Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/47/17. The contractual start date was in January 2018. The final report began editorial review in January 2019 and was accepted for publication in June 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Andrew Booth is a member of the National Institute for Health Research Complex Reviews Support Unit Funding Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Booth et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction and background
Good health and access to health care are not always equitable. There is clear evidence to link vulnerability with poorer health and poorer access to health services. People from vulnerable groups have generally worse health for diverse complex reasons and they are also known to access health care, particularly routine health care, less than people from non-vulnerable groups. 1 A notable pattern of health service use can be observed across people from vulnerable groups and, without simplifying, or conflating the needs of individual members of these groups, one of these patterns involves disproportionate use of the emergency and urgent care (EUC) system.
People from specific groups may use the EUC system more as they are engaged in behaviours that are likely to cause them harm (e.g. substance users) or they may be unable to access primary health care so use the EUC system as a proxy for routine care (e.g. homeless people, people who are geographically isolated). There is also evidence that people who are ‘low-acuity’ users of EUC (people who have medical problems that would be better addressed outside the EUC system) are more likely to come from a vulnerable group.
These reasons have stimulated interest in candidate interventions that attempt to manage demand for EUC by these vulnerable population groups. Clearly, there is potential for interventions delivered to vulnerable population groups and individuals to address wider determinants of health (and delivered outside the EUC system); however, the focus of this review is on the management of demand for EUC by the EUC system.
It is unclear whether this demand is concentrated in emergency departments (EDs) or whether it presents elsewhere within the EUC system. Rising demand is acknowledged by the NHS2 as placing pressure on frontline staff and systems. One of the 2017/18 national service improvement priorities for the NHS is ‘improving A&E performance . . . upgrading the wider urgent and emergency care system so as to manage demand’ (p. 12). 2 (Reproduced with permission from NHS England. 2 Contains public sector information licensed under the Open Government Licence v3.0.)
Vulnerability in a health-care context can be conceptualised in a variety of ways. In this study, we have chosen to use the definition from the European Union VulnerABLE project,3 which states that ‘Vulnerability is a social phenomenon, affected by multiple processes of exclusion that can lead to or result from health problems’. [Reproduced with permission. © European Union, 2017. The reuse policy of European Commission documents is regulated by Decision 2011/833/EU (OJ L 330, 14.12.2011, p. 39)]. Vulnerability is a complex phenomenon; for the purpose of the project, we are conceptualising this population as being more likely to have poor health and more likely to face problems accessing health care appropriately. The brief for the review from the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme was to focus on a set of seven priority groups as follows:
-
socioeconomically deprived individuals and families (socioeconomically deprived)
-
people living in rural/isolated areas (including coastal communities) (geographically isolated)
-
migrants (new migrants)
-
ethnic minority groups (minorities)
-
the long-term unemployed/inactive (unemployed)
-
people with an unstable housing situation who are homeless or at risk of homelessness (homeless)
-
people with substance misuse problems (substance misuse).
Two further groups may receive interventions to manage their demand and use of EUC (low-acuity users and frequent attenders). Low-acuity users of the ED tend to use the ED when their clinical problem could be more appropriately dealt with elsewhere. Diverse reasons may explain why they seek EUC rather than routine care. 4,5 Such reasons may be linked closely to population characteristics shared by our vulnerable groups. Although this low-acuity group is not a priority for this review, its inclusion in the review will aid commissioners and decision-makers to identify potential possible interventions and areas for further research.
One particular group of ED users is referred to as ‘frequent attenders’. These users visit the ED ‘often’ – defined as five or more visits a year. These users are seen as vulnerable because they ‘are more at risk of having poor social, physical and psychological health’ for a variety of reasons, which cause, and result from, their use of the ED. 6 There may well be overlap between frequent attenders, low-acuity users and the specific population groups identified above; however, it is important to be aware that the literature may describe groups in terms of their patterns of use, rather than the needs that drive this use.
Objectives
The aim of this three-stage review was to identify and map, using predefined population groups, interventions that have been developed and delivered to individuals or groups to manage their use of EUC services. These interventions may either reduce demand or ensure that populations use the appropriate EUC as needed. An additional aim was to classify these interventions, where the evidence permitted, in terms of intervention characteristics and to report headline messages of the outcomes of these interventions. Further detail on the content and delivery of these interventions was to be extracted using a Template for Intervention Description and Replication (TIDieR7). It was anticipated that the review, which also aimed to look at current UK initiatives, would help us to understand what can be learnt about delivering interventions to vulnerable service users and also to identify potential gaps within the research and practice agendas, with a view to stimulating future research and evaluation.
Research questions
The research questions for this review were as follows:
-
What interventions exist to manage use of EUC by people from vulnerable groups?
-
What are the characteristics of these interventions?
-
Is there evidence of service delivery outcomes (for patients and the health service) resulting from these interventions?
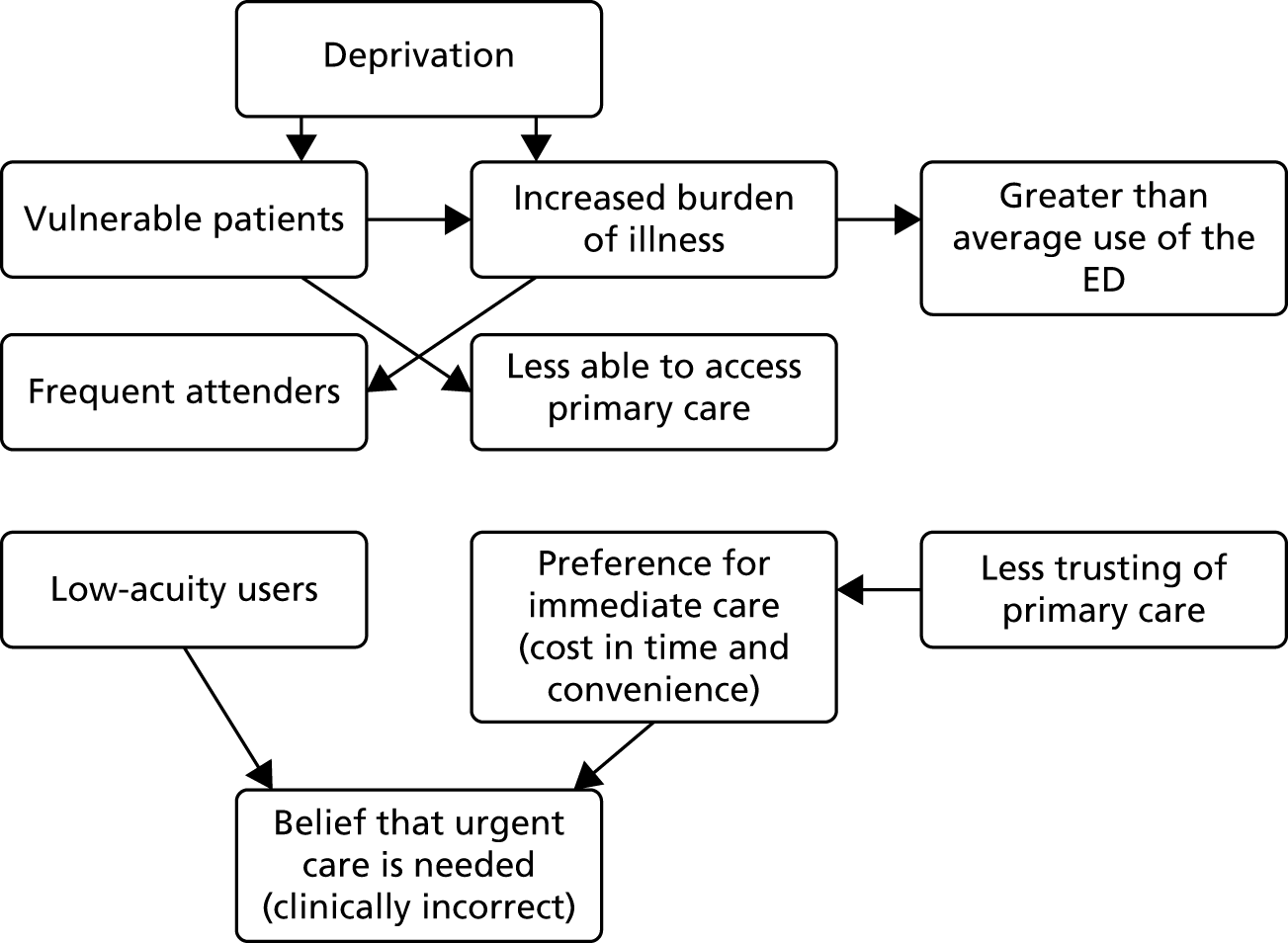
An initial model to illustrate the complexity of associations and outcomes in this research area was developed by the team from the review of reviews by Coster et al. 4 The original review of reviews had identified six themes that accounted for most factors related to ED attendance and urgent care usage: access to and confidence in primary care; perceived urgency and anxiety and the value of reassurance from emergency-based services; views of family, friends or health-care professionals; convenience (in terms of location, not having to make appointments and opening hours); individual patient factors; and perceived need for emergency medical services (EMSs) or hospital care, treatment or investigations. This initial model, which helped us to conceptualise the review, is illustrated in Figure 1. Vulnerable patients had been identified as one factor within individual patient factors, linked but not invariably associated with deprivation. The team took these factors at a disaggregated level, transforming them from the original linear framework into a conceptual model.
FIGURE 1.
Diagram illustrating the complex relationships underpinning use of emergency care.
The overall aims of the project were as follows:
-
Identify and map, using predefined population groups, interventions that have been developed and delivered to individuals or groups to manage their use of EUC services. These interventions may either reduce demand or ensure that populations use the appropriate EUC as needed.
-
When the evidence permits, classify these interventions in terms of intervention characteristics.
-
When the evidence permits, report headline messages of the outcomes of these interventions.
-
When interventions include outcomes data (evaluative), assess how the content and delivery of these interventions has been reported using the TIDieR framework. 7
-
When interventions do not report outcomes data (descriptive), report the content and delivery of the intervention using an abbreviated version of the TIDieR framework. 7
-
Understand what can be learnt about delivering interventions to vulnerable service users.
-
Identify potential gaps within the research and practice agendas with a view to stimulating future research and evaluation.
Chapter 2 Review methods
Overview
The initial phase of the project entailed carrying out a systematic mapping review, conducted in accordance with published methods. 8 This phase was followed by an intervention analysis examining the content and delivery of each intervention using the TIDieR framework. 7 The intervention analysis aimed to offer a broad overview of intervention content to facilitate further knowledge synthesis or primary research while summarising the current state of the evidence base through analysing the interventions reported. During the third and final phase of the work, we undertook a review of current UK initiatives (whether or not they have been evaluated) that had the aim of managing demand. The three phases of the project are summarised in Figure 2.
FIGURE 2.
Overview of the phases of the review.
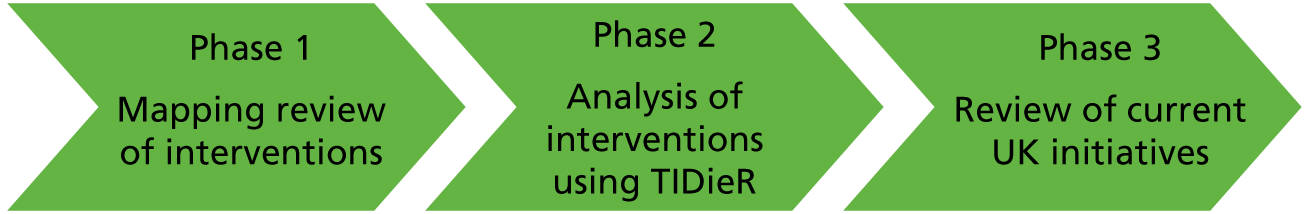
Table 1 summarises how the evidence was funnelled through the review, outlining the actions taken during each phase and the main outcomes of the work and including comments on issues and challenges encountered during each phase.
| Action | Outcome | Comments |
|---|---|---|
| Looked for all reported interventions for vulnerable groups with service delivery outcomes | Vulnerable groups tended to be reported only in terms of their ‘frequent attendance’ | In those studies in which managing use of the ED was reported, this was only in terms of clinical outcomes for the patient group. Interventions that were delivered outside the ED but that had ED service use outcomes were reported for these patient groups, but again this was outside the scope of the initial mapping review |
| Identified evidence on interventions for frequent attenders | A cumulative TIDieR7 for case management and for other interventions for frequent attenders | Users were defined by use of the ED rather than population characteristics; they tend to be from a vulnerable group but are not described as this |
| Looked for all reported but not evaluated interventions for vulnerable groups in the ED | Review of initiatives | Limited evidence on these initiatives |
Phase 1 mapping review methods
Identification of literature
A database search was undertaken in January 2018 by an experienced information specialist, who developed the search strategy using published terms for specific vulnerable groups in an iterative process, using retrieved citations to inform terms for further searching.
Sources searched
A full line-by-line search strategy is presented in Appendix 1. Searches were limited to the last 10 years and to English-language studies. Searches were limited to studies published in the last 10 years to capture the changing nature of EUC, as documented across emergency care research, and also to capture the demographic changes that have an impact on society generally and more specifically on who is vulnerable and how they are vulnerable. The search was run in MEDLINE, Web of Science (Science Citation Index Expanded, Social Sciences Citation Index, Conference Proceedings Citation Index – Science, Conference Proceedings Citation Index – Social Science & Humanities) and Cumulative Index to Nursing and Allied Health Literature (CINAHL). Retrieved references were deduplicated and saved in EndNote 11 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA]. The search process was recorded, including a list of databases searched, dates of searches, limits applied and numbers of hits and duplications, as per Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 9
Study selection
Study selection was undertaken using EPPI-Reviewer 4 software (EPPI-Centre, Social Science Research Unit, Institute of Education, University of London). Three reviewers screened the identified references, with a fourth reviewer screening 10% of the records from each of the three reviewers. A Cohen’s kappa value to measure agreement between reviewers was calculated.
Inclusion criteria
Study selection was undertaken in accordance with the inclusion criteria outlined in Table 2.
| Study aspect | Criteria |
|---|---|
| Population |
Socioeconomically deprived people and families Migrants Ethnic minority groups The long-term unemployed/inactive People with an unstable housing situation People living in rural/isolated areas People with substance abuse disorders When articles related to more than one population group, these were included When an intervention related to a group using EUC frequently and/or for low-acuity reasons, these were included |
| Setting |
Delivered within the EUC system (limited to the ED and ambulance/paramedic care) Evidence from any of the following settings: USA, UK, Canada, Australia, New Zealand or Europe |
| Outcomes | Health service outcomes (for patients and the health service) |
| Study design |
All types of study design when an intervention is reported (descriptive or evaluative) Surveys of patient experience of interventions were not included Reviews were used as a source of primary evidence |
| Data types |
Evidence from conference abstracts on interventions/populations when there is not already a published evaluation study Given the evidence generally available in conference abstracts, these are more likely to be included at the mapping stage than in intervention analysis Grey literature in the form of reports of interventions delivered in the UK |
| Other criteria |
English language only Evidence published since 2008 |
Screening process
Following screening at the title and abstract stage, the full texts of the references that were selected were scrutinised for inclusion in the review; if they did not meet the inclusion criteria, they were excluded. The screening process was divided between three reviewers, with a fourth reviewer screening 10% of each of the three reviewers’ references.
Data-collection process and data items
Data extraction was undertaken in Microsoft Word® (Microsoft Corporation, Redmond, WA, USA) using a data-extraction template designed for the mapping review. The extraction form was piloted on a small sample of papers prior to use and included paper identifying code; author; setting; study type; population; intervention; and outcomes and headline messages. In addition, during the data-extraction process, references were categorised into ‘bundles’ according to the vulnerable population group(s) that they addressed.
Methods for phases 2 and 3
Phases 2 and 3 of the project were iterative and involved two value-added synthesis processes: first, an intervention analysis to examine the components of each intervention, and, second, an initiative analysis to identify interventions in practice within a UK NHS setting. As candidate interventions from the initiative analysis were identified, the team retraced its steps to the evidence base, as captured in the EndNote database for the project and through targeted searches of the MEDLINE database, to augment the list of candidate interventions.
The intervention analysis and initiative analysis sought to add both intervention detail and UK context-sensitive breadth to the mapping review of published literature. These analyses aimed to extend the field of inquiry to include the wider whole system [e.g. not just the ED and ambulance care but also including, but not limited to, walk-in centres, urgent general practitioner (GP) access, same-day community-based nursing and telephone helplines, e.g. NHS 111] of EUC beyond the limited lens offered by the inclusion criteria of the mapping review.
Eligibility criteria for phases 2 and 3 of the project
Table 3 outlines the eligibility criteria for the intervention analysis and initiative analysis phases of the project.
| Study aspect | Criteria |
|---|---|
| Population |
Socioeconomically deprived people and families Migrants Ethnic minority groups The long-term unemployed/inactive People with an unstable housing situation People living in rural/isolated areas People with substance abuse disorders When articles related to more than one population group, these were included |
| Intervention |
Only interventions that fulfil a dedicated EUC function or for which EUC is the superordinate function were included (i.e. interventions or services that attract a small proportion of EUC cases were excluded) Interventions related to a group who use the EUC system frequently and/or for low-acuity reasons were included |
| Setting |
Delivered within the wider whole system of EUC (extending beyond the narrower definition in the mapping review) Evidence from any of the following settings: USA, UK, Canada, Australia, New Zealand or Europe |
| Outcomes | Health service outcomes (for patients and the health service), e.g. reduction in the number of presentations in the ED, reduction in the number of emergency admissions made through the ED |
| Study design | All types of study design when an intervention is reported (descriptive or evaluative) |
| Data types | Evidence on intervention components from published studies of interventions or from less formal (grey literature) descriptions of current practice (e.g. from ‘good practice casebooks’, general practice and health service newspapers and magazines). Evaluation data from health service newspapers and magazines were reported but not considered as authoritative evidence |
| Other criteria |
English language only Evidence published since 2008 |
Identification process for phases 2 and 3
Given the comprehensive nature of the search for the mapping review, in which the search strategy was designed to be comprehensive (with only the synthesis and analysis conducted at a more superficial level), it was decided that there was no need to extend the bibliographic search process, a decision verified by confirming the presence of references, tracked through additional search methods, within the original EndNote database.
Coverage of the relevant literature for the intervention analysis and initiative analysis was therefore provided in three main ways:
-
by using Google and Google Scholar (Google Inc. Mountain View, CA, USA) to find unpublished and published descriptions of interventions designed to address frequent users of emergency services, including, but not exclusive to, the identified list of vulnerable groups
-
by revisiting the extensive EndNote database (of more than 18,000 references) for occurrences of specific named interventions from (1) above, supplemented by targeted searches for these named interventions in MEDLINE to retrieve suboptimally indexed or recent occurrences of these interventions
-
by examining relevant reviews and systematic reviews for single instances of eligible interventions.
To supplement information retrieved, an additional search was undertaken of UK grey literature for the initiatives review. A Google search using key terms for each focal population, together with ‘emergency department’, ‘accident and emergency’ or ‘A&E’, focusing on sites within the nhs.uk domain, was undertaken. In addition, the websites of the Royal College of Emergency Medicine and the Care Quality Commission were searched for interventions delivered to frequent attenders/vulnerable groups.
As each new candidate intervention was identified, for example ‘front of accident and emergency (A&E) general practice’, ‘care navigator’ or ‘rapid access doctor’, these phrases were entered into Google and Google Scholar to retrieve extra supporting detail. When the phrase alone was not sufficiently distinct, for example ‘care navigator’, the phrase was combined with ‘emergency department’, ‘accident and emergency’ or ‘A&E’. Individual initiatives were examined to establish whether they were, in fact, homogeneous or whether they contained essential differences (e.g. an acute visiting service being delivered by a GP as opposed to a paramedic). For this reason, more than one entry may be present in the list of initiatives but present as a single entry within the intervention descriptions. Finally, we returned to the published literature using the specific phrase for the intervention to establish the existence of systematic review or quantitative research evidence supporting the intervention.
Study selection
Candidate interventions identified from the initiative analysis were selected according to the above eligibility criteria by a single reviewer. Heterogeneity of interventions and of outcome data meant that meta-analysis was neither feasible nor appropriate.
Data-collection process
The team used an abbreviated version of the TIDieR framework7 to analyse intervention content. A template was created for each type of intervention; therefore, the intervention was the unit of analysis, not the individual study report. A single reviewer extracted data against the TIDieR framework, using multiple data sources to triangulate intervention descriptions across study reports and resolve any inconsistencies. The abbreviated TIDieR was typically populated from key studies describing the intervention, descriptions of initiatives from news articles or grey literature on good practice or, most frequently, by combining multiple sources.
Data items
Each intervention template (modified TIDieR) included the author and date, a brief name for the intervention, the intervention purpose (why), the intervention materials and procedures (what), who provided the intervention, how and where the intervention was delivered and with what frequency (when) and intensity (how much) the intervention was delivered, together with details of any tailoring or modifications. The template concluded with evaluative details on how well (planned) and the degree to which these plans were realised – how well (actual).
For the initiatives, we extracted the following: name, setting (location), setting (geographical), aim of the initiative, initiative details, reported outcomes, evaluation of the initiative, where next and headline message.
Risk of bias
The mapping review aimed to provide an overview of the amount and characteristics of the literature and, therefore, in line with normal mapping review methods we did not include a quality appraisal of individual studies. Given the inclusive nature of the literature on interventions and initiatives, we provided an overview of the included study designs, including reporting when evidence was from higher-quality empirical work, rather than completing individual quality appraisals for each study. The likely risk of bias was, however, considered during our evaluation of each study using the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) approach, as outlined in the following section.
Methods of analysis
Few accepted ways exist for summarising findings from a mixed body of evidence. Outcomes from quantitative studies may be summarised using the GRADE system,10 whereas qualitative findings can be summarised using the related GRADE-CERQual (Confidence in the Evidence from Reviews of Qualitative Research) approach. 11 The focus of both tools is on the outcomes/findings and they are not designed for use at an intervention level. However, preliminary attempts in other reviews carried out by the team (e.g. Sworn and Booth12) suggest that the domains/constructs from these grading systems may offer a useful overarching structure for analysis. We therefore decided to use the five domains of the GRADE approach10 to summarise the diverse and diffuse evidence underpinning each intervention, across the published literature and yet including unpublished initiatives. We summarised the collective evidence for each intervention according to the likely risk of bias, the degree of imprecision, the inconsistency surrounding the estimate of effect, the likely indirectness and the potential for publication bias. Although not designed to provide a definitive assessment of the evidence base, this overarching system can indicate the need for further research (to reduce uncertainties around the risk of bias and imprecision), the need for further synthesis (to reconcile uncertainties around inconsistency and contextual variation), the need for more rigorous evaluation (to address publication bias) and the need for UK-specific initiatives (to address indirectness, i.e. lack of direct relevance for a UK context).
Protocol and registration
Given the iterative nature of the work, and that the initial element was a mapping review, which is not eligible for PROSPERO registration, the study was not formally registered as a systematic review. A study protocol was drafted in advance of the work and was available on the NIHR HSDR programme website.
Involvement of stakeholders
A patient and public involvement group provides ongoing advice to projects that are being carried out at the Sheffield HSDR Evidence Synthesis Centre. The group has eight members, with national representation. The second meeting of the group, held in February 2018, included discussion of this project, with public members reporting that research on EUC services is of particular interest to them, particularly given the high-profile nature of these services in the media. Input from the public advisors highlighted the need to avoid conveying a negative perception of vulnerable people during the review, as vulnerability could result from circumstances over which people have no control. The advisors perceived that vulnerable groups were generally under-researched and reported how public understanding may be unclear regarding how vulnerability may lead to discrimination and poorer health outcomes.
The group cautioned that it would be important to think about the impact of austerity on these populations during the review, both in terms of a general decrease in wealth in society and the differential impact that this might have on these groups and also in terms of the cuts to services, particularly those upstream that might have an impact on increased use of the health-care system. Input from the group highlighted the need to look for examples of interventions that had failed, as well as those that had been successful. The advisors also mentioned that the criminal justice system, in particular the police, often took a role in health and social services and that it might be worth looking at interventions delivered by the police to these groups in emergency settings. Notes from this meeting are available (see Report Supplementary Material 1).
In addition to our discussions with our patient and public involvement panel, we also sought advice from clinical academics within the School of Health and Related Research (ScHARR), University of Sheffield, who are involved in the delivery of care within the ED to ensure that our understanding of vulnerability made sense and that we were conceptualising the scope of EUC in an understandable manner.
Chapter 3 Results
Overview
The results from the three phases of the work are outlined separately in sequence in the following sections. The main findings and recommendations are combined in Chapter 4.
Studies included in the mapping review
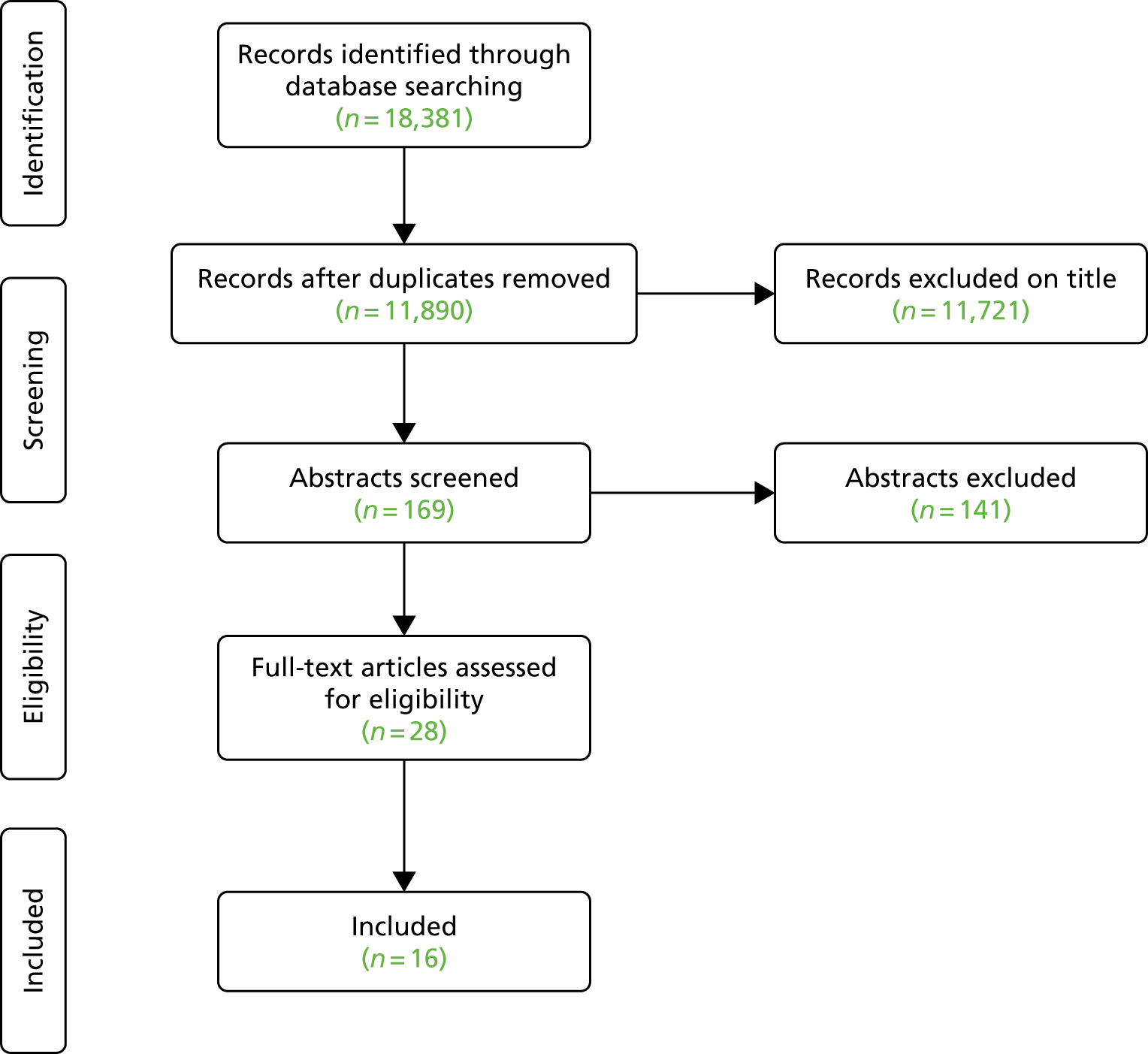
The database search identified 18,381 records (MEDLINE Epub Ahead of Print, MEDLINE In-Process & Other Non-Indexed Citations, MEDLINE Daily and MEDLINE – 6210; CINAHL – 3647; and Web of Science and Conference Proceedings Citation Indexes – 8524). Following deduplication, a total of 11,890 records remained for screening. Figure 3 provides a summary of the process of study selection. A total of 169 references were initially screened as ‘include’. On further scrutiny, 141 of these were excluded. The most common reason for exclusion related to the study outcomes reported as clinical outcomes for patients with no health service-demand-related outcomes reported. Any paper that included an outcome that could be related to the use of or demand for UEC was included. The full texts of 28 papers were screened, with 16 included in the mapping review. 13–28 Full details of these papers are included in Report Supplementary Material 1.
FIGURE 3.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram illustrating the process of mapping review study selection.
Characteristics of studies included in the mapping review
The primary study papers that met the inclusion criteria all used an evaluative design. There were four randomised controlled trials (RCTs),14,22,26,28 three non-randomised trials19,23,24 and three cohort studies. 15,17,21 The majority of the literature was from North America, with three studies from the UK,13,15,21 a single study from Australia28 and a single study from Switzerland. 14
Synthesis of mapping review findings
Table 4 summarises the data extraction for the mapping review. None of the study populations was described in terms of being ‘vulnerable’. Included studies referred to participants as being frequent users or frequent callers,14,15,17,20–27 young people with alcohol-related presentations,28 people with high opioid use,22 people at high risk of drug-seeking behaviour16 or people on a low income. 18
| Study | Setting | Study type | Population | Intervention | Outcomes (headline message) | |||
|---|---|---|---|---|---|---|---|---|
| Country | UEC setting | Description of population | Intervention group size (control group size) | Description or evaluation | Description of the intervention | |||
| Baker et al. (2013)13 | UK | ED | Cohort study | ‘people in an acute phase of representations’ | 20 | Evaluation | Care plans including cognitive–behavioural therapy to address reported mental health and physical health problems | Reduction in attendances for all 20 patients enrolled in the study (estimated as 245 attendances displaced) |
| Bodenmann et al. (2016)14 | Switzerland | ED | RCT, 12-month follow-up | Frequent users (five or more visits in the previous 12-month period) aged > 18 years | 125 (125) | Evaluation | Case management in addition to emergency care at 1, 3 and 5 months. Interdisciplinary mobile team | Intervention group made 19% fewer visits – not statistically significant (odds ratio 0.81, 95% CI 0.63 to 1.02; p = 0.08) |
| Edwards et al. (2015)15 | UK | Ambulance | Pilot study | Frequent ambulance callers, mostly with multiple and complex reasons for calling and who required multiple interventional strategies | 110 | Evaluation | Case management intervention | Significant reduction in median call volume observed as a result of the individualised case management programme. The programme found that these callers had complex unmet medical, mental health, social and personal care needs |
| Fiesseler et al. (2015)16 | USA | ED | Retrospective cohort study | ‘Patients at high risk for drug seeking behavior’ | 53 | Evaluation | Care plan initiated by an ED staff member. Primary care physician contacted and if agreed an ED care plan was put in place. The plan directed patients to visit the ED for new or recurring symptoms but outlined that they would be screened on arrival and if there was no new disease there would be no opioid administration or limited opioid administration | Prior to intervention – mean annual visits 7.6 (95% CI 6.3 to 9.1); 1 year post intervention – mean visits decreased to 2.3 (95% CI 1.5 to 3.1; p ≤ 0.0001); 2 years post intervention – mean visits declined to 1.5 (95% CI 0.9 to 2.1; p ≤ 0.0001) |
| Garbers and Peretz (2016)17 | USA | ED | Pre/post design | Patients without a primary care provider, without insurance or who had visited the ED more than once in the preceding 12 months | 75,765 patients who did not receive patient navigator services | Evaluation | Patient navigator programme aimed to work with providers, nurses, social workers and care managers to support patients to best understand, access and utilise the health-care system, along with family members | ‘Findings demonstrate that patients who had frequent ED T&R [treat and release] visits before navigation had significantly fewer visits in year after navigation. Among 535 navigated patients who had 3–5 ED visits in the year pre-navigation, on average, number of visits decreased by 1.68 visits in the year after navigation – a difference of 898 visits within this subset alone’ |
| Kim et al. (2015)18 | USA | ED | Unclear/cross-sectional study | Low income/uninsured | 10,761 | Evaluation | Hospital EDs linked to local primary care providers. ED staff referred patients to clinics. Describes a number of sites that implemented similar models. ‘Navigators’ in hospitals and clinics | 71% of patients did not have a subsequent ED visit during the study period. Much of the analysis considers the variance in visits between the study population. Authors report no reduction in ED visits overall, but a reduction for those with chronic or behavioural conditions or more frequent users, although data are not presented in the paper |
| McCormack et al. (2013)19 | USA | ED | Prospective, non-equivalent control group trial | Patients with at least five ED visits annually for 2 consecutive years and one within 6 months, alcohol dependence and undomiciled without shelter use for 9 out of 24 months | 20 participants with the highest baseline ED visits compared with 20 patients who received standard care and 20 patients from the previous year | Evaluation | Social worker and outreach team met with participants, guided by previous care plans, to offer shelter on discharge. Caseworkers relocated participants into increasingly supportive settings, co-ordinated multidisciplinary care and updated plans during biweekly interagency meetings about participants’ medical, psychosocial and housing needs | Differences in attendance between intervention and prospective patients and retrospective control patients were –12.1 (95% CI –22.1 to –2.0) and –12.8 (95% CI –26.1 to 0.6) for ED visits and –8.5 (95% CI –22.8 to 5.8) and –19.0 (95% CI –34.3 to –3.6) for inpatient days, respectively; 18 participants accepted shelter; no control patients were housed. ED use decreased and housing placements were achieved |
| Michelen et al. (2006)20 | USA | ED | Unclear – retrospective cohort study | ED frequent fliers – patients using the ED three or more times in the past 6 months (age range 0–95 years) | 539 at baseline, 537 at 3 months, 177 at 6 months | Evaluation | Health priority specialist, working in an ED diversion programme. On a visit to the ED the health priority specialist was informed that a patient had attended the ED. The health priority specialist then made contact to attempt to identify the reasons for use of the ED and manage frequent use of the ED | Including patients seen at all three assessment points, there was a significant decrease in ED use and referral to primary care providers. Provision of health education and counselling were linked to reduced ED use |
| Ng et al. (2015)21 | UK | ED | Cohort study | 7 of the 20 most frequent ED attenders over the last 12 months who were causing the greatest challenges for the team | 7 patients (no control group) | Evaluation | Comprehensive medical assessment of patients by an ED clinician followed by a biopsychosocial assessment. A patient-centred plan was then drawn up (working with patients and carers) for any contact with health and social services, including future ED visits | As a result of the Frequent Attendances programme, there was a significant decrease in presentations to the ED. The authors propose that this may be related to the addition of a liaison psychiatry clinician (working at the interface between physical and mental health) to the intensive case management team |
| Rathlev et al. (2016)22 | USA | ED | Randomised non-blinded two-group parallel design | Patients with opioid use disorder and high-frequency ED use; three affiliated hospitals with identical electronic health records | 20 assigned to the care plan group and 20 assigned to the usual care group | Evaluation | Care plan instituted and added to the electronic health record | Primary outcome was opioid use (not relevant for this study). Also collected information on secondary outcomes, including number of ED visits. Care plans did not alter the number of ED visits |
| Seaberg et al. (2017)23 | USA | ED | Prospective RCT | Superutilisers of the ED (five or more visits to the ED in the last 12 months) | 148 in the treatment group (134 in the control group) | Evaluation | A patient navigator worked with ED patients to review diagnoses and prescriptions and arrange follow-up appointments, etc. Delivered in the ED at the time of the initial appointment, at follow-up appointments and via telephone calls (2 weeks–12 months following the initial visit) | All reported results were statistically significant – overall ED visits decreased for both groups but there was a greater decrease in the intervention group. The same pattern was observed for decrease in costs and increase in primary care physician use. There was no difference in patient satisfaction pre and post intervention for either group |
| Shnowske et al. (2018)24 | USA | ED | Retrospective cohort analysis of electronic care records | Aged > 18 years, assigned a care guide as identified as having recurrent visits for non-emergent complaints | 287 | Evaluation | Case management via a care guide who assisted patients with barriers to finding non-emergent care, such as identifying primary care, scheduling appointments, educating patients and helping with financial management of medical care | Care guide initiation does reduce ED use by at least 40% for non-emergent and chronic complaints; however, these patients were not being directed back to primary care instead |
| Shumway et al. (2008)25 | USA | ED | 24-month randomised trial with interviews and service usage and cost data from administrative records | 252 frequent users | 167 case management, 85 usual care | Evaluation | Long-term clinical case management including assessment, crisis intervention, individual and group supportive therapy, assistance in obtaining stable housing and income entitlements, linkage to medical care providers, referral to substance abuse services as needed, and ongoing assertive community outreach | Case management was associated with statistically significant reductions in psychosocial problems that are common among ED frequent users (homelessness, alcohol use, lack of health insurance and social security income, and financial need). Case management was associated with statistically significant reductions in ED use and cost. No differences in use or cost of other hospital services |
| Stergiopoulous et al. (2017)26 | Canada | ED | RCT | Adults (aged > 18 years) with five or more visits in the past 12 months, with at least one visit for mental health or addiction | 83 brief case management and 83 usual care | Evaluation | Brief intensive case management offering a wide range of services to participants, including medical and social support | Primary outcome was frequency of ED visits in the 12 months following the intervention. Compared with usual care, the intervention group saw a 14% reduction in the frequency of ED visits during the post-randomisation process; however, this was not statistically significant |
| Tadros et al. (2012)27 | USA | EMSs transport | Pilot study | Adults with ≥ 10 EMSs transports in 12 months or patients a with significant recent increase in transport use | 51 (sequentially recruited) | Evaluation | Resource Access Program – surveillance, case management and referral to identify and modify medical and social factors leading to increased calls to EMSs | Evidence of a decrease in EMSs transports but limited impact on use of hospital services (authors suggest that care may have been displaced) |
| Tait et al. (2016)28 | Australia | ED | RCT (cost-effectiveness data) | 12- to 19-year-olds with an alcohol-related presentation | 60 (67) | Evaluation | Link worker, brief intervention and referral. The link worker carried out follow-up contacts, made appointments with services and attended appointments if required | No difference at the 10-year follow-up in the cost of ED presentations between the intervention and the control group (AU$4266 vs. AU$4150; p = 0.916). No significant difference in number of ED events between groups (p = 0.849). ED attendances and rates of presentation specifically with an alcohol or other dependency mental health diagnosis were significantly reduced in the intervention group (0.03 vs. 0.25, p = 0.010; 0.03 vs. 0.25, p = 0.010, respectively) |
The interventions evaluated in the primary studies included provision of a link worker for young people with an alcohol-related presentation, combined with a brief intervention and referral,28 and introduction of a system for people on a low income or who were uninsured whereby hospital EDs were linked to local primary care providers and ED staff referred patients to these clinics18 (both subsequently classified under ‘outreach services and teams’). Interventions also included a care plan initiated by ED staff for patients at high risk of drug-seeking behaviour. 16 Case management, which could include offering additional social support to patients, was described in four studies. 14,15,24,26 The difference between interventions described as case management and those referred to as care plans was not always clearly distinguishable, as establishing a plan was often a main component of management.
A care plan intervention was reported to have resulted in a significant reduction in mean annual ED visits among the 53 patients in the study group, from 7.6 visits [95% confidence interval (CI) 6.3 to 9.1 visits] to 2.3 visits (95% CI 1.5 to 3.1 visits; p ≤ 0.0001) at 1 year of follow-up and 1.5 visits (95% CI 0.9 to 2.1 visits; p ≤ 0.0001) at 2 years’ follow-up. 16
The link worker intervention was evaluated in a RCT. 28 The authors reported no difference at 10 years’ follow-up in the cost of ED presentations between the intervention group and the control group (AU$4266 vs. AU$4150; p = 0.916). There was also no significant difference in the number of ED events between groups (p = 0.849). However, ED attendances and rates of presentation specifically with an alcohol or other dependency mental health diagnosis were significantly reduced in the intervention group compared with the control group (0.03 vs. 0.25, p = 0.010; 0.03 vs. 0.25, p = 0.010, respectively).
The linking system intervention18 similarly appeared to have resulted in no reduction in ED visits overall, although the authors reported that there was a reduction for those with chronic or behavioural conditions or more frequent users (however, data for this finding were not provided in the paper).
A RCT evaluating case management for frequent attenders who had mental health or addiction difficulties found a 14% reduction in frequency of ED visits during the post-randomisation process; however, in line with the studies described above, this reduction did not reach statistical significance. 26 A pilot study of frequent ambulance callers suggested that case management was promising as a method to reduce the median call volume, although the authors highlighted the complex range of needs of patients. 15
Of the 16 included studies, there was overall uncertainty regarding the effectiveness of interventions aiming to reduce UEC use, with five studies indicating a reduction in service use16,17,20,21,23 and six studies suggesting no significant reduction in service use. 18,22,24,26–28 There appeared to be no clear pattern regarding which types of interventions reported positive outcomes, although studies indicating effectiveness tended to be of a non-comparative design.
The mapping review identified the extremely limited evidence regarding interventions and outcomes for people who might be classified as being ‘vulnerable’. The paucity of empirical evidence suggested that a further full systematic review of interventions for vulnerable patients was not indicated. The review identified the lack of clarity regarding intervention types and components, with a potentially useful direction for further work being to unravel elements of the interventions evaluated. It was anticipated that further exploration of the detail of interventions aimed at reducing UEC usage in patients more generally might assist in understanding which interventions may be promising for vulnerable groups. Given the limited available evidence in academic journals, it was also anticipated that grey literature and other sources of reporting may be a worthwhile avenue of exploration.
Developing a typology: the intervention and initiative analyses
The phase 2 intervention search focused on further exploring the characteristics of existing interventions aiming to reduce the use of UEC services. Following the iterative process described in Chapter 2, the review team developed a typology of nine different intervention types (Table 5). In addition to the literature found during the mapping review, the phase 2 intervention analysis identified four additional articles: three were related to multicomponent packages, including case management, case finding, care planning and outreach for the homeless and those with substance use problems,29–31 and one reported a programme to prevent less serious, and therefore potentially inappropriate, cases from presenting at an ED. 32
| Intervention type | Mapping review | Analysis | |
|---|---|---|---|
| Intervention | Initiative | ||
| Care navigators | ✓ | ✓ | |
| Care planning | ✓ | ||
| Case finding | ✓ | ✓ | |
| Case management | ✓ | ✓ | |
| Front of A&E general practice/front-door streaming model | ✓ | ||
| Migrant support programme | ✓ | ||
| Outreach services and teams | ✓ | ||
| Rapid access doctor/paramedic/urgent visiting service | ✓ | ||
| Urgent care clinics | ✓ | ✓ | |
To supplement the evidence from the initial mapping review and phase 2 intervention search, in phase 3 of the study we sought further evidence from the grey literature and other sources beyond academic journals. In phase 3, we identified 22 further documents33–54 relating to 15 UK initiatives. Data from these documents were extracted against an abbreviated version of the TIDieR framework and examined to further develop and refine our understanding of the intervention characteristics and components.
Primary sources of these initiatives were good-practice case books and rapid reviews, commissioning plans and news articles, either in the GP press (e.g. Pulse) or in local newspapers. It was not always possible to determine the extent to which initiatives were truly innovative and the extent to which they had been developed elsewhere and then implemented in a new location. The method by which each type of intervention was identified is indicated in Table 5.
The following sections provides a summary description of each intervention in our typology, drawing on information from the three phases of the review. Completed TIDieRs for the interventions are available in Report Supplementary Material 1. For illustrative purposes only, a sample abbreviated TIDieR for targeted case management is provided in Table 6.
| Item | Details |
|---|---|
| Studies | Hudon et al.;29,30 Grover et al.31 |
| Item 1. Brief name | Case management |
| Item 2. Why | Intensive personalised management (through a care plan) enables co-ordination of services and appropriate targeting of care |
| Item 3. What (materials) | Care plan |
| Item 4. What (procedures) | Composite package of interventions, which may include:
|
| Item 5. Who provided | Health-care professionals, typically specialist nurses with medical support |
| Item 6. How | In an ED context, initial contact is within the ED and then follow-up may occur following discharge and may involve multiple health and social care agencies |
| Item 7. Where | May be delivered face to face in a patient’s home or in an ED setting or by telephone |
| Item 8. When and how much | Frequency and duration of contacts varies according to need |
| Item 9. Tailoring | At intervals determined by the case manager; may also be patient initiated |
| Item 10. Modifications | Components from the above list vary according to setting, skill mix and target population |
Further details of the sources by which the initiatives were identified are available in Appendix 2. Table 7 summarises the key details of each intervention.
| Intervention | What (procedures) | What (materials) | Who provided | Where |
|---|---|---|---|---|
| Acute visiting service/rapid access doctor | Responds to clinically appropriate green category triaged calls from 999, uniquely dispatched from an ambulance service clinical decision-making hub. Supports locally based ambulance crews – assesses, diagnoses, prescribes and treats at home, without requiring paramedic response, conveyance to hospital or subsequent admission | Mobile directory of services | Dedicated GP with a driver in a non-ambulance service vehicle | Community |
| Alcohol Intoxication Management Services | Alternative care pathway to divert acute alcohol-related attendances from the ED | Care pathway | Not stated | ED and diverted from the ED |
| Case management | Composite package including case finding; assessment; care planning; care co-ordination, including but not limited to medication management, self-care support, advocacy and negotiation, psychosocial support, monitoring and review and case closure. May include self-management, patient education and disease management | Care plan | Health-care professionals, typically specialist nurses with medical support | Face to face in a patient’s home or in an ED setting or by telephone |
| Frequent Attenders Programme | Biopsychosocial assessment; frequent attenders clinic for brief interventions and monitoring of subsequent attendances | Care plan | Doctor and senior nurse clinical leads | ED |
| Front of A&E general practice/front-door streaming model | Provision of alternative primary care-based services to patients not requiring ED admission | Hospital has a co-located urgent GP centre, open from 08.00 to 24.00 every day of the year | Two or three GPs work in the centre daily, with a minimum of two GPs working at any one time | ED |
| Health Diversity Initiative | Addresses confusion over GP out-of-hours services and poor rates of registration from migrant groups | Includes community education sessions (6-week courses) and bilingual advocacy and interpretation services | Multidisciplinary team of nurses, health coaches, paramedics, pharmacists, midwives, nutritionists and falls specialists | Multiple settings |
| High Impact User Team | Management of top 100 most frequent attending patients | Support plans, behavioural contracts, signposting | Multidisciplinary group of ED and other medical staff alongside police, ambulance and other staff | ED |
| High Intensity User Programme | Tackles problems of patients with complex psychosocial problems as an alternative to A&E presentation. Uses personal mentoring and one-to-one coaching | No details | No details | ED |
| Homeless Hospital Discharge Programme (care navigators) | Works as part of the hospital discharge team to proactively identify homeless patients and establish their ongoing care needs | No details | Works with a community-based ‘broker’ to find out what help is available and the barriers to be addressed | ED and hospital |
| GSTT@home (Guy’s and St Thomas’ NHS Foundation Trust @home service; GSTT@home service) | Service for the prevention of admission and the provision of early discharge; provides intensive care for short episodes through multidisciplinary teamwork, with the aim of returning patients to their prior health status following an acute episode of ill health | Care pathway | Senior nurses with acute hospital ED nursing experience skilled at managing complex, acutely unwell patients. Nurses were usually at master’s level with advanced differential diagnostic skills and were non-medical prescribers | Community |
| Multidisciplinary integrated care | Integrated care | Integrated care plan | Not stated | ED |
| Non-clinical care navigator | Screens and offers signposting to services outside hospital as appropriate:
|
Signposting | Team including doctors, nurses, physiotherapists, triage nurses and the A&E rapid response team | ED and medical assessment unit within a hospital setting |
| Positive Lives | Focuses on individuals who present at A&E with a non-medical need (e.g. anxiety, unemployment, homelessness or depression) and aims to change the way they are supported. Individuals are offered access to appropriate support to address their issues and improve well-being. Ongoing support provided if needed | No details | The Positive Lives lead works one-to-one with individuals to uncover the underlying cause of their crisis | ED |
| The Sociolance | On-the-spot care or transport to a care provider. Referrals to other services | Emergency medical dispatch centre | Sociolance | Community |
| Urgent care clinics | Service that primarily treats injuries or illnesses requiring immediate care, but not serious enough to require a visit to an ED | Treatment facility – may also include diagnostic services | General practice teams | Often located near A&E departments. See Front of accident and emergency general practice for co-located services |
| Urgent visiting service | GP-led rapid assessment service for patients unwell at home who might otherwise call an ambulance | Utilises mobile SystmOne (The Phoenix Partnership, Horsforth, UK) application to enable access to records | Locums deployed to backfill sessions to free up GPs to lead the service | Community |
| Working Together to Connect Care | Case review and referral to community services | Case management | ED staff | ED |
Care navigators (non-clinical)
Care navigators are increasingly seen across a wide diversity of health-care settings and their existence attests to the increasing complexity of comorbidities and interacting health and social problems and the bewildering complexity of how health services are organised and how interagency relationships present themselves to a service user. 37 Within the specific context of the ED, the care navigator can fulfil a twofold function, referring the service user to other services that may be useful, together with information on access and eligibility (a casebook describes how a long-term visitor to London was advised on temporary registration with a GP and on which GPs accepted temporary registrants), and acting as a liaison point with members of the ED team. 36 The care navigator role is formally recognised by a task specification and associated competencies. This role can be of particular value to those with limited familiarity with the organisation of health services, whatever the reason, together with those with languages other than English, those with learning difficulties and those with poor health literacy.
Care planning
Frequently a component of wider case management initiatives, care planning is an approach of choice when the complex needs of a particular type of patient are semipredictable. 30 Groups of patients who have shared needs, for example those with substance use disorders or those who are homeless, benefit from a standardised approach. 43 Pascal et al. 55 invoke knowledge management by identifying a shared care plan as a ‘knowledge object’, that is ‘information solidified into a pure and objective form [that] . . . takes the form of text or can be embedded in physical artefacts such as machinery or tools’. 54 As a standalone knowledge object, a shared care plan serves to structure and contextualise the patient–practice relationship through creation of an actual document, prompting referral to other agencies and proceduralising less familiar areas of care. 55
Case finding
Frequent attenders typically fall into recognisable groups; some of these correspond to the categories of vulnerable populations identified for this report. Case finding may be of benefit when populations have complex, non-medical psychological or social needs that cannot be met or resolved by repeated presentation at an ED, for example in the unemployed, those with substance use disorders or those who are homeless. 30,31 By ‘breaking’ a vicious cycle of presentation and re-presentation, the intervention may help to reduce inappropriate reattendance.
Case management (targeted)
Case management may include elements of care planning and case finding. It represents another form of personalised care by which needs that are not resolved through inappropriate presentation to an ED are channelled to more appropriate outlets. Thus, there is an element of care navigation included in the role.
Front of accident and emergency general practice
Front of A&E general practice represents a generic approach to inappropriate presentation at an ED for minor conditions and injuries. For this reason, it is not yet clear whether or not the vulnerable groups targeted by this review are particularly likely to benefit from such provision. In theory, provision of single-site services should be valuable for those who have difficulty navigating primary care or more general health service provision, such as migrants or those whose first language is not English. 44 However, this approach would be of limited value to other vulnerable groups for whom access to EDs located in a major population area is already problematic, such as those living in rural areas or those without transportation (e.g. the homeless). As some commentators have observed, notwithstanding the rhetoric of ‘front of A&E services’, permanent provision of GP services alongside an ED becomes a de facto extended ED, the main attraction of which lies in the provision of a small percentage of appropriate primary care services from a primary care (i.e. commissioning), not acute, hospital budget.
@home
The service receives referrals from GPs and two major hospitals. 52 A clinical lead nurse, with experience of establishing new services, leads and develops the team strategically and operationally, with consultant geriatrician support within a multidisciplinary team (senior nurses led by matrons together with GPs, rehabilitation support workers, physiotherapists, an occupational therapist, social workers and a pharmacist). The multidisciplinary team assesses, initiates and implements treatment, and meets daily to discuss the progress of the patient. Owing to the acuity of the patients, most nurses are at band 6 or 7 (supported by a few band 5 nurses and placements from student nurses.
The GSTT@home service pursues three specific aims:
-
identifying people at risk of a hospital admission and providing care that prevents their condition from worsening
-
allowing people to be given a high level of care in their own home instead of being admitted unnecessarily to hospital
-
allowing for advanced discharge from hospital so that patients can recuperate in the comfort of their home while receiving high-quality care.
The service is designed for 260–80 referrals each month and operates 24 hours per day, 7 days per week, with the overnight service mainly focused on palliative and end-of-life care or an acute medical emergency such as a blocked urinary catheter. The main referral criteria are adults aged ≥ 18 years living with an acute onset of illness (including acute exacerbations of chronic conditions). Most patients can be classified as either ‘early discharge’ (following a medical procedure in hospital and requiring further nursing care or therapy) or ‘admission avoidance’ (at high risk of requiring a hospital admission). All referrals are triaged by the GSTT@home duty clinician (matron or GP) or, if referrals are for inpatients, they are reviewed and assessed by a GSTT@home in-reach nurse. The in-reach nurses review patients in the ED and acute assessment wards and on post-take rounds identify suitable patients as quickly as possible. The GSTT@home duty clinician or in-reach nurse determines if a referral is appropriate and fits the acceptance criteria (i.e. patients requiring short-term care in their own home that can be provided by the team). The patient is then transferred to the appropriate team where he or she is assessed by a senior nurse/GP. The patient’s GP is informed that the patient has been seen by the GSTT@home team and is sent an intervention summary on discharge from the service.
Migrant support programme
Migrants and those from ethnic minorities with a first language other than English are likely to benefit from a support programme that fulfils a dual role of literacy and health literacy, as typically provided by a diversity inclusion programme. 45
Outreach services and teams
Outreach services are potentially useful for those for whom presentation at an ED represents an acute phase of more pervasive underlying chronic issues, such as those relating to psychological health and social challenges. Outreach to the homeless, to those with substance abuse problems, to the long-term unemployed and to other targeted groups of the population, such as ethnic minorities and migrants, can offer both ongoing monitoring and co-ordination of health and social care services. 28 However, outreach services are considered potentially very intensive and expensive and so must be targeted judiciously.
Rapid access doctor/paramedic/urgent visiting service
Physical access barriers to EUC are manifest in multiple ways; they may result in either inappropriate calls to ambulance services or non-use of services at an acute setting. Services that can visit patients in the community, in their own home if appropriate, can provide an early assessment of clinical need and reduce presentation at EDs when not required. Patients who are vulnerable because of access difficulties may benefit from such services. 41 In addition, rapid access services may be perceived as being more accessible or more locally sensitive. However, such services do not necessarily address difficulties around care navigation as patients have to be familiar with the available service and know how to access it. Furthermore, our review of initiatives found variation in whether rapid access services were initiated by general practices or ambulance services. This could have a differential effect on perceived eligibility for those who are homeless or who are not registered with a general practice.
Urgent care clinics
Limited evidence from the USA suggests that urgent care centres (walk-in clinics outside a traditional ED) may be disproportionately used by the homeless. 32 However, it is unclear whether this simply reflects the same patterns of frequent use encountered by EDs or whether it captures some added relative advantage that such clinics might offer. A high percentage (69%) of users of an urgent care clinic in the USA were not registered with a doctor, suggesting that they are attractive to a homeless or migrant population. 32 However, it is unclear to what extent this would be equally true in the UK. In theory, the local positioning of these centres offers a more accessible point of contact than an acute hospital, and such services may be perceived as being more context sensitive.
Vulnerable subpopulations
Table 8 summarises the vulnerable population subgroups included in studies of each type of initiative, indicating either reports of positive outcomes or when uncertainty was reported.
| Intervention type | Vulnerable population subgroup | ||||||
|---|---|---|---|---|---|---|---|
| Socioeconomically deprived | Migrants | Ethnic minority groups | Long-term unemployed | Unstable housing situations | Rural/isolated areas | Substance abuse disorders | |
| Care navigators (non-clinical) | ? | ✓ | ✓ | ✓ | |||
| Care planning | ? | ✓ | ✓ | ✓ | |||
| Case finding | ✓ | ✓ | ✓ | ✓ | |||
| Case management (targeted) | ? | ✓ | ✓ | ✓ | |||
| Front of A&E general practice | ? | ? | ✓ | ||||
| Migrant support programme | ✓ | ✓ | |||||
| Outreach services and teams | ✓ | ✓ | ✓ | ✓ | |||
| Rapid access doctor/paramedic/urgent visiting service | ? | ✓ | |||||
| Urgent care clinics | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
Evaluation of the strength of evidence
Table 8 illustrates how some interventions, such as case management and care planning, have been demonstrated to be effective across diverse contexts. These contexts include some that are specific to the vulnerable populations covered by this review. In contrast, locally driven NHS solutions, such as the rapid access doctor and the diversity action service for migrants, have demonstrated good locally relevant results but are lacking in rigorous evaluations. Furthermore, such initiatives may reveal a systematic publication bias in celebrating ‘local success stories’. Similarly, we can observe extensive roll-out of the Blackpool model42 of case finding and the Luton and Dunstable model46 of front of A&E general practice, stimulated by local enthusiasm for adoption or by government endorsement and mandate. Table 9 seeks to consolidate and evaluate the disparate evidence from multiple sources by using a ‘light’ version of the GRADE domains. Risk of bias relates to the methodological quality of the supporting studies whereas imprecision is determined by the uncertainty around the likely overall strength of effect. Inconsistency conveys the degree to which different studies demonstrate a consistent pattern of effect whereas indirectness relates to the relevance of the included studies to a UK context. Finally, publication bias examines the likelihood of selective reporting of results, a particular concern when alleged ‘good-practice’ initiatives are being reported in professional journals (e.g. Health Service Journal or Nursing Times), on websites or in casebooks. Collectively, these five components contribute to an overall assessment that is rated as very low (the true effect is probably markedly different from the reported effect), low (the true effect might be markedly different from the reported effect), moderate (the authors believe that the true effect is probably close to the reported effect) or high (the authors have a lot of confidence that the true effect is similar to the reported effect). Note that we use the phrase ‘reported effect’ in preference to ‘estimated effect’ to convey that the evidence base includes both quantitative and qualitative data. Similarly, the assessment is considered to be ‘GRADE light’ because the quality, strength, consistency, relevance and selectivity of the evidence base are explored at the level of the intervention, not the individual study finding, as the originators of GRADE intended.
| Intervention type | Number of studies | Number of participants | Risk of bias | Imprecision | Inconsistency | Indirectness | Publication bias | Overall assessment | Notes |
|---|---|---|---|---|---|---|---|---|---|
| Care navigators | 3 | 76,334 | * | * | ** | ** | * | Moderate | Generic care navigator role is common. Limited evidence of specific ED application |
| Care planning | 3 | 113 | ** | ** | *** | ** | ** | High | Supported by SR evidence, generically. More evidence required for specific groups. Component of case management |
| Case finding | 5 | 1045 | * | * | ** | *** | * | Moderate | Effective in some circumstances. Component of case management. Interpreted locally (Blackpool model) with strong social support element |
| Case management | 4 | 688 | ** | ** | ** | *** | *** | High | Supported by SR evidence, generically. More evidence required for specific groups |
| Front of A&E general practice/front-door streaming model | 1 | N/A | * | * | * | * | * | Low | Limited evidence. Differential success across hospitals. Partially covered by a Cochrane review. Likely to be context specific |
| Migrant support programme | 1 | N/A | * | * | ** | *** | * | Low | Single case study with limited evaluation. Context-sensitive solution |
| Outreach services and teams | 2 | 10,888 | * | * | * | *** | ** | Moderate | Some evidence for outreach teams. Unclear the extent to which they are effective for specific populations within this review |
| Rapid access doctor/paramedic/urgent visiting service | 1 | N/A | * | * | * | * | * | Low | Limited examples of initiatives. Not exclusively for rural areas. Different mechanisms apply for different contexts |
| Urgent care clinics | 1 SR | N/A | * | ** | ** | ** | ** | Moderate | Substantive US evidence. Large number of UK sites. Unclear whether or not theoretical benefits for specific vulnerable populations are realised in practice |
Although the meaning of the results presented in Table 9 are explored in detail in Chapter 4, it is nevertheless worth observing a polarisation between interventions that are supported at a systematic review level through multiple consistent studies, derived mainly from non-UK settings, and initiatives, largely at the pilot or non-evaluated stage, that show promise within a UK context. This trade-off between likely rigour and likely relevance makes it particularly challenging to interpret the evidence base, compounded by the fact that even UK studies describing promising initiatives tend to frame the discourse in the language of ‘frequent attenders’ rather than as interventions targeting vulnerable populations.
Chapter 4 Discussion
This discussion looks at the overall take-home messages from the three phases of the review and seeks to draw together some general observations and conclusions.
What interventions were identified?
As previously mentioned for the mapping review, it is extremely challenging to identify interventions that are targeted specifically at the vulnerable groups nominated for this review. Interventions may not specifically identify vulnerability as the feature to be addressed by their programme theory. Alternatively, interventions may target the population generally, with the implication that vulnerable populations may benefit equally or even may benefit more than the general population. In some cases, we had to work backwards from interventions employed by initiatives introduced by specific health communities to target vulnerable populations (e.g. urgent care clinics) to look at the associated evidence for that intervention.
The shortlist of nine intervention types identified from the multiple routes used for this review, namely the mapping review, the intervention analysis and the survey of initiatives, comprises:
-
care navigators
-
care planning
-
case finding
-
case management
-
front of A&E general practice/front-door streaming model
-
migrant support programme
-
outreach services and teams
-
rapid access doctor/paramedic/urgent visiting services
-
urgent care clinics.
A previous narrative review of reviews56 categorised interventions to reduce frequent attendance at EDs into six types:
-
cost sharing
-
strengthening primary care
-
pre-hospital diversion (including telephone triage)
-
co-ordination
-
education and self-management support
-
barriers to access EDs.
The intervention typology developed during our review adds to this previous work by providing discrete types of interventions outlined in the literature, rather than categorising general approaches. The diversity of intervention types that we identified indicates different conceptualisations of the exact nature of the problem of frequent attendance and, consequently, a differential ability for these interventions to benefit vulnerable groups. Interventions relating to cost sharing or co-ordination may result in more efficient and more appropriate utilisation of care but are unlikely to benefit vulnerable populations directly unless specifically targeted at these groups (e.g. case management of the homeless).
More promising, particularly for vulnerable populations for whom physical access is an issue, are those interventions that challenge difficulties relating to the proximity of services, such as strengthening primary care (e.g. urgent care clinics) or pre-hospital diversion (e.g. telephone services, including triage). It should be noted that stereotypical representations of vulnerable populations may impede identification of potential interventions, for example a systematic review of access to health services by homeless people using technology found high rates of mobile phone and technology ownership. 57 Education and self-management support can prove challenging to several of the identified vulnerable groups, for example those with low levels of health literacy, those with a first language other than English and those with an itinerant lifestyle. The final category of interventions that address barriers to access overlaps partially with those interventions that address physical access or navigation barriers, as mentioned above, but, more widely, may address systemic difficulties, such as the requirement to provide proof of residence or the unsympathetic or unwelcoming attitudes of ED staff. 58
Why are these groups vulnerable/at higher risk?
The heterogeneous grouping of vulnerable patients specified for this review recognises that vulnerability presents in many forms. Indeed, one common form of vulnerability – frailty among older and chronically unwell patients – was specifically excluded from this review, having previously been separately targeted by the evidence synthesis programme. 59 In trying to conceptualise vulnerability at a level superordinate to the list of included groups, we identify the following ‘vulnerabilities’:
-
vulnerability in terms of a limited ability to navigate the health system (either through language challenges or through limited health literacy)
-
vulnerability in terms of constrained physical access to current health provision (e.g. rural communities, those likely to encounter transportation difficulties)
-
vulnerability in terms of difficulties in demonstrating eligibility for current health services (e.g. migrants and the homeless)
-
vulnerability in terms of having a higher likelihood of complex psychological and social issues not adequately or appropriately addressed by health services and requiring multiagency involvement (e.g. long-term unemployed, those in a non-stable housing situation, those experiencing substance use disorders)
-
vulnerability in terms of requiring a higher degree of social or emotional support (a proportion of those from among the long-term employed, those experiencing substance use disorders, those from ethnic minorities and migrants).
These different vulnerabilities are addressed by different mechanisms present within the different interventions; for example, issues around physical access may be addressed by the provision of ‘more-local’ urgent care centres or an urgent visiting service. Conversely, an intervention may activate multiple mechanisms; for example, the particular type of case finding activated by the paramedic from Blackpool42 offers elements of navigation, outreach and social and emotional support. Finally, how an initiative is set up may differentially address different vulnerabilities; for example, a rapid access doctor accessed through participating general practices may result in the persistence and extension of an existing barrier of limited eligibility (based on practice registration and having a permanent address), whereas the same service accessed as an extension of the ambulance service would be equally available to the homeless and to migrants.
In a twist on the perspective presented in this report, Couture et al. 60 argue that frequent use of health services is itself a marker of vulnerability. Such frequent users, they maintain, deserve attention because of high costs and negative outcomes, such as lower quality of life and higher mortality. For this reason, they contend that health-care systems should offer interventions tailored to the needs of frequent users and to their level of health literacy, including strategies to promote activation. Such an approach is best evidenced in the health diversity initiative for migrants,44 but, it could be argued, it has wider applications for populations in whom health literacy, not language proficiency, remains a key issue.
A further paradox relates to the fact that the provision of multiple channels for accessing services may maximise the chances of certain vulnerable populations being able to access an appropriate service while, at the same time, adding to the complexity facing those vulnerable populations for whom being able to navigate the health-care system is the more significant problem. For example, one of the experiences of the pilot front of A&E services initiative was poor uptake related to poor awareness of the role of the new service compared with the existing ED. 46–49 Other services and initiatives specifically exclude specific vulnerable groups; for example, the Guy’s and St Thomas’ and King’s College Hospitals rapid response service40 excludes patients for whom the primary diagnosis is a mental health or substance disorder problem.
Strengths and limitations of this review
This three-stage review has optimised the use of resources by, first, undertaking a mapping phase, before undertaking more intensive analytical phases, ensuring that the final review approach is meaningful and potentially useful. As anticipated by the review team and HSDR programme commissioners, there is a limited body of evidence on interventions for vulnerable people who have service delivery outcomes. Findings from papers included in the mapping review confirmed the existence of evidence for the interventions used having a positive effect on ED attendance, although, as noted, many of these interventions did include an ‘outside the ED’ element. This finding, in turn, justified our widened scope for the subsequent phases of the review.
The mapping review looked only at interventions for vulnerable groups that are delivered within the EUC system. We were aware that interventions that are being delivered outside the EUC system, within acute or primary care, offer the potential to reduce ED use by these groups. For our intervention analysis, we imposed a more forgiving requirement in recognition that (1) interventions may be triggered within the ED but followed up in primary care, (2) re-presentation and/or readmission of frequent users made such a distinction somewhat arbitrary and (3) the EUC system could conceivably include extensions offered in primary care that are conceived as operating seamlessly as part of an extended EUC system (e.g. rapid access doctors, urgent care clinics and front of A&E general practice).
Although, as reported in Chapter 1, it is acknowledged that patients in these vulnerable groups are frequent and heavy users of the EUC system, there is limited evidence to show that interventions specifically target use of services by these groups. The screening process for this review indicated that interventions are often reported in terms of patient outcomes, rather than health system or service delivery outcomes, thus limiting the number of papers included in this review.
The intervention analysis ensured that details of the interventions can be identified and explored and differences manifest at a local level can be identified and clearly flagged. A major contribution of this overall review (particularly given the dearth of specifically targeted interventions identified from the literature) is the review of current practice (like many researchers, we resist the label of ‘good practice’ for promising and yet superficially evaluated or unevaluated initiatives). This has expanded our pool of candidate interventions, although, once again, evidence of specific targeting is limited and the vulnerable populations from our target list benefit, if at all, only collaterally from initiatives and, within these initiatives, differentially according to the specific nature of their vulnerabilities. This additional searching (citation and reference list checking) highlighted additional interventions to include in the review and the full intervention analysis has highlighted germane aspects of the interventions of interest. By combining the publication and practice evidence bases, we have been able to offer a potentially valuable perspective on the current landscape, where work is being done and where future work is required.
Weaknesses relate to the diverse nature of the evidence, ranging from published studies to brief mentions in news stories or ‘good-practice’ casebooks. This poses particular challenges for synthesis, especially as this tends to polarise the twin considerations of rigour and relevance, which, ideally, should be complementary when characterising the evidence base. The trialled interventions typically originate from the USA, and the locally sensitive initiatives from the UK are likely to be vulnerable to risk of bias, particularly selective reporting bias. Furthermore, initiatives that are evaluated in the short term are vulnerable to several implementation biases compared with routine roll-out and adoption, for example the disproportionate influence of the ‘hero innovator’ and the enthusiasms of early adopters. This narrative may partly, although not entirely (see below), explain the differential success of the front of A&E streaming initiatives at Luton and Dunstable, and Frimley Park. 46–49
Initiatives of alleged good practice carry known limitations in frequently displaying the presence of reporting bias, in the use of relative measures of performance (e.g. percentages) with inadequate measures of baseline performance and in limited evaluation objectives and time frames. As a consequence, they do not necessarily depict an accurate picture of real-world implementation. In particular, they typically invoke cost savings without presenting the actual cost of designing, planning and introducing the intervention. Nevertheless, they do indicate potential candidate interventions that might benefit from more rigorous evaluation. An illustrative example in this review is the front of A&E general practice initiative, which yielded vastly different results in Luton and Dunstable, and Frimley Park, leading at least one commentator to highlight the likely context sensitivity of such interventions. 50 Indeed, Edwards50 reminds us that there are no simple solutions or policies for complex problems. Notwithstanding a letter in 2017 from the chief executives of NHS England and NHS Improvement, instructing trusts to ensure that every hospital in England should use hospital-based GPs to triage and redirect patients as they are first seen in A&E,47 commentators could point to a differential effect between well-suited hospitals serving populations that use A&E extensively for primary care concerns48 and areas where GPs see a high proportion of emergency cases on the same day. 46 This context sensitivity provides a strong indicator for further realist evaluation61,62 and realist synthesis approaches63 within an ED context.
Chapter 5 Conclusions
This review was conducted against a backdrop of the emergency system experiencing higher demand. Reasons include more patients, an ageing population (more older people with more complex health issues), more patients with increasingly complex and co-morbid health issues (across the general population) and a decrease in the availability of other services. However, despite conclusive evidence of disproportionate use of the ED by certain groups of people, the majority of interventions appear either to tackle the problem at a general population level, for example front of A&E general practice or urgent care clinic approaches, or to target frequent attenders as a discrete group.
Although one would expect a proportion of the vulnerable populations identified in this report to benefit from population-based solutions and, indeed, these vulnerable populations to figure in frequent attender case-finding approaches, neither of these approaches tackles the specific needs of and barriers for each specific population. Such an approach requires a more sophisticated and nuanced understanding of how vulnerability is to be interpreted in these diverse populations. Our patient and public involvement group further identified that vulnerability may hold a temporal dimension. Although they expressed this in terms of population characteristics, this is likely to be equally true with regard to patterns of ED utilisation (i.e. a frequent attender during one measurement period will not necessarily figure during a previous or subsequent measurement period). Frequent attendance is not necessarily inappropriate attendance and several vulnerable groups are known to have more complex or more serious physical problems. Nevertheless, a substantive part of the problems facing certain vulnerable groups is social and non-medical and can benefit from co-ordination with, and navigating to, other non-health agencies.
Reasons for increased patterns of use of the ED for vulnerable groups are complicated and encompass a wide variety of drivers (burden of disease, access to primary care, patient preference). Indeed, our patient and public involvement group identified additional types of vulnerability that potentially would invoke an even wider diversity of drivers of ED use. A wider understanding of what exactly is meant by ‘vulnerability’ could potentially lead to the inclusion of other subpopulation groups, such as people with dementia, and thus broaden the richness of potential solutions to address these vulnerabilities. This, in turn, would acknowledge that ‘vulnerable populations’ is an even more heterogeneous grouping than implemented in this review and that nuanced understandings and tailored interventions are strongly indicated.
As a consequence of a research agenda articulated around the phenomenon of frequent attendance, we have identified a distinct shortage of interventions designed specifically to reduce demand for ED services from the identified list of vulnerable groups. Interventions that do exist are mostly delivered within the community setting. This justifies our decision to interpret an extended conception of EUC services for the intervention and initiative analysis, while preserving the focus on health service outcomes, particularly relating to presentation at an ED or admission via an ED.
Interventions and initiatives offering alternatives to presentation at an ED or admission via an ED currently trade between rigour and relevance. In particular, front of A&E services have received ministerial endorsement in advance of a detailed examination of their implications, particularly with regard to their context sensitivity. Further research is needed to challenge the ‘one-size-fits-all’ models implied by blanket endorsement, particularly to explore variation by setting and variation according to different conceptions of vulnerability.
Of particular interest are initiatives identified as ‘bottom-up’ locally generated solutions that offer a response to frequent attendance. Such initiatives as that generated in Blackpool42 for frequent attenders draw from an established menu of intervention components to compile a locally sensitive package of actions. Many of these intervention components are comparatively well tested but little knowledge is available on which component to select under which circumstances. This is particularly important given that multicomponent interventions invariably contribute to increased costs in the absence of data on which components are essential or desirable and, indeed, which components are ‘active’. Complex systems thinking emphasises that a model of cumulation may be inappropriate when it is interaction (e.g. synergy or antagonism) that may be most relevant. Resource implications should also be examined through rigorous economic evaluation.
Practicable steps shared by local initiatives include (1) an analysis of frequent attenders; (2) formation of a multidisciplinary, indeed multisector, team, to ensure that social needs are addressed alongside health-care needs; (3) a case management approach with nominated co-ordination and responsibility; and (4) shared documentation allowing a holistic picture of patient contacts to be accessed by all relevant professionals. Once these prerequisites have been put in place, service response and improved access can be targeted, looking, in particular, at improved access to services, alternatives to ambulance conveyance and emergency admission, and delivering non-urgent responses through primary or community care.
Some of the uncertainties identified by this report are being addressed by current research in progress.
Implications for health care
-
The evidence highlights that the reasons for the increased patterns of use of the ED by vulnerable groups are complicated and encompass a wide variety of drivers, including burden of disease, access to primary care and patient preference.
-
The evidence indicates that the specific needs of and barriers for each subpopulation among those categorised as vulnerable may differ, requiring a nuanced understanding of these diverse populations. Decision-makers need to gain an accurate picture of the distribution of specific vulnerable populations in order to target service responses appropriately.
-
The review found a notable shortage of interventions designed specifically to reduce demand for ED services from vulnerable groups, with existing interventions being mostly delivered within the community setting. Front of A&E services are being strongly promoted but there is little evidence that they particularly address the needs of vulnerable populations. Indeed, they may share some of the physical and geographical barriers to access typically encountered in connection with EDs.
-
The review found that the majority of interventions aim to tackle the problem of increased patterns of ED use by vulnerable groups at a general population level (such as front of A&E general practice or urgent care clinic approaches) or target frequent attenders as a discrete group. Health-care decision-makers could seek to monitor the prevalence of identified vulnerable groups presenting at EDs and primary care alternatives and seek to avoid local barriers to appropriate use.
-
The review identifies common components of interventions targeting frequent users: (1) analysis of frequent attenders, (2) multisectoral teams, (3) case management approaches and (4) shared documentation. Health-care providers can select from these core components to construct a locally sensitive package of responses and submit these for ongoing evaluation.
Recommendations for research
-
The review found that interventions specifically targeting the vulnerable groups identified in this report need to be co-designed,64 developed, trialled and rigorously evaluated. A particular need was identified for further research on the clinical effectiveness and cost-effectiveness of promising UK initiatives.
-
The evidence indicates that evaluations of these types of interventions will probably require mixed-methods approaches, with an important contribution to be made by qualitative inquiry.
-
The review suggests that interventions may also require an explicit and conceptually sound theoretical basis, particularly in understanding vulnerability and how it affects ED use.
-
The role of technology and health informatics, briefly touched on by this report, requires further examination, particularly relating to the identification and co-ordination of frequent users. 64
-
The findings of the review further indicate the potential for realist evaluation approaches,63,65,66 especially as several interventions identified seem to be heavily context dependent.
Acknowledgements
Contributions of authors
Andrew Booth (Reader) co-led the study, including contributing to data analysis and report writing.
Louise Preston (Research Fellow) co-led the study, including contributing to data analysis and report writing.
Susan Baxter (Senior Research Fellow) contributed to the mapping review and report writing.
Ruth Wong (Information Specialist) contributed to the electronic database searching.
Duncan Chambers (Research Fellow) contributed to the review processes, including sifting and data extraction.
Janette Turner (Reader in Emergency and Urgent Care Research) provided topic expertise.
Data-sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- McCormick B, Hill P-S, Poteliakhoff E. Are Hospital Services Used Differently in Deprived Areas? Evidence to Identify Commissioning Challenges. Oxford: Centre for Health Service Economics & Organisation (CHSEO); 2012.
- NHS . Next Steps on the Five Year Forward View 2018.
- Balfour R, Arora L, Farrar P, Hughes P, Morosi M. VulnerABLE: Pilot Project Related to the Development of Evidence-Based Strategies to Improve the Health of Isolated and Vulnerable Persons 2017. https://ec.europa.eu/health/sites/health/files/social_determinants/docs/2017_vulnerable_literaturereview_en.pdf (accessed 7 September 2019).
- Coster JE, Turner JK, Bradbury D, Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med 2017;24:1137-49. https://doi.org/10.1111/acem.13220.
- Scherer M, Lühmann D, Kazek A, Hansen H, Schäfer I. Patients attending emergency departments. Dtsch Arztebl Int 2017;114:645-52. https://doi.org/10.3238/arztebl.2017.0645.
- Iglesias K, Baggio S, Moschetti K, Hugli O, Daeppen JB. Using case management in a universal health coverage system to improve quality of life of frequent emergency department users: a randomized controlled trial. Qual Life Res 2018;27:503-1. https://doi.org/10.1007/s11136-017-1739-6.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- James KL, Randall NP, Haddaway NR. A methodology for systematic mapping in environmental sciences. Environ Evid 2016;5. https://doi.org/10.1186/s13750-016-0059-6.
- Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328. https://doi.org/10.1136/bmj.328.7454.1490.
- Lewin S, Bohren M, Rashidian A, Munthe-Kaas H, Glenton C, Colvin CJ. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 2: how to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0689-2.
- Sworn K, Booth A. Scoping Review: Patient Safety Outcomes and Nursing Skill Mix Interventions. Sheffield: University of Sheffield, School of Health and Related Research (ScHARR) for the RCN Strategic Research Alliance; 2019.
- Baker M, Stallard J, Gibson S. A pilot project targeting frequent attenders at the emergency department with medically unexplained symptoms. Emerg Med J 2013;30:866-66. https://doi.org/10.1136/emermed-2013-203113.2.
- Bodenmann P, Velonaki VS, Griffin JL, Baggio S, Iglesias K, Moschetti K, et al. Case management may reduce emergency department frequent use in a universal health coverage system: a randomized controlled trial. J Gen Intern Med 2017;32:508-15. https://doi.org/10.1007/s11606-016-3789-9.
- Edwards MJ, Bassett G, Sinden L, Fothergill RT. Emerg Med J 2015;32:392-6. https://doi.org/10.1136/emermed-2013-203496.
- Fiesseler F, Riggs R, Salo D, Klemm R, Flannery A, Shih R. Care plans reduce ED visits in those with drug-seeking behavior. Am J Emerg Med 2015;33:1799-801. https://doi.org/10.1016/j.ajem.2015.08.038.
- Garbers S, Peretz P. Urban patient navigator program associated with decreased emergency department use, and increased primary care use, among vulnerable patients. J Community Med Health Educ 2016;6. https://doi.org/10.4172/2161-0711.1000440.
- Kim TY, Mortensen K, Eldridge B. Linking uninsured patients treated in the emergency department to primary care shows some promise in Maryland. Health Aff 2015;34:796-804. https://doi.org/10.1377/hlthaff.2014.1102.
- McCormack RP, Hoffman LF, Wall SP, Goldfrank LR. Resource-limited, collaborative pilot intervention for chronically homeless, alcohol-dependent frequent emergency department users. Am J Public Health 2013;103:221-4. https://doi.org/10.2105/AJPH.2013.301373.
- Michelen W, Martinez J, Lee A, Wheeler DP. Reducing frequent flyer emergency department visits. J Health Care Poor Underserved 2006;17:59-6. https://doi.org/10.1353/hpu.2006.0010.
- Ng A, Nadarajan V, McIver S, Reid C, Schofield E, Sachar A. Frequent attendances to a London emergency department: a service improvement project embedding mental health into the team. London J Prim Care 2015;7:70-7. https://doi.org/10.1080/17571472.2015.11493438.
- Rathlev N, Almomen R, Deutsch A, Smithline H, Li H, Visintainer P. Randomized controlled trial of electronic care plan alerts and resource utilization by high frequency emergency department users with opioid use disorder. West J Emerg Med 2016;17:28-34. https://doi.org/10.5811/westjem.2015.11.28319.
- Seaberg D, Elseroad S, Dumas M, Mendiratta S, Whittle J, Hyatte C, et al. Patient navigation for patients frequently visiting the emergency department: a randomized, controlled trial. Acad Emerg Med 2017;24:1327-33. https://doi.org/10.1111/acem.13280.
- Shnowske K, Berg DD, Guntern P, Hop D. Care guide use for repeated non-emergent complaints and its effect on emergency department visit frequency. Am J Emerg Med 2018;36:1697-8. https://doi.org/10.1016/j.ajem.2018.01.036.
- Shumway M, Boccellari A, O’Brien K, Okin RL. Cost-effectiveness of clinical case management for ED frequent users: results of a randomized trial. Am J Emerg Med 2008;26:155-64. https://doi.org/10.1016/j.ajem.2007.04.021.
- Stergiopoulos V, Gozdzik A, Cohen A, Guimond T, Hwang SW, Kurdyak P, et al. The effect of brief case management on emergency department use of frequent users in mental health: findings of a randomized controlled trial. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0182157.
- Tadros AS, Castillo EM, Chan TC, Jensen AM, Patel E, Watts K, et al. Effects of an emergency medical services-based resource access program on frequent users of health services. Prehosp Emerg Care 2012;16:541-7. https://doi.org/10.3109/10903127.2012.689927.
- Tait RJ, Teoh L, Kelty E, Mountain D, Hulse GK. Emergency department-based intervention with adolescent substance users: 10 year economic and health outcomes. Drug Alcohol Depend 2016;165:168-74. https://doi.org/10.1016/j.drugalcdep.2016.06.005.
- Hudon C, Chouinard MC, Lambert M, Dufour I, Krieg C. Effectiveness of case management interventions for frequent users of healthcare services: a scoping review. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012353.
- Hudon C, Courteau J, Krieg C, Vanasse A. Factors associated with chronic frequent emergency department utilization in a population with diabetes living in metropolitan areas: a population-based retrospective cohort study. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2453-3.
- Grover CA, Sughair J, Stoopes S, Guillen F, Tellez L, Wilson TM, et al. Case management reduces length of stay, charges, and testing in emergency department frequent users. West J Emerg Med 2018;19:238-44. https://doi.org/10.5811/westjem.2017.9.34710.
- Scott DR, Batal HA, Majeres S, Adams JC, Dale R, Mehler PS. Access and care issues in urban urgent care clinic patients. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-222.
- Harcourt D, McDonald C, Cartlidge-Gann L, Burke J. Working Together to Connect Care: a metropolitan tertiary emergency department and community care program. Aust Health Rev 2018;42:189-95. https://doi.org/10.1071/AH16236.
- Irving A, Goodacre S, Blake J, Moore SC. Managing alcohol-related attendances in emergency care: can diversion to bespoke services lessen the burden?. Emerg Med J 2017;35:79-82. https://doi.org/10.1136/emermed-2016-206451.
- West of England Academic Health Science Network . Implementing a High Impact User Team Toolkit 2018. https://www.weahsn.net/wp-content/uploads/hiu_toolkit_FINAL.pdf (accessed 18 September 2019).
- Garner A, Cahill M, Holt V. Non-clinical navigators can ease pressures in A&E. HSJ 2015. www.hsj.co.uk/commissioning/non-clinical-navigators-can-ease-pressures-in-aande/5081937.article (accessed 18 September 2019).
- NHS Arden and Greater East Midlands Commissioning Support Unit . Homeless Hospital Discharge Programme n.d. www.ardengemcsu.nhs.uk/case-studies/homeless-hospital-discharge-programme/ (accessed 7 September 2019).
- Pitalia P. How our acute visiting service reduced emergency admissions by 30 per cent. Pulse 2013. http://www.pulsetoday.co.uk/home/practical-commissioning/how-our-acute-visiting-service-reduced-emergency-admissions-by-30-per-cent/20002277.article (accessed 18 September 2019).
- Duffin C. GPs provide full-time visiting service in bid to cut emergency admissions. Pulse 2013. www.pulsetoday.co.uk/news/commissioning/commissioning-topics/emergency-admissions/gps-provide-full-time-visiting-service-in-bid-to-cut-emergency-admissions/20002219.article (accessed 18 September 2019).
- Woodward M, Proctor N. Avoiding A&Amp;E Through Rapid Response Teams and See and Treat Models: A Rapid Review of Existing Evidence 2016. www.healthylondon.org/wp-content/uploads/2017/11/Rapid-review-Rapid-response-teams-and-see-and-treat-models.pdf (accessed 9 September 2019).
- Connor R. Supporting Sustainable General Practice. Innovation in Primary Care – Examples and Case Studies for General Practice. London: NHS England; 2015.
- Monteith R. Bridlington Free Press 2018. www.bridlingtonfreepress.co.uk/news/health/blackpool-nurse-helps-reduce-a-e-visits-from-a-group-of-frequent-callers-by-90-per-cent-1-9172448 (accessed 25 June 2019).
- Kelly J. Project Aiming to Reduce A&Amp;E Pressures n.d. www.thenorthernecho.co.uk/news/16351024.project-aiming-to-reduce-ae-pressures/ (accessed 25 June 2019).
- Ford A, de Silva D, Haririan S. Cutting A&E use and health inequalities. Nurs Times 2013;109:14-6.
- Ford A, de Silva D, Archer D. How to reduce A&E use by targeting diversity. HSJ 2012. www.hsj.co.uk/technology-and-innovation/how-to-reduce-aande-use-by-targeting-diversity/5052217.article (accessed 18 September 2019).
- Gregory J. NHS England pilot area found front-door A&E GPs ‘did not work’. Pulse 2017. www.pulsetoday.co.uk/news/commissioning/commissioning-topics/urgent-care/nhs-england-pilot-area-found-front-door-ae-gps-did-not-work/20035884.article (accessed 18 September 2019).
- Iacobucci G. All emergency departments must have GP led triage by October. BMJ 2017;356. https://doi.org/10.1136/bmj.j1270.
- Khan H. How hospital-based GPs can ease the A&E crisis. The Guardian 2015.
- Wickware C. Nearly 420 extra GPs needed across country to deliver A&E streaming service. Pulse 2017. www.pulsetoday.co.uk/news/gp-topics/employment/nearly-420-extra-gps-needed-across-country-to-deliver-ae-streaming-service/20034234.article (accessed 18 September 2019).
- Edwards N. Lesson 1: Avoid the Temptations of the Grand Plan. London: The Nuffield Trust; 2018.
- Lee GA, Titchener K. The Guy’s and St Thomas’s NHS Foundation Trust @home service: an overview of a new service. London J Prim Care 2017;9:18-22. https://doi.org/10.1080/17571472.2016.1211592.
- Lee G, Sakone P, Mulhall H, Kelleher K, Burnett K. Using hospital at home to reduce admissions. Nurs Times 2015;111:12-5.
- Pickstone N, Lee GA. Does the @home team reduce local emergency department attendances? The experience of one London service [published online ahead of print 22 May 2019]. Int Emerg Nurs 2019. https://doi.org/10.1016/j.ienj.2019.04.003.
- Hislop D. Mission impossible? Communicating and sharing knowledge via information technology. J Inf Technol 2002;17:165-77. https://doi.org/10.1080/02683960210161230.
- Pascal CJ, McInerney C, Orzano J, Clark EC, Clemow L. The use of knowledge management in healthcare: the implementation of shared care plans in electronic medical record systems at one primary care practice. J Inf Knowl Manag 2013;12. https://doi.org/10.1142/S0219649213500408.
- Van den Heede K, Van de Voorde C. Interventions to reduce emergency department utilisation: a review of reviews. Health Policy 2016;120:1337-49. https://doi.org/10.1016/j.healthpol.2016.10.002.
- McInnes DK, Li AE, Hogan TP. Opportunities for engaging low-income, vulnerable populations in health care: a systematic review of homeless persons’ access to and use of information technologies. Am J Public Health 2013;103:e11-24. https://doi.org/10.2105/AJPH.2013.301623.
- Fine AG, Zhang T, Hwang SW. Attitudes towards homeless people among emergency department teachers and learners: a cross-sectional study of medical students and emergency physicians. BMC Med Educ 2013;13. https://doi.org/10.1186/1472-6920-13-112.
- Preston L, Chambers D, Campbell F, Cantrell A, Turner J, Goyder E. What evidence is there for the identification and management of frail older people in the emergency department? A systematic mapping review. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06160.
- Couture ÉM, Chouinard MC, Fortin M, Hudon C. The relationship between health literacy and quality of life among frequent users of health care services: a cross-sectional study. Health Qual Life Outcomes 2017;15. https://doi.org/10.1186/s12955-017-0716-7.
- Reddy S, Carey TA, Wakerman J. A realist case study of a regional hospital’s response to improve emergency department access in the context of Australian health care reforms. Health Serv Res Manag Epidemiol 2016;3:1-8. https://doi.org/10.1177/2333392816631101.
- Hudon C, Chouinard MC, Aubrey-Bassler K, Burge F, Doucet S, Ramsden VR, et al. Case management in primary care for frequent users of healthcare services with chronic diseases and complex care needs: an implementation and realist evaluation protocol. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-026433.
- Nielsen K, Miraglia M. What works for whom in which circumstances? On the need to move beyond the ‘what works?’ question in organizational intervention research. Hum Relat 2016;70:40-62. https://doi.org/10.1177/0018726716670226.
- Hamad MMAA, Connolly VM. Ambulatory emergency care – improvement by design. Clin Med 2018;18:69-74. https://doi.org/10.7861/clinmedicine.18-1-69.
- Chambers D, Cantrell A, Booth A. Factors that facilitate the implementation of interventions to reduce preventable hospital admissions with a focus on cardiovascular or respiratory conditions: an evidence map and realist synthesis. Health Serv Deliv Res 2019.
- Cooper A, Davies F, Edwards M, Anderson P, Carson-Stevens A, Cooke MW, et al. The impact of general practitioners working in or alongside emergency departments: a rapid realist review. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-024501.
Appendix 1 Search strategy (mapping review)
The search was run in MEDLINE, Web of Science (Science Citation Index Expanded, Social Sciences Citation Index, Conference Proceedings Citation Index – Science, Conference Proceedings Citation Index – Social Science & Humanities) and CINAHL.
Date range searched: 2008–18.
Date searched: January 2018.
Search strategy
-
*Emergency Service, Hospital/
-
*Emergency Medical Services/
-
*Emergency Medicine/
-
(emergenc* adj2 service*).ti,ab.
-
emergenc* care.ti,ab.
-
((urgent or unscheduled) adj care).ti,ab.
-
emergenc* department*.ti,ab.
-
*Ambulances/
-
ambulance*.ti,ab.
-
or/1-9
-
*Vulnerable populations/
-
*Poverty/
-
*Socioeconomic Factors/
-
(vulnerable or socioeconomic* or disadvantaged or depriv* or poverty or poor or low-income* or low income* or low pay or low* paid).ti.
-
((vulnerable or socioeconomic* or disadvantaged or depriv* or poverty or poor or low-income* or low income* or low pay or low* paid) adj3 (individual* or people or person* or famil* or population* or communit* or neighbourhood* or group*)).ab.
-
((financ* or economic* or money) adj2 (hardship* or difficult* or problem* or worries or worry)).ti,ab.
-
*Social Isolation/
-
(social* adj1 (exclu* or inequalit* or isolat*)).ti,ab.
-
or/11-18
-
Rural Population/
-
(rural or remote or coast* or geographical* isolat*).ti.
-
((rural or remote or coast* or geographical* isolat*) adj3 (people or patient* or population* or communit* or neighbourhood* or group* or area*)).ab.
-
((hard* or difficult) adj2 (reach or locate or find)).ti,ab.
-
or/20-23
-
refugee*.ti,ab.
-
asylum seeker*.ti,ab.
-
(migrant* or immigrant* or emigrant*).ti,ab.
-
Refugees/
-
“Emigrants and Immigrants”/
-
“transients and migrants”/
-
((human or child or people or person) adj traffick*).ti,ab.
-
(“first generation” or “second generation” or “third generation”).ti,ab.
-
(“new arrival*” or settler* or newcomer*).ti,ab.
-
((multi or trans or cross) adj cultural*).ti,ab.
-
(multi adj (ethnic or racial or lingual)).ti,ab.
-
diaspora.ti,ab.
-
ethnic groups/
-
(traveller* or gypsies or gypsy or gipsy or gipsies or romany or romanies or romani or romanis or rromani or rromanis or roma).ti,ab.
-
(african american or african americans or asian or asians or black or blacks or hispanic or hispanics or indian or indians or latino or latina or latinos or latinas or native american or native americans).ti.
-
(bme or black ethnic minorit* or black minorit* ethnic* or south asian* or bangladeshi* or pakistani* or indian* or sri lankan* or asian* or east asian* or chinese or taiwanese or vietnamese or korean* or japanese or afro-caribbean* or african-caribbean* or caribbean or african* or black* or afro* or islam* or hindu* or sikh* or buddhis* or muslim* or moslem* or christian* or catholic* or jew*).ti.
-
or/25-40
-
*Unemployment/
-
(unemploy* or jobless or workless).mp.
-
((job* or work or employment) adj3 (redundan* or insecur* or loss* or lose or lost
-
or search* or seek* or find*)).ti,ab.
-
(economic* adj3 inactive).ti,ab.
-
or/42-45
-
exp *Homeless Persons/
-
(homeless* or rough sleep*).mp.
-
((unstabl* or emergency or temporary or inadequate or poor or overcrowd*
-
or over crowd*) adj3 (hous* or accommodation or shelter* or hostel* or dwelling*)).ti,ab.
-
runaway*.mp.
-
(street adj3 (individual* or person* or people or group* or population*)).ti,ab.
-
or/47-51
-
(addict* or ((substance* or alcohol* or drug* or cocaine or heroin or amphetamine*
-
or marijuana or cannabis) adj2 (misus* or abus* or depend* or use* or using))).ti,ab.
-
(legal high* or (psychoactive adj (substance* or product*))).ti,ab.
-
*Substance-Related Disorders/
-
*Drug Users/
-
*Alcoholics/
-
or/53-57
-
10 and (19 or 24 or 41 or 46 or 52 or 58)
-
Case report.tw.
-
Letter/
-
Historical article/
-
60 or 61 or 62
-
exp Animals/
-
Humans/
-
64 not (64 and 65)
-
63 or 66
-
59 not 67
-
limit 68 to (english language and yr = “2008 -Current”)
Appendix 2 Search results for initiatives and intervention analysis
| Delivered in EUC context | Number of search results | |||
|---|---|---|---|---|
| EndNote database | PubMed MEDLINE | Google (NHS only) | Google Scholar | |
| Care navigators | 2 | 3 | 2570 | 312 |
| Care planning | 80 | 249 | 31 | 44 |
| Case finding | 4 | 151 | 16 | 9 |
| Case management | 167 | 1071 | 57 | 70 |
| Front of A&E general practice | 0 | 0 | 2460 | 2 |
| Front-door streaming | 0 | 0 | 731 | 10 |
| Migrant support programme | 495 | 423 | 11 | 125 |
| Outreach services | 103 | 799 | 4 | 7 |
| Outreach teams | 8030 | 3180 | ||
| Rapid access doctor | 8 | 0 | 22 | 2 |
| Acute visiting service | 1 | 0 | 1550 | 21 |
| Rapid access paramedic | 8 | 0 | 0 | 0 |
| Urgent visiting service | 0 | 0 | 28 | 1 |
| Urgent care clinics | 14 | 101 | 2280 | 1630 |
List of abbreviations
- A&E
- accident and emergency
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- ED
- emergency department
- EMS
- emergency medical service
- EUC
- emergency and urgent care
- GP
- general practitioner
- GRADE
- Grading of Recommendations, Assessment, Development and Evaluations
- HSDR
- Health Services and Delivery Research
- NIHR
- National Institute for Health Research
- RCT
- randomised controlled trial
- TIDieR
- Template for Intervention Description and Replication
