Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/47/17. The contractual start date was in September 2017. The final report began editorial review in October 2018 and was accepted for publication in April 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Andrew Booth is a member of the National Institute for Health Research Complex Reviews Support Unit Funding Board (2015 to present), the Health Services and Delivery Research Funding Board (2018 to present) and the Systematic Reviews Programme Advisory Group (2019 to present).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Chambers et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Admissions to hospital increasingly contribute to pressure on health system resources internationally. In the UK NHS, changes to commissioning arrangements have increased the focus on reducing hospital admissions. 1 In 2016–17, there were 5.8 million emergency admissions to hospitals, costing approximately £13.7B. 2 This situation poses a significant challenge to health services delivery. Factors contributing to health service pressures include the high and rising unit costs of unplanned hospital admissions compared with those of other forms of care; increasing admissions of older people; and the disruption that emergency admissions cause to elective health care, most notably to inpatient waiting lists, and to the individuals admitted. 1
Unplanned hospital admission rates vary between geographical areas from 90 to 139 per 1000 people, and variation in emergency admission rates is even higher. 3 The existence of such variation across the NHS indicates that there is potential to reduce hospital admission rates. The way in which emergency admissions are recorded also varies between institutions and this makes it more difficult to get an accurate picture of the current situation.
Interest in reducing admissions focuses in particular on a group of ambulatory care sensitive conditions (ACSCs), defined as conditions for which hospital admission could be prevented with care delivered in the primary care setting. 4 These include asthma, chronic obstructive pulmonary disease (COPD), diabetes, epilepsy, hypertensive disease, dementia and heart failure. 5
The terminology in this field is complex. Terms such as ‘unplanned admissions’, ‘inappropriate admissions’, ‘unnecessary admissions’, ‘preventable admissions’ and ‘avoidable admissions’ are widely used but not always in a consistent way. Unplanned admissions may be defined as admissions or re-admissions involving an overnight stay in hospital that were not previously planned or are defined as ‘elective’. 3 The term ‘avoidable admissions’ is often used to refer to admissions via emergency departments that could potentially be avoided through interventions in the urgent and emergency care system. The focus of this evidence synthesis project is on preventable admissions, defined as admissions for ACSCs and other long-term conditions that could potentially be prevented by provision of appropriate care and services in primary care and community settings. However, the two categories are not mutually exclusive and some interventions to reduce preventable admissions or re-admissions may be delivered in pre-hospital, emergency department or other hospital settings.
Over more than a decade, the NHS has explored community-, population- and policy-level interventions aimed at reducing preventable hospital admissions, but these have had little impact on admission rates. 1 In 2012, a series of systematic reviews by Purdy et al. 3 summarised the evidence regarding interventions that had exhibited success in reducing unplanned hospital admissions. In terms of services to reduce admissions, Purdy et al. 3 found evidence of effectiveness for education, self-management, exercise and rehabilitation, and for telehealth in certain patient populations, mainly respiratory and cardiovascular. 3 Case management, community interventions and specialist clinics showed effectiveness for heart failure only. However, case management and specialist clinics overall, care pathways and guidelines, medication reviews, vaccine programmes and hospital at home did not appear to reduce preventable admissions. The reviews found insufficient evidence on the role of service combinations or co-ordinated system-wide care services, emergency department interventions, continuity of care, home visits or pay-by-performance schemes. 3
Thus, although the pattern of findings was mixed, Purdy et al. ’s3 systematic reviews revealed a consistent picture of reduction across different interventions targeting two particular types of condition, namely cardiovascular and respiratory conditions, with some of the interventions being disease-specific. By way of comparison, one of the quality measures for accountable care organisations under the US Patient Protection and Affordable Care Act6 is to reduce preventable emergency admissions for three chronic medical conditions: COPD, congestive heart failure and asthma. 7 For this interpretative review, the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme asked us to consider these as ‘proven interventions’ and to seek to provide an in-depth understanding of how interventions that have been shown to reduce admissions for cardiovascular and respiratory conditions work in practice. This includes both (1) how the interventions work to reduce unplanned admissions and (2) how they seek to ensure that admissions that are avoided are, in fact, unnecessary. The intention is also to identify some potentially transferable lessons that might determine how to achieve comparable success in other conditions or, at least, help in understanding factors that potentially explain when comparable success is not realised outside these two focal conditions.
The aim of this research was to fill a gap in the evidence base around successful implementation of admission reduction programmes by focusing on understanding what works for whom, why it works and in what contexts it works. 8 We first investigated interventions that are currently used in the NHS to manage cardiovascular or respiratory conditions using a systematic mapping approach. 9 We then used a realist approach8 to identify and explain factors that contribute to successful implementation of interventions to reduce preventable hospital admissions, looking at responses to interventions that involve different mechanisms and different contexts. To the best of our knowledge, this is the first example of a realist-based approach exploring these aspects of implementation.
Chapter 2 Methods
Overall review strategy
The overall review comprised two main phases:
-
systematic mapping of cardiorespiratory intervention studies for reducing preventable admissions
-
realist review of implementation evidence.
The overall review commenced with the decision, agreed with the NIHR HSDR programme team, to focus exploration on those conditions revealed by the 2010 Purdy review1 to demonstrate effective interventions to prevent avoidable hospital admissions. A positive effect or positive indication was consistently found for cardiorespiratory conditions and this was a focus for systematic mapping of studies.
Based on these included studies, four complementary activities were conducted (Table 1):
-
generation of if–then–leading to statements from a conceptually rich set of empirical studies and theoretical papers and selection of candidate programme theories
-
analysis of implementation studies to identify intervention components using an abbreviated version of the Template for Intervention Description and Replication (TIDieR) checklist
-
analysis of implementation studies using the Promoting Action on Research Implementation in Health Services (PARiHS) framework
-
comparison of PARiHS templates with shortlisted programme theories.
| Review component | |||||||
|---|---|---|---|---|---|---|---|
| 1. Evidence base for effectiveness | 2. Intervention map | 3. Programme theory | 4. Empirical studies | 5. PARiHS analysis | 6. Realist analysis | 7. Integration of review outputs | |
| Review activity | Selection from Purdy et al.3 review | Systematic mapping of studies | Generation of if–then–leading to selection of candidate theories |
Identification of implementation studies for mapped interventions Use of TIDieR-Lite templates |
Analysis of implementation studies for mapped interventions | Analysis of PARiHS templates against shortlisted programme theories | Analysis of map, interventions, implementations and programme theories |
| Review deliverable | Search strategy for map | Map of interventions by study characteristics | Shortlist of intervention-independent programme theories | Sets of implementation studies for each intervention | PARiHS templates for each intervention | Identification of mechanisms linked to interventions | Final report |
| Location in report | Chapter 2 | Chapter 3 | Chapter 2, Testing and refining the programme theory | Chapter 4, Number and type of UK studies sections | Chapter 4, Contextual factors sections | Chapter 4, Description of putative mechanisms sections, and Chapter 5 | Chapters 5 and 6 |
Finally, Chapters 5 and 6 provide the opportunity to integrate the diffuse review outputs.
The remainder of this chapter provides fuller details of the mapping and realist reviews.
Mapping review
The objective of the mapping review was to identify and map the literature on interventions that could be used to reduce preventable hospital admissions in the NHS, with a particular focus on cardiovascular and respiratory conditions. The included studies were to be used as a sampling frame, allowing the realist synthesis to examine the underpinning mechanisms that explain how the interventions work in practice, for whom and in what circumstances.
Inclusion criteria
Studies were included in the mapping review if they met the following criteria:
-
Published in or since 2010 in the English language.
-
Conducted in a relevant country (UK, USA, Canada, Australia or New Zealand). Canada, Australia and New Zealand were included as the countries with health systems most similar to that in the UK, and the USA was included because of the high volume of good-quality health research conducted there. We took a pragmatic decision to exclude as far as possible studies from other European countries because of differences in health service organisation. We recognise that this could involve excluding potentially relevant studies from some countries, but consider that the impact on the structure of the evidence map was likely to be relatively minor.
-
Recruited adults with a cardiovascular or respiratory condition (not cancer).
-
Evaluated or described an intervention that could reduce preventable hospital admissions or re-admissions. Based on the work of Purdy et al. ,3 the following interventions of interest were specified in advance: case management, specialist clinics, community interventions (not fitting into any other relevant category), patient education, self-management, pulmonary rehabilitation, cardiac rehabilitation and telehealth. Programmes involving combinations of these interventions were also eligible for inclusion.
-
Reported admissions/re-admissions or prevented admissions as an outcome and/or reported on implementation of the intervention (e.g. barriers and facilitators, qualitative studies of staff or patient views/experiences) in the context of reducing admissions.
The main study designs of interest were experimental studies (e.g. randomised and non-randomised trials), controlled and uncontrolled observational studies, qualitative studies and systematic reviews. We attempted to exclude editorials, letters, study protocols, papers discussing study rationale and design and other papers not reporting substantive data. Given that inclusion was based on titles and abstracts, published conference abstracts were eligible for inclusion.
Literature search
Formal bibliographic searches of MEDLINE, Cumulative Index to Nursing and Allied Health Literature, Health Management Information Consortium, EMBASE, Web of Science and The Cochrane Library were conducted in September 2017 and October 2017. The search was developed from initial scoping searches and previous systematic reviews, with search terms adapted for each information source. The search comprised terms for ACSCs combined with intervention terms and terms around admissions, implementation and research dissemination. The MEDLINE search is documented in Appendix 1. The ACSCs included the following: angina, hypertension, COPD and asthma. Intervention terms were derived from The King’s Fund report Avoiding Hospital Admissions: What Does the Research Evidence Say?. 1 The search was limited to studies published from 2010, when the Purdy report1 was published, to July 2018 and research published in the English language. Focusing on this narrower time frame is further justified by the specific focus of this review on implementation; an implementation context is a continually mutable backdrop within which to evaluate the introduction of a complex intervention.
Recent initiatives and, specifically, those that have been evaluated within a UK context were prioritised. Nevertheless, the review methodology preserved the potential to engage with the wider literature through coverage of reviews that extend the time and geographical limits beyond the formal sampling frame. The UK focus was strengthened by examination of the catalogues of the Health Services Management Centre at the University of Birmingham, The King’s Fund Library and Health Management Online (NHS Scotland).
Screening of search results and coding of included records
Bibliographic records identified by the literature research were imported into EPPI-Reviewer 4 (Evidence for Policy and Practice Information and Co-ordinating Centre, University of London, London, UK) for screening and data extraction. Records were screened for inclusion or exclusion by one reviewer, with a 10% sample being screened by two reviewers to check for consistency. Screening of search results was based on information in database records (title or title and abstract) only; we did not systematically screen full texts.
Data extraction (coding) was carried out by one reviewer in EPPI-Reviewer 4 using a mixture of tick-box selection and manual data entry. Table 2 summarises the extracted data items. We did not extract study findings or authors’ conclusions because the purpose of the review was to map interventions and not to evaluate their effectiveness.
| Data to code | Options | Comments |
|---|---|---|
| Include or exclude | Include; exclude; query |
Initial code set Include if: |
| Included studies only | ||
| Study identifier | Author, year, EndNote (Clarivate Analytics, Philadelphia, PA, USA) number | |
| Study design | Experimental; controlled observational; uncontrolled observational; qualitative; literature review; other; unclear | Broad categories for simplicity |
| Population/condition | Coronary heart disease; heart failure; hypertension; asthma; COPD; multiple; other cardiovascular; other respiratory | Coronary heart disease includes angina and post MI |
| Sample size | Number of participants | |
| Intervention | Case management; specialist clinics; community interventions; patient education; self-management; pulmonary rehabilitation; cardiac rehabilitation; telehealth; multiple; other; unclear |
Community interventions = those that do not fit into other relevant categories (Purdy et al. 3) This is based on Purdy et al. ’s3 findings of interventions with evidence of positive effect; can be added to if necessary |
| Comparator | Alternative intervention; usual care; baseline; not applicable; unclear/not reported | |
| Country | UK; USA; Canada; Australia; New Zealand; multiple countries; not applicable; unclear/not reported | |
| Access route | General practitioner; other general practice staff; emergency department; paramedic; telephone advice; outpatient appointment; hospital discharge; community service; patient-initiated; other; unclear/not reported | Who acts as ‘gatekeeper’ for the intervention? |
| Data type | Quantitative; qualitative; mixed | |
| Outcomes assessed | Admissions/re-admissions;3 prevented admissions;1 patient reported; staff reported; costs/cost-effectiveness; workforce outcomes; health system outcomes; qualitative outcomes; other | Statistical data;3 audit/judgement on specific cases1 |
| Length/period of study | Length of study | Years/months |
Mapping review synthesis
We produced a descriptive summary of key characteristics of the body of included studies as reported in Chapter 3. Summary tables were developed using the search, cross-tabulation and reporting functions of EPPI-Reviewer 4.
Realist synthesis
The mapping review revealed the coverage by journal literature of each of the main intervention types identified by Purdy et al. ,1,3 including the existence of systematic review evidence and UK-based quantitative and qualitative studies. This helped to inform the sampling frame for the subsequent realist synthesis. In contrast to a conventional systematic review, a realist synthesis is not required to examine a comprehensive and exhaustive sample from the literature; instead, it explores a judiciously and purposively selected sample favouring richer, more informative data.
The practical focus of this review required exclusion of evidence with limited transferability to the NHS, such as avoidable admissions in low- and middle-income countries. Through systematic review-level evidence, we accessed studies from four countries in addition to the UK, namely the USA, Australia, Canada and New Zealand. We also engaged with the wider evidence base (using supplementary searches) through systematic reviews, opinion pieces and direct reference to individual study reports, particularly when authors themselves established a connection to the UK context. Explicit inclusion criteria were implemented in our sampling frame to ensure consistent study selection by the review team across the nine intervention types.
Data extraction
In contrast to the mapping review, data extraction for the realist synthesis was based on the full text of each item. Purpose-designed data extraction forms drew on appropriate frameworks as structures by which to interrogate the theories and the empirical evidence. We used an experimental methodological development, previously tried in another NIHR HSDR realist synthesis,10,11 which combined use of realist synthesis methods with elements of best-fit framework synthesis. Best-fit framework synthesis involves identification of an appropriate ‘good-enough’ framework to operate as both a vehicle for data extraction and, subsequently, an analytical lens for examination of extracted data. 12 Best-fit framework synthesis is believed to expedite the data extraction process,13 with a majority of the data being handled deductively using the framework before a subsequent inductive phase to code data not explained by the categories derived from the original framework. 14
The focus of this realist synthesis on implementation encouraged the review team to focus on frameworks or models specifically derived in an implementation, knowledge translation or evidence-based health-care context. Instead of embarking on an extensive parallel process of framework identification, which was typically the case in previous uses of best-fit framework synthesis,15 the team used the sourcebook, Models and Frameworks for Implementing Evidence-Based Practice: Linking Evidence to Action,16 and rapidly reviewed the pictorial models and accompanying textual descriptions for ‘fit’ to the purpose and context of the review. A short list of candidate models was subsequently narrowed down to the PARiHS framework. Within the PARiHS framework, successful implementation is represented as a function of the nature and type of evidence (to be examined from the mapping review), the qualities of the context in which the evidence is being introduced and the way the process is facilitated17 (to be extracted from included UK studies, both quantitative and qualitative).
Previous experience of realist synthesis within complex service delivery contexts had also revealed the value of using the TIDieR as a formal framework for identifying and describing the components of included interventions. 18 We therefore decided to use a version of this template, abbreviated in recognition of both the time constraints and the generic level at which interventions have been characterised, as a structure for describing the nine intervention types. The 12-item TIDieR checklist [brief name, why, what (materials), what (procedure), who provided, how, where, when and how much, tailoring, modifications, how well (planned), how well (actual)] was therefore abbreviated in the form of the five-item ‘TIDieR-Lite’ (by whom, what, where, to what intensity, how often). Importantly, this was to be used to summarise the generic characteristics of each intervention type across multiple intervention reports, although significant areas of variation across each generic type were prompted for identification by the framework.
Finally, data relating to programme theory were extracted using an ‘if–then–leading to’ realist logic structure, pioneered by other research teams and used in previous reviews by team members. This enabled the generation of multiple programme theory statements [ultimately five in number: programme theories (PTs) 1–5; see Programme theory development] to be used to examine data from included empirical studies and to communicate programme logic to stakeholders in the form of narrative scenarios.
In summary, data extraction comprised use of:
-
an implementation framework, PARiHS, as a structure for examining how interventions are delivered
-
an intervention template, TIDieR, as a format for describing intervention components
-
a realist logic template, if–then–leading to, to elicit programme theory on how interventions might work.
Initial logic model
The team deliberated regarding whether or not logic models would be required for each intervention type, ultimately concluding that the focus on mechanisms, as opposed to outcomes, would facilitate a single inclusive logic model that could explain multiple points within the overall complex adaptive system. 19 Using barriers and facilitators identified from a rich subset of the literature, supplemented by input from team members and from the patient and public involvement (PPI) group (see Patient and public involvement), the team identified three systemic ‘problem points’:
-
Patient uncertainty about appropriate admission. This would have a direct effect on patient-centred interventions such as self-management, but also a secondary effect on health-care professional (HCP)-mediated interventions as patients attempted to resolve their initial uncertainty.
-
HCP uncertainty about appropriate admission. This revolves around the HCP’s gatekeeper role and may relate to the severity of patient symptoms, the risk-averse culture within which HCPs might operate and awareness of alternative service provision.
-
Structural barriers to appropriate admission. Patient or HCP current or previous experience of health service delivery may have an impact on the decision pathway. For example, if patients or HCPs have previously experienced delays in arrival of ambulance transport, they may factor in such delays by initiating call-out earlier than the patient’s symptoms might otherwise justify.
Based on these three potential problem points, the teams mapped the different interventions to those points that each sought to address. For example, telehealthcare may offer a ‘feedback’ loop to a patient on whether or not their current physical signs or symptoms should trigger admission and/or can offer more data to the HCPs to help them make a more informed and ‘real-time’ referral judgement. This map of barriers and the mechanisms by which interventions might address them became the initial logic model and contributed to the development of programme theories focusing on how inappropriate admissions may be facilitated or prevented at the three problem points listed above.
Programme theory development
Five programme theory components were identified following a review of published barriers, consultation with the PPI group and analysis of a rich subset of intervention studies for preventable admissions (Box 1). These are expressed in the form of hypotheses to be tested against the empirical data.
People with chronic conditions are frequently admitted to hospital when hospital is not the optimal destination for them. They may have symptoms that could be self-managed or anxieties that could be addressed by patient education or information.
Programme theory 2People with chronic conditions lack knowledge about alternative health provision and therefore draw disproportionately on well-signposted channels, such as their GP or the emergency department. Alternatively, patients perceive that presentation to an emergency department holds relative advantage (e.g. quality, ease of access, response) over GP-based or other primary or community care services. Patients pressure HCPs to admit them to hospital.
Programme theory 3HCPs lack confidence in their own diagnoses or may lack confidence in, or knowledge of, alternative sources of health-care provision and so may refer people with chronic conditions or admit them directly to hospital. HCPs feel under pressure to admit people with chronic conditions directly to hospital.
Programme theory 4People with chronic conditions use health services inappropriately, delaying their presentation to HCPs or hospital because of perceptions of the service either anticipated or based on the past experience of either themselves or others.
Programme theory 5General practitioners and other HCPs are influenced by the wider context of the health-care system, and the availability or otherwise of support and incentives may influence their adoption of interventions and pathways designed to avoid preventable referrals and admissions to hospital.
GP, general practitioner.
Synthesis
Following identification of the initial programme theories, the review team extracted data into evidence tables. The resultant hypotheses operationalised synthesised statements around which we developed an explanatory narrative referenced to the underpinning evidence base. Additional searches for mid-range theories (conceptual models or frameworks relevant to one or several of the interventions covered by the review) and overarching theories (theories relevant to the phenomenon of inappropriate admissions as a whole) were conducted using Google Scholar (Google Inc., Mountain View, CA, USA). The aim of searching for these higher-level theories was to elucidate how previous researchers have understood factors underlying inappropriate admissions and their prevention at a relatively high level of abstraction. Our EPPI-Reviewer map, reference management database and accompanying data extraction spreadsheets collectively offer a comprehensive evidence base relevant to interventions to reduce unplanned hospital admissions.
Testing and refining the programme theories
Searches for programme theories relevant to avoidable admissions were conducted using Publish or Perish 6™ software. 20 This desk-based tool offers an auditable interface to searching of the Google Scholar resource as well as allowing construction of semicomplex search strategies.
The first set of Google Scholar searches combined the term ‘ambulatory sensitive’ with terms for preventable admissions and different programme theory terms. The second set of searches combined the term ‘preventable admissions’ with ‘hospitalisation or hospitalization’ and different programme theory terms. Full details of the search terms used for each individual search and the number of results retrieved are provided in Appendix 2.
Papers retrieved from the programme theory searches were reviewed by one reviewer with experience of harvesting programme theories. Prioritising conceptually and contextually rich papers, the reviewer drafted preliminary if–then–leading to statements21 [known technically as context–mechanism–outcome (CMO) configurations] for discussion with the review team. The aim of this process was not to generate an exhaustive list of possible explanations but to generate a selection of theories of change operating variously at patient/carer, health provider and health system levels. When several programme theory components seemed to be interrelated, these were combined into a more overarching explanation.
From the papers retrieved from the programme theories searches and from the papers included in the mapping review, we developed five programme theories to guide the realist review. Details of the generic programme theories are given in Box 1. Details of the programme theories expressed as if–then–leading to statements and the probable types of evidence identified by the team by which programme theories might be supported or negated are provided in Table 3. In Chapter 4, the programme theories are considered in the specific context of each of the included interventions.
| Programme theory | Types of evidence |
|---|---|
| PT1: IF patients are equipped with knowledge/information for self-management, including seeking help as appropriate, THEN they will access hospital/health services as required LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions |
|
| PT2: IF patients feel confident and satisfied with non-secondary-care health provision THEN they will not consider it necessary to access/request secondary care services LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions |
|
| PT3: IF GPs/primary care staff feel confident in their own ability to diagnose and/or refer patients appropriately and have confidence in and knowledge of services available within primary and community care THEN they will not refer patients to hospital LEADING TO an increase in use of self-management and non-secondary-care health service provision and a reduction in unplanned admissions |
|
| PT4: IF patients delay/are delayed in accessing health services THEN patients may experience exacerbation of symptoms LEADING TO a higher level of clinical input or resource use when they finally access health care and an increase in unplanned admissions |
|
| PT5: IF clinicians and other health service staff perceive that the wider health system provides appropriate support and incentives THEN they will feel confident in implementing (and evaluating) interventions that involve changes to practice and professional roles LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions |
|
The initial programme theories were tested from the theoretical literature, empirical studies and insights from the PPI group. Programme theories were examined against the nine individual intervention types and collectively as a set. A subsequent activity involved seeking to map the elements of the programme theory to potential mid-range theories that might add greater transferability to review findings. 22 Mid-range theories could be identified serendipitously, when reviewing the empirical evidence, but more typically were identified from Google Scholar searches that combined the intervention (e.g. ‘case management’) with terms relating to models or theories (i.e. ‘theor*’ or ‘model*’ or ‘framework*’ or ‘concept*’). 23
Patient and public involvement
Members of the pre-existing Sheffield HSDR Evidence Synthesis Centre Public Involvement Advisory Group provided input to the study at various stages, including exploration of the study parameters, discussion regarding the meaning and interpretation of the study findings, drafting of the Plain English summary and help with disseminating the findings and maximising the impact of the research. The group comprised nine members, mainly from the Yorkshire and Humber region, with two members from other regions of England. Members were recruited by contacting other existing PPI groups and via a PPI website.
The project was discussed at three meetings of the advisory group. At the first meeting, the researchers introduced the topic and also provided a brief introduction to the concept of a realist review. We then discussed pathways that could potentially lead from a patient perceiving a problem to an avoidable admission or avoidance of admission. Advisory group members gave their perspective on factors that could influence patient behaviour at various stages of the pathway (e.g. ‘Patients lack confidence in their ability to self-monitor and self-manage their condition’ and ‘Patients perceive that they need to be treated in hospital’). This discussion was helpful to the research team in developing programme theories for analysis in the realist synthesis.
Before the second meeting, the researchers ‘translated’ aspects of the programme theories into ‘scenarios’ (see Appendix 3) and discussed these with the advisory group. Group members provided input on both the credibility of the scenarios and the appropriateness of the language used to describe them. Some scenarios were significantly modified as a result and this was reflected in a change in the researchers’ understanding of the corresponding programme theory.
The third advisory group meeting coincided with near-completion of the draft final report. The main findings were presented and the advisory group members discussed the draft plain English summary and channels for disseminating the research and achieving wider impact.
Changes to the protocol
Time and resource constraints meant that we were not able to engage with HCP stakeholders to the extent outlined in the protocol. Because we did not invite HCPs to participate in interviews or focus groups, we did not need to obtain ethics approval as envisaged in the protocol.
Chapter 3 Results of mapping review
Screening of literature search results
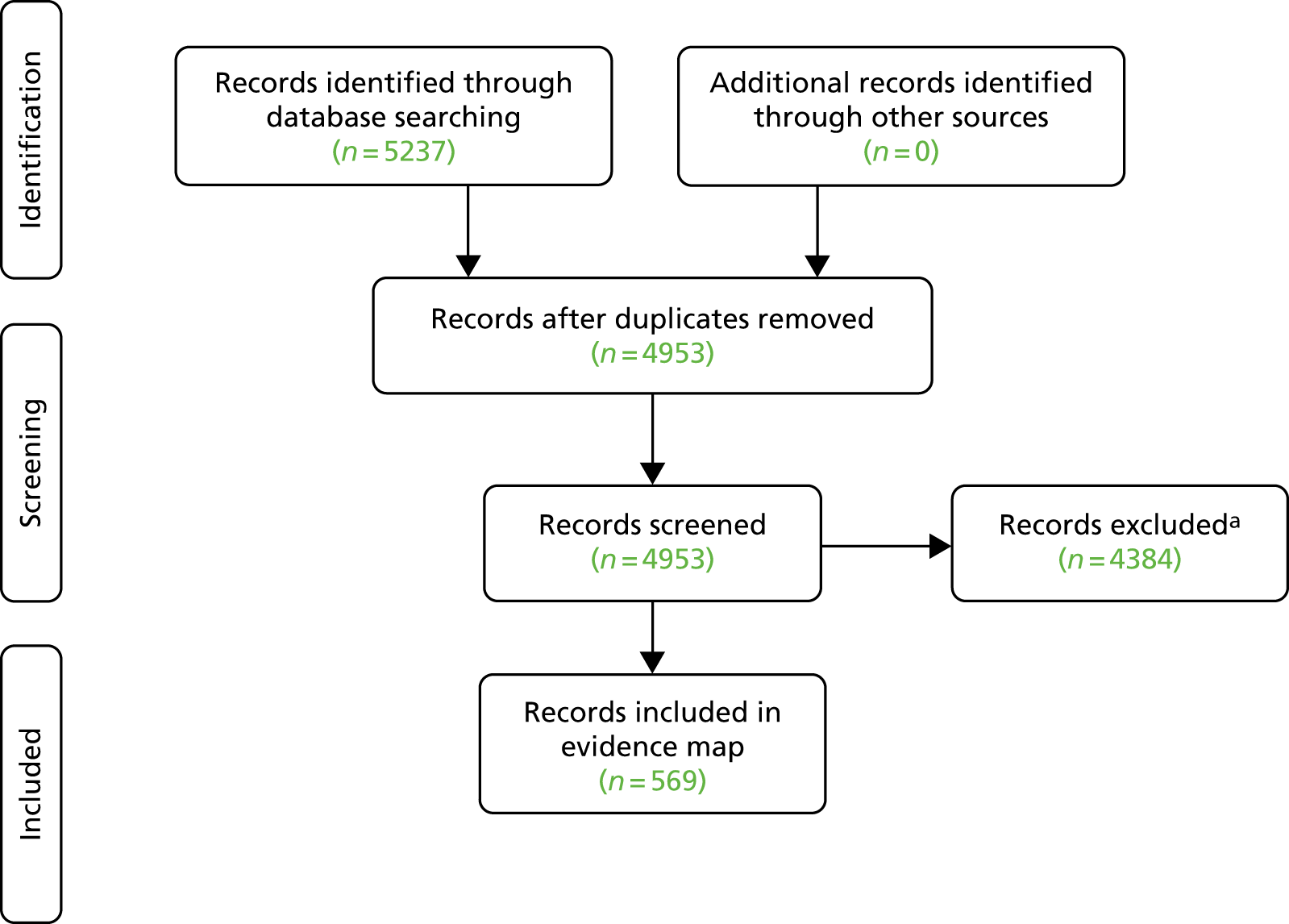
Figure 1 [adapted from the standard Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram] summarises the results of the screening process. A total of 569 publications were judged to meet the inclusion criteria (based on titles and abstracts) and were coded in EPPI-Reviewer 4. The total numbers in the following sections do not always add up 569 because of studies being coded for more than one item within a category or because studies could not be fully coded with the information available in the abstract.
FIGURE 1.
Flow of studies through the mapping review. a, Irrelevant, not country or date range of interest or additional duplicates.
Populations
The most commonly studied conditions were heart failure (238 studies) and COPD (212 studies). Other conditions with significant numbers of studies were asthma (65 studies), hypertension (44 studies) and coronary heart disease (CHD) (25 studies). Thirty-two studies were coded as covering multiple (generally three or more) conditions. Some of these studies included patients with chronic conditions outside the main focus of the mapping review (e.g. diabetes).
Interventions
The largest groups of interventions were those coded as self-management (122 studies) and telehealth (119 studies). Patient education (72 studies) was frequently linked with self-management. Pulmonary rehabilitation (53 studies) was more commonly studied than cardiac rehabilitation (24 studies). A large group of studies (87 studies) evaluated multiple interventions, notably those characterised as transitional care programmes. There were 50 studies of community-based interventions and 37 studies of case management.
Nature/amount of evidence
The numbers of included studies coded by intervention for each condition are listed in Table 4. In general, the frequency of included studies reflected the findings of Purdy et al. 3 Interventions and populations for which Purdy et al. 3 found evidence of positive effects were generally well represented in the map, as illustrated in Table 4. Examples were patient education and telehealth for heart failure (46 and 66 studies, respectively), self-management of asthma (37 studies) and pulmonary rehabilitation for COPD (59 studies). Interventions considered to have evidence of no effect (as distinct from no evidence of effect) were less well represented: we included 15 studies of case management for COPD but only three studies of community interventions for CHD and two studies of specialist asthma clinics.
| Condition | Number of studies per intervention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case management | Specialist clinics | Community interventions | Patient education | Self-management | Cardiac rehabilitation | Pulmonary rehabilitation | Telehealth | Multiple | Other | Unclear | |
| CHD | 2 | 0 | 3 | 2 | 3 | 12 | 0 | 4 | 0 | 0 | 0 |
| Heart failure | 18 | 10 | 16 | 46 | 44 | 12 | 2 | 66 | 37 | 14 | 0 |
| Hypertension | 2 | 3 | 6 | 7 | 13 | 1 | 0 | 11 | 4 | 2 | 0 |
| Asthma | 2 | 2 | 4 | 9 | 37 | 0 | 0 | 3 | 8 | 5 | 0 |
| COPD | 15 | 1 | 24 | 6 | 27 | 2 | 59 | 57 | 36 | 17 | 1 |
| Multiple | 7 | 1 | 4 | 5 | 3 | 1 | 1 | 4 | 9 | 0 | 0 |
| Other cardiovascular | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 2 | 1 | 1 | 0 |
| Other respiratory | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
Evidence by study design
Interventions not rated by Purdy et al. 3 but covered by substantial numbers of studies (≥ 20) in the mapping review included self-management for heart failure (44 studies, although many of these also included patient education) and community interventions (24 studies) and telehealth (57 studies) for COPD.
Literature reviews (including systematic reviews, narrative reviews and some conceptual or discussion papers based on literature reviews) were the most common type of literature included in the mapping review (156 studies), followed by experimental studies [randomised and non-randomised controlled trials (117) and uncontrolled observational studies (115)]. We also identified 47 controlled observational and 61 qualitative studies. As this was a mapping review, the quality of individual studies was not assessed. In the following sections, we briefly describe the composition of the main groups of included studies.
Key systematic reviews included in the mapping review are listed in Table 5. Up-to-date (2016 or 2017) systematic reviews were found for most key combinations of condition and intervention. Several were Cochrane reviews or overviews of reviews, which use standard methods and are likely to be of high quality. Although some reviews focused purely on effectiveness of interventions, other reviews attempted to assess that features were most essential to intervention effectiveness or to identify barriers to and facilitators of implementation. This latter group of reviews was most useful for the realist synthesis.
| Condition | Key reviews |
|---|---|
| CHD |
Cardiac rehabilitation: Anderson et al. (2016),24 Anderson and Taylor (2014),25 Huang et al. (2015)26 and Karmali et al. (2014)27 Telehealth: Huang et al. (2015)26 |
| Heart failure |
Case management: Huntley et al. (2016)28 and Van Spall et al. (2017)29 Specialist clinics: O’Neill et al. (2017)30 and Thomas et al. (2013)31 Community interventions: Coffey et al. (2017),32 Health Quality Ontario (2017)33 and Van Spall et al. (2017)29 Patient education: Casimir et al. (2014)34 and Zarea Gavgani et al. (2015)35 Telehealth: Clarke et al. (2011),36 Gorst et al. (2014),37 Graves et al. (2013),38 Inglis et al. (2015),39 Kitsiou et al. (2015),40 Klersy et al. (2016),41 Kotb et al. (2015),42 Lin et al. (2017),43 Pandor et al. (2013)44 and Vassilev et al. (2015)45 |
| Hypertension | Telehealth: Harrison and Wild (2017)46 |
| Asthma | Self-management: Denford et al. (2014),47 Marcano Belisario et al. (2013),48 Morrison et al. (2014),49 Pinnock et al. (2015),50 Pinnock et al. (2017),51 Ring et al. (2011)52 and Ring et al. (2012)53 |
| COPD |
Case management: Martínez-González et al. (2014)54 Self-management: Baker and Fatoye (2017),55 Clari et al. (2017),56 Harrison et al. (2015),57 Howcroft et al. (2016),58 Jonkman et al. (2016),59 Jordan et al. (2015),60 Lenferink et al. (2017),61 Wang et al. (2017)62 and Zwerink et al. (2014)63 Pulmonary rehabilitation: Alison and McKeough (2014),64 Cox et al. (2017),65 Jones et al. (2017),66 Keating et al. (2011),67 Meshe et al. (2017),68 Moore et al. (2016)69 and Puhan et al. (2016)70 |
Experimental studies generally compared an intervention with ‘usual care’. Usual care was generally not defined at all in the abstracts that we used for coding, making it difficult to compare studies. A few studies compared different interventions, although these tended to be variations of a common intervention (e.g. more vs. less intense or different durations) rather than distinctly different interventions. The distribution of experimental studies across conditions/interventions broadly reflected that of the whole group of included studies.
Controlled observational studies were less frequent in the map than experimental studies were, with no combination of condition/intervention having more than seven such studies. Similar to the experimental studies, the majority of this group compared the intervention with a ‘usual-care’ control group. By contrast, most uncontrolled observational studies (65 studies) used baseline values as a comparator, although 14 such studies also included a ‘usual-care’ group.
Qualitative studies are an important source of evidence for understanding the implementation of interventions in practice, as the views and perceptions of HCPs and patients have a strong influence on if and how interventions work in practice. The 61 qualitative studies included in the map covered the range of relevant populations and interventions, the largest single group being studies of pulmonary rehabilitation for COPD (13 studies). Other populations and interventions were covered by up to seven qualitative studies. Studies using recognised methods of qualitative analysis, such as thematic analysis, were included in this group, although the quality of individual studies was not assessed.
Setting
Most studies were conducted in the USA (207 studies), followed by the UK (103 studies), Canada (46 studies) and Australia (43 studies). Just two studies from New Zealand were included. There were 91 studies, primarily literature reviews, in which the concept of study country was considered to be not applicable, and 59 studies were conducted in multiple countries. Finally, the country was coded as unclear/not reported for 23 studies in which the reviewer’s judgement was that the setting was likely to be one of the countries included in the map. We did not systematically check the full texts of included studies to identify the authors’ country of origin, so it is possible that this group includes a few studies from outside our defined settings of interest.
In terms of how patients accessed the intervention, the largest single group was studies in which the access route was not reported or was judged as unclear (213 studies). The most common identified ways of accessing interventions were via community-based services (134 studies) and at the time of hospital discharge to reduce risk of re-admission (122 studies). General practitioners (GPs) or equivalent primary care doctors were the access route in 45 studies, and other general practice staff were the access route in 22 studies. Less frequent ways of accessing interventions were outpatient appointments (24 studies), emergency departments (15 studies) and paramedic and telephone advice (two studies each). There were no included studies in which access to the intervention was initiated by the patient.
UK evidence
We included 103 studies from the UK. The majority of these focused on a small number of interventions: self-management of COPD (12 studies), pulmonary rehabilitation for COPD (15 studies) and telehealth for COPD (26 studies) and heart failure (15 studies). Almost half of the included UK studies (49 studies) dealt with interventions classified as telehealth, primarily remote monitoring and consultation. This concentration on telehealth probably reflects strong backing for the technology from the Department of Health and Social Care through initiatives such as 3 Million Lives and the Whole System Demonstrator trial. 71 Interventions classed as effective by Purdy et al. 3 but with limited evidence from the UK included cardiac rehabilitation and telehealth for CHD (one study each), case management (one study), specialist clinics (no studies), community interventions (two studies), patient education for heart failure (two studies) and self-management of asthma (six studies).
Outcomes
We mapped two measures of effect on admissions: (1) admissions (or re-admissions) per se, based on aggregated data from trials or routinely collected data, and (2) prevented admissions, based on audit of individual cases; these outcomes were reported in 311 and three studies, respectively. This suggests that in most included studies there was an implicit assumption that admissions were prevented appropriately (i.e. the intervention did not lead to patients not being admitted when admission was the most appropriate course of action) but this was not investigated directly.
Other commonly reported outcomes were patient-reported outcomes such as quality of life (211 studies), health system outcomes such as length of stay or emergency department visits (91 studies), qualitative outcomes (themes identified by qualitative analysis) (85 studies) and costs or cost-effectiveness (73 studies). Other outcomes, including mortality, were reported in 133 studies.
Summary of findings
The mapping review allowed identification and description of a large number of studies relating to interventions to reduce preventable hospital admissions for people with cardiac or respiratory conditions. A limited number of descriptive outcomes are reported here but the features of EPPI-Reviewer allow the data to be analysed in a wide variety of ways. Unsurprisingly, the interventions identified by Purdy et al. 3 as having the best evidence of effectiveness (or no effect) were well represented in the map. The largest group of studies originated from the USA; differences between health-care systems mean that care should be taken in extrapolating the results of such studies to the UK setting. Regarding the included studies from the UK, a similar distribution of studies was shown by intervention and population to that of the map as a whole but there was evidence of some country-specific features, such as the prominence of studies of telehealth. We excluded studies from non-UK European countries based on lack of similarity between most countries’ health systems and the UK NHS. This means that some studies of interventions that could be implemented in the UK were omitted from the mapping review. However, it is unlikely that this would have led to any significant intervention being omitted from the mapping review altogether. Furthermore, studies from European countries were included indirectly via the inclusion of relevant systematic reviews in our mapping review.
Mapping reviews use systematic methods to identify, screen and code studies, but a mapping review is not a systematic review. Mapping reviews generally omit some standard features of systematic reviews, for example study quality assessment, and do not attempt to assess effectiveness. The role of mapping reviews is to provide a descriptive account of the published literature and this should be taken into account when assessing the findings of this part of the overall evidence synthesis.
The studies coded for the mapping review and stored in EPPI-Reviewer 4 represent a broad sampling frame of UK studies for use in the accompanying realist synthesis. In view of the number of studies screened for inclusion and included, we cannot rule out the possibility that some studies were included or excluded in error. Inclusion decisions were taken on the basis of information in the title and abstract only and, in some cases, important information (e.g. the study country) was not available. However, it is unlikely that any errors regarding study inclusion or exclusion would have a major effect on the overall shape of the evidence map.
Chapter 4 Analysis of UK studies
Case management
Summary
Exploration of case management reveals that the role of the specialist nurse is key to its success. The impact of the role is determined by issues relating to responsiveness (as seen in response times) and availability (as seen in the demand for 24-hour access), which themselves can be moderated by the size of the nursing caseload and the competing demands of the administrative workload. A tension may be identified between the intrinsic advantages of continuity of care, as especially evidenced in a knowledge of a patient’s symptoms and the need to provide round-the-clock coverage to patients with more severe manifestations of cardiorespiratory conditions. Case management is therefore seen to require substantive re-engineering of the health system in which it is intended to operate.
Definition
Case management is a generic term, with no single definition, described as the process of planning, co-ordinating and reviewing the care of an individual. The Case Management Society of America provides a definition on its website (www.cmsa.org; accessed 4 April 2019). This definition was operationalised by Purdy et al. 3 in their series of NIHR reviews. The literature reflects confusion between case management as an ongoing process and as an intensive time-limited intervention. 72
Case management within the NHS has been largely configured as community-based programmes, set up and funded by primary care trusts and typically (but not always) staffed by community matrons. 72 In recent years, UK initiatives have focused on multidisciplinary team (MDT)-led case management but have demonstrated little or no reduction in use of secondary care. 73 Increasingly, attention has focused on the ‘added value’ of benefits for patients and professionals. 74 Interest in case management has been revived by the new models of care initiatives, with their focus being on integrated care.
Intervention components
Rather than comprising a single intervention, case management typically describes a package of care that covers activities that vary widely between programmes; it is described as a ‘prototypical example of a complex intervention’. 75 Such variation makes case management both difficult to describe and challenging to evaluate. TIDieR-Lite components of self-management interventions are summarised in Table 6.
| Question | Characteristics |
|---|---|
| By whom? | Health-care professionals, typically specialist nurses with medical support |
| What? |
|
| Where? | May be delivered face to face in a patient’s home or in a clinic setting or via the telephone |
| To what intensity? | Frequency and duration of contacts varies according to need |
| How often? | At intervals determined by case manager; may also be patient initiated |
Several commentators72,76,77 identify the following core components as particularly important to case management programmes:
-
case-finding
-
assessment
-
care planning
-
care co-ordination (usually undertaken by a case manager within the context of a MDT), including but not limited to –
-
medication management
-
self-care support
-
advocacy and negotiation
-
psychosocial support
-
monitoring and review
-
case closure (in time-limited interventions).
-
Case management can include components such as self-management, patient education and disease management programmes,72 making it more challenging to distinguish this intervention from others reviewed in this report. Case management may be delivered in diverse ways that vary according to intensity (frequency and duration of the contacts), degree of embeddedness in the local care network, the background and training of case managers and the extent to which they work alone or within a team. Further variation is exhibited in whether or not the case manager is supported through reflexive group meetings with peers or supervisors, how the target population is identified and how the case management intervention is initiated.
Number and type of UK studies identified
The effectiveness review by Purdy1 drew on only one UK study of case management. 78 This randomised controlled trial (RCT) in a COPD population in West London found no difference between case management and usual care in terms of numbers of hospital admissions. Indeed, the primary impact of the intervention seemed to be a reduced need for unscheduled primary care consultations. For every one COPD patient receiving the intervention and self-management advice, there were 1.79 fewer unscheduled GP contacts. 78
The mapping review identified two further quantitative UK studies (three papers) of case management for cardiovascular or respiratory conditions published since 2010. One study examined a COPD population in a single general practice79 and the other study73,80 presented data on 20 ACSCs. The six conditions of relevance to this review were asthma, atrial fibrillation, CHD, COPD, heart failure and hypertension.
Three UK qualitative studies were identified (four papers/reports). One of these studies examined patients with heart failure and staff involved in their care81 and the other two initiatives targeted case management in ‘high-risk’ populations including conditions eligible for this review.
Details of the studies included in the analysis are presented in Appendix 4, Table 25.
Operating programme theories
Programme theory 2 proposes that IF patients feel confident and satisfied with non-secondary care health provision THEN they will not consider it necessary to access/request secondary care services LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions. Case management affects a patient’s perceived capability of staying in their own home. 82 Crisis situations can be anticipated, if not averted; this is particularly important in the context of exacerbations as, for example, with COPD.
However, because of its personalised, tailored nature and the involvement of multiple health and social care professionals, case management may be considered overly intrusive. 82 Others patients report that the case manager was perceived as an impediment to accessing their GP. 83 Furthermore, if a patient feels supported, they are less likely to feel a need to access sources of support from secondary care. One patient with respiratory problems74 reported past and probable future occasions when her needs might be best met in hospital. This patient perceived the hospital as a means for meeting not just her medical needs but also her holistic needs, making her feel safer and therefore less anxious. Other participants described their ‘confidence’ in local hospitals should circumstances arise in which they feel that some of their needs may be better met in hospital.
Case management also engages with PT3: IF primary care staff (in this case the case manager) feel confident in their own ability to refer patients appropriately and have confidence in and knowledge of services available within primary and community care THEN they will not refer patients to hospital LEADING TO an increase in use of self-management and non-secondary care health service provision and a reduction in unplanned admissions. In this context, the detailed knowledge of a patient’s condition and circumstances and the holistic perspective of their care enables the case manager to calibrate and negotiate appropriate thresholds for secondary care intervention. Previously, the Evercare evaluation found that, as advanced primary nurses’ knowledge of available services increased over time, they referred their patients to an increasing range of resources for support. 84 Gowing et al. 74 report that some patients may be content to trust the case manager’s judgement, but others may resolutely insist that hospital is the best place for them. A major issue was the lack of adequate social care support, although isolated instances of providing overnight care following hospital discharge were reported. 74
An important contextual variable is the need for adequate training to strengthen the case managers’ self-efficacy and confidence in the appropriateness of their situational assessments. 82 This confirms that, as case managers become more experienced, GPs are likely to spend less time liaising with other services and case managers are able to provide more patient care themselves. 85 One potential unintended consequence of case management is increased levels of case finding resulting in a non-reduction in hospital admissions. 85
Detailed knowledge of a patient’s condition and circumstances (embracing both clinical and social contextual factors) also mitigates operation of action according to PT4, that is the patient does not perceive a need to delay presentation to secondary care services; they feel empowered to elicit information from their case manager as and when required. The triad of case manager, patient and informal carer only perceives a need to escalate action when the personalised threshold has been exceeded. A key contextual factor here relates to case manager caseload: if a case manager holds responsibility for an excessive number of cases then they will be unable to determine appropriate personalised thresholds and will either admit a patient unnecessarily or cause/contribute to delays in seeking treatment. Delays in accessing services have been shown to lead to deterioration in patients’ health and are a probable cause of future hospital admission. Lack of available community-based services constitutes a major challenge to effective case management. 84,86
Description of putative mechanisms
Possible mechanisms for case management are summarised in Box 2. In theory, case management seeks to increase efficiency by reducing unnecessary contacts with the health system. 87 Such contacts include fragmented routine contacts, as well as emergency contacts caused by potentially preventable exacerbations. The goal of case management is ‘to better co-ordinate care, offering individually-tailored contacts and care planning’. 87
-
Accurate case finding; identification of top 2% of at-risk patients on at-risk register.
-
Single point of assessment.
-
[May use MDT to case manage.]
-
Joint care planning.
-
Care co-ordination.
-
Contact between case manager and patient/caregiver.
-
Regular monitoring.
-
Knowledge of referral options.
-
Incentives.
-
‘Green tape’: clear guidelines and algorithms relating to resource allocation by patients.
-
[Self-management.]
-
Knowledge and motivation of health and social care staff.
-
Clarity of role.
-
Access to training.
-
Optimised caseload levels (may not be achieved).
-
Regular and longer contact/visits.
-
Organisational structure of the programme.
-
Financial and regulatory framework.
-
Available physical and human resources.
-
Information systems to support communication.
-
Accountability of individual or team to patient (named case manager).
-
Confidence in ability to determine appropriate personalised thresholds.
-
Identification of barriers to patient remaining at home and primary, community and social care resources required to address these barriers.
-
Reduced fragmentation among services.
-
Confidence in personalised thresholds.
-
Belief in capability for self-care and remaining at home.
-
Prompt and open communication to health-care professionals of exacerbations or barriers to self-care.
-
Acceptance of care and services offered.
-
Self-efficacy (health-care professional).
-
Self-efficacy (patient/informal caregiver).
-
Increased case finding.
-
Changes to medication (to avoid adverse effects) in conjunction with GPs.
-
Case management seen as another add-on service competing for NHS resources.
-
Patients reluctant to be discharged from case management.
-
Improved functional status.
-
Improved quality of life.
Green font denotes outcomes that could be detrimental in the context of reducing inappropriate hospital admissions.
The case management model is predicated on the presence of so-called ‘super utilisers’: ‘high-risk’, high-need patients, typically with multiple health conditions, who utilise a disproportionate amount of health-care resource (with a high cost). 88 The idea behind case management is that by targeting additional and individually tailored primary care at these patients, more costly secondary care admissions (particularly emergency admissions) can be avoided. 89
However, research suggests that case management does not meet its primary aims for the patients involved, although it is associated with increased patient satisfaction. 87,90 In practice, MDT case management tends to target those identified as ‘high risk’ using a selected statistical algorithm that is validated to predict patients who are likely to have substantial future health-care use. 80 These tools generate a heterogeneous group of patients, and it may be that there are subgroups for which the direct effects of the intervention are more effective. However, as papers by Stokes et al. 73,80 reveal, it can be extremely challenging to identify so-called ‘super utilisers’ both in terms of the ‘safe’ margin of those who can be appropriately managed in primary care and, equally, in terms of those for whom the complexity of their comorbidities renders secondary care an appropriate option.
Systematic review evidence identifies continuity of care as an important influence on admissions for long-term conditions. 91 Commentators seek to distinguish continuity of relationship (a continuous caring relationship with clinicians) from continuity of management (all aspects of integration, co-ordination and sharing of information). Both mechanisms can be considered important in the context of preventable admissions. A patient must feel that they can trust the judgement of the HCP and that the HCP has a sufficient understanding of their unique personal circumstances. Practically, continuity of management is important in the context of 24-hour care and delivery of services across organisational and professional boundaries.
Case management is centred on the premise that targeted, proactive, community-based care is more cost-effective than downstream acute care. Delivering such care requires that an intervention is integrated across care providers to avoid overlap and to ensure that each care provider knows and realises what each other care provider does. Wagner et al. ’s92 chronic care model (CCM) has been proposed as a framework to restructure the health system towards integrated, proactive, consistent and continuous care, and, thus, anticipate acute exacerbations or lessen their consequences. 93 The CCM draws on six interacting elements: links with the community, the health system, self-management support, tailored delivery system design, help for decision support and adequate clinical information systems. 94 Case management for people with complex care needs offers a potential strategy for delivering this type of integrated care.
Time-limited case management targets those with the greatest risk of emergency admission. A stepped approach means that people at lower risk of admission can be targeted with disease management programmes or supported in self-management. Case management shares the patient orientation of self-management75 (see Self-management). Indeed, patients in the study by Gowing et al. 74 reported being able to take a more active role in their own planning and care, thereby promoting independence. However, independence appears context dependent: a respiratory patient in the same study described being given a rescue pack for COPD and struggling with her own judgement about when to use it. 74
Previous evaluations report that policy-makers assumed that case management would stimulate ‘service redesign beyond the introduction of case management itself’. 85 However, evidence of wider local re-engineering of primary and secondary care for older people has proved challenging to establish.
Conceptually, case management can be understood in the context of integrated care. The six dimensions of services integration suggested by the National Collaboration for Integrated Care and Support (2013)95 are:
-
consideration of patient and family needs
-
communication with the patient and between HCPs
-
access to information
-
involvement in decision-making
-
care planning
-
transitions between various HCPs.
Roland et al. 96 advance possible explanations as to why using case management to improve care integration is not guaranteed to improve outcomes. The first is a potentially faulty underlying programme theory (i.e. because supply-induced demand increases appropriate admissions and does not simply decrease inappropriate admissions). Alternatively, the implementation of case management interventions may be wanting – an explanation on which Goodwin97 and Ling et al. 98 draw to explain suboptimal achievement of effects.
Efforts to strengthen coping capability are closely linked to the self-efficacy theories propounded by Bandura99 (see Self-management).
Contextual factors
In common with other complex interventions, case management studies generally lack contextual detail. As a complex intervention, case management includes various components interacting in a non-linear way to produce outcomes that are highly dependent on context and variables across settings. Attention should focus on analysing not only if and how case management works for frequent users of health-care services, but also in what contexts it works.
Role of patient preference
Several studies reveal that patients are generally satisfied with individual case manager-led case management approaches. 87,100,101 Patients particularly appreciate increased contact with HCPs and greater proactive input85,102 and reassurance that care was being co-ordinated. 102 In their qualitative study of the Northumberland High-Risk Patient Programme (NHRPP), Gowing et al. 74 recorded that patients were generally unaware of the exact composition of the programme but, nevertheless, observed such individual features as a named GP, regular review and the occurrence of MDT meetings.
Sheaff et al. 85 report that patients and carers valued case management for improving access to health care, increasing psychosocial support and improving communication with HCPs. They also report that ‘patients were often anxious that no-one should “take their nurse away” and were often reluctant to be discharged from case management’. 85
Role of culture
This section refers primarily to organisational culture within the health-care system. See also the following section, Role of leadership.
In most cases, case management requires significant cultural change. 1 In fact, much of the relative lack of attributed success relates to the inability of case management approaches to stimulate the radical scale of change required to realise its full benefits. Ross et al. 72 observed that case management is most effective as part of a wider programme of care in which various strategies are used to integrate care. These include good access to primary care, support for health promotion and primary prevention, and co-ordinated community-based packages for rehabilitation and reablement. 72 Where these features are not present, case management may not demonstrate effects on emergency admissions. 84 In their thematic analysis of key factors of case management interventions, Hudon et al. 103 highlight how the scale of innovation must be achieved across multiple levels, including in organisational culture.
Role of leadership
Leadership and culture are closely linked, so this section should be considered in conjunction with the previous one.
Good leadership skills are required to secure the support of other members of the MDT for the case management model. In their thematic analysis, Hudon et al. 103 highlight how leadership effectiveness is a key factor of case management interventions.
Role of evaluation/measurement
Many individuals undergo repeated monitoring and review as well as further assessment and care planning until they are fit to exit the case management system (note previous discussion about time-limited vs. ongoing definitions of case management; see Definition). 72 A well-written care plan enables case managers to monitor and review whether or not an individual is receiving an appropriate package of care. Frequency of monitoring will depend on the individual’s level of need:84 daily, weekly or monthly, and directly, in the individual’s home and/or through remote monitoring (e.g. by telephone or through telemonitoring of blood pressure or other vital signs). Such monitoring can be undertaken by a MDT.
Care plans must be constantly reviewed and changed when necessary. The NHRPP incorporated a key area of monitoring: patients were to be followed up promptly within 3 days of discharge from hospital. It should be recognised that telephone contacts are likely to be under-reported because of the burden of recording. 104
Role and characteristics of facilitation
The case manager typically operates within a MDT. It is vital that those in the team, and beyond, are engaged in the programme. Primary care professionals and social care staff generally welcome the role of case managers once they have a better understanding of what they do. 105 They particularly appreciated the role of the case manager in:
-
regular monitoring of patients
-
making diagnoses and changes to medication regimens
-
addressing patients’ social isolation by spending time with them
-
co-ordinating the overall care process
-
providing a link between primary, secondary and social care.
Case managers need to work proactively with diverse health and social care professionals, requiring good working relationships and effective communication. 106
Qualitative research supports personal aspects of the case manager role; community matrons were typically perceived as ‘friends’ in the case manager role. 83 This finding corresponds to data from corresponding roles in which empathy and compassion are regarded as important attributes.
Case management facilitates access to support and care as and when required. The patient, and their informal caregiver if present, feels able to call for adequate and appropriate help. 82 There is evidence of case managers (specifically community matrons) conducting low-skill roles initially, but with the aim of these being delegated to other professionals in time or absorbed within self-care. 83 If, on the other hand, a patient feels uncertain about their capability to remain at home, notwithstanding the information with which they have been provided, they feel empowered to access relevant secondary care-based help. Initially, the case manager occupies a role as a facilitator and gatekeeper to accessing appropriate help. Over time, however, the patient and informal caregiver feel increasingly able to assess when a personalised threshold for accessing secondary care services has been crossed.
Role/skills of implementation facilitators
Care planning includes many components and may cross multiple settings rather than be episode based. Fragmentation of care remains a persistent threat given the need to co-ordinate care plans for patients with complex chronic health conditions across multiple care contexts and professional groups. Given the frequent lack of consensus among professionals, relatives, carers and clients about the proposed care plan, good negotiation and communication skills are essential.
In addition to the pivotal role of the case manager, the care plan is typically seen as an essential component of the case management process. The initial assessment is translated into the development of a care plan and then facilitated and co-ordinated by the case manager. Published studies, although agreeing on the importance of this component, typically lack detail on how this process should be undertaken.
Case management as an intervention may display considerable variation in the intensity with which it is delivered. Resource provision and the expertise of the case managers in their facilitation role are important contextual variables that may have an impact on the success of the intervention. Further important variables include the balance of the case managers’ time between co-ordinating health and community-based services and interacting directly with the patient, the time spent on administrative tasks as opposed to direct work with patients, caseload size and role conflicts associated with combining the case management role with other clinical responsibilities.
Crucial to the effective implementation of case management is case manager control over the form and content of the services provided. Does the case manager exert some control over the supply or availability of services or other resources? Alternatively, are resources allocated on a team basis or is the success of the intervention dependent on referrals to other services? This latter ‘brokerage model’ has been considered insufficient on its own to exert the requisite influence to achieve effectiveness. However, even case management programmes with relatively more budgetary control may achieve only limited success when delivered within a wider resource-constrained environment. 107
Supporting evidence
This is a brief summary of evidence from systematic reviews, concentrating on hospital (re)-admission as the outcome of interest. Key results from UK studies included in this analysis are also presented.
Case management is an area that is rich in systematic reviews and evidence syntheses. Small numbers of systematic reviews briefly addressed enabling factors of successful case management interventions in the discussion sections of their papers. In a review of the effectiveness of case management among frequent emergency department users, Kumar and Klein108 noted that ‘frequency of follow-up, availability of psychosocial services, assistance with financial issues and active engagement of the case manager and the patient were important characteristics of CM [case management] interventions’.
Huntley et al. 109 conducted a systematic review to identify observational studies conducted at a practice level that describe factors and interventions that have an impact on levels of utilisation of unscheduled secondary care. Their review was limited by the challenges of trying to review across different health systems in different contexts. They found a benefit from seeing the same HCP, thus informing debates about continuity of care. Proximity to health-care provision was another major factor. However, they found it difficult to determine factors affecting quality of care.
Huntley et al. 109 subsequently conducted a systematic review and meta-analysis of case management interventions for heart failure. They included case management within a hospital context and also studies targeting nursing homes and long-term care settings. None of their included UK studies therefore met our tighter inclusion criteria. They identified four studies of community-initiated case management versus usual care (two RCTs and two non-RCTs), with only the two non--RCTs showing a reduction in admissions. 109
Stokes et al. 87 conducted a meta-analytic review of 36 studies. Meta-analyses showed no significant differences in total cost, mortality or utilisation of primary or secondary care. They found small yet significant effects for case management in terms of self-reported health status and patient satisfaction. Interestingly, their secondary analyses indicated that ‘the effectiveness of case management may be increased when delivered by a MDT, when a social worker was involved, and when delivered in a setting rated as low in initial “strength” of primary care’. 87
In an effectiveness review that included 10 studies, none from the UK, Joo and Liu110 reported that three studies documented statistically significant reductions in hospital re-admissions. Two of these statistically significant studies fell within our 2010–18 time period. Melton et al. 111 report that participants with multiple chronic illnesses in a nurse-led case management intervention group demonstrated lower 30-day and 60-day hospital re-admission rates than participants in the control group (p < 0.05 vs. p = 0.01, respectively). Chow and Wong112 similarly report that a nurse-led case management focused on older adults with chronic illnesses in China demonstrated a significant reduction in hospital re-admission rates in the intervention group compared with the control group (p = 0.018). 112 The characteristics of these interventions indicate potential overlap in this review with the intervention labelled ‘specialist clinics’, with such clinics typically being nurse led.
Joo and Liu113 conducted a qualitative evidence synthesis, using thematic synthesis, to review 10 qualitative studies published between 2007 and 2016 for attitudes of individuals with chronic illnesses and their caregivers towards case management. Access to health-care resources, health status supports and emotional aid were identified as facilitators of case management. Low information about case management and time constraints were identified as barriers. A complementary synthesis by Joo and Huber114 looked at barriers perceived by case managers when implementing case management. This thematic synthesis of 10 qualitative studies (2007–16) identified five barriers to implementation: unclear scope of practice, diverse and complex case management activities, insufficient training, poor collaboration with other HCPs and client relationship challenges.
In summary, there is little recent evidence to suggest that case management is effective across multiple diverse contexts. The UK research is limited in both quantity and rigour and suggests that such interventions are very context specific, with the surrounding environment playing a major role in the effect of the case management intervention. The intervention is well liked by patients and, generally, by staff, although concerns persist about caseload and the ability to deliver care in a timely and accessible manner. Economic evaluations are relatively rare and it would seem that the performance of case management depends very much on how wide the evaluation framework is cast in terms of both costs and benefits.
Potential enhancements of intervention/implementation
Commentators on case management consistently point out that, although the case manager role is pivotal, ultimately, success is determined by the support available to back up the initial management. This depends not only on available primary care resources but also on further social care involvement. 74 A further consideration is the availability of a case manager. Optimally, 24-hour access to case management74 can combat the uncertainties that arise when the patient is unable to contact necessary advice and assistance. Below this very intensive level of provision, uncertainties about whether or not help is available and what to do when it is unavailable serve to subvert the very mechanisms by which case management achieves its success. Complementing availability concerns are anxieties about responsiveness. Issues relating to the overall caseload of the case manager, the level of dependency of patients within that caseload and the amount of time shared with other duties, for example administrative responsibilities, are critical to a timely response. So, specifically in connection with community matrons in a case manager role, Brown et al. 83 reported concern at the ability of community matrons to be able to respond within the patient’s perceived time scale.
Although opportunities to co-create care plans with members of the primary care team are generally welcomed by patients and family members,74 this requires sufficient time to prepare for care planning and to discuss those plans. It is therefore essential to make this planning process feel meaningful to the patient. Some patients felt that by articulating their views and voicing concerns on behalf of other patients they could advocate for those who felt unable to take an active role.
Case management is a complex activity that operates over multiple care settings. Some commentators suggest that greater integration of information technology (IT) systems, including shared electronic medical records and access to resource directories and clinical guidelines, could lead to improved patient outcomes (e.g. Lynch et al. 115). However, this may be an artefact of earlier evaluations and may now be offset, to a substantive degree, by technological developments in electronic health records, care plans and remote servers accessed through user authentication and secured, encrypted transmissions.
Previous evaluations emphasise the need for care pathways to be interpreted flexibly because patients do not fit into standard care pathway approaches. At a practical level, this meant that strict eligibility criteria and inefficient administrative procedures often led to delays in service delivery. 84 Another reason for system failure was that nurses did not always have adequate access to alternatives to admission.
In a novel attempt to bring external theory to bear on the case management phenomenon, Swanson and Weissert116 explore the principal agent framework and street-level bureaucratic theory. 116 They conclude that incentives, as well as ‘green tape’, clear rules, guidelines and algorithms relating to resource allocation among patients, would have an impact on the greater effectiveness of case management.
Evaluations have found little evidence of the systematic redesign of care aspired to by many case management programmes. The Evercare evaluation observed that ‘poor integration between primary and secondary care, and out of hours services were not focused on keeping patients out of hospital’. 84 It concluded that more radical system redesign is needed to achieve a greater impact on admissions. Such radical system redesign has not generally been achieved, notwithstanding the potential offered by new models of care initiatives. 11,117
Patient education
Summary
Patient education is seen as a key component to several interventions designed to reduce preventable admissions and, given demands on GP time, the role of the nurse is seen as critical to the delivery of such information. Three particular factors can be seen to mediate the success of patient education-based interventions (1) patient education is delivered in anticipation of exacerbations or other health incidents and so patients may not see the direct relevance of the information at the time provided or may forget it completely, (2) patient education needs to be situated within the relative experience of individual patients (e.g. ‘if your exacerbation is worse than the last one then . . .’) rather than in some impersonal absolute for all patients and (3) for many patients, self-efficacy, rather than education retention, is the issue. Many patients experience anxiety about their own ability to manage a situation and to make a correct decision. Unless this anxiety is alleviated, they will always seek a second opinion for reassurance.
Definition
A minimal definition of patient education is the teaching or training of patients concerning their own health needs. In their report, Purdy et al. 3 distinguish traditional patient education, which offers information and technical skills, from self-management education, which teaches problem-solving skills. From this perspective, self-management education complements traditional patient education in supporting patients to live the best-possible quality of life with their chronic condition. 118 Nevertheless, such a distinction is not implemented consistently throughout the literature, making the co-existence of patient education and self-management as separate intervention categories in this report particularly problematic. Self-management of multiple chronic illnesses, educating patients to monitor their own health and being able to recognise illness severity feature in current health-care policy. The boundary between providing patient information and delivering patient education may also be difficult to perceive.
Controversy in the literature surrounds whether or not adult education is an appropriate model for patient education, particularly given that patients’ health needs are contingent to particular time periods or stages in a disease or treatment pathway. The above definition conveys formality, contrasting with the ‘teachable moment’, the idea that a HCP may harness any opportunity during their therapeutic encounter to impart some education that meets a patient’s health needs. 119 Key to this process is recognition of what health needs are; a patient may not know what they need to know while a HCP may not be able to time their education intervention to a point when a patient is most attentive, receptive or responsive to a particular message.
Kongstvedt120 defines patient education as a process that involves imparting information to patients that will alter their health behaviours or improve their health. This concept of behavioural change, very visible in the literature of the ‘teachable moment‘, is fundamental to contemporary views of patient education.
The National Institute for Health and Care Excellence (NICE) guidelines for heart failure121 recommend that people with chronic heart failure should be offered:
personalised information, education, support and opportunities for discussion throughout their care to help them understand their condition . . .
The reference to ‘personalised information’ is particularly significant in this context; patients need to be able to situate the information that they have received within their own context of symptoms and disease progression.
Key challenges for patient education as an intervention relate to the fact that patient education is often an adjunct to other interventions that might be used to manage preventable admissions (e.g. cardiac rehabilitation, self-management and telehealth) and so it may be challenging to separate patient education as a discrete intervention/intervention component. The Cochrane review on patient education in the management of CHD122 does attempt to separate the educational component from other aspects of cardiac rehabilitation. Furthermore, patient education may constitute an ongoing iterative process that takes place over frequent patient–clinician interactions and therefore may be difficult to quantify.
Intervention components
The key components of patient education interventions as reflected by UK studies identified for the mapping review are summarised in Table 7. As mentioned previously, a key challenge relates to how to operationalise the concept of patient education. Within a research context, the Cochrane review definition122 requires the presence of all four of the following elements: (1) instructional activities organised in a systematic way, (2) an inpatient, outpatient or community setting, (3) structured knowledge transfer about CHD for secondary prevention and (4) face to face (group or one to one) or interactive delivery.
| Question | Characteristics |
|---|---|
| By whom? | By a HCP to a patient with or without the patient’s significant others |
| What? | Instructional activities organised in a systematic way, involving personal direct contact including structured knowledge transfer about condition, causes, treatments or methods of secondary prevention |
| Where? | Delivered as an inpatient or as an outpatient in a community-based intervention setting or programme in a face-to-face format, in groups or on a one-to-one basis. May also include alternative delivery, such as ‘telehealth’ |
| To what intensity? | Intensity varies |
| How often? | Frequency varies |
Number and type of UK studies identified
The mapping review identified three UK quantitative studies of patient education for cardiovascular or respiratory conditions. One study examined patients admitted with acute asthma,123 a further study explored COPD patients with breathlessness124 and the remaining study examined multiple conditions including the cardiac and respiratory conditions,125 which are the focus of this report.
Five UK qualitative papers were identified. Four of these papers reported findings from the HoldFAST study,126–129 and some of those identified were not from the mapping review but from supplementary follow-up of citations and references. The HoldFAST study was a multicentre study co-ordinated across the University of Bristol, the University of Oxford and Keele University and funded by NIHR. It aimed to explore the experiences of patients with heart failure from ‘multiple standpoints using ethnographic methods, combining observations, interviews and documentary data sources’. 128 It therefore offers a rich source of data on the experience of heart failure patients and particularly their experience of interventions that were commonly encountered in their ongoing care (e.g. patient education and specialist nurses). The remaining study130 examined the experience of patients who have encountered an exacerbation of COPD, particularly in relation to fear and anxiety.
Details of the studies included in the analysis are presented in Appendix 4, Table 26.
Operating programme theories
Programme theory 1 is ‘People with chronic conditions are frequently admitted to hospital when hospital is not the optimal destination for them. They may have symptoms that could be self-managed or anxieties that could be addressed by patient education or information.’. However, patients not only lack information about heart failure and self-care but, most importantly within this context, they also lack knowledge on when to seek help. 128 Patients may often, but not always, comprehend the information that they have been provided, particularly if it is given in a standardised format. However, what they may typically lack is situational knowledge (i.e. how to relate the information they have previously been given to the signs and symptoms that they are experiencing). Patients may feel confident about self-management of their medication in general, and yet not feel confident about their actions in an ‘emergency’ situation.
Access to written or verbal advice from a HCP, delivered remotely via technology and without presenting for face-to-face consultation or admission, may offer one route by which to address patient symptoms and concerns. However, there is increasing recognition that such information is effective only if the patient is receptive and the information is received at the time of need. If such information is not available, or if the patient perceives that it is not readily accessible, they may resort to easier channels of access, such as a telephone call to their GP. There is substantial evidence to indicate that human sources of information are considered more accessible than other information sources in most contexts. Increased facility to look up information, for example on the internet, may change perceptions about accessibility, particularly out of hours, but this raises associated questions about whether or not such information is authoritative and credible and concerns that such information is not typically tailored to the context-specific needs of the individual patient. Glogowska et al. 127 documents how education messages were not always received and acted on by patients, which could lead to unplanned admissions.
Patients may find it particularly challenging to assess whether or not they have reached a legitimate trigger point when first experiencing symptoms (e.g. coughing in relation to COPD131), when symptoms are of a severity not previously encountered or when symptoms include a new and unfamiliar feature. Patients may therefore delay seeking help [‘I’ll just wait to see if the symptoms get better (or worse) before seeking further help’] or they may respond to the novelty or unfamiliarity of the symptoms (‘I’ve not had one of these before, it must be bad’). Being unable to normalise their symptoms against their own experience, patients may need to normalise what they are encountering against the experience of others, either as encountered through self-help groups or secondhand via their nurse or doctor.
People with chronic conditions could lack knowledge about alternative health provision and therefore draw disproportionately on well-signposted channels, such as their GP or the emergency department (PT2). Similar concerns relate to information required for directional purposes, as opposed to information required to manage a clinical problem. Directory-type information may not be easily accessed or navigated and may not be maintained and kept up to date. If the credibility of such a source is damaged, albeit in a minor way, a patient may find themselves pursuing channels that are more likely to yield a successful response.
When patients have a good relationship with their GP, they may perceive that they are more accessible at an appointment or a home visit. 132 Other patients may feel guilty if they have to call the GP. As a consequence, they may leave the decision to the agency of another: a carer or family member. 132 Having missed the initial window for timely non-hospital intervention, they may find themselves at a point at which they are too late to avoid hospital admission.
If patients do not have written or verbal information on when to telephone for an ambulance, they may be less likely to use emergency services appropriately. One possible approach is to include such information in a written self-management plan. 132 Both primary and secondary care physicians in the HoldFAST study acknowledged that they were unsure about what services were available or that there were few services on which they could call. 129
People with chronic conditions may also use health services inappropriately, delaying their presentation to a GP or hospital (PT4) because of perceptions of the service either anticipated or based on the past experience of either themselves or others. Some patients may also feel a reluctance to seek medical advice if they perceive that their previous actions may have contributed to their condition (as in the case of smoking and COPD131).
Description of putative mechanisms
Possible mechanisms for patient education are summarised in Box 3. As noted by Fry et al. ,126 Bury133 describes the effects of chronic illness as ‘biographical disruption’ to everyday life. Disruption extends beyond the patients themselves to have an impact on their families and wider social network. In response, patients and their families may look for information, support and the most effective strategies to manage their symptoms, hoping to minimise potential future disruption.
-
Instructional activities organised in a systematic way.
-
Personal direct contact.
-
Structured knowledge transfer (e.g. condition, causes, treatments or methods of secondary prevention).
-
HCP knows patient’s personal circumstances, including comorbidities.
-
Relaxed environment in which the patient has ‘control’.
-
Patients whose first language is not English.
-
Patients who are too ill to benefit from education.
-
Patients who are in denial about their condition.
-
Patients attributing their condition to growing older.
-
Patients with learning difficulties.
-
Patients experiencing cognitive decline.
-
Patients living with addictions.
-
Good communication.
-
Tailoring of knowledge transfer to capacity and needs.
-
Sufficient time to allow tailored explanations.
-
Good communication.
-
Good situational knowledge of their condition and appropriate responses to exacerbations.
-
Challenging of ‘sick role’.
-
Increased self-sufficiency.
-
Decreased utilisation of health services.
-
Development of ‘expert patient role’.
-
Possible development of a resource for similar patients.
Green font denotes factors that could be detrimental to reducing admissions by patient education.
Symptom unpredictability reportedly leaves patients feeling helpless and completely dependent on those around them. This, in turn, can lead to a lack of control of the illness and an increased burden on families and the health-care system (Morris et al. 134). Implications for carers are that responsibility for care may shift from the patient to their spouse or immediate family. Commentators suggest that these factors may precipitate a patient to adopt the ‘sick role’, relying on their family for support with both their illness and previous responsibilities. 135
Contextual factors
The HoldFAST study found that, notwithstanding almost universal recognition of the importance of providing education to patients to help them manage their condition among secondary care physicians (specialists) and GPs, both secondary care physicians and GPs found that time pressures during consultations restricted their contribution to patient education.
Participants acknowledged that not all patients would take up the education offered. Patients who find the information difficult to assimilate would find self-management difficult. These patients were more likely to be those for whom English was not their first language, those too ill to benefit from education or in denial about their condition, people with learning disabilities and those experiencing cognitive decline or living with addictions. The specialist heart failure nurses felt that it was necessary to adapt the education they offered patients to the individual’s ability to receive it. They tried to identify issues of importance to patients as a way of personalising the information. The nurses stressed that even when patients were able to understand information, it would still be necessary to repeat those messages regularly. 126
Role of patient preference
All respondents in a HoldFAST study expressed positive views about the role within patient education of specialist heart failure nurses. 126 Specialist nurses were perceived to have more time to dedicate to patients. Their role in explaining the illness and providing support was greatly appreciated by the respondents. This additional time allowed for greater patient education on how to identify symptoms that could indicate a worsening of their illness.
The GPs expressed the view that their personal patients would be likely to receive a different response than if someone else, lacking a knowledge of individual patients’ values and clinical circumstances, handled their care. Continuity of care is, by implication, associated with appropriate targeting of health-care facilities and resources. 129 Other situational factors, not catered for by generic patient education, include when families are struggling to manage patients at home or patients are living alone without sufficient support.
Although recognition exists of the increasing role that specialist heart failure nurses and community matrons could play in supporting patients at home, this was accompanied by acceptance that they could not provide round-the-clock services and that symptoms like breathlessness required careful management in the community. 129
Role of culture
Fry et al. 126 emphasise the importance of continuity of care as an organisational backdrop against which to deliver effective patient education. This theme is specifically picked up in detail in a paper focusing on organisational management of heart failure. 128 An initial barrier relates to the initial diagnosis and labelling of the condition, with clinicians euphemistically referring to an ageing heart or a stiff heart in order to alleviate the impact of the stark term ‘heart failure’ and its connotations with terminal illness. 128 Many patients then found the level of supporting information and education unsatisfactory, often having to rely on leaflets available in the clinic or on explanations on their discharge papers. In contrast, when a specialist heart failure nurse was involved, explanations were felt to be more complete and satisfactory.
Clinicians highlighted how the organisational culture of a busy hospital was not conducive to the provision of appropriate explanations of heart failure;128 within hospital and community-based heart failure specialist nursing teams, patients reported more positive experiences. Overall, the study revealed that a lack of patient information and education was a strong theme and a key barrier to the development of patient self-help strategies to help prevent re-admissions (see Self-management). Health-care participants emphasised that patients need to be given information and guidance as part of an ‘ongoing conversation’. Use of the term ‘ongoing’ here links this to the wider theme of continuity of care, with heart failure specialist nurses and GPs being seen to be key to the success of this process.
Patient education is typically perceived as a time-consuming activity that may prove challenging to accommodate in the time-pressured environment of clinical encounters. In addition, its upstream preventative function can be seen as detached and remote from the more typical disease management activities of the clinic. Effects of patient education are not typically observable and definitive evidence on its effectiveness is lacking. As a consequence, patient education may be seen as a ‘common good’ and a patient right, but not necessarily a critical and integral component of an intervention. However, high levels of patient satisfaction from patient education activities suggest that it can be considered critical to patient-centred care.
Role of leadership
Glogowska et al. 129 emphasise how having a specialist nurse who could take the lead in co-ordinating the care of the heart failure patient was considered vital by many respondents. It is, however, unclear, whether this refers to leadership in the sense intended by the PARiHS framework or rather whether it is referring to a form of case management that is more appropriately considered as facilitation. More importantly, a specific role for leadership in the context of patient education is not identified, although it could be a collateral benefit achieved from greater integration, co-ordination and continuity of care.
Role of evaluation/measurement
Delivery of patient education is heterogeneous, not only in the form and format in which it is delivered but equally in the characteristics of the deliverer and in the potential receptivity of the recipient. It is extremely challenging to ensure the fidelity of delivery of patient education in a busy clinic setting. Minimal standards may be monitored (e.g. did the patient receive a patient education booklet?), but critical components of the patient education (e.g. did the patient receive and understand key messages and did they receive the information that they needed at that particular time?) are challenging to elicit on a routine basis.
Role and characteristics of facilitation
The HCPs accepted that heart failure patients at the end of their lives were repeatedly hospitalised, even when no further interventions would change the course of the condition, because of the lack of planning and provision that could keep them in the community. In location 2, this was attributed to patients being admitted by out-of-hours doctors who did not know them. 129
Respondents described a lack of proactive contact from the health-care system, both from hospitals and primary care, regarding scheduling appointments and the next stages in their care pathway. These respondents described a degree of uncertainty about what would happen next and whose responsibility it was to monitor and support them. They expressed uncertainty about whose responsibility it was to initiate communication when hospitals or primary care failed to send information to the respondents as they had said they would. Other respondents, however, described certain HCPs as being exceptionally efficient at facilitating direct access to themselves or other parts of the health-care system quickly. In these instances, patients expressed appreciation for the effectiveness of that particular doctor or nurse, which led to anticipation of a positive future relationship between the HCP and the patient. 126
Role/skills of implementation facilitators
Specialist heart failure nurses were perceived to have more time to dedicate to patients. The nurses’ role in explaining the illness and providing support was greatly appreciated by respondents. 126 The nurses also provided patient education on symptoms that could indicate an exacerbation of their illness. Specialist nurses are able to liaise with different clinicians co-ordinating care to participants with complex multiple comorbidities. 126,129
Supporting evidence
Numerous studies have identified a lack of patient understanding of heart failure including a lack of patient knowledge of medications and self-care. A Cochrane review of patient education in the management of CHD122 concludes that, overall, the evidence is of only very low to moderate quality. It finds that patient education, as part of a cardiac rehabilitation programme, ‘does not contribute to fewer deaths, further heart attacks, heart by-pass or angioplasty, or admission to hospital for heart-related problems’. 122 It does acknowledge that there is evidence of fewer other heart-related events and improvements in health-related quality of life with education-based interventions. It was not possible to determine an effect on individual mortality.
The current evidence base seems largely interpreted within a ‘first do no harm’ frame. In the absence of sufficient information at present, ‘to fully understand the benefits or harms of patient education for people with heart disease’, the Cochrane review122 endorses current guidelines that ‘people with heart disease should receive comprehensive rehabilitation that includes education’. Further research is needed to evaluate how education for people with heart disease can be delivered in an effective and cost-effective way.
Potential enhancements of intervention/implementation
Provision of specialist heart failure nurses, alongside GP and specialist clinician input, was recognised as an essential mechanism for ongoing patient education. Time spent in outpatient clinics is brief and highly pressurised and HCPs have to select judiciously the two or three items of information that they want the patient to recall when they get home. 127 Specialist heart failure nurses, either in clinic or in the community, were seen as having the optimal opportunity to exploit opportunities for ongoing education.
Glogowska et al. 127 report that education represented a considerable portion of the specialist heart failure nurse role. The ongoing relationship between the specialist nurse and the patient, in particular during routine home visits, where patients are more relaxed, in control and have more time to assimilate information, offered an opportunity for delivery of patient education. This was considered particularly important given that the patient can take in only a small percentage of what the HCP shares on any one occasion. 127
Further exploration is required on the degree of tailoring and personalisation required in order for patient education to be effective. Some commentators have suggested the value of the ‘information prescription’, analogous to a medication prescription, which combines a formality of exchange with personalisation to patient perspectives. 35 In connection with tailoring, a review by the Joanna Briggs Institute34 suggests that future studies might consider interventions inclusive of more diverse ethnic populations of varying literacy and socioeconomic levels.
Self-management
Summary
Self-management follows from and complements patient education. Written action plans, including information on when to seek medical help, are a key component of many self-management programmes. The key mechanism for self-management is thought to involve increasing a patient’s self-efficacy and confidence to be actively involved in managing their condition. There is strong evidence from systematic reviews of randomised trials supporting the effectiveness of supported self-management for reducing hospital admissions in respiratory conditions, such as asthma and COPD, and cardiovascular conditions, such as chronic heart failure. UK studies did not find a decrease in admissions with self-management relative to usual care, although one study suggested that self-management for COPD is likely to be cost-effective.
Self-management support is most frequently delivered by nurses, but GPs and other physicians are also involved. Some studies stress the importance of the whole team in embedding self-management support at the level of the general practice.
Definition
Purdy et al. 3 define self-management in terms of education in skills needed to manage the disease, behaviour change and emotional support for patients. Self-management education complements traditional patient education by teaching problem-solving skills alongside information and technical skills. Written action plans are a key component of many self-management programmes, especially for respiratory conditions. The plans support patients in managing both chronic conditions and acute exacerbations of their condition, including when to seek medical help.
An early review paper136 identifies three key self-management tasks (medical management, role management and emotional management) and six self-management skills (problem-solving, decision-making, resource use, formation of a patient–provider partnership, action planning and self-tailoring). Role management involves adapting behaviour and/or activities as required to manage the health condition and self-tailoring involves applying self-management knowledge and skills appropriately to a patient’s individual context.
Intervention components
The key components of self-management interventions are summarised in Table 8. This table reflects UK practice, as described in the studies selected from the mapping review (see the following section).
| Question | Characteristics |
|---|---|
| By whom? | A variety of HCPs delivered self-management support in included studies. The most frequently involved group was nurses but GPs and other physicians were also involved. Some studies stressed the importance of the whole team in embedding self-management support at the level of the general practice137,138 |
| What? | The level of self-management support offered to patients varied widely across studies and often appeared to be enhanced for research purposes rather than reflecting normal clinical practice. Key elements included training in self-management,139 remote symptom monitoring,140 action plans137,141,142 and home visits.139,140 Named interventions (GOAL and SPACE) were evaluated in three studies143–145 |
| Where? | Self-management support is most frequently co-ordinated through general practices and other primary care settings, but is also offered through specialist outpatient services |
| To what intensity? | Interventions varied in intensity, including the amount of initial training offered to participants, additional support, such as remote monitoring or home visits, and support for developing and reviewing action plans |
| How often? | Self-management support was typically offered as a ‘one-off’ intervention involving education, sometimes combined with other support, such as monitoring. By contrast, action plans are designed to last indefinitely, with regular (preferably annual) reviews to update the plan when necessary |
Number and type of UK studies identified
The mapping review identified 25 studies of self-management for cardiovascular or respiratory conditions. The largest group of studies dealt with COPD (12 studies), followed by asthma (six studies) and hypertension (five studies). One study covered both asthma and COPD. 142 The studies selected for inclusion in this analysis focused on asthma or COPD (or both) because these were the conditions with most data on the role of self-management for reducing avoidable admissions in the UK. Two studies on heart failure were excluded: one dealt largely with the development of an intervention146 and the other was used earlier in the review process to develop initial programme theories. 128 Details of the studies included in the analysis are presented in Appendix 4, Table 27.
Operating programme theories
By definition, PT1 is applicable to self-management education and support. However, the included UK studies provided mixed evidence relating to this theory. Studies generally failed to provide clear evidence of a reduction in hospital admissions associated with self-management interventions for patients with COPD or a mixture of long-term conditions. 138,139,144 There was evidence of patients feeling satisfied with non-secondary care provision of self-management support (PT2), but this referred to a service with enhanced support. 140 Implementation of asthma action plans was hindered by lack of confidence by GPs and other clinicians in the usefulness of the intervention (PT3). 141 PT4, referring to the possibility of patients delaying seeking treatment leading to greater overall use of health services, may also operate in some circumstances but we did not find evidence of this in our sample of studies.
Several studies related to PT5, which stresses the influence of the wider health-care system and the availability or otherwise of support and incentives. These included factors operating at the level of general practices, local NHS commissioners and national policies, such as the Quality and Outcomes Framework (QOF), that encourage practices to prioritise mandatory targets at the expense of other work. 137,138,144,147
Description of putative mechanisms
The key mechanism for self-management is thought to involve increasing a patient’s self-efficacy and confidence to be actively involved in managing their condition. Lorig and Holman136 state that increasing self-efficacy can be achieved through four key mechanisms: performance mastery, (role) modelling, reinterpretation of symptoms and social persuasion. Some relevant mechanisms highlighted in this analysis of UK studies are summarised in Box 4.
-
Education and training.
-
Remote symptom monitoring.
-
Home visits.
-
Action plans (including review/updating).
-
Patient age and family support.
-
Patient support for intervention.
-
Support/advice available for patients.
-
Commitment to research/evidence.
-
Active promotion of self-management.
-
Financial penalties for re-admission.
-
Whole-practice approach to implementation.
-
Support from wider health-care system (managers or commissioners).
-
Teams feel empowered to support holistic self-management.
-
Self-management incorporated into routine practice.
-
Acquire skills/knowledge.
-
Reinterpretation/reframing of symptoms.
-
Partnership with HCPs.
-
Social support.
-
Increased self-efficacy.
-
Ongoing self-management.
-
Appropriate use of health services.
-
Reduction in preventable admissions.
Contextual factors
Role of patient preference
Patient preference was generally seen as a barrier to participation in self-management, although much of the qualitative research on this topic was based on the perspective of HCPs rather than of patients. Kennedy et al. 138 noted that patients in their study had only a small amount of time in contact with HCPs and this made it difficult for them to embed self-management in their daily routine. They also suggested that patients from deprived backgrounds may have difficulty engaging with concepts such as participation in self-management and shared decision-making, particularly when they may be feeling unwell. 138
Morrow et al. ,137 Ogunbayo et al. 147 and Roberts et al. 142 all presented qualitative data on HCPs’ views of supporting self-management of COPD and/or asthma. Barriers identified included reluctance to attend review appointments, patients being ‘in denial’ about the severity of their condition, unwillingness to change behaviour, personal circumstances that made it difficult for patients to prioritise self-management and patient resistance to action plans.
In the study by Patel et al. ,140 patients who had experienced an enhanced self-management support intervention expressed concerns about continuing self-management without additional support after the study period. Some patients expressed a preference for seeing a GP rather than using rescue medication for an exacerbation, again suggesting barriers to engaging in self-management. In a study of personalised action plans,141 patients stated that they did not use the plans because they did not meet their needs; the plans focused too much on medication and management of worsening symptoms.
Data from quantitative studies also support the existence of patient preference-related barriers to self-management. Hoskins et al. 143 recruited only 48 patients for their study, compared with a target of 80. Similarly, 164 out of 464 participants who were approached declined to participate in the study by Johnson-Warrington et al. ,144 and only 14 of those who did participate expressed an interest in going on to pulmonary rehabilitation. In the Glasgow supported self-management trial,139 only a minority of those who received the intervention (75/180) were classified as ‘successful’ in self-managing their COPD after 12 months.
Some examples of patient preference facilitating self-management were also reported. Bucknall et al. 139 identified predictors of successful COPD self-management, including younger age and living with others. In the trial by Hoskins et al. ,143 those patients who agreed to take part were highly motivated, resulting in low rates of attrition. Kennedy et al. 138 recruited 43% of eligible patients to their study, which the authors considered a high participation rate for a primary care-based community intervention. In studies of HCPs’ views, respondents recognised that most patients wanted information on how to manage their condition137 and that improved understanding and ownership may make patients more willing to follow self-management action plans. 142 Patel et al. 140 reported that all the patients in their study were willing to use an electronic diary to allow symptom monitoring regardless of their previous experience with the technology. The authors suggested that patients were willing to engage with self-management because they felt uncomfortable with being frequent users of health services. 140 Finally, Ring et al. 141 found that personalised action plans were perceived by both patients and HCPs to be useful for certain groups, particularly those learning about their asthma and how to manage it.
Role of culture
This section refers primarily to organisational culture within the health-care system. See also Role of leadership.
Cultural barriers to self-management support were identified in several studies. Hoskins et al. 143 found that HCPs found difficulties in producing an action plan in the time available for a consultation, perceiving that discussion of patients’ life goals complicated the process. Another study recruited patients in hospital and reported that short inpatient stays made it difficult to complete all the necessary procedures. 144 Kennedy et al. 138 and Morrow et al. 137 identified the importance of competing priorities for GPs, including a tendency to treat work that was not audited or recognised through the QOF as a lower priority. GPs were concerned about delegating self-management support to nurses but often felt that they had no alternative. Ogunbayo et al. 147 identified differences in culture between teams working in different settings. HCPs from primary care backgrounds tended to view self-management from a narrow perspective focusing on medication management and annual reviews, whereas those from specialist respiratory teams felt empowered to deliver a more ‘holistic’ style of support. 147 In Patel et al. ’s140 study of enhanced self-management support, some patients expressed frustration with the attitude of the health service, particularly GPs, in relation to waiting times for appointments and pressure to see a nurse rather than a doctor.
Ring et al. 141 found that, despite guideline recommendations, many HCPs did not fully support the use of personalised asthma action plans. This meant that they did not routinely issue plans or review them with patients. A specific cultural barrier identified by Roberts et al. 142 was lack of self-efficacy among HCPs, with one-third of respondents stating that they lacked confidence in their ability to construct an action plan. Lack of confidence was more common among doctors than among nurses. 142
Cultural facilitators of implementing self-management support included buy-in at the general practice level137,143 and support from the local health management organisation (primary care trust). 138 As noted previously, professionals working in specialist respiratory teams felt able to deliver more ‘holistic’ support compared with their primary care colleagues. 147 Research nurses were viewed positively by patients as a source of advice, although this reliance cast some doubt on patients’ ability to manage unsupported self-management after the study. 140 In studies of action plans, HCPs shared the view that such plans were appropriate for certain patients141 and were in line with the culture of evidence-based practice. 142
Role of leadership
Leadership and culture are closely linked, so this section should be considered in conjunction with the previous one.
In relation to the Good Outcomes for Asthma Living (GOAL) intervention for asthma, Hoskins et al. 143 identified the introduction of a time-consuming intervention into routine practice as a major challenge and identified leadership at the whole-practice level as a means of overcoming this. In this study, a large urban practice with a commitment to research was the only participating practice that met its target for patient recruitment. 143 Morrow et al. 137 also identified engaging the whole practice team as a way of developing and implementing asthma self-management. Kennedy et al. 138 noted that their study received support from the local primary care trust, although the significance of this declined over time as the trusts gave way to Clinical Commissioning Groups. The support was reflected in high levels of practice recruitment and staff attendance at training events.
A different form of leadership was exercised by the wider health system in the form of audit, incentives and penalties. One study’s authors noted that ‘fines’ to providers for re-admissions within 30 days of discharge may facilitate implementation of self-management interventions. 144 Practice priorities were reported to be shaped by national policies and priorities including the QOF, and there was an expectation that practices would also focus on areas of relative weakness. 137 The system of commissioning was reported to lead to lack of continuity in service provision and variation between geographical areas. 147
Role of evaluation/measurement
The included studies evaluated some combination of the effectiveness of self-management, implementation of the intervention in practice and patient or HCP views and perceptions of self-management. Only one study evaluated cost-effectiveness: Dritsaki et al. 145 found that participants who received the Self-management Programme of Activity, Coping And Education (SPACE) intervention for COPD gained 0.1 quality-adjusted life-years (QALYs) compared with usual care, at an estimated cost of £280.39 per QALY. This translated to a 97% chance of the intervention being cost-effective at a threshold of £20,000 per QALY. 145
As noted previously, Bucknall et al. 139 identified the characteristics of patients who were more likely to be successful in implementing self-management, mainly younger age and living with others. The GOAL intervention to support goal-setting for asthma self-management was successful in changing the process of asthma review, but the extra time required was a problem given the constraints of routine practice. This suggested that further refinement was required before proceeding to a definitive trial of the intervention. 143 In terms of evaluating interventions against usual care, Johnson-Warrington et al. 144 noted that participants in their study received specialist follow-up routinely, suggesting that usual care may already be close to optimum. Kennedy et al. 138 drew attention to the need to better understand the active components of interventions that contribute to effective self-management support.
Morrow et al. 137 and Ogunbayo et al. 147 both emphasised the role of measurement operating within the health system (specifically the QOF system that was formerly in operation) in influencing how self-management was implemented at the organisational (specifically the general practice) level.
Qualitative evidence on the barriers to and facilitators of self-management is discussed in Contextual factors (see Role of patient preference, Role of culture and Role of leadership). Evidence from the included studies about the effectiveness of self-management interventions for reducing hospital admissions in UK settings is discussed in Supporting evidence.
Role and characteristics of facilitation
Facilitation of the implementation of self-management operates on two levels: between the health-care system and HCPs delivering self-management support and between those HCPs and the patients they serve. The included UK studies provided examples of both levels of facilitation. In two studies, training was provided to participants in advance to enable them to participate in the study. 139,144 A third study involved time-limited support for participants, including home visits by research nurses, with the aim of self-management continuing unsupported after the end of the study period. 140
In terms of facilitation at the level of the HCP, this was provided through the research team in two studies. 138,143 Training was relatively brief (one half-day workshop and two practice-based sessions) and Kennedy et al. 138 noted that this was the maximum achievable within the constraints imposed by other demands on staff time. The role of HCPs in facilitating self-management through action plans in routine practice was explored qualitatively by Roberts et al. ;142 participants noted that GPs often delegated this work to nurses or other practice staff, but further details were not reported.
Role/skills of implementation facilitators
The role and skills of implementation facilitators were discussed in most of the included studies. Seven studies reported at least some data, as summarised in Table 9. Three of the studies involved facilitation at the level of HCPs and in four cases facilitation was delivered to patients directly in the context of research (two studies) or routine practice (two studies).
| Study | Role/skills of implementation facilitators | Who was facilitated? |
|---|---|---|
| Bucknall et al. (2012)139 | Nurses were trained to deliver structured self-management in four fortnightly home visits, each lasting about 40 minutes. Nurses’ training was based on self-regulation theory. Those without previous respiratory experience completed three half-day training sessions covering COPD and communication strategies designed to empower patients | HCPs → patients |
| Hoskins et al. (2016)143 | Training was delivered to nurses by two nurse practitioners and a health psychology researcher | HCPs → patients |
| Johnson-Warrington et al. (2016)144 | Introductory session involved a trained physiotherapist who used motivational interviewing techniques to support behaviour change, goal-setting and problem-solving. Details of staff facilitating further support were not reported | Patients |
| Kennedy et al. (2013)138 | Two facilitators employed by the primary care trust delivered training and provided access to self-management support activities and resources | HCPs → patients |
| Ogunbayo et al. (2017)147 | Participants were from primary care (n = 8), specialist respiratory (n = 7) and pulmonary rehabilitation (n = 5) teams, with highly varied professional backgrounds | Patients |
| Patel et al. (2016)140 | Research nurses monitored symptoms as reported in electronic diaries and visited patients as required | Patients |
| Roberts et al. (2012)142 | For asthma, 25% of physicians reported undertaking self-management support themselves. Support was more commonly delegated to a practice nurse or nurse specialist (64%). For COPD, 25 out of 44 physicians and 10 out of 14 nurses reported undertaking self-management support | Patients |
Supporting evidence
This is a brief summary of evidence from systematic reviews, concentrating on hospital (re-)admission as the outcome of interest. Key results from UK studies included in this analysis are also presented.
For asthma, a Cochrane review published in 2003148 found that optimal self-management for adults with asthma almost halved the risk of hospitalisation [risk ratio 0.58, 95% confidence interval (CI) 0.43 to 0.77]. Optimal self-management was defined as provision of a written action plan for self-management of exacerbations together with self-monitoring and regular medical review. The finding was based on 36 randomised trials involving 6090 participants. Supported self-management is strongly recommended in national and international guidelines, including those of the British Thoracic Society/Scottish Intercollegiate Guidelines Network. 149 These guidelines cite 261 randomised trials included in 22 systematic reviews in support of the recommendation for self-management to be provided.
In a 2014 Cochrane review,63 self-management for patients with COPD was associated with a lower probability (compared with usual care) of respiratory-related hospitalisations [odds ratio (OR) 0.57, 95% CI 0.43 to 0.75, nine studies, 1749 participants, moderate-quality evidence] and all-cause hospitalisations (OR 0.60, 95% CI 0.40 to 0.89, six studies, 1365 participants, moderate-quality evidence). The authors calculated that, over 1 year of follow-up, 8 (95% CI 5 to 14) participants with a high baseline risk of respiratory-related hospital admission needed to be treated to prevent one participant with at least one hospital admission. 63 The corresponding figure for those at low baseline risk was 20 (95% CI 15 to 35) participants.
Although heart failure was not covered in this section of the report, systematic reviews and meta-analyses suggest a benefit of self-management interventions to reduce hospital admissions in this condition also. However, interpretation of findings is complicated by heterogeneity arising from issues such as varying trial designs, intervention components, follow-up periods and methods of outcome assessment. 150
In summary, there is strong evidence from systematic reviews of randomised trials supporting the effectiveness of supported self-management for reducing hospital admissions in respiratory conditions such as asthma and COPD and cardiovascular conditions such as chronic heart failure. This evidence has resulted in strong recommendations in clinical guidelines in favour of implementing self-management as widely as possible. However, guidelines also recognise the challenges of implementing a complex intervention with limited resources and of involving patients as active partners in managing their condition.
The UK research did not entirely support the findings of the systematic reviews. None of the three studies that evaluated the outcome found a decrease in hospital admissions with self-management relative to control groups. 138,139,144 The influence of these findings on UK practice is unclear and it should be noted that we did not attempt to identify all relevant UK studies or even a representative sample of them. The only economic evaluation included in our analysis suggested that self-management for COPD is likely to be cost-effective in the UK, with an estimated cost of £280.00 per QALY gained compared with usual care. 145
Potential enhancements of intervention/implementation
Suggestions for improving the implementation of self-management came from three qualitative studies. The suggestions originated from HCPs participating in the studies or from study authors rather than from patients or the public.
Suggestions from the study by Morrow et al. 137 included emphasising the evidence for benefit and improving teamwork (including team-based education) and organisational strategies (including remote consulting), which would need to fit within existing practice routines. Technology was thought to offer some potential solutions but these must be integrated with existing practice IT systems. In Ogunbayo et al. ’s147 study, normalising self-management into routine practice was identified as a theme at the practitioner level. Participants perceived that this involved use of various self-management planning tools as well as changing practitioner or practice culture.
Finally, Ring et al. 141 discussed the potential role of a multifaceted intervention to facilitate implementation of personalised action plans by tackling identified barriers (e.g. using standard templates, electronic prompts to review plans and encouraging patients to bring plans to review appointments).
Telehealthcare
Summary
Telehealthcare appears to offer inherent advantages in terms of feedback mechanisms, condition monitoring and communication between health providers and patients. However, some systemic issues remain: either the patient has to make the decision as to when emergency admission is appropriate, based on feedback data that need to be calibrated according to probable severity, or the HCP remains in control of that decision. In the latter case, it is critical that the HCP has all the information that is required to facilitate the decision. For example, they may wish to corroborate the telemonitoring data with observation of physical signs. Provision of telemonitoring data does not address the essential issues of patient self-efficacy or practitioner efficacy, namely the confidence to make a decision about the appropriateness of admission within a risk-averse culture or a safety-first psychological state.
Definition
‘Telemedicine’ is frequently used as an umbrella term. However, this term carries unwelcome connotations by placing the doctor at the centre of the interaction. Terms such as telehealthcare, telehealth and telecare are to be preferred. Telehealth involves the remote exchange of data between a patient and HCPs as part of a patient’s diagnosis and health-care management. Examples include monitoring of blood pressure or of blood glucose for diabetes. Telehealth may facilitate an improved patient understanding of their health conditions, providing them with tools for self-monitoring, encouraging better self-management of health problems and alerting additional professional support if devices signal a problem.
A Cochrane review of services for patients with asthma151 combines both the ‘health’ suffix and the ‘care’ suffix to define ‘telehealthcare’ as ‘the provision of personalized healthcare at a distance’. 151 Telehealthcare embodies three components: (1) information obtained from the patient, (2) electronic transfer of data over a distance and (3) personalised feedback from a HCP.
‘At a distance’ requires use of a ‘tool of distance communication that works without the simultaneous physical presence of the participants in the interaction’. Such a technology might be ‘telephone, e-mail, the internet or any other networked or mobile device’. 151 The emphasis is on the nature of the interaction; the novelty or sophistication of the technology is irrelevant to an understanding of how the interaction is successful, although unfamiliarity and complexity of the technology may add further barriers to implementation. Feedback from the HCP to the patient could be synchronous or asynchronous (i.e. by store-and-forward technology, in which a patient’s data are kept in an electronic repository and forwarded to a HCP on request). Advice should be tailored to the consulting patient. Many telehealthcare interventions are designed to help patients manage their condition and, therefore, several of the underpinning mechanisms may relate to the facilitation of self-management.
There are no recommendations for telehealthcare for the management of chronic heart failure in the NICE, European Society of Cardiology or American College of Cardiology/American Heart Association guidelines. 152 Despite the lack of UK guidance, the government has vigorously advanced the telehealth agenda through the 3 Million Lives initiative. This policy initiative aspired to enhance the lives of the population by encouraging and supporting (but not directly funding) the use of telecare and telehealth applications as a vehicle for providing more person-centred and integrated care.
Intervention components
The key components of telehealthcare interventions are summarised in Table 10. This table reflects UK practice, as described in the studies selected from the mapping review (see the following section).
| Question | Characteristics |
|---|---|
| By whom? | HCPs |
| What? | Interaction including telemonitoring, feedback and provision of tailored information (e.g. symptom questions and educational messages) |
| Where? | ‘Tool of distance communication that works without the simultaneous physical presence of the participants in the interaction’. Can be ‘telephone, e-mail, the internet or any other networked or mobile device’151 |
| To what intensity? | Can be patient initiated or clinician instigated in response to monitoring |
| How often? | At intervals determined by clinician, patient or symptoms |
Number and type of UK studies identified
The mapping review identified one UK quantitative study of telehealthcare, from the Whole System Demonstrator Project,71 for COPD, diabetes and heart failure. The quantitative TELESCOT RCTs153–155 that accompanied several UK qualitative studies predated our cut-off date, being published in 2009.
The mapping review identified a total of seven UK qualitative studies: three examined COPD, one examined hypertension and the remainder explored multiple conditions. Three UK qualitative studies had been conducted alongside the TELESCOT trials. Further qualitative studies examined COPD patients receiving a community respiratory service156 and patients with hypertension,157,158 both in the West Midlands. Ure et al. 159 conducted a qualitative study examining a COPD telemonitoring service in NHS Lothian and a critical commentary160 examined transferable lessons from this experience. Finally, Williams et al. 161 examined patients’ expectations and experiences of a mHealth application for COPD in Oxfordshire.
Details of the studies included in the analysis are presented in Appendix 4, Table 28.
Operating programme theories
Crundall-Goode and Goode152 identify four types of barriers to successful implementation of telehealthcare applications for chronic health conditions: patient related, health and social care organisation related, technology related and evidence/economic related. The first and second of these barriers figure prominently among our candidate programme theories, with technology related being specific to telehealthcare interventions and evidence/economic related being picked up across all interventions in our PARiHS framework.
Specifically, telehealthcare, in the form of telemonitoring, operates within PT1. PT1 states that if patients are equipped with knowledge and information for self-management, they will access health services only when required, leading to appropriate resource use and a reduction in unplanned admissions. Telemonitoring addresses the fear and anxiety that a patient experiences if they are not sure whether or not to call the health services. They have the reassurance that their condition is being monitored, thereby accelerating the feedback loop between patient and clinician. However, telemonitoring is limited, given its focus only on specific signs, whereas the patient’s symptoms may cross a wide range of circumstances, either linked to or independent of what they are being monitored for. In this case, the telemonitor may be offering an alternative or contradictory picture that increases, rather than reduces, the uncertainty.
Alternatively, people with chronic conditions may perceive that presentation to an emergency department holds relative advantage (e.g. quality, ease of access, response) over GP-based or other primary or community care services (PT2). People with chronic conditions may pressure GPs to admit them to hospital. All of the above explanations assume that people behave in a ‘rational’ manner when seeking information. However, information need has an important affective dimension. As has already been demonstrated, much inappropriate utilisation by patients is attributable to anxiety and uncertainty. Provision of information does not always allay this; its effectiveness depends on whether it is trusted or whether it needs further verification or validation. Under such circumstances, a patient may consult an information source but have an outstanding need for a ‘second opinion’, particularly if the information they have to hand is not situated in their specific circumstances. The perceived authority of the local hospital may be seen to eclipse the less satisfactory response from local primary care provision.
Alternatively, GPs or other HCPs may lack confidence in their own diagnoses or may lack confidence in or knowledge of alternative sources of health-care provision and so may refer people with chronic conditions or admit them directly to hospital. GPs or other HCPs may feel under pressure to admit people with chronic conditions directly to hospital (PT3). In the context of patient education, and not the educational needs of the HCPs themselves, health providers may find it challenging to identify and locate information for patients, which is, again, situated within the patient’s specific needs. Alternatively, they may encounter contradictions between what the available information recommends and their own clinical judgement.
People with chronic conditions may also use health services inappropriately, delaying their presentation to a GP or hospital (PT4) because of perceptions of the service either anticipated or based on their own or others’ past experiences. Such mental imprints may exert a stronger and more powerful influence over their behaviour than the provision of patient education.
Salisbury et al. 162 identify the existence of the CCM as a dominant way of conceptualising chronic disease management. However, they highlight that this model was not designed with telehealthcare in mind and that it does not, therefore, readily accommodate considerations relating to this type of intervention.
Description of putative mechanisms
Box 5 provides a summary of putative mechanisms. We believe that telehealthcare is unique among the interventions examined in this report, given that a realist synthesis has already been conducted to identify the core mechanisms underpinning telehealthcare interventions. Vassilev et al. 45 examined three chronic health conditions, including COPD and heart failure (which are eligible for this review), and identified three concepts that suggest how telehealthcare engages with patients, carers and HCPs:
-
relationships – if and how a telehealth intervention enables or limits the possibility for relationships with professionals and/or peers
-
fit – how well telehealthcare interventions can be integrated into everyday life and health-care routines and the extent to which they are easy to use; compatible with patients’ existing environment, skills and capacity; and do not significantly disrupt patients’ lives and routines
-
visibility – visualisation of symptoms and feedback has the capacity to improve knowledge, motivation and a sense of empowerment, to engage network members and to reinforce positive behaviour change, prompts for action and surveillance.
-
Information supplied by the patient, whether orally, in written or graphical form or through some type of monitoring.
-
Electronic transfer of information to a care provider.
-
Feedback from the HCP tailored to the individual patient.
-
Integration of IT systems across sectors.
-
Reliability of technology.
-
Real-time monitoring of patient.
-
Reassurance and feedback alleviating stress and anxiety.
-
Resolution within primary care.
-
Increasing dependence on practitioner support for telemonitoring.
-
Possible over-treatment.
-
Challenges in how best to organise services to support the technology.
-
Reduced utilisation of secondary care.
-
Increased or inappropriate use of telemonitoring/practitioner support.
-
Increased health service utilisation.
-
Diversion from existing service delivery.
Green font denotes outcomes that could be detrimental in the context of reducing inappropriate hospital admissions.
These three concepts (communication, fit and visibility) clearly have a critical role in acceptance of the intervention. Our own programme theories have a different emphasis and particularly confirm aspects of visibility, namely the closure of a feedback loop so that patients and professionals can respond to current symptoms and their severity and make a judgement on whether emergency admission is indeed appropriate or whether appropriate alternatives exist. The fact that this assessment can be conducted in real time provides the additional benefit that neither the patient nor the professional has to worry about the deterioration or, indeed, improvement of the symptoms in the interval between the ‘trigger’ symptoms (e.g. an exacerbation) and contact with a HCP.
Contextual factors
Role of patient preference
Overall, patients appear more positive than professionals about using telehealth. 163,164 However, the Whole System Demonstrator project165 identified patients who resisted telehealthcare because they believed that dependence on technology would reaffirm their sick-dependency role and lack of independence. Clearly, the technology was imbued with a symbolic significance that went beyond a pattern of dependence signalled by frequent visits to a GP or other HCP or by frequent home visits. Patients were also concerned that the technology would raise their own awareness about their condition, causing increased anxiety. HCPs have also raised concerns that the creation of a person-mediated intervention role, such as a case manager, would increase patient dependence rather than facilitate self-management. This tension between monitoring and dependence, self-management and independence is central to the success of several of the included interventions.
In the specific context of telemonitoring, Crundall-Goode and Goode152 observe how some patients reported finding the daily readings/questionnaires monotonous, questioning their effectiveness owing to lack of knowledge and conflicting advice from the team. The team sought to address patient boredom by adapting care plans as much as the technology would allow, providing a more flexible and patient-sensitive approach to self-monitoring.
In other cases, the technology was seen, typically by carers, as a way of seeking to replace care already provided through face-to-face interaction with an inferior care package delivered by technology. The carer saw the visible dependence of the patient on the personalised health care as appropriate recognition of their illness state.
Role of culture
The TELESCOT studies153–155 sought to facilitate convergence between health and social care partners by making this a condition of the bidding process. According to Lluch,166 the Scottish Government believed that the funding was effective in changing how care was traditionally delivered by inducing the organisational changes needed to co-ordinate health and social care and the cultural change for stakeholders involved at a local level. The momentum of the telehealthcare projects helped to mainstream the interventions and consolidate this change. Other commentators have warned against ‘bolting on’ telehealthcare provision to existing services, emphasising the need to integrate provision in clinical pathways. 152
Concerns about increased workloads frequently feature in clinician concerns. These can be addressed to a certain extent by attention to improving clinician user interfaces. 160
The TELESCOT evaluations153–155 revealed additional issues that need to be addressed at a cultural or organisational level. According to the study authors, organisations need to devise an acceptable balance between self-care and professional support. 160 They also need to develop interventions to overcome the prejudices of HCPs towards telemonitoring technologies. In connection with patients, they need to develop effective measures to prevent patients from under-reporting their symptoms for fear of bothering their HCPs167 or to let technological readings over-ride their judgement. Other technological nuances frequently overlooked by RCTs include the need to reduce uncertainty around data transmission and to simplify self-assessment of symptoms by debilitated patients. 160
Role of leadership
Technological developments, as required for the development of telehealthcare, are seen as particularly dependent on leadership. In an analysis of telehealthcare systems for chronic conditions in England and Scotland, Lluch166 observes how the lack of strategic leadership for structural change hampers the natural uptake and diffusion of these technologies.
Role of evaluation/measurement
Investment in telehealth has often been partly justified on the basis that its cost can be recovered by reductions in the use of secondary health care. However, it is difficult to evaluate and realise the results of such an effect. Where patients selected for intervention have a history of emergency care, and in the absence of a control group, such patients tend to exhibit reductions in use of emergency care over time (i.e. regression to the mean). 71 Therefore, in the absence of a control group, whether or not observed reductions are attributable to the intervention is unclear. Telehealth service evaluations are characterised as being poorly organised, with few focusing on the economic benefits. This has probably contributed to subsequent withdrawal of funding and to the consequent paucity of peer-reviewed service evaluations in the published literature. 152 Guidance for commissioners and service providers on how best to evaluate and audit a telehealth service has been published. 168
One of the potential criticisms of the Whole System Demonstrator projects in the UK169 is that the final trial evaluation assessed the added value of telehealth and telecare over a reorganised service and not the benefits of whole-systems redesign compared with conventional care. Therefore, generalisability of the results was limited to reorganised services. 166 This observation resonates with other interventions where a whole-system redesign approach is advocated rather than ‘bolting on’ specialist interventions alongside existing service provision.
Role and characteristics of facilitation
In the context of telehealthcare, facilitation has two specific applications:
-
The added requirement to facilitate the reporting and repair of faulty equipment to minimise patient and staff dissatisfaction. 152 This requirement typically lies outside the skill sets of those delivering the clinical service.
-
There is some evidence to suggest that the valuable time and energies of HCPs may be diverted away from clinical duties and redirected to entry-level technical support. 152 Technical facilitation may therefore come at the opportunity cost of providing facilitation in the form of clinical support, patient education, etc.
Role/skills of implementation facilitators
Table 11 provides a summary of the role and skills of implementation facilitators.
| Study | Role/skills of implementation facilitators | Who was facilitated? |
|---|---|---|
| TELESCOT, reported in Lluch (2011)166 | In each pilot project, telehealthcare implementation and day-to-day activity were mainly driven by trained, community nurses. For the pilots, community nurses received additional, specific training about the conditions they were dealing with and about the telehealthcare technology | Community nurses |
| TELESCOT, reported in Lluch (2011)166 | Trained, community nurses responsible for delivering training to patients | Patients |
Supporting evidence
This is a brief summary of evidence from systematic reviews, concentrating on hospital (re-)admission as the outcome of interest. Key results from UK studies included in this analysis are also presented.
For COPD, Polisena et al. 170 showed lower rates of emergency admissions for patients receiving home monitoring plus telephone support. Their systematic review tentatively suggested that home telehealth could reduce the rate of hospitalisation for patients with COPD, but was limited by the quality of the studies included. 170
An important review outside our inclusion period, by Paré et al. ,171 reviewed 65 empirical studies across four conditions and distinguished the effects of telehealth between different conditions. They suggested that effects on reduced visits to emergency departments, hospital admissions and average length of hospital stay were more consistent in pulmonary and cardiac disorders than in diabetes and hypertension. 171
A Cochrane review of studies of heart failure reported that telemonitoring and structured telephone support reduced admissions for heart failure. 172 However, findings were based on generalising a large number of studies with a mean sample size of 330. A study of 1653 patients with heart failure found no significant effect on hospital use or mortality. 173
Data supporting the efficacy of telemonitoring in reducing hospital admissions is mixed. Clinical trials of telemonitoring reported within the inclusion period have not demonstrated the positive impact on hospital admissions found in a systematic review based on smaller studies. 174–176
Potential enhancements of intervention/implementation
Peirce et al. 177 draw on stakeholder interviews to conclude that telemonitoring systems have not overcome the drawbacks of conventional care because ‘they existed as an off-the shelf “bolt-on” and could not be connected with many of the different care services that these patients engage with’. They assert that a future early-detection telemonitoring system should be designed with high levels of user input and, therefore, be characterised by high usability and integration with multiple services. To this they add technical requirements such as more versatility of monitoring capabilities and proven automated methods of pattern detection. Crundall-Goode and Goode152 highlight how there is little guidance outside a trial context on the optimal duration of telemonitoring arrangements, citing evidence that mortality benefits may be lost past a certain duration of intervention. They therefore suggest the enhancement of a care plan that proposes when to step down telehealth and have devised their own example of this.
Cardiac rehabilitation
Summary
Cardiac rehabilitation is offered to people with cardiovascular disease, typically those who have survived a heart attack but also patients with angina or heart failure. Cardiac rehabilitation programmes typically involve tailored exercise together with education and advice to help patients reduce risk factors and recover their confidence. Cochrane reviews of cardiac rehabilitation concentrate on explaining the benefits of the intervention through the physiological effects of exercise on the cardiovascular system. However, given that most cardiac rehabilitation programmes involve interventions other than structured exercise, other mechanisms are likely to be involved in most cases.
Cardiac rehabilitation should be delivered by a MDT led by a clinical co-ordinator (a senior clinician responsible for co-ordinating, managing and evaluating the service). There is a strong international evidence base for cardiac rehabilitation but interpretation of the evidence for the UK is complicated by multiple factors, including a trial casting doubt on its effectiveness as delivered in UK practice. At a national level, the National Audit of Cardiac Rehabilitation (NACR) has provided leadership for cardiac rehabilitation programmes in most countries of the UK. The publication of regular reports and data has been accompanied by a campaign of support for cardiac rehabilitation backed by the British Heart Foundation.
Definition
Cardiac rehabilitation is an intervention offered to people with cardiovascular disease, typically those who have survived a heart attack but also patients with angina or heart failure. Cardiac rehabilitation programmes typically involve tailored exercise together with education and advice to help patients reduce risk factors and recover their confidence. More detailed definitions are available from the NACR (www.cardiacrehabilitation.org.uk/patient-information.htm; accessed 9 March 2018) and the British Association for Cardiovascular Prevention and Rehabilitation (BACPR). 178
Intervention components
The six core components of cardiac rehabilitation as defined by the BACPR are health behaviour change and education; lifestyle risk factor management; psychosocial health; medical risk management; long-term strategies; and audit and evaluation. Table 12 summarises the key features of the intervention.
| Question | Characteristics |
|---|---|
| By whom? | MDT |
| What? | Six core components: health behaviour change and education; lifestyle risk factor management; psychosocial health; medical risk management; long-term strategies; and audit and evaluation |
| Where? | Ideally setting of patient’s choice (e.g. home, community setting or hospital) |
| To what intensity? | Patients are encouraged to engage in structured exercise at least two to three times per week |
| How often? | Patient and MDT should work together for at least 8 weeks |
The BACPR standards for cardiac rehabilitation specify that the intervention should be delivered by a MDT led by a clinical co-ordinator (a senior clinician responsible for co-ordinating, managing and evaluating the service). 178 The standards acknowledge that the composition of the MDT may vary but state that, overall, the team must have appropriate knowledge, skills and competencies in line with the standards and be able to deliver the core components. 178 The disciplines considered key to the delivery of cardiac rehabilitation include dietitian, exercise specialist, nurse specialist, occupational therapist, pharmacist, physician with special interest in prevention and rehabilitation, physiotherapist and practitioner psychologist. The BACPR standards also stress the importance of active engagement with a patient’s wider care team, for example the GP, other general practice staff and social worker. 178
The content of cardiac rehabilitation programmes is designed to deliver the six core components mentioned earlier in this section while meeting individual goals and taking account of patient preference and choice. The BACPR recommend that patients should be offered a choice in terms of venue (e.g. home, community setting or hospital) and timing of sessions. Cardiac rehabilitation may be delivered in a variety of ways (centre based, home based, manual based, web based, etc.). However the programme is delivered, patients are encouraged to engage in structured exercise at least two to three times per week, with documentation of regular review, goal-setting and exercise progression. The BACPR standards specify that the patient and MDT should work together for at least 8 weeks. 178 Detailed standards for the non-exercise components of programmes are also provided.
Number and type of UK studies identified
The mapping review included just two UK studies coded for cardiac rehabilitation: a qualitative study of web-based cardiac rehabilitation in primary care179 and a pilot study of early rehabilitation for patients hospitalised for heart failure. 180 Two systematic reviews of cardiac rehabilitation provided evidence for the effectiveness of cardiac rehabilitation and identified further UK studies181,182 (see Appendix 4, Table 29), although many of these were outside the date range of interest for this review. A key UK study identified from the reviews was the Rehabilitation After Myocardial Infarction Trial (RAMIT), which concluded that ‘the value of cardiac rehabilitation as practised in the UK is open to question’. 183 The publication of RAMIT was accompanied by editorials and commentaries that, although not empirical research, provided important insights into the implementation of cardiac rehabilitation programmes in the UK. 184–186 Another randomised trial questioned the effectiveness and cost-effectiveness of exercise-based rehabilitation for elderly patients with heart failure. 187 Finally, we included the latest report from the UK NACR, which provides detailed statistical information about the delivery of cardiac rehabilitation in different regions of the UK (excluding Scotland). 188 A recent publication using NACR data identified factors influencing patient engagement with cardiac rehabilitation programmes, including service-level factors. 189
Operating programme theories
Cardiac rehabilitation is primarily concerned with preventing further events and re-admissions for people hospitalised for CHD or heart failure. As the intervention includes behaviour change and education, the overarching PT1 appears relevant. This states that IF patients are equipped with knowledge and information for self-management, they will access health services only when required, LEADING TO appropriate resource use and a reduction in unplanned admissions. The main evidence for this comes from RAMIT, in which the majority of cardiac rehabilitation patients rated 7 out of 11 elements (information on heart disease, risk factors, medication, advice on diet, exercise training, relaxation training and stress management training) as being very or fairly helpful on a four-point scale. 183 However, this finding is difficult to interpret as the study did not find evidence of a reduction in admissions in the cardiac rehabilitation group.
If patients are undergoing cardiac rehabilitation as part of a co-ordinated programme of care at home or in the community, the overarching PT2 may operate. Briefly, IF patients are satisfied with provision outside secondary care, THEN they will not feel it necessary to access secondary care services, LEADING TO appropriate use of services and reduction in unplanned admissions. Evidence on provision outside secondary care was lacking in the included studies, making the role of PT2 difficult to evaluate.
Programme theory 3, relating to clinicians’ confidence in diagnosis and referral, is of limited relevance because cardiac rehabilitation is mainly used to reduce re-admission in patients who have already been diagnosed and hospitalised. A similar statement may be made about PT4 (adverse effects of patient delays in accessing treatment), but there is evidence from the included studies of patients failing to take up cardiac rehabilitation or dropping out before completing the programme, which would prevent them from obtaining the benefits claimed for cardiac rehabilitation. 188,189
Description of putative mechanisms
Cochrane reviews of cardiac rehabilitation concentrate on explaining the benefits of the intervention through the physiological effects of exercise on the cardiovascular system. For example, Anderson et al. 181 list six direct benefits of exercise training on the heart and coronary vasculature. They also note possible indirect effects of exercise on risk factors for atherosclerotic disease, such as blood lipids, smoking and blood pressure. 181 These indirect effects include changes in behaviour as well as physiological changes.
The Cochrane review of exercise-based rehabilitation for heart failure also stresses the physiological benefits of exercise training while acknowledging that the precise mechanism(s) leading to benefits in health outcomes is unclear. 182
Given that most cardiac rehabilitation programmes involve interventions other than structured exercise, other mechanisms are likely to be involved in most cases (Box 6). Core components of cardiac rehabilitation aim to support people to change their behaviour and hence reduce their modifiable risk factors for hospital admission or re-admission and other adverse outcomes. This includes increasing participants’ knowledge but also increasing their confidence so that they continue to exercise, abstain from smoking, etc., after the end of the formal cardiac rehabilitation programme. As most cardiac rehabilitation programmes are delivered in groups, support from other group members as well as programme staff is likely to be important. 190
-
Behaviour change and education.
-
Lifestyle risk factor management.
-
Psychosocial health.
-
Medical risk management.
-
Long-term strategies.
-
Audit and evaluation.
-
(Note: exercise is also a key component, although not defined as such by the BACPR. 178)
-
Patient interest in participating.
-
Programmes offering choice reflecting patient needs and preferences.
-
Positive feedback from previous participants.
-
Multidisciplinary team delivering the programme.
-
Evidence to support effectiveness and cost-effectiveness.
-
Clinician endorsement.
-
Policy initiatives to promote cardiac rehabilitation.
-
Personal commitment to cardiac rehabilitation.
-
Diverse MDT.
-
Guidelines and standards.
-
Physiological benefits of exercise.
-
Professional support to reduce risk factors.
-
Social support in group settings.
-
Self-efficacy.
-
Continued adherence to programme.
-
Reduced hospital (re-)admissions.
-
Potential reduced mortality.
Contextual factors
Role of patient preference
Patient preference and other patient factors substantially influence the success of implementation of cardiac rehabilitation programmes. Most UK studies reported on patient preference as a barrier to implementation. Some patients were unwilling to engage in cardiac rehabilitation programmes or dropped out before completing the programme. In the latest NACR report, the percentage of patients who were not interested or declined to attend increased from 14% for early rehabilitation to 54% for long-term maintenance. 188 Factors associated with lower engagement with cardiac rehabilitation in a separate study using NACR data included increasing age, being female, socioeconomic deprivation and belonging to a minority ethnic group. 189 In a trial of a web-based cardiac rehabilitation programme, 78.6% of potential participants declined or did not respond. 191 Participants perceived lack of time, bad weather and the need for self-motivation as barriers. Older participants perceived a web-based programme as more suitable for younger people. 179 In the context of RAMIT, West et al. 183 reported that most control patients did not feel the need for further support or advice, despite being aware of the existence of cardiac rehabilitation programmes. In their study of patients with heart failure, Witham et al. 187 suggested that increases in activity due to the programme may be counterbalanced by decreases elsewhere, resulting in no overall increase in physical activity.
Factors associated with positive patient preference were also reported by most of the included studies. Al Quait et al. 189 reported that cardiac rehabilitation programmes were attractive to younger male patients. Houchen et al. 180 began rehabilitation early and reported that potential participants expressed interest in cardiac rehabilitation while they were still in hospital. Patients following a web-based programme gained confidence as they engaged with the programme and valued the fact that they were no longer coping with their condition without support. 179 RAMIT found that patients who were referred to cardiac rehabilitation programmes rated much of the content as helpful or very helpful. 183 Positive feedback from previous participants could potentially assist recruitment to cardiac rehabilitation programmes, although we are not aware of whether or not any programmes have used or evaluated this strategy. The latest NACR report emphasises the importance of cardiac rehabilitation programmes being menu based and reflecting patient preferences, which it notes are influenced by factors including age, gender and diagnosis. 188
Role of culture
See also the following section: Role of leadership.
Implementation of cardiac rehabilitation programmes is influenced by the internal culture of the NHS organisations involved, as reported in several included UK studies. Studies of both patients with angina179,191 and those with heart failure180 reported that these patients were under-represented in terms of referral to and participation in cardiac rehabilitation programmes. If cardiac rehabilitation programmes are seen as being primarily for patients recovering from a heart attack, this would be a major cultural barrier to participation by people with other cardiac conditions. One study also noted an effect of the source of referral, with patients referred by a cardiac nurse being less likely to engage with cardiac rehabilitation than those referred from other sources, whereas patients referred from general practice were more likely to engage. 189 Providing patients with a definite date for starting a programme promoted engagement.
The disciplinary make-up of teams delivering cardiac rehabilitation is likely to reflect the organisation’s culture and its perception of cardiac rehabilitation as an intervention. The NACR found considerable variation across countries in the UK in the range of professionals supporting cardiac rehabilitation, although 93% of programmes were delivered by staff from three or more disciplines. 188 However, a commentary on the publication of RAMIT noted that fewer than 5% of cardiac rehabilitation programmes in the UK have a doctor as part of the team. The authors argue that this ‘lack of medical patronage’ may partly explain why cardiac rehabilitation remains a ‘Cinderella service’. 185 Witham et al. 187 failed to show a benefit of cardiac rehabilitation for elderly patients with heart failure in their study using a level of intervention considered to reflect what is realistically achievable in routine practice.
Evidence-based (or evidence-informed) decision-making is seen as central to the culture of modern health-care systems. Cardiac rehabilitation in the UK expanded in the 1990s and was recommended in guidelines from that time. 183 However, the publication of RAMIT (2012), which appeared to question the effectiveness of UK cardiac rehabilitation programmes,183 has proved a barrier to implementation of cardiac rehabilitation. The trial results led to the evidence for cardiac rehabilitation being challenged by clinicians, managers and commissioners. 185 In particular, questions were raised about the effectiveness of cardiac rehabilitation in the context of modern medical management of myocardial infarction and the boundary between rehabilitation and ongoing secondary prevention. 183,184 Houchen et al. 180 noted the importance of evidence clearly establishing that cardiac rehabilitation can reduce re-admissions for heart failure in the context of financial penalties for 30-day re-admissions in the NHS.
Broader cultural influences on the implementation of cardiac rehabilitation mainly reflect topics discussed in Role of patient preference, for example different attitudes to exercise or different attitudes to use of online resources may influence how cardiac rehabilitation is implemented for different patient groups.
Role of leadership
Leadership and culture are closely linked, so this section should be considered in conjunction with the previous one. One study (citing other research) noted a link between individual HCPs’ endorsement of cardiac rehabilitation and its uptake by patients. 189
At a national level, the NACR has provided leadership for cardiac rehabilitation programmes in most countries of the UK (excluding Scotland). The publication of regular reports and data has been accompanied by a campaign of support for cardiac rehabilitation backed by the British Heart Foundation. The British Association for Cardiovascular Rehabilitation (now the BACPR) published its standards for cardiac rehabilitation in 2007. 186 This work has prompted policy initiatives from the Department of Health and Social Care and new guidelines are expected to reduce variation and specify minimum standards of service. 185 The NACR already provides data on services’ compliance with standards on a regional basis. 188
The included studies also identified some barriers associated with national and local leadership in the UK. West et al. 184 noted that the emerging National Service Framework for CHD was a factor in halting recruitment for RAMIT (leading to questions about the trial’s statistical power). Inadequate staffing and resourcing of many cardiac rehabilitation programmes186 may be a reflection of lack of commitment to cardiac rehabilitation by clinical leaders (hospital specialists and commissioners) at a local level.
Role of evaluation/measurement
Several included studies were pilot or uncontrolled studies and their authors noted the need for more robust evaluation of cardiac rehabilitation programmes, with randomisation and an adequate sample size. 180,191 RAMIT, by contrast, was designed to evaluate typical cardiac rehabilitation programmes as delivered in the NHS in England. 183 However, the inconclusive results of the study and its shortfall in recruitment have led to controversy about how the trial should be interpreted and its implications for implementation of current cardiac rehabilitation programmes. 184–186
As noted previously, the NACR plays a key role in measuring uptake and evaluating the quality of cardiac rehabilitation programmes. The published reports demonstrate improvements over time but, as noted by one author, they also reveal ‘daunting challenges’ and ‘substantial scope for improvement’. 186
Role and characteristics of facilitation
The included UK studies report limited information about the facilitation of implementation of cardiac rehabilitation programmes. In some studies, support was provided to participants by researchers involved in development and evaluation of the intervention under test. 191 In others, research was carried out in existing cardiac rehabilitation programmes. 180,183 A key role in facilitation is played by the NACR through its identification of variations in practice and measurement of programmes against common standards. 186,188 However, few details of the facilitation process are contained in the available reports.
Role/skills of implementation facilitators
None of the included studies reported on the role and skills of implementation facilitators as distinct from researchers conducting a study and HCPs delivering a cardiac rehabilitation service. In particular, the NACR annual reports and website do not appear to report on active facilitation other than making information available to service providers (audit and feedback).
Supporting evidence
This is a brief summary of the evidence for the effectiveness of cardiac rehabilitation in terms of reduction of hospital (re-)admissions, based on systematic reviews and guidelines.
Cardiac rehabilitation is recommended in the NICE guidelines on secondary prevention after myocardial infarction192 and management of chronic heart failure,121 and in other national and international guidelines. 193 The Department of Health and Social Care published guidance on commissioning cardiac rehabilitation in 2010. 194
There are Cochrane systematic reviews of cardiac rehabilitation (described as ‘exercise-based rehabilitation’) for CHD181 and heart failure,182 as well as numerous other systematic reviews and meta-analyses. In the review of cardiac rehabilitation for CHD, cardiac rehabilitation reduced overall risk of hospital admissions by 18% compared with no-exercise controls [15 trials; risk ratio 0.82, 95% CI 0.70 to 0.96). 181 A larger effect was seen in the Cochrane review of cardiac rehabilitation for patients with heart failure. 182 Compared with a control, exercise training reduced the rate of overall (15 trials, 1328 participants; risk ratio 0.75, 95% CI 0.62 to 0.92, fixed-effect analysis) and heart failure-specific hospitalisation (12 trials, 1036 participants; risk ratio 0.61, 95% CI 0.46 to 0.80, fixed-effect analysis).
Numerous factors complicate the interpretation of this evidence for the UK NHS setting. As noted previously, RAMIT questioned the effectiveness of cardiac rehabilitation programmes as delivered to patients with CHD in NHS hospitals. This prompted a considerable amount of discussion. Some authors questioned the relevance of the Cochrane reviews on the grounds that they include older studies that do not reflect the improved treatment offered to patients receiving ‘usual care’ in modern practice. However, advocates of cardiac rehabilitation point out that there is no strong evidence of a decline in the effect of cardiac rehabilitation on mortality over time. 185 The issue remains unresolved and appears to be a potential barrier to full implementation of cardiac rehabilitation in the NHS.
Potential enhancements of intervention/implementation
Factors favouring successful implementation were identified as follows:
Pulmonary rehabilitation
Summary
The British Lung Foundation’s definition of pulmonary rehabilitation is an exercise and education programme for people with long-term lung conditions. 195 UK programmes are diverse in setting; length, type and intensity of exercise; and provision of education. A key mechanism for the effect of pulmonary rehabilitation appears to be increased self-efficacy for both exercise and self-management. There is strong evidence for the effectiveness of pulmonary rehabilitation (including reducing re-admissions) from systematic reviews of RCTs of pulmonary rehabilitation for COPD. 70,186,187,192,193,196 However, further research is needed to investigate the components of COPD that are most important, how long the programme should be and the frequency of the training.
Definition
The British Lung Foundation’s definition of pulmonary rehabilitation is ‘a programme of exercise and education for people with a long-term lung condition’. 195 Pulmonary rehabilitation consists of a tailored physical exercise programme combined with general health advice and education on managing the condition and associated symptoms. 195
The British Thoracic Society Guideline on pulmonary rehabilitation for adults (2013) has recommendations for the physical exercise training and education components of pulmonary rehabilitation. 197
Intervention components
The updated Cochrane review highlights how pulmonary rehabilitation programmes (PRPs) offer diverse components. 70 They can be based in inpatient or outpatient settings, or at home. The length of the programmes can also differ, ranging from 6 weeks to 6 months, and training intensity can range from daily to twice weekly. The exercise training component can include endurance or strength training or both, with specific exercise training selected to best meet the needs of each individual patient. In addition, the patient education component of the programme can extend from basic advice through to more extensive self-management programmes. All of these differences in the components can influence their effectiveness and contribute to the complexity of implementation. Key components of pulmonary rehabilitation are detailed in Table 13. This reflects UK practice as described in the studies selected from the mapping review.
| Question | Characteristics |
|---|---|
| By whom? | A range of HCPs, including physiotherapists, nurses, nurse specialists, occupational therapists and dietitians. Practice nurse and physiotherapist,198–200 occupational therapists,201 pulmonary rehabilitation team on acute ward consisting of physiotherapists and nurses,202,203 physiotherapist team204 |
| What? | Programmes consist of group sessions that include physical exercise training, patient education, dietary advice and psychological and emotional support |
| Where? | Outpatient departments or community settings including community halls, leisure centres and health centres. Primary care setting (cluster),198–200 community gym facilities,201 lung centre,205 web based,206 hospital as acute admission,203 community settings204 |
| To what intensity? | The British Thoracic Society 2013 guideline found that ‘In the UK, for practical and economic reasons, programmes lasting longer than 6–8 weeks are not standard; however, there is some ongoing debate as to the efficacy of programmes lasting less than 6 weeks’.197 The guideline states that ‘Pulmonary rehabilitation programmes of 6–12 weeks are recommended. (Grade A)’.197 Eight-week programme with follow-up (cluster),198–200 7 weeks,206 8 weeks,207 6 weeks201,203,204 |
| How often? | The British Thoracic Society 2013 guideline recommends ‘Pulmonary rehabilitation programmes including the attendance at a minimum of 12 supervised sessions are recommended, although individual patients can gain some benefit from fewer sessions. (Grade A)’.197 Twice weekly,201,204 weekly 2-hour session (cluster)198–200 |
Number and type of UK studies
The mapping review identified 17 papers of 15 UK studies for pulmonary rehabilitation for COPD; one of the studies was for exacerbations of chronic respiratory disease but the majority of the patients had a primary diagnosis of COPD. 203 In addition, three systematic reviews of pulmonary rehabilitation were identified. 69,196,208 These reviews demonstrated the effectiveness of pulmonary rehabilitation and helped with the identification of further UK studies, although many were outside the date range of interest for this review. Five qualitative studies and 11 quantitative studies are included in the realist synthesis (see Appendix 4, Tables 30a and 30b). One of the quantitative studies is reported in three papers. 198–200
Operating programme theories
Pulmonary rehabilitation programmes aim to improve the length of time that patients with COPD can exercise for without feeling out of breath and to improve their symptoms, self-confidence and emotional well-being. According to the Cochrane review by McCarthy et al. ,196 pulmonary rehabilitation is likely to achieve its effect through several mechanisms. Collectively, pulmonary rehabilitation seeks ‘to reduce COPD symptoms, re-establish and improve functional ability, enhance participation in everyday life, promote autonomy and improve [quality of life]’. Pulmonary rehabilitation focuses on systemic aspects of the disease common among patients with COPD. The three principal components are (1) an exercise component, (2) an educational component and (3) a behaviour change element.
The exercise component of pulmonary rehabilitation targets physical improvement by increasing inspiratory volume and reducing dynamic hyperinflation. Exercise increases muscle function, delaying fatigue and resulting in increased exercise tolerance. 196 Simultaneously, the educational component of pulmonary rehabilitation focuses on collaborative self-management and behaviour change. Patients are provided with information and knowledge regarding COPD, building skills such as goal-setting, problem-solving and decision-making, and developing action plans that allow them to better recognise and manage their disease. The behaviour change element focuses on modifying nutritional intake and smoking patterns; adhering to medication and regular exercise; and utilising effective breathing techniques and energy-saving strategies. These last two elements emphasise the similarities of pulmonary rehabilitation to other interventions, such as patient education and self management.
As PRPs include patient education, PT1 resonates as one possible theory of change. When patients are equipped with knowledge/information for self-management of COPD, including when and where to seek help as appropriate, they will hopefully access the hospital/health services as required. This, in turn, could lead to appropriate utilisation of health resources and a reduction in unplanned admissions. Participants in one programme198–200 described how their relationship with HCPs changed to a more collaborative relationship and that they felt that they now knew what to ask HCPs for and how to self-manage their condition, which was empowering for them.
One study worked with GPs and practice nurses to develop strategies that would influence and consequently increase their referrals to pulmonary rehabilitation. 209 This relates to PT5 when GPs and other HCPs are influenced by the wider context of the health-care system and the availability or otherwise of support and incentives may influence their adoption of pulmonary rehabilitation, which could help to avoid unnecessary referrals and admissions to hospital.
Programme theory 4 refers to the possibility of patients delaying seeking treatment, which then leads to greater overall use of health services; this could happen with patients with COPD, and one of the UK studies investigating the way in which professionals introduce the possibility of a pulmonary rehabilitation-affected uptake discussed this. 202 The study found that COPD patients are often self-conscious about their condition; this can be related to shame or stigmatisation and they can believe that the COPD is their own fault. This can be associated with a reluctance to ask for help from HCPs, which could lead them to not taking up pulmonary rehabilitation or not completing it, which could then mean that their health deteriorates and they then need to access other services. Their reluctance to ask for help could therefore lead to them making greater use of the health service or to unavoidable admissions.
Description of putative mechanisms
Pulmonary rehabilitation consists of two components: exercise and patient education (Box 7). The patient education component can be basic information or advice about COPD or medication or a more extensive self-management programme. One mechanism in self-management involves enabling participants to successfully understand the need for change, to appreciate the benefits of change and to live with the change long term. This mechanism took place in the UK study in which occupational therapists delivered a participant-empowered approach to pulmonary rehabilitation that built on traditional models of self-management. 201 The programme was highly beneficial and patients improved their physical fitness, well-being and confidence to manage their condition.
-
Patient exercise programme.
-
Patient education.
-
Emotional and psychological support.
-
Accessible location.
-
Location where participants feel comfortable.
-
Access to follow-up.
-
Available physical and human resources.
-
Organisational structure of the programme.
-
Patient age and family support.
-
Patient support for intervention.
-
Support/advice available for patients.
-
Belief in capacity for exercise.
-
Belief in ability to self-manage.
-
Acceptance of care and services offered.
-
Improved skills and self-efficacy of facilitators.
-
Improved quality of life.
-
Improved functional status.
-
Improved self-efficacy.
-
Improved confidence in ability to exercise.
-
Improved ability to self-manage.
-
Appropriate utilisation of health resources.
-
Reduction in preventable admissions.
Self-management programmes also work on increasing the patients’ self-efficacy and confidence in managing their own condition. 210,211 Through completing a self-management programme and the exercise component, patients could also increase their confidence in their ability to exercise, meaning that they will then exercise more. Enhanced understanding of the benefits of regular activity as part of disease management prompted increased participation. 212
Pulmonary rehabilitation programmes are provided to patients in groups and exercising in a group can have important benefits for the patients:
The key premise of social identity theory is that group membership (e.g. exercise group) to which a person belongs can provide an individual with a sense of who they are in terms of a defined group identity (i.e. ‘we’ and ‘us’ rather than ‘I’ and ‘me’), that is, the way person feels and thinks about self is derived from their social groupings.
The operation of social identity theory can be demonstrated in UK studies on pulmonary rehabilitation. A qualitative study considering the barriers and facilitators for patients continuing to exercise following the programme found that continued peer and professional support was important to participants. 212 Participants on another programme199,200 described how working in the group helped them by making them motivated to continue with the programme and helped them to focus on what they wanted to achieve. One qualitative study found that professional and peer support were important aspects of the programme. Participants want to exercise in a peer group and saw this as an opportunity for social interaction. 212
Contextual factors
Role of patient preference
The location of the PRP and how easily accessible it is for patients can help the programme to succeed or can act as a barrier to patients. To make the programmes more accessible to patients, health services have started to try to run programmes in community settings. One programme provided by general practices in Ireland used inexpensive equipment and trained practice nurses and physiotherapists with no prior COPD expertise to facilitate a PRP in primary care. 200 Another programme that was offered in the local community gym facilities received very positive patient feedback. 201
A qualitative study considering the barriers and facilitators for patients continuing to exercise following the programme found that continued peer and professional support was important. 212 Participants that attended maintenance sessions stayed more physically active than participants who were offered only a list of facilities where they could exercise. Participants wanted facilities where they could exercise with people with a similar condition. 212 Participants also wanted to exercise in a peer group and saw this as an opportunity for social interaction. 212
Participants in another programme198–200 discussed how working in the group made them more motivated to continue attending the programme and helped them to focus on what they wanted to achieve. Another study214 found that the facilitators of exercise included encouragement, company, professional support, goal-setting, personal attributes and availability of a range of exercise options.
The venue used for pulmonary rehabilitation can also be a barrier. One qualitative study212 suggested facilities where programme participants could exercise following completion of the programme but found that participants felt unsure about using such facilities owing to the environment and the perceived healthier, fitter members. The exercise facility presented a possible barrier to attendance owing to its potential to provoke feelings of embarrassment or intimidation. Familiarity with staff helped to ease anxiety associated with moving to a new venue. Supervision, albeit in a less intensive form than during pulmonary rehabilitation, was important for guiding components of the exercise programme with which participants lacked confidence – such as the cooldown – or for altering or progressing regimens.
Participants in one programme198–200 described how their relationship with HCPs developed into a more collaborative relationship, that they know what to ask HCPs for and how to self-manage their condition.
Patients’ reasons for not exercising were often related to symptoms of their COPD or stigma about their disease. Breathlessness was a common reason for not participating in exercise. In addition, how symptoms varied or started unexpectedly could influence activity. The education aspects of the programme improved their knowledge and understanding of symptom management, leading to greater control over breathlessness. Education about the benefits of regular activity as part of self-management of COPD led to increased participation in exercise. 212
Role of culture
To encourage programme accessibility, one study206 offered a web programme, which was a popular choice. However, this could be a barrier for some groups of patients because, to participate, patients had to have internet access and be web literate.
How professionals introduce the possibility of pulmonary rehabilitation was found to affect uptake. 202 The study found that COPD patients are often self-conscious about their condition; this can be related to shame or stigmatisation and they can believe that the COPD is their own fault. This can be associated with a reluctance to ask for help from HCPs or socially. All of these feelings of low self-worth can make their interactions with HCPs difficult, potentially seeing them as critical or judgemental, which may mean that they will not seek help or might refuse pulmonary rehabilitation. When introducing pulmonary rehabilitation, professionals should be aware of such sensitivities and facilitate open discussion that offers time, compassion and understanding as a means of facilitating uptake.
The role of the group was important to participants. Professional and peer support were identified as key elements; participants expressed a desire to exercise in a peer group, which was combined with an opportunity for social interaction. 212
Role of leadership
The role of leadership was not investigated in the included studies.
Role of evaluation/measurement
Future trials could investigate choice-based pulmonary rehabilitation, enabling patients to choose location-based or web-based programmes. 206
One study203 investigated whether or not introducing rehabilitation while in hospital for an acute exacerbation of COPD could reduce risk of re-admission. The study found that early rehabilitation did not reduce the risk of subsequent re-admission and concluded that the results from their study suggest that, beyond current standard physiotherapy practice, progressive exercise rehabilitation should not be started during the early stages of the acute illness.
Patients who decline referral to pulmonary rehabilitation described feelings of shame, guilt and fear of others’ opinions of them, which related to their lowered self-worth and led them to decline interventions or reduce their help-seeking from HCPs. 202 Another study found that people with COPD experienced difficulties in maintaining an active lifestyle and the findings suggest that confidence is an important determining factor in physical activity participation in patients with COPD. 212 When introducing pulmonary rehabilitation, HCPs need to be mindful of patients’ feelings about their COPD and could try to enable an open discussion with patients, which offers time, compassion and understanding of their feelings as a means of facilitating pulmonary rehabilitation uptake. 202
Role and characteristics of facilitation
Findings from a qualitative study suggest that people with COPD perceive peer and professional exercise-focused support to be important for maintaining an active lifestyle after pulmonary rehabilitation. 212 The study data highlight the difficulties experienced by people with COPD in maintaining an active lifestyle and suggest that confidence is an important determining factor in physical activity participation in people with COPD. The study authors suggested that health services should look to work in collaboration with local authorities and voluntary organisations to increase opportunities for people with COPD to be physically active, recognising the importance of continued peer and professional support. People with COPD can suffer from breathlessness, which can worsen in certain circumstances, and access to advice and reassurance from skilled staff was very valuable to improve pulmonary rehabilitation participatants’ confidence in their ability to exercise.
Role/skills of implementation facilitators
Hospital-based PRPs generally use expensive equipment and are delivered by respiratory specialists. The Structured Education Pulmonary Rehabilitation Programme (SEPRP) used inexpensive equipment and trained practice nurses and physiotherapists with no prior COPD expertise to facilitate the PRP in primary care. Training the practice nurses and physiotherapists increased their skills and ensured that the knowledge gained remained within primary care so that it could potentially have a longer-lasting impact. 198–200
In an initial discussion about starting a PRP, professionals need to give time, compassion and understanding to their patients, which could potentially facilitate pulmonary rehabilitation uptake. 202
Supporting evidence
Three systematic reviews of pulmonary rehabilitation were identified. 69,70,196 Two are updated Cochrane systematic reviews, published in 2015196 and 2016. 70
The 2015 updated review reviewed RCTs that found that pulmonary rehabilitation improves the health-related quality of life of people suffering from COPD and that it should be part of the management and treatment of patients with COPD. 196 Further research in this area could beneficially consider which components of pulmonary rehabilitation are the most important, the ideal length of the programme, the intensity of training required and how long the programme benefits actually last.
The second updated Cochrane review70 and the other review69 considered the effect of pulmonary rehabilitation following acute exacerbations of COPD. Puhan et al. 70 found that pulmonary rehabilitation improves quality of life and exercise capacity and is a safe intervention for patients with COPD following an exacerbation. However, the reasons for diverse effects on hospital re-admissions and mortality shown in the studies are not fully clear and future studies should research whether or not the extent of the rehabilitation programme and the organisation of such programmes in specific health-care systems (e.g. in the rehabilitation setting vs. embedded in the continuum of care from hospital to home to outpatient care) influences the effects of rehabilitation after COPD exacerbations. The third review69 reviewed the results from 10 RCTs, which suggested that pulmonary rehabilitation reduces subsequent admissions, but pooled results from the three cohort studies did not. This could possibly be explained by the heterogeneous nature of individuals included in observational research and the varying standard of PRPs.
Potential enhancements of intervention/implementation
A study investigating the impact of deprivation on pulmonary rehabilitation completion found that patients living in more deprived areas are less likely to complete a PRP. 215 However, people in deprived areas who completed a PRP had similar clinical outcomes to patients in more affluent areas. Therefore, interventions targeted at enhancing referral, uptake and completion of pulmonary rehabilitation among patients living in deprived areas could reduce morbidity and health-care costs in this hard-to-reach population. Another study found that introducing strategies that are relatively easy to implement lead to the potential for more patients to access the health and quality-of-life benefits that pulmonary rehabilitation offers. 209
A large well-conducted RCT compared the efficacy of pulmonary rehabilitation delivered in a community setting with pulmonary rehabilitation delivered in a more traditional hospital-based setting. 204 Both settings produced significant improvements in terms of exercise capacity and quality of life acutely and after long-term follow-up. The costs of the two programmes were similar. The choice of model will therefore depend on local factors of convenience, existing availability of resources and incremental costs. Another RCT found that a primary care-based structured education PRP is feasible and may increase local accessibility to people with moderate and severe COPD. 198–200
Occupational therapists can deliver a participant-empowered approach to pulmonary rehabilitation that builds on traditional models of self-management. Critically, this approach enables participants to successfully understand the need for change, appreciate the benefits of change and live with the change long term. 201
Introducing the group opt-in session improved the graduation rates at The North Bristol Lung Centre pulmonary rehabilitation course and reduced wasted assessments. 205
Professionals should facilitate an open discussion, which offers time, compassion and understanding, with patients as a means of facilitating pulmonary rehabilitation uptake. 202 For patients who refused referral to pulmonary rehabilitation, had not completed a course or had yet to be referred, the way the service was introduced was an important determinant of willingness to participate. 216 Recognition of the role that uncertainty plays in patients with COPD is the first step towards developing interventions focused on reducing this uncertainty, thereby reducing the burden of the disease for the individual patient and facilitating pulmonary rehabilitation attendance. 217
Smoking status, availability of social support and markers of disease severity were predictors of attendance and adherence to pulmonary rehabilitation. 218
Specialist clinics
Summary
Specialist clinics provide advanced diagnostic or treatment services for specific conditions, often in primary care or community settings, with care delivered by specialist nurses or MDTs. Possible mechanisms for effectiveness of specialist clinics include improved self-efficacy and open communication with HCPs, especially specialist nurses. Limited UK research on specialist clinics was identified. Systematic review evidence supported their effectiveness for heart failure but evidence for hypertension was less clear. Potential enhancements to improve effectiveness include clinics being run by nurses already known to the patient and a high intensity of contact immediately after discharge, decreasing over time.
Definition
Specialist clinics provide advanced diagnostic or treatment services for specific conditions. Such clinics exist in both primary and secondary care settings. They may use nurses to lead clinics or MDTs to help manage long-term conditions. 3
Intervention components
Specialist clinics are provided by a range of HCPs trained in the specialist care of the specific condition or patient type. The clinics are provided in the community and can include staff from primary and secondary care. The clinics are of varying intensity and comprise different components of care. More details of the key components of specialist clinics are provided in Table 14. This reflects UK practice, as described in the studies selected from the mapping review.
| Question | Characteristics |
|---|---|
| By whom? | Nurses led specialist nurse-led clinics with consultant backup219 or multidisciplinary care teams that can include staff from primary and secondary care220 |
| What? | Treatment and management of condition, including education for patient and family or carer about the condition and any medication |
| Where? | Primary care settings,219,220 Purdy and Huntley4 also include studies in secondary care settings |
| To what intensity? | Specialist clinics research included in Purdy and Huntley4 varied in intensity from weekly to fortnightly to monthly. Both of the included UK studies had one clinic appointment with follow-up as required by individual patient219,220 |
| How often? | A hypertension clinic offered follow-up by the specialist nurse on a monthly basis for a maximum of 6 months or until blood pressure was below the optimal target. Monthly appointments include motivational interviews and encouraged behavioural changes to reduce cardiovascular risk factors. Following a reduction in the patient’s blood pressure to below the target, the nurse had a short telephone call with the patient on a monthly basis to remind and promote continuation of agreed lifestyle and medication changes. Following the 6-month trial, the specialist nurse had no further contact with the patients, who were then asked to see their usual HCPs when required219 |
Number and type of UK studies identified
Two UK research studies on specialist clinics published from 2010 onwards were identified from the mapping review. 219,220 One of the clinics was for patients with hypertension219 and one was for high-risk respiratory patients with COPD or asthma. 220 The research studies were both quantitative: one was a RCT219 and the other was an uncontrolled observational study. 220 A summary table of the included studies is provided (see Appendix 4, Table 31).
Operating programme theories
Specialist clinics included education about the chronic condition and any medication that relates to PT1. If the specialist clinics can educate patients about their condition, this can lead to self-management, which could then lead to a reduction in unplanned admissions. The RCT for hypertension219 found a reduction in systolic blood pressure; this reduction potentially means that the condition is being appropriately managed and thus should mean that these patients will not have unplanned admissions. The observational study found a reduction in acute respiratory exacerbations, unscheduled visits to GPs and hospital admissions for acute respiratory exacerbations. 220
Linking to the GP programme theory, PT5, potentially several aspects of the UK RCT219 had a beneficial effect on patient blood pressure. One aspect was a letter about the clinic and explaining that they had been invited as their last recorded blood pressure reading was higher than recommended levels. Although they might not attend the clinic, they might more regularly take their tablets and see their own GP for regular blood pressure checks. Patients who did attend might start taking their medication more regularly as they learnt more about the risks of cardiovascular disease and because their blood pressure was being monitored on a regular basis. Motivational interviews conducted by the nurse could also have helped to reinforce regular taking of medication and lifestyle changes. In addition, in this study, the patients with blood pressure above the target were being regularly followed up, which might not be the norm in primary care. This links to the idea of clinical inertia, and if nurse-led specialist clinics can overcome clinical inertia, then they could be effective. 221
In addition, for PT5, if clinicians and other health service staff believe that specialist clinics provide appropriate support, then they will refer patients to them if they are established or will implement the setting up of specialist clinics where appropriate, which, through the changes to practice and their professional role, will lead to appropriate utilisation of health resources and, potentially, a reduction in unplanned admissions.
The two included studies offered specialist clinics in the primary care setting, which links to PT2. The provision of a specialist clinic in the primary care setting will hopefully mean that the patients feel confident and satisfied with the care offered to them and will continue to use these services and not request secondary care services. Positive written feedback from patients indicated that the patients found the joint clinics provided by primary and secondary care professionals for high-risk respiratory patients acceptable and that they were satisfied with health services provided. 220 This observational study found a reduction in hospital admissions, indicating that the clinic was potentially effective. Satisfaction with the clinic was also demonstrated by the high attendance levels, and some of the patients attending had previously missed their routine annual COPD check-up.
Programme theory 3 could potentially be relevant in terms of GPs and primary care staff. If GPs and primary care staff have confidence in and knowledge of specialist clinics available within primary care, then they will be more likely to refer patients to the specialist clinics instead of secondary health-care provision. Diffusion of innovation is relevant here: if roles (i.e. specialist nurse clinics) are not supported and embedded into the existing system, then patients will not be referred to them. A case study of consultant nurse posts discussed how they developed in an ad hoc manner and that new posts need to be supported by HCPs and embedded into the system to succeed. 222 This diffusion of innovation is based on an earlier systematic review by Greenhalgh et al. 223
Description of putative mechanisms
Possible mechanisms of action are summarised in Box 8.
-
Identification of appropriate patients.
-
Specialist nurse as main contact.
-
GP or consultant backup.
-
Regular monitoring.
-
Regular support.
-
Knowledge of referral options.
-
Knowledge and motivation of specialist or practice nurse.
-
Clarity of nurse role.
-
Clarity of GP and consultant backup role.
-
Access to training for nurse.
-
Accountability of nurse to patient.
-
Reduced fragmentation among services.
-
Belief in capacity for self-care.
-
Prompt and open communication to nurse of exacerbations or barriers to self-care.
-
Confidence in self-management.
-
Acceptance of care and services offered.
-
Improved skills of nurses.
-
Improved self-efficacy of nurses.
-
Changes to medication in conjunction with GP or consultant.
-
Ongoing self-management.
-
Improved quality of life.
-
Improved functional status.
-
Improved self-management.
-
Self-efficacy of patient and informal caregiver.
-
Appropriate use of health services.
Contextual factors
Both of the included studies discussed how patient preference could work as either a barrier to or a facilitator of the operation of specialist clinics. Feedback from patients who attended the joint clinics for high-risk respiratory patients220 was positive. All patients described attending the clinic as a positive experience in terms of patient experience of the clinic and the interventions made. The reduction in hospital admissions indicated in this study suggests that the clinic was potentially effective. Satisfaction with the clinic was also demonstrated by the high attendance levels, and some of the patients attending had previously missed their routine annual COPD check-up.
The RCT researched patients from two inner-city practices who were invited to a specialist nurse-led hypertension clinic or received usual care. 219 Eighty-two patients were randomised to the specialist nurse-led hypertension clinic; of these, 27 (33%) chose not to attend. The study authors thought that the attendance would potentially have been higher if the clinic was run by a practice nurse with whom patients were familiar.
Role of culture
The specialist nurse-led hypertension clinic was conducted in two London inner-city practices, with > 40% of participants being of black African, black Caribbean or Asian ethnicities. 219 The study found that the intervention was associated with reduced systolic blood pressure. However, the results could be different between practices with different ethnic groups.
Role of leadership
The role of leadership as a barrier to or facilitator of the operation of specialist clinics was not reported in the included studies.
Role of evaluation/measurement
The role of evaluation/measurement in specialist clinics was not reported in the included studies.
Role and characteristics of facilitation
The integrated model of care provided in a joint clinic by primary and secondary care professionals for patients with high-risk respiratory problems220 allowed for shared learning between primary and secondary care, and intra-organisationally, within the MDT:
Initiative placed strong emphasis on importance of patient and carer education. The emphasis on education for patients was intended to leave a legacy of patients who are able to self-manage more effectively and healthcare professionals who are upskilled in the management of patients with respiratory disease and more technically assured in performing specialist respiratory assessment.
Role/skills of implementation facilitators
The joint clinic intervention220 increased the skills of HCPs in the management of patients with respiratory diseases, enabling them to become more competent in conducting specialist respiratory assessments.
The specialist clinic for hypertension trial219 was conducted by an experienced cardiovascular research nurse with backup from a consultant physician who had a specialist interest in hypertension. It was conducted in just two inner-city London general practices, meaning that the findings may not be applicable to other clinical staff or populations.
Supporting evidence
Evidence for specialist clinics was found in the series of systematic reviews by Purdy et al. 3 and one conference abstract of a review on specialist clinics for hypertension. 224
Purdy et al. 3 found that specialist clinics for patients with heart failure can decrease the risk of unplanned admission, being most effective when patients had frequent appointments close to the time of discharge, which then reduced during follow-up.
The other review224 considered the involvement of nurses in the management of hypertension, particularly in the UK. The systematic review found evidence of improved outcomes with nurse prescribers from non-UK health-care settings. However, the review was able to identify only one trial of adequate size recruiting patients with hypertension in UK primary care, and found that, although it is currently practice for hypertension management to move from GPs to nurses in the UK, there is actually no good-quality trial evidence from UK primary health care that supports the widespread employment of nurses in hypertension management.
Potential enhancements of intervention/implementation
The RCT authors220 suggested that a specialist clinic run by a practice nurse known to patients might increase uptake.
Purdy et al. 3 found that specialist clinics were most effective when there was a high intensity of appointments immediately after discharge from hospital that then steadily reduced.
Community interventions
Summary
Community interventions are interventions that take place in community settings but do not primarily involve case management, attending a specialist clinic, education or exercise/rehabilitation. Examples were identified from the UK for heart failure and COPD, including a ‘natural experiment’ comparing different COPD service models commissioned in demographically similar areas of Wales. A key component is providing support to people living in the community, often through home visits. Possible mechanisms of action depend on formation of a trusting relationship between the patient and the HCP (usually a nurse) delivering the service.
Overall, the systematic review evidence identified by our mapping review is not strongly supportive of the effectiveness of community interventions for reducing hospital admissions. However, this may reflect the inherent clinical heterogeneity of the interventions in this group. Study authors have suggested a diverse range of possible enhancements to interventions, without any clear themes emerging.
Definition
Community interventions are defined by exclusion as those that take place in community settings but do not primarily involve case management, attendance at a specialist clinic, education or exercise/rehabilitation. 3
Intervention components
Key components are summarised in Table 15 based on the TIDieR-Lite checklist. This is based on our sample of included UK studies.
| Question | Characteristics |
|---|---|
| By whom? | Most interventions are delivered by nurses, sometimes as part of a MDT. Nurses may have specialist training in, for example, COPD or heart failure. One included study compared interventions delivered by specialist and generically trained nurses with and without links to secondary care225 |
| What? | Most community interventions involve providing support for patients living in the community. In the case of heart failure specialist nurses, this involves providing education to help patients manage their condition but also liaising with other HCPs to ensure co-ordination and continuity of care. ‘Hospital at home’ as an alternative to admission or to support patients after discharge may also be considered to belong to this group of interventions |
| Where? | Community interventions are often delivered in patients’ own homes |
| To what intensity? | Varies between interventions/populations. For heart failure, community-based specialist nurse services may operate alongside other services such as cardiac rehabilitation in community settings. The intensity of interventions that can be offered to patients is limited by caseload and availability of administrative support |
| How often? | Varies between interventions/populations. Specialist nurse services generally aim to offer patients at least one home visit, with any subsequent appointments either at home or in a clinic setting. Care is planned on an individual basis, with provision for discharge of stable patients to standard primary care and liaison with palliative care for those approaching the end of life |
Number and type of UK studies identified
The mapping review identified eight UK studies covering community interventions. Two were qualitative studies of specialist heart failure nurse services in the community. 127,226 Both studies presented HCPs’ perspectives only.
Three other studies dealt with COPD. A qualitative study of barriers to and facilitators of physical activity for patients in primary care227 appeared relevant to designing community interventions that might be less demanding for patients than full pulmonary rehabilitation. An evaluation of a telephone alert service provided by the Met Office228 differs from other community intervention studies in that the intervention was not provided by the NHS (although it was commissioned by multiple primary care trusts) and did not involve home visits. The service reduced hospital admissions when admissions with a comorbid diagnosis of COPD were included. 228 It was discontinued in 2013 and evaluated retrospectively. Flood-Page225 used a ‘natural experiment’ to compare different models of community care implemented in neighbouring areas with similar demographic characteristics. The authors suggested that service models with close links between primary and secondary care may be more effective in reducing hospital admissions than those involving primary care alone.
Appendix 4, Table 32, summarises the included studies. A news article,229 a narrative literature review230 and a conference abstract231 were excluded on the grounds of being too short to provide relevant data for this analysis.
Purdy et al. ’s3 review of community interventions included only one UK study. This was a randomised trial of home-based support for older patients with heart disease following hospital discharge. 232 The study fell outside the time period for inclusion in our review. A citation search of this study did not identify any more recent relevant community intervention studies.
Operating programme theories
The relevant programme theories are as follows:
-
PT1 – IF patients are equipped with knowledge/information for self-management, THEN they will access hospital/health services as required, LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions. Increased patient knowledge could result from working with specialist nurses or other community-based HCPs, but this was not reported in our included studies, which concentrated on the perspectives of HCPs.
-
PT2 – IF patients feel satisfied with non-secondary care provision, THEN they will not consider it necessary to access secondary care services, LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions. The included studies from the UK do not directly support this theory because they do not include data on patient satisfaction and related outcomes.
-
PT3 – IF GPs/primary care staff feel confident in their own ability to diagnose and/or refer patients appropriately and have confidence in and knowledge of services available within primary and community care, THEN they will not refer patients to hospital, LEADING TO an increase in use of self-management and non-secondary care services and a reduction in unplanned admissions. This theory appears relevant to some of the studies included in Supporting evidence. Flood-Page225 found that services with close links between primary and secondary care appeared to be most effective for reducing COPD admissions. 225 Similarly, MacKenzie et al. 226 highlighted the improving relationships between GPs and specialist nurses over time following implementation of a specialist nurse service and the role of the nurses in providing co-ordination and continuity of care for patients with heart failure.
-
PT5 – IF clinicians and other health service staff perceive that the wider health system provides appropriate support and incentives, THEN they will feel confident in implementing (and evaluating) interventions that involve changes to practice and professional roles, LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions. Again, support for this programme theory comes from studies of HCPs’ perspectives on the implementation of new services, generally based on specialist nurses working in the community as part of a MDT covering COPD or heart failure. 127,226
Description of putative mechanisms
Box 9 summarises key mechanisms to explain how the intervention is believed to work.
-
Patient education and support.
-
Co-ordination of services.
-
Ongoing relationship with patient.
-
Ongoing relationship with patient.
-
Home visits.
-
National policies/guidelines.
-
Acceptance of nurse role.
-
Effective communication within MDTs.
-
Developing relationship with nurse.
-
Improved patient knowledge and self-efficacy.
-
Secondary care and GP satisfaction with care quality.
-
Improved care co-ordination and continuity.
-
Reduction in inappropriate admissions.
Contextual factors
Role of patient preference
Just two studies reported on patient preference as a barrier to implementing community interventions. Glogowska et al. 127 reported that the challenging nature of the information supplied about patients’ conditions may be a barrier to some patients working with community specialist nurses. This suggests that, for some patients, knowledge of and information about self-management may not translate to behavioural change leading to more appropriate use of services, as suggested by PT1. For patients with COPD, Kosteli et al. 227 identified both personal factors and social factors that could influence patients against engaging in physical activity programmes. In terms of programme theories, this again potentially relates to PT1, because knowledge of and information about self-management may not be sufficient to overcome barriers such as patients’ perceived physical limitations and lack of motivation, as well as social barriers, such as overprotective family members and perceived lack of time.
Kosteli et al. 227 identified facilitators of physical activity arising from patients’ personal choice and feelings of obligation to others. Support from family members and/or other people in a similar situation was identified as a social facilitator. This again relates to PT1 and suggests that whether or not patients are willing to engage in physical activity to reduce their risk of hospital admission may depend on the balance between barriers and facilitators in their personal circumstances.
Role of culture
Some of the patient-related and socially mediated barriers and facilitators identified by Glogowska et al. 127 and Kosteli et al. 227 might also be considered as influenced by culture in its broadest sense. Glogowska et al. 127 also identified ‘heart failure’ as a ‘loaded term’ that could negatively influence patients’ perception of the condition and their ability to manage it.
Organisational culture as a barrier was addressed only by MacKenzie et al. 226 They reported that nurses running a community-based service found it difficult to gain trust from GPs, and some GPs considered that the nurses’ role was unclear and the service disjointed. However, other GPs found the service valuable and nurses reported that relations with GPs improved over time, suggesting that the cultural barriers were mainly short term. Participants in the study by Glogowska et al. 127 saw home visits as an important facilitator of their service, perceiving patients to feel more relaxed in their own home than in a hospital or other clinical setting.
Role of leadership
The study by Flood-Page et al. 225 was possible because different local health boards in Wales developed different models for community-based services for people with COPD. This is an example of the importance of local decision-making for implementing effective interventions in a devolved health-care system such as the UK NHS: national guidelines and policy initiatives will have little impact unless they are taken up at the local level. At the local level, both Glogowska et al. 127 and MacKenzie et al. 226 noted tensions between professional groups and/or teams about who has ‘control’ of a patient’s treatment. This type of leadership (or cultural) problem could hinder effective implementation of interventions, which is facilitated when HCPs work effectively together in MDTs. 127 GPs appeared ready to provide leadership on heart failure in the study by MacKenzie et al. ,226 with 70 out of 84 GPs reporting that they had read the latest national guidance. 226
Role of evaluation/measurement
The included studies took a variety of approaches to evaluation and measurement. Flood-Page et al. 225 analysed routine NHS data and emphasised that their study was a service evaluation rather than research. Sarran et al. ’s228 study of a telephone alert service for COPD patients was one of several that evaluated this intervention, so its findings should not be considered definitive. The authors noted that it was important to take account of patients with a comorbid diagnosis of COPD as well as those with a primary diagnosis in evaluating the intervention. 228 The remaining three studies used qualitative methods, with two investigating the perspective of HCPs127,226 and one investigating the perspective of patients. 227
Role and characteristics of facilitation
The studies reported limited data about facilitation. Flood-Page et al. 225 explicitly stated that they were investigating services as implemented in routine NHS practice. This meant that services were delivered by different groups in each area, as described in the following section. The heart failure specialist nurses in the service examined by Glogowska et al. 127 worked with patients from initial diagnosis and were generally regarded as the lead clinicians for their patients. MacKenzie et al. 226 examined a similar specialist nurse service and reported that nurses perceived that better pre-launch planning would have facilitated implementation of the service.
Role/skills of implementation facilitators
Flood-Page et al. 225 identified several different models of service delivery. In Caerphilly Local Health Board, COPD was managed by COPD nurse specialists working, essentially, in isolation. In Newport and Monmouthshire, generically trained nurses managed COPD and other long-term conditions, working alongside GPs without direct secondary care input. In Torfaen and Blaenau Gwent, COPD was managed by nurse specialists, GPs and consultant chest physicians around a weekly outpatient clinic. Consultants provided telephone advice at other times. In two studies of heart failure specialist nurses, one identified the nurses’ role as a link between secondary and primary care,127 whereas the other, set in Scotland, emphasised co-operation between nurses and GPs to facilitate evidence-based management of patients with heart failure. 226 Thus, this small sample of studies suggests that a wide range of models of facilitation of community interventions exists in the UK NHS, which is reflected in the different roles and skills of the staff involved (primarily nurses).
Supporting evidence
Evidence on the effectiveness of community interventions (including hospital at home) comes from Cochrane and other systematic reviews. Cochrane reviews have assessed hospital at home interventions for admission avoidance233 and early discharge,234 and specifically for acute exacerbations of COPD. 235 Although the interventions were delivered in the patient’s home, staff delivering the service could be community based, hospital based or a mixture of the two. Of the three reviews, only the one covering acute exacerbations of COPD found a significant effect on reducing hospital re-admissions compared with hospital inpatient treatment. 235 It should be noted that Purdy et al. 3 treat hospital at home separately from community interventions.
Health Quality Ontario33 systematically reviewed studies of early follow-up (within 7 or 30 days) after hospital discharge for heart failure or COPD in reducing re-admissions. Follow-up could be conducted by telephone or by home visits, so the review scope was relatively broad. Early follow-up was associated with reduced all-cause re-admissions after adjusting for confounders, but the strength of evidence was classed as low to very low on the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system. A Cochrane review by Wong et al. 236 examined home care by outreach nurses for people with COPD. This review also failed to find a significant effect of the intervention on hospital admission or mortality. Significant heterogeneity was present for hospital admissions, possibly related to the presence of one outlying study with a large decrease in admissions whereas other studies showed an increase.
Other reviews identified by the mapping review focused on community-based programmes for hypertension but with a focus on Canada237 and on transitional care interventions, which are dealt with in the next section.
Overall, the systematic review evidence identified by our mapping review is not strongly supportive of the effectiveness of community interventions for reducing hospital admissions. Most of the evidence relates to heart failure or COPD. The definition of community interventions covers a mixed group of interventions and the limitations of the evidence base may reflect the inherent clinical heterogeneity of this group.
Potential enhancements of intervention/implementation
Study authors suggested a diverse range of possible enhancements without any clear themes emerging. Flood-Page et al. 225 emphasised the importance of links between primary and secondary care, whereas MacKenzie et al. 226 pointed to the need to consider urban versus rural settings, as GPs see their roles differently in the two settings. Participants also mentioned the need for effective planning and preparation before implementing a new community service. Glogowska et al. 127 stressed the importance of both the nurse’s ongoing relationship with the patient and their role in co-ordinating and ensuring continuity of care.
Multiple/other interventions
Summary
It is difficult to provide a formal definition of this group of miscellaneous interventions. Most examples of multiple interventions involve co-operation between different elements of the health-care system/workforce. Other interventions are generally simpler interventions not covered by any of the other groups of interventions in the review. Five UK studies were included, of which three involved multiple interventions (two for COPD and one for heart failure) and two were classified as ‘other interventions’. Two studies included explicit statements about how the intervention is believed to work, both relating to PT1 and PT2. The disparate nature of the interventions in this group makes it difficult to identify relevant systematic reviews and other sources of synthesised evidence. Contextual factors around implementation were relatively well reported for this group of studies, with differences in facilitation between interventions implemented across a whole area and those implemented at a smaller scale (e.g. a single hospital or practice).
Definition
It is difficult to provide a formal definition of this group of miscellaneous interventions. Most examples of multiple interventions involve co-operation between different elements of the health-care system/workforce, in some cases affecting all stages of the patient pathway from diagnosis to the end of life. 238 ‘Other’ interventions are generally simpler interventions not covered by any of the other groups of interventions in the review.
Intervention components
The key components of each included UK study are summarised in Table 16 based on the TIDieR-Lite checklist.
| Study | Question | ||||
|---|---|---|---|---|---|
| By whom? | What? | Where? | To what intensity? | How often? | |
| Multiple interventions | |||||
| Roberts et al. (2010)238 | Whole system | Five stages focusing on prevention/accurate diagnosis; treatment and management of stable disease; enhanced services for severe/complex disease; specialist and generalist unscheduled care; community and hospital end-of-life care |
|
Not reported | Not reported |
| Williams et al. (2010)239 | Clinical nurse specialist | Transitional care comprising discharge planning, patient education and follow-up | Hospital and home/community | Regular visits during hospital stay; follow-up in nurse-led clinics or via home visits | Not reported |
| Ghosh et al. (2016)240 | Clinical commissioning group and community NHS trust plus commercial partners | Telemonitoring; case management by respiratory specialist nurses; health coaching to increase knowledge and confidence, leading to more effective self-management | Home | Variable intensity (except telehealth) but averaged seven patient contacts per month | Not reported |
| Other interventions | |||||
| Wilkinson et al. (2014)241 | Project team (consultant, respiratory nurse specialist and registrar) working with existing community teams and general practice staff | Two workstreams:
|
1.5-hour consultant-led appointment followed by open access to services (respiratory centre and community nursing team) | Not reported | |
| Cope et al. (2015)242 | Respiratory clinical nurse specialist and community early assisted discharge service | Hospital in-reach service to optimise management and support early discharge | Large acute county hospital |
|
Monday to Friday only |
Number and type of UK studies identified
Five studies were included, of which three involved multiple interventions238–240 and two were classified as ‘other interventions’. 241,242 Two of the multiple intervention studies were for COPD and one was for heart failure. All three studies used an observational design and only one had a control group (see Appendix 4, Table 33).
The intervention reported by Roberts et al. 238 was an integrated COPD service covering the inner-city area of Salford. Ghosh et al. 240 evaluated a complex intervention involving telehealth, health coaching and a specialist nurse service, also in an urban setting (Leicester). The heart failure transitional care service evaluated by Williams et al. 239 involved discharge planning, patient education and follow-up. Patients received regular visits during their hospital stay and follow-up in nurse-led clinics or home visits. This study had a historical control group.
The two other interventions involved a consultant-led community-based service for COPD patients with frequent admissions and education, spirometry training and case-finding for primary care241 and a hospital in-reach service to optimise management and support early discharge to community services. 242
Operating programme theories
The overarching programme theories appear to operate to different extents in different interventions. PT1 (patient knowledge for self-management) was part of the interventions reported by Williams et al. ,239 Cope et al. 242 and Ghosh et al. 240 The studies by Cope et al. 242 and Ghosh et al. 240 reported increases in patient confidence to self-manage their condition, although based on a small sample, whereas the study by Williams et al. 239 assessed only patient satisfaction. As this was a short-term study of a transitional care service, it appears to have limited relevance to PT2 (patient satisfaction with non-secondary care provision). Other studies did not report data relevant to PT2.
Programme theory 3 (GP/primary care staff confidence) appears relevant to those studies in which enhanced education and training for HCPs was part of the intervention. 238,241 However, outcomes related to increased HCP confidence were not reported in these studies. PT4 (patient delay in seeking treatment) appears relevant to the work of Wilkinson et al. ,241 who identified a group of patients with frequent admissions who had become disengaged from primary care and were more likely to visit the emergency department. PT5 (wider health system support and incentives) appears to operate in those studies in which new services were implemented across a broad area with input from a range of relevant stakeholders. This is exemplified by the studies of Ghosh et al. ,240 Roberts et al. 238 and Wilkinson et al. 241
Description of putative mechanisms
Two studies included explicit statements about how the intervention is believed to work. Williams et al. 239 invoke the health belief model, arguing that support in the transition from hospital to community would increase patients’ self-efficacy and develop their confidence to make decisions about their health. Cope et al. 242 state that early assessment followed by supported discharge is thought to work through patients being more aware of the community services available to them and therefore having the confidence to access such services again in the future. Patients have a better understanding and ability to self-manage their respiratory condition. These mechanisms relate to PT1 and PT2. Other relevant factors identified from the included studies are summarised in Box 10.
-
Telehealth, clinical coaching, specialist nurses (Ghosh et al. 240).
-
Discharge planning, nurse-led follow-up (Williams et al. 239).
-
Integrated service model (Roberts et al. 238).
-
Hospital in-reach, early assisted discharge (Cope et al. 242).
-
Community service for people with repeat admissions, primary care education and case finding (Wilkinson et al. 241).
-
Partnership between NHS organisations (Ghosh et al. 240 and Roberts et al. 238).
-
Patient involvement in intervention design (Ghosh et al. 240 and Roberts et al. 238).
-
Intensive support (Ghosh et al. 240).
-
Partnership with industry (Roberts et al. 238).
-
Awareness of problem, support from national policy initiatives (Williams et al. 239 and Cope et al. 242).
-
Project team working with both patients and HCPs (Wilkinson et al. 241).
-
Urban setting with ‘critical mass’ of patients (Ghosh et al. ,240 Roberts et al. 238 and Wilkinson et al. 241).
-
Early contact with patients (Williams et al. 239 and Cope et al. 242).
-
Engagement in education/training (Roberts et al. 238 and Wilkinson et al. 241).
-
Identification of patients with greatest needs (Wilkinson et al. 241 and Ghosh et al. 240).
-
Integration with other services (Ghosh et al. ,240 Wilkinson et al. 241 and Roberts et al. 238).
-
Increased knowledge of condition and treatment.
-
Awareness of community services.
-
Increased self-efficacy (patients).
-
Satisfaction with information and services provided.
-
Services appropriate for patient needs.
-
Fewer unplanned admissions.
-
Improved health outcomes.
-
Potential cost savings.
Contextual factors
Role of patient preference
Ghosh et al. 240 and Roberts et al. 238 reported that patient representatives were involved in the development of the intervention, helping to ensure that services were in line with patient needs and preferences. Wilkinson et al. 241 identified a barrier around patient preference, in that patients with frequent admissions had become disengaged from primary care and were often admitted after attending an emergency department. Studies generally found high levels of satisfaction with interventions designed to avoid re-admission compared with alternatives. 242
Role of culture
Organisational culture was identified as a barrier in the studies of transitional care239 and in-reach services242 with community-supported discharge. The transitional care service required nurses to play a more prominent role in the MDT, whereas the in-reach service was limited to weekdays because the MDT did not operate a 7-day service. Wilkinson et al. 241 noted that their intervention may not be transferable to less well-resourced or rural settings and also that 2 out of 36 general practices declined to take part. However, the fact that a pilot 7-day service was subsequently started242 and that the great majority of practices took part241 suggested that organisational culture was able to respond to the demands of new services.
Role of leadership
Ghosh et al. 240 and Roberts et al. 238 emphasised the role of different NHS organisations and other stakeholders in working together to implement new services across a whole area. For change on a smaller scale, two studies saw the support provided by national guidelines and policy documents as important. 239,242
Role of evaluation/measurement
All of the studies in this group showed the value of using routinely collected data and audits to identify problems and to support the effectiveness/cost-effectiveness of interventions (while recognising problems with the data for demonstrating causal links).
Role and characteristics of facilitation
Facilitation in the three studies of large-scale interventions238,240,241 involved education and support to help HCPs to deliver the intervention. Wilkinson et al. 241 also provided education to patients who had experienced repeated hospital admissions for COPD. The transitional care and in-reach studies involved facilitation by specialist nurses working in MDTs. 239,242
Role/skills of implementation facilitators
As above, there was a difference between the larger- and smaller-scale interventions. Facilitators in the former group possessed a wide range of skills and included people from outside the NHS (e.g. employees of technology or pharmaceutical companies). 238,240,241 The other studies saw individual nurses acting as implementation facilitators. 239,242
Supporting evidence
The disparate nature of the interventions in this group makes it difficult to identify relevant systematic reviews and other sources of synthesised evidence. For example, one of the included studies evaluated a transitional care intervention for heart failure patients. 239 Although there are several published systematic reviews of transitional care interventions,243–245 their scope is generally wider than that of Williams et al. ,239 making their relevance to implementation of this specific intervention uncertain.
Potential enhancements of intervention/implementation
In relation to community services for COPD, suggested enhancements were improved access to smoking cessation services, especially in deprived areas,238 and support for practice nurses in primary care. 241
For transitional care and early supported discharge, authors suggested support for 7-day working239,242 and agreed diagnostic criteria and treatment guidelines for heart failure between primary and secondary care. 239
Chapter 5 Synthesis of findings: common mechanisms and links to mid-range theory
This chapter seeks to advance findings from the review of individual interventions by attempting cross-intervention synthesis. In doing so, it aims to move from the specifics of individual interventions to the identification of contexts, intervention components and mechanisms that are likely to contribute to intended or unintended outcomes. 246
Three approaches were used to facilitate the synthesis of findings:
-
Implementation factors were mapped from individual studies into the PARiHS framework.
-
Intervention components were mapped from intervention types into a common five-item TIDieR-Lite framework.
-
Programme theory components (PT1–5) were interpreted for each intervention type and connections to mid-range theory were actively sought.
In each case, the available data were constrained by both the level of reporting present in individual included studies and the degree to which those studies focused on implementation aspects.
Insights from the PARiHS framework
Evidence
The clinical conditions selected as the focus for this report, namely cardiac and respiratory conditions, were purposively prioritised to represent areas with strong evidence of effectiveness in terms of the reduction of avoidable admissions. However, studies that demonstrated a positive effect had not necessarily demonstrated an effect in a UK context. Indeed, only a very small proportion of the studies identified by Purdy et al. 3 and adopted by us as a supposed robust evidence base had been conducted in a UK setting. Furthermore, the types of evidence available to explore implementation constitute a far less robust source of evidence than that for interventions.
Context
A typical limitation of the health services and delivery evidence base is its dependence on studies from the USA. This complicates interpretation of intervention studies, because the US-managed care system is so markedly different from the UK NHS, and this challenge is accentuated when examining implementation evidence. We have had to restrict implementation evidence used, at least to a large part, to insights from the UK. However, such a pragmatic decision should not be allowed to mask the fact that, even within the NHS, contexts may be markedly different in terms of culture, organisation and resources, so pilots or initiatives evaluated in one area may not readily transfer even to adjacent NHS constituencies.
Facilitation
The PARiHS framework emphasises the need for appropriate facilitation to increase the likelihood of a successful outcome. 17 The type of facilitation and the role and skills of the facilitator are determined by the specific needs of the organisation. Facilitators work with individuals and teams to enhance the implementation process. In the included studies, the most common mode of facilitation was training of staff. This can be challenging to achieve in an NHS environment alongside ongoing delivery of health services. Training was largely procedural, with little evidence of attempts to change the organisational culture in which preventable admissions take place. This deficiency may be addressed in the new models of care initiative,247 which targets widespread organisational change with preventable admissions as a shared priority.
Much of the evidence on facilitation related to the initiation of the intervention in the context of an experimental evaluation, with the expectation that additional resources for facilitation might be available in the trial setting, rather than in subsequent sustainability and spread. Despite extensive attempts to follow up citations from trials and other experimental studies, we found few examples of the implementation of interventions as trial results were rolled out more widely. Those accounts that do exist tend to focus on packages of care that have progressed a relatively long way down the diffusions of innovations curve, such as case management and cardiac rehabilitation. This probably reflects the focus on publishing generalisable results from empirical studies in the research literature rather than on examining implementation issues related to sustainability and spread.
Insights from the TIDieR-Lite framework
The five-item TIDieR-Lite framework enabled us to capture key features of the interventions and their delivery in a format that allowed comparison across the range. Many of the included interventions were highly variable in terms of setting, delivery, content and duration. This was particularly true of case management and patient education programmes. By contrast, cardiac rehabilitation had a set of national standards and a national audit programme to assess adherence to those standards. However, the actual delivery of programmes showed variation in the professionals delivering the intervention, generally through a MDT. The standards state that patients should have a choice of settings for cardiac rehabilitation, although the extent to which this is available in practice was unclear. The field of pulmonary rehabilitation also had guidelines for intensity and duration of the intervention, perhaps reflecting the need for patients to participate in these interventions by exercising outside formal supervised sessions. Self-management interventions often included time-limited support for patient education and behaviour change combined with an action plan designed to last indefinitely and be reviewed on a regular basis.
A second key insight was the considerable degree of overlap that often existed between interventions from different groups. In particular, patient education to support self-management was present in programmes labelled as case management, patient education, self-management and telehealth. Education was also key to transitional care interventions designed to reduce re-admissions by supporting patients’ discharge from hospital and providing appropriate support in the community. Telehealth interventions were distinctive mainly in their mode of delivery, minimising face-to-face interaction between patients and HCPs. This contrasted with some community-based interventions, which took place in patients’ own homes and involved a co-operative relationship between patients and individual HCPs.
The role of specialist nurses in co-ordinating care for patients as well as delivering care to patients was a key feature of many interventions, particularly case management, self-management support and specialist clinics. Specialist nurses with expertise in heart failure or COPD and other respiratory conditions have become increasingly common in the UK NHS over recent years. These nurses may work in primary, secondary or community care settings. An interesting ‘natural experiment’ in Wales225 suggested that services with close links between primary and secondary care may be most effective for reducing hospital admissions for COPD.
In summary, TIDieR-Lite provided a valuable descriptive framework for understanding key features of the interventions and their implementation. Examination of the summary tables for the different interventions highlighted some patterns and contrasts. The roles of national standards and disease-focused specialist nurses in some interventions were of particular interest.
Insights from the programme theories
Evidence supporting the programme theories is summarised in Table 17.
| Programme theory | Supporting evidence |
|---|---|
| PT1: IF patients are equipped with knowledge/information for self-management, including seeking help as appropriate, THEN they will access hospital/health services as required, LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions |
|
| PT2: IF patients feel confident and satisfied with non-secondary care health provision, THEN they will not consider it necessary to access/request secondary care services, LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions | |
| PT3: IF GPs/primary care staff feel confident in their own ability to diagnose and/or refer patients appropriately and have confidence in and knowledge of services available within primary and community care, THEN they will not refer patients to hospital, LEADING TO an increase in use of self-management and non-secondary care health service provision and a reduction in unplanned admissions |
|
| PT4: IF patients delay/are delayed in accessing health services, THEN patients may experience exacerbation of symptoms, LEADING TO a higher level of clinical input or resource use when they finally access health care and an increase in unplanned admissions | A lack of timely and accurate diagnosis of exacerbations resulted in unplanned admissions128 |
| PT5: IF clinicians and other health service staff perceive that the wider health system provides appropriate support and incentives, THEN they will feel confident in implementing (and evaluating) interventions that involve changes to practice and professional roles, LEADING TO appropriate utilisation of health resources and a reduction in unplanned admissions | Health care delivered across multiple services, confusion about eligibility for specialist heart failure services and relational/managerial discontinuity of care added additional complexity and likelihood of suboptimal management and unplanned admissions128 |
Programme theory 1
Programme theory 1: people with chronic conditions are frequently admitted to hospital when hospital is not the optimal destination for them. People with chronic conditions may have symptoms that could be self-managed or anxieties that could be addressed by patient education or information.
We found evidence to support PT1. Challenges for people with chronic conditions related less to being ill-equipped for self-management and more to difficulties in situating their symptoms within the information with which they have been provided. People with chronic conditions are typically able to interpret their symptoms relative to only their own past experience or the observed experience of others, not against some absolute ‘trigger point’.
There was some evidence to suggest that being equipped with action plans or personalised self-management plans can help people with chronic conditions to assess whether or not external intervention is required. A similar challenge with patient education related to the need to locate available information within the context of what the patient already knows and what they perceive they need to know. There was some evidence to suggest that patients are not typically well equipped to process information on a just-in-case basis, particularly as this may result in a form of information overload. Again, the facility to access contextually sensitive information at the time it is required, whether this be available as a personalised action plan or as telephone advice, rather than being expected to absorb it within a short period of time and then recall it when needed, was positively indicated. The likelihood that a patient’s personal experience serves as a benchmark for their decisions about the need for future intervention indicates the potential value of using a trajectory-based approach to the identification of trigger points (e.g. ‘if you either experience these symptoms that you have previously experienced again or start to experience these specific new symptoms then you should . . .’).
Programme theory 2
Programme theory 2: people with chronic conditions lack knowledge about alternative health provision and therefore draw disproportionately on well-signposted channels, such as their GP or the emergency department.
Alternatively, patients perceive that presentation to an emergency department holds relative advantage (e.g. quality, ease of access and response) over GP-based or other primary or community care services (PT2). People with chronic conditions pressure HCPs to admit them to hospital.
We did not find substantive evidence to suggest that patients exert direct pressure on the decision for emergency admission primarily on the basis of relative advantage. On the contrary, we found that people with chronic conditions often resisted admission to an emergency department. Structural constraints, such as distance from home, distance from family, the alien (i.e. non-homely) hospital environment and the complexity and duration of the transport and admission process, may combine to make emergency admission an unattractive option. It therefore seems that concerns associated with anxiety and risk may constitute a more important driver. Hospitals are seen as a safe place that can offer security and reassurance. However, the presence of perceived, implicit or indirect pressure cannot be underplayed. HCPs may be influenced by personal factors in their relationship with a specific patient (‘soft’ factors) or by fear of litigation, and, ultimately, this could have an impact on the appropriateness of hospital referrals.
Programme theory 3
Programme theory 3: HCPs lack confidence in their own diagnoses or may lack confidence in or knowledge of alternative sources of health-care provision and so may refer people with chronic conditions or admit them directly to hospital. HCPs feel under pressure to admit people with chronic conditions directly to hospital (PT3).
Simmonds et al. 128 use the expression ‘decision flashpoints’ and highlight how clinical misdiagnosis of symptoms (typically breathlessness in the case of comorbid heart failure) can send the patient along a different disease pathway until they require emergency admission. Simmonds et al. 128 emphasise that inappropriate resolution of ‘decision flashpoints’ is perhaps more likely to happen when there is a lack of relational continuity with a GP.
Simmonds et al. 128 further report that ‘some GPs lacked knowledge of heart failure and specialist services, resulting in “mismanaged patients” ’. 128 Conversely, they report that GPs could also be ‘possessive of their patients’,128 reducing the likelihood of referral to specialist heart failure nurses.
Programme theory 4
Programme theory 4: people with chronic conditions use health services inappropriately, delaying their presentation to HCPs or hospital because of perceptions of the service either anticipated or based on the past experience of either themselves or others.
Programme theory 5
A weakness of the above programme theories is the extent to which they imply the availability of choice and rational decision-making in determining the decision to admit. This is addressed, at least to a certain extent, by the inclusion of PT5, namely that GPs and other HCPs are influenced by the wider context of the health-care system, and the availability or otherwise of support and incentives may influence their adoption of interventions and pathways designed to avoid preventable referrals and admissions to hospital (PT5). An exploration of organisational aspects of the management of heart failure concludes that:
Different service providers and professional groups had unintentionally co-created structures, systems and professional hierarchies that militated against the provision of seamless care.
Simmonds et al. 128
Such fragmentation and compartmentalisation not only presents barriers within particular episodes of care (e.g. interactions between GPs and specialist heart failure nurses or between GPs and medical specialists), but also undermines more whole-system-based interventions, such as patient education, which requires coherence and consistency across organisational boundaries and telemedicine, which logistically requires IT systems and procedures to be joined up. 166
Simmonds et al. 128 offer evidence that carers adopt an unofficial ‘ambassadorial’ role to help the patient navigate organisational fragmentation and unravel problems caused by poor communication and co-ordination. Carers grew in confidence and proficiency, subsequently being able to become more proactive in challenging the organisation and provision of care on behalf of the person they cared for. However, this added undesirable extra stress and responsibility for carers who often had their own health problems with which to contend.
Within a publicly funded health service such as the NHS, structural constraints and limited availability of alternatives may influence the ultimate decision as to what care is provided. Few resources can be accessed urgently (i.e. within 1 day), and those urgent-access resources that do exist have limited capacity. 249 Clinicians and patients may factor in anticipated system delays into their decision-making processes and develop compensatory strategies, for example if a ‘tipping point’ is likely to occur within a particular period. For some patients, admission to an acute hospital becomes the only option available if other services cannot be accessed sufficiently rapidly.
Resource-related constraints, such as the limited capacity of health and social services, and suboptimal communication between primary and secondary care clinicians may equally affect the clinical pathway. Initiatives that offer better coverage of clinical care, yet at the associated expense of a loss of continuity of care, may increase the likelihood of preventable admissions. For example, changes to the provision of out-of-hours services have led to concerns that deputising locums (with less familiarity with the patient’s medical or social history) might refer patients to another service or hospital more often than established counterparts. 250 Conversely, specialist nursing provision, seen by many as a potential way of reducing inappropriate admissions, may constitute an early and easy target for budgetary cuts when resources are limited. 249
Insights from mid-range theory
We searched for papers describing conceptual models or frameworks relevant to each of the interventions included in the synthesis. For pragmatic reasons, we aimed to identify five or six theories per intervention, but, in some cases, fewer were found. The findings are briefly summarised in the following sections.
Case management
The search located four theoretical/conceptual papers, which were published between 2001 and 2018 (Table 18). The majority of the frameworks and models focused on the health provider, although the earliest theories were targeted at an individual patient level and the most recent focused on a complex health system model. A total of seven models were identified in the four included papers.
| Study | Theory/conceptual model | Focus of theory or model |
|---|---|---|
| Enguidanos (2001)251 | Theory of planned behaviour | Patient |
| Transtheoretical model | Patient | |
| O’Brien et al. (2018)252 | Engagement through CARInG (Communication and actions to improve health; Relationships built on trust in Intensive outpatient care program staff; and Insight and goal-setting ability) framework | Health system |
| Swanson and Weissert (2018)116 | Principal–agent framework | Health provider |
| Street-level bureaucratic theory | Health provider | |
| Van Durme et al. (2016)82 | Conceptual framework of integrated care253 | Health provider |
| Wagner et al.’s92 CCM | Health provider |
A recent realist synthesis82 focusing on the case management of a different population, namely the frail elderly, nevertheless reveals two potentially useful frameworks/models. According to the conceptual framework of integrated care,253 the patient’s perception of their own capability, informed by the perception of informal caregivers, can lead them to accept the primary care services offered as an alternative to hospital admission and to believe that they are able to manage their condition at home. 82 This framework links closely to the self-efficacy beliefs of Bandura,99 which figure prominently in connection with other intervention types, such as self management and patient education. Indeed, these efficacy expectations are central to PT1 when a patient does not feel equipped with sufficient situational knowledge to manage their own decision on hospital admission. The converse of this is that self-efficacy, when coping with one’s chronic conditions, will have an impact on the extent to which a patient, and their caregiver, feels sufficiently equipped to continue to manage from home.
For the second theory, from the realist synthesis of case management of the frail elderly,82 the review team draws on Wagner et al. ’s222 CCM to identify perceived social support as a mediator for helping patients to stay at home. Several of our own programme theory components draw on perceived levels of support, available in primary and community care, as an important factor in the decision of whether or not to admit to hospital. These perceptions can be held by the patient, the informal caregiver or the health provider. Key for this intervention are the skills of the case manager, who should be facilitated by access to adequate training and sufficient time to fulfil the case management function. A related consideration is the extent to which patients associate their routine care with a local primary/community care community or the extent to which the acute hospital is viewed as the hub for their care. This latter consideration can be managed by engaging with the expectations of peers within the community and may be modified by the ongoing interactions with the case manager.
Patient education
Patient education is extremely well theorised and our review team felt that there would be little benefit to be gained by engaging with the totality of this theorisation. Instead, the search for theories, conceptual frameworks and models in connection with patient education focused on reviews or compendia covering multiple frameworks. We located three reviews, published between 2008 and 2017 (Table 19). All of the frameworks and models focused on the patient (e.g. by seeking to understand and/or explain patient behaviour in relation to the operation of patient education). We were surprised not to identify more transactional-based models regarding the mutual reciprocity of information exchange between the patient and the health provider.
| Study | Theory/conceptual model | Focus of theory or model |
|---|---|---|
| John et al. (2011)254 | Common sense model of illness perceptions | Patient |
| Social cognition theory | Patient | |
| Theory of planned behaviour | Patient | |
| The stages of change model (or transtheoretical model) | Patient | |
| Syx (2008)255 | Health belief model | Patient |
| EuroMed Info (2017)256 | Health belief model | Patient |
| Cognitive dissonance theory | Patient | |
| Diffusion theory | Patient | |
| Stress and coping theory | Patient | |
| Self-efficacy theory | Patient | |
| Locus of control theory | Patient | |
| Adult learning theory | Patient |
Self-management
The search located six papers, published between 1998 and 2016 (Table 20). The majority of the frameworks and models focused on the patient (e.g. by seeking to understand and/or explain patient behaviour in relation to the intervention).
| Study | Theory/conceptual model | Focus of theory or model |
|---|---|---|
| Ryan and Sawin et al. (2009)257 | Individual and family self-management theory | Patient |
| Williams et al. (2004)258 | Self-determination theory | Patient |
| Lorig et al. (1999)259 | Bandura self-efficacy99 | Patient |
| Bandura (1998)260 | Social cognitive theory | Patient/health system/society |
| Heisler et al. (2002)261 | Unnamed conceptual model | Patient |
| Hoskins et al. (2016)143 | Goal-setting theory; Leventhal’s self-regulation model; health action process approach | Health system/patient |
The earliest paper to be published (in 1998)260 covered a wide range of topics under the broad heading of ‘social cognitive theory’, suggesting that theoretical treatment of self-management has a long history. The frameworks used in five further studies were diverse (see Table 20). These studies involved patients with chronic health conditions, diabetes or asthma. Heisler et al. 261 described a conceptual model that focused on how provider behaviour can influence self-management via its influence on self-efficacy. Williams et al. 258 used a self-determination theory based on the concepts of autonomous or controlled motivation and perceived competence or incompetence in a study of people with type 2 diabetes. The theory was useful for relating changes in self-management behaviour to changes in glycaemic control. The individual and family self-management theory described by Ryan and Sawin257 emphasises the role of dyads within a family and the family as a whole, as well as individuals, in supporting self-management.
Finally, in a recent empirical study, Hoskins et al. 143 evaluated a self-management intervention for asthma based on multiple theoretical models. The study suggested that the theory-based intervention was promising but the need for additional time in appointments was a potential barrier to implementation.
Telehealthcare
Telehealthcare, particularly telemonitoring, is a well-theorised area requiring some selectivity when mapping interventions to underpinning mid-range theories. The following list is, therefore, an indicative summary that seeks to extend across different foci and disciplines. A recent review of numerous theoretical frameworks extends this coverage further. 262
The search located five papers, published between 2010 and 2016 (Table 21). The majority of the frameworks and models focused either on the patient (e.g. by seeking to understand and/or explain patient behaviour in relation to the intervention) or on health providers whose attitudes to adoption and acceptance of technology are critical to the intervention success.
| Study | Theory/conceptual model | Focus of theory or model |
|---|---|---|
| Sharma et al. (2010)263 | Giddens’s structuration theory and consequence of modernity264,265 | Health providers |
| Shankel and Wofford (2016)266 | Symptom management theory | Patients |
| Asua et al. (2012)267 | Theory of reasoned action | Health providers |
| Gagnon et al. (2012)268 | Technology acceptance model | Health providers; patients |
| Asua et al. (2012)267 | Theory of interpersonal behaviour | Health providers |
The earliest paper to be published was published in 2010, meaning that more long-standing theories of telehealthcare (particularly telemonitoring) have not been picked up by this report. Most of these frameworks are used in providing a theoretical basis for intervention development, with a recent review demonstrating a higher prevalence of theory-informed interventions than in many comparable areas of health care.
Cardiac rehabilitation
The search located eight papers, published between 1994 and 2010 (Table 22). The majority of the frameworks and models focused on the patient (e.g. by seeking to understand and/or explain patient behaviour in relation to the intervention).
| Study | Theory/conceptual model | Focus of theory or model |
|---|---|---|
| Goud et al. (2010)269 | Cabana et al.270 | Health provider |
| Blanchard et al. (2003)271 | Theory of planned behaviour | Patient |
| Grace et al. (2004)272 | Behavioural model of health services utilisation | Patient |
| Jeng and Braun (1994)273 | Bandura’s self-efficacy theory99 | Patient |
| Lau-Walker (2006)274 | Interactive care model | Patient |
| Allen et al. (2004)275 | PRECEDE–PROCEED model | Patient and system |
| Johnson et al. (1998)276 | Andersen and Newman277 | Patient and system |
| Kitson et al. (1998)278 | Early version of PARiHS? | Whole system |
The earliest paper to be published (in 1994)273 used the Bandura self-efficacy theory99 as a basis for predicting patient behaviour and planning interventions, including methods of increasing self-efficacy and, hence, optimising outcomes. The frameworks used in three further studies, although named differently, were similar in structure, consisting of predisposing, enabling and reinforcing/need factors. 272,275,276 These studies involved diverse populations, including white and African American women and rural US populations.
Blanchard et al. 271 found that the theory of planned behaviour was a useful framework for understanding adherence to cardiac rehabilitation, with perceived behavioural control making the largest contribution to adherence. Lau-Walker274 combined illness representation and self-efficacy theories to produce an interactive care model as a framework for research into intervention design for rehabilitation.
Other conceptual models focused on the wider health system. Kitson et al. 278 used cardiac rehabilitation as an exemplar to test an early version of the PARiHS framework for research implementation. Finally, Goud et al. 269 used a framework developed by Cabana et al. 270 to study HCPs’ adherence to guidelines related to cardiac rehabilitation. The framework includes both internal and external barriers to guideline implementation.
Pulmonary rehabilitation
We identified two mid-range theory papers for pulmonary rehabilitation,212,213 both of which used social identity theory (Table 23).
Specialist clinics
We found no relevant mid-range theory papers for specialist clinics.
Community interventions
Only two relevant papers were located for this group of interventions (Table 24). This may reflect a paucity of literature or the challenges of searching in this area in a limited time frame, or both.
| Study | Intervention | Theory/conceptual model | Focus of theory or model |
|---|---|---|---|
| Community | |||
| Falk Rafael (2000)279 | Community nursing | Watson’s theory of human caring280 | Patient and nurse |
| May (2006)281 | Any complex intervention | Normalisation process model | Health system |
| Miscellaneous | |||
| Wee and Vrijhoef (2015)282 | Transitional care | Unnamed: ‘conceptualisation, implementation and evaluation’ | Health system |
| Williams et al. (2010)239 | Transitional care | Health belief model | Patient |
Falk Rafael279 used Watson’s theory of human caring280 to investigate community nursing and the importance of the nurse–patient relationship. The normalisation process model described by May281 can be applied to any complex intervention in health-care settings. The paper includes the example of nurse-led home telecare for COPD, which is described in terms of the theory’s constructs as moderate for interaction, high for relational integration and skill-set workability, and moderate for contextual integration between primary and secondary care.
Multiple/other interventions
Transitional care is an example of a multiple-component intervention not covered by any of the other categories. Wee and Vrijhoef282 described a conceptual framework for evaluating the development, implementation and performance of transitional care interventions (see Table 24). The model seeks to explain why and how the interventions should work to minimise re-admissions for patients admitted to hospital who need to be transferred between different settings or levels of care during their admission.
Overarching theories
Several areas of supporting theory may help to explain the phenomenon of inappropriate admissions. We have focused on four particular lines of exploration:
-
clinical inertia and admission as ‘the default position’
-
candidacy and ‘deservedness’
-
continuity and personalisation of care
-
sick dependency role and reliance on primary health-care professionals.
Clinical inertia and admission as ‘the default position’
Engaging with the included studies at the level of mechanisms, rather than simply at an intervention level, revealed the importance of the concept of ‘clinical inertia’ in relation to the phenomenon of emergency admissions, especially re-admissions. Clinical inertia is defined as the failure to establish appropriate targets and escalate treatment to achieve treatment goals. This concept appears to have gained initial traction in the context of diabetes,283 which, along with the conditions covered by this review, figures among the most prominent of ACSCs. It has subsequently been promoted in evidence-based health care as an explanation for lack of clinical uptake of clinical decision tools rooted in a lack of confidence in their content and concerns about potential disruption to workflows. 284 Could a similar lack of confidence, this time in primary care provision, and concerns about disruptive change offer one possible explanation for clinicians’ apparent ‘reluctance’ to explore alternatives to emergency admission? Elwyn et al. 284 subsequently linked clinician inertia to the related phenomenon of ‘organisational inertia’, which seems to be at play in this particular arena.
It is interesting to observe that other comparable forms of inertia, attributable to other key protagonists in the decision to admit, are evoked in other included studies. In their Cochrane review, Glynn et al. 285 seek to explain why frequent contact with HCPs does not guarantee better blood pressure control by drawing on the observations of some commentators to suggest that this may be attributable to ineffective management and inadequate practice organisation (i.e. ‘clinical inertia’). When monitoring is shifted from HCPs to patients themselves, Jones et al. 157 remark on a patient phenomenon comparable to clinicians’ clinical inertia, with patients being reluctant to increase medication further in the face of borderline readings, a form of participant inertia.
Generically, the phenomenon of ‘clinical inertia’ is addressed by encouraging patients and physicians to communicate more effectively and respond appropriately to changes in patient circumstances. It may appear paradoxical to be considering clinical inertia in the context of inappropriate escalation of treatments, namely in referring a patient from primary to secondary care. However, failure to establish appropriate targets and to respond appropriately to changes in patient circumstances are equally at the heart of what we observe for inappropriate emergency admissions. We have identified a further variant of clinical inertia of particular relevance in the context of emergency admissions, namely as inertia by remaining within admission as the ‘default position’. As a health improvement document286 states, the culture of an organisation can often be to admit patients as a default position, which can result in admission rates being higher than they need to be.
Consequently, County Durham and Darlington NHS Foundation Trust has implemented measures to minimise admission rates to accident and emergency (A&E), with particular focus on the interaction between the A&E department and the acute medical unit (AMU). These measures include:
-
ensuring that all admissions are discussed with a senior decision-maker prior to admission, including out-of-hours admissions
-
developing processes to allow direct referrals to the AMU rather than requiring admittance to A&E as a preliminary, unnecessary step
-
ensuring a regular, ongoing two-way dialogue between A&E and AMU staff to ensure that referral/admittance decisions are reviewed and challenged
-
AMU consultants regularly coming into the A&E department to aid assessment and ‘pull’ patients from A&E when appropriate.
Early access to senior decision-makers and appropriate selection processes287 feature prominently in many of the intervention types identified in this report.
Supplementary ways of addressing clinical inertia are identified in the literature288 (Box 11) and may serve as a basis for developing new or improved interventions to address this ‘default’ variant.
-
Assessment of performance.
-
Evidence-based education.
-
Flow sheets, automated reminders.
-
Periodic feedback: content, timing and format.
-
Treatment algorithms.
-
Patient education.
-
Treatment targets.
-
Side effects, costs, complexity.
Information drawn from Phillips et al. 288
According to Phillips et al. ,288 clinical inertia is due to at least three problems: overestimation of care provided; use of ‘soft’ reasons to avoid intensification of therapy; and lack of education, training and practice organisation aimed at achieving therapeutic goals. For that variant of clinical inertia whereby HCPs adopt emergency admission as a default position, there is a related pathology, but one that may relate to the converse of the original ‘clinical inertia’. For example, the primary health-care professional may underestimate the care that is currently being provided (or that might be available) in primary care, or overestimate the additional care that may be provided in secondary care. In addition, the HCP may use ‘soft’ reasons to justify and initiate intensified intervention in an emergency department. Finally, they may require recalibration, through education and training, with regard to realistic expectations from intervention. Phillips et al. 288 locate the overcoming of clinical inertia in the context of the benefits of treating to therapeutic targets and the need to structure routine practice to facilitate effective management of disorders for which resolution of patient symptoms is not a sufficient indicator of optimal care. Such systems require sophisticated and reliable mechanisms of feedback and performance evaluation.
Although the emphasis on education of GPs, supported by evidence-based guidelines, clearly offers a potential to overcome a lack of knowledge of the condition and the available services to which GPs might refer, it is worthy to note that a qualitative synthesis of GPs’ barriers to managing heart failure in primary care289 reports ongoing difficulties with information overload. It appears that, just as patients do not experience an absence of information, so much as it not being tailored and personalised to their own specific requirements, GPs do not require yet more educational strategies around greater numbers of evidence-based guidelines so much as the facility to have guidelines tailored to their own local context.
In the context of emergency department-based interventions, the concept of ‘appropriate deliberate clinical inertia’ has been framed in recognition of the need to resist inappropriate or unnecessary interventions. 290 It appears that this concept may be appropriated in primary care to recognise situations in people with chronic conditions that do not result, for example, in any change in the dose or nature of medications. Clear agreement between patients and HCPs that emergency admission will not resolve or in any way modify their symptoms or treatment can act as a sound basis for ‘shared decision-making to improve patient care with the use of clinical judgement’. 290
Candidacy and ‘deservedness’
Another important concept relates to ‘candidacy’, which has previously been explored in relation to access to and utilisation of health care in general. The concept suggests that an individual’s identification of his or her ‘candidacy’ for health services is structurally, culturally, organisationally and professionally constructed. 291 An unintended consequence of several interventions identified in this report is the ‘legitimisation’ of use of services, leading to a possible increase, rather than decrease, in the number of inappropriate admissions. Exactly how this works may vary; initial use of emergency services, either appropriately or inappropriately, may be seen as opening up a pathway of ‘deservedness’ for future entitlement. The initial episode may be seen as legitimised as a ‘one-off’ or it may open the way for ‘similar’ utilisation in the future. More constructively, appropriate use, as confirmed or ratified by HCPs during admission or subsequently during follow-up, may help a patient to ‘benchmark’ their personalised symptoms and set thresholds for external involvement. The complication here is that patients with chronic conditions typically have multiple symptoms and so the ‘benchmark’ directly relates only to those specific symptoms that precipitated admission. This may result in empirical ‘trial and error’ around emergency admissions for distinct yet potentially related symptoms.
Continuity and personalisation of care
Continuity of care is revealed as an important influence on admissions for long-term conditions. 91 The distinction between continuity of relationship (a continuous caring relationship with clinicians) and continuity of management (all aspects of integration, co-ordination and sharing of information) was helpful when completing this analysis, recognising that both mechanisms are revealed as important in the context of preventable admissions. Systematic reviews have found that relational continuity was associated with lower rates of emergency department attendance and hospital admissions. 3,109 Other likely benefits include improved outcomes for patients, including in medication adherence. 128,292
However, Simmonds et al. 128 also illustrate how relational continuity may be unhelpful, for example when a GP is reluctant to refer a patient to a specialist nurse either because they wanted to hold on to management of the patient themselves or because they had little knowledge of the available services. This results in an unhelpful ‘default’ position and can lead to yet another form of ‘clinical inertia’.
Sick dependency role and reliance on primary health-care professionals
Interventions introduced to prevent emergency admissions can have a disruptive effect on the sickness role of the affected patients. For example, the Whole System Demonstrator project165 reported that patients believed that dependence on technology would reaffirm their sickness role and lack of independence. It would also be a visible reminder of their own condition, with the potential to cause increased anxiety.
HCP-mediated intervention roles, such as case manager, also hold a disruptive potential. HCPs were concerned that such roles would increase patient dependence rather than facilitate self-management. In particular, it is challenging to manage the balance between offering improved access to support and reassurance when needed and creating a dependence on the HCP that subverts self-management. This links back to the earlier consideration of candidacy: provision of a specialist service and a ‘passport’ to entitlement of follow-up services when necessary and appropriate may be seen as legitimising contact with secondary care and lead to increased, rather than reduced, utilisation.
In other cases, the technology was seen, typically by carers, as a way of seeking to replace care already provided through face-to-face interaction with an inferior care package delivered by technology. The carer saw the visible dependence of the patient on the personalised health care as appropriate recognition of their illness state.
Finally, the addition of specialist intervention alongside existing provision can lead to perceptions that levels of health care are excessive or superfluous. 165 For example, when a patient is already in regular contact with HCPs, perhaps for comorbid conditions, there may appear to be little need for additional telemonitoring. Such views may reflect actual redundancy and overlap, due to poor integration of specialist services with usual care, or may simply reflect the patient’s perception (i.e. where similar-looking interventions have clearly distinct clinical functions), resulting in poor compliance. Experimental interventions, from pilot studies through to full trials, are more likely to result in such perceived duplication than established services but, nevertheless, the integration of specialist and general care, or between different forms of specialist care for comorbid conditions, is an issue of which those implementing specialist interventions should be aware.
The role of integrated care mid-range theories
The fundamental move towards transformation of current models of primary care by means of implementing proactive integrated care hints at the future potential of integrated care approaches to analysing and resolving the systemic issues revealed by the phenomenon of preventable admissions. Attempts to understand the effects of integrated primary care approaches and underlying mechanisms in relation to other populations, such as frail community-living older adults, may translate to the condition-specific contexts of COPD and heart failure that are the focus of this report. For example, a theory-based evaluation called ‘Finding and Follow-up of Frail older persons’293 offers a theoretical model that incorporates interrelated elements of integrated primary care approaches: (1) proactive case-finding, (2) case management, (3) medication review, (4) self-management support and (5) working in multidisciplinary care teams. Furthermore, this model recognises the importance of cognitive and behavioural components of both HCPs and patients, targeted by so many of the individual mid-range theories identified for each intervention type. Seemingly intractable problems may well be amenable to analytical lenses developed in alternative arenas.
Chapter 6 Discussion and conclusions
Main findings
Mapping review
The mapping review of studies of interventions to reduce preventable admissions published since 2010 identified 569 publications, predominantly related to heart failure or COPD. The interventions identified by Purdy et al. 3 as having the best evidence of effectiveness (or no effect) were well represented in the map. The largest group of studies originated from the USA. The included studies from the UK showed a similar distribution of studies by intervention and population to that of the map as a whole, but there was evidence of some country-specific features, such as the prominence of studies of telehealth. The findings of the mapping review were helpful in informing the sampling frame for the subsequent realist synthesis.
The mapping review and subsequent analysis of UK studies for each intervention (see Chapter 5) revealed that, in many cases, a strong international evidence base for effectiveness of an intervention existed alongside limited evidence specific to the UK context. Cardiac rehabilitation (see Chapter 4, Cardiac rehabilitation) perhaps illustrated this phenomenon most clearly. We often found limited information to help understand how particular interventions have been implemented in the UK NHS and which approaches to implementation work best in NHS contexts. Information on the role of leadership and approaches to facilitating the implementation of interventions was often lacking.
Implementation framework
Within the PARiHS framework, successful implementation is represented as a function of the nature and type of evidence (to be examined from the mapping review), the qualities of the context in which the evidence is being introduced and the way the process is facilitated17 (to be extracted from included UK studies, both quantitative and qualitative). We found that interventions with strong evidence of effectiveness overall had not necessarily demonstrated effectiveness in UK settings; that the largest proportion of the evidence came from the USA, where the context for delivery of health care is very different from that of the UK; and that facilitation of the implementation of interventions was often not reported or inadequately reported in UK studies, which generally focused mainly on effectiveness or qualitative evidence of the patient and HCP experience of service delivery.
Descriptive framework
The TIDieR-Lite framework provided a useful descriptive framework for recording key elements of the interventions and their delivery. Many of the included interventions were highly diverse in the way they were delivered, the main exceptions being cardiac and pulmonary rehabilitation. There was also considerable overlap between interventions in terms of their key components. The role of specialist nurses in providing continuity of care and links between primary and secondary care was highlighted in multiple studies.
Programme theories
We identified and tested five programme theories (using the sequence CMO) to explain how the interventions might work (see Box 1). The programme theories, expressed as scenarios, were refined and endorsed by our PPI group. We found evidence to support PT1, which suggests that hospital admissions could be reduced by optimal self-management. Considering PT2, we did not find substantive evidence to suggest that patients may seek hospital admission primarily on the basis of relative advantage. It seems that concerns associated with anxiety and risk may constitute a more important driver, hospitals being seen as safe places that can offer security and reassurance. However, the presence of perceived, implicit or indirect pressure cannot be ruled out. PT3 relates to clinicians’ confidence in their own diagnoses and ability to refer appropriately to services that might avoid admission. In the context of cardiovascular and respiratory disease, this is relevant to patients with symptoms, such as breathlessness, that could result from various underlying causes.
Direct evidence for PT4 (admissions resulting from patient delay in seeking treatment) was limited in our sample of studies. One study128 noted that a lack of timely and accurate diagnosis contributed to exacerbations of heart failure. Finally, PT5 (influence of the broader health system context) addressed the limitations on rational decision-making around hospital admissions. This was reflected in our studies. For example, heart failure care delivered across multiple services, confusion about eligibility for specialist care and relational/managerial discontinuity of care increased the likelihood of suboptimal management and unplanned admissions. 128
Overall, we believe that the programme theories considered in this realist synthesis are valuable for understanding why unplanned and avoidable admissions occur and the facilitators of and barriers to reducing them.
Mid-range theories
We found numerous examples (both descriptive and empirical studies) of mid-range theories relevant to the interventions under review. The largest group focused on the patient, for example factors influencing adherence to recommended interventions, but theories related to HCPs’ behaviour and the overall health system were also located. Some theories were cited in relation to several interventions (e.g. Bandura’s self-efficacy theory). However, it is unclear whether the prevalence of efficacy/coping theories reflects their greater utility in this context or simply their higher profile. Nevertheless, self-efficacy was revealed as a key component to PT1, not only determining the level of comfort that a patient had with coping with their own condition but also, more importantly, how well equipped the patient feels they are to be able to manage their own exacerbations without resorting inappropriately to primary care health provision or to admission to an acute hospital.
Overarching theories
The overarching theories discussed in Chapter 5 may be considered as more exploratory than the programme and mid-range theories. In general, these theories may help to understand the underlying mechanisms at the level of the patient and HCP in the presence and absence of interventions designed to avoid admissions.
Strengths and limitations
The double evidence mismatch
In theory, seeking UK-focused implementation evidence to accompany interventions that had previously been demonstrated as effective in preventing inappropriate hospital admissions for cardiorespiratory conditions appears both a coherent and an easily manageable literature review task. In practice, however, we encountered a logic problem that we have labelled the ‘double evidence mismatch’. First, the 2010 review by Purdy1 demonstrated the average effectiveness of the candidate interventions based on a comprehensive sample of international studies, within which UK studies constituted a small and largely insignificant part. The quest for implementation evidence might therefore largely focus on UK studies that had a small effect, negative effect or a statistically insignificant effect. Second, the fact that our review team focused on studies published since 2010 means that interventions being implemented during this period may not resemble the interventions being trialled during evaluation of the original intervention. Indeed, this situation was compounded by the profound shortage of implementation evidence for UK initiatives between 2010 and 2018. Qualitative evidence constituted a large part of our recent evidence base and may not necessarily be intervention focused, nor linked to relevant trials. This type of evidence ‘mismatch’ is considered rare; we have previously encountered such a mismatch only when trying to map international RCTs from a Cochrane review against a qualitative research evidence base restricted to the UK and similar health systems. We therefore make the methodological recommendation that the scope of intervention and implementation evidence, or indeed quantitative and qualitative evidence, seeks to be as coterminous as possible so as not to artificially constrain the evidence base. However, we also acknowledge that, by its nature, implementation evidence may need to be more current than the original effectiveness studies.
Value of the PARiHS framework
We were unable to exploit the full value of the PARiHS framework, not through any limitations of the framework itself but because of constraints in the reporting of the individual interventions. Limitations encountered tended to fall into three categories:
-
Published reports did not articulate implementation issues in terms of evidence, context and facilitation or did not cover the range of aspects of these dimensions included in PARiHS (e.g. ‘evidence’ is not limited to research evidence).
-
Published reports covered one or more of these issues but reports were not structured in a way in which such data were straightforward to extract.
-
Published reports focused on implementation at a level that excluded some of the important PARiHS concepts. For example, only a study specifically on organisational aspects included data on organisational culture, whereas leadership issues were almost entirely absent.
This confirms observations previously made in relation to frameworks (i.e. that frameworks derived for use in primary research studies may not represent a good match for the level of granularity sustained by their use in synthesis activities, with syntheses typically covering issues at a broader level of detail). The version of PARiHS that we chose was not the most recent but we believe that limitations in the reporting of implementation in the included studies mean that little would have been gained by using a more refined version of the framework.
We had reviewed a range of candidate frameworks before selecting the PARiHS framework as our eventual choice. Analysis of included literature during the subsequent realist process revealed use of alternative frameworks,98 specifically when exploring implementation issues, notably May et al. s’294 normalisation process model295 and a framework of barriers to and facilitators of quality improvement projects from a systematic review led by Kaplan et al. 296 It is presently unclear whether or not these frameworks would share similar limitations with regard to the granularity of synthesised data or, indeed, if selection of these alternative evaluation ‘lenses’ would have yielded more insightful observations.
Value of the TIDieR-Lite template
In contrast, the TIDieR-Lite framework proved particularly useful both as a means of exploring variation within intervention groups and when seeking to delineate between interventions. It became apparent that several interventions labelled in their own right were also included within other interventions; for example, patient education is a key component in self-management. Similarly, self-management is a key function of much telehealthcare. Specialist clinics may hold a primary function in providing patient education and supporting self-management. Use of the framework therefore revealed the difficulties in attributing an effect to particular interventions and in isolating which components are most essential in delivering an effect. The limitations of the classification of interventions further confirmed the value of moving from an intervention-based approach towards the realist synthesis based on mechanisms. Phenomena such as clinical inertia and the default position, the effects, intended and unintended, of candidacy and the pivotal role of continuity and personalisation of care transcend the seven intervention types and therefore offer more transferable messages.
Implications for service delivery
We have identified the following implications for service delivery:
-
Our findings suggest that some evidence-based interventions may have limited evidence for effectiveness in the UK context. All available evidence and data sources should be considered alongside other relevant factors in deciding which interventions and service models to implement.
-
Implementation of supported self-management programmes reflects an approach that is supported by both theory and empirical evidence. Patients may need to be reassured that they will not be totally unsupported at the end of time-limited interventions.
-
Service delivery would benefit from better description and specification of both interventions and associated implementation strategies. This includes documentation of service delivery in routine practice as well as in research or demonstration projects. The development of standards and auditing of service delivery by the NACR for cardiac rehabilitation appears to be a useful exemplar.
-
Specialist nurses with expertise in heart failure or COPD make a major contribution to implementation of interventions to reduce avoidable admissions. Specialist nurses can work in a variety of settings and service models depending on the local context. They can support evidence- and theory-informed implementation of relevant interventions by, for example, supporting self-management and signposting patients to appropriate community-based services.
-
Many contextual factors operating at the level of the patient and the health system tend to promote referral and possible admission to hospital as the default course of action for people with exacerbations of a chronic disease. In particular, difficulties in navigating between complex and fragmented services need to be addressed if avoidable admissions are to be reduced. The increasing incidence of multimorbidity means that it will be important to ensure that patients are not excluded by inappropriately strict criteria for access to specialist services. Literacy and language issues can also create barriers to patients accessing appropriate services that can reduce their risk of hospital admission.
Implications for research
We have identified the following implications for research:
-
There is a clear mismatch between the international and national evidence base for some interventions designed to reduce avoidable admissions. This can be a barrier to implementation in practice. Although funding of new trials is unlikely to be a priority, research should focus on understanding and interpreting existing evidence and the transferability of findings between different health systems and contexts (including changes in usual care for chronic conditions).
-
Research on effective implementation of interventions and its barriers and facilitators continues to lag behind research on intervention effectiveness. Theory can help to inform design of promising implementation strategies that can be evaluated using appropriate study designs. Depending on the context, evaluation could range from randomised trials to before-and-after studies (preferably controlled) and audits of local or national data. Researchers could consider conducting process evaluations alongside trials in line with the Medical Research Council recommendations for evaluating complex interventions.
-
Health services researchers should be encouraged to provide clear description/reporting of implementation strategies used in their research, using appropriate reporting guidelines and frameworks.
-
Qualitative research is required to investigate patients’ and HCPs’ decision-making around hospital referrals and admissions, including the impact of specific interventions and the current context of pressure on the NHS workforce and resources.
Conclusions
Preventable hospital admissions for chronic cardiovascular and respiratory conditions are common and are costly for both the health service and the patient/family involved. Systematic reviews have identified interventions with strong evidence of effectiveness in reducing such admissions. However, the synthesised evidence may not be supported by evidence of effectiveness in a specific setting or of how best to implement the intervention in routine practice. Our mapping review and supplementary searching indicated that this was the case for some interventions that are widely recommended and employed in the UK health system. The subsequent realist data extraction and synthesis used diverse frameworks and levels of theory to examine how interventions might work and factors that support or hinder their implementation. The TIDieR-Lite framework proved useful in characterising interventions and indicated that interventions with different names often contain the same or overlapping components. The programme theories we developed from the literature were supported to varying degrees by empirical evidence, but all provided valuable insights.
Overall, implementation of interventions to reduce avoidable admissions for cardiovascular and respiratory conditions appears to be favoured by:
-
Support for self-management by patients and their families/carers, including ability to recognise when they need to seek further help.
-
Support for services that signpost patients to consider using less familiar services when appropriate rather than treating GP appointments/referral as the default option.
-
Recognition of possible drivers leading patients to seek admission, for example the need for security and reassurance at a difficult time.
-
Support for GPs and other HCPs to diagnose and refer patients appropriately and with confidence. This includes creation of a supportive background context and set of incentives in the health system.
-
Support for workforce roles, commonly filled by specialist nurses, that promote continuity of care and co-ordination between different services across primary, secondary and community care.
Acknowledgements
We gratefully acknowledge the contributions of the Sheffield Evidence Synthesis Centre public involvement group, which discussed and validated early and subsequent versions of the programme theory. We also acknowledge the invaluable support and input from Dr Susan Baxter, who facilitated the public involvement group, and from Janette Turner and Dr Emma Knowles, who provided topic-specific input into the PPI group meetings. We thank Susan Croft and Janette Turner for their comments on sections of the draft report and the external peer reviewers for their thorough and constructive feedback.
Contributions of authors
Duncan Chambers (https://orcid.org/0000-0002-0154-0469) managed the mapping review and led on analysis of mapping data.
Anna Cantrell (https://orcid.org/0000-0003-0040-9853) led the literature search processes for both the mapping review and the realist synthesis.
Andrew Booth (https://orcid.org/0000-0003-4808-3880) developed the realist synthesis protocol and designed the working methods for the realist synthesis, including the TIDieR-Lite and intervention templates. He also generated the embryonic programme theory, which was refined and finalised by all of the review team.
All team members contributed equally to the analysis and writing of the final report.
Data-sharing statement
No new data have been created in the preparation of this report; therefore, there is nothing available for access and further sharing. All queries should be submitted to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Purdy S. Avoiding Hospital Admissions: What Does the Research Evidence Say?. London: The King’s Fund; 2010.
- National Audit Office . Reducing Emergency Admissions 2018.
- Purdy S, Paranjothy S, Huntley A, Thomas R, Mann M, Huws D, et al. Interventions to Reduce Unplanned Hospital Admission: A Series of Systematic Reviews. Bristol: University of Bristol; 2012.
- Purdey S, Huntley A. Predicting and preventing avoidable hospital admissions: a review. J R Coll Physicians Edinb 2013;43:340-4. https://doi.org/10.4997/JRCPE.2013.415.
- NHS England . Emergency Admissions for Ambulatory Care Sensitive Conditions – Characteristics and Trends at National Level 2014.
- Office of the Legislative Counsel . Patient Protection and Affordable Care Act 2010.
- Wallace E, Smith SM, Fahey T, Roland M. Reducing emergency admissions through community based interventions. BMJ 2016;352. https://doi.org/10.1136/bmj.h6817.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- James KL, Randall NP, Haddaway NR. A methodology for systematic mapping in environmental sciences. Environ Evid 2016;5. https://doi.org/10.1186/s13750-016-0059-6.
- Turner A, Mulla A, Booth A, Aldridge S, Stevens S, Battye F, et al. An evidence synthesis of the international knowledge base for new care models to inform and mobilise knowledge for multispecialty community providers (MCPs). Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0346-x.
- Turner A, Mulla A, Booth A, Aldridge S, Stevens S, Begum M, et al. The international knowledge base for new care models relevant to primary care-led integrated models: a realist synthesis. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06250.
- Booth A, Carroll C. How to build up the actionable knowledge base: the role of ‘best fit’ framework synthesis for studies of improvement in healthcare. BMJ Qual Saf 2015;24:700-8. https://doi.org/10.1136/bmjqs-2014-003642.
- Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-39.
- Carroll C, Booth A, Cooper K. A worked example of ‘best fit’ framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-29.
- Carroll C, Booth A, Leaviss J, Rick J. ‘Best fit’ framework synthesis: refining the method. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-37.
- Rycroft-Malone J, Bucknall T. Models and Frameworks for Implementing Evidence-based Practice: Linking Evidence to Action. Chichester: John Wiley & Sons; 2010.
- Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implement Sci 2008;3. https://doi.org/10.1186/1748-5908-3-1.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Martin C, Vogel C, Hederman L, Smith K, Zarabzadeh A, Grady D, et al. Handbook of Systems and Complexity in Health. New York, NY: Springer; 2012.
- Harzing AW. Publish or Perish 2007. https://harzing.com/resources/publish-or-perish (accessed 27 August 2019).
- Pawson R, Sridharan S, Killoran A, Kelly MP. Evidence-Based Public Health: Effectiveness and Efficiency. Oxford: Oxford University Press; 2010.
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38. https://doi.org/10.1136/bmjqs-2014-003627.
- Booth A, Carroll C. Systematic searching for theory to inform systematic reviews: is it feasible? Is it desirable?. Health Info Libr J 2015;32:220-35. https://doi.org/10.1111/hir.12108.
- Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta-analysis. J Am Coll Cardiol 2016;67:1-12. https://doi.org/10.1016/j.jacc.2015.10.044.
- Anderson L, Taylor RS. Cardiac rehabilitation for people with heart disease: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev 2014;12. https://doi.org/10.1002/14651858.CD011273.pub2.
- Huang K, Liu W, He D, Huang B, Xiao D, Peng Y, et al. Telehealth interventions versus center-based cardiac rehabilitation of coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol 2015;22:959-71. https://doi.org/10.1177/2047487314561168.
- Karmali KN, Davies P, Taylor F, Beswick A, Martin N, Ebrahim S. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev 2014;6. https://doi.org/10.1002/14651858.CD007131.pub3.
- Huntley AL, Johnson R, King A, Morris RW, Purdy S. Does case management for patients with heart failure based in the community reduce unplanned hospital admissions? A systematic review and meta-analysis. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010933.
- Van Spall HGC, Rahman T, Mytton O, Ramasundarahettige C, Ibrahim Q, Kabali C, et al. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis. Eur J Heart Fail 2017;19:1427-43. https://doi.org/10.1002/ejhf.765.
- O’Neill I, Gale C, McCallum A, McIntyre H, Squire I, Cherif M. Impact of mode of delivery of disease management programmes on clinical outcomes among patients following hospitalised heart failure: a systematic review and meta-analysis. Eur J Heart Fail 2017;19:5-601.
- Thomas R, Huntley A, Mann M, Huws D, Paranjothy S, Elwyn G, et al. Specialist clinics for reducing emergency admissions in patients with heart failure: a systematic review and meta-analysis of randomised controlled trials. Heart 2013;99:233-9. https://doi.org/10.1136/heartjnl-2012-302313.
- Coffey A, Mulcahy H, Savage E, Fitzgerald S, Bradley C, Benefield L, et al. Transitional care interventions: relevance for nursing in the community. Public Health Nurs 2017;34:454-60. https://doi.org/10.1111/phn.12324.
- Health Quality Ontario . Ontario health technology assessment series: Effect of early follow-up after hospital discharge on outcomes in patients with heart failure or chronic obstructive pulmonary disease: a systematic review. Ont Health Technol Assess Ser 2017;17:1-37.
- Casimir YE, Williams MM, Liang MY, Pitakmongkolkul S, Slyer JT. The effectiveness of patient-centered self-care education for adults with heart failure on knowledge, self-care behaviors, quality of life, and readmissions: a systematic review. JBI Database System Rev Implement Rep 2014;12:188-262. https://doi.org/10.11124/jbisrir-2014-1438.
- Zarea Gavgani V, Kazemi Majd F, Nosratnejad S, Golmohammadi A, Sadeghi-Bazargani H. The efficacy of written information intervention in reduction of hospital re-admission cost in patients with heart failure; a systematic review and meta-analysis. J Cardiovasc Thorac Res 2015;7:1-5. https://doi.org/10.15171/jcvtr.2015.01.
- Clarke M, Shah A, Sharma U. Systematic review of studies on telemonitoring of patients with congestive heart failure: a meta-analysis. J Telemed Telecare 2011;17:7-14. https://doi.org/10.1258/jtt.2010.100113.
- Gorst SL, Armitage CJ, Brownsell S, Hawley MS. Home telehealth uptake and continued use among heart failure and chronic obstructive pulmonary disease patients: a systematic review. Ann Behav Med 2014;48:323-36. https://doi.org/10.1007/s12160-014-9607-x.
- Graves BA, Ford CD, Mooney KD. Telehealth technologies for heart failure disease management in rural areas: an integrative. Online J Rural Nurs Health Care 2013;13:56-83.
- Inglis SC, Clark RA, Dierckx R, Prieto-Merino D, Cleland JG. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst Rev 2015;10. https://doi.org/10.1002/14651858.CD007228.pub3.
- Kitsiou S, Paré G, Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: an overview of systematic reviews. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4174.
- Klersy C, Boriani G, De Silvestri A, Mairesse GH, Braunschweig F, Scotti V, et al. Effect of telemonitoring of cardiac implantable electronic devices on healthcare utilization: a meta-analysis of randomized controlled trials in patients with heart failure. Eur J Heart Fail 2016;18:195-204. https://doi.org/10.1002/ejhf.470.
- Kotb A, Cameron C, Hsieh S, Wells G. Comparative effectiveness of different forms of telemedicine for individuals with heart failure (HF): a systematic review and network meta-analysis. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0118681.
- Lin MH, Yuan WL, Huang TC, Zhang HF, Mai JT, Wang JF. Clinical effectiveness of telemedicine for chronic heart failure: a systematic review and meta-analysis. J Investig Med 2017;65:899-911. https://doi.org/10.1136/jim-2016-000199.
- Pandor A, Thokala P, Gomersall T, Baalbaki H, Stevens JW, Wang J, et al. Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation. Health Technol Assess 2013;17. https://doi.org/10.3310/hta17320.
- Vassilev I, Rowsell A, Pope C, Kennedy A, O’Cathain A, Salisbury C, et al. Assessing the implementability of telehealth interventions for self-management support: a realist review. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0238-9.
- Harrison CE, Wild K. Using telehealth in the management of hypertension. Nurs Stand 2017;31:44-9. https://doi.org/10.7748/ns.2017.e10618.
- Denford S, Taylor RS, Campbell JL, Greaves CJ. Effective behavior change techniques in asthma self-care interventions: systematic review and meta-regression. Health Psychol 2014;33:577-87. https://doi.org/10.1037/a0033080.
- Marcano Belisario JS, Huckvale K, Greenfield G, Car J, Gunn LH. Smartphone and tablet self management apps for asthma. Cochrane Database Syst Rev 2013;11. https://doi.org/10.1002/14651858.CD010013.pub2.
- Morrison D, Wyke S, Agur K, Cameron EJ, Docking RI, Mackenzie AM, et al. Digital asthma self-management interventions: a systematic review. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.2814.
- Pinnock H, Epiphaniou E, Pearce G, Parke H, Greenhalgh T, Sheikh A, et al. Implementing supported self-management for asthma: a systematic review and suggested hierarchy of evidence of implementation studies. BMC Med 2015;13. https://doi.org/10.1186/s12916-015-0361-0.
- Pinnock H, Parke HL, Panagioti M, Daines L, Pearce G, Epiphaniou E, et al. Systematic meta-review of supported self-management for asthma: a healthcare perspective. BMC Med 2017;15. https://doi.org/10.1186/s12916-017-0823-7.
- Ring N, Jepson R, Hoskins G, Wilson C, Pinnock H, Sheikh A, et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Couns 2011;85:e131-43. https://doi.org/10.1016/j.pec.2011.01.025.
- Ring N, Jepson R, Pinnock H, Wilson C, Hoskins G, Wyke S, et al. Developing novel evidence-based interventions to promote asthma action plan use: a cross-study synthesis of evidence from randomised controlled trials and qualitative studies. Trials 2012;13. https://doi.org/10.1186/1745-6215-13-216.
- Martínez-González NA, Berchtold P, Ullman K, Busato A, Egger M. Integrated care programmes for adults with chronic conditions: a meta-review. Int J Qual Health Care 2014;26:561-70. https://doi.org/10.1093/intqhc/mzu071.
- Baker E, Fatoye F. Clinical and cost effectiveness of nurse-led self-management interventions for patients with copd in primary care: a systematic review. Int J Nurs Stud 2017;71:125-38. https://doi.org/10.1016/j.ijnurstu.2017.03.010.
- Clari M, Matarese M, Ivziku D, De Marinis MG. Self-care of people with chronic obstructive pulmonary disease: a meta-synthesis. Patient 2017;10:407-27. https://doi.org/10.1007/s40271-017-0218-z.
- Harrison SL, Janaudis-Ferreira T, Brooks D, Desveaux L, Goldstein RS. Self-management following an acute exacerbation of COPD: a systematic review. Chest 2015;147:646-61. https://doi.org/10.1378/chest.14-1658.
- Howcroft M, Walters EH, Wood-Baker R, Walters JA. Action plans with brief patient education for exacerbations in chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2016;12. https://doi.org/10.1002/14651858.CD005074.pub4.
- Jonkman NH, Westland H, Trappenburg JC, Groenwold RH, Bischoff EW, Bourbeau J, et al. Do self-management interventions in COPD patients work and which patients benefit most? An individual patient data meta-analysis. Int J Chron Obstruct Pulmon Dis 2016;11:2063-74. https://doi.org/10.2147/COPD.S107884.
- Jordan RE, Majothi S, Heneghan NR, Blissett DB, Riley RD, Sitch AJ, et al. Supported self-management for patients with moderate to severe chronic obstructive pulmonary disease (COPD): an evidence synthesis and economic analysis. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19360.
- Lenferink A, Brusse-Keizer M, van der Valk PD, Frith PA, Zwerink M, Monninkhof EM, et al. Self-management interventions including action plans for exacerbations versus usual care in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2017;8. https://doi.org/10.1002/14651858.CD011682.pub2.
- Wang T, Tan JY, Xiao LD, Deng R. Effectiveness of disease-specific self-management education on health outcomes in patients with chronic obstructive pulmonary disease: an updated systematic review and meta-analysis. Patient Educ Couns 2017;100:1432-46. https://doi.org/10.1016/j.pec.2017.02.026.
- Zwerink M, Brusse-Keizer M, van der Valk PD, Zielhuis GA, Monninkhof EM, van der Palen J, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014;3. https://doi.org/10.1002/14651858.CD002990.pub3.
- Alison JA, McKeough ZJ. Pulmonary rehabilitation for COPD: are programs with minimal exercise equipment effective?. J Thorac Dis 2014;6:1606-14.
- Cox NS, Oliveira CC, Lahham A, Holland AE. Pulmonary rehabilitation referral and participation are commonly influenced by environment, knowledge, and beliefs about consequences: a systematic review using the Theoretical Domains Framework. J Physiother 2017;63:84-93. https://doi.org/10.1016/j.jphys.2017.02.002.
- Jones AW, Taylor A, Gowler H, O’Kelly N, Ghosh S, Bridle C. Systematic review of interventions to improve patient uptake and completion of pulmonary rehabilitation in COPD. ERJ Open Res 2017;3:00089-2016. https://doi.org/10.1183/23120541.00089-2016.
- Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis 2011;8:89-9. https://doi.org/10.1177/1479972310393756.
- Meshe OF, Claydon LS, Bungay H, Andrew S. The relationship between physical activity and health status in patients with chronic obstructive pulmonary disease following pulmonary rehabilitation. Disabil Rehabil 2017;39:746-56. https://doi.org/10.3109/09638288.2016.1161842.
- Moore E, Palmer T, Newson R, Majeed A, Quint JK, Soljak MA. Pulmonary rehabilitation as a mechanism to reduce hospitalizations for acute exacerbations of COPD: a systematic review and meta-analysis. Chest 2016;150:837-59. https://doi.org/10.1016/j.chest.2016.05.038.
- Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2016;12. https://doi.org/10.1002/14651858.CD005305.pub4.
- Steventon A, Bardsley M, Billings J, Dixon J, Doll H, Hirani S, et al. Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial. BMJ 2012;344. https://doi.org/10.1136/bmj.e3874.
- Ross S, Curry N, Goodwin N. Case Management: What it is and How it Can Best be Implemented. London: The King’s Fund; 2011.
- Stokes J, Kristensen SR, Checkland K, Bower P. Effectiveness of multidisciplinary team case management: difference-in-differences analysis. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010468.
- Gowing A, Dickinson C, Gorman T, Robinson L, Duncan R. Patients’ experiences of a multidisciplinary team-led community case management programme: a qualitative study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012019.
- Köpke S, McCleery J. Systematic reviews of case management: too complex to manage?. Cochrane Database Syst Rev 2015;1. https://doi.org/10.1002/14651858.ED000096.
- Kodner DL. Consumer-directed services: lessons and implications for integrated systems of care. Int J Integr Care 2003;3. https://doi.org/10.5334/ijic.80.
- Challis D, Hughes J, Berzins K, Reilly S, Abell J, Stewart K, et al. Implementation of case management in long-term conditions in England: survey and case studies. J Health Serv Res Policy 2011;16:8-13. https://doi.org/10.1258/jhsrp.2010.010078.
- Sridhar M, Taylor R, Dawson S, Roberts NJ, Partridge MR. A nurse led intermediate care package in patients who have been hospitalised with an acute exacerbation of chronic obstructive pulmonary disease. Thorax 2008;63:194-200. https://doi.org/10.1136/thx.2007.077578.
- Gruffydd-Jones K, Richman J, Jones RC, Wang X. A pilot study of identification and case management of high-risk COPD patients in a general practice. Fam Pract 2010;27:494-8. https://doi.org/10.1093/fampra/cmq045.
- Stokes J, Kristensen SR, Checkland K, Cheraghi-Sohi S, Bower P. Does the impact of case management vary in different subgroups of multimorbidity? Secondary analysis of a quasi-experiment. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2475-x.
- Close H, Hancock H, Mason JM, Murphy JJ, Fuat A, de Belder M, et al. ‘It’s Somebody else’s responsibility’ – perceptions of general practitioners, heart failure nurses, care home staff, and residents towards heart failure diagnosis and management for older people in long-term care: a qualitative interview study. BMC Geriatr 2013;13. https://doi.org/10.1186/1471-2318-13-69.
- Van Durme T, Schmitz O, Ces S, Lambert A-S, Billings JR, Anthierens S, et al. Why is case management effective? A realist evaluation of case management for frail, community-dwelling older people: lessons learned from Belgium. Open J Nurs 2016;6:863-80. https://doi.org/10.4236/ojn.2016.610085.
- Brown K, Stainer K, Stewart J, Clacy R, Parker S. Older people with complex long-term health conditions. Their views on the community matron service: a qualitative study. Qual Prim Care 2008;16:409-17.
- Boaden R, Dusheiko M, Gravelle H, Parker S, Pickard S, Roland M, et al. Evaluation of Evercare: Final Report 2006.
- Sheaff R, Boaden R, Sargent P, Pickard S, Gravelle H, Parker S, et al. Impacts of case management for frail elderly people: a qualitative study. J Health Serv Res Policy 2009;14:88-95. https://doi.org/10.1258/jhsrp.2008.007142.
- Russell M, Roe B, Beech R, Russell W. Service developments for managing people with long-term conditions using case management approaches, an example from the UK. Int J Integr Care 2009;9. https://doi.org/10.5334/ijic.303.
- Stokes J, Panagioti M, Alam R, Checkland K, Cheraghi-Sohi S, Bower P. Effectiveness of case management for ‘at risk’ patients in primary care: a systematic review and meta-analysis. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0132340.
- Price-Haywood EG, Petersen H, Burton J, Harden-Barrios J, Adubato M, Roberts M, et al. Outpatient complex case management: health system-tailored risk stratification taxonomy to identify high-cost, high-need patients. J Gen Intern Med 2018;33:1921-7. https://doi.org/10.1007/s11606-018-4616-2.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83:457-502. https://doi.org/10.1111/j.1468-0009.2005.00409.x.
- Gravelle H, Dusheiko M, Sheaff R, Sargent P, Boaden R, Pickard S, et al. Impact of case management (Evercare) on frail elderly patients: controlled before and after analysis of quantitative outcome data. BMJ 2007;334. https://doi.org/10.1136/bmj.39020.413310.55.
- Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord 2006;6. https://doi.org/10.1186/1471-2261-6-43.
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q 1996;74:511-44. https://doi.org/10.2307/3350391.
- Askerud A, Conder J. Patients’ experiences of nurse case management in primary care: a meta-synthesis. Aust J Prim Health 2017;23:420-8. https://doi.org/10.1071/PY17040.
- Van Durme T, Schmitz O, Cès S, Anthierens S, Maggi P, Delye S, et al. A comprehensive grid to evaluate case management’s expected effectiveness for community-dwelling frail older people: results from a multiple, embedded case study. BMC Geriatr 2015;15. https://doi.org/10.1186/s12877-015-0069-1.
- National Collaboration for Integrated Care and Support . Integrated Care and Support: Our Shared Commitment 2013.
- Roland M, Lewis R, Steventon A, Abel G, Adams J, Bardsley M, et al. Case management for at-risk elderly patients in the English integrated care pilots: observational study of staff and patient experience and secondary care utilisation. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.850.
- Goodwin N. Reviewing the evidence on case management: lessons for successful implementation. Int J Integr Care 2011;11. https://doi.org/10.5334/ijic.825.
- Ling T, Brereton L, Conklin A, Newbould J, Roland M. Barriers and facilitators to integrating care: experiences from the English Integrated Care Pilots. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.982.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. https://doi.org/10.1037/0033-295X.84.2.191.
- Hudon C, Chouinard MC, Diadiou F, Lambert M, Bouliane D. Case management in primary care for frequent users of health care services with chronic diseases: a qualitative study of patient and family experience. Ann Fam Med 2015;13:523-8. https://doi.org/10.1370/afm.1867.
- Williams V, Smith A, Chapman L, Oliver D. Community matrons – an exploratory study of patients’ views and experiences. J Adv Nurs 2011;67:86-93. https://doi.org/10.1111/j.1365-2648.2010.05458.x.
- Sandberg M, Jakobsson U, Midlöv P, Kristensson J. Case management for frail older people – a qualitative study of receivers’ and providers’ experiences of a complex intervention. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-14.
- Hudon C, Chouinard MC, Lambert M, Diadiou F, Bouliane D, Beaudin J. Key factors of case management interventions for frequent users of healthcare services: a thematic analysis review. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-017762.
- Gagnon AJ, Schein C, McVey L, Bergman H. Randomized controlled trial of nurse case management of frail older people. J Am Geriatr Soc 1999;47:1118-24. https://doi.org/10.1111/j.1532-5415.1999.tb05238.x.
- Chapman L, Smith A, Williams V, Oliver D. Community matrons: primary care professionals’ views and experiences. J Adv Nurs 2009;65:1617-25. https://doi.org/10.1111/j.1365-2648.2009.05002.x.
- McEvoy P, Escott D, Bee P. Case management for high-intensity service users: towards a relational approach to care co-ordination. Health Soc Care Community 2011;19:60-9. https://doi.org/10.1111/j.1365-2524.2010.00949.x.
- Reilly S, Hughes J, Challis D. Case management for long-term conditions: implementation and processes. Ageing Soc 2010;30:125-55. https://doi.org/10.1017/S0144686X09990183.
- Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med 2013;44:717-29. https://doi.org/10.1016/j.jemermed.2012.08.035.
- Huntley A, Lasserson D, Wye L, Morris R, Checkland K, England H, et al. Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-004746.
- Joo JY, Liu MF. Case management effectiveness in reducing hospital use: a systematic review. Int Nurs Rev 2017;64:296-308. https://doi.org/10.1111/inr.12335.
- Melton LD, Foreman C, Scott E, McGinnis M, Cousins M. Prioritized post-discharge telephonic outreach reduces hospital readmissions for select high-risk patients. Am J Manag Care 2012;18:838-44.
- Chow SK, Wong FK. A randomized controlled trial of a nurse-led case management programme for hospital-discharged older adults with co-morbidities. J Adv Nurs 2014;70:2257-71. https://doi.org/10.1111/jan.12375.
- Joo JY, Liu MF. Experiences of case management with chronic illnesses: a qualitative systematic review. Int Nurs Rev 2018;65:102-13. https://doi.org/10.1111/inr.12429.
- Joo JY, Huber DL. Barriers in Case managers’ roles: a qualitative systematic review. West J Nurs Res 2018;40:1522-42. https://doi.org/10.1177/0193945917728689.
- Lynch JP, Forman SA, Graff S, Gunby MC. High-risk population health management – achieving improved patient outcomes and near-term financial results. Am J Manag Care 2000;6:781-91.
- Swanson J, Weissert WG. Case Managers for high-risk, high-cost patients as agents and street-level bureaucrats. Med Care Res Rev 2018;75:527-61. https://doi.org/10.1177/1077558717727116.
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. Understanding new models of integrated care in developed countries: a systematic review. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06290.
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA 2002;288:2469-75. https://doi.org/10.1001/jama.288.19.2469.
- Lawson PJ, Flocke SA. Teachable moments for health behavior change: a concept analysis. Patient Educ Couns 2009;76:25-30. https://doi.org/10.1016/j.pec.2008.11.002.
- Kongstvedt P. The Managed Health Care Handbook. Aspen, CO: Aspen Publishers; 2001.
- National Institute for Health and Care Excellence (NICE) . Management of Chronic Heart Failure in Adults in Primary and Secondary Care (Clinical Guidance 108) 2010.
- Anderson L, Brown JP, Clark AM, Dalal H, Rossau HK, Bridges C, et al. Patient education in the management of coronary heart disease. Cochrane Database Syst Rev 2017;6. https://doi.org/10.1002/14651858.CD008895.pub3.
- Das LM, Murray J, Ajmal M, Wolstenholme N, Jayaratnam A. Are acute asthma admissions preventable with improved patient education?. Eur Respir J 2013;42.
- Howard C, Dupont S. ‘The COPD breathlessness manual’: a randomised controlled trial to test a cognitive–behavioural manual versus information booklets on health service use, mood and health status, in patients with chronic obstructive pulmonary disease. NPJ Prim Care Respir Med 2014;24. https://doi.org/10.1038/npjpcrm.2014.76.
- Steventon A, Tunkel S, Blunt I, Bardsley M. Effect of telephone health coaching (Birmingham OwnHealth) on hospital use and associated costs: cohort study with matched controls. BMJ 2013;347. https://doi.org/10.1136/bmj.f4585.
- Fry M, McLachlan S, Purdy S, Sanders T, Kadam UT, Chew-Graham CA. The implications of living with heart failure; the impact on everyday life, family support, co-morbidities and access to healthcare: a secondary qualitative analysis. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0537-5.
- Glogowska M, Simmonds R, McLachlan S, Cramer H, Sanders T, Johnson R, et al. Managing patients with heart failure: a qualitative study of multidisciplinary teams with specialist heart failure nurses. Ann Fam Med 2015;13:466-71. https://doi.org/10.1370/afm.1845.
- Simmonds R, Glogowska M, McLachlan S, Cramer H, Sanders T, Johnson R, et al. Unplanned admissions and the organisational management of heart failure: a multicentre ethnographic, qualitative study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-007522.
- Glogowska M, Simmonds R, McLachlan S, Cramer H, Sanders T, Johnson R, et al. ‘Sometimes we can’t fix things’: a qualitative study of health care professionals’ perceptions of end of life care for patients with heart failure. BMC Palliat Care 2016;15. https://doi.org/10.1186/s12904-016-0074-y.
- Halpin D, Hyland M, Blake S, Seamark C, Pinnuck M, Ward D, et al. Understanding fear and anxiety in patients at the time of an exacerbation of chronic obstructive pulmonary disease: a qualitative study. JRSM Open 2015;6. https://doi.org/10.1177/2054270415614543.
- Risør MB, Spigt M, Iversen R, Godycki-Cwirko M, Francis N, Altiner A, et al. The complexity of managing COPD exacerbations: a grounded theory study of European general practice. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003861.
- Jones RC, Hyland ME, Hanney K, Erwin J. A qualitative study of compliance with medication and lifestyle modification in chronic obstructive pulmonary disease (COPD). Prim Care Respir J 2004;13:149-54. https://doi.org/10.1016/j.pcrj.2004.05.006.
- Bury M. Chronic illness as biographical disruption. Sociol Health Illn 1982;4:167-82. https://doi.org/10.1111/1467-9566.ep11339939.
- Morris RL, Sanders C, Kennedy AP, Rogers A. Shifting priorities in multimorbidity: a longitudinal qualitative study of patient’s prioritization of multiple conditions. Chronic Illn 2011;7:147-61. https://doi.org/10.1177/1742395310393365.
- Rolland JS. Chronic illness and the life cycle: a conceptual framework. Fam Process 1987;26:203-21. https://doi.org/10.1111/j.1545-5300.1987.00203.x.
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1-7. https://doi.org/10.1207/S15324796ABM2601_01.
- Morrow S, Daines L, Wiener-Ogilvie S, Steed L, McKee L, Caress AL, et al. Exploring the perspectives of clinical professionals and support staff on implementing supported self-management for asthma in UK general practice: an IMP2ART qualitative study. NPJ Prim Care Respir Med 2017;27. https://doi.org/10.1038/s41533-017-0041-y.
- Kennedy A, Bower P, Reeves D, Blakeman T, Bowen R, Chew-Graham C, et al. Implementation of self management support for long term conditions in routine primary care settings: cluster randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.f2882.
- Bucknall CE, Miller G, Lloyd SM, Cleland J, McCluskey S, Cotton M, et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ 2012;344. https://doi.org/10.1136/bmj.e1060.
- Patel N, Jones P, Adamson V, Spiteri M, Kinmond K. Chronic obstructive pulmonary disease patients’ experiences of an enhanced self-management model of care. Qual Health Res 2016;26:568-77. https://doi.org/10.1177/1049732315573013.
- Ring N, Booth H, Wilson C, Hoskins G, Pinnock H, Sheikh A, et al. The ‘vicious cycle’ of personalised asthma action plan implementation in primary care: a qualitative study of patients and health professionals’ views. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0352-4.
- Roberts NJ, Younis I, Kidd L, Partridge MR. Barriers to the implementation of self management support in long term lung conditions. London J Prim Care 2012;5:35-47. https://doi.org/10.1080/17571472.2013.11493370.
- Hoskins G, Williams B, Abhyankar P, Donnan P, Duncan E, Pinnock H, et al. Achieving Good Outcomes for Asthma Living (GOAL): mixed methods feasibility and pilot cluster randomised controlled trial of a practical intervention for eliciting, setting and achieving goals for adults with asthma. Trials 2016;17. https://doi.org/10.1186/s13063-016-1684-7.
- Johnson-Warrington V, Rees K, Gelder C, Morgan MD, Singh SJ. Can a supported self-management program for COPD upon hospital discharge reduce readmissions? A randomized controlled trial. Int J Chron Obstruct Pulmon Dis 2016;11:1161-9. https://doi.org/10.2147/COPD.S91253.
- Dritsaki M, Johnson-Warrington V, Mitchell K, Singh S, Rees K. An economic evaluation of a self-management programme of activity, coping and education for patients with chronic obstructive pulmonary disease. Chron Respir Dis 2016;13:48-56. https://doi.org/10.1177/1479972315619578.
- Greaves CJ, Wingham J, Deighan C, Doherty P, Elliott J, Armitage W, et al. Optimising self-care support for people with heart failure and their caregivers: development of the Rehabilitation Enablement in Chronic Heart Failure (REACH-HF) intervention using intervention mapping. Pilot Feasibility Stud 2016;2. https://doi.org/10.1186/s40814-016-0075-x.
- Ogunbayo OJ, Russell S, Newham JJ, Heslop-Marshall K, Netts P, Hanratty B, et al. Understanding the factors affecting self-management of COPD from the perspectives of healthcare practitioners: a qualitative study. NPJ Prim Care Respir Med 2017;27. https://doi.org/10.1038/s41533-017-0054-6.
- Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, Haywood P, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2003;1. https://doi.org/10.1002/14651858.CD001117.
- Scottish Intercollegiate Guidelines Network . British guideline on the management of asthma: 2014 update. Thorax 2014;69:i1-192.
- Jonkman NH, Westland H, Groenwold RH, Ågren S, Atienza F, Blue L, et al. Do self-management interventions work in patients with heart failure? An individual patient data meta-analysis. Circulation 2016;133:1189-98. https://doi.org/10.1161/CIRCULATIONAHA.115.018006.
- McLean S, Chandler D, Nurmatov U, Liu J, Pagliari C, Car J, et al. Telehealthcare for asthma. Cochrane Database Syst Rev 2010;10. https://doi.org/10.1002/14651858.CD007717.pub2.
- Crundall-Goode A, Goode KM. Using telehealth for heart failure: barriers, pitfalls and nursing service models. Br J Cardiac Nurs 2014;9:396-40. https://doi.org/10.12968/bjca.2014.9.8.396.
- Fairbrother P, Pinnock H, Hanley J, McCloughan L, Sheikh A, Pagliari C, et al. TELESCOT programme team . Continuity, but at what cost? The impact of telemonitoring COPD on continuities of care: a qualitative study. Prim Care Respir J 2012;21:322-8. https://doi.org/10.4104/pcrj.2012.00068.
- Fairbrother P, Pinnock H, Hanley J, McCloughan L, Sheikh A, Pagliari C, et al. Exploring telemonitoring and self-management by patients with chronic obstructive pulmonary disease: a qualitative study embedded in a randomized controlled trial. Patient Educ Couns 2013;93:403-10. https://doi.org/10.1016/j.pec.2013.04.003.
- Fairbrother P, Ure J, Hanley J, McCloughan L, Denvir M, Sheikh A, et al. Telescot programme team . Telemonitoring for chronic heart failure: the views of patients and healthcare professionals – a qualitative study. J Clin Nurs 2014;23:132-44. https://doi.org/10.1111/jocn.12137.
- Gale N, Sultan H. Telehealth as ‘peace of mind’: embodiment, emotions and the home as the primary health space for people with chronic obstructive pulmonary disorder. Health Place 2013;21:140-7. https://doi.org/10.1016/j.healthplace.2013.01.006.
- Jones MI, Greenfield SM, Bray EP, Baral-Grant S, Hobbs FD, Holder R, et al. Patients’ experiences of self-monitoring blood pressure and self-titration of medication: the TASMINH2 trial qualitative study. Br J Gen Pract 2012;62:e135-42. https://doi.org/10.3399/bjgp12X625201.
- Jones MI, Greenfield SM, Bray EP, Hobbs FR, Holder R, Little P, et al. Patient self-monitoring of blood pressure and self-titration of medication in primary care: the TASMINH2 trial qualitative study of health professionals’ experiences. Br J Gen Pract 2013;63:e378-85. https://doi.org/10.3399/bjgp13X668168.
- Ure J, Pinnock H, Hanley J, Kidd G, McCall Smith E, Tarling A, et al. Piloting tele-monitoring in COPD: a mixed methods exploration of issues in design and implementation. Prim Care Respir J 2012;21:57-64. https://doi.org/10.4104/pcrj.2011.00065.
- Cafazzo JA, Seto E, Jadad AR. Qualitative studies enrich telemonitoring research, practice, and technology design. Prim Care Respir J 2012;21:10-1. https://doi.org/10.4104/pcrj.2012.00023.
- Williams V, Price J, Hardinge M, Tarassenko L, Farmer A. Using a mobile health application to support self-management in COPD: a qualitative study. Br J Gen Pract 2014;64:e392-400. https://doi.org/10.3399/bjgp14X680473.
- Salisbury C, Thomas C, O’Cathain A, Rogers A, Pope C, Yardley L, et al. TElehealth in CHronic disease: mixed-methods study to develop the TECH conceptual model for intervention design and evaluation. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006448.
- Pope C, Rowsell A, O’Cathain A, Brownsell S. For Want of Evidence: A Meta-review of Home-based Telehealth for the Management of Long-term Conditions. Findings from the Evidence Synthesis. Bristol: University of Bristol; 2010.
- Rowsell AC, Pope C, O’Cathain A. Briefing Report on Evidence from Systematic Reviews of Telehealth for and Computerised Web-Based Interventions for Depression and Mental Health Problems 2011.
- Sanders C, Rogers A, Bowen R, Bower P, Hirani S, Cartwright M, et al. Exploring barriers to participation and adoption of telehealth and telecare within the Whole System Demonstrator trial: a qualitative study. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-220.
- Lluch M. Empowering PATIENTS through ICT, organisational impact on healthcare systems in England and Scotland. Commun Strat 2011;83:37-58.
- Green CA, Johnson KM, Yarborough BJ. Seeking, delaying, and avoiding routine health care services: patient perspectives. Am J Health Promot 2014;28:286-93. https://doi.org/10.4278/ajhp.120702-QUAL-318.
- Goode KM, Crundall-Goode A, Barrett DI. Measuring the effectiveness of home telemonitoring. Br J Healthc Management 2014;20:165-71. https://doi.org/10.12968/bjhc.2014.20.4.165.
- Bower P, Cartwright M, Hirani SP, Barlow J, Hendy J, Knapp M, et al. A comprehensive evaluation of the impact of telemonitoring in patients with long-term conditions and social care needs: protocol for the whole systems demonstrator cluster randomised trial. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-184.
- Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K, et al. Home telehealth for chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Telemed Telecare 2010;16:120-7. https://doi.org/10.1258/jtt.2009.090812.
- Paré G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inform Assoc 2007;14:269-77. https://doi.org/10.1197/jamia.M2270.
- Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev 2010;8. https://doi.org/10.1002/14651858.CD007228.pub2.
- Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, et al. Telemonitoring in patients with heart failure. N Engl J Med 2010;363:2301-9. https://doi.org/10.1056/NEJMoa1010029.
- Bekelman DB, Plomondon ME, Carey EP, Sullivan MD, Nelson KM, Hattler B, et al. Primary results of the Patient-Centered Disease Management (PCDM) for Heart Failure Study: a randomized clinical trial. JAMA Intern Med 2015;175:725-32. https://doi.org/10.1001/jamainternmed.2015.0315.
- Blum K, Gottlieb SS. The effect of a randomized trial of home telemonitoring on medical costs, 30-day readmissions, mortality, and health-related quality of life in a cohort of community-dwelling heart failure patients. J Card Fail 2014;20:513-21. https://doi.org/10.1016/j.cardfail.2014.04.016.
- Inglis SC, Clark RA, McAlister FA, Stewart S, Cleland JG. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: Abridged Cochrane Review. Eur J Heart Fail 2011;13:1028-40. https://doi.org/10.1093/eurjhf/hfr039.
- Peirce SC, Hardisty AR, Preece AD, Elwyn G. Designing and implementing telemonitoring for early detection of deterioration in chronic disease: defining the requirements. Health Informatics J 2011;17:173-90. https://doi.org/10.1177/1460458211409717.
- British Association for Cardiovascular Prevention and Rehabilitation . BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation 2017.
- Devi R, Carpenter C, Powell J, Singh S. Exploring the experience of using a web-based cardiac rehabilitation programme in a primary care angina population: a qualitative study. Int J Ther Rehabil 2014;21:434-40. https://doi.org/10.12968/ijtr.2014.21.9.434.
- Houchen L, Watt A, Boyce S, Singh S. A pilot study to explore the effectiveness of ‘early’ rehabilitation after a hospital admission for chronic heart failure. Physiother Theory Pract 2012;28:355-8. https://doi.org/10.3109/09593985.2011.621015.
- Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016;1. https://doi.org/10.1002/14651858.CD001800.pub3.
- Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJ, Dalal H, et al. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev 2014;4. https://doi.org/10.1002/14651858.CD003331.pub4.
- West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 2012;98:637-44. https://doi.org/10.1136/heartjnl-2011-300302.
- West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT). Heart 2013;99. https://doi.org/10.1136/heartjnl-2012-302961.
- Doherty P, Lewin R. The RAMIT trial, a pragmatic RCT of cardiac rehabilitation versus usual care: what does it tell us?. Heart 2012;98:605-6. https://doi.org/10.1136/heartjnl-2012-301728.
- Wood D. Is cardiac rehabilitation fit for purpose in the NHS: maybe not. Heart 2012;98:607-8. https://doi.org/10.1136/heartjnl-2012-301811.
- Witham MD, Fulton RL, Greig CA, Johnston DW, Lang CC, van der Pol M, et al. Efficacy and cost of an exercise program for functionally impaired older patients with heart failure: a randomized controlled trial. Circ Heart Fail 2012;5:209-16. https://doi.org/10.1161/CIRCHEARTFAILURE.111.963132.
- National Audit of Cardiac Rehabilitation (NACR) . Annual Statistical Report 2017 2017.
- Al Quait A, Doherty P, Gutacker N, Mills J. In the modern era of percutaneous coronary intervention: is cardiac rehabilitation engagement purely a patient or a service level decision?. Eur J Prev Cardiol 2017;24:1351-7. https://doi.org/10.1177/2047487317717064.
- Clark AM, Whelan HK, Barbour R, MacIntyre PD. A realist study of the mechanisms of cardiac rehabilitation. J Adv Nurs 2005;52:362-71. https://doi.org/10.1111/j.1365-2648.2005.03601.x.
- Devi R, Powell J, Singh S. A web-based program improves physical activity outcomes in a primary care angina population: randomized controlled trial. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3340.
- National Institute for Health and Care Excellence (NICE) . Secondary Prevention in Primary and Secondary Care for Patients Following a Myocardial Infarction (Clinical Guidance 172) 2013.
- Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ 2015;351. https://doi.org/10.1136/bmj.h5000.
- Department of Health and Social Care . Cardiac Rehabilitation Commissioning Pack 2010.
- British Lung Foundation . Pulmonary Rehabilitation or PR 2018. www.blf.org.uk/support-for-you/keep-active/pulmonary-rehabilitation (accessed 20 March 2018).
- McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015;2. https://doi.org/10.1002/14651858.CD003793.pub3.
- Bolton CE, Bevan-Smith EF, Blakey JD, Crowe P, Elkin SL, Garrod R, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults: accredited by NICE. Thorax 2013;68:ii1-30. https://doi.org/10.1136/thoraxjnl-2013-203808.
- Casey D, Murphy K, Cooney A, Mee L. Developing a structured education programme for clients with COPD. Br J Community Nurs 2011;16:231-7. https://doi.org/10.12968/bjcn.2011.16.5.231.
- Casey D, Murphy K, Cooney A, Devane D, McCarthy B, Kirwan C, et al. A cluster randomised controlled trial evaluating the effectiveness of a structured pulmonary rehabilitation education programme for improving the health status of people with chronic obstructive pulmonary disease (COPD): the prince study. Am J Respir Crit Car Med 2012. https://doi.org/10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A2400.
- Casey D, Murphy K, Devane D, Cooney A, McCarthy B, Mee L, et al. The effectiveness of a structured education pulmonary rehabilitation programme for improving the health status of people with moderate and severe chronic obstructive pulmonary disease in primary care: the PRINCE cluster randomised trial. Thorax 2013;68:922-8. https://doi.org/10.1136/thoraxjnl-2012-203103.
- Easthaugh S, Farmer J. Sustained health behaviour: an OT led community pulmonary rehabilitation programme. Br J Occup Ther 2016;79:21-2.
- Harrison SL, Robertson N, Apps L, M CS, Morgan MD, Singh SJ. ‘We are not worthy’ – understanding why patients decline pulmonary rehabilitation following an acute exacerbation of COPD. Disabil Rehabil 2015;37:750-6. https://doi.org/10.3109/09638288.2014.939770.
- Greening NJ, Williams JE, Hussain SF, Harvey-Dunstan TC, Bankart MJ, Chaplin EJ, et al. An early rehabilitation intervention to enhance recovery during hospital admission for an exacerbation of chronic respiratory disease: randomised controlled trial. BMJ 2014;349. https://doi.org/10.1136/bmj.g4315.
- Waterhouse JC, Walters SJ, Oluboyede Y, Lawson RA. A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation, followed by telephone or conventional follow-up. Health Technol Assess 2010;14. https://doi.org/10.3310/hta14060.
- Graves J, Sandrey V, Graves T, Smith DL. Effectiveness of a group opt-in session on uptake and graduation rates for pulmonary rehabilitation. Chron Respir Dis 2010;7:159-64. https://doi.org/10.1177/1479972310379537.
- Chaplin E, Hewitt S, Apps L, Edwards K, Brough C, Glab A, et al. An interactive web-based pulmonary rehabilitation programme: a randomised controlled feasibility trial. Eur Respir J 2016;48. https://doi.org/10.1183/13993003.congress-2016.PA2064.
- Faulkner J, Walshaw E, Campbell J, Jones R, Taylor R, Price D, et al. The feasibility of recruiting patients with early COPD to a pilot trial assessing the effects of a physical activity intervention. Prim Care Respir J 2010;19:124-30. https://doi.org/10.4104/pcrj.2010.00008.
- Santus P, Bassi L, Radovanovic D, Airoldi A, Raccanelli R, Triscari F, et al. Pulmonary rehabilitation in COPD: a reappraisal (2008–2012). Pulm Med 2013;2013. https://doi.org/10.1155/2013/374283.
- Foster F, Piggott R, Riley L, Beech R. Working with primary care clinicians and patients to introduce strategies for increasing referrals for pulmonary rehabilitation. Prim Health Care Res Dev 2016;17:226-37. https://doi.org/10.1017/S1463423615000286.
- Bentsen SB, Wentzel-Larsen T, Henriksen AH, Rokne B, Wahl AK. Self-efficacy as a predictor of improvement in health status and overall quality of life in pulmonary rehabilitation – an exploratory study. Patient Educ Couns 2010;81:5-13. https://doi.org/10.1016/j.pec.2009.11.019.
- Lox CL, Freehill AJ. Impact of pulmonary rehabilitation on self-efficacy, quality of life, and exercise tolerance. Rehabil Psychol 1999;44. https://doi.org/10.1037/0090-5550.44.2.208.
- Hogg L, Grant A, Garrod R, Fiddler H. People with COPD perceive ongoing, structured and socially supportive exercise opportunities to be important for maintaining an active lifestyle following pulmonary rehabilitation: a qualitative study. J Physiother 2012;58:189-95. https://doi.org/10.1016/S1836-9553(12)70110-8.
- Levy AR, Matata B, Pilsworth S, Mcgonigle A, Wigelsworth L, Jones L, et al. An intervention for pulmonary rehabilitators to develop a social identity for patients attending exercise rehabilitation: a feasibility and pilot randomised control trial protocol. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-018-0238-z.
- Lewis R, Cramp F. Facilitators and barriers to exercise maintenance in chronic obstructive pulmonary disease: patient views. Physiotherapy Ireland 2010;31:19-24.
- Steiner MC, Lowe D, Beckford K, Blakey J, Bolton CE, Elkin S, et al. Socioeconomic deprivation and the outcome of pulmonary rehabilitation in England and Wales. Thorax 2017;72:530-7. https://doi.org/10.1136/thoraxjnl-2016-209376.
- Moore L, Hogg L, White P. Acceptability and feasibility of pulmonary rehabilitation for COPD: a community qualitative study. Prim Care Respir J 2012;21:419-24. https://doi.org/10.4104/pcrj.2012.00086.
- Lewis A, Bruton A, Donovan-Hall M. Uncertainty prior to pulmonary rehabilitation in primary care: a phenomenological qualitative study in patients with chronic obstructive pulmonary disease. Chron Respir Dis 2014;11:173-80. https://doi.org/10.1177/1479972314539981.
- Hayton C, Clark A, Olive S, Browne P, Galey P, Knights E, et al. Barriers to pulmonary rehabilitation: characteristics that predict patient attendance and adherence. Respir Med 2013;107:401-7. https://doi.org/10.1016/j.rmed.2012.11.016.
- Dean SC, Kerry SM, Khong TK, Kerry SR, Oakeshott P. Evaluation of a specialist nurse-led hypertension clinic with consultant backup in two inner city general practices: randomized controlled trial. Fam Pract 2014;31:172-9. https://doi.org/10.1093/fampra/cmt074.
- Gillett K, Lippiett K, Astles C, Longstaff J, Orlando R, Lin SX, et al. Managing complex respiratory patients in the community: an evaluation of a pilot integrated respiratory care service. BMJ Open Respir Res 2016;3. https://doi.org/10.1136/bmjresp-2016-000145.
- Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010;3. https://doi.org/10.1002/14651858.CD005182.pub4.
- Drennan VM, Goodman C. Sustaining innovation in the health care workforce: a case study of community nurse consultant posts in England. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-200.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Clark C, Smith L, Harding G, Taylor R, Campbell J. Nurse led hypertension clinics: evolving ahead of the evidence?. J Hum Hypertens 2011;25:625-36. https://doi.org/10.1038/jhh.2011.74.
- Flood-Page P. Comparing community models of COPD care. Br J Healthc Management 2016;22:355-9. https://doi.org/10.12968/bjhc.2016.22.7.355.
- MacKenzie E, Smith A, Angus N, Menzies S, Brulisauer F, Leslie SJ. Mixed-method exploratory study of general practitioner and nurse perceptions of a new community based nurse-led heart failure service. Rural Remote Health 2010;10.
- Kosteli MC, Heneghan NR, Roskell C, Williams SE, Adab P, Dickens AP, et al. Barriers and enablers of physical activity engagement for patients with COPD in primary care. Int J Chron Obstruct Pulmon Dis 2017;12:1019-31. https://doi.org/10.2147/COPD.S119806.
- Sarran C, Halpin D, Levy ML, Prigmore S, Sachon P. A retrospective study of the impact of a telephone alert service (Healthy Outlook) on hospital admissions for patients with chronic obstructive pulmonary disease. NPJ Prim Care Respir Med 2014;24. https://doi.org/10.1038/npjpcrm.2014.80.
- Annandale J, Hurlin C, Lewis K. Reducing COPD admissions with a specialist chronic disease management team. Nurs Times 2009;105.
- Bades A. Effective management of COPD. J Community Nurs 2012;26:4-8.
- Hunt V, Anderson D, Lowrie R. Specialist domiciliary pharmacy intervention may reduce exacerbation frequency and hospitalisation in patients with severe chronic obstructive pulmonary disease. Thorax 2016;71. https://doi.org/10.1136/thoraxjnl-2016-209333.287.
- Sinclair AJ, Conroy SP, Davies M, Bayer AJ. Post-discharge home-based support for older cardiac patients: a randomised controlled trial. Age Ageing 2005;34:338-43. https://doi.org/10.1093/ageing/afi116.
- Shepperd S, Iliffe S, Doll HA, Clarke MJ, Kalra L, Wilson AD, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev 2016;9. https://doi.org/10.1002/14651858.CD007491.pub2.
- Gonçalves-Bradley DC, Iliffe S, Doll HA, Broad J, Gladman J, Langhorne P, et al. Early discharge hospital at home. Cochrane Database Syst Rev 2017;6. https://doi.org/10.1002/14651858.CD000356.pub4.
- Jeppesen E, Brurberg KG, Vist GE, Wedzicha JA, Wright JJ, Greenstone M, et al. Hospital at home for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012;5. https://doi.org/10.1002/14651858.CD003573.pub2.
- Wong CX, Carson KV, Smith BJ. Home care by outreach nursing for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012;4. https://doi.org/10.1002/14651858.CD000994.pub3.
- Kaczorowski J, Del Grande C, Nadeau-Grenier V. Community-based programs to improve prevention and management of hypertension: recent Canadian experiences, challenges, and opportunities. Can J Cardiol 2013;29:571-8. https://doi.org/10.1016/j.cjca.2013.02.011.
- Roberts JA, Maslin TK, Bakerly ND. Development of an integrated chronic obstructive pulmonary disease service model in an inner-city region in the UK: initial findings and 12-month results. Prim Care Respir J 2010;19:390-7. https://doi.org/10.4104/pcrj.2010.00071.
- Williams G, Akroyd K, Burke L. Evaluation of the transitional care model in chronic heart failure. Br J Nurs 2010;19:1402-7. https://doi.org/10.12968/bjon.2010.19.22.1402.
- Ghosh S, O’Kelly N, Roberts E-J, Barker C, Swift J. Combined interventions for COPD admissions within an urban setting. Br J Healthc Management 2016;22:123-31. https://doi.org/10.12968/bjhc.2016.22.3.123.
- Wilkinson T, North M, Bourne SC. Reducing hospital admissions and improving the diagnosis of COPD in Southampton City: methods and results of a 12-month service improvement project. NPJ Prim Care Respir Med 2014;24. https://doi.org/10.1038/npjpcrm.2014.35.
- Cope K, Fowler L, Pogson Z. Developing a specialist-nurse-led ‘COPD in-reach service’. Br J Nurs 2015;24:441-5. https://doi.org/10.12968/bjon.2015.24.8.441.
- Feltner C, Jones CD, Cené CW, Zheng ZJ, Sueta CA, Coker-Schwimmer EJ, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med 2014;160:774-84. https://doi.org/10.7326/M14-0083.
- Vedel I, Khanassov V. Transitional care for patients with congestive heart failure: a systematic review and meta-analysis. Ann Fam Med 2015;13:562-71. https://doi.org/10.1370/afm.1844.
- Albert NM. A systematic review of transitional-care strategies to reduce rehospitalization in patients with heart failure. Heart Lung 2016;45:100-13. https://doi.org/10.1016/j.hrtlng.2015.12.001.
- Denyer D, Tranfield D, Buchanan DA, Bryman A. The SAGE Handbook of Organizational Research Methods. London: Sage Publications Ltd; 2009.
- NHS England . New Care Models n.d. www.england.nhs.uk/new-care-models/ (accessed 29 September 2019).
- Clark AP, McDougall G, Riegel B, Joiner-Rogers G, Innerarity S, Meraviglia M, et al. Health status and self-care outcomes after an education-support intervention for people with chronic heart failure. J Cardiovasc Nurs 2015;30:S3-1. https://doi.org/10.1097/JCN.0000000000000169.
- Hammond CL, Pinnington LL, Phillips MF. A qualitative examination of inappropriate hospital admissions and lengths of stay. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-44.
- Roberts E, Mays N. Can primary care and community-based models of emergency care substitute for the hospital accident and emergency (A. E) department?. Health Policy 1998;44:191-214. https://doi.org/10.1016/S0168-8510(98)00021-9.
- Enguidanos S. Integrating behavior change theory into geriatric case management practice. Home Health Care Serv Q 2001;20:67-83. https://doi.org/10.1300/J027v20n01_04.
- O’Brien CW, Breland JY, Slightam C, Nevedal A, Zulman DM. Engaging high-risk patients in intensive care coordination programs: the engagement through CARInG framework. Transl Behav Med 2018;8:351-6. https://doi.org/10.1093/tbm/ibx004.
- Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care 2013;13. https://doi.org/10.5334/ijic.886.
- John H, Hale ED, Bennett P, Treharne GJ, Carroll D, Kitas GD. Translating patient education theory into practice: developing material to address the cardiovascular education needs of people with rheumatoid arthritis. Patient Educ Couns 2011;84:123-7. https://doi.org/10.1016/j.pec.2010.06.023.
- Syx RL. The practice of patient education: the theoretical perspective. Orthop Nurs 2008;27:50-4. https://doi.org/10.1097/01.NOR.0000310614.31168.6b.
- EuroMed Info . The Theoretical Basis of Patient Education – Introduction n.d. www.euromedinfo.eu/theoretical-basis-of-patient-education-introduction.html/ (accessed 3 October 2019).
- Ryan P, Sawin KJ. The individual and family self-management Theory: background and perspectives on context, process, and outcomes. Nurs Outlook 2009;57:217-25.e6. https://doi.org/10.1016/j.outlook.2008.10.004.
- Williams GC, McGregor HA, Zeldman A, Freedman ZR, Deci EL. Testing a self-determination theory process model for promoting glycemic control through diabetes self-management. Health Psychol 2004;23:58-66. https://doi.org/10.1037/0278-6133.23.1.58.
- Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care 1999;37:5-14. https://doi.org/10.1097/00005650-199901000-00003.
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health 1998;13:623-49. https://doi.org/10.1080/08870449808407422.
- Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 2002;17:243-52. https://doi.org/10.1046/j.1525-1497.2002.10905.x.
- Wade V, Gray L, Carati C. Theoretical frameworks in telemedicine research. J Telemed Telecare 2017;23:181-7. https://doi.org/10.1177/1357633X15626650.
- Sharma U, Barnett J, Clarke M. Clinical users’ perspective on telemonitoring of patients with long term conditions: understood through concepts of Giddens’s structuration theory & consequence of modernity. Stud Health Technol Inform 2010;160:545-9.
- Giddens A. Central Problems in Social Theory: Action, Structure and Contradiction in Social Analysis. Berkeley, CA: University of California Press; 1980.
- Giddens A. The Consequences of Modernity. Hoboken, NJ: John Wiley & Sons; 2013.
- Shankel EC, Wofford LG. Symptom management theory as a clinical practice model for symptom telemonitoring in chronic disease. J Theory Constr Test 2016;10.
- Asua J, Orruño E, Reviriego E, Gagnon MP. Healthcare professional acceptance of telemonitoring for chronic care patients in primary care. BMC Med Inform Decis Mak 2012;12. https://doi.org/10.1186/1472-6947-12-139.
- Gagnon MP, Orruño E, Asua J, Abdeljelil AB, Emparanza J. Using a modified technology acceptance model to evaluate healthcare professionals’ adoption of a new telemonitoring system. Telemed J E Health 2012;18:54-9. https://doi.org/10.1089/tmj.2011.0066.
- Goud R, van Engen-Verheul M, de Keizer NF, Bal R, Hasman A, Hellemans IM, et al. The effect of computerized decision support on barriers to guideline implementation: a qualitative study in outpatient cardiac rehabilitation. Int J Med Inform 2010;79:430-7. https://doi.org/10.1016/j.ijmedinf.2010.03.001.
- Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999;282:1458-65. https://doi.org/10.1001/jama.282.15.1458.
- Blanchard CM, Courneya KS, Rodgers WM, Fraser SN, Murray TC, Daub B, et al. Is the theory of planned behavior a useful framework for understanding exercise adherence during phase II cardiac rehabilitation?. J Cardiopulm Rehabil 2003;23:29-3. https://doi.org/10.1097/00008483-200301000-00007.
- Grace SL, Evindar A, Kung TN, Scholey PE, Stewart DE. Automatic referral to cardiac rehabilitation. Med Care 2004;42:661-9. https://doi.org/10.1097/01.mlr.0000129901.05299.aa.
- Jeng C, Braun LT. Bandura’s self-efficacy theory: a guide for cardiac rehabilitation nursing practice. J Holist Nurs 1994;12:425-36. https://doi.org/10.1177/089801019401200411.
- Lau-Walker M. A conceptual care model for individualized care approach in cardiac rehabilitation – combining both illness representation and self-efficacy. Br J Health Psychol 2006;11:103-17. https://doi.org/10.1348/135910705X41914.
- Allen JK, Scott LB, Stewart KJ, Young DR. Disparities in women’s referral to and enrollment in outpatient cardiac rehabilitation. J Gen Intern Med 2004;19:747-53. https://doi.org/10.1111/j.1525-1497.2004.30300.x.
- Johnson JE, Weinert C, Richardson JK. Rural residents’ use of cardiac rehabilitation programs. Public Health Nurs 1998;15:288-96. https://doi.org/10.1111/j.1525-1446.1998.tb00352.x.
- Andersen R, Newman J. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc 1973;51:95-124. https://doi.org/10.2307/3349613.
- Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care 1998;7:149-58. https://doi.org/10.1136/qshc.7.3.149.
- Falk Rafael A. Philosophy, science, and theory of human caring as a conceptual framework for guiding community health nursing practice. Advances Nurs Sci 2000;23:34-49. https://doi.org/10.1097/00012272-200012000-00005.
- Watson J. The theory of human caring: retrospective and prospective. Nurs Sci Q 1997;10:50-2. https://doi.org/10.1177/089431849701000114.
- May C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-86.
- Wee SL, Vrijhoef HJ. A conceptual framework for evaluating the conceptualization, implementation and performance of transitional care programmes. J Eval Clin Pract 2015;21:221-8. https://doi.org/10.1111/jep.12292.
- Knecht LA, Gauthier SM, Castro JC, Schmidt RE, Whitaker MD, Zimmerman RS, et al. Diabetes care in the hospital: is there clinical inertia?. J Hosp Med 2006;1:151-60. https://doi.org/10.1002/jhm.94.
- Elwyn G, Scholl I, Tietbohl C, Mann M, Edwards AG, Clay C, et al. ‘Many miles to go . . .’: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-S2-S14.
- Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Self-monitoring and other non-pharmacological interventions to improve the management of hypertension in primary care: a systematic review. Br J Gen Pract 2010;60:e476-88. https://doi.org/10.3399/bjgp10X544113.
- NHS Improvement . A&Amp;E Improvement Programme North Region n.d. https://improvement.nhs.uk/documents/720/ae-improvement-programme-good-practice-in-the-north.pdf (accessed 3 October 2019).
- Hamad MMAA, Connolly VM. Ambulatory emergency care – improvement by design. Clin Med 2018;18:69-74. https://doi.org/10.7861/clinmedicine.18-1-69.
- Phillips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, et al. Clinical inertia. Ann Intern Med 2001;135:825-34. https://doi.org/10.7326/0003-4819-135-9-200111060-00012.
- Smeets M, Van Roy S, Aertgeerts B, Vermandere M, Vaes B. Improving care for heart failure patients in primary care, GPs’ perceptions: a qualitative evidence synthesis. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-013459.
- Egerton-Warburton D, Cullen L, Keijzers G, Fatovich DM. ‘What the hell is water?’ How to use deliberate clinical inertia in common emergency department situations. Emerg Med Australas 2018;30:426-30. https://doi.org/10.1111/1742-6723.12950.
- Mackenzie M, Conway E, Hastings A, Munro M, O’Donnell C. Is ‘candidacy’ a useful concept for understanding journeys through public services? A critical interpretive literature synthesis. Soc Policy Adm 2012;47:806-25. https://doi.org/10.1111/j.1467-9515.2012.00864.x.
- Uijen AA, Bosch M, van den Bosch WJ, Bor H, Wensing M, Schers HJ. Heart failure patients’ experiences with continuity of care and its relation to medication adherence: a cross-sectional study. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-86.
- Vestjens L, Cramm JM, Birnie E, Nieboer AP. Evaluating an integrated primary care approach to improve well-being among frail community-living older people: a theory-guided study protocol. BMC Geriatr 2018;18. https://doi.org/10.1186/s12877-018-0832-1.
- May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, et al. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Serv Res 2007;7. https://doi.org/10.1186/1472-6963-7-148.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q 2010;88:500-59. https://doi.org/10.1111/j.1468-0009.2010.00611.x.
- Hall Aitken . Central Manchester Practice Integrated Care Team Report 2014.
- Beacon A. Practice-integrated care teams – learning for a better future. J Integr Care 2015;23:74-87. https://doi.org/10.1108/JICA-01-2015-0005.
- Hanley J, Pinnock H, Paterson M, McKinstry B. Implementing telemonitoring in primary care: learning from a large qualitative dataset gathered during a series of studies. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-018-0814-6.
- May CR, Finch TL, Cornford J, Exley C, Gately C, Kirk S, et al. Integrating telecare for chronic disease management in the community: what needs to be done?. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-131.
- Condon C, Moloney E, Lane S, Stokes E. Pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: an audit of referral and uptake. Physiother Pract Res 2015;36:115-9. https://doi.org/10.3233/PPR-150058.
Appendix 1 Search strategy for the mapping review
MEDLINE
Databases: Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R).
Date range searched: 1946 to present.
Date searched: September 2017.
Search strategy
-
ambulatory care sensitive condition$.ab,ti. (399)
-
“Ambulatory care sensitive conditions”.kw. (37)
-
ACSC.ab,ti. (210)
-
primary care sensitive condition$.ab,ti. (39)
-
PCSC.ab,ti. (63)
-
exp Angina Pectoris/ (44,306)
-
angina.ab,ti. (51,535)
-
heart failure/or heart failure, diastolic/or heart failure, systolic/ (108,637)
-
((heart or cardiac or myocardial) and fail$).ab,ti. (207,554)
-
Hypertension/ (227,011)
-
hypertension.ab,ti. (347,343)
-
Asthma/ (118,479)
-
asthma$.ab,ti. (143,461)
-
Pulmonary Disease, Chronic Obstructive/ (32,875)
-
(copd or “chronic obstructive pulmonary disease$”).ab,ti. (52,948)
-
Lung Diseases, Obstructive/ (18,640)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 (903,975)
-
Case Management/ (9789)
-
case management.ab,ti. (9810)
-
“specialist clinic$”.ab,ti. (1226)
-
“Drug Utilization Review”/ (3572)
-
((medication or drug) adj3 review$).ab,ti. (7588)
-
self care/or self administration/ (41,630)
-
self-care.ab,ti. (14,579)
-
self-management.ab,ti. (14,098)
-
pulmonary rehabilitation.ab,ti. (2824)
-
Influenza Vaccines/ (20,563)
-
influenza vaccin$.ab,ti. (15,110)
-
flu vaccin$.ab,ti. (1062)
-
Practice Guidelines as Topic/ (104,685)
-
care pathway$.ab,ti. (3000)
-
care guideline$.ab,ti. (1663)
-
Community Health Services/ (30,426)
-
community intervention$.tw. (1653)
-
House Calls/ (3093)
-
home visit$.ab,ti. (7640)
-
Patient Education as Topic/ (81,677)
-
patient education.ab,ti. (15,166)
-
cardiac rehabilitation/or exercise therapy/ (36,370)
-
exercise based cardiac rehabilitation.ab,ti. (169)
-
Telemedicine/ (17,189)
-
telemedicine.ab,ti. (8638)
-
or/18-42 (381,151)
-
17 and 43 (31,399)
-
Patient Admission/ (22,420)
-
(prevent$ or avoid$ or reduc$ or unplanned or unnecessary or unscheduled).ab,ti. (4,125,882)
-
45 and 46 (4775)
-
((prevent$ or avoid$ or reduc$ or unplanned or unnecessary or unscheduled) adj3 admission$).ab,ti. (4908)
-
hospitalization/or patient readmission/ (104,518)
-
46 and 49 (25,222)
-
47 or 48 or 50 (32,244)
-
(implementation or implementing).ab,ti. (230,025)
-
(dissemination or disseminating).ab,ti. (52,450)
-
(research adj2 integration).ab,ti. (589)
-
(transfer$ adj2 knowledge).ab,ti. (2249)
-
barrier$.ab,ti. (237,473)
-
facilitator$.ab,ti. (19,882)
-
sustainability.ab,ti. (15,412)
-
((change or changing) adj (behavio?r or practice)).ab,ti. (2509)
-
(research adj2 utili?ation).ab,ti. (1214)
-
“research into practice”.ab,ti. (783)
-
“knowledge to action”.ab,ti. (559)
-
52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 (529,378)
-
51 or 63 (559,087)
-
44 and 64 (3868)
-
limit 65 to (english language and yr = “2010 -Current”) (1943)
Appendix 2 Publish or Perish searches
Searches conducted in Publish or Perish
2026 results copied into Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and EndNote.
Date range searched: inception to 19 September 2017.
Search date: 19 September 2017.
| Query number | All of the words | Any of the words | Exact phrase | Results retrieved |
|---|---|---|---|---|
| 1 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | logic model | 462 |
| 2 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | logic models | 159 |
| 3 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | program theories | 21 |
| 4 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | program theory | 85 |
| 5 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | programme theory | 38 |
| 6 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | programme theories | 12 |
| 7 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | theory of change | 161 |
| 8 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | theory of action | 129 |
| 9 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | outcomes chain | 3 |
| 10 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | program logic | 86 |
| 11 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | programme logic | 9 |
| 12 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | logical framework | 155 |
| 13 | ambulatory sensitive | preventable unexpected unplanned admissions hospitalisation hospitalization | logical frameworks | 7 |
| 14 | preventable admissions | hospitalisation hospitalization | logic model | 326 |
| 15 | preventable admissions | hospitalisation hospitalization | logic models | 89 |
| 16 | preventable admissions | hospitalisation hospitalization | program theories | 8 |
| 17 | preventable admissions | hospitalisation hospitalization | program theory | 31 |
| 18 | preventable admissions | hospitalisation hospitalization | programme theory | 10 |
| 19 | preventable admissions | hospitalisation hospitalization | programme theories | 7 |
| 20 | preventable admissions | hospitalisation hospitalization | theory of change | 75 |
| 21 | preventable admissions | hospitalisation hospitalization | theory of action | 25 |
| 22 | preventable admissions | hospitalisation hospitalization | outcomes chain | 2 |
| 23 | preventable admissions | hospitalisation hospitalization | program logic | 39 |
| 24 | preventable admissions | hospitalisation hospitalization | programme logic | 6 |
| 25 | preventable admissions | hospitalisation hospitalization | logical framework | 78 |
| 26 | preventable admissions | hospitalisation hospitalization | logical frameworks | 3 |
Appendix 3 Admissions are possible: some realist(ic) scenarios
Scenario 1: self-managing Sarah
After visiting her GP because of breathlessness and a persistent cough, Sarah was diagnosed with COPD. With help from her general practice and community respiratory nurse service, Sarah started a personal self-management plan. Sarah had to give up smoking, take regular exercise, eat a balanced diet and take regular medication. Sarah was also prescribed standby medication to be taken if her symptoms suddenly got worse (exacerbation). She was worried that the standby medication might be risky but she knew she could always phone the community nurse service for advice or, if necessary, call NHS 111. After 3 months on the plan, Sarah’s COPD is getting slowly worse but she increases her dose of regular medication as advised by the plan and her symptoms return to their previous level after a couple of days. So far, Sarah has not had to use her standby medication but she feels confident to do so if necessary rather than go straight to A&E.
-
Is the scenario realistic? Would you change anything about how it is written?
-
From Sarah’s perspective what might make it easier or more difficult for her to follow her self-management plan?
Scenario 2: case management for Kareem
Kareem has recently been in hospital because of a serious heart problem. Now that he is back at home, his care is co-ordinated by Mark, a community-based specialist nurse. Mark acts as a case manager for Kareem. Mark visits Kareem regularly at home to talk about his condition and to check his medication. Mark also keeps in touch with Kareem’s general practice, so that he does not have to go there so often. Kareem is ultimately under the care of a specialist at the local teaching hospital but he is happy with Mark as a first point of contact. He knows that Mark can arrange for him to have an outpatient appointment at the hospital if he needs it.
-
Is the scenario realistic? Would you change anything about how it is written?
-
From the perspective of a patient what are the possible advantages and disadvantages of this case management approach?
Scenario 3: doctor Donna’s dilemma
Donna, a GP in a medium-sized practice, is already running late with her appointment schedule. She looks at the records of her next patient. Joseph has recently been in hospital because of a serious heart problem. The hospital prescribed a number of drugs for Joseph to take but there are many options for treating his condition, for example changing doses or switching to a different drug if he experiences harmful side effects. Donna has seen patients with Joseph’s condition before, but not many.
Donna knows about a community specialist nurse who would be able to co-ordinate Joseph’s care, but the nurse is part of a new service and she has never met him. On the other hand, Donna knows that the hospital cardiology department has an excellent reputation and they are already familiar with Joseph. If her patient’s symptoms are getting worse, might it be best to send Joseph directly to the hospital and let them sort him out?
-
Is the scenario realistic? Would you change anything about how it is written?
-
What influence do you think a patient might have over the doctor’s final decision?
Scenario 4: delaying Doug
Doug has been coping with a chronic disease for just over 10 years. Last night, his symptoms were very bad, causing him discomfort, pain and considerable anxiety. He was wondering whether he should call 111 or wait until morning to see his GP. When morning came he decided not to visit his GP. He recalled a similar occasion in the past when he had made an urgent visit to his GP. The GP had called an ambulance and, after waiting quite some time for the ambulance to arrive, he was taken to hospital to undergo what felt like an endless series of tests. In the end, none of the tests seemed to add very much to what he and the doctor already knew. ‘None of us was any the wiser’, he says.
-
Is the above scenario realistic? Would you change anything about how it is written?
-
Put yourself in Doug’s position, why might you be reluctant to call 111 or to visit your GP in this situation?
Appendix 4 Study summary tables
| Study | Setting | Study design | Aims | Results/findings | Implications |
|---|---|---|---|---|---|
| Gruffydd-Jones et al. (2010)79 | Eleven patients in a single general practice | Pilot study | To examine the effect of case management in primary care of patients with COPD at high risk of hospital admission, identified using a novel multidimensional index of disease severity (DOSE index) | No improvement in health status, but non-significant reduction in total hospital admissions (three vs. zero) and total bed-days (16 vs. 0) compared with same reference period in previous year. Increase in self-management knowledge | RCT required |
| Stokes et al. (2016)73 | Single Clinical Commissioning Group in UK NHS; 2049 intervention patients were compared using propensity scoring one to one with control patients. At the practice level, 30 practices were compared using natural experiment through staged implementation. Twenty ACSCs | Comparative observational study | To evaluate MDT case management intervention at individual (direct effects of intervention) and practice (potential spillover effects) levels | Slight, clinically trivial increases in inpatient non-elective admissions (+ 0.01 admissions per patient per month, 95% CI 0.00 to 0.01; ES 0.02) and 30-day re-admissions (+ 0.00, 95% CI 0.00 to 0.01; ES 0.03). No indication that highest-risk patients benefited more from intervention. At the practice level, there was a small decrease in inpatient non-elective admissions (–0.63 admissions per 1000 patients per month, 95% CI –1.17 to –0.09; ES –0.24). However, result did not withstand robustness check; estimate may have absorbed differences in underlying practice trends |
Intervention does not meet its primary aim. Clinical significance and cost-effectiveness of small practice-level effects is debatable Ongoing need to develop effective ways to reduce preventable attendances in secondary care for high-risk population |
| Stokes et al. (2017)80 | Extended previous analysis (see Stokes et al.73) with 2049 propensity-matched case management intervention patients, adding an additional interaction term to determine subgroup effects (difference-in-difference-in-differences) by different definitions of multimorbidity. Outcome measures included diverse secondary care utilisation and cost measures | Comparative observational study | To explore whether or not effects of case management vary in patients with different types of multimorbidity | Where results were significant, the vast majority of ESs identified in either direction were very small. Trend for very slight increases of admissions with treatment for the most complex patients (highest risk). Patients with a Charlson Comorbidity Index score of > 5 may benefit slightly more from case management with decreased ACSC admissions (ES –0.06) and inpatient re-admissions (30 days, ES –0.05). Patients with only cardiovascular/metabolic cluster conditions may benefit slightly more, with decreased inpatient non-elective admissions (ES –0.12) | Results indicate no appropriate multimorbidity subgroup at which to target case management in terms of secondary care utilisation/cost outcomes. The most complex, highest-risk patients may legitimately require hospitalisation, and intensified management may better identify these unmet needs. End-of-life patients (e.g. Charlson Comorbidity Index score of > 5)/those with only conditions particularly amenable to primary care management (e.g. cardiovascular/metabolic cluster conditions) may benefit very slightly more than others |
| Study | Setting | Study design | Aims | Intervention | Results/findings | Implications |
|---|---|---|---|---|---|---|
| Close et al. (2013)81 | 17 patients, 8 care home staff, 5 GPs and 3 HF nurses in residential care | Interview study | To examine experiences and expectations of clinicians, care home staff and residents in interpreting suspected symptoms of HF and deciding if and how to intervene | Tailored, consultant-led management plan delivered by HF nurses | Participants perceived no clear lines of responsibility in providing HF care in care facilities. Many clinical staff had negative views of the acceptability and utility of interventions. Some staff inappropriately limited residents’ access to HF diagnosis and treatment. Care facility staff and residents welcomed intervention but felt that there was no opportunity for dialogue about balance of risks and benefits. Most residents wanted to be involved in health-care decisions but this was not possible because of physical, social and organisational barriers. An on-site HF service was acceptable to residents and care facility staff | HF diagnosis and management is of variable quality in long-term care. Conflicting expectations and a lack of co-ordinated responsibility for care contribute to a culture of benign neglect that excludes the wishes and needs of residents. A greater focus on rights, responsibilities and co-ordination may improve health-care quality for older people in care |
| Gowing et al. (2016)74 | Community patients receiving primary care in Northumberland, England | To explore views and experiences of patients on care received while enrolled on the Northumberland High-Risk Patient Programme | Case finding using a MDT-led community case management programme, and support of patients through care planning and regular reviews by primary, community, secondary and social care professionals | Four themes: awareness and understanding of Northumberland High-Risk Patient Programme, confidence in primary health-care team, limitations of home care and active role of being a patient. Participants lacked detailed awareness of the Northumberland High-Risk Patient Programme but agreed with its broad aim. They were highly satisfied with their care and access to team members. Limitations of alternatives to hospital were related to patients’ psychological needs, importance of overnight care and needs of those without informal carers. Participants recognised the need for Northumberland High-Risk Patient Programme patients to be active in contributing to planning and managing their own care | MDT-led case management was generally well received by patients and their families | |
| Hall Aitken (2014)297 and Beacon (2015)298 | No details | To present a case study of development of multidisciplinary Practice-Integrated Care Teams in central Manchester | There has been an overall reduction in secondary care activity for patients the teams have been working with, with the largest reduction being in emergency admissions. Patient feedback indicates increased overall satisfaction with care and advice received from health-care/social care professionals. Evaluation demonstrated a strong professional commitment to principles of integrated care, improved team confidence and skills, and cost savings from secondary care | This GP-centred model has enabled primary care to take a key role in development of an out-of-hospital integrated care system. Community professionals such as nurses and social workers have been able to build stronger relationships with general practice, enabling system linkages essential to delivery of integrated health and social care |
| Study | Setting | Aims | Results/findings | Implications |
|---|---|---|---|---|
| Das et al. (2013)123 | Retrospective audit of case notes for all patients admitted with acute asthma (September to October 2012) | To review asthma admissions to investigate whether or not they may have been preventable with better management in the community. Management in the acute setting was audited against the British Thoracic Society guidelines | Of 41 patients identified, 56% were on treatment step 1 or 2 of the British Thoracic Society’s guidelines, 37% were on step 3 and the remaining 7% were on steps 4 and 5. At discharge, only two patients had a medication dose increase and six had a new medication added. Documentation of treatment and provision of self-management plans were poor | Asthma exacerbations requiring admission can reflect poor disease control. Poor compliance and inhaler technique, limited use of self-management plans and lack of patient education contributed to these admissions. Suggested that GPs should ensure that regular asthma reviews are undertaken in the community. The authors propose a checklist to improve adherence to British Thoracic Society guidance |
| Howard and Dupont (2014)124 | 220 COPD patients in Hillingdon, Uxbridge, randomly allocated to receive either the COPD breathlessness manual (case management) or information booklet. Patients were instructed to work through their programme at home, over 5 weeks. Guidance from a facilitator was provided at an initial home visit plus two telephone follow-ups | To compare a cognitive–behavioural manual vs. information booklets on health service use, mood and health status | After 12 months, total A&E visits had reduced by 42% in the case management group, compared with a 16% rise in the information booklet group. Reductions in hospital admissions and bed-days were greater in the case management group. Estimated savings at 12 months were greatest in the case management group, amounting to £30,000 or £270 per participant | Suggested that the COPD manual is a straightforward cost-effective intervention worth offering to COPD patients primary or secondary care |
| Steventon et al. (2013)125 | Community-based intervention in a large English city with industry | To test the effect of a telephone health coaching service (Birmingham OwnHealth) on hospital use and associated costs | Matched controls and intervention patients were similar before the date of enrolment. After enrolment, emergency admissions, outpatient attendances and secondary care costs increased more quickly among intervention participants than among controls. Checks showed that reductions in emergency admissions were unlikely to have been missed because of unobserved differences between the intervention and control groups | The intervention did not lead to the expected reductions in hospital admissions or secondary care costs over 12 months, and could have led to increases |
| Study | Setting | Aims | Results/findings | Implications |
|---|---|---|---|---|
| Fry et al. (2016) (HoldFAST cluster)126 | Three geographical locations in the UK: the Midlands, South Central England and the south-west of England. Qualitative interviews with 11 patients who had participated in HoldFAST, a multicentre NIHR-funded ethnographic study of heart failure focusing on unplanned hospital admissions involving Bristol, Oxford and Keele Universities | To use secondary analysis to interrogate a qualitative data set to explore the experiences of patients living with heart failure | Respondents described how disruption of routine activity due to their symptoms caused them to seek medical care. Respondents disclosed difficulties of living with other comorbidities (managing multiple and complex medication regimes and negotiating multiple appointments). Many respondents described uncertainty around diagnosis and delays in communication from HCPs | Facilitated access to health care, through good communication between services and having a strong support network of both family and clinicians can reduce the impact of heart failure on lives of patients and those around them |
| Glogowska et al. (2015) (HoldFAST cluster)127 | Three geographical locations in the UK: the Midlands, South Central England and the south-west of England. The HoldFAST, multicentre NIHR-funded study involving Bristol, Oxford and Keele Universities. Qualitative in-depth interviews with 24 clinicians across primary, secondary, and community care | To explore perceptions and experiences of health-care clinicians working in MDTs that include specialist heart failure nurses when caring for management of heart failure patients | Identified two particular challenges when working with heart failure patients:
|
Highlights the role of specialist heart failure nurses in delivering education tailored to patients and facilitating better liaison among all clinicians, particularly in managing comorbidities and drug regimens. A specialist nurse role as caseworkers for their patients was perceived as a way of ensuring co-ordination and continuity of care |
| Glogowska et al. (2016) (HoldFAST cluster)129 | Qualitative in-depth interviews with 24 HCPs across primary, secondary and community care in three locations in England: the Midlands, South Central and the south-west. Within HoldFAST, a multicentre study involving Bristol, Oxford and Keele Universities, funded by NIHR | To explore perceptions and experiences of HCPs working with patients with heart failure around end-of-life care | HCPs discussed their struggle to find alternatives to hospital admission for patients at the end of their life. Patients may be hospitalised because of a lack of planning, which would enable them to die at home if they so wished | HCPs regarded opportunities for patients with heart failure to have ongoing discussions about their end-of-life care with clinicians they know as essential. These key professionals can help co-ordinate care and support in the terminal phase of the condition. Links between heart failure teams and specialist palliative care services appear to benefit patients. Further sharing of expertise between teams is recommended |
| Halpin et al. (2015)130 | District General Hospital, Exeter, Devon | To determine the importance of fear and anxiety at the time of an exacerbation of COPD. To assess the influence of carers and HCPs on this fear and anxiety | Four themes emerged: panic and fear; anxiety management techniques used during an exacerbation; intervention from family members and carers; and response to medical services. Panic and fear are important emotions prior to admission | Many patients recognised a link between panic/fear and worsening symptoms. Some were able to use self-management techniques to reduce their panic/fear. Some relatives were seen as helping and others were seen as exacerbating the symptoms. The emergency services were seen as providing reassurance and a sense of safety |
| Simmonds et al. (2015) (HoldFAST cluster)128 | 31 patients with severe or difficult-to-manage heart failure were followed up for up to 11 months; 9 carers; 55 HCPs across three geographical locations in the UK: the Midlands, South Central England and the south-west of England. The HoldFAST multicentre study involving Bristol, Oxford and Keele Universities, funded by NIHR | To identify critical points on patient pathways where risk of admission is increased and identify barriers to implementation of evidence-based interventions | Fragmentation of health care, inequitable provision of services and poor continuity of care presented barriers to interventions for heart failure. Critical points affecting risk of current/future admission occurred throughout the pathway. Some patients did not receive a formal clinical diagnosis. Patients lacked information about heart failure, self-care and when to seek help. Some clinicians lacked knowledge about diagnosis and management. Approaching the end of life, patients were admitted when other options (e.g. palliative care) could have been appropriate | Fragmented health care and discontinuity of care add complexity and increase the likelihood of suboptimal management and unplanned admissions. The need for clinician education about heart failure and specialist services was acknowledged |
| Study and population | Study design | Results/findings | Implications |
|---|---|---|---|
|
Bucknall et al. (2012)139 Population/condition: COPD |
Experimental | Supported self-management had no effect on time to first re-admission or death due to COPD. Exploratory subgroup analysis revealed a minority of intervention participants who successfully self-managed their COPD. These patients had a significantly reduced rate of COPD re-admission than other intervention patients. Successful self-management was associated with being younger and living with others | Authors concluded that supported self-management cannot be recommended for the general population of patients hospitalised for COPD exacerbations in the UK |
|
Dritsaki et al. (2016)145 Population/condition: COPD |
Other economic evaluation | Participants in the intervention group gained 0.1 QALYs compared with the usual-care group at an estimated cost of £280.39 per QALY | There was a 97% chance of the intervention being cost-effective at a threshold of £20,000 per QALY and a 99% chance at £30,000 per QALY |
|
Hoskins et al. (2016)143 Population/condition: asthma |
Experimental | The GOAL intervention changed the process of asthma review and was well received by patients, but required additional time, which was problematic within the limitations of the traditional nurse appointment | Changes to recruitment methods and further development of the intervention are needed before proceeding to a definitive cluster RCT |
|
Johnson-Warrington et al. (2016)144 Population/condition: COPD |
Experimental | The SPACE intervention did not reduce re-admission at 3 months compared with usual care. The intervention provided some benefits in quality of life and increasing time to first re-admission with no increase in mortality | Authors noted that all participants received specialist follow-up as part of usual care; hence, their care may already be optimum |
|
Kennedy et al. (2013)138 Population/condition: multiple |
Experimental | 4533 patients (81%) completed 6-month follow-up and 4076 (72.8%) completed 12-month follow-up. There were no differences between intervention and control practices for any outcome measure | Authors concluded that the active components needed to support self-management are not sufficiently understood at either the primary care or patient level |
|
Morrow et al. (2017)137 Population/condition: asthma |
Qualitative | Supported self-management was largely a nurse-led task within clinic-based annual reviews. Barriers included poor attendance at asthma clinics, lack of time, demarcation of roles, limited access to a range of tailored resources and competing agendas in consultation, often due to multimorbidity | Suggestions of initiatives to improve the provision of supported self-management included emphasising the evidence of benefit and improving teamwork (including team-based education), organisational strategies (including remote consulting) that need to fit within existing practice routines. Technology was thought to offer some potential solutions but must be integrated with existing practice IT systems |
|
Ogunbayo et al. (2017)147 Population/condition: COPD |
Qualitative | Factors affecting self-management support implementation were categorised as patient, practitioner or system level. Patient-level factors, including knowledge and understanding of COPD and personal circumstances, were mainly seen as barriers. Practitioners saw their own specialty, interest and experience as an overarching factor in how they provided support to patients | Authors identified multiple organisational-/system-level factors, including inconsistency of referral pathways and the widespread use of different self-management planning tools. The authors concluded thatall three levels need to be considered for optimal implementation |
|
Patel et al. (2016)140 Population/condition: COPD |
Qualitative | Patients responded positively to the use of technology and valued the perceived support from remote monitoring. No patient required hospital admission during the study. Awareness of COPD symptoms and confidence in self-management increased during the study | Patients valued the support of the research nurses and some felt concern about managing COPD at home without this support |
|
Ring et al. (2015)141 Population/condition: asthma |
Qualitative | Primary care implementation of PAAPs is characterised by a vicious cycle whereby negative views/actions of patients and HCPs reinforce one another. Twenty-five years after PAAPs were recommended, many organisational and practical barriers remain | Authors recommend a whole-system approach, using multifaceted interventions to tackle identified barriers |
|
Roberts et al. (2012)142 Population/condition: asthma and COPD |
Uncontrolled observational | The questionnaire response rate was 33% (58/175). Respondents expressed strong support for guideline recommendations, but implementation in routine practice was patchy | Identified barriers included time constraints, lack of training/resources, concerns about patients’ ability to self-manage and lack of confidence among clinicians for completing self-management plans |
| Study | Setting | Aims | Results/findings | Implications |
|---|---|---|---|---|
| Steventon et al. (2012)71 |
179 general practices in three areas of England COPD, diabetes and heart failure |
To assess the effect of home-based telehealth interventions on the use of secondary health care and mortality | Patient characteristics were similar at baseline. Compared with controls, the intervention group had a lower admission proportion within the 12-month follow-up (OR 0.82, 95% CI 0.70 to 0.97; p = 0.017). Mortality at 12 months was lower for intervention patients than for control patients (4.6% vs. 8.3%; OR 0.54, 95% CI 0.39 to 0.75; p < 0.001). Differences in admissions and mortality remained significant after adjustment. Mean number of emergency admissions per head differed between groups (crude rates, intervention 0.54 vs. control 0.68); these changes were significant in unadjusted comparisons (incidence rate ratio 0.81, 95% CI 0.65 to 1.00; p = 0.046) and after adjusting for a predictive risk score, but not after adjusting for baseline characteristics. Observed differences in other forms of hospital use, including notional costs, were not significant. Differences in emergency admissions were greatest at the beginning of the trial, with a particularly large increase for the control group | Telehealth is associated with lower mortality and emergency admission rates. Reasons for short-term increases in admissions for the control group are not clear, but trial recruitment processes may have had an effect |
| Study | Setting | Study design | Aims | Results/findings | Implications |
|---|---|---|---|---|---|
| Crundall-Goode and Goode (2014)152 | Overview of advantages and disadvantages of different nursing telehealth service models in use in the UK | Qualitative review | To guide nurses and their managers on how to meet challenges of implementing a telehealth service for CHF management by exploring possible barriers to and pitfalls of its introduction | ||
| Fairbrother et al. (2012)153 | Telemonitoring service for patients with COPD introduced in Lothian, Scotland, in 2009 | Qualitative study nested within the TELESCOT COPD RCT | To explore the views of patients and professionals on telemonitoring, including perceived impact of telemonitoring on continuity of care |
Patients and HCPs considered relationship-based continuity of care important in delivering telemonitoring services Managers placed emphasis on improved continuity of clinical management to reduce health-care costs. However, professionals described operational challenges when ‘bolting on’ telemonitoring provision to usual-care provision, leading to additional managerial discontinuities |
Managers and HCPs face major challenges in meeting demands for both relationship continuity and continuity of clinical management when developing telemonitoring services |
| Fairbrother et al. (2013)154 | Patients with COPD and HCPs participating in a RCT of telemonitoring in Lothian, Scotland | Semistructured interviews | To explore patient and professional views on self-management in the context of telemonitoring in COPD | Patients considered that telemonitoring empowered self-management by enhancing their understanding of COPD and providing additional justification for their decisions to adjust treatment or seek professional advice. Professionals discussed telemonitoring as promoting compliance with medical advice and encouraged patients to exercise personal responsibility within clinical parameters, but expressed concerns about promoting the sick role and creating dependence on telemonitoring. Patients and professionals shared responsibility for prompt management of exacerbations of COPD | Care is needed to minimise risk in some patients of increasing dependence on practitioner support. Many patients were able to embrace greater responsibility for their health. The model of service provision remained clinician centred. A medical model of ‘compliant self-management’ may paradoxically promote dependence on professionals |
| Fairbrother et al. (2013)155 | A chronic heart failure telemonitoring service set up by NHS Lothian, Scotland | Semistructured interviews with 18 patients and five professionals participating at different time points in this new service | To understand the views of patients and professionals on the acceptability and perceived usefulness of telemonitoring in the management of CHF in the context of day-to-day care provision | Five main themes were identified:
|
Patients and professionals considered telemonitoring useful in managing CHF, but with caveats. Patients felt reassured by what was perceived as continuous practitioner surveillance. Professionals expressed concern regarding perceived patient dependence on practitioner support. Increased workload was also a concern. Both groups acknowledged need for improved technology and changes to service provision to better meet intended objectives of the service Professionals emphasised importance of case selection and adequate training and support, both for patients and themselves, to maximise expected benefits of the service |
| Gale and Sultan (2013)156 | COPD patients receiving a community respiratory service in Sandwell, West Midlands | In-depth, qualitative, situated interviews with COPD patients receiving the service | To document the experience and interaction with the technology of people with COPD in order to understand how they negotiated incorporating telehealth technologies into their everyday life and home space, and to understand why they valued it | Telehealth brought peace of mind through two mechanisms: legitimising contact with HCPs and increased patient confidence in the management of their condition. When the home is the primary health space, the introduction of telehealth can modify emotional and bodily experiences to an extent that is significant for people with COPD | Process by which technology can provide ‘peace of mind’ to people with long-term conditions should be taken into account when designing or commissioning a service |
| Hanley et al. (2018)299 | Large data set from TELESCOT series of studies (181 patients and 109 professionals) | Qualitative interview and focus group data from the TELESCOT programme | To explore what drove changes to how telemonitoring was implemented, compare experience of telemonitoring across diverse long-term conditions and identify what issues, in the experience of the participants, need to be considered in implementing new telemonitoring systems | Four major themes were identified: using data, empowering patients, adjusting the model of care and system design | Telemonitoring was valued by patients who found it empowering and convenient. Professional concerns centred on whether or increased surveillance may create dependency. However, despite initial concerns being addressed as the service evolved, primary care professionals identified persistent barriers to widespread routine adoption requiring improved system design |
| Jones et al. (2012)157 | 24 general practices in the West Midlands | Qualitative study embedded within a RCT (Telemonitoring and Self Management in the Control of Hypertension) of patient self-management of hypertension | To explore patients’ views of self-monitoring blood pressure and self-titration of antihypertensive medication |
Patients were confident about self-monitoring. Many felt that their multiple home readings were more valid than single office readings taken by their GP. Although many patients self-titrated medication when required, others lacked the confidence to increase medication without reconsulting with their GP. Patients were more comfortable with titrating medication if blood pressure readings were substantially above target. Patients were reluctant to implement a change if readings were borderline. Many planned to continue self-monitoring after the study finished and report home readings to their GP, but few wished to continue with a self-management plan Participants valued the additional information. Many felt confident in both self-monitoring blood pressure and self-titrating medication |
Reluctance to change medication for borderline readings suggests behaviour similar to the clinical inertia seen for physicians Additional support for those lacking in confidence to implement prearranged medication changes may allow more patients to undertake self-management |
| Jones et al. (2013)158 | 24 West Midlands general practices | Qualitative study embedded within RCT of HCPs participating in the TASMINH2 trial of patient self-monitoring with self-titration of antihypertensives | To explore HCPs’ views and experiences of patient self-management, particularly with respect to future implementation into routine care | Professionals were positive about self-monitoring, but procedures for ensuring that patients measured blood pressure correctly were haphazard. GPs interpreted home readings variably, with many not adjusting for lower home blood pressure. Interviewees were satisfied with patient training and arrangements for blood pressure monitoring and self-titration of medication during the trial, but less sure about implementation into routine care. A need for training of both patients and professionals was identified | HCPs wanted more patient involvement in hypertension care. They needed a framework to work within. Training for patients in how to measure blood pressure and how home readings become part of their care is required before self-monitoring and self-titration can be implemented widely. As home monitoring becomes more widespread, the development of patient self-management, including self-titration of medication, should follow, but this may take time |
| May et al. (2011)300 | 221 HCPs, managers, patients and carers; social care professionals and managers; and service suppliers and manufacturers for telecare services in community and domestic settings in England and Scotland | Large-scale comparative study using qualitative data collection techniques: semistructured interviews with key informants, task groups and workshops; framework analysis of qualitative data informed by normalisation process theory | To identify factors inhibiting the implementation and integration of telecare systems for chronic disease management in the community | Key barriers to integration were uncertainties about coherent and sustainable service and business models; lack of co-ordination across social and primary care boundaries, lack of financial or other incentives to include telecare within primary care services; a lack of a sense of continuity with previous service provision and self-care work undertaken by patients; and general uncertainty about adequacy of telecare systems. These problems led to poor integration of policy and practice | Telecare services may offer a cost-effective and safe form of care for some people living with chronic illness. Slow and uneven implementation and integration does not stem from problems of adoption. It results from incomplete understanding of the role of telecare systems and subsequent adaption and embeddedness to context, and uncertainties about the best way to develop, co-ordinate, and sustain services to assist with chronic disease management. Interventions are needed to:
|
| Peirce et al. (2011)177 |
26 key informants from across the UK. 18 had a clinical background, seven in nursing, with four working as community-based nurses providing care for patients with chronic diseases. Eight informants had experience in health informatics, four policy leads in NHS and nine with recent experience of telehealth programmes. Two academics Interviews took place from June to November 2008 (approximately 90 minutes each) |
Qualitative study using stakeholder interviews | To define current standards of care and user requirements for improved early-detection telemonitoring | Early detection has not informed technology or service design. Telemonitoring is driven by available technology rather than by users’ needs. Describes set of requirements questions to inform design and implementation of telemonitoring systems and suggests research needed to develop successful early-detection telemonitoring | User-centred design and genuine interdisciplinary approaches are needed to create solutions that are fit for purpose, sustainable and address real needs of patients, clinicians and health-care organisations |
| Sanders et al. (2012)165 (Whole System Demonstrator project cluster) | Participants were recruited from four trial groups (with diabetes, COPD, heart failure or social care needs) from three trial areas (Cornwall, Kent, east London) | Qualitative semistructured interviews conducted with people who declined to participate in the trial or who withdrew. Observations of home visits were conducted by shadowing eight members of health and social care staff visiting people at home. Fieldnotes were made of observational visits and explored alongside interview transcripts | To explore barriers to participation and adoption of telehealth and telecare from the perspective of people who declined to participate or withdrew from the trial | Barriers to adoption of telehealth and telecare were identified: requirements for technical competence and operation of equipment; threats to identity, independence and self-care; expectations and experiences of disruption to services. Respondents held concerns that special skills were needed to operate equipment, often based on misunderstandings. Respondents’ identified threats to identity associated with positive ageing and self-reliance. Interventions could also undermine self-care and coping. Participants were reluctant to risk potentially disruptive changes to often highly valued existing services | Findings regarding perceptions of potential disruption of interventions to identity and services go beyond common expectations that concerns about privacy and dislike of technology deter uptake. These insights indicate that more detailed information and time for discussion could be valuable, especially on introduction. Potential recipients should have the opportunity to discuss their expectations and such views might usefully feed back into design and implementation |
| Sharma et al. (2010)263 | Prior to launch of telehealth service in Nottingham | Focus group discussions with clinical users (nurses and technicians) | To elicit initial perceptions about the service and describe findings from the preliminary phase of a larger longitudinal study | Trust and sense of security are two very salient aspects that govern adoption of new technological innovation. Unattended, these aspects contribute to arousal of conflict and contradiction within a system | Successful telehealth implementations in health-care setting require providers of the service to focus on how clinical users’ trust can be gained and sense of security promoted while using telehealth services and technology |
| Ure et al. (2012)159 (commentary160) | NHS Lothian COPD telemonitoring service incorporating touch-screen computer for daily recording of symptoms and weekly oximetry and spirometry measurement | In-depth interviews with patients and professionals before/after installation of telemonitoring equipment. Interviews recorded, transcribed and thematically analysed. Data on use of health-care resources obtained from primary care records | To explore perceptions of patients and professionals about pilot implementation of COPD telemonitoring service | Patients were generally positive about technology (enabled earlier recognition of exacerbations and access to clinical advice). Clinicians had concerns about false-positive symptom scores, difficulties in interpreting physiological data, overtreatment (large increase in antibiotics and steroid prescribing) and increased workload | Telemonitoring was perceived by patients as improving access to professional care, but raised concerns for clinicians about possible overtreatment and how best to organise services to support the technology |
| Williams et al. (2014)161 | Oxfordshire primary care | An embedded qualitative study using interviews with patients with COPD from various community NHS services | To explore patients’ expectations and experiences of using a mobile telehealth-based (mHealth) application and to determine how such a system may have an impact on their perceived well-being and ability to manage their COPD | Patients identified no difficulties in using the mHealth application. Patients who used the application reported increased awareness of variability of their symptoms (onset of exacerbation and recovery time) and reassurance through monitoring (continuity of care) | Patients could use the mHealth application, interpret clinical data and use the data for self-management without previous knowledge. Telehealth interventions can complement current clinical pathways for self-management |
| Study | Study design | Results/findings | Implications |
|---|---|---|---|
| Al Quait et al. (2017)189 |
Uncontrolled observational Logistic regression modelling study |
Based on data on 59,807 patients, CR engagement decreases by 1.2% per year of age (OR 0.98) and is approximately 7% lower (OR 0.93) in female patients, and patients are 4.4 times more likely to engage if they receive a confirmed joining date (OR 4.4) | Engagement with CR is not purely a patient decision but is related to service-level factors, over which health-care systems have more control |
| Devi et al. (2014)191 | Experimental | In a randomised trial of a web-based CR programme for people with angina, significant benefits were seen at 6-week follow-up, with effects on angina frequency and social quality-of-life score persisting at 6 months | The intervention may be appropriate to offer to people with angina. The programme is likely to be cheaper to operate and run than conventional alternatives but a larger trial is required to demonstrate effectiveness and cost-effectiveness |
| Devi et al. (2014)179 | Qualitative | The web-based programme was accepted and valued by participants. Participants suggested that the programme should be provided at the time of diagnosis | Barriers to participation were similar to those identified for traditional programmes |
| Doherty and Lewin (2012)185 | Other editorial comment on RAMIT (West et al. 2012183) | RAMIT was not designed to evaluate the efficacy of CR. The evidence that CR reduces mortality and is highly cost-effective remains little changed | There is unjustifiable variation in CR services across the UK but the RAMIT results should not be generalised to ‘CR as practised in the UK’. Clinical audit and observational analysis of NACR data will help to identify how best to deliver CR services |
| Houchen et al. (2012)180 | Uncontrolled observational | Early rehabilitation significantly improved exercise capacity and depression and reduced heart failure-associated health-care utilisation in patients who had recently been hospitalised. The intervention was safe | However, the sample size was small and results were not compared with a control group. Therefore, the effects of natural recovery are unknown |
| NACR (2017)188 |
Uncontrolled observational UK national audit |
Over 100,000 patients were registered with the audit. The age of patients receiving CR ranged from 18 to 108 years, with a mean age of 70 years for females and 66 years for males. Just under 30% of patients were women. The percentage of patients starting and completing core CR was 77% and group CR was the predominant mode of delivery. The audit reported tangible gains compared with the previous report | Recommended actions include positive action to recruit more female patients, changing the type of programme offered if necessary; increased referral of patients with HF; offering a wider range of programme options; ensuring assessment of patients as they complete programmes; and increasing the duration and frequency of sessions if programmes are not meeting minimum standards |
| West et al. (2012)183 | Experimental | There were no significant differences between groups in mortality at 2 years (RR 0.98, 95% CI 0.74 to 1.30) or after 7–9 years (RR 0.99, 95% CI 0.85 to 1.15), cardiac events, seven of eight domains of the health-related quality-of-life scale or in psychological general well-being. Rehabilitation patients reported slightly less physical activity. No differences between groups were reported in perceived quality of care | Rehabilitation programmes may contribute to ‘seamless patient care’ and they are appreciated by many patients but evidence of objective benefit is weak relative to the proven benefits from other aspects of cardiac management |
| West et al. (2013)184 | Other authors’ response to comments on the RAMIT publication | Not applicable | Findings of RAMIT, together with other recent trials, support the efficacy and effectiveness of typical courses of outpatient CR |
| Witham et al. (2012)187 |
Experimental Randomised trial |
Results do not support the usefulness of a tailored exercise programme for older patients with HF | More work is needed, possibly involving more intensive exercise, better targeting of patients with breathlessness or combining exercise with education and behavioural interventions |
| Wood (2012)186 | Other editorial comment on RAMIT (West et al. 2012183) | Not applicable | The results of RAMIT should lead CR programmes to re-evaluate their service and outcomes. Although current programmes are appreciated by patients, they are not ‘fit for purpose’ and need to change. This will require both reconfiguration of services and cultural change, as well as investment by the NHS |
| Study | Setting | Aims | Results/findings | Implications |
|---|---|---|---|---|
| Casey et al. (2012)199 | General practices (clusters) in the western region of Ireland | To evaluate the effectiveness of a structured pulmonary rehabilitation education programme on the health status of people with COPD | Participants allocated to the intervention group had statistically significant higher mean CRQ-D score [mean 4.42 (SD 0.36) vs. mean 3.85 (SD 0.45)], baseline and covariate adjusted mean difference TM49 (95% CI aTM2, 0.78) and CRQ Physical scores (mean 4.62 vs. mean 4.2), baseline and covariate adjusted mean difference aTM37 (95% CI TM4, 0.6). No other statistically significant difference between groups was seen | The SEPRP delivered in the primary care setting is effective in improving the health status of people with COPD as measured by the CRQ |
| Casey et al. (2013)200 | General practices (clusters) in the western region of Ireland | To evaluate the effectiveness of a structured pulmonary rehabilitation education programme on the health status of people with COPD | Participants allocated to the intervention group had statistically significant higher mean change total CRQ scores (adjusted mean difference 1.11, 95% CI 0.35 to 1.87). However, the CI does not exclude a smaller difference than the one that was prespecified as clinically important. Participants allocated to the intervention group also had statistically significant higher mean CRQ-D scores after intervention (adjusted mean difference 0.49, 95% CI 0.20 to 0.78) and CRQ Physical scores (adjusted mean difference 0.37, 95% CI 0.14 to 0.60). However, CIs for both the CRQ-D and CRQ Physical subscales do not exclude smaller differences prespecified as clinically important. No other statistically significant differences between groups were seen | A primary care-based structured education PRP is feasible and may increase local accessibility to people with moderate and severe COPD |
| Casey et al. (2011)198 | General practices (clusters) in the western region of Ireland | To describe the development of a SEPRP for the PRINCE |
All participants had enjoyed the programme; the involvement of different HCPs and the teaching strategies used were appropriate The findings indicate that nurse-led primary care-based structured education programmes have the potential to empower clients with COPD to better self-manage their chronic health condition. The PRINCE study has demonstrated that nurses working in primary care can have a key role in pulmonary rehabilitation. Their expertise was essential to the development of the PRINCE SEPRP, and they also were able to facilitate the programme effectively. The philosophy of PRINCE was based on empowerment, with the programme activities designed to give clients the knowledge, confidence and skills they need to self-manage |
Nurses working in the community have the opportunity to work with people in empowering ways, and PRINCE is one example of how this can be put into practice |
| Chaplin et al. (2016)206 (conference abstract) | Not reported. | To determine if an interactive web-based PRP is a feasible alternative to conventional PR | 103 patients were recruited. The largest proportion of patients randomised wanted the web programme (n = 38%). A statistically significant improvement (p < 0.01) was observed within each group in the ESWT (web programme: mean change 189 ± 211.1; PR classes: mean change 184.5 ± 247.4 seconds) and CRQ-D (WEB: mean change 0.7 ± 1.2; PR classes: mean change 0.8 ± 1.0). There were no significant differences between the groups in any outcome | A web-based PRP is feasible and acceptable when compared with conventional PR. Future trials maybe around choice-based PR, enabling stratification of patient care |
| Condon et al. (2015)301 | Two academic teaching hospitals in Dublin, Ireland | To identify referral, uptake and PR completion rates over a 3-month period | Of 183 people with confirmed COPD, 98 (54%) met the HSE’s model of care criteria for PR. Thirty-nine (21%) were not functionally limited by the disease and 23 (12%) were considered not suitable for PR. Approximately half (n = 50) of those eligible were referred for assessment but after 6 months, only seven people had completed a PRP | Referral to PR was adequate but timely uptake by patients remains poor. Low uptake has implications for the effectiveness of PR in reducing mortality and hospital re-admissions |
| Easthaugh and Farmer (2016)201 | Community gym facilities in the borough of Gateshead | To determine whether or not a PRP provided in community gym facilities can lead to sustainable behaviour change to support effective self-management of patients with mild to moderate symptoms of COPD | The programme has proved to be highly beneficial and very positive participant feedback has been received. A significant number of patients have sustained long-term genuine health behaviours. Participants have benefited by having greater knowledge and understanding of the management of their condition with improved physical fitness and well-being and have been able to achieve personal goals. In addition, participants have the long-term sustainable benefits of maintaining progress and confidence to manage their condition, which represents improved outcomes for patients, and potentially demonstrates economic value, with decreased need for social/medical care | Occupational therapists can deliver a participant-empowered approach to PR that builds on traditional models of self-management. Critically, this approach enables participants to successfully understand the need for change, appreciate the benefits of change and to live the change long term |
| Faulkner et al. (2010)207 | General practices in Exeter | To determine the feasibility of recruiting patients with early COPD to the Health Enhancing Activity in Lung THerapy (HEALTH) exercise and education programme | Of 27 practices approached, 16 (59.3%) agreed to participate. Of 215 potentially eligible patients contacted, 60 (27.9%) replied. Twenty (33.3%) were randomised to either the HEPA intervention (n = 10) or usual care (n = 10). Fourteen patients attended a postintervention assessment | This study provides important evidence that may inform future recruitment strategies for PR for patients with GOLD stage II COPD. Based on these study findings, the authors estimate that to recruit 100 patients it would be necessary to approach approximately 7000 patients on a COPD register and a multicentre trial would be required to achieve a suitable sample. Given the evidence of the effectiveness of PR in patients with more severe COPD, there is now an urgent need to determine whether or not similar observations apply in the larger group of individuals with earlier disease characteristics |
| Foster et al. (2016)209 | Eight general practices in Stoke | To work with primary care clinicians (GPs and practice nurses) from eight practices, to develop strategies for influencing clinician and patient behaviours to increase referral rates for PR | The baseline survey of clinicians (n = 22) revealed inadequate knowledge about PR, particularly among GPs. Actionable changes recommended included in-house education sessions, changes to practice protocols, and ‘pop-ups’ and memory aids (mugs and coasters) to prompt clinician/patient discussions about PR. Audit findings resulted in changes to improve the quality and availability of coded information about patients eligible for PR. These changes, supported by clinicians (n = 9) in the follow-up survey, aimed to facilitate and increase the quality of patient/clinician discussions about PR. Findings from the patient survey (n = 126, response rate 25.7%) indicate that such changes will increase the uptake of PR, as patients who accepted a referral for PR provided more positive feedback about their discussions with clinicians | The strategies introduced were relatively easy to implement and the anticipated advantage is more patients accessing the health and quality-of-life benefits that PR offers |
| Graves et al. (2010)205 | PR courses at The North Bristol Lung Centre | To determine the effect on course uptake and completion of a GOIS before baseline assessment for a PR course | The proportion of referred patients taking up the offer of individualised baseline assessment or a GOIS was similar (75% vs. 72.2%; p-value not significant). However, since in the GOIS group the opt-in session preceded the individualised baseline assessment and some patients opted out, a smaller proportion of referred patients underwent this assessment than in the non-GOIS group (58.7% vs. 75%; p < 0.001). In addition, dropouts following individualised baseline assessments were also reduced (7% vs. 22%; p < 0.001). Both of these factors reduced ‘wasted’ assessments. Similar proportions of patients referred began the PR course in both groups (53% vs. 51.7%; p-value not significant), but a higher proportion of patients graduated in the GOIS group (87.9% vs. 76.4%; p < 0.05). Drop-out rates due to illness were similar in both groups (8.5% pre vs. 6.8% post; p-value not significant). However, drop-out rates not due to illness were much higher in the non-GOIS group (15.1% vs. 5.3%; p < 0.001). In the GOIS group, patients who did not attend the GOIS were, on average, younger (64.6 vs. 69.7 years; p < 0.001) and had a higher mean per cent predicted forced expiratory volume (50.6% vs. 43.8%; p < 0.05) than those who did attend. A greater proportion of patients who opted in to the GOIS and attended the PR course lived < 25 minutes from the PR centre than either those who did not attend the GOIS or those who attended and then opted out (77.4% vs. 63%; p < 0.005) | The GOIS improved the graduation rates at The North Bristol Lung Centre PR course and reduced wasted assessments. There was no effect on initial uptake. Analysis of the behaviour of patients invited to a GOIS suggested that age, lung function and travel distance were important factors influencing patient choice. Since the introduction of the GOIS, the authors have treated more patients without increasing staffing. They commend this approach to others providing PR courses |
| Greening et al. (2014)203 | An acute cardiorespiratory unit in a teaching hospital and an AMU in an affiliated teaching district general hospital, UK | To investigate whether or not an early rehabilitation intervention initiated during acute admission for exacerbations of chronic respiratory disease reduces the risk of re-admission over 12 months and ameliorates the negative effects of the episode on physical performance and health status | Of the 389 participants, 320 (82%) had a primary diagnosis of COPD. 233 (60%) were re-admitted at least once in the following year (62% in the intervention group and 58% in the control group). No significant difference between groups was found (hazard ratio 1.1, 95% CI 0.86 to 1.43; p = 0.4). An increase in mortality was seen in the intervention group at 1 year (OR 1.74, 95% CI 1.05 to 2.88; p = 0.03). Significant recovery in physical performance and health status was seen after discharge in both groups, with no significant difference between groups at 1 year | Early rehabilitation during hospital admission for chronic respiratory disease did not reduce the risk of subsequent re-admission or enhance recovery of physical function following the event over 12 months and mortality at 12 months was higher in the intervention group. The results suggest that beyond current standard physiotherapy practice, progressive exercise rehabilitation should not be started during the early stages of the acute illness |
| Hayton et al. (2013)218 | Norwich | To assess predictors of attendance and adherence of PR | Of patients referred for PR, 31.8% did not attend and 29.1% were non-adherent. Multiple logistic regression revealed that LTOT use and living alone were independent predictors of poor attendance. Current smoking, poor shuttle walking distance and hospitalisations were independent predictors of poor adherence | Smoking status, availability of social support and markers of disease severity were predictors of attendance and adherence to PR |
| Steiner et al. (2017)215 | PR services across England and Wales | To investigate whether or not socioeconomic deprivation is associated with rates of completion of PR or the clinical benefits bequeathed by PR | 210 PRPs enrolled 7413 patients. Compared with the general population, the PR sample lived in relatively deprived neighbourhoods. There was a statistically significant association between rates of completion of PR and quintile of deprivation (70% in the least and 50% in the most deprived quintiles). After baseline adjustments, the risk ratio for patients in the most deprived relative to the least deprived quintile was 0.79 (95% CI 0.73 to 0.85; p < 0.001). After baseline adjustments, IMD was not significantly associated with improvements in exercise performance and health status | Patients living in more deprived areas are less likely to complete PR. However, deprivation was not associated with clinical outcomes in patients who complete therapy. Interventions targeted at enhancing referral, uptake and completion of PR among patients living in deprived areas could reduce morbidity and health-care costs in such hard-to-reach populations |
| Waterhouse et al. (2010)204 | Hospitals or community sites in Sheffield | To determine whether or not pulmonary rehabilitation carried out in a community setting is more effective than that carried out in a standard hospital setting and which is more cost-effective; also whether or not telephone follow-up is both cost-effective and useful in prolonging the beneficial effects of a PRP |
Patients in the hospital rehabilitation group increased the distance they could walk at the post-rehabilitation follow-up by 283 m (SD 360 m), an increase relative to baseline of 109% (SD 137%). Patients in the community rehabilitation group increased the distance they could walk at the post-rehabilitation follow-up by 216 m (SD 340 m), an increase relative to baseline of 91% (SD 133%). There was no statistically significant difference between the groups (17.8%, 95% CI –24.3% to 59.9%; p = 0.405). For longer-term outcomes at 6, 12 and 18 months post rehabilitation, there was no evidence of a rehabilitation group effect After allowing for the initial post-rehabilitation baseline distance walked, time (follow-up visit) and the factorial design (telephone follow-up group), the average difference in the post-rehabilitation follow-up distance walked on the ESWT between the hospital and community rehabilitation groups was 1.5 m (95% CI –82.1 to 97.2 m; p = 0.971), and between the telephone and no-telephone groups it was 56.9 m (95% CI –25.2 to 139 m; p = 0.174). There was no difference between hospital or community groups in terms of acute effect or persistence of effect. Health economic analysis favoured neither hospital nor community settings, nor did it clearly favour telephone follow-up or routine care |
PR delivered in a community setting has similar efficacy to that produced in a more traditional hospital-based setting; both settings producing significant improvements in terms of exercise capacity and quality of life acutely and after long-term follow-up. Health economic analysis showed that neither hospital nor community programmes were greatly favoured. The choice of model will depend on local factors of convenience, existing availability of resources and incremental costs. Staff characteristics may be important in gaining optimal outcome, and care should be taken in staff recruitment and training |
| Study | Aims | Results/findings | Implications |
|---|---|---|---|
| Harrison et al. (2015)202 | To explore how patients who refuse referral to PR appraise acute exacerbations of COPD, in the context of having considered and declined PR | Three conceptual themes emerged: ‘construction of the self’, ‘relinquishing control’ and ‘engagement with others’. Prominent in the participants’ narratives are self-conscious cognitions, which appear founded in shame and stigmatisation. Perceived personal culpability for COPD appears to sensitise participants’ towards their interactions with HCPs, construed as critical and judgemental, which may increase avoidant behaviours, such as refusal of PR | When introducing PR, HCPs need to be mindful of patients’ sensitivities to being shamed, which stem from perceived culpability for COPD. Compassion-focused interventions that encourage trust and safety may promote active partnership working and facilitate engagement with PR |
| Hogg et al. (2012)212 | What are the views and perceptions of people with COPD regarding maintaining an active lifestyle following a course of PR? | Five main themes emerged: value of PR, ongoing exercise, professional support, peer social support and health status. PR was seen as enabling a more active lifestyle by improving physical ability and confidence to manage breathlessness, and reducing fear of exertion. An exercise routine following rehabilitation was seen as essential for maintaining activity. Participants identified a need for ongoing, structured and supervised sessions to maintain new-found abilities. The exercise facility presented a possible barrier to attendance because of its potential to provoke feelings of embarrassment or intimidation. Professional and peer support were identified as key elements and participants wanted to exercise in a group that offered an opportunity for social interaction. COPD symptoms had a negative impact on physical activity participation. Confidence or self-efficacy for physical activity emerged as prominent factors in main themes | The opportunity for structured exercise with peer and professional support, in a suitable venue, is perceived as important for supporting an active lifestyle following PR. The desire for such opportunities may be related to individuals’ self-efficacy towards physical activity |
| Lewis et al. (2014)217 | To explore COPD patient experiences during the key period from referral to initiation of PR in the UK | Twenty-five COPD participants aged 42–90 years were interviewed. ‘Uncertainty’ affected participants throughout their lived experience of COPD, which negatively affected illness perceptions, PR perceptions and increased participants’ panic and anger. Participants who perceived COPD less as a chronic condition and more as a cyclical process experienced fewer feelings of panic or anger. The experience of uncertainty was disabling for these COPD participants. Recognition of the role that uncertainty plays in patients with COPD is the first step towards developing interventions focused on reducing this uncertainty, thereby reducing the burden of the disease for the individual patient and facilitating PR attendance | Recognition of the role that uncertainty plays in patients with COPD is the first step towards developing interventions focused on reducing this uncertainty, thereby reducing the burden of the disease for the individual patient and facilitating PR attendance |
| Lewis and Cramp (2010)214 | To explore the attitudes of people with COPD to exercise and reasons for non-concordance with exercise maintenance post PR | From the focus group discussion, three main themes were identified: effects of exercise, facilitators of exercise and barriers to exercise. The effects of exercise were perceived to be mainly positive, although tiredness was also mentioned. Facilitators of exercise included encouragement, company, professional support, goal-setting, personal attributes and availability of a range of exercise options. Barriers to exercise included changing health status, fear, lack of support and environment. A range of exercise options need to be available and combined with professional support, goal-setting, encouragement, company and a suitable environment | The above themes may guide service providers in planning maintenance exercise sessions and in assisting people with COPD to strengthen exercise facilitators and overcome barriers to exercise. As individuals have different needs, and as their health status and circumstances change, communication needs to be ongoing and the exercise maintenance adaptable. A range of exercise options needs to be available and combined with professional support, goal-setting, encouragement, company and a suitable environment |
| Moore et al. (2012)216 | To assess the obstacles to participation in PR among COPD patients in a community-based PR programme and associated general practices | Twenty-four patients (13 male, 12 not referred) were interviewed. There were major concerns about the acceptability of PR. Some were concerned about the feasibility of attending the sessions. Other barriers included perceptions of PR and of exercise, how a smoker might be seen and the suitability of group activity. The views of professionals were influential, as were recommendations from other patients. The location of the centre was important. Participants’ willingness or reluctance to take on something new was a central element of the decision. Many saw a role for experienced patients in introducing the treatment | For patients who refused referral to PR, had not completed a course or had yet to be referred, the way the service was introduced significantly influenced their willingness to participate |
| Study | Setting | Aims | Results/findings | Implications |
|---|---|---|---|---|
| Dean et al. (2014)219 | Two inner-city general practices in London | To evaluate the effect of a specialist nurse-led hypertension clinic with consultant backup on change in systolic blood pressure | Follow-up was 89% (313/353). There was greater reduction in systolic blood pressure in the clinic group (n = 144) than in the usual-care group (n = 169) (adjusted difference 4.4 mmHg; 95% CI 0.7 to 8.2 mmHg) | Invitation to a specialist nurse-led hypertension clinic with consultant backup was associated with reduced systolic blood pressure |
| Gillett et al. (2016)220 | To evaluate an integrated service managing high-risk respiratory patients at risk of poor outcomes | Two general practices in the UK region of Wessex. One urban and one rural practice | 82 patients were identified, 55 attended. 13 (23.6%) had their primary diagnosis changed. In comparison with the seasonally adjusted baseline period, in the 9-month follow-up there was an increase in inhaled corticosteroid prescriptions of 23.3%, a reduction in short-acting beta-agonist prescription of 33.3%, a reduction in acute respiratory exacerbations of 67.6%, a reduction in unscheduled GP surgery visits of 53.3% and acute respiratory hospital admissions reduced from three to zero. Only four patients (7.3%) required referral to secondary care. Health economic evaluation showed respiratory-related costs per patient reduced by £231.86 | This service development evaluation demonstrates that patients with respiratory disease at risk of suboptimal outcomes can proactively be identified for management by an integrated team in the community without the need for extensive, expensive secondary care technologies and warrants further evaluation at scale to determine its impact in other regions to fully determine health economic outcomes |
| Study | Study design | Results/findings | Conclusions |
|---|---|---|---|
|
Flood-page (2016)225 Population/condition: COPD |
Controlled observational | Between 2003 and 2009 there was a 5.5% increase in COPD admissions across Gwent and a 5% increase for Wales as a whole. LAB admissions increased in all bar two areas, where they fell by 4.6% and 4.3%, respectively | Authors (while acknowledging limitations of the study) concluded that services with close links between primary and secondary care may be more effective than those based around primary care alone |
|
Glogowska et al. (2015)127 Population/condition Heart failure |
Qualitative | Specialist heart failure nurses have key roles in delivering education to patients and facilitating communication among the clinicians involved in their care. Participants perceived the nurse role as important for ensuring co-ordination and continuity of care | |
|
Kosteli et al. (2017)227 Population/condition: COPD |
Qualitative | Understanding patient-specific social cognitive influences on physical activity participation can inform planning of tailored interventions for people with COPD | |
|
MacKenzie et al. (2010)226 Population/condition: heart failure |
Qualitative | GP response rate was 32%. Despite strong supporting evidence, the nurse-led service was not welcomed by all doctors | Authors suggest that commissioners and service providers should be aware of the different roles of urban and rural GPs when designing such services. Service models designed from experience in urban areas may not be directly transferable to rural settings |
|
Sarran et al. (2014)228 Population/condition: COPD |
Controlled observational | The difference between intervention and control practices for admissions with a primary diagnosis of COPD was –0.8 percentage points (95% CI –1.8 to 0.2 percentage points). For admissions with a primary or comorbid diagnosis, the corresponding values were –2.3 percentage points (95% CI –4.2 to –0.4 percentage points) | Authors concluded that Healthy Outlook reduced hospital admissions for COPD when comorbid diagnoses were included |
| Study | Study design | Results/findings | Conclusions |
|---|---|---|---|
| Multiple interventions | |||
|
Ghosh et al. (2016)240 Population/condition: COPD |
Uncontrolled observational | Eligible patients had two or more unscheduled admissions for COPD in the previous 12 months. Over the 12-month intervention period, admissions decreased from 3.13 to 1.02 per patient. There was a net saving to the clinical commissioning group of £117,550 | The intervention as a whole was significantly associated with reduced admissions, but components such as specialist nurse home visits and health coaching were not |
|
Roberts et al. (2010)238 Population/condition: COPD |
Uncontrolled observational | Implementation of the new service model was associated with an increase in COPD diagnoses, with reductions in unplanned hospital admissions (935 to 840) and average length of stay (8.3 to 7.7 days). Costs associated with COPD management fell from £1.78M to £1.53M | Authors stressed the importance of liaising with a wide range of stakeholders and collaborating with the pharmaceutical industry in an ethical way. The POINTS software facilitated change by providing data on the patient population and current management practices |
|
Williams et al. (2010)239 Population/condition: heart failure |
Controlled observational | The number of re-admissions was lower in the intervention group than in the control group (4/47 vs. 7/50) but the sample size was too small for statistical significance. Questionnaire responses indicated that patients were satisfied with the new service | |
| Other interventions | |||
|
Cope et al. (2015)242 Population/condition: COPD |
Uncontrolled observational | Compared with pre-service data, the in-reach service reduced average length of stay by 2.53 days. Re-admissions within 30 days were reduced from 8.1 per month in 2012/13 to 3.9 in 2013/14. Numbers discharged to the early assisted discharge service increased from 9 to 79, representing 17% of admitted patients | Authors stated that the in-reach service model would be applicable to other long-term conditions and hospital sites |
|
Wilkinson et al. (2014)241 Population/condition: COPD |
Uncontrolled observational | Thirty-four patients were found to be responsible for 176 admissions (22% of total COPD admissions) to the hospital. These patients required 185 active interventions during the 12-month study period but only 39 hospital admissions. The 30-day re-admission rate decreased from 13.4% to 1.9% (p < 0.01) | Authors concluded that the use of medical intelligence data to identify factors underlying frequent admission allowed an effective intervention to be delivered in a consultant-led model |
List of abbreviations
- A&E
- accident and emergency
- ACSC
- ambulatory care sensitive condition
- AMU
- acute medical unit
- BACPR
- British Association for Cardiovascular Prevention and Rehabilitation
- CCM
- chronic care model
- CHD
- coronary heart disease
- CI
- confidence interval
- CMO
- context–mechanism–outcome
- COPD
- chronic obstructive pulmonary disease
- GOAL
- Good Outcomes for Asthma Living
- GP
- general practitioner
- HCP
- health-care professional
- HSDR
- Health Services and Delivery Research
- IT
- information technology
- MDT
- multidisciplinary team
- NACR
- National Audit of Cardiac Rehabilitation
- NHRPP
- Northumberland High-Risk Patient Programme
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- PARiHS
- Promoting Action on Research Implementation in Health Services
- PPI
- patient and public involvement
- PRP
- pulmonary rehabilitation programme
- PT
- programme theory
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- RAMIT
- Rehabilitation After Myocardial Infarction Trial
- RCT
- randomised controlled trial
- SEPRP
- Structured Education Pulmonary Rehabilitation Programme
- SPACE
- Self-management Programme of Activity, Coping and Education
- TIDieR
- Template for Intervention Description and Replication
