Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/136/93. The contractual start date was in January 2014. The final report began editorial review in July 2017 and was accepted for publication in December 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Macfarlane et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
When this project was first designed, in 2012, a succession of analyses showing raised mortality among patients admitted to hospital at weekends was being published, and so-called ‘weekend effects’ were prominent on the policy agenda in England. Five years later, the number of published studies on these topics has grown and arguments about their interpretation and policy relevance continue. Maternity and neonatal services have always had to operate 24 hours a day, 7 days a week. Analyses of births and their outcome by time of day, day of the week and season have a longer history and are vital for informing the adequacy of arrangements for staffing and safety.
In designing this research project, we aimed to explore the implications of patterns of birth timing for NHS maternity and neonatal services, using administrative data for births in England and Wales in the early years of the 21st century. The research questions arose from previous research undertaken by two of the co-investigators, from the 1970s onwards,1–4 combined with the current policy focus on improving safety, extending midwifery-led care and choice of place of birth, and ensuring quality 24-hour care.
The funding for this research was both timely and relevant to proposed changes in maternity service provision. To carry out this study, we planned to draw on and extend data linkage developed in two previous projects. The first project linked data recorded at birth registration with data recorded at birth notification, at which point babies’ NHS numbers are allocated. 5,6 The second project linked these linked data to records of hospital care at birth in England7 and in Wales8 to create a new linked dataset bringing together the relevant data from several sources.
Unfortunately, this project has been seriously undermined by a series of obstacles. In our second project, we experienced delays in getting permission to access data from what was then the Health and Social Care Information Centre (HSCIC). We attempted to learn from this and use our experience to prevent similar problems from occurring again, but prior knowledge was insufficient to keep this project to schedule. We have experienced substantial delays and barriers as a consequence of the impact on data access of the implementation of the Health and Social Care Act 20129 and the wider implications of the unsuccessful attempt to establish the care.data system. 10,11 These barriers, followed by information technology (IT) infrastructure problems, slowed us down and meant that, despite an extension to the original time frame, our funding ended while we were still in the relatively early stages of the analysis. Regrettably, having created a unique and reliable 10-year database, we have not had time to complete many of the planned analyses, particularly analyses of outcomes. We are applying for further funding to complete these.
After setting the scene in Chapter 1, by describing the health policy context of our project and the previous work on the timing of birth and on data linkage, we go on in Chapter 2 to describe the methods and results of our data linkage and quality assurance work. In Chapter 3, we describe the methods of our planned analyses, before presenting and discussing the results of those analyses that have been completed. Chapter 4 explains how patient and public involvement (PPI) was integral to our project. In Chapter 5, we discuss the results of our linkage work and analyses and the gaps left by the work we were unable to do. The implications of our experiences for health care and for further research using administrative data are set out in Chapter 6. Appendix 1 describes the barriers that impeded our research and our attempts to overcome them.
Health policy context
To set policies about the 24-hour health service and its relevance to maternity care in context, we start with a broad overview of the ways in which policies for maternity care in England and Wales have developed in the longer term and then review the new policies set in train in recent years while our project has been under way.
Confidential enquiries
Quality health care has been defined as care that is safe and effective and results in a positive experience. 12
There has been a longstanding concern about the safety of maternity care, in terms of maternal mortality and of stillbirths and neonatal mortality. The UK has the longest-running programmes of confidential enquiries into pregnancy-related deaths in the world. After earlier developments in Scotland, Confidential Enquiries into Maternal Deaths have been run in England and Wales since 1928. 13 Following confidential enquiries into perinatal deaths at regional and local levels, the Confidential Enquiry into Stillbirth and Deaths in Infancy was set up nationally in 1993. 14,15 Learning from the enquiries regarding ways to reduce preventable factors associated with deaths has led to considerable improvements in service quality. Following a retendering exercise, the MBRRACE-UK (Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK) consortium is now responsible for these enquiries and has a key role in monitoring current policies. 15
Choice of settings for birth
At the beginning of the 20th century, nearly all women gave birth at home; by the end of the century, hospital birth was almost universal. Many factors contributed to this major change, but from 1970 onwards there was an explicit policy that all births in England should take place in hospital. In response to this, the proportion of births occurring at a mother’s home in England and Wales fell from 13% in 1970 to < 1% of all births in 1987, before starting to rise again. The rise was already occurring when the House of Commons Health Committee reviewed available evidence in its Inquiry into Maternity Services. 16 The Inquiry’s conclusions were wide-ranging, but it is perhaps best remembered for its conclusion that:
The policy of encouraging all women to give birth in hospital cannot be justified on grounds of safety.
Although limited, the evidence, coupled with demand from women and support from maternity charities and the Royal College of Midwives (RCM), led to changes in government policy in both England and Wales during the 1990s. 16,17 The Welsh Office issued the Protocol for Investment in Health Gain, which emphasised the need for women to have more control and an informed choice about the care given in pregnancy and childbirth. 18 In England, the Department of Health and Social Care responded to the report by setting up the Expert Maternity Group. Its report, Changing Childbirth,19 published in 1993, endorsed many of the policy changes set out in the Health Committee’s report, moving towards woman-centred care and a greater role for midwives, with at least 30% of women having a midwife as the lead professional.
These policies continued after the change of government in 1997. They were set out in detail in 2007 in Maternity Matters,20 after the aims had been outlined earlier in the National Service Framework for Children, Young People and Maternity Services. 21
The policy called explicitly for ‘an evidence-based culture’, which learned from adverse events and highlighted the value of routine data collection and analysis. 20
There was a strong emphasis on choice and this included a ‘choice guarantee’ on place of birth and other aspects of maternity care. 20 The Maternity Matters document stated that a ‘guiding principle’ for the modern maternity services was that:
All women will need a midwife and some need doctors too.
Although the proportion of births taking place at the mother’s home rose to well over 2% in the decade after the Changing Childbirth report was published, this was followed by a small decrease from 2008 to 2012. The number of alongside midwifery units (AMUs) rose from 26 in 2007 to over 100 in 2016, whereas the number of freestanding midwifery units (FMUs) rose slightly from 56 to 62 over the same time period (Miranda Dodwell, BirthChoiceUK, 2016, personal communication). In 2012, an estimated 9% of women gave birth in an AMU and 2% of women gave birth in a FMU. 22 This represented some change but fell well short of the 30% proposed in Changing Childbirth. 19
In 2002, the Welsh Assembly Government set a target of 10% for home births by 2007 as part of its strategy to develop midwifery-led care and access to services that were unfamiliar to many communities. 23 The National Service Framework for Children, Young People and Maternity Services in Wales24 had similar ambitions to those for England. This was followed by Strategic Vision for Maternity Services in Wales, the cornerstone of which continued to be tackling health inequalities. 25 Choice of place of birth and access to midwifery care pathways were part of the plan.
In response to the limited nature of the previous evidence and a recommendation by the National Institute for Health and Care Excellence (NICE) for further research, the Birthplace Programme of Research, a large-scale prospective cohort study, was funded. It aimed to evaluate and compare the risks and benefits for healthy women with straightforward pregnancies, who are at ‘low risk’ of complications, of giving birth at home or in FMUs, AMUs or obstetric units (OUs), focusing in particular on birth outcomes. 26 The Birthplace research found that outcomes for babies were similar for women planning birth in all settings but compared with women planning a hospital birth, women planning a home birth or birth in a midwifery unit had a lower risk of having a caesarean section, an assisted delivery or a haemorrhage.
The research also found that women planning a home birth or midwifery unit birth were more likely than women planning for birth in an OU to have a ‘normal’ birth. 26
This research was used as a basis for the 2014 revision to the NICE Intrapartum Care Guideline. 27 Birthplace26 also confirmed that the policy of choice of place of birth was safe, and that planning care in midwife-led care settings at home and in FMUs or AMUs for women at low risk of developing complications during labour and birth resulted in fewer invasive and costly medical procedures. 27
Health inequalities
One of the themes in the House of Commons Health Committee’s report that received less attention was health inequalities and maternity care for disadvantaged women. This reflects the extent to which the degree of emphasis placed on preventing health inequalities, investing in public health and improving access to maternity care has varied over time and between governments.
From 1997 to 2010, during the 13 years of Labour government, there was a clear emphasis on inequalities in health outcomes and the need to know where specific health ‘gains’ could be achieved. The National Service Framework for Children, Young People and Maternity Services, published in 2004,21 followed frameworks for other key areas of health care, including cancer, heart disease and diabetes. It looked at perinatal mortality and morbidity, and other aspects of child health, in relation to structural inequalities, as well as at the impact of poverty and disadvantage succeeding from one generation to the next. 28 There was an emphasis on cross-departmental policies to reduce the number of children living in poverty. 29 A key strategy for improving maternity experiences included improving maternity rights and pay.
The strategic review of health inequalities in England, chaired by Michael Marmot, emphasised the social determinants of health and health inequality. 30 The review team concluded that, in addition to the social justice argument for addressing health inequalities, there was also a pressing economic imperative for change as annual costs to the exchequer attributable to inequality in illness were estimated to be £31–33 billion in productivity losses, £20–32 billion in lost taxes and higher welfare payments and over £5.5 billion in additional NHS costs. 30 It was therefore also necessary to engage members of the public in protecting and promoting their own health.
Reducing the costs of litigation
Broader sociopolitical changes were also influential, including the regulation of hours by the European Working Time Directive,31 reductions in the numbers of junior doctors and the increasing cost of maternity litigation. A report by the NHS Litigation Authority showed that between 2000 and 2009, 5087 claims for injury were made against the NHS, for which it paid out £3.1B in damages. 32 The three most frequent categories of claim were those relating to the management of labour, caesarean section and cerebral palsy. 32 Improving the overall quality of maternity care and reducing deaths and injury are important, as is the need to make the best use of limited resources.
Recent policy developments
After the change in government in 2010, it was several years before new maternity policies were developed. The NHS Five Year Forward View,33 published in October 2014, set out a vision for how the NHS in England would have to adapt to meet the needs of a changing population and committed further funding for the NHS. It stated that a ‘one size fits all’ approach to health care was no longer applicable to a diverse population and proposed new models of care, including in relation to maternity care. Speaking of the need to move away from a factory-like model of ‘care and repair’, the NHS Five Year Forward View set out a greater focus on community engagement and prevention of disease through improved public health, although its view of this was based more on individual than on structural measures.
It also spelled out the considerable growing demands on the service as a result of people living longer, opportunities and pressures to provide ever more complex science- and technology-led interventions and the continuing impact of smoking, alcohol use, lack of exercise and rising levels of obesity on levels of diabetes, stroke, heart disease and cancer. A national maternity review was subsequently commissioned to investigate the changes to maternity services needed to meet the needs of the population. 33
It was also asked to ensure that the recommendations of the Morecambe Bay investigation34 of ‘serious failures of clinical care’, which led to avoidable deaths of mothers and babies in one maternity unit, could be embedded throughout the NHS in England. 35
The review’s findings were incorporated in a Five Year Forward View for maternity, Better Births,35 a strategic framework with many broad-ranging aims. It aimed to make a significant culture change, based on two fundamental principles, described as being:
The importance of women being able to make choices about their care, and the safety of the mother and baby being paramount.
This safer, more personalised care, in which maternity services are responsive to the needs and circumstances of individual mothers and babies, would be focused on reducing avoidable deaths and damage through a focus on acute services delivered by multidisciplinary teams. In addition to the distress caused to families by negligence during maternity care, compensation costs the NHS an average of £560M per year. 35 This care would also encompass more community-based and midwife-led services for women with a straightforward pregnancy who are at low risk of complications. Better Births35 also preserved the commitment to the choice of place of birth given in Maternity Matters. 20
Meanwhile, the Welsh Government set out its strategic vision for maternity services in 201125 and set up the Maternity Network Wales in 2015. 36 This has three main priority areas: (1) to lead on a number of interventions to reduce stillbirth rates in Wales, (2) to improve the quality of maternity services by implementing the recommendations made by the Quality and Safety subgroup of the All Wales Maternity Service Implementation Group in its report published in June 201337 and (3) to work in partnership with women and families. 38 This is to be achieved through a number of subgroups set up by the Network.
NHS care at weekends
From 2001 onwards, a considerable number of analyses have shown higher mortality rates among patients admitted to hospital at weekends than on weekdays and there has been considerable debate about how to interpret these rates. 39,40
We have not attempted to summarise them here, as we are aware that a systematic review is under way. 41 Instead, we have given examples that highlight some of the arguments. For example, a study using routinely collected data for over 4 million emergency admissions found that the overall adjusted odds of death was 10% higher for weekend admissions than for weekday admissions. 42 Another study using patient records for 14 million hospital admissions found a higher risk of in-hospital death within 30 days of admission for weekend admissions than for weekday admissions, but the chance of actually dying at the weekend was lower than the chance of dying mid-week. 43 In contrast, a prospective cohort study with 74,000 stroke patients showed no difference between 30-day survival at weekends and on weekdays. 44
Even if there are weekend effects, it is unclear if they reflect differences in quality of care or differences in case mix. For example, one study found that patients admitted at the weekend were more seriously ill than those admitted during the week. 45 Another suggested that the weekend effect arises from patient-level differences at admission rather than reduced hospital staffing or services. 46 Even where it is suspected that staffing makes a difference, there are questions about whether this reflects numbers or type of staff or their seniority. One study examining nearly 4 million elective procedures concluded that consultant seniority has no impact on predicting 30-day mortality. 47
These uncertainties have not impeded calls from politicians and others for a 7-day health service. NHS England established a Seven Days a Week Forum and its report, published in November 2013,48 was cited prominently in the report of the Review Body on Doctors’ and Dentists’ Remuneration published in 2015. 49
Despite the conflicting evidence, in the NHS Mandate published in 2015, the Secretary of State for Health for England, called for ‘a truly seven-day health service’:
The NHS should be there for people when they need it; this means providing equally good care seven days of the week, not just Monday to Friday.
Although these policies have been labelled ‘24/7’, the analyses have been largely restricted to differences between days. As we show in the following section, this is not the case for analyses of births, and times of day have been taken into account when discussing the staffing of maternity services. Although it is self-evident that maternity services need to operate 24 hours a day, 7 days a week, there are still many questions about the type and seniority of staff needed.
Staffing of maternity hospitals
Although adequate staffing is central to delivering high-quality, efficient health care, most of the debates have been about medical staffing and have mainly related to consultants, although they featured in negotiations about revisions to junior doctors’ contracts49 and their decision to take industrial action in response. Although the RCM repeatedly expresses concern about shortfalls in midwifery staffing, it has not been in this context. This is a matter of concern to the College and it has supported our project at each stage, stating that the information we aimed to produce would have been useful to it.
The National Patient Safety Agency ‘Hospital at Night’ Programme,50,51 set up in 2005, proposed that the way to achieve safe clinical care was to have out-of-hours care delivered by a multiprofessional team with the full range of skills and competencies across a whole range of disciplines in a hospital to meet the immediate needs of patients. This did not apply to obstetrics as, according to the Royal College of Obstetricians and Gynaecologists (RCOG),51 women in labour needing medical care would be managed by obstetricians within the department and not by the Hospital at Night team. Thus, the emergency obstetric rota would be staffed for 168 hours a week (‘24/7’) from within the discipline of obstetrics and gynaecology.
For a number of years, the RCOG advocated increasing the hours of consultant presence in maternity units. 52,53 Initial recommendations were for units to have a minimum of 40 hours of consultant obstetrician cover a week, with exceptions for units with fewer than 1000 births a year and those with low complication rates. In addition, units with > 5000 births were to have 60 hours of consultant cover a week. The Healthcare Commission’s maternity services report, Towards Better Births, reported that only 68% of trusts reported meeting this standard in 2007, with some trusts reporting a very minimal presence, as low as 10 hours per week. 54
In 2007, new recommendations were made for a minimum of 60 hours of consultant presence in all OUs, with a specific recommendation of 98 hours for units with 4000–5000 births. For units with over 5000 births per annum, the RCOG recommended consultant presence on the labour ward both day and night, for 168 hours per week, referred to as ‘24/7’ cover, by 2010. For the largest units with over 6000 births, the suggested time frame for implementation was earlier, by 2008. 55
This drive for increased consultant presence came at a time when there were also increasing pressures on the workforce. The RCOG report High Quality Women’s Health Care56 identified the impact of the European Working Time Directive on women’s health care, and specifically the introduction of the 48-hour week, which led to a need to increase the numbers of consultants to provide cover. The RCOG report, The Future Workforce in Obstetrics and Gynaecology,57 calculated that 168 hours’ cover for a delivery suite, along with other clinical activity, would require the employment of 18–21 consultants per OU. This led to proposals for obstetric services to be centralised, with the closure of small OUs, as these might be uneconomic to run with the recommended level of consultant presence.
In terms of obstetric staffing, the Strategic Vision for Maternity Services in Wales policy referred to compliance with the European Working Time Directive, the need for services to comply with the RCOG guidance for 40 hours of consultant labour ward presence per week, depending on the number of deliveries per year, and for a middle-grade doctor at level Specialty Trainee 3 or higher or at Staff Grade, Associate Specialist and Specialty Doctor grades to cover the labour ward at all times at which a consultant is not present. 25
By 2014, only two units in the UK had achieved 168 hours per week of consultant presence58 even though numbers of consultant obstetricians and gynaecologists in England had risen substantially. Over the years between 2002 and 2017, numbers of full-time equivalent staff had almost doubled, with an increase of 20% in the last 5 years of this period. 59,60
Despite the decisive strategic direction taken by the RCOG, the evidence that these levels of consultant presence would increase safety for mothers and babies was not clear, particularly in relation to the increase in size of OUs resulting from this policy. 61,62 A systematic review and related case studies from England, France and Sweden concluded that ‘A model considered equitable by consultants and which includes prospective cover for holidays, thus truly providing continuous consultant labour ward presence, requires 26 consultants’. 63 This would be possible only within current budgets for England only in very large, tertiary level units providing care for a disproportionately large number of women with complex care, and so attracting the higher tariffs available for paying for their care.
Based on several factors, including limited available evidence on the impact of 24-hour consultant presence, with little to show that this improves the quality of care, together with competing arguments for deploying any additional staffing, such as employment of more midwives or having greater consultant obstetrician presence at weekends, the authors concluded that the case for 24-hour consultant obstetrician presence on the labour ward had so far not been demonstrated. 63
Given the lack of evidence that 24-hour resident consultant presence on the labour ward has any impact on women’s outcomes, the RCOG subsequently produced a report to update its guidance on obstetric staffing. 64 It stated that:
It is recognised that there is huge variability of service provision around the country in terms of workload complexity, geography and current middle grade staffing. For this reason, there is no single staffing model which is suitable for all UK units . . . Within obstetrics it is no longer possible to make recommendations about hours of consultant presence on the labour ward based on number of deliveries because of the diversity of consultant contracts and working practices.
Royal College of Obstetricians and Gynaecologists. Providing Quality Care for Women: Obstetrics and Gynaecology Workforce. London: RCOG; 2016. 64 Royal College of Obstetricians and Gynaecologists © 2018
It did, however, strongly recommend that all OUs should have a minimum labour ward consultant presence during working hours between Monday and Friday, with the aim of extending this to every day of the week. 64
Reducing stillbirths and neonatal deaths
As well as the focus on keeping care for healthy women straightforward and on avoiding iatrogenic effects and rising costs, there has been a concurrent focus on a traditional cornerstone of quality maternity care, that is, improving safety by reducing avoidable maternity and perinatal injuries and deaths. This comes at a time of rising birth rates, rising ages at childbirth and increasing rates of obesity and other clinical and social complexity. These factors have led to greater demands on the service, and an increased proportion of women needing medical care and more intensive midwifery support. The Morecambe Bay Inquiry34 highlighted the importance of careful needs assessment and close interdisciplinary working to ensure consistent and improving levels of safety in maternity care. These are all drivers affecting commissioning priorities and strategic decision-making in service delivery.
As part of the Five Year Forward View, the government’s ambition is to halve the rates of stillbirth and neonatal death in England by 2030;65 the Saving Babies’ Lives Care Bundle is designed to guide commissioners and clinicians on how to develop services to make this happen. 66 It brings together four elements of care: (1) reducing smoking in pregnancy, (2) risk assessment and surveillance for fetal growth restriction, (3) raising awareness of reduced fetal movement and (4) effective fetal monitoring during labour.
In 1928, the stillbirth rate for England and Wales was 40.1 per 1000 total births and this fell steadily from the 1950s to the turn of the century, but then levelled off and thus became a cause for concern. In 2012, the stillbirth rate started to fall again, reaching 4.5 per 1000 total births in 2015. Even before the implementation of the government’s strategy, over the period 2013–15, the stillbirth rate in the UK as a whole, published by MBRRACE-UK, fell by almost 8%, largely because of a reduction in antepartum stillbirths at gestational ages of 32 weeks and over. 67
The neonatal mortality rate for England and Wales (i.e. deaths in the first month of life) fell more steadily from 30.9 per 1000 live births in 1928 to 2.7 per 1000 live births in 2013 and 2.5 per 1000 live births in 2014, although the decline had become less marked and the rate increased slightly to 2.6 in 2015. Data for the UK as a whole, published by MBRRACE-UK, showed that neonatal death rates fell marginally from 1.84 per 1000 live births in 2013 to 1.74 per 1000 live births in 2015. 67 In 2015, nearly two-thirds of these neonatal deaths were of babies who were born preterm and two-thirds of the stillbirths occurred before the pregnancy reached full term. 67 Rates published by MBRRACE-UK differ from those from civil registration as MBRRACE-UK systematically excludes events following the termination of pregnancy at ≥ 24 weeks of gestation and the deaths of babies born before 24 weeks of gestation. 67
Preterm birth and congenital anomalies account for a significant proportion of neonatal deaths and stillbirths, but the causes of preterm birth are poorly understood. Some countries, notably the Nordic countries, whose stillbirth and neonatal mortality rates our politicians aspire to emulate, have much lower rates of preterm birth and also lower rates of obstetric intervention than the countries of the UK. 68 A better understanding of the causes of preterm birth and the development of interventions to prevent them are urgently needed. This requires research programmes to evaluate the efficacy of both preventative and ‘rescue’ interventions.
The MBRRACE-UK consortium has led a coalition of stakeholders in developing a national, standardised Perinatal Mortality Review Tool to support local review processes. This is expected to improve assessments of the quality of care and postmortem investigations. The quality and incompleteness of data are also issues, preventing a full picture from being known, and also preventing accurate monitoring of changes.
In 2014, the RCOG launched a long-term quality improvement programme, Each Baby Counts, with the aim of halving the number of babies who die or are left severely disabled as a result of preventable incidents occurring during term labour, by 2020. Each Baby Counts is a measure that brings together the number of babies who are stillborn at term, who die within the first week of life or who are diagnosed with severe brain injuries. 69
In Wales, the National Assembly’s Health and Social Care Committee held an inquiry into stillbirths in 2012, which was reported in February 2013. It made a number of recommendations to reduce stillbirth rates,70 including the setting up of the Maternity Network Wales to take this work forward. 38
Variations in the patterns of the time when babies are born may affect stillbirth and neonatal mortality rates and can have implications for the staffing needs of maternity services. This can affect the care that women receive and their experience of that care. Investigations into patterns of birth timing and subsequent outcomes may inform changes in service provision that can improve care to make it safer and more personalised.
In particular, the strategy to reduce stillbirths may increase rates of induction of labour, which would have implications for the proportion of women eligible for midwifery-led care and for the pattern and timing of births in different settings. 66,69
Previous research on the timing of birth
Time of day of birth
Up to the middle of the 20th century, there was a popular assumption that times of birth and death were by and large predetermined, although it was recognised that unexpected, possibly untoward, events could change them. The second half of the century saw increasing use of medical intervention to influence the time of birth and to prolong the lives of babies born very preterm or with conditions previously thought to be incompatible with life.
It was established in the 19th century that numbers of spontaneous births varied by time of day and were higher at night than during the day. 71–73 For example, in his Essai de physique sociale,74 published in 1835, Adolf Quetelet cited data from Brussels and Hamburg, which showed that the numbers of live births in the 6-hour periods before and after midnight were higher than those in the corresponding periods before and after noon. An exception was found in the Hamburg data, which were subdivided by season and which showed that numbers of live births were high on winter mornings.
In the 20th century, data from a special birth certificate in use in Buffalo City, New York, showed that numbers of spontaneous births in 1937 were highest in the early hours of the morning from 03.00 to 05.00, whereas the much smaller numbers of births involving obstetric intervention peaked from 09.00 to 11.00. 75 A study of over 16,000 births in Birmingham, England, in the early 1950s focused on the time of onset of spontaneous labour and found that it peaked in the middle of the night, around 02.00, especially for primiparous women, with numbers of births peaking from 03.00 to 05.00. 76 Intervention rates were low in this period but caesarean sections were more likely to occur during the day.
Reviews published in the 1960s and 1970s found that, in previous studies, births were most likely to occur between 01.00 and 06.00. 71,73 Further studies in the 1960s pointed out that this peak was apparent only in predominantly normal births, which did not involve invasive clinical procedures. Some of the rationale for the rising rates of induction, acceleration and caesarean section from the 1970s onwards was an intention to concentrate births into conventional working hours in order to optimise access to clinical care. 77–79
The impact of these rising rates was to move the peak in overall numbers of births into daytime hours. For example, studies in Switzerland of births from 1979 to 1981 showed that the highest numbers of births occurred on weekdays between 08.00 and 16.00,80 but this analysis did not subdivide births by mode of onset and birth. An analysis of all births in the state of Massachusetts, USA from 1989 to 1995 showed a peak between 07.00 and 09.00, the times associated with planned caesarean section. 81 When the analysis was restricted to singleton vaginal births of spontaneous onset without stimulation, the variations were less marked but numbers of births were slightly higher in the daytime between 09.00 and 15.00, with a peak from 11.00 to 13.00.
Other US states now record times of birth79 and an analysis of births in 2013 in 41 states plus the District of Columbia showed that overall numbers of hospital births were concentrated into daytime and early evening hours. 82 Elective caesarean sections were concentrated into mornings with two peaks at 08.00 and 12.00, whereas numbers of emergency caesarean sections were highest during late afternoons and early evenings. Numbers of both induced and non-induced vaginal births were highest between 12.00 and 18.00, although the numbers of non-induced births varied considerably less.
In the USA, only out-of-hospital births showed a pattern similar to that in earlier analyses, with numbers of births being highest between 03.00 and 05.00. 82 In contrast, a study in a hospital in Spain with a high caesarean section rate showed that overall numbers peaked during morning hours, but unlike in the USA, numbers of spontaneous births were still highest in the early hours of the morning. 83 Similarly to this, an earlier study in Norway found that numbers of spontaneous births peaked in the early hours of the morning, especially for births to multiparous women, whereas numbers of births to primiparous women peaked later in the day. 84
A similar effect was seen in the Netherlands in a study that compared vertex singleton term births without oxytocic drugs to women having care from midwives with those births to women having care from obstetricians. 85 Among women cared for by midwives, numbers of births to primiparous women peaked between 08.00 and 09.00 and births to multiparous women peaked at 05.00. For women cared for by obstetricians, the corresponding peaks were several hours later, between 14.00 and 15.00 for primiparous women and between 08.00 and 09.00 for multiparous women.
An unpublished study of births in seven hospitals in northern Portugal after spontaneous onset of labour showed that neither spontaneous nor operative births peaked in the early hours of the morning (Cristina Teixeira, Polytechnic Institute of Bragança, 2015, personal communication).
These comparisons raise questions about styles of practice and settings for care. A particular question is why the timing of spontaneous births has retained its traditional early morning peak in some settings, but not in others. Another question is about the extent to which births following induction are concentrated into daytime hours.
Day of birth
In England and Wales, a study of daily variations in numbers of births in the 1970s found a pronounced weekly cycle, with numbers of births being lowest on Sundays, followed by Saturdays, and the highest numbers of births occurring from Tuesday to Friday. Numbers of births were low on public holidays, with Christmas Day and Boxing Day having the lowest numbers of births in each year. 1,86 Similar patterns were observed in a number of other countries87–95 and an analysis of births in Israel showed a deficit on Saturdays. 96
The patterns of birth in England and Wales changed over the 7-year period of 1970–6. The ratio of the average numbers of births on Saturdays to the overall daily average for the year decreased from 1.00 in 1970 to 0.93 in 1976, while the corresponding ratio for births on Sundays fell from 0.88 in 1970 to 0.77 in 1976. The ratio for births on Mondays rose from 0.92 in 1970 to 0.97 in 1976. It was not possible to tabulate these births by method of onset of labour or delivery, but data from a different source, the Hospital In-Patient Enquiry (HIPE), showed that induction rates rose steeply in the early 1970s, from 23% in 1970 to 39% in 1974, and then fell slightly, reaching 35% in 1976. 97
Data from other countries,87,90,93 and a subsequent special analysis of HIPE data for England and Wales,98 suggested that day of the week variations in both elective caesarean section and induction made a major contribution to the daily variations observed in births. In particular, a study in France compared data for 1946–50, when there was little day of the week variation, with data for 1968–75, by which time a deficit of births on Sunday had become well established. 95
Further analyses of patterns of birth in England and Wales showed that over the period 1979–96, weekly patterns of birth in England and Wales were more stable than they had been in the 1970s. The ratio of the average numbers of births on Saturdays to the overall daily average for the year ranged between 0.92 and 0.94 over the period, and the corresponding ratio for births on Sundays rose from 0.79 in 1979 to 0.83 in 1996. The ratio for births on Mondays rose slightly from 0.97 to 0.99 over the period. 2 A second, more detailed, analysis was undertaken of births over this period but the birth registration data again took the form of counts and were not linked to data about methods of delivery. 2 Separately from this, tabulations of data from the Hospital Episode Statistics (HES) for England from the mid-2000s showed the extent to which elective caesarean sections and, to a lesser extent, births following induction are more likely to occur on weekdays than at weekends. 99
Births in midwife-led settings
There has been very limited recent work on births in out-of-hospital settings. Births in midwife-led settings, including home births, are now low in number compared with births in OUs and, therefore, are more difficult to analyse.
The local study of births in Birmingham, England, in 1950 and 1951 referred to previously (see Time of day of birth) showed that numbers of domiciliary births, which accounted for a much larger proportion of all births than they do now, peaked from 02.00 to 07.00 and spontaneous births, which formed a majority of births in this analysis, followed the same pattern. 76
The analysis of day of the week variation in births in the 1970s found some day of the week variation in births occurring at home, but it was very much less marked than in hospital births. 100
More recently, additional analyses of the Birthplace data looked at timing of births planned in midwife-led settings in alongside and freestanding midwifery units and at home and compared them with hospital births in terms of likelihood of having a caesarean section, an instrumental delivery, a ‘straightforward’ birth or a ‘normal birth’. Times of births were subdivided into weekdays during ‘office hours’ from 09.00 to 16.59, weekday nights and weekends. 101
Women planning OU birth were less likely to have a birth without obstetric intervention if their birth occurred on a weekday during ‘office hours’ than if they gave birth at night. In births planned in AMUs and at home, there was no difference between time of day or day of the week and any of the main outcome measures.
Nulliparous women who planned to give birth in FMUs and who gave birth during weekday ‘office hours’ were less likely to give birth by caesarean section than nulliparous women who gave birth at night. Multiparous women who gave birth on weekdays during ‘office hours’ or at weekends were less likely to have a normal birth than those who gave birth on a weekday at night.
Overall, the authors suggested that their findings could be interpreted as consistent with a possible effect of non-clinical factors on intervention, but that there were other possible explanations and that further research was warranted. 101
Birth outcomes in relation to time and day of birth
Analyses of stillbirth and neonatal mortality by time of day and day of birth has a long history. Some early studies analysed outcomes by time of day of birth. The 19th century Brussels data included numbers of stillbirths, which were higher in the afternoons. 74 Stillbirth and neonatal mortality rates were the focus of an analysis in the early 20th century of births in New York State in 1929102 and 1936,75,103 and of an analysis of data from an unspecified location in the UK,104 which also found higher rates in the afternoon.
Subsequent analyses of mortality by time of day later in the 20th century found different patterns. Studies in Switzerland found that perinatal mortality rates were higher at night and that rates rose in births occurring through the late afternoon and the early evening and then began to fall in births occurring after midnight. 80,105,106 An analysis of births in Sweden from 1973 to 1995 found higher mortality rates among babies born at night, from 17.00 to 01.00, followed by a minimum around 04.00 and a second peak around 09.00, especially for preterm births. 107 In contrast, an analysis of neonatal deaths in California found that neonatal mortality rates were slightly higher in babies born at night, but were higher among babies born in the early hours of the morning than among those born before midnight. 106 A further study subdivided births in Sweden from 1991 to 1997 by risk of death and suggested that babies born at night were at higher risk of early neonatal death but not of intrapartum death. 108
A number of studies from the 1970s onwards analysed the outcome of pregnancy by day of the week of birth. An analysis of perinatal mortality in England and Wales among births in the years 1970–61,86,100 showed a weekly cycle, with higher rates among babies born at weekends, but warned that these were crude rates, so no conclusions could be drawn. A subsequent analysis of data for England and Wales for the years 1979–962 used more advanced statistical modelling techniques and found that stillbirth and early neonatal mortality rates tended to be higher among births on Saturdays and Sundays, respectively, than among births on other days, but this was also restricted to crude rates.
The findings of other studies were inconsistent. A study in Canada found slightly higher crude rates of stillbirths and neonatal deaths among births at weekends, but the difference disappeared after adjustment for gestational age,109 and a study in Australia found no difference after adjustment for birthweight. 2,91
An analysis by day of the week published while this project was under way used unlinked HES data for England and concluded that perinatal mortality was highest at the weekend,62 although the authors’ analysis and interpretation of their results was highly criticised in subsequent rapid responses. 110–112 Like past analyses of rates of stillbirth and perinatal mortality in England and Wales, this analysis made no distinction between intrapartum and antepartum stillbirths.
Data about the exact timing of death, subdivided into before labour, during labour or not known, are recorded on the medical certificate of stillbirth. The completeness of these data has improved in recent years but the quality has not been reassessed. Better quality data are available, however, from confidential enquiries. 113–115
An analysis of data for 1993–5 from the All Wales Perinatal Survey had pointed to higher rates of mortality related to intrapartum asphyxia in the holiday months of July and August and suggested a possible association with the rotation of junior doctors to new posts in August, but this was based on relatively small numbers of deaths. 116 Similar effects were reported in intrapartum-related deaths in Scotland. 117 The analysis of data for England and Wales for 1979–96 showed that all perinatal mortality rates varied depending on the time of year. 2
Like previous analyses for England and Wales, this did not take account of the time of day of birth as it was not included in routine data systems at the time. Analyses by day of birth and time of day by method of onset of labour and gestational age were not possible, as all the relevant data items were not recorded at a national level for England and Wales, even though they have long been recorded locally.
More recent analyses of the outcome of births by day of week and time of day from Scotland118 and the Netherlands119 that have dichotomised time of day and day of the week as ‘in hours’ and ‘out of hours’ have attracted considerable media attention and raised questions about the safety of ‘out-of-hours’ care. Both studies reported raised mortality rates among babies born outside usual weekday working hours. The analysis of Scottish singleton birth and neonatal mortality data for the years 1985–2004 showed raised neonatal mortality attributed to asphyxia at weekends and on weekdays outside the hours of 09.00 to 17.00. 118 The authors found no changes over time and suggested that the findings were also true in other countries of the UK.
A ‘rapid response’ based on data from the West Midlands from 1995 to 2009 showed, however, that similar patterns were found in the region in the late 1990s but had subsequently disappeared, and there was no evidence of a raised mortality rate ‘out of hours’ in the years 2005–9. 120
The inconsistent nature of previous findings could reflect the underlying complexity of contributory factors and the challenges inherent in examining cause of death questions. The provision of care, in particular the provision of facilities to allow rapid delivery and prompt resuscitation, would be expected to affect different types of death in different ways. These provisions might be crucial in the response to an acute event, such as uterine rupture. They would not, however, alter the course of a baby affected by, for example, renal agenesis, which is invariably fatal. Furthermore, there is considerable potential for bias within any such analysis. For example, both planned caesarean delivery at term, which carries a low risk of stillbirth,91,100,109 and high-risk births, such as elective preterm births, tend to take place during the normal working week and could contribute to either an overestimate or an underestimate of the relative risk of giving birth out of hours. Finally, stillbirths and neonatal deaths are rare events, especially intrapartum stillbirth, which accounted for only around 9% of stillbirths reported to MBRRACE-UK. Therefore, a large dataset is needed to analyse births and their outcome by day of the week and hour of the day. Recent developments in data recording and linkage in England and Wales mean that these analyses are now possible for large numbers of births from 2005 onwards, as are analyses of data about any subsequent hospital care for mothers and babies. As a result of the novel data linkage work described here, the analysis planned for the project and completed in part is the first to be undertaken.
Data linkage
This project built on two preceding data linkage projects in England and in Wales5–8 and on earlier developments in routine linkage of infant, childhood and maternal mortality.
Previous analyses of data for England and Wales for the years 1970–61 and 1979–962 were based on aggregated counts. Although there was limited use of mortality data linked to births in the second of these analyses,2 mortality was not disaggregated by cause. Analyses by time of day, method of onset of labour and gestational age were not possible in these analyses, as the relevant data items were not available at a national level for England and Wales.
Recent developments in data recording and linkage have changed this. As a by-product of the change to birth notification to enable the allocation of babies’ NHS numbers at birth in 2002, a small set of variables not recorded at birth registration, including the time of day of birth and gestational age, are now recorded in the national birth notification dataset. 121 A series of collaborative projects led by City, University of London, was undertaken to build a database of linked datasets. The first two piloted the linkages and explored their potential for use in research and the production of national statistics.
In the first project, the NHS number, a unique identifier, and other common data items, such as the mothers’ and their babies’ dates of birth, were used to match the birth notification records to birth registration records for individual mothers and their babies. The methods and linkage rates are described in published articles. 5,6 This linkage, piloted using data about births in 2005, made it possible for the first time to analyse birth registration data on the basis of the gestational age at birth. The Office for National Statistics (ONS) has mainstreamed this linkage and uses the linked data to publish annual statistics, which have also been used for international comparisons by Euro-Peristat. 68 The linked data were also used for analyses of preterm birth rates in babies of black Caribbean and black African ethnicity who were born in England and Wales from 2005 to 2007 by their mothers’ countries of birth. These showed considerable differences between babies with mothers born in different parts of Africa. 122
In the second project, funded by the Medical Research Council (MRC) and also led by City, University of London, the previously linked data were further linked with the Maternity HES for England, and corresponding data for Wales. This meant that the birth data were linked to data about the onset of labour and mode of birth for most, although not all, women giving birth in the years from 2005 to 2007. 7,8,123 More generally, this linkage made it possible to analyse data about the care given at birth in relation to the parents’ sociodemographic background and also to variables such as birthweight and gestational age, which are poorly reported in Maternity HES.
These two projects laid a useful foundation for the work described in this report in which the techniques used previously were enhanced and used to link these data for births in the years 2005 to 2014. As morbidity in mothers and babies is also a matter of concern, the current project has extended the database by linking births to data about subsequent hospital admissions and readmissions of mothers and babies recorded in HES and the Patient Episode Database for Wales (PEDW).
While this project was under way, another project, Tracking the Impact of Gestational Age on health, educational and economic outcomes: a longitudinal Record linkage (TIGAR),124 was funded by the MRC and is being led by Maria Quigley of the National Perinatal Epidemiology Unit (NPEU). It is making use of birth and hospital data linked for this project about preterm births and subsequent hospital admissions of children. These data will be linked further to education data from the National Pupil Database for England, to look at the educational performance of children born preterm. Alison Macfarlane and Nirupa Dattani are among the co-investigators for the TIGAR project.
Our own project provided a unique opportunity to use previously unavailable data to identify any differences in outcome associated with ‘out-of-hours’ care for specific groups of women and babies, and to consider the impact of staffing levels. It was considered that this would provide a useful resource to inform the process of future reconfiguration and staffing of maternity services, including increases in consultant numbers, as well as providing some evidence of the impact of these processes on women’s experiences of care. The focus on reducing stillbirth by referring more women for induction of labour also makes it timely to have detailed data on this particular aspect of care.
Aims and objectives
Aims
To build on work done in a previous project to link data from civil registration, notification of birth to allocate NHS numbers to babies and data about care during delivery in order to analyse linked maternity and neonatal data for England and Wales about births in the years 2005–14 to compare daily, weekly and yearly variations in numbers of spontaneous and other births by time, day and season of birth and to compare variations in rates of adverse outcome.
Objectives
To achieve these aims, the objectives were to answer the following questions:
-
How do numbers of births vary depending on time of day, day of the week and time of year of birth and how does this relate to methods of onset of labour and delivery and multiplicity?
-
Subject to the availability of data, how do patterns of birth vary between maternity services in relation to variations in medical and midwifery staffing, patterns of intervention and size of unit?
-
How does the outcome of pregnancy in terms of rates of cause-specific intrapartum stillbirth and neonatal and infant mortality rates and rates of morbidity recorded at birth and at hospital admission in the first year of life vary depending on the time of day, day of the week and time of year of delivery in relation to gestational age and intervention in the onset of labour and delivery?
-
Have the patterns observed changed over the years 2005–14?
The project aimed to inform decision-making by providing information about how the numbers of births in England and Wales vary by time of day, day of week and day of the year. It separately analysed births before term and post-term births occurring after 42 weeks. In addition, it took account of whether labour and birth occurred spontaneously or whether their timing was affected by inducing labour or by undertaking either a planned caesarean section or an unplanned or ‘emergency’ caesarean section during labour, or before the onset of labour.
It was intended that the rates of death and severe problems in babies or their mothers would be analysed in relation to these factors and that the results would be related to information about midwifery and obstetric staffing in maternity units and NHS trusts and to their overall rates of induction and caesarean section. This information could have been used by the NHS in planning both levels of staffing in terms of midwives and obstetricians and in detailed rostering, with the aim of trying to match the numbers of women in labour and giving birth with the numbers of midwives available and the availability of specialist obstetric care should complications arise.
Challenges and barriers
There is a common misconception in some circles that administrative data are in the public domain and are readily available for analysis. In reality, especially in cases in which analyses draw on individual records, there are many protections in place, as well as administrative barriers, limiting access to such data to ensure the confidentiality of personally identifiable data. Although these protections are necessary, this can delay projects for many months and can make it impossible to complete scheduled research on time, as happened with this project.
In order to access the data, researchers are required to work in a controlled environment in which the security and confidentiality of the data are safeguarded. Researchers in this project used the ONS Virtual Microdata Laboratory (VML), which is run by an experienced and helpful team of staff, but which at the time of our project had an IT infrastructure inadequate to cope with a project of this scale. Many months of IT problems led to further delays. Further details and the impact of these barriers on the project, which made it impossible to complete it within the fixed-term funding period, are described in Appendix 1. Since 1 November 2017, after our funded project finished, the VML has been known as the Secure Research Service (SRS), but in this report we have retained the original name.
Chapter 2 Data acquisition and linkage, quality assurance and organisation
This chapter describes the data acquired for the project, the methods used to link the data and to assure the quality of the linkages when possible, together with the results of the linkages and the quality assurance. The many problems and setbacks that delayed this process are described in Appendix 1. The methods for analysing the data and the results of the analyses can be found in Chapter 3.
Study design
The study design was a retrospective birth cohort analysis of linked routinely collected data about births, maternity care in labour and at birth, and any subsequent hospital admissions of mothers or babies after birth. We used the REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement, the checklist of items extended from the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement, which should be reported in observational studies using routinely collected health data. 125 This can be found on the project’s page on the National Institute for Health Research (NIHR) Journals Library website. 126
Setting and population
The target population was the 7,013,804 registered births that occurred in England and Wales in the years 2005–14 (Table 1).
| Year | Number of births |
|---|---|
| 2005 | 649,371 |
| 2006 | 673,069 |
| 2007 | 692,653 |
| 2008 | 711,820 |
| 2009 | 709,434 |
| 2010 | 722,081 |
| 2011 | 723,339 |
| 2012 | 732,826 |
| 2013 | 701,376 |
| 2014 | 697,835 |
Data used in the project
When a baby is born in England and Wales, data are recorded in several separate information systems. When babies’ parents register the birth, mainly socio-demographic data are collected. A smaller set of data are recorded when the birth is notified to the NHS by the midwife or other birth attendant and the NHS number, a unique identifier, is issued. The ONS links the deaths of babies and children who die up to the age of 18 years with their corresponding birth registration records. It also links deaths of women occurring within a year of giving birth to the corresponding baby’s birth record. In addition, information on causes of maternal death, stillbirth and neonatal death is collected through the relevant confidential enquiries.
Data about care at delivery are recorded in the Maternity HES if the birth occurs in England. For births in Wales, data about care at delivery are recorded in PEDW, which is linked to the National Community Child Health Database (NCCHD). HES and PEDW collect data about all hospital admissions including maternity admissions.
The maternity datasets relevant to this project are described in more detail in the following sections, starting with the main data available for England and Wales as a whole, followed by the data available for England only or for Wales only, and finishing with additional datasets identified as being useful to add to our analyses.
Data for England and Wales
Birth registration
It is a legal requirement to register all live births within 42 days of birth. The definition of a live birth, the legal basis for registration, the process and a complete list of data items collected, are described in detail elsewhere. 127 The information is obtained, usually from one or both parents, by the local registrar of births, marriages and deaths. The local child health department passes some information from the birth notification it receives from the midwives to the registrar to verify the birth. This has included the baby’s birthweight since 1975 and the NHS number, since 2002, as described below.
The process for registration of stillbirths is similar to that for live births, except that registrars do not retain the NHS number for a stillbirth and the informant will also give the registrar a medical certificate of stillbirth completed by the attending midwife or doctor. This certifies the cause of death and includes an assessment of gestational age at birth and birthweight.
The information recorded at birth registration is collected centrally by the General Register Office and made available to the ONS for the production of statistics.
Birth notification
Since 1915, midwives or other birth attendants have been required to notify births to local health services. In the early 2000s, the route of notification changed so that NHS numbers could be issued to babies at birth instead of at registration, which could be up to 6 weeks later. To enable this, an interim system, the NHS Numbers for Babies (NN4B) service, was instituted in 2002 with a small dataset, which was of limited use on its own but contained important data items not available elsewhere. This provided the opportunity to obtain information such as time of birth, gestational age, a baby’s ethnicity and birth order within multiple births. Information on gestational age at birth is of key importance, as babies born preterm, that is before 37 completed weeks of gestation, are at particularly high risk of morbidity and mortality in early years of life. 128–130
Death registration
Baby and child deaths
All deaths should be registered within 5 days of occurrence and the person registering a death must produce a medical certificate of death completed by the medical practitioner who was present at, or examined the body after, death. Since 1975, deaths of babies before they reach the age of 1 year have been routinely linked to their corresponding birth registration records. The linkage was extended in the 1990s and the ONS now links deaths of all children aged under 16 years born from 1993 onwards to their birth records.
Maternal deaths
Since 1994, deaths of women within a year of giving birth are linked to the corresponding births by the ONS for use in confidential enquiries into maternal deaths.
Data for England only
Maternity Hospital Episode Statistics
Maternity HES contain data for births occurring in NHS hospitals in England. It is not designed to collect data about births in private or other hospitals, at home or elsewhere, even though it was originally envisaged that information about all births should be compiled. 131 HES includes a range of information on care at birth such as the mode of onset of labour and birth clinical complications, gestational age and the mother’s ethnicity as well as information about the baby, such as date of birth, sex, birthweight and geographical information on where the baby was born.
There are two types of maternity records in HES: the delivery record and the birth record. Both types of records consist of a core Admitted Patient Care (APC) record with an additional 19 fields, in an appended baby ‘tail’, also known as a ‘maternity tail’.
The HES delivery record is a mother-based record containing the mother’s details with a baby tail, which can accommodate up to nine babies born in one delivery episode. In contrast, the birth registration and notification linked data consist of one record per baby.
A HES birth record is generated for the baby. It contains the baby’s details and it also has a baby tail containing the same type of information that is recorded in the corresponding baby tail of the mother’s delivery record. It is also sometimes referred to as a HES baby record.
The baby tail data coverage is not as complete as the rest of the HES data. There are a number of reasons for the incompleteness and data quality issues, such as:
-
Trusts submitting a significantly higher number of delivery episodes than birth episodes.
-
Trusts failing to submit data on the number of birth episodes where they record a high number of delivery episodes.
-
Trusts failing to submit any delivery records. This can happen when trusts have standalone maternity systems that are not linked to their hospital systems.
The HES Patient Identifier (HESID) is a pseudonymised number used to uniquely identify a patient without the necessity of viewing or using patient-identifiable information such as the NHS number. This identifier can be used to track patients through the HES database or for linkage to other datasets such as mortality. HESID is derived using a matching algorithm that looks at various combinations of the following patient-identifiable fields:
-
NHS number
-
date of birth
-
sex
-
postcode
-
local patient identifier.
The HESIDs are stored nationally in the HES index. This is updated monthly and older versions are not kept.
For each episode of care with a particular consultant or midwife, a HES record is created, but each time this record is updated with new information, a new version of the record can be created. As a result, several versions of the HES record for the same episode of care are created.
Data for Wales only
Patient Episode Database for Wales
The Patient Episode Database for Wales (PEDW) is a database of individual hospital patient records. It includes all records of inpatient and day case activity in the NHS in Wales and data on Welsh residents treated in English NHS trusts. In 1997, the mandated inpatient and day case dataset was changed to the APC record used in Maternity HES. The decision to adopt the APC was to align the Welsh inpatient and day case dataset with that of England to allow benchmarking. The APC contains demographic, clinical and administrative data items, such as the age and sex of the patient and the diagnostic and operative procedures undertaken during the episode of care in hospital.
The APC extracts received from the Welsh NHS organisations and from English NHS organisations that treat Welsh residents are used to update the PEDW.
Individual records are submitted to the PEDW on the basis of a patient’s consultant episode, which is a record of the care an admitted patient receives in the continuous care of one consultant within one Local Health Board. If the patient is transferred to the care of another consultant, either in the same or another specialty or if they are transferred to another Local Health Board for continuing inpatient care, another consultant episode will start and another PEDW record will be generated. 132
Patients whose episodes are captured by the PEDW are classified as inpatients, day cases, maternity patients and regular attendees. A maternity patient is defined as a pregnant or recently pregnant woman admitted to a maternity ward including delivery facilities. Every hospital birth in Wales should have a PEDW record. The record consists of general information, diagnosis and procedure information for the mother. A maternity tail is attached to each general record for each baby born and contains fields with data relating to the relevant mother and babies. The completeness and quality of data in the maternity tail of the record are known to be poor. 133
National Community Child Health Database
The NCCHD is Wales’ first national community child health system and contains anonymised records for all children born after 1987 who were resident, or treated, in Wales. It has been created by bringing together selected information from locally managed community child health databases. Since 2002, community child health database records have been initiated from the birth notification records but may subsequently be amended locally. The database has been used to produce maternal and child health statistics for Wales, as well as to support the administration of child immunisation and health surveillance programmes. From 2017, however, annual published maternity statistics for Wales were produced using a new Maternity Indicators DataSet. 134
Additional data
Centre for Maternal and Child Enquiries, England and Wales
Prior to 2012, the Centre for Maternal and Child Enquiries (CMACE) collected epidemiological and clinical data on all stillbirths and neonatal deaths in England, Wales, Northern Ireland, the Crown Dependencies of the Channel Islands and the Isle of Man. These data were collected by a network of local health professionals co-ordinated by the CMACE local offices. Data were compiled centrally and cross-matched with statutory registration data on stillbirths and neonatal deaths from the ONS. A key part of CMACE’s work was the perinatal mortality surveillance system. The aim of this was to ensure that all data collected on stillbirths and neonatal deaths were validated, analysed and published in reports. Since 2012, this work has been done by MBRRACE-UK. 15
Workforce data
Data compiled by the NHS for England and Wales separately
There are no routinely collected data about numbers of staff on duty by time of day and day of the year.
Other staffing data that are available come from the annual medical and non-medical workforce censuses of numbers and full-time equivalent staff in post in England and in Wales on 30 September each year. In England, these data are available only for trusts as a whole rather than for each maternity unit within a trust.
In England, annual workforce censuses were superseded by monthly workforce data for management purposes, which have been compiled since 2009. These were incomplete at the outset and changes were made over the time period. The primary area of work, that is ‘obstetrics and gynaecology’, may be subdivided into secondary and tertiary areas such as obstetrics, gynaecology, maternity and neonatal intensive care. ‘Fetal medicine’ was categorised separately. Thus, although midwives can be identified by their occupation codes, it is unclear to what extent doctors, nurses and other staff working in obstetrics and gynaecology are involved in maternity care.
Data from professional organisations
The RCOG compiles two-yearly reports based on asking each maternity unit to report on numbers of consultants in post and numbers of Specialty Trainees. The RCOG census for 2011 reported that data for earlier years were incomplete, but this report and the report for 2013 indicate those units that satisfy the RCOG’s recommendations for consultant staffing. 135,136
The Royal College of Paediatrics and Child Health (RCPCH) has been undertaking two-yearly censuses of the paediatric workforce since 1999, which include information about UK neonatal staffing. 137
Data acquired for the project
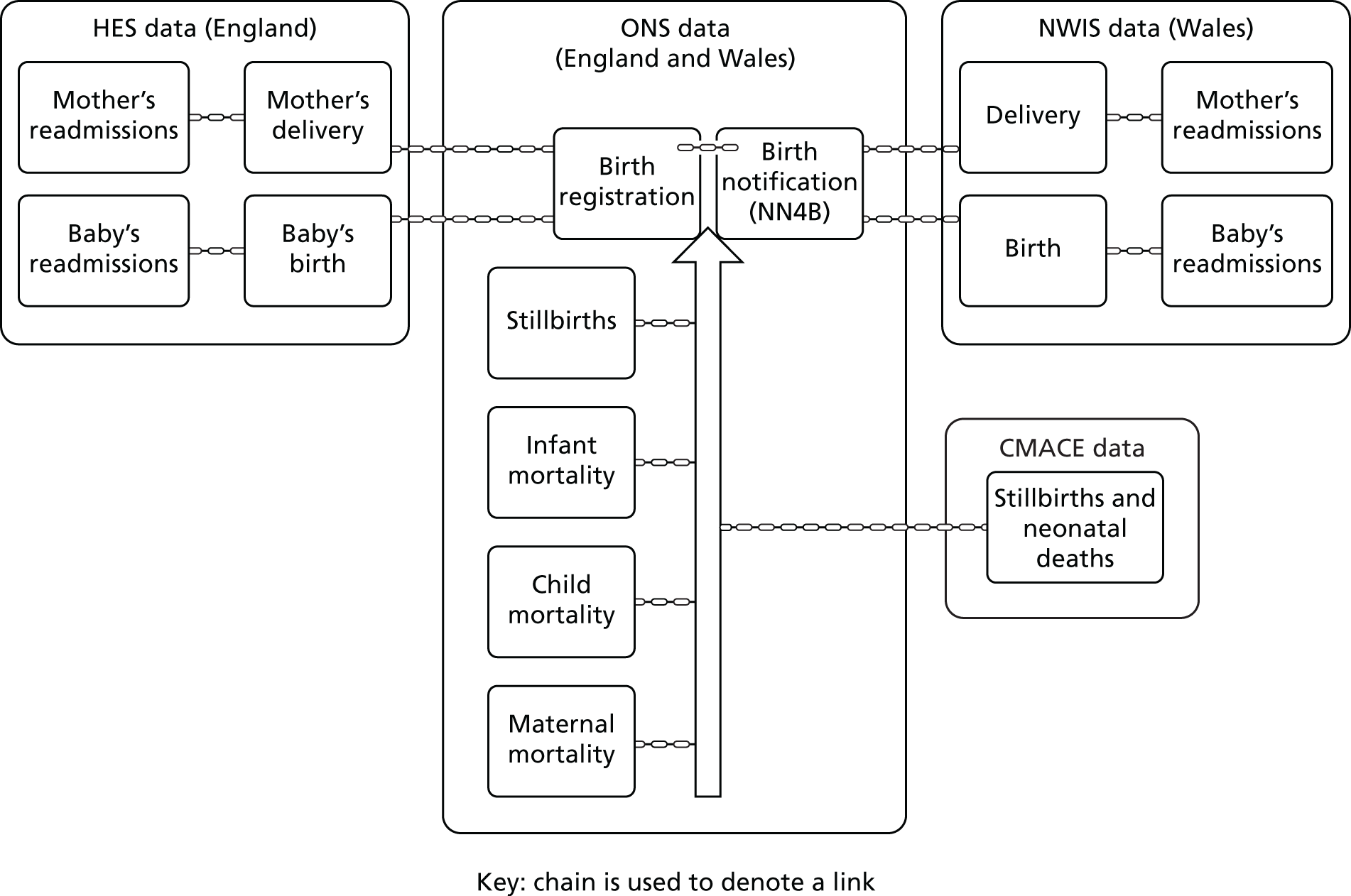
An overview of the datasets used in the project is shown in Figure 1 and the data acquired are summarised in Table 2.
FIGURE 1.
Overview of datasets used in the project. NWIS, NHS Wales Informatics Service.
| Name of dataset | Source | Years of birth | Coverage |
|---|---|---|---|
| Data from civil registration | |||
| Birth registration linked to birth notification | ONS | 2005–14 | All births in England and Wales |
| Maternal deaths linked to births | ONS | 2008–14 | Deaths of women of childbearing age within a year of giving birth in England and Wales linked to births |
| Infant deaths linked to births | ONS | 2005–14 | Deaths in the first year of life of babies born in England and Wales linked to birth records |
| Childhood deaths linked to births | ONS | 2005–14 | Deaths of children aged 1 year or over born in England and Wales linked to birth records |
| Stillbirths reported to confidential enquiries | CMACE | 2005–9 | England and Wales |
| Neonatal deaths in England and Wales reported to confidential enquiries | CMACE | 2005–9 | Neonatal deaths in England and Wales reported to confidential enquiries |
| Hospital data | |||
| Maternity HES | HSCIC | 2005–14 | England: linked and unlinked delivery and birth records |
| HES | HSCIC | 2005–14 | England: subsequent admissions of babies |
| HES | HSCIC | 2005–14 | England: subsequent admission of mothers |
| NCCHD/PEDW | NWIS | 2005–14 | Wales: linked and unlinked records |
| PEDW | NWIS | 2005–14 | Wales: subsequent admissions of babies |
| PEDW | NWIS | 2005–14 | Wales: subsequent admission of mothers |
| Workforce data | |||
| Annual workforce census | HSCIC | 2005–14 | England: aggregated annual census of numbers of staff by staff group and trust |
| Annual workforce statistics | NWIS | 2005–14 | Wales: aggregated annual census of numbers of staff by staff group and trust |
Birth registration and birth notification (‘ONS birth records’)
As a result of a project led by City, University of London, to link birth registration data with the birth notification dataset,5 the ONS now routinely links these two datasets and uses the linked data in its annual publications. 138 Linked data from this source for the years 2005–14 were provided to the project (see Figure 1). Linked birth registration/birth notification records are referred to in this report as ‘ONS birth records’.
Linked-in mortality data
Data from death registration had already been linked to ONS birth records (see Figure 1).
Data about deaths of babies under 1 year of age, linked to the corresponding ONS birth record, were provided to the project by the ONS for births in 2005 to 2014. The ONS also provided data for deaths at 1 year or over of age of children born from 2005 to 2014 occurring up to the age of 9 years.
The ONS provided records of deaths of mothers within a year of giving birth linked to the corresponding ONS birth records for births from 2008 onwards.
Data for linkage
Maternity Hospital Episode Statistics
We made an application to the HSCIC, now known as NHS Digital, for HES data for the financial years from 1 April 2004 to 31 March 2015 to cover the ONS calendar year data for 2005–14. We applied for delivery ([EPITYPE] = 2 or 5) and birth ([EPITYPE] = 3 or 6) records. The lists of fields requested are shown in Appendix 2 (see Tables 39, 41, 45, 52 and 57). We also requested mothers’ and babies’ non-delivery records. For mothers, this consisted of antenatal admissions, postnatal admissions and admissions unrelated to maternity. For babies, this included postnatal admissions and subsequent admissions unrelated to the child’s birth, for example as a result of accidents.
Patient Episode Database for Wales/National Community Child Health Database
Information from NCCHD and PEDW was provided by the NHS Wales Informatics Service (NWIS). As for HES, data were received from PEDW for financial years from 1 April 2004 to 31 March 2015. Data items included demographic and administrative fields as well as clinical fields, such as diagnoses and operative procedures during the delivery episode. NCCHD data included information about gestational age, onset of labour, the number of babies born and each baby’s birthweight, sex, live birth or stillbirth status, mode of delivery, ethnicity, birth location, breastfeeding at birth and breastfeeding at 6/8 weeks.
Centre for Maternal and Child Enquiries
Centre for Maternal and Child Enquiries data without patient identifiers, such as the NHS number, date of birth and postcode, were available for the years 2005–9 from the Healthcare Quality Improvement Partnership (HQIP). These records were acquired for linkage to ONS stillbirth records to distinguish between antepartum and intrapartum stillbirths and also to ONS neonatal death records.
Data to be used in future analyses
Workforce data
As there are no routinely collected data about numbers of staff on duty by time of day and day of the year, the only way such data could be obtained would be by doing an extensive and expensive prospective data collection exercise. In the absence of such data, we identified the available data with the aim of using them to assess overall levels of staffing.
We identified the NHS annual medical and non-medical workforce censuses of numbers and full‐time equivalent staff data for England and planned to download them from the HSCIC website. We downloaded the data for Wales, which are held online in open data format. Our plan was to send these aggregated data to the VML, so that we could use them in our location-based analysis.
We had been advised by reviewers to consider using the monthly workforce data. The underlying data themselves are available only to designated NHS staff, although aggregated monthly data are published online by the HSCIC. We discussed them by telephone with a relevant member of HSCIC staff as well as downloading files for selected months. The data were not available for the whole period we were studying and were incomplete at the outset and changes were made over time. More fundamentally, the way in which the workforce data were categorised by areas of work made it difficult to distinguish between staff working in maternity care and staff working in gynaecology.
We took advice from the member of RCOG staff responsible for its workforce censuses and downloaded the data. We planned to take advice about use of the RCPCH workforce censuses.
Record linkage
This section describes the main data linkages undertaken in the project, starting with the largest dataset, the linkage of ONS records of births occurring in England with Maternity HES, and the quality assurance of this linkage, described in detail in Quality assurance of the linkage to delivery records. This is followed by the linkage of ONS birth records of births occurring in Wales with PEDW/NCCHD records. Finally, we provide a description of linkage of stillbirths and neonatal deaths among births registered in England and Wales with the CMACE data. These linkages are summarised in Appendix 2 (see Table 34).
Linkage of ONS birth records for England with Maternity HES delivery records
Linkage identifiers and algorithms
Several variables are common to all three data sources, as can be seen in Table 3. In addition, some data items are unique to each data source and linkage enables new analyses using these combined data. For example, it is now possible to compare time of birth with birth outcomes and to report on the outcomes of birth by type of care at birth in terms of onset of labour and mode of delivery by gestational age, time of day and day of the week.
| Data items | Data sources | ||
|---|---|---|---|
| Birth registration | Birth notification | Maternity HES | |
| Baby’s NHS number | ✓ | ✓ | ✓ |
| Mother’s NHS number | ✓ | ✓ | |
| Birth date of baby | ✓ | ✓ | ✓ |
| Delivery time | ✓ | ||
| Birthweight | ✓ | ✓ | ✓ |
| Gestational age (stillbirth) | ✓ | ✓ | ✓ |
| Gestational age (live birth) | ✓ | ✓ | |
| Sex of baby | ✓ | ✓ | ✓ |
| Number of babies born | ✓ | ✓ | ✓ |
| Live or stillbirth | ✓ | ✓ | ✓ |
| Parity/number of previous childrena | ✓ | ✓ | |
| Baby’s/mother’s postcode of usual residence | ✓ | ✓ | ✓ |
| Ethnic category of baby | ✓ | ||
| Ethnic category of mother | ✓ | ||
| Country of birth of mother | ✓ | ||
| Country of birth of father | ✓ | ||
| Parents’ socio-economic status | ✓ | ||
| Type of delivery place | ✓ | ✓ | ✓ |
| Mother’s date of birth | ✓ | ✓ | ✓ |
| Marital status of mother | ✓ | ||
| Method of delivery | ✓ | ||
| Complications in pregnancy | ✓ | ||
Patient identifiers, including the mother’s and baby’s NHS numbers [NHSNO], postcode of residence [POSTCODE], the mother’s and baby’s [DoB] and baby’s sex [SEX] together with a unique record identifier [ONS_id] were extracted by the ONS from the linked birth registration and notification file if the place of birth was England and sent to the data linkage team at the HSCIC.
The linkage algorithm that had been previously used to link births in 2005–77 was used to link further data for the years 2008–14. ONS identifiers were first linked to the most recent version of the HES index to obtain the HES patient identifiers known as [HESID]s. 139 These were then linked to the HES delivery records. The number of ONS birth records linked to more than one HES delivery record was, however, very much higher than it had been when the data for 2005–7 were linked. The HSCIC therefore recommended using its in-house linkage algorithm, which is used routinely to link ONS death registration data to HES140 apart from step 8 of its algorithm, which was replaced with a step where only the NHS number was matched, as shown in Table 4. A pilot study was carried out using the 2005 data and the number of duplicate HES delivery records linked to the ONS birth record, and the linkage rate was ascertained before data for 2006–14 were linked. The same algorithm was used to link ONS birth records to HES birth records.
| Step | NHSNO | DOB | SEX | POSTCODE | Additional information |
|---|---|---|---|---|---|
| 1 | Exact | Exact | Exact | Exact | |
| 2 | Exact | Exact | Exact | ||
| 3 | Exact | Partial | Exact | Exact |
Two components (i.e. YYYY, MM, DD) of the two date of birth values match or two components of the two date of birth values match when the MM and DD parts of one of them are swapped |
| 4 | Exact | Partial | Exact | ||
| 5 | Exact | Exact | |||
| 6 | Exact | Exact | Exact | Where NHSNO does not contradict the match and date of birth is not 1 January and the postcode is not in the ‘ignore’ list | |
| 7 | Exact | Exact | Exact | Where NHSNO does not contradict the match and date of birth is not 1 January | |
| 8 | Exact |
The linked data provided by the HSCIC consisted of four files with data for the financial years 2004/5 to 2014/15. One file contained [ONS_id] linked to HES delivery records, a second file consisted of [ONS_id] linked to HES baby records, a third file consisted of [ONS_id] linked to [HESID] and a fourth file contained unlinked HES delivery and birth records.
Results
For the pilot study using the 2005 data, the file sent to the HSCIC by the ONS consisted of identifiers for the 617,613 babies who were either born in England or whose mother was resident in England. The resident in England category was used for births in the ONS linked dataset that occurred at home. The HSCIC first linked these to the HES index to get the [HESID] and then to the HES delivery records. The file returned to the ONS consisted of 624,326 ONS birth records linked to a [HESID] and a second file of 582,963 ONS birth records that were linked to a HES delivery record. This included 25,188 records in which the ONS birth record was linked to more than one HES delivery record (Table 5).
| Year | Number of births from the ONS | Number of ONS birth records linked to HES delivery records (excluding duplicate HES delivery records) | Number of duplicate HES delivery records (i.e. more than one HES delivery record per ONS birth record) | Never linked to HES delivery record | Percentage linked | Linked HES delivery records after quality assurance process | Percentage linked after quality assurance |
|---|---|---|---|---|---|---|---|
| 2005 | 617,613 | 582,963 | 25,188 | 34,650 | 94.4 | 571,775 | 92.6 |
| 2006 | 640,271 | 607,649 | 23,582 | 32,622 | 94.9 | 592,028 | 92.5 |
| 2007 | 659,061 | 632,039 | 27,207 | 27,022 | 95.9 | 614,542 | 93.2 |
| 2008 | 676,999 | 655,511 | 24,192 | 21,488 | 96.8 | 640,900 | 94.7 |
| 2009 | 675,330 | 657,622 | 40,575 | 17,708 | 97.4 | 642,508 | 95.1 |
| 2010 | 687,100 | 673,566 | 50,086 | 13,534 | 98.0 | 662,014 | 96.3 |
| 2011 | 688,681 | 674,751 | 45,005 | 13,930 | 98.0 | 663,135 | 96.3 |
| 2012 | 698,457 | 681,677 | 41,373 | 16,780 | 97.6 | 668,055 | 95.6 |
| 2013 | 668,433 | 651,957 | 42,656 | 16,476 | 97.5 | 641,108 | 95.9 |
| 2014 | 664,967 | 647,047 | 46,932 | 17,920 | 97.3 | 635,692 | 95.6 |
| Total | 6,676,912 | 6,464,782 | 366,796 | 212,130 | 96.8 | 6,331,757 | 94.8 |
Using the revised linkage algorithm reduced the number of ONS birth records linked to more therefore than one HES delivery record from 6% to 4%. Data for births in 2006–14 were therefore then linked to HES delivery records using the revised linkage algorithm shown in Table 4.
In the pilot study using 2005 data, around 66% of the previously linked ONS birth registration and notification records were linked to the HES delivery records in stage 1 of the linkage algorithm shown in Table 6. This matched records that had the same mother’s NHS number, the exact mother’s date of birth, sex and full postcode. A further 29% of the ONS birth records were matched to HES delivery records using the exact mother’s date of birth, postcode of residence of the mother and sex (stage 6 of the algorithm). About 5% of the records were linked using a combination of the mother’s NHS number, exact or partial date of birth, sex and postcode. ONS birth records that were not linked to HES accounted for 3% of all records.
| Year | Match rank (%) | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
| 2005 | 66.0 | 2.6 | 1.0 | 0.1 | 0.9 | 28.8 | 0.6 | 0.1 | 100.0 |
| 2006 | 69.4 | 2.6 | 1.0 | 0.1 | 1.2 | 25.1 | 0.5 | 0.1 | 100.0 |
| 2007 | 73.5 | 2.9 | 1.2 | 0.1 | 0.5 | 21.3 | 0.4 | 0.0 | 100.0 |
| 2008 | 77.3 | 2.9 | 1.3 | 0.1 | 0.4 | 17.6 | 0.4 | 0.0 | 100.0 |
| 2009 | 81.7 | 2.8 | 1.4 | 0.1 | 0.3 | 13.4 | 0.3 | 0.0 | 100.0 |
| 2010 | 85.5 | 2.5 | 1.5 | 0.1 | 0.3 | 10.0 | 0.2 | 0.0 | 100.0 |
| 2011 | 88.2 | 2.5 | 1.5 | 0.1 | 0.3 | 7.2 | 0.2 | 0.0 | 100.0 |
| 2012 | 90.5 | 2.5 | 1.6 | 0.1 | 0.3 | 4.9 | 0.1 | 0.0 | 100.0 |
| 2013 | 92.0 | 2.5 | 1.7 | 0.1 | 0.2 | 3.5 | 0.1 | 0.0 | 100.0 |
| 2014 | 92.7 | 2.7 | 1.8 | 0.1 | 0.3 | 2.5 | 0.1 | 0.0 | 100.0 |
Linkage of ONS birth records to HES delivery records for births from 2005 to 2014 showed that the number of records linked using stage 1 of the algorithm increased from 66% in 2005 to 92.7% in 2014. There was a corresponding decrease in the number of records linked in stage 6 of the algorithm, which does not use the mother’s NHS number, from 28.8 to 2.5% (see Table 6).
For each year’s births, on average about 36,000 ONS birth records, ranging from 23,582 to 50,086, were linked to more than one HES delivery record and the quality assurance procedure described in Quality assurance of the linkage to delivery records selected the most appropriate of these linked records to be maintained for analysis. This resulted in 92–6% of the ONS birth records being linked to the correct HES delivery record after quality assurance (see Table 5).
Linkage bias
To check for linkage bias, the distributions by multiplicity, age of mother, ethnicity and region of residence of numbers of records that linked to HES delivery records and those that did not were compared and are shown in Appendix 2 (see Table 28). Although the linkage rate increased from 94% in 2005 to 97% in 2014 (see Table 5), there were statistically significant differences between the distributions. The linkage rate was 3% lower for multiple births, 2% lower for babies with mothers aged under 15 years and 3% lower for those with mothers aged 40 years and above. Over 2% of babies of black African ethnicity were not linked to Maternity HES. More than 98% of the babies whose mothers were resident in the East Midlands, North West, South Central, South West, West Midlands, and Yorkshire and the Humber regions were successfully linked to Maternity HES, but this proportion was slightly lower, at 95%, among babies whose mothers were resident in London.
Linkage of ONS birth records for England with Maternity HES birth records
Linkage identifiers and algorithms
The identifiers and algorithm and methods for linking HES birth records to ONS birth records were the same as for the linkage to HES delivery records described above (see Tables 3 and 4).
Results
The HES birth records were much more straightforward to link than the delivery records as this involved a one-to-one link between an ONS birth record and a HES birth record. The numbers of HES birth records linked to ONS birth records, for each year from 2005 to 2014, were higher than the numbers of HES delivery records linked to the ONS birth records (Table 7).
| Year | Numbers of births from the ONS | ONS births linked to HES birth records | Percentage linked |
|---|---|---|---|
| 2005 | 617,613 | 609,778 | 98.73 |
| 2006 | 640,271 | 633,183 | 98.89 |
| 2007 | 659,061 | 651,551 | 98.86 |
| 2008 | 676,999 | 668,967 | 98.81 |
| 2009 | 675,330 | 669,926 | 99.20 |
| 2010 | 687,100 | 682,261 | 99.30 |
| 2011 | 688,681 | 683,768 | 99.29 |
| 2012 | 698,457 | 693,221 | 99.25 |
| 2013 | 668,433 | 662,963 | 99.18 |
| 2014 | 664,967 | 659,192 | 99.13 |
Quality assurance of the linkage to delivery records
This section describes the extensive quality assurance process for the linked HES delivery records and ONS birth records only. Similar quality assurance of the linked HES birth records and ONS birth records could not be achieved within the project time scale. The aim was to assess the linked records to efficiently identify and preserve one correctly linked HES delivery record with the maximum amount of delivery information from all possible links to create a file to be used in analysis.
Only the ONS birth records that linked to a mother’s [HESID] and HES delivery record could be quality assured. There were instances where the linkage algorithm did not link an ONS registered birth to a HES delivery record. This could be because no delivery record existed. For example, the majority of home births and births in private health facilities are not usually captured by HES. In addition, some trusts may not have submitted HES data at particular times, possibly if they were experiencing problems with their IT systems. There may also have been a linkage error. Overall, 1.7% of singleton and 4.3% of multiple ONS birth records without a link to a HES delivery record did have a link to the mother’s [HESID]. There has not been time to investigate these problems further.
The quality assurance work was carried out in the secure environment of the ONS VML. Microsoft Access® (Microsoft Corporation, Redmond, WA, USA) database software was used as it was the only database software available in the VML at that time, and Structured Query Language (SQL) code was used for replicability. The relatively large size of the data files and restrictions on database size and processing speed constrained the design of the methods used. These are described further in Appendix 1.
Data preparation and data quality checks are described in Appendix 2.
A pilot was initially carried out on data for 2005 to help formulate the methodology. The procedure described below in this section is the final version that was used for the linked ONS births and HES delivery data for births in all of the 10 years. Clerical checks were carried out throughout the development phase using relevant variables and identifiers to inform and improve the procedure.
To determine which links to preserve or discard, the links between the ONS birth records and HES delivery records were categorised either as ‘same mother same baby’ or ‘same mother different baby’. The latter category accounts for instances in which the same mother has given birth to another baby within the 10-year study period. The category ‘wrong link’ was used when neither of the previous categories applied, suggesting incorrect maternal linkage or data quality problems. These scenarios are summarised in Table 8. They exclude occasions when a birth registration record did not link to any HES delivery records.
An ONS birth record may link to one correct or incorrect HES delivery record, or to more than one HES delivery record. Reasons for one, none or some of these records being correct are shown in Table 8.
| Category | Summary | Details | Action |
|---|---|---|---|
| SMSB | ONS birth record linking to one relevant HES delivery record | One-to-one linkage as expected | Keep link |
| SMSB | ONS birth record linking to many relevant HES delivery records, with no clear episode order sequence | Due to duplicate HES records, or pre- and post-delivery HES records |
Keep link to one of the duplicates or the most appropriate delivery record Move others to unlinked file |
| SMSB | ONS birth record linking to many relevant HES records, with a clear episode order sequence | Due to multiple episodes as part of a hospital spell |
Keep link to one episode record and maximise delivery information Move others to unlinked file |
| SMDB | ONS birth record linking to one or more incorrect HES delivery record (same mother) | Another birth to the same mother within the study period | Move to unlinked file |
| WL | ONS birth record linking to one or more incorrect HES delivery record | The maternal linkage is incorrect or poor data quality | Move to unlinked file |
The quality assurance exercise aimed to keep ‘same mother same baby’ linked records and move all others to the unlinked file. If more than one correct link was available, only one linked delivery record containing the maximum amount of delivery information was chosen. This was to create a one-to-one relationship and support ease of analysis.
Baby data items were compared to ascertain that the linked records related to the same baby. These were the baby’s date of birth, sex, gestational age, birthweight and location of birth.
The codes used for locations of birth differed between the datasets and also varied over time as a result of organisational changes within the NHS. These were translated into a consistent common location code, the ‘derived location code’, and allocated to an ‘assigned trust’ designed specifically for the study, as described in Derivation of variables and in Appendix 2. Lookup tables were created to map all the location of birth codes ([CESTRSS] from birth registration records, [ORGCODEZ] from birth notification records and [PROCODE]/[SITETRET] combinations from HES delivery records) to ‘assigned trusts’. If ‘assigned trusts’ matched, this indicated a linkage match. This proved to be a test that was too sensitive, resulting in too many false negatives where the assigned trust of birth did not match when all the other baby items matched. This may have resulted from women transferring between nearby units or coding conventions between trusts in a local neighbourhood. A further lookup table was therefore created, which resulted in a ‘geographic match’ where the main OU in a trust was within 25 miles of an OU within another trust. This distance was reduced to 10 miles for London, and greater distances were used in rural areas such as Wales and South West England. This was developed using latitude and longitude co-ordinates from the BirthChoiceUK maternity unit database (used with the permission of Rod Gibson Associates Ltd) to calculate a matrix of distances between each trust’s OU. Home births and births taking place elsewhere were designated geographic matches by default as the codings in the birth notification and HES datasets did not distinguish these birth locations well.
Four combinations of the baby data items were used to check whether or not a linked ONS birth record and HES delivery record related to the same baby, in order of decreasing certainty from 1 to 4, as shown in Table 9. Combination 1 required all the data items to match. Combination 2 required geographic location and date of birth to match plus either birthweight or gestational age or sex. Combination 3 required only geographic location and date of birth to match and birthweight, gestational age and sex will not match in these cases. Combinations 2 and 3 took into account the high occurrence of missing values and poor data quality in HES. Combination 4 accounted for a degree of data entry error in the date of birth by allowing it to differ by up to 4 days, but only if backed up by a matching geographic location of birth, and with birthweight, gestational age and sex not differing very much between ONS and HES if the values were present. If they were different and the date of birth was not an exact match, it was considered to be a different baby. The four combinations were applied in order so that the most reliable matches were identified first.
| Combination | ONS birth record and HES delivery location of birth matches | ONS birth record and HES delivery baby date of birth matches | ONS birth record and HES delivery birthweight matches | ONS birth record and HES delivery gestational age matches | ONS birth record and HES delivery sex of baby matches | ||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | Exact | and | Exact | and | Exact | and | Exact | and | Exact |
| 2 | Exact | and | Exact | and | Exact | or | Exact | or | Exact |
| 3 | Exact | and | Exact | ||||||
| 4 | Exact | and | Differs by up to 4 daysa | and | Missing or not completely different | and | Missing or not completely different | and | Missing or not completely different |
If the linked records referred to the same baby and there was more than one linked HES delivery record to choose from, then the record with the most onset of delivery and delivery method information was chosen, as these variables were of key importance for the analysis. The presence of valid values in these and other fields were used to inform this.
The procedure was implemented using deterministic stepwise rules to be carried out in order, with any linked records dealt with at each stage excluded from subsequent stages. A summary is given in Box 1. Fuller details are provided in Appendix 2 (see Table 29). It differed slightly between singleton and multiple births to account for the greater complexity of linkage of multiple births.
-
Exclude links to invalid HES delivery records.
-
Exclude links to surplus × 6 or × 9 duplicate HES delivery records.
-
Exclude links to HES delivery records where the HES baby date of birth is too far away from the ONS baby date of birth to be the same birth.
-
Keep if baby data items match.
-
Exclude if baby data items do not match.
-
Keep episode if baby data items match and contains maximum delivery information.
-
Exclude episode(s) if baby data items do not match and/or episode contains less delivery information.
-
Keep record if baby data items match with latest episode dates.
-
Exclude record(s) if baby data items do not match and/or earlier episode dates.
-
Keep record if baby data items match and contains maximum delivery information.
-
Exclude record(s) if baby data items do not match and/or contains less delivery information.
The first two rules cleaned the HES delivery data by eliminating invalid linked records and duplicates. It is known that some trusts generate multiple copies of the same delivery episode record, usually six or nine copies of the same record. In these cases, only one was kept to be quality assured and the others were discarded for efficiency.
Once all rules in the procedure had been carried out, it was confirmed that all linkages had been assigned a decision, and that there were no more records to check.
Further checks were made on the following:
-
Private hospital births should not have a link to a HES delivery record unless the mother or baby were later transferred to a NHS hospital for any reason.
-
Each HES delivery record should link to the correct number of ONS birth records depending on whether it is for a singleton or multiple delivery.
-
The baby’s date of birth in the ONS birth record should fall within the HES delivery admission period. This was not always the case even when it was a confident link. The check could not be made for home births as there were no admission dates.
-
If there was more than one correct and relevant linked HES delivery record for an ONS birth record, any missing onset of delivery and method of delivery information was filled in from these.
The quality assurance procedure took the equivalent of 55 working days for singleton births and 16 days for multiple births. Microsoft database software and processing limitations of the VML at that time slowed the procedure down. Microsoft SQL Server has since been made available in VML and would speed up this process considerably.
Seventeen per cent of linked records for singleton births were dealt with in the first two cleaning stages, and a further 80% were dealt with by rules 3 and 4. All the remaining rules were required to deal with the residual 3% of more complex cases.
Five per cent of linked records for multiple births were dealt with in the first two cleaning stages, and a further 60% were dealt with by rules 3 and 4. This left 35% as residual records, reflecting the greater complexity inherent in records of multiple births.
For each year of birth, the complex residual cases were clustered within particular trusts. This was probably attributable to IT problems and changes to systems in those trusts.
A summary of the results for singleton and multiple births by calendar year is given in Appendix 2 (see Table 30).
Of the total 6,468,586 singleton ONS birth records, 97% had been linked to one or more HES delivery records and could be quality assured. Of these, 98% remained linked to one HES delivery record and 2% had all HES links discarded after quality assurance. Ninety-five per cent of all ONS singleton birth records overall were left with a link to a HES delivery record for analysis.
Of the 208,326 multiple births, 95% were linked to one or more HES delivery records and could be quality assured. Of these, 98% remained linked to one HES delivery record and 2% had all HES links discarded after quality assurance. Ninety-three per cent of all ONS multiple birth records overall were left with a link to a HES delivery record for analysis.
For singleton births, the percentage of all birth records left linked to one HES delivery record after quality assurance increased fairly consistently over time, from 93% in 2005 to 95% in 2014. For multiple births, the rate increased from 94% in 2005 to 97% in 2010, but then started to decrease again to 87% in 2014. This reflects the same patterns as the percentage of ONS birth records that were originally linked to a HES delivery record and are biased by the number of records that linked to a [HESID] but not that delivery record, were excluded from quality assurance.
The majority (76%) of the discarded linked records for singleton births were attributable to duplicate copies of HES delivery episodes and were dealt with in the preliminary cleaning stage of the quality assurance procedure. The remaining reasons for discarding links are discussed in detail in Appendix 2. Of interest are the 4,854 links categorised as ‘no-matches’. Although they are relatively small in number, they give insight into linkage error and quality assurance error. Some missed links were also discovered, raising further questions about the quality of the linkage, discussed in Appendix 2. General insights into data quality issues that were revealed by the quality assurance are also given.
Certain features were more common in incorrectly linked records than in correctly linked ONS birth records. These included births linked using a less reliable stage of the linkage algorithm that excludes the NHS number, births at home and in the London region, and births where the birthweight or gestational age was missing in HES. This suggests some bias in the linkage and often relates to data quality issues. These patterns differed between singleton and multiple births. Fuller details are given in Appendix 2.
Quality assurance of HES birth records linkage
The quality of linkage of the baby file has yet to be assessed.
Linkage of ONS birth records for Wales to Patient Episode Database for Wales/National Community Child Health Database
Linkage identifiers and algorithms
A number of variables are common to all the four sources of data for Wales (birth registration, birth notification, PEDW and NCCHD) as can be seen in Table 10. In addition, some data items are unique to each data source and linkage enables new analyses using these linked data.
| Data items | Data sources | |||
|---|---|---|---|---|
| Birth registration | Notification | NCCHD | PEDWa | |
| Baby’s NHS number | ✓ | ✓ | ✓ | |
| Mother’s NHS number | ✓ | ✓ | ✓ | |
| Birth date of baby | ✓ | ✓ | ✓ | ✓ |
| Delivery time | ✓ | ✓ | ||
| Birthweight | ✓ | ✓ | ✓ | |
| Gestational age (stillbirth) | ✓ | ✓ | ✓ | ✓ |
| Gestational age (live birth) | ✓ | ✓ | ✓ | |
| Sex of baby | ✓ | ✓ | ✓ | |
| Number of babies born | ✓ | ✓ | ✓ | ✓ |
| Live or stillbirth | ✓ | ✓ | ✓ | |
| Parity/number of previous childrenb | ✓ | ✓ | ||
| Baby’s/mother’s postcode of usual residence | ✓ | ✓ | ✓ | ✓ |
| Ethnic category of baby | ✓ | ✓ | ||
| Ethnic category of mother | ||||
| Country of birth of mother | ✓ | |||
| Country of birth of father | ✓ | |||
| Parents’ socioeconomic status | ✓ | |||
| Type of delivery place | ✓ | ✓ | ✓ | |
| Mother’s date of birth | ✓ | ✓ | ✓ | ✓ |
| Marital status of mother | ✓ | ✓ | ||
| Method of delivery | ✓ | ✓ | ||
| Complications in pregnancy | ✓ | |||
Patient identifiers, including the mother’s and baby’s NHS numbers, postcode of residence, mother’s and baby’s date of birth and baby’s sex, together with a unique record ID, were extracted by the ONS from the linked birth registration and notification file when the place of birth was Wales and were sent to the NWIS, for linkage to the NCCHD and PEDW.
The NCCHD contains records for individual children, whereas maternity records in PEDW relate primarily to mothers. The first phase of the linkage involved linking the birth registration/notification dataset to NCCHD using the baby’s NHS number. The next phase of the linkage involved using the mother’s NHS number from NCCHD to link to the mother’s records in PEDW.
In records where the mother’s NHS number was missing, combinations of the mother’s date of birth and full or partial postcode with either Office of Population Censuses and Surveys Classification of Interventions and Procedures Version 4 (OPCS-4) operation codes R14–R27 (which code for deliveries) or International Classification of Diseases, 10th Revision (ICD-10) diagnostic codes O00–O99 (which code for conditions in pregnancy and childbirth) were used.
The linkage algorithm that was used to link to the PEDW is:
-
mother’s NHS number with operation code R14–R27
-
date of birth and postcode with operation code R14–R27
-
date of birth and partial postcode with operation code R14–R27
-
mother’s NHS number with diagnosis code O00–O99
-
date of birth and postcode with diagnosis code O00–O99
-
date of birth and partial postcode with diagnosis code O00–O99.
Results
In the first phase of the linkage, over 99% of records from the NCCHD were linked to birth registration/notification data for births occurring in the years 2005–14 (Table 11). Nearly 95% of these records were further linked to PEDW for 2005–12. The linkage rates for 2013 and 2014 were much lower, at 78 and 82%, respectively.
| Year | Number of ONS birth records | Number linked to NCCHD | Percentage linked to NCCHD | Number linked to NCCHD and PEDW | Percentage linked to NCCHD and PEDW |
|---|---|---|---|---|---|
| 2005 | 31,758 | 31,723 | 99.89 | 30,042 | 94.70 |
| 2006 | 32,798 | 32,762 | 99.89 | 31,152 | 95.09 |
| 2007 | 33,592 | 33,263 | 99.02 | 30,739 | 92.41 |
| 2008 | 34,821 | 34,793 | 99.92 | 33,149 | 95.27 |
| 2009 | 34,104 | 34,071 | 99.90 | 32,357 | 94.97 |
| 2010 | 34,981 | 34,959 | 99.94 | 33,346 | 95.39 |
| 2011 | 34,658 | 34,638 | 99.94 | 33,013 | 95.31 |
| 2012 | 34,369 | 34,359 | 99.97 | 32,882 | 95.70 |
| 2013 | 32,943 | 32,789 | 99.53 | 25,647 | 78.22 |
| 2014 | 32,868 | 32,865 | 99.99 | 27,072 | 82.37 |
There were no ONS birth registration/notification records linked to more than one record from NCCHD or PEDW in the files provided by NWIS. Quality assurance was carried out by assessing whether or not some or all of the stated common data items, such as date of birth, multiplicity, sex, gestational age and birthweight, matched across datasets. This was much more straightforward than for the English dataset.
Linkage to CMACE stillbirth and neonatal death records
In this project, the CMACE stillbirth and neonatal death data for England and Wales were linked to stillbirth registration records in order to distinguish between antepartum and intrapartum stillbirths, as at registration this information is incomplete and, where coded, the quality has not been assessed. For neonatal deaths, CMACE used a different classification to record the cause of death information and it was considered that this would provide a useful comparison to the information recorded on the death certificate.
Linkage identifiers and algorithms
As the CMACE data did not yet have patient identifiers, a linkage algorithm had to be developed, using data items that were available in the registration and CMACE datasets. CMACE data for 2008 and 2009 included registration details in the form of registration district and subdistrict and entry numbers, which are also recorded on the ONS birth and death registration records so that these data were linked by the ONS. CMACE data for 2010 did not include any unique data items that could be used for linkage. Data collection for 2011 and 2012 was incomplete owing to a delay in the retendering process for the confidential enquiries and consequently in transferring work from CMACE to MBRRACE-UK. The 2013 and 2014 data from MBRRACE-UK were not available, as there had not yet been time to develop metadata and also because for just over 4% of stillbirths, it was not possible to distinguish whether they were intrapartum or antepartum because of problems with the coding system used. 114,115
The CMACE data for 2005 were used in a pilot to develop a stepwise linkage algorithm using a combination of day of birth, month of birth, age of mother, gestational age and organisation code for the location of birth for linking the CMACE data to the stillbirth and neonatal death registration records, as shown in Table 12. In response to organisational changes in the NHS, new variables described as ‘assigned trusts’ and ‘derived location codes’ were derived and further details on this can be found in Derivation of variables. The quality of linkage was assessed at each stage of the algorithm.
| Step | Day of birth | Month of birth | Age of mother | Time of birth | Gestational age | Organisation code | Assigned trust code | Derived location code |
|---|---|---|---|---|---|---|---|---|
| 1 | Exact | Exact | Exact | Exact | Exact | |||
| 2 | Exact | Exact | Exact | Exact | ||||
| 3 | Exact | Exact | Exact | Exact | ||||
| 4 | Exact | Exact | Exact | Exact | ||||
| 5 | Exact | Exact | Exact | Exact | ||||
| 6 | Exact | Exact | Exact | Exact |
Results
There were 3,484 stillbirth and 2,211 neonatal death registrations in 2005. More than 83% of these records were linked to CMACE using steps 1, 2 and 5 of the linkage algorithm, including day and month of birth of the baby, age of mother and other unique data items such as organisation or assigned trust code (see Derivation of variables) and time of birth or gestational age (Table 13). A further 9% of the records were linked using steps 3 and 4 of the algorithm, which excluded the age of the mother. The overall linkage rate for 2005 was 93%.
| Year | Match rank | Registration details | Unlinked records | Total | Linkage rate | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |||||
| 2005 | 2,080 | 2,035 | 437 | 58 | 631 | 65 | – | 389 | 5,695 | 93.2 |
| 2006 | 2,177 | 2,001 | 536 | 54 | 560 | 61 | – | 483 | 5,872 | 91.8 |
| 2007 | 2,265 | 1,871 | 294 | 72 | 786 | 88 | – | 384 | 5,760 | 93.3 |
| 2008a | – | – | – | – | – | – | 5,206 | 960 | 6,166 | 84.4 |
| 2009a | 649 | 526 | 26 | 51 | 88 | 79 | 4,186 | 605 | 6,210 | 90.3 |
Similar percentages of records were linked at different stages of the algorithm for 2006 and 2007, and the overall linkage rates were similar to those for 2005.
The data items used in the linkage algorithm were not available for deaths in 2008, so the 2008 CMACE data were linked by the ONS using registration details, including registration district and subdistrict number as well as the entry number on the register. The linkage rate for 2008 was lower at 84%.
There were 6,210 stillbirths and neonatal deaths in the 2009 registration file. Of these, 4,186 records were linked to CMACE records by the ONS using registration details. The remaining 2,024 records did not include registration details so these were linked using the linkage algorithm. In total, 5,605 registration records were linked to CMACE records for 2009, giving a linkage rate of 90%.
Organisation of data for England for analysis
Database construction
In order to hold the data for analysis, database structures were needed. For much of the duration of the project, the only available database was Microsoft Access®. As Microsoft Access® databases have limited capacity, they are unsuitable for holding large datasets, so subsets of data had to be physically stored in individual annual files. This led to a network of 50 or more interlinked databases, making processing very slow. It was not until relatively late in the project, in the summer of 2016, that Microsoft SQL Server was made available to us. This allowed all the ONS data for England and Wales combined and the HES data for England, including readmission data, to be stored in a single database and be processed at speeds that were previously unimaginable.
The implications of this in terms of delay to the project, notably the slow processing when using Microsoft Access® and the need to spend time re-programming for Microsoft SQL Server, are described more fully in Appendix 1. As the initial importing of much of the data was performed in Microsoft Access®, this is explained in some detail in Appendix 2 to facilitate the audit trail back to the original data. Appendix 2 also describes how the linked data received from the HSCIC were prepared for storage in the database.
The following datasets were stored in the database environment:
-
Birth registration records linked to birth notification records provided by the ONS.
-
Stillbirth, infant and child mortality and maternal mortality records provided by the ONS.
-
Mothers’ HES delivery records.
-
Mothers’ HES non-delivery admission records. These consisted of antenatal admissions, postnatal admissions and admissions unrelated to maternity.
-
Babies’ HES birth records.
-
Babies’ HES subsequent admission records. These included postnatal admissions and subsequent admissions unrelated to the child’s birth, for example as a result of accidents.
The structure of these records has considerable numbers of many-to-one relationships, for example successive births to the same mother, more than one birth record in a multiple delivery and successive subsequent admissions of mothers and babies. This structure is supported in the relational database environment, summarised in Figure 2. In this, each box refers to a separate table in the SQL database. This is essentially identical to the Microsoft Access® data structure except it now includes readmissions and data for births in all the years are in one table.
FIGURE 2.
Relational database structure for HES delivery and birth records linked to ONS linked birth notification/birth registration records.
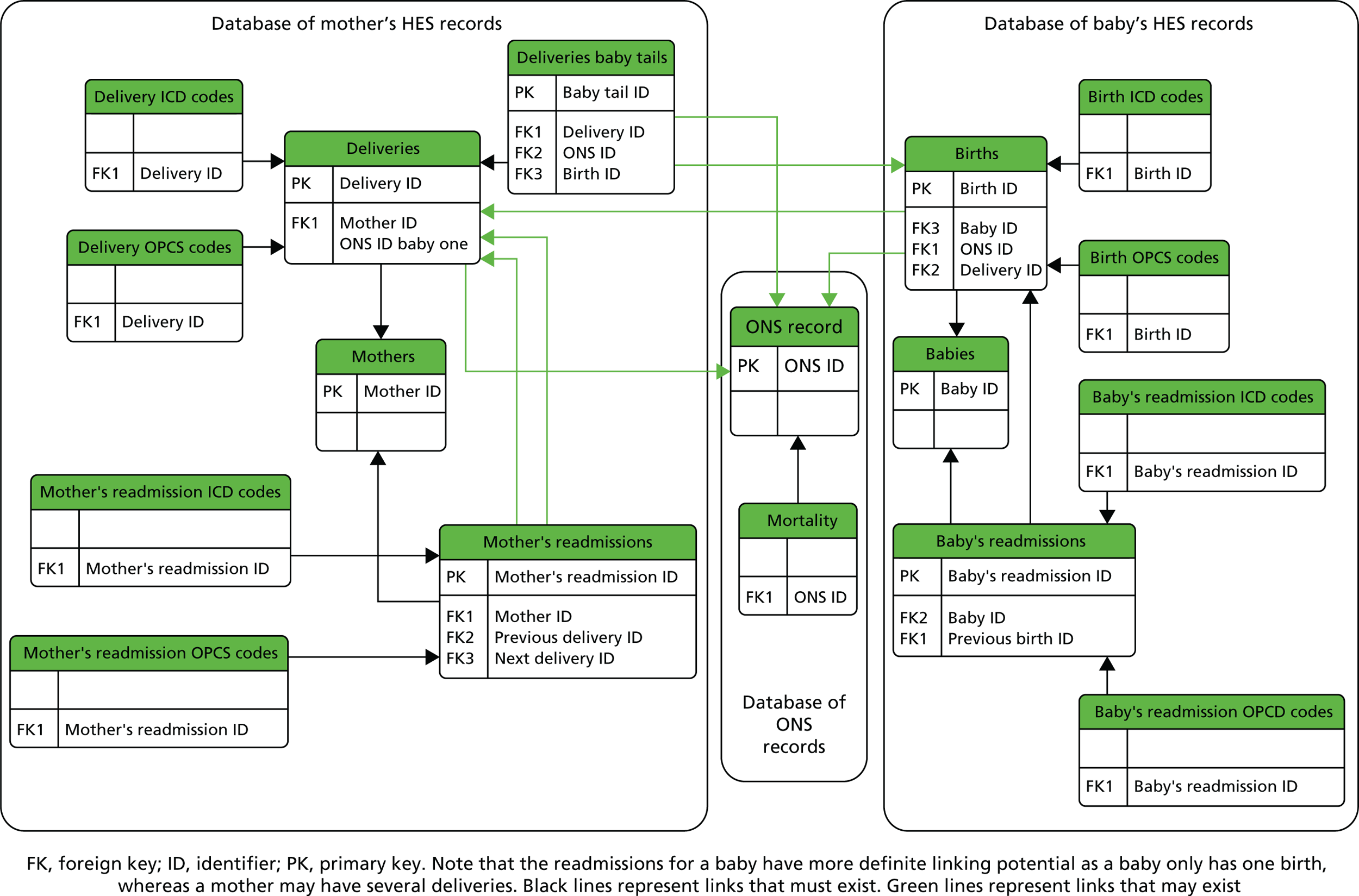
In the following text, the names of database fields are enclosed in square brackets. The word linkage is taken to mean the link between database tables using unique keys and the phrase ‘record linkage’ to mean the matching of ONS to HES records.
In Figure 2, arrows represent possibilities for linking tables using keys. Black lines represent links that must exist, for instance every delivery ICD-10 code record must be associated with a particular delivery record. Green lines represent links that may exist. For example, a delivery record may link to an ONS record. The primary key (PK) is unique. An example of a foreign key (FK) would be [Delivery ID] in the Deliveries Baby Tails table. For twins, this table had two records each with the same [Delivery ID] pointing to the same delivery record. Although labelled FK in this diagram as this is their role, these are not declared as FKs in the database. FKs impose referential integrity, which is not a function that was required in this project but these fields have been indexed. Appendix 2 lists all the unique PKs in each database table.
In HES, a mother or baby may be diagnosed with a variety of conditions and undergo a number of procedures. There is space for up to 20 diagnostic codes and 24 procedure codes. To efficiently analyse these records, it is necessary to normalise the data so that questions can be asked of them without having to consider the multiplicity of the many-to-one relationship. For example, to determine if a mother had an episiotomy it is tedious to work through all 24 fields for operation codes in her HES record, but if the data are normalised in a relational database this is reduced to one question on a single field.
Derivation of variables
New variables were derived in the ONS and HES delivery datasets based on standardising or combining the original values in the data fields to create better quality or more useful variables. These are listed in detail in Appendix 2. Some derived variables involved fairly minor manipulation, but much more work was required to impute the two key variables of parity and location of birth codes. Parity is very incompletely recorded in HES and was not recorded for all births at birth registration until May 2012. Location codes for maternity units were derived to overcome the many changes in organisation codes resulting from NHS reorganisations over the period and the different ways of coding for site of birth in the datasets used.
Parity
Parity is usually defined as the number of previous registrable live births and stillbirths. HES records the numbers of previous pregnancies leading to one or more registrable live births or stillbirths in the field [NUMPREG]. Unfortunately, some trusts fail to complete this field correctly. A few declare all their mothers to be either primiparous or having their second child. Others simply do not assign any value at all to this field. The trusts affected were identified and parity was set to unknown for the years in question. See Appendix 2, Table 37, for the estimated proportions of primiparous women by trust and year.
Some information about parity can be gleaned from the ICD-10 codes in the diagnostic fields. For instance, a mention of a previous caesarean section indicates that the current birth is not the mother’s first baby.
Because the HES dataset consists of data for births over a period of 10 years, it was possible to look back through a mother’s birth history and count forward from her first recorded baby to the current baby to estimate the number of births she has had. This does not provide a good estimate for births in the early years and in later years the estimate is suspect for women who are of high parity. The length of the time period is more than sufficient to distinguish primiparous women from multiparous women. In practice, the marginal differences in estimated outcome are inversely proportional to parity.
Birth registration records contain a field called [PREVCH]. Before May 2012, parents registering a birth within marriage were asked about the numbers of previous live births or stillbirths to the current or any previous husband. There was increasing confusion about this question, which was formulated in the 1930s. Since May 2012, under the Population (Statistics) Act 1938 as amended by the Welfare Reform Act 2009, all women have been asked about their number of previous live and still births, irrespective of whether the births were inside or outside marriage. 127,141 This should align the data recorded at registration with those used in clinical practice but some unanticipated discrepancies arose and the ONS has been working with the General Register Office to train local registrars in asking the new questions. 141
[NUMPREG] is a count of the number of deliveries a woman has had, whereas [PREVCH] reports the number of births, so [NUMPREG] will deviate from parity for multiple births. Over the period covered by this project, it can be assumed that a married mother has had at least this many children, and [PREVCH] can be used as a lower bound on a woman’s parity. This information can be factored into the estimation of parity along with the HES data so that whenever it exceeds the HES-only estimate it is used to overwrite it.
Because information is propagated forward, values of [PREVCH] in earlier years can influence the estimate of parity in later years. This has the potential to introduce a slight bias, with the parity of unmarried women being artificially depressed from the true value relative to married women. If the analysis is restricted to later years of the period and uses only a primiparous/multiparous split, then this should not be too serious an issue.
It is computationally efficient to simultaneously derive whether a woman has had a previous caesarean section at the same time as estimating parity, as both require propagating information forward through a woman’s delivery history.
The steps taken to estimate parity based on HES only and then by making use of the birth registration data are described in Appendix 2. The derived fields are [Derived Parity] and [Derived Parity (ONS)], respectively.
Coding location of birth
Over the period 2005–14, the vast majority of women over 95% gave birth in NHS hospitals142 but some women gave birth in other places. Between 2.3% and 2.9% gave birth at home and less than 0.5% gave birth outside hospital or in non-NHS establishments.
Women give birth in NHS hospitals in one of three types of maternity unit: an obstetric (consultant-led) unit, an alongside (co-located) midwifery unit or a freestanding midwifery unit. According to data for England collected by the National Audit Office, in 2012, 87% of women gave birth in an OU, 9% gave birth in an AMU and 2% gave birth in a freestanding midwifery unit. 22 The definitions of these units are given in Appendix 2 (see Box 2).
NHS hospital maternity services are generally provided by NHS acute trusts, although before the Health and Social Care Act came into force in April 2013,9 some services were provided by primary care trusts. NHS trusts may have one or more OUs, with or without an AMU and may or may not also have one or more FMUs. Some trusts have up to five FMUs. Almost all trusts have an OU, although there are two trusts, in Weston-super-Mare and Bournemouth, which only have a FMU.
Women can only give birth in an AMU or FMU if they do not require obstetric care. Women who are admitted to an AMU or FMU may need to transfer to an OU to give birth if complications arise. If this is the case, then the birth should be recorded as taking place at the OU.
Establishing the location of birth was useful for assessing the quality of the linkage within ONS birth records and also the quality of the linkage of these records with the HES records. Location of birth can then be used further to undertake analyses by maternity unit, by NHS trust or type of unit, for example anOU or midwife-led unit.
Much of the work done on the location of birth relied on previous work undertaken by the public information service BirthChoiceUK and its historical maternity unit database held by Rod Gibson Associates Ltd. The project was given permission to use some of the data from the database, which includes a list of maternity units that opened between 2001 and March 2015, with dates of significant events such as openings, closings and changes in location, unit type or administering trust.
Establishing location of birth within the project was complicated by some inaccurate coding and by discrepancies between the different datasets. This can be masked by differences in how location of birth is coded in these. In the linked ONS births dataset, location of birth is represented by the communal establishment code [CESTRSS] in the registration records and by two fields [ORGCODEZ] and [DELPLAZ] in the notification dataset. This prevents a direct comparison of location of birth.
Even if these codes can be mapped to specific maternity units, there is a further problem for data analysis as the administrative arrangements for both trusts and maternity units can change over time. NHS trusts have undergone a number of changes between 2005 and 2014, including a number of mergers and changes of responsibility for maternity services, for example from primary care trusts to acute trusts. Furthermore, maternity units themselves can change with openings, closures and changes of unit type, for example from an OU to a FMU or from an OU on its own to an OU with an AMU. In addition, maternity units may physically move to a new site or be transferred to another trust administratively.
To allow for such changes, it was necessary to create three new variables (Assigned Trust, Derived Location of Birth and Unit Type) and add them to birth registration records for England and Wales and to HES delivery records. The methods developed to do this are described in Appendix 2.
Database documentation
All database tables, fields and descriptions are listed in Appendix 2. This includes the metadata obtained from the ONS about birth registration, birth notification and death registration, as well as metadata about variables obtained from the HSCIC in HES delivery and birth records and in records of subsequent admissions of mothers and babies after birth.
The list of preferred variables for use in analysis is given in Appendix 2, Preferred variable list and the means of accessing these from standard statistical packages are given in Appendix 2, ODBC link.
The relational database brings together the three datasets – birth registration, birth notification and HES – for England for the 10 years from 2005 to 2014 together with linkages to mortality data and readmission records. Because of the structure of the database and the new facilities in the VML, it is now possible to perform complex analyses with relatively little processing time. Using Open Database Connectivity (ODBC), data can be extracted from the database directly into other statistical software applications. SQL tables can be linked to using Microsoft Access®, or applications such as Statistical Analysis System [SAS® (SAS Institute Inc., Cary, NC, USA)], Stata® (StataCorp LP, College Station, TX, USA) and R (The R Foundation for Statistical Computing, Vienna, Austria) can import entire datasets.
Summary and conclusions
The linkages described in this chapter are summarised in Appendix 2 (see Table 34). This shows that we have done all the linkage of individual-level records set out in our proposal, although some of the quality assurance of linkage remains to be done. Linking over 6 million HES delivery and birth records and over 300,000 PEDW and NCCHD records to ONS birth records has been challenging. Building the relational database has been a major achievement and will make it simpler to do the analyses we planned. The only data we have yet to acquire are the workforce data for England, but these aggregated data are in the public domain and are readily available for downloading.
Chapter 3 describes the analyses we planned and those we have done using the quality assured linked data.
Chapter 3 Analysis of data
Introduction
This chapter describes the methods and approaches used for the analyses that were done, and presents the results. It also describes the methodological approaches planned for those analyses for which there was not time to complete. The complete set of proposed analyses is given in Appendix 3 (see Table 72). This was drawn up at NIHR’s request to support the application it invited the team to make for further funding. It was subdivided into the analyses that could be completed by 31 March 2017 and those that could not be completed without the proposed second extension, which NIHR decided not to fund.
The proposal for this project stated that the focus would be on singleton births, because of concerns about the quality of data for multiple births, but that this would be investigated to enable analysis if possible. The quality assurance process described in Chapter 2 concluded that the analysis of linked multiple births is feasible, but this was done after the quality assurance of singleton births because of its greater complexity. As shown in Table 72, the analysis of multiple births was scheduled to be done after 31 March 2017 if a Variation to Contract had been agreed. As a result, these analyses have not been done. Therefore, most of the analyses described here were based on singleton births.
This chapter starts with descriptive analyses of numbers of births in England and Wales by time of day and day of the week based on ONS birth record data (linked birth registration and notification data) only. This is followed by a much more detailed analysis of birth data for England, which are linked to HES to enable the analysis of births by mode of onset of labour and time of day and day of the week using statistical modelling. The section on patterns of birth concludes with analyses of the smaller numbers of births in Wales by time of day and day of the week and then analyses of births at home in England and Wales combined.
Unfortunately, because of external delays described in Appendix 1, there was not time to do most of the proposed analyses of variations in the outcome of birth. As set out in the project proposal, planned analyses of stillbirths included only intrapartum stillbirths, as the timing of antepartum stillbirths is not known and is not directly affected by the same factors. Descriptive analyses of intrapartum stillbirth rates are included. The chapter closes with an overview of the other planned outcome measures and the analyses that had to be set aside.
Descriptive analyses
Number of observations used in the analysis
There were 7,013,804 births registered in England and Wales that occurred from 1 January 2005 to 31 December 2014. Of these, there were 6,676,912 babies whose mothers were resident in England and 336,892 babies whose mothers were resident in Wales. Multiple and singleton births were identified using information on multiplicity recorded at birth registration. There were 6,468,586 singleton and 208,326 multiple birth records in England that were linked to HES delivery records by HSCIC. After quality assurance, which was described in detail in Chapter 2, 6,138,487 singleton births and 193,270 multiple birth records remained linked to HES delivery records (Figure 3).
FIGURE 3.
Births registered in England and Wales by multiplicity and linked to the hospital delivery records: 2005–14. QA, quality assurance.
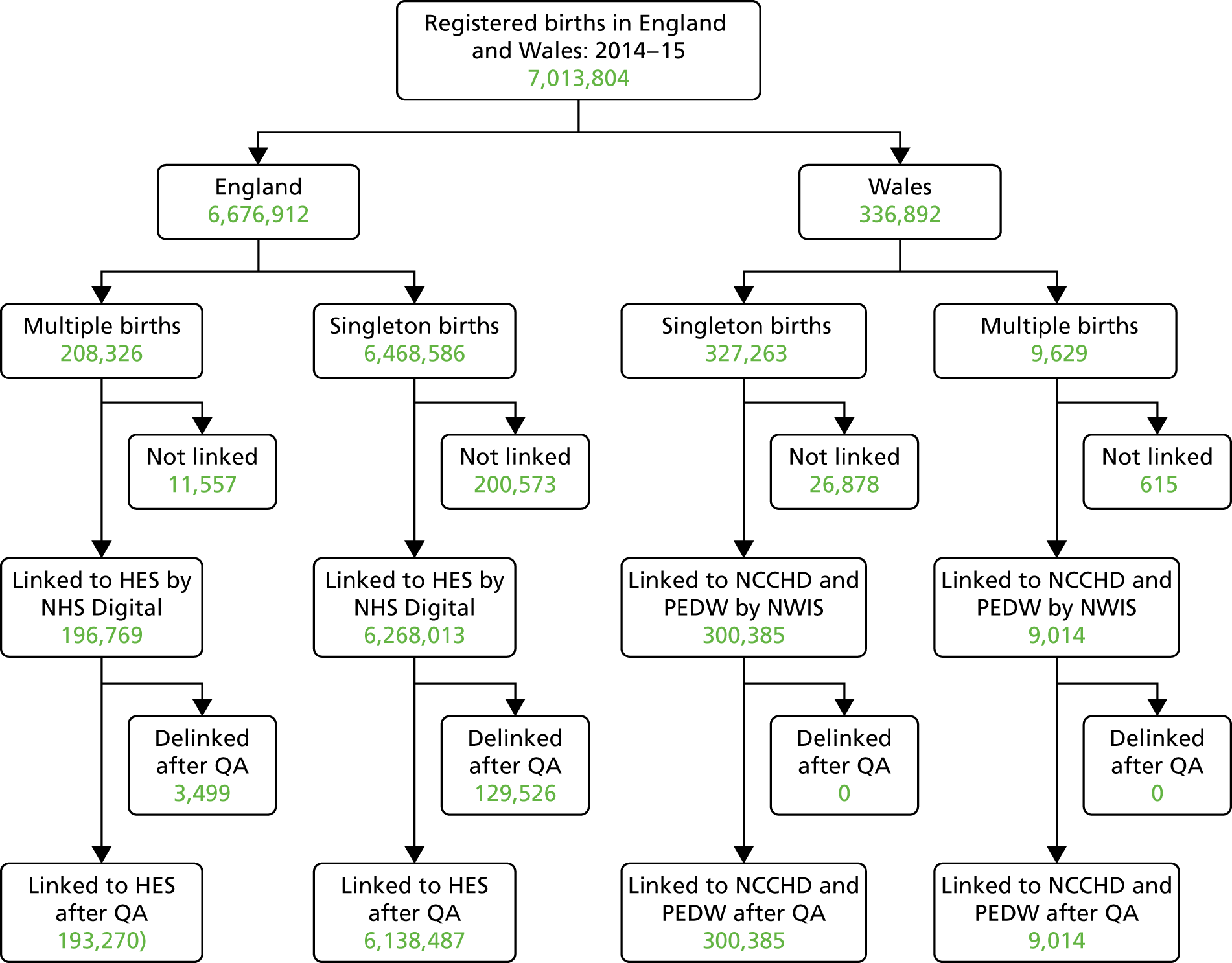
Of the 327,263 singleton babies either resident or born in Wales, 300,385 birth records were linked to the NCCHD and PEDW by NWIS. There were no duplicates and the quality of linkage was good; therefore, no records were removed after quality assurance. Similarly, 9014 multiple birth records were linked to the NCCHD and PEDW by NWIS and all records remained linked after quality assurance (see Figure 3).
Variations in overall numbers of births in England and Wales by time of day and day of the week
Over the period from 2005 to 2014, the overall numbers of births in England and Wales showed the same pattern as in preceding years, with a regular weekly cycle with the numbers of births each day increasing from Mondays to Fridays, with lower numbers of births on Saturdays and the lowest numbers of births on Sundays. In addition, numbers of births varied seasonally, with a peak in late September. As shown in Figure 4, this pattern was interrupted by public holidays, with the lowest numbers of births in most years being on Christmas Day and Boxing Day.
FIGURE 4.
Daily live births in England and Wales: 2005–14.

To illustrate this, data for 1 year, 2011, are shown in Figure 5, in which it can be seen that numbers were relatively low at New Year, at Easter and on other public holidays, including in early May when the usual pattern of public holidays was disrupted by an extra public holiday related to a royal wedding. Visual inspection suggests that these dips were preceded by short-term increases in numbers of births. This was investigated in the analyses described below.
FIGURE 5.
Number of live births by day, England and Wales: 2011.
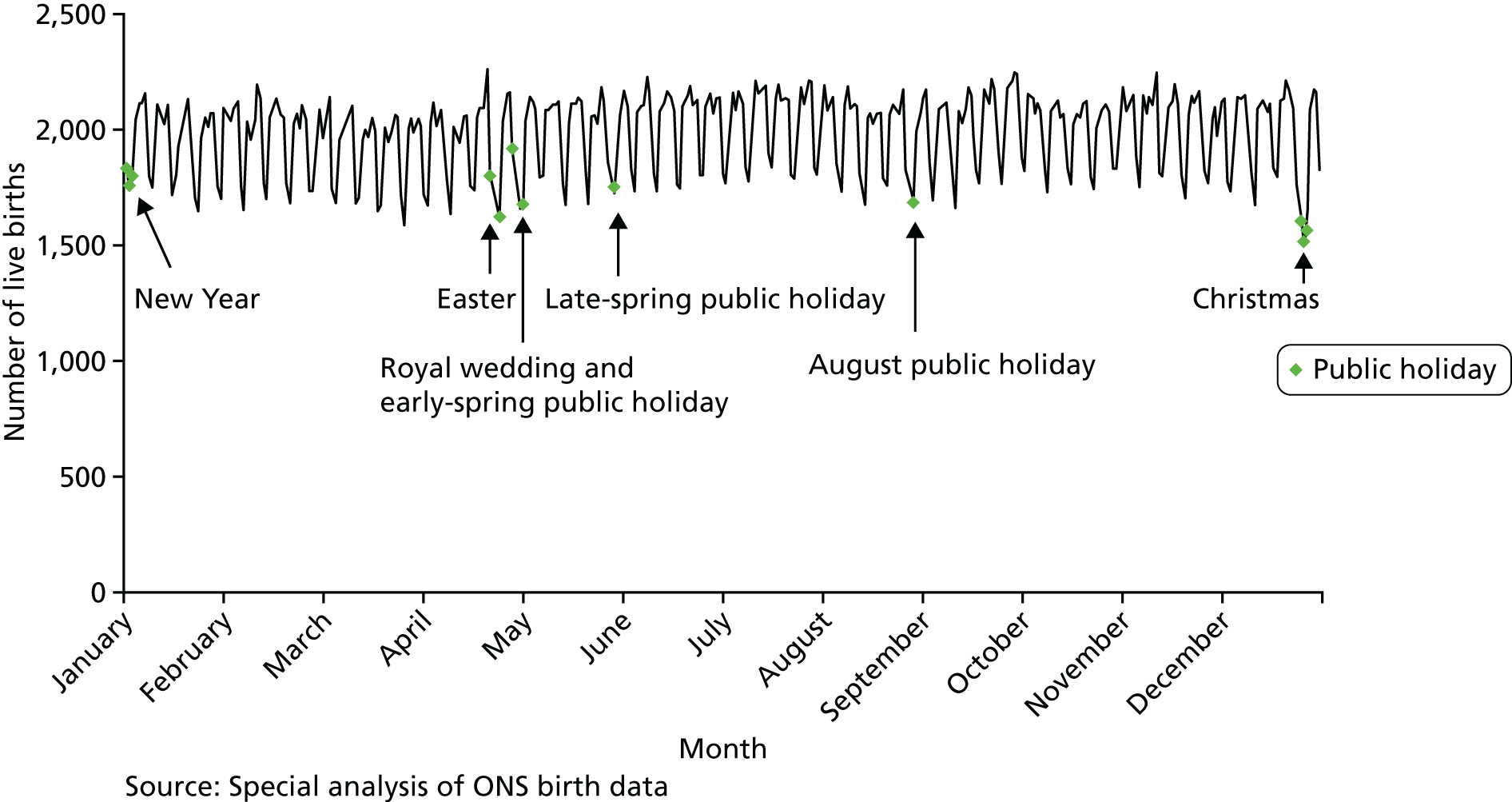
The overall numbers of births each year between 2005 and 2012, apart from a slight decrease in 2009, and then fell slightly in 2013 and 2014. To investigate whether or not the daily patterns changed over time, the average numbers of births on each type of day were compared with the daily average for the corresponding year.
The daily pattern changed very little over the period 2005–14 (see Appendix 3, Table 73). This is illustrated in Figure 6. For clarity, it shows only 2005, 2009 and 2014, namely the first, middle and final years of the project period.
FIGURE 6.
Ratios of average numbers of daily live births to overall average for the year, England and Wales: 2005, 2009 and 2014.
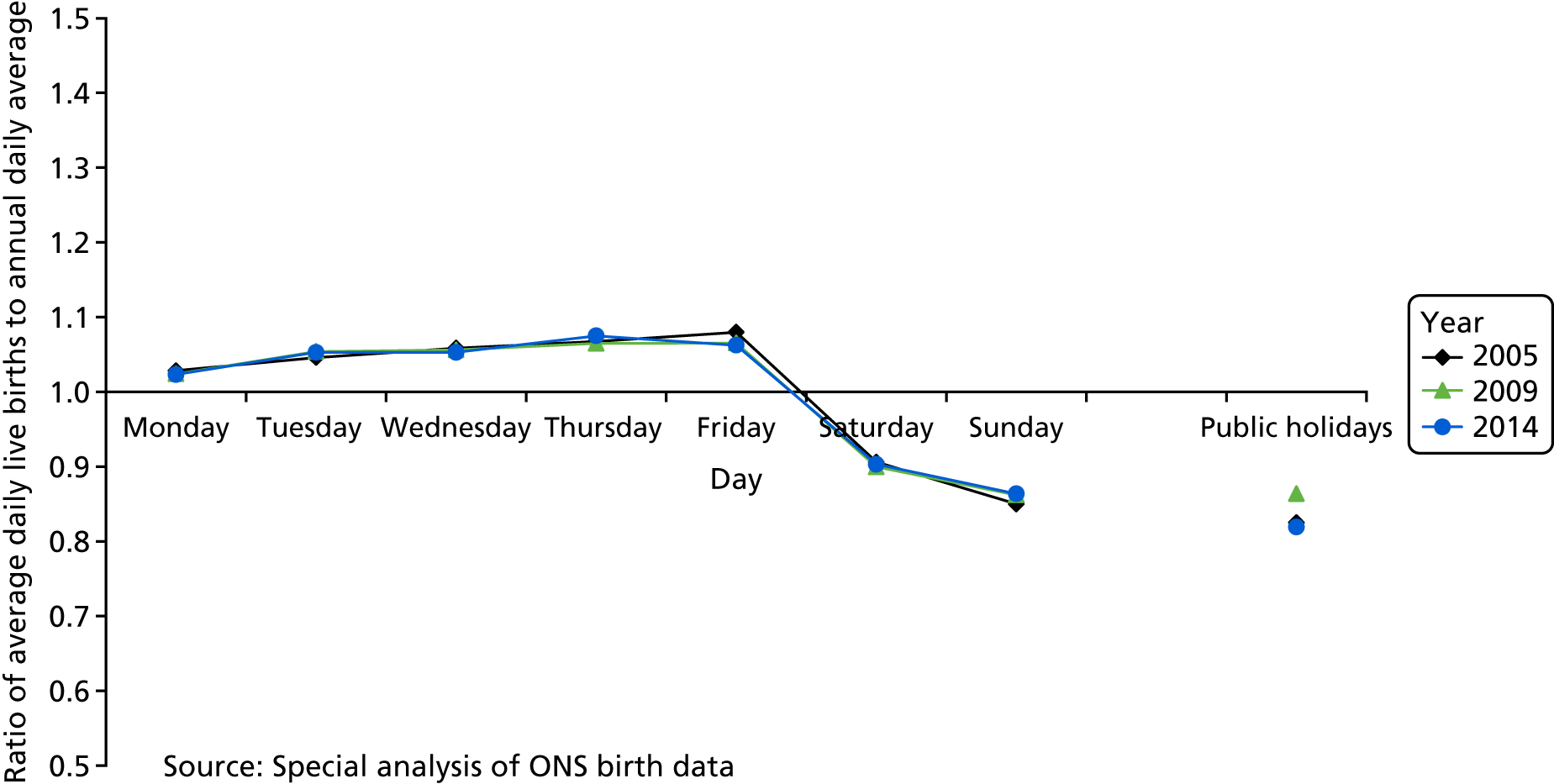
The data in Figures 5 and 6 come from a special analysis by the ONS of all live births. In what follows, we have used the data acquired for the project to describe variations in singleton births, as described earlier.
Variations in numbers of singleton births in England and Wales by day of birth and by time of day of birth
Variations over time
It has already been shown above that the daily variations in numbers of live births were stable over the period 2005–14. The overall hourly pattern for all singleton births is shown in Appendix 3, Table 74, which shows the ratio of average numbers of births per hour to the overall average for the year for 2005–14. As with data for daily variations in numbers of births, data about hourly patterns are shown for births in 2005, 2009 and 2014 in Figure 7. Again, because the overall numbers of births each year rose and fell over the study period, we have expressed the average numbers of births each hour as a percentage of the overall hourly average. There was relatively little change over the years studied.
FIGURE 7.
Average numbers of singleton births per hour in relation to overall hourly average for each year, England and Wales: 2005, 2009 and 2014.
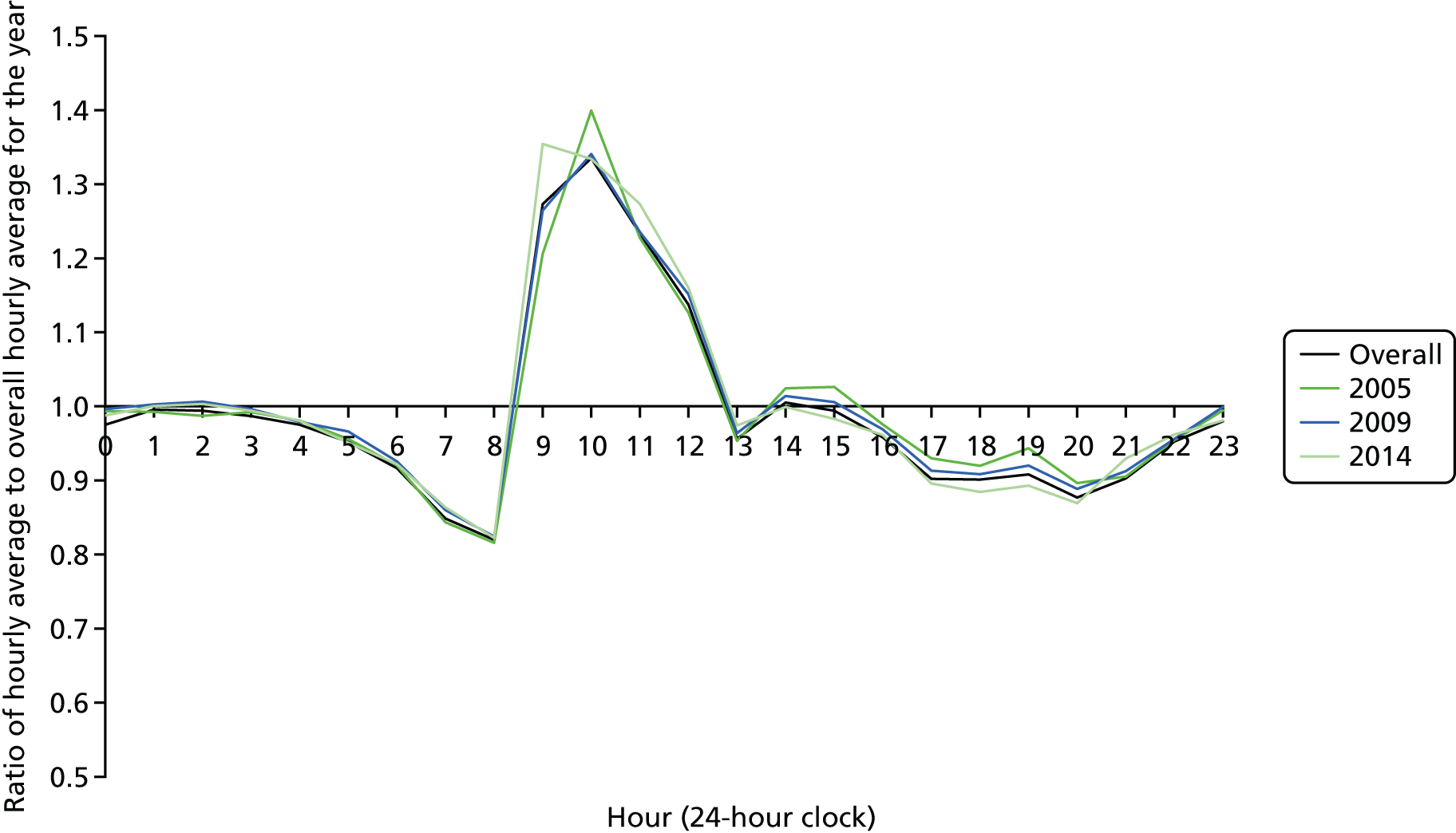
The exception was that in 2005 and other early years of the period, there was a sharp peak in numbers of births between 10.00 and 10.59. This changed slightly over the 10-year period and by 2014 and immediately preceding years, this had broadened out to cover the time period from 09.00 to 11.59, and the smaller peaks early and late in the afternoon had become less prominent.
Variations by time of day and month
Singleton births were tabulated by month and time of day. The average numbers of births per hour were then calculated. As there is known seasonality in numbers of births, the ratios of the hourly averages to the overall monthly averages were then calculated for the years 2005–14 combined. This was done separately for term births, late preterm births and very preterm births (Figures 8–10). Although ratios were calculated for all 12 months, only 4 months’ ratios are shown. They were chosen to be December, containing the shortest day, June, containing the longest day, and March and September, containing the spring and autumn equinoxes, respectively. The time of day of births in October 2008 were known to be missing, so these births were omitted from analyses of time of day but not from analyses of day of birth.
FIGURE 8.
Average numbers of singleton births at 37–42 weeks of gestation or more per hour in relation to overall hourly average for each month, England and Wales: 2005–14.
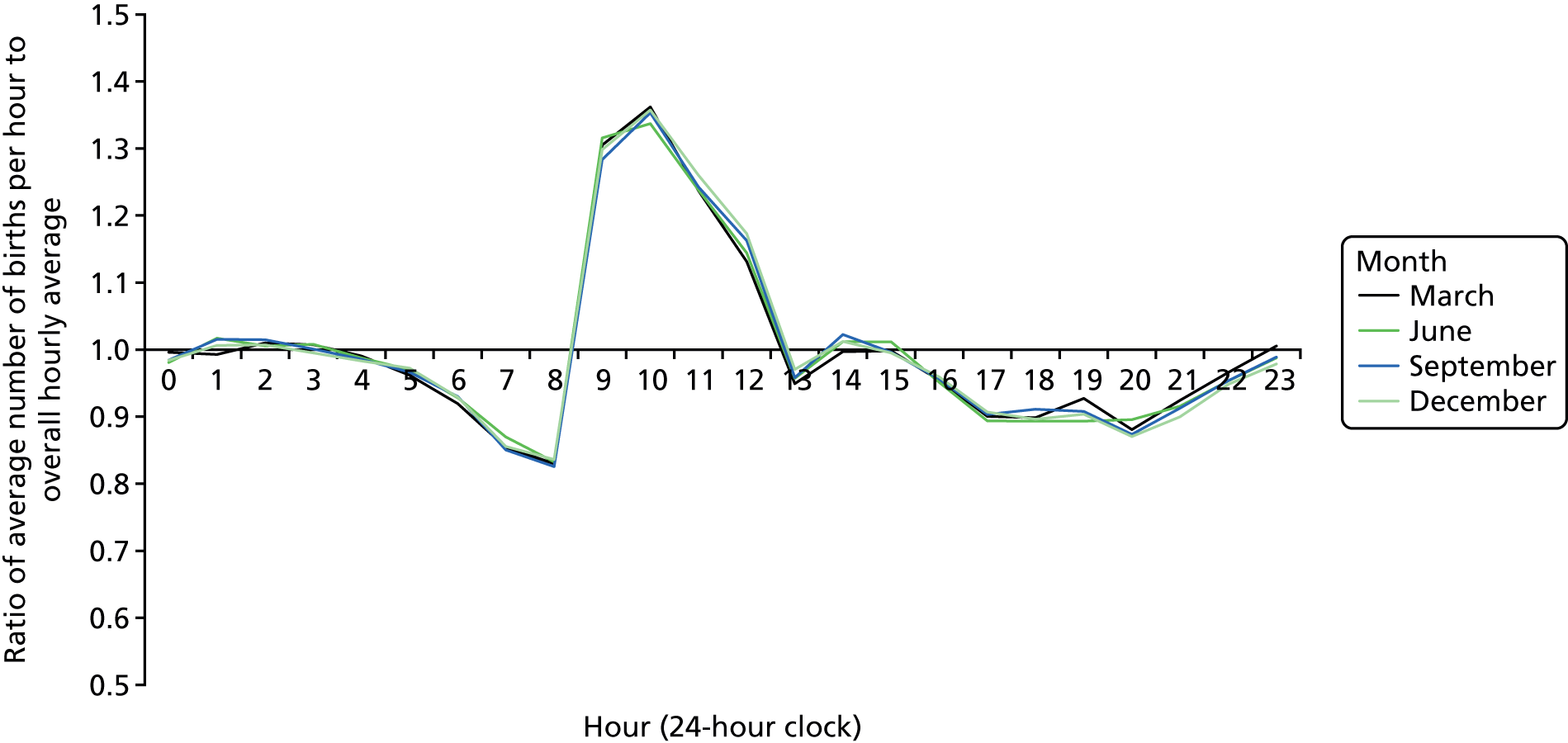
FIGURE 9.
Average numbers of singleton births at 32–36 weeks of gestation per hour in relation to overall hourly average for each month, England and Wales: 2005–14.
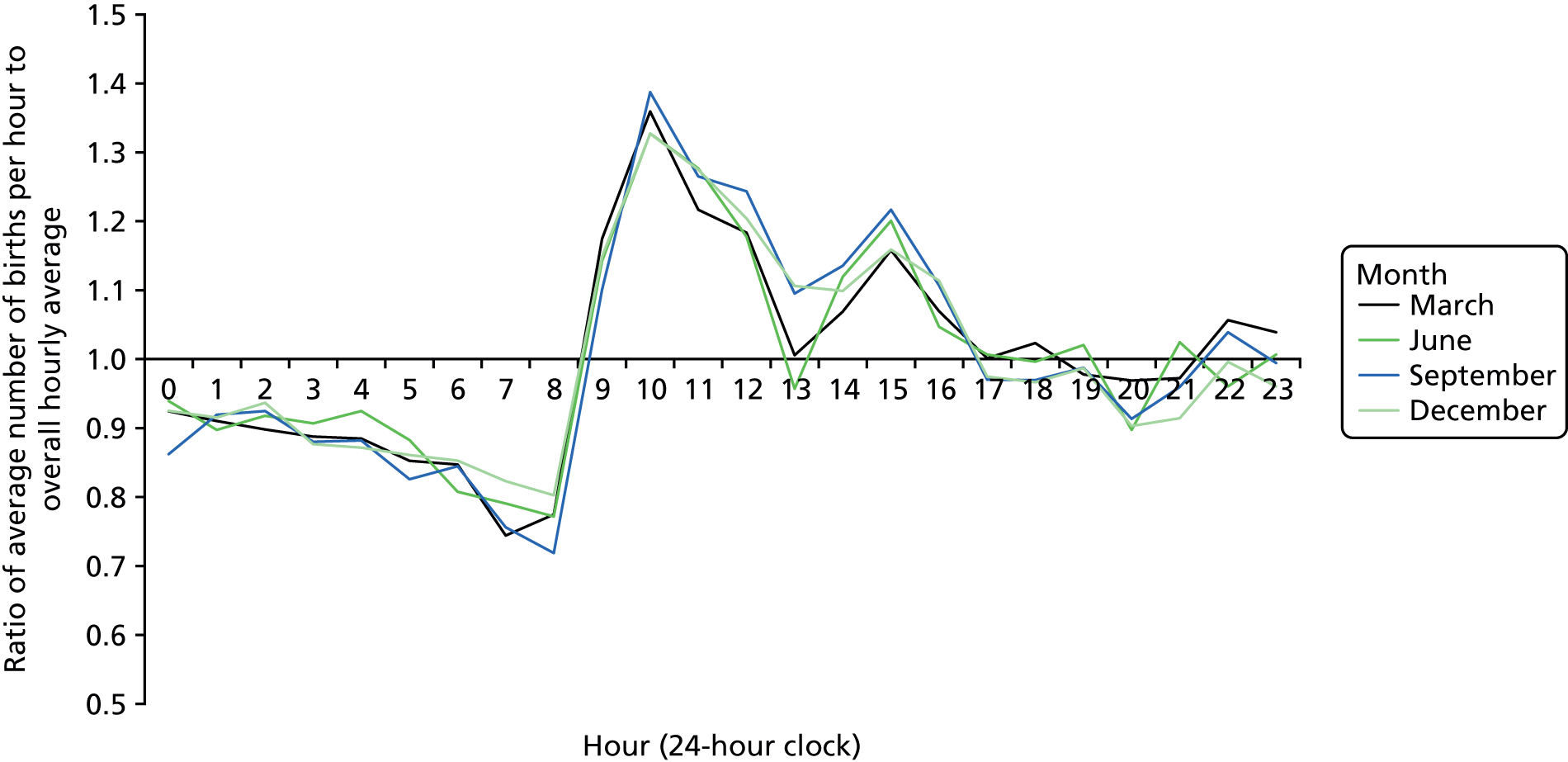
FIGURE 10.
Average numbers of singleton births at 23–31 weeks of gestation per hour in relation to overall hourly average for each month, England and Wales: 2005–14.
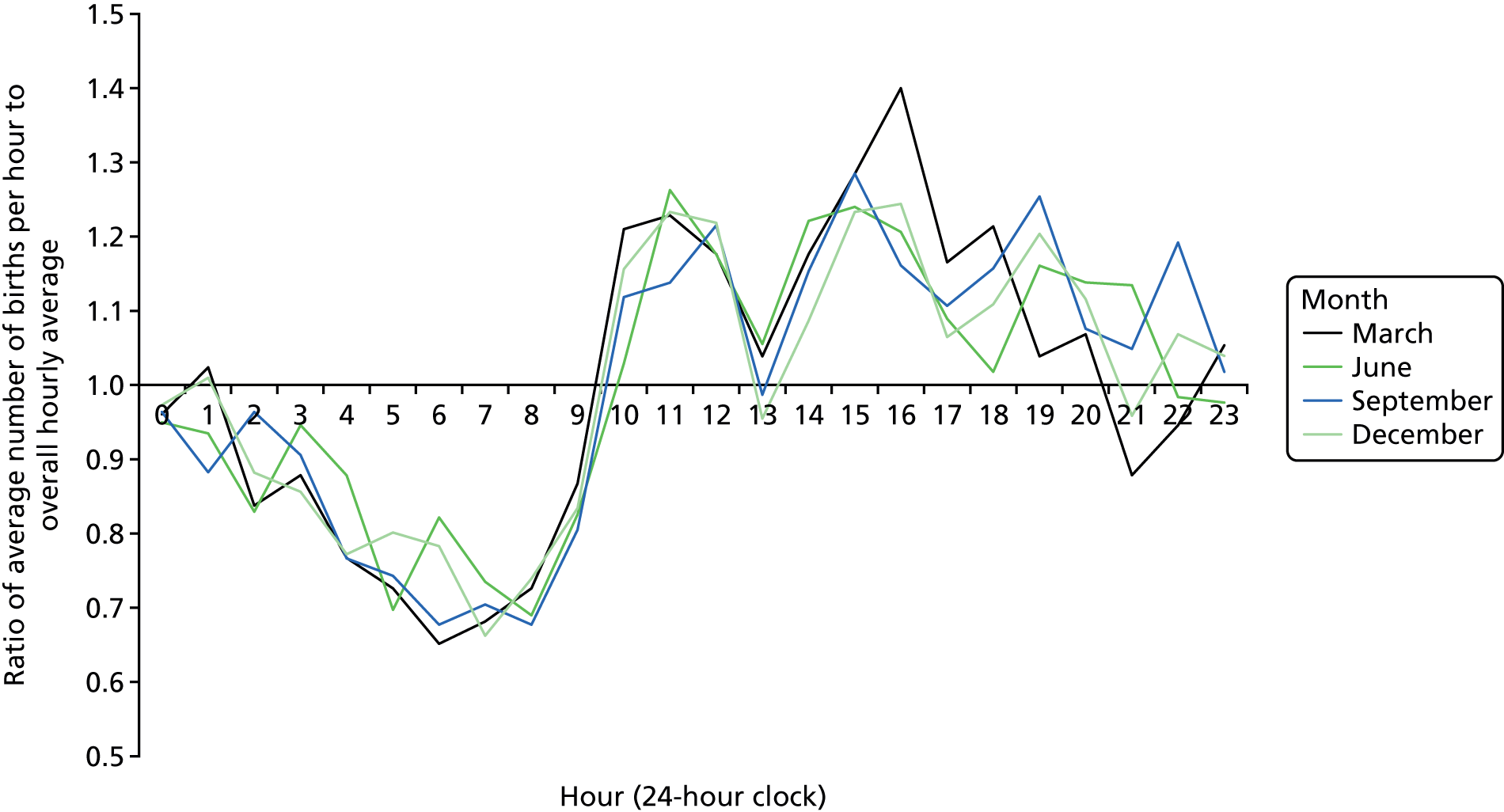
Numbers of term births showed a pronounced peak in the morning and a smaller peak in the afternoon (see Figure 8), as with all singleton births (see Figure 7). There was little sign of any differences between months of birth.
Numbers of late preterm births also peaked in the afternoon, but to a much greater extent than term births (see Figure 9). Although there appeared to be greater differences between the months of birth, these did not show a recognisably consistent pattern and further analysis is needed to assess whether or not the differences were bigger than would be expected by chance.
The very much smaller numbers of early preterm births showed a more erratic pattern, with signs of three peaks, in the morning, the early afternoon and the early evening, in some months and four peaks in others (see Figure 10). Without further analysis, it is impossible to assess the extent to which these were compatible with random variation. It was clear, however, that hourly numbers of births were below average from midnight to 09.00 and tended to be above average between 09.00 and midnight. This pattern was discernible but much less marked for late preterm births.
Characteristics of mothers and babies
Mothers’ ages
When numbers of singleton births were analysed by day and by mothers’ ages grouped into 5-year age groups, marked differences were apparent. Initially, mothers aged under 15 years and those aged 45 years and over were tabulated separately, but as the numbers were small they were combined with adjoining age groups.
Variations by day of birth are shown in Table 14 and Figure 11. These show the same overall patterns as for all births, but there is a considerable age gradient, with relatively small daily differences for women aged under 20 years to a much larger concentration of births to women aged 35 years and over onto weekdays.
| Day of the week | Age group (years) | ||||||
|---|---|---|---|---|---|---|---|
| Under 20 | 20–24 | 25–29 | 30–34 | 35–39 | 40 and over | All | |
| Monday | 102 | 344 | 513 | 551 | 317 | 75 | 1,902 |
| Tuesday | 106 | 356 | 526 | 559 | 319 | 76 | 1,942 |
| Wednesday | 108 | 358 | 530 | 561 | 319 | 76 | 1,952 |
| Thursday | 109 | 363 | 538 | 568 | 324 | 77 | 1,979 |
| Friday | 110 | 365 | 537 | 566 | 322 | 78 | 1,978 |
| Saturday | 105 | 333 | 474 | 477 | 253 | 57 | 1,699 |
| Sunday | 100 | 317 | 450 | 450 | 238 | 52 | 1,607 |
| Public holiday | 107 | 336 | 474 | 477 | 253 | 57 | 1,705 |
| All | 106 | 348 | 509 | 531 | 297 | 70 | 1,861 |
FIGURE 11.
Ratio of average daily numbers of births to overall daily average by age of mother, England and Wales: 2005–14.
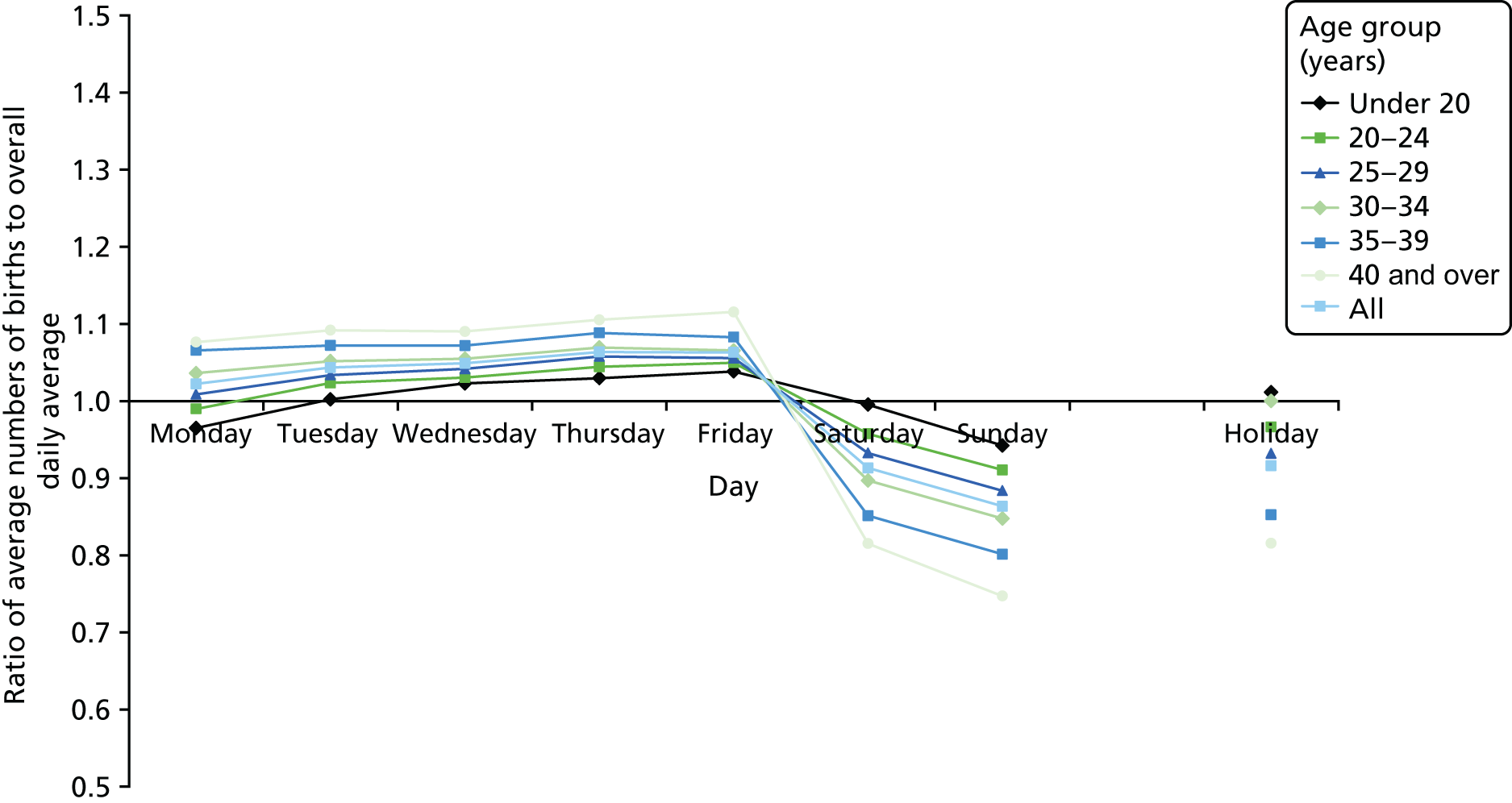
The same applies to variations by time of day (Figure 12). Numbers of births show a morning peak and a smaller afternoon peak, but the variation is much less marked in births to younger women than in births to older women.
FIGURE 12.
Ratio of average hourly numbers of births to overall hourly average by age of mother, England and Wales: 2005–14.
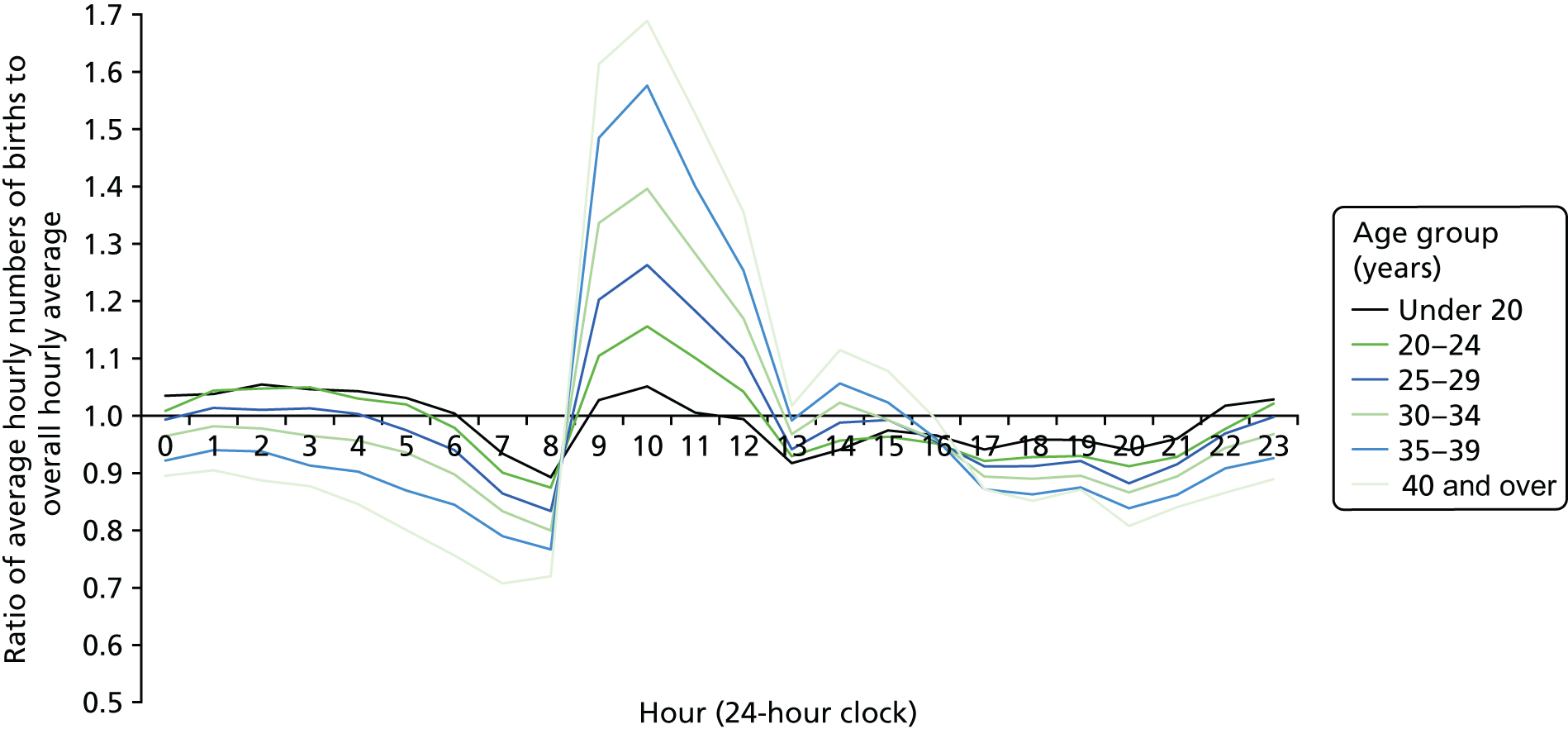
Babies’ ethnicity and mothers’ countries of birth
We analysed daily and hourly numbers of births by babies’ ethnicity as reported at birth notification and mothers’ countries of birth, dichotomised as born inside and outside the UK. Some of these categories contained small numbers of births. These 18 tabulations did not show a clear picture. It was clear that a more focused analysis is needed, taking into account other variables, notably onset of labour and mode of birth.
Gestational age and birthweight
Singleton births are analysed by gestational age and birthweight by day in Figure 13. As 91% of babies born at 22–31 weeks’ gestation weighed less than 2,500 g, they are not subdivided by birthweight (see Figure 13c), although it may be useful to subdivide this group in future analyses to gain an insight by the timing of the most preterm births.
FIGURE 13.
Ratio of average numbers of singleton births to overall daily average by birthweight, England and Wales: 2005–14.
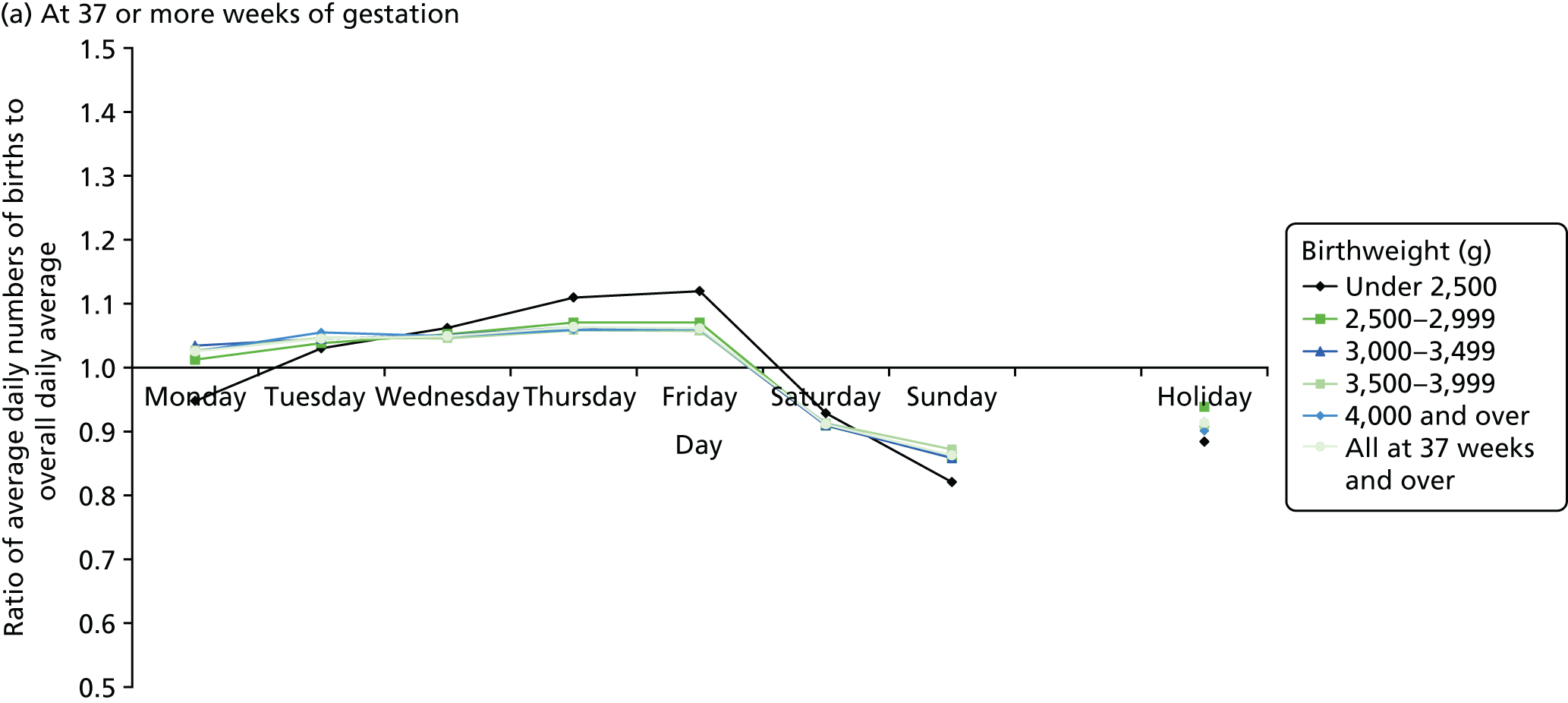
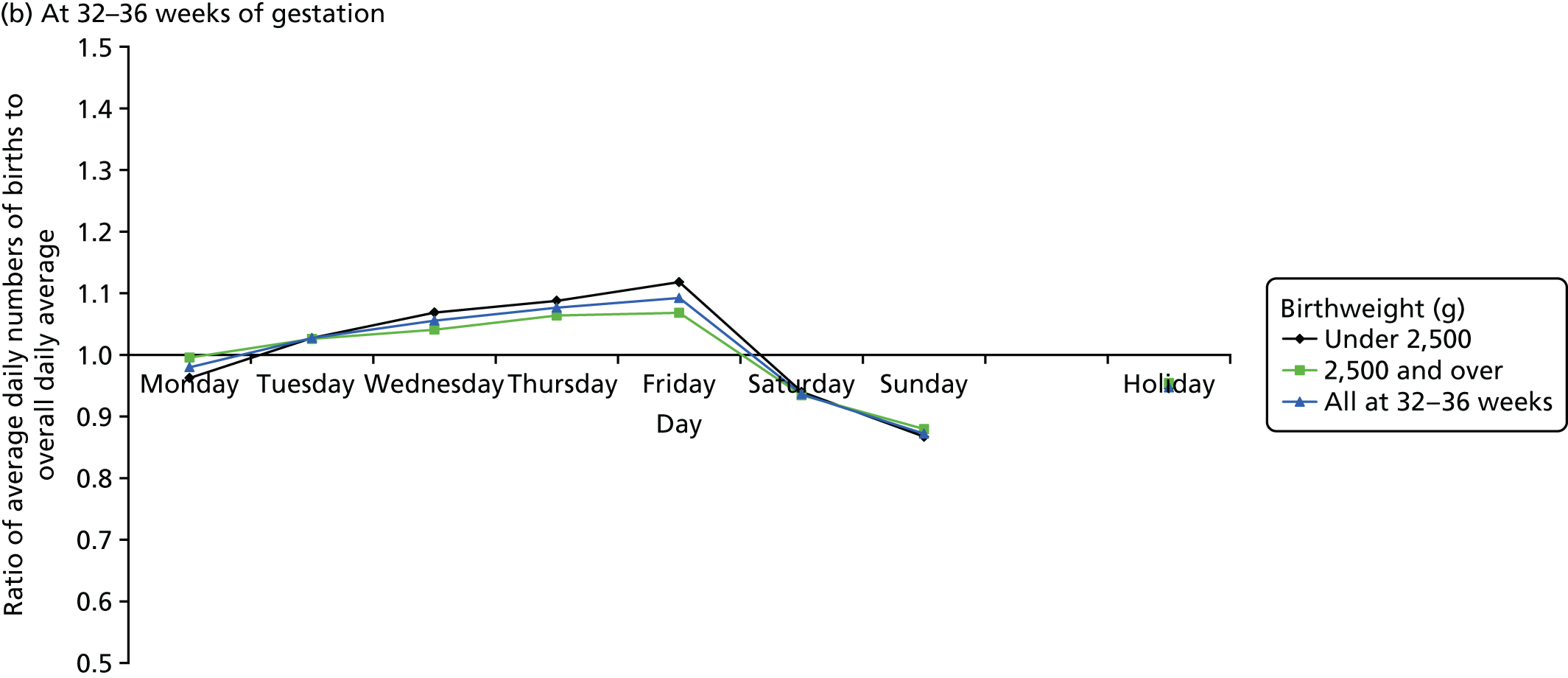
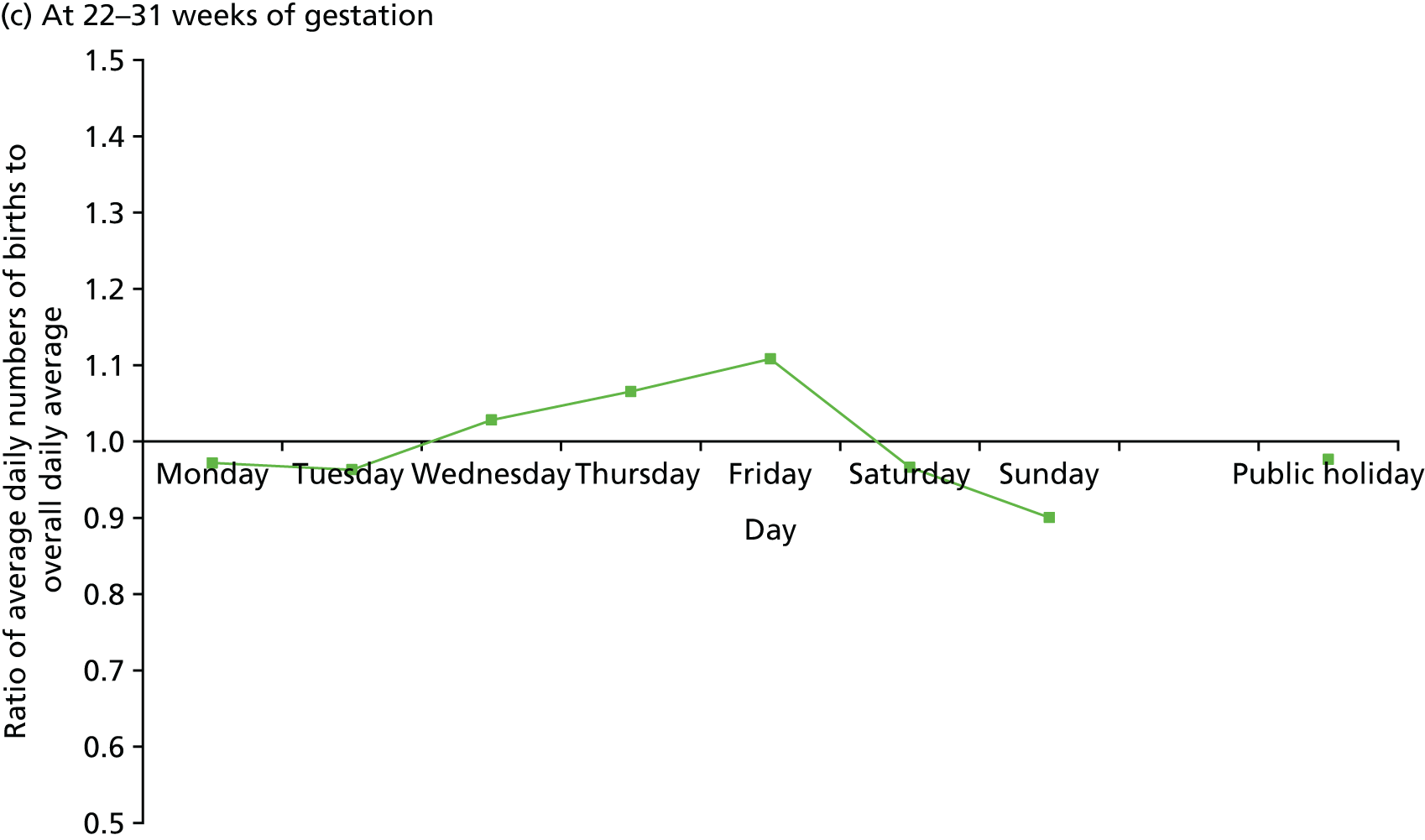
These analyses suggest that, for term and late preterm births, babies weighing under 2,500 g are more likely to be born on Thursdays and Fridays and less likely to be born on Sundays and Mondays than heavier babies. Variations by time of day, shown in Figure 14, show differences within both late preterm and term births between low birthweight babies and those weighing 2,500 g or more. They were more likely to be born between 09.00 and 12.00, in the afternoons and in the hours around midnight.
FIGURE 14.
Ratio of average hourly numbers of singleton births to overall daily average by birthweight, England and Wales: 2005–14.
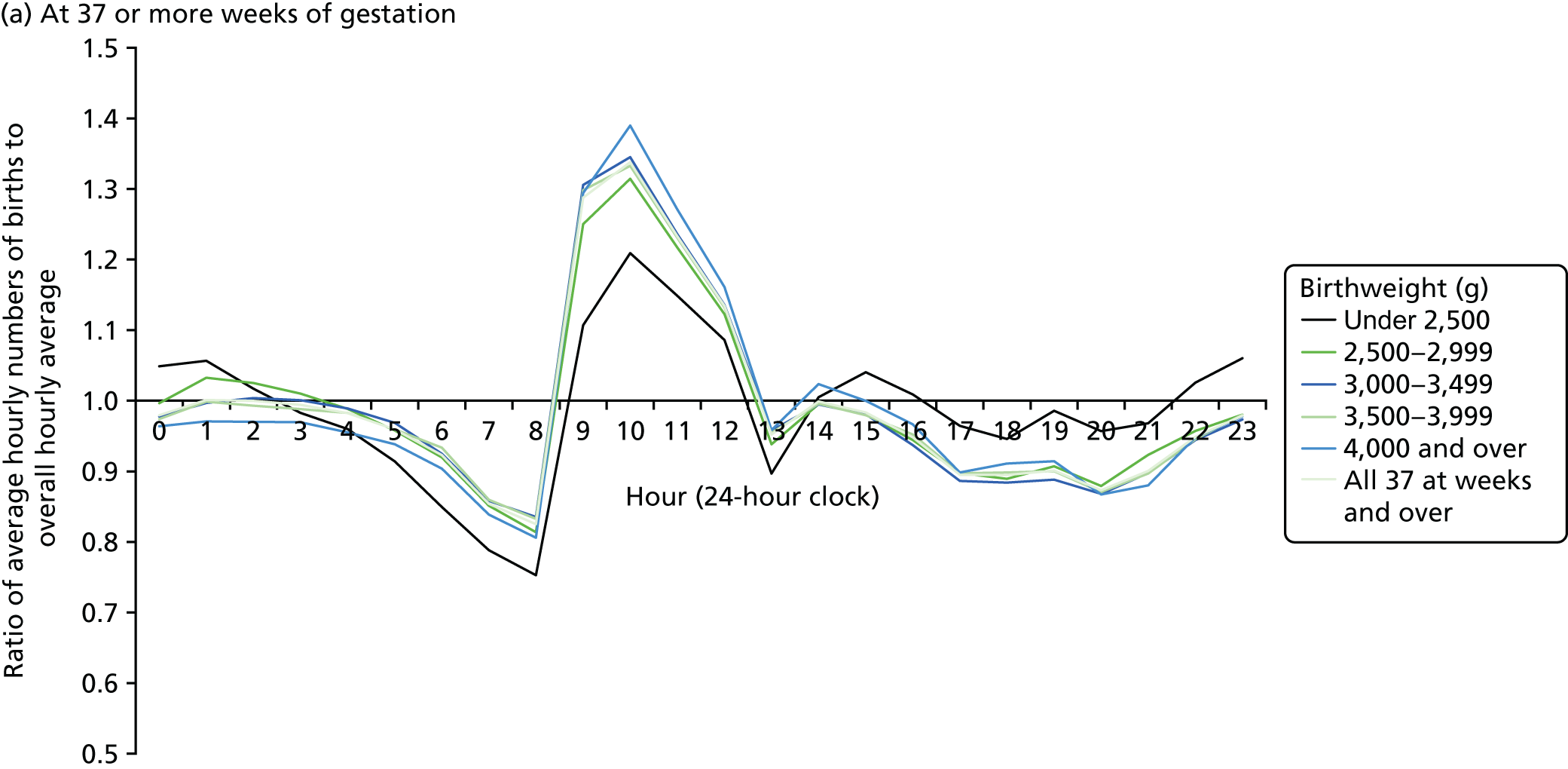
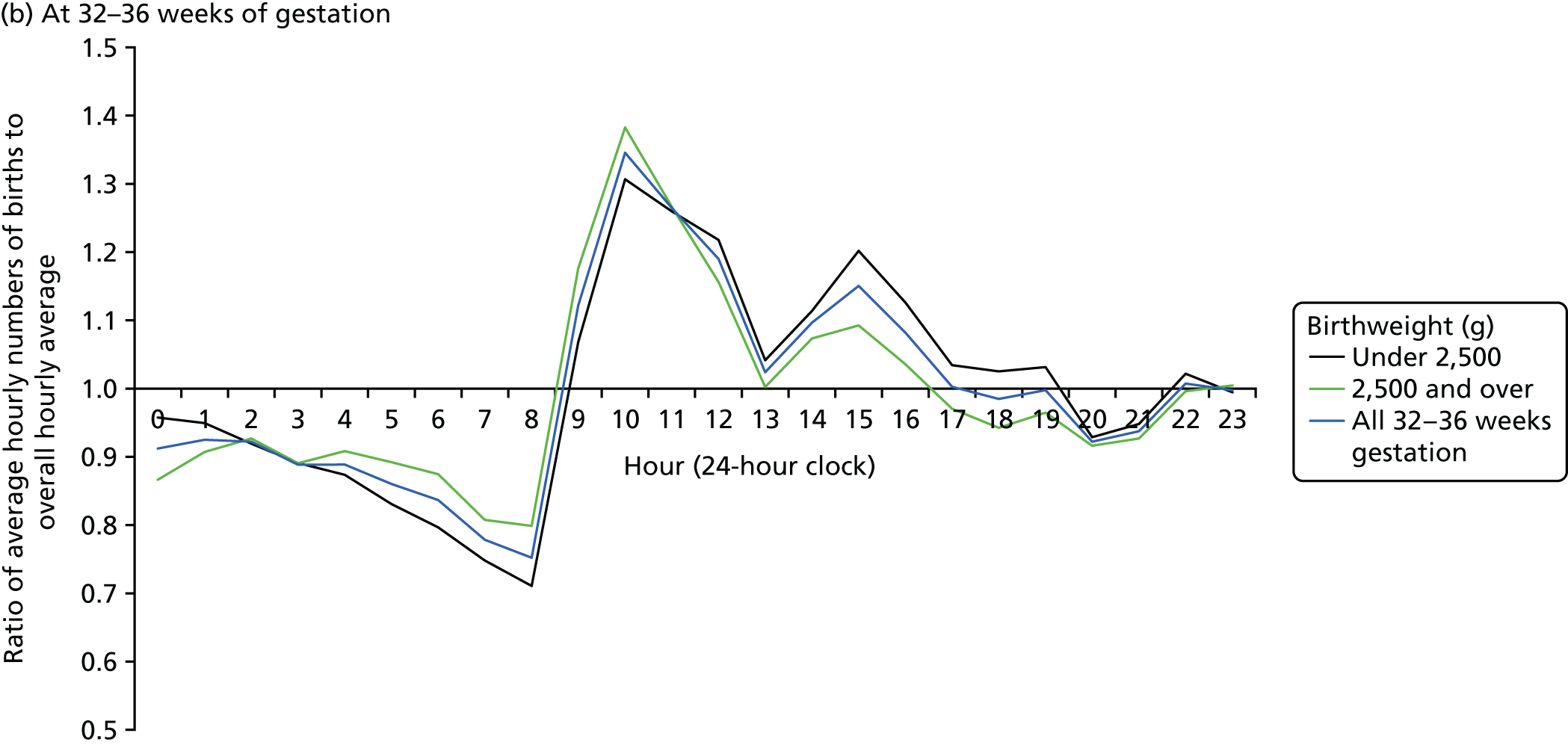
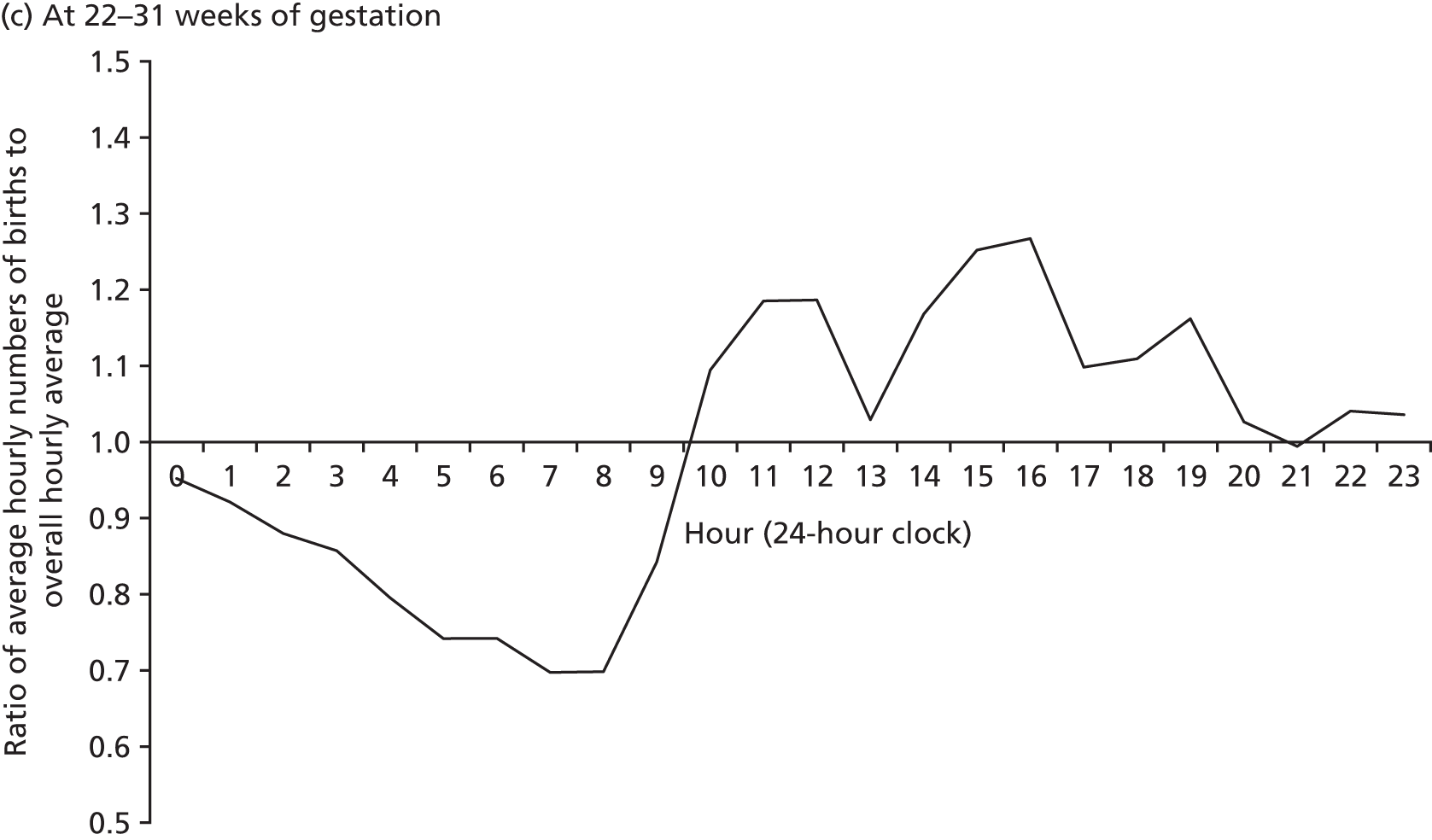
Settings for birth
Using the derived location codes, all singleton births were analysed by time of day and day of the week for each type of birth setting. As described in Chapter 2 (see also Appendix 2), maternity units with a consultant OU were subdivided according to whether or not they also had an AMU within the same hospital. Unfortunately, it was not possible to distinguish between births occurring in an OU or an AMU on the same site. FMUs at premises without a consultant OU are shown separately. There were relatively small numbers of births in private and military hospitals and even smaller numbers of births in hospitals with no maternity facilities (Table 15). There were also a few births recorded as taking place ‘elsewhere’, that is, in a range of other places, including in transit to maternity facilities. There is a marked day of the week pattern, with numbers of births in hospitals with OUs increasing from Monday to Friday (Figure 15a). The numbers are considerably lower on Saturdays and public holidays and much lower on Sundays. Although there is a weekly cycle in numbers of births at home and in FMUs, it is much less marked and there is no deficit in numbers of births on public holidays. Daily variations in other types of birth setting (see Figure 15b) are much wider, but are based on much smaller numbers and so would have had much wider confidence intervals. Births in private and military hospitals are much more heavily concentrated into weekdays than those in NHS hospitals and show much bigger deficits at weekends. Numbers of births in the other settings show weekly cycles that are less pronounced.
| Day | Birth setting | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| OU | OU with AMU | FMU | Private unit | Military hospital | Not a maternity unita | Home | Elsewhere outside hospital | All places | |
| Monday | 1,027.5 | 777.7 | 35.7 | 6.8 | 1.3 | 0.5 | 49.4 | 3.2 | 1,902.1 |
| Tuesday | 1,069.6 | 774.6 | 35.7 | 6.6 | 1.6 | 0.5 | 49.7 | 3.5 | 1,941.6 |
| Wednesday | 1,066.7 | 787.5 | 36.3 | 6.2 | 1.5 | 0.5 | 49.7 | 3.4 | 1,951.9 |
| Thursday | 1,085.3 | 796.9 | 36.1 | 6.8 | 1.5 | 0.5 | 49.0 | 3.2 | 1,979.3 |
| Friday | 1,084.4 | 797.4 | 35.9 | 6.7 | 1.5 | 0.5 | 48.5 | 3.1 | 1,978.0 |
| Saturday | 927.0 | 681.7 | 34.7 | 5.5 | 0.9 | 0.4 | 46.3 | 2.9 | 1,699.4 |
| Sunday | 868.6 | 651.2 | 34.0 | 3.5 | 0.8 | 0.4 | 45.1 | 3.1 | 1,606.7 |
| Public holiday | 924.7 | 686.9 | 36.1 | 3.3 | 1.1 | 0.3 | 48.6 | 3.6 | 1,704.8 |
| All | 1,015.8 | 750.4 | 35.5 | 5.9 | 1.3 | 0.5 | 48.2 | 3.2 | 1,860.8 |
FIGURE 15.
Variations in singleton births by day of the week, England and Wales: 2005–14.
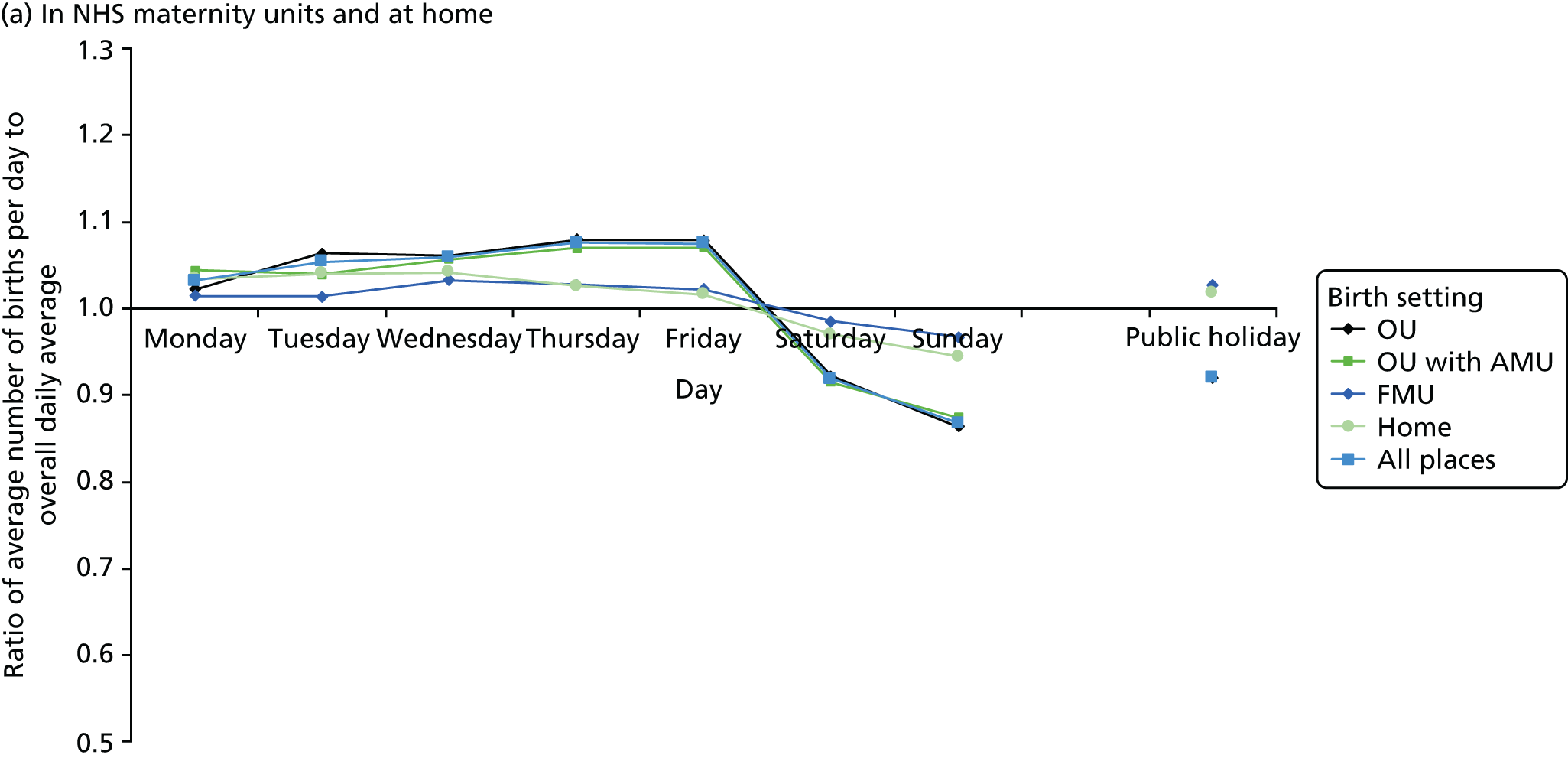
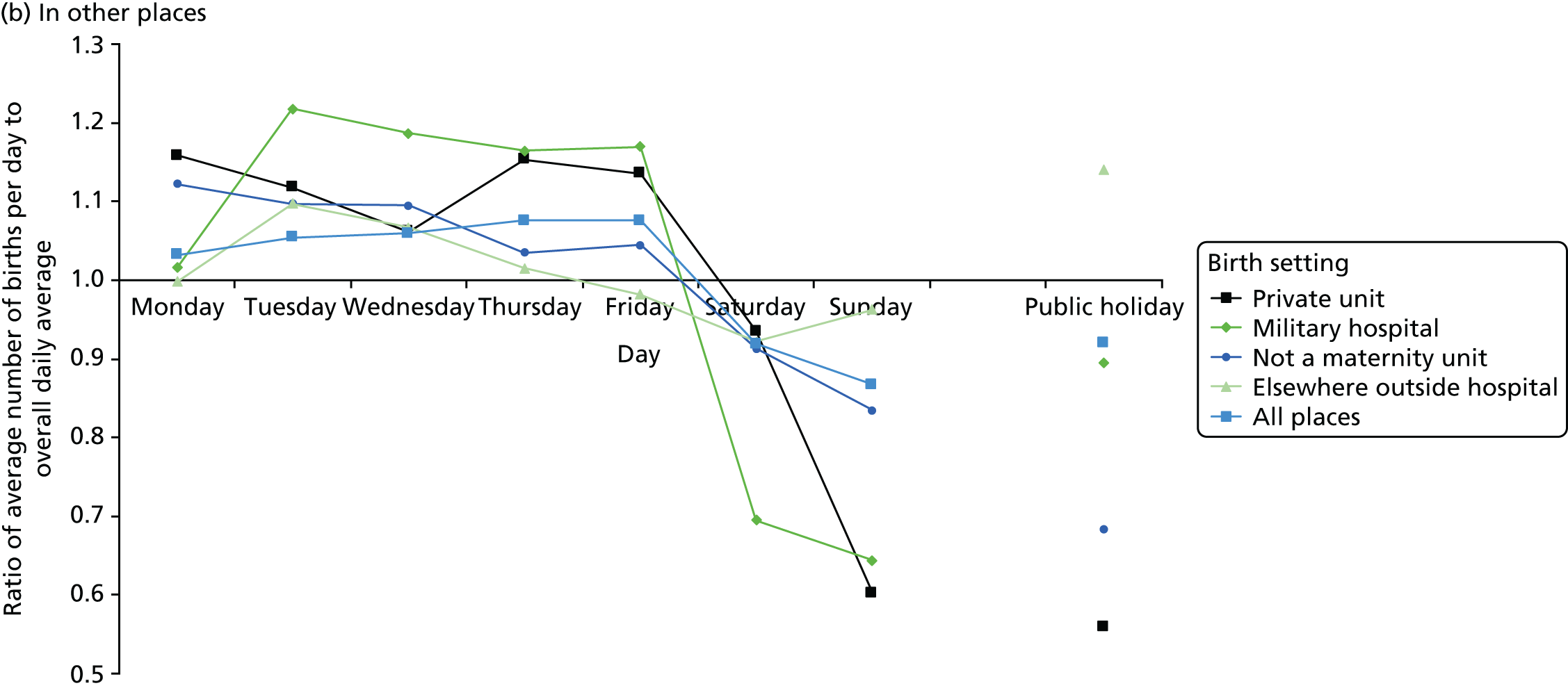
When numbers of births are plotted by time of day, they also show different patterns. In Figure 16, they are also shown as ratios. Numbers of births in hospitals with OUs peak in the mornings from 09.00 onwards, then, after a much smaller afternoon peak, they decrease after 17.00 and increase again up to midnight and then fall off after 05.00–06.00 (see Figure 16a). Numbers of births in FMUs and at home were highest from midnight to 10.00, peaking from 04.00 to 06.00. They were lowest during the day and during the hours up to midnight (see Figure 16a). The patterns in the other settings are much less distinct, as they are based on small numbers, but there is a sharp peak at 08.00 in births in military hospitals and morning peaks followed by early and late afternoon peaks in private hospitals (see Figure 16b). Births that occur either in hospitals without maternity units or elsewhere are unlikely to have occurred there intentionally and it is notable that those in non-maternity units tend to occur in the morning, whereas those ‘elsewhere’ follow similar patterns to births at home and in FMUs, although they have a flatter peak from 04.00 to 08.00.
FIGURE 16.
Variation in singleton births by time of day, England and Wales: 2005–14.
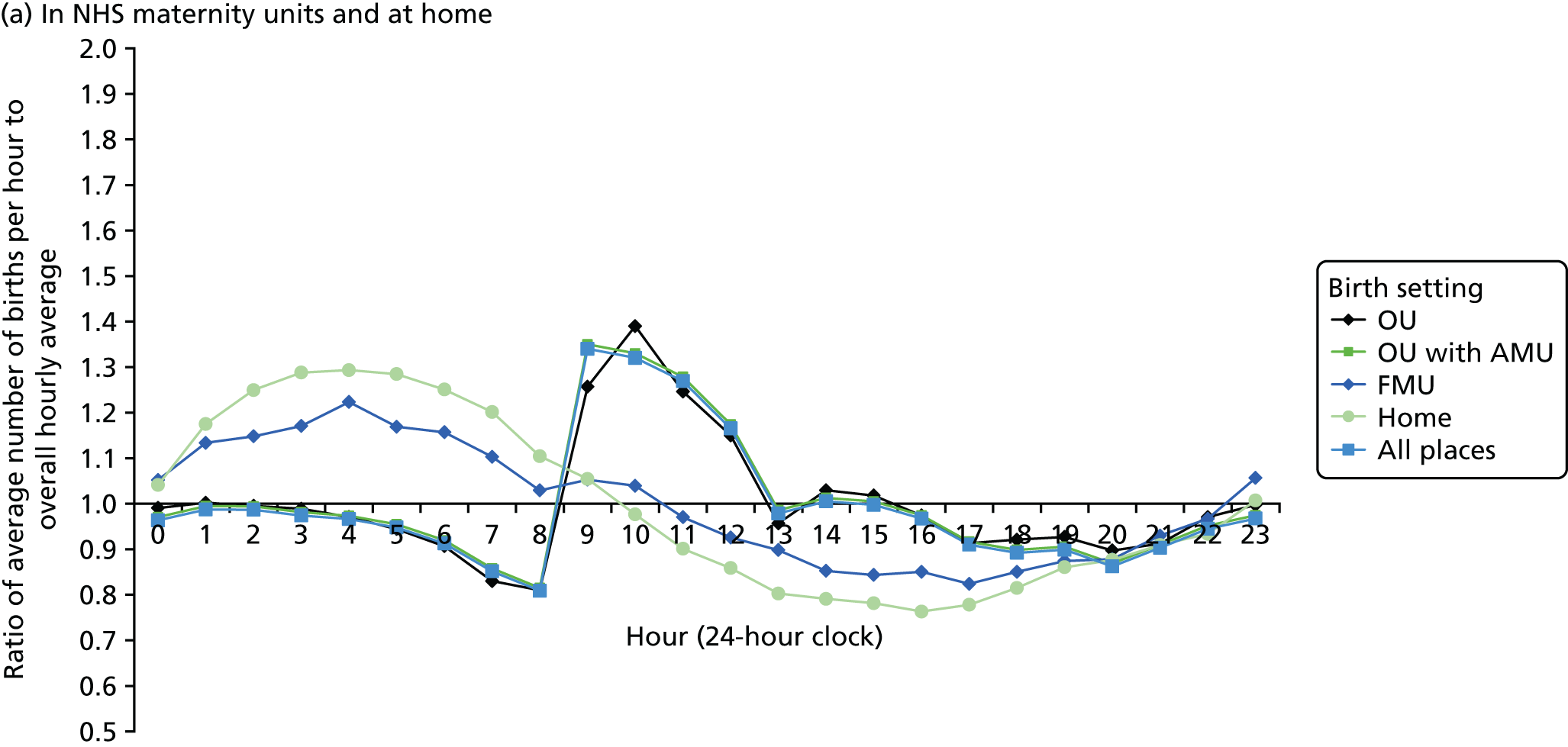
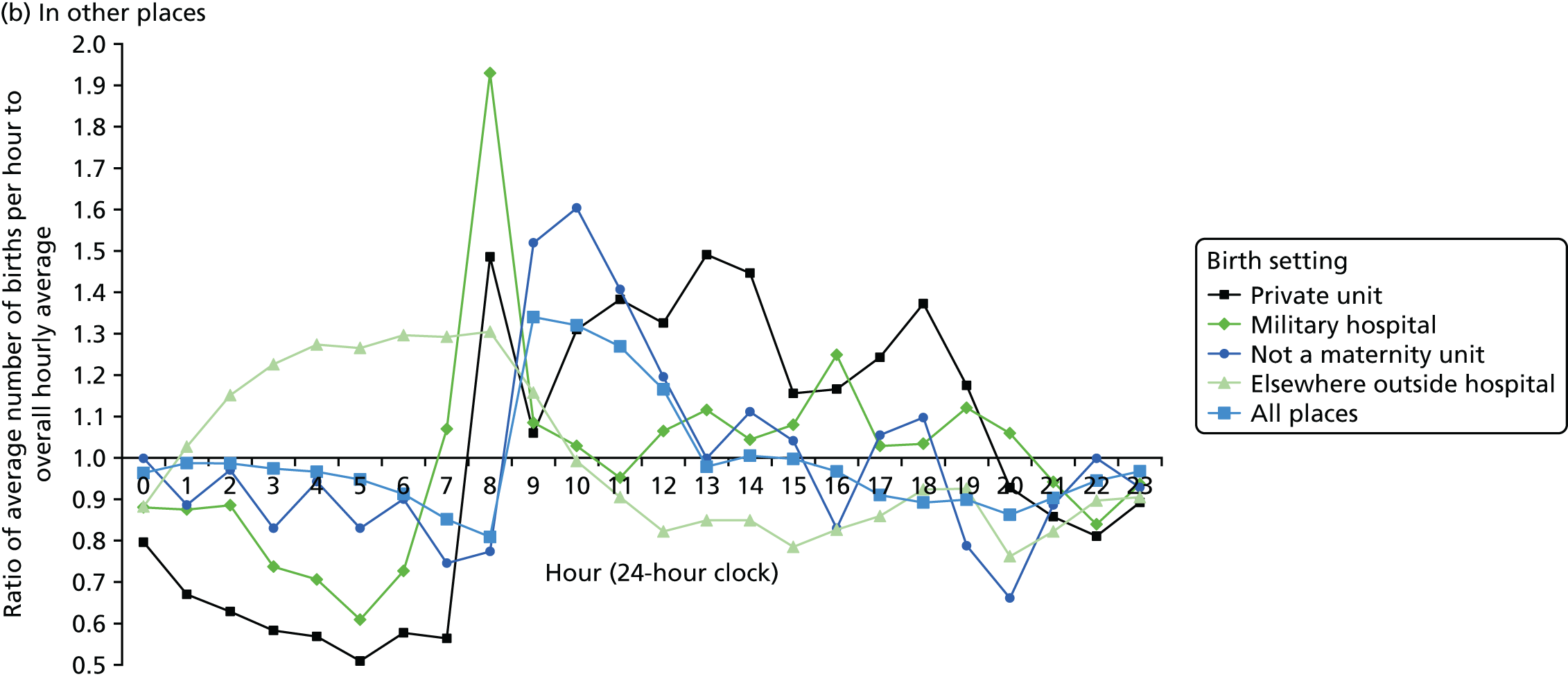
It is clear that the patterns observed for hospital births are related to obstetric intervention and that the hourly patterns vary by day of the week. Singleton births in hospital were analysed for England and Wales separately in what follows, as information on onset of labour and method of delivery was coded differently in HES and the PEDW.
Births in NHS hospitals in England by onset of labour and method of delivery
This section of the analysis describes in detail how day and time of birth vary by onset of labour, mode of birth and gestational age in NHS maternity units in England.
Methods
Data for analysis
The steps taken to derive a subset of data for analysis are illustrated in Figure 17. The source dataset consisted of all 6,468,586 registered singleton births occurring from 1 January 2005 to 31 December 2014 in England. After linkage and quality assurance, 6,138,487 singleton births were judged to be linked to the correct HES delivery record. A total of 542 additional records were excluded because, after a careful comparison of the records, it was ascertained that the linkage between birth registration and birth notification records was incorrect. As shown in Figure 17 and Table 77, the resulting subset contained 6,137,945 records, that is, 94.9% of the source dataset. Further investigation was carried out to assess whether or not the births in this subset differed from the source dataset with respect to region of residence, year, month, type of day and hour of birth, age of mother, sex and gestational age of baby. These analyses are reported in detail in Appendix 3, Table 78. For each of these variables, there was a statistically significant difference between the distributions of births included in and excluded from the derived subset. Births in the years from 2009 onwards were more likely to be linked than those in the years up to 2008. However, the differences between the source dataset and the derived subset were small: below 1 percentage point for any category.
FIGURE 17.
How the subset was derived for analysis.
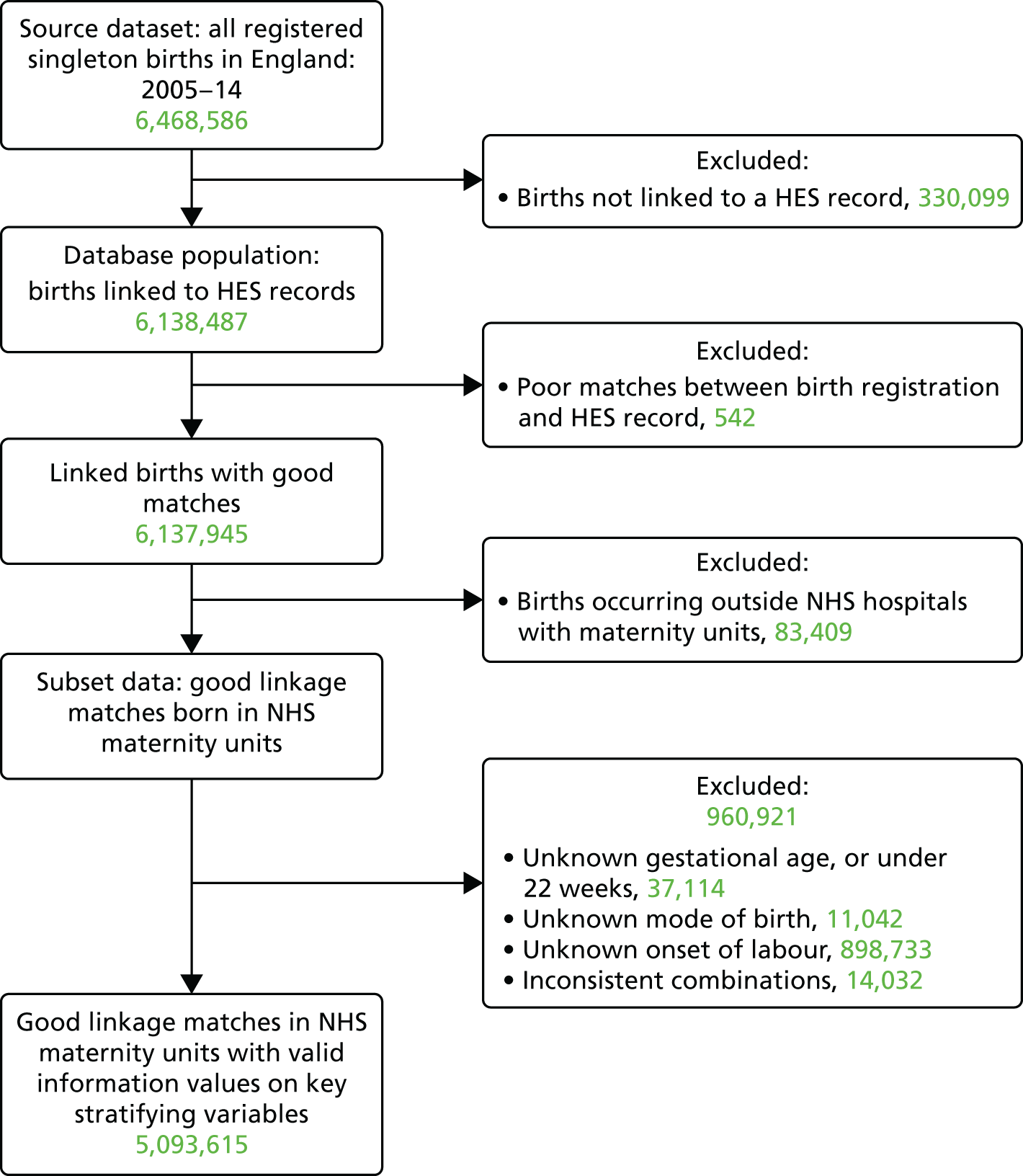
The subset used for these analyses included 6,054,536 births recorded as having taken place in NHS maternity units, excluding 83,409 births that took place at home, in private hospitals, in NHS hospitals without maternity facilities, or elsewhere outside a hospital. Births outside hospitals and those occurring at home have low rates of inclusion in Maternity HES and, as a consequence, low rates of linkage, so overall data quality would have suffered had they been included in the analysis.
Finally, 960,921 birth records with missing or inconsistent data were excluded from the subset. These records included 898,733 with missing data about the onset of labour, a key variable, 11,042 with mode of birth missing, 37,114 with gestational age missing and 14,032 with inconsistent combinations of data items. The excluded births made up 15.9% of the subset, leaving data for 5,093,615 births, as shown in Figure 17 and Table 16. The records excluded because of missing information were compared with those retained to see if this changed the distribution of births with respect to region of residence, year, month, type of day and hour of birth, age of mother, sex and gestational age of baby.
These comparisons are reported in detail in Appendix 3, Table 80, and show statistically significant differences between included and excluded births for all variables, except the baby’s sex. Nonetheless, differences between all linked NHS hospital births and the subset were small, the biggest difference being 1.02 percentage points for a category. Relatively fewer births in later years had to be excluded, compared with births in earlier years, as the completeness of data had improved.
Descriptive analysis
Descriptive analyses by time of birth and day of the week were done separately for eight combinations of onset of labour and mode of birth. In the descriptive summaries, the mean number of births in a particular hour of the week was calculated. For example, ‘Monday 00.00 to 00.59’ records the mean number of births in the first hour of a non-holiday Monday. The mean number of births is a suitable statistic, because it allows direct comparison between the mean number of births per hour on different types of day, taking into account differences in numbers of each type of day in the study period. For example, there were more non-holiday Tuesdays than non-holiday Mondays.
Statistical modelling
Appropriate statistical techniques were used to fit models to describe daily, weekly and yearly cycles in births and the outcomes of pregnancy. Circular data, also known as angular, harmonic, cyclical, periodic, directional or seasonal data, often consist of dates or hours of the day. 143 The measurement scale is cyclic and is expressed, mathematically, as angles within the unit circle. As cyclical patterns are dominated by the mathematical properties of trigonometric functions, typically harmonic terms based on the sine and cosine functions, analytical methods required to summarise, visualise and model these circular data differ substantially from those used in linear statistics. 144
Statistical analyses of seasonal patterns in epidemiology focus on (1) cyclical events, such as incidence of births, or (2) cyclical risk factors for an event, such as day of the week of birth, as independent predictors of events. The first case refers to cyclical response variables, usually dates. The analysis of such variables requires special descriptive and modelling methods, for instance circular histograms, rose diagrams and models based on circular random variables. 144
For the analysis of cyclical risk factors for numbers of births, we used spectral analysis145 to describe the incidence of births, adjusting for daily, weekly and yearly patterns. Secular and cyclical birth trends were modelled using generalised linear models with a Poisson or a negative binomial distribution, the latter being preferred if there is overdispersion in the data. Both probability models use a logarithmic link, which is suitable for modelling birth counts as it guarantees that the mean, and the model predictions, will be positive.
Non-parametric spline regression functions were used to account for overall trends in the study period. These trends arise from sociodemographic fluctuations that reflect changes in immigration and macroeconomic variables. Daily, weekly and yearly cycles corresponding to hour of birth, day of the week of birth and date of birth were modelled using trigonometric functions (sine and cosine) appropriate for the length of the period. These functions take into account the cyclical nature of changes and incorporated non-standard features of the data, for example clock changes, movable holidays and leap years. 146
There were 3,652 days from 1 January 2005 to 31 December 2014. Our model aimed to predict the numbers of births on each of these days separately for each of the eight combinations of onset of labour and mode of birth defined in Table 16. We fitted negative binomial regression models with a logarithmic link, and included the following predictor variables to define the models’ linear predictors:
-
Type of day as described above.
-
Harmonic terms to account for the yearly cycle of birth frequencies. This is important, as without this adjustment our model would not be able to distinguish seasonal variations in birth frequencies from the effects of public holidays, such as Christmas. We used spectral methods based on empirical periodograms145 to identify relevant cyclical frequencies and set up the harmonic terms as follows. The days of the year from 1 January to 31 December were transformed into angles on the radian scale, from 0 to just under 2π. The sine and cosine of the angles were then added as predictor variables in the model, at all frequencies from 1 to 9 (where 1 signifies a 12-month cycle, and 9 signifies a 1.33-month cycle).
-
A non-parametric, natural cubic spline term146 to control for trends over time, estimated using the 120 months from January 2005 to December 2014, whereby the months were coded sequentially 0 to 119. We allowed 3 degrees of freedom per year. Without this adjustment, trends in numbers of births and trends in intervention rates over our study period could have confounded our estimates of holiday effects.
-
Two dummy variables identifying days of clock changes. Days on which the clock changes to British Summer Time have 23 hours and thus a lower expected number of births; days on which the clock changes back to Greenwich Mean Time have 25 hours and a higher expected number of births.
Models fitted and interpretation
Negative binomial models were used because frequencies of live births were overdispersed and this required further parameters than those provided by Poisson models.
In our statistical models, estimates were presented as rate ratios (RRs): the ratio of the expected number of births on one type of day over the mean number of births per day. For example, a RR of 1.10 for a Friday means that the expected number of births on Fridays is 10% higher than the mean. A RR of 0.88 for a Sunday means that the expected number of births on Sundays is 12% lower than the mean. All RRs were adjusted for yearly cycles, trend and clock changes, as described earlier. Model comparisons were performed using likelihood ratio tests.
We calculated 99% confidence intervals around parameter estimates, and, for hypothesis tests, used a significance level of α = 0.01. All statistical analyses were carried out in R version 3.1.2. 147
Results
Daily and weekly patterns of births by onset and delivery
Table 16 shows the number of births by onset of labour, mode of birth and gestational age group.
| Onset of labour | Mode of birth | Number of births | Percentage | |||
|---|---|---|---|---|---|---|
| Gestational age | Total | |||||
| Term | Preterm | Post-term | ||||
| Spontaneous | Spontaneous | 2,401,010 | 121,915 | 45,487 | 2,568,412 | 50.4 |
| Emergency caesarean section | 308,248 | 29,440 | 11,121 | 348,809 | 6.8 | |
| Instrumental | 425,955 | 21,542 | 12,472 | 459,969 | 9.0 | |
| Induced | Spontaneous | 577,544 | 38,249 | 60,075 | 675,868 | 13.3 |
| Emergency caesarean section | 188,413 | 11,913 | 38,335 | 238,661 | 4.7 | |
| Instrumental | 162,882 | 7,168 | 28,006 | 198,056 | 3.9 | |
| No laboura | Elective caesarean sectiona | 441,500 | 23,879 | 4,614 | 469,993 | 9.2 |
| Emergency caesarean section | 84,384 | 44,465 | 4,998 | 133,847 | 2.6 | |
| Total | 4,589,936 | 298,571 | 205,108 | 5,093,615 | 100.0 | |
| Percentage | 90.1 | 5.9 | 4.0 | 100.0 | ||
Figure 18 shows the average number of births per hour in NHS maternity units in England over the course of the week and on public holidays. The pattern is the same, whether we look at all singleton births in NHS maternity units in England (green line), or the somewhat smaller subset of births for which we have complete data and that we could include in our analyses (black line). This suggests that our subset is representative of the timing of births in NHS maternity units in England from 2005 to 2014.
FIGURE 18.
Average number of singleton births in NHS maternity units per hour over the week, England: 2005–14.
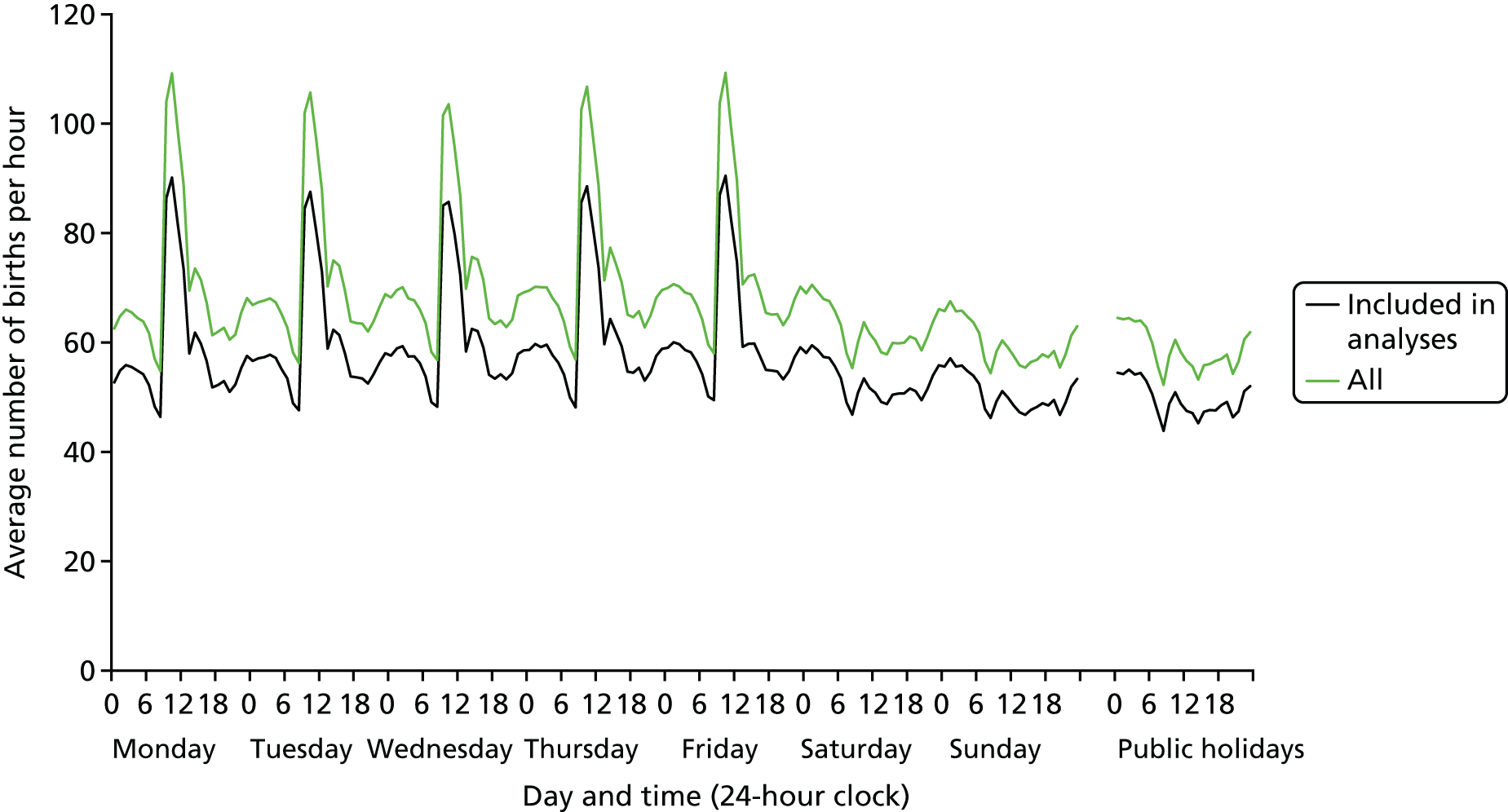
The peaks in mean frequencies occur on weekdays between 09.00 and 12.59, with a smaller secondary peak between 14.00 and 14.59 on weekdays. A second period of relatively high numbers of births, although with a much smaller peak, occurs between 22.00 and 06.59, regardless of the type of day. Low numbers of births can be seen between 08.00 and 08.59 on weekdays and also at weekends and on public holidays.
It is important to consider the proportion of births that occur outside ‘usual’ working hours. Overall, 71.4% of all singleton births in NHS maternity units and 71.5% of those in the analysis subset occurred ‘out of hours’, that is at weekends, on public holidays or on weekdays between 17.00 and 08.59. Conversely, 28.6% of all births in NHS hospitals and 28.5% of births in the analysis subset occurred within ‘usual’ working hours, that is on weekdays between 09.00 and 16.59. As in a ‘normal’ 40-hour week, ‘usual’ working hours account for 23.8% of the total of 168 hours in a week, the extent to which births have been concentrated into ‘usual’ working hours is limited.
Figure 18 shows the overall daily and weekly cycles of births, whereas Figure 19 demonstrates how these cycles differ by onset of labour and mode of birth. There are clear differences in circadian and weekly patterns. For a more detailed view of average numbers of births per hour in each of the eight combinations of mode of onset and births, for a typical weekday (Thursday), see Appendix 3, Figure 27. Graphical data exploration, which is not shown here, suggested that the circadian patterns do not vary appreciably by gestational age group. We therefore concentrated on circadian patterns in term births in this analysis but we also compared weekly patterns of births in preterm, term and post-term gestational age groups (see Figure 20).
FIGURE 19.
Average number of term births per hour by type of day, onset of labour and mode of birth, England: 2005–14.
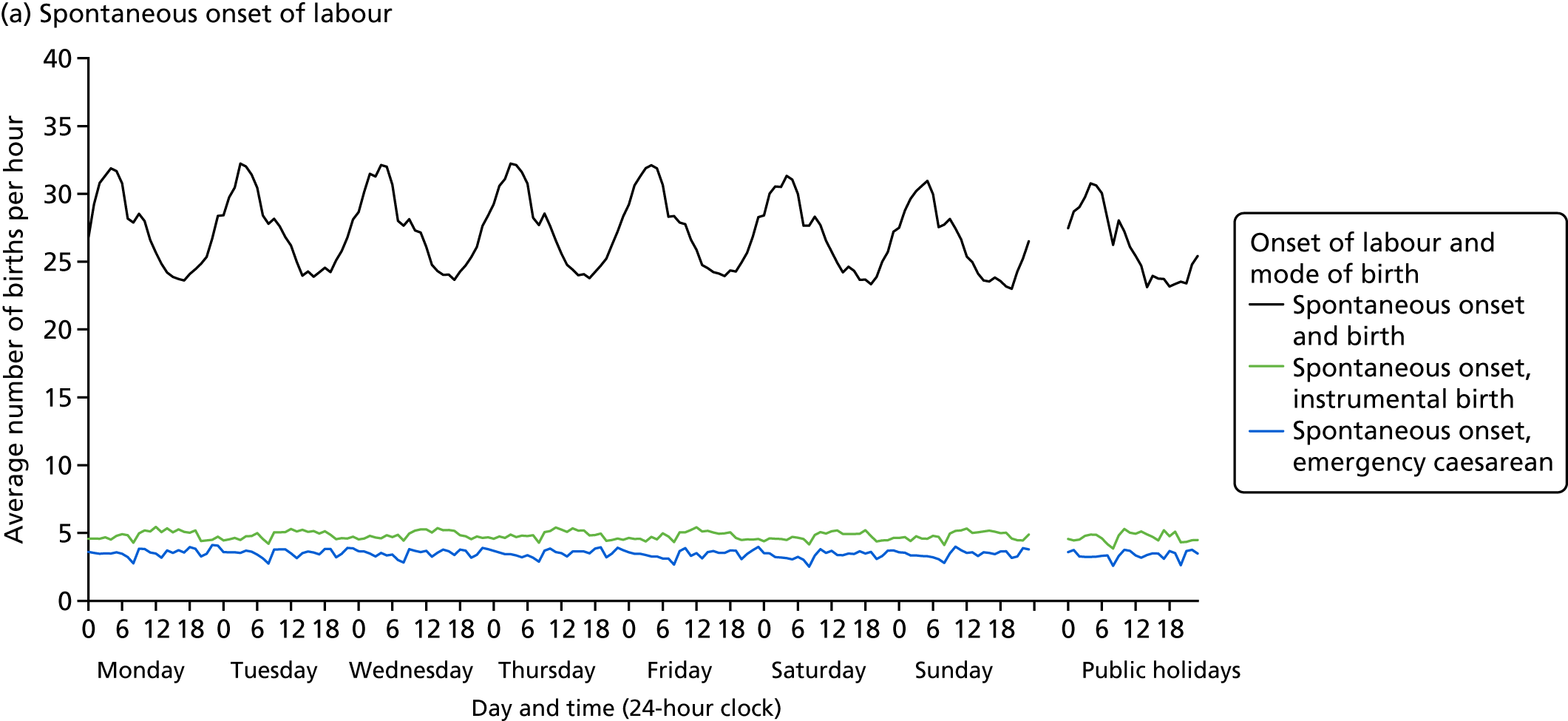
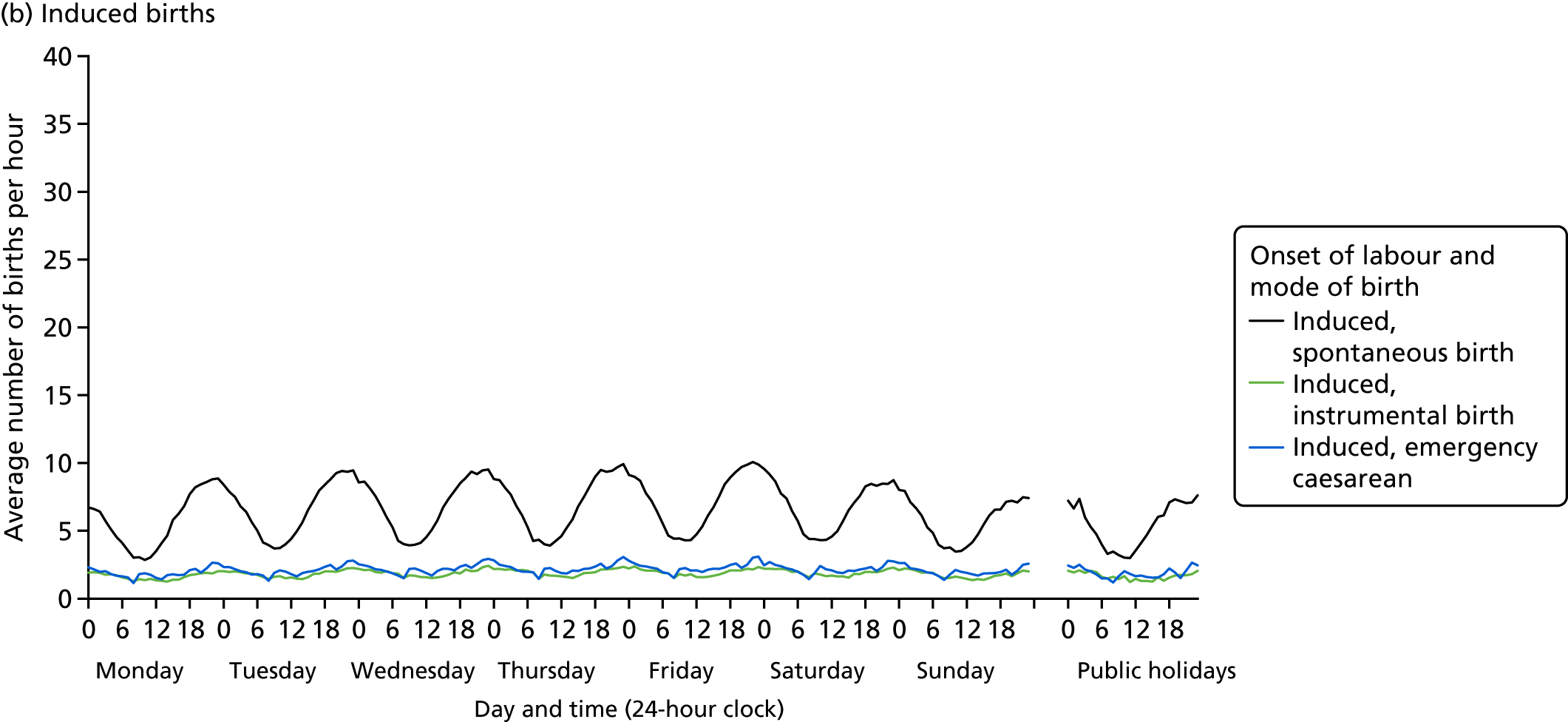
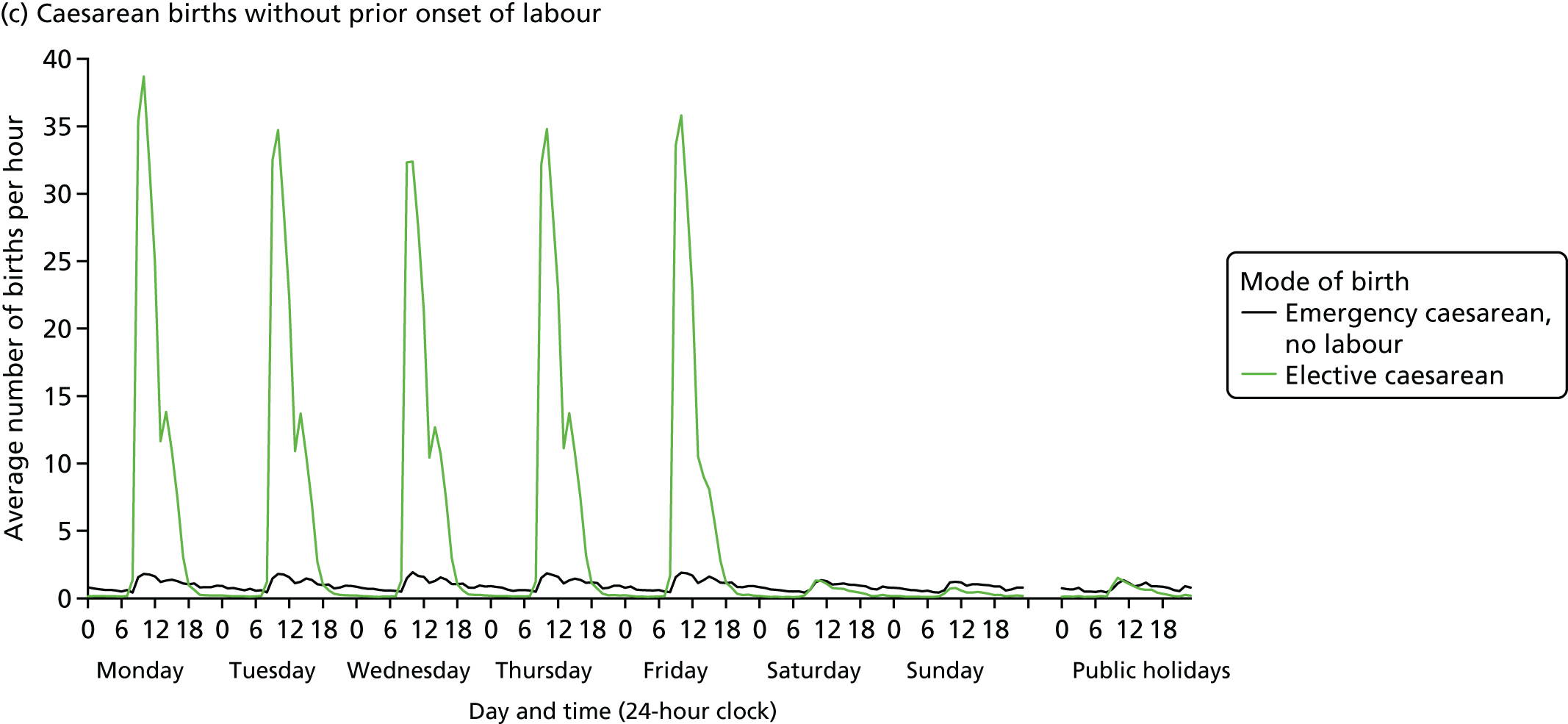
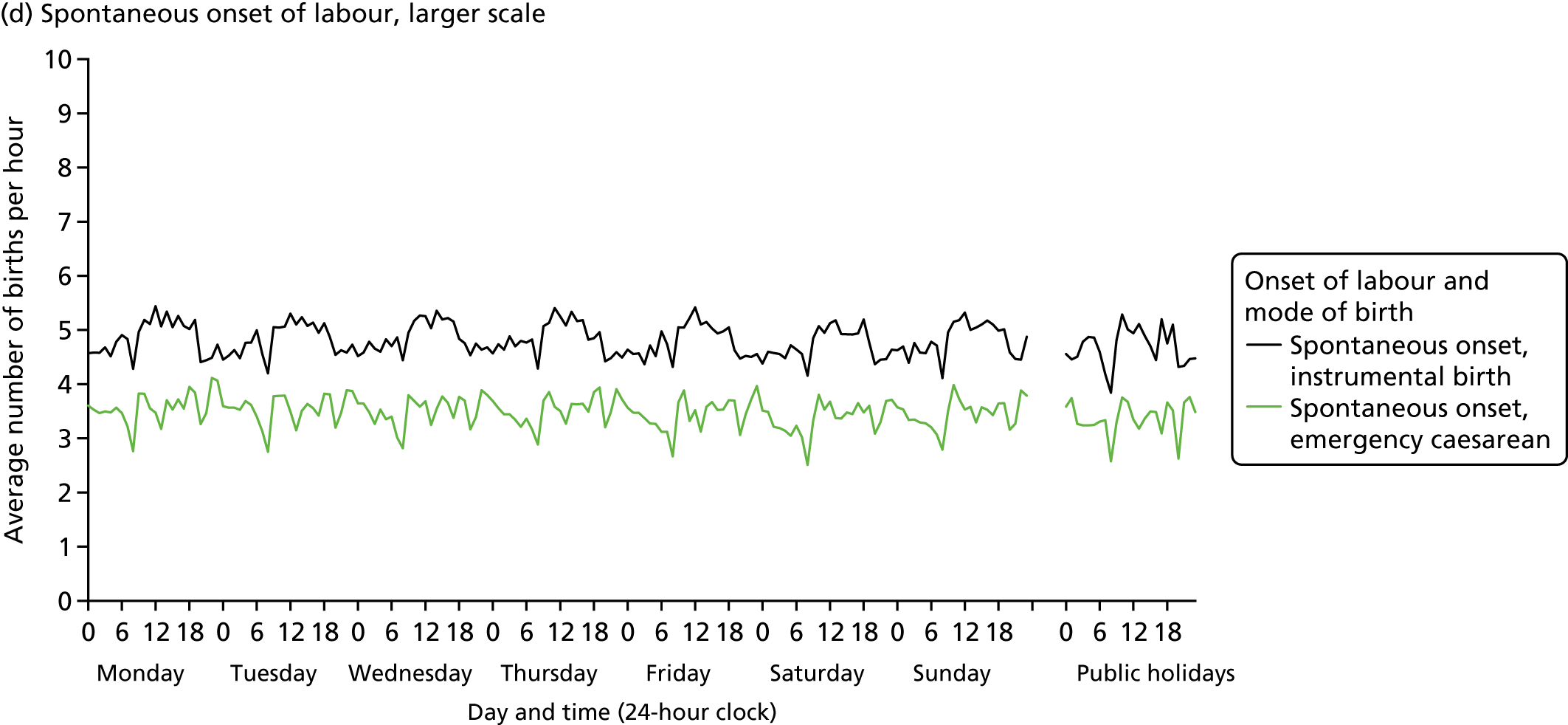
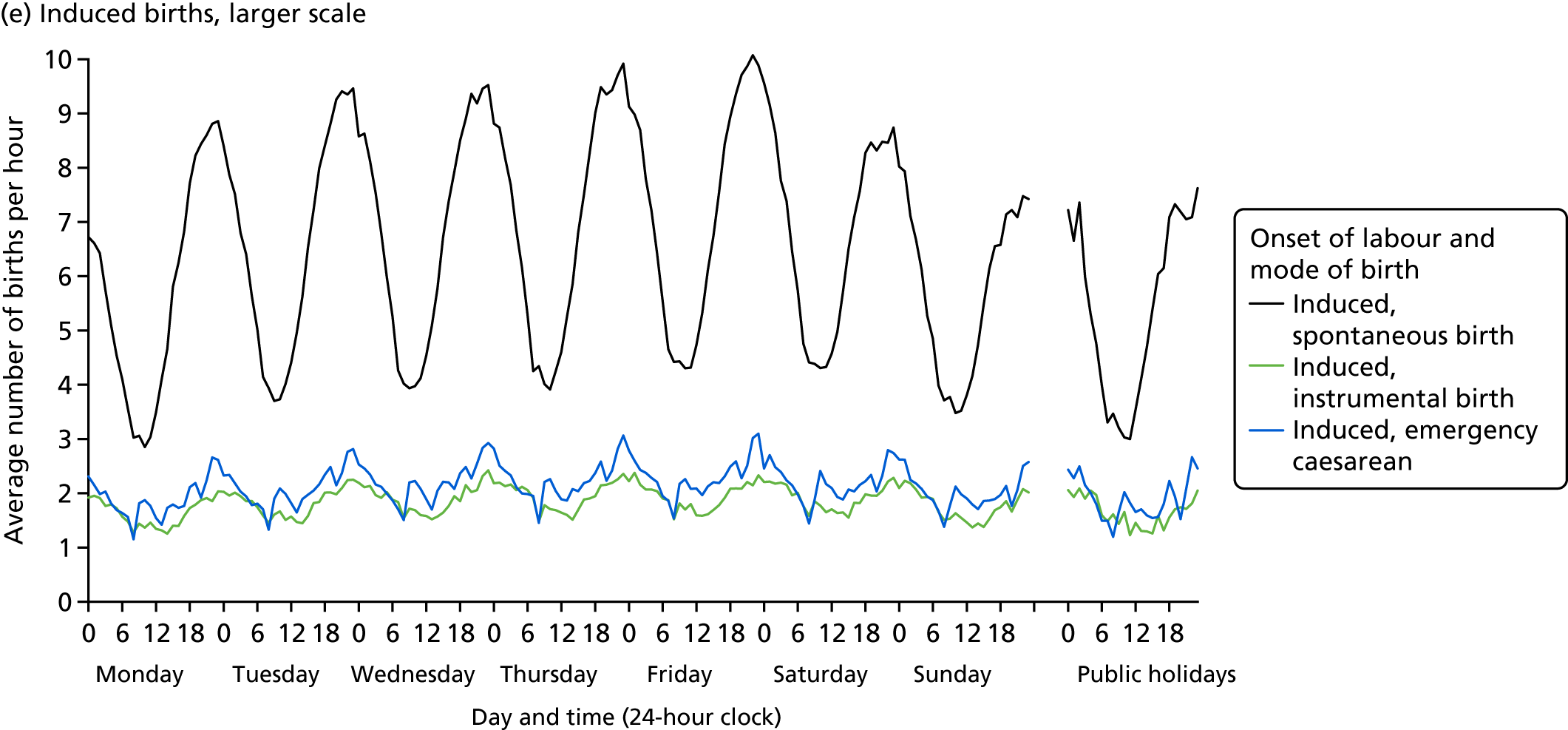
Spontaneous onset
Figure 19a shows the average numbers of births per hour with spontaneous onset over the course of a week, by mode of birth. Figure 19d then shows instrumental births and emergency caesarean sections on a larger scale to bring out their patterns more clearly. Just over half of all births in our dataset are spontaneous births following spontaneous onset of labour. These have a roughly sinusoidal pattern and are most likely to occur between 01.00 and 07.00, with a peak around 04.00, and a trough in the afternoon. In addition, there is a small but noticeable interruption of the sinusoidal pattern at 08.00.
In contrast, instrumental births after spontaneous onset of labour are more likely to occur between 09.00 and 17.00 than in the night and early morning. The least frequent time for births in this group is 08.00. Births where spontaneous onset of labour was followed by an emergency caesarean section are more frequent between 09.00 and 00.00 than in the early hours of the morning. There are three distinct dips in the distribution, the most pronounced of which is seen at 08.00, with somewhat smaller dips at 13.00 and 20.00.
In general, the patterns of births after spontaneous onset over the course of the day do not vary much between weekdays, weekends and public holidays. Nonetheless, numbers of spontaneous births after spontaneous onset are slightly lower on Sundays and public holidays than on weekdays, as we explore in detail below.
Induced onset
Figure 19b shows the average number of induced births per hour over the course of a week, by mode of birth. Figure 19e then shows instrumental births and emergency caesarean sections within this group on a larger scale. Spontaneous births after induced onset of labour follow a sinusoidal pattern, with a peak during the hour before midnight and a trough just before noon.
The same midnight peak appears when inductions are followed by instrumental births or emergency caesarean sections, although in these groups the patterns are less regular than for induced spontaneous births. The three groups of induced births share a weekly cycle that has its highest peak on Friday night and its trough on Monday morning.
Caesarean births
Figure 19c shows the distribution of caesarean births without prior onset of labour separately for elective and emergency caesarean sections. Elective caesarean sections are mostly carried out on weekdays between 09.00 and 12.00, with a pronounced peak between 09.00 and 10.59. Very few occur between 17.00 and 07.00 on weekday evenings and nights, and even fewer at any time at weekends and on public holidays.
Emergency caesarean sections without prior onset of labour follow a somewhat similar pattern to elective caesarean sections, with a pronounced peak between 09.00 and 12.00. There is a difference, however, as average numbers of emergency caesarean sections without prior onset of labour are higher than average numbers of elective caesarean sections in the evening, at night and in the early morning, and the same applies to weekends and public holidays.
Day of the week differences
Statistical models were fitted to estimate differences in the daily numbers of singleton term births by type of day, separately for each of the eight combinations of onset of labour and mode of birth, adjusted for yearly cycles in numbers of births and trends over time. Results are presented in Table 17. This uses RRs, together with 99% confidence intervals, to compare the predicted average numbers of births in each category of onset and birth on each type of day to the overall daily average for the category.
| Day | Onset of labour, RR (99% confidence interval) | |||||||
|---|---|---|---|---|---|---|---|---|
| Spontaneous | Induced | No labour | ||||||
| Spontaneous | Emergency caesarean section | Instrumental | Spontaneous | Emergency caesarean section | Instrumental | Elective caesarean section | Emergency caesarean section | |
| Monday | 1.00 (0.99, 1.00) | 1.02 (1.01, 1.04) | 1.01 (0.99, 1.02) | 0.87 (0.86, 0.88) | 0.89 (0.87, 0.90) | 0.88 (0.87, 0.90) | 1.53 (1.52, 1.55) | 1.05 (1.01, 1.09) |
| Tuesday | 1.01 (1.00, 1.01) | 1.02 (1.00, 1.03) | 1.00 (0.99, 1.01) | 1.02 (1.01, 1.03) | 0.98 (0.97, 1.00) | 0.99 (0.97, 1.01) | 1.38 (1.37, 1.40) | 1.06 (1.02, 1.09) |
| Wednesday | 1.01 (1.01, 1.02) | 1.01 (1.00, 1.02) | 1.01 (1.00, 1.02) | 1.05 (1.04, 1.06) | 1.04 (1.02, 1.05) | 1.03 (1.01, 1.05) | 1.36 (1.34, 1.37) | 1.07 (1.03, 1.10) |
| Thursday | 1.01 (1.01, 1.02) | 1.01 (1.00, 1.02) | 1.01 (1.00, 1.02) | 1.07 (1.06, 1.08) | 1.06 (1.04, 1.07) | 1.06 (1.04, 1.08) | 1.41 (1.40, 1.43) | 1.08 (1.05, 1.12) |
| Friday | 1.01 (1.01, 1.02) | 0.99 (0.98, 1.01) | 1.00 (0.99, 1.01) | 1.10 (1.09, 1.11) | 1.09 (1.07, 1.10) | 1.06 (1.04, 1.07) | 1.36 (1.35, 1.38) | 1.09 (1.06, 1.13) |
| Saturday | 0.99 (0.99, 1.00) | 0.97 (0.95, 0.98) | 0.98 (0.97, 0.99) | 1.04 (1.03, 1.05) | 1.03 (1.01, 1.05) | 1.04 (1.03, 1.06) | 0.08 (0.08, 0.09) | 0.86 (0.84, 0.89) |
| Sunday | 0.98 (0.97, 0.98) | 0.99 (0.98, 1.00) | 1.00 (0.99, 1.01) | 0.88 (0.87, 0.89) | 0.95 (0.93, 0.96) | 0.96 (0.94, 0.97) | 0.06 (0.05, 0.06) | 0.83 (0.80, 0.86) |
| Public holiday | 0.98 (0.97, 0.99) | 0.99 (0.96, 1.02) | 0.98 (0.96, 1.01) | 0.88 (0.86, 0.91) | 0.92 (0.88, 0.96) | 0.92 (0.88, 0.97) | 0.09 (0.08, 0.10) | 0.84 (0.76, 0.92) |
| Christmas | 0.93 (0.90, 0.95) | 0.88 (0.82, 0.95) | 0.97 (0.92, 1.03) | 0.61 (0.57, 0.65) | 0.79 (0.72, 0.87) | 0.81 (0.74, 0.90) | 0.05 (0.04, 0.06) | 0.72 (0.58, 0.88) |
| Day before public holiday | 1.00 (0.98, 1.01) | 0.96 (0.92, 1.00) | 1.00 (0.97, 1.04) | 1.10 (1.06, 1.13) | 1.08 (1.03, 1.13) | 1.08 (1.03, 1.14) | 1.43 (1.39, 1.48) | 1.11 (1.01, 1.21) |
| Day after public holiday | 0.99 (0.97, 1.00) | 1.02 (0.99, 1.06) | 1.00 (0.97, 1.03) | 0.87 (0.84, 0.90) | 0.86 (0.82, 0.91) | 0.88 (0.83, 0.93) | 1.62 (1.58, 1.67) | 0.99 (0.90, 1.10) |
| Adjusted R2 | 0.843 | 0.423 | 0.623 | 0.826 | 0.664 | 0.737 | 0.972 | 0.628 |
| Percentage deviance | 1.5 | 1.9 | 0.4 | 18.7 | 7.2 | 4.6 | 94.6 | 9.3 |
| Number of births | 2,401,010 | 308,248 | 425,955 | 577,544 | 188,413 | 162,882 | 441,500 | 84,384 |
The models fitted well. Residuals were approximately normally distributed for all models, and there were no influential outliers. Adjusted R2 values ranged from 0.42 for spontaneous onset and emergency caesarean section to 0.97 for elective caesarean sections. Type of day differences were statistically significant (p < 0.001) for all groups, but the strength of the relationship varied considerably. Type of day accounted for 94.6% of the variation in daily numbers of elective caesarean births, but only for 0.4% of the variation among instrumental births after spontaneous onset of labour.
The estimated adjusted RRs in Table 17 point to differences in the numbers of term births by type of day. As well as births on each day of the week, births on Christmas Day and Boxing Day, public holidays and on days immediately before and after a public holiday are shown. For births after the spontaneous onset of labour, differences by type of day were small. Numbers of spontaneous births after spontaneous onset of labour were higher on weekdays, especially from Wednesday to Friday, than on Sundays and public holidays. An estimated 7% fewer babies were born on Christmas Day and Boxing Day than on an average day. Similar, but smaller, differences between types of day were found for emergency caesarean sections and instrumental births after spontaneous onset.
As shown in Figure 19, numbers of births after the induction of labour differed more strongly by type of day than births after spontaneous onset. There was a weekly cycle with a peak on Friday and a trough on Sunday and Monday. Holidays and Sundays had similar rates but there were far fewer induced births on Christmas Day and Boxing Day than on any other type of day. Like Mondays, days after public holidays had low numbers of births, whereas days before public holidays were similar to Fridays in having high rates. This general pattern was the same for all induced births, although the size of these differences varied by mode of birth, with the widest differences between days being among spontaneous births.
Differences between days were most pronounced among elective caesarean births, which rarely occurred at weekends or on public holidays. Numbers of elective caesarean sections tended to be highest on Mondays and on weekdays after a holiday period, followed by Thursdays and weekdays before a public holiday, and then Tuesday, Friday and Wednesday.
Numbers of caesarean sections without prior onset of labour were also higher on weekdays than on weekends and holidays, although the differences were small compared with differences in numbers of elective caesarean sections. Numbers of emergency caesarean sections without prior labour were highest on Mondays, Tuesdays and weekdays after public holidays.
Differences between preterm, term and post-term births
Next we considered whether or not the differences by type of day within each combination of onset of labour and mode of birth for preterm and post-term births were similar to those for term births. Estimated RRs and their confidence intervals, and p-values relating to the interaction effect for all eight combinations of onset of labour and mode of birth, are shown in Figure 20. Our analysis suggests that in six of the eight combinations of onset of labour and mode of birth, differences by type of day were not the same for all gestational age groups. The exceptions were emergency caesarean sections and, to a lesser extent, instrumental births after spontaneous onset. For these, the interactions between gestational age and ‘type of day’ in predicting number of births per day were not statistically significant (see Figures 20b and 20c).
FIGURE 20.
Estimated RRs and 99% confidence intervals by type of day and gestational age group, England: 2005–14.
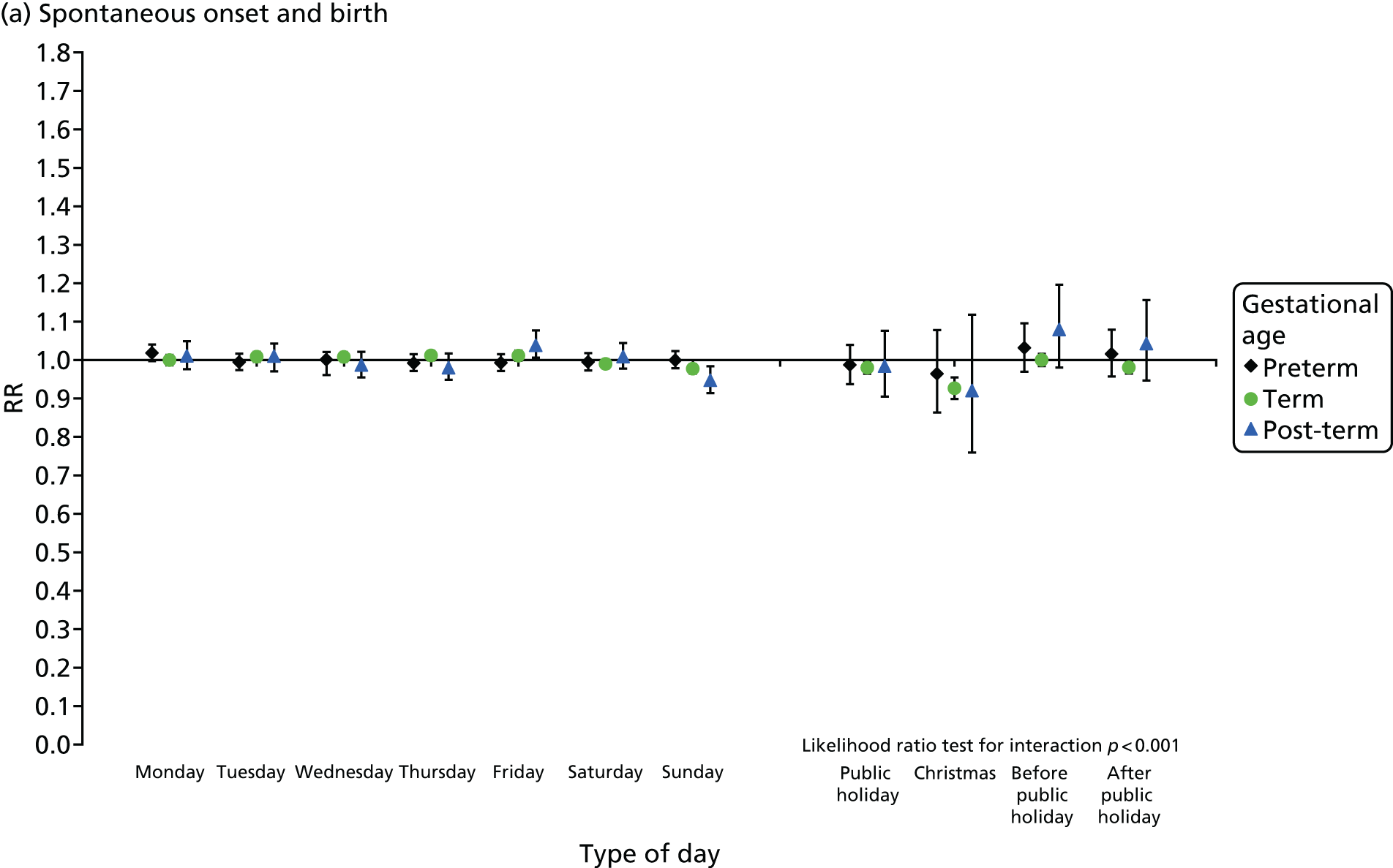
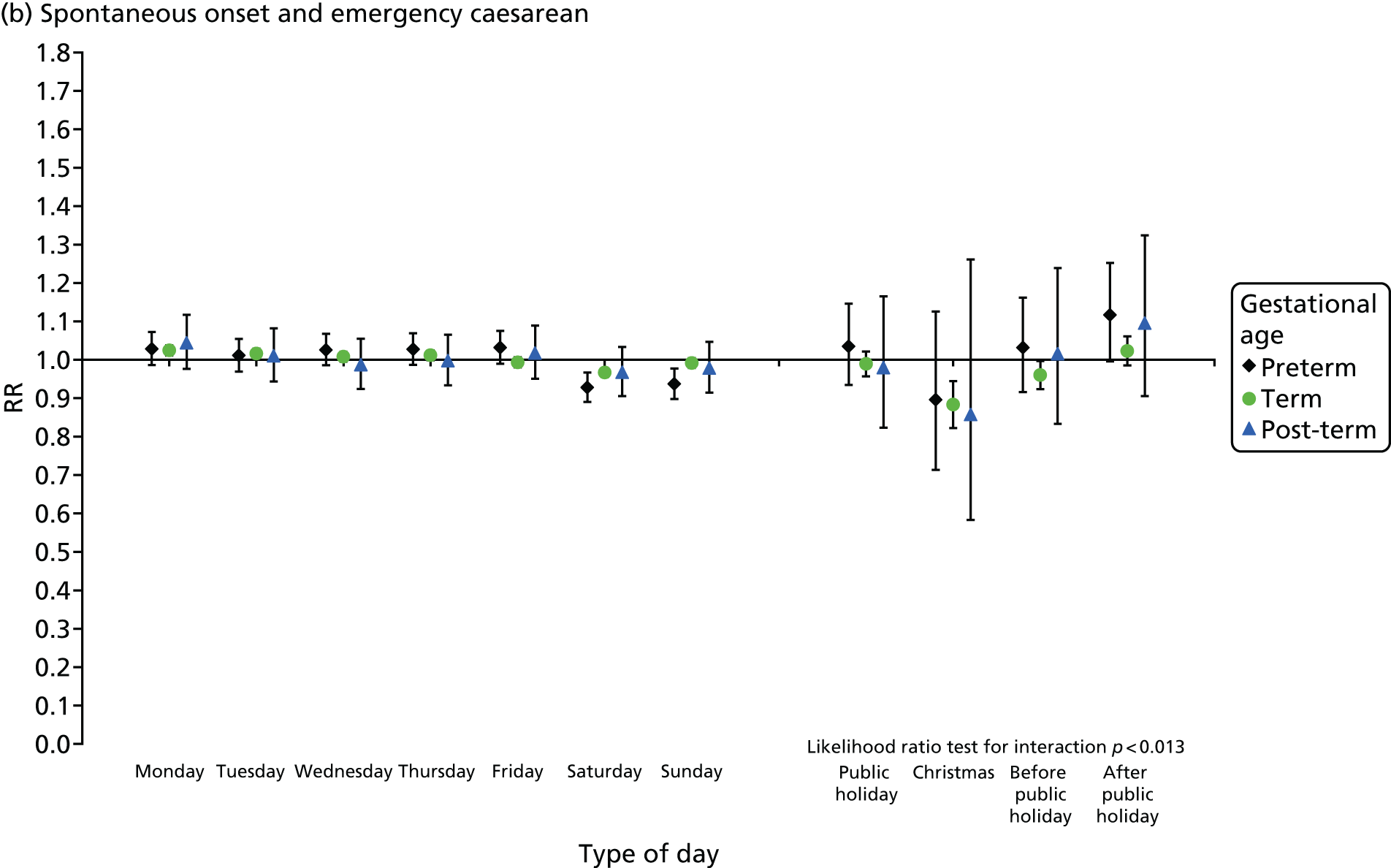
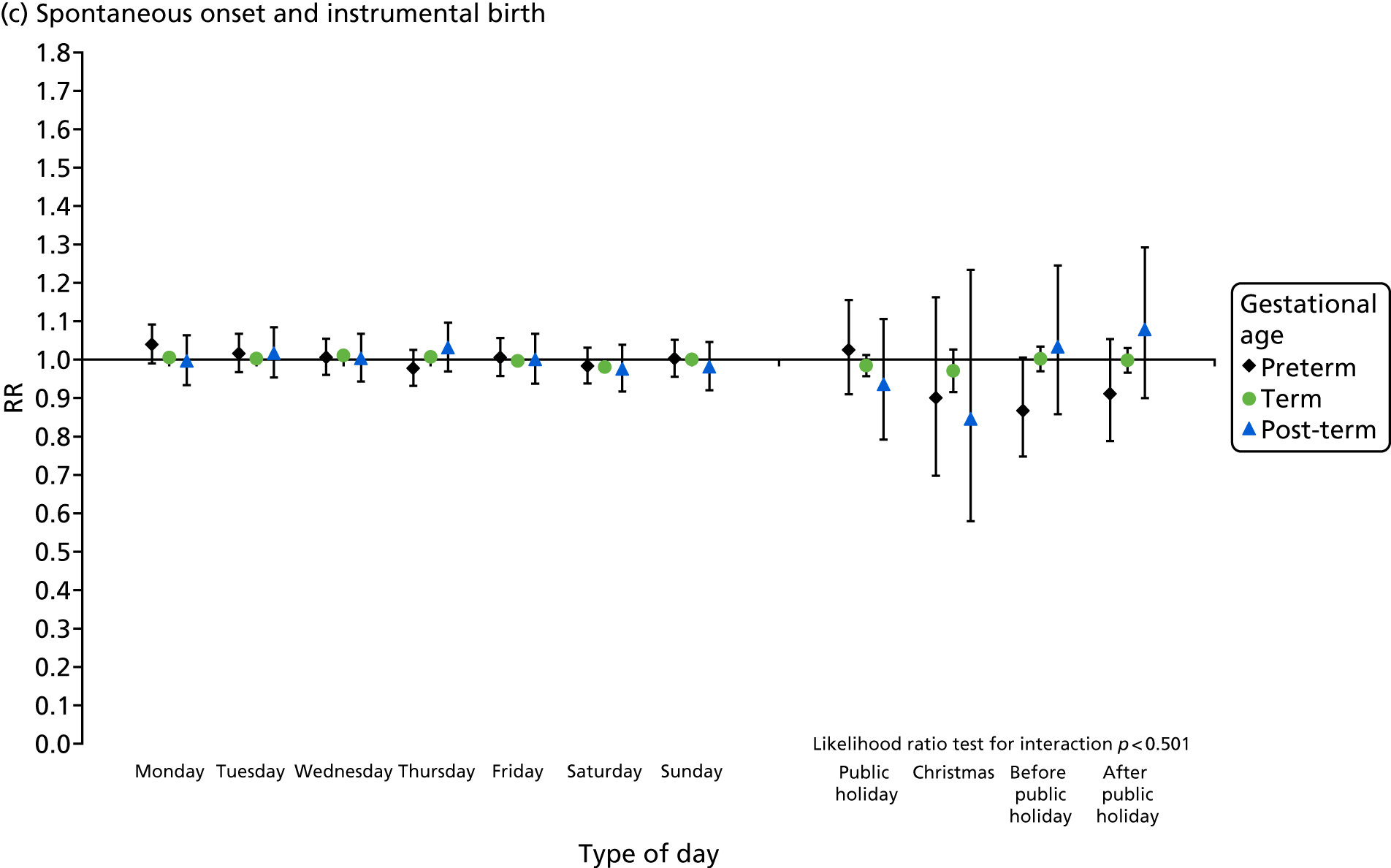
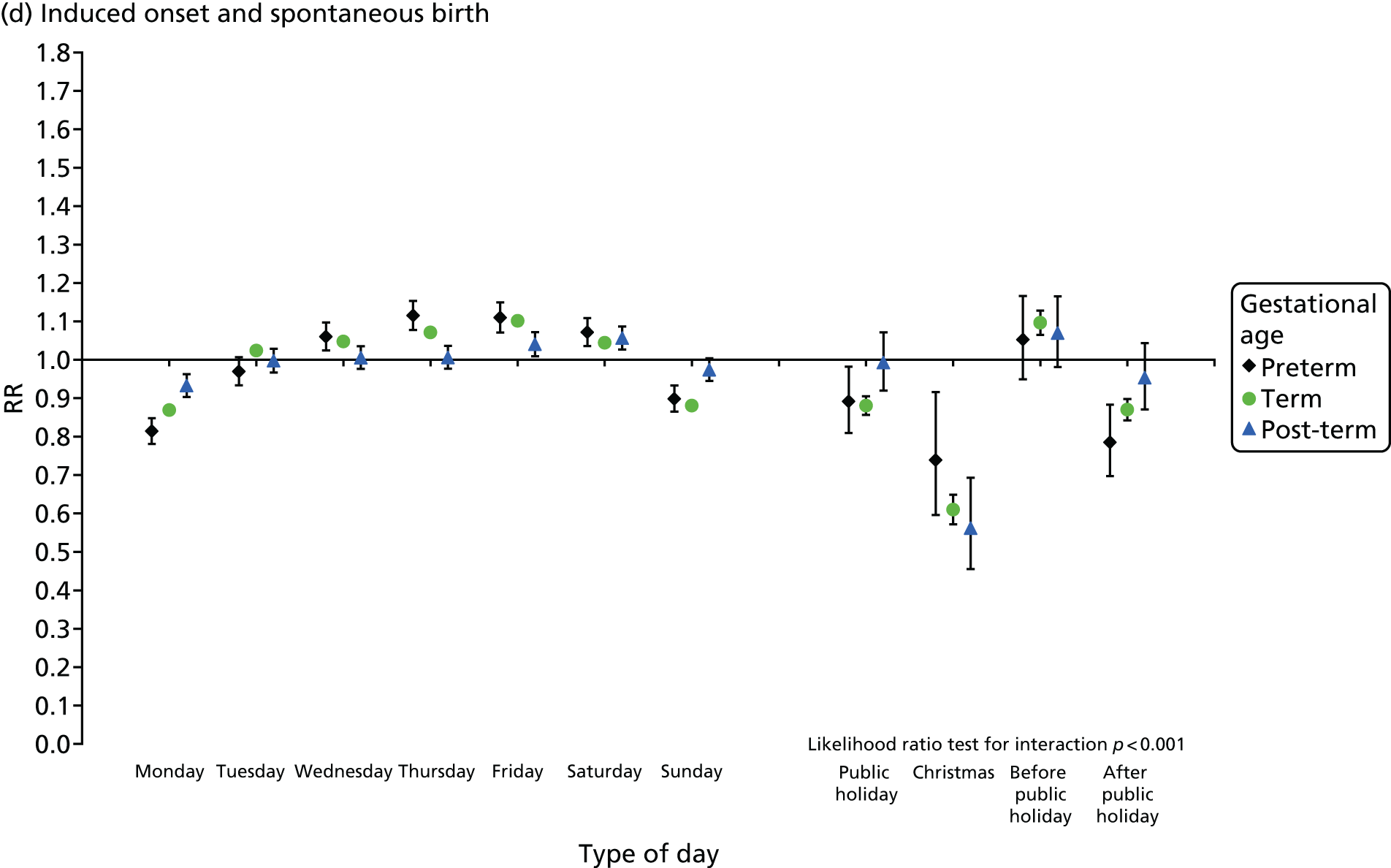
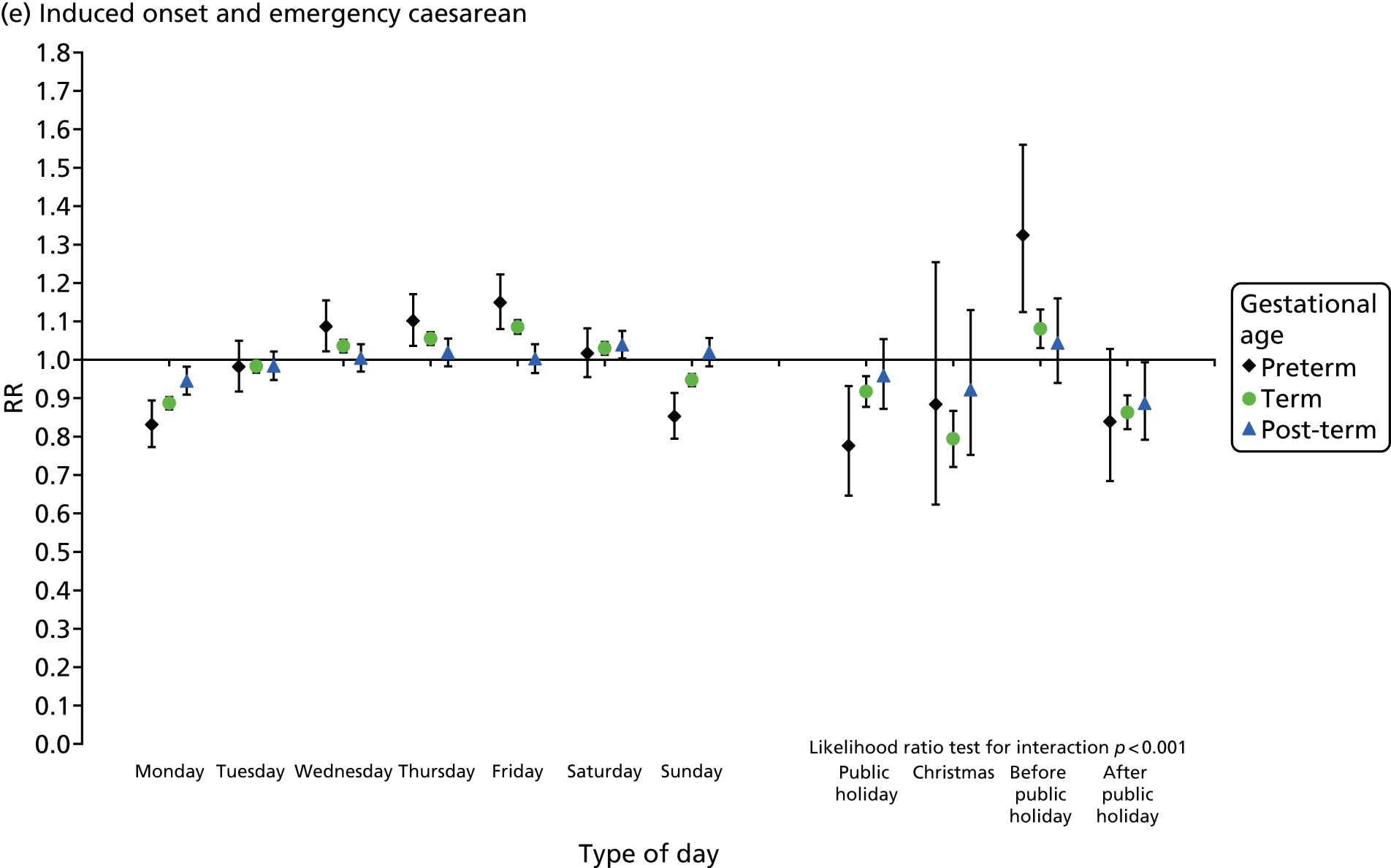
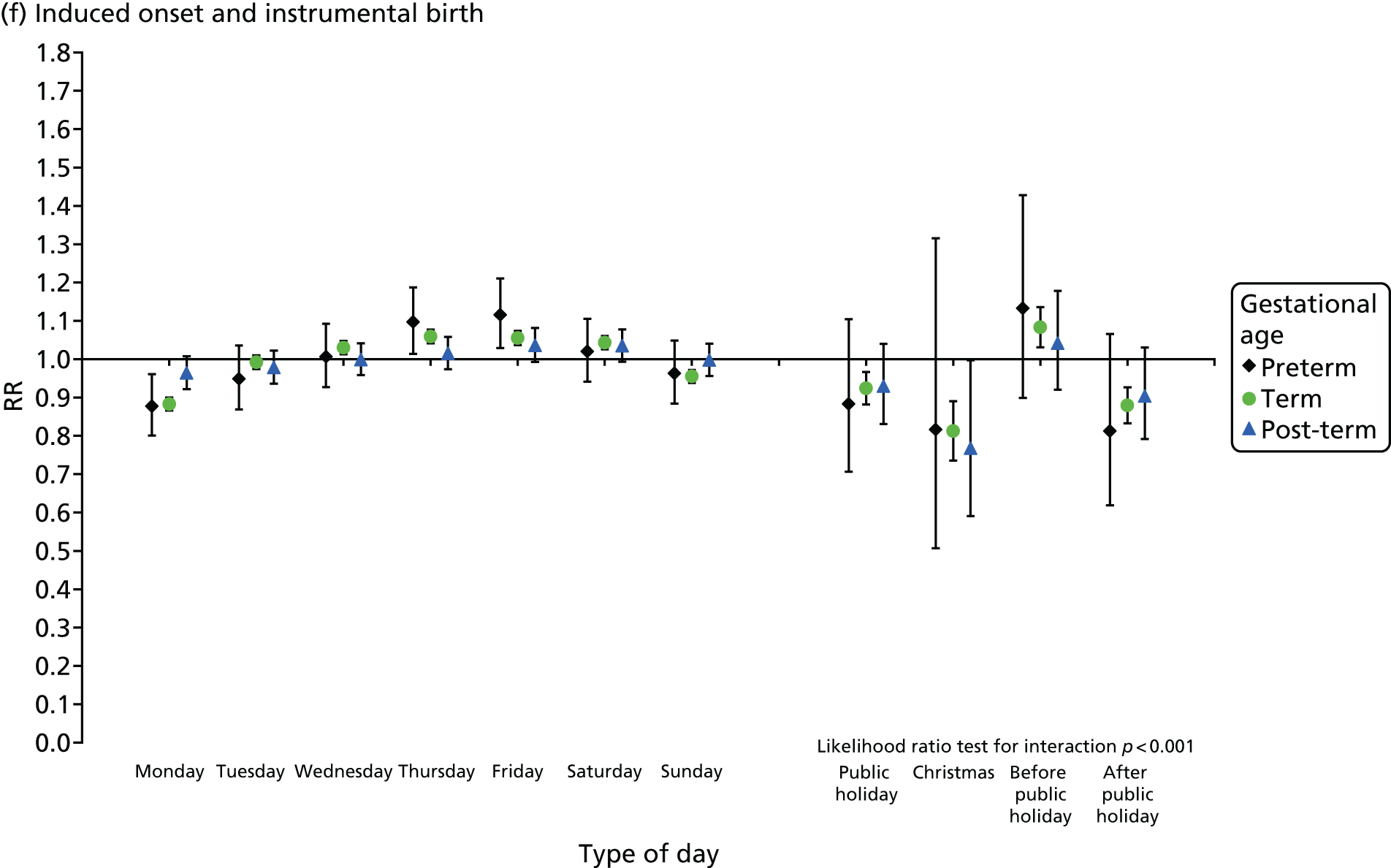
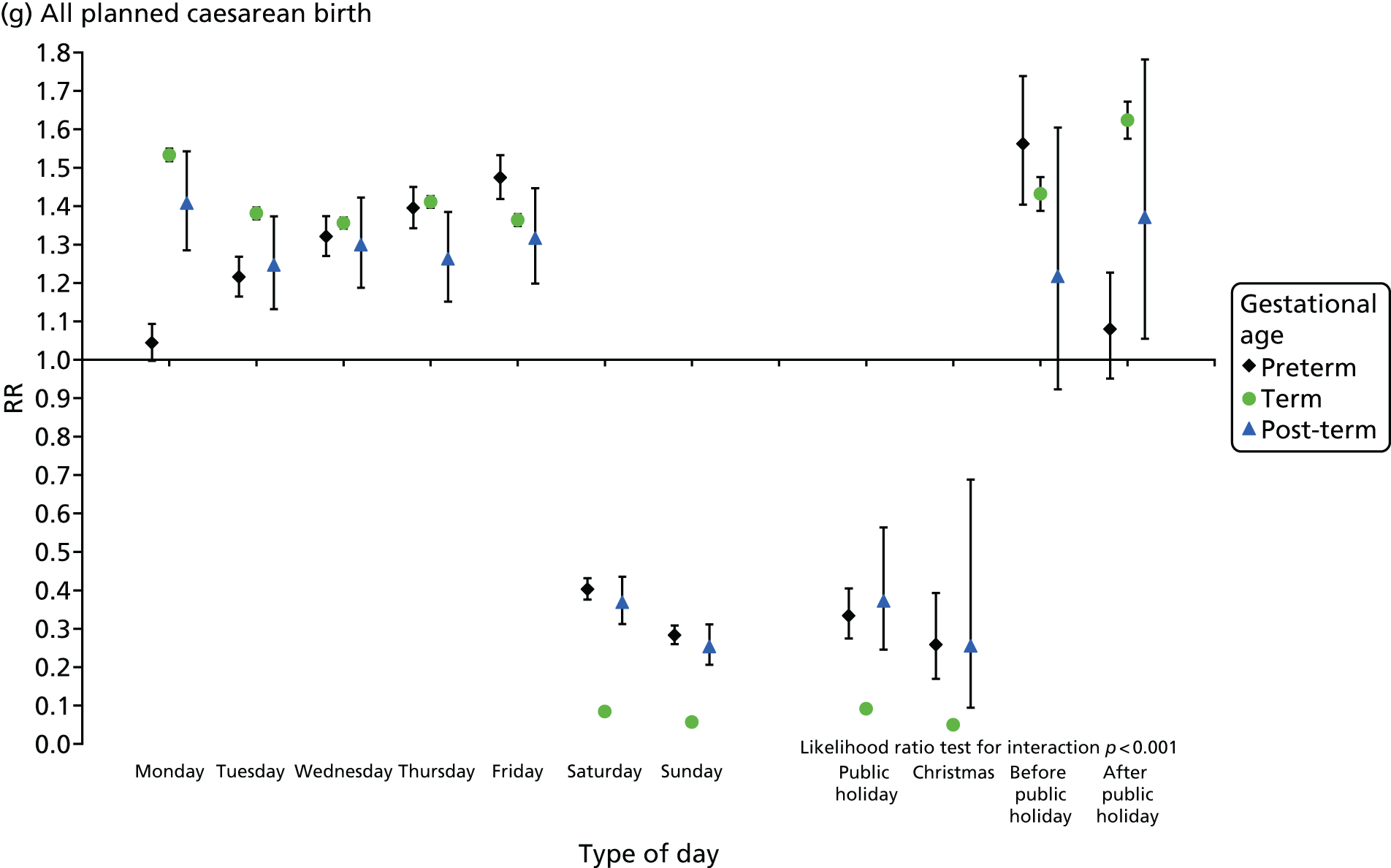
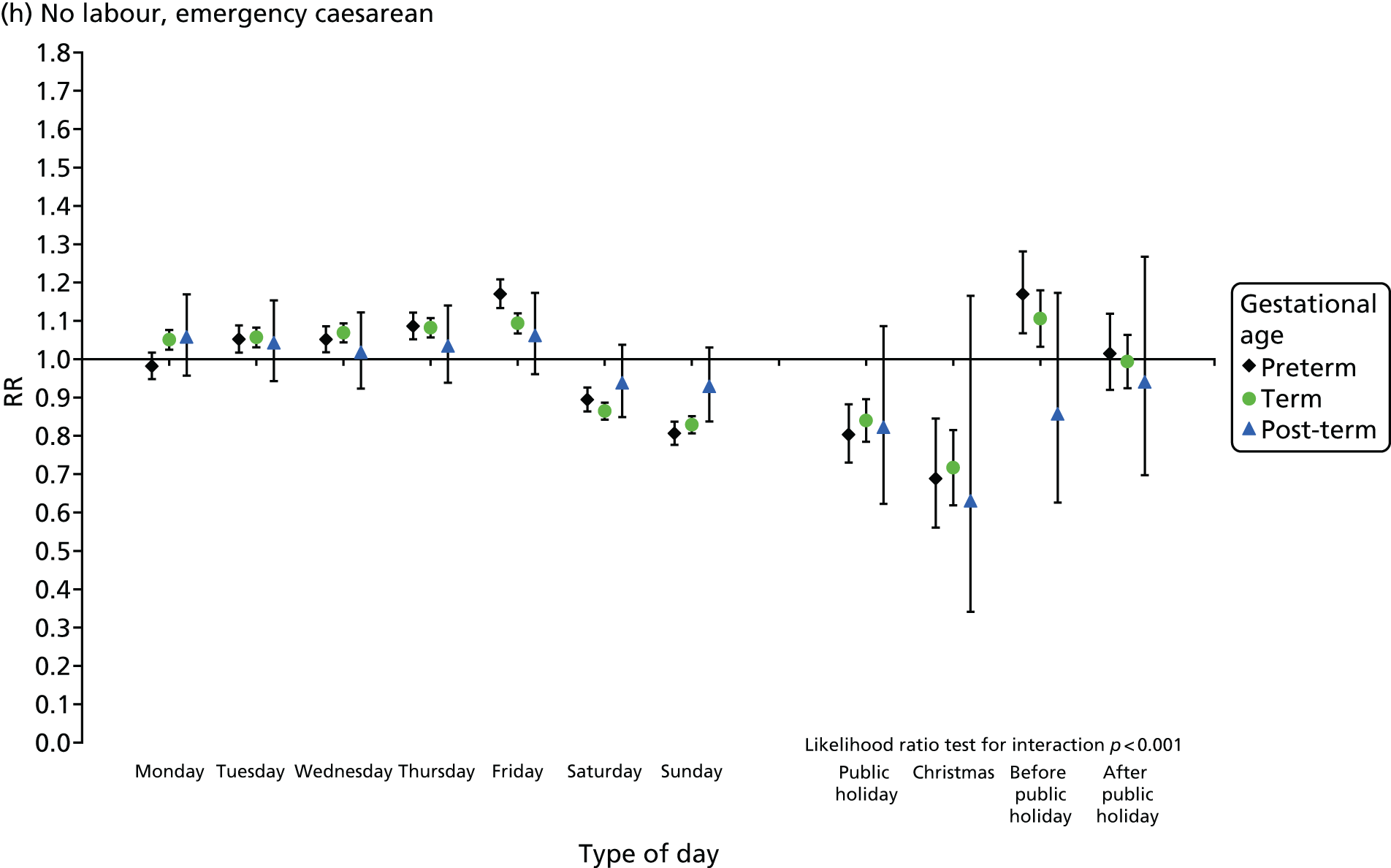
For spontaneous births after spontaneous onset, shown in Figure 20a, there was evidence of differences by type of day for term births, as reported above. However, there was no evidence of differences by type of day among preterm births. As numbers of post-term births were much lower, all the confidence intervals for post-term births were wider than, and included, the intervals for term births. This meant that no statistically reliable differences could be detected between these two groups.
Among induced births (see Figures 20d–f), the average numbers of births by day followed the same overall pattern regardless of gestational age group, but differences between types of days tended to be widest among preterm births and narrowest among post-term births.
For elective caesarean sections (see Figure 20g), the pattern among post-term births was similar to that among term births, although differences between types of days were somewhat smaller for post-term births. Preterm elective caesarean sections, followed a different pattern, however, with numbers being highest on Fridays and on weekdays before a public holiday, and lower on Mondays and weekdays after a public holiday than on other weekdays.
Finally, in emergency caesarean sections without prior onset of labour, again, there is little to suggest differences between post-term and term births. Preterm births in this group followed a similar pattern to preterm elective caesarean sections, however, with numbers being highest on Fridays and on days before public holidays.
Births in NHS hospitals in Wales by mode of birth
Methods
Data used
The data used for analysis were singleton live birth registration records linked to birth notification, NCCHD and PEDW records for births that occurred in NHS hospitals in Wales from 1 January 2005 to 31 December 2014.
In Wales, information on the induction of labour and mode of birth is recorded in the maternity tail as part of the PEDW, but data completeness and quality are poor and cannot be used to provide accurate statistics. 133 Therefore, it was decided in Wales some years ago to count inductions as those deliveries for which procedures R14 and R15 are recorded on the patient record. The OPCS-4 classification includes augmentation (speeding up of labour) within the induction codes, as the procedures undertaken are the same for induction and augmentation of labour. Welsh coders are, however, instructed via a Welsh Coding Standard not to use these codes for augmentation of labour; they must assign the codes only when procedures are undertaken to induce (start) labour.
Similarly, information on mode of birth is derived using procedure codes R17 to R25, shown in Table 18, rather than using the variable from the ‘maternity tail’ in the PEDW.
| Procedure codes | Method of delivery |
|---|---|
| R14 | Surgical induction |
| R15 | Other induction |
| R17 | Elective caesarean section |
| R18 | Emergency caesarean section |
| R19, R20 | Spontaneous or assisted breech |
| R21 | Forceps delivery |
| R22 | Ventouse delivery |
| R23 | Face to pubis delivery |
| R24 | Normal delivery |
| R25 | Caesarean hysterectomy |
In the PEDW, there is normally one procedure code present on the record. Therefore, it is not possible to analyse births in NHS hospitals in Wales by both onset of labour and mode of birth. Instead, the analysis considered only mode of birth.
The time of day was taken from the birth notification dataset in which it is recorded as hours and minutes of the day. This was coded into hourly intervals, with hours running from 0 to 23, where 0 means 00.00–00.59. The day of birth was derived using the date of birth recorded at birth registration, which is the most complete and accurate record of dates of birth in England and Wales.
Descriptive analysis
The numbers of births in Wales were tabulated by gestational age and mode of birth. Then, the average numbers of births on each day of the week by mode of delivery were calculated for preterm, term and post-term births.
Results
In Wales, 6% of births in NHS hospitals were preterm (before 37 weeks), 89% occurred at term (37–41 weeks) and 5% were post-term (42 weeks or more). Just over half of all preterm births occurred spontaneously compared with 64% of term births. For post-term births, over 51% of babies were born instrumentally and 26% were born by emergency caesarean section (Table 19).
| Mode of birth | Preterm | Term | Post-term |
|---|---|---|---|
| Elective caesarean section | 1,720 | 29,602 | 494 |
| Emergency caesarean section | 4,799 | 32,846 | 3,678 |
| Spontaneous | 8,242 | 163,091 | 2,548 |
| Instrumental | 1,361 | 29,789 | 7,284 |
| All | 16,170 | 256,111 | 14,156 |
As in England, these differences in mode of birth were associated with differences in the timing of birth, as can be seen in Table 20 and Figures 21–23. Because the numbers of births in Wales were smaller than for England, the numbers of births on public holidays were not shown separately, being extremely small.
| Day | Mode of birth | All | |||
|---|---|---|---|---|---|
| Elective caesarean section | Emergency caesarean section | Spontaneous | Instrumental | ||
| Preterm births | |||||
| Monday | 0.45 | 1.28 | 2.26 | 0.35 | 4.35 |
| Tuesday | 0.62 | 1.27 | 2.30 | 0.37 | 4.58 |
| Wednesday | 0.57 | 1.37 | 2.31 | 0.39 | 4.65 |
| Thursday | 0.69 | 1.36 | 2.32 | 0.45 | 4.83 |
| Friday | 0.66 | 1.48 | 2.34 | 0.35 | 4.84 |
| Saturday | 0.20 | 1.31 | 2.31 | 0.36 | 4.19 |
| Sunday | 0.14 | 1.20 | 2.09 | 0.36 | 3.82 |
| All | 0.48 | 1.33 | 2.28 | 0.38 | 4.47 |
| Term births | |||||
| Monday | 10.45 | 8.82 | 43.05 | 7.90 | 70.42 |
| Tuesday | 13.11 | 9.23 | 45.58 | 8.08 | 76.24 |
| Wednesday | 7.68 | 9.33 | 46.56 | 8.16 | 71.98 |
| Thursday | 13.84 | 9.51 | 46.68 | 8.41 | 78.65 |
| Friday | 10.42 | 9.50 | 46.75 | 8.62 | 75.49 |
| Saturday | 0.99 | 8.74 | 44.59 | 8.41 | 62.96 |
| Sunday | 0.76 | 8.36 | 42.08 | 8.01 | 59.42 |
| All | 8.18 | 9.07 | 45.04 | 8.23 | 70.73 |
| Post-term births | |||||
| Monday | 0.18 | 1.01 | 0.64 | 1.96 | 3.83 |
| Tuesday | 0.18 | 1.02 | 0.69 | 2.01 | 3.94 |
| Wednesday | 0.15 | 1.00 | 0.69 | 2.16 | 4.05 |
| Thursday | 0.16 | 1.05 | 0.73 | 2.05 | 4.03 |
| Friday | 0.16 | 1.08 | 0.72 | 2.06 | 4.06 |
| Saturday | 0.08 | 1.03 | 0.71 | 2.03 | 3.90 |
| Sunday | 0.04 | 0.93 | 0.75 | 1.81 | 3.56 |
| All | 0.14 | 1.02 | 0.70 | 2.01 | 3.91 |
FIGURE 21.
Singleton preterm births by time of day, day of the week and mode of birth, Wales: 2005–14.
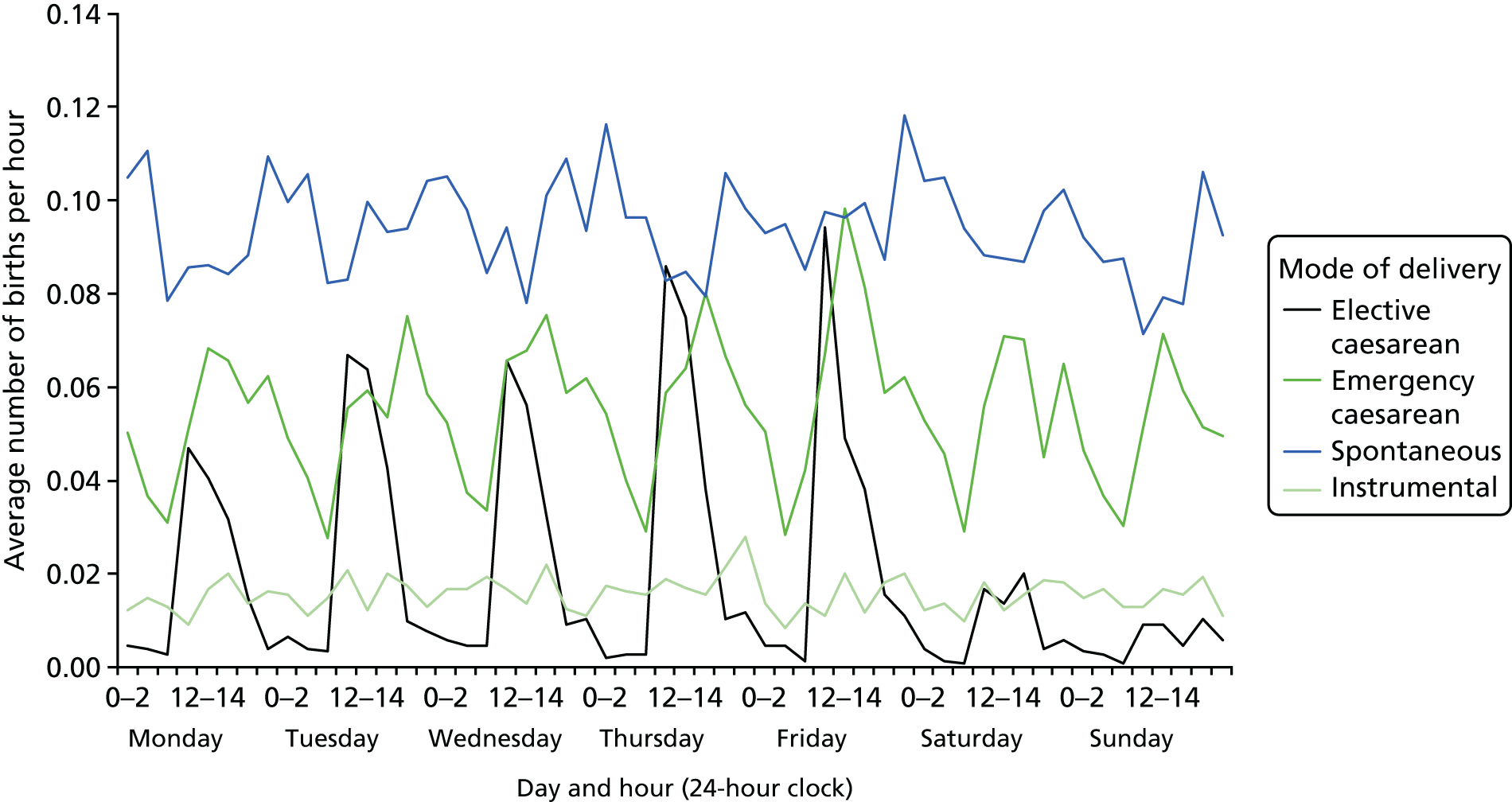
FIGURE 22.
Singleton term births by time of day, day of the week and mode of birth, Wales: 2005–14.
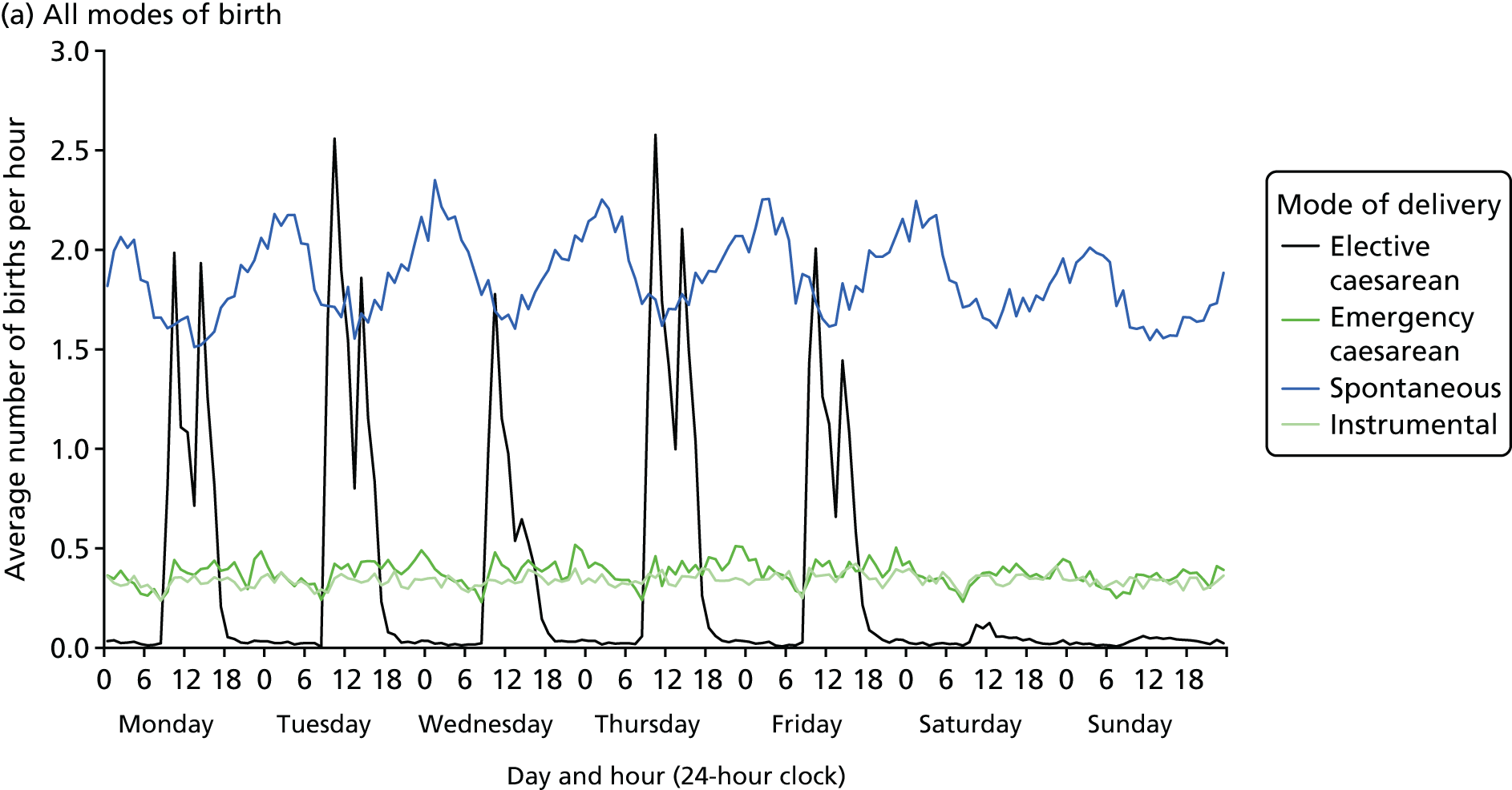
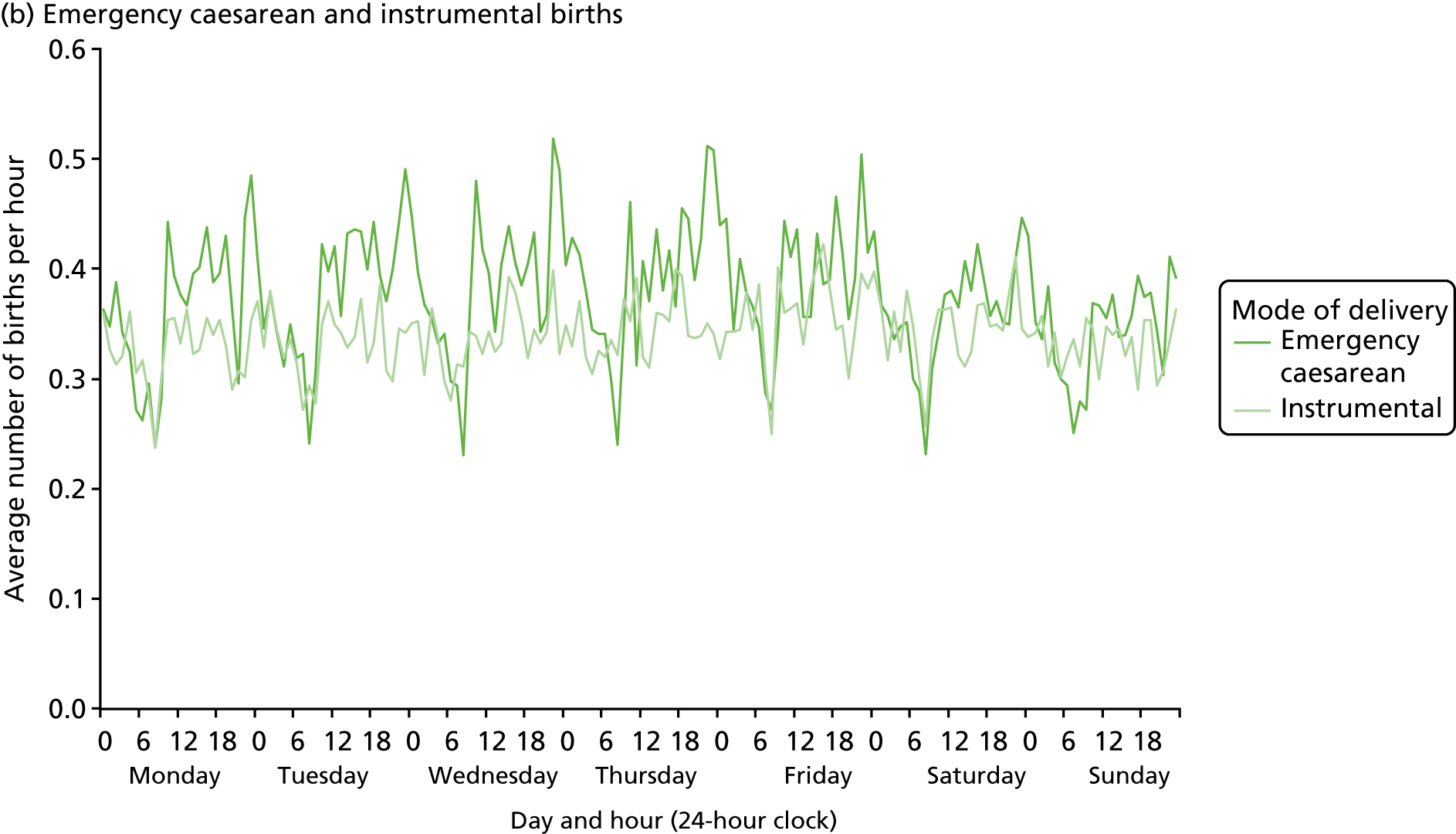
FIGURE 23.
Singleton post-term births by time of day, day of the week and mode of birth, Wales: 2005–14.
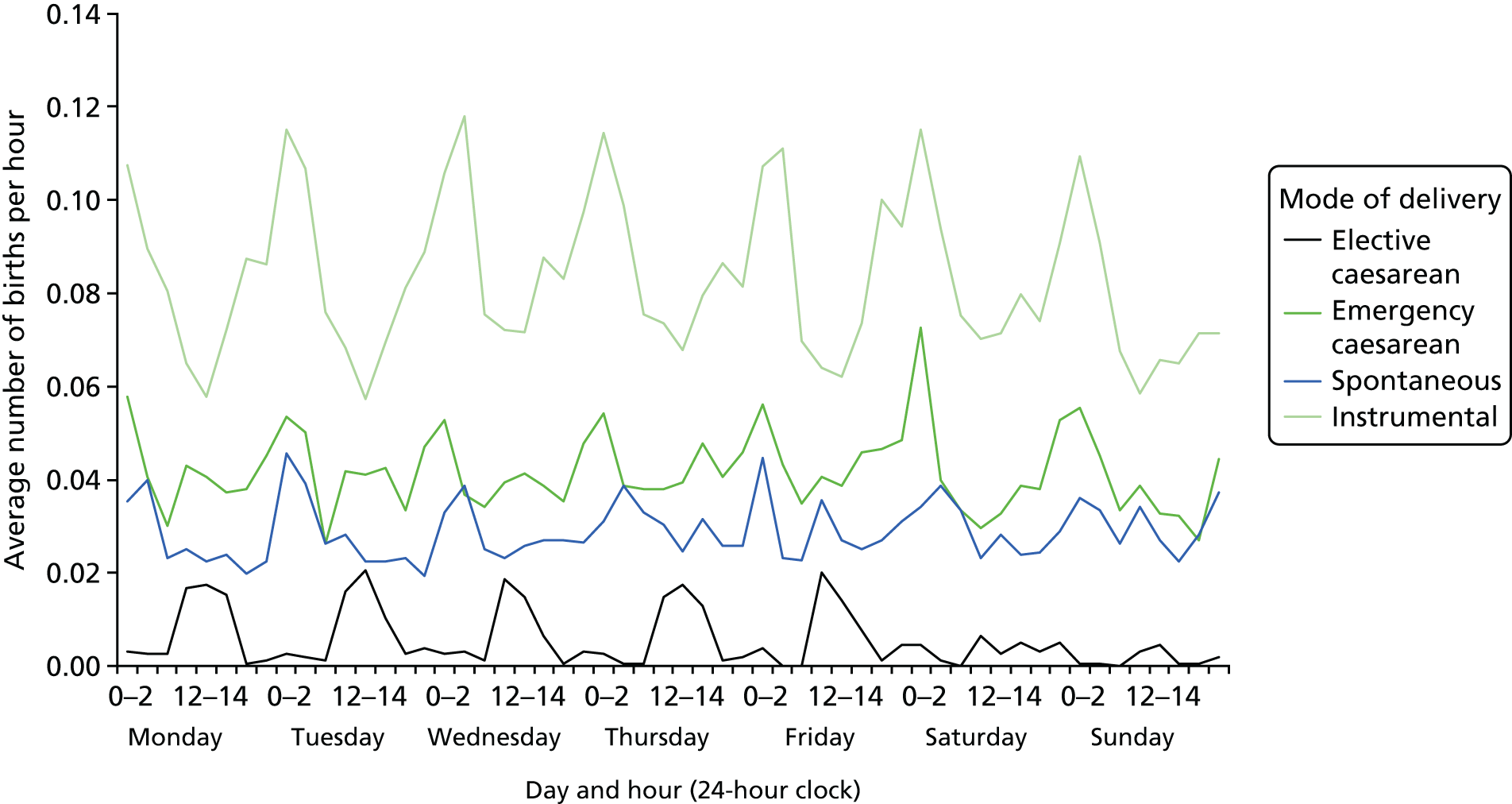
Numbers of preterm births remained at fairly similar levels from Monday to Saturday, but were lower on Sundays. Numbers of both elective and emergency caesarean sections increased from Monday to Fridays and were highest on Thursdays and Fridays. The variations by time of day and day of the week are shown in Figure 21. Along with post-term births, they were aggregated into 3-hour time slots, as the numbers were small. This shows that numbers of emergency caesarean section peaked later in the day than elective caesarean section and that numbers of spontaneous preterm births peaked in the early hours of the morning, as Figure 22a shows.
Among term births, spontaneous births predominate and show similar patterns to those in England as Figure 22a shows. The much smaller numbers of instrumental and emergency caesarean births are plotted on a larger scale in Figure 22b. Numbers of both are relatively high early in the morning then reach a low at 07.00–08.00 before numbers rise again.
Post-term births, shown in Figure 23, show high rates of intervention, with most births being assisted vaginal births, involving the use of forceps or ventouse. These births exhibit similar time of day patterns. Along with spontaneous births, emergency caesarean section peaked in the early hours of the morning. In contrast, the relatively small numbers of elective caesarean section took place during daytime hours.
Births at home in England and Wales
Method
Data used
The dataset used for analysis included birth registration records linked to birth notifications, previously known as NN4B, for all births that occurred in England and Wales from 1 January 2005 to 31 December 2014. The planned place of birth at the onset of labour care, the key variable used in the Birthplace study,26 is not recorded in the linked dataset used. Instead, at birth registration, births taking place at the mother’s usual place of residence are categorised as occurring at home, irrespective of where they were planned to occur. This was used as the best available indicator of home births, but it will include both planned home births occurring at home and unplanned home births. There are no recent data about the extent of unplanned home births, but it appears from past data that they accounted for 0.36–0.5% of all births. 148–150 It excludes those planned home births at the start of labour care where the mother transfers to hospital during labour. In nulliparous women, the Birthplace study found that this was the case for 45% of planned home births. 26
Time of day was taken from the birth notification dataset in which it is recorded as hours and minutes of the day. We coded this into hourly intervals, with hours running from 0 to 23, where 0 means 00.00 to 00.59. Day of birth was derived using the date of birth recorded at birth registration, which is the most complete and accurate record of dates of birth in England and Wales.
Descriptive analysis
The numbers of births at home by day of the week were tabulated for England and Wales from 1 January 2005 to 31 December 2014. Then, the average numbers of home births on each day of the week and the overall daily average for each year were calculated to produce RRs. Similarly, RRs for all live births by day of the week were produced for comparison. For example in Table 21, a RR of 1.05 for a Friday means that the average number of births on Fridays was 5% higher than the overall mean. A RR of 0.93 for a Sunday meant that the average number of births on Sundays was 7% lower than the mean in Table 21.
| Year | Day of the week | ||||||
|---|---|---|---|---|---|---|---|
| Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday | |
| Home births | |||||||
| 2005 | 0.98 | 1.01 | 0.99 | 1.06 | 1.05 | 0.98 | 0.93 |
| 2006 | 1.06 | 1.02 | 1.04 | 1.02 | 0.99 | 0.94 | 0.94 |
| 2007 | 1.03 | 1.01 | 1.01 | 1.00 | 1.01 | 0.97 | 0.97 |
| 2008 | 1.03 | 1.02 | 1.05 | 0.98 | 0.99 | 0.96 | 0.97 |
| 2009 | 1.03 | 1.05 | 1.05 | 1.02 | 0.99 | 0.93 | 0.94 |
| 2010 | 0.99 | 1.04 | 1.02 | 1.03 | 1.00 | 0.99 | 0.93 |
| 2011 | 1.03 | 1.00 | 1.01 | 1.04 | 1.01 | 0.96 | 0.96 |
| 2012 | 1.01 | 1.06 | 1.03 | 0.99 | 1.03 | 0.94 | 0.95 |
| 2013 | 1.00 | 1.04 | 1.05 | 1.02 | 0.99 | 0.99 | 0.92 |
| 2014 | 1.02 | 1.04 | 1.03 | 1.01 | 1.02 | 0.94 | 0.94 |
| All live births | |||||||
| 2005 | 0.98 | 1.04 | 1.05 | 1.06 | 1.10 | 0.91 | 0.85 |
| 2006 | 1.00 | 1.03 | 1.05 | 1.06 | 1.07 | 0.91 | 0.87 |
| 2007 | 1.01 | 1.04 | 1.05 | 1.06 | 1.07 | 0.92 | 0.86 |
| 2008 | 1.02 | 1.04 | 1.05 | 1.05 | 1.06 | 0.91 | 0.87 |
| 2009 | 1.01 | 1.05 | 1.05 | 1.06 | 1.05 | 0.91 | 0.87 |
| 2010 | 1.00 | 1.05 | 1.04 | 1.06 | 1.05 | 0.91 | 0.88 |
| 2011 | 1.01 | 1.04 | 1.04 | 1.06 | 1.05 | 0.91 | 0.88 |
| 2012 | 1.01 | 1.03 | 1.04 | 1.07 | 1.06 | 0.91 | 0.87 |
| 2013 | 1.02 | 1.03 | 1.04 | 1.07 | 1.05 | 0.91 | 0.88 |
| 2014 | 1.01 | 1.05 | 1.04 | 1.06 | 1.05 | 0.91 | 0.87 |
Results
In England and Wales, just over 2% of all live births from 2005 to 2014 occurred at home and 99.7% of these were singleton births (Table 22).
| Year of birth | Number of live births | Proportion multiple | |
|---|---|---|---|
| Singletons | Multiples | ||
| 2005 | 16,474 | 53 | 0.32 |
| 2006 | 18,080 | 41 | 0.23 |
| 2007 | 19,508 | 62 | 0.32 |
| 2008 | 20,169 | 56 | 0.28 |
| 2009 | 19,103 | 36 | 0.19 |
| 2010 | 17,933 | 56 | 0.31 |
| 2011 | 17,036 | 55 | 0.32 |
| 2012 | 16,570 | 40 | 0.24 |
| 2013 | 15,504 | 45 | 0.29 |
| 2014 | 15,758 | 56 | 0.36 |
| All | 176,135 | 500 | 0.28 |
There was considerable regional variation in the proportion of all live births occurring at home. This ranged from about 1% of births in the North East region to 4% in the South West region. All regions showed similar time trends, with a steady decline from 2008 to 2012, followed by a levelling off (Figure 24).
FIGURE 24.
Home births as a percentage of all live births by region, England and Wales: 2005–14.
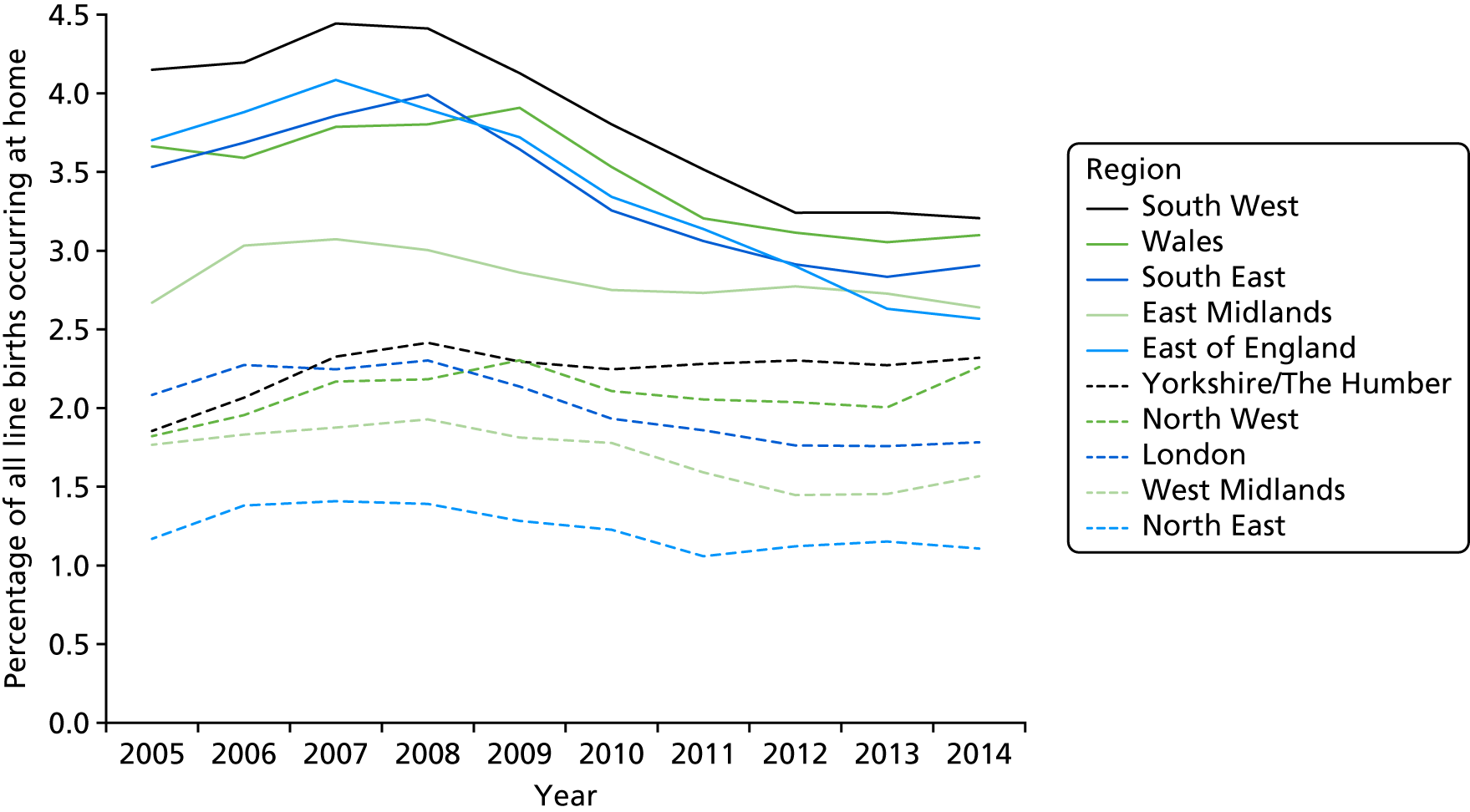
There was a slight deficit in the average numbers of home births on Saturdays and Sundays compared with on weekdays (Table 23). Although very small, this was also observed in the 1970s. 100 This meant that the RRs of the average number of home births on each day of the week to the overall daily average for each year (Table 21) showed similar patterns as those for all live births, but the differences were much narrower. Although the RR for Friday births fluctuated from 0.99 to 1.05 for home births, it varied from 1.05 to 1.10 for all live births. On Saturday, the RR ranged from 0.93 to 0.99 for home births and from 0.91 to 0.92 for all live births. The difference was most marked on Sundays when the RR varied from 0.92 to 0.96 for home births and 0.85 to 0.88 for live births.
| Year | Day of the week | ||||||
|---|---|---|---|---|---|---|---|
| Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday | |
| 2005 | 2,249 | 2,326 | 2,280 | 2,437 | 2,401 | 2,287 | 2,140 |
| 2006 | 2,716 | 2,613 | 2,681 | 2,611 | 2,536 | 2,424 | 2,459 |
| 2007 | 2,911 | 2,803 | 2,811 | 2,768 | 2,809 | 2,683 | 2,679 |
| 2008 | 2,955 | 2,980 | 3,053 | 2,803 | 2,824 | 2,743 | 2,784 |
| 2009 | 2,794 | 2,847 | 2,855 | 2,817 | 2,696 | 2,515 | 2,542 |
| 2010 | 2,525 | 2,651 | 2,614 | 2,619 | 2,610 | 2,525 | 2,368 |
| 2011 | 2,488 | 2,419 | 2,435 | 2,516 | 2,444 | 2,372 | 2,331 |
| 2012 | 2,423 | 2,478 | 2,417 | 2,326 | 2,410 | 2,208 | 2,268 |
| 2013 | 2,196 | 2,331 | 2,309 | 2,251 | 2,181 | 2,186 | 2,019 |
| 2014 | 2,285 | 2,327 | 2,342 | 2,268 | 2,278 | 2,114 | 2,105 |
| Total | 25,542 | 25,775 | 25,797 | 25,416 | 25,189 | 24,057 | 23,695 |
Approximately 97% of home births occurred at term (37–42 weeks of pregnancy), 2% were preterm (before 37 weeks) and under 0.5% were post-term (over 42 weeks).
Average numbers of term births varied by time of day and day of week (Figure 25) and were highest in the early hours of weekday mornings between 01.00 and 07.00.
FIGURE 25.
Average numbers of term births at home by hour of day and day of the week, England and Wales: 2005–14.
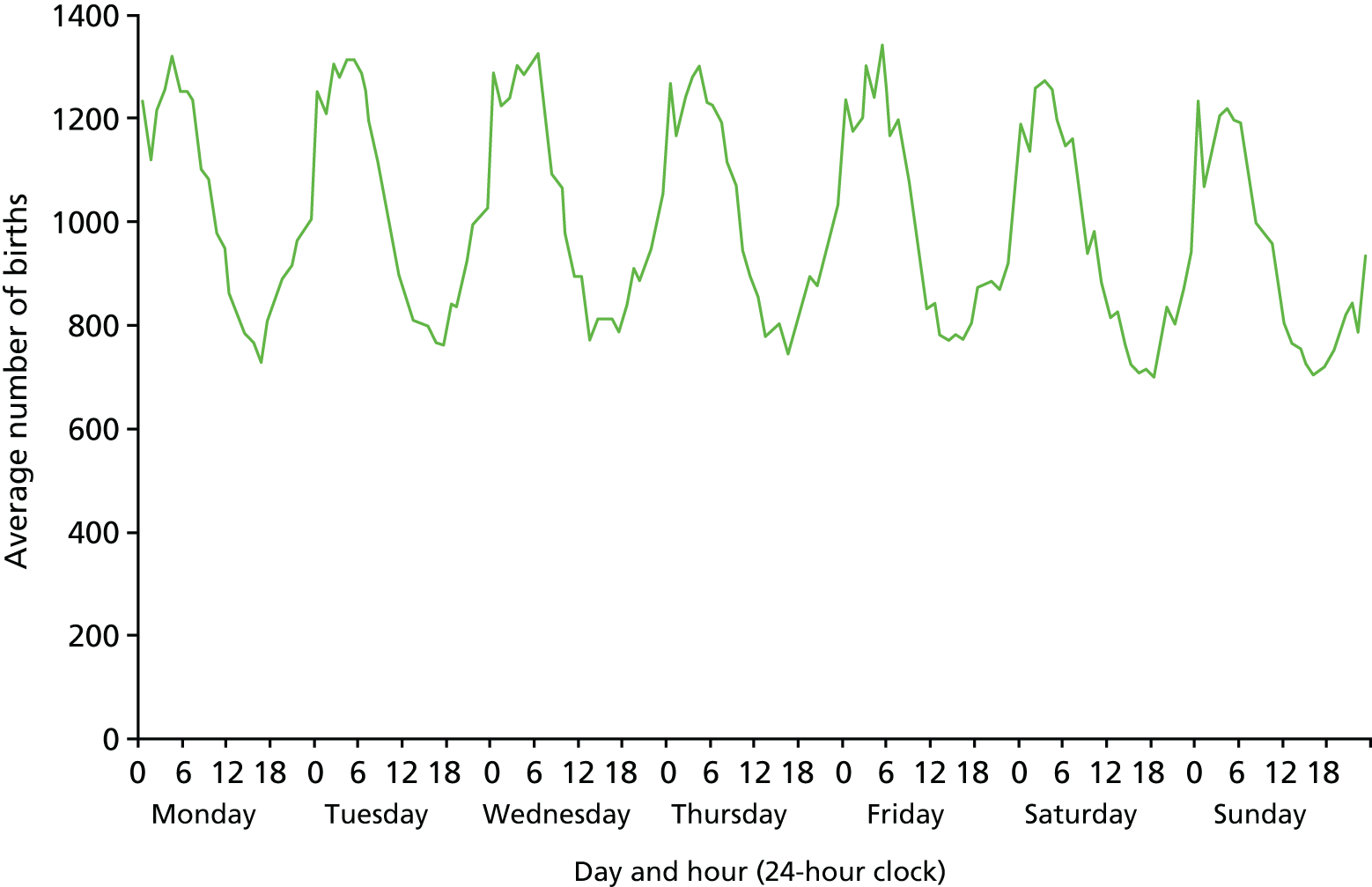
The much smaller numbers of preterm births fluctuated much more widely by time and day of week, so the times of birth have been aggregated into 3-hour groups (Figure 26). Although overall numbers of births did not vary by day of the week, and average numbers were highest in early mornings between 03.00 and 08.00, this varied by day of the week, with the most marked peak being on Sunday and Monday mornings, followed by Saturdays.
FIGURE 26.
Average numbers of preterm births at home by hour of the day and day of week, England and Wales: 2005–14.
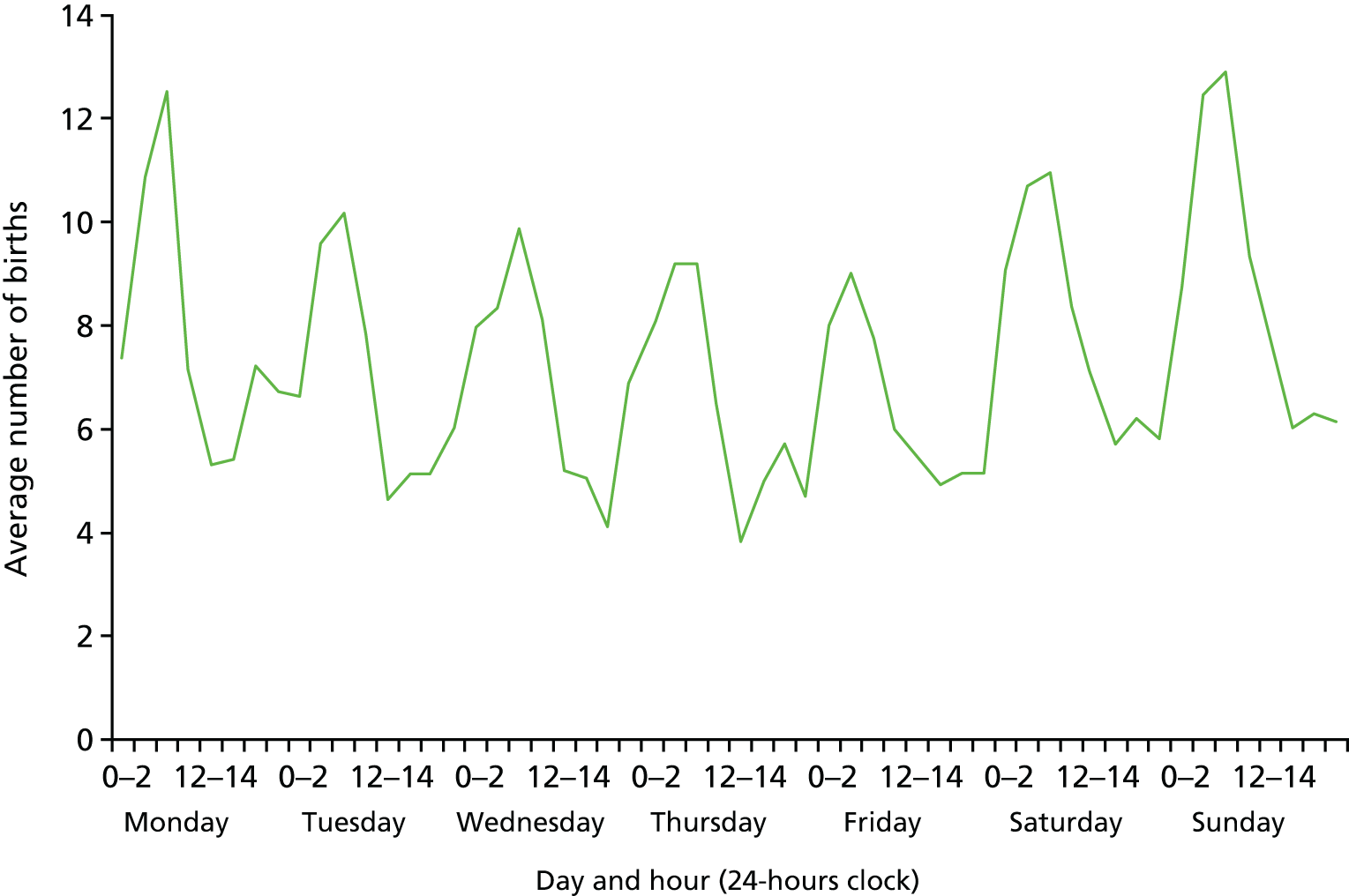
Outcome of births by time of day and day of the week
We planned to use a number of outcome measures from the linked dataset to reflect the safety and quality of maternity care received by women. These included significant harms to mothers and babies. For babies, these included intrapartum stillbirth, neonatal and infant mortality rates, survival to the age of 2 years and morbidity recorded by ICD-10 codes in hospital records of admissions to neonatal units and any subsequent readmissions to hospital, together with rates of medical intervention.
For mothers, these measures included death within a year of giving birth and morbidity recorded in HES records of any subsequent hospital episodes of readmissions of mothers.
We also planned to investigate the use of positive outcome measures for babies and mothers, starting with births without obstetric intervention or ‘normal’ birth rates and measures such as the well-baby flag and bodily integrity, building on quality indicators developed for a maternity workforce project in which two members of the project team (RG and MD) had previously been involved at King’s College London. 151
We planned to stratify outcomes by mothers’ characteristics, gestational age and obstetric or medical risk factors, using ICD-10 and OPCS-4 codes to identify women who were at higher risk of complications according to criteria set out in the NICE intrapartum care guideline. 27
A key analysis was to group maternity units and trusts by levels of obstetric intervention to look at possible associations with pattern of the timing of birth. We also planned to use this to look at possible association between levels of midwife and obstetric staffing and outcomes, although we were aware that the available workforce data are limited.
Unfortunately, because of external delays (described in Appendix 1), there was not time to undertake most of the proposed analyses of variations in the outcome of birth apart from preliminary descriptive analyses of intrapartum stillbirth rates.
Intrapartum stillbirths in England and Wales: 2005–9
To examine the question of how birth outcomes vary by time of day and day of the week, the data in the current study provided relatively detailed information on the causes of stillbirth, with information on the obstetric characteristics of all mothers, including those whose babies died, for a large number of births.
As stated earlier, the analysis was restricted to intrapartum stillbirth. It was pointed out by the project Study Advisory Group that the ONS classification of the causes of stillbirth does not adequately distinguish between intrapartum and antepartum stillbirth. This distinction was made possible using data from CMACE. Therefore, arrangements were made to acquire and link in these data. As described in Chapter 2, these data were available only for the years 2005 to 2009.
In England and Wales, there were 17,817 registered stillbirths that occurred from 1 January 2005 to 31 December 2009 and 15,240 of these were successfully linked to CMACE data (see Chapter 2). Of these, 1,255 (8.2%) were intrapartum stillbirths (Table 24).
| Year | Total number of ONS stillbirths | Number linked to CMACE | Percentage intrapartum |
|---|---|---|---|
| 2005 | 3,484 | 3,150 | 8.4 |
| 2006 | 3,604 | 3,166 | 8.9 |
| 2007 | 3,533 | 3,076 | 7.5 |
| 2008 | 3,568 | 2,601 | 7.8 |
| 2009 | 3,628 | 3,247 | 8.7 |
Intrapartum stillbirths by time of day and day of week
The preliminary descriptive analysis presented here is very tentative and further work is required to interpret these findings and their implications for policy.
As the numbers of intrapartum stillbirths were small, analysis by time of day and day of week involved grouping births between 09.00 and 17.00 on Monday to Friday and births at all other times including weekends, defined as ‘all other times’. In the study period, 282 intrapartum stillbirths, a rate of 0.28 per 1000 live births and stillbirths, occurred from Monday to Friday from 09.00 and 17.00, and 973, a rate of 0.40 per 1000, occurred at all other times (Table 25).
| Characteristics | Timing of birth | |||
|---|---|---|---|---|
| Monday to Friday, 09.00–17.00 | All other times | |||
| Number | Ratea | Number | Ratea | |
| Total | 282 | 0.28 | 973 | 0.40 |
| Gestational age | ||||
| Preterm | 161 | 1.98 | 532 | 3.00 |
| Term | 120 | 0.13 | 439 | 0.20 |
| Sex | ||||
| Male | 146 | 0.29 | 517 | 0.42 |
| Female | 134 | 0.28 | 456 | 0.39 |
| Birthweight (g) | ||||
| Under 1,500 | 124 | 8.67 | 404 | 13.27 |
| 1,500–2,499 | 37 | 0.56 | 137 | 0.95 |
| 2,500 and over | 119 | 0.13 | 423 | 0.19 |
| Not stated | 2 | 0.23 | 9 | 0.44 |
| Mother’s age (years) | ||||
| Under 20 | 24 | 0.45 | 78 | 0.47 |
| 20–24 | 49 | 0.29 | 180 | 0.38 |
| 25–29 | 70 | 0.28 | 242 | 0.37 |
| 30–34 | 76 | 0.26 | 245 | 0.37 |
| 35–39 | 49 | 0.26 | 179 | 0.48 |
| 40 and over | 14 | 0.31 | 49 | 0.62 |
Intrapartum stillbirth rates were consistently higher at ‘all other times’ than on Monday to Friday between 09.00 and 17.00, particularly among preterm babies and very low birthweight babies weighing under 1,500 g. Similarly, rates by mothers’ age were consistently higher for all age groups, except mothers aged 40 and over, which are based on small numbers (Table 26).
| Day of week/time of birth | Total number | Ratea | Cause of stillbirths (ONS classification) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Congenital anomalies | Antepartum infections | Asphyxia, anoxia or trauma | External conditions | Other specific conditions | Other conditions | Not known | |||
| Weekday, 09.00–17.00 | 282 | 0.28 | 28 | 15 | 74 | 2 | 8 | 150 | 5 |
| Weekday, 17.00–08.59 | 613 | 0.39 | 60 | 10 | 184 | 0 | 13 | 342 | 4 |
| Weekend, 09.00–08.59 | 360 | 0.42 | 37 | 9 | 104 | 0 | 8 | 199 | 3 |
| Total | 1,255 | 0.37 | 125 | 34 | 362 | 2 | 29 | 691 | 12 |
The risk of intrapartum stillbirths appears to be higher among births occurring outside the hours of the normal working week. The excess risk was slightly higher for births at the weekend than for births between 17.01 and 08.59 from Monday to Friday. This was associated with an increased risk of stillbirths attributed to asphyxia, anoxia or trauma and ‘other conditions’ (see Table 13).
Further work
There was not time to do the intended next step of the analysis. The intention had been to perform statistical analysis involving modelling with logistic regression to explain the preliminary and tentative finding of an apparent excess risk of intrapartum stillbirths to women giving birth outside ‘office hours’, particularly at weekends and in the evenings and at night on weekdays. In the absence of this analysis, it is not possible to draw any firm conclusions.
Early neonatal, neonatal and infant mortality in England and Wales
Although descriptive analyses of neonatal and infant mortality were well under way by the time the project funding ended, they need further work, so we have not included them in this report.
It was intended that we would to go on to analyse mortality by fitting logistic regression models equivalent to a Poisson general linear model. These models are along the same lines as those we used for analysing births by onset of labour and mode of birth, as described earlier. They were to include the same categories of covariates and their interactions and follow the same model selection strategy. If overdispersion were apparent, we would use negative binomial models with a logarithmic link. These models would have produced RRs for stillbirth rates and for neonatal, infant and postneonatal mortality. We intended to exclude deaths attributable to congenital anomalies as they are not immediately preventable by care during pregnancy and birth. For other mortality outcomes, time and date of birth might operate as risk factors whose effects might potentially be mitigated.
To model survival up to 1 and 2 years of age, as well as maternal and infant morbidity, we would fit Cox proportional hazard regression models using the same framework to define the linear predictors. The assumptions of proportionality of hazards were to be tested using methods based on extensions of the Cox models. 152
Other planned outcome measures
Time did not allow us to analyse any of the other outcome measures that we had identified. We did, however, do some groundwork, following research elsewhere about the extent to which the morbidity information needed to construct both positive and negative indicators was captured in HES.
A major analysis by the NPEU153 compared maternal morbidity reported in HES with the types of morbidity that had been the subject of studies by the UK Obstetric Surveillance System (UKOSS). 154 This showed that although the quality and completeness of Maternity HES improved during the time period of the analysis, from April 2003 to March 2013, there were discrepancies in the data from HES. We planned to take this work into account in our analyses. As partners in Euro-Peristat, we also followed the progress of the work of the EUROpean NETwork on Severe Acute Maternal Morbidity, which focuses on using routine data to report severe maternal morbidity. 155
Members of our Study Advisory Group suggested neonatal follow-up studies, which had developed indicators that we could consider using. We investigated these and found that many were based on primary data collection and, were thus based on data that are not recorded in HES.
Nevertheless, there is considerable scope for using the data we have linked to derive both short-term and long-term positive indicators of the outcome of indicators that we have identified and to undertake the outstanding analyses set out in Appendix 3. We shall be applying for funding to do this.
Chapter 4 Patient and public involvement
Active user involvement has been at the heart of our project. PPI is now recognised as a vital component of health research. 156 The national advisory group INVOLVE defines public involvement in research as research being carried out ‘with’ or ‘by’ members of the public rather than ‘to’, ‘about’ or ‘for’ them. 156 As pregnancy is not an illness, the term ‘service user’ rather than ‘patient’ is used in the context of maternity care. By involving women who had used maternity services or who had experience of being maternity service user representatives, we hoped to gain a different perspective on our research and make our research more relevant by addressing the needs and views of those using maternity services. We also hoped to improve the quality of our research by ensuring that the methods we were using were acceptable, particularly regarding our use of sensitive medical records, and to ensure that our analyses were appropriate and our outputs were accessible.
Patient and public involvement plans set out in the protocol
Over a number of years prior to the project, the chief investigator developed strong links with service user groups and representatives. This enabled service users’ views on the project to be sought at an early stage in the design. The aims of active involvement were to ensure that the needs of maternity services users to have access to safe midwifery, obstetric and neonatal care 24 hours a day, 7 days a week and throughout the year were addressed throughout the research project.
Our approach to PPI was to include three different areas for input. First, two experienced maternity service user representatives collaborated on the project as co-investigators. Further collaboration was made possible by inviting another four service user representatives to be in the Study Advisory Group. Involvement with the public was then extended by holding meetings to consult with a wider range of women involved with local maternity services, often as members of Maternity Service Liaison Committees (MSLCs). These events were held in accessible venues in different areas of the country, following the principle of ‘go to where they are’. They were designed to be attractive events at which attendees could meet other MSLC service user members and network.
This approach was supported by including budgets for meetings and travel expenses in the initial bid to NIHR, as well as a salary or consultancy fee for those with a significant input and time commitment.
The two service user representatives who were co-applicants to the project were involved in the study design at the outset. We planned for them to have active involvement at all stages of the project. Miranda Dodwell, a service user researcher and subject expert, who, as co-founder of BirthChoiceUK (see www.birthchoiceuk.com), has made HES maternity data accessible to the public, was employed so that she could join the project team as a researcher and attended regular executive meetings to discuss the direction of the research and to analyse and interpret results as they become available. In particular, she has expertise in identifying outcome measures derived from routine data, which assess quality of maternity care from a woman’s perspective. Mary Newburn’s role as co-investigator was to represent and facilitate the involvement of NCT, the UK’s pregnancy and parenting charity. Mary has a background in policy, service user research, service user advocacy and the development of evidence-informed information for women and their partners. We planned to involve women with an expressed interest in maternity services, indicated by their membership of a local maternity group or committee, or an organisation related to seeking improved maternity services. At ‘involvement meetings’, planned and organised with NCT, we intended to involve women in the design of the study, its communication to the public, in active discussion about the results as they emerged, and in plans for further analysis.
The team planned for all written output from the project to be reviewed by service users to ensure that service users’ concerns and questions were addressed. It was intended that both Mary Newburn and Miranda Dodwell would have a key role involving service users during each year of the project, by organising face-to-face meetings, making presentations with other researchers at these meetings, facilitating discussion and analysing feedback from small group work and discussion.
Plans to make the results accessible to the public included providing a summary of the research and links to the research outputs on the BirthChoiceUK website, once papers were published. NCT will disseminate the findings to parent representatives and to ‘patient’ advocates serving on MSLCs, and labour ward forums, as well as publishing in magazines and journals for parents and NCT practitioners.
Both NCT and BirthChoiceUK planned to use their social media presence on Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) and Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) to alert their followers to summaries of research on the BirthChoiceUK website, papers in peer-reviewed journals and NIHR published reports.
Patient and public involvement input on the project
As intended, service users have been involved in the research from the design and funding application stage onwards, as described below and in Appendix 4.
Patient and public involvement in the project team
Miranda Dodwell and Mary Newburn have worked as co-investigators throughout the project, attending project team meetings, at which they have helped to shape the analyses, contributed to the interpretation of findings and been involved in the writing of project reports and papers for publications. In addition, Miranda has used her knowledge of maternity data gained from her maternity user work with BirthChoiceUK to contribute to the data preparation, working in the VML as an approved researcher on the location of maternity units. Although Rod Gibson, another member of the project team, was not engaged specifically for PPI, his background with data analysis for BirthChoiceUK has also meant that his contribution has a PPI element to it.
Miranda Dodwell and Mary Newburn also organised and, along with Alison Macfarlane, participated in engagement and involvement activities.
Patient and public involvement in the Study Advisory Group
A Study Advisory Group was formed for the project (see Appendix 5). Its membership included service users recruited from four different areas of England: Liverpool, Coventry, West Middlesex and Surrey. These women had different interests and backgrounds. They all had experience of involvement in maternity services planning and service user feedback in their local areas, through membership of their MSLC. One is a leading member of the Association for Improvements in the Maternity Services (AIMS); one was invited to join the Study Advisory Group as a parent representative; one who, in her employment, holds a senior position in public health, was invited to join as the public health representative; and one who has specific experience relating to breastfeeding, was particularly valued for her knowledge of infant feeding issues and how these may be related to mode of birth, time of birth and staffing.
Involvement meetings
Together with NCT staff, Miranda Dodwell and Mary Newburn organised three meetings with service users and third-sector groups. A further meeting was organised in conjunction with the Mother and Child Research group at City, University of London (@City_CMCHR). These were all used to involve women in the planned analysis and the presentation and reporting of the emerging findings.
Meeting 1: November 2014 in Birmingham, jointly with NCT
The first meeting, held on Saturday 29 November 2014 in Birmingham, was used to consider the ethics of the data linkage study, to gather service users’ views and to enable PPI in the design of a poster to describe the study methods.
The meeting in Birmingham was attended by about 35 people, including about 20 members and chairpersons of MSLCs, six NCT policy and research staff, three other NCT staff involved with commissioning maternity services/NHS trusts, two researchers from the project team at City, University of London, and the head of patient experience for children, young people and maternity at NHS England.
Alison Macfarlane led a presentation and facilitated group discussion about the project. Although the methodology of the project was complex, it was explained so that people with no statistical background could understand it. Participants were told how the project was designed to proceed through a number of stages in order to assess the extent to which services provide care to women and babies on the basis of their needs, at the times of the day and night, and day of the week, when care is needed. First, the researchers would gain approval to allow them to access three different large databases with information for each of 10 years. We explained that there were serious delays with this part of the process. Second, the three databases had to be linked so that the data from each could be combined. This was a new and complex process made more difficult and slow by the strict data security required and limited computer capacity at the permitted data access facility. Third, the data had to be ‘cleaned’, which meant checking for duplicate cases, missing information and inconsistencies and either correcting or removing each case before analysis was carried out. This was also time-consuming, especially given that we were dealing with > 7 million records. We also provided service users with some results from previous projects relating to seasonal and daily patterns of birth to show them the type of analyses that would be done.
Participants joined enthusiastically and knowledgeably in the question and answer session after hearing the summary, with personal experiences and observations, feedback from women in antenatal/postnatal NCT groups and queries about related aspects of care. With increasing numbers of births involving elective procedures such as induction and planned caesarean section, and a simultaneous shortage of midwifery staff in most parts of the country, the questions about quality of care for women in labour outside ‘normal working hours’ were thought to be highly pertinent and all the representatives present were keen to hear more about the study and its potential findings.
The discussion about confidentiality and use of data also elicited vigorous debate. The methodology outlined for the study was thought to be quite complex but those present, especially the ‘research networkers’ (NCT members with an expressed interest in research, who are supported to learn more about research in a participative way), demonstrated high levels of appreciation about the challenges and solutions when analysing data for approximately 7 million births. They were happy for women’s data to be used in the way that was planned and did not feel that this was a breach of confidentiality. Feedback from the discussion was presented at the Study Advisory Group meeting held on 9 January 2015.
We were required as a condition of permission to process patient-identifiable data without consent under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (‘section 251 support’) to take steps to inform parents about how their data would be used for our project and details on how they could register their objection to the processing of their personally identifiable data. Researchers therefore produced a draft poster that was sent to the Confidentiality Advisory Group (CAG) of the NHS Research Authority on 2 April 2014. We asked for comments on the draft poster at the meeting with service user representatives and were able to use this feedback to make changes to the poster. Following this, it was distributed to all the maternity units in England and Wales, using address labels produced from the BirthChoiceUK database of maternity units (used with the permission of Rod Gibson Associates Ltd), for display in waiting areas and other public places.
Meeting 2: November 2015 in Wakefield, West Yorkshire, jointly with NCT
Continuing the approach used in 2014, the following year we decided to meet once again with women serving on MSLCs. In collaboration with NCT, we invited MSLC service user members from all parts of England to a one-day meeting held on a Saturday 21 November 2015 in Wakefield for networking, support and presentations.
The event was advertised as a support and information day, a familiar concept, so people knew what to expect. NCT’s events manager organised the practical aspects. Two co-investigators (MN and MD) liaised with NCT’s research engagement officer to plan the programme and promoted the event using social media and the hashtag #MSLC. The purposes of the day were to:
-
bring together maternity services user representatives, activists, maternity researchers and policy staff to share intelligence and MSLC good practice, and to facilitate mutual support
-
enable the NIHR-funded researchers at City, University of London, whose project funded the day, to seek input and feedback from service user representatives
-
increase service user representatives’ confidence and motivation by providing an opportunity for them to share their work and learn new skills.
The programme was designed to meet the priorities of the delegates and provide a good lunch as well as discuss the study. Approximately 30 people attended the day, from areas as diverse as North Cumbria, Leeds, Wakefield, Norfolk, South London, Sussex and Blackpool.
One of the researchers (MD) gave an introductory talk about the study. In our experience, maternity services users are often interested in, and more familiar with, research questions that are amenable to qualitative research, such as ‘how do women feel?’ or ‘why do some units have higher intervention rates?’. So, she explained the kinds of question that can be addressed by large datasets and the potential provided by a data linkage project, showing a preliminary analysis of births at home as an example. MSLC maternity user representatives were very interested.
She acknowledged the issues identified by service users at the previous year’s meeting and gave everyone copies of the study poster, which had been circulated for display in local maternity units. Delegates then formed small groups to discuss their experience of maternity services in the evening, during the night and at weekends. A fuller report of the issues discussed is included in Appendix 4. In short, service users expressed concerns about temporary midwifery unit closures and midwifery units operating an ‘on-call’ model in the evening, during the night and at weekends, staffing shortages and cuts to budgets, the need for specialist perinatal mental health services, and staff going off duty, thereby influencing the course of labour. There were concerns that non-English speakers might suffer ‘out of hours’ owing to a lack of interpreters and that vulnerable women might be most affected by any weaknesses in the system, such as decisions about the need for interventions, and the urgency of any interventions, being taken by junior obstetricians without good consultant or senior midwife support.
Women shared their perceptions and stories from their local service. Some said that they wanted care based on their needs, not the constraints of the service. They said that they could feel pressured if they are told for example that ‘The obstetric unit will be best, there are not many midwives in the freestanding midwifery unit’. It was also suggested that sometimes the caesarean section rate drops when a consultant unit is very busy as there is less chance to intervene. A participant reported that an obstetrician had once suggested this.
There was concern and anxiety about recent news reports of research findings suggesting that more deaths occur in hospitals at the weekend. It is noted that the study from which these results came62 stated explicitly that there had been no PPI. A few women said that they had chosen an elective caesarean birth or induction mid-week because they were worried about poor staffing and lack of support at the weekend.
Meeting 3: June 2016 in London, arranged by City, University of London Centre for Maternal and Child Health Research
The next involvement meeting, held in London on a weekday evening on 21 June 2016, was arranged in conjunction with the City, University of London Centre for Maternal and Child Health Research parents’ advisory group. Four or five mothers of young children were expected and two attended. Both had given birth within the past 2 years. One had two children. One was Eastern European. Miranda Dodwell and Mary Newburn ran the session, combining introductions, presentation of the aims and methods of the research, some predictions, discussion, and some specific questions to the women about their experiences, perceptions and any concerns. This included asking the women about experiences known to them of differences in care by time of the day and day of the week. They reported accounts of poorer care in the early evening and at night because of lower staffing levels, reducing support to women who had just given birth, including help in establishing breastfeeding. They also cited other women who had not experienced problems at night. They also said that women may feel apprehensive because of reports of lower staffing levels ‘out of hours’. In areas of London in which there are many women who do not speak English, and many more who do not have English as their first language, they pointed to problems with access to language support at night and the stress that this might cause.
Meeting 4: November 2016 in Bristol, jointly with NCT
The fourth and final involvement day was held in Bristol on Saturday 12 November 2016. The decision to host the meeting in Bristol was taken to make the meeting accessible to women living in the south-west of England. An innovation at the 2016 meeting was to hold ‘speed dating’ sessions, enabling delegates to choose a programme of practical ‘taster’ activities to meet their particular interests and needs. These were flexible, enabling delegates to move around freely; empowering, as many delegates led sessions; interactive; and responsive to the questions and interests of those attending. The aim was to create a day that service users would be motivated to come to. The tactic was successful, as 33 people attended the meeting, including 17 service user members of MSLCs. Other attendees included NCT staff members, the mother of a child with Down syndrome, a Positive Birth Movement member, Healthwatch, two young and newly qualified midwives, a health visitor, the chairperson of the RCOG’s Women’s Network, a NHS England representative a NIHR representative and one or two other researchers.
The study session was made up of a presentation by Alison Macfarlane and discussion in small groups. The presentation included descriptive analysis showing the timing of spontaneous onset/spontaneous birth labours, the timing of births at home, and the timing of births with induction, and planned or unplanned caesarean sections. Service users were struck by how much maternity care activity there is – and should be, on the basis of normal circadian patterns – in the evening and at night. There was discussion about the impact of darkness and light on the labour and birth behaviour of mammals, informed by one person’s work with laboratory rats. She described how days and nights for the rats were reversed by lighting so that researchers could observe births during their working day, the message being that darkness stimulates labour and birth. The discussion focused on appropriate messages for the public, what service users would like to see communicated to commissioners and service managers and how the emerging findings relate to Better Births35 recommendations for maternity services, and their priorities for future research. Further detail is available in Appendix 4.
One particularly pertinent issue raised was the extent to which the current campaign to reduce stillbirths66 is driving up rates of induction of labour. Service users questioned whether or not women were able to exercise their autonomy and to make truly informed choices. Their perception was that women with and without complications or risk factors are being offered induction earlier in pregnancy, once they had reached ‘term’. ‘How many say no, they don’t want to be induced?’ was a question asked by service users.
There was also concern in one area that, because a maternity unit was closing, choice of place of birth was diminishing rather than increasing. In other areas, service users felt that information on Better Births recommendations35 had not ‘percolated down to midwives, let alone others’. They commented that for midwives there is ‘no such thing as “out of hours” for birth’ and wondered if it was appropriate for maternity units to have fewer midwives at night given the additional demands of physiological labour during the hours of darkness. In terms of messages for commissioners:
-
Service users felt that there was a need to ‘create more midwife places’ to meet present needs ‘let alone to create continuity’. There was discussion about too few midwives (‘60–80 women each per year’) and this causing burnout.
-
Service users noted that there are pilot studies for service development work but then funding stops, and they wanted to know why.
Feedback from each of the involvement days was reported and discussed further at the following Study Advisory Group meeting. Some of the suggested further research questions that were discussed at the fourth and final involvement meeting are included in our recommendations in Chapter 6.
Dissemination
Thus far, dissemination via NCT and BirthChoiceUK has been limited because the study has experienced delays and barriers and there have been only preliminary results to share. Several articles have now been published in peer-reviewed journals. 157–159 Publication, which puts the methodology and results in the public domain, allows the results to be shared with the wider public.
Social media
Real-time information about the first involvement day was tweeted and retweeted by participants including Mary Newburn, BirthChoiceUK and other participants who between them have more than 10,000 Twitter followers and so have considerable reach among the maternity community. Further activity has been generated around subsequent meetings.
We have used the short, accessible title ‘Birth Timing’, and the hashtag #BirthTiming when communicating to service users about the study, and #MSLC, which draws in service users on these multidisciplinary forums. In England, MSLCs are being replaced by Maternity Voices Partnerships (MVPs). Now, the hashtag #MVP is therefore used alongside or instead of #MSLC.
Both NCT and BirthChoiceUK will continue to use their social media presence on Facebook and Twitter to alert their followers to summaries of research on the BirthChoiceUK website, papers in peer-reviewed journals and NIHR published reports.
Patient and public involvement in outputs and dissemination
Both Mary Newburn and Miranda Dodwell have been actively involved in the writing up of the paper describing patterns of births, something that is reflected in the authorship. They have contributed to two additional articles on linkage methods and data cleaning, making detailed comments on the draft. The time of birth analyses were presented to service users at the fourth involvement day and points raised have contributed to the discussion section of the paper. There have also been opportunities to contribute to the creation of research posters for the International Population Data Linkage Conference (Swansea, 24–26 August 2016) and the RCM annual conference (Harrogate, 19–20 October 2016) and the 12th International Normal Labour and Birth Research Conference, (Grange over Sands, 2–4 October 2017).
Feedback from service users will inform our dissemination in terms of messages and target audience. Learning from the patterns of planned home birth, during which women are not affected by an institutional environment, and births in all settings studied, which peak during night-time hours, service users wanted commissioners and professionals to be made aware of the impact of institutional care, and to consider critically issues such levels of lighting, privacy and intimacy. They felt that it was very important for research studies to differentiate by place of labour and birth. In terms of messages for the public, service users wanted positive messages to be the focus of the story, rather than risks and harms, which could undermine confidence and self-efficacy. Concerned that media reporting cannot be relied on to convey positive, or even balanced and accurate messages, they urged that dissemination:
-
should tell ‘the story’ to women directly (so no gatekeeping effect); for example, via YouTube (YouTube, LLC, for example, San Bruno, CA, USA), Facebook, blogs and MSLC networks
-
should provide bite-sized messages for women (i.e. give very clear conclusions).
Planned dissemination beyond the lifetime of the project
Now that the results have been published, BirthChoiceUK will provide a summary of the research and links to the research outputs on its website. NCT will disseminate the findings to parent representatives and to ‘patient’ advocates serving on MSLCs, MVPs160 and labour ward forums, as well as publishing in magazines and journals for parents and NCT practitioners.
BirthChoiceUK (@BirthChoiceUK), Miranda Dodwell (@mirandadodwell1) and Mary Newburn (@MaryNewburn1) have a substantial lay following on Twitter. A posting will also be made on the Facebook discussion of National Maternity Voices, and London MVP Network.
The NCT will disseminate the findings to parent representatives and ‘patient’ advocates serving on MVPs and labour ward forums. This will have the effect of highlighting research findings and service users’ views and priorities to clinical managers and commissioners.
The NCT plans to post results on its parent-facing website and on ‘babble’, its intranet for NCT practitioners and other workers. An article will be published in Perspective, NCT’s continuing professional development journal for NCT practitioners (antenatal teachers, breastfeeding counsellors and postnatal leaders). Despite there being no additional funding, it may be possible to arrange for a ‘Birth Timing’ speaker to present results and facilitate discussion at a further involvement meeting in 2018, convened by NCT for service user members of MVPs and labour ward forums. Now that the results have been published, a telephone journal club discussion is being arranged. 159 NCT may also be able to incorporate the findings into conference presentations and talks to policy-makers and professionals, such as the All Party Parliamentary Group on Maternity, which was set up with the support of NCT, and continues to be serviced by NCT. All dissemination activities will be enhanced and reach a wider audience with the use of social media such as Facebook and Twitter.
Planned activities that have not been possible
It was not possible to complete all of the planned analyses and writing up, so opportunities for dissemination to the public have been more limited. There was no further funding for work to continue beyond the end of June 2017. As a result, some planned activities were not possible, such as disseminating a short summary of findings via NCT local branch newsletters.
Unplanned dissemination activity
The NCT organised a meeting on 17 October 2017 with the University of Birmingham entitled ‘Monitoring babies during labour: What are the issues for pregnant women and their health professionals?’, a dissemination event for the INtelligent Fetal AssessmeNT Monitoring (INFANT) randomised controlled trial. 161 Two posters containing project results and lay summaries of key findings of the project were shared at the event and attracted considerable interest.
Further research questions
The service user involvement meeting discussions generated further research questions. These included:
-
Can we get real data on length of labour (with the start of labour decided by women)?
-
What is/is there a physiological basis for birth at night? Why does it happen? How can the right conditions be created to support physiology?
-
Does the time of day at which women labour and give birth affect their experiences of labour?
-
Does continuity of care affect experiences of labour and birth timing?
-
Are transfer rates from midwifery units affected by time of day?
-
Is there a correlation between declining postnatal care quality and declining subsequent birth rates?
-
Do we need to rethink birth environments for women needing medical interventions?
-
Do we need to rethink the timing of induction so that this does not result in a problematic staffing model?
-
How does physiology affect birth timing? What are the roles of female physiology and baby physiology? In each case, what is the mechanism?
-
Does having fewer staff at night pose a problem for women/childbirth?
-
Is 24/7 consultant cover justified?
-
What is the right staffing model to provide safe care?
Strengths and weaknesses of patient and public involvement in the study
The PPI in the study has been strong in many respects. Two service user researchers have been co-investigators, influencing the research design from the very beginning, and one (MD) has taken an active role in data linkage, creating assigned trusts based on her previous knowledge of, and work with, an online community organisation (www.birthchoiceuk.com). The other service user researcher (MN) successfully facilitated recruitment of service users who have been active members of the research advisory group. Both service user researchers have participated fully in the writing up of the data linkage and quality assurance processes, thus helping to ensure that the language is accessible and clear, as well as in the writing up of papers submitted for publication.
There have been four face-to-face involvement meetings to discuss pertinent issues, involving around 65 service users directly, including women with experience of perinatal bereavement, women with English as a second language, women not born in the UK, a Muslim community leader, a woman originally from Eastern Europe and many leaders of local MVPs or MSLCs.
The pertinent issues discussed have included the ethics of using population data for retrospective study without obtaining consent from each individual but instead using an opt-out model and posters to advertise this for display in health facilities; the co-design of the explanatory posters; presentations about population-level studies, so that those giving their time learned more about research and thus gained knowledge and skills; sharing of descriptive statistics and small group work in issues of importance to women, to service delivery and to research.
Women have advised on how to communicate the study findings and further research questions. Interestingly, the small group work highlighted the need to find ways to circumnavigate traditional print and broadcast media, which often present alarmist or ‘worst case’ messages which make arresting headlines. Although newsworthy, these may be less accurate than moderate or positively framed messages, and may be alarming for pregnant women. The groups felt that researchers should summarise their own findings in a balanced and reliable way and use social media to publicise them. Although research teams and research funders may not have the social media profile to do this effectively at present, this approach to communication has been very much in the news during and since the 2017 general election.
The weaknesses of the PPI include limited success in reaching black and minority ethnic women. As there are many different groups with different experiences and concerns, it is always an advantage to speak to numerous different groups in order to truly reflect the diversity of service users, and to engage women equally in publicly funded research. It is unfortunate that, because analyses were delayed and the planned analyses were not completed, we have been able to share and discuss fewer findings with maternity service users than might otherwise have been the case. If a further extension had been funded to complete the planned analyses, another PPI meeting would have been arranged to discuss these results.
Chapter 5 Discussion
Principal findings
To our knowledge, this is the first study to analyse, at a national level for England and Wales, data showing how numbers of births vary by time of day and day of the week, throughout the week and the year, and how these patterns vary by gestational age, onset of labour and mode of birth. Having a large dataset with > 7 million births over a 10-year period made it possible to analyse the effects of time of day and day of the week, and to produce estimates with good precision, even for the less common combinations of mode of labour onset and mode of birth.
This was made possible through data linkage. Linkage of birth registration with birth notification data made it possible to analyse births and infant deaths by gestational age and time of day along with the demographic and other data recorded at birth registration. Further linkage to data recorded at birth in England and Wales and to data about subsequent admissions to hospital has created a new linked database and made it possible to analyse these births by mode of labour onset and mode of birth.
Day of birth
The overall patterns of numbers of births by day in our study are similar to those seen in analyses of registered births in England and Wales by day from 1970 to 19761,86 and from 1979 to 1996,2 which showed pronounced weekly cycles and lower numbers of births on public holidays, particularly in NHS hospitals with consultant units. Marked day of the week differences in patterns of birth after induced labour or birth by elective caesarean section were also apparent in tabulations of HIPE data for 198098 and in tables published in reports of Maternity HES for the years from 1994/5 to 2005/6. 99,162
Similar patterns have also been seen in many other countries90,91,94,95 and the consensus is that they reflect staff working patterns, especially the concentration of elective caesarean sections onto weekday mornings. In contrast, emergency caesarean sections would be expected in response to an urgent clinical need and thus be independent of the day of the week. Yet, we found that the relatively small numbers of emergency caesarean sections without prior onset of labour were considerably lower on Sundays and public holidays than on weekdays, and that their numbers were highest on days immediately preceding weekends and public holidays.
It is also difficult to find a ready explanation for the finding that the numbers of spontaneous births after spontaneous onset of labour varied by days of the week, although to a much lesser extent. Over the years in our study period, average numbers of these births were about 1% lower on Saturdays, 2% lower on Sundays and public holidays apart from Christmas, and 7% lower on Christmas Day and Boxing Day than the overall daily average. It may be that women who are in labour on a Friday or a day before a public holiday may be more likely to be subject to intervention to bring forward their birth before the weekend or a public holiday. This is an important question for women using the services but research of a different kind is needed to try to answer it. Data from the Birthplace in England study suggest that this may vary depending on the setting in which women receive care. 101
The pattern observed was not surprising, however, as it was already apparent in the 1970s. Among births occurring at home or in NHS hospitals without consultant OUs from 1970 to 1976, numbers of births were lower at weekends100,163 and all the differences widened as induction rates rose from 1970 to 1976. 100 The patterns were also apparent in the HIPE and HES data referred to above. A possible explanation for the relative deficit in births at home at weekends is that some maternity units may be short staffed and midwives may not be available to provide care at women’s homes at weekends. Other possible suggestions were made at our PPI meetings, however, and some had already been made in the 1970s.
A Lancet editorial commenting on the earlier data and pointing to the higher proportions of low birthweight babies among those born at weekends suggested that this might reflect the selective induction of term babies during the week164 and prompted correspondence suggesting possible explanations. One letter reporting similar patterns in Scotland in 1980 suggested that women’s stress levels may differ between weekends and weekdays and that these differences may have an impact on the onset of labour. 88 Another letter165 pointed to research showing that the relationship between stress and onset of labour becomes less important as pregnancies approach term. 166 In the current project, service user representatives raised questions about the physiology of labour and the impact of the time of day, as well as the day of the week, on the onset of labour and mode of birth.
Preterm births
Unlike the earlier analyses, we had data available to analyse preterm, term and post-term births separately. We found that, unlike those births at term, numbers of spontaneous preterm births after spontaneous onset of labour did not vary by time of day and were not lower at weekends and on public holidays. A similar result was found in a study of 2,005,096 births from 1 January 1960 to 30 September 1994 in Denmark. Lower than usual numbers of term births occurred on Christmas Eve, when the most important family gathering takes place in the evening, and the following 3 days, but there was no reduction in numbers of preterm births. 167
Hour of birth
This study showed that spontaneous births after spontaneous onset of labour showed broadly the same sinusoidal patterns (i.e. peaking at night) seen in local analyses in England in 1950 and 1951. 76,168
Although patterns of timing of spontaneous birth have remained unchanged in England, overall patterns of birth have changed with the rise in rates of obstetric intervention. The rising rates of elective caesarean section have concentrated increasing numbers of births into weekday mornings.
In contrast, although the rationale for increasing rates of induction in the 1970s was to concentrate births into daytime hours, our data show that numbers of induced births peak at night, around midnight, irrespective of the mode of birth. Rates of induction of labour rose from 23% of all births in England in the financial year 2012/13 to 29% in 2016/17. 169 It seems likely that they will continue to rise in the light of the drive to reduce intrapartum stillbirths, with interventions being identified as the mechanisms to achieve this aim. 35,66,69 The Saving Babies’ Lives Care Bundle describes four elements of care designed to bring this about. 66 Of these, both risk assessment and surveillance for fetal growth restriction and raising awareness of reduced fetal movement are likely to have an impact on the induction of labour. A third factor, namely ‘effective fetal monitoring during labour’, may influence the number of assisted births overall, and, as assisted births are more usual after induction of labour, there may be an additional effect among women whose labour is induced. There may, therefore, be an additional need for midwifery and medical staffing around midnight. In addition, the likelihood of a night-time birth should be taken into account when planning the induction of a baby with a condition for which specialist care will be needed after birth. A systematic review comparing morning and evening induction of labour for improving outcomes170 found only two trials that used prostaglandins and one that used intravenous oxytocin. These found few clinically significant differences, but one of the trials using prostaglandins found that women preferred to start induction in the morning.
Patterns of spontaneous birth similar to those seen in England were also visible among spontaneous births in a hospital in Spain in 1991, 2005 and 2007. 83 In contrast, although data about spontaneous births in New York State in 1929 and 1936 showed these same patterns,75,103 they were no longer visible among spontaneous births in hospitals in the USA in 2013, when numbers of spontaneous births were higher between 12.00 and 17.00 than at other times. These patterns were still present in out-of-hospital births, which showed a pattern similar to that in earlier data, with numbers of births being highest between 03.00 and 05.00. 82
Detailed distributions varied because, in the USA, elective caesarean sections were concentrated into mornings, with two peaks at 08.00 and 12.00, whereas numbers of emergency caesarean sections were highest during late afternoons and early evenings. Numbers of induced vaginal births showed a very different pattern from those in England, being highest between 12.00 and 18.00. Numbers of vaginal births after spontaneous onset of labour varied considerably less but numbers were higher between 12.00 and 17.00 than at other times.
A study in the Netherlands suggested another factor that may affect the time of birth, along with the timing of onset of labour. Women without obstetric intervention who had care from midwives had shorter labours than those who had care from obstetricians. 85 Among women receiving care from midwives, numbers of births to primiparous women peaked between 08.00 and 09.00 and births to multiparous women peaked at 05.00. For women cared for by obstetricians, the corresponding peaks were > 5 hours later, between 14.00 and 15.00 for primiparous women and between 08.00 and 09.00 for multiparous women.
Although other factors may have played a part, these comparisons raise questions about differences in styles of practice and settings for care. It is notable that in the USA, the proportion of women giving birth in hospital who have midwifery care is low, whereas in England, midwives are the lead carers for most women who do not have obstetric intervention.
Births in hospital in Wales
Our analyses of births in NHS hospitals in Wales were by mode of birth, as data about the onset of labour were less reliable and there was not time for a closer examination of the data or for implementation of our plan to derive a subset of data items common to both England and Wales. In addition, these data were based on much smaller numbers of births. By and large, births in Wales showed similar patterns to those in England, with numbers of elective caesarean sections peaking in mornings and numbers of spontaneous births peaking in the early hours of the morning.
Births outside hospital in England and Wales
Births at home in England and Wales from 2005 to 2014, which we have analysed separately, also show similar patterns to those for home births in Birmingham in 1950 and 1951. 76
In England and Wales, information on the planned place of birth at the onset of labour care is not recorded on any of the linked administrative datasets used in the study and the majority of births occurring at home are not included in the Maternity HES for England. This means that the analyses presented here include unplanned home births and exclude those for which the woman was planning a home birth but transferred to hospital during labour, because she developed complications for which hospital care was needed. No information about this was available in the datasets we analysed.
In the Birthplace study,26 35.1% of nulliparous and 6.4% of multiparous healthy women with low-risk pregnancies planning a home birth transferred to hospital during labour. As only 25% of them were nulliparous, the overall transfer rate was 14.2%. The question of whether or not transfer rates varied by time of day and day of the week was explored in a set of follow-on analyses from the Birthplace study and no difference was found by day of week. An apparent peak in transfers from home in the early hours of the morning was not statistically significant. 101 This tends to suggest that higher numbers of transfers in labour are not the main cause of lower numbers of home births at the weekend.
Intrapartum stillbirth
The analyses presented in this report are very preliminary and need more rigorous analysis before any conclusions can be drawn.
Data linkage
As well as analysing patterns of birth, this project has undertaken, and evaluated methods of, data linkage. Although this was not one of its stated aims, the linkage has been innovative. As well as producing linked data, which can be used for further research, it has produced a relational database to hold HES data for England and linked birth registration and notification data linked to death registration data for England and Wales combined. It has also led to important findings about the linkage processes, some of which are applicable more widely.
Data linkage for England
Linked birth registration and notification records from ONS were linked to HES delivery and birth records by the data linkage team at the HSCIC. Although this team has extensive experience of linking external datasets to HES, this project offered new challenges. We used a linkage algorithm, which was similar to that routinely used by the HSCIC, to link ONS death records to HES records, but there were issues with the quality of linkage. In the period 2005–14, 4–6% of the ONS birth records for each year were incorrectly linked to the HES delivery record and 4–7% of HES delivery records were linked to more than one ONS birth record.
The number of birth registration and notification records linked to the HES delivery records using the NHS number increased over the years from 2005 to 2014. This was not surprising, as completeness of the mother’s NHS number in the registration and notification linked records increased over time. In 2005, the mother’s NHS number was present in more than two-thirds of the records, and this increased to over 90% in 2014.
In addition, the mother’s NHS number was missing from a small proportion of HES records. A further one-quarter of the registration and notification linked records in 2005 were linked using exact date of birth, sex and postcode and this decreased to 3% in 2014. There were concerns about using the postcode in the linkage algorithm for linking data for earlier years, as the HES index may not hold all historical postcodes of residence of the mother and the postcode on registration and notification linked data was recorded at the time of registration. It is possible that the mother could have moved since having the baby and this variable is also subject to recording and reporting errors.
Overall, a linkage rate of over 90% was achieved and it improved over time, especially in 2014, when there had been a shorter time between birth and the data linkage being carried out, meaning that the [HESID] encrypted identifier derived from patient identifiers, including postcodes, would have been less likely to have changed. This suggests that [HESID] at birth should be retained as a separate field for linkage.
Although ONS birth registration data have remained of consistently high quality, there have been issues with data quality and completeness in Maternity HES. The numbers of births and deliveries in London are under-represented in Maternity HES, which could be attributable to under-reporting, or complete lack of reporting, of births by several hospitals. 171 In addition, HES currently captures few home births and none occurring in private hospitals, even though data about all births should be submitted to Maternity HES.
Quality assurance of linkage
The aim of the quality assurance was to prepare the linked dataset for analysis but the results also shed light on the quality of the data and the linkage itself. This makes it informative for other users of similarly linked data and for HSCIC staff doing the linkage.
The method adopted compares common baby data items, giving most importance to matching babies’ dates of birth and locations of birth. Altogether, 98% of births originally linked to HES were left with one preserved link. This meant that 95% of all singleton births and 93% of all multiple births in England in the period of 2005–14 were linked to one correct HES delivery record after quality assurance.
Administrative duplicate HES records were found to be the main reason for discarding links. Other reasons were other births to the same mother within the study period, the presence of multiple HES records per delivery for various reasons, and error in the linkage and in the quality assurance method itself.
Certain features were more common in incorrectly linked records than in correctly linked records. Compared with correctly linked records, incorrectly linked records were more likely to have been linked using a less reliable stage of the linkage algorithm or to relate to births occurring at home or to residents of the London region or to births for which the birthweight or gestational age was missing from HES records. This suggests some bias in the linkage and often relates to data quality issues. These patterns differed between singleton and multiple births. Missed links were also discovered, which together with the previous findings, provide additional evidence on the quality of the linkage.
The linkage error identified by quality assuring the linked dataset suggests that linkage carried out using similar algorithms and by ‘trusted third parties’ generally cannot be assumed to be error-free and may affect any analyses carried out on them. The ‘trusted third party’ model replaces identifiers with an encrypted code, and the de-identified data only are made available to researchers in a secure environment. This has implications for other research projects that are not informed of the quality of the linkage, or do not have the means to quality assure the data themselves using identifiers. In particular, no assessment of the quality of the linkage algorithm is routinely published by HSCIC. We were able to detect this through using the VML to access personally identifiable data.
Data linkage for Wales
The linkage rate was approximately 95%, which was similar to the rate achieved in linking birth registration and notification linked records to Maternity HES. However, the quality of linkage to the NCCHD and PEDW was much better than Maternity HES and the data in all the fields of interest in the NCCHD were much more complete than in the corresponding fields in Maternity HES. The PEDW data are equivalent to Maternity HES but their completeness could not be assessed and compared for the reasons stated earlier, because the key data items were not obtained from the PEDW.
Generalisability
The findings apply to England and Wales as a whole. We did not have time to investigate variations between maternity units as planned.
Strengths and limitations
These analyses were based on a large dataset, derived from over 7 million births as a whole and over 5 million births in the subset used for analyses by onset of labour and mode of birth in England, giving sufficient numbers of births for detailed analyses. By linking three datasets together, we have greatly increased the numbers of variables available for analysis and there is scope for further analysis to look at social, demographic and clinical factors, which we have not touched on here. Linkage has also made it possible to use the much more complete data on gestational age recorded at birth notification to compensate for the poor-quality data about gestational age recorded in HES.
On the other hand, we had to exclude 15.9% of the births in England in our linked subset from analysis, mainly because data about onset of labour were missing. This mainly resulted from the fact that the key data items were missing from HES records for a number of maternity units as well as for some individual births. This has been a longstanding problem172 but the situation improved considerably over the years 2003–10. 171 Unfortunately, the situation began to deteriorate at the end of our study period and in subsequent years. 173
In addition, there are questions about the quality of data in HES submitted by some maternity units, but we could not directly evaluate the recording quality of key variables, particularly gestational age, onset of labour and mode of birth. Even after using data linkage, some key variables used in previous analyses elsewhere were not available to us. Analyses in the Netherlands showed differences by parity in the timing of birth, but parity is missing from many HES records and was not recorded for all births at registration until May 2012. 141 As part of our project, methods have been developed for imputing parity, which could be used in future analyses. In addition, the time of onset of labour is not recorded in any of the datasets that we have linked, perhaps because it is often difficult to obtain an accurate measure of the time when labour starts. Although there has been considerable investment since the mid-2000s in a new Maternity Services DataSet174 containing a much wider range of data than Maternity HES, it is still very incomplete, so Maternity HES is still needed to monitor trends at a national level as well as variations between maternity units and to allow it to decline in quality and completeness at this point would be very shortsighted.
There are no recent data on the extent to which births at home are unplanned, although it is likely that preterm births at home are unintended. Some unplanned births at home are likely to occur before the arrival of a midwife and may be categorised as ‘birth before arrival’. This term has no clear definition and can also include births that occur while a woman is on her way to her planned place of birth. The numbers of births that take place ‘elsewhere’ outside hospital premises but not at the woman’s usual place of residence are low in England and Wales, but has risen from 0.1% of all births in the 1980s and 1990s to 0.2% in 2013 and 2014. Increases in births before arrival as a whole have been reported in other countries, such as Norway, which have centralised their maternity services and studies, along with an analysis based in a large English maternity unit, show that such births tend to be more common at night. 175,176 Our analysis of births ‘elsewhere’ in England and Wales showed that numbers of births ‘elsewhere’ were highest in the early hours of the morning, peaking between 04.00 and 07.00.
To answer some of the questions raised here, data are needed about planned place of birth at the onset of labour. Since 2015, a much wider range of data is now being collected through the new Maternity Services DataSet174 for England. Like HES, it did not record the planned place of birth at the onset of labour care in version 1, although it is hoped to implement this in version 2. Wales is also developing a new maternity dataset but this does not currently record the planned place of birth at the onset of labour care either.
The analysis of intrapartum stillbirths was restricted to 2005–9 as CMACE data were not available for all the years of the study period. CMACE data for 2010 did not include any unique data items that could be used for linkage. Data collection for 2011 and 2012 was incomplete owing to a delay in the retendering process for the confidential enquiries and consequently in transferring work from CMACE to MBRRACE-UK. The 2013 and 2014 data from MBRRACE-UK were not available as the team had not yet had time to develop metadata to enable the data to be used by others. In any case, problems had arisen with the Cause Of Death and Associated Conditions (CODAC) system177 introduced to classify causes of death, so for 4.9% of stillbirths in 2013 and 3.8% of stillbirths in 2014, it was not possible to ascertain whether they were antepartum or intrapartum in Version 1, although it is hoped to implement this in Version 2. 114,115
On the medical certificate of stillbirth, the completeness of recording of the information about the timing of death as before labour, during labour or not known has increased over the time period of our project, but its quality has not been reassessed.
Chapter 6 Conclusions and recommendations
Conclusions
Timing of birth
In England and Wales, over the years 2005–14, numbers of births varied by day of the week. Numbers were highest on weekdays and increased through the week, with the highest numbers of births on Fridays. Numbers were lower at weekends, reaching a minimum on Sundays, and low on public holidays, with the lowest numbers on Christmas Day and Boxing Day. This is in line with patterns established from the 1970s onwards and did not change over the period studied.
Numbers of births varied by time of day. On weekdays, numbers peaked sharply from 09.00 to 11.00, with much smaller peaks in the afternoon. Every day, numbers of births then reached much broader maxima at night and were highest in the early hours of the morning. This is the first time that births in England and Wales have been analysed by time of day at a national level.
The overall patterns were dominated by births in NHS hospitals with OUs, in which the majority of births took place. Numbers of births in FMUs and at home varied much less by day of the week, but were still slightly lower at weekends than on weekdays. There was no morning peak in numbers of births in these settings, which showed a sinusoidal pattern, with numbers of births per hour being highest at night, reaching a maximum in the early hours of the morning.
Singleton births at term in England were analysed by method of onset and mode of birth. Just over half of these births were spontaneous after the spontaneous onset of labour and they showed similar patterns to births in FMUs, with average numbers of births per hour being highest in the early hours of the morning. Just over one-fifth of births followed induced labours and their numbers reached were highest in the hours around midnight, regardless of the mode of birth. Nearly 12% of births were by planned caesarean section and were concentrated between 09.00 and 12.00. Analyses of term births in Wales by mode of birth showed similar patterns.
It was planned to analyse the outcome of births in terms of mortality and morbidity in mothers and babies by time of day and day of the week, but the project was severely delayed by problems in accessing data and by subsequent IT infrastructure problems in handling large files of data for more than 7 million births in the 10-year period. Although patterns of birth have been described, more rigorous statistical analysis of some topics is needed. Analyses of the outcome of pregnancy had only just started when the funding period ended and analyses of differences between trusts and their maternity units had yet to be done.
Data linkage
To prepare the data for analysis, we have successfully acquired and linked birth registration and notification data for more than 7 million births in England and Wales for a 10-year period (2005–14). We have linked these to Maternity HES records for births in England. For births in Wales, we have linked them to PEDW records, which are linked to the NCCHD records. For births in both countries, we have also linked in records of subsequent admissions of mothers and babies. This work has been done in the secure setting of the ONS VML to ensure the confidentiality of personally identifiable data.
To hold the hospital data for England and the registration and notification data for England and Wales and organise them for analysis, we have built an innovative relational database. Outside this, we have organised the hospital data for Wales for analysis. These data can now also be used for other analyses of births and their outcome.
Although the linkage was successful, the overall quality was dependent on the quality and completeness of Maternity HES data. This improved considerably up to 2010, but then declined at the end of the study period and subsequently. Although the new, more wide-ranging, Maternity Services DataSet174 is being implemented, it is still very incomplete and it would be short sighted to abandon Maternity HES unless the new data for England are complete.
We have evaluated the linkage and found it to be of good quality. The quality assurance also identified a technical problem with the ‘trusted third party’ model, which is planned to be used increasingly under the Digital Economy Act 2017. 178 This replaces identifiers with an encrypted code, and the deidentified data only are made available to researchers in a secure environment. Quality assurance of the linked dataset identified some linkage errors. This was possible because of our ability to access personal identifiers in the secure environment of the VML. This suggests that linkage carried out using similar algorithms and by ‘trusted third parties’ generally cannot be assumed to be error-free and may affect any analyses carried out on the data.
The VML is an invaluable facility and the ONS has more than 10 years’ experience of running it. The disadvantage is that even after an upgrade, its infrastructure is limited in relation to the increasing number of users. The problems we encountered may, to some extent, have been a consequence of the size and complexity of our project but work of this sort is likely to increase in the future, given plans to increase the extent of data linkage under the Digital Economy Act 2017. 178
The relational database and the linked data for Wales are valuable assets for future research both by our team and by other researchers. To ensure timeliness, resources and mechanisms are needed to routinely update the linked data on a regular basis, rather than relying on one-off applications for data access, which may be subject to delays.
Data for subsequent years are likely to be affected by ‘opt-outs’ by people who are unwilling for their data to be used for purposes other than their health care. As these opt-outs tend to be clustered in particular areas, withdrawal of their data is likely to lead to bias. 179
The wider context of health data for England
The problems we have encountered should be set in the wider context of the way in which the Health and Social Care Act 20129 has led to a fragmentation of public health data analysis in England. A major consequence has been the barriers to data access, not only for academic researchers but also for public health analysts who were moved out of the health service to local authorities and Public Health England.
Although the Health and Social Care Act 20129 designated the HSCIC as the main authority responsible for health information, in practice there has been fragmentation and duplication. For example, the HQIP is responsible for commissioning clinical audits, and many other organisations have responsibilities for the collection and analysis of data, including NHS England, the Department of Health and Social Care, NHS Improvement, Public Health England and the Care Quality Commission, whereas the ONS analyses birth and death data. It is very apparent that England has fallen well behind Wales and Scotland, and behind other countries internationally, in its linkage and analysis of data.
Implications for practice
The findings have a number of implications for practice. A minority of births, mainly elective caesarean sections, can be scheduled to take place during daytime hours. Spontaneous births after labours of spontaneous onset, which make up just over half of singleton term births, peak in the early hours of the morning. This may have implications for staffing, especially midwifery staffing, particularly in view of the policies in Better Births35 to increase the proportion of normal births without obstetric intervention.
Patterns of birth following the induction of labour all show that numbers of births are at their highest in the hours around midnight, irrespective of the mode of birth. Numbers of inductions of labour are rising as a consequence of the drive to reduce stillbirths. 66,69 This may have implications for midwifery and medical staffing around midnight.
Recommendations for research
This section focuses on completing and developing the project described in this report. It is also important, however, to consider the research questions raised at our public involvement meetings. They are summarised briefly in Chapter 4 and more fully in Appendix 4. These were much more wide-ranging and included the relationships between the physiology of birth and its timing, developing woman-centred measures of the duration of labour, and ways in which staffing levels and continuity of care at night could affect women’s experiences of care. Participants in public involvement meetings also raised questions about the extent to which organisational factors, such as arrangements for transfer to obstetric care from midwifery units or women’s homes, could differ by time of day or night. These are all important questions and would need different research approaches from those used in this project.
Research using the linked data in the relational database
Questions about the timing of birth and its outcome are as relevant now as they were 5 years ago when the project was first designed. Although an analysis of perinatal mortality by day of the week was published in 2015,62 this was widely criticised and the responses to it raised questions for further investigation. We shall, therefore, be seeking additional funding to finish our proposed analyses of the outcome of pregnancy in terms of mortality and morbidity and of the variations between maternity units.
Further questions have arisen in the course of the project. In particular, the Saving Babies’ Lives safer baby care package is based on four inter-related approaches, the second of which is likely to increase the already rising proportion of births in which labour is induced. This may have implications for the time of day and day of week on which births occur. We recommend that further research is carried out to monitor changes in induction rates in relation to changing maternity policy such as the Saving Babies’ Lives Care Bundle.
The database we have created would be useful to explore this question. More generally, it is a resource that can be used for other purposes and by other researchers. One project, TIGAR,124 has been funded by the MRC to use the database and is under way. Alison Macfarlane and Nirupa Dattani are among the co-investigators. Another researcher has now submitted a funding application that includes further linkage to housing data from the 2011 Census180 to investigate children’s respiratory problems and analyses of associations with air pollution.
So far, our analyses of timing of birth in relation to onset of labour and mode of delivery have focused on singleton births. As we have found that the data on multiple births are of much better quality than we had been led to believe, and there are major gaps in knowledge about the outcome of multiple pregnancy, there is scope for analyses of data about children from multiple births, both in relation to the timing and mode of birth and more generally.
Development of the linkage
To maintain timeliness, the database should be updated regularly, with Data Sharing Agreements that allow for the routine provision of data rather than one-off operations, which are vulnerable to delays. Strategies are also needed to deal with the consequences of opt-outs from use of data for research and planning as this will lead to bias. In the longer term, changes to give potential objectors the option to distinguish between research and other uses of their data would be useful, given the considerable extent of public support for health research.
There is also scope to build on our linkage by further linkage to other data. A strength of our linked dataset is that it starts from birth registration, which is statutory. It contains demographic data that are more robust than those in clinical datasets, which have other priorities. When the new datasets being implemented in England and in Wales are more complete, it would be beneficial to link them in as well in order to link a wider range of clinical data to complete population-based demographic information.
Research resources
Our ability to do the work described here has relied on access to the VML. After its upgrade in the summer of 2015, the numbers of users increased and its infrastructure became overloaded, leading to delays in our project, despite the measures that the ONS VML team took to help us. The size and complexity of our project gave rise to particular challenges, but we thought that it would not be surprising if there were other users with projects on a similar scale in the future. This is an important resource run by an experienced and supportive team of staff, so we considered that further enhancement and development of its IT infrastructure and geographical accessibility would be a worthwhile investment.
Since our project ended, and in response to feedback from users, ONS is improving the connectivity and capacity of its secure research service (SRS), formerly known as the VML. These developments enable accredited researchers to securely access the SRS from organisations that can demonstrate they meet the security requirements for trusted access. In addition, the new technology refresh ensures the service can accommodate multiple simultaneous complex analytical research projects without any loss of performance to other researchers.
The wider context
The problems encountered by researchers and public health analysts in accessing and analysing data have now been recognised by the UK Statistics Authority and the Office for Statistics Regulation, following representations by the Health Statistics User Group, the Royal Statistical Society and the Faculty of Public Health, in which we have been involved. At the time of writing this report, the UK Statistics Authority had just launched a consultation on a revised Code of Practice, based on three pillars of trustworthiness, quality and value and this code has now been published. 181 We hope that research funders will engage with this to ensure that the funding they devote to the secondary analysis of routine health data can be used better in the future than has been possible in recent years.
Acknowledgements
The authors would like to thank all their colleagues in the ONS, NHS Wales Digital (HSCIC) and the NWIS for their help. In particular, they would like to thank Emma Gordon, Joanne Evans, Claudia Wells, Alex Lloyd, Justine Pooley, Elizabeth McLaren and members of the VML team at the ONS, Ariane Alamdari and Garry Coleman at the HSCIC and Gareth John at the NWIS. We would like to thank everyone who took part in our PPI activities for the advice and insights they gave and the members of our Study Advisory Group for their help and advice.
Contributions of authors
Alison Macfarlane (Professor of Perinatal Health, Epidemiology) acted as principal investigator and led on writing the report.
Nirupa Dattani (Senior Research Fellow in Perinatal Health, Data Analysis and Epidemiology) led on the data linkage, undertook descriptive analysis and contributed to writing the report.
Rod Gibson (Data Analyst) constructed a relational database to hold the data, organised the data for analysis and contributed to writing the report.
Gill Harper (Research Fellow and Data Analyst, Quantitative Geography) quality assured the linkage and contributed to writing the report.
Peter Martin (Research Fellow, Statistics) contributed to statistical modelling, descriptive analysis and to writing the report.
Miranda Dodwell (Senior Research Fellow and Maternity Service User Representative, BirthChoiceUK) took part in the project as a subject expert and service user researcher. She devised and quality assured the assigned codes for NHS trusts and contributed to writing the report.
Mary Newburn (Maternity Service Researcher, NCT) led on the PPI activities and contributed to the proposal and to writing the report.
Mario Cortina-Borja (Professor of Biostatistics, Statistics) led on the statistical methods and contributed to writing the report.
Publications
Articles
Macfarlane A, Dodwell M, Newburn M, Gibson R, McMullen S. Re: Association Between Day of Delivery and Obstetric Outcomes: Observational Study. BMJ Rapid Response 25 November 2015. 351: www.bmj.com/content/351/bmj.h5774/rr-7.
Dattani N, Macfarlane A. Linkage of Maternity Hospital Episode Statistics data to birth registration and NHS Numbers for births in England 2005–2014: methods. A population-based birth cohort study. BMJ Open 2018;8:e017897. https://doi.org/10.1136/bmjopen-2017-017897
Harper G. Linkage of Maternity Hospital Episode Statistics data to birth registration and notification records for births in England 2005–2014: quality assurance of linkage of routine data for singleton and multiple births. BMJ Open Mar 2018;8:e017898. https://doi.org/10.1136/bmjopen-2017-017898
Martin P, Cortina-Borja M, Newburn M, Harper G, Gibson R, Dodwell M, et al. Timing of singleton births by onset of labour and mode of birth in NHS maternity units in England, 2005–2014: a study of linked birth registration, birth notification, and hospital episode data. PLOS ONE 2018;13:e0198183. https://doi.org/10.1371/journal.pone.0198183
Posters
How We Use and Protect Information from the NHS About Births. Poster sent to every maternity unit. Sent on 28 July 2014.
Dattani N, Macfarlane A. Analysis of births at home in England and Wales by time of day and day of the week using linked administrative data. Poster presented at Farr Institute International Conference, University of St Andrews, St Andrews, 26–28 August 2015.
Macfarlane A, Dattani N. Using data linkage to build a national database of data about birth and its outcome for policy analysis in England and Wales. Poster presented at Farr Institute International Conference, University of St Andrews, St Andrews, 26–28 August 2015.
Harper G, Macfarlane A, Dattani N, Dodwell M, Newburn M, Gibson R, et al. Analysing the Daily, Weekly and Yearly Cycles of Births and their Implications for the NHS Using Linked Data. Poster presented at the International Population Data Linkage Conference, Swansea, 24–26 August 2016.
Macfarlane A, Dattani N, Harper G, Cortina-Borja M, Martin P, Gibson R, Dodwell M, Newburn M. Births and their Outcome: Analysing the Daily, Weekly and Yearly Cycles and their Implications for Midwifery Care. Poster presented at the Royal College of Midwives Annual Conference, Harrogate, 19–20 October 2016.
Macfarlane A, Martin P, Cortina-Borja M, Newburn M, Harper G, Gibson R, et al. ‘A Time to be Born?’. Poster presented at the 12th International Normal Labour and Birth Research Conference, Grange Over Sands, 2–4 October 2017 (winner of the Scientific Review Team Prize).
Macfarlane A, Martin P, Cortina-Borja M, Newburn M, Harper G, Gibson R, et al. Births: the Weekly Cycle. Poster presented at the 12th International Normal Labour and Birth Research Conference, Grange Over Sands 2–4 October 2017.
Conferences and presentations
Dattani N, Macfarlane A, Datta-Nemdharry P. Using Data Linkage to Create a National Database of Birth and Maternity Data. Paper presented at the Royal Statistical Society Conference, Sheffield, September 2014.
Macfarlane AJ. ‘Care.data’: Bungled Opportunity or Unjustified Intrusion? Invited presentation to the Royal Statistical Society meeting, London, 7 October 2014.
Macfarlane A, Dattani N. Using Linkage of Administrative Data to Build a National Database for Analysis of Birth and its Outcome in England and Wales. Presentation at the Administrative Data Research Network Conference, Edinburgh, 1–2 June 2017.
Harper G. Quality Assuring Linked Birth Registration and Hospital Episode Statistics Delivery Records – Results and Lessons Learned. Presentation at the Administrative Data Research Network Conference, Edinburgh, 1–2 June 2017.
Harper G. Insights on Third Party Linkage and Data Quality from Quality Assuring Linked Birth Registrations and HES Delivery Records in England 2005 to 2014. Presentation at the Royal Statistical Society International Conference, University of Strathclyde, Glasgow, 4–7 September 2017.
Macfarlane A, Martin P, Cortina-Borja M, Dattani N, Harper G, Newburn M. Gibson R. ‘A Time to be Born’? Presentation at the Royal Statistical Society International Conference, University of Strathclyde, Glasgow, 4–7 September 2017.
Martin P, Cortina-Borja M, Dattani N, Harper G, Gibson R, Newburn M, et al. Variations in Numbers of Births by Day of the Week in Relation to Onset of Labour and Mode of Giving Birth, England 2005–2014. Presentation at the Royal Statistical Society International Conference, University of Strathclyde, Glasgow, 4–7 September 2017.
Disclaimers
The data were processed in the secure environment of the ONS VML and the following disclaimer applies.
This work contains statistical data from ONS, which is Crown Copyright. The use of the ONS statistical data in this work does not imply the endorsement of the ONS in relation to the interpretation or analysis of the statistical data. This work uses research datasets, which may not exactly reproduce National Statistics aggregates.
Approvals
Ethics approval (reference number 05/Q0603/108) and subsequent substantial amendments were granted by East London and City Local Research Ethics Committee 1 and its successors.
Permission to use patient-identifiable data without consent under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (‘section 251 support’) was initially granted by the Patient Information Advisory Group PIAG 2-10(g)/2005. Renewals and amendments and a second permission, CAG 9-08(b)2014, under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (or ‘same legislation’) were granted by the Secretary of State for Health and the Health Research Authority following advice from the CAG.
A second permission CAG 9-08(b)2014 to use patient-identifiable data without consent under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 and create a research database held at the ONS for analyses relating to inequalities in the outcome of pregnancy and to inform maternity service users about the outcome of midwifery, obstetric and neonatal care was granted by the Health Research Authority.
Permission to access data from the ONS in the VML was granted by the ONS Microdata Release Panel. All members of the research team successfully applied for ONS Approved Researcher Status.
Permission to link and analyse data held by the HSCIC, now NHS Digital, was granted under Data Sharing Agreement NIC-273840-N0N0 N.
Data-sharing statement
The authors do not have permission to supply data or identifiable information to third parties, including other researchers, but they have permission under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 to analyse patient-identifiable data for England and Wales without consent and create a research database that could be accessed by other researchers using the SRS at the ONS. Anyone wishing to access the linked datasets for research purposes should apply via the CAG to the Health Research Authority to access patient-identifiable data without consent and then to the ONS and NHS Digital. Discussions with the ONS and NHS Digital about the application process are under way. In the first instance, enquiries about access to the data should be addressed to the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives Readers can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Macfarlane A. Variations in number of births and perinatal mortality by day of week in England and Wales. Br Med J 1978;2:1670-3. https://doi.org/10.1136/bmj.2.6153.1670.
- Hawe E, Macfarlane A, Bithell J. Daily and seasonal variation in live births, stillbirths and infant mortality in England and Wales, 1979–96. Health Stat Q 2001;9:5-15.
- Salib E, Cortina-Borja M. Effect of month of birth on the risk of suicide. Br J Psychiatry 2006;188:416-22. https://doi.org/10.1192/bjp.bp.105.009118.
- Cortina-Borja M, Haigh J. The birthday problem. Significance 2007;4:124-7. https://doi.org/10.1111/j.1740-9713.2007.00246.x.
- Hilder L, Moser K, Dattani N, Macfarlane A. Pilot linkage of NHS Numbers for babies data with birth registrations. Health Stat Q 2007;33:25-33.
- Moser K, Macfarlane A, Chow YH, Hilder L, Dattani N. Introducing new data on gestation-specific infant mortality among babies born in 2005 in England and Wales. Health Stat Q 2007;35:13-27.
- Dattani N, Datta-Nemdharry P, Macfarlane A. Linking maternity data for England, 2005–06: methods and data quality. Health Stat Q 2011;49:53-79. https://doi.org/10.1057/hsq.2011.3.
- Datta-Nemdharry P, Dattani N, Macfarlane A. Linking maternity for Wales, 2005–07: methods and data quality. Health Stat Q 2012;54:1-24.
- Health and Social Care Act 2012. London: The Stationery Office; n.d.
- Freeman G. Written Statement to Parliament: Review of Health and Care Data Security and Consent. London: Department of Health and Social Care; 2016.
- Macfarlane A. Lack of Trust, Not Privacy, Underpins Fears About Care Data 2014. http://theconversation.com/lack-of-trust-not-privacy-underpins-fears-about-care-data-22971 (accessed 9 July 2017).
- Darzi L. High Quality Care for All: NHS Next Stage Review Final Report. London: The Stationery Office; 2008.
- Macfarlane A, Lewis G. Why Mothers Die: The Confidential Enquiries into Maternal Deaths in the United Kingdom. London: RCOG Press; 2001.
- Macintosh MCM. The Lessons of CESDI. Obstetr Gynaecol 1999;1:13-7. https://doi.org/10.1576/toag.1999.1.2.13.
- Kurinczuk JJ, Draper ES, Field DJ, Bevan C, Brocklehurst P, Gray R, et al. Experiences with maternal and perinatal death reviews in the UK – the MBRRACE-UK programme. BJOG 2014;121:41-6. https://doi.org/10.1111/1471-0528.12820.
- House of Commons . Health Committee Enquiry on Maternity Services 1991. www.publications.parliament.uk/pa/cm200203/cmselect/cmhealth/796/796we27.htm (accessed 13 July 2017).
- Campbell R, Macfarlane A. Where to be Born? The Debate and the Evidence. Oxford: National Perinatal Epidemiology Unit; 1994.
- Protocol for Investment in Health Gain: Maternal and Early Child Health. Cardiff; 1992.
- Changing Childbirth: Report of the Expert Committee on Maternity Care. London: Department of Health and Social Care; 1993.
- Maternity Matters: Choice, Access and Continuity of Care in a Safe Service. London: Department of Health and Social Care; 2007.
- The National Service Framework for Children, Young People and Maternity Services. London: Department of Health and Social Care; 2004.
- Maternity Services in England HC794. London: The Stationery Office; 2013.
- Delivering the Future in Wales: A Framework for Realising the Potential of Midwives in Wales. Briefing Paper 4. Cardiff: Welsh Assembly Government; 2002.
- National Service Framework for Children, Young People and Maternity Services in Wales. Cardiff: Welsh Assembly Government; 2004.
- A Strategic Vision for Maternity Services in Wales. Cardiff: Welsh Assembly Government; 2011.
- Brocklehurst P, Hardy P, Hollowell J, Linsell L, Macfarlane A, McCourt C, et al. Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort study. BMJ 2011;343. https://doi.org/10.1136/bmj.d7400.
- Intrapartum Care for Healthy Women and Babies. Clinical Guideline CG190. London: NICE; 2014.
- Griggs J, Walker R. The Costs of Child Poverty for Individuals and Society: A Literature Review. York: Joseph Rowntree Foundation; 2008.
- Ending Child Poverty: Everybody’s Business. London: HM Treasury; 2008.
- Fair Society, Healthy Lives: The Marmot Review. London: The Marmot Review; 2010.
- European Parliament . Directive 2003 88 EC of the European Parliament and of the Council of 4 November 2003 Concerning Certain Aspects of the Organisation of Working Time 2003. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:32003L0088:EN:HTML (accessed 13 July 2017).
- Ten Years of Maternity Claims: An Analysis of NHS Litigation Authority Data. London: NHS Litigation Authority; 2012.
- Five Year Forward View. London: NHS England; 2014.
- Kirkup B. The Report of the Morecambe Bay Investigation. London: The Stationery Office; 2015.
- Better Births. Improving Outcomes of Maternity Services in England. A Five Year Forward View for Maternity Care. London: NHS England; 2016.
- A Maternity Network for Wales. Cardiff: Welsh Government; 2013.
- Welsh Government Maternity Strategy. Report from Quality and Safety Sub-Group. Cardiff: Welsh Government; 2013.
- About Maternity Network Wales. Cardiff: Public Health Wales; 2015.
- Bray BD, Steventon A. What have we learnt after 15 years of research into the ‘weekend effect’?. BMJ Qual Saf 2017;26:607-10. https://doi.org/10.1136/bmjqs-2016-005793.
- Wise J. The weekend effect – how strong is the evidence?. BMJ 2016;353. https://doi.org/10.1136/bmj.i2781.
- Chen YF, Boyal A, Sutton E, Armoiry X, Watson S, Bion J, et al. The magnitude and mechanisms of the weekend effect in hospital admissions: a protocol for a mixed methods review incorporating a systematic review and framework synthesis. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0260-2.
- Aylin P, Yunus A, Bottle A, Majeed A, Bell D. Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 2010;19:213-17. https://doi.org/10.1136/qshc.2008.028639.
- Freemantle N, Richardson M, Wood J, Ray D, Khosla S, Shahian D, et al. Weekend hospitalization and additional risk of death: an analysis of inpatient data. J R Soc Med 2012;105:74-8. https://doi.org/10.1258/jrsm.2012.120009.
- Bray BD, Cloud GC, James MA, Hemingway H, Paley L, Stewart K, et al. Weekly variation in health-care quality by day and time of admission: a nationwide, registry-based, prospective cohort study of acute stroke care. Lancet 2016;388:170-7. https://doi.org/10.1016/S0140-6736(16)30443-3.
- Freemantle N, Ray D, McNulty D, Rosser D, Bennett S, Keogh BE, et al. Increased mortality associated with weekend hospital admission: a case for expanded seven day services?. BMJ 2015;351. https://doi.org/10.1136/bmj.h4596.
- Walker AS, Mason A, Quan TP, Fawcett NJ, Watkinson P, Llewelyn M, et al. Mortality risks associated with emergency admissions during weekends and public holidays: an analysis of electronic health records. Lancet 2017;390:62-7. https://doi.org/10.1016/S0140-6736(17)30782-1.
- Ruiz M, Bottle A, Aylin PP. Exploring the impact of consultants’ experience on hospital mortality by day of the week: a retrospective analysis of hospital episode statistics. BMJ Qual Saf 2016;25:337-44. https://doi.org/10.1136/bmjqs-2015-004105.
- NHS Services Seven Days a Week Forum . Summary of Initial Findings 2013. www.england.nhs.uk/wp-content/uploads/2013/12/forum-summary-report.pdf (accessed 9 July 2017).
- Contract Reform for Consultants and Doctors & Dentists in Training – Supporting Healthcare Services Seven Days a Week CM9108. London: The Stationery Office; 2015.
- Hospital at Night. Patient Safety Risk Assessment Guide. London: NHS Modernisation Agency; 2005.
- Royal College of Obstetricians and Gynaecologists . Hospital at Night n.d. www.rcog.org.uk/en/careers-training/resources--support-for-trainees/training-guidelines/hospital-at-night/ (accessed 2 July 2017).
- Towards Safer Childbirth: Minimum Standards for the Organisation of Labour Wards. Report of Joint Working Party. London: RCOG; 1999.
- Royal College of Obstetricians and Gynaecologists . The Future Role of the Consultant 2005. www.rcog.org.uk/globalassets/documents/guidelines/wprfutureroleconsultant2005.pdf (accessed 13 July 2017).
- Towards Better Births. A Review of Maternity Services in England. London: Healthcare Commission; 2008.
- Safer Childbirth: Minimum Standards for the Organisation and Delivery of Care in Labour. Working Party Report. London: RCOG; 2007.
- High Quality Women’s Health Care: A Proposal for Change. London: RCOG; 2011.
- The Future Workforce in Obstetrics and Gynaecology. London: RCOG; 2009.
- Royal College of Obstetricians and Gynaecologists Census Report 2014/15. London: RCOG; 2016.
- Health and Social Care Information Centre . NHS Hospital and Community Health Service (HCHS) Workforce Statistics in England, Medical and Dental Staff – 2002-2012, As at 30 September 2013. http://content.digital.nhs.uk/catalogue/PUB10394 (accessed 3 July 2017).
- Workforce and Facilities Team, NHS Digital . NHS Workforce Statistics - March 2017, Provisional Statistics 2017. http://content.digital.nhs.uk/pubs/hchsworkmar17prov (accessed 3 July 2017).
- Knight HE, van der Meulen JH, Gurol-Urganci I, Smith GC, Kiran A, Thornton S, et al. Birth ‘out-of-hours’: an evaluation of obstetric practice and outcome according to the presence of senior obstetricians on the labour ward. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1002000.
- Palmer WL, Bottle A, Aylin P. Association between day of delivery and obstetric outcomes: observational study. BMJ 2015;351. https://doi.org/10.1136/bmj.h5774.
- Knight M, Henderson J, Kurinczuk J. Evidence Review to Support the National Maternity Review 2015. Report 3: Systematic Review and Case Studies to Assess Models of Consultant Resident Cover and the Outcomes of Intrapartum Care; and Two International Case Studies of the Delivery of Maternity Care. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2015.
- Providing Quality Care for Women: Obstetrics and Gynaecology Workforce. London: RCOG; 2016.
- Hunt Rt Hon J. Department of Health and Social Care . New Ambition to Halve Rate of Stillbirths and Infant Deaths 2015. www.gov.uk/government/news/new-ambition-to-halve-rate-of-stillbirths-and-infant-deaths (accessed 3 July 2017).
- Saving Babies’ Lives: A Care Bundle for Reducing Stillbirth. Leeds: NHS England; 2016.
- Manktelow B, Smith L, Prunet C, Smith P, Boby T, Hyman-Taylor P, et al. Perinatal Mortality Surveillance Report: UK Perinatal Deaths for Births from January to December 2015. Leicester: The Infant Mortality and Morbidity Studies, Department of Health Sciences, University of Leicester; 2017.
- Euro-Peristat project with SCPE and Eurocat . European Perinatal Health Report. The Health of Pregnant Women and Babies in Europe in 2010 2013. www.europeristat.com/reports/european-perinatal-health-report-2010.html (accessed 2 July 2017).
- Each Baby Counts: 2015 Summary Report. London: RCOG; 2017.
- Inquiry into Stillbirths in Wales: Key Conclusion and Recommendations. Cardiff: National Assembly for Wales; 2013.
- Smolensky M, Halberg F, Sargent F, Itoh S, Ogatu K, Yoshimura H. Advances in Climatic Physiology. New York, NY: Springer; 1972.
- Jolly A. Hour of birth in primates and man. Folia Primatol 1972;18:108-21. https://doi.org/10.1159/000155472.
- Kaiser IH, Halberg F. Circadian periodic aspects of birth. Ann N Y Acad Sci 1962;98:1056-68. https://doi.org/10.1111/j.1749-6632.1962.tb30618.x.
- Quetelet A. Sur l’homme et le développement de ses facultés ou essai de physique sociale. Paris: Bachelier; 1835.
- Yerushalmy J. Hour of birth and stillbirth and neonatal mortality rates. Child Dev 1938;9:373-8. https://doi.org/10.2307/1125565.
- Charles E. The hour of birth; a study of the distribution of times of onset of labour and of delivery throughout the 24-hour period. Br J Prev Soc Med 1953;7:43-59. https://doi.org/10.1136/jech.7.2.43.
- Fraser W, Usher RH, McLean FH, Bossenberry C, Thomson ME, Kramer MS, et al. Temporal variation in rates of cesarean section for dystocia: does ‘convenience’ play a role?. Am J Obstet Gynecol 1987;156:300-4. https://doi.org/10.1016/0002-9378(87)90272-9.
- Webb DA, Culhane J. Time of day variation in rates of obstetric intervention to assist in vaginal delivery. J Epidemiol Community Health 2002;56:577-8. https://doi.org/10.1136/jech.56.8.577.
- Young D. When was the baby born? Reflecting on the time of day, day of week, mode of delivery, and birth outcomes. Birth 2011;38:1-2. https://doi.org/10.1111/j.1523-536X.2010.00448.x.
- Paccaud F, Martin-Béran B, Gutzwiller F. Hour of birth as a prognostic factor for perinatal death. Lancet 1988;1:340-3. https://doi.org/10.1016/S0140-6736(88)91130-0.
- Anderka M, Declercq ER, Smith W. A time to be born. Am J Public Health 2000;90:124-6. https://doi.org/10.2105/AJPH.90.1.124.
- Mathews TJ, Curtin S. When are babies born: morning, noon, or night? Birth certificate data for 2013. NCHS Data Brief 2015;200.
- Bernis C, Varea C. Hour of birth and birth assistance: from a primate to a medicalized pattern?. Am J Hum Biol 2012;24:14-21. https://doi.org/10.1002/ajhb.21228.
- Glattre E, Bjerkedal T. The 24-hour rhythmicity of birth. A populational study. Acta Obstet Gynecol Scand 1983;62:31-6. https://doi.org/10.3109/00016348309155754.
- Heres MH, Pel M, Borkent-Polet M, Treffers PE, Mirmiran M. The hour of birth: comparisons of circadian pattern between women cared for by midwives and obstetricians. Midwifery 2000;16:173-6. https://doi.org/10.1054/midw.1999.0210.
- Macfarlane A, Thew P. Births: the weekly cycle. Population Trends 1978;13:23-4.
- Chan A, Keane RJ, Scott J. Elective caesarean section and child deprivation. Lancet 1996;347. https://doi.org/10.1016/S0140-6736(96)90660-1.
- Cole S. Weekend births. Lancet 1984;2. https://doi.org/10.1016/S0140-6736(84)90504-X.
- Paccaud F, Neury JJ, Ackermann-Liebrich U. Weekend births (letter). Lancet 1984;324. https://doi.org/10.1016/S0140-6736(84)92949-0.
- Rindfuss RR, Ladinsky JL. Patterns of births: implications for the incidence of elective induction. Med Care 1976;14:685-93. https://doi.org/10.1097/00005650-197608000-00005.
- Mathers CD. Births and perinatal deaths in Australia: variations by day of week. J Epidemiol Community Health 1983;37:57-62. https://doi.org/10.1136/jech.37.1.57.
- Wells R. Still never on Sundays. Med J Aust 1980;2:160-1.
- Rindfuss RR, Ladinsky JL, Coppock E, Marshall VW, Macpherson AS. Convenience and the occurrence of births: induction of labor in the United States and Canada. Int J Health Serv 1979;9:439-60. https://doi.org/10.2190/C8CF-GLPC-6LBW-9KWA.
- Martins JM. Never on Sundays. Med J Aust 1972;1:487-8.
- Calot G. Le mouvement journalier des naissances à l’intérieur de la semaine. Population (French Edition) 1981;1:9-40. https://doi.org/10.2307/1532429.
- Cohen A. Seasonal daily effect on the number of births in Israel. J R Stat Soc Ser C Appl Stat 1983;32:228-35. https://doi.org/10.2307/2347945.
- Macfarlane A, Mugford M, Henderson J, Furtado A, Stevens J, Dunn A. Birth counts: statistics of pregnancy and childbirth Volume 2, Tables. London: The Stationary Office; 2000.
- Macfarlane A. Hospital In-patient Enquiry Maternity Tables. London: HMSO; 1986.
- Statistical Bulletin 1997/28. London: Department of Health and Social Care; 1997.
- Macfarlane A. Day of the week variations in numbers of births and perinatal mortality rates. J Matern Child Health 1979;4:415-16.
- Hollowell J, Rowe R, Townend J, Knight M, Li Y, Linsell L, et al. The Birthplace in England national prospective cohort study: further analyses to enhance policy and service delivery decision-making for planned place of birth. Health Serv Deliv Res 2015;3.
- DePorte J. The prevalent hour of stillbirth. Am J Obstet Gynecol 1932;23:31-7. https://doi.org/10.1016/S0002-9378(32)90240-3.
- Yerushalmy J. Neonatal mortality by order of birth and age of parents. Am J Hyg 1938;28:244-70.
- Hill AB. Principles of Medical Statistics. London: The Lancet; 1937.
- Ruffieux C, Marazzi A, Paccaud F. The circadian rhythm of the perinatal mortality rate in Switzerland. Am J Epidemiol 1992;135:936-52. https://doi.org/10.1093/oxfordjournals.aje.a116389.
- Gould JB, Qin C, Chavez G. Time of birth and the risk of neonatal death. Obstet Gynecol 2005;106:352-8. https://doi.org/10.1097/01.AOG.0000168627.33566.3c.
- Luo ZC, Karlberg J. Timing of birth and infant and early neonatal mortality in Sweden 1973–95: longitudinal birth register study. BMJ 2001;323:1327-30. https://doi.org/10.1136/bmj.323.7325.1327.
- Stephansson O, Dickman PW, Johansson AL, Kieler H, Cnattingius S. Time of birth and risk of intrapartum and early neonatal death. Epidemiology 2003;14:218-22. https://doi.org/10.1097/01.EDE.0000037975.55478.C7.
- Luo ZC, Liu S, Wilkins R, Kramer MS. Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System . Risks of stillbirth and early neonatal death by day of week. CMAJ 2004;170:337-41. https://doi.org/10.1097/00006254-200407000-00010.
- Richmond D, Knight HE, Cameron A, Currie I, Smith GC, Cromwell D, et al. Re: Association Between Day of Delivery and Obstetric Outcomes: Observational Study. BMJ Rapid Response 25 November 2015 2015. www.bmj.com/content/351/bmj.h5774/rr-13 (accessed 4 July 2017).
- Freudenthal B. Editorial Double-Standards for Dr Foster – a Major Fail for BMJ. BMJ Rapid Response 25 November 2015 2015. www.bmj.com/content/351/bmj.h5774/rr-8 (accessed 4 July 2017).
- Macfarlane A, Dodwell M, Newburn M, Gibson R, McMullen S. Re: Association Between Day of Delivery and Obstetric Outcomes: Observational Study, BMJ Rapid Response 25 November 2015 2015. www.bmj.com/content/351/bmj.h5774/rr-7 (accessed 4 July 2017).
- Perinatal Mortality 2009: United Kingdom. London: CMACE; 2011.
- Manktelow B, Smith L, Evans T, Hyman-Taylor P, Kurinczuk J, Field D, et al. Perinatal Mortality Surveillance Report: UK Perinatal Deaths for births from January to December 2013. Leicester: The Infant Mortality and Morbidity Group, Department of Health Sciences, University of Leicester; 2015.
- Manktelow BM, Smith LK, Evans TA, Hyman-Taylor P, Kurinczuk JJ, Field DJ, et al. Perinatal Mortality Surveillance Report, UK Perinatal Deaths for Births from January to December 2014. Leicester: The Infant Mortality and Morbidity Group, Department of Health Sciences, University of Leicester; 2016.
- Stewart JH, Andrews J, Cartlidge PH. Numbers of deaths related to intrapartum asphyxia and timing of birth in all Wales perinatal survey, 1993–5. BMJ 1998;316:657-60. https://doi.org/10.1136/bmj.316.7132.657.
- Chalmers JW, Shanks E, Paterson S, McInneny K, Baird D, Penney G. Scottish data on intrapartum related deaths are in same direction as Welsh data. BMJ 1998;317:539-40. https://doi.org/10.1136/bmj.317.7157.539.
- Pasupathy D, Wood AM, Pell JP, Fleming M, Smith GC. Time of birth and risk of neonatal death at term: retrospective cohort study. BMJ 2010;341. https://doi.org/10.1136/bmj.c3498.
- de Graaf JP, Ravelli AC, Visser GH, Hukkelhoven C, Tong WH, Bonsel GJ, et al. Increased adverse perinatal outcome of hospital delivery at night. BJOG 2010;117:1098-107. https://doi.org/10.1111/j.1471-0528.2010.02611.x.
- Gardosi J, Tonks A, Francis A. Risk of Neonatal Death Due to Intrapartum Anoxia in Out of Hours Deliveries in the West Midlands. BMJ Rapid Response 2 September 2010 2010. www.bmj.com/rapid-response/2011/11/02/risk-neonatal-death-due-intrapartum-anoxia-out-hours-deliveries-west-midla (accessed 4 July 2017).
- Personal Demographics Service Birth Notification Data Set Overview. Leeds: NHS Digital; 2017.
- Datta-Nemdharry P, Dattani N, Macfarlane AJ. Birth outcomes for African and Caribbean babies in England and Wales: retrospective analysis of routinely collected data. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2012-001088.
- Dattani N, Datta-Nemdharry P, Macfarlane AJ. Linking maternity data for England 2007: methods and data quality. Health Stat Q 2012;53:4-21.
- TIGAR: Tracking the Impact of Gestational Age on Health, Educational and Economic Outcomes: A Longitudinal Record Linkage. Oxford: NPEU; n.d.
- Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001885.
- National Institute for Health Research . Births and Their Outcome: Analysing the Daily, Weekly and Yearly Cycles and Their Implications for the NHS: Study Documentation 2017. www.journalslibrary.nihr.ac.uk/programmes/hsdr/1213693/#/ (accessed 15 November 2017).
- User Guide to Birth Statistics. Newport: ONS; 2017.
- Brocklehurst P. Infection and preterm delivery. BMJ 1999;318:548-9. https://doi.org/10.1136/bmj.318.7183.548.
- Scottish Perinatal and Infant Mortality and Morbidity Report 2003. Edinburgh: NHS Scotland; 2004.
- Stillbirth, neonatal and postneonatal mortality 2000-02, England, Wales and Northern Ireland. London: Confidential Enquiry into Maternal and Child Health; 2004.
- Supplement to the First and Fourth Reports to the Secretary of State. London: Steering Group on Health Services Information; 1985.
- NHS Wales Informatics Service . Information and Statistics n.d. www.infoandstats.wales.nhs.uk/page.cfm?pid=41012&orgid=869 (accessed 26 June 2017).
- Maternity Statistics, Wales: Method of Delivery 2001–2011. Cardiff: Welsh Government; 2012.
- Welsh Information Standards Board . Maternity Indicators Data Set: Data Standards Change Notice 2016. www.nwisinformationstandards.wales.nhs.uk/sitesplus/documents/299/20160629%2DDSCN%202016%2002%2DMaternity%20Indicators%20Data%20Set%2DFinal%20v1.1.pdf (accessed 6 July 2017).
- Medical Workforce in Obstetrics and Gynaecology. 20th RCOG Report. London: RCOG; 2012.
- Royal College of Obstetricians and Gynaecologists Census Report 2013. London: RCOG; 2015.
- Royal College of Paediatrics and Child Health (RCPCH) . Previous Workforce Censuses n.d. www.rcpch.ac.uk/improving-child-health/better-nhs-children/workforce-planning/workforce-census-2017/previous-censuse (accessed 6 July 2017).
- Birth Characteristics in England and Wales, 2015, Table 7: Live births and Stillbirths by Gestational Age at Birth, 2015 Birth Cohort. Newport: ONS; 2016.
- HES Data Dictionary Admitted Patient Care. Leeds: NHS Digital; 2017.
- A Guide to Linked Mortality Data from Hospital Episode Statistics and the Office for National Statistics. Leeds: Health and Social Care Information Centre; 2015.
- Quality Assurance of New Data on Birth Registrations, as a Result of Changes to the Population Statistics Act – from May 2012 Onwards. Newport: ONS; n.d.
- Birth Characteristics in England and Wales, 2014, Table 16: Maternities: Place of Birth and Whether Area of Occurrence is the Same as Area of Usual Residence, or Other Than Area of Usual Residence, 2014. Newport: ONS; 2015.
- Barnett AG, Dobson AJ. Analysing seasonal health data. New York, NY: Springer Science & Business Media; 2010.
- Fisher NI. Statistical Analysis of Circular Data. Cambridge: Cambridge University Press; 1995.
- Brockwell PJ, Davis RA. Time series: theory and methods. New York, NY: Springer Science & Business Media; 2013.
- Wood SN. Generalized Additive Models: An Introduction with R. Boca Raton, FL: CRC Press; 2017.
- R: A Language and Environment for Statistical Computing. Vienna: The R Foundation for Statistical Computing; 2013.
- Murphy JF, Dauncey M, Gray OP, Chalmers I. Planned and unplanned deliveries at home: implications of a changing ratio. Br Med J 1984;288:1429-32. https://doi.org/10.1136/bmj.288.6428.1429.
- Northern Region Perinatal Mortality Survey Coordinating Group . Collaborative survey of perinatal loss in planned and unplanned home births. BMJ 1996;313:1306-9. https://doi.org/10.1136/bmj.313.7068.1306.
- Gyte G, Dodwell M, Newburn M, Sandall J, Macfarlane A, Bewley S. Estimating intrapartum-related perinatal mortality rates for booked home births: when the ‘best’ available data are not good enough. BJOG 2009;116:933-42. https://doi.org/10.1111/j.1471-0528.2009.02147.x.
- Sandall J, Murrells T, Dodwell M, Gibson R, Bewley S, Coxon K, et al. The efficient use of the maternity workforce and the implications for safety and quality in maternity care: a population-based, cross-sectional study. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02380.
- Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. New York, NY: Springer Science & Business Media; 2013.
- Nair M, Kurinczuk JJ, Knight M. Establishing a national maternal morbidity outcome indicator in England: a population-based study using routine hospital data. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0153370.
- UK Obstetric Surveillance System (UKOSS). Oxford: NPEU; n.d.
- Euro-Peristat . EURONET-SAMM Project: EUROpean NETwork on Severe Acute Maternal Morbidity 2016. www.europeristat.com/images/Paris_2016_meeting/Collaborations/Presentation_EURONET-SAMM_for_EURO-Peristat_april_2016.pdf (accessed 12 July 2017).
- Briefing Notes for Researchers: Involving the Public in NHS, Public Health and Social Care Research. Eastleigh: INVOLVE; 2012.
- Dattani N. Macfarlane A. Linkage of Maternity Hospital Episode Statistics data to birth registration and NHS Numbers for births in England 2005–2014: methods. A population-based birth cohort study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-017897.
- Harper G. Linkage of Maternity Hospital Episode Statistics data to birth registration and notification records for births in England 2005–2014: quality assurance of linkage of routine data for singleton and multiple births. BMJ Open Mar 2018;8. https://doi.org/10.1136/bmjopen-2017-017898.
- Martin P, Cortina-Borja M, Newburn M, Harper G, Gibson R, Dodwell M, et al. Timing of Singleton Births by Onset of Labour and Mode of Birth in NHS Maternity Units in England, 2005–2014: A Study of Linked Birth Registration, Birth Notification, and Hospital Episode Data. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0198183.
- Implementing Better Births: A Resource Pack for Local Maternity Systems. London: NHS England; 2017.
- Brocklehurst P. The INFANT Collaborative Group . A study of an intelligent system to support decision making in the management of labour using the cardiotocograph – the INFANT study protocol. BMC Preg Childbirth 2016;16. https://doi.org/10.1186/s12884-015-0780-0.
- Richardson A, Mmata C. NHS Maternity Statistics, England: 2005–06. Leeds: The Information Centre; 2007.
- Macfarlane A. Day of birth. Lancet 1984;2. https://doi.org/10.1016/S0140-6736(84)91250-9.
- Anonymous . Birth counts. Lancet 1984;1:1448-9.
- Newton R. Weekend birth. Lancet 1984;2.
- Newton RW, Hunt LP. Psychosocial stress in pregnancy and its relation to low birth weight. Br Med J 1984;288:1191-4. https://doi.org/10.1136/bmj.288.6425.1191.
- Melbye M, Wohlfahrt J, Westergaard T, Jensen AK, Koch A, Hjalgrim H, et al. Births at Christmas are different: population based survey of 2 million deliveries. Christmas Paper Study Group. BMJ 1997;315:1654-5. https://doi.org/10.1136/bmj.315.7123.1654.
- Simpson AS. Are more babies born at night?. Br Med J 1952;2. https://doi.org/10.1136/bmj.2.4788.831.
- NHS Maternity Statistics, 2016–17. Leeds: NHS Digital; 2017.
- Bakker JJ, van der Goes BY, Pel M, Mol BW, van der Post JA. Morning versus evening induction of labour for improving outcomes. Cochrane Database Syst Rev 2013;2. https://doi.org/10.1002/14651858.CD007707.pub2.
- Ghosh RE, Ashworth DC, Hansell AL, Garwood K, Elliott P, Toledano MB. Routinely collected English birth data sets: comparisons and recommendations for reproductive epidemiology. Arch Dis Child Fetal Neonatal Ed 2016;101:F451-7. https://doi.org/10.1136/archdischild-2015-309540.
- Macfarlane A. At last – maternity statistics for England. BMJ 1998;316:566-7. https://doi.org/10.1136/bmj.316.7131.566.
- Secondary Care Analysis Team NHS Digital . Hospital Maternity Activity 2015–16 2016. www.content.digital.nhs.uk/catalogue/PUB22384 (accessed 14 November 2017).
- Maternity and Children’s Data Set. Leeds: NHS Digital; n.d.
- Vik ES, Haukeland GT, Dahl B. Women’s experiences with giving birth before arrival. Midwifery 2016;42:10-5. https://doi.org/10.1016/j.midw.2016.09.012.
- Ford J, Pett G. ‘BBA’ birth. Analysis of one year’s ‘born before arrival’ births and trends in BBA birth 2000–07 in a large English maternity unit. MIDIRS Midwifery Digest 2008;18:217-23.
- Froen JF, Pinar H, Flenady V, Bahrin S, Charles A, Chauke L, et al. Causes of death and associated conditions (Codac) – a utilitarian approach to the classification of perinatal deaths. BMC Preg Childbirth 2009;9. https://doi.org/10.1186/1471-2393-9-22.
- Digital Economy Act 2017. London: The Stationery Office; 2017.
- National data opt-out programme. Leeds: NHS Digital; 2018.
- Energy Performance of Buildings Data: England and Wales. London: Ministry of Housing, Communities and Local Government; n.d.
- Code of Practice for Statistics: Ensuring Official Statistics Serve the Public. n.d.
- Moser KA, Dattani N, Leon DA, Stanfield KM. Data on births by ethnic group now available for England and Wales. BMJ 2008;337. https://doi.org/10.1136/bmj.a1967.
- Moser K, Macfarlane A, Dattani N. Survival rates in very preterm babies in England and Wales. Lancet 2008;371:897-8. https://doi.org/10.1016/S0140-6736(08)60411-0.
- Moser K, Stanfield KM, Leon DA. Birthweight and gestational age by ethnic group, England and Wales 2005: introducing new data on births. Health Stat Q 2008;39:22-31.
- Oakley L, Maconochie N, Doyle P, Dattani N, Moser K. Multivariate analysis of infant death in England and Wales in 2005–06, with focus on socio-economic status and deprivation. Health Stat Q 2009;42:22-39. https://doi.org/10.1057/hsq.2009.15.
- Leon DA, Moser KA. Low birth weight persists in South Asian babies born in England and Wales regardless of maternal country of birth. Slow pace of acculturation, physiological constraint or both? Analysis of routine data. J Epidemiol Community Health 2012;66:544-51. https://doi.org/10.1136/jech.2010.112516.
- Moser K, Hilder L. Assessing quality of NHS Numbers for Babies data and providing gestational age statistics. Health Stat Q 2008;37:15-23.
- Health Service (Control of Patient Information) Regulations 2002. London: The Stationery Office; 2002.
- House of Commons Health Committee . Handling of NHS Patient Data 2014. www.parliament.uk/business/committees/committees-a-z/commons-select/health-committee/news/14-04-04-handling-of-nha-patient-data/ (accessed 12 July 2017).
- Data Access Request Service (DARS). Leeds: NHS Digital; n.d.
- Independent Group Advising on the Release of Data (IGARD). Leeds: NHS Digital; n.d.
- Pregnancy and Ethnic Factors Influencing Births and Infant Mortality: 2013. Newport: ONS; 2015.
- Rowe R. Birthplace Terms and Definitions: Consensus Process. Birthplace in England Research Programme. Final Report Part 2. London: HMSO; 2011.
- Organisation Data Service. Leeds: NHS Digital; n.d.
Appendix 1 Challenges and barriers
A description of how the data were acquired for the project, and of the processes of linkage, quality assurance and organisation of data for analysis, was given in Chapter 2. This was followed by Chapter 3, which described the methods of analyses of births and their outcomes and gave the results of the analyses that were undertaken. This was quite deliberately separated from descriptions of the processes of obtaining permission to do the work. Although some of these application processes worked smoothly, the application for access to Maternity HES delayed the project for many months. Another key factor outside our control was the limitations of the IT infrastructure of the ONS secure setting, the VML. These problems prevented us from completing the work on time and within budget, despite the considerable efforts made by individual members of ONS and HSCIC staff to help us overcome the barriers.
Experience from preceding maternity data linkage projects
Linkage of birth registration data to birth notification data
As described in Chapters 1 and 2, the data linkage aspects of the project built on two preceding projects. The first of these, which linked birth registration data to birth notification data held in the interim NN4B system, made data about the timing of birth, gestational age and other key variables available at a national level. The linkage was done within ONS, where Nirupa Dattani was head of Child Health Statistics. She was able to make arrangements for a researcher employed and funded by City, University of London, to design the project, develop the linkage methods and assess the quality of the birth notification data. 5,6 The data were used in a number of analyses both at the time and subsequently. 122,182–187
The ONS mainstreamed the linkage and used the linked data in its publications. The collaboratively written articles about the linkage contributed to the success of City, University of London, the Nursing and Midwifery Unit of Assessment of the 2008 Research Assessment Exercise.
From the start, the project was designed to include further linkage to the Maternity HES for England and maternity data from the NCCHD/PEDW for Wales. We did not have the funds needed to do this immediately but we included the full plans in our applications for ethics and other approvals. In 2005, we obtained ethics approval for this (reference number 05/Q0603/108) from East London and the City Local Research Ethics Committee and approval from the Patient Information Advisory Group under Section 60 of the Health and Social Care Act 2001 (PIAG 2–10(g) 2005). To prepare for applications for further funding, permission was also obtained from the Information Centre’s Security and Confidentiality Advisory Group to link birth registration and notification data to Maternity HES.
The Information Centre, as it was originally called, was being established at the time this project was being set up. The Department of Health and Social Care statistician responsible for analyses of Maternity HES transferred to the new organisation and continued to take an active interest in the project, as did his counterparts in Wales.
Linkage to data about maternity care in England and Wales
The opportunity for a second project to do the next stage of the linkage came in July 2008, when funding was obtained from the MRC through a successful application to the Joint Wellcome Trust/MRC Electronic Patient Data Linkage Initiative. By this time, Nirupa Dattani had left the ONS as her post had been relocated to Newport. This meant that the work could no longer be done within the ONS and permission was requested to use the ONS secure setting, the VML.
Before starting work on the second project, all the approvals obtained previously were renewed. This included successful applications for a substantial amendment to the ethics approval and for further permission to process patient-identifiable data without consent, now under Regulation 5 of the Health Service (Control of Patient Information) Regulation 2002. 188 ONS Approved Researcher Status was obtained for the project and for all the staff who would be accessing data in the VML. Approval was also obtained from the Caldecott Guardian for Wales.
The former Department of Health and Social Care statistician responsible for Maternity HES had left the Information Centre when his post was relocated to Leeds and, for many years, no externally identifiable member of staff had long-term responsibility specifically for Maternity HES. Although a senior member of the Information Centre staff joined the project as co-applicant, this was on the understanding that he would not be able to devote much time to the project. He did, however, give key help with data access problems. In contrast to the situation in England, we continued to have longstanding named contacts in Wales.
The application for HES data was submitted to the Information Centre’s Data Management Subgroup, which had superseded the Security and Confidentiality Advisory Group. The new body confirmed that permission to link civil registration and registration data to Maternity HES was still valid; therefore the path appeared clear to appoint a researcher, who started in July 2008.
Unfortunately, however, when a meeting was held with Northgate Solutions to which HES data processing had been outsourced, it transpired that a new committee, the Data Access Advisory Group (DAAG), had superseded the Data Management Subgroup. It was necessary to reapply for access to HES data, a process that delayed the project by 4 months and increased the costs of accessing the data. Although we were able to successfully complete and document the data linkages,7,8,123 losing 4 months of the 2-year funding period severely restricted our ability to make use of the linked data for analysis as planned.
These first two projects showed that it is feasible to link data from several sources to derive an enhanced database that contains a much wider range of data than any of the original datasets individually. 6–8,123,187 The second project also highlighted the danger that valuable project time could be wasted by the delays involved in applications for access to data from Maternity HES. We tried to learn from both the positive and negative experiences when designing the project that forms the subject of this report.
The current project
Application to the National Institute for Health Research for funding
The successive stages of our application to NIHR took place over the period from December 2012 to September 2013, which was a time of considerable organisational change. As a result of the implementation of the Health and Social Care Act 2012, the Information Centre for Health and Social Care, as it was then known, was taken over by Connecting for Health, which had previously been responsible for NHS IT infrastructure, to form a new organisation, the HSCIC. By and large, most of the senior management of the new organisation came from an IT infrastructure background and key people were unfamiliar with data access issues.
The National Information Governance Board was abolished and the staff responsible for overseeing ‘Section 251 approvals’ were transferred to the CAG of another new organisation, the Health Research Authority. The administration of Research Ethics Committees was centralised. The longstanding administrative staff of our local Research Ethics Committees, based in Mile End Hospital, were replaced by new staff based in Bristol. In view of all these changes, we made sure that we maintained contact with the key staff, including data providers, and discussed our proposal with them at each stage of the application process in an attempt to avoid the problems we had experienced previously. This included attending the Data Linkage Stakeholder Forum which the HSCIC held in October 2013 to encourage the use of data linkage and which gave an opportunity for informal discussions about our project.
Approvals
Our project funding started in January 2014 and NIHR encouraged us not to delay the start. Before the project started, we applied for a substantial amendment to our ethics approval and a second approval (CAG 9–08(b)/2014) under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 to link in data from the HES for England and the PEDW about subsequent admissions of mothers and babies without patient consent. This second application for ‘Section 251’ approval took the form of an application to form a database to be held in the secure environment of the VML at the ONS along with the previously linked data. We obtained approvals for the amendment to our ethics approval and the new ‘Section 251’ application during the first month, although the latter applied only to England. We were told that this was pending the completion of new arrangements being made for accessing data for Wales, which had been disrupted by the implementation of the Health and Social Care Act.
On the advice of our Study Advisory Group, we applied to the HQIP for access to data about stillbirths and neonatal deaths from the CMACE, held by the NPEU, which had taken over responsibility for the confidential enquiries into stillbirths and neonatal deaths from CMACE. As explained in Chapter 3, this was to obtain more reliable data about intrapartum deaths than was available from ONS cause of death coding procedures. Successful applications were made to amend our ethics and ‘Section 251’ approvals to support this.
Owing to an oversight, we had not included data on deaths of children aged over one year and deaths of mothers within 1 year of giving birth in our earlier applications. These data are routinely linked by ONS to the corresponding birth records and are thus readily available, subject to permission. We therefore applied for amendments to our ethics and ‘Section 251’ approvals and ONS Microdata Release Panel for access to these data. In addition, we applied for ONS Approved Researcher Status for the project and all members of the project team.
All these applications went smoothly in a timely manner. During the course of the project, we renewed these approvals and also our first ‘Section 251’ approval annually. The barrier that delayed the project was gaining access to data from HES and, to a lesser extent, to NHS data for Wales.
Application for Hospital Episode Statistics data for England
We arranged to meet the staff from the HSCIC with whom we had discussed the project during the application process in late March 2014, to finalise arrangements and our application to the DAAG for HES data.
On 17 March 2014, the HSCIC staff contacted us to cancel the meeting. They told us that this was because of a review and suggested that we contact them 2 months later, at the end of May, to rearrange the meeting. The next day, three members of the project team attended the NIHR welcome meeting at which NIHR’s concern that projects are completed on time and within budget was stressed. We told our programme manager about the latest developments, pointed out that they were entirely outside our control and shared our concerns about the delay.
We arranged a meeting with the HSCIC manager in charge of the data applications and he offered to try to arrange access to data. He made an arrangement to telephone the principal investigator on 9 April 2014, but this call did not take place.
It became clear that other circumstances were affecting our communication with HSCIC. In previous months, NHS England had been heavily criticised in the media and more widely for the approaches it was using to inform the public about its plans to use data from general practice and link them to hospital data in its new care.data system. High-profile press reports about data leaks and the sale of personally identifiable data to private companies undermined public confidence about the use of NHS data. This led to an inquiry by the House of Commons Health Committee into the handling of NHS patient data. Kingsley Manning, Chairperson of the HSCIC, and Max Jones, Director of Information Services, were invited to appear at a hearing on 8 April 2014,189 the day before the promised telephone call.
After this, we had no further contact from the HSCIC. No explanations were given either proactively or in response to e-mail enquiries. We therefore resorted to the HSCIC’s formal complaints procedure, and made a complaint on the grounds that it was advertising services on its website and elsewhere but not providing them. There was no further news until 9 May 2014 when a letter from the Director of Data and Information Services was posted on HSCIC’s website, announcing the review of processes and governance for the sharing of data releases. In response to our complaint, we subsequently received a letter from him dated 30 May 2014 saying that the review was necessary to improve the process of application for data.
The HSCIC’s moratorium was still under way in early June 2014, so we were still unable to arrange a meeting to discuss our application. We therefore decided to submit our application without meeting HSCIC to discuss it.
At the time HSCIC stopped processing applications, in April 2014, it had already built up a backlog of applications and this continued to grow during the hiatus that followed. It then set out to implement a completely new ‘one size fits all’ application system to process the wide range of applications for data it receives.
Once the moratorium was over, we had a number of contacts with HSCIC staff, some of whom appeared to be working in parallel with each other and giving us conflicting messages on the progress of our application. Most told us that the sender had checked that our application was in the queue but was not in a position to tell us when it would be processed. This lack of information made it impossible to plan work or to keep NIHR informed about likely progress with the project. To add to our frustration, we, and our university’s IT department, received repeated requests to delete data that HSCIC’s records said we had received in 2007. We presumed that this was a consequence of our application to the Security and Confidentiality Advisory Group, which had been approved in 2007, as described above. We were unable to comply with requests to delete data we had never held and, in any case, had never intended to hold at the university.
Lobbying for access to data
The DAAG published its minutes on its website and at some points published data about numbers of applications awaiting consideration. It was very apparent that numbers of applications in the queue were growing, so we joined together with other affected researchers to lobby for access to data, initially through the Health Statistics User Group, which then made representations to other organisations.
As the HSCIC senior management came mainly from an IT infrastructure background, there was limited experience of how data are used in health research or public health analysis. In particular, there appeared to be a lack of awareness that research applications would have already been scrutinised by funders and their reviewers, by ethics committees and, in most cases, also by the Health Research Committee’s CAG. As a result, the checks made by these organisations were repeated, even though most applicants to DAAG included these approvals with their applications.
In contrast, the misuses of data that had caused concern in the press and in parliament had not been subjected to this level of scrutiny and were largely from the private sector. Alison Macfarlane contributed to letters sent from the Health Statistics User Group to the Chief Executive of the HSCIC and from the President of the Faculty of Public Health to the Secretary of State for Health proposing that the applicants who have obtained permissions should be subjected to a streamlined process that did not replicate approval processes already successfully completed. This did not appear to have any impact.
It also appeared from the DAAG minutes that applications were not being dealt with in chronological order. Through convening meetings with other affected researchers, we found that the Wellcome Trust, the research councils and the cancer research charities were taking active approaches to the HSCIC. We therefore asked if NIHR could approach HSCIC to make the case for all the researchers it funded, as we felt that this would have more impact than approaches from individual researchers. Our programme manager told us that NIHR staff had been told not to approach the HSCIC as the matter was being dealt with at the highest level.
Despite the continuing uncertainty, we were given the go-ahead to rearrange our technical meeting with the Data Linkage and Extract Service and a useful telephone meeting was held. We were unable to send a representative to the HSCIC’s stakeholder meeting on 21 July 2014 as we were told it was oversubscribed.
We did not receive any news about our application until mid-September when we were told that the HSCIC wanted to submit our application to the 24 or 29 September meetings of DAAG and wanted a telephone meeting to clarify some details. This took place on 17 September 2014 and we were told that a draft application document would arrive by the end of the week to be checked and amended before submission. The document did not arrive and we continued to ask about it for some weeks. We noted from the online minutes that on 24 September, DAAG considered other applications, while on 29 September it set aside all applications to devote the entire meeting to discussing the data needs of Genomics England Ltd.
Finally, in early November, Alison Macfarlane, who was visiting Leeds for other reasons on 10 November 2014, e-mailed the HSCIC to say that she would be calling at its office at 17.00 to discuss our application. Two members of HSCIC staff met her with a draft document. They discussed the details in it and e-mailed it to her straight away. This made it possible to get back to them quickly with further corrections.
The application was then considered at the DAAG meeting on 18 November 2014, but was not approved, as the committee wanted further information and had questions such as regarding the details of the Section 251 approvals. Although we had passed this information to the HSCIC, it seems that it was not shown to the committee. We provided answers to the questions very quickly and the application was resubmitted to the DAAG the following week and approved at its meeting on 25 November 2014, subject to information being checked with the CAG. Our application was finally approved on 16 December 2014.
Negotiating data-sharing agreements
Although we had now obtained permission to access the data we needed, the project still could not start until overarching data-sharing contracts at organisational level and project-specific contracts, originally known as Data Re-use Agreements and now known as Data Sharing Agreements, were signed.
In our case, the organisational level contract, known as a Data Sharing Framework Contract, was between the ONS, which is holding the data for the project in its secure facilities, and the HSCIC. It forms part of a wider service-level agreement, which was under renegotiation in early 2015. As part of its support for our project, the ONS negotiated with the HSCIC to deal with the Data Sharing Framework Contract in advance of the rest of the agreement and this went through smoothly.
Unfortunately, this was not the case with the Data Re-use Agreement, which arrived from the HSCIC with numerous drafting errors, which we corrected. This was followed by a long delay, after which the HSCIC told us that it had not understood our application and so had returned it to its committee, the DAAG. We then found that the version it agreed lacked one of two required technical appendices and we were not allowed access to data until the full document was approved.
There was a further wait until the HSCIC sent a revised version, now described as a Data Sharing Agreement, using a completely different form. As well as containing further new drafting errors, this new form did not cover our situation, in which the data are held at ONS but the work is done by the City, University of London, project team using the VML.
While we were waiting for these problems to be resolved, we were asked by our NIHR programme manager to document the problems we were experiencing. We hoped that this might lead to help in dealing with the problems, so were disappointed to receive an e-mail informing us that NIHR intended to discontinue the project unless we could arrange immediate access to the data.
We forwarded this e-mail to the HSCIC and also gave notice that we intended to make a Stage 2 complaint, following on from the Stage 1 complaint we had made early in 2014. The matter was escalated to a more senior member of HSCIC staff who quickly redrafted the contract in a way that made it possible for work to finally start in June 2015. Although this solved our immediate problems, we found, when we came to try to renew the Data Sharing Agreement 2 years later, that it had been incorrectly drafted.
Access to data for Wales
As was mentioned above, the Health and Social Care Act 2012 disrupted aspects of data flow between England and Wales. This meant that when our second Section 251 approval was granted in early 2014, it did not apply to Wales. When we queried this with our contacts at the NWIS, we were told that the problem was being discussed at a very senior level and that primary legislation in the Welsh Assembly might be needed to resolve it.
We explored the possibility of accessing data for Wales via the Secure Anonymised Information Linkage (SAIL) Databank, based at the University of Swansea. It transpired that the SAIL anonymisation process includes removing all dates, so data from it would not enable us to do our current project for which dates were a key data item.
Fortunately, pending primary legislation, the NWIS made an application for a ‘Section 251’ application to share data outside Wales. This was considered by the CAG in November 2014. Eventually it was decided that the two countries could sign a Memorandum of Understanding to cover the situation until legislation was enacted. Early in 2015, we were given to understand that linkage could proceed and in February 2015 we met the NWIS to take this forward and enable linkage with Welsh data.
Recruitment of staff
Our initial plan, set out in our application to NIHR, was to use the data from our previous projects for further analysis while obtaining and linking data for more recent years. At the start of the project, we therefore started to recruit the project researcher and part-time administrator. We advertised both posts in February 2014 and received over 30 applications for each. Cecile Bremont took up the appointment of part-time project administrator in April 2014. The post of project researcher was offered to an excellent applicant but she subsequently withdrew as she was offered a post elsewhere. By this time, the HSCIC moratorium was under way, and we were told by NIHR not to offer the post to another applicant at this stage. Although this was understandable, not having a researcher in post severely restricted our capacity to undertake the analyses we had identified that could be done with ONS data alone.
By the time we were in a position to start work on the data linkage in 2015, only 6 months remained on our contract, although application for a Variation to Contract was under discussion with NIHR. As recruitment processes can take at least 3 months if the successful candidate has to give notice from another post, we discussed with NIHR the possibility of employing a highly experienced applicant from the previous recruitment process, who had not been available for interview and was only available part time. As she was still available and was willing to come for 6 months in the first instance, we interviewed and appointed her, with the aim of extending her appointment and recruiting a second member of staff whose skills complemented her if our application for Variation to Contract was successful. This had the advantage that we were immediately able to appoint an experienced person, but of course the disadvantage was that being part time meant that the work she did progressed more slowly than if she had been employed full time.
Data items needed for quality assurance
We were in active contact with colleagues at ONS and with the HSCIC’s Data Linkage Service during the protracted process of gaining access to data, so that the groundwork was laid to start work on our project as soon as permissions were finally granted. The HSCIC provided the linked data for England and work started in the VML to assure the quality of the linkage. As this got under way, it became apparent that further data items that we had not requested were needed for this. The only way to obtain these was to request a re-issue of the data.
We were reluctant to take this course because of the earlier delays, and discussed this with the Head of Data Access at the HSCIC. We pointed out that changing our specification would mean agreeing a new Data Sharing Agreement and expressed our concern that this might add further delay. He commented that our work has indicated a need for additional fields in order to improve the linkage and hence data quality and went on to suggest that this in itself is an interesting finding. He added that this could have an impact on other research in this area and this is discussed in Chapter 2.
Although the revised Data Sharing Agreement did not have to go back to DAAG, this revision took longer than originally suggested because it co-incided with a rush of applications for data before the HSCIC was required to start deleting the records of ‘Type 2 objectors’. These were people who had objected to their records being used for purposes other than their health care, including secondary analysis, because of concerns about the data being used for commercial purposes. This short-term increase in numbers of applications introduced a further delay, although we were able to get on with other work while the revision was under way. The data linkage work was also done in parallel, so the HSCIC provided the revised extract to the project in March 2016, as soon as authorisation was given.
Using the Office for National Statistics’ secure setting
This project has involved linking and analysing personally identifiable data, including data items recorded at birth registration under the Population (Statistics) Acts. We were able to do this and our previous project only because we were able to access the data in the secure setting of the ONS VML. This is its facility for providing secure access to sensitive detailed data. Access is provided for approved researchers working on defined and approved non-commercial projects, which are judged to serve the public good. Data cannot be downloaded, but users can access the data at their desk if they are part of a government organisation, or otherwise in a ‘safe room’ at one of the ONS sites. In our case, going from the university to the VML access point in Pimlico involved a journey of around 30 minutes by public transport or bicycle. A member of the project team who lives in Gloucestershire drove to the ONS building in Newport to use the VML.
Before outputs can be released from the secure environment of the VML, they have to be scrutinised and cleared by VML staff before being e-mailed to the person who generated the output. Usually, this is dealt with promptly, typically on the next working day, but occasionally there have been longer delays, resulting in further delays if outputs have to be discussed with other members of the project team.
At the time this project started, the VML had been in operation for over 10 years without upgrading and there were frequent problems with its servers, creating major challenges for the team responsible for keeping it up and running. In the summer of 2015, it was upgraded, and projects were migrated to new facilities, but the upgrading increased the extent to which it was used, particularly within government.
The data for the project related to over 7 million babies and their mothers, with numerous ‘many-to-one’ relationships. As described in Chapter 2, the best way to hold such data is in a relational database. At the start of the project, the only relational database software available was Microsoft Access®. Although this software has many useful features, it is limited in its file sizes. This meant that the data for each year had to be split into an ONS birth registration file, a HES delivery record file and a HES birth record file. The result was a large number of separate databases, which then had to be interlinked. Although this provided a workable solution, setting up the infrastructure was labour intensive. Because the VML’s facilities are shared between many users, the processing speeds were mostly very slow.
Unfortunately, this was exacerbated by a succession of problems. These were discussed at each stage with members of the ONS VML team, which made considerable effort to support our project and help to resolve them.
The first was a technical problem, which caused work to be lost up to 10 to 20 times a day, and which made it impossible to run programmes that needed to run for many hours. It is possible that this was caused by very short-term outages. Microsoft Access® is particularly sensitive to this as it expects to maintain continuous access to data discs and is intolerant to outages of even a millisecond, which do not affect other software. This problem lasted several months, despite the best efforts of a project member and the VML team to identify the cause. It was possible to continue work on the project by dividing tasks into many short stages and logging progress in detail. Although progress was made during this period, it was painfully slow.
Shortly after the outage problem was solved, processing speeds in the VML plummeted, probably owing to an increase in the number of users rather than any specific technical issue. Logging of computational tasks showed that, on occasion, processing speeds sometimes fell to 100 times slower than normal. The problem was discussed with the VML team, which responded in July 2016 by providing us with a separate server box. Although this helped to some extent, our data remained on the same network drive and it was access to this drive that was causing the bottleneck.
In a further attempt to help us manage the very large database, the VML team made Microsoft SQL Server available to the project in June 2016. This had not been available earlier as there were a number of security issues to be resolved. Despite an initial reluctance on our part to switch technologies at this stage in the project, some experimentation made it clear that this was a fast and robust platform to use for storing and manipulating the data. The change entailed a considerable amount of work to design a new database, reimport the data and rewrite some of the code. Microsoft improved performance in terms of speed and reliability made the move to the new database platform worthwhile. Meanwhile, other members of the team had to continue their analysis work on the old server while the database was being transferred to the SQL system and they were not able to benefit immediately from the improvements.
Despite all of these problems, the project team produced a relational database of good-quality linked data, including data for England from the three main datasets (birth registration, birth notification and HES) for the 10-year period 2005–14, together with additional linkages relating to mortality and location of births. Non-delivery admissions of mothers and subsequent admissions of babies were also included, linked in by [HESID]. The database could be updated with data for more recent years using the same techniques. In future, this can be achieved much more efficiently given the additional software and processing power available in the VML as a result of the improvements prompted by this project.
Impact on progress with the project
In our progress report to NIHR in August 2016, we said that we hoped to be able to answer the main research questions by the end of the funded project, but would need to seek further funding to complete all the analyses. It soon became apparent, in view of the problems described above, that this was overoptimistic and we discussed the situation with our programme manager. This led to a meeting in Southampton on 24 October 2016, as a result of which we were invited to apply for a second Variation to Contract. This entailed a considerable amount of work and led to several requests for further detailed information. The net result of all this was being informed on 17 March 2017, 2 weeks before the funding ended, that we had not been successful and that no further funding would be available.
Comments
We have set out the above in considerable detail, as it is clear that problems of these types are not typical of those dealt with previously by NIHR programme managers who have had limited experience of what is involved. This reflects the fact that secondary analysis of routine data is a form of research that is not usually funded by NIHR and it has complex constraints that can be out of the researchers’ control.
This project started at a time when access to routine data was receiving considerable hostile media attention and at a time when the HSCIC was a relatively new and inexperienced organisation. In our attempts to gain access to data for analysis, we have been in touch with many other researchers who planned to use HSCIC data. As a result, we know that this project is among many others that have been adversely affected and that considerable sums of research money have been wasted as a consequence. As well as public funds, this has included money donated by the public to research charities. Members of the public have been invited to object to the use of their personal data for purposes other than their health care, without distinguishing between the purposes. It is clear from the level of donations to health research charities and also from surveys that health research enjoys considerable public support, although use of people’s data for commercial purposes does not.
At meetings and conferences that we have attended, it has become increasingly apparent that although Wales and Scotland are among world leaders in the innovative use of data linkage for analysis of health problems, and Northern Ireland is moving forward rapidly, England is well behind. In addition, data access is a problem, not only for research, but for public health analysis more generally. Public health analysts, who were moved out of the NHS to local authorities and Public Health England, have found themselves no longer able to access the data they need for their work. We have been involved in the widespread lobbying that has prompted the UK Statistics Authority to act on this and, in the wake of a series of meetings to identify the problems, an English Health Statistics Steering Group has been set up.
At the time we submitted this report in July 2017, we were aware that over the past 2 years, the HSCIC has taken steps to improve its application processes. An online application system has been introduced190 and a new committee, the Independent Group Advising on the Release of Data (IGARD),191 with wider representation and a lay chairperson has replaced DAAG. At the time we submitted this report in July 2017, we were not yet in a position to comment on the impact of this change, although we were about to apply to IGARD to renew our Data Sharing Agreement. When we did so, we experienced many problems.
If NIHR does want to encourage the researchers it funds to make greater use of routine data, we would suggest that it could include people with routine data experience among its staff. It would also be useful to make it possible to delay the starts of projects until access to routine data has been secured. We were under considerable pressure to start in January 2014, by which time we had ethics and ‘Section 251’ approvals, although we did not yet have permission to access HES and the data for Wales. Although we built a delay of 4 months into our project management plans, this was in line with our previous experience rather than the unexpectedly dysfunctional circumstances that we actually encountered.
We are extremely disappointed that, having got to the stage at which we had acquired the data, linked them, quality assured the main linkages, built the innovative relational database and started the analyses, we were unable to continue and complete them. As soon as this report was submitted, we started looking for sources of additional funding to do this, but a year had passed before we were able to identify a source for which we were eligible to apply and this opportunity arose as a result of changes in eligibility criteria.
Access to the linked data by other researchers
The relational database holding the high-quality linked data for the 10-year period 2005–14 is potentially an extremely useful resource for future maternity researchers. As a result of the work of the project team in piloting linkage techniques, acquiring the necessary data and working on linkage algorithms, followed by the extensive quality assurance and the technical achievement of creating a database to hold the linked data, it is now possible to undertake complex analyses that were not possible before the creation of the database. Our second ‘Section 251’ approval was for a database that other researchers can apply to access.
To date, one request has been successfully made for access to the linked data and another is in the pipeline. In both cases, this involves collaboration with members of our team. The first request relates to a project to investigate hospital care and the educational attainment of children born preterm by analysing the data we have linked and making further linkage to the National Pupil Database. Maria Quigley of the NPEU is Principal Investigator of TIGAR,124 funded by the MRC, and Alison Macfarlane and Nirupa Dattani are among the co-investigators. This project was specifically mentioned in our Data Sharing Agreement. Although subsequent hospital episodes have been successfully analysed, it was not possible to obtain permission for linkage with the National Pupil Database.
A researcher from University College London has now applied for funds to use the linked data to investigate childhood illnesses leading to hospital care among children from minority ethnic groups. She was in the position of applying for her own ethics and ‘Section 251’, but wanted to do preliminary analyses to inform the development of her application, so we arranged for her to have an honorary contract with City, University of London. She already had Approved Researcher Status and so should have been in a position to apply to access the data in the VML. This approach was proposed by the Head of Data Access at the the HSCIC but was subsequently vetoed when we applied to renew our Data Sharing Agreement.
In response to NIHR’s request to describe how data may be accessed more generally, following the end of this project, we have had discussions with both the ONS and HSCIC. Over a year later, it was still too soon to give a definitive response. We therefore suggest that any researcher wanting to access the data should contact the corresponding author in the first instance to discuss ways of making the application to take their proposals forward.
Changes to the project protocol
The original protocol was written in 2013 before the implications of the Health and Social Care Act 2012 and the establishment of the HSCIC became fully apparent. The work has been severely delayed by factors outside the control of the project team and this led to a number of changes to this protocol, which are documented in the final report of the project.
The major changes were caused by the delays to the project timeline. We made several attempts during the course of the project to update this timeline, and did update it when we applied for a Variation to Contract in June 2015. From that point onwards, further uncertainties meant that work had to be rescheduled. It is inherent in projects of this type that timing can be altered by factors outside the researchers’ control. As a result, the analyses of outcome and of differences between maternity units were not done during the funding period. We have now applied for further funding to do them.
We made two amendments to the data requested. The first was to compensate for an oversight. The data provided to us by the ONS automatically included infant deaths linked to births. For completeness, we subsequently also requested data on the deaths of children aged over a year, which the ONS routinely links to children’s birth records. To investigate the deaths of mothers, we requested the data about deaths of women during childbirth or within a year after giving birth, which the ONS routinely links to the corresponding birth records. This involved obtaining the necessary permissions, but as the data were already linked these requests did not significantly add to the work of the project.
The second addition was made at the suggestion of a member of our Study Advisory Group. He pointed out that that the Wigglesworth classification used by the ONS to classify causes of stillbirth and neonatal death is unable to differentiate reliably between antepartum and intrapartum stillbirth and that the classification used by the Centre for Maternal and Child Enquiries, which had been responsible for national confidential enquiries up to 2010, made a much better distinction. He advised us to request and link in these data for the years 2005–9 to analyse intrapartum stillbirths and we implemented his suggestion, as described in Chapters 2 and 3.
In our previous linkage project, a nine-step algorithm made up of a combination of patient identifiers such as mother’s and baby’s NHS number, dates of birth and postcode was used to link the linked birth registration/birth notification records for births occurring in 2005–7 to Maternity HES records. 7,123 In this project, we were advised by the HSCIC to compare this with its standard linkage algorithm, as described in Chapter 2. We found that this performed better and so we used it for linkage of data for the whole 10-year period.
We also found that the ‘filters’, that is, the criteria used to select records for inclusion, which we had used in our previous project on the recommendation of Northgate Solutions, performed marginally less well than those used by the HSCIC. We had not intended to make any changes, but as we requested revised data with additional variables, we took the opportunity to use the opportunity to change the filters and also to request data up to the most recently available year, 2014, to compensate for delays to the project.
There were changes over the period 2005–14 in the ways in which workforce data are compiled and published. As acknowledged in our proposal, a major change was the new monthly reporting system introduced in 2009. It has undergone a number of changes since then. Our examination of the data and discussions with the member of HSCIC staff responsible led us to suspect that analyses may not be possible for the whole 10-year period, but we had not reached definitive conclusions at the time the project ended.
Our proposal did not specify how the data were to be held in the VML. For reasons given in Chapter 2, because of the volume and complexity of the data, a relational database was built to hold the data and this was a major achievement of the project.
Changes to the dissemination plans
Our original dissemination strategy was based on the assumption that we would produce three papers, one describing patterns of births, one giving results of analyses of mortality and one giving results of analyses of morbidity, to be submitted to peer-reviewed journals before disseminating their content more widely. We have not changed our plans for methods of dissemination, apart from trying to learn from the adverse consequences of the way in which a related article in the British Medical Journal62 was reported in the popular media.
As work progressed, we became aware of interest in the data linkage aspects of the project, notably the changes made since our previous project, the methods for which were described in three articles. 7,8,123 Because these are referenced and also mentioned in discussions with us, it seems important to update the information in them. As a result, two further articles on linkage methods and quality assurance were submitted for publication and have now been published. 157,158 Work on describing patterns of births was subdivided into two separate articles. One article describing the timing of singleton births in NHS maternity units in England has now been published. 159 The second, focusing on home births and other births outside NHS maternity units was initially rejected but will be resubmitted following the journal’s suggestions.
As we did not complete analyses of mortality and morbidity, these articles will be dependent on obtaining additional funding, as will articles on multiple births. We still plan to submit an article presenting some of our published findings about patterns of birth to Significance, the Royal Statistical Society’s magazine, which aims to popularise statistics and has a very wide international circulation.
The results of the descriptive analyses of patterns of births were presented in 2016 as posters at the International Population Data Linkage Conference and the RCM annual conference. Analyses of patterns of births at home were presented as a poster at the 2-yearly international data linkage conference hosted by the Scottish Health Informatics Programme in Scotland in 2015. Oral presentations of the quality assurance methods and of the series of linkage projects as a whole were made at the Administrative Data Research Network conference in Edinburgh in June 2017 and three oral presentations were made at the Royal Statistical Society’s conference in September 2017. Two posters, one on the time of day of birth and one on the day of birth were presented at the 12th International Normal Labour and Birth Research Conference in October 2017 and the first of these won the Scientific Review Team prize. We had intended to aim for a presentation at an obstetric conference, but there was not a timely conference to which we could submit an abstract.
Patient and public involvement is an important component of our dissemination plan and is described in Chapter 4.
Appendix 2 Data linkage and organisation
Linkage and quality assurance
Linkage bias (England only)
There was a statistically significant difference in distribution between ONS birth records that were linked to HES delivery records by the HSCIC and those that were not linked in terms of multiplicity, age of mother, ethnicity and region of residence, as shown in Table 27.
| Variable | Number of ONS birth records | Linked to HES delivery record | Never linked to HES delivery record | Linkage rate |
|---|---|---|---|---|
| Year of birth | ||||
| 2005 | 617,613 | 582,963 | 34,650 | 94.39 |
| 2006 | 640,271 | 607,649 | 32,622 | 94.90 |
| 2007 | 659,061 | 632,039 | 27,022 | 95.90 |
| 2008 | 676,999 | 655,511 | 21,488 | 96.83 |
| 2009 | 675,330 | 657,622 | 17,708 | 97.38 |
| 2010 | 687,100 | 673,566 | 13,534 | 98.03 |
| 2011 | 688,681 | 674,751 | 13,930 | 97.98 |
| 2012 | 698,457 | 681,677 | 16,780 | 97.60 |
| 2013 | 668,433 | 651,957 | 16,476 | 97.54 |
| 2014 | 664,967 | 647,047 | 17,920 | 97.31 |
| Total | 6,676,912 | 6,464,782 | 212,130 | 96.82 |
| χ2 test | p < 0.0001 (χ2 = 39689.65, df = 9) | |||
| Multiplicity | ||||
| Singletons | 6,468,586 | 6,268,013 | 200,573 | 96.90 |
| Multiples | 208,326 | 196,769 | 11,557 | 94.45 |
| Total | 6,676,912 | 6,464,782 | 212,130 | 96.82 |
| χ2 test | p < 0.0001 (χ2 = 3928.09, df = 1) | |||
| Age of mother (years) | ||||
| Under 15 | 1,739 | 1,653 | 86 | 95.05 |
| 15–19 | 206,936 | 200,367 | 6,569 | 96.83 |
| 20–24 | 1,218,562 | 1,186,178 | 32,384 | 97.34 |
| 25–29 | 1,812,830 | 1,764,402 | 48,428 | 97.33 |
| 30–34 | 1,926,290 | 1,865,427 | 60,863 | 96.84 |
| 35–39 | 1,092,622 | 1,048,332 | 44,290 | 95.95 |
| 40–44 | 245,526 | 232,397 | 13,129 | 94.65 |
| 45 and over | 15,821 | 14,020 | 1,801 | 88.62 |
| Not stated | 156,586 | 152,006 | 4,580 | 97.08 |
| Total | 6,676,912 | 6,464,782 | 212,130 | 96.82 |
| χ2 test | p < 0.0001 (χ2 = 12579.68, df = 8) | |||
| Ethnicity of baby | ||||
| Bangladeshi | 93,074 | 91,081 | 1,993 | 97.86 |
| Indian | 199,963 | 194,212 | 5,751 | 97.12 |
| Pakistani | 272,457 | 266,007 | 6,450 | 97.63 |
| Black African | 215,621 | 203,962 | 11,659 | 94.59 |
| Black Caribbean | 65,048 | 62,685 | 2,363 | 96.37 |
| White British | 4,239,203 | 4,140,349 | 98,854 | 97.67 |
| White Other | 547,384 | 523,826 | 23,558 | 95.70 |
| Other | 628,556 | 602,162 | 26,394 | 95.80 |
| Not stateda | 415,606 | 380,498 | 35,108 | 91.55 |
| Total | 6,676,912 | 6,464,782 | 212,130 | 96.82 |
| χ2 test | p < 0.0001 (χ2 = 61433.75, df = 8) | |||
| Baby’s sex | ||||
| Female | 3,253,584 | 3,149,797 | 103,787 | 96.81 |
| Male | 3,423,327 | 3,314,985 | 108,342 | 96.84 |
| Not stated | 1 | 0 | 1 | 0.00 |
| Total | 6,676,912 | 6,464,782 | 212,130 | 96.82 |
| χ2 test | p < 0.0001 (χ2 = 33.90, df = 2) | |||
| Gestational age | ||||
| Missing or under 22 weeks | 53,236 | 50,420 | 2,816 | 94.71 |
| Preterm | 506,206 | 486,517 | 19,689 | 96.11 |
| Term | 5,861,275 | 5,678,501 | 182,774 | 96.88 |
| Post-term | 256,195 | 249,344 | 6,851 | 97.33 |
| Total | 6,676,912 | 6,464,782 | 212,130 | 96.82 |
| χ2 test | p < 0.0001 (χ2 = 1884.07, df = 3) | |||
| Hour of birth | ||||
| 00.00–02.59 | 816,647 | 791,373 | 25,274 | 96.91 |
| 03.00–05.59 | 801,801 | 776,911 | 24,890 | 96.90 |
| 06.00–08.59 | 711,622 | 687,834 | 23,788 | 96.66 |
| 09.00–11.59 | 1,094,422 | 1,061,279 | 33,143 | 96.97 |
| 12.00–14.59 | 869,441 | 840,948 | 28,493 | 96.72 |
| 15.00–17.59 | 795,151 | 769,329 | 25,822 | 96.75 |
| 18.00–20.59 | 743,832 | 719,896 | 23,936 | 96.78 |
| 21.00–23.59 | 782,848 | 758,454 | 24,394 | 96.88 |
| Not stated | 61,148 | 58,758 | 2,390 | 96.09 |
| Total | 6,676,912 | 6,464,782 | 212,130 | 96.82 |
| χ2 test | p < 0.0001 (χ2 = 334.96, df = 8) | |||
| SHA region of usual residence | ||||
| East Midlands | 456,324 | 448,489 | 7,835 | 98.28 |
| East of England | 672,006 | 652,543 | 19,463 | 97.10 |
| London | 1,298,130 | 1,227,661 | 70,469 | 94.57 |
| North East | 307,532 | 301,141 | 6,391 | 97.92 |
| North West | 867,881 | 850,726 | 17,155 | 98.02 |
| South Central | 462,848 | 455,243 | 7,605 | 98.36 |
| South East | 514,289 | 503,042 | 11,247 | 97.81 |
| South West | 566,860 | 559,043 | 7,817 | 98.62 |
| West Midlands | 709,445 | 695,469 | 13,976 | 98.03 |
| Yorkshire/The Humber | 645,649 | 635,293 | 10,356 | 98.40 |
| Elsewhere | 10,989 | 9,507 | 1,482 | 86.51 |
| Home | 164,954 | 126,622 | 38,332 | 76.76 |
| Not stated | 5 | 3 | 2 | 60.00 |
| Total | 6,676,912 | 6,464,782 | 212,130 | 96.82 |
| χ2 test | p < .0001 (χ2 = 269313.43, df = 12) | |||
Data preparation and quality checks
Both mothers’ and babies’ identifiers were available for the ONS birth and HES delivery records to use in the quality assurance process. These were mother’s date of birth, NHS number and postcode of usual residence, and baby’s date of birth, NHS number and sex.
It was necessary to normalise the baby information in the maternity tail section of each HES delivery record so that the data could be stored and interrogated efficiently in the database environment. This meant that if information was held on more than one baby in the maternity tail part of a delivery record, this was transformed into separate records for each baby. For example, this meant that there were two records, one for each of the two babies in a twin delivery. Each record contained the same common episode identifier, APC fields and maternity tail fields, but with the respective baby’s information in each one.
For variables common to birth registration and birth notification, the maximum amount of reliable information was derived from the two sources. The baby’s date of birth, birthweight and sex were taken from birth registration, and gestational age was taken from birth notification, unless values were missing.
Inconsistencies were found between ONS records and HES records in the data types and formats used for variables such as dates and the baby’s sex. These variables were recorded into common formats for use in the linked database.
The extent of missing values for key items of data about the baby in the ONS birth records for 1 January 2005 to 31 December 2014 and HES normalised records for 1 April 2004 to 31 March 2015 is given in Table 28.
| Variable | ONS singleton birth records | HES singleton delivery records | ONS multiple birth records | HES multiple delivery records |
|---|---|---|---|---|
| Total | 6,468,586 | 7,040,590 | 208,326 | 230,019 |
| Percentage with missing values for | ||||
| Baby’s date of birth | 0.00 | 19.4 | 0.00 | 16.3 |
| Sex of baby | 0.00 | 23.1 | 0.00 | 16.1 |
| Gestational age | 0.71 | 37.2 | 0.80 | 27.8 |
| Birthweight | 0.56 | 22.7 | 1.70 | 15.3 |
A value would have to be missing on both birth registration and birth notification to be considered missing overall on ONS birth records in Table 28. Although the total numbers may not be directly comparable as a result of definitional and date differences, the percentages of missing values per variable gives an indication of differences in data completeness.
The HES delivery data have a much higher proportion of records with missing values than ONS birth records, for example up to 37% for gestational age in singleton births. The proportion of records with missing information is lower for multiple births in HES, as data items for the first baby are often repeated for their siblings in the same delivery.
When a baby’s date of birth was missing on HES, it was derived from operation dates if a delivery code was present. If sex of baby, gestational age or birthweight were missing, they could not be derived.
Data about gestational age and birthweight are known to have problems, notably implausible values, truncation and rounding in HES. ONS birth records can also have implausible values for birthweight but this has been improving with the introduction of ‘warning’ edits to birth notification systems.
Full quality assurance procedure
Quality assurance procedures for singleton and multiple births to select only one correct linked HES delivery record for each ONS birth record and to discard incorrect linkages (detailed version) are shown in Table 29.
| Rule | Category | Applies to | Keep the link | Discard the link | Notes |
|---|---|---|---|---|---|
| Singleton births | |||||
| 1 | Cleaning | Linked to HES records that have no birth or operation dates or is an invalid delivery | HES records where baby date of birth = null or valid delivery = false | ||
| 2 | Cleaning | Duplicate HES records (typically × 6 or × 9) linked to same ONS birth record when baby tail information and identifier is identical | The first version of the duplicate HES record goes through to the subsequent cleaning stages | All other versions of the duplicate HES record | Caused by IT administrative issues in some NHS trusts |
| 3 | SMDB | ONS birth record linked to HES record when baby date of birth differs between them by 24 weeks (168 days) or more | If HES baby date of birth 24 weeks (168 days) or more from ONS birth record for baby date of birth | The size of the date difference implies a different birth to the same mother | |
| 4 | SMSB | ONS birth record linked to one HES record (originally or remaining) | If ONS birth and HES variables match as listed in Table 9 | If ONS birth and HES variables do not match as listed in Table 9 | |
| 5 | SMSB | ONS birth record linked to more than 1 HES record all from same spell with genuine epiorder sequence (or a combination of genuine spell and additional delivery records) | If ONS birth and HES variables match as listed in Table 9 (baby date of birth must be exact match) and episode is part of spell and onset of delivery and delivery method and birth status values are valid | If ONS birth and HES variables do not match as listed in Table 9 or are the other episodes in that spell |
Identifies where ONS birth records are linked to more than 1 HES record because some or all form a hospital spell. A spell is identified as an episode that has a sequence of epiorder numbers (e.g. 1 and 2) and the episode start date of the subsequent episode = the episode end date of the previous episode, all have the same admission date, and the discharge date is recorded only on the final episode The episode in the spell with the maximum and valid delivery information is chosen |
| 6 | SMSB | ONS birth record linked to more than 1 HES record with different epikeys but duplicate (admidate, disdate, epistart, epiend, epiorder, date of birth, gestat, birweit, baby sex, numbaby, birstat, birordr, delonset, delmeth, ICD-10 code count, OP code count, procode, sitetret) | If ONS birth and HES variables match as listed in Table 9 and highest epikey | If ONS birth and HES variables do not match as listed in Table 9 or if not highest epikey | Highest epikey is the latest HES record and should contain the most information |
| 7 | SMSB |
ONS birth record linked to > 1 HES record with different epikeys but duplicate (epiorder, date of birth, gestat, birweit, baby sex, numbaby, birstat, birordr, delonset, delmeth, procode, sitetret) Different admidate, disdate, epistart, epiend, ICD-10 code count, OP code count |
If ONS birth and HES variables match as listed in Table 9 and highest epikey | If ONS birth and HES variables do not match as listed in Table 9 or if not highest epikey |
Highest epikey is the latest HES record and should contain the most information The additional HES records can be pre- or post-hospital admissions relating to a delivery |
| 8 | SMSB | ONS birth record linked to > 1 HES record with different epikeys not duplicates | If ONS birth and HES variables match as listed in Table 9 (baby date of birth must be exact match) and ONS and onset of delivery and delivery method and birth status and birth order values are valid | If ONS birth and HES variables match as listed in Table 9 but baby date of birth is not an exact match (or HES baby date of birth is null) and onset of delivery and delivery method and birth status and birth order values are not valid and there is a corresponding Keep record | Chooses the linked HES record with the maximum valid delivery information |
| 10 | SMSB | ONS birth record linked to two HES records, both of which match on baby date of birth and location of birth | If ONS birth and HES variables match as listed in Table 9 (HES-derived and original baby date of birth must be exact match to ONS) and onset of delivery and delivery method and birth status and birth order values are valid. Most escalated onset of delivery and delivery method | If ONS birth and HES variables match as listed in Table 9 (HES derived baby date of birth is exact match to ONS but HES original baby date of birth is null) and onset of delivery and delivery method and birth status and birth order values are valid (but less escalated) | A small number of records that can be differentiated by one containing maximum delivery information and one does not when they both match on location of birth and baby date of birth |
| 11 | SMSB | ONS birth record linked to HES records with differing baby date of birth values (within 14 days of ONS baby date of birth) | If ONS birth and HES variables match as listed in Table 9 (baby date of birth must be exact match) and valid onset of delivery and delivery method value | If HES baby date of birth ≤ –14 days from ONS baby date of birth or HES baby date of birth ≤ –1 and > –14 days before ONS baby date of birth or if already a Keep record and HES baby date of birth ≥ 1–14 days from ONS baby date of birth |
Differentiates between the HES linked records by HES baby date of birth. The HES records that have HES baby date of birth ≤ –14 days from ONS baby date of birth, then ≤ –1 and > –14 days before ONS baby date of birth, then ≥ 1–14 days from ONS baby date of birth, are discarded and the remaining one linked HES record with HES baby date of birth = ONS baby date of birth and valid method of delivery value is kept (if matching) The discarded HES records look like maternal pregnancy care records based on ICD-10 codes |
| 12 | SMWB | ONS birth record linked to HES records with differing baby date of birth values (within 15 to 168 days of ONS baby date of birth) | If ONS birth and HES variables match as listed in Table 9 (baby date of birth must be exact match) and valid onset of delivery and delivery method value | If already a Keep record and HES baby date of birth more than 14–168 days from ONS baby date of birth and different baby tail values |
The discarded records look like different births approximately 2 or 3 months later to the same mother, some of which are clearly premature births Could have been incorporated in Rule 3 |
| 13 | ONS birth record linked to more than 1 HES record with different epikeys but duplicate (date of birth, gestat, birweit, baby sex, delonset, delmeth) | If ONS birth and HES variables match as listed in Table 9 and highest epikey | If not highest epikey | ||
| 14 | SMSB | Clerical check to identify potential multiple birth records when more than 1 HES baby tail with same epikey linking to ONS birth record and/or where HES multibirth ICD-10 is true and/or the epikey is linked to more than 1 ONS birth record, but not attributable to SMDB |
Keep as a singleton matched birth if ONS birth and HES variables match as listed in Table 9 and HES multiple birth ICD-10 but matches only one ONS birth record or either ONS birth or HES say multiple or stillbirth, baby tails identical, keep only one HES record with field order 1 (genuine duplicates) or ONS birth singleton and HES multiple, treat as singleton if baby tails are the same |
Identify as potential multiple birth if: epikey links more than 1 ONS birth record with same baby date of birth or two different HES baby tails, one stillbirth, and only one ONS birth record for livebirth or HES multiple birth ICD-10 and HES baby tails different Discard all if ONS birth and HES variables do not match as listed in Table 9 |
Any records identified as potential multiple births are separated and given to ONS to check |
| 15 | Check | If previous stages have kept more than correct number of linked HES records per ONS birth | The highest epikey | Version(s) with earlier or other epikeys | |
| 16 | Check | If previous stages have kept no links per ONS birth |
If birth location match, ONS baby date of birth within HES admission date ranges, and gestation, birthweight and sex match or are null and match rank 1 and is not a SMDB or invalid record or if birth location does not match but everything else does |
Clerical | |
| Multiple births | |||||
| 1 | Cleaning | Linked to HES records that are invalid deliveries | HES records where valid delivery = false | Do not exclude those where HES baby date of birth = null because they may be ghost baby tail records | |
| 2 | Cleaning | Duplicate HES records (typically × 6 or × 9) linked to same ONS birth record where baby tail information and identifier are identical | The first version of the duplicate HES record goes through to the subsequent cleaning stages | All other versions of the duplicate HES record | Caused IT administrative issues in some NHS trusts |
| 3 | SMDB | ONS birth record linked to HES record when baby date of birth differs between them by 24 weeks (168 days) or more | If HES baby date of birth 24 weeks (168 days) or more from ONS birth record baby date of birth | The size of the date difference implies a different birth to the same mother | |
| 4 | SMSB |
ONS birth records in MULTBTNO linked to one epikey and the correct number of baby tails (originally or remaining) Correct number of baby tails Correct number of ONS birth records One epikey per MULTBTNO |
If ONS birth and HES variables match as listed in Table 9 and field order 1 for first baby, field order 2 for second baby, etc., so that ONS birth record corresponds to correct baby tail |
If ONS birth and HES variables do not match as listed in Table 9 or field and birth orders do not match and sex and birthweight are wrong way round and there are already two correct Keep records |
|
| 5 | SMSB |
ONS birth records in MULTBTNO linked to one epikey and more than the correct number of baby tails More than the correct number of baby tails (duplicates) Correct number of ONS birth records One epikey per MULTBTNO |
If ONS birth and HES variables match as listed in Table 9 and field order 1 (or lowest) for first baby, field order 2 (or plus 1) for second baby, etc., so that birth record corresponds to correct baby tail |
If ONS birth and HES variables do not match as listed in Table 9 or field and birth orders do not match and sex and birthweight are wrong way round and there are already two correct Keep records |
|
| 6 | SMSB |
ONS birth records in MULTBTNO linked to more than one epikey Correct number of ONS birth records More than one epikey per MULTBTNO |
Where epikey matches by baby date of birth, ONS baby date of birth is within HES admission date range, and has valid/most escalated onset of delivery and delivery method | All others |
Births with more than 1 epikey correctly associated with them, but not spells Owing to first baby linked to 1 epikey and the second baby to the other or duplicates with epikey number increasing by one each time, or non-delivery records |
| 7 | SMSB | Remaining MULTBTNO with fewer than the correct number of ONS birth records | If ONS birth and HES variables match as listed in Table 9 | Some of the missing ONS birth records found in singleton file and unlinked file | |
| 8 | Check | If previous stages have kept more than the correct number of links per MULTBTNO. Epikeys are exact duplicates | Version with highest epikey or version within admission date range | Version(s) with earlier or other epikeys | |
| 9 | Check | If previous stages have kept no links per MULTBTNO |
If birth location match, ONS baby date of birth within HES admission date ranges, and gestation, birthweight and sex match or are null and match rank 1 and is not a SMDB or invalid record or if birth location does not match but everything else does |
Clerical | |
Quality assurance results
For a summary of quality assurance results for singleton and multiple births linked to HES delivery records by calendar year, see Table 30.
| Year | Total singleton ONS birth records | Total singleton ONS births linked to any HES delivery records by HSCIC | Percentage of total singleton ONS births linked to any HES delivery records by HSCIC | Of singleton ONS births linked to any HES delivery records by HSCIC, number left with link to one HES delivery record after QA | Of singleton ONS births linked to any HES delivery record by HSCIC, percentage left with link to one HES delivery record after QA | Of singleton ONS births linked to any HES delivery records by HSCIC, number left with no links to HES delivery records after QA | Of singleton ONS births linked to any HES delivery records by HSCIC, percentage left with no links to HES delivery records after QA | Percentage of all total singleton ONS births left with link to one HES delivery record after QA | Percentage of all total singleton ONS births left with no links to HES delivery records after QA |
|---|---|---|---|---|---|---|---|---|---|
| Singleton births | |||||||||
| 2005 | 599,237 | 565,559 | 94.4 | 554,566 | 98.1 | 10,993 | 1.9 | 92.5 | 7.5 |
| 2006 | 620,730 | 589,127 | 94.9 | 573,770 | 97.4 | 15,357 | 2.6 | 92.4 | 7.6 |
| 2007 | 638,995 | 612,782 | 95.9 | 595,585 | 97.2 | 17,197 | 2.8 | 93.2 | 6.8 |
| 2008 | 656,196 | 635,411 | 96.8 | 621,006 | 97.7 | 14,405 | 2.3 | 94.6 | 5.4 |
| 2009 | 653,322 | 636,284 | 97.4 | 621,423 | 97.7 | 14,861 | 2.3 | 95.1 | 4.9 |
| 2010 | 665,599 | 652,533 | 98.0 | 641,167 | 98.3 | 11,366 | 1.7 | 96.3 | 3.7 |
| 2011 | 666,582 | 653,552 | 98.0 | 642,263 | 98.3 | 11,289 | 1.7 | 96.4 | 3.6 |
| 2012 | 676,399 | 661,511 | 97.8 | 648,501 | 98.0 | 13,010 | 2.0 | 95.9 | 4.1 |
| 2013 | 647,666 | 633,222 | 97.8 | 622,943 | 98.4 | 10,279 | 1.6 | 96.2 | 3.8 |
| 2014 | 643,860 | 628,032 | 97.5 | 617,263 | 98.3 | 10,769 | 1.7 | 95.9 | 4.1 |
| All years | 6,468,586 | 6,268,013 | 96.9 | 6,138,487 | 97.9 | 129,526 | 2.1 | 94.9 | 5.1 |
| Year | Total multiple ONS birth records | Total multiple ONS births linked to any HES delivery records by HSCIC | Percentage of total multiple ONS births linked to any HES delivery records by HSCIC | Of multiple ONS births linked to any HES delivery records by HSCIC, number left with link to one HES delivery record after QA | Of multiple ONS births linked to any HES delivery record by HSCIC, percentage left with link to one HES delivery record after QA | Of multiple ONS births linked to any HES delivery records by HSCIC, number left with no links to HES delivery records after QA | Of multiple ONS births linked to any HES delivery records by HSCIC, percentage left with no links to HES delivery records after QA | Percentage of all total multiple ONS births left with link to one HES delivery record after QA | Percentage of all total multiple ONS births left with no links to HES delivery records after QA |
| Multiple births | |||||||||
| 2005 | 18,376 | 17,404 | 94.7 | 17,209 | 98.9 | 195 | 1.1 | 93.6 | 1.1 |
| 2006 | 19,541 | 18,522 | 94.8 | 18,258 | 98.6 | 264 | 1.4 | 93.4 | 1.4 |
| 2007 | 20,066 | 19,257 | 96.0 | 18,957 | 98.4 | 300 | 1.6 | 94.5 | 1.5 |
| 2008 | 20,803 | 20,100 | 96.6 | 19,894 | 99.0 | 206 | 1.0 | 95.6 | 1.0 |
| 2009 | 22,008 | 21,338 | 97.0 | 21,085 | 98.8 | 253 | 1.2 | 95.8 | 1.1 |
| 2010 | 21,501 | 21,033 | 97.8 | 20,847 | 99.1 | 186 | 0.9 | 97.0 | 0.9 |
| 2011 | 22,099 | 21,199 | 95.9 | 20,872 | 98.5 | 327 | 1.5 | 94.4 | 1.5 |
| 2012 | 22,058 | 20,166 | 91.4 | 19,554 | 97.0 | 612 | 3.0 | 88.6 | 2.8 |
| 2013 | 20,767 | 18,735 | 90.2 | 18,165 | 97.0 | 570 | 3.0 | 87.5 | 2.7 |
| 2014 | 21,107 | 19,015 | 90.1 | 18,429 | 96.9 | 586 | 3.1 | 87.3 | 2.8 |
| All years | 208,326 | 196,769 | 94.5 | 193,270 | 98.2 | 3,499 | 1.8 | 92.8 | 1.7 |
Reasons for discarding Hospital Episode Statistics records linked to an Office for National Statistics birth
Table 31 shows a breakdown of reasons for discarding HES delivery records linked to an ONS birth excluding duplicate copies of HES delivery episodes and invalid deliveries for singleton births in England by year.
| Year | All | a | b | c | d | e | f |
|---|---|---|---|---|---|---|---|
| Total links broken (excluding exact duplicates and invalid records) | Same mother different baby | Multiple episodes – pre-/post-delivery admission | Multiple episodes – part of spell | Multiple episodes – exact duplicates with different epikeys | No match | Potential multiple birth | |
| 2005 | 46,164 | 24,457 | 14,941 | 5,805 | 104 | 817 | 40 |
| 2006 | 49,706 | 25,082 | 16,565 | 6,984 | 204 | 782 | 89 |
| 2007 | 48,999 | 26,304 | 13,187 | 8,301 | 323 | 799 | 85 |
| 2008 | 47,748 | 26,032 | 9,466 | 11,473 | 89 | 614 | 74 |
| 2009 | 40,519 | 25,688 | 6,137 | 7,680 | 283 | 673 | 58 |
| 2010 | 37,007 | 24,993 | 5,176 | 5,819 | 366 | 599 | 54 |
| 2011 | 37,013 | 24,679 | 6,033 | 5,367 | 741 | 145 | 48 |
| 2012 | 36,176 | 24,966 | 5,899 | 4,298 | 838 | 146 | 29 |
| 2013 | 34,285 | 23,071 | 5,709 | 5,018 | 281 | 169 | 37 |
| 2014 | 31,690 | 21,980 | 3,662 | 3,957 | 1,863 | 110 | 118 |
| All years | 409,307 | 247,252 | 86,775 | 64,702 | 5,092 | 4,854 | 632 |
| Percentage | 100 | 60.41 | 21.20 | 15.81 | 1.24 | 1.19 | 0.15 |
An ONS birth record may have been linked to one or more HES delivery records for a variety of reasons given in Table 31. After quality assurance, some or all of the available linked HES delivery records will have been discarded, leaving a link to one correct HES delivery record or to none at all. Discarding all the linked HES delivery records for a birth suggests incorrect linkage and is discussed in the next section.
Overall 76% of all the linked HES delivery records that were discarded were duplicate copies of HES delivery episodes, and 0.5% were invalid delivery records, dealt with in cleaning stages 1 and 2 of the methodology. A summary of the remaining reasons by year for singleton births is given in Table 31.
Same mother different baby
This accounted for 60% of all discarded links. This is expected when the study period covers 10 years and each birth is linked by the mothers’ identifiers to all other deliveries to that mother in that period.
Multiple episodes – pre/post delivery admission
This accounted for 21% of discarded links. It arose where additional episodes relating to a delivery, usually relating to a pre- or post-delivery admission. The numbers of these generally decreased over time, suggesting that data quality is a factor.
Multiple episodes – part of spell
The third main reason for discarding links, accounting for 16%, was links to other episodes in a spell having been discarded, keeping only the link to the episode with the most amount of delivery information.
Other reasons
The remaining three reasons each accounted for less than 2% of discarded links. The sixth column shows when multiple delivery records contained the same information and links to superfluous records were discarded. This is also a data quality issue. There was a large increase in these in 2014. The eighth column relates to a small number of linked singleton birth records that were identified as ‘potential multiple births’, described below (see Data and linkage quality issues).
The seventh column shows ‘no matches’; links discarded when there are no matching variables or insufficient numbers of matching variables according to the quality assurance methodology, and the baby’s date of birth did not indicate a ‘same mother different baby’. This group is of interest because it could indicate erroneous false positive links by the linkage algorithm, or it could indicate erroneous false negatives in the quality assurance methodology. Fifty-seven percent (2,743) of this group were linked by match rank 1 of the linkage algorithm, the most reliable stage of the linkage algorithm that matches all available identifiers including the NHS number, suggesting that they should be correct maternal linkages. These were checked in greater detail clerically for explanations.
Of these, 2,323 (85%) were true no matches, whereby none of the five baby data items matched at all or only the place of birth matched, or only the sex matched or only the gestation matched. In these cases, the baby’s date of birth had not been transposed nor was it a different baby to the same mother. This suggested that incorrect maternal linkage or some other data quality issue has been involved. This accounted for 0.04% of all singleton birth records originally linked to a HES delivery record.
It appeared that 366 links (13%) were potential false negatives made in error by the quality assurance methodology. The dates of birth in these do not match owing to transposition in the date of birth elements. If this had been factored into the methodology, these links would have not been discarded.
The remaining 94 links (3%) were undeterminable, with some discriminatory baby data items matching and some not. For example, the date of birth may match or have been transposed, but birthweight and/or place of birth may be very different.
Some of the categories of problems shown in Table 31 may have been restricted to particular NHS trusts but further investigation would be needed to check this.
Data and linkage quality issues
Quality assurance of the linked dataset for such a large population revealed issues with the quality of the data within each of the datasets and also the quality of linkage that otherwise might not be detectable. Although it is already known that HES has data quality issues, issues were found in the ONS birth records that warranted further investigation.
First, the consistent common location code that was assigned to the place of birth codes was found not to match between birth registration and notification for 22% of the singleton births with a correct HES delivery link after quality assurance. This suggested that the linkage between birth registration and notification could be incorrect. A sample of these records that also had very discordant mother and baby identifiers and baby tail information was given to the ONS, which carried out this linkage, for checking.
The ONS confirmed that the baby NHS number or the sequence number192 matched for these cases and, therefore, that the linkage was correct between ONS birth registration and birth notification, regardless of the discordant variables. However, no quality assessment of the sequence number assignment process was available, so 542 of the most suspect cases were flagged. It was decided to exclude these from analyses.
Second, a small number of singleton birth records appeared to be multiple birth records (see Table 31) based on a combination of HES variables suggesting a multiple birth delivery, and other birth registrations existing to the same mother on the same day, yet these were not labelled as a multiple birth by the ONS. Again, these cases were checked by the ONS, which confirmed that they should be multiple births. The error was explained by a delay in some records being registered and received, possibly causing issues with finding the corresponding record in its system.
Third, after quality assurance, a small number of multiple births did not have all the expected number of ONS birth records, for example, a twin birth had only one ONS birth record associated with it rather than two. These were not always explained by stillbirths prior to 24 weeks’ gestation, which should not be registered as births. Investigation revealed that the missing ONS birth records could often be found in the ‘unlinked’ ONS birth records file, to which no HES records were linked. This could be the case even if the mothers’ identifiers, including NHS number, clearly matched.
This was discussed with our contact at the HSCIC, who investigated this. It was explained that these missed links were attributable to either the HES patient index having been updated since the linkage was done originally or linkage error. The project did not attempt to find any further missing links.
The advantage of having the identifiers available to the project team for both ONS birth and HES delivery records made it possible to investigate and explain the above issues, but other research projects may not. Overall, this highlights how researchers and analysts should not assume that any routinely collected administrative datasets and linkages carried out between them are error-free.
Differences between records with correct and incorrect linkage
Checks were carried out to ascertain if the ONS birth records that remained correctly linked to one HES delivery record after the quality assurance procedure, and the ONS birth records with all links to HES delivery records discarded after the quality assurance procedure, differed significantly by key variables. Discarding all links could indicate linkage error, data quality issues or false negatives in the quality assurance methodology.
Table 32 compares the proportions of values for the key variables for both groups, and chi-squared tests were used to test the null hypothesis that the distribution of a variable is the same in the two groups. Variables from the ONS birth records include the match rank of the linkage algorithm, the region of birth, the year of birth, the month of birth, the day of birth based on an 8-day categorisation (including public holidays), the day of birth based on an 11-day categorisation (including specific public holidays and the days before and after them), the hour of birth, the age of the mother, the sex of the baby, the ethnicity of the baby, gestational age, if the birth was a stillbirth and the location of birth. Missing gestational age and missing birthweight in HES were also included.
| Variable | Singleton births | Multiple births | Difference between no link to HES delivery and linked to HES delivery after QA | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Percentage distribution of variables | Percentage distribution of variables | |||||||||
| All birth registrations | All birth registrations linked to HES by HSCIC with a HES delivery record | Linked to HES delivery after QA | No link to HES delivery after QA | All birth registrations | All birth registrations linked to HES by HSCIC with a HES delivery record | Linked to HES delivery after QA | No link to HES delivery after QA | Singletons | Multiples | |
| Match rank | ||||||||||
| 1 | 80.51 | 81.92 | 82.06 | 75.13 | 80.3 | 81.4 | 81.4 | 80.9 | –6.93 | –0.59 |
| 2 | 2.65 | 2.67 | 2.65 | 3.68 | 2.0 | 2.1 | 2.1 | 2.8 | 1.03 | 0.71 |
| 3 | 1.39 | 1.42 | 1.42 | 1.27 | 1.3 | 1.3 | 1.3 | 1.1 | –0.15 | –0.16 |
| 4 | 0.06 | 0.06 | 0.06 | 0.09 | 0.0 | 0.0 | 0.0 | 0.1 | 0.03 | 0.08 |
| 5 | 0.45 | 0.46 | 0.46 | 0.51 | 0.4 | 0.4 | 0.4 | 0.5 | 0.06 | 0.14 |
| 6 | 13.26 | 13.16 | 13.05 | 18.40 | 14.3 | 14.4 | 14.4 | 13.6 | 5.35 | –0.85 |
| 7 | 0.28 | 0.27 | 0.27 | 0.38 | 0.3 | 0.3 | 0.3 | 0.1 | 0.11 | –0.25 |
| 8 | 0.05 | 0.04 | 0.03 | 0.53 | 0.0 | 0.0 | 0.0 | 0.9 | 0.50 | 0.93 |
| Null | 1.36 | 0.00 | 0.00 | 0.00 | 1.3 | 0.0 | 0.0 | 0.0 | 0.00 | 0.00 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p <0 .001 (χ2 = 11,815.13, df = 7) | p < 0.001 (χ2 = 903.69, df = 7) | ||||||||
| Region of birth | ||||||||||
| East Midlands | 6.84 | 6.95 | 7.02 | 3.56 | 6.61 | 6.66 | 6.64 | 7.66 | –3.46 | 1.02 |
| East of England | 10.05 | 10.08 | 10.12 | 8.09 | 10.50 | 10.46 | 10.43 | 12.35 | –2.03 | 1.92 |
| London | 19.36 | 18.92 | 18.93 | 18.34 | 21.91 | 21.14 | 21.03 | 26.86 | –0.59 | 5.83 |
| North East | 4.61 | 4.66 | 4.73 | 0.97 | 4.62 | 4.75 | 4.81 | 1.54 | –3.77 | –3.26 |
| North West | 13.02 | 13.18 | 13.32 | 6.63 | 12.35 | 12.49 | 12.52 | 10.89 | –6.69 | –1.63 |
| South Central | 6.92 | 7.03 | 7.08 | 4.56 | 7.39 | 7.47 | 7.47 | 7.69 | –2.52 | 0.22 |
| South East | 7.68 | 7.76 | 7.83 | 4.38 | 8.48 | 8.53 | 8.52 | 8.72 | –3.45 | 0.19 |
| South West | 8.48 | 8.63 | 8.73 | 3.74 | 8.91 | 9.17 | 9.25 | 4.74 | –5.00 | –4.51 |
| West Midlands | 10.64 | 10.78 | 10.93 | 3.83 | 10.03 | 10.05 | 10.09 | 7.75 | –7.09 | –2.35 |
| Yorkshire/The Humber | 9.69 | 9.85 | 9.97 | 4.07 | 8.92 | 9.05 | 9.07 | 8.46 | –5.90 | –0.61 |
| Elsewhere | 0.17 | 0.15 | 0.10 | 2.34 | 0.05 | 0.04 | 0.04 | 0.43 | 2.24 | 0.39 |
| Home | 2.54 | 2.01 | 1.22 | 39.49 | 0.23 | 0.19 | 0.14 | 2.92 | 38.27 | 2.77 |
| Not known | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 992,568.53, df = 11) | p < 0.001 (χ2 = 1768.25, df = 11) | ||||||||
| Year of birth | ||||||||||
| 2005 | 9.26 | 9.02 | 9.03 | 8.49 | 8.82 | 8.84 | 8.90 | 5.57 | –0.55 | –3.33 |
| 2006 | 9.60 | 9.40 | 9.35 | 11.86 | 9.38 | 9.41 | 9.45 | 7.55 | 2.51 | –1.90 |
| 2007 | 9.88 | 9.78 | 9.70 | 13.28 | 9.63 | 9.79 | 9.81 | 8.57 | 3.57 | –1.23 |
| 2008 | 10.14 | 10.14 | 10.12 | 11.12 | 9.99 | 10.22 | 10.29 | 5.89 | 1.00 | –4.41 |
| 2009 | 10.10 | 10.15 | 10.12 | 11.47 | 10.56 | 10.84 | 10.91 | 7.23 | 1.35 | –3.68 |
| 2010 | 10.29 | 10.41 | 10.45 | 8.78 | 10.32 | 10.69 | 10.79 | 5.32 | –1.67 | –5.47 |
| 2011 | 10.30 | 10.43 | 10.46 | 8.72 | 10.61 | 10.77 | 10.80 | 9.35 | –1.75 | –1.45 |
| 2012 | 10.46 | 10.55 | 10.56 | 10.04 | 10.59 | 10.25 | 10.12 | 17.49 | –0.52 | 7.37 |
| 2013 | 10.01 | 10.10 | 10.15 | 7.94 | 9.97 | 9.52 | 9.40 | 16.29 | –2.21 | 6.89 |
| 2014 | 9.95 | 10.02 | 10.06 | 8.31 | 10.13 | 9.66 | 9.54 | 16.75 | –1.74 | 7.21 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p <0 .001 (χ2 = 4645.84, df = 9) | p < 0.001 (χ2 = 811.59, df = 9) | ||||||||
| Month of birth | ||||||||||
| January | 8.28 | 8.27 | 8.26 | 8.46 | 8.35 | 8.38 | 8.39 | 8.09 | 0.20 | –0.30 |
| February | 7.59 | 7.58 | 7.56 | 8.40 | 7.57 | 7.56 | 7.57 | 6.97 | 0.84 | –0.60 |
| March | 8.29 | 8.26 | 8.21 | 10.19 | 8.22 | 8.20 | 8.17 | 9.89 | 1.98 | 1.72 |
| April | 8.00 | 7.99 | 8.00 | 7.56 | 7.95 | 7.97 | 7.94 | 9.43 | –0.44 | 1.49 |
| May | 8.43 | 8.44 | 8.45 | 7.72 | 8.38 | 8.38 | 8.39 | 7.92 | –0.74 | –0.48 |
| June | 8.27 | 8.28 | 8.29 | 7.91 | 8.55 | 8.52 | 8.52 | 8.57 | –0.38 | 0.06 |
| July | 8.68 | 8.69 | 8.70 | 8.10 | 8.68 | 8.70 | 8.70 | 8.92 | –0.60 | 0.22 |
| August | 8.60 | 8.61 | 8.62 | 8.17 | 8.07 | 8.14 | 8.15 | 7.57 | –0.45 | –0.58 |
| September | 8.65 | 8.67 | 8.68 | 8.21 | 8.39 | 8.43 | 8.46 | 6.89 | –0.47 | –1.57 |
| October | 8.67 | 8.69 | 8.70 | 8.24 | 8.97 | 8.91 | 8.91 | 9.03 | –0.46 | 0.12 |
| November | 8.21 | 8.22 | 8.22 | 8.08 | 8.43 | 8.40 | 8.41 | 7.89 | –0.14 | –0.53 |
| December | 8.32 | 8.32 | 8.30 | 8.95 | 8.44 | 8.39 | 8.38 | 8.83 | 0.65 | 0.45 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 1072.06, df = 11) | p < 0.001 (χ2 = 42.23, df = 11) | ||||||||
| Day of birth: 8-day categorisation | ||||||||||
| Monday | 13.25 | 13.25 | 13.25 | 13.27 | 13.75 | 13.76 | 13.74 | 14.49 | 0.02 | 0.75 |
| Tuesday | 14.63 | 14.64 | 14.64 | 14.53 | 16.41 | 16.38 | 16.39 | 15.72 | –0.11 | –0.67 |
| Wednesday | 14.90 | 14.90 | 14.90 | 14.86 | 16.74 | 16.80 | 16.80 | 16.29 | –0.04 | –0.51 |
| Thursday | 15.03 | 15.03 | 15.04 | 14.87 | 17.31 | 17.29 | 17.29 | 17.63 | –0.17 | 0.35 |
| Friday | 14.73 | 14.73 | 14.73 | 14.65 | 16.66 | 16.65 | 16.68 | 15.06 | –0.08 | –1.62 |
| Saturday | 12.96 | 12.95 | 12.94 | 13.32 | 9.77 | 9.76 | 9.74 | 10.95 | 0.38 | 1.21 |
| Sunday | 12.14 | 12.15 | 12.15 | 12.10 | 7.75 | 7.75 | 7.75 | 8.00 | –0.05 | 0.25 |
| Public holiday | 2.36 | 2.36 | 2.36 | 2.40 | 1.61 | 1.62 | 1.61 | 1.86 | 0.04 | 0.25 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 36.20, df = 7) | p = 0.0333 (χ2 = 15.22, df = 7) | ||||||||
| Day of birth: 11-day categorisation | ||||||||||
| Monday | 13.05 | 13.05 | 13.05 | 12.99 | 13.54 | 13.55 | 13.54 | 14.32 | –0.07 | 0.78 |
| Tuesday | 13.32 | 13.33 | 13.33 | 13.26 | 14.95 | 14.92 | 14.93 | 14.58 | –0.06 | –0.35 |
| Wednesday | 14.59 | 14.59 | 14.59 | 14.46 | 16.37 | 16.43 | 16.44 | 16.00 | –0.12 | –0.43 |
| Thursday | 14.55 | 14.56 | 14.56 | 14.24 | 16.78 | 16.76 | 16.76 | 16.95 | –0.32 | 0.19 |
| Friday | 13.59 | 13.59 | 13.59 | 13.55 | 15.39 | 15.37 | 15.40 | 13.63 | –0.04 | –1.77 |
| Saturday | 12.96 | 12.95 | 12.94 | 13.47 | 9.77 | 9.76 | 9.74 | 10.95 | 0.53 | 1.21 |
| Sunday | 12.14 | 12.15 | 12.15 | 12.24 | 7.75 | 7.75 | 7.75 | 8.00 | 0.09 | 0.25 |
| After public holiday | 1.68 | 1.68 | 1.69 | 1.62 | 1.89 | 1.88 | 1.88 | 1.60 | –0.07 | –0.28 |
| Before public holiday | 1.75 | 1.75 | 1.75 | 1.72 | 1.95 | 1.96 | 1.96 | 2.11 | –0.03 | 0.16 |
| Christmas | 0.43 | 0.43 | 0.43 | 0.50 | 0.29 | 0.29 | 0.29 | 0.37 | 0.07 | 0.09 |
| Public holiday | 1.93 | 1.93 | 1.93 | 1.95 | 1.33 | 1.33 | 1.33 | 1.49 | 0.03 | 0.16 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 60.47, df = 10) | p = 0.0525 (χ2 = 18.15, df = 10) | ||||||||
| Hour of birth | ||||||||||
| 00.00–02.59 | 12.35 | 12.36 | 12.35 | 12.84 | 8.42 | 8.46 | 8.45 | 9.00 | 0.49 | 0.56 |
| 03.00–05.59 | 12.15 | 12.15 | 12.12 | 13.75 | 7.74 | 7.82 | 7.81 | 8.06 | 1.64 | 0.25 |
| 06.00–08.59 | 10.79 | 10.76 | 10.73 | 12.53 | 6.67 | 6.69 | 6.67 | 8.03 | 1.80 | 1.36 |
| 09.00–11.59 | 16.06 | 16.10 | 16.13 | 14.39 | 26.62 | 26.56 | 26.53 | 27.98 | –1.74 | 1.45 |
| 12.00–14.59 | 12.88 | 12.87 | 12.90 | 11.80 | 17.35 | 17.27 | 17.28 | 16.95 | –1.10 | –0.33 |
| 15.00–17.59 | 11.86 | 11.85 | 11.87 | 10.93 | 13.41 | 13.37 | 13.40 | 11.77 | –0.94 | –1.63 |
| 18.00–20.59 | 11.19 | 11.18 | 11.19 | 11.02 | 9.65 | 9.65 | 9.67 | 8.49 | –0.16 | –1.19 |
| 21.00–23.59 | 11.81 | 11.81 | 11.81 | 11.80 | 9.18 | 9.21 | 9.22 | 8.69 | –0.01 | –0.53 |
| Null | 0.91 | 0.91 | 0.91 | 0.93 | 0.96 | 0.96 | 0.96 | 1.03 | 0.03 | 0.07 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 1146.18, df = 8) | p = < 0.001 (χ2 = 26.99, df = 8) | ||||||||
| Age of mother (years) | ||||||||||
| Under 15 | 0.03 | 0.03 | 0.03 | 0.02 | 0.01 | 0.01 | 0.01 | 0.00 | –0.01 | –0.01 |
| 15–19 | 3.16 | 3.16 | 3.18 | 2.28 | 1.24 | 1.26 | 1.27 | 0.86 | –0.89 | –0.41 |
| 20–24 | 18.48 | 18.57 | 18.59 | 17.39 | 11.14 | 11.41 | 11.46 | 8.75 | –1.20 | –2.72 |
| 25–29 | 27.29 | 27.42 | 27.42 | 27.44 | 22.70 | 23.10 | 23.19 | 18.12 | 0.01 | –5.07 |
| 30–34 | 28.72 | 28.73 | 28.70 | 30.39 | 32.75 | 32.85 | 32.83 | 33.98 | 1.69 | 1.16 |
| 35–39 | 16.13 | 15.99 | 15.96 | 17.20 | 23.75 | 23.44 | 23.40 | 25.81 | 1.24 | 2.41 |
| 40–44 | 3.60 | 3.53 | 3.54 | 3.19 | 5.99 | 5.64 | 5.57 | 9.46 | –0.35 | 3.89 |
| 45 and over | 0.20 | 0.19 | 0.19 | 0.19 | 1.34 | 1.17 | 1.15 | 2.14 | 0.00 | 0.99 |
| Null | 2.39 | 2.39 | 2.40 | 1.91 | 1.08 | 1.12 | 1.12 | 0.89 | –0.49 | –0.24 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 716.36, df = 8) | p < 0.001 (χ2 = 196.19, df = 8) | ||||||||
| Sex of baby | ||||||||||
| Female | 48.69 | 48.69 | 48.66 | 49.65 | 49.87 | 49.91 | 49.93 | 48.84 | 0.99 | –1.09 |
| Male | 51.31 | 51.31 | 51.34 | 50.35 | 50.13 | 50.09 | 50.07 | 51.16 | –0.99 | 1.09 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3499 | ||
| χ2 test | p < 0.001 (χ2 = 49.40, df = 1) | p = 0.2018 (χ2 = 1.63, df = 1) | ||||||||
| Ethnicity of baby | ||||||||||
| Bangladeshi | 1.41 | 1.43 | 1.43 | 1.00 | 0.86 | 0.89 | 0.89 | 0.69 | –0.43 | –0.20 |
| Indian | 3.00 | 3.02 | 3.04 | 1.90 | 2.73 | 2.62 | 2.60 | 3.63 | –1.14 | 1.03 |
| Pakistani | 4.12 | 4.15 | 4.18 | 2.81 | 2.98 | 2.99 | 2.98 | 3.06 | –1.37 | 0.07 |
| Black African | 3.21 | 3.14 | 3.12 | 3.90 | 3.73 | 3.67 | 3.64 | 5.54 | 0.77 | 1.91 |
| Black Caribbean | 0.97 | 0.97 | 0.97 | 0.91 | 1.09 | 1.09 | 1.10 | 0.97 | –0.06 | –0.13 |
| White British | 63.44 | 63.99 | 63.97 | 64.75 | 65.11 | 65.85 | 65.90 | 62.79 | 0.78 | –3.12 |
| White other | 8.19 | 8.10 | 8.13 | 6.75 | 8.38 | 8.21 | 8.23 | 7.14 | –1.38 | –1.08 |
| Other | 9.43 | 9.34 | 9.35 | 8.71 | 8.85 | 8.65 | 8.65 | 8.69 | –0.64 | 0.03 |
| Not known | 6.20 | 5.87 | 5.80 | 9.21 | 6.26 | 6.02 | 5.99 | 7.40 | 3.41 | 1.41 |
| Null | 0.02 | 0.01 | 0.01 | 0.07 | 0.02 | 0.01 | 0.01 | 0.09 | 0.06 | 0.08 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 4730.98, df = 9) | p < 0.001 (χ2 = 151.29, df = 9) | ||||||||
| Gestational age | ||||||||||
| Missing or less than 22 weeks | 0.79 | 0.78 | 0.76 | 1.29 | 0.93 | 0.92 | 0.90 | 1.83 | 0.53 | 0.92 |
| Preterm | 6.08 | 6.07 | 6.05 | 7.13 | 54.10 | 53.86 | 53.84 | 54.93 | 1.08 | 1.09 |
| Term | 89.17 | 89.18 | 89.19 | 88.63 | 44.85 | 45.09 | 45.12 | 43.13 | –0.56 | –2.00 |
| Post-term | 3.96 | 3.97 | 4.00 | 2.95 | 0.13 | 0.13 | 0.13 | 0.11 | –1.04 | –0.01 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 1048.57, df = 3) | p < 0.001 (χ2 = 35.71, df = 3) | ||||||||
| Stillbirth | ||||||||||
| No | 99.52 | 99.53 | 99.58 | 97.30 | 98.87 | 98.88 | 98.92 | 96.46 | –2.28 | –2.47 |
| Yes | 0.48 | 0.47 | 0.42 | 2.70 | 1.13 | 1.12 | 1.08 | 3.54 | 2.28 | 2.47 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 205,684 | 193,270 | 12,414 | ||
| χ2 test | p < 0.001 (χ2 = 14,053.04, df = 1) | p < 0.001 (χ2 = 188.14, df = 1) | ||||||||
| Variable | All birth registrations | All birth registrations and HES links by HSCIC | Linked to HES after QA | Broken links after QA | All birth registrations | All birth registrations and HES links by HSCIC | Linked to HES after QA | Broken links after QA | Singletons | Multiples |
| Gestational age missing on HES | ||||||||||
| No | 68.94 | 73.50 | 52.70 | 74.18 | 79.73 | 68.86 | –20.80 | –10.87 | ||
| Yes | 31.06 | 26.50 | 47.30 | 25.82 | 20.27 | 31.14 | 20.80 | 10.87 | ||
| Total | 6,468,586 | 7,862,903 | 6,138,487 | 1,724,416 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 272,051.09, df = 1) | p < 0.001 (χ2 = 6086.08, df = 1) | ||||||||
| Birthweight missing on HES | ||||||||||
| No | 80.69 | 83.38 | 71.12 | 85.88 | 89.52 | 82.40 | –12.26 | –7.13 | ||
| Yes | 19.31 | 16.62 | 28.88 | 14.12 | 10.48 | 17.60 | 12.26 | 7.13 | ||
| Total | 6,468,586 | 7,862,903 | 6,138,487 | 1,724,416 | 208,326 | 395,202 | 193,270 | 201,932 | ||
| χ2 test | p < 0.001 (χ2 = 129,812.25, df = 1) | p < 0.001 (χ2 = 4814.69, df = 1) | ||||||||
| Location of birth Assigned Trust code | ||||||||||
| MMC | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| MML | 0.07 | 0.00 | 0.00 | 0.04 | 0.04 | 0.00 | 0.00 | 0.00 | 0.04 | 0.00 |
| MMS | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| PPJ | 0.04 | 0.01 | 0.00 | 0.26 | 0.00 | 0.00 | 0.00 | 0.06 | 0.26 | 0.06 |
| PPL | 0.30 | 0.04 | 0.00 | 1.74 | 0.40 | 0.05 | 0.00 | 2.52 | 1.74 | 2.51 |
| PPN | 0.00 | 0.00 | 0.00 | 0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.00 |
| PPT | 0.00 | 0.00 | 0.00 | 0.08 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.00 |
| R1F | 0.18 | 0.18 | 0.18 | 0.27 | 0.18 | 0.18 | 0.18 | 0.31 | 0.09 | 0.13 |
| RA2 | 0.48 | 0.49 | 0.49 | 0.21 | 0.57 | 0.59 | 0.60 | 0.23 | –0.28 | –0.37 |
| RA4 | 0.22 | 0.23 | 0.23 | 0.11 | 0.18 | 0.19 | 0.18 | 0.37 | –0.12 | 0.19 |
| RA7 | 0.84 | 0.86 | 0.87 | 0.35 | 0.84 | 0.89 | 0.90 | 0.23 | –0.52 | –0.67 |
| RA9 | 0.35 | 0.35 | 0.35 | 0.10 | 0.33 | 0.33 | 0.33 | 0.11 | –0.25 | –0.22 |
| RAE | 0.89 | 0.91 | 0.92 | 0.43 | 0.66 | 0.69 | 0.68 | 1.00 | –0.49 | 0.32 |
| RAJ | 0.54 | 0.55 | 0.55 | 0.24 | 0.57 | 0.56 | 0.55 | 0.86 | –0.31 | 0.31 |
| RAL | 0.48 | 0.48 | 0.49 | 0.13 | 0.44 | 0.44 | 0.44 | 0.34 | –0.36 | –0.10 |
| RAP | 0.55 | 0.55 | 0.55 | 0.21 | 0.49 | 0.49 | 0.49 | 0.34 | –0.34 | –0.15 |
| RAS | 0.60 | 0.61 | 0.62 | 0.15 | 0.57 | 0.59 | 0.59 | 0.40 | –0.47 | –0.19 |
| RAX | 0.83 | 0.84 | 0.85 | 0.32 | 0.99 | 0.93 | 0.93 | 1.23 | –0.52 | 0.30 |
| RBA | 0.47 | 0.47 | 0.48 | 0.27 | 0.55 | 0.55 | 0.55 | 0.46 | –0.21 | –0.09 |
| RBD | 0.30 | 0.31 | 0.32 | 0.04 | 0.31 | 0.32 | 0.33 | 0.14 | –0.28 | –0.18 |
| RBK | 0.61 | 0.63 | 0.64 | 0.13 | 0.50 | 0.51 | 0.51 | 0.29 | –0.50 | –0.23 |
| RBL | 0.52 | 0.53 | 0.54 | 0.14 | 0.52 | 0.53 | 0.53 | 0.26 | –0.40 | –0.28 |
| RBN | 0.50 | 0.49 | 0.50 | 0.08 | 0.41 | 0.41 | 0.41 | 0.06 | –0.43 | –0.36 |
| RBT | 0.42 | 0.42 | 0.42 | 0.45 | 0.39 | 0.39 | 0.39 | 0.37 | 0.02 | –0.02 |
| RBZ | 0.23 | 0.24 | 0.24 | 0.10 | 0.21 | 0.22 | 0.22 | 0.29 | –0.14 | 0.07 |
| RC1 | 0.46 | 0.46 | 0.46 | 0.39 | 0.48 | 0.46 | 0.46 | 0.60 | –0.07 | 0.14 |
| RC3 | 0.43 | 0.40 | 0.40 | 0.09 | 0.35 | 0.33 | 0.33 | 0.40 | –0.32 | 0.07 |
| RC9 | 0.74 | 0.75 | 0.76 | 0.50 | 0.81 | 0.80 | 0.80 | 0.66 | –0.25 | –0.15 |
| RCB | 0.49 | 0.50 | 0.51 | 0.05 | 0.48 | 0.51 | 0.51 | 0.34 | –0.46 | –0.17 |
| RCC | 0.25 | 0.25 | 0.23 | 1.04 | 0.17 | 0.17 | 0.16 | 0.69 | 0.81 | 0.52 |
| RCD | 0.29 | 0.30 | 0.31 | 0.04 | 0.25 | 0.26 | 0.27 | 0.00 | –0.27 | –0.27 |
| RCF | 0.36 | 0.37 | 0.38 | 0.08 | 0.31 | 0.32 | 0.32 | 0.06 | –0.30 | –0.27 |
| RCX | 0.34 | 0.34 | 0.35 | 0.05 | 0.33 | 0.34 | 0.34 | 0.06 | –0.30 | –0.29 |
| RD1 | 0.72 | 0.72 | 0.72 | 0.43 | 0.74 | 0.75 | 0.76 | 0.34 | –0.29 | –0.42 |
| RD3 | 0.72 | 0.73 | 0.74 | 0.18 | 0.72 | 0.74 | 0.75 | 0.26 | –0.57 | –0.49 |
| RD7 | 0.75 | 0.76 | 0.78 | 0.16 | 0.69 | 0.69 | 0.68 | 0.74 | –0.61 | 0.06 |
| RD8 | 0.55 | 0.55 | 0.54 | 1.02 | 0.52 | 0.51 | 0.50 | 1.23 | 0.48 | 0.73 |
| RDD | 0.64 | 0.66 | 0.67 | 0.11 | 0.61 | 0.64 | 0.65 | 0.14 | –0.57 | –0.51 |
| RDE | 0.56 | 0.57 | 0.57 | 0.31 | 0.58 | 0.58 | 0.57 | 0.80 | –0.26 | 0.23 |
| RDU | 0.72 | 0.74 | 0.75 | 0.31 | 0.79 | 0.80 | 0.80 | 0.69 | –0.43 | –0.11 |
| RE9 | 0.22 | 0.23 | 0.23 | 0.05 | 0.16 | 0.17 | 0.17 | 0.06 | –0.18 | –0.11 |
| REF | 0.62 | 0.64 | 0.64 | 0.30 | 0.59 | 0.61 | 0.62 | 0.34 | –0.34 | –0.27 |
| REP | 1.22 | 1.24 | 1.26 | 0.20 | 1.59 | 1.64 | 1.66 | 0.74 | –1.07 | –0.91 |
| RF4 | 1.35 | 1.32 | 1.35 | 0.34 | 1.35 | 1.31 | 1.31 | 1.09 | –1.01 | –0.23 |
| RFF | 0.42 | 0.43 | 0.43 | 0.11 | 0.37 | 0.38 | 0.39 | 0.11 | –0.33 | –0.27 |
| RFR | 0.42 | 0.42 | 0.42 | 0.12 | 0.41 | 0.41 | 0.41 | 0.46 | –0.30 | 0.05 |
| RFS | 0.43 | 0.44 | 0.45 | 0.09 | 0.38 | 0.40 | 0.41 | 0.11 | –0.36 | –0.29 |
| RFW | 0.64 | 0.63 | 0.62 | 1.13 | 0.54 | 0.49 | 0.47 | 1.23 | 0.51 | 0.76 |
| RGC | 0.77 | 0.76 | 0.77 | 0.33 | 0.74 | 0.72 | 0.72 | 0.80 | –0.43 | 0.08 |
| RGN | 0.64 | 0.65 | 0.66 | 0.11 | 0.60 | 0.60 | 0.60 | 0.63 | –0.54 | 0.03 |
| RGP | 0.32 | 0.33 | 0.33 | 0.06 | 0.29 | 0.29 | 0.29 | 0.17 | –0.27 | –0.12 |
| RGQ | 0.54 | 0.52 | 0.48 | 2.48 | 0.53 | 0.49 | 0.46 | 1.94 | 2.00 | 1.48 |
| RGR | 0.37 | 0.38 | 0.39 | 0.04 | 0.35 | 0.36 | 0.36 | 0.17 | –0.34 | –0.19 |
| RGT | 0.80 | 0.82 | 0.84 | 0.08 | 1.05 | 1.10 | 1.11 | 0.11 | –0.76 | –1.00 |
| RH8 | 0.58 | 0.59 | 0.60 | 0.16 | 0.65 | 0.67 | 0.68 | 0.40 | –0.44 | –0.28 |
| RHM | 0.85 | 0.86 | 0.87 | 0.45 | 0.86 | 0.87 | 0.88 | 0.34 | –0.42 | –0.54 |
| RHQ | 1.03 | 1.05 | 1.07 | 0.20 | 1.16 | 1.14 | 1.13 | 1.74 | –0.87 | 0.62 |
| RHU | 0.86 | 0.87 | 0.88 | 0.30 | 0.95 | 0.99 | 1.00 | 0.40 | –0.58 | –0.60 |
| RHW | 0.83 | 0.85 | 0.86 | 0.39 | 0.95 | 0.99 | 0.99 | 0.74 | –0.48 | –0.25 |
| RJ1 | 0.97 | 0.98 | 0.99 | 0.30 | 1.24 | 1.26 | 1.28 | 0.49 | –0.70 | –0.79 |
| RJ2 | 0.55 | 0.53 | 0.53 | 0.46 | 0.52 | 0.53 | 0.53 | 0.29 | –0.07 | –0.25 |
| RJ6 | 0.65 | 0.65 | 0.65 | 0.68 | 0.61 | 0.61 | 0.59 | 1.91 | 0.03 | 1.33 |
| RJ7 | 0.74 | 0.75 | 0.76 | 0.26 | 0.99 | 1.00 | 1.01 | 0.77 | –0.50 | –0.24 |
| RJC | 0.40 | 0.41 | 0.41 | 0.14 | 0.36 | 0.36 | 0.36 | 0.29 | –0.27 | –0.07 |
| RJD | 0.31 | 0.31 | 0.32 | 0.08 | 0.28 | 0.27 | 0.28 | 0.06 | –0.24 | –0.22 |
| RJE | 0.85 | 0.86 | 0.87 | 0.29 | 0.77 | 0.79 | 0.80 | 0.31 | –0.58 | –0.48 |
| RJF | 0.54 | 0.54 | 0.54 | 0.46 | 0.48 | 0.50 | 0.50 | 0.34 | –0.09 | –0.16 |
| RJL | 0.69 | 0.70 | 0.71 | 0.46 | 0.59 | 0.61 | 0.61 | 0.57 | –0.24 | –0.04 |
| RJN | 0.30 | 0.31 | 0.31 | 0.02 | 0.30 | 0.31 | 0.32 | 0.09 | –0.29 | –0.23 |
| RJR | 0.47 | 0.48 | 0.49 | 0.08 | 0.47 | 0.48 | 0.49 | 0.11 | –0.41 | –0.37 |
| RJZ | 0.74 | 0.73 | 0.73 | 0.47 | 1.02 | 0.97 | 0.97 | 0.89 | –0.26 | –0.09 |
| RK5 | 0.46 | 0.47 | 0.48 | 0.19 | 0.41 | 0.43 | 0.43 | 0.06 | –0.29 | –0.38 |
| RK9 | 0.66 | 0.67 | 0.66 | 1.15 | 0.74 | 0.72 | 0.72 | 1.03 | 0.49 | 0.31 |
| RKB | 0.83 | 0.85 | 0.87 | 0.25 | 0.89 | 0.92 | 0.93 | 0.11 | –0.62 | –0.82 |
| RKE (Whittington) | 0.56 | 0.48 | 0.40 | 4.43 | 0.59 | 0.47 | 0.40 | 4.34 | 4.03 | 3.94 |
| RL4 | 0.57 | 0.58 | 0.59 | 0.12 | 0.60 | 0.62 | 0.62 | 0.43 | –0.47 | –0.19 |
| RLN | 0.50 | 0.50 | 0.51 | 0.06 | 0.44 | 0.45 | 0.46 | 0.00 | –0.45 | –0.46 |
| RLQ | 0.27 | 0.28 | 0.29 | 0.07 | 0.26 | 0.25 | 0.25 | 0.29 | –0.22 | 0.03 |
| RLT | 0.35 | 0.36 | 0.36 | 0.05 | 0.29 | 0.31 | 0.31 | 0.11 | –0.32 | –0.20 |
| RLU | 1.11 | 1.10 | 1.11 | 0.52 | 1.32 | 1.27 | 1.26 | 1.91 | –0.58 | 0.66 |
| RM1 | 0.84 | 0.86 | 0.88 | 0.04 | 0.82 | 0.86 | 0.87 | 0.20 | –0.84 | –0.67 |
| RM2 | 0.56 | 0.56 | 0.55 | 1.04 | 0.55 | 0.52 | 0.50 | 1.43 | 0.49 | 0.93 |
| RM4 | 0.11 | 0.11 | 0.11 | 0.24 | 0.08 | 0.08 | 0.08 | 0.17 | 0.13 | 0.09 |
| RMC | 0.74 | 0.76 | 0.78 | 0.13 | 0.61 | 0.63 | 0.64 | 0.11 | –0.64 | –0.53 |
| RMP | 0.40 | 0.41 | 0.41 | 0.12 | 0.31 | 0.32 | 0.32 | 0.17 | –0.30 | –0.15 |
| RN1 | 0.41 | 0.42 | 0.43 | 0.16 | 0.44 | 0.44 | 0.44 | 0.51 | –0.27 | 0.07 |
| RN3 | 0.63 | 0.65 | 0.66 | 0.17 | 0.62 | 0.66 | 0.66 | 0.26 | –0.49 | –0.41 |
| RN5 | 0.42 | 0.42 | 0.43 | 0.07 | 0.45 | 0.48 | 0.48 | 0.06 | –0.36 | –0.43 |
| RN7 | 0.59 | 0.60 | 0.62 | 0.07 | 0.52 | 0.54 | 0.55 | 0.11 | –0.54 | –0.43 |
| RNA | 0.68 | 0.69 | 0.70 | 0.21 | 0.60 | 0.59 | 0.60 | 0.54 | –0.50 | –0.05 |
| RNH | 0.82 | 0.79 | 0.78 | 1.18 | 0.63 | 0.61 | 0.61 | 0.63 | 0.40 | 0.02 |
| RNJ | 0.68 | 0.69 | 0.70 | 0.14 | 0.57 | 0.57 | 0.57 | 0.49 | –0.56 | –0.09 |
| RNL | 0.47 | 0.46 | 0.46 | 0.51 | 0.42 | 0.41 | 0.41 | 0.66 | 0.05 | 0.25 |
| RNQ | 0.56 | 0.57 | 0.57 | 0.12 | 0.54 | 0.55 | 0.56 | 0.09 | –0.45 | –0.48 |
| RNS | 0.65 | 0.66 | 0.67 | 0.13 | 0.72 | 0.75 | 0.75 | 0.57 | –0.54 | –0.18 |
| RNZ | 0.34 | 0.35 | 0.35 | 0.08 | 0.43 | 0.45 | 0.45 | 0.06 | –0.27 | –0.40 |
| RP5 | 0.79 | 0.81 | 0.82 | 0.13 | 0.70 | 0.71 | 0.71 | 0.71 | –0.69 | 0.01 |
| RPA | 0.68 | 0.69 | 0.70 | 0.25 | 0.73 | 0.76 | 0.76 | 0.51 | –0.45 | –0.25 |
| RQ8 | 0.64 | 0.64 | 0.62 | 1.30 | 0.70 | 0.65 | 0.63 | 2.17 | 0.68 | 1.55 |
| RQM | 0.81 | 0.81 | 0.82 | 0.49 | 1.15 | 1.11 | 1.11 | 1.00 | –0.33 | –0.11 |
| RQQ | 0.36 | 0.37 | 0.37 | 0.09 | 0.34 | 0.35 | 0.35 | 0.11 | –0.28 | –0.24 |
| RQW | 0.56 | 0.55 | 0.56 | 0.19 | 0.59 | 0.57 | 0.57 | 0.69 | –0.37 | 0.12 |
| RQX | 0.74 | 0.74 | 0.73 | 1.02 | 0.97 | 0.97 | 0.97 | 0.86 | 0.29 | –0.12 |
| RR1 | 1.60 | 1.64 | 1.66 | 0.62 | 1.34 | 1.38 | 1.39 | 0.89 | –1.04 | –0.50 |
| RR7 | 0.28 | 0.28 | 0.29 | 0.05 | 0.29 | 0.29 | 0.29 | 0.29 | –0.24 | 0.00 |
| RR8 | 1.40 | 1.38 | 1.39 | 0.64 | 1.47 | 1.43 | 1.43 | 1.34 | –0.76 | –0.08 |
| RRF | 0.45 | 0.45 | 0.46 | 0.20 | 0.42 | 0.43 | 0.43 | 0.40 | –0.26 | –0.03 |
| RRV | 0.74 | 0.75 | 0.76 | 0.37 | 1.35 | 1.35 | 1.36 | 0.94 | –0.38 | –0.42 |
| RTD | 0.97 | 0.98 | 1.00 | 0.26 | 1.25 | 1.29 | 1.30 | 0.57 | –0.74 | –0.73 |
| RTE | 0.93 | 0.95 | 0.97 | 0.11 | 0.98 | 1.03 | 1.04 | 0.17 | –0.86 | –0.87 |
| RTF | 0.47 | 0.48 | 0.49 | 0.08 | 0.34 | 0.35 | 0.36 | 0.00 | –0.42 | –0.36 |
| RTG | 0.84 | 0.86 | 0.87 | 0.32 | 0.79 | 0.79 | 0.78 | 1.17 | –0.55 | 0.39 |
| RTH | 1.26 | 1.28 | 1.27 | 1.43 | 1.56 | 1.52 | 1.50 | 3.06 | 0.16 | 1.56 |
| RTK | 0.59 | 0.60 | 0.61 | 0.07 | 0.77 | 0.79 | 0.81 | 0.06 | –0.54 | –0.75 |
| RTP | 0.64 | 0.63 | 0.64 | 0.31 | 0.70 | 0.69 | 0.69 | 0.71 | –0.33 | 0.02 |
| RTR | 0.80 | 0.80 | 0.81 | 0.20 | 0.91 | 0.93 | 0.95 | 0.17 | –0.61 | –0.77 |
| RTX | 0.51 | 0.52 | 0.52 | 0.25 | 0.41 | 0.42 | 0.43 | 0.23 | –0.27 | –0.20 |
| RV8 | 0.74 | 0.75 | 0.76 | 0.27 | 0.61 | 0.59 | 0.60 | 0.49 | –0.49 | –0.11 |
| RVJ | 0.87 | 0.89 | 0.91 | 0.21 | 1.02 | 1.05 | 1.06 | 0.29 | –0.70 | –0.77 |
| RVL | 0.96 | 0.93 | 0.90 | 2.27 | 0.95 | 0.89 | 0.87 | 2.26 | 1.37 | 1.39 |
| RVR | 0.75 | 0.75 | 0.76 | 0.27 | 0.86 | 0.85 | 0.86 | 0.63 | –0.49 | –0.23 |
| RVV | 1.03 | 1.03 | 1.02 | 1.90 | 1.05 | 1.00 | 0.96 | 3.14 | 0.89 | 2.19 |
| RVW | 0.53 | 0.53 | 0.54 | 0.08 | 0.51 | 0.53 | 0.54 | 0.06 | –0.46 | –0.48 |
| RVY | 0.45 | 0.44 | 0.45 | 0.09 | 0.39 | 0.39 | 0.39 | 0.57 | –0.37 | 0.18 |
| RW3 | 1.27 | 1.27 | 1.28 | 0.93 | 1.48 | 1.43 | 1.41 | 2.52 | –0.35 | 1.11 |
| RW6 | 1.52 | 1.55 | 1.58 | 0.24 | 1.20 | 1.24 | 1.25 | 0.77 | –1.34 | –0.47 |
| RWA | 0.84 | 0.86 | 0.87 | 0.16 | 0.79 | 0.81 | 0.82 | 0.37 | –0.71 | –0.45 |
| RWD | 0.86 | 0.86 | 0.85 | 0.97 | 0.72 | 0.74 | 0.73 | 1.26 | 0.12 | 0.53 |
| RWE | 1.54 | 1.56 | 1.57 | 0.96 | 1.44 | 1.42 | 1.40 | 2.37 | –0.61 | 0.97 |
| RWF | 0.76 | 0.77 | 0.78 | 0.33 | 0.98 | 1.01 | 1.02 | 0.51 | –0.45 | –0.50 |
| RWG | 0.82 | 0.84 | 0.85 | 0.33 | 0.91 | 0.89 | 0.88 | 1.03 | –0.52 | 0.15 |
| RWH | 0.80 | 0.80 | 0.78 | 1.73 | 0.94 | 0.94 | 0.92 | 2.00 | 0.95 | 1.08 |
| RWJ | 0.54 | 0.56 | 0.57 | 0.08 | 0.52 | 0.55 | 0.55 | 0.40 | –0.49 | –0.15 |
| RWP | 0.87 | 0.87 | 0.89 | 0.28 | 0.89 | 0.83 | 0.84 | 0.71 | –0.60 | –0.12 |
| RWW | 0.48 | 0.49 | 0.50 | 0.22 | 0.44 | 0.45 | 0.46 | 0.23 | –0.28 | –0.23 |
| RWY | 0.86 | 0.87 | 0.88 | 0.43 | 0.78 | 0.79 | 0.79 | 0.86 | –0.46 | 0.07 |
| RX1 | 1.50 | 1.53 | 1.55 | 0.77 | 1.60 | 1.58 | 1.57 | 2.03 | –0.78 | 0.46 |
| RXC | 0.58 | 0.59 | 0.60 | 0.13 | 0.49 | 0.49 | 0.49 | 0.54 | –0.47 | 0.06 |
| RXF | 0.98 | 1.00 | 1.02 | 0.19 | 0.79 | 0.83 | 0.84 | 0.20 | –0.83 | –0.64 |
| RXH | 0.83 | 0.82 | 0.83 | 0.33 | 1.08 | 1.07 | 1.06 | 1.51 | –0.50 | 0.45 |
| RXK | 0.89 | 0.89 | 0.90 | 0.43 | 0.68 | 0.67 | 0.66 | 1.00 | –0.47 | 0.34 |
| RXL | 0.44 | 0.45 | 0.46 | 0.16 | 0.39 | 0.41 | 0.41 | 0.17 | –0.30 | –0.24 |
| RXN | 0.67 | 0.68 | 0.69 | 0.52 | 0.61 | 0.62 | 0.61 | 0.74 | –0.16 | 0.13 |
| RXP | 0.83 | 0.85 | 0.86 | 0.19 | 0.72 | 0.74 | 0.74 | 0.40 | –0.67 | –0.34 |
| RXQ | 0.81 | 0.82 | 0.83 | 0.30 | 0.78 | 0.80 | 0.81 | 0.29 | –0.53 | –0.53 |
| RXR | 0.97 | 0.96 | 0.97 | 0.88 | 0.82 | 0.84 | 0.84 | 0.69 | –0.09 | –0.15 |
| RXW | 0.75 | 0.77 | 0.78 | 0.18 | 0.76 | 0.79 | 0.80 | 0.46 | –0.60 | –0.34 |
| RYJ | 1.43 | 1.44 | 1.46 | 0.47 | 2.38 | 2.32 | 2.33 | 1.69 | –0.99 | –0.65 |
| RYQ | 1.50 | 1.53 | 1.55 | 0.48 | 1.61 | 1.67 | 1.68 | 0.80 | –1.07 | –0.88 |
| RYR | 0.79 | 0.80 | 0.80 | 0.47 | 0.81 | 0.80 | 0.80 | 0.69 | –0.33 | –0.11 |
| XXX | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Total | 6,468,586 | 6,268,013 | 6,138,487 | 129,526 | 208,326 | 196,769 | 193,270 | 3,499 | ||
| χ2 test | p < 0.001 (χ2 = 6,267,610.79, df = 151) | p < 0.001 (χ2 = 9154.95, df = 151) | ||||||||
The null hypothesis is rejected for all variables except for sex, day of birth based on an 8-day categorisation and day of birth based on an 11-day categorisation in multiple births. Finding significant differences is to be expected because the dataset is large and the chi-squared test can pick up subtle differences, but this does not tell us very much. Comparing the difference in the percentage distribution of values for each variable for the two groups provides more information on how they differ. This information is given in Table 33 for singleton and multiple births for which the difference is over 1%.
| Variable | Singleton births | Multiple births | ||
|---|---|---|---|---|
| Value | Difference in percentagesa | Value | Difference in percentagesa | |
| Match rank of linkage algorithm | 6 | 5.4 | ||
| Region of birth | Elsewhere | 2.3 | East of England | 1.9 |
| Home | 38.3 | London | 5.8 | |
| Home | 2.8 | |||
| Year of birth | 2006 | 2.5 | 2012 | 7.4 |
| 2007 | 3.6 | 2013 | 6.9 | |
| 2009 | 1.4 | 2014 | 7.2 | |
| Month of birth | March | 2.0 | March | 1.7 |
| April | 1.5 | |||
| Day of birth (8-day categorisation) | Saturday | 1.2 | ||
| Day of birth (11-day categorisation) | Saturday | 1.2 | ||
| Hour of birth | 03.00–05.59 | 1.7 | 06.00–08.59 | 1.4 |
| 06.00–08.59 | 1.8 | 09.00–11.59 | 1.5 | |
| Sex of baby | Male | 1.1 | ||
| Age of mother (years) | 30–34 | 1.7 | 30–34 | 1.2 |
| 35–39 | 1.3 | 35–39 | 2.4 | |
| 40–44 | 3.9 | |||
| Ethnicity of baby | Not known | 3.4 | Black African | 1.9 |
| Not known | 1.4 | |||
| Gestational age | Preterm | 1.1 | Preterm | 1.1 |
| Stillbirth | Yes | 2.3 | Yes | 2.5 |
| Gestational age missing on HES | Yes | 20.1 | Yes | 10.9 |
| Birthweight missing on HES | Yes | 12.3 | Yes | 7.0 |
| Trust | PPL (Portland) | 1.7 | PPL (Portland) | 2.5 |
| RGQ (Ipswich) | 2.0 | RGQ (Ipswich) | 1.5 | |
| RKE (Whittington) | 4.0 | RJ6 (Croydon) | 1.3 | |
| RVL (Barnet and Chase Farm) | 1.4 | RKE (Whittington) | 3.9 | |
| RQ8 (Mid Essex) | 1.6 | |||
| RTH (Oxford University Hospitals) | 1.6 | |||
| RVL (Barnet and Chase Farm) | 1.4 | |||
| RVV (East Kent) | 2.0 | |||
| RW3 (Central Manchester) | 1.1 | |||
| RWH (East and North Hertfordshire) | 1.1 | |||
Table 32 breaks down the proportions of each group by the match rank of the HSCIC linkage algorithm, providing useful information about the quality of their linkage at each stage. It shows a comparison of distributions of key variables for singleton and multiple births in England from 2005 to 2014, for four groups of data:
-
All birth registrations (n = 6,468,586 singleton births, n = 208,326 multiple births)
-
All birth registrations linked to HES by the HSCIC with a HES delivery record (n = 6,268,013 singleton births, n = 196,769 multiple births)
-
Those of group 2 that remain linked to HES after quality assurance (n = 6,138,487 singleton births, n = 193,270 multiple births)
-
Those of group 2 left with no link after quality assurance (n = 129,526 singleton births, n = 3,499 multiple births).
The data in Table 32 for gestational age missing in HES and birthweight missing in HES are based on total links (a birth registration record can link to more than one HES record):
-
All birth registrations (n = 6,468,586 singleton births, n = 208,326 multiple births)
-
All birth registrations and HES links by the HSCIC (n = 7,862,903 singleton births, n = 395,202 multiple births)
-
Those of group 2 that remain linked to HES after quality assurance (n = 6,138,487 singleton births, n = 193,270 multiple births)
-
Those of group 2 total broken links after quality assurance (n = 1,724,416 singleton births, n = 201,932 multiple births).
Total numbers of links are inflated for multiple births because each birth registration within a multiple delivery links with every possible HES baby tail (i.e. a minimum of four linked records).
Chi-squared tests were conducted to test the null hypothesis that the distribution of a demographic variable was the same in the ‘linked to HES after QA’ as in the ‘No link to HES after QA’. Any rows with values of 0 were excluded from the chi-squared tests.
These differences give an indication of when either incorrect linkage, or false negatives are more likely to occur in the quality assurance. Differences between singleton and multiple births are seen. Some of these associations with incorrect linkage make sense. Home births are less likely to have a HES delivery record as many are not captured by hospital-based clinical systems from which HES records are derived. Match rank 6 is a less reliable stage of the linkage algorithm because it does not match on the NHS number. HES data quality is known to be poorer in years 2006 and 2007, although for multiple births, years 2012–14 are more likely to be incorrectly linked. Missing data for gestational age and birthweight in HES values mean that there is less information to make a correct link. The other factors require more investigation or could be simply due to chance, with the large numbers involved.
Linkage summary
| Linkage | Dataset 1 | Dataset 2 | Geographical area | Time period for births | Linkage done? | Quality assurance done? | Analyses started? | In draft final report? | Article by end of March 2017? | Article after end of March 2017? | Presentation after end of March 2017? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 1. Birth registration linked to birth notification | 7. Maternity HES delivery and birth records | England | 2005–14 | Yes | Completed for singleton and multiple births linked to HES delivery records | Yes for singletons, no for multiples. Analyses of singletons published in PLOS1 June 2018 and presented at conferences | Yes | Two articles, one on linkage and one on quality assurance drafted by March 2017 and published in BMJ Open, March 2018 | Single article to be written for submission to Archives of Disease in Childhood, focusing on data | Presentations on quality assurance given at ADRN conference June 2017, RSS conference September 2017 |
| B | 1. Birth registration linked to birth notification | 10. NCCHD/PEDW | Wales | 2005–14 | Yes | Yes | Yes | Yes | No | Yes, probably as part of article on analyses for Wales | |
| C | 1. Birth registration linked to birth notification | 5. Stillbirths reported to confidential enquiries | England and Wales | 2005–9 | Yes | Yes | Yes | Yes | No | Yes, as part of article on analyses | |
| D | 1. Birth registration linked to birth notification | 6. Neonatal deaths in England and Wales reported to confidential enquiries | England and Wales | 2005–9 | Yes | Yes | No, as found that classifications used were not relevant to research questions | Brief mention | No | Possibly brief mention in article on neonatal deaths | |
| E | 7. Maternity HES delivery records | 8. HES, subsequent admissions of mothers | England | 2005–14 | Yes | No | No | Brief mention of linkage | No | Yes | |
| F | 7. Maternity HES birth records | 9. HES, subsequent admissions of babies | England | 2005–14 | Yes | No | No | Brief mention of linkage | No | Yes | |
| G | 10. PEDW delivery records | 11. PEDW, subsequent admissions of mothers | Wales | 2005–14 | Yes | No | No | Brief mention of linkage | No | Yes | |
| H | 10. PEDW baby records | 12. PEDW, subsequent admissions of babies | Wales | 2005–14 | Yes | No | No | Brief mention of linkage | No | Yes |
Data organisation
Importing source data files
For ONS records, mothers’ HES delivery records and babies’ HES birth records source data were initially imported into Microsoft Access® where many manipulations were then performed. At a later stage of the project, the Microsoft Access® tables were imported into Microsoft SQL Server. To perform the import into Microsoft SQL Server, it was first necessary to convert the Access® ‘.accdb’ files into the older Access® ‘.mdb’ file format.
Importing data into Microsoft Access® files was quite involved and is described below.
Office for National Statistics data
Office for National Statistics birth registration linked to birth notification
Formally, an ONS record consists of the birth notification record linked to birth registration and, where appropriate, to the baby’s mortality record.
For the years 2005–12, CSV files were created from SAS® files of registration data linked to birth notification for births in England and Wales. SAS® files were used as a number of additions had been made to the files, which was not always reflected in source CSV files (2007 – postcodes missing).
For 2013 and 2014, CSV files were created from IBM SPSS Statistics files (IBM Corporation, Armonk, NY, USA) of registration data linked to birth notification (2014 – postcode of baby for birth notification truncated). For 2014, MULTIBTNO was taken from another CSV file.
The CSV files were stored in a folder for ONS birth records by year.
These files were linked into the Microsoft Access® file ‘ONS Link File’. An import specification was used to force all fields to be short text irrespective of their native format.
The SQL queries implemented in Visual Basic for Applications code were then used to import records into the native Microsoft Access® table ‘ONS yy’. At this stage, string values of ‘NULL’ and ‘.’ were converted to database NULL. Fields that were integer in their native format were converted to type Long Integer. The target Microsoft Access® table had text fields set to represent the length of the text string that they were designed to hold.
The ONS file names varied across the years; all years were mapped to the 2006 ONS file name convention.
The unique record identifier [ID] supplied with the ONS data was not unique across all years. For 2005–7, the identifier started at 1 every year. For 2008 onwards, the identifier was prefixed by the year, so record 1 appeared as 2008000001. This was too long to be cast as a Long Integer. A new unique identifier was created by taking the supplied ID, stripped of the year if relevant, and prefixing with the last two digits of the year, that is [ONS ID] = yy × 107 + [ID]. So, the first record had an identifier of 80000001.
The source files did not uniformly contain the mother’s or baby’s NHS number. For England, these data were obtained from the CSV files containing identifiers. The field [Country] was set to ‘E’ if a record appeared in these files containing English identifiers. For 2013 and 2014, CSV files were created from SAS® files.
For Wales, the NHS number was not found in the data, so records set for linking could be identified; the [County] field was set to ‘W’ if a record appeared in CSV files originating from NWIS’ for years 2005–12. For 2013 and 2014, CSV files were created from the SAS® files for Wales. Any record that had already been marked as English would have been marked with a ‘B’ for both but this did not occur.
Office for National Statistics mortality records
Because mortality records were very few, these fields were all put in one table: ‘Mortality yy’. For many years: the mortality fields were full of the text string NULL; these fields were filtered out.
Each record then consisted of a triplet of identifying information:
[ONS ID], which linked back to the baby’s core ONS record.
[Mortality Field], which took values from the list (ICD10, DI10P, DI10PF).
[Field Order], which was a number from 1 to 15.
The mortality fields [AGEC], [AGECUNIT], [DWIGS10], [ICD10U] and [ICD10UF] were included in the ONS core record.
Office for National Statistics stillbirth records
Imported directly into the SQL Server from CSV file ‘Still Births All (CSV).csv’ and built by concatenating the individual annual spreadsheets of stillbirths.
Office for National Statistics infant mortality records
Age: 0 years.
Wigglesworth codes were imported into the table [Wigglesworth Codes] in the database ‘ONS Link File’. Using a query, these were subsequently manually copied into the appropriate [ONS yy] table.
Office for National Statistics childhood mortality records
Age: 1–15 years.
Taken from the two spreadsheets ‘Child deaths 2005 to 2007’ and ‘Child deaths 2008 to 2014’. These contained only death registration records that had been linked to birth registration/notification records.
The day, month and year fields in the date of death and those in the date of birth were each concatenated to form standard date fields. In some years there were a few records for which the date of birth on the death registration did not fully match the date of birth on the birth registration. On inspection, these appeared to be errors or births that occurred around midnight, so the following day’s date had been entered.
Office for National Statistics maternal mortality records
The Office for National Statistics provided about deaths of women who gave birth within the 12 months preceding their death, linked to data from the baby’s birth records. Its documentation explained that in some cases, the deceased may have given birth twice in the year proceeding her death, in which case there were two records. These records were imported from a file of maternal deaths. Each worksheet related to births within that year. For example, the records on the 2013 page related to women who died within 1 year of giving birth in 2013. This meant that the 2014 worksheet may not have been complete, as there may have been deaths in 2015 of women who gave birth in 2014, which had not yet been registered.
The matching was done by extracting the first name, surname and date of birth of the mother, plus the date of birth of the child, from each birth record within the stated year, then using the first name, surname and date of birth of the mother, searching for any matching death record within 1 year of the date of birth/stillbirth of the child(ren) when the age of the deceased was in the range of 10–65 years.
Hospital Episode Statistics data
Mothers’ delivery records
Mothers’ deliveries records were linked into the database ‘HES Deliveries Link File’ using the import specification ‘MOTHER _ APC Link Specification’. With the exception of dates, the majority of fields were characterised as text even if the native format was numeric. This policy proved more resistant to corruption.
The linked tables were subsequently imported into the associated Microsoft Access® tables [Delivery yyyy], [Deliveries Baby Tails yyyy], [Deliveries OPCS yyyy] and [Deliveries ICD yyyy]. The HES field EPIKEY is numerically too large to use as a long integer, hence, it was imported as a text string. This makes it unsuitable for using as an index. It is essential that an index is unique across all years. To arrange this, a temporary autonumber field (Temp ID]) was included. From this a unique identifier across all years was generated from the formula [Delivery ID] = yy × 107 + [Temp ID]. To avoid confusion and mistakes, [Temp ID] was subsequently deleted. [Delivery ID] was manually turned into a primary key.
During the import process the following field manipulations took place:
All dates were reformatted on importing to standard Microsoft Access® format.
It was desirable to have [NUMBABY] as a numeric value. This was achieved by mapping the value representing unknown ‘X’ into ‘–1’.
For the same reason, [BIRORDR_n] was treated in the same fashion.
OPCS-4 codes in the procedure codes that take values ‘-’ or ‘&’ were ignored.
The ICD-10 codes in the diagnostic codes were limited to four characters and if any of (‘+’, ‘–’, ‘X’) was on the end of the code, it was stripped off.
The relational tables [Deliveries Baby Tails yyyy], [Deliveries OPCS yyyy] and [Deliveries ICD yyyy] were populated by using EPIKEY as a unique identifier, as this was the only available identifier field in the source text file. Baby tails with [BIRORDR] = ‘X’ were not imported as it is known that when this is the case the rest of the field contains no useful information.
The ONS-HES linkage file was imported in an analogous fashion, first, in to the table [Full Mother HES ONS Linkage]. This was subsequently copied to the table [Mother HES ONS Linkage] excluding match rank zero (see Match rank zero).
Babies’ birth records
This proceeded in an analogous manner to mothers’ deliveries except there is only one baby tail so this was incorporated into the baby’s core birth record.
Mothers’ readmission records
Later on in the project, these text files were imported directly into Microsoft SQL Server.
Babies’ readmission records
Later on in the project, these text files were imported directly into Microsoft SQL Server.
Preparing the linked data received from the Health and Social Care Information Centre
Office for National Statistics to Hospital Episode Statistics mother linkage
The HSCIC provided the project with a standard HES extract plus three additional text files:
-
MOTHER_LINKAGE provided the map between each ONS record and the mother’s HES ID.
-
MOTHER_OLD_NEW provided the map between old and new HES ID.
-
MOTHER_UNMATCHED listed the ONS records that failed to link to a mother in HES.
The table [Full Mother HES ONS Linkage] holds the entirety of the original HSCIC text file MOTHER_LINKAGE. The table [Mother HES ONS Linkage] is a copy of the records in [Full Mother HES ONS Linkage], excluding match rank zero. See the section below to see why. The handful of records with missing HES ID or [ONS Link ID] was also excluded. It is this table that was used for linkage.
The table [Mother HES ONS Linkage] has the following relevant fields:
-
[Mother ID] – this should be used in preference to HES ID. If it was not for the inclusion of old HES ID the two would be in one-to-one correspondence but the former is computationally more efficient.
-
[ONS ID] – this is unique over all years and should be used in preference to [ONS Link ID] as it is computationally more efficient.
Match rank zero
The HSCIC assigns a unique identifier called HES ID to every patient. When the HSCIC receives a new record it attempts to locate the patient within their existing list of HES IDs. This is a complex process depending on identifiers such as NHS number, postcode, date of birth and local hospital identifiers. If it fails to find a match, a new HES ID is assigned.
Because the information that HSCIC receives is occasionally incomplete or incorrect, this matching procedure is imperfect. On occasions it is retrospectively realised that two distinct HES IDs actually represent the same patient. When this occurs, the two HES IDs are added to a file that provides a lookup table relating the old HES ID that appears in the HES records to the HES ID that has most recently been assigned.
This affects the project in two ways. First, by taking this lookup into account the linking of ONS records to HES can be improved. Second, when estimating a woman’s parity or any other factor that depends on her history, the lookup provides a more reliable way of gathering and inspecting a woman’s complete record set.
Every year, around 2000–5000 old HES IDs appear in the delivery records (i.e. slightly less than 1%). There were a few problems in the lookup file. For instance, 739 old HES IDs were associated with one new HES ID and a considerable number had multiple matches. A conservative approach was adopted whereby any link between old and new HES ID that was not bijective was ignored. The table also contains many duplicate entries; these were eliminated at the import stage.
It is this association between HES IDs that is responsible for match rank zero in the linking between ONS records and HES ID. Any current HES ID that matches an ONS record using match rank 1 to 8 and also has an associated old HES ID implies that there should exist a match between the same ONS record and the old HES ID. This implied linkage is included in the linkage algorithm and designated with match rank being set to zero.
Because there is a one-to-one correspondence between [HES ID] and [Mother ID], substituting new HES IDs for old is equivalent to substituting new Mother IDs for old. To accommodate this link between old and new HES IDs, both the [Deliveries] table and the [Mother HES ONS Linkage] table have any old [Mother ID] replaced by the new [Mother ID]. Note that the HES ID that appears in these tables is not changed. Because of this substitution it is now possible to ignore ONS linkages to HES that have a match rank of zero.
Linking the Office for National Statistics record to the Hospital Episode Statistics delivery record baby tail
There is one ONS record for each baby’s birth and one HES record for each mother’s delivery episode, so in the case of multiple births several ONS records link to the same HES delivery record. However, each delivery record has a separate baby tail for each baby, so it is natural to link each ONS birth record to the appropriate baby tail in the HES delivery record.
Multiple births were linked in the ONS record with the field [MULTBTNO]. Because the time of each birth is recorded in the ONS record, the birth order can be determined. Each baby tail in the HES delivery record also records the birth order, so, where this information exists, it is simple to assign the correct ONS record to the appropriate baby tail.
Unfortunately, the birth order in HES is not always recorded. Two situations occur: (1) the baby tail is missing and (2) the baby tail exists but the birth order is unknown. When this is the case all other information in the baby tail is also missing.
When the baby tail is missing from the HES record, a new tail is generated and tagged as an ONS ghost record. This allows the HES delivery record to retain its link to the ONS record in a consistent manner.
When the baby tail exists and the birth order is not recorded, the position of the index position of the baby tail in the record is used as a proxy for birth order.
Primary keys in each database table
Table: ONS
The linked birth registration birth notification records all live births in the table called ONS. Each record has a unique identifier [ONS ID] that is used for all linkages to other tables.
The field [ONS Link ID], when used in association with [ONS Link Year], allows the table to be linked back to the original source data. Note that for earlier years this key is not unique between years. This field should not be used for any table linkages.
Table: ONS mortality
Each record can be linked back to the ONS birth registration/notification records using the field [ONS ID].
Table: mothers
Each patient in HES is represented by a unique 31-character-long text string. This is unwieldly to work with so each mother in HES is assigned a unique integer identifier [Mother ID]. These were in one-to-one correspondence with the mother’s HES ID.
This field is necessary when considering the relationship between a mother’s delivery records and her readmission records.
Primary key: [Mother ID].
Table: deliveries
Primary key: [Delivery ID].
Foreign keys:
-
[Mother ID] – each record also holds the [Mother ID], which allows deliveries to be chained and facilitates linkage to readmissions.
-
[ONS ID Baby One] – this is identical to the value of [ONS ID] in the first baby tail. It is provided as a short cut for when it is the mother’s characteristics that are being investigated and there is no need to invoke the baby tail record.
Table: deliveries baby tails
Primary key: [Baby Tail ID].
Foreign keys:
-
[Delivery ID] – use to link baby tail to delivery record.
-
[ONS ID] – when the record linkage exists, this points to the matched ONS record.
-
[Birth ID] – when the record linkage of the ONS record to both the delivery record and the birth record exists then the link between the baby tail of the delivery record and the baby’s birth record can be inferred. This link was not inferred during this project, but a field was provided in the database to allow this to happen in the future.
Table: delivery ICD codes
Foreign key: [Delivery ID] – use to link to delivery record.
Table: delivery OPCS codes
Foreign key: [Delivery ID] – use to link to delivery record.
Table: deliveries indicators
Primary key: [Delivery ID].
For every record in the deliveries table there is a corresponding record in this table. The table’s purpose is to provide a home for indicators that were calculated throughout the project and hence require additional columns.
Table: mothers’ readmissions
This table contains antenatal admissions, postnatal readmissions and admissions unrelated to maternity. Although a link is provided to previous and next delivery records further work needs to be done before the record can be categorised as ante, post or unrelated.
Primary key: [Mothers Readmissions ID].
Foreign keys:
-
[Mother ID].
-
[Previous Delivery ID] – links the readmission record to the last previous delivery record. Quality needs to be assessed as there were readmission records on the day of delivery.
-
[Next Delivery ID] – links the readmission record to the first next delivery record. Quality needs to be assessed.
Table: mothers’ readmission ICD codes
Foreign key: [Mother’s Readmissions ID] – use to link to readmission record.
Table: mothers’ readmission OPCS codes
Foreign key: [Mother’s Readmissions ID] – use to link to readmission record.
Table: babies
In the real world a baby is only born once. In HES, a baby can have many birth records, hence the need to have separate IDs to represent the baby and to represent each of its birth records.
This table plays an analogous part to the table Mothers.
Primary key: [Baby ID].
Table: births
Primary key: [Birth ID].
Foreign keys:
-
[Baby ID] – facilitates link to babies’ readmissions.
-
[ONS ID] – when the record linkage exists, this points to the matched ONS record.
-
[Delivery ID] – when an ONS record links to both the delivery record and the birth record then the link between the baby’s birth record and the delivery record can be inferred.
-
[Baby Tail index] – identifies the baby tail in the delivery record that the birth record is linked to when an ONS record is linked to both a delivery record and a birth record. Should be linked to the field [Field Order] in the table of baby tails.
-
[Mother ID] – when an ONS record links to both the delivery record and the birth record then the link between the baby’s birth record and the mother can be inferred. This can be used to link siblings.
Table: births ICD codes
Foreign key: [Birth ID] – use to link to birth record.
Table: births OPCS codes
Foreign key: [Birth ID] – use to link to birth record.
Table: birth indicators
Primary key: [Birth ID].
For every record in the Births table there is a corresponding record in this table. The table’s purpose is to provide a home for indicators that were calculated throughout the project and hence require adding columns.
Table: babies’ readmissions
This table contains postnatal readmissions and admissions unrelated to maternity.
Primary key: [Baby’s Readmissions ID].
Foreign keys:
-
[Baby ID].
-
[Previous Birth ID] – links the readmission record to the baby’s birth. Although the use of the word ‘previous’ is superfluous it is retained for consistency with the mother’s readmissions records. Quality needs to be assessed.
Table: babies’ readmissions ICD codes
Foreign key: [Baby’s Readmissions ID] – use to link to readmission record.
Table: babies’ readmissions OPCS codes
Foreign key: [Baby’s Readmissions ID] – use to link to readmission record.
Deriving new variables from Office for National Statistics data
Derived variables contain new values based on standardising or combining the original values in the data fields to create better quality or more useful variables.
[Age Father]
Age in years with months converted to decimal years.
[Age Mother]
Age in years with months converted to decimal years.
[Multiple]
Multiple birth, defined if [MULTTYPE] is not NULL.
[Birth Order]
Field derived using birth notification fields DOBZ and DELTIMEZ. This replicates the birth notification field [CONFORDZ]. The ONS have not quality checked this field and it was found to contradict the birth order derived using [DOBZ] and [DELTIMEZ] on rare occasions. Because in theory a multiple birth could span midnight on New Year’s Eve, the calculation should be done on all data years simultaneously. This proved impossible in the VML so each year was done individually. This is very unlikely to cause a problem. Because babies born by caesarean section can share the same time of birth, the algorithm has to appeal to [CONFORDZ] to distinguish the birth order when this situation occurs. This situation occurs around 20 times per year (i.e. ≈0.1% of multiple birth records).
[Babies in Delivery]
Field derived from count of set of records with common entries in MULTBTNO. Replicates the birth notification field [CONFNUMZ].
[Babies in Delivery from MULTTYPE]
Derived from a lookup table using MULTTYPE. This will indicate 4 only if the multiplicity is greater than or equal to 4.
[Gestational Age]
For birth registration, gestational age is reported only for stillbirths, so use birth notification (GN) over birth registration gestational age (GR) unless:
-
IF GN is NULL or GR = 0 AND GR > 0 THEN use GR.
-
IF GN = 0 (unknown) then set to NULL.
[Birth Weight]
Use birth registration weight (WR) over birth notification weight (WN) unless:
-
IF WR = 9998 OR WR = 9999 OR WR = 0 OR WR = NULL OR WR < 100 THEN
-
(IF WN = > 100 AND WN <> 9998 AND WN <> 9999 THEN use WN ELSE set to NULL)
-
IF WR < 1000 AND WN = 10 × WR THEN use WN (least significant digit occasionally dropped).
[Baby Sex]
Use birth registration but translate (1, 2) to (M, F). If missing, revert to birth notification if this is one of (M, F). Note that data suggest that sex is always allocated by time of birth registration.
Ethnicity
[Ethnicity], [Ethnicity 9], [Ethnicity 5]
The 100 one- or two-letter codes were mapped onto the standard 17 one-letter codes. In 2005 the text description often appeared instead of the code. This is mapped to the one-letter code. These codes can then be further mapped to the ONS-9 and ONS-5 category systems. The ONS-9 codes cannot be mapped directly onto the ONS-5 codes (Table 35).
| Ethnicity | Ethnicity 9 | Ethnicity 5 | |||
|---|---|---|---|---|---|
| Code | Text | Code | Text | Code | Text |
| A | White British | 6 | White British | 1 | White |
| B | White Irish | 7 | White other | 1 | White |
| C | Any other white background | 7 | White other | 1 | White |
| D | Mixed white and black Caribbean | 8 | Other | 4 | Other |
| E | Mixed white and black African | 8 | Other | 4 | Other |
| F | Mixed white and Asian | 8 | Other | 4 | Other |
| G | Any other mixed background | 8 | Other | 4 | Other |
| H | Asian Indian | 2 | Indian | 2 | Asian |
| J | Asian Pakistani | 3 | Pakistani | 2 | Asian |
| K | Asian Bangladeshi | 1 | Bangladeshi | 2 | Asian |
| L | Any other Asian background | 8 | Other | 2 | Asian |
| M | Black Caribbean | 5 | Black Caribbean | 3 | Black |
| N | Black African | 4 | Black African | 3 | Black |
| P | Any other black background | 8 | Other | 3 | Black |
| R | Chinese | 8 | Other | 4 | Other |
| S | Any other ethnic group | 8 | Other | 4 | Other |
| Z | Not known | 9 | Not known | 5 | Not known |
The map between the birth notification field [ETHCATZ] and the reduced categories can be found in the SQL table [AA Ethnicity Codes Map].
Dates of birth
[Baby DoB Birth Notification]
[DOBZ] date formatted pre 2013, otherwise copied.
As time of birth comes from birth notification, then, for consistency, this date should be used when timing information is being modelled rather than the date of birth available from birth registration. When a CSV file is exported, this date is used to generate the day, month and year of birth. It is also the date that is used to link to public holidays.
[Baby DoB Birth Registration]
[Date of birth] date formatted.
[Mother DoB Birth Notification]
[DOBMZ] date formatted pre 2013, otherwise copied.
[Mother DoB Birth Registration]
[DOBM] date formatted.
[Baby DoB]
IF [Baby Date of Birth Birth Registration] is NULL THEN use [Baby Date of Birth Birth Notification].
[Mother DoB]
IF [Mother DoB Birth Registration] is NULL THEN use [Mother Date of Birth Birth Notification].
Place of residence
[Baby Post Code Birth Notification]
Cleaned version of [PCDRBZ] with a single space located at the fourth to last position. Text is converted to uppercase and postcodes that take on the value ‘X X’ or contain commas or double quotation marks were replaced with NULL.
[Mother Post Code Birth Registration]
Cleaned version of [PCDRM] with a single space located at the forth to last position.
[Post Code]
[Mother Post Code Birth Registration] unless missing, otherwise [Baby Post Code Birth Notification] if its string length is > 5. This field is designed to create a single complete postcode for the record. This should be used with care as there may be good reason why the mother’s and baby’s postcodes were different.
[Region Code of Country of Birth of Mother]
Originated from ONS country codes recorded in [CTRYPOBM] using the lookup table found in the Ethnicity database. The coding system changed after 2006; however, some post-2006 codes leaked into 2006. For 2006 only, if a country code could not be found in the earlier codes then the post-2006 codes were tried. Note that some countries have several valid codes.
[Region Code of Country of Birth of Father]
Originated from ONS country codes recorded in [CTRYPOBF] using the lookup table found in the Ethnicity database. The coding system changed after 2006; however, some post-2006 codes leaked into 2006. For 2006 only, if a country code could not be found in the earlier codes then the post-2006 codes were tried. Note that some countries have several valid codes.
[Location Code Birth Registration]
A unique code identifying the maternity unit where the birth occurred, according to birth registration field [CESTRSS]. NULL values were mapped to ‘XXX-XX’.
Note: codes for 2005–14 have been mapped but if new data for subsequent years are added, they should be checked for new [CESTRSS] codes.
[Location Code Birth Notification]
A unique code identifying the maternity unit where the birth occurred, according to birth notification. Derived from the Birth Notification field [ORGCODEZ] and lookup tables. NULL values were mapped to ‘XXX-XX’.
Note: codes for 2005–14 have been mapped but if new data for subsequent years are added, they should be checked for new [CESTRSS] codes.
[Location Code DELPLAZ]
A unique code identifying the maternity unit where the birth occurred according to the free-text field [DELPLAZ] in birth notification. NULL values were mapped to ‘XXX-XX’.
Note: because of the free-text nature of [DELPLAZ] it requires the mapping of all the variations and misspelling of hospital names. This was done for 2005–14 but future years will require this map to be updated.
[Location Code]
The best estimate of where the birth occurred based on birth notification and registration. Taken as [Location Code Birth Registration] unless either of [Home Birth] or [Elsewhere Birth] was true, in which case replaced by codes representing these locations.
[Pseudo Trust Birth Registration]
Mapping of [Location Code Birth Registration] onto assigned trust.
[Pseudo Trust Birth Notification]
Mapping of [Location Code Birth Notification] onto assigned trust.
[Pseudo Trust DELPLAZ]
Mapping of [Location Code DELPLAZ] onto assigned trust.
[Pseudo Trust]
Mapping of [Location Code] onto assigned trust.
[Home Birth]
True if [Location Code Birth Registration] = ‘XXX-HX’.
[Elsewhere Birth]
True if [Location Code Birth Registration] = ‘XXX-EX’.
[Country]
If Health Region of Place of Birth is in Wales ([HROPOB] = Q99) or is unknown ([HROPOB] is NULL) and if Health Region of Mother is in Wales ([HRORM] = Q99), then designated as a Welsh birth. Designate a birth as English if not Welsh. Note that for some years [HRORM] the source files reads ‘NUL’ instead of ‘NULL’, hence avoided being set to database NULL during the import phase. This value was set to NULL during the country assignment.
Takes values E or W.
[Unit Type]
Looks up [Location Code Birth Registration] in the table [Unit Type] found in the database AA Unit Type. Constrained by using [Baby Date of Birth] to lie between [Start Date] and [End Date] of the unit’s existence in the given configuration.
Takes values OU, OU + AMU, FMU, Elsewhere, Home, not a maternity hospital (NAMH), Private, Military, Unknown.
Mortality
[Birth Status Birth Notification]
For 2005–7, LSBTHZ values of (NULL, Live, Still Birth ante-partum, Still Birth intra-partum, Still Birth indeterminate, Dead) were mapped to (NULL, 1, 2, 3, 4, 5).
For later years, LSBTHZ values of (NULL, 1, 2, 3, 4, 5) were mapped to (NULL, 1, 2, 3, 4, 5).
[AGECUNIT]
This field is an ONS field and is not derived. It is included here for convenience.
Definitions:
[AGECUNIT]: 4 = days, [AGEC] = 0 to 6.
[AGECUNIT]: 3 = weeks, [AGEC] = 1 to 4.
[AGECUNIT]: 2 = months, [AGEC] = 1 to 11.
[AGECUNIT]: 1 = years, [AGEC] ≥ 1.
Date of Birth counted as day zero.
Early neonatal: [AGECUNIT] = 4 and [AGEC] < 7.
Late neonatal: [AGECUNIT] = 3 and [AGEC] < 4 (weeks 1–3).
Neonatal: Early neonatal and late neonatal. [AGECUNIT] = 2 or ([AGECUNIT] = 3 and [AGEC] < 4).
Post neonatal: [AGECUNIT] = 2 or ([AGECUNIT] = 3 and [AGEC] = 4) (i.e. > 3 weeks and < 1 year).
Infant: [AGECUNIT] ≠ 1.
Deriving new variables from Hospital Episode Statistics data
Mothers’ Hospital Episode Statistics delivery record
[Delonset 2]
Where there were several HES records per delivery the ‘best’ record may not actually contain the onset method. When this is so, the onset method is taken from an alternative record. Otherwise this field is set to [DELONSET].
[Induction or Acceleration (OPCS)]
True if one of the OPCS codes for the record is equal X35.1 or like R14.* or like R15.*
[Induction or Acceleration]
True if either [Delonset 2] one of (1, 2, 3) or [Induction or Acceleration OPCS] is True.
[Multiple ICD]
True if record has one or more of the following ICD-10 codes indicating a multiple is in the record:
-
Z37.(2–7); Z38.(3–8); O84*
[HES Multiple]
True if [Multiple ICD] is True or ([NUMBABY] > 1 but not equal 6 or 9).
[Episiotomy]
True if one of the OPCS codes for the record is like R27.*
Parity
[Derived Parity]
See section on Calculating parity below.
[Nulliparous]
[Derived Parity] = 0.
[Derived Parity (ONS)]
See section on Calculating parity below.
[Nulliparous (ONS)]
[Derived Parity (ONS)] = 0.
Miscellaneous fields
[Baby Tails Count]
This is a count of the number of baby tails that a delivery record contains.
[OPCS Code Count]
This is a count of the number of OPCS procedure codes that the mother’s delivery record contains.
[ICD Code Count]
This is a count of the number of ICD-10 diagnostic codes that the mother’s delivery record contains.
[Valid Delivery]
Set to false if induced abortion if Q14 in procedure codes or diagnostic codes O00 to O08. Code ‘:Ab’ inserted into [Exclude Reason] field.
[Post Code]
Cleaned version of [HOMEADD] with single space in the fourth from last position.
[Episode Start]
Cleaned version of [EPISTART]. If [EPISTART] is > 1 year before the date associated with the beginning of the file, NULL is substituted {i.e. for the data file 06/07 if [EPISTART] is before 1/April/2005, NULL is used}. This is acceptable for maternity records.
[Episode End]
Cleaned version of [EPIEND]. [EPIEND] is used to allocate the record to the correct HES file, so by definition it will fall between 1/4/yy and 31/3/yy+ 1. However 1/1/1800 and 1/1/1801 were used as unknown dates so a lower cut-off of 1/4/20yy is used.
[Location Code HES]
Populated by linking [PROCODE] and [SITETRET] to the lookup linked table [HES (PC and ST) to Location Code]. The case where [SITETRET] is NULL has to be treated separately.
[Pseudo Trust Code HES]
Populated by searching for [Location Code HES] in the lookup table [Location Codes].
Baby tail in mother’s delivery record
[Baby Sex]
[SEXBABY] values of (1, 2) transposed to (M, F) in [Baby Sex]. Values of (M, F) in [SEXBABY] transferred directly.
Values of 0 = Not known, 3 = Indeterminate, 9 = Not specified, all set to NULL.
[Stillbirth]
Set to TRUE if BIRSTAT in (‘2’, ‘3’, ‘4’), False otherwise.
[Birth Weight]
In HES [BIRWEIT] = 9999 denotes unknown, 7000 denotes ≥ 7 kg.
If [Birth Weight] is set equal to [BIRWEIT] if the latter is < 7000 else set to NULL.
Low birthweights not cleaned as yet.
[Assumed HES Baby’s DoB]
When available this is set to the first baby’s date of birth [DOBBABY_1]. Failing this, the derived field [Delivery Procedure Date] is used. For a first episode, if [DOBBABY_1] falls outside the cleaned episode start and end dates ([Episode Start], [Episode End]) and [Delivery Procedure Date] does not, the latter is used in preference to the recorded baby’s date of birth.
If still no date available, then revert to using episode dates. This date only needs to be approximate so working on the premise that a woman will spend longer in hospital after a birth than before the following rule is applied:
If [Episode Start] = [Episode End] OR [Episode Start] + 1 = [Episode End].
Then set [Assumed HES Baby’s DoB] = [Episode Start].
ELSE
Then set [Assumed HES Baby’s DoB] = [Episode Start] + 1.
It is observed that sometimes the [Assumed HES Baby’s Date of Birth] lies outside the episode dates.
[Valid Baby Tail]
Some trusts complete either six or nine baby tails even for a singleton delivery. Baby tail records were marked as invalid in accordance with to the following rules.
There were six or nine baby tails and [NUMBABY] ≠ 9 (i.e. known) then baby tails after [NUMBABY] were marked invalid.
Where there were nine baby tails and [NUMBABY] = 9 (unknown) and [BIRORDR] = –1 (birth order unknown) then baby tails marked as invalid. This rule relies on the observation that if birth order is unknown, invariably all other fields in the baby tail were also unknown so no information is lost.
[ONS Ghost]
In the case of multiple births some trusts did not complete all the required baby tails. Where a HES delivery record was linked to an ONS record that indicates a multiple birth and the HES delivery has insufficient baby tails then new (ghost) baby tails were generated. All data fields retain NULL values.
Delivery Indicators
[Delmeth OPCS]
Synthetic version of DELMETH generated using procedural codes (Table 36).
| [Delmeth OPCS] | Method | OPCS code | Assignment order |
|---|---|---|---|
| 0 | Spontaneous vertex | R24* | 9 |
| 1 | Spontaneous cephalic | R23* | 8 |
| 2 | Lower forceps | R215 or R218 or R219 | 3 |
| 3 | Other forceps | R211 or R212 or R213 or R214 | 4 |
| 4 | Ventouse | R22* | 5 |
| 5 | Breech other | R20* | 7 |
| 6 | Breech extraction | R19* | 6 |
| 7 | Elective caesarean section | R17* | 1 |
| 8 | Emergency caesarean section | R18* | 2 |
| 9 | Other | R25* | 10 |
| X | Unknown | Otherwise | 11 |
Some records have several delivery codes; this could be because of a multiple birth, failed forceps or erroneous data entry. The most severe mode is chosen as the delivery mode on the basis of the order caesarean section, instrumental, spontaneous vaginal.
[Delmeth Best]
If [Delmeth OPCS] is known (i.e. ≠ X or 9) then this is used, else [DELMETH_1] is used from the first baby tail. The source is recorded in [Delmeth Source].
[Delmeth Best 2]
Where there were several HES records per delivery, the ‘best’ record may not actually contain the delivery method. When this is so, the delivery method is taken from an alternative record. Otherwise this field is set to [Delmeth Best].
[Current CS]
Mention of caesarean section in DELONSET, [DELMETH Best] or diagnostic codes.
[Previous CS (ICD)]
A previous caesarean section indicated in current record’s diagnostic codes. See section on Calculating parity.
[Previous CS]
Caesarean section in a previous delivery recorded in HES or a previous caesarean section mentioned in the diagnostic codes. See section on Calculating parity.
[Multiple ICD]
The diagnostic codes in the delivery record indicate a multiple birth.
[HES Multiple]
Either the diagnostic codes in the delivery record or the HES field NUMBABY indicate a multiple birth.
[OPCS Code Count]
This is a count of the number of OPCS-4 procedure codes that the baby’s birth record contains.
[ICD Code Count]
This is a count of the number of ICD-10 diagnostic codes that the baby’s birth record contains.
Calculating parity
One of the problems with calculating parity in HES is the identification of a delivery event and the removal of the duplicate records before the calculation can proceed. Because of the linkage of ONS birth records to HES delivery records this task has already been completed in a manner superior to the usual method applicable for unlinked HES.
As subsequent analyses of the data are restricted to linked HES records, the estimation of parity is restricted to those HES records that link to an ONS record.
Variable definitions
[Recorded Parity] – the value reported in the HES field NUMPREG unless the delivery is in a trust that misreports parity.
[ONS Pseudo Parity] – the Birth Registration field [PREVCH] that represents the total number of previous either live or stillborn children born within marriage.
[Previous CS (ICD)] – set to True if an ICD-10 code within the HES delivery record indicates a previous caesarean section has taken place.
[Current CS] – set to True if there is evidence within the current HES delivery record indicating that a caesarean section has taken place in the current delivery.
[Previous Pregnancy (ICD)] – set to True if an ICD-10 code within the HES delivery record indicates a previous delivery has taken place.
[Recorded Order] – this represents the sequential numbering of a woman’s delivery records as recorded in the HES extract available to the project.
[Previous CS] – this is derived by propagating information about previous and current caesarean sections forwards through a woman’s delivery history.
[Derived Parity] – this is the estimation of parity derived from all the information available in HES, but excluding any information from birth registration.
[Derived Parity (ONS)] – this is the estimation of parity derived from all the information available in HES along with any information that can be harvested from the corresponding linked birth registration record. The value will never be less than [Derived Parity].
Step 1: identifying trusts that misreport parity
The unit of analysis is taken to be assigned trusts. This is used in preference to units as this avoids considering midwife-led units, which will undoubtedly often have a skewed parity distribution.
For each assigned trust with more than 100 records of known parity and for each year, the percentage of nulliparous women was calculated. If this percentage fell outside the range 20–70% then the parity for the women who gave birth in that assigned trust during the given year was set to unknown. This updated parity was stored in the field [Recorded Parity].
Step 2: determining information about previous pregnancies from the current pregnancy
A mention of any of the following ICD-10 codes indicates that this is not a woman’s first pregnancy. The first two codes also indicate a previous caesarean section:
-
O34.2 – maternal care due to uterine scar from previous surgery
-
O75.7 – vaginal delivery following previous caesarean section
-
Z35.4 – supervision of pregnancy with grand multiparity
-
Z64.1 – problems related to multiparity
-
Z87.5 – personal history of complications of pregnancy, childbirth and the puerperium
-
Z87.6 – personal history of certain conditions arising in the perinatal period.
Step 3: determining information about the current pregnancy
As previously discussed, [NUMPREG] reports a woman’s parity, although some trusts misreport this.
There are no other indicators of parity in the current pregnancy; however, there are four places in which a caesarean section in the current pregnancy is mentioned. This is needed to propagate forward to a woman’s next delivery so as to be aware of previous caesarean sections.
[DELONSET] = 2. Elective caesarean section recorded in method of onset.
[DELMETH Best] = either 7 or 8. This field has the field [DELMETH] and OPCS procedure codes for delivery method rolled into one variable. Either an elective or an emergency caesarean section is looked for.
A mention of an ICD-10 codes starting with O82. These codes are rarely used, but were included for completeness.
Step 4: counting forward deliveries
A mother is assumed to have the same HES ID throughout her obstetric history. All of a mother’s deliveries were placed in date order. For each delivery the [Recorded Order] is set to the delivery’s place in the sequence.
For the first delivery if the [Recorded Parity] ([NUMPREG] unless from a trust with suspect data) is greater than zero then this value is assumed to be correct and is placed in the field [Derived Parity]. If [Recorded Parity] is zero or unknown and there is no evidence in the ICD codes that there was a previous pregnancy, then [Derived Parity] is set to zero. If there is evidence of a previous pregnancy then [Derived Parity] is set to one. The ICD codes are not specific about the number of previous pregnancies and some clearly indicate many. However, the marginal effect of parity rapidly decreases with increasing parity so parity of one was assumed in all cases.
For successive deliveries the parity is assumed to be one more than the last delivery unless the value of [Recorded Parity] exceeds this, in which case the [Recorded Parity] is assumed correct. There were quite legitimate reasons why this could occur. For example, a mother may have her second baby in Wales, hence in HES her recorded parity would be zero followed by two for successive deliveries.
Step 5: factoring in birth registration
The value reported in in the Birth Registration field [PREVCH] represents the minimum parity a woman may possess.
For the first delivery if [PREVCH] exceeds [Derived Parity] then [Derived Parity (ONS)] is set equal to [PREVCH] otherwise it is set to the [Derived Parity] as determined by Step 4.
For successive deliveries [Derived Parity (ONS)] is set equal to the maximum of the three values:
-
[Derived Parity (ONS)] for the last delivery + 1
-
[Derived Parity] for this delivery
-
[PREVCH] for the ONS record linked to this delivery.
| Assigned trust | Code | 2004–5 | 2005–6 | 2006–7 | 2007–8 | 2008–9 | 2009–10 | 2010–11 | 2011–12 | 2012–13 | 2013–14 | 2014–15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Airedale NHS Foundation Trust | RCF | 44 | 44 | 43 | 44 | 46 | – | – | – | – | – | 43 |
| Ashford and St Peter’s Hospitals NHS Foundation Trust | RTK | 32 | 34 | 36 | 49 | – | – | 46 | 48 | 47 | 47 | 45 |
| Barking, Havering and Redbridge University Hospitals NHS Trust | RF4 | 32 | 33 | 32 | 32 | 34 | – | – | – | – | – | 67 |
| Barnet and Chase Farm NHS Hospitals Trust | RVL | 37 | 36 | 37 | 35 | 45 | 46 | 50 | 43 | 45 | 45 | 45 |
| Barnsley Hospital NHS Foundation Trust | RFF | 36 | 46 | 43 | 36 | 36 | 33 | 32 | 33 | 32 | 0 | 0 |
| Barts and The London NHS Trust | RNJ | 32 | 29 | 31 | 32 | 32 | 33 | 32 | 31 | 36 | 37 | 29 |
| Basildon and Thurrock University Hospitals NHS Foundation Trust | RDD | 41 | 40 | 39 | 34 | 32 | 31 | 29 | 31 | 31 | 0 | 0 |
| Basingstoke and North Hampshire NHS Trust | RN5 | 32 | 31 | 30 | 31 | 32 | 35 | 36 | 35 | 34 | – | – |
| Bedford Hospital NHS Trust | RC1 | 42 | 43 | 42 | 44 | 50 | 55 | 54 | 53 | 53 | 47 | 42 |
| Birmingham Women’s NHS Foundation Trust | RLU | 42 | 41 | 37 | – | 0 | 36 | 37 | 4 | 18 | 39 | 40 |
| Blackpool Teaching Hospitals NHS Foundation Trust | RXL | – | 43 | 35 | 35 | 38 | 83 | 45 | 42 | 33 | 31 | 33 |
| Bolton NHS Foundation Trust | RMC | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Bradford Teaching Hospitals NHS Foundation Trust | RAE | 37 | 37 | 33 | – | 29 | 28 | 27 | 26 | 27 | – | – |
| Brighton and Sussex University Hospitals NHS Trust | RXH | – | – | – | – | 72 | 64 | 59 | 56 | 55 | 0 | 0 |
| Buckinghamshire Healthcare NHS Trust | RXQ | 46 | 46 | 43 | 39 | 22 | 16 | 31 | 44 | 44 | 45 | 42 |
| Burton Hospitals NHS Foundation Trust | RJF | 45 | 47 | 46 | 41 | 45 | 44 | 46 | 45 | 40 | 42 | 40 |
| Calderdale and Huddersfield NHS Foundation Trust | RWY | – | – | – | – | 36 | 36 | 35 | 33 | 42 | 43 | 43 |
| Cambridge University Hospitals NHS Foundation Trust | RGT | 46 | 48 | 47 | – | 50 | 49 | 49 | 51 | 50 | 49 | 55 |
| Central Manchester University Hospitals NHS Foundation Trust | RW3 | 36 | 35 | 35 | 38 | 42 | 43 | 44 | 46 | 0 | 0 | 0 |
| Chelsea and Westminster Hospital NHS Foundation Trust | RQM | – | 41 | 45 | 11 | 60 | – | – | – | – | – | 56 |
| Chesterfield Royal Hospital NHS Foundation Trust | RFS | 39 | 44 | 46 | 48 | – | – | – | – | 44 | 44 | 0 |
| City Hospitals Sunderland NHS Foundation Trust | RLN | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 38 | 0 |
| Colchester Hospital University NHS Foundation Trust | RDE | 35 | 35 | 36 | – | – | – | – | – | – | – | 36 |
| Countess Of Chester Hospital NHS Foundation Trust | RJR | 48 | 47 | 46 | 47 | 49 | 48 | 47 | 46 | 46 | 0 | 0 |
| County Durham and Darlington NHS Foundation Trust | RXP | 44 | 39 | – | – | – | 39 | 36 | 36 | 34 | 31 | 0 |
| Croydon Health Services NHS Trust | RJ6 | 31 | 37 | 32 | – | 33 | 33 | 33 | 31 | 100 | 100 | – |
| Dartford and Gravesham NHS Trust | RN7 | 35 | 38 | 37 | 37 | 36 | 37 | 36 | 9 | 33 | 32 | 31 |
| Derby Teaching Hospitals NHS Foundation Trust | RTG | 39 | 36 | 43 | 41 | 37 | 37 | 36 | 35 | 36 | 34 | 34 |
| Doncaster and Bassetlaw Hospitals NHS Foundation Trust | RP5 | 43 | 44 | 44 | – | 44 | 44 | 44 | 43 | 42 | 37 | 41 |
| Dorset County Hospital NHS Foundation Trust | RBD | – | – | – | – | – | – | – | – | – | – | 0 |
| Ealing Hospital NHS Trust | RC3 | 35 | 35 | 33 | 35 | 33 | – | – | – | – | 2 | 0 |
| East and North Hertfordshire NHS Trust | RWH | 46 | 44 | 45 | 45 | – | – | – | 47 | 48 | 46 | 46 |
| East Cheshire NHS Trust | RJN | 37 | 37 | 35 | – | – | – | 36 | 35 | 34 | 32 | 33 |
| East Kent Hospitals University NHS Foundation Trust | RVV | 41 | 39 | 42 | 45 | 31 | 37 | 33 | 32 | 32 | 0 | 0 |
| East Lancashire Hospitals NHS Trust | RXR | 32 | 32 | 33 | 34 | 33 | 32 | 32 | 30 | 30 | 29 | 0 |
| East Sussex Healthcare NHS Trust | RXC | 41 | 43 | 44 | 45 | 44 | 44 | 45 | 42 | 42 | 0 | 0 |
| Epsom and St Helier University Hospitals NHS Trust | RVR | 35 | 30 | – | – | 36 | 33 | 33 | 32 | 32 | 31 | 30 |
| Frimley Park Hospitals NHS Foundation Trust | RDU | 38 | 36 | 37 | 38 | 38 | 36 | 38 | 35 | 36 | 33 | 35 |
| Gateshead Health NHS Foundation Trust | RR7 | – | – | – | – | – | 75 | 53 | 46 | 52 | 45 | 47 |
| George Eliot Hospital NHS Trust | RLT | 37 | 38 | 35 | 67 | 100 | 100 | 100 | 100 | 100 | 100 | 79 |
| Gloucestershire Hospitals NHS Foundation Trust | RTE | – | – | – | – | 14 | 48 | 48 | 46 | 45 | 44 | 45 |
| Great Western Hospitals NHS Foundation Trust | RN3 | 1 | 1 | 1 | 1 | 4 | 7 | 9 | 5 | 18 | 37 | 0 |
| Guy’s and St Thomas’ NHS Foundation Trust | RJ1 | 0 | 0 | 0 | 0 | – | – | – | – | – | 0 | 0 |
| Harrogate and District NHS Foundation Trust | RCD | – | – | – | – | 59 | 47 | 0 | 0 | 0 | 0 | 0 |
| Heart Of England NHS Foundation Trust | RR1 | 60 | 50 | 31 | 97 | 51 | 34 | 32 | 33 | 32 | 31 | 23 |
| Heatherwood and Wexham Park Hospitals NHS Foundation Trust | RD7 | 46 | 45 | 46 | – | 46 | 44 | – | – | – | – | – |
| Hinchingbrooke Health Care NHS Trust | RQQ | 100 | 100 | 100 | 100 | 100 | – | 47 | 50 | 56 | 62 | 66 |
| Homerton University Hospital NHS Foundation Trust | RQX | 0 | 27 | 31 | 46 | 30 | 29 | 31 | 31 | 30 | 30 | 32 |
| Hull and East Yorkshire Hospitals NHS Trust | RWA | – | – | – | – | – | – | – | 33 | 32 | 33 | 33 |
| Imperial College Healthcare NHS Trust | RYJ | 47 | 45 | 51 | – | – | – | – | – | – | – | 67 |
| Ipswich Hospital NHS Trust | RGQ | 34 | 37 | 35 | – | 35 | 7 | 35 | – | – | 0 | 0 |
| Isle of Wight NHS Trust | R1F | 34 | 38 | 38 | 39 | 40 | 42 | 36 | 38 | 38 | 45 | 3 |
| James Paget University Hospitals NHS Foundation Trust | RGP | 43 | 44 | 42 | 45 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Kettering General Hospital NHS Foundation Trust | RNQ | – | – | – | – | – | – | – | – | 0 | 0 | 0 |
| King’s College Hospital NHS Foundation Trust | RJZ | 34 | 32 | 31 | 60 | 38 | 43 | 54 | – | – | – | – |
| Kingston Hospital NHS Foundation Trust | RAX | 36 | 36 | 36 | 38 | 38 | 39 | 37 | 38 | 35 | 36 | 35 |
| Lancashire Teaching Hospitals NHS Foundation Trust | RXN | 41 | – | – | – | 37 | 36 | 31 | 31 | 54 | 30 | 32 |
| Leeds Teaching Hospitals NHS Trust | RR8 | 39 | 43 | 43 | 43 | 42 | 46 | 41 | 39 | 37 | 37 | 20 |
| Lewisham and Greenwich NHS Trust | RJ2 | – | – | – | – | – | – | – | – | – | 41 | – |
| Liverpool Women’s NHS Foundation Trust | REP | – | 0 | 0 | – | – | – | 0 | 0 | 0 | 28 | – |
| Luton and Dunstable University Hospital NHS Foundation Trust | RC9 | 30 | 31 | 32 | 32 | 32 | 31 | 30 | 30 | 29 | 26 | 0 |
| Maidstone and Tunbridge Wells NHS Trust | RWF | 59 | 32 | 33 | 33 | 29 | 35 | 33 | 33 | 32 | 28 | 0 |
| Medway NHS Foundation Trust | RPA | 76 | 74 | 74 | 72 | 81 | 92 | 83 | 87 | 95 | 87 | – |
| Mid Cheshire Hospitals NHS Foundation Trust | RBT | – | – | – | – | – | – | 100 | 100 | 100 | 100 | 100 |
| Mid Essex Hospital Services NHS Trust | RQ8 | 37 | 35 | 35 | 33 | 35 | 37 | 34 | 34 | 34 | 33 | 33 |
| Mid Staffordshire NHS Foundation Trust | RJD | 100 | 100 | 100 | 100 | – | – | – | – | – | 100 | 100 |
| Mid Yorkshire Hospitals NHS Trust | RXF | 41 | 43 | 41 | 42 | 42 | 44 | 40 | 40 | 44 | 43 | – |
| Milton Keynes University Hospital NHS Foundation Trust | RD8 | 48 | 45 | – | – | – | – | – | – | – | – | – |
| Newham University Hospital NHS Trust | RNH | 0 | 31 | 30 | – | 34 | 32 | 34 | 35 | 34 | 31 | 38 |
| Norfolk and Norwich University Hospitals NHS Foundation Trust | RM1 | 35 | 36 | 33 | 32 | 34 | 34 | 32 | 33 | 33 | 31 | 32 |
| North Bristol NHS Trust | RVJ | – | – | – | – | 100 | 63 | 73 | 33 | 38 | 46 | 54 |
| North Cumbria University Hospitals NHS Trust | RNL | – | – | – | – | – | – | – | – | – | – | – |
| North Middlesex University Hospital NHS Trust | RAP | 100 | 100 | 100 | 98 | – | – | – | – | – | – | 32 |
| North Tees and Hartlepool NHS Foundation Trust | RVW | 40 | 43 | 43 | – | 34 | 39 | 35 | 34 | 33 | 37 | 35 |
| North West London Hospitals NHS Trust | RV8 | – | – | – | – | 100 | 46 | 100 | 44 | 44 | 45 | 43 |
| Northampton General Hospital NHS Trust | RNS | 47 | 45 | 46 | 45 | 46 | 44 | 41 | 34 | 34 | 0 | 0 |
| Northern Devon Healthcare NHS Trust | RBZ | – | 42 | 48 | – | 47 | 43 | 44 | 45 | 43 | 43 | 42 |
| Northern Lincolnshire and Goole NHS Foundation Trust | RJL | 45 | 45 | 43 | – | 42 | 73 | 47 | – | – | – | – |
| Northumbria Healthcare NHS Foundation Trust | RTF | 46 | 44 | 44 | 43 | 44 | 42 | 38 | 36 | 35 | 38 | 41 |
| Nottingham University Hospitals NHS Trust | RX1 | – | – | – | – | 43 | 41 | 42 | 37 | 31 | 33 | 32 |
| Oxford University Hospitals NHS Foundation Trust | RTH | 42 | 45 | 46 | 46 | 46 | 46 | 47 | 45 | 38 | 37 | 40 |
| Pennine Acute Hospitals NHS Trust | RW6 | 32 | 34 | 39 | 31 | 32 | 30 | 29 | 28 | 29 | 27 | 26 |
| Peterborough and Stamford Hospitals NHS Foundation Trust | RGN | 34 | 34 | 34 | 34 | 34 | 33 | 32 | 33 | 32 | 32 | 31 |
| Plymouth Hospitals NHS Trust | RK9 | – | – | – | – | – | – | – | – | – | – | – |
| Poole Hospital NHS Foundation Trust | RD3 | 30 | 30 | 34 | – | 40 | 41 | 40 | 37 | 37 | 35 | 34 |
| Portsmouth Hospitals NHS Trust | RHU | 35 | 33 | 33 | 33 | 33 | 33 | 34 | 34 | 33 | 32 | 4 |
| Royal Berkshire NHS Foundation Trust | RHW | – | – | – | – | – | 47 | 48 | 46 | 46 | 42 | 0 |
| Royal Cornwall Hospitals NHS Trust | REF | 50 | 47 | 46 | 47 | – | 45 | 45 | 44 | 44 | 44 | 42 |
| Royal Devon and Exeter NHS Foundation Trust | RH8 | – | – | – | – | – | 46 | 48 | 49 | 47 | 40 | 0 |
| Royal Free London NHS Foundation Trust | RAL | 70 | 72 | 69 | 53 | 45 | 37 | 37 | 35 | 34 | 36 | 35 |
| Royal Surrey County Hospital NHS Foundation Trust | RA2 | 39 | 37 | 39 | 39 | 42 | – | – | – | – | – | – |
| Royal United Hospitals Bath NHS Foundation Trust | RD1 | – | – | – | – | – | – | – | 4 | 2 | 2 | 38 |
| Salisbury NHS Foundation Trust | RNZ | – | – | 41 | – | 38 | 32 | 34 | 30 | 30 | 31 | 29 |
| Sandwell and West Birmingham Hospitals NHS Trust | RXK | 23 | 36 | 35 | 35 | 20 | 32 | 32 | 33 | 34 | 34 | 74 |
| Scarborough and North East Yorkshire Health Care NHS Trust | RCC | – | – | – | – | – | – | – | – | – | – | – |
| Sheffield Teaching Hospitals NHS Foundation Trust | RHQ | 37 | 35 | 35 | 35 | 34 | 35 | 38 | 36 | 36 | 31 | 31 |
| Sherwood Forest Hospitals NHS Foundation Trust | RK5 | 47 | 44 | 44 | 44 | 44 | 44 | 46 | 46 | 44 | 45 | 46 |
| Shrewsbury and Telford Hospital NHS Trust | RXW | – | – | – | – | 35 | 34 | 34 | 33 | 32 | 32 | 30 |
| South Devon Healthcare NHS Foundation Trust | RA9 | – | – | – | – | 50 | 51 | 46 | 46 | 45 | 44 | 43 |
| South London Healthcare NHS Trust | RYQ | 30 | 31 | 30 | – | 23 | 20 | 26 | 32 | 44 | 29 | 0 |
| South Tees Hospitals NHS Foundation Trust | RTR | 43 | 37 | 35 | 37 | 35 | 36 | 36 | 35 | 33 | 0 | 0 |
| South Tyneside NHS Foundation Trust | RE9 | – | – | – | – | 92 | 95 | 100 | 97 | 75 | 89 | 0 |
| South Warwickshire NHS Foundation Trust | RJC | 34 | 37 | 55 | 100 | 100 | 69 | – | – | – | 45 | 45 |
| Southend University Hospital NHS Foundation Trust | RAJ | 3 | 3 | 58 | 36 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Southport and Ormskirk Hospital NHS Trust | RVY | 32 | 32 | 32 | 34 | – | – | – | – | – | – | 39 |
| St George’s University Hospitals NHS Foundation Trust | RJ7 | 42 | 43 | 39 | 38 | 40 | 39 | – | – | – | – | – |
| St Helens and Knowsley Hospital Services NHS Trust | RBN | 37 | 39 | 35 | – | – | 45 | 43 | 45 | 46 | 77 | – |
| Stockport NHS Foundation Trust | RWJ | 36 | 36 | 36 | 38 | 38 | 38 | 36 | 32 | 32 | 31 | 30 |
| Surrey and Sussex Healthcare NHS Trust | RTP | 100 | 100 | 100 | 100 | – | 33 | 40 | 100 | 43 | 32 | 31 |
| Tameside Hospital NHS Foundation Trust | RMP | 100 | 100 | 100 | – | 100 | 100 | 100 | 100 | 100 | 40 | – |
| Taunton and Somerset NHS Foundation Trust | RBA | – | – | – | – | – | 34 | 82 | 33 | 33 | 30 | 30 |
| The Dudley Group NHS Foundation Trust | RNA | – | – | – | – | 58 | 54 | 54 | 55 | 48 | 49 | 46 |
| The Hillingdon Hospitals NHS Foundation Trust | RAS | – | – | – | – | 100 | 100 | 100 | 34 | 36 | 3 | 1 |
| The Newcastle upon Tyne Hospitals NHS Foundation Trust | RTD | 0 | 20 | 47 | 48 | 0 | 24 | 53 | 53 | 54 | 0 | 0 |
| The Princess Alexandra Hospital NHS Trust | RQW | 20 | 21 | 17 | 14 | 26 | 25 | 24 | 24 | 28 | 24 | 30 |
| The Queen Elizabeth Hospital, King’s Lynn, NHS Foundation Trust | RCX | 37 | 32 | 33 | 34 | 36 | 36 | 32 | 36 | 36 | 35 | 35 |
| The Rotherham NHS Foundation Trust | RFR | 45 | 45 | 44 | 45 | 44 | 43 | 43 | 42 | 43 | – | 40 |
| The Royal Wolverhampton NHS Trust | RL4 | – | – | – | – | 45 | 44 | 44 | 44 | 43 | 42 | 42 |
| The Whittington Hospital NHS Trust | RKE | 32 | 26 | 30 | 29 | 29 | 30 | 32 | 50 | 48 | 35 | 33 |
| Trafford Healthcare NHS Trust | RM4 | 31 | 35 | 32 | 33 | 34 | 42 | – | – | – | – | – |
| United Lincolnshire Hospitals NHS Trust | RWD | 48 | 44 | 43 | 46 | 45 | 47 | 46 | 45 | 44 | – | – |
| University College London Hospitals NHS Foundation Trust | RRV | 28 | 5 | 69 | 66 | – | – | – | – | – | – | 100 |
| University Hospital Of North Staffordshire NHS Trust | RJE | 33 | 34 | 33 | – | – | 47 | 47 | 45 | 39 | 24 | 31 |
| University Hospital Of South Manchester NHS Foundation Trust | RM2 | 0 | 0 | 0 | 100 | 100 | – | – | 100 | 100 | 100 | 37 |
| University Hospital Southampton NHS Foundation Trust | RHM | 34 | 35 | 37 | – | – | 35 | 34 | 0 | 44 | 43 | 40 |
| University Hospitals Bristol NHS Foundation Trust | RA7 | 47 | 47 | 47 | 46 | 47 | 47 | 48 | 49 | 27 | 23 | 20 |
| University Hospitals Coventry and Warwickshire NHS Trust | RKB | 5 | 5 | 6 | 37 | 37 | 35 | 34 | 32 | 31 | 31 | 33 |
| University Hospitals Of Leicester NHS Trust | RWE | 43 | 43 | – | – | – | 0 | 33 | 33 | 32 | 33 | 31 |
| University Hospitals Of Morecambe Bay NHS Foundation Trust | RTX | – | – | 100 | 100 | 100 | 100 | 43 | 33 | – | 0 | 0 |
| Walsall Healthcare NHS Trust | RBK | 33 | – | 33 | 32 | 32 | 31 | 31 | 31 | 32 | 0 | 0 |
| Warrington and Halton Hospitals NHS Foundation Trust | RWW | – | – | – | – | – | – | – | – | – | – | – |
| West Hertfordshire Hospitals NHS Trust | RWG | 0 | 52 | 45 | 47 | 46 | 46 | 46 | – | – | 44 | 44 |
| West Middlesex University Hospital NHS Trust | RFW | 42 | 47 | 48 | 46 | 46 | 48 | 49 | 48 | 45 | 47 | 44 |
| West Suffolk NHS Foundation Trust | RGR | 42 | 43 | 42 | 45 | 44 | 45 | 45 | 44 | 45 | 41 | 0 |
| Western Sussex Hospitals NHS Foundation Trust | RYR | 64 | 76 | 100 | – | 100 | 99 | 94 | 96 | 100 | 100 | 100 |
| Whipps Cross University Hospital NHS Trust | RGC | 29 | 32 | 34 | 33 | 34 | 34 | 34 | 32 | 30 | 30 | 50 |
| Winchester and Eastleigh Healthcare NHS Trust | RN1 | 42 | 41 | 42 | – | – | 38 | 31 | 35 | 36 | – | – |
| Wirral University Teaching Hospital NHS Foundation Trust | RBL | – | – | – | – | – | – | 0 | 0 | 0 | 62 | 44 |
| Worcestershire Acute Hospitals NHS Trust | RWP | 100 | 94 | 78 | 72 | 57 | – | – | – | – | – | 43 |
| Wrightington, Wigan and Leigh NHS Foundation Trust | RRF | 38 | 38 | 39 | 37 | 37 | 37 | 37 | 36 | 34 | 34 | 31 |
| Wye Valley NHS Trust | RLQ | 36 | 34 | 62 | 100 | – | – | 100 | 100 | 100 | 100 | 89 |
| Yeovil District Hospital NHS Foundation Trust | RA4 | – | – | – | – | 44 | 45 | 48 | 54 | 42 | 43 | 37 |
| York Teaching Hospital NHS Foundation Trust | RCB | – | – | – | – | – | – | – | – | – | – | – |
Assigned trust, derived location of birth and unit type
These variables were required to undertake analyses by NHS trusts, maternity unit or type of unit (e.g. OU or midwifery unit) but presented some challenges. Once these variables were created, they could be used to determine if they were the same in each dataset and, if not, which was the most accurate Assigned Trust, Location of Birth and Unit Type to use for analysis. Definitions of types of maternity unit are given in Box 2.
-
Obstetric unit (OU): a NHS clinical location in which care is provided by a team, with obstetricians taking primary professional responsibility for women at high risk of complications during labour and birth. Midwives offer care to all women in an OU, whether or not they are considered at high or low risk, and take primary responsibility for women with straightforward pregnancies during labour and birth. Diagnostic and treatment medical services including obstetric, neonatal and anaesthetic care are available on site, 24 hours a day.
-
Alongside midwifery unit (AMU): a NHS clinical location offering care to women with straightforward pregnancies during labour and birth in which midwives take primary professional responsibility for care. During labour and birth diagnostic and treatment medical services, including obstetric, neonatal and anaesthetic care are available, should they be needed, in the same building, or in a separate building on the same site. Transfer will normally be by trolley, bed or wheelchair.
-
Freestanding midwifery unit (FMU): a NHS clinical location offering care to women with straightforward pregnancies during labour and birth in which midwives take primary professional responsibility for care. General practitioners may also be involved in care. During labour and birth, diagnostic treatment medical services including obstetric, neonatal and anaesthetic care, are not immediately available but are located on a separate site should they be needed. Transfer will normally involve care or ambulance.
Definitions taken from Rowe. 193 This report may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising.
Rowe R. Birthplace Terms and Definitions: Consensus Process. Birthplace in England Research Programme. Final Report Part 2. London: HMSO; 2011.
Creating derived variables was required because:
-
The place of birth codes within each dataset are not directly comparable, so it is necessary to translate each type of code into a common code for each birth location by mapping to a definitive list of locations.
-
Locations of birth are not fixed over the period 2005–14, as hospitals open, close, move site, move trust or change status (e.g. from OU to FMU). Some of these changes result in changes to postcodes, communal establishment codes or ODS codes. For example, Frome hospital has moved site once and has been managed by four different trusts, resulting in five potential hospital codes, each relevant only for a certain period of time. When there are hospital changes (e.g. a change of trust or site), old codes and new codes may be used in parallel for some time or changes might occur at different times in the different datasets.
Coding of place of birth is different in each of the three datasets: birth registration (ONS), birth notification (NN4B) and HES.
Birth registration
This is based on a numerical Communal Establishment code [CESTRSS] of up to five digits. Every birth registration record has a communal establishment code. Communal establishments include:
-
NHS hospitals with maternity provision
-
NHS hospitals without maternity provision
-
non-NHS hospitals (private/military)
-
communal establishments that are not hospitals (e.g. schools and care homes).
Births occurring at home or elsewhere are denoted by a H or E, respectively. Types of establishment are designated using [ESTTYPEB] 1–5. NHS communal establishments are denoted by [NHSIND] = 1 (non-NHS = 2).
Birth notification
This is recorded in two fields: [ORGCODEZ] and [DELPLAZ].
[ORGCODEZ] is based on a hospital’s ODS code,194 a five-digit alphanumeric code in the form RWD01, in which the first three characters indicate a NHS trust and the last two indicate a particular hospital site. In some cases, this may be entered as free text.
[DELPLAZ] is a free-text field that usually gives the name of hospital of birth, but may only give the name of the trust. Some hospitals in different areas of the country have the same name and are, therefore, indistinguishable from each other based on the [DELPLAZ] field alone (e.g. there are several hospitals with the name St Mary’s).
Home births or those taking place elsewhere may not have an [ORGCODEZ] or may use the [ORGCODEZ] of the hospital responsible for the home birth service. The place of birth may be recorded in [DELPLAZ] (e.g. ‘home delivery’ or the actual address ‘72 High Street, PO2 8LT’ [not a real address]).
Hospital Episode Statistics
This is recorded in two fields [PROCODE] and [SITETRET]. These are both based on a hospital’s ODS code, but may use different ones from those used for birth notification. The [PROCODE] may identify the site or only the trust (e.g. RWD00). The combination of [PROCODE] and [SITETRET] will usually determine the hospital site of birth.
Home births are poorly recorded in HES and are often recorded as taking place at one of the hospital sites or are given a non-specific trust code. A very few trusts use particular [SITETRET] codes to denote home births.
Four Microsoft Access® lookup tables were created:
-
[CESTRSS] to location code (Fields: CESTRESS, Derived Location code).
-
[ORGCODEZ]/[DELPLAZ] combination to location code (Fields: [ORGCODEZ], [DELPLAZ], Derived Location code). This was originally done separately as two tables.
-
[PROCODE]/[SITETRET] to location code (Fields: [PROCODE], [SITETRET], Derived Location code).
-
Location codes (Fields: Location code, Location Name, Assigned Trust, Project Postcode, Service Group Code).
This enabled each of three datasets making up the linked records to have a comparable Location of Birth and Assigned Trust.
Assigned Trusts
In order to perform analyses using NHS trust as a variable, it was necessary to assign maternity units to only one trust each for the period 2005–14, even if the trust providing maternity services had varied over the course of the study period. These are referred to as ‘Assigned Trusts’. The majority of maternity units (125) were administered by a single trust over this period and were naturally assigned to this trust. When groups of maternity units were transferred from trust to trust in a group, they were assigned to the most recent trust. For example, the Wiltshire midwifery units and the OU in Bath were administered by four different trusts between 2005 and 2014, and were assigned to the administering trust in 2014, Royal United Hospitals Bath NHS Foundation Trust. Where trusts merged early on in the study period, units were assigned to the merged trust (e.g. two trusts in Nottingham merged on 1 April 2006 and the maternity units within these were both assigned to the merged Nottingham University Hospitals NHS Trust). When trusts merged late on in the study period, units were assigned to the pre-merged trusts (e.g. the three trusts that merged to form Barts Health NHS Trust on 1 April 2012 were treated as three separate trusts).
Overall, there were 196 trusts in England and Wales, which were treated as 150 Assigned Trusts. For ease of analysis, the 150 Assigned Trusts were grouped into 138 ‘Service Groups’, which reflected larger groups of trusts with a relationship. For example, the three trusts merging to form Barts Health NHS Trust on 1 April 2012 were treated as three separate Assigned Trusts but formed one Service Group.
Assigned Trusts were also allocated to one of the 10 Strategic Health Authority regions in England in existence between April 2006 and March 2013 for regional analysis. Welsh Trusts were allocated to a single region of Wales.
A lookup table mapping Assigned Trusts to actual trusts based on baby’s date of birth was also created.
Derived location codes
All maternity units held in the BirthChoiceUK database already had a unique ID. These were collated to create a fixed location code based on a hospital site or maternity service offered to women in a local area during the study period.
A mapping system using a lookup table for each type of code enabled the translation of the different coding systems into a common language. These lookup tables were based on the BirthChoiceUK historical maternity unit database, used with the permission of Rod Gibson Associates Ltd. These database contains details of all maternity units, NHS trusts and service configurations over the past 15 years with dates of opening and closures, changes of trust and unit type.
A large amount of mapping of ODS, HES and [CESTRSS] codes had previously been undertaken by BirthChoiceUK and this work was supplemented by further work for this project, particularly in relation to birth notification, where [ORGCODEZ] and [DELPLAZ] were mapped to maternity units.
A maternity unit that moved entirely to a new site in the locality was regarded as a single birth location, continuous with the previous site. A unit that changed from being an OU to a FMU was also treated as being the same location with the same code with the date of change of status noted. A maternity unit that moved to a different trust also kept the same code. This is in contrast to the ODS codes, which can change when a maternity unit moves site or trust.
Derived location codes were also devised for locations of birth that were not NHS maternity units included in the BirthChoiceUK database. This included private maternity hospitals, military hospitals, NHS hospitals that did not have maternity units and communal establishments that were not NHS hospitals, such as care homes or schools. Location codes for NHS hospitals were allocated to the correct Assigned Trust. For completeness an additional location code was also used for a home birth or a birth taking place ‘elsewhere’ – for example in an ambulance or at the roadside.
Each location code was also allocated a location name to help with any visual checking of discrepancies, on the basis that it is easier to see the difference between CF1 and CM1 if one is also displayed as Cardiff and one as Chelmsford, or similarities between TN2 and ME16 if they are displayed as Tunbridge Wells and Maidstone. Derived location codes were allocated to Assigned Trusts. When the location of birth was ‘private’, ‘military’, ‘home’, ‘elsewhere’ or ‘not known’, an Assigned Trust code based on NHS Trust could not be allocated.
Most likely location of birth
In a number of cases, linkages between birth registrations, notifications and HES records looked to be correct but the location of birth did not match exactly based on the four different codes used for location. Work was undertaken to determine which was the most reliable code to use to determine location of birth, which would have consequences for analyses based on Assigned Trust and on Unit Type (e.g. OU or midwifery unit). There were a number of challenges in determining the accurate location of birth:
-
Some codes are used by more than one maternity unit and sometimes by more than one trust, and some maternity units use more than one code in each of the datasets.
-
Some place of birth codes are not specific to a particular site. Birth registrations are site specific, but birth notification and HES codes sometimes use service provider/trust codes or text instead of being site specific.
-
Place of birth codes in the different datasets sometimes conflict with each other. In birth notification record, the organisation code and place of delivery (in text), sometimes conflict with each other within the dataset. This may be due to poor linkage, but often is due to coding issues.
-
For all four types of codes there is no reliable way to establish if births are in the OU or AMU if a hospital has both types of unit.
-
In birth notification and HES, there is no standard designated code for a home birth or births taking place elsewhere.
England and Wales
Birth registration/notification linked records
For birth registration/notification linked records that had undergone quality assurance, [CESTRSS] was found to be the most reliable source of place of birth (Table 38). It was complete (2 ‘not known’ out of over 7 million birth registration records) and always specific to a maternity unit (rather than NHS trust) or to another communal establishment, home or ‘elsewhere’. [DELPLAZ] was not always specific to a maternity unit and as this was a free-text field this was difficult to code reliably. [ORGCODEZ] had almost no codes for home births or births taking place ‘elsewhere’ and was sometimes missing or was contradictory with [DELPLAZ]. Using a combination of [ORGCODEZ] and [DELPLAZ] increased the completeness of the location field but there were still over 100,000 unknown locations of birth and over 150,000 records for which only the trust and not the site of birth was known.
| Birth setting | Birth registration | Birth notification (combined) | Birth notification [ORGCODEZ] | Birth notification [DELPLAZ] |
|---|---|---|---|---|
| Maternity unit | 6,796,550 | 6,712,081 | 6,506,418 | 5,780,848 |
| Known trust (site not known) | – | 158,361 | 355,645 | 838,674 |
| Home | 176,635 | 6,018 | 11 | 6,014 |
| Elsewhere | 11,803 | 1,162 | – | 1,150 |
| Private | 22,535 | 22,290 | 9116 | 22,290 |
| Military | 4,816 | 4,824 | 181 | 4,824 |
| Not a maternity hospital | 1,463 | 624 | 96 | 603 |
| Not known | 2 | 108,444 | 142,337 | 359,401 |
| Total births | 7,013,804 | 7,013,804 | 7,013,804 | 7,013,804 |
On the basis of completeness and specificity of coding, it was decided that for analyses based on birth registration/notification records only, [CESTRSS] would be used as the source of location. The location code for the registration record was recorded in the database and was used for analysis based on location of birth.
Derived location codes matched between birth registration and birth notification records in 94.5% of cases. In cases in which a derived location code was a NHS maternity unit, Assigned Trust codes matched in 99.9% of these cases.
Unit type
If one is using only the birth registration/notification dataset, then esttypeb is a useful variable to separate out births in NHS hospitals and exclude births in communal establishments that are not hospitals (e.g. care homes and schools) as well as births in non-NHS hospitals.
However, because we had mapped the communal establishment codes to the BirthChoiceUK historical database, we were able to do a much more detailed coding of where births took place.
A separate variable, UNIT TYPE, was used to determine the unit type (e.g. OU, OU+AMU, private, other communal establishment NAMH). A lookup table was created, mapping maternity unit types to location code based on dates of opening and closing. For example, if a maternity unit changed from being an OU to a FMU on the same site (i.e. the same location code) the type of unit could be determined by looking up the baby’s date of birth.
The lookup table used dates of opening and closing from the BirthChoiceUK historical maternity unit database. Once in the VML, every birth registration record was allocated a type of Unit Type based on location of birth (as determined by the [CESTRSS] code) and the baby’s date of birth. This was recorded in the database for each birth record to allow complex analyses based on changes in trust organisation and service configuration to be performed.
England
In birth registration/notification and HES delivery, linked singleton records that had undergone quality assurance HES records were more complete and specific than birth notification records but not as much as birth registration records (Table 39). It was decided that the location code for the registration record would also be used for the registration/notification and HES delivery linked record as having been derived from the most reliable source of place of birth information.
| Birth setting | Birth registration | Birth Notification (combined) | HES delivery |
|---|---|---|---|
| Maternity unit | 6,248,732 | 6,121,852 | 6,248,881 |
| Known trust | – | 149,384 | 81,882 |
| Home | 75,371 | 3,011 | 481 |
| Elsewhere | 6,457 | 640 | – |
| Not a maternity hospital | 1,198 | 402 | 516 |
| Not known | 2 | 56,471 | – |
| Total births | 6,331,760 | 6,331,760 | 6,331,760 |
Derived location codes matched between birth registration and HES delivery records in 97.1% of cases. When a derived location code was a NHS maternity unit, Assigned Trust codes matched in 99.97% of cases.
List of all database tables
-
AA CESTRSS to Location Code
-
AA DELPLAZ to Location Code
-
AA Distance Match
-
AA Ethnicity Codes 17
-
AA Ethnicity Codes 5
-
AA Ethnicity Codes 9
-
AA Ethnicity Codes Map
-
AA HES (PC and ST) to Location Code
-
AA ICD 10
-
AA Location Codes
-
AA MultType
-
AA ORGCODEZ to Location Code
-
AA Post Code to LSOA
-
AA Unit Type
-
Babies
-
Baby HES ONS Linkage
-
Baby Old to New HES ID
-
Babys_Readmissions
-
Babys_Readmissions_ICD
-
Babys_Readmissions_OPCS
-
Births
-
Births ICD & OPCS Flat
-
Births_ICD
-
Births_Indicators
-
Births_OPCS
-
Deliveries
-
Deliveries ICD & OPCS Flat
-
Deliveries_Baby_Tails
-
Deliveries_ICD
-
Deliveries_Indicators
-
Deliveries_OPCS
-
Mother HES ONS Linkage
-
Mother HES ONS Linkage Cleaned
-
Mother Old to New HES ID
-
Mothers
-
Mothers_Readmissions
-
Mothers_Readmissions_ICD
-
Mothers_Readmissions_OPCS
-
ONS
-
ONS Mortality
-
ONS Mortality Cause of Death
-
ONS Records Unmatched to Baby
-
ONS Records Unmatched to Mother
-
X Parity
Detailed description of database tables and fields
Source fields are in upper case and derived fields are in title case. When a field is referred to in the text it is enclosed in square brackets.
ONS database tables
Tables 40–42 show detailed descriptions of database tables and fields from the ONS dataset.
| Database table name: ONS | ||
|---|---|---|
| Field name** | Description | Data type |
| MNHSNOZ | Mothers NHS number (BN). (Too large to cast as Integer) | varChar(10) |
| NHSNOZ | Baby NHS number (BN) | varChar(10) |
| DOBZ# | Baby’s date of birth (BN) Cleaned version [Baby Date of Birth Birth Notification]. Note change of format in 2013 | varChar(10) |
| DELTIMEZ | Delivery time (BN) | varChar(8) |
| SEXZ# | Baby gender (BN), 0 = not known, 9 = not specified | varChar(1) |
| LSBTHZ# |
Birth status (BN). Coding changes in 2008. Cleaned version [Birth Status Birth Notification] Warning: this field has commas in that even when wrapped in quotes when exporting CSV files causes R to read incorrectly. These must be replaced when creating export files |
varChar(26) |
| BTHWGTZ# | Birth weight, 9999 & 9998 not knowns (BN). Cleaned version [Birth Weight] | Integer |
| GESTZ# | Gestation age, Zero = unknown (BN). Cleaned version [Gestational Age] | Integer |
| SUSCONAZ | Suspected congenital anomaly indicator (BN) | varChar(1) |
| ETHCATZ# |
Ethnicity (BN) Non-standard coding in 2005. Cleaned version [Ethnicity] Warning: this field has commas in that even when wrapped in quotes when exporting CSV files causes R to read incorrectly. These must be replaced when creating export files |
varChar(31) |
| PCDRBZ# |
Postcode of usual residence of baby (BN). Cleaned version [Baby Post Code Birth Notification] Warning: this field has commas and double quotes in that even when wrapped in quotes when exporting CSV files causes R to read incorrectly. These must be replaced when creating export files |
Char (10) |
| ORGCODEZ# | Organisation code (BN). Cleaned version [Location Code Birth Notification] | varChar(5) |
| DELPLAZ |
Organisation name (BN) Warning: this field has commas in that even when wrapped in quotes when exporting CSV files causes R to read incorrectly. These must be replaced when creating export files |
varChar(63) |
| DELTYPEZ | Delivery place type (BN) | varChar(40) |
| DOBMZ# | Mother’s date of birth (BN). Cleaned version [Mother Date of Birth Birth Notification]. Note change of format in 2013 | varChar(10) |
| CONFORDZ# | Cleaned version [Birth Order] | Integer |
| CONFNUMZ# | Cleaned version [Babies in Delivery] and [Babies in Delivery from MULTTYPE] | Integer |
| GPCODEZ | GP code (BN) | |
| CHORGZ | Child health system organisation code (BN) | |
| INTERFZ | Interface (BN) | |
| AGEBF# | Age of father/parent at time of birth of child. Format: yymm (BR). Cleaned version [Age Father] | varChar(4) |
| AGEBFIND | Whether age of father/parent imputed (1) or not (NULL) (BR) | varChar(1) |
| AGEBM# | Age of mother at time of birth of child. Format: yymm (BR). Cleaned version [Age Mother] | varChar(4) |
| AGEBMIND | Whether age of mother imputed (1) or not (NULL) (BR) | varChar(1) |
| AGEBMGRP | Quinary age grouping of mother (BR) | varChar(5) |
| BIRTHWGT# | Birth weight, 9998/9(?): indicates that no birth weight (BR). Cleaned version [Birth Weight] | Integer |
| CESTRSS# | Communal establishment code (BR). Cleaned version [Location Code Birth Registration] | varChar(5) |
| CTRYPOBF# | Country code of place of birth of father of child (BR). Cleaned version [Region Code of Country of Birth of Father] | varChar(4) |
| CTRYPOBM# | Country code of place of birth of mother of child (BR) Cleaned version [Region Code of Country of Birth of Mother] | varChar(4) |
| CTRYRM | County code of usual residence of mother of child (BR) | varChar(2) |
| DOB# | Baby’s date of birth (BR). Cleaned version [Baby Date of Birth Birth Registration] | varChar(8) |
| DOBDY | Day of birth of child (BR) | varChar(2) |
| DOBMT | Month of birth of child (BR) | varChar(2) |
| DOR | Date of registration. Yyyymmdd (BR) | varChar(10) |
| REGYR | Year of registration (BR) | Integer |
| BTHIMAR | Birth in marriage indicator | Integer |
| DURMAR | Duration of marriage. Format: yymm (NOT decimal) (BR) | varChar(4) |
| DOBM# | Mother’s date of birth (BR). Cleaned version [Mother Date of Birth Birth Registration] | varChar(10) |
| NHSIND | NHS establishment indicator. 1 NHS, 2 non-NHS, or NULL (BR) | Integer |
| ESTTYPEB | Establishment type where birth occurred (BR) | varChar(1) |
| GESTATN# | Gestation period (BR). Cleaned version [Gestational Age] | Integer |
| HROPOB | Health regional office code for place of birth | varChar(3) |
| HRORM | Health regional office code for usual residence of mother of child. Derived from PCDRM | varChar(3) |
| HAUTRM | Health authority code for usual residence of mother of child (BR) | |
| GORRM | Regional code of usual residence of mother of child (BR) | varChar(1) |
| STREGRM | Standard region code of usual residence of mother of child | varChar(1) |
| WARDRM | Ward code of usual residence of mother of child | varChar(6) |
| MULTTYPE | Multiple birth type (BR) | varChar(2) |
| MULTBTNO* | Unique ID for each delivery involving multiple births. (BR) | varChar(15) |
| MATTAB | Maternity tabulation selection indicator. Set to 1 on all single births and to 1 on one birth/stillbirth in a multiple | Integer |
| PCDPOB | Postcode of place of birth of child (BR) | varChar(10) |
| PCDRM# | Postcode of usual residence of mother of child (BR). Cleaned version [Mother Post Code Birth Registration] | Char (10) |
| PREVCH | Previous children born, total (BR) | Integer |
| PREVCHL | Previous children live born (BR) | Integer |
| PREVCHS | Previous children stillborn (BR) | Integer |
| PRCHLIND | Previous children live born, number imputed indicator | |
| PRCHSIND | Previous children stillborn, number imputed indicator | |
| SBIND | Still birth indicator (BR) | varChar(1) |
| EMPSECF | Employment status (ONS code) of father of child for SOC 2000 (BR) | Integer |
| EMPSECM | Employment status (ONS code) of mother of child for SOC 2000 (BR) | Integer |
| EMPSTF | Employment status (ONS code) of father of child (BR) | Integer |
| EMPSTM | Employment status (ONS code) of mother of child (BR) | Integer |
| OCC90F | Occupational code of father of child | varChar(3) |
| OCC90M | Occupational code of mother of child | varChar(3) |
| SECCATF | NS SEC operational category for father of child (BR) | Integer |
| SECCATM | NS SEC operational category for mother of child (BR) | Integer |
| NSSEC _ COMB | Combined NS SEC at birth | Integer |
| SECCLRF (also called SCLASF) | Social class of father of child (BR) | varChar(1) |
| SECCLRM (also called SCLASM) | Social class of mother of child (BR) | varChar(1) |
| SOC2KF | Standard occupation classification (2000) for father of child | varChar(4) |
| SOC2KM | Standard occupation classification (2000) for mother of child | varChar(4) |
| SEX# | 1 = M, 2 = F, 3 = Indeterminate (BR). Cleaned version [Baby Sex] | varChar(1) |
| TBTHTM | Total births to mother, live and still in this delivery episode (BR) | Integer |
| SOURCETABLE | Year of creation of births dataset | Integer |
| Age Father | Father/parent’s age, months as decimal years | Single |
| Age Mother | Mother’s age, months as decimal years | Single |
| Baby Date of Birth Birth Notification | Derived from DOBZ | Date |
| Baby Date of Birth Birth Registration | Derived from Date of Birth | Date |
| Baby Date of Birth | From Birth Registration unless missing then Notification | Date |
| Mother Date of Birth Birth Notification | Derived from DOBMZ | Date |
| Mother Date of Birth Birth Registration | Derived from DOBM | Date |
| Mother DoB | From Birth Registration unless missing then Notification | Date |
| Multiple | More than one baby in delivery episode | Bit |
| Birth Order | Derived from DOBZ and DELTIMEZ. This replicates the birth notification field CONFORDZ. ONS have not quality checked this field and it was found to contradict the birth order derived using DOBZ and DELTIMEZ on rare occasions | Integer |
| Babies in Delivery | Derived from count of set of records with common entries in MULTBTNO. Replicates the birth notification field CONFNUMZ | Integer |
| Babies in Delivery from MULTTYPE | This will only indicate 4 if the multiplicity is > 4 | Integer |
| Birth Status Birth Notification |
2005–07 text entries mapped onto 1 to 5 that appear in later years 1 = live 2 = still birth, antepartum 3 = still birth, intrapartum 4 = still birth, indeterminate 5 = dead |
Integer |
| Ethnicity | Cleaned [ETHCATZ] mapped to ONS 17 categories | varChar(7) |
| Ethnicity 9 | Cleaned [ETHCATZ] mapped to ONS 9 categories | varChar(1) |
| Ethnicity 5 | Cleaned [ETHCATZ] mapped to ONS 5 categories | varChar(1) |
| Gestational Age | Cleaned and combined [GESTZ] and [GESTATN] | Integer |
| Birth Weight | Cleaned and combined [BTHWGTZ] and [BIRTHWGT] | Integer |
| Baby Sex | Cleaned and combined [SEXZ] and [SEX] (M/F) | varChar(1) |
| Baby Post Code Birth Notification | PCDRBZ with all spaces removed | varChar(8) |
| Mother Post Code Birth Registration | PCDRM with all spaces removed | varChar(8) |
| Post Code | Use [Mother Post Code Birth Registration] unless missing | varChar(8) |
| LSOA 2001 | Mother Post Code Birth Registration mapped onto 2001 LSOA (derived) | varChar(9) |
| LSOA 2011 | Mother Post Code Birth Registration mapped onto 2011 LSOA (derived) | varChar(9) |
| Region Code of Country of Birth of Mother | varChar(3) | |
| Region Code of Country of Birth of Father | varChar(3) | |
| Location Code Birth Notification | Unique maternity unit identifier for Birth Notification place of birth | varChar(7) |
| Location Code Birth Registration | Unique maternity unit identifier for Birth Registration place of birth | varChar(7) |
| Location Code DELPLAZ | Unique maternity unit identifier for Birth Notification free text field [DELPLAZ]place of birth | varChar(7) |
| Location Code | Best guess at place of birth | varChar(7) |
| Pseudo Trust Birth Notification | Derived from map of Location Code to Pseudo Trust | varChar(3) |
| Pseudo Trust Birth Registration | Derived from map of Location Code to Pseudo Trust | varChar(3) |
| Pseudo Trust DELPALZ | Derived from map of Location Code to Pseudo Trust | varChar(3) |
| Pseudo Trust | Derived from map of Location Code to Pseudo Trust | varChar(3) |
| Home Birth | Derived from [Location Code Birth Registration] (i.e. CESSTRESS) | Bit |
| Elsewhere Birth | Derived from [Location Code Birth Registration] (i.e. CESSTRESS) | Bit |
| Unit Type | Type of maternity unit derived from [Location Code Birth Registration]. OU, OU+AMU, FMU and other settings | varChar(15) |
| Country | E if submitted to HSCIC, W if submitted to NWIS, B if submitted to both | varChar(1) |
| Discordant | Set to True if it looks like the birth notification is incorrectly linked to the birth registration record | Bit |
| ONS Link ID | Original ID created by ONS. Only use to link back to source data. Note that this is not unique across years and must be used alongside [ONS Link Year]. For linking tables within database use [ONS ID] | varChar(31) |
| ONS Link Year* | ONS year used for linkage | Integer |
| Is Linked to HES Delivery | True if the ONS record is linked to a HES delivery record after linkage cleaning | Bit |
| Is Linked to HES Birth | True if the ONS record is linked to a HES birth record after linkage cleaning. Not current set | Bit |
| Originally Linked to HES Mother | Record linked to a mother in original linkage performed by HSCIC | Bit |
| Originally Linked to HES Baby | Record linked to a baby in original linkage performed by HSCIC | Bit |
| ONS Link Mother Match Rank | Integer | |
| ONS Link Baby Match Rank | Integer | |
The database tables described in Table 41 store the core section of all types of mortality record (i.e. stillbirth, infant, child and maternal). The type of mortality determines which fields are populated.
| Database table name: ONS mortality | ||
|---|---|---|
| Field name | Description | Data type |
| ONS ID* | This is not a primary key as both the mother and the child can both die. It is, however, clustered for efficiency | Integer |
| Is Stillbirth | Equals 1 if a stillbirth | Bit |
| Is Infant | Equals 1 if child died before 1st birthday | Bit |
| Is Neonatal Infant | Equals 1 if child died before 4 weeks | Bit |
| Is Post Neonatal Infant | Equals 1 if child survived 4 completed weeks and died before first birthday | Bit |
| Is Child | Equals 1 if child survived 1 year. This field is naturally right censored | Bit |
| Is Maternal | Equals 1 if mother died of any cause within 1 year of childbirth | Bit |
| Is Final | There is a set of causes of final causes of death ICD codes in addition to the original set of causes | Bit |
| NHSNO | NHS number. (Maternal & child mortality) | varChar(10) |
| PCDR (Death) | Postcode of usual residence of deceased. (Maternal mortality only) | varChar(10) |
| CESTRSS (Death) | Communal establishment place of death code. (Child mortality only) | varChar(5) |
| AGEC | Ages at death in units given by AGECUNIT. (Infant & child mortality) | Int |
| AGECUNIT | 4 = days, 3 = weeks, 2 = months, 1 = years (Infant & child mortality) | Int |
| ICD10U | Original underlying cause of death. (Post neonatal Infant, child & maternal mortality) | varChar(4) |
| ICD10UF | Final underlying cause of death (after postmortem) (Post neonatal Infant, child & maternal mortality) | varChar(4) |
| WIGS10 | Wigglesworth code. National Statistics Hierarchical classification of mortality for ICD10 | Int |
| DoD | Date of death | Int |
| DoB Child (Mortality) | Date of birth of child as given in mortality record. Occasionally differs from birth record. (Child mortality) | Date |
| DoB Mother (Mortality) | Date of birth of mother. (Maternal mortality) | Date |
| IMLINKNO | Infant mortality link number. (Child mortality only) | varChar(6) |
| ONS Link ID | Original unique(-ish) ID used by ONS. Use field [ONS ID] unless linking back to source data | varChar(31) |
| ONS Link Year | Year of file in which record was originally received from. These correspond to date of birth of child or last delivery of mother | Int |
Stillbirth: 2005–14. Note that approximately 200 ONS stillbirth records for 2007 are missing from this dataset.
Infant: 2005–14.
Child: 2005–14.
Maternal: 2008–14.
Table 42 relates to the underlying cause of death for all types of mortality record, that is stillbirth, infant, child and maternal. The Final cause should be used if it exists, otherwise the Original cause should be used.
| Database table name: ONS mortality cause of death | ||
|---|---|---|
| Field name | Description | Data type |
| ONS ID* | This is not a primary key as both the mother and the child can both die | Integer |
| Is Juvenile | Equals 1 if record belongs to a child (stillbirth, infant or child) | Bit |
| Is Maternal | Equals 1 if a maternal death | Bit |
| Is Original Cause | Equals 1 if original cause | Bit |
| Is Final Cause | Equals 1 if final cause (i.e. original cause modified by postmortem or coroner’s report) | Bit |
| Cause ICD Code | ICD-10 code | varChar(4) |
| Field Order | 1 to 15 | Bit |
Mothers’ tables
Table 43–55 show detailed descriptions of database tables and fields from the HES records relating to the mother.
The Deliveries database table forms core delivery record. It holds the important fields from the mother’s HES delivery record. See Deriving new variables from Office for National Statistics data and Deriving new variables from Hospital Episode Statistics data for definitions of derived fields.
| Database table name: deliveries | ||
|---|---|---|
| Field name | Description | Data type |
| Delivery ID** | Primary key. Note that this is unique to a delivery record but because of duplicate HES records may not be unique to an actual mother’s delivery | Integer |
| Mother ID* | Foreign key that identifies mother | Integer |
| HES ID | ENCRYPTED _ HESID | varChar(32) |
| NEWNHSNO | Patient’s NHS number | varChar(10) |
| PROCODE | Organisation acting as a health care provider | varChar(5) |
| SITETRET | Site code of treatment | varChar(5) |
| PROCODET | Type of provider code | varChar(5) |
| PROTYPE | Provider type | varChar(10) |
| HOMEADD# | Patient’s home postcode. Cleaned version [Post Code] | varChar(8) |
| SEX | Patient’s sex (cleaned by HSCIC to be female) | varChar(1) |
| NUMPREG | Parity as reported in HES. 99 = Unknown | Integer |
| NUMBABY | Number of babies reported by HES in delivery episode | Integer |
| DOMPROC | Dominant procedure (operation) code | varChar(1) |
| DELONSET | HES field indicating method of onset of labour | varChar(1) |
| DELPREAN | Anaesthetic given during labour or delivery | varChar(1) |
| DELPOSAN | Anaesthetic given post-labour or delivery | varChar(1) |
| ETHNOS | Ethnicity | varChar(2) |
| ANASDATE | Date of first antenatal appointment | Date |
| ANAGEST | Gestational age at 1st antenatal appointment | Integer |
| ADMIDATE | Admission date | Date |
| DISDATE | Date of discharge. Only present for last episode in a spell | Date |
| ADMIMETH | How the patient was admitted to hospital | varChar(2) |
| ADMISORC | Identifies where the patient was immediately prior to admission | varChar(2) |
| DISDEST | Destination on discharge | varChar(2) |
| DISMETH | Method of discharge | varChar(1) |
| ANTEDUR | Antenatal days of stay | Integer |
| POSTDUR | Postnatal stay | Integer |
| EPISTART# | Episode start date. Cleaned version [Episode Start] | Date |
| EPIEND# | Episode end date. Cleaned version [Episode End] | Date |
| EPIORDER | The number of the episode within the current spell | Integer |
| EPISTAT | Episode status. 1 represents unfinished episode, 3 finished | varChar(1) |
| EPITYPE | Episode type | varChar(1) |
| HRGLATE | varChar(3) | |
| HRGLATE35 | varChar(3) | |
| HRGNHS | Trust derived HRG value | varChar(3) |
| HRGNHSVN | Version number of Trust derived HRG value | varChar(3) |
| GPPRPCT | Primary Care Trust area in which patient’s GP was registered. 59,898 = Not applicable (non-England), 59,999 = Unknown | varChar(5) |
| PROVSPNOPS (PROVSPNO) | A number to provide a unique identifier for each Hospital Provider | varChar(12) |
| LSOA01 | Lower Super Output Area | varChar(9) |
| IMD04RK | IMD Overall Rank | Integer |
| DELINTEN | Delivery place (intended) | varChar(1) |
| DELCHANG | Delivery place change reason | varChar(1) |
| MATAGE | Mother’s age at delivery | Integer |
| DOB | Patient’s date of birth | |
| MOTDOB | Mother’s date of birth | Date |
| EPIKEY | Unique HES record ID. Cast as text as too long for 4-byte integer, consequently not used as primary key. Although unique to HES the files supplied by HSCIC have multiple of some HES records of the link to ONS | varChar(14) |
| Trust Code | First three characters of PROCODE | varChar(3) |
| Location Code HES | varChar(7) | |
| Pseudo Trust Code HES | varChar(3) | |
| Post Code | Derived from HOMEADD with single space as fourth to last character | varChar(8) |
| Episode Start | Date | |
| Episode End | Date | |
| Assumed Delivery Date | The baby’s date of birth or if missing the date associated with the OPCS delivery cod | Date |
| ONS ID Baby One* | Copy of the ONS ID of 1st baby. Sometimes it is only the characteristics of the mother being looked at so this provides a convenient short cut as the mother’s details should be the same in all the ONS records of a multiple birth | Integer |
| ONS Link Year Baby One | Calendar year of ONS record that is linked to the first baby | Integer |
| ONS Link match _ rank | The link is with the mother so appears here and not in baby tail | Integer |
| Year of Data* | Financial year episode completed in. Format. Relates to year of source file | varChar(5) |
| Valid Delivery | Delivery represents a registrable birth | varChar(1) |
The following fields were not imported.
| Field name | Description | Reason not imported |
|---|---|---|
| EPIS _ CLF | Episode start date check flag | Redundant |
| EPIE _ CFL | Episode end date check flag | Redundant |
| CAUSE | Copy of the first diagnosis code that represents an external cause | Not Supplied |
| OACODE6 | Census Output Area | |
| RESCTY | County of residence | |
| MSOA01 | Using postcode to link back ONS source files of IMD, etc. | |
| rururb _ ind | Rural urban indicator | Using postcode to link back ONS source files of IMD, etc. |
| imd04c etc | IMD | Using postcode to link back ONS source files of IMD, etc. |
| Neodur | Age of baby in days if < 28 days | Baby only |
| Neocare | Baby only | |
| well _ baby _ ind | Baby only |
Database Table 44 is essentially a sideways continuation of the Deliveries database table. The records are in one to one correspondence. Because Table 44 needs frequent structural modifications it is stored as a separate table rather than as part of the Deliveries database table. See Deriving new variables from Hospital Episode Statistics data.
| Database table name: Deliveries_Indicators | ||
|---|---|---|
| Field name | Description | Data type |
| Delivery ID** | Primary key | Integer |
| Delivery Procedure Field Order | Index position of delivery code in procedure codes field list | Integer |
| Delivery Procedure Date | Date associated with delivery procedure | Date |
| Delmeth OPCS | Synthetic version of DELMETH, (method of delivery) derived from procedure codes | varChar(1) |
| Delmeth Best | [Delmeth OPCS] if available else DEMETH _ 1 | varChar(1) |
| Delmeth Source | Origin of data used in [Delmeth Best] (OP = Delmeth OPCS, BT = DELMETH _ 1) | varChar(2) |
| Delmeth Best 2 | Where there are several HES records per delivery the ‘best’ record may not actually contain the delivery method. When this is so the delivery method is taken from an alternative record. Otherwise this field is set to [Delmeth Best] | varChar(1) |
| DELONSET 2 | Where there are several HES records per delivery the ‘best’ record may not actually contain the onset method. When this is so the onset method is taken from an alternative record. Otherwise this field is set to [DELONSET] | varChar(1) |
| Induction or Acceleration (OPCS) | OPCS indicators indicate induction or acceleration | Bit |
| Induction or Acceleration | True if either [Delonset] or [Induction or Acceleration (OPCS)] is True | Bit |
| Episiotomy | Derived from OPCS codes | Bit |
| Derived Parity | Best estimate of parity from HES | Integer |
| Nulliparous | Derived Parity = 0 | Bit |
| Derived Parity (ONS) | Parity calculated using the additional information available in the ONS record | Integer |
| Nulliparous (ONS) | Derived Parity (ONS) = 0 | Bit |
| Previous CS (ICD) | Evidence of a previous CS found in current record diagnostic codes | Bit |
| Previous CS | Evidence of a previous CS found | Bit |
| Current CS | A CS mentioned in diagnostic codes, procedure codes, DELMETH _ 1 or DELONSET | varChar(1) |
| Baby Tails Count | Number of populated baby tails in record | Integer |
| Multiple ICD | Delivery is a multiple birth as reported by diagnostic codes | varChar(1) |
| HES Multiple | Delivery is a multiple birth derived from consideration of diagnostic codes and NUMBABY | varChar(1) |
| ONS Multiple | If ONS record indicates a multiple birth | varChar(1) |
| OPCS Code Count | Number of OPCS codes reported in procedure fields | Integer |
| ICD Code Count | Number of ICD-10 codes reported in diagnostic fields | Integer |
| Unit Type | Type of maternity unit derived from [Location Code HES]. OU, OU+AMU, FMU and other settings | varChar(15) |
| Pre-existing diabetes | Bit | |
| Gestational diabetes | Bit | |
| Pre-existing hypertension | High blood pressure | Bit |
| Pre-eclampsia | Bit | |
| Eclampsia | Bit | |
| Placenta | Either praevia or abruption | Bit |
| Polyhydramnios | Excess of amniotic fluid | Bit |
| Oligohydramnios | Deficiency of amniotic fluid | Bit |
Database Table 45 relates to the populated baby tails of which there can be up to nine in the mother’s delivery record.
| Database table name: Deliveries_Baby_Tails | ||
|---|---|---|
| Field name | Description | Data type |
| Delivery ID* | Foreign key linking baby tail to parent delivery record in Deliveries table | Integer |
| ONS ID* | Foreign key inking baby tail to corresponding ONS birth record in ONS table | Integer |
| Birth ID* | Foreign key linking to HES birth record for the baby. It may not always be possible to establish this link | Integer |
| DOBBABY | Baby’s date of birth as reported by HES in baby tail | Date |
| BIRORDR | Birth order (X mapped to –1 so that field can be cast as long.) 8,9 represents not knowns | Integer |
| SEXBABY# | 1 Male, 2 Female, 9 not specified. Standardised version [Baby Sex] | varChar(1) |
| DELMETH | Delivery method | varChar(1) |
| BIRWEIT | Birth weight. 7000 = 7000 g or more, 9999 = Not known | Integer |
| GESTAT | Length of gestation, 99 = Not known | Integer |
| BIRSTAT# | Birth status, 1 = live | varChar(1) |
| BIRESUS | Resuscitation method | varChar(1) |
| DELPLAC | Delivery place (intended) | varChar(1) |
| DELSTAT | Status of person conducting delivery | varChar(1) |
| Assumed HES Baby Date of Birth | Best estimate of baby’s date of birth using HES record | Date |
| Assumed HES Baby Date of Birth Source | (Date of Birth = DOBBABY, OP = Delivery Procedure Date, OP* = OP overwritten) Date of Birth as Date of Birth outside episode, Ep = Episode Dates | varChar(3) |
| Baby Sex | M or F or NULL | varChar(1) |
| Stillbirth | True when BIRSTAT = 2, 3, 4 | Bit |
| Birth Weight | Integer | |
| Gestational Age | Integer | |
| ONS Ghost | New baby tail generated as place holder when ONS indicates more babies in delivery than HES baby tails | Bit |
| ONS Link Year | Required to know which file to link to | Integer |
| Field Order* | Number representing the position of the baby tail in the delivery record, 1–9. This is usually the same as birth order, but not necessarily so | Integer |
| Valid Tail | True if genuinely populated | Bit |
Database Table 46 relates to the ICD-10 diagnostic codes that appear in the mother’s delivery record.
| Database table name: Deliveries_ICD | ||
|---|---|---|
| Field name | Description | Data type |
| Delivery ICD Code ID* | Primary key | Integer |
| Delivery ID** | Foreign key linking to core delivery record [Deliveries] | Integer |
| ICD Code* | varChar(4) | |
| Field Order | Number representing position of the diagnostic code in the delivery record. Range 1–20 | Integer |
Database Table 47 relates to the OPCS codes that appear in the mother’s delivery record.
| Database table name: Deliveries_OPCS | ||
|---|---|---|
| Field name | Description | Data type |
| Delivery OPCS Code ID* | Primary key | Integer |
| Delivery ID** | Foreign key linking to core delivery record [Deliveries] | Integer |
| OPCS Code* | varChar(4) | |
| OP Date | Date of procedure | Date |
| Field Order | Number representing position of the diagnostic code in the delivery record. Range 1–24 | Integer |
Some statistical packages prefer to work with flat files rather than linked relational files. This file holds the ICD-10 and OPCS codes in a flat file format.
| Database table name: Deliveries ICD & OPCS Flat | ||
|---|---|---|
| Field name | Description | Data type |
| Delivery ID* | Primary key | Integer |
| DIAG _ nn | Diagnostic code nn = 1 to 20 | varChar(4) |
| OPERTN _ nn | Operation or procedure codes nn = 1 to 24 | varChar(4) |
| OPDATE _ nn | Date of procedure nn = 1 to 24 | Date |
Table 49 will contain antenatal admissions, postnatal readmissions and admissions unrelated to maternity.
| Database table name: Mothers_Readmission | ||
|---|---|---|
| Field name | Description | Data type |
| Mothers Readmission ID** | Primary key | Integer |
| Mother ID* | Mother id | Integer |
| ENDAGE | Age at end of episode | Integer |
| STARTAGE | Age at start of episode | Integer |
| NEODUR | Age of baby in days | Integer |
| DOB | Patient’s date of birth | Date |
| DOB _ CFL | Date of birth check flag – patient | Integer |
| ETHNOS | Ethnicity | varChar(2) |
| NEWNHSNO | Patient’s NHS number | varChar(10) |
| HES ID | ENCRYPTED _ HESID | varChar(32) |
| HOMEADD | Patient’s home postcode | varChar(8) |
| SEX | Patient’s sex | varChar(1) |
| ADMIDATE | Admission date | Date |
| ADM _ CFL | Admission date check flag | Integer |
| ELECDATE | Date of decision to admit | Date |
| ELEC _ CFL | Date of decision to admit check flag | Integer |
| ADMIMETH | How the patient was admitted to hospital | varChar(2) |
| ADMISORC | Identifies where the patient was immediately prior to admission | varChar(2) |
| FIRSTREG | First regular day or night admission | Integer |
| ELECDUR | Waiting time | Integer |
| DISDATE | Date of discharge. Only present for last episode in a spell | Date |
| DIS _ CFL | Discharge date check flag | Integer |
| DISDEST | Destination on discharge | varChar(2) |
| DISMETH | Method of discharge | varChar(1) |
| BEDYEAR | Bed-days within the year | Integer |
| SPELBGIN | Beginning of spell | Integer |
| EPIEND | Episode end date | Date |
| EPISTART | Episode start date | Date |
| SPELDUR | Duration of spell | Integer |
| SPELEND | End of spell | varChar(1) |
| EPIDUR | Episode duration | Integer |
| EPIORDER | The number of the episode within the current spell | Integer |
| EPIE _ CFL | Episode end date check flag | Integer |
| EPIS _ CFL | Episode start date check flag | Integer |
| EPISTAT | Episode status. 1 represents unfinished episode, 3 finished | varChar(1) |
| EPITYPE | Episode type | varChar(1) |
| PROVSPNOPS | A number to provide a unique identifier for each Hospital Provider. (PROVSPNO) | varChar(12) |
| DIAG _ nn nn from 01 to 20 | Diagnostic (ICD-10) code. These codes are also stored in a relational table | varChar(4) |
| DIAG3 _ 01 | Diagnosis 3 character ICD9 or ICD10 code | varChar(3) |
| DIAG4 _ 01 | Diagnosis 4 character codes | varChar(4) |
| CAUSE | External cause of injury or poisoning | varChar(6) |
| CAUSE4 | External cause code 4 characters | varChar(4) |
| CAUSE3 | External cause code 3 characters | varChar(3) |
| OPERTN _ nn nn from 01 to 24 | Operational or procedural codes. These codes are also stored in a relational table | varChar(4) |
| OPDATE _ nn nn from 01 to 24 | Date of procedure | Date |
| OPERSTAT | Operation status code | Integer |
| POSOPDUR | Post-operative duration | Integer |
| PREOPDUR | Pre-operative duration | Integer |
| CLASSPAT | Patient classification | Integer |
| INTMANIG | Intended management | Integer |
| MAINSPEF | Main specialty | varChar(3) |
| TRETSPEF | Treatment specialty | varChar(3) |
| DOMPROC | Dominant procedure (operation) code | varChar(4) |
| HRGLATE35 | varChar(3) | |
| HRGNHS | Trust derived Health Resource Group value | varChar(3) |
| HRGNHSVN | Version number of Trust derived Health Resource Group value | varChar(3) |
| SUSCOREHRG | SUS generated core spell Health Resource Group | varChar(5) |
| SUSHRG | SUS generated Health Resource Group | varChar(5) |
| SUSHRGVERS | SUS generated Health Resource Group version number | varChar(3) |
| SUSSPELLID | SUS generated spell id | varChar(10) |
| PCTCODE | Primary care trust of responsibility | varChar(3) |
| PCTCODE06 | Primary care trust of responsibility current | varChar(5) |
| PROCODE | Organisation acting as a health care provider | varChar(5) |
| SITETRET | Site code of treatment | varChar(5) |
| PROTYPE | Provider type | varChar(10) |
| RESLADST | Local authority district | varChar(4) |
| PCTNHS | Primary care trust in the NHS | varChar(3) |
| LSOA01 | Lower Super Output Area | varChar(9) |
| MSOA01 | Middle Super Output Area 2001 | varChar(9) |
| RURURB _ IND | Rural/Urban indicator | Integer |
| IMD04C | Index of Multiple Deprivation crime domain | Float |
| IMD04ED | Index of Multiple Deprivation education training and skills domain | Float |
| IMD04EM | Index of Multiple Deprivation employment deprivation domain | Float |
| IMD04HD | Index of Multiple Deprivation health and disability domain | Float |
| IMD04HS | Index of Multiple Deprivation barriers to housing and service domain | Float |
| IMD04I | Index of Multiple Deprivation income domain | Float |
| IMD04IA | Index of Multiple Deprivation income affecting adults domain | Float |
| IMD04IC | Index of Multiple Deprivation income affecting children domain | Float |
| IMD04LE | Index of Multiple Deprivation living environment domain | Float |
| IMD04 | IMD Index of Multiple Deprivation | Float |
| IMD04RK | Index of Multiple Deprivation Overall Rank | Integer |
| IMD04 _ DECILE | Index of Multiple Deprivation decile group | varChar(20) |
| ACPLOC _ n n from 1 to 9 | Augmented care location | varChar(2) |
| ACPDQIND _ n n from 1 to 9 | Augmented care period data quality indicator | varChar(2) |
| ACPDISP _ n n from 1 to 9 | Destination of a discharged patient after a period of augmented care | varChar(2) |
| ACPEND _ n n from 1 to 9 | Augmented care period end date | Date |
| ACPPLAN _ n n from 1 to 9 | Indicates whether any part of the ACP was planned in advance of admission to the ACP location | varChar(1) |
| ACPN _ n n from 1 to 9 | Order of an episode within a sequence of episodes that make up a period of augmented care | Integer |
| ACPOUT _ n n from 1 to 9 | Augmented care period outcome indicator | varChar(2) |
| ACPSOUR _ n n from 1 to 9 | Where the patient was immediately before the period of augmented care | varChar(2) |
| ACPSPEF _ n n from 1 to 9 | Main specialty of the consultant clinically managing the period of augmented care | varChar(3) |
| ACPSTAR _ n n from 1 to 9 | Start date of a period of augmented care | Date |
| DEPDAYS _ n n from 1 to 9 | High-dependency care level | Integer |
| INTDAYS _ n n from 1 to 9 | Intensive care level days | Integer |
| NUMACP | Number of augmented care periods within episode | Integer |
| OPCS43 | OPCS43 flag indicates whether at least one operative procedure code is present in the OPCS4.3 set and not in the OPCS4.2 set | varChar(2) |
| EPIKEY | Unique HES record ID. Cast as text as too long for 4-byte integer, consequently not used as PK. Although unique to HES the files supplied by HSCIC have multiple of some HES records of the link to ONS | varChar(14) |
| Year of Data* | Financial year episode completed in. Format yyxx. Relates to year of source file | varChar(4) |
| Previous Delivery ID* | Points to the last delivery before this readmission. NULL if none exists. Does not imply a postnatal readmission | Integer |
| Days Since Previous Delivery | This can be large if the admission was unrelated to the last delivery | Integer |
| Next Delivery ID* | Points to the next delivery after this admission. NULL if none exists. Does not imply an antenatal readmission | Integer |
| Days To Next Delivery | This can be large if the admission was unrelated to the next delivery (e.g. the admission could be a postnatal admission from a previous delivery) | Integer |
Database Table 50 will contain the ICD-10 diagnostic codes that appear in the mother’s readmission record.
| Database table name: Mothers_Readmission_ICD_Codes | ||
|---|---|---|
| Field name | Description | Data type |
| Mother’s Readmission ICD Code ID* | Primary key | Integer |
| Mother’s Readmission ID** | Foreign key linking to core mother’s readmission record [Mother’s Readmission] | Integer |
| ICD Code* | varChar(4) | |
| Field Order | Number representing position of the diagnostic code in the readmission record | Integer |
Database Table 51 will contain the OPCS diagnostic codes that appear in the mother’s readmission record.
| Database table name: Mothers_Readmission_OPCS_Codes | ||
|---|---|---|
| Field name | Description | Data type |
| Mother’s Readmission OPCS Code ID* | Primary key | Integer |
| Mother’s Readmission ID** | Foreign key linking to core mother’s readmission record [Mother’s Readmission] | Integer |
| OPCS Code* | varChar(4) | |
| OP Date | Date of procedure | Date |
| Field Order | Number representing position of the diagnostic code in the readmission record | Integer |
As database Table 52 shows, [Mother ID] is in one-to-one correspondence with [HES ID] but is computationally more efficient.
| Database table name: Mother | ||
|---|---|---|
| Field name | Description | Data type |
| Mother ID** | Primary key | Integer |
| HES ID | HES Extract ID | varChar(32) |
Database Table 53 relates to the linkage with match rank zero removed.
| Database table name: Mother’s HES ONS Linkage | ||
|---|---|---|
| Field name | Description | Data type |
| Mother ID | Integer | |
| ONS ID | Integer | |
| HES ID | HES Extract ID | varChar(32) |
| ONS Link ID | varChar(31) | |
| ONS Link Year | Integer | |
| ONS Link match _ rank | Integer | |
Database Table 54 relates to the remaining good links after cleaning.
| Database table name: Mother’s HES ONS Linkage Cleaned | ||
|---|---|---|
| Field name | Description | Data type |
| ONS ID | Integer | |
| Delivery ID* | Integer | |
| Field Order | Identifies which baby tail in the delivery record ONS record is linked to | Integer |
| Batch | S = singletons cleaning batch, M = multiple cleaning batch. For database maintenance only | varchar(1) |
Database Table 55 provides the map between old and new HES ID. Duplicate entries have been removed.
| Database table name: Mother’s Old to New HES ID | ||
|---|---|---|
| Field name | Description | Data type |
| Mother ID* | Integer | |
| HES ID | HES Extract ID | varChar(32) |
| Old Mother ID | Integer | |
| Old HES ID | HES Extract ID | varChar(32) |
| Use | Set to False if the HES ID links to more than one old HES ID | Bit |
Babies’ tables
Tables 56–66 show detailed descriptions of database tables and fields from the HES records relating to the baby.
Database Table 56 shows key fields from the baby’s HES birth record plus derived fields.
| Database table name: Births | ||
|---|---|---|
| Field name | Description | Data type |
| Birth ID** | Primary key | Integer |
| ONS ID* | Foreign key that links to the corresponding ONS birth record [ONS All Years] | Integer |
| Baby ID* | Although a baby is only born once, it may still have several HES birth records. [Baby ID] is unique to the baby while [Birth ID] is unique to each of its HES birth records | |
| Delivery ID* | Foreign key that identifies the mother’s delivery episode in which the baby was born. Inferred from Linkage to ONS records | Integer |
| Deliveries Baby Tail Field Order* | Identifies which baby tail in the delivery record the birth corresponds to. Inferred from Linkage to ONS records | Integer |
| Mother ID* | Identifies the mother of the baby as she appears in the delivery records. Could potentially be used to identify siblings. Inferred from Linkage to ONS records | |
| HES ID | ENCRYPTED _ HESID | varChar(32) |
| Trust Code | First three characters of PROCODE | varChar(3) |
| PROCODE | Organisation acting as a health care provider | varChar(5) |
| SITETRET | Site code of treatment | varChar(5) |
| NUMBABY | Number of babies reported by HES in delivery episode. Compared to delivery record understates multiple births | Integer |
| DELONSET | HES field indicating method of onset of labour | varChar(1) |
| DELPREAN | Anaesthetic given during labour or delivery | varChar(1) |
| DELPOSAN | Anaesthetic given post-labour or delivery | varChar(1) |
| ETHNOS | Ethnicity | varChar(2) |
| ADMIDATE | Admission date | Date |
| DISDATE | Date of discharge. Only present for last episode in a spell | Date |
| ADMIMETH | How the patient was admitted to hospital | varChar(2) |
| ADMISORC | Identifies where the patient was immediately prior to admission | varChar(2) |
| DISDEST | Destination on discharge | varChar(2) |
| DISMETH | Method of discharge | varChar(1) |
| ANTEDUR | Antenatal days of stay | Integer |
| POSTDUR | Postnatal stay | Integer |
| EPISTART | Episode start date | Date |
| EPIEND | Episode end date | Date |
| EPIORDER | The number of the episode within the current spell | Integer |
| EPISTAT | Episode status. 1 represents unfinished episode, 3 finished | varChar(1) |
| EPITYPE | Episode type | varChar(1) |
| PROVSPNOPS (PROVSPNO) | A number to provide a unique identifier for each Hospital Provider | varChar(12) |
| LSOA01 | Lower Super Output Area | varChar(9) |
| IMD04RK | IMD Overall Rank | Integer |
| DELINTEN | Delivery place (intended) | varChar(1) |
| MOTDOB | Mother’s date of birth | Date |
| DOBBABY_1 | Baby’s date of birth as reported by HES in baby tail | Date |
| BIRORDR_1 | Birth order (X mapped to –1 so that field can be cast as long.) 8, 9 represents not knowns. Similar to NUMBABY in not being as well reported as delivery record | Integer |
| SEXBABY_1 | 1 Male, 2 Female, 9 not specified | varChar(1) |
| DELMETH_1 | Delivery method | varChar(1) |
| BIRWEIT_1 | Birth weight. 7000 = ≥ 7000 g, 9999 = Not known | Integer |
| GESTAT_1 | Length of gestation, 99 = Not known | Integer |
| BIRSTAT_1 | Birth status, 1 = live | varChar(1) |
| BIRSUS_1 | Resuscitation method | varChar(1) |
| DELPLAC_1 | Delivery place (intended) | varChar(1) |
| DELSTAT_1 | Status of person conducting delivery | varChar(1) |
| NEOCARE | Neonatal level of care | varChar(1) |
| NEODUR | This field contains the age in days of a baby admitted as a patient. It is derived from admission date (admidate) and date of birth. If the baby is older than 27 days, neodur is not calculated | Integer |
| WELL_BABY_IND | Neonate receiving normal levels of care. This is incorrectly calculated in HES | Bit |
| EPIKEY | Unique HES record ID. Cast as text as too long for 4-byte integer, consequently not used as PK. Although unique to HES the files supplied by HSCIC have multiple of some HES records of the link to ONS | varChar(14) |
| Location Code | varChar(7) | |
| Pseudo Trust Code | varChar(3) | |
| Year of Data* | Financial year episode completed in. Format. Relates to year of source file | varChar(5) |
Database Table 57 is essentially a sideways continuation of the Births table. The records are in one to one correspondence. Because this table needs frequent structural modifications it is stored as a separate table rather than as part of the Births table.
| Database table name: Birth_Indicators | ||
|---|---|---|
| Field name | Description | Data type |
| Birth ID** | Primary key | Integer |
| OPCS Code Count | Number of OPCS codes reported in procedure fields | Integer |
| ICD Code Count | Number of ICD-10 codes reported in diagnostic fields | Integer |
| Baby Sex | Values M or F or NULL | varChar(1) |
| Stillbirth | BIRSTAT _ 1 = 2, 3 or 4 | Bit |
Database Table 58 contains the ICD-10 diagnostic codes that appear in the baby’s birth record.
| Database table name: Birth_ICD | ||
|---|---|---|
| Field name | Description | Data type |
| Birth ICD Code ID* | Primary key | Integer |
| Birth ID** | Foreign key linking to core HES birth record [Births] | Integer |
| ICD Code* | varChar(4) | |
| Field Order | Number representing position of the diagnostic code in the birth record | Integer |
Database Table 59 contains the OPCS codes that appear in the baby’s birth record.
| Database table name: Birth_OPCS | ||
|---|---|---|
| Field name | Description | Data type |
| Birth OPCS Code ID* | Primary key | Integer |
| Birth ID** | Foreign key linking to core HES birth record [Births] | Integer |
| OPCS Code* | varChar(4) | |
| OP Date | Date of procedure | Date |
| Field Order | Number representing position of the diagnostic code in the birth record | Integer |
Some statistical packages prefer to work with flat files rather than linked relational files. Table 60 holds the ICD-10 and OPCS codes in a flat file format.
| Database table name: Births ICD and OPCS Flat | ||
|---|---|---|
| Field name | Description | Data type |
| Delivery ID* | Primary key | Integer |
| DIAG_nn | Diagnostic code. nn = 1 to 20 | varChar(4) |
| OPERTN_nn | Operation or procedure codes nn = 1 to 24 | varChar(4) |
| OPDATE_nn | Date of procedure nn = 1 to 24 | Date |
Database Table 61 will contain postnatal readmissions and admissions unrelated to maternity.
| Database table name: Baby’s_Readmissions | ||
|---|---|---|
| Field name | Description | Data type |
| Baby’s Readmission ID* | Primary key | Integer |
| Baby ID* | Baby ID | Integer |
| Birth ID* | This can only be assigned once one of the possible several HES birth records has been designated the ‘best’ record | Integer |
| ENDAGE | Age at end of episode | Integer |
| STARTAGE | Age at start of episode | Integer |
| NEODUR | This field contains the age in days of a baby admitted as a patient. It is derived from admission date (admidate) and date of birth. If the baby is older than 27 days, neodur is not calculated | Integer |
| DOB | Patient’s date of birth | Date |
| DOB_CFL | Date of birth check flag – patient | Integer |
| ETHNOS | Ethnicity | varChar(2) |
| NEWNHSNO | Patient’s NHS number | varChar(10) |
| HES ID | ENCRYPTED _ HESID | varChar(32) |
| HOMEADD | Patient’s home postcode | varChar(8) |
| SEX | Patient’s sex | varChar(1) |
| ADMIDATE | Admission date | Date |
| ADM_CFL | Admission date check flag | Integer |
| ELECDATE | Date of decision to admit | Date |
| ELEC_CFL | Date of decision to admit check flag | Integer |
| ADMIMETH | How the patient was admitted to hospital | varChar(2) |
| ADMISORC | Identifies where the patient was immediately prior to admission | varChar(2) |
| FIRSTREG | First regular day or night admission | Integer |
| ELECDUR | Waiting time | Integer |
| DISDATE | Date of discharge. Present only for last episode in a spell | Date |
| DIS_CFL | Discharge date check flag | Integer |
| DISDEST | Destination on discharge | varChar(2) |
| DISMETH | Method of discharge | varChar(1) |
| BEDYEAR | Bed-days within the year | Integer |
| SPELBGIN | Beginning of spell | Integer |
| EPIEND | Episode end date | Date |
| EPISTART | Episode start date | Date |
| SPELDUR | Duration of spell | Integer |
| SPELEND | End of spell | varChar(1) |
| EPIDUR | Episode duration | Integer |
| EPIORDER | The number of the episode within the current spell | Integer |
| EPIE_CFL | Episode end date check flag | Integer |
| EPIS_CFL | Episode start date check flag | Integer |
| EPISTAT | Episode status. 1 represents unfinished episode, 3 finished | varChar(1) |
| EPITYPE | Episode type | varChar(1) |
| PROVSPNOPS | A number to provide a unique identifier for each Hospital Provider (PROVSPNO) | varChar(12) |
| DIAG_nn nn from 01 to 20 | Diagnostic (ICD-10) code. These codes are also stored in a relational table | varChar(4) |
| DIAG3_01 | Diagnosis 3 character ICD9 or ICD10 code | varChar(3) |
| DIAG4_01 | Diagnosis 4 character codes | varChar(4) |
| CAUSE | External cause of injury or poisoning | varChar(6) |
| CAUSE4 | External cause code 4 characters | varChar(4) |
| CAUSE3 | External cause code 3 characters | varChar(3) |
| OPERTN_nn nn from 01 to 24 | Operational or procedural codes. These codes are also stored in a relational table | varChar(4) |
| OPDATE_nn nn from 01 to 24 | Date of procedure | Date |
| OPERSTAT | Operation status code | Integer |
| POSOPDUR | Post-operative duration | Integer |
| PREOPDUR | Pre-operative duration | Integer |
| CLASSPAT | Patient classification | Integer |
| INTMANIG | Intended management | Integer |
| MAINSPEF | Main specialty | varChar(3) |
| TRETSPEF | Treatment specialty | varChar(3) |
| DOMPROC | Dominant procedure (operation) code | varChar(4) |
| HRGLATE35 | varChar(3) | |
| HRGNHS | Trust derived HRG value | varChar(3) |
| HRGNHSVN | Version number of Trust derived HRG value | varChar(3) |
| SUSCOREHRG | SUS generated core spell Health Resource Group | varChar(5) |
| SUSHRG | SUS generated Health Resource Group | varChar(5) |
| SUSHRGVERS | SUS generated Health Resource Group version number | varChar(3) |
| SUSSPELLID | SUS generated spell ID | varChar(10) |
| PCTCODE | Primary care trust of responsibility | varChar(3) |
| PCTCODE06 | Primary care trust of responsibility current | varChar(5) |
| PROCODE | Organisation acting as a health care provider | varChar(5) |
| SITETRET | Site code of treatment | varChar(5) |
| PROTYPE | Provider type | varChar(10) |
| RESLADST | Local authority district | varChar(4) |
| PCTNHS | Primary care trust in the NHS | varChar(3) |
| LSOA01 | Lower Super Output Area | varChar(9) |
| MSOA01 | Middle Super Output Area 2001 | varChar(9) |
| RURURB_IND | Rural/Urban indicator | Integer |
| IMD04C | Index of Multiple Deprivation crime domain | Float |
| IMD04ED | Index of Multiple Deprivation education training and skills domain | Float |
| IMD04EM | Index of Multiple Deprivation employment deprivation domain | Float |
| IMD04HD | Index of Multiple Deprivation health and disability domain | Float |
| IMD04HS | Index of Multiple Deprivation barriers to housing and service domain | Float |
| IMD04I | Index of Multiple Deprivation income domain | Float |
| IMD04IA | Index of Multiple Deprivation income affecting adults domain | Float |
| IMD04IC | Index of Multiple Deprivation income affecting children domain | Float |
| IMD04LE | Index of Multiple Deprivation living environment domain | Float |
| IMD04 | IMD Index of Multiple Deprivation | Float |
| IMD04RK | IMD Overall Rank | Integer |
| IMD04_DECILE | Index of Multiple Deprivation decile group | varChar(20) |
| ACPLOC_n n from 1 to 9 | Augmented care location | varChar(2) |
| ACPDQIND_n n from 1 to 9 | Augmented care period data quality indicator | varChar(2) |
| ACPDISP_n n from 1 to 9 | Destination of a discharged patient after a period of augmented care | varChar(2) |
| ACPEND_n n from 1 to 9 | Augmented care period end date | Date |
| ACPPLAN_n n from 1 to 9 | Indicates whether any part of the ACP was planned in advance of admission to the ACP location | varChar(1) |
| ACPN_n n from 1 to 9 | Order of an episode within a sequence of episodes that make up a period of augmented care | Integer |
| ACPOUT_n n from 1 to 9 | Augmented care period outcome indicator | varChar(2) |
| ACPSOUR_n n from 1 to 9 | Where the patient was immediately before the period of augmented care | varChar(2) |
| ACPSPEF_n n from 1 to 9 | Main specialty of the consultant clinically managing the period of augmented care | varChar(3) |
| ACPSTAR_n n from 1 to 9 | Start date of a period of augmented care | Date |
| DEPDAYS_n n from 1 to 9 | High-dependency care level | Integer |
| INTDAYS_n n from 1 to 9 | Intensive care level days | Integer |
| NUMACP | Number of augmented care periods within episode | Integer |
| OPCS43 | OPCS43 flag indicates whether at least one operative procedure code is present in the OPCS4.3 set and not in the OPCS4.2 set | varChar(2) |
| EPIKEY | Unique HES record ID. Cast as text as too long for 4-byte integer, consequently not used as PK. Although unique to HES the files supplied by HSCIC have multiple of some HES records of the link to ONS | varChar(14) |
| Year of Data* | Financial year episode completed in. Format yyxx. Relates to year of source file | varChar(4) |
Database Table 62 holds the ICD-10 diagnostic codes that appear in the baby’s readmission record.
| Database table name: Baby’s_Readmissions_ICD_Codes | ||
|---|---|---|
| Field name | Description | Data type |
| Baby’s Readmission ICD Code ID* | Primary key | Integer |
| Baby’s Readmission ID** | Foreign key linking to core baby’s readmission record [Baby’s Readmission] | Integer |
| ICD Code* | varChar(4) | |
| Field Order | Number representing position of the diagnostic code in the readmission record | Integer |
Database Table 63 holds the OPCS codes that appear in the baby’s readmission record.
| Database table name: Baby’s_Readmission_OPCS_Codes | ||
|---|---|---|
| Field name | Description | Data type |
| Baby’s Readmission OPCS Code ID* | Primary key | Integer |
| Baby’s Readmission ID** | Foreign key linking to core baby’s readmission record [Baby’s Readmission] | Integer |
| OPCS Code* | varChar(4) | |
| OP Date | Date of procedure | Date |
| Field Order | Number representing position of the diagnostic code in the readmission record | Integer |
As Database Table 64 shows, [Baby ID] is in one-to-one correspondence with [HES ID] but is computationally more efficient.
| Database table name: Babies | ||
|---|---|---|
| Field name | Description | Data type |
| Baby ID* | Primary key | Integer |
| HES ID | HES Extract ID | varChar(32) |
Database Table 65 relates to the linkage with match rank zero removed.
| Database table name: Baby’s HES ONS Linkage | ||
|---|---|---|
| Field name | Description | Data type |
| Baby ID* | Integer | |
| ONS ID* | Integer | |
| HES ID | HES Extract ID | varChar(32) |
| ONS Link ID | varChar(31) | |
| ONS Link Year | Integer | |
| ONS Link match_rank | Integer | |
Database Table 66 provides the map between old and new HES ID. Duplicate entries have been removed.
| Database table name: Old to New Baby’s HES ID | ||
|---|---|---|
| Field name | Description | Data type |
| Baby ID* | Integer | |
| HES ID | HES Extract ID | varChar(32) |
| Old Baby ID | Integer | |
| Old HES ID | HES Extract ID | varChar(32) |
| Use | Set to False if the HES ID links to more than one old HES ID | Bit |
Code lookup tables
There are a number of lookup tables that match codes to descriptions. Their names are prefixed with ‘AA’ so that they all appear at the top of the table list. These are shown in Table 67 (location codes), Table 68 (ethnicity codes) and Table 69 (other miscellaneous codes).
| Field name | Description | Data type |
|---|---|---|
| Database table name: AA location codes | ||
| Location Code** | Unique code for every maternity unit. See Location Code documentation | varChar(7) |
| Location Name | Description of location code | varChar(63) |
| Pseudo Trust | Pseudo Trust (Assigned Trust) to which unit belongs | varChar(3) |
| Project Postcode | varChar(15) | |
| Service Group Code | varChar(63) | |
| SHA Code | varChar(3) | |
| SHA Region | varChar(31) | |
| Area Team Code | varChar(3) | |
| Area Team | varChar(127) | |
| Region (Geography) Code | varChar(3) | |
| Region (Geography) | varChar(64) | |
| Country | Country that maternity unit is in (England, Wales) | varChar(15) |
| Database table name: AA CESTRSS to Location Code | ||
| CESTRSS** | Birth Registration code for place of birth | varChar(5) |
| Location Code | Map to [Location Code] | varChar(7) |
| Database table name: AA ORGCODEZ to Location Code | ||
| ORGCODEZ** | Birth Notification code for place of birth | varChar(5) |
| Location Code | Map to [Location Code] | varChar(7) |
| Database table name: AA DELPLAZ to Location Code | ||
| DELPLAZ | Birth Notification description of place of birth | varChar(?) |
| Location Code | Map to [Location Code] | varChar(7) |
| Database table name: AA HES (PC and ST) to Location Code | ||
| PROCODE* | varChar(5) | |
| SITETRET* | ||
| Location Code | Map to [Location Code] | varChar(7) |
| Database table name: AA Distance Match | ||
| Gives an approximate Euclidean distance between two assigned trusts. Used in the cleaning of ONS to HES linkage | ||
| Pseudo Trust 1* | varChar(3) | |
| Pseudo Trust 2* | varChar(3) | |
| Distance | In miles | Float |
| Match | Designates the type of match | varChar(31) |
| Cleaning Match | Yes/No | varChar(3) |
| Database table name: AA Post Code to LSOA | ||
| Post Code | varChar(8) | |
| LSOA01 | varChar(9) | |
| LSOA11 | varChar(9) | |
| Database table name: AA Unit Type | ||
| Location Code* | varChar(7) | |
| Start Date | First day unit was in specified configuration | Date |
| End Date | Last day unit was in specified configuration | Date |
| Birth Setting | Configuration of unit. Birth Setting: OU, OU+AMU, FMU, Home, Elsewhere, Private, Military, NAMH Unknown | varChar(15) |
| Field name | Description | Data type |
|---|---|---|
| Database table name: AA Ethnicity codes map | ||
| ETHCATZ** | Two letter codes found in birth notification field ETHCATZ plus text description found in 2005 file | varChar(31) |
| Ethnicity Code 17 | Map to single letter codes for 17 category system | varChar(1) |
| Ethnicity Code 9 | Map to 9 category system | varChar(1) |
| Ethnicity Code 5 | Map to 5 category system | varChar(1) |
| Database table name: AA Ethnicity Codes 17 | ||
| Ethnicity Code 17** | ONS 17 category system | varChar(1) |
| Category | Description | varChar(31) |
| Ethnicity Code 9 | Map to 9 category system | varChar(1) |
| Ethnicity Code 5 | Map to 5 category system | varChar(1) |
| Database table name: AA Ethnicity Codes 9 | ||
| Ethnicity Code 9** | varChar(1) | |
| Category | Description | varChar(31) |
| Database table name: AA Ethnicity Codes 5 | ||
| Ethnicity Code 5** | varChar(1) | |
| Category | Description | varChar(31) |
Table 69 includes admissible values for ONS field [MULTTYPE]. For years 2009 to 2012 only the leading zero was omitted in ONS data, so this table includes a single character code that duplicates the double character code with a leading zero.
| Field name | Description | Data type |
|---|---|---|
| Database table name: AA MultType | ||
| MultType* | Two letter code designating birth status of multiple birth | varChar(2) |
| Description | varChar(63) | |
| Male | Number of males in multiple, live or still | Integer |
| Female | Number of females in multiple, live or still | Integer |
| Total | Number of babies in multiple, live or still | Integer |
| Live | Number of live births | Integer |
| Stillbirth | True if any baby still born | Bit |
| Database table name: AA ICD-10 diagnostic codes | ||
| Contains a description of all ICD-10 codes | ||
| ICD Code** | Primary key | varChar(4) |
| Description | ||
Preferred variable list
There are often several sources for the same data item. Table 70 indicates the preferred source recommended for this project.
| Variable required | Source | Variable name |
|---|---|---|
| Time of birth | Birth notification | DELTIMEZ |
| Date of birth | Birth registration | DOBr |
| Sex of baby | Birth registration | SEX |
| Holidays | Derived | |
| NHS births | Birth registration | NHSIND |
| Gestation age | Birth notification | GESTZ |
| Birthweight | Birth registration | BTHWGTR |
| Ethnicity | Birth notification | ETHCATZ |
| Country of birth | Birth registration | MCOB |
| Stillbirth indicator | Birth registration | SBIND |
| Parity | Derived | Still an open question which version we use |
| Onset of labour | HES | Delonset 2 |
| Method of delivery | HES | Delmeth Best 2 |
| Region of residence | Birth registration | HRORM |
| Unit type | Derived from CESTRESS | |
| Pseudo trust code | Derived from CESTRESS | |
| Singleton/multiple | Birth registration | MULTTYPE |
| Acceleration/induction (England) | Derived | |
| Mother’s age | Birth registration | AGEBM. Note that this is in the format yymm. The field [Age Mother] holds this field in decimal years |
| IMD | Derived |
ODBC link
Using ODBC it is possible to extract data from the database directly into other applications.
Importing data into statistical software programmes
Structure query language tables can be linked to using Microsoft Access®, or applications such as SAS®, Stata and R can import entire datasets. As of 2016, there were difficulties using ODBC with SPSS but this should be fixable by the VML team.
SAS
An example of SAS® code:
/*Loads in English ONS records for 2014, should take just a couple of mins*/
PROC SQL;
Connect to ODBC(‘DSN=vmlsql01;’||’Trust _ Connection = Yes’);
Create Table Work.ONS2014 AS Select * FROM Connection to ODBC
(SELECT * FROM ONS AS S WHERE [ONS Link Year] = 2014 AND Country = ‘E’;);
QUIT;
This imports entire English 2014 ONS records directly from the SQL Server table and places the data in the SAS® table ‘ONS2014’. From this point onwards a conventional SAS® session can take place. Be sure to include the many semicolons. The import will take only a minute or two.
R
An example in R code:
The library RODBC has to be installed.
library(RODBC)
dnHandle <-odbcConnect(‘vmlsql01’)
myExample<-sqlQuery(dnHandle,’SELECT * FROM ONS AS S WHERE [ONS Link Year] = 2014’)
odbcClose(dnHandle)
This will load 2014 ONS records into the data frame ‘myExample’. Note that while importing R converts suitable variables into category variables which can be very time-consuming.
Stata
Stata has first to be told about the ODBC link. One trick that works is to go to File > Import > ODBC data source. Once any table has been loaded in the following code will work for the remainder of the session.
An example in Stata:
odbc load, clear exec(“SELECT * FROM ONS AS S WHERE [ONS Link Year]=2014”)
This will import the 2014 ONS records into a Stata table where it can be manipulated or saved as a Stata dataset.
Importing all 10 years of ONS data will take a couple of minutes.
SPSS
From the main menu chose File > Import > Databases > New Query. Then select VMLSQL01 as the ODBC Source and tick the Views checkbox. At the time the project ended, there was a problem with ODBC links to SQL. This has now been resolved and users can use the link from the desktop within the project. Researchers should arrange with ONS to set up this link for each researcher separately.
SQL views
To make accessing data easier, a number or database Views have been constructed, which have the linkages hardwired into them. A database view from the perspective of a user just extracting data looks the same as a database table while hiding from the user the complexity of linking several database tables. Other useful tasks are also embedded into the view. For example, some of the ONS fields have commas or double quotation marks in the data. This can confuse some software packages, particularly R. The view removes the offending characters.
Resolving name clashes
Occasionally a HES field will have the same name as a ONS field, for example, SEX and [Birth Weight]. In views that link ONS to HES the following system is used to resolve name clashes. The HES field name is modified by placing its originating table in brackets. The following shorthand is used: BT = Baby Tail, D = Delivery, DI = Delivery Indicator. So, for example, the HES variable SEX becomes SEX (D).
View: ODBC all ONS
This view extracts all ONS records, but, like in the above example, conditions can be attached that restrict the data to a subset. For example, substituting the line below in the above SAS® code would give the sex and birthweight of Welsh stillbirths:
View: ODBC-linked HES singleton deliveries
This returns the mother’s HES delivery record for records that were successfully linked to English singleton ONS records. To avoid creating excessively wide data files it returns only the [ONS ID] and does not return the entire ONS record. The ONS record can of course be imported into another SAS® table and the link made with the SAS® Merge command or similar in other applications.
View: ODBC-linked HES multiple deliveries
This is the same as above but now returns HES records that link to English multiple deliveries. Now for, say, twins there are two separate ONS records and one delivery record with two relevant baby tails. The view will return the same core delivery record twice with each of the baby tails appended to each. An example is shown in Table 71.
| [ONS ID] | [Delivery ID] | [Field Order] (baby tail) |
|---|---|---|
| 10 | 123456 | 1 |
| 11 | 123456 | 2 |
| 117 | 988213 | 1 |
| 118 | 988213 | 2 |
The total number of records will correspond to the number of babies, not the number of deliveries.
View: ODBC-linked HES singleton deliveries and indicators
There are a number of derived variables that are stored in the table [Deliveries_Indicators]. This view returns the same data as in the view [ODBC Linked HES Singleton Deliveries] but now with these additional fields appended to the side.
View: ODBC all English singleton ONS and linked HES deliveries
Returns all ONS fields and records and all HES delivery fields, including derived ones for English singletons. Note that for records for which the ONS record is not linked to a delivery record, the HES fields will all be null.
This query can take some minutes to run.
View: ODBC all English singleton ONS and linked HES deliveries with ICD and OPCS
Same as view [ODBC All English Singleton ONS and Linked HES Deliveries] but with the flat file of ICD-10 diagnostic codes and OPCS procedural codes attached to each delivery record.
Appendix 3 Analysis of data
Proposed analyses
Table 72 shows the complete set of proposed analyses, both those that were done, and those that were planned but that there was not time to complete. This was drawn up at NIHR’s request to support the application it invited the team to make for further funding. It was subdivided into the analyses that could be completed by 31 March 2017 and those that could not be completed without the proposed second extension, which NIHR decided not to fund. It was amended at proof stage to described the position in late 2018.
| Analysis | Dataset | Subset | Time period | Area | Relationships | Type of analysis | In draft final report? | Presentation by end of March 2017? | Article by end of March 2017? | Article after end of March 2017? |
|---|---|---|---|---|---|---|---|---|---|---|
| Objective 1: Variations in birth by time of day and day of the week | ||||||||||
| 1 | Birth registration linked to birth notification | Births at home | 2005–14 | England and Wales | Births by time of day, day of week of birth, gestational age | Descriptive analysis | Yes | Conference poster 2015 | Drafted March 2017 | Article submitted for publication but rejected. To be revised and resubmitted |
| 2 | Birth registration linked to birth notification | Other births outside NHS hospitals | 2005–14 | England and Wales | Births by time of day, day of week of birth, gestational age | Descriptive analysis | Yes | As part of a larger article after March 2017. To be included in revised article on home births | ||
| 3 | Birth registration linked to birth notification linked to Maternity HES delivery records | Singleton births in NHS hospitals | 2005–14 | England | Births by time of day, day of week of birth, gestational age, mode of onset of labour, mode of delivery | Descriptive analysis | Yes | Posters at international Population Data Linkage Conference and RCM conference, 2016 | Presented at RSS conference September 2017 and posters at International Normal Birth Conference, October 2017. Article to be drafted for ‘Significance’ | |
| 4 | Birth registration linked to birth notification linked to Maternity HES delivery records | Singleton births in NHS hospitals | 2005–14 | England | Births by time of day, day of week of birth, gestational age, mode of onset of labour, mode of delivery | Statistical modelling | Yes | Article drafted by March 2017 | Article published June 2018 in BMJ Open | |
| 5 | Birth registration linked to birth notification linked to Maternity HES delivery records | Multiple births | 2005–14 | England | Births by time of day, day of week of birth, gestational age, mode of onset of labour, mode of delivery | Descriptive analysis plus modelling if found appropriate | No | No | Further funding needed for analysis | |
| 6 | Birth registration linked to birth notification linked to PEDW/NCCHD | Singleton and multiple births | 2005–14 | Wales | Births by time of day, day of week of birth, gestational age, mode of onset of labour, mode of delivery | Descriptive analysis plus modelling if found appropriate | No | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2018 | |
| Objective 2: Differences between maternity services | ||||||||||
| 7 | Birth registration linked to birth notification linked to Maternity HES delivery records | Singleton and multiple births in NHS hospitals | 2005–14 | England | Use 17. Database of trust and maternity unit site codes to derive and group maternity units by numbers of births and intervention rates to analyse associations between size and intervention rates of maternity units and patterns of births by time of day and day of the week of birth | Descriptive analysis | No | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | |
| 8 | Deaths linked to birth registration linked to birth notification linked to Maternity HES delivery records | Singleton and multiple births in NHS hospitals | 2005–14 | England | Use results of above plus staffing level data to analyse outcome by time of day and day of week of birth by characteristics of maternity units | Descriptive analysis and statistical modelling | No | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | |
| 9 | Birth registration linked to birth notification linked to PEDW/NCCHD | Singleton and multiple births in NHS hospitals | 2005–14 | Wales | Use database of trust and maternity unit site codes to derive and group maternity units by numbers of births and intervention rates to analyse associations between size and intervention rates of maternity units and patterns of births by time of day and day of the week of birth | Descriptive analysis | No | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | |
| 10 | Deaths linked to birth registration linked to birth notification linked to PEDW/NCCHD | Singleton and multiple births in NHS hospitals | 2005–14 | Wales | Use results of above plus staffing level data to analyse outcome by time of day and day of week of birth by characteristics of maternity units | Descriptive analysis and statistical modelling | No | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | |
| Objective 3: Outcome by time of day and day of the week | ||||||||||
| Outcomes for babies | ||||||||||
| 11 | Birth registration linked to birth notification linked to CMACE | Intrapartum stillbirths | 2005–9 | England and Wales | Intrapartum deaths by time of day, day of week of birth, gestational age, cause of death and other factors | Descriptive analysis | Yes | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | ||
| 12 | Birth registration linked to birth notification linked to Maternity HES delivery records | Infant deaths linked to births, singletons only | 2005–14 | England | Neonatal deaths by time of day, day of week of birth, gestational age, cause of death and other factors | Descriptive analysis only | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | ||
| 13 | Birth registration linked to birth notification linked to Maternity HES delivery records | Childhood deaths linked to births, singletons only | 2005–14 | England | Survival to the age of two by time of day, day of week of birth, gestational age, cause of death and other factors | Descriptive analysis only | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | ||
| 14 | Birth registration linked to birth notification linked to Maternity HES delivery records | Infant and childhood deaths linked to births, singletons only | 2005–14 | England | Neonatal and infant deaths and survival to the age of two by time of day, day of week of birth, gestational age, cause of death and other factors | Statistical modelling based on descriptive analysis | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | ||
| 15 | Birth registration linked to birth notification linked to Maternity HES delivery records | Infant and childhood deaths linked to births, multiple births | 2005–14 | England | Neonatal and infant deaths and survival to the age of two by time of day, day of week of birth, gestational age, cause of death and other factors | Descriptive analysis plus modelling if found appropriate | No | Further funding needed for analysis | ||
| 16 | Birth registration linked to birth notification linked to PEDW/NCCHD | Infant and childhood deaths linked to births, multiple births | 2005–14 | Wales | As above, but less detailed as numbers smaller | Descriptive analysis plus modelling if found appropriate | No | Further funding needed for analysis | ||
| 17 | Birth registration linked to birth notification linked to Maternity HES baby records linked to subsequent admissions of babies | Admissions of babies up to two years after birth | 2005–12 births | England | Morbidity leading to hospital admission up to the age of two by time of day, day of week of birth, gestational age and other factors | Descriptive analysis plus modelling if found appropriate | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | ||
| 18 | Birth registration linked to birth notification linked to PEDW baby records linked to subsequent admissions of babies | Admissions of babies up to two years after birth | 2005–12 births | Wales | Morbidity leading to hospital admission up to the age of two by time of day, day of week of birth, gestational age and other factors | Descriptive analysis plus modelling if found appropriate | No | Further funding needed for analysis. Singletons included in application funded by ESRC, May 2019 | ||
| Outcomes for mothers | ||||||||||
| 19 | Birth registration linked to birth notification | Deaths of women within a year of giving birth linked to births | 2005–14 | England and Wales | Maternal mortality by cause, time of day and day of the week of birth | Descriptive analysis plus modelling if found appropriate | No | Included in application funded by ESRC, May 2019 | ||
| 20 | Birth registration linked to birth notification linked to Maternity HES delivery records | 2005–14 | England | Births without obstetric intervention by time of day and day of the week of birth | Descriptive analysis plus modelling if found appropriate | Yes | Included in application funded by ESRC, May 2019 | |||
| 21 | Birth registration linked to birth notification linked to PEDW/NCCHD | 2005–14 | Wales | Births without obstetric intervention by time of day and day of the week of birth | Descriptive analysis plus modelling if found appropriate | No | Included in application funded by ESRC, May 2019 | |||
| 22 | Birth registration linked to birth notification linked to Maternity HES delivery records linked to subsequent admissions of mothers | Subsequent admissions of mothers within a year of giving birth | 2005–13 | England | Maternal morbidity by time of day and day of the week of birth | Descriptive analysis plus modelling if found appropriate | No | Included in application funded by ESRC, May 2019 | ||
| 23 | Birth registration linked to birth notification linked to PEDW delivery records linked to subsequent admissions of mothers | Subsequent admissions of mothers within a year of giving birth | 2005–13 | Wales | Maternal morbidity by time of day and day of the week of birth | Descriptive analysis plus modelling if found appropriate | No | Included in application funded by ESRC, May 2019 | ||
| Objective 4: Changes over time | ||||||||||
| Subsumed in other analyses | ||||||||||
Descriptive analysis of births by day of the week and time of day
Table 73 gives the daily pattern of live births per day and ratio by year for England and Wales for the years 2005–14, showing that this has changed very little over the period. Further information is shown in Chapter 3, Variations in overall numbers of births in England and Wales by time of day and day of the week.
| Day | Total | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Average numbers of live births per day | |||||||||||
| Monday | 1,963 | 1,819 | 1,876 | 1,936 | 1,991 | 1,981 | 2,022 | 2,038 | 2,044 | 1,970 | 1,949 |
| Tuesday | 2,006 | 1,850 | 1,913 | 1,974 | 2,031 | 2,039 | 2,083 | 2,086 | 2,080 | 1,996 | 2,005 |
| Wednesday | 2,015 | 1,873 | 1,940 | 1,995 | 2,035 | 2,043 | 2,075 | 2,076 | 2,098 | 2,013 | 2,005 |
| Thursday | 2,045 | 1,888 | 1,956 | 2,006 | 2,052 | 2,060 | 2,115 | 2,123 | 2,139 | 2,060 | 2,047 |
| Friday | 2,042 | 1,910 | 1,966 | 2,026 | 2,073 | 2,061 | 2,105 | 2,101 | 2,128 | 2,028 | 2,023 |
| Saturday | 1,733 | 1,603 | 1,666 | 1,723 | 1,752 | 1,740 | 1,800 | 1,799 | 1,801 | 1,728 | 1,720 |
| Sunday | 1,651 | 1,504 | 1,574 | 1,619 | 1,671 | 1,668 | 1,720 | 1,725 | 1,721 | 1,656 | 1,645 |
| Public holidays | 1,623 | 1,460 | 1,533 | 1,618 | 1,635 | 1,671 | 1,688 | 1,707 | 1,715 | 1,621 | 1,560 |
| All | 1,914 | 1,769 | 1,834 | 1,890 | 1,936 | 1,934 | 1,981 | 1,983 | 1,992 | 1,914 | 1,904 |
| Ratio of average numbers of live births per day to overall daily average for the year | |||||||||||
| Monday | 1.03 | 1.03 | 1.02 | 1.02 | 1.03 | 1.02 | 1.02 | 1.03 | 1.03 | 1.03 | 1.02 |
| Tuesday | 1.05 | 1.05 | 1.04 | 1.04 | 1.05 | 1.05 | 1.05 | 1.05 | 1.04 | 1.04 | 1.05 |
| Wednesday | 1.05 | 1.06 | 1.06 | 1.06 | 1.05 | 1.06 | 1.05 | 1.05 | 1.05 | 1.05 | 1.05 |
| Thursday | 1.07 | 1.07 | 1.07 | 1.06 | 1.06 | 1.06 | 1.07 | 1.07 | 1.07 | 1.08 | 1.07 |
| Friday | 1.07 | 1.08 | 1.07 | 1.07 | 1.07 | 1.07 | 1.06 | 1.06 | 1.07 | 1.06 | 1.06 |
| Saturday | 0.91 | 0.91 | 0.91 | 0.91 | 0.91 | 0.90 | 0.91 | 0.91 | 0.90 | 0.90 | 0.90 |
| Sunday | 0.86 | 0.85 | 0.86 | 0.86 | 0.86 | 0.86 | 0.87 | 0.87 | 0.86 | 0.87 | 0.86 |
| Public holidays | 0.85 | 0.83 | 0.84 | 0.86 | 0.84 | 0.86 | 0.85 | 0.86 | 0.86 | 0.85 | 0.82 |
| All | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
Table 74 gives the ratio of average births per hour to the overall average for the year for England and Wales for the years 2005–14. Further information is shown in Chapter 3, Variations in numbers of singleton births in England and Wales by day of birth and by time of day of birth, Variations over time.
| Hour of birth | Total | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 00.00–00.59 | 0.98 | 0.99 | 0.99 | 0.98 | 0.99 | 1.00 | 0.97 | 0.97 | 0.98 | 0.97 | 0.99 |
| 01.00–01.59 | 1.00 | 0.99 | 1.01 | 1.00 | 1.01 | 1.00 | 1.01 | 1.01 | 1.00 | 1.01 | 1.00 |
| 02.00–02.59 | 0.99 | 0.99 | 0.99 | 1.00 | 1.02 | 1.01 | 1.00 | 1.00 | 1.01 | 1.00 | 1.00 |
| 03.00–03.59 | 0.99 | 0.99 | 0.99 | 0.99 | 1.00 | 1.00 | 1.01 | 0.99 | 0.99 | 0.99 | 0.99 |
| 04.00–04.59 | 0.98 | 0.98 | 0.98 | 0.99 | 0.98 | 0.98 | 0.98 | 0.99 | 0.99 | 0.98 | 0.98 |
| 05.00–05.59 | 0.95 | 0.96 | 0.96 | 0.96 | 0.97 | 0.97 | 0.96 | 0.96 | 0.96 | 0.95 | 0.95 |
| 06.00–06.59 | 0.92 | 0.92 | 0.93 | 0.93 | 0.93 | 0.93 | 0.93 | 0.93 | 0.92 | 0.92 | 0.92 |
| 07.00–07.59 | 0.85 | 0.84 | 0.86 | 0.85 | 0.84 | 0.86 | 0.86 | 0.86 | 0.85 | 0.86 | 0.86 |
| 08.00–08.59 | 0.82 | 0.82 | 0.83 | 0.83 | 0.84 | 0.82 | 0.82 | 0.83 | 0.84 | 0.83 | 0.82 |
| 09.00–09.59 | 1.27 | 1.21 | 1.23 | 1.25 | 1.24 | 1.26 | 1.28 | 1.32 | 1.33 | 1.35 | 1.35 |
| 10.00–10.59 | 1.34 | 1.40 | 1.39 | 1.36 | 1.35 | 1.34 | 1.33 | 1.32 | 1.33 | 1.33 | 1.33 |
| 11.00–11.59 | 1.23 | 1.23 | 1.23 | 1.24 | 1.24 | 1.24 | 1.24 | 1.24 | 1.25 | 1.26 | 1.27 |
| 12.00–12.59 | 1.14 | 1.13 | 1.12 | 1.14 | 1.14 | 1.15 | 1.15 | 1.16 | 1.16 | 1.16 | 1.16 |
| 13.00–13.59 | 0.96 | 0.95 | 0.96 | 0.96 | 0.98 | 0.96 | 0.96 | 0.96 | 0.98 | 0.97 | 0.97 |
| 14.00–14.59 | 1.01 | 1.02 | 1.02 | 1.02 | 1.02 | 1.01 | 1.02 | 1.01 | 1.00 | 1.01 | 1.00 |
| 15.00–15.59 | 0.99 | 1.03 | 1.00 | 1.02 | 1.01 | 1.01 | 1.01 | 1.00 | 1.00 | 0.99 | 0.98 |
| 16.00–16.59 | 0.96 | 0.98 | 0.97 | 0.97 | 0.98 | 0.97 | 0.97 | 0.96 | 0.96 | 0.95 | 0.96 |
| 17.00–17.59 | 0.90 | 0.93 | 0.91 | 0.91 | 0.91 | 0.91 | 0.92 | 0.91 | 0.90 | 0.90 | 0.90 |
| 18.00–18.59 | 0.90 | 0.92 | 0.92 | 0.93 | 0.91 | 0.91 | 0.91 | 0.91 | 0.90 | 0.90 | 0.88 |
| 19.00–19.59 | 0.91 | 0.94 | 0.93 | 0.94 | 0.92 | 0.92 | 0.91 | 0.92 | 0.90 | 0.90 | 0.89 |
| 20.00–20.59 | 0.88 | 0.90 | 0.90 | 0.90 | 0.89 | 0.89 | 0.88 | 0.88 | 0.88 | 0.87 | 0.87 |
| 21.00–21.59 | 0.90 | 0.91 | 0.90 | 0.90 | 0.89 | 0.91 | 0.91 | 0.92 | 0.92 | 0.92 | 0.93 |
| 22.00–22.59 | 0.95 | 0.95 | 0.96 | 0.96 | 0.97 | 0.96 | 0.96 | 0.95 | 0.96 | 0.97 | 0.96 |
| 23.00–23.59 | 0.98 | 0.99 | 0.99 | 0.98 | 0.99 | 1.00 | 0.99 | 0.99 | 0.98 | 0.98 | 0.98 |
Births in NHS hospitals in England by onset of labour and method of delivery
Structure of records in Maternity Hospital Episode Statistics
Records of delivery episodes in the Maternity HES should have information about the birth coded in the ‘maternity tail’ appended to the standard APC record, which includes codes for diagnoses in accordance with the ICD, as well as codes for procedures carried out during the episode, using the OPCS-4 Classification of Interventions and Procedures. In some cases, the maternity tail is missing for whole maternity units and in other cases it is missing for individuals.
Onset of labour
Information about the onset of labour is included in the variable DELONSET in the HES maternity tail and coded as shown in Table 75.
| Variable DELONSET in HES maternity tail | Onset of labour |
|---|---|
| 1 = Spontaneous: the onset of regular contractions whether or not preceded by spontaneous rupture of the membranes | Spontaneous |
| 2 = Any caesarean section carried out immediately following the onset of labour, when the decision was made before labour | Caesarean section |
| 3 = Surgical induction by amniotomy | Induced |
| 4 = Medical induction, including the administration of agents either orally, intravenously or intravaginally with the intention of initiating labour | |
| 5 = Combination of surgical induction and medical induction | |
| 8 = Not applicable (from 1996–97 onwards) | Missing |
| 9 = Not known: validation error |
Mode of birth
Coding of mode of birth is shown in Table 76. Mode of birth is recorded in the variable DELMETH_1 in the HES maternity tail. OPCS-4 codes for any procedures undertaken are included in the core HES record and are available for most births. Since the mid-1990s, the procedure codes have been used for mode of birth in routine Maternity HES publications. 99
| Code | Categories used in DELMETH_1 in HES maternity tail | OPCS-1 code | Mode of birth |
|---|---|---|---|
| 0 | Spontaneous vertex (normal vaginal delivery, occipitoanterior) | R24* | Spontaneous |
| 1 | Spontaneous other cephalic (cephalic vaginal delivery with abnormal presentation of head at delivery, without instruments, with or without manipulation) | R23* | |
| 2 | Low forceps, not breech, including forceps delivery not otherwise specified (forceps, low application, without manipulation) | R215 or R218 or R219 | Instrumental |
| 3 | Other forceps, not breech, including high forceps and mid forceps (forceps with manipulation) | R211 or R212 or R213 or R214 | |
| 4 | Ventouse, vacuum extraction | R22* | |
| 5 | Breech, including partial breech extraction (spontaneous delivery assisted or unspecified) | R20* | Spontaneous |
| 6 | Breech | R19* | Instrumental |
| 7 | Elective caesarean section | R17* | Elective caesarean section |
| 8 | Emergency caesarean section | R18* | Emergency caesarean section (and other surgical) |
| 9 | Other | R25* | Missing |
| X | Not known | Otherwise |
Mode of birth was therefore derived using the OPCS-4 procedure codes, which were recorded in the core record for 98% of births. There were, however, some records with more than one delivery code. These could have arisen because of a multiple birth, failed forceps or erroneous data entry. In these cases, the most invasive mode was chosen as the mode of birth in the order caesarean section, instrumental and spontaneous vaginal. For records for which the mode of birth was coded as 9 or X to denote it was missing, the information recorded in DELMETH_1 in the maternity tail was used. For 0.1% of births, mode of birth was not recorded in either place but there were several episode records for the same delivery, the record with the mode of birth coded in the range 0–8 was used. For records for which the mode of birth was elective caesarean section, we grouped 445,453 births in which the onset was recorded as ‘caesarean’ with 24,450 births in which the onset was recorded as spontaneous because exploratory analysis suggested that there was no difference between these groups of births with respect to time and day of birth.
Checking singleton births for linkage bias
Table 77 defines ‘ONS births’ and the two subsets of births defined according to the outcome of linkage and quality assurance procedures summarised in Figure 17. The distributions of these two subsets according to demographic and other relevant variables were compared in Table 78. This also shows the results of chi-squared tests conducted to test the hypothesis that the distributions were the same.
| Category | Definition | Number of records |
|---|---|---|
| ONS birth records | All registered births linked to notified births | 6,468,586 |
| Linked and matched births | ONS birth records included in the study | 6,137,945 |
| Unlinked or unmatched births | ONS births excluded from the study because they were unlinked or unmatched | 330,641 |
| Variable | Percentage distribution | ||
|---|---|---|---|
| Linked and matched births | Unlinked or unmatched births | All ONS birth records | |
| Year of birth | |||
| 2005 | 9.03 | 13.55 | 9.26 |
| 2006 | 9.35 | 14.24 | 9.60 |
| 2007 | 9.70 | 13.16 | 9.88 |
| 2008 | 10.12 | 10.66 | 10.14 |
| 2009 | 10.12 | 9.66 | 10.10 |
| 2010 | 10.45 | 7.39 | 10.29 |
| 2011 | 10.46 | 7.36 | 10.30 |
| 2012 | 10.57 | 8.44 | 10.46 |
| 2013 | 10.15 | 7.48 | 10.01 |
| 2014 | 10.06 | 8.05 | 9.95 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 6,137,945 | 330,641 | 6,468,586 |
| Note: χ2 test (H0: distribution of linked and matched births is the same as the distribution of unlinked or unmatched births): p < 0.001 (χ2 = 29,363.2, df = 9) | |||
| Month of birth | |||
| January | 8.26 | 8.55 | 8.28 |
| February | 7.56 | 8.21 | 7.59 |
| March | 8.21 | 9.75 | 8.29 |
| April | 8.00 | 7.85 | 8.00 |
| May | 8.45 | 8.11 | 8.43 |
| June | 8.28 | 7.97 | 8.27 |
| July | 8.70 | 8.37 | 8.68 |
| August | 8.62 | 8.18 | 8.60 |
| September | 8.68 | 8.10 | 8.65 |
| October | 8.69 | 8.27 | 8.67 |
| November | 8.22 | 8.08 | 8.21 |
| December | 8.31 | 8.55 | 8.32 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 6,137,945 | 330,641 | 6,468,586 |
| Note: χ2 test (H0: distribution of linked and matched births is the same as the distribution of unlinked or unmatched births): p < 0.001 (χ2 = 1,513.1, df = 11) | |||
| Region of residence | |||
| East Midlands | 7.39 | 3.71 | 7.20 |
| East of England | 9.75 | 8.56 | 9.69 |
| London | 19.30 | 27.27 | 19.71 |
| North East | 4.73 | 2.24 | 4.61 |
| North West | 13.32 | 7.44 | 13.02 |
| South Central | 7.49 | 3.96 | 7.31 |
| South East | 7.74 | 4.97 | 7.60 |
| South West | 8.06 | 3.50 | 7.82 |
| West Midlands | 10.93 | 5.41 | 10.64 |
| Yorkshire/The Humber | 9.97 | 4.51 | 9.69 |
| Home | 1.23 | 27.05 | 2.55 |
| Elsewhere | 0.11 | 1.39 | 0.17 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 6,137,943 | 330,638 | 6,468,581 |
| Note: five births had an unknown birth region and were excluded from this table. Note: χ2 test (H0: distribution of linked and matched births is the same as the distribution of unlinked or unmatched births): p < 0.001 (χ2 = 915877.2, df = 11) | |||
| Gestational age group | |||
| Missing or below 22 weeks | 0.76 | 1.32 | 0.79 |
| Preterm | 6.05 | 6.73 | 6.08 |
| Term | 89.19 | 88.71 | 89.17 |
| Post-term | 4.00 | 3.23 | 3.96 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 6,137,945 | 330,641 | 6,468,586 |
| Note: χ2 test (H0: distribution of linked and matched births is the same as the distribution of unlinked or unmatched births): p < 0.001 (χ2 = 1,947.9, df = 3) | |||
| Mother’s age (years) | |||
| Under 15 | 0.03 | 0.03 | 0.03 |
| 15–19 | 5.58 | 4.98 | 5.55 |
| 20–24 | 18.59 | 16.41 | 18.48 |
| 25–29 | 27.42 | 24.89 | 27.29 |
| 30–34 | 28.69 | 29.27 | 28.72 |
| 35–39 | 15.96 | 19.15 | 16.13 |
| 40–44 | 3.54 | 4.81 | 3.6 |
| 45 and over | 0.19 | 0.47 | 0.2 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 6,468,584 | 330,639 | 6,137,945 |
| Note: two unlinked records had no information about mother’s age. χ2 test (H0: distribution of linked and matched births is the same as the distribution of unlinked or unmatched births): p < 0.001 (χ2 = 6,433.4, df = 7) | |||
| Baby’s sex | |||
| Female | 48.66 | 49.20 | 48.69 |
| Male | 51.34 | 50.80 | 51.31 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 6,137,945 | 330,641 | 6,468,586 |
| Note: two unlinked records had no information about mother’s age. χ2 test (H0: distribution of linked and matched births is the same as the distribution of unlinked or unmatched births): p < 0.001 (χ2 = 36.09, df = 1) | |||
| Day of birth | |||
| Monday | 13.05 | 13.00 | 13.05 |
| Tuesday | 13.33 | 13.25 | 13.32 |
| Wednesday | 14.59 | 14.59 | 14.59 |
| Thursday | 14.56 | 14.40 | 14.55 |
| Friday | 13.59 | 13.55 | 13.59 |
| Saturday | 12.94 | 13.32 | 12.96 |
| Sunday | 12.15 | 12.06 | 12.14 |
| Public holidays | 1.93 | 1.98 | 1.93 |
| Christmas | 0.43 | 0.46 | 0.43 |
| Last weekday before a holiday period | 1.75 | 1.73 | 1.75 |
| First weekday after a holiday period | 1.69 | 1.66 | 1.68 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 6,137,945 | 330,641 | 6,468,586 |
| Note: χ2 test (H0: distribution of linked and matched births is the same as the distribution of unlinked or unmatched births): p < 0.001 (χ2 = 58.9, df = 10) | |||
| Hour of birth | |||
| 00.00–02.59 | 12.46 | 12.55 | 12.47 |
| 03.00–05.59 | 12.23 | 12.84 | 12.26 |
| 06.00–08.59 | 10.82 | 12.03 | 10.89 |
| 09.00–11.59 | 16.28 | 14.88 | 16.21 |
| 12.00–14.59 | 13.01 | 12.74 | 13.00 |
| 15.00–17.59 | 11.98 | 11.74 | 11.97 |
| 18.00–20.59 | 11.29 | 11.36 | 11.29 |
| 21.00–23.59 | 11.92 | 11.84 | 11.92 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 6,092,298 | 237,145 | 6,409,443 |
| Note: 59,143 of all registered births had no information on the time of birth. χ2 test (H0: distribution of linked and matched births is the same as the distribution of unlinked or unmatched births): p < 0.001 (χ2 = 921.2, df = 7) | |||
Checking for bias between singleton births included and excluded from the study dataset
As shown in Figure 17, 83,409 births were excluded as they occurred in places other than NHS hospitals with maternity units. Table 79 compares the two subsets of singleton births in NHS maternity units in relation to the inclusion criteria for the study dataset. The distributions of these two subsets according to demographic and other relevant variables were compared in Table 80. This also shows the results of chi-squared tests conducted to test the hypothesis that the distributions were the same.
| Category | Definition | Number of records |
|---|---|---|
| Births in NHS maternity units | All singleton births in NHS maternity units | 6,054,536 |
| Study dataset | Subset of births in NHS maternity units, after excluding births with information about gestational age, onset of labour or mode of birth missing | 5,093,615 |
| Birth in NHS maternity units excluded from study dataset | Births in NHS maternity units excluded because information about gestational age, onset of labour or mode of birth was missing | 960,921 |
| Variable | Singleton births in NHS maternity units | ||
|---|---|---|---|
| Included in study dataset | Excluded from study dataset | All | |
| Year of birth | |||
| 2005 | 8.53 | 11.99 | 9.08 |
| 2006 | 8.69 | 13.05 | 9.38 |
| 2007 | 8.43 | 16.58 | 9.73 |
| 2008 | 9.63 | 12.68 | 10.11 |
| 2009 | 10.52 | 7.88 | 10.10 |
| 2010 | 10.98 | 7.44 | 10.42 |
| 2011 | 11.12 | 6.87 | 10.44 |
| 2012 | 11.26 | 6.80 | 10.55 |
| 2013 | 10.60 | 7.71 | 10.14 |
| 2014 | 10.24 | 8.98 | 10.04 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 5,093,615 | 960,921 | 6,054,536 |
| Note: χ2 test (H0: distribution of births in study dataset is the same as the distribution of excluded births): p < 0.001 (χ2 = 142,070, df = 9) | |||
| Month of birth | |||
| January | 8.18 | 8.72 | 8.27 |
| February | 7.44 | 8.23 | 7.57 |
| March | 8.01 | 9.35 | 8.22 |
| April | 8.06 | 7.69 | 8.00 |
| May | 8.51 | 8.11 | 8.45 |
| June | 8.35 | 7.90 | 8.28 |
| July | 8.79 | 8.18 | 8.69 |
| August | 8.73 | 8.07 | 8.63 |
| September | 8.76 | 8.28 | 8.68 |
| October | 8.72 | 8.56 | 8.69 |
| November | 8.20 | 8.30 | 8.22 |
| December | 8.24 | 8.63 | 8.31 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 5,093,615 | 960,921 | 6,054,536 |
| Note: χ2 test (H0: distribution of births in study dataset is the same as the distribution of excluded births): p < 0.001 (χ2 = 4343.6, df = 11) | |||
| Region of birth | |||
| East Midlands | 8.31 | 3.15 | 7.49 |
| East of England | 10.43 | 6.98 | 9.88 |
| London | 18.98 | 22.64 | 19.56 |
| North East | 4.71 | 5.25 | 4.80 |
| North West | 14.51 | 8.10 | 13.49 |
| South Central | 7.64 | 7.31 | 7.59 |
| South East | 6.92 | 12.76 | 7.84 |
| South West | 7.57 | 11.30 | 8.17 |
| West Midlands | 10.98 | 11.58 | 11.07 |
| Yorkshire/The Humber | 9.95 | 10.94 | 10.11 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 5,093,615 | 960,921 | 6,054,536 |
| Note: the categories ‘Home’, ‘Elsewhere’, and ‘Not known’ have been excluded from this table (they are excluded from the study by design). χ2 test (H0: distribution of births in study dataset is the same as the distribution of excluded births): p < 0.001 (χ2 = 119,121, df = 9) | |||
| Gestational age group | |||
| Preterm | 5.86 | 7.67 | 6.14 |
| Term | 90.11 | 88.15 | 89.81 |
| Post-term | 4.03 | 4.19 | 4.05 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 5,093,615 | 914,676 | 6,008,291 |
| Note: births with unknown gestational age or gestational age below 22 weeks have been excluded from this table. χ2 test (H0: distribution of births in study dataset is the same as the distribution of excluded births): p < .001 (χ2 = 4503.2, df = 2) | |||
| Mother’s age (years) | |||
| Under 15 | 0.03 | 0.03 | 0.03 |
| 15–19 | 5.60 | 5.72 | 5.62 |
| 20–24 | 18.78 | 18.07 | 18.66 |
| 25–29 | 27.61 | 26.66 | 27.46 |
| 30–34 | 28.61 | 28.80 | 28.64 |
| 35–39 | 15.72 | 16.71 | 15.88 |
| 40–44 | 3.48 | 3.79 | 3.53 |
| 45 and over | 0.18 | 0.21 | 0.19 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 5,093,615 | 960,921 | 6,054,536 |
| Note: χ2 test (H0: distribution of births in study dataset is the same as the distribution of excluded births): p < 0.001 (χ2 = 1,269.7, df = 7) | |||
| Baby’s sex | |||
| Female | 48.64 | 48.64 | 48.64 |
| Male | 51.36 | 51.36 | 51.36 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 5,093,615 | 960,921 | 6,054,536 |
| Note: χ2 test (H0: distribution of births in study dataset is the same as the distribution of excluded births): p = 0.996 (χ2 = 0.00003, df = 1) | |||
| Day of birth | |||
| Monday | 13.04 | 13.12 | 13.06 |
| Tuesday | 13.30 | 13.47 | 13.33 |
| Wednesday | 14.57 | 14.69 | 14.59 |
| Thursday | 14.55 | 14.68 | 14.57 |
| Friday | 13.57 | 13.76 | 13.60 |
| Saturday | 12.97 | 12.71 | 12.93 |
| Sunday | 12.20 | 11.77 | 12.13 |
| Public holiday | 1.94 | 1.85 | 1.92 |
| Christmas | 0.43 | 0.44 | 0.43 |
| Last weekday before a holiday period | 1.74 | 1.80 | 1.75 |
| First weekday after a holiday period | 1.68 | 1.71 | 1.69 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 5,093,615 | 960,921 | 6,054,536 |
| Note: χ2 test (H0: distribution of births in study dataset is the same as the distribution of excluded births): p < 0.001 (χ2 = 281.6, df = 10) | |||
| Hour of birth | |||
| 00.00–02.59 | 12.51 | 12.08 | 12.44 |
| 03.00–05.59 | 12.26 | 11.72 | 12.17 |
| 06.00–08.59 | 10.83 | 10.43 | 10.77 |
| 09.00–11.59 | 16.17 | 17.19 | 16.34 |
| 12.00–14.59 | 12.96 | 13.54 | 13.05 |
| 15.00–17.59 | 11.95 | 12.31 | 12.01 |
| 18.00–20.59 | 11.33 | 11.10 | 11.30 |
| 21.00–23.59 | 11.98 | 11.63 | 11.93 |
| All | 100.00 | 100.00 | 100.00 |
| Total number | 5,048,369 | 951,563 | 5,999,932 |
| Note: χ2 test (H0: distribution of births in study dataset is the same as the distribution of excluded births): p < 0.001 (χ2 = 1,344.5, df = 7) | |||
The average number of births per hour on non-holiday Thursdays
Figure 27 shows the distributions of mean number of births per hour on non-holiday Thursdays. This allows the reader to view in more detail the distributions shown in Figure 19 in the main text. Thursday was chosen as an example day.
FIGURE 27.
Mean number of singleton births per hour on a non-holiday Thursday in NHS maternity units by method of onset of labour and mode of birth, England: 2005–14.
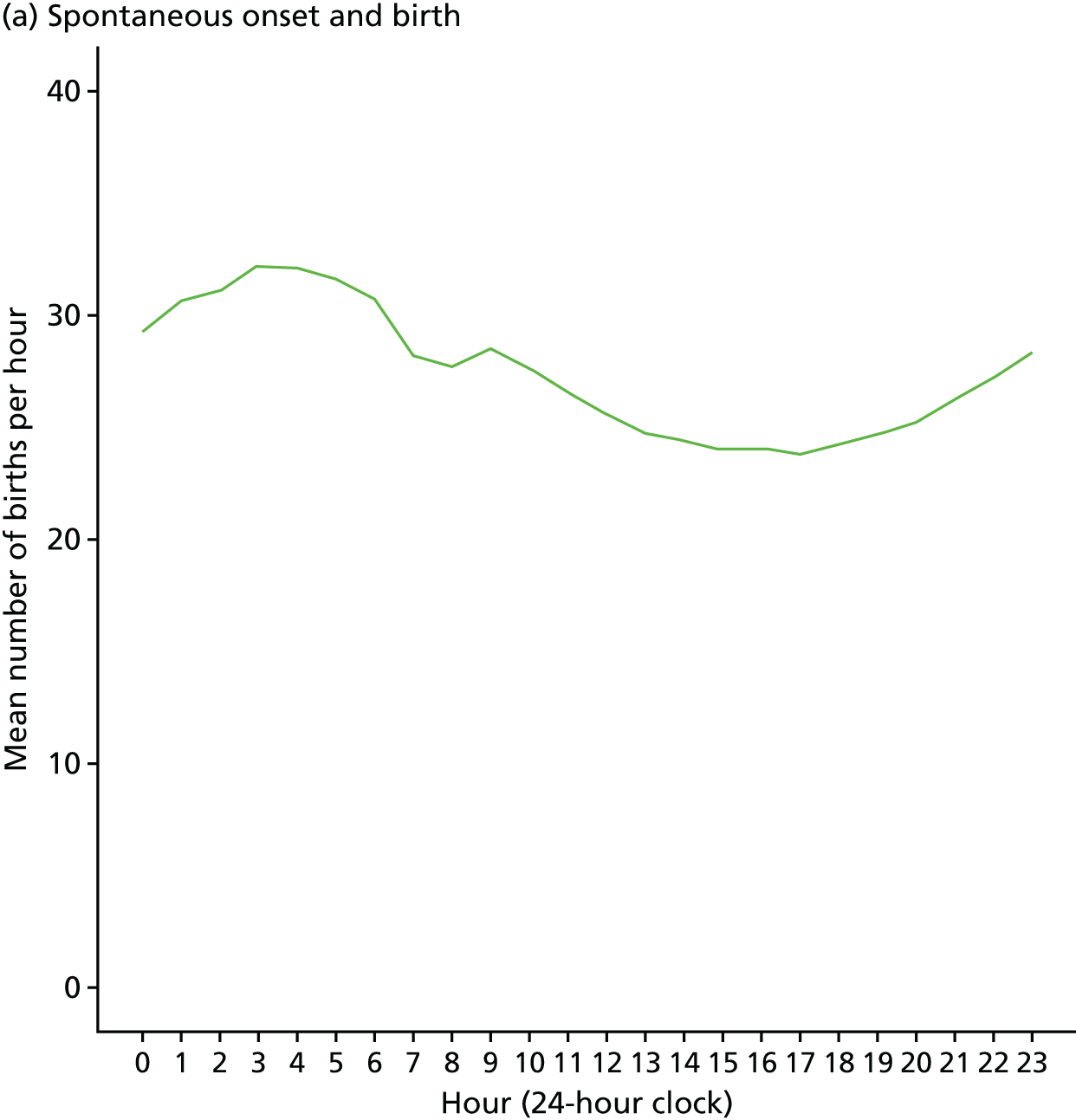
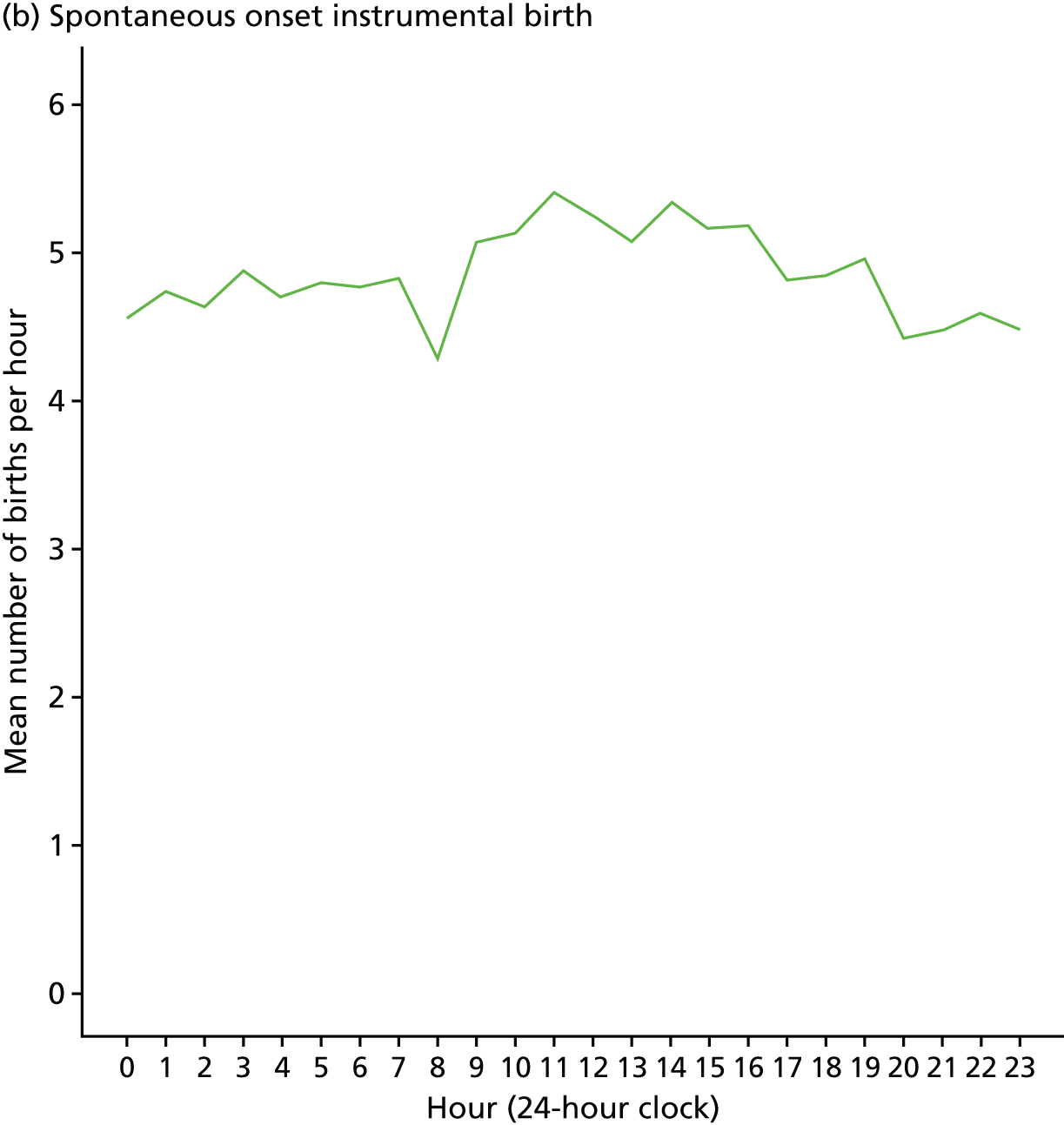
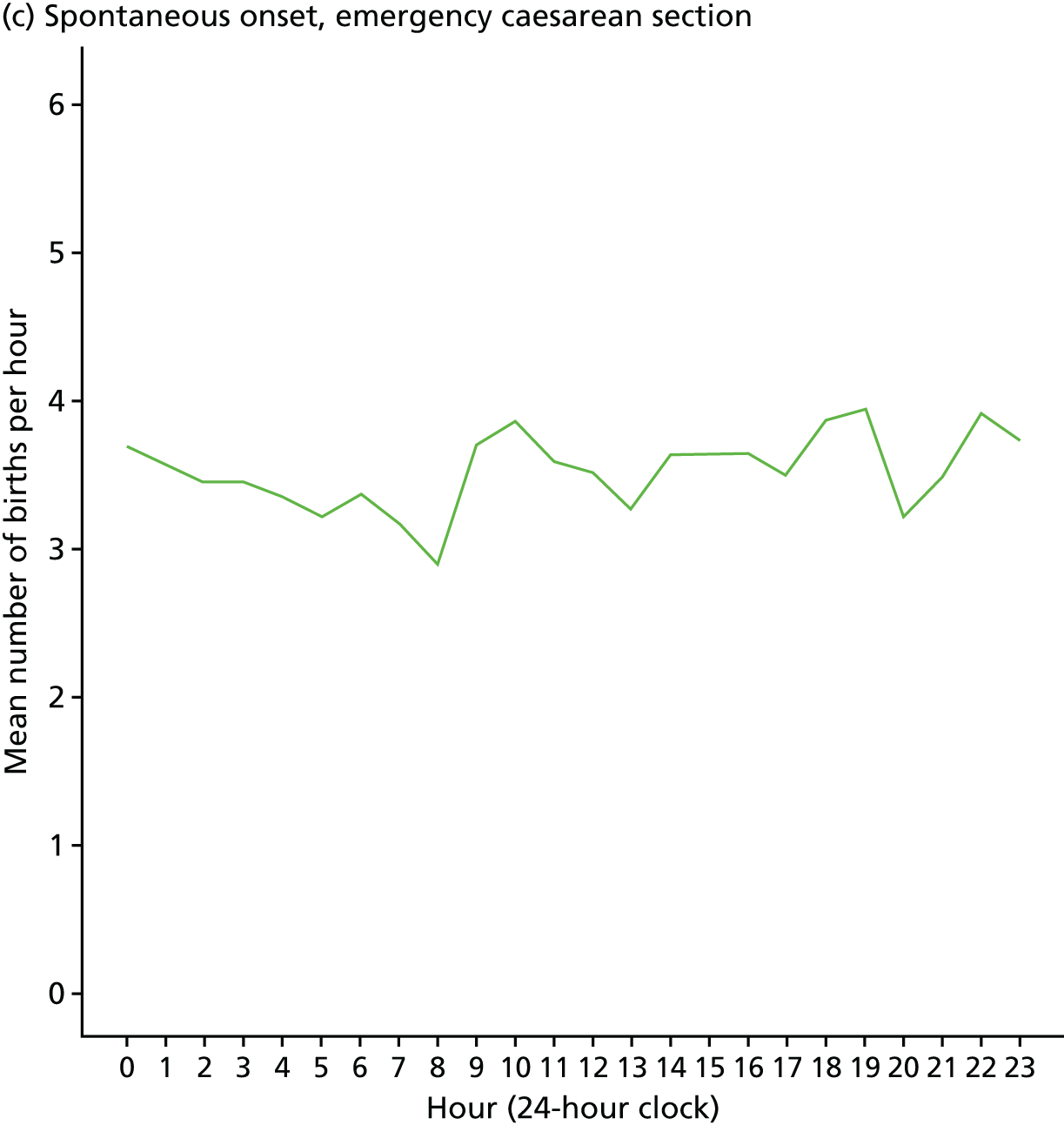
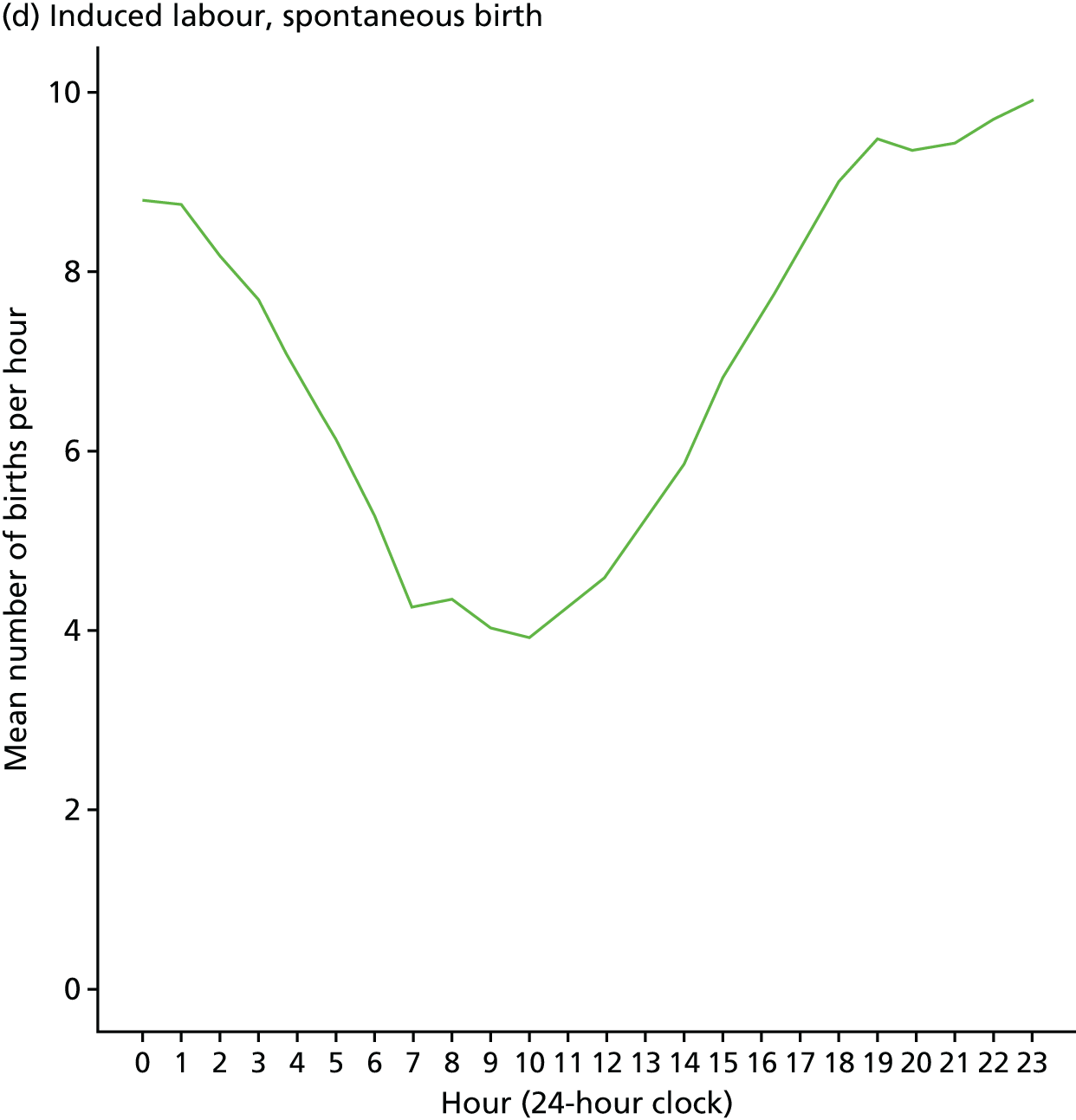
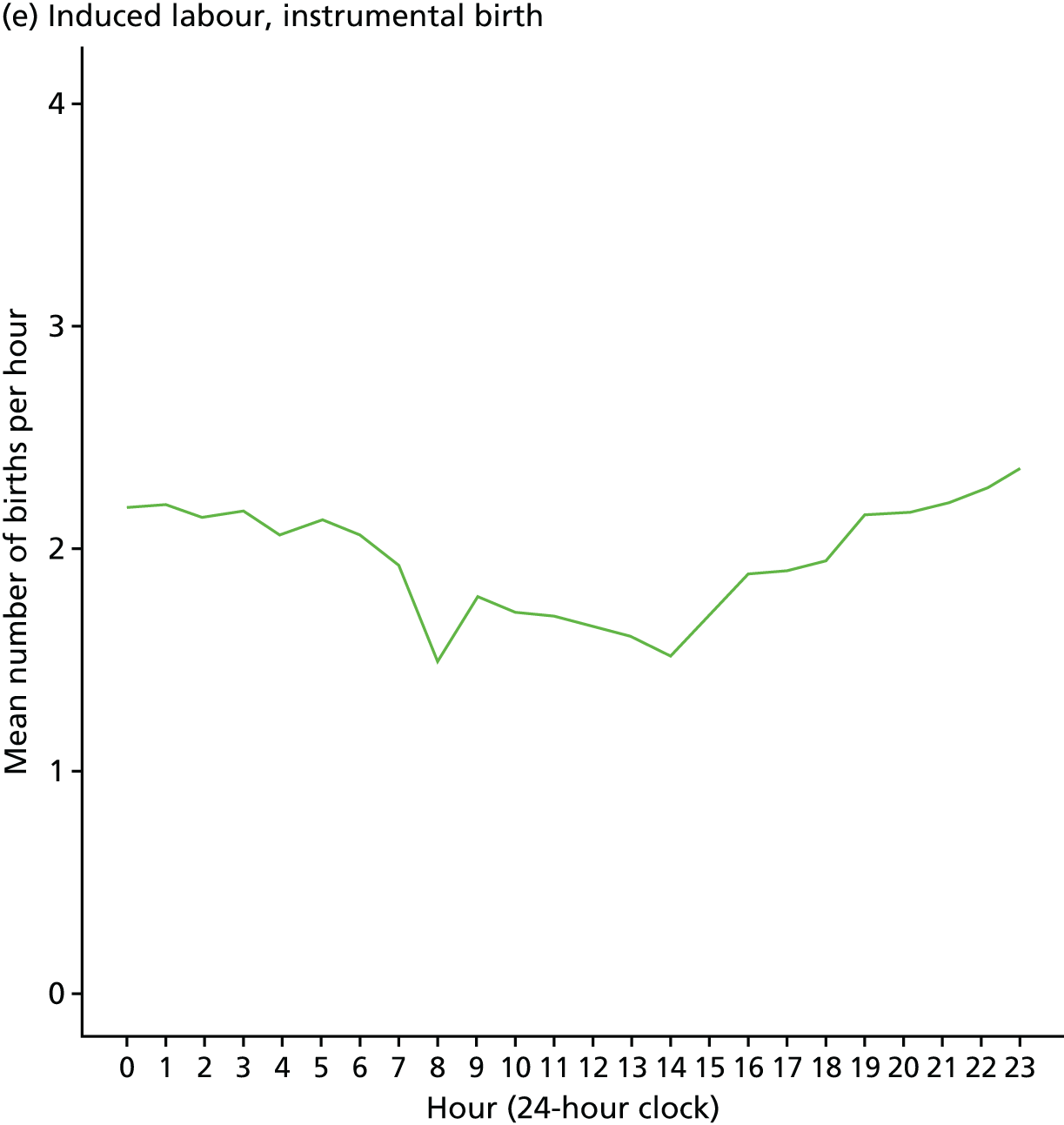
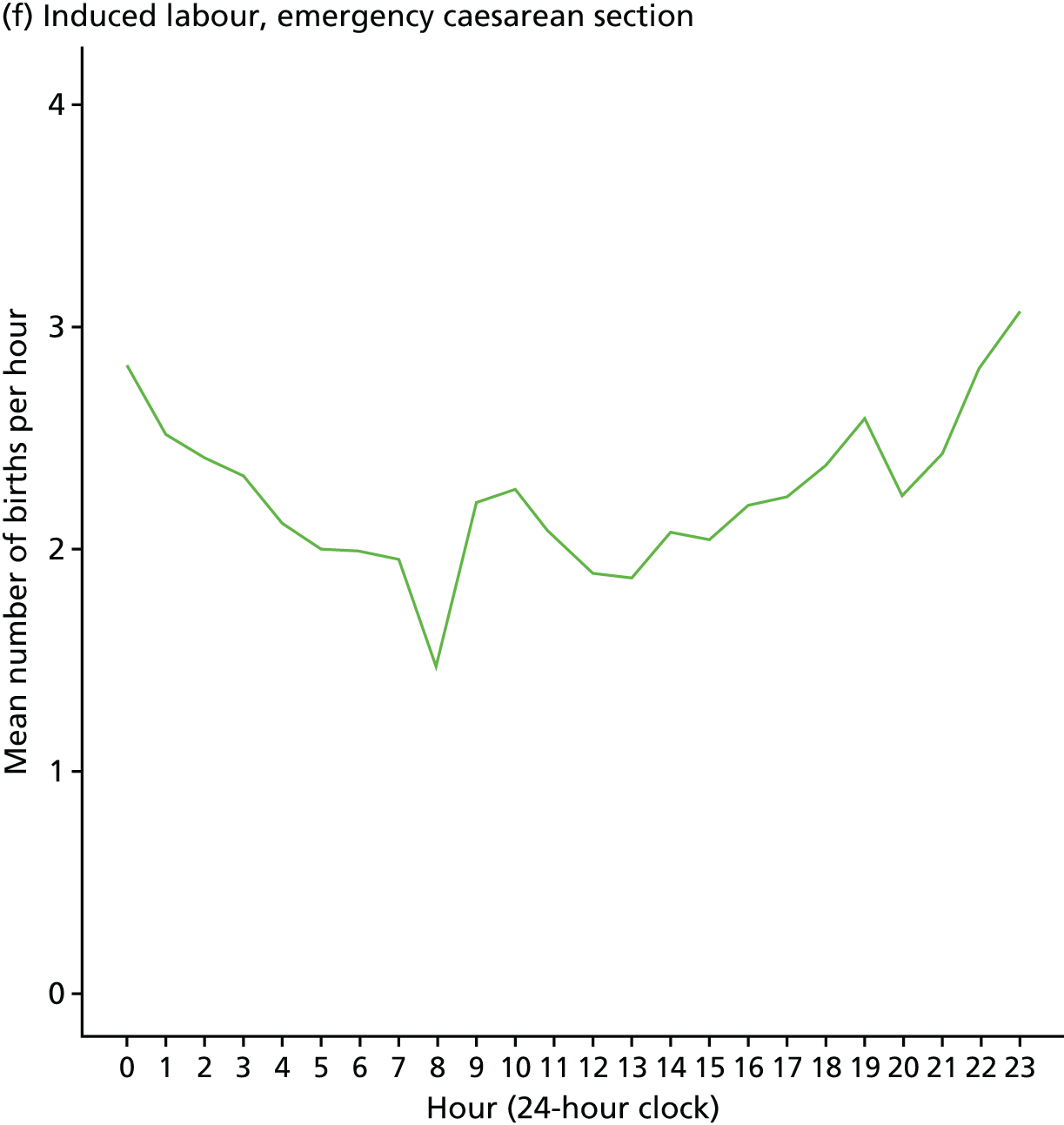
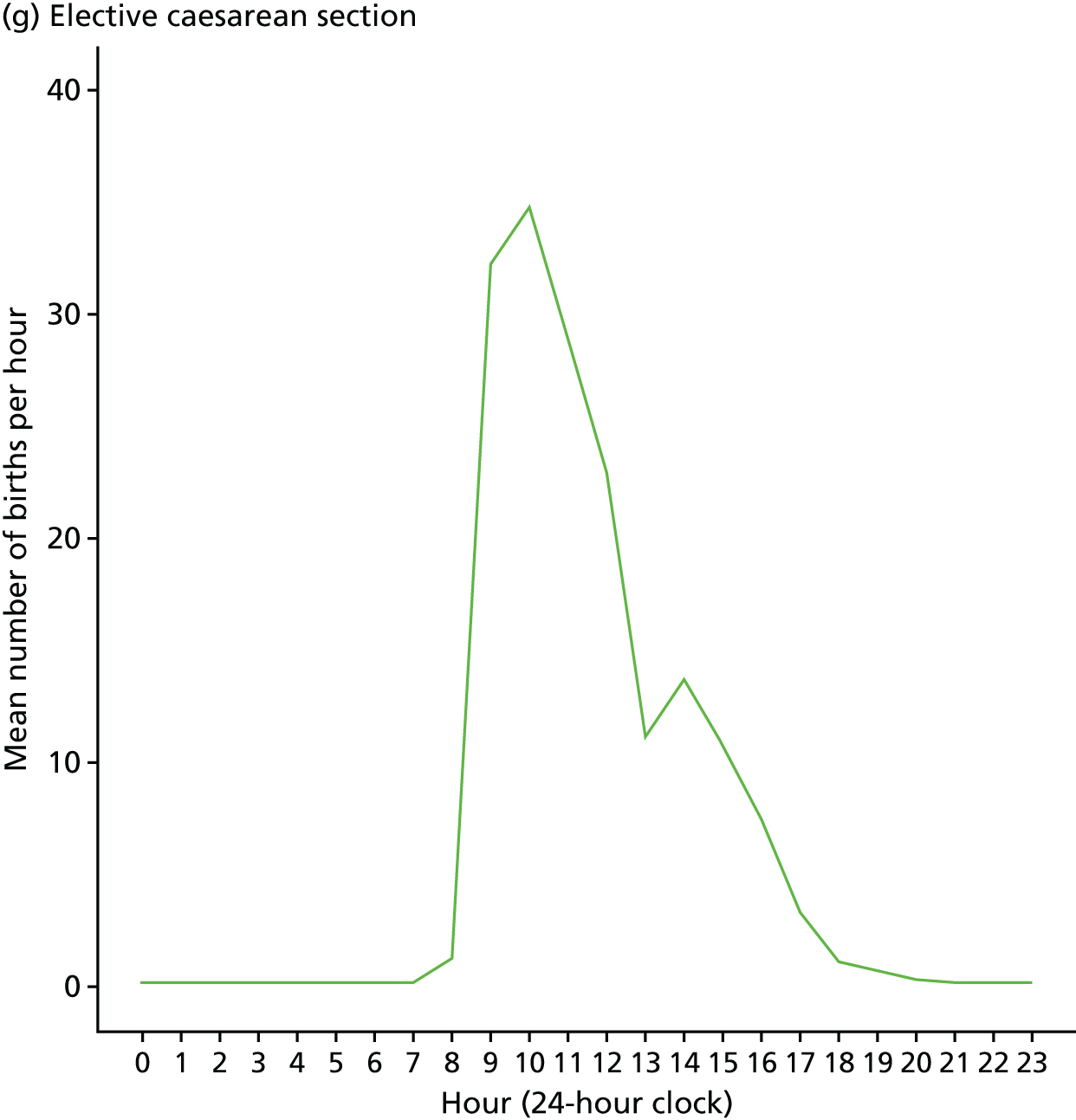
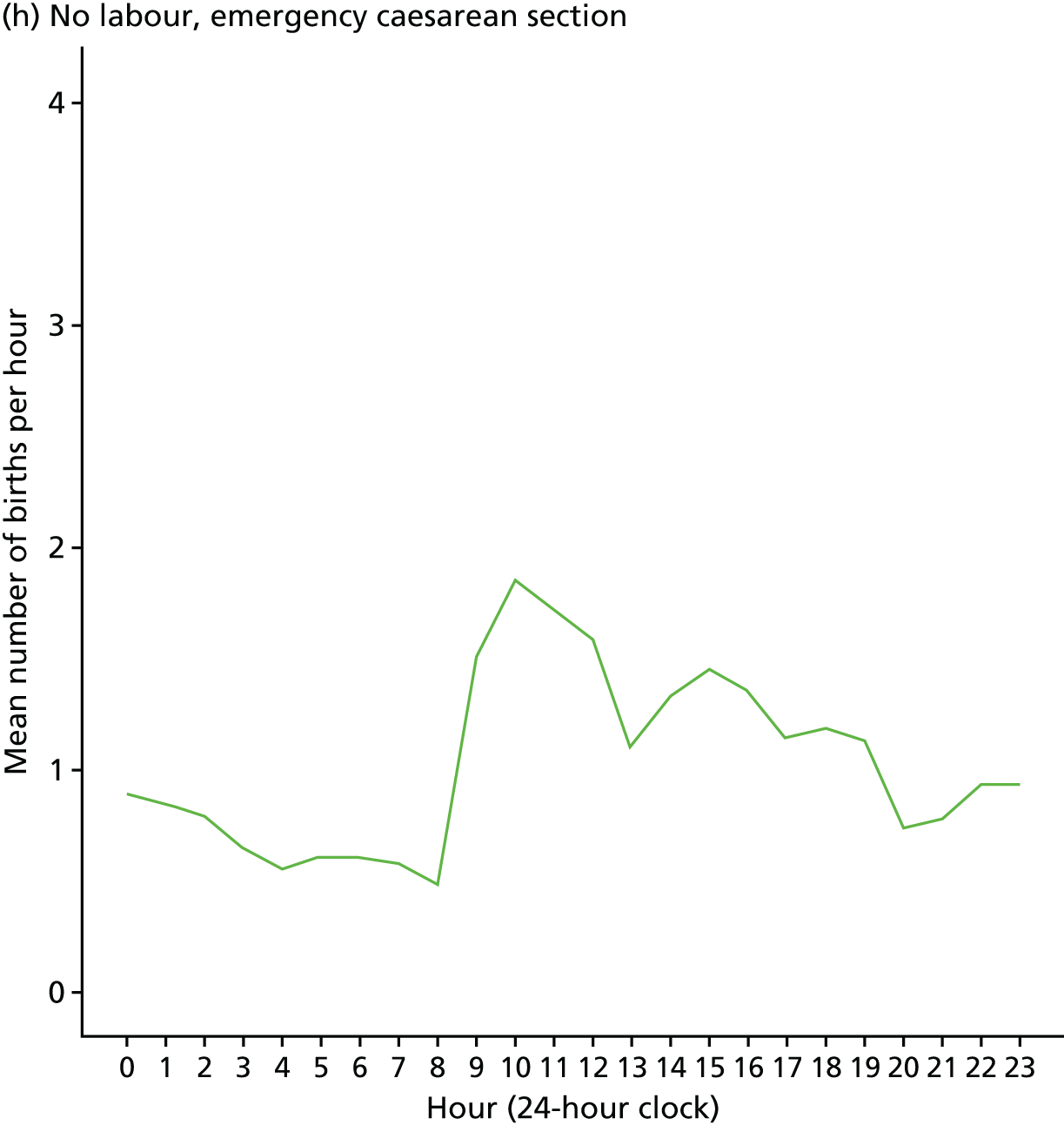
Appendix 4 Patient and public involvement
Appeal for service users to become study advisors
Service user involvement meetings
Service user involvement day, Saturday 29 November 2014, held in Birmingham
Around 35 women booked to attend the day, organised by NCT, the maternity and parenthood charity, and almost all of these attended for all or part of the day. This included about 20 members and chairpersons of MSLCs, six NCT policy and research staff, three other NCT staff involved with CCGs/trusts, City, two University of London, academics, and Kath Evans, Experience of Care Lead – Maternity, Infants, Children and Young People at NHS England. She and Mary Newburn were among those who tweeted about the day and the study. Kath Evans has almost 8000 Twitter followers, so her reach is very considerable. @marynewburn1 tweeted and retweeted and is followed by many NCT branches.
The format of the day worked very well. This involved combining a focus on the Birth Timing maternity statistics study in the afternoon a Microsoft Powerpoint assisted presentation, prepared and recorded by Miranda Dodwell, small group work for answering questions and discussion, followed by a plenary report-back and, in the morning, activities to respond to the expressed needs and interests of maternity services user representatives. There were introductions and agenda-setting for the day, keynote speaker presentations, sharing of experiences and concerns, networking and focused discussion on issues of concern. The lunch period was an important opportunity for mutual support, further discussion and networking.
There was a lot of interest in the Birth Timing study and real engagement with all of the issues and questions. Representatives had many observations to make in terms of what happens in hospitals at different times of the day and night. Some felt that units could be difficult to get into out of office hours owing to security systems and low levels of staffing, and that there were often agency midwives working who perhaps provided lower-quality care (emotionally) than permanently employed staff. Conversely, the view was expressed that as hospitals are quieter at night when procedures like the induction of labour, planned caesarean section and discharge home of mothers and babies are not taking place, the unit was a more peaceful place, more conducive to undisturbed labour and birth (women might be left undisturbed and be able to get on with it, or possibly be more likely to have one-to-one care as there were fewer routine procedures taking midwives’ time and attention).
The service users worked in small groups to discuss a series of questions about the current study and maternity services. Questions for consideration were:
-
What are your experiences of maternity staffing outside ‘normal working hours’?
-
How much do you think ‘out-of-hours’ care affects women’s experiences of maternity care and birth outcomes?
-
What are your concerns, if any, about ‘out-of-hours’ care?
-
Are there any particular areas you would like us to concentrate on in our research about birth timing and outcomes for women and babies, subject to our research protocol and the limitations of available routine data?
-
Do you think we have taken enough care to ensure the privacy of women’s and babies’ records?
Discussion feedback
Birth Timing poster: representatives discussed the issues of confidentiality and use of data in the Birth Timing study, and gave feedback on the poster to be displayed in NHS clinics and waiting areas. They were happy that women’s data were to be used in the way that was planned and did not feel that this was a breach of confidentiality.
Concerns about quality of care: the groups expressed a number of concerns about quality of care, including concerns about quality of staffing at night (lack of specialist care or senior staff), limits to choice and threats to choice of birth place in some areas (e.g. a midwife-led unit closed to keep the OU open), and concerns about postnatal care, including lack of out-of-hours breastfeeding support, issues with partners being sent home at night (postnatally), there being not enough midwifery staff on the postnatal ward, or feeling that the staff were too stretched or too tired to be asked for help and support.
‘Out-of-hours’ care: as well as noting concerns about lack of specialist care or senior staff at night, a number of positive observations were made about care ‘out of hours’ when the maternity unit was less busy. These included ‘parking is easier at night!’, ‘staff are less busy at night’, ‘The labour ward is quieter and more conducive to undisturbed labour and birth’, ‘You are more likely to get one-to-one care’, ‘24-hour consultant presence – could be reassuring for all staff’.
Research questions: the women were concerned about the whole continuum of care and wanted more research on the impact of postnatal care, and, in particular, readmissions for feeding-related issues. (Are these indicators of poor postnatal care? Do they vary by staffing levels or by time of day of first feed, or day of week?)
The Head of Patient Experience at NHS England attended the meeting and heard first-hand about the interests and concerns of parent representatives on MSLCs from across the country. Mary Newburn had approached her about the need for more structured support for PPI in maternity services. Following the meeting, Mary Newburn submitted a successful funding bid to NHS England for a project to provide maternity PPI networking opportunities, development of maternity PPI guidance and briefings, and some VOICES training in specific skills and knowledge to help MSLC service user leaders feel more confident and supported, and to work more effectively.
Service user involvement day, 21 November 2015, held in Wakefield
Continuing the approach used in 2014, we decided to meet with women serving on MSLCs. In collaboration with NCT, we invited MSLC service user members from all parts of England to a 1-day meeting for networking, support and presentations. This approach follows the principle of ‘go to where they are’. Although we could not, with a widely dispersed group, go to where all representatives live, we went to a central place that they could access easily (with travel costs subsidised where necessary), where they would want to go to in order to meet other representatives and network.
The event was advertised as a representatives’ support and information day, a familiar concept, so people knew what to expect and felt that it would be worthwhile. NCT’s events manager organised the practical aspects (venue hire, refreshments, marketing using NCT databases, delegate bookings, delegate packs and name badges). Two co-investigators, Mary Newburn and Miranda Dodwell, liaised with NCT’s Research Engagement Officer to plan the programme and promoted the event using social media and the hashtag #MSLC.
The purpose of the day was to:
-
bring together maternity services’ user representatives, activists, maternity researchers and policy staff to share intelligence and MSLC good practice, and facilitate mutual support
-
enable the NIHR-funded Birth Timing researchers at City, University of London, from the project funding the day, to seek input and feedback from service user representatives
-
increase representatives’ confidence and motivation by providing an opportunity for them to share their work and learn new skills.
The programme was designed to meet the priorities of the delegates and provide a good lunch as well as discuss the Birth Timing study. Approximately 30 people attended the day, from areas as diverse as North Cumbria, Leeds, Wakefield, Norfolk, South London, Sussex and Blackpool.
One of the researchers, Miranda Dodwell, gave an introductory talk about the Birth Timing study. In our experience, maternity services users are often interested in research questions that are suitable for qualitative research, such as ‘how do women feel?’ or ‘why do some units have higher intervention rates?’. So, Miranda talked about that and then explained the kinds of questions that can be addressed by large datasets and the potential provided by a data linkage project. She acknowledging the issues flagged by service users at the meeting the previous year and gave everyone copies of the study poster for display in local maternity units. She explained that there had been hold-ups in the previous 12 months and shared preliminary analysis of actual home birth numbers across all days of the year, pointing out the patterns occurring on public holidays and at the weekend. MSLC maternity user representatives were very interested.
Delegates then formed small groups to discuss their experience of maternity services out of hours and at weekends. Issues discussed included:
-
A tendency for midwifery units or other community services to be closed if the OU was short of midwives. ‘Staff are drawn out of the community into the acute unit, affecting provision of home birth services.’
-
The impact of austerity budgets and limited staffing, causing unit closures and reducing the quality or availability of postnatal care. ‘We have had closure of units due to staff shortages. There is a lack of (midwifery) staff on the postnatal wards. And at the weekend, postnatal (home) visits are not the same as mid-week.’.
-
Lack of specialist mental health services: ‘There is no one with an interest in perinatal mental health.’.
-
News coverage about more deaths occurring at the weekend. 62 Mothers are anxious because of media coverage of this question.
-
Women are offered, and have, pain relief sooner than they otherwise might. ‘They have an epidural before staff go off duty.’ Variation in when services are available is confusing for parents/unacceptable. ‘Our MLU is “on-call only” from 8am – 8pm weekdays and at weekends. ☹‘
-
A perception that ‘There is a bias in the rate of induction over the week.’.
-
Concern about both lower staffing levels and staff tiredness out of hours.
-
Midwives staffing both the midwife-led unit (MLU) and home births being too stretched and often unavailable to provide both services to different women in labour at the same time.
-
Non-English speakers suffer out of hours owing to a lack of interpreters; this applies also to ‘out-of-area’ and non-booked women.
-
Concerns about how vulnerable women might be affected most of all by, for example, decisions taken by junior obstetricians without good support.
-
A few women choose a caesarean section or induction of labour midweek because they are worried about poor staffing and lack of support (e.g. on a Saturday).
-
Women want care based on their needs, not constraints of the service, but can be pressured: ‘The obstetric unit will be best, there are not many midwives in the FMU . . .‘. Sometimes the caesarean section rate drops when the unit is very busy as there is less chance to intervene. (An obstetrician suggested this once.)
Service user involvement meeting, 21 June 2016, City, University of London
The London meeting was arranged in conjunction with the City, University of London Centre for Maternal and Child Health Research parents’ advisory group. Face-to-face meetings are held several times a year. The organiser, a lecturer in maternal and child health at City, University of London, told us, ‘We usually fit 2–3 different projects into these meetings . . . You will get either 35 or 55 minutes to discuss your project with the group. Please consider an activity, so that this is not just simply a Q&A [question and answer] session. We usually have 4–8 mums attending, ready to give their opinion.’.
The group is promoted via a blog (https://blogs.city.ac.uk/surf/) and Twitter. The blog says:
We are looking for parents or parents-to-be who want to be involved in our research to improve the health of children and their families. You can participate through e-mail, Skype, phone or by coming to our meetings. We meet every second month in central London and can pay any reasonable travel costs for those who travel within London. We will pay £15/hour for your help.
The advisory group’s Twitter account, @City_CMCHR has 219 followers (accessed 3 August 2016). Four or five women were expected on the evening of the Birth Timing meeting and two attended. Both had had a baby within the past 2 years. One had two children. One was Eastern European. Miranda Dodwell and Mary Newburn ran the session, combining introductions, presentation of the aims and methods of the Birth Timing research, some predictions, discussion and some specific questions to the women about their experiences, perceptions and any concerns.
We asked: in your experience, how much is women’s experience of maternity care affected by the calendar and the clock (i.e. day of week and time of day)?
Themes included ‘fewer staff out of hours can affect experience and quality’. The women said:
-
Yes, day of week and time of day has an impact.
-
There is less support available as a result of low staffing levels, especially in the evening.
-
At weekends, one said, waiting times were long as ‘more urgent’ cases were prioritised. For her, this resulted in a longer hospital stay.
-
In the special care baby unit, she went on, ‘there were no nurses to cannulise so the paediatrician had to cannulise, but had to rush off as the unit was unstaffed and day staff had not arrived for handover’. Interruptions and lack of care/support reported (in the early hours before breakfast).
-
The other participant said that there were no problems during the night when she had a caesarean section with her first child.
-
More recently, with her second baby, there were issues during labour/birth during the week (after 17.00). (Baby was eventually born by caesarean section.)
-
Mum recalled being told off by the ‘night nurse’ and being rushed.
-
Breastfeeding advice – midwives were there only sporadically, and a mum recalls having to wait too long (12 hours) for specialist staff and advice.
-
In response to the question ‘How much do you think it affects women?’, one participant noted ‘no long-term impact on my bonding with child and health, but the first week could have been better’. She added ‘I still feel a bit traumatised.’.
-
‘If you know you’re going to have a C-section then you might feel very stressed or stressed to some extent “What if it’s on the weekend? What if there’s less staff?” ‘.
-
Mum’s awareness of pre-existing conditions can be anxiety-provoking and exacerbated by lack of staff at certain points, such as the weekend.
-
It was noted that it is important not to make false assumptions about cause and effect: ‘I feel like I’m making assumptions about certain aspects of care that I perceive as “substandard”, and its associations with time and day.’. For 2 nights, this mum experienced pelvic pain ‘I felt like I had to “grin and bear it”, and I’m not sure if it would have been different during the day, as it might be that in the night, it’s just dark and I’m alone and I would just like my partner to be there.’.
-
‘I hadn’t had lunch when I gave birth. The midwives gave me a sandwich. It wasn’t enough when I was really hungry. I expected better. It might not be to do with time of day or the day itself; it might just be about general lack of care and compassion for the woman.’.
-
In response to the question ‘How do you think maternity care affects babies’ health and wellbeing?’, it was noted that one mum’s sister-in-law had a caesarean section and lacked breastfeeding support. She stopped breastfeeding completely at 3 months. Had she had more support, she could have carried on breastfeeding, especially at night.
-
At night-time (in hospital), it is quieter, as there are not many admissions, so midwives could then provide specialist feeding support and, ‘check-in with women about how they are feeling’ as, ‘It’s not like you’re sleeping!’ Night-time is a really good time to provide support. It would be extremely helpful, including postnatal depression.’.
The presenter explained that the research team have to follow strict rules about confidentiality and need special permission to access medical records (these are securely kept at the ONS). Asked after the presentation, ‘Do you think we have taken enough care to ensure the privacy of women’s and babies’ records?’ the women said ‘yes’. They also felt that the research was ‘important, especially if it helps improve outcomes’.
In response to the question ‘Are there any particular areas that you would like us to concentrate on in our research about birth timing and outcomes for women and babies, subject to our research protocol and the limitations of available routine data?’, the women noted the following:
-
Outcomes for caesarean births – I am interested in finding out whether the service women are getting out of hours is still fine (or the same quality as the service during the day); and the same for weekend/public holidays and during the week. ‘If there’s any impact it’s something I would be worried about in terms of the care I receive.’.
-
Birth timing associations with breastfeeding – does support in the early hours after birth (or lack of it, e.g. at night) affect length of breastfeeding, and exclusive/mixed feeding? (The Birth Timing study probably cannot answer this). There would need to be a further data linkage to breastfeeding at 6–8 weeks.
-
Staffing patterns around birth – is there a less specialist staff presence at night and does it make a difference to measurable outcomes? ‘If I had seen a consultant at night then I would have relaxed.’.
In response to the question ‘Can you give us any feedback from your Trust about the effect on more vulnerable women or those with more complex needs (e.g. younger, older, socially deprived, non-English speakers)?’, the women had concerns. One noted:
both my sisters-in-law are Polish – generally language is not an issue but when it comes to medical terms, illnesses, procedures they might not be familiar with terms. Individual midwives need to take into consideration the vulnerabilities of the woman. There is likely to be less access to translators out of hours, and – particularly when a woman is exhausted and medicated – it might be more difficult for her to communicate and really understand what is being said to her when English is not her first language.
Service user involvement day, Saturday 12 November 2016, held in Bristol
Building on the involvement approaches used in 2014 and 2015, plans for the 2016 PPI meeting organised by NCT staff in collaboration with researchers included inviting women serving on MSLCs, other relevant charities, voluntary organisations and interest groups. As the format seemed to work well in previous years, the Birth Timing research discussions were part of a 1-day programme on maternity services topics. In addition to MSLC service user members from different parts of England, there were a small number of service user advocates from Wales, Scotland and Northern Ireland.
Previous PPI meetings had been held in Birmingham, Wakefield and East London. The decision to host the meeting in Bristol was specifically designed to make the meeting accessible to women living in the south-west of England, and specifically to reduce journey times. An innovation at the 2016 meeting was to hold ‘speed dating’ sessions, enabling delegates to choose a programme of practical ‘taster’ activities to meet their particular interests and needs and to be active, interactive and responsive. The aim was to create a day that service users involved with multi-disciplinary maternity services committees in their local area would be motivated to come to. The tactic was successful as 33 people attended the meeting, including 17 service user members of MSLCs. Others included NCT staff members, the mother of a child with Down syndrome, a Positive Birth Movement member, Healthwatch, two young, newly qualified, midwives, a health visitor, the chairperson of the Royal College of Obstetricians’ Women’s Network, a NHS England representative and a NIHR representative and researchers.
Social media [the Facebook MSLC members and leaders group and Twitter (#BirthTiming and #MSLC)] were used to communicate about the meeting and the study.
The Birth Timing session was made up of a presentation by Professor Alison Macfarlane and discussion in small groups. The presentation included descriptive analysis showing the timing of spontaneous onset/spontaneous birth labours, the timing of births at home, the timing of births with induction, and planned or unplanned caesarean sections. Service users were struck by how much maternity care activity there is – and needs to be – in the evening and at night. There was discussion about the impact of darkness and light on the labour and birth behaviour of mammals, informed by one person’s work with laboratory rats, whose days and nights were manipulated so that researchers could observe births during their working day. The message was that darkness stimulates parturition. The discussion focused on appropriate messages for the public, and what service users would like to see communicated to commissioners and service managers and how the emerging findings relate to Better Births35 recommendations for maternity services.
In group 1, there was discussion about messages for pregnant women based on the research findings. Service users felt that some important messages were ‘you don’t need a consultant for all births’, ‘for safety, midwives are experts when birth is straightforward’. They wondered how evidence on place of birth was being presented to women and asked ‘Are e-services websites presenting sound messages about evidence?’. In terms of messages for commissioners:
-
Service users wanted to ask service managers if attention was paid to ensuring continuity of midwifery care for women having induction of labour.
-
Service users expressed the view that home assessment in early labour can make a positive difference to women’s experiences, in terms of feeling supported.
The group’s further research questions were:
-
Can we get real data on length of labour (with the start of labour decided by women)?
-
What is/is there a physiological basis for birth at night? Why does it happen? How can the right conditions be created to support physiology?
-
Does the time of day when women are in labour and give birth affect their experiences of labour?
-
Are transfer rates from midwifery units affected by time of day?
In group 2, there was concern that induction rates were rising as a result of the drive to reduce stillbirth. This means that induction is offered sooner for women with and without complications or risk factors. ‘How many say no, they don’t want to be induced?’. ‘Do women have accurate information to make decisions?’. There was concern in one area that because a birth unit was closing, choice of place of birth was diminishing rather than increasing. In other areas, service users felt that information on Better Births35 recommendations had not ‘percolated down to midwives, let alone others’. They commented that, for midwives, there is ‘no such thing as “out of hours” for birth’ and wondered if it was appropriate in birth units to have ‘fewer midwives at night’. In terms of messages for commissioners:
-
Service users felt that there was a need to ‘create more midwife places’ to meet present needs ‘let alone to create continuity’. There was discussion about too few midwives (‘60–80 women each per year’) and this causing burnout.
-
Service users noted that there were pilot studies for service development work but then funding stops, and they wanted to know why.
The group’s further research questions were about breastfeeding, the impact of partners being present during labour, the size of midwifery caseloads and the impact of poor postnatal care (if any) on future birth rates. They included:
-
Why do so many women . . . feel they don’t have enough milk? . . . experience sore nipples? . . . have babies that do not ‘latch’ themselves?
-
Is there a correlation between areas with comprehensive breastfeeding support as in NICE guidance and breastfeeding rates over the years?
-
What are partners’ ideas about labour and birth? What influence does this have on labour and birth, and how do partners influence mental health?
-
What is the ideal caseload size for midwives looking after different groups of women, including those with straightforward pregnancies, and those with additional social or health factors?
-
Is there a correlation between ‘declining postnatal care’ and declining birth rates?
In group 3, there was discussion about the impact of daylight and bright hospital lighting on labour and birth, and noted that ‘normal birth hours are not normal working hours’. They felt that it was very important for research studies to differentiate by place of labour and birth. In terms of messages for commissioners:
-
Service users felt that it was important to ‘commission for reality i.e. provide more staff at night, if more babies are being born then’.
In terms of messages for women, the group felt that it was valuable to focus on positive messages about birth (rather than on risks and harms), ‘press release a good news story and the data’. They also said:
-
Tell ‘the story’ to women directly (so no gatekeeping effect) (e.g. via YouTube, Facebook, blogs and MSLC lines).
-
Provide bite-sized messages for women (i.e. really clear conclusions).
It was suggested that when MSLCs ask women about their labour and birth experiences they might ask in future the time of day when labour and birth occurred.
The group’s further research questions were:
-
If light affects labour, might there be seasonal changes, differentiating in summer and winter?
-
Are transfer times from midwife-led units affected by the time of day?
-
Does continuity of carer affect experiences and birth timing?
-
Is it possible to determine how changes in induction policy affect the physiology of birth and timing of birth (i.e. more or fewer early-morning births)?
Group 4 also discussed ‘normal birthing hours’ versus ‘normal working hours’. They felt that there was an ‘easy win: turning down the lights’ in hospitals.
The group’s further research questions were:
-
Do we need to rethink birth environments for women needing medical interventions?
-
Do we need to rethink the timing of induction so that this does not result in a problematic staffing model?
-
How does physiology affect birth timing? What are the roles of female maternal physiology and of baby physiology? In each case, what is the mechanism?
-
Does having fewer staff at night pose a problem for women/childbirth?
-
Is 24/7 consultant cover justified?
-
What is the right staffing model to provide safe care?
Appendix 5 Study Advisory Group membership
| Name | Role | Organisation | Role in group |
|---|---|---|---|
| Rona McCandlish | Midwife | Independent Consultant in Maternity Care | Chairperson |
| Debbie Chippington Derrick | Maternity service user representative | AIMS | Member |
| Kate Bedding | Maternity service user representative | Member | |
| Helen Castledine | Public health, maternity service user representative | MLSC co-chairperson | Member |
| Eleanor Molloy | Maternity service user representative | Breastfeeding counsellor, NCT | Member |
| Graham Cookson | Professor of Economic & Public Policy | University of Surrey | Member |
| Jenny Kurincuk | Professor of Perinatal Epidemiology | Director, NPEU | Member |
| Shantini Paranjothy | Clinical Senior Lecturer | Cardiff University | Member |
| Dharmintra Pasupathy | Consultant in Maternal & Fetal Medicine & Perinatal Epidemiology | King’s College London | Member |
| Jane Sandall | Professor of Social Science and Women’s Health | King’s College London | Member |
| Martin Ward-Platt | Consultant Paediatrician | Consultant in neonatal paediatrics in Newcastle upon Tyne; Clinical Lead for the National Congenital Anomaly and Rare Disease Registration Service | Member |
| Kate Brintworth | Midwife | Head of Maternity Commissioning North East London | Member |
| Matteo De Martino | Registrar, ST2 Obstetrics & Gynaecology | Royal Free NHS Foundation Trust | Member, invited but unable to attend |
| Nilum Patel | Maternity policy | Department of Health and Social Care | Observer, invited but unable to attend |
| Andrew James | Maternity policy | Department of Health and Social Care | Observer |
| Alex Lloyd | Manager, Child Health Statistics Team | ONS | Observer, up to September 2016 |
| Elizabeth McLaren | Statistician, Vital Statistics Outputs Branch ONS | ONS | Observer, from September 2016 |
| Justine Pooley | Head of Life Events Data Management | ONS | Observer, from September 2016 |
| Giovanna-Maria Polato | Team Leader – Intelligence Mental Health, Learning Disabilities and Community Services | Care Quality Commission | Observer |
| Claudia Wells | Head of Mortality Statistics | ONS | Observer, up to September 2016 |
| Jane Winter | Statistician | Head of HES analysis team, HSCIC | Observer |
Glossary
- Adjusted R2 value
- A goodness-of-fit statistic, normally interpreted as the percentage of variance in the response variable, which is explained by the model, penalised by a function of its complexity (normally the number of parameters).
- Rowe R. Birthplace Terms and Definitions: Consensus Process. Birthplace in England Research Programme. Final Report Part 2. London: HMSO; 20112018Queen’s Printer and Controller of HMSO 2011Alongside midwifery unit
- A NHS clinical location offering care to women with straightforward pregnancies during labour and birth in which midwives take primary professional responsibility for care. During labour and birth, diagnostic and treatment medical services, including obstetric, neonatal and anaesthetic care are available, should they be needed, in the same building, or in a separate building on the same site. Transfer will normally be by trolley, bed or wheelchair. See Box 2.
- Anoxia
- A condition characterised by an absence of oxygen supply to an organ or tissue.
- Antepartum
- Before the onset of labour.
- Asphyxia
- Lack of air; suffocation.
- Birth notification
- When a midwife or other health professional notifies the Personal Demographic Service of a birth so that a NHS number is issued.
- Birth registration
- The process by which a child’s birth is recorded in the civil register. This is required for the child to obtain a birth certificate.
- Caesarean birth
- Surgical delivery of a baby through the mother’s abdomen.
- Centre for Maternal and Child Enquiries record
- Epidemiological and clinical data about a stillbirth or neonatal death in England, Wales, Northern Ireland, the Crown Dependencies of the Channel Islands and the Isle of Man. Collected by the Centre for Maternal and Child Enquiries prior to 2012.
- Confidence interval
- An interval estimate of a population parameter, typically regression coefficients in this study. The 95% confidence interval (e.g. calculated using the mean proportion and its standard error) would contain the true value (e.g. population proportion) on 95 occasions (out of 100) if the same study were repeated 100 times on different randomly drawn samples.
- Congenital
- Existing at the time of birth.
- Cubic spline term
- A flexible way of modelling long-term non-cyclical changes in the distribution of frequencies.
- Elective caesarean section
- Caesarean birth planned prior to labour.
- Elsewhere
- Births that occur outside communal establishments but not at a mother’s home.
- Emergency caesarean section
- Caesarean birth undertaken after labour has commenced.
- Rowe R. Birthplace Terms and Definitions: Consensus Process. Birthplace in England Research Programme. Final Report Part 2. London: HMSO; 20112018Queen’s Printer and Controller of HMSO 2011Freestanding midwifery unit
- A NHS clinical location offering care to women with straightforward pregnancies during labour and birth in which midwives take primary professional responsibility for care. General practitioners may also be involved in care. During labour and birth, diagnostic and treatment medical services including obstetric, neonatal and anaesthetic care, are not immediately available but are located on a separate site should they be needed. Transfer will normally involve car or ambulance. See Box 2.
- Gestational age
- The duration of the pregnancy measured in completed weeks since the first day of the last menstrual period.
- Harmonic variable
- A variable that can account for cyclical effect in a statistical model (e.g. those of day of the year or hour of the day).
- Health and Social Care Information Centre
- An arms-length body of the Department of Health and Social Care. Under the Health and Social Care Act, it is the national provider of information, data and information technology systems for commissioners, analysts and clinicians in health and social care. Since 1 August 2016, it has been known as NHS Digital, although Health and Social Care Information Centre remains its legal name.
- HESID
- Hospital Episode Statistics patient identifier, which is derived from several different patient identifiers and provides a way of tracking patients through the Hospital Episode Statistics database without identifying them.
- Hospital Episode Statistics
- A data warehouse containing details of all admissions, outpatient appointments and accident and emergency attendances at NHS hospitals in England, commonly referred to as ‘HES’. The data are held in a core record for each hospital episode.
- Hospital Episode Statistics birth record
- A Hospital Episode Statistics health record relating to the birth of a baby. The record relates to the baby but has some details of the mother held in a maternity tail.
- Hospital Episode Statistics delivery record
- A Hospital Episode Statistics health record relating to a mother giving birth. The record relates to the mother but has some details of the baby held in a maternity tail.
- Induction of labour
- Procedures for artificially initiating the onset of labour.
- Instrumental birth
- Delivery assisted by ventouse or forceps.
- Intrapartum
- During labour.
- Maternity Hospital Episode Statistics
- Hospital Episode Statistics that relate to delivery and birth records. These have an additional part called the maternity tail appended to the core record, with details of the baby and birth.
- Maternity tail
- An additional record appended to a core Hospital Episode Statistics record for episodes relating to a delivery or birth.
- Multiparous
- Term describing a pregnant woman who has previously given birth.
- Negative binomial regression model
- A statistical model to account for datasets in which there is a greater variability than would be expected under a Poisson model (overdispersion).
- NHS Digital
- An arms-length body of the Department of Health and Social Care. Under the Health and Social Care Act, it is the national provider of information, data and information technology systems for commissioners, analysts and clinicians in health and social care. Before 1 August 2016, it was known as the Health and Social Care Information Centre and that is still its legal name.
- Normal birth
- A birth where labour starts spontaneously and progresses spontaneously without drugs and is achieved without a caesarean section, use of forceps or ventouse or an episiotomy.
- Nulliparous
- Term describing a woman who had not previously given birth.
- Rowe R. Birthplace Terms and Definitions: Consensus Process. Birthplace in England Research Programme. Final Report Part 2. London: HMSO; 20112018Queen’s Printer and Controller of HMSO 2011Obstetric unit
- A NHS clinical location in which care is provided by a team, with obstetricians taking primary professional responsibility for women at high risk of complications during labour and birth. Midwives offer care to all women in an obstetric unit, whether or not they are considered at high or low risk, and take primary responsibility for women with straightforward pregnancies during labour and birth. Diagnostic and treatment medical services including obstetric, neonatal and anaesthetic care are available on site, 24 hours a day. See Box 2.
- Office for National Statistics birth record
- A birth registration record linked with a birth notification record, as provided to the project by the Office for National Statistics.
- Parity
- Total number of previous live births and stillbirths. This does not include abortions or miscarriages.
- Patient Episode Database for Wales/National Community Child Health Database record
- Delivery and birth records for babies born in Wales or born to mothers resident in Wales, held in the Patient Episode Database for Wales linked to information held in the National Community Child Health Database.
- Periodogram
- A plot used to explore possibly important cyclical patterns.
- Post-term pregnancy
- Gestational age of 42 or more completed weeks.
- Preterm birth
- Birth occurring before 37 completed weeks of gestation.
- Primiparous
- Term describing a pregnant woman who has not previously given birth.
- p-value
- The probability that the observed value of a test statistic would occur, assuming that the null hypothesis is correct. A measure of the support provided by the data to the null hypothesis. If it is smaller than a prespecified significance level then the risk of incorrectly rejecting this hypothesis is considered sufficiently small.
- Rate ratio
- The ratio of the expected number of births on one type of day over the mean number of births per day.
- Registrable birth
- A stillbirth after 24 completed weeks of pregnancy or a live-born baby.
- Spontaneous onset labour
- Term describing a labour that is not induced.
- Stillbirth
- ‘A child which has issued forth from its mother after the 24th week of pregnancy and which did not at any time after being completely expelled from its mother breathe or show any other signs of life.’ [Definition taken from Section 41 of the Births and Deaths Registration Act 1953, as amended by the Stillbirth (Definition) Act 1992.]
- Term pregnancy
- Gestational age from 37 completed weeks to under 42 completed weeks.
- Trauma
- Wound or injury.
- Trusted Third Party linkage
- Data linkage by an organisation that has been authorised by another organisation to process identifiable data for linkage.
- Type 2 objectors
- People who have opted out of their personal confidential information being shared by NHS Digital for purposes other than their own direct care. This is the term which was in use at the time this project was under way.
- Ventouse
- Equipment used for the vacuum extraction of a baby during birth.
List of abbreviations
- AIMS
- Association for Improvements in the Maternity Services
- AMU
- Alongside midwifery unit
- APC
- Admitted Patient Care
- CAG
- Confidentiality Advisory Group
- CESDI
- Confidential Enquiries into Stillbirths and Deaths in Infancy
- CMACE
- Centre for Maternal and Child Enquiries
- CQC
- Care Quality Commission
- DAAG
- Data Access Advisory Group
- FK
- Foreign Key
- FMU
- Freestanding midwifery unit
- GP
- General practitioner
- HES
- Hospital Episode Statistics
- HESID
- Hospital Episode Statistics patient identifier
- HIPE
- Hospital In-Patient Enquiry
- HQIP
- Healthcare Quality Improvement Partnership
- HSCIC
- Health and Social Care Information Centre
- ICD-10
- International Classification of Diseases, 10th Revision
- IGARD
- Independent Group Advising on the Release of Data
- IMD
- Index of Multiple Deprivation
- MBRRACE-UK
- Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK
- MRC
- Medical Research Council
- MSLC
- Maternity Service Liaison Committee
- MVP
- Maternity voices partnership
- NCCHD
- National Community Child Health Database
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NN4B
- NHS Numbers for Babies
- NPEU
- National Perinatal Epidemiology Unit
- NWIS
- NHS Wales Informatics Service
- ODBC
- Open Database Connectivity
- ONS
- Office for National Statistics
- OPCS-4
- Office of Population Censuses and Surveys Classification of Interventions and Procedures, Version 4
- OU
- Obstetric unit
- PEDW
- Patient Episode Database for Wales
- PK
- Primary key
- PPI
- Patient and public involvement
- RCM
- Royal College of Midwives
- RCOG
- Royal College of Obstetricians and Gynaecologists
- RCPCH
- Royal College of Paediatrics and Child Health
- RR
- Rate ratio
- SAS®
- Statistical Analysis System
- SQL
- Structured Query Language
- SRS
- Secure Research Service
- TIGAR
- Tracking the Impact of Gestational Age on health, educational and economic outcomes: a longitudinal Record linkage
- VML
- Virtual Microdata Laboratory
