Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/47/11. The contractual start date was in June 2018. The final report began editorial review in December 2018 and was accepted for publication in May 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Rodgers et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background
NHS England uses the term ‘digital-first primary care’ to refer to delivery models through which a patient can receive the advice and treatment they need from their home or place of work via online symptom checking and remote consultation. 1 In these models, the patient’s first point of contact with a general practitioner (GP) is through a digital channel, rather than a face-to-face consultation, although the latter may remain an option if required.
Since 2015, NHS England has invited a number of organisations to become new care model vanguard sites, each:
. . . taking a lead on the development of New Care Models, which will act as the blueprints for the NHS moving forward and the inspiration to the rest of the health and care system.
NHS England’s Harnessing Digital Technology workstream seeks to provide support to these organisations focusing on implementing digital solutions:
. . . to rethink how care is delivered, given the potential of digital technology to deliver care in radically different ways, [and] help organisations to more easily share patient information.
The Health Innovation Network was commissioned by the Harnessing Digital Technology workstream to undertake a review of the evidence base for technology-enabled care services. The review, which was published in 2017, looked for evidence on short messaging service (SMS), video consultation, digital health applications (apps), web-based interventions and telemonitoring. 3
However, this review did not look exclusively at digital innovations in primary care, such as ‘digital-first primary care’, as conceptualised by NHS England. As digital-first services have increased in number and reach, so have questions about the implementation and effects of such services. For example, the implications of digital-first primary care for general practice payments was the subject of a national consultation undertaken in July–August 2018. 1
In October 2018, a the UK government published a policy document on the use of technology, digital and data within health and care to meet the needs of all users. 4 The stated objective is the provision of care and improved health outcomes for people in England. To achieve this, a clear focus is needed on improving the technology used by NHS staff, social care workforce and the different groups who deliver and plan health and care services for the public. The document sets out a vision to develop a new approach collaboratively and setting clear standards for the use of technology in health care. 4
NHS England initially approached the Health Services and Delivery Research (HSDR) Evidence Synthesis Centre to help identify published evidence of potential relevance to digital-first primary care. An iterative process of scoping the literature was agreed. The first stage, to scope and summarise existing evidence, was undertaken and the findings discussed with NHS England, resulting in further refinement of the research questions of interest to be undertaken in the second stage.
Chapter 2 Methods
Stage 1: scoping and summary of the evidence
Initially, NHS England requested a map of the available published literature relevant to digital health in primary care. Given the limited resources and likely large volume of literature, this primarily focused on secondary research.
Identification of evidence
Scoping searches were carried out during July 2018 to identify systematic reviews relating to digital health in primary care. The search strategy consisted of terms for digital health combined with terms for primary care. No date or geographical limitations were applied. In MEDLINE a further set of terms were added to the strategy to limit retrieval to systematic reviews. The following databases were searched: MEDLINE, Cochrane Database of Systematic Reviews (CDSR), Database of Abstracts of Reviews of Effects (DARE) and the Health Technology Assessment database. Searches were conducted in July 2018, without any date restrictions. The PROSPERO database was also searched to identify protocols of ongoing systematic reviews.
In addition, a range of research, policy and government websites were searched to identify relevant reports. Authors of ongoing work were contacted. Search strategies can be found in Appendix 1.
Selection criteria
Two reviewers screened the title and abstracts of retrieved records against the following inclusion criteria.
Study design
-
Systematic reviews, meta-analyses and other forms of evidence syntheses. Reviews could include primary studies of any design. Though the searches focused on evidence syntheses, any related primary studies incidentally encountered were also included when relevant. However, this study did not systematically search for relevant primary research evidence.
Population
-
Primary care medical staff and (1) patients (or their caregivers) of any age and/or (2) other medical professionals.
Interventions
-
As the known literature rarely conceptualised interventions as ‘digital primary care’, any form of non-face-to-face interaction, including e-mail, online/video, messaging and artificial intelligence-led systems or triage, were included. Reviews that included telephone consultation alongside digital forms of interaction were included at this stage. Reviews focusing predominantly or solely on the following were excluded:
-
improving adherence to treatment or rates of attendance through the use of reminders
-
remote monitoring or self-management of conditions without some form of two-way interaction being a key component
-
remote treatment, coaching or rehabilitation-focused interventions (e.g. remote therapy for mental health conditions).
-
Outcomes
-
Outcomes were not restricted but could include impact on care in terms of effectiveness and safety; patient access/convenience; and system-level efficiencies and related issues, such as workforce retention, training and satisfaction. In terms of patient access, this includes a better understanding of which patients are able to use digital consultations and what conditions are/are not appropriate for non-face-to-face engagement.
Stage 2: narrowing the evidence base – rapid evidence synthesis
NHS England requested a very rapid, brief and high-level overview of the evidence retrieved in stage 1. Although a full systematic review was not possible, given the time and resources available, the HSDR Evidence Synthesis Centre attempted to introduce a level of transparency and reproducibility not typically associated with these kinds of briefings. Therefore, aspects of systematic review methodology, such as a priori inclusion criteria, critical appraisal of included evidence, and process measures to avoid bias and errors, were introduced.
Revised research questions
After examining the retrieved scoping materials, NHS England refined their initial list of questions to the following:
-
What are the benefits of digital modes and models of engagement between patients and primary care? To patients, GPs, the system?
-
As GP workload and workforce is the main threat to primary care, how do we use these innovations to alleviate this, rather than only increase patient convenience and experience?
-
Which patients can benefit from digital (online) modes and models of engagement between patients and primary care?
-
What channels work best for different patient needs and/or conditions?
-
Are there differences in synchronous and asynchronous models?
-
-
How to integrate ‘digital-first’ models of accessing primary care within wider existing face-to-face models?
-
How to contract such models and how to deliver: what geography size, population size?
We conducted a rapid synthesis of the most relevant evidence identified during the scoping exercise (stage 1) to establish if and to what extent these questions can be answered by the identified research. Given the limited time and resources, a comprehensive systematic review was not attempted.
Revised selection criteria
To understand what evidence might be available to address each of these questions, we further refined the list of documents to the following:
-
systematic reviews/evidence syntheses, including evidence on the use of digital (online) modes and models of engagement between patients and primary care (telephone/audio alone was excluded unless it was alongside digital modes)
-
ongoing research and any incidentally identified primary studies focused on the use of digital (online) modes and models of engagement in any health-care setting.
When evidence was available to address one of the above questions, the relevant results/conclusions were extracted. When no evidence was available from the included documents, this was made clear.
Selection procedure
All records were screened by two reviewers, with disagreements resolved by consensus or consulting a third reviewer.
Data extraction
For each included record, data were extracted on study/review methods, type of digital intervention, patient population(s), outcomes and authors’ conclusions. Data were extracted by one reviewer and checked by a second.
Critical appraisal
Critical appraisal of included evidence was facilitated by relevant assessment tools and reporting standards. These included the DARE database selection criteria for systematic reviews,5 the Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) for the reporting of realist syntheses6 and the Critical Appraisal Skills Programme checklist for qualitative research. 7 The quantitative studies were assessed by reviewers for adequacy of reporting of methods used. Assessments were conducted by one reviewer and checked by a second.
No evidence was rejected on the basis of critical appraisal. Findings of the critical appraisal were tabulated and used to inform judgements about the internal and external validity of included research results presented in the thematic synthesis. A brief narrative summary of the main concerns raised by the critical appraisal process is presented in Chapter 3, Critical appraisal and limitations of the secondary data and Critical appraisal and limitations of the primary study data.
Synthesis
The seven research questions identified by NHS England formed the basis of a thematic framework. When empirical evidence and/or related conclusions were identified in the evidence, they were coded, grouped and synthesised according to the following themes.
-
Benefits of digital modes and models of engagement between patients and primary care:
-
issues relating to GP workload and workforce
-
patients subgroups that can(not) benefit
-
the effects of different channels for different groups/settings
-
differences between synchronous and asynchronous models.
-
-
Integration of digital-first models within wider existing face-to-face models.
-
Issues relevant to contracting delivering digital-first models (e.g. geography size, population size).
When included publications looked at health care in general, only evidence applicable to primary care was coded and synthesised. Similarly, when publications included evidence relating to traditional telephone consultations, this was coded only when the data could also be applicable to digital modes of engagement.
External engagement
As described in Stage 2: narrowing the evidence base – rapid evidence synthesis, this work was conducted for NHS England, which was contacted at the start and end of each major iteration of the project.
After receiving a very brief outline of the topic area via the National Institute for Health Research (NIHR), the research team arranged a teleconference with several NHS England representatives to establish the goals and methods of the original scoping work. On the basis of this call, the research team wrote a brief research protocol, undertook the scoping exercise, and produced an interactive spreadsheet and brief summary document for NHS England.
After reviewing the scoping materials, the research team and NHS England held another teleconference, after which NHS England provided a revised set of research questions (see Revised research questions). The research team updated the research protocol to outline methods to be used in stage 2.
After submitting a written report on the results of stage 2, the research team made a presentation on the findings of both stages 1 and 2 to NHS England representatives. Following this presentation and subsequent discussions, the research team drew together the materials from each stage of the process to produce the current report.
Although this report summarises some evidence relating to patient and public views, patient and public representatives were not directly involved in the development of this work.
Chapter 3 Results
Stage 1: results of the initial scoping work
In total, 2846 records were retrieved and screened, and 92 included. All the included documents were summarised in a brief narrative overview, alongside an annotated spreadsheet that could be ordered or filtered according to the following characteristics:
-
reference number
-
author
-
funder/document source
-
country
-
year
-
title
-
nature of document (e.g. primary study, systematic review, review of reviews, realist review, call for proposals)
-
publication status (published, ongoing)
-
technology(ies) of interest
-
primary focus of document (e.g. primary care, emergency care, health care in general)
-
health condition(s) or population of interest
-
nature of evidence: effects (e.g. efficacy/effectiveness/risks/harms), implementation (e.g. enablers/barriers), cost-effectiveness, qualitative data
-
link to full text (when available)
-
notes.
The spreadsheet was sent to NHS England together with abstracts for all retrieved publications and an overview of the evidence. A copy of the spreadsheet is available from the authors and the overview is presented in Chapter 3, Stage 1: summary of key evidence from scoping work.
Stage 1: summary of key evidence from scoping work
A brief textual summary of key evidence was submitted alongside the annotated spreadsheet. The spreadsheet was intended to allow NHS England to interrogate the literature at a high level. The summary was intended to draw attention to the documents likely to be of greatest interest to them:
-
There are many reviews of digital alternatives to face-to-face consultations; however, many are primarily concerned with ‘mainstream’ technologies, such as telephone consultation/triage. Only a minority specifically focus on primary care.
-
Most very narrowly evaluate the introduction or use of a class of technology (e.g. internet video consultation), rather than the integration of such technologies as part of a broader reorganisation or reimagining of services.
-
The Technology Enabled Care Services review commissioned by NHS England and published in April 2017 provides a good overview of these broader reviews, and discusses the available evidence in the context of the new care models vanguard sites. 3
-
A report by the Nuffield Trust, published in November 2016, although not a formal evidence synthesis, cited a small amount of ‘evidence of impact’ relating to wearables/monitoring technology, online triage tools, online information/advice/targeted interventions/peer support, online booking/transactional services, remote consultations, online access to records/care plans and apps. 8
-
Much of the most recent work relevant to digital-first consultations in primary care has been undertaken by Helen Atherton from Warwick Medical School. Among other publications, she has co-authored two recent (February 2018 and June 2018) NIHR HSDR-funded projects on the potential of alternatives to face-to-face consultation in general practice9–11 and the role of digital clinical communication for NHS providers of specialist clinical services for young people. 12–14 The first of these included a realist review to identify explanations of why and how various alternatives to face-to-face consultations might work (or not) in primary care. 9–11 The second aimed to provide an overview of how video is actually being used in health-care settings, by reviewing the existing published reviews. 12–14 An ongoing NIHR-funded systematic review to explore patient and clinical experiences with two-way synchronous video consultations in health care was due to be completed by this group in July 2019. 15
-
In addition to the Warwick projects, the NIHR HSDR programme has funded a systematic review of digital and online symptom checkers and health assessment/triage services. This work was being completed by the NIHR HSDR Evidence Synthesis Centre in Sheffield. 16 We corresponded with the authors who said that, although the remit was limited to systems that attempt to direct people to appropriate services based on information about their symptoms, some of the studies looked at these as part of broader digital primary care systems (Duncan Chambers, University of Sheffield, 2018, personal communication). This systematic review searched for evidence on both generic and named systems (e.g. askmyGP, webGP, WebMD, GP at hand, Push Doctor, Engage Consult), and was undergoing peer review, though the authors were happy to share the final draft report (which has subsequently been published).
-
Our searches also encountered several recent or ongoing primary studies that have been conducted alongside evidence syntheses. Although not focused on primary care, a recently published NIHR HSDR study (June 2018)17 used multilevel mixed methods to examine remote video consultations in three contrasting clinical settings (diabetes, antenatal diabetes and cancer surgery) in an NHS acute trust. 17
-
We also identified two currently open NIHR calls for proposals (Digital Technologies to Improve Health and Care;18 and Evaluating the Digital 111 Offer: NHS 111 Online). 19
Stage 2: narrowing the evidence base – rapid evidence synthesis
Included studies
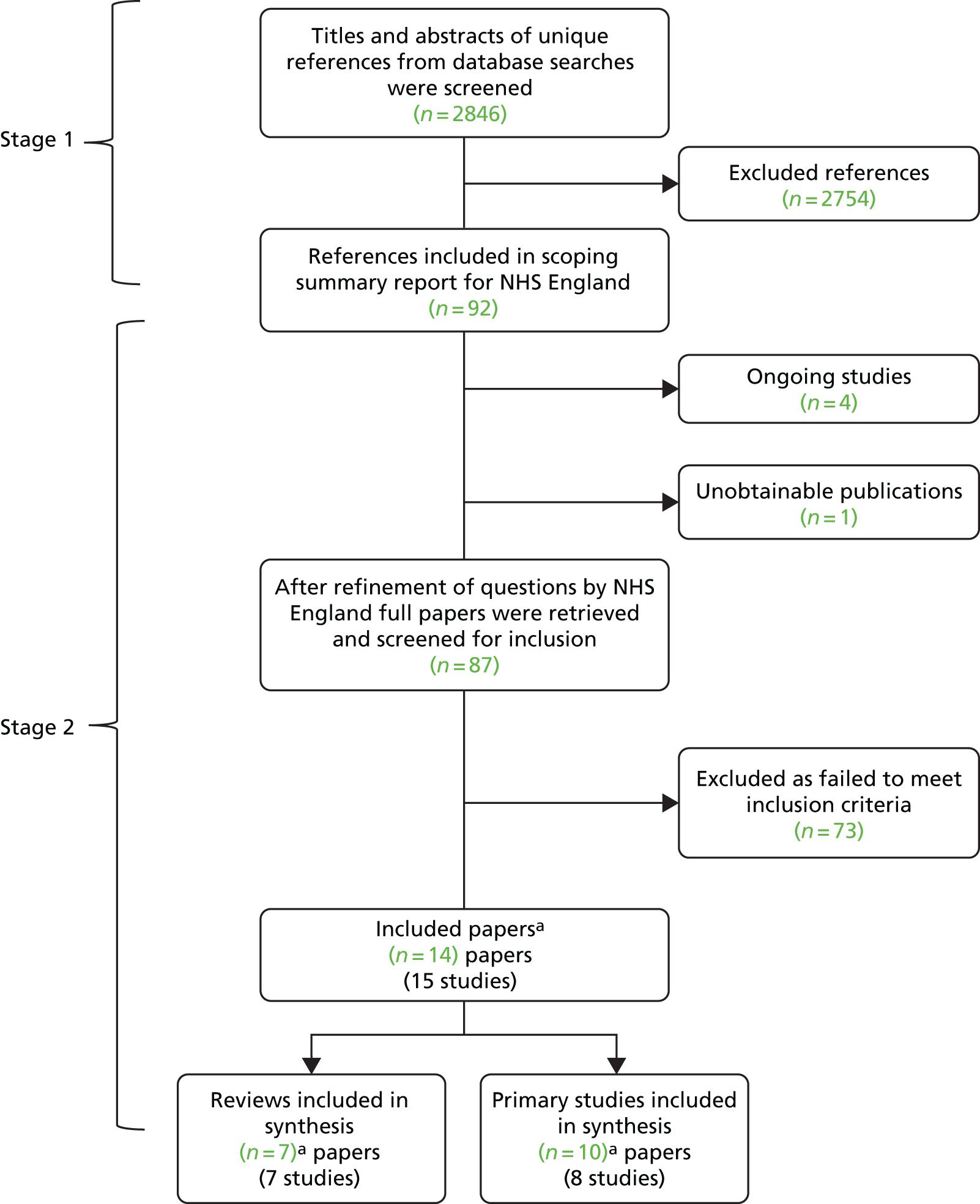
Ninety-two papers were included in stage 1 (scoping and summary of evidence). After further assessment of full papers, a total of 15 reviews and studies (in 14 publications8–11,20–29) were included in stage 2. One project (Atherton et al. 9) contributed to more than one form of evidence (i.e. a conceptual review, survey, case study and analysis of routine data) in multiple publications. Seven studies provided review evidence8,9,20–24 and eight studies9–11,25–29 provided primary quantitative and qualitative evidence (Figure 1). A number of ongoing studies were also identified and are listed in Appendix 2 together with details of one paper we were unable to obtain, despite e-mailing the author.
Stage 2: overview of included evidence
Characteristics of included reviews
The seven8,9,20–24 included reviews were published between 2012 and 2018. Out of the seven reviews, two were systematic reviews,21,24 two were realist reviews9,23 and three were produced in a ‘literature review’ style format. 8,20,22 When reported, the publication dates of studies included in the reviews ranged from 1995 to 2018.
The authors of five reviews were UK based. 8,9,21,23,24 Two of the UK-based reviews were funded by the NIHR HSDR programme,9,24 one by the Cochrane Collaboration21 and one by the Arden Cluster Research Capability Fund. 23 The review by Castle-Clarke and Imison8 was published by the Nuffield Trust and based, in part, on research commissioned by NHS England.
Type(s) of technology
In terms of technology, two reviews20,21 focused on e-mail communication only between patients and physicians20 and any health-care professionals. 21 The review by Hickson et al. 22 examined the use of e-visits, which were defined as any online consultation between patient and clinician. However, the review excluded any study related to care delivered via video, teleconferencing or telephone. It therefore may have been predominantly focused on communication via e-mail, although this is not stated in the review. Atherton et al. 9 examined alternatives to face-to-face consultations, which included telephone consultations (but not triage), e-mail, e-consultations, video, SMS text messaging, telehealth and any other form of ‘care at a distance’ apps. Similarly, Huxley et al. 23 included a range of digital technologies potentially used for patient–clinician communication: video, e-mail, internet forums and SMS text messaging. Chambers et al. 24 reviewed the evidence in relation to digital and online symptom checkers and health advice/triage services for urgent care. The review by Castle-Clarke and Imison8 focused on seven different digital services offered by the NHS, but only two (online triage and remote consultations) are relevant to the current review.
Relevance to primary care
Of the reviews which examined clinical communication between patient and health-care professionals, only two were exclusively limited to research related to primary care and general practice. 22,23 Other reviews included some evidence from other settings, such as secondary and tertiary care. The Cochrane review by Atherton et al. ,21 on clinical communication via e-mail, included nine studies of which only three were primary care based. In addition, Antoun20 also included studies that focused on the use of e-mail for broader communication purposes, such as co-ordinating health-care appointments, reminding individuals to attend appointments, providing health promotion information and communicating the results of diagnostic tests. All of the issues above potentially limit the relevance of reported findings to the current review questions.
Populations included in reviews
Huxley et al. 23 included studies conducted with various marginalised populations, whereas the other reviews appeared to focus more generally on any adults (patients, parents or adult caregivers). Only two reviews21,24 provided specific details about the countries in which included studies were conducted. The review by Chambers et al. 24 was the only one to clearly identify UK evidence. Nine out of 27 studies included in this review were conducted in the UK. Of the three primary care-based studies included in the review by Atherton et al. ,21 two were from the USA and one from Norway. Huxley et al. 23 was the only other review to report any geographical detail, with the review authors stating that the reported evidence came from high-income countries.
Outcomes
In terms of the main outcomes of interest examined, reviews commonly reported on patient access and equity, specifically the characteristics of individuals using alternative communication methods and/or which patients could potentially benefit the most from digital consultations. 8,9,20,22,24 In addition, Huxley et al. 23 reported evidence on the potential of digital patient–clinician communication to remove key barriers to accessing general practice for marginalised groups.
Most reviews reported findings in relation to implementation, including barriers to use, or outcomes related to service delivery, safety, harms or quality of care. 8,9,20–22,24 Six reviews8,9,20–22,24 examined patient health service use or the impact of digital communication on patient demand. Stakeholder views or experience of alternative consultation methods or levels of satisfaction were reported in five reviews. 8,9,21,22,24 Five reviews8,20–22,24 also examined evidence in relation to patient health outcomes or clinical effectiveness. The potential impact of digital methods of consultation on health professionals (e.g. knowledge, behaviour, workload) or consultation dynamics was examined in four reviews. 8,9,20,21 Fewer reviews examined evidence in relation to financial costs or cost-effectiveness. 22,24 Chambers et al. 24 reported a number of other outcomes: diagnostic accuracy, accuracy of signposting and compliance with triage advice. A table presenting the characteristics of each review is provided in Appendix 3, Table 3.
Critical appraisal and limitations of the secondary data
The two systematic reviews conducted by Atherton et al. 21 and Chambers et al. 24 were methodologically rigorous. Both were supported by a comprehensive search of academic databases, as well as an online search for grey literature. Inclusion/exclusion criteria were clearly stated in each review and an appropriate quality and risk of bias assessment of included studies was conducted. An appropriate synthesis of findings was also conducted in both cases, and adequate study details reported. Two reviewers were involved at key stages of the review process, which reduced the potential for bias and error. Findings and conclusions of both reviews are potentially generalisable across countries. However, all of the included studies in the review by Atherton et al. 21 were assessed as being at risk of bias. Furthermore, the three studies based in primary care were assessed at risk of multiple sources of bias. Aside from two randomised trials, all studies in the review by Chambers et al. 24 were judged as having at least a moderate risk of bias. In addition, the overall strength of evidence was assessed by the review authors as being ‘weak’.
Reviews by Antoun,20 Castle-Clarke and Imison,8 and Hickson et al. 22 were assessed as being of low quality, owing to poor reporting. In all three reviews,8,20,22 there was limited reporting of both the methodological process and study details. However, the DARE criteria were not well suited to the appraisal of the Castle-Clarke and Imison8 report, which combined the findings of a literature review with case studies and expert interviews.
The lack of study details made it difficult to determine accurately the reliability or generalisability of many findings. However, given the technological focus of the reviews, it is likely that some findings potentially have relevance across countries.
The realist reviews conducted by Atherton et al. 9 and Huxley et al. 23 were assessed as ‘adequate’ or ‘good’ for the majority of the RAMESES quality standards criteria. However, it was possible to identify some limitations in both reviews, including a lack of study details. Findings in the review by Huxley et al. 23 also appeared to be based on a database search that was restricted to a very narrow date range, covering 1 year only (2013–14). Furthermore, the review by Atherton et al. 9 included opinion pieces, as well as primary studies, and many of the individual findings were drawn from a small number of studies of unknown design and origin. Although the country and setting of the included studies is uncertain, it is likely that the findings are potentially generalisable. The findings of the Huxley et al. 23 review related to various marginalised groups within high-income countries and are likely to be generalisable to a UK setting. See Tables 5 and 6 in Appendix 4 for critical appraisal assessments of included reviews.
Characteristics of included primary studies
The HSDR report by Atherton et al. 9 examined the potential of alternatives to face-to-face consultations in UK general practice. It comprised one conceptual review and three primary studies. The primary studies comprised (1) focused ethnographic case studies conducted in general practices in England and Scotland (qualitative data were collected from staff and adult patients/carers, with a particular focus on gaining the involvement of ‘hard-to-reach’ groups; (2) a quantitative cross-sectional scoping survey of general practices and individual GPs in England and Scotland; and (3) secondary analysis of patient health record data from general practices in England and Scotland. Each of the primary studies focused on a range of alternative consultation technologies, such as telephone consultation, e-consultations, e-mail, text messaging and video. The results of the scoping survey and case study research have also been published in journal articles. 10,11 Key outcomes of interest reported across the three primary studies included the extent of use of alternatives to face-to-face consultations; motives and rationale for use; stakeholder experiences or views, including on the types of patients who potentially benefit the most; characteristics of patients who use alternatives; and implementation issues. The methodology and methods used across the three primary studies were appropriate to the stated aims. The authors acknowledged some limitations to the research, but overall this UK-based report is highly relevant and addresses key questions of interest to the current review.
In total, five other primary studies were included. 25–29 Two of the studies were conducted in the UK25,29 and the other three were based in the USA. 26–28 Funding for the two UK studies25,29 was provided by the NHS Northern, Eastern and Western Devon Clinical Commissioning Group (CCG)25 and the Scottish Government/Chief Scientist Office. 29 Donaghy et al. 29 focused on video consulting (the Attend Anywhere system) between patients (aged ≥ 16 years) and clinicians for follow-up appointments in general practices in Lothian, Scotland. Carter et al. 25 evaluated webGP, which is an e-consultation and self-help web service for adult patients. The webGP e-consult service involves patients completing an online form which is reviewed by a practice GP. The patient then receives a response from the practice (e.g. they are asked to collect a prescription or offered a telephone or face-to-face consultation). Studies from the USA focused on adults’ use of e-visits28 and Teladoc (Westchester County, NY, USA; URL: www.teladoc.com). 26,27 Like webGP, the Teladoc system requires a patient to submit an online request for a consultation. A participating physician then reviews the patient’s medical history and contacts them to hold a consultation, which may be via telephone, internet or mobile app. It was reported that Teladoc physicians respond to requests 24 hours a day, 7 days a week. For e-visits, a patient submits information about their condition via an online portal. This information along with the patient’s medical record is reviewed by a physician who makes a diagnosis and then replies to the individual through the portal within several hours. 26
Both Carter et al. 25 and Donaghy et al. 29 employed a mixed-method design, whereas the three studies26–28 from the USA adopted a quantitative approach and involved secondary data analysis. Mehrotra et al. 28 analysed the data of patients with sinusitis and urinary tract infection only. Similarly, the two studies26,27 by Uscher-Pines et al. were also restricted to patients with a small number of specific health conditions: acute respiratory illnesses, urinary tract infections and skin problems;27 or lower back pain, pharyngitis and acute bronchitis. 26 No restrictions were placed on the types of patients who participated in either of the UK-based studies.
All five studies25–29 reported on the characteristics of individuals utilising digital forms of consultation and/or which patients could potentially benefit the most from their use. Other outcomes reported included the extent of alternative technology use;25–27 stakeholder views and experiences/satisfaction;25,29 impact on quality of care;26 implementation issues, consultation content and health service use. 29 A table presenting the characteristics of each primary study is provided in Appendix 3, Table 4.
Critical appraisal and limitations of the primary study data
The studies by Carter et al. 25 and Donaghy et al. 29 used appropriate methodology for the research aims, and methods were clearly described. These two studies25,29 were conducted in the UK, so the results will have a high degree of relevance. However, data collection in both studies was limited to a small number of practices. Furthermore, practices participating in the study by Carter et al. 25 were located in only one CCG area and had a predominantly white British population. Donaghy et al. 29 stated that the case-mix variation between groups potentially limits the conclusions that can be drawn. Limiting the focus to follow-up appointments was justified by the authors on the grounds of helping to control case-mix variation. It was also reported that clinicians had difficulties in recruiting patients to video consulting. Consequently, this resulted in a self-selecting sample comprising mainly younger and more ‘tech-savvy’ individuals.
Both studies by Uscher-Pines et al. 26,27 were based on data from patients enrolled in one US health insurance programme. The authors cautioned, therefore, that the results may not be generalisable outside California or to different patient populations. Analyses in both studies also focused on a small number of health conditions only. In addition, almost all patients (98–99%) had a consultation via telephone rather than through video, internet or the Teladoc app and, consequently, the results are of limited direct relevance. Limitations of the study by Mehrotra et al. 28 included being restricted to patients in a small number of practices in Pittsburgh and focusing on only two health conditions. The generalisability of the results may again be limited, but the broad conclusions related to the types of patients who used the e-visits technology, which could potentially have UK relevance. See Table 7 in Appendix 4 for critical appraisal assessment of UK qualitative studies.
Stage 2: thematic synthesis of included evidence
A large proportion of material in this synthesis is derived from a recent NIHR-funded project by Atherton et al. 9 on alternatives to face-to-face consultation in general practice. This project included a conceptual review of the literature, a survey of UK general practice staff, a series of focused ethnographic case studies in eight UK general practices and an analysis of routine consultation data. Material throughout this report has been reproduced with permission from Atherton et al. 9,10
We have also included a second NIHR-funded project – a systematic review of digital and online symptom checkers and health assessment and triage services for urgent care – by Chambers et al. 24 This review includes evidence more closely aligned with the concept of ‘digital-first’ primary care, although does not focus on alternative consultation methods.
Taken together, these two publications9,24 represent the most robust, comprehensive and up-to-date source of evidence on this topic and include important evidence that could not be entirely reported here. The rapid synthesis below draws together some findings and conclusions from these publications, alongside other recent evidence of potential relevance to the research questions identified by NHS England. A summary of findings is available in Appendix 5.
Benefits of digital modes and models of engagement between patients and primary care
Absence of reliable evidence
It is clear from recent reviews that there is very little reliable data on the effects of alternative models of consultation. As will become apparent in this synthesis, much of the existing data are qualitative, providing some insight into the perceptions of patients and health professionals. However, objective measurement of the impact of alternative consultation models is lacking for most relevant outcomes.
The reviews undertaken by Atherton et al. 9,21 noted the dearth of evidence relating to alternatives to face-to-face consultations in general. They found little quantitative research either on the impact of e-mail on GP workload, or on analysis of the content of e-mails in comparison with face-to-face and telephone consulting for similar problems. A separate group of reviewers also reported a lack of robust evidence on the impact of e-mail on patient outcomes, health services outcomes (e.g. service use) or health-care professional outcomes (professional knowledge, behaviours and performance). 20 They also reported very limited evidence on safety, quality of care, privacy issues and appropriateness of e-mail communication.
Atherton et al. 9 noted that much of the literature on video consulting in primary care was focused on the potential of the technology, rather than exploring its impact on the content of the consultation or on GP workload or patient satisfaction. Although uptake of alternative consultation technologies in primary care was found to be low, it was unclear if this was due to GPs applying the use of alternatives selectively, patients not being aware of their availability or not wishing to use them, or problems with implementation. The authors also noted a lack of evidence relating to the roles of team members, such as reception staff, in delivering alternatives to the face-to-face consultation. 9
In 2015, Hickson et al. 22 noted that the delivery of primary care via e-visits on mobile platforms was still in its adolescence, with few methodologically rigorous analyses of outcomes of efficiency, patient health or satisfaction. No significant new evidence appears to have been found in subsequent reviews or in this current rapid evidence synthesis.
Looking specifically at digital and online symptom checkers and health advice/triage services, Chambers et al. 24 noted the weakness of existing evidence, being based largely on observational studies. In particular, Chambers et al. 24 highlighted that major uncertainties surround the likely impact of ‘digital 111’ services on most outcomes.
Uptake of alternative consultation models
From a scoping survey of UK GPs and practice managers, Atherton et al. 9 found that the majority of practices routinely offered telephone consultations (211/318, 66%) and few (6%) reported facilitating e-mail consultations (20% of practices intended to offer e-mail consultations in the future, but 53% had no such plan). None of the respondent practices reported offering internet video consultations and very few (4%) reported any plans to do so in the future. There was also evidence that 21% of practices had previously offered e-mail and that 10% had previously offered internet video, but that they had subsequently withdrawn these services. 9
Most GPs reported personally providing telephone consultations on most working days or every working day (79%). Only 8% of GPs reported providing e-mail consultations on most working days or every working day, whereas 45% did so rarely or sometimes and just under half (47%) never provided e-mail consultations. Furthermore, 99% stated that they never conduct consultations via internet video. Provision of telephone, e-mail or video consultations did not vary by GP age or sex, or by study site. 9
The authors concluded that unless, or until, uptake of e-consultations or video consultations increases, it will be impossible to measure their impact. 9 They added that these systems incur a subscription charge, and, to be cost-effective, would have to be both widely used and reduce practice workload considerably. 9
A 2016 review similarly concluded that physicians’ use of e-mail with patients is low and lags behind the willingness of patients to communicate with their physicians through e-mail. 20
When Skype™ (Microsoft Corporation, Redmond, WA, USA) video consultations were first introduced in a Manchester primary care practice in 2013, there was an initial increase in overall demand, with the same number of face-to face appointments being provided alongside additional Skype consultations. 8 However, increasing access to face-to-face appointments reduced the uptake of Skype consultations, as patients preferred face-to-face consultation. 8
A US study reported that ‘Teladoc’ visits accounted for a very small proportion of health-care use. Thirty-four per cent of all Teladoc visits occurred on weekends and holidays, in contrast to 8% of office visits. The timing of Teladoc visits closely resembled the timing of emergency department visits. 27 However, almost all (98–99%) Teladoc visits occur by telephone. Therefore, results are of limited direct relevance to digital modes of engagement.
Impact on clinical practice and patient health outcomes
The Atherton et al. 9 conceptual review noted evidence of ‘safety-netting’ behaviour, in which, for example, primary care doctors were more likely to prescribe antibiotics during an e-visit than a face-to-face consultation. The review authors suggested that this may reflect uncertainty about the medico-legal consequences of this form of prescribing. 9 A US primary study26 reported a similar finding, in which face-to-face office consultations more frequently avoided inappropriate prescribing of antibiotics for acute bronchitis than did Teladoc consultation (telephone, internet or mobile app).
Only two studies included in the Chambers et al. 24 review of digital symptom checkers and health advice and triage services reported on clinical effectiveness outcomes, making it difficult to draw conclusions. One study indicated that users of the ‘Internet Doctor’ website had longer illness duration and more days of illness rated moderately bad or worse than the usual care group, but the difference was not statistically significant. 24 Several patients using the ‘webGP’ system were reported to have received advice to seek treatment for serious symptoms that might otherwise have been ignored. 24 Evidence on patients’ reactions to online triage advice and whether they follow the advice or seek further help or information was very limited. Only two of the included studies reported specifically on patients’ compliance (or intention to comply) with advice received. The authors state that preliminary evidence from NHS England evaluation of NHS 111 online suggested that patients may be more likely to seek further advice for more urgent conditions. 24
Safety, harms and quality-of-care outcomes
A 2012 Cochrane review21 of e-mail consultation found that trials did not report any harms, though this is not the same as stating with confidence that no harms occurred. In their 2018 conceptual review,9 the same authors stated that much more work is required to identify potential patient safety issues and mitigate any associated risks.
None of six included studies reporting on safety-related outcomes identified any problems or differences in outcomes between digital/online symptom checkers and health professionals. 24 However, studies evaluating safety were generally short term and small scale. Some were limited to people with specific types of symptoms (e.g. influenza-like illness or respiratory infections) and others recruited from specific population groups (e.g. students) that were not representative of typical users of urgent care services. Like Atherton et al. ,9 Chambers et al. 24 advised that the evidence should be interpreted as a lack of evidence on harms rather than evidence showing no harm.
Elsewhere, Hickson et al. 22 reported evidence that e-visits can improve quality of care, access to care and continuity of transitions in care, but provided no further details.
The Atherton et al. 9 conceptual review noted that patient privacy and confidentiality are described as being important, but reports of privacy and confidentiality breaches are few and collection of these data is uncommon.
Impact on consultation dynamic
The Atherton et al. 9 conceptual review noted that alternatives to face-to-face communication can change the dynamic of consultations, so that elements may be lost or may need to be expressed in different ways or at different times for the doctor–patient relationship to be maintained. Some studies in this review noted particular uncertainty around the ‘rules of engagement’ for e-mail and video consultations. Other publications noted that typical face-to-face consultations allow for diagnostic cues, such as smelling a patient’s breath, noting how a patient walks into the room, as well as using casual contact, such as shaking hands, that enables assessment of skin temperature and tone. The loss of non-verbal communication may also diminish the ability to check a patient’s understanding. However, authors report that there is little research indicating whether misunderstandings are increased or diminished with alternatives to the face-to-face consultation. 9
Conversely, some responders to Atherton et al. ’s scoping survey9 described benefits of digital consultations, such as patients being able to send pictures of a transient rash or an audio file of a child’s cough. Other respondents preferred to use e-mail because of communication difficulties or disabilities that made it difficult to get to the surgery.
Huxley et al. ’s review23 focusing specifically on the impact of digital communication on marginalised groups included a study reporting that both clinicians and patients need the rich stimuli (e.g. auditory, visual, tactile and olfactory) of face-to-face contact to build the therapeutic relationship. One included review suggested that face-to-face consultations are essential for communication about emotional states, though evidence from single studies suggested that patients do communicate their emotional states with GPs via e-mail and are able to discuss embarrassing or sensitive questions. One study suggested that patients consulting for physical problems can feel less intimidated via video link and feel able to ask more questions.
There was some evidence to suggest that reducing the need for patients to engage with receptionists and other health centre staff may reduce apprehension for some patients. 23
A recent unpublished study, conducted in a Scottish primary care setting, reported that face-to-face consultations were longer and more problems were raised and addressed than in telephone and video consultations of similar duration. 29 The types of problems addressed were similar across the three consultation types and were typical of general practice.
During face-to-face consultations, patients’ health understanding was more likely to be sought and the problem placed into a psychosocial context at least once than in telephone or video consultations. Face-to-face consultations were also associated with more overall ‘information giving’ by both patients and clinicians (but this may partly reflect the number of problems raised). The authors noted that increased confidence and experience with video consultations might lead to different consultation dynamics in the future. 29
Financial costs or cost-effectiveness
Evidence on cost or cost-effectiveness is largely absent from the identified literature.
The review of digital and online symptom checkers and health advice and triage services for urgent care identified cost-effectiveness data from two studies (both produced by digital system manufacturers). 24 Based on 6 months of pilot data, webGP was estimated to provide £11,000 savings annually for an average general practice (6500 patients) compared with current practice. A saving to commissioners equivalent to £414,000 annually for a CCG covering 250,000 patients was also suggested. The Babylon Check app (Babylon, London, UK) claimed to provide average savings of over £10/triage compared with NHS 111 by telephone, based on a higher proportion of patients being recommended to self-care. A third study found that potential savings to practices from using e-consultation depended on the percentage of face-to-face appointments avoided. 24
One review identified a limited number of US data on costs-applied reimbursements for e-visits to a fee-for-service model of patient payment, but this is not generalisable to an NHS funding model. 22
Diagnostic accuracy
One review suggested that digital and online systems have yet to achieve a high level of accuracy in the diagnosis of specific conditions. This applies both to ‘general purpose’ symptom checkers and to those limited to particular conditions. 24 Most studies reported that the diagnostic accuracy of symptom checkers was poor in absolute terms, though two studies found evidence that symptom checkers performed relatively well when complaints were generally common and uncomplicated. 24
Another overview concluded that diagnosis apps are not always accurate, which may encourage patients to use the health system unnecessarily. 8
Information, triage and signposting
The accuracy of signposting of patients to the most appropriate level of service was inconsistent between studies evaluating digital and online symptom checkers and triage services. 24 Algorithm-based triage tended to be inferior and more risk averse than that of health professionals, with 85% of respondents being advised to visit their doctor in one study. 24 The only studies to find clearly equal or superior accuracy of triage and signposting to appropriate services using an automated system were the evaluations of ‘Babylon Check’ produced by the company that developed the system. The app gave an accurate triage outcome in 88.2% of cases, compared with 75.5% for doctors and 73.5% for nurses (one study). 24
The realist review by Huxley et al. 23 found no evidence that digital communication will improve knowledge about health services and how to access them.
Health professional experience and satisfaction
Atherton et al. ’s ethnographic case studies9 in eight UK general practices found that clinicians use e-mail to share and gather information when co-ordinating complex health-care packages. For nurses, telephone and e-mail consultations were valued in the management of diabetes (e.g. for discharge checks and medication reviews). For GPs, the main motivation for using alternatives to face-to-face consultation was to help manage their workload.
On the basis of a survey of over 300 UK general practices, the authors concluded that:
Despite policy pressure to introduce consultations by email and internet video, there is a general reluctance among GPs to implement alternatives to face-to-face consultations. This identifies a substantial gap between rhetoric and reality in terms of the likelihood of certain alternatives (email, video) changing practice in the near future.
Clinicians from a recent study conducted in Scottish general practice reported that video consultation appeared to be of less utility in managing patient problems, largely because of technical issues (B McKinstry, personal communication). Overall, 62% of clinicians rated video consultation as ‘very useful’ (29/47), compared with 85% for face-to-face consultations (29/47) and 76% for telephone consultations (38/50). In addition, 62% of clinicians would ‘absolutely’ choose video consultations, again compared with 94% for face-to-face consultations and 90% for telephone consultations. In contrast to other more positive views, some clinicians felt that video consultations did not add anything advantageous to telephone consultations. Interviews confirmed findings from the other data collection methods that face-to-face remained the ‘gold standard’ and that, like telephone consultations, video consultations tended to be limited to a single problem. Furthermore, the lack of a physical examination prevented clinicians from spontaneously addressing other health issues. 29
Another recent primary study, evaluating the ‘webGP’ e-consultation approach in Devon, found that in the majority of cases (37/61, 63%), the GP reported being ‘not at all familiar with the patient’, with only three (5%) reporting being ‘very familiar’. In virtually all cases (58/61, 97%), GPs reported feeling either ‘very confident’ or ‘confident’ about managing the e-consult request. 25
Patient experience and satisfaction
Two studies in the Atherton et al. 9 conceptual review reported that when patients had been offered an alternative to the face-to-face consultation, they usually report liking them. 9 Patients viewed the removal of the necessity to attend the GP or nurse’s professional space as a benefit of e-mail and telephone consultations. Other reported benefits included the convenience of being able to consult while at work, to choose when and how to consult, and the perceived advantage of avoiding the practice receptionist. 9
Patients interviewed in the 2018 UK case studies were interested in using these technologies (particularly telephone and e-mail), which they saw as a means of reducing the time they had to expend arranging to see and consult clinicians (particularly for what they termed ‘simple’ problems). 9 The use of alternatives to the face-to-face consultation could also be much more convenient, as well as time saving, for people who have difficulty physically getting to a surgery, either for geographical reasons or because of illness. The asynchronous nature of some alternatives, such as e-mail, meant that patients could send a message at a time that suited them and then read the response later, rather than having their diary dictated by appointment availability. 9
One overview noted that the developers of webGP and askmyGP reported patients being satisfied with their services. 8 It was suggested that patient satisfaction may be related to the use of professional review in the service. 8
In uncontrolled studies identified in one systematic review, study participants generally expressed high levels of satisfaction with digital and online triage services. 24 These studies appeared to be rating usability rather than satisfaction with the advice received or the degree of reassurance provided. One study identified in the review, an evaluation of NHS 111, reported that patients tend to be less satisfied with triage services when they have been auto-routed from another health service, such as a GP out-of-hours service. 24
Patients in the recent Scottish primary care study reported that they were generally happy with all available forms of consultation, which were considered equally useful, but face-to-face scored consistently higher than video and telephone consultations in a number of domains: health professionals giving enough time; asking about symptoms; listening; explaining tests and treatments; involving patients in decisions; treating patients with care and concern; and taking problems seriously. 29 Technical problems were more common with video consultations: some patients had significant problems with insufficient bandwidth and occasionally the connection failed and telephone consultation was used instead. The biggest perceived advantage for patients of video consultation was time saving. 29
The recent evaluation of webGP by Carter et al. 25 reported substantial differences (> 10% between groups) between e-consulters and face-to-face consulters for reported problem resolution (55% vs. 33% ‘completely resolved’, respectively) and seeing or speaking to a GP following the consultation request (52% vs. 93.8%, respectively). e-consulters also reported being less satisfied than face-to-face consulters with their ability to consult their preferred GP (44% vs. 57%, respectively). Although satisfaction rates were generally high, some patients had concerns about confidentiality, particularly around reception staff reading confidential medical information submitted via web requests. 25
Issues relating to general practitioner workload and workforce
Impact on service use and professional workload
The Atherton et al. 9 conceptual review of alternatives to face-to-face consultation found limited evidence from three studies suggesting that the availability of e-mail consultations had not ‘opened the floodgates’ for patient demand and these alternatives have not been widely used where patients have been able to e-mail family doctors for some time. 9 In one US study, patient use of secure e-mail with clinicians was not found to be associated with an increase in the use of clinical services 7–18 months after first use. Although it was associated with an initial increase in activity by e-mail users, this did not persist beyond 6 months (though it is unclear if this study relates to primary care). 9 Although studies have examined the association between e-mail and outcomes, there is limited evidence about the organisational and relational dynamics that contribute to change. 9
Interviews with UK primary care staff reported that alternative consultation methods could offer flexibility to both staff and patients depending on how practices organised the working day, with GPs and nurses being able to choose when, and in what order, to reply to messages or make telephone calls. 9 Other themes included telephone consultations taking longer than expected, lengthening the working day; some telephone consultations were converted to face to face, increasing the overall number of consultations with that patient.
Based on the evidence as a whole, Atherton et al. 9 concluded that there is little quantitative research on the impact of e-mail on workload and on the analysis of the content of e-mails in comparison with face-to-face and telephone consulting for similar problems. The authors did not find evidence to determine whether or not the provision of alternatives to face-to-face consultation leads to supply induced demand. 9
Hickson et al. 22 found studies with conflicting findings on the impact of e-visits on face-to-face consultation rates and Castle-Clarke and Imison8 reported mixed evidence on the capacity of online triage tools to manage demand. Some evidence suggested that interactive symptom checkers are often risk averse, recommending professional care when self-management is appropriate, and inaccurate diagnosis apps might potentially encourage patients to use the health system unnecessarily. 8
Chambers et al. 24 provided more detailed evidence on the influence of symptom checkers on the pattern of service use. One randomised controlled trial (RCT) focused on promoting self-care and covered respiratory symptoms only. The results showed that the intervention group had fewer contacts with doctors (but more contact with NHS Direct) than controls, despite having a longer duration and greater severity of illness. It was unclear if this finding is generalisable to systems covering the full range of urgent care. An NHS England evaluation of NHS 111 online found that online/digital triage was associated with a small shift towards self-care when compared with telephone triage (18% vs. 14%). In addition, online and digital triage directed a smaller proportion of patients to other primary care services, such as GPs, dental and pharmacy (40 vs. 60%). A pilot evaluation of the webGP system by its developers reported that 18% of patients had been diverted away from requesting a GP appointment for that consultation. In addition, 14% of patients reported that they would have attended a walk-in centre or other urgent care service if they had not had access to the webGP system. However, the report provides few details of the methodology used. Data provided by the manufacturer of the ‘Babylon Check’ app indicated that patients were more likely to be triaged to self-care by the app than with NHS 111 by telephone (40% vs. 14%). One further study suggested that students had a stronger intention to seek treatment for a hypothetical illness when the diagnosis was made using WebMD or Google (Google Inc., Mountain View, CA, USA) than with no electronic aid.
The recent UK study by Donaghy et al. 29 reported that video consultation was generally time neutral for clinicians.
Some UK primary care respondents suggested that webGP had increased the workload for GPs and administrative staff, whereas others suggested that webGP was shifting workload from the GP to the patient. 25
Impact on follow-up consultations
The analysis of routinely collected UK primary care data by Atherton et al. 21 found that most consultations by telephone, e-mail or e-consult are followed by another consultation (around 62%, often face to face) within 14 days, and this is more common than after an initial face-to-face consultation (48%). Therefore, the authors concluded that any analysis of the use of alternatives to face-to-face consultations needs to take account of knock-on effects in the following 2 weeks. 21
In the 2014 US evaluation,27 initial Teladoc visits were less likely than emergency department or physician office visits to result in a follow-up visit for a similar condition in any setting (6% vs. 20% vs. 13%, respectively). It could not be established whether fewer follow-up appointments with Teledoc was attributable to higher rates of clinical resolution, or to an increase in initial consultations for minor complaints that would not require follow-up. 27
The UK study25 of webGP reported that, in 72% of e-consults, the GP suggested a subsequent face-to-face or telephone consultation with a GP or nurse.
Atherton et al. ’s 2012 Cochrane review21 reported inconsistent findings on the impact of e-mail consultation on subsequent consultations of different types.
Data on the duration of follow-up consultations were sparse. One study of telephone triage in a general practice reported that, despite a clinician speaking with patients during a telephone triage encounter, the subsequent face-to-face consultation was no shorter. 21
Patients subgroups that can(not) benefit
Compared with patients using traditional face-to-face consultations, evidence from multiple sources indicates that users of alternative methods are more likely to be younger,8,9,20,25,27–29 healthier,20,27 female8,25,27 and have higher levels of education, employment or income. 8,9,20,25,27
Patients who used video consultations in primary care in Scotland were more likely to be working and to have experienced other video technologies, such as Skype and FaceTime (Apple Inc., Cupertino, CA, USA), and clinicians stated that, while trying to be inclusive of all patients, they were more likely to attempt to recruit patients who were more technology savvy. 29
Although health professionals raise concerns that older patients, disabled patients, people without literacy skills and patients who are less educated may be disadvantaged through alternatives to the face-to-face consultation,10 there is some evidence that, among those who have internet access, patients who are disabled, elderly, less confident or living at some distance from the practice are often among those who are particularly keen to use e-mail consultations. 10
A case study conducted in a Manchester primary care practice found that Skype consultations most benefited patient groups with additional needs (e.g. those with mobility problems and parents of autistic children who find attending the practice distressing) and those not in the local area (e.g. students wanting ongoing care from their usual GP). 8 For some patients in the recent Scottish study, video consultation was less stressful and more practical (e.g. patients with mobility problems or anxiety disorders). 29 A UK study of webGP reported similar findings. 25
Huxley et al. 23 concluded that digital communication technology offers marginalised groups increased opportunities to access health care. The removal of the patient ‘being seen’ seeking help potentially removes the embarrassment, social disapproval and stigma that some patients may experience at health-care centres, and anonymity of digital communication could encourage groups who wish to remain hidden to seek help. Digital communication provides an increased feeling of privacy when an interpreter is not physically present, which increases patient willingness to discuss sensitive issues; however, loss of visual information can reduce interpretation quality. People who do not have English as a first language are not heavy users of digital communications in English-speaking countries, so the advantages may be lost. In addition, the authors concluded that, as benefits of digital communication also apply to non-marginalised groups, patient–clinician communication could potentially be monopolised by those who are already well able to access services. 23
Atherton et al. 9 noted that much of the evidence about potential benefits and disadvantages for patients and particular subgroups of patients has been written from the health-care professional perspective and credible empirical evidence from patients is very limited.
The effects of different channels for different groups and settings
There is little direct evidence on the differential effects of different consultation channels and how these vary among groups and settings.
Routine data reported by Atherton et al. 9 indicated that face-to-face consultation rates were slightly higher in the least deprived areas and telephone consultations slightly higher in the most deprived areas, but otherwise there was no strong relationship with deprivation for these consultation types. 9 However, for electronic consultations, some of these patterns were reversed, with the highest rates in young adults and white patients. There was also a clear trend towards higher rates of e-mail consultations in the less deprived areas. 9 The demography of patients using telephone consulting was largely similar to that of patients attending the surgery and there were insufficient instances of use of video consulting to determine the demography of users with confidence.
As might be expected, telephone consultations are more challenging for people who have communication difficulties (primarily those who did not use English as a first language or who had hearing or speech problems), learning difficulties or cognitive impairment. 9
For some of these groups, written communication, such as webmail or e-mail and e-consulting systems, might be helpful. 9 e-mail exchanges can provide a consultation record, and possibly clearer explanations and subsequent understandings than information obtained during face-to-face contact. This may be particularly advantageous to those who are less articulate or confident in person, those who wish to discuss their consultation with others and those who need help with translation. 9
Some patients may be more willing to disclose intimate or sensitive information via an e-mail than in person or over the telephone, especially if they are at work or in a public place. 9
One overview mentioned studies indicating that patients are often more honest with digital tools than with a professional, but no further details were reported. 8
Atherton et al. 9 note that that practice staff, and sometimes patients, can blur the distinction between telephone consultation and telephone triage, and it is unclear whether or not policy-makers have made the distinction.
Differences between synchronous and asynchronous models
Conceptually, asynchronous text-based models of communication, such as e-mail and e-consultation, have been recognised as useful for people who are very anxious, find face-to-face contact difficult, have hearing or communication difficulties or struggle to express themselves. 9 Asynchronicity allows both patients and health-care professionals to send and act on contacts at a time that suits them, enabling health-care professional to draw on external resources or check evidence and providing sources of information for the patient. With e-mail, patients can also attach photographs and other digital files, such as audio recordings. For patients preparing for a hospital visit or recovering afterwards, these forms of consultation provide a way to communicate without having to visit. 9
Although asynchronous models work poorly for health conditions that require urgent care,22 they can potentially reduce the need to negotiate with receptionists, deal with appointment systems, travel to surgery and use waiting rooms. 23 Whereas synchronous models, such as video consultation, can retain some aspects of face-to-face consultation through real-time interpersonal interaction, these aspects are lost with asynchronous approaches. However, as elsewhere in the literature, quantification of the purported advantages and disadvantages of synchronous and asynchronous methods is largely absent.
Integration of digital-first models within wider existing face-to-face models
The identified publications did not provide information on how to integrate digital models into primary care, but a number of barriers to implementation of digital modes and models of engagement have been identified.
Health professional concerns about alternative consultation models
A possible barrier to implementation of alternative consultation or digital-first models is concern among primary care staff about possible adverse consequences.
Concerns about increases in demand and workload (both in terms of increased consultations and administrative load) were commonly reported in the literature. 9,20,22 Specific concerns included ‘lowering the bar’ to consultation, inappropriate use of e-mail as a means of fast-tracking a face-to-face appointment and concerns about introducing a new means of accessing a service that is already failing to cope with patient demand. 9 As mentioned in Issues relating to general practitioner workload and workforce, evidence on the actual impact of alternative models on demand and workload is extremely limited.
Some GPs expressed concerns about patient access and equity: although some had experience of some vulnerable and older people who preferred alternative consultation methods, others thought that these same groups would be disadvantaged. 9 In interviews, staff and patients concurred that alternatives to face-to-face consultation might be unsuitable if a new health problem was being presented, if the patient was older or confused, or if the patient was using a complex array of medicines. Clinicians varied in their views about which patients were most likely to be suitable for an alternative consultation; in some cases these decisions were based on age, socioeconomic status or ethnic group. 9
Security, confidentiality and privacy issues have also been identified as important concerns for physicians that act as barriers to implementation. 9,20 In one e-mail study,20 some physicians feared receiving spam e-mails, viruses or being hacked. Others were concerned about the uncertainty of e-mail receipt by patients and the lack of integration with medical records. 20
Concerns around medico-legal issues in handling sensitive and urgent matters have also been raised by clinicians. 9,20 These include concerns about content and the suitability of e-mail for discussing sensitive issues and addressing new or urgent symptoms using an asynchronous method. Some physicians reported fear of medical errors owing to the absence of physical examinations, as well as potential miscommunication and litigation for medical negligence. 9
Infrastructure and logistics
One barrier noted by Atherton et al. 9 was the technical difficulties that may be encountered ‘working within the heavily firewalled, low bandwidth systems of the NHS’. 9 Examples included inadequate technology and long set-up times, resulting in some planned video consultations defaulting to telephone. 9 The authors noted the importance of reliable contingencies being in place in case of technological failure, as there may be clinical consequences (e.g. it may be particularly distressing for people with mental illness). 10
The recent UK study of video consultation concluded that rising ownership of smart devices and experience of video calling will increase demand for such services, but further investment in information technology (IT) infrastructure in general practices would be required to enable video consultation to become a routine service. 29 Video consultation may also require practices to allocate a well-lit, private area for staff to use. 9
Beyond having adequate IT infrastructure to provide digital consultations, primary care staff felt that any future implementation of these systems should be properly integrated with desktop personal computers used for consulting, as well as with current appointment and electronic record systems. 22,25,29
Patient–professional relationships
Clinicians reported that having an established relationship with the patient is an important facilitator of implementing alternative consultation models, including video consultation,29 telephone and e-mail. 9 Continuity also mattered to patients: for certain health problems, it might be important to know the clinician who would be consulted remotely. 9 There was some evidence that patients try to see trusted GPs for mental health issues rather than the most available GP, thereby prioritising relationship over convenience. 23 Huxley et al. 23 reported that text-based communication leaves room for interpretation; therefore, communication between patients and clinicians with well-established relationships is more likely to be successful than that between strangers. 23 One study noted potential inequalities in delivery of care in which clinicians chose which patients they would consult with on this basis. 9
Professional identity
Atherton et al. 9 noted the role of professional identity as an implementation issue in both their conceptual review and case studies. Some interviewees perceived the core tenet of general practice as the doctor–patient relationship, as conducted in the face-to-face consultation, ‘Medicine’s about relationships really and getting to know your patient as a person’. 9 Other research suggests that any new technology needs to be seen to enhance what the professional sees as their core role, otherwise it is unlikely to be accepted into practice. 9
Similarly, the few studies that have collected the views and experiences of practice nurses on alternative consultation models suggested that nurses feel that their role requires proximity to the patient. 9 In a study of a telehealth self-care support system for people with chronic health problems, the nurses who were providing the service positioned their work as ‘proper nursing’, whereas nurses who were using the telecare system suggested that the calls with patients were ‘just chat’ and doubted that real nursing could be delivered via the telephone. 9 A Norwegian study of nurses working in emergency medicine found that the approach of nurses changed when they consulted remotely; they were more assertive and gave more advice. 9
Two studies found that some health-care professionals were worried that their lack of confidence with technology might be exposed and that such exposure may undermine their authority. 9 One study reported that the balance of power within the consultation may change if the primary care professional’s skills come under patient scrutiny. However, it was suggested that this would not necessarily be damaging and could result in a helpful shift in relationship dynamics over the longer term. 9
Policies and procedures around the implementation of alternative consultation models
There is some evidence that the effective implementation of alternative consultation models can be hindered by the absence of relevant policies, procedures and guidance. In the UK case study practices observed by Atherton et al. ,9 policies about e-mailing patients were not in place, not known about or not followed. Contradictions were evident; for example, one GP explained that their practice was trying to discourage patients from engaging in two-way e-mail communication with the practice, yet the GP used e-mail with ‘selected’ (trusted) patients. 9 The authors concluded that robust systems for handling e-mail have not been established in practices and this would be difficult to achieve using standard e-mail (e.g. establishing with confidence the identity of patients using the system). Even when more secure alternatives can be provided by practices, effective triage systems would need to be implemented to determine the suitability of the medium (e.g. urgency of response, need for physical examination). 8,9 If patients can choose from a range of consultation options that are equally available, then the patient group using each type of consultation will be determined by patients themselves. If use of alternatives to the face-to-face consultation is mandated by the practice as the default way to gain access to care, it will be important to facilitate other routes to care to avoid marginalisation of groups with particular needs. 9
It was also observed that e-mail consultations were not consistently recorded in the medical record. 9 Three studies reported potential inefficiencies that included duplicate consultations for patients who consult remotely and then attend the practice or require a home visit. 9
Other studies reported concerns about what would happen if a part-time member of staff fails to pick up an urgent e-mail. 9
Some evidence related specifically to the process of integrating traditional and alternative consultation models in practice may be important. Increasing the availability of face-to-face appointments by offering a walk-in clinic was seen to reduce the number of Skype consultations in a UK general practice,8 and procedures around organisation of appointments was considered potentially important for successful implementation of webGP. 25
Better awareness and understanding among staff and patients about alternative consultation models may facilitate implementation. UK case studies suggested that primary care staff encounter difficulties in making patients aware of the alternative consultation options and getting them to engage with these alternatives when face-to-face consultation is still seen as the ‘gold standard’. 10
Atherton et al. 9 concluded that lack of targeted training and investment may be a barrier to the implementation of alternative consultation models. 9 Receptionists and administrators have a key role in ensuring that new consultation methods are taken up by, and delivered to, patients, but this is not always acknowledged or considered by other members of the practice. Receptionists were not offered training and practices were reluctant to invest financially in training for any staff members, sometimes delivering ad-hoc or in-house training, or in the case of e-consultation training only the GPs. 10 The authors noted that the GP Access Fund is an important facilitator of implementation, because it provides a rationale, financial support and training. 10
One study recommended that patients be shown how to use a system at a point when it is relevant to them, rather than as part of a general induction to their health-care organisation. If the information does not come at the right time, the patient may not remember the system, or (as is likely in a fast-moving field) the system may have changed by the time they come to use it. 10
Unintended consequences
Integration of new consultation models with existing practices can have unintended consequences. Some studies reported that e-mail and e-consultations were used by patients to bypass the gatekeeping role of the reception staff to gain direct contact with a primary care professional, or otherwise circumvent existing systems within the practice, such as appointments and telephone consultations. 9,25 This prospect was sometimes viewed as unacceptably disruptive by clinicians. 9 Some interviewees were also critical of the types of problems reported by patients via webGP incurring unnecessary delays in care. 25
Issues relevant to contracting delivering digital-first models (for example geography size, population size)
The evidence identified in this rapid review was typically focused on the introduction of alternative consultation models within individual primary care practices. Consequently, no evidence was identified to inform contracting these models at a regional or national level.
Chapter 4 Discussion
Principal findings
There appears to be very little evidence exclusively evaluating ‘digital-first’ models of health-care delivery. The existing review literature is rarely characterised in terms of ‘digital first’ or even ‘digital’ consultation models. More commonly, reviews focus on alternative channels for triage or face-to-face consultation, only a subset of which relate to purely digital technologies. Similarly, although the focus of this review was on primary care, the review literature sometimes combined data from interventions that were implemented in wider health-care settings.
Although there appears to be consistent evidence that users of alternatives to face-to-face consultations are likely to be younger, healthier females with higher levels of education and employment, the included evidence was often small scale or qualitative in nature. Empirical evidence is either lacking or contradictory for health-related and service delivery outcomes, and quantitative evidence on the benefits and disadvantages for different patient groups is lacking. Consequently, although the concerns of potential users are well documented, there is little evidence to support or refute their validity. In some instances it was difficult to untangle more robust qualitative evidence from simple opinion.
Much of the most recent and higher-quality work in this area has been funded by the NIHR HSDR programme. This includes a major programme of work conducted at Warwick Medical School, which specifically examined the potential of alternatives to face-to-face consultations in UK general practice. 9 The NIHR HSDR programme also funded the recent systematic review of digital and online symptom checkers and health assessment/triage services from the University of Sheffield’s School of Health and Related Research). 24
Limitations of the identified evidence
The quality of the included reviews was variable and the majority had significant limitations. Poor reporting of methodology and a lack of adequate study details were common issues. This made it difficult to assess the reliability of many of the reported findings. Two higher-quality reviews considered the primary studies they included as being at risk of bias9,24 and the primary studies identified by the current scoping exercise were typically small scale and rarely replicated.
The scoping stage of this project identified many reviews of alternatives to face-to-face consultations. Many of these were primarily concerned with ‘mainstream’ technologies, such as telephone consultation and triage, and only a minority specifically focused on primary care. Most reviews very narrowly evaluated the introduction or use of a class of technology (e.g. internet video consultation), rather than the integration of such technologies as part of a broader reorganisation or reimagining of services. Much of the evidence is characterised in terms of alternatives to face-to-face consultation, rather than ‘digital-first primary care’. An exception may be the review of digital and online symptom checkers and health assessment and triage services by Chambers et al. 24
Much of the evidence on digital forms of consultation relates to long-established technology, including e-mail and telephone consultation. There is some systematic review evidence on live video consultation and online triage tools, but nothing on, for example, consultation via mobile telephone health-care apps. Nor does there currently appear to be a great deal of evidence evaluating methods that employ ‘next-generation’ forms of technology (e.g. artificial intelligence, advanced messaging platforms). The timelines for RCTs and other population-based evaluations mean that this form of evidence will always lag behind technological innovation and evolution. However, RCTs are not necessarily the most appropriate form of evaluation in this area and timelines for gathering evidence cannot be an excuse for not fully evaluating new technologies. In October 2016, the Accelerated Access Review recommended that the National Institute for Health and Care Excellence should review its health technology assessment processes and methods to ensure they are fit for purpose to assess new types of emerging products and enable access to the products the NHS needs. 30
Limitations of the scoping exercise and thematic synthesis
This report describes a novel approach to rapid evidence-gathering for a policy audience. Although the topic, scope and outputs were determined by the requirements of a policy-making body (NHS England), the work was undertaken by an independent academic research centre with a long-established international reputation for evidence synthesis (Centre for Reviews and Dissemination, University of York). Although the former group required a very rapid, brief and high-level overview of the evidence, the latter attempted to introduce a level of transparency and reproducibility not typically associated with these kinds of briefings. Consequently, this draft report reflects some of the necessary compromises that had to be made to meet the objectives of both groups.
The first stage of this project was a rapid scoping exercise to identify published secondary research of broad relevance to the topic area of interest, the original objective being to classify the retrieved evidence in terms of broad descriptive characteristics. In response to the subsequent requirements of the policy customer, the second stage of the project provided a rapid synthesis of the themes that emerged from the key material identified in the scoping exercise. Despite stage 2 incorporating a thematic synthesis of the evidence identified during the basic scoping exercise, from a methodological standpoint, stage 2 should be considered an extension of the scoping review, rather than a true qualitative synthesis. In addition, some of the questions asked before stage 2 were very broad in scope and/or not well suited to empirical investigation. The authors have therefore been careful not to make claims on the basis of an enhanced scoping review that could be supported only by a more conventional, rigorous and properly resourced qualitative review.
Given the limited available time and resources, a pragmatic decision was made to limit the searches to a small number of databases and focus on identifying secondary evidence, with only targeted searching for the most recent and relevant primary studies. We therefore cannot rule out the existence of other primary research evidence not identified either by these searches or by the included reviews. However, wherever possible within the constraints of the project, we applied robust and transparent methods for the identification, selection, critical appraisal and synthesis of the evidence. As well as identifying ongoing research, we incorporated the findings of unpublished evidence (at the time of writing) that we obtained directly from the research authors. 24,29
Chapter 5 Conclusions
Rapid scoping of the literature suggests that there is little high-quality evidence relating to ‘digital-first primary care’, as defined by NHS England. The broader evidence on alternatives to face-to-face consultation addresses certain policy-maker concerns, such as the possible impact of new technologies on workload and workforce, inequalities, local implementation and integration with existing services. However, although this evidence gives an insight into the views and experiences of health professionals in relation to such concerns, quantitative empirical data are lacking.
What are the benefits of digital modes and models of engagement between patients and primary care?
Nature of the identified evidence
It should be noted that much of the literature on digital modes and models of engagement focus either on the inherent characteristics of the technology (e.g. text-based consultations have obvious advantages for some patient groups and obvious disadvantages for others) or on the views and perceptions users (clinicians or patients). Unfortunately, there are few objective outcome data to evaluate the benefits and risks of digital modes and models of engagement against standard practice in primary care. Where evidence is available, it is extremely limited, often from just one or two studies, and often from studies conducted in a non-UK primary care setting.
Consequently, the evidence is either sparse or contradictory for patient health outcomes; quality of care; access to care; continuity of care; breaches of privacy or confidentiality; financial costs and cost-effectiveness; diagnostic accuracy; accuracy of triage; and signposting.
The available evidence suggests that the uptake of existing digital modes and models of engagement is currently very low, which may have limited the opportunity to undertake robust research on potential benefits. However, the current low rate of uptake may represent an opportunity for the growth of digital modes and models of engagement.
Effects of digital modes and models
Alternative modes and models of engagement change the interpersonal dynamic of the traditional primary care consultation. Many of the rich sense stimuli of a face-to-face consultation are lost, although digital modes of engagement allow patients to share recorded images and sounds to aid remote assessment and diagnosis. Some evidence suggests that video consultations are shorter and result in less information being shared and fewer problems being discussed than face-to-face consultations. However, other evidence suggests that video consultation may be preferable for patients who feel apprehensive about face-to-face encounters with GPs or other practice staff.
Patients were often satisfied with alternatives to face-to-face consultation that provided convenience, flexibility and control, particularly when dealing with ‘simple’ problems. Some evidence suggested that face-to-face consultations were more highly rated than alternatives when time was needed for discussion, making decisions and taking problems seriously. Patients expressed concerns about confidentiality, for example in relation to web requests being viewed by non-clinical staff. GPs satisfaction rates suggested that face-to-face remains the preferred ‘gold standard’, with substantially lower ratings for video consultation. Both patients and GPs commonly encountered technical problems with video consultation.
There does not appear to be evidence to suggest harms, but the few studies measuring this for digital modes of engagement were generally short term and small scale. There is also some evidence to suggest increased GP caution when using alternative consultation models, leading to ‘safety netting’ behaviours, such as higher than usual antibiotic prescribing.
Issues relating to general practitioner workload and workforce
There appears to be little quantitative evidence on the impact of e-mail on overall workload in primary care, whereas findings on e-visits and e-consultation are mixed. There is some evidence that online triage tools can divert demand away from primary care services, but results vary between interventions and outcome measures. One recent UK study suggested that video consultations are time neutral for clinicians.
The impact of alternative consultations on the number and duration of follow-up consultations is not well established, and the authors of the most recent UK studies recommend that future evaluations specifically measure any ‘knock-on’ effects in the 2 weeks following a digital consultation.
Which patients can benefit from digital (online) modes and models of engagement between patients and primary care?
The available evidence consistently suggests that patients who use alternative consultation methods are younger and healthier and have higher levels of education, employment and income than patients who use traditional primary care services. This particularly appears to be the case for digital modes of communication. This has raised concerns about the potential for digital modes and models of engagement in primary care to reduce access for older patients with complex health needs, as well as patients from more deprived areas. However, there is some evidence that – for those with access and the ability to use digital services – alternative consultation methods may be popular among some older patients and patients with mobility or anxiety issues.
It should be noted that much of the empirical evidence about the impact on subgroups is from a health professional perspective, rather than a patient perspective.
What channels work best for different patient needs and/or conditions?
There appears to be little in-depth comparison of the differential effects of different channels of engagement in primary care. The main distinction in the literature is between technologies that rely primarily on verbal or textual interaction. Often the advantages and disadvantages of each mode are theoretical rather than empirical.
Telephone consultations are challenging for people with hearing or speech problems, learning difficulties or cognitive impairment, or who do not have English as a first language. There does not appear to be strong evidence about whether or not digital modes of engagement can mitigate any of these challenges.
Are there differences in synchronous and asynchronous models?
Much of the identified literature emphasises the theoretical rather than empirical differences between synchronous and asynchronous models. Synchronous models retain some advantages of interpersonal interaction between patient and clinician. Asynchronous models lose these advantages and are generally unsuitable for urgent health needs. However, asynchronous models can provide flexibility for both clinicians and patients, and may be preferred by patients with anxiety or communication difficulties.
How to integrate ‘digital-first’ models of accessing primary care within wider existing face-to-face models
A number of barriers to implementation of digital modes and models of engagement have been identified.
Health professionals have expressed concerns about workload changes; patient access and equity; security, confidentiality and privacy issues; and medico-legal concerns around medical errors and medical negligence owing to the absence of physical examinations and the potential for miscommunication. With the possible exception of patient access and equity, there appear to be limited empirical data to either substantiate or allay these concerns.
Several studies identified technical barriers to the implementation of digital models of engagement, with one author citing ‘the heavily firewalled, low bandwidth systems of the NHS’. 9 Beyond having adequate IT infrastructure to deliver digital engagement, primary care staff felt that adequate implementation of such technology would also require integration with established appointment and electronic record systems.
Some studies observed that the presence of an established relationship between GP and patient facilitated alternative forms of consultation.
General practitioners and nurses value the clinician–patient relationship and some have identified physical proximity as an important factor in its development. One author suggests that ‘any new technology needs to enhance what the professional sees as their core role, otherwise it is unlikely to be accepted into practice’. 9
The absence of clear policies, procedures and guidance relating to alternative models of engagement can create inconsistencies in practice that lead to inefficiency and inequality. Problems noted in the literature include unclear contingency planning for staff absence or technical failure, lack of promotion of consultation options to eligible patient groups and lack of targeted training for administrative staff.
How to contract such models and how to deliver: what geography size, population size?
Available evidence typically focused on the impact of alternative consultation models in the context of individual primary care practices. No evidence was identified to inform contracting these models at a regional or national level.
Chapter 6 Implications for policy
As well as obtaining better empirical data on the effects of ‘digital primary care’, policy-makers may want to engage directly with the concerns of health professionals around practitioner core roles, workload, medico-legal issues, patient access, equity, security, confidentiality and privacy issues. Engagement with professionals might also address the perceived technological barriers to implementation.
Some of the questions of interest to policy-makers – such as how the delivery and funding of primary care services might be reconfigured as a consequence of digital consultation methods – cannot be answered by research evidence alone, and may require in-depth engagement with all primary care stakeholders.
Chapter 7 Implications for research
A broad scope qualitative or mixed-methods review of the literature is unlikely to be of great value in informing future decisions about digital-first primary care. This exercise has identified recent reviews of both digital and online symptom checkers and triage services, and alternatives to face-to-face communication. However, much of the primary evidence relates to approaches and technologies that have changed since their evaluation, and new technologies continue to emerge.
A major difficulty for establishing an evidence base relating to digital technologies, in general, is the rate of innovation and the time needed for evaluation. Individual primary studies take time, particularly when a period of follow-up is required to capture clinical outcomes. Yet more time is required for replication studies to be conducted and for systematic reviews to collate and evaluate a body of evidence.
The immediate outcome of interest to developers of digital interventions is likely to be usability. A digitally delivered service with potential to be highly effective may prove unsuccessful because it is unusable or unfit for use in realistic contexts. Usability testing, as implemented by software developers, typically follows a different paradigm to most clinical research, whereby better designs are derived from identifying single failures, rather than establishing effectiveness through repeated success. Future research into the digital delivery of clinical interventions may need to reconcile these ‘digital’ and ‘clinical’ evaluation paradigms.
Although developers focus on measures of usability and user satisfaction, these alone will not capture the clinical consequences of new forms of engagement, both for patients who use these interventions and forthose who do not. Evaluation of any new health technology that changes the means of triage, diagnosis or consultation needs to measure outcomes that matter to patients, professionals and the broader health service. Alternative forms of engagement may impact on clinical practice, diagnostic accuracy, safety, harms, quality of care, consultation dynamic, costs and organisational factors. Future studies should carefully consider the proximal and distal impacts of new engagement technologies to ensure that appropriate forms of outcome data are collected. Some phenomena (e.g. the impact of digital communication interventions on clinician–patient consultation dynamic) may benefit from further qualitative primary research.
Acknowledgements
Contributions of authors
Mark Rodgers (https://orcid.org/0000-0002-5196-9239) (Research Fellow, Evidence Synthesis) contributed to the protocol, drafted the protocol and carried out study selection, evidence synthesis and write up of the report.
Gary Raine (https://orcid.org/0000-0002-0354-0518) (Research Fellow, Evidence Synthesis) contributed to the protocol, carried out study selection, data extraction, critical appraisal and write up of the report.
Sian Thomas (https://orcid.org/0000-0003-0917-0068) (Research Fellow, Evidence Synthesis) contributed to the protocol, carried out study selection, data extraction, critical appraisal and write up of the report.
Melissa Harden (https://orcid.org/0000-0003-2338-6869) (Information Specialist) contributed to the protocol, conducted all searching, wrote the search sections of the report and commented on the draft report.
Alison Eastwood (https://orcid.org/0000-0003-1079-7781) (Professor, Research) contributed to the protocol, oversaw the project, contributed advice and expertise and commented on all drafts of the report.
Data-sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- NHS England . Digital-First Primary Care and Its Implications for General Practice Payments 2018. www.engage.england.nhs.uk/survey/digital-first-primary-care/user_uploads/digital-first-access-to-gp-care-engagement-v2.pdf (accessed 9 October 2018).
- NHS England . New Care Models: Vanguards – Developing a Blueprint for the Future of NHS and Care Services 2016.
- Health Innovation Network . TECS Evidence Base Review. Findings and Recommendations 2017.
- Department of Health and Social Care . The Future of Healthcare: Our Vision for Digital, Data and Technology in Health and Care 2018.
- Chambers D, Wade R, Wilson P. Training Manual for Selecting Reviews and Writing Abstracts for the Database of Abstracts of Reviews of Effects (DARE). York: Centre for Reviews and Dissemination, University of York; 2012.
- Wong G, Greenhalgh T, Westhorp G, Pawson R. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: the RAMESES (Realist And Meta-narrative Evidence Syntheses – Evolving Standards) project. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02300.
- Critical Appraisal Skills Programme . CASP Appraisal Checklists 2018. https://casp-uk.net/casp-tools-checklists/ (accessed 9 October 2018).
- Castle-Clarke S, Imison C. The Digital Patient: Transforming Primary Care?. London: Nuffield Trust; 2016.
- Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, et al. The potential of alternatives to face-to-face consultation in general practice, and the impact on different patient groups: a mixed-methods case study. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06200.
- Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, et al. Alternatives to the face-to-face consultation in general practice: focused ethnographic case study. Br J Gen Pract 2018;68:e293-e300. https://doi.org/10.3399/bjgp18X694853.
- Brant H, Atherton H, Ziebland S, McKinstry B, Campbell JL, Salisbury C. Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice. Br J Gen Pract 2016;66:e460-6. https://doi.org/10.3399/bjgp16X685597.
- Armoiry X, Sturt J, Phelps EE, Walker CL, Court R, Taggart F, et al. Digital clinical communication for families and caregivers of children or young people with short- or long-term conditions: rapid review. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.7999.
- Griffiths F, Armoiry X, Atherton H, Bryce C, Buckle A, Cave J. The role of digital communication in patient-clinician communication for NHS providers of specialist clinical services for young people [the Long-term conditions Young people Networked Communication (LYNC) study]: a mixed-methods study. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06090.
- Atherton H, Huxley C, Court R, Taggart F, Turk A, Ha J, et al. A Rapid Review of the Impact of Communication Technologies on Clinical Outcomes for Young People With Diabetes 2018. www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018086259 (accessed 8 May 2018).
- Thiyagarajan A, Atherton H, Griffiths F, Fleming J. To Explore Patient and Clinician Experience WITH Video Consultation: A Systematic Review 2018. www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018100032 (accessed 6 July 2018).
- Chambers D, Cantrell A, Booth A, Preston L, Baxter S, Johnson M, et al. Digital and Online Symptom Checkers and Health Assessment Triage Services: Systematic Review 2018. www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018093564 (accessed 8 May 2018).
- Shaw S, Wherton J, Vijayaraghavan S, Morris J, Bhattacharya S, Hanson P, et al. Advantages and limitations of virtual online consultations in a NHS acute trust: the VOCAL mixed-methods study. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06210.
- NIHR . Call for Proposals: 18 89 Digital Technologies to Improve Health and Care 2018. www.nihr.ac.uk/funding-and-support/documents/current-funding-opportunities/Digital%20technologies/18-89-digital-technologies.pdf (accessed 12 December 2018).
- National Institute for Health Research . Call for Proposals: Evaluating the Digital 111 Offer: NHS 111 Online 2018. www.nihr.ac.uk/funding-and-support/documents/current-funding-opportunities/hsdr/hsdr-online-111-highlight-notice.pdf (accessed 12 December 2018).
- Antoun J. Electronic mail communication between physicians and patients: a review of challenges and opportunities. Fam Pract 2016;33:121-6. https://doi.org/10.1093/fampra/cmv101.
- Atherton H, Sawmynaden P, Sheikh A, Majeed A, Car J. Email for clinical communication between patients/caregivers and healthcare professionals. Cochrane Database Syst Rev 2012;11. https://doi.org/10.1002/14651858.CD007978.pub2.
- Hickson R, Talbert J, Thornbury WC, Perin NR, Goodin AJ. Online medical care: the current state of ‘eVisits’ in acute primary care delivery. Telemed J E Health 2015;21:90-6. https://doi.org/10.1089/tmj.2014.0022.
- Huxley CJ, Atherton H, Watkins JA, Griffiths F. Digital communication between clinician and patient and the impact on marginalised groups: a realist review in general practice. Br J Gen Pract 2015;65:e813-21. https://doi.org/10.3399/bjgp15X687853.
- Chambers D, Cantrell AJ, Johnson M, Preston L, Baxter SK, Booth A, et al. Digital and online symptom checkers and assessment services for urgent care to inform a new digital platform: a systematic review. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07290.
- Carter M, Fletcher E, Sansom A, Warren F, Campbell J. Feasibility, acceptability and effectiveness of an online alternative to face-to-face consultation in general practice: a mixed methods study of webGP in six Devon practices. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-018688.
- Uscher-Pines L, Mulcahy A, Cowling D, Hunter G, Burns R, Mehrotra A. Access and quality of care in direct-to-consumer telemedicine. Telemed J E Health 2016;22:282-7. https://doi.org/10.1089/tmj.2015.0079.
- Uscher-Pines L, Mehrotra A. Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Aff 2014;33:258-64. https://doi.org/10.1377/hlthaff.2013.0989.
- Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. Characteristics of patients who seek care via eVisits instead of office visits. Telemed J E Health 2013;19:515-19. https://doi.org/10.1089/tmj.2012.0221.
- Donaghy E, Atherton H, Hammersley V, McNeilly H, Bikker A, Robbins L, et al. Br J Gen Pract 2019;69:e586-e594. https://doi.org/10.3399/bjgp19X704141.
- GOV.UK . Accelerated Access Review: Final Report 2016. www.gov.uk/government/publications/accelerated-access-review-final-report (accessed 12 December 2018).
- Atherton H, Ziebland S. Digit Health 2016;2. https://doi.org/10.1177/2055207616675559.
- Katz SJ, Moyer CA, Cox DT, Stern DT. Effect of a triage-based e-mail system on clinic resource use and patient and physician satisfaction in primary care: a randomized controlled trial. J Gen Intern Med 2003;18:736-44. https://doi.org/10.1046/j.1525-1497.2003.20756.x.
- Katz SJ, Nissan N, Moyer CA. Crossing the digital divide: evaluating online communication between patients and their providers. Am J Manag Care 2004;10:593-8.
- Kummervold PE, Trondsen M, Andreassen H, Gammon D, Hjortdahl P. Patient–physician interaction over the internet. Tidsskr Nor NorskeLaegeforen 2004;124:2633-6.
Appendix 1 Scoping searches
Searches were conducted for reviews related to digital alternatives to face-to face consultations in primary care. In addition to records directly focused on alternatives to face-to-face communication, searches also identified related reviews addressing broader issues around digital innovation in primary care, including computerised clinical decision support systems, ‘e-health’ and electronic health records.
MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, and Daily
Via Ovid http://ovidsp.ovid.com/.
Date range searched: 1946 to present.
Date searched: 5 July 2018.
Records retrieved: 1491.
Search strategy
-
Medical Informatics/ (10,660)
-
exp Medical Informatics Applications/ (415,196)
-
exp Computer Systems/ (163,773)
-
exp Software/ (139,951)
-
Automation/ (16,345)
-
Man-Machine Systems/ (2634)
-
exp Artificial Intelligence/ (76,164)
-
algorithms/ (225,494)
-
exp Medical Records Systems, Computerized/ (35,178)
-
exp Health Records, Personal/ (1444)
-
Medical Record Linkage/ (4430)
-
Electronic Prescribing/ (878)
-
Health Information Exchange/ (607)
-
exp Telecommunications/ (80,668)
-
wearable electronic devices/or fitness trackers/ (512)
-
exp Monitoring, Ambulatory /(26,109)
-
‘Referral and Consultation’/ (60,838)
-
(digital$ or digitis$ or digitiz$).ti,ab. (129,852)
-
(ehealth or e-health or electronic health).ti,ab. (14,141)
-
((automat$ or information or computer$ or electronic$ or software or expert) adj2 system$).ti,ab. (68,020)
-
(ICT or ((information or communication) adj2 technolog$)).ti,ab. (18,686)
-
health information technology.ti,ab. (2296)
-
(artificial intelligence or (AI adj2 system$)).ti,ab. (2876)
-
algorithm$.ti,ab. (206,169)
-
decision support system$.ti,ab. (4499)
-
clinical decision support.ti,ab. (3408)
-
(econsult$ or e-consult$).ti,ab. (181)
-
((video$ or virtual$ or electronic$ or online or on-line or internet or web or email$ or e-mail$ or remote$ or technolog$) adj6 (consult$ or refer$ or communicat$ or access$)).ti,ab. (38,923)
-
((mobile$ or app or apps or application$ or telephone$ or phone$ or smartphone$ or iphone$ or android or ipad$) adj6 (consult$ or refer$ or communicat$ or access$)).ti,ab. (14,657)
-
(text messag$ or texting or short message$ or SMS).ti,ab. (7564)
-
(videoconferenc$ or video conferenc$ or skype).ti,ab. (2497)
-
(evisit$ or e-visit$ or (electronic$ adj2 visit)).ti,ab. (59)
-
(eappointment$ or e-appointment$ or ((electronic$ or online or on-line or internet or web or virtual or video$) adj2 appointment$)).ti,ab. (104)
-
(teleconsult$ or tele-consult$).ti,ab. (1068)
-
(telerefer$ or tele-refer$).ti,ab. (6)
-
non-face-to-face.ti,ab. (79)
-
((asynchronous or synchronous) adj2 communicat$).ti,ab. (155)
-
(eprescri$ or e-prescri$ or electronic$ prescri$).ti,ab. (1209)
-
(econsult$ or e-consult$).ti,ab. (181)
-
(ereferral$ or e-referral$).ti,ab. (56)
-
electronic medical record$.ti,ab. (11,852)
-
electronic health record$.ti,ab. (10,193)
-
electronic patient record$.ti,ab. (1765)
-
personal health record$.ti,ab. (853)
-
(computer$ adj (patient or health or medical) adj record$).ti,ab. (1177)
-
(telemedicine or telehealth or telehealthcare or telecare or telemental or telemanagement or telerehabilitation or telepsychology or teletherapy or tele-medicine or tele-health or tele-healthcare or tele-care or tele-management or tele-mental or tele-rehabilitation or tele-psychology or tele-therapy).ti,ab. (13,506)
-
(mhealth or m-health or mobile health).ti,ab. (2983)
-
((video$ or virtual$ or electronic$ or online or on-line or internet or web or email$ or e-mail$ or remote$) adj3 (service$ or deliver$ or care or healthcare)).ti,ab. (14,301)
-
((mobile$ or app or apps or application$ or telephone$ or phone$ or smartphone$ or iphone$ or android or ipad$) adj3 (service$ or deliver$ or care or healthcare)).ti,ab. (15,377)
-
((mobile or online or on-line or internet or web or remote$) adj3 (platform$ or system or technolog$)).ti,ab. (17,346)
-
or/1-50 (1,251,298)
-
Primary Health Care/ (68,274)
-
General Practice/ (11,558)
-
Family Practice/ (63,928)
-
General Practitioners/ (6221)
-
Physicians, Family/ (15,805)
-
Physicians, Primary Care/ (2624)
-
Primary Care Nursing/ (386)
-
(primary adj2 care).ti,ab. (116,110)
-
primary healthcare.ti,ab. (4330)
-
general practitioner$.ti,ab. (45,738)
-
general practice$.ti,ab. (37,186)
-
(GP adj (surger$ or service$ or trust$ or provider$ or practice$)).ti,ab. (1511)
-
family physician$.ti,ab. (13,483)
-
(physician$ adj2 (group$ or practice$)).ti,ab. (11,128)
-
(Clinical commissioning group$ or CCG or CCGs).ti,ab. (2090)
-
or/52-66 (256,375)
-
51 and 67 (40,732)
-
(GP consult$ adj2 (app or apps or application$)).ti,ab. (3)
-
GP at hand.ti,ab. (3)
-
GP hub$.ti,ab. (2)
-
68 or 69 or 70 or 71 (40,735)
-
systematic$ review$.ti,ab. (126,630)
-
meta-analysis as topic/ (16,282)
-
meta-analytic$.ti,ab. (5931)
-
meta-analysis.ti,ab,pt. (134,378)
-
metanalysis.ti,ab. (166)
-
metaanalysis.ti,ab. (1444)
-
meta analysis.ti,ab. (110,631)
-
meta-synthesis.ti,ab. (635)
-
metasynthesis.ti,ab. (249)
-
meta synthesis.ti,ab. (635)
-
meta-regression.ti,ab. (5570)
-
metaregression.ti,ab. (519)
-
meta regression.ti,ab. (5570)
-
(synthes$ adj3 literature).ti,ab. (2614)
-
(synthes$ adj3 evidence).ti,ab. (7915)
-
integrative review.ti,ab. (2131)
-
data synthesis.ti,ab. (9842)
-
(research synthesis or narrative synthesis).ti,ab. (2088)
-
(systematic study or systematic studies).ti,ab. (10,510)
-
(systematic comparison$ or systematic overview$).ti,ab. (2852)
-
evidence based review.ti,ab. (1794)
-
comprehensive review.ti,ab. (11,861)
-
critical review.ti,ab. (14,084)
-
quantitative review.ti,ab. (602)
-
structured review.ti,ab. (702)
-
realist review.ti,ab. (214)
-
realist synthesis.ti,ab. (146)
-
or/73-99 (273,757)
-
review.pt. (2,397,048)
-
medline.ab. (94,233)
-
pubmed.ab. (81,475)
-
cochrane.ab. (61,692)
-
embase.ab. (65,543)
-
cinahl.ab. (20,444)
-
psyc?lit.ab. (908)
-
psyc?info.ab. (23,392)
-
(literature adj3 search$).ab. (47,808)
-
(database$ adj3 search$).ab. (46,362)
-
(bibliographic adj3 search$).ab. (2078)
-
(electronic adj3 search$).ab. (17,254)
-
(electronic adj3 database$).ab. (21,989)
-
(computeri?ed adj3 search$).ab. (3298)
-
(internet adj3 search$).ab. (2726)
-
included studies.ab. (16,899)
-
(inclusion adj3 studies).ab. (12,687)
-
inclusion criteria.ab. (66,696)
-
selection criteria.ab. (27,072)
-
predefined criteria.ab. (1673)
-
predetermined criteria.ab. (939)
-
(assess$ adj3 (quality or validity)).ab. (65,256)
-
(select$ adj3 (study or studies)).ab. (56,445)
-
(data adj3 extract$).ab. (49,685)
-
extracted data.ab. (11,542)
-
(data adj2 abstracted).ab. (4650)
-
(data adj3 abstraction).ab. (1399)
-
published intervention$.ab. (150)
-
((study or studies) adj2 evaluat$).ab. (157,808)
-
(intervention$ adj2 evaluat$).ab. (9438)
-
confidence interval$.ab. (345,570)
-
heterogeneity.ab. (138,313)
-
pooled.ab. (72,823)
-
pooling.ab. (10,532)
-
odds ratio$.ab. (226,154)
-
(Jadad or coding).ab. (160,764)
-
or/102-136 (1,214,999)
-
101 and 137 (209,235)
-
review.ti. (391,379)
-
139 and 137 (105,264)
-
(review$ adj4 (papers or trials or studies or evidence or intervention$ or evaluation$)).ti,ab. (157,635)
-
100 or 138 or 140 or 141 (469,678)
-
letter.pt. (991,994)
-
editorial.pt. (461,929)
-
1comment.pt. (722,222)
-
143 or 144 or 145 (1,640,316)
-
142 not 146 (458,626)
-
exp animals/not humans/ (4,469,565)
-
147 not 148 (446,603)
-
72 and 149 (1491)
Cochrane Database of Systematic Reviews
Via Wiley http://onlinelibrary.wiley.com/.
Date range searched: Issue 7 of 12, July 2018.
Date searched: 5 July 2018.
Records retrieved: 414.
Search strategy
-
#1 MeSH descriptor: [Medical Informatics] this term only (84)
-
#2 MeSH descriptor: [Medical Informatics Applications] explode all trees (12,397)
-
#3 MeSH descriptor: [Computer Systems] explode all trees (5103)
-
#4 MeSH descriptor: [Software] explode all trees (3032)
-
#5 MeSH descriptor: [Automation] this term only (278)
-
#6 MeSH descriptor: [Man-Machine Systems] this term only (62)
-
#7 MeSH descriptor: [Artificial Intelligence] explode all trees (1179)
-
#8 MeSH descriptor: [Algorithms] this term only (3716)
-
#9 MeSH descriptor: [Medical Records Systems, Computerized] explode all trees (639)
-
#10 MeSH descriptor: [Health Records, Personal] explode all trees (137)
-
#11 MeSH descriptor: [Medical Record Linkage] this term only (35)
-
#12 MeSH descriptor: [Electronic Prescribing] this term only (30)
-
#13 MeSH descriptor: [Health Information Exchange] this term only (5)
-
#14 MeSH descriptor: [Telecommunications] explode all trees (5806)
-
#15 MeSH descriptor: [Wearable Electronic Devices] this term only (6)
-
#16 MeSH descriptor: [Fitness Trackers] this term only (29)
-
#17 MeSH descriptor: [Monitoring, Ambulatory] explode all trees (3144)
-
#18 MeSH descriptor: [Referral and Consultation] this term only (1980)
-
#19 (digital* or digitis* or digitiz*):ti,ab,kw (8121)
-
#20 (ehealth or e-health or ‘electronic health’):ti,ab,kw (1455)
-
#21 ((automat* or information or computer* or electronic* or software or expert) near/2 system*):ti,ab,kw (4050)
-
#22 (ICT or ((information or communication) near/2 technolog*)):ti,ab,kw (1069)
-
#23 (‘artificial intelligence’ or (AI near/2 system*)):ti,ab,kw (223)
-
#24 algorithm*:ti,ab,kw (10,244)
-
#25 ‘decision support’ next system*:ti,ab,kw (1235)
-
#26 ‘clinical decision support’:ti,ab,kw (434)
-
#27 (econsult* or e-consult*):ti,ab,kw (16)
-
#28 ((video* or virtual* or electronic* or online or on-line or internet or web or email* or e-mail* or remote* or technolog*) near/6 (consult* or refer* or communicat* or access*)):ti,ab,kw (4315)
-
#29 ((mobile* or app or apps or application* or telephone* or phone* or smartphone* or iphone* or android or ipad*) near/6 (consult* or refer* or communicat* or access*)):ti,ab,kw (1832)
-
#30 (text next messag* or texting or short next message* or SMS):ti,ab,kw (2541)
-
#31 (videoconferenc* or video next conferenc* or skype):ti,ab,kw (609)
-
#32 (evisit* or e-visit* or (electronic* near/2 visit*)):ti,ab,kw (29)
-
#33 (eappointment* or e-appointment* or ((electronic* or online or on-line or internet or web or virtual or video*) near/2 appointment*)):ti,ab,kw (13)
-
#34 (teleconsult* or tele-consult*):ti,ab,kw (501)
-
#35 (telerefer* or tele-refer*):ti,ab,kw (1)
-
#36 non-face-to-face:ti,ab,kw (18)
-
#37 ((asynchronous or synchronous) near/2 communicat*):ti,ab,kw (16)
-
#38 (eprescri* or e-prescri* or electronic* next prescri*):ti,ab,kw (104)
-
#39 (econsult* or e-consult*):ti,ab,kw (16)
-
#40 (ereferral* or e-referral*):ti,ab,kw (11)
-
#41 ‘electronic medical’ next record*:ti,ab,kw (1407)
-
#42 ‘electronic health’ next record*:ti,ab,kw (958)
-
#43 ‘electronic patient’ next record*:ti,ab,kw (155)
-
#44 ‘personal health’ next record*:ti,ab,kw (86)
-
#45 (computer* next (patient or health or medical) next record*):ti,ab,kw (62)
-
#46 ‘health information technology’:ti,ab,kw (114)
-
#47 (telemedicine or telehealth or telehealthcare or telecare or telemental or telemanagement or telerehabilitation or telepsychology or teletherapy or tele-medicine or tele-health or tele-healthcare or tele-care or tele-management or tele-mental or tele-rehabilitation or tele-psychology or tele-therapy):ti,ab,kw (3920)
-
#48 (mhealth or m-health or mobile health):ti,ab,kw (2394)
-
#49 ((video* or virtual* or electronic* or online or on-line or internet or web or email* or e-mail* or remote*) near/3 (service* or deliver* or care or healthcare)):ti,ab,kw (3271)
-
#50 ((mobile* or app or apps or application* or telephone* or phone* or smartphone* or iphone* or android or ipad*) near/3 (service* or deliver* or care or healthcare)):ti,ab,kw (2732)
-
#51 ((mobile or online or on-line or internet or web or remote*) near/3 (platform* or system or technolog*)):ti,ab,kw (2593)
-
#52 {or #1-#51} (61,013)
-
#53 MeSH descriptor: [Primary Health Care] this term only (4424)
-
#54 MeSH descriptor: [General Practice] this term only (437)
-
#55 MeSH descriptor: [Family Practice] this term only (2220)
-
#56 MeSH descriptor: [General Practitioners] this term only (228)
-
#57 MeSH descriptor: [Physicians, Family] this term only (488)
-
#58 MeSH descriptor: [Physicians, Primary Care] this term only (149)
-
#59 MeSH descriptor: [Primary Care Nursing] this term only (30)
-
#60 (primary near/2 care) (22,531)
-
#61 primary next healthcare (591)
-
#62 general next practitioner* (7196)
-
#63 general next practice* (7401)
-
#64 (GP next (surger* or service* or trust* or provider* or practice$)) (243)
-
#65 family physician* (5512)
-
#66 (physician* near/2 (group* or practice*)) (3035)
-
#67 ((Clinical next commissioning next group*) or CCG or CCGs) (282)
-
#68 33-#67-#67 (34,692)
-
#69 #52 and #68 (6423)
-
#70 ((GP next consult*) near/2 (app or apps or application*)) (0)
-
#71 ‘GP at hand’ (0)
-
#72 GP next hub* (1)
-
#73 {or #69-#72} (6424)
-
#74 {or #69-#72} in Cochrane Reviews (Reviews and Protocols) (414)
Database of Abstracts of Reviews of Effects
Via www.crd.york.ac.uk/CRDWeb/.
Date range searched: inception to 31 March 2015.
Searched on: 5 July 2018.
Records retrieved: 313.
The strategy below was used to search DARE and the HTA database.
Search strategy
-
MeSH DESCRIPTOR Medical Informatics (23)
-
MeSH DESCRIPTOR Medical Informatics Applications EXPLODE ALL TREES (3879)
-
MeSH DESCRIPTOR Computer Systems EXPLODE ALL TREES (357)
-
MeSH DESCRIPTOR Software EXPLODE ALL TREES (174)
-
MeSH DESCRIPTOR Automation (35)
-
MeSH DESCRIPTOR Man-Machine Systems (2)
-
MeSH DESCRIPTOR Artificial Intelligence EXPLODE ALL TREES (295)
-
MeSH DESCRIPTOR algorithms (473)
-
MeSH DESCRIPTOR Medical Records Systems, Computerized EXPLODE ALL TREES (111)
-
MeSH DESCRIPTOR Health Records, Personal EXPLODE ALL TREES (42)
-
MeSH DESCRIPTOR Medical Record Linkage (7)
-
MeSH DESCRIPTOR Electronic Prescribing (8)
-
MeSH DESCRIPTOR Health Information Exchange (1)
-
MeSH DESCRIPTOR Telecommunications EXPLODE ALL TREES (664)
-
MeSH DESCRIPTOR fitness trackers (0)
-
MeSH DESCRIPTOR Monitoring, Ambulatory EXPLODE ALL TREES (159)
-
MeSH DESCRIPTOR Referral and Consultation (335)
-
(digital* or digitis* or digitiz*) (497)
-
(ehealth or e-health or ‘electronic health’) (121)
-
(((automat* or information or computer* or electronic* or software or expert) NEAR2 system*)) (497)
-
(system* NEAR2 (automat* or information or computer* or electronic* or software or expert)) (327)
-
(ICT) OR ((information or communication) NEAR2 technolog*) OR (technolog* NEAR2 (information or communication)) 179 (‘health information technology’) (11)
-
(‘artificial intelligence’) OR (AI NEAR2 system*) OR (system* NEAR2 AI) (7)
-
(algorithm*) (899)
-
(decision support system*) (148)
-
(clinical decision support) (62)
-
(econsult* or e-consult*) (3)
-
((video* or virtual* or electronic* or online or on-line or internet or web or email* or e-mail* or remote* or technolog*) NEAR (consult* or refer* or communicat* or access*)) (800)
-
((consult* or refer* or communicat* or access*) NEAR (video* or virtual* or electronic* or online or on-line or internet or web or email* or e-mail* or remote* or technolog*)) (450)
-
((mobile* or app or apps or application* or telephone* or phone* or smartphone* or iphone* or android or ipad*) NEAR (consult* or refer* or communicat* or access*)) (164)
-
((consult* or refer* or communicat* or access*) NEAR (mobile* or app or apps or application* or telephone* or phone* or smartphone* or iphone* or android or ipad*)) (118)
-
(text messag* or texting or short message* or SMS) (80)
-
(videoconferenc* or video conferenc* or skype) (56)
-
(evisit* or e-visit*) OR (electronic* NEAR2 visit*) OR (visit* NEAR2 electronic*) (8)
-
((eappointment* or e-appointment*) OR ((electronic* or online or on-line or internet or web or virtual or video*) NEAR appointment*) OR (appointment* NEAR (electronic* or online or on-line or internet or web or virtual or video*))) (2)
-
(teleconsult* or tele-consult*) (19)
-
(telerefer* or tele-refer*) (0)
-
(non-face-to-face) (4)
-
((asynchronous or synchronous) NEAR2 communicat*) OR (communicat* NEAR2 (asynchronous or synchronous)) (4)
-
(eprescri* or e-prescri* or electronic* prescri*) (16)
-
(econsult* or e-consult*) (3)
-
(ereferral* or e-referral*) (2)
-
(electronic medical record*) (37)
-
(electronic health record*) (53)
-
(electronic patient record*) (11)
-
(personal health record*) (3)
-
((computer* NEAR1 (patient or health or medical) NEAR1 record*)) (15)
-
(telemedicine or telehealth or telehealthcare or telecare or telemental or telemanagement or telerehabilitation or telepsychology or teletherapy or tele-medicine or tele-health or tele-healthcare or tele-care or tele-management or tele-mental or tele-rehabilitation or tele-psychology or tele-therapy) (471)
-
(mhealth or m-health or mobile health) (33)
-
((video* or virtual* or electronic* or online or on-line or internet or web or email* or e-mail* or remote*) NEAR3 (service* or deliver* or care or healthcare)) (136)
-
((service* or deliver* or care or healthcare) NEAR3 (video* or virtual* or electronic* or online or on-line or internet or web or email* or e-mail* or remote*)) (160)
-
((mobile* or app or apps or application* or telephone* or phone* or smartphone* or iphone* or android or ipad*) NEAR3 (service* or deliver* or care or healthcare)) (174)
-
((service* or deliver* or care or healthcare) NEAR3 (mobile* or app or apps or application* or telephone* or phone* or smartphone* or iphone* or android or ipad*)) (142)
-
((mobile or online or on-line or internet or web or remote*) NEAR3 (platform* or system or technolog*)) (67)
-
((platform* or system or technolog*) NEAR3 (mobile or online or on-line or internet or web or remote*)) (41)
-
#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 (8475)
-
MeSH DESCRIPTOR Primary Health Care (856)
-
MeSH DESCRIPTOR General Practice (47)
-
MeSH DESCRIPTOR Family Practice (261)
-
MeSH DESCRIPTOR General Practitioners (26)
-
MeSH DESCRIPTOR Physicians, Family (50)
-
MeSH DESCRIPTOR Physicians, Primary Care (16)
-
MeSH DESCRIPTOR Primary Care Nursing (3)
-
(primary NEAR2 care) (3872)
-
(primary healthcare) (34)
-
(general practitioner*) (1060)
-
(general practice*) (605)
-
(GP NEAR1 (surger* or service* or trust* or provider* or practice*)) (79)
-
(family physician*) (87)
-
(physician* NEAR2 (group* or practice*)) OR ((group* or practice*) NEAR2 physician*) (430)
-
(Clinical commissioning group* or CCG or CCGs) (13)
-
#58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #72 (4976)
-
#57 AND #73 (1129)
-
(GP consult* NEAR (app or apps or application*)) (0)
-
(GP at hand) (0)
-
(GP hub*) (0)
-
#74 OR #75 OR #76 OR #77 (1129)
-
(*) IN DARE (45,418)
-
#78 AND #79 (313)
-
(*) IN HTA (17,351)
-
#78 AND #81 (9114)
Health Technology Assessment database
Via www.crd.york.ac.uk/CRDWeb/.
Date range searched: inception to 31 March 2018.
Searched on: 5 July 2018.
Records retrieved: 114.
See Database of Abstracts of Reviews of Effects, Search strategy for search strategy used.
PROSPERO
Via www.crd.york.ac.uk/PROSPERO/.
Date range searched: inception to 5 July 2018.
Searched on: 5 July 2018.
Records retrieved: 681.
Search strategy
-
#1 MeSH DESCRIPTOR medical informatics (12)
-
#2 MeSH DESCRIPTOR Medical Informatics Applications EXPLODE ALL TREES (240)
-
#3 MeSH DESCRIPTOR computer systems EXPLODE ALL TREES (292)
-
#4 MeSH DESCRIPTOR software EXPLODE ALL TREES (112)
-
#5 MeSH DESCRIPTOR automation (1)
-
#6 MeSH DESCRIPTOR man-machine systems (0)
-
#7 MeSH DESCRIPTOR artificial intelligence (4)
-
#8 MeSH DESCRIPTOR algorithms (20)
-
#9 MeSH DESCRIPTOR medical records systems, computerized EXPLODE ALL TREES (41)
-
#10 MeSH DESCRIPTOR Health Records, Personal EXPLODE ALL TREES (34)
-
#11 MeSH DESCRIPTOR medical record linkage (1)
-
#12 MeSH DESCRIPTOR electronic prescribing (9)
-
#13 MeSH DESCRIPTOR health information exchange (2)
-
#14 MeSH DESCRIPTOR telecommunications EXPLODE ALL TREES (355)
-
#15 MeSH DESCRIPTOR fitness trackers (6)
-
#16 MeSH DESCRIPTOR Monitoring, Ambulatory EXPLODE ALL TREES (35)
-
#17 MeSH DESCRIPTOR Referral and Consultation EXPLODE ALL TREES (85)
-
#18 digital* or digitis* or digitiz* (950)
-
#19 ehealth or e-health or ‘electronic health’ (384)
-
#20 (automat* or information or computer* or electronic* or software or expert) ADJ2 system* (654)
-
#21 (ICT or ((information or communication) ADJ2 technolog*)) (230)
-
#22 ‘health information technology’ (22)
-
#23 (‘artificial intelligence’ or (AI ADJ2 system*)) (15)
-
#24 algorithm* (602)
-
#25 ‘decision support’ ADJ system* (70)
-
#26 ‘clinical decision support’ (54)
-
#27 econsult* or e-consult* (11)
-
#28 (video* or virtual* or electronic* or online or on-line or internet or web or email* or e-mail* or remote* or technolog*) ADJ6 (consult* or refer* or communicat* or access*) (1343)
-
#29 (mobile* or app or apps or application* or telephone* or phone* or smartphone* or iphone* or android or ipad*) ADJ6 (consult* or refer* or communicat* or access*) (179)
-
#30 text messag* or texting or short message* or SMS (324)
-
#31 ((text ADJ (message or messages or messaging)) or texting or (short ADJ (message or messages or messaging)) or SMS) (397)
-
#32 videoconferenc* or video conferenc* or skype (115)
-
#33 (evisit* or e-visit* or (electronic* ADJ2 visit*)) (5)
-
#34 (eappointment* or e-appointment* or ((electronic* or online or on-line or internet or web or virtual or video*) ADJ2 appointment*)) (1)
-
#35 teleconsult* or tele-consult* (18)
-
#36 telerefer* or tele-refer* (0)
-
#37 non-face-to-face (8)
-
#38 (asynchronous or synchronous) ADJ2 communicat* (5)
-
#39 eprescri* or e-prescri* or electronic* prescri* (17)
-
#40 econsult* or e-consult* (11)
-
#41 ereferral* or e-referral* (5)
-
#42 ‘electronic medical’ ADJ record* (44)
-
#43 ‘electronic health’ ADJ record* (67)
-
#44 ‘electronic patient’ ADJ record* (12)
-
#45 ‘personal health’ ADJ record* (16)
-
#46 computer* ADJ (patient or health or medical) ADJ record* (5)
-
#47 telemedicine or telehealth or telehealthcare or telecare or telemental or telemanagement or telerehabilitation or telepsychology or teletherapy or tele-medicine or tele-health or tele-healthcare or tele-care or tele-management or tele-mental or tele-rehabilitation or tele-psychology or tele-therapy (313)
-
#48 mhealth or m-health or ‘mobile health’ (242)
-
#49 (video* or virtual* or electronic* or online or on-line or internet or web or email* or e-mail* or remote*) ADJ3 (service* or deliver* or care or healthcare) (369)
-
#50 (mobile* or app or apps or application* or telephone* or phone* or smartphone* or iphone* or android or ipad*) ADJ3 (service* or deliver* or care or healthcare) (158)
-
#51 (mobile or online or on-line or internet or web or remote*) ADJ3 (platform* or system* or technolog*) (468)
-
#52 #51 OR #50 OR #49 OR #48 OR #47 OR #46 OR #45 OR #44 OR #43 OR #42 OR #41 OR #40 OR #39 OR #38 OR #37 OR #36 OR #35 OR #34 OR #33 OR #32 OR #31 OR #30 OR #29 OR #28 OR #27 OR #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 (4939)
-
#53 MeSH DESCRIPTOR primary health care (2800)
-
#54 MeSH DESCRIPTOR general practice (330)
-
#55 MeSH DESCRIPTOR Family Practice (33)
-
#56 MeSH DESCRIPTOR general practitioners (33)
-
#57 MeSH DESCRIPTOR Physicians, Family (7)
-
#58 MeSH DESCRIPTOR Physicians, Primary Care (6)
-
#59 MeSH DESCRIPTOR Primary Care Nursing (1)
-
#60 primary ADJ2 care (2176)
-
#61 primary healthcare (81)
-
#62 general ADJ practitioner* (353)
-
#63 general ADJ practice* (512)
-
#64 GP ADJ (surger* or service* or trust* or provider* or practice*) (61)
-
#65 family ADJ physician* (114)
-
#66 physician* ADJ2 (group* or practice*) (45)
-
#67 ‘Clinical commissioning’ ADJ group* (36)
-
#68 CCG or CCGs (41)
-
#69 #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 (2713)
-
#70 #69 AND #52 (681)
-
#71 ‘GP consult’ ADJ2 (app or apps or application*) (0)
-
#72 GP at hand (1)
-
#73 GP hub* (0)
-
#74 GP consult* ADJ2 (app or apps or application*) (0)
-
#75 #70 OR #71 OR #72 OR #73 OR #74 (681).
Website searches
The following online sources were searched for relevant documents:
-
Agency for Healthcare Research and Quality. Health Information Technology. URL: https://healthit.ahrq.gov/ (accessed 5 July 2018).
-
Deloitte. URL: https://www2.deloitte.com/uk/en/pages/life-sciences-and-healthcare/solutions/deloitte-uk-centre-for-health-solutions.html (accessed 5 July 2018).
-
European Commission. Digital Single Market. URL: https://ec.europa.eu/digital-single-market/ (accessed 5 July 2018).
-
European Commission. EU Reports and Studies on eHealth. URL: https://ec.europa.eu/digital-single-market/en/reports-and-studies/75992/3553 (accessed 5 July 2018).
-
HIMSS Europe. HIMSS Analytics Annual European eHealth Survey. URL: www.himss.eu/himss-analytics-annual-european-ehealth-survey (accessed 5 July 2018).
-
Good eHealth. URL: http://good-ehealth.org/ (accessed 5 July 2018).
-
The Health Foundation. URL: www.health.org.uk/ (accessed 5 July 2018).
-
Health Innovation Network. URL: https://healthinnovationnetwork.com/ (accessed 5 July 2018).
-
HealthIT.gov. URL: www.healthit.gov/ (accessed 5 July 2018).
-
HIMMS Europe. URL: www.himss.eu/ (accessed 5 July 2018).
-
mHealth Evidence. URL: www.mhealthevidence.org/ (accessed 5 July 2018).
-
Nesta. Digital Health. URL: www.nesta.org.uk/project/digital-health/ (accessed 5 July 2018).
-
NHS Digital. URL: https://digital.nhs.uk/ (accessed 5 July 2018).
-
NHS England. General Practice Forward View. URL: www.england.nhs.uk/gp/gpfv/ (accessed 5 July 2018).
-
NIHR Journals Library. URL: www.journalslibrary.nihr.ac.uk/ (accessed 5 July 2018).
-
NIHR ongoing research (Ellie Fairbank, 13 June 2018, NIHR HSDR Research Manager-Monitoring, personal communication).
-
NIHR School of Primary Health Research. URL: www.spcr.nihr.ac.uk/ (accessed 5 July 2018).
-
Nuffield Department of Primary Care Health Sciences. Digital Health and Innovation. URL: www.phc.ox.ac.uk/research/research-themes/digital-health-and-innovation (accessed 5 July 2018).
-
Rand Corporation. Benchmarking deployment of eHealth among GPs. URL: www.rand.org/randeurope/research/projects/benchmarking-ehealth-among-general-practitioners.html (accessed 5 July 2018).
-
Royal Australian College of General Practitioners. URL: www.racgp.org.au/your-practice/ehealth/additional-resources/racgp-technology-survey/ and https://www.racgp.org.au/your-practice/ehealth/ (accessed 5 July 2018).
-
The King’s Fund. URL: www.kingsfund.org.uk/ (accessed 5 July 2018).
-
The Nuffield Trust. URL: www.nuffieldtrust.org.uk/ (accessed 5 July 2018).
-
University College London. Institute of Digital Health. URL: www.ucl.ac.uk/digital-health (accessed 5 July 2018).
-
NIH U.S. National Library of Medicine. National Information Center on Health Services Research and Health Care Technology. URL: www.nlm.nih.gov/hsrinfo/informatics.html (accessed 5 July 2018).
-
World Health Organization. eHealth. URL: www.who.int/ehealth/en / (accessed 5 July 2018).
Appendix 2 Ongoing studies
| Ongoing study | Web link |
|---|---|
| Atherton H, Eccles A, Car M, Goyder C, Heneghan C, Majeed A, et al. Email for Clinical Communication Between Patients/Caregivers and Healthcare Professionals. PROSPERO: CRD42017075291 | An update of a 2012 Cochrane review21 (included in synthesis). URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017075291 (accessed 12 December 2018) |
| Mold F, Lai Y-L, Hendy J, Lusignan Sd. A Systematic Review to Investigate the Usefulness of Remote Consultation Systems for Patients and Professionals in Primary Care: Existing Challenges and Future Health Care in the UK. PROSPERO: CRD42015019152 | Awaiting publication. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015019152 (accessed December 2018) |
| Thiyagarajan A, Atherton H, Griffiths F, Fleming J. To Explore Patient and Clinician Experience with Video Consultation: A Systematic Review. PROSPERO: CRD42018100032 | URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018100032 (accessed December 2018) |
| Warwick Medical School. Content Analysis of E Mail Consultations Between General Practitioners and Patients | URL: https://warwick.ac.uk/fac/sci/med/research/hscience/apc/digitalhealth/contact (accessed December 2018) |
| Publication details | Comment |
|---|---|
| Castle-Clarke S, Kumpunen S, Machaqueiro S, Curry N, Imison C. Digital Requirements for New Primary Care Models: A Briefing for Clinicians and Managers. London: Nuffield Trust; 2016. URL: www.nuffieldtrust.org.uk/files/2017-01/digital-technology-primary-care-web-final.pdf | A briefing report was available, but did not meet our inclusion criteria. On consulting with the author, the literature review associated with this briefing was not published and, therefore, not included in the synthesis |
Appendix 3 Tables of study characteristics
Parts of Appendix 3 have been reproduced with permission from the following studies:
-
Atherton et al. 9 (this contains information licensed under the Non-Commercial Government Licence v2.0).
-
Castle-Clarke and Iminson8 (The Digital Patient: Transforming Primary Care? London: Nuffield Trust; 2016).
-
Carter et al. 25 [© Carter M, Fletcher E, Sansom A, Warren F, Campbell J. 2018. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/].
-
Huxley et al. 23 [© Huxley CJ, Atherton H, Watkins JA, Griffiths F. 2015. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/licenses/by-nc/3.0/].
-
Atherton and Ziebland31 [© Atherton H and Ziebland S. 2016. Reproduced from Atherton and Ziebland. 31 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 3.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/3.0/].
-
Atherton et al. 10 [© Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A. 2018. Reproduced from Atherton et al. 10 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/].
-
Donaghy et al. 29 [© Donaghy E, Atherton H, Hammersley V, McNeilly H, Bikker A, Robbins L, et al. 2019. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/].
-
Brant et al. 11 Republished with permission of Royal College of General Practitioners from Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice, Brant et al. , 66, 648, 2016; permission conveyed through Copyright Clearance Center, Inc.
-
Uscher-Pines and Mehrotra. 27 Republished with permission of Project Hope/Health Affairs Journal from Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider, Uscher-Pines and Mehrotra et al. , 33, 2, 2018; permission conveyed through Copyright Clearance Center, Inc.
| General | Methods | Intervention | Population | Reported outcomes |
|---|---|---|---|---|
|
First author (year of publication): Antoun (2016) 20 Country: Lebanon Aims of the review: to present an overview of the current literature about e-mail communication between physicians and patients; current challenges and propose opportunities for future research Funding: none |
Search range of dates: NR Language limitations: NR Number of included primary studies: NR Date range of included studies: NR Country of included studies: NR Primary study designs: NR Inclusion/exclusion criteria: NR |
Type/focus: e-mail Interface: asynchronous Communication with health professional(s): physicians |
Target patient population: all patients Patient characteristics: age, NR; sex, NR; SES, NR; health condition(s), NR |
Patient access/equity Service performance and efficiency Implementation (barriers and opportunities) |
|
First author (year of publication): Atherton (2018) 9 Country: UK Aims of the review: to identify and synthesise articles that explore, or test, the effects of alternatives to face-to-face consultations with regard to patient and staff experiences, or describe theories or ideas about the potential effects Overall project aim: to review existing evidence about alternatives to face-to-face consultation; conduct a scoping exercise to identify ways in which general practices currently provide these alternatives; recruit eight general practices as case studies for focused ethnographic research, exploring how practice context, patient characteristics, type of technology and the purpose of the consultation interact to determine the impact of these alternatives; and synthesise the findings in order to develop a website resource about the implementation of alternatives to face-to-face consultations and a framework for subsequent evaluation Funding: NIHR HSDR programme; Atherton received funding from the NIHR School for Primary Care Research during the conduct of the study |
Search range of dates: from inception to 2015, then applied a filter to identify those from 2012 onwards Language limitations: NR Number of included primary studies: n = 149. Thirty-six articles explicitly stated to be in primary care, although some were in multiple health settings. Fifty-six of 149 were used in identifying themes and devising the conceptual map Date range of included studies: unclear Country of included studies: NR Primary study designs: any study or article design, including opinion pieces. (Note: this has implications for findings as some references cited may not relate to research studies) Inclusion/exclusion criteria: mainly focused on studies from 2012, but included pre-2012 when relevant Setting of interest was primary care, but material from related settings (e.g. e-mail consultation between patients and specialists) was included when it provided lessons directly relevant to primary care Eligible technologies: telephone consultations (but not those used to triage all requests for consultations before offering any face-to-face appointments), e-mail, e-consultations and internet video (e.g. Skype) technologies, SMS, telehealth and any other ‘care at a distance’ app |
Type/focus: telephone consultations (but not triage), e-mail, e-consultations and internet video, SMS, telehealth and any other ‘care at a distance’ app Interface: synchronous and asynchronous Communication with health professional(s): reception staff, nurses, GPs, practice managers. Also included other groups (secondary care clinicians, policy-makers, professional bodies) and also acknowledging roles that apply outside a UK setting (e.g. service manager and primary care physician) |
Target patient population: patients (particularly disadvantaged groups) and carers Patient characteristics: age, NR; sex, NR; SES, NR; health condition(s), NR |
Organisational disruptions and dynamics Professional disruptions and dynamics Spatial disruptions and dynamics |
|
First author (year of publication): Atherton (2012) 21 Country: UK Aims of the review: to assess the effects of health-care professionals and patients using e-mail to communicate with each other, on patient outcomes, health service performance, service efficiency and acceptability Funding: N/A (Cochrane Collaboration) |
Search range of dates: inception to January/February 2010 Language limitations: no language restrictions Number of included primary studies: nine included in total, but only three were primary care based. Two studies (Katz 200332 and Katz 200433) based in primary care clinics affiliated with a US university. One study (Kummervold 200434) was based in a general practice Date range of included studies: 1995–2009 Country of included studies: USA (n = 5); Norway (n = 2); Canada (n = 1); Australia (n = 1). Of the three studies based in primary care, two were in the USA and one in Norway Primary study designs: all of the included studies were RCTs Inclusion/exclusion criteria: RCTs; quasi-RCTs; controlled before and after with at least two intervention and two control sites; interrupted time series with at least three time points before and after intervention All health-care professionals, patients and caregivers regardless of age, sex and ethnicity. Studies in all settings, that is primary care settings (services of primary health care), outpatient settings (outpatient clinics), community settings (public health settings) and hospital settings Included studies in which e-mail was used for two-way clinical communication between patients/caregivers and health-care professionals. Could be encrypted or unencrypted or based on web messaging Considered comparisons between outcomes of e-mail communication and no intervention, as well as other modes of communication, such as face to face, postal letters, telephone calls to a landline or mobile telephone, text messaging using a mobile telephone and automated vs. personal e-mails |
Type/focus: e-mail Eight studies compared e-mail with standard methods of communication. One study compared e-mail with telephone for the delivery of counselling Interface: asynchronous Communication with health professional(s): all health-care professionals |
Target patient population: all patient groups Patient characteristics: Age: all participants in the three primary care studies were adults. Five out of the other six studies also involved adults only. Participants in one study were parents/caregivers of children attending a paediatric dermatology clinic Sex: NR, assumed to be mixed SES:NR Health condition(s): in Kummervold 2004,34 participants were patients at the general practice – no specific health conditions stated In non-primary care studies: physical disabilities (n = 1); obesity (n = 1); patients referred for thyroid or parathyroid surgery (n = 1) Staff characteristics: in two primary care studies, adult participants were physicians, staff and resident physicians (Katz 200433), and faculty and resident physicians in primary care (Katz 200332) |
Primary outcomes: whether or not the e-mail was understood and acted on correctly by the recipient as intended by the sender, specifically in relation to:
|
|
First author (year of publication): Castle-Clarke (2016) 8 Country: UK Aims of the review: to ‘pull together’ the evidence that exists about digital services offered by the NHS Note, this review covered seven technologies. In this data extraction we focus on only two: online triage and remote consultations. Other findings are reported for monitoring and wearable technology; online sources of health information; targeted interventions and peer support; online appointment booking and repeat prescription ordering; online access to records; and ‘apps’ to help patients manage their conditions or stay well Funding: partly based on research commissioned by NHS England |
Search range of dates: NR Language limitations: NR Number of included primary studies: NR Date range of included studies: NR Country of included studies: NR Primary study designs: NR Inclusion/exclusion criteria: NR Minimal information about methods was reported: the authors report conducting a literature review, interviewing 21 experts (including representatives from technology companies, policy, academia, patient organisations and health-care providers) and held a workshop to test and refine four future scenarios. They also undertook four case studies comprising desk research and one or more interviews with key people at the featured organisations Note, authors report that the focus is largely on primary care, but evidence from secondary care has also been reported in the report |
Type/focus: online triage; remote consultations Interface: synchronous/asynchronous Communication with health professional(s): primarily primary care centres, though some other results refer to secondary care Case study: Moss Side Health Centre, Manchester, introduced Skype consultations to its patients in January 2013. It is a single practice in inner-city Manchester and employs six GPs, one nurse, two practice pharmacists, a practice manager and an administrative team. Authors report the use of Skype at the practice has been driven by one dedicated individual and relied on an investment of personal time |
Target patient population: NR Patient characteristics: age, NR; sex, NR; SES, NR; health condition(s): NR |
Online triage tools: managing demand on professional time; interview data from staff; patient experience; health outcomes Remote consultations (case study site): impact Managing demand on professional time (literature review evidence): patient experience; health outcomes |
|
First author (year of publication): Chambers (2019) 24 Country: UK Aims of the review: to conduct an independent review of digital and online symptom checkers and health advice/triage services for urgent health to inform strategic decision-making and service design Funding: HSDR programme (HSDR16/47/17) |
Search range of dates: not stated (but search not restricted by date) Language limitations: none Number of included primary studies: 29 publications from 27 studies. Four were from the grey literature Date range of included studies: 2006–18 Country of included studies: NR for all studies; nine studies were conducted in the UK Primary study designs: simulation (n = 5); experimental (n = 4); qualitative (n = 2); uncontrolled observational (n = 10); controlled observational (n = 3); other (survey) (n = 3): (numbers collated from tables 1–3) Inclusion/exclusion criteria: general population seeking information online or digitally to address an urgent health problem, including adults and children and issues arising from both acute and long-term chronic illness. Non-urgent problems, such as possible Asperger’s syndrome or memory loss/early dementia, were excluded Intervention: any online or digital service designed to assess symptoms, provide health advice and direct patients to appropriate services. This reflects the role of the NHS 111 telephone service Services that provide only health advice were excluded, as were those that offer treatment (e.g. online CBT services) Comparator: the ‘gold standard’ comparator is current practice of telephone assessment (e.g. NHS 111) or face-to-face assessment (e.g. general practice, urgent care centre or emergency department). However, studies with other relevant comparators (e.g. comparative performance in tests or simulations) or with no comparator were included if they addressed the research questions Outcomes: see Reported outcomes Study design: inclusion was not restricted by study design but included studies had to evaluate (quantitatively or qualitatively) some aspect of an online/digital service Studies from any high-income country health-care system were eligible for inclusion Excluded: studies that merely describe services without providing any quantitative or qualitative outcome data; conceptual papers and projections of possible future developments; studies conducted in low- or middle-income country health systems |
Type/focus: digital and online symptom checkers and health advice/triage services for urgent care Interface: synchronous/asynchronous Communication with health professional(s): unclear if all included studies involved automated schemes |
Target patient population: NR Patient characteristics: Age: adults (including parents or adult caregivers) Sex: NR, assumed to be mixed SES: NR Health condition(s): 17 studies were focused on the general population and 10 studies focused on a specific condition |
Safety; clinical effectiveness; diagnostic and triage accuracy; accuracy of signposting; compliance with advice; use of, and contacts with, health services; costs/cost-effectiveness; equity and inclusion; patient/carer satisfaction |
|
First author (year of publication): Hickson (2015) 22 Country: USA Aims of the review: the purpose of this review is to systematically analyse the current literature on the state of e-visit utilisation, with focus specifically on non-urgent primary care practice settings Funding: NR |
Search range of dates: NR Language limitations: NR Number of included primary studies: n = 24 Date range of included studies: 1998–2014 Country of included studies: NR Primary study designs: NR Inclusion/exclusion criteria: explicit inclusion criteria not reported Papers were excluded if the focus was on care for chronic conditions; care delivery via video, teleconferencing or telephone; or papers were editorial/opinion pieces |
Type/focus: e-visit (e-mail) Interface: asynchronous Communication with health professional(s): physicians |
Target patient population: primary care Patient characteristics: age, NR; sex, NR; SES, NR; health condition(s): NR |
Patient access/equity Efficiency and continuity of care Quality of care Health services use Patient satisfaction Implementation barriers (structural and human capital) |
|
First author (year of publication): Huxley (2015) 23 Country: UK Aims of the review: assess the potential impact of the availability of digital clinician–patient communication on marginalised groups’ access to general practice in the UK Funding: Arden Cluster Research Capability Fund. H. Atherton is funded by a NIHR School for Primary Care Research fellowship |
Search range of dates: 1 January 2013 to 7 February 2014 Language limitations: English language only Number of included primary studies: Review 1: what are the barriers to accessing general practice for marginalised groups? Forty-three studies identified from database searches (carers n = 6; people with mental health problems n = 20; refugees, homeless people, Gypsies and Travellers n = 17) Review 2: what impact would the use of digital communication between clinician and patient have on the ability of marginalised groups to access general practice? Seventeen studies identified from database searches An additional 10 studies were identified from purposive searching Date range of included studies: NR Country of included studies: reported as being from ‘high-income countries’ for both reviews Primary study designs: Review 1: reported to be predominantly qualitative and cross-sectional Review 2: reported to be theory, experimental, qualitative and systematic reviews Inclusion/exclusion criteria: derived from scoping process, studies of technologies that included video, e-mail, internet forums and SMS. Participants from marginalised groups including those with mental illness, refugees, asylum-seekers, homeless people, Travellers, and carers |
Type/focus: studies of technologies that included, video, e-mail, internet forums and SMS Interface: synchronous/asynchronous Communication with health professional(s): general practice clinicians |
Target patient population: participants from marginalised groups, including those with mental illness, refugees, asylum-seekers, homeless people, Travellers and carers Patient characteristics: reported only by group – those with mental illness, refugees, asylum-seekers, homeless people, Travellers and carers. Age, NR; sex, NR; SES, NR; health condition(s): NR |
Patient access/equity Barriers to access: Patient-related barriers: |
| General | Methods | Intervention | Population | Reported outcomes |
|---|---|---|---|---|
|
First author (year of publication): Atherton (2018) 9 , 10 Country/region: England and Scotland Study aim: to understand how, under what conditions, for which patients and in what ways, alternatives to face-to-face consultations present benefits and challenges to patients and practitioners in general practice Funding: NIHR HSDR programme; Atherton received funding from the NIHR School for Primary Care Research during the conduct of the study |
Study design (as described by authors): part of a larger review using realist methodology Focused ethnographic case studies in eight UK general practices between June 2015 and March 2016, using realist approach Participants: patients were selected using purposive sampling, ensuring that patients had different characteristics in relation to age, sex, ethnicity, disability, frequency of attendance and whether or not they had long-term health conditions. Specifically included were people in ‘hard-to-reach’ groups with regard to accessing general practice (e.g. young males, the vulnerably housed and minority ethnic groups). All patients invited to participate in interviews had experience of using an alternative to the face-to-face consultation within the practice It was not compulsory to disclose any long-term condition or disability Sample size: staff members n = 45; patient and carers n = 39 Data collection method: non-participant observation, informal conversations with staff, and semistructured interviews with staff and patients were conducted. Practice documents and protocols were reviewed Data analysis: data were analysed through charting and the ‘one sheet of paper’ mind-map method to identify the line of argument in each thematic report Response rate (surveys): N/A |
Type/focus description: the participating practices used a varied range of alternatives to the face-to face consultation, including telephone, e-consult, video and e-mail in varying degrees of frequency Interface: synchronous/asynchronous Communication with health professional(s): six practices in England and two practices in Scotland (derived from approaches to practices included in the scoping survey) Practices included some from the most and least deprived areas in terms of deprivation deciles Implementation: NR Comparators (if reported): N/A |
Target population of intervention:NR Patient characteristics: age, NR; sex, NR; SES, NR; health condition(s): NR |
Service delivery: rationale of general practice plans to introduce alternatives to face-to face communications Outcomes important to participants (staff and patients) |
|
First author (year of publication): Atherton (2018) 9 and Brant (2016) 11 Country, region: UK (Areas of Bristol, Oxford, Lothian and Highlands & Western Islands of Scotland) Study aim: to identify the frequency and range of ways in which general practices are providing (or planning) alternatives to face-to-face consultations Funding: NIHR HSDR programme; Atherton received funding from the NIHR School for Primary Care Research during the conduct of the study |
Study design (as described by authors): part of a larger review using realist methodology (see other data extraction forms) A scoping survey Participants: GPs and practice managers Sample size: practices n = 421; individuals n = 2719 Data collection method: a postal survey was sent to all practice managers, GP partners and salaried GPs in all practices around Bristol, Oxford, and Lothian and Highlands & the Western Islands of Scotland Questions used a 5-point Likert Scale and a free-text box Various other methods were used to identify any practices using alternatives to face-to-face consultations. This including accessing each of the practice websites in the three study areas. Websites were identified for 368 practices Data analysis: Primary analysis was at practice level, with analysis of GPs’ personal use of alternative forms of consultation at an individual level. Numerical data were analysed using simple statistical methods. When different responses were given by responders within the same practice the authors used the mean result at practice level. The extent of variation in response by different individuals within the same practice was explored using the within-practice standard deviation (SD) and the intraclass correlation coefficient (ICC). Responses regarding GPs’ own use of alternatives to face-to-face consultation were analysed at individual responder level, and responses from practice managers were excluded from these analyses The results from the free-text box were analysed thematically Response by practice: overall 319/421 (76%); England 163/186 (88%); Scotland 156/235 (66%) Response by individual: overall 889/2719 (33%); England 40%; Scotland 25% Free-text responses on survey: 249/889 (28%) Number of responses per practice ranged from 1 to 11 |
Type/focus description: Email, video, telephone and text (telephone triage was excluded) Interface: Synchronous/Asynchronous Communication with health professional(s): GPs and Practice Managers Implementation: NR Comparators (if reported): N/A |
Target population of intervention: NR Patient characteristics: age, NR; sex, NR; SES, NR; health condition(s): NR |
Service delivery: GP Practice plans to introduce alternatives to Face-to-Face communications (e-mail, video, telephone, text (sms messages) Current provision of alternatives to face-to-face consultations at an individual general practitioner level Concerns for GPs, practices and patients 249/889 of the responses included some form of free text Concerns of GPs, for practices and patients Perceived benefits of the introduction of alternatives to face to face consultations Benefits for GPs, practices and patients Exploration of practice websites |
|
First author (year of publication): Atherton (2018) 9 Country, region: UK (England and Scotland) Study aim: to examine the feasibility of using routinely collected data to assess the number of consultations of different types in UK general practice Funding: NIHR HSDR programme; Atherton received funding from the NIHR School for Primary Care Research during the conduct of the study |
Study design (as described by authors): part of a larger review using realist methodology Routine data collection Participants: all patients within participating case study practices. Further data are provided in tables throughout the report Sample size: unclear Data collection method: researchers assessed practice policies in the practice and, when possible, audited reliability of the data. Patient data were also extracted from the EMIS. Searches on data were carried out from 11 November 2015 and 7 March 2016 at different practices. Data collected included patient details, details of appointments and consultations. Analysis was restricted to the 6-month period from 11 May 2015 to 11 November 2016 Data analysis: Data were coded as:Professional types were coded as:Various statistical analyses were conducted to compare consultation rates Response rate (surveys): N/A |
Type/focus description: telephone, e-consult, e-mail, face to face in surgery or at home Interface: synchronous/asynchronous Communication with health professional(s): eight GP primary care practices (six in England; two in Scotland) Implementation: N/A Comparators (if reported): N/A |
Target population of intervention: further details are provided in the report Patient characteristics: age, NR; sex, NR; SES, NR; health condition(s): NR |
Proportion of consultations conducted by various methods Number of consultations and number of patients reconsulting within 14 days |
|
First author (year of publication): Carter 2018 25 Country, region: UK, Devon Study aim: to evaluate the feasibility, acceptability and effectiveness of webGP as piloted by six general practices Funding: NHS NEW CCG |
Study design (as described by authors): mixed Participants: six practices participating in the NEW CCG webGP pilot were approached by e-mail Sample size: data collection method: data from practice databases, GP completion of case reports, patient questionnaires and staff interviews Collected approximately 6 months after implementing webGP (February–July 2016) Six practices provided retrospective data on consultations (before and after implementation); 20 GPs completed case reports (regarding 61 e-consults); 81 patients completed questionnaires; five GPs and five administrators were interviewed Data analysis: statistical analysis was conducted on quantitative data, whereas qualitative data were analysed thematically Response rate (surveys): N/A |
Type/focus description: webGP Interface: asynchronous GP e-consultation and self-help web service accessed by adult patients (aged ≥ 18 years) via their practice’s web (webGP) Provides five services which are available from participating general practices’ websites:webGP had been in use at five of the practices for at least 3 months and for the remaining practice for just over a month. All practices had promoted webGP via a large poster and/or television screen in the waiting room and the practice website. One practice had also added information about webGP to the bottom of prescriptions and to the telephone answerphone message Communication with health professional(s): general practices in NEW CCG’s area Implementation: NR Comparators (if reported): NR |
Target population of intervention: area deprivation score for practices ranged from 14.9 to 34.5 (higher numbers indicate greater deprivation); deprivation deciles ranged from 2 to 8 (lower number indicates greater deprivation) Patient characteristics: case report forms were completed Age: adults (aged ≥ 18 years) Sex: mixed SES: see Target population of intervention above Health condition(s): NR |
Number of consultations (face to face and telephone) and differences between groups Case report forms completed by GPs for patients using e-consult system Timings of an e-consult request and the delay between its receipt and the GP’s response Patient satisfaction: five GPs, five administrators/receptionists; three in person, seven by telephone, with a mean interview length of 14 minutes (SD 6 minutes, range 5–27 minutes). Patients provided comments in free-text boxes as part of their questionnaire survey Feasibility of webGP Acceptability of webGP Effectiveness of webGP |
|
First author (year of publication): Donaghy (2019) 29 Country, region: Scotland, Lothian Study aim: to assess the feasibility, acceptability and utility to patients and clinicians of video consultation, and the potential differences between such consultations and TCs and FTFC by comparing the duration and content of VCs and their impact on subsequent use of services Funding: Scottish government, Chief Scientist Office |
Study design (as described by authors): mixed methods Participants: clinicians and practice patients Sample size: 13 clinicians and 162 patients in six practices (10 GPs and three practice nurses) Data collection method: audio-recordings of consultations; semistructured interviews (VC patients and clinicians) questionnaires (both patients and clinicians) Data analysis: content analysis of audio-recordings Interviews were analysed thematically Descriptive analysis of questionnaire data. Some opened ended responses, listed in report appendix Response rate: 12 practices expressed interest and 6 participated (13 clinicians) 203 patients were recruited, 162 gave consent. 149 recordings obtained from consultations with 162 patients Questionnaire data obtained from 118 out of the 149 patients with a recorded consultation (79%) Twenty-one out of 45 VC patients were interviewed (52% male, age range 22–76 years). Semistructured interviews were completed with all participating clinicians, either individually or in small groups |
Type/focus description: VC/Attend Anywhere (URL: www.attendanywhere.com) Interface: synchronous communication Communication with health professional(s): GPs or practice nurses Implementation: clinicians asked eligible patients if they had the necessary equipment to conduct a VC. If so, they offered a choice of VC, FTFC or TC for follow-up and requested permission to record this consultation. VC occurred via the Attend Anywhere website In total, 45 VC, 53 TC and 51 FTFC consultations were conducted Comparators (if reported): TCs and FTFCs |
Target population of intervention: patients requiring a follow-up consultation who had access to an internet-connected computer with a camera and sound capability, tablet or 4G and/or Wi-Fi-enabled smartphone (running Google Chrome; Google Inc., Mountain View, CA, USA) and a working e-mail address Patient characteristics: Age: > 16 years (mean age = 49.71 years) Sex: both (sex assessed as factor influencing use) SES: mixed (deprivation assessed as factor influencing use) Health condition(s): mixed |
Patient experience/satisfaction Patient access/equity Consultation content Clinician experience/implementation Implementation Type of patient/problem Service use |
|
First author (year of publication): Mehrotra (2013) 28 Country, region: USA, Pittsburgh, PA Study aim: to examine who seeks care via an e-visit instead of an in-person office visit Funding: National Institutes of Health, Career Development Award and internal University of Pittsburgh Medical Center funding |
Study design (as described by authors): quantitative Participants: adult patients with a Pennsylvanian post code registered at study practices Sample size: N/A Data collection method: secondary analysis of data from medical records Data analysis: the characteristics of patients who had an e-visit or office visit for two conditions were compared using bivariate analyses (chi-squared test). A multivariate model was then devised to predict e-visit use Response rate (surveys): NA |
Type/focus description: e-visits Interface: asynchronous Communication with health professional(s): physicians at four primary care practices Implementation: all office visits and e-visits for sinusitis and urinary tract infections provided at study practices between January 2010 and May 2011 were identified from medical records (index visit). For each patient with an index visit, data on all encounters in the electronic medical record were identified (2009–11). Goal was to identify first visits for the condition. Demographic data were then extracted from medical records Comparators (if reported): e-visits vs. office visits |
Target population of intervention: N/A Patient characteristics: Age: adults Sex: both SES: employment status and income examined Health condition(s): sinusitis and urinary tract infection |
Patient access/equity: use by different patient groups/conditions (bivariate and multivariate analysis) |
|
First author (year of publication): Uscher-Pines (2016) 26 Country, region: USA, California Study aim: to compare the quality of care at Teladoc (www.teladoc.com) with that at physician offices and compare access to care for Teladoc users and nonusers Funding: California Health Care Foundation and National Institutes of Health |
Study design (as described by authors): quantitative Participants: adults enrolled in California Public Employees’ Retirement System health maintenance organisation Sample size: N/A Data collection method: secondary analysis of health plan claims data and enrolment details from April 2012 to October 2013 Data analysis: geographic information system-based analyses were used to compare Teladoc users and non-users with respect to location and proximity to alternative sites of care. On five access variables Teladoc users and non-users were compared using chi-square. Logistic regression models were used to predict Teladoc use The performance of Teladoc and physician offices was compared using chi-square on three Healthcare Effectiveness Data and Information Set measures Response rate (surveys): N/A |
Type/focus description: Teladoc Interface: synchronous communication Communication with health professional(s): primary care physicians Implementation: Teladoc-registered patients request a consult with a Teladoc physician via telephone, internet or mobile app. The patient is assigned to an available physician licensed to practice in the patient’s state of residence. If the patient is judged to need testing, follow-up care or immediate medical attention, the patient is directed to contact their primary care physician or to visit an emergency department Study: California Public Employees’ Retirement System patients were divided into Teladoc users (n = 3043) and non-users (n = 230,872). Non-users included those with no health-care use during the study period. Teladoc users had at least one visit to Teladoc from April 2012 through to October 2013 Comparators (if reported): physician office consultations |
Target population of intervention: N/A Patient characteristics: Age: 18–64 years Sex: mixed SES: NR Health condition(s): lower back pain; pharyngitis; acute bronchitis |
Patient access/equity Access for underserved populations Performance on Healthcare Effectiveness Data and Information Set measures |
|
First author (year of publication): Uscher-Pines (2014) 27 Country, region: USA, California Study aim: to explore the reasons patients sought Teladoc consults and compare the sociodemographic characteristics and care patterns of enrolees who used Teladoc with those of enrolees who used emergency departments and physicians’ offices for similar conditions Funding: California Health Care Foundation |
Study design (as described by authors): quantitative Participants: individuals enrolled in California Public Employees’ Retirement System health maintenance organisation Sample size: N/A Data collection method: secondary analysis of health plan claims data and enrolment details from April 2012 to February 2013 Utilised the medical claims of 2718 Teladoc users, as well as the medical claims of a random sample of 72,191 non-users of Teladoc from the 306,027 eligible enrolees with Teladoc coverage Data analysis: patterns of Teladoc use among children and adults were examined Average monthly Teladoc visits were compared with average monthly emergency department and office visits among adults (not children), who sought care for the three leading conditions during the study period [acute respiratory illnesses; urinary tract infections (and urinary symptoms); skin problems] Baseline demographic, socioeconomic, comorbidity and utilisation variables were compared for adults who visited Teladoc, the emergency department or physicians’ offices, using chi-square and t-tests Multivariable logistic regression was used to test for an independent relationship between the type of index visit (Teladoc vs. office visit) and follow-up visit to any location within 21 days for a diagnosis in the same diagnostic category, adjusting for age, sex and Charlson comorbidity score Response rate (surveys): N/A |
Type/focus description: Teladoc Interface: synchronous communication Communication with health professional(s): primary care physicians Implementation: Teladoc-registered patients request a consult with a Teladoc physician via telephone or internet. The patient is assigned to an available physician licensed to practice in the patient’s state of residence Comparators (if reported): physician office and emergency department consultations |
Target population of intervention: N/A Patient characteristics: Age: comparisons made for adults only Sex: mixed SES: NR Health condition(s): comparisons made for acute respiratory illnesses, urinary tract infections (and urinary symptoms) and skin problems |
Teladoc use Characteristics of Teladoc users |
Appendix 4 Critical appraisal of included evidence
| Critical appraisal criterion | Atherton (2012)21 | Antoun (2016)20 | Chambers (2019)24 | Hickson (2015)22 | Castle-Clarke (2016)8 |
|---|---|---|---|---|---|
| 1. Was the search adequate? | Yes | Yes | Yes | Yes | NR |
| 2. Were inclusion/exclusion criteria reported? | Yes | No | Yes | No | No |
| 3. Were the data synthesised? | Yes | No | Yes | Yes | No |
| 4. Was the review quality assessed? | Yes | No | Yes | No | No |
| 5. Were adequate study details reported? | Yes | No | Yes | No | No |
| Comments | Cochrane review. In addition, more than one author was involved in each stage of review process, reducing the potential for error and bias | Literature review. One database (MEDLINE and reference checking. OVID not a database but a gateway) | More than one author involved in each stage of review process, reducing the potential for error and bias | USA | UK report including a literature review and case studies |
| Critical appraisal criterion | Huxley (2015)23 | Atherton (2018)9 |
|---|---|---|
| The research topic is appropriate for a realist approach | Adequate | Adequate |
| The research question is constructed in such a way as to be suitable for a realist synthesis | Adequate | Adequate |
| The review demonstrates understanding and application of realist philosophy and realist logic which underpins a realist analysis | Good | Good |
| The review question is sufficiently and appropriately focused | Adequate | Adequate |
| An initial realist programme theory is identified and developed | Adequate | Adequate |
| The search process is such that it would identify data to enable the review team to develop, refine and test programme theory or theories | Adequate | Good |
| The selection and appraisal process ensures that sources relevant to the review containing material of sufficient rigour to be included are identified. In particular, the sources identified allow the reviewers to make sense of the topic area; to develop, refine and test theories; and to support inferences about mechanisms | Inadequate | Adequate |
| The data extraction process captures the necessary data to enable a realist review | Unclear | Adequate |
| The realist synthesis is reported using the items listed in the RAMESES reporting standards for realist syntheses | The authors do not report using RAMESES reporting standards | The authors do not report using RAMESES reporting standards |
| Critical appraisal criterion | Atherton (2018)9,10 | Carter (2018)25 | Donaghy (2019)29 |
|---|---|---|---|
| Was there a clear statement of the aims of the research? | Yes | Yes | Yes |
| Is a qualitative methodology appropriate? | Yes | Yes | Yes |
| Was the research design appropriate to address the aims of the research? | Yes | Yes | Yes |
| Was the recruitment strategy appropriate to the aims of the research? | Yes | Yes | Yes |
| Was the data collected in a way that addressed the research issue? | Yes | Yes | Yes |
| Has the relationship between researcher and participants been adequately considered? | Cannot tell | Cannot tell | Cannot tell |
| Have ethical issues been taken into consideration? | Yes | Yes | Cannot tell |
| Was the data analysis sufficiently rigorous? | Yes | Yes | Yes |
| Is there a clear statement of findings? | Yes | Yes | Yes |
| How valuable is the research? | a | b | c |
Appendix 5 Summary of findings
Parts of Appendix 5 have been reproduced with permission from the following studies:
-
Atherton et al. 9 (this contains information licensed under the Non-Commercial Government Licence v2.0).
-
Castle-Clarke and Iminson8 (The Digital Patient: Transforming Primary Care? London: Nuffield Trust; 2016).
-
Carter et al. 25 [© Carter M, Fletcher E, Sansom A, Warren F, Campbell J. 2018. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/].
-
Huxley et al. 23 [© Huxley CJ, Atherton H, Watkins JA, Griffiths F. 2015. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/licenses/by-nc/3.0/].
-
Atherton and Ziebland31 [© Atherton H and Ziebland S. 2016. Reproduced from Atherton and Ziebland. 31 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 3.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/3.0/].
-
Atherton et al. 10 [© Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A. 2018. Reproduced from Atherton et al. 10 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/].
-
Donaghy et al. 29 [© Donaghy E, Atherton H, Hammersley V, McNeilly H, Bikker A, Robbins L, et al. 2019. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/].
-
Brant et al. 11 Republished with permission of Royal College of General Practitioners from Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice, Brant et al. , 66, 648, 2016; permission conveyed through Copyright Clearance Center, Inc.
-
Uscher-Pines and Mehrotra. 27 Republished with permission of Project Hope/Health Affairs Journal from Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider, Uscher-Pines and Mehrotra et al. , 33, 2, 2018; permission conveyed through Copyright Clearance Center, Inc.
| First author (year of publication) | Relevant outcomes as reported | Summary of findings |
|---|---|---|
| Antoun (2016)20 | Patient access/equity | Most patients who have used e-mail with their physicians are younger, are healthier (one study) and have higher education and income (one study). Ethnic minority patients are less likely to use physician–patient e-mail communication. Black women, older patients and patients with Medicaid are also less likely to have e-mail than their counterparts (one study). One study highlighted potential inequity of access for those without internet access, such as poor people and elderly people. In three studies (two US based; one UK based), a majority of patients expressed a willingness to communicate with health-care providers via e-mail communication. One further US study found that almost half of respondents aged > 65 years were willing to participate in e-mail communication with a physician |
| Service performance and efficiency | Lack of robust evidence on physician–patient communication, including patient outcomes, health services outcomes (e.g. services use) and health-care professional outcomes (professional knowledge, behaviours and performance). In addition, there was very limited evidence on safety, quality of care, privacy issues and appropriateness of e-mail communication. Findings from three studies of early adopters found that e-mail communication did not increase physicians’ workload. However, this related mainly to opportunistic communication rather than the effect on workload of more frequent systematic adaption of e-mail communication | |
| Implementation (barriers and opportunities) |
Potential for increase in workload identified by physicians as a barrier to use (three studies). Apprehension about information overload, and patients’ demands Lack of reimbursement is one of the issues that may discourage physicians from using e-mail communication with patients (three studies). Some models for reimbursing e-mail consultations have been developed. In Denmark, e-mail communication with patients is reimbursed by the national health coverage Security, confidentiality and privacy issues identified as important concerns for physicians that act as barriers in three studies. In one study, some physicians also feared receiving spam e-mails or viruses or being hacked. Others were concerned about the uncertainty of e-mail receipt by patients and the lack of integration with medical records Fear of medico-legal issues in handling sensitive and urgent matters were a concern for physicians in three studies. This includes concerns about content and the suitability of e-mail to discuss sensitive issues; and addressing new or urgent symptoms (one study). Some physicians reported fear of medical errors as a result of the absence of physical examinations, as well as potential miscommunication and litigation for medical negligence (two studies). Concern about impact on patient–physician relationship due to lack of face-to-face interaction was also reported (one study) |
|
| Atherton (2018)9 | Service delivery/organisational: uptake and awareness | Patients’ lack of awareness of the possibility of an e-mail consultation was reported to be a reason for non-use (one study). Two studies reported selectively offering alternatives to patients who the primary care professionals felt were able to use them appropriately. Review authors reported a lack of material relating to perspectives of reception staff (who have a patient-facing role) and their contribution to uptake and awareness |
| Organisation of alternatives to face-to-face consultation in a health-care setting |
One study reported concerns about what happens if a part-time member of staff fails to pick up an urgent e-mail and if alternatives to face-to-face consultation introduce inefficiencies for the practice Concerns among staff whether or not patients will treat the options responsibly, with fears that the relative ease of sending e-mails may lead to some patients overconsulting or misrepresenting their symptoms (two studies). However, limited evidence from three studies suggested that e-mail consultations have not ‘opened the floodgates’ for patient demand (one study) and the alternatives have not been widely used in which patients have been able to e-mail family doctors for some time (two studies) E-mail consultations are a standard part of primary care in Denmark and some doctors have admitted managing their patients’ expectations by deliberately delaying their responses to non-urgent e-mails (one study) There is little evidence about how best to time, conduct and record other forms of consultation (aside from face to face) (three studies). This makes changes to service delivery difficult (two studies). Three studies reported potential inefficiencies, including duplicate consultations for patients who consult remotely and then attend the practice or require a home visit One study of telephone triage in a general practice reported that despite a clinician speaking with patients during a telephone triage encounter, the subsequent face-to-face consultation was no shorter Two studies found that e-mail can allow patients to bypass the gatekeeping role of the reception staff and have direct contact with the primary care professional, or whoever replies to the e-mail. This prospect is sometimes viewed as unacceptably disruptive by clinicians (one study). Authors reported a lack of evidence relating to the roles of team members, such as reception staff, in delivering alternatives to the face-to-face consultation |
|
| Organisation of space | Two studies found that to benefit from video conferencing, practices may need to allocate a well-lit, private area for the staff to use, as well as reliable connections, so that screens do not freeze mid-consultation. This applies to the systems patients use as well (one study). Reliable contingencies need to be in place in case of technological failure as there may be clinical consequences (e.g. it can be particularly disturbing for people with mental illness) (one study) | |
| Professional disruptions and dynamics: proximity in the consultation |
A medium other than face-to-face consultations changes some aspects of the performance of the consultations, elements may be lost or may need to be expressed in different ways or at different times for the doctor–patient relationship to be maintained (two studies). There is particular uncertainty of the ‘rules of engagement’ for e-mail and video consultations (three studies). Traditional face-to-face consultations allow for diagnostic cues, such as smelling a patient’s breath, noting how a patient walks into the room, as well as using casual contact, such as shaking hands, enabling assessment of skin temperature and tone (two studies). Health-care professionals may lose some of the ability to check a patient’s understanding which can be conveyed via non-verbal communication (two studies) Authors report that there is little research indicating whether misunderstandings are increased or diminished with alternatives to the face-to-face consultation |
|
| Safety/harms | Despite one study citing patient safety as a reason to be wary of introducing alternatives to the face-to-face consultation, there is very little documentation of what these concerns are. Patient privacy and confidentiality are described as being important, but reports of privacy and confidentiality breaches are few and collection of these data are uncommon (unclear which studies this comment relates to). The Cochrane review of trials relating to e-mail for consultation found that the trials did not report any harms, but this is not the same as stating with confidence that no harms occurred. Conceptual review authors stated that much more work is required to identify potential patient safety issues and mitigating any associated risks | |
| Professional indemnity | Related to the lack of guidance or consensus on best practice, patient safety and the risk of litigation are often raised when alternatives to the face-to-face consultation are proposed (two studies). One study found there is also some evidence that clinicians’ safety concerns are leading to safety-netting, demonstrated by prescribing behaviour: for example, primary care doctors are more likely to prescribe antibiotics during an e-visit than when they consult face to face. Authors suggested that this may reflect uncertainty about the medico-legal consequences of this form of prescribing | |
| Health-care professional attitudes |
When asked about their views on using alternatives to face-to-face consultation, health-care professionals raised concerns focused on whether or not their clinical duty to provide safe and effective care may be compromised (two studies). Another study reported that much of this concern relates to the potential impact of additional consultation methods on their workload. Fears included increases in consultation volume (two studies) and increased administrative load (one study) Among health-care professionals with experience of successfully using alternatives to face-to-face consultation in their practices, one study reported that there were still feelings of uncertainty about the long-term effects on workload and, consequently, on their patients Research suggests that any new technology needs to be seen to enhance what the professional sees as their core role (one study), otherwise it is unlikely to be accepted into practice (two studies) Few studies have collected the views and experiences of practice nurses on alternatives to face-to-face consultation, but evidence from four studies suggests that nurses feel that their role requires proximity to the patient. In a study of a telehealth self-care support system for people with chronic health problems, the nurses who were providing the service positioned their work as ‘proper nursing’, whereas nurses who were using the telecare system suggested that the calls with patients were ‘just chat’ and doubted that real nursing could be delivered via the telephone. A Norwegian study of nurses working in emergency medicine found that the approach of nurses changed when they consulted remotely: they were more assertive and gave more advice |
|
| Health-care professional skills |
Two studies found that some health-care professionals were worried that their lack of confidence with technology might be exposed and that such exposure may undermine their authority. One study reported that the balance of power within the consultation may change if the primary care professional’s skills come under patient scrutiny. However, it was suggested that this would not necessarily be damaging and could result in a helpful shift in relationship dynamics over the longer term Lactation consultants in one study of breastfeeding support via video consultation were concerned about technical issues, such as the quality of images, and were not confident about undertaking clinical assessments via video. However, the patients were very satisfied with the remote consultations |
|
| Spatial disruption and dynamics | Asynchronicity allows both patients and health-care professionals to send and act on contacts at a time that suits them, enabling health-care professional to draw on external resources or check evidence and providing sources of information for the patient (two studies) | |
| Patient interface with alternatives to the face-to-face consultation |
Two studies reported that when patients had been offered an alternative to the face-to-face consultation, they usually report liking them. Patients viewed the removal of the necessity to attend the GP or nurse’s professional space as a benefit of e-mail and telephone consultations (three studies). Others reported that benefits included the convenience of being able to consult while at work (one study), to choose when and how to consult and the perceived advantage of avoiding the practice receptionist (two studies) With e-mail, patients can communicate with a doctor outside office hours, and exchange information with personal contacts regarding symptoms or health and care decisions. Patients can also attach photographs and other digital files, such as audio-recordings (two studies). For patients preparing for a hospital visit or recovering afterwards, these forms of consultation provide a way to communicate without having to visit (one study) E-mail exchanges can provide a consultation record, and possibly clearer explanations and subsequent understandings than information obtained during face-to-face contact (one study). This may be particularly advantageous to those who are less articulate or confident in person, those who wish to discuss their consultation with others and those who need help with translation (one study). Some patients may be more willing to disclose intimate or sensitive information via an e-mail than in person or over the telephone, especially if they are at work or in a public place (one study) Health professionals raise concerns that older patients, disabled patients, people without literacy skills and patients who are less educated may be disadvantaged through alternatives to the face-to-face consultation (three studies). Although, there is some evidence that those who have internet access, patients who are disabled, elderly, less confident or living at some distance from the practice are often among those who are particularly keen to use e-mail consultations (one study) One study recommend that patients should be shown how to use a system at a point when it is relevant to them, rather than as part of a general induction to their health-care organisation. If the information does not come at the right time, the patient may not remember the system, or (as is likely in a fast-moving field) the system may have changed by the time they come to use it Authors report that much of the evidence about potential benefits and disadvantages for patients and particular subgroups of patients has been written from the health-care professional perspective and credible empirical evidence from patients is very limited |
|
| Evidence in relation to specific technologies |
The conceptual review highlighted a lack of evidence about the use of video consultation in primary care settings9 There are examples of use in mental health conditions and palliative care, for which pilot studies have explored the feasibility of using video (three studies). The first evaluation of the GP Access Fund found that video consultations had a low rate of patient uptake and were yet to show benefits. The results of the second evaluation are pending. Review found no published studies related to e-consultations, but authors report that several local evaluations of e-consult use were being conducted in England Despite the low level of uptake, video consultation is still regarded as transformative in general practice. However, findings (of the whole Atherton 2018 review9) suggest that the reality of trying to implement video consultations is very different from the theory of what it might offer, and this has implications for practice and service delivery Authors state that practice staff and sometimes patients often blurred the distinction between telephone consultation and telephone triage, and it is unclear whether or not policy-makers have made the distinction US-based studies of e-mail consultation have explored associations between the use of patient–clinician e-mail and a range of outcomes. In one study, patient use of secure e-mail with clinicians was not found to be associated with an increase in the use of clinical services 7–18 months after first use. Although it was associated with an initial increase in activity by e-mail users, this did not persist beyond 6 months (but unclear if this study relates to primary care). Although studies have examined the association between e-mail and outcomes, there is limited evidence about the organisational and relational dynamics that contribute to change Concern about whether improving access through use of alternatives to the face-to-face consultation will increase or decrease workload pressure is also evident in much previous research on the use of alternatives, such as telephone (one study) or e-mail consultations (one study) |
|
| Atherton (2012)21 | Patient/caregiver outcomes | Not measured for primary care. One study in a community setting found that telephone counselling for lifestyle modification had a greater effect than e-mail counselling for some measures of patient health status and well-being. Individuals in the telephone counselling group also had a significantly greater number of website logins than those in the e-mail group. Other evidence from non-primary care settings indicated that e-mail communication with health professionals did not have an effect on whether or not patients used the internet for finding out about their disease or where to seek treatment |
| Health-care professional outcomes | None of the trials measured how e-mail affects health-care professionals. Two studies based in primary care reported health professional perceptions. The results indicated that professional acceptability and satisfaction was higher for physicians in the e-mail group than the standard methods of communication. No significant difference between groups in either study for physician satisfaction with patient communication outside clinical visits | |
| Health service outcomes: resource use (patients) | One primary care study found that the reduction in the mean number of contacts to the GP and front office was greater in the e-mail group. The reduction was also greater in office visits per patient per year and in telephone consultations | |
| Health service outcomes: resource use (health-care professionals) | Results from two primary care studies suggested that e-mail intervention leads to an increased number of e-mails and telephone calls received by health-care professionals than the standard method of communication | |
| Harms | In one of the primary care studies, many patients reported having insufficient web experience to navigate the intervention website. It was not clear if this had any impact on the health of the patient or the quality of health care. One community-based study found no difference between e-mail and telephone counselling groups in terms of harm | |
| Effect on patient–professional communication | Effect on patient–professional communication is unclear, but some evidence from one study in an ambulatory internal medicine practice that participant satisfaction with communicating non-urgent messages to a doctor and/or nurse was rated excellent/very good by more people in the e-mail than the standard group. However, there was no difference between groups for those rating it as poor | |
| Value of service | Evidence from one primary care study was that e-mail may have an impact on how patients perceive the value of a service. Participants in the e-mail group were willing to pay less for an online consultation than the standard group who had not received the intervention | |
| Castle-Clarke (2016)8 | Online triage tools: managing demand on professional time |
There was mixed evidence on the capacity of online triage tools to manage demand, and effects were dependent on the type of triage tool used There is limited evidence that support for self-management can reduce demand. One study (a large survey in the USA, 2013) found that 59% of participants had gone online during the previous year to look for health information. Thirty-five per cent of participants had gone online specifically to diagnose a condition; of these, 46% concluded they needed to see a medical professional, whereas 38% believed that the problem could be dealt with at home A pilot study of webGP (2014) reported that for every user requiring a GP response via e-consultation, five users require online self-help only. An online system ‘askmyGP’, which takes information about a patient’s condition, found that providers using the system are better able to manage demand during the day (unclear if this is the same study) One trial (2003) of an e-mail triage system reported that e-mail increased the communication burden on clinicians and staff and did not substitute for telephone consultations. More recent evidence from one study (2016) suggested that GP telephone triage is not associated with a reduction in clinical contact time for GPs, although nurse-led telephone triage is ‘Significant potential’ was reported for interactive symptom checkers to increase demand (unclear which study reported this). Two studies appeared to report that interactive symptom checkers are often risk-averse, recommending professional care when self-management is appropriate (one study, 2015), and diagnosis apps are not always accurate (one study 2014), which may encourage patients to use the health system unnecessarily |
| Interview data | Several interviewees felt that online triage, if handled correctly, has a big role to play in managing demand in the future. There was a sense that being able to actively intercept patients who are about to make an appointment, potentially through the practice website, offers ‘significant gains’:[For] people who have actively decided to come to your practice website, usually to find your opening hours and your phone number [to] book an appointment . . . that’s your opportunity to intercept . . . to walk them past a series of offers that mean self-help, signposting, symptom checking . . . that actually means you can pull out six per cent or seven per cent of demand right off the bat | |
| Patient experience |
There is little evidence about how patients experience online triage tools. It was reported that much depends on the type of triage tool used. The developers of webGP and askmyGP have reported that patients are satisfied with the service. It was suggested that patient satisfaction may be related to the use of professional review in the service A survey (2009) of 515 people found that 40% felt more anxious about their medical condition when viewing information online, prior to accessing the health-care system One study (2014), an evaluation of NHS 111, reported that patients tend to be less satisfied with triage services when they have been auto-routed from another health service, such as a GP out-of-hours service Authors reported that patients suffering from depression or anxiety may prefer online symptom checkers, rather than revealing their problems to a professional (unclear which study reported this evidence). Several studies (number not reported) found that patients are often more honest with digital tools than with a professional |
|
| Health outcomes | Authors reported that robust evaluations are lacking and there is no evidence on the impact of online triage tools on health outcomes | |
| Remote consultations (case study site): impact |
When Skype consultations were initially introduced in the case study site at Moss Side Health Centre, Manchester, they were received very positively by patients, who reported high levels of satisfaction. They were used by approximately 10–15% of registered patients (which at the time totalled 6000–7000). However, after the practice offered a walk-in clinic between 8.30 a.m. and 9.30 a.m., guaranteeing access to a GP, the number of Skype consultations has declined to approximately 5% of registered patients (one or two consultations per week). The practice concluded that the ‘gold standard’ for patients is a face-to-face appointment when it comes to clinical assessment The practice found that Skype consultations mostly benefited patient groups with additional needs (e.g. those with mobility problems and parents of autistic children who find attending the practice distressing). Skype also worked well for those who are not in the local area (e.g. students wanting ongoing care from their usual GP) When Skype consultations were first introduced, there was an increase in demand, with the same number of face-to face appointments being provided, as well as additional Skype consultation. However, now there is greater access to face-to-face appointments, uptake is low as patients prefer a face-to-face consultation However, GPs do feel that Skype and e-consultations have helped the practice to manage its workload better, due to the flexibility and choice in how to consult with the patient Benefits included:Challenges included: |
|
| Managing demand on professional time (literature review evidence) |
One study (2015) reported that remote consultations have variously been found to increase workload, increase workload temporarily and decrease workload, although one study (2010) found that remote consultations are usually quicker than face-to-face visits Much depends on the context, patient type and the health problem. Essential to have effective triage systems to ensure that remote consultations are offered only to patients most likely to benefit |
|
| Patient experience |
Three primary care studies (2004, 2010 and 2015) reported that patients often feel more comfortable to ask questions and welcome the ability to save the clinician’s message and return to it at a later time. Though patient satisfaction tends to improve when professionals respond to their queries quickly (one study, 2015) Two studies (2000 and 2015) reported that video consultations can offer improved convenience and flexibility, although they tend to be most valued by those who struggle to access care in person (one study 2010) |
|
| Health outcomes | One study (Atherton 201221 – included as a separate review in our evidence summary) reported evidence on the clinical outcomes of remote consultations is generally inconclusive due to low-quality evidence. A review (2012) of the clinical use of Skype found no hard evidence in favour of it or against it. Although one study (2013) reported that in some cases professionals may be better able to make clinical assessments when face to face | |
| Chambers (2019)24 | Safety | None of the six included studies reporting on safety-related outcomes identified any problems or differences in outcomes between symptom checkers and health professionals. However, studies evaluating safety were generally short term and small scale. Some were limited to people with specific types of symptoms (e.g. influenza-like illness or respiratory infections) and others recruited from specific population groups (e.g. students) that were not representative of typical users of urgent care services. Review authors advised that the evidence should be interpreted cautiously, indicating that there is no evidence of a detrimental impact on safety rather than evidence of no detrimental effect |
| Clinical effectiveness | Only two studies reported on clinical effectiveness outcomes, making it hard to draw conclusions. One study compared the Internet Doctor website with usual care. Results showed that users of the website had longer illness duration and more days of illness rated moderately bad or worse than the usual care group, but the difference was not statistically significant. Several patients using the webGP system were reported to have received advice to seek treatment for serious symptoms that might otherwise have been ignored | |
| Diagnostic accuracy | Highly variable between different systems, but generally low. The evidence from eight studies included in the review suggested that digital and online systems have yet to achieve a high level of accuracy in the diagnosis of specific conditions. This applies both to ‘general purpose’ symptom checkers and to those limited to particular conditions. Most studies reported that the diagnostic accuracy of symptom checkers was poor in absolute terms. However, two studies found evidence that symptom checkers performed relatively well when complaints were generally common and uncomplicated | |
| Accuracy of signposting | Accuracy of signposting of patients to the most appropriate level of service was inconsistent between seven included studies. Algorithm-based triage tended to be inferior to and more risk-averse than that by health professionals, with 85% of respondents being advised to visit their doctor in one study. The only studies to find clearly equal or superior accuracy of triage and signposting to appropriate services using an automated system were the evaluations of Babylon Check produced by the company that developed the system. The app gave an accurate triage outcome in 88.2% of cases, compared with 75.5% for doctors and 73.5% for nurses (one study) | |
| Compliance with triage advice | Very limited evidence on patients’ reactions to online triage advice and whether they follow the advice or seek further help or information. Only two of the included studies reported specifically on patients’ compliance (or intention to comply) with advice received. Preliminary evidence from NHS England evaluation suggested that patients may be more likely to seek further advice for more urgent conditions | |
| Service use | Some indication that symptom checkers can influence the pattern of service use. One RCT focused on promoting self-care and covered respiratory symptoms only. Results showed that the intervention group had fewer contacts with doctors (but more contact with NHS Direct) than controls, despite having a longer duration and greater severity of illness. Unclear if this finding is generalisable to systems covering the full range of urgent care. Further evidence from two grey literature reports. An NHS England evaluation found that online/digital triage was associated with a small shift towards self-care when compared with telephone triage (18% vs. 14%). In addition, online/digital triage directed a smaller proportion of patients to other primary care services, such as GPs, dental and pharmacy (40% vs. 60%). A pilot evaluation of the webGP system by its developers reported that 18% of patients had been diverted away from requesting a GP appointment for that consultation. In addition, 14% of patients reported that they would have attended a walk-in centre or other urgent care service if they had not had access to the webGP system. However, the report provides few details of the methodology used. Data provided by the manufacturer of the ‘Babylon Check’ app indicated that patients were more likely to be triaged to self-care by the app than by NHS 111 by telephone (40% vs. 14%). One further study that students had a stronger intention to seek treatment for a hypothetical illness when the diagnosis was made using WebMD or Google than with no electronic aid | |
| Cost-effectiveness/costs | Cost-effectiveness data were reported in two studies produced by system manufacturers. Based on 6 months of pilot data, webGP was estimated to provide £11,000 savings annually for an average general practice (6500 patients) compared with current practice. A saving to commissioners equivalent to £414,000 annually for a CCG covering 250,000 patients was also suggested. The ‘Babylon Check’ app was claimed to provide average savings of over £10/triage compared with NHS 111 by telephone, based on a higher proportion of patients being recommended to self-care. A third study found that potential savings to practices from using e-consultation depended on the percentage of face-to-face appointments avoided. However, findings from this study have limited relevance as the focus was not on symptom checkers | |
| Access/inclusion | Over half of the included studies considered equity and inclusion issues either directly or by comparing users and non-users of digital triage systems. Younger (four studies) and employed (three studies) people were more likely to use these services. Women were also more likely to use these services than men. Older and less educated patients more likely to prefer telephone or face-to-face contact. Potential implications for health equity if urgent care pathways prioritise (or appear to prioritise) requests originating from digital sources. In primary care issues have arisen because patients using e-consultation systems to request an appointment following online triage may be seen more quickly than those contacting the practice by telephone | |
| Patient/carer satisfaction | Ten of the 27 included studies had an outcome of patient/carer satisfaction. Study participants generally expressed high levels of satisfaction with digital and online triage services, albeit in uncontrolled studies. The studies appeared to be rating usability rather than satisfaction with the advice received or the degree of reassurance provided | |
| Hickson (2015)22 | Patient access/equity | In five studies, women used e-visit technologies more frequently than men. Mixed evidence in relation to age. Two e-visit studies reported that middle-aged patients used the service more often than younger individuals. Four other studies reported that younger patients used e-visits more often. Older patients were less likely to use the service when there was a fee (one study). Inconsistent evidence on whether healthier patients are more likely to use e-visits and related technologies. Lack of data on e-visit patient/user health literacy, socioeconomic indicators and differences in rural vs. urban populations |
| Efficiency and continuity of care | Evidence that mobile e-visit technologies can improve efficiency (three studies) (no details reported). Three other US studies reported cost savings for providers from e-visits. One study estimated that an e-visit prevented an office visit in approximately 40% of patients and decreased financial loss from Medicaid reimbursement. One study indicated that cost saving can be achieved while maintaining the same level of care. However, most of the included studies that focused on costs applied e-visit reimbursements to a fee-for-service model of patient payment. Therefore, cost findings are not generalisable to other payment models | |
| Quality of care | Evidence that e-visits can improve quality of care (two studies), access to care (two papers) and also continuity with transitions in care (two papers) (no details reported). Patients must be educated about proper use of e-visits because the asynchronous nature of the communication works poorly for health conditions that require urgent care (two papers). The use of triage systems may be used to address this issue and improve physician workflow | |
| Health services use | One US study found that e-visits did not significantly decrease the frequency of face-to-face primary care office visits. It was suggested that patients may treat e-visits as supplementary to rather than a substitute for traditional care delivery | |
| Patient satisfaction | Patient satisfaction has rarely been addressed in acute primary care e-visit implementation analyses. Only one study of patient satisfaction with e-visit acute primary care services was identified (results not reported) | |
| Implementation barriers (structural and human capital) | Physicians have expressed concern about the lack of an established model for insurance reimbursement, the lack of integration with electronic medical records, workflow and other existing systems and legal/security concerns. In terms of a lack of integration with electronic medical records, one study found that there were significant costs associated with transferring the e-mail content into electronic medical records and vice versa. To overcome this issue, template-driven systems that eliminate the need for free text have been used. Structured, template-driven systems are potentially more efficient in providing the clinician with pertinent information without back-and-forth communications. These systems also integrate with medical records more effectively than e-mail. Patient perceptions and concerns about privacy reported to be mixed. Patient health literacy, physician technological literacy and concerns about overuse also identified in the review as potential barriers to e-visit implementation. In terms of overuse, one study found that there was no undue burden from electronic communication, as it took less time to respond than answering telephone messages. Evidence from three studies indicated that patients do not misuse e-visits. One survey of physicians identified concerns that patients under-report their conditions or request inappropriate advice | |
| Huxley (2015)23 | Patient access/equity: practical access issues | For carers, people with mental health problems: three studies found that e-mail offered efficiency, speed and flexibility (e.g. could be used to communicate while patients working). Asynchronous technology can also reduce the need to negotiate with receptionists, appointment systems, travel to surgery and use waiting rooms (two studies) |
| Lack of candidacy | Carers: no increase in carer perceived candidacy despite an increase in channels for access to general practice, as it is first necessary for the carer to identify as a candidate for health care before starting the help-seeking process (one study) | |
| Lack of ability to communicate with health professionals | Refugees, asylum-seekers and people with mental health problems: digital communication provides an increased feeling of privacy when an interpreter is not physically present, which increases patient willingness to discuss sensitive issues; however, loss of visual information can reduce interpretation quality (one study). People who do not have English as a first language are not heavy users of digital communications in English-speaking countries (two studies), so the advantages may be lost | |
| Patient-related barriers | Refugees and asylum-seekers, homeless people, Gypsies and Travellers: communication technology was found to facilitate continuity of care (three studies). Anonymity of digital communication could encourage groups who wish to remain hidden to seek help (two studies). No evidence was found to indicate that digital communication will improve knowledge about health services and how to access them | |
| Negative experiences with health-care service and staff |
People with mental health problems, refugees and asylum-seekers, homeless people, Gypsies and Travellers: patients try to see trusted GPs for mental health issues rather than the most available GP, thereby prioritising relationship over convenience (two studies) Text-based communication leaves room for interpretation; therefore, communication between patients and clinicians with well-established relationships is more likely to be successful than that between strangers (two studies) One study reported that to build the therapeutic relationship, both clinicians and patients need to have face-to-face contact for the richness of stimuli available (e.g. auditory, visual, tactile and olfactory) Digital communication would reduce the need for patients to engage with receptionists and other health centre staff, reducing apprehension about negative experiences with staff (three studies) No evidence was found that digital communication in itself will improve patients’ trust in the GP or increase health services’ awareness of patients’ rights |
|
| Stigmatising and negative reaction to patients |
People with mental health problems, refugees and asylum seekers, homeless people, Gypsies and Travellers: one review suggested that face-to-face consultations were essential for communication about emotional states. Other evidence suggests that patients do communicate their emotional states with GPs via e-mail (one study) and are able to discuss embarrassing or sensitive questions (one study) Patients consulting for physical problems can feel less intimidated via video link and feel able to ask more questions (one study) One review reported that teenage girls willingly e-mailed a health professional in a magazine column to discuss problems/queries that they would not necessarily talk about face to face The removal of the patient ‘being seen’ to seek help potentially removes the embarrassment, social disapproval and stigma that some patients may experience at health-care centres (two studies) |
| First author (year of publication) | Description of patients and primary care providers (if reported) | Summary of interventions and comparators | Reported outcomes | Summary of findings |
|---|---|---|---|---|
| Atherton (2018)9,10 (ethnographic case study) |
Patients: n = 39 Thirteen male, 25 female and one transgender Ten identified as carers Seven had restricted mobility Thirty had a long-term condition Six had a mental health condition (where a condition was disclosed) Fifteen had multimorbidity (where conditions were disclosed) Sixteen were educated to degree level or above Primary care providers: the participating practices had a range of list sizes, from 1938 to 18,353. One was in a rural area, two in semi-rural areas and five in the inner city In total, 45 staff members were interviewed. Staff participants included 19 GPs, 10 practice managers or deputies, one practice co-ordinator, one nurse practitioner, five practice nurses, one rural health worker, five receptionists, one patient service manager, one practice administrator, and an IT manager |
The participating practices used a varied range of alternatives to the face-to-face consultation, including telephone, e-consult, video and e-mail in varying degrees of frequency |
Service delivery: rationale of general practice plans to introduce alternatives to face-to face communications Outcomes important to participants (staff and patients) |
Data largely taken from journal article Rationale given for introducing an alternative to the face-to-face consultation included:Rationales differed between practices, but also within practices, with different team members having differing perceptions and understandings. In many practices the decision to implement alternative forms of consultation was in the context of a perception of increasing demand and external encouragement from policy to introduce alternatives. For some the introduction was triggered by the offer of financial support |
| Practice organisation | In practices without a formal e-consultation system, members of the practice team did not always know whether or not other staff were, for example, in e-mail contact with their patients. One GP, during an interview, said:I do the same as everyone else in the practiceGP1, Practice C, inner city, mixedHowever, accounts from other staff members and observations by the ethnographer suggested otherwise. In the case study practices, policies about e-mailing patients were either not in place, not known about or not followed. Contradictions were evident; for example, one GP explained that their practice was trying to discourage patients from engaging in two-way e-mail communication with the practice, yet he used e-mail with ‘selected’ (trusted) patients:What we’re envisaging is . . . saying, ‘No reply @ X Medical Practice,’ to make it a bit more obvious that you’re not meant to replyGP3, Practice F, semi-rural, affluentInformal discussions and interviews with staff and patients identified different views about the boundaries of a consultation. Patients described using telephone and e-mail for background information, a perspective that was reinforced if the patient was then asked to attend a face-to-face consultation. There were inconsistencies in staff recording consultations in the medical record (e.g. it was observed that not all e-mail consultations were necessarily included in the medical record) | |||
| Staff and patient experiences | Patients could express a preference for an alternative to a face-to-face consultation only if they were aware that the practice offered it, and this was not always the case. Telephone consultations were well integrated within the practices studied but the ethnographic observations suggested that patients rarely asked for a non-face-to-face consultation and receptionists offered them only as a last resort when all appointments were taken. This was consistent with the staff belief ‘that patients prefer to see the doctor’ or, as one of the patients put it, a telephone consultation was:. . . better than nothing, but not 100 per cent50-year-old female patient, Practice D, rural, mixedOther interviews suggested that, depending on the health issues, some patients preferred to avoid coming to the practice. Alternatives could offer flexibility to both staff and patients depending on how practices organised the working day. GPs and nurses were able to choose when and in what order to reply to messages or make telephone calls:I’m able to manage my time a bit betterGP 2, Practice H, inner city, affluentOther themes emerged regarding telephone consultations, including telephone consultations taking longer than expected, lengthening the working day; some telephone consultations were converted to face-to-face, increasing the overall number of consultations with that patient | |||
| For which patients and problems |
In interviews, staff and patients concurred that alternatives to face-to-face consultation might be unsuitable if a new health problem was being presented, if the patient was older or confused, or if the patient was using a complex array of medicines. Clinicians varied in their views about which patients were most likely to be suitable for an alternative consultation; in some cases these decisions were based on age, socioeconomic status or ethnic group (e.g. telephone consultations were best used with patients who had been born in the UK) Clinicians felt more confident to gather information via telephone or e-mail if the patient was known to be sensible and deemed to use the system in a judicious manner. Continuity mattered to patients too: for certain health problems, it might be important to know the clinician who would be consulted remotely |
|||
| Implementation |
Barriers to implementation included difficulties in making patients aware of the option to use an alternative to the face-to-face consultation and getting them to engage with these alternatives when the face-to-face consultation was still seen as the ‘gold standard’; lack of understanding within practices about the role of alternatives to the face-to-face consultation and how they might impact on the practice and the staff which could increase workload via conversions to face-to-face consultations; and potential inequality of delivery of care in which clinicians chose which patients they would consult with this way Receptionists and administrators had a key role in ensuring that new consultation methods were taken up by and delivered to patients, but this was not always acknowledged or considered by other members of the practice. Receptionists were not offered training and practices were reluctant to invest financially in training for any staff members, sometimes delivering ad-hoc or in-house training, or in the case of e-consultation training only the GPs. Training was:Staff member, Practice F, semi-rural, affluentOther factors relating to implementation included the use of ‘out-of-office’ messages to avoid patients having a long wait for a reply to an e-mail. However, others were not adequately considered beforehand, such as inadequate technology, length of time to set up video consultations, etc., meaning some consultations defaulted to telephone. Other barriers included not enough telephone lines, difficulty recording during consultation. More subtle factors included the impact on professional identity, with the core tenet of general practice being the doctor–patient relationship, as conducted in the face-to-face consultation:GP3, Practice C, inner city, mixedFacilitators of implementation included the GP Access Fund, which was an important facilitator to implementation because it provided a rationale, financial support and training In several practices the introduction was driven by one or two ‘innovators’ who got alternatives to the face-to-face consultation implemented. Other facilitators included identification of a clear role for alternatives to the face-to-face consultation in some conditions and for certain patients. Patients were positive about the use of alternatives to the face-to-face consultation; both staff and patients shared an understanding about the limitations of these mediums, which made implementation smoother. Flexibility of alternatives to the face-to-face consultation made them easier to ‘slot’ into day-to-day practice. A willingness to adapt their use once introduced was a key facilitator:Practice administrator, Practice D, rural, mixed |
|||
| Outcomes important to participants (staff and patients) |
For clinicians: using e-mail to share and gather information when co-ordinating complex health-care packages For nurses: using telephone and e-mail consultations for management of diabetes (e.g. for discharge checks and medication reviews) For GPs: the main motivation was to help them manage their workload For patients: liked the efficiency and convenience offered by alternatives. Some thought that an e-mail that went directly to the GP avoided involving the receptionist in the decision about whether or not the patient needed to be seen:76-year-old male patient with comorbidities, Practice F, semi-rural, affluentIn addition, for patients of alternatives to the face-to-face consultation, benefits related to certain elements of the medium, for example e-mail and e-consultation offered an asynchronous and text-based approach, which was recognised as useful for people who were very anxious, or found face-to-face contact difficult, who had hearing or communication difficulties and those who struggled to express themselves |
|||
| Atherton (2018)9 and Brant (2016)11 (a scoping survey) |
Patients: not reported Primary care providers: participating practices were significantly larger (in terms of numbers of registered patients and doctors per practice p < 0.01 for both results) than those that did not participate. No significant differences between responding and non-responding practices in terms of their deprivation score. Of the 696 respondents who reported their sex, 59% (413/696) were female. Respondents categorised their ages as 25–34 years (90/889, 10%), 35–44 years (239/889, 27%), 45–54 years (362/889, 41%) or ≥ 55 years (189/889, 21%). Of all the responses, 12% (105/889) came from practice managers and 88% (784/889) from doctors |
E-mail, video, telephone and text (telephone triage was excluded) – no further details reported |
Service delivery: GP plans to introduce alternatives to Face-to-Face communications (e-mail, video, telephone, text (sms messages) Information provided on practice websites for patients |
Although the majority of practices reported routinely offering telephone consultations (211/318, 66%), few (6%) reported facilitating e-mail consultations; 20% of practices intended to offer e-mail consultations in the future, but 53% had no such plan. None of the respondent practices reported offering internet video consultations, and very few (4%) reported any plans to do so in the future. There was also evidence that 21% of practices had previously offered e-mail, and that 10% had previously offered internet video, but that they had subsequently withdrawn these services. There were some inconsistencies between respondents within the same practice about their practice’s use of telephone (within practice SD 0.91, ICC 0.53) and e-mail consultations (SD 1.1, ICC 0.39). There was less variation between respondents about their practice’s use of video consultation (SD 0.52, ICC 0.20), related to the limited use of this consultation method in general |
| Current provision of alternatives to face-to-face consultations at an individual general practitioner level | Most GPs reported personally providing telephone consultations on most working days or every working day (79%). Only 8% of GPs reported providing e-mail consultations on most working days or every working day, while 45% did so rarely or sometimes and just under half (47%) never provided e-mail consultations. Furthermore, 99% stated that they never conduct consultations via internet video. Provision of telephone, e-mail or video consultations did not vary by GP age or sex, or by study site (data not reported) | |||
| Concerns for GPs, practices and patients 249/889 of the responses included some form of free text |
The free-text responses revealed concerns about the perceived risks to patients, the organisation and practice staff Concerns expressed included the view that adopting e-mail or video consultation would be inefficient for the practice, would increase demand, would be a challenge in terms of privacy and confidentiality, and would increase clinical risk, with medicolegal consequences A few GPs had experience of some vulnerable and older people who preferred alternative consultation methods, while others thought that these same groups would be disadvantaged. Practical issues, such as the reliance on appropriate internet provision and broadband reliability, the financial outlay and local concerns about information governance, were mentioned as further barriers to implementation 21% of practices reported having tried using e-mail, and 10% using internet video, despite a general antipathy towards their introduction, and had since reduced such use. This may provide support for these concerns |
|||
| Views of GPs: concerns for GPs (from free-text box on survey, see box 1 of journal article) | Increased access:Increasing access options increases GP stresse-mail is a nightmare – access all the time, and hundreds of e-mailsIncrease clinical risk:It’s a personal preference, but I find the increased access too intrusive and increases risk of information getting lost/filed with other documentsWe have discussed use of e-mail communication but find there is a risk of e-mails not being acted upon when certain GPs are on leave, leading to unnecessary risk and delayI feel the level of risk with these are higher than a face-to-face or phone | |||
| Concerns for practices | Increased workload:If we take on e-mail consultations, we will have possibly hundreds of e-mails. Who will deal with them? . . . medico-legal consequences of delay. We have no capacity. This will possibly increase workloadWe already get more than 100 emails EACH daily. This would open the floodgates and we would drown. It is unmanageablePrivacy and confidentiality:Issue with confidentiality using e-mailQuery issues with medico-legal problems and confidentialityChallenge of technology:Internet connection currently barely up to current software requirements for e-referrals, etc. Don’t have software and hardware capacity for more modern techniques | |||
| Concerns around patients | Disadvantage certain groups, such as the older people:Concern that most vulnerable (deaf/blind/elderly/demented/mentally ill) least able to access, and so unintentionally disadvantagedVery elderly population – technology difficult | |||
| Perceived benefits of the introduction of alternatives to face to face consultations | A few responders mentioned experience of benefits, such as patients being able to send pictures of a transient rash or an audio file of a child’s cough, or those who preferred to use email because of communication difficulties or disabilities that made it difficult to get to the surgery. Some also mentioned using email with particular ‘selected’ patients, and being in email contact with their own GPs | |||
| Benefits for GPs | From box 2 of journal article: used to support the face-to-face consultation:I think patients using media – for example, bringing in photos of their transient rashes, or recordings of their babies cough – are great‘In combination with phone consult (and with consent), I have got patients to text me photos of problem – for example, rash, eye inflammation – to help confirm diagnosis or whether need to be seen, etc.Would be good to do one way doc–patient communications instead of letters | |||
| Benefits for practices | Workload management:We encourage patients to use email to send info to us (stops clogging up the phone lines) | |||
| Benefits for patients | Advantage for those with physical or communication difficulties:I use email for one patient who has MND [motor neurone disease] and so cannot speak on phoneEmail really helpful for deaf patients (who sometimes send me an email before attending a consultation to save time), and for tracheostomy patients | |||
| Exploring practice websites | 128 out of 184 English and 125 out of 184 Scottish practices stated they offered telephone consultations (not including those used for triage), ranging from same-day call-back to booking a telephone consultation in advance. Five English practices and one Scottish practice offered an electronic messaging service (e-consultations), and four English practices and one Scottish practice invited patients to e-mail their doctor; however, for one there did not appear to be an e-mail address provided, and one English practice had a ‘webform’ box on their site for non-urgent messages. None mentioned offering video consultations. Although some of this information was clearly displayed, for some of the alternatives to the face-to-face consultation offered, particularly e-mail, it was difficult to find the information on practice websites. Authors noted it was useful to cross-reference the findings from the website search with those from the survey, as sometimes websites were out of date | |||
| Atherton (2018)9 (routine data collection) |
Patients: details provided in table in final report Primary care providers: GPs or nurse |
Telephone, e-consult, e-mail, face-to-face in surgery or at home | Proportion of consultations conducted by various methods |
The proportion of all consultations conducted by telephone varied from 8% to 31%. Among practices offering e-mail consultations, the highest proportion of consultations conducted was 0.58% in one practice, with other practices conducting only 0.02% of consultations. e-consultations also appear to be very rarely used, accounting for 0.22% and 0.23% of consultations in those practices that offer them. It is important to note that, across all practices, face-to-face consultations in surgery still account for the vast majority (79.8%) of all consultations, with home visits accounting for another 1.4% of consultations. The use of alternatives to face-to-face consultations in our case study practices was higher than the national average, but among the case study practices chosen because of their interest in the use of alternatives, such approaches account for only a small proportion (18.7%) of all consultations, and 98.6% of these were telephone consultations Females had higher rates of most types of consultation than males. Patients from non-white ethnic groups had a higher rate of telephone consultations and a lower rate of home visits and electronic consultations than white patients Rates of surgery consultations and e-mails appeared to be highest in the least deprived quintile, but this analysis does not take account of confounding factors, such as age |
| Number of consultations | Electronic consultations were less common in children and more common in patients who were white and those who lived in more affluent areas | |||
| Number of patients reconsulting within 14 days | Fifty per cent of patients having a telephone consultation had a subsequent surgery consultation within 14 days and 29% had another telephone consultation. Some patients will have had both, so 62% of patients had another consultation (compared with 48% of patients who had a surgery consultation then having another consultation within 14 days). For patients having an e-consult, 39% also had a surgery consultation and 31% also had a telephone consultation (62% had at least one additional consultation) within 14 days | |||
| Carter (2018)25 |
Patients: from study practices Primary care providers: general practices in NHS NEW CCG’s area |
GP e-consultation and self-help web service accessed by adult patients (aged ≥ 18 years) via their practice’s web | Number of consultations (face to face and telephone) and differences between groups |
Only four practices reported data for face-to-face and telephone consultations separately. The rate of face-to-face consultations with a GP within the data extraction period decreased slightly, but consistently, over the 4-year period. Consultation rates for combined GP face-to-face and telephone consultations increased in two practices, but decreased in the other four All six practices offered nurse face-to-face consultations. There were mixed results for rates of such consultations within the data extraction period. Rates increased in three practices and decreased in the remaining three. When it was possible to calculate combined consultation rates for face-to-face and telephone consultations with nurses, rates decreased in two practices (practices 3 and 6) and increased in one (practice 1) Using data provided by the webGP developers to the CCG, the calculated consultation rate for practice patients having e-consults during January, February and March 2016. The consultation rate for documented webGP consultations averaged seven (range across practices 1–11) Differences between e-consulters and face-to face consulters:substantial differences (> 10% between groups) existed between e-consulters and face-to-face consulters for reported problem resolution (55% vs. 33% ‘completely resolved’) reported seeing or speaking to a GP following the consultation request (52% vs. 93.8%). Other small differences were reported (see paper) e-consulters also reported being less satisfied than face-to-face consulters with their ability to consult their preferred GP (44% vs. 57%) Other results reported in the paper |
| Case report forms completed by GPs for patients using e-consult system |
Sixty-one out of 77 e-consult requests submitted by patients across all practices during the data collection period were completed by GPs (79%). Case report forms were completed for more female patients (n = 45) than for male patients (n = 16). The largest number was for patients in the age group 25–34 years (n = 18). The smallest number was for patients in the age groups 65–74 years (n = 1) and ≥ 85 years (n = 1). The number of GPs in each practice who completed case report forms ranged from two (who completed a total of five case report forms) to five (who completed a total of 35 case report forms). The number of case report forms completed during a 4-week period ranged from 4 to 35 per practice From the discussion:Result of e-consult (e.g. further face-to-face consultation, nurse visit):For the majority of cases (37/61, 61%), the GP reported being ‘not at all familiar with the patient’; only three (5%) reported being ‘very familiar’. In virtually all cases (58/61, 95%), GPs reported feeling either ‘very confident’ or ‘confident’ about managing the e-consult request |
|||
| Timings of an e-consult request and the delay between its receipt and the GP’s |
Response:Authors reported that in 16 cases, there were discrepancies in recorded delay between e-consult and time of GP response between GP collected data and patient survey, although this may be as a result of the data collection process Patient survey (e-consulters and face-to-face consulters):Of the e-consulter respondents:Principal reasons for using webGP were: |
|||
| Patient satisfaction | Eighty-six per cent of respondents reported being satisfied with their overall experience of using webGP; 86% reported being likely to use webGP in the future; 79% would recommend webGP to their family/friends | |||
| Qualitative data | Five GPs, five administrators/receptionists; three in person, seven by telephone, with a mean interview length of 14 minutes (SD 6 minutes, range 5–27 minutes). Patients provided comments in free-text boxes as part of their questionnaire survey | |||
| Feasibility of webGP |
Many interviewees voiced concerns about webGP and how it was being used by patients. Some felt that patients were using webGP to circumvent existing systems within the practice, such as appointments and telephone consultations:P3 01/GPSome interviewees were also critical about the types of problems reported by patients via webGP and unnecessary delays in care which may be incurred Through free-text comments, some patients confirmed that they were using webGP as an alternative to existing, less efficient systems:60201_webGPAlthough, conversely, the efficiency of other systems in the practice (such as telephone consulting) was cited by one staff interviewee as a possible reason for the low rate of use |
|||
| Acceptability of webGP | Staff interviewees perceived benefits for particular groups of patients, such as the flexibility of using webGP for working people:For people who work it’s sometimes difficult to sit on a phone and make a phone call, whereas you can sit and type an email quite quicklyP1_02/administratorSome also mentioned particular conditions and situations for which webGP may be advantageous, such as problems with mental health:There’s one really good example . . . It was a girl with anxiety . . . She got embarrassed easily and stumbled over her words and that was her barrier to actually coming and discussing it in the first placeP2_02/GPPatients concurred with this view through free-text comments (one patient comment available in paper):I find the online consultation option very convinient as I can give all the information I want to give and it saves me anxiety and having to travel or make a phone call. My partner is physically disabled so this will be useful for him too40291_webGP | |||
| Effectiveness of webGP | Interviewees expressed a range of views on the impact of webGP on GP/practice staff workload. Some respondents suggested that webGP had increased the workload for administrative staff:So it’s giving us more work, cos we’re ringing them, to make them an appointment, rather than them ringing us to make an appointmentP1_02/administratorThere was also a suggestion that webGP was shifting workload from the GP to the patient:. . . you’re shifting time and effort to the patient’s . . . responsibility, who can afford to spend an extra couple of minutes here and there at the expense of saving time for the GPs . . .P2_02/GPOthers were concerned that the anticipated reduction in GP workload had not materialised and that webGP had in fact increased the GP’s work:I think it might give extra work to the GP, because they’ve then got to access the document that we’ve attached, read it, phone the patientP2_01/receptionistSeveral interviewees suggested improvements to the webGP programme, such as a way of alerting patients to expect a call from their practice following submission of an e-consult request:I think quite often you need to make a very quick phone call to the patient to clarify a detail or to explain a plan and that is often a problem. They don’t answer the phone, it’s not at a convenient time for them, they’re not expecting it . . . I wonder whether a more ready way of being able to reply by e-mail25P4 01/PPatients too were concerned about some aspects of webGP in its current form:Although I agree with the concept of webGP, it is not yet an alternative. I gave confidential information via a web request, only to be then contacted by a female receptionist. What confidentiality does that offer!60331_webGPFrom discussion (p. 9):GPs feel confident in dealing with this new way of consulting, but frequently decide that the patient needs to see or speak to a GP or a nurse. The responsibility for conveying this decision to the patient is often given to an administrator, shifting such workload towards non-clinical staff25 | |||
| Donaghy (2019)29 | Thirteen clinicians and 162 patients in six primary care practices in Lothian, Scotland | VC compared with FTFC and TCs | Patient experience/satisfaction |
Patients who participated in VCs mainly found the experience positive. Patients reported that they were generally happy with all three forms of consultation, which were considered equally useful, but FTFC scored consistently higher than VC and TC in a number of domains: doctor/nurse giving enough time; asking about symptoms; listening; explaining tests and treatments; involving in decisions; treating with care and concern; taking problems seriously. In total, 71% of FTFCs and TCs were rated as being ‘very useful’ compared with 63% of VCs Technical problems were more common with VC than TC. Some patients had significant problems with insufficient bandwidth and occasionally the connection failed and TC was used. The biggest perceived advantage for patients of VC was time saving. For some patients, VC was less stressful and more practical (e.g. patients with mobility problems or anxiety disorders). Patients who participated in interviews were all happy to use VC again |
| Patient access/equity | Patients participating in VC were generally younger (VC 42.0 years, TC 54.34 years, FTFC 52.33 years); more likely to be female [VC 54% (28/52), TC 55% (31/56), FTFC 39% (21/54)]. However, it was reported that once age was considered, sex ‘dropped out’ as a factor. VC patients were similar in terms of deprivation and a large proportion were white British (87%). Patients who used VC were more likely to be working and to have experienced other video technologies such as Skype/FaceTime. Clinicians stated that although trying to be inclusive of all patients, they were more likely to attempt to recruit patients who were more technology savvy. Clinicians and patients felt that having an established relationship facilitated VCs | |||
| Consultation content |
On average, FTFCs were longer and more problems were raised and addressed than TCs and VCs (which were similar). The types of problems addressed were similar across the three consultation types and were typical of general practice. During FTFCs, patients’ health understanding was more likely to be sought and the problem placed into a psychosocial context at least once, than in TCs or VCs (which were similar). FTFCs were also associated with more overall ‘information giving’ by both patients and clinicians (but this may partly reflect the number of problems raised) From discussion: |
|||
| Clinicians experience/implementation | Patients were more positive about the technology than clinicians, and clinicians reported that VC appeared to be of less utility in managing patient problems. This was largely because of technical issues. Overall, 62% of clinicians rated VC as ‘very useful’ (29/47) compared with 85% of FTFCs (29/47) and 76% of TCs (38/50). In addition, 62% of clinicians would ‘absolutely’ choose VCs again compared with 94% for FTFCs and 90% TCs. Clinicians felt that future VC systems would have to seamlessly integrate with current IT and appointment systems to be adopted at scale and main streamed. All clinicians stated that current IT systems would need to be significantly improved and any future VC function integrated into the desktop PC used for consulting. In contrast to other more positive views, some clinicians felt that VCs did not add anything advantageous to TCs. Interviews confirmed findings from the other data collection methods that FTFC remained the ‘gold standard’ and that like TC, VC tended to be limited to one problem. Furthermore, the lack of a physical examination prevented clinicians from spontaneously addressing other health issues. Clinicians were generally of the opinion that VC was time neutral for them; however, they recognised the benefit for patients in terms of absence from work and travel time. Although technical problems emerged as a bigger issue for clinicians than patients, it improved with their increasing experience. There was an acknowledgement that increasing familiarity with VCs was likely to resolve this issue | |||
| Type of patient/problem | Clinicians and patients reported that VC was helpful for working people and for people with mobility or mental health problems. VC was considered particularly suitable for medication reviews and test results. VC was seen to be superior to TC in terms of rapport, reassurance, general health assessment, communication, checking understanding and body language assessment. For ‘very serious or sensitive’ issues, patients still preferred a FTFC | |||
| Service use | Around half of the patients were seen in the subsequent 4 weeks. Apart from three patients (who had multiple contacts), consultation frequencies were similar across the three types of consultations. A similar proportion of subsequent consultations were for follow-up of the index consultation | |||
| Mehrotra (2013)28 | Patients in four primary care practices in Pittsburgh, PA, USA | e-visits vs. office visits | Patient access/equity |
Out of 5165 visits for sinusitis, 465 (9%) were e-visits. Of the 2954 visits for UTIs at the four practices, 99 were via an e-visit (3%). Bivariate analyses found notable differences between e-visit and office visit patients across various characteristics Women were more likely to use an e-visit than men: For sinusitis (female): 77% e-visits vs. 69% office visits. For UTI (females) 98% e-visits vs. 78% office visits (p < 0.001 for both). Older (aged ≥ 65 years) patients were less likely to use an e-visit: sinusitis 6% e-visits vs. 13% office visits; UTI 9% e-visits vs. 27% office visits (p < 0.001 for both). Patients with more visits (three or more visits for any reasons) in the prior year were more likely to use an e-visit: sinusitis 85% e-visits vs. 76% office visits; UTI 87% e-visits vs. 74% office visits (p < 0.01 for differences) Employed patients were more likely to use an e-visit: sinusitis 75% e-visits vs. 62% office visits; UTI 60% e-visits vs. 46% office visits (p < 0.01 for both) The differences in patient characteristics observed in bivariate analyses were largely confirmed in multivariate models. The exception is that employed patients were not more likely to use an e-visit. Average income in the patient’s zip code was not associated with e-visit use Using multivariate models to control for other patient factors, the variables most strongly associated with a patient initiating an e-visit vs. an office visit were age [18–44 years vs. ≥ 65 years: sinusitis, odds ratio 1.65 (95% CI 0.97 to 2.81); UTI, odds ratio 2.97 (95% CI 1.03 to 8.62)] and longer travel distance to clinic [> 10 miles from patient home to clinic vs. 0–5 miles: sinusitis, odds ratio 6.54 (95% CI 4.68 to 9.16); UTI, odds ratio 3.25 (95% CI 1.74 to 6.07)] |
| Uscher-Pines (2014)27 | Adults enrolled in California Public Employees’ Retirement System health maintenance organisation | Teladoc | Use of Teladoc |
A total of 2718 adult and child members of the California Public Employees’ Retirement System (0.9% of all eligible members) had a total of 3701 Teladoc visits with an average of 1.36 visits per Teladoc user. Across the sample of 74,550 adult enrolees, (including both users and non-users of Teladoc), the average number of monthly visits for all conditions were 291 Teladoc visits, 39,431 office visits and 883 emergency department visits. Thus, Teladoc visits accounted for a very small proportion of health care use. Thirty-four per cent of Teladoc visits occurred on weekends and holidays, in contrast to 8% of office visits. The timing of Teladoc visits closely resembled the timing of ED visits. Across the 3 leading health conditions, Teladoc visits were less likely than visits to the ED or physicians’ offices to result in a follow-up visit for a similar condition in any setting. 6% of Teladoc visits resulted in a follow-up visit for a similar condition, in contrast to 13% of office visits and 20% of ED visits. The lower follow-up visit rate for Teladoc visits versus office visits was also seen after adjustment for age, sex and comorbidity score (odds ratio 0.44; p < 0.01) From discussion: if follow-up is considered to be a rough proxy for clinical resolution, there is little evidence of misdiagnosis or treatment failure in Teladoc visits. Teladoc providers may be successfully diagnosing and treating a wide range of illnesses via telephone consultations. However, it is also possible that Teladoc patients are seeking care for complaints that are so minor that follow-up visits are not necessary |
| Characteristics of Teladoc users | Teladoc users were more likely to be younger than individuals who visited physicians’ offices for similar conditions. Teladoc users were also more likely to be healthier (ie have fewer chronic conditions and to not have used health care in 2011) compared to patients who visited the ED or physicians’ offices for similar conditions. Women made up a larger percentage of Teladoc users, compared to individuals who visited the ED and physicians’ offices. Furthermore, Teladoc users lived in slightly more affluent communities than users of other settings. (All differences reported as p < 0.01.) |
Appendix 6 Authors conclusions, implications for research and practice: reviewer comments
Parts of Appendix 6 have been reproduced with permission from the following studies:
-
Atherton et al. 9 (this contains information licensed under the Non-Commercial Government Licence v2.0).
-
Castle-Clarke and Iminson8 (The Digital Patient: Transforming Primary Care? London: Nuffield Trust; 2016).
-
Carter et al. 25 [© Carter M, Fletcher E, Sansom A, Warren F, Campbell J. 2018. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/].
-
Huxley et al. 23 [© Huxley CJ, Atherton H, Watkins JA, Griffiths F. 2015. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/licenses/by-nc/3.0/].
-
Atherton and Ziebland31 [© Atherton H and Ziebland S. 2016. Reproduced from Atherton and Ziebland. 31 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 3.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/3.0/].
-
Atherton et al. 10 [© Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A. 2018. Reproduced from Atherton et al. 10 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/].
-
Donaghy et al. 29 [© Donaghy E, Atherton H, Hammersley V, McNeilly H, Bikker A, Robbins L, et al. 2019. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/].
-
Brant et al. 11 Republished with permission of Royal College of General Practitioners from Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice, Brant et al. , 66, 648, 2016; permission conveyed through Copyright Clearance Center, Inc.
-
Uscher-Pines and Mehrotra. 27 Republished with permission of Project Hope/Health Affairs Journal from Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider, Uscher-Pines and Mehrotra et al. , 33, 2, 2018; permission conveyed through Copyright Clearance Center, Inc.
| First author (year of publication) | Summary of authors’ conclusions and implications for research and health care as reported by authors | Reviewer comments: (1) brief interpretation of internal validity; (2) issues relevant to external validity |
|---|---|---|
| Antoun (2016)20 |
Physicians’ use of e-mail with patients is low and lags behind the willingness of patients to communicate with their physicians through e-mail. Factors behind this lag include physician and patient characteristics, lack of robust evidence and perceived barriers Further research is needed to better understand the factors behind the slow and scarce adoption of e-mail use, and test currently available and proposed opportunities that may enhance it |
(1) An adequate search was conducted using one database, as well as backward and forward reference searching. The search terms used were also reported, but it is unclear if any attempt was made to identify unpublished material or if date/language restrictions were applied. Inclusion/exclusion criteria were not reported and no details provided on any other aspect of the methodological process, including quality assessment. There was inadequate reporting of study details and the overall number of included studies was not provided. The findings were written in a ‘literature review’ format and an adequate data synthesis was not provided. The review was not limited to e-mail communication as an alternative to face-to-face consultations. Also, cited research focusing on e-mail communication for: the provision of information on disease prevention and health; communicating results of diagnostic investigations; co-ordination of health-care appointments and attendance reminders (2) Some of the primary research cited appear to have been conducted in the UK. Despite the poor quality of reporting, it is feasible, given the topic, that findings related to equity and implementation issues potentially have relevance across countries |
| Atherton (2018)9 |
The conceptual review identified and synthesised material relating to patient and staff experiences of alternatives to the face-to-face consultation, along with theories and ideas about the potential effects. Key questions to be asked when researching alternatives to the face-to-face consultation were applied in devising a case study guide, which was used by the focused ethnographers in guiding data collection at case study sites Implications for research (note, no specific recommendations from the conceptual review, these cover the entire project): Authors report their research as hypothesis-generating, to create a logical framework for future evaluations Further research on a range of questions is required Is it possible to improve uptake of alternatives to face-to-face consultations and, if so, does this lead to benefits for patients and general practices? What is the impact on access to care as perceived by patients (speed of access, convenience, timely access to care that meets their perceived needs)? What is the impact on NHS workload and, in particular, the impact on different sectors of the NHS (primary and secondary care) and different professional groups (doctors, nurses, receptionists and administrative staff)? What is the impact on the quality and safety of patient management? For which patients and for which conditions are different forms of alternatives most efficient and effective? How do different forms of consultation change the content of the consultation? How satisfied are clinicians and patients with different forms of alternative to the face-to-face consultation? Future research may need to explore different questions for each of the different technologies. However, unless or until uptake of e-consultations or video consultations increases, it will be impossible to measure impacts There are three types of alternatives to the face-to-face consultation that are priorities for robust evaluation because they are being widely implemented in the absence of evidence, these are:Research design for all three types of consultation should focus more on how the service, including relationships, expectations and patterns of work, is redesigned, than on the nature of the technology itself Implications for practice and service delivery: authors devised a web resource for GPs, practice staff and commissioners. The principle of the resource was to provide a self-appraisal and guidance tool and covered the following: Why do you want to introduce an alternative to face-to-face consultations? |
(1) Mixed-methods review: a conceptual review informed by realist review methods, survey and studies. Part of a larger review using realist methodology The review adequately met the criteria in the RAMESES appraisal tool A range of databases were searched from inception and then a filter applied to identify those from 2012 onwards. It should be noted that opinion pieces were included, which may have implications for findings as some references cited may not be research studies. A list of included studies was not provided so it is not possible to assess the potential impact A formal critical appraisal of the included studies was not undertaken, but authors state they assessed studies for relevance and rigour, although results of this are not reported The methods of synthesis were appropriate. It appears that more than one researcher was involved in each stage of the review Not all the included studies related to primary care research. Most of the evidence was for e-mail and telephone consultations, with very little evidence on video consultation. Many of the individual findings were drawn from one or two studies of unknown design, which may impact the reliability of the findings (2) The country and setting of the included studies is uncertain; however, it is likely that the findings are generalisable |
| Atherton (2012)21 |
The evidence base was limited, with variable results and missing data. Therefore, it was not possible to adequately assess the effect of e-mail for clinical communication between patients/caregivers and health-care professionals Owing to the inconclusive evidence, recommendations for clinical practice could not be made. However, there is no evidence of harms caused by e-mail interventions Future research should ideally address the issue of missing data and methodological concerns by adhering to published reporting standards |
(1) This Cochrane review was methodologically rigorous. A comprehensive list of academic databases was searched and a search of the grey literature was also conducted. Reference lists of relevant studies were checked and authors of included studies contacted for details of any further research or unpublished data. Inclusion and exclusion criteria were reported. Included studies were assessed appropriately for risk of bias and adequate study details reported. The authors conducted an appropriate synthesis of the findings. More than one author was involved in each stage of review process, reducing the potential for error and bias. However, only three out of the nine included studies were conducted in a primary care setting All of the included studies were assessed to be at risk of bias. The three studies based in primary care were assessed at risk of multiple sources of bias (2) Findings and conclusions are potentially generalisable across countries |
| Castle-Clarke (2016)8 |
Authors stated there is a lack of robust evidence on the impact that many technologies will have and in which contexts. In particular, a lack of evidence of the potential impact on health outcomes and, to a lesser extent, demand remains somewhat unclear for a range of technologies. Although there is much that is still not known, there are many promising areas and a number that urgently require further research The authors report a list of implications for practice across all the technologies included (further details can be found in the report) |
(1) This is a report including a literature review, case studies and interviews. However, no methods are detailed, so it is not possible to determine the reliability of the findings The results are based, in the main, on single studies of unknown design (2) Although a small number of patient experience data were derived from secondary care settings, the report authors have clarified that the majority of evidence directly relates to primary care |
| Chambers (2019)24 |
Strength of evidence is weak, being based largely on observational studies Major uncertainties surround the likely impact of ‘digital 111’ services on most outcomes. It will be important to monitor and evaluate the services using all available data sources and by commissioning high-quality research |
(1) The review was supported by a comprehensive search of seven academic databases and an internet search. No restrictions on language or date were applied. Reference lists of included studies and key reviews were checked and contact also made with service providers. Inclusion/exclusion criteria were clearly stated and a quality assessment of included studies conducted Adequate details about included studies were reported. An assessment of the overall strength (quality and relevance) of evidence for each outcome was also made. The authors conducted an appropriate synthesis of the findings. More than one author was involved in screening, data extraction and quality/strength of evidence assessment. The extent of involvement of the second reviewer was limited to screening or checking 10% of the sample (2) Nine out of the 27 included studies were conducted in the UK. Findings and conclusions are potentially generalisable across countries |
| Hickson (2015)22 |
e-visits and online care technology, particularly through mobile devices, offer the promise of increasing patient engagement and strengthening acute primary care services The delivery of primary care via e-visits on mobile platforms is still in adolescence, with few methodologically rigorous analyses of outcomes of efficiency, patient health and satisfaction Patient satisfaction should be measured and reported in future evaluations to assist in the development of the technologies |
(1) An adequate search was conducted using two databases and additional research was identified through cross-referencing. The search terms used were reported, but it is unclear if any attempts were made to identify unpublished material or if date/language restrictions were applied. Inclusion/exclusion criteria were not adequately reported and no details provided on any other aspect of the methodological process, including quality assessment. There was inadequate reporting of study details, including study designs, country of origin and participant information. Not all included papers were primary studies, with several appearing to be ‘literature review’-type papers. The review authors provide an adequate synthesis of findings from included papers. The conclusions reported are weak In view of the issues above, the findings and conclusions from this review should be treated with caution (2) It is unclear in which country most of the included primary studies were conducted. Despite the poor quality of reporting, the nature of the topic means that some findings potentially have relevance across countries. The authors stated that findings on cost savings/efficiency will not be generalisable beyond the ‘fee-for-service model’ of patient payment |
| Huxley (2015)23 |
Digital communication technology offers marginalised groups increased opportunities to access health care. However, it cannot remove all barriers to care for these groups. It is likely that they will remain disadvantaged relative to other population groups after their introduction There is widespread expectation that the use of digital communication between clinician and patient will improve access to health care for marginalised groups. This review suggests there are likely to be some benefits, but many barriers will remain and not all marginalised groups will gain benefit, owing to their limited access to digital technology. As benefits also apply to non-marginalised groups then patient-clinician communication could potentially be monopolised by those who are already well able to access services and have good access to digital technology. This needs further investigation. Costs to health service providers and patients will also have implications on patterns of access. There is a need to evaluate the impact of the introduction of digital clinician–patient communications on population patterns of access to health care. Further research is required to understand how digital communication can impact on the acceptability and quality of health care, including the impact on patient–clinician communication and the relative advantages and disadvantages of communication with and without visual cues |
(1) This was a realist review. The review was coded ‘adequate’ or ‘good’ to most of the criteria of the RAMESES quality standards. However, overall methods were not reported in detail and it was not possible to assess fully. The review searched a number of databases and the authors consulted a number of health-care professionals and patients to help define the scope of the review. Only studies in English were included Inclusion criteria were not reported in full The quality of the included reviews and studies was reported as being assessed to aid contextualising the results. The results of this assessment were not reported in full, but authors report many had methodological weaknesses It is unclear, overall, how many reviews or studies were included in the review, nor which countries studies were conducted in, although authors state they were all ‘high-income countries’. Details of individual studies were not reported (2) It is unclear how many of the included studies were conducted in the UK. However, the findings relate to several marginalised groups within high-income countries and are likely to be generalisable to a UK setting |
| First author (year of publication) | Summary of authors’ conclusions and implications for research and health care as reported by authors | Reviewer comments |
|---|---|---|
| Atherton (2018)9,10 (ethnographic case study) |
Authors reported that experience of implementing alternatives to the face-to-face consultation suggests that changes in patient access and staff workload may be both modest and gradual. Practices planning to implement them should consider carefully their reasons for doing so and involve the whole practice team Summary of implications: Intervention studies should focus on the consequences for professional relationships, expectations and patterns of work of using technology The low rates of usage of alternative forms of consultation, other than telephone, need further investigation to understand to what extent this relates to a lack of patient awareness or demand, problems of implementation, or simply slow adaptation leading to increased uptake in time Areas to consider include why do you want to do this, which type of alternative are you interested in, who is it for and why, how do we get it right and how will we know if it has worked? When introducing an alternative to the face-to-face consultation the potential for unintended consequences should be considered, as these may have a bearing on the potential success of these forms of consultation |
A well-reported ethnographic case study of eight UK general practices. Provided pertinent data on the rationale for introduction of alternatives to face-to-face consultations, barriers to and facilitators of implementation, as well as GP and patient views Authors note that only one practice served a community with a high proportion of patients from ethnic minority backgrounds |
|
Atherton (2018)9 and Brant (2016)11 (scoping survey) Note, data largely extracted from journal article |
Despite policy pressure to introduce consultations by email and internet video, there is a general reluctance among GPs to implement alternatives to face-to-face consultations. This identifies a substantial gap between rhetoric and reality in terms of the likelihood of certain alternatives (email, video) changing practice in the near futureImplications for research: authors state that the concerns listed are based primarily on perception and anecdote. The general reluctance to adopt alternatives to face-to-face consultations is therefore unlikely to change without a change in policy. More evidence is required before email or internet video consultations can be recommended as a routine part of primary care |
The authors appear to have taken adequate steps to recruit a range of GP practices across geographical and social boundaries and a large number of practices were recruited Reporting of methods used during data extraction are minimally reported Some information relating to GPs recruited is reported but no patient data are available in the report or journal article The statistical methods used appear appropriate The authors acknowledge a risk of response bias, particularly with free text responses. Respondents may have a particular standpoint on the subject. The authors therefore acknowledge that the findings from the survey may not necessarily be generalisable. However, they offer an insight into current use of alternatives to face to face consultations Authors acknowledge that shortly after conducting the survey, many practices introduced e-consult methods, precipitated by the GP Access Fund. These developments were not be reflected in survey results |
| Atherton (2018)9 (routine data collection) |
Authors note that these analyses should be considered as being exploratory, given the small numbers of consultations within some cells, the issues about the reliability of coding and the fact that not all types of alternative were offered in all practices Authors’ conclusions (p. 71):Telephone consultations are much more established and have been used for many years, but, even so, account for only 18% of all consultations, with a maximum of 31% in the practice that used the telephone to the greatest extent. The key finding is that the vast majority (80%) of consultations are still conducted face to face in surgery, even in case study practices selected because they were attempting to make more use of alternatives to face-to-face consultations The pattern of consultation rates in relation to patient characteristics was broadly as expected, with higher rates in children and the elderly, women, patients from ethnic minority groups and patients with multimorbidity. Face-to-face consultation rates were slightly higher in the least deprived areas and telephone consultations slightly higher in the most deprived areas, but otherwise there was no strong relationship with deprivation for these consultation types However, for electronic consultations, some of these patterns were reversed, with the highest rates in young adults and white patients. There was also a clear trend towards higher rates of e-mail consultations in the less deprived areas Most consultations by telephone, e-mail or e-consult are followed by another consultation (often face to face) within 14 days, and this is more common than after an initial face-to-face consultation. Therefore, any analysis of the use of alternatives to face-to-face consultations needs to take account of knock-on effects in the next 2 weeks Further data are provided in the report |
Study methods were reported, and methods of statistical analysis appear appropriate Author highlighted the limitations of the data due to the small number of practices included, differing technology, differences between practices in recording data, missing data and that not all practices offered all types of alternatives The data were collected in the UK |
| Carter (2018)25 |
There is potential to assess the impact of new systems on consultation patterns by extracting routine data from practice databases. Staff and patients noticed subtle changes to responsibilities associated with online options. Greater uptake requires good communication between practice and patients, and organisation of systems to avoid conflicts and misuse. Further research is required to evaluate the full potential of webGP in managing practice workload Implications for research: Future research might recruit practices in which webGP has been used more frequently and for a longer period of time Although case report forms provided valuable information on clinical decisions, not all were completed. A more robust system for the collection of completed forms from participating GPs would be advisable in any future study Implications for practice: Promotion of a shared message among practice staff and with patients, about the introduction of new systems for telephone triage and real time may help overcome some issues, such as staff being protective of their existing systems and wary about patients using webGP gaining an unfair advantage over other patients who are non-users Authors noted that the overall uptake and workload was less than was anticipated by some practice staff, and better communication with and marketing to patients may result in increased use They also noted that webGP did not easily integrate with some existing practice IT systems, and more consideration may be needed in respect of the organisation of appointments and for providing guidance to patients as to when to consult online |
Study was described as mixed-methods design with data from practice databases, GP completion of case reports, patient questionnaires and staff interviews The study was conducted in the south-west of England and will be very relevant The methods used were appropriate for the study and were well described. The qualitative part of the study met most of the criteria for the Critical Appraisal Skills Programme. However, the patient data were taken from free-text boxes in surveys, which may not be considered as in depth as interview data Authors note the evaluation was limited, however, to a small group of practices participating in the webGP pilot implementation in just one CCG area, with a predominantly white British population. Owing to the small population they acknowledge that this does not allow them to assume saturation of themes Uptake of webGP was varied, with very few patients in most practices making use of the new system. Authors also noted that the completeness of consultation data varied between practices. There were also changes within GP practices reported to have taken place during the study period |
| Donaghy (2019)29 |
For follow-up consultations, VC has distinct advantages over TC and, if integrated with current practice IT systems, will provide an alternative to FTFC, where formal physical examination is not required, particularly when discussing test results, medication changes and in some mental health consultations, with considerable time saving to patients VC shows promise for many types of consultation in primary care. Rising ownership of smart devices and experience of video calling will increase demand for such services. However, further investment in IT infrastructure in general practices is required to enable VC to become a routine service Authors expressed intention to conduct further research in a larger number of practices with better integrated VC systems and exploring both acute and follow-up consultations |
Described as a feasibility/pilot study. The research was conducted with a small number of practices and involved follow-up appointments only. However, it is UK based, so findings have a high degree of relevance Methodology appropriate for the study aims and clearly described. Characteristics of participants provided Two researchers were involved in analysing the qualitative data, reducing the potential for bias and error. A summary of the analysis was also fed back to clinicians and patient participants to check agreement with findings and assist interpretation A high proportion of patients with an audio consultation recording completed a questionnaire. No audio-recording was obtained 54 out of 203 recruited patients. Reasons for loss of participants were given. In the largest proportion of cases (21/54, 39%) it was due to the consultation not being audio-recorded by a clinician Authors stated that in a feasibility study, where participants are not randomised, case-mix variation between groups potentially limits the conclusions that can be drawn Limiting to follow-up appointments was justified by the authors on the grounds of helping to control case-mix variation. Text indicates that there was an intention (at least initially) to trial the system on some acute appointments, but the process was considered too complex to be explained and organised by busy reception staff Clinicians found it difficult to recruit people to VC, inevitably resulting in a self-selected group who were largely younger and ‘tech-savvy’ Practices were recruited through a local GP newsletter Some practices declined to participate citing concerns about increased workload and disruption to practice working Appropriate ethics approvals were obtained, as well as patient consent. However, other ethical issues related to data collection/storage, anonymity, etc., were not reported |
| Mehrotra (2013)28 | At the four primary care study practices, e-visits accounted for almost 7% of visits for sinusitis and UTIs. e-visits attract a younger patient population who might use e-visits for convenience reasons. No ‘digital divide’, as employment status and income were not associated with e-visits use in multivariate analyses |
US setting and not based on primary data, but the broad findings in terms of the types of patients who used the technology potentially have UK relevance Paper authors identified a number of limitations. Analysis was based on diagnostic codes, rather than presenting symptoms. For example, among the patients who initiated an e-visit on the patient portal, only 80% were given a diagnosis of sinusitis Comparing e-visits with office visits may not have been the most appropriate comparison, as many physicians utilised telephone care for the two conditions. Urgent care centres and retail clinics are also becoming more popular |
| Uscher-Pines (2016)26 |
Teladoc providers were less likely to order diagnostic testing and had poorer performance on appropriate antibiotic prescribing for bronchitis. Teladoc users were not preferentially located in underserved communities. It appears that Teladoc is primarily serving those in urban areas in close proximity to a range of alternatives for acute care Short-term needs include ongoing monitoring of quality and additional marketing and education to increase telemedicine use among underserved patients Teladoc visits were associated with less diagnostic testing than consultations in physician offices. This has different implications for quality, depending on the condition, as diagnostic testing is recommended for streptococcal pharyngitis but discouraged for lower back pain. Owing to a lack of on-site testing, Teladoc physicians tell patients to seek testing via their primary care physician or an emergency department. Results suggest that patients infrequently do so and, therefore, treatment of conditions where testing is necessary may be inappropriate for this model of care at this time. Authors indicated that Teladoc is developing protocols for physicians to order test directly |
This is a US study based on secondary data analysis Results potentially of limited direct relevance because the vast majority of Teladoc visits occur via telephone rather than by video or app (Uscher-Pines 201427 stated that 98–99% of Teladoc visits for CalPERS enrolees occur by telephone) Authors identified a number of limitations. For example, study focused only on CalPERS patients so results may not be generalised outside California, to different types of patient populations or to telemedicine companies with different features |
| Uscher-Pines (2014)27 |
Teladoc appears to be expanding access to patients who are not connected to other providers. Additional work is needed to fully explore the impact of Teladoc on access, quality and costs. However, findings suggests that Teladoc is offering a useful and potentially cost-effective service Authors make the point that the patients attracted to Teladoc – a more affluent and likely more technologically savvy group – might have fewer access needs then people living in areas characterized by a shortage of primary care or socioeconomic disadvantage. Further research is needed to understand whether Teladoc might be improving access for patients with lower incomes and those in rural areas and, if not, whether it could be positioned to do so in the future It is unclear to what extent Teladoc visits are substituting for office or emergency department visits and to what extent they represent new use of health care for conditions that would have resolved themselves without intervention. If Teladoc visits do represent new use, they could lead to increased utilisation and costs Teladoc providers saw patients with many diagnoses that typically require a physical exam, diagnostic testing, or both. Without the use of additional technology, Teladoc will continue to be limited in its ability to support the diagnosis and management of many conditions Additional research is needed to address questions about the quality of care, such as rates of antibiotic prescribing across settings, the management of conditions that require physical exams or diagnostic testing, and the use of Teladoc by patients with potentially emergent conditions |
Almost all (98–99%) of Teladoc visits for CalPERS enrolees occur by telephone. Therefore, results are of limited direct relevance Study focused only on CalPERS patients so results may not be generalised outside California |
Glossary
- Asynchronous models
- Includes text-based models of communication, such as e-mail or e-consultations via a website.
- Primary care
- The first point of contact for patients and includes general practices [with general practitioners (doctors) and nurses], pharmacy, dentistry and optometry.
- Synchronous models
- Includes voice and video models of communication, including video consulting, face-to-face and telephone consultations. Synchronous text-based communication may include instant messaging and web-based ‘live chat’ applications.
List of abbreviations
- app
- application
- CCG
- Clinical Commissioning Group
- DARE
- Database of Abstracts of Reviews of Effects
- GP
- general practitioner
- HSDR
- Health Service and Delivery Research
- IT
- information technology
- NIHR
- National Institute for Health Research
- RAMESES
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
- RCT
- randomised controlled trial
- SMS
- short messaging service