Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/177/04. The contractual start date was in July 2014. The final report began editorial review in November 2018 and was accepted for publication in July 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Claire Hulme was a member of the National Institute for Health Research (NIHR) Commissioning Board over the life of the project (from 2013 to 2017). Mary Godfrey reports grants from NIHR for Health Services and Delivery Research (HSDR) 12/209/66, HSDR 12/5003/01, Health Technology Assessment 11/143/01 and Programme Grants for Applied Research RP-PG-1210-12017 during the conduct of the study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Young et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background and rationale to study
Nearly 12 million people in the UK are aged ≥ 65 years, which is projected to increase by 5.5 million in the next 20 years, and the number of people aged ≥ 85 years is projected to double to 4 million. 1 An increasingly older population, along with improvements in the management of chronic conditions, will result in more people living to very old age with one or more chronic conditions. 2 As multimorbidity increases with age, over half of those aged ≥ 85 years will have four or more chronic conditions (complex multimorbidity). 3 Furthermore, among more than one-third of those with complex multimorbidity, the burden is exacerbated by mental ill health (e.g. depression and dementia). 3 Multimorbidity is associated with secondary care utilisation, complications during a hospital stay, reduced functional capacity and increased need for co-ordinated care and support to facilitate safe hospital discharge. 4 Multimorbidity therefore poses considerable challenges for appropriate models of treatment and rehabilitation during and following an acute illness and for ongoing support from health and social care services. This is a major issue and decision-makers across the NHS are attempting to reconfigure services to deal with the year-on-year increase in hospital admissions, often with inadequate evidence to inform their decisions.
Community hospitals are a long-established health-care facility in the UK, as well as internationally. They can be loosely defined as small hospitals that provide a wide range of locality-based outpatient and inpatient services such as health promotion, rehabilitation, day hospital and diagnostic services. Specific service configurations differ between community hospitals as a result of local history, proximity to a larger general acute hospital and perceived need. The policy direction for community hospitals was contained in the white paper Our Health, Our Care, Our Say: A New Direction for Community Services. 5 It was expected that primary care trusts would engage in an ‘ambitious’ shift of resources from secondary care to community services over a 10-year period. A new generation of community hospitals was proposed as an important component of the vision for community services within the umbrella term, ‘intermediate care’. The new format for the community hospital was that they should be locally led, of high quality and focus on older people. It was expected that they would provide new care pathways, adopt new technologies, minimise acute hospital admissions, promote integrated solutions and be affordable for the whole health economy. 5
There is high-quality evidence that supports the community hospital as an effective bed-based rehabilitation service for older people. A multicentre study in England randomised patients (n = 490) either to remain in a general hospital ward or to transfer to one of seven community hospitals. 6 The main finding was a significantly greater functional independence at 6 months for the patients allocated to the community hospital group,6 with similar cost-effectiveness. 7 A similar single-centre randomised controlled trial in Norway (n = 142) reported lower mortality and indirect evidence for increased independence for the community hospital group than for the group receiving continued care in a general hospital. 8 There is also evidence that older people are in favour of and, if given the choice, would prefer community hospital ward care. 9–11
This evidence suggesting superior outcomes for older people receiving rehabilitation in a community hospital, at an affordable cost, is encouraging, particularly as most of ≈400 community hospitals in the UK provide inpatient rehabilitation. 12 Thus, community hospitals remain an important provision for health care in the NHS. Considerable additional information describing the contemporary community hospital is available from two other national surveys from the NHS Benchmarking Network (NHSBN): the NHSBN Community Hospitals Project (begun in 2012);13 and the National Audit of Intermediate Care (NAIC). 14 These complementary surveys provide information on 180 community hospitals (approximately two-thirds of all community hospitals in England). Two findings are prominent. First, it is clear that a core function of the contemporary community hospital is rehabilitation for older people: ‘general rehabilitation’ is provided in 97% of the community hospitals. This is in accord with strong policy directives from the Department of Health and Social Care relating to intermediate-care services for older people. 15,16 Second, the contemporary community hospital is characterised by extreme variation in provision [e.g. bed provision per 100,000 weighted population (range < 10–70); clinical leadership (50% nurse led; 50% consultant led); average length of stay (LOS) (11–58 days); cost per admission (£3700–17,500); and cost per day (£140–450)].
This variation in the community hospital was highlighted by the NHS Institute for Innovation and Improvement but, despite provider engagement with their Productive Community Hospital initiative,17 the wide variations have continued. There is evidence that some features might be associated with performance, for example the lack of ward leadership,18 excessive waiting times for admission19 and underprovision of the Comprehensive Geriatric Assessment. 20 However, our knowledge of the features that characterise optimum community hospital ward performance is incomplete as no large-scale study has been designed to systematically investigate the issue. In addition, there is a paucity of information available to service planners about the comparative outcomes and efficiencies of community hospitals in relation to alternative forms of community services, such as home-based rehabilitation and social service enablement services. Thus, when this study began, nearly 10 years on from the white paper Our Health, Our Care, Our Say: A New Direction for Community Services,5 the ‘ambitious’ shift of care focus for older people from secondary care to the community had not been realised. 21
Community hospitals and intermediate care
A prominent and sustained health-care policy for older people during the last decade has been that of intermediate care. Consistent with the established policy direction of increasing the provision of community-based services for older people, intermediate-care policy has been partly driven by the acknowledgement that large general hospitals comprise an environment in which unintended harms (e.g. increased risk of falls, delirium and increased dependency) are common for this vulnerable patient group, and the proposition that intermediate care might be less expensive.
Intermediate care comprises a range of service models designed to provide community-based, short-term rehabilitation with the aim of preventing admission to hospital and/or facilitating early discharge. Intermediate care was first proposed in the National Beds Inquiry,22 became a formal health-care policy in the NHS Plan of 2000,23 and was implemented as part of the National Service Framework for Older People in 2001. 15 Subsequently, intermediate care formed part of a wider health and social care policy loosely summarised as care closer to home. 16 The new role for community hospitals was specifically highlighted in these policy documents and, later, in implementation guidance. However, despite the successful achievement of intermediate-care expansion targets, and release of substantial capital monies for community hospital new-builds, the strategic objective of intermediate care to reduce pressures on acute hospital beds was not realised. ‘Refreshed’ guidance was produced that, once again, encompassed community hospital provision. 24 Acute services continue to be hard pressed, largely owing to a continuing year-on-year increase in acute admissions of older people. 25,26 Despite a decade of consistently applied policy, investment in intermediate-care services to provide short-term rehabilitation for older people appears to have stalled. The NAIC obtained information in 2014 from 62 commissioning and 112 provider organisations (327 intermediate-care services). 27 An important finding was that intermediate-care capacity nationally was around half that required to address the anticipated need for inappropriate admissions and post-acute care for older people. This mismatch of demand and supply has been a constant finding in the subsequent rounds of the national audit. 28,29 In addition, it was apparent that there is considerable scope to free up capacity in many services by simply addressing excessive lengths of intermediate-care stay. The average LOS was considerably longer than those given in the Department of Health and Social Care guidelines: ‘They (intermediate care) are time-limited, normally no longer than six weeks and frequently as little as 1 to 2 weeks or less’ (© Crown copyright 2009. Contains public sector information licensed under the Open Government Licence v3.0). 24 In the national audit,27 75% of patients in bed-based intermediate care had a LOS of > 2 weeks, and 9% of patients had a LOS of > 90 days. Specifically, for a community hospital with 20 beds and 90% occupancy, if the hospital is performing at the 75% quartile (LOS = 31 days) and improved to the 25% quartile (LOS = 21 days), it would be able to treat approximately 100 more patients per year (48% increase). Alternatively, if a 20-bedded community hospital is performing at the 75% quartile for cost per occupied bed-day (£200 per day) and improves to the 25% quartile (£110 per day), the annual cost saving is approximately £650,000.
From a whole-systems perspective, subsequent rounds of the NAIC reported no relationship between the scale of local intermediate-care provision and its impact on secondary care utilisation. 28,29 It was concluded that the case for further investment required new local evaluations to provide better evidence that future increases in intermediate-care capacity would indeed favourably affect secondary care utilisation. Until, and unless, this evidence is available, it will be difficult for commissioners to justify pro-active reductions in the secondary care bed base. In relation to community hospitals, this means that capital investment in new community hospitals will continue to be sporadic and opportunistic rather than strategically planned, and that some community hospitals will close or have bed reductions because of uncertainty over their contribution to the whole-system approach.
Community hospitals are part of this general uncertainty about intermediate care. Indeed, even producing a unifying definition for community hospitals has proved problematic, mostly because there are different models or subtypes of community hospital. This lack of agreement for community hospitals is important because it limits the potential of the commissioning process to shape the service to be delivered and leaves unanswered questions such as ‘what are the critical parameters of a community hospital?’ and ‘what are the tolerances to these parameters?’. For example, some community hospitals are nurse led and some medically led, but nurse-led rehabilitation units (where the admission, assessment, monitoring and discharge of patients are organised by senior nurses, and doctors have an advisory role) have been associated with weak evidence of increased mortality, and may operate at considerably higher unit costs. 18 Not surprisingly, this leads to uncertainty among commissioners and planners about the possible contribution of community hospitals. The number of community hospitals declined slightly between 1998 and 2008 (334 to 296),12 and again up to 2017, but this headline finding disguises a mixed picture of closures offset by newly opened facilities, which reflects an inconsistent approach to the provision of community services for older people.
A popular alternative bed-based form of intermediate care is the model of care home-based rehabilitation. Although widely used (as evidenced in the NAIC), little is known about its effectiveness, cost-effectiveness or safety. Only one randomised controlled trial has been conducted. 30 The NAIC reported that care home-based intermediate care was provided at considerably lower unit costs than community hospital care (£136 compared with £252 per day). 28
Robust comparison studies of different models of community hospital care are needed to provide confidence to patients, practitioners and commissioners in an evidenced-based selection approach that favours community hospital with specific criteria known to be associated with cost-effectiveness. Improved understanding of the role, external relationships, staffing structures and care processes in community hospitals providing intermediate care would clarify their contribution.
Aims and objectives of the research programme
Aims
The Models of Community Hospital Activity (MoCHA) study addressed deficiencies in the existing community hospital evidence base. This study aimed to explore the core unifying function of the contemporary community hospital: rehabilitation for older people. Thus, the key aim was to understand the features that optimise or detract from efficiency of community hospital ward care.
Objectives
-
To measure the current relative performance (cost efficiency) of community hospital inpatient care for older people (studies 1 and 2).
-
To identify the characteristics of community hospital inpatient care for older people that optimise performance (studies 1 and 3).
-
To develop web-based interactive toolkits for use by local commissioners and community hospital teams that support operational changes to optimise performance (study 4).
-
To investigate the current impact of community hospital inpatient care for older people on secondary care and the potential impact if the community hospital care was optimised to best practice nationally (study 5).
-
To determine if there is an association between the configuration (capacity and proportions) of short-term, community-based services (i.e. community hospital wards, home-based rehabilitation, care home rehabilitation and enabling services) and reduction in secondary care bed utilisation by older people (study 5).
Overview of method
The underpinning objectives of the project were addressed through a mixed-methods project design, consisting of five interdependent studies. This approach used existing data alongside complementary prospective data to produce insights that could not be achieved by the study of the components alone, and represents an efficient and effective research design.
-
Study 1: an analysis of cost efficiency of community hospitals (see Chapter 2).
-
Study 2: a national survey of community hospitals (see Chapter 3).
-
Study 3: comparative case study of community hospitals (see Chapter 4).
-
Study 4: development of toolkits for commissioners and community hospital providers to optimise performance (see Chapter 5).
-
Study 5: an analysis of the impact of intermediate-care services on secondary care utilisation (see Chapter 6).
Study team
The co-applicants comprised a team of health economists and efficiency analysis experts led by Claire Hulme; the Patients Association (led by Heather Eardley); the Community Hospitals Association (CHA) (led by Helen Tucker); a social scientist with experience in older people’s services (Mary Godfrey); and academic clinicians with experience in community hospital care delivery (John Young, John Gladman, Elizabeth Teale and Pam Enderby).
Patient and public involvement
Through the participation of the Patients Association and CHA, patient and public involvement was an integral feature of the study from conception and development of the research design to conduct of the research and interpretation and development of the interactive toolkit. Representatives of both (Heather Eardley and Helen Tucker) were co-applicants in the research and their contributions were critical in ensuring that the study engaged with the needs of patients and current quality and performance issues in this service sector. We worked with the Patients Association to produce a ‘primer’ that described the concepts that underpinned the economic efficiency work, concepts that would be unfamiliar to most people (see Appendix 1). This was used as an introduction during two workshops we held at consecutive CHA annual conferences during 2015 and 2016 attended by practitioners and NHS managers.
For all aspects of the study, we engaged with members of the CHA through sequential participation in their annual conferences from 2015 to 2017, where we delivered presentations and workshops, inviting feedback to inform the content and format of the interactive toolkit. Study progress was also conveyed on the CHA website.
In addition, for study 3, we involved our well-informed local older person’s group (approximately 15 people) with which we have a long-standing relationship. This is a subgroup of a forum established by the local authority that comprised approximately 300 retired local people who have been consulted on health and social policy issues. The subgroup has been acting as an advisory body in all aspects of our research with older people since July 2007. Meetings of the group took place to inform data collection methods and contribute to the ethics application, and following conclusion of data collection to reflect on the emerging findings and their implications. We also presented our initial findings to staff groups involved in each of our three case study sites towards the end of the study to further inform our interpretations and conclusions.
Ethics
Ethics approval was required only for study 3 (ethnographic case studies); all of the other studies were based on anonymised, aggregate data. Ethics approval was obtained via the Health Research Authority that governs research ethics in the UK (reference number: 15/YH/0062). The main ethics issues were securing the consent of patients to take part in specific ward observations, conversations and interviews, especially those who might lack capacity on account of dementia or delirium; not seeking formal consent for the general observations of ward routines; and maintaining anonymity of hospitals, wards, trusts/health boards, staff and patients.
Patient consent
The consent procedures adhered to the Mental Capacity Act (2005)31 and accompanying Code of Practice. 32 Consent was an ongoing process. The researchers repeatedly checked with participants that they were happy to continue and were sensitive to any signs of distress or unwillingness to proceed. If any such signs, verbal or non-verbal, were present, we discontinued.
General ward observations
As observations were unobtrusive, carried out in public or semi-public spaces, and did not identify individual staff, patients or visitors by name, we considered that it would be impractical and probably more intrusive to seek formal written consent from all those present. Instead, we sought informal, verbal consent. Prior to each observation, the researcher reported to a senior staff member and introduced themselves to staff not previously met at an opportune moment so as not to interfere with the work flow. At the end of each observation period, the researcher ‘signed out’ with the senior staff member. Emphasis throughout was that observations were conducted with the full knowledge, support and co-operation of ward staff. If anyone appeared unhappy, distressed or uncomfortable, we did not include them in the observation.
Privacy and anonymity
We have used pseudonyms throughout for community hospitals, wards, trusts/health boards, staff, patients and caregivers, and have altered some biographical details to protect anonymity, privacy and confidentiality.
Summary
Community hospitals continue to provide an important function for the NHS. There is high-quality evidence that supports the community hospital as an effective bed-based rehabilitation service for older people. Nevertheless, the contemporary community hospital is characterised by extreme variation in provision and there is evidence that some features may be associated with ward-level performance. Our knowledge of the features that characterise optimum community hospital ward performance is incomplete. In a number of sequential and overlapping studies, and employing mixed methods, this research aimed to understand the features of community hospital ward care that optimise or detract from optimum performance, through the lens of rehabilitation for older people, the core unifying function of the contemporary community hospital, and to provide a resource for community hospitals to inform practice. It also sought to investigate the impact on secondary care of community hospital inpatient care for older people. Patient and public involvement was an integral feature of all aspects of the study through the participation of the Patients Association and CHA and a local older person’s group.
Chapter 2 An analysis of the cost efficiency of community hospitals (study 1)
Introduction
As discussed in Chapter 1, there is a growing body of evidence to support community hospitals as an effective bed-based alternative to rehabilitation in the acute setting in terms of patient outcomes. However, in terms of economic outcomes, the evidence base is much weaker. One study reported community hospital rehabilitation to be cost-effective relative to secondary care in England. 7 Elsewhere, a national study of 180 community hospitals found considerable variation in the provision of services. 26 However, there is only speculation as to the causes of the variation. Finally, on the basis of cost comparisons, it was estimated that there were achievable savings of £1.2–1.8B in community services in general. 33 With a total spend of £8.4B across these services, this represents a potential for cost reduction of around 15%.
In the study presented here, we sought to extend the understanding of community hospitals in respect of the drivers of costs, economies of scale and bed occupancy. Furthermore, we assessed the relative efficiency of ward providers. In collaboration with the NHSBN, we made use of the NHSBN Community Hospital Programme data set encompassing hospitals in England, Scotland and Wales. 13 We adopted a stochastic frontier framework approach, which allowed both the cost structure and cost efficiency to be analysed.
Specifically, study 1 considered the following objectives:
-
study objective 1 – to measure the current relative performance (cost efficiency) of community hospital inpatient care for older people
-
study objective 2 – to identify the characteristics of community hospital inpatient care for older people that optimise performance.
We start with a general description of cost efficiency analysis based on frontier techniques that includes a discussion of the econometric approach to efficiency analysis. We then describe the data and categorisation of the variables to construct the final data set used for modelling. The specific methods and empirical specification of models are described in detail. Finally, we report the results of the analyses and diagnostic statistics with a discussion of interpretation and limitations.
Stochastic frontier analysis for community hospital costs and efficiency
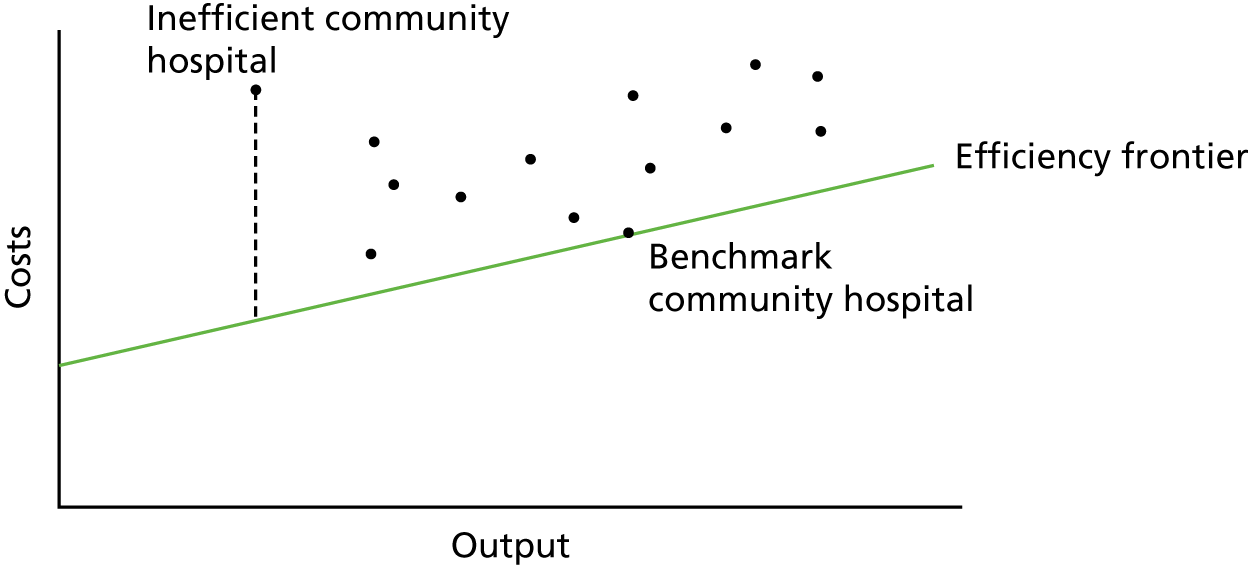
Frontier techniques have a long history of use in efficiency analysis, following pioneering work by Farrell. 34 The principle behind frontier techniques is very simple: an efficiency or ‘best-practice’ frontier is defined, representing full efficiency, and then distances from the frontier are measured, representing inefficiency. That is, the further from the frontier, the higher the inefficiency. This is shown for the case of community hospitals in Figure 1.
FIGURE 1.
Conceptual features of frontier-based efficiency analysis as applied to community hospitals.
Frontiers are regarded as the foremost hospital efficiency analysis tool and are seen to have great potential in health-care markets more widely. 35,36 Frontier techniques have been applied widely in health for measuring efficiency. 36–41 There are, broadly, two approaches to frontier analysis, both of which have been deployed repeatedly to analyse efficiency in health-care markets. The first is an approach based on mathematical programming, data envelopment analysis (DEA), and the second is based on econometric estimation, stochastic frontier analysis (SFA). We make use of SFA in this study because, unlike DEA, it enables us to analyse both costs and efficiency, which are of interest to managers and policy-makers. Furthermore, it enables removal of statistical noise from the predictions of efficiency, which is a key advantage over DEA. 41
The stochastic frontier (SF) model for costs defines the efficiency frontier as a cost function (based on outputs, input prices, environmental variables and quality, thus allowing for variables not in control of the decision-making unit. The frontier assumes the shape of the cost function. The frontier represents the minimum attainable cost for a firm, given its levels of outputs and input prices (and other features defined by the cost function noted above). Deviations of firms from the frontier are considered to be, in part, due to inefficiency, where the distance to the frontier represents the magnitude of the inefficiency. In addition, the SF model allows for the removal of random statistical noise in the data from inefficiency estimates.
The SF model can be computed mathematically as:
where care costs are a function represented as f (. . .) in Equation 1 of output (y), input prices (w), environmental influences (z) and quality (q). The ε term is the observed deviation from the frontier; it comprises both inefficiency (u) and random noise (v) to a firm’s (in this context, a hospital ward’s) production that impinges on its costs, as in Equation 2. Figure 2 shows the conceptual features of the SF model.
FIGURE 2.
Diagrammatic representation of the stochastic cost frontier model.
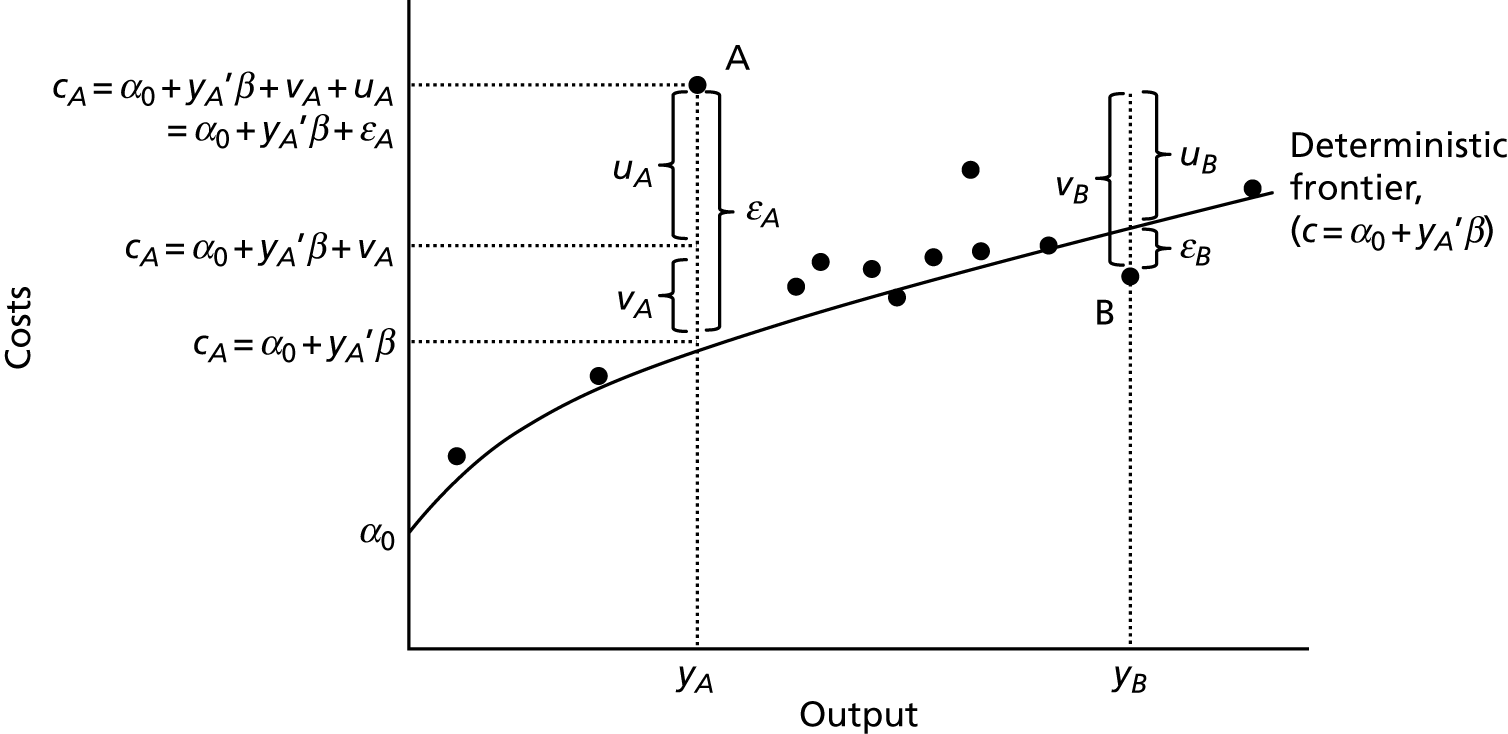
The gradient of the frontier in Figure 2 is defined according to the cost function and is the deterministic element of the model. In this case, costs (c) are defined as a function of outputs (), namely c=α0+y’β.
We consider observation A, representing a specific community hospital A. Here, as shown, community hospital A has output yA, at which the minimum attainable costs for community hospital A (shown via the cost frontier) are cA=α0+ y’Aβ. The observed value is in fact point A, which is higher than the deterministic frontier for community hospital A, given its level of output. Then, the community hospital-specific observed deviation ϵA comprises both the community hospital’s inefficiency uA and random statistical noise vA. In this case, both noise and inefficiency have a positive influence on costs.
In some cases, community hospitals are observed to be below the deterministic frontier, as in observation B for which the observed deviation from the frontier εB is negative. This is the result of a noise component vB, which is negative and greater than the community hospital’s (positive) inefficiency uB. Here, community hospital B has output yB at which the cost frontier is cB=α0+y’Bβ.
Random noise can encompass a number of features. In non-health-care settings, these typically comprise random ‘shocks’ to production that include untoward events, such as strikes, unusual weather, force majeure, etc. In addition, this component can account for measurement error and approximation error (from the choice of functional form). 41 The defining feature of the SF model is its ability to remove these factors so that they do not distort the underlying metric of interest: inefficiency.
Although we had originally planned to use DEA as a cross-check for ranking efficiency scores, we did not apply DEA because the method does not deal well with random noise in the data and also because we were interested in establishing the relationship between costs and cost drivers, which DEA does not support. We therefore decided to focus on econometric methods as the most appropriate method for the research objectives.
NHS hospital efficiency studies
Although there is no previous evidence on cost efficiency for community hospital wards, there is a wealth of econometric evidence for the general hospital setting. We did not undertake a full systematic review. Instead, a scoping search was carried out in MEDLINE in 2015. The search included all relevant publications published up to 30 September 2015. In addition, research papers already known to the authors of this study were included and citation tracking of identified papers used. A list and summary review of these studies42–53 is provided in Table 1. This will facilitate later comparisons between the two types of inpatient ward provision.
| Year | Authors | Methods | Unit of analysis | Sample size (n) | Years | Observations (n) | Findings |
|---|---|---|---|---|---|---|---|
| 2001 | Harper et al.42 | COLS | General surgery specialties | 31 | 1998/9–1999/2000 | 62 | No efficiency predictions reported; rank correlations only, which were highly correlated between models |
| 2002 | Street and Jacobs43 | COLS; SFA | Whole hospital | 217 | 1999 | 217 | Average inefficiency: 0.74 COLS; 0.90–0.92 for SFA |
| 2003 | Street44 | COLS; SFA | Whole hospital | 236 | 1999 | 236 | Average inefficiency: 0.69 COLS; 0.87–0.90 for SFA |
| 2006 | Ferrari45 | SFA (distance function approach) | Whole hospital | 52 | 1991/2–1996/7 | 312 | Productivity gain average 3% per annum; no time-varying inefficiency; no efficiency estimates reported |
| 2006 | Jacobs et al.46 | COLS; SFA | Whole hospital | 185 | 1994/5–1997/8 | 740 | Mean efficiency across range: COLS 0.69; SFA cross-section 0.87–0.90; panel 0.61–0.92 |
| 2010 | Laudicella et al.47 | 2SLS cost function | Obstetrics | 136 hospitals; 952,273 patients | 2005/6 | 952,273 | More and less efficient units identified; efficiency itself not quantified explicitly |
| 2012 | Cooper et al.48 | Difference-in-differences | Individual procedure | 161 hospitals; 1,882,750 patients | 2002/3–2010/11 | 1,882,750 | Competition appeared to induce efficiency improvements |
| 2013 | Daidone and Street49 | 2SLS cost function | Specialised services | 163 hospitals; 12,154,599 patients | 2008/9 | 12,154,599 | Some variation in hospital efficiency but not reported |
| 2013 | Gutacker et al.50 | Multilevel cost function | Individual procedure | 147 hospitals; 194,570 patients | 2009/10 | 194,570 | For hip replacement, 95% of providers within a range of –£2740 to £3690 (mean £6335) |
| 2015 | Buckell et al.51 | SFA | Pathology laboratories | 57 hospitals | 2006/7–2010/11 | 187 | Efficiency of around 0.87; efficiency decreased over time; multifactor productivity increased over time |
| 2015 | Moran and Jacobs52 | Ordered probit; linear model | Mental health | 58 providers; 185,281 patients | 2011/12–2012/13 | 342,288 | Performance based on outcomes; variation of around 11% in ordered probit and around 2% in linear model attributable to providers |
| 2015 | Smith et al.53 | SFA | Pathology laboratories | 57 hospitals | 2006/7–2010/11 | 187 | Variation in efficiency at different levels in the organisation; average efficiency around 0.77 |
We note the link between the cost function methods used and the SFA literature. In several studies, a hospital-specific effect from a cost function is used as the measure of hospital efficiency (some authors use the term performance). 47,49,50,52 In this sense, they are akin to the panel data SF models that measure time-invariant inefficiency. 41,47
Community hospital data set
The NHSBN is the in-house benchmarking service of the NHS. The Network has 270 members including Clinical Commissioning Groups (CCGs), acute and mental health trusts and community providers, and runs a range of benchmarking projects across all sectors of NHS provision. Members submit locally collected data to participate in the projects. Participation is not compulsory and incomplete data submissions are accepted.
The NHSBN Network Community Hospital Programme was instigated at the request of the network members to provide a structured comparison using key metrics that include workforce, activity, investment levels and quality measures. However, the granularity of the NHSBN Network Community Hospital data set at the ward level for older people was insufficient for the analysis. Further questions were therefore added to the data collection process for the 2013/14 survey13 to enable capture of data at a level to facilitate the analyses, namely at ward level. However, this meant that only this version of the Community Hospitals Project was used for this study, which collected data on 158 community hospitals from the financial year 2013/1413 (not the 3 years originally anticipated).
We started by categorising the variables into general features of the community hospital, information on patient access, services provided, workforce characteristics, activity of community hospitals, financial data and service quality. The nature of the variables includes continuous, categorical, binary and qualitative data.
Our unit of analysis was the community hospital ward for older people. Provision of services on older people’s wards is the core activity of community hospitals. We adopted this approach for a variety of reasons. First, it allowed us to maximise the sample size, as there was a high number of missing data for variables at the whole-hospital level (Table 2 shows a variable summary of missing data). Second, this allowed us to better control for the issue of heterogeneity between providers than would be the case at the whole-hospital level 54 (there is less heterogeneity in the provision of services on the ward). This is important as we have a limited number of variables on patient characteristics, quality, hospital characteristics and input prices. Third, following an initial modelling exercise, results indicated that models at the whole-hospital level yielded questionable results in terms of parameter estimates and, consequentially, efficiency predictions, probably because of the high number of missing data. Fourth, by focusing on wards, managers are better placed to understand the source of inefficiency than with whole-hospital analysis, in which the source of inefficiency may be unclear.
| Variable | Description | Categorya | Variable type | Wards (n) | Missing (n) |
|---|---|---|---|---|---|
| Community hospital older people’s ward costs (£) | Operating costs for older people’s wards | c | Continuous | 129 | 28 |
| Total number of admissions to all older people’s wards in this community hospital (2013/14) | Total admissions | y | Continuous | 143 | 15 |
| Occupied bed-days (all older people’s wards) (2013/14) | Total occupied bed-days | y | Continuous | 139 | 19 |
| Materials input prices (£) | Non-staff operating costs divided by the number of beds | w | Continuous | 119 | 39 |
| London weight | Binary variable taking the value of 1 if the London wage supplement is received | w | Binary | 113 | 45 |
| Staff mix (average annual salary of clinical staff, £) | Total staff costs divided by the number of staff in whole-time equivalent terms | z | Continuous | 130 | 28 |
| Bed occupancy (%) (all older people’s wards) (2013/14) | Ratio of used to available beds | z | Continuous | 138 | 20 |
| Average LOS for older people’s wards (2013/14) | Average number of days patients stay on the ward | z | Continuous | 139 | 19 |
| Number of services | Number of services provided by the community hospital | z | Continuous | 158 | 0 |
| Number of beds on older people’s wards | Number of beds on wards | z | Continuous | 158 | 0 |
| Approximately how old is your community hospital? (< 20, 20–50, 50–100, > 100 years) | Age of the community hospital, years, by category | z | Categorical | 141 | 17 |
| Does this community hospital have specific admission criteria set out in a formal policy or service level agreement? (Y/N) | Patient selection criteria, may be indicative of higher-severity patients where true | z | Binary | 120 | 38 |
| Diagnostics (Y/N) | Diagnostic services provided – proxy for case mix | z | Binary | 114 | 44 |
| Proportion of senior staff (%) | Ratio of senior staff to total staff | q | Continuous | 142 | 16 |
| Proportion of physiotherapists and occupational therapists (%) | Ratio of physiotherapists and occupational therapists to total staff | q | Continuous | 141 | 17 |
| MDT meetings weekly? (Y/N) | Proxy for quality | q | Binary | 133 | 25 |
| Has the community hospital been involved in any research programmes during the previous year? (Y/N) | Proxy for quality | q | Binary | 120 | 38 |
| Frequency of clinical governance meetings (no meetings, monthly, quarterly, annually) | Proxy for quality | q | Categorical | 137 | 21 |
Our data set comprises 158 community hospital wards from 158 NHS providers and 18 variables per ward. Of these, 11 were continuous variables, five were binary variables and two were categorical variables. The continuous variables comprise what can be seen as core variables (i.e. the dependent variable and variables on outputs and input prices) and some environmental variables (these include, for example, patient selection policy and provision of diagnostic services). There are also continuous quality variables. See Table 2 for the list of variables, their descriptions, classification and missing data.
Some of the variables we used were constructed from other variables in the data set. Materials input prices were defined as the non-labour operating costs divided by the number of beds. Staff costs were calculated by the total labour costs divided by the number of staff, in whole-time equivalent (WTE) terms. The proportion of physiotherapy/occupational therapy staff and senior staff was defined as the ratio of each of these to the total number of staff.
We removed 14 outliers from the data set. For materials input prices, there were two clear outliers (around £100,000; the mean for this variable is around £9000). For staff mix, observations in excess of £50,000 were removed (i.e. where average wages were > £50,000). In this case, 12 observations were removed. All other variables appeared to have plausible distributions. Furthermore, we tested models that included the outliers and estimates did not appear to be sensitive. After cleaning the data set for missing values and outliers (some remained unverified), 101 community hospital wards were available for analysis. Thus, we undertook a complete-case analysis (having also removed outliers from the data set).
Descriptive statistics
The descriptive statistics for the 101 community hospital wards are presented in Table 3. For each variable, the category (see Equation 1), mean, standard deviation, minimum, maximum and number are reported.
| Variable | Mean | Standard deviation | Minimum | Maximum |
|---|---|---|---|---|
| CH ward costs (£) | 2,255,170 | 1,504,690 | 624,526 | 7,970,050 |
| Number of admissions to CH ward | 417 | 254.65 | 107 | 1499 |
| Occupied bed-days | 10,671 | 7324.06 | 2886 | 47,295 |
| Materials input prices (£) | 9293 | 9855.11 | 1989 | 50,998 |
| London weighting | 0.10 | 0.30 | 0.00 | 1.00 |
| Staff mix (average annual salary of clinical staff, £) | 31,617 | 9646.70 | 5291 | 48,935 |
| Bed occupancy (%) | 89.69 | 6.59 | 68.90 | 100 |
| Average LOS (days) | 26 | 7.82 | 12 | 53 |
| Number of services provided by CH | 14 | 5.99 | 3 | 27 |
| Number of beds in ward | 31 | 20.49 | 4 | 130 |
| Approximately how old is your CH? (< 20, 20–50, 50–100, > 100 years) | 2.50 | 1.08 | 1.00 | 4.00 |
| Does this CH have specific admission criteria set out in a formal policy or service level agreement? (Y/N) | 0.71 | 0.45 | 0.00 | 1.00 |
| Diagnostics available (Y/N) | 0.48 | 0.50 | 0.00 | 1.00 |
| Proportion of senior nursing staff (%) | 0.16 | 0.09 | 0.02 | 0.46 |
| Proportion of physiotherapists and occupational therapists (%) | 0.18 | 0.18 | 0.00 | 0.91 |
| MDT meetings weekly? (Y/N) | 0.88 | 0.33 | 0.00 | 1.00 |
| Has the CH been involved in any research programmes during the last year? (Y/N) | 0.24 | 0.43 | 0.00 | 1.00 |
| Frequency of clinical governance meetings (no meetings, monthly, quarterly, annually) | 2.93 | 0.49 | 1.00 | 4.00 |
We can see that, on average, the annual expenditure for the provision of a community hospital ward is £2.3M.
For the output variables, on average, 417 patients were treated each year, accounting for around 11,000 occupied bed-days.
The London weighting variable suggests that around 10% of our sample are based in London (we do not have any further geographical information).
For the environmental variables, average bed occupancy reveals that community hospital wards are close to capacity, with an occupancy rate close to 90%. The National Audit Office (NAO) suggest that bed shortages may occur when bed occupancy is in excess of 85%. 55
Community hospital age is a categorical variable for which categories reflect incrementally older community hospitals.
The remaining environmental variables show various environmental aspects of the sample of community hospitals. Around 70% have a patient selection policy, and around half provide diagnostic services.
For the measures of quality, on average, senior staff occupy 16% of the workforce. There is a range from around 2% up to around 46%. Although the mean is approximately the same for the ratio of physiotherapy and occupational therapy (18%), the range is much greater: from 0% up to 91%. It appears that most community hospitals hold regular governance meetings (88%) and that around one-quarter have been involved in research programmes (24%).
Methods for model specification and estimations
Functional form and inefficiency
Having specified the form of our economic model (see Equation 1), and detailed the data, we now move to the specification of our econometric model. We begin with a Cobb–Douglas functional form. The Cobb–Douglas form allows the estimation of a linear function when log-transformed. Thus, the Cobb–Douglas realisation of Equation 1 is:
where:
-
ci – operating costs of older people’s wards for community hospital i
-
yi – output of older people’s wards for community hospital i
-
wi – input prices of older people’s wards for community hospital i
-
zi – environmental variables of older people’s wards for community hospital i
-
qi – quality of older people’s wards for community hospital i
-
ui – inefficiency of community hospital i.
α0 is the intercept and vi is the random noise in the data. ln(·) denotes that the variable is in natural logarithms.
To retrieve community hospital-specific predictions of inefficiency, ui above, it is necessary to make distributional assumptions about both ui and vi.The standard assumptions are that inefficiency is distributed with half-normal truncated at zero, and noise is normally distributed with zero mean. This is referred to as the normal-half normal model.
Then, using the method of Jondrow et al. ,56 community hospital-specific prediction of inefficiency, u^i, can be computed as:
where i is the number of observations, σ2=σu2+σv2 and λ2=σu2/σv2. When λ2 = 0, the variance is due solely to random noise – there is no inefficiency. 39 The disturbance is defined as εi=vi+ui=c−α0−x’β. Φ(x) is the cumulative distribution function of the standard normal variable evaluated at x. ϕ(x) is the corresponding probability density function.
Finally, the estimate of cost efficiency from the SF model is:
The βs are the first derivatives of cost with respect to each variable and so, for example, in the case of output ∂ln(c)∂ln(y)=β1. This allows direct interpretation of the parameter estimates as cost elasticities. Using the coefficient on output, we can observe the economies of scale properties in the provision of services. In addition, using natural logarithms is useful for technical issues, such as helping to reduce heteroscedasticity. 57
It is possible to examine the properties of the cost function in greater detail by using more complex functional forms. A common form used in the literature is the transcendental logarithmic, or translog. 46 As with the Cobb–Douglas form, natural logarithms are taken. This form differs through the addition of both higher order and interaction terms between variables. A translog has some appealing empirical and economic features: its flexible nature means it provides a second-order differential approximation to any unknown function (.);58 it does not impose restrictions on substitution possibilities and allows economies of scale to vary with output levels. This is likely to provide a better empirical approximation of the unknown cost function than the Cobb–Douglas form. The price is the addition of variables, which may affect the precision of estimates. The translog realisation of Equation 1 is:
where variables are as in Equation 7.
An appealing feature of these specifications is that the translog nests the Cobb–Douglas form. That is, the Cobb–Douglas form is a special case of the translog in which the squared and interaction terms are all equal to zero. In the empirical setting, it is possible to use a Wald test to test this restriction and, thus, as a means of deciding between specifications. We report the results of these tests in the following section.
Estimation results, community hospital ward costs and efficiency
Estimation outputs
Table 4 reports the six estimated models. Although we tested the complete set of variables in Table 3, we did not find that all variables were significant. We began with a full model and tested down to arrive at a parsimonious specification including only variables that were significant. Four variables were retained as statistically significant, namely the number of occupied bed-days (that relates lengths of stay and number of admissions), bed occupancy rate, nursing staff skill mix and materials input prices. We report models after having applied a Wald test to decide between specifications. In all cases, the translog was rejected, meaning that the Cobb–Douglas form was adopted in all cases. The exception to this was that the higher-order term for bed occupancy was retained as it was found to be significant.
| Regressors | COLS | Half normal | Truncated normal | Exponential | Gamma | Rayleigh | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | Significance | Coefficient | Significance | Coefficient | Significance | Coefficient | Significance | Coefficient | Significance | Coefficient | Significance | |
| Constant | 1.57243 (0.869) | * | 1.20133 (0.926) | 1.23144 (0.998) | 1.42859 (1.056) | 1.54492 (0.904) | * | 1.10161 (0.989) | ||||
| Log-(occupied bed-days) | 0.8451 (0.050) | *** | 0.851935 (0.051) | *** | 0.846839 (0.0540 | *** | 0.853875 (0.051) | *** | 0.852711 (0.051) | *** | 0.846726 (0.054) | *** |
| Log-(materials input prices) | 0.19074 (0.040) | *** | 0.197202 (0.038) | *** | 0.193506 (0.039) | *** | 0.203948 (0.039) | *** | 0.205231 (0.038) | *** | 0.195717 (0.038) | *** |
| Log-(staff mix) | 0.29368 (0.062) | *** | 0.34732 (0.069) | *** | 0.346611 (0.062) | *** | 0.32774 (0.076) | *** | 0.320843 (0.056) | *** | 0.346643 (0.061) | *** |
| Log-(bed occupancy) | –1.24419 (0.511) | ** | –0.943673 (0.511) | * | –0.998334 (0.642) | –0.9678 (0.547) | * | –0.98829 (0.560) | * | –1.00774 (0.601) | * | |
| [Log-(bed occupancy)]2 | –13.5702 (3.081) | *** | –13.2466 (2.946) | *** | –13.6751 (2.817) | *** | –12.6519 (3.090) | *** | –12.6581 (2.573) | *** | –13.7243 (2.670) | *** |
| λ/θ | 2.0511 (0.519) | *** | 2.08783 (1.256) | * | 6.337 (2.527) | ** | 5.51691 (2.578) | ** | ||||
| σ | 0.36822 (0.003) | ** | 0.32454 (0.109) | *** | 0.20249 (0.039) | *** | 0.21320 (0.032) | *** | 0.34629 (0.069) | *** | ||
| μ | 0.199992 (0.451) | |||||||||||
| Probability | 0.61667 (0.235) | *** | ||||||||||
| R 2 | 0.79 | |||||||||||
| Log-likelihood | –5.0826 | –4.06141 | –4.03529 | –4.27569 | –3.49423 | –4.007 | ||||||
| AIC | 24.1 | 26.1 | 24.6 | 25.0 | 24.0 | |||||||
| Log-likelihood vs. OLS | 2.043 | * | 2.095 | 1.614 | 3.443 | * | 2.151 | * | ||||
| Degrees of freedom | 6 | 8 | 9 | 8 | 9 | 8 | ||||||
Number of log-likelihood versus ordinary least squares is a statistical test of the stochastic frontier model versus the basic cost function
Cost elasticities
We now consider the cost elasticities. Elasticity refers to the relative rate of change of outputs and costs. If the cost elasticity with respect to outputs is < 1, then outputs are rising at a faster rate than costs. This implies that there are economies of scale present. If the elasticity is > 1, then costs are rising at a faster rate than outputs. Here, diseconomies of scale are present.
The parameter estimates appear to be consistent with each other and with the ordinary least squares (OLS) estimates in the corrected ordinary least squares (COLS) model. This is important as the COLS model does not impose the distributional assumptions that the SF models do, meaning that the parameter estimates are more reliable. Moreover, the parameter estimates appear to be in a plausible range and consistent with expectations, which we discuss below. The R2 for the COLS model reveals that the model has good explanatory power, accounting for 79% of the cost variation in the sample, even with a fairly limited number of variables.
The cost elasticity with respect to output is highly significant and consistent across all models, at around 0.85. This suggests that a 1% rise in output is associated, on average across the sample, with a 0.85% increase in costs. This, in turn, suggests that output is rising (in terms of proportion) more quickly than costs, implying that there are some economies of scale in the provision of services in older people’s wards. One outstanding issue is that no evidence was found to support variation in economies of scale across the output range: higher-order terms were not found to be significant. It was suggested that the economies of scale properties were likely to vary between community hospitals, but no evidence was found to support this.
Cost elasticity with respect to input prices is, as with output, highly significant and consistent between models, at around 0.20. This suggests that, on average, an increase in materials prices of 1% is associated with a 0.2% rise in costs, all other things remaining equal. Prices are similar for different regions across the country.
For staff mix, the parameter estimates are all positive and highly significant, reflecting that use of a higher proportion of staff on higher bands inflates costs, which is unsurprising. There is slight variation between models, where coefficient estimates are in the range 0.29–0.35. This suggests that a 1% increase in spend per staff is associated with a 0.29% to 0.35% increase in costs.
Bed occupancy has been specified with the addition of a higher-order term, which was the preferred specification in all cases. The variables have been mean-scaled to allow direct interpretation of the first-order term (they represent the cost elasticity at the sample mean). Therefore, the parameter estimates on the bed occupancy variables can be discussed directly. The coefficients suggest that a 1% increase in bed occupancy is associated with a 0.94–1.24% decrease in operating costs. That the data supported a second-order term implies that the relationship is non-linear. The results suggest that the second-order term is negative. Then, the second derivative is also negative, implying negative concavity in the relationship. This implies that the elasticity at the higher end of the range will be lower than at the lower end of the range. This suggests that the effect on costs of having higher bed occupancy is greater for community hospitals with bed occupancy levels that are at the lower end of the range.
Overall, that the parameter estimates are reasonable, the R2 value is high and that the parameter estimates are consistent between models suggest that the models are good representations of the underlying cost function.
Model testing
For functional form, as noted, we made use of a Wald test to decide between a Cobb–Douglas and translog specification. The joint test on the higher order and interaction terms rejected their inclusion. We further tested down by individually testing each of the translog terms. The only term that we found to be significant was the second-order term on bed occupancy. We therefore retained this variable in our final specification.
We used a likelihood ratio procedure (LR) to test for the presence of inefficiency. 59 This involves a test of the SF against its OLS counterpart (the SF nests the OLS model). The LR test statistic is:
which has an asymptotic distribution, which is a 50 : 50 mixture of χ02 and χ12. 46 LOLS is the log-likelihood for OLS, and LSF is the log-likelihood for the SF model at hand.
Rejection of the null, H0 : LOLS = LSF, in favour of the SF indicates that the SF model is a better fit of the data. Our interpretation of this result is the presence of inefficiency.
This procedure was applied to the full set of models estimated and the results are reported in Table 3. With the exceptions of the truncated-normal and normal-exponential SF, all null hypotheses are rejected at the 10% level (given the relatively small sample size). That is, three out of five of our models support the presence of inefficiency in the data.
Although it is not possible to statistically test between SF models directly (they are not nested), it is possible to use information criteria to identify a preferred model. In this case, using the Akaike information criterion (AIC) (see Table 3), the Rayleigh SF is preferred as its AIC value is lowest. We note, however, the similarity between SF models in respect of LR, AIC and parameter estimates, rendering this choice somewhat irrelevant. This is one reason why we use the full range of efficiency estimates in making judgements about community hospital efficiency.
Community hospital ward efficiency
Descriptive statistics for efficiency predictions from the range of models are presented in Table 5. Corresponding kernel densities are presented in Figure 3.
| Efficiency specification | Meana | Standard deviation | Minimum | Maximum |
|---|---|---|---|---|
| COLS | 0.560 | 0.138 | 0.263 | 1.000 |
| Half normal | 0.808 | 0.087 | 0.514 | 0.940 |
| Truncated normal | 0.823 | 0.083 | 0.524 | 0.943 |
| Exponential | 0.878 | 0.063 | 0.575 | 0.952 |
| Gamma | 0.921 | 0.049 | 0.645 | 0.975 |
| Rayleigh | 0.724 | 0.087 | 0.458 | 0.888 |
| Mean | 0.831 | 0.543 | 0.939 |
FIGURE 3.
Kernel densities for efficiency predictions. HN, half normal; TN, truncated normal.
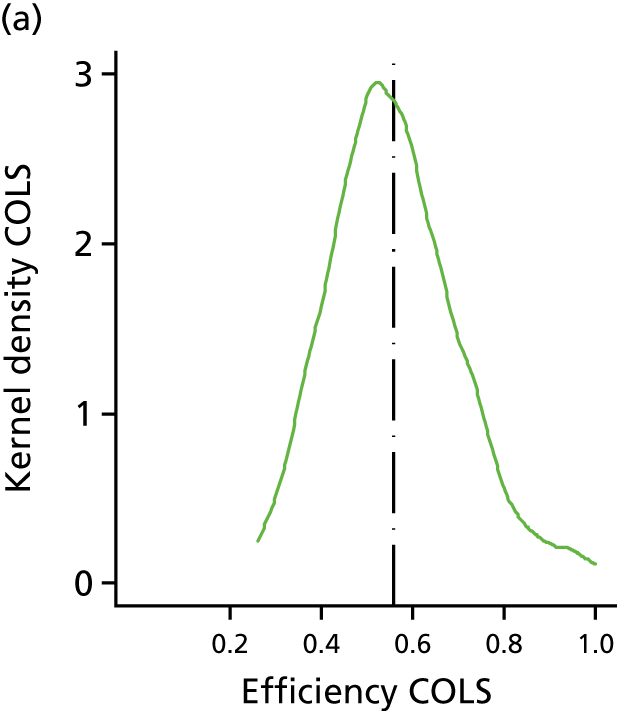
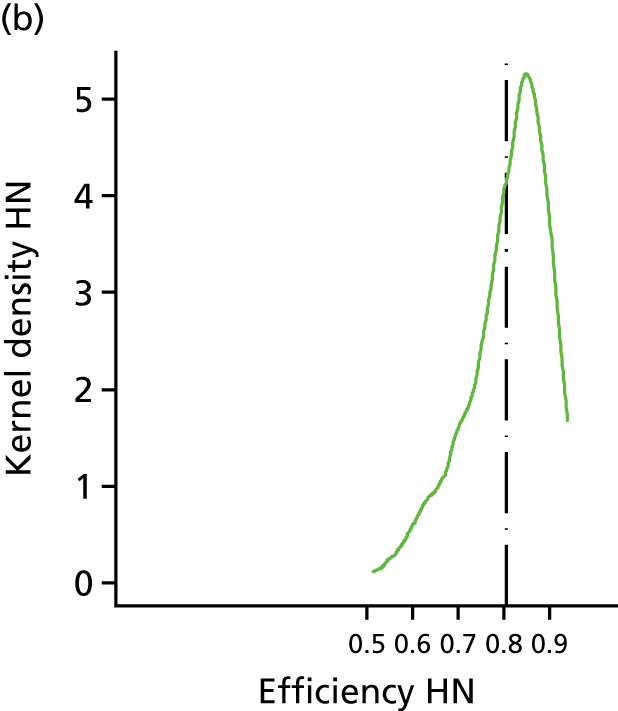
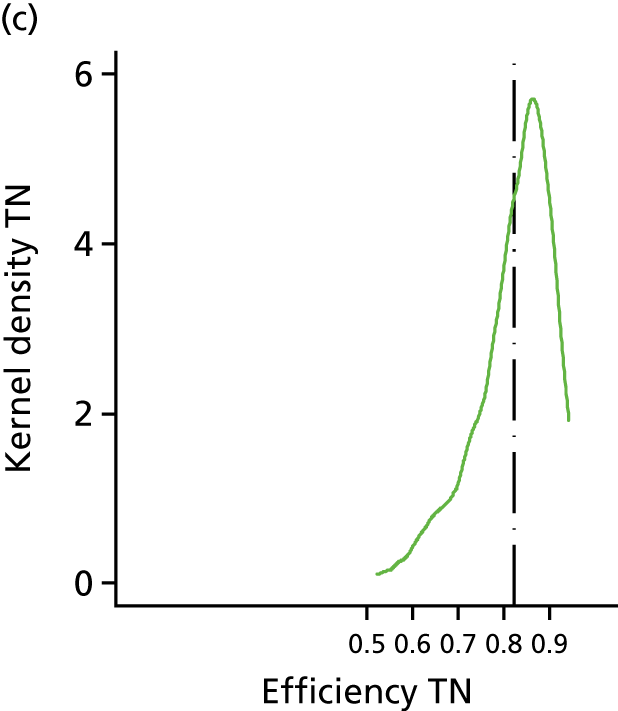
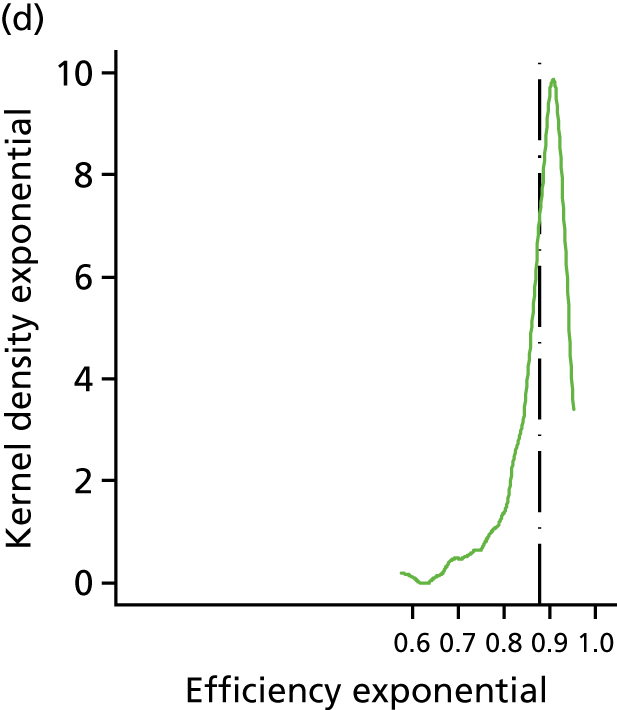
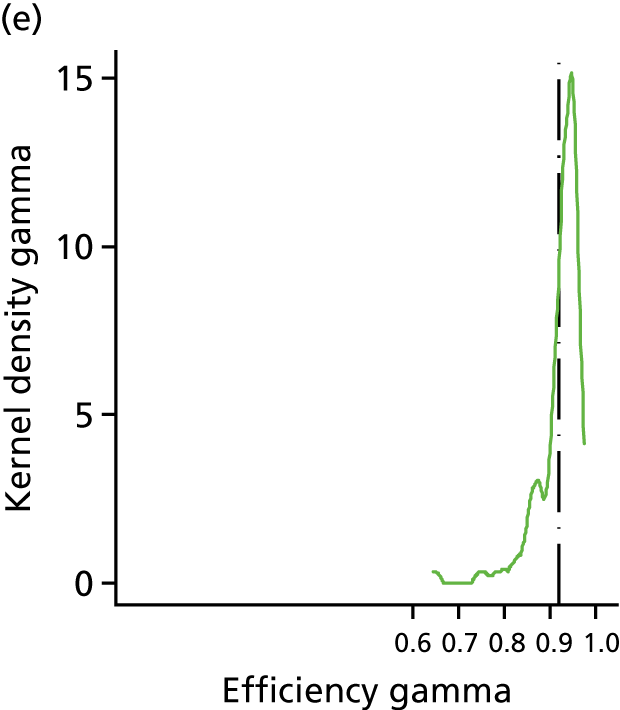
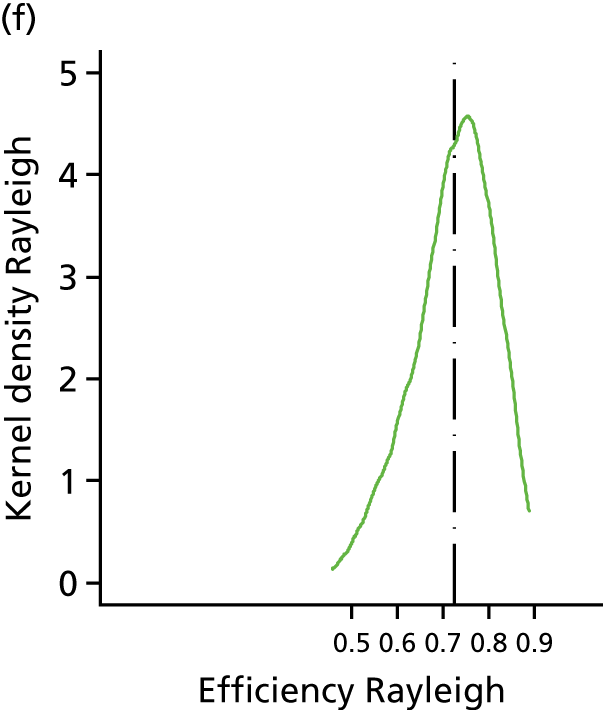
In Table 4 we can see that, in three out of five specifications, the SF model was preferred to OLS. As expected, the COLS average efficiency is much lower than the remaining models, owing to the failure to separate statistical noise from efficiency. Indeed, the minimum value is much lower than those of comparator models. Specifically, a value of 0.26 suggests that this community hospital ward could reduce its costs by 74% if it brought its performance in line with best practice. This result seems rather implausible, particularly as the analysis is focused on the ward rather than the whole community hospital. For these reasons, the efficiency predictions from the COLS model have been discarded.
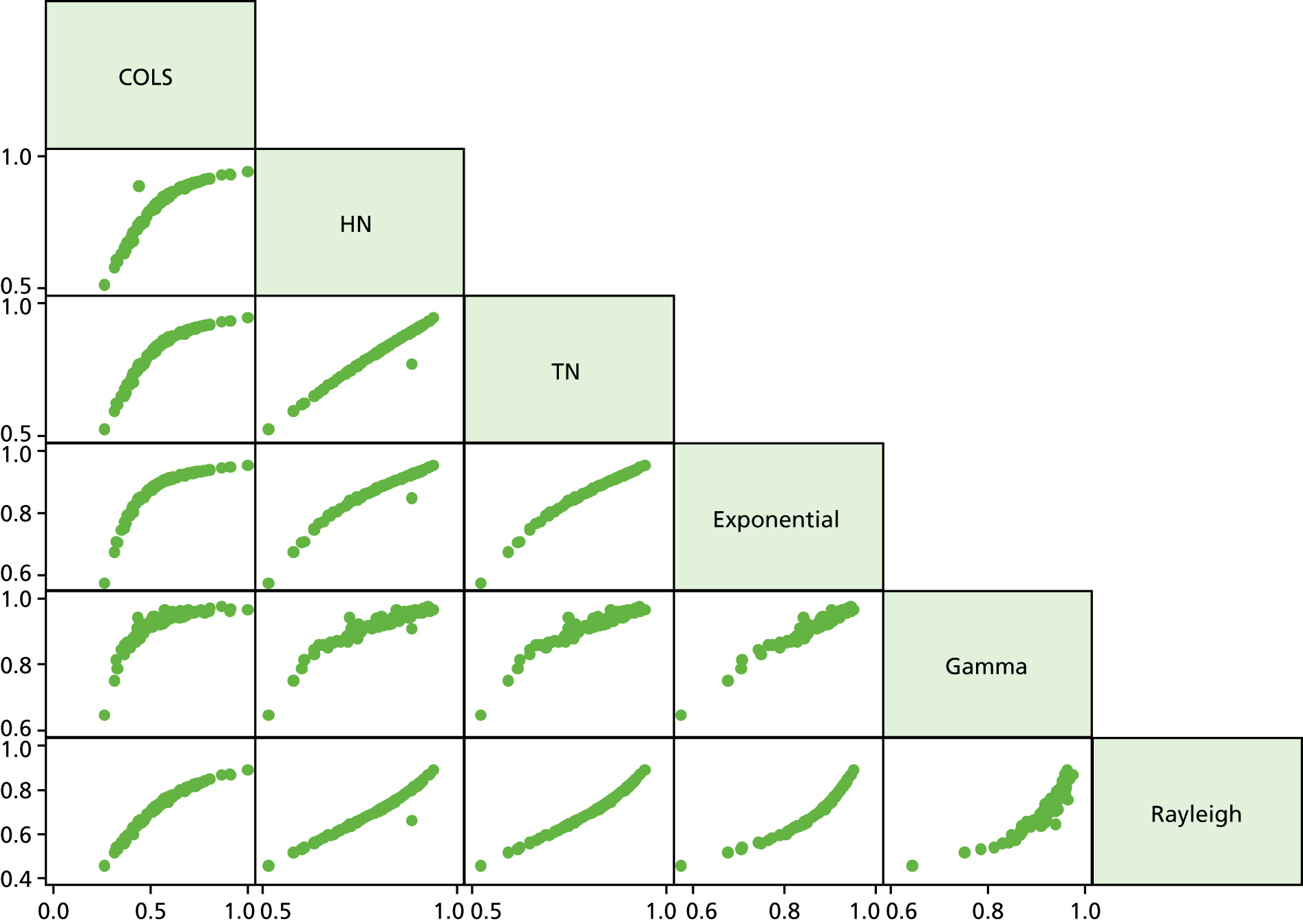
For the remaining models, the mean efficiency predictions are in the range of 0.72–0.92, with an average of 0.83. The interpretation of this number is that, on average, community hospital wards could reduce operating costs by 17% if the performance of all community hospitals was brought in line with best practice. The minimum ranged from 0.46 to 0.58 with an average of 0.54, and the maximum ranged from 0.89 to 0.98 with an average of 0.94. There was some variation in the standard deviations between model predictions, which can be seen in the kernel densities in Figure 3. Some of the models yield predictions with similar average efficiency, whereas others do not. The range in mean predictions of efficiency of 20% (0.72–0.92) is rather large. Therefore, there is a question as to how the efficiency predictions correlate between models. We examine this issue in detail in Tables 5 and 6, by looking at models’ efficiency prediction correlation in terms of absolute values and rank. Figure 4 shows the correlation matrix graphically.
| Correlation | COLS | Half normal | Truncated normal | Exponential | Gamma | Rayleigh |
|---|---|---|---|---|---|---|
| COLS | ||||||
| Half normal | 0.91 | |||||
| Truncated normal | 0.91 | 0.99 | ||||
| Exponential | 0.84 | 0.96 | 0.98 | |||
| Gamma | 0.77 | 0.91 | 0.93 | 0.97 | ||
| Rayleigh | 0.96 | 0.98 | 0.99 | 0.95 | 0.89 |
FIGURE 4.
Correlation matrix absolute efficiency predictions. Note that all of the cells in the figure are actually an individual graph themselves. All are showing efficiency: both x- and y-axes. HN, half normal; TN, truncated normal.
It is unsurprising that the Rayleigh model predicts the lowest efficiency given that this distribution allows for a non-zero modal value. Although this is also true for the truncated-normal model, this does not appear to be the case. We note, however, that the mu parameter is not significant in this model, which may explain this finding. Indeed, using the LR test, the half-normal model is preferred to its truncated-normal alternative.
Tables 6 and 7 and Figure 4 show pairwise correlation between the predictions of efficiency, which is high. Farsi et al. 54 suggest that values in excess of 0.90 denote concordance between models. That almost all pairs of efficiency predictions are over 0.90 in Table 6 reflects similarity between models’ predictions. Moreover, in terms of rank correlation, as shown in Table 7, not only are correlation coefficients high, they are statistically significant across all pairs of predictions. This high correlation is visible in Figure 4. These results hold for the COLS model, which may be expected to give different results because of its composed error. We do not find any evidence of this in this instance.
| Kendall’s tau | COLS | Half normal | Truncated normal | Exponential | Gamma | Rayleigh |
|---|---|---|---|---|---|---|
| COLS | ||||||
| Half normal | 0.93*** | |||||
| Truncated normal | 0.95*** | 0.97*** | ||||
| Exponential | 0.96*** | 0.96*** | 0.99*** | |||
| Gamma | 0.80*** | 0.77*** | 0.80*** | 0.80*** | ||
| Rayleigh | 0.95*** | 0.97*** | 0.99*** | 0.98*** | 0.80*** |
Overall, although the average predicted efficiency spanned a range of 20%, the correlation, and in particular the ranks, between model predictions were very similar. The ranks of the predictions are particularly important because the goal of this exercise is to identify high and low performers. We turn to this issue in the discussion.
Discussion
Results from the models are, overall, encouraging from several perspectives. First, the parameter estimates are sensible and plausible. Importantly, the results appear to be consistent over a range of specifications and with the OLS base case, which does not impose the distributional assumptions that the SF models do. The base model, a limited number of variables notwithstanding, had considerable explanatory power, which is a good sign for the reliability of the estimates.
Our testing procedure indicated that our functional form was appropriate. All but one of the models detected the presence of inefficiency. Predictions of inefficiency are within a plausible range, and the models’ predictions of inefficiency are highly correlated. This finding supports previous studies in that ranks are not affected by distributional assumptions. This is key here: our cross-sectional results appear robust to the specification of efficiency distribution. This further implies that models agreed as to high and low performers and it proved possible to rank-order the cost efficiency of the included community hospital wards, but the rank-order was not declared as we received deidentified data for this research study. Nonetheless, in a situation of formal benchmarking, providing a rank order would be a simple procedure based on the models and data inputs described here. In terms of other efficiency studies, the results from our SFA analysis were comparable with those from previous studies43,44,46,51,53 of NHS general hospital efficiency (0.61–0.92; see Table 1). This suggests that the cost efficiency of community hospital wards is similar to that of general hospital wards. The COLS estimates were below those presented in studies elsewhere. Our COLS result was 0.56; results from other studies42–44,46 ranged from 0.69 to 0.74. However, the COLS models are more susceptible to outliers. Moreover, our testing procedure favoured the use of SFA, the results of which accord with prior studies. Importantly, the results here seem to accord with those of community hospitals more generally. 33
There are some methodological points for discussion. First, being a cross-sectional analysis, there are concerns over uncertainty; as we have one observation only per ward, we do not see the precision of the efficiency estimates increase per ward as the sample size increases. 44,60 We did not calculate prediction intervals around our estimates, although this may be an important avenue for future development so as to assess the extent of the uncertainty. However, that the ranks of providers are consistent across models helps to allay this issue insofar as we are able to assess the general level of efficiency and identify high and low performers.
Second, there is an issue around unobserved heterogeneity (when the variance, or standard deviation, of a variable varies across the range of the variable), particularly as the model did not support the inclusion of variables as proxies for case mix, patient severity and quality. We note that we are analysing costs at ward level, where there is likely to be much less heterogeneity than if we were modelling at the whole-hospital level. Indeed, the OLS results indicate that much of the variation has been explained. Moreover, by allowing for noise and removing it from our measure of inefficiency, it may well be that some unobserved influences are captured here. 41
We were able to utilise a unique data set on community hospitals that facilitated an econometric efficiency analysis on this part of the NHS for the first time. The data set suffered, to an extent, from missing values leading to a reduced sample with which to estimate models. We do not know the reason for the missing data; we have assumed it to be missing at random for the purposes of this analysis. We attempted an imputation exercise in preliminary work, which did not yield plausible results.
There may also be other more practical considerations. For example, although the NHSBN Community Hospital Programme included WTEs for staffing levels, there is the potential for over- or underestimation for staff who have responsibilities across sites or hospitals.
We considered that there might be selection effects of hospitals that chose deliberately not to report on the basis of their own poor performance. But to know this, they would need to have an intimate knowledge of their own and other wards’ operations in order to make a reasonable determination of this. Thus, it seems unlikely that they would be able to do this (although they might have considered themselves to be a poor performer). Moreover, if this was the case, we surely would not observe the range of efficiency estimates that we did: those that genuinely performed poorly would drop out of the sample.
The restricted sample size may be one reason why it was not possible to use a translog functional form and, thus, allow some flexibility in the cost function. In particular, no evidence was found to support variation in the cost elasticity over the output range. Of course, it may be that the cost elasticity is constant over the output range, but this view was not supported by community hospital staff. The other complication to this issue is the lack of a capital component in our cost variable. We note that, in this regard, we are not truly measuring the economies of scale, more a measure of size. This may an explanation for the finding on the cost elasticity with respect to output.
Our general view is that, given the data available, the models are well specified and are a good approximation of the underlying cost function. We thus have confidence in our predictions of inefficiency. The level of efficiency is high and the results are in keeping with those found elsewhere in the general hospital sector. Furthermore, we are able to identify high and low performers from the models, meaning that managerial effort can be targeted effectively to maximise gains across the sector.
The average predicted efficiency among community hospital wards was 0.83, implying that, on average, community hospitals could reduce operating costs in the provision of service on older people’s wards by 17% if performance was in line with best practice. If community hospitals were able to extinguish this inefficiency, there would be around £47M of available gains; total spend is around £227M. There was a range of performance, with the lowest-performing community hospital operating at around 0.55, whereas the highest-performing community hospitals were operating at around 0.94. That is, the models indicate that all community hospitals can improve efficiency on their wards.
Using a price year of 2013/14, in terms of input prices and staff mix, the results were unsurprising. Those community hospitals that faced higher input prices appeared to have higher costs; those community hospitals that employed a more experienced staff force also appeared to have higher costs. In terms of output, the results appeared to suggest that there were reasonable economies of scale at the sample mean, with a beta coefficient on output of around 0.85. This suggests that, for wards with bed size below the mean, marginal costs can be reduced by increasing the scale of the operation; for those above the mean, the scale at which the all-important cut-off point of 1 is reached is unclear. We note a slight limitation here, which is that, as suggested by staff working in community hospitals at a workshop held at the 2016 CHA conference (13–15 May, Bristol, UK)), we did not find variation in economies of scale between smaller and larger community hospitals (we did not find a statistically significant squared term on the output variable). However, the main finding was in keeping with what had been proposed: that there were economies of scale present. For bed occupancy, it appears that increasing bed occupancy rates are associated with lower costs. This may reflect that spare capacity is costly. However, this needs to be balanced against the effect on the service of high occupancy, which may be disruptive to service provision; we note that our sample mean is around 90%. Indeed, the NAO have suggested that services in which bed occupancy levels are in excess of 85% may experience disruption (in the general hospital setting). 55 This would be an interesting area for future work.
Summary
In the analyses described in this chapter we have applied econometric techniques to NHS community hospitals for the first time using a unique data set collected by NHSBN. The analyses suggest the potential for economies of scale in the provision of community hospital services for older people. As expected, higher input prices and a more experienced staff mix were associated with higher costs, and costs appeared to be lower when bed occupancy was higher.
We used a range of models to predict efficiency in our sample of community hospitals. Under differing assumptions, models’ predictions varied somewhat. Their average was 0.83, implying that, on average, community hospitals could reduce operating costs in the provision of service on older people’s wards by 17% if performance was in line with best practice. There was a range of performance, with the lowest-performing community hospital operating at around 0.55, whereas the highest performing community hospitals were operating at around 0.94. The predictions of efficiency were found to be highly correlated between models, in terms of both absolute values and ranks. Policy implications of our findings are discussed in Chapter 7.
Chapter 3 National survey of community hospitals (study 2)
Introduction
According to the CHA, there are > 500 community hospitals in the UK: 346 in England, 101 in Scotland, 44 in Wales and 13 in Northern Ireland. However, not all community hospitals have inpatient beds and the numbers fluctuate because of closures and newly commissioned facilities. 12 From this national pool of community hospitals, 158 elected to participate in the Community Hospitals Project run by the NHSBN for the financial year of 2013/14. 13 Of these 158 hospitals, 101 returned questionnaires with the required information for the health economics analyses to determine key performance features (see Chapter 2, Community hospital data set). This sample comprises approximately 25% of community hospitals across England. Community hospitals across England will have a range of (unknown) reasons to participate in the NHSBN Community Hospitals Project and this may lead to a sample bias, for example over-representation of more adventurous community hospitals with high cost efficiencies. To address this, and to obtain more generalisable estimates of cost efficiency, we designed a national survey of community hospitals.
The intention of the survey was to augment the NHSBN Community Hospitals Project data set through a greater representation of community hospitals not only in England but across the UK. This study therefore contributed to the following project objectives:
-
to measure the current relative performance (cost efficiency) of community hospital inpatient care for older people
-
to identify the characteristics of community hospital inpatient care for older people that optimise performance.
Method
The focus of the national community hospital survey was to collect data from a larger and more representative sample of community hospitals that provide rehabilitation to older people in the UK. The aim was to develop a brief postal survey instrument that focused only on the four key cost efficiency parameters identified in study 1: bed occupancy, input prices, LOS and staff mix (see Chapter 2). Questions relating to these four parameters were extracted from the existing items in the NHSBN Community Hospitals Project, to ensure comparability. The survey instrument therefore comprised a covering letter and four questions presented in four A4 pages (see Appendix 3).
Sampling frame for the national community hospitals survey
The sampling frame used for the piloting and administration of the national community hospitals survey was developed using a three-stage process.
Stage 1
The first stage entailed the receipt of a list of community hospitals in the UK from the University of Birmingham community hospitals project team. The list had been sourced by the University of Birmingham from NHS Digital (formerly known as the Health and Social Care Information Centre) and was an accurate listing of community hospitals in 2012/13. This initial list contained 404 hospitals (559 rehabilitation/older people’s wards) of which 258 were in England, 11 were in Northern Ireland, 40 were in Wales and 95 were in Scotland.
Stage 2
The second stage involved a reconciliation process to ensure that the list excluded hospitals that had been closed or lost their beds or changed ownership. This was done in conjunction with the CHA, which provided business intelligence on recent hospital closures, and supplemented through internet searches and telephone calls to 291 individual community hospitals. The final list to be used for the postal survey contained 423 community hospitals (284 in England, 10 in Northern Ireland, 91 in Scotland and 38 in Wales), and an estimated 582 rehabilitation/older people’s wards in the UK.
Stage 3
To develop a contact list for the community hospitals, we sought the name of the matron/charge nurse/ward manager at each of the 423 sites. This information was obtained through internet searches and telephone calls.
The intention of this was to personalise the covering letter that accompanied the survey to facilitate improved completion and return rates.
Survey pilots
The survey instrument was sense-checked using 10 community hospitals selected at random from the ‘CHA Research Group’ (a list of community hospitals interested in research). We requested feedback on content and format. The feedback received was incorporated into a revised version of the survey instrument and then sent to a random selection of 10 community hospitals from the study sampling frame. The community hospitals used in the piloting of the questionnaire were selected using random number generating in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA). The pilot sample was weighted according to the number of community hospitals in each country (five in England, one in Northern Ireland, three in Scotland and two in Wales).
The covering letter that described the rationale for the survey accompanied the questionnaire and a request for feedback on the individual questions was included also.
The pilot sites that did not respond were contacted again after 2 weeks. All information received was included in the final version of the study survey.
Main survey
The covering letter and survey instrument (see Appendix 3), addressed to the persons identified in stage 3, were posted to the 423 community hospitals (587 rehabilitation/older people’s wards) identified during stage 2. The covering letter and questionnaire were accompanied by a stamped addressed envelope, for the return of completed survey instrument to the study team. A reminder letter was sent to non-responding sites at 2 weeks from the initial mail-out.
Returned questionnaires were logged and the information they contained entered on a central secure database for analysis.
Results
The pilot of the questionnaire had three returns (response rate 33.3%) from a sample of 10 community hospitals.
The initial mailing of the questionnaires to 587 rehabilitation/older people’s wards (423 community hospitals) resulted in only 17 responses (2.9%). We therefore contacted, by telephone, the ward managers/matrons for a selection of the non-responding sites to establish reasons for not completing the survey. The reasons provided included:
-
‘too busy on the ward to keep up with “non-essential” admin[istration]’
-
‘survey isn’t a priority’
-
‘no incentive to complete the survey’
-
‘don’t have information readily available to enable easy completion’
-
‘financial information not immediately available’
-
‘terminology (e.g. what do we mean by indirect costs?)’
-
‘needed manager‘s approval to complete survey’
-
‘information requested on finances is confidential’.
We subsequently modified the administration method by adopting a more focused approach that included only the non-participants of the NHSBN Community Hospitals Project. In this way, we hoped to learn something about these ‘non-responders’ and to determine if they were systematically different from the responding hospitals across our four key variables.
As part of this method we contacted approximately 10% of the non-responding hospitals (30 in England, 11 in Wales and 27 in Scotland). This resulted in an additional seven questionnaires from wards being returned.
Thus, we received a total of 24 survey questionnaires from the first and second methods of administration: 17 from the first method and seven from the second method. This represented a return rate of 4.1% from the overall 587 community hospital wards surveyed (Figure 5).
FIGURE 5.
Number and response rates for the national community hospitals survey.
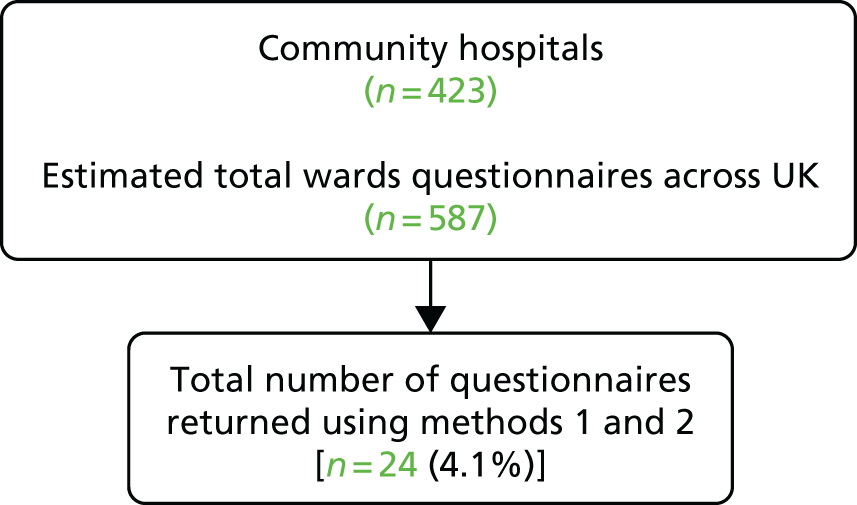
Discussion
Our ambition had been to augment the NHSBN Community Hospitals Project data set using updated information obtained from a new national survey. It was hypothesised that the ‘more engaged’ hospitals might be over-represented in the existing NHSBN Community Hospitals Project data set. It was envisaged that the administration of the specifically developed MoCHA survey questionnaire would provide a more representative sample of community hospitals wards across the UK.
However, despite the active and helpful assistance of the CHA, and using the questions that had been previously tested in the NHSBN Community Hospitals Project, and despite a reasonably successful pilot survey (33% return rate) that allowed us to improve our methods, the main survey response rate was insufficient to allow us to re-calculate the estimates of cost efficiency – the main purpose of the national survey. This result was both disappointing and unexpected. National surveys of community hospitals have been conducted regularly by the CHA and there have been excellent response rates. It might have been that the purpose of our survey was either misunderstood, or understood but perceived as being of low value to the respondents. Feedback from some respondents supported the latter, which included comments such as: ‘too busy on the ward to keep up with “non-essential” admin[istration]’, ‘survey isn’t a priority’ and ‘no incentive to complete the survey’. It is also possible that the data we were seeking were not easily or consistently accessible at ward level.
Chapter 4 Comparative case study of community hospitals (study 3)
Study objective 2: to identify the characteristics of community hospital inpatient care for older people that optimise performance.
Introduction
We anticipated that some components of community hospital ward care would not be captured or adequately summarised through the quantitative indicators of performance available for the cost-efficiency analysis described in the preceding chapter. Study 3 therefore sought to provide insight into the dimensions of rehabilitation practice as accomplished on community hospital wards with older people.
Community hospitals provide an important intermediate-care function within a repertoire of services aimed at providing transitional or time-limited support to people at a critical point on either side of the policy fulcrum that is the acute hospital (i.e. on the cusp of a shift from independence to dependence, following an acute event or exacerbation of chronic illness or illness in context of frailty). Rehabilitation to facilitate recovery is a major part of the intermediate-care function. Nevertheless, research on patients’ experiences of community hospitals primarily focuses on factors such as the ‘homely’ nature of the environment (physical and social: size and atmosphere); the localism or closeness of the community hospital to their own home and family; and the interpersonal, social and psychological aspects of care delivery (i.e. care as human connection). 9,10,61,62 Although central to the patient experience of care, less clear is how the work to facilitate recovery is actually accomplished. 63–66
There is broad agreement in research and policy on what is good rehabilitation practice. 67,68 It should be multidisciplinary, co-ordinated and patient centred: encompassing comprehensive need assessment; collaborative active engagement of the person in establishing goals for recovery in their terms; and provide enabling support, skills development, and emotional and practical assistance. Understanding what this ‘good practice’ actually looks like in the community hospital setting in respect of older people and how it is organised, would provide new insight into qualitative aspects of community hospital performance and what shapes it (objective 2). This understanding could also be incorporated into the interactive toolkits for use by local commissioners and community hospital teams to support operational changes to optimise performance (objective 4). To achieve these objectives, we undertook in-depth case studies of four wards in three community hospitals.
Aims of study 3
-
To provide a descriptive and explanatory account of how care supported recovery of frail, older people with rehabilitation needs in the context of community hospital wards.
-
To identify dimensions of care quality as understood by staff and experienced by older patients and their informal caregivers.
-
To examine how people access community hospitals and, conversely, the resources and support at local level to facilitate timely discharge.
Methodology
We performed a multimethod, comparative case study design. Case study research69–72 is characterised by the depth and detail of information collected within naturally occurring, bounded settings, although the boundary between the setting and focus of analytic interest is permeable. 71 In this study, analytic focus was care delivery to older people with rehabilitation needs on community hospital wards. This is one aspect of the work of community hospitals that is also affected by external factors (e.g. referral practices and resources within the health and social care system). The distinctiveness of the case study method is its systemic and holistic perspective. 69 It facilitates in-depth and context-specific understanding of practice and how it is experienced in real time.
Methods
Sampling and recruitment
We purposively selected three community hospitals providing inpatient rehabilitation based on their relative cost efficiency from study 1 (see Chapter 2), namely two ‘high performers’ and one ‘low performer’. This was to enable in-depth exploration of how cases that differed in respect of performance varied in the quality of their care processes and delivery.
We had originally planned to include a hospital in each of three UK countries: England, Scotland and Wales. Following initial interest, we sought appropriate ethics and governance approvals to pursue the research. Of the three community hospitals that expressed interest in taking part, one of the English hospitals was forced to withdraw on account of major building works that would take months to complete. Following lengthy negotiations, the Scottish hospital was not pursued as the time involved in securing appropriate ethics and governance agreements meant that it would not be possible to undertake fieldwork within the study time scale. We found ourselves locked in a debate with different authorities in Scotland about whether the proposed study was research or audit (see Appendix 4, Figure 11). We finally recruited two English and one Welsh community hospitals (four wards) that met our cost-efficiency performance criteria. Face-to-face meetings were held with senior staff at hospital/ward level to discuss participation and to gather information on ward organisation, staffing, patient profile and the spatial environment of the ward/hospital.
The selected community hospitals were all managed by NHS provider organisations: two by community health trusts and one by a combined organisation (health board) providing health services across the spectrum of acute, specialist, primary and community services, and integrated health and social care provision for older people with frailty.
In the case studies, we purposively selected ward staff to ensure inclusion of individuals from different disciplines and seniority levels. We also identified senior managers in each provider trust/health board, either through informants at senior level in trusts and health boards or by who emerged during observation as being central to providing and managing services in the transition to and from community hospitals. Our aim was to recruit around six staff in each case study.
We employed typical and critical case sampling to identify patients admitted to each community hospital ward and their caregivers to explore their journey into, through and discharge from the community hospital. We sought to recruit five patient/caregiver dyads from each ward: patients who were regarded as typical of those on community hospital wards and those viewed as complex in that they posed challenges for delivery, on account of multimorbidities including cognitive impairment.
In this chapter, we have used pseudonyms throughout (i.e. for community hospital/wards, trusts/health board, staff, patients and caregivers) and have altered some biographical details to protect anonymity, privacy and confidentiality.
Data collection methods
We employed mixed methods encompassing quantitative and qualitative data collection to build up a picture of each community hospital ward, including how rehabilitation practice was enacted by staff and the meaning and experience of patients (and carers) to whom it was delivered.
Case profiles
Patient profiles were constructed from routinely collected anonymised data. Ward culture was partly derived from a structured questionnaire on care culture (shared philosophy, leadership, mutual support and teamworking) completed anonymously by ward staff73 and from observation and staff interviews, and documents were collected relating to policy, procedures, care processes and priorities.
We asked hospitals to complete a common pro forma on an Excel spreadsheet for patients admitted to the included wards in the 12 months prior to fieldwork. For each patient, we sought to collect demographic (age, gender, residence prior to admission), clinical (reason for admission, dementia diagnosis) and service variables (source of referral, date of admission and discharge, length of inpatient stay and discharge destination). We were only partially successful. Not all of the information required was readily available and/or it proved time-consuming to put together. We therefore had to negotiate what was feasible and possible in each site. In Castle and Lawrence community hospitals, most data were provided over 9 and 8 months, respectively, although in Castle community hospital this was for one ward only (male ward) and in Lawrence community hospital for one female ward. In Ramsay community hospital, senior ward staff completed the pro forma from referral sheets held in the hospital, which was a time-consuming effort, for 3 winter and 3 summer months. Caution is therefore required and the findings here are indicative, but consistent with the other data sources.
Ward practices
We employed ethnographic methods (observation, informant interviews, shadowing staff, conversation and documents)74–77 to observe and experience ‘first hand’ the organisation and delivery of rehabilitation care to patients. This included knowledge-sharing, decision-making, action and interaction between therapists, nursing, care and medical staff, and between staff and patients. We observed decision-making and action in multidisciplinary forums, the composition varying with purpose. These included multidisciplinary team (MDT), board and handover meetings during which care and rehabilitation were planned and reviewed, and discussion and action on discharge took place. Descriptions of settings, events, interactions and activities were captured in contemporaneous jottings and written up subsequently as expanded accounts. 74,77 Researchers maintained a chronological field journal for each case, which included their impressions and reactions. Observation was conducted over different times of the day and evening, including weekends, typically in 3- to 4-hour blocks over approximately 10 weeks (226 hours in total). We also observed various types of formal MDT forums (a total of 18). In the course of observation and sensitive to the demands on staff, we engaged in informal conversations with individuals to clarify issues raised. This provided a rich account of what was happening and how it was understood by those involved.
Staff
We collected data via qualitative interviews78 with 25 ward staff, including therapists, using a topic guide to examine their views on the patient profile, care processes, multidisciplinary working and discharge-planning. This included how the work of rehabilitation and care for older people was understood, what made it work and for whom, the resources available and the professional, organisational, cultural and other contextual factors affecting delivery from their different perspectives. Through discussion of anonymised cases we explored the kinds of patients perceived as best suited to the service and those most likely to benefit. Similar interviews were conducted with 18 senior trust and health board managers and middle managers responsible for delivering transitional care (community-based intermediate-care services). The former conveyed an overview of policy and strategic direction relating to the community hospital, including local initiatives to facilitate the smooth flow of patients into and through the wards; and the latter provided perspective on the interface between the community hospital and the wider health and care system.
Patient/relative case studies
Data were collected about the experience of care from a patient and caregiver perspective via observation of ward care delivery, attendance at MDT and family meetings, contemporaneous conversations with patients and examination of case notes. The method of ‘conversations in the moment’ alongside observation with patients was particularly valuable in respect of those who had cognitive problems or were living with dementia. As data were collected in real time, the method of ‘conversations in the moment’ required neither verbal facility nor ability to recall. 79 When possible, we followed patients from near admission to discharge. We interviewed patients selected for observation and their caregivers (when available) in each case study site shortly before discharge from the community hospital to facilitate near experience accounts. The interviews examined patients’ lives prior to admission, the precipitating event, the meaning attached to recovery and the function rehabilitation performed in that. A total of 16 patient case studies (including seven separate carer interviews) were completed employing these multiple methods. For a summary of data collection by case study site, see Appendix 5.
Analysis
Data analysis proceeded at multiple levels and stages with the ward as the unit of analysis. We developed a narrative description of the structure (bed base, staffing, patient profile), activities (throughput) and care culture of each ward. Quantitative data from hospital admission systems (age, sex, reason for admission, type of residence, length of inpatient stay, discharge destination, hospital mortality) were analysed to provide descriptive statistics; qualitative interview and observational data were drawn on to examine how staff meanings, beliefs and values were shaped by the organisational context and articulated in practice in each organisation.
Employing grounded theory analytical techniques80 such as concurrent data collection and analysis, constant comparison and search for negative cases, we examined the process of delivery of rehabilitation care to patients with different characteristics and needs in context of the ward environment, drawing on the observational data and conversations with staff and patients. Such techniques provide a robust approach to analysis and direct attention on conditions, processes and consequences pertinent to ward practices and care delivery. Ideas about the emerging data were continuously tested out through discussions among the research team, further focused observation, interviews and informant conversations.
With the patient as the unit of analysis, we similarly employed grounded theory analytical techniques to compare and contrast experiences and outcomes across patients similar to, and different from, each other in the event that precipitated admission, their prior social engagement and their physical, cognitive and health status, including comorbidities. We drew on previous research64 on recovery trajectories in intermediate care to examine the pattern of recovery for patients, taking into account the diversity of patient characteristics and what recovery meant to them.
Using analytic induction, we compared and contrasted the study wards in their structure, culture and process of delivery, drawing on the narrative descriptions of each community hospital case. The general analytic categories subsuming the work of rehabilitation developed from the data were interdisciplinary working and co-ordination at ward level; communication and information-sharing; engagement of patients and caregivers in decision-making; attention to the relational, emotional and practical aspects of care, including for patients with different needs; and the systems and practices for effecting a smooth and timely patient journey into and from the ward. The varied ways in which these were understood and accomplished were set within professionals‘ understanding, meanings, knowledge, skills and resources with regard to the patients with whom they worked.
Research team
The team comprised two investigators who conducted the case studies (Elizabeth Lavender and Rosemary Shannon), both with qualitative research expertise, and MG, the academic lead, an experienced qualitative researcher and teacher of qualitative methods. All three met regularly (approximately fortnightly) to consider emerging ideas and directions to pursue. Meetings, telephone conversations and e-mail discussions enabled dialogue and mutual support. The wider research team, including the chief investigator, met every 2 months to discuss progress, in addition to receiving advice and support from the Programme Management Group (including representatives of the Patient Association and CHA), and our local older person’s group.
Findings
In the first section, we present the descriptive context of the three community hospitals. We then examine staff conceptions and delivery of rehabilitation and care, including with respect to people with complex needs, and identify quality dimensions of practice that emerged from the study. Finally, we draw together how therapy and care supported recovery and the processes for effecting ‘safe’, timely discharge, including how transitional and follow-on support was negotiated and organised.
Description of the community hospitals
As indicated above, to maintain anonymity, each community hospital and parent NHS organisation has been given a fictitious name. Each hospital was managed and delivered by an NHS organisation, whether a community trust (Ramsay community hospital), community and mental health trust (Lawrence community hospital) or health board (Castle community hospital). All were part of networks of community hospitals in the geographical area covered by the parent organisation. Even so, the service models within each network were also shaped by their historical origins, albeit strategic initiatives at senior management level were directed at melding them into an overarching system of transitional care, not always in alignment with their local communities (Table 8).
| Case study | Organisational location | Geographical setting | Service model |
|---|---|---|---|
| Castle CH |
Castle CH is managed by Brandon Health Board, one of seven health boards in Wales. Each health board plans, secures and delivers all health-care services in their areas including acute, primary, community and mental health Brandon serves a population of > 600,000, spread over scattered rural areas, villages and urban centres. It employs > 14,000 staff |
The CH is located in the middle of a housing development on the outskirts of a relatively affluent town. It is one of five local CHs in the geographic area covered by the health board |
Castle CH opened in 2000. It operates as a base for a wide array of health, social care and support services for its local population (town and rural hinterland). The inpatient unit operates as two wards There is an older people’s acute mental health ward on site, which is separately managed and staffed Co-location of health services for a local population was part of a strategic initiative of the board for over a decade. It involved the closure or redesignation of several traditional CHs. The integrated model of service spanning health and social care for older people with frailty was a more recent innovation, with pooled health and social care budgets |
| Ramsay CH | Ramsay CH is managed by Coastal Community Partnership NHS Trust in the south of England. The trust plans and delivers community health services across the age spectrum, serving a population of around 1 million spread over urban centres and a rural and coastal hinterland. It employs nearly 5000 people | This CH is located in a prosperous village, in a large Victorian building off the main street. It is the largest of 11 local CHs in the geographical area covered by the trust | Ramsay CH has been a health resource for the local community in different guises since the 1930s, when established with philanthropic funding: a convalescent home for mothers and babies; a maternity hospital; then reborn as a CH in the late 1970s. With strong roots in the local community, referrals are now drawn from a wider area. It has been extensively renovated in recent years. No other services are provided at the site. The nearest general hospital with diagnostic facilities is around 8 miles distant |
| Lawrence CH |
Lawrence CH is managed by Midland Partnership Community and Mental Health NHS Trust in the centre of England. The Trust plans and delivers community, learning disability and mental health services across the age spectrum The Trust serves a population of around one million spread over a large, rural county and an ethnically diverse city. It employs around 5500 staff |
This CH is located on the edge of a large, ethnically diverse city in a 1970s building Lawrence CH is one of eight in the geographical area of the trust. Apart from Lawrence, all the other CHs are located in rural areas/small towns |
Lawrence CH provides subacute medical and general rehabilitation for older people primarily from across the city (and, on occasion, the county, depending on bed availability). It operates as two separate wards. It is physically located in a building that also houses three wards for older people with acute mental health needs provided by the same trust, albeit separately organised, staffed and managed. Located on the same site (but not the same building) are offices of teams providing intermediate-care services and the smaller of two city-based general hospitals The development of Lawrence CH was part of a process of reorganisation (and some closures) of CHs across the county and city. Many were small, GP-led cottage hospitals providing recuperation and rehabilitation and with strong, historical attachments to their local communities. The reorganisation was driven strategically by the need to reduce length of acute hospital stay and needs of a complex patient population who required a further period of recovery |
Castle community hospital in Brandon Health Board in Wales was opened in 2000 and operates as a hub for the co-location of community, primary, outpatient and some secondary health services for a geographically defined population that is not age specific. Furthermore, it extends beyond health to encompass peer support and voluntary sector providers in respect of life difficulties. It is also a base for the local community resource team, a component of an integrated model of health and social care for people with frailty, spanning acute, transitional, reablement and community services. The bed-base comprises three wards, two of them (referred to as Castle community hospital) are for transitional care and were the focus of our case study; the third is a ward for older people with acute mental health needs. In this respect, the wider hospital site serve both a geographic- and age-related purpose.
Established with a philanthropic legacy in the 1930s, Ramsay community hospital, now managed by Coastal Community Partnership NHS Trust in England, was initially a convalescence home for mothers and babies and then a maternity hospital. It has operated as an inpatient resource for older people requiring rehabilitation and palliative care for a mainly rural community for about five decades. No other health services are provided from the site. Ramsay community hospital has strong roots in the local community – several patients commented that their children were born there. More recently, referrals have been drawn from a wider geographic area.
Lawrence community hospital, managed by Midland Community and Mental Health NHS Trust, is a relatively recent development (from 2012). Previously on the site was a bed-based resource for older people with long-term care needs and a social care/therapy unit managed by the local authority. This community hospital is a city-wide resource within a predominantly rural community hospital network. It was described as ‘subacute’, providing medical and general rehabilitation to meet the needs of an increasingly complex older patient profile and to facilitate their medical and functional recovery to enable a ‘safe’ discharge. It did not identify as a ‘local’ resource in that patients might come from any part of the city (and on occasion, from the county). Its purpose was age related, albeit for frail older people with medical and rehabilitation needs.
As organisations, the three hospitals varied in their degree of autonomy, in staffing and in operating systems. Although Castle wards had their own dedicated nursing and care staff, physiotherapists also provided input into outpatient therapy clinics on the wider community hospital site. In addition, occupational therapists were integrated within community resource teams as part of the frailty service so that they could follow patients from hospital into, and through, transitional enablement support. A feature of the organisational model of community hospitals in the Midland Community and Mental Health Trust was the priority attached to, and systems in place for, standardisation of practices and procedures across the network (same referral criteria, working patterns, services provided, staff skillset, etc.). In addition to their management role in their own hospital, each community hospital matron had specific areas of responsibility for all hospitals in the network. These could embrace organisational features (e.g. staff recruitment and training) or responsibility for quality assurance in a specific clinical area (e.g. falls, pressure sores). Of the three hospitals, Ramsay community hospital operated as a relatively autonomous service, reinforced by its long-standing senior nursing team (see Table 8 for a summary description and comparison of each community hospital organisational location and service model).
Ward organisation and staff profile
The three hospitals had evolved as primarily ‘step-down’ facilities located in the virtual space between secondary and primary care. Their main function, therefore, was to support early discharge of patients from acute hospitals, predominantly older people who required further inpatient nursing, therapy and medical oversight to pursue recovery, functional improvement and to enable a ‘safe’ discharge.
The ward bed base varied between 26 beds in Ramsay, 32 in Castle and 42 in Lawrence; Castle and Lawrence were organised as two single-sex wards. They shared some characteristics and diverged on others (Table 9).
| Community hospital | Spatial organisation | Ward team |
|---|---|---|
| Castle |
32 beds across two single-sex wards 18–20 female beds; 14–12 male beds Female ward: four × 4-bed bays, one × 2-bed rooms, four × single rooms Male ward: three × 4-bed bays, four × single rooms |
Senior staff: ward manager, who manages both wards and a deputy sister Ward clerk for each team Female ward: nursing/care staff-to-patient ratio –Male ward: nursing/care staff-to-patient ratio –Skill mix on both wards, % nurse/HCA: 40/60 Each ward is staffed separately although staff are encouraged to work shifts on both Therapists: 1.8 FTE PTs; 1 FTE therapy technician; 1.5 FTE OTs; 1.5 FTE therapy technician/therapy assistant Registrar and junior doctor provide medical cover 09.00–17.00 on weekdays; consultant overview |
| Ramsay |
26 beds across one ward Five × 4-bed bays, two × 2-bed rooms, two × single rooms |
Senior ward staff: ward manager and two ward sisters Ward clerk Nursing/care staff-to-patient ratio:Skill mix, % nurse/HCA: 42/58 Therapists: 1.5 FTE PT; 2 FTE OT; 3 FTE therapy technicians GP (employed by the trust) provides medical cover 09.00–17.00 on weekdays; consultant overview |
| Lawrence |
23-bed male ward One × 4-bed bay, three × 2-bed rooms, 13 × single rooms |
Senior ward staff: ward manager and three deputy sisters Ward clerk Nursing/care staff-to-patient ratio:Skill mix, % nurse/HCA: 42/58 Therapists: 1 FTE PT, 1.5 FTE technical instructors; 2 FTE OTs. 1 OT and 1 PT team leaders work across both wards Advanced nurse practitioners provide medical cover 09.00–17.00 on weekdays; consultant overview |
Nursing and care staffing complement and profile were somewhat similar across the three hospitals (an approximate staff-to-patient ratio of 1 : 4 during the day), albeit higher in Lawrence community hospital (1 : 3.3). The proportion of qualified to unqualified staff was similar for the three hospitals (around 40%/60% qualified to unqualified staff). During fieldwork, Castle and Lawrence community hospitals were very understaffed and relied on bank and/or agency staff to provide cover, usually also involving substitution of unqualified for qualified staff. The problem was exacerbated in Lawrence by high demand pressures reflecting the fact that fieldwork was conducted during the winter months (December–March). By contrast, fieldwork in Castle and Ramsay community hospitals was carried out during the summer months (June–September).
In Lawrence, both the staff group and its patient profile were ethnically diverse. This contrasted with Castle and Ramsay, where both staff and patients were predominantly white.
Each hospital was nurse-led with a multidisciplinary skill mix. Nurses, therapists and care staff primarily worked in an integrated and interdisciplinary manner to provide general nursing, personal care, rehabilitation and palliative care. Onsite medical cover was provided weekdays, 09.00 to 17.00, although its form varied between sites. In Ramsay community hospital, a general practitioner (GP) was employed by the trust on a full-time basis; in Castle community hospital, a registrar and junior doctor covered both wards; and in Lawrence community hospital, advanced nurse practitioners (ANPs) (senior nurses who, through additional training and qualifications, were able to diagnose and prescribe medication) provided ‘medical’ cover. In each site as well, there was sessional consultant oversight from the local acute hospital, typically once-weekly attendance at the MDT meeting and board round. Castle and Ramsay community hospitals had a social worker based on the unit employed by the local authority Adult Social Care agency: their contiguous physical location and continuous presence facilitated shared knowledge of patients and informal relationships with staff. In Lawrence, social workers were not hospital based: two part-time social workers employed by the city local authority worked with patients within the city catchment; patients from the county were referred to the relevant county social work team.
Their physical environments varied. Castle community hospital was modern and bright; most of the beds were arranged in 4- and 2-bed bays, with four single rooms in each ward. It had a day room and a relatives’ meeting room, and led onto a courtyard garden. Ramsay community hospital was an attractive, bright, late-Victorian building, which was extensively decorated in recent years. It was mainly arranged in 4-bed bays, with a couple of double rooms and two single rooms. All patient rooms had windows or glass doors that led out to a covered veranda at the front of the building and onto an open grass area. There was a large communal dining room, family meeting room and chapel. In both community hospitals, the organisation of internal space facilitated sociability between patients and encouraged movement. The physical environment of Lawrence community hospital was spacious with multiple rooms for meetings, including a relatives’ room, although the decor was ‘tired’. The ward comprised 13 single rooms, three 2-bed rooms and one 4-bed room. It looked out over a pleasant, grassed area. Inside, the spatial organisation could contribute to patient isolation and meant that staff were in near continuous motion between spaces, affecting the amount of time they could spend with individuals. In contrast to many acute wards,79 the spatial ‘footprint’ of each community hospital ward was generous, although their multifunctional spaces were primarily used for meetings rather than for therapeutic or social activities.
In each site, mechanisms existed in the local acute hospitals to identify patients considered suitable for referral to the community hospital or other transitional services. These comprised individuals or teams (their designation and precise remit varied) who operated at the ‘front end’ of the acute hospital either to prevent an acute admission or to in-reach into wards to identify patients for discharge and with ongoing support needs.
A discharge liaison practitioner working across the frailty service and the main catchment hospital filtered referrals to Castle community hospital: the value from the community hospital staff perspective was that the post-holder’s in-depth knowledge of local transitional and community services meant that they had confidence that relevant information about the patient’s medical circumstances and discharge plan accompanied the referral. Here, daily discussion of patient flow from the general hospital to the community hospital and subsequent return home occurred informally between the liaison practitioner and the ward manager.
A team of nurses based in the acute hospital performed a similar function regarding referrals to Lawrence community hospital. Employed by the community and mental health trust, a distinctive feature of this team was that individuals rotated between the acute hospital, community hospitals and intermediate-care services. The rationale for the model was that knowledge-sharing about working practices, care cultures and the range of resources available facilitated collaboration and service integration, reducing overlaps and identifying gaps. Such mechanisms also reinforced the alignment of the community hospitals with the acute pathway.
In Ramsay, a team employed by Coastal Community Trust worked in the acute hospital to identify patients suitable for referral to one of the community hospitals with a vacant bed, unless a patient expressed a preference for a specific community hospital and a vacancy was imminent.
Patient profiles
In terms of the patient profile (Table 10), patients in advanced older age predominated, although this was most pronounced in Ramsay, where over two-thirds of those admitted were aged ≥ 85 years (probably reflecting the locality population profile). By contrast, around half of patients admitted to Castle and under half those admitted to Lawrence were aged > 85 years. A minority of admissions to each hospital were younger men with multiple health and social needs, with, for example, amputations as a consequence of diabetes, and/or alcohol-related chronic conditions including homelessness. Their particular combination of needs typically resulted in prolonged LOSs, often as a consequence of unsuitable, rented accommodation or being of ‘no fixed abode’.
| Patient characteristics | Castle CH (N = 147) | Ramsay CH (N = 84) | Lawrence CH (N = 191) |
|---|---|---|---|
| Age range (years), n (%) | |||
| ≤ 64 | 8 (5) | 3 (4) | 16 (8) |
| 65–74 | 13 (9) | 3 (4) | 26 (13) |
| 75–79 | 22 (15) | 10 (12) | 26 (13) |
| 80–84 | 28 (19) | 12 (14) | 34 (17) |
| 85–89 | 36 (24) | 28 (34) | 40 (20) |
| ≥ 90 | 40 (27) | 28 (34) | 47 (24) |
| Median (range) | 85 (37–100) | 87 (57–103) | 82 (39–97) |
| Prior residence, n (%) | No information on prior residence – most patients came from their own homes | ||
| Home | 130 (88) | 62 (74) | |
| Assisted living | 0 (0) | 3 (4) | |
| Care home | 9 (6) | 18 (21) | |
| Other | 0 (0) | 1 (1) | |
| No information | 8 (5) | 0 (0) | |
| Source of admission, n (%) | |||
| Acute hospital ward | 129 (87) | 53 (63) | 190 (98) |
| A&E | 1 (1) | 11 (13) | 0 (0) |
| GP | 6 (4) | 19 (23) | 5 (2) |
| Care home | 0 (0) | 1 (1) | 0 (0) |
| No information | 11 (7) | 0 (0) | 0 (0) |
| Discharge destination, n (%) | |||
| Home | 93 (63) | 50 (60) | 117 (61) |
| Acute ward | 22 (15) | 14 (17) | 34 (17) |
| Care home | 11 (8) | 10 (12) | 22 (11) |
| Assisted living | 1 (1) | 3 (4) | 0 (0) |
| Died | 18 (12) | 0 (0) | 3 (2) |
| Temporary residence | 0 (0) | 0 (0) | 14 (7) |
| Other | 0 (0) | 2 (92) | 0 (0) |
| No information | 2 (1) | 0 (0) | 0 (0) |
| Median LOS (days) (minimum, maximum) | 29 (3, 206) | 25 (1, 108) | 21 (1, 67) |
Between one-fifth and one-quarter of patients had a documented diagnosis of dementia, which, based on our observations, understated its prevalence.
A common theme among staff at all levels within and across sites was that the patient profile had become more complex because of population ageing, the discharge of patients from acute hospital earlier in their recovery pathway and policy changes that had resulted in the expansion of community-based rehabilitation services in the person’s own home. For example, the development of an integrated frailty system of care across Brandon Health Board, referred to earlier, spanning acute, reablement, rehabilitation and community services in the person’s home meant that patients who could go home from the acute hospital with support were more likely to do so. The combined and interactive effect of these developments contributed to the fact that those using inpatient rehabilitation were frailer and had multiple and chronic difficulties.
The dominance of the acute hospital in directing patients to the community hospitals is reflected in referral patterns. Fewer than 5% of referrals to Castle and Lawrence community hospitals originated directly from GPs. The rate of GP referral to Ramsay, based on winter months data, is comparatively high in comparison, and senior ward staff reported that it was very variable.
Nearly two-thirds of patients admitted to each community hospital returned to their own homes on discharge, with some intrahospital variation. Under one-fifth of those admitted to each community hospital were discharged back to acute care, either within days of their admission on account of acute medical need or after a lengthy inpatient episode, as a result of illness deterioration.
The median LOS on community hospital wards varied between 21 days in Lawrence, 25 days in Ramsay and 29 days in Castle. This conceals enormous variation and does not elucidate the factors contributing to extended LOSs, thereby identifying action to address them. The interactive effect of patient-related and organisational factors contributing to lengthy inpatient episodes are considered in more depth in Trajectories of recovery, drawing on patient case studies.
The high proportion of patient deaths in Castle compared with the other community hospitals (and wide range in inpatient stay) was a legacy of the ward model operating on one of the two words in which an important function was the provision of long-term palliative care.
Care culture
Each hospital had experienced change over time (i.e. in their patient profile, purpose and role in the local health system) and this had a direct impact on their staff group. In Castle and Ramsay community hospitals, many current members of staff worked in the hospital when it had a different purpose or patient profile, posing challenges in forging a common ethos and practice.
In Castle, the two wards had different origins and functions: one was a merged long-term subacute unit with GP-managed beds and the other had been a stroke rehabilitation ward until 18 months prior to the research. Whereas nursing and care staff in the former brought skills in working with older people, therapists considered that they adopted a more ‘caring’-for than an enabling approach with patients. On the other hand, it was reported (and illustrative episodes were observed) that support staff who had previously worked on the stroke rehabilitation ward adopted a more consistent enabling practice. Some of these staff, however, appeared less comfortable working with older people who had complex needs. During fieldwork, training specifically in the care of people with dementia was being introduced in Castle. In addition, access to advice and specialist assessment of patients with mental health problems had been initiated via a psychiatric liaison service. Across the two wards in Castle community hospital, the adoption of a consistent enablement approach remained work in progress.
In Ramsay community hospital, long-standing members of staff, including senior nurses and therapists, retained memories of a more community responsive service and a patient group for whom rehabilitation meant intensive work to improve strength, balance and functionality following a fracture to resume previous life routines. In both Ramsay and Castle community hospitals, there was, among some staff, a harking back to a time when they could do ‘proper’ rehabilitation; by contrast, they felt limited in what they could achieve, and evinced a sense of discomfort in working with some patients with complex needs.
In Lawrence, there was a common sense of purpose on care delivery to patients with combined medical, therapy and social needs within a delimited time, preparatory to effecting transition on to community-based services. This care culture was supported through staff training and skills development to respond to patient complexity. For nurses and health-care assistants (HCAs), the training programme included care of people with dementia, recognising and managing deteriorating patients, and end-of-life care.
Process of care delivery
Enacting rehabilitation
It is argued that the process of rehabilitation is at the heart of ‘best practice’ for older people. 81 Forging a shared understanding of the purpose of rehabilitation in the context of a changing patient profile and interdisciplinary working practices emerged as a key issue for staff. Staff in Lawrence community hospital were explicit that their patients were best described as ‘acute with frailty’, and that this had implications for the purpose and goals of rehabilitation:
We’re a medical step-down ward, with a little bit of rehabilitation. Patients are more poorly and acute than we’ve seen for a long time . . . that’s because of earlier discharges [from hospital] . . . would you call it a ‘left shift’ . . . complex discharges as well including dementia patients . . . they are more dependent . . . [I mean] more frail . . . the amount of hoists and rotundas, we have very few who are independent . . . patients coming in who are high falls risk.
Senior ward nurse 05, Lawrence community hospital
Rehabilitation in the sense of work to optimise functional ability in context of medical needs and frailty to achieve a ‘safe’ discharge remained a goal, albeit the meaning of ‘safe’ varied with the environment to which patients were being discharged (e.g. home or long-term care). There was recognition that the time frame within which the unit operated meant that more sustained, preventative work was not possible:
. . . functional is about can they mobilise, can they get around their house, get washed and dressed, get in and out of their bath . . . We can get them to do those things to the best they can whilst they’re here . . . some patients you do want longer with them . . . who come because of falls . . . balance work, strengthening, gait pattern, things like that, and we don’t really get the chance to implement those kind of things properly.
Therapist 09, Lawrence community hospital
The limits of what could be achieved within the supportive environment of the community hospital for patients with complex needs meant that the work involved contributed to, but did not complete the process of, ‘recovery’. Thus, it highlighted the need for support and resources for patients to pursue ‘recovery’ in transitioning from hospital and back home.
In Castle community hospital, senior ward staff and therapists commented on the impact that the frailty service had on its purpose and function. As the frailty service had expanded the range of community-based acute, transitional and enablement services, patients who could go home from hospital with support were more likely to do so. As a consequence, those referred to the inpatient unit were patients:
. . . from the local area who need further medical intervention but they’re medically stable . . . have complex discharge-planning needs . . . because of multiple chronic conditions; or are palliative . . . [They come] mostly from acute wards or via bed management . . .
Senior ward staff 09, Castle community hospital
The community hospital and the rehabilitation resource offered benefit for such patients:
. . . they have more intense physio[therapy] here and they’re more directed on what patients need at home.
Senior ward staff 11, Castle community hospital
But the patients also benefited at the end of their community hospital episode because, according to staff, the transition home was eased as a consequence of the diverse services that could be accessed during the transition from an inpatient bed to getting back home. In addition, occupational therapists in Castle community hospital worked across the hospital and patient’s home as part of an integrated reablement team:
Here we work on daily tasks . . . able to go to the toilet independently . . . to manage getting in and out of the bed, getting on and off a chair . . . to get the person home safely. Sometimes it’s: ‘I want to be able to go to the shops like I used to’ or go to church that . . . you can break down and say ‘well in order to go to [do those] you need to be able to transfer and to walk so far and get in and out of the car’ . . . Because we are an integrated team we see people in hospital . . . and [continue] . . . when they go home with reablement . . . short term assessment and continuing rehab[ilitation] [at home]. Then, we might . . . look at those goals more closely . . . and work on them at home.
Therapists 12 & 13, Castle community hospital
In Ramsay community hospital, therapy and nursing staff conveyed the difficulties of a model of rehabilitation that aimed to maximise independence, given the time targets to achieve it with their patients:
[The occupational therapist role focuses] on preparing patients and family for discharge from hospital to home and back to the home environment with the level of support that they’ve got there . . . [Now] you’re aiming for . . . a smooth discharge and for them to be as safe and as independent as possible at home. But obviously a lot of what you do . . . will depend on how long you’re given to do it . . . in the past when you had much lengthier stays you’d be doing a lot more rehab[ilitation] with the patient, trying to get them back to a high level. Whereas now, they might have to go home before they get back to their baseline or to their maximum potential. But you’ve still got to get them home safely . . . it used to be 5 weeks . . . now the aim is 2 weeks . . .
Therapist 07, Ramsay community hospital
For these staff, the problem of securing ‘safe’ discharge was exacerbated by lack of knowledge about what transitional support was provided and for which patients. Moreover, senior staff suggested a need for greater clarity as to what patients and relatives could be expected to achieve in a community hospital in terms of ‘recovery’. Emphasis on such performance targets as reduced LOS and re-admission avoidance, it was argued, needed to take account of what was achievable in terms of recovery with their emerging patient profile:
We need honesty . . . and . . . the patient and their families need . . . to know what [can be expected] . . . what we get is a patient that has lots of complex needs, lots of comorbidities, has a bit of a nightmare at home if they’ve got a home . . . to sort out . . . . The pressure to look at length of stay as being the all-important thing . . . when . . . a patient might not happen to fit into a pathway or they might change pathways once they’re here because of something else happening . . . people don’t look wide enough to think, ‘actually yes, we might extend their stay by another week’ but if it stops them going back into hospital or it stops them coming back in here, then that’s time well spent.
Senior nurse 06, Ramsay community hospital
These varied perspectives in part reflected the challenges experienced by staff in responding to the needs of patients with multiple and complex needs. In all three community hospitals, forging a joint and collaborative approach to rehabilitation as ‘enabling’ and patient-centred work for their emerging patient group posed tricky issues related to staffing, the physical ward environment, knowledge and skills deficits.
An enabling approach to practice is central to rehabilitation. We noted earlier that prior experience, beliefs and knowledge of the patient group contributed to the way care staff pursued a primarily caring- for or enabling approach. In Castle, the routine use of ‘Stedys’ (Invacare Corporation, Elyria, OH, USA) (a standing and wheeled transfer frame) to transport patients from bed to bathroom was commented on by therapists:
Normally ‘Stedys’ are just used for transferring from . . . one chair to another, and that was [therapist’s experience of their use in previous work settings] but here . . . because the legs splay they can use them to transport patients . . . It wouldn’t be my means of transporting somebody . . . It’s beneficial if that’s what they’ve been assessed for . . . and that’s what we’ve advised the nurses to use . . . but if we’ve progressed them and said, ‘This patient can stand and step around,’ then it’s negative . . . as patients . . . isn’t it, because instead you’re only standing, you’re on wheels, you’re turning, you know, you’ve got your sit to stand, stand into a [walking] frame that you learn to use at home probably anyway, stepping around, maintaining your balance, you’ve got, you know, and then they can practice that . . . when they need the toilet rather than [be transported] but you know it depends on staffing on the ward . . .
Therapist 14, Castle community hospital
Although staffing was implicated, it was noted that practice was very variable because of prior experience caring for very dependent older people. Nevertheless, in all three community hospitals, there were accounts of creative approaches to rehabilitation relating to problem-focused strategies to support patients with multiple health problems including dementia:
A patient . . . 96 and not great at doing anything with her hands because of arthritis and had poor eyesight . . . Her knee . . . was so deformed that it was very unstable . . . I tried . . . a splint which did the job . . . the problem was putting it into practical use as the patient couldn’t put it on herself . . . so we had to go back and think what can we do. So . . . we modified it, sewed Velcro to the strap . . . and a green fabric on top of it so it was easy to see and she could feel it and we practised with her and she could take it off and put it on by herself . . . For patients . . . with memory problem . . . I look at . . . not just what they’re doing physically, but observing their communication . . . what words they use, what cues help them to remember . . . . There was a patient who had poor memory and didn’t remember to take her frame with her . . . we put a sign on her frame saying, ‘Use me’ . . . on a yellow background with black letters ‘cause it’s easier for her to see that . . . which was enough to help her remember to use the frame . . . There’s no textbook that tells you how to do those things . . . and they don’t work for everyone . . . it’s trying out what makes it easier for the patient . . .
Therapist 10, Ramsay community hospital
Responding empathically to patients with dementia or memory problems, and trying out tailored strategies to resolve problems limiting a patient‘s participation in ‘recovery work’, as in the above, reinforced the significance of specific knowledge and skills on the part of staff and the consequences of deficits in both. We could identify a continuum of practices reflecting available support and investment in training and specialist resources for patients with particular needs.
Some, but not all, staff viewed patients who exhibited ‘problem behaviours’ in the context of dementia and delirium, as ‘inappropriate’ admissions. In Ramsay, for example, such patients were ‘cohorted’ (the term that was employed) into one of the bays and a worker, often a bank or agency staff member, sat in the bay. There was little or no communication between the staff member and patients, save to admonish the person (e.g. ‘don’t get up’, ‘don’t do that’), which was reported also among some staff in acute and palliative hospital wards. 79,82,83 This was in contrast to individual staff members, described as having a ‘magic touch’, who engaged empathically with such patients using touch and voice to provide a physical and metaphorical ‘handhold’ to assuage distress. It was also in stark contrast to staff’s typical interactions with patients generally, which were suffused with warmth and sociability. Although there was acknowledgement among senior trust managers that this ‘controlling’ approach was problematic, training to enhance skills and change the care culture had not been put in place during fieldwork. At the other end of the spectrum, dedicated training in the care of people with dementia was part of a mandatory training programme in Lawrence and beginning in Castle. In Lawrence too, there were patients who cried out in distress, were agitated and disruptive of others and were nursed together in one of the bays. Here, however, one or two staff members sat with them for long periods, engaging in conversation, playing games, playing music and employing their knowledge of the individuals to draw them in. Staff here could also access specialist support from the adjacent mental health ward. There was an expectation on staff that this work was a necessary and legitimate feature of ward work, hence the importance attached to equipping staff with the skills and support to do it effectively.
Key dimensions of care quality
In the three community hospitals, progressing recovery to secure a ‘safe’ discharge was seen to require a co-ordinated, collaborative endeavour involving medical, nursing and therapy staff. In each hospital, direct therapy input, either on the ward or in a gym/therapy space, occurred approximately once daily (weekdays) for those patients who were well enough and for whom the plan was to return home. In addition, it was expected that nursing and care staff would support rehabilitation goals through encouraging and supporting mobility and self-care.
Interdisciplinary working
Across the three case studies, high value was placed on interdisciplinary working between staff as an aspiration and as a valued practice accomplishment.
The MDT meeting and board/ward round were formal mechanisms used by each ward for information-sharing and decision-making about therapy, care and discharge-planning. The ward round involved reviewing each patient in person by their bed; the board round was briefer and the patients were reviewed in absentia away from the bedside.
In Ramsay and Castle community hospitals, the MDT occurred once weekly, as did the board/ward round. Typically, attendees were the ward sister, therapists (physiotherapists and occupational therapists), social worker, hospital-based doctor (GP in Ramsay) and link consultant from the acute hospital. Each patient was discussed briefly. In Castle, the consultant provided the steer and set the pace eliciting an update on goals and progress from the doctor and therapists, movement on place of discharge, feedback on (or plans for) patient/caregiver meetings and any medical/nursing issues, including mental health assessments that might affect next steps. In Ramsay, the senior nurse took the lead and the content was similar. In both, staff shared personally meaningful knowledge of the patient and family either conveyed by HCAs and nurses from observations and conversations with patients and families or participants’ own encounters with them.
In addition, in both community hospitals, a meeting involving members of the MDT, but without the consultant, occurred weekly. In Ramsay, this was described as a ‘board’ meeting, and in Castle, it was referred to as a ‘patient flow’ meeting. Their purposes were broadly similar in both community hospitals: to translate decision-making taken at the MDT meeting regarding patients into firm action plans and allocate responsible individuals to ensure progress with mobilising the probable support required, and to highlight those patients for whom a discharge outcome was yet to be agreed. Progress on associated action in respect of resources to achieve movement forward was then discussed. The content of both meetings served the broad focus on securing timeliness of decision-making and action, maintaining momentum and avoiding planning ‘drift’.
In Lawrence, weekly MDT meetings included the ANP, senior nurse (ward manager/sister), therapists and social worker. A consultant from the acute hospital had recently been appointed to provide medical cover but was not observed at MDT meetings. During fieldwork, consultant engagement primarily involved conducting joint ward rounds once or twice weekly with the ANP, and providing medical advice at the ANP‘s request. In addition, short board meetings occurred daily from Monday to Friday. Participation extended beyond senior ward staff to include a staff nurse, therapy technicians and ward clerk. A social worker and member of the Intensive Community Support team (a virtual ward with over 250 beds across the city and county) were frequently in attendance. Focus was primarily on a patient’s current situation, readiness for, and plans towards discharge, including identifying those who might be able to go home with support from the Intensive Community Support team. Aspects considered included current physical and mental health, mood, engagement in and progress with therapy and specific actions to move forward discharge. The meeting was more inclusive of staff directly involved in delivering care and therapy, plans were considered in more detail than at the MDT meeting and responsibilities for action were assumed by individuals attending. These board meetings were well attended, contributed to a collaborative stance towards delivery and reinforced a model of collegiate interprofessional working, characterised by distributed authority and flexible leadership. 84 Staff from different disciplines took turns to lead the discussion.
Across the three hospitals, different professionals were viewed as having a particular domain of expertise, and so the decision-making and action drew on all of them. The following is illustrative:
Elsie was an 80-year-old woman with spinal compression and advanced cancer referred by the GP for ‘general rehabilitation’. She had been admitted to the community hospital some 31 days previously. The therapist reported that she was now able to walk to and from the toilet independently with support of a walking frame. The senior nurse added that Elsie had started chemotherapy and was due a session the coming week. She continued that background work had involved organising transport to and from the general hospital [the ward clerk had made the arrangements]. Discussion centred on how nursing and therapy staff needed to organise her therapy sessions for optimum times between chemo and to protect her. ‘Anne [ward clerk] is chasing her chemo dates for us now’, and ‘when Elsie feels most nauseous and fatigued, we must let her hibernate’ (Senior Nurse). ‘She can still walk but fatigue is high. She banks her energy for what she needs to do’ (OT). The consultant was to clarify with oncology whether treatment goals were palliative.
Fieldnote: Ramsay MDT
Collaboration in routine practices
In Lawrence, the strong ethos of interdisciplinary working reflected in formal meetings was carried through to, and reinforced by, collaborative ward practices. Therapists were a visible presence on the ward from early morning (08.00 start) to mid-to-late afternoon (around 16.30):
As things crop up in the day, there’s certain nurses that are allocated to certain patients, we’ll just go and speak to the nurse that is allocated to specific patients . . . everyone’s really approachable, we’ll just hand it over verbally, but I think generally the communication is quite good . . . if we’ve got an issue to raise with a relative, they would do that for you . . . Especially the more senior nurses that have worked here quite a long time, you can rely on them to relay the information.
Therapist 08, Lawrence community hospital
Staff (i.e. nurses, HCAs and therapists) reported that they identified as a team. It was observed and recounted in interviews with nurses that therapists were cognisant of the demands on ward staff and would help out when they were seen to be stretched, for example if a patient needed to go to the toilet:
Yes of course . . . if a patient needs the toilet, then they need it. Yesterday we were hoisting someone and he said he needed the toilet so we got him on the bed pan . . . that helps us as well . . . we can look at their rolling, their movement . . . how far they can walk, their exercise tolerance . . . independence with their toilet hygiene for home . . . you can take it as an opportunity . . . when they’re pulling their things up, then I can look at how they balance without holding onto their walking frame . . . , you’ve got to take your opportunities, because then sometimes they’re here and they don’t actually want to do anything.
Therapist 09, Lawrence community hospital
The routine and taken-for-granted character of these practices is illustrated below:
The physio[therapist] makes a drink for a patient, she explains to the HCA doing the drinks as she does this that he missed the drinks because she had taken him to practise stairs. Later at the therapy team meeting, one of the issues raised following a request from the matrons was supporting patients to become independent at mealtimes. Therapists agreed that the OT and PT [occupational therapist and physiotherapist] would be available to encourage patients walking to the dining room. There was no discussion or debate.
Fieldnote, Lawrence community hospital
In Castle and Ramsay community hospitals, although collaborative working was a feature of practice, relationships tended not to be as close and reciprocal as in Lawrence. In Castle, this was partly shaped by the organisational context. The downside of the occupational therapy integrated model was that therapists were not as visible a presence on the ward and likewise for the physiotherapists, given their wider role in the hub. Therapists here did not rely on ward staff to take patients to the gym/therapy rooms as porters were available to do this. In Ramsay, therapists tended to adopt more defined professional boundaries. For example, care staff considered that therapists and therapy technicians could provide assistance with mobility for patients to go to eat in the dining room; both therapists and technicians regarded it as outside their respective roles. Whereas situational factors such as staffing difficulties were experienced in both Ramsay and Lawrence, the effect on multidisciplinary working were very different: boundary demarcation in Ramsay and an interdisciplinary, collegiate approach in Lawrence.
In all three hospitals, physiotherapists and occupational therapists indicated that they valued working jointly: initial assessments were often conducted together, meaning that patients did not have to repeat information and the assessment paperwork was completed jointly. Some aspects of the information gathering were carried out by one or the other, reflecting their areas of expertise (e.g. the physiotherapist did a strength assessment and the occupational therapist took a social history).
Interprofessional communication
Systems for interprofessional communication varied across hospitals. In Castle and Ramsay, notations and symbols alongside each patient name on the whiteboard and updated following MDT and board meetings communicated what kind of assistance was required from staff to support therapy goals, patients‘ specific needs for support (e.g. because of dementia, nutritional difficulties) and estimated discharge date. It was noted during fieldwork that there was often a delay between decisions arrived at during MDT meetings and what was written on the whiteboard, although informal knowledge-sharing could bridge the gap.
Lawrence community hospital had implemented an electronic real-time communication system for use by all staff, including those directly providing care. There were also robust collaborative mechanisms in place at different levels to facilitate use. Each MDT and board meeting had a different designated professional responsible for inputting actions and decisions directly onto a hand-held computer (i.e. the ‘nerve centre’) that linked in real time to the central patient system and electronic patient board at the nurses’ station. This also served the purpose of communicating action in relation to individual patients to members of the ward team, who also carried their own hand-held computer. The same system was used to record action points from handover meetings and relevant knowledge about patients and families (even as they made quick notes on handover sheets). Ward staff were observed using the system to check on a patient’s health status or progress with discharge.
Meaningful engagement of patients and families
Staff in all three hospitals placed high value on engagement with patients and families. Acquiring knowledge about the individual as patient and person from a myriad of sources was part of the admission process, and was built on subsequently. Knowledge acquisition encompassed medical, social, psychological, emotional and functional aspects, as well as family circumstances and relationships, that, in turn, informed shared clinical, care and therapy goals.
Ongoing, pro-active involvement with family members from admission was partly to develop understanding of the patient in their biographical, relational and environmental context and to elicit a picture of how the person managed prior to the event that brought them into hospital to inform a plan of action towards recovery. It was also to provide close family with informational, emotional and practical support and to engage them in encouraging their relative in the rehabilitation process.
Formal mechanisms existed for knowledge-sharing, decision-making and action. Castle community hospital had introduced a goal-setting meeting early in the admission with the patient, relatives, senior nurse, physiotherapist and social worker, although during fieldwork, staff pressures had extended the period of time during which it occurred. This was intended as an open discussion to share knowledge, consider preferences, valued goals and the steps necessary to work towards them. It primarily served the purpose of engaging family members in supporting the patient’s goals and in sustaining the person’s motivation to persist with the work. From interviews with therapists, the work of assessment and developing a treatment plan with the patient did not wait on the goal-planning meeting, it began at admission alongside the doctor’s clerking of the patient:
At the nursing station, I chat to the OT [occupational therapist] and physio[therapist]. One of the physios notes the importance of involving the family and patients’ wishes in order to work out what the patients‘ goals are for when they go home, commenting: ‘It’s no good them getting home and then realising they want to go into the garden which has steps, if they haven’t thought about and practised steps first’.
Fieldnote, Castle community hospital
In Castle and Ramsay community hospitals, progress and discharge-planning meetings were held with patients and families. It was reported that everyone had at least two meetings during their stay, either a goal-setting or a progress meeting and a discharge-planning meeting. In practice, the number depended on the complexity of the issues involved in decision-making and the degree to which there was consensus between the relevant parties (i.e. staff, patients and family members) on the goals for treatment and therapy and the plan for discharge. In Lawrence, most patients had at least one family meeting and, depending on the complexity of discharge arrangements, might have more than one.
On a routine day-to-day basis, ward staff in each hospital provided reassurance and celebrated advances, however small, which was aimed at building up confidence and hope. Therapists in Ramsay, for example, had implemented a system for communicating patients’ need for assistance with mobilising. The traffic light system – using symbols on assistive devices – was a clearly observable and simple means of conveying to ward staff the level of assistance patients required with mobilising (e.g. red2 indicated need for assistance of two staff and green meant that the person was independently mobile). For patients, the symbols were a measure of their progress, a marker of their nearness/distance from discharge and, therefore, a source of conversation and social comparison:
Two patients are in conversation about the status of the coloured stickers on their frames – both yellow. One comments to the other: ‘don’t worry, we’ll get there in the end’.
Fieldnote, Ramsay community hospital
Therapists were aware that the point of transition could be a source of anxiety. The following exchange occurred after the therapy technician had spent time with Isobel working with her to identify what assistive devices she might need at home:
As the therapy technician talks to Isobel, she asks her how she felt walking the distance to the bathroom. Isobel replies that she felt all right and then asks the therapist a little uncertainly: ‘do you think I’m doing all right’? The therapist replies that she was and changes the sticker on the walking frame from yellow to green: ‘you can go on our own now, but if you feel a bit wobbly just ring the bell and we’ll come’.
Fieldnote, Ramsay community hospital
Agnes’s daughter reassured her mother that moving on to the green sticker was not a pre-condition for going home:
She continued with the physio[therapy] and she was then promoted to the yellow sticker which was a big, big thing . . . that meant we were looking at discharge. Then the therapist rang me and said because of her Parkinson’s and her issues with balance, they didn’t feel they could ever put her on the green to mean that she was totally safe which I agreed with . . . so we never got the green sticker . . . Mum was desperate to get the green; [two other patients] in her room had got the green . . . I didn’t tell her that she wasn’t safe, just that she wasn’t as mobile as [the other two] but ‘it won’t matter because you’ll go home and you will deal with your home situation and you’ll be fine . . . ’ And we worked out what to do at night to make her safer.
Patient case study 01, Ramsay
In all three hospitals, occupational therapists assumed a key role in communicating with families and facilitated knowledge-sharing between family members, patients and staff. There were circumstances in which these therapists adopted the lead role in planning for discharge, for example where there was no social worker involved as when the patient’s primary needs related to housing and adaptations and not packages of personal care. Informal discussion with family members was regarded as a valued and legitimate investment of ward staff time. Senior staff pro-actively engaged with family members during visiting times. They also conveyed in their stance openness and accessibility to being approached, which, in turn, mirrored their expectations on the staff team as a whole. In handover meetings, for example, HCAs would often provide relevant knowledge about the patient, gleaned from conversations with relatives or the patient as they went about their day-to-day business. In Castle community hospital, the fact that staff tended to live locally meant that patients were often known to them, whether this was as acquaintances, through family connections or their positions in the community. This was reflected in an atmosphere of familiarity and shared understanding of values and experiences of living in a small town. A different kind of familiarity was observed in Lawrence: the ethnically diverse staff group meant that individual staff could communicate with patients in their own language and were sensitive to cultural and religious sensibilities.
These varied formal and informal mechanisms for knowledge-sharing between ward staff and between staff, patients and relatives are illustrated in vignettes (see Figures 6–8) as features of good practice.
Trajectories of recovery
We noted from patient profile data that median LOS in all community hospital wards concealed considerable intrahospital variation. Patient case studies were aimed at illuminating the factors that contributed to this. Although the trajectory of recovery for patients with different characteristics and needs contributed to variation in LOS and destination outcome, organisational barriers and resource gaps, often operating cumulatively and interactively, were also implicated. From patient case studies, we can identify a number of distinct recovery trajectories as well as the critical conjunctures that shaped them.
Working at recovery: towards resumption of previous routines
Isobel is illustrative of this trajectory. Prior to the health event that precipitated community hospital admission, Isobel was fit and active and enjoyed an ‘out-and-about’ lifestyle. She and her spouse had a shared interest in gardening. The couple had close family nearby and had a wide circle of friends and long-standing neighbours. They received no formal services. At 85 years, a fall resulted in an admission by ambulance to accident and emergency with a cracked pelvis and a 1-week stay on an acute hospital ward. This was her first overnight stay in hospital for many years (a broken arm several years previously had not involved an inpatient stay).
In her first week on the community hospital ward, Isobel was in considerable pain that affected her mobility. She described ‘not being allowed’ to go to the toilet on her own and was ‘told to ring the bell’. As the pain subsided with medication, she was encouraged by the therapy technician to use a walking frame; a yellow sticker conveyed that she required supervision with mobility. Sociable and enjoying the company of others (‘I wouldn’t like to be on my own’), she walked to the dining room with her frame, usually sitting with the same people. Towards the end of her second week, the therapy technician changed her yellow sticker to a green one, reassuring her that if she felt unsafe, to ask for assistance. After being assessed for assistive devices that would help her recovery at home, she was anxious to get home and knew that there was still a way to go to get back to where she had been but felt that being in a familiar environment would help her regain self-confidence. The assistive devices were delivered as planned and she was discharged 17 days following admission with no other services.
Trajectory: non-linear and remitting
A non-linear and remitting trajectory was a common trajectory type among patients in all three community hospitals. This trajectory involved a pattern of recovery that was non-linear and remitting: with alternate periods of progress and deterioration, and which typically contributed to long LOSs. This could result in a level of stability that opened up a window of opportunity in which to plan for supported discharge home (illustrated, for example, in Figure 7a). Often, such patients required a complex package of supportive arrangements combining intensive formal and informal care, at least in the transition phase.
Alternatively, this trajectory resulted in a downwards spiral involving a shift in objective from return home to planning for long-term care, as illustrated in the case study of Peter. He had been admitted to the community hospital from an acute ward when he had fallen and fractured his hip. This was the most recent of several falls, with the most serious consequences. Prior to this event, Peter (aged 81 years) and his wife were receiving considerable formal support on account of his physical needs and dementia: carers three times daily, and 2 hours weekly respite for his wife. Initially assessed for support with mobilising with the perspective of returning home – it was what he and his wife wanted – alternate periods of agitation and unresponsiveness over several weeks disrupted rehabilitation work and he deteriorated physically and cognitively. Meetings and conversations involving nurses and therapists with Peter, his wife and son concluded that he would not be able to return home, a decision arrived at within 3 weeks of admission, and the continuing health-care eligibility assessment was initiated. He was still on the ward 60 days later. Organisational factors prolonged the community hospital episode. The lengthy process of assessment of eligibility for continuing health-care funding was unsuccessful when presented at the funding panel; an assessment for NHS-supported nursing care in a care home was then conducted. A simultaneous search by the family, with support from community hospital staff, for a care home that would provide for his needs ensued. A nursing home, following assessment, agreed to take him and a place was available. The planned move was put on hold as the panel had not yet made a decision on funding. Peter had been in the community hospital for 81 days.
Fragile recovery: getting home to keep going
This was another common trajectory recovery pattern. Here, patients’ conception of ‘recovery’ was to make sufficient progress that they could just return home having regained sufficient strength and ‘wellness’ to keep going. Simultaneously, they were anxious and fearful that they might not manage it.
Margaret (aged 90 years), similar to Isobel, had a fall resulting in a cracked pelvis. Unlike Isobel, she lived alone and had multiple chronic health conditions (cardiac problems, osteoporosis and hearing impairment) and active breast cancer for which she had chosen not to undergo treatment. Prior to the fall, she was restricted to her home. She had a private carer for 1 hour daily and a private physiotherapist to sustain mobility fortnightly, used a microwave to heat up ready meals and did her own shopping by telephone. She was supported by family and ‘good neighbours’ (‘elderly like myself’).
Margaret’s recovery was slow. She was helped daily by therapists, first to transfer between bed and chair, then, when stronger, she was encouraged to walk with a frame. She enjoyed the company of the other patients with whom she shared a bay, stating that it helped to keep her spirits up. Two weeks into her stay, she remarked: ‘they say I’m getting there but I don’t see it’. She was anxious to return home but equally anxious about managing again, yet adamant she did not want to go into a care home: ‘If I’m on my last legs, I’ll go into a hospice’. After 31 days, Margaret was discharged home with support from the reablement service for up to 6 weeks.
In both this and the non-linear and remitting trajectory, the pattern of complex multimorbidity necessitated in-depth and ongoing planning and, for those going home, typically required mobilisation of intermediate-care support and/or negotiation of increased packages of care. Nevertheless, overall destination outcomes from each of the community hospitals suggested that around two-thirds of patients return to their own home.
Moving on from the community hospital
Among the three community hospitals, discharge was not a single event. It was a process that was pursued over time. Thus, the organisation of clinical, care and therapy work with patients on the ward through such collaborative and knowledge-sharing mechanisms as MDTs, handovers and board and ‘flow’ meetings drove goal-planning and action forward. Engagement of patient and family members through formal and informal encounters involved the elicitation, negotiation and renegotiation of options and choices in line with the patient’s recovery trajectory and available resources, including local service systems with their varied agencies and services, eligibility criteria and timescales. These, in turn, established a framework for progress review and identified the support necessary to facilitate ‘safe’ discharge. In all three hospitals, discharge-planning was both an end point in the hospital episode and a critical juncture in the patient journey whether to resume prior routines, facilitate keeping going with enhanced formal support, initiate entry into a care home, or provide assistance in managing a newly acquired disability.
Patients and families sometimes reported that they were in the dark about plans for moving on from the community hospital. Often underpinning such communication gaps were staff’s own lack of knowledge about, or absence of control in the context of, multiple-level negotiations occurring within and between agencies and services about follow-on support. It could also reflect uncertainty among staff as to whether or not the person was ‘sufficiently’ safe to go home, which involved a combination of their stage of recovery and their home situation, including access to informal support and availability of formal services. The depth and breadth of local family networks in the locality of Castle community hospital, for example, meant that staff would ‘try out’ a patient at home for several days, but this was less common in the other sites.
For many patients in community hospitals, ‘moving on’ required not only packages of social care in the longer term to enable them to remain at home, but support and resources to pursue their recovery in the transition from the ‘protected’ environment of the community hospital to their familiar home environment. ‘Safe’ discharge, particularly for those with complex needs, was predicated on the availability of appropriate assistance to manage this transition. This included, for example, therapy to sustain and build on functional progress achieved in the community hospital, particularly important in that regular community therapy provision had waiting lists of up to 6 months, or enablement support to restore confidence in managing tasks of daily living. Two inter-related factors affected availability of transitional support: (1) comprehensiveness and capacity of the health and social care services to provide such support and (2) effectiveness of the mechanisms in place to facilitate continuity between sectors and services. Both factors required shared knowledge about what was available and appropriate for patients with different types of need.
In this respect then, ‘moving on’ had an individual and systemic meaning. For those patients with frailty/in advanced older age, moving on to pursue recovery in their own environment was likely to require an additional bit of help to manage the transition. At a system level, seamless and co-ordinated transition of patients from the hospital required appropriate services to enable it and the local knowledge and networks of staff to navigate through it.
Summary
In this study, we sought to provide insight into the less tangible components of community hospital working that might be incorporated into the interactive toolkits for use by local commissioners and community hospital teams to support operational changes to optimise performance. Our conclusions are based on the analysis of 226 patient observation episodes obtained from three study sites, and a total of 66 interviews with staff, senior managers and patients/carers. In many aspects, the three community hospital wards were very different: in the model of operation of the community hospital, in their physical environments and in the resources and support available to facilitate transitional and ongoing support, particularly for older people with frailty. This is not surprising, as a multimethod review of community hospitals in the UK and in other high-income countries concluded: ‘such hospitals exist in a variety of forms and encompass a varied range of services, diverse models of ownership and management and different degrees of co-ordination with general hospitals on the one hand, and with primary and community services, on the other’. 85
Even so, despite their differences, each community hospital was undergoing a process of change as a consequence of several linked strategic drivers: more effective and efficient use of acute hospitals; delivering health care ‘closer to home’, particularly for older people with complex needs; and an integrated response between sectors and services for those needing time, space and transitional support to recover from illness. Responding to the specific needs of patients with multiple and complex comorbidities made particular demands on community hospital ward staff’s knowledge, skills and resources in terms of how the clinical, care and therapy work with patients on the ward was organised and the engagement of family members and patients was pursued. Each of them adopted systems and mechanisms to facilitate interdisciplinary working, care co-ordination and patient/family engagement, which varied in content reflecting local circumstance, although their underpinning purpose and functions were similar. Nevertheless, forging an enabling and patient-centred rehabilitation ethos and practice across the whole of their patient population was a work in progress. In each case study, features of the physical environment, knowledge and skill deficits vis a vis the emerging patient group affected rehabilitation practice in ways that did not clearly differentiate the ‘cost-efficient performers’ and the less ‘cost-efficient performers’.
In each community hospital, there existed formal structures reflecting and reinforcing distributive forms of leadership stretching across the medical, nursing, therapy and care functions of the setting. These extended beyond the traditional MDT meeting that typically involved medical expertise and oversight to encompass arenas for in-depth progress review, concerted, interdependent action and co-ordination of work to effect movement in the patient ‘recovery journey’, including organising support to manage transition beyond the hospital.
Limitations
Findings are drawn from three community hospitals only and so they cannot be regarded as representative; however, this was not our purpose. Even so, the findings did capture something of the diversity of community hospitals in terms of historical origins, organisation, rehabilitation practice and what shapes them. We were unable to secure as much information about patient profiles as we had hoped. It did not appear, for whatever reason, that wards could easily access such data.
Chapter 5 To develop a toolkit for commissioners and community hospital providers to optimise performance (study 4)
Introduction
Continuing pressures on limited NHS finances and increased demand for services have led the NHS to consider ways by which to improve operational efficiency. The NHS Five Year Forward View86 sets out an ambition to achieve 2% net efficiency gains across the NHS each year for the rest of the decade.
A report by Monitor in 2013 estimated achievable savings of £1.2–1.8B in community services in general. 33 Given a total spend of £8.4B across these services, this represents around a 15% potential for cost reduction.
In this chapter we set out how we developed a toolkit for commissioners and community hospital providers to support operational changes to optimise the cost efficiency of community hospital ward care for older people. This is the final stage of our programme of work and related to objective 3 (study 4): to develop toolkits for commissioners and community hospital providers to optimise performance.
Methods
A web-based interactive toolkit for use by local commissioners and community hospital teams was formulated by integrating the outputs from the econometrics analysis (study 1, see Chapter 2), the data collected by the NHSBN and the outputs from the qualitative case studies (study 3, see Chapter 4).
The content of the toolkit was co-produced and iteratively modified by the Project Management Group, the CHA (lead Helen Tucker) and the Patients Association (lead Heather Eardley). The toolkit was based on previous similar work conducted by NHSBN for other clinical service areas. The toolkit comprises a database in structured query language server, an application interface built in a Node.js framework and a front end (user interface) built using Angular 2 technology. The toolkit is hosted on a Windows® (Microsoft Corporation) server within Internet Information Services (Microsoft Corporation).
Initial testing was conducted by the NHSBN analytics team. The web pages were then published to the testing area of the NHSBN server. A further round of testing took place with three community hospital sites. Amendments were made at this stage to ensure that the toolkits functioned correctly as specified and met user requirements.
The toolkit was launched for discussion and feedback at the 2017 CHA Annual Conference (2–4 June, Manchester, UK) in the format of an interactive workshop. Delegates’ suggestions for further modification were recorded and incorporated into the final version.
Once testing was complete, the toolkit was published on the NHSBN live web and database environment and is now being promoted nationally through the CHA.
Toolkit content
The toolkit comprises three key components:
-
an efficiency calculator
-
scenario calculator
-
case studies.
Efficiency calculator
The efficiency calculator was developed to facilitate the assessment by local teams of their relative community hospital ward cost compared with other community hospital wards in the UK.
The calculator generates an ‘efficiency score’ for any community hospital for which data are entered into the tool by the user. The resulting efficiency score is then benchmarked against efficiency scores of other community hospitals derived from the analysis of community hospital data from the NHSBN’s 2014 Community Hospitals Project.
The formula used to calculate the efficiency score is:
Formula reference examples:
-
c – costs of staff, materials, and so forth
-
y – a string of cost drivers such as the number of patients treated
-
w – input prices, wages, capital costs
-
z – environmental variables such as bed occupancy, mix of services provided
-
q – quality of clinical audit results, research activities, meticillin-resistant Staphylococcus aureus (MRSA) occurrence, pressure sores, patient-reported experience measure
-
ε – variables of inefficiency.
Scenario-based calculator
The key characteristics (indicators) of community hospital wards that optimise performance, as identified in study 1, are analysed in detail by the scenario calculator.
The characteristics considered in the calculator are pay cost per occupied bed-day, bed occupancy, nursing ratio, staffing levels and LOS. The tool allows the user to enter values for a community hospital ward for each of the indicators to assess the resource implications of moving to national average or target values.
The calculator shows the gap between local and national average or target levels for community hospital ward performance and the investment required to meet these levels or the potential savings available.
Case studies
A workshop was arranged at the 2016 CHA Annual Conference (13–15 May, Bristol, UK) attended by community hospital staff of various grades. Participants were clear that aspects of quality of care were important and needed to be incorporated into the proposed toolkit. Different methods of presenting the findings from the case studies were discussed including self-assessment questionnaires that explored ward culture and processes, checklists and training programmes. The favoured solution, however, was a series of case vignettes that demonstrated the findings from the case studies. The participants felt that this would be a familiar format for them and would allow the staff to reflect on their own practices in relation to the key rehabilitation care characteristics that had emerged. Subsequent meetings and feedback on the content and presentation of illustrative vignettes involved reciprocal exchange between researchers and leading members of the CHA. These were further tested out in workshops at the 2017 CHA Annual Conference.
Notwithstanding the diversity of their service models and the dynamic of health and social care systems within which the community hospitals operated, the critical features of quality practice, which framed the vignettes, resonated with participants. As elaborated on in Chapter 4, these embraced mechanisms for interdisciplinary working and communication, meaningful engagement with patients and families and goal-directed, purposive action to move patients forward to secure a ‘safe’ discharge.
The vignettes have been provided in Figures 6–8. The vignette in Figure 6 is intended to set the scene by describing the organisational context, model of service provision, patient profile and patient and service outcomes for the three case studies. It highlights the ways in which community hospitals appear to be undergoing a process of change in some respects, although there is continuity in others. It also sets out the quality criteria that we employed (i.e. criteria that broadly reflect a consensus in policy and research), although here specifically pertaining to the work with older people with rehabilitation needs in a community hospital environment. The scenarios conveyed in Figures 7 and 8 set out practices, patient experiences and discussion points relating to features of the work of community hospitals that staff indicated were challenging: the increased complexity of their patient profile, the dynamic and non-linear nature of recovery of patients with complex needs, and the demands on them in terms of skill and creativity in responding to the multiple and complex needs of these patient. They are not intended to convey one ideal solution; on the contrary, they are intended to prompt discussion of locally relevant solutions to similar issues encountered.
FIGURE 6.
Qualitative case studies: organisation, model of delivery, patient profile and outcomes, and quality criteria.
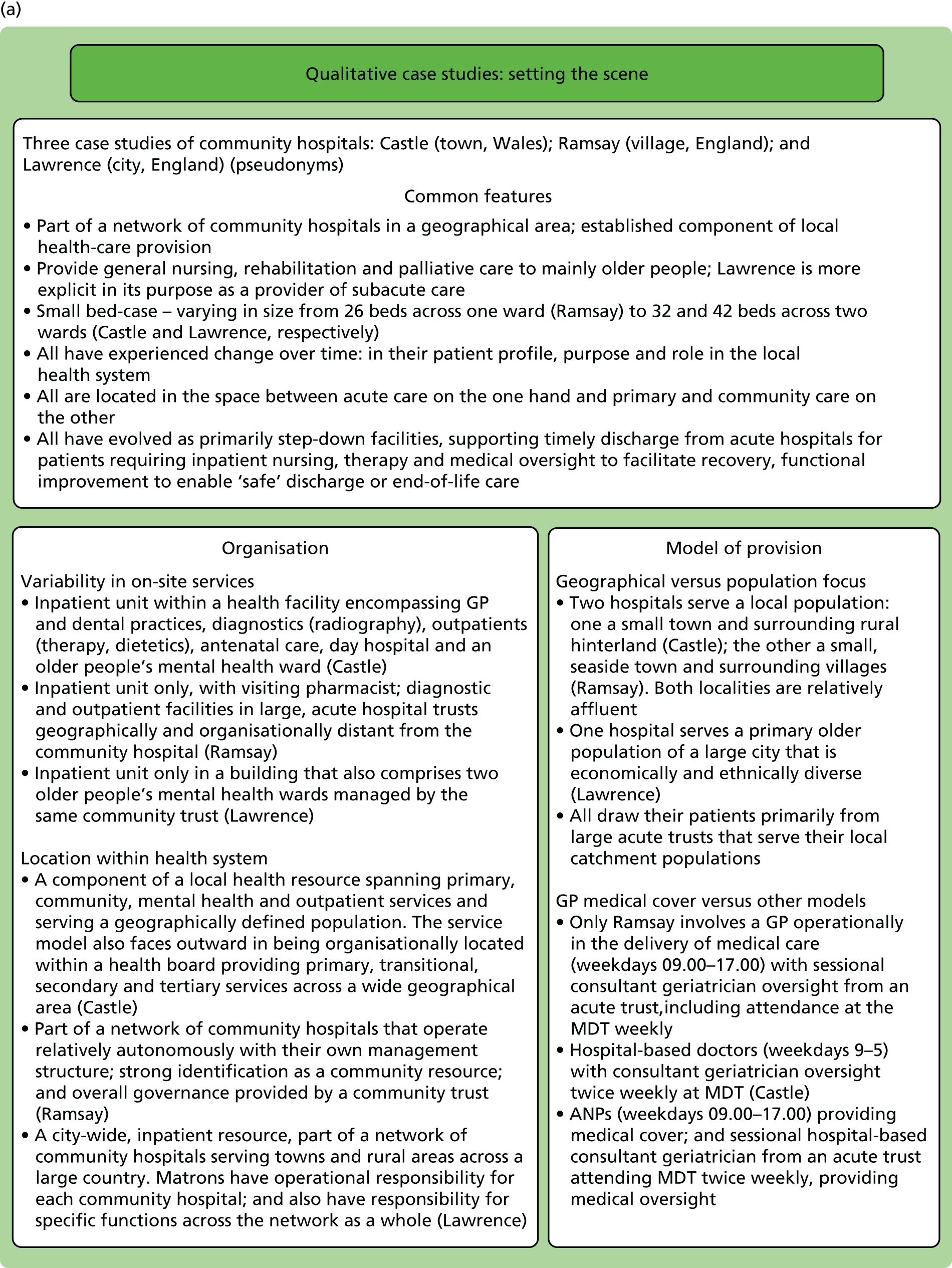
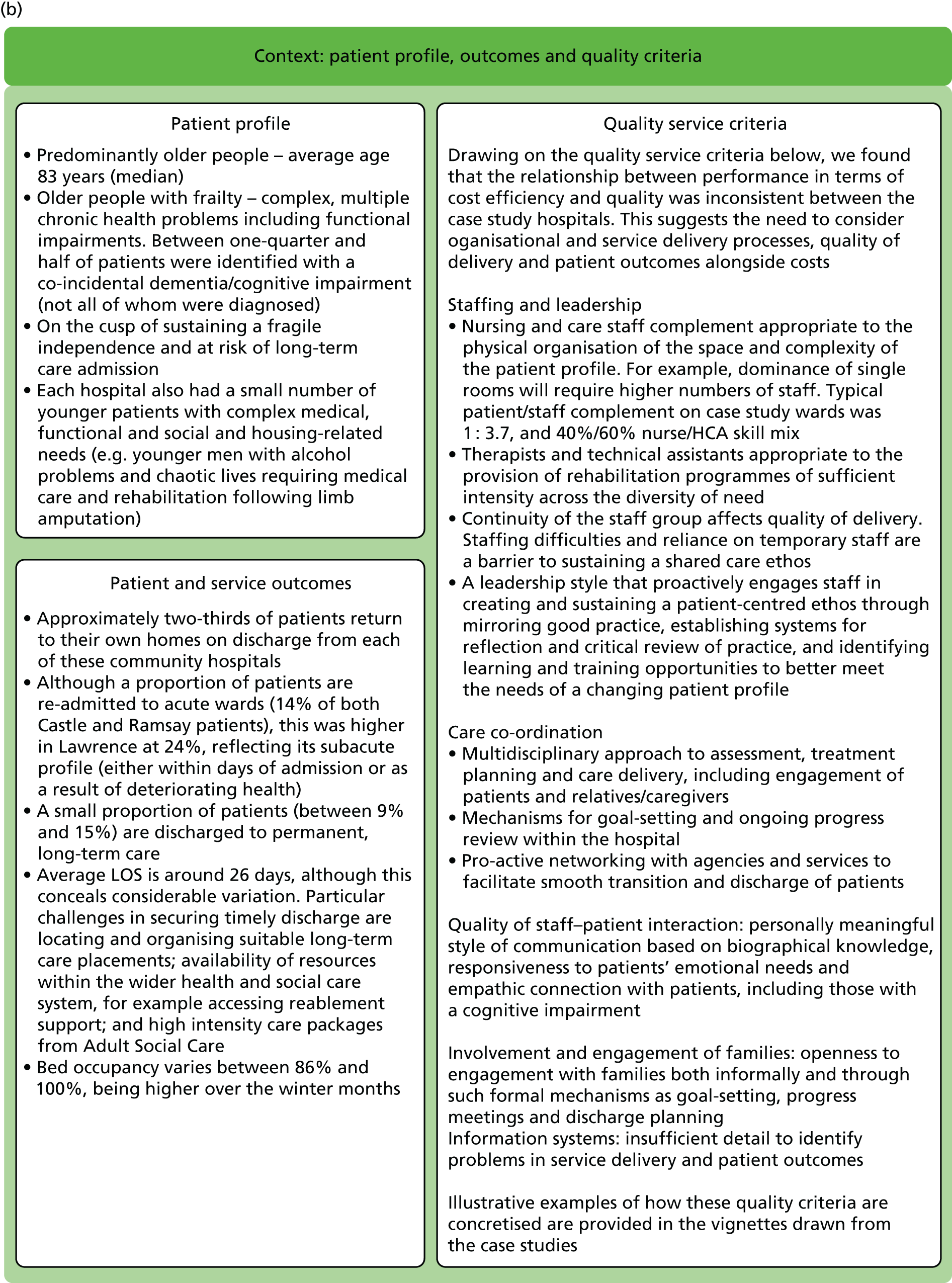
FIGURE 7.
Rehabilitation: a patient with frailty. A&E, accident and emergency; OT, occupational therapist; PT, physiotherapist.
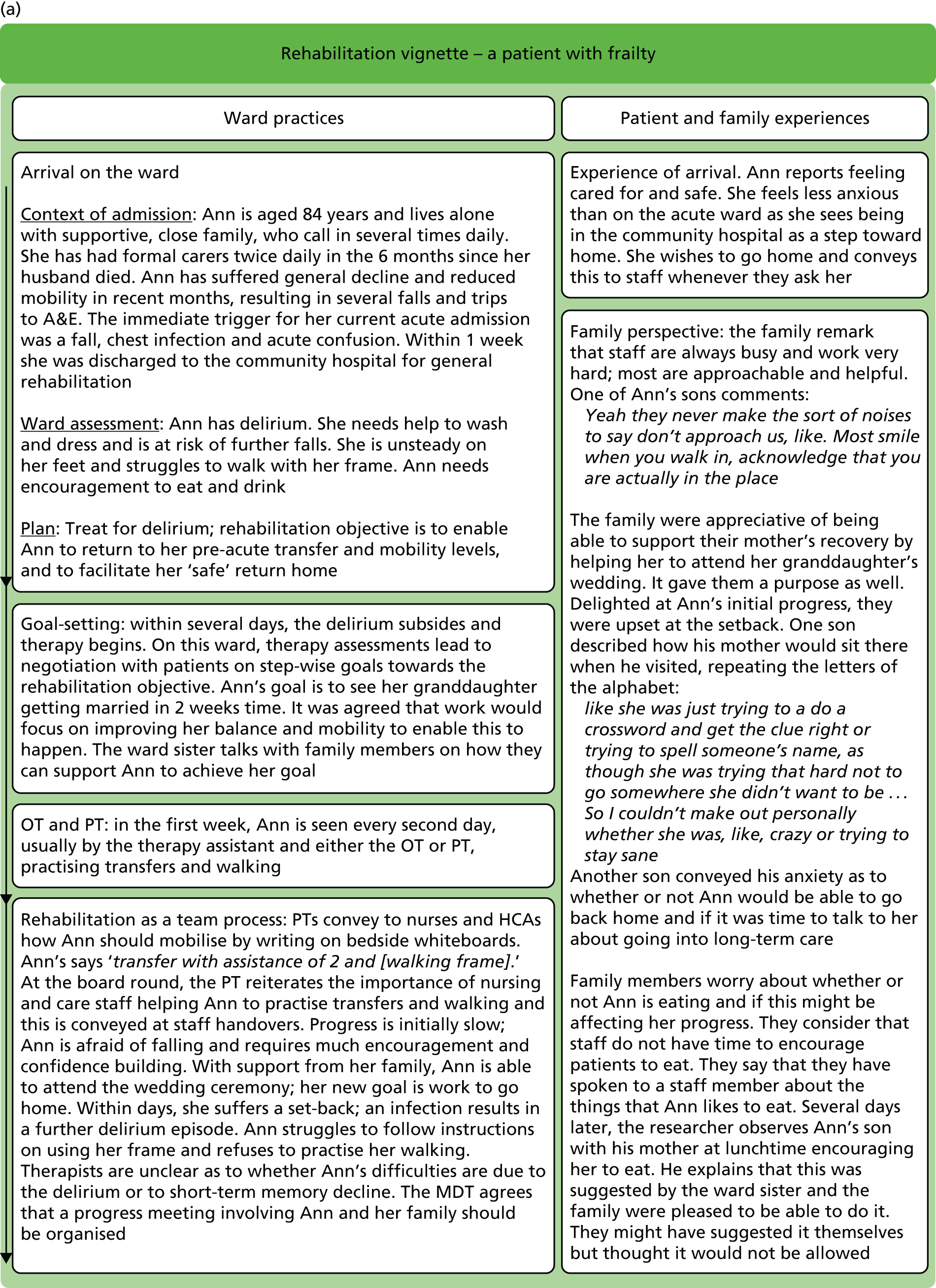
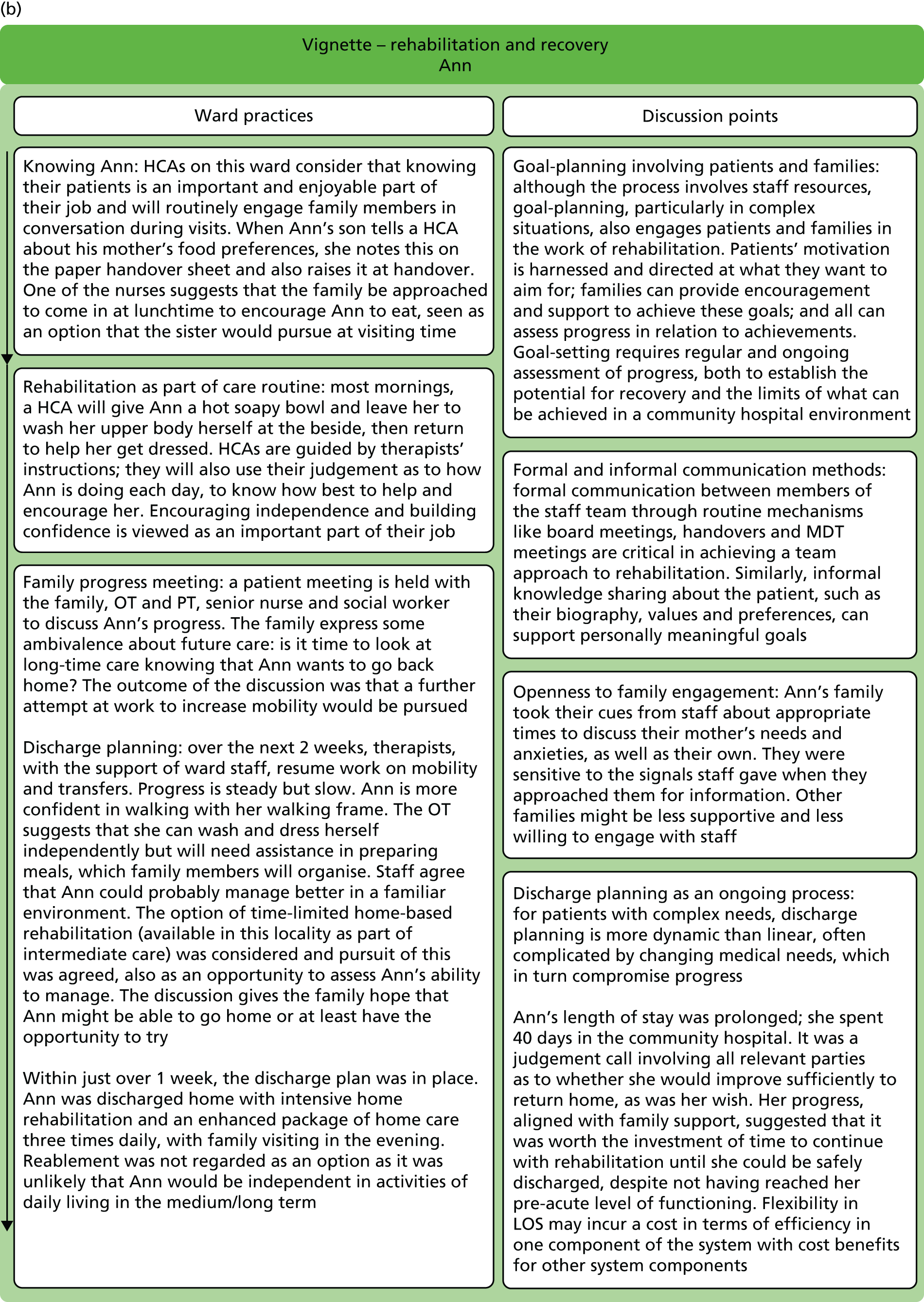
FIGURE 8.
Complexity of patient need: a patient with coincidental dementia. OT, occupational therapist; PT, physiotherapist.

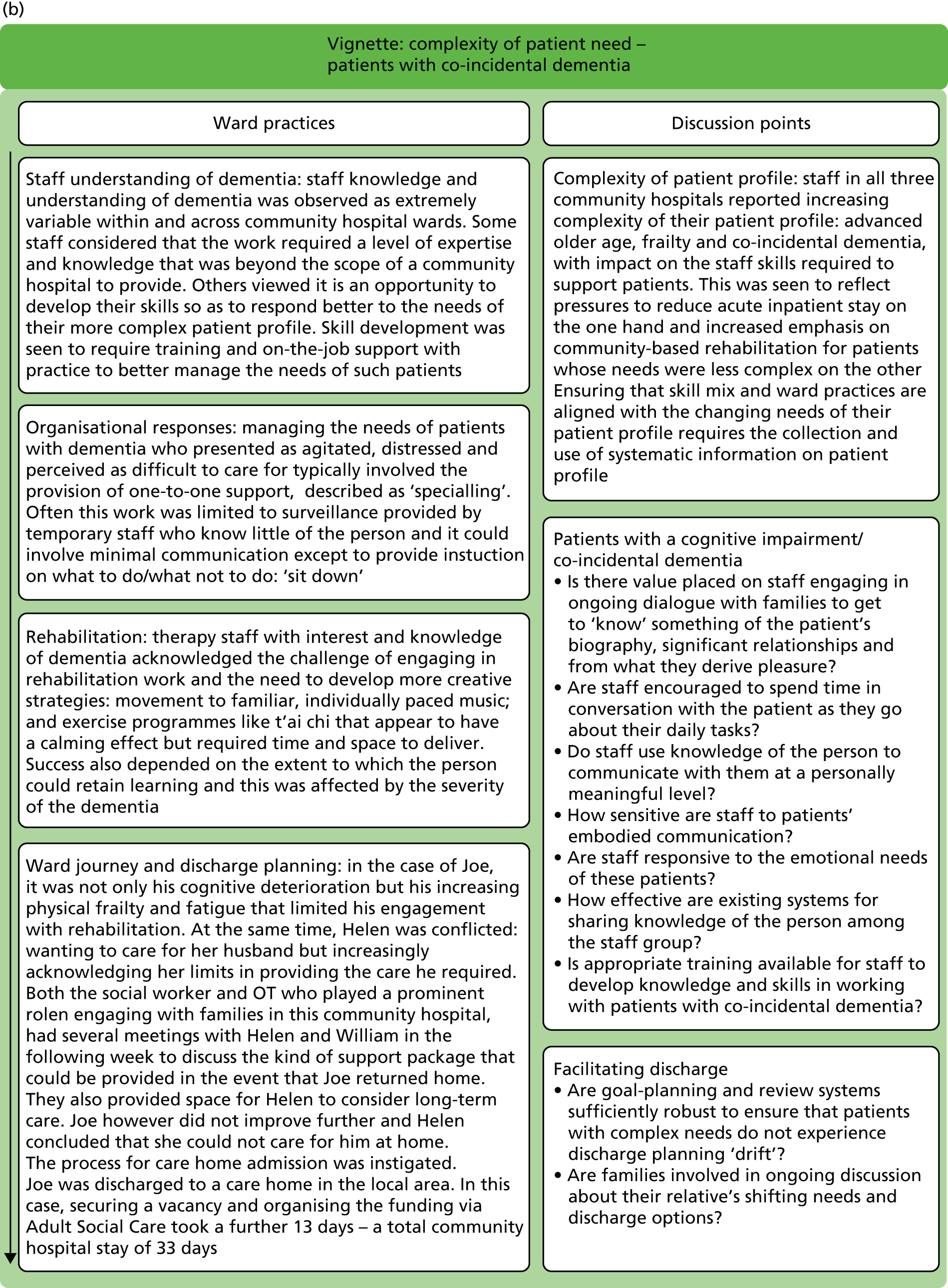
Publication
A full version of the toolkit can be found at http://mocha.nhsbenchmarking.nhs.uk/. 87
Discussion
The toolkit contains an important practical output available from the MoCHA study. It enables a summative, user-friendly resource, which allows the project outputs to be more accessible to a wider audience. Feedback on the toolkit was regularly sought from commissioners, community hospital teams and other stakeholders throughout the toolkit development process. Hence, the finalised toolkit will be in line with the users’ requirements.
The efficiency page of the toolkit enables community hospital staff to produce an efficiency score, using the equation developed during study 1 of the project. It was considered that a simplified approach to presenting this information was preferable. Thus, the efficiency calculation is hidden and users are required to enter only the relevant data for their community hospital. The score is then generated by the user selecting a ‘calculate’ tab. The efficiency score provides the percentage of savings that could be achieved if the community hospital was working in line with the most efficient hospital. The limitation of this approach, however, is that a proportion of the toolkit users may be interested in viewing the efficiency score calculation and information on how this calculation was produced. To mitigate against this limitation, a link with further information on the calculation is provided on the toolkit’s efficiency page.
The economic analysis used data sets collected from the NHSBN 2013/14 Community Hospitals survey13 and the 2014 NAIC survey27 to produce the efficiency score. However, the toolkit requires the community hospital staff to input the most recent data available to calculate a local efficiency score. This discrepancy is outlined in the toolkit. Annual updates are possible but would require a source of funds.
The toolkit’s calculations page reviews the metrics that were identified in the economic analysis as having the greatest influence on a community hospital ward efficiency score. These were input prices, nursing staff skill mix, bed occupancy and LOS. The resources required to bring the index community hospital ward current values in line with a national average or target rate is assessed. The nursing ratio in a community hospital ward is also included in the calculations page. To easily assess the impact of changing certain metrics, they are reviewed in isolation. The impact on a wider range of metrics needs to be fully considered before any changes in service delivery are made.
The case studies developed to fulfil the requirements for study 3 of the project identified working practices and service delivery that may have contributed to differences in cost efficiency that were not accounted for in the quantitative health economic analyses. The practices identified were distinctive for each of the three case studies but have not been formally linked to cost efficiency. They were, however, greatly valued by the community hospital staff involved in developing the toolkit.
The qualitative nature of the case study material was not easily captured for use within the otherwise quantitative toolkit. The case study information is supplied as downloadable Portable Document Format (PDF) files. 87 Alternative formats were considered but they were not achievable because of the limited resources available. A more interactive presentation of the qualitative information might be considered for future projects.
Chapter 6 An analysis of the impact of intermediate-care services on secondary care utilisation (study 5)
Introduction
Increasing emergency admissions to hospital is an established issue facing health-care systems internationally. A key factor underpinning the increase is the complex needs of older people with frailty and multimorbidity. 88 The continuing global demographic transition89 implies that urgent solutions are required. In England, the NAO has reported that over half of the growth in emergency admissions is related to older people. 55 More detailed analysis demonstrated that an important subgroup of emergency admissions comprised patients with very short LOSs: 79% of the increase in emergency admissions between 2013/14 and 2016/17 was caused by people who did not stay overnight, such that nearly one-third of emergency admissions in 2016/17 did not stay overnight. 90 However, there is evidence from national data in England that this subgroup of emergency admissions involving older people varies substantially across local areas with a 9.3-fold variation. 91 This suggests that some areas have developed services, or have care systems in place, that are capable of addressing the needs of patients who would otherwise be admitted to hospital for < 24 hours.
The term intermediate care refers to a range of community services that have formed part of national health-care policy in England since 2001. 24 The defining characteristics of intermediate care are that they are community-based services, they are multiagency and multidisciplinary, and they provide a support and rehabilitation model of care that is time limited (generally up to 2 weeks and no more than 6 weeks). 24
A practical typography of intermediate care has been developed27 that identifies four common types of intermediate care:
-
bed-based intermediate care comprising community hospitals and short-term care home admissions
-
home-based intermediate care comprising ‘hospital at home’ services
-
crisis response teams (CRTs) that aim to respond within 48 hours of referral
-
reablement services, which are similar to ‘hospital at home’ services but primarily funded by local councils rather than health-care commissioners.
Department of Health and Social Care policy stipulated that one function of intermediate care is a focus on admission avoidance. 24 It is therefore plausible to consider that one explanation of the national variation in emergency admissions with short LOSs might relate to the deployment of these services in terms of scale and type. However, the effectiveness of intermediate-care services for hospital admission avoidance is unknown. 92 To investigate this aspect of intermediate care, we used national data sets to explore the relationship between the provision of intermediate care in local areas and emergency admissions to hospital.
This study related to:
-
research objective 4 – to investigate the impact of community hospital care for older people on use of secondary care
-
research objective 5 – to determine if there is an association between short-term, community-based services and reduction in secondary care utilisation by older people.
Method
Our plan was to use multiple regression analyses to investigate the relationship between the dependent variables (indicators of secondary care utilisation) and independent variables characterising the quantum of intermediate-care service types in local areas. We anticipated that the independent variables would relate to measures of intermediate-care service type activity and that the data used in this work were aggregated to the level of a CCG.
Sources of data
The analyses used the NAIC, first introduced in 2012. 26 The audit includes bed- and home-based intermediate-care services provided by a range of health and social care providers, including acute trusts, community service providers, local authorities and independent providers. These services are delivered in a range of health and social care settings including service users’ own homes, general hospitals and community hospitals, nursing and residential care homes.
The audit is structured with organisational- and patient-level components. Patient demographic information includes age, gender, pre-admission accommodation and place of referral. There is a practitioner-completed assessment that places the patient into one of 10 categories depending on their service need: no intervention needed; prevention/maintenance programme; convalescence; slow stream rehabilitation; regular rehabilitation; intensive rehabilitation; specific treatment for an individual condition (e.g. wound care); medical care and rehabilitation; rehabilitation for a complex disabling condition; and palliative care. Each category has a clear definition for accurate completion. The assessment is completed on arrival and at discharge from the service. Service outcome is assessed by recording the place of residence at discharge and whether that is consistent with improved/maintained function (return to pre-admission accommodation) or deterioration in function (new care home or change from care home to nursing home).
Thus, information is collected on the four commonest types of intermediate-care service: bed-based intermediate care (community hospitals and care home beds); CRTs; home-based intermediate care; and reablement services. The first three services are delivered by health providers, and the last is delivered by local councils or jointly by local councils and health agencies. All the services aim to provide out-of-hospital comprehensive geriatric assessment with personal support and rehabilitation. The CRT differs in that it is solely directed to admission avoidance; the other services combine admission avoidance ‘step-up’ care with post-discharge ‘step-down’ care. 24
The audit encompasses the core community services that are essential to improve and/or maintain the independence of older people with dementia, multimorbidity and frailty after an acute illness or injury, or potentially to provide an urgent response to prevent hospital admission. The audit provides clear guidance on the definition of each intermediate-care service and there is a telephone support line available to assist enrolling sites with service characterisation. The analyses use the 2014/15 data set. 28 It was originally planned that data on secondary care utilisation would be derived from NHS Digital, and indeed we requested a bespoke data set from NHS Digital to obtain CCG-level activity data for numbers of emergency admissions for people aged ≥ 75 years with a LOS of > 24 hours, and duration of acute stay. However, negotiating the data specifications proved a laborious process that ran over the time window we had available to us. Thus, taking a pragmatic approach, data on the secondary care utilisation outcome for older people were obtained from the Atlas of Variation in Healthcare 2015. 91 The Atlas is a collaboration between NHS England, Public Health England and NHS Right Care and reports a range of health-care indicators.
There were five ‘Maps’ of potential interest to us in the Atlas of Variation:
-
Map 61 – rate of emergency admission to hospital for people aged ≥ 75 years with a LOS of < 24 hours per 100,000 population per CCG.
-
Map 62 – rate of admission to hospital for people aged ≥ 75 years from nursing home and residential care setting per 100,000 population per CCG.
-
Map 63 – rate of council-supported permanent admissions of people aged ≥ 65 years to nursing home and residential care home setting per 100,000 population by upper-tier local authority (UTLA).
-
Map 64 – percentage of people aged ≥ 65 years who were discharged from hospital into reablement/rehabilitation services by UTLA.
-
Map 65 – percentage of people aged ≥ 65 years who are still at home 91 days after discharge from hospital into reablement/rehabilitation services.
The community-based indicator used in the analyses was ‘emergency admission with a stay of < 24 hours for people aged ≥ 75 years per 100,000 population’ (Map 61). This indicator was selected as it might plausibly be related to the admission avoidance function of intermediate care. The indicator is collected and reported at the level of a CCG.
Maps 63–65 are reported at UTLA level (i.e. local authority footprints). We attempted to link these into the CCG-level data contained in the NAIC data set. This linkage proved challenging. In many cases, we found that several CCGs, with differing intermediate-care service profiles, related to a single UTLA, and CCG boundaries were not coterminous with the UTLA. There may have been more than one general hospital in a single UTLA boundary, making it problematic to apportion hospital activity. We attempted to simplify the cross-mapping process by reducing the Atlas of Variation data set to situations in which one UTLA related to a single CCG, but this resulted in too few cases for analysis.
The two data sets were combined by mapping the emergency admissions outcome indicator to the measures of intermediate service provision obtained from the NAIC for each CCG that had participated in the audit. This was done by the NHSBN organisation so that the researchers were blinded to CCG identification.
Analyses
The analyses used the following regression specification:
where Yi is emergency admission with a stay of < 24 hours for patients aged ≥ 75 years per 100,000 population; Xi is a vector of explanatory variables related to intermediate-care service activity data, namely, admissions to bed-based intermediate-care services; referrals to CRTs; referrals to home-based intermediate-care services; and new assessments carried out by reablement services; β the vector of coefficient to be estimated; and εi the residuals. Thus, we were investigating the extent to which increasing the activity of a specific type of intermediate-care service might be associated with an increase or decrease in emergency admissions for older people. We initially investigated the functional relationship using the OLS method for each intermediate-care service, and for combinations of services. However, we anticipated non-linear associations and were mindful of potential biases due to heteroscedasticity: the situation in which the variability of a variable is unequal across the range of values of a second variable. The Breusch–Pagan test was used to test for heteroscedasticity93 and the Zarembka Box–Cox test used to compare goodness of fit: the extent to which observed data matches values expected by theory. 94 If significant heteroscedasticity was demonstrated, we planned to investigate different functional forms by transforming the data and retesting for heteroscedasticity and goodness of fit to ensure robustness of results.
Results
The Atlas reported the emergency admission indicator (‘Map 61’) for all CCGs (n = 211) with a mean of 5261 admissions per year (standard deviation 2046 admissions per year; range 1186–11,011 admissions per year) per 100,000 population per CCG. However, data on intermediate-care service provision from the NAIC were restricted to the CCGs that had enrolled in the audit and not all of the participating CCGs provided the full range of intermediate-care service types (Table 11).
| Statistics | Bed-based intermediate-care services | CRT | Home-based intermediate-care services | Reablement services | Total |
|---|---|---|---|---|---|
| Number of admissions or referrals per index year | Mean 767, SD: 964 | Mean: 2468, SD: 2957 | Mean: 2625, SD: 3777 | Mean: 1246, SD: 787 | Mean: 6232, SD: 2351 |
| Emergency admission (‘Map 61’) | Mean 6057, SD: 2854 | Mean: 5851, SD: 2529 | Mean: 5967, SD: 2737 | Mean: 5912, SD: 2554 | Mean: 6051, SD: 2034 |
| Number of CCGs | 54 | 42 | 50 | 41 | 23 |
Ordinary least squares results
The OLS linear regression analyses for each of the four intermediate-care service types, and all types combined, showed that none of the estimated coefficients was statistically significant but that only the referrals to the CRTs (model 1) and new assessments carried out by reablement services (model 4) had a negative impact on emergency admissions (Table 12). Bed-based and home-based intermediate-care services had no significant effect. Owing to the relatively small size of the sample, especially when the services are pooled, we must stress that the absence of significance does not mean an absence of effect of a service, but rather that the model fails to detect any effect. Yet the limited number of observations should not impact the validity of a statistically significant relationship.
| Dependent variable Map 61 | Model | ||||
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| CRT | –0.192* (SE 0.108) | –0.203 (SE 0.238) | |||
| Bed-based intermediate-care services | 0.065 (SE 0.297) | 1.002 (SE 0.771) | |||
| Home-based intermediate-care services | –0.065 (SE 0.077) | 0.19 (SE 0.271) | |||
| Reablement services | –0.770* (SE 0.443) | –0.428 (SE 0.654) | |||
| Constant | 6324.937*** (SE 413.636) | 6006.477*** (SE 363.391) | 6138.435*** (SE 353.895) | 6871.334*** (SE 651.104) | 5863.132*** (SE 1155.067) |
| R 2 | 0.073 | 0.001 | 0.015 | 0.072 | 0.123 |
Transformation of the variables
Thus, despite the fact that the coefficients are not significant, when running OLS linear regression analyses for the four types of intermediate-care services, we found that CRTs and reablement services have a negative impact on emergency admissions of older people. We investigated this result further by developing more robust models that accounted for non-linear effects. Standard approaches to variable transformation were used.
Initially, we conducted logarithmic and quadratic transformation of the variables on the basis that the logarithmic transformation has variance-stabilising properties and both the logarithmic and quadratic transformations enabled us to account for non-linear effects. The logarithmic transformation captures non-linear average effects and the quadratic one non-linear marginal effects. Because the variable was normalised by the sample mean, the coefficient for Ln CRT can be interpreted straight away as the average marginal effect.
This demonstrated a statistically significant relationship with emergency admissions for the CRT type of intermediate care, but not for the other three types of intermediate care (Table 13). Despite the statistically significant coefficient, the Breusch–Pagan test indicated that the results might be biased by heteroscedasticity (Breusch–Pagan Test: χ2 = 3.99; p-value = 0.0459).
| Intermediate care service | Dependent variable logarithm of Map 61 |
|---|---|
| Ln CRT | –0.217** (SE 0.080) |
| (Ln CRT)2 | –0.080*** (SE 0.029) |
| Constant | 8.609*** (SE 0.163) |
| Number of CCGs | 42 |
| R 2 | 0.189 |
We investigated solutions to correct for the heteroscedasticity. We noted that the Box–Cox test (for ‘goodness of fit’) had a θ value of 1, indicating that no transformation of the dependent variable was required (θ = 1.101; SE = 0.316; z = 3.2; p > 0.001). A reverse semi-logarithm form was therefore used in which the dependent variable (number of emergency admissions) was not transformed. The Breusch–Pagan test was repeated and confirmed that the reverse semi-logarithm model solved the heteroscedasticity issue (χ2 = 0.00; p-value = 0.959). The results of the reverse semi-logarithm transformation are shown in Table 14. Using the same transformation process for the other types of intermediate care, we did not find significant relationships with emergency admissions.
| IC services | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| Ln CRT | –978.253** (SE 368.359) | |||
| (Ln CRT)2 | –358.755** (SE 133.387) | |||
| Ln bed-based IC | 140.866 (SE 375.110) | |||
| (Ln bed-based IC)2 | –160.865 (SE 233.264) | |||
| Ln home-based IC | –256.956 (SE 315.723) | |||
| (Ln home-based IC)2 | –211.608 + (SE 129.030) | |||
| Ln reablement IC | –1,168.800 + (SE 706.408) | |||
| (Ln reablement)2 | –482.857 (SE 541.546) | |||
| Constant | 5,666.895*** (SE 744.889) | 4,688.853** (SE 2,096.550) | 6,634.959*** (SE 909.437) | 5,934.763*** (SE 420.142) |
| Number of CCGs | 42 | 54 | 50 | 41 |
| R 2 | 0.184 | 0.026 | 0.069 | 0.073 |
A caveat to the use of the reverse semi-logarithm model is that the coefficients cannot be interpreted directly. In the case at hand, the coefficients for model 1 suggest that a 1% increase in the activity of CRTs decreases, by 9.73, the emergency admissions for < 24 hours for patients aged ≥ 75 years per 100,000 population. Similarly, the coefficients for model 4 suggest an 11.63 decrease of emergency admissions when reablement intermediate-care services are increased by 1%, but this result is weakly significant.
Discussion
This study investigated the impact of different types of intermediate-care services (including community hospitals) on secondary care utilisation. Intermediate-care services have been established in many health-care systems internationally. They operate in the ‘virtual space’ between primary and secondary care and are directed especially, but not exclusively, on the needs of older people with, or recovering from, acute illness or injury. Prevention of emergency admissions to hospital is a stated ambition for intermediate-care services in the NHS in England and Wales. 24 It is unclear to what extent they fulfil this function. We believe this to be the first large-scale study to investigate this issue. It was considered an important question for service commissioners who wish to understand not simply the effect of services on clinical outcomes, but how services might be inter-related and the extent to which services might operate as a substitutes for one another.
Our starting point was a national data set: the Atlas of Variation. 91 This reports population-level outcome indicators for each CCG in England. We selected Map 61 as the one most likely to be influenced by the provision of local intermediate-care services. This indicator, ‘emergency admission with a stay of < 24 hours for people aged ≥ 75 years per 100,000 population’, reports on a group of patients who will be familiar to health-care professionals working in acute care. These patients present to hospital acutely but are well enough to return home the following day. We hypothesised that this patient group would represent an ideal population for intermediate-care services and that increased intermediate-care activity might decrease these brief admissions. However, we recognised that intermediate care is an umbrella term that includes several service models. For this reason we investigated the four most common forms of intermediate care, as described and defined in the NAIC. 28 These were bed-based intermediate care (community hospitals and care home beds); CRTs; home-based intermediate care; and reablement services.
Our main finding was that the CRT type of intermediate care, and only the CRT type, had a statistically significant negative association with the emergency admission indicator. Thus, as CRT activity increased (quantified by referrals to the CRTs), there was an associated decrease in emergency admissions with a LOS of < 24 hours for people aged ≥ 75 years. This result is based on CRT activity data from 42 CCGs. We anticipated a non-linear relationship and indeed this was so. But the final regression model we developed dealt effectively with the critical statistical issues of heteroscedasticity and goodness of fit and the results can therefore be considered robust. It is reasonable to assume that the CRT form of intermediate care can function as a substitution service for brief emergency admissions to hospital for older people.
It should also be noted that we did not find an effect of community hospitals (bed-based intermediate care) on admission avoidance. In National Audit of Intermediate Care 2014: Key Findings,27 it was reported that the largest source of referrals for bed-based intermediate-care services was acute wards (60%), followed by GPs (18%) and social care (6%). Thus, admission avoidance represents a minority function for bed-based intermediate-care services.
Study limitations
This study is based on data obtained from a sample of < 50 CCGs. Although this represents a reasonable sample, ideally the findings should be confirmed using a larger group of CCGs to ensure that they are both robust and generalisable. Caveats should also be placed around linking CRT activity to reductions in admissions, given the absence of information on the profile and quality of intermediate-care services, or conversion rates from referrals to assessment. This may be possible if the NAIC becomes more widely adopted.
In addition, our findings relate to one narrowly defined indicator of emergency admissions (LOS of < 24 hours). Future studies should investigate more broadly defined indicators of emergency care and indicators of, for example LOS. Our study does not address the financial opportunity costs of providing a substitute service for emergency admissions for older people. This will require cost comparison studies, such as randomised controlled trials with embedded cost-effectiveness components.
Use of a bespoke data set from NHS Digital to obtain CCG-level activity data for numbers of emergency admissions for people aged ≥ 75 years with a LOS of > 24 hours, and duration of admission, might lead to a better understanding of the contribution of the four types of intermediate care separately, and in combination, on secondary bed use. However, negotiating the data specifications proved a laborious process that ran over the time window we had available to us.
Conclusion
To our knowledge, this is the first study to suggest that CRT type of intermediate care can act as a substitution service for older people and reduce emergency hospital admissions. Nevertheless, how it does so, whether this is through direct service provision or via mobilisation of other services, requires further study. The finding does not extend to other common forms of intermediate care (e.g. bed-based care, home-based care or reablement services).
Chapter 7 Discussion
Introduction
Community hospitals are small hospitals with a range of locally provided inpatient and outpatient services95 and are established health-care facilities in the UK and internationally. 85 Although they can provide a range of local services (e.g. minor injury units, day hospitals, satellite secondary care clinics), 98% of community hospitals in the UK provide inpatient rehabilitation for older people. 26–29 In the context of an ageing population, this is a potentially valuable health service function. Indeed, high-quality evidence supports community hospitals as a clinically effective bed-based rehabilitation service for older people when compared with larger general hospitals,6,8 and there is evidence that inpatient community hospital rehabilitation for older people is cost-effective relative to secondary care in England. 7 However, survey information from 180 community hospitals in England indicates considerable variation in operating costs and outputs of these hospitals. 13 This is an important consideration for health-care planners who need to make decisions on how to deploy resources optimally for local populations.
We developed several inter-related studies to explore and understand more fully the nature of these variations in community hospital performance. The previous chapters have presented and discussed the constituent studies that constituted our programme of work. They have also conveyed the reasons why we were unable to pursue aspects of the intended study that are set out in the published protocol. Here, we return to our research objectives to discuss the key findings and implications for community hospital delivery and organisation.
Research objective 1
To measure the current relative performance (cost efficiency) of community hospital inpatient care for older people (studies 1 and 2).
Cost efficiency
Efficiency represents how well inputs such as labour, capital and materials are used to produce outputs. In the case of inpatient community hospital rehabilitation, outputs are the treatment of patients. Cost efficiency is producing a given output at lowest cost. Frontier techniques have been applied widely in health care to measure cost efficiency,36–40 including estimates of the cost efficiency for inpatient care in large hospitals. 43,44,46 To our knowledge, this is the first study to investigate the cost efficiency of inpatient community hospital rehabilitation using frontier analysis techniques.
The modelling process can be thought of conceptually as having two stages (although estimation proceeds in a single stage). In the ‘first stage’, an equation is estimated that describes the relationships between the costs of a case and its outputs, inputs, environmental influences and quality variables – these relationships are referred to as elasticities (how much costs change as the variables change). The ‘second stage’ calculates the efficiency of each case, using the elasticities (the relationships between costs, outputs and other variables) from the first stage. The SFA techniques attempt to mathematically distinguish the efficiency of a case from random factors that might also have affected its outputs (e.g. bad weather, industrial action). Figures 1 and 2 provide a visual representation of the concept with an efficiency ‘frontier’ demonstrating the minimum possible cost for different output levels (bed-days). Each of the points represents a hospital. The vertical distance of each hospital from that frontier is made up of deviations resulting from random factors (noise) and also lower efficiency that may affect costs in a given year, as noted above.
Because the ‘second stage’ of the analysis (i.e. the estimation of efficiency) is dependent on the assumed distributions of efficiency and random factors, it is usual in this second stage to use several different sets of assumptions about these distributions, thereby producing several different estimates of efficiency, testing whether the estimates are stable over a range of assumptions, or whether they are dependent on certain assumptions. We therefore developed six different models (COLS and five SFA models), each with a different assumption about the distribution of efficiency of community hospitals (the distributions used for the SFA models were half normal, truncated normal, exponential, gamma and Rayleigh) to examine whether or not the estimates were robust to changes in the distributional assumptions.
The results of this SFA analysis suggest that cost efficiency in community hospital wards in the UK is comparable with that of the NHS acute hospital sector (albeit previous studies have considered the whole hospital rather than analysis at the ward level). 43,44,46 Overall, the results from the models were robust. The parameter estimates were within plausible ranges and the results appeared to be consistent over a range of specifications and with the COLS base case, which does not impose the distributional assumptions that the SF models do. The models’ predictions of efficiency were highly correlated. Furthermore, our finding of economies of scale was supported when results were presented to community hospital staff workshops. The estimated frontier model reported enables community hospitals in the sample to observe their relative efficiency against the estimated cost frontier (representing the most cost efficient hospitals). It should also be noted that those hospitals operating at the highest cost efficiency can be readily distinguished (but were not identified in our study because of our use of anonymised records), which is useful to facilitate learning across the sector. Moreover, the cost frontier was translated into a practical web-based tool (study 4), meaning that community hospitals can now benchmark their performance after inputting their individual characteristics.
The findings have several important policy implications. The efficiency estimates imply that, on average, community hospitals could reduce operating costs in the provision of inpatient wards by 17% if performance was in line with the most cost-efficient hospitals in the data set. This would result in around £47M of available annual gains in relation to our sample of 101 community hospital wards. There was a range of performance, with the lowest-performing community hospital operating at around 0.55 efficiency, although the highest-performing community hospitals were operating at around 0.94 (Figure 9). That is, the model indicates that all community hospitals can improve efficiency on their wards.
FIGURE 9.
Distribution of the community hospital ward (n = 101) efficiency estimates. Dotted lines are minimum, mean and maximum values. HN, half normal.
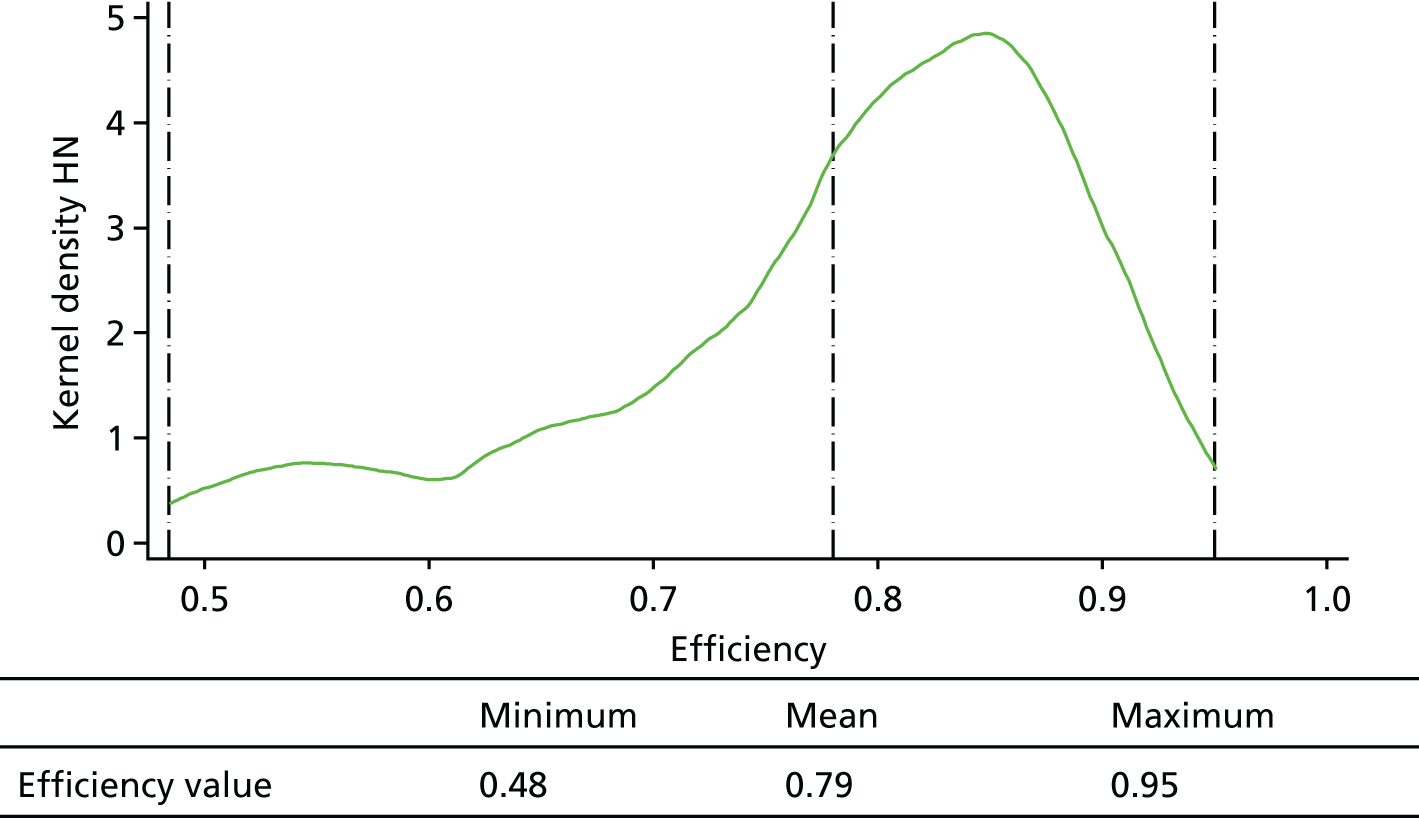
The economies of scale findings suggest that, for wards with size below the mean, average costs can be reduced by increasing the scale of the operation. We found that a 1% increase in bed occupancy is associated with a 0.94–1.24% decrease in operating costs. However, this is not simply a question of increasing bed occupancy. The NAO has suggested that services in which bed occupancy levels are in excess of 85% may experience disruption (in the general hospital setting)55 and we note that our sample mean for bed occupancy is around 90%. More importantly, we found that a 1% rise in output is associated with an average 0.85% increase in costs, that is, output can rise more quickly than costs. This again points to opportunities for efficiency gains.
The interpretation of the efficiency estimate is as follows. An estimate of 1 means that the community hospital is fully efficient, otherwise it is not. So, taking 0.8 as an example, a community hospital could reduce its costs by 20% (i.e. 1 – 0.8 = 0.2) if it were to improve its performance in line with best practice.
National survey
The distribution of cost-efficiency values presented in Figure 9 summarises the findings from the 101 community hospital wards for which we had data available from NHSBN. We do not know the extent to which our sample of community hospital wards was representative of the current national stock of community hospitals. It might be that there are a greater number of highly cost-efficient services or, more plausibly, that there are more community hospitals operating with a low cost efficiency and perhaps not minded to subscribe and contribute to the Community Hospital Programme run by NHSBN. Unfortunately, the national survey we developed to address this issue did not succeed. This was surprising as the survey instrument was carefully developed with considerable input from the Patients Association and the CHA. We aimed to collect information only on the four key variables identified as the main drivers of cost efficiency in the econometric study, not the full data set collected by NHSBN. Subsequent investigation of the non-responders, and the experience of researchers in the case study sites in securing routine ward data for the patient profiles, suggested that the problem may relate to the way community hospital wards collect and use data. Some wards collect data that are centrally aggregated to contribute to performance targets, but not presented back to wards to inspect and use (e.g. for quality improvement); some community hospitals with more than one ward may aggregate ward data at only hospital and not ward level; and some ward managers/matrons may have particular interest in examining patterns in admissions over time and may periodically carry out an audit of admissions, or enlist the help of performance staff to make sense of it (i.e. reports are not continuous). Each of these patterns was visible in our three case studies; hence, the work involved at ward level to access data for the case studies was facilitated only through the relationships built up by researchers with staff on site. However, the important implication is that we cannot extrapolate reliably from our sample of 101 community hospital wards to present estimates for potential efficiency savings for the national stock of community hospitals, either for England or for the UK. The CHA conducts regular national surveys with excellent response rates from its membership (e.g. see the CHA website12). It would therefore be possible to incorporate our brief survey instrument in a future CHA-conducted survey. In this way, updated estimates for community hospital cost efficiency might be obtained.
Research objective 2
To identify the characteristics of community hospital inpatient care for older people that optimise performance (studies 1 and 3).
Cost-efficiency study
Four inter-related factors were identified that were statistically significantly associated with community hospital ward performance: number of occupied bed-days (this is derived from lengths of stay and number of admissions), bed occupancy rate, nursing staff skill mix and ward staffing levels. From a practical point of view, these factors are all potentially modifiable by ward staff and hospital managers. There is much that might be done on the ground to optimise efficiency and the web-based tool allows an exploration of ‘what if?’ scenarios.
Comparative case studies
Three case studies were conducted with a purposeful sample: two community hospitals with high cost- efficiency performance and one with low performance. An important finding was that the field researchers were unable to discern the performance categories from their observations and interviews. This is perhaps reassuring for several reasons. First, it supports our proposition that the performance of community hospital wards is only partly explained by ‘collectable’ factors. Second, some form of a qualitative analysis is required to understand and rank performance status of a community hospital ward. Third, and perhaps most importantly, the aspects that are most obvious to direct ward observation are more related to the quality of the care experience and processes and action to effect the patient recovery journey than measurable performance parameters. Thus, we found that less tangible aspects of the organisation and delivery of the rehabilitation process were the ‘missing’ ingredients to our otherwise formulaic approach to community hospital performance. These aspects were endorsed and readily understood by practitioners in our CHA workshops.
Perhaps we should not have been surprised at the endorsement of less tangible rehabilitation parameters as essential to a more complete understanding of community hospital performance. The process of rehabilitation lies at the heart of ‘best practice’ for older people. 67 Rehabilitation has been defined by The King’s Fund as ‘an often complex process which enables individuals after impairment by illness or injury to regain as far as possible control over their own lives‘. 68 Rehabilitation has historically been an integral function of acute hospital care, particularly in care of older people departments. However, an established pattern of rising emergency admissions for older people, despite a steady reduction in acute hospital beds, has inevitably resulted in shorter LOSs, making general hospital rehabilitation especially vulnerable. 67 Community hospitals nationally and internationally have been taking up this care gap. 85 Our ward observations and staff and patient/carer interviews identified several key aspects of rehabilitation: interdisciplinary working that included collaboration in routine practices and effective interprofessional communication, meaningful engagement of patients and families, identifying and working with recovery trajectories, and care transitions. We explored several approaches to systematically including these aspects into the web-based tool we developed. Questionnaires, inventories and checklists were considered but seemed to lack the complexity that was at the core of these topics. At a practitioner workshop held during the 2016 CHA annual conference, the idea of a selection of vignettes emerged as a potential solution (see Chapter 4). These were co-produced with the CHA. They appeared to encourage and empower the ward teams to reflect on their core ward practices.
The importance of reflective local practice was supported through other findings from the case studies. Localism and pressures to change were strong themes in all three sites. Irrespective of their particular service model, each hospital functioned within a national and local dynamic and changing health and social care system. This shaped how people were routed into the hospital, the performance standards it was expected to achieve and the resources available to carry out its purpose, including facilitating the seamless and co-ordinated transition of patients from it. This dynamic had affected the patient profiles in each of the three community hospitals (multiple comorbidities and frailty) and shaped a conception of rehabilitation as contributory to a process of recovery that would continue in the person’s own familiar environment or provide opportunity and space for patients and families to come to terms with a move to long-term care.
The specific systems and mechanisms adopted reflected local circumstances, but their underpinning purpose and functions were similar. Thus, the ongoing organisation of clinical, care and therapy work with patients on the ward through such collaborative and knowledge-sharing mechanisms as MDTs, handovers, board and ‘flow’ meetings drove goal-planning and action forward. Engagement of patient and family members through formal and informal encounters involved the elicitation, negotiation and renegotiation of options and choices in line with the patient’s recovery trajectory and available resources, including local service systems with their varied agencies and services, eligibility criteria and time scales. These, in turn, established a framework for progress review and identified the support necessary to facilitate ‘safe’ discharge. In all three hospitals, discharge-planning was both an end point in the hospital episode and a critical juncture in the patient journey to resume prior routines, facilitate keeping going with enhanced formal support, initiate entry into a care home or provide assistance in managing a newly acquired disability. In their developed form, formal structures and informal processes for communication, decision-making and conjoint, interdependent and co-ordinated action stretching across the medical, nursing, therapy and care functions of the setting were more akin to a distributive form of leadership84 that included patients and caregivers, than to a singular model of nurse-led leadership. 18
There were aspects of practice that required further development, including investment in training and support to provide appropriate and effective care to patients with multiple and complex needs. At the same time, better understanding of appropriate outcomes and time scales to achieve them needs to draw on multiple quality measures of ‘best’ performance and ‘recovery trajectories’ pertaining to patients with varied needs.
However, the issues posed here have implications for the broader question of the meanings of community hospitals for their local communities, addressed in the two linked research studies. 62,85 There is a perception within the community hospital sector that the provision of local services for local people has, in large part, contributed to their community value, attachment and engagement of local people actively in supporting them. Therefore, their development within a wider, more integrated system of care has been viewed as a threat that has been reinforced by the support function they are increasingly obliged to perform as providers of step-down intermediate care to acute hospitals.
Research objective 3
To develop web-based interactive toolkits for use by local commissioners and community hospital teams that support operational changes to optimise performance (study 4).
From a community hospital care delivery perspective, this was regarded as an important output of our programme of work. Essentially, this is a practical tool for use by front-line community hospital staff and service managers that operationalised the evidence base developed in our research studies. This work was led by NHSBN which has considerable experience in building, testing and launching this type of interactive toolkit. Involvement of the membership of the CHA and subsequent endorsement and promotion of the toolkit was similarly vital to our shared work. The toolkit is now available at http://mocha.nhsbenchmarking.nhs.uk/. 87
Research objectives 4 and 5
To investigate the current impact of community hospital inpatient care for older people on secondary care and the potential impact if the community hospital care was optimised to best practice nationally (study 5).
To determine if there is an association between the configuration (capacity and proportions) of short-term, community-based services (i.e. community hospital wards, home-based rehabilitation, care home rehabilitation and enabling services) and reduction in secondary care bed utilisation by older people (study 5).
These were demanding and ambitious objectives for which we made important but incomplete progress. 96 We successfully utilised data from the Atlas of Variation91 and linked this to the NAIC data set available to us from NHSBN. Thus, we took a broader perspective than solely the contribution of community hospitals. Rather, we wished to consider the range of community services under the umbrella term intermediate care. Many definitions of intermediate care have been proposed. For the English NHS, the Department of Health and Social Care published a definition of intermediate care:15
. . . a range of integrated services to promote faster recovery from illness, prevent unnecessary acute hospital admission and premature admission to long-term residential care, support timely discharge from hospital and maximise independent living.
Department of Health and Social Care. 15
These services have undergone rapid expansion nationally since they were promoted in the National Service Framework for Older People in 2001. 15
The NAIC data set is a unique community service data set that contains descriptive, activity, process and outcome variables on four well-categorised and nationally common types of intermediate care: bed-based intermediate care (community hospitals and care home beds), CRTs, home-based intermediate care and reablement services (delivered by local councils). Thus, the audit encompasses the core community services that are essential to improve and/or maintain the independence of older people with dementia, multimorbidity and frailty after an acute illness or injury, or potentially to provide an urgent response to prevent hospital admission.
Although our eventual research focus on Map 61 was pragmatic, it also made good sense from a health services policy perspective. One of the founding ambitions of intermediate care was that it would lead to reduced demand for emergency hospital admissions for older people. 15 As far as we are aware, this ambition for intermediate care has not been subjected to robust scrutiny. And if intermediate-care services are indeed able to reduce demand for acute hospital care, it seemed it would be most likely to affect transient emergency admissions (LOSs of < 24 hours), as this population of older people might be most readily supported in the community (i.e. admission avoidance).
Our main finding was that the CRT type of intermediate care had a statistically significant negative association with the emergency admission indicator. Thus, as CRT activity increased, there was an associated decrease in emergency admissions with a LOS of < 24 hours for people aged ≥ 75 years. It should be noted that none of the other types of intermediate-care activity was associated with a reduction in emergency admissions. Thus, for bed-based (that includes community hospitals) and home-based intermediate care, and reablement services, no statistical link to admission avoidance was found in our analyses.
The modest sample size of 42 CCGs precluded a reliable calculation of effect size. This would be a useful future extension of our work. A further extension would be to examine a broader definition of secondary care utilisation. We requested a bespoke data set from NHS Digital to obtain CCG-level activity data for numbers of emergency admissions for people aged ≥ 75 years with a LOS of > 24 hours, and duration of admission. We believed this might lead to a better understanding of the contribution of the four types of intermediate care separately, and in combination, on secondary bed use. For example, it might then be possible to understand the role of community hospitals in supporting the general hospital in terms of releasing beds through discharge support (‘step-down’ care). However, negotiating the data specifications proved a laborious process that ran over the time window we had available to us.
There is much uncertainty about how best to address the pressing issue of admission avoidance. 97 Our finding that the CRT form of intermediate care can function as a substitution service for brief emergency admissions to hospital for older people is therefore an important one for commissioners. It provides greater confidence that investment in these types of services can indeed reduce secondary care utilisation for a growing and vulnerable population group. Our findings are in accord with findings from the NAIC, which enrolled 60 CRTs with 60,384 associated patients and reported that only 10% subsequently required admission to hospital. 28 This was interpreted as evidence that CRTs can support the majority of patients referred to them within their own homes.
Conclusions
The main results suggest that efficiency of community hospital wards in the NHS is comparable with that of the NHS acute sector. Furthermore, they suggest economies of scale in the provision of ward services and potential efficiency savings that might be augmented by economies of scale. As a top-down analysis, it therefore serves as a challenge for further research as to how less efficient community hospitals might reduce costs. We also present the first evidence to confirm the admission avoidance function of the intermediate-care service model of CRTs. This finding did not apply to the current configuration of community hospitals, which are currently more frequently used as step-down facilities. Given the still increasing demands on acute care internationally, the strategic role of community hospitals for admission avoidance remains an important area for future research. The work described here indicates the practical and methodological challenges involved in combining data sets that employ different service models and different geographical footprints. The NAIC currently combines data for all types of bed-based services. Future rounds of the audit might usefully separate out the different bed-based service models to facilitate learning.
The case studies reinforced the significance of a whole-system approach to understanding community hospital performance. How people were routed into community hospitals, the characteristics of such patients, the performance standards they were expected to achieve and the resources available to carry out their intended purpose were affected by dynamic national and local health and social care factors. The increasing complexity of patients, in turn, shaped a conception of rehabilitation as contributory to a process of recovery that would continue in the person’s own familiar environment or provide opportunity and space for patients and families to come to terms with a move to long-term care.
The quality dimensions of practice identified were integral to securing ‘timely’, safe discharge: conjoint, interdependent and interprofessional working and knowledge-sharing drove goal-planning and action forward, informed by engagement of patient and family members. These mechanisms and practices established a framework for ongoing progress review and identifying support necessary to facilitate ‘safe’ discharge, both an end point in the hospital episode and a critical juncture in the patient journey.
Research implications
-
Future research should be based, when possible, on panel data sets that follow key variables over time. This would allow increased analytic power and should be possible given the NAIC is now in its seventh iteration, and that the Atlas of Variation is regularly updated.
-
Future national surveys of community hospitals should include our four key variables so that cost efficiency can be calculated as a new summary outcome for community hospital ward performance.
-
A programme of development work could be initiated to examine the extent to which community hospital wards are able to optimise their quality and efficiency using the published toolkit. This might include new training programmes for staff working in this sector that take account of the increased complexity of patients.
-
Community hospitals tend to be considered in isolation. We recommend more whole-system analyses, possibly using other national ‘Maps’ available in the Atlas of Variation, to further investigate the impact of community hospital activity on secondary care utilisation. Our preliminary econometric analyses suggest that this is methodologically feasible.
-
At care-delivery level, there is need for in-depth research into the relationship between patient profile, mechanisms and practices for delivering rehabilitation, patient-recovery trajectories and destination outcomes.
-
There is need for the development of a more granular understanding of intermediate-care service use in respect of different service models and their combinations to better understand how to optimise outcomes for patients with particular characteristics.
Acknowledgements
We are pleased to acknowledge the work of Heather Eardley who led the contribution from the Patients Association and helped with conceptual thinking, study design and improving research materials. We are grateful to the many community hospital staff who contributed to the NHSBN Community Hospital Programme, and to the staff who provided data to the NAIC. We thank the staff at the Atlas of Variation for providing us with data on secondary care utilisation. In addition, we thank the practitioners who engaged with us during workshops held at several CHA annual conferences and helped to improve our work.
We owe particular thanks to the NHS organisations and community hospitals that took part in the case studies. The requirements of anonymity mean that we cannot name them; only they know who they are. They include the NHS managers and local collaborators who facilitated and took part in the research and the ward managers and staff in our participating wards. Invariably, community hospital staff made us welcome; they answered our questions with patience, interest and good humour as they went about their tasks; and they tolerated our ongoing presence even though being observed might have felt intrusive at times. We are also very grateful to those staff who gave their time to take part in interviews and shared their views and experiences with us. We felt privileged to share the experiences of patients and their relatives and learned an enormous amount from them.
Finally, we acknowledge with thanks the contributions made by the following colleagues and research staff: Satti Saggu, Elizabeth Lavender, Rosemary Shannon and Sylvia Nikolova.
The published protocol can be found in Gladman et al. 96
Contributions of authors
John Young (https://orcid.org/0000-0003-4085-9306) prepared the Abstract, Plain English summary, Scientific summary, and Chapters 1, 3 and 7, which were then improved and edited by the other authors. He also edited Chapters 2, 3 and 6.
Claire Hulme (https://orcid.org/0000-0003-2077-0419) co-wrote a larger report from which Chapter 2 was drawn, and also wrote a larger report (alongside the health economics team) from which Chapter 6 was drawn.
Andrew Smith (https://orcid.org/0000-0003-3668-5593) co-wrote a larger report from which Chapter 2 was drawn.
John Buckell (https://orcid.org/0000-0002-4157-4217) co-wrote a larger report from which Chapter 2 was drawn.
Mary Godfrey (https://orcid.org/0000-0002-2408-534X) wrote Chapter 3, with Helen Tucker (https://orcid.org/0000-0003-2829-9115) contributing to the writing of the case study scenarios.
Claire Holditch (https://orcid.org/0000-0002-9250-952X) and Jessica Grantham (https://orcid.org/0000-0003-0759-676X) co-wrote Chapter 5.
Pam Enderby (https://orcid.org/0000-0002-4371-9053) and John Gladman (https://orcid.org/0000-0002-8506-7786) provided specific input into Chapters 1 and 7.
Elizabeth Teale (https://orcid.org/0000-0002-5923-3170) provided specific input into Chapter 1 and the Scientific summary.
Jean-Christophe Thiebaud (https://orcid.org/0000-0003-0331-4753) wrote the econometric analysis section of Chapter 6.
All chapters were reviewed by all authors.
Data-sharing statement
No new quantitative data were generated by this programme of work. The data sets we used for the econometric analyses are the property of the NHSBN. The qualitative (case study) material is held by Mary Godfrey (Academic Unit of Elderly Care & Rehabilitation, University of Leeds). The toolkit is published on the NHSBN website and available to use after prior registration. All data requests should be submitted to the corresponding author for consideration.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data are vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Office for National Statistics . National Population Projections: 2016-Based Statistical Bulletin 2017. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/nationalpopulationprojections/2016basedstatisticalbulletin (accessed 26 June 2019).
- Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet 2009;374:1196-208. https://doi.org/10.1016/S0140-6736(09)61460-4.
- Kingston A, Robinson L, Booth H, Knapp M, Jagger C. MODEM project . Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing 2018;47:374-80. https://doi.org/10.1093/ageing/afx201.
- Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing 2016;45:431-5. https://doi.org/10.1093/ageing/afw044.
- Department of Health and Social Care . White Paper. Our Health, Our Care, Our Say: A New Direction for Community Services 2006. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/272238/6737.pdf (accessed 30 October 2018).
- Young J, Green J, Forster A, Small N, Lowson K, Bogle S, et al. Postacute care for older people in community hospitals: a multicenter randomized, controlled trial. J Am Geriatr Soc 2007;55:1995-2002. https://doi.org/10.1111/j.1532-5415.2007.01456.x.
- O’Reilly J, Lowson K, Green J, Young JB, Forster A. Post-acute care for older people in community hospitals – a cost-effectiveness analysis within a multi-centre randomised controlled trial. Age Ageing 2008;37:513-20. https://doi.org/10.1093/ageing/afn120.
- Garasen H, Winspoll Johnsen R. Long term outcomes after intermediate care at a community hospital for elderly patients: 12 months follow up of a randomised controlled trial. Scan J Public Health 2008;36:197-204. https://doi.org/10.1177/1403494808089685.
- Small N, Green J, Spink J, Forster A, Lowson K, Young J. The patient experience of community hospital – the process of care as a determinant of satisfaction. J Eval Clin Pract 2007;13:95-101. https://doi.org/10.1111/j.1365-2753.2006.00653.x.
- Small N, Green J, Spink J, Forster A, Young J. Post-acute rehabilitation care for older people in community hospitals and general hospitals – philosophies of care and patients’ and caregivers’ reported experiences: a qualitative study. Disabil Rehabil 2009;31:1862-72. https://doi.org/10.1080/09638280902847002.
- Green J, Forster A, Young J, Small N, Spink J. Older people’s care experience in community and general hospitals: a comparative study. Nurs Older People 2008;20:33-9. https://doi.org/10.7748/nop2008.07.20.6.33.c6617.
- Community Hospitals Association . Profiling Community Hospitals n.d. www.communityhospitals.org.uk/profiling-community-hospitals.html (accessed 7 June 2019).
- NHS Benchmarking Network . Community Hospitals Overview Benchmarking Report 2015. www.wnecumbria.nhs.uk/wp-content/uploads/2016/09/NHS-Benchmarking Community-Healthcare.pdf (accessed 28 October 2018).
- NHS Benchmarking Network . National Audit of Intermediate Care n.d. www.nhsbenchmarking.nhs.uk/ (accessed 30 October 2018).
- Department of Health and Social Care . National Service Framework for Older People 2001. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/198033/National_Service_Framework_for_Older_People.pdf (accessed 24 June 2019).
- Department of Health and Social Care . Delivering Care Closer to Home: Meeting the Challenge 2008. https://webarchive.nationalarchives.gov.uk/20130124043303/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_086051.pdf (accessed 24 June 2019).
- NHS Institute for Innovation and Improvement . The Productive Ward Series n.d. http://webarchive.nationalarchives.gov.uk/20120502150329/http://www.institute.nhs.uk/quality_and_value/productivity_series/the_productive_series.html (accessed 30 October 2018).
- Griffiths PD, Edwards MH, Forbes A, Harris RL, Ritchie G. Effectiveness of intermediate care in nursing-led in-patient units. Cochrane Database Syst Rev 2007;2. https://doi.org/10.1002/14651858.CD002214.pub3.
- Young J, Forster A, Green J, Bogle S. Post-acute transfer of older people to intermediate care services: the sooner the better?. Age Ageing 2007;36:589-92. https://doi.org/10.1093/ageing/afm057.
- Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev 2017;9. https://doi.org/10.1002/14651858.CD006211.pub3.
- Audit Commission . More for Less 2009 10: Are Efficiency and Productivity Improving in the NHS? 2010. https://webarchive.nationalarchives.gov.uk/20101218023001/http://www.audit-commission.gov.uk/SiteCollectionDocuments/AuditCommissionReports/NationalStudies/20101216moreforless200910.pdf (accessed 27 June 2019).
- Department of Health and Social Care . Shaping the Future NHS: Long Term Planning for Hospitals and Related Services Consultation Document on the Findings of The National Beds Inquiry 2000. www.nhshistory.net/nationalbeds.pdf (accessed 23 August 2019).
- Department of Health and Social Care . The NHS Plan: A Plan for Investment, a Plan for Reform 2000. https://navigator.health.org.uk/content/nhs-plan-plan-investment-plan-reform-2000 (accessed 27 August 2019).
- Department of Health and Social Care . Intermediate Care: Halfway Home: Updated Guidance for the NHS and Local Authorities 2009. https://webarchive.nationalarchives.gov.uk/20130124050747/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@pg/documents/digitalasset/dh_103154.pdf (accessed 27 June 2019).
- Imison C, Poteliakhoff E, Thompson J. Older People and Emergency Bed Use: Exploring Variation. London: The King’s Fund; 2012.
- Holditch C. Intermediate Care. London: Findings presented to The King’s Fund; 2017.
- NHS Benchmarking Network . National Audit of Intermediate Care 2014: Key Findings 2014. https://static1.squarespace.com/static/58d8d0ffe4fcb5ad94cde63e/t/58f08f872994ca3c1de69eee/1492160402738/naic-provider-report-2014.pdf (accessed 30 October 2018).
- NHS Benchmarking Network . National Audit of Intermediate Care 2015: Key Findings 2015. https://static1.squarespace.com/static/58d8d0ffe4fcb5ad94cde63e/t/58f08efae3df28353c5563f3/1492160300426/naic-report-2015.pdf (accessed 30 October 2018).
- NHS Benchmarking Network . National Audit of Intermediate Care 2017: Key Findings 2017. https://s3.eu-west-2.amazonaws.com/nhsbn-static/NAIC%20(Providers)/2017/NAIC%20England%20Summary%20Report%20-%20upload%202.pdf (accessed 30 October 2018).
- Fleming SA, Blake H, Gladman JR, Hart E, Lymbery M, Dewey ME, et al. A randomised controlled trial of a care home rehabilitation service to reduce long-term institutionalisation for elderly people. Age Ageing 2004;33:384-90. https://doi.org/10.1093/ageing/afh126.
- Great Britain . Mental Capacity Act 2005 2005.
- Great Britain . Mental Capacity Act 2005 Code of Practice 2007.
- Monitor . Improvement Opportunities in the NHS: Quantification and Evidence 2013. www.monitor.gov.uk/sites/all/modules/fckeditor/plugins/ktbrowser/_openTKFile.php?id=37844 (accessed 23 February 2014).
- Farrell MJ. The measurement of productive efficiency. J Royal Stat Soc 1957;120:253-90. https://doi.org/10.2307/2343100.
- Lovell C. Frontier analysis in healthcare. Int J Healthcare Technol Manage 2006;7:5-14. https://doi.org/10.1504/IJHTM.2006.007870.
- Mutter RL, Rosko MD, Greene WH, Wilson PW. Translating frontiers into practice: taking the next steps toward improving hospital efficiency. Med Care Res Rev 2011;68:3-19. https://doi.org/10.1177/1077558710384878.
- Hollingsworth B, Dawson PJ, Maniadakis N. Efficiency measurement of health care: a review of non-parametric methods and applications. Health Care Manag Sci 1999;2:161-72. https://doi.org/10.1023/A:1019087828488.
- Hollingsworth B. Non-parametric and parametric applications measuring efficiency in health care. Health Care Manag Sci 2003;6:203-18. https://doi.org/10.1023/A:1026255523228.
- Hollingsworth B, Peacock S. Efficiency Measurement in Health and Health Care. Abingdon: Routledge; 2008.
- Worthington AC. Frontier efficiency measurement in health care: a review of empirical techniques and selected applications. Med Care Res Rev 2004;61:135-70. https://doi.org/10.1177/1077558704263796.
- Coelli TJ, Rao D, O’Donnell C, Battese GE. An Introduction to Efficiency and Productivity Analysis. New York, NY: Springer; 2005.
- Harper J, Hauck K, Street A. Analysis of costs and efficiency in general surgery specialties in the United Kingdom. January 2001. HEPAC Health Econ Prevent Care 2001;2:150-7. https://doi.org/10.1007/s10198-001-0077-2.
- Street A, Jacobs R. Relative performance evaluation of the English acute hospital sector. Appl Econ 2002;34:1109-19. https://doi.org/10.1080/00036840110088100.
- Street A. How much confidence should we place in efficiency estimates?. Health Econ 2003;12:895-907. https://doi.org/10.1002/hec.773.
- Ferrari A. The internal market and hospital efficiency: a stochastic distance function approach. Appl Econ 2006;38:2121-30. https://doi.org/10.1080/00036840500427437.
- Jacobs R, Street A, Smith P. Measuring Efficiency in Health Care. Cambridge: Cambridge University Press; 2006.
- Laudicella M, Olsen KR, Street A. Examining cost variation across hospital departments – a two-stage multi-level approach using patient-level data. Soc Sci Med 2010;71:1872-81. https://doi.org/10.1016/j.socscimed.2010.06.049.
- Cooper Z, Gibbons S, Jones S, McGuire A. Does Competition Improve Public Hospitals’ Efficiency? Evidence from a Quasi-experiment in the English National Health Service. London: London School Economics; 2012.
- Daidone S, Street A. How much should be paid for specialised treatment?. Soc Sci Med 2013;84:110-18. https://doi.org/10.1016/j.socscimed.2013.02.005.
- Gutacker N, Bojke C, Daidone S, Devlin NJ, Parkin D, Street A. Truly inefficient or providing better quality of care? Analysing the relationship between risk-adjusted hospital costs and patients’ health outcomes. Health Econ 2013;22:931-47. https://doi.org/10.1002/hec.2871.
- Buckell J, Smith A, Longo R, Holland D. Efficiency, heterogeneity and cost function analysis: empirical evidence from pathology services in the National Health Service in England. Appl Econ 2015;47:3311-31. https://doi.org/10.1080/00036846.2015.1013617.
- Moran V, Jacobs R. Comparing the performance of English mental health providers in achieving patient outcomes. Soc Sci Med 2015;140:127-35. https://doi.org/10.1016/j.socscimed.2015.07.009.
- Smith A, Buckell J, Wheat P, Longo R, Greene WH, Khalaf L, et al. Productivity and Efficiency Analysis. Switzerland: Springer International Publishing; 2015.
- Farsi M, Filippini M, Kuenzle M. Unobserved heterogeneity in stochastic cost frontier models: an application to Swiss nursing homes. Appl Econ 2005;37:212-41. https://doi.org/10.1080/00036840500293201.
- National Audit Office . Emergency Admissions to Hospital : Managing the Demand, London 2013. www.nao.org.uk/wp-content/uploads/2013/10/10288-001-Emergency-admissions (accessed 25 October 2018).
- Jondrow J, Knox Lovell CA, Materov IS, Schmidt P. On the estimation of technical inefficiency in the stochastic frontier production function model. J Econometrics 1982;19:233-38. https://doi.org/10.1016/0304-4076(82)90004-5.
- Kumbhakar SC, Hjalmarsson L. Labour-use efficiency in Swedish social insurance offices. J Appl Econometrics 1995;10:33-47. https://doi.org/10.1002/jae.3950100104.
- Christensen LR, Greene WH. Economies of scale in U.S. electric power generation. J Polit Econ 1976;84:655-76. https://doi.org/10.1086/260470.
- Coelli T. Estimators and hypothesis tests for a stochastic frontier function: Monte Carlo analysis. J Product Anal 1995;6:247-68. https://doi.org/10.1007/BF01076978.
- Wheat P, Greene W, Smith ASJ. Understanding prediction intervals for firm specific inefficiency scores from parametric stochastic frontier models. J Product Anal 2014;42:55-6. https://doi.org/10.1007/s11123-013-0346-y.
- Lappegard Ø, Hjortdahl P. Perceived quality of an alternative to acute hospitalization: an analytical study at a community hospital in Hallingdal, Norway. Soc Sci Med 2014;119:27-35. https://doi.org/10.1016/j.socscimed.2014.08.014.
- Davidson D, Ellis Paine A, Glasby J, Williams I, Tucker H, Crilly T, et al. Analysis of the profile, characteristics, patient experience and community value of community hospitals: a multi-method study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07010.
- Hart E, Lymbery M, Gladman JR. Away from home: an ethnographic study of a transitional rehabilitation scheme for older people in the UK. Soc Sci Med 2005;60:1241-50. https://doi.org/10.1016/j.socscimed.2004.07.007.
- Godfrey M, Townsend J. Older people in transition from illness to health: trajectories of recovery. Qual Health Res 2008;18:939-51. https://doi.org/10.1177/1049732308318038.
- Trappes-Lomax T, Hawton A. The user voice: older people’s experiences of reablement and rehabilitation. J Integ Care 2012;20:181-95. https://doi.org/10.1108/14769011211237528.
- Pearson M, Hunt H, Cooper C, Shepperd S, Pawson R, Anderson R. Providing effective and preferred care closer to home: a realist review of intermediate care. Health Soc Care Community 2015;23:577-93. https://doi.org/10.1111/hsc.12183.
- Young J, Robinson J, Dickinson E. Rehabilitation for older people. BMJ 1998;316:1108-09. https://doi.org/10.1136/bmj.316.7138.1108.
- Nocon A, Baldwin S. Trends in Rehabilitation Policy: A Review of the Literature. London: King’s Fund Publishing; 1998.
- Ragin C, Byrne D, Ragin C. The Sage Handbook of Case – Based Methods. London: Sage Publications Ltd; 2013.
- Stake R. The Art of Case Study Research. London: Sage Publications Ltd; 1995.
- Yin R. Case Study Research: Design and Methods. London: Sage Publications Ltd; 2009.
- Byrne D, Byrne D, Ragin C. The Sage Handbook of Case–based Methods. London: Sage Publications Ltd; 2013.
- Patterson M, Nolan M, Rick J, Brown J, Adams R, Mussen G. From Metrics to Meaning: Culture Change and Quality of Acute Hospital Care for Older People. London: HMSO; 2011.
- Spradley JP. Participant Observation. Wadsworth: Belmont, CA; 1980.
- Lofland J, Snow D, Anderson L, Lofland LH. Analysing Social Settings: A Guide to Qualitative Observations and Analysis. Belmont CA: Wadsworth; 2006.
- Gobo G. Doing Ethnography. London: Sage Publications Ltd; 2008.
- Emerson RM, Fretz RI, Shaw LL. Writing Ethnographic Fieldnotes. Chicago, IL: University of Chicago Press; 1995.
- Mishler EG. Research Interviewing Context and Narrative. Cambridge, MA: Harvard University Press; 1991.
- Godfrey M, Young J, Shannon R, Skingley A, Woolley R, Arrojo F, et al. The Person, Interactions and Environment Programme to improve care of people with dementia in hospital: a multisite study. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06230.
- Charmaz K. Constructing Grounded Theory. Thousand Oaks, CA: Sage Publications Ltd; 2014.
- Nolte E, McKee M. Caring for People with Chronic Conditions: a Health System Perspective. Maidenhead: Open University Press; 2008.
- Tolson D, Smith M, Knight P. An investigation of the components of best nursing practice in the car of acutely ill hospitalized older patients with coincidental dementia: a multi-method design. J Adv Nurs 1999;30:1127-36. https://doi.org/10.1046/j.1365-2648.1999.01194.x.
- Hosie A, Agar M, Lobb E, Davidson PM, Phillips J. Improving delirium recognition and assessment for people receiving inpatient palliative care: a mixed methods meta-synthesis. Int J Nurs Stud 2017;75:123-9. https://doi.org/10.1016/j.ijnurstu.2017.07.007.
- Gronn P. Distributed leadership as a unit of analysis. Leadership Quart 2002;13:423-51. https://doi.org/10.1016/S1048-9843(02)00120-0.
- Pitchforth E, Nolte E, Corbett J, Miani C, Winpenny E, . Community hospitals and their services in the NHS: identifying transferable learning from international developments – scoping review, systematic review, country reports and case studies. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05190.
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 21 August 2017).
- Bradford Teaching Hospitals NHS Foundation Trust, Benchmarking Network . MOCHA: Models of Community Hospital Activity n.d. http://mocha.nhsbenchmarking.nhs.uk/ (accessed 9 September 2019).
- Royal College of Physicians . Future Hospital; Caring for Medical Patients. A Report From the Future Hospital Commission to the Royal College of Physicians 2013. www.rcplondon.ac.uk/projects/outputs/future-hospital-commission (accessed 27 August 2019).
- World Health Organization . World Report on Ageing and Health 2015. http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=8E5E52AFE9A84F5B0165F82F733E3B6A?sequence=1 (accessed 9 April 2018).
- National Audit Office . Reducing Emergency Admissions n.d. www.nao.org.uk/wp-content/uploads/2018/02/Reducing-emergency-admissions.pdf (accessed 7 October 2019).
- Public Health England/NHS England . The NHS Atlas of Variation in Healthcare Compendium 2015 n.d. http://tools.england.nhs.uk/images/atlas15/atlas.html (accessed 27 August 2019).
- Shepperd S, Iliffe S, Doll HA, Clarke MJ, Kalra L, Wilson AD, et al. Admission avoidance hospital at home. Cochrane Database Sys Rev 2016;9. https://doi.org/10.1002/14651858.CD00791.pub2.
- Breusch T, Pagan A. A simple test for heteroscedasticity and random coefficient variation. Econometrica 1979;47:1287-94. https://doi.org/10.2307/1911963.
- Zarembka P, Zarembka P. Frontiers of Econometrics. New York, NY: Academic Press; 1974.
- Seamark D, Moore B, Tucker H, Church J, Seamark C. Community hospitals for the new millennium. Br J Gen Pract 2001;51:125-7.
- Gladman J, Buckell J, Young J, Smith A, Hulme C, Saggu S, et al. Understanding the Models of Community Hospital rehabilitation Activity (MoCHA): a mixed-methods study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2015-010483.
- Huntley AL, Chalder M, Shaw ARG, Hollingworth W, Metcalfe C, Benger JR, et al. A systematic review to identify and assess the effectiveness of alternatives for people over the age of 65 who are at risk of potentially avoidable hospital admission. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016236.
- Hajargasht G. Stochastic frontiers with a Rayleigh distribution. J Prod Anal 2015;44:199-208. https://doi.org/10.1007/s11123-014-0417-8.
- Greene W. LIMDEP Econometric Modeling Guide. New York, NY: Econometric Software, Inc.; 2012.
Appendix 1 Economic efficiency of community hospitals’ inpatient beds
Introduction
This paper provides an introduction to the economic analysis tool SFA that is being used in the Community Hospitals Research Programme on Efficiency by a team of researchers at Leeds University. This briefing paper provides supporting information for a presentation and workshop prepared for the CHA conference.
The researchers are interested in feedback from practitioners working in community hospitals on their view of which factors can influence efficiency in practice. We are also interested in ‘variables’ that may affect the service. We are available for any questions and further discussion on this tool and its application to community hospitals in practice.
Please contact: XXXX.
Fundamentals of economics
In the language of economics, firms are said to be operating a production process that uses inputs (labour, capital, materials) to produce outputs. In the case of community hospitals, inputs might include the costs of employing staff, buying medicines and running the premises, whereas outputs will typically include the health service provided (i.e. treating patients) and will incorporate aspects of service quality. We can examine this ‘production process’ through cost and other key data. Some community hospitals are adept at converting their inputs into outputs, that is, they are efficient. Other community hospitals are less so, that is, they are inefficient. We are interested in quantifying this efficiency/inefficiency spectrum. If a community hospital’s costs are our measure of interest, then we are measuring cost efficiency.
Measuring cost efficiency
In order to measure cost efficiency, we can construct an efficiency line or a ‘frontier’ that represents the minimum possible cost for a community hospital given its output. The line advances upwards as the number of cases treated increases and, therefore, some of the costs also increase (e.g. medicines used). This line would represent the most cost-efficient community hospital and can be viewed as a benchmark against which other community hospitals can be compared. We can therefore plot other community hospitals in relation to this most cost-efficient line. The further the particular community hospital lies above this line or frontier, the more that particular community hospital can be said to be cost inefficient. If we plot data from lots of community hospitals, we can measure relative cost efficiency. This is shown in Figure 10.
FIGURE 10.
The efficiency frontier line. For simplicity, the frontier is shown as a straight line but it is more commonly a curved line.
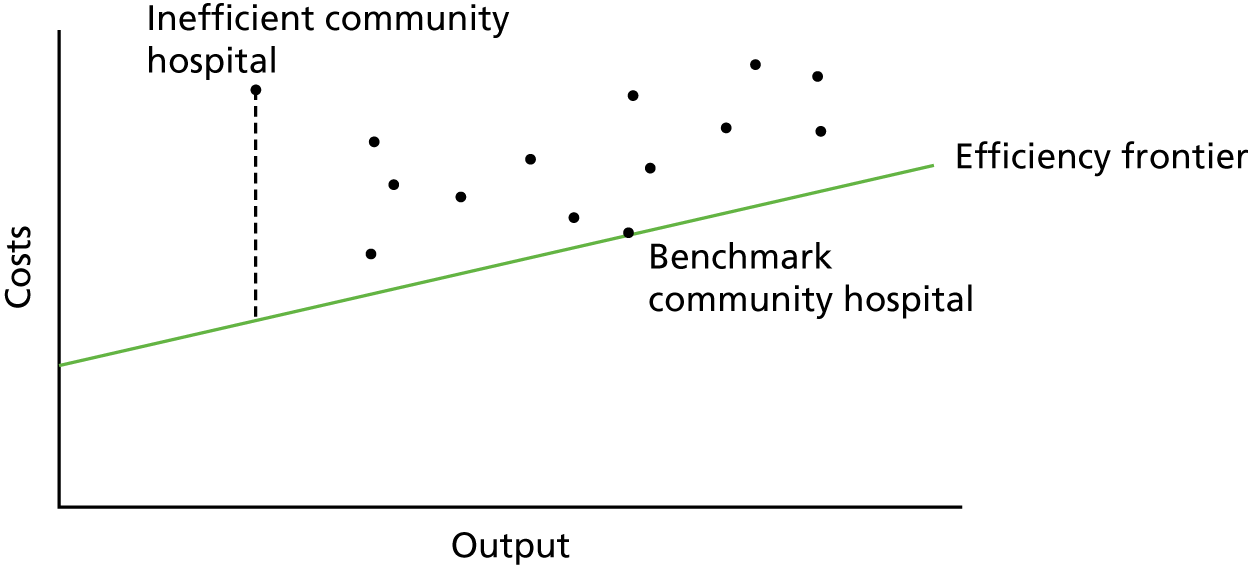
The cost function
The shape of the efficiency frontier is defined using a cost function that shows how costs (c) are related to a string of cost drivers including outputs (y) (e.g. the number of patients treated), input prices (w) (e.g. wages, capital costs), environmental variables (z) (e.g. bed occupancy, mix of services provided) and quality (q) (e.g. clinical audit results, research activities, MRSA occurrence, pressure sores, patient-reported experience measure)
Appendix 2 Stochastic frontier analysis: distributional assumptions
Distributional assumptions
One issue with the SF model is the need to make distributional assumptions and the effect of the assumption on the prediction of inefficiency. Because of this, there has been some concern around the prediction of inefficiency. 42 It is possible to use a number of different assumptions for the inefficiency term and, therefore, to make a number of assumptions about the form of inefficiency and then to test between models. Moreover, it is possible to test the correlation between models’ predictions, both in terms of absolute results and rank, to assess robustness. Therefore, the following models are tested (Table 15).
| Model | Assumptions about distribution |
|---|---|
| COLS | No decomposition of the model error into noise and inefficiency, and does not impose distributional assumptions on the components of the error |
| Half normal | Noise is normally distributed with zero mean; inefficiency assumed to be distributed as half normal |
| Truncated normal | Same form as the half normal, except that the mode of inefficiency is allowed to be non-zero |
| Exponential | Distribution is akin to the half normal, but its shape is different. The modal value of inefficiency is zero |
| Gamma | Allows the form of inefficiency to vary. The modal value of inefficiency is zero |
| Rayleigh | Allows for a modal value of inefficiency that is non-zero without the need to estimate an additional parameter, as is the case with the truncated-normal model |
For further discussion of distributional assumptions, see Coelli et al. 41 For the Rayleigh distribution, see Hajargasht. 98
To test for inefficiency, we test each model against the OLS as a base model. We adopt a LR for this purpose.
In total, we estimate 12 models (six specifications of the distribution of inefficiency; two functional forms). We report the results for six models, having applied the test for functional form.
We use LIMDEP version 10 (Econometric Software, Inc., Plainview, NY, USA) for estimations. 99
The full report of this analysis, written by Claire Hulme and economics colleagues, may be obtained if requested from the authors.
Appendix 3 National community hospitals survey
Appendix 4 Scottish community hospital ethics journey
FIGURE 11.
Scottish community hospital ethics journey. AWI, adults with capacity; IRAS, Integrated Research Application System; R&D, research and development; REC, Research Ethics Committee.
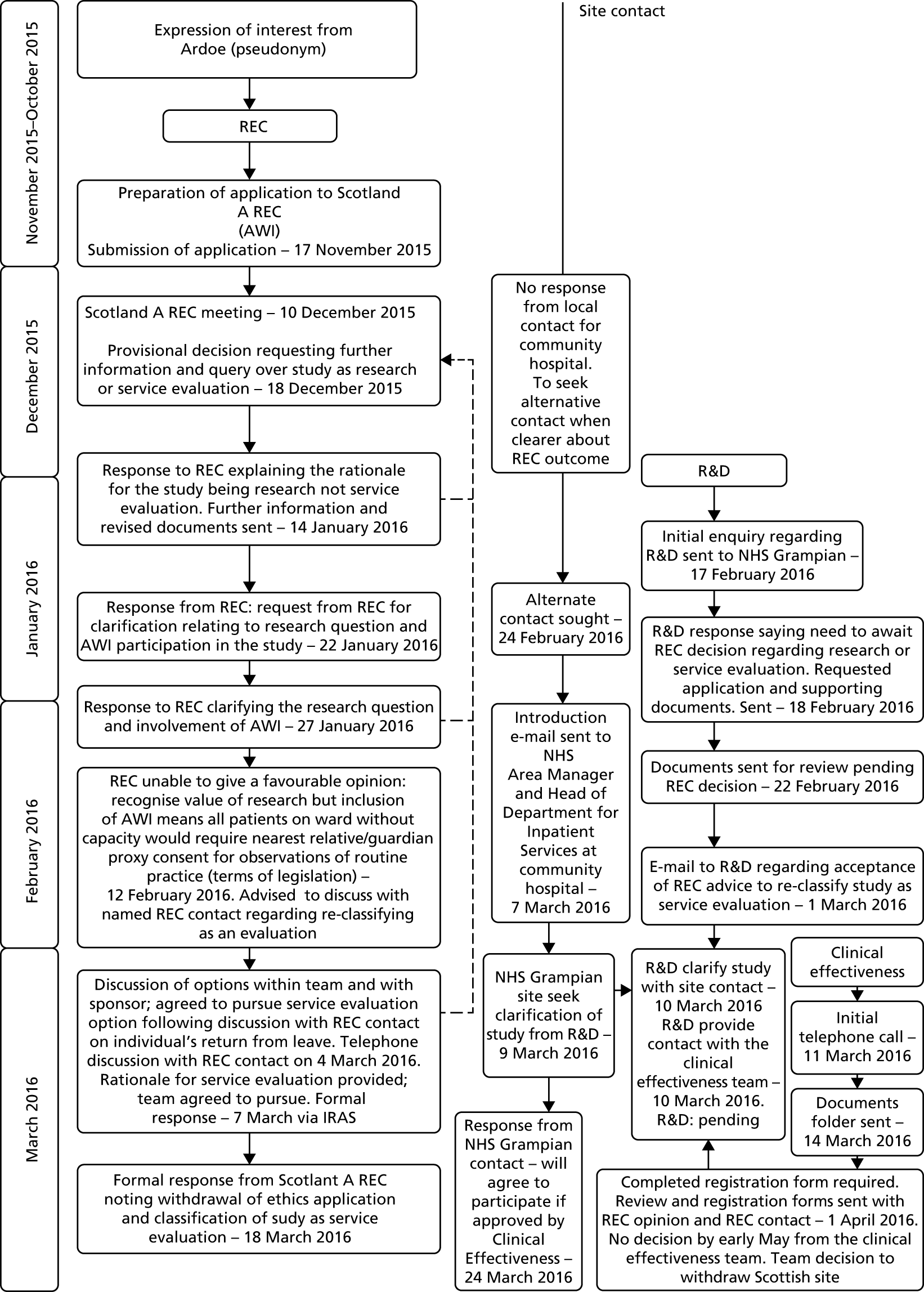
For ethics documentation, see www.journalslibrary.nihr.ac.uk/programmes/hsdr/1217704/#/ (accessed 28 August 2019).
Appendix 5 Summary of data collection for study 3
| Dates | Castle (n) | Ramsay (n) | Lawrence (n) | Total (n) |
|---|---|---|---|---|
| May–August 2016 | End July–November 2016 | December 2016–March 2017 | ||
| Observation (hours) | 80 | 85 | 61 | 226 |
| Interviews: ward staff | 11 | 8 | 6 | 25 |
| Interviews: senior trust managers/intermediate-care middle managers | 9 | 5 | 4 | 18 |
| Patient case studies | 4 (including 3 carers) | 8 (including 3 carers) | 4 (including 1 carer) | 16 |
| Staff questionnaires | 18 | 12 | 9 | 39 |
List of abbreviations
- AIC
- Akaike information criterion
- ANP
- advanced nurse practitioner
- CCG
- Clinical Commissioning Group
- CHA
- Community Hospitals Association
- COLS
- corrected ordinary least squares
- CRT
- crisis response team
- DEA
- data envelopment analysis
- GP
- general practitioner
- HCA
- health-care assistant
- LOS
- length of stay
- LR
- likelihood ratio procedure
- MDT
- multidisciplinary team
- MoCHA
- Models of Community Hospital Activity
- MRSA
- meticillin-resistant Staphylococcus aureus
- NAIC
- National Audit of Intermediate Care
- NAO
- National Audit Office
- NHSBN
- NHS Benchmarking Network
- OLS
- ordinary least squares
- SF
- stochastic frontier
- SFA
- stochastic frontier analysis
- UTLA
- upper-tier local authority
- WTE
- whole-time equivalent
