016 and 2017 tariffs (total sample).
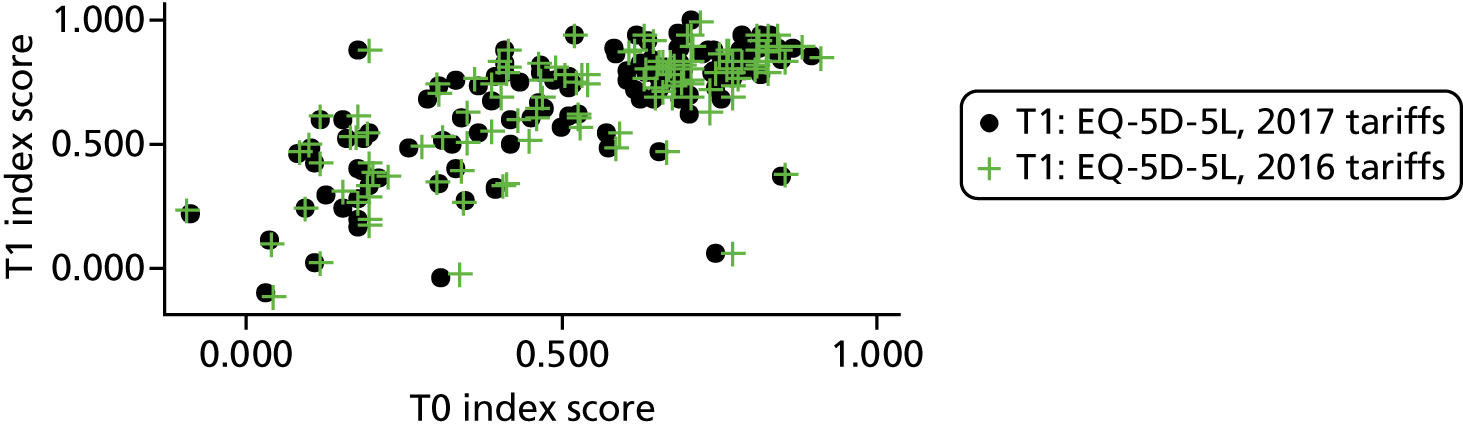
Outcomes data
FIGURE 14.
The EQ-5D-5L index scores: distributions at T0 and T1 (total samples).
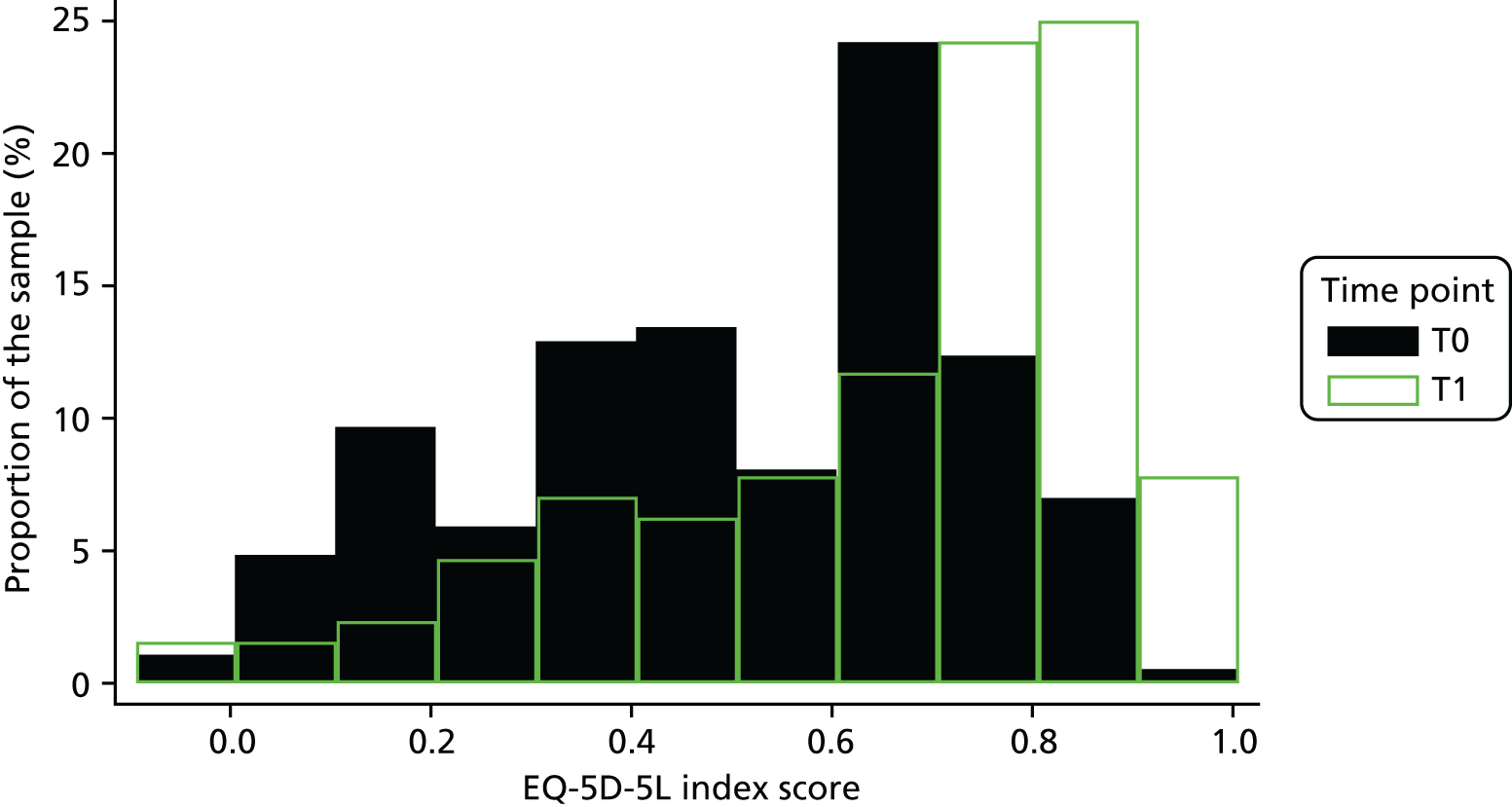
FIGURE 15.
The EQ VAS scores: distributions at T0 and T1 (total samples).
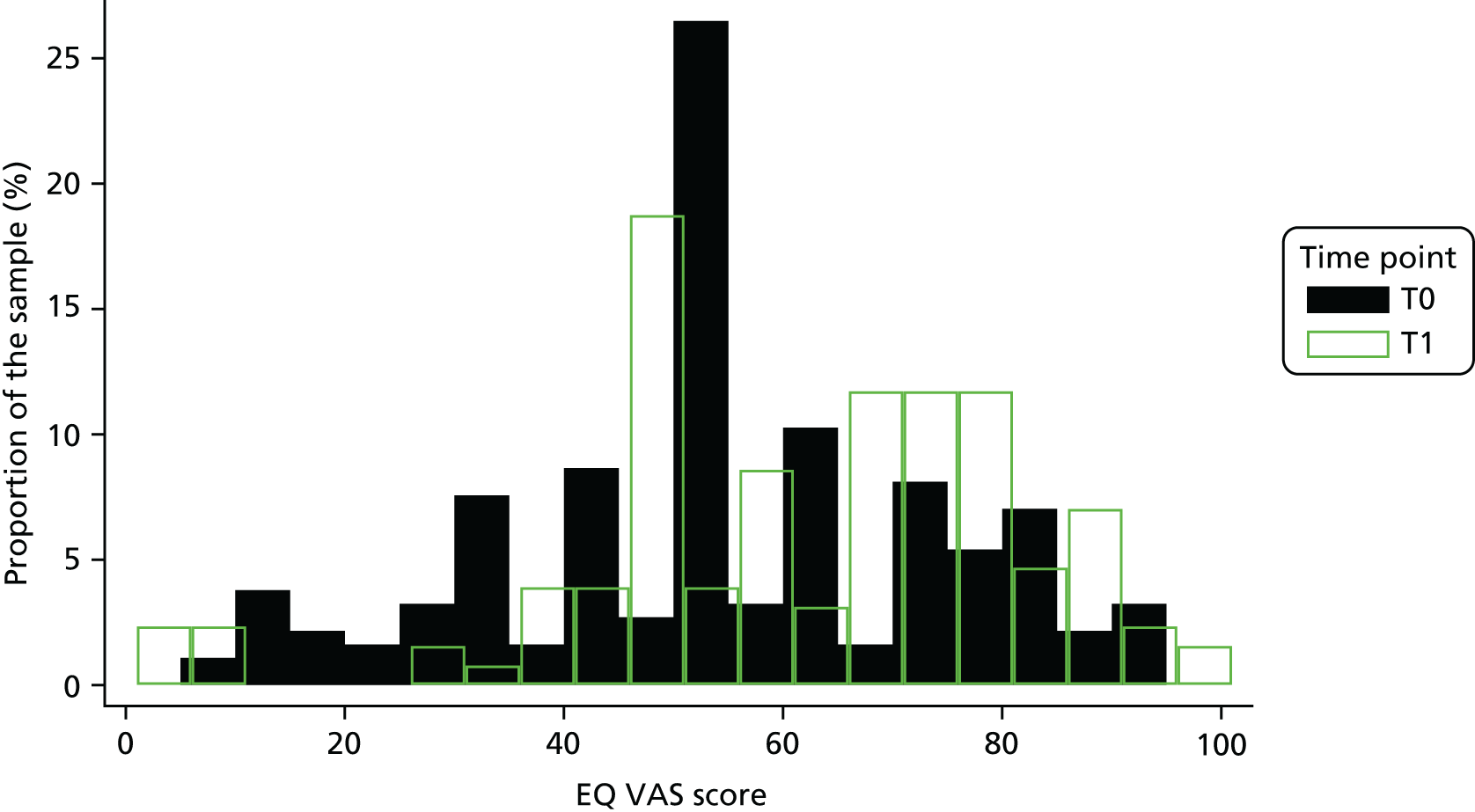
FIGURE 16.
Distribution of EQ VAS scores: at T1 and T2 (total samples).
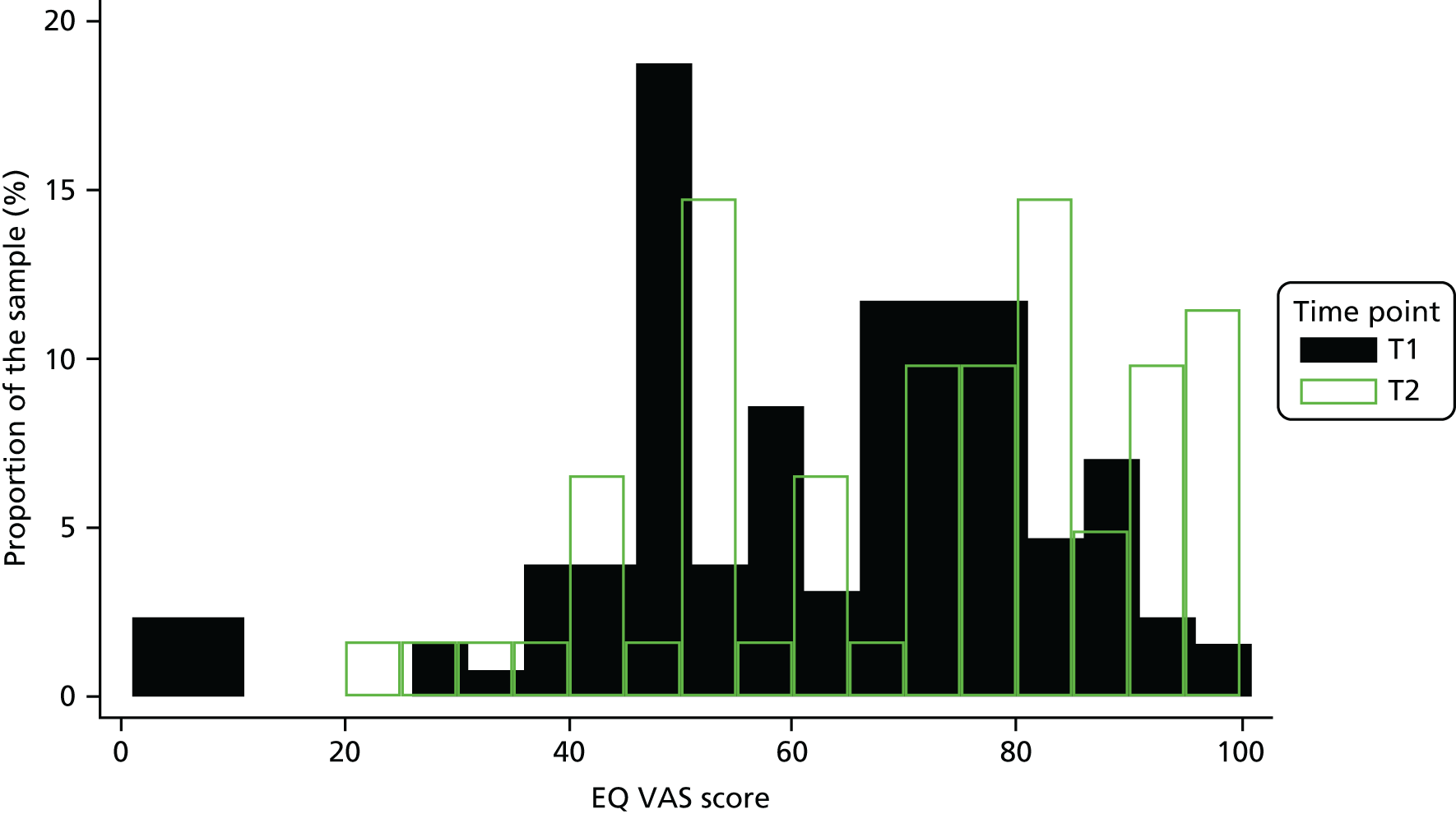
| Change | T0 to T1, n (%) | T1 to T2, n (%) |
|---|---|---|
| EQ-5D-5L index | ||
| Deterioration | 16 (13) | 21 (43) |
| Maintenance | 4 (3) | 3 (6) |
| Improvement | 108 (84) | 25 (51) |
| Total | 128 (100) | 49 (100) |
| EQ VAS | ||
| Deterioration | 17 (13) | 20 (39) |
| Maintenance | 4 (3) | 10 (20) |
| Improvement | 107 (84) | 21 (41) |
| Total | 128 (100) | 51 (100) |
| Change | EQ-5D-5L domain, n (%) | ||||
|---|---|---|---|---|---|
| Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | |
| Deterioration | 12 (9) | 3 (2) | 9 (7) | 18 (14) | 22 (17) |
| Maintenance | 50 (39) | 34 (27) | 48 (38) | 63 (49) | 61 (48) |
| Improvement | 66 (52) | 91 (71) | 71 (55) | 47 (37) | 45 (35) |
| Total | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) |
Appendix 8 Work package 2a: Adult Social Care Outcomes Toolkit – self-completed data – figures and tables
FIGURE 17.
The ASCOT-SCT4 index scores: distributions at T0 and T1 (total samples).
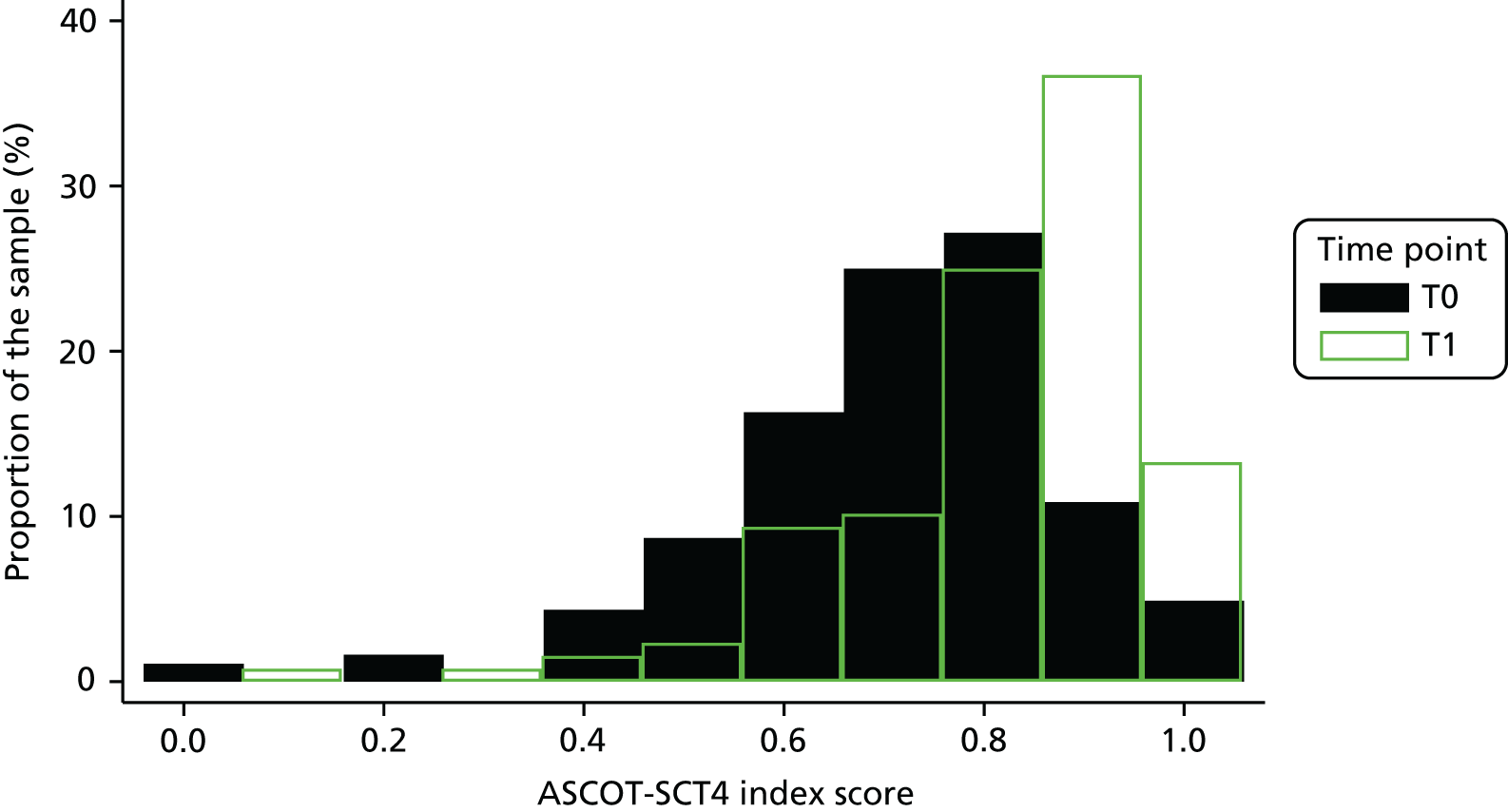
FIGURE 18.
The ASCOT-SCT4 index scores: distributions at T1 and T2 (total samples).
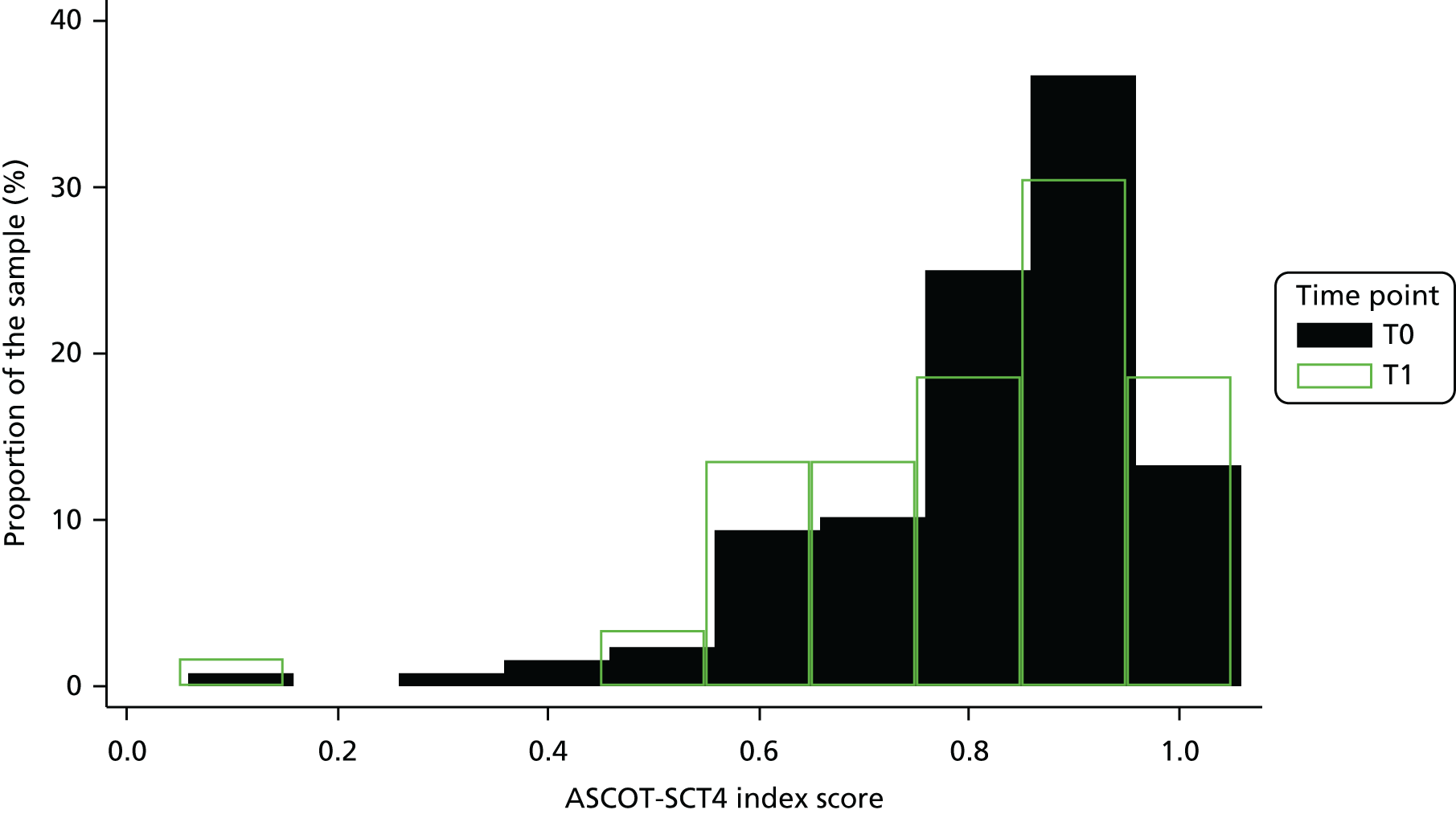
| Change | T0 to T1, n (%) | T1 to T2, n (%) |
|---|---|---|
| Deterioration | 31 (24) | 21 (45) |
| Maintenance | 4 (3) | 3 (6) |
| Improvement | 93 (73) | 23 (49) |
| Total | 128 (100) | 47 (100) |
| Change | ASCOT-SCT4 domain, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | Personal appearance | Food and drink | Safety | Social contact | Time | Accommodation | Feeling about having help | Feeling about help | |
| Deterioration | 13 (10) | 7 (5) | 5 (4) | 19 (15) | 24 (19) | 16 (13) | 11 (9) | 7 (5) | 13 (10) |
| Maintenance | 60 (47) | 62 (48) | 78 (61) | 87 (68) | 55 (43) | 58 (45) | 80 (63) | 88 (69) | 93 (73) |
| Improvement | 55 (43) | 59 (46) | 45 (35) | 22 (17) | 49 (38) | 54 (42) | 37 (29) | 33 (26) | 22 (17) |
| Total | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) |
Appendix 9 Work package 2a: Barthel Index descriptive data – figure and tables
FIGURE 19.
Barthel Index scores: distributions at T0 and T1 (total samples).
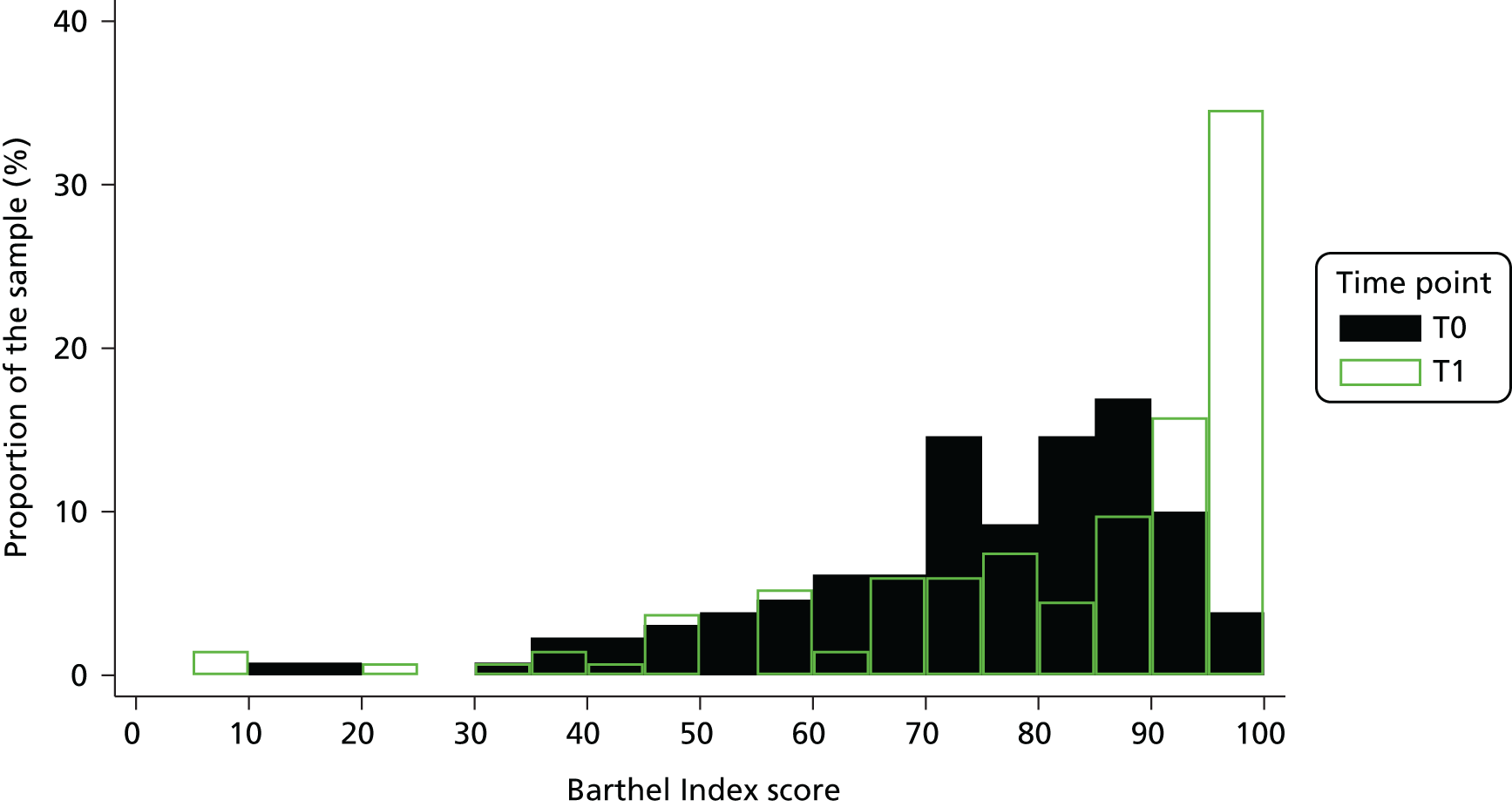
| Change | n (%) |
|---|---|
| Deterioration | 22 (23) |
| Maintenance | 11 (11) |
| Improvement | 63 (66) |
| Total | 96 (100) |
| Change | Barthel Index domain, n (%) | Total score, N (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Feeding | Bathing | Grooming | Dressing | Bowels | Bladder | Toilet use | Transfers | Mobility | Stairs | ||
| Deterioration | 5 (5) | 8 (8) | 9 (9) | 7 (7) | 10 (10) | 7 (7) | 13 (14) | 14 (15) | 18 (19) | 15 (16) | 22 (23) |
| Maintenance | 72 (75) | 43 (45) | 53 (55) | 38 (40) | 76 (79) | 73 (76) | 70 (73) | 58 (60) | 67 (70) | 61 (64) | 11 (11) |
| Improvement | 19 (20) | 45 (47) | 34 (35) | 51 (53) | 10 (10) | 16 (17) | 13 (14) | 24 (25) | 11 (11) | 20 (21) | 63 (66) |
| Total | 96 (100) | 96 (100) | 96 (100) | 96 (100) | 96 (100) | 96 (100) | 96 (100) | 96 (100) | 96 (100) | 96 (100) | 96 (100) |
Appendix 10 Work package 2a: Nottingham Extended Activities of Daily Living scale data – figure and tables
FIGURE 20.
The NEADL total scores: distributions at T0 and T1 (total samples).
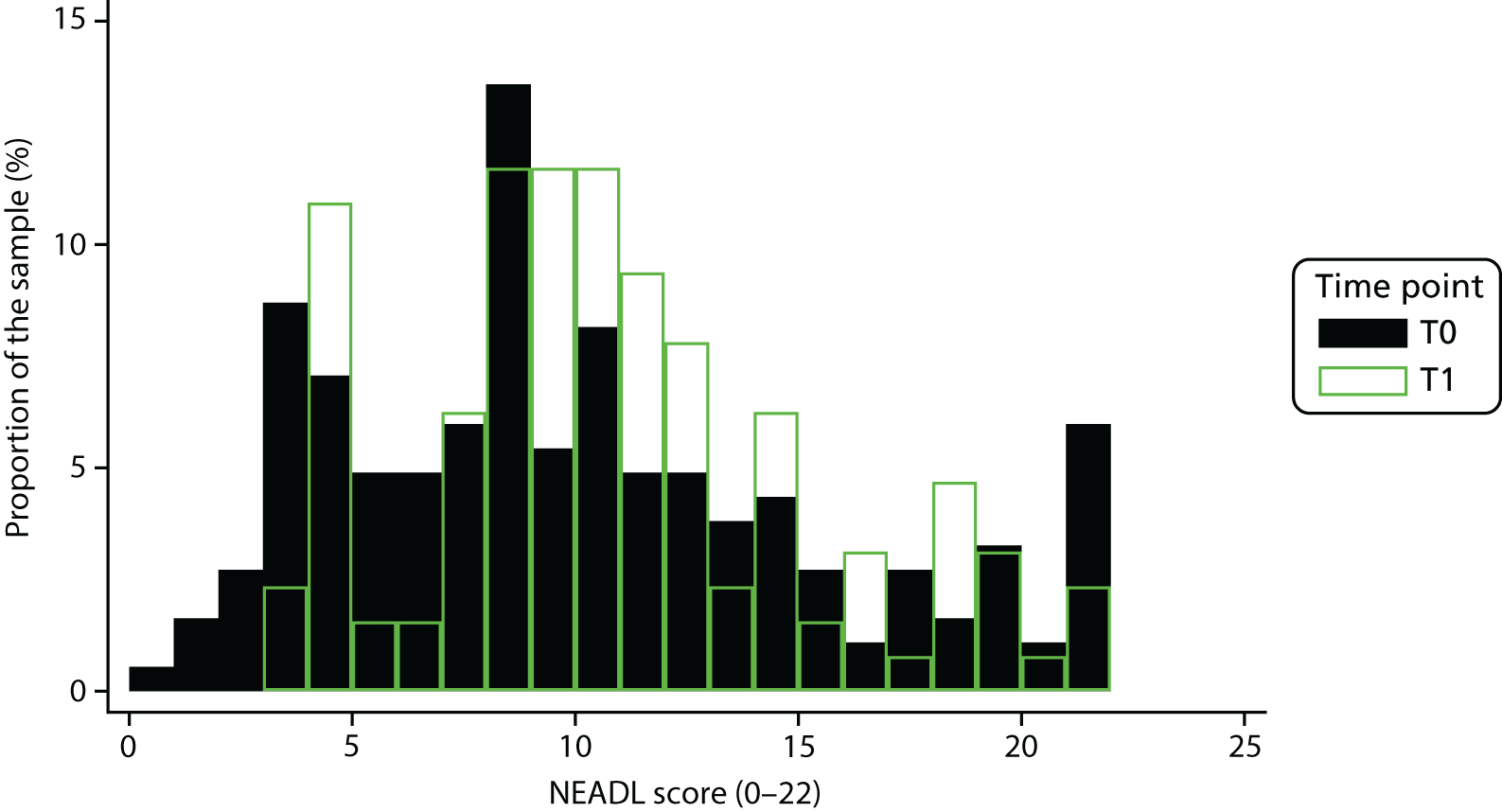
| Type of change | T0 to T1, n (%) | T1 to T2, n (%) |
|---|---|---|
| Deterioration | 39 (30.5) | 14 (26.9) |
| Maintenance | 18 (14.1) | 4 (7.7) |
| Improvement | 71 (55.5) | 34 (65.4) |
| Total | 128 (100.0) | 52 (100.0) |
| Type of change | Domain, n (%) | Total score | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mobility | Kitchen | Domestic | Leisure | ||||||||||||||||||||
| Walk | Climb | In/out car | Uneven | Cross roads | Transport | Feed oneself | Make drink | Carry drink | Wash up | Make snack | Money | Small wash | Housework | Shopping | Clothes wash | Read | Use telephone | Write letters | Socialise | Gardening | Driving | ||
| Deterioration | 21 (17) | 9 (7) | 22 (17) | 18 (14) | 17 (13) | 13 (10) | 1 (1) | 3 (2) | 4 (3) | 1 (1) | 3 (2) | 17 (13) | 3 (2) | 10 (8) | 11 (9) | 17 (13) | 3 (2) | 0 (0) | 0 (0) | 11 (9) | 9 (7) | 11 (9) | 39 (30) |
| Maintenance | 87 (69) | 106 (83) | 85 (67) | 90 (71) | 98 (77) | 108 (85) | 120 (94) | 110 (86) | 103 (80) | 108 (84) | 108 (84) | 95 (74) | 100 (78) | 111 (87) | 106 (83) | 89 (70) | 116 (91) | 124 (97) | 108 (84) | 108 (84) | 115 (90) | 113 (88) | 18 (14) |
| Improvement | 19 (15) | 12 (9) | 20 (16) | 19 (15) | 12 (9) | 6 (5) | 7 (5) | 15 (12) | 21 (16) | 19 (15) | 17 (13) | 16 (13) | 25 (20) | 7 (5) | 11 (9) | 21 (17) | 9 (7) | 4 (3) | 20 (16) | 9 (7) | 4 (3) | 4 (3) | 71 (55) |
| Total | 127 (100) | 127 (100) | 127 (100) | 127 (100) | 127 (100) | 127 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 127 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) | 128 (100) |
Appendix 11 Work package 2a: 12-item General Health Questionnaire – figure and table
FIGURE 21.
Distribution of GHQ-12 scores: at T0 and T1 (total samples).
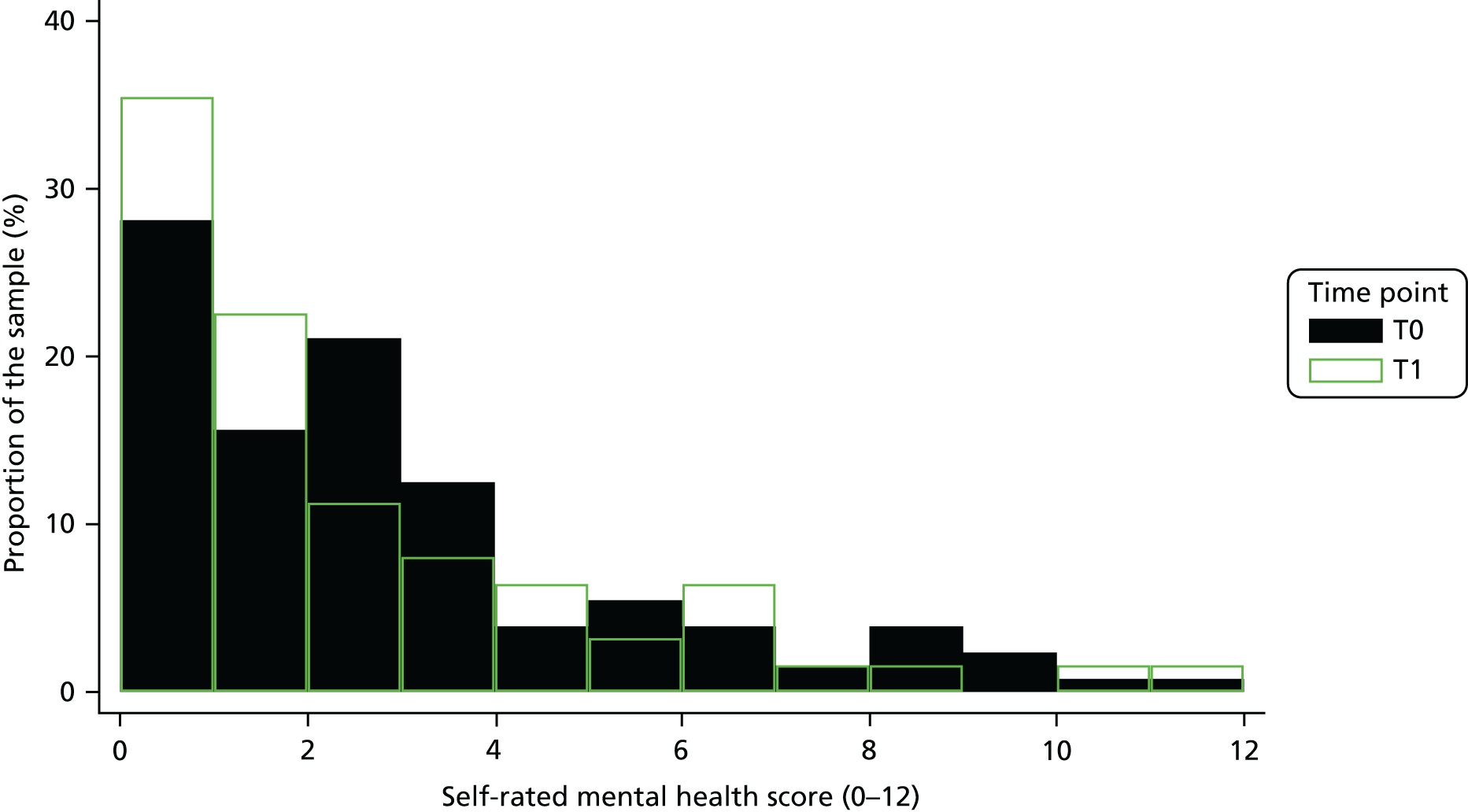
| Type of change | T0 to T1, n (%) | T1 to T2, n (%) |
|---|---|---|
| Deterioration | 23 (18.0) | 12 (24.0) |
| Maintenance | 16 (12.5) | 13 (26.0) |
| Improvement | 89 (69.5) | 25 (50.0) |
| Total | 128 (100) | 50 (100) |
Appendix 12 Work package 2a: factors associated with T1 outcomes – regression models
| Outcome: health-related quality of life at discharge | Version | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Aa | Bb | |||||||||
| Coefficient | p-value | 95% CI | llik | BIC | Coefficient | p-value | 95% CI | llik | BIC | |
| Explanatory variables | ||||||||||
| Model 1: 128 | ||||||||||
| Health-related quality of life at baseline | 0.707 | < 0.001 | 0.573 to 0.84 | 47.9 | –607.8 | 0.677 | < 0.001 | 0.603 to 0.752 | 53.2 | –612.9 |
| Individual-level characteristics | ||||||||||
| Model 2: 128 | ||||||||||
| Health-related quality of life at baseline | 0.705 | < 0.001 | 0.569 to 0.842 | 48.06 | –607.8 | 0.676 | < 0.001 | 0.6 to 0.753 | 53.4 | –608.1 |
| Sex (reference: female vs. male) | 0.018 | 0.009 | 0.004 to 0.031 | 0.015 | 0.233 | –0.01 to 0.039 | ||||
| Model 3: 128 | ||||||||||
| Health-related quality of life at baseline | 0.719 | < 0.001 | 0.591 to 0.847 | 48.2 | –607.8 | 0.696 | < 0.001 | 0.623 to 0.77 | 54.2 | –608.1 |
| Living alone (reference: no vs. yes) | –0.024 | < 0.001 | –0.03 to –0.019 | –0.042 | 0.033 | –0.08 to –0.003 | ||||
| Model 4: 124 | ||||||||||
| Health-related quality of life at baseline | 0.671 | < 0.001 | 0.519 to 0.823 | 48.4 | –584.8 | 0.62 | < 0.001 | 0.582 to 0.657 | 55.2 | –585.1 |
| Sufficient money (reference: no vs. yes) | 0.081 | < 0.001 | 0.063 to 0.098 | 0.102 | < 0.001 | 0.049 to 0.155 | ||||
| Model 5: 128 | ||||||||||
| Health-related quality of life at baseline | 0.713 | < 0.001 | 0.582 to 0.844 | 49.1 | –607.9 | 0.683 | < 0.001 | 0.606 to 0.76 | 53.8 | –608.1 |
| Referral reason (reference: return to home vs. remain at home) | 0.046 | 0.313 | –0.043 to 0.134 | 0.032 | 0.313 | –0.03 to 0.094 | ||||
| Model 6: 128 | ||||||||||
| Health-related quality of life at baseline | 0.702 | < 0.001 | 0.55 to 0.854 | 48.1 | –607.8 | 0.667 | < 0.001 | 0.58 to 0.754 | 54.1 | –608.1 |
| Informal carer involved (reference: no vs. yes) | –0.033 | 0.653 | –0.179 to 0.112 | –0.062 | 0.221 | –0.161 to 0.037 | ||||
| Model 7: 128 | ||||||||||
| Health-related quality of life at baseline | 0.713 | < 0.001 | 0.576 to 0.849 | 48.74 | –607.8 | 0.678 | < 0.001 | 0.612 to 0.73 | 53.5 | –608.1 |
| Physical health key comorbidities (reference: none vs. one) | 0.025 | 0.514 | –0.049 to 0.098 | 0.007 | 0.832 | –0.057 to 0.071 | ||||
| None vs. two or more | –0.025 | 0.602 | –0.118 to 0.068 | –0.034 | 0.545 | –0.145 to 0.077 | ||||
| Model 8: 128 | ||||||||||
| Health-related quality of life at baseline | 0.659 | < 0.001 | 0.615 to 0.703 | 50.1 | –607.9 | 0.645 | < 0.001 | 0.612 to 0.678 | 54.5 | –608.2 |
| Age (years) | 0.004 | 0.291 | –0.003 to 0.01 | 0.003 | 0.293 | –0.002 to 0.008 | ||||
| Model 9: 87 | ||||||||||
| Health-related quality of life at baseline | 0.733 | < 0.001 | 0.539 to 0.927 | 34.2 | –377.3 | 0.701 | < 0.001 | 0.564 to 0.837 | 36.6 | –377.4 |
| Assessor-reported functional status at baseline (Barthel Index) | 0.001 | 0.212 | –0.001 to 0.003 | 0.001 | 0.141 | –0.000 to 0.003 | ||||
| Model 10: 128 | ||||||||||
| Health-related quality of life at baseline | 0.669 | < 0.001 | 0.572 to 0.767 | 0.628 | < 0.001 | 0.592 to 0.664 | 55.0 | –608.2 | ||
| Self-reported functional status at baseline (NEADL) | 0.004 | 0.015 | 0.001 to 0.007 | 0.005 | 0.091 | –0.001 to 0.011 | ||||
| Model 11: 128 | ||||||||||
| Health-related quality of life at baseline | 0.622 | < 0.001 | 0.517 to 0.726 | 50.6 | –607.9 | 0.606 | < 0.001 | 0.538 to 0.674 | 55.3 | –608.2 |
| (Worse) mental health at baseline (GHQ-12) | –0.014 | 0.017 | –0.025 to –0.003 | –0.012 | 0.001 | –0.019 to –0.005 | ||||
| Model 12: 108 | ||||||||||
| Health-related quality of life at baseline | 0.64 | < 0.001 | 0.584 to 0.696 | 61.9 | –499.0 | 0.639 | < 0.001 | 0.588 to 0.689 | 62.3 | –498.9 |
| Engagement with reablement (HRERS-RV) | 0.009 | < 0.001 | 0.008 to 0.01 | 0.01 | < 0.001 | 0.008 to 0.012 | ||||
| Service-level characteristics | ||||||||||
| Model 13: 127 | ||||||||||
| Health-related quality of life at baseline | 0.698 | < 0.001 | 0.591 to 0.805 | 48.9 | –602.1 | 0.674 | < 0.001 | 0.604 to 0.745 | 52.9 | –607.1 |
| Single team model (reference: no vs. yes) | 0.034 | 0.545 | –0.057 to 0.125 | –0.013 | < 0.001 | –0.015 to –0.010 | ||||
| Intervention characteristics | ||||||||||
| Model 14: 128 | ||||||||||
| Health-related quality of life at baseline | 0.711 | < 0.001 | 0.578 to 0.843 | 48.2 | –607.8 | 0.679 | < 0.001 | 0.601 to 0.758 | 53.3 | –608.1 |
| Intervention fidelity (reference: partial vs. complete) (ERPC) | 0.025 | 0.7 | –0.102 to 0.152 | 0.011 | 0.842 | –0.094 to 0.116 | ||||
| Model 15: 128 | ||||||||||
| Health-related quality of life at baseline | 0.711 | < 0.001 | 0.547 to 0.876 | 47.9 | –607.8 | 0.677 | < 0.001 | 0.576 to 0.778 | 53.2 | –608.1 |
| Duration of reablement (weeks) | 0.002 | 0.796 | –0.015 to 0.019 | 0 | 0.986 | –0.013 to 0.013 | ||||
| Model 16: 127 | ||||||||||
| Health-related quality of life at baseline | 0.699 | < 0.001 | 0.604 to 0.793 | 49.5 | –602.1 | 0.673 | < 0.001 | 0.600 to 0.745 | 52.9 | –607.1 |
| In-house vs. outsourced reablement workers | –0.049 | 0.413 | –0.165 to 0.068 | 0.017 | < 0.001 | 0.013 to 0.022 | ||||
| Characteristic | ASCOT-SCT4 index score | |
|---|---|---|
| Without controlling for site | Controlling for site | |
| Service user characteristics | ||
| Age (years) | 0.001 (0.000 to 0.002) | 0.001 (–0.001 to 0.002) |
| Sex | 0.024 (–0.001 to 0.050) | 0.021 (–0.004 to 0.045) |
| Key physical health comorbidities | ||
| Coefficient on one key comorbidity | 0.031 (–0.016 to 0.078) | 0.019 (–0.029 to 0.067) |
| Coefficient on two or more key comorbidities | 0.015 (–0.008 to 0.037) | 0.010 (–0.009 to 0.029) |
| Living situation | 0.003 (–0.024 to 0.031) | –0.009 (–0.058 to 0.040) |
| Perceived financial situation | 0.017 (–0.018 to 0.051) | 0.031 (0.016 to 0.045) |
| Supported by family and friends | –0.029 (–0.061 to 0.003) | –0.046 (–0.104 to 0.013) |
| Mental health at baseline (GHQ-12) | –0.014 (–0.019 to –0.009) | –0.013 (–0.017 to –0.009) |
| Functional status at baseline (modified Barthel Index) | –0.001 (–0.002 to –0.000) | –0.001 (–0.002 to –0.000) |
| Health-related quality of life (EQ-5D-5L) | 0.050 (–0.107 to 0.207) | 0.046 (–0.084 to 0.175) |
| Functional status at baseline (NEADL) | 0.000 (–0.006 to 0.006) | 0.000 (–0.007 to 0.007) |
| Engagement with reablement (HERS) | 0.006 (0.002 to 0.010) | 0.006 (0.001 to 0.010) |
| Reason for referral | 0.039 (–0.001 to 0.078) | 0.034 (0.008 to 0.060) |
| Service/intervention characteristics | ||
| Duration of reablement | 0.007 (0.004 to 0.011) | 0.006 (0.002 to 0.010) |
| Intervention fidelity | 0.033 (0.009 to 0.058) | 0.024 (–0.001 to 0.050) |
| Type of provider (outsourced vs. in-house) | –0.041 (–0.093 to 0.012) | –0.011 (–0.014 to 0.008) |
| Single vs. multiple team model | 0.034 (0.000 to 0.070) | 0.000 (–0.003 to 0.003) |
| Assessor-reported functional status at discharge (Barthel Index) | Version | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Aa | Bb | |||||||||
| Coefficient | p-value | 95% CI | llik | BIC | Coefficient | p-value | 95% CI | llik | BIC | |
| Explanatory variables | ||||||||||
| Model 1: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.629 | < 0.001 | 0.359 to 0.899 | –407.9 | 27,179.5 | 0.601 | < 0.001 | 0.305 to 0.898 | –406.7 | 26,479.7 |
| Individual-level characteristics | ||||||||||
| Model 2: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.625 | < 0.001 | 0.351 to 0.900 | –407.9 | 27,158.5 | 0.598 | < 0.001 | 0.298 to 0.899 | –406.7 | 26,466.2 |
| Sex (reference: female vs. male) | –1.008 | 0.42 | –1.980 to –0.036 | –0.937 | 0.024 | –1.749 to –0.126 | ||||
| Model 3: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.597 | < 0.001 | 0.354 to 0.840 | –406.5 | 26,352.0 | 0.549 | < 0.001 | 0.294 to 0.804 | –404.3 | 25,138.6 |
| Living alone (reference: no vs. yes) | 5.991 | 0.278 | –4.834 to 16.816 | 7.900 | 0.083 | –1.040 to 16.841 | ||||
| Model 4: 93 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.664 | < 0.001 | 0.413 to 0.915 | –393.7 | 25,481.3 | 0.643 | < 0.001 | 0.372 to 0.914 | –393.1 | 25,120.4 |
| Sufficient money (reference: no vs. yes) | 6.246 | < 0.001 | 3.650 to 8.841 | 5.256 | < 0.001 | 4.466 to 6.047 | ||||
| Model 5: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.633 | < 0.001 | 0.368 to 0.899 | –407.9 | 27,142.3 | 0.604 | < 0.001 | 0.320 to 0.888 | –406.7 | 26,476.7 |
| Referral reason (reference: return to home vs. remain at home) | 1.268 | 0.532 | –2.708 to 5.243 | 0.583 | 0.735 | –2.794 to 3.961 | ||||
| Model 6: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.619 | < 0.001 | 0.395 to 0.843 | –405.9 | 25,681.9 | 0.587 | < 0.001 | 0.341 to 0.833 | –404.0 | 24,978.5 |
| Informal carer involved (ref: no vs. yes) | –12.94 | < 0.001 | –16.592 to –9.291 | –13.21 | < 0.001 | –15.59 to –10.83 | ||||
| Model 7: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.611 | < 0.001 | 0.379 to 0.843 | –405.8 | 25,980.4 | 0.596 | < 0.001 | 0.348 to 0.844 | –405.3 | 25,665.6 |
| Physical health key comorbidities (ref: none vs. one) | –7.036 | 0.002 | –11.516 to –2.555 | –5.739 | < 0.001 | –8.942 to –2.536 | ||||
| None vs. two or more | –7.865 | 0.092 | –17.026 to 1.295 | –7.128 | 0.112 | –15.924 to 1.668 | ||||
| Model 8: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.626 | < 0.001 | 0.350 to 0.902 | –407.7 | 27,044.8 | 0.602 | < 0.001 | 0.300 to 0.904 | –406.6 | 26,410.6 |
| Age (years) | 0.144 | 0.009 | 0.036 to 0.253 | 0.110 | 0.199 | –0.058 to 0.279 | ||||
| Model 9: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.442 | < 0.001 | 0.200 to 0.684 | –398.4 | 22,184.1 | 0.388 | < 0.003 | 0.133 to 0.643 | –396.0 | 21,097.5 |
| Self-reported functional status at baseline (NEADL) | 1.327 | < 0.001 | 0.910 to 1.744 | 1.412 | < 0.001 | 1.048 to 1.776 | ||||
| Model 10: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.535 | < 0.001 | 0.239 to 0.830 | –404.4 | 25,184.9 | 0.518 | < 0.001 | 0.204 to 0.831 | –403.4 | 24,650.1 |
| Health-related quality of life at baseline (EQ-5D-5L) | 19.690 | < 0.001 | 12.423 to 26.957 | 19.081 | < 0.001 | 11.424 to 26.738 | ||||
| Model 11: 96 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.629 | < 0.001 | 0.352 to 0.907 | –407.1 | 26,662.0 | 0.601 | < 0.001 | 0.298 to 0.904 | –405.7 | 25,878.4 |
| (Worse) mental health at baseline (GHQ-12) | –0.841 | < 0.001 | –1.238 to –0.445 | –0.914 | < 0.001 | –1.407 to –0.421 | ||||
| Model 12: 76 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.623 | < 0.001 | 0.498 to 0.749 | –308.7 | 14,680.5 | 0.594 | < 0.001 | 0.558 to 0.631 | –307.8 | 14,319.7 |
| Engagement with reablement (HRERS-RV) | 1.693 | < 0.001 | 1.471 to 1.915 | 1.702 | < 0.001 | 1.501 to 1.904 | ||||
| Service-level characteristics | ||||||||||
| Model 13: 95 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.626 | < 0.001 | 0.308 to 0.944 | –402.1 | 25,996.5 | 0.659 | < 0.001 | 0.353 to 0.965 | –399.9 | 24,815.9 |
| Single team model (ref: no vs. yes) | –1.939 | 0.721 | –12.576 to 8.697 | 5.337 | 0.029 | 0.544 to 10.130 | ||||
| Intervention characteristics | ||||||||||
| Model 14: 75 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.676 | < 0.001 | 0.460 to 0.893 | –315.8 | 19,611.8 | 0.654 | < 0.001 | 0.416 to 0.891 | –315.4 | 19,407.2 |
| Intervention fidelity (ref: partial vs. complete) (ERPC) | 0.952 | 0.664 | –3.348 to 5.253 | 1.302 | 0.475 | –2.267 to 4.871 | ||||
| Model 15: 95 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.631 | < 0.001 | 0.468 to 0.793 | –402.8 | 26,349.3 | 0.611 | < 0.001 | 0.417 to 0.805 | –401.9 | 25,872.5 |
| Duration of reablement (weeks) | –0.602 | 0.288 | –1.711 to 0.507 | –0.414 | 0.386 | –1.352 to 0.523 | ||||
| Model 16: 104 | ||||||||||
| Assessor-reported functional status at baseline (Barthel Index) | 0.635 | < 0.001 | 0.351 to 0.918 | –402.2 | 26,040.9 | 0.632 | < 0.001 | 0.330 to 0.934 | –400.5 | 25,100.9 |
| In-house vs. outsourced reablement workers | 1.279 | 0.760 | –6.937 to 9.495 | –1.358 | 0.602 | –6.461 to 3.745 | ||||
| Self-reported functional status at discharge (NEADL) | Version | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Aa | Bb | |||||||||
| Coefficient | p-value | 95% CI | llik | BIC | Coefficient | p-value | 95% CI | llik | BIC | |
| Explanatory variables | ||||||||||
| Model 1: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.493 | < 0.001 | 0.484 to 0.503 | –340.8 | 927.9 | 0.515 | < 0.001 | 0.451 to 0.579 | –335.3 | 796.1 |
| Individual-level characteristics | ||||||||||
| Model 2: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.489 | < 0.001 | 0.465 to 0.514 | –340.1 | 911.0 | 0.512 | < 0.001 | 0.444 to 0.581 | –335.0 | 795.2 |
| Sex (reference: female vs. male) | –0.782 | 0.241 | –2.088 to 0.524 | –0.461 | 0.413 | –1.566 to 0.644 | ||||
| Model 3: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.479 | < 0.001 | 0.438 to 0.519 | –339.7 | 902.3 | 0.497 | < 0.001 | 0.402 to 0.592 | –333.4 | 760.7 |
| Living alone (reference: no vs. yes) | 0.931 | 0.237 | –0.612 to 2.474 | 1.194 | 0.075 | –0.119 to 2.506 | ||||
| Model 4: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.475 | < 0.001 | 0.458 to 0.492 | –331.1 | 925.8 | 0.499 | < 0.001 | 0.447 to 0.551 | –326.0 | 806.0 |
| Sufficient money (reference: no vs. yes) | 0.776 | 0.027 | 0.089 to 1.462 | 0.664 | 0.008 | 0.171 to 1.157 | ||||
| Model 5: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.500 | < 0.001 | 0.481 to 0.519 | –340.3 | 916.3 | 0.519 | < 0.001 | 0.460 to 0.578 | –335.1 | 796.6 |
| Referral reason (reference: return to home vs. remain at home) | 0.618 | 0.025 | 0.076 to 1.159 | 0.383 | 0.344 | –0.410 to 1.175 | ||||
| Model 6: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.493 | < 0.001 | 0.483 to 0.504 | –340.6 | 923.5 | 0.515 | < 0.001 | 0.447 to 0.583 | –335.1 | 796.4 |
| Informal carer involved (reference: no vs. yes) | –0.616 | 0.467 | –2.276 to 1.044 | –0.631 | 0.372 | –2.014 to 0.753 | ||||
| Model 7: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.489 | < 0.001 | 0.486 to 0.493 | –340.7 | 925.7 | 0.517 | < 0.001 | 0.455 to 0.580 | –335.2 | 799.5 |
| Physical health key comorbidities (reference: none vs. one) | –0.302 | 0.594 | –1.411 to 0.808 | 0.179 | 0.656 | –0.608 to 0.966 | ||||
| None vs. two or more | –0.119 | 0.868 | –1.517 to 1.280 | 0.271 | 0.573 | –0.673 to 1.216 | ||||
| Model 8: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.490 | < 0.001 | 0.481 to 0.500 | –340.7 | 925.0 | 0.512 | < 0.001 | 0.450 to 0.574 | –335.1 | 797.0 |
| Age (years) | –0.017 | < 0.001 | –0.022 to –0.011 | –0.020 | 0.022 | –0.037 to –0.003 | ||||
| Model 9: 87 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.387 | < 0.001 | 0.291 to 0.483 | –229.5 | 617.1 | 0.439 | < 0.001 | 0.331 to 0.548 | –224.5 | 509.2 |
| Assessor-reported functional status at baseline (Barthel Index) | 0.071 | 0.011 | 0.016 to 0.127 | 0.043 | < 0.001 | 0.024 to 0.061 | ||||
| Model 10: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.472 | < 0.001 | 0.440 to 0.504 | –340.4 | 917.4 | 0.497 | < 0.001 | 0.432 to 0.562 | –335.0 | 794.0 |
| Health-related quality of life at baseline (EQ-5D-5L) | 1.314 | 0.107 | –0.283 to 2.911 | 1.082 | 0.040 | 0.048 to 2.115 | ||||
| Model 11: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.499 | < 0.001 | 0.459 to 0.539 | –340.7 | 925.8 | 0.515 | < 0.001 | 0.427 to 0.603 | –335.3 | 800.9 |
| (Worse) mental health at baseline (GHQ-12) | 0.047 | 0.739 | –0.229 to 0.323 | –0.005 | 0.967 | –0.232 to 0.222 | ||||
| Model 12: 108 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.474 | < 0.001 | 0.464 to 0.484 | –285.6 | 751.6 | 0.500 | < 0.001 | 0.406 to 0.595 | –278.9 | 606.4 |
| Engagement with reablement (HRERS-RV) | 0.147 | < 0.001 | 0.096 to 0.199 | 0.176 | < 0.001 | 0.148 to 0.204 | ||||
| Service-level characteristics | ||||||||||
| Model 13: 127 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.495 | < 0.001 | 0.458 to 0.531 | –336.2 | 875.1 | 0.510 | < 0.001 | 0.445 to 0.574 | –332.3 | 782.9 |
| Single team model | –1.184 | 0.198 | –2.988 to 0.620 | 0.174 | < 0.001 | 0.156 to 0.192 | ||||
| Intervention characteristics | ||||||||||
| Model 14: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.498 | < 0.001 | 0.477 to 0.518 | –340.4 | 917.8 | 0.516 | < 0.001 | 0.447 to 0.585 | –335.2 | 800.0 |
| Intervention fidelity (reference: partial vs. complete) (ERPC) | –0.595 | 0.487 | –2.273 to 1.083 | –0.189 | 0.737 | –1.293 to 0.914 | ||||
| Model 15: 128 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.486 | < 0.001 | 0.473 to 0.500 | –339.9 | 905.7 | 0.510 | < 0.001 | 0.446 to 0.574 | –334.9 | 792.6 |
| Duration of reablement (weeks) | –0.263 | 0.361 | –0.827 to 0.301 | –0.163 | 0.506 | –0.642 to 0.316 | ||||
| Model 16: 127 | ||||||||||
| Self-reported functional status at baseline (NEADL) | 0.490 | < 0.001 | 0.464 to 0.516 | –337.8 | 915.9 | 0.510 | < 0.001 | 0.446 to 0.575 | –332.3 | 782.9 |
| In-house vs. outsourced reablement workers | –0.182 | 0.777 | –1.446 to 1.082 | –0.156 | < 0.001 | –0.203 to –0.110 | ||||
Appendix 13 Work package 2b: analytical frameworks
Staff interviews: analytical framework
Identifiers
-
Site/service.
-
Staff group.
-
Focus group size.
Delivery of reablement
-
Barriers/sticking points in reablement pathway and perceived reasons:
-
referral
-
assessment
-
handover from assessor to reablement workers
-
monitoring and review
-
discharge
-
access to specialist support
-
interfacing with other statutory services
-
local voluntary sector context.
-
-
Working well/perceived good practice in reablement pathway (include exemplars):
-
referral
-
assessment
-
handover from assessor to reablement workers
-
monitoring and review
-
discharge
-
access to specialist support
-
interfacing with other statutory services
-
local voluntary sector context.
-
-
Changes over time:
-
direction of change
-
perceived reasons.
-
-
The ideal pathway:
-
features
-
rationale.
-
The impact of reablement
-
Views on outcomes:
-
anticipated
-
unanticipated.
-
-
Views on effectiveness:
-
comparisons with home care and other models of support.
-
-
Views on active ingredients:
-
the approach
-
the staff
-
the relationship between the individual and staff.
-
Factors that have an impact on outcomes
-
Individual.
-
Family.
-
Organisational context.
-
Delivery issues.
-
Staff.
Other
-
Other issues/topics.
-
Researcher reflections.
Service user interviews: analytical framework
Identifiers
-
ID number.
-
Site.
-
Sex: F/M.
-
Age.
-
RT (returner); RM (remainer).
-
Previous reablement use: FU (first use)/PU (previous use).
-
Household composition: lives alone/lives with (relationship).
Sheet 1: understanding of reablement
-
Reason for referral to the reablement service.
-
Finding out about the service and initial understanding/expectations.
-
Views on referral (good idea or not).
-
Evidence of goals-focused approaches.
-
Understanding of the reablement approach and objectives of the intervention.
Sheet 2: the experience of receiving the service
-
Support provided.
-
Support not provided.
-
Ways reablement worker worked with clients.
-
How easy/difficult was it to work with the workers?
-
Involvement of others in reablement activities.
-
Changes over time.
Sheet 3: perceived outcomes
-
Difference service made.
-
Most important outcome/most difference.
-
Most enjoyable aspect.
-
Most difficult aspect.
-
Impact on close family members.
Sheet 4: factors having an impact on outcomes
-
Relationship with reablement workers (including companionship).
-
Workers’ qualities, attitudes, approaches, knowledge and skills.
-
Timing, frequency and duration of visits.
-
Service delivery issues.
-
Other (including changes in health).
Sheet 5: end of service and reflections
-
Narrative of service stopping.
-
Feelings when service stopped.
-
How managing now.
-
Reasons would recommend service (or not).
-
Suggested ways to improve service.
-
Researcher reflections.
Appendix 14 Work package 2c: Services and Care Pathway Questionnaire development and piloting
Introduction
This questionnaire was developed to capture service users’ resource use of statutory and voluntary- and private-sector services, out-of-pocket costs and informal carer involvement. We could not identify an existing tool that collected this information with respect to the target population and that was sufficiently relevant to the intervention under investigation. Therefore, a questionnaire was developed and piloted before it was taken into the field. The content of the questionnaire was informed by the data needed by the project and by existing tools. 75,94–98
Testing and adapting the draft versions
A first draft was shared with the members of the SSC for comment. At the same time, the patient and public involvement representatives on the SSC offered to complete the questionnaire and then comment. Comments from the SSC led us to simplify the format to enable self-completion, should study participants choose this option.
This redrafted version (see the end of this appendix) was then administered to 13 reablement service users as part of our wider piloting work. We observed that all of these individuals were able to complete the form either independently or with some assistance. As they completed the form, they talked through their experiences of using services. In nine of the interviews, this narrative of service use highlighted some issues that the research team needed to consider in finalising the questionnaire. These included how the complexity of service provision and use could be captured most simply without double-counting, the parameters of particular questions, and how best to format the questionnaire to minimise burden and confusion and thus maximise completion. We consider reporting each of these issues in turn.
Double-counting
Discussions with pilot participants indicated two places in the questionnaire that might be susceptible to double-counting:
-
‘In the past 7 days, have you used a local authority transport service/taxi vouchers, etc.?’ and ‘In the past 7 days, have you used a voluntary transport service?’
-
‘Since [April], have you attended an outpatient appointment? (includes mental health and consultant appointments in clinics or in GP practices)’ and ‘In the past 7 days, have you had an appointment with a GP?’
In the first example, we were concerned about double-counting because often voluntary-sector transport is funded wholly or in part by social services. Unsurprisingly, participants were not aware of funding arrangements: they could not distinguish between the types of transport and/or could not provide the name of the transport service (which would have allowed us to investigate who provided/funded the services). In this instance, we decided to remove the question about voluntary-sector transport and during training we advised LSOs to guide participants to list other transport in the section on ‘other services’ if they wished.
In the second example, we removed reference to general practices from the question about outpatient appointments to avoid confusion for participants and possible double-counting.
Parameters and clarification of particular questions
Nine pilot participants indicated some degree of confusion about whether or not the location of the service affected whether or not they should report its use, and also whether or not they should include particular services.
For example, participants were not sure whether they should include telephone appointments with clinicians as well as face-to-face appointments. We amended the questionnaire to make it clear to include both methods of having a GP consultation. One participant explained that she had had a planned stay in a rehabilitation community hospital after a planned hospital stay for a surgical procedure. She was not clear about whether or not the days in the community hospital should be included in the numbers of nights’ stay for her planned admission. Based on the team’s experience, we were aware that rehabilitation inpatient stays are common for this group of clients and we amended the questionnaire to include a question specifically about rehabilitation/recuperation inpatient stays. In response to participants being unsure whether or not they should include calls to 111 as well as calls to 999, we added a question about calling 111.
Two pilot participants were not sure which people to include when completing the question about help from family and friends (section 5). For example, they were not sure if they should include neighbours and family who ‘popped around’ to keep them company rather than doing anything practical for them. For the purposes of this project, we were focused on costing the more practical elements of care and support. In the training delivered to LSOs, we made it clear that support that was solely focused on providing company should not be reported.
Other queries were dealt with by ensuring that we trained the LSOs to know how to respond if similar questions were raised again. For example, participants who had microwave meals provided and delivered by a private company or supermarket online/delivery services should not include information about these in their responses, unless these were social service funded. Responding to one pilot participant’s query, we advised LSOs that if a participant was given and used a piece of equipment but also returned it within the timescale stated in the question, this should still be recorded because, for cost purposes, we were interested in whether or not that piece of equipment was used at all.
Wider learning and formatting the questionnaire
The piloting indicated that participants could accurately recall the use of non-hospital-based health services for a longer time frame than we had originally planned. We amended these questions to ask about use of services over a longer time frame than originally planned, namely 14 days rather than 7 days.
Those participants who contributed to the cost of a service did not always pay for it in the same timescales as those about which we asked. For example, they might pay monthly or 3-monthly for a service but we were asking about service use and payment over a fortnight. In their training LSOs were advised to pay attention to the possible differing timescales of payments and the question, and to calculate the cost for the question timescale.
Given that some participants in the pilot had several family members and friends providing support, we changed the format of the question to enable them, or the LSO, to make notes and then sum the total hours of practical support that they had received in the previous 7 days.
The question about transport use was reworded to provide clarity for completion and analysis. We amended it to ask about the number of journeys taken and whether these were one-way or return journeys, rather than how many times transport had been used.
The draft questionnaire was taken forward to piloting. This is presented on the following page.
Appendix 15 Work package 2c: additional information
Unit costs
| Item | Unit cost, 2016 (£) | Source | Notes |
|---|---|---|---|
| Hospital services | |||
| Hospital outpatient appointment | 119.70 | NHS Reference Costs 2015–2016 53 | Average consultant-led, non-consultant-led and outpatient procedures |
| Day case | 733.31 | NHS Reference Costs 2015–2016 53 | Average day case |
| Excess bed stay for planned hospital admission | 361.67 | NHS Reference Costs 2015–2016 53 | Over four nights (average length of stay) |
| Transfer to another hospital for recovery | 331.63 | NHS Reference Costs 2015–2016 53 | Average unit cost for rehabilitation |
| Excess bed stay for unplanned hospital admission | 298.41 | NHS Reference Costs 2015–2016 53 | Over eight nights (average length of stay) |
| Other hospital admissions | 389.10 | NHS Reference Costs 2015–2016 53 | Regular day or night admissions |
| A&E or walk-in centre | 137.74 | NHS Reference Costs 2015–2016 53 | Emergency medicine |
| 999 or 111 calls | 7.00 | NHS Reference Costs 2015–2016 53 | Ambulance calls |
| Other health-care services (rounded to units) | |||
| GP appointment | 36 | PSSRU 2016,52 p. 154 | Per surgery consultation of 9.22 minutes, including direct care staff costs and qualification costs |
| Nurse appointment | 11 |
PSSRU 2016,52 p. 152 PSSRU 2015, p. 183 |
Nurse based at GP practice, including qualification costs: £44 per hour Average contact duration is 15.5 minutes99 |
| Nurse specialist appointment | 13 |
PSSRU 2016,52 p. 151 PSSRU 2015,99 p. 184 |
Nurse band 7, including qualification costs: £52 per hour Assumes average contact duration is 15.5 minutes,99 as per nurse based at GP practice |
| Therapist: OT, physiotherapist, speech therapist, chiropodist, podiatrist | 9 | PSSRU 2016,52 p. 194 |
Allied health professionals band 5: £34 per hour Assumes average contact duration is 15.5 minutes,99 as per nurse based at GP practice |
| Social-care services | |||
| Home care, per appointment | 12.00 | PSSRU 2016,52 p. 169 |
Face-to-face weekday: £24 per hour Assume 30 minutes per session100 |
| Day care, per hour | 13.00 | PSSRU 2016,52 p. 37 |
£61 per client attendance 2.88 hours per attendance |
| Meals, per meal | 4.00 | Glendinning et al.,20 p. 201, inflated to 2015–16 | |
| Social service appointment: social worker | 15.5 | PSSRU 2016,52 pp. 165 and 168 |
Average between social worker cost (per hour of client-related work) and OT cost Assumes average contact duration is 15.5 minutes (PSSRU 2015), as per nurse based at GP practice |
| Sitting service, per hour | 21.00 | PSSRU 2016,52 p. 94 | Home sitting for disabled children, assumed generalisable for sitting service to older adults |
| LA transport service, per journey | 0.55 | Research briefings to parliament101 |
In 2013/14, > 15 million passenger trips were provided by community transport organisations In 2015, the Department for Transport estimated that £7.8M was paid to community transport services from the Bus Service Operator’s Grant + £200,000/year to the Community Transport Association = £8M/15 million trips = 55 pence per trip Inflated to 2016 |
| Services provided by voluntary organisations or charities | |||
| Befriending service, per session | 7.7 | PSSRU 2016,52 p. 55 | £92/12 hours |
| Shopping service, per session | 3.00 | Supermarkets’ average delivery charges | Range is £1–6; mid-point £3 selected |
| Advice service, per session | 32.00 | PSSRU 2016,52 p. 131 | Budgeting advice service for families |
| Cleaner, per hour | 21.00 | PSSRU 2016,52 p. 146 | Housekeeping assistant is at Agenda for Change band 1. Mid-point band 1 is £15,500 per year.102 Calculated from the ratio of wages to hourly cost band |
| Informal care | |||
| Informal care, per hour | 15.72 | ONS55 | Average hourly pay (gross) |
| Adaptations to home | |||
| Downstairs conversion for WC/washroom | 10,134 | PSSRU 2016, pp. 106–752 | |
| Downstairs extension for bedroom | 27,468 | PSSRU 2016, pp. 106–752 | |
| Downstairs extension for en-suite bedroom | 34,587 | PSSRU 2016, pp. 106–752 | |
| Downstairs extension for WC/washroom | 23,199 | PSSRU 2016, pp. 106–752 | |
| Level access shower | 4782 | PSSRU 2016, pp. 106–752 | |
| Stair lift (straight) | 1927 | PSSRU 2016, pp. 106–752 | |
| Stair lift (complex) | 4693 | PSSRU 2016, pp. 106–752 | |
| Bed moved to downstairs room | 40 | PSSRU 2016, pp. 106–752 | |
| External handrail fitted | 42 | PSSRU 2016, pp. 106–752 | |
| Internal handrail fitted | 28 | PSSRU 2016, pp. 106–752 | |
| Outside lighting installed | 256 | PSSRU 2016, pp. 106–752 | |
| Over-bath shower fitted | 108 | PSSRU 2016, pp. 106–752 | |
| Ramp to front/back door created | 316 | PSSRU 2016, pp. 106–752 | |
| Raise/lower electrical/light switches | 80 | PSSRU 2016, pp. 106–752 | |
| Step to front/back door created | 481 | PSSRU 2016, pp. 106–752 | |
| Equipment | |||
| Adapted telephone | 23 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Bath seat | 40 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Commode chair | 188 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Entry phone | 119 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Grab rail | 112 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Hoist | 1123 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Keysafe | 47 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Magnifier | 9 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Pendant alarm | 100 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Perching stool | 58 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Portable ramp | 95 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Raised chair seat | 51 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Raised toilet seat | 30 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Raising chair seat | 743 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Shower chair on wheels | 356 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Shower seat | 49 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Special tin opener | 14 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Tap turners | 16 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Transfer boards | 61 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Walking frame | 69 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Walking stick | 14 | Glendinning et al.,20 p. 202, inflated to 201652 | |
| Wheelchair (manual), per year | 95 | PSSRU 2016, p. 9652 | |
| Wheelchair (active user), per year | 191 | PSSRU 2016, p. 9652 | |
| Wheelchair (electric powered), per year | 443 | PSSRU 2016, p. 9652 | |
| Profiling bed | 1139 | Health and Safety Laboratory RR764 2010, p. 37, inflated to 201652 | Mid-point of the observed range of costs for electric profiling beds |
| Pressure mattress | 13.5 | NICE CG179 2014, p. 279,103 inflated to 201652 | Average of rental cost per day for constant and alternating pressure mattresses |
| Pressure cushion | 29 | Supplier online104 | Invacare Propad profile pressure cushion (Invacare Ltd, Bridgend, UK) |
Services and Care Pathway Questionnaire: extent of missing data
FIGURE 22.
Missing information: resource use – T0 and T1. (a) T0; and (b) T1.
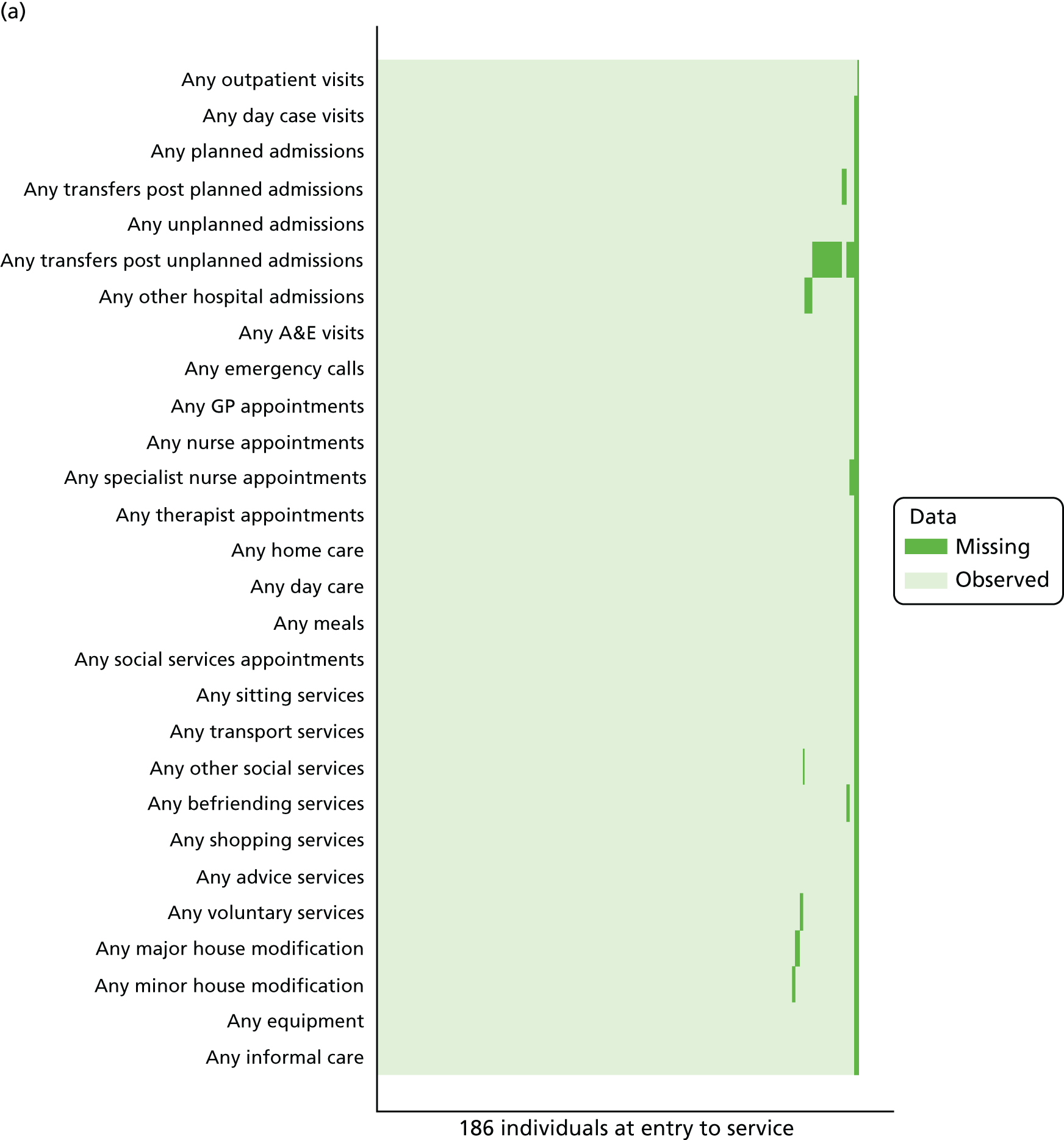
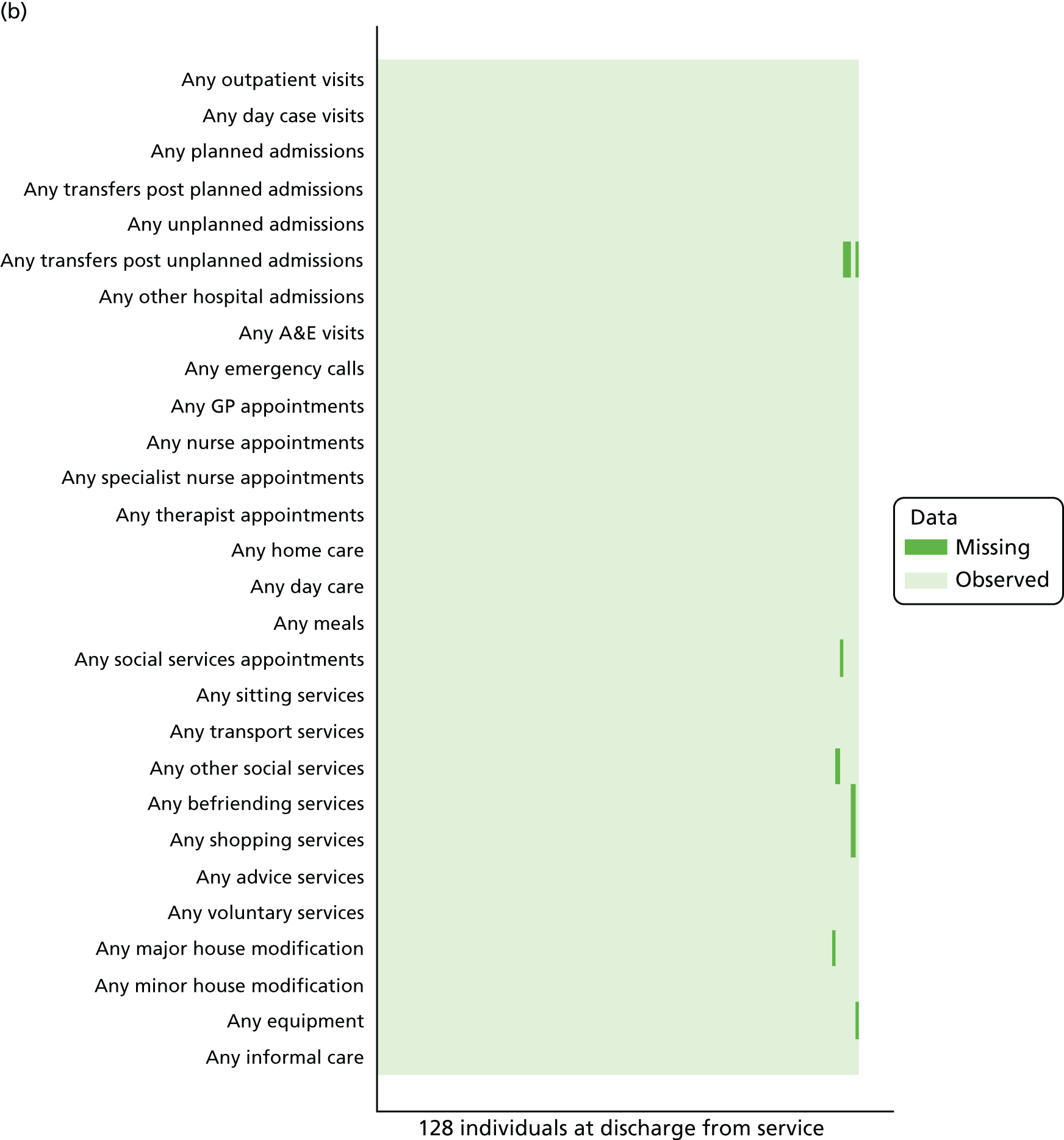
FIGURE 23.
Missing information: intensity of resource use – T0 and T1. (a) T0; and (b) T1.
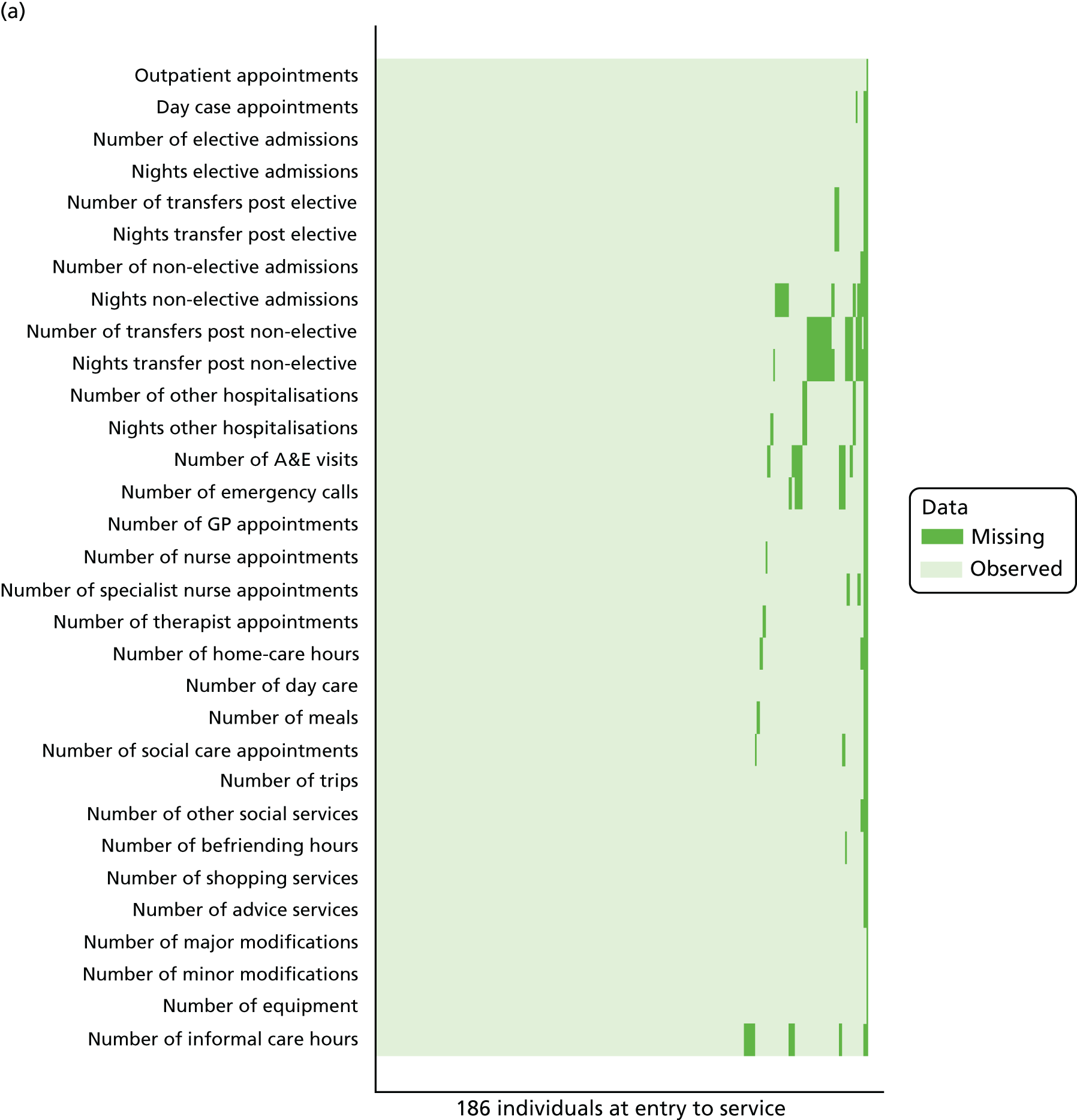
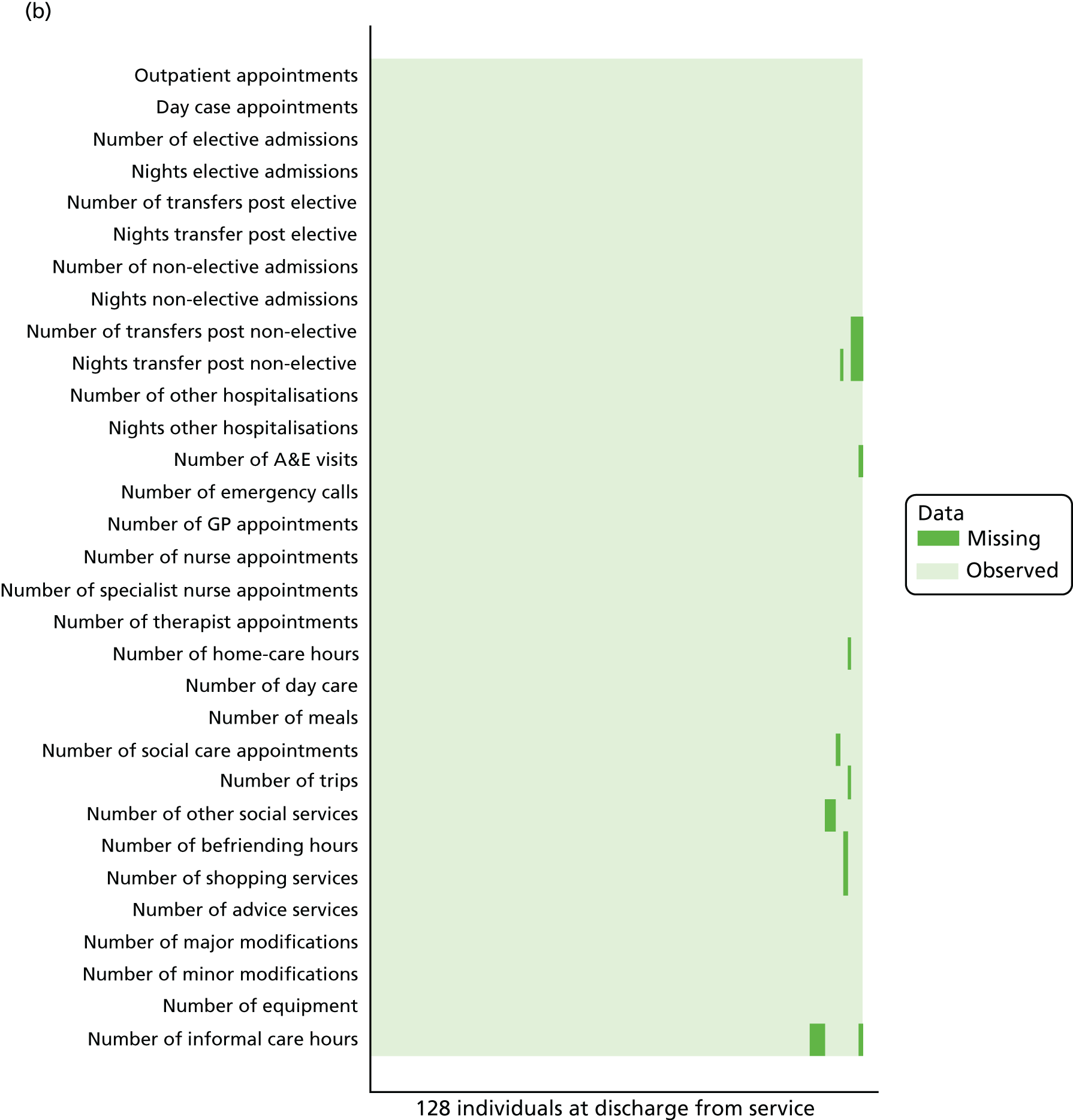
FIGURE 24.
Missing information: resource use and the intensity of resource use – T2.
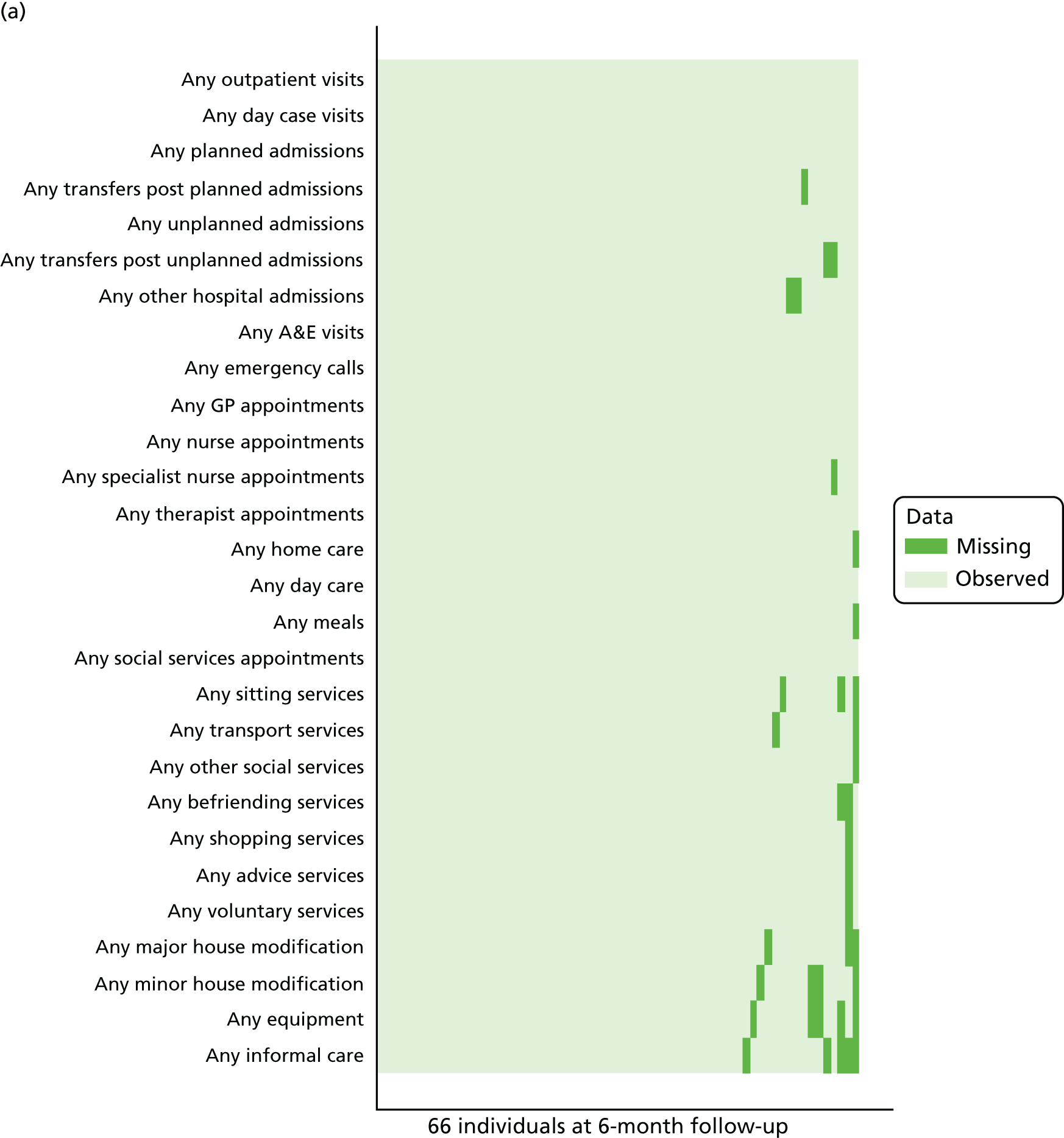
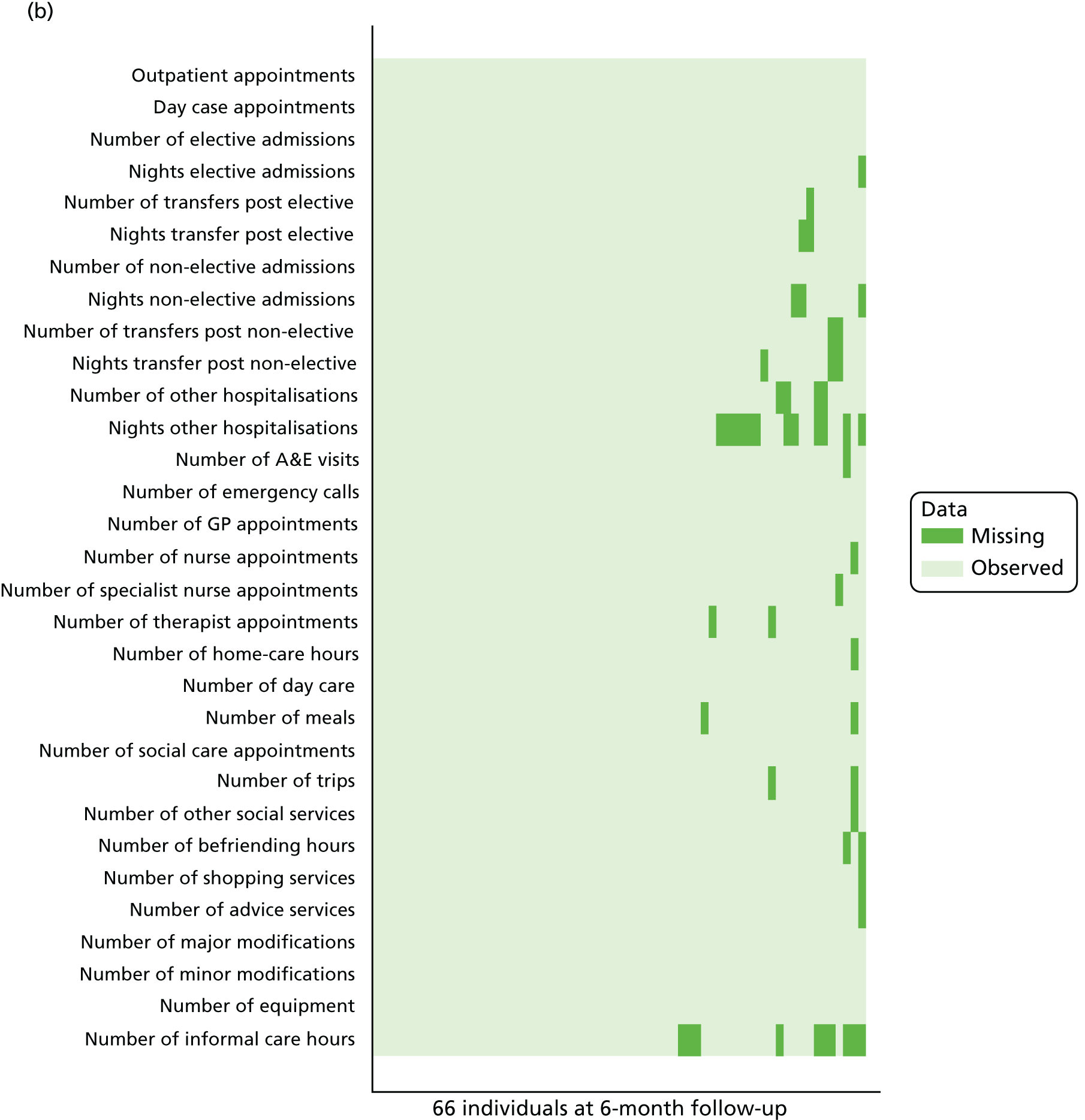
Appendix 16 Work package 3: analytical frameworks
Service lead/manager interviews: analytical framework
Chart 1: history and context
-
Interviewee title/background/experience.
-
Year service set up and how long service offered to people with dementia.
-
Aims/objectives of the service for people with dementia.
-
Funding and commissioning arrangements (e.g. started as a pilot or mainstream funding).
-
Barriers to/facilitators of setting up the service.
-
Changes in service design since started.
Chart 2: description of the service
-
Inclusion/exclusion criteria (including how these decisions are made and views on appropriateness of criteria).
-
Knowledge of who has/does not have dementia and problems arising.
-
Referral routes.
-
Types of interventions and the duration of the intervention.
-
Ways the service organised/adapted to accommodate the needs of people with dementia (e.g. longer sessions, same person visiting, more experienced person).
-
Advantages and disadvantages of organising/adapting the service in this way.
-
How goals are set, who is involved and how (including details provided by any other organisation).
-
Details of ongoing assessments and monitoring progress.
-
What happens at the end, when clients are discharged, when clients need ongoing support.
-
Existence and details of any follow-up support provided.
Chart 3: staff, training and link with other services
-
Professional skills within the team.
-
Details of training opportunities.
-
Any differences between training for managers/all staff/staff working with people with dementia.
-
Views on adequacy of staff training and issues arising.
-
Suggestions for any useful dementia-specific training.
-
Working with professional skills outside the service.
Chart 4: views on the advantages and disadvantages of different types of reablement services supporting people with dementia
-
Dementia-specific reablement service.
-
Generic reablement with protocol.
-
Generic reablement without protocol.
Chart 5: outcomes, barriers/facilitators
-
Views on positive outcomes to assess the success of reablement for people with dementia.
-
Views on reablement working for people with dementia.
-
Views on user-centred facilitators of/barriers to reablement working for people with dementia.
-
Views on organisational facilitators of/barriers to reablement working for people with dementia.
-
Views on the extent to which the service has met its desired/intended objectives.
-
Views on the extent to which the NHS supports specialised services.
Chart 6: messages for other services and suggestions for improvement
-
Messages for meeting the reablement needs of people with dementia.
-
What would have been done differently with hindsight.
-
Suggestions for improvement.
Chart 7: cost of the service
-
Details of any database/record of service users kept (including how many use the service and time spent with and contacts per user).
-
Details of records of what other services people with dementia use/how is it recorded/how linked up the service is to other services people with dementia might use.
-
Number of people with dementia receiving the service per month.
-
Existence/details of waiting list for the service – how many people and how long on the waiting list.
-
Existence/details of a separate budget.
-
Changes to the budget in the last 12 months and reasons for that.
-
Cost estimates of providing the service to people with dementia.
-
Views on whether providing a specialist service is more costly than providing a generic service.
-
Existence/details of additional resources required for people with dementia (e.g. staff time, more skilled staff, equipment).
-
Views on how any additional financial resources would be spent – in the reablement service in general or in the reablement service for people with dementia (including reasons for that).
-
Existence/details of any financial constraints the service is currently facing.
Reablement worker interviews: analytical framework
Chart 1: history and context
-
Interviewee title/background/experience (including length of time working in the reablement team in general/in the team supporting people with dementia).
-
Current caseload.
-
Interviewee roles/responsibilities (supporting all/people with dementia).
-
Training opportunities (including any specific dementia training).
Chart 2: reablement in practice
-
Types of intervention.
-
Differences in the way they work with people with dementia (e.g. longer sessions, more visits).
-
Knowledge of client’s condition (degree of dementia progression), including problems arising when there is a lack of knowledge.
-
Goal setting (who is involved, how goals are decided and access to life stories).
-
Details of ongoing assessments and monitoring progress.
-
Existence/details of any outcomes measures used for people with dementia (including views on adequacy of tools).
-
What happens at the end, when clients are discharged, when clients need ongoing support (including % discharged altogether).
-
Any delays in securing appropriate support for people with dementia (including issues arising).
-
Existence and details of any follow-up support provided.
-
Details of any reablement work with the family.
Chart 3: experiences and views about reablement working for people with dementia
-
Does it work equally/differently with different groups of people with dementia (e.g. level of progression, family circumstances, age, referral route).
-
Views on positive outcomes to assess the success of reablement for people with dementia.
-
Details of actual benefits of reablement for people with dementia (e.g. changes in functional ability, independence, quality of life, risk of entering residential care, social life).
Chart 4: facilitators and barriers
-
Views on the advantages and disadvantages of having a specialist service/protocol for people with dementia.
-
Views on user-centred factors enhancing/constraining the benefits of the reablement for people with dementia.
-
Views on organisational factors enhancing/constraining the benefits of the reablement for people with dementia.
Chart 5: messages for other services and suggestions for improvement
-
Messages for meeting the reablement needs of people with dementia.
-
Suggestions for improving the potential benefits of the reablement for people with dementia.
List of abbreviations
- ADL
- activities of daily living
- A&E
- accident and emergency
- ASCOT
- Adult Social Care Outcomes Toolkit
- ASCOT-SCT4
- Adult Social Care Outcomes Toolkit – self-completed
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- df
- degrees of freedom
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ VAS
- EuroQol visual analogue scale
- ERPC
- Experiences of Reablement Practice Checklist
- GHQ-12
- 12-item General Health Questionnaire
- GP
- general practitioner
- HRERS
- Hopkins Rehabilitation Engagement Rating Scale
- HRERS-RV
- Hopkins Rehabilitation Engagement Rating Scale – Reablement Version
- HSDR
- Health Services and Delivery Research
- LA
- local authority
- LASSD
- local authority social services department
- LSO
- local study officer
- NAIC
- National Audit of Intermediate Care
- NEADL
- Nottingham Extended Activities of Daily Living
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OT
- occupational therapist
- SCPQ
- Services and Care Pathway Questionnaire
- SD
- standard deviation
- SSC
- Study Steering Committee
- WP
- work package
