Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/07/87. The contractual start date was in September 2014. The final report began editorial review in April 2018 and was accepted for publication in January 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Robert Grant reports grants from King’s College London during the conduct of the study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Harris et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
This mixed-methods realist evaluation of intentional rounding (IR) in acute hospital wards in England, conducted in four phases, was designed to address the research question: what is it about IR in hospital wards that works, for whom and in what circumstances? This chapter describes the background to IR in England and the structure of the report.
Background
State-funded systems of health care in advanced economies are facing unprecedented challenges arising from ageing populations and increasing demands for care in the context of stretched resources. The revelations of the systemic and appalling failures of compassion and care at the Mid Staffordshire NHS Foundation Trust that took place between 2005 and 2009 were a profound shock to the public, government, health-care system and professions, and led to Sir Robert Francis’ landmark inquiry, report1 and recommendations to improve accountability and governance for the paramount purpose of protecting the interests of patients. The Francis report1 raised fundamental questions about the nature of compassionate organisational cultures and nursing care in the NHS and called for more research.
In response, the National Institute for Health Research Health Services and Delivery Research programme commissioned a stream of new research intended to generate evidence to meet the gaps in knowledge of service delivery, and to discover what worked well for whom and at what cost. The call, After Francis: Research to Strengthen Organisational Capacity to Deliver Compassionate Care in the NHS [see the commissioning brief on the project web page; URL: www.journalslibrary.nihr.ac.uk/programmes/hsdr/130787/#/ (accessed 4 July 2019)], invited robust evaluations of interventions to improve the leadership, organisational culture and quality of front-line care across a broad range of staff. One of the concerns of the Francis report1 was the neglect of some patients by dysfunctional nursing that failed to respond to fundamental needs, such as pain, hydration, hygiene and comfort, and failed to ensure patient safety. One of the 290 wide-sweeping recommendations made by Francis in his final report (Volume 3, p. 1610) was that:
Regular interaction and engagement between nurses and patients and those close to them should be systematised through regular ward rounds.
Francis. 1
Regular patient rounds, often called back rounds or comfort rounds, have always been a plank of nursing care and have recently received renewed interest in the USA and the UK with what has become known as ‘intentional rounding’ (IR), a structured intervention that systematises regular nursing ward rounds. It was this model of regular rounding that attracted attention from policy-makers, triggered by public-interest concerns following the publication of the Francis report. 1
The origins and meanings of intentional rounding
The specific intervention recognised as IR was developed in 2007 in the USA by the Studer Group,2 a private, for-profit health-care consultancy company (Pensacola, FL, USA), and the Alliance for Health Care Research. The term ‘intentional rounding’, originally coined by the Owensboro Medical Health System Inc. (Owensboro, KY, USA), is not universally used and IR has also been called ‘hourly rounding’,2 ‘proactive patient rounds’,3 ‘comfort rounds’4 or ‘rounds with intent to care’. 5 IR is a timed, planned intervention that sets out to address fundamental elements of nursing care, typically by means of a regular bedside ward round. The aim is to proactively identify and meet patients’ fundamental care needs and psychological safety. The typical format of IR, as developed by the Studer Group, is based on the 4Ps (Box 1), although there are lesser-used variants based on 3Ps (pain, position and personal needs),9,10 5Ps (potty, position, pain, possessions and patient focus)11 and 6Ps (pain, positioning, proximity, personal care, pumps and promise). 12
During each round, the following standardised protocol is used by a nurse for each patient.
-
An opening phrase is used by the nurse to introduce his or herself and to put the patient at ease.
-
Scheduled tasks are then performed.
-
A discussion follows of the four key elements of the round, often called the ‘4Ps’:
-
positioning – making sure the patient is comfortable and assessing the risk of pressure sores
-
personal needs – assessing a patient’s personal needs, including whether or not they need assistance with getting to the toilet
-
pain – asking patients to rate their level of pain on a scale of 0–10
-
placement – ensuring that any items a patient needs are within easy reach.
-
-
An assessment of the care environment, such as checking the temperature of the room or any fall hazards.
-
Ending the interaction with a closing phrase such as ‘Is there anything else I can do for you before I go?’.
-
The patient is informed of when the nurse will return.
-
The nurse documents the round.
If patients are unable to respond during the round, the nurse may follow this process with family members. 7
Reproduced from Harris et al. 8 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
The policy context for the introduction of intentional rounding in England
Even before Sir Robert Francis’ recommendations, and in anticipation of his report,1 emerging concerns about what had happened at the Mid Staffordshire NHS Foundation Trust increased the level of concern about patient care and patient safety among the public, health-care professionals and politicians. Interest in IR began when it was identified by The King’s Fund Point of Care programme as a possible way of improving the patient experience of care. Around this time, some senior nurse managers in the UK had visited the USA and had been exposed to IR, as expounded by the Studer Group. 13
Prime minister announcement
In January 2012, while visiting Salford Royal Hospital, in the Salford Royal NHS Foundation Trust, the then prime minister David Cameron announced a raft of changes, including measures designed to bolster leadership, improve care and allow patients to rate their care. 14 He stated that nurses should make hourly rounds to ensure that each patient was comfortable. In the same speech in 2012, he set up a new national body called the Nursing and Care Quality Forum (NCQF) to promote ‘best practice’ among staff.
As the study was nearing its end, we were able to talk to an official who was close to implementation of the policy about the circumstances of the introduction of IR. The policy development was rapid and took place over the Christmas/new year break to be included, together with the formation of the NCQF, in an announcement by the then prime minister David Cameron on 6 January 2012 as part of the plans to manage the expected messages in the Francis report. 1 The ideas were generated at speed and were not given the usual time for the measured, consultative and thoughtful processes expected of policy development. Although not a statutory requirement (and, therefore, not mandatory), it was supported by the chief nursing officer (CNO) at the time and, therefore expected to happen. Not surprisingly, there were no guidelines to support its implementation and IR was not defined other than as an intervention to be delivered by registered nurses (RNs) in order to see their patients hourly using the 4Ps as discussed in the US evidence (see Box 1). It was expected that RNs would use their professional judgement about how to deliver IR, what to ask the patients and how to interpret and act on the subsequent interaction. Interestingly, it was envisaged that IR would not be explicitly documented on a specific IR form, although documentation about care delivered and patient condition was expected to be written in a patient’s notes, which could be done retrospectively at the end of a shift as long as the evidence was recorded. Furthermore, there were no resources to support the development and implementation of IR, as it was thought that RNs would be regularly checking their patients anyway. There was no expectation that progress with implementation of IR would be reported back to the Department of Health and Social Care. The NCQF was tasked with supporting IR implementation as part of its ‘having time to care’ workstream.
Role of the Nursing and Care Quality Forum
When the NCQF was convened, it inherited supporting the implementation of IR as part of its role. Some NHS trusts were early adopters, piloting and implementing aspects of IR in 2011 before the majority of other trusts,15 so some of the key aspects of structured rounds were already under way in a few places. The NCQF was well informed by the experience of IR in early-adopter trusts and endorsed the implementation of IR as part of their workstream on making time to care,5 in which they planned to:
. . . accelerate the implementation of person centred approaches such as ‘rounding with intention to care’ – where every individual receiving care knows they will have at least hourly contact with staff . . .
NCQF. 5
The forum of nursing experts were concerned that IR could easily become a tick-box exercise; however, it was thought that it would support nurses in prioritising talking to their patients. Therefore, the content of IR was considered less important than the interaction that it would enable and so the 4Ps structure was not expected to be used rigidly. The NCQF assumed that there would be a form to document IR. However, there were no guidelines for trusts about how to implement IR or recommended documentation. Furthermore, there was no evidence of a strategy for introducing IR across the country or for overseeing its development and impact. To address this, the NCQF supported the development of seven ‘demonstrator sites’ for IR, chosen to reflect a variety of health-care and social care providers in a range of geographical locations to support implementation of IR.
The NCQF commissioned a small study4 to learn from these sites, the findings of which noted the potential benefits and limitations of IR, variations in practice and included recommendations of how to conduct IR. This was released in August 20134 as widespread national implementation of IR was already under way and a new CNO was appointed at NHS England, who launched a new vision for nurses called Compassion in Practice. 16 At this point, the role of the NCQF became unclear and it is not known how widely this report was circulated. It was available on an NHS website (www.6cs.england.nhs.uk) until 2016, but is no longer publicly available. A freedom of information request was submitted to the Department of Health and Social Care in January 2018 for the report and minutes of NCQF meetings, but no documents were available.
Structure of the report
This report is structured as follows:
-
Chapter 2 reports the study aims and objectives, and the methodological approach used to address these.
-
Chapter 3 describes the first phase of the study, the realist synthesis of the evidence for IR. The aim of this phase was to generate hypotheses on what the mechanisms of IR may be, what particular groups may benefit most or least and the contextual factors that might be important to its success or failure.
-
Chapter 4 describes the second phase of the study, the national survey of non-specialist NHS acute trusts in England. This survey explored how IR was being implemented and supported across England and the way in which organisational context (or features of services and health-care organisations) influenced its implementation.
-
Chapter 5 gives an overview of the three case study sites and their staff data, describing how IR has been implemented, developed and supported at each site. This chapter also investigates trends in patient outcomes and provides an analysis of the costs and benefits of IR.
-
Chapter 6 explores nursing staff and other clinical, management and administrative staff experiences of IR, how they believed it affected the way they delivered care and the barriers and facilitators they experienced. Through observations of nursing staff undertaking IR and of the care that patients received, Chapter 6 also highlights how IR has been implemented on the ground.
-
Chapter 7 explores patients’ and carers’ experiences and perceptions of how IR influences their experiences of care.
-
Chapter 8 synthesises the data from each phase of the study to identify what aspects of IR work, for whom, in what circumstances and why.
-
Chapter 9 sets out the key messages from the study, reviews the approach and methods used and discusses the implications of the findings for policy, practice and research.
Chapter 2 Methods
This chapter reports the study aims and objectives and the methodological approach used to address these.
Aims and objectives
The overall aim of the study was to investigate the impact and effectiveness of IR in hospital wards in England on the organisation, delivery and experience of care from the perspective of patients, their carers and staff. The research question was ‘what is it about IR in hospital wards that works, for whom and in what circumstances?’ We investigated this at four levels of the organisation and delivery of health services – (1) national, (2) service provider organisation, (3) individual ward/unit and (4) individual person – to identify the ways in which the context (i.e. the environment and organisation) at each of these levels influenced the mechanisms (i.e. the assumptions and theories about the ways in which IR achieved its objectives) and the outcomes or impact. The study objectives were to:
-
determine the number of NHS trusts in England that had implemented IR and analyse how this had been developed and supported
-
identify how IR had been implemented on the ground and evaluate its contribution to the delivery of patient care as a whole and how it fits in alongside other approaches to improving quality and safety
-
explore nursing staff, health-care assistants’ (HCAs’) and other clinical and management staff experiences of IR and how it affects the way they deliver care
-
explore patients’ and their carers’ experiences and perceptions of how IR influences their experiences of care
-
investigate trends in patient outcomes (retrieved from routinely collected NHS ward data) in the context of the introduction of IR and other care improvement initiatives that have been introduced by using statistical process control methods such as cumulative sum charts
-
examine the barriers to and facilitators of the successful implementation of IR
-
conduct a bottom-up analysis of the costs of IR by identifying the resources used by case study wards to develop and implement it
-
synthesise the data from each of the study phases to identify which aspects work, for whom and in what circumstances.
Project methodology
Study design and conceptual basis
A multimethod study design was undertaken using realist evaluation methodology17 to evaluate the implementation of IR in England. Realist evaluation is a theory-driven approach designed for evaluating complex social interventions, such as IR. 18,19 It does not seek to answer the question ‘does this intervention work?’ but instead acknowledges that complex social interventions only ever work for certain people in particular circumstances. The key task of a realist evaluation is to therefore understand and explain the patterns of success and failure by asking the exploratory question: ‘what is it about this intervention that works, for whom and in what circumstances?’17,19 It achieves this through the identification of causal explanations of how an intervention or programme is anticipated to work, known as context–mechanism–outcome (CMO) configurations.
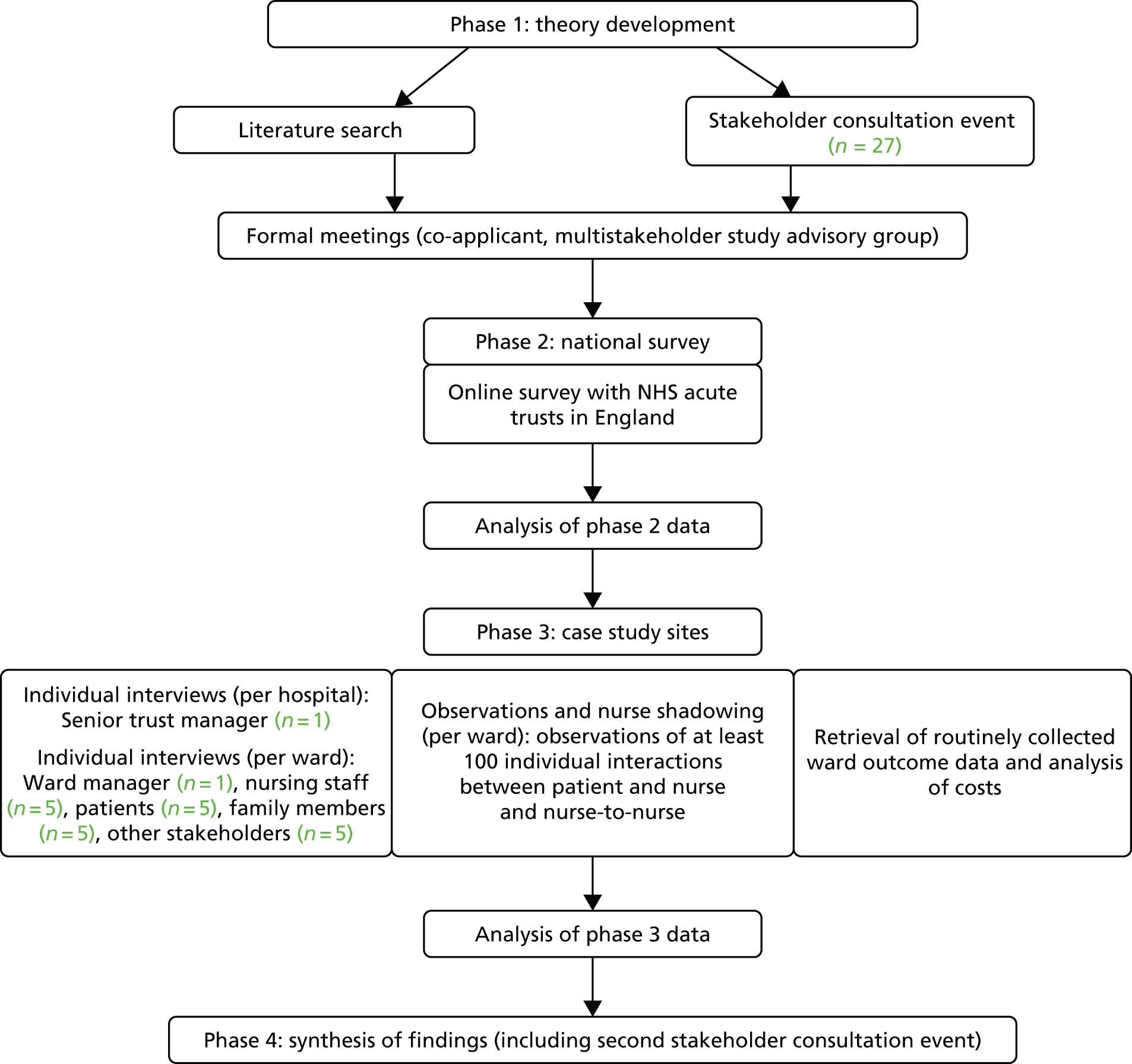
The study was conducted in four phases: (1) theory development; (2) a national survey of all NHS acute trusts in England; (3) in-depth case studies of six wards in three NHS acute trusts involving individual interviews with health-care staff, patients and their carers, observations of IR and nurse shadowing, retrieval of routinely collected ward outcome data and analysis of costs; and (4) synthesis of study findings. Figure 1 shows the study flow diagram. More detailed descriptions of the methodology for each phase is provided in individual phase chapters.
FIGURE 1.
Study flow diagram. Reproduced from Harris et al. 8 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Ethics and dissemination
The study was approved by the NHS Health Research Authority South East Coast – Surrey Research Ethics Committee (reference number 14/LO/1977). All participants were informed that they were free to refuse to participate or withdraw from the study at any time.
Patient and public involvement in the research
Patient and public involvement was an integral part of this study; it was guided throughout the study duration by a multistakeholder advisory group consisting of NHS senior managers and health-care professionals and patient and carer representatives. Nine patient and carer representatives were recruited from local voluntary sector organisations and other networks, where role descriptions were circulated. The advisory group met three times over the course of the study and meetings were chaired by Sally Brearley, who has worked with patients and carers on a variety of research and service improvement projects. Other members of the research team assisted by facilitating small group discussions and taking notes. Service user representatives in the group were paid an honorarium of £100 per meeting for their time and contribution. All travel expenses for attending the meetings were paid from the research budget and a newsletter was distributed in between meetings to keep members updated with study progress. The input of the advisory group was of great value to the study. The group came together at key points in the process and contributed to all aspects of the research, including commenting on the study mechanisms, national survey questions, interview schedules, data analysis and dissemination strategy, and ensuring that the study was grounded in the issues and perspectives of key stakeholders.
Chapter 3 Phase 1: theory development – a realist synthesis of the evidence
This chapter describes the first phase of the study: the realist synthesis of the evidence for IR. The aim of this phase was to generate hypotheses on what the mechanisms of IR may be, what particular groups may benefit most or least, the contextual factors that might be important to its success or failure and the associated outcomes. This theory development drew on principles of realist synthesis18 and the subsequent framework was to be tested in phases 2 and 3 of the study.
Method
In stage 1, a search of academic, policy and grey literature was undertaken to develop initial programme theories of IR. Expert advice was sought from library and information science specialists around generating relevant search terms, and between June and July 2014 four electronic databases were searched [Allied and Complementary Medicine Database (AMED), Cumulative Index to Nursing and Allied Health Literature (CINAHL), MEDLINE and the Royal College of Nursing Archive] alongside searches of Google and Google Scholar (Google Inc., Mountain View, CA, USA), InterNurse, Social Care Institute for Excellence (SCIE) and NHS Evidence using the strategies highlighted in Table 1. Relevant documents were independently examined by two researchers to identify any purported mechanisms of IR (i.e. theories or assumptions about why/how IR worked/was expected to work).
| Strategy for searches in AMED, CINAHL, MEDLINE, RCN Archive, PsycINFO, HMIC, EMBASE, Scopus, BMJ Journals and The Cochrane Library |
|---|
| Free-text terms and operators |
|
“Intentional round*” OR “hourly round*” OR “patient round*” OR “purposeful round*” OR “nursing round*” OR “comfort round*” AND “nurs*” [Limiters: Abstract only (where applicable), English language only] |
| Strategy for searches in Google, Google Scholar, InterNurse, SCIE, NHS Evidence (each search undertaken separately) |
|
“Intentional round” “Hourly round” “Patient round” “Purposeful round” “Nursing round” “Comfort round” |
Between October and November 2014, stage 2 of the synthesis was undertaken, with the aim of identifying empirical research that either supported or refuted the mechanisms identified in stage 1, or identified any new mechanisms. A comprehensive search for empirical research was undertaken using the search strategy highlighted in Table 1. Snowball searches and citation searches in CINAHL and Scopus were also conducted. A structured data extraction form was completed for every paper, recording either salient details on the study design, objectives and participants, or the reason for its exclusion. Broad inclusion criteria were used, meaning that a paper was included if it described nursing rounds occurring every 2 hours or less and highlighted empirical evidence of any associated context, outcome or mechanism. In line with realist synthesis methodology, conventional approaches to quality appraisal were not used;21 instead, each study’s ‘fitness for purpose’ was assessed by considering its relevance and rigour. The evidence collected from these papers was synthesised by drawing together all information on contexts, mechanisms and outcomes. Similarities and differences in findings were sought in order to build a comprehensive description of each mechanism and its role in IR. Focused literature searches were also conducted for mechanisms for which little evidence was found.
A third and final search of the literature was undertaken in February 2016 to ensure that the synthesis was up to date and that no research published in the interim period had been missed. Searches were repeated as in stage 2, but focused only on research published between December 2014 and February 2016. Snowball searches and hand-searches were also undertaken. In addition to the review of the relevant literature, a stakeholder consultation event was held in February 2015, at which key figures associated with IR (e.g. Directors of Nursing of NHS hospitals, health-care staff) plus members of the study’s advisory group were asked to discuss their understanding of IR and their reasoning for its implementation, to further elicit realist theories on the mechanisms.
Findings
This section presents the findings of the realist synthesis. A total of 44 papers were included in the realist synthesis, drawn from a variety of sources [i.e. the professional press (n = 21),3,7–9,22–38 peer-reviewed journals (n = 18),39–56 study reports (n = 4)4,57–59 and one doctoral thesis]. 60 The research was primarily undertaken in the USA (n = 25)3,7–9,22,25–27,32,33,35–42,44,47,48,52–54,60 but also included research from the UK (n = 12),4,23,24,28,30,31,34,46,51,57–59 Australia (n = 5),43,45,49,50,55 Canada (n = 1)29 and Iran (n = 1). 56 Studies were conducted in a variety of settings, including accident and emergency, intensive care, mental health, maternity, orthopaedics and medical-surgical units and used both qualitative and quantitative research methods. The papers were published between 2006 and 2017, with a peak in publication in 2012. The two earliest published papers (2006 and 2007) were authored by Meade (and colleagues),22,39 who was directly connected to the Studer Group; these papers were heavily cited by authors publishing at later dates. The 44 papers were written by a total of 168 authors, with only three authors (Meade,22,39,40 Braide23,24 and Neville25,41) authoring or co-authoring more than one paper. This suggested that there had not been a major programme of research by one group of researchers in IR.
Eight potential mechanisms of IR were identified in the first stage of the literature search; these are highlighted in Table 2, along with their provisional descriptions. In Table 3, the programme theories for each of the eight mechanisms are presented in descending order according to the number of papers addressing them and the CMOs are summarised. A number of individual CMO configurations were identified and examples of these have been provided for selected mechanisms in Boxes 2 and 3. It must be noted that these programme theories were not mutually exclusive, with one context and/or mechanism feeding into another or becoming an outcome of a third. However, they have been separated here for clarity.
| Mechanism title | Mechanism (resources) | Mechanism (reasoning/responses) |
|---|---|---|
| Consistency and comprehensiveness* |
|
This provides reassurance and confidence in the quality of care to patients, their carers and staff |
| Allocated time* | IR gives nurses allocated ‘time to care’ (i.e. gives time to check that patients are comfortable and their needs are being met, thereby treating patients with dignity, and replaces ‘presumed care’) | This helps nurses to organise their work and feel able to prioritise this aspect of nursing care |
| Accountability* | Staff are required to complete and sign the IR document to say that they have carried out hourly checks |
|
| Nurse–patient relationships and communication* |
|
This enables staff to get to know patients better and become more aware of their needs, notice unusual behaviours/appearances and detect subtle/significant changes that can affect comfort and safety |
| Visibility* | IR increases the visibility/presence of nurses within a unit by increasing the time that nurses spend in the direct vicinity of their patients (i.e. it gets nurses to the patient’s bedside) |
|
| Anticipation* | IR enables nurses to anticipate/pre-empt and proactively address patient needs instead of being reactive and waiting for patient call bells and alarms | This ensures that all patients receive regular care instead of unequally distributed care among patients focused towards those who have frequent call bell use |
| Staff communication and/or teamworking | IR provides health-care professionals with documented evidence | This is used to enhance staff communication, teamwork and prioritise care in future rounds |
| Patient empowerment | IR provides an opportunity for nursing staff, patients and carers to get to know each other better | This empowers patients to ask for what they need in order to maintain their comfort and well-being |
| Mechanism title | Context | Mechanism (resources) | Mechanism (reasoning/responses) | Outcomes (from literature) |
|---|---|---|---|---|
| CMO 1: consistency and comprehensiveness |
|
|
|
|
| CMO 2: allocated time |
|
IR gives nurses allocated ‘time to care’ (i.e. time to check that patients are comfortable and their needs are being met, thereby treating patients with dignity and replaces ‘presumed care’) | This helps nurses to organise their work and to feel able to prioritise this aspect of nursing care |
|
| CMO 3: accountability |
|
Staff are required to complete and sign the IR document to say they have carried out hourly checks |
|
|
| CMO 4: nurse–patient relationships and communication |
|
|
This enables staff to get to know patients better and become more aware of their needs and, through this knowledge, nurses can gather a keen sense of unusual behaviours and appearances and detect subtle/significant changes that can affect comfort and safety |
|
| CMO 5: visibility | Ward setting/layout | IR increases the visibility/presence of nurses in a unit by increasing the time that nurses spend in the direct vicinity of their patients (i.e. it gets nurses to a patient’s bedside) |
|
|
| CMO 6: anticipation |
|
IR enables nurses to anticipate/pre-empt and proactively address patient needs instead of being reactive and waiting for patient call bells and alarms |
|
|
| CMO 7: staff teamwork and communication |
|
IR provides health-care professionals with documented evidence | . . . that can be used to prioritise care in future rounds | . . . and this leads to improved staff communication and teamwork |
| CMO 8: patient empowerment |
|
IR provides an opportunity for nursing staff, patients and carers to get to know each other better | This empowers patients to ask for what they need in order to maintain their comfort and well-being | . . . and this leads to higher levels of patient and carer satisfaction with care |
Using a repeated-measures design, fall rates and risk assessment data were collected at three time points (before, during and 1 year post implementation of IR) in two postoperative orthopaedic units in a large academic medical centre in the USA. Four focus groups were also held with 14 nurses several weeks post intervention. 42
-
Context: postoperative orthopaedics setting, where a number of procedures are elective in otherwise healthy patients.
-
Consistency and comprehensiveness mechanism present: otherwise healthy patients are asked about toileting every hour.
-
Outcome: nurse feels ‘silly’ and uncomfortable asking these questions, which results in her not asking patients toileting questions during IR.
Interviews with 15 RNs from one public hospital in Australia were reported, with data arising from a larger research project examining missed nursing care. Relevant IR policy documents, charts and notes were also gathered and reviewed. 43
-
Context: IR is considered as ‘fundamental nursing care’ by management.
-
Allocated time mechanism absent: the time required to undertake rounding is not factored into the nursing workload and attempts to factor rounding into staffing numbers are unsuccessful.
-
Outcomes: increased nursing workload, which means either that IR is omitted or the documentation is completed at the end of the shift.
Programme theories
Context–mechanism–outcome 1: intentional rounding ensures that consistent and comprehensive care is delivered to all patients by all nurses
A total of 21 papers4,9,11,24,26–32,41–47,57,58,60 highlighted the link between IR and consistent and comprehensive care. The structured, systematic approach to IR prompted and guided the delivery of care to a required standard, helped staff to remember to conduct all aspects of care on each round4,58 and identified tasks that might otherwise be missed. 9 The format helped ensure continuity of care across staff members, which was thought to be particularly important for guiding junior/unqualified staff and those less familiar with patients. 4 IR enabled staff to speak regularly to all patients, which helped prevent quieter patients from being overlooked. 4
However, in most studies there was recognition that a dependence on standardisation did not always ensure successful IR and that a flexible approach may be more appropriate. 28,41,43–45,47 Nurses were reported to use their clinical judgement and professional autonomy to modify the rounding process, assessing patients on an individual basis and making informed choices about how frequently to conduct rounds and what questions to ask. 4,24,27,32,41,42,44,45,60 Others highlighted how the breadth of care elements covered in IR could be modified in order to comprehensively address all potential patient needs and make it relevant to individual settings. 4,26 The setting of care was an important influencing context for this mechanism. For example, in mental health wards, there were reports of IR being disproportionate for ‘low-risk’ patients4 or too intrusive for those experiencing psychotic symptoms. 32 Other influencing contexts were time limitations, low staffing levels and conflicting priorities; all of these made IR more difficult. 31,41,57,60 Understanding of the principle and practice of IR was also reported to vary according to individual staff characteristics. 4
Context–mechanism–outcome 2: intentional rounding gives nurses allocated ‘time to care’
A total of 19 papers4,9,22,24,28,29,31,33,39–41,43,45,48–50,57,58,60 discussed the ‘allocated time’ mechanism. There was no indication that nurses were given specifically allocated time in which to conduct IR (i.e. no discussion of other aspects of nursing workload being reduced or extra resources being provided). There was, however, some evidence that IR could have time-saving benefits for nurses, enabling them to better organise their workload and free up more ‘time to care’. 4,9,57 No other descriptions of the mechanism were highlighted and reported outcomes were limited, although some reported improved staff satisfaction22,39 reflective staff practice4 and positive patient feedback. 57
There was more empirical evidence regarding the absence of the mechanism, with some staff stating that IR was ‘nothing new’, that it was akin to what they were already doing or that made no difference to their practice. 4,28,31,40,45,50 There was also evidence that staff believed that IR resulted in less ‘time to care’ and added to, rather than reduced, their workload. 24,28,43,45,50 It was felt by some that the documentation associated with IR took nurses away from delivering patient care28 and others talked about having to fit in rounds around the rest of their workloads. 29,43,60 In these situations, higher-priority duties could take precedence33 and more complex patients could be prioritised. 24,41,49,60 The need for cultural change in an organisation was an important influencing context for this mechanism,4,24,28,48,49 as was successful teamworking. 41
Context–mechanism–outcome 3: intentional rounding increases nurses’ accountability for the standard of care provided
A total of 19 papers4,9,24,30–33,41–45,47,48,50,51,57,58,60 discussed this mechanism. Accountability was perceived by some to underpin IR;4,9,33,43,48,60 however, there was no evidence that increased personal accountability led to the delivery of higher standards of care, as the accountability of staff generally related only to responsibility for ensuring that they completed the IR documentation, rather than responsibility for carrying out high-quality rounds. Similarly, although the documentation associated with IR did enable care delivery to be audited, there were concerns that such audits provided information only about staff compliance with documentation procedures and not evidence of rounding quality or confirmation that any action(s) required had taken place. 4,24,31,58 There were also concerns that such audits may provide an incentive for staff to simply ‘tick boxes’ on the documentation, rather than completing the task in full,30 and incidents were reported of nurses completing all documentation at the beginning/end of their shift4,43–45,48 or falsifying information on IR documentation when they had forgotten to complete it. 43
The suitability of rounding documentation was an important context for this mechanism, with evidence that, where documentation was not ‘fit for purpose’ or duplicated nursing effort, non-compliance with IR protocols was more likely to occur. 4,31,41,42,57 The visibility and placement of rounding documentation was also an important context,9,44 with evidence that keeping documentation physically close to patients helped to ensure that it was completed as required. 9,45 Finally, leadership and management support was also an influencing factor. 4,9,42,45,47,60 Few studies discussed the outcomes of the mechanism, but some reported that nurses felt patronised, insulted or untrusted,31,43,50,60 and one study43 reported that it was believed that IR devalued nursing work by focusing on processes rather than professional judgement. 43
Context–mechanism–outcome 4: intentional rounding enhances nurse–patient communication and/or relationships
A total of 17 papers highlighted the positive impact that IR could have on nurse–patient communication. 4,22,24,28,30,34,35,40,41,43,45–47,57–60 It was widely reported that IR increased the frequency of nurse–patient communications;4,28,34,40,47,57,58 staff believed that this was welcomed by patients and their carers,24,28,40,46 making them feel more involved in their care,28 more likely to voice concerns40 and less likely to feel ignored/neglected. 57 There was less evidence that IR improved the quality of nurse–patient communication, although some staff felt that it was the final question (‘Is there anything else I can do for you?’) that was crucial, perceiving this to demonstrate respect and compassion. 45 There was little discussion of the impact of IR on nurse–patient relationships. Some staff felt that IR helped them to get to know patients better57 and made them more aware of patients’ conditions and needs,28,40,45 which could potentially affect patient outcomes28 and lead to better teamworking,57 fewer patient complaints and increased nurse satisfaction. 24,28,45,57 However, not all outcomes were positive and there were reports of patients being irritated or annoyed by IR. 28 Some staff felt that using predetermined scripts stripped communications of authenticity and made nurse–patient contacts a matter of routine,43 whereas some patients highlighted the importance of quality interactions with staff, noting the value of meaningful contacts and feeling connected. 30,57,59
Context–mechanism–outcome 5: intentional rounding increases nurse visibility and/or presence
A total of 11 papers9,23,24,28,40,45,47,49,57,58,60 discussed this mechanism. Some staff believed that IR increased the visibility of nurses on a unit;40,45 this was generally viewed positively, with perceived benefits such as enhanced nurse–patient communication,28 helping patients to feel well cared for and increasing staff satisfaction. 47 However, some negative outcomes of increased visibility were also reported by staff, including an increase in non-urgent requests from patients. 49 It was noted that rounding could be particularly challenging in rehabilitation settings, with reports that increased visibility of staff led to patients doing less for themselves and instead waiting for staff to assist them during their rounds. 28 Some staff questioned any association between IR and increased visibility, believing that they were visible to patients even when they were not undertaking rounds. They could not, however, confirm whether this was also the patients’ perception. 57 In the few studies that did explore patient and carer perceptions, it was generally agreed that increased visibility of nursing staff was valued by both patients and their carers. 9,23,24
Context–mechanism–outcome 6: intentional rounding enhances a nurse’s ability to anticipate and proactively address patient needs
A total of 11 papers4,9,25–27,43,46,48,57,58,60 addressed this mechanism. A number of staff identified IR as an intervention that enabled them to be proactive in anticipating patient needs, as opposed to being reactive to patient call bells or requests for help. 9,27,43,46,48,60 There were a number of staff-reported outcomes associated with this mechanism, including increased patient satisfaction,27 reduced anxiety,46 increased reassurance,4,46 reduced call bell usage4,57 and an overall sense of calm on the ward. 4 IR was also reported to enable nurses to intervene earlier when a patient’s medical condition was deteriorating46 and to prevent quieter patients from being overlooked. 4,43,57 Few studies reported patient experiences of the mechanism, although patient questionnaires demonstrated an improvement in patient satisfaction25 and patient perceptions of nursing proactivity following the implementation of IR. 57 One influencing context was the type of patient on the ward where IR was being carried out and their particular needs. For example, changing position and getting in and out of bed were identified as activities that could be anticipated and addressed by hourly rounding, whereas pain management and toileting could not be anticipated by hourly rounding. The layout of the ward was also an influencing context, with IR helping to ensure that patients in side rooms were not forgotten. 58
Context–mechanism–outcome 7: intentional rounding enhances staff communication and/or teamworking
A total of nine studies9,27,29,32,40,41,47,57,60 discussed this mechanism. Several studies9,29,32,47,57 discussed staff communication and its interconnecting relationship with IR (i.e. strong staff communication was perceived to be crucial for effective rounding, and rounding was perceived to improve staff communication). In addition to communication, some studies also noted the relationship between IR and staff teamworking (both unidisciplinary and mulitidisciplinary);9,40,41,60 once again, an interconnecting relationship was noted between the two (i.e. teamworking was perceived to be crucial to successful IR60, and effective rounding was perceived to improve staff teamworking). 9 Some staff believed that rounding improved ‘camaraderie’ on a unit; led to a calmer, less ‘chaotic’ atmosphere; and helped prevent tasks being missed. 9 When staff communication and teamworking were deemed to be ineffective, this caused frustration and concern among staff and reduced the effectiveness of IR. Some highlighted nurses’ reluctance to ask other team members for help as a barrier to effective IR;60 other influencing contexts were staff involvement, ownership of practice29,47 and the busyness of the ward. 27
Context–mechanism–outcome 8: intentional rounding fosters patient empowerment
Overall, the evidence related to this mechanism was weak, with only four studies4,25,28,57 identified and no detailed descriptions provided. The brief definition of the mechanism was supported only by limited empirical evidence, primarily drawn from one UK study. 4 This reported that individuals in care homes became more ‘forthcoming’ when they knew that staff were coming to see them regularly, empowering them to ask for what they needed. 4 As in the original definition, this study4 also found patient empowerment to be closely entwined with nurse–patient communication and relationships. Tentative evidence related to patient empowerment as an outcome of IR was identified by three other studies. 25,28,57
Influencing contexts and outcomes of intentional rounding
Although the aim of realist syntheses is to better understand the interplay of how a particular context affects a specific mechanism to produce outcomes,61 this review has found that such detailed theoretical explanations of IR are rarely provided in the literature. A list of potential ‘backdrops’ believed by authors to influence IR and a list of potential outcomes reported to arise from it were, however, identified and are highlighted in Appendices 1 and 2. The findings of this synthesis echo those of a systematic review of the barriers to effective implementation and sustainment of IR on medical and surgical wards,62 as well as identifying additional barriers. In Table 3, the theories by which IR may work are made explicit, and CMO configurations that are to be tested and refined in later phases of the study are summarised.
Discussion
The absence of any theoretical development of IR was notable in the synthesis, as many studies reported only the outcomes of implementing IR without providing any explanation of how or why these outcomes occurred. Similarly, many studies discussed the contexts that influenced IR but failed to explain how these conditions interacted with mechanisms to produce specific outcomes. This poor understanding of how IR works poses a major challenge to learning, replication and sustainability of the intervention.
The synthesis identified a number of discrepancies between how IR is purported to work and how it operates in practice, as well as international differences in how the intervention has been implemented. For example, guidance from the US states that the intervention should be utilised in a standardised manner so that all patients receive the same input. 2 Yet other countries, including the UK, appear to have adopted a more flexible approach, based on nurses’ clinical judgements of patient needs and preferences. The intervention has, therefore, not been consistently implemented across settings, but has been adapted and extended to suit local circumstances. This leads to an important question of how flexible the approach to the delivery of IR can be before it can no longer be considered IR.
Managing risk has also been acknowledged as an important driver for the introduction of IR. Assumptions have been made that IR will increase the personal accountability of nurses and raise the overall standard of nursing care. However, this synthesis has identified that this is not necessarily the case. IR may assist organisations to monitor and audit the care provided by their nursing staff, but evidence suggests that these audits focus on compliance with documentation procedures rather than on the quality of the rounds. This illustrates another ambiguity in the purpose of IR: is it to support nurses to improve the care they deliver, or to provide nursing managers with detailed evidence of nursing activity? Or is it an assurance tool for nurse directors seeking to report the quality of care to their boards and the public?
Summary
-
Despite the widespread use of IR, there is ambiguity surrounding its purpose and limited evidence of how it works in practice.
-
Differences in the implementation of IR demonstrate the importance of care delivery context and highlight that IR has been adapted in different contexts and as time has progressed.
-
This synthesis generated eight CMO configurations (see Table 3), which were tested and refined in subsequent phases of the study.
Chapter 4 Phase 2: a national survey of NHS acute trusts in England
This chapter describes the second phase of the study: the national survey of NHS acute trusts in England. This chapter addresses objective 1 of the study, exploring how IR was being implemented and supported across England and the way in which organisational context (or features of services and health-care organisations) influenced its implementation.
Method
In phase 2, a national survey of NHS acute trusts in England was conducted to explore how IR was being implemented and supported. A structured questionnaire to be administered online via SurveyMonkey® (Palo Alto, CA, USA) was developed and piloted in a local hospital trust. Following feedback from this pilot and the study advisory group, the survey was amended and shortened to maximise the response rate (see Report Supplementary Material 1). It included questions about:
-
when IR was implemented
-
provision of staff training/education opportunities to prepare staff to conduct IR
-
specific details about how the intervention was being implemented, which members of staff conducted rounds, how often they were conducted and how the rounds were documented and audited.
Details of NHS trusts in England were accessed online from the NHS website (www.nhs.uk; accessed 1 September 2015) and e-mail addresses for each chief nurse (often called ‘executive director of nursing’) were obtained from a list supplied by the CNO at NHS England to enable each director of nursing to be contacted directly. The list of trusts and contact details were compiled based on trust configuration, giving a total of 155 acute trusts. Trust acquisitions and mergers, and organisational and leadership changes occurring at this time were not insubstantial, meaning a dynamic approach during the data collection phase had to be adopted to maximise the response rate. An invitation to participate in the study with the link to the online survey was sent directly to each chief nurse in April 2015, with the request that they completed it themselves or forwarded the link to an alternative senior nurse with responsibility for implementing nursing services. Up to three reminders were sent by e-mail or telephone. Information about the survey was circulated and promoted by regional directors of nursing in England at their regular meetings with trust chief nurses, by the chief nurse at Health Education England and by the NHS Trust Development Agency in their newsletter to directors of nursing. Responses to the survey were collected in a SurveyMonkey web form, stored by SurveyMonkey in a secure, EU-based server and downloaded by the researchers when the collection was complete. The findings were then analysed in Stata® version 12 (StataCorp LP, College Station, TX, USA). The questions were a mix of multiple choice and free-text entry. Categorical questions were counted and percentages were calculated after allocating free text. Numerical questions were summarised with histograms, medians and quartiles. Free-text answers were examined and used to inform the qualitative research that followed.
Findings
Sample and respondent characteristics
Responses were received from 108 (70%) of the 155 English NHS hospital trusts that were sent the survey, of which 76 (70%) were acute trusts, 23 (21%) were integrated acute and community trusts and nine (8%) were specialist trusts. The mean number of beds in the responding trusts was 709 (range 39–2000) and 98 (91%) trusts had wards that were structured as predominantly smaller bays (typically 4–6 beds in a bay); 44 (41%) had wards that were made up of predominantly single rooms and 26 (24%) had wards that were predominantly Nightingale wards (i.e. the majority of beds in one large ward area). A total of 102 respondents provided their job title, which showed that the majority of the surveys [N = 89 (87%)] were completed by corporate-level nursing leaders in the trust, that is chief nurses (n = 31), deputy chief nurses (n = 43) or another corporate-level senior nurse (n = 15). The remaining 13 questionnaires were completed by divisional or directorate level heads of nursing. At the beginning of the survey, a brief definition of IR was given:
. . . a structured process whereby nurses in hospitals carry out regular checks, usually hourly, with individual patients using a standardised protocol to address issues of positioning, pain, personal needs and placement of items.
A total of 103 respondents (95%) indicated that this was their understanding of IR; there were four missing responses, and one respondent thought that the definition made the interaction sound mechanistic and failed to capture the essence of IR (i.e. showing patients, at regular intervals, that staff are concerned about meeting their needs).
Descriptive statistical analysis
Implementation of intentional rounding
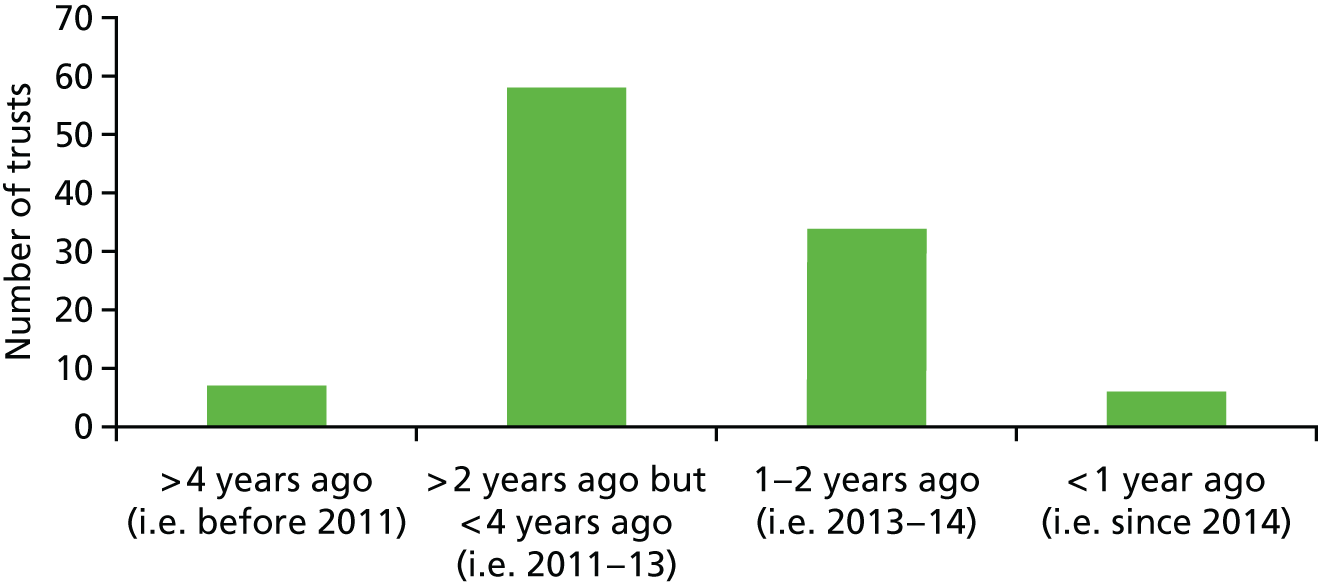
A total of 105 (97%) trusts stated that they had implemented IR in some way, although details around how and when it was implemented varied widely. For example, the vast majority of trusts implemented IR between 2011 and 2014. Seven trusts could be considered ‘pioneers’ or ‘innovators’, having implemented IR before 2011, and six could be considered late adopters, stating that IR had been adopted after 2014. Further breakdown is shown in Figure 2.
FIGURE 2.
When was IR implemented?
Once IR had been implemented, few trusts [n = 18 (17%)] reported that it had been interrupted for any length of time. Those that did gave the following reasons for the interruption: difficulty in implementing/sustaining IR, with several changes to documentation and pilots (n = 9); to review that IR was meeting its objectives (n = 3); staff shortages (n = 2); winter bed pressures (n = 1); ward managers deciding to stop IR and then re-introduce it (n = 1); poor understanding of the structured approach (n = 1); and to transfer documentation to an electronic record (n = 1).
Most trusts used the term ‘intentional rounding’ [n = 54 (53%)], although a large number of other different terms were also used, with ‘comfort rounds’ being the most common alternative [n = 14 (14%)] (Table 4).
| Alternative name | Trusts, n (%) |
|---|---|
| Comfort rounds | 14 (14) |
| Care round or Care rounding | 11 (11) |
| Hourly rounding or Hourly rounds or Hourly care rounds | 4 (4) |
| Essential care rounds | 2 (2) |
| Care and comfort rounding | 2 (2) |
| Patient contact round | 1 (1) |
| Rounding | 1 (1) |
| Intentional safety care bundle | 1 (1) |
| Better-care rounding tool | 1 (1) |
| Patient-focused rounding | 1 (1) |
| Time to care | 1 (1) |
| I-Care | 1 (1) |
| Safety and comfort checks | 1 (1) |
| Care and comfort checks | 1 (1) |
| Around-the-clock care | 1 (1) |
| Patient-focus rounding | 1 (1) |
| Well-being standards | 1 (1) |
| Caring around the clock | 1 (1) |
| Rounding with a reason | 1 (1) |
| Quality rounds | 1 (1) |
The majority [n = 67 (64%)] had implemented IR on all wards in the trust, although 18 trusts (17%) had implemented it on specific wards only and 20 (19%) had other more specific arrangements (Table 5).
| Clinical area | Trusts, n (%) |
|---|---|
| All adult inpatient areas | 101 (96) |
| Acute admissions | 91 (87) |
| Emergency department | 80 (76) |
| Maternity areas | 74 (70) |
| Day-care areas | 74 (70) |
| Paediatric wards | 72 (69) |
A few trusts had implemented IR in only a small number of clinical areas (e.g. in surgical wards only). Other trusts had implemented IR in specific areas, such as intensive therapy units (n = 1), operating theatres (n = 1), surgical assessment units (n = 1) and outpatient waiting areas (n = 1). Some trusts indicated that there was variation in where and how IR was implemented in their organisation. For example, one trust chose not to mandate IR but to leave it up to ward managers to decide. Another trust had initially implemented IR on all wards for all patients, but revised this to select patients ‘at risk’ (e.g. those with confusion or dementia, those post surgery or those at a high risk of falling).
A total of 84 (80%) trusts reported that, on the wards where IR had been implemented, it occurred for all patients. Where IR did not occur for all patients [n = 21 (20%)], this was mainly based on patient need, with nine responses indicating that patients who were assessed as being at higher risk/vulnerable received IR and seven responses stating that patients who were self-caring or mobile did not receive IR. One respondent said that some patients opted out of IR.
In 93 trusts (89%), a mix of RNs and unregistered nursing support staff conducted IR. In one trust (1%), only RNs conducted IR, and in two trusts only unregistered staff (2%) conducted IR. Nine (9%) trusts responded that allied health professionals (AHPs) were also involved in IR, with two trusts adding that doctors had occasionally been involved.
There was some variation among trusts regarding the frequency with which IR was carried out during the day on wards where IR was implemented. Twenty-three (22%) trusts implemented IR hourly, 21 (20%) implemented IR every 2 hours on all wards and 29 (28%) implemented IR hourly for some wards and every 2 hours on other wards. Thirty-two (30%) trusts had some variation in frequency, usually dependent on individual patient risk/needs. One trust specified that frequency was prescribed by a RN and another that need was assessed daily. Six trusts did not specify a frequency but said that it was dependent on patient need. Other variations were indicated, for example that IR should be conducted five or six times per day (n = 1), that it should be conducted hourly for high-risk patients and three times in 7 hours for other patients (n = 1), or that it was ward specific (n = 1).
A similar varied pattern was found for the frequency with which IR was conducted during night-time on wards where IR was implemented. Ten trusts (10%) implemented IR hourly, 26 (25%) implemented IR every 2 hours on all wards and 26 (5%) conducted IR hourly for some wards and every 2 hours for other wards. A total of 43 (41%) trusts had some variation in frequency, usually dependent on individual patient risk/needs, as during the day. Several respondents indicated that staff made hourly checks but that patients would not be disturbed or woken up to do IR.
A total of 85 (81%) trusts said that they had a structured protocol, script or procedure in place during IR. Table 6 shows the aspects of care included as part of IR. The most frequently included items were personal needs, positioning and pain assessment, which are in keeping with the accepted definition of IR. The majority of trusts also included placement of patient items, environmental safety checks and checking pressure areas. However, there were a significant number of items not usually considered part of IR that were also included [e.g. interactions with carers and checking fluid balance and intravenous (i.v.) lines and infusions], suggesting that the IR protocol was adapted by many trusts to address additional patient needs. Additional items that other trusts included were continence, nutrition, falls risk assessment, cognitive status and mouth care.
| Aspect of care | On all wards, n (%) | On some wards, n (%) | On no wards, n (%) |
|---|---|---|---|
| Items in Studer version of IR | |||
| Placement of patient items | 62 (83) | 9 (12) | 4 (5) |
| Positioning | 77 (92) | 8 (10) | 0 (0) |
| Checking of pressure areas | 61 (81) | 12 (16) | 2 (3) |
| Pain assessment | 75 (90) | 6 (7) | 0 (0) |
| Personal needs (e.g. toileting) | 78 (93) | 6 (7) | 0 (0) |
| Environmental safety checks | 61 (82) | 8 (11) | 6 (7) |
| Items in trust adaptations of IR | |||
| Checking vital signs | 13 (25) | 12 (23) | 28 (53) |
| Checking i.v. lines and infusions | 19 (33) | 15 (26) | 24 (41) |
| Checking fluid balance | 36 (55) | 12 (18) | 17 (26) |
| Interactions with carers | 37 (58) | 10 (16) | 17 (26) |
A total of 50 (48%) trusts reported that individual wards had flexibility about what they included in the IR. This flexibility included wards adding to the standard content of IR for their specific patient group or specialty (n = 9), staff using ‘common sense’ to ask only relevant questions (n = 7), adaptation of IR questions for specific patient groups (n = 8) and having a free-text option to record additional information.
Most trusts documented IR [n = 101 (96%)]. The majority used paper documentation kept by the patient’s bedside [n = 90 (86%)] or at the nurses’ station (n = 6). Some used electronic documentation at the bedside using a mobile device (n = 4) or at the nurses’ station (n = 1). One trust documented IR on a whiteboard and 10 trusts used a combination of paper and electronic documentation. Documentation was supposed to occur after every round in most trusts [n = 91 (87%)] or at the end of the shift at five trusts (5%). Timely documentation after every round was seen as better, but five trusts acknowledged that, in reality, staff documented IR at the end the shift some or most of the time.
Intentional rounding was audited by the majority of trusts [n = 68 (65%)], although five respondents did not know if IR was audited or not. Audits tended to be part of monthly general nursing compliance and metrics audits (n = 13), weekly or fortnightly senior nurse/ward manager quality rounds or documentation audits (n = 8) or spot-checked on daily ward manager/matron rounds (n = 9). Other, less frequent, responses included that IR was not audited formally, but was used in the management of incidents and complaints (n = 3); that IR was looked at as part of 6-monthly or annual reviews (n = 7); that IR was assessed as part of patient experience surveys (n = 2); and that it was reviewed in ‘Back to the Floor’ senior nurse reviews (n = 1).
The majority of respondents perceived that IR had a positive impact on patient experience (82%) and safety (79%) or had made no difference (Table 7). They thought that IR had less of an impact on carers’ experiences, but that the impact it did have was positive (55%). IR was thought to have some positive impact on staff experience (44%), although 10 respondents thought that IR had a negative impact on staff experience. The majority thought that IR had a positive impact on accountability (66%), although 34% thought that it made no difference to staff accountability. Some trusts perceived improvements in the number of falls and pressure ulcers; however, 19 trusts thought it was very difficult to say whether or not any improvements were due to IR, as other initiatives undertaken may also have had an impact.
| Area of change | Change, n (%) | ||
|---|---|---|---|
| Positive impact | Negative impact | No difference | |
| Patient experience | 77 (82) | 0 (0) | 17 (18) |
| Patient safety | 75 (79) | 0 (0) | 20 (21) |
| Carer experience | 48 (55) | 0 (0) | 39 (45) |
| Organisation of care | 61 (66) | 1 (1) | 30 (33) |
| Staff experience | 39 (44) | 10 (11) | 39 (44) |
| Accountability | 61 (66) | 0 (0) | 31 (34) |
Sixty-three (60%) trusts provided education for staff when IR was introduced and 52 (50%) trusts made IR education mandatory as part of the induction of new staff. Only 18 (17%) trusts provided education about IR as an ongoing requirement for all staff, although 27 trusts (26%) said that education was locally arranged in ward areas/specialties. Some trusts provided more than one approach to education and 15 trusts (14%) had no planned programme to educate and prepare staff for using IR. Two (2%) respondents did not know whether or not IR education was provided for staff.
The survey included opportunities to provide additional information about how IR was implemented. A total of 108 trusts responded to the survey; of these, 94 provided a free-text response to at least one question. These responses were analysed to search for examples of contexts, mechanisms or outcomes associated with IR; this is reported in Appendix 3.
Summary
-
A total of 70% of all NHS acute trusts in England responded to the national survey.
-
Of these
-
97% said that they had implemented IR in some way
-
89% had a mix of registered and unregistered nursing staff conducting IR
-
81% had a structured protocol, script or procedure in place for IR
-
96% documented IR.
-
-
Large variations were noted across trusts as to when, on which wards and for which patients IR was implemented; how regularly IR was conducted; what aspects of care were included in IR; and what educational opportunities staff received about IR.
Chapter 5 Phase 3: in-depth case studies – ward profile data, patient outcomes, and costs and benefits
This chapter addresses objectives 2, 5 and 7 and gives an overview of the three case study sites and their staff data, describing how IR has been implemented, developed and supported at each site. This chapter also investigates trends in patient outcomes (retrieved from routinely collected NHS ward data) in the context of the introduction of IR and other care improvement initiatives that have been introduced. An analysis of the costs and benefits of IR is also provided.
Ward profile data method
In phase 3, in-depth case studies were conducted to explore the extent to which the CMO configurations of IR identified in the literature and from the stakeholder consultation event were compatible with or relevant to modern health service delivery and the experiences of health-care staff and those of patients and their carers. The results from the survey, alongside NHS trust characteristics such as location and number of beds, were used to select the case study sites to be as broadly representative as possible, while maintaining the diversity necessary for qualitative data. The co-investigators discussed and agreed the selection of trusts together to identify sites where IR had been implemented differently (e.g. hourly versus every 2 or 4 hours), sites with different ward layouts (e.g. predominantly single rooms vs. Nightingale layouts) and sites of different sizes. Two trusts were approached and declined to participate in the study before the three case study sites were finalised.
Two wards were identified by senior trust staff in each hospital (one acute and one care of older people, to reflect the areas of concern in the Francis inquiry1). Trusts were able to choose their own wards and were not given any other criteria for how to do so by the study researchers. The research team spent 2–3 weeks based on each ward to undertake data collection.
To map the organisational and service delivery context in which IR was implemented, individual interviews were undertaken with directors of nursing/senior nurse managers and ward managers at each of the case study sites and a matron at site 3. A topic guide (see Appendix 4) was designed for this purpose, to collect information about the implementation and development of IR in each trust, details about how IR was undertaken, monitored and evaluated and any future development plans for the intervention. A total of 17 individual interviews were undertaken with trust and ward managers and a matron (Table 8). Audio files were transcribed and examined to produce a detailed description of the organisational context in which IR was introduced at each site.
| Case study site | Staff interviewed (n) | ||
|---|---|---|---|
| Senior nurse manager (Director of Nursing) | Ward manager | Matron | |
| 1 | 3 | 2 | 0 |
| 2 | 3 | 2 | 0 |
| 3 | 4 | 2 | 1 |
Ward and trust managers at each case study site were also asked to provide any documents that they could that contained information on their team or service, including nursing shift patterns, staffing information, sickness levels and vacancy rates. Researchers prepared ward layout maps to highlight the ecology of each case study ward, including the layout of patient beds. Detailed ward profiles including the ward layouts can be seen in Appendix 5 and a summary is provided in Tables 9–12. Reproduced examples of the IR documents for each site are provided in Appendices 6–9.
| Trust characteristic | Site 1 | Site 2 | Site 3 |
|---|---|---|---|
| Size | Large (> 800 beds) | Large (> 800 beds) | Very Large (> 1000 beds) |
| Location | Urban | Urban with rural catchment area | Urban |
| Bed occupancy (%) | > 90 | > 90 | > 90 |
| Ward characteristic | Site 1 | Site 2 | Site 3 | |||
|---|---|---|---|---|---|---|
| Ward a | Ward b | Ward a | Ward b | Ward a | Ward b | |
| Specialty | Health care for older people | Acute medicine, endocrinology | Acute trauma orthopaedic | Health care for older people | Acute medicine, cardiac and respiratory | Health care for older people |
| Number of beds | 24 | 24 | 32 | 32 | 26 | 18 |
| Predominant ward layout | 3–7 bed bays | 3–7 bed bays | Single, en suite rooms | Single, en-suite rooms | 4 bed bays | Nightingale |
| Nursing organisation | NS | Three teams | NS | Four teams | NS | NS |
| Shift pattern | 12-hour shifts | 12-hour shifts | Combination of 12-hour shifts and early (07.00–13.30) and late (13.00–19.30) shifts | Combination of 12-hour shifts and early (07.00–13.30) and late (13.00–19.30) shifts | 12-hour shifts | 12-hour shifts |
| Nursing team | Site 1 | Site 2 | Site 3 | |||
|---|---|---|---|---|---|---|
| February 2017 | January 2017 | April 2017 | May 2017 | July 2017 | July 2017 | |
| Nursing staff establishment at the time of data collection | ||||||
| Band 7 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Band 6 | 2.0 | 2.0 | 3.6 | 3.6 | 4.9 | 2.1 |
| Band 5 | 15.19 | 17.29 | 17.2 | 20.9 | 21.5 | 12.7 |
| Band 4 | 9 | 0 | 2.6 | 6.6 | 0 | 0 |
| Band 3 | 0 | 0 | 6.5 | 5.8 | 0 | 0 |
| Band 2 | 15.09 | 11.09 | 19.6 | 7.1 | 9.5 | 12.4 |
| Total | 33.28 | 31.38 | 50.5 | 45.0 | 36.9 | 28.2 |
| Vacancy rate | 4 (FTE) | 4 (FTE) | 4.4 (FTE) | 8.1 (FTE) | 19.78% | 9.69% |
| Agency/bank use | 127 shifts covered by temporary staff | 82 shifts covered by temporary staff | 6.7 (FTE)
|
11.4 (FTE)
|
8.06 (FTE) | 4.57 (FTE) |
| Sickness |
RN: 19.74% HCA: 0% |
RN: 11.56% HCA: 45.08% |
1.1 (FTE); 3.0% | 2.2 (FTE); 5.4% | 2.54 (FTE) | 0.38 (FTE) |
| Implementation of IR | Site 1 | Site 2 | Site 3 |
|---|---|---|---|
| When introduced | Some discrepancy; some time between 2009 and 2012, most likely 2011 | Some discrepancy, some time between 2014 and 2016, most likely 2014 | Because of staff changes, the exact date is unclear; it was around 2012/13 |
| Circumstances | Part of a strategy to reduce patient harm and increase care quality | Part of the strategy to reduce increased falls risk due to a predominantly single-room environment and develop compassionate care | Ward managers able to decide whether to implement IR or not. The majority of wards were thought to be implementing it at the time of the study |
| Staff involvement | Not initially, but recognised that this was ill-judged and staff were involved to redesign the IR process and documentation, which was piloted on some wards before roll-out to all wards | Managers reported a period of testing and piloting, although they think that IR was probably implemented too quickly across the trust | Owing to staff changes, it is unclear the degree to which staff were involved in implementation |
| Documentation | Four-page A4 booklet. Has been frequently revised according to perceived need. Includes 4Ps questions and the ‘Is there anything else I can do for you?’ question | Two-sided form. Includes 4Ps questions and the ‘Is there anything else I can do for you?’ question |
|
| Trust IR policy | Detailed trust policy | Detailed trust standard operating procedure | No formal IR policy |
| Frequency of IR | Hourly between 8.00 and 22.00, every 2 hours between 22.00 and 8.00 hours. Time intervals pre-written onto form | Frequency could vary according to risk assessment as long as rationale was recorded. Minimum frequency of every 4 hours. Time of IR was not specified, so specific time was entered by staff |
|
| Who does IR | Both HCAs and RNs. RN required to complete IR at 2.00, 8.00, 12.00, 16.00, 20.00 hours | Any member of clinical staff who had read the IR standard operating procedure and had received training in SKIN and Falls bundles | Both RN and HCA staff |
| Adaptation of IR beyond Studer format | IR documentation included questions about mobility, bed rail position, special mattress, body map to record skin integrity and presence of medical devices | IR documentation included questions offering drinks/snacks, falls prevention, body map to record skin integrity and presence of medical devices. Space available to document any actions resulting from IR | IR form for patients with a Waterlow score of ≥ 10 included assessing skin inspection, nutrition and special mattress needs |
The method of retrieval of routinely collected outcome data
Routinely collected outcome data from the NHS Safety Thermometer were retrieved for each of the case study wards. The NHS Safety Thermometer (www.safetythermometer.nhs.uk; accessed 13 September 2017) is a measurement tool to monitor commonly occurring patient harms in the NHS. It is used locally to support improvement in the delivery of harm-free care. Safety thermometer data were requested from case study trusts. The data received were analysed separately for each trust because of inconsistencies in the way in which they were recorded and aggregated. The main goal of this part of the analysis was to triangulate with the observational data. There were limitations because of the design of the study itself. Many things had changed at the same time in the health service and it would be hard to say that any pattern over time was due to IR, unless one could compare hospitals doing IR with others not doing IR. However, there were no controls (i.e. hospitals that did not undertake IR at all). It was hoped that some hospitals might have adopted early and others might have suspended IR for various reasons, giving us enough of a mixture to do a ‘synthetic controls’ analysis, which is increasingly used in economics, but this was limited as there were only six case study wards. Furthermore, safety thermometer data were collected on only 24 patients per month; analysis was, therefore, exploratory. Each of the various harms were summarised as line charts showing the percentage over time, with 95% binomial confidence intervals superimposed. Autocorrelation charts were generated to check for any persisting patterns over time, when one month seemed to influence the next. All data handling and analysis was done in Stata version 14.
The goal of quantitative analysis in this project was to fit within the realist evaluation framework. IR has not been implemented as a universal intervention that could be expected to show a homogeneous effect in all settings and times, like the introduction of a vaccine. Therefore, these quantitative analyses attempted neither causal inference nor estimation of the effect of IR. The purpose was to explore and understand patterns in the survey, Care Quality Commission (CQC) ratings and safety thermometer data, and to provide stimulus for qualitative data collection and interpretation. 63
Safety thermometer data
Safety thermometer data were obtained from the three case study sites. Each hospital aggregated, labelled and shared the data in a different way, which limited analysis. Ideally, the data would have been combined into one table and then trends over time that might relate to IR would have been explored, for example a decrease in harms such as pressure sores at the time of IR being initiated in each hospital. However, the site differences meant that each hospital had to be analysed separately. There were also the following additional limitations:
-
The data from different sites covered different time periods.
-
IR was implemented before the safety thermometer data that could be accessed (there may be older, similar audit indicators, but not in a consistent format that could be compared across sites and months).
-
Two sites gave aggregate data only, not at patient level.
-
Case mix could not be considered with the safety thermometer data as there were no variables to give context for each patient, such as demographics, prescriptions and diagnoses.
-
Sample size was small, at about 24 per month.
-
An assumption that there were no inclusion biases was required.
Charts of the various harms were drawn as percentages, changing over time, for each ward. On these, the 95% CI is shown: this is the range of percentages that could contain a true rate of harms, given that sometimes the safety thermometer data will, by chance, pick up too many harms and sometimes too few. If a horizontal line can be drawn across the chart that does not leave that green area, then that means that the data obtained were not inconsistent with there having been no trend over time at all. However, even this basic form of statistical inference needs a further caveat: examining several wards over many months on several indicators is likely to produce an apparently interesting pattern just by chance. For this reason, these charts were used simply to feed into discussions in interviews and to contextualize observational data. Figure 3 shows the percentages of any new harms for each ward (anonymised) that provided data. In each case, IR had been initiated before the safety thermometer data began.
FIGURE 3.
Percentages of any new harms for each case study ward.
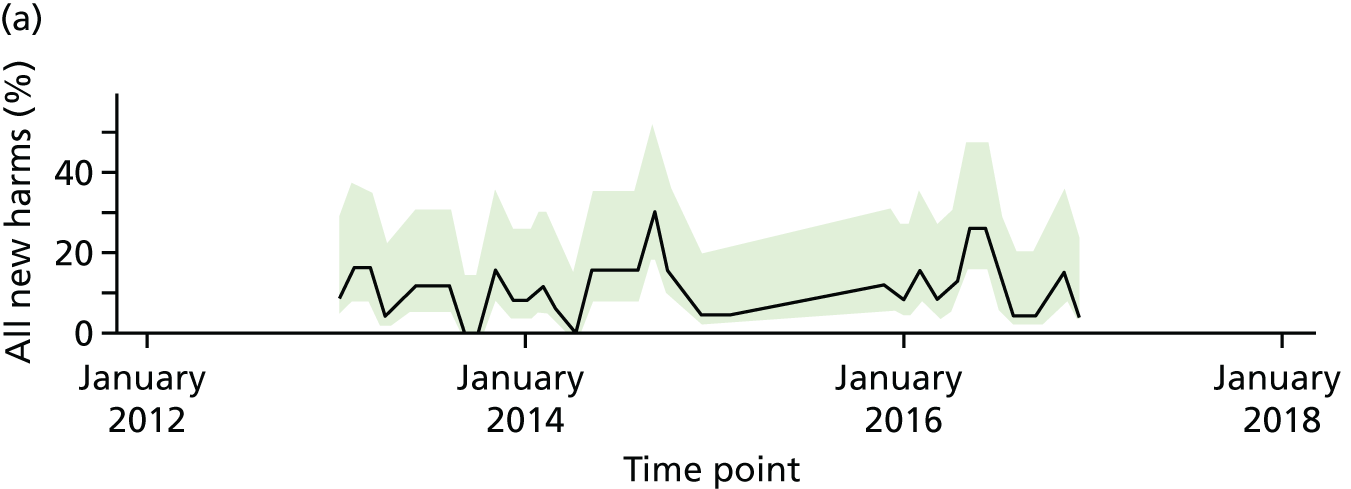

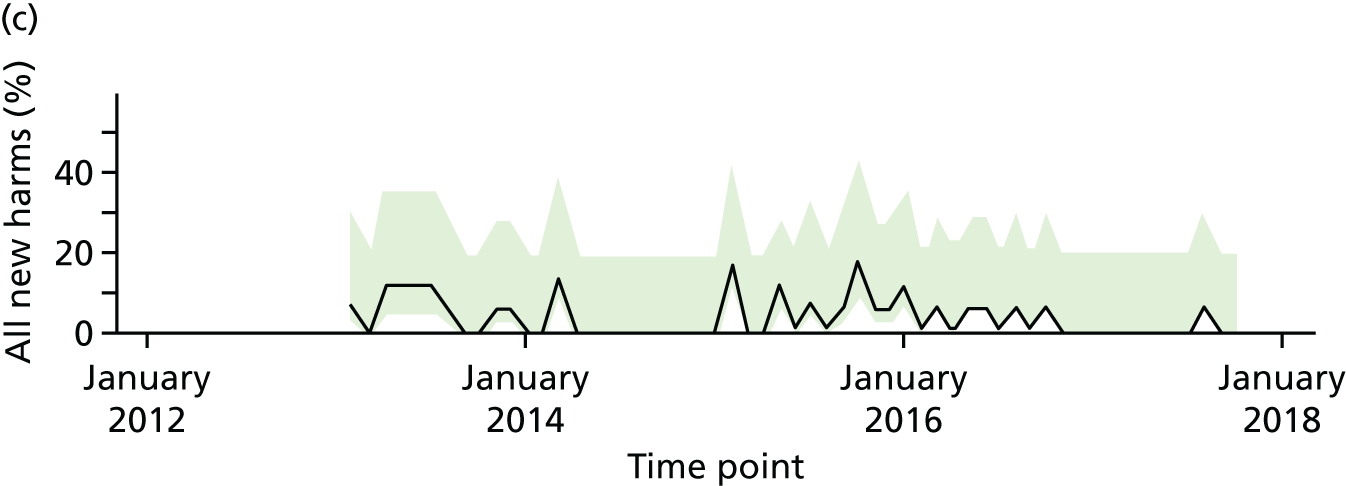
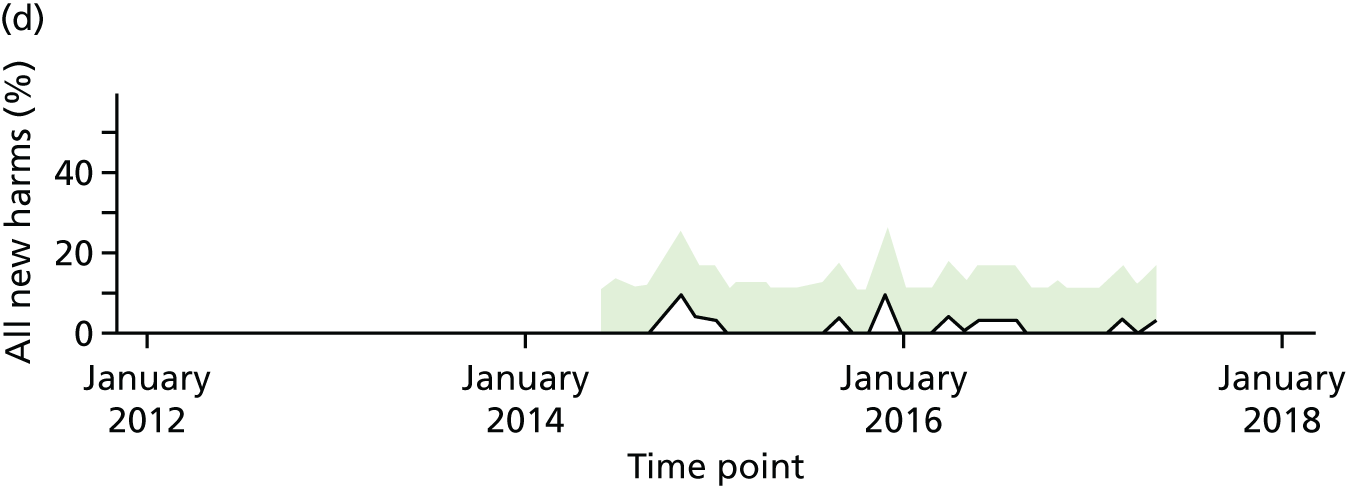
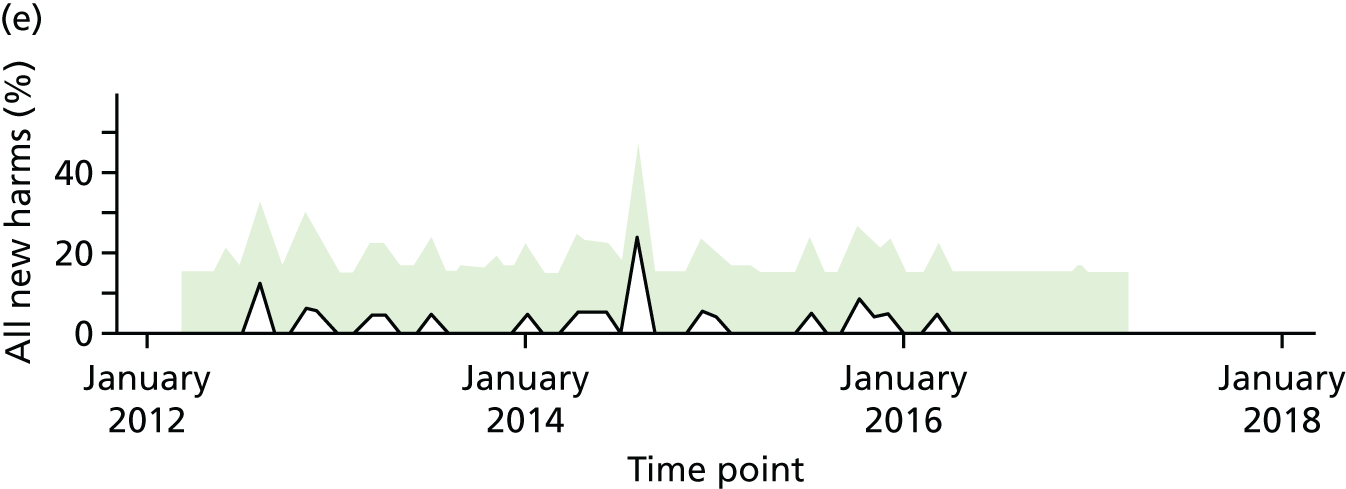
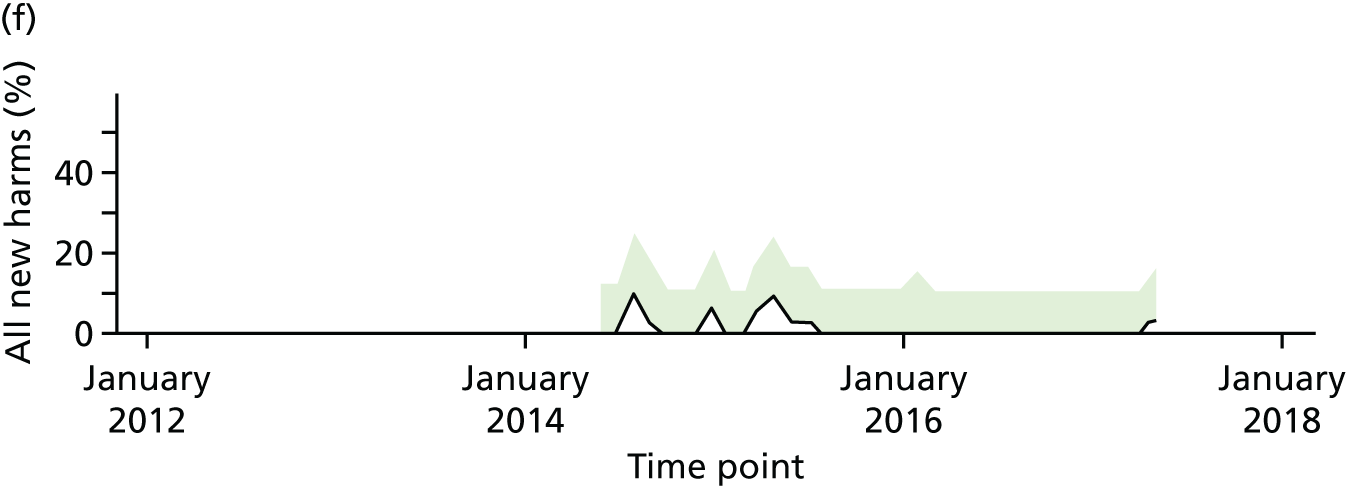
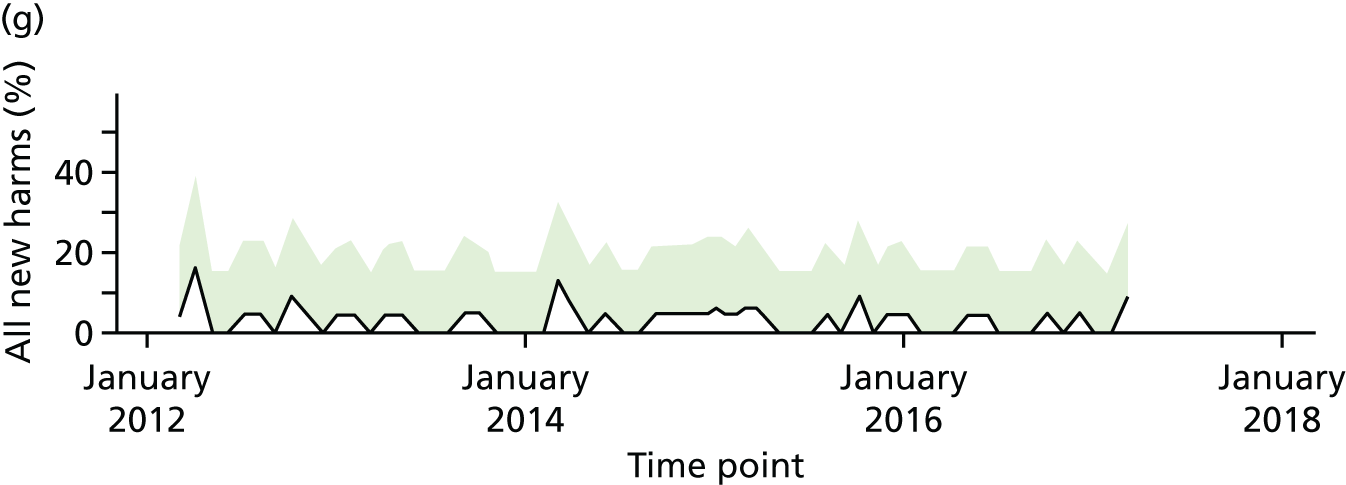
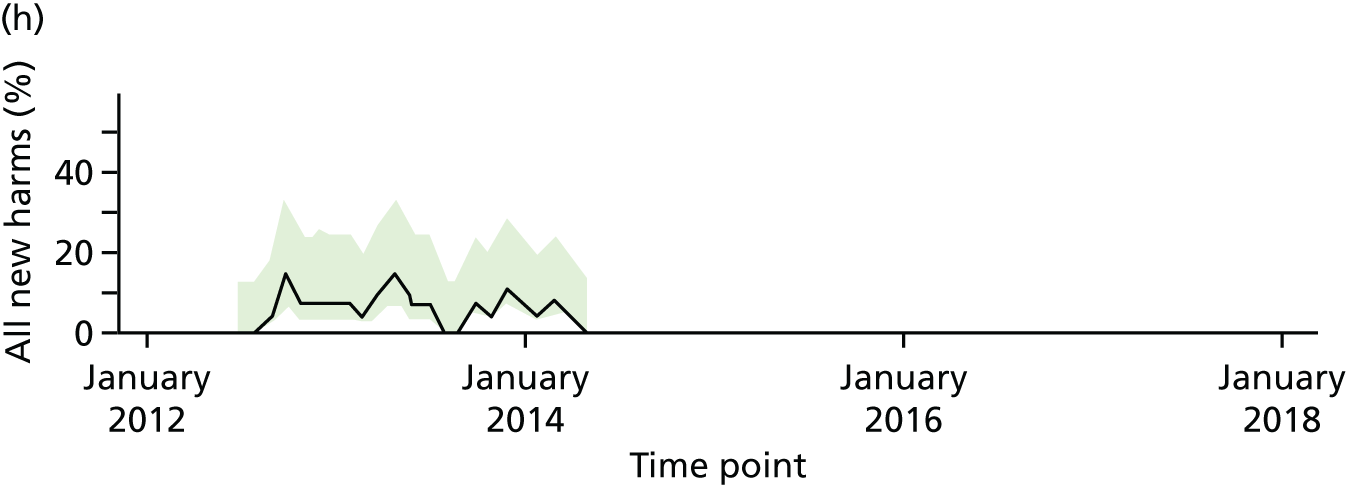
One case study site (site 2) identified wards as having different identities before and after a change of building location; the data were analysed on this basis. There are, therefore, eight wards highlighted in Figure 3 instead of six.
Method of cost analysis
A bottom-up approach to costing of IR activity was intended, using resource data collected in the staff interviews, non-participant observation and shadowing, and detailed information about ward context. However, this was not possible because of the difficulty in observing IR as a discrete activity and a lack of organisational memory of how IR was implemented. Therefore, the aim of this analysis was to calculate the incremental cost to the NHS of conducting IR in the wards included in the study, instead of not conducting IR (see Appendix 10). Three main types of cost were included in the analysis to estimate the total incremental costs:
-
direct costs – the cost of any consumable resource directly used for the implementation of IR
-
opportunity cost – the value of an alternative service that was given up as a result of performing IR
-
indirect costs – cost of start-up, development and training not directly attributable to IR.
Costs and benefits
The incremental costs amounted to £8.27 per patient-day for hourly IR. Incremental costs dropped to almost half (£4.47 per patient-day) if IR was conducted every 2 hours. This difference should be expected, as the opportunity cost of nursing time drives ≈90% of the total incremental costs of IR. The dominance of nursing time costs makes a formal sensitive analysis irrelevant. Total incremental costs of IR are directly correlated with the frequency of IR and the hourly wage of the nurses dedicated to it. Total incremental cost and frequency of IR seem to be linearly correlated: by reducing the frequency by 50%, the total incremental costs dropped by a similar percentage. Total incremental costs of IR are less sensitive to the hourly pay of nursing staff, as the assumption used in the base case already allocates 70% of IR to HCAs (bands 2 and 3). By allocating 100% of IR to HCAs, total incremental costs would drop to £7.19 for hourly IR and to £3.96 for IR every 2 hours.
The results of this incremental cost analysis lead to a relevant conclusion: IR rounding imposed on the NHS an increase in the daily cost of hospitalisation in the range of £4.47–8.27 per patient, depending on the frequency of IR. For a ward of similar size to the ones included in this study, this would represent an annual increase in hospitalisation costs, estimated to be in the range of £38,164–70,609. Because NHS costs are calculated on full absorption basis, which includes the allocation of all overhead costs to health services produced, the annual incremental costs of IR could exceed £100,000 per hospital ward in the case of hourly IR.
This cost analysis shows that total incremental costs imposed by IR on the NHS budget would require a full economic evaluation of its value for money.
Chapter 6 Professional perspectives of intentional rounding and observations of its delivery
This chapter addresses objectives 2, 3 and 6, exploring nursing staff and other clinical, management and administrative staff experiences of IR; how they believed it affected the way they delivered care; and the barriers to and facilitators of IR that they experienced. This chapter also highlights how IR has been implemented on the ground, exploring the contribution of IR to the delivery of patient care as a whole; this is possible because of the observations that were carried out of nursing staff undertaking IR and of the care that patients received.
Method
On each ward, individual qualitative interviews were conducted with the ward manager (n = 1), ward nursing staff and HCAs (n = 5), and other stakeholders, such as doctors and therapy staff (n = 5). Health-care staff were purposively sampled to attain a range of professions and grades. Generally, most staff who were approached agreed to participate in the research and only three members of staff across all the sites declined to participate in an interview.
Interview schedules were informed by the findings of phase 1 and specifically designed to elicit detailed reflections on how the different mechanisms and contexts of IR influenced the interviewee and others around them. Individual interviews were transcribed and analysed using framework analysis64 to identify themes in the data and to test and refine the causal explanations, expressed as the CMO configurations identified in phase 1.
Perspectives of senior nurses and ward managers
Participant characteristics
Seventeen senior nurses and ward managers participated in individual, semistructured interviews (see Appendix 11). Table 13 highlights their participant characteristics, in terms of their role. It should be noted that none of the senior nurses interviewed personally delivered IR and so often talked in interviews about how they thought IR was delivered or how they expected it should work.
| Profession/role | Number of interviews |
|---|---|
| Senior nurse | 10 |
| Ward manager | 6 |
| Matron | 1 |
Findings
Mechanism: accountability (n = 17)
All senior nurse participants mentioned accountability during the interview. Eight participants were clear that IR was the responsibility of the RN and, although IR was frequently carried out by HCAs, this was under the supervision of the RN. However, in two of the case study sites, when IR was first implemented, it was found that RNs did not complete it, because they thought that it was a task for HCAs, a view that senior staff felt needed to be addressed. In one trust, the documentation was revised to specify that RNs were required to complete IR every 4 hours.
Intentional rounding documentation
Accountability was seen to be demonstrated primarily by documentation of IR:
. . . from an exec[utive] nurse’s perspective, gives me some assurance that if you’ve ticked box then you’ve done it, and if not ticked box, you haven’t.
Executive Director of Nursing
This need to focus on documentation was commonly explained by the widely accepted mantra of ‘if it’s not documented, it’s not done’, although some participants expressed the view that the act of documenting did not always make someone feel accountable. There were varied views about the format of IR documentation. Some senior staff thought that it brought together lots of different forms, including IR, in an easy format that everyone could follow. There was an understanding of the need to streamline documentation to reduce the burden of paperwork; however, there were also concerns that the IR form could reduce the scope of nursing care provided to patients:
. . . so we’ve got kind of one kind of uniform approach, and it’s all in one booklet. But then there’s certain things that aren’t in the booklet, so then there’s risk of, if it’s not in the booklet we don’t have to do it, does that make sense?
Matron
In all sites, documentation had been designed and subsequently adapted, involving groups of nurses usually adding components not typically associated with IR (e.g. pressure sore risk assessment, food and fluid charts) to increase the clinical utility of the intervention. Several senior nurses shared unease about whether or not too much had been included, so that the form became unwieldy and more confusing to complete, as different elements needed to be completed at different time intervals. Furthermore, there was a lot of duplication with other documents and assessment, resulting in information being recorded in two or more places at times.
Benefits of intentional rounding documentation
Senior nursing staff gave a very clear view that one of the benefits of IR was the documented evidence that it provided. This evidence was thought to be useful to ward-based nursing staff as it demonstrated care delivered, including where care delivery was delegated to HCAs, and provided them with what one participant called ‘psychological safety’, making sure that they were doing the right things, intentionally, for their patients. This highly structured and standardised evidence was very useful to senior nursing staff, as it gave them assurance of a minimum standard of care delivered to all patients, particularly in unstable environments when there were shortages of staff and increased numbers of temporary staff. This evidence was found to be useful in dealing with untoward incident reporting, answering complaints and cases referred to the coroner:
I have been sat in meetings where we’ve had to talk to families before coronial processes and it’s been a relief to the family, and to me as a Director of Nursing, to be able to take those charts and say ‘But this is the care that was provided to your loved one, this is the way in which we diligently cared for them, this is the way in which they interacted with the nurses on an hourly basis or a 2-hourly basis during the night’. When, sometimes, those families walk away, they’ve got some peace because we’ve got an ability to say that we did and we provided care that was to an appropriate standard when they’ve sometimes been worried we haven’t.
Director of Nursing
One participant also thought that IR could counteract a lack of skill in the nursing workforce:
. . . it’s a prop to good nurse education, so if we structure this in such a way, the IR is a prop to any gaps we might have in the knowledge and skills of our nurses.
Director of nursing
Limitations of intentional rounding documentation
Although IR documentation was considered a useful source of information by some participants in order to respond to complaints, the majority of participants voiced concern about how accurately IR documentation reflected care delivered to the patient:
. . . from what I see on an audit, it literally is a tick, tick, tick, tick, tick, tick, tick, tick, tick. Now, for me, that doesn’t necessarily mean it was done . . .
Matron
As a result, few relied on IR alone to respond to a complaint, but instead they looked at the entire patient record. Senior staff were aware that nurses were frequently interrupted or had other priorities in caring for a group of patients that sometimes hampered timely documentation, even though IR had been done. Senior nurses, particularly in sites 2 and 3, also expressed concern that the principle of regularly checking patients inherent in IR was being lost in the focus on completion of documentation and whether or not IR was completed in a cursory way. They were unsure of what nurses did as a result of checking the patients’ needs, as this follow-up information was rarely documented:
. . . the task had become the documentation, not the actual conversation or the care.
Director, service development
Auditing intentional rounding
There was variation in the approach to auditing IR. Site 1 had a very structured approach as part of a well-defined, trust-wide quality assurance programme, but the senior nurses at sites 2 and 3 were unclear about how IR was audited. One participant at site 3 spoke about a large trust-wide audit conducted on the quality of staff interaction with patients, which included observation of care episodes. This prompted a realisation that IR had not been mentioned at all in the findings of this audit.
The influence of policy on intentional rounding
Six participants talked directly about the political origins of IR with the publication of the Francis report1 and the government’s response to this being very influential. All those who talked about the report described the findings as shocking, and four participants thought that the introduction of IR was either strongly recommended or mandatory as a result. One participant did not perceive it as an NHS ‘must do’, but saw it as an important response to restore public confidence and trust. In one trust, preparations for IR had already started prior to the report’s publication. Several participants talked about the ongoing influence of the Francis report1 on nursing and IR, and participants from all sites talked about their aspirations to develop nurses and nursing. In two sites, participants talked about how they wanted to get to the point where IR was not needed and the approach to regular, individualised contact with patients was the cultural norm for nursing staff. At the third site, this was not talked about. One participant talked about the need for nursing to evolve and become accountable for outcomes of care rather than processes of care (i.e. IR):
. . . I think the horror that was the findings of the Francis report was horrific and everyone knows that, it’s the bit where even team members will say ‘well if you don’t do this, it’ll be like Francis’ . . . I guess, for me, Francis is old now and we need to, as a profession, be evolving in, and measuring ourselves and deciding going forward, you know, how do you we demonstrate good-quality care, what is, what is an outcome that we want to see, rather than a measure that we want to implement that would give us an outcome.
Director of nursing
However, several participants talked of IR as a safety net or safety valve that reduces the pressure on the trust and the directors of nursing in a financially challenged health system with increasing shortages of staff, and how it would take a brave person to stop doing it. Although it was no longer thought to be required or audited by the CQC, there was the perception that if something went wrong, there would be the expectation that IR should have been in place.
Mechanism: consistency and comprehensiveness (n = 16)
Sixteen senior nurse participants discussed the consistency and comprehensiveness of IR in some way. Thirteen described it as a ‘checklist’, an ‘aide memoire’ or a ‘framework’, which supported staff to deliver care and prompted them to think about safety aspects of patient care. It was thought to be particularly helpful for junior and temporary staff or those unfamiliar to the ward to know what they should be doing. Furthermore, it was thought to support standardised care and be an important way of checking if care was delivered and ensuring that it was documented, which was important for governance. An important perceived benefit of the IR checklist was alerting nurses to safety risks (e.g. falls risk assessment, pressure risk assessment, pressure-relieving equipment, food and fluid intake). However, many of the prompts that were considered useful were local adaptations and additions to the original US model of IR.
Although the ‘checklist’ function was considered useful, there was also concern that it would be a prescriptive, task-orientated way of asking set questions. Instead, it was thought that IR should be delivered as part of a nurse–patient conversation to identify and meet individual patient needs. None of the participants thought that IR should be delivered in a standardised, rigid way at every round, as this would compromise holistic care. They felt that IR needed to be adapted so that questions were appropriate to the care being provided and tailored to each individual patient’s needs. For instance, it was not thought necessary to always ask all of the questions, but that nurses should be able to use their clinical judgement (or common sense, at times) to determine which questions were appropriate. One participant also emphasised the word ‘intentional’:
And I think it’s all about the word ‘intentional’, we intended to ask you this and we’ve found that out and so we intend to ask you whether you’re comfortable, we intend to find that out, so it’s our intention to do that as opposed to it’s our intention just to tick a box and we’ll just make sure that’s done on every ward for everybody.
Director, service development
Should intentional rounding be delivered to all patients?
Eight participants considered that IR should be delivered to all patients. This was thought to be particularly important for site 2, where there was a large number of single rooms. In site 1 the importance of ‘eyeballing’ every patient was emphasised, and IR was seen as facilitating this by one participant:
Sometimes, or you’ll be assessing them at a level that actually is probably a bit of overkill, do you know what I mean? But you will know that everybody got it.
Executive director of nursing
Senior staff in site 3 were more amenable to the idea that not all patients needed IR. One participant thought that some patient groups, typically younger, self-caring patients and some services (e.g. short stay or day surgery) did not need IR, although they were cautious of having some patients on the ward receiving IR while others on the same ward did not. Another participant in site 3 thought that conducting IR with young, self-caring patients took time away from more vulnerable patients whose needs were for fundamental care.
Flexibility of the frequency of IR was also discussed and there were different views at the three sites. Most participants from site 1 expected IR to be delivered every hour, although one member of senior staff had a different view and said that the frequency of IR was decided at ward level, in partnership with matrons and also with individual patients, on the premise that ‘one size doesn’t fit all’. Senior staff at site 2 thought that it was unrealistic to do IR at a fixed time every 1 or 2 hours, and so were clear that IR should be recorded at the actual time that patients were seen by nursing staff. Three participants explained that few nurses told patients when they would return to do the next IR because some patients have high expectations and would expect the nurses to be back at the exact time and would be unhappy if this did not happen.
Fewer senior staff discussed the comprehensiveness of IR, although those who did acknowledged that IR was adapted to include other aspects of care beyond the 4Ps (e.g. skin bundle, food and fluid charts, body map, invasive devices, elimination, hearing aids and dentures) in order to make it a more holistic framework. However, the tension of adding more elements to what was essentially a quick check was highlighted. Furthermore, there was concern that the focus on IR had reduced the scope of nursing practice to a narrow focus on the fundamentals, as well as the prevention of adverse events, leading to degradation of individualised care management:
. . . I mean, I don’t want it to be important because it shows that we are at a state in our evolution that that’s the minimum standard, in a sense. I would rather have nurses who are able to articulate, ‘Mr Smith, I need to be doing this, this and this because I spotted that’s what’s going to make the difference for him while he’s in hospital.’ . . . otherwise, we have people sitting in hospital for ages because all we’re doing is the fundamentals.
Executive director of nursing
Mechanism: staff communication (n = 12)
Twelve participants discussed staff communication and teamworking. IR was thought to facilitate some communication between nurses and HCAs, although this tended to focus on whether or not patients had been checked (i.e. IR documentation was completed), rather than on sharing information about the patient or facilitating the way staff worked together. One participant could see how IR documentation would help the nurse in charge keep up to date with care delivery for patients, but did not see how it would help nurses working together.
Intentional rounding was seen by six participants as helpful in supporting RNs to supervise the work of unqualified staff, both in terms of knowing what they had done and, particularly for newly qualified nurses, in delegating work to very experienced HCAs:
I think, you know, when you’re delegating care, I think it works well, if you’re working with a HCA workforce, because they’ve got evidence that they’ve delivered the care they were expected to deliver, and that can be reviewed.
Executive director of nursing
Although IR was seen as an intervention that could be undertaken by members of the multidisciplinary team, it was acknowledged that only nursing staff delivered IR and, therefore, IR had little impact on communication within the wider team.
Mechanism: nurse–patient communication (n = 12)
Three participants thought that IR increased the frequency of communication between nursing staff and patients, although none thought that it would improve the quality of that communication. Few participants thought that IR facilitated communication with carers; those that did focused on carers being reassured by IR documentation, indicating that patients had been seen and had received food and drinks, rather than IR facilitating conversations. Four participants thought that IR had no influence on nurses’ communication with patients and their carers, reducing nursing interaction to a list of tasks or closed questions to complete rather than the opportunity to talk with the patient:
. . . the contact becomes transactional rather than enriching, so you’re not having a conversation with that patient.
Director of nursing
Four participants said that they did not think IR was explained to patients.
Mechanism: allocated time (n = 11)
Eleven participants talked about the allocated time mechanism, but did not see IR as providing nurses with ‘time to care’. They were aware of time constraints that nurses experienced in delivering care, particularly when wards were short-staffed, and how that perceived lack of time influenced the way IR was conducted:
I won’t ask the questions or I won’t look at the, because they’re going to ask me and I haven’t got time to answer those questions. They might ask me, I might have to go and find someone else and I haven’t got time to do it, you know, I’ve heard that, staff say that.
Director, service development
Four participants described IR as encouraging the conversation rather than following a script:
. . . they’re just questions that you should ask, along with other things as well, so then you just complete that you’ve done it, rather than stand there and be like, ‘do you want the toilet?’ and tick, you know?
Ward manager
Senior staff talked about their expectation that IR would be incorporated into other clinical or care activities (e.g. helping a patient to wash or doing a dressing). The majority thought that staff were already delivering this care to patients and that the IR paperwork supported what they were already doing:
I’ve been sort of saying, you’re doing it as part of your care at the same time, you know, particularly when you’re also washing somebody, you’re doing one of your intentional roundings then.
Deputy director of nursing
I think staff are doing it anyway, staff are in the rooms and they’re delivering that care, it’s just a case of signing that paper, ‘cause they’re doing it . . .
Executive director of nursing
Mechanism: visibility (n = 9)
Seven participants thought that IR increased the visibility of nurses:
. . . if we didn’t have intentional rounding . . . what would I use to understand whether nurses were sat around a nursing station or they were actually in a bay working with our patients and their families? IR for me is the hook that keeps nurses going to the bedside, I guess.
Executive director of nursing
This was thought to be particularly important in environments with a large proportion of single rooms, irrespective of whether patients were fully dependent on nurses for their physical needs or self-caring. Even in a Nightingale ward structure, where nurses were already visible to patients, IR was still considered important to facilitate direct contact, as patients were sometimes reluctant to disturb busy nurses to ask for help. However, in wards with four- to six-bedded bays, IR was not thought to increase visibility, as nurses spent most of their time in the bay (which had a computer and phone extension in it) already, and they had no reason to leave.
Mechanism: anticipation (n = 8)
Five senior nurses thought that IR may enable staff to be proactive and anticipate patients’ needs ‘as long as they’re not just going through the motions’. However, this was thought to be restricted if patients were not aware that a nurse would be returning at a specific time, if nurses were delayed because they were with another patient or if something unexpected happened on the ward. Furthermore, one participant was unconvinced that patients waiting for a nurse to return to ask for something was a good thing:
. . . I don’t want somebody to wait for an hour for the toilet because they think someone’s coming back, I want them to press their buzzer when they want it.
Ward manager
Mechanism: patient empowerment (n = 3)
Of the three participants that mentioned patient empowerment, one thought that IR could empower patients if it was conducted in the right way and two said that patients and carers were aware of the IR documentation and sometimes read the forms. There was no evidence that senior nursing staff thought or expected IR to empower patients.
General contexts and outcomes
General contexts
In addition to the contexts linked with specific mechanisms already discussed, interviewees discussed some more general contexts that influenced IR as a whole, for instance ward culture and leadership, and staff education and training. Senior nurses thought that ward culture and leadership had a key influence on the nursing care delivered and on how IR was delivered, that is, not as a tick-box exercise, although IR was not thought to contribute to this ward culture. Senior nurses considered staff development had a more important influence on quality of nursing care than IR and some talked about their longer-term plans to do this. Although a couple of senior nurses thought that training had been provided when IR was first introduced, they were not able to provide details of this. Another senior nurse recalled seminars with nurses to discuss how they wanted to implement IR. However, the majority thought that formal training had not been provided, and that ward managers had explained how to complete the IR documentation to their teams, described by one senior nurse as ‘there was no roll-out so it was the blind leading the blind a bit to start with’.
All senior nurses thought, but were not sure, that subsequent ‘on-the-job’ training was delivered locally, arranged by ward managers as part of staff induction. However, this training focused on how to complete the documentation rather than the purpose of IR and what the anticipated outcomes would be. As one ward manager said:
It’s actually good to think about IR, because it’s not something that I’ve ever sat down and really thought about and scrutinised, because I think, as a band 5, it was just something that we had to do, you just did it because that’s what you’re told to do. So it’s never, it’s not something that I’ve ever sat and thought about as to why we do it and what the benefits are and, but it’s good to.
Ward manager
Senior staff were aware that nurses were concerned initially about the additional paperwork required by IR, that they did not see the point of it and that they thought they should be spending their time doing something more important. However, with time IR was thought to have become embedded, not questioned, ‘done without a second thought’ and, according to one ward manager, ‘I don’t think it makes any difference any more.’ Senior nurses talked about their ambition to develop the quality of nursing care provision so that IR would not be needed through staff development, nursing leadership development and being very clear about what good nursing care looks like.
General outcomes
Although there was acknowledgement that determining the causal effect of IR on specific patient outcomes would be very difficult, senior staff did think that IR could have an impact on falls and pressure ulcers. Several also thought that IR had an impact on nutrition, hydration and pain reduction. However, these perspectives focused mainly on the patient outcomes that IR could potentially influence rather than having evidence that it did influence these outcomes. IR was not thought to influence ward atmosphere or call bell use, as found in the US evaluation studies. 8,22,26,37,39,40,47
Summary
-
All senior trust and ward managers mentioned accountability in some way during the interview. Accountability was seen to be demonstrated primarily by documentation of IR. Senior staff felt that one of the benefits of IR was the documented evidence it provided, although they acknowledged that this evidence was not always sufficient/reliable.
-
Most senior staff described IR as a checklist, aide memoire or a framework that supports nursing staff to deliver care. However, there were concerns that it could be used in a prescriptive, task-orientated way, when it should be delivered in a conversational way, tailored to individual patient needs. None of the senior staff interviewed thought that IR should be delivered in a standardised, rigid way at every round.
-
Intentional rounding was thought to facilitate some communication between nursing staff, although this tended to focus on whether or not patients had been checked.
-
Few senior staff believed that IR increased the frequency or quality of staff communications with patients.
-
Senior staff did not see IR as providing nurses with ‘time to care’. The majority thought that staff were delivering care to patients and that the IR paperwork supported what they were already doing.
Perspectives of nursing staff
Participant characteristics
An opportunity sample of nursing staff was identified, based on who the research team met while collecting data on the wards and who agreed to participate in the research. Thirty-three front-line nursing staff members participated in an individual, semistructured interview (see Appendix 12); Table 14 summarises these interviewees’ level of seniority and education. All of the nursing staff interviewed were aware of and had personally undertaken IR.
| Seniority/education | Number of interviews |
|---|---|
| Senior staff nurse/junior ward sister (band 6) | 8 |
| Staff nurse (band 5) | 13 |
| HCA (bands 2 and 3) | 12 |
Findings
Mechanism: accountability (n = 33)
All nursing staff mentioned accountability in some way during the interview. Four participants mentioned the political origins of IR, believing this was the reason why it was implemented in the UK:
. . . I’m aware this came out as a pre-emptive thing, didn’t it? In light of the Francis report, a pre-emptive strike by David Cameron to show that we’re actually doing something after the horse had bolted, before it broke in the press.
Staff nurse, band 5
Others thought it had been implemented as a ‘standard-setter’ for nursing care across hospital settings, in order to ensure that patients were ‘safe’ and ‘not neglected’. However, most participants did not talk about IR as influencing their own personal accountability for the standards of care delivered. Only six said that IR made themselves or other nursing staff feel more accountable for the standard of care they were providing, whereas three believed that they would provide the same standard of care with or without IR. Some acknowledged that IR may improve standards in hospitals that were providing poor care, but did not see how it could benefit their hospitals, as they rated their institutions highly.
Audits of intentional rounding
Some participants were aware that IR documentation was being audited in their trust. Two senior staff nurses were able to identify positive outcomes associated with this, such as being able to identify and improve poor care and celebrate and reward good care. However, others (including a ward sister) were not clear whether or not IR was audited, and, if so, who audited it and what information they reviewed. Some staff also queried the usefulness of auditing IR documentation without assessing the quality of the round delivered:
. . . it’s just a tick and you can’t assume that someone’s done a good job because of a tick.
Staff nurse, band 5
Intentional rounding documentation
Although IR documentation varied between sites (see Appendices 6–9) broadly, opinion on the format of IR documentation was divided. Some (but not all) HCAs and newly qualified staff liked the format, appreciating that it was fairly concise and had a ‘tick-box’ style that was quick and easy to complete. Others did not like the tick-box format, stating that the documentation missed important information about patients and did not demonstrate the variety of tasks that nursing staff had undertaken. Some also said that they would prefer more open space on the documentation to add more detailed text.
Benefits of the intentional rounding documentation
Sixteen staff felt that a positive outcome of IR was that it provided ‘evidence’ or ‘proof’ that nursing care had been delivered. The need to evidence the care one delivers seems to have been entrenched into participants’ way of thinking, with many repeating a particular phrase, or words to this affect: ‘. . . if you haven’t written it down, you haven’t done it’. That is not to say that nurses changed their actions because of IR: they said they were working as they always had done, but the IR documentation now gave them written proof of this:
Do you think if you didn’t have to sign it, you might not go in [to a patient’s room to do IR]?
‘Oh, no, I think I would go in but I think it’s a good way of showing that I’ve gone in.
Most appeared to be accepting of this need to evidence care, acknowledging that this was the current nature of the NHS, although some expressed dismay that nursing care had moved in this direction. Two nurses saw the IR documentation as a means of positively highlighting how much time they do spend with their patients or as a way to ‘emphasise the good work that we do’, but the majority viewed it as a means of protecting or ‘covering’ oneself following an incident or complaint. The need for written evidence in the light of complaints suggested that nursing staff felt that their testimony alone would be insufficient in these circumstances. A number of examples of specific aspects of care that should be evidenced were provided, including the need to prove that nursing staff had been inspecting patients’ skin and changing their positions regularly, offering them food and drink and asking about their pain. For others, because nurses were required to initial each round, the IR documentation offered a means of proving which nurses had been delivering attentive patient care and identifying those who had not.
Ten participants said that IR documentation provided staff with a useful picture of each patient over the course of the day, identifying how much food and fluid they had consumed and how often they had passed urine or opened their bowels. (Staff mainly referred to the food and fluid balance records when discussing this, which is not part of the Studer Group IR protocol, but is an additional item that many of the case study sites had added into their IR documentation.) Staff found this to be useful because it enabled them to identify and respond to potential problems.
Five participants felt that a benefit of the IR documentation was that carers could read through it and find out what had happened with patients outside visiting hours. (Again, however, this tended to be associated with the information stored on the food and fluid chart, which is not part of the Studer Group IR protocol.) This was felt to be particularly important for patients who had dementia or other conditions that meant that they could not feed back this information to carers themselves. They thought that being able to access this information would be reassuring to family members (hereafter referred to as ‘carers’), enabling them to feel confident that the patient was receiving good care in their absence and would also mean that carers did not have to keep asking nursing staff for this information.
Problems with the intentional rounding documentation
Only three participants said that they always completed the IR documentation at the time of interaction. Contextual factors that facilitated the completion of IR documentation included locating it at the bedside, being reminded by management to complete IR documentation in a timely manner and ensuring that everyone had sufficient and suitable training in IR so that they knew how and when to complete it. For some, personal beliefs about the importance of nursing documentation also influenced their likelihood to prioritise its completion.
One-third of participants said that they or their colleagues often completed IR documentation later in their shift, after the round had taken place. These staff were clear that they had completed the round itself, but they just had not had time to document it. They therefore felt that this was an acceptable and inevitable part of the IR process, so long as the documentation was up-to-date before the end of their shift (even if this meant that they had to stay back late to complete it). Nevertheless, for some, this lack of compliance with documentation procedures led to anxiety, as they knew that this was not how the IR documentation was supposed to be completed and they worried about the potential consequences. Other concerns arose when participants were providing more frequent care to patients than the IR procedures implied (i.e. more frequently than once or twice hourly). In these cases, nurses were not writing down every time they assisted a patient; therefore, they worried that the IR documentation was not an accurate reflection of the care a patient had actually received.
For almost all of these participants, a lack of time, created either because of staff shortages or through conflicting tasks and priorities, was the main reason that they either forgot or chose not to complete their IR documentation on interaction and instead completed it later in their shift. In such busy working environments, nursing staff felt that they needed to use their professional judgement in order to decide which tasks to prioritise, and IR was often felt to be a lower priority.
Six participants said that they or their colleagues had either completed the IR documentation prospectively or completed it without undertaking the round. Prospective completion of the documentation involved either writing all of the times of interaction with patients onto the form in advance, at the start of the day and then filling the rest in later or writing the incorrect time of interaction onto the form, in order to fit within the allocated hourly slot. Others admitted that the IR documentation was sometimes completed without the round even being undertaken:
. . . when we first started doing the intentional rounding, I think me and everybody was doing it where we would just write every hour and tick it, just tick it, every hour, and just tick, tick, tick all the way down.
Without asking?
Well, without asking yeah, that’s the truth of it, just tick and tick and tick.
Again, a lack of time was reportedly the main reason why nursing staff chose to complete the IR documentation prospectively or completed it without undertaking the round, as, when time was scarce, they were more likely to perceive IR as a tick-box exercise. This temptation to document rounds prospectively, or without completing the round, was exacerbated by senior management pressure to ensure that documentation was always up to date. At one site, a number of staff mentioned that management had instructed them to be honest on their IR documentation and record it for the exact time at which the round had taken place. Staff at this site appreciated this and felt that inaccuracies on the IR documentation were decreasing following this guidance. They also felt that it was important for their trust to see an accurate picture of how often they were able to interact with patients, so that they were aware of the reality of their busy workloads.
Six participants said that the IR documentation could lead to negative consequences for nursing staff, making them feel scrutinised or worried that they would face disciplinary action if they did not complete it. This was particularly notable when wards were short staffed or busy workloads had prevented nurses from undertaking IR or completing the IR documentation.
Five participants struggled with balancing their desire to spend time with patients and their requirement to complete documentation. Others noted the difference between ‘a good nurse’ and ‘a good documenter’ and felt frustrated when colleagues appeared to prioritise their documentation over their patients. One nurse concluded that implementing IR documentation alone was not sufficient to ensure compassionate patient care:
. . . there’s no documentation that’s going to go along and say ‘hey, you should care more about your patients and check out if they’ve got water’; you’ve either got that passion and you’re already going to do that . . . and you’ve got that caring, compassionate nature that nurses have or you don’t.
Staff nurse, band 5
Mechanism: consistency and comprehensiveness (n = 33)
Intentional rounding as a checklist or ‘checking’ mechanism
All nursing staff mentioned the consistency and comprehensiveness mechanism in some way during their interview. Eighteen participants referred to IR as either a ‘checklist’ or a system for ‘checking’ on a wide variety of patient needs. Some participants felt that this checklist was more beneficial for new/inexperienced members of staff and for agency/bank staff. Others felt that there was a greater need to regularly ‘check’ on patients in single rooms, as nurses could not see how they were doing without physically entering their rooms. It was also noted that regular checks worked successfully only if there were sufficient staff on duty. Generally, the perceived outcomes of such checking were to ensure that the patients were ‘comfortable’ or ‘OK’, but a small number of participants felt that regular checking could help prevent pressure sores, reduce the number of falls and ensure that patients were eating and drinking sufficiently. Others also felt that these checks could be satisfying for nursing staff, enabling them to leave a patient knowing that they were comfortable and had everything they needed.
Some participants said that the tasks undertaken in IR were ‘things that we should be doing anyway’ but 17 participants felt that IR offered a useful reminder or prompt to prevent staff from forgetting these tasks. Again, some felt that these reminders were more useful for bank/agency and new/recently qualified staff and less necessary for permanent members of staff or those with more experience. In busy working environments, where staff were juggling many different tasks, some also said that they found the IR documentation useful to remind themselves of what they had previously done with a patient (e.g. what side they had last been turned on to), although again this refers to additional checks and detail not usually associated with IR.
The role of flexibility
Opinion was mixed on whether or not IR should be applied to all patients, but the belief that IR should be applied to all patients was more frequently aired by staff from case study site 1. These participants said that applying IR to all patients resulted in less confusion for staff and ensured that all patients received comprehensive care without anyone being missed. However, these staff had also experienced problems with this approach and sometimes saw it as additional, unnecessary work. The notion that IR was not suitable for all patients was more commonly raised by staff from case study site 3, who felt that IR was more beneficial for some patients (e.g. higher-risk, elderly, unwell, bed-bound patients and those with dementia, cognitive impairment or pressure ulcers) than others (e.g. younger, more mobile, independent patients or those who were more ‘well’). Some nursing staff said that it was not possible to ask all patients the IR questions because some lacked the capacity to answer. Therefore, nursing staff were required to use their observational skills and professional judgement to answer the questions for them or ask their carers’ advice.
No one said that IR was or should be applied using a structured, systematic approach at every round. Instead, staff talked about using their clinical judgement and their common sense to tailor IR to each individual patient. Such flexibility was regularly applied, in terms of how the questions were posed, what was asked and how often they were asked.
No one felt that it would be appropriate for nursing staff to simply read out the questions to patients from the IR documentation; participants instead preferred to incorporate them as part of a friendly conversation. They felt that doing so was more genuine and was more likely to help build a rapport with patients, whereas asking them ‘parrot fashion’ was more likely to cause irritation.
Some staff said that they chose not to ask every question at every round because they did not think it was necessary or because they felt that it would become ‘tedious’ for everyone involved. Others questioned whether or not it was realistic to expect nurses to be able to complete IR as intended, saying that they simply did not have the time to ask each patient every question because of their busy workloads, lack of staff and other demands on their time:
I think if you . . . did it asking each question how you’re supposed to do it, you would never do anything else.
Senior staff nurse, band 6
One participant felt that the question ‘is there anything else I can do for you?’ was the most useful question on the IR form, and helped identify those issues that were important to patients but which might otherwise be missed (e.g. did the patient need something from the shop? or did they want to read a newspaper?, etc.). Some people said that they asked this question more indirectly or more casually, with statements such as ‘do you need anything?’ or ‘can I help you?’, but others said they chose not to ask patients this question at all, simply because they did not have the capacity to respond to their answer:
. . . sometimes that’s not a question you want to ask, ‘is there anything else I can do for you?’, because you don’t want to know the answer [laughs].
Senior staff nurse, band 6
Many participants felt that there should be flexibility in how often IR was conducted with patients and that some patients needed it more frequently than others, depending on their health needs and other personal circumstances. For some, this flexibility was simply a practical solution to the fact that each day was different and you could never guarantee being able to check on each patient at the same interval each day. At case study sites 2 and 3, nursing staff had a degree of flexibility around how often they could undertake IR and many said that they did vary the regularity of their rounds depending on individual need. However, some participants from these sites did acknowledge that using this flexible approach could be confusing for nursing staff, as everyone did IR slightly differently and they were not always sure how frequently they were supposed to round each patient. At case study site 1, staff did not have any flexibility around the regularity of IR as they were all aware that it was supposed to be hourly, although some staff still tried to carve out an element of flexibility within these boundaries.
Fewer staff discussed the comprehensiveness of IR and whether or not it was able to help identify all patient needs (n = 9). Most felt that the breadth of areas included in IR was very good and that everything included in a round was an important component of positive patient care.
Mechanism: nurse–patient communication and relationships (n = 30)
Two ways in which IR could potentially influence nurse–patient communication were identified. These were as follows.
Intentional rounding could increase the frequency of nurse–patient communication
Eleven participants said that IR increased the frequency of nurse communication with patients. Busy working environments and a general lack of nursing time was the key context for this, as some felt that, in the light of the competing demands on their time, IR enabled them to ensure that they returned to their patients regularly. Others said that without IR they would spend less time talking with their patients and more time responding to their other tasks. However, the communications that arose from IR were generally seen as brief, with nurses describing just ‘popping in’ to check that patients were OK rather than having lengthy discussions with them. Nevertheless, some staff felt that brief but more frequent communication was appreciated by patients and their carers, making them feel ‘cared for’ and ‘valued’ and giving them confidence that they would not be ‘forgotten’. One nurse referred to this as offering ‘good customer service’ to patients and their carers. Others believed that IR made patients feel more comfortable with nursing staff and more confident to approach them with any problems they may have or any issues they would like to discuss.
However, not all outcomes of more frequent communication were positive, as some said that nursing staff and patients (particularly those who had been on the ward for longer periods of time) found the increased frequency of communication to be a ‘nuisance’. A further unanticipated negative outcome was that IR could raise patients’ and carers’ expectations of how much time nursing staff should be spending with patients, an expectation that, in reality, nursing staff were not able to meet.
Intentional rounding could improve the quality of nurse–patient communication
Only three participants believed that IR improved the quality of nurse–patient interactions. These participants felt that the process of IR helped them to open up lines of deeper communication with patients (particularly those who were less vocal or had communication difficulties), enabling them to focus on each person’s individual needs.
Few participants talked of the impact IR could have on nurse–patient relationships and only four participants said that IR could be beneficial for improving these relationships. Some said that the process of IR made patients feel more cared for and considered by nursing staff, which enabled positive relationships to develop. For others, the increased regularity of communication with patients due to IR helped nursing staff get to know their patients better, enabling them to detect subtle, significant changes that could affect safety.
Some overall contexts that influenced nurse–patient communication and relationships were identified by nursing staff. For example, a lack of time generally made participants feel that nurse–patient communication and relationships suffered. The personal characteristics of staff were also felt to be important, with some staff being identified as more approachable and chatty than others. It was acknowledged that some staff were better at starting conversations with patients; therefore, IR may be more useful for those that struggle to communicate (or are less experienced at communicating) with patients than for those who do this naturally. Equally, some patients were felt to be chattier than others and IR could be useful for encouraging quieter patients to make their voices heard.
Mechanism: allocated time (n = 29)
All but four participants discussed the allocated time mechanism, but they focused, not on the presence of this mechanism, but the absence. No one felt that they had been given specific, allocated time in which to undertake IR. In fact, a small number of participants (including both qualified and non-qualified staff) perceived IR to be ‘additional work’, which took up more of their time. Others believed that they would be doing the tasks included in IR anyway, even if it had not been introduced:
. . . I just feel like it’s a term that’s been coined for something that we’re already doing, they’re just putting a name on it.
Senior staff nurse, band 6
But most participants said that IR did not take up too much of their time because they simply incorporated it alongside other aspects of their workload. For example, RNs talked about fitting IR in alongside their medication rounds and HCAs talked of incorporating it into the daily patient washes and bed linen changes. Generally, these participants said that they had chosen to incorporate IR alongside their other tasks because there was not the time or number of staff required to do it any other way. At case study site 2, staff were told that they should be doing IR every time they entered a patient’s room; therefore, they usually combined IR alongside whatever other task they had entered the room to undertake.
Only one participant felt that IR enabled them to prioritise patients’ basic care needs. However, one experienced nurse disagreed with the idea that RNs should be prioritising basic care when, in reality, they often needed to be focused on more clinical aspects of care and could delegate basic care to unqualified staff. Nine participants discussed the idea that IR might affect the organisational or time management skills of nursing staff and two (both band 5 nurses) felt that IR could have a beneficial impact on this. Seven said that certain tasks/patients have to be prioritised over others and that choosing not to undertake IR was often a demonstration of good time management/prioritisation skills.
Mechanism: staff communication and teamworking (n = 24)
Twenty-four participants discussed this mechanism; 16 felt that IR encouraged or improved staff communication, usually in terms of an improved handover of information about patients between nursing staff or across shifts. Others felt that IR enabled nursing staff to better share their tasks and responsibilities among each other and pick up on any tasks that their colleagues may have missed. Six participants also felt that IR was useful for RNs as a day-to-day supervisory tool for more junior or unqualified staff. These participants said that the IR documentation was checked by senior members of staff to ensure that those under their supervision were working as expected and completing their allocated tasks.
Although everyone acknowledged that IR was, first and foremost, a nursing document, used mainly by nursing staff, a few participants did feel that their non-nursing colleagues (mainly doctors and dietitians) did refer to the IR documentation for information about patients (however, this was generally the food and fluid parts of the form, which, again, are not part of the original US protocol). Some felt that there was a missed opportunity for good interprofessional teamworking and that it would be beneficial if other health-care workers also completed the IR form when they were with the patient. This seemed particularly relevant to therapy staff, who were reported to spend longer periods of time with patients than nurses could often manage. It was felt that therapy staff could undertake some of the tasks on the IR form (e.g. offer a drink, ask about the toilet) as part of their therapy session and document this so that it offered a more realistic picture of the number of people who had visited the patient each day.
A relationship between IR and teamworking was identified by some participants (i.e. not only was IR perceived to improve staff communication and teamworking, but strong staff communication and teamworking were perceived to be important for effective IR). Good teamworking, which assisted IR, involved reminding colleagues when they had forgotten to undertake IR, offering assistance to others when they were too busy to undertake rounds or taking the initiative to help colleagues with particular aspects of the IR load. The only other influencing context of the mechanism was individual staff personalities and characteristics, as some team members were naturally more proactive and better team players than others.
Mechanism: visibility (n = 21)
Twenty-one participants discussed this mechanism, although only five believed that IR actively increased nurse visibility. These participants talked of their busy working environments, which involved many tasks to be completed away from patients’ bedsides (e.g. taking telephone calls, working in the clinic, documenting on the computer). They felt that IR offered a clear reason for nursing staff to ‘keep going back’ to patients, thereby increasing their visibility. This was believed to be ‘comforting’ to both patients and nurses, making patients less anxious about being left alone and reassuring nurses that their patients were OK. However, one HCA found that increasing her visibility meant that she was being asked to do additional, non-urgent tasks by patients.
Not everyone agreed that IR increased nurse visibility and four participants (who all worked on wards with bay layouts) said that they rarely left their bay anyway, and were, therefore, visible to patients most of the time. Indeed, 15 participants talked of the important context of ward layout and its impact on nurse visibility, with most stating that IR may be a more useful means of increasing nurse visibility in single room wards or side rooms, rather than bay-based settings (as patients in single/side rooms did not see nursing staff as often as those in bays). However, not everyone agreed with this and one participant felt that IR did not even increase nurse visibility in single/side room settings.
Mechanism: anticipation (n = 20)
Twenty participants discussed this mechanism and five felt that IR enabled staff to better anticipate and proactively address patient needs. This was believed to be beneficial for toileting, avoiding falls and overall experience of care, as well as enabling nursing staff to identify any issues before they escalated. One participant believed that, by enabling nursing staff to anticipate patient needs, IR resulted in fewer patient call bells; however, two disagreed, stating that IR had no impact on call bell use. This may be because call bell use was perceived to be complex and dependent on the personal characteristics of the patients or the variety of needs and requests they may have. Eight participants felt that IR did not influence how proactive they were or affect their ability to anticipate patient needs. In particular, some staff felt that it was not possible to anticipate patients’ toileting requirements or whether or not they would like a hot drink, as these needs could change rapidly. Instead, these staff informed patients to use their call bell should such needs arise. Others felt that anticipating patients’ needs was already part of their nursing skill or personal characteristics and something they would be doing with or without IR.
The key context of the mechanism was associated with patients’ and carers’ understanding and awareness of IR. When asked if they told patients and their carers about the process of IR and what it entailed, all but three said that they did not tell them unless a patient or carer specifically asked. For some, this also included not telling them when they would be back to see them next. Generally, nursing staff said that they did not tell patients and their carers about IR because they did not think that they would care about the working processes nurses were undertaking or that they would not understand them. However, in most cases, the anticipation mechanism could not be triggered for patients and carers as they were unaware that IR was taking place and, as such, could not anticipate when a nurse would return. The layout of the ward was the only other influencing context in the anticipation mechanism, as having a nurse based in a bay was felt to be more beneficial for nursing staff to observe patients closely and proactively identify any requirements they might have.
Mechanism: patient empowerment (n = 8)
Only eight participants discussed the patient-empowerment mechanism. On the basis of participants’ responses, patient empowerment appeared not to be an independent mechanism of IR, but a possible outcome of the increased frequency of communication that IR promoted. Four participants said that IR enabled nursing staff to go to a patient’s bedside more regularly and, as a consequence of this, patients became more familiar and confident with the nursing staff and more likely to ask them for what they needed. However, four participants disagreed with this and felt that IR made no difference to patient empowerment. One staff nurse said that IR could not empower patients because they did not know that it was happening, whereas others said that the patients on their ward were already confident enough to ask for what they needed, regardless of IR. No other contexts or outcomes associated with the mechanism were identified.
General contexts and outcomes
General contexts
In addition to the contexts linked with specific mechanisms already discussed (e.g. staff shortages, lack of time, ward layout), all interviewees also highlighted some of the more general contexts that influenced the intervention of IR as a whole. This included the amount of training and education nursing staff received around IR. Although some participants remembered attending training or lectures about IR, many said that no formal training had been provided, perhaps because the intervention was viewed as ‘self-explanatory’ (senior staff nurse, band 6) or something that, ‘anyone can use’ (senior staff nurse, band 6). Instead, it was more common for staff to receive informal training from their colleagues, with more experienced nursing staff explaining the IR paperwork to new team members and demonstrating how they undertook IR. However, this sometimes posed problems as the training they delivered depended on the trainer’s own understanding of the intervention, which meant that they could sometimes pass on incorrect guidance and information:
. . . I suppose there’s no hard and set rule of how to do it, so they’ll talk them through how they do it.
Staff nurse, band 5
There was also a sense that many staff did not know why they were delivering IR and had not received any training around its purpose or why particular components of care had been included. Participants said they delivered IR ‘because I have to’ (staff nurse, band 5) and had never really formed much of an opinion or reaction to it. Others said that they undertook IR because that was just ‘how we work’ (staff nurse, band 5) and that it was a ‘process that’s automatic’ (staff nurse, band 5) and so embedded in their daily routine that it was not something they ever gave much thought to:
. . . I don’t think about doing it, yeah, more like it’s just a bit of a routine, it’s ingrained.
Staff nurse, band 5
. . . I just do it second nature.
HCA
Some participants, therefore, felt that it was important for nursing staff to develop a greater understanding of ‘why it’s so important’ (staff nurse, band 5) so that they all delivered IR as intended and did not view it as extra work that was a hindrance or nuisance. This links to another important influencing context: the level of engagement that staff felt around the implementation or process of IR. Few staff said that they were involved in the implementation of IR or influenced it in any way, but it was felt that improving staff engagement in IR would improve nursing staff understanding of its benefits:
. . . I think just probably ensuring people understanding fully what the tool is used for and making sure that they’re supported just to sort of use it properly and then allowing them to see the benefits of use.
Senior staff nurse, band 6
Individual staff characteristics, such as having good communication skills and empathy, as well as the amount of experience nurses had in working with patients, were also felt to be important contexts in the success of IR.
General outcomes
Generally, staff did not associate IR with any specific outcomes, although some nursing staff felt that it could be a helpful tool for reducing pressure sores and falls, which could possibly lead to a quicker discharge from hospital. Others said that IR helped them feel satisfied that they were delivering good patient care.
Summary
-
All nursing staff mentioned accountability in some way during their interview. However, most nursing staff did not talk about IR influencing their own personal accountability for standards of care delivered, although some acknowledged that it may improve standards in hospitals that were providing poor care.
-
Half of all nursing staff interviewed felt that a positive outcome of IR was that it provided evidence that nursing care had been delivered. Most viewed this as a means of protecting oneself following an incident or complaint.
-
All nursing staff mentioned the consistency and comprehensiveness mechanism in some way during their interview. Many participants referred to IR as a checklist or system for checking on a wide variety of patient needs. They also felt that IR offered a useful prompt or reminder to prevent staff from forgetting to undertake particular tasks.
-
Opinion was divided on whether or not IR should be applied to all patients, but no nursing staff felt that IR should be applied using a structured, systematic approach at every round. Instead, nursing staff talked about using their clinical judgement and common sense to tailor IR to each patient.
-
Some nursing staff felt that IR increased the frequency of nurse–patient interactions, although these communications were usually brief, rather than lengthy discussions. Few nursing staff believed that IR could improve the quality of nurse–patient interactions.
-
No nursing staff felt that they had been given specific, allocated time in which to undertake IR.
-
Half of all nursing staff felt that IR encouraged or improved staff communication, generally in terms of an improved handover of information about patients between nursing staff or across shifts.
-
Few nursing staff felt that IR affected nurse visibility, anticipation of needs or patient empowerment.
Perspective of other health-care professionals
Participant characteristics
An opportunity sample of non-nursing health-care staff was identified, based on who the research team met while collecting data on the wards and who agreed to participate in the research. Twenty-eight other (i.e. non-nursing or managerial) health-care staff participated in an individual, semistructured interview (see Appendix 13), some of whom had direct experience of conducting IR. Table 15 shows the participant characteristics of the other health-care staff interviewed in terms of their profession/role and whether or not they had direct experience of undertaking IR.
| Profession/role | Number of interviews | Experience of doing IR |
|---|---|---|
| Medical consultant/trainee | 6 | No |
| Occupational therapist | 4 | No |
| Physiotherapist | 2 | No |
| Dietitian | 1 | No |
| Pharmacist | 1 | No |
| Student nurse | 5 | Yes |
| Ward clerk/receptionist | 4 | Yes |
| Housekeeper | 4 | Yes |
| Rehabilitation support worker | 1 | Yes |
Findings
Mechanism: comprehensiveness and consistency (n = 20)
Intentional rounding is/should be applied to all patients
Opinion was split on whether or not IR should be applied to all patients. Even interviewees who said that they thought that it should be applied to everyone gave examples of it being more beneficial for certain patients or in certain settings. The key arguments in favour of applying IR to all patients in a ‘standardised and formalised’ way, is that no one and nothing ‘gets missed’.
Intentional rounding benefits some patients more than others
Participants highlighted those patients who they felt were most in need of IR, which included those who were not independent or were at risk of pressure damage, falls or malnutrition; elderly patients, especially those with dementia; patients who wandered or were in need of enhanced care; patients who needed turning; stroke patients; and those with difficulties communicating verbally. It was felt that IR checks could be done less frequently for those patients who were relatively well or those who were waiting to go home. Participants who suggested changing the frequency of IR said that it should be done through individual risk assessments, as a patient’s condition could change unexpectedly. They felt that using IR flexibly allowed nurses to use their clinical judgement to determine the frequency of IR needed for each patient. If IR was used for all patients, regardless of risk, interviewees argued that it may be viewed as time-consuming, frustrating and monotonous, rather than useful for patient safety.
Intentional rounding as a memory aid/checklist
On the whole, having a checklist to act as a ‘visual reminder’ was seen as beneficial for everyone, especially when working in environments where there was likely to be constant distractions. Interviewees felt that IR checks were helpful as a memory aid to avoid things being missed and/or overlooked, although not everyone agreed that this was necessary:
. . . I think everybody probably needs documentation and structure to the thinking, to think ‘OK continence, pain, food and fluid’.
Consultant in geriatric medicine
I don’t think a lot of these things would be addressed without this document, because it’s just, it’s a visual reminder, isn’t it, to address.
Housekeeper
Rigid, scripted versus conversational style of intentional rounding
Opinion was divided on whether IR should be done in a rigid or flexible way (i.e. in terms of the specific questions asked, how frequently, and if and how it should be adapted). For example, as people became used to doing IR, they developed their own style and form of wording, rather than using a formal script:
. . . but I literally used to do everything by the book and said every single question and made sure I said ‘is there anything else that I can do?, even though most of the time people said, ‘no, no, I’m fine’.
Student nurse
Others recognised that not all IR questions would be relevant to all patients and there was a need to use a conversational style and open questions when doing IR to encourage a dialogue:
That’s a difficult one because there’s a part of you that thinks it should be done rigidly, because it’s our job to make sure that we cover all bases, but then at the same time it’s that, that relationship between nurse and patient that you don’t want it to seem like the patient can’t tell you their concern and their worries.
Trainee doctor
Mechanism: accountability (n = 19)
Although it was understood that the responsibility and accountability for IR lay with the RNs, it was not always obvious how this worked in practice. Some interviewees noticed that IR was often completed by HCAs and checked by RNs and ward managers. In one site, the IR form was changed so RNs were required to sign it every 4 hours to say that they had checked their patients themselves and to check that the day’s intentional rounds were up to date. All student nurses interviewed said that they had completed IR checks and documentation ‘to help out’.
Importance of intentional rounding documentation
There was a consensus among the ‘other health-care’ professionals that IR documentation was valued because it provided evidence of nursing care having been delivered, should that be required at a later date for responding to patient complaints and coroners’ inquests:
. . . some patients you think ‘oh they’ll be fine’, but once they go home they might complain and that’s when you want to look at IRs as well.
Ward receptionist
The majority of interviewees mentioned that nursing staff needed to provide evidence that care had been delivered in order to protect themselves in case ‘something terrible happens’:
. . . obviously to cover your back I suppose, and to make sure that you’ve got proof that they’ve been rolled if they develop a further pressure sore, or if they get moisture damage because they’ve been left incontinent, so that you’ve got documentation to show, I guess.
Student nurse
Where IR documentation was enhanced with site-specific adaptations, this was regarded as helpful of keeping track of care provided (e.g. last skin check, positioning changes, food and fluid balance).
Accuracy and completeness of documentation
A few interviewees who completed IR themselves and/or checked IR documentation reported that they had noticed gaps and realised that nurses completed it retrospectively, particularly when the ward was short-staffed:
. . . I certainly can say that I’ve filled a form in and I’ve not completed it when the times have been there. But we have just been so short-staffed . . . when the ward’s up to staff, it’s not a problem, they do get it done.
Housekeeper
A student nurse explained that they would not sign IR documentation if they had not done the round, but would put a line through the box to show that they had not done it. One consultant said that they had confidence in the accuracy and completeness of the IR documentation on the case study ward:
. . . I know on [the ward] it’s very well filled in and it’s complete. I’ve worked on a couple of other wards in the trust and it’s not always so complete, so I wouldn’t be asking on (the ward) about the quality of information because I’d know it would be correct.
Consultant
Some interviewees spoke of the dangers of IR becoming a tick-box exercise and the balance between making it feasible to do, yet sufficiently detailed to be meaningful:
. . . it is a bit of a tick-box exercise and, but, in a way, that’s the same with most documentation is you can only go on what’s been documented; I mean, technically people can write whatever they want so . . . [laughter] . . . there has to be an element of trust that what’s being written down is what’s actually being done.
Pharmacist
Tick-box completion – can be misleading if don’t know story behind the ticks.
Occupational therapist
One medical consultant spoke about the dangers of not detecting changes over a longer time period because the focus was on task completion.
Mechanism: allocated time (n = 16)
A total of 16 ‘other health-care staff’ referred to this mechanism; none thought that IR provided allocated time to care and two interviewees thought that IR would involve extra work or was ‘sometimes a hindrance’:
. . . obviously it will take them, it must take time to do the IR and make sure it’s regularly up to date . . . the actual process and documentation of itself, it might be adding to the workload if the ward’s understaffed.
Core medical trainee
Mechanism: staff communication/teamworking (n = 15)
Knowledge and understanding about the purpose of intentional rounding
All other health-care staff interviewees were able to give some explanation of what IR was, although a few interviewees admitted that they had been prompted to ask their nursing colleagues what it was having seen our research posters. Eleven interviewees were able to speak knowledgably because of their direct experience of doing IR (as a student nurse, or through previously working as a HCA). The types of IR descriptions and explanation they gave were as follows:
It’s to make sure that the patient’s OK, the call bell’s in reach if they need anything, any pain management because some people might not ask for it, positional changes, pressure relief, that’s a big one as well, people might not be able to move, it just prompts to keep on top of changes.
Student nurse
Well, it’s mainly falls and pressure areas and if you see anybody walking about in the bay, you know, should they be up? So it gives me the idea of looking on there, should they be walking about?
Ward receptionist
Others learned about it through their own observations and reflections of nursing care:
I think it’s just where the nursing staff just do regular checks to check their patients are all right, so literally just popping their heads into the room and asking them if they’re OK and if they need anything, and then continuing on to the next person.
Physiotherapist
Views on uses of intentional rounding
Intentional rounding documentation directly used by non-nursing staff
It was rare for other health-care staff to directly refer to IR documentation. In one case study site, several interviewees said that they had referred to IR documentation, but they were referring to ‘enhanced, site-specific IR add-ons’. Other health-care staff recognised that they asked patients the same IR questions, but said that they preferred to do this rather than look at IR documentation. Alternatively, they said that they would speak directly to a nurse on duty to get the information they required:
No. If we needed more information, we tend to just ask the nurses or ask the patient, quite often, or ask them if they’ve been up to the toilet and in any pain and things like that, rather than looking at the sheet.
Physiotherapist
Improved quality and frequency of nurse–patient relationships
A consultant felt that IR allowed patients to say if they needed anything when asked directly and two student nurses felt that IR helped them build rapport with their patients through regular, one-to-one interaction, but they also recognised that using IR to build rapport was unusual:
I’m quite happy with doing it and it allows me to actually build rapport with the patient, whilst I’m speaking to them, I can do the documentation; but, in practical terms, once you’re a nurse and you’re looking after patients all on your own, then it happens to be the case that it’s not such a rapport-building activity, because I don’t see any nurses interacting and filling them out really, I don’t see that happening.
Student nurse
Perceived benefits of intentional rounding for carers
Participants perceived the main advantage for carers to be that when IR documentation was visible (e.g. placed outside a patient’s room or at the end of the bed) it had the potential to reassure them that patients were being seen and regularly monitored. However, these benefits were dependent on how IR was done and, particularly, how visible the IR checks and interaction were to others:
I’ve seen nurses and HCAs filling them out . . . I’ve seen occasionally where they’ll ask questions, but most of the time when I see it they’re just looking at the patient in their bed space.
Pharmacist
. . . it tends to be quite yes and no rather than an open, more open conversation.
Occupational therapist
Unfortunately, taking this approach created problems because when it was not obvious that IR checks had been done while carers were visiting, and/or the IR documentation was not up to date, this led to worries and complaints to other health-care staff, for instance:
. . . yesterday a patient’s friend looked at the chart and was quite worried because, according to the chart, the patient hadn’t had anything to eat or drink for quite a few hours, so then that made the relative worried . . . they mentioned it to the staff on the ward and they mentioned it to me and I think they were told by the staff that the chart may have been incomplete, so they, the patient probably did have something to eat or drink but it was just, it looked like it may not have been filled on the chart.
Core medical trainee
Mechanism: anticipation (n = 4)
A few interviewees were familiar with the theory that IR led to a more efficient use of nursing resources by pre-empting problems, (e.g. preventing incontinence or dehydration). Some interviewees also thought that IR might lead to nurses referring high-risk patients on for further interventions:
. . . nurse can get dietitian involved if they see patient not eating or drinking enough.
Dietitian
Mechanism: patient empowerment (n = 4)
There was virtually no support that this mechanism played a role in IR, although two interviewees said that they had been asked by patients about IR or had seen patients completing a food–fluid chart (an IR add-on at one site).
General contexts and outcomes
General contexts
Other health-care staff spoke about the general contexts that they felt influenced IR. Most usually, they mentioned the success of IR being influenced by wider infrastructure of organisation, for example being short staffed, winter pressures, patients who require closer attention:
. . . at the moment we’re short [staffed] again because they’ve potentially tried to deprive us of nurses, but because we’ve had to work more beds due to winter pressures, the nurses have been pushed across the organisation and the numbers are swollen. So I expect they’re struggling at the moment doing IR.
Consultant in geriatric medicine
There was a lack of awareness in multidisciplinary teams of IR generally, and, for those who had experience of doing IR, a lack of guidance, leading to confusion on how it should be done:
I think it would be really useful to understand how nurses are meant to be doing their rounds . . . sometimes we don’t know how other professions operate and it’s really important.
Junior doctor
General outcomes
Given this lack of general awareness of IR, other health-care staff guessed what the intended outcomes of IR might be. These included improvements in patient safety and care (i.e. reductions in dehydration, falls, toileting accidents, incontinence, and monitoring pain, skin integrity, mood and well-being) and a better patient experience because it shows patients that you’re really thinking about them. They thought that IR would be good for less cognitively able patients who would not necessarily press the call bell and actively seek help.
One doctor reflected that:
I don’t know. I would say that, over the course of the last 10 years or so, I think the nurses have got better in this particular environment, in this particular ward at things like the MDT [multidisciplinary team]. So, for example, when I ask ‘is she eating?’, ‘is she confused?’, ‘is she continent?’, I do get better answers these days. I’m not sure that’s down to, necessarily, IR; I couldn’t say.
Consultant geriatric medicine
Summary
-
The understanding of IR in this sample of interviewees was mixed, because although some had had direct experience of doing IR, others had learned about it only through their own observations of nursing care.
-
It was rare for other health-care staff to directly refer to IR documentation. Although some health-care staff realised that they ask patients similar questions, it was more usual for other health-care staff to find a nurse on duty to speak to.
-
Other health-care staff recognised the dilemma between having a structure that was used in a standardised and formal way for everyone verses the need for flexibility to adapt to suit patient need.
-
Other health-care professionals saw the value of having documented evidence of nursing care having been delivered.
Observations of intentional rounding (nurse shadowing and non-participant observation of direct patient care)
This section addresses objectives 2 and 6, utilising non-participant observation to highlight how IR had been implemented on the ground, exploring its contribution to the delivery of patient care as a whole and how it fitted alongside other approaches to improving quality and safety.
Method
Two approaches to non-participant observation were conducted:
-
’Shadowing’ nursing staff to explore how they interacted with patients and each other in relation to IR, and how IR contributed to the way they worked. Nursing staff were purposively sampled to attain a range of grades and levels of experience. All participants provided informed consent and researchers took narrative field notes of what they observed. These narrative field notes of nursing staff observations were then used to complete two protocols, one to record individual IR interactions and the other to assess fidelity to the original IR intervention, as set out by the Studer Group.
-
‘Shadowing’ patients to observe individual interactions between patients and nurses. To facilitate this, the researchers undertook a Quality Patient Care Scale (Qualpacs) for five patients in each ward. Qualpacs65 is an established instrument for assessing the quality of care a patient receives from a nurse, using 68 items across the following areas of care: physical, general, psychosocial, communication and professional implications. The instrument is patient focused, with observations based on who attends a patient’s bedside to provide care and how frequently. 66 The observer(s) watched the care received by selected patients over a 2–4 hour period and rated each aspect of this care on a scale of 1 (poorest care) to 5 (best care). 66,67 To complete the Qualpacs observations, researchers (who were both RNs) had access to patients’ nursing care plans and notes to assess how the care delivered addressed a patient’s individual plan for nursing care. In sites 1 and 2, two observers scored independently and met to discuss and agree scores. In site 3, owing to staff changes, one observer conducted the Qualpacs observations.
Researchers planned to observe up to 100 individual IR interactions between the patient and nurse and interactions between nurses on each ward using these various methods. In all observations, the researcher recorded how often interactions occurred, what patients were asked during their interactions, what care was provided and, when possible, the duration of each individual interaction. External factors that affected the delivery of IR were also recorded to help establish how the intervention fitted within the whole nurse experience of the delivery of care and the whole patient experience of receiving care. Researchers made as few interruptions as possible when shadowing nursing staff and refrained from asking questions. The observation data entered into the ‘fidelity to original intervention’ protocol were analysed using descriptive statistics. The data entered into the ‘individual IR interactions’ protocol and the Qualpacs descriptions of interactions were thematically analysed using the coding framework developed to analyse the individual staff interview data, which covered the contexts, mechanisms and associated outcomes of IR and how these were linked.
Participant characteristics
A total of 188 hours of care delivery was observed by four research staff. Observations were undertaken throughout the day and evening shifts (ranging between 07.00 and 01.15) on both weekdays and weekends. Thirty-nine nursing staff were ‘shadowed’ during this time, with researchers following them for several hours at a time and recording how they interacted with patients and each other in relation to IR. Table 16 highlights the participant characteristics of those staff who were shadowed, in terms of their profession/role.
| Profession/role | Number of observations |
|---|---|
| Sister/junior sister | 3 |
| RN | 24 |
| HCA | 10 |
| Assistant practitioner/trainee assistant practitioner | 2 |
For the Qualpacs observations, researchers observed direct patient care from the perspective of 28 patients. They did this by sitting unobtrusively near each patient’s bedside and recording the time and the nature of the interactions they had with nursing staff (interactions with non-nursing were noted but not scored in the Qualpacs analysis) over 2–4 hours. A Qualpacs (see Report Supplementary Material 2) was completed for each patient to assess the quality of care they received; average care is assessed as the quality of care expected to be delivered by a newly registered nurse, and given a score of 3.
Findings
Mechanism: allocated time
Range of tasks
Staff were very busy and were seen to carry out a wide range of tasks including technical clinical care (e.g. medication administration, i.v. medication, dressings, cannula insertion), assessments (e.g. manual handling, nutrition, pressure areas), personal care (e.g. helping patients to wash/shower, clean teeth, go to the toilet; feeding patients) and administration (e.g. ward rounds, taking telephone calls, updating senior staff on bed availability/transfers, handovers). Some tasks were scheduled at routine times (e.g. drug rounds, washing patients) whereas others were performed as needed.
Staff were undertaking many tasks in addition to intentional rounding
Intentional rounding was sometimes a stand-alone activity, but staff often multitasked and combined IR with other activities:
-
RNs sometimes completed IR as they did drug rounds, focusing on aspects that may require adjustments to medication, such as pain or whether or not patients had opened their bowels.
-
Inspecting pressure areas when helping patients wash or moving and turning them.
-
Checking pain level and food and fluid intake when doing observations (e.g. blood pressure, measuring blood sugar).
-
Distributing meals and taking note (mentally and written) of what patients were given.
-
Removing cannulas, and recording this on the medical devices adaption on the IR form.
-
Making and answering telephone calls.
-
Responding to patient and carer queries.
Staff were frequently interrupted by patients, carers and other health-care staff, and sometimes nurses interrupted themselves (e.g. to check a call bell, answer the telephone or to find someone to help them with a patient). Particularly in site 1, where IR was hourly, staff were observed retrospectively documenting rounds or catching up. This suggests that nurses did not have sufficient time to do IR as they were having to prioritise other activities. In addition, some patients needed additional care beyond the expected allocation of time. Sometimes staff spent a lot of time with certain patients to meet their needs for clinical care and/or reassurance.
Mechanism: visibility
Intentional rounding was not observed to make a difference on the extent to which nurses were seen as having a presence or being visible to patients and ward layout had a bigger influence. In wards with bays or a Nightingale layout, patients were seen to speak to nurses/ask for things because they could see them. Nurses were also seen to act responsively and intervene/help patients because they could see help was needed. In wards with a large number of single rooms, nurses were less visible to patients and other staff. IR was not observed to increase the frequency of direct interaction between patients and nurses as nurses were with patients or were visible to them for a variety of purposes far more often than the IR was completed.
Mechanism: consistency and comprehensiveness
Considerable variation in the practice of IR, in relation to its consistency, comprehensiveness and the documentation of rounds, was observed. However, it remains challenging to distinguish between the types of variation and the reasons for differences in practice, and, in particular, whether variations were attributable to deliberate patient-centred flexibility or to different interpretations of what was expected. It is also apparent that some variations seemed to be influenced by different degrees of staff buy-in or to contextual factors such as staff shortage or lack of time. Relevant observations are grouped under a series of headings, as follows.
Intentional rounding embedded into routine practice
In some cases, there was little or no evidence of a standardised or scripted round, as nurses engaged informally with patients as they assisted with tasks such as repositioning without any evidence of a linear or structured way of asking questions of the patient. The nurse would then complete the IR form while engaging with the patient. Staff were sometimes observed delivering comprehensive care to patients. For example, for one particular patient, care delivered, which included detailed assessments and completion of IR, took 45 minutes.
Intentional rounding as a system for ‘checking’ on patients
Staff were observed to check on patients during their rounds, asking them both general questions and more specific questions. Although this checking seemed mainly positive, there was one instance in which a HCA seemed so focused on checking specific aspects of the IR documentation that she did not react to other concerns raised by a patient. There was also evidence that staff used IR as a mental checklist for all the different tasks that they needed to undertake with every patient. Although this may ensure that nothing was missed, occasionally this checklist made some staff appear particularly task orientated in their approach.
Flexibility and variation in the style and content of rounds
Across all case study sites, staff demonstrated a flexible approach to how IR was delivered and a scripted approach to IR was never used. For more details of how staff used flexibility and variation in the style and content of their rounds, see Chapter 8, Fidelity to the original intervention.
Flexibility around frequency of rounds
At case study site 1, less flexibility was observed around how often IR was undertaken, as it was usually conducted hourly. In case study site 2, staff were instructed to undertake IR every time they went into a patient’s room rather than at specific timed intervals. This might explain why we observed differences in the regularity with which IR documentation was completed for different patients at case study site 2 and why there was some confusion in case study site 2 as to how often IR was supposed to be conducted. Some staff recorded the actual time of rounds whereas others recorded the time the round was supposed to take place, notwithstanding that every patient could not be seen at the same time. Some staff at this site also appeared to worry that they were not undertaking IR as often as they should.
Consistency/inconsistency of documentation
The IR documentation was comprehensive with all the elements of IR (as described by the Studer Group) included in the form. All documentation had site-specific IR additions; thus, they were more comprehensive than IR. However, this structured, comprehensive approach was not observed to be consistently delivered.
Different pattern of rounding at night
Regular checks continued during night shifts. On the whole, IR documentation was observed to be completed sensitively and proportionately during the night. No patients were observed to be woken up to do IR, although staff regularly walked around the ward areas observing patients. In the Nightingale ward in site 3, one HCA sat at the far end of the ward to keep an eye on patients. An assistant practitioner said that IR was difficult at night as they needed to watch patients who were at a high risk of falls so they do a very quick walk around the ward to check everyone else and may not be able to document IR at the time.
Temporary staff
Few temporary staff were seen working on the ward areas, and permanent staff sometimes covered unfilled shifts. One bank nurse was seen completing IR without talking to the patient, so there was no indication that IR was helping her provide care on this occasion. However, it was not clear whether or not she knew the IR policy.
Mechanism: staff communication/teamworking
Good teamworking as important for successful intentional rounding
There was some evidence of teamworking among staff when delivering IR. For example, at case study site 2, staff were allocated a certain number of patient rooms each day and focused their time on the patients in these rooms. However, when other staff were busy, a HCA was observed to attend a patient to whom she was not allocated, assisting him to use the bedpan and then completing his IR documentation. There was also evidence of teamwork when staff shared out the different components of IR between themselves. However, occasionally this made IR difficult to observe (and perhaps more complex to undertake), as it was sometimes difficult to distinguish who was completing what parts of the documentation, for whom and why. This also sometimes led to errors being made, such as IR documentation not being completed for some patients, or a duplication of effort by nursing staff.
Lack of evidence of beneficial impact on team communication/teamwork
In other instances, IR was not observed to be particularly beneficial for team communication/teamworking. Nursing staff working together were seen catching up/updating each other at regular intervals during shifts but IR was rarely seen to be mentioned. This tended to be focused on progress with patient care tasks rather than IR, although updating each other on a patient’s condition was sometimes observed. All sites had a form of bedside handover, but IR was rarely discussed at this handover between shifts. When IR was discussed in relation to managing work, it often appeared to be seen as a task (e.g. how to allocate rounds between staff). In one instance, a staff nurse and HCA were talking about what they needed to do next and the HCA stated that he had ‘done all the ticks’.
Sharing aspects of intentional rounding
Some aspects of the IR form were completed by different members of staff (e.g. the RN would ask about pain during the drug round, and the HCA would complete the pressure area parts of the form after helping a patient wash and complete the food and fluid parts of the form after meals). How this was agreed was not observed, although there was some indication that this evolved over a period of working together. In most wards, unqualified staff were observed to complete a large proportion of the IR forms. On one ward, which was more acute and had a higher skill mix, IR was seen as predominantly a RN task. On this ward, one HCA told the observer that she would fill in the IR chart/skin bundle chart if she had time and knew the patient.
Lack of evidence of intentional rounding as a supervisory or management tool
There was little evidence of IR and its documentation being used as a supervisory/management tool for RNs to check on the work that unqualified staff had done, although during informal conversations with staff, some RNs said that they did use it in this way.
Intentional rounding and other members of the health-care team
Intentional rounding documentation was occasionally observed to be looked at by other members of the multidisciplinary team (e.g. consultants). However, on one occasion, it was the additional food and fluid part of the form that was referred to and not the IR intervention as defined by the Studer Group. IR was never observed to be completed by anyone other than the nursing team.
Mechanism: nurse–patient communication and relationships
Nurse–patient communication during rounds
Nursing staff and patients were observed to talk to each other often. The majority of interactions were not observed to be part of an intentional round, although it is possible that any information discussed/observed by nurses may contribute in some way to completing IR documentation. Some interactions, although not all, were very short, sometimes just passing comments as nurses were working in the bays. Patients were often seen to start conversations/make requests when nurses were in the vicinity, but opportunities for ad hoc conversation were fewer for patients in single rooms. Longer conversations between nurses and patients were infrequent, but were observed (not as part of IR). However, communication was also observed during IRs. Regardless of ward layout, nursing staff in all settings were seen to communicate with patients during IR.
Sometimes the focus was on the content of the round and communication was very short, with nurses asking if the patient was OK or had any pain. Longer conversations tended to occur when patients were having a wash or other procedure (e.g. dressings, putting up i.v. lines, feeding). During these times, some staff were observed having general social conversations or chats with patients about their carers, pets or plans for the weekend; during other times, staff were observed to be less chatty or focused on patients’ health needs/conditions. In some instances, no specific IR questions were asked and the interaction was more akin to a general conversation, but pertinent aspects of IR were assessed. Nursing care frequently focused on addressing physical needs (e.g. helping patients to wash or to go to the toilet, giving medications, feeding and undertaking observations). Nursing staff were rarely seen to address psychological care needs (e.g. talk about patients’ concerns and anxieties, providing information about treatment plans and conduct detailed assessment of a patient’s nursing needs). On one occasion, a patient was observed to be very distressed about a cancelled operation. During an interaction with a student nurse, the opportunity to talk to the patient about this was missed and the completion of IR, which apparently took precedence, seemed unhelpful at this time.
Doing intentional rounding without including patients
On a number of occasions, nursing staff were observed to complete the IR documentation when patients were asleep or when patients were not at their bedside:
Some staff were even observed to complete the IR documentation without communicating with patients who were awake and next to them. Furthermore, on one occasion, a HCA was observed to complete IR documentation after asking another member of staff the question, rather than the patient themselves:
[HCA] is outside bed [X] and next to the domestic. She asks the domestic ‘did she drink her cup of tea?’ and the domestic says yes. [HCA] completes the fluid balance for this patient.
Not all patients want to communicate with staff during rounds
Some patients did not appear to want to communicate with nursing staff as they undertook their rounds, perhaps because they were making a telephone call or watching television. Occasionally, patients were unpleasant to nursing staff, making communication difficult. One patient was observed to be sexually inappropriate in their conversation, to which the nurse skilfully and kindly redirected the conversation. In a ward caring for older people, some of the more confused patients were also aggressive when nurses were delivering fundamental care.
Nurse–carer communication
Staff were less frequently observed to interact with carers during IR, mainly because carers were often not present. However, when they were present, carers were observed asking staff questions and staff tried to answer any queries they had. On one ward with a large number of single rooms, the ward manager stated that staff were sometimes reluctant to go into patient rooms when carers were there and that she had had to tell them that they must.
Mechanism: anticipation
Evidence of anticipating patient needs
There was some evidence that nursing staff were anticipating patient needs, but it was difficult to say if this was due to IR. There were occasions when patients were observed to press their call bell shortly after an intentional round had been conducted (e.g. to go to the toilet). However, in one instance when this was observed it is not known if IR would have anticipated this need as the HCA did not ask the patient if he needed to go to the toilet. There was some evidence that nursing staff were anticipating patients’ needs for water, as some would top up patients’ glasses without being asked. On one occasion, a RN was observed to anticipate a patient’s future need for pain relief, although this was likely to be because she was doing the drug round, rather than IR. Call bells were often observed to be placed where patients could reach them, especially at site 2, which had a high proportion of single rooms. One member of staff was concerned that a patient did not know how to use the call bell, despite it being explained.
On site 2, there were no apparent guidelines about how often IR should be done. Staff were told to complete IR every time they went into a patient’s room/bed area, so this did not change practice and staff saw patients when they had something else to do for them. Staff were sometimes heard telling patients that they would see them later, but a time for this was never specified, which limited the anticipation mechanism. Nurses often told patients to let them know or to press the buzzer if they needed anything. Observations demonstrated little other evidence of the anticipation mechanism in action. As previously stated, staff never told patients a specific time that they would return. Instead, staff were regularly observed to tell their patients to call them or to use the call bell if they needed anything. In one example, when there had been no use of call bells on a particular morning, the HCA and nurse agreed that this was because there was always a clinical staff member in the bay.
Mechanism: accountability
Accuracy of documentation
The potential for IR to contribute for accountability in relation to care was observed to be somewhat constrained by the ways in which IR was documented. The completion of IR documentation was observed, but it was rare that all the components of IR were done, although most of the time they were documented as being done. Sometimes staff would put a dash for an item that was not asked/assessed at the time of documentation. Sometimes staff completed the documentation without asking any of the questions. Sometimes documentation was incomplete or filled in for only some of the times for which rounding was supposed to have taken place.
Completion of aspects of intentional rounding, but without documentation
On occasion, staff delivered what looked like components of IR but did not complete the IR documentation. This was more common in case study site 3, where clear examples of IR were very difficult to observe. Staff were often seen to incorporate aspects of IR into their general interactions with patients (e.g. ensuring that patients were comfortable, asking them about their eating and drinking, ensuring that they could reach everything they needed), but not documenting this as IR, so care was sometimes delivered to patients and nursing staff talked to patients and checked if they needed anything, but IR was not documented.
Sometimes nurses attended to patients’ needs, such as providing water, or moving possessions within reach, but this was not recorded. It is not clear in such instances if the interaction was seen as part of an intentional round or, possibly, seen as part of some other interaction such as a medicine round, or simply as an unstructured interaction with patients to meet their needs as they arose. Staff were aware of the issue of not completing documentation. During an observation session, the observer asked the RN about the issue with documentation and was told that time was a big issue; staff do not have the time to document rounds and there are constant interruptions and other demands. The staff member realised that this was not ideal but ‘patients come first’.
There were a number of instances observed when IR documentation was complete and up-to-date. However, some errors in the IR documentation were identified, for example in relation to the risk of falls.
Retrospective and prospective completion of intentional rounding documentation
On one ward in site 3, a RN told the observer that she rarely had time to complete IR during the shift so she usually completed it retrospectively at the end of the shift. Staff were observed both retrospectively and prospectively completing IR documentation. Examples included:
The HCA asked the patient about their food: ‘I weren’t on this morning and no one’s filled it in’ (the IR chart) she says to the patient. She asked for details about what the patient ate for breakfast and lunch and fills in the chart.
[Nurse] moved on to the next patient’s room and picked up the notes from outside the room. She flicked through and started filling in the IR form outside the room. She told the observer she likes to look at and complete the IR form just before she goes in; otherwise, she says ‘you get a barrage of questions’ and it disturbs her completion of it.
At case study site 2, where IR documentation tended to be kept outside the patients’ private room, some staff were observed to complete the IR documentation just before they entered the room to undertake the round. Frequently, nursing staff were observed to complete several time slots in one go. This occurred more often with hourly IR and where times were specified on the form (i.e. 08.00, 09.00, 10.00, 11.00) rather than have a space to write the actual time.
Completing intentional rounding documentation without asking the questions
Staff were additionally observed to complete sections of the IR documentation without asking the questions, or asking a general ‘everything alright?’ and then completing all of the boxes from there. For example, an observer noted that all of their boxes had been completed on the front page of the IR chart, even though the patient was asked only about her food and drink. In another instance, the HCA asked the patient if everything was all right and then completed the form to indicate ‘8am. Drink ‘Y’, Toilet ‘N’, Pain ‘Y’, Anything else ‘N’.
In other instances, staff were observed to complete charts at the end of their shift, sometimes ticking to indicate that checks had been done, but sometimes marking ‘not seen’ if that was the case. One observer, in conversation with a staff nurse in a site where patients were looked after in side rooms, noted that the nurse explained that when she began her shift she would complete the IR forms for the eight patients she was looking after first but would insert ‘N’ or ‘/’ if it had not been checked (e.g. something like a pressure sore, which will probably be checked by HCAs during the washes and can be completed then). The reason for doing all the IR forms immediately was because it looked ‘nicer’ having the chart filled in first thing in the morning and she did not want it to appear that a patient has been neglected if left until 9/10 a.m. when the medication round was completed and washes began.
Complaints handling and evidence of care
On one occasion, the influence of IR in handling a complaint was observed. A matron came in and started to ask a nurse about a patient complaint. The family had complained that care had not been delivered and the matron had looked at the IR chart and found it to be empty. The nurse was visibly concerned and could not remember the patient. She told the observer it may have been the day when the ward was very short staffed and she had 16 patients to look after. On another occasion, the observer spoke to a band 6 RN about the use of IR as evidence and the nurse said that IR was important as evidence to demonstrate care had been delivered. She placed this in the context of carers complaining a lot and making assumptions that people were not doing their job properly, not just nurses but doctors as well. IR enabled staff to demonstrate that they have done their jobs.
Lack of auditing of intentional rounding documentation
No evidence of auditing IR was seen by the observers.
Mechanism: patient empowerment
Observers noted that patient empowerment would be difficult to observe. Although patients and carers were observed asking questions or asking for specific things (e.g. drinks, or to go to the toilet) there was little evidence of patients asking for more than the usual care that nurses were providing anyway. Overall, there was little evidence of patients being empowered by IR, although on one occasion, a nurse was asking a patient about their pain during IR and this seemed to assist the patient in asking about his other needs. Both patients and their carers were observed to ask nursing staff questions and queries throughout the day, calling them over as and when required, rather than waiting until rounds took place.
Non-participant observation of direct patient care and staff interactions with patients (Qualpacs)
Although researchers had previous experience of using Qualpacs, they found it to be a challenging tool to use in this study. Qualpacs relied on assessing whether or not the care observed addressed the patients’ needs as planned in their nursing care plans (the research team did not have access to the medical notes). However, the nursing documentation for all the observed patients was standardised nursing care plans, none of which had been personalised for the patient and no additional care plans had been written. So researchers were unclear of what nursing care should be delivered to each patient and whether or not the care observed met a patient’s individualised needs. Researchers made assessments on the appropriateness of care, which may not be accurate; this is a limitation of the study. As a result, there were concerns about the validity of the Qualpacs scores as a measure of the quality of nursing care. Therefore, these scores have not been reported. However, as part of the Qualpacs methodology, the start time of each interaction between patients and health-care staff and a description of each interaction was recorded (Table 17).
| Number of interactions by RNs | Number of interactions by unregistered staff | |
|---|---|---|
| Site 1 | ||
| Ward a: older people | ||
| Observation session 1 | 1 | 3 |
| Observation session 2 | 4 | 4 |
| Observation session 3 | 4 | 9 |
| Observation session 4 | 4 | 4 |
| Observation session 5 | 5 | 5 |
| Ward b: acute | ||
| Observation session 1 | 6 | 7 |
| Observation session 2 | 5 | 3 |
| Observation session 3 | 2 | 0 |
| Observation session 4 | 4 | 10 |
| Observation session 5 | 2 | 0 |
| Site 2 | ||
| Ward a: acute | ||
| Observation session 1 | 2 | 4 |
| Observation session 2 | 2 | 3 |
| Observation session 3 | 2 | 5 |
| Observation session 4 | 4 | 1 |
| Observation session 5 | 2 | 5 |
| Ward b: older people | ||
| Observation session 1 | 4 | 3 |
| Observation session 2 | 3 | 4 |
| Observation session 3 | 3 | 2 |
| Observation session 4 | 5 | 5 |
| Observation session 5 | 3 | 4 |
| Site 3 | ||
| Ward a: acute | ||
| Observation session 1 | 9 | 1 |
| Observation session 2 | 4 | 1 |
| Observation session 3 | 6 | 1 |
| Observation session 4 | 10 | 8 |
| Ward b: older people | ||
| Observation session 1 | 4 | 7 |
| Observation session 2 | 2 | 10 |
| Observation session 3 | 7 | 8 |
| Observation session 4 | 2 | 5 |
Researchers recorded the time intervals between every interaction (Table 18). Patients were seen frequently by staff: between every 12.5 and 16.8 minutes by any member of hospital staff, between every 16.5 and 22.9 minutes by any member of nursing staff and between every 28.0 and 49.8 minutes by a RN.
| Participants | Duration of observation (minutes) | Time interval between interactions between patients and all staff members (minutes) | Time interval between interactions between patients and all nursing staff members (minutes) | Time interval between interactions between patients and RNs (minutes) | |||
|---|---|---|---|---|---|---|---|
| Range | Mean | Range | Mean | Range | Mean | ||
| Site 1 | |||||||
| Ward a: older people | |||||||
| Patient 1 | 120 | 2–40 | 9.2 | 2–40 | 9.2 | 12–60 | 24 |
| Patient 2 | 150 | 0–88 | 30 | 0–88 | 30 | 20–130 | 75 |
| Patient 3 | 150 | 1–39 | 13.6 | 1–55 | 18.8 | 5–73 | 30 |
| Patient 4 | 180 | 0–38 | 13.8 | 3–54 | 22.5 | 3–105 | 45 |
| Patient 5 | 180 | 2–50 | 13.8 | 5–70 | 22.5 | 9–92 | 45 |
| Total | 780 | 0–88 | 16.08 | 0–88 | 20.6 | 3–130 | 43.8 |
| Ward b: acute | |||||||
| Patient 1 | 150 | 0–69 | 15 | 0–69 | 16.7 | 1–84 | 25 |
| Patient 2 | 120 | 0–56 | 12 | 0–56 | 12 | 5–96 | 30 |
| Patient 3 | 180 | 0–40 | 11.3 | 0–40 | 11.3 | 0–130 | 20 |
| Patient 4 | 150 | 13–72 | 37.5 | 31–72 | 50 | 31–72 | 50 |
| Patient 5 | 150 | 3–50 | 25 | 3–50 | 25 | 3–50 | 25 |
| Total | 750 | 0–72 | 12.5 | 0–72 | 23 | 0–130 | 30 |
| Site total | 1530 | 0–88 | 14.29 | 0–88 | 21.8 | 0–130 | 36.9 |
| Site 2 | |||||||
| Ward a: acute | |||||||
| Patient 1 | 120 | 0–35 | 13.3 | 0–35 | 13.3 | 4–43 | 20 |
| Patient 2 | 150 | 1–30 | 13.6 | 1–39 | 18.8 | 1–89 | 37.5 |
| Patient 3 | 120 | 0–37 | 17.1 | 0–44 | 20.0 | 5–63 | 30 |
| Patient 4 | 150 | 0–37 | 10.7 | 0–37 | 11.5 | 1–47 | 21.4 |
| Patient 5 | 150 | 0–31 | 10.0 | 1–45 | 18.8 | 10–60 | 37.5 |
| Total | 690 | 0–37 | 12.94 | 0–45 | 16.48 | 1–89 | 29.28 |
| Ward b: older people | |||||||
| Patient 1 | 120 | 0–35 | 15.0 | 0–68 | 20.0 | 0–69 | 24.0 |
| Patient 2 | 150 | 0–28 | 10.7 | 0–38 | 15.0 | 0–62 | 30.0 |
| Patient 3 | 150 | 0–33 | 10.7 | 1–43 | 21.4 | 24–102 | 50.0 |
| Patient 4 | 150 | 1–39 | 13.6 | 5–41 | 21.4 | 46–52 | 37.5 |
| Patient 5 | 150 | 0–39 | 11.5 | 3–39 | 15.0 | 30–120 | 75.0 |
| Total | 720 | 0–39 | 12.3 | 0–68 | 18.56 | 0–120 | 43.3 |
| Site total | 1410 | 0–39 | 12.62 | 0–68 | 17.52 | 0–120 | 36.29 |
| Site 3 | |||||||
| Ward a: acute | |||||||
| Patient 1 | 180 | 0–71 | 22.5 | 0–71 | 30.0 | 0–87 | 36.0 |
| Patient 2 | 180 | 0–47 | 12.9 | 0–53 | 16.4 | 0–53 | 18.0 |
| Patient 3 | 215 | 2–43 | 19.5 | 5–83 | 30.7 | 5–116 | 35.8 |
| Patient 4 | 245 | 1–30 | 12.25 | 1–48 | 14.4 | 1–109 | 22.3 |
| Total | 820 | 0–71 | 16.79 | 0–83 | 22.88 | 0–113 | 28.03 |
| Ward b: older people | |||||||
| Patient 1 | 215 | 1–61 | 17.9 | 1–61 | 17.9 | 6–72 | 43.0 |
| Patient 2 | 180 | 2–35 | 18.0 | 2–35 | 18.0 | 35–108 | 60.0 |
| Patient 3 | 250 | 0–41 | 13.2 | 0–60 | 17.9 | 34–131 | 62.5 |
| Patient 4 | 270 | 0–29 | 11.25 | 3–35 | 15.0 | 10–65 | 33.75 |
| Total | 915 | 0–61 | 15.09 | 0–61 | 17.2 | 6–131 | 49.81 |
| Site total | 1735 | 0–71 | 15.94 | 0–83 | 20.04 | 0–131 | 38.92 |
Summary
-
Staff were observed to be very busy and to carry out a wide range of tasks. IR was usually combined with other activities and staff were frequently interrupted when undertaking IR, which meant that they were observed to document IR retrospectively. On occasion, staff delivered what looked like IR but did not complete IR documentation.
-
Considerable variation in the practice of IR in relation to its consistency and comprehensiveness was observed. Across all sites, staff demonstrated a flexible approach to how IR was delivered and a scripted approach to IR was never used.
-
Intentional rounding was never observed to be completed by anyone other than nursing staff (RNs and HCAs); non-nursing staff rarely looked at it.
-
Nursing staff and patients were observed to talk to each other often, although the majority of interactions were not observed to be part of an intentional round.
-
There was some evidence that nursing staff were anticipating patient needs, but it was difficult to say if this was due to IR.
-
Intentional rounding was not observed to make any difference to nurse visibility or patient empowerment.
-
On average, patients have a direct interaction with a member of hospital staff (e.g. a member of medical staff, nursing staff, AHP staff, housekeeping staff, phlebotomist) every 12.62 to 15.94 minutes.
-
On average, patients have a direct interaction with a member of nursing staff (e.g. RN, HCA, student nurse) every 17.52 to 21.8 minutes, which is considerably more frequent than the recommended frequency of IR.
-
On average, patients have a direct interaction with a member of registered nursing staff (e.g. staff nurse, ward manager, clinical nurse specialist) every 36.29 to 38.92 minutes, which is considerably more frequent than the recommended frequency of IR.
-
Although there is similarity between the time intervals of direct interactions with all staff and all nursing staff between acute wards and care of older people wards, there is a marked difference in the time intervals of interactions with RNs. Patients in acute wards have a direct interaction with a RN, on average, every 29.03 to 30 minutes, whereas the average is every 43.30 to 49.81 minutes for patients on care of older people wards. The reasons for this are unclear; there are no obvious trends in nursing establishment and skill-mix data, as presented in Appendix 5.
Chapter 7 Patient and carer perspectives of intentional rounding
This chapter addresses objective 4, by exploring patients’ and carers’ experiences and perceptions of how IR influences their experiences of care.
Method
On each ward, individual qualitative interviews were conducted with up to five patients and five family carers. Researchers were guided by the nurse in charge of the ward about which patients and carers were appropriate to invite to take part. All participants gave informed consent and all interviews were audio-recorded and transcribed, unless the interviewee requested otherwise.
It was anticipated that patients and their carers might not be explicitly aware of the term ‘intentional rounding’; when this occurred, the interviewer asked about ‘hourly nursing rounds’ or about the regular contact that the patient or their carer had with nursing staff. Individual interviews were transcribed and analysed using framework analysis64 to identify themes in the data and to test and refine the causal explanations expressed as the CMO configurations identified in phase 1.
Perspectives of patients and carers
Participant characteristics
A total of 34 patients and 28 carers participated in semistructured interviews (see Appendices 14 and 15). A further 19 patients and 12 carers were approached but declined to participate in an interview. Interviews were mostly conducted with one person, but in two instances one patient was interviewed alongside two carers, and in one instance two carers were interviewed together. Table 19 highlights the number and type of interviews undertaken at each site.
| Site | Number of interviews | Number of people interviewed | Number of patients interviewed | Number of carers interviewed |
|---|---|---|---|---|
| 1 | 18 | 20 | 12 | 8 |
| 2 | 22 | 25 | 13 | 12 |
| 3 | 17 | 17 | 9 | 8 |
| Total | 57 | 62 | 34 | 28 |
Interpreting data from patients and carers
Before presenting the findings from the patient and carer interviews, a few cautionary notes should be made. Interviews with patients and carers provided a range of useful observations about daily care. Some people made astute observations and had practical suggestions for how services could be improved. The interviews also provided a reality-check on how nursing practices and ward regimes were experienced by patients and those close to them. Generally, similar themes emerged across interviews, with differences possibly reflecting the diversity at each site in terms of how IR had been implemented and other factors such as ward layout. However, there were a number of factors that require caution in the interpretation of data from patients and carers. First, half of the wards selected for observation and interviews were care of the elderly wards. Many patients on those wards were frail and/or had cognitive difficulties, as indeed did some of the patients on general medical wards. For some patients, and some carers, cognitive difficulties and other personal challenges appeared to affect their ability to understand questions or to stay on the topic. Second, patients and carers often made comments of a general nature, or answered questions with simple affirmative or negative responses, without giving sufficient details to enable researchers to put a high level of confidence in their recall. Sometimes patients agreed with what they believed to be the point of the question, for example simply answering ‘yes’ to a question about nurse visibility, or whether they could communicate with them. In those cases, it was difficult to assess the patient’s level of insight or understanding.
Third, there were sometimes contradictory statements in an interview, or some ambiguity about which staff patients had seen and how often. Many patients were unsure of the professional identity or designation of staff, so they did not always understand whether or not a particular person’s presence at their bedside was part of regular rounding or for some other purpose. Nor did patients necessarily make a distinction between nurses, doctors and other health-care professionals. Fourth, patients and carers were not always clear on what had happened on their current admission or what had taken place on previous admissions (or on previous wards in this admission), or indeed what had happened to someone else. Fifth, the overwhelming majority of patients and carers did not recall an explanation of IR (by that or any other name). Although there is room for argument on how much a lack of appreciation of IR by patients or carers affects its implementation, it may well affect the recognition or perception of IR. Linked to this point is the difficulty of understanding whether or not comments from patients and carers reflected the practice of IR and any of its associated mechanisms, or lack thereof. Patients and carers were often eloquent and perceptive about the quality of care that they perceived, but it was often difficult or impossible to know whether or not, or to what extent, the care they described had taken place in an IR context.
Finally, in view of the above, it is not surprising that patients and carers had explicit views on a limited number of mechanisms, and a few contexts. Outcomes were sometimes implicit but rarely explicit. Unsurprisingly, patients and carers did not perceive what went on around them in terms of mechanisms, although they were sometimes quite tuned in to the contexts within which care was being delivered. When it had seemed reasonably safe to infer that comments were relevant to the mechanisms, contexts and outcomes reported in other parts of this report, this was done. However, in order to make the most of patient/carer information, it is also necessary and reasonable to take careful note of their broader comments on care in general, while being cautious about how this relates to the mechanisms, contexts and outcomes of IR.
Findings
Mechanism: accountability (n = 0)
This mechanism was not evident, as such, to patients and carers, although one carer noted confidence as an outcome of seeing that nurses took responsibility and knew what they were doing. Another commented on ‘red tape’ as contextual, saying:
I know they’ve got an awful lot of paperwork, sometimes you wonder if it’s too much but, you know, it’s like anything, isn’t it, maybe some of it is red tape, maybe some of it is to cover themselves, some of it is obviously because they need information and they need to pass it on to other people.
Carer
Mechanism: consistency and comprehensiveness (n = 48)
Many patients and carers made comments about consistency and comprehensiveness in their care. Some 25 comments were made about consistent monitoring, but 17 comments were made about variations in the frequency and practice of nurses coming to the bedside, for example:
. . . it’s almost like a glance, rather than a look, so it’s just ‘Oh, that’s OK, let’s go, don’t have to go in there’, that’s the sort of feeling you get.
Carer
Thirty-one people felt that regular rounding was useful for checking on specifics, with general observations and hydration mentioned most frequently. Positive outcomes of consistent and comprehensive care included confidence and reassurance, particularly for carers, and patients, while one patient felt that disturbance from night-time observations was a negative but necessary feature of regular attention.
Mechanism: nurse–patient and nurse–carer communication and relationships (n = 50)
A large number of comments were made about communication and relationships, with both patients and carers making positive comments about communication and engagement with staff, but it was rarely possible to link such comments to IR. Positive comments from patients often highlighted the relational aspects of communication:
. . . Oh yeah, you can have a laugh, yeah, you can have a good laugh with them you know, because otherwise you’re just sort of sat here and you know, growing cobwebs, but no, you can have a good laugh with them because you need it.
Patient
You know, you’re not just, to them you’re not a patient, you are a person, that’s the, I think that’s the thing, you are a person, not a patient.
Patient
No carers and only four patients felt that IR had been explained to them, whereas 18 patients and 17 carers specifically said that IR had not been explained to them. Positive outcomes of good communication were mentioned nine times, almost always in relation to feeling better and feeling reassured:
Well, it just means that I can sleep at night, really. You know, that nothing horrible is going on, you know, that they listened to her, you know, and they don’t fob her off, which is good.
Carer
Mechanism: allocated time (n = 0)
There were no comments directly relating to this mechanism, although some patients and carers reported having to wait for care, which might be construed as a negative observation in relation to this mechanism.
Mechanism: staff communication and teamworking (n = 0)
No comments were made on this mechanism.
Mechanism: visibility (n = 45)
Forty-five of the patient/carer interviews included positive comments about nurse visibility/presence, whereas eight participants made negative comments. However, this is the mechanism for which it was most difficult to be confident that patient/carer observations were evidence of a mechanism for IR, as many people seemed to be commenting on the general visibility of staff:
Ever since I’ve been here, there’s always someone in the vicinity or in here, you know.
Carer
Nonetheless, staff visibility was clearly one of the aspects of care that patients valued most, whether or not in the context of IR:
. . . there’s something to be said about just being in a bay and actually seeing faces, so I think maybe the nurses do also kind of know that they are going to be seen by maybe four or five patients when they enter the bay and kind of make it a point to go, you know, ‘Hi, how are you?’, as well, so it’s better.
Carer
Mechanism: anticipation (n = 45)
The issue of whether or not IR had an impact on anticipating needs was discussed in 45 interviews, but the majority felt that regular rounds may be useful for addressing immediate needs, rather than future needs, such as going to the toilet or aspects of comfort that might arise suddenly or unpredictably. As one patient explained:
To be really, really truthful, I think possibly regarding going to the toilet, I probably call them, they don’t, they wouldn’t necessarily come and ask if I want to go to the toilet, but they would probably say ‘are you in pain?’ They’re more likely to concentrate on the medical side there and, you know, giving out pills and things, whereas going to the toilet, it’s probably, would be more up to us to let them know.
Patient
So, call bells were still needed in such instances, and patients referred to staff telling them to use the call bell if needed. However, some patients did not like to use the call bell or reported dissatisfaction with delays in responding to it. Occasionally, patients also implied that they felt that they had a responsibility to alert staff to changes in their condition:
. . . and yes, if you don’t ask every single question every time it actually doesn’t matter, because let’s be honest, everybody has a voice, if somebody didn’t say ‘are you in severe pain and would you like some morphine?’, then you can say ‘could I have some morphine today, please?’. People are capable of asking, even in the baddest, you know, the worst state.
Patient
Mechanism: patient and carer empowerment (n = 25)
Twenty-five interviews elicited comments about patient and carer empowerment, but twice as many people felt that IR did not empower patients or carers than felt it might. Nor did the majority engage with IR charts:
I did have a look at it, but it’s got codes on and things like that, and I had a look at them and I thought ‘well it’s nothing to do with me really’; all I know is I’m getting better, I’ll be going home.
Patient
Carers only very rarely saw IR as an enabler of their involvement in the patient’s care. Because IR had rarely been explained to patients and they were often unaware that it was an aspect of their care and of its documentation, it is not surprising that this was so.
General comments about care
Almost all patients and carers made some general comments about their care that were not necessarily directly related to IR. Broadly positive comments were made twice as often as negative comments. Positive comments tended to be generic in nature, often commending friendly and attentive staff:
. . . they all seem to be very nice, you know, I’ve never seen anybody nasty.
Patient
I found them very friendly. I got here today and it was lunchtime and they were about to help her with her lunch, but I usually try to come at lunchtime so that I can feed her and then they can feed someone else. But I found them to be very helpful, she’s always been clean. Yeah, I feel they’ve taken care of her when I’m not here, I don’t feel anxious when I leave.
Carer
Adverse comments tended to focus on poor communication or inattentive staff, or about inadequate care on other wards and poor access to other services such as primary care and community services. Commonly, individuals made both positive and negative comments, sometimes suggesting that mitigating circumstances were responsible for shortcomings:
. . . occasionally my grandmother might comment on the fact that if she has pressed the call button, it might have been a little while before somebody comes by or it might be the case that if she’s asked for something . . . they kind of go off and forget about her, which isn’t, of course, their fault, but it’s just the case that everybody’s really, really, really busy.
Carer
Overwhelmingly, patients and carers welcomed and were reassured by the visibility of nursing staff and by friendly communication, and perhaps a bit of banter. One patient said:
Yes, I mean I always sort of say, ‘when are you kicking me out?’, and they usually sort of say, ‘as soon as possible’, you know, it’s that type of rapport that makes the day go by because it’s a long day here when you can’t move and all you’ve got to do is look at the sky.
Patient
Patients clearly wanted to be able to get attention when they needed it, but were less concerned about the precise regularity or form of rounding, so long as needs were met and they felt that they were being treated with respect and good humour. Indeed, one carer, when told by the interviewer about the existence of scripted rounds, commented:
I don’t think that’s very people friendly, really.
Carer
General contexts
Patients and carers noted some of the contextual factors that influenced their care, some of which applied to IR as well as to wider aspects of their care. Patients and carers rarely linked contexts to particular mechanisms of IR, although some inferences could be drawn, for example when comments were made about the need for regular rounding varying according to a patient’s condition or stage of recovery. By far the most frequent contextual factors were staff being busy and/or wards being understaffed, which affected mechanisms including consistency and comprehensiveness and nurse–patient and nurse–carer communication. Ward layout was also significant (e.g. whether or not there were single rooms, the proximity of a patient to the nurses’ station, whether or not staff were based in bays), in so far as it affected staff visibility.
Summary
-
Interviews with patients and carers provide insight into what patients and carers value, although it is less clear how much IR is the best vehicle for delivering these attributes of nursing care.
-
There is no convincing evidence that IR is widely understood or perceived by patients, and its potential for empowering patients is limited as a stand-alone approach to engaging and empowering patients and those close to them.
-
In so far as IR may help to bring nurses regularly to patients’ bedsides to attend to their current needs, it may be welcomed by patients and carers, although it is unlikely to be the only means of achieving regular contact, nor a reliable way of anticipating future needs.
Chapter 8 Realist evaluation of intentional rounding: data synthesis
This chapter addresses objectives 6 and 8, reporting the key findings from the realist evaluation to examine the barriers to and facilitators of the successful implementation of IR and synthesising the data from each phase of the study to identify what aspects of IR work, for whom, in what circumstances and why. As part of the synthesis process, a second stakeholder consultation event took place, where attendees considered the findings and how they fitted with their own knowledge and experience of IR. The data reported here includes interview and observation data from the six wards in the three case study sites.
Aims and objectives
The study aims to understand how IR ‘works’ in England, for whom and in what circumstances; to suggest ways to improve its effectiveness; to inform decisions about its implementation in other contexts; and to understand what was causing variations in implementation or outcomes.
Findings
This section is divided into four parts. First, the initial and revised, evidence-informed programme theory is presented to give a broad overview of how IR ‘works’. Second, more detail is provided by outlining the four layers of contextual factors that enable or inhibit the activation of mechanisms. Third, implementation fidelity in England and adaption of the US version of IR (i.e. the Studer Group’s protocol) is examined, followed by a final description of detailed CMO configurations and supporting data.
Programme theory
All programmes (henceforth called ‘interventions’) will implicitly or explicitly have a programme theory or theories68 about how the intervention is expected to cause its intended outcomes. When an intervention such as IR is implemented, it is testing a theory about what ‘might cause change’, even though that theory may not be explicit. 69 As previously explained, in the first phase of the research, the initial theories of IR, or mechanisms by which change might occur, were not very explicit (see Chapter 3). Thus, a key task in the realist synthesis was to make the theories in the intervention explicit, by developing clear hypotheses about how and for whom IR might ‘work’ and why. Data used to develop the initial programme theory included analysis of academic peer-reviewed articles, policy documents and grey literature, and discussion in an initial stakeholder consultation event involving service user representatives and NHS clinical staff. These approaches enabled the development of initial programme theories about how, for whom and under what circumstances IR helps nurses with their work (Box 4).
Our initial programme theories of how IR ‘works’ (highlighting the underlying mechanisms providing the active ingredients to facilitate change) were expressed by identifying eight a priori propositions:
-
Consistency and comprehensiveness – when implemented in a comprehensive and consistent way, IR improves health-care quality, satisfaction and reduces potential harms.
-
Allocated time to care – embedding IR into daily routine practice gives nurses allocated time to care.
-
Accountability – documenting IR checks increases accountability and raises fundamental standards of care.
-
Nurse–patient relationships and communication – when workload and nursing staffing levels permit, more frequent nurse–patient contact improves relationships and communication and increases awareness of patient comfort and safety needs.
-
Visibility of nurses – increasing visibility, time when nurses are in the direct vicinity of patients, promotes vigilance, provides reassurance and reduces potential harms.
-
Anticipation – more frequent nurse–patient contact enables nurses to anticipate patient needs and take pre-emptive action.
-
Multidisciplinary teamwork and communication – IR documentation facilitates teamwork and communication.
-
Patient empowerment – IR empowers patients to ask for what they need to maintain their comfort and well-being.
Revised evidence-informed programme theory
The revised evidence-informed programme theory is presented in Box 5. An iterative CMO configuration process was used, distilling from the CMOs how IR (the intervention) causes its intended outcomes, based on an analysis of the data. In particular, the degree of support for each CMO configuration was examined within different data sources (e.g. nurses, managers, patients, carers, other health-care professionals) and obtained by different data collection methods (e.g. interviews, observations, national survey).
Some evidence. IR documentation usually covered all core IR components (as described by the Studer Group protocol). The IR core components had sometimes been adapted and expanded (e.g. by the inclusion of additional site-specific ‘comfort and safety’ checks). There was considerable variability in how IR had been implemented between and within sites. IRs were not carried out in a structured, comprehensive and consistent way. Although the IR documentation was usually completed, there was evidence that it was not being completed comprehensively; it was completed retrospectively or, occasionally, prospectively. When the consistency and comprehensiveness mechanism was activated, this contributed to the following outcomes:
-
Senior nurse managers and front-line nurses said that IR helped nurses (especially new, temporary and junior nurses) know what was required to deliver basic, fundamental patient care to a minimum standard.
-
Senior nurse managers and front-line nurses said that IR led to improvements in health-care quality and satisfaction and reduced potential harms.
Mechanism partially activated.
Allocated time to careThere was no evidence that it gave nurses allocated time to care as IR was often completed quickly, embedded in daily routine practice and not prioritised over other tasks. No outcomes were associated with this mechanism.
Mechanism not activated.
AccountabilityThere was some evidence that, when documented ‘authentically’, IR provided nurses and ward and senior nursing managers with reassurance and evidence that basic, fundamental patient care had been delivered. When the accountability mechanism was activated, this contributed to the following outcome:
-
Nurses said they could use IR documentation to provide evidence that they had delivered basic, fundamental patient care to a minimum standard.
There was no evidence that IR increased personal accountability, as nurses said they already felt a professional accountability for the care they delivered.
Mechanism partially activated.
Nurse–patient relationships and communicationThere was no evidence that IR was a vehicle for meaningful nurse–patient conversations, even if nurses deviated from script/set questions and developed their own style of doing IR. No outcomes were associated with this mechanism.
Mechanism not activated.
Visibility of nursesEvidence is inconclusive. Nurse presence and visibility was important to patients and their carers but the specific contribution of IR to this was unclear. Often, IR was completed at the same time as other patient bedside duties and ward layout (bays) facilitated increased nurse presence and visibility rather than IR. Uncertain outcomes were associated with this mechanism.
Unclear if mechanism is activated.
AnticipationEvidence is inconclusive. There was some evidence that nursing staff anticipated patient needs and took pre-emptive action; however, it was hard to say if this was due to IR (as IR was completed alongside other patient bedside duties). There was some evidence that patients had to ask for what they needed immediately after IR had been done (e.g. when IR had been completed without asking all ‘4 P’ questions, using call bell to ask to go to the toilet, asking for pain medication, etc.). Uncertain outcomes associated with this mechanism.
Unclear if mechanism activated.
Multidisciplinary teamwork and communicationThere was minimal evidence that IR checks or documentation were used in informal or formal nursing or multidisciplinary discussions and handovers to facilitate teamwork and communication. No outcomes were associated with this mechanism.
Mechanism not activated.
Patient empowermentThere was no evidence that IR empowered patients to ask for what they needed to maintain their comfort and well-being, as currently implemented. No outcomes were associated with this mechanism.
Mechanism not activated.
There was some evidence to suggest that the ‘consistency and comprehensiveness’ and ‘accountability’ mechanisms were at least partially activated, in some contexts. Both CMOs were considerably more complex than the initial programme theories and CMOs had implied. Some nurses said IR helped them ‘communicate with their colleagues and within teams’, but this was not supported through the observations or any other source. When activated, the outcomes that were most closely linked to these mechanisms were as follows:
-
All nurses knew what was required to deliver basic, fundamental patient care to a minimum standard.
-
Nurses said that they could use IR documentation to provide evidence that they had delivered basic, fundamental patient care to a minimum standard.
-
Nurses said that they thought that IR led to improvements in levels of patient comfort and safety.
The evidence was inconclusive around whether or not the ‘anticipation’ and ‘visibility and presence’ mechanisms were activated, because, in practice, it was often hard or impossible to separate IR from nurses delivering usual care. Finally, there was no evidence to support the activation of the ’nurse–patient relationships’, ‘allocated time to care’ or ‘patient empowerment’ mechanisms. No additional CMOs were identified during the national survey of senior nursing managers or in the case study fieldwork. The reasons for these findings will be explored in the remainder of this chapter.
Contextual factors influencing variation in implementation and outcomes of intentional rounding
In this section, four layers of context that activate mechanisms and lead to outcomes of IR are examined. Pawson70 and Pawson et al. 71 identified four contextual layers that influence variation in outcomes:
-
individual capabilities and characteristics of key actors
-
interpersonal relationships
-
organisational setting
-
intrastructural setting
This section builds on and refines the contextual factors previously identified in the realist synthesis, based on the case study fieldwork. In Chapters 6 and 7 the perspectives of patients, carers, front-line nurses, senior management and other health-care professionals on organising, delivering and receiving IR were presented. Here, these perspectives are synthesised to describe the enabling and inhibiting factors that determined whether or not mechanisms were activated, operating at each contextual layer. These contextual factors are based on data presented in preceding chapters and/or have been theorised on the basis of these data. For example, the patients and carers whom we interviewed had not received an information leaflet on admission to the wards (as recommended in some of the individual trust IR policy documents from the case studies), but if they had been, we would have inferred that it was more probable that they would have had an awareness of IR.
Individual capabilities and characteristics of key actors
Type of patients
-
Enabling: IR was most beneficial when patients –
-
were elderly and/or vulnerable (e.g. dementia, at risk of falls, wandering, need turning)
-
had difficulties verbally communicating.
-
-
Inhibiting: IR was least beneficial –
-
when IR was carried out rigidly and not adapted to suit patient needs (see Intentional rounding adaptations)
-
for patients who were relatively well, independent or waiting to go home.
-
Patient and carer awareness, understanding and involvement
-
Enabling: patients and carers were aware of IR because –
-
they had received a leaflet about IR on admission
-
they were given a verbal explanation about what it was and why it was being done
-
they had engaged in conversations that were prompted by the IR process
-
they had been told when nurses would be coming back to see them as part of IR
-
IR documentation could be easily accessed by patients and their carers (e.g. kept at the end of the bed, as paper copies), so patients and carers had the opportunity and felt able to see what was being recorded, if they wanted to.
-
-
Inhibiting: patients and carers were not aware of IR. This ‘invisibility’ of IR may have been because –
-
they did not know about IR because they had not been given a written or verbal explanation of it
-
patients were too unwell to comprehend or remember explanations or information about IR
-
they could not distinguish between IR and usual care, because nurses did not ask questions while completing IR (e.g. if they were silently working through a mental IR checklist, or it was done at same time as another nursing task)
-
the IR documentation was not physically accessible for patients and carers to inspect, and/or is considered ‘out of bounds’ to patients and carers.
-
Nursing staff characteristics
-
Enabling: setting out minimum standards of care for IR could be of most use for nurses who –
-
are unfamiliar with a ward and/or a type of patient (e.g. new or temporary nurses)
-
have less training and/or experience (e.g. HCAs, student nurses)
-
are not performing to the expected minimum standard of care.
-
-
Inhibiting: setting out minimum standards of care for IR could be of least use for –
-
RNs who had developed their own strategies, practices or mental checklists for ensuring patient comfort and safety. Formal IR processes were unnecessary as they were either already meeting or exceeding the minimum standards of care. Put succinctly, they were doing it already.
-
HCAs who were very experienced and closely supervised by RNs.
-
Leadership characteristics
-
Enabling: when senior nursing managers –
-
could clearly articulate how IR fitted within the trust’s overall vision and philosophy of nursing care
-
were instrumental in embedding IR in wider organisational processes for ensuring that fundamentals of care were given priority (e.g. documentation, IR part of package of measures for minimising harms)
-
encouraged IR uptake and staff ‘buy-in’, through reminders, tips for success, monitoring performance, rounds experts and senior management walkabouts.
-
-
Inhibiting: when senior nursing managers –
-
did not support the implementation of IR.
-
Interpersonal relationships and organisational setting
In Chapter 5, the three case studies were described in terms of their ward profiles, safety thermometer data and costing. In the following sections, comparisons are made across organisational settings in relation to implementation, environmental and structural factors.
Implementation factors
-
Staged or simultaneous implementation.
-
Staff engagement and motivation.
-
Staff education, training and understanding.
-
Fidelity and adaptation (see Fidelity to the original intervention).
-
Design and suitability of IR documentation.
Environmental and structural factors
-
Ward setting and layout.
-
Job demands, workload and nurse staffing levels.
-
Skill mix.
Staged or simultaneous implementation approach
-
Enabling: implementation was most effective when –
-
IR was introduced locally via multidisciplinary staff working groups to develop documentation, piloting and staff consultation on revising documentation.
-
There was widespread roll-out and testing in specific settings, wards and with different types of patients.
-
There was an ongoing programme of auditing, reviewing and adapting.
-
-
Inhibiting: implementation was least effective when –
-
IR was introduced with minimum preparation, multidisciplinary staff involvement or consultation.
-
IR was introduced simultaneously to all wards.
-
Staff engagement and motivation
-
Enabling: IR was most useful when nurses and other health-care staff saw and appreciated the benefits of IR (e.g. as a prompt to remember specific items to maintain care and minimise harms).
-
Inhibiting: IR was least useful when nurses and other health-care staff did not see or appreciate the purpose and benefits of IR (e.g. when they saw it as a, ‘tick-box exercise’).
Staff education, training and understanding of intentional rounding
-
Enabling: nurses and other health-care staff had a high level of IR knowledge and understanding of IR. This may be for a number of reasons –
-
IR awareness was embedded in staff inductions.
-
There was clarity in IR instructions and guidance (e.g. for dealing with certain scenarios).
-
There was staff training.
-
Role models were on the ward who could demonstrate and reinforce how to do IR for specific patients.
-
The benefits of IR processes and documentation were obvious to all (e.g. the ward manager gave specific feedback and encouragement, IR was regularly referred to by colleagues).
-
-
Inhibiting: nurses and other health-care staff had limited knowledge and understanding of IR. This may be because –
-
There was no formal training on IR.
-
Staff were not sure how to complete IR in certain circumstances (e.g. the form did not fit all patients or all wards).
-
There was a lack of effective role models for IR.
-
Staff did not see purpose of IR.
-
Design and suitability of intentional rounding documentation
-
Enhancing: when documentation layout and instructions –
-
were clear to promote accurate completion
-
were clear on how to adapt (e.g. do risk assessments, determine frequency, decide if not applicable)
-
were adapted to suit ward/patients
-
had high face and content validity.
-
-
Inhibiting: when documentation was not fit for purpose (for further descriptions of IR documentation variability, see Intentional rounding adaptations).
Environmental and structural factors
-
Enabling: IR was most useful where –
-
ward layout included or consisted entirely of single rooms, so there was scope to increase nursing presence and visibility through IR
-
there was a lack of other initiatives/systems to ensure that nurses were visible and could closely monitor patients.
-
-
Inhibiting: IR was least useful where –
-
The ward layout used modern design with bays (in our case study sites, bays of 6–8 patients), or in Nightingale wards (where patients were in one large room without subdivisions). This was because nurses were already highly visible to patients in such wards. IR had an added benefit of increasing nursing presence only if it involved nurses speaking directly to patients as part of the process (and not merely looking to assess levels of comfort and safety).
-
Other initiatives/systems were in place to ensure that nurses were visible and closely monitored patients (e.g. in one case study site, the hospital with bays had introduced ‘bay-tagging’ to ensure that there was always a nurse present in the bay, to increase vigilance and to prevent patients getting out of bed unaided, and falling).
-
-
Enabling: IR was most useful when –
-
staffing levels and job demands enabled nurses to complete and document IR without continuous interruptions or having to prioritise other duties
-
nurses were able to document IR at the same time, rather than completing forms retrospectively.
-
-
Inhibiting: IR was least useful when –
-
it was inhibited because nurses faced competing workload priorities caused by busy wards, interruptions, emergencies or having a high number of complex patients
-
job demands and/or staffing levels meant that nurses had to complete IR forms retrospectively.
-
-
Enabling: IR was most useful when –
-
the workforce was unstable (e.g. new, temporary, high turnover)
-
there was a high proportion of nurses who were inexperienced and/or junior on the ward.
-
-
Inhibiting: IR was least useful when –
-
the workforce was stable
-
nurses already used their education, skills, knowledge and experience to exceed the minimum standard of fundamental patient care, as set out by IR.
-
-
Enhancing: IR was most useful when –
-
guidance from senior nursing management and IR organisational policies on what was expected was clear, consistent and realistically achievable.
-
-
Inhibiting: IR was least useful when –
-
guidance from senior nursing management and IR organisational policies were incompatible and/or open to different interpretations.
-
Intrastructural setting
There were a number of other contextual factors influencing the implementation of IR in England, which are discussed throughout this report and only briefly summarised here.
NHS context
The public inquiry1 led by Sir Robert Francis identified the causes and failings in patient care at Mid Staffordshire NHS Foundation Trust. The report, in three volumes, focused on the neglect of patients, poor standards of care and the adequacy of regulatory and supervisory systems. The inquiry also highlighted issues of negative culture, tolerance of poor standards and disengagement from managerial and leadership responsibilities. Local organisations were asked to take action to strengthen the patient voice, improve front-line care and change culture through leadership. Although there were a few early pioneers of IR in England, having implemented it prior to 2011, widespread adoption of IR occurred only between 2011 and 2014.
Health policy
The level of concern about patient care and patient safety among the public, health-care professionals and politicians was such that it was necessary for the UK government to act quickly to convince the public that the failings identified at the Mid Staffordshire NHS Foundation Trust were being taken seriously and that the recommendations in the Francis report1 were being acted on. Following an announcement by the then prime minister, David Cameron, directors of nursing were told explicitly that they should ‘comply or explain’ why they were not implementing IR. In practice, this meant that many directors of nursing in NHS hospitals perceived the implementation of IR to be mandatory. Our national survey of directors of nursing showed that 97% of trusts had implemented IR in some form, and in at least some wards.
NHS culture
Increasingly, the NHS is described as having a ‘blame culture’, characterised by staff reporting a lack of trust, living with a threat of litigation and fear of reprisals for ‘mistakes’ and that organisations are risk-averse and have a tendency to look for individual ‘mistakes’ rather than for environmental-/system-level explanations. The senior nursing manager interviewees in this study explained at length the daily and ever-increasing challenges they faced in supporting the nursing workforce to deliver high-quality patient care and their fear of ‘being the next Mid Staffs’:
. . . everyone was wary and conscious of Mid-Staffs anyway, and also it was one of those things that, I’m sure every trust and every management team and every organisation did not want Mid-Staffs to be happening in their place.
English implementation fidelity and adaption to the US version of intentional rounding
Fidelity to the original intervention
As stated in Observations of intentional rounding (nurse shadowing and non-participant observation of direct patient care), 188 hours of care delivery were observed by four research staff. A total of 240 IRs were observed in this time, delivered by RNs, HCAs, ward sisters, assistant practitioners and trainee assistant practitioners, and both bank and permanent members of staff. Observations were undertaken throughout the day and evening shifts (ranging between 07.00 and 01.15) on both weekdays and weekends. At every round, researchers recorded whether or not each member of staff conducted the core components of IR according to the Studer Group’s protocol. The following examination of fidelity has been conducted to explore how observations of IR delivered in the English case study sites compare to the original IR intervention as promoted by the Studer Group.
In each intentional round, researchers looked for an opening phrase, examples of the ‘4 P’s’ (pain, positioning, personal needs and placement of items), an environmental assessment, a closing phrase and information about when the staff member would return. Researchers noted whether or not each of these components was observed ‘fully’ (as per the Studer Group protocol), ‘partially’ (notable but not as defined as in the Studer Group protocol) or ‘not observed’. To increase inter-rater reliability between observers, we discussed and agreed how to define each of these categories in the research team; the definitions are provided in Appendix 16 for the sake of transparency.
Researchers also recorded details of when staff members completed the IR documentation (this referred to either ‘immediately after the round’; ‘retrospectively’, i.e. at a later time in the day; ‘prospectively’, i.e. before the round took place; or ‘not at all’. The ‘not at all’ category meant that researchers did not see the nursing staff complete the documentation for the duration of the observation session. The researchers can therefore not be sure that documentation was not completed after the observation session had ended, e.g. at the end of the nursing staff shift). Researchers also recorded any observations of RNs checking that IR had been completed by HCAs (i.e. checking IR documentation to see if HCAs had completed it). On occasion, researchers were unable to determine whether or not a component of IR had been delivered. This was usually because IR was being undertaken at the same time as personal care delivery and the patient and staff member were either behind a drawn curtain or in a single room with the door closed, leaving researchers unable to see or hear the care being delivered. When this was the case, the instances have been recorded in the fidelity table as ‘unable to observe’.
As Appendix 16 highlights, there are a number of caveats to these data. Just because researchers did not observe nursing staff asking patients directly about each of the IR components, one cannot assume that they were not internally assessing them and making clinical judgements as to their relevance. Nursing staff may have felt (rightly or wrongly) that they already knew the answer to some of these questions and, therefore, did not need to ask the patients directly. Similarly, nursing staff may have assessed that particular aspects of the IR protocol were not pertinent to some patients and, therefore, they did not vocalise them. Researchers did not ask nursing staff why they behaved as they did after each round, meaning that they could not be sure what nursing staff were thinking as they performed IR. This is a possible methodological limitation in the study, although it is probable that nursing staff would not have had the time or capacity to debrief with researchers after each round. A further point to remember is that, in some cases, nursing staff were delivering IR when patients were either asleep or away from their bed. In these instances, protocols stated that nursing staff should still complete the IR documentation even though they could not ask patients any of the questions. Instead, they were to mark on their documentation either ‘patient asleep’ or ‘off ward’. Similarly, there were occasions when nursing staff were unable to directly ask patients IR questions either because patients could not speak English/had health issues that made them incapable of responding or because patients had expressed a desire not to be disturbed, yet on these occasions nursing staff were still required to complete the IR documentation. These issues all explain part of the reason why the completion of documentation was observed more commonly than the asking of questions. With these caveats in mind, Table 20 demonstrates how regularly nursing staff were observed to ask patients about or, in the case of environmental assessment, undertake each aspect of the IR protocol.
| Observation | Studer Group protocol, n/N (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Opening phrase in which nurse introduces self | Positioning (check comfortable, assess pressure sore risk) | Personal needs (assess personal needs, assist with toileting) | Pain (ask patient to rate pain on a scale of 0–10) | Placement (ensure any items are in easy reach) | Environment (assess care environment e.g. temperature of room, fall hazards) | Closing phrase (e.g. ‘is there anything else I can do for you before I go?’) | Patient informed of when the nurse will return | Documents round immediately after interaction | Documents round retrospectively (within observation period) | Documents round prospectively (i.e. before talking to patient) | Does not document at all (within observation period) | |
| Fully observed | 39/240 (16) | 48/240 (20) | 54/240 (23) | 15/240 (6) | 51/240 (21) | 13/240 (5) | 6/240 (3) | 2/240 (0.8) | 181/240 (75) | 21/240 (9) | 4/240 (2) | 31/240 (13) |
| Partially observed | 87/240 (36) | 16/240 (7) | 8/240 (3) | 48/240 (20) | 3/240 (1) | 7/240 (3) | 15/240 (6) | 7/240 (3) | – | – | – | – |
| Observed in any form (full/partial) | 126/240 (53) | 64/240 (27) | 62/240 (26) | 63/240 (26) | 54/240 (23) | 20/240 (8) | 21/240 (9) | 9/240 (4) | 206/240 (86) | – | – | – |
| Not observed | 113/240 (47) | 171/240 (71) | 173/240 (72) | 173/240 (72) | 183/240 (76) | 215/240 (90) | 217/240 (90) | 229/240 (95) | – | – | – | – |
| Unable to observe | 1/240 (0.4) | 5/240 (2) | 5/240 (2) | 4/240 (2) | 3/240 (1) | 5/240 (2) | 2/240 (0.8) | 2/240 (0.8) | 2/240 (0.8) | 1/240 (0.4) | – | – |
| Site 1 | ||||||||||||
| Observed | 4/89 (4) | 13/89 (15) | 11/89 (12) | 5/89 (6) | 14/89 (16) | 4/89 (4) | 1/89 (1) | 1/89 (1) | 76/89 (85) | 5/89 (6) | 1/89 (1) | 7/89 (8) |
| Partially observed | 20/89 (22) | 4/89 (4) | 1/89 (1) | 14/89 (16) | 1/89 (1) | 3/89 (3) | 1/89 (1) | 0/89 (0) | – | – | – | – |
| Observed in any form (full/partial) | 24/89 (27) | 17/89 (19) | 12/89 (13) | 19/89 (21) | 15/89 (17) | 7/89 (8) | 2/89 (2) | 1/89 (1) | 82/89 (92) | – | – | – |
| Not observed | 65/89 (73) | 70/89 (79) | 75/89 (84) | 68/89 (76) | 74/89 (83) | 80/89 (90) | 86/89 (97) | 87/89 (98) | – | – | – | – |
| Unable to observe | 0/89 (0) | 2/89 (2) | 2/89 (2) | 2/89 (2) | 0/89 (0) | 2/89 (2) | 1/89 (1) | 1/89 (1) | 0/89 | 0/89 | – | – |
| Site 2 | ||||||||||||
| Observed | 19/108 (18) | 27/108 (25) | 25/108 (23) | 6/108 (6) | 26/108 (24) | 5/108 (5) | 5/108 (5) | 0/108 (0) | 83/108 (77) | 9/108 (8) | 3/108 (3) | 11/108 (10) |
| Partially observed | 51/108 (47) | 7/108 (6) | 4/108 (4) | 26/108 (24) | 2/108 (2) | 2/108 (2) | 12/108 (11) | 3/108 (3) | – | – | – | – |
| Observed in any form (full/partial) | 70/108 (65) | 34/108 (31) | 29/108 (27) | 32/108 (30) | 28/108 (26) | 7/108 (6) | 17/108 (16) | 3/108 (3) | 95/108 (88) | – | – | – |
| Not observed | 37/108 (34) | 72/108 (67) | 77/108 (71) | 74/108 (69) | 79/108 (73) | 100/108 (93) | 90/108 (83) | 104/108 (96) | – | – | – | – |
| Unable to observe | 1/108 (1) | 2/108 (2) | 2/108 (2) | 2/108 (2) | 1/108 (1) | 1/108 (1) | 1/108 (1) | 1/108 (1) | 1/108 (1) | 1/108 (1) | – | – |
| Site 3 | ||||||||||||
| Observed | 16/43 (37) | 8/43 (18) | 18/43 (42) | 4/43 (9) | 11/43 (26) | 4/43 (9) | 0/43a (0) | 1/43 (2) | 22/43 (51) | 7/43 (16) | 0/43 (0) | 13/43 (30) |
| Partially observed | 16/43 (37) | 5/43 (12) | 3/43 (7) | 8/43 (19) | 0/43 (0) | 2/43 (5) | 2/43 (5) | 4/43 (9) | – | – | – | – |
| Observed in any form (full/partial) | 32/43 (74) | 13/43 (30) | 21/43 (49) | 12/32 (28) | 11/43 (26) | 6/43 (14) | 2/43 (5) | 5/43 (12) | 29/43 (67) | – | – | – |
| Not observed | 11/43 (26) | 29/43 (67) | 21/43 (49) | 31/43 (72) | 30/43 (70) | 35/43 (81) | 41/43 (95) | 38/43 (88) | – | – | – | – |
| Unable to observe | 0/43 (0) | 1/43 (2) | 1/43 (2) | 0/43 (0) | 2/43 (5) | 2/43 (5) | 0/43 (0) | 0/43 (0) | 1/43 (2) | 0/43 (0) | – | – |
Table 20 shows that 240 individual IR interactions were observed over a period of 188 hours: 89 intentional rounds were observed at case study site 1 (during 68 hours of observation), 108 intentional rounds were observed at case study site 2 (during 60 hours of observation) and 43 intentional rounds were observed at case study site 3 (during 60 hours of observation). A number of other (non IR-related) interactions were also observed in this time frame; these are discussed in Chapter 6, Perspective of other health-care professionals, General contexts and outcomes. Although similar numbers of observational hours were undertaken at each site, far fewer IRs were observed at case study site 3 because clear examples of IR were very difficult to identify. Staff were often seen to incorporate aspects of IR into their general interactions with patients but not to refer to this as IR or document it as such.
Across all sites, the most frequently observed aspect of IR was the completion of IR documentation. Overall, 86% of all IR interactions were observed to be documented. Seventy-five per cent of rounds were documented immediately after they were undertaken, whereas 9% of rounds were documented retrospectively and 2% were documented prospectively. Case study sites varied markedly in their approach towards documentation of IR. Documentation was completed most regularly at case study site 1, where 92% of rounds observed were documented, usually immediately after the round had taken place (85%). In comparison, 67% of rounds observed at case study site 3 were documented and 51% were completed immediately after the round. More rounds were completed retrospectively at case study site 3 (16%) than at sites 1 (6%) or 2 (8%), and rounds were also more likely to go undocumented in site 3 (30%) than at site 1 (8%) or site 2 (10%). The majority of rounds were documented at case study site 2 (88%), although only 77% were completed immediately after the round and prospective completion was noted more often here than at other sites (3%, compared with 1% at site 1 and 0% at site 3). This was because case study site 2 consisted primarily of single rooms, with IR documentation stored outside a patient’s room. Staff were therefore occasionally observed to complete the IR documentation before they entered the room to undertake the round.
The only other aspect of IR that was more commonly observed than not was the use of an opening phrase. Nursing staff used an opening phrase in 53% of the intentional rounds observed. However, it was rare for nursing staff to introduce themselves by name (as per the Studer Group protocol); this occurred in only 16% of interactions. Nursing staff tended to introduce themselves by name when meeting a patient for the first time, when the patient had new visitors with them or when a period of time had lapsed since they had last seen the patient (e.g. if the staff member had not been on shift for a couple of days). It was far more common (in 36% of interactions) for nursing staff to simply use a generic opening statement, such as ‘Morning’, ‘Hello’, ‘Are you allright?’ or ‘How are you feeling?’ when they entered the room or approached a patient’s bed. Occasionally, nursing staff opened the conversation with a direct question, such as did they want to get back into bed or had they opened their bowels, rather than begin with a greeting, per se. However, in 47% of rounds observed, no opening phrase was used by nursing staff at all – they simply approached the patient and started undertaking their tasks. Again, there were notable differences between sites in the use of opening phrases. Nursing staff at case study sites 2 and 3 were far more likely to use any form of opening statement than those at site 1, with opening phrases observed in 74% of IR interactions at site 3, 65% of IR interactions at site 2 and 27% of IR interactions at site 1.
Findings for all ‘4 P’s’ of IR were similar, in that these issues were rarely observed to be asked about by nursing staff. ‘Positioning’, ‘personal needs’, ‘pain’ and ‘placement of items’ questions were observed to be asked in 27%, 26%, 26% and 23% of rounds, respectively. This pattern of not asking about the ‘4 P’s’ was noted across all sites, although staff at case study site 1 were less likely to ask any of the ‘4 P’s’ questions than staff at the other sites. One other notable difference was that staff at case study site 3 were more likely to ask about personal needs (49%) than staff at sites 1 (13%) or 2 (27%). Environmental assessments were also uncommon, with these being observed in only 8% of all IR interactions. Again, staff at case study site 3 were observed to undertake environmental assessments more often (14%) than staff at sites 1 (8%) or 2 (6%).
A closing phrase, in any form, was observed in only 9% of all interactions. According to the Studer Group protocol, nursing staff are required to ask the question ‘Is there anything else I can do for you?’, but the staff in this study were observed asking this question (or words to that affect, e.g. ‘Do you need anything?’) in only 3% of rounds. Staff at case study site 2 were more likely (5%) to ask this question than staff at sites 1 (1%) or 2 (0%), although there may be some reasonable explanations for this finding (e.g. a larger number of single rooms). As shown in Table 12, staff at case study site 3 were not required to ask this question; therefore, it is unsurprising that no one did. Furthermore, case study site 2 was the only site where staff were required to sign the IR documentation to confirm that they had asked this question, whereas staff at site 1 were supposed to ask it but did not need to document it. This requirement to document the closing phrase on the form may explain why staff at site 2 were more likely to ask this question than those from other sites. However, it is questionable why only 5% of nursing staff were observed to ask this question, given their requirement to document this on the IR form. Using a generic closing statement to end rounds was observed slightly more often (in 6% of all rounds observed) than asking the Studer Group closing question. Statements such as ‘thanks’, ‘bye’ or ‘shout me if you want anything’ were used and others informed patients to use their call bell if they required any assistance. However, in 90% of rounds observed, nursing staff used no closing statement at all; they simply completed the round and left. Occasionally, this was because the nurse had been interrupted by another member of staff at this point and had terminated the round prematurely in order to provide assistance elsewhere. However, leaving without saying anything was less common in case study site 2 (83%) than in sites 1 (97%) or 3 (95%); this may be because of the predominance of single rooms in this site. It may be that it feels less comfortable for nursing staff to leave a single room without giving a closing statement than it does for those leaving a bedside in a shared bay. The end of an intentional round delivered in a single room may feel more finite to staff when they have to physically leave the room, rather than for those working in a bay setting, who may simply be returning to their bay-based desk or moving to the patient in the next bed.
Finally, Studer Group protocols state that nursing staff should inform the patient when they will next return to them, but this was observed in < 1% of all interactions (0.8%). It was slightly more common (3%) for staff to give a vague suggestion that they would be returning to the patient (e.g. ‘see you later’ or ‘see you in a bit’) but far more common (95%) for staff not to mention anything about coming back. This propensity for staff to not mention when they would be returning to the patient was observed across all sites, but was slightly less common at case study site 3 (88%) than at sites 1 (98%) or 2 (96%). It was also rare for RNs to be observed checking HCA’s IR documentation, as this was observed on only three occasions (once at site 1 and twice at site 2).
Overall, Table 20 demonstrates that IR was not being delivered in the English case study sites in the same manner promoted by the Studer Group. In these sites, the main focus of IR appeared to be in the completion of IR documentation, regardless of whether or not the IR questions had been asked. What is clear from these findings is that the successful completion of IR paperwork is not necessarily indicative of fundamental care being delivered by nursing staff during the rounds. At case study site 1, where the regular completion of IR documentation was most successful (i.e. completed for 92% of observed interactions), nursing staff were the least likely to ask patients about any aspect of the four P’s and least likely to open their interactions with any form of greeting or inform patients when they would return. Indeed, staff at this site were observed more than at any other to simply complete IR documentation without asking patients any of the questions on the form. Comparatively, at case study site 3, where the regular completion of IR documentation was least successful (i.e. completed for only 67% of interactions), nursing staff were the most likely to be observed undertaking a number of aspects of IR (e.g. using an opening phrase, asking about personal needs, undertaking an environmental assessment and informing patients when they would return) – they just did not always document to say that they had done so. These findings suggest that health-care managers should exercise some caution when relying on IR documentation for audit purposes or in response to incidents or complaints: the completion of IR documentation does not necessarily mean that fundamental care has been delivered and vice versa.
Intentional rounding adaptations
In England, IR implementers have adapted the version of IR that was originally promoted by the Studer Group in six different ways:
-
reach
-
frequency
-
content
-
style
-
responsibility
-
documentation.
Reach
In theory, if IR was conceptualised, broadly and simply, to mean checking regularly to ensure that patients were comfortable, safe, not in pain and had everything they needed, all patients would benefit from IR and this would mean that no one would be missed or neglected. Towards the end of this study, we learned that this was all that was originally intended by UK policy-makers when introducing IR in England. In practice, however, the Studer Group protocol for IR is more specific and less relevant for some patients and in some settings.
Frequency
The regularity of IR varied according to:
-
patient characteristics
-
patient ‘risk’ assessment
-
time of day/night.
Content
During English implementation, the Studer Group protocol content had been adapted in the following ways:
-
Irrelevant questions had been omitted (e.g. mobile/independent patients were not asked if they needed a change of position or to go to the toilet).
-
Patient-relevant questions/checks were added (e.g. vital signs, food–fluid charts, skin checks, wound care, i.v. lines and infusions, pressure ulcer risk assessment, incontinence check, nutrition check, falls prevention).
-
Response format had changed (e.g. Y = yes, N = no, UC = unable to communicate, NA = not applicable vs. tick for yes, cross for no, etc.).
Style
Intentional rounding could be carried out using a script and asking closed questions or by being incorporated into a general conversation and asking open questions. For a variety of reasons, some nurses undertook IR in a task-orientated, tick-box way, rather than using it as an opportunity to engage the patient in conversation to find out more about them and develop a rapport/relationship.
Responsibility
The responsibility for completing IR was shared between HCAs and RNs (and sometimes student nurses), but the proportion of IR that was done by each group varied. Furthermore, the strategies for ensuring that RNs took overall responsibility for IR differed (e.g. one site changed their documentation layout to ensure that RNs signed to say they had taken overall responsibility, even if some IR checks were completed by HCAs).
Documentation
Adaptations were made to IR documentation in a variety of ways:
-
Layout – whether staff had to enter the specific time the round was completed or if time slots of every 1 or 2 hours were already recorded on the form; certain components of the form were colour coded to ensure that they were completed by RNs, etc.
-
Clarity of instructions/guidance – for example where there was the inclusion of a body map to note pressure damage areas and the presence of devices.
-
Instructions on the regularity of specific aspects of IR adaption – where pressure ulcer checks were included in IR the frequency of these checks was dependent on patients’ assessed risk, for example ‘high risk’ (every 2 hours minimum), ‘medium risk’ (every 4 hours) or ‘low risk’ (daily).
-
Complexity – for example, with regard to documentation, ‘keys’ such as ‘position or links to other screening tools embedded in IR (e.g. Nutrition Malnutrition screening tool).
-
IR follow-up identified and documented – whether or not there was space for nursing staff to record any variation/deviance or any actions resulting from rounding (e.g. pain control, medication administered).
-
Ease of access – whether or not IR documentation was kept at end of patients’ beds, outside their room or at the nursing station.
-
Where IR is recorded – for example, was it recorded on a separate form or in a nursing document bundle of other assessments and records, etc.?
-
Form – whether IR documentation was kept in an electronic or paper format.
Detailed revised contexts–mechanisms–outcomes
A detailed exploration of the refined CMOs that informed the revised programme theory are provided in Table 21.
| Mechanism title | Context (i.e. describes enabling and inhibiting contexts that activate or fail to activate ‘mechanisms’) | Mechanism (resources) | Mechanism (reasoning/responses) | Outcomes (anticipated outcomes) |
|---|---|---|---|---|
|
CMO 1: consistency and comprehensiveness Partially activated |
|
|
|
|
|
CMO 3: accountability Partially activated |
|
|
|
. . . and provides a protection for nurses if needed for patient/carer complaints, incidents, coroner’s inquests (i.e. they can provide evidence that they have delivered basic fundamental patient care) |
|
CMO 7: multidisciplinary teamwork and communication Minimally activated |
|
IR provides nurses and other health-care professionals with written record of the fundamental, basic care that has been delivered that can be handed over and/or referred to in their absence |
|
. . . and this leads to improved nursing and multidisciplinary communication and teamwork |
|
CMO 5: visibility of nurses Inconclusive |
|
|
|
|
|
CMO 4: nurse–patient relationships and communication Not activated |
|
|
This enables nurses to get to know patients better and become more aware of their needs, notice unusual behaviours/appearances and detect subtle/significant changes that affect comfort and safety |
|
|
CMO 2: allocated time to care Not activated |
|
IR gives nurses allocated ‘time to care’ for fundamental, basic care (i.e. time to check that patients are comfortable and their needs are being met, thereby treating patients with dignity and replacing ‘presumed care’) | This helps nurses to organise their work and feel able to prioritise this aspect of nursing care |
. . . and leads to nurses becoming empowered . . . and to increased staff, patient and carer satisfaction with care and fewer patient complaints |
|
CMO 6: anticipation Not activated |
|
IR enables nurses to anticipate/pre-empt and proactively address patient needs instead of being reactive and waiting for patient call bells and alarms | This ensures that all patients receive regular care instead of unequally distributed care among patients focused towards those who have frequent call bell use |
|
|
CMO 8: patient empowerment Not activated |
|
IR provides an opportunity for nurses, patients and carers to get to know each other better |
|
. . . and this leads to higher patient and carer satisfaction with care |
Using theories to develop contexts–mechanisms–outcomes
The national survey of senior nursing managers, interviews (with front-line nurses, senior nursing managers, other health-care staff, patients and carers), observation of patients (to complete Qualpacs) and shadowing of individual nurses all provided data to support and refute the CMOs. The findings of this study support other work that suggests that some mechanisms operate on a continuum, rather than simply the mechanism ‘firing’ or ‘not firing’. 72 In this section, the existing literature and theories are drawn on to develop two of the eight mechanisms that we have concluded were partially activated, namely CMO 1, ‘consistency and comprehensiveness’, and CMO 3, ‘accountability’.
Context–mechanism–outcome 1: consistency and comprehensiveness
Is intentional rounding a task-orientated or worker-orientated activity?
One of the tensions underpinning IR is the degree to which it should be structured, standardised and applied to everyone in a consistent and comprehensive way or used in a selective and flexible way. When analysing jobs, occupational psychologists make the distinction between jobs or roles that are primarily task-orientated activities (i.e. anyone can do it if they have a checklist) and worker-orientated activities (i.e. requires knowledge and skill that goes beyond any checklist). 73
In its original US form, IR falls nearer the task-orientated end of the continuum. This study has revealed the huge variation in the way IR has been implemented in England and the many site-specific adaptations that have extended the remit of IR beyond the original US form. These site-specific adaptations include additional comfort and safety checks (e.g. vital signs, food and fluid charts, wound care, i.v. lines and infusions, pressure ulcer risk assessment, falls prevention) and the using of IR selectively. Arguably, these additional comfort and safety checks and the tailoring of IR to particular patients, settings and circumstances require additional nursing knowledge, skill and professional judgement, meaning that IR then becomes more of a ‘worker-orientated activity’. This has implications for practice, in terms how the work is allocated and supervised and what additional knowledge, skill and professional judgement is required to conduct IR.
Use of checklists to improve safety
Checklists have been used to improve safety in the aviation industry and imported into health care, for example in the World Health Organization surgical safety checklist. 74 IR would be an example of a checklist that is used for normal everyday procedures. Normal everyday checklists are effective whenever there are:
. . . advantages to standardising performance, time is not critical, the series of tasks is too long to be committed to memory (or there are likely to be interruptions to execution of the task that might interfere with memory retrieval), and the environment enables a physical list to be accessed and used.
Clay-Williams and Colligan75
Intentional rounding checklists differ from those used in aviation in a number of ways, outlined in the following sections.
Standardising performance
The nursing environment requires an approach with more flexibility than that found on the flight deck. Although every flight is different, there is more variation in hospitals (e.g. types of patients, settings, ward layouts) than on the flight deck. When the IR tasks become more complex, the role of nursing staff in completing and/or supervising IR tasks and completing documentation needs to be clear.
Time
This study has shown that nurses are encouraged to conduct IR around other tasks, rather than as a discreet activity. Although IR is not a time-critical activity, it is conducted regularly on an hourly basis or every 2 hours.
Series of tasks
The IR checklist in its original US form is not long (e.g. the 4Ps, an opening and closing phrase, an environmental scan and telling the patient when the nurse will return).
Ongoing versus one-off
Unlike aviation checklists, which are designed for one-off specific occasions (pre flight, after take-off, before landing), IR checklists are used repeatedly throughout the day and night.
Context–mechanism–outcome 3: accountability
Another tension underpinning IR is its contribution to supporting accountability for nursing care. This exists at several levels, including from the point of care to senior management and commissioning.
Accountability for own actions, covered by the Nursing and Midwifery Council code (2018)
There are numerous definitions of individual accountability, but, essentially, it is each nurse accepting responsibility for their nursing practice. RNs, as well as being legally accountable, are accountable to several stakeholders: their employer, regulator [the Nursing and Midwifery Council (NMC)] and the person receiving care, whose requirements may at times conflict.
Delegating authority, covered by the Nursing and Midwifery Council code
The NMC also requires a RN to retain accountability for nursing tasks delegated to other staff. 76 Delegation was not specifically mentioned in the Francis report,1 although staffing policies of reducing the skill mix of registered to unregistered staff were considered to have contributed to declining professionalism and tolerance of poorer standards of care. The NMC code77 requires that nurses delegate tasks that are within the competence of the other person, to supervise and support them so that they can provide safe and compassionate care and to confirm that the completed task has been delivered to the required standard. This is a challenge, particularly when wards are short staffed and the team includes temporary staff. Little is known about how care is delegated, which is usually locally determined,78 although it can cause anxiety for newly qualified RNs. 79 This study has demonstrated that IR is predominantly valued by nurses as a way of providing this evidence for care delivered by themselves and, to a larger degree, that they have delegated to an unregistered nursing assistant. It is argued that the risk-averse and blame culture in the nursing and health-care environment leads to RNs needing evidence that the care they are accountable for providing has been delivered and IR does provide them with this reassurance.
Evaluating performance, a trust requirement
Evidence in this study suggests that IR documentation is being used to demonstrate that care has been delivered when performance is being challenged, for example complaints, inquests and untoward incidents. However, this study has demonstrated that documentation, for various reasons, does not reflect the care that was delivered at the time. Furthermore, senior nurses were aware of this and did not rely on IR alone but reviewed the whole patient record.
One case study trust used the IR documentation as a performance measurement in their service development programme. This raises the question of whether or not IR is a ‘good’ or ‘adequate’ measure of performance. In a review of metrics for nursing, indicators were seen to provide information about care delivery and how it can be improved, and to monitor performance against agreed standards. 80 They advised against the use of measures that focus on care processes rather than outcome, as they were most vulnerable to what they called gaming and/or perverse incentives. This study has shown that the standard to which IR should be delivered is ambiguous, with nurses and senior nurses valuing flexibility in conducting IR, contrary, in some cases, to explicit hospital policy. Furthermore, IR is vulnerable to intentional and unintentional gaming; thus, it is argued that IR is a poor measure of nursing performance. Approaches to evaluating the effectiveness of performance should involve proper evaluation techniques that are capable of measuring performance through the use of clearly defined, achievable and measurable goals that set out what ‘good performance’ looks like. Currently, it is not surprising that nurses have concluded that ‘good performance’ in relation to IR means completing IR documentation, as this is what is audited by senior nursing staff.
Summary
-
In the revised, evidence-informed programme theory, only two of the original eight mechanisms were partially activated (‘consistency and comprehensiveness’ and ‘accountability’). The evidence for two mechanisms was inconclusive (‘visibility of nurses’ and ‘anticipation’). There was minimal evidence for one mechanism (multidisciplinary teamwork and communication) and no evidence for the remaining three (‘allocated time to care’, ‘nurse–patient relationships and communication’ and ‘patient empowerment’).
-
The four layers of contextual factors that enabled or inhibited the activation of mechanisms were explored. These included type of patients; patient and carer awareness, understanding and involvement; nursing staff characteristics; leadership characteristics; implementation factors, such as staged or simultaneous implementation; staff engagement and motivation; staff education, training and understanding of IR; design and suitability of IR documentation; and environmental and structural factors, such as ward setting/layout, job demands and staffing levels, skill mix/workforce stability, senior nursing management/IR organisational policies, NHS context health policy and NHS culture.
-
A total of 240 IR interactions were observed over the course of 188 hours of care delivery observation. Although 86% of all IR interactions were observed to be documented, fidelity to the original intervention (i.e. the Studer Group protocol) was generally low.
Chapter 9 Conclusions
In Chapter 8, the findings of the realist evaluation were presented and it was shown how the complex processes inherent in IR contributed to the delivery of nursing care to patients in acute hospitals in England. This research offers unique perspectives on the effectiveness of IR, in particular what works, for whom and in what circumstances. Its strengths are the careful analysis and unpacking of views of IR through multiple and multidisciplinary lenses at both national and granular levels of three case studies. The extensive observation of nursing practice, as well as the results of the national survey, analysis of case study interviews and quality outcomes, provide a significant contribution to the knowledge and understanding of the practice of nursing, as it is played out through IR. The aim of this chapter is to set out the key messages from the study, review the approach and methods used and discuss the implications of findings for policy, practice and research.
Key messages
Nursing care was observed to be generally good and, at times, excellent; unsafe care or care that neglected a patient’s fundamental needs was not observed
Intentional rounding was introduced into nursing practice as a response to the extreme and shocking failures of care at the Mid Staffordshire NHS Foundation Trust. It was intended to improve nursing interaction and engagement with patients to restore confidence and trust and ensure patient safety. Senior nursing managers told us that they encouraged IR to be integrated into other activities; therefore, it is reassuring that IR was rarely observed as a discrete activity, but instead emerged as part of the process of getting to know, looking after and responding to patients within a continuous nurse–patient relationship. Drawing from the extensive observation data, we suggest that, although the Studer Group protocol of IR was rarely observed, the quality of nursing care was generally good and, at times, excellent.
Intentional rounding makes a minor overall contribution to the delivery of nursing care
Patients were observed to be seen by a RN, on average, every 37 minutes and by a member of nursing staff, on average, every 20 minutes. Therefore, nurses interacted with patients far more often than required as part of an intentional round. Furthermore, the frequency of these interactions was very similar on each of the three sites, even though on one site IR was hourly, on another every 2 hours and unspecified on another. This suggests that nursing staff work in similar ways to be available to patients and monitor what is happening with them. In this context, IR can be seen to make a small contribution, and is only part of the process of the way in which nursing staff engage with patients.
Intentional rounding is not visible to patients and carers
Patients and carers were usually not aware that nursing staff were undertaking IR. This is perhaps not surprising as patients, carers and nursing staff alike all said that IR was rarely explained to patients and carers, despite the requirement to do so in hospital policy (in the two sites that had a specific IR policy). This also supports our conclusion that nurses were more likely to absorb IR into their other activities and practice. However, nurses also rarely told patients when they would be returning to check them again, mainly because they were managing competing priorities, could not be confident that they would be available at a specific time and were careful not to raise expectations that might not be possible to meet and, therefore, could potentially result in a complaint. Thus, the opportunity offered by IR to reassure patients and carers of regular, time-specific contact was rarely realised. However, this finding needs to be understood, first, in the context of the frequent contact observed in the case study wards reported above, and, second, that patients and carers who were interviewed valued and were generally satisfied with the level of contact they had with nursing staff. Ironically, patients valued the relational elements of interactions with nursing staff, which, as the findings show, is not a prominent feature of the IR protocol. Many of the IRs observed had very little relational interaction and often involved asking closed questions or simply completing documentation without any communication at all; therefore, it is probable that the interactions in which nurses develop a relationship with patients occur when nurses are delivering other nursing care activities and not IR.
Intentional rounding is used by nursing staff as a defence/safety net
A strong theme emerging from the data was that IR provided evidence of accountability for care delivered, which was reassuring for nursing staff working in NHS organisational cultures preoccupied by the management of risk. However, at times, nurses expressed views and some anxiety that they were unable to conduct IR at the frequency required by their trust or to document IR in real time, as a result of time pressures and interruptions. This was justified in terms of nurses having been with patients anyway and already knowing what their patients needed. Anxiety to provide ‘proof that shows that we’ve been in and we’ve had the conversations with the patient’ was expressed as ‘if it’s not documented, it’s not been done’. It should be noted that bed occupancy on each case study site was > 90%, which is above the recommended rate of 85%. 81 This study has shown that nurses carry out nursing activities included in IR without completing the documentation and, conversely, complete IR documentation without carrying out the nursing care activities required. However, the observational data shows clearly that a lack of documenting IR does not necessarily mean the absence of an encounter or that patients have not been checked in some way. Furthermore, documenting IR does not necessarily mean that the IR care activities have been done.
Although senior nursing managers expressed reticence about the accuracy of IR records on the delivery of nursing care, it was clear that it provided them with reassurance that care had been delivered, with some acknowledging that IR was used as a safety net or as a defence against allegations of poor practice at an individual practitioner, ward and organisational level. Senior nursing managers expressed ambitions to develop nursing practice beyond the confines of IR, which was seen as a minimum standard and not something to aspire to, but felt restricted by a performance management approach in the NHS that perpetuated an ethos of compliance and risk aversion that inhibited innovation. 82 The emphasis on IR documentation by most nursing staff demonstrated that nurses were behaving consistently in the prevailing NHS organisational culture that values counting and transactional activity as a measure of risk mitigation rather than relationship-based care.
The intentional rounding protocol as defined by the Studer Group is not sufficient in England
The majority of trusts nationally have adapted the IR protocol, as defined by the Studer Group, in six different ways: reach, frequency, style, responsibility, content and documentation. This is often in consultation with clinical staff to improve usability in the clinical setting. These adaptations, which varied within and between acute trusts, demonstrated that the Studer Group IR format of the 4Ps is not sufficient in the English health-care context. There are notable differences in service delivery contexts between the USA and England, with the USA having hospitals that provide almost exclusively single room environments. However, in this study, the case study hospital with predominantly single rooms (site 2) also adapted the IR protocol to include more clinical components, such as food and fluid charts, wound care, incontinence checks, falls prevention and pressure ulcer risk assessments, which are all still referred to as ‘IR’.
Furthermore, hospital finance in the USA is more market driven, which is likely to have influenced the development of IR. The Studer Group’s developments coincided with Medicare stopping reimbursement for the treatment of injuries resulting from preventable inpatient falls. Health-care reimbursement is also linked to patient satisfaction surveys of nursing responsiveness, motivating providers to improve patient satisfaction with nursing care. 83
This indicates the need for caution when considering the implementation of interventions from other international health-care systems. Introducing new ways of working in complex, organisational and professional structures needs wide consultation, careful planning and piloting. This was circumvented in the case of the widespread introduction of IR in England. Announced for political expediency to contribute to managing poor public opinion in the anticipation of the publication of the Francis report,1 it is argued that IR was taken up unquestioningly by the majority of trusts and took root in a culture of fear, blame and regulation.
Intentional rounding adds to the tension inherent in the delivery of systematised care versus individual patient care
Nursing has long struggled to articulate a unified, collective position on what it uniquely contributes to patient care, experience and outcome. What is rarely disputed, however, is the centrality and importance of the relationship between the patient and nurse to the delivery of care that benefits patient recovery. Kitson et al. 84 identify an ongoing tension in nursing practice between a task-orientated, ‘mechanistic’ approach to delivering fundamental care and the need for consistency in managing the relational aspects of providing patient care. They assert that there is a need to acknowledge the:
. . . inherent systemic tension between the task and time approach to ‘getting the job done’ and the need for someone (on the patient’s behalf) to be integrating and personalizing the experience through thinking about the whole experience and linking activities into a series of meaningful encounters.
The systematised, structured approach to IR was seen to emphasise transactional care delivery rather than relational, individualised patient care. The flexibility with which IR was seen to be delivered, endorsed by senior nursing managers, was potentially a way of managing this tension by allowing nurses to individualise the care they provided to some degree while still being compliant to organisational expectations.
Intentional rounding is poorly understood by staff
Despite the widespread implementation of IR, it is noteworthy that the purpose of IR was poorly understood and valued by many front-line nursing staff, compounded, perhaps, by the lack of training and explanation provided. Our findings estimate that the annual incremental costs of IR could exceed £100,000 per hospital ward in the case of hourly IR. But there were no additional resources to support the policy directive, probably because it was thought that nurses were providing this care already, which adds a further constraint on implementation. Many nurses thought that IR was the form that documented the actions taken, rather than a vehicle for having a conversation with patients regularly to ensure that their needs were being met.
Intentional rounding does not contribute to multidisciplinary care
The Department of Health and Social Care’s85 response to the Francis report1 stressed the need for greater interprofessional collaboration:
. . . we will work together, collaborating on behalf of patients, combining and coordinating our strengths on their behalf, sharing what we know and taking collective responsibility for the quality of care that people experience.
Despite efforts to improve the communication across professional groups in the interests of patients, it is disappointing that progress is slow. Members of the multidisciplinary team and other staff were often not aware of IR and did not contribute to conducting it. Those who were saw the potential for improving patient care, but rarely accessed the information it provided. Thus, this could be seen as a missed opportunity for multidisciplinary collaboration. 86
Strengths and limitations
A key strength of the study was the use of mixed methods and their integration, guided by the realist evaluation approach. The realist synthesis comprehensively reviewed all available international literature and provided an initial programme theory for the impact of IR that was largely missing in the existing literature. Using this initial programme theory to underpin the main study ensured that the study directly built on what was already known, thereby advancing knowledge.
The high response rate for the national survey of English acute trusts (70%) gives confidence that the findings provide an accurate account of the implementation of IR, and is unique in that it gives a comprehensive and reliable overview.
The study captured the experiences and perceptions of multiple stakeholders and has provided a comprehensive view of IR, seen through the lens of those leading, implementing, delivering and receiving it. Researchers spent 2–3 weeks on each case study ward to ensure that the evaluation was focused on the delivery of IR on the ground. This benefited the study hugely. During interviews with senior nurse managers, researchers were frequently directed to interview other senior nurses; they therefore interviewed more managers than intended. This gave additional richness to the data on nursing leaders and executive perspectives of IR, often a hard-to-reach group. 87
A limitation of the study was that, because IR was often delivered alongside other care activities and in a flexible way, it was sometimes difficult to identify when IR was occurring. During the observation, it was important that the researchers did not interrupt nurses, so asking questions was kept to a minimum. However, interviewing nursing staff immediately after shadowing them would have enabled researchers to follow up on nurses’ reasoning for the care delivered and how IR contributed to this. Furthermore, nurses kept a lot of information about patients in their heads and often worked with patients for several days at a time, which influenced the interactions they had with patients. It was not possible for researchers to observe how this knowledge affected the delivery of IR. It was discussed in Chapter 8 how IR is often difficult for researchers to observe, as it was rarely delivered as a discrete activity, but was instead undertaken alongside other nursing activities, an approach encouraged by senior nursing managers and leaders. Furthermore, the lack of findings about the influence of IR on patient outcomes included in the safety thermometer data limits inferences on how mechanisms link to clinical outcomes for patients.
Case study sites were selected using the responses to the national survey to provide breadth of context within which IR was implemented. However, being able to achieve the depth of data required for detailed examination of how IR worked limited the number of case study sites that could feasibly be included. Therefore, there may be some important contextual factors that we were unable to select for and this may limit the generalisability of findings. Furthermore, trust nursing managers selected the wards to be included in the research, which may have introduced bias.
There were also some disparities between sources of data from the different methods used (e.g. what staff talked about in the interviews and what researchers observed). 88
Implications for policy and practice
The evidence from this study, to our knowledge the first national evaluation of IR worldwide, demonstrates that the effectiveness of IR is very weak. However, there is also clear evidence for a lack of clarity in the purpose and expectations of IR, lack of education and preparation of staff nationally and locally and a lack of resources to support the introduction and sustainability of IR. It is probable that the way in which the policy was developed, disseminated, implemented and supported influenced the effectiveness of the delivery of IR. It is clear that guidelines for good policy-making89 were not adhered to in this case. In the following sections, we set out the implications for the management of health-care services and for nursing through the voices of senior managers, the stakeholder advisory group and others.
Implications for nurses to take charge of nursing practice
The consistently strong message coming through the survey and interviews was the view of nurse leaders that IR, as an exemplar of nursing practice, should be shaped by the profession and not others:
. . . we need to, as a profession, be evolving in, and measuring ourselves and deciding going forward, you know, how do . . . we demonstrate good quality care . . . what is an outcome that we want to see, rather than a measure that we want to implement that would give us an outcome.
Director of nursing
. . . the risk of that is we won’t sort our own problems out. . . . what percentage of the workforce is graduates? Probably about 45, 50%? We’re not using the brains of those people because we haven’t created an environment where we’ve got leaders who are thinkers and doers.
Director of nursing
Some perceived that failure to do so had, in part, contributed to the political imperative to implement IR. We propose that the results of this study should inform a national nursing conversation about the future of IR in England. This would help NHS trusts and senior nursing managers decide which direction they want to take to respond to this new evidence and to consider whether or not there are alternative interventions that support the delivery of fundamental nursing care to patients.
Implications for nursing leadership: ‘If I were you, I wouldn’t start from here’
At our final study advisory group, where the recommendations from the study were discussed, a service user member recalled the joke about a tourist who asks for directions and received the reply ‘Well sir, if I were you, I wouldn’t start from here’. As explained earlier (see Chapter 1, Prime minister announcement), IR was hastily introduced at a time when government needed to be seen to be acting in response to the Francis report. 1 As borne out by these findings, IR as an intervention to address patient need is highly contestable. The implications for nurse leaders is to consider how to take the findings in a review that may recommend ‘de-implementation’ or ‘stopping practices that are not evidence-based’90 or ‘to abandon care that wastes resources or delivers no benefit to patients’. 91 We suggest that there is a need for a national discussion/debate within the nursing profession to consider whether or not IR is the best way of achieving desired outcomes, and what the desired outcomes are. It may be better to start afresh, rather than attempting to tweak a system that has been implemented. This is, arguably, an activity rarely undertaken by the profession. A director of nursing in this study said:
. . . we don’t have these professional conversations . . . we don’t have those types of forums because we’re so caught up just trying to keep it safe at the moment in most organisations . . . there’ll be more and more decisions that are made politically because we don’t have those right conversations and we’re caught on the back foot and because we don’t have a vision and a plan and a visual sense of how you do it; they can walk all over us and they implement these things because they can. That’s a cynical view.
Director of nursing
A decision to discontinue IR would be a bold undertaking and would need to be adequately resourced and supported. The NHS is under immense pressure and it is anticipated that the reassurance of the evidence that IR provides nurses would be difficult to relinquish:
. . . it is quite difficult because once things are in place, it’s really a brave person that says ‘right, stop doing that, let’s do this’.
Director of nursing
Implications for an improvement agenda: intentional rounding needs to be more purposeful and rationalised, that is ‘intentional’
An alternative to discontinuation is to lead a review to implement improvements that address shortcomings identified in this research. A relaunch of IR could consider renaming and site-specific adaptations, which often exceed the US version of IR. A broader umbrella term would reflect this (e.g. ‘comfort and safety rounds’). This study has identified lessons about implementation that should be considered if IR was relaunched:
-
Review the purpose of IR and the level of flexibility that is acceptable. Consider the criteria for how a flexible approach should be implemented.
-
Education should be provided to all nursing staff (and other staff if involved in IR) about the purpose of IR and how it should be delivered.
-
The purpose of IR should be explained to patients and their carers.
-
Consider involving other non-nursing staff in contributing to the record of when patients are seen and care activities undertaken.
-
Documentation should not have set hourly intervals but instead have space for staff to write the specific time when the patient was attended to.
-
Areas of duplication between different elements of documentation should be reduced.
-
Audits of IR should focus on the delivery of IR, not the documentation of IR.
-
Review the status of IR as a ‘comply or explain’ intervention and devise guidelines on how IR should be included in CQC inspections.
Implications of rapid policy development to complex problems
We have argued that hasty policy-making ‘on the hoof’ as a response to political crises is problematic. The development and implementation of IR as a national policy was done in a vacuum and involved importing an untested US model. A period of piloting, evaluation and refinement would support the integration of a policy of intervention into a complex system. Manski92 proposes ‘adaptive policy’ that remains flexible as the mechanisms and impacts become evident in different settings, and argues against the notion that research leads to a single true number that captures the effectiveness of policy, however seductive this may appear. This study provides evidence of the need for caution in using IR documentation as a performance indicator. Much has been written about the unintended consequences of measuring activities and setting targets, and, given the evident weakness of the documentation, it would be unwise to co-opt this as any kind of data on processes of care. 93
Recommendations for further research
The implications for policy and practice discussed above are wide-ranging and, as we have suggested, contingent on discussion by senior nursing managers and leaders on how to respond to this evaluation of IR. However, what is clear is the need to identify what patients and their carers would value and expect from nursing interventions that support fundamental care delivery, whether a revised form of IR or an alternative intervention. Furthermore, it would be valuable to explore the extent to which patients and their carers want or need to understand nursing processes in order to have a good experience and/or outcome of care. 94
This study has identified that further research is needed in the following areas:
-
Identify and evaluate the effectiveness of approaches to strengthening the relational aspects of nurse–patient relationships, taking into account the complexity of the care provision (i.e. what works, for whom and in what circumstances).
-
As the number of unregistered nursing roles increases, identify and evaluate the methods of RN supervision of patient care.
-
Implement and evaluate a community of nursing practice and change supported by an effective learning/buddy network.
Conclusions
This is the first theory-informed, large-scale, mixed-methods evaluation of IR, to our knowledge. It makes a significant contribution to our understanding of the delivery of nursing care in the NHS. The evidence shows the effectiveness of IR, as adapted in England, is very weak and suggests that there is a need for a national discussion about whether or not IR is the optimum intervention to support the delivery of fundamental nursing care to patients. This is a long-standing priority for nursing and this study of IR demonstrates the challenge of how national nursing initiatives permeate to the frontline of care provision. Furthermore, it demonstrates the lack of organisational resilience insofar as IR is not stable when the acute wards are under pressure.
If we want dignity and respect, we need to focus on nurses and the care they deliver . . .
David Cameron, 201214
Although patients were observed as having contact with a RN every 37 minutes on average, and were generally positive about their experience with nursing care, we have demonstrated that IR, in isolation, is not sufficient. To uphold dignity and respect, more is needed than a tick-box approach. Nurses themselves recognised this and were ambivalent at best about the value of IR. This is a watershed moment that requires us to think again, putting the focus on the patient and the nursing care that they want, and that nurses want to give.
Acknowledgements
We extend our thanks to all the patients, carers and members of staff who participated in the study, to the members of the study advisory group and all the attendees at the stakeholder consultation events. We are also grateful for the advice and support of our research collaborators on the study: Katy Schnitzler and Felicity Mayer.
Contributions of authors
Ruth Harris (Professor of Health Care for Older Adults) designed the study, provided overall direction, conducted the realist synthesis, collected and analysed data and drafted sections of the report.
Sarah Sims (Project Co-ordinator) designed the study, conducted the realist synthesis, collected and analysed data and drafted sections of the report.
Mary Leamy (Lecturer in Mental Health) collected and analysed data and drafted sections of the report.
Ros Levenson (Independent Consultant) designed the study, analysed data and drafted sections of the report.
Nigel Davies (Principal Lecturer) designed the study, conducted the realist synthesis, collected and analysed data and reviewed the report.
Sally Brearley (Patient and Public Involvement Fellow) designed the study, planned and chaired the advisory group and stakeholder events and reviewed the report.
Robert Grant (Freelance Statistician) designed the study, analysed data and drafted sections of the report.
Stephen Gourlay (Associate Professor of Management) designed the study, contributed to data analysis and reviewed the report.
Giampiero Favato (Professor of Accounting and Finance) designed the study, analysed data and drafted sections of the report.
Fiona Ross (Professor of Health Research) designed the study, contributed to data analysis and drafted sections of the report.
Publications
Schnitzler K, Davies N, Ross F, Harris R. Using Twitter™ to drive research impact: a discussion of strategies, opportunities and challenges. Int J Nurs Stud 2016;59:15–26.
Harris R, Sims S, Leveson R, Gourlay S, Ross F, Davies N, et al. What aspects of intentional rounding work in hospital wards, for whom and in what circumstances? A realist evaluation protocol. BMJ Open 2017;7:e014776.
Sims S, Leamy M, Davies N, Schnitzler K, Levenson R, Mayer F, et al. Realist synthesis of intentional rounding in hospital wards: exploring the evidence of what works, for whom, in what circumstances and why. BMJ Qual Saf 2018;27:743–57.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review. Exclusive use will be retained until the publication of major outputs.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry 2013.
- Studer Group . Best Practices: Sacred Heart Hospital, Pensacola, Florida. Hourly Rounding Supplement 2007.
- Tea C, Ellison M, Feghali F. Proactive patient rounding to increase customer service and satisfaction on an orthopaedic unit. Orthop Nurs 2008;27:233-40. https://doi.org/10.1097/01.NOR.0000330305.45361.45.
- Levenson R. A Report on the Implementation of Intentional Rounding at Demonstrator Sites for the Nursing and Care Quality Forum 2013. www.6cs.england.nhs.uk/pg/cv_blog/content/view/81314/76110?ctype=blog&container=76110&cview=81300 (accessed 1 September 2015).
- Nursing and Care Quality Forum . Letter to Prime Minster 2012. www.gov.uk/government/uploads/system/uploads/attachment_data/file/216812/NCQF-letter-to-PM.pdf (accessed 25 August 2019).
- Bartley A. The Hospital Pathways Project. Making it Happen: Intentional Rounding. London: The King’s Fund Point of Care and The Health Foundation; 2011.
- Halm M. Hourly rounds: what does the evidence indicate?. Am J Crit Care 2009;18:581-4. https://doi.org/10.4037/ajcc2009350.
- Harris R, Sims S, Levenson R, Gourlay S, Ross F, Davies N, et al. What aspects of intentional rounding work in hospital wards, for whom and in what circumstances? A realist evaluation protocol. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014776.
- Kessler B, Claude-Gutekunst M, Donchez AM, Dries RF, Snyder MM. The merry-go-round of patient rounding: assure your patients get the brass ring. Medsurg Nurs 2012;21:240-5.
- Bourgault AM, King MM, Hart P, Campbell MJ, Swartz S, Lou M. Circle of excellence. Does regular rounding by nursing associates boost patient satisfaction?. Nurs Manage 2008;39:18-24. https://doi.org/10.1097/01.NUMA.0000340814.83152.35.
- Sherrod BC, Brown R, Vroom J, Sullivan DT. Round with purpose. Nurs Manage 2012;43:32-8. https://doi.org/10.1097/01.NUMA.0000409925.39096.19.
- London Health Sciences Centre . Hourly Comfort Rounding Toolkit n.d. www.lhsc.on.ca/doc/orientation/falls/presentation_content/external_files/LHSC%20Hourly%20Comfort%20Rounding%20Toolkit_May%202016v1.pdf (accessed 25 August 2019).
- Fitzsimons B, Bartley A, Cornwell J. Intentional rounding: its role in supporting essential care. Nurs Times 2011;107:18-21.
- Topping A. Nurses to make hourly rounds under Cameron plans. The Guardian 2012. www.theguardian.com/society/2012/jan/06/nurses-hourly-rounds-cameron-hospitals (accessed 13 September 2019).
- Rogers E. Diffusion of Innovations. New York, NY: Free Press of Glencoe; 1962.
- NHS Commissioning Board . Compassion in Practice: Nursing, Midwifery and Care Staff. Our Vision and Strategy 2012.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications Ltd; 1997.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. ESRC Research Methods Programme Methods Paper 2 2004. www.ccsracuk/methods/publications/documents/RMPmethods2.pdf (accessed 2 September 2013).
- Hewitt G, Sims S, Harris R. The realist approach to evaluation research: an introduction. Int J Ther Rehabil 2012;19:250-9. https://doi.org/10.12968/ijtr.2012.19.5.250.
- Sims S, Leamy M, Davies N, Schnitzler K, Levenson R, Mayer F, et al. Realist synthesis of intentional rounding in hospital wards: exploring the evidence of what works, for whom, in what circumstances and why. BMJ Qual Saf 2018;27:743-57. https://doi.org/10.1136/bmjqs-2017-006757.
- Pawson R. Digging for nuggets: how ‘bad’ research can yield ‘good’ evidence. Int J Soc Res Methodol 2006;9:127-42. https://doi.org/10.1080/13645570600595314.
- Meade CM. Round bounty. One-hour rounding positively influences patients and nursing staff members. Mark Health Serv 2007;27:23-7.
- Braide M. The effect of intentional rounding on essential care. Nurs Times 2013;109:16-8.
- Dix G, Phillips J, Braide M. Engaging staff with intentional rounding. Nurs Times 2012;108:14-6.
- D’Alessio E, Magsalin M, Neville KL, Patten C. Enhancing nursing’s presence. Nurs Manag 2010;41:16-8. https://doi.org/10.1097/01.NUMA.0000390468.21033.f1.
- Berg K, Sailors C, Reimer R, O’Brien Y, Ward-Smith P. Hourly rounding with a purpose. Iowa Nurse Reporter 2011;24:12-4.
- Blakley D, Kroth M, Gregson J. The impact of nurse rounding on patient satisfaction in a medical-surgical hospital unit. Medsurg Nurs 2011;20:327-32.
- Dewing J, O’Meara BL. Introducing intentional rounding: a pilot project. Nurs Stand 2013;28:37-44. https://doi.org/10.7748/ns2013.10.28.6.37.e7652.
- Dyck D, Thiele T, Kebicz R, Klassen M, Erenberg C. Hourly rounding for falls prevention: a change initiative. Creat Nurs 2013;19:153-8. https://doi.org/10.1891/1078-4535.19.3.153.
- Kenny R, Norton C. Staff and patient views on intentional rounding. Nurs Times 2015;111:16-9.
- Lowe L, Hodgson G. Hourly rounding in a high dependency unit. Nurs Stand 2012;27:35-40. https://doi.org/10.7748/ns2012.10.27.8.35.c9362.
- Moran J, Harris B, Ward-Miller S, Radosta M, Dorfman L, Espinosa L. Improving care on mental health wards with hourly nurse rounds. Nurs Manag 2011;18:22-6. https://doi.org/10.7748/nm2011.04.18.1.22.c8412.
- Sobaski T, Abraham M, Fillmore R, McFall DE, Davidhizar R. The effect of routine rounding by nursing staff on patient satisfaction on a cardiac telemetry unit. Health Care Manag 2008;27:332-7. https://doi.org/10.1097/HCM.0b013e31819179a1.
- Hutchings M. Caring around the clock: rounding in practice. Nurs Times 2012;108:12-4.
- Olrich T, Kalman M, Nigolian C. Hourly rounding: a replication study. Medsurg Nurs 2012;21:23-6.
- Culley T. Reduce call light frequency with hourly rounds. Nurs Manage 2008;39:50-2. https://doi.org/10.1097/01.NUMA.0000313098.19766.d0.
- Woodard JL. Effects of rounding on patient satisfaction and patient safety on a medical-surgical unit. Clin Nurse Spec 2009;23:200-6. https://doi.org/10.1097/NUR.0b013e3181a8ca8a.
- Goldsack J, Bergey M, Mascioli S, Cunningham J. Hourly rounding and patient falls: what factors boost success?. Nursing 2015;45:25-30. https://doi.org/10.1097/01.NURSE.0000459798.79840.95.
- Meade CM, Bursell AL, Ketelsen L. Effects of nursing rounds on patients’ call light use, satisfaction, and safety: scheduling regular nursing rounds to deal with patients’ more mundane and common problems can return the call light to its rightful status as a lifeline. Am J Nurs 2006;106:58-71. https://doi.org/10.1097/00000446-200609000-00029.
- Meade CM, Kennedy J, Kaplan J. The effects of emergency department staff rounding on patient safety and satisfaction. J Emerg Med 2010;38:666-74. https://doi.org/10.1016/j.jemermed.2008.03.042.
- Neville K, Lake K, LeMunyon D, Paul D, Whitmore K. Nurses’ perceptions of patient rounding. J Nurs Adm 2012;42:83-8. https://doi.org/10.1097/NNA.0b013e318243365e.
- Tucker SJ, Bieber PL, Attlesey-Pries JM, Olson ME, Dierkhising RA. Outcomes and challenges in implementing hourly rounds to reduce falls in orthopedic units. Worldviews Evid Based Nurs 2012;9:18-29. https://doi.org/10.1111/j.1741-6787.2011.00227.x.
- Willis E, Toffoli L, Henderson J, Couzner L, Hamilton P, Verrall C, et al. Rounding, work intensification and new public management. Nurs Inq 2016;23:158-68. https://doi.org/10.1111/nin.12116.
- Fabry D. Hourly rounding: perspectives and perceptions of the frontline nursing staff. J Nurs Manag 2014;23:200-10. https://doi.org/10.1111/jonm.12114.
- Flowers K, Wright K, Langdon R, McIlwrath M, Wainwright C, Johnson M. Intentional rounding: facilitators, benefits and barriers. J Clin Nurs 2016;25:1346-55. https://doi.org/10.1111/jocn.13217.
- Kirk K, Kane R. A qualitative exploration of intentional nursing round models in the emergency department setting: investigating the barriers to their use and success. J Clin Nurs 2016;25:1262-72. https://doi.org/10.1111/jocn.13150.
- Rondinelli J, Ecker M, Crawford C, Seelinger C, Omery A. Hourly rounding implementation: a multisite description of structures, processes, and outcomes. J Nurs Adm 2012;42:326-32. https://doi.org/10.1097/NNA.0b013e31824ccd43.
- Deitrick LM, Baker K, Paxton H, Flores M, Swavely D. Hourly rounding: challenges with implementation of an evidence-based process. J Nurs Care Qual 2012;27:13-9. https://doi.org/10.1097/NCQ.0b013e318227d7dd.
- Harrington A, Bradley S, Jeffers L, Linedale E, Kelman S, Killington G. The implementation of intentional rounding using participatory action research. Int J Nurs Pract 2013;19:523-9. https://doi.org/10.1111/ijn.12101.
- Walker K, Duff J, Fitzgerald K. ‘Rounding’ for better patient care: an evaluation of an improvement intervention implementation. Int J Nurs Pract 2015;21:207-13. https://doi.org/10.1111/ijn.12244.
- Morgan L, Flynn L, Robertson E, New S, Forde-Johnston C, McCulloch P. Intentional rounding: a staff-led quality improvement intervention in the prevention of patient falls. J Clin Nurs 2017;26:115-24. https://doi.org/10.1111/jocn.13401.
- Emerson BL, Chmura KB, Walker D. Hourly rounding in the pediatric emergency department: patient and family safety and satisfaction rounds. J Emerg Med 2014;47:99-104. https://doi.org/10.1016/j.jemermed.2013.11.098.
- Krepper R, Vallejo B, Smith C, Lindy C, Fullmer C, Messimer S, et al. Evaluation of a standardized hourly rounding process (SHaRP). J Healthc Qual 2014;36:62-9. https://doi.org/10.1111/j.1945-1474.2012.00222.x.
- Brosey LA, March KS. Effectiveness of structured hourly nurse rounding on patient satisfaction and clinical outcomes. J Nurs Care Qual 2015;30:153-9. https://doi.org/10.1097/NCQ.0000000000000086.
- Gardner G, Woollett K, Daly N, Richardson B. Measuring the effect of patient comfort rounds on practice environment and patient satisfaction: a pilot study. Int J Nurs Pract 2009;15:287-93. https://doi.org/10.1111/j.1440-172X.2009.01753.x.
- Negarandeh R, Hooshmand Bahabadi A, Aliheydari Mamaghani J. Impact of regular nursing rounds on patient satisfaction with nursing care. Asian Nurs Res 2014;8:282-5. https://doi.org/10.1016/j.anr.2014.10.005.
- Lucas B. Proactive Patient Rounding: Developing Nursing Pratice to Improve the Quality of Patient Care 2010. www.fons.org/Resources/Documents/Project%20Reports/PFProactivePatientRoundingNov2010.pdf (accessed 25 August 2019).
- Luxton S. Foundation of Nursing Studies. Patients First Programme – Project Report. The Introduction of Intentional Rounding to Aid Falls Prevention in an Acute Stroke Unit 2012. http://fons.org/Resources/Documents/Project%20Reports/PFTauntonJan2013.pdf (accessed 25 August 2019).
- Maben J, Griffiths P, Penfold C, Simon M, Pizzo E, Anderson J, et al. Evaluating a major innovation in hospital design: workforce implications and impact on patient and staff experiences of all single room hospital accommodation. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03030.
- Sullivan T. Emergency Department Nurses’ Perceptions of the Benefits and Challenges of Hourly Rounding. Minneapolis, MN: Walden University; 2013.
- Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist Synthesis: Rameses Training Materials 2013. www.ramesesproject.org/media/Realist_reviews_training_materials.pdf (accessed 25 August 2019).
- Toole N, Meluskey T, Hall N. A systematic review: barriers to hourly rounding. J Nurs Manag 2016;24:283-90. https://doi.org/10.1111/jonm.12332.
- Grant RL, Hood R. Complex systems, explanation and policy: implications of the crisis of replication for public health research. Critical Public Health 2017;27:525-32. https://doi.org/10.1080/09581596.2017.1282603.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analyzing Qualitative Data. London: Routledge; 1994.
- Wandelt MA, Slater Stewart D. Slater Nursing Competencies Rating Scale. New York, NY: Appleton-Century-Crofts; 1975.
- Spilsbury K, Adamson J, Atkin K, Bartlett C, Bloor K, Borglin G, et al. Evaluation of the Development and Impact of Assistant Practitioners Supporting the Work of Ward-based Registered Nurses in Acute NHS (Hospital) Trusts in England. Southampton: NIHR Service Delivery and Organisation Programme; 2010.
- Norman IJ, Redfern SJ. The validity of Qualpacs. J Adv Nurs 1995;22:1174-81. https://doi.org/10.1111/j.1365-2648.1995.tb03120.x.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0643-1.
- Westhorp G, Prins E, Kusters C, Hultink M, Guijt I, Brouwers J. Realist Evaluation: An Overview Report from an Expert Seminar With Dr Gill Westhorp 2011.
- Pawson R. Evidence Based Policy: A Realist Perspective. London: Sage Publications Ltd; 2006.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Pearn M, Kandola R. Job Analysis: A Practical Guide for Managers. London: Institute of Personnel Management; 1988.
- Sivathasan N, Rakowski KRM, Robertson BF, Vijayarajan L. The World Health Organization’s ‘Surgical Safety Checklist’: should evidence-based initiatives be enforced in hospital policy?. JRSM Short Rep 2010;1. https://doi.org/10.1258/shorts.2010.010007.
- Clay-Williams R, Colligan L. Back to basics: checklists in aviation and healthcare. BMJ Qual Saf 2015;24:428-31. https://doi.org/10.1136/bmjqs-2015-003957.
- Nursing & Midwifery Council . The Code: Professional Standards of Practice and Behaviour for Nurses and Midwives 2015.
- Nursing and Midwifery Council (NMC) . The Code: Professional Standards of Practice and Behaviour for Nurses, Midwives and Nursing Associates 2018. www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf (accessed 25 August 2019).
- Magnusson C, Allan H, Horton K, Johnson M, Evans K, Ball E. An analysis of delegation styles among newly qualified nurses. Nurs Stand 2017;31:46-53. https://doi.org/10.7748/ns.2017.e9780.
- Johnson M, Magnusson C, Allan H, Evans K, Ball E, Horton K, et al. ‘Doing the writing’ and ‘working in parallel’: how ‘distal nursing’ affects delegation and supervision in the emerging role of the newly qualified nurse. Nurse Educ Today 2015;35:e29-33. https://doi.org/10.1016/j.nedt.2014.11.020.
- Griffiths P, Jones S, Maben J, Murrells T. State of the Art Metrics for Nursing: A Rapid Appraisal. London: King’s College London; 2008.
- NHS Providers . Bed Occupancy Rates Hit Record High 2017. http://nhsproviders.org/news-blogs/news/bed-occupancy-rates-hit-record-high (accessed 25 August 2019).
- Ham C. Reforming the NHS from Within: Beyond Hierarchy, Inspection and Markets. London: The King’s Fund; 2014.
- Wolosin R, Ayala L, Fulton BR. Nursing care, inpatient satisfaction, and value-based purchasing: vital connections. J Nurs Adm 2012;42:321-5. https://doi.org/10.1097/NNA.0b013e318257392b.
- Kitson AL, Muntlin Athlin A, Conroy T. Anything but basic: nursing’s challenge in meeting patients’ fundamental care needs. J Nurs Scholarsh 2014;46:331-9. https://doi.org/10.1111/jnu.12081.
- Department of Health and Social Care . Patients First and Foremost: The Initial Government Response to the Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry 2013.
- Reeves S, Ross F, Harris R. Fostering a ‘common culture’? Responses to the Francis Inquiry demonstrate the need for an interprofessional response. J Interprof Care 2014;28:387-9. https://doi.org/10.3109/13561820.2014.921985.
- Harris R, Kelly D, Hunt JA, Plant H, Kelley K, Richardson A, et al. Accessing elite nurses for research: reflections on the theoretical and practical issues of telephone interviewing. J Res Nurs 2008;13:236-48. https://doi.org/10.1177/1744987107084671.
- Moffatt S, White M, Mackintosh J, Howel D. Using quantitative and qualitative data in health services research – what happens when mixed method findings conflict?. BMC Health Services Research 2006;6. https://doi.org/10.1186/1472-6963-6-28.
- Rutter J, Hallsworth M. Making Policy Better: Improving Whitehall’s Core Business. London: Institute for Government; 2011.
- Prasad V, Ioannidis JP. Evidence-based de-implementation for contradicted, unproven, and aspiring healthcare practices. Implement Sci 2014;9. https://doi.org/10.1186/1748-5908-9-1.
- van Bodegom-Vos L, Davidoff F, Marang-van de Mheen PJ. Implementation and de-implementation: two sides of the same coin?. BMJ Qual Saf 2017;26:495-501. https://doi.org/10.1136/bmjqs-2016-005473.
- Manski CF. Public Policy in an Uncertain World: Analysis and Decisions. Cambridge, MA: Harvard University Press; 2013.
- Smith PC, Mossialos E, Papanicolas I, Leatherman S. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Cambridge: Cambridge University Press; 2010.
- Hewitt G, Sims S, Greenwood N, Jones F, Ross F, Harris R. Interprofessional teamwork in stroke care: is it visible or important to patients and carers?. J Interprof Care 2015;29:331-9. https://doi.org/10.3109/13561820.2014.950727.
- Royal College of Nursing . NHS Pay Scales 2016–17 n.d. www.rcn.org.uk/employment-and-pay/nhs-pay-scales-2016-17 (accessed 25 August 2019).
- NHS Improvement . Approved Costing Guidance n.d. https://improvement.nhs.uk/resources/approved-costing-guidance/ (accessed 25 August 2019).
Appendix 1 Influencing contexts of intentional rounding
| Context | Description |
|---|---|
| Individual capabilities and characteristics of key actors | |
| Staff education, training and understanding of IR (n = 28)3,9–11,23–25,28,29,31–37,40,42,44,47–53,58,60 | Staff education, understanding and training in IR was commonly viewed as an important factor in its success.9,11,24,25,28,29,31,34–36,40,42,47,48,50,58,60 Methods of educating staff about IR varied, and included lectures/presentations, ward meetings, online learning modules, competency tests and feedback to staff on practice.3,9,10,23,29,32,33,36,37,40,47,51–53 Even where substantial education/training opportunities were available, not all managers participated or enabled their team to participate28 and some staff remained unprepared for IR.48 Participating in IR educational opportunities was more difficult for nurses working night shifts44 and for agency/’floating’ nurses35 |
| Staff engagement and motivation (n = 23)4,9,11,23,24,26,28–30,32,34,36,38,40,44,46–51,57,58 | IR was more successful when staff were engaged with, committed to and positive towards IR from the outset and throughout.4,9,11,23,24,26,34,38,46,47,49,51,57,58 Methods of fostering engagement varied, and included involving staff in the design and implementation of IR initiatives, sharing best practice and developing a strong sense of team.4,9,11,28,32,40,47,49,51 IR was implemented less successfully when staff were resistant towards it, perceived it as a top-down process/paper exercise or did not believe that it improved patient experience; in these situations, IR was performed irregularly/with little intention by staff and poor activity not routinely challenged4,23,30,44,48,50 |
| Staff characteristics (n = 2)4,57 | Understanding of the principles and practices of IR varied according to individual staff characteristics, including age and level of training/experience4,57 |
| Leadership/management support for IR (n = 18)3,4,10,22,24,28,32,34–36,38,42,44,45,47–49,51 | Support from nursing leadership/management was key to successful IR, with leaders being required to provide a number of functions, including encouraging staff ‘buy-in’, providing ongoing reminders and tips for success, and monitoring performance.3,4,10,22,24,32,34,38,42,47–49,51 Some papers highlighted the importance of unit champions/rounding experts/’buddy support,’4,24,35,36,48 although others did not acknowledge their value.44 Senior ‘walkabouts’ were seen as useful,4 but some reported variable long-term commitment of leaders towards IR28 |
| Type of patients (n = 15)4,24,28,30,32,41–44,46,49,50,57,58,60 | Nurses did not think that all patients required hourly rounding and some patients did not want to be seen every hour.4,24,28,30,32,42–44,46,58 Complex and demanding patients took up more of nurses’ time during IR and were prioritised over those deemed to be ‘well’.24,41,49,50,60 IR was highlighted as being most beneficial for older and vulnerable patients who required help with activities of daily living46 |
| Patient and carer education and understanding of IR (n = 1)53 | Variations in the amount of education and information around IR that patients and carers receive does not appear to have a significant impact on their perceptions of care53 |
| Ward characteristics | |
| Ward setting/layout (n = 5)4,32,40,45,46 | IR may be less suitable/more difficult to implement in some settings, including A&E and mental health.4,32,40,46 Open ward layouts facilitate IR, whereas closed or cluttered layouts inhibit it45 |
| Workload issues/lack of time (n = 13)24,27,28,30,37,41,45,46,48,50,57,59,60 | IR was inhibited when nurses faced competing tasks and priorities in their workload caused by busy wards, staff shortages, poor skill mix, high patient-to-nurse ratios, interruptions, emergencies or large numbers of complex patients24,27,28,30,37,41,45,46,48,50,57,59,60 |
| Who conducts the rounds? (n = 6)4,32,39,44,46,57 | There was variation across studies around who delivered IR (i.e. staff of all levels vs. senior staff only).4,32,39,45,57 Confusion around who should be delivering IR was a barrier to its implementation.57 IR worked best when all types of nursing, care and support staff were involved, but senior staff retained an active and visible daily role4 |
| Organisation and system characteristics | |
| Documentation associated with IR (n = 14)4,26,29–32,41,42,46,47,50,51,58,59 | Staff who did not acknowledge the benefits of IR documentation or believed it to be a burdensome, ‘tick-box exercise’ perceived the IR process negatively.4,30,41,42,50,59 Frustration occurred when IR paperwork duplicated information recorded on other charts/logs.31,32,41,59 To document IR effectively, personalised tools were required to suit the setting and needs of the ward4,26,29,32,47,51,58 |
| Presence of other organisational changes/competing initiatives/(n = 6)28,42,43,47,49,59 | Introducing multiple, simultaneous initiatives or changes alongside IR had a negative impact on its implementation28,42,43,47,49,59 |
| ‘Cultural change’ (n = 5)4,11,24,28,48 | Successful implementation of IR required cultural change in organisations.4,24,28,48 Some highlighted the importance of embedding IR within existing daily routines,28 but others felt that ward activity should be re-orientated to fit around IR24 |
| Implementation approach (n = 5)4,23,24,34,45 | Variations in the implementation approach for IR were noted: some reported a staged introduction of IR4,23,24 whereas others introduced it simultaneously across different wards and departments.4 The advantages of rolling out IR across the whole organisation outweighed the advantages of a more gradual approach4 |
| Reason for implementation (n = 2)28,59 | The reason behind the implementation of IR can influence staff perceptions of it. For example, the fact that IR was a government initiative helped some leaders to promote the concept in their clinical areas, but others reported resenting the intervention for the same reason28 |
Appendix 2 General outcomes of intentional rounding
| Outcome | Description | Expected change in outcome |
|---|---|---|
| Self-report patient and staff outcomes | ||
| Patient and carer satisfaction and perceptions of care (n = 24)3,9–11,22,24–26,32,33,35–37,39–41,43,49,52–57 | Nineteen studies reported that IR increased patient and/or carer satisfaction or improved their perceptions of care,3,9–11,22,24–26,32,33,36,37,39–41,49,54,56,57 although some had small sample sizes, low response rates, methodological concerns or did not report findings to support their claims/state whether or not any differences were statistically significant.9,36,41,54 Four studies reported no statistically significant differences in patient and/or carer satisfaction or perceptions of care following IR implementation35,52,53,55 and one found mixed results43 | Most studies reported that IR improved patient and/or carer satisfaction |
| Staff satisfaction and perceptions of care (n = 9)4,9,24,28,38,40,41,47,55 | Four studies reported that IR improved staff perceptions of care provided and/or increased job satisfaction4,9,40,55 and two associated IR with benefits to staff turnover.9,47 Two studies associated IR with more negative staff perceptions/experiences of care.24,28 One reported a statistically significant difference between nurses’ perceived benefits of IR for patients and for themselves, identifying IR as benefiting patients but not staff41 | Some evidence of improved job satisfaction and reductions in staff turnover |
| Patient uncertainty (n = 1)37 | One study reported that IR reduced patient uncertainty around whether or not a caregiver would come to their assistance for immediate needs37 | One study reported a reduction in patient uncertainty |
| Patient awareness of IR (n = 2)4,30 | There was little evidence that patients were aware of the IR process, although most felt that their needs were attended to on a regular basis or that they saw their nurse ‘enough’4,30 | Limited evidence |
| Clinical and management outcomes | ||
| Call bell use (n = 18)10,22–24,26,27,34–37,39,40,43,47,49,52,53,57 | Twelve studies reported a decrease in call bell use following the introduction of IR,10,22,24,26,27,36,37,39,40,47,49,57 although the same concerns around anecdotal reports and a lack of findings to support these claims were noted. Three studies reported an overall increase in call bell use following the introduction of IR.35,52,53 Others reported mixed results, such as variations in call bell usage across different wards in the same study.23,34 Two studies concluded IR did not reduce call bell use,23,43 but two noted a reduction in call bell duration (i.e. the length of time taken to respond to call bell activation or the length of time patients wait to have their call bells answered)23,24 | Mixed findings on whether call bell use decreases with IR |
| Pressure ulcers (n = 8)11,23,24,31,44,47,54,57 | Seven studies reported a decrease in the number of hospital-acquired pressure ulcers and/or improvements in the early detection of pressure ulcers following the implementation of IR (although, again, some of these studies had the methodological/reporting issues previously highlighted or were based on staff reports).11,23,24,44,47,54,57 One study reported mixed results around the impact of IR on pressure ulcers31 | Most studies reported a decrease in the number of pressure ulcers |
| Pain management (n = 3)44,47,57 | Three studies reported improvements in patients’ pain management following the implementation of IR, although two were based on staff reports only44,57 and one did not provide findings to support these claims47 | Some evidence reporting improvements in pain management |
| Patient falls (n = 22)9–11,22,23,29,31,34,35,37–42,44,45,47,51,53,54,58 | Thirteen studies reported a decrease in the number of patient falls following the implementation of IR,9,22,23,29,35,37,39–41,44,45,47,51 although some were based on anecdotal staff reports/perceptions only44,45 or did not report findings to support their claims/state whether or not any changes were statistically significant.9,23,29,41,47 Five studies reported no statistically significant change in the overall falls rate10,11,31,38,53 and one reported an increase.58 One study found initial positive gains, although falls rates returned to baseline levels in a 1-year follow-up.42 Others said decreased falls rates could be attributed to other initiatives and not necessarily IR34,54 | Most studies reported a decrease in patient falls |
| Walking distances (n = 2)53,59 | One study reported increased walking distances for staff as a consequence of implementing IR,59 but another found more mixed results53 | Mixed findings |
| Health economic outcomes | ||
| Costs (n = 1)4 | No clear impact of IR on hospital costs has been highlighted4 | No impact |
| Patient re-admission rates (n = 1)53 | No significant differences were found in 30-day patient re-admission rates between the IR intervention and control groups in one study53 | No impact |
| Hospital-reported patient outcomes | ||
| Leaving without being seen/against medical advice (n = 1)40 | IR reduced the number of patients leaving A&E without being seen by 23.4% and leaving against medical advice by 22.6% in one study40 | One study found a reduction in patients leaving against medical advice |
| Patient complaints (n = 5)23,24,31,32,47 | Three studies reported patient complaints reduced after implementing IR, although this was based on staff report only or findings were not reported to support this claim.23,24,47 The third study acknowledged the reduction in complaints could be attributed to other ongoing initiatives and not necessarily to IR.23 Two studies either reported no change in the overall number of patient complaints associated with IR or stated that complaints were too few in number to measure a notable difference31,32 | Mixed findings |
Appendix 3 Analysis of trusts’ additional free-text responses to national survey questions
Mechanism: consistency and comprehensiveness (n = 69)
The most frequently occurring mechanism identified in the survey was the ‘consistency and comprehensiveness’ mechanism, with staff discussing the flexible nature of IR in their trusts. Sixty-nine of the 107 respondents discussed the way in which flexibility had been incorporated into IR in their trust in some form:
. . . we have implemented a more bespoke approach depending on the patient group.
[Staff] use their professional judgement as to how often rounding is to take place i.e. hourly, 2 hourly, etc.
Nurses may ask four patients all together in a bay if they are OK or need anything.
Mechanism: accountability (n = 20)
Twenty trusts highlighted the relationship between IR and accountability. One trust stated that IR fostered a ‘greater understanding of staff accountability’, and another said it improved the accountability of RNs for the quality of care delivered by unqualified staff. One trust reported that HCAs were particularly supportive of IR implementation, as they felt that ’. . . they were able to, perhaps for the first time, document and almost “prove” that they were providing care for the patients’. However, 12 of the 20 trusts referred to IR as being/having the potential to be perceived as a ‘tick-box exercise’, with one stating that some staff completed all the documentation at the end of a shift. This respondent referred to IR as ’. . . a great concept [that] has lost its way and is now perceived negatively by many nursing staff’.
One trust said staff did not appreciate completing IR documentation and did not think it provided any reflection of the care they provided. Another was also critical of IR, describing it as a ‘political response’. However, one trust said that teaching programmes had changed nurses’ negative opinions towards IR, enabling them to recognise it as a supportive tool to good nursing care delivery as well as an excellent record of care provided. The notion that IR provides a record of care was echoed by a further four trusts, which stated that information from IR documentation had been used to answer complaints or provide reassurance to worried carers. Two trusts said they checked IR documentation following an incident such as a fall or pressure ulcer and that this provided an incentive to staff to ensure that IR was being carried out. Another trust stated that IR was a useful resource for giving visibility to wards struggling with low staffing levels, as documentation highlighting the difficulties in providing IR on a shift had been used as a way of escalating and agreeing resource allocation for the ward.
Mechanism: nurse–patient communication and relationships (n = 5)
Five trusts mentioned the relationship between IR and nurse–patient communication and relationships. Two felt that IR did not facilitate a ‘connection’ between nurses and patients, and one stated that some nurses felt that it could ‘trivialise’ nursing interactions. However, another trust associated IR with improved nurse–patient communication, stating that IR was about nurses ‘being with patients and . . . showing patients, at regular intervals, that they are concerned about meeting patients needs’. A fourth trust noted that IR should be about improving nurse–patient communication and responsiveness to individual concerns rather than about completing IR documentation, and the fifth stated they had revised their IR documentation following feedback from staff for the need for greater patient interaction.
Mechanism: visibility (n = 2)
Two trusts highlighted the relationship between IR and visibility and both said IR ensured that staff were more visible to patients. One trust said this made patients feel safe, as they believed staff would notice if they became unwell.
No other mechanisms were highlighted by staff in the free-text survey responses.
Contexts
Contexts influencing the success or failure of IR were mentioned by 23 trusts. These included the following.
Intentional rounding documentation and tools
Issues surrounding IR documentation were mentioned by seven trusts. A few trusts noted that there had initially been some resistance to IR, with staff seeing it as, ‘another form to fill in’. However, over time resistance diminished and one trust stated that, when it was highlighted that staff were simply being asked ‘to document care that they were already undertaking’, there was a greater acceptance of its implementation. One trust had tried using ‘IR clocks’, but these were not a success and were withdrawn. Another trust felt that a move towards electronic recordings of patient interactions might make the process of IR easier.
Staff engagement
Some trusts stated that staff engagement was important to the success of IR and it was noted that some staff would welcome the intervention and others reject it. One trust said the process of engaging staff took time and another said that maintaining motivation for IR could be a challenge. One trust said that IR had failed when staff and leaders were not engaged in the process, believing it to be onerous and lacking in value. In these cases, the frequency of rounds had been reduced without discussion. Another trust said that, on the wards where IR worked well, the ward manager drove the intervention on a daily basis and staff embraced the principles of IR and enjoyed the process of nursing in this way. Another trust said that teaching programmes had reversed nurses’ initial negative attitudes towards IR.
Management/leadership of the process
One trust said the value of IR had to be regularly enforced by all levels of leadership on wards in order to maintain high standards, and another talked of the importance of leadership rounds. Another said they had tried to implement IR, but ‘due to the project leads moving on to new posts, the project has not progressed’.
Reason for implementing intentional rounding
Two trusts said they were already undertaking hourly rounding prior to the Francis report,1 and its implementation was, therefore, not in response to this. Two trusts said that IR had been implemented because of a change towards a larger number of single-room accommodation.
Culture of the ward
Two trusts talked of the need to embed IR into the culture of the ward and integrate it into the daily routine. Not seeing IR as a ‘separate entity’ was perceived as important to its success, although one trust acknowledged that this could be a slow process. Another noted that IR is ‘not the panacea to all concerns and needs to be used as part of a toolkit’.
The impact of other initiatives
One trust said that with ‘so many initiatives . . . ongoing it is sometimes easy to lose the sustainability’ of IR. Two trusts had recently moved nursing desks into patient bays and felt that this had a bigger impact on care and outcomes than IR.
Type of ward
As previously mentioned, some trusts did not perceive IR as suitable for particular types of ward (such as those with a high turnover/volume of patients); therefore, IR was not implemented in these areas.
Type of patient
Again, a number of trusts felt that IR was more relevant for ‘high-risk’ or ‘vulnerable’ patients, or for patients who have high physical nursing care input requirements.
Outcomes
Outcomes resulting from the implementation of IR were mentioned by 38 trusts. Of these, 18 commented that demonstrating the impact of IR was very difficult or not possible. The reasons for this included that any impact or improvement in outcome could not be attributed solely to IR, particularly when other changes in care delivery had taken place, for example staffing, leadership, ward configuration. Health care was observed to be a complex system and assessing a direct cause and effect of IR was thought to be very difficult. It was also thought that trusts had insufficient data to evaluate the impact of IR and several trusts indicated that they had not audited the impact of IR, so the question of impact was difficult to answer.
Patient outcomes
Patient outcomes were the outcomes most commonly mentioned by trusts. Reduction in pressure ulcers was mentioned by 11 trusts and reduction in falls and/or injury as a result of a fall was mentioned by 11 trusts. An impact on aspects of patient experience/satisfaction was also mentioned by 11 trusts; this impact was seen as mainly positive with, for example, one trust saying that patient survey results showed that patients on the ward felt safe and that they thought that staff would notice if they became unwell, and another trust said that patients ‘generally liked quality rounds because they felt less isolated and know they will be checked regularly’. However, two trusts indicated that some patients reported negative outcomes of the implementation of IR when patients who were not part of the care rounds felt neglected or when patients felt that they were being disturbed too often. One trust said that patients had reported being disturbed too often and recognised nurses have ‘too much writing’. Patients ‘have started wanting to negotiate regular timings to be seen.’ Other, less frequently mentioned, outcomes included management of pain (one trust), reduction of patient complaints related directly to nursing care (two trusts) and that IR provides psychological safety for patients, carers and staff (one trust).
A few trusts reported these improved outcomes with some caveats, for example that IR needs to be adhered to correctly and closely monitored to have an impact, that improved outcomes are not always sustained and that how it is applied in practice is critical in terms of staff engagement and impact of patient outcomes. One trust said that, when IR was first implemented and carefully monitored, falls and unanswered call bells decreased; however, when implemented on a wider scale when close monitoring was not facilitated, its impact was thought to be limited as a result of IR not being conducted correctly. Another trust said that ‘On the wards where it works well (where the ward manager drives the process consistently), the patient and carer feedback is good.’
Carers’ outcomes
Outcomes for patients’ carers were infrequently mentioned in the survey open responses. Three trusts said that IR had a positive impact for carers. One said that, where IR works well, carer feedback is good. Two trusts indicated that it provides psychological safety for carers, for example ‘Relatives’ feedback is that they like the reassurance that their “loved one” is being seen on a regular basis’.
Staff outcomes
Ten trusts commented on staff outcomes; there was a mixed view of both positive and negative outcomes. Positive outcomes included that staff felt supported by the IR structured approach, that it provides psychological safety for staff (as well as patients and carers) and staff enjoy working with IR; for example, one trust said ‘those staff who truly embrace the principles enjoy the process of nursing in this way’. Two trusts commented that IR contributed to staff development; for example, one trust said ‘it has proved to be a useful vehicle for supporting the development needs of more junior staff’ and another said ‘Awareness amongst the RNs of their accountability for the practice of the unqualified staff is heightened’.
However, other trusts reported that staff did not find IR beneficial and, instead, thought that it took away their autonomy and was not a reflection of the care they provided; for example, one trust said ‘Staff do not like completing this as they feel it takes away their autonomy; however, they acknowledge there is a positive impact’. And another trust said ‘Staff do not appreciate ticking a chart and do not feel it is any reflection on the care they provided. They report wanting a system that is intuitive to patient’s needs and requests rather than a standardised approach’. Another trust said that nurses were reliant on IR to trigger activity rather than plan their day with their group of patients and team. One trust suggested that IR may increase the work pressure for staff. They said ‘Staff talk about not wanting to feel a failure when they cannot get to every patient every hour’. Another trust said that staff had not reported back either positively or negatively on the impact of IR on their time or job satisfaction.
Trust outcomes
Eight trusts mentioned an impact of IR on outcomes for trusts. The most frequently mentioned (four trusts) was a reduction in complaints. IR was described as ‘a very useful tool and has helped answer complaint responses, root-cause analysis evidence for falls and pressure ulcers’. Furthermore, IR was found to help ‘articulate that there is evidence that care interventions have taken place at designated times (or not as the case may be)’ when responding to complaints and determining actions for ward teams to address these issues. Other outcomes mentioned were ‘harm-free care’, as measured by the safety thermometer; most improved trust (from a sample of > 70 trusts) in terms of patient experience (PICKER survey); and that IR provides a structure for documentation and can generate large volumes of paper records for patients with extended stays.
Appendix 4 Contextual mapping interview topic guide
Appendix 5 Detailed ward profiles
Note that ward layouts have been made more general in some cases to ensure confidentiality of sites.
Case study site 1
Case study site 1 was a large university teaching hospital in an urban location. Two wards were studied.
Ward 1a
Ward 1a was a 24-bed ageing and complex medicine ward. The ward was divided into bays and side rooms, which were mainly used for infective patients requiring barrier nursing or patients reaching end of life.
Ward 1b
Ward 1b was a 24-bed acute medical ward with a specialty in diabetes and endocrinology. Ward 1b was split into three teams, each of which looked after a group of eight patients (made up of a bay of seven beds and a side room). Each team was led by a ward sister and comprised both RNs and HCAs. The layouts of wards 1a and 1b were the same; a map of this layout is provided in Figure 4.
FIGURE 4.
Layout of wards 1a and 1b.
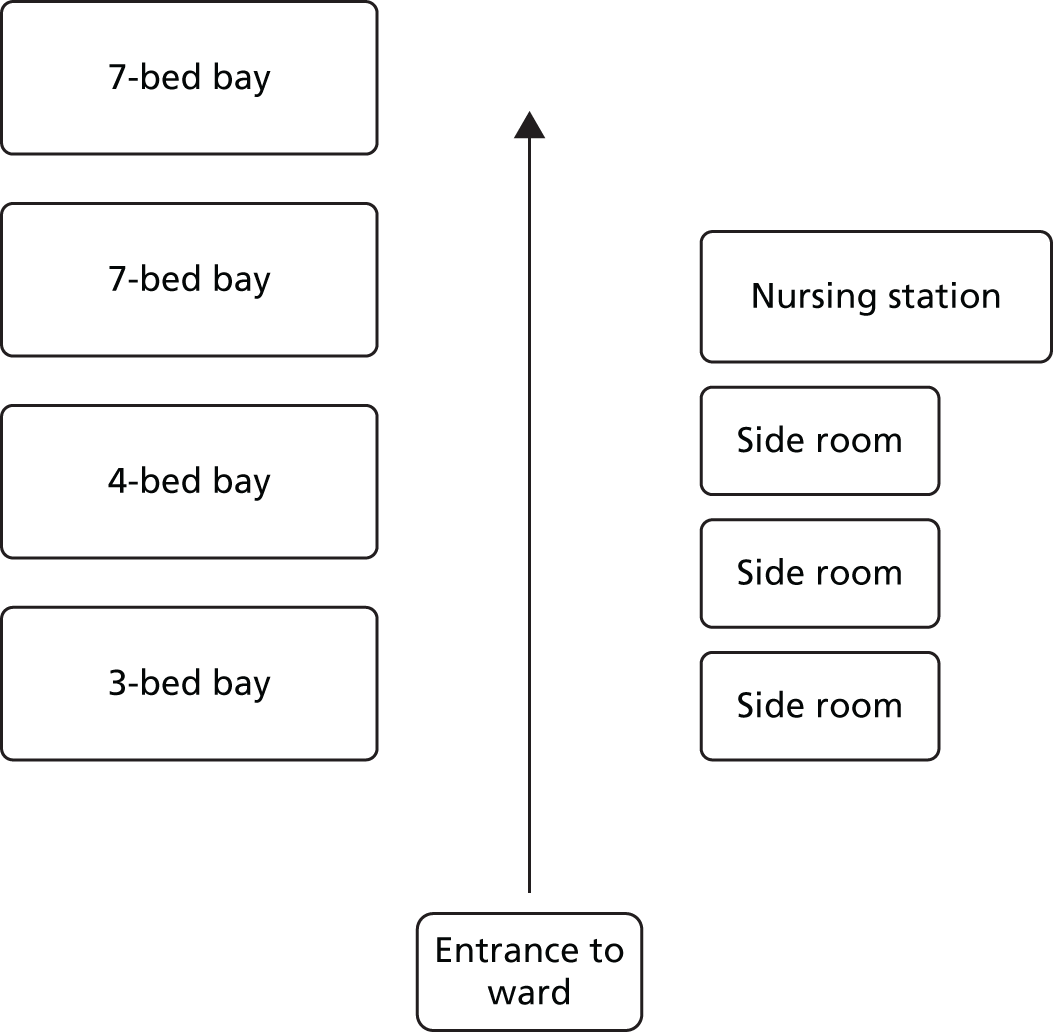
Nursing shift patterns
Staff on both case study wards worked 12-hour shifts.
Staffing information
Table 22 highlights the staffing levels on wards 1a and 1b at the time of data collection.
| Staff band | Nursing staff establishment (FTE) in January and February 2017 | |
|---|---|---|
| Ward 1a (February 2017) | Ward 1b (January 2017) | |
| 7 | 1.0 | 1.0 |
| 6 | 2.0 | 2.0 |
| 5 | 15.19 | 17.29 |
| 2 | 15.09 | 11.09 |
| Total | 33.28 | 31.38 |
| Total vacancy rate in January to February 2017 (FTE) | 3 RN vacancies | 4 RN vacancies |
| 1 HCA vacancy | 0 HCA vacancies | |
At the time of undertaking data collection at ward 1a (February 2017), 127 nursing shifts were covered by bank staff and no shifts were worked by agency staff. When undertaking data collection at ward 1b (January 2017), 81 nursing shifts were covered by bank staff and one shift was worked by agency staff.
Sickness levels
At the time of undertaking data collection at ward 1a, the sickness levels for RNs was 19.74% but there was no HCA sickness. When undertaking data collection at ward 1b, the sickness levels for RNs was 11.56% and for HCAs was 45.08%.
Vacancy rates
At the time of undertaking data collection at ward 1a, there were three RN vacancies and one HCA vacancy on the ward. During data collection at ward 1b, there were four RN vacancies and no HCA vacancies. No members of staff were on maternity leave at the time of data collection on ward 1a or 1b.
Implementation and development of intentional rounding
There was some discrepancy among senior managers as to when IR was implemented in this trust, with suggestions that it was implemented some time between 2009 and 2012, most probably 2011. One manager suggested that IR was introduced in the trust as part of a larger strategy around increasing patient safety, as a means of reducing harm (e.g. hospital-acquired pressure ulcers, falls, dehydration) and improving the quality of care and patient experience. Their memory of its introduction was that a member of staff had been to the USA and heard about IR and had brought this idea back with them to their trust. Their colleagues had then watched videos about IR on YouTube (YouTube, LLC, San Bruno, CA, USA), to find out more about the intervention:
. . . I certainly recall very clearly seeing these YouTube videos and thinking ‘do you know what, that sounds like actually quite a sound principle and a philosophy to base nursing care on’.
However, this manager felt that IR was not initially implemented particularly well in the trust, as a result of not engaging front-line nursing staff with the process, which led to hostility and mistrust:
. . . we all of a sudden . . . got this concept and decided that we were going to write a fantastic policy to support it and there was an implementation scheme that sat with that . . . But we got it wrong, because what we didn’t do was, we didn’t ask our staff to interpret it for us properly and to be able to understand how to deliver it properly.
This resulted in senior managers asking nursing staff to become involved with the process and a group of matrons joined together to re-look at the IR paperwork, with the aim of creating something that would be ‘. . . a little bit more useful and applicable within the ward and department level’. Senior managers said the IR paperwork was then re-designed, with input from front-line nursing staff and some patient involvement, and piloted on a small number of wards. They felt that this meant that the staff felt a sense of ownership over the process:
. . . what they have designed is what they believe to be important.
A policy paper was prepared by trust managers in May 2016 that was aimed at all clinical staff, including AHPs, and outlined trust expectations in relation to nursing staff undertaking IR. In this paper, IR was described as:
. . . a structured process where nursing staff carry out regular checks with individual patients at set intervals, typically hourly. The hourly check of patients follows a prescriptive format and should finish with the closing keywords, most commonly, ‘Is there anything else I can do for you?.
The paper stated that it was expected that all nursing staff should understand and adhere to the IR policy by regularly checking the ‘4Ps’ of IR, asking patients specific questions and completing a formal written checklist at each round. The policy stated that ‘It is anticipated that this approach will provide a platform for addressing the needs and concerns of patients’ and highlighted US research findings39 reporting reductions in call bell use, falls and pressure ulcers and an increase in patient satisfaction. The process of adaptation of IR was ongoing in this trust, and the IR documentation was continuously changing according to perceived need:
. . . the documentation came out and then a bit later on the policy got written and then we’ve revised the policy on from that . . . and we’ve revised the document sort of every 2 years to the document that we’ve got now.
Intentional rounding procedure and documentation
The trust policy on IR was that a welcome leaflet explaining IR should be given to every patient on admission. This was to be accompanied by a verbal explanation of the IR process. Both wards at case study site 1 used the same IR form, which was a four-page, folded, booklet-style paper document, including, on the front page, boxes to complete for the ‘4Ps’, falls risk and skin bundle questions. Intervals of 1 or 2 hours were pre-written onto the form and IR questions were to be asked on an hourly basis between 08.00 and 22.00 and every 2 hours between 22.00 and 08.00. If patients were asleep, staff were not expected to disturb them unless their care needs required this. RNs were specifically required to complete IR forms on the hours of 02:00, 08:00, 12:00, 16:00 and 20:00 and HCAs could complete it at other times. However, this was described as a ‘minimum standard’; RNs could also complete IR at other times of the day if they wanted. Staff were expected to complete each box on the form with a ‘yes’ or ‘no’ answer, depending on a patient’s response. Printed at the bottom of page 1, highlighted in red and using bold typeface, was the question, ‘Is there anything else I can do for you?’, but staff were not required to state anywhere on the documentation whether or not they had asked this question.
The second page of the IR booklet contained questions on mobility, bed rail position and a mattress guide along with a body map, on which staff could record skin integrity details and highlight if and where on the body a patient had any devices. The third page of the IR booklet was the 24-hour fluid balance chart and the final page contained the food record chart. IR forms were kept at the foot of the bed and were the only documentation in the trust that were in paper format; all other documentation was electronic. When IR forms were completed, they were filed on-site. A reproduced example of the case study site 1 IR document is provided in Appendix 6.
Case study site 2
Case study site 2 was a large hospital in an urban location with a rural catchment area. Three-quarters of the patient beds at this site were in single rooms, most with en suite bathrooms. Two wards were studied.
Ward 2a
Ward 2a was a 32-bed acute trauma orthopaedics ward and dedicated hip fracture unit with 24 single rooms and two four-bed bays. The ward had the nurses’ station in the middle, opposite the main entrance, with a four-bed bay on either side and single rooms spread across a corridor on each side. Single rooms were grouped into two sets of pairs and between each pair of rooms was a standing perch, where staff could write up notes while maintaining good observation of patients.
Ward 2b
Ward 2b was a 32-bed complex medicine for older people ward with 24 single rooms and two four-bed bays. The ward provided medicine for patients with general medical problems who had complex needs. The ward was divided into four teams, consisting of RNs and HCAs; patient care was divided between the teams each shift. The layout for ward 2b was the same as for ward 2a; a map of this layout is provided in Figure 5.
FIGURE 5.
Layout of wards 2a and 2b at case study site 2.
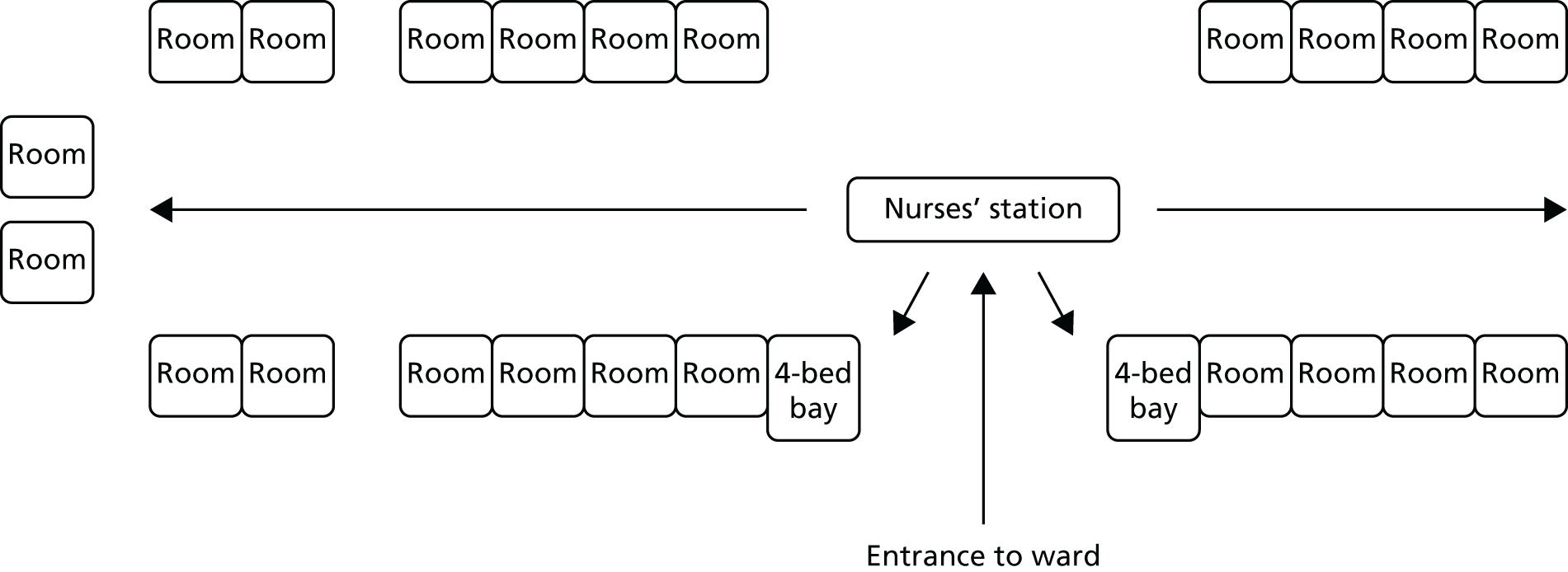
Nursing shift patterns
Staff on both wards worked a combination of shift patterns: early shifts (07:00–13:30), late shifts (13:00–19:30), long days (07:00–19:30) and nights (19:00–07:30).
Staffing information
Table 23 highlights the staffing levels on wards 2a and 2b at the time of data collection.
| Staff band | Nursing staff establishment (FTE) in April 2017 | |
|---|---|---|
| Ward 2a | Ward 2b | |
| 7 | 1.0 | 1.0 |
| 6 | 3.6 | 3.6 |
| 5 | 17.2 | 21.1 |
| 4 | 2.6 | 6.6 |
| 3 | 6.5 | 5.9 |
| 2 | 19.6 | 7.2 |
| Total | 50.5 | 45.3 |
| Total vacancy rate in April 2017 (FTE) | 4.4 | 7.9 |
| Range of total vacancy rate from May 2016 to May 2017 (FTE) | 3.0–10.9 | 4.0–8.5 |
| Total vacancy factor (%) | 8.7 | 17.4 |
| Range of total vacancy factor (%) May 2016 to May 2017 (%) | 6.0–21.6 | 8.8–18.8 |
Sickness levels
At the time of undertaking data collection at ward 2a (April 2017), the sickness level for all nursing staff was 2.18%. When undertaking data collection at ward 2b (April 2017), the sickness level for all nursing staff was 4.42%.
Vacancy rates
The vacancy rate on ward 2a was 4.4 full-time equivalent (FTE). The vacancy rate on ward 2b was 8.1 FTE.
Implementation and development of intentional rounding
Again, there was some discrepancy among senior managers as to when IR was implemented in this trust, with suggestions that it was implemented some time between 2014 and 2016. One manager believed it was implemented in 2014 when the hospital was moving to a new site with predominantly single rooms. At the time, managers were concerned that the move to single rooms would affect the patient falls risk and so were looking to proactively introduce a policy to target this:
. . . we were concerned about our rate of falls; we were looking to reduce that rate quite proactively, ahead of the move, when we knew we had a big risk coming, because we had the 70% single rooms in the new building, and we wanted to prepare for that.
After speaking with colleagues at neighbouring trusts that had already implemented IR, the rationale behind the intervention resonated with managers, who felt that this could help develop a calm and compassionate climate at their new hospital site:
. . . we heard somebody from there talk about it, and you know, that whole concept of leaving the patient with the words, very calmly spoken, to say, ‘Is there anything else I can do for you? Because I have the time,’ seemed to really resonate, and be something we wanted to make sure that that’s the way our patients would feel, too. That nurses weren’t rushed.
Managers reported a period of testing and piloting IR documentation and training staff about the process of undertaking IR, although some reported that, with hindsight, IR was probably implemented too quickly across the trust. A trust standard operating procedure document was circulated in May 2014, aimed at all clinical staff, ward receptionists, administrators and housekeepers and described IR as:
. . . the timed, planned intervention by healthcare staff in order to address common elements of in-patient care. The aim being to proactively identify and meet patients’ fundamental care needs and psychological safety. By means of a regular bedside ward round, intentional rounding is a structured way of making observations and carrying out tasks in order to ensure the patient’s comfort and wellbeing, and recording that this has been done.
The document states that the implementation of IR aimed to create a safer hospital environment and reduce patient harm by proactively checking patients. It stated that IR had been shown to reduce call bell use, falls and hospital-acquired pressure ulcers and improve patient satisfaction, pain management, nutrition and hydration. It urged that:
All patients, family members and carers will have the intentional rounding tool explained to them on first admission and on any subsequent ward to ward transfer. . . . The named nurse for the patient will identify during bedside handover, the frequency of intentional rounding required and will discuss this with the patient.
It also informs nursing staff that, ‘Each comfort question on the intentional rounding tool should be asked in order and documented on the tool’.
Intentional rounding procedure and documentation
Both wards at case study site 2 used the same IR form, which was on a two-sided sheet of paper. The front page of the documentation had boxes for patient comfort (drink/snack, toilet, pain, ‘anything else I can do for you?’), falls prevention and skin bundle questions. The second page of the IR booklet contained questions on pressure ulcers and a body map, on which staff could record skin integrity details and highlight if and where on the body map a patient had any devices. Space was also provided for staff to document any variance/deviation and any actions resulting from rounding (e.g. pain control medication administered).
Trust policy on IR stated that RNs could alter the frequency of IR to reflect other assessments as long as this was indicated on the patient’s care plan, safety briefing and patient record. Policy also stated that if patients were deemed to be at minimal risk of falls and low risk of pressure ulcers, IR could be conducted at a minimum frequency of every 4 hours. However, ward managers informed researchers that, in practice, staff were asked to complete IR every time they entered the patient’s room. The timing section at the top of the form was left blank so that nurses could enter the specific time when the interaction took place. If patients were asleep, staff were not expected to disturb them unless their care needs required this. According to trust policy, any member of clinical staff, including medical and AHP staff who had read the IR policy and received training in the SKIN bundle and Falls Bundle, could undertake IR and complete the documentation. However, again, ward managers told us it was generally nursing staff who undertook IR, although there was no minimum standard as to how often RNs should undertake it, as in site 1. Staff were expected to complete each box on the form with a ‘yes’ or ‘no’ answer, depending on the patient’s response. IR documentation was stored differently on the two case study wards. On one ward, IR was hung on a magnetic board directly outside a patient’s room and could therefore be clearly seen when at the standing perch. In the second ward, IR documentation was stored in patient care folders, alongside a number of other pieces of documentation, including the stool chart, patient care plan, 24-hour fluid balance charts and acute pain observation chart. A reproduced example of the case study site 2 IR document is provided in Appendix 7.
Case study site 3
Case study site 3 comprised two large university teaching hospitals in the same trust, spread across several sites in urban locations. Two wards were studied.
Ward 3a
Ward 3a was a 26-bed cardiac and respiratory medicine ward. A map of the layout of ward 3a is provided in Figure 6.
FIGURE 6.
Layout of ward 3a.
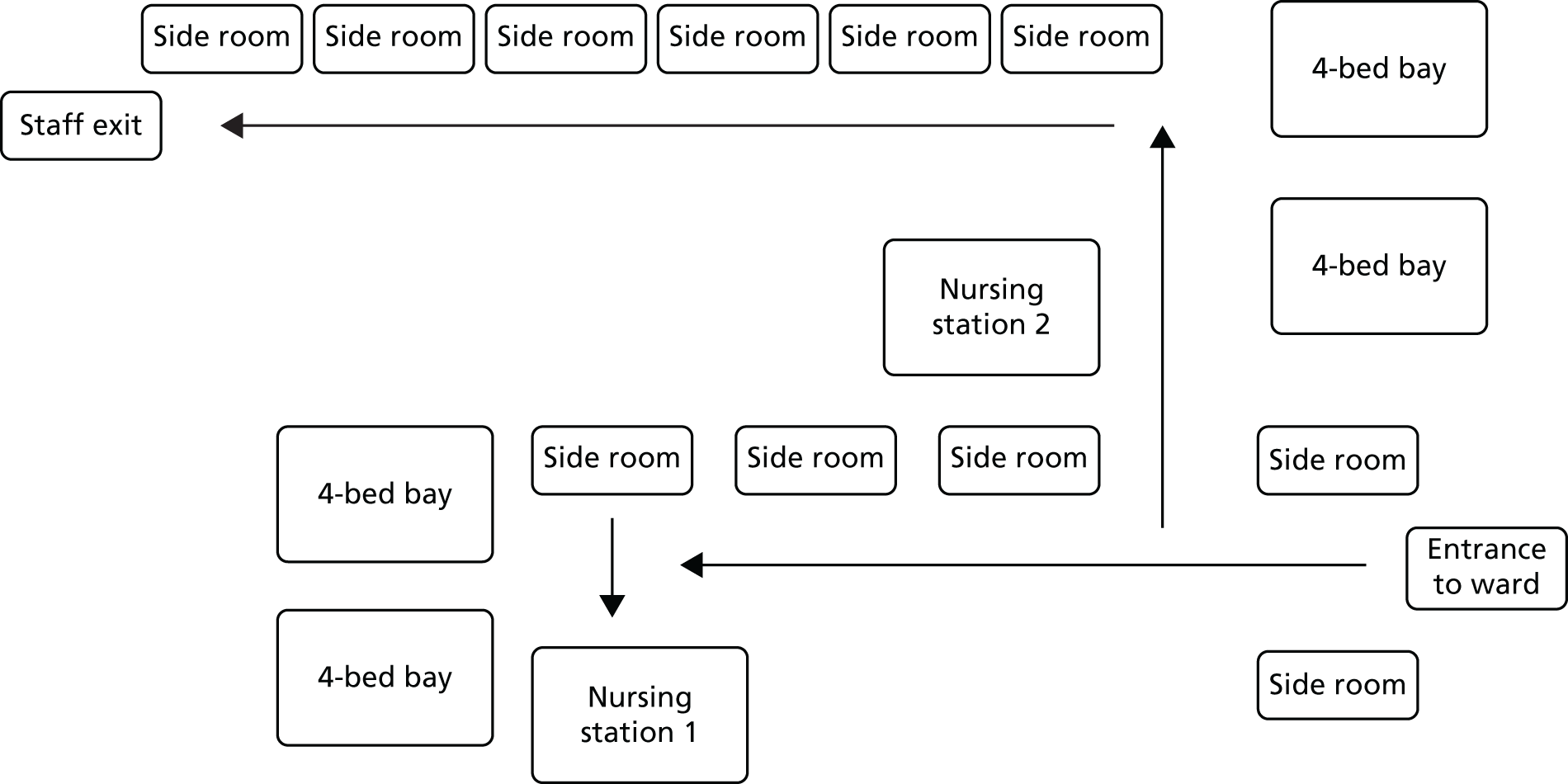
Ward 3b
Ward 3b was an 18-bed, single-sex, elderly care acute medical ward, with a modified Nightingale-style layout of three bays or sections (two with six beds and one with four beds) and two side rooms. A map of the layout of ward 3b is provided in Figure 7.
FIGURE 7.
Layout of ward 3b.
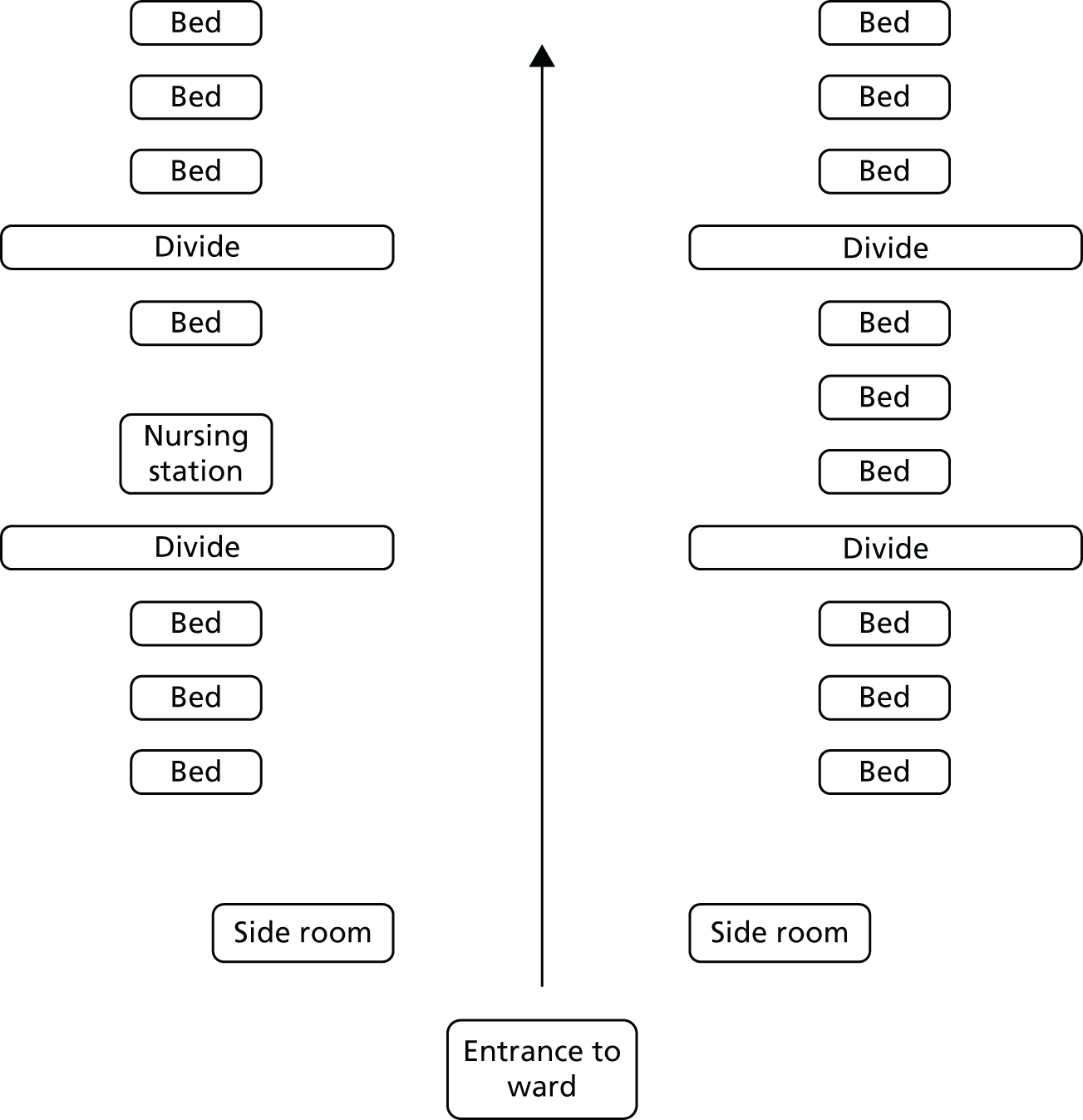
Nursing shift patterns
The majority of staff on both wards worked long days (08:00–20:30) and night shifts (20:00–08:30), although some staff worked early shifts (08:00–16:00).
Staffing information
Table 24 highlights the staffing levels on wards 3a and 3b at the time of data collection.
| Staff band | Nursing staff establishment (FTE) in July 2017 | |
|---|---|---|
| Ward 3a | Ward 3b | |
| 7 | 1.0 | 1.0 |
| 6 | 4.9 | 2.1 |
| 5 | 21.5 | 12.7 |
| 2 | 9.5 | 12.4 |
| Total | 36.9 | 28.2 |
Sickness levels
At the time of undertaking data collection at ward 3a, the sickness levels for all nursing staff was 7.30%. When undertaking data collection at ward 3b, the sickness levels for all nursing staff was 1.36%.
Vacancy rates
The vacancy rate on ward 3a was 19.78%. The vacancy rate on ward 3b was 9.69%.
Implementation and development of intentional rounding
Most of the senior managers interviewed were relatively new to the trust and IR was already in place when they joined; therefore no one was able to say when exactly IR had been implemented. However, a matron who had been working as a nurse in the trust for many years guessed that IR may have been implemented around 2012/13. This high level of change and rapid turnover was quite common in this trust and it was acknowledged that organisational memory had been affected as a result, as had the way in which new interventions were implemented:
. . . my predecessor was 6 months and her predecessor was 6 months . . . So organisational memory is, is difficult. Also this particular trust has been through quite a lot of changes and has been through quite a lot of audit and scrutiny as well, and so some of the interventions have had to be put in very quickly and kind of rolled out very quickly.
The matron’s recollection of how IR was implemented in the trust was hazy, but she felt that it was introduced quickly, without being tested or piloted in a small number of wards:
. . . I actually do not recall it being piloted . . . I’ve probably, from memory, feel that it was just, one day it was launched.
However, it was not introduced as mandatory on all wards and ward managers were given the flexibility to choose whether or not they delivered the intervention. Some ward managers, therefore, initially chose not to implement IR, although it was believed that more wards were delivering it now:
. . . it was launched and . . . some wards did it, some wards accepted it, and some of my wards at the time would not, like one manager, one in particular, refused to do it because he didn’t think it was necessary, because he felt his nurses did it . . . And it was only in recent times, and it’s now a new ward manager, that then they saw the benefits.
Senior managers did not think that nursing staff had been given any formal training in delivering IR, although it was part of ward induction:
We have a well-run ward module that teams go through which helps people to manage care and manage the environment and which IR would be part of that but I don’t think we have people going off on course on IR; I think it’s on-the-job training as far as I would be aware.
As far as senior managers were aware, there was no formal policy documentation on IR circulated to staff at this trust, other than the guidance on IR provided in the nursing documentation bundle (see Intentional rounding procedure and documentation).
Intentional rounding procedure and documentation
Both wards at case study site 3 used the same IR documentation; however, two IR forms were used: one for patients with a Waterlow score (i.e. an estimated risk for the development of a pressure sore in a given patient) of < 10 and another form for patients with a Waterlow score of ≥ 10. Both forms were incorporated into the ‘nursing documentation bundle’, a 49-page, printed booklet completed by nursing staff, which also included discharge planning documentation, the patient health record, cannula care management/care plan and skin damage body mapping, etc. The IR documentation for patients with a Waterlow score of < 10 required nursing staff to ask patients every 2 hours about their hydration needs, toileting needs, environmental assessment, movement needs (e.g. repositioning, footwear, walking aids), pain and general well-being. Timings were already included on the documentation (e.g. 08:00, 10:00, 12:00) and nursing staff were to complete each section with a ‘yes’, ‘no’ or ‘not applicable’ response and sign their name. If a patient was asleep between the hours of 00:00 and 06:00, nursing staff were advised to discuss with the nurse in charge whether or not the patient should be woken for IR.
The IR documentation for patients with a Waterlow score of ≥ 10 was more detailed, and nursing staff were advised to ‘continuously complete’ the form each day. Questions included assessing surface needs (e.g. mattress type, bed height), skin inspection, movement needs, toilet needs and nutrition. No timings were preincluded on the form and nursing staff had to write on the form the specific time when the interaction took place. Neither form required nursing staff to ask the question ‘Is there anything else I can do for you?’ At both sites, nursing bundles were kept at a patient’s bedside. An example of each IR document from case study site 3 is provided in Appendices 8 and 9.
Appendix 6 Example of intentional rounding documentation at case study site 1
Appendix 7 Example of intentional rounding documentation at case study site 2
Appendix 8 Example of intentional rounding documentation at case study site 3 (for patients with a Waterlow score of < 10)
Appendix 9 Example of intentional rounding documentation at case study site 3 (for patients with a Waterlow score of ≥ 10)
Appendix 10 Cost analysis
Incremental cost analysis of intentional rounding
Introduction
The aim of this analysis was to calculate the incremental cost to the NHS of conducting IR in the wards included in the study instead of not doing it. Three main types of cost were included in the analysis to estimate the total incremental costs:
-
direct costs – the cost of any consumable resource directly used for the implementation of IR
-
opportunity cost – the value of an alternative service given up to perform IR
-
indirect costs – cost of start-up, development and training not directly attributable to IR.
The unit of cost (total costs incurred) was reported in incremental cost per patient per day of hospitalisation. Costs and prices are reported in 2017 Great British pounds.
Method
All costs were allocated to patients hospitalised in the wards included in the analysis over different units of time. The estimate of the median number of patients per ward per day, week, month and year was calculated using bed occupancy figures. The calculations are not reported to avoid identification of the study sites.
Owing to the lack of observed data, direct costs were estimated based on the best methodological option available. As an example, the cost of printing an A4 sheet of paper was estimated by approximation, based on the unitary printing cost borne in 2017 by Kingston University (£0.20 per sheet). Storage costs were estimated based on replacement cost, the weekly cost of renting a space large enough to store a large cabinet (£6.92 per week).
Opportunity costs were estimated based on nursing time used. Median hourly wages per salary band were obtained from NHS published pay scales at national level. 95 Table 25 reports the median estimates of hourly wages of nursing staff by salary band and spine point.
| Opportunity cost: time | Median hourly pay (£) | Median pay per minute (£) |
|---|---|---|
| Ward clerk band 1 | 7.87 | 0.13 |
| HCA band 2 | 8.37 | 0.14 |
| HCA band 3 | 9.28 | 0.15 |
| RN band 5 | 12.69 | 0.21 |
| RN band 6 | 15.27 | 0.25 |
| Ward manager band 7 | 18.54 | 0.31 |
| Matron band 8 | 22.44 | 0.37 |
Indirect costs (e.g. development of IR printed material, start-up and ward training) were estimated based on time used by nursing staff as directly observed in the field work. The nursing staff of a representative ward was obtained by the FTEs reported for two wards included in the study (site 3, wards a and b). Table 26 reports details of the staffing estimate. Indirect costs were amortised over 1 year and allocated to the median number of patient-days per ward per year.
| Site 3, ward | Salary bands | FTEs | Representative ward | Nurses (n) |
|---|---|---|---|---|
| b | Nurses – band 7 | 1.0 | Band 7 | 1 |
| b | Nurses – band 6 | 2.1 | Band 5 or 6 | 21 |
| b | Nurses – band 5 | 12.7 | Band 2 or 3 | 11 |
| b | Total band 5 and 6 | 14.8 | ||
| b | Band 2 | 12.4 | ||
| a | Nurses – band 7 | 1.0 | ||
| a | Nurses – band 6 | 4.9 | ||
| a | Nurses – band 5 | 21.5 | ||
| a | Total band 5 and 6 | 26.5 | ||
| a | Band 2 | 9.5 |
Results and comments
The outcomes of the incremental cost analysis are reported in Table 27.
| Incremental costs | Type of cost | Unitary cost | Units used | Daily cost | Estimation method |
|---|---|---|---|---|---|
| Direct costs | |||||
| Printing documentation | A4 sheet | 0.20 | 2 | 0.40 | Unitary printing cost at known Institution (Kingston Business School) |
| Storage | storage | 6.92 | 0.006 | 0.04 | Weekly rental cost for storing a large cabinet/[(2 A4 per day) × 7/(mean patients per ward per day) × 2 × 7] |
| Filing | Hourly pay | 7.87 | 0.006 | 0.05 | Ward clerk 1 hour × week/[(2 A4 per day) × 7/(mean patients per ward per day) × 2 × 7] |
| Total direct costs/patient/day | 0.49 | ||||
| Opportunity cost: allocation of nursing time | |||||
| Completing IR | |||||
| Sites with hourly IR | Mean pay per minutea | 0.17 | 42 | 7.26 |
|
| Sites with IR every 2 hours | Mean pay per minutea | 0.17 | 20 | 3.46 |
|
| Auditing IR | |||||
| Ward manager | Pay per minute | 0.31 | 0.31 | 0.09 | Ward manager auditing five patient IR notes per week (10 minutes per set of notes, i.e. 50 minutes for five patients) |
| Matron | Pay per minute | 0.37 | 0.07 | 0.03 | Matron auditing five patient IR notes per month (10 minutes per set of notes, i.e. 50 minutes for five patients) |
| Total opportunity cost per patient per day of hourly IR (£) | 7.38 | ||||
| Total opportunity cost per patient per day of IR every 2 hours (£) | 3.58 | ||||
| Set-up and training costsb,c | |||||
| Multidisciplinary team meetings | Hourly pay band 7 | 18.54 | 18 | 0.04 | 3 multidisciplinary team meetings × 6 members of staff (three ward managers, band 7 and three senior nurses/allied professionals, band 8) (2 hours) |
| Hourly pay band 8 | 22.44 | 18 | 0.05 | ||
| Consultation on forms | Hourly pay band 7 | 18.54 | 16 | 0.03 | E-mail consultation with ward managers (30 minutes × all nurses in ward) |
| Ward-based IR training | Hourly pay band 7 | 18.54 | 0.25 | 0.01 | Ward manager chat with all nursing staff (all grades – HCA, band 5 and 6) – 15 minutes nursing staff – 15 minutes per staff member |
| Mean hourly pay band 5 | 13.98 | 5.16 | 0.10 | ||
| Mean hourly pay band 2 | 8.825 | 2.73 | 0.03 | ||
| Peer observation | Hourly pay band 7 | 18.54 | 0.25 | 0.01 | On-the-job training – peer observation (all grades – HCA, band 5 and 6) – 15 minutes |
| Mean hourly pay band 5 | 13.98 | 5.16 | 0.10 | ||
| Mean hourly pay band 2 | 8.825 | 2.73 | 0.03 | ||
| Total set up and training cost/patient/day | 0.41 | ||||
| Total incremental cost of hourly IR per patient per day (£) | 8.27 | ||||
| Total incremental cost of IR every 2 hours per patient per day (£) | 4.47 | ||||
The incremental costs amounted to £8.27 per patient-day for hourly IR. Incremental costs drop to almost half (£4.47 per patient-day) if IR is conducted every 2 hours. This difference should be expected, as the opportunity cost of nursing time drives ≈90% of the total incremental costs of IR. The dominance of nursing time costs makes irrelevant a formal sensitive analysis. Total incremental costs of IR are directly correlated with the frequency of IR and the hourly wage of the nurses dedicated to it. Total incremental cost and frequency of IR seem to be linearly correlated: by reducing the frequency by 50%, the total incremental costs dropped by a similar percentage. Total incremental costs of IR are less sensitive to the hourly pay of nursing staff, because the assumption used in the base case already allocates 70% of IR to HCAs (bands 2 and 3). By allocating 100% of IR to HCAs, total incremental costs would drop to £7.19 for hourly IR and 3.96 for IR every 2 hours.
The results of this incremental cost analysis lead to a relevant conclusion: IR rounding imposed on the NHS an increase in the daily cost of hospitalisation in the range of £8.27–4.47 per patient, depending on the frequency of IR. For a ward of similar size to the ones included in the study, this would represent an annual increase of hospitalisation costs estimated to be in the range of £70,609–38,164 per year. Since NHS costs are calculated on full absorption basis,96 which includes the allocation of all overhead costs to health services produced, the annual incremental costs of IR could exceed £100,000 per hospital ward in the case of hourly IR.
This cost analysis shows that total incremental costs imposed by IR on the NHS budget would require a full economic evaluation of its value for money.
Appendix 11 Interview schedule: ward managers
Appendix 12 Interview schedule: nursing staff
Appendix 13 Interview schedule: health-care staff (non-nursing)
Appendix 14 Interview schedule: patients
Appendix 15 Interview schedule: carers
Appendix 16 Definitions for observation categories
| Observation category | Definition |
|---|---|
| Opening phrase | |
| Fully observed | Nursing staff greets the patient and introduces themselves by namea |
| Partially observed | Nursing staff greets the patient but does not introduce themselves by name |
| Not observed | Nursing staff does not use any opening phrase or general greeting before starting the round |
| Positioning | |
| Fully observed | Nursing staff checks that the patient is comfortable and assesses/asks about pressure sores when appropriateb |
| Partially observed | Nursing staff either checks if the patient is comfortable or assesses/asks about pressure sores (not both) |
| Not observed | Nursing staff does not ask about comfort or assess/ask about pressure sores |
| Personal needs | |
| Fully observed | Nursing staff asks about patient’s personal needs and asks about/assists with toileting or checks catheterc |
| Partially observed | Nursing staff either asks about patient’s personal needs or asks about/assists with toileting/checks catheter (not both) |
| Not observed | Nursing staff does not ask about/assess patient’s personal needs or toileting issues |
| Pain | |
| Fully observed | Nursing staff asks patient about pain and asks them to assess their pain on a scale of 0–10d |
| Partially observed | Nursing staff asks patient about pain but does not ask them to assess/rate their level of pain |
| Not observed | Nursing staff does not ask about pain |
| Placement of items | |
| Fully observed | Nursing staff ensures that any items a patient needs (e.g. call bell, drink) are within easy reach (note that staff may or may not vocalise this – the researcher may just see nursing staff moving things closer to patient) |
| Partially observed | Nursing staff asks about/mentions any items a patient needs (e.g. call bell, drink, personal valuables) but does not ensure these are in easy reach |
| Not observed | Nursing staff does not mention personal items or ensure items a patient needs are within easy each |
| Environmental assessment | |
| Fully observed | Nursing staff is seen/heard to assess the care environment (e.g. any fall hazards, temperature of room, whether curtains need opening/closing) and rectify any issues |
| Partially observed | Nursing staff assesses some of the care environment issues but either does not assess them all or does not rectify any issues |
| Not observed | Nursing staff is not seen/heard to assess any care environment issues |
| Closing phrase | |
| Fully observed | Nursing staff says the phrase ‘Is there anything else I can do for you?’e or words to that effect |
| Partially observed | Nursing staff ends the conversation with a general closing phrase (e.g. ‘goodbye’ or ‘thanks’) |
| Not observed | Nursing staff does not use any closing phrase before completing the round |
| Patient informed of when the nursing staff will return | |
| Fully observed | Nursing staff gives a specific time when they will return to the patient |
| Partially observed | Nursing staff gives a general sense that they will return to the patient (e.g. ‘I’ll be back again soon’ or ‘See you in a bit’) |
| Not observed | Nursing staff does not mention when or if they will return to the patient |
Glossary
- 4Ps
- The four key elements of intentional rounding: (1) positioning, (2) personal needs, (3) pain and (4) placement of items.
- Context
- ‘The ‘backdrop’ of programmes and research . . . broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism’ (Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311–46).
- Mechanism
- ‘. . . mechanisms are underlying entities, processes or structures which operate in particular contexts to generate outcomes of interest’ (Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31). More specifically, ‘. . . mechanisms are a combination of resources offered by the social programme under study and stakeholders’ reasoning in response’ (Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10:49).
- Outcome
- A result of the interaction between a mechanism and its triggering context.
- Programme theory
- The programme theory specifies what is supposed to be done in a policy or programme (theory of action) and how and why that is expected to work (theory of change) [Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist Synthesis: Rameses Training Materials. 2013. URL: www.ramesesproject.org/media/Realist_reviews_training_materials.pdf (accessed 25 August 2019)].
List of abbreviations
- AHP
- allied health professionals
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMO
- context–mechanism–outcome
- CNO
- chief nursing officer
- CQC
- Care Quality Commission
- FTE
- full-time equivalent
- HCA
- health-care assistant
- IR
- intentional rounding
- i.v.
- intravenous
- MDT
- multidisciplinary team
- NCQF
- Nursing and Care Quality Forum
- NMC
- Nursing and Midwifery Council
- Qualpacs
- Quality Patient Care Scale
- RN
- registered nurse
