Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/59/40. The contractual start date was in September 2014. The final report began editorial review in July 2017 and was accepted for publication in February 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Eleanor Winpenny reports grants from UK Clinical Research Collaboration [Medical Research Council (MRC)] and grants from MRC, outside the submitted work.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Newbould et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Context
Some sections of this report have been reproduced from Newbould et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/; from Ball et al. 2 © Author(s) (or their employer(s)) 2018. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: http://creativecommons.org/licenses/by/4.0/; and from Newbould et al. 3 © British Journal of General Practice 2019 This article is Open Access: CC BY-NC 4.0 licence (http://creativecommons.org/licenses/by-nc/4.0/).
A commission on the future of the primary care workforce in England,4 published in 2015, highlighted a number of challenges for primary care, including an increasing population size, an increasing number of patients with complex needs and an increasing overall demand with growing numbers of primary care visits each year. A number of changes have taken place in primary care to respond to these changes in demand. These changes include greater use of telephone or e-mail systems for triage or telephone consultation as an alternative to face-to-face appointments.
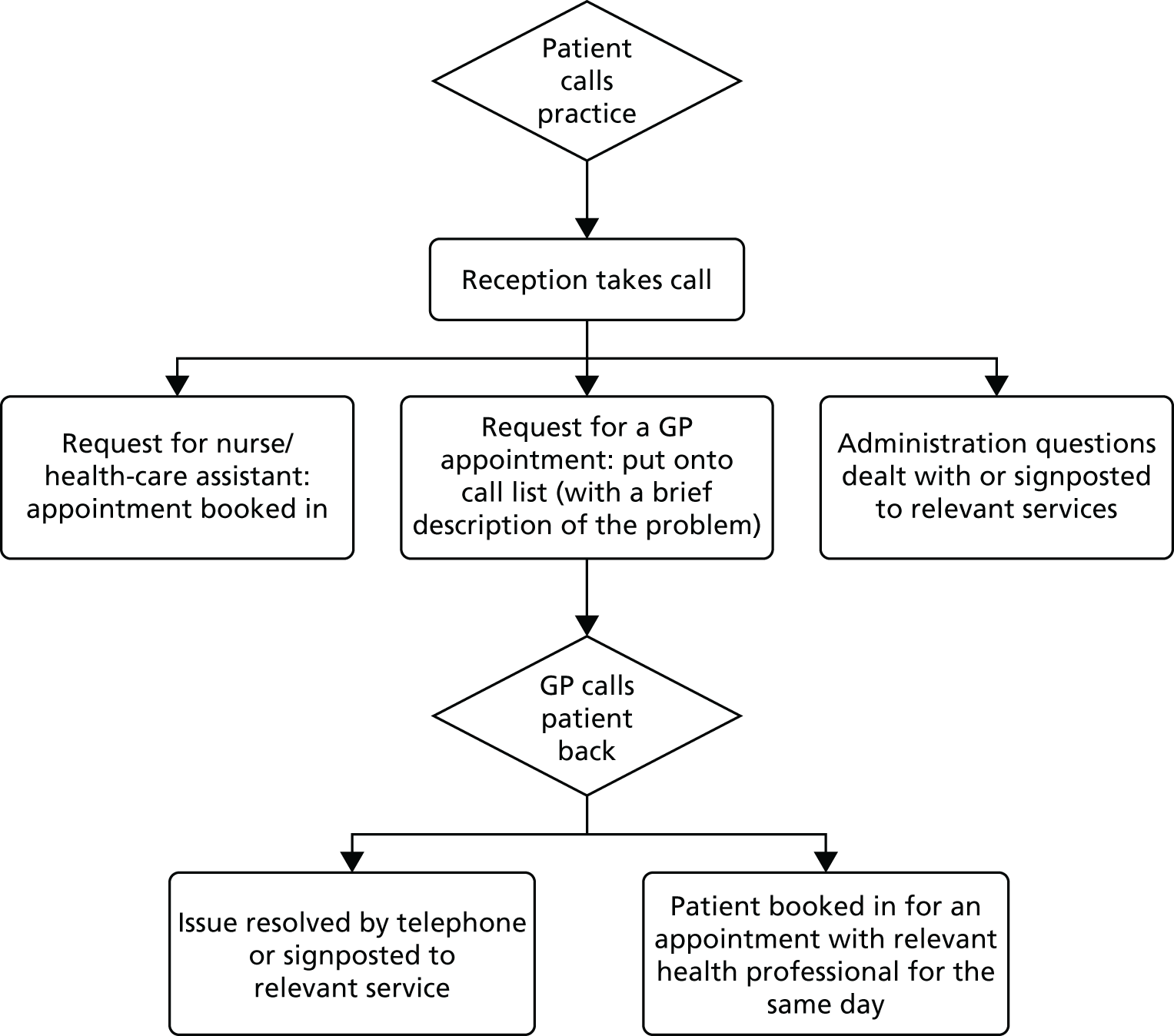
Despite the growth in the use of telephone consultations in general practice in England, there is limited evidence as regards their effectiveness in reducing overall workload in primary care, with studies suggesting that increasing the use of telephone consultations has a neutral impact on workload or may actually increase it (see Chapter 2). Currently, two commercial companies in England, GP Access Ltd (Cossington, Leicestershire) and Productive Primary Care Ltd (Woodhouse Eaves, Leicestershire; commonly known as ‘Doctor First®’), offer a new and significantly different pathway for patients seeking a face-to-face general practitioner (GP) appointment. The approach was first rolled out in 2011 and has been taken up by a small but growing number of practices (147 practices had been using the approach for ≥ 6 months at the time of this study). Starting with a detailed analysis of demand and workforce capacity, the ‘telephone first’ approach (described in detail in the following sections) promoted by these companies requires all patients requesting an appointment to first speak to a GP on the telephone rather than arranging a face-to-face consultation directly. After contacting the surgery, patients are called back on the same day by a GP and, at the end of this call, a decision is made regarding whether the patient needs to come in to see a GP face to face (usually on the same day), whether they need to be directed to an alternative health-care provider or whether their concern can be satisfactorily and appropriately dealt with on the telephone. At the start of the day, the majority of GP appointment slots are free, giving GPs the control to determine when, and for how long, to book face-to-face appointments. Patients are required to contact the surgery on the same day that they wish to be seen. It also means that all patients requesting an appointment with a GP will at least speak to a GP on the same day. Figure 1 shows how a ‘telephone first’ system typically works. We suggest the term ‘telephone first’ for this approach to differentiate it from ‘telephone triage’ or ‘telephone consultation’, which are terms used widely in the literature. ‘Telephone triage’ implies assigning priority to seeing patients, which, although this is an element of the ‘telephone first’ approach, is too limited to describe the wider system change. ‘Telephone consulting’ involves a discussion between a health professional and patient focused on the management of an existing condition or the diagnosis and treatment of a newly presented condition.
FIGURE 1.
Flow diagram of a typical ‘telephone first’ system.
Significant claims have been made as to the effectiveness of these ‘telephone first’ systems; for example, in 2013, a NHS England guide to the evidence base for urgent and emergency care5 stated that:
Proven and tested systems exist in England, where telephone consultations are used routinely in general practice, whilst other developed systems include telephone assessment of all patients prior to attending the practice [. . .]. The ‘Doctor First®’ model [one of the operating models available] has demonstrated a cost saving of approximately £100k per practice through prevention of avoidable attendance and admissions to hospital.
Reproduced with permission from NHS England. 5 Contains public sector information licensed under the Open Government Licence v3.0
These claims are based on data from companies that have a commercial interest in promoting their product. Despite this overall positive assessment of the Doctor First model, the NHS England report also highlights that there is insufficient evidence to know to what extent these systems may generate new demand through help-seeking for minor conditions, the acceptability of the non-face-to-face consultations for certain patient groups including older people and any consequences for patient safety, for example through the loss of visual clues. 5
Evaluations and academic literature have not focused on ‘telephone first’ systems to date; for example, a recent cluster randomised controlled trial (RCT) (the ESTEEM trial)6 provided robust evidence comparing nurse-led and GP-led triage systems in primary care. In contrast to the ‘telephone first’ approach, in which all requests for face-to-face GP appointments are triaged, the ESTEEM trial practices were running a traditional booking system in which the majority of appointments are booked in advance by reception staff and triage was used only for patients requesting same-day consultations within general practice. 7
As ‘telephone first’ systems are being rolled out across England, there is a need for rigorous evaluations to understand the impact of these telephone-based systems. These evaluations may include understanding patient experience, including appropriateness for hard-to-reach groups; impact on consultations from the perspective of patients and staff; and impact on subsequent use of primary and secondary care services.
It is also important to understand the cost consequences of these systems for general practice.
Study design
This evaluation of the ‘telephone first’ approach was a multimethod study. A number of methods were used to enable detailed exploration of the impacts of the ‘telephone first’ approach in general practice. The study comprised three key elements: (1) quantitative, (2) economic and (3) qualitative. The study design used a controlled before-and-after (time-series) approach using national reference data sets; this approach enabled exploration of the impacts of the ‘telephone first’ approach on primary and secondary care services; the latter was a particular focus of this study, given the claims made about ‘telephone first’ approaches in NHS England literature. 5 Such documents also advocate the cost savings of such an approach; as a result, we incorporated an economic element in the study to explore the cost consequences of the approach in general practice.
Given the radical change that a ‘telephone first’ approach has on the way a practice operates, we also wanted to identify the impacts on patients, staff and hard-to-reach groups. We used a qualitative approach for this element of the work, to enable us to explore in detail the views and experiences of staff and patients using a ‘telephone first’ approach.
Aims and objectives
Our research sought to address three main research questions:
-
How does a ‘telephone first’ approach affect patient experience and use of primary and secondary care services?
-
What is the impact of ‘telephone first’ approaches on the nature of consultations for patients and staff, and how appropriate is this approach for hard-to-reach groups?
-
What are the cost consequences of a ‘telephone first’ approach in general practice?
To address these questions, we used a combination of qualitative and quantitative approaches and a cost–consequences analysis for the economic evaluation. The research focuses on practices using a ‘telephone first’ approach provided by one of two known commercial providers in England: Doctor First (provided by Productive Primary Care Ltd) and GP Access (provided by GP Access Ltd).
Selected ‘telephone first’ approaches
Figure 1 summarises how both approaches (Doctor First and GP Access) work for patients seeking an appointment. Box 1 provides further details for patients seeking an appointment with a GP, based on the GP Access standard approach. For all contacts, patients are encouraged to telephone the practice, although exceptions are expected for patients for whom this is not feasible (e.g. deaf patients). It is important to note that systems can be adapted by practices. We found more information on a specified standard approach for GP Access than on a specified standard approach for Doctor First, and this is reflected in the detail provided in Box 1.
-
Practice receptionist will take the patient’s details (name, date of birth and contact telephone number) and may ask for a brief description of the problem and any special requests (e.g. for callback not to be at a certain time). A specific subset of calls may be directly booked in with the GP (e.g. antenatal checks).
-
The call can be directly transferred from reception to a GP or added to the GP’s callback list. GP Access specifies two approaches that a practice could use to organise callback lists: (1) a list from which all GPs pick patients (may have GP initials by patient to indicate preference) or (2) a separate list for each GP on duty for callbacks in that session.
-
The GP prioritises calling patients back based on the information provided, rather than in chronological order. GP Access specifies that a GP may decide to bring the patient in without a call, if the problem note and history mean a call would be redundant. The doctor phones the patient and together they decide if and when the patient needs to be seen face to face in the surgery (either by a GP or by another health professional) or if the issue can be dealt with via telephone or needs to be directed to another service.
-
If at the end of the telephone consultation the patient still wants to be seen, the GP will book them in for a face-to-face appointment. When a face-to-face appointment is arranged, the majority (both GP Access and Doctor First report around 80%) will be arranged to take place on the same day as the call.
Support offered by the companies
It is important to note that the two providers do not just provide a ‘telephone first’ appointment system but seek to work with practices to understand and manage demand and provide support in the implementation of and transition to their specific ‘telephone first’ approach. Doctor First has a three-stage approach for transitioning to a ‘telephone first’ approach over an 18-week period: (1) data gathering, to help practices to gain a clear understanding of activity, backlog, capacity and demand in order to identify how many clinical sessions are required per day to meet the demands of patients (takes 4–8 weeks); (2) an implementation phase, to reduce backlog of appointments and provide training to all staff to help with the smooth transition to Doctor First, inform patients of upcoming changes and clinical system configuration (takes 10 weeks); and (3) following ‘going live’, 4 weeks of patient feedback and monitoring to help gather views on the system and communicate with patients. 9
The other provider, GP Access, has a five-stage approach over 12 weeks; this is described as (1) coming to a consensus among partners and appointing a change leader (week 1), (2) preparing the whole staff team, patients and the system [includes an e-learning session for GPs on telephone consulting (weeks 1–3)], (3) support on the launch day (weeks 3–4), (4) access to rapid support by telephone following changeover (weeks 5–11) and (5) confirming decision to continue with approach 12 weeks after implementation. GP Access also offers practices a 3-month subscription to an analytical support service, which provides measurement, feedback and advice to address problems as they arise. 10
Reported benefits of the approach
Both providers report substantial benefits of the system to practices, in terms of both reduced stress for practice staff and cost savings as a result of time saved and more efficient use of time. The providers also report that practices that have switched to the new system have increased patient satisfaction. The nature of the claims made by Doctor First and GP Access on their websites are summarised in the following sections. As noted, there is no independent evaluation to date to support or refute these suggested benefits; our study seeks to address this gap in the evidence base.
Claims made by Doctor First
On its website,11 Productive Primary Care has made a range of claims relating to benefits of Doctor First for both patients and GPs/practice staff. For patients, the stated benefits include being able to see the doctor of their choice at the time they choose, greater patient satisfaction (as indicated by a reduction in complaints) and the fact that the approach ensures that the sickest patients are seen first. With respect to clinician satisfaction, claims are made regarding the system enabling a more productive and satisfying way of working, with increased knowledge of and control over workload and working life. With respect to benefits for practice staff, it is claimed that there are improvements in the work environment and satisfaction of reception staff as a result of the availability of sufficient appointments to meet the needs of all patients (so that they are no longer acting as a barrier to, but rather as a facilitator of, the patients’ journey through practice systems) and the fact that they are not required to make decisions outside their area of expertise, which would be better made by clinicians. In addition, claims are also made regarding benefits to the practice overall, including the near-complete disappearance of ‘did not attends’ (DNAs), financial savings (for reinvestment) of > £30,000 per annum per full-time GP, and a happier work environment as a result of a reduction in stress for patients, GPs and practice staff alike. 9 Finally, there are reported benefits with respect to savings for the NHS more broadly, with reference to a 20% reduction in accident and emergency (A&E) attendance for practices using Doctor First. 11
Claims made by GP Access
Similarly, GP Access has made a range of similar claims on its website. Patient satisfaction is identified as a key benefit,12 linked to reported improvements in continuity of care (e.g. an increase in continuity of care in one Norfolk practice from 53% to 60% over 6 months following the introduction of the approach, and 80% continuity being achieved in a Dorset practice that had been using this model for 11 years)13 and the claim that the approach provides the capacity for the GP to see the patients who need to be seen as soon as possible and usually on the same day. 12 With respect to benefits for GPs and practice staff, claims are made regarding the potential to raise GP productivity by 20%, leading to reduced stress, saving time and resulting in a happier practice. 10 Again, claims are made regarding benefits to the practice overall, including reductions in the numbers of DNAs14 and financial savings (with reports of a saving of £90,000 per annum in one Leicestershire practice). 15 Finally, there are reported benefits for the wider NHS, with a reported 20% reduction in emergency admissions from practices using the GP Access model. 16,17
Structure of the report
This report begins by presenting a literature review of existing evidence around telephone consultation approaches in general practice, designed to establish what is already known about our main research questions (see Chapter 2). The following chapters present the method and results from each of the main parts of the study, namely analysis of data from practices (see Chapter 3), our patient experience survey (see Chapter 4), our practice manager survey (see Chapter 5), analysis of data from the national GP Patient Survey (see Chapter 6), analysis of hospital utilisation data (see Chapter 7), economic analysis (see Chapter 8), interviews with patients (see Chapter 9) and interviews with staff (see Chapter 10). The discussion and conclusions are presented in Chapters 11 and 12.
Impact of patient and public involvement
The study team benefited from input from a number of patient and public involvement (PPI) members during the study; for example, the PPI members recommended the inclusion of out-of-pocket patient expenses in the economic analysis. We also had patient input on written documents, such as patient information leaflets and consent forms, ensuring that information disseminated to participants was suitable and understandable to a lay audience. Rather than repeating this information in each chapter, we have summarised the contribution of PPI in Chapter 11, Impact of patient and public involvement.
Ethics approval and consent
This study was reviewed and given a favourable opinion by the West of Scotland Research Ethics Committee 5 (reference number 15/WS/0088). Written informed consent was sought from all participants for participation in and audio-recording of interviews and for the publication of anonymised quotes.
All required research governance approvals were obtained.
Changes to the protocol
During the course of the study, under the guidance of our study steering committee (SSC), a number of minor changes to the original protocol18 were made regarding the design and methodology of the study. The changes relating to each element of the study, along with the rationale underlying the amendments, are set out in the following sections.
Analysis of administrative data from general practices (see Chapter 3)
Changes to the outcomes considered
In addition to the outcomes presented in Chapter 3, our original protocol stated that we would also analyse DNA rates, waiting times in surgery, recall rates and time for GPs to return calls. However, when we got into detailed discussion with the commercial provider who was making data available, it was clear that these data could not be reliably extracted and, therefore, they were not in the list of data items supplied by the company.
Patient experience survey (see Chapter 4)
Change to the number of practices surveyed
The number of practices taking part in the patient and carer survey element of the study was reduced from 28 (as specified in the original protocol) to 20, and the number of surveys sent out by each practice was increased. The rationale for this change was to ensure a more efficient use of resources without significantly affecting the power of the study to detect differences between groups. Under the original plan, we anticipated 450 responses from 28 practices; 837 responses were ultimately received from 20 practices.
Change to inclusion criteria for patients and carers
On the recommendation of the SSC, changes were made to the inclusion criteria for patients and carers to be sent a survey in order to address potential risks regarding confidentiality for particular groups of patients (e.g. teenagers, patients at risk of domestic violence and patients dealing with sensitive issues, for whom receiving a postal survey indicating that they have had a recent appointment may be a risk to confidentiality). A step was introduced into the protocol: GPs screened the list of patients selected to receive a survey and removed those patients for whom inclusion was considered to be a risk. In addition, whereas parents of patients aged ≤ 12 years were sent a survey to complete on behalf of the child, parents of teenage patients were excluded because of potential risks to patient confidentiality for this age group.
Patient experience: analysis of data from the national GP Patient Survey (see Chapter 6)
Change to included covariates in regression models
In the original protocol, practice-level covariates (practice size, rurality, deprivation and ethnicity/age/sex profile) were planned to be included in regression models along with patient-level covariates. However, on attempting to run these models they were found to be very slow to converge, making analysis impractical. As a random intercept for practice was included, the practice-level effects should already have been controlled for, and so these variables were dropped from the analysis to simplify the models. It was not expected that this would make any material difference to the results obtained.
Secondary care utilisation: analysis of Hospital Episode Statistics data (see Chapter 7)
Change to included covariates in regression models
As with the analysis of GP Patient Survey data, it was found that the models using Hospital Episode Statistics (HES) data were very slow to run and simplifications had to be made. Again, practice-level covariates were not included in line with the GP Patient Survey analysis. It was not expected that this would make any material difference to the results obtained.
Economic analysis (see Chapter 8)
Change from postal to telephone survey for collection of cost data
In developing the survey on costs (which was to be completed by practice managers at all intervention practices), it became apparent that, given the complexity of some of the answers required, and following discussion with external colleagues with experience of gathering similar data, it would be more appropriate to complete the questionnaire over the telephone than by sending it out by post. This enabled the provision of guidance and support in completing the required information that would not have been possible if it had been completed independently in paper form. Sending out a complicated questionnaire by post would have been likely to result in a low response rate.
Reduction in the number of practice managers invited to participate in the cost survey
Because it was anticipated that a better response would be achieved by using a telephone survey than by using a postal questionnaire, we revised the protocol so that we planned to approach up to 30 practice managers, selected at random from the 102 intervention practices, rather than sending a postal questionnaire to all practice managers. In total, 18 practice managers participated, and this sample was considered sufficient to gain an understanding of the costs involved.
Change to method for obtaining pricing of systems
Fees paid to the commercial providers were provided by the practice managers in the cost survey. Therefore, it was unnecessary to contact the providers for this information.
Change to analysis approach for cost survey data
Because of the anticipated difficulty in obtaining reliable quantitative data, we altered the approach to the analysis of the cost survey data to comprise a description of the cost items involved, supplemented by limited quantitative analysis (including identification of upper and lower cost bounds for sensitivity analysis) when meaningful and appropriate.
Change in the time horizon
In the original protocol,18 we proposed using data extracted for up to 3 years prior to and up to 2 years post the adoption of a ‘telephone first’ approach. Instead, we simply used Prescription Cost Analysis data (NHS Business Services Authority)19 and HES data from 2009 to 2016 in control practices and ± 12 months from the launch of ‘telephone first’ in intervention practices, mirroring the outcomes analysis.
Change to summary of results
Because we were unable to estimate a mean cost of installing and running the systems in a reliable quantitative manner, we do not present an overall cost per month but instead present a text summary of all of the cost components.
Interviews with patients and staff (see Chapters 9 and 10)
Change to the number of practices involved in the qualitative element of the study
In the original protocol, we planned to interview patients and staff at eight practices about their experiences relating to the ‘telephone first’ approach; however, in order to allow greater variation in the characteristics of the practices selected for study, because of the observed wide variation in practice setting, practice characteristics and how the approach had been implemented, we proposed to increase this number to 14 practices.
Analysis of disenrolment data (not conducted)
The original protocol included examining disenrollment data. However, because of the delays in obtaining HES data, we decided not to request additional data on disenrolment as it would have caused further delays in the delivery of the project.
Chapter 2 Literature review
The literature review aimed to review and synthesise existing evidence around telephone triage and telephone consulting in primary care settings in the UK and other high-income countries.
Methods
Our review drew on scoping review methodology20 to establish what is known about telephone triage and telephone consulting broadly, and in relation to our three main research questions. We sought to capture but did not explicitly search for or restrict our search to ‘telephone first’ approaches. Full details of the search strategy, inclusion and exclusion criteria and data extraction and synthesis are given in Appendix 1. An electronic search of the PubMed research literature database was conducted up to 9 November 2016. In addition, The King’s Fund Health Management Information Consortium (HMIC) data were searched (from 1995 to 16 January 2017). The main search terms were ‘primary care’ or ‘general practice*’ AND ‘phone’ or ‘telephon*’ AND ‘triag*’ or ‘consult*’. Studies were excluded if they had a sole focus on nurse-led, emergency or out-of-hours triage, if they were published in a language other than English and if they did not focus on high-income countries. No exclusions were made on the basis of publication type or on date of publication for PubMed. Guided by our research questions, data were extracted on study type and methods, type of telephone system (triage or consultation or both), details of telephone system, setting (geographical and health care), reported outcomes [health outcomes, patient safety, staff experience, patient experience (hard-to-reach groups), impact on service use, impact on consultation, and cost] and other notable findings. We sought to undertake a narrative synthesis rather than pool numerical results, based on our research questions and knowledge of the literature. We did not seek to exclude studies based on quality, although we noted methodological concerns in our synthesis.
Results
A total of 911 articles were identified via the database searches outlined in Methods and detailed in Appendix 1. Of these, 836 were excluded based on screening of titles/abstracts, in line with our inclusion and exclusion criteria, and 75 were selected for full-text review and data extraction. Of these, two were unavailable and 18 were excluded following full-text review, because they did not contain empirical research or only touched tangentially on telephone consulting.
Fifty-five papers were included in the review: 23 relating explicitly to telephone triage systems, 31 to telephone consultations and one to a range of primary care patient interfaces, such as e-mail. Papers came from the UK (53), the Netherlands (1) and the USA (1). These included 22 non-peer reviewed pieces (e.g. news articles, editorials, letters and opinion pieces) and 33 peer-reviewed articles. Study types included:
-
studies related to two RCTs (8 papers)
-
systematic reviews (2)
-
a literature review with undefined methods (1)
-
an audit (1)
-
qualitative interview/focus group studies (4; across 5 papers)
-
patient–doctor dialogue analyses (3)
-
studies using primary survey data (of patients, practice staff and/or GPs) (12)
-
a national retrospective analysis of the amount and nature of primary care activity (1)
-
quantitative analyses of prescribing behaviour (1) and patient recall of the content of consultations (1).
Key studies and bodies of work
The majority of studies reviewed were based in the UK (53), and among these it is worth noting two dominant bodies of work, that is, papers relating to the same study or involving the same authors.
The first is the ESTEEM trial, to which nine papers relate. 6,7,21–27 The ESTEEM trial was a cluster RCT comparing nurse-led and GP-led telephone triage systems with usual care for patients requesting same-day consultations in general practice in England. 28 The core intervention in the ESTEEM trial consisted of a number of steps. Following an initial telephone conversation with a receptionist, patients requesting a same-day face-to-face appointment with a GP were called back by either a nurse or a GP. The phoning clinician discussed the patient’s condition and chose from a range of management options, such as dispensing self-care advice, booking a same-day or future face-to-face appointment or referral to other appropriate services. 6 In addition to presenting evidence around clinical effectiveness and cost-effectiveness of GP- and nurse-led triage, papers resulting from the trial also explore patient and staff experience, patient satisfaction and impact of telephone triage on GP workload.
The second dominant body of work is a series of five papers by McKinstry and colleagues. 29–33 These include qualitative research around GPs’, other staff members’ and patients’ views on the safety and appropriateness of telephone consultations compared with face-to-face consultations, as well as a two-site RCT investigating the use of doctor time and subsequent service use for telephone consultations compared with face-to-face consultations (as a way to manage requests for same-day appointments). 31 The RCT excluded urgent cases and patients asking to speak to the GP specifically for advice. In addition to the original journal articles, the RCT also accounts for seven letters to journal editors,34–39 written in response, and one editorial40 included in our review.
Terminology
The literature refers to both ‘telephone triage’ and ‘telephone consultation’, but it can be challenging to differentiate what is meant by each. In many cases, the terms appear to be used interchangeably or are ill-defined or poorly described. 41 The term ‘telephone triage’ is generally applied to an approach in which patients requesting a face-to-face appointment are asked to first speak to a doctor by telephone before a decision is made regarding whether or not the patient needs to attend and how quickly that should happen. ‘Telephone consultation’ can be understood as a more general term, which encapsulates consultations undertaken as part of triage or consultations that are undertaken by telephone for other purposes, such as scheduled check-ups or follow-up for the management of chronic conditions. In this chapter, we use the term ‘telephone consultation’ to encompass both triage and more generic consultation systems. It was not clear if any of the systems covered in the literature related directly to ‘telephone first’ approaches as presented in this study.
Prevalence of telephone consultations
There are few empirical studies that give an indication of the level of use of telephone consultations in general practice. A survey of general practices in Devon,42 published in 2001, showed that 19% of practices (n = 15) surveyed were offering telephone consultations for patients seeking same-day appointments that were not deemed urgent. A survey of practice managers in Wales,43 published in 2008, reported that 42% of those who responded (n = 167) had introduced GP telephone consultations more systematically since 2003, when a new General Medical Services contract was introduced. More recently, a survey of the use of different forms of alternatives to face-to-face appointments30 showed that two-thirds of practices (211/318, 66%) surveyed, across south-west England and Scotland, reported that they were using telephone consultations ‘frequently’, although this was not further defined.
Before the publication of a retrospective analysis of 100 million consultations in England (2007–14)44 in 2016, information on the proportion of consultations that take place by telephone within a general practice was mainly restricted to information provided by individual GPs in letters to journals. In these,34,37,45 GPs make the claim that telephone consultations form an important part of appointment provision, accounting in one case for 43% of all appointments. 45 The much larger retrospective analysis by Hobbs et al. 44 included analysis of GP and nurse consultations for registered patients at 398 English general practices from April 2007 to March 2014. The largest change observed in patterns of consultation over this period was a doubling of GP telephone consultation rates. This increase compared with a 5.2% increase in GP face-to-face consultations over the same period, although face-to-face consultations still accounted for 90% of all consultations despite the increase in use of telephone consultations.
Impact on access to primary care
One potential advantage of telephone consultations is that they improve access, either by negating the need to travel or by increasing convenience for patients; however, there is limited research addressing this directly. A qualitative study in Scotland33 reported that GP telephone consultations were generally seen to improve patient access. For patients who worked full time, had reduced mobility, valued not needing to travel to the surgery or lived in rural and remote areas, telephone consultations were seen as a helpful way to overcome physical distance and the need to travel. In urban practices, greater emphasis was placed on using telephone consultations for acute presentations as a way of managing demand.
The ESTEEM trial of telephone consultations for patients requesting same-day appointments23 reported that, although the introduction of the telephone consulting system was associated with improved access in terms of getting through on the telephone, there was no overall difference in ease of access to prompt care, comparing patients receiving the GP-led telephone system and those receiving usual care. The study also found that the introduction of telephone consultations did not seem to alleviate the challenges faced by working patients in accessing flexible and convenient care. 23 Patients unable to take time away from work or who could do so only with difficulty reported lower satisfaction than those who did not have these challenges, and this did not vary depending on whether patients were receiving GP-led telephone consultations or usual care. 27
Perceived appropriateness of telephone consultations
Patient and doctor perceptions of the appropriateness of using telephone consultations to deliver care in general practice appear to be given most focus among earlier published studies. Two studies46,47 found little agreement between doctors and patients in perceived appropriateness of GP telephone consultations for a given complaint. Stevenson et al. 46 found that, after face-to-face consultations, doctors and patients were in agreement about only 5.5% of 1067 face-to-face consultations in terms of whether or not the issue discussed could have been dealt with by telephone. Doctors showed a greater inclination towards telephone use than patients, with consultations considered in hindsight to be appropriate for management by telephone in 13.9% of cases for GPs, as opposed to 11.4% of cases for patients. 46 The single-practice study by Kernick et al. 47 also found little agreement between patients and doctors, who were separately interviewed before booked face-to-face consultations regarding whether they felt that the patient could have been appropriately managed by a telephone consultation with the GP or a consultation with a specially trained nurse. The study reported that both patients and doctors considered that only a small number of cases were suitable for management by telephone (5.8% and 5.1%, respectively). Among GPs interviewed by Hallam,48 there was broad agreement on the types of complaint that could be appropriately handled by telephone, including minor, self-limiting conditions and certain recurring conditions, whereas those thought to be inappropriate for telephone consultation included chest pain, abdominal pain, breathing difficulties, illness in a young child or new patient, non-traumatic bleeding and high fever.
More recently, the ESTEEM trial process evaluation6 suggests that patients are more open to telephone consultations and have greater confidence in the GP assessing their problem on the telephone. Patients appreciated the convenience offered by GP telephone consultations and felt that it made sense for the doctor, rather than the patient, to decide whether or not an appointment was needed and to weed out ‘time wasters’.
Experience of patients
Patient satisfaction
A range of studies published from 1992 to 2015 report on patient satisfaction with GP telephone consultations. These studies tend to report high levels of satisfaction, although many do so without a comparator. 49–52 Jiwa et al. 49 reported that 98% of patients responding to a survey in one general practice were satisfied with the outcome of a GP telephone consultation and 84% [95% confidence interval (CI) 76% to 90%] would happily receive the service again in similar circumstances. Two RCTs21,31 reported no significant difference overall in patient satisfaction between those who received telephone consultations and those who received face-to-face consultations with their GP. Analysis from the ESTEEM trial also allowed comparison between patients managed by telephone consultation by a GP or by a nurse. Calitri et al. 21 found that, compared with GP face-to-face consultations, patients who received a nurse telephone consultation alone, or who received a nurse telephone consultation with a subsequent GP face-to-face consultation, were less satisfied than those whose telephone call was with a GP initially.
Confidentiality
One discussion paper,53 one qualitative study29 and the ESTEEM trial process evaluation6 raise specific concerns around confidentiality and telephone consultations. The qualitative study,29 involving patients, clinicians and administrative staff, reported a broad range of concerns. These related to conversations that could potentially be overheard (whether at home, in the surgery, at work or in public spaces) and the disclosure of personal information to the receptionist. In addition, difficulty of maintaining privacy in small communities, errors in identification and identity fraud, the use of answering machines, third-party conversations (e.g. between the doctor and a relative if the patient’s consent is unclear) and teenagers’ confidentiality, especially in relation to sexual health, were raised as concerns. 29
Experience of hard-to-reach and vulnerable groups
Although the introduction of telephone consulting may help to overcome some barriers to access for primary care, such as physical distance, a number of studies reflected concerns that telephone consultation systems may exacerbate access inequalities or differential experiences for hard-to-reach or potentially vulnerable groups of patients. Groups of concern in the literature include those without access to a telephone or with language or other communication difficulties,54 as well as older people, ethnic minorities and the economically deprived.
Older people
Two studies51,55 showed that older patients were one of the largest and most frequent users of telephone consultation services. Although a recent survey of general practices in England and Scotland30 highlighted concerns among some GPs that elderly patients could be disadvantaged as a result of telephone consultations, there is very little research from which to judge whether or not this concern is realised in practice. One study across five general practices56 found that older patients were not disadvantaged by telephone consultations in primary care, and that Patient Enablement Instrument (PEI) scores (a self-reported measure of a patient’s ability to cope with illness) following telephone consultations did not differ between older (aged > 70 years) and younger respondents.
Ethnicity
Two studies27,57 considered the experiences of patients from ethnic minority groups with telephone consultations and suggest that the pattern of experience is varied and sensitive to the type of health-care professional involved. In the ESTEEM trial, differences in satisfaction with different telephone consultation approaches reported between ethnic groups were generally small (with those from ethnic minority groups being less satisfied than British white patients), and substantially less than differences in overall satisfaction reported by ethnic minorities compared with white British patients. 27
However, an earlier qualitative study by Rashid and Jagger57 compared views and experiences of telephone consultations among Asian and non-Asian patients, and reported that more Asian patients disliked management of illness by telephone and consultations that did not involve GPs (e.g. with a nurse) than non-Asian patients. The authors reported that only 6% of Asian patients reported difficulty explaining their symptoms in English and concluded that cultural differences were more likely to explain the differences in experiences and views of telephone consultations and other aspects of using health care.
Deprivation
The ESTEEM trial found a non-significant difference in reported convenience for GP-led telephone consultations and nurse-led triage compared with usual care by patients in more deprived groups. 27
Experience of staff
Clinicians
Clinicians’ experiences were explored in the ESTEEM trial process evaluation,6,26 although the authors note that findings may have been affected by the implementation of telephone consultations under trial conditions.
The authors found that attitudes towards telephone consultations varied between practices and doctors. Telephone consultations were seen to benefit practices in a number of ways. They were viewed as an optimal use of resources, allowing them to allocate appointments more equitably, efficiently and rationally, and facilitating more appropriate appointments6 than before. Perceived benefits were accentuated by overwhelming demand that staff reported having experienced previously, and telephone consultations were often seen to have helped in this regard. Indeed, clinicians’ experiences of reduced pressure and stress as a result of the introduction of telephone consultations were also noted across some of the grey literature. 58
However, factors such as the effective allocation of resources and support, division of workload and roles and communication also affected successful implementation and staff acceptability. Workload disparity between clinicians was a key challenge, with some GPs taking on more calls than others, whether because of patient preference (e.g. female GPs taking on more female patients) or because of the use of a ‘duty doctor’ system, in which specific GPs were charged with taking calls at any given time. Although the latter could have the potential to even out workload, some of the staff who were interviewed felt that this placed additional burden on non-duty doctors, who had to cope with the demand for face-to-face appointments by doing additional sessions or taking paperwork home,26 thus highlighting the importance of careful planning in staff allocation in the use of telephone consultation systems. Although some GPs were entirely comfortable with using the telephone, others found the experience stressful, dissatisfying and inefficient. 6 The manner in which system change is communicated and discussed among staff was also important to how the telephone consultation approach was received,26 and a supportive staff team and culture of adaptability to change improved acceptability.
Reception staff
Two studies reported on reception staff’s experiences and showed that these were mixed, possibly dependent on the model of telephone consultation and variable roles for receptionists within these. Receptionists interviewed as part of the ESTEEM trial felt that the telephone consultation system made their job less stressful by relieving the burden of finding appointments, dealing with patient frustration or having to make judgements about the urgency of patients’ complaints;6 however, the authors also noted the importance of resource allocation to support and empower reception staff in their new roles within the telephone-based system,26 and indeed a qualitative study in Scotland29 emphasised the discomfort felt by some receptionists because of the responsibility placed on them to request information about a patient’s condition(s) for the purposes of triage.
Education and training
The importance of education regarding the proper use of telephone consultations for clinicians and staff, as well as for patients, was highlighted by some authors, although it was not the main focus of any study reviewed.
Three papers55,59,60 from the grey literature highlighted concerns regarding a lack of specialised training for clinicians delivering telephone consultations, with GPs having to learn by trial and error. 55 The lack of training for receptionists and their key role in distinguishing urgent from non-urgent cases was also seen as a potential risk to patient safety. 60
Patient education and understanding of telephone consultation systems was also a factor explored in the literature, although to a small degree. A published survey of four practices in England52 linked significant differences in levels of patient awareness of telephone consultation systems between practices to the practices’ approaches to publicity. These included receptionists telling patients, use of leaflets or posters or reliance on word of mouth. 52 The study found that only half of the total number of patient respondents (n = 1025) knew that they could speak to a doctor by telephone. More recently, the ESTEEM trial process evaluation6 found that some patients were confused about how their new consultation system worked.
Impact on the nature of consultations
Two studies in the UK that compared the nature and content of patient–doctor interactions in telephone and face-to-face consultations61,62 found that telephone interactions were shorter and largely focused on single-issue or biomedical concerns. Telephone consultations emphasised biomedical information exchange over psychosocial or affective communication, and doctors used closed questions much more commonly than they used open ones;62 however, Hewitt et al. 61 point out that brief telephone consultations are appropriate when telephone consultations for new problems would lead to a face-to-face meeting. The ESTEEM trial25 also compared nurse and doctor telephone interactions with patients in a sample of video- and audio-recorded consultations. They reported that, although the length of calls was similar, nurses asked patients more questions [mean 14.72 questions, standard deviation (SD) 6.42 questions] than GPs (mean 5.51 questions, SD 4.66 questions), on average, whereas GPs asked more questions eliciting patient concerns or expectations and to obtain medical history than nurses (43% of GPs’ questions were of this nature, compared with only 11% of nurses’ questions). In interpreting these apparently large differences, it is important to note that the nurses, but not GPs, were using computer-aided software when they took a patient history.
Patient safety and health outcomes
A number of papers raise concerns about patient safety in relation to use of the telephone as an alternative to face-to-face contact with GPs, and indeed conclusions with regard to safety have been the subject of disagreement and debate among researchers;63 however, few studies have provided empirical evidence to support these concerns. 64
Studies that reported that telephone consultations appear safe did so only on the basis that patient–doctor communication can be adequate and patient recall of safety-netting instructions is improved. Most recently, although the authors could not rule out differences between groups for measures of safety, the ESTEEM trial found that GP- and nurse-led telephone consultations appeared safe, and were not associated with excess deaths, hospital admissions or attendance at emergency departments. 23
Impact on service utilisation and delivery
Impact on primary care contacts
The impact of GP telephone consultations on primary care workload and on the number of face-to-face appointments was a key issue in a range of studies, which suggests that, although telephone consultations can result in initial reductions in primary care demand, over time this may represent a redistribution of workload rather than an overall saving. There is some evidence in small-scale studies49,65 and claims in letters34,55,66 that GP telephone consultation systems reduced patient demand for face-to-face appointments, out-of-hours services49 and home visits. 34,65 Earlier studies of patient perspectives also suggested that telephone consultations resulted in resource savings, as approximately three-quarters of patients surveyed who had received telephone consultations would have made a face-to-face appointment had they not spoken to the GP on the telephone. 51,67
However, the ESTEEM23 and McKinstry et al. 29 RCTs suggest that an initial drop in face-to-face contacts is associated with a redistribution rather than reduction of GP workload. The authors found that GP telephone consultations led to an increase in consultations (of all types) in the subsequent 2 weeks (from 0.4 to 0.6 consultations, 95% CI of difference 0.0 to 0.3 consultations)6,31,35,41 or an overall increase in combined telephone and face-to-face contacts compared with usual care. 6,23
The ESTEEM trial found that GP telephone consultations were associated with a 33% increase in the mean number of contacts over the next 28 days compared with usual care (face to face and telephone combined) [2.65 (SD 1.74) contacts (telephone consultation system) vs. 1.91 (SD 1.43) contacts (usual care), rate ratio (RR) 1.33, 95% CI 1.30 to 1.36]. Although GP telephone consultations reduced face-to-face contacts by 39% (RR 0.61, 95% CI 0.54 to 0.69), the mean number of telephone consultations per patient increased 10-fold. Thus, the authors identified an overall redistribution of GP workload with GP telephone consultations, with any time savings from reduced face-to-face contacts more than balanced by increases in the number of telephone contacts undertaken. 6
Impact on the duration of clinician contact
The ESTEEM23 and McKinstry et al. 29 RCTs also examined the impact of telephone consultations on the duration of clinician contacts, and found no significant difference and some time savings, respectively, when compared with usual care. The ESTEEM trial found no overall clinician time savings from GP telephone consultations: the composite duration of clinician–patient contact on the day of the request was 10.3 minutes for GP telephone consultations and 9.6 minutes for usual care, with no clinically significant difference in the overall GP time required between the two. 24
The two-site RCT by McKinstry et al. 31 found that the use of telephone consultations for same-day appointments was time-saving overall, in terms of patient–doctor contact, compared with those appointments that were made directly face to face, but the longest clinician contact was for those who consulted by telephone and were subsequently asked to come to the practice (mean 10.9 minutes, SD 4.4 minutes);35 however, shorter-term savings may have been offset by the higher subsequent reconsultation noted above. Two trials24,31 found that the duration of a GP face-to-face consultation combined with a preceding telephone consultation was longer than that of a face-to-face consultation in usual care.
Impact on use of out-of-hours and emergency services
Although the grey literature reviewed includes claims of lower numbers of A&E attendances as a result of the introduction of telephone consultation systems,68–70 the evidence to bear out these claims is limited, as only one study23 reported on the impact of telephone consultation systems on the use of health services outside primary care. The ESTEEM trial23 found no significant difference between the use of NHS Direct or emergency care services for patients assigned to GP- or nurse-led consultations and usual care. The authors found no significant increase in the proportion of patients with at least one emergency admission within 7 or 28 days of the consultation request, in either the GP- or nurse-led telephone groups, when compared with usual care. Additionally, similar proportions of patients reported contact with NHS Direct in the 28-day follow-up across the three groups (roughly 2%), with similar mean numbers of contacts, at 0.05 and 0.04 per person for GP telephone consultations and usual care, respectively. 23
Impact on costs
Although significantly increased telephone costs45,49,58,68,71 and concerns around the initial financial outlay30 associated with the implementation of telephone consultation systems were raised in the literature, robust evidence on costs is sparse. An economic evaluation conducted as part of ESTEEM23 found that, although GP telephone consultations were associated with increased contacts, there was no significant difference in average costs of health care over 28 days from a same-day consultation request between patients who received GP telephone consultations and usual care, possibly attributable to the reduction in GP face-to-face contacts.
The impact of telephone consultation on prescribing behaviour was raised as another concern in relation to cost. Some authors argued that a tendency for telephone consultation to foster ‘automatic’ repeats of medication would result in overprescribing and higher costs for patients and the health system. 72 Yet, studies that investigated prescribing patterns31,48 found limited use in telephone consultations or no difference in GP antibiotic prescribing behaviour compared with face-to-face consultations.
The potential for telephone consultations to offer patient cost savings, especially on travel in remote rural areas, has also been noted,73 but remains unexplored in the literature.
Summary
We have given an overview of the existing evidence base around telephone consultations in primary care as it relates to patient access, patient experience (including that of hard-to-reach and vulnerable groups), clinician and staff experience, the nature of consultations, patient safety, service utilisation (both within and outside general practice) and costs. Although the limited nature of the evidence has been noted here and elsewhere,36,54 in the last decade key studies and bodies of work, such as the ESTEEM trial23 and the work of McKinstry and colleagues,29–33 have clearly contributed towards a more robust evidence base in the UK. We did not seek to exclude studies on the basis of quality, which runs the risk of overinferring from poor-quality studies. This said, we have noted study type and any major limitations to interpreting findings throughout our synthesis.
In relation to our three research questions, the existing evidence around telephone consultation remains patchy and somewhat inconclusive. There is evidence to suggest that the content and focus of consultations is altered in telephone consultations compared with face-to-face consultations, but there is limited evidence from which to assess whether or not this has an impact on patient safety. Overall, patients seem no less satisfied with telephone consultations than with face-to-face consultations, although telephone-based systems do not appear to necessarily overcome challenges of access for those in work, or improve satisfaction for those living remotely. Nor is there evidence to suggest that particular patient groups, such as older patients, are specifically disadvantaged through the use of telephone consultation systems. Patients from ethnic minority groups may have different experiences of telephone consultations compared with white British patients, but the reasons for this need further exploration. The experience of clinicians and wider practice staff is varied and contingent on the system and practice context into which telephone consulting is introduced. In terms of resource use, although telephone consultation may reduce primary care contact (e.g. through consultation length) initially, it seems likely from the evidence that this is not sustained when subsequent contacts are taken into account. Similarly, it is not clear that telephone consultations result in changes in patients’ use of wider health services, such as emergency care, changed patterns of GP prescribing or potential cost savings. The evidence base needs to be strengthened in this regard.
Chapter 3 Analysis of administrative data from general practices
Data were provided by one commercial provider (GP Access) using data from administrative information within the clinical records of practices using the ‘telephone first’ approach. The analysis aimed to explore if, and how, appointments changed following the introduction of the approach.
Methods
Data on telephone and face-to-face appointments and on continuity of care were extracted from the practices’ computer systems by the commercial company up to 28 October 2016 and transferred to the research team as anonymised data sets for analysis. For individual appointment-level data, information was available regarding the date and time when an appointment was booked, the date and time when the appointment took place, the type of appointment (face-to-face, telephone, home visits or administrative) and who the appointment was with (GP, nurse or other). Continuity of care was measured over short time periods in the months following the introduction of the ‘telephone first’ approach. The continuity of care data included the usual provider continuity (UPC) score (the proportion of visits that are with the most frequently seen GP) and patient age. To preserve anonymity, the commercial company created the UPC score;74 this was calculated for each patient who had two or more appointments in any 1 calendar month as the number of appointments with the GP most frequently seen divided by the total number of appointments in that time period. Patients could not be linked across different months. The company also provided details on the date when the ‘telephone first’ approach was introduced and the current status of the system [i.e. whether, in their view, the practices were still running the ‘telephone first’ system per protocol, running a hybrid system (e.g. permitting some degree of advance booking) or had ceased using the approach]. Only practices that launched the ‘telephone first’ approach before 31 December 2015 were included in the final data set to allow sufficient time for the system to have bedded in (potentially allowing ≥ 10 months of post-intervention data for each practice, although in reality this was often less).
As data were available for intervention practices from only one commercial company, there are no control practices. Care must therefore be taken in attributing changes to the intervention, as outside factors (e.g. other contemporaneous changes in the NHS) could have had an influence on the results. We examined changes in the following outcomes (see Table 1 for full definitions):
-
number of appointments
-
time waited for an appointment
-
length of appointment
-
total time spent consulting (by GPs) per day
-
continuity of care.
Inclusion and exclusion criteria are outlined in Table 1. The reason for excluding appointments that took place on Saturdays or Sundays (and appointments booked on these days when considering the time waited for an appointment) was that the very small numbers compromised statistical modelling. Given their rarity, excluding these appointments was unlikely to have had an important overall effect on our conclusions. Consultation lengths were determined by how long patient records were open for each consultation, rather than the actual time spent consulting. Although consultations lasting > 30 minutes do take place, we considered that recorded durations of > 30 minutes were more likely to reflect a record being left open beyond the end of a consultation and so, when considering the length of appointments or the total time spent consulting per day by practice GPs, appointments lasting > 30 minutes were excluded from the analysis.
| Outcome | Definition | Inclusion criteria | Model | Unit of analysis |
|---|---|---|---|---|
| Number of appointments | The total number of appointments (face to face, telephone or home visits) with a GP per practice per day |
|
Mixed-effects Poisson regression | Each day in each practice |
| Time waited for an appointment | The number of days between booking the appointment (face to face or by telephone) and the time the patient had the appointment with the GPa |
|
Linear mixed model | Individual appointments |
| Length of appointment | The time in minutes between the start and the end of an appointment (either face to face or by telephone) with a GP |
|
Linear mixed model | Individual appointments |
| Total time spent consulting (by GPs) per day | The total time in minutes that GPs spent in appointments (face to face and by telephone) with patients per practice per day |
|
Log-transformed for analysis Linear mixed-effects regression model |
Each day in each practice |
| Continuity of care | For patients with two or more appointments in 1 month, the proportion of appointments that are with the GP most frequently seen in that month (score from 0 to 1) |
|
Linear mixed-effects regression | Individual patients in each month |
Statistical analysis
Two types of analysis were carried out for each of the outcomes. The first was a before-and-after analysis, illustrated by the ‘superposed epoch graphs’ which (see Figures 2–4) in the chapter where the introduction of the system in each practice is set at time zero. A superposed epoch graph is a way of visually representing changes that take place over time in a number of practices when an intervention took place in all of the practices but at different times. The plots show trends over time relative to the time at which the intervention started, which is defined as time zero, enabling visual inspection of changes before and after the intervention. Second, an interrupted time-series regression analysis was performed for each outcome, looking (1) for within-practice step changes at the time when the intervention was introduced and (2) for a within-practice change in the preceding trend (e.g. slowing down of a previous increase). We also model heterogeneity in these changes to examine whether or not the intervention has a different effect in different practices. Full details of the statistical analysis are given in Appendix 2.
A large proportion (30%) of data on length of appointment were missing from the practice data provided by the commercial company, especially for telephone consultations (52% compared with 18% for face-to-face consultations). Ignoring appointments with missing durations would have led to a systematic underestimation of the total time spent consulting. To overcome this, appointment length was imputed for those appointments with missing length and then added to the observed lengths to obtain a better estimate of the total time spent consulting for each day in each practice. Because we were imputing individual consultation lengths rather than total time spent consulting per day in a practice, a single imputation was made using a linear regression model similar to that used in the analysis of individual consultation lengths, but with fixed effects for practice rather than random effects, and stratified by before and after the intervention launch. Single, rather than multiple, imputation was used because of the computational burden. The use of single imputation will not lead to a biasing of estimates but may lead to an underestimate of standard errors (SEs). To combat this, the imputed SEs were multiplied by the square root of the ratio of the proportion of cases requiring no imputation.
Our main analyses were all done on an intention-to-treat basis. This included all practices identified by the commercial company as having used the ‘telephone first’ approach, even when the practices were using a hybrid form of the approach (e.g. by allowing some prebooked appointments) or had since ceased using it altogether. In this and other analyses, a sensitivity analysis (see Appendix 3) was performed, restricting the analysis to practices in which we believed, on the basis of information provided by the commercial company, that the system was being run consistently with the company’s protocols. The companies were asked to classify all practices that had used their ‘telephone first’ approach as ‘running’, ‘hybrid’ (i.e. allowing some additional degree of advance booking of appointments) or ‘reverted’ (i.e. had stopped using the ‘telephone first’ approach). In the per-protocol sensitivity analyses, we included only practices classified by the companies as ‘running’.
Results
The main intention-to-treat analysis included data from 59 practices with 1,926,979 appointments spread over 16,795 practice-days. The sensitivity ‘per-protocol’ analysis (see Appendix 3) included data from 27 practices covering 997,772 appointments over 8158 practice-days.
Number of appointments
Superposed epoch analysis
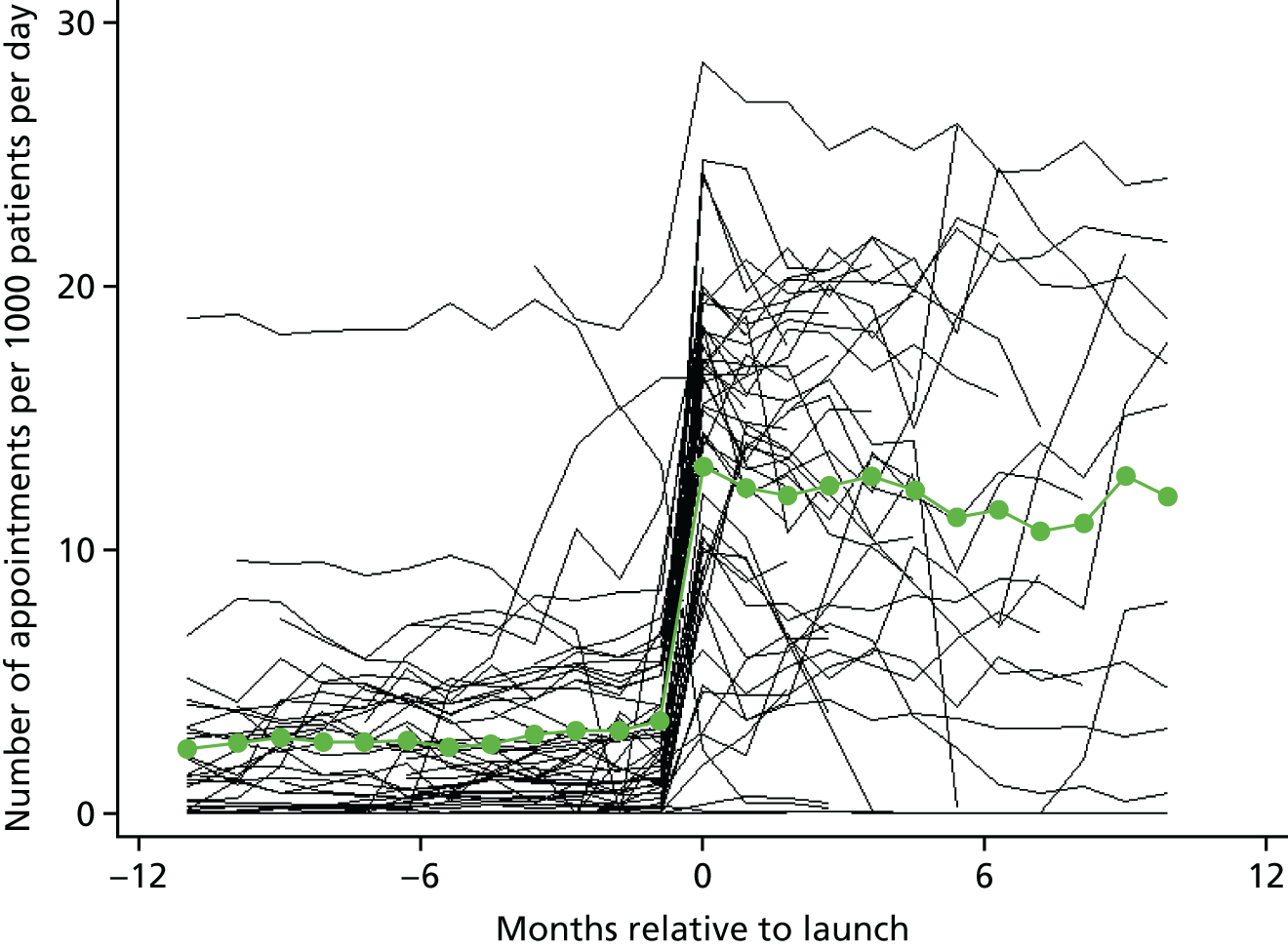
The mean number of appointments per 1000 patients per day was 16.5 (SD 6.3) before the intervention started; this increased to 21.8 appointments (SD 8.1 appointments) post intervention (Figure 2). This increase differed by appointment type, with decreases seen in the number of face-to-face appointments, from a mean of 13.0 appointments (SD 4.5 appointments) to a mean of 9.3 appointments (SD 5.5 appointments) (Figure 3), and increases seen in the number of telephone appointments, from a mean of 3.0 appointments (SD 4.0 appointments) to a mean of 12.2 appointments (SD 7.5 appointments) (Figure 4).
FIGURE 2.
Superposed epoch analysis showing the change in the total number of appointments per 1000 patients per day relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
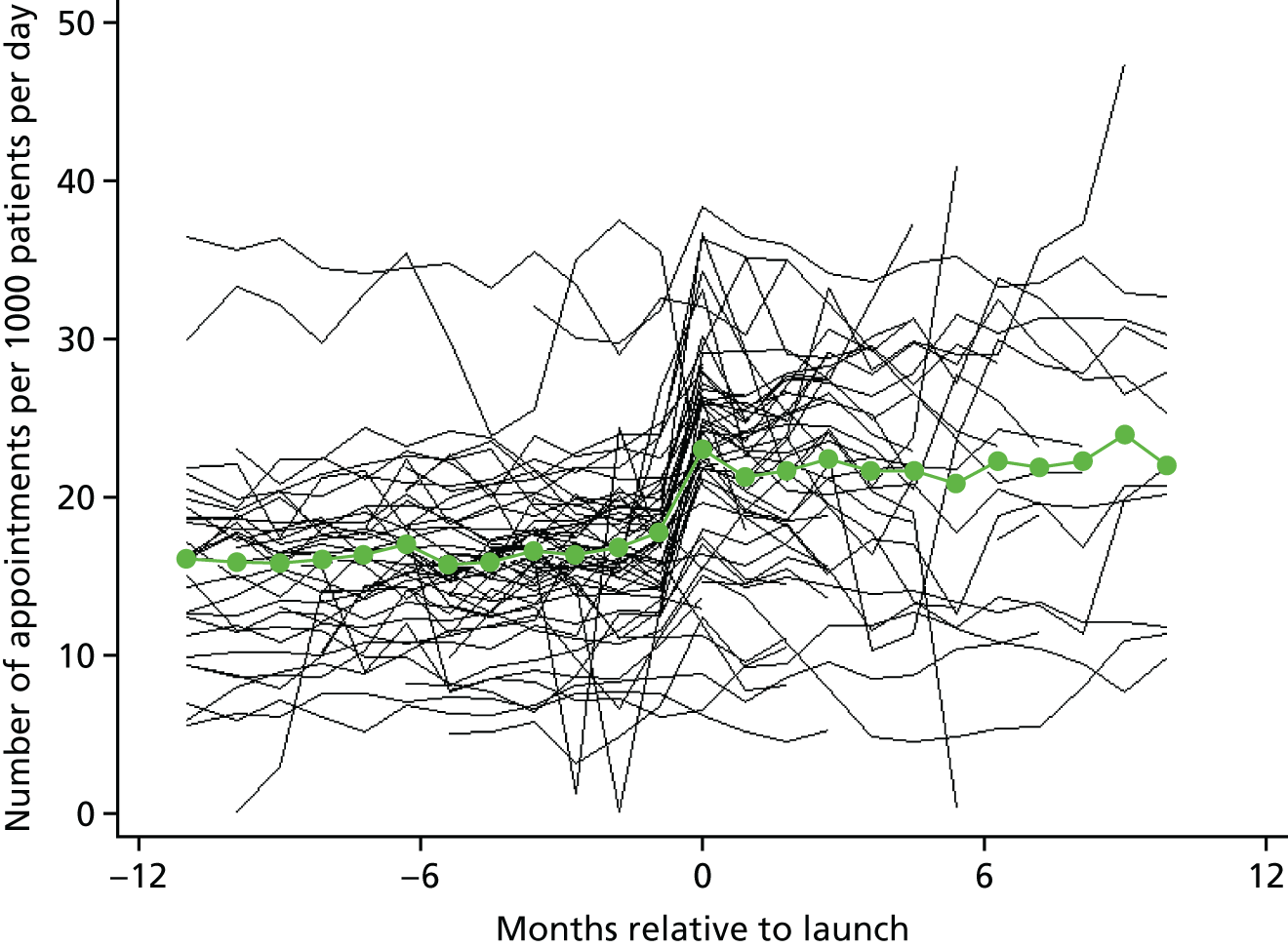
FIGURE 3.
Superposed epoch analysis showing the change in the number of face-to-face appointments per 1000 patients per day relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means. Reproduced from Newbould et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
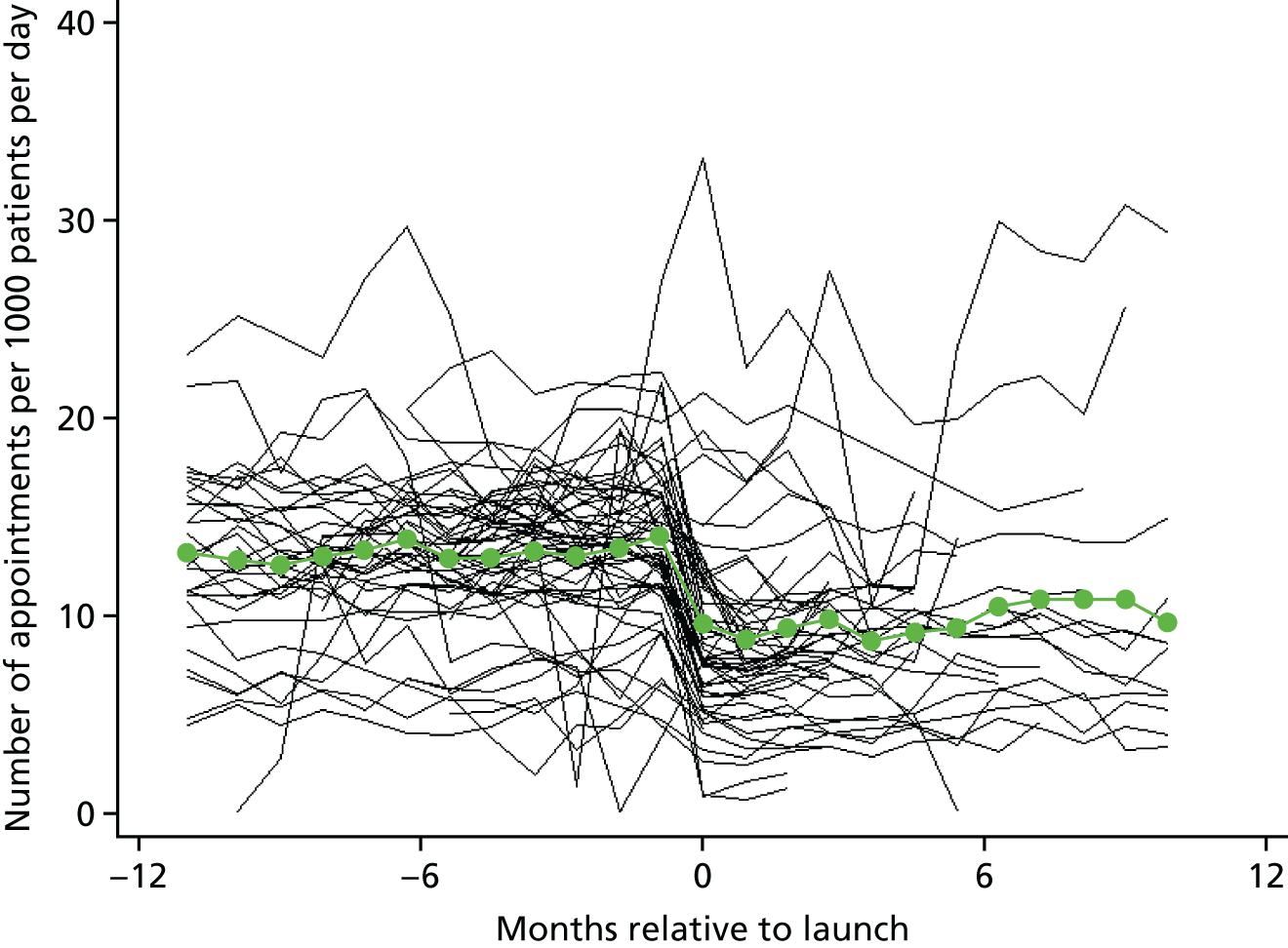
FIGURE 4.
Superposed epoch analysis showing the change in the number of telephone appointments per 1000 patients per day relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means. Reproduced from Newbould et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Regression analysis
The changes observed in the superposed epoch analysis are reflected in the regression analyses (Table 2). There was a 28% increase in all appointments following the introduction of the intervention (RR at step change 1.28, 95% CI 1.17 to 1.39; p < 0.0001), which comprised a 38% drop in face-to-face appointments and a 12-fold increase in the number of telephone consultations (RRs for step change are presented in Table 2; p < 0.0001 for all appointment types). It should be noted that the large relative change in telephone appointments in part reflects small numbers pre launch and that this relative increase is larger than the change in average figures as it represents the average within-practice change (the mean rate of telephone consultations pre launch will be more strongly influenced by those practices already doing many telephone consultations). Although there was a slight slowing in the initial rate of increase, the total number of appointments continued to increase post intervention by 4% per year (RR 1.04, 95% CI 1.04 to 1.05; p < 0.0001). There was considerable heterogeneity between practices in the changes in total number of appointments with the 95% reference ranges suggesting that some practices reduced overall appointment numbers by up to 32%, whereas for others the total number of appointments increased by a factor of 2.4. The per-protocol sensitivity analysis produced broadly consistent findings (see Appendix 3).
| Appointment type | Step change at transition | Trend | Interaction p-valueb | |||||
|---|---|---|---|---|---|---|---|---|
| Pre transition | Post transition | |||||||
| RR (95% CI) | p-value | Heterogeneitya | RR (95% CI) | p-value | RR (95% CI) | p-value | ||
| All | 1.28 (1.17 to 1.39) | < 0.0001 | 0.68 to 2.39 | 1.07 (1.06 to 1.08) | < 0.0001 | 1.04 (1.04 to 1.05) | < 0.0001 | < 0.0001 |
| Face to face | 0.62 (0.55 to 0.71) | < 0.0001 | 0.24 to 1.62 | 1.03 (1.01 to 1.04) | < 0.0001 | 0.98 (0.97 to 0.99) | < 0.0001 | < 0.0001 |
| Telephone | 12.04 (6.33 to 22.90) | < 0.0001 | 0.10 to 1467.39 | 1.11 (1.09 to 1.12) | < 0.0001 | 1.46 (1.43 to 1.49) | < 0.0001 | < 0.0001 |
Time waited for an appointment
Superposed epoch analysis
The mean number of days between booking an appointment and having an appointment across all intervention practices was 4.0 (SD 7.0) prior to the intervention and 0.9 (SD 3.9) after the intervention (Figure 5). Similar drops in time between booking and having an appointment are seen when restricting to face-to-face appointments [from a mean of 4.5 days (SD 7.4 days) to a mean of 1.8 days (SD 5.6 days)] and telephone appointments [from a mean of 1.8 days (SD 4.2 days) to a mean of 0.3 days (SD 1.7 days)].
FIGURE 5.
Superposed epoch analysis showing the change in the mean time between booking and having an appointment of any type relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
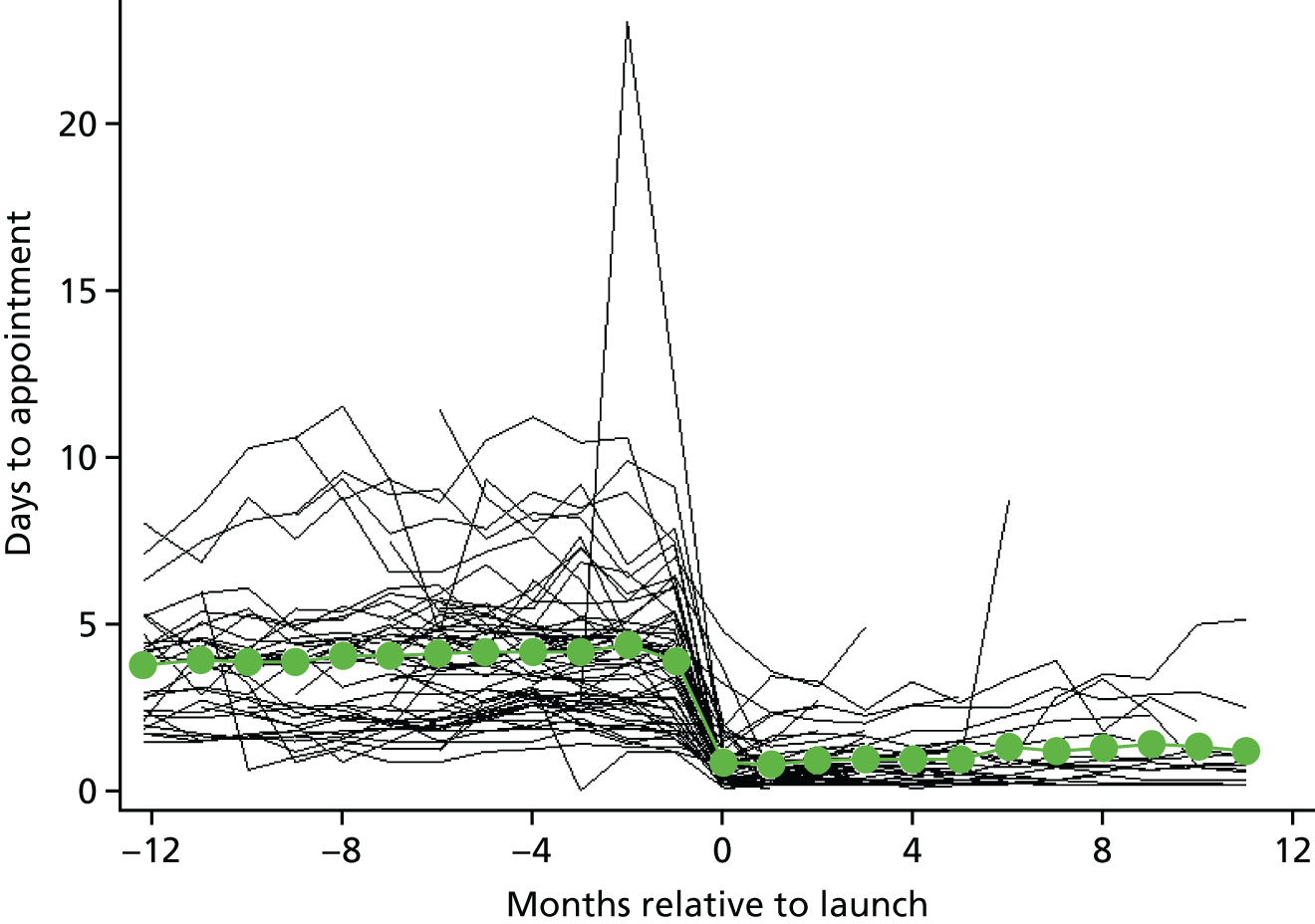
Regression analysis
Decreases in the number of days to an appointment, seen in the superposed epoch graphs, are reflected in the regression analysis (Table 3). The time between booking and having an appointment dropped, on average, by 3.3 days (95% CI –3.8 to –2.8 days; p < 0.0001) after initially switching to the intervention (step change). The same decrease is seen for face-to-face appointments and a smaller reduction is seen for telephone consultations. The time between booking and having an appointment continued to increase over time following the introduction of the intervention; however, given that the annual increase in time waited is much smaller than the initial step decrease in time waited following the introduction of the intervention, it would take many years for the waiting time in the average practice to return to pre-intervention levels. Again, the 95% reference ranges show that there was substantial heterogeneity between practices in the reduction in length of time waited between booking and having an appointment; however, all practices show a decrease in the time between booking and having an appointment.
| Appointment type | Step change at transition | Trend | Interaction p-valueb | |||||
|---|---|---|---|---|---|---|---|---|
| Pre transition | Post transition | |||||||
| Mean time to appointment (days) (95% CI) | p-value | Heterogeneitya | Mean change in time to appointment (days/year) (95% CI) | p-value | Mean change in time to appointment (days/year) (95% CI) | p-value | ||
| All | –3.30 (–3.80 to –2.80) | < 0.0001 | –5.91 to –0.71 | 0.20 (0.16 to 0.25) | < 0.0001 | 0.22 (0.16 to 0.27) | < 0.0001 | 0.6928 |
| Face to face | –3.31 (–3.89 to –2.72) | < 0.0001 | –6.31 to –0.31 | 0.53 (0.47 to 0.59) | < 0.0001 | 0.49 (0.40 to 0.58) | < 0.0001 | 0.4982 |
| Telephone | –0.78 (–1.07 to –0.48) | < 0.0001 | –2.21 to 0.71 | –0.21 (–0.26 to –0.16) | < 0.0001 | 0.15 (0.12 to 0.18) | < 0.0001 | < 0.0001 |
The per-protocol sensitivity analysis produced broadly consistent findings for the step change in time waited immediately following the introduction of the intervention, but there was evidence that the time waited between booking and getting an appointment of any type continued to decrease slightly post intervention in these practices (see Appendix 3).
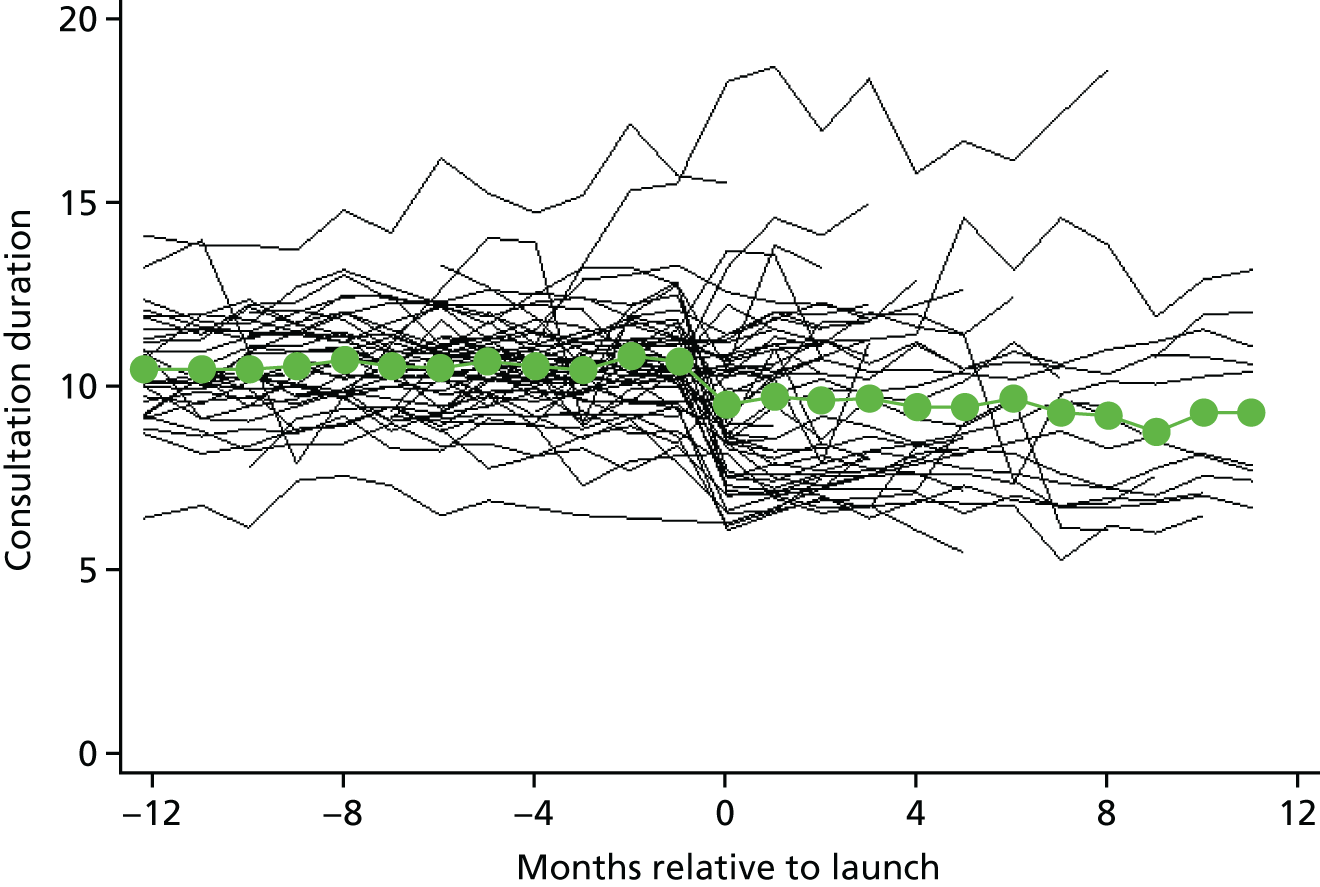
Length of appointment
Superposed epoch analysis
On average, the duration of appointments decreased from 10.5 minutes (SD 6.0 minutes) pre intervention to 8.5 minutes (SD 6.2 minutes) post intervention (Figure 6). The change in duration was less when restricting to face-to-face appointments [from a mean of 10.9 minutes (SD 5.9 minutes) to a mean of 10.2 minutes (SD 6.4 minutes)] or telephone appointments [from a mean of 7.7 minutes (SD 6.0 minutes) to a mean of 6.2 minutes (SD 5.1 minutes)], suggesting that much of the overall reduction in average appointment duration is due to a change in the proportion of appointments that are telephone appointments. It is worth bearing in mind that patients who had a face-to-face appointment may also have had a telephone appointment. For this reason, it is likely that the total consultation duration for each patient increases for patients who had both telephone and face-to-face appointments; however, as we cannot link telephone and face-to-face appointments, we cannot demonstrate that this is actually the case.
FIGURE 6.
Superposed epoch analysis showing the change in appointment duration relative to the intervention launch: face-to-face and telephone. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
Regression analysis
The regression analysis suggests that the differences observed in the superposed epoch analysis exaggerate the effect of the intervention somewhat (Table 4). Across all appointment types there was a mean decrease in appointment duration of 0.9 minutes (95% CI 1.43 to 0.33 minutes; p = 0.0024) immediately following the introduction of the intervention. There was no significant evidence of a change in the duration of face-to-face appointments (p = 0.18), whereas telephone appointments decreased in duration by about 0.5 minutes. The 95% reference ranges indicate that there was considerable heterogeneity between practices, with some practices reducing the durations of appointments and others increasing the durations of appointments. For all appointments, there was a reversal in the pre-intervention trend of increasing appointment duration to a post-intervention trend of decreasing appointment duration such that, on average, over the year following the intervention launch there was an additional reduction of around 0.3 minutes.
| Appointment type | Step change at transition | Trend | Interaction p-valueb | |||||
|---|---|---|---|---|---|---|---|---|
| Pre transition | Post transition | |||||||
| Mean change in length of appointment (minutes) (95% CI) | p-value | Heterogeneitya | Mean change in length of appointment (minutes/year) (95% CI) | p-value | Mean change in length of appointment (minutes/year) (95% CI) | p-value | ||
| All | –0.88 (–1.43 to –0.33) | 0.0024 | –3.67 to 1.91 | 0.19 (0.14 to 0.25) | < 0.0001 | –0.28 (–0.35 to –0.21) | < 0.0001 | < 0.0001 |
| Face to face | 0.22 (–0.11 to 0.55) | 0.1800 | –1.41 to 1.86 | 0.35 (0.29 to 0.41) | < 0.0001 | –0.34 (–0.43 to –0.24) | < 0.0001 | < 0.0001 |
| Telephone | –0.51 (–0.89 to –0.13) | 0.0096 | –1.79 to 0.77 | 0.42 (0.28 to 0.57) | < 0.0001 | –0.39 (–0.50 to –0.29) | < 0.0001 | < 0.0001 |
The per-protocol sensitivity analysis produced estimates in the same direction, but the decrease in average appointment length was smaller. This smaller decrease, combined with larger SEs as a result of the decreased sample size, meant that the decrease in appointment duration was no longer statistically significant, either for all appointments or for telephone consultations (see Appendix 3).
Total time spent consulting per day by general practitioners
Superposed epoch analysis
The mean time spent consulting per 1000 patients increased slightly from 7.8 hours (SD 2.5 hours) per day pre intervention to 8.5 hours (SD 4.0 hours) post intervention (Figure 7). It should be noted that the number of practices providing data decreased rapidly in the months after the launch. The reason for this is that, although we had a minimum cut-off point for the ‘after’ period of data collection, some practices had longer periods of data available for the period after the change. For this reason, some medium- or long-term effects might not be evident.
FIGURE 7.
Superposed epoch analysis showing the change in the total time spent consulting relative to the intervention launch: hours per 1000 patients per day. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
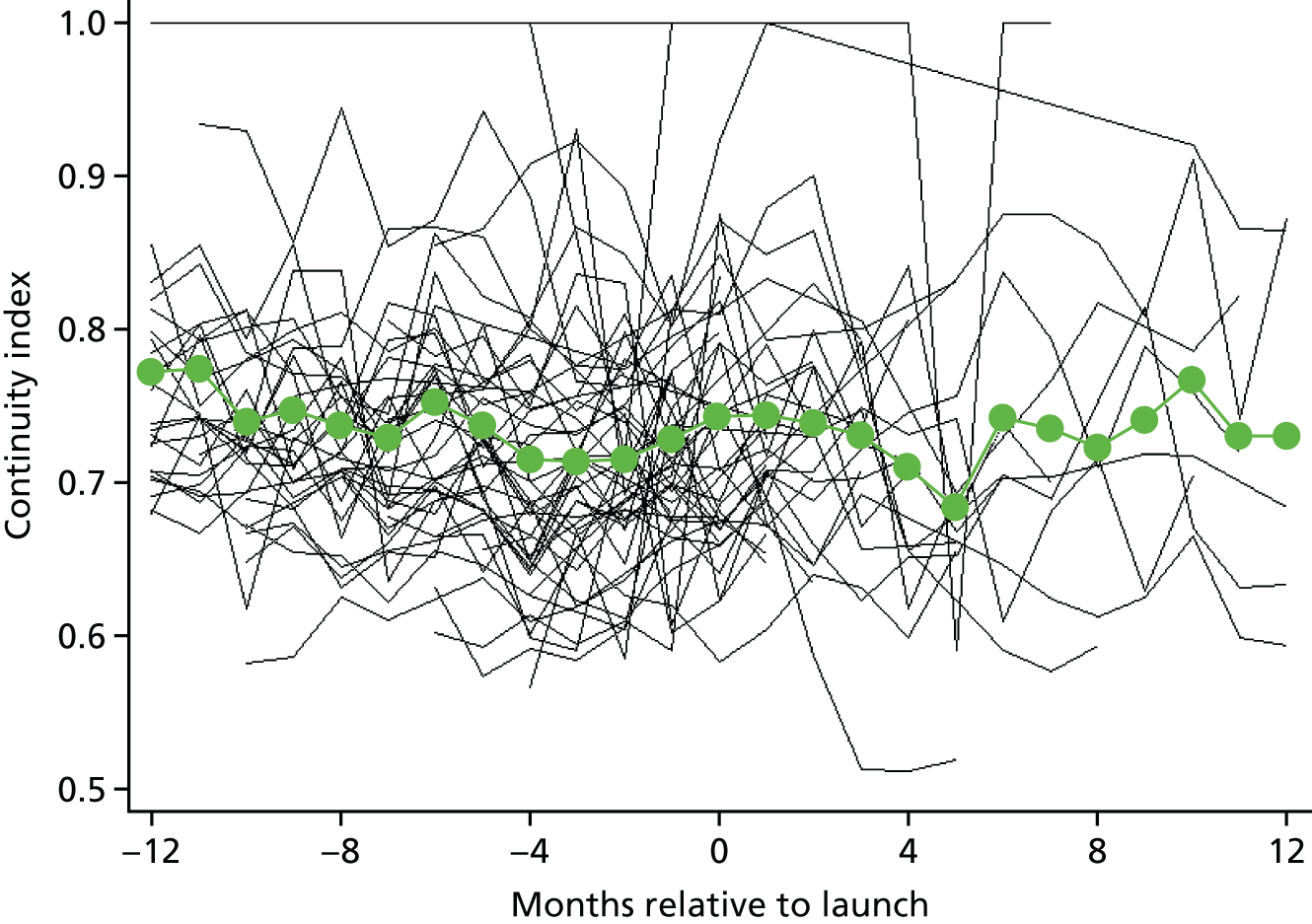
Regression analysis
There was only very weak evidence (p = 0.088) of any change in the total time spent consulting by GPs each day on average, with an estimated increase of 8% (ratio of time 1.08, 95% CI 0.99 to 1.17) (Table 5). Consistent with the analysis on the number of appointments, the total time spent consulting decreased for face-to-face appointments and increased for telephone appointments. As with other outcomes, large heterogeneity in the effect was seen; some practices experienced an increase in the total time spent consulting of up to 79%, whereas others saw decreases up to 35% (as illustrated by the 95% reference range).
| Appointment type | Step change at transition | Trend | Interaction p-valueb | |||||
|---|---|---|---|---|---|---|---|---|
| Pre transition | Post transition | |||||||
| Ratio | p-value | Heterogeneitya | Ratio | p-value | Ratio | p-value | ||
| All | 1.08 (0.99 to 1.17) | 0.0883 | 0.65 to 1.79 | 1.00 (0.94 to 1.05) | 0.8728 | 1.05 (1.02 to 1.09) | 0.0051 | 0.0856 |
| Face to face only | 0.60 (0.52 to 0.70) | < 0.0001 | 0.23 to 1.57 | 1.09 (1.03 to 1.14) | 0.0018 | 0.99 (0.96 to 1.03) | 0.6398 | 0.0045 |
| Telephone | 5.45 (3.41 to 8.72) | < 0.0001 | 0.54 to 55.6 | 0.97 (0.87 to 1.08) | 0.5921 | 1.50 (1.38 to 1.63) | < 0.0001 | < 0.0001 |
Continuity of care
Superposed epoch analysis
Continuity of care data were available for 50 practices (100,367 data points pre launch and 27,847 data points post launch). The mean continuity index (which takes possible values between 0 and 1) in practices was very similar before and after the launch of the intervention: 0.728 (SD 0.08) and 0.731 (SD 0.79), respectively. This can be seen in the superposed epoch analysis (Figure 8), in which there is some fluctuation over time but values are roughly equal before and after launch. It is also worth noting that the data become sparse at > 5 months post launch.
FIGURE 8.
Superposed epoch analysis showing the continuity index relative to the months to launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
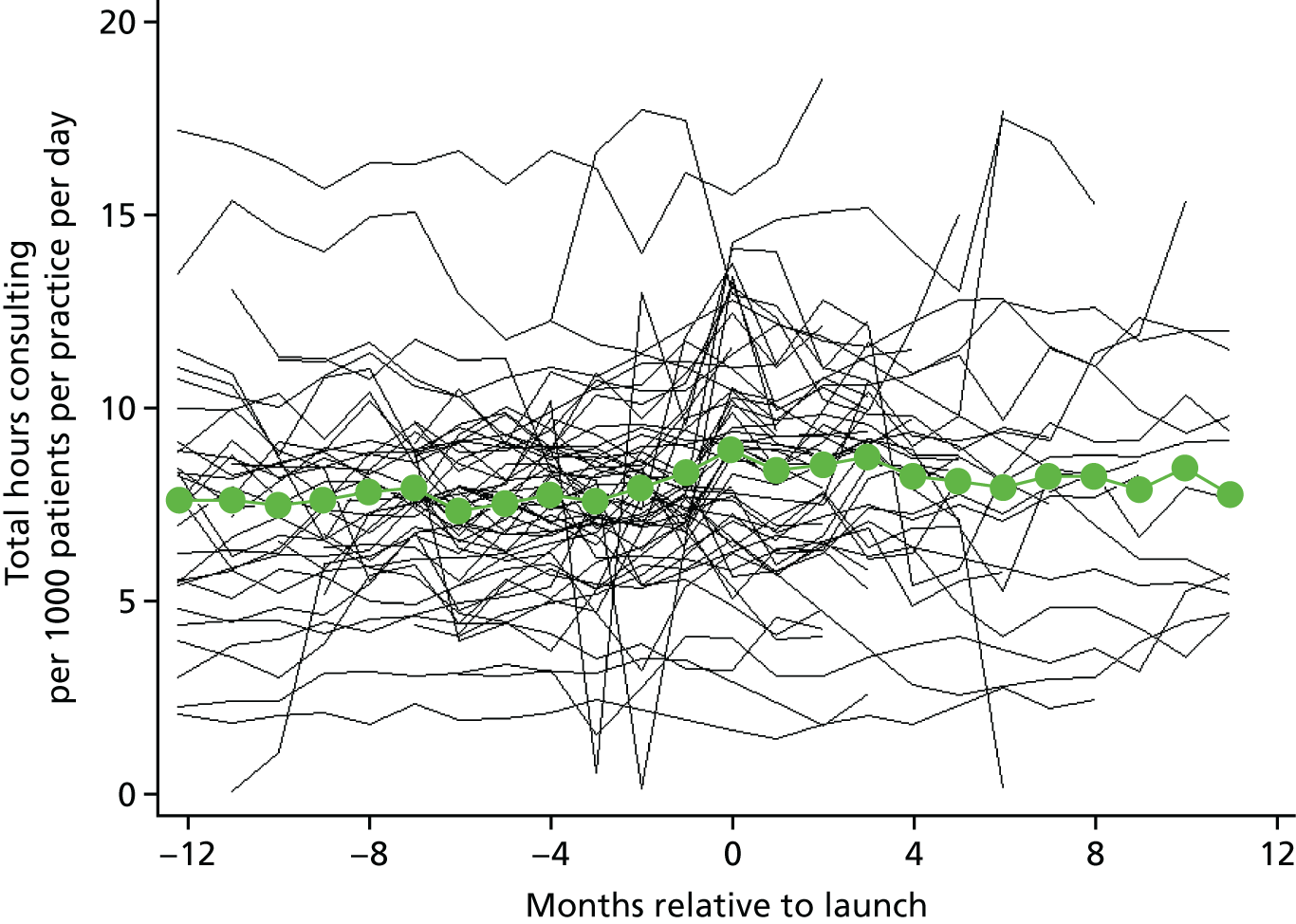
Regression analysis
The regression analysis provides evidence (p < 0.001) that continuity improves after starting the intervention but only by a small amount (difference of 0.06, 95% CI 0.04 to 0.08 on a scale from 0 to 1). Although there is evidence of a subsequent decrease in continuity, it would take around 10 years to erode the initial gains made if this decline were to continue. As with other outcomes, there is strong heterogeneity in the effect of the intervention between practices, with continuity increasing in most practices but decreasing in some (illustrated by the 95% reference range shown in Table 6).
| Step change at transition | Trend | Interaction p-valueb | |||||
|---|---|---|---|---|---|---|---|
| Pre transition | Post transition | ||||||
| Change in continuity index | p-value | Heterogeneitya | Change in continuity index per year | p-value | Change in continuity index per year | p-value | |
| 0.058 (0.037 to 0.081) | < 0.001 | –0.074 to 0.191 | –0.0001 (–0.0002 to 0.0001) | 0.40 | –0.006 (–0.006 to –0.005) | < 0.001 | < 0.001 |
Summary
The analysis presented here demonstrates an increase in the total number of GP appointments with the introduction of the telephone system. This is composed of a substantial increase in telephone appointments and smaller decreases in face-to-face appointments. This is what one would expect from the ‘telephone first’ approach, given that its central mechanism is the use of telephone consultations to reduce the need for face-to-face consultation. These findings are also in line with previous work on telephone triage systems. 23
Associated with an increase in the number of consultations is a decrease in the average overall length of consultations. Rather than being driven by shorter face-to-face consultations, this is driven by a shift from predominantly face-to-face consultations to a mix of telephone and face-to-face consultations. Although it would be useful to know whether individual patients used more or less GP time to deal with their problems, these data do not allow us to address that question directly as the anonymisation process meant that it was not possible to link telephone consultations to subsequent face-to-face consultations for individual patients. However, we have been able to look at the impact on total GP workload by considering changes in the total time spent consulting. Here, the uncertainty in our estimates is large, with a best estimate of an 8–9% increase in the total workload of GPs following the start of the ‘telephone first’ approach; again there is wide variation between the experiences of different practices.
Given that the ‘telephone first’ approach does not allow patients to book GP appointments in advance (except in a few circumstances), it is not surprising that we find a dramatic drop in the time between booking an appointment and the appointment taking place (to a mean of < 1 day), a finding that is consistent with our analysis of the GP Patient Survey (see Chapter 6). In contrast, improvements to continuity of care were, at best, modest.
Among all of the findings presented here, there is large heterogeneity in the effect of the intervention with, for example, some practices experiencing substantial reductions in overall workload and others finding that there were large increases in overall workload.
Finally, it is worth noting that almost half of the practices that had started the ‘telephone first’ approach had either adopted a hybrid approach in which there was some limited availability of prebooked appointments or had reverted to standard practice. Nevertheless, our sensitivity analysis, which was restricted to those still running the system ‘per protocol’, did not lead to substantially different conclusions.
Chapter 4 Patient experience survey
A descriptive patient survey was undertaken to understand patients’ perspectives and experiences at 20 practices using the ‘telephone first’ approach supported by the commercial providers. The survey questions were designed to understand patients’ experiences of booking an appointment and their satisfaction with the approach. The aim of the survey was to capture an in-depth understanding of patients’ recent experiences of booking an appointment. Later, we present an analysis of data from the national GP Patient Survey (see Chapter 6). Although that analysis allows for a controlled comparison between practices using the ‘telephone first’ approach and those not using the ‘telephone first’ approach, the survey reported in this chapter is a general survey of patients’ experiences with primary care services. For this reason, the GP Patient Survey does not focus on issues specific to the ‘telephone first’ approach.
Methods
Survey development
The survey was designed by the evaluation team, informed by a review of the literature and with reference to a number of existing surveys (including the GP Patient Survey, the General Practice Assessment Questionnaire, the out-of-hours patient questionnaire and the survey used in the ESTEEM trial) from which questions were sourced or adapted. Survey questions were first tested in cognitive interviews with 16 patients in the waiting room of a single practice to determine whether or not they were being interpreted as intended. A revised survey and covering letter were reviewed by PPI representatives on the study advisory committee before full-scale piloting of the survey by post was undertaken (according to the dissemination method outlined in the following sections). Only minor revisions were made following piloting; therefore, pilot data were included in the overall analysis.
Practice selection, sampling and recruitment
The two commercial companies provided a list of practices known to be running the ‘telephone first’ approach. The sampling frame was restricted to practices that had been operating the ‘telephone first’ approach since 24 June 2015 (n = 101) (i.e. those that had been operating the approach for ≥ 6 months at the time of recruitment) in order to ensure that the new appointment system had been given enough time to ‘bed in’. Initially, a stratified random sampling method was used to recruit practices; however, the low participation rate meant that, ultimately, all practices were approached in order to reach our recruitment target. Practices were approached in batches (initially of 10 surgeries and then of five surgeries) by letter; a researcher followed up with a telephone call until either a response was received or researchers had been chasing for 3 months (when attempts were abandoned). This was followed by a mail-out to all of the remaining 61 practices in the final batch. With the final batch for chasing, we randomised the order of the list and worked our way through it, chasing by telephone until we had a sufficient number of practices. The response rate from practices was 20%.
The characteristics of practices that participated in the survey are shown in Table 7. Although there is variation across most of these characteristics, it should be noted that only one rural practice was recruited.
| Practice identification number | Provider | Launch date | Practice characteristic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Practice size (n) | GP count (n) | Payer | Rurality | Deprivation (more or less deprived than average) | Ethnicity (above or below average % of population of England that are white) | Sample size (n) | Number of responders | Response rate (%) | |||
| 100 | GPA | 7 July 2014 | 8093 | 7 | Self-pay | Urban | Less | Above | 96 | 51 | 53.13 |
| 101 | GPA | 1 October 2012 | 6672 | 7 | Self-pay | Urban | Less | Above | 86 | 42 | 48.84 |
| 102 | DF | 15 April 2013 | 2347 | 3 | CCG | Urban | Less | Above | 91 | 54 | 59.34 |
| 103 | DF | 17 June 2013 | 7312 | 6 | CCG | Urban | More | Above | 88 | 34 | 38.64 |
| 104 | GPA | 25 July 2011 | 4913 | 3 | Self-pay | Urban | Less | Below | 85 | 29 | 34.12 |
| 105 | DF | 1 February 2013 | 11,484 | 10 | Self-pay | Urban | Less | Above | 97 | 49 | 50.52 |
| 106 | DF | 24 April 2013 | 16,072 | 13 | Self-pay | Urban | Less | Above | 92 | 43 | 46.74 |
| 108 | DF | 11 February 2013 | 4913 | 4 | CCG | Urban | More | Above | 100 | 35 | 35.00 |
| 110 | GPA | 31 March 2014 | 8639 | 8 | CCG | Urban | More | Above | 100 | 38 | 38.00 |
| 111 | DF | 20 May 2013 | 11,489 | 9 | CCG | Urban | More | Above | 80 | 34 | 42.50 |
| 112 | DF | 1 July 2014 | 7934 | 8 | CCG | Urban | More | Below | 79 | 18 | 22.78 |
| 113 | GPA | 25 June 2012 | 6128 | 4 | Self-pay | Urban | Less | Above | 98 | 48 | 48.98 |
| 114 | GPA | 16 July 2013 | 8364 | 7 | Self-pay | Urban | Less | Above | 90 | 53 | 58.89 |
| 115 | DF | 1 July 2014 | 4538 | 4 | CCG | Urban | Less | Above | 97 | 52 | 53.61 |
| 116 | GPA | 16 April 2012 | 6553 | 8 | Self-pay | Urban | More | Above | 100 | 40 | 40.00 |
| 117 | DF | 23 April 2013 | 7888 | 7 | Self-pay | Urban | Less | Above | 100 | 50 | 50.00 |
| 118 | DF | 19 November 2012 | 5738 | 6 | CCG | Urban | More | Above | 100 | 34 | 34.00 |
| 119 | DF | 1 April 2013 | 13,166 | 10 | CCG | Urban | More | Above | 97 | 52 | 53.61 |
| 120 | DF | 16 June 2014 | 13,703 | 17 | CCG | Urban | Less | Above | 97 | 33 | 34.02 |
| 121 | DF | 30 April 2012 | 11,525 | 11 | Self-pay | Rural | Less | Above | 100 | 48 | 48.00 |
Because of the likelihood that practices that agreed to take part in the survey were more successful in operating the ‘telephone first’ approach than those that declined, we compared the two sets of practices using nationally reported GP Patient Survey data from 2015/16 (weighted for non-response and design). The mean percentage of patients reporting being seen or spoken to on the same or next day was 81.5% (SD 4.2%) for participating practices and 68.6% (SD 14.6%) for those practices that were not recruited. For ‘good’ or ‘very good’ ratings of overall experience, the mean was 86.4% (SD 7.7%) in participating practices and 79.9% (SD 11.4%) in those practices that were not recruited. This confirmed our concern that responses from practices that agreed to take part in this survey were likely to be more positive than other practices using the ‘telephone first’ approach.
Survey distribution
For each of the 20 practices, the survey was distributed by post to a random sample of between 80 and 100 patients who had received a telephone consultation with a GP during the day preceding the survey mail-out. The mail-out day was selected by the practices. Surveys were distributed between 23 November 2015 and 27 October 2016.
Details of patients who had received a telephone consultation in the day preceding the survey mail-out (or the previous Friday if the mail-out was on a Monday) were extracted into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet. These details included:
-
patient name
-
NHS number
-
sex
-
age
-
ethnicity (if available)
-
GP seen
-
date and time (a.m. or p.m.) of appointment (if available)
-
home address
-
usual GP (if available).
Duplicates, based on NHS number, were removed. Children aged between 13 and 17 years were excluded in order to avoid compromising confidentiality when approaching patients in this age group. If the number of patients remaining was < 80, data were extracted on all patients who had spoken to a GP in the 2 days prior to the survey mail-out. If there were > 100 patients (either in a single day or across multiple days needed to get to a sample size of ≥ 80), a random sample of 100 patients was taken. The final sample was reviewed by GPs, who removed any patients for whom they had concerns related to vulnerability.
The survey was posted to patients (or the parents of patients aged < 13 years) with a letter from the practice inviting them to respond. Patients were encouraged to ask for assistance to complete the survey if required. A reminder was posted to non-responders 2 weeks after the original mail-out.
Analysis
Survey responses have been summarised using descriptive statistics. Some patients did not answer all of the survey questions; consequently, the total number of responses presented varies for each question as we present the results based on all those who answered it. In order to account for non-response bias, the results have been weighted based on the age and sex of the patients who were sent a survey. There were insufficient data on ethnicity to include in the weighting. The weighted results represent the views of the patients consulting, which might not be representative of all patients registered at the practice; however, this difference also reflects the fact that some groups of patients are more likely to contact the practice than others.
In order to investigate whether or not certain patient groups had different experiences of the ‘telephone first’ approach, we used logistic regression models. We created six dichotomous outcomes:
-
Was the patient expecting a callback? (Yes compared with no/unsure.)
-
How did the patient rate the length of time to be called back? (Good/excellent compared with acceptable/poor/very poor.)
-
How convenient was it speaking to a GP on the telephone? (More convenient compared with less convenient/no difference.)
-
How difficult was it communicating with a GP on the telephone? (More difficult compared with less difficult/no difference.)
-
Did the patient receive a face-to-face appointment with someone? (Yes compared with no.)
-
Would the patient prefer to return to the old appointment system? (Yes/do not mind compared with no.)
Each outcome was modelled in a separate logistic regression, which included age (categorised into nine age bands), sex (male/female), health status (five categories from poor to excellent), ethnicity (white/non-white), primary language (English/other), ability to take time off work (four categories: not relevant, no, yes with difficulty and yes easily) and a random effect for practice.
Results
The survey was sent to 1873 patients from 20 practices. Overall, 837 responses were received; the response rate was 45% (837/1873). Response rates varied between practices, from 23% to 60% (see Table 7), and were slightly higher for female patients than for male patients. Furthermore, older patients were more likely to respond to the survey: the mean age of responders was 17 years higher than the mean age of non-responders (56.2 years compared with 38.9 years, respectively). The demographic characteristics of those responding to the survey are presented in Appendix 4.
Descriptive analysis
Patient experience of using the ‘telephone first’ approach
Of the total sample of respondents, 85.0% (707/831, 82.0% weighted) were calling to discuss their own health (i.e. they were the patient), 9.0% (75/831, 13.0% weighted) were calling on behalf of their child, 4.2% (35/831, 3.5% weighted) were calling on behalf of an adult for whom they cared and 1.7% (14/831, 1.2% weighted) were calling for another reason.
The vast majority of respondents, (91.0%) initially contacted the practice by telephone (753/825, 92.0% weighted), 1.7% initially contacted the practice online (14/825,1.4% weighted) and 5.7% initially contacted the practice in person (47/825, 5.4% weighted). Only around two-thirds (69.0%; 569/825, 67.0% weighted) of respondents expected to receive a callback from the GP.
The length of time that patients waited for a callback from the GP varied considerably: 23% (189/814, 21% weighted) waited for < 20 minutes, 44% (360/814, 44% weighted) waited for 20–60 minutes and 32% (256/814, 34% weighted) waited > 1 hour. In addition, 1.1% of respondents (9/814, 1.1% weighted) reported that they did not receive a callback. The majority of patients who were called back within 20 minutes of the initial contact rated the waiting time as excellent (71%, 75% weighted). Patients called back within 20–60 minutes most commonly rated the callback waiting time as excellent (33%, 38% weighted) or good (36%, 34% weighted). The majority of those who waited for > 1 hour considered this acceptable (43%, 41% weighted) or good (24%, 25% weighted). The waiting times before receiving a callback and how the respondents rated these are presented in Table 8.
| Waiting time for callback | Rating of waiting time, % of patients (n/N) | Total, N (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Very poor | Poor | Acceptable | Good | Excellent | |||||||
| Absolute | Weighted | Absolute | Weighted | Absolute | Weighted | Absolute | Weighted | Absolute | Weighted | ||
| < 20 minutes | 2.1 (4/189) | 2.1 | 0.5 (1/189) | 0.4 | 2.7 (5/189) | 2.2 | 24 (45/189) | 20 | 71 (134/189) | 75 | 189 (100) |
| 20–60 minutes | 0.3 (1/360) | 0.3 | 1.9 (7/360) | 1.4 | 29 (104/360) | 26 | 36 (129/360) | 34 | 33 (119/360) | 38 | 360 (100) |
| > 1 hour | 6.3 (16/256) | 6.5 | 16 (41/256) | 16 | 43 (110/256) | 41 | 24 (61/256) | 25 | 11 (28/256) | 11 | 256 (100) |
| No callback | 33 (3/9) | 31 | 33 (3/9) | 23 | 22 (2/9) | 39 | 11 (1/9) | 6.9 | 0 (0/9) | 0 | 9 (100) |
| Total | 3.0 (24/814) | 3.1 | 6.4 (52/814) | 6.4 | 27 (221/814) | 27 | 29 (236/814) | 28 | 35 (281/814) | 36 | 814 |
Overall, 50.0% of calls (421/837, 50.0% weighted) resulted in the patient being asked to come to the practice for a face-to-face consultation: 44.0% (367/837, 44.0% weighted) for a GP appointment and 7.3% (61/837, 6.6% weighted) for a nurse appointment. The outcomes of calls are listed in Table 9 (88 respondents listed more than one outcome). Overall, 89.0% of respondents (695/784, 89.0% weighted) were satisfied with the outcome of their call, whereas 7.9% (62/784, 7.9% weighted) thought that they should have received a face-to-face appointment, 1.2% (9/784, 0.9% weighted) thought that a follow-up call should have been arranged and 2.3% (18/784, 2.2% weighted) chose the ‘other’ option.
| Outcome of call | % of participants | n/N, % weighted |
|---|---|---|
| Advice only | 17 | 145/837, 17 |
| Prescription | 22 | 183/837, 22 |
| GP face-to-face appointment | 44 | 367/837, 44 |
| Nurse face-to-face appointment | 7 | 61/837, 7 |
| Follow-up call with GP | 4 | 30/837, 4 |
| Follow-up call with nurse | 2 | 17/837, 2 |
| Other | 8 | 67/837, 8 |
The majority of participants found speaking to a GP by telephone before having a face-to-face appointment more convenient than just attending a face-to-face appointment without being able to talk to the doctor on the telephone first (55%, 56% weighted); 22% of participants (22% weighted) reported that it was less convenient and 23% (22% weighted) reported that there was no difference. Respondents’ weighted ratings of the convenience of talking to a doctor on the telephone before making an appointment are illustrated in Figure 9.
FIGURE 9.
Weighted rating of the convenience of being table to talk to a GP on the telephone first compared with attending a face-to-face appointment without being able to speak to the doctor on the telephone first.
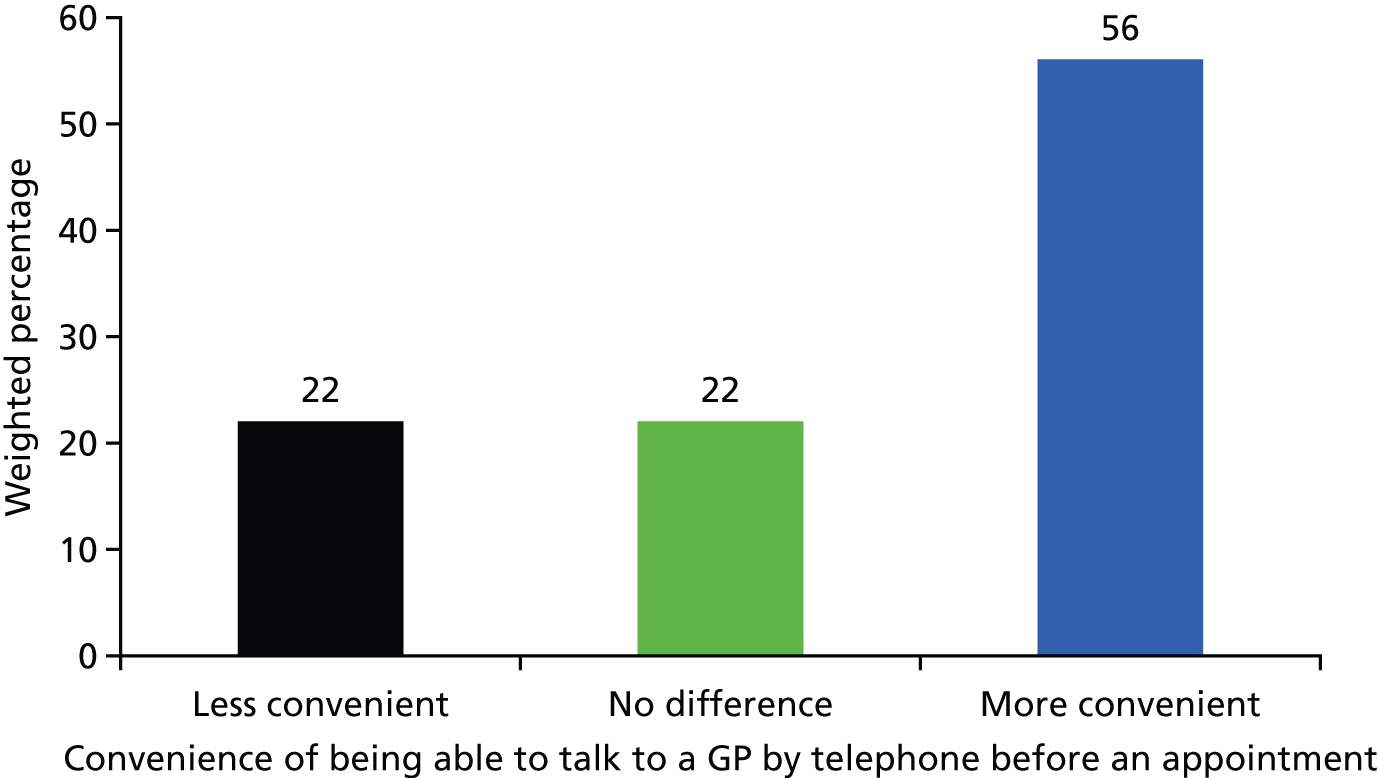
The majority of patients reported finding no difference between their ability to communicate with the GP over the telephone and their ability to communicate with the GP in person (65%, 64% weighted); 23% (24% weighted) reported that it was more difficult and 12% (12% weighted) reported that it was less difficult. Respondents’ perceptions of their ability to communicate with the GP by telephone is illustrated in Figure 10. For those who reported that it was more difficult to communicate with the GP over the telephone than face to face, the reasons for their answers are provided in Table 10.
FIGURE 10.
Weighted rating of the difficulty of communicating with the GP by telephone compared with in person.
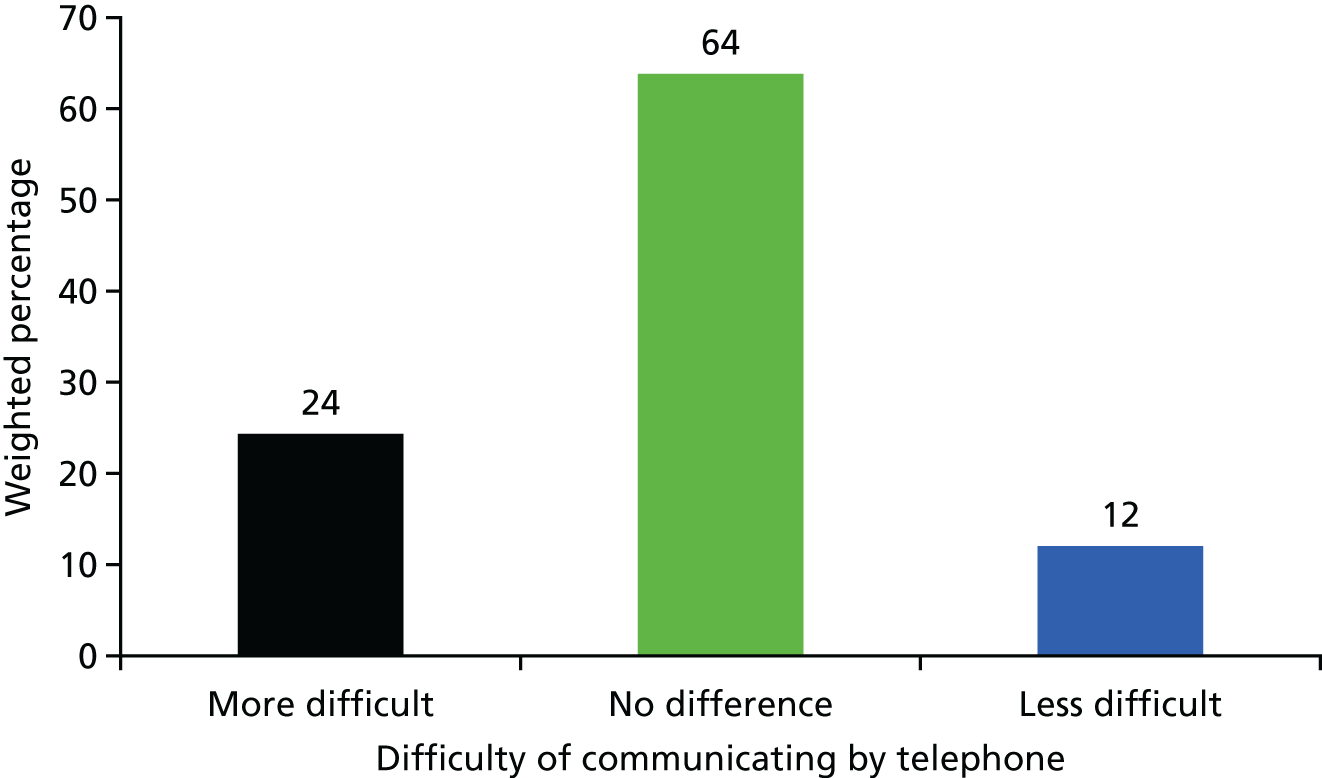
| Reason | % of participants | n/N, % weighted |
|---|---|---|
| English is not my first language | 0 | 0/0, 0 |
| Doctor could not see my health problem | 29 | 52/182, 28 |
| Telephone line was not clear | 8 | 15/182, 8 |
| Patient had impaired hearing | 3 | 5/182, 2 |
| Difficult to explain the problem | 47 | 85/182, 49 |
| Other | 2 | 4/182, 2 |
Overall, 31% of respondents (250/816, 32% weighted) reported that they preferred the ‘telephone first’ approach to the previous appointment system used by the practice, 33% (267/816, 30% weighted) would prefer to return to the old system and 37% (299/816, 38% weighted) reported that they did not have a preference.
Regression analysis
The results of the regression analysis exploring whether or not patient demographic and social factors are associated with their reported experience of the ‘telephone first’ approach are presented in Table 11. The survey was not designed to be sufficiently large to reliably look at the experiences of individual patient subgroups, and in most cases the differences we found in this post-hoc analysis were not statistically significant. Given this lack of power, we note that there is a lack of statistical significance even when large coefficients are seen [e.g. odds ratios (ORs) as large as 2]. One statistically significant effect is that women are less likely to report it being more convenient to speak to a GP on the telephone (OR 0.57, 95% CI 0.41 to 0.82; p = 0.002).
| Patient factors | Experience | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Expecting a callback (n = 660) | Rating of waiting time for callback (n = 656) | Convenience of speaking to GP on telephone (n = 640) | Difficulty of communicating by telephone (n = 647) | Got a face-to-face appointment (n = 663) | Prefers old system (n = 656) | |||||||
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age (years) | ||||||||||||
| < 18 | 1.32 (0.59 to 2.94) | 0.33 | 1.25 (0.53 to 2.93) | 0.68 | 0.64 (0.29 to 1.40) | 0.64 | 1.18 (0.34 to 4.13) | 0.84 | 1.74 (0.80 to 3.84) | 0.060 | 1.49 (0.69 to 3.24) | 0.37 |
| 18–24 | 0.85 (0.32 to 2.29) | 1.15 (0.37 to 3.63) | 0.76 (0.27 to 2.10) | 1.17 (0.23 to 5.98) | 1.60 (0.58 to 4.43) | 1.74 (0.61 to 4.99) | ||||||
| 25–34 | 0.83 (0.41 to 1.71) | 1.18 (0.54 to 2.58) | 1.00 (0.48 to 2.08) | 1.99 (0.70 to 5.64) | 0.58 (0.28 to 1.21) | 1.25 (0.60 to 2.61) | ||||||
| 35–44 | 0.71 (0.35 to 1.44) | 1.31 (0.61 to 2.82) | 0.92 (0.45 to 1.90) | 1.97 (0.69 to 5.61) | 0.67 (0.32 to 1.37) | 0.79 (0.39 to 1.61) | ||||||
| 45–54 | Baseline | Baseline | Baseline | Baseline | Baseline | Baseline | ||||||
| 55–64 | 1.75 (0.93 to 3.27) | 0.64 (0.34 to 1.18) | 0.55 (0.31 to 1.00) | 1.45 (0.58 to 3.58) | 1.38 (0.77 to 2.48) | 1.80 (0.98 to 3.30) | ||||||
| 65–74 | 1.14 (0.59 to 2.22) | 0.92 (0.46 to 1.82) | 0.84 (0.43 to 1.61) | 1.73 (0.67 to 4.47) | 1.48 (0.78 to 2.80) | 1.43 (0.75 to 2.73) | ||||||
| 75–84 | 0.96 (0.49 to 1.88) | 0.78 (0.39 to 1.57) | 0.67 (0.35 to 1.31) | 1.00 (0.35 to 2.83) | 1.59 (0.83 to 3.04) | 1.48 (0.77 to 2.86) | ||||||
| ≥ 85 | 0.82 (0.34 to 1.96) | 0.79 (0.31 to 2.00) | 0.60 (0.25 to 1.43) | 1.51 (0.43 to 5.25) | 0.71 (0.30 to 1.72) | 2.60 (1.01 to 6.72) | ||||||
| Sex | ||||||||||||
| Male | Baseline | 0.33 | Baseline | 0.21 | Baseline | 0.002 | Baseline | 0.88 | Baseline | 0.12 | Baseline | 0.20 |
| Female | 1.19 (0.84 to 1.69) | 0.79 (0.54 to 1.15) | 0.57 (0.41 to 0.82) | 1.04 (0.62 to 1.73) | 0.76 (0.54 to 1.08) | 1.26 (0.89 to 1.78) | ||||||
| Health status | ||||||||||||
| Excellent | Baseline | 0.91 | Baseline | 0.83 | Baseline | 0.059 | Baseline | 0.083 | Baseline | 0.37 | Baseline | 0.58 |
| Very good | 0.89 (0.42 to 1.90) | 1.00 (0.45 to 2.26) | 0.37 (0.17 to 0.82) | 0.79 (0.26 to 2.39) | 1.08 (0.51 to 2.27) | 1.58 (0.76 to 3.27) | ||||||
| Good | 0.93 (0.44 to 1.95) | 0.81 (0.37 to 1.77) | 0.51 (0.24 to 1.10) | 0.75 (0.26 to 2.19) | 0.73 (0.36 to 1.51) | 1.70 (0.84 to 3.46) | ||||||
| Fair | 0.82 (0.38 to 1.79) | 0.81 (0.35 to 1.84) | 0.56 (0.25 to 1.25) | 0.87 (0.29 to 2.66) | 0.69 (0.32 to 1.47) | 1.43 (0.68 to 2.99) | ||||||
| Poor | 1.10 (0.45 to 2.69) | 0.68 (0.27 to 1.70) | 0.34 (0.14 to 0.83) | 2.05 (0.63 to 6.61) | 0.62 (0.26 to 1.44) | 1.85 (0.78 to 4.34) | ||||||
| Ethnicity | ||||||||||||
| White | Baseline | 0.75 | Baseline | 0.18 | Baseline | 0.13 | Baseline | 0.15 | Baseline | 0.65 | Baseline | 0.24 |
| Other | 1.13 (0.53 to 2.40) | 0.59 (0.27 to 1.28) | 0.56 (0.26 to 1.19) | 1.95 (0.79 to 4.80) | 1.19 (0.55 to 2.56) | 1.61 (0.72 to 3.59) | ||||||
| Primary language | ||||||||||||
| English | Baseline | 0.48 | Baseline | 0.52 | Baseline | 0.65 | Baseline | 0.97 | Baseline | 0.24 | Baseline | 0.56 |
| Other | 1.45 (0.52 to 4.04) | 0.72 (0.26 to 1.96) | 0.80 (0.26 to 1.19) | 1.03 (0.29 to 3.63) | 1.85 (0.67 to 5.09) | 1.36 (0.49 to 3.79) | ||||||
| Ability to take time away from work | ||||||||||||
| Yes, easily | Baseline | 0.36 | Baseline | 0.064 | Baseline | 0.074 | Baseline | 0.39 | Baseline | 0.40 | Baseline | 0.48 |
| Yes, with some difficulty | 1.33 (0.77 to 2.29) | 0.63 (0.35 to 1.14) | 0.52 (0.30 to 0.90) | 0.69 (0.30 to 1.62) | 1.01 (0.58 to 1.74) | 1.43 (0.83 to 2.46) | ||||||
| No | 1.02 (0.53 to 1.98) | 0.45 (0.22 to 0.91) | 0.46 (0.23 to 0.92) | 1.52 (0.63 to 3.67) | 0.62 (0.32 to 1.22) | 1.60 (0.80 to 3.17) | ||||||
| Not relevant | 1.54 (0.91 to 2.61) | 0.99 (0.56 to 1.75) | 0.63 (0.37 to 1.08) | 1.00 (0.47 to 2.12) | 0.80 (0.47 to 1.34) | (0.69 to 1.95) | ||||||
There was weak evidence that working status was associated with convenience of speaking to a GP on the telephone (p = 0.07) and ratings of waiting times (p = 0.06). In particular, those who could not take time away from work to receive a callback were less likely to report it to be more convenient to speak to a GP on the ‘telephone first’ (OR 0.46, 95% CI 0.23 to 0.92) and less likely to rate the waiting time as being satisfactory than those who were more easily able to take time away from work (OR 0.45, 95% CI 0.22 to 0.91). There was also weak evidence (p = 0.06) that respondents with less than excellent self-reported health were less likely to report that it was more convenient to speak to a GP by telephone than those who reported being in excellent health (e.g. poor vs. excellent OR 0.34, 95% CI 0.14 to 0.83). There was also weak evidence (p = 0.08) that self-reported health status was associated with the reported ease of communicating with a GP by telephone. Respondents with very good/good/fair self-reported health status were less likely to report that it was easier to communicate by telephone and those in poor health were more likely to report that it was easier to communicate by telephone than those in excellent health (e.g. poor vs. excellent OR 2.05, 95% CI 0.63 to 6.61). Given that there was no correction for multiple testing, these results should be treated with caution.
Space was available at the end of the questionnaire to add free-text comments; these comments showed a wide range of views, which, consistent with the patient interviews (see Chapter 9), included both very positive and very negative views. An illustrative selection of these comments is presented in Box 2.
I think to be able to pick up a phone and speak to your GP who will either see you, leave a prescription or advise you to see a nurse is excellent.
Practice 104
On the rare occasions it’s been an emergency, the ring back has been almost immediate – I cannot fault the system.
Practice 105
It saves wasting the time of the GP if the matter can speedily be dealt with over the phone.
Practice 116
Excellent service. It’s much easier to speak to doctor and the few times I’ve phoned in, my problem has been sorted out over the phone which saves time for both parties.
Practice 117
With this system if it’s necessary, you usually get to see the doctor the same day – it saves time for serious cases to see the doctor. Much better than the old system.
Practice 108
Examples of negative comments
Speaking to the doctor isn’t the problem: it’s getting through on the phone that’s the difficulty.
Practice 111
I think this system is stupid. Once I waited 6 hours for a callback – I could have been dead.
Practice 110
The callback system is truly awful – I cannot plan my day as I work from site to site over long distances.
Practice 103
If you work in a job where you can’t take phone calls it can be almost impossible to get a callback from a doctor.
Practice 121
The only difficulty for me is that it’s sometimes difficult to explain more intimate matters to a GP over the phone – I work in an office with other people and it can be difficult to find a quiet confidential place to talk.
Practice 116
Reproduced from Newbould et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Summary
Just under one-third of patients surveyed preferred the ‘telephone first’ approach to the previous system, with the rest almost equally split between wanting to return to the previous system or having no preference.
Around two-thirds of people surveyed expected to receive a callback from the GP before making a face-to-face appointment. Patients were more likely to give a positive rating if the callback was received within 1 hour, with 95% of people who were called back within 20 minutes rating this as excellent or good. However, even when the wait was > 1 hour, nearly 80% of participants thought that this was at least ‘acceptable’ and more than one-third thought that it was good or excellent, a finding that could be because some people specifically wanted a delayed callback, as noted in our patient interviews (see Chapter 9). There was some evidence that those who found it harder to take time away from work and those not in work (including retirees) were less likely to rate the callback time as good or excellent.
Half of the patients surveyed were called in for a face-to-face appointment with either a GP or a nurse. This conversion rate is above the threshold suggested by both commercial companies. A large majority of patients were satisfied with the outcome of the GP call, although just under 10% thought that they should have been called in for a face-to-face appointment.
Most respondents reported that it was more convenient to be able to speak to a GP on the telephone before an appointment than just attending a face-to-face appointment without being able to talk to the doctor on the telephone first. However, there were indications that women, people with worse self-reported health and those less able to take time away from work were less likely to report that it was convenient. Although most people found no difference in communicating with the GP by telephone compared with communicating face to face, a substantial minority said that they found it more difficult. The most common reason for finding it more difficult was that the patient found it difficult to explain the problem or felt that they needed to show the doctor their health problem. Interestingly, those who reported being in ‘poor’ health were less likely to report difficulty than those in excellent health, which could reflect an existing rapport between frequent users and the practice doctors.
When considering the generalisability of these results, we should bear in mind that we did not achieve a representative sample of practices taking part in the survey. Only one rural practice was selected and the national GP Patient Survey scores were, on average, substantially better in those practices that participated than in those that declined to take part. Given this, it seems likely that our sample over-represents those practices in which the ‘telephone first’ approach was working well. For this reason, our findings may provide an overoptimistic view of patients’ experiences.
Chapter 5 Practice manager survey
The practice manager survey aimed to understand the practice’s experience of setting up and using a ‘telephone first’ approach, as well as the perceived advantages and disadvantages of the approach for both practice staff and patients, from the practice staff’s perspective.
Methods
Survey development
The development of the survey was informed by themes emerging from the qualitative element of the study (based on interviews with GPs and practice staff, and with patients). Survey questions were first tested in a cognitive interview with a practice manager to determine whether or not they were being interpreted as intended, before piloting the revised survey with a small sample of practice managers (n = 3).
Practice selection and sampling
The two commercial companies provided a list of practices known to be running the ‘telephone first’ approach. The sample frame was restricted to practices that had been operating the ‘telephone first’ approach since 24 June 2015 (n = 101 practices).
Survey distribution
A paper-based survey was sent by post and addressed to the practice manager in September 2016 alongside a letter from the study’s principal investigator. When relevant, the letter was tailored to account for whether the practice had already participated or declined to participate in other elements of the study. A reminder survey was sent 4 weeks later, followed by an opportunity to fill in the survey online 6 weeks after the initial mail-out.
Analysis
Survey responses have been summarised using descriptive statistics. Some practice managers did not answer all of the survey questions; consequently, the total number of responses presented varies for each question as we present the results based on all those who answered it. Free-text responses were read and grouped into overarching themes.
Results
In total, 42 practice managers responded; the response rate was 41% (42/102). Of these, 16 respondents (38%, 16/42) were from a practice that had participated in at least one other component of our study. All respondents reported that their practice either was currently using the ‘telephone first’ approach (81%, 34/42) or had previously used it (19%, 8/42).
For the 34 practices currently using the ‘telephone first’ approach, the average length of time that the system had been in place was just over 3 years, ranging from 0.2 to 5 years. All practice managers reported that telephone consultations were conducted by GPs, and an additional 13 practice managers (39%) reported that nurse practitioners also conducted some telephone consultations.
Respondents were asked to mark on a scale from 0 to 100 the percentage of requests for same-day appointments and advance appointments preceded by a telephone consultation. All practice managers reported that, for ≥ 20% of requests for same-day appointments, a telephone consultation preceded a face-to-face appointment, and 78% of practice managers (25/32) reported that ≥ 90% requests for same-day appointments were preceded by a telephone consultation. There were lower levels of telephone consultation prior to advanced appointments: 17% of practice managers (5/30) reported that no requests for advanced appointments were preceded by a telephone consultation, but 70% (21/30) reported that ≥ 90% of requests for advance appointments were preceded by a telephone consultation before an appointment was given. Over half of practice managers surveyed (53%, 17/32) reported that the way they used telephone consultations had changed since they began using the approach.
Over three-quarters of practices that responded (76%, 31/41) reported that they had received help from a commercial company to switch to the ‘telephone first’ approach. Seventy per cent of practice managers (28/40) described problems or challenges when setting up the new service (Table 12).
| Challenges | n |
|---|---|
| Ensuring that patients understand the system | 6 |
| Adapting to increase in demand from patients/GP’s workload | 5 |
| Catching up with backlog prior to the system launch | 4 |
| Dealing with patient dissatisfaction with new system | 4 |
| Need for additional telephone lines | 2 |
| Retraining staff | 2 |
| Adapting GP rotas to the new system | 2 |
| Very stressful for staff because of feeling constantly ‘on call’ | 1 |
| Outgoing calls match incoming calls at peak times | 1 |
| Knowing at what stage of the day to revert to urgent only | 1 |
| High cost of telephone calls | 1 |
Practice managers were asked about the advantages and disadvantages of using the ‘telephone first’ approach for GPs and practice staff. All practice managers reported advantages or disadvantages of the new system. Overall, 88% (36/41) reported that they had found advantages for GPs and practice staff, and 78% (32/41) reported that they had found disadvantages for GPs and practice staff (Table 13).
| Advantages and disadvantages | n |
|---|---|
| Advantages | |
| GPs can manage their own time | 9 |
| Increased capacity for appointments (more appointment slots available per day) | 5 |
| Less pressure on receptionist to decide who gains access to limited appointments/receptionist no longer acting as gatekeeper to appointments | 4 |
| Less confrontation for reception staff | 3 |
| Better use of GPs’ time | 3 |
| GPs need to see fewer patients face to face | 2 |
| Reduced DNAs | 2 |
| Improved staff satisfaction | 1 |
| Patients can always get an appointment | 1 |
| Patients are not waiting outside the surgery before the surgery opens | 1 |
| GPs can access patients’ information before seeing them, enabling them to direct the patient to the right clinician | 1 |
| No wasted face-to-face appointments | 1 |
| Practice staff are able to better manage demand | 1 |
| Helped GPs reduce their amount of work | 1 |
| More flexible approach | 1 |
| No overflowing prebooked sessions to cancel if GP is sick | 1 |
| Disadvantages | |
| Increased/more intense workload for GPs and more stress | 11 |
| Fuels demand from patients (sometimes for trivial telephone conversations) | 9 |
| Increased patient complaints | 4 |
| Increased patients’ expectations | 3 |
| Practice’s telephone bill rose | 3 |
| Frequent need to call patient twice (e.g. if missed callback) | 2 |
| Changed the way doctors see patients/GPs dissatisfied with less face-to-face contact | 2 |
| Increased workload for reception staff | 2 |
| Need more telephone lines | 2 |
| GPs found it difficult to get through the list of patients | 1 |
| GPs do not like unpredictable nature of the day | 1 |
| Changing patient behaviour, with many ringing late in the day | 1 |
| Patients exaggerate the urgency of their issue in order to receive a face-to-face appointment | 1 |
| Patients do not appreciate how good their access is now | 1 |
| Patients initially not happy, but gradually accepted new system | 1 |
| Does not suit everyone or every practice | 1 |
Summary
Over half of practices using a ‘telephone first’ approach reported that the practice had modified the way the system originally operated. For example, in contrast to the approach promoted by the two commercial companies, some practices were using a nurse practitioner as well as GPs for telephone consultations prior to offering a face-to-face appointment.
Practice managers identified a range of advantages and disadvantages of the approach both for staff working at the practice and for patients. The same factors were often identified as both advantages and disadvantages; for example, it was easier under the ‘telephone first’ approach for a GP to be in control of their working day but, conversely, there was a level of unpredictability as to what the day would bring because GPs did not know what was going to come up until they were speaking to patients on the telephone. Likewise, some practice managers considered that the system was better for working patients, who then did not have to take time off work to speak to a doctor, whereas others noted that it could be more challenging for patients who had difficulty receiving a telephone call at work.
Chapter 6 Patient experience: analysis of data from the national GP Patient Survey
We undertook a controlled analysis to examine changes in patients’ self-reported experiences of care in intervention practices before and after the introduction of the ‘telephone first’ approach compared with data from a random sample of control practices; this analysis used data from the national GP Patient Survey.
Methods
Data source and sampling
The GP Patient Survey is a national postal survey of patients’ experiences of primary care in England. The survey is sent twice a year (July to September and January to March) to ≈2.8 million adult patients per year. A stratified sample of patients aged ≥ 18 years who have been continuously registered with a general practice for ≥ 6 months is drawn from the practice list of each general practice in England, with patients from practices that are known from prior surveys to have low response rates being oversampled. Full details of the sampling strategy have been published. 75
We used data from July 2011 to April 2016. The contents of the survey remained largely consistent over this time period. Response rates have fluctuated over the period: falling from 38% in 2011/12 (1,037,946 responses) to 33% in 2014/15 (858,381 responses) and recovering to 39% in 2015/16 (836,312 responses) following the introduction of a reminder postcard in addition to the two reminder surveys already used. The data period included data from a total of 8323 practices, but not all practices had data for each wave of the survey; the number of practices contributing data varied between 8243 and 7687 in any one wave. This variation is primarily due to practice closures and openings.
Practices using a ‘telephone first’ approach between 2011 and 2016 were identified based on information provided by the two commercial companies providing support for implementing this service. The companies provided details on the practices that were using their system, the date when the ‘telephone first’ approach was introduced and the current status of the system (i.e. whether still running a full ‘telephone first’ system, running a hybrid system or if the practices had abandoned the system). Only practices that launched the ‘telephone first’ approach before 31 December 2015 were included in the analysis to allow sufficient time for the system to have bedded in; those with later launch dates were classified as non-intervention practices in this analysis. In total, 146 intervention practices were identified in the GP Patient Survey data set. This was considerably larger than the expected number of 90 practices used in our original sample size calculations. The number of practices receiving the intervention varied over time (Table 14), and only one practice was using the ‘telephone first’ approach throughout the entire data period. For the intervention practices, we had data from between 0 and 4.5 years pre intervention and 0.5 and 5 years post intervention (nine GP Patient Survey waves in each case). Analysis was restricted to survey respondents who had indicated that they had attempted to see or speak to a GP in the previous 6 months. This restriction allowed us to attribute reported experiences to the time period of the survey. A total of 29,472 surveys were available from intervention practices post launching the ‘telephone first’ approach. To inform selection of control practices, we undertook a survey of 500 practices to establish how widespread approaches similar to the ‘telephone first’ approach were (see Appendix 5). Based on our findings that such approaches were rare, controls were selected at random from all practices classified as non-intervention practices (i.e. any practice in England not on the list provided by the commercial companies or practices that launched the ‘telephone first’ approach after 31 December 2015). For computational reasons, our analysis was restricted to data from all 146 intervention practices and a random 10% sample of control practices, with between 778 and 976 control practices providing data at any one time.
| Wave | Year (number of practices) | ||||
|---|---|---|---|---|---|
| 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | |
| July–September | 1 | 22 | 74 | 105 | 140 |
| January–March | 6 | 44 | 79 | 122 | 144 |
Analysis
We used seven measures of patient experience from the GP Patient Survey in this analysis:
-
Last time you saw or spoke to a GP from your GP surgery, how good was that GP at each of the following?
-
giving you enough time
-
listening to you
-
explaining tests and treatments
-
involving you in decisions about your care
-
treating you with care and concern.
-
-
Generally, how easy is it to get through to someone at your GP surgery on the telephone?
-
Would you recommend your GP surgery to someone who has just moved to your local area?
-
How often do you see or speak to the GP you prefer?
-
How long after initially contacting the surgery did you actually see or speak to them?
-
How convenient was the appointment you were able to get?
-
Overall, how would you describe your experience of making an appointment?
In each case, responses were rescaled between 0 (poor experience) and 100 (good experience). In the case of the first question above on GP communication, a composite variable was created to take the mean of all informative responses as long as three or more informative responses were given. For the fifth question, a binary outcome was created of whether or not the patient was ‘seen or spoken to on the same day’ as the initial contact. The reason for also looking at ‘time until seen or spoken to’ as a binary variable is that the protocol recommended by the commercial companies is that all requests for an appointment with a GP should be dealt with on the same day.
Two types of analysis were carried out for each of the outcomes. The first was a before-and-after analysis, illustrated by the superposed epoch graphs (see Figures 11–18) in which the introduction of the system in each practice is set at time zero. Second, a regression analysis was performed for each outcome, looking (1) for step changes at the time when the intervention was introduced and (2) for a change in the preceding trend (e.g. slowing down of a previous increase). We also model heterogeneity in these changes to examine whether or not the intervention has a different effect in different practices. Adjustment was also made for season and national trends along with adjustment for person-level factors (age, sex, ethnicity and deprivation level). Full details of the statistical analysis are given in Appendix 6.
Our main analysis was conducted on an intention-to-treat basis. It includes all practices identified by the commercial companies even when the companies informed us that the practices were running a hybrid form of the system or were no longer running the system. This was done in order to avoid selection bias, whereby only the successful practices continue with the system in the recommended form. A sensitivity analysis (see Appendix 6) was also performed, restricting the analysis to the 89 practices in which we believed, on the basis of information provided by the commercial companies, that the system was being run consistent with the companies’ protocols.
Results
The intention-to-treat analysis is presented in the following sections: (1) the superposed epoch analysis and (2) the regression analysis. The sensitivity analysis restricted to practices in which we believed, on the basis of information provided by the commercial companies, that the system was being run consistent with the companies’ protocols is presented in Appendix 7.
Before-and-after analysis of GP Patient Survey score (intervention practices only)
Figures 11–18 show the changes in score relative to intervention launch (the superposed epoch analysis) for the seven measures of patient experience. For each graph, the black lines represent the mean score of patients within a single intervention practice relative to the launch time. The green dots represent the mean score of patients in all intervention practices combined relative to the launch time. In all cases, large variation in scores between practices can be seen by the spread in the black lines.
FIGURE 11.
Superposed epoch analysis of GP communication composite mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
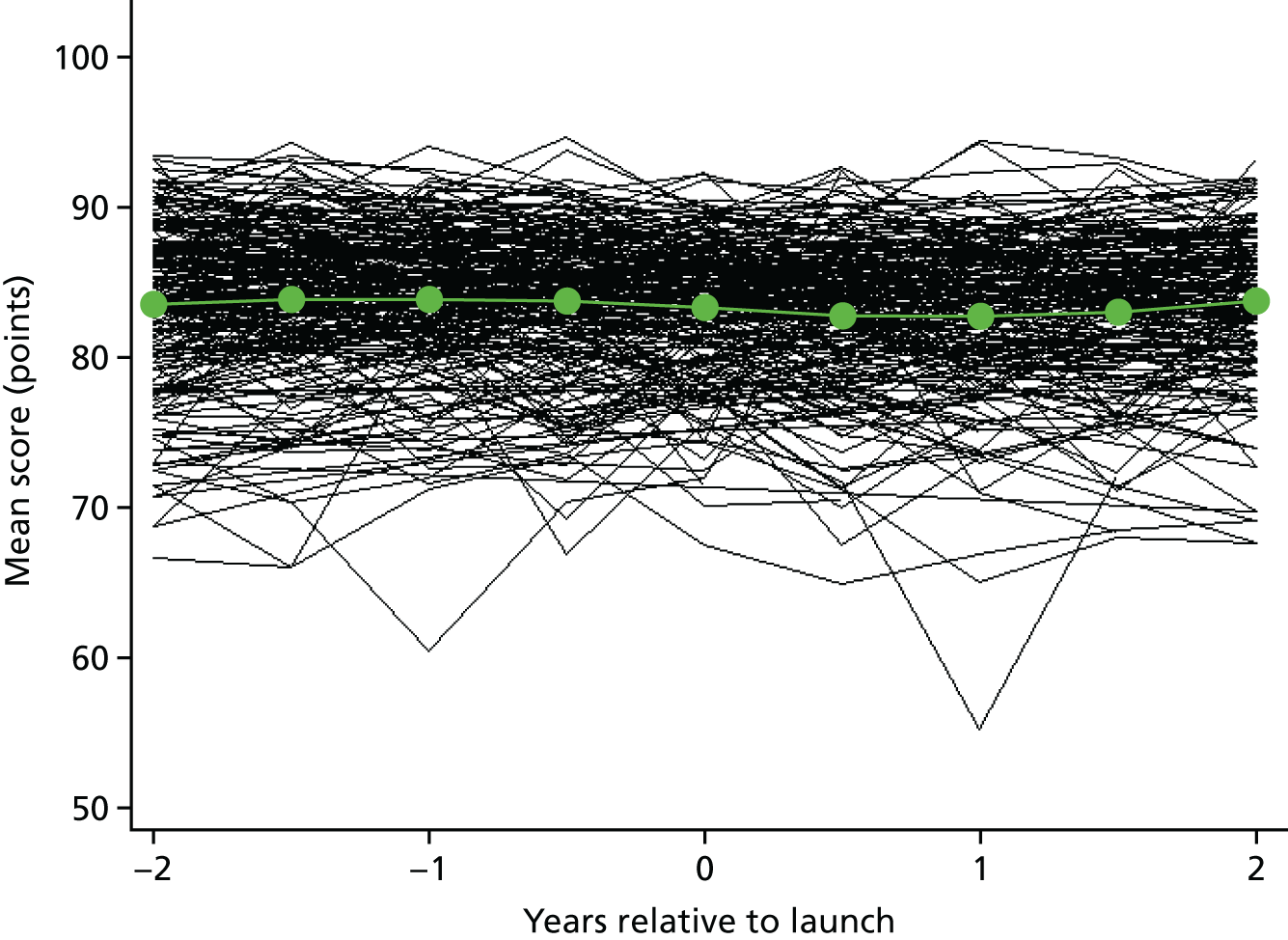
FIGURE 12.
Superposed epoch analysis of ease of getting through on the telephone mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
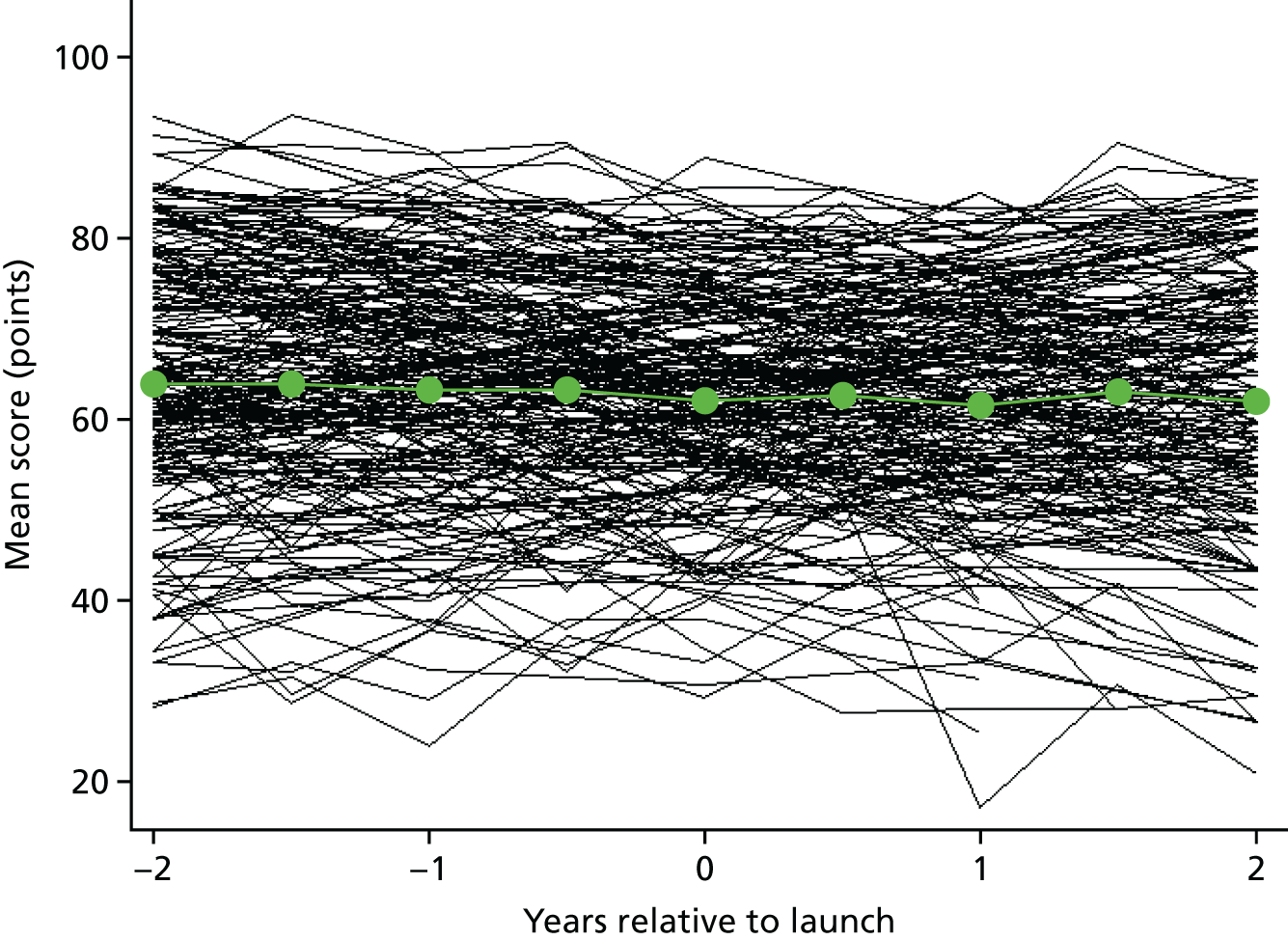
FIGURE 13.
Superposed epoch analysis of mean score on ‘recommending GP surgery to someone who has just moved into the area’ relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
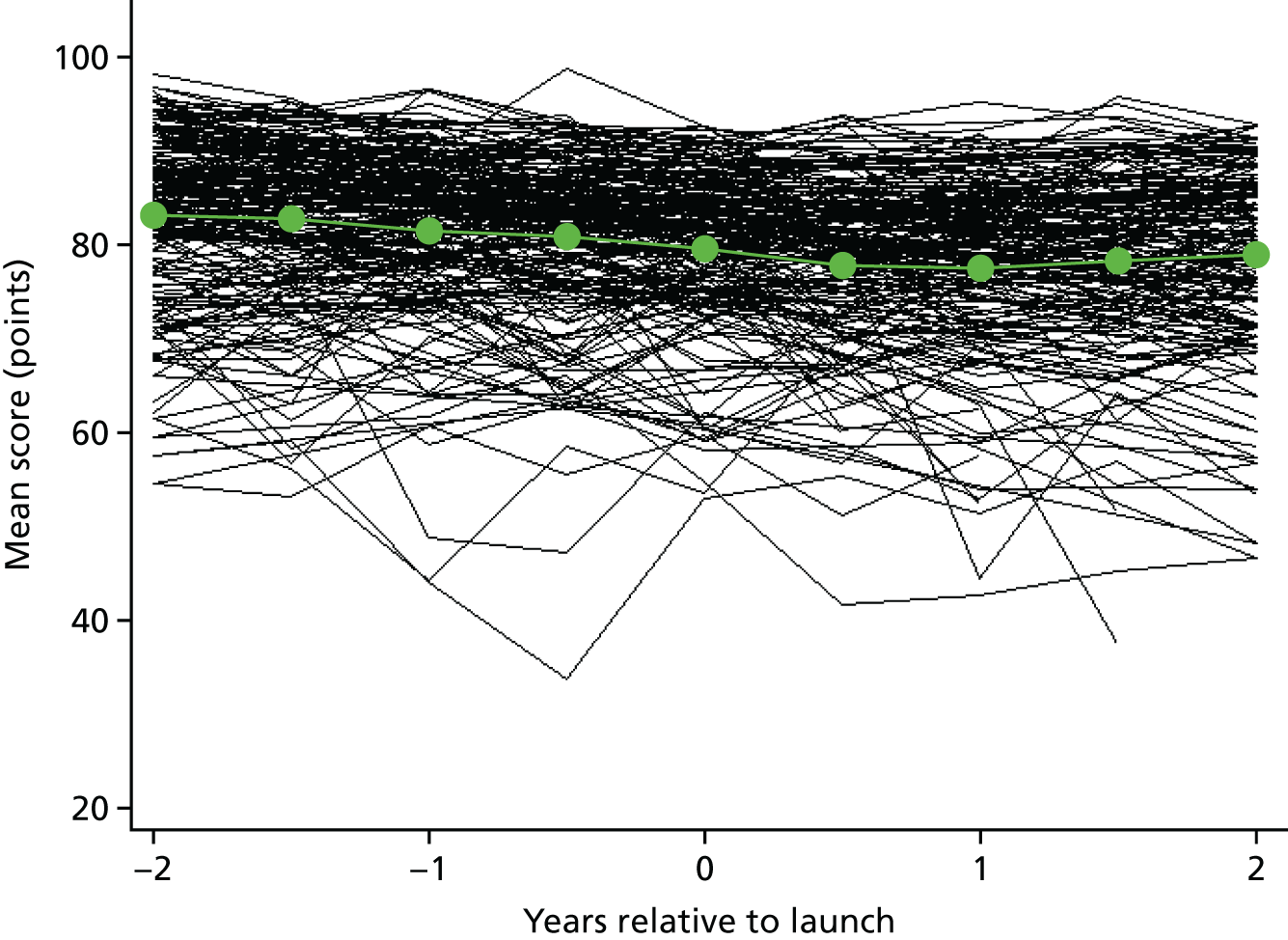
FIGURE 14.
Superposed epoch analysis of ability to see preferred GP mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
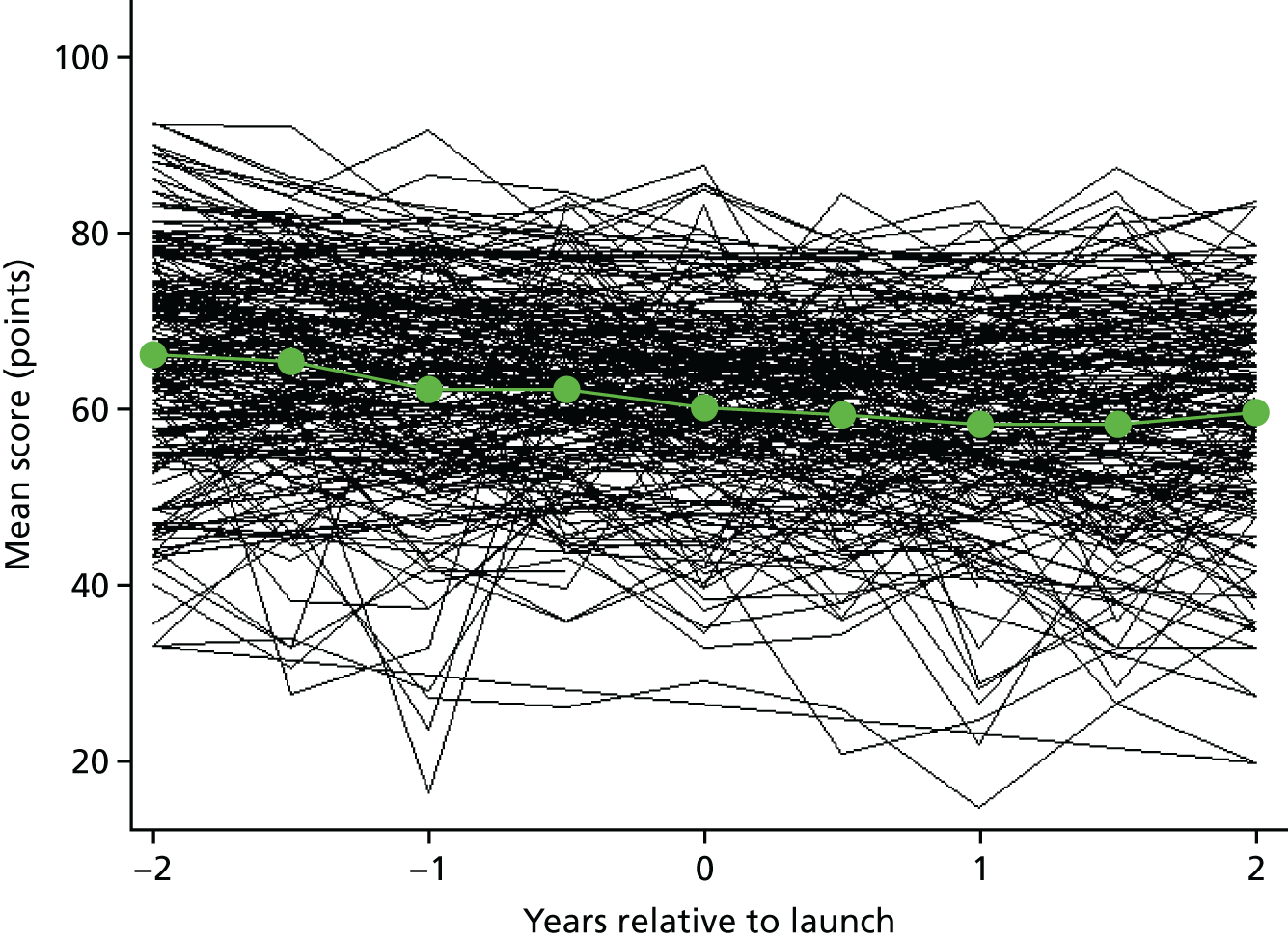
FIGURE 15.
Superposed epoch analysis of time until seen or spoken to mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
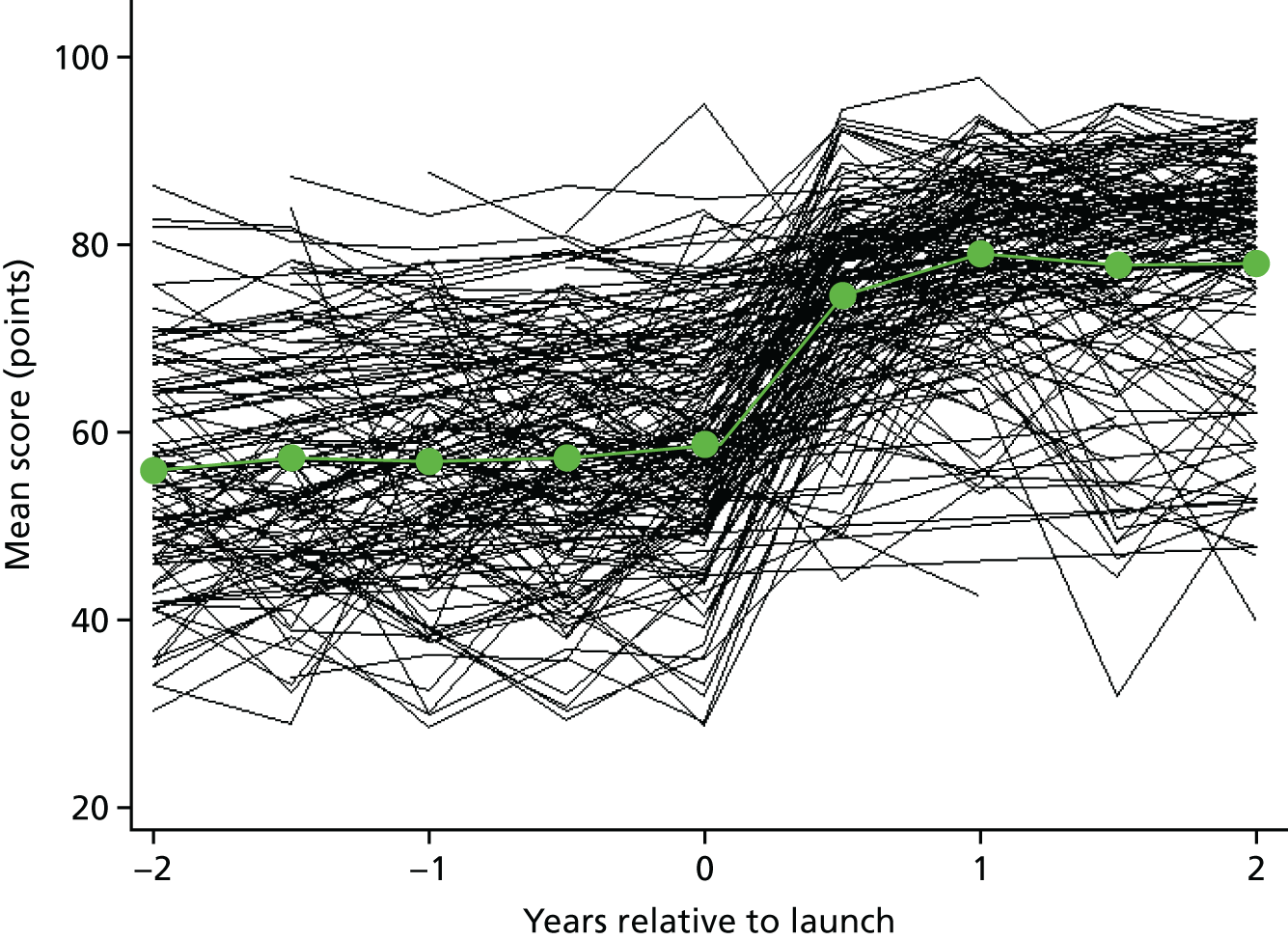
FIGURE 16.
Superposed epoch analysis of percentage of people seen or spoken to on the same day relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
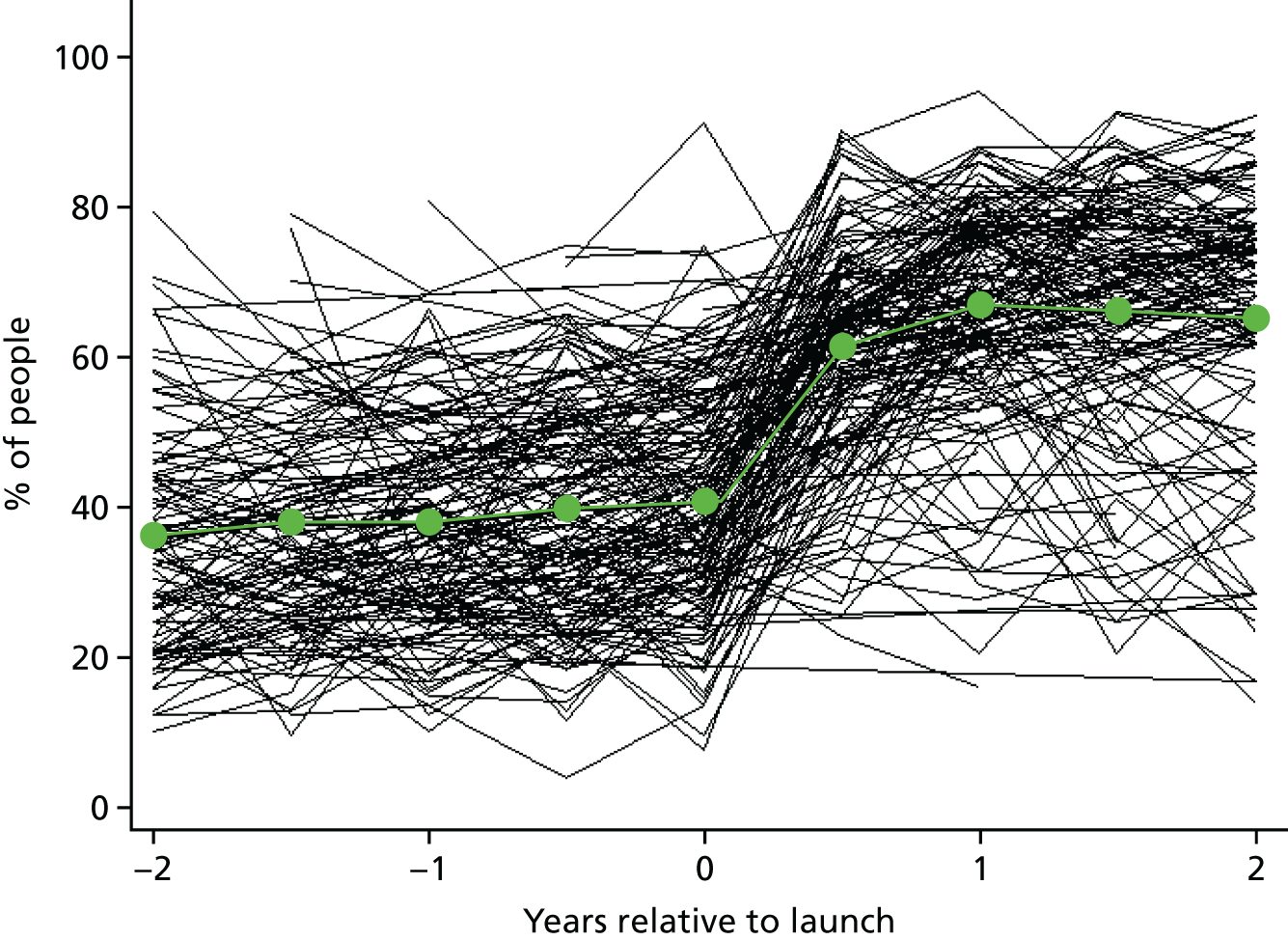
FIGURE 17.
Superposed epoch analysis of convenience of appointment mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
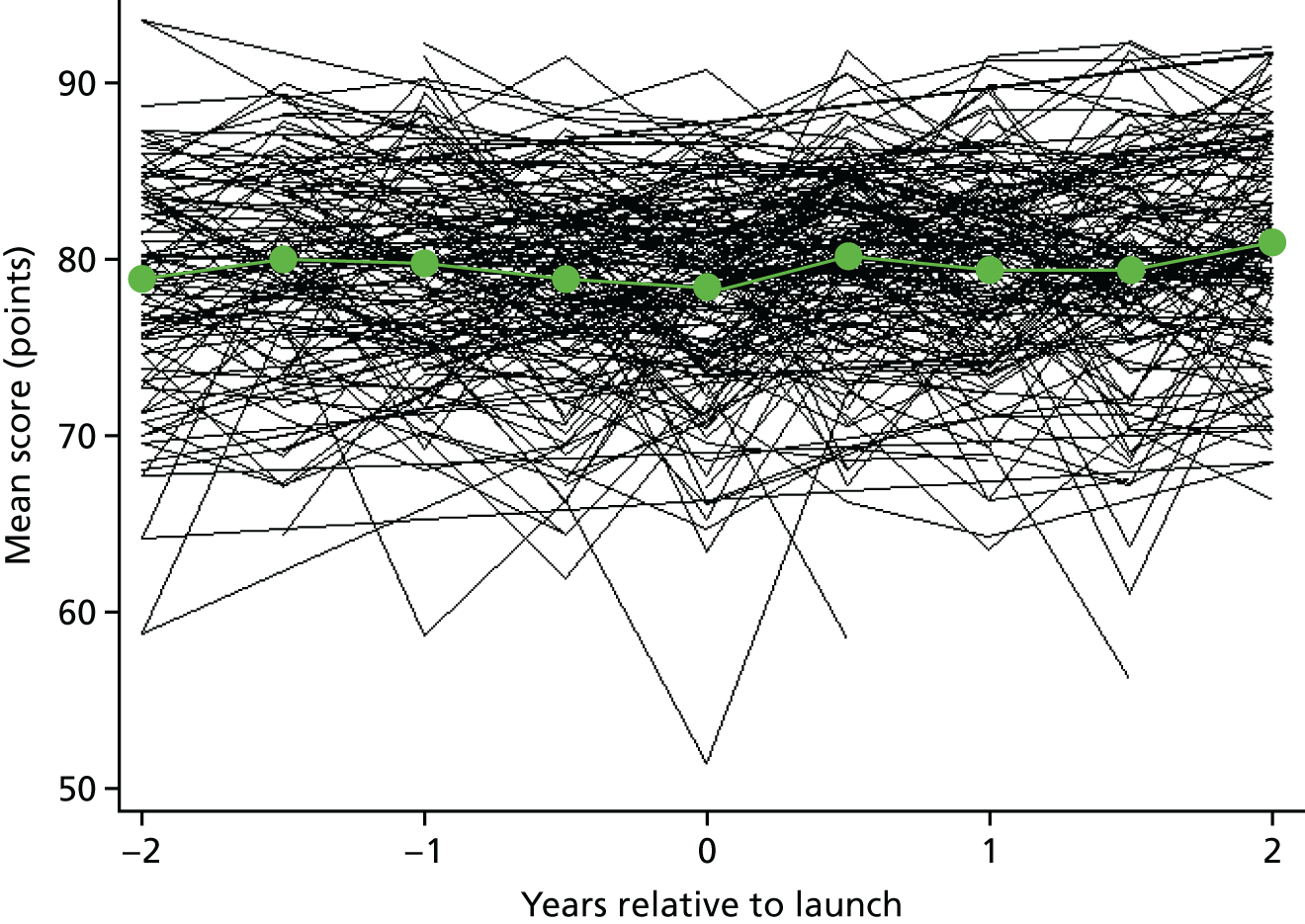
FIGURE 18.
Superposed epoch analysis of overall experience of making an appointment mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
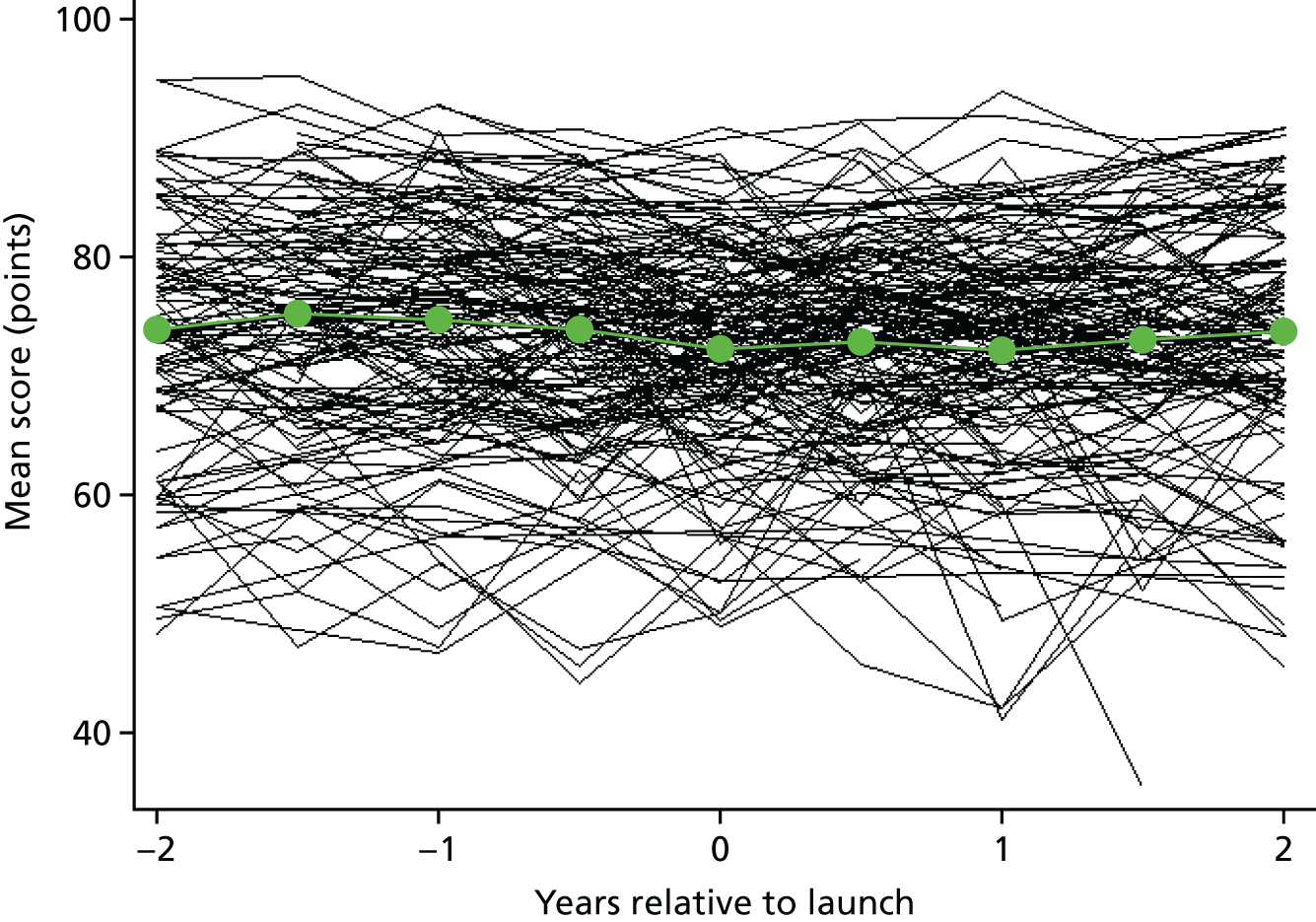
The most obvious change in score was seen for the patients’ rating of time until seen or spoken to (see Figure 15). The mean score increased from 58.6 points (SD 11.7 points) (on a scale from 0 to 100) before the launch to 74.5 points (SD 10.0 points) immediately after launch (year 0.5 in Figure 15), and increasing to 79.0 points (SD 10.0 points) in the next wave (year 1 in Figure 15). The proportion of patients being seen or spoken to on the same day as making initial contact with the surgery increased from 40.9% (SD 14.1%) before the launch to 67.2% (SD 14.9%) in the year following launch. This change is substantial compared with the background variation between practices.
For other outcomes, changes were far more modest and often not easily discernible from background trends. Scores increased for one of the six other outcomes considered: convenience of appointment [from a mean of 78.3 points (SD 5.7 points) at the time of the launch to a mean of 79.3 points (SD 5.7 points) 1 year post launch; see Figure 17]. Scores decreased for the other five measures considered: (1) GP communication [from a mean of 83.3 points (SD 4.9 points) at the time of the launch to a mean of 82.7 points (SD 5.4 points) 1 year post launch; see Figure 11], (2) ease of getting through on the telephone [from a mean of 62.2 points (SD 12.4 points) at the time of the launch to a mean of 61.5 points (SD 12.9 points) 1 year post launch; see Figure 12], (3) recommend GP surgery [from a mean of 79.4 points (SD 8.9 points) at the time of the launch to a mean of 77.4 points (SD 9.9 points) 1 year post launch; see Figure 13], (4) ability to see preferred doctor [from a mean of 60.1 points (SD 11.5 points) at the time of the launch to a mean of 58.5 points (SD 12.1 points) 1 year post launch; see Figure 14] and (5) rating of overall experience of making an appointment [from a mean of 72.2 points (SD 8.7 points) at the time of the launch to a mean of 72.0 points (SD 9.4 points) 1 year post launch; see Figure 18]. These differences are all very small compared with the mean reduction in time until being seen or spoken to (20.4 points on a 0–100 scale; see Figure 15), the largest being the 1.0-point increase in convenience of appointment time and the 1.6-point reduction in patients who would recommend the practice to someone who has just moved into the area.
Comparison with other practices in England (controlled regression analysis)
The results of the mixed-effects regression analyses for the seven patient experience measures are presented in Table 15. The coefficient for the step change following the intervention can be interpreted as the effect on the intervention immediately following the launch being the difference between the observed scores and that expected had the intervention not happened. Consistent with the graphical analysis, there is a very strong effect seen in the rating of time until being seen or spoken to, which increases by 20.0 points (95% CI 18.2 to 21.9 points; p < 0.001) on the 0–100 scale, and when considered as a binary outcome, we see an increased percentage of patients being seen or spoken to on the same day as making contact, with an OR of 2.70 (95% CI 2.41 to 3.01; p < 0.001). There is also evidence of decreases in the GP communication score (–0.89 mean points, 95% CI –1.40 to –0.38 points; p < 0.001), recommending GP surgery (–2.37 mean points, 95% CI –3.22 to –1.52 points; p < 0.001) and ability to see the preferred GP (–1.25 mean points, 95% CI –2.41 to –0.08 points; p = 0.035). There is no evidence of a change in the other three outcomes considered (p > 0.3).
| GP Patient Survey outcome | Change following intervention | |||||
|---|---|---|---|---|---|---|
| Step | Additional yearly | |||||
| Difference (95% CI) | p-value | Heterogeneity (95% reference range)a | Difference (95% CI) | p-value | Heterogeneity (95% reference range)a | |
| GP communication composite | –0.89 (–1.40 to –0.38) | < 0.001 | –3.83 to 2.05 | –0.03 (–0.29 to 0.23) | 0.82 | –0.52 to 0.46 |
| Ease of getting through on the telephone | 0.49 (–0.58 to 1.57) | 0.37 | –9.07 to 10.05 | 0.18 (–0.57 to 0.93) | 0.64 | –5.82 to 6.18 |
| Would you recommend your GP surgery? | –2.37 (–3.22 to –1.52) | < 0.001 | –9.11 to 4.37 | 0.24 (–0.24 to 0.72) | 0.34 | –2.54 to 3.02 |
| Seeing preferred GP | –1.25 (–2.41 to –0.08) | 0.035 | –7.78 to 5.28 | 0.050 (–0.65 to 0.75) | 0.89 | –3.24 to 3.34 |
| Time until being seen or spoken to | 20.04 (18.16 to 21.93) | < 0.001 | 1.44 to 38.64 | 0.12 (–0.87 to 1.11) | 0.81 | –7.62 to 7.86 |
| Convenience of appointment | 0.38 (–0.35 to 1.10) | 0.31 | –5.11 to 5.87 | 0.41 (0.08 to 0.75) | 0.016 | –0.84 to 1.66 |
| Overall experience of making an appointment | –0.44 (–1.46 to 0.57) | 0.39 | –9.73 to 8.85 | 0.86 (0.32 to 1.40) | 0.002 | –2.65 to 4.37 |
| Binary outcome: ORb | ||||||
| Seen or spoken to on same day | 2.70 (2.41 to 3.01) | < 0.001 | 1.15 to 6.31 | 1.01 (0.95 to 1.07) | 0.82 | 0.62 to 1.60 |
For five of the seven continuous outcomes and the binary outcome of being seen or spoken to on the same day, there is no evidence of a differential trend between the intervention practices and that which would have been expected (additional yearly change following intervention in Table 15, p > 0.3). For the convenience of making an appointment and the overall experience of making an appointment, there is a small additional positive trend (p = 0.016 and p = 0.002, respectively).
In addition to the average differences, Table 15 also shows that there was evidence of strong heterogeneity in the effect of the intervention, demonstrated by the random effects. For all but one of the outcomes considered, the SD of the random slope for both the step change following intervention and the differential slope following intervention was larger than the main effect, meaning that substantial numbers of practices saw an improvement, whereas others saw declines in scores (see the 95% reference ranges in the step change column in Table 15). For the rating of time until being seen or spoken to, improvement was seen across the board, but with large variations in magnitude: the middle 95% of practices showed increases of between 1.4 points and 38.6 points for the continuous outcome (ORs between 1.15 and 6.31).
Finally, the supplementary analysis found no evidence that the effect of the intervention was different between those in work or not in work (p > 0.1 for all; results not shown). The sensitivity per-protocol analysis (see Appendix 7) produced broadly consistent findings, but with some small differences: there was evidence of an increase in the step change for ease of getting through on the telephone (mean 1.79 points, 95% CI 0.44 to 3.13 points; p = 0.009) and the differential trend in time until being seen or spoken to (mean 1.91 points, 95% CI 0.90 to 2.93 points; p < 0.001 as a continuous outcome and OR of 0.24, 95% CI 0.62 to 1.60; p < 0.001 as a binary outcome).
Summary of findings
The ‘telephone first’ approach appears to have had little, or no, impact on the reported experience of patients attending those practices, except for the outcome of ‘time until a patient is seen or spoken to after initially contacting a practice’, in which a dramatic increase in the percentage of patients being seen on the same day is seen following the introduction of the ‘telephone first’ approach. This is perhaps not surprising given that same-day access is the fundamental aim of the approach, but the fact that such a dramatic change is seen demonstrates that these data are sensitive to such changes. The small changes seen in other items suggest that improvement in timely access is not significantly detrimental to other dimensions of patient experience; however, there were small initial reductions in the proportion of patients who would recommend their practice to someone moving into the area and in patients’ ability to see their preferred GP. However, it is equally important to note the lack of substantial improvements apart from timely access. Thus, although there is little detriment, there appear to be no additional benefits to patient experience.
Chapter 7 Secondary care utilisation: analysis of Hospital Episode Statistics data
In order to examine the effect of the ‘telephone first’ approach on secondary care utilisation, we undertook a controlled analysis of A&E attendances, outpatient attendances and inpatient admissions. This compared the number of attendances/admissions by patients registered in practices known to be using the approach before and after the launch of the system, and compared these changes to a random selection of control practices across England using HES data.
Methods
Accident and emergency, outpatient and inpatient HES data were obtained from NHS Digital covering the period from April 2008 to March 2016.
Accident and emergency and outpatient attendances are recorded as attendances in HES, whereas inpatient HES data are recorded as a series of ‘Finished Consultant Episodes’ (i.e. time spent under a particular consultant’s care). Prior to analysis, we linked these episodes together to form single admissions using the University of York Centre for Health Economics Continuous Inpatient Spell definition. Admissions were flagged if they were related to an ambulatory care sensitive (ACS) condition based on the classification used by Bardsley et al. 76 Furthermore, admissions were defined either as elective or emergency admissions based on the HES data classification (a small number of admissions were defined as ‘other’ in the HES data and, although they are included in the all-admissions counts, they are not included in the elective or emergency counts).
For all observations in which a patient’s general practice was recorded, patient age, sex and Index of Multiple Deprivation (IMD) (a measure of small-area-level deprivation of the patient’s home address) were extracted. Age groups were then defined as 5-year age groups up to the age of 19 years, then 10-year bands up to the age of 89 years, with a further group containing all ages of ≥ 90 years. IMD was classified into five groups with quintile defining cut-off points, from most to least deprived. The number of attendances/admissions per calendar month in each age group, by sex and by IMD strata, were calculated within each practice separately for each year and month of data for the following outcomes:
-
A&E attendances
-
outpatient attendances
-
all inpatient admissions
-
all inpatient admissions for ACS conditions
-
elective inpatient admissions
-
emergency inpatient admissions.
To inform selection of control practices, we undertook a survey of 500 practices to establish how widespread approaches that were similar to the ‘telephone first’ approach were. Based on our findings that such approaches were rare, control practices were selected from all practices not on the list provided that were understood to be using the ‘telephone first’ approach. For computational reasons, we did not use all practices in England as controls, but rather used a random 10% sample of practices in England that we did not believe had used a ‘telephone first’ approach. Based on practice denominator files of age and gender profiles extracted from the National Health Application and Infrastructure Services systems (‘Exeter system’) annually from 1 April 2008 to 1 April 2015, we excluded all control practices whose list size was < 1000 in at least 1 year of the study from the initial sample because very small practices are often atypical or may indicate new or closing practices. No intervention practices had a list size of < 1000 at any time in the study period. We also excluded data from practices in years in which their practice code did not appear in the Exeter system denominator files, even when attendances/admissions were attributed to patients at the practice. Furthermore, we excluded the data from practices in the year preceding a year in which the practice did not appear in the system, in order to exclude practices in which mergers or closures may have taken place during the year of analysis. One intervention practice was excluded on the basis of this criterion: the launch date was in September but the practice no longer appeared in the Exeter denominator files in the following April. This gives a final analysis sample of 841 control practices and 145 intervention practices. This was considerably larger than the expected number of 90 practices used in our original sample size calculations.
Finally, the data in intervention practices were restricted to between 1 year before and 1 year after the practice launch date. This was to focus on changes that were attributable to the ‘telephone first’ approach rather than any other factors, including potential concerns about the impact of practice mergers and closures. Data for control practices were included for the whole time period to give the best characterisation of background trends and variability.
In some months, practices included in the analysis had no relevant admissions or attendances for A&E, inpatient or outpatient data in one or more age, sex and IMD combination (there are 120 possible combinations). For each of these practice-months in which there were no attendances or admissions for a particular stratum, we include the strata with a count of ‘0’ admissions or attendances.
Practices using a ‘telephone first’ approach during the data period were identified based on information provided by the two commercial companies providing support for implementing this service. The companies provided details on the practices that were using their system, the date when the ‘telephone first’ approach was introduced and the current status of the system (i.e. whether the practice was still running a full ‘telephone first’ system, a hybrid system or if the practice had abandoned the system). Only practices that launched the ‘telephone first’ approach before 31 December 2015 were included in the analysis to allow sufficient time for the system to have bedded in; those with later launch dates were excluded (from both the intervention practices and the control practices).
Two types of analysis were carried out for each of the outcomes. The first was a before-and-after analysis, in which the introduction of the system in each practice is set at time zero. Second, a regression analysis was performed for each outcome looking (1) for step changes at the time when the intervention was introduced and (2) for a change in the preceding trend (e.g. slowing down of a previous increase). We also model heterogeneity in these changes to examine whether or not the intervention has a different effect in different practices. Full details of the statistical analysis are provided in Appendix 8.
Our main analysis was conducted on an intention-to-treat basis. It included all practices identified by the commercial companies even when the companies informed us that the practices were running a hybrid form of the system or were no longer running the system. This was done in order to avoid selection bias, whereby only the successful practices continue with the system in the recommended form. A sensitivity analysis (see Appendix 9) was also performed, restricting the analysis to the 89 practices in which we believed, on the basis of information provided by the commercial companies, that the system was being run consistent with the companies’ protocols.
Results
The intention-to-treat analysis is presented in the following sections: (1) the superposed epoch analysis and (2) the regression analysis. The intention-to-treat analysis included > 13 million A&E attendances, > 78 million outpatient attendances and > 13 million inpatient admissions linked to around 80,000 practice-months. The sensitivity analysis is presented in Appendix 9 and shows broadly consistent findings with the main analysis.
Before-and-after analysis (intervention practices only)
The superposed epoch analysis of A&E attendances for intervention practices is shown in Figure 19. There is no clear change in the rate of A&E attendances at the time of intervention launch. The mean rate of A&E attendances is 35.9 (SD 10.8) per 1000 patients per month in the year prior to the launch of the ‘telephone first’ approach and 36.7 attendances (SD 11.3) per 1000 patients per month in the year after the launch.
FIGURE 19.
Superposed epoch analysis of A&E attendances relative to the intervention launch. The black lines represent the attendances within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
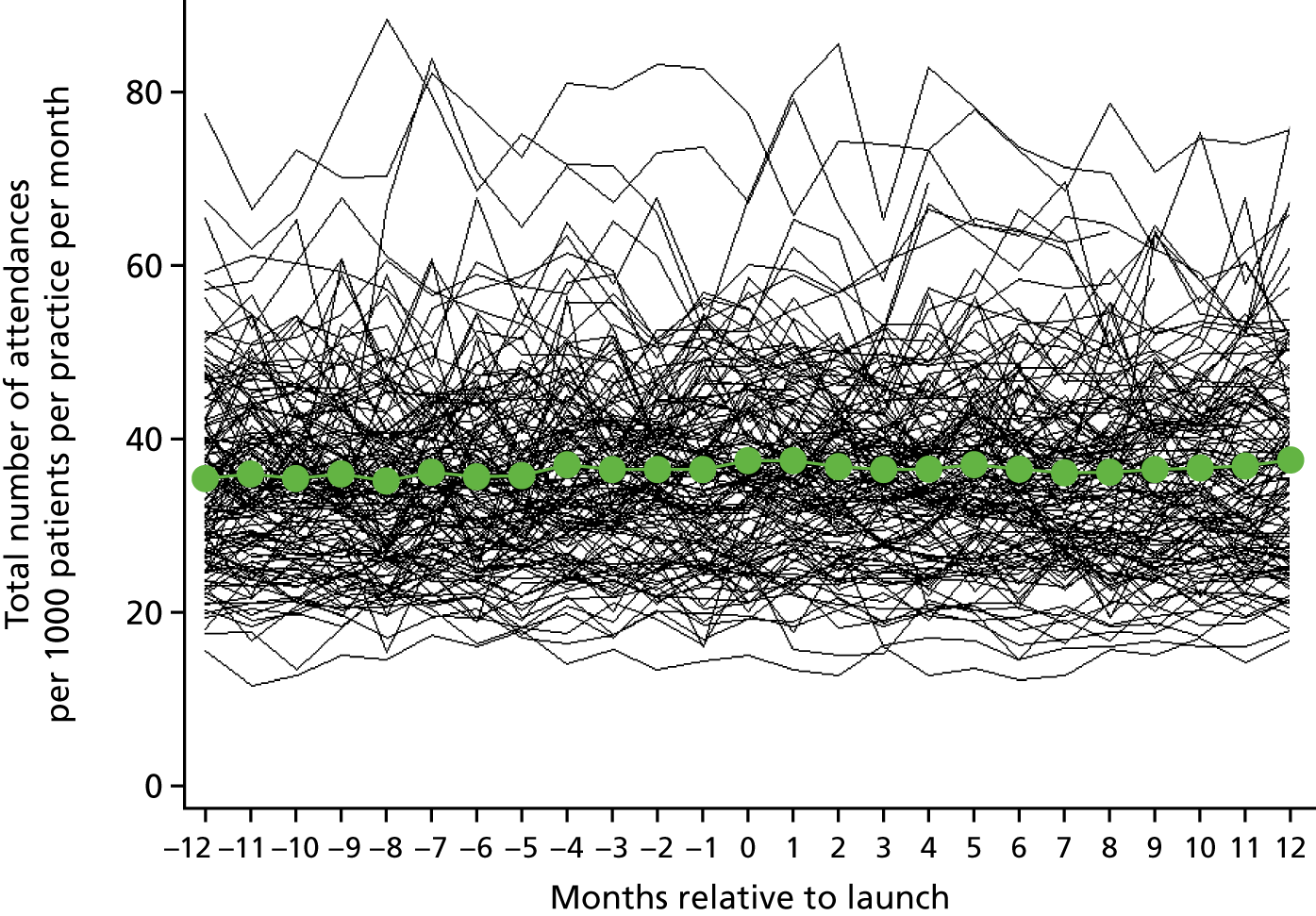
The superposed epoch analysis of outpatient attendances for intervention practices is shown in Figure 20. As with A&E attendances, there is no clear change in the rate of outpatient attendances at the time of intervention launch. The mean rate of A&E outpatient attendances is 196.1 (SD 49.9) per 1000 patients per month in the year prior to the launch of the ‘telephone first’ approach and 207.8 attendances (SD 55.9) per 1000 patients per month in the year after the launch.
FIGURE 20.
Superposed epoch analysis of outpatient attendances relative to the intervention launch. The black lines represent the attendances within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
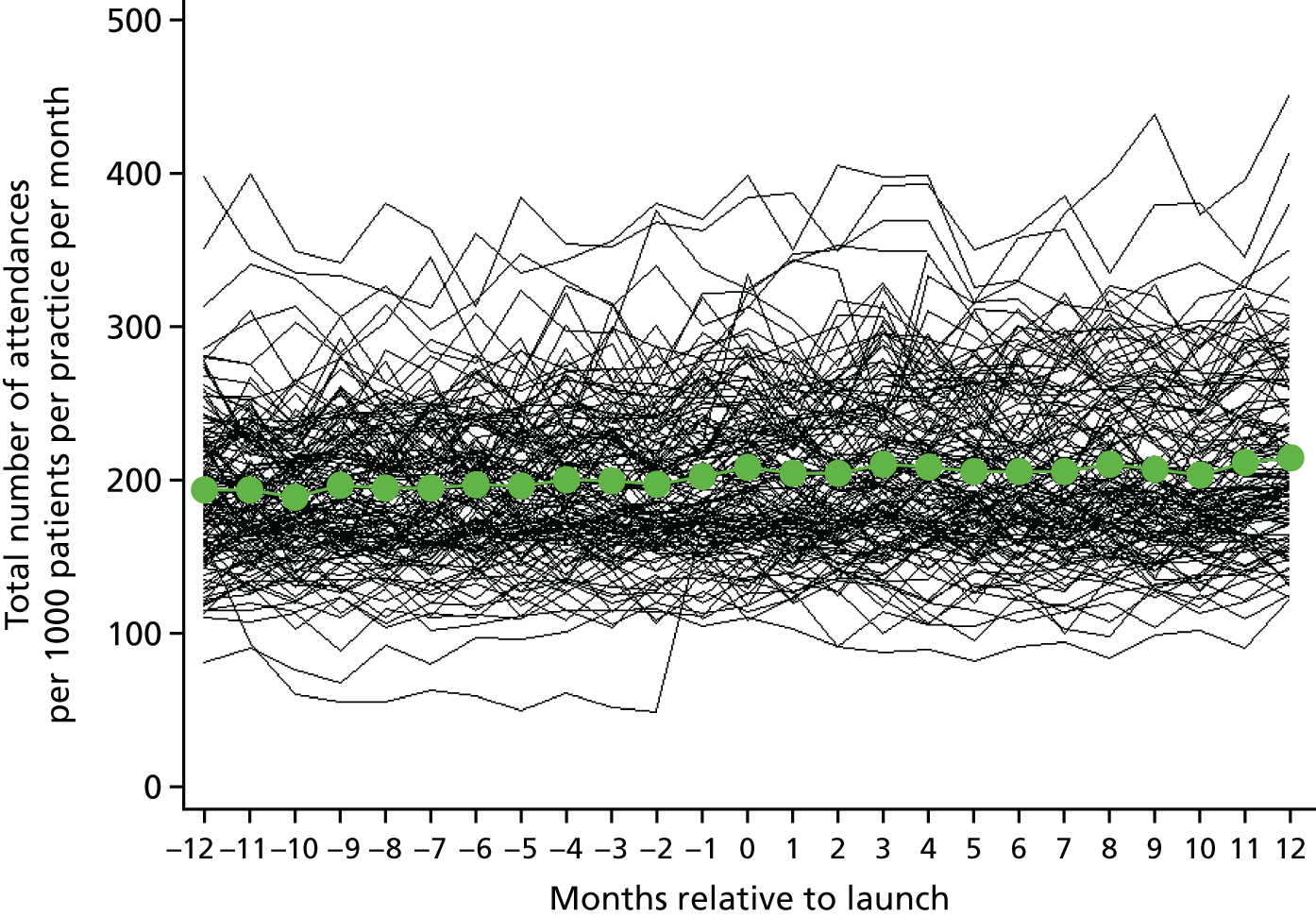
The superposed epoch analysis of inpatient admissions for intervention practices is shown in Figure 21. Again, there is no clear change in the rate of admissions around the time of intervention launch. The mean admission rate is 31.3 attendances (SD 6.53) per 1000 patients per month in the year prior to the launch of the ‘telephone first’ approach and 32.2 attendances (SD 7.0) per 1000 patients per month in the year after the launch.
FIGURE 21.
Superposed epoch analysis of all inpatient admissions relative to the intervention launch. The black lines represent the admissions within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
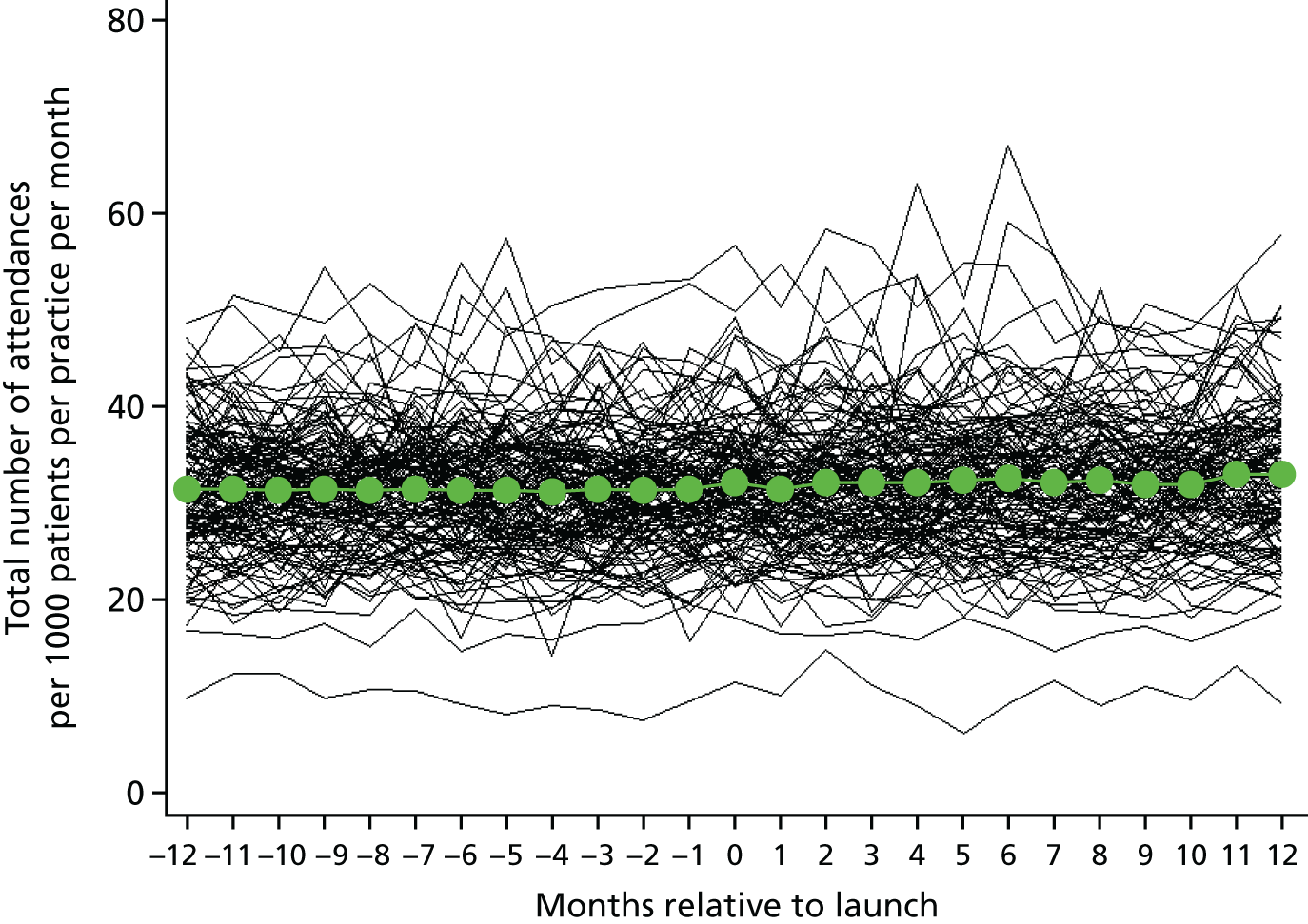
The superposed epoch analyses of inpatient admissions for ACS conditions, elective admissions and emergency admissions are shown in Figures 22–24. As with the other admissions, no clear change is seen that corresponds with the start of the ‘telephone first’ approach. The mean rates of admissions for ACS conditions, elective admissions and emergency admissions are 3.1 (SD 1.2), 17.8 (SD 5.0) and 10.5 (SD 2.7) admissions per 1000 patients per month, respectively, in the year prior to the launch of the ‘telephone first’ approach and 3.2 (SD 1.3), 18.0 (SD 5.1) and 10.9 (SD 2.9) admissions per 1000 patients per month, respectively, in the year after the launch.
FIGURE 22.
Superposed epoch analysis of all inpatient admissions for ACS conditions relative to the intervention launch. The black lines represent the admissions within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
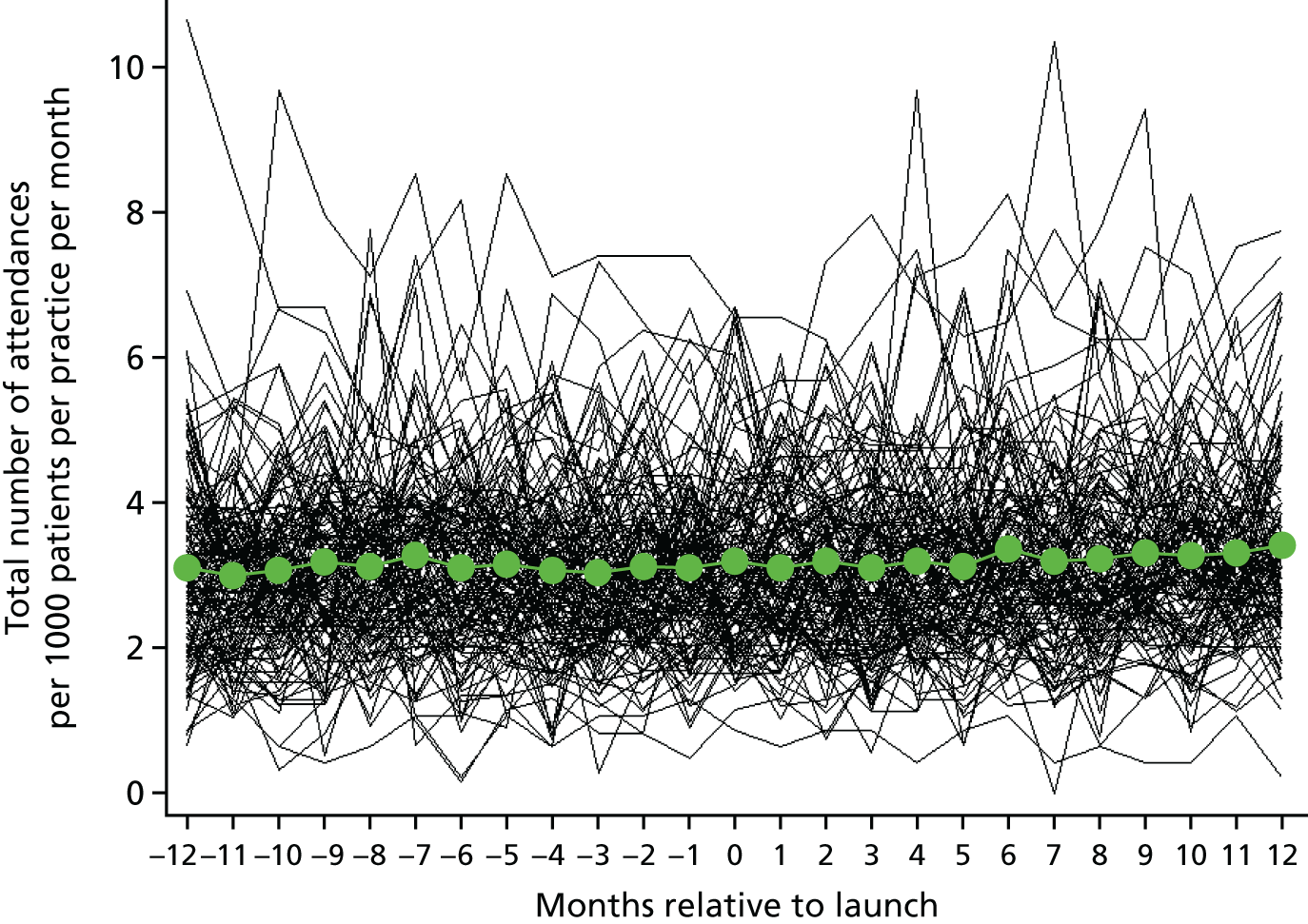
FIGURE 23.
Superposed epoch analysis of elective inpatient admissions relative to the intervention launch. The black lines represent the admissions within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
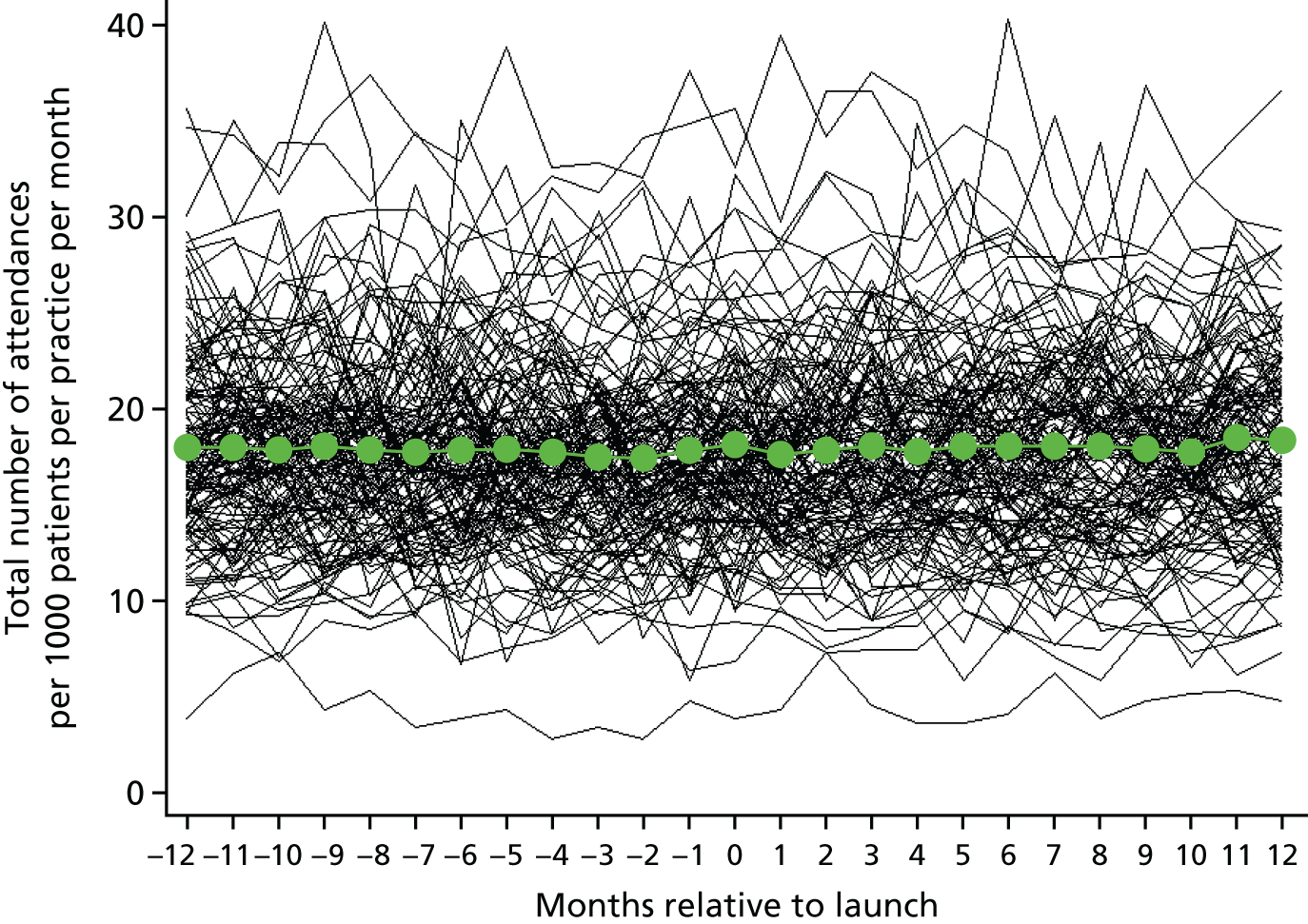
FIGURE 24.
Superposed epoch analysis of emergency inpatient admissions relative to the intervention launch. The black lines represent the admissions within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
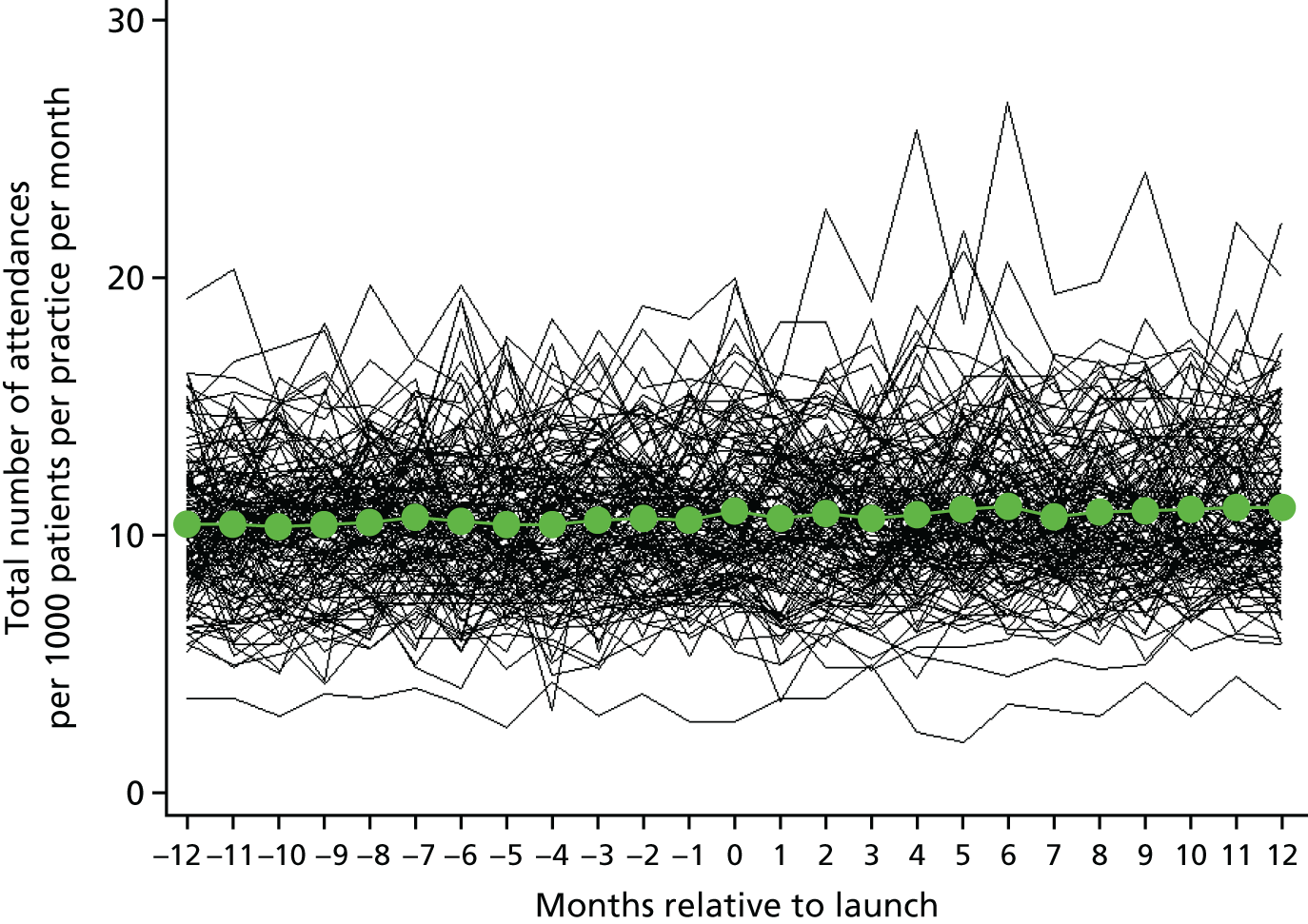
Regression analysis (using randomly sampled practices in England as controls)
The results of the regression analysis are shown in Table 16. There is no evidence of a step change in A&E attendance associated with the start of the ‘telephone first’ approach (p = 0.68). There is, however, strong evidence (p = 0.005) that, following the start of the ‘telephone first’ approach, the intervention practices’ rate of increase is slower than that expected given their pre-intervention trends and national trends, although this differential trend is small, at around 2% per year (RR 0.98, 95% CI 0.97 to 0.99) and against a background of A&E attendances that increased by approximately 100% across the study period from April 2008. Although on average there was no change seen in A&E attendances coinciding with the launch of the intervention, there was moderate heterogeneity (variation) in the effect of the intervention. The model suggests that, although on average there was no step change at the transition to the ‘telephone first’ approach, some practices saw increases in A&E attendance of up to 10%, whereas others saw decreases of up to 8% (95% reference range RR 0.92 to 1.10). The results for outpatient attendances are almost identical to those seen for A&E attendances: there was no evidence of a step change at the transition and there was a 2% decrease relative to background trends per year, with slightly greater heterogeneity between practices.
| Outcome | Step change at transition | Additional yearly change following intervention | |||
|---|---|---|---|---|---|
| RR (95% CI) | p-value | Heterogeneitya | RR per year (95% CI) | p-value | |
| A&E attendances | 1.00 (0.99 to 1.02) | 0.68 | 0.92–1.10 | 0.98 (0.97 to 0.99) | 0.0046 |
| Outpatient attendances | 1.00 (0.99 to 1.02) | 0.63 | 0.89–1.13 | 0.98 (0.97 to 0.98) | < 0.0001 |
| All inpatient admissions | 1.02 (1.01 to 1.03) | 0.0058 | 0.98–1.05 | 1.01 (1.00 to 1.02) | 0.2 |
| ACS condition inpatient admissions | 1.04 (1.00 to 1.08) | 0.032 | 0.87–1.24 | 1.06 (1.02 to 1.11) | 0.0073 |
| Elective inpatient admissions | 1.01 (0.99 to 1.02) | 0.56 | 0.90–1.13 | 1.02 (1.00 to 1.04) | 0.015 |
| Emergency inpatient admissions | 1.02 (1.00 to 1.04) | 0.016 | 0.96–1.09 | 1.00 (0.98 to 1.03) | 0.86 |
There is evidence that inpatient admissions increase, on average, by about 2% following the transition to the ‘telephone first’ approach (RR 1.02, 95% CI 1.01 to 1.03; p = 0.006); this increase is twice as large in the case of admissions for ACS conditions (RR 1.04, 95% CI 1.01 to 1.03; p = 0.032). There is no evidence that inpatient admissions further change relative to the background trend, although there is an additional increase of around 6% per year for the ACS admissions (RR 1.06, 95% CI 1.02 to 1.11; p = 0.007). When admissions are split into elective and emergency admissions, there is evidence of a step increase in emergency admissions in line with that seen for all admissions (transition RR 1.02, 95% CI 1.00 to 1.04; p = 0.02), and there is no evidence (p = 0.56) of a step change in elective admissions. However, care must be taken to not interpret the lack of evidence of a change in elective admissions as evidence of an absence of a change due to the reduced sample size in these analyses, in which the CIs are wide and substantially overlapping and may be consistent with a common change across the two admission types. There is evidence that elective admissions continue to increase beyond background trends post transition, but no evidence of a similar increase in emergency admissions; again, there is a substantial overlap in CIs. As with A&E and outpatient appointments, heterogeneity in the step change was seen, such that for each outcome considered there were practices that had increased admissions at the transition and others that had decreased admissions at the transition.
Summary of findings
There was no evidence that the use of the ‘telephone first’ approach was associated with any initial reduction in secondary care utilisation; rather, there were small increases in admissions, especially those for ACS conditions. The increase in inpatient admissions was seen as both a step change at the transition and a continued increase above national trends following the transition (for admissions associated with ACS conditions and elective admissions). For both A&E attendances and outpatient attendances, there was no immediate change, but the rate of attendances subsequently rose more slowly in the intervention practices than the national trend, reducing by about 2% less per year than the national trend in each case. Although these changes are seen on average, there was considerable heterogeneity in the changes seen between practices, such that, for each of the outcomes, some practices had increased utilisation whereas others had decreased utilisation.
Chapter 8 Economic analysis
Introduction
The objective of the economics component is to estimate the costs of introducing a ‘telephone first’ approach and compare these with any benefits obtained. A conventional cost–utility analysis is inappropriate for this as it is not possible to capture any improvements in health-related quality of life from increased access to primary care in a meaningful or reliable way. We therefore conducted a cost–consequences analysis, in which the costs of introducing a ‘telephone first’ approach were compared with any benefits obtained.
Method
The cost perspective of the analysis is that of the NHS. The costs measured are those of implementation and operation of the scheme, changes in other primary care costs (prescriptions and time spent consulting), and changes in secondary care costs (referrals and A&E attendances) attributable to the ‘telephone first’ approach.
Primary care costs
Costs of initiating and operating the ‘telephone first’ approach
A telephone survey on the costs of the intervention was based on a previous survey undertaken by members of the research team. 77 The survey was administered in 20 intervention practices taking part in the survey of patient experience (see Chapter 4). Each questionnaire was completed during a single telephone call with the practice manager, or a colleague nominated by the practice manager, between March 2015 and December 2016.
The questionnaire was divided into two parts: (1) non-staff costs and (2) staff costs. Costs are reported as stated by respondents, inclusive of VAT (value-added tax; at 20%) and adjusted when necessary to the 2015/16 price year using the Hospital and Community Health Services inflation index. 78 Staffing costs were estimated based on the mid-point of the respective staff grade for 2015/16. 78 Capital costs were uprated to 2015/16 costs using the Hospital and Community Health Services inflation index. 78 Respondents were invited to indicate the level of certainty about cost estimates provided on a scale of 1 (least certain) to 10 (most certain).
Cost of primary care consultations
Changes in total consultation time per day by practice GPs reported in Chapter 3 were costed at national 2015/16 prices,78 assuming an 8-hour working day (£171 per hour of patient contact, excluding direct care staff costs and qualification costs). 78
Prescription costs
Quantities of prescriptions and net ingredient cost data were extracted from publicly available data for prescriptions written in England and dispensed in the community in the UK79 between August 2010 and December 2016 for intervention practices and a random sample of 10% of all other practices in England that were selected as controls for the analysis of hospital utilisation data (n = 829; see Chapter 7). Data on all items, and items commonly prescribed for ACS conditions80 (see Table 17) and for antibiotics, were summarised by month. Costs were inflated to 2016 prices based on the Consumer Price Index (CPI)81 of pharmaceutical products for items within British National Formulary (BNF),82 chapters 1–19, and the CPI of other medical and therapeutic equipment for items within BNF,82 chapters 20–23.
A log-linear random effects model was applied, adjusting for time period as fixed effects and a random intercept and slope. Adjustment for age/sex/deprivation level was not possible because data were on a per-practice level only.
Secondary care costs
Hospital Episode Statistics data were obtained from NHS Digital between April 2008 and March 2016 for intervention and control practices, as described in Chapter 7. The field ‘SUSHRG’ (secondary uses service health resource group) was matched to the relevant Healthcare Resource Group (HRG) 2015/16 reference cost83 for A&E, outpatient contacts and inpatient episodes of care (finished consultant episodes). When there was no valid HRG, a weighted average cost of the HRG stem (e.g. AA23) or HRG root (e.g. AA) was applied. When there was still no valid HRG, an average unit cost for an A&E, outpatient or inpatient cost was applied. 83 To provide context, the mean cost in 2015/16 was £138 for an A&E attendance, £137 for an outpatient procedure and £3750 for an elective inpatient admission. The cost of referrals per 1000 patients in intervention practices was then calculated for the 12 months prior to and the 12 months post the introduction of ‘telephone first’, and the crude change was calculated. The step change attributable to ‘telephone first’ was then calculated by multiplying the costs in the 12 months prior to the introduction by RR – 1, where RR is the proportionate step change reported in Table 16. The slope change attributable is calculated by multiplying the cost in the 12 months prior to the introduction by exp[ln(RR)/2] – 1, where RR is the proportionate slope change reported in Table 17. The total change is the sum of the two.
| Condition | BNF82 chapters/sections |
|---|---|
| Asthma | 3.1, 3.2 and 3.3 |
| Congestive heart failure | 2.1.1, 2.2.2, 2.2.3.3b, 2.4, 2.5.5 and 2.6.1 |
| Diabetes mellitus complications | 2.6.4 |
| Chronic obstructive pulmonary disease | 3.6 |
| Angina | 2.6.2, 2.6.3, 2.9b, 2.9c and 2.10.1 |
| Iron-deficiency anaemia | 9.1.1 |
| Hypertension | 2.2, 2.5.2, 2.5.3 and 2.5.4 |
| Nutritional deficiencies | 9.4, 9.5 and 9.6 |
Table 18 summarises each component of the analysis, the method of analysis and data sources.
| Item | Data sources | Approach to analysis |
|---|---|---|
| Primary care costs | ||
| Cost of implementation and operation in intervention practices | Telephone interview with intervention practices using structured telephone questionnaire | Costs reported as non-staff fixed and variable costs related to the implementation and routine operation of the ‘telephone first’ approach, and costs of any staffing changes |
| Consultations | Data from GP Access practices | Overall change in minutes spent consulting multiplied by cost per minute |
| Prescribed medications per month by practice | General practice prescribing data – all intervention practices and 829 randomly sampled control practices for 2008 to 2016 | Analysis of quantity and cost of drugs monthly from 2010 to 2016 in control practices and ±1 year of commencement in intervention practices. Subanalyses for ACS conditions and antibiotic prescriptions |
| Secondary care costs | HES data – all intervention practices and 829 randomly sampled control practices for 2008 to 2016 | Application of unit costs to calculate cost of A&E and outpatient attendances and inpatient admissions (all, elective and emergency, and for ACS conditions). Application of proportionate changes (see Table 16, Chapter 7) to calculate change in cost attributable to ‘telephone first’ |
Additional cost analyses
At the request of the study PPI group, we included some exploratory analyses of patient out-of-pocket costs. These were limited to travel costs, because a more thorough investigation of, for example, loss of earnings was beyond the scope of this study. Car travel was costed at Her Majesty’s Revenue and Customs (HMRC)-approved mileage rates. 84 Bus travel costs were obtained from Department for Transport statistics. 85
Results
Eighteen out of 20 intervention practices agreed to take part in the telephone survey. The duration of the telephone calls ranged from 15 to 40 minutes.
Costs of initiating and operating the ‘telephone first’ approach
Non-staff costs
Contract with the commercial company
Sixteen (out of 18) practices reported that they (n = 3) or their Clinical Commissioning Group (CCG) (n = 13) paid a one-off charge to one of the commercial companies for design and implementation of the ‘telephone first’ approach. Three CCG-funded practices felt that the services were not value for money as they were already using similar (or better) systems.
The median charge from the commercial companies was £10,810 per practice (range £7200–13,803; 12 practices provided information with high certainty). The fees partially reflected the size of the practice, although there was some variation in services provided. Services included introductory meetings for staff to explain the ‘telephone first’ approach; meetings to discuss the existing booking system, analysis of performance data and potential system modifications; training for practice staff in telephone consultations and communication skills; advice on setting up the system (including dealing with any prior backlog of bookings); and methods for eliciting patient feedback and monitoring performance.
Other costs incurred by the practices
Practices incurred a range of further costs that were mainly related to telephones, computer hardware (including headsets) and marketing materials.
Ten out of the 18 practices purchased new telephone equipment (internet telephones, mobile telephones or landlines): four practices installed new telephone landlines at £100 per line (median 4 new lines, range 4–10 new lines). One practice expanded internet telephone capability and five purchased new mobile telephones. These were provided to GPs and nurses in the practice for when the main telephone lines were busy: these practices found that the mobile telephones were better value for money than landlines, and added flexibility (e.g. for home/car working). The mean annual cost per mobile (including calls) was £512 (range £188–840). One practice reported that they had purchased mobile telephones on the advice of the commercial company, but these were eventually found to be unnecessary and were returned before the end of the contract.
Three out of 18 practices reported that their landline telephone bill had doubled: ranging from an additional £500 to £1000 per month. One already used mobile telephones, but had noted an increase in use because existing landlines were now often in use. Landline and mobile telephone contracts were under regular review because of initially unpredictable costs. The substantial initial rise in the cost of calls may have been a short-term issue before more suitable contracts were negotiated. Practices kept their telephone costs under regular review.
No practices purchased new computer hardware or software, as existing systems were able to implement the new approach. Seven practices purchased new headsets (range £100–182 per headset), which were provided to all receptionists and, in some cases, to all GPs and nurses.
No practices reported any additional formal training sessions over and above those provided by the commercial company; however, some informal ‘learning on the job’ was necessary, taking place during routine office hours. Some practices updated staff induction materials, with one practice estimating that this took 20 hours of an administrator’s time. Some practices also recognised the need for ongoing training for new and existing members of staff to ensure that the benefits of the system were fully realised.
Six practices incurred costs related to informing patients about the new system, including updating the practice website, newspaper advertisements and leaflets. When such tasks were undertaken in-house, this did not incur any additional cost other than the opportunity cost of the administrator time. One practice mailed all their patients with information about the new system, at a cost of £7600 (covered by the CCG).
No practice reported any office reconfiguration costs attributable to the ‘telephone first’ approach.
Staff costs
Very few practices were able to attribute specific staff changes to the adoption of the ‘telephone first’ approach, although working patterns or hours had changed for some staff. Five of the 18 practices made concurrent additions to staffing (reception, administration and dispensing staff as well as nurses and GPs), but stated that these could not be attributed directly to the ‘telephone first’ approach. However, two of these practices reported that they had increased staff numbers because of an increased list size, which they attributed to patients switching from other practices, because of easier access to GPs in their surgeries.
Only two practices reported that additional staff had been employed as a direct result of the ‘telephone first’ approach. One practice employed one additional full-time receptionist and one additional full-time nurse as a result of a perceived increase in consultations, although it was subsequently decided that the additional nurse was excess to requirements. Another practice reported that an additional nurse practitioner had been employed.
Six practices reported that additional appointments were scheduled to clear backlogs prior to the switchover. In two cases, this was managed in-house by cancelling all holiday leave and training for a 2-week period. In three cases, an additional locum doctor was required for a period of between 1 and 10 days.
Other primary care costs
Consultations
There was no statistically significant change in overall consulting time (see Chapter 3, Total time spent consulting per day by practice GPs).
Prescriptions
The introduction of the ‘telephone first’ approach was not associated with any differences in cost or numbers of prescriptions, except for the cost (but not the number of items prescribed) of prescriptions for iron-deficiency anaemia (Tables 19 and 20). There is no clinical reason for this observation and, because it is not reflected in the quantities prescribed, it is likely to be a spurious observation.
| Drug type | Step change at transition | Change in slope following transitiona | 95% reference range for step change transitionb | ||
|---|---|---|---|---|---|
| RR (95% CI) | p-value | RR per year (95% CI) | p-value | ||
| All | 0.986 (0.940 to 1.035) | 0.572 | 0.963 (0.893 to 1.039) | 0.333 | 0.986 to 0.986 |
| Asthma | 0.992 (0.961 to 1.024) | 0.601 | 0.981 (0.934 to 1.031) | 0.452 | 0.992 to 0.992 |
| Congestive heart failure | 0.994 (0.960 to 1.030) | 0.749 | 0.988 (0.935 to 1.044) | 0.657 | 0.994 to 0.994 |
| Angina | 0.999 (0.968 to 1.031) | 0.940 | 0.988 (0.940 to 1.037) | 0.622 | 0.999 to 0.999 |
| Iron-deficiency anaemia | 0.982 (0.954 to 1.011) | 0.213 | 0.993 (0.950 to 1.037) | 0.738 | 0.982 to 0.982 |
| Hypertension | 0.999 (0.970 to 1.028) | 0.927 | 0.998 (0.954 to 1.045) | 0.942 | 0.999 to 0.999 |
| Antibacterial drugs | 1.018 (0.984 to 1.053) | 0.295 | 0.958 (0.909 to 1.010) | 0.114 | 1.018 to 1.018 |
| All ACS condition drugs | 0.988 (0.948 to 0.029) | 0.562 | 0.977 (0.916 to 1.042) | 0.478 | 0.988 to 0.988 |
| Drug type | Step change at transition | Change in slope following transitiona | 95% reference range for step change transitionb | ||
|---|---|---|---|---|---|
| RR (95% CI) | p-value | RR per year (95% CI) | p-value | ||
| All | 0.987 (0.939 to 1.037) | 0.596 | 1.003 (0.927 to 1.085) | 0.941 | 0.987 to 0.987 |
| Asthma | 1.000 (0.965 to 1.037) | 0.998 | 0.984 (0.930 to 1.041) | 0.566 | 1.000 to 1.000 |
| Congestive heart failure | 0.977 (0.941 to 1.015) | 0.232 | 1.043 (0.983 to 1.105) | 0.163 | 0.977 to 0.977 |
| Angina | 0.997 (0.962 to 1.096) | 0.889 | 1.036 (0.980 to 1.096) | 0.212 | 0.997 to 0.997 |
| Iron-deficiency anaemia | 0.963 (0.924 to 1.003) | 0.069 | 1.098 (1.035 to 1.164) | 0.002 | 0.896 to 1.117 |
| Hypertension | 1.001 (0.964 to 1.039) | 0.949 | 1.033 (0.976 to 1.093) | 0.267 | 1.001 to 1.001 |
| Antibacterial drugs | 1.017 (0.975 to 1.060) | 0.438 | 0.997 (0.934 to 1.064) | 0.926 | 1.017 to 1.017 |
| All ACS condition drugs | 0.990 (0.947 to 1.035) | 0.665 | 1.000 (0.933 to 1.035) | 0.991 | 0.990 to 0.990 |
Secondary care costs
The analysis of HES in Chapter 7 shows that there was, on average, a small (2%) increase in admissions when practices moved to the ‘telephone first’ approach; this increase was mainly concentrated in emergency admissions. Subsequently, the introduction of the new system was associated with a small (2%) reduction in the rate of increase in A&E attendances and a small (2%) increase in the previous rate of increase for elective admissions.
Table 21 shows the changes in costs of secondary care utilisation. Combining the step change at the introduction of the ‘telephone first’ approach with the change in the underlying trend over the subsequent year, there were small non-significant reductions in costs for A&E and outpatient attendance and a significant increase in costs of admissions, leading to an estimated overall increase in secondary care costs of £11,776 per 1000 patients in the first year after changing to the new approach (aggregating A&E and outpatient attendance and admissions coded as emergency or elective).
| Cost category | Cost (£), mean (95% CI) | |||||
|---|---|---|---|---|---|---|
| Over 12 months prior to transition to the ‘telephone first’ approach | Over 12 months post transition to the ‘telephone first’ approach | Crude change | Initial change attributablea to the ‘telephone first’ approach | Change over the next 12 months attributablea to the ‘telephone first’ approach | Total change over the first 12 months attributablea to the ‘telephone first’ approach | |
| A&E attendance | 57,546 (54,948 to 60,144) | 59,555 (56,847 to 62,264) | 2009 (1074 to 2944) | 2 (–853 to 866) | –578 (–870 to –287) | –577 (–1481 to 335) |
| Outpatient attendance | 275,673 (264,037 to 287,309) | 293,408 (280,283 to 306,534) | 17,735 (12,868 to 22,602) | 8 (–4086 to 4148) | –2770 (–3483 to –2064) | –2762 (–6921 to 1434) |
| Inpatient admissions for ACS conditionsb | 99,821 (94,340 to 105,302) | 104,997 (99,109 to 110,885) | 5176 (1851 to 8500) | 4013 (73 to 8083) | 2957 (800 to 5160) | 6970 (2464 to 11,600) |
| Inpatient admissions coded as ‘elective’ | 399,822 (384,057 to 415,587) | 42,1051 (403,406 to 438,695) | 21,228 (13,437 to 29,019) | 4009 (–1987 to 10,077) | 3984 (39 to 7966) | 7993 (807 to 15,249) |
| Inpatient admissions coded as ‘emergency’ | 354,384 (335,309 to 373,459) | 35,0183 (331,767 to 368,598) | –4201 (–12,739 to 4337) | 7105 (66 to 14,272) | 7 (–4385 to 4439) | 7112 (–1192 to 15,531) |
Patient out-of-pocket costs
An exploratory analysis was performed to predict the impact of the introduction of the ‘telephone first’ approach on patient out-of-pocket costs. We limited these costs to travel costs, which were calculated assuming that travel was by car or bus; we did not attempt to calculate other costs (e.g. loss of earnings). Travel by car was costed at £0.45 per mile, multiplied by the mean distance of the patient’s home address from a GP surgery within each lower-layer super output area (LSOA). 86
The mean distance to the closest GP surgery across all LSOAs was 1.587 km (SE 0.00845 km) (0.986 miles). Multiplied by £0.45 per mile, this results in a round trip cost of £0.89 for each car-based trip to see a GP face to face. The mean cost per bus passenger journey is £1.53, or £3.06 for a return journey, for each face-to-face GP appointment. 85 The mean number of primary care visits per patient per year in 2008/9 was 5.5 (median 5.46 visits, interquartile range 4.85–6.22 visits), equating to a cost of £4.90 (for travel by car) or £16.83 (for travel by bus) per year. This represents the maximum out-of-pocket saving to a patient should all of their consultations be via telephone rather than face to face. For the estimate of a 28% average reduction in face-to-face consultations (see Chapter 3), this would be equivalent to an average annual saving of £1.38 (for travel by car) or £4.71 (for travel by bus).
This estimate assumes that people will choose to go to their nearest GP surgery. As there are many other factors influencing GP choice that could result in a patient choosing a more distant GP, the distance and, hence, cost savings could be higher than estimated. The potential savings would also be higher for those who visit their GP more frequently.
In summary, this exploratory analysis suggests that the potential for out-of-pocket savings for patients as a result of a ‘telephone first’ approach is small. Other factors, such as convenience and waiting time to see a GP, are likely to have a larger influence on patient preferences.
Summary
According to the practices that responded to our cost survey, the commercial companies providing management support for the ‘telephone first’ approach charged around £10,000 for setting up the system in the practice. For this payment, practices typically received analysis of their current booking systems and performance data, training for practice staff and tailored advice on implementing the system, and methods for eliciting patient feedback and performance monitoring. In addition, some practices needed to install additional land or mobile telephone lines. Marketing expenses were relatively low, although one of the effects of this may have been initial low awareness of the new system among patients: only two-thirds of survey respondents who called for an appointment were expecting the GP to call them back (see Chapter 4, Descriptive analysis). Staffing changes were minimal, with changes to working patterns being more common than hiring new staff.
The ‘telephone first’ approach was not associated with any clinically significant changes in numbers or costs of prescriptions.
The adoption of the ‘telephone first’ approach was associated with non-significant decreases in the cost of A&E and outpatient attendance over the first year (but the significant slope effect suggests that these may reach statistical significance over a longer time horizon). The approach was associated with an increase in the cost of inpatient admissions. Overall, there were no major changes associated with the introduction of the ‘telephone first’ approach in secondary care costs; therefore, we found no evidence to support the claims, repeated in NHS England literature,5 that the introduction of the ‘telephone first’ approach was associated with secondary care cost savings of £100,000 (see Chapter 1). Bearing in mind the heterogeneity that we observed, savings may have been achieved in some practices, but, on average, would have been cancelled out by increased secondary care costs in other practices.
Chapter 9 Interviews with patients on the implementation of a ‘telephone first’ approach in general practice
Introduction
Among the benefits of the ‘telephone first’ approach reported by the commercial companies providing support to practices adopting it were improvements in patient satisfaction (associated with timeliness of access and improved continuity of care) and a reduction in the number of complaints received. As outlined in Chapter 2, published studies of patient satisfaction with GP telephone consultations,29,30,51–54,57 in general, have also tended to report positive findings. However, there has also been a range of concerns expressed in the literature regarding the acceptability of the approach (particularly with respect to the issue of confidentiality29,53 and the potential to exacerbate access inequalities or differential experiences for hard-to-reach or vulnerable groups of patients27,30,54,57).
In this chapter, we report the findings of qualitative interviews conducted with patients and carers to explore their views on and experiences of the ‘telephone first’ approach, as implemented within the general practices they attended.
Methods
Site selection, sampling and recruitment
Qualitative interviews with patients were undertaken in 12 GP surgeries. The participating practices were located in a number of areas of England: the north-east, the north-west, the Midlands, East Anglia, London, the south-east and the south-west. These practices formed a subset of the practices that were sampled for the patient and carer survey. Surgeries were selected from the sample of 20 to include those with a range of experiences in adopting the ‘telephone first’ approach, including those with positive experiences and those that had experienced or overcome problems. However, it should be noted that the practices that agreed to take part in this element of the study were probably those in which the appointment systems were working better than the appointment systems in those practices that declined to participate (see further details in Chapter 4).
In the first instance, patients who were potential participants indicated their interest in being contacted for an interview by returning a reply slip that accompanied the patient and carer survey (see Chapter 4). Purposive sampling of those who expressed an interest was carried out by the research team, based on survey responses. We sought to gain a range of views and to ensure that the following groups of people were included: older people, people who work outside the home, people with disabilities, people with chronic conditions and people whose first language was not English. Selected interested participants were contacted by a member of the research team by the preferred contact mode (telephone or e-mail) indicated in the reply slip and were invited to take part in an interview.
Data collection
Semistructured interviews were conducted by four researchers (SB, JN, JC and JE), either at the patient’s home (n = 12) or at his/her GP surgery, as requested by the patient. All interviewees gave written consent to be interviewed. A common interview guide informed by the literature was used for each interview, although emphasis was given to allowing participants to talk from their own perspective. The focus of the interview was on patients’ and carers’ views of the advantages and disadvantages of the ‘telephone first’ approach, including its convenience, perceptions of quality of care and impacts on the doctor–patient relationship. Interviews were audio-recorded with the participants’ permission, and transcribed verbatim. Transcripts were anonymised by removing references to identifiable names and places.
Data analysis
Data analysis proceeded in parallel with data collection and informed the iterative development of the interview topic guide and observation protocol. Thematic analysis of the data was conducted based on the principles outlined by Boyatzis. 87 Transcripts were read and re-read, and codes were applied to meaningful sections of text. Coding was conducted by Sarah Ball, Jennie Corbett, Josephine Exley, Jennifer Newbould and Emma Pitchforth. As analysis progressed, codes were organised into overarching or organising themes using NVivo version 10 (QSR International, Warrington, UK). Data within themes were scrutinised for confirming and disconfirming views across the range of participants. The emerging findings were shared and discussed regularly among the study team.
Results
Four researchers conducted interviews with a total of 43 patients from 12 general practice sites. Interviews lasted between 17 and 54 minutes. Between two and five patients (and their carers) were interviewed at each site; participants were selected to represent a broad range of the characteristics described in Site selection, sampling and recruitment. Table 22 summarises the self-reported characteristics of the participants who were interviewed and the practices with which they were registered.
| Specific characteristics of the ‘telephone first’ approach (patient perspective) | Participant characteristics | ||||||
|---|---|---|---|---|---|---|---|
| Identification number | Agea (years) | Sexa | Ethnicitya | Health statusa | Employment status; nature of health concerns; frequency of GP use; additional notesa,b | Approach preferenceb | |
Practice 100 (urban, list size 9093)
|
100_1004 | 71 | Female | White British | Fair | Retired; multiple chronic health issues; frequent user | ‘Telephone first’ |
| 100_1006 | 79 | Male | White British | Good | Retired; multiple chronic health issues; infrequent user | ‘Telephone first’ | |
| 100_1064 | Adultc | Female | White British | Fair | Carer for 85-year-old mother with dementia; both have chronic health issues; frequent user | ‘Telephone first’ | |
| 100_1086 | 63 | Male | White British | Good | Recently retired; infrequent user | ‘Telephone first’ | |
Practice 101 (urban, list size 6672)
|
101_1002 | 76 | Male | White British | Very good | Retired; minor health issues requiring specialist input; infrequent user; hearing impairment | ‘Telephone first’ |
| 101_1006 | 65 | Male | White British | Very good | Full-time carer for spouse; ongoing health issue requiring specialist input; infrequent user | ‘Telephone first’ | |
| 101_1024 | 50 | Female | Other black | Fair | Early retirement due to ill health; frequent user | ‘Telephone first’ | |
| 101_1086 | 37 | Male | White British | Good | Works full time; ongoing mental and physical health issues; regular review by GP | ‘Telephone first’ | |
Practice 102 (urban, list size 2347)
|
102_1014 | 77 | Female | White British | Fair | Retired; multiple chronic conditions; frequent user | ‘Telephone first’ |
| 102_1019 | 67 | Male | White British | Poor | Retired; multiple chronic conditions; regular user of GP; seeing a specialist, lives alone | Conventional | |
| 102_1031 | 47 | Female | White British | Poor | Works part time; ongoing mental and physical health issues; frequent user; hearing impairment | ‘Telephone first’ | |
| 102_1064 | 65 | Female | White British | Good | Retired; infrequent user of GP | ‘Telephone first’ | |
Practice 103 (urban, list size 7312)
|
103_1030 | 41 | Female | White British | Fair | Mother of two disabled children; frequent user, often for advice by telephone | ‘Telephone first’ |
| 103_1034 | 78 | Male | White British | Fair | Retired; very frequent user | ‘Telephone first’ | |
| 103_1042 | 50 | Female | White British | No response | Does not work; mental and chronic physical health problems; frequent user | Conventional | |
| 103_1053 | 71 | Female | White British | Good | Retired; frequent user | ‘Telephone first’ | |
| 103_1074 | 67 | Female | White British | Fair | Retired; infrequent user | ‘Telephone first’ with modifications | |
Practice 104 (urban, list size 4913)
|
104_1070 | 54 | Female | White British | Fair | Does not work due to chronic health problems; infrequent user as condition is well controlled | ‘Telephone first’ |
| 104_1087 | 74 | Female | White British | Good | Retired; increasing frequency of GP visits with age | ‘Telephone first’ | |
Practice 105 (urban, list size 11,484)
|
105_1040 | 79 | Female | White British | Good | Retired; chronic health issues; frequent user; hearing impairment | ‘Telephone first’ |
| 105_1043 | Adultc | Female | White British | N/A | Does not work – mother of young child; chronic health issues (self and child); frequent user | ‘Telephone first’ | |
| 105_1090 | 78 | Male | White British | Fair | Retired; multiple chronic health issues; frequent user | ‘Telephone first’ | |
| 105_1099 | 78 | Male | White British | Very good | Retired; fit and active; infrequent user of GP | ‘Telephone first’ | |
Practice 106 (urban, list size 16,072)
|
106_1013 | 53 | Female | White British | No response | Works flexibly from home; chronic health issue, anxiety; frequent user; previous missed cancer diagnosis | Conventional |
| 106_1025 | 78 | Female | White British | Fair | Retired; chronic health issue; frequent user | ‘Telephone first’ | |
| 106_1026 | 45 | Female | White British | Good | Not currently working because of ill health; infrequent user | ‘Telephone first’ | |
| 106_1064 | 68 | Female | White British | Fair | Retired; chronic health issues; but infrequent user | ‘Telephone first’ | |
| 106_1077 | 61 | Female | White British | Fair | Does not work; mental health and multiple chronic physical health problems; frequent user | ‘Telephone first’ | |
Practice 108 (urban, list size 4913)
|
108_1032 | 59 | Female | White British | Good | Works full time but finds it easy to take calls or make appointments; chronic condition; carer for elderly parents (with hearing impairment); frequent user for self and as carer | ‘Telephone first’ |
| 108_1090 | 66 | Female | White British | Good | Retired; infrequent user | Conventional | |
| 108_1099 | 28 | Female | Chinese | Good | Student – some difficulty taking calls or making appointments; frequent contact with GP; speaks English as second language; unfamiliar with UK health system | N/A (only experienced this system) | |
Practice 110 (urban, list size 8639)
|
110_1007 | 60 | Female | White British | Fair | Early retirement due to ill health; frequent user | Conventional |
| 110_1026 | 74 | Male | White British | Poor | Retired; multiple chronic conditions requiring specialist input; mental health issues; reports limited use of GP due to telephone; lives alone | Conventional | |
| 110_1095 | 63 | Female | White/black | Fair | Part-time/voluntary work; ongoing mental health issues; reports limited use of GP due to telephone | Conventional | |
Practice 112 (urban, list size 7934)
|
112_1015 | 65 | Female | White British | Good | Retired; infrequent user | ‘Telephone first’ |
| 112_1046 | Adultc | Male | Other | N/A | Working parent; speaks English as second language | ‘Telephone first’ | |
Practice 114 (urban, list size 8364)
|
114_1008 | 48 | Male | White British | Good | Works, easy to take calls or make appointments; chronic health issues; frequent user | ‘Telephone first’ |
| 114_1029 | Adultc | Female | White British | N/A | Carer for elderly father; works from home; frequent user of GP for self and as carer | ‘Telephone first’ | |
| 114_1058 | 72 | Female | White British | Poor | Retired; chronic health issues; frequent user | Conventional | |
Practice 117 (urban, list size 7888)
|
117_1027 | 51 | Female | White British | Very good | Works, difficult to take calls; infrequent user | ‘Telephone first’ |
| 117_1029 | 60 | Female | White British | Poor | Does not work because of ill health and caring responsibilities; multiple chronic conditions; very frequent user | ‘Telephone first’ | |
| 117_1066 | 32 | Female | White British | Good | Single mother/part-time voluntary work; infrequent user | ‘Telephone first’ | |
| 117_1073 | 86 | Male | White British | Good | Retired; recent hospital stay but previously in good health; infrequent user | ‘Telephone first’ | |
Does the ‘telephone first’ approach work for patients?
The nature of the responses of patients to the ‘telephone first’ approach was extremely varied: although some patients reported being highly satisfied with the approach, others found it to be unacceptable or that it did not meet their needs. Many participants provided strong positive endorsements:
I really don’t find anything difficult [about the system] – I really don’t. I think that it works so well.
105_1040
In contrast, a small number of patients reported being so dissatisfied with the approach that they were considering moving to a different practice. Others were ambivalent, considering the new approach to be the least bad option:
I’m prepared to stick with it because, I mean, going back to the old system, no. That’s even worse.
106_1077
In describing their experiences of the approach, patients outlined a broad range of advantages and disadvantages across five distinct categories: (1) access to care, (2) quality of consultation, (3) continuity of care, (4) patient safety and (5) confidentiality. Within each of these categories, there were contrasting views with respect to whether the introduction of a ‘telephone first’ approach was perceived to represent an improvement or a hindrance.
Access to care
Although some patients reported that the new approach made it easier and quicker to access care when required, others had the opposite experience, with many describing one or more disadvantages regarding access to care.
Acceptability of the booking process
Although several patients described how the initial contact with the practice to request an appointment was more streamlined following the changes, and others commented on a perceived positive change in the attitudes or approaches of the reception staff, many reported difficulties with or objections to the new booking process (such as long waits for calls to be answered, restricted opening times for telephone lines and a lack of clarity around how the system worked or when to call):
Tried for 2 days, press 2 [for automatic redial], still off – and on the Thursday someone actually answered. [. . .] Said ‘what is it?’ so I said what [was wrong] and I need to see the doctor. They phoned me back then. She says well Doctor [name redacted] is not in today – phone tomorrow. Bump. So I phoned the next morning 8 o’clock. Phones off. I phoned every 5 minutes till 8.30 a.m. – it came on, ‘surgery’s now full, phone Monday’.
110_1026
Responsiveness and flexibility of the approach
Many patients commented on the prompt response of GPs following their initial call to the surgery. Guaranteed same-day callbacks (in some cases within minutes, or within an agreed time slot) reassured patients who were anxious about what might be wrong with them and the availability of timely face-to-face appointments (if required) was appreciated by many. One patient commented that ‘apart from just jumping in the car and going walking into a doctor’s, there’s no other way you could improve that’ (101_1002).
However, some of those interviewed described a delayed or unpredictable response:
You wait for sometimes 7 hours and then they’ll say ‘I’m sorry, you’re going to have to make the appointment to come and see me tomorrow. I can’t book it, you’ll have to phone up tomorrow morning at 8.30 again’ and start the process all over again.
103_1034
Equitable/fair access to care
A number of patients indicated that they appreciated that effective triage using the ‘telephone first’ approach led to more efficient use of resources and improved access for patients with the greatest need for urgent care, and recognised that this, in turn, conferred benefits on them as individuals (ensuring prompt access if required):
I mean sometimes if he’s [the GP] really busy, you don’t hear from him for a couple of hours but then he’s obviously got patients there that are a priority. They know how to prioritise them which is good.
102_1014
Many patients described receiving prompt face-to-face appointments when they felt they needed them:
I’ve not felt brushed off with just an answer on the phone. Whenever I’ve said ‘I think I need to come down and see you’ or whatever, ‘I’d like to come and talk’, then yes, that’s never been a problem.
102_1064
Convenience of the approach
Many patients reported that they found that the ‘telephone first’ approach enabled more convenient access to advice and care, with benefits including being able to get on with daily activities rather than having to wait for long periods in the surgery (instead waiting at home or elsewhere, with the availability of mobile telephone contact), a reduced need to travel to the surgery unnecessarily and access to medication without the need for a face-to-face appointment:
I like the fact that on a day like today, it is chucking it down, it’s miserable, it’s cold, if my mum had had to come to the doctor instead of a phone call on any day where the weather was like this, it would have caused her a lot of pain.
102_1031
In addition, a number of patients reported that the introduction of the ‘telephone first’ approach had enhanced their experience of visiting the surgery (when they were required to do so) by, for example, reducing waiting time and freeing up space in the waiting room and car park.
However, others found the approach (or elements of it) to be inconvenient for a range of reasons, including not being able to book appointments in advance (a particular issue for working people and people dependent on others for transport); not being able to drop into the surgery when passing to make an appointment; not knowing when to expect a callback and receiving a callback at inconvenient times (when shopping, on public transport or at work) or having poor mobile phone reception; and having to stay at home to wait for the call, particularly if it was regarding a personal issue that would be difficult to discuss in public:
You can’t sit glued to your phone all day waiting for a call, even if you’ve got a mobile phone, you might be in the shower, or you might be in a shop or on the other phone or something. So it doesn’t work . . . and how people who are working expect to get an appointment, I don’t know really.
110_1007
Quality of consultation
With respect to the quality of the GP consultations experienced when using the ‘telephone first’ approach, patients described both the advantages and disadvantages of consulting by telephone rather than face to face and the impact of the new approach on face-to-face appointments that followed an initial telephone consultation.
Changes to the nature of face-to-face appointments
Although most patients did not report changes in the nature of face-to-face appointments following the introduction of the ‘telephone first’ approach, a small number noted improvements, such as reduced waiting times in their surgery and a calmer, more relaxed atmosphere, with patients experiencing less time pressure during appointments:
You see the doctor on time. They don’t seem to rush because there’s not 20 people in the waiting room.
101_1002
Some patients suggested that the approach led to GPs being better prepared and, as a result, appointments being more streamlined:
They already know exactly what you’re going for, so obviously they’ve got your notes. Well, it’s all computer now, isn’t it; they’ve got everything ready and they know who they’re going to see, which is a lot better. [. . .] They’re pre-warned really, aren’t they, and what they’re looking at.
104_1087
However, a few patients commented that having to repeat details that they had already given over the telephone in the face-to-face appointment was an annoyance and appeared to be inefficient.
Continuity of care
Given the claims made by the commercial providers of the ‘telephone first’ approach regarding its potential to improve continuity of care for patients, interviewees were specifically asked about changes in the ease with which they were able to see a preferred GP (relational continuity).
Relational continuity
A small number of patients reported finding it easier to see or speak to their preferred GP with the ‘telephone first’ system than with the traditional system, as a result of the way in which calls were allocated within the practice, with patients being able either to specify which GP they would like to call them back or, if this was not possible, to request a face-to-face appointment with their preferred GP during the telephone call. However, many patients reported the opposite experience, finding it harder to see their preferred GP, and observing a trade-off between being seen or spoken to quickly and seeing their preferred GP.
Several patients expressed concern about whether or not an unfamiliar GP could effectively assess an issue over the telephone, and they worried about the lack of opportunity to develop or sustain a relationship with a GP (a particular concern for vulnerable patients such as older people or those with mental health issues):
I think that if people, you know, are suffering from some form of mental health issues that if you have got a rapport with someone they could then pick that up and say, ‘Are you OK today?’ [. . .] you know, ‘You look a bit down’, or if somebody’s in a dishevelled, sort of, way that are not normally like that you would pick that up as well. [. . .] Whereas the way that this is operating at the moment I don’t think that that always happens. It’s just whichever day you ring in, you’ll get that particular doctor that’s on duty.
102_1019
Patient safety
Patient views on the impact (or potential impact) of the ‘telephone first’ approach on patient safety (as a result of the changes in accessibility of care, quality of consultation and continuity described in the previous sections) also varied considerably between patients and across practices. Although some patients expressed concerns regarding the impact on patient safety, others perceived the approach to be safer for patients with respect to improvements in emergency response, preventing the escalation of minor ailments and infection control, which are each discussed in the following sections.
Emergency response
The timely access to a GP under the new system served to reassure patients who were anxious about what may be wrong with them, with one patient describing how the prompt response had been potentially life-saving:
So I phoned up and it was early in the morning and I mentioned to the receptionist what the problem was, and so within minutes another doctor phoned back and he said, ‘you had better come down, I want to have a look at you’. So I went down and then he said, ‘you are looking a bit peaky’ and I said to him, ‘will you do some blood tests on me?’ [. . .] I got a callback from them at 4 in the afternoon, saying to get an ambulance. [. . .] I had to have a transfusion, within an hour I was in the hospital on a drip.
117_1029
However, although most patients reported that urgent cases were prioritised and dealt with quickly, patients at one surgery described extreme difficulty with getting through to the practice by telephone after the introduction of the telephone system, which left them feeling vulnerable and dependent on emergency services.
Preventing escalation
Some patients reported that they believed that prompt, equitable and convenient access to a GP under the new system increased the likelihood of dealing with issues in a timely manner and preventing escalation:
Well I think you get to talk to your doctor when you need to talk to him or her, rather than having a long wait and perhaps getting progressively worse. Certainly if it’s an acute condition, it can make a difference, can’t it?
100_1004
Other patients described being put off from visiting the GP as a result of the perceived inconvenience of the ‘telephone first’ approach or the belief that appointments were available only for those with an urgent need, potentially leading to the escalation of minor ailments:
I would say I’m probably less inclined [to contact the GP] [. . .] because of the inconvenience of it. So I might leave something and see if it gets better on its own for a while whereas, perhaps before, I would have left it less time.
114_1058
Confidentiality
A significant proportion of patients expressed concerns regarding confidentiality associated with the ‘telephone first’ approach, with respect to both the provision of details to reception staff in advance of the GP consultation and the telephone consultation itself.
Providing details to reception staff
Many patients commented that they felt uncomfortable with providing details of their medical conditions to reception staff, maintaining the belief that only the GP should be privy to such information, and expressing concern about whether or not the information they provided would be treated in confidence (a particular issue for patients in tight-knit communities, who knew receptionists outside the setting of the surgery):
You know that whatever you say to a doctor is going to stay with the doctor; with the receptionist, you are never quite sure if it’s going to stay there.
117_1066
This discomfort was often expressed very strongly [e.g. one patient described the approach as ‘absolutely disgusting’ (103_1042)] and was reported even among some patients who acknowledged the benefit of providing the information in order to enable the prioritisation of calls.
Confidentiality of the telephone consultation
A number of patients reported confidentiality concerns associated with the telephone consultation itself, some reporting difficulties with receiving the callback at a time when and/or in a location where their conversation could be overheard (whether at home with family members present, in a work setting or in public, such as when shopping or on public transport). One patient described the difficulty she experienced when attempting to talk to a GP regarding concerns about her husband’s poor memory:
I have to choose, I either have to go into the surgery and talk to the receptionist in front of everybody there and say, I need to see a doctor, and this is what I want to come and talk to them about, or I’ve got to choose a time when my husband is not in, and he’s very rarely out so, there are disadvantages in some ways.
114_1058
What factors influence whether or not the ‘telephone first’ approach works for patients?
As outlined in the previous sections, there were a range of patient views regarding the nature of the advantages and disadvantages of the ‘telephone first’ approach; however, it was also apparent that the weight or value given to particular advantages and disadvantages varied significantly. For example, a disadvantage that represents a mild annoyance for one patient could represent a ‘deal-breaker’ for another, rendering the approach completely unacceptable. With reference to the descriptions given by patients regarding how the ‘telephone first’ approach worked in the practice they attended (see Table 22), it is clear that there was considerable variation between practices in how the approach was implemented and the nature of the challenges experienced by patients using it.
Practice and system characteristics
Capacity of the system to meet demand
Differing reports by patients regarding ease of access to care and the perceived safety of the approach reflected differences in the capacity of the practices using the ‘telephone first’ approach to meet demand. Although some practices were positively described by patients as being highly responsive to their needs, other practices seemed to be unable to provide a timely service, with patients describing being unable to get through to book a callback from a GP, and insufficient callback slots or same-day appointments being available.
Of the eight patients who stated that they would prefer to return to a traditional system, six were attending practices described by patients as having difficulty with meeting demand (practices 103, 106, 108 and 110).
Flexibility of the approach
The varied responses regarding the convenience of the ‘telephone first’ approach reflected variation in the degree to which practices allowed flexibility in the approach in order to meet patients’ needs. Some practices made exceptions to the system (such as allowing a limited number of advance bookings or direct face-to-face bookings), whereas others were rigid in their application of the rules, leading to inconvenience and frustration for patients. One patient described how the practice had revised its approach and become more flexible over time, resulting in increased acceptability:
Initially that was quite frustrating when you rang up [. . .] and I said [when told there were no appointments available that day] ‘Well can I make an appointment?’ and they say ‘Well no, you need to ring back tomorrow’. That was quite frustrating but now they have addressed that; I think it’s the flexibility and the access you get. I find it very easy to access. I think that’s what the telephone appointment system gives you.
101_1086
Capacity to preserve patient choice/continuity of care
Contrasting reports regarding the effect of the approach on continuity of care reflected variation in the capacity of the particular approach that was implemented to enable patients to choose their preferred GP for a callback or face-to-face appointment. Based on patient reports, practices varied considerably in the degree to which they were organised to accommodate such requests.
Extent of patient engagement and education
The degree to which patients reported that they had been consulted (or at least informed) ahead of the introduction of the new approach also varied considerably. Many patients reported having a lack of awareness of how the approach would work from the outset (e.g. the booking process and when to call), and were unhappy with the lack of consultation around its introduction, which led to confusion, anxiety and misconceptions regarding the purpose behind the introduction of the approach. However, several patients commented that their initial misgivings had not, by and large, been realised.
Patient characteristics and resources
In addition to the effects of the practice and system characteristics described in the previous sections, interviewees also described a range of patient characteristics and resources (relating to themselves or others); the presence of these were perceived to enable effective engagement with their practice via the ‘telephone first’ approach, whereas their absence served as potential barriers. These are outlined in Table 23.
| Patient characteristics | Enablers | Potential barriers |
|---|---|---|
| Communication skills | Being articulate with good communication skills | Experiencing communication or comprehension difficulties [e.g. as a result of hearing impairment; having English as second language; illness or disability (motor neurone disease, dementia); nervousness or anxiety regarding use of the telephone] |
| Confidence/assertiveness | Having the confidence to request the desired outcome (e.g. a face-to-face appointment or consultation with preferred GP) | Lacking confidence to express or push for desired outcome, tendency to play down symptoms, not wanting to waste doctors’ time |
| Flexibility of daily schedule | Having the flexibility in one’s daily schedule to fit around the time constraints of using the system (e.g. being at home during the day/retired/self-employed/working flexibly) | Lacking flexibility in daily schedule [e.g. working in a job that it is difficult to take time away from or being dependent on others for transport (requiring planning ahead)] |
| Access to mobile telephone | Being accessible on a mobile telephone | Not having access to a mobile telephone (e.g. older people, those unable to take calls at work) |
| Ease of access to surgery | Living/working close to the surgery (so can get to same-day appointment quickly) | Commuting to work; difficulty getting to the surgery without arranging transport (e.g. as a result of mobility issues) |
| Nature of health complaint | Having particular conditions that are more amenable to the ‘telephone first’ approach, (e.g. chronic conditions or familiar symptoms) | Having sensitive or personal health issues that are difficult to discuss in public setting/with receptionist |
| Nature of relationship with GP or surgery | Having a longstanding relationship with doctor, trusting that they know when you need to be seen and feeling comfortable communicating with them | Being unfamiliar with doctor/lacking trust in telephone consultation |
| Patient expectations and experience | Low expectations regarding access (e.g. based on previous experience of poor access) |
High expectations regarding access Anxiety regarding system safety based on previous bad experience |
Suitability for potentially disadvantaged patients
Potentially disadvantaged patients, such as older people, those who are deaf or hearing impaired and those for whom English is not their first language, are more likely to lack many of the characteristics or resources required to successfully engage with the ‘telephone first’ approach. However, based on the interviews conducted, although many patients expressed concerns on behalf of these patient groups regarding the suitability of the approach, patients within these groups themselves did not, in general, report particular disadvantages that could not be overcome by minor adjustments and accommodation of their needs.
With regard to older patients, for example, none of the nine patients aged ≥ 75 years who took part in the study stated that they preferred the previous system to the new approach. However, nearly half of those interviewed who were aged between 50 and 74 years would have preferred to return to the previous system, possibly indicating that those in work found the ‘telephone first’ approach less convenient.
With respect to patients with communication difficulties, in the case of the two patients interviewed for whom English was not their first language, any difficulty with communication by telephone appeared to be overcome simply by the GP offering a face-to-face appointment once the difficulty had become apparent. Similarly, three of the five patients with a hearing impairment who were interviewed described measures that they were able to take to use the system successfully (such as finding a quiet place to take the call from the GP); however, two patients suggested that communication was impaired, with the practice failing to make adjustments. One patient described the difficulties experienced by her mother, and how this had required her to intervene:
There are times when she doesn’t understand. So if she’s said to me, ‘I didn’t understand that’, I then ring up and ask the question and I do ring on their behalf if I think that they’re not getting [. . .] service that they need [. . .] they don’t appear to treat mum any differently because she is deaf.
108_1032
Suitability for patients who work
In addition to concerns expressed regarding the suitability of the approach for patients in the ‘hard-to-reach’ groups discussed in Suitability for potentially disadvantaged patients, many patients worried about how the approach would function for working people. Among the patients who were working, the flexibility of their daily schedule, proximity of their place of work to the GP surgery and ease of using a mobile telephone while at work were factors that had an impact on the acceptability of the system. However, some reported that they found the approach more convenient than the previous system, with telephone consultations replacing the need for face-to-face appointments in many instances, meaning that they were not required to take time out of work to attend the surgery in person.
Interplay between patient characteristics and how the ‘telephone first’ approach was implemented
Although both the way in which the ‘telephone first’ approach was implemented and characteristics of the patients themselves contributed to the acceptability of the approach to individual patients, the interplay between these two sets of factors also appeared to be important.
In considering the acceptability of the ‘telephone first’ approach, patients weighed up the advantages and disadvantages they experienced as a result of its introduction. The reason that was most consistently cited for preferring the new system over the previous approach was being able to gain prompt access to a GP (initially by telephone, and face to face if required). If the system delivered this, then patients tended to tolerate the disadvantages and inconveniences. Many patients provided long lists of annoyances (difficulty with getting through on the telephone, confidentiality concerns when talking to receptionists, not being able to book in advance and not liking waiting for the callback) and still concluded that they preferred the new approach because they could speak to a doctor within hours and see them on the same day if they needed to.
Conversely, patients reporting that they found the approach to be unacceptable tended to be those who, as a result of a combination of personal characteristics and features of the particular approach taken by the practice, were left feeling vulnerable and unsupported. These included patients with mental health issues in practices using approaches that seemed unresponsive or in which there was little provision for continuity of care.
The observed variation between patients with respect to the perceived acceptability, advantages and disadvantages of the approach supports the idea that many of the reported problems related to how the approach had been implemented rather than the ‘telephone first’ approach in principle, thus indicating potential for the challenges to be overcome, for example by tailoring the approach to best meet the needs of vulnerable patients.
Summary of findings
The response of patients to the ‘telephone first’ approach was extremely varied, with some patients reporting that they were very satisfied and others expressing major concerns. Based on patient reports, practices appeared to vary considerably in how they had implemented the approach, and the nature of challenges experienced by patients also differed. Patients reported a wide range of advantages and disadvantages in five main categories [(1) access to care, (2) consultation quality, (3) continuity of care, (4) patient safety and (5) confidentiality), but with contrasting views in each case regarding whether the approach led to improvements or was a hindrance. The factors that were identified as having an impact on acceptability included characteristics of the practice and how the approach was implemented (e.g. capacity to meet demand and system flexibility) and patient characteristics and resources (e.g. communication skills, confidence/assertiveness, flexibility of daily schedule, mobile telephone access and ease of access to the surgery). The acceptability of the approach with respect to particular ‘hard-to-reach groups’ was considered in relation to these characteristics.
Although this study shows the potential for a significant proportion of patients’ problems to be dealt with on the telephone, this approach suits some patients well, whereas others find it much less acceptable. There were variations in the way the approach had been implemented within practices, with some practices catering considerably better than others for the needs of particular patient groups (such as those with mental health issues and other vulnerable groups).
Chapter 10 Staff interviews
Introduction
This chapter explores the views of administrative staff, GPs, practice managers and a small number of practice nurses. The benefits of the ‘telephone first’ approach, as reported by commercial companies, include practice staff experiencing less stress and cost savings from the efficient use of staff time. In the ESTEEM trial6,26 of telephone triage for on-the-day appointments, clinicians had varied views of the approach. Some reported that telephone triage had enabled equitable use of appointments, with patients being efficiently managed, whereas others noted that a key challenge was workload disparities between clinicans, with some undertaking more telephone calls than others. The ESTEEM trial also noted that reception staff reported less stress in their job,6 although another study by McKinstry et al. 29 indicated that reception staff felt uncomfortable with the responsibility placed on them. This chapter reports the views of staff from a range of practices on the adoption of a ‘telephone first’ approach.
Methods
Site selection, sampling and recruitment
Qualitative interviews were undertaken with staff at 12 GP surgeries from which patients were recruited. The methods for practice selection are described in Chapter 4. Up to five members of staff were recruited from each practice. Practices selected staff to participate based on who they deemed most suitable to talk about the ‘telephone first’ approach within their practice. In general, two GPs, a practice manager and a receptionist/administrative staff member were interviewed.
Data collection
Semistructured face-to-face interviews were conducted by four researchers (SB, JN, JC and JE). Two interviews, both with GPs, were conducted by telephone (by JN and EP): in one case, the GP was not at work because of sickness and asked to be interviewed over the telephone, and, in the other case, the interview was held after the practice visit at a more convenient time for the GP. All participants gave written consent to be interviewed. A common interview guide informed by the literature was used for each interview. The interview explored the reasons for switching approach, the setting-up process, perceptions of quality of care and safety as well as impacts on the doctor–patient and intrapractice staff relationships. The advantages and disadvantages of the ‘telephone first’ approach were also discussed.
With participants’ permission, interviews were audio-recorded and transcribed verbatim. For one practice, audio-recordings were unavailable because of technical problems, and detailed notes were taken. All transcripts and notes were anonymised. Data analysis followed the same methods as those described for the patient interviews (see Chapter 9).
Results
Respondents interviewed
A total of 49 members of staff from the 12 practices were interviewed. The number of staff members interviewed in a single practice ranged from three to five, with four interviews being completed in the majority of practices. Twenty-one (43.8%) of the interviews were conducted with a GP, 14 (29.2%) with reception/administrative staff, 10 (20.8%) with practice managers, two (4.2%) with a nurse and one (2.1%) was a joint interview with the practice manager and an administrator.
The 12 practices were located in a variety of geographical locations across England and were from seven Clinical Research Network areas. Seven practices had paid for the support of commercial companies to adopt a ‘telephone first’ approach; for five of these, fees were paid by the CCG. Practices varied regarding the level of deprivation in the areas they served, with two practices noting particular deprivation among their practice populations, with high rates of unemployment (practice 103) and high numbers of refugees and immigrants (practice 108). Seven practices had been supported by Doctor First and five were supported by GP Access. Some additional characteristics, such as practice size, of the practices from which staff were from are given in Table 22.
This chapter explores staff views on the adoption of a ‘telephone first’ approach in primary care. The chapter first examines why practices chose to implement a ‘telephone first’ approach and their experiences of adopting the system. We then explore the implications for staff and the practice and staff perceptions of the impact on patients. The chapter concludes with the enablers of and barriers to the adoption of a ‘telephone first’ approach in general practice.
Why adopt a ‘telephone first’ approach?
In all 12 practices, participants identified problems meeting demand as a key reason for changing to a ‘telephone first’ approach, including that, under their previous systems, patients had often had to wait a long time to see a GP:
So, you know, it was getting up to, sort of, 3 or 4 weeks, you know, before people would get a routine appointment and we had a duty doctor system, where the duty doctor was here and booked on the day. We were finding that was getting incredibly onerous and stressful for the duty doctor because he might get, oh I don’t know, 70, 80 sometimes even 100 calls in a day.
Practice manager 5001, practice 105
A number of respondents, from different practices, described how, over time, the practice had struggled with demand for appointments and had added extra face-to-face appointments or telephone appointments to manage demand. GPs in particular often mentioned that struggling with their workload was a motivator for trying a different approach:
I think the thing which worked for everyone was obviously altruistic motives like ‘yes we want to see patients who need to be seen’. But also managing our own workload and knowing what comes through the doors was the most important selling point if I can remember all the years back, what worked for others.
GP 5001, practice 108
. . . our system was ‘ring a week ahead’, so ‘ring on Monday for the following Monday’, but the phone lines opened at 8 and by 5 past all the appointments were gone. And we would get a huge queue; people would start queuing before 7 o’clock, so you’d get this awful queue at the door and you’d finish your morning surgery and there’d be like 30 extras waiting to be seen.
GP 5003, practice 112
Often, the decision to change approach related to a number of factors, but some participants described something that made the situation come to a head, for example a member of staff leaving. Two GPs noted particular cases in which patients had waited an unacceptably long time to see a GP as being factors in their decision to change to the ‘telephone first’ approach. In one case, a patient had died, possibly as a result of delays in being seen, and, in another, the patient had waited for an appointment for a condition that required urgent attention.
A concern for fairness and equity in the system was also often mentioned by staff. Many felt that a traditional booking system favoured those who were quickest to call the surgery rather than those in the most clinical need:
Just a feeling of unsustainable demand and also a real feeling of sort of unfairness in our access to the surgery, we had patients who shouted loudest at the desk got seen for things that weren’t urgent and things that potentially should have been seen quickly waited 2 or 3 weeks.
GP 5004, practice 101
Other reasons for changing to the ‘telephone first’ approach included a large number of appointments that patients sometimes do not attend, and CCGs offering funding to cover input from the commercial companies.
During interviews, a number of practice staff mentioned that one person at the practice had led the introduction of a ‘telephone first’ approach; this was usually a GP, but sometimes a practice manager. As well as researching the concept and liaising with the commercial companies, this individual often provided enthusiasm and leadership for the change, which enabled other staff to learn about the approach and raise queries or concerns.
Participants described the process by which practices had made the decision to switch to a ‘telephone first’ approach. For some practices, this involved doing research and visiting other practices using the approach. Many participants stressed the importance of all practice staff being brought into the discussion as an enabler of successful adoption. In a number of practices, particular individuals, usually GPs, had been reluctant to change to the ‘telephone first’ approach.
Implementing the ‘telephone first’ approach
Practices varied in the extent to which they were using telephone consulting prior to the adoption of the ‘telephone first’ approach. Some had a conventional booking system, in which all patients were pre-booked into face-to-face appointments. Others were already using some form of telephone triage for appointments, for example emergency appointments or when face-to-face slots were fully booked.
All participating surgeries had used a commercial company (Doctor First or GP Access) to support the transition to the ‘telephone first’ approach. Over time, most practices had modified the ‘telephone first’ approach they had adopted, although all practices had largely maintained the key component that face-to-face appointments with a GP had to be preceded by a telephone conversation with a GP. Exceptions to this were usually very limited, for example 6-week baby checks being pre-booked. However, there was some variation between practices, with some GPs booking some patients into slots in advance.
Practices varied in the extent to which they would make modifications to the way the ‘telephone first’ approach was outlined by the commercial companies. A number of practices had made a number of modifications to the ‘telephone first’ approach, and one surgery was continuing to make modifications to the approach. Although deviation from the ‘prescribed’ approach was sometimes described as being discouraged by the commercial companies offering support, some practices felt that modifications helped them to overcome challenges and tailor the approach for their population and staff.
It was evident from the interviews that the ‘telephone first’ approach was operating more smoothly in some practices than in others. In nine practices (100, 101, 103, 104, 105, 106, 108, 112 and 114), staff, overall, felt that the ‘telephone first’ approach was working well, although they had experienced a number of challenges. In one practice (110), all staff identified problems with the approach; this was also evident in interviews with patients (see Chapter 9). In two practices (102 and 117), there was a varied response to how the ‘telephone first’ approach was working. Even in practices in which it was felt that the approach was working, there was variation between staff members: although one GP might feel that the ‘telephone first’ approach was working well, another GP in the same surgery might have found the new system more challenging. At the end of the interview, all participants were asked if, given the choice, they would prefer to retain the ‘telephone first’ approach or revert to a conventional appointment system. Of the 46 participants who answered this question, 41 replied that they would prefer to stay with the ‘telephone first’ approach, one was unsure and four preferred to revert to a traditional appointment system, three of whom were from the same practice. However, it should be noted that the practices that agreed to take part in this element of the study were probably those in which the appointment systems were working better than those that declined to participate (see further details in Chapter 4). However, even those participants who indicated that they would like to keep the ‘telephone first’ approach noted ongoing challenges:
Whenever we’ve talked about it we’ve said that we’d stick and I think that’s because of this . . . it’s worry about if we didn’t speak to them today we’d be back to this 3-week thing [wait to see the GP].
GP 5004, practice 105
Yes, I mean it is fraught with difficulties and problems but there is no way we would go back, no way.
GP 5002, practice 112
Patient safety
Given the literature on concerns about safety regarding telephone triage approaches, all respondents were asked about this issue during the interviews. The majority of GPs felt that a ‘telephone first’ approach was safer than a traditional booking system because all patients who want an appointment with a GP would, at a minimum, speak to a GP on the same day:
. . . our health system is changing, there isn’t enough time, so you’ll either change with it. Or you let it crumble and the doctors who are saying, ‘Well, we don’t think it’s safe’, well, they’ve got 4-week waits to be seen. And, well, you’ve got all those patients who you’re holding back onto [an] iceberg; you don’t know what’s wrong with them, so how’s it safe to have them waiting 4 weeks? So it doesn’t make sense to have that argument.
GP 5002, practice 104
Several GPs spoke about how they dealt with safety when speaking to the patient by telephone and the importance of ‘safety netting’; for example, many GPs stated they had a low threshold for bringing people in for a face-to-face consultation and would call a patient in if anything concerned them:
I mean, I feel if there’s any, sort of, if I’m speaking to someone and I’m not sure what’s going on and I just don’t quite trust what I’m hearing I would always then get them in.
GP 5003, practice 105
A few GPs who were interviewed spoke of individual attitude to risk as being particularly important when using a ‘telephone first’ approach, and also in general practice more widely. Some GPs were said to be more comfortable with risk than others. This might be influenced by how long the doctor had been a GP, how well they knew the patient, how much telephone consulting they had done previously and their personality:
So the people who have done a lot more telephone triage are probably . . . it’s all about you managing risk. So it’s about how much risk you’re willing . . . I suppose that’s being a GP is we manage risk.
GP 5004, practice 106
General practitioners’ experiences of the ‘telephone first’ approach
The GPs were asked how the ‘telephone first‘ approach had affected their working day, compared with working with a traditional appointment system.
All GPs were speaking to more patients than under the traditional system, but they were seeing fewer patients face to face. For some GPs, this was a better way of working:
. . . it’s still hard work, and sometimes it’s hard in different ways because you’re making more decisions because you’re dealing with more patients, so it actually can be quite exhausting even though you aren’t seeing as many patients . . . It’s really nice, so at the end of the day if it’s gone to plan we’ve spoken to everybody that wants to be spoken to that day . . . we’re sort of on top of our demand – that psychologically is a real plus to think that’s it, we’re done, we’re sorted.
GP 5004, practice 101
Some mentioned that face-to-face appointments, under the ‘telephone first’ approach, tended to be more intense than under a traditional appointment system:
So one of the big problems with it is the appointments we do book are much more intensive. So, you know, under our previous system I would pretty, much every surgery, have a couple of catch-up appointments. You know, I’d have somebody just needed their sick note renewing for whatever reason and sometimes it could take a long time but quite often that would be very quick, or a pill check . . . Whereas, all that now is gone because it’s done over the phone. So actually the only people who make it through the door are the people . . . none of those really short, dead easy, ‘I’m going to catch back a bit of time’. They’ve all gone because it’s all done on the phone.
GP 5004, practice 117
There was considerable variation in individual views about changes in workload. For GPs at one surgery, the ‘telephone first’ approach meant less stress, less workload and shorter working days:
We definitely go home earlier, definitely. At the time [before the ‘telephone first’ approach], 3 years ago, I used to work a Monday evening and, in theory, we should finish at 6.30 [p.m.], I was still here at 8 o’clock most Monday evenings. Now, our Monday evening team, by a quarter to seven, they are gone, and all the patients have been managed and seen.
Administrator/receptionist 5001, practice 114
However, in some other practices, GPs were concerned about increases in demand:
So my main worry about this is that demand has increased and continues to increase because we are so accessible and there is no barrier there.
GP 5004, practice 117
Despite implementation of the ‘telephone first’ approach, a few practices noted that they were overwhelmed by demand. They had experienced days when there were too many requests for telephone calls and not enough slots for GPs to call them all back, even if GPs were willing to work late. In such instances, practices often had an approach of turning the telephone lines to ‘emergency calls only’. The time of day when this took place varied: for some it was 5 p.m., for others it was 3 p.m. and for one surgery, which was struggling with the approach, it was quite early in the morning:
. . . when telephone triage first started the latest was 2 p.m., now the latest is probably 11:30 a.m. and that’s an exception.
That’s when you go through to emergencies only?
Yeah, I mean this morning it was, oh my god I’m not sure what time it was this morning, I wasn’t . . . I didn’t really keep an eye on it. Quite often it’s before 9 a.m.
Practice manager 5001, practice 110
A few GPs reported that patients had started to telephone them about things because they were available, for example to tell them about having a poor night’s sleep or to ask for advice when their child had diarrhoea for half an hour:
I think there is evidence that we take calls about things which are basically because we’re so easy to access. In years gone by, you know, I’m not sure I would have had people ringing up and just checking about the ingredients of their shampoo or their medication. Just because they couldn’t have done.
GP 5004, practice 117
In contrast, one GP did not feel that demand had increased and, in fact, noted a decline in demand as a result of the telephone first approach:
And I think we’re now, I think 2 years in, I think we’re seeing a reduction in demand, and there is some evidence that this does happen, I think we’re seeing a reduction in demand for things that we don’t need to see.
GP 5004, practice 101
Some GPs liked the flexibility that the ‘telephone first’ approach afforded them to arrange their workload and felt that it gave them more control over their day as it was them who called patients and allocated them, if appropriate, to face-to-face appointment slots. Others liked, on occasion, being able to book longer face-to-face slots for complex cases. Conversely, other GPs reported that they found the system harder in terms of balancing the callbacks with other tasks such as supervising students, home visits and paperwork. Practices and individuals had varied approaches to address such problems, for example by not having any face-to-face appointments until later in the day.
Many GPs mentioned the unpredictable nature of the day. Unlike a traditional appointment system, in which a GP comes in to a diary full of appointments each day, under the ‘telephone first’ approach, the diary started empty of appointments each morning. Telephone consultations then began and face-to-face appointment slots would begin to be booked in. Some respondents liked the unpredictable nature of the day, whereas for others it brought some anxiety about the day ahead. Some GPs felt that the fact that calls came in continually throughout the day was a strain:
And things like meetings; you know you have a meeting and you can see that people are sitting there getting twitchy, you know, looking at their watch thinking I’ve been in this meeting an hour, how many more telephone calls are going to be on my screen now than there were an hour ago and how much time have I got to deal with them, am I actually going to be able to get through before 7 o’clock or whatever.
GP 5002, practice 102
A number of GPs felt that they were working in a more isolated way under the ‘telephone first’ approach, as they spent more time on their own in their rooms making telephone calls rather than seeing patients face to face. A number of surgeries had introduced measures to try to mitigate this, for example joint coffee and lunch breaks so that GPs could talk to each other or shared call lists to increase the feeling of teamwork.
The experiences of reception staff
One component of the ‘telephone first’ approach, as advocated by the two commercial providers, is for reception staff to take a brief note of the patient’s problem. This is to assist GPs with deciding in which order to call back patients, with patients with more serious complaints being called back first. From interviews at different surgeries, it became clear that the role of the receptionist in the ‘telephone first’ approach varied. In one surgery, the receptionists took no details of the patient’s complaint; in some surgeries, they took minimal details about the condition. In other surgeries, reception staff had been trained to take a brief reason for the call and to signpost patients to alternative routes of care if appropriate. Some practices had modified the system so that the GP could flag patients they wished the receptionist to book for a face-to-face appointment based on the description taken by receptionists. When reception staff had more of an active role, it appeared to alleviate some of the pressures from the GP and was seen as an enabler of the successful adoption of a ‘telephone first’ approach.
Reception staff spoke about the change in their role and the increased responsibility now that they were taking details of the condition from the patient. Most reception staff felt empowered by this enhanced role, although a few felt associated anxiety about potentially serious cases:
Chest pain or symptoms of like a stroke but again it’s really hard but if we are just worried then we can let the doctor know because we’ve got instant message as well, we can always just do, or ‘Not sure about this call. You might need to take it’ or we could just simply pop them on hold, give the doctor a ring and then the doctor can say ‘Well I’ll call them back or I’ll take it’.
Administrator/receptionist 5003, practice 108
Some reception staff felt that their role was less pressured as they no longer had to spend the day telling patients that there were no longer any appointments available, as had happened under the previous system. Several staff who were interviewed spoke of how the ‘telephone first’ approach had led to a happier reception team:
. . . the admin staff like it in the fact that they don’t have patients shouting at them now, like, ‘What do you mean you haven’t got any appointments? It’s only, you know, 8:45 a.m. and how can you have run out of appointments already?’ That sort of thing.
Practice manager 5001, practice 102
Although the nature of the working day had changed for reception staff, there was a consensus among surgery staff that the overall workload of reception staff had remained the same; in particular, the telephone lines often continued to be busiest at the very start of the day.
Changes in practice culture
Some respondents commented on how the ‘telephone first’ approach had altered the culture of the practice, sometimes for better and sometimes for worse. Some felt that the staff had become more cohesive. For example, in one practice, clinicians and administrative staff felt that there was greater appreciation of each other’s roles because the duty GP now took calls in the reception office. Others felt that it had brought staff together in a shared commitment to try to make ‘telephone first’ approach work:
The doctors now, sounds horrible if you say they look out for each other now, not that they didn’t before but they are far more supportive of each other than they were before.
Practice manager 5003, practice 106
Some participants spoke of the importance of the practice agreeing rules of how the system would work so that patients negotiated the system in the same way each time, and they saw this as an enabler of the successful adoption of the approach:
. . . someone who has got a sore throat will ring up the GP instead of going to the pharmacy. I think we circumvent that, partly . . . we do limit the call numbers, partly ‘cause we are reasonably singing from the same hymn sheet; so, if you do ring up with a sore throat you know you’re going to get told to go to the pharmacy, so you know people don’t tend to do that.
GP 5003, practice 112
There were a number of reported conflicts in situations in which not all GPs used the ‘telephone first’ approach as intended. In one practice, one particular GP opted out of the ‘telephone first’ approach and had turned all his appointments into face-to-face appointments; that GP had since left the practice. In another practice, one GP refused to use the ‘telephone first’ approach, and so saw patients only face to face, booked in through telephone consultations by other GPs, and this had caused some confusion for the patients.
In some practices, respondents described how the ‘telephone first’ approach had led to greater divisions between administrative and health-care staff, with GPs rarely leaving their rooms. This contrasts with the practice reported above, in which staff had become more cohesive; this emphasises the large variation between practices in how the ‘telephone first’ approach had worked for them.
Staff perceptions of implications for patients
We asked staff about the effect of the ‘telephone first’ approach on groups of patients who might be adversely affected by the approach, including patients for whom English was not their first language, older people, deaf or hearing-impaired people and patients without telephones. Respondents often commented on the nature of the population that the surgery served and the impacts this had on the implementation of the ‘telephone first’ approach. For some practices, the population they served acted as an enabler of the approach, for example if most patients spoke English as their first language or had their own transport.
Two practices in deprived areas identified elements of their populations that were challenges to the ‘telephone first’ approach:
The population which it really doesn’t work with is our, kind of, immigrant population, our asylum seekers and refugees. Sometimes there’s language problems and problem with expectations; we have a low threshold for calling them in. The only [way] it helps is that we can arrange [an] interpreter for them, so rather than them booking an appointment and turning up without an interpreter.
GP 5001, practice 108
For other practices, challenges were identified to be high numbers of people receiving state benefits, unemployed people or people with learning difficulties. Perhaps surprisingly, these practices had successfully adopted the ‘telephone first’ approach and noted that they had made adaptations to the system for these groups. In fact, for those with a chaotic lifestyle, the immediacy of having the appointment on the same day was said to have been advantageous.
All practices had systems in place for deaf or hearing-impaired people. These included the ability to book straight into face-to-face consultations, being able to text the practice to request an appointment or a carer or relative being able to speak to the GP on a patient’s behalf.
Respondents spoke of services that were available for individuals who may find it challenging to navigate the ‘telephone first’ approach in the traditional way:
. . . some of them we have a flag on [the clinical system] saying ‘if this person rings up for a consultation just book them in’ because sometimes, particularly when we have say hard-of-hearing, deaf patients, vulnerable, learning difficulties, we just book those in, they don’t have a call anyway. And there are some patients that don’t fall into these groups that still it doesn’t work on the phone. But they are few and far between really and most people . . . we’re all used to using the phone now.
GP 5004, practice 101
In addition to provision for patients with certain conditions, staff often spoke about individual patients for whom an alternative system had been set up, for example for a homeless patient and for a patient with memory problems. The default was often that such groups would get booked directly in for a face-to-face consultation.
It has been suggested that elderly patients may be disadvantaged by increased use of telephone consulting, but the majority of staff who were interviewed felt that this was not the case and that most elderly people liked the system once they had experienced it. A few GPs did note that some elderly patients missed the contact that a face-to-face consultation afforded. Some participants noted making special arrangements for elderly patients who relied on family and friends or public transport to visit the surgery, as they were less able to come to the surgery immediately if a face-to-face consultation with the GP was thought necessary.
Owing to the nature of the ‘telephone first’ approach, which relies on the patient being available to take a telephone call from a GP, other groups of people for whom the system may be a challenge were identified. A number of respondents mentioned the need to help patients who worked in roles in which they were unable to take telephone calls during the day:
. . . then you have doctors, teachers, call-centre workers, taxi drivers, HGV [heavy goods vehicle] drivers, policemen, people who work in large open-plan offices who are very unhappy.
GP 5004, practice 105
Some surgeries, in such situations, asked patients to indicate a time during the day during when they could be contacted, for example during their lunchbreak or once they had finished work.
A number of participants reflected on the provision of a service for hard-to-reach groups that took away the telephone call element of the approach. Although necessary for some patients, there was concern that it provided an inequitable service for a group of patients who automatically would be given a face-to-face consultation:
Yeah and sometimes, I mean, we’ve discussed that whether it’s . . . that it’s an unfair advantage to them because there’s language problems, they get appointments.
GP 5001, practice 108
In the case of some groups, such as patients who claimed to not have a telephone, there was sometimes concern that patients were using this excuse as a way to directly obtain a face-to-face appointment without the need for a telephone call with a GP. There was also a feeling, among some participants, that the system would not work if too many patients were exempt from the telephone call element of the approach.
Staff perceptions of patients’ opinions of the system
Many staff felt that patients were pleased with the ‘telephone first’ approach, and they reported positive feedback from patients. Respondents also pointed to positive feedback from NHS Friends and Family Tests and NHS Choices indicating patients’ satisfaction with the ‘telephone first’ approach. One practice had noticed an increase in the number of patients registering with them who had previously been registered with another local practice. Again, in interpreting these data, it should be noted that the practices that agreed to take part in this element of the study were probably those in which the appointment systems were working better than in those that declined to participate.
Some respondents felt that patients preferred the ‘telephone first’ approach, but that it sometimes took time for them to get used to it:
I think the hardest part at first was obviously make sure the patients understood how it worked. Obviously information had gone out to them prior, etc., but obviously there’s always a little bit of confusion . . . So I think it was probably a little bit more time-consuming at the beginning and obviously to have a few patients who weren’t very happy. But I think as time went on and obviously people became aware of the system and realised that actually they get to speak to a doctor quite quickly. If they need to be seen they get seen more soon, you know, I think that resistance tapered away and people came to realise that actually it’s a better system.
Administrator/receptionist 5003, practice 101
One respondent felt that the approach took a while to settle in, and that it took 2 years to see benefits. Practices varied in their approach to determining if a face-to-face consultation was required. One practice had a policy of ending all telephone consultations by checking that the patient was happy to not be seen face to face. In others, the decision was solely that of the GP.
In one practice that was struggling with the approach, respondents believed that the number of patients was declining as a result of the ‘telephone first’ approach, because patients had disenrolled to register at other local surgeries. Patient feedback had been very negative in this practice:
. . . we’ve had an awful lot of complaints but, I mean we seem to have a very complaining population anyway. We were getting very demoralised with NHS Choices, all the sort of comments on there, I think we ourselves sympathise with some of the patients’ comments.
Practice manager 5001, practice 110
Impacts of the ‘telephone first’ approach on the nature of consultations
Some GPs did not like communicating on the telephone and preferred face-to-face consultations, although a number of GPs felt that their telephone consultations had improved as they had become more experienced. A few GPs reported that the ‘telephone first’ approach had enabled them to practise medicine in a different way to that enabled by a traditional appointment system. For example, they could give a patient advice in the morning and then call them back in the afternoon to see if there was any improvement or if additional treatment was required. Some GPs also felt that they had more control over which patients were seen, rather than the reception team acting as a gatekeeper as is the case in a traditional appointment system.
The opportunity to educate patients was also mentioned, with more frequent contact meaning that there was the opportunity to teach patients about conditions or when they needed to contact a GP. One practice reported that demand had gone down, which a GP attributed to better patient education:
So the sort of education about the role of antibiotics in ear infections in children, you know very limited evidence, . . . if you’re otherwise happy with the child, they’re not unwell, we’re probably not going to do anything different today, call us back in a couple of days. So that message I think has got through . . . Certainly I feel I’m speaking to less people that really I think why did they phone about that, you know, I think those calls do . . . I think patients learn that they don’t need to call.
GP 5004, practice 101
Some GPs noted that the ‘telephone first’ approach also enabled them to appropriately book patients into appointments with other practitioners, such as practice nurses, for issues for which it was not necessary for the patient to see a GP:
We’ve realised; some of them can be directed to other people. Previously they just ended up with appointments with a GP when they actually could have gone and seen the practice nurse or the HCA [health-care assistant]. So we found that takes out a workload, it’s a better management of other clinicians’ appointments.
GP 5002, practice 104
One GP felt that the ‘telephone first’ approach led him to do more medical tests than perhaps were necessary:
. . . the ultimate is face-to-face consultations, but if you can’t do face to face maybe telephone is the best option in a way. But I think you need to do a lot more training. But then if you have 40 phone calls and you want to spend 10 minutes on a phone call to try and make sure you’ve not missed anything or do you go the other way and say well actually she’s complaining of this I’d better do all the blood tests in the world and then think well clinically why have I done those, well it’s cleared me as a conscience?
GP 5004, practice 110
Continuity of care
The GP respondents were asked about the impacts of the ‘telephone first’ approach on continuity of care. A number of respondents felt that there was no real difference in continuity of care under a ‘telephone first’ approach compared with a traditional booking system:
I suppose I don’t know. I don’t think that’s much different from our old system to the new one to be honest, with our particular group of patients anyway.
GP 5003, practice 105
Some GPs noted that continuity of care was becoming harder to deliver, but felt that this was related more to issues such as more part-time working than to factors associated with the ‘telephone first’ approach. When interviewed, several reception staff talked about trying to ensure that patients saw their preferred doctor if possible:
So like when they register the doctor’s names are on there and they can ask what days their doctor works, so most of the patients know what days their doctors work, so they’ll probably only phone on those days that they want a specific doctor, not if their doctor is not working then usually they don’t phone.
Administrator/receptionist 5002, practice 105
It was evident that practices varied in their policies; for example, some practice staff would ask the patient which doctor they would prefer to see or speak to, whereas others would give an appointment with a named GP only if it was specifically requested by a patient.
Patient education and knowledge of the ‘telephone first’ approach
Patient education and knowledge of the system was seen by respondents as an enabler of the successful adoption of the ‘telephone first’ approach. Prior to launching the ‘telephone first’ approach, practices had communicated the change to patients in a variety of ways, often using material provided by the commercial companies. There was variation in the extent to which this was done: some practices had written to every patient registered with them, whereas others had put notices up in the practice. Respondents also varied in the importance they placed on patient education:
So it was planning and patient education – patient education I think was the most important part I think. I know one of our neighbouring practices tried it and didn’t get on and I think that’s where they fell down was the patients didn’t understand what they were trying to do.
Administrator/receptionist 5003, practice 101
Some respondents spoke of explaining to patients the importance of telling the receptionist the nature of their problem in order for them to be triaged appropriately. At times, patients struggled to understand elements of the system, such as the inability to pre-book for appointments on different days:
We do try and keep to the appointments that we like, the calls that we take today, are for today, not trying to overflow onto the next day. Because otherwise we get to the same point where we’re full again and it’s just, you know, it just goes on and on and on. But they [patients] do struggle with the ‘oh well why can’t you just put me down for tomorrow?’ And then we have to say sorry you have to call back from half past eight in the morning. They really struggle with that.
Administrator/receptionist 5002, practice 103
Practices that had attempted to adopt a ‘telephone first’ approach but had ceased using it
In our qualitative analysis, we were aware that the majority of staff from GP surgeries that were involved in the study had felt that the adoption of the ‘telephone first’ approach had been broadly successful. There was also evidence, from our quantitative data, that practices that took part in that element of the study had a somewhat more positive patient experience than those that declined to participate. As a result, we sought to conduct interviews with staff from two general practices that had adopted a ‘telephone first’ approach but had then stopped using it.
Using information from the commercial companies on practices that they knew had stopped using the approach, and practices identified from the practice manager survey as no longer using a ‘telephone first’ approach, practice managers were phoned and invited to participate in the study. As in the main study, recruiting to this element of the project was challenging, but two practices agreed to participate. Interviews were conducted as in the main study, with the topic guide modified accordingly. Interviews were transcribed verbatim and analysed following the same approach (see Chapter 10, Methods, for more detail).
Four interviews were conducted with five members of staff from two GP surgeries. Interviews were conducted with GPs (n = 3) and one joint interview was conducted with an administrative manager and member of the administrative team. Three interviews were conducted face to face and one was conducted by telephone.
As in the main study, staff from both practices described being motivated to adopt a ‘telephone first’ approach because of problems with demand and concern that patients were waiting a long time for appointments with a GP. However, all staff reported how the ‘telephone first’ approach had been challenging from the start as a result of the high number of telephone calls it generated. All of those interviewed spoke about the pressure on GPs, with GPs reporting not enjoying their work as much, feeling stressed and feeling more isolated:
. . . it also felt sometimes there was so much work and you just saw a growing list of patients and you were just trying to get through it and you were trying not to bring people down [to the surgery].
GP 5001, practice 201
Participants at both practices mentioned challenges with staff retention as a factor that had an impact on use of the ‘telephone first’ approach. In one practice, two partners and four salaried GPs left in a 2-year period. The other practice lost two partners in quick succession. Respondents noted that reasons for GPs leaving were not solely attributable to the ‘telephone first’ approach, but they often commented that it had not helped. Matching capacity to demand is key to the ‘telephone first’ approach as outlined by the commercial companies; this is something that both practices had struggled with because of staff shortages.
Both practices also attributed the challenging patient populations they served as a reason why the ‘telephone first’ approach had not worked:
We broke a lot of doctors by employing that particular service [telephone first] in the context of our patient population.
GP 5003, practice 202
Although they were in different geographical locations, both practices reported that their patient population was in an area with a high level of deprivation, with a high prevalence of drug and alcohol problems and many patients experiencing mental health challenges. Nevertheless, it should be noted that the main study included practices with similar challenging patient demographics, and they had successfully adopted the approach. Two GPs, from different practices, commented that when they had abandoned the approach they saw patients who had not contacted them under the ‘telephone first’ approach:
It was interesting when we changed back to a different system, there are a whole load of really vulnerable people who we were suddenly seeing again that we hadn’t been seeing.
GP 5001, practice 201
All staff who were interviewed, particularly GPs, had found admitting that the ‘telephone first’ approach had not worked distressing:
I think it was hard to admit it because you feel like it should work . . . you know you do not want to be the one who has failed at something. I guess that’s part of being a doctor is not it? That we are quite competitive . . . you know saying you cannot do something is a difficult thing to say.
GP 5001, practice 202
I did not want to say anything because I felt like everybody else was probably fine and it was just me and then I had one of those unintended conversations with one of the other partners . . . so I said to her [that I was not coping with ‘telephone first’] and I just saw this kind of massive sense of relief and she said, ‘do you know I hate it and I think I’m going to have to leave if it carries on’.
GP 5001, practice 201
A decision to abandon the ‘telephone first’ approach posed challenges for all staff at the practices, and the period when practices decided how they would reconfigure the appointment system was described as difficult. Morale was often low because the ‘telephone first’ approach had not succeeded. Both practices had stopped using the ‘telephone first’ approach but had decided not to revert to a traditional booking system using all face-to-face consultations, but instead decided to retain some elements of telephone consultations. Both had adopted a hybrid approach, with telephone consulting used for on-the-day appointments and face-to-face appointments being available in advance with pre-bookable slots.
Although participants were upbeat about the future and the new approaches they had implemented, it was evident that for staff in practices that had unsuccessfully tried to implement the ‘telephone first’ approach, there could be considerable negative impacts on individual staff members and the practice as a whole.
Summary of findings
This chapter has highlighted that there was great variety in the views of staff towards the adoption of the ‘telephone first’ approach. Although staff in the majority of practices felt that the approach was working successfully, they also described challenges. Even for those who felt that the approach was successful, there were a number of implications for staff, practice management, practice culture, the nature of consultations and continuity of care, as well as for considerations regarding hard-to-reach groups and patient education.
Table 24 draws together the enablers of and barriers to the successful adoption of a ‘telephone first’ approach in primary care, as outlined by practice staff in the interviews. Staff often articulated these barriers and enablers as factors that had assisted in the successful adoption of the approach or that were challenges to it. Several practices had explored ways to overcome what they considered to be barriers to the successful implementation of the ‘telephone first’ approach, often in the form of modifications to the approach.
| Enablers of the successful implementation of a ‘telephone first’ approach | Barriers to the successful implementation of a ‘telephone first’ approach |
|---|---|
|
|
This research has shown that practices’ experiences of the ‘telephone first’ approach were varied. Even in practices in which the adoption is broadly viewed as a success, there are challenges that may be mitigated by the consideration of enablers and barriers, as outlined in Table 24. The majority of staff who were interviewed indicated that they would prefer to retain the ‘telephone first’ approach rather than to revert to a traditional appointment system, showing the potential for the approach to be acceptable to GPs, practice managers and reception staff in primary care. However, as previously noted, practices that took part in this part of the study were those in which the appointment systems appeared to be working better than in those that declined to take part.
Chapter 11 Discussion
Background
In recent years, an expanding population, rising demand for care and increasing numbers of patients with complex problems have combined to present a challenge for general practice: a situation that some have described as a crisis.
NHS England responded in 2016 with the General Practice Forward View,88 which promised increased funding including commitments to an expanded multidisciplinary workforce, although such measures will take time to show benefits. Many general practices have sought ways to manage the challenges of demand, including by diversifying the workforce and increasing the use of alternatives to face-to-face consultations. Telephone triage and telephone consulting approaches have also been advocated. However, to date, none of these has had a radical impact on demand for care. In particular, a 2014 major RCT of telephone triage by GPs and nurses for patients requesting same-day appointments (ESTEEM23) found that overall GP workload was increased by introducing telephone triage, with no reduction in costs.
A number of practices in England have adopted a whole-system change, a ‘telephone first’ approach in which telephone consultations with a GP take place prior to all face-to-face consultations. After telephoning the practice, patients are called back by a GP and, at the end of this call, a decision is made regarding whether the patient needs to come in for a face-to-face consultation or whether their concern has been satisfactorily and appropriately dealt with on the telephone. Practices are offered management support with introducing this system by two commercial providers (Doctor First and GP Access); this support includes detailed analysis of workload patterns to enable practices to match capacity to demand. Data from the companies suggest reduced practice workload, improved continuity of care, reduced A&E attendances, financial savings and improved patient and staff satisfaction. The ‘telephone first’ approach is advocated in NHS England literature. 5 However, until this study was conducted, no independent evaluation of these approaches had been undertaken.
Our research sought to address three main research questions in relation to the ‘telephone first’ approach as offered by Doctor First and GP Access:
-
How does the ‘telephone first’ approach affect patient experience and use of primary and secondary care services?
-
What is the impact of the ‘telephone first’ approach on the nature of consultations for patients and staff, and how appropriate is this approach for hard-to-reach groups?
-
What are the cost consequences of the approach?
Summary of findings
Summary of quantitative findings
In our quantitative analyses, we principally report an intention-to-treat analysis, including the 89 practices that were operating the system as recommended by the companies alongside those practices that had modified the ‘telephone first’ approach and were using a hybrid form of telephone consulting and a small number of practices that had ceased running the system altogether. We also included a sensitivity analysis that was restricted to practices that we believed were running the system as recommended by the companies throughout the data collection period. In general, these two analyses produced similar findings.
Data from the computer systems of practices using one of the commercial companies showed that there had been a major effect on patterns of consultation as a result of the introduction of the ‘telephone first’ approach, with a 12-fold increase in telephone consultations and a 38% reduction in face-to-face consultations. There was an overall increase in the total number of consultations (face to face and telephone) of 28%. There were equally dramatic changes in time from booking to appointment time – from an average of 4 days for face-to-face appointments before the change to an average of 0.9 days after the change. The length of consultations was similar before and after the change (10.9 minutes before and 10.2 minutes after for face-to-face consultations and 7.7 minutes before and 6.2 minutes after for telephone appointments), with an overall increase in length of surgery consulting time of around 8% following the change (face-to-face and telephone consultations combined). Although these results were broadly similar in the sensitivity analyses that were restricted to practices operating the new system throughout the period of data collection, there was wide variation in patterns of consulting in individual practices, with some experiencing a marked decrease in overall consulting time and others experiencing a substantial increase. Practices also varied greatly in the proportion of telephone consultations that were followed by a face-to-face consultation.
In the controlled analysis of A&E attendances with use of HES, the numbers of A&E attendances before and after the launch for patients registered in practices using a ‘telephone first’ approach were compared. There was no evidence that use of a ‘telephone first’ approach led to a change in the average rate of A&E attendances. There was evidence of a slower increase in attendances for intervention practices than for control practices, but the trend was very small. We also noted small increases in emergency admissions following the introduction of the ‘telephone first’ approach, which were associated with small net increases in secondary care costs. Although, again, there was wide variation between individual practices, we found no evidence to support the claims of widespread cost savings from the new approach.
An analysis of patient experience from the national GP Patient Survey compared ‘telephone first’ practices with control practices in England. The biggest difference by far was a 20-percentage-point improvement in intervention practices in responses to the GP Patient Survey question on length of time to see or speak to a doctor or nurse. This was equivalent to an average improvement of nearly one full category in the four-point scale used in this national survey (the question was ‘How long after initially contacting the surgery did you actually see or speak to them?’ and the answers were ‘on the same day’/‘next working day’/‘a few days later’/‘a week or more later’). Other differences were small in comparison, and included an increase in the convenience of the appointment (0.38 percentage points more positive), small but statistically significant reductions in overall experience of making an appointment (0.44 percentage points more negative), reported doctor–patient communication (0.89 percentage points more negative) and ability to see the patient’s preferred doctor (1.25 percentage points more negative). Patients were also 2.4 percentage points less likely to recommend their GP surgery to others after the intervention.
In the patient survey that we conducted of people who had recently had a telephone consultation in ‘telephone first’ practices, 21.6% reported that the telephone consultation was less convenient, 23% reported that there was no difference, and over half (55.4%) said that it was more convenient; however, we have evidence that the practices that agreed to take part in this survey had more positive experiences than those that declined to take part.
One factor that is likely to influence patients’ reported experiences is whether or not they were expecting to have to speak to a GP before making an appointment. Of patients surveyed, 70% of those who phoned expected to get a callback, but 25% did not. Those who were least likely to expect a call were those who visited the surgery to request an appointment.
As in the patient survey, patients expressed a wide range of views in the interviews we conducted. One of the most striking features of these interviews was the extremes of responses, as exemplified in the following patient quotations: ‘I have rang the GP’s surgery at 8.30 a.m. and redialled 152 times before getting through to surgery then waited till 5.30 p.m. for callback from a doctor’ and ‘This new system has proved truly excellent and my doctor has seen me on the same day if she has thought it necessary’. The ‘telephone first’ approach clearly suited some people by reducing the need for them to come into the surgery, but it was problematic for others (e.g. when it was difficult for someone working in an open-plan office to take a callback). However, a substantial proportion of negative comments were about the operation of the scheme itself rather than the principles behind it. So, for example, patients may not have minded being phoned back by a GP, but they complained about the difficulty of getting through on the telephone, restricted times when the telephone lines were open, lack of flexibility in scheduling the callback from the GP and lengthy delays before the callback was made.
Summary of qualitative findings
Patients also described the characteristics that made it easier for them to use the ‘telephone first’ approach. These included being articulate and having the confidence to press for the outcome they wanted, having flexibility in their daily schedule and having an existing trusting relationship with the GP who was deciding whether or not a face-to-face consultation was necessary. Some practices had clearly organised themselves so that it was easier for the patient to see a doctor of their choice; in others it was harder. Not having English as a first language was identified as a problem by patients but, contrary to our expectations and concerns expressed in the literature,30 older people expressed generally positive views about the new system. Indeed, none of the nine patients aged > 75 years who we interviewed said that they would prefer to return to the old system. Patients who were at work found it less easy to manage the new system (e.g. not knowing when the GP would call back). A few practices were able to give patients a specific time when the doctor would call, but others were unable to do this.
A wide range of opinions were also expressed in staff interviews. These included examples of practices in which the approach appeared to be working well and others where it was working less well. Within practices, individual staff members also expressed strong views about liking or disliking the new approach. For some GPs, the ‘telephone first’ approach had meant that they were able to go home earlier, whereas others felt overwhelmed by increased demand. For most GPs, the new scheme involved a major change in the way they worked. It also involved redistribution of work, especially in practices in which partners took the telephone calls but salaried or locum doctors saw a higher proportion of patients who came for a face-to-face consultation. Practices were generally noted to be quieter during the day, with fewer patients attending for face-to-face appointments.
Receptionists had a very important role in implementing the new system and most of those interviewed welcomed the increased responsibility that they were given and the increased ability to offer patients appointments (albeit not face-to-face appointments). Practice managers were key to the effective implementation of the ‘telephone first’ approach and described the importance of understanding patterns of demand before deciding how to introduce the new approach.
Concerns were sometimes expressed about the safety of telephone consulting. The doctors we interviewed did not see this as a major problem. Indeed, they thought that the new system was safer because patients were able to have contact with a doctor much more quickly (by telephone) – they could then be given a face-to-face appointment rapidly if needed. Patients also commented that the new system avoided delays in speaking to someone about a problem that could be serious.
Members of staff who were interviewed also described changes in the culture of practices, including greater cohesiveness, with staff being more supportive of each other. However, again, there was a wide range of views including descriptions of tension within the team, especially when one GP was opposed to the new system. For staff in practices that had unsuccessfully tried to implement the ‘telephone first’ approach, there could be considerable negative impacts on individual staff members and the practice as a whole.
There were parallels between the staff and patient interviews in that when the ‘telephone first’ approach was successful it often worked for both staff and patients. Yet when the system was strained, for example when there were not enough slots on the day for telephone calls or difficulties with patients getting through on the telephone, both staff and patients struggled with the approach. Overall, the majority of patients and staff interviewed would choose to keep the ‘telephone first’ approach over a ‘traditional’ appointment system.
Summary of the cost–consequences analysis
The cost–consequences analysis reported a median cost of £10,810 paid by practices to commercial providers for support with adopting the ‘telephone first’ approach, but other set-up costs for practices were generally small, and few made staffing changes when they introduced the new system. We found no evidence to support claims of major reductions in secondary care costs, although, as with other aspects of the study, there was wide variation between individual practices with, for example, practice patients making substantially more, or less, use of A&E after the ‘telephone first’ system was introduced.
Interpretation of findings
This study has identified a wide range of views (both positive and negative) expressed by patients and staff about the introduction of a ‘telephone first’ approach. The quantitative results, when examined at an individual practice level, also show that there can be substantial benefits of the approach to some practices but considerable challenges for others.
At first glance, such variation may be surprising; however, given the amount of variation between GP surgeries across the country, perhaps this should not be unexpected. General practice surgeries are small organisations and often have unique cultures shaped by history, individuals, norms and local influences.
Differences between general practices are seen in a wide range of clinical areas, such as rates of prescribing, referral rates and access to diagnostic tests, which are attributable to a variety of factors including individual clinician attitudes and local infrastucture. 89–91
Such variation in practice culture may determine the extent to which the ‘telephone first’ approach is successful. For example, if a practice has struggled with patient access to appointments for a long time, it may be that once the ‘telephone first’ approach is introduced the practice becomes overwhelmed with patient requests for appointments.
A related challenge of this approach may be the concept of the ‘symptom iceberg’, as described by McAteer et al. ,92 who note that many symptoms are common among the population but that not all symptoms are presented to a medical professional. A system, such as ‘telephone first’, that increases access to GPs could potentially result in a greater number of people presenting symptoms to clinicians for which they would otherwise not have consulted a professional. This is echoed by our data: GPs felt that, under the ‘telephone first’ approach, patients contacted them about symptoms that they would not usually have consulted them about, or would usually have waited longer to consult about, and these symptoms may have disappeared in the meantime.
The concept of supplier-induced demand may also explain the challenges to some general practices of a ‘telephone first’ approach. When additional services are provided, demand for care does not necessarily decrease, a phenomenon seen in other areas of the NHS. For example, the introduction of NHS Direct has been shown to have no effect on use of emergency care,93 and NHS walk-in clinics have been shown not to affect out-of-hours consultations94 or to reduce waiting times for primary care. 95
What is clear for the ‘telephone first’ approach (or any other system) is that it will not work if there is a fundamental mismatch between demand for care and capacity to meet that demand. An important question is whether or not the new approach is an effective solution to the problem of demand for care exceeding the capacity of practices to meet that demand. Our overall estimation of an 8% increase in total consultation time suggests that it does not. Nevertheless, this figure masks large variation between practices in which both patients and staff seemed to be happy and others in which patients were dissatisfied and staff described being at breaking point.
Our impression, based on our data, many hours spent in the practices, and two learning events we held as part of the project, is that the ‘telephone first’ approach works best in practices that are highly organised. The practices least likely to succeed are ones with a large backlog of unmet need that is suddenly released by making telephone consultations available and ones that are poorly organised or unable to recruit and, therefore, unable to match staff resources to patient need. Therefore, the most ‘successful’ practices were ones that entered into discussion with the commercial companies with a clear understanding of their workload and with the means to meet demand. We have concerns that CCGs may have commissioned services from the commercial providers hoping that they will ‘sort out’ chaotic practices in which workloads are clearly out of control. As an approach to demand management, the schemes possibly work best for practices that need them least.
There is then a range of practice cultural factors that have a major influence on subsequent progress. The first of these is agreement among the staff about the approach to be taken. The practice manager is key to this, and most practices in which the scheme operated well had highly organised practice managers, often with sophisticated data systems of their own. Indeed, we are aware of other practices that have adopted the approach successfully on their own without the support of external consultancy. It was also important that there was shared understanding and support for the new approach among staff, and in particular among GP partners in the practice.
Practical issues were very important. These include information being provided to patients on how the scheme works and how to navigate it, putting sufficient time into reception staff training, having sufficient telephone lines and staff to answer calls to deal with demand at all times, and ensuring training and support for GPs in telephone consulting (especially locums and registrar doctors). Likewise, the schemes could be operated to improve continuity of care, with the doctor taking a telephone consultation directing patients to a face-to-face appointment with a doctor they knew. However, in many practices, a number of face-to-face consultations were carried out by salaried doctors and locums, with partners being responsible for the telephone calls – this could make continuity of care for patients more difficult.
We noted in our qualitative work that practices had often made slight changes to the approach from that advocated by the commercial companies. In some practices, nurses conducted some of the telephone triage, an approach not advocated by either commercial company. Although this change may appear interesting in potentially reducing the cost of running the ‘telephone first’ approach, it should be noted that findings from the ESTEEM trial22 show that increases in nursing workload were much greater when nurses took triage calls than when GPs did. This suggests that such an approach may not lead to overall financial savings.
It was also clear that the new approach worked better for some patients than for others. It worked well for patients who had the flexibility to be available when the GP phoned back, and elderly people in general felt that the scheme worked well for them. It worked less well for some working people who needed to schedule their days ahead or found it difficult to take telephone calls at work. We found that the ‘telephone first’ approach could be operated in a way that was flexible for ‘hard-to-reach’ groups, such as those who did not speak English as a first language, and all practices had made modifications for patients who were deaf or had hearing difficulties.
Finally, we have limited data on the outcomes of care. The study was not designed to detect important but infrequent events, such as threats to patient safety from telephone consulting. However, we note the views expressed that if such risks exist (which they may do on occasion), they are likely to be offset by patients being able to speak to a doctor on the telephone much more promptly rather than having to wait much longer to see a GP, which was often the situation prior to the introduction of the ‘telephone first’ approach. Our study found no evidence that use of a ‘telephone first’ approach led to a change in the average rate of A&E attendance. This is in contrast to the claims of commercial companies, also quoted in NHS England literature,5 and this suggests a limited impact of a ‘telephone first’ approach on secondary care utilisation and, thus, limited financial savings for the wider NHS.
Impact of patient and public involvement
Patient and public involvement representatives were closely involved in the study throughout its development and delivery. At the outline proposal stage, we received written comments from our PPI panel and some small changes were made to our application as a result. A face-to-face meeting was held with seven members of Inspire (our local PPI group) once we were invited to submit a full proposal.
The PPI members were very engaged in the topic at this meeting, with several commenting on the importance of this research for patients. A number of proposed changes to the research were discussed with the group. In response to these discussions, two substantial changes were made to the application. The first was in response to a concern that not enough patients would be interviewed as part of the qualitative element and that there was an imbalance because fewer patient interviews than staff interviews were proposed. In response to this comment, we increased the number of patient interviews from three per surgery to four per surgery. Participants also recommended an increase in the number of lay members in the SSC. In response to this, we increased the number of lay members in the SSC from two to four.
The study team benefited from input from four PPI members throughout the course of the study. PPI representatives were members of the SSC, alongside staff from GP surgeries and GPs. The SSC attended three meetings, one in each year of the study, in which the project team presented the research and obtained input from SSC members; members also participated in wider discussion about the project and the interpretation of its findings.
The involvement of PPI members led to a number of small but significant modifications to the project. For example, out-of-pocket patient expenses were included in the cost–consequences analysis after the idea was suggested by a PPI member during a SSC meeting. The exclusion of 13- to 17-year-olds from the patient survey was also added when a PPI member expressed concern regarding a young person having consulted with a GP without the knowledge of their parents and then being sent a survey by the general practice.
Between face-to-face meetings, input on written documents designed for patients, such as patient information leaflets, was obtained from PPI members. This ensured that the information disseminated to participants was suitable and understandable to a lay audience. One PPI member wrote the Plain English summary for the final report to ensure that this too was understandable by a lay audience.
The attendance of PPI members from our SSC, and patient representatives from practices using a ‘telephone first’ approach, at the second study learning event enabled the voice of patients as well as staff to be represented at this event at which we discussed how the approach had worked for some practices but not for others, and explored the potential reasons for this variation.
Robustness of results and limitations
This study is the first independent evaluation of a ‘telephone first’ approach. The evaluation used a multimethod approach with in-depth qualitative and quantitative aspects including the use of large independently collected national data sets (the GP Patient Survey and HES). We acknowledge a number of limitations to our approach. Our study design was not theory-driven, it therefore provides insights into the way in which ‘telephone first’ was embedded differently in different practices and modified, but it was not designed as a full implementation study. The literature review in Chapter 2 was detailed but was not a full systematic review and we have drawn attention to some issues relating to the quality of some studies. The data collected from clinical administrative records in practices were not originally collected for research purposes and so we had no means of, for example, checking on the accuracy of coding or accounting for missing data in some cases. Furthermore, there were no control data for this aspect of the study; we used data from practices using only one commercial provider (GP Access). For the analysis of continuity of care, we used shorter time periods than is common for this type of analysis. In our analysis of patient survey data, we conducted some post hoc analyses to explain variations in the responses of different population groups but we acknowledge in the relevant sections that these analyses were underpowered. In no cases did we have data collected from practices before they introduced the ‘telephone first’ approach; doing so would have allowed us to explain the substantial heterogeneity seen between practices in almost all aspects of the findings. In the economic analysis, we relied on practice managers’ perceptions of staff changes that they were able to attribute to the ‘telephone first’ approach without any independent evidence. In our qualitative work and our own patient survey, we have some evidence that practices that participated in that element of the study had a somewhat more positive patient experience than those that did not participate. However, we are reassured that our sample included practices that were having success with the approach, those struggling with it and some that had abandoned the approach. We acknowledge that some groups that are defined as hard to reach, for example those with learning difficulties or who have difficulties with speaking English, may have been less likely to participate in interviews or to have completed the patient survey, and as a result their views may not be adequately represented. Although we acknowledge these limitations, there was a high degree of consistency between different aspects of the study (e.g. between our own survey and the GP Patient Survey analysis, and between the quantitative and qualitative findings). We are, therefore, confident in the overall robustness of our findings.
Chapter 12 Conclusions
A range of approaches are needed to meet demand for care in general practice. Some of these involve increasing the size and disciplinary mix of the general practice workforce, addressed in part in NHS England’s General Practice Forward View. 88 Telephone consultations are another approach to reducing the demand for face-to-face consultations. This study evaluates a more radical ‘telephone first’ approach, which is founded on the principle that a substantial proportion of regular general practice workload can be dealt with via telephone and, therefore, requires that all requests for a consultation should initially involve a telephone consultation with a GP.
Our study shows that the ‘telephone first’ approach results in considerable improvements in patients’ ability to access care from their general practice, and that a substantial proportion of problems can be dealt with on the telephone. The introduction of the system was associated with a small increase in total consulting time (telephone and face-to-face consulting combined), albeit with wide variation between practices. Some practices experienced large decreases in workload and others experienced substantial increases, possibly attributable to the increased availability of telephone consultations where there had previously been high levels of unmet need. Views on this new approach varied widely among both staff and patients. In practices using the ‘telephone first’ approach, over half of patients felt that it was more convenient, and for patients who find it easy to receive a callback from the doctor or in practices in which a callback can be arranged at a particular time, the new approach represented a service with which patients were generally satisfied. As with patients, strong views, both for and against the new approach, were expressed by staff, although staff from most practices operating the system in our study said that they would not return to their previous approach. Compared with other practices in England, patients in practices using the ‘telephone first’ approach expressed somewhat more negative views about a range of aspects of their care including doctor–patient communication and the ability to see a GP of their choice, although they found appointments much more convenient to arrange. Overall, patients responding to the national GP Patient Survey were less likely to recommend practices that had adopted the new approach, compared with other practices in England. We found no evidence that the ‘telephone first’ approach would, on average, result in significant reduction in secondary care costs.
An approach that requires patients to be called back by a GP before any face-to-face appointment can be booked suits some patients better than others (e.g. those who have flexibility in their day and can easily be called back). Some practices have therefore modified their original approach to allow limited advance booking of appointments. However, this works only if there is sufficient capacity to deal with both telephone and face-to-face consultations on the day. The ‘telephone first’ approach also crucially needs patients to be able to get through to their practice on the telephone and for practices to provide capacity for telephone consultations at all times, including periods of peak demand. Therefore, as an approach to demand management, it is possible that the approach may work best for practices that need it least.
Findings from this research suggest that the ‘telephone first’ approach is not a panacea for meeting demand for general practice care. However, it does demonstrate the opportunity for a substantial proportion of patients’ needs to be met without a face-to-face consultation.
It is clear from this and other studies that telephone consulting forms a useful part of the services that a practice offers to patients, and it is also clear from our results that a substantial amount of GPs’ workload and patients’ problems can be dealt with on the telephone. However, neither telephone triage (as in the ESTEEM6 trial) nor the ‘telephone first’ approach evaluated here are a solution to meeting demand for care in general practice.
Recommendations for future research
A key question for practice that could be addressed by future research is how to develop systems that are flexible enough to meet the needs of all their patients. A rigid ‘telephone first’ approach for all consultations does not do this, but we observed practices that were modifying this approach (often on an ongoing basis) to meet the needs of patients as closely as they could. Successful approaches are likely to be different in different practices and more work could be done to identify what works best in different circumstances.
A second issue that we have not addressed in this study relates to the approach that practices take to matching capacity to demand. The commercial companies offering management support to practices adopting the ‘telephone first’ approach stress that understanding patterns of demand and allocating resources to meet them are critical to the success of the approach (e.g. having sufficient staff for predictably busy times/days of the week). More work could be done to investigate how predictable patterns of demand are, and to what extent reallocation of human resources could reduce the pressures that practices feel they are under.
Acknowledgements
We thank all members of the SSC, chaired by Dr Peter Bailey. This committee included patient members Brett Collard, Margaret Johnson, Graham Rhodes and Nick Roberts, alongside professional members who provided advice during the course of the study. We would particularly like to thank Margaret Johnson, who wrote the Plain English summary for this report. We are grateful to the commercial companies (Productive Primary Care and GP Access) that provided contact details of practices using their approaches. We are enormously grateful to the staff and patients from practices that took part in the study. We are thankful to Dr Rupert Payne, who acted in a quality assurance role on this report.
Contributions of authors
Jennifer Newbould (Research Leader) was the project leader. She was a co-applicant and contributed to design of the project. She led the qualitative elements of the study, contributed to Chapters 4, 5 and 9, was the lead author of Chapter 10 and a co-author of Chapters 11 and 12. She contributed to the final report writing and the assimilation of the final report.
Sarah Ball (Analyst) was the project manager. She was the lead author of Chapter 9 and contributed to Chapters 4, 5 and 10. She contributed to the assimilation of the final report.
Gary Abel (Senior Lecturer in Medical Statistics) was a co-applicant and contributed to design of the project. He led the quantitative elements of the study. He was the lead author of Chapters 3, 6 and 7 and contributed to Chapters 4 and 8.
Matthew Barclay (Statistician) contributed to Chapter 8.
Tray Brown (National Institute for Health Research Methods Fellow in Health Economics) contributed to Chapter 8.
Jennie Corbett (Analyst) was a co-author of Chapter 2 and a contributor to Chapters 4, 9 and 10.
Brett Doble (Research Associate in Health Economics) contributed to Chapter 8.
Marc Elliott (Distinguished Chairperson in Statistics) contributed to Chapters 3, 4, 6 and 7.
Josephine Exley (Senior Analyst) was the lead author for Chapters 4 and 5 and a contributor to Chapters 3, 6, 7, 9 and 10.
Anna Knack (Research Assistant) contributed to Chapter 2 and to the assimilation of the final report.
Adam Martin (Analyst) contributed to Chapter 8.
Emma Pitchforth (Associate Research Group Director) was a co-applicant and contributed to the design of the project. She was the lead author of Chapter 1, a co-author of Chapter 2 and a contributor to Chapters 9 and 10.
Catherine Saunders (Senior Research Associate) contributed to Chapters 3, 7 and 8.
Edward CF Wilson (Senior Research Associate) was a co-applicant and contributed to the design of the project. He led the economic element of the study and was the lead author of Chapter 8.
Eleanor Winpenny (Analyst) contributed to Chapter 6.
Miaoqing Yang (Analyst) contributed to Chapter 8.
Martin Roland (Emeritus Professor of Health Services Research) was the principal investigator with oversight of all elements of the project. He co-designed the project, was the lead author of Chapters 11 and 12 and a contributing author to Chapters 3–7. He contributed to the final report writing and the assimilation of the final report.
Publications
Newbould J, Abel G, Ball S, Corbett J, Elliott M, Exley J, et al. Evaluation of telephone first approach to demand management in English general practice: observational study. BMJ 2017;358:j4197.
Ball SL, Newbould J, Corbett J, Exley J, Pitchforth E, Roland M. Qualitative study of patient views on a ‘telephone-first’ approach in general practice in England: speaking to the GP by telephone before making face-to-face appointments. BMJ Open 2018;8:e026197.
Newbould J, Exley J, Ball S, Corbett J, Pitchforth E, Roland M. GPs’ and practice staff’s views of a telephone first approach to demand management: a qualitative study in primary care [published online ahead of print April 23 2019]. Br J Gen Pract 2019.
Data-sharing statement
There are no data available for further access or sharing because of the nature of the study. This research used both commercially sensitive data and data subject to a confidentiality agreement with NHS Digital, which prevents wider distribution beyond the study team. All queries should be submitted to the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Newbould J, Abel G, Ball S, Corbett J, Elliott M, Exley J, et al. Evaluation of telephone first approach to demand management in English general practice: observational study. BMJ 2017;358. https://doi.org/10.1136/bmj.j4197.
- Ball SL, Newbould J, Corbett J, Exley J, Pitchforth E, Roland M. Qualitative study of patient views on a ‘telephone-first’ approach in general practice in England: speaking to the GP by telephone before making face-to-face appointments. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-026197.
- Newbould J, Exley J, Ball S, Corbett J, Pitchforth E, Roland M. GPs’ and practice staff’s views of a telephone first approach to demand management: a qualitative study in primary care [published online ahead of print April 23 2019]. Br J Gen Pract 2019. https://doi.org/10.3399/bjgp19X702401.
- The Future of Primary Care: Creating Teams for Tomorrow. Leeds: Health Education England; 2015.
- NHS England . Urgent and Emergency Care Review: Evidence Base Engagement Document 2013. www.england.nhs.uk/wp-content/uploads/2013/06/urg-emerg-care-ev-bse.pdf (accessed 8 March 2017).
- Campbell JL, Fletcher E, Britten N, Green C, Holt T, Lattimer V, et al. The clinical effectiveness and cost-effectiveness of telephone triage for managing same-day consultation requests in general practice: a cluster randomised controlled trial comparing general practitioner-led and nurse-led management systems with usual care (the ESTEEM trial). Health Technol Assess 2015;19. https://doi.org/10.3310/hta19130.
- Campbell JL, Britten N, Green C, Holt TA, Lattimer V, Richards SH, et al. The effectiveness and cost-effectiveness of telephone triage of patients requesting same day consultations in general practice: study protocol for a cluster randomised controlled trial comparing nurse-led and GP-led management systems (ESTEEM). Trials 2013;14. https://doi.org/10.1186/1745-6215-14-4.
- Longman H, Coupe S, Peteron C, Singh K. Proposal to Study a System of Access in General Practice Involving a Rapid Telephone Response by a GP 2014. http://gpaccess.uk/wordpress/wp-content/uploads/2013/02/PA-System-study-proposal-v3G.pdf (accessed 3 February 2016).
- Productive Primary Care Ltd . Improving Patient Access to Primary Care Services n.d. http://productiveprimarycare.co.uk/doctor-first.html (accessed 1 November 2017).
- GP Access . What We Do n.d. http://gpaccess.uk/what-we-do/launch/ (accessed 2 November 2017).
- Productive Primary Care Ltd . Productive Primary Care n.d. http://productiveprimarycare.co.uk/index.html (accessed 2 November 2017).
- GP Access . Who We Are n.d. http://gpaccess.uk/about-us/who-we-are/ (accessed 2 November 2017).
- GP Access . Continuity n.d. http://gpaccess.uk/research/continuity/ (accessed 2 November 2017).
- GP Access . An Empty Waiting Room – What’s Not to Like? n.d. http://gpaccess.uk/case-studies/empty-waiting-room-whats-not-like/ (accessed 2 November 2017).
- GP Access . Practices n.d. http://gpaccess.uk/case-studies/practices/ (accessed 2 November 2017).
- GP Access . A&Amp;E Effects n.d. http://gpaccess.uk/research/a-e-effects/ (accessed 2 November 2017).
- GP Access . Comparison of Mode of Access to GP Telephone Consultation and Effect on A&Amp;E Usage 2012. http://gpaccess.uk/wordpress/wp-content/uploads/2013/01/Comparison-of-access-modes-AE-effect-v3-GPA.pdf (accessed 31 October 2017).
- Wilson E, Pitchforth E, Head F, Abel G, Newbould J. Tele-First: Telephone Triage As an Alternative to Face to Face Contact in General Practice 2014. www.journalslibrary.nihr.ac.uk/programmes/hsdr/135940/#/ (accessed 2 November 2017).
- NHS Business Services Authority . Prescription Cost Analysis Data n.d. www.nhsbsa.nhs.uk/prescription-data/dispensing-data/prescription-cost-analysis-pca-data (accessed 26 September 2018).
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-69.
- Calitri R, Warren FC, Wheeler B, Chaplin K, Fletcher E, Murdoch J, et al. Distance from practice moderates the relationship between patient management involving nurse telephone triage consulting and patient satisfaction with care. Health Place 2015;34:92-6. https://doi.org/10.1016/j.healthplace.2015.04.002.
- Campbell J, Warren F, Taylor R, Green C, Salisbury C. Patient perspectives on telephone triage in general practice – authors’ reply. Lancet 2015;385. https://doi.org/10.1016/S0140-6736(15)60283-5.
- Campbell JL, Fletcher E, Britten N, Green C, Holt TA, Lattimer V, et al. Telephone triage for management of same-day consultation requests in general practice (the ESTEEM trial): a cluster-randomised controlled trial and cost–consequence analysis. Lancet 2014;384:1859-68. https://doi.org/10.1016/S0140-6736(14)61058-8.
- Holt TA, Fletcher E, Warren F, Richards S, Salisbury C, Calitri R, et al. Telephone triage systems in UK general practice: analysis of consultation duration during the index day in a pragmatic randomised controlled trial. Br J Gen Pract 2016;66:e214-8. https://doi.org/10.3399/bjgp16X684001.
- Murdoch J, Barnes R, Pooler J, Lattimer V, Fletcher E, Campbell JL. Question design in nurse-led and GP-led telephone triage for same-day appointment requests: a comparative investigation. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-004515.
- Murdoch J, Varley A, Fletcher E, Britten N, Price L, Calitri R, et al. Implementing telephone triage in general practice: a process evaluation of a cluster randomised controlled trial. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0263-4.
- Warren FC, Calitri R, Fletcher E, Varley A, Holt TA, Lattimer V, et al. Exploring demographic and lifestyle associations with patient experience following telephone triage by a primary care doctor or nurse: secondary analyses from a cluster randomised controlled trial. BMJ Qual Saf 2015;24:572-82. https://doi.org/10.1136/bmjqs-2015-003937.
- ESTEEM. Exeter: University of Exeter Medical School; 2016.
- McKinstry B, Watson P, Pinnock H, Heaney D, Sheikh A. Confidentiality and the telephone in family practice: a qualitative study of the views of patients, clinicians and administrative staff. Fam Pract 2009;26:344-50. https://doi.org/10.1093/fampra/cmp032.
- Brant H, Atherton H, Ziebland S, McKinstry B, Campbell JL, Salisbury C. Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice. Br J Gen Pract 2016;66:e460-6. https://doi.org/10.3399/bjgp16X685597.
- McKinstry B, Walker J, Campbell C, Heaney D, Wyke S. Telephone consultations to manage requests for same-day appointments: a randomised controlled trial in two practices. Br J Gen Pract 2002;52:306-10.
- McKinstry B, Watson P, Elton RA, Pinnock H, Kidd G, Meyer B, et al. Comparison of the accuracy of patients’ recall of the content of telephone and face-to-face consultations: an exploratory study. Postgrad Med J 2011;87:394-9. https://doi.org/10.1136/pgmj.2010.101287.
- McKinstry B, Watson P, Pinnock H, Heaney D, Sheikh A. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. Br J Gen Pract 2009;59:e209-18. https://doi.org/10.3399/bjgp09X420941.
- Doublet-Stewart M. Telephone consultations. Br J Gen Pract 2002;52:501-2.
- Innes M. Telephone consultations. Br J Gen Pract 2002;52.
- Jiwa M. Telephone consultations. Br J Gen Pract 2002;52:852-3.
- Joesbury H. Telephone consultations. Br J Gen Pract 2002;52.
- McKinstry B, Walker J. GP telephone consultations. Br J Gen Pract 2002;52:585-6.
- McKinstry BH. Telephone consultations may not save time. BMJ (Clinical Researched) 2002;325. https://doi.org/10.1136/bmj.325.7374.1242.
- McKinstry B, Sheikh A. Unresolved questions in telephone consulting. J R Soc Med 2006;99:2-3.
- Bunn F, Byrne G, Kendall S. The effects of telephone consultation and triage on healthcare use and patient satisfaction: a systematic review. Br J Gen Pract 2005;55:956-61.
- Luthra M, Marshall MN. How do general practices manage requests from patients for ‘same-day’ appointments? A questionnaire survey. Br J Gen Pract 2001;51:39-41.
- Edwards A, Neal RD. The effect of the new GMS contract on GP appointment provision in Wales: postal questionnaire survey of practice managers. BMC Res Notes 2008;1. https://doi.org/10.1186/1756-0500-1-117.
- Hobbs FDR, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. National Institute for Health Research School for Primary Care Research . Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet 2016;387:2323-30. https://doi.org/10.1016/S0140-6736(16)00620-6.
- Brown A. Telephone consultations. Br J Gen Pract 2002;52.
- Stevenson M, Marsh J, Roderick E. Can patients predict which consultations can be dealt with by telephone?. Br J Gen Pract 1998;48:1771-2.
- Kernick DP, Reinhold DM, Mitchell A. How should patients consult? A study of the differences in viewpoint between doctors and patients. Fam Pract 1999;16:562-5. https://doi.org/10.1093/fampra/16.6.562.
- Hallam L. Patient access to general practitioners by telephone: the doctor’s view. Br J Gen Pract 1992;42:186-9.
- Jiwa M, Mathers N, Campbell M. The effect of GP telephone triage on numbers seeking same-day appointments. Br J Gen Pract 2002;52:390-1.
- Stuart A, Rogers S, Modell M. Evaluation of a direct doctor–patient telephone advice line in general practice. Br J Gen Pract 2000;50:305-6.
- Nagle JP, McMahon K, Barbour M, Allen D. Evaluation of the use and usefulness of telephone consultations in one general practice. Br J Gen Pract 1992;42:190-3.
- Hallam L. Access to general practice and general practitioners by telephone: the patient’s view. Br J Gen Pract 1993;43:331-5.
- Sokol D, Car J. Protecting patient confidentiality in telephone consultations in general practice. Br J Gen Pract 2006;56:384-5.
- Chapman JL, Zechel A, Carter YH, Abbott S. Systematic review of recent innovations in service provision to improve access to primary care. Br J Gen Pract 2004;54:374-81.
- Patel H, Patel M, Car J. Telephone consultations in general practice: areas for improvement. J Telemed Telecare 2005;11:265-6. https://doi.org/10.1258/1357633054471876.
- Jiwa M, Freeman J, Coleman M, Joesbury H. Do older patients feel able to cope with illness following telephone consultations? A multi-practice survey in the UK. Curr Med Res Opin 2005;21:339-44. https://doi.org/10.1185/030079905X26225.
- Rashid A, Jagger C. Attitudes to and perceived use of health care services among Asian and non-Asian patients in Leicester. Br J Gen Pract 1992;42:197-201.
- Benson L. Improving access with triage. General Practitioner n.d.:30-1.
- Car J, Freeman GK, Partridge MR, Sheikh A. Improving quality and safety of telephone based delivery of care: teaching telephone consultation skills. Qual Saf Health Care 2004;13:2-3. https://doi.org/10.1136/qshc.2003.009241.
- Chou J. UK Telephone Triage on the Rise 2013. www.nursinginpractice.com/article/uk-telephone-triage-rise (accessed 29 October 2018).
- Hewitt H, Gafaranga J, McKinstry B. Comparison of face-to-face and telephone consultations in primary care: qualitative analysis. Br J Gen Pract 2010;60:e201-12. https://doi.org/10.3399/bjgp10X501831.
- Innes M, Skelton J, Greenfield S. A profile of communication in primary care physician telephone consultations: application of the Roter Interaction Analysis System. Br J Gen Pract 2006;56:363-8.
- Gray DP, Wilkie P. Patient perspectives on telephone triage in general practice. Lancet 2015;385:687-8. https://doi.org/10.1016/S0140-6736(15)60282-3.
- Gillam S. Telephone triage in-hours: does it work?. Br J Gen Pract 2014;64:327-8. https://doi.org/10.3399/bjgp14X680377.
- Khan MN. Telephone consultations in primary care, how to improve their safety, effectiveness and quality. BMJ Qual Improv Rep 2013;2. https://doi.org/10.1136/bmjquality.u202013.w1227.
- Oldham J. Telephone use in primary care. Programme to shape demand has been started in several practices. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7363.547.
- Brown A, Armstrong D. Telephone consultations in general practice: an additional or alternative service?. Br J Gen Pract 1995;45:673-5.
- Singh K. How we saved 90,000 a year through GP phone triage. Pulse 2012;72:34-5.
- Swage T, Longman H. Hanging on the telephone. Health Serv J 2013;123:24-5.
- Longman H. How doctor–patient phone calls can cut unnecessary emergency care attendances. Health Serv J 2012;122:22-4.
- Longman H. GP, Phone Home 2012. www.hsj.co.uk/technology-and-innovation/gp-phone-home/5052766.article (accessed 25 September 2018).
- Haaijer-Ruskamp FM, Stewart R, Wesseling H. Does indirect consultation lead to overprescribing in general practice?. Soc Sci Med 1987;25:43-6. https://doi.org/10.1016/0277-9536(87)90205-X.
- Curtis P, Evens S. Doctor–patient communication on the telephone. Can Fam Physician 1989;35:123-8.
- Breslau N, Reeb KG. Continuity of care in a university-based practice. J Med Educ 1975;50:965-9. https://doi.org/10.1097/00001888-197510000-00006.
- NHS England . Surveys and Reports n.d. https://gp-patient.co.uk/SurveysAndReports (accessed 21 June 2017).
- Bardsley M, Blunt I, Davies S, Dixon J. Is secondary preventive care improving? Observational study of 10-year trends in emergency admissions for conditions amenable to ambulatory care. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-002007.
- RAND Europe, Ernst & Young LLP . National Evaluation of the Department of Health’s Integrated Care Pilots: Appendices, RAND Europe 2012. www.rand.org/content/dam/rand/pubs/technical_reports/2012/RAND_TR1164z2.pdf (accessed 2 November 2017).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- NHS Digital . GP Practice Prescribing Data n.d. https://data.gov.uk/dataset/prescribing-by-gp-practice-presentation-level (accessed 21 June 2017).
- Tian Y, Dixon A, Gao H. Data Briefing April 2012. Emergency Hospital Admissions for Ambulatory Care-Sensitive Conditions: Identifying the Potential Reductions 2012. www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/data-briefing-emergency-hospital-admissions-for-ambulatory-care-sensitive-conditions-apr-2012.pdf (accessed 2 November 2017).
- Office for National Statistics . Inflation and Price Indices n.d. http://gpaccess.uk/wordpress/wp-content/uploads/2013/01/Comparison-of-access-modes-AE-effect-v3-GPA.pdf (accessed 21 June 2017).
- British National Formulary. London: BMJ Group and Pharmaceutical Press; n.d.
- Department of Health and Social Care . NHS Reference Costs 2015 to 2016 2016. www.gov.uk/government/uploads/system/uploads/attachment_data/file/577084/National_schedule_of_reference_costs_-_main_schedule.xlsx (accessed 2 November 2017).
- Her Majesty’s Revenue and Customs . Travel – Mileage and Fuel Rates and Allowances n.d. www.gov.uk/government/publications/rates-and-allowances-travel-mileage-and-fuel-allowances/travel-mileage-and-fuel-rates-and-allowances (accessed 2 November 2017).
- Department for Transport Statistics . Table BUS0402a. Operating Revenue Per Passenger Journey at Current Prices on Local Bus Services by Metropolitan Area Status and Country: Great Britain. Annual from 2004 05 n.d. www.gov.uk/government/statistical-data-sets/bus04-costs-fares-and-revenue (accessed 9 January 2017).
- Office for National Statistics . Changes to Output Areas and Super Output Areas in England and Wales, 2001 to 2011 2012. www.ons.gov.uk/ons/guide-method/geography/products/census/report--changes-to-output-areas-and-super-output-areas-in-england-and-wales--2001-to-2011.pdf (accessed 21 June 2017).
- Boyatzis R. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: SAGE Publications; 1998.
- NHS England . General Practice Forward View 2016. www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf (accessed 21 June 2017).
- Watkins C, Harvey I, Carthy P, Moore L, Robinson E, Brawn R. Attitudes and behaviour of general practitioners and their prescribing costs: a national cross sectional survey. Qual Saf Health Care 2003;12:29-34. https://doi.org/10.1136/qhc.12.1.29.
- Rossdale M, Kemple T, Payne S, Calnan M, Greenwood R. An observational study of variation in GPs’ out-of-hours emergency referrals. Br J Gen Pract 2007;57:152-4.
- Nicholson BD, Oke JL, Rose PW, Mant D. Variation in direct access to tests to investigate cancer: a survey of English general practitioners. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0159725.
- McAteer A, Elliott AM, Hannaford PC. Ascertaining the size of the symptom iceberg in a UK-wide community-based survey. Br J Gen Pract 2011;61:e1-1. https://doi.org/10.3399/bjgp11X548910.
- Munro J, Sampson F, Nicholl J. The impact of NHS Direct on the demand for out-of-hours primary and emergency care. Br J Gen Pract 2005;55:790-2.
- Chalder M, Sharp D, Moore L, Salisbury C. Impact of NHS walk-in centres on the workload of other local healthcare providers: time series analysis. BMJ 2003;326. https://doi.org/10.1136/bmj.326.7388.532.
- Maheswaran R, Pearson T, Munro J, Jiwa M, Campbell MJ, Nicholl J. Impact of NHS walk-in centres on primary care access times: ecological study. BMJ 2007;334. https://doi.org/10.1136/bmj.39122.704051.55.
- NHS Digital . Quality and Outcomes Framework (QOF) – 2013–14 2014. https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/quality-and-outcomes-framework-qof-2013-14 (accessed 29 October 2018).
Appendix 1 Method of carrying out the scoping review for the literature review in Chapter 2
Our approach followed the principles of a systematic review in terms of having systematic and replicable search strategies and explicit inclusion and exclusion criteria. Unlike a systematic review, we did not seek to exclude studies based on quality, although we noted methodological concerns in our synthesis. We sought to undertake a narrative synthesis rather than pool numerical results, based on our research questions and knowledge of the literature.
Search strategy
An electronic search of the PubMed research literature database was conducted up to 9 November 2016. In addition, The King’s Fund HMIC data were searched (from 1995 to 16 January 2017). The HMIC combines records from the Department of Health and Social Care’s Library and Information Services and The King’s Fund Information and Library Services and provides access to official publications and a range of grey literature in addition to journal articles. Table 25 details the search terms used for each database. Searches of eligible studies’ reference lists were also conducted.
| Database | Search terms |
|---|---|
| PubMed |
general practic*[Title/Abstract] OR primary care[Title/Abstract] OR general practice[MeSH Terms] AND consult*[Title/Abstract]) OR triag*[Title/Abstract] AND telephon*[Title/Abstract] OR phone[Title/Abstract] |
| HMIC |
su: (general practice or general practitioners or primary care) AND su: (consultation or consultations) AND su: (triage or telephone) |
Inclusion and exclusion criteria
Table 26 summarises the inclusion and exclusion criteria used.
| Category | Criteria | |
|---|---|---|
| Inclusion | Exclusion | |
| Setting | General practice | Centralised rather than practice-based triage (e.g. NHS Direct) |
| Types of triage |
GP-led triage Consultation when with triage |
Sole focus on nurse-led triage Emergency triage Sole focus on out-of-hours triage Triage of referrals from primary to secondary care |
| Means of communication | Telephone |
Communication not involving telephone No mention of telephone |
| Language | English | Any language other than English |
| Country setting | High-income countries | Low- and middle-income countries |
| Document type | All | N/A |
| Date of publication |
Any for PubMed 1995 or later for HMIC |
N/A for PubMed Pre 1995 for HMIC |
Any type of study published in English that examined telephone triage or telephone consulting delivered by GPs in a high-income country was eligible for inclusion. We placed no date restriction on the PubMed search, but for HMIC we excluded publications before 1995. This was a pragmatic decision, based on the research team’s knowledge of the patterns of use of telephone consultations in general practice in England. Studies that only examined nurse-led, emergency or out-of-hours telephone consultations were not included. Studies that focused solely on centralised telephone triage systems, such as NHS Direct, were also excluded. Knowing the evidence base to be relatively early in development, the type of publication was not restricted and included observational studies, literature reviews, editorials and letters. Therefore, studies did not need to have a comparator.
Study selection
Records identified by the searches were managed in EndNote X6.0.1 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] and assessed for inclusion by scanning titles and abstracts against the inclusion and exclusion criteria. This was initially done by one reviewer (SB for PubMed and JC for HMIC) against the stated inclusion and exclusion criteria, and uncertainties were resolved through discussion with the wider study team. Another reviewer (EP) independently screened the included studies and those whose eligibility was uncertain based on the initial screening to determine the final list of potentially eligible studies. Full-text screening of potentially eligible studies was undertaken as part of the data extraction.
Data extraction
Data from studies identified as eligible were extracted into a Microsoft Excel spreadsheet template. Guided by our research questions, data were extracted on study type and methods, type of telephone system (triage/consultation/both), details of telephone system, setting (geographic and health care), reported outcomes [health outcomes, patient safety, staff experience, patient experience (hard-to-reach groups), impact on service use, impact on consultation, and cost] and other notable findings. The data extraction template was piloted on a small number of studies and refined. Data extraction was undertaken by three researchers (JC, EP and AK).
Synthesis
We undertook a narrative synthesis of the evidence in relation to our research questions and identified additional themes arising from the literature. The results are presented by prevalence of telephone consultations in general practice, impact of telephone consultations on patient access to the GP, appropriateness of telephone consultations, experience of patients, experience of hard-to-reach and vulnerable groups, experience of staff (GPs and reception staff), impact on the nature of consultations, patient safety and health outcomes, impact on service utilisation, and cost consequences. This is preceded by an overview of the literature, including a discussion of the dominant bodies of work included and a discussion of terminology.
Appendix 2 Statistical methods used for analysing administrative data from practices
Two types of analysis were carried out for each of the outcomes. The first was a before-and-after analysis, illustrated by the ‘superposed epoch graphs’ in which the introduction of the system in each practice is set at time zero. Second, a regression analysis was performed for each outcome, looking (1) for step changes at the time the intervention was introduced and (2) for a change in the preceding trend (e.g. slowing down of a previous increase). We also model heterogeneity in these changes to examine whether or not the intervention has a different effect in different practices.
Before-and-after analysis
Graphical superposed epoch analyses were performed for the five outcomes presented in Chapter 3 to illustrate the unadjusted change in outcomes before and after the introduction of the intervention. For all outcomes except continuity of care, the average of the outcome was calculated over 30-day periods relative to the launch date; with the practice launch date defining time zero for individual practices. For continuity of care, the calculation was based on calendar months due to the format of data provided. Given that the intervention started at different time points in each practice, different relative time periods include data from different periods of time.
For each outcome, we calculated (1) the mean within an individual practice for each 30-day period and (2) the mean of individual practice means with available data for each time period. These means were plotted as time relative to launch.
Regression analysis
Mixed-effects regression analysis was used to investigate changes associated with the intervention. The models used, essentially interrupted time-series analyses, all take a similar form, but different types of model were used depending on the outcome. In brief, the models captured a step change associated with the start of the intervention as well as a change in trend; for example, the intervention may have led to an immediate increase relative to the background trend, which was then eroded by a reduction over time. We also model heterogeneity in these changes to examine whether or not the intervention has a different effect in different practices.
Each model contained a categorical variable for month to account for seasonality, and a categorical variable for day of week to account for variations across the week (noting that for continuity of care in which data are monthly, day of week was not included). Continuous time relative to launch date (in years) was included to account for underlying secular trends. A random intercept was included to account for differing baselines by practice and the resulting clustering of observations within practices. A binary variable indicating when the intervention was present captured any instantaneous ‘step’ change in the outcome at the start of the intervention. An interaction between time relative to launch and the intervention indicator captured whether or not the linear trend changed following the intervention. For continuity of care models only, the age of the patient was also included as a third-order (cubic) polynomial in addition to the variables described above. Analyses were performed for all types of appointments combined as well as separately by type of appointment (face to face or telephone; see Chapter 3 for details).
To better approximate normal distributions, data were log-transformed prior to analysis. For the ease of interpretation, exponentiated coefficients are presented as duration ratios (i.e. the relative change in total time spent consulting by a practice).
Our main analysis was done on an intention-to-treat basis. It includes all practices identified by the commercial company, even when the practices were using a hybrid form of the ‘telephone first’ approach or had since ceased using it altogether. A sensitivity analysis (see Appendix 3) was performed, restricting the analysis to practices in which we believed, on the basis of information provided by the commercial company, that the system was being run consistent with the company’s protocols.
Appendix 3 Sensitivity per-protocol analysis of practice administrative data
This appendix presents findings from the sensitivity analysis for the analysis of appointment data. The sensitivity analysis followed the same methods as those reported in Appendix 2, but the data were restricted to practices in which we believed, on the basis of information provided by the commercial company, that the system was being run consistent with the company’s protocols. The companies were asked to classify all practices that had used their ‘telephone first‘ approach as ‘running’, ‘hybrid’ (i.e. allowing some additional degree of advance booking of appointments) or ‘reverted’ (i.e. had stopped using the ‘telephone first‘ approach). We included only practices classified by the companies as ‘running’ in the per-protocol sensitivity analyses. The sensitivity analysis included data from 27 practices covering 997,772 appointments over 8158 practice-days.
Number of appointments
Superposed epoch analysis
FIGURE 25.
Superposed epoch analysis showing the change in total number of appointments per 1000 patients per day relative to the intervention launch: practices with status ‘running’. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
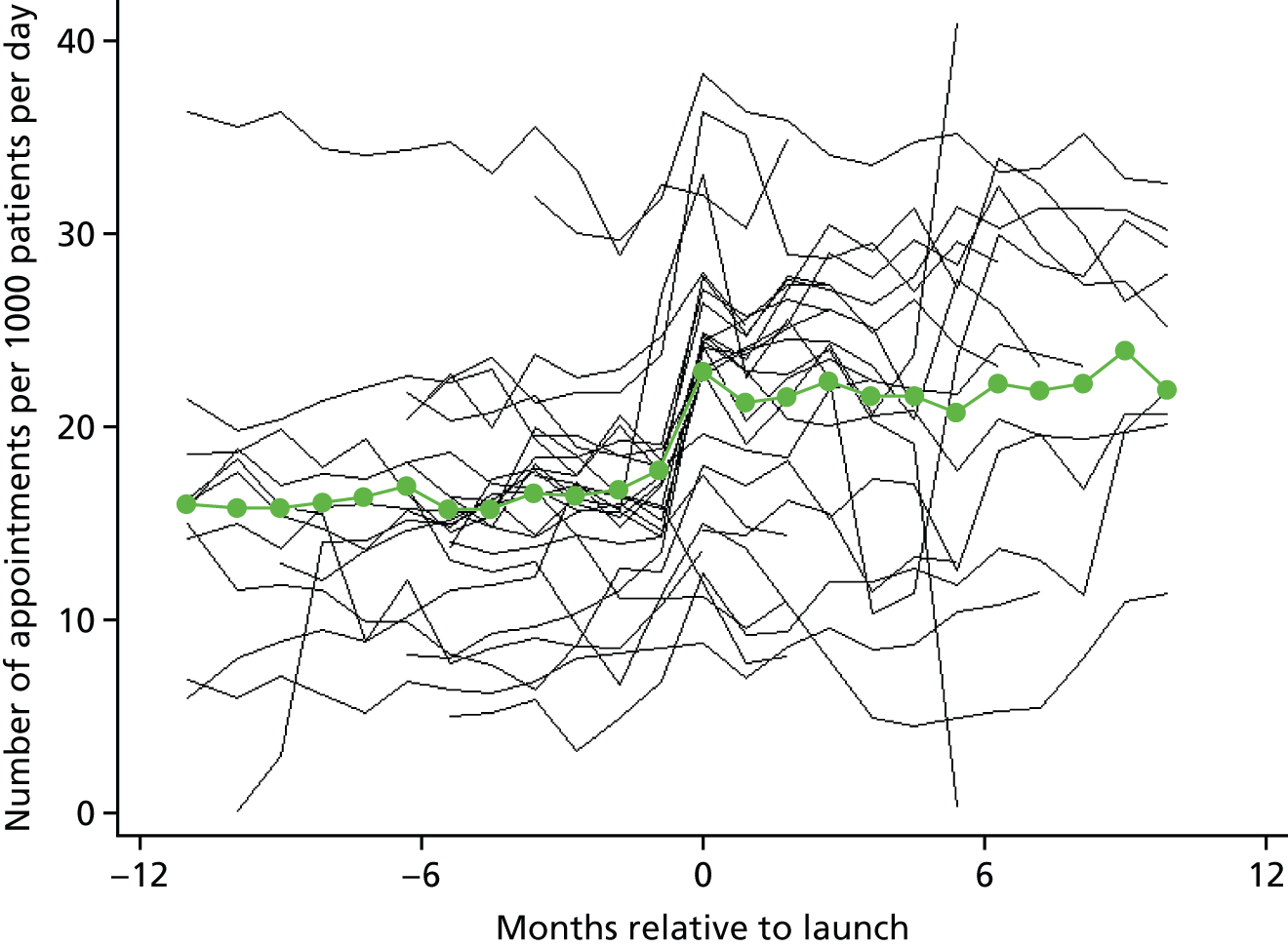
FIGURE 26.
Superposed epoch analysis showing the change in the number of face-to-face appointments per 1000 patients per day relative to the intervention launch: practices with status ‘running’. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
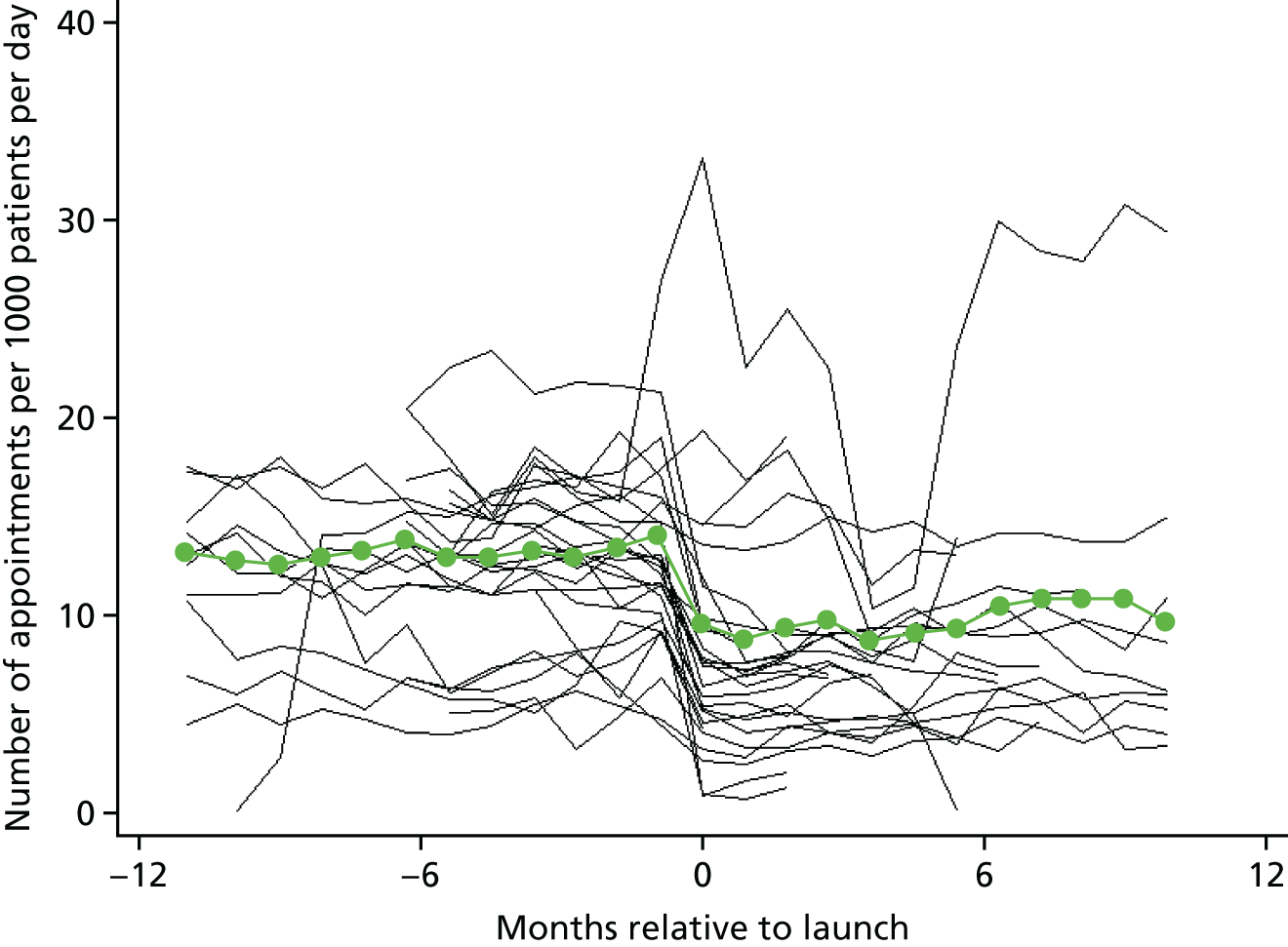
FIGURE 27.
Superposed epoch analysis showing the change in the number of telephone appointments per 1000 patients per day relative to the intervention launch: practices with status ‘running’. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
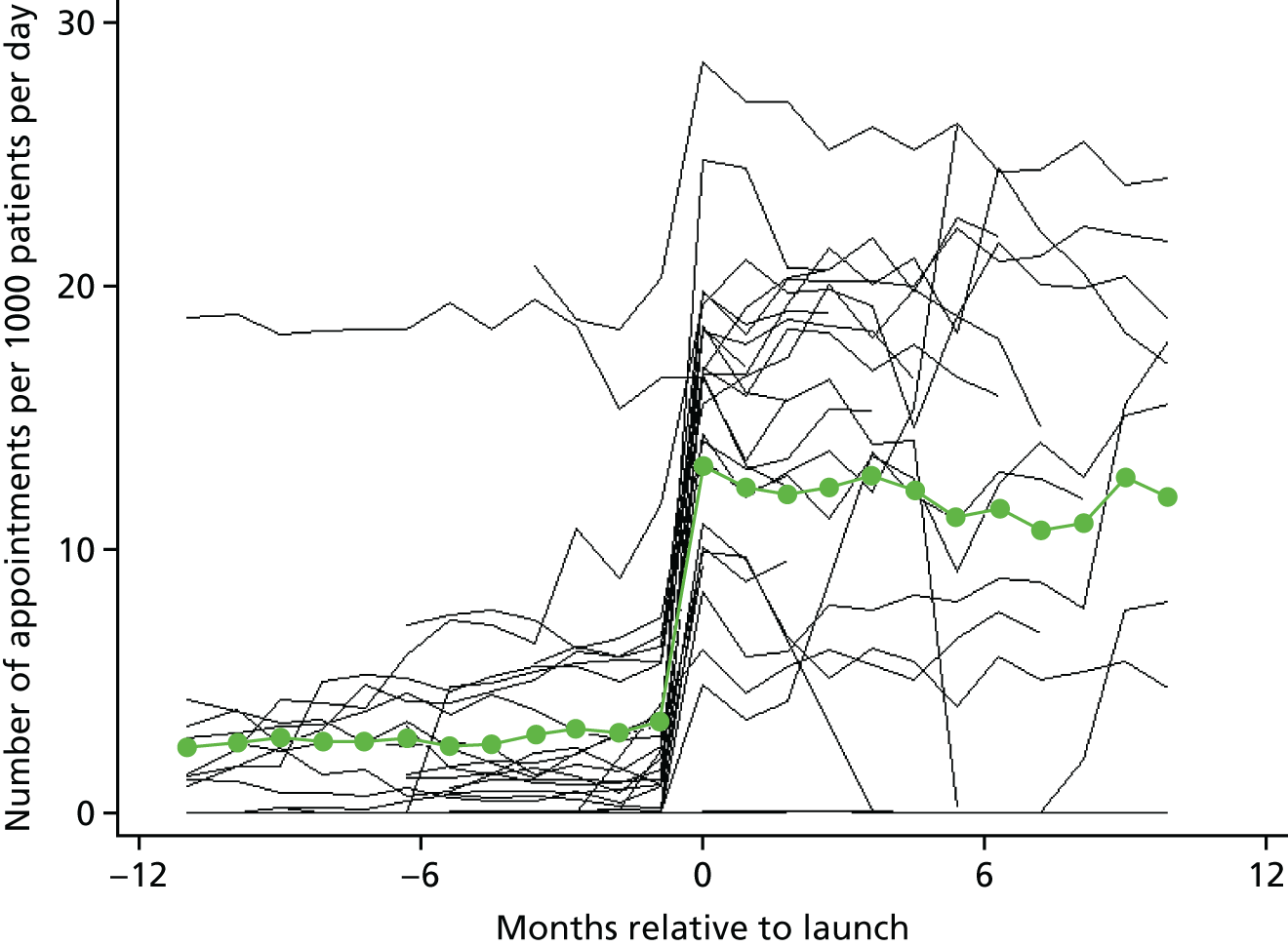
Regression analysis
| Appointment type | Transition | Interaction p-valuea | 95% reference range for step change transition | |||||
|---|---|---|---|---|---|---|---|---|
| Step change at | Pre | Post | ||||||
| RR (95% CI) | p-value | RR (95% CI) | p-value | RR (95% CI) | p-value | |||
| All appointments | 1.28 (1.13 to 1.46) | < 0.001 | 1.10 (1.09 to 1.11) | < 0.0001 | 1.02 (1.01 to 1.04) | < 0.0001 | < 0.0001 | 0.66 to 2.47 |
| Face to face | 0.54 (0.42 to 0.68) | < 0.0001 | 1.03 (1.01 to 1.05) | 0.003 | 0.97 (0.96 to 0.99) | < 0.0001 | < 0.0001 | 0.16 to 1.82 |
| Telephone | 14.35 (5.52 to 37.30) | < 0.0001 | 1.14 (1.13 to 1.16) | < 0.0001 | 1.30 (1.27 to 1.34) | < 0.0001 | < 0.0001 | 0.12 to 1740.59 |
Time waited for an appointment
Superposed epoch analysis
FIGURE 28.
Superposed epoch analysis showing the change in the mean time between booking and having an appointment relative to the intervention launch: practices with status ‘running’. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
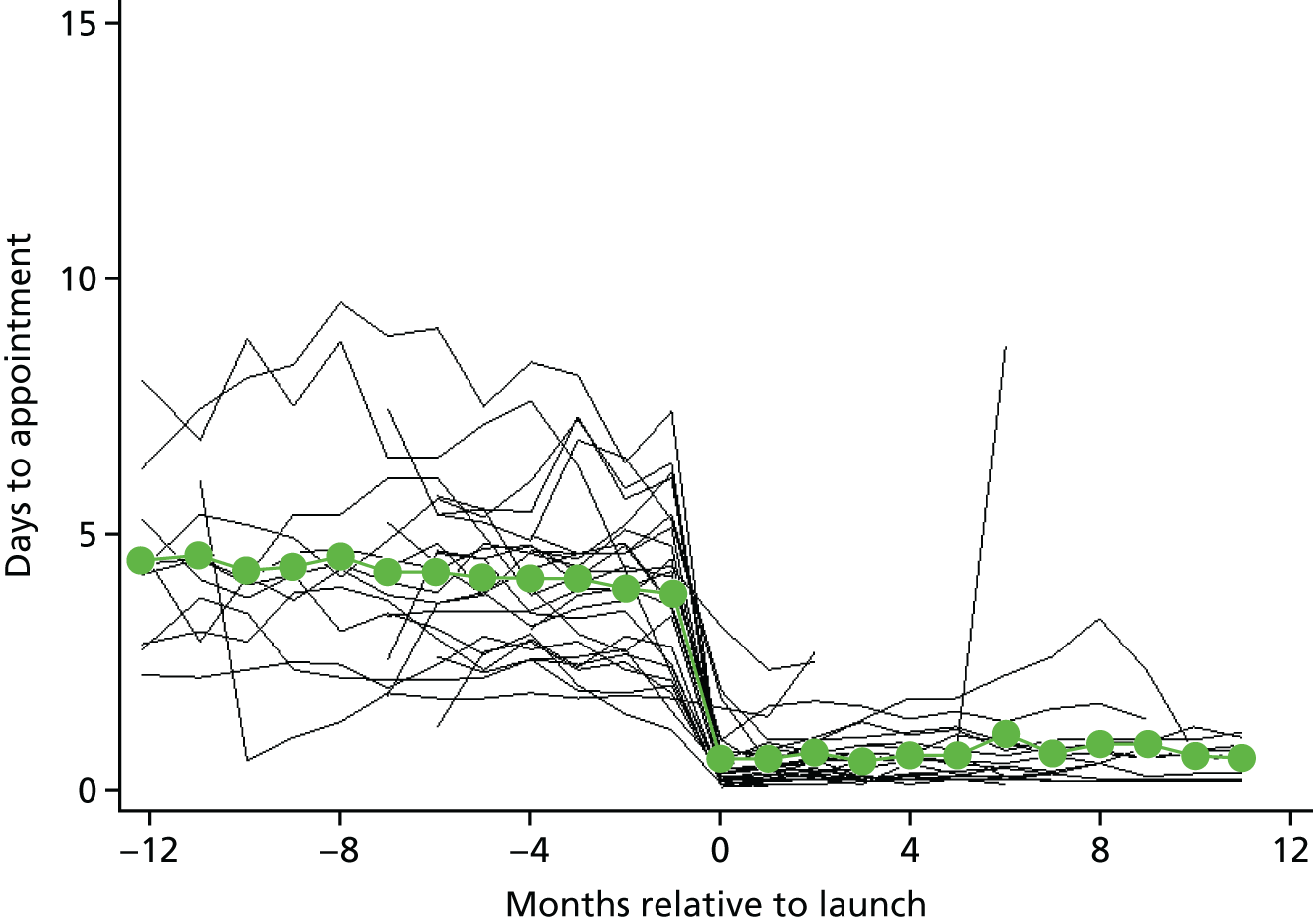
Regression analysis
| Appointment type | Step change at transition | Trend | Interaction p-valuea | 95% reference range for step change transition | ||||
|---|---|---|---|---|---|---|---|---|
| Pre transition | Post transition | |||||||
| Time to appointment, mean difference in days (95% CI) | p-value | Change in time to appointment in days/year (95% CI) | p-value | Change in time to appointment in days/year (95% CI) | p-value | |||
| All | –3.48 (–4.11 to –2.84) | < 0.0001 | –0.14 (0.07 to 0.20) | < 0.0001 | –0.13 (–0.18 to –0.07) | < 0.0001 | < 0.0001 | –5.71 to –1.31 |
| Face to face | –3.67 (–4.55 to –2.79) | < 0.0001 | 0.73 (0.63 to 0.82) | < 0.0001 | –0.10 (–0.22 to 0.01) | 0.0665 | < 0.0001 | –6.71 to –0.61 |
| Telephone | –0.62 (–1.10 to –0.15) | 0.0123 | –0.34 (–0.40 to –0.28) | < 0.0001 | –0.00 (–0.04 to 0.03) | 0.9246 | < 0.0001 | –2.11 to 0.91 |
Length of appointment
Superposed epoch analysis
FIGURE 29.
Superposed epoch analysis showing the change in appointment duration relative to the intervention launch: practices with status ‘running’. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
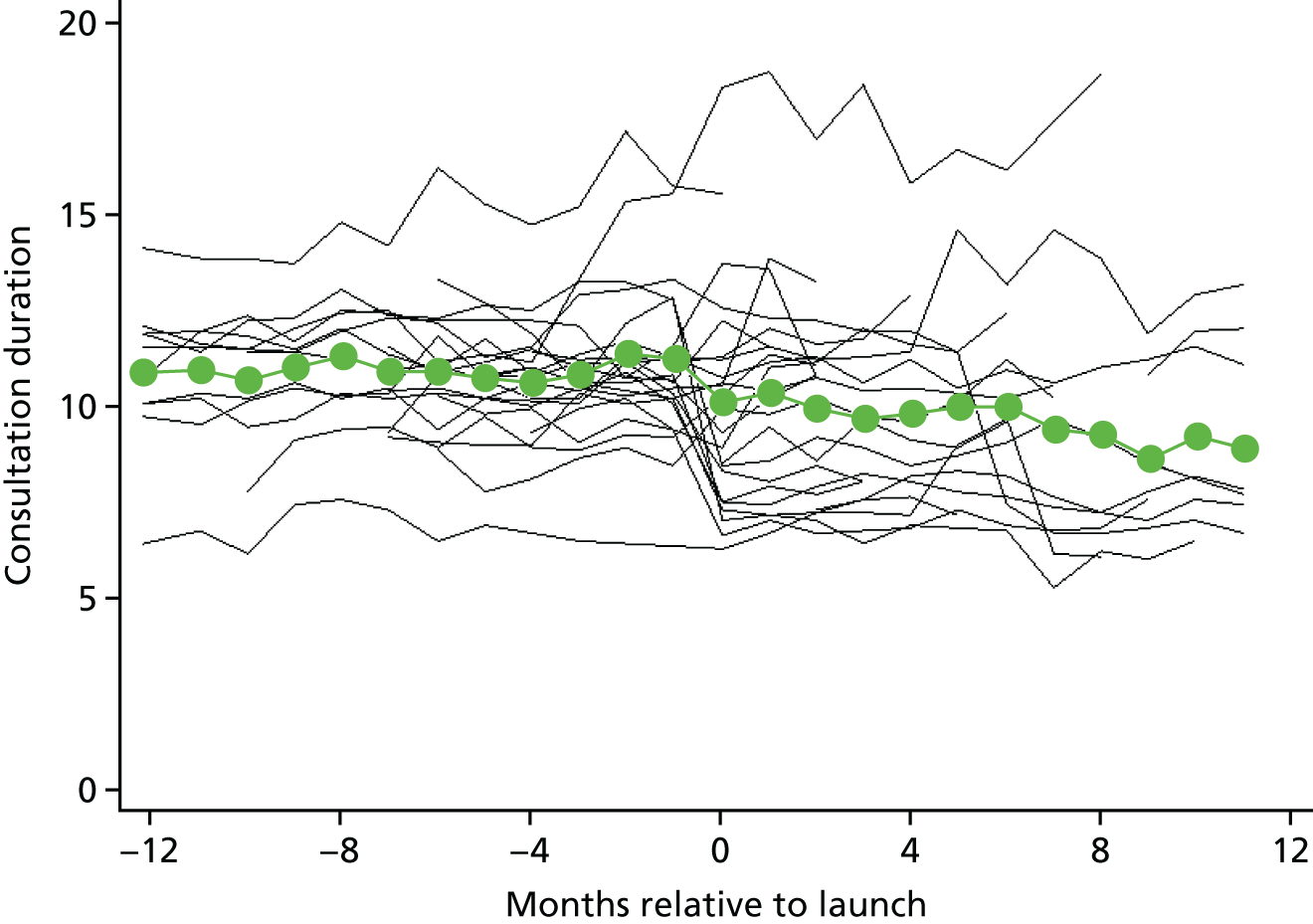
Regression analysis
| Appointment type | Step change at transition | Trend | Interaction p-valuea | 95% reference range for step change transition | ||||
|---|---|---|---|---|---|---|---|---|
| Pre transition | Post transition | |||||||
| Change in length of appointment (minutes) (95% CI) | p-value | Change in length of appointment (minutes/year) (95% CI) | p-value | Change in length of appointment (minutes/year) (95% CI) | p-value | |||
| All | –0.39 (–1.42 to 0.64) | 0.4414 | 0.30 (0.20 to 0.39) | < 0.0001 | –0.85 (–0.95 to –0.75) | < 0.0001 | < 0.0001 | –3.68 to 2.90 |
| Face to face only | 0.84 (0.28 to 1.41) | 0.0052 | 0.47 (0.37 to 0.58) | < 0.0001 | –1.03 (–1.16 to –0.90) | < 0.0001 | < 0.0001 | –0.91 to 2.59 |
| Telephone | –0.66 (–1.53 to 0.22) | 0.1244 | 0.53 (0.34 to 0.73) | < 0.0001 | –0.67 (–0.80 to –0.54) | < 0.0001 | < 0.0001 | –2.08 to 0.76 |
Total time spent consulting
Superposed epoch analysis
FIGURE 30.
Superposed epoch analysis showing the change in total time spent consulting relative to the intervention launch: practices with status ‘running’. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
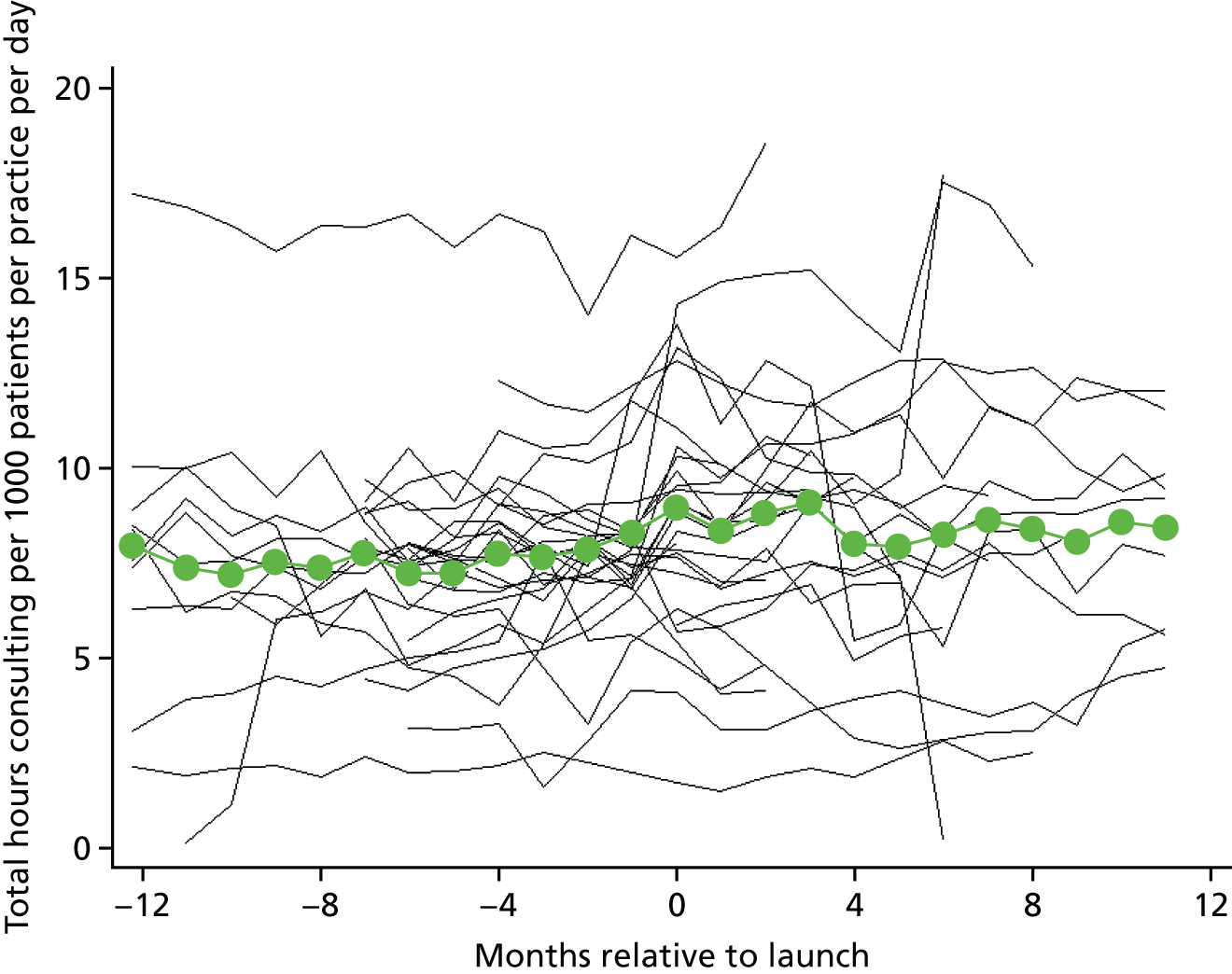
Regression analysis
| Appointment type | Step change at transition | Trend | Interaction p-valuea | 95% reference range for step change transition | ||||
|---|---|---|---|---|---|---|---|---|
| Pre transition | Post transition | |||||||
| Ratio (95% CI) | p-value | Ratio (95% CI) | p-value | Ratio (95% CI) | p-value | |||
| All | 1.07 (0.93 to 1.24) | 0.3369 | 1.04 (0.97 to 1.12) | 0.2587 | 1.08 (1.01 to 1.15) | 0.0285 | 0.4841 | 0.62 to 1.86 |
| Face to face only | 0.53 (0.40 to 0.70) | < 0.0001 | 1.11 (1.04 to 1.19) | 0.0021 | 1.00 (0.94 to 1.07) | 0.9625 | 0.0238 | 0.15 to 1.82 |
| Telephone | 6.15 (3.08 to 12.29) | < 0.0001 | 1.12 (.98 to 1.28) | 0.0863 | 1.35 (1.18 to 1.54) | < 0.0001 | 0.0478 | 0.74 to 51.37 |
Continuity of care
Superposed epoch analysis
FIGURE 31.
Superposed epoch analysis showing the continuity index relative to the months to launch: practices with status ‘running’. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
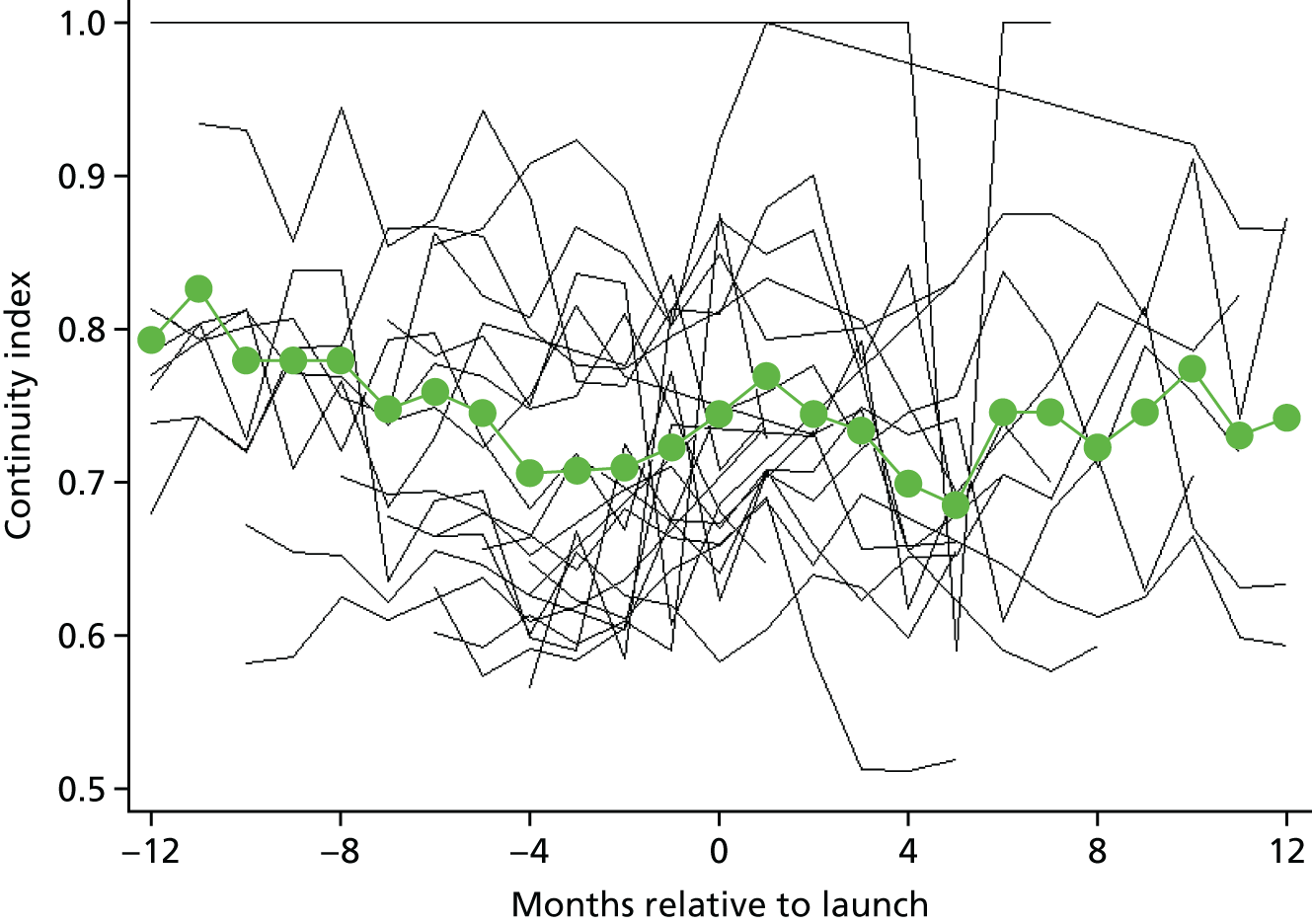
Regression analysis
| Step change at transition | Trend | Interaction p-value | 95% reference range for step change transition | ||||
|---|---|---|---|---|---|---|---|
| Pre transition | Post transitiona | ||||||
| Change in continuity index (95% CI) | p-value | Change in continuity index per year (95% CI) | p-value | Change in continuity index per year (95% CI) | p-value | ||
| 0.067 (0.029 to 0.105) | < 0.001 | 0.0003 (0.0000 to 0.0007) | 0.072 | –0.006 (–0.007 to –0.006) | < 0.001 | < 0.001 | –0.103 to 0.237 |
Appendix 4 Demographic characteristics of responders to the patient survey
Overall 63% of patients who responded to the survey were female (528/837), which was slightly higher than the percentage of patients sampled who were female (61%), reflecting a slightly higher response rate for females than for males. The age distribution of patients who responded is presented in Figure 32. Responders were, on average, older than non-responders (mean age 56.2 years and 38.9 years, respectively).
FIGURE 32.
Age range of patients surveyed.
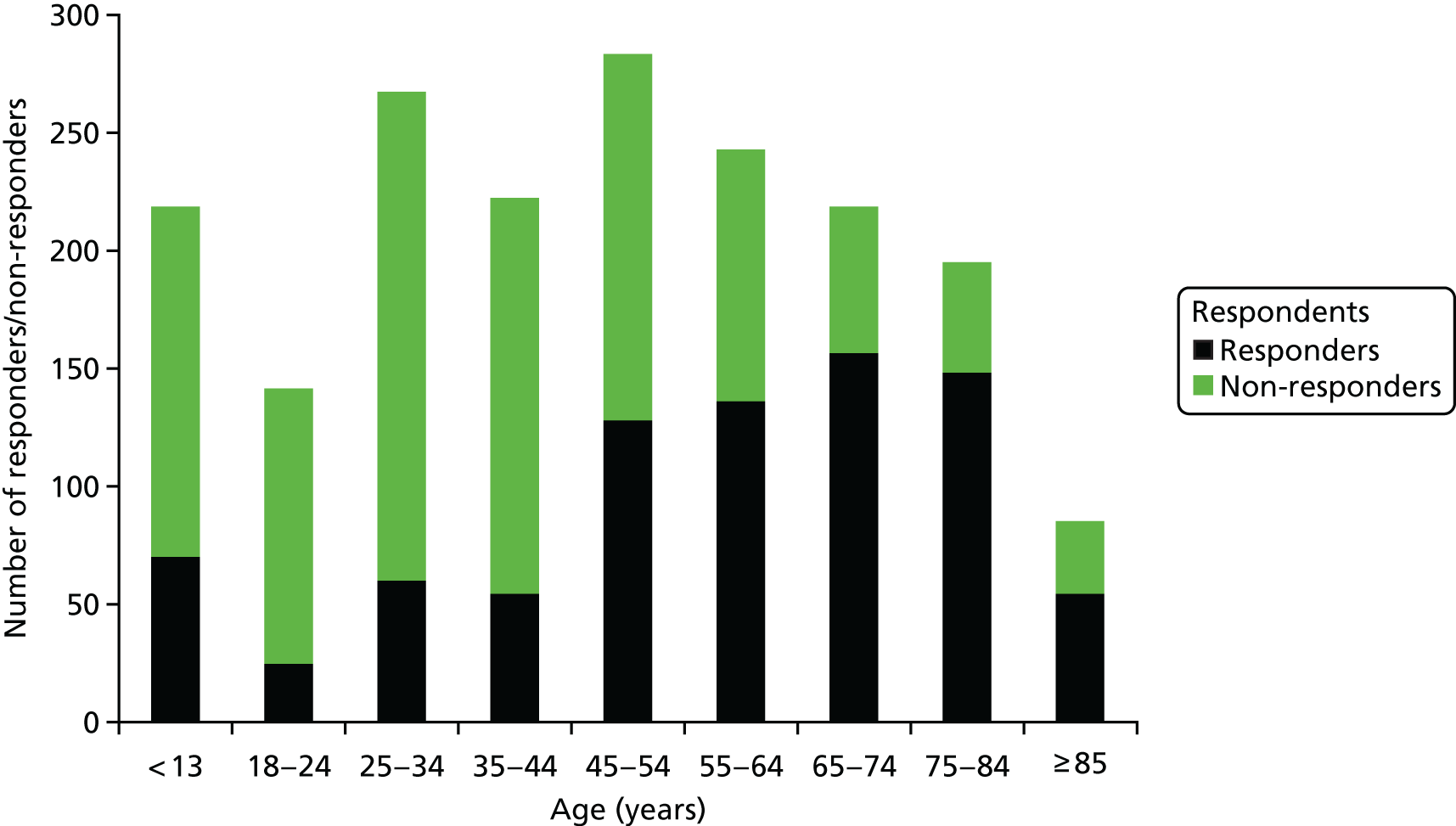
Respondents were asked to rate their health (or the health of the patient they were responding on behalf of) on a five-level Likert scale, from poor to excellent: 26% (201/787) reported very good or excellent health and 13% (98/787) reported poor health (Figure 33). Overall, 64% of respondents (499/779, 57% weighted) stated that they (or the patient who they were responding on behalf of) had a long-standing illness, disability or infirmity (defined in the survey as ‘anything that has troubled you over a period of time, or that is likely to affect you over a period of time’).
FIGURE 33.
Weighted health status of patients surveyed.
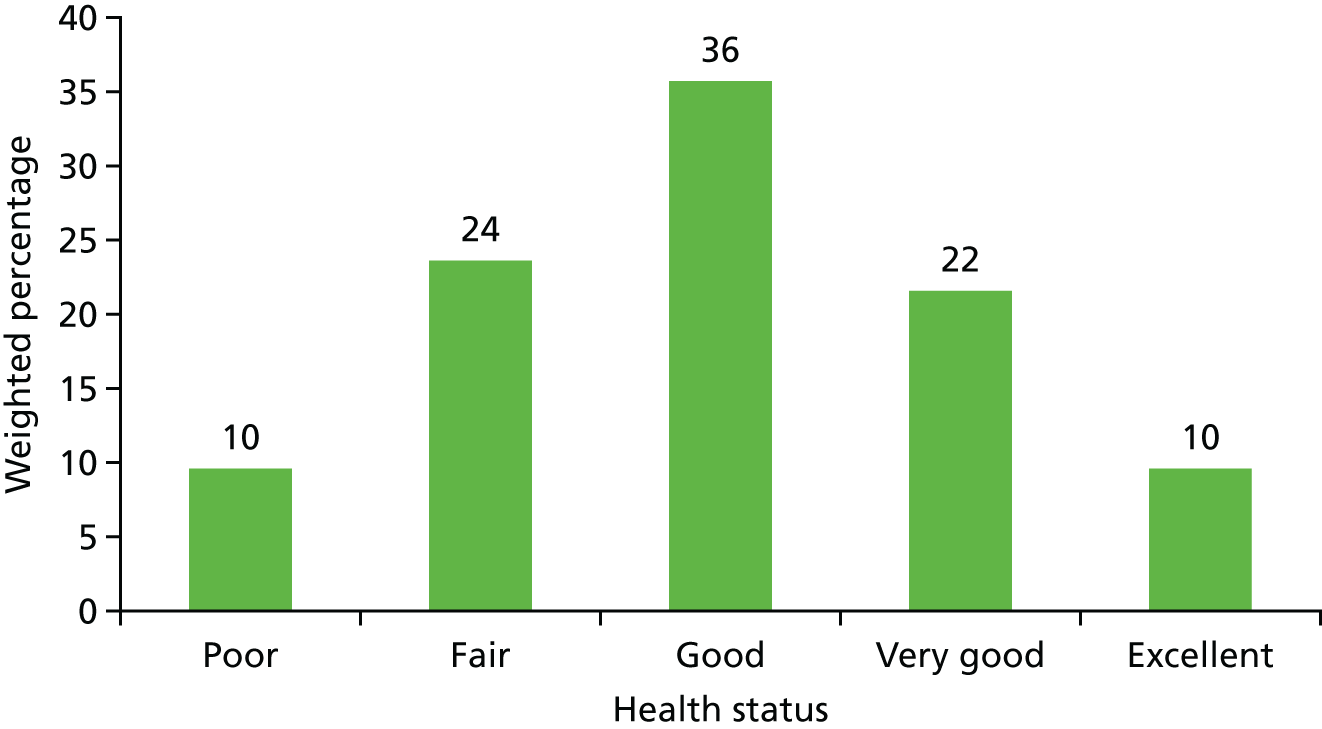
Eighty-nine per cent of respondents (697/780, 87% weighted) identified themselves (or the patient who they were responding on behalf of) as white British. Ninety-seven per cent of patients (or the patient they were responding on behalf of) (778/805, 97% weighted) surveyed spoke English as their main language. For the 27 patients who did not speak English as their main language, 22% (6/27, 27% weighted) reported that they spoke English very well, 44% (40% weighted) reported that they spoke English well, 19% (12% weighted) reported that they did not speak English well and 15% (22% weighted) reported that they did not speak English at all.
The majority of respondents reported that they (or the patient who they were responding on behalf of) did not work (54%, 43% weighted). For the remaining respondents, 15% (18% weighted) reported that if they need to see a GP during working hours they can easily take time away from work to do so, 22% (29% weighted) reported that they could do so with some difficulty, whereas 9.4% (11% weighted) reported that they could not take time away from work (Figure 34).
FIGURE 34.
Weighted percentage of respondents’ self-reported ability to take time away from work to see a GP.
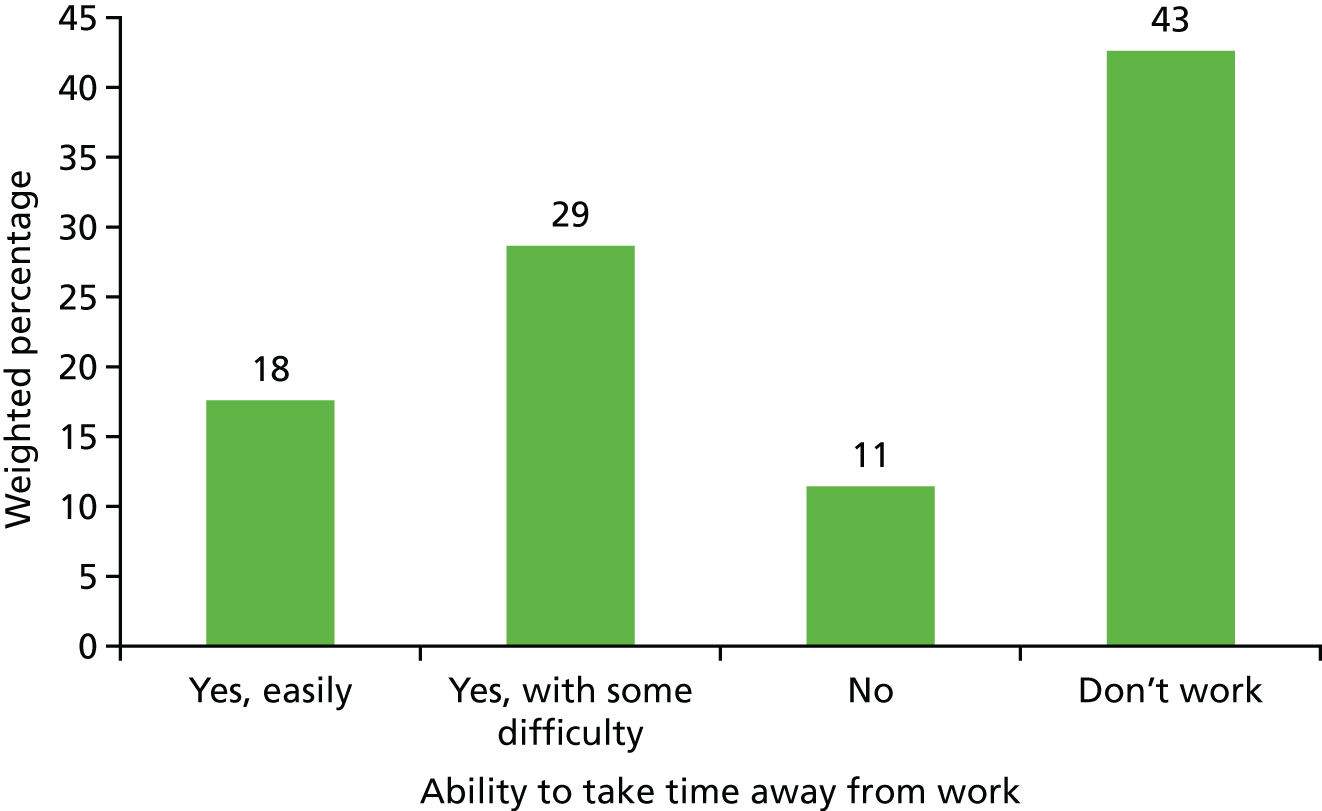
Appendix 5 Initial survey of practices to inform selection of control practices for main analysis of patient experience and secondary care utilisation
Methods
We performed a postal survey of 500 general practices asking about their use of telephone triage in order to inform our analysis of GP Patient Survey data and HES data. Practices were selected at random from those listed in the 2013/14 Quality and Outcomes Framework data set after first excluding those practices with a registered list size of fewer than 1000 patients. 96 Paper surveys were mailed to practice managers on 23 January 2015, with a single reminder sent after 4 weeks to practices that had not yet responded. The survey included the following questions:
-
Does your surgery use telephone triage for patients asking for an appointment with the GP?
-
Who conducts this telephone triage?
-
What % of face-to-face appointments are triaged by telephone by a GP? (a) Pre-bookable appointments and (b) same-day appointments.
-
When did your surgery begin triaging requests for appointments in the manner currently used?
-
Have you received help from a commercial company in adopting telephone triage? If yes, which company?
Results
We received 198 responses to the survey (response rate 39.6%). Of responding practices, 47.5% (94/198) reported using some form of telephone triage for patients wanting an appointment with a GP. Of those practices using telephone triage, the vast majority used GPs to conduct the triage (79/94, 84%), with 30.8% (29/94) and 16.0% (15/94) of practices using nurse practitioners or practice nurses, respectively (with a number of practices using multiple staff types).
Although 14.1% of all responding practices (28/198) reported using telephone triage for at least half of same-day appointments, only 6.1% (12/198) reported using telephone triage for more than half of appointments booked in advance. When restricting to the vast majority of appointments (≥ 80%), these figures fell to 10.6% (21/198) and 5.1% (10/198), respectively. Only four practices (2.0%) reported using telephone triage for 100% of all appointments. Only two practices reported being helped by a commercial company to adopt telephone triage.
Conclusions
Although telephone triage was not rare in our sample, it was very uncommon to find it being used for the vast majority of appointments, particularly pre-bookable appointments. Given that the ‘telephone first’ approach requires all patients to first speak to a GP on the telephone, this suggest that such an approach is not widely used. For this reason, for the analysis of GP Patient Survey data and HES data, we used a random sample of general practices as our control group on the basis that the very low numbers of practices using this approach not included in our intervention sample would have a minimal impact on attenuating any observed differences.
Appendix 6 Statistical methods used in the analysis of GP Patient Survey data
Before-and-after analysis of GP Patient Survey scores (intervention practices only)
Graphs have been produced that illustrate changes in patient experience scores in intervention practices before and after the introduction of the intervention. A superposed epoch analysis is performed whereby the number of survey waves relative to the intervention launch date is calculated for each practice: the survey immediately preceding the intervention launch date is defined as time zero, the survey wave immediately following intervention launch date is time period one, and the survey following that time is period two, etc. Given that the intervention started at different time points in each practice, different relative time periods include data from different periods of time. Furthermore, not all practices had data for all time periods relative to intervention launch. The analysis was restricted to data 2 years either side of the launch date.
For each of the seven GP Patient Survey experience measures, we calculated (1) the mean score within each intervention practice for each relative time period and (2) the mean score across all intervention practices with available data for each relative time period. These means were plotted as time relative to launch.
Comparison with other practices in England (controlled regression analysis)
The superposed epoch analysis does not control for what is happening external to the intervention and may also be confounded by a number of factors, for example the timing of intervention launch relative to nationwide trends and other NHS initiatives. In the second stage of the analysis, we undertook a controlled regression analysis to estimate a difference-in-difference effect of the intervention. Controls were selected at random from all practices classified as non-intervention practices (i.e. any practice in England not on the list provided by commercial companies or practices that launched the ‘telephone first’ approach after 31 December 2015). For computational reasons, our analysis was restricted to data from all intervention practices and a random 10% sample of non-intervention practices, with between 778 and 976 control practices providing data at any one time.
For each continuous GP Patient Survey experience measure, a separate mixed-effects linear regression model was used. With the exception of changing the outcome (patient experience measure), the structure of the models is otherwise the same. Patient-level adjustment is made for self-reported sex, age (eight groups) and ethnicity (five groups) taken from GP Patient Survey responses and IMD (a small-area measure of socioeconomic deprivation based on a patient’s postcode of residence) using groups defined by national quintiles. There is an indicator variable for survey wave capturing both seasonal differences and longer-term trends. Variations in baseline levels for each practice resulting in clustering are accounted for using a random intercept for practice, as well as a random slope for time allowing for differential trends. This modelling allows us to capture the background scores against which the effect of the intervention can be measured. A similarly structured mixed-effects logistic regression model was used to model the binary ‘seen or spoken to on the same day’ outcome.
The effect of the intervention is captured using two fixed-effect variables. The first is an indicator variable that takes the value of 1 when the practice was an intervention practice and the survey was mailed after the intervention had started, and a value of zero otherwise. This term is intended to capture a step change in experience measure after starting the ‘telephone first’ approach. The second variable is equal to the time (in years) since the intervention started at a practice and survey mail-out. When the practice is a non-intervention practice, or the survey mail-out precedes the intervention, this variable equals zero. This variable is intended to capture a change in trend of patient experience scores post intervention. Furthermore, random slopes are included for both of these variables to allow for heterogeneity in the effect of the intervention between practices. The estimated SD of these random slopes is combined with the fixed effects to calculate a 95% reference range (i.e. the range of intervention effect we expect to see across most practices).
Finally, a supplementary analysis was performed to investigate if the effect of the intervention was differential between those in work or not in work by including a main effect for working status (based on GP Patient Survey responses) and an interaction between working status and the intervention variable. This analysis was motivated by early findings from the qualitative workstream.
Appendix 7 Sensitivity per-protocol analysis of GP Patient Survey data
This appendix presents findings from the sensitivity analysis for the GP Patient Survey data. The sensitivity analysis followed the same methods as those reported in Appendix 6, but the data were restricted to practices in which, to the best of our knowledge, the system was being run consistent with the method proposed by the commercial companies (i.e. practices that were no longer using a ‘telephone first’ approach or practices running a ‘hybrid’ system were removed from the analysis). The results are very similar to those presented in the main report, with a large improvement in patients’ rating of time to be seen and small decreases in numbers of patients recommending their surgery to others and to their ability to see a GP of their choice. However, as with the main analyses, initial decreases in reported experience for these last two aspects showed some evidence of recovery over subsequent years.
| Wave | Number of practices | ||||
|---|---|---|---|---|---|
| 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | |
| July–September | 1 | 16 | 47 | 63 | 85 |
| January–March | 4 | 28 | 51 | 78 | 89 |
Results
Before-and-after analysis of GP Patient Survey scores (intervention practices only)
FIGURE 35.
Superposed epoch analysis of GP communication composite mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
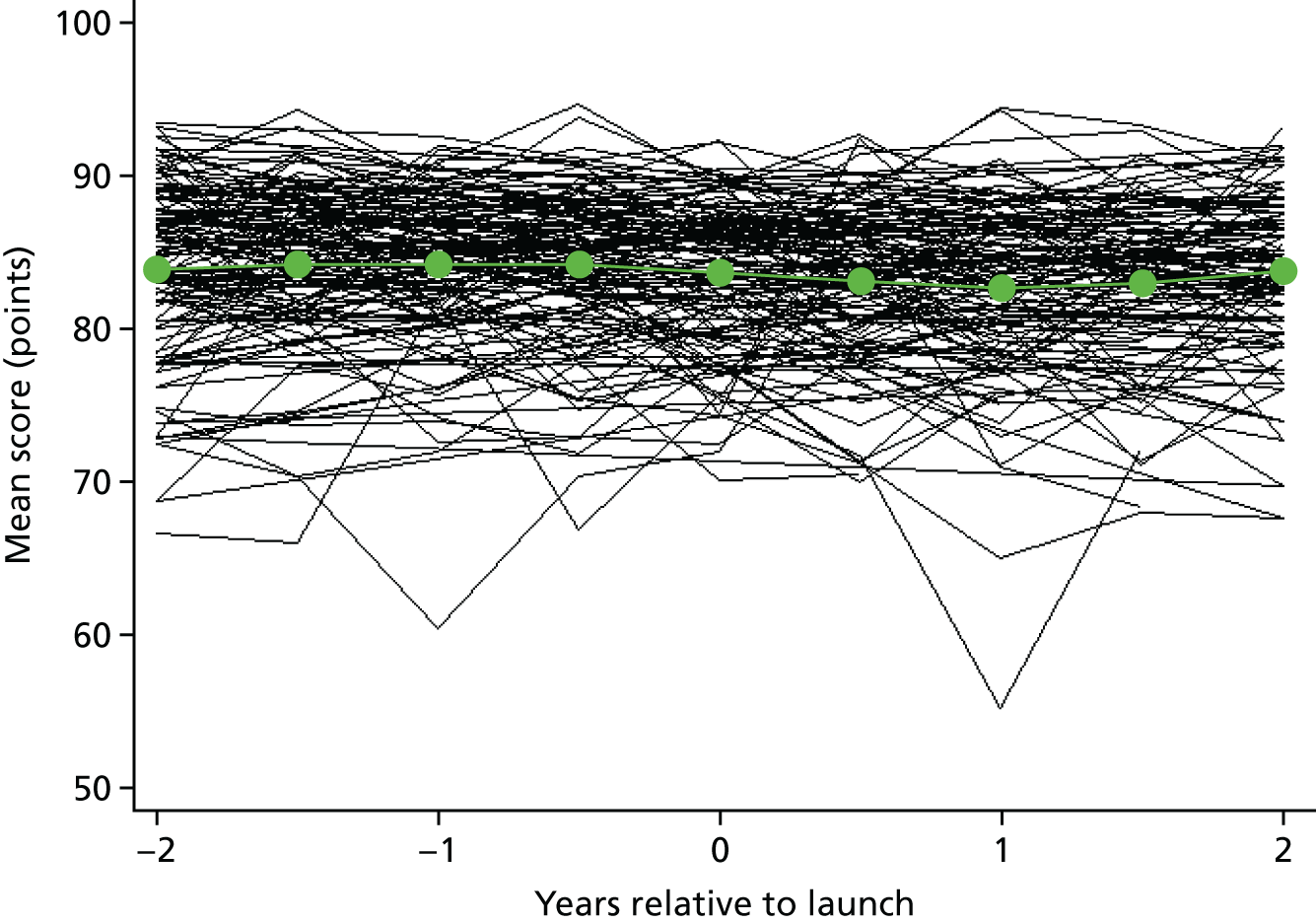
FIGURE 36.
Superposed epoch analysis of ease of getting through on the telephone mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
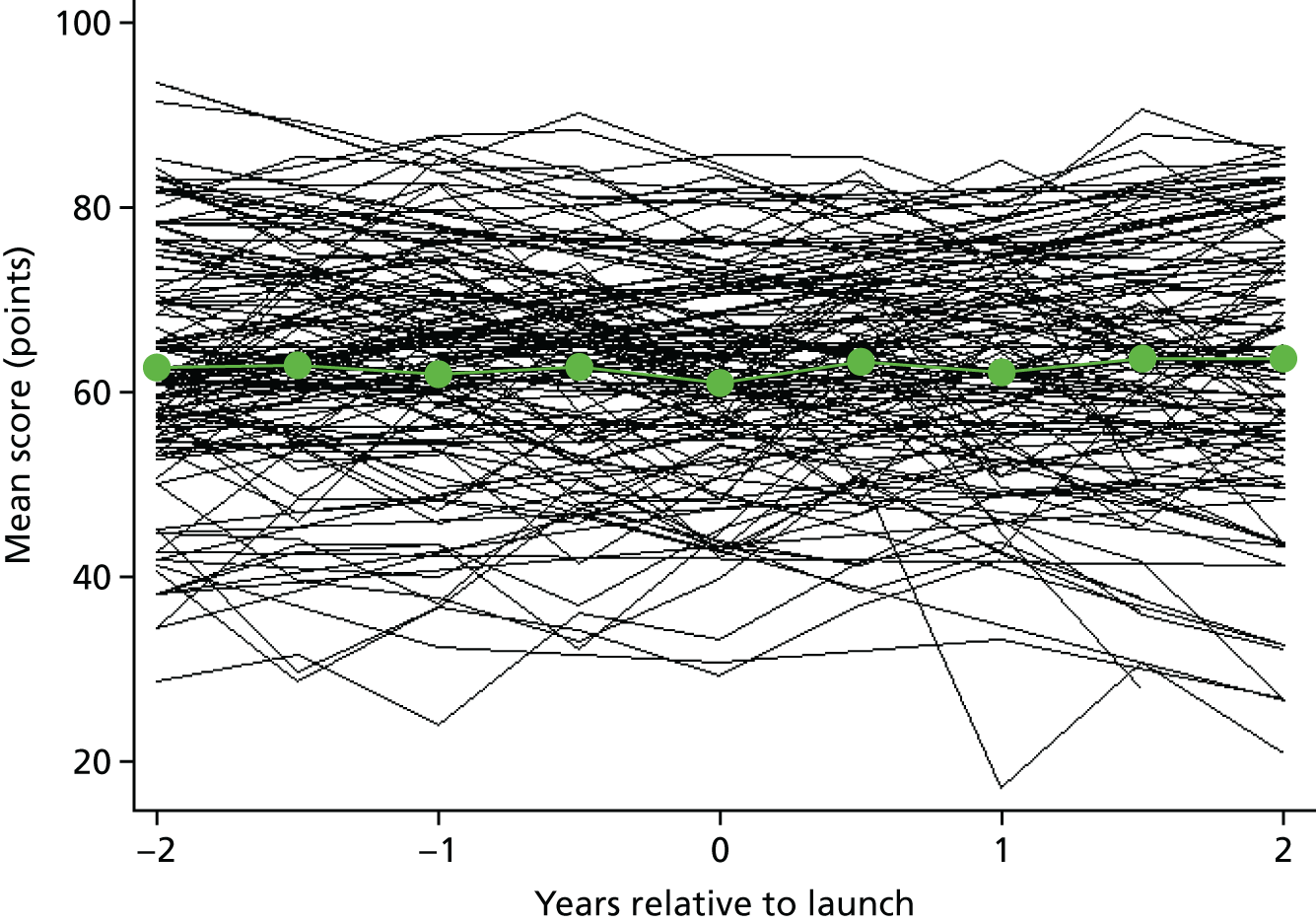
FIGURE 37.
Superposed epoch analysis of recommending GP surgery mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
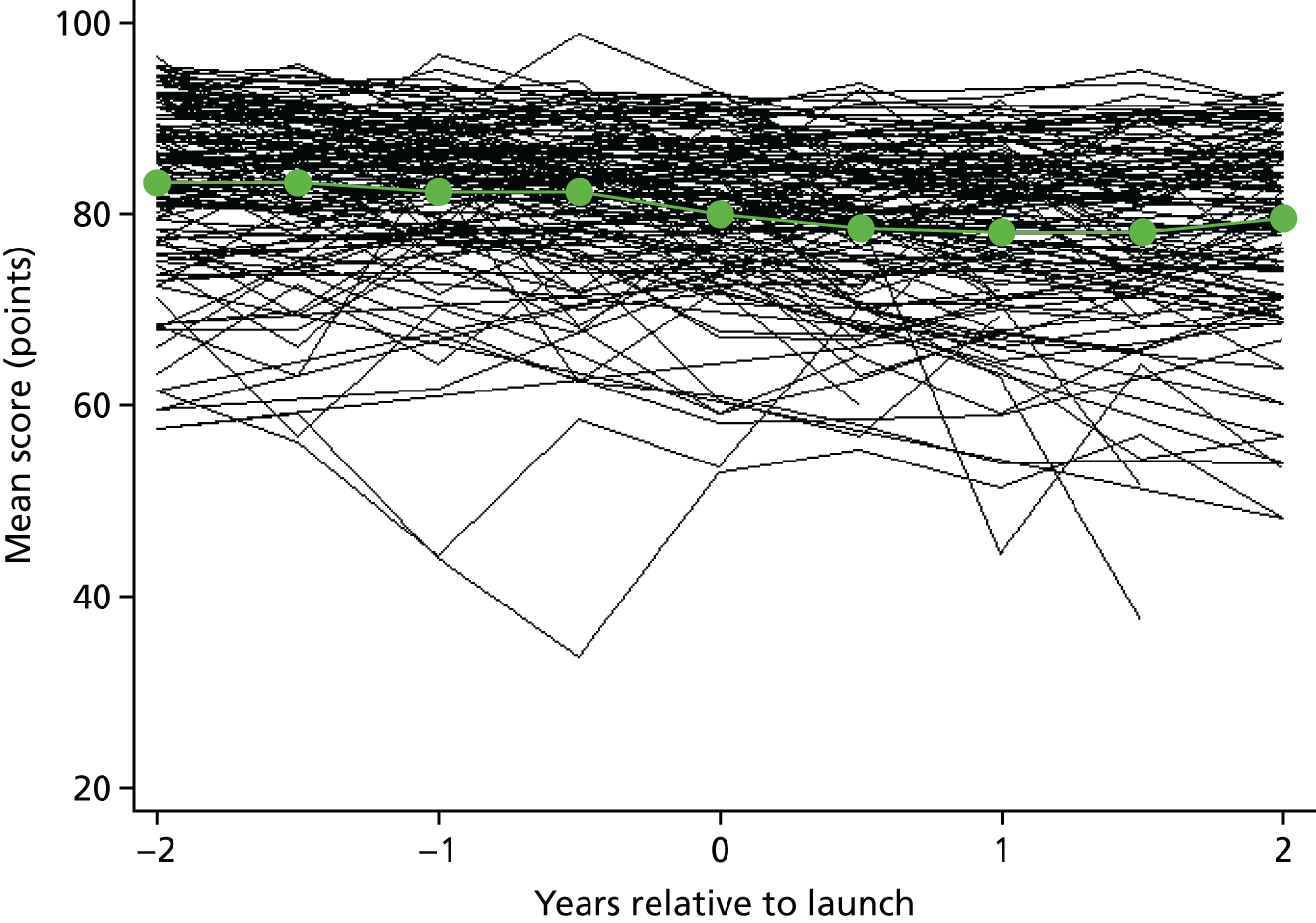
FIGURE 38.
Superposed epoch analysis of ability to see preferred GP mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
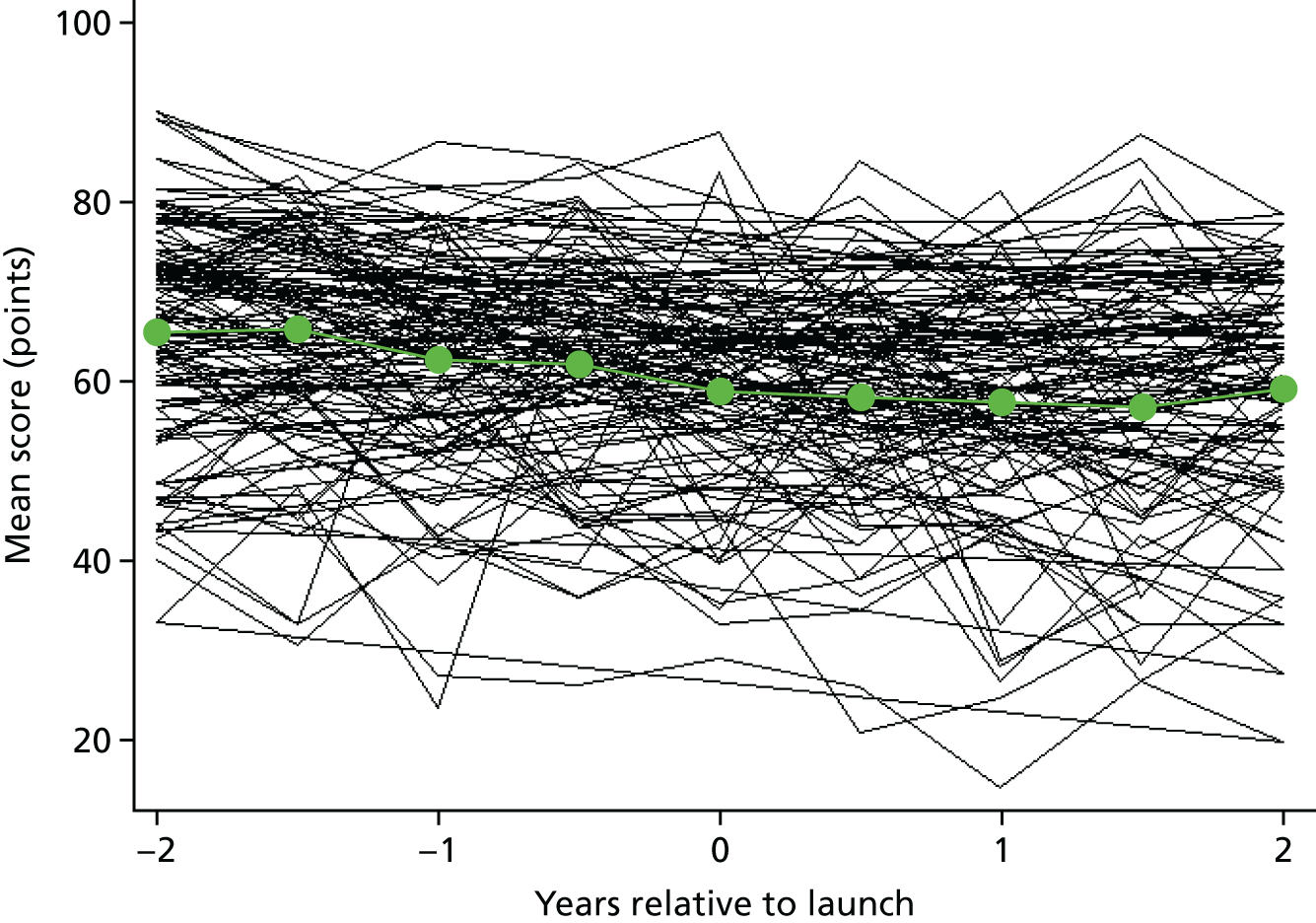
FIGURE 39.
Superposed epoch analysis of time until seen or spoken to mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
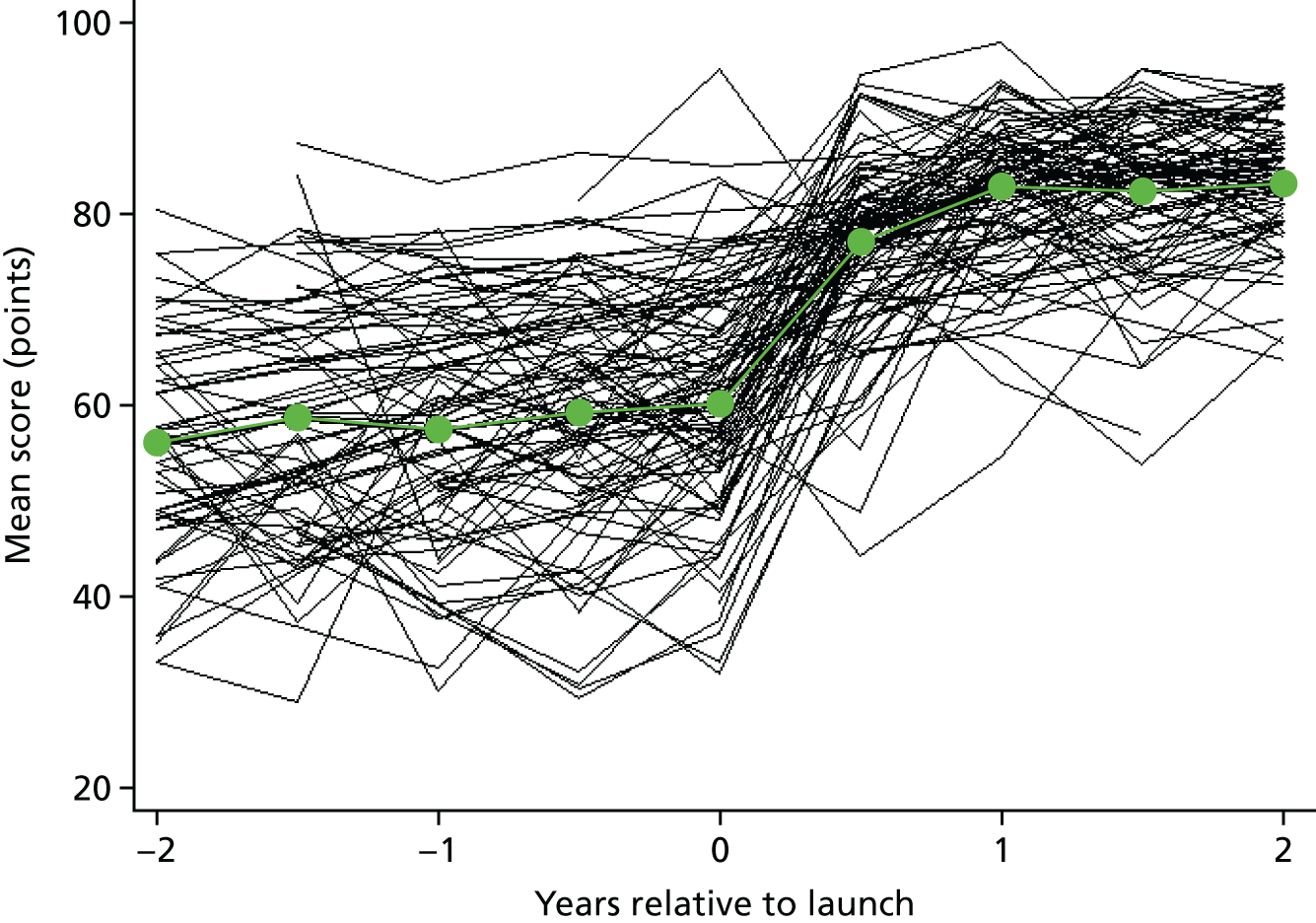
FIGURE 40.
Superposed epoch analysis of percentage of people seen or spoken to on the same day relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
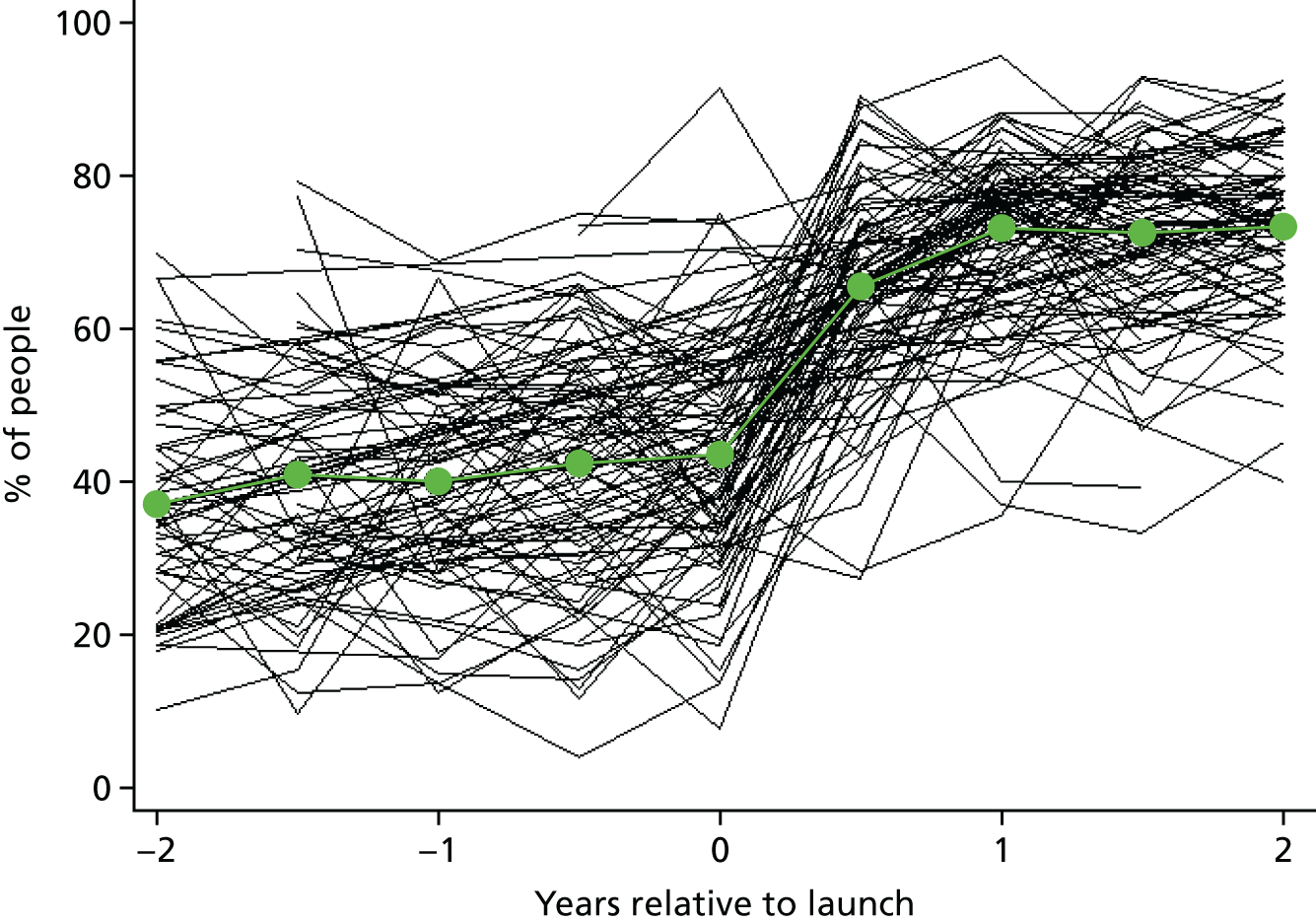
FIGURE 41.
Superposed epoch analysis of GP convenience composite mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
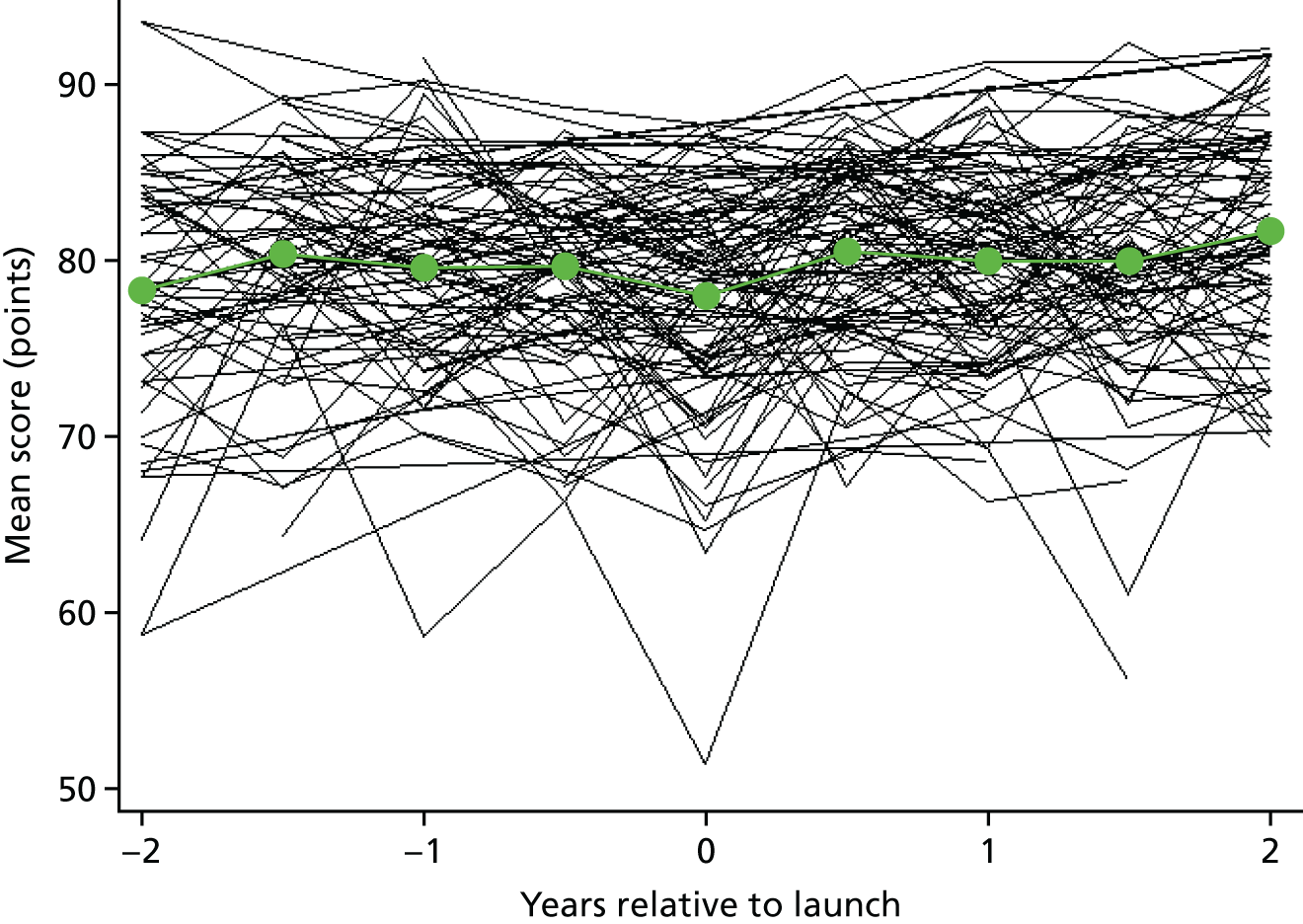
FIGURE 42.
Superposed epoch analysis of overall experience of making an appointment mean score relative to the intervention launch. The black lines represent the mean within a single practice relative to the launch time, with each black line representing a single intervention practice. The green dots represent the mean of individual practice means.
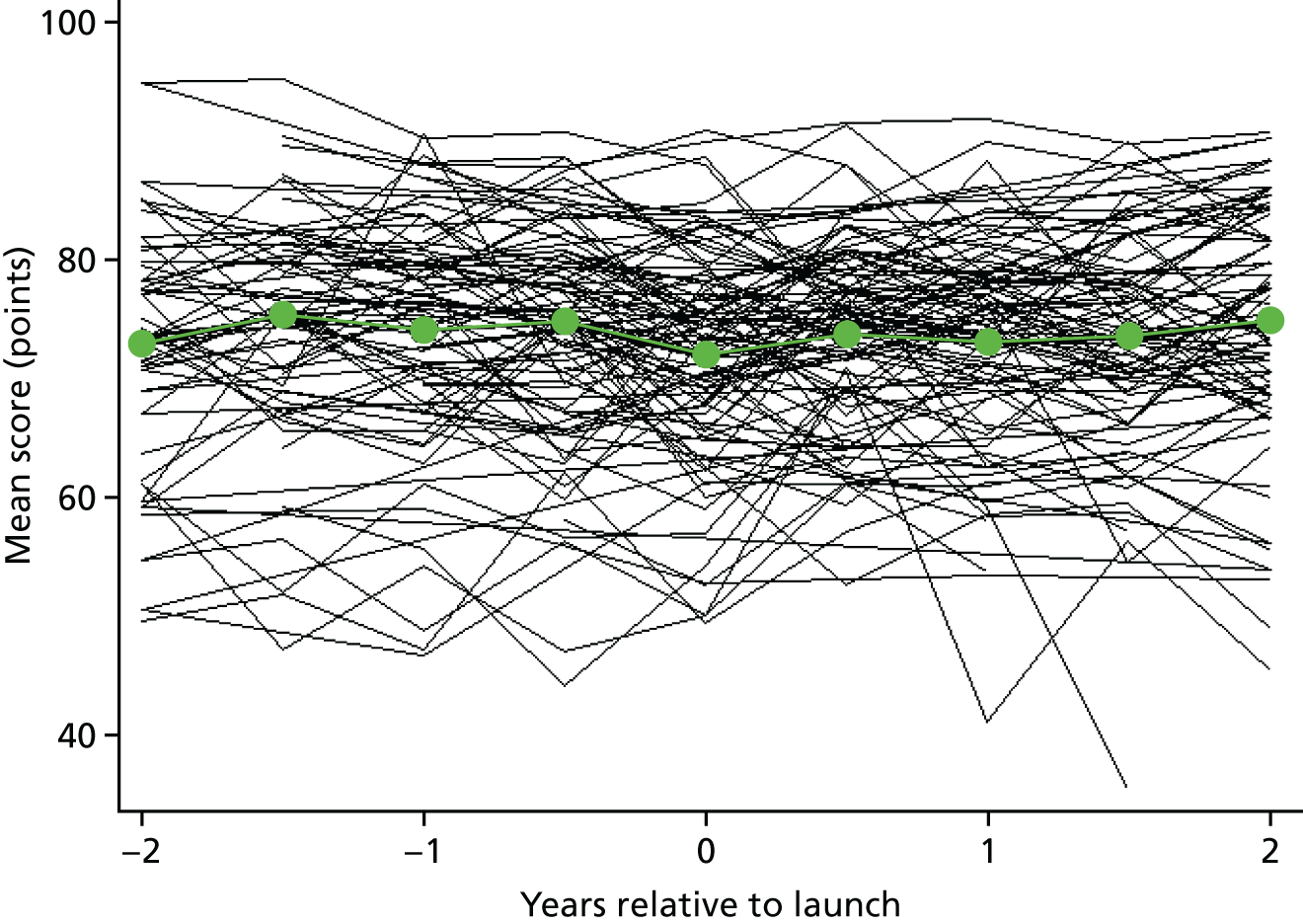
Comparison with other practices in England (controlled regression analysis)
| GP Patient Survey outcome | Change following intervention (95% CI) | |||
|---|---|---|---|---|
| Step | p-value | Additional yearly | p-value | |
| Continuous outcomes: difference on 0–100 scale | ||||
| GP communication composite | –1.36 (–2.01 to –0.71) | < 0.001 | 0.16 (–0.16 to 0.47) | 0.33 |
| Ease of getting through on the telephone | 1.79 (0.44 to 3.13) | 0.009 | 0.41 (–0.51 to 1.33) | 0.39 |
| Would you recommend your GP surgery? | –2.70 (–3.77 to –1.63) | < 0.001 | 0.24 (–0.34 to 0.82) | 0.42 |
| Seeing preferred GP | –1.75 (–3.32 to –0.18) | 0.03 | 0.37 (–0.48 to 1.22) | 0.39 |
| Time until seen or spoken to | 21.27 (18.87 to 23.67) | < 0.001 | 1.91 (0.90 to 2.93) | < 0.001 |
| Convenience of appointment | 0.69 (–0.19 to 1.57) | 0.12 | 0.70 (0.33 to 1.07) | < 0.001 |
| Overall experience of making an appointment | 0.29 (–1.03 to 1.61) | 0.67 | 0.98 (0.33 to 1.63) | 0.003 |
| Binary outcome: ORa | ||||
| Seen or spoken to on same day | 3.33 (2.83 to 3.91) | < 0.001 | 1.11 (1.04 to 1.19) | 0.002 |
| GP Patient Survey outcome | Change following intervention | |||
|---|---|---|---|---|
| Step | Additional yearly | |||
| SD | 95% reference range | SD | 95% reference range | |
| Continuous outcomes: difference on 0–100 scale | ||||
| GP communication composite | 1.52 | –4.34 to 1.62 | 0.28 | –0.34 to 0.71 |
| Ease of getting through on the telephone | 4.69 | –7.40 to 10.98 | 2.94 | –5.35 to 6.17 |
| Would you recommend your GP surgery? | 3.36 | –9.29 to 3.89 | 1.31 | –2.33 to 2.81 |
| Seeing preferred GP | 4.17 | –9.92 to 6.42 | 1.52 | –2.61 to 3.35 |
| Time until seen or spoken to | 9.57 | 2.51 to 40.03 | 2.71 | –3.40 to 7.22 |
| Convenience of appointment | 2.57 | –4.35 to 5.73 | 0.26 | 0.19 to 1.21 |
| Overall experience of making an appointment | 4.92 | –9.35 to 9.93 | 1.64 | –2.23 to 4.19 |
| Binary outcome: ORa | ||||
| Seen or spoken to on same day | 0.54 | 1.14 to 9.68 | 0.19 | 0.61 to 1.31 |
Appendix 8 Statistical methods used in the analysis of Hospital Episode Statistics data
Two types of analysis were carried out for each of the outcomes. The first was a before-and-after analysis, illustrated by the ‘superposed epoch graphs’, in which the introduction of the system in each practice is set at time zero. Second, a regression analysis was performed for each outcome, looking (1) for step changes at the time when the intervention was introduced and (2) for a change in the preceding trend (e.g. slowing down of a previous increase). We also model heterogeneity in these changes to examine whether or not the intervention has a different effect in different practices.
Our main analysis was conducted on an intention-to-treat basis. It includes all practices identified by the commercial companies, even when the companies informed us that the practices were running a hybrid form of the system or were no longer running the system. This was done in order to avoid selection bias, whereby only the successful practices continue with the system in the recommended form. A sensitivity analysis (see Appendix 9) was also performed, restricting the analysis to practices in which we believed, on the basis of information provided by the commercial companies, that the system was being run consistent with the companies’ protocols.
Before-and-after analysis (intervention practices only)
Graphs have been produced illustrating changes in A&E attendances and admissions in intervention practices before and after the introduction of the intervention (see Chapter 7, Figures 19–24). These superposed epoch analyses calculate the time relative to the intervention launch date for each month individually for each practice. So the month including the intervention launch date is defined as time zero, the month immediately following the intervention launch date is defined as time period one, and the month following that is defined as time period two, etc. Given that the intervention started at different time points in each practice, different relative time periods include data from different months and years. Furthermore, not all practices had data for all time periods relative to intervention launch, particularly those that started using the ‘telephone first’ approach later in the study (although all practices had at least 3 months of data post intervention, with most practices having > 3 months of data). The analysis was restricted to data from 1 year either side of the launch date.
For each outcome considered, we calculated (1) the number of attendances/admissions per month per 1000 patients within each intervention practice for each relative time period and (2) the mean of practice attendance/admission rates across all intervention practices with available data for each relative time period. These means were plotted as time relative to launch.
Comparison with other practices in England (controlled regression analysis)
The superposed epoch analysis does not control for what is happening external to the intervention practices and could be confounded by a number of factors, for example the timing of the intervention launch in relation to nationwide trends or other NHS initiatives. In the second stage of the analysis, we therefore undertook a controlled analysis to estimate a difference-in-difference effect of the intervention practices compared with control practices in the rest of England.
A mixed-effects Poisson regression was used, adjusting for patient age, sex, deprivation and time period (96 dummy variables, one for each month from April 2008 to March 2016) as fixed effects, a random intercept to account for different baseline rates between practices, and a random slope for a continuous time variable allowing for different trends between practices. The effect of the intervention is captured using two fixed-effect variables. The first is an indicator variable that takes the value of 1 when the practice was an intervention practice and the HES data related to a time period after the intervention had started, and a value of zero otherwise. This term is intended to capture a step change in attendances after starting the ‘telephone first’ approach. The second variable is equal to the time (in years) since the intervention started at a practice. When the practice is a non-intervention practice, or the data relate to a period preceding the intervention, this variable equals zero. This variable is intended to capture a change in trend of patient experience scores post intervention.
We additionally included a second time period variable, with time pre and post intervention in intervention practices only, and zero in control practices, to allow for a differential trend in admissions or attendances in control practices compared with intervention practices overall, unrelated to the intervention start date.
Furthermore, a random slope is included for the step change variable to allow for heterogeneity in the effect of the intervention between practices. The estimated SD of these random slopes is combined with the fixed effects to calculate a 95% reference range (i.e. the range of intervention effect we expect to see across most practices).
Appendix 9 Sensitivity per-protocol analysis of Hospital Episode Statistics data
This appendix presents findings from the sensitivity analysis for the secondary care data, restricting the analysis to practices that we believed, on the basis of information provided by the commercial companies, were running the ‘telephone first’ approach consistent with the companies’ protocols. The sensitivity analysis followed the same methods as those reported in the main analysis (see Chapter 7 and Appendix 8). The results are very similar to those presented in the main report, with no evidence of a step change in A&E and outpatient attendances, but evidence of a slower increase over time in intervention practices than in the background trend. We also find evidence of step increases in inpatient admissions.
FIGURE 43.
Superposed epoch analysis of A&E attendances relative to the intervention launch. The black lines represent the attendances within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
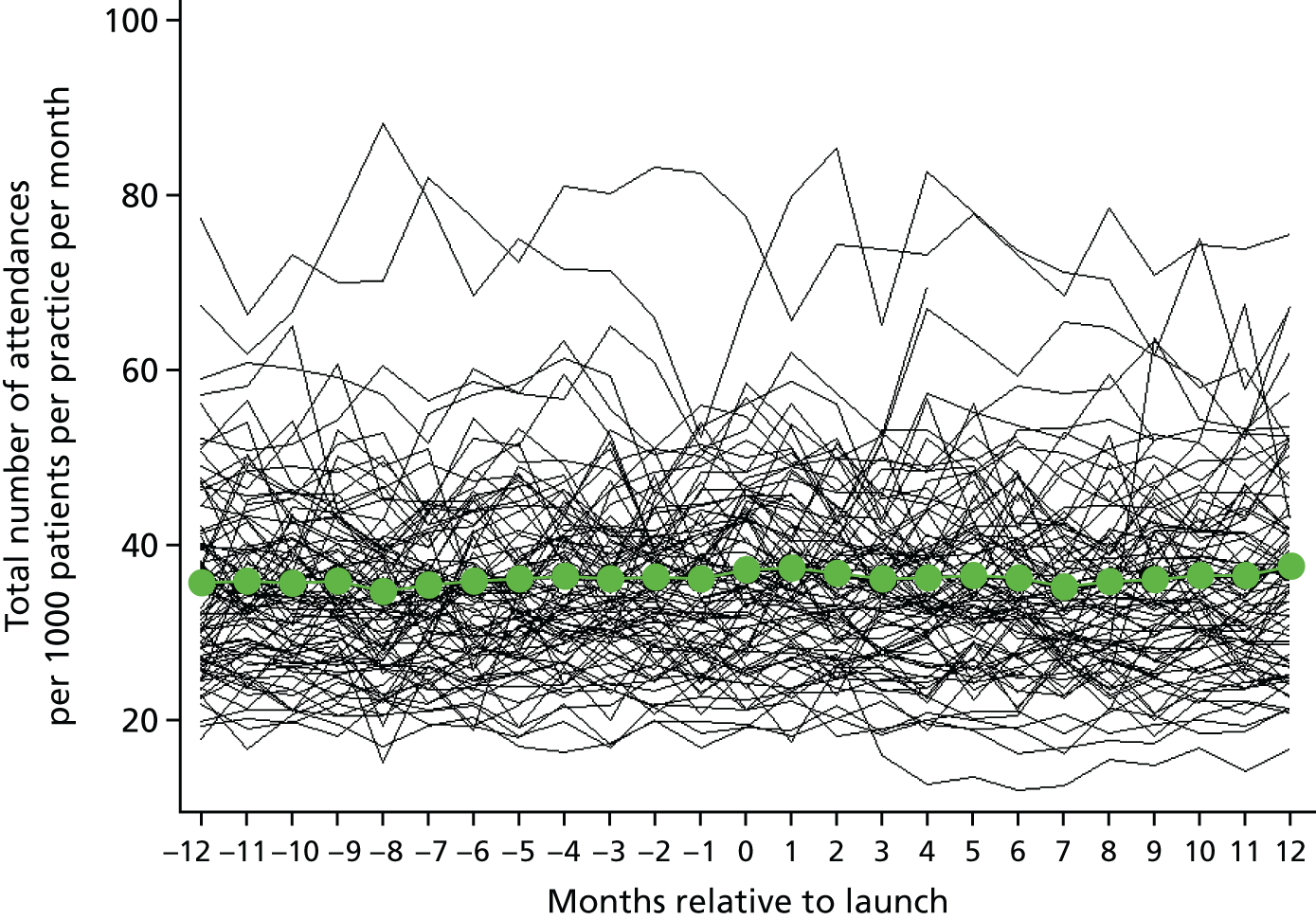
FIGURE 44.
Superposed epoch analysis of outpatient attendances relative to the intervention launch. The black lines represent the attendances within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
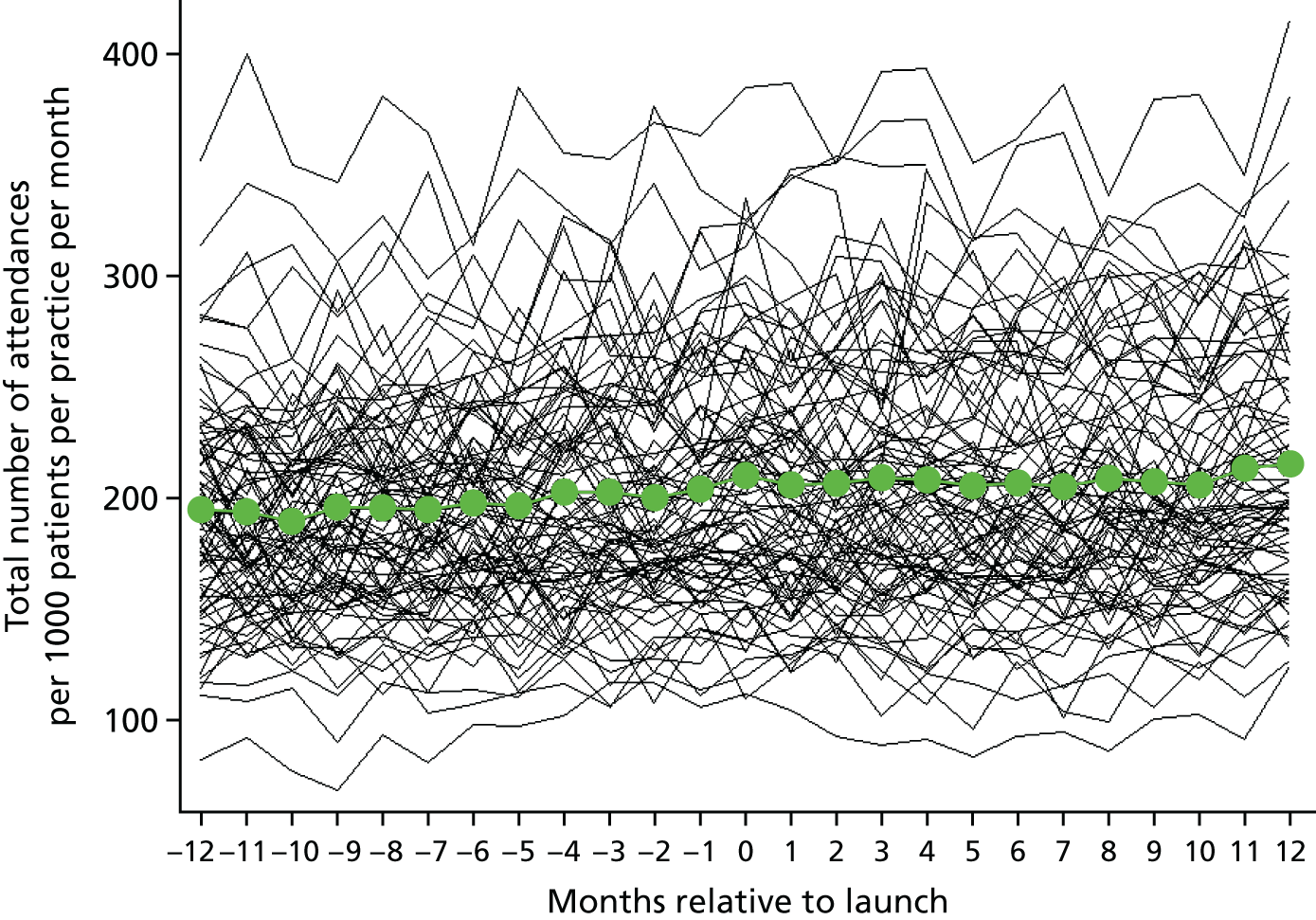
FIGURE 45.
Superposed epoch analysis of all inpatient admissions relative to the intervention launch. The black lines represent the admissions within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
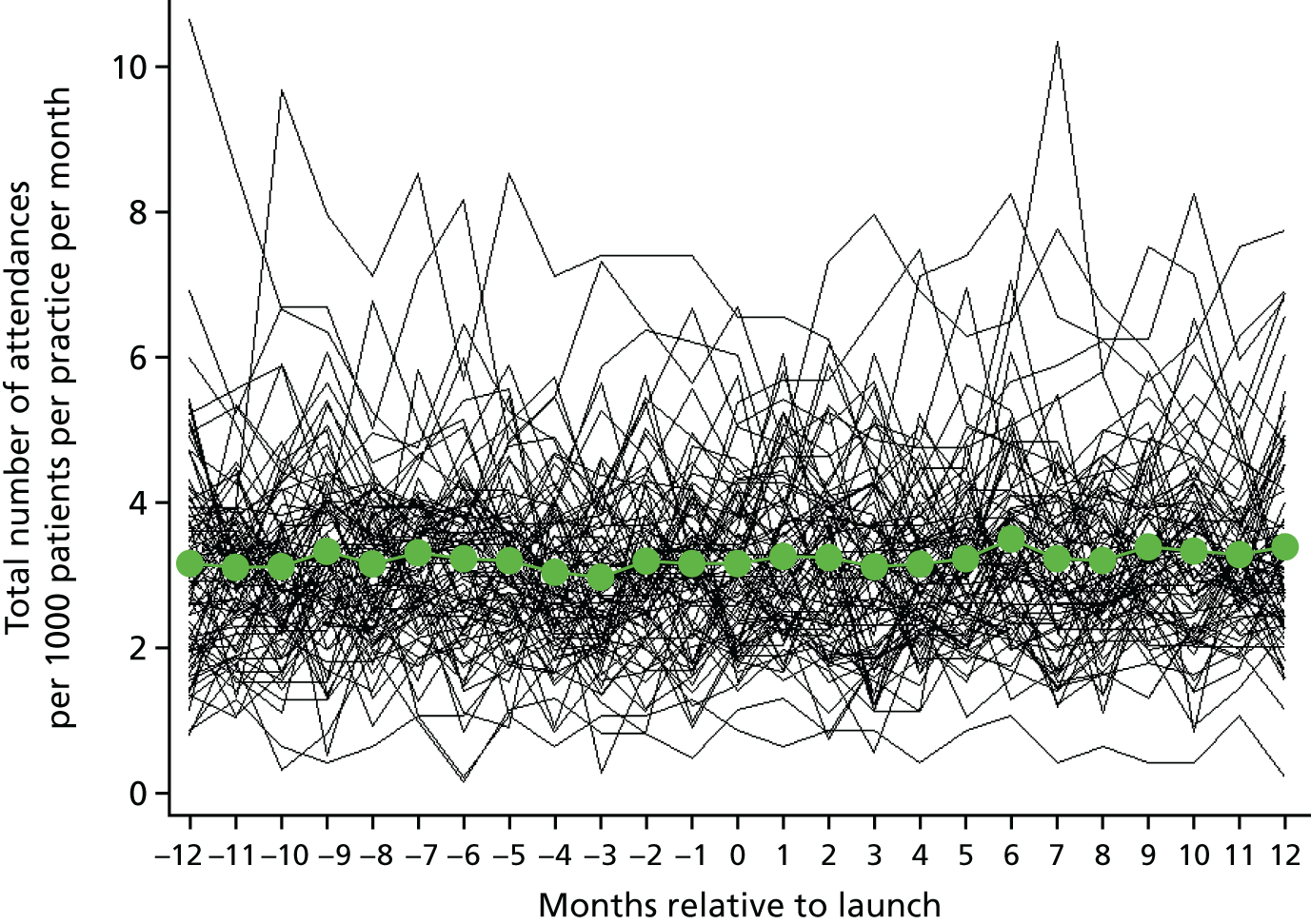
FIGURE 46.
Superposed epoch analysis of all inpatient admissions for ACS conditions relative to the intervention launch. The black lines represent the admissions within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
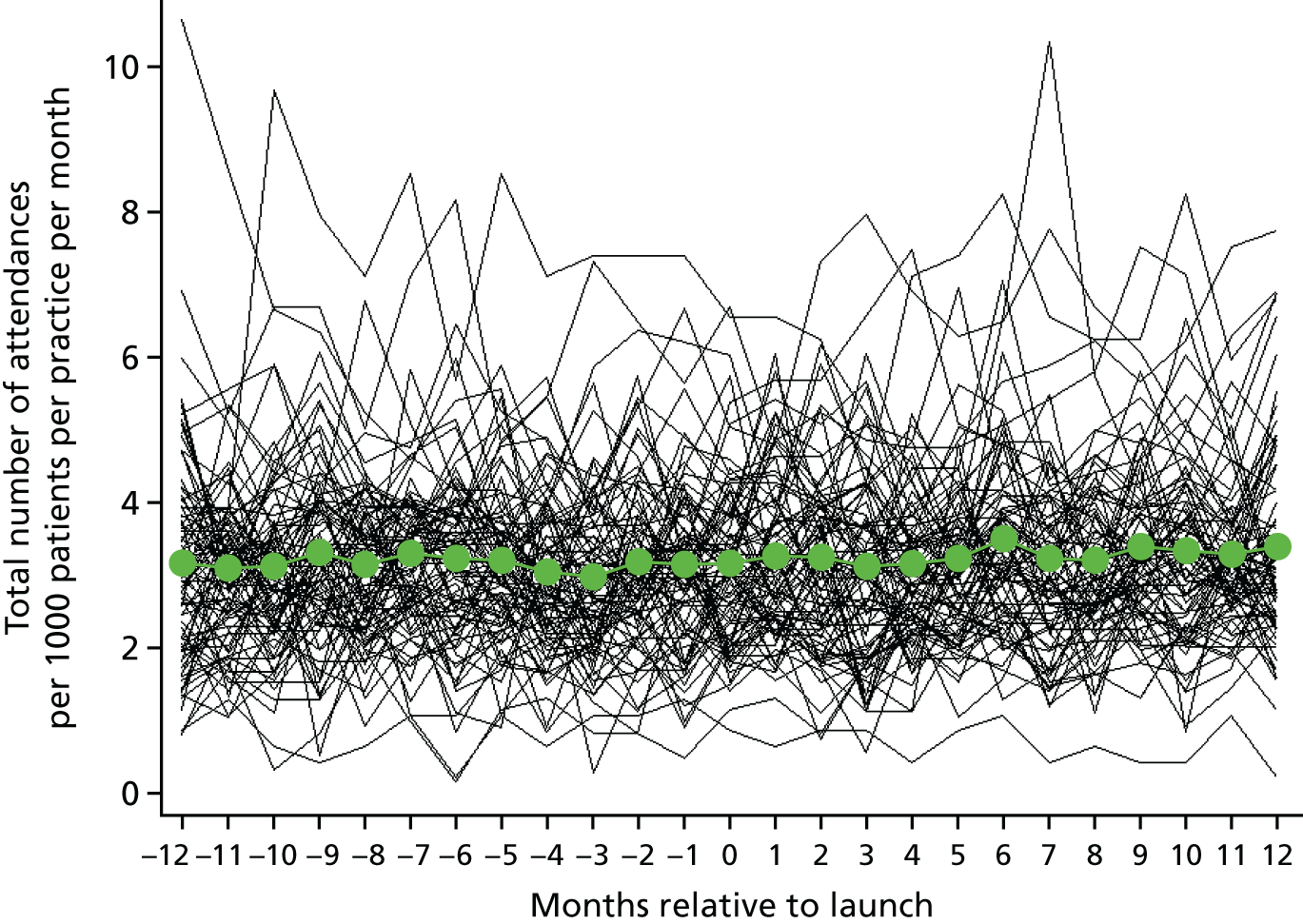
FIGURE 47.
Superposed epoch analysis of elective inpatient admissions relative to the intervention launch. The black lines represent the admissions within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
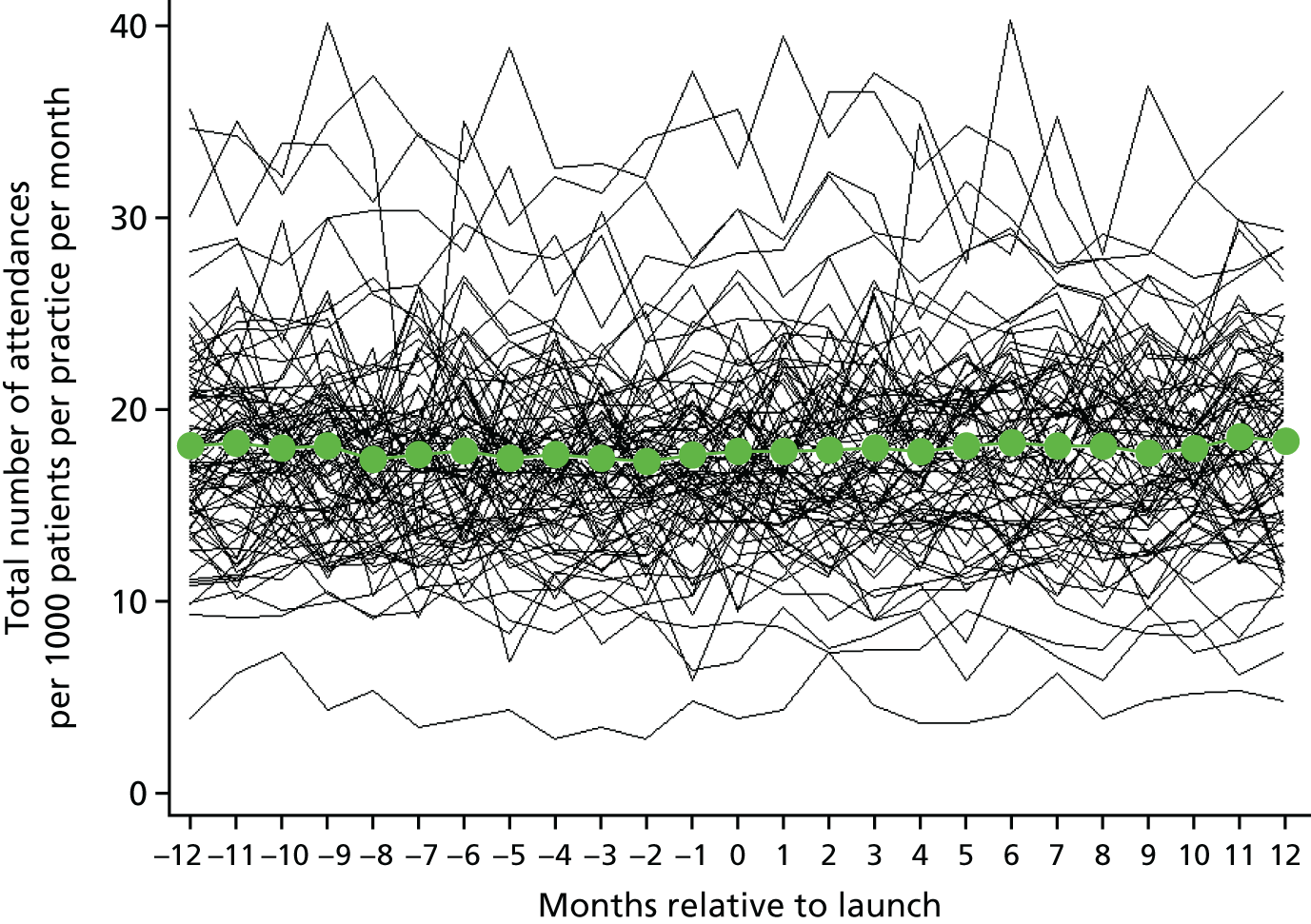
FIGURE 48.
Superposed epoch analysis of emergency inpatient admissions relative to the intervention launch. The black lines represent the admissions within a single practice relative to the launch time, with each black line representing a different intervention practice. The green dots represent the mean of individual practice means.
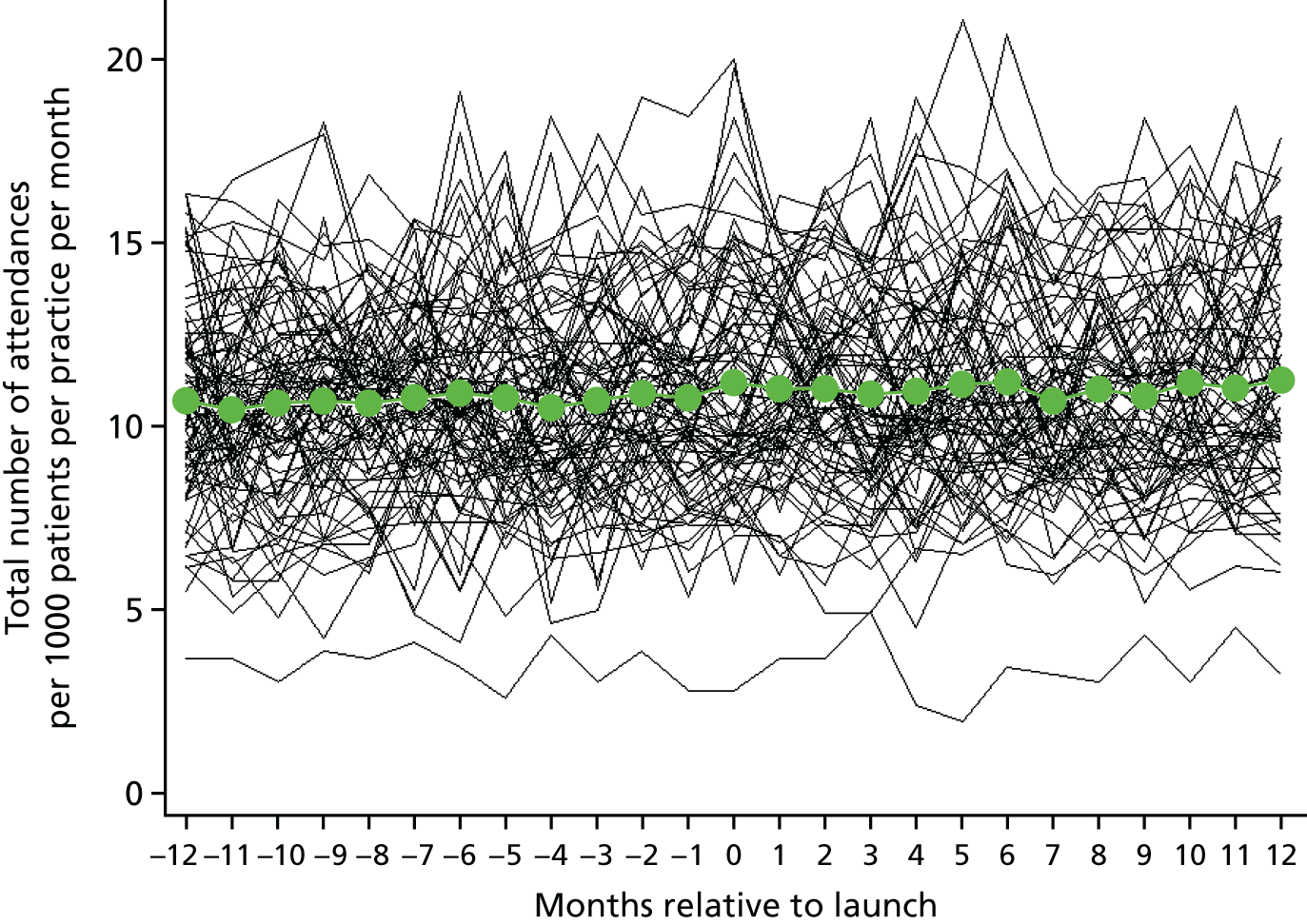
| Outcome | Step change at transition | ||||
|---|---|---|---|---|---|
| Additional yearly change following transition | |||||
| RR (95% CI) | p-value | Heterogeneitya | RR per year (95% CI) | p-value | |
| A&E attendances | 1.00 (0.99 to 1.02) | 0.71 | 0.92–1.10 | 0.98 (0.96 to 1.00) | 0.012 |
| Outpatient attendances | 0.99 (0.98 to 1.00) | 0.19 | 0.91–1.08 | 0.97 (0.96 to 0.97) | < 0.0001 |
| All inpatient admissions | 1.00 (1.01 to 1.04) | 0.0013 | 0.97–1.08 | 1.02 (1.00 to 1.03) | 0.1 |
| ACS condition inpatient admissions | 1.05 (1.01 to 1.10) | 0.026 | 0.87–1.27 | 1.10 (1.04 to 1.17) | 0.0009 |
| Elective inpatient admissions | 1.03 (1.01 to 1.05) | 0.0082 | 0.93–1.14 | 1.04 (1.02 to 1.07) | 0.0012 |
| Emergency inpatient admissions | 1.02 (1.00 to 1.04) | 0.056 | 0.97–1.08 | 0.99 (0.96 to 1.02) | 0.59 |
List of abbreviations
- A&E
- accident and emergency
- ACS
- ambulatory care sensitive
- BNF
- British National Formulary
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CPI
- consumer price index
- DNA
- did not attend
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- HMIC
- Health Management Information Consortium
- HRG
- Healthcare Resource Group
- IMD
- Index of Multiple Deprivation
- LSOA
- lower-layer super output area
- OR
- odds ratio
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- RR
- rate ratio
- SD
- standard deviation
- SE
- standard error
- SSC
- study steering committee
- UPC
- usual provider continuity
