Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/182/14. The contractual start date was in September 2017. The final report began editorial review in June 2018 and was accepted for publication in September 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Rodgers et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background and research questions
The volume of crisis calls related to people with serious mental ill health is an increasing challenge for police services. The limited training that these services have in mental health care can affect the appropriateness of their response in some circumstances. Often police officers have to decide on the management of mental ill health on the spot with limited options available to them other than temporary detention for assessment.
In February 2014, 22 national bodies involved in health, policing, social care, housing, local government and the third sector came together and signed the Mental Health Crisis Care Concordat: Improving Outcomes for People Experiencing Mental Health Crisis that set out how public services should work together to respond to people who are in a mental health crisis. 1
Although people experiencing a mental health crisis can be identified through primary care or hospital emergency contacts, in many cases, the affected people themselves or members of the public may call 111 or 999. Consequently, police officers often become the first responders to mental health-related incidents and thus a common gateway to care. This has raised concerns about the use of police resources and police officers’ relative lack of knowledge, skills and support when handling the mental health needs of individuals in crisis.
If a police officer believes that someone is experiencing a mental health crisis in a public place and is deemed to be in immediate need of care or control, section 136 of the Mental Health Act 1983 (S136)2 provides the officer authority to take that person to a ‘place of safety’ so that their mental health needs can be properly assessed. In the past, this has meant that people often ended up in a police cell, which could be frightening and could potentially precipitate a worse outcome. The Mental Health Act 1983: Code of Practice 20153 required the specific use of health-based places of safety (HBPOS) where mental health services can be provided. In practice, psychiatric units and hospital accident and emergency (A&E) departments are commonly used as HBPOS. In January 2017, the Policing and Crime Act4 resulted in a number of changes to S136. These were (1) police must consult mental health professionals (MHPs), if practicable, before using S136, (2) police stations cannot be used as a place of safety for people under the age of 18, (3) police stations can only be used as a place of safety in specific ‘exceptional’ circumstances for adults and (4) the period of detention is reduced from 72 hours to 24 hours with the possibility of a 12-hour extension under certain defined circumstances. 2,4–6
In May 2015, the Department of Health and Social Care (DHSC) made available £15M in capital funding to improve the provision, capacity and quality of HBPOS to better support people detained under S136. 7 A further £15M of funding was announced in October 2017 through the Beyond Places of Safety grant scheme. 8
Previously, S136 applied only to people who were encountered in a public place; section 135 of the Mental Health Act 1983 (S135) required a magistrate-issued warrant when police officers intended to enter private premises to remove a person to a place of safety for assessment. The Policing and Crime Act 20174 changes to S135 and S136 now allow an assessment to take place in the premises/home under certain circumstances (S135), removing the need to be in a place to which the public has access (S136).
In part, the Mental Health Crisis Care Concordat: Improving Outcomes for People Experiencing Mental Health Crisis1 was established to promote local multiagency arrangements to improve the quality of care for people experiencing a mental health crisis and to ensure that they are diverted to health rather than police settings. Mental health ‘street triage’ schemes were established in a DHSC pilot in 2013 and an evaluation was published in 2016. 9 Street triage, as piloted in England, typically takes the form of MHPs supporting police officers when they respond to emergency calls for cases that involve a person who may be suffering from a mental illness. These individuals often come into contact with the police despite not necessarily having committed an offence, and street triage interventions aim to direct these people to appropriate services, thereby avoiding inappropriate further interaction with the criminal justice system (CJS). 10 In such interventions, MHPs may be deployed to an incident with police officers and/or be situated in police force control rooms, where they can help monitor emergency calls and provide advice and support to call handlers and officers who may be interacting with a person in mental distress or crisis.
Another approach closely related to street triage is the Crisis Intervention Team (CIT) model. This involves specially trained police officers responding to calls involving suspected mental ill health either alone or alongside mental health and addiction professionals. As with street triage, the aim is to divert persons with mental ill health from the CJS to mental health treatment, when appropriate. 11,12 This approach was pioneered in the USA and there is an increasing interest in the UK in mental health training for front-line police officers. 11–13
In contrast to street triage, liaison and diversion (L&D) services are typically concerned with helping people when they are suspected of having committed an offence. Teams of specialist mental health-trained staff are located at police custody suites or courts to give an assessment and refer the person on to more appropriate mental health services outside the justice system. Alternatively, these specialist teams may support an individual while they remain in the justice system if their index offence or risk means that they cannot be diverted immediately. 11,12 However, it is conceivable that in the future L&D service providers, in agreement with local police forces and health commissioners, could extend their role to cover street triage objectives. 10
There is no universally accepted taxonomy of interventions in this area. A recent scoping review of interagency collaboration models between the police and other agencies for people with apparent mental ill health identified a range of possible models. 14 These included:
-
Pre-arrest diversion – providing police officers with specialist mental health training to better manage situations involving people with mental ill health and to offer treatment as an alternative to arrest, such as CIT.
-
Co-response – a shared protocol pairing specially trained police officers with MHPs to attend police call-outs involving people with mental ill health (often how UK street triage pilot schemes have been conceptualised).
-
Information-sharing agreements – information about people with mental ill health being shared between police and other agencies or between the individual with mental ill health and the police and other agencies.
-
Co-location – MHPs being employed by police departments to provide on-site and telephone consultations to officers in the field.
-
Consultation – police agencies accessing advice from MHPs when working with people with mental ill health, often via telephone.
Schemes that have described themselves as street triage can incorporate aspects of some or all of the above approaches; it can be seen that street triage is often used to describe one form of intervention that belongs to a larger cluster of interventions with similar aims. This rapid evidence synthesis will, therefore, use the term police-related mental health triage (PRMHT) interventions rather than street triage. This study is interested in all intervention models that aim to improve outcomes when police officers are called to incidents primarily relating to mental health rather than criminal concerns.
Initial scoping work
Scoping searches
To inform the protocol development, we undertook initial scoping work to gauge the focus and extent of the current evidence base. Scoping searches were carried out in August 2017 to identify existing reviews, primary studies and ongoing research relating to PRMHT interventions. The following databases were searched: Epistemonikos (a source of systematic reviews relevant to health decision-making; The Epistemonikos Foundation, Santiago, Chile), MEDLINE, Applied Social Sciences Index and Abstracts (ASSIA) and PROSPERO. In total, 498 records were identified and scanned for relevance. In addition, a variety of approaches for identifying further relevant material were utilised, such as contact with experts, reference checking of relevant studies and web searching.
Results of scoping work
Initial scoping work identified five systematic reviews that described and evaluated PRMHTs. 11,15–18 In addition, a number of non-systematic literature reviews also described relevant intervention models. 19–22
The existing reviews incorporated overlapping literature searches, the most recent of which was completed in June 2016. Although these reviews provided a useful overview of the existing evidence, the reviews also highlighted the methodological inadequacy of many existing evaluations for drawing firm conclusions about the effects of PRMHT interventions. Consequently, a new systematic review of the literature on effectiveness is unlikely to add much additional knowledge.
In addition to these evaluations, several qualitative and mixed-methods primary studies focused on PRMHT interventions that have been published, although scoping searches did not identify any published syntheses of these data. A rapid evidence synthesis of the existing primary research data in this area was considered to be of value.
Further details of the initial scoping work are provided in the protocol. 23
Research questions
What is the evidence base for models of PRMHT interventions?
-
Which models have been described in the literature?
-
What evidence is there on the effects of these models?
-
What evidence is there on the acceptability and feasibility of these models?
-
What evidence is there on the barriers to, and facilitators of, the implementation of these models?
Chapter 2 Methods
Synthesis approach
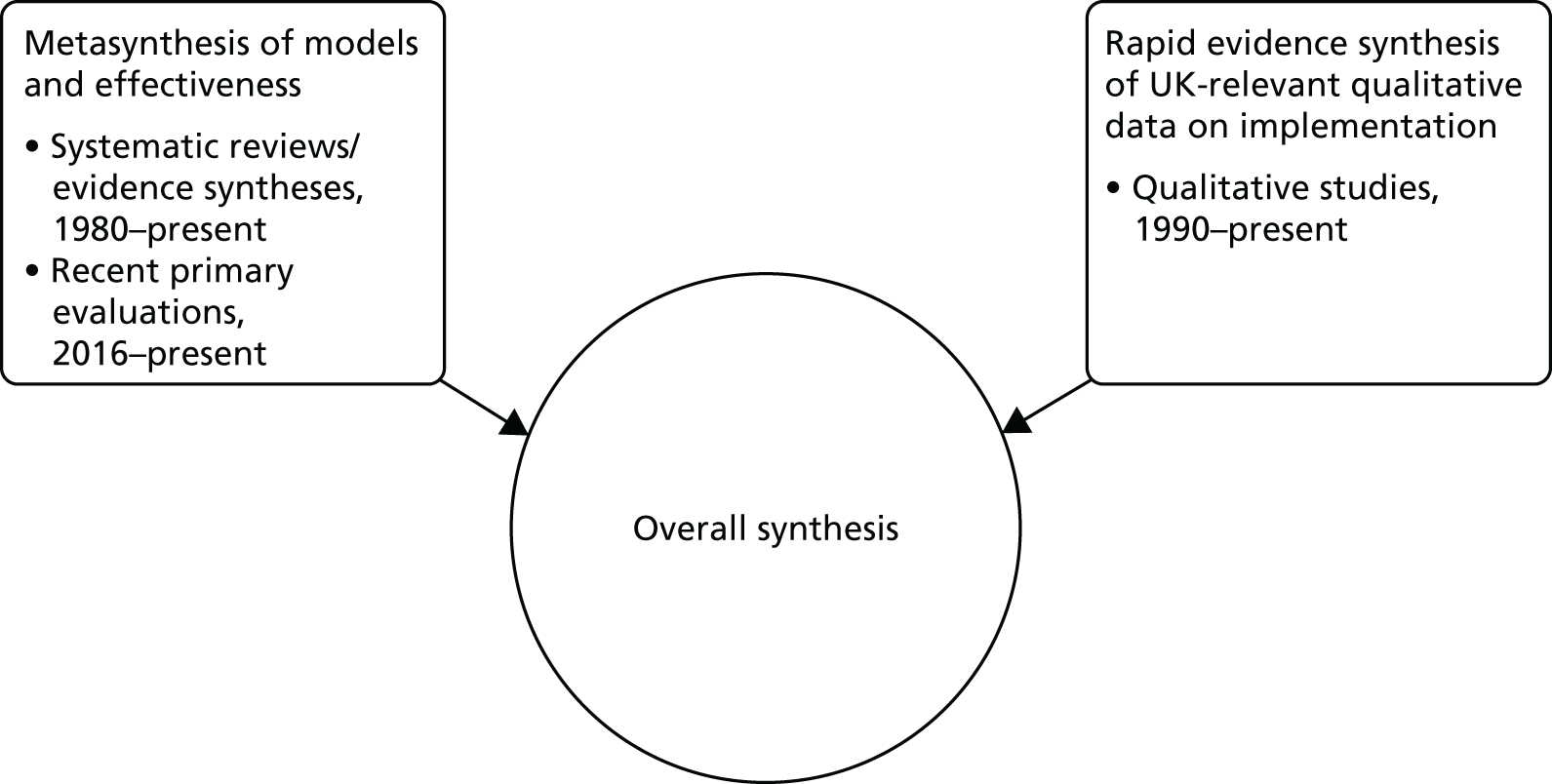
Based on the findings of the scoping work, we undertook a three-part evidence synthesis of evidence on PRMHT interventions:
-
Metasynthesis of evidence on the effects of PRMHT intervention models –
-
undertook a taxonomy of evaluated PRMHT interventions and described the different underlying intervention models
-
summarised quantitative evidence on the effects of PRMHT interventions.
-
-
Rapid evidence synthesis of UK-relevant qualitative data on implementation.
-
Overall synthesis –
-
combined the findings from the quantitative and qualitative components in a narrative synthesis
-
outlined the evidence for what works in what circumstances and for whom, potentially setting the scene for further research (outside the scope of this project) to develop programme theories of the more successful models.
-
Literature searching
Evidence on the effects of police-related mental health triage intervention models
Search strategies from an ongoing systematic review by Park et al. 16 were used as a basis for the literature search to identify recent reviews or primary evaluations of PRMHT interventions.
The following databases were searched in November 2017: ASSIA, Criminal Justice Abstracts, EMBASE, MEDLINE, PAIS Index, PsycINFO, Scopus, Social Care Online, Social Policy & Practice, Social Sciences Citation Index and Social Services Abstracts. Searches were limited to English-language studies published from 2016 onwards.
Additional web searching was undertaken. Relevant UK reports were identified through searches of the following websites:
-
College of Policing (see www.college.police.uk/)24
-
Mental Health Foundation (see www.mentalhealth.org.uk/)25
-
Crisis Care Concordat (see www.crisiscareconcordat.org.uk/)26
-
Centre for Mental Health (see www.centreformentalhealth.org.uk/)27
-
Connect Evidence Based Policing (see http://connectebp.org)28
-
the East Midlands Police Academic Collaboration (see www.empac.org.uk/). 29
A focused search of Google (Google Inc., Mountain View, CA, USA), using the advanced search interface, was also undertaken to identify any further UK-relevant reports.
UK-relevant qualitative data on implementation
The literature search aimed to identify qualitative primary studies of PRHMT interventions. The search strategy from the ongoing review by Park et al. 16 was used with the addition of a previously tested search strategy designed to limit retrieval to qualitative studies. 30 Limits were applied to restrict retrieval to English-language studies published from 1990 onwards. Preliminary searches indicated an absence of relevant evidence prior to this date; even if evidence were to exist, the difference in service delivery context from the present day would limit its value. The search was not limited by geographical location or setting.
The following databases were searched on 9 November 2017: ASSIA, Criminal Justice Abstracts, MEDLINE, PsycINFO and the Social Sciences Citation Index.
As for quantitative data, additional web searching and a focused search of Google, using the advanced search interface, were also undertaken to identify any further UK-relevant reports.
Full search strategies can be found in Appendix 1.
Selection criteria
Evidence on the effects of police-related mental health triage intervention models
A metasynthesis of existing reviews, identified through initial scoping searches, was undertaken, supplemented with an updated search of the literature to consolidate the most recent evidence on the effects of known models of PRMHT.
Population
Reviews and studies were included if they evaluated interventions relating to individuals who are perceived (by themselves, by others or by police officers) to be experiencing mental ill health or a mental health crisis and who come into contact with the police.
Interventions
Reviews and studies were included if they described interventions that met the following definition of PRMHT:
-
Police officers responding to calls involving individuals perceived to be suffering from mental ill health or a mental health crisis.
-
A judgement about the most appropriate route of care for the person concerned is made in the absence of suspected criminality or a criminal charge (e.g. the use of L&D services to assess and refer individuals to an appropriate non-CJS treatment or support service, would be relevant; L&D services related to out of court disposals, case management and sentencing would not be relevant).
Study design and comparators
Reviews/evidence syntheses and recent relevant primary studies (those that were published after the search dates of included evidence syntheses) were included. Emphasis was placed on reviews that use transparent or reproducible methods [as determined by the Database of Abstracts of Reviews of Effects (DARE) criteria]. 31 It is mandatory that reviews demonstrated adequate inclusion and exclusion criteria, a literature search and a synthesis. In addition, a formal quality assessment of primary studies and/or sufficient study details must have been reported. Further details of the assessment are available from the review authors. Reviews that failed to meet these standards were tabulated and referenced. For recent primary studies, inclusion was restricted to quantitative evaluative methods, either as a stand-alone methodology or as a discrete part of a larger mixed-method study. Non-evaluative descriptive publications were excluded but recorded for information; details can be found in Appendix 2. Ongoing studies are listed in Appendix 3.
Outcomes
Inclusion was not restricted by outcome. Outcomes of interest were the:
-
rate of utilisation of police cells in relation to S135 and S136
-
quality and timeliness of assessment, referral and treatment
-
mental health outcomes
-
demand on police resources and police officer time
-
demand for community mental health services
-
rates of hospitalisation via A&E or acute mental health services
-
level of service engagement
-
rates of reoffending or arrest
-
changes in case-finding and access to health services (e.g. mental health, substance misuse, sexual health and contraception)
-
experience of services for service users
-
experiences of police and mental health staff (including future staff training needs) and other relevant stakeholders
-
costs to health and police services.
Settings
Inclusion was not restricted by country or setting.
UK-relevant qualitative data on implementation
A rapid evidence synthesis of qualitative and mixed-methods primary studies was undertaken to identify factors affecting implementation. Given the differences in service organisation and wider cultural differences between countries, this part of the work was restricted to UK evidence.
Population
Studies were included if they reported data on interventions relating to individuals who are perceived (by themselves, by others or by police officers) to be suffering from mental ill health or a mental health crisis and who come into contact with the police.
Interventions
Studies were included if they described interventions that met the following definition of PRMHT:
-
Police officers responding to calls involving individuals perceived to be suffering from mental ill health or a mental health crisis.
-
A judgement about the most appropriate route of care for the person concerned is made in the absence of suspected criminality or a criminal charge (e.g. the use of L&D services to assess and refer individuals to an appropriate non-CJS treatment or support service would be relevant; L&D services related to out of court disposals, case management and sentencing would not be relevant).
Study design
Inclusion was restricted to well-reported qualitative studies that collected data using specific qualitative techniques (such as unstructured interviews, semistructured interviews or focus groups, either as a stand-alone methodology or as a discrete part of a larger mixed-method study) and from which the data were analysed qualitatively (e.g. using thematic analysis, content analysis or other recognised qualitative method). Studies that collected data using qualitative methods but then analysed these data using quantitative methods were excluded.
Outcomes
Inclusion was not restricted by outcome. Outcomes of interest included stakeholder (including service users’ and providers’) perspectives on the acceptability and feasibility of PRMHT, with specific reference to:
-
attitudes, beliefs and experiences about the use of the intervention
-
perceived facilitators of and barriers to implementation (e.g. willingness, capability and capacity of both police and mental health workforces, organisational and procedural factors)
-
health equity issues [e.g for black, Asian and minority ethnic (BAME) communities, people without English as their first language, people with neurodevelopmental disabilities]
Settings
Given the unique governance arrangements for delivering a mental health triage service in the UK, as well as important differences in social context and the delivery of health and criminal justice services between countries, inclusion was restricted to qualitative data on interventions that were undertaken in the UK.
Selection procedure
Three reviewers screened the results of the literature searches in EndNote X7 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA]. Each record was screened by one reviewer, with clearly irrelevant records rejected. The remaining records were classified as clearly relevant or of borderline relevance and were independently assessed by a second reviewer. Any disagreements were resolved by consensus with a third reviewer.
All studies included on the basis of title and abstract were screened again based on the full publication and following the same procedure.
Records that were initially classified as ‘borderline’ but ultimately excluded can be found in Appendix 4.
Data extraction and risk-of-bias assessment
Key review and primary evaluation characteristics were extracted and tabulated.
Risk of bias in reviews was assessed using the Egan et al. -adapted criteria32 previously used in a Health Services and Delivery Research metasynthesis on support for informal carers and the provision of services in the UK for armed forces veterans with post-traumatic stress disorder. 33,34 As part of a methodological piece of work, we had also intended to use the ROBIS assessment tool35 which is a more detailed and nuanced assessment, but because of a lack of time and resources it was not used.
The risk of bias of primary evaluations of effects was to be assessed using study design-specific tools. The quality of the more robust primary study designs was critically appraised, conventionally considered to be randomised controlled trials (RCTs) and controlled trials, using the Cochrane Effective Practice and Organisation of Care risk-of-bias tool for controlled studies. 36 However, many of the remaining studies were predominantly single-group designs based on retrospective data collection from routine sources. When comparisons were reported, these often used historical data prior to the intervention. These designs are typically considered less methodologically robust. Although these single-group studies were not formally assessed for methodological quality, the adequacy and clarity of reporting on context, methods and impact was considered.
The methodological quality of qualitative studies was assessed using the Critical Appraisal Skills Programme (CASP) checklist for qualitative research. 37
Data coding and synthesis
Evidence on the effects of police-related mental health triage intervention models
The aims, characteristics, results and risks of bias of included reviews and recent primary evaluations of effects were tabulated and combined in a narrative synthesis. This describes the most prominent models of intervention alongside evidence on the nature, strength and direction of observed effects for these interventions.
UK-relevant qualitative data on implementation
Characteristics of included studies were extracted and tabulated and their full text entered into NVivo version 11 (QSR International, Warrrington, UK) for coding and thematic analysis. 38 Texts were coded by one reviewer and checked by another. Descriptive and analytical themes were developed using the themes reported by Reveruzzi and Pilling9 as a framework. This framework was selected because it allowed us to rapidly integrate additional primary research evidence with that derived from the DHSC pilot studies.
Overall synthesis
An overall narrative synthesis (Figure 1) drew together evidence from the effects of PRMHT interventions in the UK using UK-relevant qualitative data on implementation, to address the stated research questions:
-
Which models have been described in the literature?
-
What evidence is there on the effects of these models?
-
What evidence is there on the acceptability and feasibility of these models?
-
What evidence is there on the barriers to, and facilitators of, the implementation of these models?
FIGURE 1.
Structure of the rapid evidence synthesis.
In the absence of adequate evidence, detailed recommendations were made for the design and conduct of any future evaluations in this area.
Advisory group
A project advisory group was convened to help to provide expert advice and input. This involved researchers from primary evaluations of PRMHT interventions and police staff, including a control room sergeant and a street triage supervisor. The advisory group were free to comment on any aspect of the rapid evidence synthesis, including, but not limited to:
-
refining the definition of PRMHT if necessary
-
identifying the highest-priority outcomes
-
identifying UK-relevant data from the international literature
-
discussing findings
-
developing practical recommendations for the various stakeholder audiences
-
identifying highest-priority areas for further research.
Comments and suggestions from the advisory group were incorporated into the final report.
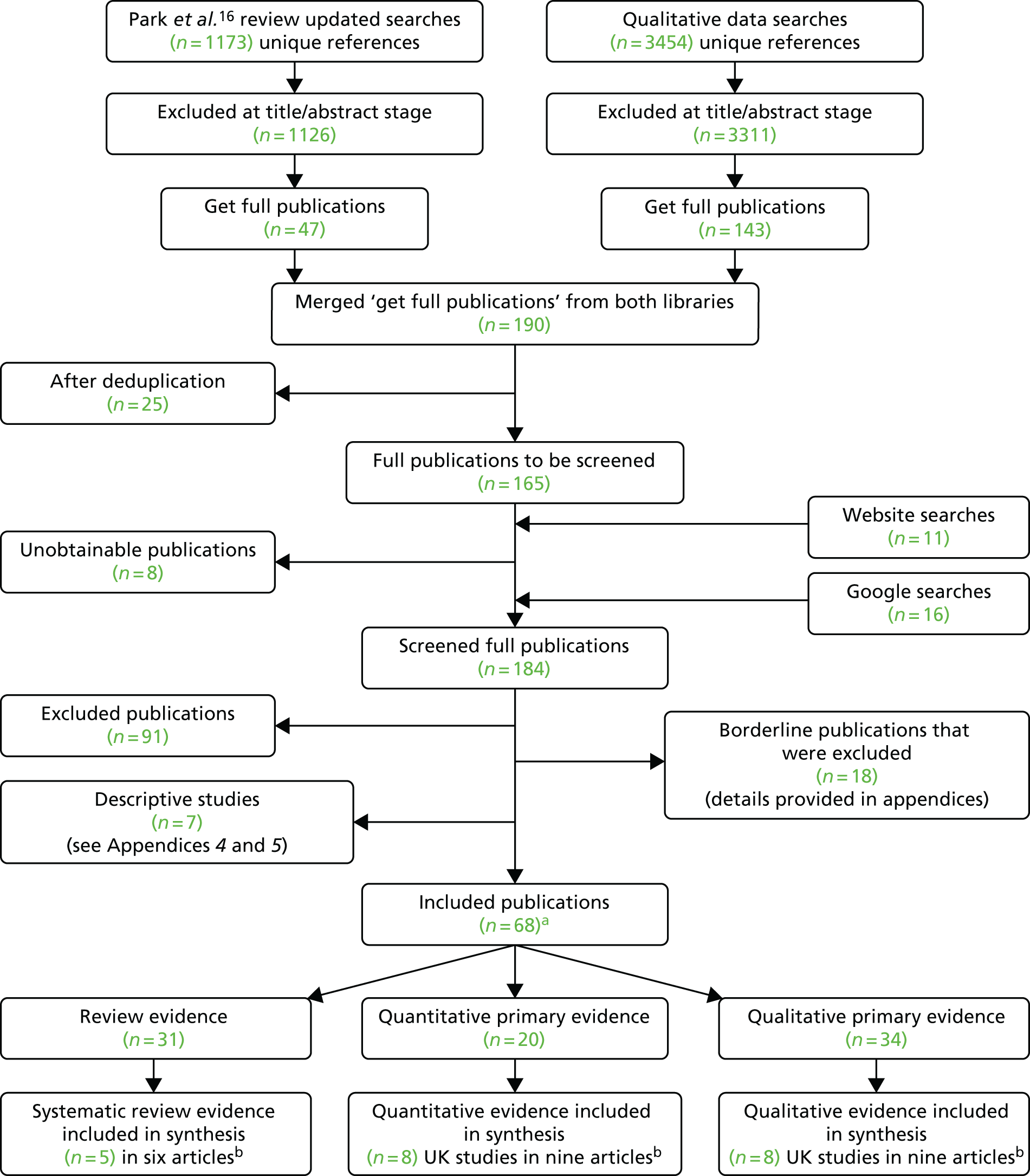
Chapter 3 Search results
Sixty-eight publications were included. Any one paper may have contributed to more than one section of evidence (e.g. provided systematic review, quantitative or qualitative evidence). Thirty-one publications provided review evidence, 20 publications provided quantitative evidence and 34 publications provided qualitative evidence (Figure 2).
FIGURE 2.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart. a, Any one paper may have contributed to more than one section of evidence [hence, the total number (n) increases from 68 to 85]; b, studies not included in the synthesis are detailed in the appendices.
Chapter 4 Metasynthesis of evidence on the effectiveness of models
Systematic reviews
Overall, 31 review articles evaluating PRMHT interventions were identified. This study focused on those reviews that used systematic, transparent or reproducible methods, as determined by the DARE criteria. 31 This resulted in five reviews being included in the synthesis. 11,12,14,15,39,40 There were six articles published for the five reviews as Kane et al. 11 also published their review protocol. The remaining 25 review articles were excluded from the synthesis as their methods were deemed less robust (according to DARE criteria) or were not reported. These reviews are listed in Appendix 5 and DARE assessments for all identified reviews are presented in Appendix 6.
Below is a summary of the five included systematic reviews. Three reviews were evaluations of PRMHT interventions,11,12,15,40 one review evaluated mental health training programmes for PRMHT39 and one was a scoping review of interagency collaboration models for PRMHT. 14 Details of the study characteristics are also provided in Table 1. The level of detail of participants, interventions, comparators, outcomes and findings varied between reviews. Terminology also differed and was often undefined. We have endeavoured to report the findings in as much detail as was available from the original reviews.
| Reference details of included studies: countries, study designs, number of studies, date range of studies | Review objective/aim and inclusion/exclusion criteria | Full description of intervention(s) and comparator(s) (when reported) | Summary of authors’ conclusions and summary of implications for research and health care, as reported by the authors | Commentary: (1) brief interpretation of internal validity and (2) issues relevant to external validity |
|---|---|---|---|---|
| Systematic reviews of interventions | ||||
| aKane et al.11,12 | ||||
|
Countries: unclear, although appears to include Australia, Canada, the USA and the UK (England) Street triage: (when reported) Australia, Canada, the USA and the UK (England) CIT: Australia and USA Multiple intervention comparison: USA Study designs: L&D – controlled studies (n = 5), pre–post studies (n = 2) Street triage – controlled studies (n = 3), pre–post comparison studies (n = 2) CIT – meta-analysis (n = 1), controlled studies (n = 6), pre–post studies (n = 2) Comparison across intervention types – unclear Number of studies: 23 L&D (n = 7) Street triage (n = 5) CIT (n = 9) Comparison across intervention types (n = 1) (two papers) Date range of studies: L&D: 2005–15 Street triage: 2000–16 CIT: 2004–16 Comparison across intervention types: 1999–2000 |
To evaluate the effectiveness of police–mental health service interventions for responding to ‘people with mental disorder and suspected offending or public safety problems’ Included studies had to relate to an intervention for those with mental ill health or a ’problem’; report objective outcome measures regarding offending or mental health; involve participants aged > 18 years; the design had to be experimental/quasi-experimental and had to include an intervention and comparison group(s) or a pre/post comparison; comparison group members had to be individually matched to intervention participants, or baseline comparability was demonstrated, or allocation of participants was random PhD theses and articles not in English were excluded, as were papers published before 1980 |
Street triage: various, including a mobile crisis unit that provides two police officers and one nurse from 15.00 to 22.30 for 7 days a week, with a psychiatrist available for telephone consultation and an initial response to 911 calls identified as psychiatric emergency situations is also provided; mental health mobile crisis unit partnership between mental health services, police and emergency health services offering short-term crisis management, using a mobile team that consists of a plain-clothes police officer and a MHP; and PACER; street triage pilot schemes in England (no further detail reported) Comparisons (when reported) included areas with no service or retrospective data collected from a time when teams were not on duty CIT: in some studies officers had 40 hours of training Comparators (when reported) appeared to be no training Studies on L&D services were also reported |
Authors’ conclusions: the studies reviewed offer some positive evidence for the interventions. However, the research base remains underdeveloped, needing more large-scale, well-designed trials. Only two studies looked at the differences between approaches, and neither one is conclusive. CIT is the intervention with the most robust evidence underpinning it but is not widely used outside the USA. In England and Wales, although not operating with any design fidelity to the CIT model, there is some local integration of approaches that are elsewhere delivered as discrete interventions Implications for research and health care: future services should take note of the current research and seek to capitalise on what works, and further build the evidence to refine and develop integrated interventions |
|
| bPaton et al.15 | ||||
|
Countries: the UK, Canada, the USA and Australia Study designs: mainly descriptive studies (n = 2) and quasi-experimental (n = 4) Number of studies: six (relevant to our rapid evidence synthesis) Date range of studies: 2000–14 |
To conduct a rapid synthesis of evidence on the clinical effectiveness and cost-effectiveness of models of care (at each of the four stages of the care pathway identified by the Crisis Concordat) for treatment and support of people experiencing a mental health crisis For urgent and emergency access to crisis care: eligible for inclusion were quantitative (controlled) and qualitative studies of people with mental health problems accessing emergency services and emergency department care. Eligible interventions were those designed at service level (including training) to improve service and service user outcomes (e.g. waiting times, hospital admissions, reduced use of force/restraint, self-harm, violence, mental health outcomes and service user experience) |
Street triage or telephone triage by health or social care professionals in collaboration with police officers (some in receipt of CIT training) Various, including a telephone triage service (RAID); a street triage crisis partnership involving mental health services, municipal policy and emergency health services; and a comparison of interventions including police officers with mental health training and assistance provided to police by community service officers; and a mobile crisis team Comparators included nothing (or pre-intervention data only), areas with no access to services, or interventions compared with each other Police officers receiving training in mental health Training interventions were based on CITs or MHIT Comparators included none (or pre-intervention data only); or police officers not in receipt of training |
Authors’ conclusions: there is very limited evidence for support (via training, street or telephone triage) to police officers from MHPs. Street triage and training of police offers were both associated with reduced police time at the scene of mental health-related incidents; street triage may also improve user engagement with outpatient treatment services. People with mental health problems were more likely to be taken to a health-care setting (as opposed to being arrested) as a result of mental health training undertaken by police officers. There was no evidence of intervention effect on levels of force used by police officers in mental health-related calls Implications for research and health care: rigorous, high-quality evaluation is needed. The authors did not report any implications for practice |
This data extraction focuses on only data presented for urgent and emergency access to crisis care (including street triage) as part of a wider review, which also addressed access to support before crisis point, quality treatment and care in crisis, promoting recovery/preventing future crisis
|
| cTaheri40 | ||||
|
Countries: the USA and Australia Study designs: quasi-experimental (including two studies with matched control) Number of studies: eight Date range of studies: 2006–14 |
To evaluate the evidence on the effects of CITs, with a specific focus on its effects on the core elements set forth by the Memphis model Included studies had to use a quasi-experimental or experimental design (at the very least involving a post-intervention measure of outcomes and a comparable control group), with a focus on CIT in individuals with mental ill health (all definitions included) Outcomes of interest were official or officer-reported arrests of a person with mental ill health, police officer use of force or of police officer injury |
CIT: although the characteristics of included CIT models were not reported, an operational definition of CIT was provided for the review (i.e. any specialised, police-based, jail diversion response to persons with mental ill health following the Memphis model) All included studies evaluated a CIT programme implemented by law enforcement Comparators: included matched controls (two studies: one matching police districts, one matching individual officers); six studies compared CIT-trained officers with non-matched samples of non-CIT trained officers |
There is insufficient evidence to conclude if CIT models reduce officer injury when police officers encounter people with mental ill health. There appears to be some evidence of no effect in relation to CIT and arrest outcomes or officer use of force; overall, findings are mixed. This result does not indicate that CIT programmes should be discontinued Higher-quality evaluative research should attempt to use matched control designs, record both pre- and post-intervention data and use both official and self-reported measures |
|
| Scoping review of interagency collaboration models | ||||
| dParker et al.14 | ||||
|
Countries: Australia, Canada, the USA, the UK and the Netherlands Study designs: (overall review) various, mostly – descriptive, mixed-methods, service evaluations, controlled before and after studies. Other designs – survey, qualitative, case study, audit, scoping review, prospective observational study Number of studies: 125 Date range of studies: not reported |
To identify and map the evidence on interagency collaboration models/mechanisms, the broad areas/issues covered and views/experiences connected to the models Eligible for inclusion were English-language studies of empirical evaluations or descriptions of interagency collaboration models Evidence had to be UK based or from any Organisation for Economic Co-operation and Development country Models had to include police engagement with members of the public with apparent mental ill health, mental vulnerabilities or learning disabilities Any outcome was considered. Studies published before 1995 were excluded |
Pre-arrest diversion (43 articles): first-line response police officers with special mental health training who liaise with mental health services. Most widely reported was the CIT model (17 articles) Comparators: not reported Co-response (36 articles): a shared protocol between specially trained police officers and MHPs. Three articles focused on UK-based ‘street triage’ involving initial police call handlers referring to the street triage team (a dedicated police officer and a psychiatric nurse working together) or (when the team was busy) telephone support to police attending an incident Comparators: not reported Co-location (five articles): MHPs employed by police departments to provide assistance (on-site and over the telephone) to police officers attending an incident Comparators: not reported Consultation model (three articles): typically, telephone advice (e.g. a dedicated 24-hour contact number) providing police access to advice from MHPs Comparators: not reported Service integration models (three articles): multiagency integrated service (e.g. community-care networks) involving a network co-ordinator (often a community psychiatric nurse), a personalised action plan for the individual in mental distress and active follow-up with signposting to the relevant agency Comparators: not reported |
Authors’ conclusions (overall): 13 different interagency collaboration models to deal with various mental health-related interactions were identified (12 models involved the police and mental health services/MHPs) Implications for research and health care (overall): a systematic review of effectiveness would be possible for some service models, others warrant more robust evaluation (such as a RCT). Future evaluation should target health-related outcomes and have an impact on key stakeholders |
This data extraction focuses on models of interest to our rapid evidence synthesis, as follows: pre-arrest diversion, co-response, co-location, consultation model; service integration models (Other models included in the scoping review: information sharing agreement models; court diversion models; comprehensive systems model; special protective measures; joint investigation training; re-entry programmes; integrated model) 1. The scoping review contained an appropriately broad question and a corresponding search strategy covering published and unpublished literature. Selection criteria were clearly stated. The review process demonstrated attempts to minimise error and bias. An established framework was used to map the literature and the results of this were clearly presented The authors acknowledge absence of study quality assessment and synthesis of the findings as a limitation of the review, thus precluding conclusions about the effectiveness of individual service models 2. The map of literature was sufficiently detailed to allow an assessment of generalisability to other countries and settings |
| Systematic review of training interventions | ||||
| eBooth et al.39 | ||||
|
Countries: the USA, Canada, the UK, Sweden and Australia Study designs: Police training – systematic review (n = 1), RCT (n = 12), prospective non-RCTs (n = 3) mental health-related training specifically for police in England: non-comparative evaluations (n = 3) Number of studies: 19 Date range of studies: 2001–15 |
To evaluate the effectiveness of training programmes and/or training resources aimed at increasing knowledge and/or behaviour or attitudes of the trainees about ill health, mental vulnerability and learning disabilities and of satisfaction with training and barriers to, and facilitators of, effective training Eligible for inclusion were studies of police officers; other police staff engaging with the public; members of the CJS; health professionals (non-mental health trained) in acute care; education workers; and other relevant professions/organisations/mental health charities Interventions of interest were any specific mental health training or learning resources aimed at improving attitudes, knowledge and skills of professionals dealing with members of the public (any age) with mental health issues or learning disabilities Comparators of interest were no training, usual practice or different modalities of training Primary outcomes of interest included changes in practice (behaviour) and outcomes for members of the public Secondary outcomes included satisfaction with training, shifts in attitude towards mental health, and changes in confidence, knowledge and skills Systematic reviews, RCTs and qualitative studies of views and experiences were eligible for inclusion Additionally (for police-related interventions only), non-RCTs, observational studies and published/unpublished audits and evaluations in England and Wales were eligible |
Interventions with a broad mental health focus For police officers CIT programmes (course content not reported) Education (including mental ill health, substance abuse, medication, treatment, civil commitment law, intervention techniques) mental health awareness training (including S136 procedures, meetings with MHPs, interactive teaching and role play) Various anti-stigma courses (including education, practical training and psychiatry lectures, workshops about mental health problems and how police can support people); online training (delivered by a combination of personal experience and information giving) MHIT (course content not reported) Comparators: when reported/when applicable, no training or alternative training For other non-mental health trained professionals Caseworker training and consultation model ‘Project Focus’ (including awareness of mental health needs, effective mental health treatment and developing action plans for youths in the community) MHFA with emphasis on self-help, including a five-step action plan (‘ALGEE’) aimed at University Resident Advisors MHFA (translated to Swedish) aimed at public sector staff Modified version of the Youth MHFA course (with ‘ALGEE’ action plan) aimed at teachers and students Peer Hero Training aimed at University Resident Assistants (including dramatisations, counselling sessions, interviews with parents of students/senior residence life professionals) Comparators: waiting list, usual practice Interventions with a specific mental health focus For police officers Awareness training on intellectual disabilities (including community-based role-play) Web-based/online video education on autism spectrum disorder – ‘Law Enforcement: Your Piece to the Autism Puzzle’ Comparators: no training, waiting list For other non-mental health trained professionals Classroom-based information on the autism spectrum disorder aimed at trainee teachers Alternatives for Families: Cognitive-Behavioural Therapy (AF-CBT) aimed at community clinicians ‘The student body; promoting health at any size an online programme’ aimed at teachers and public health professionals (comprising six modules covering media and peer pressure, healthy eating, active living, teasing, adult role models and school climate) Education on adolescent depression aimed at teachers (delivered in three parts: introduction, case vignettes, discussion of specific issues) Modified Barkley’s parent-training programme adapted for teachers (and aimed at teachers and parents) to help children with attention deficit hyperactivity disorder Comparators: alternative training, usual practice |
Authors’ conclusions: various training programmes exist for non-MHPs engaging with people with MH issues. Evidence indicates some short-term behaviour change for trainees Implications for research and health care: longer-term follow-up of training programmes is needed, as is better quality research evaluating training for UK police officers Note: authors report that included studies were poorly reported, with various omissions making it difficult to extract or calculate an intervention effect. The systematic review and primary studies also had poor reporting of methods |
|
Characteristics of systematic reviews
The reviews of PRMHT effects included studies conducted in Australia, Canada, the Netherlands, Sweden, the USA and the UK, published between 1999 and 2016 (when reported).
Study designs of the included primary studies varied across the reviews. The reviews of PRMHT interventions included a meta-analysis, controlled studies, quasi-experimental controlled studies, pre–post comparisons and descriptive studies. The review of training programmes for PRMHT included a systematic review, RCTs and prospective non-RCTs. Most studies in the scoping review of interagency collaboration models were descriptive but this review also included mixed-methods studies, service evaluations, scoping reviews and observational studies.
Police-related mental health triage interventions
Details of the interventions of PRMHT were generally only briefly reported in the reviews and included the following.
Pre-arrest diversion
Control room call-handlers identify incidents when people are in a mental health crisis and to which they can despatch unaccompanied police officers with special mental health training who can then refer to mental health services [e.g. CIT or a Mental Health Intervention Team (MHIT)]. 11,12,14,15,39,40
Co-response
Co-response includes front-line police officers being supported by a MHP as a joint, on-scene response (hours may be restricted, i.e. co-response with MHPs may be operated only during night shifts) and/or a MHP in a control room [e.g. street triage teams in the UK11,12,14,15 or a police, ambulance and clinical early response (PACER) in Australia]. 12 The Parker et al. 14 scoping review described interventions in which the MHP exclusively provided advice from a separate location (e.g. via telephone) as befitting a ‘consultation’ model.
Service integration models
This intervention was described in the scoping review of models of interagency collaborations. 14 The model describes multiagency integrated services to create a network to bridge gaps between services, decrease arrest, decrease violence, improve educational attendance and completion, and reduce symptoms of mental ill health and psychological distress. These may typically involve a network co-ordinator (often a MHP), a personalised action plan for individuals in mental distress and active follow-up with signposting to the relevant agency. This is somewhat broader than the focus of the current review as it encompasses far more than triage and/or crisis work.
Training programmes and resources
Training and resources were described for the various PRMHT interventions, which had either a specific or a broad mental health focus. 39
Mental health triage providers and users
Whenever reported, the providers of the PRMHT interventions (service providers) were police officers,11,12,14,15,40 community service officers15 and MHPs. 15 The scoping review by Parker et al. 14 reported a wide range of relevant agency collaborators from health, welfare and social care services. The review by Booth et al. 39 evaluated training programmes and described a range of trainers, such as police officers, MHPs, educators and service users. Trainees included police officers as well as others from areas such as education, welfare and social care. 39
People coming into contact with PRMHT interventions (service users) were described in only two of the reviews. Taheri40 evaluated CIT interventions and broadly described service users as those diagnosed with mental ill health. The scoping review by Parker et al. 14 described service users as adults, children, young people and mixed populations. No further details on participants were reported in any of the reviews.
Outcomes
Organisational- and service-level outcomes were the most frequently reported across the reviews. These included rates of detention,11,12,15 use of HBPOS,11,12 arrest rates,40 mental health referrals, police officer time dealing with events and police officer safety. 11,12,15
The review of training by Booth et al. 39 reported on effects on police officer awareness, attitudes, beliefs and knowledge as a result of mental health training. A range of outcomes was also reported for the training of those in education, welfare and social care including awareness, knowledge, self-efficacy and changes to the environment. 39
Approach to synthesis
Only the review by Taheri40 conducted a meta-analysis. The remaining review authors conducted narrative syntheses because of the diversity of the primary studies and PRMHT interventions.
Overlap of primary studies within the review
There was some overlap of primary studies among the reviews themselves, and also in the additional primary studies included. The overlapping studies identified are listed in Table 1.
A summary assessment of the overlap indicates that a number of studies appeared in one or more of the effectiveness reviews. 11,12,15,40 The review by Taheri40 was also included in the Kane et al. 11,12 review. Studies in the review of training by Booth et al. 39 appeared in some of the effectiveness reviews. Some of the studies in the scoping review by Parker et al. 14 were also included in the effectiveness reviews, but findings were not reported. 39
Although there was some evidence of overlap of primary studies between the reviews, it is interesting that there was not a greater overlap given that all the reviews met our inclusion criteria. This perhaps illustrates the variety in forms of PRMHT interventions that have been evaluated and the lack of consistent nomenclature in this area in general.
Quality of the systematic reviews
The reviews were assessed for risk of bias using the Egan et al. criteria. 32 Most had some potential for error and bias in the review process. Table 2 provides details for each review.
| Egan et al.’s32 quality assessment tool questions | Systematic review | ||||
|---|---|---|---|---|---|
| Booth et al.39 | Kane et al.11,12 | Parker et al.14 | Paton et al.15 | Taheri40 | |
| Is there a well-defined question? | Yes | Yes | Yes | Yes | Yes |
| Is there a defined search strategy? | Yes | Yes | Yes | Yes | Yes |
| Are the inclusion/exclusion criteria stated? | Yes | Yes | Yes | Yes | Yes |
| Are study design and number of studies clearly stated? | Yes | Partial | Yes | Yes | Yes |
| Have the primary studies been assessed for risk of bias/quality? | Yes | No | No | Yes | No |
| Have the studies been appropriately synthesised? | Yes | Yes | Yes | Yes | Yes |
| Has more than one person been involved at each stage of the review process? | Yes | Partial | Yes | Partial | No |
Booth et al. 39 fulfilled all the criteria. Paton et al. 15 met all the criteria but did not report if more than one person was involved at each stage of the review process, which means that there is potential for reviewer error and bias in the selection of studies. Kane et al. 11,12 met some of the criteria but despite reporting the intention to assess the risk of bias of included studies, the results of this assessment were not reported and did not appear to inform the findings. The authors also did not clearly report the study designs or number of included studies. These omissions mean that it is difficult to judge the reliability of the individual studies. The involvement of more than one reviewer was reported for only some parts of the review process, meaning that there is the potential for reviewer error and bias. Taheri40 was the sole author, so there is the potential for error and bias in the selection of studies, data extraction and synthesis. Risk of bias of the primary studies was not assessed, meaning that it is not possible to judge the reliability of the results from the meta-analysis.
The scoping review by Parker et al. 14 met all the criteria apart from assessment of primary studies, which is acceptable for a scoping review that does not report effectiveness findings. 14
Findings from the reviews
We have focused on the outcomes relevant to our review questions. Two of the included reviews had broader objectives and we have only used the sections relevant to PRMHT interventions. 14,15 A summary of the relevant findings are reported in Table 3.
| First author | Description (when reported) of service users, service providers, region | Summary of interventions and comparators (e.g. street triage, CIT) | Outcomes and measures (if reported) | Summary of results (if reported) |
|---|---|---|---|---|
| Systematic reviews of interventions | ||||
| Kane et al.11,12 |
Street triage: Service users: unclear. Most studies appear to use retrospective data collection from data on service users and clients Service providers: not reported Regions: not reported |
Street triage: Comparators: very limited reporting. Reported comparators included areas with no service or retrospective data collected from a time when teams were not on duty Number of studies – five (three controlled, two pre–post comparison) |
Street triage: rates of detention under S136 (UK), psychiatric hospitalisations, outpatient contacts, length of hospital stay, referral to place of safety other than a police station, arrests. Police officer length of time on-scene, length of time to assist |
Street triage: overall, the studies reported that street triage teams provided a quicker and more appropriate response (one study of a mobile crisis unit in the USA, one study of a mental health mobile crisis team in Canada, one study of a PACER team in Australia) Street triage can improve outcomes, including reducing the use of formal detention (one study of a pilot street triage service in Cleveland, England) or increasing use of health-based places of safety (one study evaluating nine street triage schemes in England) and reducing contact time with treatment services (one study of a mental health mobile crisis team in Canada) |
|
CIT: Service users: not reported Service providers: unclear but appears to be largely police officers and correctional officers |
CIT: Comparators: non-trained officers Number of studies: nine (one meta-analysis, six controlled studies, two pre–post studies) |
CIT: direction of individuals with mental ill health to mental health services, hospital attendance time, officer self-efficacy and perceptions of verbal de-escalation |
CIT: there were mixed findings suggesting that CIT-trained officers differed from untrained officers for a number of outcomes; for example, a greater proportion of people with mental ill health were directed to mental health services by CIT-trained officers than by non-trained officers (three studies). This was influenced by the nature of the incident and the local services available CIT-trained officers demonstrated different approaches towards individuals encountered with mental ill health (three studies). This was suggested to be an existing difference between trained and non-trained officers, influencing their decision to take up such training (one study and one meta-analysis). There is also some suggestion in these studies of diffusion of benefit from CIT- to non-CIT-trained officers regarding knowledge of mental health and approaches to incidents (one study) |
|
|
Service users: not reported Service providers: not reported Regions: not reported |
Comparison of three different interventions: (1) involving civilian police employees with additional training to assist police officers in mental health emergencies and difficult to resolve calls (2) a CIT unit (3) a Mobile Crisis Unit Comparators were data from usual police response Number of studies: unclear (two articles) |
Mental disturbances requiring a response, dispositions, arrest rates |
Review authors report that the structure, approach and resources of each programme suggested that although the approaches can be effective, not all were equally effective. Statistically significant differences across the three sites examined were reported for the proportion of mental disturbance calls eliciting a specialised response (Birmingham 28%, Knoxville 40%, Memphis 95%) (one study) The dispositions (final determination) of cases handled by the specialised response personnel were found to be related to the programme type. All three programmes reported average rates of arrests (featuring mental ill health) as 7%. Key factors of success included the existence of a psychiatric triage or drop-off centre where police can transport individuals in crisis, and community partnerships so that the police response is part of a wider response involving relevant agencies |
|
| Paton et al.15 |
Service users: not clearly reported Service providers: police officers and MHPs, community service officers Regions: Canada, the USA and the UK (Greater Manchester) |
Street triage or telephone triage by health or social care professionals in collaboration with police officers (some in receipt of CIT training) Various collaborative partnerships Comparator: none (or pre-intervention data), comparisons within multicomponent model, no street triage Number of studies: three (one descriptive and two described as quasi-experimental) |
Use of Mental Health Act 19832 detention, police time on-scene, engagement with outpatient treatment, taken to treatment location, situation resolved on-scene, referred to treatment, arrested | Street triage [officers receiving telephone triage (RAID)] was associated with reduced S136 detentions and a number of calls were successfully converted to hospital admissions. Police officers felt the intervention also improved communication, co-ordination and timeliness of work, although some officers cited operational difficulties with the intervention. There were positive intervention effects on police time at the scene of a suicide call (at 24 months), and improved engagement with outpatient treatment. Areas focusing on police with mental health training were more likely (than community service officers or mobile crisis teams) to transfer people to mental health services. Community service officers were more effective at resolving a crisis at the scene; arrests were highest in this context |
|
Service users: not clearly reported Service providers: police/special weapons and tactics officers, members of MHIT Other agencies reported to be involved – health participants, non-government organisations Regions: Australia (NSW) and the USA |
Police officers receiving training in mental health CIT MHIT Comparator: none (or pre-intervention data), police officers not in receipt of training Number of studies: six (two descriptive and four described as experimental) |
Level of force (including during Mental Health Act 19832 events), referral/transport to mental health services, arrests, inpatient referrals, time (including ‘dead time’ at Mental Health Act 19832 events) | No differences were found in the level of force used by police officers, or in cases resolved at the scene, following mental health training. However, compared with no training, training seemed to result in higher levels of verbal engagement and negotiation, and in more referrals/transport for treatment. Lower arrest rates and reduced referrals to intensive psychiatric services were reported. MHIT did not show significant differences in the use of force or in the quality of the relationships between police officers receiving training and health-care staff. Trained police officers spent less time dealing with Mental Health Act 19832 events and had less dead time before handing over to health professionals | |
| Taheri40 |
Service users: broadly defined, including ‘mentally ill people’, ‘diagnosis of major mental illness’; people suffering from acute mental breakdown Service providers: police officers (when reported, were male and white) Regions: US studies (three in the mid-west, four in the south-east) and Australia (one study in NSW) |
CIT (with a specific focus on the Memphis model) compared with matched-control groups, or comparisons of CIT-trained officers with non-matched samples of non-CIT-trained officers Number of studies: eight (quasi-experimental) |
Arrest outcome (official report, arrest rate, officer self-report) Use of force outcome (use of force unspecified, official report, use of force rate, officer self-report) Officer injury outcome (police injuries not specified, official incident report) |
Findings of the review and meta-analysis (of seven studies) show null effects of CITs on arrests of people with mental ill health (d = 0.180, p = 0.495) and on police officer safety (d = –0.301, p = 0.191) Note: findings on officer injuries were reported in only two studies, but there were not enough data to conduct a meta-analysis. Therefore, findings for this outcome are not reported |
| Scoping review of models of interagency collaboration | ||||
| Parker et al.14 |
Service users: adults, children and young people, mixed (adults and children) Service providers: the scoping review included the following agency collaborators relevant to PRMHT interventions – addiction services, ambulance, community organisations, emergency services, mental health clinicians, mental health services, police, schools/colleges, nurses, social workers/social services, children and family services, hospitals (acute general), housing services, welfare services Regions: not reported |
Pre-arrest diversion: police officers with mental health training liaising with mental health services (e.g. CIT) Comparators: not reported Number of studies: 43 |
Organisational/service-level outcomes Views and experiences of agency staff (e.g. police officers) Views and experiences of people in the community (e.g. service users, families and carers) Service user mental health outcomes (e.g. improvement in mood) Cost-effectiveness or wider economic costs |
Results and synthesis of the included studies were not reported (scoping review) |
|
Co-response: shared protocol between police and MHPs (e.g. street triage) Comparators: not reported Number of studies: 36 |
Organisational/service-level outcomes Views and experiences of agency staff (e.g. police officers) Views and experiences of people in the community (e.g. service users, families and carers) Service user mental health outcomes (e.g. improvement in mood) Cost-effectiveness or wider economic costs |
Results and synthesis of the included studies were not reported (scoping review) | ||
|
Co-location: MHPs employed by police departments Comparators: not reported Number of studies: five |
Organisational/service-level outcomes Views and experiences of agency staff (e.g. police officers) Views and experiences of people in the community (e.g. service users, families and carers) |
Results and synthesis of the included studies were not reported (scoping review) | ||
|
Consultation model: police access to advice (e.g. by telephone) from MHPs Comparators: not reported Number of studies: three |
Organisational/service-level outcomes | Results and synthesis of the included studies were not reported (scoping review) | ||
|
Service integration models: co-ordinated, multiagency integrated service networks Comparators: not reported Number of studies: three |
Organisational/service-level outcomes | Results and synthesis of the included studies were not reported (scoping review) | ||
| Systematic review of training interventions | ||||
| Booth et al.39 |
Training providers: not reported Training recipients: police officers Region: USA |
CITs Comparator: none specified Number of studies: one systematic review of 12 studies |
Not reported (review of systematic review) |
CIT may be effective in connecting (via police officers) people with mental ill health with appropriate psychiatric services in the USA, but this was based on limited and poor-quality primary research CIT may also have a positive effect on officers’ attitudes, beliefs and knowledge relating to interacting with people with mental ill health, although again this was based on limited and poor-quality primary studies On a systems level, CIT – in comparison with other pre- and post-diversion programmes – may be associated with a lower arrest rate and lower associated criminal justice costs |
|
Training providers: video only, online or by trainers Training recipients: police officers, student teachers, teachers and public health professionals Region: the USA, Canada and the UK (Scotland) |
Education (including web-based/online/video) and classroom-based delivery Comparators: waiting list, alternative training Number of studies: four RCTs |
Questionnaires to measure confidence and knowledge to recognise and identify attitudes towards people with autism spectrum disorder Various survey instruments to measure satisfaction with training, changes in attitudes, knowledge, skills, behaviour and confidence in teachers and health professionals Change in practice measured by the percentage of pupils reported by teachers as being depressed (lists of class cohort). Unpiloted attitudes questionnaire |
Various successes were reported following training for police offers about autism, including improved knowledge, confidence in identifying people with autism spectrum disorder and engaging with them. Training in autism delivered by podcast was significantly more effective in changing knowledge than written communication. Following an intervention to help prevent eating disorders, statistically significant improvements were reported in the knowledge of teachers in relation to restrictive dieting and peer influence. Self-efficacy to combat weight bias was improved for public health professionals. Most participants also said the intervention would encourage improvement in school environment and curriculum delivery. In another study, an education intervention to target adolescent depression resulted in increased confidence, but did not improve ability to recognise pupils suffering from depression | |
|
Training providers: mental health liaison police officers, police trainers responsible for teaching S136 procedures, MHPs or police trainers Training recipients: police officers Region: UK (England) |
Awareness training in mental health Comparator: no comparator Number of studies: two non-comparative |
Feedback form to measure the quality of presentation/content Survey measuring understanding, skills and awareness |
High satisfaction with training, better understanding of mental health services and increased awareness of the role and pressures faced by police were reported, together with an increased ability to deal with people with mental ill health | |
|
Training providers: unclear Training recipients: police officer trainees Region: UK (Northern Ireland) |
Awareness training on intellectual disabilities Comparators: no training Number of studies: one non-RCT |
‘Attitudes towards Mental Retardation and Eugenics’ validated questionnaire | A statistically significant improvement in attitudes was reported compared with control | |
|
Training providers: mental health lecturers, service users, carers, social workers, voluntary sector staff Training recipients: police officers Region: Sweden, the UK (England) and the USA |
Anti-stigma courses Comparator: alternative training or no training, or no comparator Number of studies: three (two non-RCTs, one non-comparative study) |
CAMI and WPA (2000) questionnaires, Modified Attribution Questionnaire and other validated scales measuring attitudes and behaviour towards mental ill health | Team-based approaches using mixed teaching methods showed variable success. Improved attitudes, mental health literacy and knowledge, and an increased willingness to interact with people with mental ill health after the intervention were seen in one study. In another study, a positive impact on police work was reported because of improved understanding and communication, but no effect was noted for changes in practice. In another study there were no reported differences in changed attitudes between anti-stigma videos of personal experience and information giving | |
|
Training providers: training designers were providers Training recipients: front-line police officers including constables, senior constables and sergeants Region: Australia |
MHIT Comparator: no training Number of studies: one prospective non-RCT |
Surveys (number of items and validation not reported) to measure change in practice, outcomes for people the trainees come into contact with, satisfaction with training and change in skills/behaviour | No substantial changes were observed in practice or relationship quality between police and other stakeholders. No significant differences were reported between MHIT-trained and non-MHIT-trained officers in relation to skills (except that trained officers reported less time spent at Mental Health Act 19832 events) | |
|
Training providers: PhD-level psychologists and a social worker with experience in mental health Training recipients: child welfare caseworkers Region: USA |
Caseworker training and consultation model Comparators: waiting list Number of studies: one RCT |
Questionnaire to measure change in practice | Increased awareness of evidence-based practice was reported, but no significant changes in practice or skills were noted following a child welfare caseworker training and consultation model | |
|
Training providers: trainers from the Department of Education & Children’s Services and Child & Adolescent Mental Health Service, behavioural health clinicians, experience in mental health work (health-care staff or volunteers) Training recipients: teachers, university resident advisors, public sector staff (social workers, human resource managers and employment managers) Region: Australia, the USA and Sweden |
MHFA or modified MHFA Comparators: usual practice Number of studies: three RCTs |
Strengths and Difficulties questionnaire to measure change in outcomes for people the trainees came into contact with, vignette-based knowledge test to measure changes in attitude towards mental health, questionnaires to measure change in confidence, knowledge and skills/behaviour, various other validated/non-validated questions and scales to measure change in practice, outcomes, satisfaction, attitudes, knowledge and behaviour | Team-based MHFA was associated with increased confidence and knowledge compared with control. Other benefits included readiness of public sector staff to provide help to people in a mental health crisis; students of trained teachers more frequently reported receiving information on mental health difficulties than control recipients. Effects on change in attitude were mixed. Training for resident advisors resulted in no change in practice or in the take-up of mental health services by students under their care | |
|
Training providers: online Training recipients: university resident advisors Region: USA |
Peer Hero Training Comparators: usual practice Number of studies: one RCT |
Survey to measure change in practice, referral efficacy (five-point Likert scale) to measure change in confidence | Resident advisors involved in Peer Hero Training were more likely to attend first-aid encounters with students than those receiving training as usual, they also reported improved confidence and skills | |
|
Training providers: unclear Training recipients: community practitioners (clinicians) Region: USA |
AF-CBT Comparators: usual practice Number of studies: one RCT |
35-item AF-CBT implementation measure to measure changes in practice and in skills/behaviour; 13-item training evaluation developed by the National Child Trauma Stress Network to measure satisfaction with training; 25-item CBT Knowledge questionnaire | Short-term (6 months) significant differences were noted between the intervention and control group for greater increases in teaching process, knowledge about CBT, skills (general psychological, specific skills to deal with abuse history). A high level of satisfaction with training was reported. However, these differences were no longer significant at 18 months post training | |
|
Training providers: ‘well-trained’ group leaders Training recipients: teachers and parents Region: Sweden |
Parental training programme adapted for teachers Comparators: waiting list Number of studies: one RCT |
Change in outcomes for people the trainees came into contact with was measured by attention deficit hyperactivity disorder DSM-IV scales, and the Strengths and Difficulties questionnaire | Team-based training for teachers and parents resulted in a significant reduction in parent-rated attention deficit hyperactivity disorder symptoms and problematic behaviours at 3 months | |
The authors of the reviews reported on variations of PRMHT interventions in primary studies of various designs. It is, therefore, not possible to group the studies by model of PRMHT or outcome; the findings for each review are reported separately below.
Kane et al. (2017)
The most recently published systematic review, by Kane et al. ,11,12 included studies that reported on-street triage and CIT, plus one study that compared three different approaches with police involvement.
As a result of street triage co-response interventions, a quicker and more appropriate response by the teams was reported overall. Reductions were reported in single studies for formal detentions, an increased use of HBPOS and a reduction in time spent on-scene by the team.
Kane et al. 11,12 also reported findings for comparisons between CIT-trained officers and non-trained officers. Trained officers were more likely than non-trained officers to direct people with mental ill health to mental health services, but this depended on local services available. Trained officers also demonstrated different approaches to people with mental ill health. Although it should be noted that police officers self-selected for training, that might indicate an existing difference between trained and non-trained officers, which could have an impact on approaches and attitudes.
One study in Kane et al. 11,12 reported on a comparison of three different models operating in the USA, including civilian police employees with additional training to assist police officers in mental health emergencies, a CIT unit and a mobile crisis unit. Authors reported that ‘the dispositions of cases handled by the specialised response personnel were found to be related to the programme type’12 (no further details reported), although all three models reported an average rate of arrests of 7%. Factors reported to be related to success were the existence of a psychiatric triage or drop-off centre to which the police could transport individuals in crisis, and community partnerships in which police response is part of a wider response involving relevant agencies.
Taheri (2016)
Taheri40 reported that there were no statistically significant effects of CIT interventions, between CIT-trained and non-trained officers, on official or officer-reported accounts of arrests of people with mental ill health. However, the studies were heterogeneous and reported conflicting results. 40
Paton et al. (2016)
The review by Paton et al. 15 evaluated on-scene co-response or telephone triage by health or social care professionals in collaboration with police officers (some of whom were in receipt of CIT training). 15 These included various collaborative partnerships. One UK study of a street triage intervention, in which officers received telephone triage, was associated with a reduction in S136 detentions and a number of calls were successfully converted to hospital admissions. 42 There were also improvements in police time on the scene of a suicide call, and improvements in engagement with outpatient treatment by service users, although these findings were reported only in one or two studies.
Paton et al. 15 also reported the effects of police officers receiving training in mental health. The interventions included CIT-trained officers and a MHIT. In one study, training seemed to result in higher levels of verbal engagement and negotiation, and more referrals to and transport for treatment. Lower arrest rates and reduced referrals to intensive psychiatric services were also reported in one study. In another study, a MHIT intervention found no significant differences in the use of force before and after training, and no perceived improvement in the quality of the relationship between officers receiving training and health-care staff. Trained officers spent less time dealing with events that related to the Mental Health Act 1983. 2
Booth et al. (2017)
A review of mental health training of service providers reported findings across several interventions. 39 The review found that CIT training may be effective in connecting people with mental ill health with appropriate psychiatric services via police officers. The training may also have had an effect on officers’ attitudes, knowledge and beliefs. However, the review authors state that these findings were based on limited- and poor-quality studies. No comparison groups were reported in the primary studies.
Education, awareness training and anti-stigma courses aimed at a range of trainees including police officers, MHPs, teachers, public health officials and voluntary sector staff reported various successes following training, including positive changes in awareness, knowledge and attitudes.
A study of the training for MHIT teams of front-line police officers in Australia found no substantial changes in practice or relationship quality compared with no training. There were also no significant differences in skills.
A number of other training programmes, not directly aimed at PRMHT, were also reported in the paper.
Parker et al. (2018)
The scoping review by Parker et al. 14 did not report any findings from primary studies.
Primary studies
As the most recent search date in the included systematic reviews was 2016,12 the metasynthesis of systematic reviews was supplemented with primary studies published in 2016 or later. The aim was to consolidate the most recent evidence of the effectiveness of PRMHT interventions. As the primary studies provided greater detail about specific interventions, participants and results than the systematic reviews, these studies are discussed at greater length in this report. However, it should be borne in mind that these studies represent a much smaller body of evidence than the published systematic reviews summarised in Systematic reviews.
Overall, 20 primary studies were identified. The studies included PRMHT interventions from the USA, Australia and the UK.
We chose to focus on the UK studies because the context in which interventions are evaluated will vary by country. For example, there are important differences between the UK and the USA in terms of funding, delivery and governance of criminal justice and health services, as well as wider societal differences.
Although we focus our synthesis on UK studies, this report provides summary details of the other studies in Appendix 7.
Eight primary studies undertaken in the UK were identified in nine articles. One trial contributed two articles, including one on methodological and practical challenges of undertaking the trial. Articles were published between 2016 and 2017. All of the studies evaluated schemes in England. Table 4 provides summary details of the study characteristics. Further details of the findings from each primary study are available in Appendix 8. The level of detail when reporting on participants, interventions, comparators, outcomes and findings varied between primary studies. Terminology also differed and was often undefined. We have endeavoured to report the findings in as much detail as was available from the primary studies.
| Reference, country (region, city or locality) | Study methods | Interventions and comparators (when reported) | Summary of authors’ conclusions and summary of implications for research and health care, as reported by authors |
|---|---|---|---|
| Studies that contributed to the main synthesis | |||
| Heslin et al.43 | |||
|
Region: the UK; south-east England, Sussex (Eastbourne and wider) Also included in qualitative synthesis: no Also included in a systematic review: no |
Evaluation type/study design as described by authors: a pragmatic evaluation Brief description of methods including data sources: routine data from 6 months before (1 April to 30 September 2013) and 6 months after (1 April to 30 September 2014) implementation of street triage were obtained from the Sussex Partnership NHS Trust and used to assess detentions under S136, response to mental health-related incidents (available for only 4 months, so data were extrapolated to 6 months), and to populate a decision-analytic model To explore whether differences were caused by the street triage scheme or other factors, data on S136 detentions were also used from the rest of Sussex over the same time periods Economic evaluation: cost-offset analysis. This took a NHS and criminal justice sector perspective (full details provided in the paper) |
Description of intervention: street triage where both a police officer and a psychiatric nurse attended incidents. If the team are already attending an incident, then telephone support is provided. The team respond in an unmarked police car (officer wears standard uniform, nurse wears lanyard and arm band with ‘nurse’ printed on it) Call handlers filter calls to the street triage team. The team will not be the initial response to emergency or life-threatening events Street triage is available during peak hours of need: Wednesday–Friday 16.30–00.00 and Saturday–Sunday 09.00–00.00 Outside operating hours and prior to street triage implementation the usual response to mental health incidents would be police attendance at all incidents, where officers then make a decision whether to detain the person under S136 and take them to a place of safety or to take no further action The street triage scheme began in October 2013. Data from 1 April to 30 September 2014 were used in the evaluation Comparator (when reported): used pre-intervention data (from 1 April to 30 September 2013) Implementation details (when reported): not reported |
Authors’ conclusions: savings offset investment in street triage as a result of reduced S136 detentions, particularly those in custody. A full evaluation was not possible because of a lack of available data on patient outcomes Summary of implications for research and health care: further research is needed and future evaluations should collect data on mental health and quality-of-life outcomes, including preference-based measures capable of generating QALYs to enable full assessment of the cost-effectiveness and cost–utility of street triage Future research should also seek to capture data on the number and proportion of incidents that do not result in a detention under S136 |
| Jenkins et al.44 | |||
|
Region: the UK; England, Norwich, Norfolk and Ipswich and Suffolk Also included in qualitative synthesis: no Also included in a systematic review: no |
Evaluation type/study design as described by authors: retrospective study, assessing pre and post intervention in two areas and comparison between areas Brief description of methods including data sources: the study compared numbers and outcomes of S136 assessments Authors state data were obtained prior to and following differing changed practices within the trusts for the two areas. Numbers of S136 detentions were gained from local S136 suite records and cross-referenced with data gathered at trust level for both Ipswich and Norwich. Data for each individual were then collected retrospectively from hospital records using electronic notes Data were gathered for two 6-month periods: (before) 1 June to 30 November 2013 and (after) 1 June to 30 November 2014 |
Description of intervention: Ipswich – funded by Commissioning and Quality, developed between Norfolk and Suffolk NHS Foundation Trust and Suffolk Constabulary. Scheme commenced on April 2014 Two experienced mental health nurses working on alternate shifts alongside front-line police officers, 7 days a week from 14.00 to 00.00, to help assess and appropriately divert members of the public who present with potential mental health-related emergencies. Individual officers vary depending on the shift Comparator (when reported): Norwich established a police liaison service (funded by the police service). Not reported when this scheme commenced Four mental health nurses on rotation provided support to the local police force between 08.00 and 22.00, 7 days a week, based in the police control room and offered telephone advice to police officers without face-to-face contact with the public Implementation details (when reported): not reported |
Authors’ conclusions: the authors concluded that mental health nurses working alongside front-line police officers can help improve S136 numbers and outcomes Summary of implications for research and health care: the study lacked a detailed analysis of the work done directly by the mental health nurses and police officers involved. Future studies should include these data alongside qualitative feedback from relevant professionals and individuals to enable a fuller understanding of the impact of such a service |
| Keown et al.45 | |||
|
Region: the UK; England, Northumberland and Tyne and Wear Also included in qualitative synthesis: no Also included in a systematic review: no |
Evaluation type/study design as described by authors: a comparative descriptive study Brief description of methods including data sources: routine data were obtained from – Northumbria Police, including the monthly number of S136 detentions between September 2013 and September 2015 Data were collected by the police as a part of their own evaluation of street triage The NHS, including the mental health service provider (NTW) and one A&E Department (Sunderland Royal Hospital) The social work department of one local authority (Sunderland) Population data from the 2011 census were used to calculate the rate of S136 detentions and street triage contacts per 100,000 whole population in each locality and across the whole area covered by NTW The absolute numbers of S136 detentions and street triage contacts were collected and percentage changes were calculated. Total number of street triage contacts and S136 detentions were calculated in 3-month blocks; these were compared with a corresponding 3-month block in the previous year Absolute and percentage changes in rates were calculated, and parametric tests were used to analyse changes and associations |
Description of intervention: street triage services comprised a mental health nurse working alongside a dedicated police officer in mobile community units. Street triage operated between 10.00 and 03.00, 7 days a week Introduced over a period of time to: North Tyne (from July 2015), including Northumberland, Newcastle and North Tyneside South Tyne (from September 2014), including South Tyneside, Sunderland and Gateshead Comparator (when reported): data from street triage period were compared with pre-street triage period Implementation details (when reported): not reported |
Authors’ conclusions: there was a reduction in the rate and number of S136 detentions following the introduction of street triage. This applied to S136 detentions in police custody, A&E and S136 suites. The reduction in S136 only occurred when street triage was operating in that particular area, and the more street triage was delivered the greater the reduction The number of S136 detentions fell as soon as street triage was introduced and continued to fall steadily through the first year. Outcomes of S136 assessments did not change, but there was a reduction in admissions following a S136 assessment Results support the hypothesis that street triage leads to a reduction in S136 detentions Summary of implications for research and health care: the authors express surprise that the outcomes of S136 detentions were not significantly different after street triage implementation. Further investigation would be needed to explain this. Patterns may change with a greater understanding of street triage as the schemes progress and if hours of operation are extended Further research is needed to evaluate outcomes of street triage contacts and whether or not street triage leads to improved patient outcomes, and to delineate when street triage is the best option and when S136 might be the preferred pathway There were reported reductions in voluntary admissions and section 2 detentions, but unchanged rates of detention under section 3. Further research should examine these results using a wide range of data, preferably prospective studies, to see if they can be replicated in other areas. Further research should examine the findings using a wider range of data, preferably prospective studies |
| Reveruzzi and Pilling9 | |||
|
Region: the UK; BTP, Devon and Cornwall, Metropolitan Police (London), Sussex, West Yorkshire, North Yorkshire, Thames Valley, Derbyshire and the West Midlands Also included in qualitative synthesis: yes Also included in a systematic review: yes (Kane et al. 12) |
Evaluation type/study design as described by authors: exploration and analysis of quantitative data from nine pilot areas Brief description of methods including data sources: the period data were collected across the nine pilot areas varied, but was generally between October 2013 and April 2015 and ranged from 10 to 19 months Pilot areas were asked to collect data for all incidents with which the street triage team had contact. Depending on the local arrangements, data were collected by either police or health staff. Amendments or additions were made to the data sets depending on concerns with regard to such things as confidentiality. Therefore, data were not always collected consistently across the pilot areas. All pilot forces reported challenges with data collection and the percentage of missing data are reported. Data sets cover only incidents captured during hours of operation for each pilot area. This differed between forces and changed throughout the evaluation period |
Description of intervention: Control room, telephone response – BTP Control room and face to face – Devon and Cornwall Police (based in police control room), Metropolitan Police Service, London (based in Mental Health Trust) MHP responding when requested by officer – West Yorkshire Police, North Yorkshire Police Police officer and MHP responding together – Sussex Police, Thames Valley Police, Derbyshire Constabulary Police officer, MHP and paramedic – West Midlands Police Comparator (when reported): data from year previous to street triage interventions (only reported for S136 detention data) Implementation details (when reported): not reported |
Authors’ conclusions: analysis of the quantitative data demonstrates that the introduction of the street triage pilots led to a reduction in the use of S136 detentions. Street triage also led to an increase in the use of HBPOS overall Limitations of the evaluation included the mainly retrospective nature of the data and a lack of robust comparators for each site. This means that it was not possible to use the data to determine whether or not a particular model or models should be adopted as the standard model for street triage. In addition, the likely different populations engaged by the schemes and the quality and availability of local mental health community services were likely to have had an impact on the effectiveness of the schemes. Although no particular model seems to be associated with a more favourable outcome, it should be noted that two schemes were associated with an increase in S136 detentions during the pilot period and that this may be attributed to the focus of the team, other available mental health services and problems with the staffing of the services Conclusions relating to qualitative data are reported as part of the qualitative evidence synthesis Note: authors report that there was a lack of funding for administrative support that had an impact on the completeness of data collection. This resulted in inconsistent data reporting and some missing data. Although S136 data were generally complete, information relating to the processes of care and action taken by the street triage teams was often more limited. There were also no concurrent comparator data collected, which limits the conclusions that can be drawn. No cost-effectiveness evaluation was undertaken for this review Summary of implications for research and health care: the implications relate to the qualitative evidence that is reported separately in the qualitative evidence synthesis |
| Senker and Scott46 | |||
|
Region: the UK; England, Essex Also included in qualitative synthesis: yes Also included in a systematic review: no |
Evaluation type/study design as described by authors: single group evaluation with some comparison data across time periods when there was variation in the service provided (e.g. pilot and full street triage) Brief description of methods including data sources For the quantitative evaluation, data from the following periods were used: Pilot street triage service – 4 months from December 2014 to March 2015 Full street triage service – 1 April 2015 to 30 September 2015 Latest 2 months – October and November 2015 Cost–benefit analysis: data from the full street triage project analysis were compared with the same period the previous year (1 April 2014 to 30 September 2014) Data were collected from: South Essex Partnership University NHS Foundation Trust, North Essex Partnership University NHS Foundation Trust, Essex Police, Athena, Storm, S136 database; Essex County Council EDS data, unit costs from a range of other evaluations of Street Triage Nottinghamshire, Essex’s 4-month pilot, Devon Police, Kent Police, Pennine Police, etc. Locally accepted costs (as used in Essex Police’s 4-month pilot evaluation) were applied to the data for the two time periods analysed in the cost–benefit analysis |
Description of intervention: Street triage pilot – 4 months from December 2014 to March 2015. Nurses were on patrol with police officers on Friday, Saturday and Sunday nights between 18.00 and 02.00. A telephone line was also available between these hours Monday–Thursday Full street triage – implemented from April 2015 with one nurse and one officer on shift 18.00–02.00 daily. Two shifts – North of Essex and South of Essex counties. Officers opt into street triage as overtime. Clinicians have street triage factored into the rota or bank staff are used. Marked police car used to collect the nurse at the start of the shift, the nurse can then be contacted via Force Control Room to request attendance at an incident. Another police unit is on-scene before street triage team arrive to assess risk and confirm the need for street triage Comparator (when reported): no comparator except for cost–benefit analysis for which data from 1 April 2014 to 30 September 2014 were used Implementation details (when reported): not reported |
Authors’ conclusions: the authors concluded that the data demonstrated that there were ‘significant benefits’ from the street triage scheme in directly preventing the use of S136, as well as having a wider impact on reducing the use of S136 across Essex. This was set against a rising national trend in the use of S136. Projecting for a full year from these figures shows that street triage in Essex is likely to produce a range of savings and benefits Conclusions relating to the qualitative data are reported separately in the qualitative evidence synthesis Summary of implications for research and health care: the implications relate to the qualitative evidence that is reported separately in the qualitative evidence synthesis |
| RCT of a training programme for front-line officers | |||
| Scantlebury et al., 2017,47,48 | |||
|
Region: the UK; England, North Yorkshire Also included in qualitative synthesis: no (authors report that a manuscript has been submitted for publication) Also included in a systematic review: no |
Evaluation type/study design as described by authors: pragmatic, two-armed cluster RCT Brief description of methods including data sources: police stations in one police force were randomised with front-line police officers receiving either a bespoke mental health training package or routine training A total of 12 police stations were recruited and randomised. Final follow-up was at 6 months post training. Front-line police officers eligible included the ranks of police Constable, Sergeant and Inspector, as well as Police Community Support Officers Routinely collected data were used to assess outcomes Data are at incident level rather than caller level because of the nature of the data collected |
Description of intervention: bespoke mental health training, at six police stations, involved 1-day face-to face training in a classroom setting, delivered by qualified and experienced MHPs from the local NHS mental health trust. This was delivered to front-line police officers in addition to routine training Courses ran between May and August 2016 The aim of the training was to enhance officers’ understanding of and ability to identify mental vulnerability, record relevant information using relevant systems, respond using appropriate resources, refer vulnerable people to services that provide longer-term assistance, review incidents to ensure that risks have been effectively managed Further details are reported in the paper Comparator (when reported): routine training only, provided at six police stations Implementation details (when reported): the intervention was delivered across 25 training days at three police locations in North Yorkshire between May and August 2016 |
Authors’ conclusions: there was no evidence that a 1-day bespoke mental health training package delivered to front-line police officers by MHPs had an effect on the number of incidents reported to the police control room. However, there may be a positive effect on how officers record incidents involving individuals with mental health issues Summary of implications for research and health care: Further research should be conducted in the police setting given the amount of routinely collected police data Future research should consider issues of contamination and difficulties of obtaining reliable and meaningful outcome measures Future studies should consider follow-up of at least 1 year to allow any changes to be detected Other research recommendations are reported in the paper A supplementary paper was published on the challenges of conducting a RCT in a police setting. 47 Challenges included establishing the unit of randomisation, population of interest and sample size, understanding the policing context, time frame and set-up, and outcomes and organisational issues |
| Studies that met our inclusion criteria but only provide ‘snapshot’ (one time only) data | |||
| Brace49 | |||
|
Region: the UK; area not reported Also included in qualitative synthesis: no Also included in a systematic review: no |
Evaluation type/study design as described by authors: dissertation Brief description of methods including data sources: Mixed methods including questionnaires, interviews and call data were used Questionnaires and call data were used to assess if there has been a reduction in demand at practitioner level. Data were collected by inviting staff who regularly interact with people in mental health crises to complete a questionnaire A further data set was obtained using the most available call figures that were received in the police control room over a time period from January 2014 to June 2016 Questionnaires were distributed via supervisor briefings and returned via e-mail or hard copy Call data were provided by an internal change team who had been gathering the data as part of the review and implementation of the street triage project |
Description of intervention: street triage consisting of a mental health nurse working in the police control room between the hours of 22.00 and 07.00, and a joint police officer and mental health nurse in a police vehicle available to attend incidents 7 days a week between the hours of 17.00 and 04.00. This was intended to provide an out-of-hours service, as office hours are covered by mental health crisis teams Force control room triage nurse introduced in October 2015 and street triage car introduced in April 2016 Comparator (when reported): none Implementation details (when reported): not reported |
Authors’ conclusions: the street triage model improved multiagency working and services provided to the public. However, the model did not reduce the demand on the police in relation to the number of calls received The collective perception and belief of the police officers was that the police force is not the correct service to respond to people in a mental health crisis; however, on many occasions they are the only service equipped to respond to this need Summary of implications for research and health care: none |
| Callender and Cole50 | |||
|
Region: the UK; Northamptonshire Also included in qualitative synthesis: yes Also included in a systematic review: no |
Evaluation type/study design as described by authors: described as an assessment and evaluation Brief description of methods including data sources: a mixed-methods approach was used, including an analysis of police data records of activities during two 1-week time periods. Data was collected from Northamptonshire Police Control Room and from mental health data held by Northamptonshire Police, which were stated to mirror data compiled by MHPs (e.g. Northamptonshire Healthcare NHS Trust data) Periods covered (both during the street triage scheme) were: time 1 – between 1 February 2016 and 7 February 2016 (7 days); time 2 – between 7 March 2016 and 13 March 2016 (7 days). Authors note that these data may not be fully representative of the scope, scale and nature of incidents but should be considered as ‘a snapshot’ of the data available Comparison between police and mental health data: authors noted that there were fewer incidents identified in mental health data compared with police control room data |
Description of intervention: not clearly reported, although appears to involve police officers, control room staff and MHPs over certain time periods each week (not reported) Comparator (when reported): none Implementation details (when reported): not reported |
Authors’ conclusions: the conclusions related entirely to the qualitative data are reported separately in the qualitative evidence synthesis Authors note that data recording was inaccurate, meaning that comprehensive reporting of the evidence of actions, values and outcomes was not possible Summary of implications for research and health care: authors recommend that data-recording procedures be reviewed as streamlined, with clear expectations and accountabilities for all parties with regard to documentation |
Characteristics of primary studies
The included studies were of varying designs. One RCT evaluated a training programme for front-line officers,47,48 although the remaining studies were largely descriptive, reporting little comparative data. Single studies used the following designs: a comparison of two different models of PRMHT interventions,44 a largely single-group evaluation during a PRMHT intervention with some comparison data from a cost–benefit analysis,46 an evaluation across multiple areas of PRMHT pilot interventions that reported comparative data only for some outcomes (e.g. S136 detentions),9 a descriptive study comparing data before and after an intervention,45 a pragmatic evaluation using a decision-analytic model exploring costs,43 a non-comparative assessment and evaluation of two areas implementing a PRMHT intervention,50 and a dissertation reporting data during the period of an intervention. 49
One of these studies (Reveruzzi and Pilling)9 was also included in one of the reviews in the metasynthesis. 12 Three studies that reported quantitative data9,46,50 also informed our synthesis of qualitative evidence (see Chapter 5).
Police-related mental health triage interventions
Eight studies (in nine articles) evaluated PRMHT interventions. 9,43–50 Most studies evaluated variations of co-response or consultation models that were often referred to as street triage. The intervention characteristics varied across the studies, but all could be broadly classified in terms of the primary role of MHPs (Table 5). These fell into the following categories.
| MHP role | Region/programme name | Dedicated personnel | MHP location | Specific components |
|---|---|---|---|---|
| Joint on-scene response with police officers |
Derbyshire pilot9 Thames Valley pilot9 West Midlands pilot9 Essex46 Ipswich44 Northumberland, Tyne and Wear45 |
Three specially trained police officers and three nurses One police officer and one nurse (Thames Valley; Sussex; Essex; Northumberland and Tyne and Wear) One police officer, one nurse and one paramedic (West Midlands) |
Police car |
Act as secondary response when requested by police officers initially attending the incident (Derbyshire, Thames Valley, Essex) First response when calls not considered emergency or life-threatening (Sussex) Deployed via 999 police/ambulance control room staff; paramedic provided on-scene support to reduce inappropriate A&E attendance (West Midlands) Developed partnerships with mental health liaison team, crisis home treatment team, local ambulance service and the Samaritans (Derbyshire) Active follow-up to ensure that service users engage with health services and/or attend appointments (Sussex, West Midlands) Wrote to GPs following contact (Sussex, West Midlands) Out-of-hours service provided advice line operated via mental health crisis team (Thames Valley) Embedded into crisis and liaison pathways Links with housing, employment and education training support services (West Midlands) |
| Telephone support alone |
BTP pilot9 Norwich44 |
Four nurses, three BTP civilian staff, one police officer (BTP) Four nurses on rotation to local police force (Norwich) |
Control room |
Provided information on places of safety and mental health history (BTP) Follow-up calls to individuals (BTP) Local crisis team liaison and referrals (BTP) Built relationships with local mental health charities, local authorities and HBPOS (BTP) |
| Telephone support to on-scene police officers and attend scene if necessary |
D&C pilot9 MPS pilot9 Operation Alloy (Northamptonshire)50 |
Four nurses (D&C) Four nurses with relevant prior experience (MPS) Nurse and/or police officer (Northamptonshire and Cleveland) |
Control room (D&C) Mental Health NHS Trust (MPS) |
Alongside street triage, nurses retained their existing roles within local L&D services (D&C) MHP has full access to police command and control system (D&C) 24-hour advice and support helpline integrated into NHS trust’s existing Crisis Service Line and crisis care pathways (MPS) Referrals generated by front-line police officers to street triage nurses (MPS) Referrals to health care, social care and third sector agencies (MPS) |
| Telephone and/or on-scene response without police presence |
North Yorkshire pilot9 West Yorkshire pilot9 |
One nurse and one support worker (North Yorkshire) One nurse/approved MHP/occupational therapist and one support worker |
Office in local hospital (North Yorkshire) Crisis Assessment Service (West Yorkshire) |
A dedicated telephone line receiving calls from police control room (North Yorkshire) or front-line police officers (West Yorkshire) Vehicle equipped with police airwave radio Access to local patient information system and permission to receive information from police records (North Yorkshire) Street Triage Discharge plan outlines next steps and up to three follow-up contacts per incident Adult support only; young people aged < 18 years are referred via Child and Adolescent Mental Health Services (West Yorkshire) Embedded into crisis and liaison pathways |
| Telephone support and on-scene response with police presence | UK (area unclear)49 |
One nurse and one police officer One nurse |
Police car Control room |
|
| Provision of specialist mental health training to police officers | North Yorkshire | Qualified and experienced MHPs | Classroom setting |
Bespoke mental health training involving 1-day face-to-face training in a classroom setting Delivered to front-line police officers in addition to routine training |
Joint on-scene response with police officers (five studies)
Mental health professionals were partnered with police officers to jointly attend incidents. Schemes varied across the studies, with police officers attending in uniform and teams arriving in marked or unmarked police vehicles or community vehicles. Hours of operation varied and were often limited to ‘peak response’ hours. Outside the hours of street triage operation, ‘usual response’ from police officers and access to mental health services continued. 9,43,45,46 One study reported a telephone line also being made available during peak hours to provide support to officers. 46 In one study, joint on-scene attendance of MHPs and police officers in one county in England was compared with telephone support only from a mental health nurse in another county. 44 In this intervention, a police unit would be on-scene before the street triage team arrive to assess the risk and confirm the need for the street triage car. This is to ensure that risk assessments are carried out before MHPs arrive at the scene, as police have a duty of care towards colleagues who have not had the same degree of training in conflict management, and who do not have the clothing and/or equipment to manage such situations. The studies covered a number of areas across England including parts of Derbyshire, Essex, Northumberland, Tyne and Wear, Norfolk, Suffolk, Sussex, Thames Valley and the West Midlands.
Telephone support alone (one study)
A model in which telephone support was provided by a MHP from a police control room was employed by the British Transport Police (BTP) service, which covers large parts of England across many health trust and police service boundaries. 9 The study by Jenkins et al. 44 compared the joint on-scene response of MHP and police officers in Ipswich, Suffolk, with telephone support only from a mental health nurse in Norwich, Norfolk.
Joint on-scene response and telephone support (one study)
A dissertation by Brace49 evaluated a street triage scheme in England (area not reported) that consisted of a MHP working in the police control room as well as a joint MHP and police officer on-scene response, both overnight. The aim was to provide an out-of-hours service because during office hours a service is provided by police officers and the mental health crisis team.
Telephone advice to on-scene officers and attend if necessary (two studies)
Two studies9,50 used this model of intervention in which MHPs did not routinely attend incidents but were available to do so if required. One study, covering part of Northamptonshire, was not clearly reported in terms of the intervention but appeared to involve police officers, a MHP and control room staff over certain periods of operation each week (details not reported). 50 The other study covered parts of Devon and Cornwall, where the MHP was based in the control room, and also the area covered by the Metropolitan Police Service, where the MHP was based in a mental health trust. 9
Telephone and/or on-scene response without police presence (one study)
A telephone and/or on-scene response without police presence was reported in two pilot evaluations. MHPs were situated in a local hospital (North Yorkshire) or a Crisis Assessment Service (West Yorkshire). 9
Training programme for police officers (one study)
The RCT by Scantlebury et al. 47 evaluated a training programme conducted in North Yorkshire that was aimed at front-line police officers who come into contact with people with mental health problems. A qualified and experienced MHP delivered the 1-day face-to-face mental health training in addition to routine police training.
Mental health triage providers and users
There was a lack of information regarding participant characteristics.
Brace49 reported service providers as police officers with the rank of Constable or Sergeant, who had regular interactions with people in a mental health crisis. The remaining studies did not report any details of service providers of street triage interventions. 9,43–46,50
Data on service user characteristics were similarly limited. Reveruzzi and Pilling9 reported the age of service users who came into contact with street triage teams in pilot areas across England, with 29% of service users aged between 18 and 30 years, and over half (52%) of service users aged between 30 and 65 years. Jenkins et al. 44 reported no significant differences between service users for age or gender before or after a street triage intervention, and that most service users were of a white British background. The remaining studies did not report any data on service users who came into contact with street triage teams. 43,45,46,49,50
Three studies reported some limited population data about areas of operations of the street triage schemes that were largely figures often gathered from National Census data. 9,43,44
The RCT on the training of officers reported trainers as qualified and experienced MHPs and trainees as front-line officers of the rank of Constable, Sergeant, Inspector and Police Community Support Officers. 47,48
Outcomes
Outcomes varied widely across the included primary studies. Very few outcomes were evaluated using concurrent comparative data. Most outcomes were collected at an organisational or service level. All authors reported using routinely collected data from police and health trust records.
Outcomes included:
-
national trends across England
-
numbers and rates of S136 detentions
-
number of assessments taking place in police stations
-
number of assessments/detentions taking place in hospital
-
number of admissions to hospital as a result of S136 assessment
-
contact with community mental health teams or follow-up services
-
costs.
The RCT of a bespoke training programme for police officers reported on:
-
the number of incidents reported to a control room resulting in a police response
-
the likelihood of incidents having a mental health tag applied (i.e. a tag applied by police officers to indicate that mental health is a factor in an incident)
-
the number of individuals with a mental health warning marker involved in any incident with a police response (i.e. a marker applied by police officers to an individual’s record to indicate they have mental health problems).
Many studies recorded the above outcomes during the period of the street triage interventions but without any concurrent comparative data.
Quality assessment of the primary studies
The RCT by Scantlebury et al. 47,48 was rated as having a low risk of bias for most criteria. However, there may have been the potential for some contamination between intervention and control sites, and it was unclear whether or not incomplete outcome data were adequately addressed. Details are provided in Table 6.
| First author, year, reference | Was the allocation sequence adequately generated? | Was the allocation adequately concealed? | Were baseline outcome measurements similar? | Were baseline characteristics similar? | Were incomplete outcome data adequately addressed? | Was knowledge of the allocated interventions adequately prevented during the study? | Was the study adequately protected against contamination? | Was the study free from selective outcome reporting? | Was the study free from other risks of bias? |
|---|---|---|---|---|---|---|---|---|---|
| Scantlebury et al. 201747,48 | Low | Low | Low | Low | Unclear | Low | Unclear | Low | Low |
The remaining primary studies were at risk of multiple biases because of their designs and a lack of reporting of methods, which undermined the reliability of their findings. A summary of individual study methods is reported below.
The study by Heslin et al. 43 used routinely collected data on S136 detentions before and after a street triage intervention. A number of the data were available only for 4 months, so authors extrapolated these data for the 6-month evaluation period; a cost-offset analysis was also conducted.
Jenkins et al. 44 compared two separate models of street triage in different areas using routine data from police and health trust records, collected retrospectively at time points before and after each intervention.
The study by Keown et al. 45 used routine data collected retrospectively from police and health trust records before and after a street triage intervention.
A report by Reveruzzi and Pilling9 collected data across nine pilot areas of street triage in England. Data were collected prospectively across all areas by either police or health staff, depending on the area. However, data were not collected consistently across the pilot areas. The only comparative data provided were for S136 detentions, for which there was a high proportion of missing data in some areas.
A report by Senker and Scott46 was a single-group evaluation of both a pilot period and a full street triage service. It is unclear whether data were collected prospectively or retrospectively. The only comparative data reported were for the cost–benefit analysis.
One report50 and a dissertation49 provided no comparative data at all and are not included in the synthesis of findings.
Findings from the primary studies
To be able to answer the research question regarding the evidence of the effectiveness of the PRMHT models, we focused on comparative data. Two studies provided a ‘snapshot’ of the schemes, with only cross-sectional data collected during the operation of a scheme or pilot study, with no comparison data from before the intervention or from another model. 49,50 Although these data are interesting, it is not possible to determine the effectiveness of the interventions they describe. These studies are, therefore, not included in the findings below.
The text below summarises the findings of the primary studies. Appendix 8 provides further details.
Number and rates of section 136 detentions under the Mental Health Act 1983 (four studies)
It should be noted that some authors indicated that these data were gathered at the incident level, not the individual level. Therefore, one individual may have received more than one S136 detention.
Reveruzzi and Pilling9 evaluated the nine pilot areas of various models of street triage implemented in England. Street triage schemes in the West Midlands, Derbyshire and Thames Valley (all joint co-response schemes) saw the largest reductions in S136 detentions, with decreases of 27.5%, 25.3% and 22.7%, respectively. Significant reductions in S136 detentions were also found in West Yorkshire of 19.8% (MHP telephone and/or on-scene response without police presence), in Sussex of 18.3% (joint on-scene co-response scheme) and in Devon and Cornwall of 15.5% (MHP telephone advice to on-scene officers). The Metropolitan Police Service (MHP telephone advice to officers and attend if necessary) and North Yorkshire (MHP telephone and/or on-scene response without police presence) increased S136 detentions by 15.1% and 19.4%, respectively. BTP (MHP telephone support only) results were not included in these figures.
There were significantly fewer S136 detentions after the introduction of the street triage intervention (joint on-scene co-response) in Eastbourne and Sussex than before the intervention. 43 However, the authors noted that in only 6% of cases people were detained under S136 by street triage teams, whereas the remaining cases were made by officers during shifts when the street triage team was unavailable. The authors also noted that across the rest of Sussex S136 detentions increased, although this was not statistically significant. This study evaluates the area of Eastbourne, an area that was also included in Reveruzzi and Pilling9 as reported above, although some figures differ. This may be because each study referred to different years of census data to calculate some findings.
Two street triage schemes were compared by Jenkins et al. 44 The team in Ipswich, Suffolk, was a joint on-scene co-response team intervention, compared with a MHP telephone support-only scheme in Norwich, Norfolk. 44 Over the total evaluation time period (pre and post intervention), the telephone support team had statistically significantly fewer S136 assessments per 100,000 people than the joint on-scene co-response team (p = 0.01). The difference was statistically significantly greater between the areas in the pre-intervention period (p < 0.01). Post intervention there was a small, non-significant increase in those detained under S136 in the telephone support-only area but a large reduction in S136 assessments in the co-response team area (p = 0.01).
There was a 60% reduction in the rate of S136 detentions in the first year of a street triage scheme (joint on-scene co-response) reported by Keown et al. 45 in areas of Northumberland, Tyne and Wear. The greater the rate of street triage in an area, the greater the reduction in the rate of S136 detentions in the same area (p = 0.003). Data across three of the areas (Gateshead, South Tyneside and Sunderland) that first introduced a street triage scheme showed a statistically significant progressive reduction in the number of S136 detentions during each subsequent 3-month period in the first year of the street triage scheme compared with the previous year. This resulted in a 65% reduction in the first 3 months, 73% reduction at 6 months, 83% reduction at 9 months and 88% reduction at 12 months (p = 0.001). Additional data for Sunderland were available and authors reported a 78% average monthly reduction in S136 assessments following the introduction of street triage.
Number of assessments/detentions taking place in police stations (two studies)
Keown et al. 45 reported that only a small number of assessments were conducted in police stations both before and after the introduction of a street triage scheme (joint on-scene co-response) in one area of the intervention (Sunderland).
In Eastbourne, Sussex, there were significantly fewer detentions in custody after the introduction of a street triage (joint on-scene co-response) than the usual response before street triage (p < 0.05), as reported by Heslin et al. 43 Although because the street triage hours of operation were limited, a number of the detentions in custody during this period were by usual response.
Number of assessments in hospital (one study)
Keown et al. 45 reported that most S136 assessments were conducted in a dedicated S136 suite in a psychiatric hospital in Sunderland (just one area reported in the study), as they had been before the introduction of a street triage scheme (joint on-scene response). There were also no significant changes in the proportion of individuals detained in hospital, voluntarily admitted or with no admission after the intervention.
Detentions taking place in hospital (one study)
There were fewer detentions in hospital after the introduction of a street triage scheme (joint co-response) in Eastbourne, Sussex (reported in Heslin et al. 43), than before the intervention, but this difference was not statistically significant. Across the rest of the county, the number of people detained in hospital increased but this was not statistically significant. As reported above, because the street triage hours of operation were limited, a number of the detentions during this period were by usual response.
Number of admissions to hospital as a result of a section 136 assessment (one study)
There were no significant differences in admissions to hospital following S136 assessment reported in Jenkins et al. 44 before the introduction of street triage schemes in Ipswich, Suffolk, and Norwich, Norfolk. After the implementation of street triage, there was a statistically significant higher conversion to admissions for a joint on-scene co-response in Ipswich than pre intervention (p = 0.01), but there were no significant differences for admissions before and after the telephone support-only scheme in Norwich. After the interventions, there was also a significantly higher admission rate following S136 assessment in Ipswich than in Norwich (p = 0.04).
The same study also reported that the proportion of individuals who were not admitted to hospital following a S136 assessment but had at least one subsequent S136 assessment in the following 4 weeks decreased in both street triage schemes, but the decrease was only statistically significant for the telephone support-only scheme in Norwich (p = 0.01 vs. p = 0.14). The authors reported that there were more individuals in Norwich who had some contact with community mental health services in the 2 weeks prior to a S136 assessment than there were in Ipswich, and that there were more individuals in Norwich who had some contact with community mental health services before the introduction of a street triage intervention as opposed to after this introduction than there were in Ipswich (p = 0.01). Whereas, in Ipswich, there were no statistically significant differences between contact before or after the street triage intervention. There was also no evidence to suggest that individuals assessed in Ipswich were more likely to have been deemed to have ‘no mental illness’44 before the introduction of street triage than after, but in Norwich there was evidence to the contrary (p < 0.01).
Contact with community mental health teams or follow-up services (one study)
There was some evidence in Jenkins et al. 44 to suggest that if people in Ipswich were not admitted to hospital, they were more likely to be offered follow-up from secondary mental health services after the introduction of a street triage scheme (joint on-scene co-response) than before the intervention (p = 0.04). If follow-up was offered in Ipswich, there was evidence to suggest that the first follow-up appointment was more likely to be kept after the street triage scheme than before (p < 0.01). In Norwich, evidence from the street triage scheme (telephone support only) suggested that a person was more likely to be offered a follow-up before as opposed to after the intervention (p = 0.02), but there was no evidence of any difference between compliance rates before or after street triage implementation.
Costs (two studies)
Senker and Scott46 reported costs of a street triage scheme that had both a joint on-scene response unit and MHP telephone support in Essex. The authors reported potential annual benefits from street triage preventing the use of S136 and the wider impact of its use. These potential annual benefits included gross realisable savings for NHS trusts or Clinical Commissioning Groups of £347,200, with benefit to the value of £99,650 for the Essex police force in terms of reduced use of custody and reduced officer time attending S136 incidents, which realised a gross benefit value estimate of £446,850 and a net benefit of £179,758 when accounting for costs of running the street triage scheme.
Over the period of a street triage (joint on-scene co-response) evaluation of 26 weeks in Eastbourne by Heslin et al. ,43 the total cost of the scheme was estimated to be £148,785. The street triage team attended a total of 233 incidents, giving an estimated unit cost of £630 per incident attended.
The study calculated average costs to payers resulting in £1043 per person for street triage and £1077 for usual response; CJS: £470 for street triage and £559 for usual response (representing a cost saving of £31,862 over a 6-month period); and NHS: £574 for street triage and £517 for usual response (an additional cost of £20,406 over a 6-month period to the NHS for the street triage arm).
Other outcomes (one study)
After a 1-day bespoke training programme for front-line officers, Scantlebury47,48 reported that there were no significant differences in the number of incidents requiring a police response between those police stations receiving officer training and those police stations that did not. There was also no significant difference between the intervention and control arm stations in the number of people with mental health warning markers on their record. However, there was evidence that incidents at stations randomised to the intervention arm were more likely to have a mental health tag (applied by officers to indicate that mental health is a factor in an incident) applied than incidents assigned to control arm stations (p = 0.001).
Metasynthesis
Which models have been described in the literature?
Models described in the systematic reviews:
-
pre-arrest diversion models (which include CIT)
-
co-response and/or consultation models (which include street triage)
-
service integration models (which include multiagency integrated services).
Models described in the primary studies:
-
pre-arrest diversion –
-
MHPs delivering a 1-day bespoke training programme for front-line officers.
-
-
co-response and/or consultation models often described as street triage –
-
MHP joint on-scene co-response with police officers
-
MHP telephone support alone for on-scene police officers
-
MHP telephone support plus on-scene co-response with police officers
-
MHP telephone support and attending scene only if necessary
-
MHP telephone and/or on-scene response without police presence.
-
What evidence is there on the effectiveness of these models?
There was a paucity of evidence on the effectiveness of PRMHT interventions from the included systematic reviews. Most of the outcomes were at an organisational or service level, with many of the data relating to S136 assessments or detentions. Overall, reductions in formal detentions and an increase in the use of HBPOS were reported, but results for other outcomes were mixed. Most of these results were based on the findings of just one or two primary studies of unknown or poor quality.
Review authors reported that few studies were of robust design, many were uncontrolled single-group studies often using retrospective, routinely collected data. Very few details of the context or content of the interventions were reported. Service users were described only generically. Authors of all of the reviews acknowledge the lack of robustness in much of the available evidence and have provided recommendations for future research.
Much of the evidence in the most recent primary studies relates to the MHP joint on-scene co-response with police officers. Although there were several reported reductions in S136 detentions, fewer detentions in hospital, higher admission rates and greater likelihood of being followed up by secondary mental health services (if not admitted), these results were not always consistent. Evidence on costs is limited and somewhat contradictory in relation to the possibility of costs shifting between agencies. However, these findings were largely from one or two studies with major methodological limitations that preclude strong inferences being drawn.
Few studies reported comparative data, making it difficult to determine the relative effectiveness of different models of PRMHT against each other or against usual practice.
Recommendations for research
Authors’ recommendations from the systematic reviews:
-
Higher-quality evaluations are needed and should use self-report and official measures. 40
-
Future evaluations should target health-related outcomes and have an impact on key stakeholders. 14
-
Further build evidence to refine and develop integrated interventions. 11,12
-
Longer-term follow-up of training programmes is needed, as is better-quality research evaluating training for UK police officers. 39
Authors’ recommendations from the primary studies:
-
Evaluate outcomes of street triage contacts and whether or not the schemes lead to improved patient outcomes, and delineate when street triage is the best option and when S136 might be a preferred pathway. 45
-
Examine findings using a wider range of data, preferably prospective studies. 45
-
Data-recording procedures should be reviewed and streamlined with clear expectations and accountabilities for all parties. 50
-
Data should be collected on mental health and quality-of-life outcomes, including quality-adjusted life-years, to enable full assessment of cost-effectiveness and cost–utility of street triage. 43
-
Capture data on the number and proportion of incidents that do not result in a detention under S136. 43
-
Capture feedback from relevant professionals and individuals to enable a fuller understanding of the impact of the service. 44
Chapter 5 Rapid evidence synthesis of UK-relevant qualitative data
Volume of included evidence
A total of 34 publications including qualitative evidence on PRMHT interventions were identified. Of these, nine publications related to interventions that were implemented in the UK. 9,41,42,46,50–53 The characteristics of studies reporting non-UK qualitative data are presented in Appendix 9.
One publication was a 2016 report commissioned by NHS England (Reveruzzi and Pilling)9 that evaluated the nine street triage pilots originally funded by the DHSC in 2013. The remaining eight publications provided qualitative data on seven interventions, two of which51,52 were included in the Reveruzzi and Pilling9 report, and a further six publications provided qualitative data on five interventions which were not included. 41,42,46,50,53
Themes from UK-relevant qualitative data
The rapid evidence synthesis presented here expands the themes and findings from Reveruzzi and Pilling’s9 evaluation of DHSC-funded pilots to incorporate the five additional UK interventions. These themes were:
-
organisational objectives
-
assessment and identification of service user needs
-
pathways through the care system
-
care co-ordination and effective interagency working
-
quality of care provided
-
attitudes to service users with mental health problems
-
availability of resources
-
staff support, supervision and training needs.
Quality and methods of included qualitative studies
Table 7 summarises a brief CASP checklist evaluation for each study reporting UK qualitative data.
| CASP checklist questions | Study | |||||
|---|---|---|---|---|---|---|
| Callender and Cole50 | Dyer et al.41 | Edmondson and Cummins42 | Horspool et al.53 | Reveruzzi and Pilling9 | Senker and Scott46 | |
| 1. Was there a clear statement of the aims of the research? | Y | Y | Y | Y | Y | Y |
| 2. Is a qualitative methodology appropriate? | Y | Y | Y | Y | Y | Y |
| 3. Was the research design appropriate to address the aims of the research? | Y | Y | Y | Y | Y | Y |
| 4. Was the recruitment strategy appropriate to the aims of the research? | Y | C | Y | Y | C | Y |
| 5. Was the data collected in a way that addressed the research issue? | Y | Y | Y | Y | Y | Y |
| 6. Has the relationship between researcher and participants been adequately considered? | N | N | C | C | N | N |
| 7. Have ethical issues been taken into consideration? | Y | C | Y | Y | C | C |
| 8. Was the data analysis sufficiently rigorous? | C | C | Y | Y | C | C |
| 9. Is there a clear statement of findings? | Y | Y | Y | Y | Y | Y |
| 10. How valuable is the research? | a | b | c | d | e | f |
Reveruzzi and Pilling’s9 evaluation reviewed and synthesised qualitative data provided by pilot schemes in their individual reports. Each pilot scheme report provided data on the local experience of the services and presented a range of qualitative material, including comments received from service users, families, carers, community members, police officers, MHPs and senior colleagues. An inductive approach was used to identify codes and themes progressively throughout the analysis. The thematic framework developed by the NICE Service User Experience in Adult Mental Health: Improving the Experience of Care for People Using Adult NHS Mental Health Services guideline54 was adapted and used to index and organise all relevant themes and subthemes. Following initial analysis, the results were discussed with the research team and gaps were identified in the existing data in terms of understanding the implementation, objectives, outcomes and longevity of the pilot schemes from a senior organisational perspective. As a result, six additional senior stakeholder interviews, covering five schemes, were conducted with individuals directly involved with existing street triage schemes. A schema of questions was developed according to the set of themes identified in existing qualitative feedback; the results of these interviews were combined with qualitative data obtained from the pilot sites.
Six publications evaluated five further PRMHT schemes that were undertaken independently of the DHSC-funded pilot evaluations. These were conducted in Essex,46 Oldham,42 Northamptonshire,50 Cleveland41 and a service running PRMHT schemes in two unnamed locations. 53 These were published in 2014 and 2016; four were evaluation reports (ranging from 22 to 92 pages in length)41,42,46,50 and two were journal articles. 41,53 All the studies clearly stated their aims and collected data appropriate to those aims. However, the brevity of most reports meant that the collected data were rarely presented in detail, and few studies addressed concerns about reflexivity and rigour in the data collection and analysis procedures. Consequently, this synthesis relies on data and themes obtained from relatively few stakeholders, and the limited reporting of primary studies precludes a thorough interrogation of the underlying evidence.
Description of the intervention models and specific details
Full details of the nine pilots can be found in the 2016 evaluation report. 9 Very little detail was reported on intervention objectives and procedures from the schemes that were not part of the DHSC-funded pilot programme. However, what little information was available for all included interventions is presented in Table 8. Although there was considerable variation in how the interventions were implemented in different regions, they could be broadly classified as co-response models, consultation models or a combination of the two. More specifically, interventions could be described in terms of the primary role and/or location of the MHPs. These were:
-
co-response models in which MHPs partnered with police officers to jointly attend incidents
-
telephone-support-only consultation models in which MHPs stationed in either police control rooms or hospital premises handled tasks, such as advising officers, consulting health records, undertaking liaison and referrals, and making follow-up calls to service users
-
predominantly telephone support with the option of joining police officers at incidents when necessary
-
telephone support and/or attending incidents without the presence of police officers when considered appropriate.
| MHP role | Region/programme name | Dedicated personnel | MHP location | Specific components |
|---|---|---|---|---|
| Joint on-scene response with police officers |
|
Police car |
|
|
| Telephone support alone |
|
|
|
|
| Telephone support to on-scene police officers and attend scene if necessary |
|
|
|
|
| Telephone and/or on-scene response without police presence |
|
|
|
Although these interventions were often referred to as street triage, in some models the dedicated MHP(s) were not deployed to the street. It was also apparent that triage-related decisions were sometimes made on private premises, which has important implications for the use of S136 (see the following section).
Thematic synthesis of UK qualitative data
The 2016 evaluation9 of the nine DHSC-funded pilots coded collected qualitative data according to eight identified themes:
-
organisational objectives
-
assessment and identification of service user needs
-
pathways through the care system
-
care co-ordination and effective interagency working
-
quality of care provided
-
attitudes to service users with mental health problems
-
availability of resources
-
staff support, supervision and training needs.
The results of each theme from the DHSC-funded pilots’ evaluation are summarised below, incorporating additional published qualitative data from the additional UK interventions identified during the current rapid evidence synthesis. Studies were inductively coded to identify subthemes that emerged within the eight original themes.
Organisational objectives
Section 136 rates and related objectives
The primary objective of most PRMHT interventions was to reduce the number of S136 detentions during which police custody was used as a place of safety, with the ultimate aim of reducing demands on the police service. 9,50 Strong partnerships between police and health services were seen as crucial to achieving this objective, with co-location being described as one means of building trust, confidence and understanding within teams. 9 The authors of the Northampton evaluation noted that other objectives held by individuals and their respective organisations could relate to service quality, longer-term resolution and reduction of ‘regular callers’. 50
Shared information
A highly valued core characteristic of PRMHT interventions among police and MHPs was the ability to share information. This was seen to inform and improve the professional judgements of both police and mental health staff, thereby reducing reliance on S136. 9,42,50 When S136 was used, access to information via telephone facilitated discussions about the preferred and appropriate place of safety. 42
Role and location of mental health professionals
The most notable difference in terms of the service delivery model between the evaluated PRMHT interventions was the role and/or location of the MHP(s). In one study, opinions about how best to utilise mental health staff varied. Among control room staff, deployment with the mental health car was seen as being more closely linked with a successful resolution of the incident:
I’d like to see a bit more, I don’t know, resolution involved. ‘Cause it’s fine giving advice, I must admit I’d like to see them out more, deploy more.
However, opinions among mental health staff were somewhat more varied. Some commented on how they would deploy to ‘see what they could do’; others saw their role as being more beneficial in the control room, where they have access to patient records and can advise officers on-scene. 50
Challenges of and barriers to the delivery of organisational objectives
Challenges and barriers identified in the DHSC-funded pilots included clarifying the purpose of the scheme, educating local services about its function and clarifying police officers’ role in private premises. 9 Although some schemes were characterised as street triage, many call-outs were to people who were not in a public place. This raised issues about the limits set to police power under S136, particularly when people were in their own homes and would not come voluntarily to hospital. 46 Police officers considered it important that health professionals involved in PRMHT interventions are made aware of these limits. Conversely, concerns have been raised that control room staff may fail to request a PRMHT team to attend incidents in the home if the intervention had been promoted to them purely in terms of street triage. 46
Barriers to evaluation against organisational objectives
A challenge to showing whether or not objectives had been met was collecting evidence on the impact of interventions beyond S136 rates or other simple measures. Even when data sets were predefined, a lack of administration funds meant that data collection was often incomplete9 or inaccurate. 50 In another study, the mechanisms to identify measurable impact were suggested to be inefficient and tiring. 50
Assessment and identification of service user needs
Immediate access to accurate health information
Police officers considered the ability to have immediate access to relevant information vital to making judgements about risk and potential courses of action. 9 Information that mental health staff could provide from NHS systems [e.g. SystmOne (The Phoenix Partnership, Leeds, UK)] was seen as informing the dynamics of risk (e.g. the meaning and implications of specific mental illnesses within the context of an incident). 50 Officers expressed greater confidence in decision-making as a result of being offered immediate reliable information, including summaries about an individual’s current circumstances, information on access to services and care planning, guidance and advice on options and alternatives available on the day, and advice about how to proceed. 42 In one co-response scheme, MHPs felt pressure from control rooms to attend incidents first and a relative discomfort at this as it limited the amount of information they could ascertain before they arrived. 46
Beneficial role of mental health professionals in user needs assessment
The involvement of a PRMHT team helped better identify the needs of service users and improve access to care, perhaps especially when decisions were not straightforward. 9 In one study, MHPs described how their familiarity and knowledge of mental health conditions meant that their judgements differed from those of police officers, particularly in terms of risk. In such cases, officers often assessed an individual to be a higher risk than did the MHPs. 50 A by-product of this approach was a sharing of knowledge about mental health with individual officers, which varied according to the officers’ levels of engagement and interest. 50 Another study gave the example of someone threatening suicide as historically being enough for officers to use S136, because of a lack of alternatives and an emphasis on being risk-averse. 46 Officers involved in this co-response intervention reported feeling uncomfortable leaving someone alone if they were threatening self-harm or suicide, but also that they had historically been ‘overcautious’ when using the power to section, resulting in it being used too frequently. 46
Other perceived benefits of involving PRMHT teams in user needs assessments included increased time efficiency by freeing up other response officers while the PRMHT team dealt with mental health-specific issues (although this would not apply to forces where police officers retain ownership of an incident until its resolution), and increased knowledge and confidence regarding their available options. 9 Some health staff felt that, in their absence, police officers would still be likely to use S136 to ensure quicker assessment. 9
Service user feedback on needs assessment
Very little service user feedback was available across the studies. When this was reported in relation to the assessment of user needs, opinions were mixed. Although some service users expressed problems around communication (e.g. difficulties understanding the nurse or being told the same things that they had heard in the past – that no immediate help was available),9 some people who had previously been sectioned found the experience of street triage to be consistently better. 46 Some individuals felt reassured and calmed by the nurse’s presence and appreciated the fact that the incident was often resolved in their own home without having to go to hospital or be held in custody. 46
Identifying needs of new and repeat service users
Police-related mental health triage interventions raised implications for identifying the needs of both new and repeat service users. In some cases, street triage led to individuals being identified in the community who had previously not had input from services. 46 Elsewhere, the demand on the control room caused by regular callers and missing persons was a continual cause of frustration, with the operation failing to resolve repeat cases. 50 Although MHPs did report ongoing work with these individuals (demonstrating a willingness to develop a longer-term relationship with service users), this was done beyond the bounds of the operation. 50 One telephone-based scheme deliberately identified individuals who frequently came into contact with services via the police in order to inform interagency responses and risk planning. When utilised effectively, this appeared to reduce re-presentation and significantly support more effective management of police time and resources. 42 One co-response scheme developed a dedicated ‘Integrated Recovery Programme’ to address the high demand created by frequent service users who would regularly call the police and mental health services for support. 53
Pathways through the care system
Establishing links with other relevant services
Positive changes in pathways to care were often reported. 9 This included better police links with home treatment or crisis teams. 9 The facilitation of a wider range of pathways to emergent incidents was considered critical to reducing the number of S136 arrests that are used unnecessarily:50
It’s about opening up the pathways and the communication and liaison between various services in support of each other, really, for the best of the client to ensure that pathway is timely and consistent.
MHP.
Crisis teams’ fears of a deluge of potentially inappropriate calls were not realised, as better officer understanding meant that calls were appropriate. 9 Other perceived improvements to pathways included follow-up of referrals where none had previously existed and better pathways for people who are unengaged or unknown to services. 9
However, where crisis teams were the services originally responsible for responding to crisis situations, including calls from the police, the introduction of street triage could initially create confusion about the roles and responsibilities within the available pathways:
. . . and the police brought a gentleman . . . if you self-present, it’s like you see the crisis team but because the police had brought . . . the crisis team asked us . . . there’s nothing set in stone that because the police have brought him it has to be street triage. He’d actually self-presented and wanted to come here to see the crisis team because he thought he was in psychiatric crisis but [street triage] assessed him.
Street triage staff.
Barriers to accessing other relevant services
Some views identified systemic barriers to desired outcomes because of factors that lay outside the PRMHT interventions. Owing to long waiting times, referrals did not necessarily mean that service users received the intended mental health care or treatment, so there was a limit to what the mental health workers could guarantee the patient would receive. 53 Examples were given of some patients still getting ‘stuck’ at A&E and then being sent home after a long wait. 46 PRMHT referrals also had the potential to cause an increased workload for other services. 53
Wider strategic considerations around the role of police in mental health-care pathways
Senior staff alluded to strategic considerations around sustainability and longevity. 9 The existing PRMHT arrangements were sometimes referred to as a ‘short-term fix’ or ‘sticking plaster’. 9 Some police officers believed that they personally should be bypassed whenever possible when incidents are clearly health related. 9 One police manager described a long-term aim of moving to a situation when a police response is only required in the presence of immediate safety concerns for a client or the public:53
So one of the objectives of [project name], is the long term, almost a generational piece of work, to actually place mental health risk, mental health responsibility, back into the NHS, because it has never been in the NHS, because culturally the wider thing is the police in the UK scoop up everything.
05, police, manager, location 1.
One strategic mental health police lead described their aim of moulding ‘a single acute care pathway’ that takes account of L&D, triage, rapid assessment, intervention and discharge within a primary care health setting, while also looking at the S136 and S135 processes. 9
Pathways for intoxicated individuals present a recurring issue in one study, with there being some deliberation as to the best place to support such individuals. 46
Care co-ordination and effective interagency working
Benefits of interagency co-ordination
The most commonly reported themes related to perceived improvements in care planning, co-ordination and effective interagency relationships. 9 Stakeholders in one scheme perceived that collaborative working at operational and managerial levels led to an improved understanding between the different organisations by dispelling misconceptions and building rapport between operational staff. 53 Police officers in another scheme reflected that access to telephone support had improved mutual respect between police and psychiatric health staff, and increased reciprocal awareness of each other’s professional knowledge, skills and work pressures. 42
The combination of police and MHPs within other schemes was viewed as being complementary, and enabled police to utilise different options to achieve positive incident outcomes when they may previously have exercised S136 powers. 50,53 In one study, police officers were perceived to be less risk-averse when decision-making was shared,53 although, in another, officers felt that the responsibility for S136 cases was not fully shared, and despite taking the advice of the nurse, officers still felt that their ‘neck is on the line’, which can make them reluctant to not use S136. 46 Nurses, nevertheless, reported improved partnership working with police and more appropriate use of S136. 46
In one telephone support scheme, when S136 was initiated, handovers from police to health professionals were seen to be improved in terms of risk and potential harm, being better managed with assessments completed more speedily. 42
Other perceived benefits of improved interagency working included improved responsiveness from hospitals when MHPs were involved,9 and triage nurses gaining a better understanding of the limits to police powers. 9 The presence of MHPs was also thought to help calm situations when problems arose around police uniforms. 9 It was recognised that mental health staff were perceived less confrontationally than police officers by people in need; the fluorescent jackets and stab vests worn by officers were viewed as both presenting a physical barrier and heightening anxiety within certain situations. 50
Staffing and co-ordinated working
Staffing of the schemes was mentioned in terms of both facilitators of and barriers to successful implementation. In one case, it was strongly indicated that more consistent staffing arrangements would be welcomed, as it was recognised that staffing of the operation was irregular from both police and mental health perspectives. 50 Consistent staffing on this scheme was considered to enable the formation of stronger relationships and result in better outcomes for individuals in need. 50 Conversely, inconsistent staffing arrangements resulted in less effective utilisation of time, as expressed by police officers not knowing what to do or how to add value within the control room during quiet periods. This was equally the case during incidents when an assessment was being completed. 50 The benefits of consistent staffing may be linked to the extent of police staff enthusiasm for mental health-related work, with clinicians in one scheme reporting a qualitative difference between officers who were motivated to learn about mental health and those who were attracted to the scheme as a result of overtime payments (which led to the police officer sometimes acting simply as a ‘chauffeur’). 46 One study noted that a minority of police colleagues felt that mental health should be the responsibility of the health service. Thus, a less enthusiastic response from some officers may pose challenges to the implementation of PRMHT services. 53
Information shared by police and health colleagues
Again, police officers noted the sharing of information as a key component of effective interagency working, increasing their confidence and knowledge around mental health-related incidents and awareness of appropriate outcomes for users. 9 Officers in one study said that although the provision of advice and information from MHPs might simply be seen as a ‘nice-to-have’ resource, it was actually recognised to potentially make ‘the difference between life and death’ within certain incidents. 50 Elsewhere, the ability of police and nurses to work together when presented with someone in distress was said to facilitate the ‘bigger picture’, ensuring that more accurate decisions were made around risk. Police could provide information on an individual’s offending history, risk of assault and use of weapons, while the nurse could provide information around medication, diagnosis and care plans. 46 Police officers have expressed confidence and gratitude in receiving support from triage nurses. 9
In one case, managerial staff highlighted how the establishment of a co-response scheme had initiated a review of local agreements related to collaborative working with MHPs, police and emergency care. This led to improvements, such as a new information-sharing agreement that clarified the types of information that could be shared, and enhanced access to information that was felt to improve police decision-making, both during and outside street triage hours. 53
Barriers to effective interagency working
A number of challenges around joint working were also raised. Although police officers expressed a respect for the judgements of mental health staff, there was confusion (and sometimes tension) in relation to the decision-making processes around deployment. This was heightened when resources were scarce on the ground and control room staff saw the car/team as a deployable resource. 50 One study noted occasional disagreements about the most appropriate place of safety, which significantly impeded and delayed the progress of assessments and ultimately the resolution of incidents. This seemed particularly the case when alcohol, drugs and/or risk of violent behaviour were significant, and there was disagreement about the level of risk presented and the appropriate setting for a person to be located at. 42
One study raised the importance of establishing lines of accountability and responsibility for such decision-making. For instance, it is critical to consider who holds responsibility for the shared decision to withdraw officers from the scene of an incident (i.e. taking no further action) in which a person expressing suicidal thoughts then goes on to commit suicide. This type of dilemma directly relates to the gap in police powers between S135 and S136, an unplanned detention of an individual to a place of safety. 50 Officers in one study felt more comfortable leaving an individual threatening self-harm or suicide if the nurse had conducted their assessment and felt that it was safe to do so. 46
Poor co-ordination between external organisations was a noted challenge. For example, a ‘lack of join up’ between different NHS trusts led to delays in both patient care and the release of officers from incidents. 9 In one scheme, police service boundaries encompassed many NHS trusts and police officers would need to identify which NHS trust was responsible for care when responding to a mental health incident. 53 Staff on one scheme noted the difficulty of maintaining a complex set of inter- and intra-agency relationships, including those with police officers and mental health service providers in the voluntary and statutory sectors, as well as managing their own internal networks. 50
Quality of care provided
Positive effects on quality of care
Police, health staff and service users all noted an improvement in the quality of care with PHMRT schemes. 9 Participants in one study frequently emphasised the importance of the scheme in delivering a better-quality service to people in need, rather than simply freeing up resources. 50 It was felt that individuals in need responded more positively to MHPs on the ground, with the MHPs’ communication skills being critical to the positive resolution of specific incidents. 50
Elsewhere, the positive impact on service users was acknowledged by police officers:
. . . when the street triage team go, they get a better service. Certainly get better handling . . . wherever the person is at a time of crisis, and threatening to harm themselves, saying, I want to hang myself . . . I just want to kill myself, leave me alone . . . then giving them a bit of a brief intervention, talking to them, and making arrangements for them, their care, moving forward, to speak to their family has to be a good thing. For a mental health professional to be able to do that is fantastic because that person then does not go into detention, they do not end up in police cell or a hospital where they don’t want to be . . . whereas the police couldn’t make those sorts of judgement calls, so the service user often ends up in custody at the police station.
Police officer,
Officers noted that an asset of one telephone-based service was the ability, when appropriate, to pass their mobile phone to the person who was the subject of the call so that they could talk to the MHP. 42 This was considered to have the following advantages:
-
The distressed person could immediately speak with a trained MHP, which tended to calm situations.
-
It demonstrated that the police officers were taking seriously both the person’s views and the difficulty of their circumstances.
-
Police officers were seen as more welfare focused.
-
Officers felt that they were more frequently trusted and that any proposed plans to take people to hospital were seen to be more believable. 42
Police-related mental health triage schemes were seen as generating a positive cultural change that has benefited users. 9 One officer said that they would never previously have taken people home as they would have lost S136 powers on entering the premises, thereby potentially losing what had been seen as ‘the safest option’. 9
An additional consequence of more contacts in private dwellings was that individuals’ families were more frequently included in the care pathway, instead of people being isolated. 9 In particular, this was observed in the de-escalation of domestic situations, leading to fewer young people being seen in custody. 9 The involvement of PRMHT was reported as reassuring for family or friends who were often at the scene, which was predominantly the service user’s home. 46
Reports on the DHSC-funded schemes noted fewer S136 assessments presenting in hospitals. 9 PRMHT nurses reported that this helps prevent service users from feeling criminalised for their mental health problem. Service users in one study felt reassured and calmed by the nurse’s presence and appreciated the fact that the incident was often resolved in their own home, without having to go to hospital or be held in custody. 46 When issues could not be resolved in the home, other service users expressed relief at being taken to hospital instead of police custody, as this was less shameful. 9
Service users generally (although not universally) commented that follow-up calls were valued. 9
Attitudes to service users with mental health problems
Service users expressed negative experiences of being detained in police cells, with one person describing feeling degraded by having had to strip and change clothing. 9 Some service users felt that the police needed to work on building trust,9 for example by ‘speaking the same language’ and not asking for personal details. 9 Some service users also held negative views towards authority. This point was echoed by police officers, who particularly noted the impact of arriving in police uniform as a barrier. 9 In one study, police officers reported how competent mental health staff were when communicating with service users, striking a balance between empathy and assertiveness in resolving incidents. 50
Availability of resources
Resource savings
One study42 noted resource savings from a telephone support-based PRMHT intervention, with officers reporting that it had saved police time when responding to and dealing with calls when mental health challenges were present. This was particularly the case when an individual required hospital assistance. Prior to the PRMHT scheme, when S136 was used to remove someone to a designated place of safety (typically an A&E department), officers would have to wait a considerable amount of time until a medical doctor and a social worker were available to make an assessment and a decision. 42
Unused resource
Another study, in which a qualitative researcher shadowed a co-response team, reported some apparent ‘down-time’ between jobs, alongside occasional long journeys to attend incidents. 46 The presence or absence of such factors would need to be considered when planning for efficient PRMHT resource use. However, it was noted in the same study that individuals did not seem to mind waiting some time to be seen by the team. However, there were resource implications for the other officers on-scene who could not leave until the PRMHT team attended. 46
Availability of mental health professionals
Police officers in two studies41,42 noted the importance of MHPs being immediately available through the PRMHT scheme. In one, the services offered by a PRMHT co-response team were considered to be different from those offered by existing services, such as the crisis team, because nurses based with police officers were available to immediately respond (providing that they were on duty) to police requests for assistance. 41 The second study noted the particular importance of being able to call PRMHT telephone support in ‘real time’ at the scene of an incident (24 hours a day, 7 days a week). 42 Although there were occasions when officers did not access support because the line was engaged or not answered, this was generally the exception and became less frequent over the final period of the pilot. 42 A direct, dedicated PRMHT line was seen as a preferred route to bypass switchboards and non-emergency services and talk to a trained individual who had access to health records and quite often knew, or knew of, the person who was the subject of the call and could respond and advise quickly. 42
Police officers considered the unavailability of PRMHT staff to be a significant barrier to access and felt that additional resources were needed to ensure that staff are available to respond when needed. 9 There was some suggestion that the control room might be reluctant to deploy mental health staff to incidents because of the risk of them becoming unable to respond to other requests while deployed at the scene. 9
One study reported related concerns about staff availability and a perceived rise in the number of people driven to the hospital by police officers and left at the front desk. 41 Some police officers were suggested to have bypassed the PRMHT service when it was unavailable. Some police officers argued that it was easier and quicker to take a person directly to hospital if they agreed to attend on a voluntary basis, rather than wait for PRMHT staff to attend the scene; in other cases, the police officers disagreed with the advice given by the nurse. 41
Both police and health staff expressed disappointment at PRMHT services not being available around the clock. 9,41 A nurse noted the potential waste of resources in promoting a service that officers found not to be consistently available, leading to the risk that officers learn to ‘do without’ it. 9
Allocation of staff resources to police-related mental health triage teams
Some respondents raised concerns about the reallocation of staff resources to PRMHT from elsewhere. In one study,50 some police response officers felt that they were letting down their Incident Resolution Team (e.g. exposing their colleagues to a greater degree of risk) when deployed to PRMHT duties, rather than adding wider, systemic value. From the mental health perspective, it was indicated that, more recently, ‘bank staff’ were increasingly assigned to the operation. 50
When one co-response PRMHT service was adopted as ‘routine’, it was staffed by an officer from the regular shift. 53 Some interviewees felt that, at busy times, losing one officer from the shift compromised their ability to respond to incoming police incidents. 53 Managers were aware of this criticism but justified the decision with evidence suggesting that having one officer dedicated to mental health incidents would reduce the workload associated with mental health for other colleagues on the shift. 53 Health staff also raised concerns about competing demands when people were reallocated from existing mental health teams to PRMHT. 53 This was compounded by perceived additional demand created by PRMHT referrals. 53
Technological resource considerations
One of the DHSC-funded teams highlighted that it was crucial to develop a means of sharing electronic information on different information technology (IT) platforms or within a single shared IT platform. 9 One scheme developed models for effective record keeping and information exchange. 42 Another developed new information-sharing agreements,53 but there remained examples of incompatible technology hampering the expansion of the service. Police interviewees who proposed minimising police involvement in mental health response acknowledged that transferring this workload to health-based services would be challenging for technological reasons, such as incompatible computer systems and limitations in the call transfer systems (but the key challenge would be the absence of additional funding for mental health services to do this work). 53
Other technological considerations included the means of communication with remote mental health support. Police officers in one study expressed a preference for a dedicated mobile phone rather than contact via their radio sets. 42 This was because (1) the mobile phone could be passed to a service user if they needed to speak directly with the mental health practitioner, without having to share the officer’s personal radio earpiece, and (2) allowed officers to safely retain their radio set in case they urgently needed to call for assistance from colleagues. 42 However, some officers were unsure whether or not their use of personally owned mobile phones would be considered inappropriate and, in another scheme, limited local mobile signal coverage was reported as an occasional barrier to contact. 53 One study of a co-response model suggested that portable electronic devices might allow nurses to record notes between jobs, rather than doing this without pay after the end of a shift. 46
Staff support, supervision and training needs
Recruitment
Several respondents across the studies discussed recruitment considerations. One particular difficulty in this respect was recruitment delays caused by the strict police vetting process. 9 The procedures for recruitment to PRMHT teams were rarely reported, except for one pilot, in which a senior nurse, police officer and paramedic were all involved in appointing people to the relevant roles. 9
Both police and mental health respondents from one primarily telephone-based scheme said that they would welcome more consistent staffing arrangements, because irregular staffing adversely affected continuity. 50 However, it was acknowledged that a downside of this might be that the benefits for staff, in terms of increased knowledge between the organisations, might be more isolated to a core set of individuals. 50 Respondents in another study discussed the implications of making PRMHT involvement obligatory for all staff, expressing concern about a negative impact on motivation levels, while recognising the benefit of spreading knowledge about mental ill health more widely across the force. 46
In terms of personal characteristics, stakeholders in one PRMHT scheme described the police and mental health staff as compassionate and motivated individuals who work on the service and described these attributes as being important to the success of the service. 53
Learning and sharing of knowledge within police-related mental health triage teams
A number of comments around knowledge and learning were presented across the studies. In the case of co-response models, ongoing learning was developed through continual discussion and debriefing between the police officer and nurse sharing a response car for several hours. 9
Another study53 noted the importance of PRMHT mental health staff having appropriate knowledge of, and access to, existing mental health services (e.g. community-based mental health teams). This was more easily facilitated if the MHPs were familiar with services because they had worked with them previously.
One scheme9 began work on a joint training initiative to address confusion around the powers and procedures of both police and health organisations (e.g. the limits to police powers to detain to a place of safety when most face-to-face assessments are made within private dwellings).
Other training and support issues
One study50 suggested that better communication about the PRMHT scheme to front-line officers would support how the scheme is perceived and valued within incident resolution teams.
Service users in one police force evaluation believed that police officers needed more face-to-face contact with service users and suggested on-the-job training. 9
The idea of providing nurses with protective clothing received mixed views, with some concerned that it would affect the rapport that a lack of uniform provides. 46 Others pointed out that although MHPs did not wear protective clothing in the course of their PRMHT duties, police officers sometimes felt concerned about operating as a single-crewed unit with a civilian on board. 46
Recommendations for future implementation of police-related triage interventions
The evaluation of the government-funded pilot schemes made the following recommendations for practice:9
-
An extension of the hours of all street triage schemes should be considered, so that the schemes can provide a 24-hour service 7 days a week.
-
The role of street triage schemes should be reviewed in relation to referrals from, and contacts in, private settings.
-
A number of key functions appear to be associated with better outcomes and operation of the services; these functions should be considered when developing or extending street triage schemes, which includes:
-
joint ownership of the scheme at a senior management level to support the development of effective partnerships
-
regular reviews of joint working arrangements
-
clarity about the population to be served by street triage
-
effective information sharing between services; in particular, access to health information
-
provision of timely advice to police officers at the point of initial contact and during the assessment process
-
integration of street triage schemes with the health service-based crisis pathway
-
provision of information on agreed referral pathways to health and community services at the point of crisis or after its resolution
-
joint training programmes for street triage staff
-
improved recording of causes of crises so that this information can be presented to the local safeguarding board and be included in the Joint Strategic Needs Assessments chapters on mental health prevention.
-
-
Co-location of health and police staff (e.g. linked to a control room) or dedicated telephone line(s) appear to be an important component of effective street triage schemes and could support a cost-effective roll-out of the programme.
-
New and existing technologies to support effective information sharing could be used both within and between health and police services.
-
A national curriculum and associated training materials for street triage staff and enhanced mental health training for all police officers should be developed.
Primary evaluations of other UK-based PRMHT schemes also made implementation recommendations, some of which were more specific than those from the wider evaluation. These included:
-
Improved communication and dissemination. Specific recommendations were:
-
a communication strategy to disseminate operational effectiveness, both in terms of inward value (e.g. resource vs. outcome, frequency of S136 reduction/avoidance) and outward value (e.g. longer-term resolution for individuals in need)50
-
promote the PRMHT schemes more actively across the police force to maximise the use and efficiency of the service. 46
-
-
Ensure inclusion of ambulance services in the planning of future PRMHT pilots and schemes. 42
-
Focus on reducing frequent callers and work towards reduced police input for mental health incidents when there are no immediate safety concerns. 53
-
Providing co-response MHPs with the equipment to facilitate access to notes and allow police to scan live jobs while on shift. 46
-
Improve rota management on co-response schemes, pairing clinicians and police officers more efficiently according to locality. 46
-
Removing PRMHT duties as an overtime option to ensure that it continues to attract appropriately motivated individuals and spread a positive reputation of the service among the wider force. 46
-
Allow the ambulance service to request the attendance of the PRMHT co-response team. 46
-
Provide nurses with the option of using protective clothing. 46
Recommendations for future research from qualitative evidence
The evaluation of the government-funded pilot schemes made the following recommendations for research:9
-
A common data set should be developed, and the appropriate resources monitored to ensure that data are collected consistently and support a review of the cost-effectiveness of the scheme, which should be undertaken to provide evidence for its long-term sustainability.
-
The review could take the form of an evaluation based on routinely collected data. Alternatively, a formal research study that tests different models of PRMHT (e.g. control room-based models vs. community team-based models) could be undertaken.
Other studies highlighted the importance of improved data collection to support evaluation and other objectives. Specific recommendations were:
-
The review and streamlining of data-recording procedures. As part of this, clear formulation of the expectations and accountabilities for all parties in terms of documentation. 50
-
Improve data capture for all S136s and PRMHT attendances, to allow for a more accurate and ongoing evaluation of the scheme’s impact. 46
The recommendations from the included qualitative studies appeared to be appropriate and follow on from the presented evidence. This report provides a number of observations that emerged during the synthesis of these studies in Chapter 6.
Chapter 6 Overall synthesis, discussion and conclusions
Most PRMHT interventions involved police officers working in partnership with MHPs, although the role, responsibilities and location of MHPs varied. There is very little UK-based evidence on the alternative model of providing specialist mental health training to police officers. Interventions were generally valued by staff and showed some positive effects on procedures (e.g. rates of detention) and resources, although these results were not entirely consistent and not all important outcomes were measured. In particular, mental health service-related and individual service user outcomes were largely absent.
As PRMHT interventions sit at the intersection of criminal justice and mental health services, their successful implementation may depend on strategic integration of these services at the relevant local or regional level. Effective sharing of information and integration of knowledge among police and MHPs appears to be crucial. There is some evidence on how partnerships, protocols and technology can influence integration and implementation.
Most of the evidence was at risk of multiple biases due to design flaws and/or a lack of reporting of methods, which might affect the results. All the included primary research was conducted in England and health equity data were largely absent.
What is the evidence base for models of police-related mental health triage interventions?
Which models have been described in the literature?
The schemes evaluated in UK studies were typically described as street triage; however, these incorporated aspects from a range of different models described by Parker et al. 14 These included co-response (e.g. police officers and MHP jointly attending incidents), information-sharing agreements (e.g. information-sharing protocols and joint needs assessments), co-location (e.g. MHPs in police control rooms) and consultation (e.g. telephone advice and assistance from MHPs). All UK PRMHT schemes incorporated aspects of co-response and/or consultation, with a key difference being the role and location of MHPs. Roles of MHPs included joint in-person response to incidents alongside a police officer, providing telephone support with or without the ability to join police officers at an incident, or providing telephone and/or on-scene response without being accompanied by police. Locations of MHPs included a dedicated police car, police control room and an office in a local hospital, mental health trust or crisis assessment service.
Parker et al. 14 identified ‘pre-arrest diversion models’ as those involving police officers with special mental health training serving as the first-line police response to mental health crises in the community and acting as liaisons to the formal mental health system. In these models, such as the US-based CIT model, MHPs may provide the initial specialist training but are not routinely involved in attending incidents or directly informing assessments. There is currently an absence of UK-based qualitative data on this particular model, and there are limited quantitative data from only one UK study. 47
This report describes and classifies the different models of PRMHT on the basis of descriptions provided by study authors. However, none of the models appeared to have an explicit theoretical basis or followed a particular logic model. This has implications for evaluating the implementation of such models (see Limitations of the evidence and synthesis).
What evidence is there on the effectiveness of these models?
Whereas the scoping review by Parker et al. 14 focused on the description and classification of PRMHT models, this current rapid evidence synthesis attempts also to draw together evidence on the effects and implementation of such models.
There is little robust evidence on the effectiveness of the PRMHT models. The limited quantitative evidence available suggests reductions in formal detentions, higher hospital admission rates, increased likelihood of follow-up by secondary mental health services if patients are not admitted, and an increase in the use of HBPOS. However, the results were not entirely consistent, with some regions seeing increases in S136 rates after introducing PRMHT interventions. A single study noted that far fewer S136 detentions were made during PRMHT operating hours than outside those hours. 41 However, the absence of concurrent control groups in most evaluations means that it is difficult to separate any true effects of PRMHT interventions from statistical phenomena, such as confounding and regression to the mean. In addition, most included studies implied that a reduction in S136 rates was a desirable outcome, although this might not necessarily be true for every setting and context.
There is minimally reported, heterogeneous and conflicting evidence on the effects of PRMHT interventions on outcomes, such as on the quality/timeliness of assessment, referral and treatment, access to services, demand for police resources and number of repeated contacts with individuals.
There is limited qualitative evidence that PRMHT interventions may help identify people with mental health needs that have not previously been in contact with mental health services. However, there is a near-total absence of reliable quantitative evidence on measures such as individual mental health outcomes, changes in demand for mental health services and changes to case-finding or level of access to health services.
Although PRMHT might be conceived as a means to reduce longer-term police, health and social care costs at the expense of possible increased short-term costs, no true cost-effectiveness analyses of PRMHT schemes were found in this rapid evidence synthesis. Two studies reported police force cost savings43,46 (one46 noting that savings came from lower custody rates and reduced officer time attending S136 incidents), but these studies had conflicting findings with regard to NHS costs.
What evidence is there on the acceptability and feasibility of these models?
We identified several UK studies reporting qualitative evidence on the implementation of PRMHT models, but it should be borne in mind that this mostly consists of views from a relatively small number of police and mental health staff directly involved in delivering pilot interventions.
Acceptability
In general, police staff appeared to value PRMHTs, both officers with an interest in mental health and those who felt that mental health should not be a police responsibility. Both police and health staff noted an improvement in quality of care.
Although some service users reported improved experiences with PRMHT teams compared with previous arrangements, service user feedback was rare. Some qualitative evidence suggested that service users preferred to interact with MHPs rather than police officers. This was attributed to MHP communication skills and the association of police uniforms with authority and criminalisation. Any future provision of protective clothing (e.g. stab vests) for MHPs responding to incidents may need to consider the impact on user perceptions of MHPs as well as MHPs’ safety.
Feasibility
Most evaluated PRMHT models only addressed immediate concerns around the use of S136 by police called to mental health-related incidents. However, there are wider consequences of introducing these schemes for both police and health services, particularly risks of displacement or duplication of existing services. Strategic response to mental health-related incidents may need to consider, at the highest level, which pathways prove to be most effective for service users and make the most appropriate and efficient use of both police and NHS resources. Some barriers to successful outcomes lay outside the control of police or even PRMHT staff (e.g. lack of co-ordination between neighbouring NHS trusts). Similarly, the availability and resources of local services need to be taken into account. For example, PRMHT’s attempts to reduce the number of repeated crisis calls from an individual may prove unsuccessful if they are referred to local mental health services with long waiting times.
The reported advantages and disadvantages of retaining consistent staff on PRMHT duties may be of interest to service managers. Advantages may include enhanced relationships and understanding, greater efficiency and less frequent issues around police vetting procedures. However, disadvantages could include mental health knowledge being restricted to fewer police staff and poorer integration with the wider force. The service impact of reallocating police and MHP staff to PRMHT from other active roles should also be carefully considered.
What evidence is there on the barriers to, and facilitators of, the implementation of these models?
As for acceptability and feasibility issues, evidence on barriers and facilitators was based mostly on the views of a relatively small number of police and mental health staff directly involved in delivering pilot interventions.
Barriers
Some comments indicated uncertainty about how and when it is best to deploy MHPs to the scene of an incident. There may be a trade-off between MHPs having better access to records in a hospital/control room and using their hands-on skills to aid in incident resolution. In conjunction with other information-sharing measures, this kind of barrier might potentially be overcome by providing MHPs with improved mobile information technology. PRMHT staff from our advisory group have noted the value of being able to obtain information while en route to a service user.
Reveruzzi and Pilling’s9 evaluation appropriately recommended that the role of street triage schemes should be reviewed in relation to referrals from, and contacts in, private settings. However, since the recommendation was originally made, the Policing and Crime Act 20174 has resulted in changes to S135 and S136. 2 In theory, these changes should mitigate some of the previously identified problems around police officers being unable to enter private premises to make an assessment. However, the effect of these changes has yet to be properly established. In addition, it was clear from the evidence that not all staff were aware of the nature of police powers in public places and private premises. All MHPs and control room staff involved in PRMHT interventions being knowledgeable about the constraints on police powers may prevent misunderstandings or inappropriate recommendations for action.
Data collection is often incomplete and restricted in scope, which limits the opportunity to continuously evaluate and improve services. Methods for comprehensive, accurate and efficient data collection (that do not place undue additional demands on front-line police or health staff) may need to be developed. As PRMHT interventions are multiagency, data collection and evaluation may benefit from being correspondingly integrated and strategic. Data collection (like information-sharing) may also benefit from being governed by relevant protocols and facilitated by appropriate technology. As well as routine data collection of outcomes, such as S136 rates, future evaluations would benefit from data on quality and timeliness of assessment, referral and treatment, mental health outcomes, demand on police resources and police officer time, demand for community mental health services, rates of hospitalisation via A&E or acute mental health services, level of service engagement, experience of services for service users, and costs and savings to health and police services, including estimates of skill mix and other workforce resources. One barrier to effective interagency data collection may be obtaining the necessary staffing and resources across all of the relevant services. Other barriers include a lack of clarity from commissioners about why certain data should be recorded, obtaining consent to share individuals’ data between services and difficulties where boundaries are not coterminous (e.g. different NHS trusts overlapping one police force area or people being referred to out-of-area hospital beds).
Some qualitative studies noted the challenge of disproportionately high demand created by repeat service users. Some comments suggested that efforts could be made to work towards a distinctive and separate partnership between police and health-care services for repeat callers,50 or towards reduced police input for callers for whom there are no immediate safety concerns. 53
Such efforts may be worth further consideration and evaluation in any future implementation of PRMHT interventions.
Facilitators
The qualitative evidence as a whole emphasised Reveruzzi and Pilling’s9 conclusions around the importance of strong partnerships between police and health services, co-location of services and the value of shared information. The latter point in particular crossed several themes; shared information underpins the achievement of organisational objectives, such as reducing S136 arrests, speeding up user needs assessment and enhancing collaborative working. Future PRMHT interventions would probably benefit from immediate access to shared information across the police/health interface, facilitated by agreed protocols and underpinned by appropriate technology that permits compatibility of data across police and health systems.
In all cases, lines of accountability and responsibility need to be clear among all PRMHT staff. This is because differences in attitudes to risk between police officers and MHPs have been observed (e.g. around threats of self-harm and suicide), and because the presence of factors such as alcohol, drugs and/or the risk of violent behaviour can increase the complexity and difficulty of making judgments about the best course of action. Similarly, roles, responsibilities and reciprocal arrangements need to be clearly defined between PRMHT services, crisis teams and other related health services.
Immediate and consistent availability of MHP support was very important to police officers who were responding to mental health-related incidents, with immediacy sometimes seen as a key difference between PRMHT and crisis teams. As stated by Reveruzzi and Pilling,9 24-hour availability appears to be crucial to providing officers with a resource that is considered reliable. Appropriate communication technology may improve accessibility, such as mobile phones dedicated to the task of consulting MHPs that can have some advantages over police radio sets, although difficulties may be encountered in rural locations with poor signal coverage.
Many resource savings attributed to PRMHT interventions stem from their value in accelerating the assessment of user needs. Whereas most UK interventions have focused on retaining MHP partnerships to facilitate assessments, the US literature is more focused on interventions where police officers receive mental health training without the same level of ongoing specialist support from MHPs. No evidence was found comparing these two models, despite their potential to have quite different costs and benefits.
Limitations of the evidence and synthesis
The DHSC-funded street triage pilots were managed by local police forces in partnership with Clinical Commissioning Groups (CCGs), NHS England and Police and Crime Commissioners. Given the unique governance arrangements for delivering a mental health triage service in the UK, as well as important differences in social context and the delivery of health and criminal justice services between countries, qualitative data from non-UK settings were not incorporated. However, all identified studies evaluated PRMHT schemes in England alone, so care should be taken when extrapolating this evidence to other UK regions.
Discussion of health equity issues (e.g. for BAME communities, people for whom English is not their first language, people with neurodevelopmental disabilities) was largely absent from existing evidence. Similarly, when service user groups were involved in research, they were generally not well described.
We excluded traditional L&D services from our rapid evidence synthesis, but it is clear that many PRMHT schemes are closely integrated with L&D and are often conceptualised as a way of bringing some L&D functions to an earlier point in the pathway (e.g. assessing and referring individuals to an appropriate non-CJS treatment or support service). As such, the boundaries between PRMHT and L&D may be somewhat artificial.
Only a few systematic reviews met the inclusion criteria and there were variations between them in terms of the type of studies included and the nature of the interventions and outcomes, making it difficult to synthesise the evidence. The review authors similarly commented on the lack of robust primary evidence, which made it difficult to draw conclusions. Across the reviews, there were calls for more relevant and robust research, and a number of recommendations for research and practice were provided.
The included primary studies were limited, with very little concurrent comparative data and a wide variation in interventions generically labelled ‘street triage’ by study authors. This made it difficult to draw conclusions about effectiveness in our evidence synthesis. However, conclusions and recommendations by study authors for research and practice echoed those of the systematic reviews.
The methodological quality of the systematic reviews was formally assessed, with some having limitations that made it difficult to judge the reliability of the evidence presented. Although there were limitations in the reported review process, the authors reasonably stated that there were no robust studies to rigorously test the evidence.
The primary studies were also methodologically limited. One RCT was assessed using a recognised assessment tool, which indicated that it was largely at a low risk of bias. The remaining studies were largely descriptive with few concurrent comparisons, which made it difficult to evaluate the effectiveness across the interventions or of any particular model. Most studies included relatively small numbers of service users, precluding the generation of robust quantitative estimates of effects.
The volume of qualitative evidence presented in PRMHT studies in general is relatively limited. Even within the DHSC-funded evaluation of pilots, some of the subthemes are based on statements from just one or two individuals. Studies did not provide interview transcripts or other means of interrogating the primary study data, and it is unclear whether or not important perspectives have been overlooked. Given the lack of richness of data in individual studies, it was not possible to construct definitive context–mechanism–outcome configurations explaining why the observed outcomes developed as they did and how interventions reacted to underlying mechanisms and in what contexts. However, it was possible to identify recurrent themes across studies and further refine themes identified in previous research.
The methodological quality of included qualitative studies was evaluated using the CASP checklist. This used studies as the unit of analysis rather than outcomes, as is done in the more comprehensive GRADE-Confidence in the Evidence from Reviews of Qualitative Research (CERQual) approach. 55 However, given the relatively small volume of evidence and the rapid nature of the current synthesis, CASP is likely to have captured the main relevant quality issues.
As well as the methodological limitations described above, the nature of the different sources of evidence (e.g. systematic reviews, primary quantitative studies and primary qualitative studies) precluded us from being able to consistently structure our synthesis across sections; in some cases, evidence could feasibly be presented only by intervention, and in others only by outcome.
Owing to time and resource limitations, our project advisory group included police and research professionals only. The lack of advisory group input from MHPs and service users should be considered a limitation.
Implications for future research
Although there is published evidence that aims to describe and evaluate various models of PRMHT interventions, most evaluations are limited in scope and methodologically weak.
As we have seen, most evaluations of PRMHT interventions have focused on the use of S136 and HBPOS as primary outcomes. At the same time, separate legislation4 and capital funding schemes7,8 have been directed specifically at ensuring that there are improvements on these outcomes. However, it is clear that PRMHT interventions have wider objectives and potential benefits.
All the systematic reviews in the synthesis, published between 2016 and 2018, recommended higher-quality evaluations of PRMHTs that measure outcomes beyond simple procedural measures, such as S136 rates. 11,12,14,15,39,40
With the exception of one RCT of training,47 we have not identified any strong additional evidence in the most recent evaluative primary studies. These recent studies have echoed the recommendations of the systematic reviews, calling for prospective, comprehensive and streamlined collection of a wider variety of data to evaluate the impact of PRMHT interventions. In particular, there is a lack of information on the impact of these interventions on individuals in terms of their mental health and quality-of-life outcomes.
One frequently raised issue was that of people who often and repeatedly come into contact with services via the police. This is one important objective on which PRMHT interventions (and evaluations) could potentially focus. Some existing schemes already aim to work proactively with various partners (e.g. health, social care, local policing teams, ambulance service) on this issue.
Barriers to collecting such data may include the time and resources needed to obtain necessary ethics approval and the nature of routine police data collection. These and other methodological and practical challenges have been discussed by the authors of the only RCT in this area. 48 They recommend that police IT systems should be designed with operational and research purposes in mind, as data (which may not be fully accurate or complete) is currently stored on a number of different and poorly integrated systems. Problems around the collection of police-related data fall into three categories: (1) the nature of the data being collected (e.g. routine procedural data vs. person-centred outcomes), (2) data collection procedures (e.g. how data collection has an impact on the workload of front-line police officers) and (3) data analytic considerations (e.g. the accessibility and usefulness of data for research). In order for researchers to understand the context in which interventions are being implemented, Scantlebury et al. 48 appropriately recommend collaboration between the police and academia, with police officers embedded within trial management groups.
The available qualitative data around the implementation of PRMHTs are also relatively sparse, but provided clearer insights into possible future directions for research. Although police and health staff directly involved with PRMHTs seem to consider these interventions to be of value, the objective impact of PRMHTs (especially on wider services) is less clear. Although some, very limited, evidence suggests that PRMHT schemes may result in an overall saving of police resources, this same evidence paints a more mixed picture in terms of NHS resources, with the potential for increased resource use as well as savings. This, perhaps, should not be surprising given that co-response/consultation PRMHT models require the allocation of MHPs from elsewhere in mental health services. However, whether the impact of PRMHTs on case detection and referral pathways increases or decreases, the demand on health services remains unclear.
On the basis of the evidence included in this rapid evidence synthesis, future evaluations would be more informative if they addressed the following:
-
Clearly articulate the objectives of the PRMHT intervention.
-
Articulating the logic model underpinning the intervention may help illustrate the relationship between objectives and outcomes.
-
Involve all stakeholders (including people with mental health issues) in the design and evaluation of interventions, including the identification of these objectives.
-
Collect and analyse outcomes that relate directly to the stated objectives. Quantitative data should extend beyond S136 rates, places of safety and process data, to measuring the outcomes that are most important to the police, mental health and social-care services, and individual service users. These might provide greater insights into:
-
quality and timeliness of assessment, referral and treatment
-
mental health outcomes for service users
-
experience of services for service users
-
level of service engagement after encounters with PRMHT
-
characteristics and needs of people who frequently and repeatedly come into contact with services via the police
-
changes in case-finding and access to health services (e.g. mental health, substance misuse, sexual health and contraception)
-
demands on police resources and police officer time
-
demands for community mental health services
-
rates of hospitalisation via A&E or acute mental health services
-
costs and savings to health and police services.
-
-
Similarly, evaluations should take into consideration the shorter-, medium- and longer-term effects of PRMHT interventions, for example by evaluating the consequences of PRMHT referrals on individuals beyond the initial number and type of referral.
-
Evaluations of services to understand and address the needs of frequent/repeat service users who create a disproportionately large demand on resources may be of particular value.
-
Researchers need to make realistic allowance for data collection in budget allocations for new studies.
-
As stated in previous publications, it is likely that better data collection processes will be needed. However, these processes should not be overly burdensome to front-line police or health staff.
-
When possible, study designs should have an appropriate concurrent comparator. Although street triage interventions have been implemented in a number of ways (e.g. incorporating co-response, consultation and information-sharing components to different degrees), there may be an interest to compare the pragmatic implementation of such an approach with ‘pre-arrest diversion’ models that emphasise specialist training of police officers over ongoing collaboration with MHPs.
-
The collection of qualitative data may help better understand which approaches work best and why, although such research should capture dissenting views as well as those of advocates.
-
Given their potential to both incur costs and accrue benefits across multiple services, any future cost-effectiveness analysis of PRMHT should take a multiagency perspective to understand the relative impact of introducing a particular model on the resource use across police, health and social services.
Acknowledgements
We would like to thank the following people for their comments and suggestions in relation to draft versions of this report:
-
Richard Poole, Devon and Cornwall Police Federation
-
Anonymous Street Triage Supervisor, English Territorial Police Service
-
Alison Booth, Research Fellow, York Trials Unit, University of York
-
Annie Irvine, Research Fellow, Social Policy Research Unit, University of York
-
Nicola Moran, Lecturer/Senior Researcher, Social Policy and Social Work, University of York.
Contributions of authors
Mark Rodgers (Research Fellow, Evidence Synthesis) drafted the protocol and carried out study selection, data extraction, critical appraisal and the write-up of the report.
Sian Thomas (Research Fellow, Evidence Synthesis) carried out study selection, data extraction, critical appraisal and the write-up of the report.
Jane Dalton (Research Fellow, Evidence Synthesis) carried out study selection, data extraction and critical appraisal.
Melissa Harden (Information Specialist) conducted all searching, wrote the search sections of the report and commented on the draft report.
Alison Eastwood (Professor, Research) oversaw the project, contributed advice and expertise and commented on all drafts of the report.
All authors commented on the protocol.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Mental Health Crisis Care Concordat. Improving Outcomes for People Experiencing Mental Health Crisis. London: DHSC; 2014.
- Mental Health Act 1983. Section 136. London: The Stationery Office; 1983.
- Mental Health Act 1983: Code of Practice. Norwich: The Stationery Office; 2015.
- Policing and Crime Act 2017, Part 4, Chapter 4. London: The Stationery Office; 1983.
- Chalmers J. Changes to Sections 135 and 136 of the Mental Health Act are Coming! An Extremely Brief Summary. London: Royal College of Psychiatrists; 2017.
- Mental Health Act 1983: Section 135. London: The Stationery Office; 1983.
- Improving Health-Based Places of Safety: Guidance for Capital Funding Applications. London: DHSC; 2016.
- Beyond Places of Safety. London: DHSC; n.d.
- Reveruzzi B, Pilling S. Street Triage. Report on the Evaluation of Nine Pilot Schemes in England. London: Department of Clinical, Health and Educational Psychology, University College London; 2016.
- NHS England . Liaison and Diversion. Frequently Asked Questions n.d. www.england.nhs.uk/commissioning/health-just/liaison-and-diversion/ld-faqs/ (accessed 5 September 2017).
- Kane E, Evans E, Shokraneh F. Effectiveness of current policing-related mental health interventions in England and Wales and Crisis Intervention Teams as a future potential model: a systematic review. Syst Rev 2017;6. https://doi.org/10.1186/s13643-017-0478-7.
- Kane E, Evans E, Shokraneh F. Effectiveness of current policing-related mental health interventions: a systematic review. Crim Behav Ment Health 2018;28:108-19. https://doi.org/10.1002/cbm.2058.
- Mental Health Training for Non-mental Health Trained Professionals. A Systematic Review of the Effectiveness of Mental Health Training Programmes. York: University of York and Connect, Evidence Based Policing; 2017.
- Parker A, Scantlebury A, Booth A, MacBryde JC, Scott WJ, Wright K, et al. Interagency collaboration models for people with mental ill health in contact with the police: a systematic scoping review. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019312.
- Paton F, Wright K, Ayre N, Dare C, Johnson S, Lloyd-Evans B, et al. Improving outcomes for people in mental health crisis: a rapid synthesis of the evidence for available models of care. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20030.
- Park A, Webber M, Booth A, Hughes-Morley A, Clarke A, Wright K. Mental Health Triage for Individuals in Contact With the Police Who May Be Experiencing Mental Health Crisis: A Systematic Review n.d. www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016042008 (accessed 18 August 2017).
- Booth A, Wright K, Clarke A, Hughes-Morley A, McDaid C. Mental Health Training Programmes for Non-Mental Health Trained Professionals Coming into Contact With People With Mental Ill Health: Protocol for a Systematic Review of Effectiveness n.d. www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015015981 (accessed 18 August 2017).
- What Models or Mechanisms for Inter-Agency Collaboration Between the Police or Law Enforcement and Other Statutory Agencies for People with Mental Problems Have Been Evaluated, and What Evidence is Available on Their Effectiveness? A Systematic Scoping Review. York: York Trials Unit, Department of Health Sciences, University of York; 2017.
- Watson AC. Research in the real world: studying Chicago Police Department’s Crisis Intervention Team program. Res Soc Work Pract 2010;20:536-43. https://doi.org/10.1177/1049731510374201.
- Shapiro GK, Cusi A, Kirst M, O’Campo P, Nakhost A, Stergiopoulos V. Co-responding police-mental health programs: a review. Adm Policy Ment Health 2015;42:606-20. https://doi.org/10.1007/s10488-014-0594-9.
- Winters S, Magalhaes L, Kinsella EA. Interprofessional collaboration in mental health crisis response systems: a scoping review. Disabil Rehabil 2015;37:2212-24. https://doi.org/10.3109/09638288.2014.1002576.
- Cummins ID, Edmondson D. Policing and Street Triage. Manchester: University of Salford; 2016.
- York Health Services and Delivery Research Evidence Synthesis Centre . Police-Related Mental Health Triage Interventions: A Rapid Evidence Synthesis 2017. www.york.ac.uk/media/crd/Protocol-police-related-triage.pdf (accessed 19 February 2019).
- College of Policing. Coventry: College of Policing; 2017.
- Mental Health Foundation. London: Mental Health Foundation; 2017.
- Crisis Care Concordat . Crisis Care Concordat 2017. www.crisiscareconcordat.org.uk/ (accessed 13 August 2018).
- Centre for Mental Health. London: Centre for Mental Health; 2017.
- Connect Evidence Based Policing. York: Connect Evidence Based Policing; 2017.
- The East Midlands Police Academic Collaboration . The East Midlands Police Academic Collaboration 2017. www.empac.org.uk/ (accessed 13 August 2018).
- Shaw RL, Booth A, Sutton AJ, Miller T, Smith JA, Young B, et al. Finding qualitative research: an evaluation of search strategies. BMC Med Res Methodol 2004;4. https://doi.org/10.1186/1471-2288-4-5.
- Chambers D, Wade R, Wilson P. Training Manual for Selecting Reviews and Writing Abstracts for the Database of Abstracts of Reviews of Effects (DARE). York: Centre for Reviews and Dissemination, University of York; 2012.
- Egan M, Tannahill C, Petticrew M, Thomas S. Psychosocial risk factors in home and community settings and their associations with population health and health inequalities: a systematic meta-review. BMC Public Health 2008;8. https://doi.org/10.1186/1471-2458-8-239.
- Thomas S, Dalton J, Harden M, Eastwood A, Parker G. Updated meta-review of evidence on support for carers. Health Serv Deliv Res 2017;5.
- Dalton J, Thomas S, Melton H, Harden M, Eastwood A. The provision of services in the UK for UK armed forces veterans with PTSD: a rapid evidence synthesis. Health Serv Deliv Res 2018;6.
- Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 2016;69:225-34. https://doi.org/10.1016/j.jclinepi.2015.06.005.
- Cochrane Effective Practice and Organisation of Care (EPOC) . Suggested Risk of Bias Criteria for EPOC Reviews. EPOC Resources for Review Authors 2017. http://epoc.cochrane.org/resources/epoc-resources-review-authors (accessed 8 June 2018).
- Critical Appraisal Skills Programme . CASP Qualitative Research Checklist 2018. www.casp-uk.net/casp-tools-checklists (accessed 13 August 2018).
- Houghton C, Murphy K, Meehan B, Thomas J, Brooker D, Casey D. From screening to synthesis: using NVivo to enhance transparency in qualitative evidence synthesis. J Clin Nurs 2017;26:873-81. https://doi.org/10.1111/jocn.13443.
- Booth A, Scantlebury A, Hughes-Morley A, Mitchell N, Wright K, Scott W, et al. Mental health training programmes for non-mental health trained professionals coming into contact with people with mental ill health: a systematic review of effectiveness. BMC Psychiatry 2017;17. https://doi.org/10.1186/s12888-017-1356-5.
- Taheri SA. Do crisis intervention teams reduce arrests and improve officer safety? A systematic review and meta-analysis. Crim Justice Policy Rev 2016;27:76-9. https://doi.org/10.1177/0887403414556289.
- Dyer W, Steer M, Biddle P. Mental Health Street Triage . Policing J Policy Pract 2015;9:377-87. https://doi.org/10.1093/police/pav018.
- Edmondson D, Cummins I. Oldham Mental Health Phone Triage/Raid Pilot Project. Evaluation Report. Manchester: Manchester Metropolitan University and University of Salford; 2014.
- Heslin M, Callaghan L, Packwood M, Badu V, Byford S. Decision analytic model exploring the cost and cost-offset implications of street triage. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009670.
- Jenkins O, Dye S, Obeng-Asare F, Nguyen N, Wright N. Police liaison and section 136: comparison of two different approaches. Br J Psych Bull 2017;41:76-82. https://doi.org/10.1192/pb.bp.115.052977.
- Keown P, French J, Gibson G, Newton E, Cull S, Brown P, et al. Too much detention? Street triage and detentions under section 136 Mental Health Act in the North East of England: a descriptive study of the effects of a street triage intervention. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011837.
- Senker S, Scott M. Essex Street Triage Evaluation December 2015. Witham: Police, Fire and Crime Commissioner for Essex; 2016.
- Scantlebury A, Fairhurst C, Booth A, McDaid C, Moran N, Parker A, et al. Effectiveness of a training program for police officers who come into contact with people with mental health problems: a pragmatic randomised controlled trial. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0184377.
- Scantlebury A, McDaid C, Booth A, Fairhurst C, Parker A, Payne R, et al. Undertaking a randomised controlled trial in the police setting: methodological and practical challenges. Trials 2017;18. https://doi.org/10.1186/s13063-017-2369-6.
- Brace MS. An Assessment of the Efficacy of the ‘Street Triage’ Model Adopted by the Police in Response to Mental Health Crisis: Does the ‘Street Triage’ Model Reduce Demand from People Suffering from a Mental Health Crisis on the Police Service and Are the Police the Correct Service to Respond to This Demand? 2016.
- Callender M, Cole S. Assessing the Role, Value and Effectiveness of Mental Health Triage: Operation Alloy. Northampton: Institute for Public Safety, Crime and Justice, University of Northampton; 2016.
- Irvine AL, Allen L, Webber MP. Evaluation of the Scarborough, Whitby and Ryedale Street Triage Service. Research Report. York: Department for Social Policy and Social Work, University of York; 2015.
- Hobson Z, Grossmith L, Dawson P. Research into the London Mental Health Street Triage Pilot. London: Mayor of London Office for Policing and Crime; 2015.
- Horspool K, Drabble SJ, O’Cathain A. Implementing street triage: a qualitative study of collaboration between police and mental health services. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1026-z.
- Service User Experience in Adult Mental Health: Improving the Experience of Care for People Using Adult NHS Mental Health Services. London: NICE; 2011.
- GRADE-CERQual . GRADE-CERQual 2018. www.cerqual.org/ (accessed 13 August 2018).
- Abbott SE. Evaluating the Impact of a Jail Diversion Program on Police Officer’s Attitudes Toward the Mentally Ill 2011.
- Arey JB, Wilder AH, Normore AH, Iannazzo MD, Javidi M. Crisis Intervention Teams: an evolution of leadership in community and policing. Policing J Policy Pract 2016;10:143-9. https://doi.org/10.1093/police/pav037.
- Barcelos NM. The Impact of Crisis Intervention Team (CIT) Training on Law Enforcement Officers in Connecticut 2015.
- Browning SL, Van Hasselt VB, Tucker AS, Vecchi GM. Dealing with individuals who have mental illness: the Crisis Intervention Team (CIT) in law enforcement. Br J For Pract 2011;13:235-43. https://doi.org/10.1108/14636641111189990.
- Compton MT, Bahora M, Watson AC, Oliva JR. A comprehensive review of extant research on Crisis Intervention Team (CIT) programs. J Am Acad Psychiatry Law 2008;36:47-55.
- Cummins I, Edmondson D. Policing and street triage. J Adult Protect 2016;18:40-52. https://doi.org/10.1108/JAP-03-2015-0009.
- Davidson ML. A criminal justice system-wide response to mental illness: evaluating the effectiveness of the Memphis Crisis Intervention Team training curriculum among law enforcement and correctional officers. Crim Justice Policy Rev 2016;27:46-75. https://doi.org/10.1177/0887403414554997.
- Hannig L. Program Evaluation of Chicago’s Crisis Intervention Team Curriculum: Training Implementation Effectiveness 2015.
- Helfgott JB, Hickman MJ, Labossiere AP. A descriptive evaluation of the Seattle Police Department’s crisis response team officer/mental health professional partnership pilot program. Int J Law Psychiatry 2016;44:109-22. https://doi.org/10.1016/j.ijlp.2015.08.038.
- Kalinich AO. Crisis Intervention Team (CIT): Perspectives from Mental Health Professionals 2010.
- Lancaster A. Evidence for joint police and mental health responses for people in mental health crisis. Ment Health Pract 2016;19:20-6. https://doi.org/10.7748/mhp.2016.e1067.
- Mulay AL, Vayshenker B, West ML, Kelly E. Crisis intervention training and implicit stigma toward mental illness: reducing bias among criminal justice personnel. Int J Forensic Ment Health 2016;15:369-81. https://doi.org/10.1080/14999013.2016.1208308.
- Norris JN. Effects of Crisis Intervention Team Training and Simulated Auditory Hallucinations on Self-Efficacy, Empathy, Attitudes, and Stigma Toward Severe Mental Illness 2015.
- Prince JL. A Phenomenological Study of the Impact of Crisis Intervention Team Training on Washington, D.C. Police Officers 2012.
- RiCharde SG. American and Australian Communications Officers: Mental Health Stigma and Crisis Intervention Team 2016.
- Rodriguez VM. The Impact of Psychiatric Emergency Response Team (PERT) Training on Law Enforcement Officers on Time and Disposition Responding to Mental Health Related Emergencies in Urban, Suburban, and Rural Communities 2016.
- Stewart C. Police Intervention in Mental Health Crisis: A Case Study of the Bloomington Crisis Intervention Team (CIT) Program 2009.
- Thomas S, Watson A. A focus for mental health training for police. J Criminol Res Policy Pract 2017;3:93-104. https://doi.org/10.1108/JCRPP-01-2017-0005.
- Tucker AS, Van Hasselt VB, Russell SA. Law enforcement response to the mentally ill: an evaluative review. Brief Treat Crisis Interv 2008;8:236-50. https://doi.org/10.1093/brief-treatment/mhn014.
- Weller J. Evaluating the Responses of San Francisco Police Officers to Mental Health-Related Calls 2015.
- Woods P, Leidl D, Butler L, Stonechild J, Luimes J. Police services detention centres: a proposed solution for action. Police Pract Res 2017;18:119-31. https://doi.org/10.1080/15614263.2016.1230852.
- Young J. A Comparison Between the Effects of the One-Hour and Twelve-Hour Massachusetts Municipal Basic Recruit Officer Course Mental Health Training on Officer’s De-Escalation Skills, Self-Efficacy, and Stigmatizing Attitudes 2014.
- Lamanna D, Shapiro GK, Kirst M, Matheson FI, Nakhost A, Stergiopoulos V. Co-responding police-mental health programmes: service user experiences and outcomes in a large urban centre. Int J Ment Health Nurs 2018;27:891-900. https://doi.org/10.1111/inm.12384.
- Compton MT, Bakeman R, Broussard B, D’Orio B, Watson AC. Police officers’ volunteering for (rather than being assigned to) Crisis Intervention Team (CIT) training: evidence for a beneficial self-selection effect. Behav Sci Law 2017;35:470-9. https://doi.org/10.1002/bsl.2301.
- Compton MT, Anderson S, Broussard B, Ellis S, Halpern B, Pauselli L, et al. A potential new form of jail diversion and reconnection to mental health services: II. Demonstration of feasibility. Behav Sci Law 2017;35:492-500. https://doi.org/10.1002/bsl.2319.
- Khalsa HK, Denes AC, Pasini-Hill DM, Santelli JC, Baldessarini RJ. Specialized police-based mental health crisis response: the first 10 years of Colorado’s crisis intervention team implementation. Psychiatr Serv 2018;69:239-41. https://doi.org/10.1176/appi.ps.201700055.
- Kubiak S, Comartin E, Milanovic E, Bybee D, Tillander E, Rabaut C, et al. Countywide implementation of crisis intervention teams: multiple methods, measures and sustained outcomes. Behav Sci Law 2017;35:456-69. https://doi.org/10.1002/bsl.2305.
- Tyuse SW, Cooper-Sadlo S, Underwood SE. Descriptive study of older adults encountered by crisis intervention team (CIT) law enforcement officers. J Women Aging 2017;29:281-93. https://doi.org/10.1080/08952841.2016.1174513.
- Boscarato K, Lee S, Kroschel J, Hollander Y, Brennan A, Warren N. Consumer experience of formal crisis-response services and preferred methods of crisis intervention. Int J Ment Health Nurs 2014;23:287-95. https://doi.org/10.1111/inm.12059.
- Evangelista E, Lee S, Gallagher A, Peterson V, James J, Warren N, et al. Crisis averted: how consumers experienced a police and clinical early response (PACER) unit responding to a mental health crisis. Int J Ment Health Nurs 2016;25:367-76. https://doi.org/10.1111/inm.12218.
- Herrington V, Pope R. The impact of police training in mental health: an example from Australia. Policing Soc 2014;24:501-22. https://doi.org/10.1080/10439463.2013.784287.
- Hollander Y, Lee SJ, Tahtalian S, Young D, Kulkarni J. Challenges relating to the interface between crisis mental health clinicians and police when engaging with people with a mental illness. Psychiatr Psychol Law 2012;19:402-11. https://doi.org/10.1080/13218719.2011.585131.
- Lee SJ, Thomas P, Doulis C, Bowles D, Henderson K, Keppich-Arnold S, et al. Outcomes achieved by and police and clinician perspectives on a joint police officer and mental health clinician mobile response unit. Int J Ment Health Nurs 2015;24:538-46. https://doi.org/10.1111/inm.12153.
- McKenna B, Furness T, Oakes J, Brown S. Police and mental health clinician partnership in response to mental health crisis: a qualitative study. Int J Ment Health Nurs 2015;24:386-93. https://doi.org/10.1111/inm.12140.
- Kirst M, Francombe Pridham K, Narrandes R, Matheson F, Young L, Niedra K, et al. Examining implementation of mobile, police-mental health crisis intervention teams in a large urban center. J Ment Health 2015;24:369-74. https://doi.org/10.3109/09638237.2015.1036970.
- Kisely S, Campbell LA, Peddle S, Hare S, Pyche M, Spicer D, et al. A controlled before-and-after evaluation of a mobile crisis partnership between mental health and police services in Nova Scotia. Can J Psychiatry 2010;55:662-8. https://doi.org/10.1177/070674371005501005.
- Silverstone PH, Krameddine YI, DeMarco D, Hassel R. A novel approach to training police officers to interact with individuals who may have a psychiatric disorder. J Am Acad Psychiatry Law 2013;41:344-55.
- Sestoft D, Rasmussen MF, Vitus K, Kongsrud L. The police, social services and psychiatry cooperation in Denmark – a new model of working practice between governmental sectors. A description of the concept, process, practice and experience. Int J Law Psychiatry 2014;37:370-5. https://doi.org/10.1016/j.ijlp.2014.02.007.
- Canada KE, Angell B, Watson AC. Crisis Intervention Teams in Chicago: successes on the ground. J Police Crisis Negot 2010;10:86-100. https://doi.org/10.1080/15332581003792070.
- Canada KE, Angell B, Watson AC. Intervening at the entry point: differences in how CIT trained and non-CIT trained officers describe responding to mental health-related calls. Community Ment Health J 2012;48:746-55. https://doi.org/10.1007/s10597-011-9430-9.
- Compton MT, Halpern B, Broussard B, Anderson S, Smith K, Ellis S, et al. A potential new form of jail diversion and reconnection to mental health services: I. Stakeholders’ views on acceptability. Behav Sci Law 2017;35:480-91. https://doi.org/10.1002/bsl.2320.
- Doulas AV, Lurigio AJ. Juvenile Crisis Intervention Teams (CITs): a qualitative description of current programmes. Police J 2014;87:114-25. https://doi.org/10.1350/pojo.2014.87.2.534.
- Hanafi S, Bahora M, Demir BN, Compton MT. Incorporating Crisis Intervention Team (CIT) knowledge and skills into the daily work of police officers: a focus group study. Community Ment Health J 2008;44:427-32. https://doi.org/10.1007/s10597-008-9145-8.
- McGriff JA, Broussard B, Demir Neubert BN, Thompson NJ, Compton MT. Implementing a Crisis Intervention Team (CIT) police presence in a large international airport setting. J Police Crisis Negot 2010;10:153-65. https://doi.org/10.1080/15332581003756885.
- Skubby D, Bonfine N, Novisky M, Munetz MR, Ritter C. Crisis Intervention Team (CIT) programs in rural communities: a focus group study. Community Ment Health J 2013;49:756-64. https://doi.org/10.1007/s10597-012-9517-y.
- Tully T, Smith M. Officer perceptions of crisis intervention team training effectiveness. Police J 2015;88:51-64. https://doi.org/10.1177/0032258X15570558.
- Watson AC, Angell B, Morabito MS, Robinson N. Defying negative expectations: dimensions of fair and respectful treatment by police officers as perceived by people with mental illness. Adm Policy Ment Health 2008;35:449-57. https://doi.org/10.1007/s10488-008-0188-5.
Appendix 1 Search strategies
Search strategies for the metasynthesis of evidence on the effectiveness of models
The following search strategies are designed to update the previous searches used for an ongoing review of PRMHT interventions. 16
MEDLINE [Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)]
Via Ovid (see URL: http://ovidsp.ovid.com/).
Date range: 1946 to present.
Date searched: 7 November 2017.
Records retrieved: 314.
Search strategy
| 1 | mental health crisis.ti,ab. (204) |
| 2 | mental health crises.ti,ab. (69) |
| 3 | (mental health emergency or mental health emergencies).ti,ab. (114) |
| 4 | (psychiatric adj (crisis or crises or emergency or emergencies)).ti,ab. (1899) |
| 5 | 1 or 2 or 3 or 4 (2237) |
| 6 | Police/ (4562) |
| 7 | (police$ or policing).ti,ab. (14,093) |
| 8 | (law enforcement adj (staff or personnel or officer$ or official$ or worker$)).ti,ab. (694) |
| 9 | 6 or 7 or 8 (15,833) |
| 10 | 5 and 9 (137) |
| 11 | Mental disorder/ (158,383) |
| 12 | mental health.ti,ab. (118,368) |
| 13 | (mental$ adj disorder$).ti,ab. (34,306) |
| 14 | (mental$ adj ill$).ti,ab. (33,531) |
| 15 | Schizophrenia/ (98,309) |
| 16 | schizophren$.ti,ab. (116,520) |
| 17 | exp Personality Disorders/ (40,504) |
| 18 | 11 or 12 or 13 or 14 or 15 or 16 or 17 (421,560) |
| 19 | 9 and 18 (1594) |
| 20 | Triage/ (10,278) |
| 21 | mental health triage.ti,ab. (51) |
| 22 | street triage.ti,ab. (11) |
| 23 | 20 or 21 or 22 (10,293) |
| 24 | 9 and 23 (50) |
| 25 | Crisis Intervention/ (5747) |
| 26 | (crisis adj3 (response or co-response or coresponse or intervention$ or partnership$ or program$)).ti,ab. (2300) |
| 27 | 25 or 26 (6833) |
| 28 | 9 and 27 (254) |
| 29 | interprofessional relations/ (49,613) |
| 30 | 9 and 29 (128) |
| 31 | ((collaborat$ or partner$ or interagency or multidisciplinary or co-respon$) adj2 (police$ or policing)).ti,ab. (73) |
| 32 | 30 or 31 (198) |
| 33 | (Diversion$ or divert$).ti,ab. (53,317) |
| 34 | 18 and 33 (580) |
| 35 | 10 or 19 or 24 or 28 or 32 or 34 (2396) |
| 36 | limit 35 to yr = ‘2016 -Current’ (321) |
| 37 | limit 36 to english language (314) |
Applied Social Sciences Index and Abstracts
Via ProQuest (see URL: www.proquest.com/).
Date searched: 8 November 2017.
Records retrieved: 137.
Search strategy
| Set number | Searched for | Databases | Results |
|---|---|---|---|
| S5 | ((TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR (((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)) OR (MAINSUBJECT.EXACT(‘Triage’) OR TI,AB,IF(‘mental health triage’) OR TI,AB,IF(‘street triage’)) OR (MAINSUBJECT.EXACT(‘Crisis intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*)))) AND (MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*)))) OR ((MAINSUBJECT.EXACT(‘Diversion schemes’) OR TI,AB,IF(diversion* OR divert*)) AND (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)))) AND pd(20160101-20171231)) AND la.exact(‘ENG’) | Applied Social Sciences Index & Abstracts | 137 |
Criminal Justice Abstracts
Via EBSCOhost (see URL: www.ebsco.com/).
Date range: inception to 6 November 2017.
Date searched: 7 November 2017.
Records retrieved: 349.
Search strategy
| S1 | TX mental health crisis OR TX mental health crises | 370 |
| S2 | TX mental health emergenc* | 62 |
| S3 | TX (psychiatric N1 (crisis or crises)) OR TX (psychiatric N1 (emergency or emergencies)) | 94 |
| S4 | S1 OR S2 OR S3 | 478 |
| S5 | SU police | 19,944 |
| S6 | TX (police* or policing) | 51,273 |
| S7 | TX ((law enforcement) N2 (staff or personnel or officer* or official* or worker*)) | 10,494 |
| S8 | S5 OR S6 OR S7 | 52,086 |
| S9 | S4 AND S8 | 137 |
| S10 | TX (mental N2 health) OR TX ((mental* N2 (ill* or disorder* or distress*))) OR TX schizophren* | 37,881 |
| S11 | SU ‘mental illness’ OR SU ‘mental health’ | 14,966 |
| S12 | SU ‘Distress (Psychology)’ | 863 |
| S13 | (ZU ‘schizophrenia’) | 903 |
| S14 | S10 OR S11 OR S12 OR S13 | 38,444 |
| S15 | S8 AND S14 | 1576 |
| S16 | TX triage | 221 |
| S17 | S8 AND S16 | 43 |
| S18 | TX crisis N3 (response or co-response or coresponse or intervention* or partnership* or program*) | 1187 |
| S19 | S8 AND S18 | 357 |
| S20 | TX (collaborat* or partner* or interagency or multidisciplinary or co-respon*) N2 (police* or policing) | 470 |
| S21 | TX diversion* or divert* | 4424 |
| S22 | S14 AND S21 | 663 |
| S23 | S9 OR S15 OR S17 OR S19 OR S20 OR S22 | 2864 |
| S24 |
S9 OR S15 OR S17 OR S19 OR S20 OR S22 Limiters - Publication Date: 20160101-20171231; Language: English |
349 |
EMBASE
Via Ovid (see URL: http://ovidsp.ovid.com/).
Date range: 1974 to 6 November 2017.
Date searched: 7 November 2017.
Records retrieved: 315.
Search strategy
| 1 | mental health crisis.ti,ab. (199) |
| 2 | mental health crises.ti,ab. (70) |
| 3 | (mental health emergency or mental health emergencies).ti,ab. (126) |
| 4 | (psychiatric adj (crisis or crises or emergency or emergencies)).ti,ab. (2354) |
| 5 | 1 or 2 or 3 or 4 (2694) |
| 6 | Police/ (10,154) |
| 7 | (police$ or policing).ti,ab. (17,558) |
| 8 | (law enforcement adj (staff or personnel or officer$ or official$ or worker$)).ti,ab. (831) |
| 9 | 6 or 7 or 8 (20,635) |
| 10 | 5 and 9 (137) |
| 11 | Mental disease/ (206,258) |
| 12 | mental health.ti,ab. (137,789) |
| 13 | (mental$ adj disorder$).ti,ab. (40,741) |
| 14 | (mental$ adj ill$).ti,ab. (39,123) |
| 15 | Schizophrenia/ (162,958) |
| 16 | schizophren$.ti,ab. (145,599) |
| 17 | exp Personality Disorder/(56,264) |
| 18 | 11 or 12 or 13 or 14 or 15 or 16 or 17 (524,016) |
| 19 | 9 and 18 (1923) |
| 20 | emergency health service/and procedures/ (2032) |
| 21 | mental health triage.ti,ab. (56) |
| 22 | street triage.ti,ab. (11) |
| 23 | 20 or 21 or 22 (2093) |
| 24 | 9 and 23 (25) |
| 25 | Crisis Intervention/ (6144) |
| 26 | (crisis adj3 (response or co-response or coresponse or intervention$ or partnership$ or program$)).ti,ab. (2760) |
| 27 | 25 or 26 (7357) |
| 28 | 9 and 27 (250) |
| 29 | ((collaborat$ or partner$ or interagency or multidisciplinary or co-respon$) adj2 (police$ or policing)).ti,ab. (84) |
| 30 | (Diversion$ or divert$).ti,ab. (63,529) |
| 31 | 18 and 30 (763) |
| 32 | 10 or 19 or 24 or 28 or 29 or 31 (2831) |
| 33 | limit 32 to yr = ‘2016 -Current’ (323) |
| 34 | limit 33 to english language (315) |
PAIS Index
Via ProQuest (see URL: www.proquest.com/).
Date searched: 7 November 2017.
Records retrieved: 16.
Search strategy
| Set number | Searched for | Databases | Results |
|---|---|---|---|
| S1 | (TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR ((MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*))) AND ((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Forensic Psychiatry’) OR MAINSUBJECT.EXACT(‘Mental Illness’) OR MAINSUBJECT.EXACT(‘Mental Health’) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR TI,AB,IF(‘personality disorder’ OR ‘personality disorders’)) OR (TI,AB,IF(triage) OR TI,AB,IF(‘street triage’) OR TI,AB,IF(‘mental health triage’)) OR (MAINSUBJECT.EXACT(‘Crisis Intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*))))) OR ((MAINSUBJECT.EXACT(‘Forensic Psychiatry’) OR MAINSUBJECT.EXACT(‘Mental Illness’) OR MAINSUBJECT.EXACT(‘Mental Health’) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR TI,AB,IF(‘personality disorder’ OR ‘personality disorders’)) AND TI,AB,IF(diversion* OR divert*))) AND pd(20160101-20171107) | PAIS Index | 160 |
PsycINFO
Via Ovid (see URL: http://ovidsp.ovid.com).
Date range: 1806 to October (week 5) 2017.
Date searched: 7 November 2017.
Records retrieved: 289.
Search strategy
| 1 | mental health crisis.ti,ab. (254) |
| 2 | mental health crises.ti,ab. (74) |
| 3 | (mental health emergency or mental health emergencies).ti,ab. (82) |
| 4 | (psychiatric adj (crisis or crises or emergency or emergencies)).ti,ab. (1783) |
| 5 | 1 or 2 or 3 or 4 (2140) |
| 6 | Police Personnel/ (8247) |
| 7 | (police$ or policing).ti,ab. (20,588) |
| 8 | (law enforcement adj (staff or personnel or officer$ or official$ or worker$)).ti,ab. (1345) |
| 9 | 6 or 7 or 8 (21,741) |
| 10 | 5 and 9 (145) |
| 11 | Mental disorders/ (77,006) |
| 12 | mental health.ti,ab. (150,101) |
| 13 | (mental$ adj disorder$).ti,ab. (45,884) |
| 14 | (mental$ adj ill$).ti,ab. (44,162) |
| 15 | Schizophrenia/ (80,171) |
| 16 | schizophren$.ti,ab. (110,682) |
| 17 | exp Personality Disorders/(32,178) |
| 18 | 11 or 12 or 13 or 14 or 15 or 16 or 17 (364,962) |
| 19 | 9 and 18 (2087) |
| 20 | triage.ti,ab. (1216) |
| 21 | mental health triage.ti,ab. (35) |
| 22 | street triage.ti,ab. (4) |
| 23 | 20 or 21 or 22 (1216) |
| 24 | 9 and 23 (21) |
| 25 | Crisis Intervention/(3273) |
| 26 | (crisis adj3 (response or co-response or coresponse or intervention$ or partnership$ or program$)).ti,ab. (4377) |
| 27 | 25 or 26 (5839) |
| 28 | 9 and 27 (375) |
| 29 | ((collaborat$ or partner$ or interagency or multidisciplinary or co-respon$) adj2 (police$ or policing)).ti,ab. (152) |
| 30 | (Diversion$ or divert$).ti,ab. (4614) |
| 31 | 18 and 30 (755) |
| 32 | 10 or 19 or 24 or 28 or 29 or 31 (3118) |
| 33 | limit 32 to yr = ‘2016 -Current’ (326) |
| 34 | limit 33 to english language (289) |
Scopus
Via Elsevier (see URL: www.elsevier.com).
Date range: inception to 6 November 2017.
Date searched: 7 November 2017.
Records retrieved: 538.
Search strategy
((((TITLE-ABS-KEY (‘mental health crisis’) OR TITLE-ABS-KEY (‘mental health crises’))) OR (TITLE-ABS-KEY (‘mental health emergenc*’)) OR ((TITLE-ABS-KEY (‘psychiatric crisis’) OR TITLE-ABS-KEY (‘psychiatric crises’))) OR (TITLE-ABS-KEY (‘psychiatric emergenc*’))) AND (((TITLE-ABS-KEY (police) OR TITLE-ABS-KEY (policing))) OR ((TITLE-ABS-KEY (law AND enforcement AND staff) OR TITLE-ABS-KEY (law AND enforcement AND personnel) OR TITLE-ABS-KEY (law AND enforcement AND officer*) OR TITLE-ABS-KEY (law AND enforcement AND official*) OR TITLE-ABS-KEY (law AND enforcement AND worker*))))) OR (((TITLE-ABS-KEY (‘psychiatric disorder*’)) OR (TITLE-ABS-KEY (‘mental health’)) OR (TITLE-ABS-KEY (‘mental disease*’)) OR (TITLE-ABS-KEY (‘mental* ill*’)) OR (TITLE-ABS-KEY (schizophren*)) OR (TITLE-ABS-KEY (‘personality disorder*’))) AND (((TITLE-ABS-KEY (police) OR TITLE-ABS-KEY (policing))) OR ((TITLE-ABS-KEY (law AND enforcement AND staff) OR TITLE-ABS-KEY (law AND enforcement AND personnel) OR TITLE-ABS-KEY (law AND enforcement AND officer*) OR TITLE-ABS-KEY (law AND enforcement AND official*) OR TITLE-ABS-KEY (law AND enforcement AND worker*))))) OR (((TITLE-ABS-KEY (triage) OR TITLE-ABS-KEY (‘street triage’) OR TITLE-ABS-KEY (‘mental health triage’))) AND (((TITLE-ABS-KEY (police) OR TITLE-ABS-KEY (policing))) OR ((TITLE-ABS-KEY (law AND enforcement AND staff) OR TITLE-ABS-KEY (law AND enforcement AND personnel) OR TITLE-ABS-KEY (law AND enforcement AND officer*) OR TITLE-ABS-KEY (law AND enforcement AND official*) OR TITLE-ABS-KEY (law AND enforcement AND worker*))))) OR (((TITLE-ABS-KEY (‘crisis intervention*’)) OR (TITLE-ABS-KEY (‘crisis response*’)) OR (TITLE-ABS-KEY (‘crisis coresponse*’)) OR (TITLE-ABS-KEY (‘crisis program*’))) AND (((TITLE-ABS-KEY (police) OR TITLE-ABS-KEY (policing))) OR ((TITLE-ABS-KEY (law AND enforcement AND staff) OR TITLE-ABS-KEY (law AND enforcement AND personnel) OR TITLE-ABS-KEY (law AND enforcement AND officer*) OR TITLE-ABS-KEY (law AND enforcement AND official*) OR TITLE-ABS-KEY (law AND enforcement AND worker*))))) OR ((TITLE-ABS-KEY (collaborat* W/2 police*)) OR (TITLE-ABS-KEY (partner* W/2 police*)) OR (TITLE-ABS-KEY (interagency W/2 police*)) OR (TITLE-ABS-KEY (multidisciplinary W/2 police*)) OR (TITLE-ABS-KEY (corespons* W/2 police*))) OR (((TITLE-ABS-KEY (divert*) OR TITLE-ABS-KEY (diversion*))) AND ((TITLE-ABS-KEY (‘psychiatric disorder*’)) OR (TITLE-ABS-KEY (‘mental health’)) OR (TITLE-ABS-KEY (‘mental disease*’)) OR (TITLE-ABS-KEY (‘mental* ill*’)) OR (TITLE-ABS-KEY (schizophren*)) OR (TITLE-ABS-KEY (‘personality disorder*’)))) AND (LIMIT-TO (PUBYEAR, 2017) OR LIMIT-TO (PUBYEAR, 2016)) AND (LIMIT-TO (LANGUAGE, ‘English’))
Key
-
TITLE-ABS-KEY = terms in either title or abstract or keyword fields
-
* = truncation
-
W/2 = terms within two words of each other (any order).
Social Care Online
See URL: www.scie-socialcareonline.org.uk.
Date searched: 7 November 2017.
Records retrieved: 21.
Search strategy
- SubjectTerms:’police’ including this term only - AND AllFields:’mental or psychiatr* or schizophreni*’ - AND PublicationYear:’2016 2017’
Fifteen records.
- AllFields:’crisis intervention*’ or triage’ - AND AllFields:’police* or policing’ - AND PublicationYear:’2016 2017’
Six records.
Key
-
Subject Terms = subject heading search
-
All Fields = search of all text fields
-
* = truncation.
Social Policy & Practice
Via Ovid (see URL: http://ovidsp.ovid.com/).
Date range: inception to October 2017.
Date searched: 7 November 2017.
Records retrieved: 43.
Search strategy
| 1 | mental health crisis.mp. (115) |
| 2 | mental health crises.mp. (21) |
| 3 | (mental health emergency or mental health emergencies).mp. (7) |
| 4 | (psychiatric adj (crisis or crises or emergency or emergencies)).mp. (57) |
| 5 | 1 or 2 or 3 or 4 (187) |
| 6 | (police$ or policing).mp. (7547) |
| 7 | (law enforcement adj (staff or personnel or officer$ or official$ or worker$)).mp. (41) |
| 8 | 6 or 7 (7577) |
| 9 | 5 and 8 (31) |
| 10 | mental health.mp. (38,912) |
| 11 | (mental$ adj disorder$).mp. (6244) |
| 12 | (mental$ adj ill$).mp. (5662) |
| 13 | schizophren$.mp. (1943) |
| 14 | personality disorder$.mp. (1249) |
| 15 | 10 or 11 or 12 or 13 or 14 (43,335) |
| 16 | 8 and 15 (582) |
| 17 | Triage.mp. (76) |
| 18 | mental health triage.mp. (2) |
| 19 | street triage.mp. (5) |
| 20 | 17 or 18 or 19 (76) |
| 21 | 8 and 20 (9) |
| 22 | (crisis adj3 (response or co-response or coresponse or intervention$ or partnership$ or program$)).mp. (684) |
| 23 | 8 and 22 (40) |
| 24 | ((collaborat$ or partner$ or interagency or multidisciplinary or co-respon$) adj2 (police$ or policing)).ti,ab. (54) |
| 25 | (Diversion$ or divert$).ti,ab. (859) |
| 26 | 15 and 25 (185) |
| 27 | 9 or 16 or 21 or 23 or 24 or 26 (802) |
| 28 | limit 27 to yr = ‘2016 -Current’ (43) |
Social Sciences Citation Index
Via Web of Science, Clarivate Analytics (see URL: https://clarivate.com/).
Date range: 1956 to 6 November 2017.
Date searched: 7 November 2017.
Records retrieved: 374.
Search strategy
| # 14 | 374 | (#12 OR #10 OR #9 OR #7 OR #5 OR #3) AND LANGUAGE: (English) |
| Timespan = 2016–17 | ||
| # 13 | 2391 | #12 OR #10 OR #9 OR #7 OR #5 OR #3 |
| # 12 | 617 | #11 AND #4 |
| # 11 | 5993 | TS = (diversion* or divert*) |
| # 10 | 275 | TS = ((collaborat* or partner* or interagency or multidisciplinary or co-response*) NEAR/2 (police* or policing)) |
| # 9 | 151 | #8 AND #2 |
| # 8 | 3738 | TS = (crisis NEAR/3 (intervention* or response* or co-response* or coresponse* or partnership* or program*)) |
| # 7 | 27 | #6 AND #2 |
| # 6 | 2398 | TS = (triage) OR TS = (street triage) OR TS = (mental health triage) |
| # 5 | 1537 | #4 AND #2 |
| # 4 | 321,021 | TS = (psychiatric disorder*) OR TS = (mental NEAR/1 (health OR disorder* or disease*)) OR TS = (mental* NEAR/1 ill*) OR TS = (schizophren*) OR TS = (personality disorder*) |
| # 3 | 320 | #2 AND #1 |
| # 2 | 30,606 | TS = (police* or policing) OR TS = (law enforcement staff) OR TS = (law enforcement personnel) OR TS = (law enforcement officer*) OR TS = (law enforcement official*) OR TS = (law enforcement worker*) |
| # 1 | 7378 | TS = (mental health crisis) OR TS = (mental health crises) OR TS = (mental health emergenc*) OR TS = (psychiatric NEAR/1 (crisis or crises or emergenc*)) |
Social Services Abstracts
Via ProQuest (see URL: www.proquest.com/).
Date searched: 8 November 2017.
Records retrieved: 47.
Search strategy
| Set number | Searched for | Databases | Results |
|---|---|---|---|
| S7 | (TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR (((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Mental Illness’) OR MAINSUBJECT.EXACT(‘Mental Health’) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality Disorders’) OR MAINSUBJECT.EXACT(‘Paranoia’) OR MAINSUBJECT.EXACT(‘Psychosis’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR TI,AB,IF(‘personality disorder’ OR ‘personality disorders’)) OR (TI,AB,IF(triage) OR TI,AB,IF(‘street triage’) OR TI,AB,IF(‘mental health triage’)) OR (MAINSUBJECT.EXACT(‘Crisis Intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*)))) AND (MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*)))) OR (TI,AB,IF(diversion* OR divert*) AND (MAINSUBJECT.EXACT(‘Mental Illness’) OR MAINSUBJECT.EXACT(‘Mental Health’) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality Disorders’) OR MAINSUBJECT.EXACT(‘Paranoia’) OR MAINSUBJECT.EXACT(‘Psychosis’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR TI,AB,IF(‘personality disorder’ OR ‘personality disorders’)))) AND pd(20160101-20171108) | Social Services Abstracts | 47 |
Search strategies for the rapid evidence synthesis of UK-relevant qualitative data on implementation
The following search strategies are based on those used for an ongoing review of PRMHT interventions. {Park, 2016 #702} In addition, they include a previously tested search strategy designed to limit retrieval to qualitative studies. 30
MEDLINE [Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)]
Via Ovid (see URL: http://ovidsp.ovid.com/).
Date range: 1946 to present.
Date searched: 9 November 2017.
Records retrieved: 990.
Search strategy
| 1 | mental health crisis.ti,ab. (209) |
| 2 | mental health crises.ti,ab. (69) |
| 3 | (mental health emergency or mental health emergencies).ti,ab. (116) |
| 4 | (psychiatric adj (crisis or crises or emergency or emergencies)).ti,ab. (1911) |
| 5 | 1 or 2 or 3 or 4 (2253) |
| 6 | Police/ (4597) |
| 7 | (police$ or policing).ti,ab. (14,188) |
| 8 | (law enforcement adj (staff or personnel or officer$ or official$ or worker$)).ti,ab. (700) |
| 9 | 6 or 7 or 8 (15,939) |
| 10 | 5 and 9 (139) |
| 11 | Mental disorder/ (160,044) |
| 12 | mental health.ti,ab. (120,248) |
| 13 | (mental$ adj disorder$).ti,ab. (34,636) |
| 14 | (mental$ adj ill$).ti,ab. (34,074) |
| 15 | Schizophrenia/ (98,834) |
| 16 | schizophren$.ti,ab. (117,201) |
| 17 | exp Personality Disorders/ (40,773) |
| 18 | 11 or 12 or 13 or 14 or 15 or 16 or 17 (425,488) |
| 19 | 9 and 18 (1615) |
| 20 | Triage/ (10,365) |
| 21 | mental health triage.ti,ab. (51) |
| 22 | street triage.ti,ab. (11) |
| 23 | 20 or 21 or 22 (10,380) |
| 24 | 9 and 23 (50) |
| 25 | Crisis Intervention/ (5775) |
| 26 | (crisis adj3 (response or co-response or coresponse or intervention$ or partnership$ or program$)).ti,ab. (2317) |
| 27 | 25 or 26 (6869) |
| 28 | 9 and 27 (259) |
| 29 | interprofessional relations/ (49,993) |
| 30 | 9 and 29 (129) |
| 31 | ((collaborat$ or partner$ or interagency or multidisciplinary or co-respon$) adj2 police).ti,ab. (68) |
| 32 | 30 or 31 (194) |
| 33 | (Diversion$ or divert$).ti,ab. (54,320) |
| 34 | 18 and 33 (589) |
| 35 | 10 or 19 or 24 or 28 or 32 or 34 (2422) |
| 36 | exp qualitative research/ (39,002) |
| 37 | Nursing Methodology Research/ (17,038) |
| 38 | ‘Surveys and Questionnaires’/ (418,726) |
| 39 | Self Report/ (23,013) |
| 40 | exp Attitude/ (333,788) |
| 41 | Focus Groups/ (25,338) |
| 42 | Ethnology/(1650) |
| 43 | discourse analysis.mp. (1551) |
| 44 | content analysis.mp. (21,331) |
| 45 | ethnographic research.mp. (831) |
| 46 | ethnological research.mp. (7) |
| 47 | ethnonursing research.mp. (50) |
| 48 | constant comparative method.mp. (1413) |
| 49 | qualitative validity.mp. (14) |
| 50 | purposive sample.mp. (2865) |
| 51 | observational method$.mp. (660) |
| 52 | field stud$.mp. (14,050) |
| 53 | theoretical sampl$.mp. (582) |
| 54 | phenomenology.mp. (8141) |
| 55 | phenomenological research.mp. (405) |
| 56 | life experience$.mp. (4670) |
| 57 | cluster sampl$.mp. (6102) |
| 58 | or/36-57 (765,476) |
| 59 | findings.af. (1,849,993) |
| 60 | interview$.af. or interviews/or Interviews as Topic/ (349,102) |
| 61 | qualitative.af. (205,338) |
| 62 | or/59-61 (2,250,699) |
| 63 | 58 or 62 (2,789,177) |
| 64 | ethnonursing.af. (143) |
| 65 | ethnograph$.mp. (9467) |
| 66 | phenomenol$.af. (23,401) |
| 67 | grounded theory.mp. (9947) |
| 68 | (grounded adj (theor$ or study or studies or research or analys?s)).af. (10,099) |
| 69 | (life stor$ or women$ stor$).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] (1197) |
| 70 | (emic or etic or hermeneutic$ or heuristic$ or semiotic$).af. (15,721) |
| 71 | (data adj1 saturat$).tw. (896) |
| 72 | participant observ$.tw. (4016) |
| 73 | (social construct$ or postmodern$ or post-structural$ or post structural$ or poststructural$ or post modern$ or post-modern$ or feminis$ or interpret$).mp. (500,681) |
| 74 | (action research or cooperative inquir$ or co operative inquir$ or co-operative inquir$).mp. (3657) |
| 75 | (humanistic or existential or experiential or paradigm$).mp. (137,914) |
| 76 | (field adj (study or studies or research or observation$)).tw. (18,102) |
| 77 | human science.tw. (258) |
| 78 | biographical method.tw. (17) |
| 79 | theoretical sampl$.af. (582) |
| 80 | (purpos$ adj4 sampl$).af. (11,538) |
| 81 | (focus adj group$).af. (42,824) |
| 82 | (account or accounts or unstructured or open-ended or open ended or text$ or narrative$).mp. (575,275) |
| 83 | (life world or life-world or conversation analys?s or personal experience$ or theoretical saturation).mp. (14,416) |
| 84 | lived experience$.tw. (4268) |
| 85 | (theme$ or thematic).mp. (84,043) |
| 86 | categor$.mp. (314,804) |
| 87 | (observational adj (method$ or research or stud$)).af. (118,928) |
| 88 | questionnaire$.mp. (656,944) |
| 89 | content analysis.af. (21,336) |
| 90 | thematic analysis.af. (11,601) |
| 91 | discourse analys?s.af. (1590) |
| 92 | ((discourse$ or discurs$) adj3 analys?s).tw. (1883) |
| 93 | (constant adj (comparative or comparison)).af. (3979) |
| 94 | narrative analys?s.af. (999) |
| 95 | heidegger$.tw. (631) |
| 96 | colaizzi$.tw. (548) |
| 97 | speigelberg$.tw. (2) |
| 98 | (van adj manen$).tw. (346) |
| 99 | (van adj kaam$).tw. (42) |
| 100 | (merleau adj ponty$).tw. (206) |
| 101 | husserl$.tw. (232) |
| 102 | giorgi$.tw. (605) |
| 103 | foucault$.tw. (763) |
| 104 | (corbin$ adj2 strauss$).tw. (279) |
| 105 | glaser$.tw. (933) |
| 106 | or/64-105 (2,269,801) |
| 107 | 63 or 106 (4,216,855) |
| 108 | (mixed method$ or multimethod$ or multi-method$ or multi method$).mp. (16,355) |
| 109 | (attitude$ or belief$ or believ$ or choice$ or choos$ or experienc$ or opinion$ or perceiv$ or percept$ or prefer$ or view$).ti. (556,545) |
| 110 | 107 or 108 or 109 (4,558,138) |
| 111 | 35 and 110 (1108) |
| 112 | limit 111 to yr = ‘1990 -Current’ (1045) |
| 113 | limit 112 to english language (990) |
Applied Social Sciences Index and Abstracts
Via ProQuest (see URL: www.proquest.com/).
Date searched: 9 November 2017.
Records retrieved: 828.
Owing to problems with the search interface and problems downloading records, the search had to be split into smaller sections, with six sets of results downloaded individually and deduplicated in EndNote [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA].
Search strategy
| Set number | Searched for | Databases | Results |
|---|---|---|---|
| S21 | (TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR (((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)) OR (MAINSUBJECT.EXACT(‘Triage’) OR TI,AB,IF(‘mental health triage’) OR TI,AB,IF(‘street triage’)) OR (MAINSUBJECT.EXACT(‘Crisis intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*)))) AND (MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*)))) OR ((MAINSUBJECT.EXACT(‘Diversion schemes’) OR TI,AB,IF(diversion* OR divert*)) AND (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)))) AND ((MAINSUBJECT.EXACT(‘Qualitative data’) OR MAINSUBJECT.EXACT(‘Qualitative methods’) OR MAINSUBJECT.EXACT(‘Qualitative research’) OR MAINSUBJECT.EXACT(‘Qualitative analysis’)) OR MAINSUBJECT.EXACT.EXPLODE(‘Questionnaires’) OR (MAINSUBJECT.EXACT.EXPLODE(‘Attitudes’) OR (MAINSUBJECT.EXACT(‘Focus group interviews’) OR MAINSUBJECT.EXACT(‘Focus groups’))) OR MAINSUBJECT.EXACT(‘Discourse analysis’) OR MAINSUBJECT.EXACT(‘Content analysis’) OR MAINSUBJECT.EXACT.EXPLODE(‘Ethnography’) OR (MAINSUBJECT.EXACT.EXPLODE(‘Observation’) OR MAINSUBJECT.EXACT(‘Observational research’)) OR (MAINSUBJECT.EXACT.EXPLODE(‘Phenomenology’) OR MAINSUBJECT.EXACT(‘Life experiences’))) AND pd(19900101-20171231) |
Applied Social Sciences Index & Abstracts These databases are searched for part of your query |
81 |
| S22 | (TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR (((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)) OR (MAINSUBJECT.EXACT(‘Triage’) OR TI,AB,IF(‘mental health triage’) OR TI,AB,IF(‘street triage’)) OR (MAINSUBJECT.EXACT(‘Crisis intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*)))) AND (MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*)))) OR ((MAINSUBJECT.EXACT(‘Diversion schemes’) OR TI,AB,IF(diversion* OR divert*)) AND (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)))) AND (TI,AB,IF(‘personal experience’ OR ‘personal experiences’ OR ‘theoretical saturation’ OR (lived NEAR/1 experience*) OR theme* OR thematic OR categor* OR discurs*) OR TI,AB,IF(heidegger* OR colaizzi* OR speigelberg* OR van manen* OR van kaam* OR merleau ponty* OR husserl* OR giorgi* OR foucault* OR corbin* OR strauss* OR glaser*) OR TI,AB,IF((mixed NEAR/1 method*) OR multimethod* OR multi-method* OR multi NEAR/1 method*) OR ti((attitude* OR belief* OR believ* OR choice* OR choos* OR experienc* OR opinion* OR perceiv* OR percept* OR prefer* OR view*)) OR TI,AB,IF(findings OR interview*)) AND pd(19900101-20171231) |
Applied Social Sciences Index & Abstracts These databases are searched for part of your query |
458 |
| S23 | (TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR (((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)) OR (MAINSUBJECT.EXACT(‘Triage’) OR TI,AB,IF(‘mental health triage’) OR TI,AB,IF(‘street triage’)) OR (MAINSUBJECT.EXACT(‘Crisis intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*)))) AND (MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*)))) OR ((MAINSUBJECT.EXACT(‘Diversion schemes’) OR TI,AB,IF(diversion* OR divert*)) AND (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)))) AND (TI,AB,IF(qualitative OR ‘nursing methodology research’ OR questionnaire* OR attitude* OR ‘focus group’ OR ‘focus groups’ OR ‘discourse analysis’ OR ‘discourse analyses’ OR ‘content analysis’ OR ethnograph* OR ‘ethnological research’ OR ethnonursing) OR TI,AB,IF(‘constant comparative’ OR (purposive NEAR/1 sampl*) OR (observational NEAR/1 (research* OR method* OR stud*)) OR ‘field study’ OR ‘field studies’ OR (theoretical NEAR/1 sampl*) OR phenomenol* OR ‘life experience’ OR ‘life experiences’ OR (cluster NEAR/1 sampl*))) AND pd(19900101-20171231) |
Applied Social Sciences Index & Abstracts These databases are searched for part of your query |
175 |
| S24 | (TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR (((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)) OR (MAINSUBJECT.EXACT(‘Triage’) OR TI,AB,IF(‘mental health triage’) OR TI,AB,IF(‘street triage’)) OR (MAINSUBJECT.EXACT(‘Crisis intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*)))) AND (MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*)))) OR ((MAINSUBJECT.EXACT(‘Diversion schemes’) OR TI,AB,IF(diversion* OR divert*)) AND (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)))) AND TI,AB,IF((grounded NEAR/1 theor*) OR (grounded NEAR/1 stud*) OR ‘grounded research’ OR ‘grounded analysis’ OR ‘grounded analyses’ OR (life NEAR/1 stor*) OR (women* NEAR/1 stor*) OR emic OR etic OR hermeneutic* OR heuristic* OR semiotic* OR (data NEAR/1 saturat*) OR (participant NEAR/1 observ*)) AND pd(19900101-20171231) |
Applied Social Sciences Index & Abstracts These databases are searched for part of your query |
14 |
| S25 | (TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR (((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)) OR (MAINSUBJECT.EXACT(‘Triage’) OR TI,AB,IF(‘mental health triage’) OR TI,AB,IF(‘street triage’)) OR (MAINSUBJECT.EXACT(‘Crisis intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*)))) AND (MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*)))) OR ((MAINSUBJECT.EXACT(‘Diversion schemes’) OR TI,AB,IF(diversion* OR divert*)) AND (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)))) AND TI,AB,IF((social NEAR/1 construct*) OR postmodern* OR post-structural* OR (post NEAR/1 structural*) OR poststructural* OR (post NEAR/1 modern*) OR post-modern* OR feminis* OR interpret* OR ‘action research’ OR (cooperative NEAR/1 inquir*) OR (‘co operative’ NEAR/1 inquir*) OR (co-operative NEAR/1 inquir*) OR humanistic OR existential OR experiential OR paradigm* OR (field NEAR/1 (research OR observation*)) OR ‘human science’) AND pd(19900101-20171231) |
Applied Social Sciences Index & Abstracts These databases are searched for part of your query |
27 |
| S26 | (TI,AB,IF((collaborat* OR partner* OR interagency OR multidisciplinary OR co-respons*) NEAR/2 (police* OR policing)) OR (((TI,AB,IF(‘mental health crisis’) OR TI,AB,IF(‘mental health crises’) OR TI,AB,IF(‘mental health emergency’) OR TI,AB,IF(‘mental health emergencies’) OR TI,AB,IF(psychiatric NEAR/1 (crisis OR crises OR emergency OR emergencies))) OR (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)) OR (MAINSUBJECT.EXACT(‘Triage’) OR TI,AB,IF(‘mental health triage’) OR TI,AB,IF(‘street triage’)) OR (MAINSUBJECT.EXACT(‘Crisis intervention’) OR TI,AB,IF(crisis NEAR/3 (response OR co-response OR coresponse OR intervention* OR partnership* OR program*)))) AND (MAINSUBJECT.EXACT(‘Police’) OR TI,AB,IF(police* OR policing) OR TI,AB,IF(‘law enforcement’ NEAR/1 (staff OR personnel OR officer* OR official* OR worker*)))) OR ((MAINSUBJECT.EXACT(‘Diversion schemes’) OR TI,AB,IF(diversion* OR divert*)) AND (MAINSUBJECT.EXACT(‘Psychiatric disorders’) OR MAINSUBJECT.EXACT(‘Mental health’) OR TI,AB,IF(mental NEAR/1 (disorder* OR disease* OR health)) OR TI,AB,IF(mental* NEAR/1 ill*) OR TI,AB,IF(schizophren*) OR MAINSUBJECT.EXACT(‘Schizophrenia’) OR MAINSUBJECT.EXACT.EXPLODE(‘Personality disorders’)))) AND TI,AB,IF(‘biographical method’ OR account OR accounts OR unstructured OR open-ended OR ‘open ended’ OR text* OR narrative* OR ‘life world’ OR life-world OR ‘conversation analysis’ OR ‘conversation analyses’) AND pd(19900101-20171231) |
Applied Social Sciences Index & Abstracts These databases are searched for part of your query |
73 |
Criminal Justice Abstracts
Via EBSCOhost (see URL: www.ebsco.com/).
Date range: inception to 6 November 2017.
Date searched: 9 November 2017.
Records retrieved: 1330.
Search strategy
| S1 | TX mental health crisis OR TX mental health crises | 370 |
| S2 | TX mental health emergenc* | 62 |
| S3 | TX (psychiatric N1 (crisis or crises)) OR TX (psychiatric N1 (emergency or emergencies)) | 94 |
| S4 | S1 OR S2 OR S3 | 478 |
| S5 | SU police | 19,944 |
| S6 | TX (police* or policing) | 51,273 |
| S7 | TX ((law enforcement) N2 (staff or personnel or officer* or official* or worker*)) | 10,494 |
| S8 | S5 OR S6 OR S7 | 52,086 |
| S9 | S4 AND S8 | 137 |
| S10 | TX (mental N2 health) OR TX ((mental* N2 (ill* or disorder* or distress*))) OR TX schizophren* | 37,881 |
| S11 | SU ‘mental illness’ OR SU ‘mental health’ | 14,966 |
| S12 | SU ‘Distress (Psychology)’ | 863 |
| S13 | (ZU ‘schizophrenia’) | 903 |
| S14 | S10 OR S11 OR S12 OR S13 | 38,444 |
| S15 | S8 AND S14 | 1576 |
| S16 | TX triage | 221 |
| S17 | S8 AND S16 | 43 |
| S18 | TX crisis N3 (response or co-response or coresponse or intervention* or partnership* or program*) | 1187 |
| S19 | S8 AND S18 | 357 |
| S20 | TX (collaborat* or partner* or interagency or multidisciplinary or co-respon*) N2 (police* or policing) | 470 |
| S21 | TX diversion* or divert* | 4424 |
| S22 | S14 AND S21 | 663 |
| S23 | S9 OR S15 OR S17 OR S19 OR S20 OR S22 | 2864 |
| S24 | SU qualitative | 2861 |
| S25 | SU questionnaire | 6263 |
| S26 | SU attitude | 10,318 |
| S27 | SU focus group | 906 |
| S28 | SU discourse analysis | 310 |
| S29 | SU content analysis | 732 |
| S30 | SU ethnographic | 181 |
| S31 | SU ethnological | 5 |
| S32 | SU ethnonursing | 0 |
| S33 | SU constant comparative method | 312 |
| S34 | SU qualitative validity | 171 |
| S35 | SU purposive sample | 230 |
| S36 | SU observational method | 499 |
| S37 | SU field study | 1180 |
| S38 | SU theoretical sample | 439 |
| S39 | SU phenomenology | 454 |
| S40 | SU phenomenological research | 419 |
| S41 | SU life experience | 503 |
| S42 | SU cluster sample | 526 |
| S43 | S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 | 19,675 |
| S44 | TX findings | 56,010 |
| S45 | TX interview* | 28,255 |
| S46 | SU interview* | 6967 |
| S47 | TX qualitative | 10,541 |
| S48 | S44 OR S45 OR S46 OR S47 | 80,618 |
| S49 | S43 OR S48 | 90,518 |
| S50 | TX ethnonursing or ‘nursing methodology research’ | 1476 |
| S51 | TX ethnograph* | 3689 |
| S52 | TX phenomenol* | 1216 |
| S53 | TX grounded N1 (theor* or study or studies or research or analys?s)) | 958 |
| S54 | TX life N1 stor* OR TX women* N1 stor* | 311 |
| S55 | TX emic or etic or hermeneutic* or heuristic* or semiotic* | 995 |
| S56 | TX data N1 saturat* | 3 |
| S57 | TX participant observ* | 1149 |
| S58 | TX (social N1 construct* or postmodern* or post-structural* or post N1 structural* or poststructural* or post N1 modern* or post-modern* or feminis* or interpret*) | 20,779 |
| S59 | TX ‘action research’ or cooperative N1 inquir* or co N1 operative N1 inquir* or co-operative N1 inquir* | 595 |
| S60 | TX humanistic or existential or experiential or paradigm* | 5592 |
| S61 | TX field N1 (study or studies or research or observation*) | 2097 |
| S62 | TX ‘human science’ | 36 |
| S63 | TX ‘biographical method’ | 1 |
| S64 | TX ‘qualitative validity’ | 1 |
| S65 | TX theoretical N1 sampl* | 28 |
| S66 | TX purpos* N4 sampl* | 747 |
| S67 | TX focus N1 group* | 2689 |
| S68 | TX account or accounts or unstructured or open-ended or ‘open ended’ or text* or narrative* | 26,142 |
| S69 | TX ‘life world’ or life-world or conversation N1 analys?s or personal N1 experience* or ‘theoretical saturation’ | 895 |
| S70 | TX lived N1 experience* OR TX life N1 experience* OR TX cluster sampl* | 1377 |
| S71 | TX theme* or thematic | 7182 |
| S72 | TX categor* | 10,433 |
| S73 | TX observational N1 (method* or research or stud*) | 802 |
| S74 | TX questionnaire* | 13,511 |
| S75 | TX ‘content analysis’ | 1866 |
| S76 | TX ‘thematic analysis’ | 1225 |
| S77 | TX (discourse* or discurs*) N3 analys?s) | 667 |
| S78 | TX constant N1 (comparative or comparison) | 100 |
| S79 | TX ‘narrative analys?s’ | 176 |
| S80 | TX heidegger* | 65 |
| S81 | TX colaizzi* | 5 |
| S82 | TX speigelberg* | 0 |
| S83 | TX van N1 manen* | 3 |
| S84 | TX van N1 kaam* | 2 |
| S85 | TX merleau N1 ponty* | 27 |
| S86 | TX husserl* | 38 |
| S87 | TX giorgi* | 261 |
| S88 | TX foucault* | 531 |
| S89 | TX corbin N2 strauss* | 15 |
| S90 | TX glaser* | 205 |
| S91 | S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 OR S85 OR S86 OR S87 OR S88 OR S89 OR S90 | 86,077 |
| S92 | S49 OR S91 | 145,703 |
| S93 | TX mixed method$ or multimethod* or multi-method* or multi method* | 1581 |
| S94 | TI attitude* or belief* or believ* or choice* or choos* or experienc* or opinion* or perceiv* or percept* or prefer* or view* | 22,164 |
| S95 | S92 OR S93 OR S94 | 156,561 |
| S96 | S23 AND S95 | 1089 |
| S97 | S23 AND S95 Limiters - Publication Date: 19900101-20171231; Language: English | 1035 |
PsycINFO
Via Ovid (see URL: http://ovidsp.ovid.com/).
Date range: 1806 to October (week 5) 2017.
Date searched: searched on 9 November 2017.
Records retrieved: 1578.
Search strategy
| 1 | mental health crisis.ti,ab. (254) |
| 2 | mental health crises.ti,ab. (74) |
| 3 | (mental health emergency or mental health emergencies).ti,ab. (82) |
| 4 | (psychiatric adj (crisis or crises or emergency or emergencies)).ti,ab. (1783) |
| 5 | 1 or 2 or 3 or 4 (2140) |
| 6 | Police Personnel/ (8247) |
| 7 | (police$ or policing).ti,ab. (20,588) |
| 8 | (law enforcement adj (staff or personnel or officer$ or official$ or worker$)).ti,ab. (1345) |
| 9 | 6 or 7 or 8 (21,741) |
| 10 | 5 and 9 (145) |
| 11 | Mental disorders/ (77,006) |
| 12 | mental health.ti,ab. (150,101) |
| 13 | (mental$ adj disorder$).ti,ab. (45,884) |
| 14 | (mental$ adj ill$).ti,ab. (44,162) |
| 15 | Schizophrenia/ (80,171) |
| 16 | schizophren$.ti,ab. (110,682) |
| 17 | exp Personality Disorders/ (32,178) |
| 18 | 11 or 12 or 13 or 14 or 15 or 16 or 17 (364,962) |
| 19 | 9 and 18 (2087) |
| 20 | triage.ti,ab. (1216) |
| 21 | mental health triage.ti,ab. (35) |
| 22 | street triage.ti,ab. (4) |
| 23 | 20 or 21 or 22 (1216) |
| 24 | 9 and 23 (21) |
| 25 | Crisis Intervention/ (3273) |
| 26 | (crisis adj3 (response or co-response or coresponse or intervention$ or partnership$ or program$)).ti,ab. (4377) |
| 27 | 25 or 26 (5839) |
| 28 | 9 and 27 (375) |
| 29 | ((collaborat$ or partner$ or interagency or multidisciplinary or co-respon$) adj2 (police$ or policing)).ti,ab. (152) |
| 30 | (Diversion$ or divert$).ti,ab. (4614) |
| 31 | 18 and 30 (755) |
| 32 | 10 or 19 or 24 or 28 or 29 or 31 (3118) |
| 33 | qualitative research/ (7638) |
| 34 | questionnaires/ (16,753) |
| 35 | exp attitudes/ (314,113) |
| 36 | discourse analysis/ (7594) |
| 37 | content analysis/ (4980) |
| 38 | ethnology/ (1961) |
| 39 | ethnography/ (7721) |
| 40 | focus group$.mp. (29,177) |
| 41 | nursing methodology research.mp. (2) |
| 42 | discourse analysis.mp. (10,795) |
| 43 | content analysis.mp. (22,511) |
| 44 | ethnographic research.mp. (2478) |
| 45 | ethnological research.mp. (11) |
| 46 | ethnonursing research.mp. (19) |
| 47 | constant comparative method.mp. (1568) |
| 48 | qualitative validity.mp. (8) |
| 49 | purposive sample.mp. (2135) |
| 50 | observational method$.mp. (993) |
| 51 | field stud$.mp,md. (22,180) |
| 52 | theoretical sampl$.mp. (480) |
| 53 | phenomenology/ (12,246) |
| 54 | observation methods/(5101) |
| 55 | phenomenological research.mp. (1376) |
| 56 | life experience$.mp. (31,512) |
| 57 | cluster sampl$.mp. (1283) |
| 58 | or/33-57 (457,531) |
| 59 | findings.af. (875,563) |
| 60 | interview$.af. or interviews/or interviewing/ (557,029) |
| 61 | qualitative.af. (323,479) |
| 62 | or/59-61 (1,329,601) |
| 63 | 58 or 62 (1,570,844) |
| 64 | ethnonursing.af. (134) |
| 65 | ethnograph$.mp. (25,194) |
| 66 | phenomenol$.af. (98,007) |
| 67 | grounded theory.mp. (13,398) |
| 68 | (grounded adj (theor$ or study or studies or research or analys?s)).af. (47,646) |
| 69 | (life stor$ or women$ stor$).mp. [mp = title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (3573) |
| 70 | (emic or etic or hermeneutic$ or heuristic$ or semiotic$).af. (78,854) |
| 71 | (data adj1 saturat$).tw. (222) |
| 72 | participant observ$.tw. (7823) |
| 73 | (social construct$ or postmodern$ or post-structural$ or post structural$ or poststructural$ or post modern$ or post-modern$ or feminis$ or interpret$).mp. (217,174) |
| 74 | (action research or cooperative inquir$ or co operative inquir$ or co-operative inquir$).mp. (7781) |
| 75 | (humanistic or existential or experiential or paradigm$).mp. (121,531) |
| 76 | (field adj (study or studies or research or observation$)).tw. (10,471) |
| 77 | human science.tw. (604) |
| 78 | biographical method.tw. (55) |
| 79 | theoretical sampl$.af. (800) |
| 80 | (purpos$ adj4 sampl$).af. (7919) |
| 81 | (focus adj group$).af. (46,843) |
| 82 | (account or accounts or unstructured or open-ended or open ended or text$ or narrative$).mp. (315,661) |
| 83 | (life world or life-world or conversation analys?s or personal experience$ or theoretical saturation).mp. (13,277) |
| 84 | lived experience$.tw. (10,654) |
| 85 | (theme$ or thematic).mp. (110,853) |
| 86 | categor$.mp. (152,396) |
| 87 | (observational adj (method$ or research or stud$)).af. (42,827) |
| 88 | questionnaire$.mp. (35,1647) |
| 89 | content analysis.af. (46,748) |
| 90 | thematic analysis.af. (15,483) |
| 91 | discourse analys?s.af. (19,688) |
| 92 | ((discourse$ or discurs$) adj3 analys?s).tw. (7932) |
| 93 | (constant adj (comparative or comparison)).af. (4730) |
| 94 | narrative analys?s.af. (5920) |
| 95 | heidegger$.tw. (1684) |
| 96 | colaizzi$.tw. (405) |
| 97 | speigelberg$.tw. (0) |
| 98 | (van adj manen$).tw. (440) |
| 99 | (van adj kaam$).tw. (362) |
| 100 | (merleau adj ponty$).tw. (791) |
| 101 | husserl$.tw. (1110) |
| 102 | giorgi$.tw. (855) |
| 103 | foucault$.tw. (2601) |
| 104 | (corbin$ adj2 strauss$).tw. (551) |
| 105 | glaser$.tw. (1183) |
| 106 | or/64-105 (1,319,692) |
| 107 | 63 or 106 (2,203,951) |
| 108 | (mixed method$ or multimethod$ or multi-method$ or multi method$).mp. (22,343) |
| 109 | (attitude$ or belief$ or believ$ or choice$ or choos$ or experienc$ or opinion$ or perceiv$ or percept$ or prefer$ or view$).ti. (353,207) |
| 110 | 107 or 108 or 109 (2,315,694) |
| 111 | 32 and 110 (1805) |
| 112 | limit 111 to yr = ‘1990 -Current’ (1661) |
| 113 | limit 112 to english language (1578) |
Social Sciences Citation Index
Via Web of Science, Clarivate Analytics (see URL: https://clarivate.com/).
Date range: 1956 to 8 November 2017.
Date searched: 9 November 2017.
Records retrieved: 1330.
Search strategy
| # 26 | 1330 | (#23 AND #13) AND LANGUAGE: (English) Timespan = 1990-2017 |
| # 25 | 1372 | #23 AND #13 Timespan = 1990-2017 |
| # 24 | 1378 | #23 AND #13 |
| # 23 | 1,971,772 | #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 |
| # 22 | 708,438 | TS = (findings or interview*) |
| # 21 | 406,341 | TI = (attitude* or belief* or believ* or choice* or choos* or experienc* or opinion* or perceiv* or percept* or prefer* or view*) |
| # 20 | 59,659 | TS = (mixed method* or multimethod* or multi-method* or multi method*) |
| # 19 | 11,665 | TS = (heidegger* or colaizzi* or speigelberg* or van manen* or van kaam* or merleau ponty* or husserl* or giorgi* or foucault* or corbin* or strauss* or glaser*) |
| # 18 | 261,109 | TS = (personal experience* or theoretical saturation or lived experience* or theme* or thematic or categor* or discurs*) |
| # 17 | 365,494 | TS = (biographical method OR account OR accounts OR unstructured OR open-ended OR open ended OR text* OR narrative* OR life world OR life-world OR conversation analys?s) |
| # 16 | 395,327 | TS = (social construct* or postmodern* or post-structural* or post structural* or poststructural* or post modern* or post-modern* or feminis* or interpret* or action research or cooperative inquir* or co operative inquir* or co-operative inquir* or humanistic or existential or experiential or paradigm* or field research or field observation* or observational stud$ or human science) |
| # 15 | 125,496 | TS = (grounded theor* or grounded stud* or grounded research or grounded analys?s or life stor* or women* stor* or emic or etic or hermeneutic* or heuristic* or semiotic* or data saturat* or participant observ*) |
| # 14 | 740,655 | TS = (qualitative or nursing methodology research or questionnaire* or attitude* or focus group* or discourse analys?s or content analysis or ethnograph* or ethnological research or ethnonursing or constant comparative or purposive sampl* or observational research or observational method* or field stud* or theoretical sampl* or phenomenol* or life experience* or cluster sampl*) |
| # 13 | 2392 | #12 OR #10 OR #9 OR #7 OR #5 OR #3 |
| # 12 | 617 | #11 AND #4 |
| # 11 | 5997 | TS = (diversion* or divert*) |
| # 10 | 275 | TS = ((collaborat* or partner* or interagency or multidisciplinary or co-response*) NEAR/2 (police* or policing)) |
| # 9 | 151 | #8 AND #2 |
| # 8 | 3739 | TS = (crisis NEAR/3 (intervention* or response* or co-response* or coresponse* or partnership* or program*)) |
| # 7 | 27 | #6 AND #2 |
| # 6 | 2398 | TS = (triage) OR TS = (street triage) OR TS = (mental health triage) |
| # 5 | 1538 | #4 AND #2 |
| # 4 | 321,300 | TS = (psychiatric disorder*) OR TS = (mental NEAR/1 (health OR disorder* or disease*)) OR TS = (mental* NEAR/1 ill*) OR TS = (schizophren*) OR TS = (personality disorder*) |
| # 3 | 320 | #2 AND #1 |
| # 2 | 30,620 | TS = (police* or policing) OR TS = (law enforcement staff) OR TS = (law enforcement personnel) OR TS = (law enforcement officer*) OR TS = (law enforcement official*) OR TS = (law enforcement worker*) |
| # 1 | 7385 | TS = (mental health crisis) OR TS = (mental health crises) OR TS = (mental health emergenc*) OR TS = (psychiatric NEAR/1 (crisis or crises or emergenc*)) |
Further searching
Website searches
College of Policing
See URL: www.college.police.uk/.
Browsed the Research/What Works Centre sections and any subsections of the following: systematic review series, college published research, What Works briefings, what works in policing to reduce crime.
Used the Research/National Police Library section/Police Library Search function using the terms ‘street triage’ OR ‘mental health’. Browsed all documents found while searching.
Mental Health Foundation
See URL: www.mentalhealth.org.uk/.
Browsed the full list in the publications section.
Crisis Care Concordat
See URL: www.crisiscareconcordat.org.uk/.
Selected ‘Explore the map’ and browsed all counties for relevant documents and the research section.
Centre for Mental Health
See URL: www.centreformentalhealth.org.uk/.
Used the search box on the main page and first searched for ‘mental health’ then browsed the results. Next searched for ‘street triage’ and browsed the results. Then also browsed the following sections in ‘Publications’: criminal justice, physical and mental health, mental health policy and archive.
Connect Evidence Based Policing
See URL: http://connectebp.org.
Used the search box on the main page and first searched for ‘mental health’ and browsed the search results, next searched for ‘street triage’ and browsed the search results, then also browsed the ‘Research Streams’ section.
The East Midlands Police Academic Collaboration
See URL: www.empac.org.uk/.
Used the search box on the main page and first searched for ‘mental health’ and browsed the results; next searched for ‘street triage’ and browsed the results, then also browsed the ‘Research Networks’ section.
Google search
See URL: www.google.com/advanced_search.
-
‘street triage’ OR ‘mental health triage’, limited to English, region set to UK, portable document files (PDF), first 100 results downloaded
-
‘crisis intervention’ AND ‘police’, in English, region set to UK, PDF, 43 results returned, all downloaded.
Appendix 2 List of excluded non-evaluative descriptive publications
Adelman J. Study in Blue and Grey. Police Interventions with People with Mental Illness: A Review of Challenges and Responses. Vancouver, BC: Canadian Mental Health Association; 2003.
Durcan G. Review of Sections 135 & 136 of the Mental Health Act. The Views of Professionals, Service Users and Carers on the Codes of Practice and Legislation. London: Centre for Mental Health; 2014.
Kini R, King R, Khouja A. The Cleveland Mental Health Street Triage Pilot. Middlesbrough, OH: Police and Crime Commissioner for Cleveland; 2013.
NHS Health Scotland. Community Justice Practice Spotlight Summary 1. NHS Greater Glasgow & Clyde Police Liaison Distress Service Pilot 2015. Edinburgh: NHS Health Scotland; 2017.
O’Connor T. Liaising between the police and mental health. Nurs N Z 2004;10:15.
Solar C, Smith M. Policy Brief #1. Austerity, Decentralisation, and Local Governance: Examining Interagency Working in Policing and Mental Health. York: University of York and Connect Evidence Based Policing; 2016.
Watson AC. Research in the real world: studying Chicago Police Department’s Crisis Intervention Team program. Res Soc Work Pract 2010;20:536–43. 19
Appendix 3 List of ongoing studies
Studies that were identified as potentially relevant via web searches but had not been completed in time to include data in this report.
| Organisation | Title | Weblink |
|---|---|---|
| College of Policing |
From the What Works crime reduction systematic review series: No. 6 Police responses to people with mental health problems: a systematic map No. 7 A systematic review of the impact of police pre-arrest diversion |
URL: http://whatworks.college.police.uk/Research/Systematic_Review_Series/Pages/default.aspx (accessed 13 August 2018). |
| The Street Triage Project, conducted by the University of Sheffield | URL: http://whatworks.college.police.uk/Research/Research-Map/Pages/ResearchProject.aspx?projectid=615 (accessed 13 August 2018). | |
| East Midlands Police Academic Collaboration | Evaluation of Leicestershire Police Integrated Vulnerability and Mental Health Management Initiative | URL: www.empac.org.uk/research-networks/victims-witnesses-public-protection/evaluation-leicestershire-police-integrated-vulnerability-mental-health-management-initiative (accessed 13 August 2018). |
| Connect Project | Models of mental health triage for individuals coming to the attention of the police who may be experiencing a mental health crisis: a scoping review |
URL: http://connectebp.org/research/stream-two/ (accessed 13 August 2018). URL: www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42016042008 (accessed 13 August 2018). |
Appendix 4 Articles that were initially classified as ‘borderline’ but were ultimately excluded from the evidence synthesis
Bouveng O, Bengtsson FA, Carlborg A. First-year follow-up of the Psychiatric Emergency Response Team (PAM) in Stockholm County, Sweden: a descriptive study. Int J Ment Health 2017;46:65–73.
Cooke D. Diversion from Prosecution: A Scottish Experience. In: What Works: Reducing Reoffending – Guidelines from Research and Practice. Oxford: John Wiley & Sons; 1995. pp. 173–92.
Cowell AJ, Broner N, Dupont R. The cost-effectiveness of criminal justice diversion programs for people with serious mental illness co-occurring with substance abuse: four case studies. J Contemp Crim Justice 2004;20:292–315.
Fellow-Smith E, Hindley P, Hughes N. Defining a Health-based Place of Safety (S136) and Crisis Assessment Sites for Young People Under 18. London: Royal College of Psychiatrists; 2016.
Girard V, Bonin JP, Tinland A, Farnarier C, Pelletier JF, Delphin M, et al. Mental health outreach and street policing in the downtown of a large French city. Int J Law Psychiatry 2014;37:376–82. https://doi.org/10.1016/j.ijlp.2014.02.008
Gregory MJ, Thompson A. From here to recovery: one service user’s journey through a mental health crisis – some reflections on experience, policy and practice. J Soc Work Pract 2013;27:455–70.
Hansson L, Markström U. The effectiveness of an anti-stigma intervention in a basic police officer training programme: a controlled study. BMC Psychiatry 2014;14:55. https://doi.org/10.1186/1471-244X-14-55
Kaur S. Mental Illness and Interrogation: How Police Officers’ Confidence Measures Up. PsyD thesis. Chicago, IL: The Chicago School of Professional Psychology; 2016.
Lattimore PK, Broner N, Sherman R, Frisman L, Shafer MS. A comparison of prebooking and postbooking diversion programs for mentally ill substance-using individuals with justice involvement. J Contemp Crim Justice 2003;19:30–64.
Leason K. Police, Release Me. MA Education; 2005. URL: www.communitycare.co.uk/2005/03/10/police-release-me/ (accessed 5 February 2018).
Lord VB, Bjerregaard B, Blevins KR, Whisman H. Factors influencing the responses of crisis intervention team-certified law enforcement officers. Police Q 2011;14:388–406.
McGilloway S, Donnelly M. Mental illness in the UK criminal justice system: a police liaison scheme for mentally disordered offenders in Belfast. J Ment Health 2004;13:263–75.
Morgan J, Cordingly J. Police referrals – a crisis intervention approach. Psychiatr Bull R Coll Psychiatr 1991;15:465–8.
Noga HL, Walsh EC, Shaw JJ, Senior J. The development of a mental health screening tool and referral pathway for police custody. Eur J Public Health 2015;25:237–42. https://doi.org/10.1093/eurpub/cku160
Oxburgh L, Gabbert F, Milne R, Cherryman J. Police officers’ perceptions and experiences with mentally disordered suspects. Int J Law Psychiatry 2016;49:138–46.
Pinto SM. Police Response to Mentally Ill Persons in Crisis. PsyD thesis. Chicago, IL: The Chicago School of Professional Psychology; 2004.
Price M. Commentary: the challenge of training police officers. J Am Acad Psychiatry Law 2005;33:50–4.
Watson AC, Swartz J, Bohrman C, Kriegel LS, Draine J. Understanding how police officers think about mental/emotional disturbance calls. Int J Law Psychiatry 2014;37:351–8. https://doi.org/10.1016/j.ijlp.2014.02.005
Appendix 5 List of review evidence that failed Database of Abstracts of Reviews of Effects criteria and were excluded from evidence synthesis
| First author, year of publication (country of publication) | Aim/objective | Review design | Population (when reported) | Intervention (when reported) | Comparators (when reported) | Outcomes reported (when reported) |
|---|---|---|---|---|---|---|
| Abbott, 201156 (USA) | To evaluate the impact of a jail diversion programme on police officers’ attitudes towards those with a mental illness | Dissertation (general literature review) | Police officers | – | – | – |
| Arey, 201657 (USA) | To trace the historical context of CIT and present various elements of the models | Literature review | – | CIT | – | Descriptive text on the impact of CIT on officers’ attitudes and behaviour |
| Barcelos, 201558 (USA) | Impact of CIT training on police officers | Dissertation (general literature review) | Police officers | CIT | – | Attitudes and perceptions of self-efficacy of officers |
| Brace, 201649 (UK) | To assess the efficacy of street triage models | Dissertation (general literature review) | – | – | – | – |
| Browning, 201159 (USA) | To review the efficacy of CIT | Literature review | – | CIT | – | Various, including officer perspectives |
| Compton, 200860 (USA) | Review of CIT interventions | Literature review | Police officers | CIT | – | – |
Appendix 6 Database of Abstracts of Reviews of Effects quality appraisal of included reviews
| First author, year of publication | Question | |||||
|---|---|---|---|---|---|---|
| (1) Was the search adequate? | (2) Were inclusion/exclusion criteria reported? | (3) Were the data synthesised? | (4) Was the review quality assessed? | (5) Were adequate study details reported? | Is the review included in the evidence synthesis? | |
| Abbott, 201156 | No | No | No | No | No | No |
| Arey, 201657 | No | No | No | No | No | No |
| Barcelos, 201558 | Yes | No | No | No | No | No |
| Booth, 201739 | Yes | Yes | Yes | Yes | Yes | Yes |
| Brace, 201649 | No | No | No | No | No | No |
| Browning, 201159 | No | No | No | No | No | No |
| Compton, 200860 | Yes | No | No | No | No | No |
| Cummins, 201661 | No | No | No | No | No | No |
| Cummins, 201622 | No | No | No | No | No | No |
| Davidson, 201662 | No | No | No | No | No | No |
| Edmondson, 201442 | No | No | No | No | No | No |
| Hannig, 201563 | No | No | No | No | No | No |
| Helfgott, 201664 | No | No | No | No | No | No |
| Kalinich, 201065 | No | No | No | No | No | No |
| Kane, 201812 | Yes | Yes | Yes | Yes | Yes | Yes |
| Lancaster, 201666 | Yes | No | No | No | No | No |
| Mulay, 201667 | No | No | No | No | No | No |
| Norris, 201568 | No | No | No | No | No | No |
| Parker, 201814 | Yes | Yes | Yes | No | Yes | Yes |
| Paton, 201615 | Yes | Yes | Yes | Yes | Yes | Yes |
| Prince, 201269 | No | No | No | No | No | No |
| RiCharde, 201670 | Yes | No | No | No | No | No |
| Rodriguez, 201671 | No | No | No | No | No | No |
| Shapiro, 201520 | Yes | No | No | No | Yes | No |
| Stewart, 200972 | No | No | No | No | No | No |
| Taheri, 201640 | Yes | Yes | Yes | No | Yes | Yes |
| Thomas, 201773 | No | No | No | No | No | No |
| Tucker, 200874 | No | No | No | No | No | No |
| Weller, 201575 | No | No | No | No | No | No |
| Woods, 201776 | Yes | No | No | No | No | No |
| Young, 201477 | No | No | No | No | No | No |
Appendix 7 List of primary quantitative evidence not included in the evidence synthesis
| First author, year of publication | Aim/objective | Study design (as described by the author) | Type of data | Population | Intervention | Comparators (when applicable) | Outcomes reported |
|---|---|---|---|---|---|---|---|
| Australia and USA | |||||||
| aRiCharde, 201670 | To evaluate components of mental health stigma, attitudes and social distance among CIT/MHIT communication officers | Quasi-experimental | Survey | Communications officers (call takers, dispatchers or emergency operators) | CIT/MHIT training for communication officers | No CIT/MHIT training | Attitudes to mental ill health, social distance from people with mental ill health, differences in attitudes between New South Wales (Australia) communication officers and Virginia (USA) communication officers |
| Canada | |||||||
| aLamanna, 201878 | Service user experiences of co-responding police and mental health programmes | Retrospective data analysis | Administrative data | Service users | Mobile CIT (police and MHPs) | Police-only teams | Response times, rates of service user injury, emergency department handover times, service user experiences |
| USA | |||||||
| Compton, 201779 | To assess differences between CIT officers who self-select (volunteer) and those who are assigned | Retrospective data analysis | Used data from 2014 | Police officers assigned to CIT and police officers volunteering for CIT | CIT | None | Knowledge, attitudes, skills, level of force, disposition of subjects |
| aCompton, 201780 | Demonstration of feasibility for a jail diversion programme | Quantitative feasibility study | Linked data from patients/police/MHPs | Patients | Pre-booking jail diversion (police and mental health linkage system) | None | Number of calls |
| aDavidson, 201662 | Evaluating the effectiveness of CIT | Panel research design | Survey data | Police officers | CIT | None | Self-efficacy and management of crises, perceptions of de-escalation |
| aHelfgott, 201664 | Evaluation of the Seattle Police Department’s crisis response team officer/MHP partnership pilot programme | Descriptive process evaluation | Incident and supplemental reports | N/A (process evaluation using data from records) | CIT | None | Case type, nature, disposition, resolution, repeat contacts, community relations |
| aKhalsa, 201881 | To examine the implementation of crisis intervention teams by law enforcement agencies in Colorado | Not reported | Police CIT records | Police officers | CIT | None | Rates of SWAT use, arrests, use of force and injuries |
| aKubiak, 201782 | Presents the countywide implementation of CIT, prevalence of officer interaction with persons with mental health issues and CIT training outcomes | Case study | Pre and post surveys | Police officers | CIT | None | Knowledge and skills from training, officer opinions of psychiatric treatment, officer perceptions of mental ill health |
| aRodriguez, 201671 | Impact of psychiatric training on law enforcement officers | Retrospective study | Archival data | Law enforcement officers | PERT academy training | None | Number of emergency despatch calls: suicides, mental ill health cases, violent mental ill health cases |
| Tyuse, 201783 | Profiles older adults encountered by CIT officers | Descriptive statistics | Routine data | Older adult service users | CIT | None | Older person’s characteristics, reasons for calls and predictors of dispositions |
Appendix 8 Summary of findings from quantitative primary studies
| First author, year of publication | Description (when reported) of regional data service users and service providers (e.g. details of officers, MHPs) | Summary description of interventions (e.g. ST) and comparators (when reported) | List outcomes reported | Summary of findings |
|---|---|---|---|---|
| Studies that contributed to the main synthesis | ||||
| Heslin, 201643 |
Regional data: Eastbourne, Sussex. Described as a ‘somewhat deprived’ area in Sussex. It was reported to have a similar population size to other local authority districts in the county Eastbourne described as mainly an urban area like many of the other districts in Sussex Service users: Anyone thought to have mental health needs who came to the attention of the police and who was subject to detention, or could have potentially been subject to detention under S136 The population for Eastbourne was 99,412, and for the rest of the county of Sussex it was 688,654 (total 778,066 for the county). Based on 2011 census data |
Description of intervention: ST Comparator (when reported): Usual response – 6-months pre-intervention data |
National trends | Not reported |
| Number of call-outs/incidents |
The total number of attendances ‘after’ ST was 233 for the ST team and 125 for police officer response outside ST operating hours The ‘before’ data are unclear |
|||
| Service providers: Not reported | Outcomes of call-outs/incidents (number/rates) | |||
| Service users detained under S136 |
There were statistically significantly fewer S136 detentions during the ‘after’ ST period than the ‘before’ usual response period (118 vs. 194 cases; p < 0.001) In the ‘after’ ST period, the ST team was available for approximately 30% of the time. The remainder of the time the usual response would have been police officers in attendance. This means that the ‘after’ figures include ST team response AND usual response outside ST operating periods. Therefore, of the 118 ‘after’ S136 detentions, 7 were made by ST teams and the remaining 111 were made by police officers outside ST operating hours Note: authors report that only 6% (7/118) of cases were detained under S136 by ST teams; the remainder were detained by police officers outside ST operating hours Across the rest of Sussex, the total number of S136 applications increased by 10%, but this increase was not statistically significant (559 vs. 614; p > 0.05) Increases in the rest of Sussex could include incidents in the ST catchment area (e.g. outside normal operating hours) |
|||
| Detentions in custody |
There were also significantly fewer detentions in custody during the ST period ‘after’ than the ‘before’ usual response (56 vs. 119 cases; p < 0.05). Of the 56 cases, five were detained by the ST team and 51 by police officers outside ST operating hours Across the rest of Sussex, the number of people detained in custody increased by 6%, but this increase was not statistically significant (341 vs. 363; p > 0.05) |
|||
| Detentions in hospital |
There were fewer detentions in hospital during the ST ‘after’ period than the usual response, but this difference was not statistically significant (62 vs. 75; p > 0.05). As above, of the 62 ‘after’ cases, two were detained by the ST team and the remaining 60 by police officers outside ST team operating times Across the rest of Sussex, the number of people detained in hospital increased by 15%, but this increase was not statistically significant (218 vs. 251; p > 0.05) |
|||
| Note: authors report that it was not possible to control for various factors that may influence the results, such as geographical boundaries | ||||
| Referrals |
For the 4-month period (June–September 2014) ‘after’ period: Referrals by the ST team were largely to a GP (55%), A&E (14%) or other community services (14%). There were 6% of individuals (n = 9) admitted to hospital on an informal basis No ‘before’ data were recorded, although the clinical team advised that approved MHPs who see people in custody always refer them to their GP as a minimum, and sometimes to community mental health or drug and alcohol services Data to cover the 6-month period were extrapolated and reported in the paper |
|||
| Cost of street triage | The total cost of ST during the 26-week period of the evaluation was estimated to be £148,785. The ST team attended a total of 233 incidents, giving an estimated unit cost of £630 per incident attended | |||
| Average cost per person | Usual response arm cost £1077 compared with ST arm cost of £1043; this estimates a cost saving of £12,172 in the ST arm over the 6-month study period | |||
| Average costs per payer |
CJS: usual response arm – £559; ST arm – £470. Over a 6-month period this represents a cost saving of £31,862 to the CJS NHS: usual response arm – £517; ST arm – £574. This represents an additional cost over a 6-month period of £20,406 to the NHS in the ST arm Other results were reported in the paper |
|||
| Jenkins, 201744 |
Regional data: Population estimates from the 2011 census for the two urban areas Population (local authority data): Ipswich – 442,000, Norwich – 483,000 Index of deprivation ranking: Ipswich – 72, Norwich – 61 (lower value indicates higher deprivation rating) White British (%): Ipswich – 82.94%, Norwich – 83.65% Service users: Data were obtained from records of those individuals detained under S136 for assessment. There were no significant differences reported in participants’ age or gender pre intervention compared with post intervention in either area or between areas. There were no significant differences in ethnicity, with the majority being of white British background Mean age [years (SD)] Pre intervention: Ipswich 34.7 (13.3), Norwich 37.7 (14.0) Post intervention: Ipswich 37.5 (14.9), Norwich 37.7 (14.0) Males (%) Pre intervention: Ipswich 58.0, Norwich 47.6 Post intervention: Ipswich 51.0 Norwich 52.7 Service providers: Not reported |
Description of intervention: Officer and MHP in car (Ipswich) (joint on-scene co-response) Comparator (when reported): MHP in control room (Norwich) (MHP telephone support only) |
National trends | Not reported |
| Individuals detained under S136 and assessed per year per 100,000 population |
Over the total time period (pre and post intervention) Norwich (MHP telephone support only) had statistically significantly fewer S136 assessments per 100,000 population than Ipswich (p = 0.01). The difference was statistically significantly greater in the pre-intervention period (p < 0.01) Between the two 6-month periods there was a small, non-significant increase in those detained under S136 in Norwich (MHP telephone support only) but a large reduction in S136 assessments in Ipswich (joint on-scene co-response) post intervention (p = 0.01) Pre intervention, n (%): Ipswich 169 (77%); Norwich 87 (36%) – (p < 0.01) Post intervention, n (%): Ipswich 104 (47%); Norwich 93 (39%) – no significant differences |
|||
| Admission to hospital |
Over all the data collected for both areas, there was no significant difference in admission to hospital following S136 assessment between Ipswich and Norwich. Before the intervention, there were no significant differences between Ipswich and Norwich for admission In Ipswich (joint on-scene co-response), there was a statistically higher conversion to admissions post intervention than pre intervention (p = 0.01), but not for Norwich (MHP telephone support only) Post intervention there was a significantly higher admission rate following S136 in Ipswich (joint on-scene co-response) than Norwich (MHP telephone support only) (p = 0.04) |
|||
| Any contact with community mental health services in the 2 weeks prior to a S136 assessment | Data provided evidence that in the pre-intervention period there were more individuals in Norwich (MHP telephone support only) who had some contact with community mental health services than in the post-intervention period (p = 0.01) and when compared with Ipswich (joint on-scene co-response) (p = 0.01). In Ipswich there was no evidence of any difference between contact pre vs. post intervention | |||
| Not admitted to hospital following a S136 assessment but had at least one subsequent S136 assessment in the following 4 weeks | The proportion decreased in both groups post intervention, but the decrease was statistically significant only in Norwich (MHP telephone support only) compared with Ipswich (joint on-scene co-response) (p < 0.01 vs. p = 0.14) | |||
| Not admitted but offered follow-up by secondary mental health services |
In Ipswich (joint on-scene co-response), evidence suggested that if not admitted, people were more likely to be offered follow-up from secondary mental health services post intervention rather than pre intervention (p = 0.04). If follow-up was offered in Ipswich, there was strong evidence to suggest that the first follow-up contact was more likely to be kept post intervention than pre intervention (p < 0.01) In Norwich (MHP telephone support only) there was evidence that a person was more likely to be offered follow-up prior to the intervention than after the intervention (p = 0.02), but no evidence to suggest any difference between compliance rates pre vs. post intervention |
|||
| Diagnosis | There was no evidence to suggest that individuals assessed in Ipswich were more likely to have been deemed to have ‘no mental illness’ before the introduction of ST than after, but in Norwich there was evidence to the contrary (p < 0.01) | |||
| Keown, 201645 |
Regional: Not reported Service users: Not reported Service providers: Not reported |
Description of intervention: ST Comparator (when reported): Data from pre-ST scheme |
National trends | Not reported |
| Monthly number and annual rate of S136 detentions before and after ST across the NTW Trust area |
In the 12 months prior to the initiation of ST (September 2013–August 2014), the mean monthly number of S136 detentions across NTW was 70.8 (SD 11.0) When ST was introduced in South of Tyne (September 2014–June 2015), the mean monthly number of S136 detentions fell across NTW to 35.5 (SD 8.5), an overall reduction of 49.9% From July 2015, ST was in operation in both South and North of the Tyne. The mean monthly number of S136 detentions fell further to 18.0 (SD 2.2) over the following 4 months, an overall reduction of 74.9% There was a statistically significant reduction of 75% in the numbers of S136 detentions in the South of Tyne during the first 10 months (September–June 2015) of ST operating, compared with a fall of only 3% in the North of Tyne during the same period, where no ST was in operation yet (p < 0.001) During the first year, the rate of ST was 138.7 per 100,000 population. The rate of S136 detentions in NTW fell from 59.8 per 100,000 population prior to the introduction of ST, to 26.4 per 100,000 population in its first year, a 55.9% reduction. There was a statistically significant correlation (p = 0.003) between the rate of ST and the reduction in rate of S136 detentions in each of the six areas, indicating that the higher the rate of ST in an area, the greater the reduction in the rate of S136 detentions in the same area Linear regression indicated an association between three and a half ST contacts and one fewer S136 detention (p = 0.003) |
|||
| Change in S136 detentions in the three South of Tyne localities (Gateshead, South Tyneside and Sunderland) over the first year of ST |
Change in S136 detentions in the three South of Tyne localities (Gateshead, South Tyneside and Sunderland) over the first year of ST. Data compared were from pre intervention (September 2013–August 2014) and post intervention (September 2014–August 2015) There was a statistically significant reduction in the number of S136 detentions during each 3-month period in the first year of ST compared with the previous year. A 65% reduction in the first 3 months, 73% in the next 3 months, 83% in the following 3 months and 88% in the final 3 months (p = 0.001) During the first year, there were 1623 ST contacts for South of Tyne residents, and 403 fewer S136 detentions than in the previous year, providing a ratio of 4 : 1 or four STs for one fewer S136 detention (‘number needed to triage’ of 4) In the first 3 months, the number needed to triage was 4.7 (range: 4.2 in Sunderland to 5.5 in South Tyneside) and had reduced to 3.5 in the final 3 months (range: 2.2 in South Tyneside to 4.2 in Gateshead and Sunderland) |
|||
| The number, setting and outcome of S136 (assessments recorded by Sunderland Local Authority) | ||||
| S136 assessments |
Data were 24 months before ST, and 13 months after ST Total number of S136 assessments: 369 (before ST) and 43 (after ST) Average monthly number of assessments and SD of S136 fell from 15.4 (3.9) before ST to 3.3 (3.5) following the introduction of ST – a reduction of 78% |
|||
| Assessments in police stations |
Data were 24 months before ST, and 13 months after ST Total number of assessments prior to ST 18 (5%), fell to 1 (2%) after ST; this was recorded in the first month of ST, a reduction of 90%. The remaining assessments were conducted in hospital (before ST, n = 351, 95%; after ST, n = 42, 98%) |
|||
| Assessments in a dedicated S136 suite in a psychiatric hospital | The majority of S136 assessments occurred in a dedicated S136 suite in a psychiatric hospital – before ST (89%) and after ST (93%) | |||
| Type of A&E attendance at Sunderland Royal Infirmary |
Before data: September 2013–August 2014 After data: September 2014–August 2015 There were a total of 13 S136 assessments with police attendance in A&E prior to ST, and only two after ST. This was a statistically significant reduction of 85% (p < 0.001) Other attendance at A&E with police resulted in an increase ≥ 4 after ST compared with before ST. There was also an increase of 14% for the total number of attendances (including for other reasons) before ST compared with after ST |
|||
| Outcomes of S136 assessments |
Despite the statistically significant reduction in the rate of S136 detentions reported above, there were no significant changes in the proportion of outcomes of the assessments after ST Data were collected over 24 months before ST and 13 months after ST No admission before ST 194 (53%) compared with 26 (60%) after ST Detention in hospital before ST 56 (15%) compared with 8 (18%) after ST (p = 0.41) |
|||
| Number of admissions (typically for patients aged 18–65 years) |
Data were collected over 20 months before ST and 12 months after ST Total number of admissions to acute adult wards (voluntary and involuntary) fell by 29% in the first year of ST compared with the 20 months before ST Admissions resulting from S136 detentions fell by 84% after ST, compared with a 17% reduction in admissions where S136 was not a factor (p < 0.01) |
|||
| Number of adults < 65 years of age detained under any civil sections of the Mental Health Act 19832 |
Data appear to be collected 24 months before ST and 13 months after ST Short-term detentions (72 hours) for sections 4 and 136 fell by 72% after ST implementation (p < 0.001) Medium- to long-term detentions (≥ 28 days) for sections 2 and 3 fell by 21%, although this was not statistically significant The number of section 4 detentions increased by 72% from a monthly average of 0.6 (SD 0.8) to 1.1 (SD 0.9; not significant) The use of section 2 fell by 28% (p = 0.03), whereas the use of section 3 detentions (initially 6 months, thereafter renewable) did not change significantly |
|||
| Reveruzzi, 20169 |
Regional data Total population within the pilot areas: BTP – not applicable as they have a travelling population Derbyshire – 779,000 (2014 estimate) Devon and Cornwall – 1,135,700 (estimated by the police force) MPS – 1,288,727 (2014 estimate) North Yorkshire – 114,000 (estimated by the police force) Sussex – 101,547 (2014 estimate) Thames Valley – 666,100 (2013 estimate) West Midlands – 1,300,000 (estimated by the police force) West Yorkshire – 848,140 (approximate figure by CGG) Service users: Age of service users who were in contact with ST teams across the pilot areas – < 18 years (4%), 18–30 years (29%), 30–65 years (52%), > 60 years (5%) Service providers: Not reported |
Description of intervention: Control room – telephone response – BTP Control room and face to face – Devon and Cornwall Police (based in police control room); MPS, London (based in a Mental Health Trust) MHP responding when requested by officer – West Yorkshire Police, North Yorkshire Police Police officer and MHP responding together – Sussex Police, Thames Valley Police, Derbyshire Constabulary Police Officer, MHP and paramedic responding – West Midlands Police Comparator (when reported): Data from year previous to ST interventions (only reported for S136 detention data) |
National trends |
S136: 23,036 place of safety orders were made, resulting in the increased use of hospital-based places of safety, compared with police custody. From 64% (14,053) during 2012/13 (note: pre-nine pilot areas data) to 74% (17,008) from 2013/14 (note: post ST pilot data). This reflected a 21% increase in the use of hospital-based places of safety and a 24% decrease in police custody-based places of safety orders Over the last 10 years (up to 2016), there was a 30% increase in patients detained in hospitals as a place of safety. This number has continued to rise. The largest increase occurred after 2007, corresponding with an increased investment in HBPOS. Using police data, it was reported that at least 3% of S136 detentions resulted in people < 18 years old being detained in police custody, compared with at least 2% in HBPOS Data collection is limited but S136 detentions have been shown to vary widely across the country and are likely to depend on the local level of provision of suitable health facilities, in concurrence with the findings of this evaluation (2016) During 2013/14, when data were available, use of S136 detentions was recorded more than 1000 times in 11 policing areas, whereas the remaining 21 policing areas recorded fewer than 500 S136 detentions over the same period |
| S136 detentions (comparative data) |
Data from pilot evaluation period and same timeframe a year earlier Mean total S136 before ST, n = 458.8; mean total S136 after ST, n = 374.4 West Midlands, Derbyshire and Thames Valley saw the largest reductions in S136 detentions, with decreases of 27.5%, 25.3% and 22.7%, respectively. Significant reductions were also found in West Yorkshire (19.8%), Sussex (18.3%) and Devon and Cornwall (15.5%). Overall, the mean difference across the pilot schemes was 11.8% (excluding BTP), and if MPS and North Yorkshire are excluded this leads to a reduction of 21.5%. MPS and North Yorkshire increased S136 detentions by 15.1% and 19.4%, respectively. BTP was not included in these figures Other results reported per 100,000 and absolute numbers Note: authors report some differences in police force final reports compared with this evaluation due to how police forces collect data, as well as variation in reporting periods and geographical areas |
|||
| Outcomes of contact with ST teams (not comparative data) | In some cases, actions taken by the ST team were unreported, resulting in a proportion of missing data averaging 34.2%, with a range between 11.6% and 88.3% [e.g. data from BTP (65.6% missing) and Devon and Cornwall (88.3% missing data)] | |||
| S136 detentions | Results show that the use of S136 detentions following contact with the ST teams were relatively low across the forces, ranging from 2.0% (North Yorkshire) to 15.6% (West Yorkshire). However, the MPS scheme reported S136 detentions in 53.5% of cases following the use of the more complex stepped-care system where ST nurses responded independently and advised police. Authors note that the data should be interpreted in light of the numbers seen by the teams and the proportion of the population seen by the teams | |||
| S135 detentions | The percentage ranged from 0% in North Yorkshire to 1% (n = 8) in Derbyshire | |||
| A&E/hospital | The percentage ranged from 0% in BTP and North Yorkshire to 23.8% (n = 743) in West Midlands | |||
| Arrested | The percentage ranged from 0% in Devon and Cornwall, North Yorkshire, Thames Valley and West Yorkshire to 1.9% (n = 16) in Sussex | |||
| Detained under Mental Health Act 19832 | The percentage ranged from 0% in BTP, Devon and Cornwall, North Yorkshire, West Midlands and West Yorkshire to 1.1% (n = 9) in Derbyshire | |||
| Not detained | The percentage was 0% in all areas except BTP 0.2% (n = 5) and Derbyshire 15.6% (n = 125) | |||
| Referral to mental health service or community and mental health service (undefined) | The percentage ranged from 1.5% (n = 15) in Devon and Cornwall to 56.5% in West Yorkshire | |||
| Referral community | The percentage ranged from 0% in West Yorkshire to 37.2% in Sussex | |||
| Telephone advice | The percentage ranged from 0% in BTP, Sussex, West Midlands and West Yorkshire to 24.3% in Thames Valley | |||
| Triage discharge | The percentage ranged from 0% in BTP, Devon and Cornwall, North Yorkshire, Thames Valley and West Yorkshire to 30.2% in Derbyshire | |||
| Other (unspecified) | The percentage ranged from 0% in Devon and Cornwall and West Yorkshire to 11% (n = 345) in West Midlands | |||
| Rates per 100,000 of the population for S136 and S135 |
Authors report differences from the percentages MPS (49.0%), Sussex (26.6%), West Yorkshire (25.2%) and West Midlands (22.8%) had the highest reported numbers of S136 detentions following contact with the ST teams Sussex (72.9%) and West Midlands (57.2%) reported the highest number of admissions to A&E or hospital among the schemes For all force areas, S135 detentions following contact with the ST teams were very rare. Referrals to mental health and community services (including GPs) were common outcomes for service users in contact with ST schemes, particularly for North Yorkshire (57.2%), Sussex (54.4%) and West Yorkshire (56.5%) |
|||
| Transportation of S136 and S136 following contact with ST teams | Note: authors report a significant level of missing data | |||
| By police car | Transportation by police car was highest in Devon and Cornwall (84.6%, n = 33), Sussex (72.4%, n = 21) and Derbyshire (62.5%, n = 20) | |||
| By ambulance | Transportation by ambulance was highest in West Midlands (40.9%, n = 121), MPS (34.8%, n = 220) and BTP (31.6%, n = 120) | |||
| By triage vehicle | Transportation by triage vehicle was highest in West Midlands (50.3%, n = 149) and West Yorkshire (20.6%, n = 44); the remaining areas were 0 | |||
| Location of S135 and S136 detentions | HBPOS were most commonly used places of safety during the pilot period (68.4%). Authors report that, overall, the use of HBPOS increased during the pilot period (no data presented). When police custody (6.9%) was used to detain people under S136, it was often reported that this was because of a lack of capacity within the health-care setting. Figures were reported across force pilot areas | |||
| Duration of S135 and S136 across a 24-hour period | Data were also presented across ST areas | |||
| Current or previous contact with mental health services |
On average, 60.6% of service users who came into contact with ST were already known to mental health services. Figures ranged from 30.8% (BTP) to 80.5% (North Yorkshire) The average number of service users currently engaged with services was described as relatively low (19.2%) within a wide range from 0.0% (West Midlands, likely a data-recording problem) to 55.9% (West Yorkshire) From the nine pilot schemes, an average of 33.9% of service users had a care plan within a range from 0.9% (BTP) to 49.9% (Thames Valley) Overall, 15.3% of service users had a previous S136 detention within a range from 3.4% (BTP) to 32.3% (West Yorkshire). ST forces also recorded where subsequent sections were made under the Mental Health Act 19832 and where subsequent informal admissions were made; however, these data may have been under-reported. In the Derbyshire sample, a high proportion (39.9%) of service users were identified as having a previous conviction |
|||
| Children and young people < 18 years of age from June 2015 to March 2015 |
BTP had the highest number of contacts (telephone) with young people < 18 years of age, of which four of these contacts were with children < 12 years of age. Thames Valley saw 70 (5.2%) young people over the 10-month period, with the youngest reported to be aged 11 years. In Thames Valley, young people < 18 years of age were immediately referred to CAMHS. The Devon and Cornwall scheme reported having contact with one person < 12 years of age, and the Derbyshire scheme reported that the youngest person contacted by the team was 9 years old. The West Yorkshire scheme was primarily available to adults (aged ≥ 18 years); however, for those < 18 years of age the teams provided advice to officers and endeavoured to find an alternative care pathway through CAMHS When looking at the rate of change per 100,000 of the population, North Yorkshire (17.5%), Sussex (12.8%) and Thames Valley (10.5%) had the highest proportion of contacts with young people < 18 years of age. West Yorkshire (0.4%) had the lowest number of reported contacts with young people < 18 years of age per 100,000 of the population Other data were reported during the pilot ST schemes as ‘snapshot’ data rather than as before and after evaluation data covering: |
|||
| Note | Authors report a large number of incidents that occurred in private premises where police officers’ legal powers are often less clear. The MPS and Sussex were the only force areas to report a higher number of contacts in public spaces. The majority of BTP encounters indicate that they were in public places, although they may have begun on a train line (i.e. a private place) | |||
| Senker, 201646 |
Regional: Not reported Service users: Not reported Service providers: Not reported |
Description of intervention: ST Comparator: None |
National trends |
Rates of detention in hospitals in England under S136 increased from 1959 detentions in 1984 to 12,038 in 2009/10 and then to 17,008 in 2013/14. Note: rates of S135 detentions remained low throughout. Rates for section 2, 3, 4 and 5 also reported In Essex, the number of S136 cases was approximately 860 in 2013–14 (unclear where held); > 200 cases were held in custody in 2012–13 |
| Full ST service period | Number of call-outs during April–September 2015 | |||
| Number of call-outs/incidents |
Attended 548 call-outs (n = 265 in North Essex; n = 283 in South Essex) Number and rate of call-outs varied across Essex, ranging from the most frequent areas: Southend (18%), Basildon (17%), Chelmsford (15%), Tendring (11%), Colchester (11%) and Thurrock (10%), totalling 81% overall. Braintree, Harlow, Epping Forest, Uttlesford, Brentwood, Maldon and Rochford cumulatively account for only 16% |
|||
| Number of individuals assessed |
Sex: female, n = 277; male, n = 270 n = 203 (37%) were under the influence of drugs or alcohol |
|||
| Number of repeat call-outs/’frequent flyers’ | Seen by ST on at least two occasions: 51 people (11% of the total) during the 6-month period, with n = 8 being seen three times, n = 6 being seen four times, and n = 4 being seen five or more times | |||
| Outcomes of call-outs/incidents (number/rates) | N (%) | |||
| Admitted | 60 (11) | |||
| Service users detained under S136 | 42 (8) | |||
| Discharged | 1 (0) | |||
| No action | 127 (23) | |||
| Other (various, including signposting, followed up by community mental health team, referred to GP) | 186 (34) | |||
| Referred | 132 (24) | |||
| S136 prevented by ST (self-assessed by police officers) | 103 (19) (Note: monthly figures available. Numbers vary month to month with no specific trend up or down) | |||
| Arrested | 15 (3) | |||
| A&E | 41 (7) | |||
| Informal/voluntary admission | 38 (7) | |||
| Taken to a custody suite | 6 (1) | |||
| Taken to a HBPOS | 61 (11) | |||
| Outcomes across multiple time periods | (a) 4-month pilot: limited hours and variation in service from December 2014 to November 2015; (b) full ST service April–September 2015; and (c) last 2 months October–November 2015 | |||
| ST call-outs |
Note: authors state that this is lower for full ST than expected given the increased operating hours over the pilot, indicating that there may be some spare capacity in the model to respond to more cases Note: authors report calculations for the full ST service; this means that two-thirds (68%) of team time is ‘up time’ spent travelling to or attending incidents and one-third (32%) of team time is spent in ‘down time’ |
|||
| Prevented S136 |
|
|||
| Percentage of call-outs where S136 was prevented |
|
|||
| Per month average call-outs |
|
|||
| Per month average number of prevented S136s |
|
|||
| Cost–benefit analysis (full ST data compared with pilot and pre-pilot data) |
Using data from pre-ST (1 April 2014–30 September 2014; pilot: December 2014–March 2015 and full ST 1 April 2015–30 September 2015) Authors report potential annual benefits from ST directly preventing the use of S136 and a wider impact on reducing the overall use of S136, including the estimated gross realisable savings for NHS trusts/CCGs of £347,200 and benefit to the value of £99,650 to Essex Police in terms of reduced use of custody and reduced officer time attending S136 incidents, giving a gross benefit value estimate of £446,850 and a net benefit of £179,758 (when accounting for the cost of running the ST project). Other areas of potential benefit to CCGs may arise from the reduced use of the Mental Health Act 1983,2 assessments, ambulance call-outs, A&E attendances and non-elective admissions to hospital. (Further costs are reported in the paper) |
|||
| RCT on the training of front-line police officers | ||||
| Scantlebury, 201747,48 |
Region: North Yorkshire, England, UK Trainers: Qualified and experienced MHPs Trainees: Included rank of Constable, Sergeant, Inspector and Police Community Support Officers |
Description of intervention: Bespoke mental health training Comparator (when reported): Routine training |
National trends | Not reported |
| Number of incidents reported to the North Yorkshire Police control room resulting in a police response | At the 6-month follow-up, a median of 397 incidents had been assigned to bespoke training trial stations and 498 to the routine training control group stations (adjusted IRR 0.92, 95% CI 0.61 to 1.38; p = 0.69) | |||
|
Likelihood of incidents having a mental health tag applied Mental health tag applied by police officers to indicate that mental health is a factor in an incident |
Incidents assigned to bespoke training stations were more likely to have a mental health tag applied to them than incidents assigned to the routine training control group stations (adjusted odds ratio 1.41, 95% CI 1.16 to 1.71; p = 0.001) | |||
|
Number of individuals with a mental health warning marker involved in any incident Mental health warning marker applied by police officers to an individual’s record to indicate that they have mental health problems |
At the 6-month follow-up, there were no statistically significant differences between the intervention and control groups for the number of people with mental health warning markers involved in incidents (IRR 1.30, 95% CI 0.91 to 2.10; p = 0.13) | |||
| A random sample of 100 incidents (50 from baseline and 50 from follow-up) were reviewed by an independent MHP | The review of 100 incidents by a MHP suggests that there may be incidents involving individuals with mental health issues that are not being recorded as such | |||
| Studies reporting ‘snapshot’ single time only with no context. These findings are not included in the main synthesis | ||||
| Brace, 201649 |
Region: Not reported Service users: Not reported Service providers: Respondents to questionnaires were front-line officers from intervention/response and safer neighbourhood teams who have regular interaction with people in a mental health crisis. This included the rank of Constable and Sergeant for the quantitative data analysis |
Description of intervention: ST Comparator (when reported): None |
National trends | Not reported |
| Total mental health-related calls to police (covers January 2014–June 2016) |
2014/15: n = 6687 2015/16: n = 7428 2016 (to June): n = 3508 |
|||
| Police use of S136 |
2014/15: n = 345 2015/16: n = 511 2016 (to June): n = 282 It can be seen from the call data that the introduction of the ST services did not result in a reduction in demand (calls to service from the public) on the police service. The data also shows that if the rate of calls and S136s were to remain constant, then the end of the year total for 2016 would increase from 2015 Fifty questionnaires were distributed and 39 were returned (78% response rate). Note: responses represent the percentage of the 39 returned questionnaires. All responses were from Constables and Sergeants |
|||
| Approximately what percentage of your time is spent dealing with people suffering from a mental health crisis? | None of the officers stated that this took up 81% to 100% of their time, 5% said that it took up between 61% and 80% of their time, 25% said that it took up between 21% to 40% of their time, 31% said that it took up 0% to 20% of their time and 39% said that it took up between 41% to 60% of their time | |||
| How much demand do you feel people suffering from a mental health crisis have on front-line policing and has this remained constant over the past 5 years? | Over half of the respondents (51%) responded ‘no’, 26% of the respondents were unsure, 13% responded with ‘yes’ and 10% responded with ‘don’t know’ | |||
| In your opinion, are the police the correct service to deal with people suffering from a mental health crisis? | The overwhelming response was 92% ‘no’ from Constables and Sergeants, with the remaining 8% responding as ‘unsure’ | |||
| Those who responded ‘No’ to the ‘Are the police the correct service . . .’ question were then asked: why do you think the police are not the correct service to deal with people suffering from a mental health crisis? | Of the ‘no’ respondents, most (76%) felt that it was not core police business, 74% of respondents felt that there was a lack of resources, 51% of respondents felt that there was a lack of training and 48% of respondents felt that police officers had insufficient powers | |||
| Those who responded ‘No’ to the ‘Are the police the correct service . . .’ question were then asked: which service do you think should be responsible for responding to people suffering from a mental health crisis? Respondents could select more than one answer | All (100%) respondents stated that mental health services should be responsible for people in a mental health crisis, 71% responded that health services and ambulance services should be responsible; 66% responded that GP services should be responsible and 51% responded that social services should be responsible | |||
| Does the ST model reduce the demand on front-line policing? | The majority of respondents (87%) said ‘yes’, 11% said ‘don’t know’ and 2% were ‘unsure’ | |||
| Do you think that the ST project has reduced the demand from people suffering a mental health crisis on front-line policing? |
Only 34% of respondents (Constables and Sergeants) said ‘yes’. More officers responded ‘no’ (43%), with 15% responding ‘don’t know’ and 8% ‘unsure’ Therefore, the consensus among the participants was that the ST model was beneficial to front-line police officers |
|||
| Do front-line officers receive adequate training to effectively respond to people suffering from a mental health crisis? | Over half (51%) of respondents felt there was insufficient training | |||
| Callender, 201650 |
Regional data: Not reported Service users: Not reported, although some diagnosis data are provided in findings Service providers: Not reported |
Description of intervention: ST Comparator (when reported): No comparator |
National trends | Not reported |
| Nature of call-outs |
T1 (operational 5/7 days): eight incidents; vehicle deployed on 2 days; > 5.5 hours spent on dedicated incidents; no S136 detentions were completed T2 (operational 4/7 days): 11 incidents; vehicle deployed on 2 days; under 7 hours spent on dedicated incidents; no S136 detentions were completed Authors note that there were inconsistencies in data recording, with cells in forms left blank or other members of the mental health team completing forms. Therefore, it is unclear if blank means ‘no’ Across the two time points there were 19 incidents in total; general health/diagnosis were flagged as unknown in nine, the remaining 10 cases varied widely: with two each flagged bipolar or alcohol issues and single incidents flagged as epilepsy, social communication disorder, good, depression, suicidal thoughts or schizophrenia |
|||
| Service users detained under S136 | None | |||
| Service users detained under S135 | Not reported | |||
| Referrals | The most common outcomes across T1 and T2 were GP and police referrals. Police referrals appeared to be when the community psychiatric nurse on shift provided information to officers on the scene and they resolved the incident. Other referrals included Primary Care Liaison Services and Community Mental Health Teams, A&E and ambulance services | |||
| Number of assessments that were completed by a community psychiatric nurse | Only 6 out of the 19 incidents were formally assessed across T1 and T2. There is no information provided on the lack of assessment | |||
| Incident type (from control room data) | ‘Public safety and welfare’ was the most frequently logged incident type (no further details available). Others included domestic incident (n = 4) and missing person (n = 3); and single incidents included suspicious circumstances, violence, harassment and antisocial behaviour | |||
Appendix 9 List of primary qualitative studies excluded from evidence synthesis
| First author, year of publication | Study objective | Population | Intervention | Comparators (when applicable) | Outcomes reported |
|---|---|---|---|---|---|
| Australia | |||||
| Boscarato, 201484 | To explore consumer experience of crisis response service | Consumers of combined police and mental health services | Police Crisis Assessment and Treatment teams | None | Consumer experiences and opinions of the service(s) |
| Evangelista, 201685 | How consumers experience PACER | Consumers | A-PACER | None | Outcomes of contact with A-PACER, consumer experiences |
| aHerrington, 201486 | The impact of police training in mental health | Police officers | Mental health intervention training (similar system to CIT in USA) | Neighbouring sites to intervention areas | Interactions between police officers and people with mental ill health |
| aHollander, 201287 | How crisis mental health clinicians and police officers experience the service interface to identify perceived challenges to collaboration and possible solutions | Police and mental health service staff | Mobile psychiatric crisis assessment and treatment teams (work independently of police but responsive to police requests for shared management of people with mental ill health) | None | Frequency of contact, confidence in decision-making, experience of interface, knowledge and ability |
| aLee, 201588 | To evaluate an Australian, joint, police–mental health mobile response unit that aimed to improve the delivery of a community-based crisis response | Staff at Crisis and Intervention Treatment Centre and police officers | A-PACER | None | Reasons for and outcomes of following A-PACER referral, Police and Clinical Early Response clinician feedback |
| McKenna, 201589 | To describe the perceptions of major stakeholders on the ability of the N-PACER model to reduce behavioural escalation and improve the service utilisation by people in a mental health crisis | Consumer advisors as the voice of consumers, carer advisors as the voice of carers, mental health staff, emergency department staff, police officers and ambulance officers | N-PACER | Police-only teams | Challenge of PACER compared with police-only teams, collaboration, improvements to a person’s pathway, ways to improve PACER |
| Canada | |||||
| Kirst, 201590 | To understand processes of implementation of a multisite mobile CIT programme in a large urban centre, to identify programme strengths and challenges and to identify levels of satisfaction in service delivery | Stakeholders within the health system and at the community, managerial, team and consumer levels | Mobile CIT | None | Programme satisfaction, programme strengths, challenges in implementation/service delivery |
| aKisely, 201091 | To examine the impact of an integrated mobile crisis team formed in partnership between mental health services, municipal police and emergency health services | Service recipients, family, front-line workers and referral sources | Integrated mobile crisis team | No service | Number of calls, number of visits, acceptability, availability and satisfaction with service |
| aLamanna, 201778 | Service user experiences of co-responding police and mental health programmes | Service users | Mobile CIT (police and MHPs) | Police-only teams | Response times, rates of service user injury, emergency department handover times, service user experiences |
| aSilverstone, 201392 | Evaluating the training of police officers who may interact with people with a psychiatric disorder | Police officers | Training police officers to interact with people with psychiatric disorders | None | Benefits and acceptance of training, satisfaction |
| Denmark | |||||
| Sestoft, 201493 | Concept, process, practice and experience of the collaborative model known as PSP teams | Unclear | Collaboration between police department, social services and psychiatric/mental health services | None | Implementation, practice, process issues |
| USA | |||||
| Canada, 201094 | To evaluate CIT | Police officers | CIT | None | Application of CIT skills and knowledge, diversion from arrest to mental health services, responses to calls, perceived impediments to implementation |
| Canada, 201295 | To assess differences between CIT-trained officers and non-CIT-trained officers | Police officers | CIT-trained officers | Non-CIT-trained officers | Assessment, response tactics, disposition |
| aCompton, 201796 | Stakeholders’ views on the accessibility of a prebooking jail diversion programme (CIT) | Patients, police officers (CIT-trained and non-CIT-trained), mental health administrators | Prebooking jail diversion (police and mental health linkage system) | None | Expectations about acceptability, concerns about system |
| Doulas, 201497 | A description of current programmes | Anyone involved in the programming of CIT for juveniles | J-CIT | None | Programme features and philosophy, programme jurisdiction, origins of J-CIT; training focus and topics, client characteristics, mechanisms of intervening in crisis situations, role of family participation services, obstacles to programme implementation, programme evaluation and future goals |
| Hanafi, 200898 | How does CIT training affect police officers’ interactions with individuals with mental ill health in their daily work? | Police officers | CIT | None | Knowledge and awareness of mental ill health, ability to recognise and respond, stereotyping and stigmatisation, empathy, patience, arrests and redirection |
| Hannig, 201563 | To determine the success of the Chicago Police Department’s CIT training and curriculum | Police officers | CIT | None | Officer views on individual aspects of training, such as different mental illnesses, risk assessment, legal issues |
| aKalinich, 201065 | To explore the role of MHPs partnered with the CIT programme | MHPs from CIT schemes | CIT | None | Perceptions and experiences |
| aKubiak, 201782 | Presents the countywide implementation of CIT, prevalence of officer interaction with persons with mental health issues and CIT training outcomes | Police officers | CIT | None | Knowledge and skills from training, officer opinions of psychiatric treatment, officer perceptions of mental ill health |
| McGriff, 201099 | To understand the application of CIT in an airport setting and to elicit suggestions for improvements to the CIT programme from the perspective of police officers stationed in an airport | Police officers | CIT at an international airport | None | Motivation for participation in CIT, perceived benefits of training, special issues relevant to an airport setting, areas for improvement specifically in an airport setting |
| aPrince, 201269 | The impact of CIT training on police officers | Police officers | CIT training | None | Dispositions, policies and protocol, professional awareness, skill set, training |
| Skubby, 2013100 | To better understand the challenges of CIT programmes | Law enforcement officers, community MHPs, system administrators, consumer advocates | CIT | None | Barriers to implementation, overcoming barriers to implementation, effects of implementation |
| aStewart, 200972 | A study of a police intervention in mental health crisis | Police officers | CIT | None | Implementation and management of the programme (qualitative data), number of calls received, response time, length of call, frequency of police intervention, perception of mental ill health, incident characteristics (quantitative outcomes) |
| aTully, 2015101 | To examine officer perception of preparedness after receiving CIT training | Police officers | CIT training | None | Perceptions of preparedness |
| Watson, 2008102 | To explore experiences of people with mental ill health and their encounters with police officers | Service users | CIT | None | Nature of police encounters, vulnerability and negative expectations of police, evaluation of police encounters, advice for police officers |
Glossary
- Co-location model
- An approach in which mental health professionals are employed by police departments to provide on-site and telephone consultations to officers in the field.
- Consultation model
- An approach in which police agencies access advice from mental health professionals when working with people with mental ill health, often via telephone.
- Co-response model
- A shared protocol pairing specially trained police officers with mental health professionals to attend police call-outs involving people with mental ill health. This is often how UK ‘street triage’ pilot schemes have been conceptualised.
- Crisis Intervention Team
- Specially trained police officers respond to calls involving suspected mental ill health either alone or alongside mental health and addiction professionals. The aim is to divert persons with mental ill health from the criminal justice system to mental health treatment when appropriate. This model is commonly used in the USA.
- Health-based place of safety
- A term commonly used to describe a safe place where a person detained under section 135/136 of the Mental Health Act 1983 [Great Britain. Mental Health Act 1983. Section 136. London: The Stationery Office; 1983. URL: www.legislation.gov.uk/ukpga/1983/20/section/136 (accessed October 2017)] can be taken for assessment conducted by mental health professionals (e.g. accident and emergency department, social care or provided by a third-sector organisation).
- Information-sharing agreement model
- An approach in which information about people with mental ill health is shared between police and other agencies or between the individual with mental ill health and the police and other agencies.
- Liaison and diversion services
- Services typically concerned with helping people with mental ill health when they are suspected of having committed an offence.
- Mental Health Act 1983
- Legislation (in England and Wales) that informs people with mental ill health what their rights are regarding assessment and treatment in hospital, treatment in the community and pathways into hospital, which can be civil or criminal. [Mind. Mental Health Act 1983. 2018. URL: www.mind.org.uk/information-support/legal-rights/mental-health-act-1983/#.WxqDkIpKiM8 (accessed 8 June 2018).]
- Police-related mental health triage interventions
- A generic term used to include all intervention models that aim to improve outcomes when police officers are called to incidents primarily relating to mental health rather than criminal concerns.
- Policing and Crime Act 2017
- Contains reforms of police powers under sections 135 and 136 of the Mental Health Act 1983 (Her Majesty’s Stationery Office, 2017), including stopping detention in police cells of those aged < 18 years who are experiencing a mental health crisis, and restricting the circumstances when adults can be taken to police stations. [Great Britain. Policing and Crime Act 2017. London: The Stationery Office; 2017. URL: www.gov.uk/government/collections/policing-and-crime-bill (accessed 7 June 2018).]
- Pre-arrest diversion
- The provision of police officers with specialist mental health training to better manage situations involving people with mental ill health and offer treatment as an alternative to arrest, such as Crisis Intervention Teams in the USA.
- QALY (quality-adjusted life-year)
- A measure of the state of health of a person or group, in which the benefits, in terms of length of life, are adjusted to reflect the quality of life. One QALY is equal to 1 year of life in perfect health. [National Institute for Health and Care Excellence. Glossary. 2018. London: NICE. URL: www.nice.org.uk/glossary?letter=q (accessed 8 June 2018).]
- Section 135 of Mental Health Act 1983
- Legislation under which a warrant is sought from a court to enable a police Constable on receipt of information from a mental health professional to enter (private) premises (by force if necessary), where a person thought to be suffering from a mental disorder is believed to be, to remove them and take them to a place of safety. [Great Britain. Mental Health Act 1983. Section 135. London: The Stationery Office; 1983. URL: www.legislation.gov.uk/ukpga/1983/20/section/135 (accessed 8 June 2018).]
- Section 136 of Mental Health Act 1983
- Legislation under which a police constable may remove a person who appears to be suffering from a mental health disorder and in immediate need of care or control and take them to a place of safety to protect them or other people. This section typically relates to incidents in public spaces. [Great Britain. Mental Health Act 1983. Section 136. London: The Stationery Office; 1983. URL: www.legislation.gov.uk/ukpga/1983/20/section/136 (accessed 8 June 2018).]
- Street triage
- As piloted in England, typically takes the form of mental health professionals supporting police officers when responding to emergency calls for cases that involve a person who may be suffering from a mental illness.
List of abbreviations
- A&E
- accident and emergency
- ASSIA
- Applied Social Sciences Index and Abstracts
- BAME
- black, Asian and minority ethnic
- BTP
- British Transport Police
- CASP
- Critical Appraisal Skills Programme
- CCG
- Clinical Commissioning Group
- CIT
- Crisis Intervention Team
- CJS
- criminal justice system
- DARE
- Database of Abstracts of Reviews of Effects
- DHSC
- Department of Health and Social Care
- HBPOS
- health-based places of safety
- IT
- information technology
- L&D
- liaison and diversion
- MHIT
- Mental Health Intervention Team
- MHP
- mental health professional
- PACER
- police, ambulance and clinical early response
- portable document file
- PRMHT
- police-related mental health triage
- RCT
- randomised controlled trial
- S135
- section 135 of the Mental Health Act 1983
- S136
- section 136 of the Mental Health Act 1983
