Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/33/45. The contractual start date was in September 2014. The final report began editorial review in November 2017 and was accepted for publication in April 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Christopher Vernazza reports a grant from GlaxoSmithKline (GSK) (Brentford, London, UK) during the conduct of the study. Girvan Burnside reports a grant from GSK during the conduct of the study. Susan Higham reports grants from Unilever UK Limited (London, UK) and GSK and an Engineering and Physical Sciences Research Council (Swindon, UK) and GSK CASE (formerly known as Collaborative Awards in Science and Engineering) Studentship during the conduct of the study.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Harris et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background and introduction
Risk and responsibility in the NHS
Defining risk
Risk is the possibility that something unpleasant or unwelcome will happen. 1 Therefore, risk carries two elements: the probability of an adverse outcome happening and how important or troublesome the outcome would be. 2 Linguists have identified the word as originating from the world of navigation (the Latin word ‘risicum’ meaning sailing into uncharted waters, and the Greek ‘rhiza’ meaning the hazards of sailing too near to the cliffs, contrary tides, turbulent downdraughts, etc.). However, scholars have noted that the word risk is often used very loosely in everyday parlance and, as a conceptual phenomenon, is open to multiple interpretations. 3 Giddens, for example, argues that in traditional cultures, and in the Middle Ages, there was no such notion as risk (because troubles were understood to come from God, or simply to be part of a world that one takes as granted). 4 Rather, the idea of risk is ‘bound up with an aspiration to control and particularly with the idea of controlling the future’. 4 Lupton also identifies that the concept of risk in late modernity assumes that ‘something can be done’ to prevent misfortune. 5 She observes that ‘the notion of risk is associated with notions of choice, responsibility and blame, and has become a means by which institutions and authorities are held accountable and encouraged to regulate themselves’. 5 The term ‘risk society’ has been coined to describe modern ideas of the nature of and attitudes to risk. 6
General policy context: discourse on risk and individual responsibility
Public health in the UK and other Western countries currently operates within a neoliberal model. 7–10 Here, neoliberalism refers to a ‘system of thoughts and beliefs’7 about the role of the state that includes ‘shrinking state mandate, deregulation and privatisation, a faith in markets to govern social life, and an increased emphasis on personal choice and freedom’. 11 Using this definition to think about health, neoliberal approaches emphasise the role and responsibility of individuals to make healthy choices and, subsequently, to accept the blame for their failure in order to become a ‘good’ citizen. 12,13 As such, citizens have a duty to be well. 14 Neoliberal approaches to health in the UK are readily seen in governmental policy documents with references to an onus on the public ‘to take personal responsibility for their own health’. 15 Although the recent UK White Paper states that responsibility for health should be shared, it also emphasises the need for approaches to ‘empower individuals to make healthy choices’. 16
In a ‘risk society’ where personal responsibility for health is emphasised, experts are essential in order to provide knowledge to guide individual decision-making. Psychologists largely follow this tradition, tending to focus on risk behaviours and ways in which individuals’ responses to risks can be improved. 17 This, however, assumes that risk is an objective reality that can be measured, controlled and managed. 3 Although this ‘technicoscientific’ perspective18 on risk predominates in science and medicine, there is a danger that this approach overplays certainty when there is none. 6,19,20
An alternative standpoint is to understand risk as socially constructed within cultures,21–24 an approach emphasising that risk-taking is a form of social action that involves individuals facing challenges and making decisions that contribute to their social identity. 17 Anthropologists, for example, identify that there is often a bias ‘highlighting certain risks and downplaying others’. 21 For example, the focus on young people’s drinking in the context of excessive drinking among the middle-aged. 25 Advocates of the sociocultural perspective are concerned when, because risk tends to relate to danger and thus has a negative valence,21,26 objects, behaviours and groups are described as ‘risky’ and inevitably associated with badness, danger, being morally flawed7 and deviant. 27 Current policy discourse tends to encourage people to ‘define themselves in part by how well they succeed or fail in adopting healthy practices’. 28 Where certain groups are being defined as ‘high risk’, a rounded perspective on risk should therefore consider who is being judged, who is being blamed and who is labelling them as dangerous. 21
Rationing through risk assessment
Rationing (a process that restricts access to potentially beneficial but scarce resources) is inexorably linked to risk assessment; when professionals judge people to be at a ‘high risk’ of some disorder, they invariably seek to target scarce services at the selected population. 29 Being labelled ‘at risk’ can result in individuals being targeted for ‘expert advice, surveillance and control’. 30,31 ‘Low risk’ patients may be allocated proportionally fewer resources, even though they may have benefited from these. 29
Within a context of neoliberal responsibilisation, however, ‘high-risk’ individuals might also face restrictions on certain types of care. This is because a multiplicity of responsibilities exist. 11 Neoliberal ‘responsible’ citizens exist within a matrix of dependencies. While patients share responsibility with clinicians for their health, clinicians have wider responsibilities too, to other patients, to the state and to society in general for their use of scarce resources. Thus, fertility treatment is restricted for women over a certain body mass index,32 priority scoring tools including positive exercise tests, non-smoking habits are introduced to deal with elective surgical waiting lists,33 and root canal treatment, crowns and bridges are restricted for ‘red’ patients within prototypes of the new NHS dental contract being tested. 34 Risk is a notion that is relevant to almost every aspect of modern health care; its relevance extends beyond a means to improve the way patients look after their own health and it has a significant impact on the way health services themselves are delivered, especially in NHS dentistry.
Dental policy context
Since the 1990s, there have been various models of contract-governing work undertaken in NHS dental practice. All have been met with unintended consequences and have led to further reform. 35 Two prototypes of a new model contract are currently being tested in > 80 English dental practices. 34 Both are based on the principle of allocating patients to clinical care pathways according to an oral health risk assessment undertaken at a dental check-up. 36 Information on the patient’s medical history, social history (self-care, e.g. toothbrushing habits) and clinical examination findings determine whether the patient is categorised as red (high risk), amber (medium risk) or green (low risk) within the traffic light [red–amber–green (RAG)] system. In the prototypes and earlier pilot practices, software with a RAG algorithm was used to generate the red–amber–green rating of risk, which was then ‘fed back to the patient and used for appropriate advice and treatment’. 37 Data from new contract pilot practices indicates that 16% of adult NHS patients are green (have healthy mouths and virtually no signs of disease), 56% are amber and 28% are red. 37
Risk communication
Risk communication is something that most clinicians do every day. 38 In dentistry, risk communication is even recommended as something which ‘should form part of every patient interaction’. 39 This is because, first, patients’ risk perception, and how this balances with benefits, lies at the heart of helping patients make informed choices between treatment options and, second, because self-care and self-management behaviour is underpinned by how patients perceive threats to their health. 40,41 Risk communication is also the concern of public health practitioners, where it is seen as crucial to the prevention and co-operative management of health risks, and ‘at least equally essential to outbreak control as epidemiological training and laboratory analysis’. 42 While this study is concerned with risk communication with patients in a health-care setting to prompt improvements in self-care behaviour, its findings have relevance to other activities involving communication of health risk messages in other contexts.
Recent systematic reviews of risk work in health-care settings have found a deficit of research looking at how risk is acted on, and communicated, in routine practice. 1
Tailoring of risk information
‘Tailoring’ refers to methods of creating communications that are individualised to the receivers, with the intention that this increases impact. 43 Studies generally show that tailoring of information is beneficial. 43–45 Tailoring of risk information for health education purposes is thought to be especially important, because people are found to report their own risk of experiencing a health problem as less than that of an average person, even when given information about the average person’s risk or behaviour. 46 This systematic underestimate of personal risk is a barrier to the adoption of all types of precautionary health behaviour. 46
Individualised health communication can range from personalised generic communication (e.g. using someone’s name to personalise the message) to targeted communication (composing the message with a particular group or segment of the population in mind, an approach that is the basis of many public health education and social marketing campaigns), through to truly personalised communication that provides information based on characteristics that are unique to a person (e.g. as in brief counselling interventions). These approaches involve tailoring, which is based on characteristics beyond broad demographic categories such as age or gender and, therefore, depend on some sort of individual assessment. However, with the advent of computer-based tailoring, the population reach can still be wide. 47,48
Social marketing, which takes lessons from commercial marketing and applies them to the health and social sectors,49 takes a targeted communication approach out of concern that health messages, given inadequate understanding of the groups they are meant to serve, can result in a widening of health inequalities between the rich and poor. 50 It divides populations into ‘audience segments’ according to shared characteristics and behaviours, and then explores what each target audience prefers to do and what affects their behaviour and preferences. 51 The emphasis is on developing a whole understanding of consumers’ complexities of life, and how people choose to navigate these. 50 Pricing is a major device in the social marketing toolbox, which sums up the costs that the target audience will ‘pay’ for adopting the desired behaviour that leads to the promised benefits. Taking a ‘value to user’ approach as opposed to an ‘expert defined product’ approach lies at the heart of social marketing approaches that aim to design programmes which make changing behaviour easy. 49 Health information preferences is one way in which populations may be segmented, with this directly informing how health promotion approaches might be best applied. 52 Although many studies report area-based differences in oral health and behaviour, with application in identifying small areas that may benefit from health promotion activities,53 relatively little information exists concerning the value that people in deprived areas place on interventions that aim to improve their oral health. More work is also needed about the type and amount of information people want concerning their oral health, and whether or not this varies according to different psychographic (attitudes, values, lifestyle) groups. This study therefore has relevance, not just to inform the giving of risk information to individual patients in NHS dental practices, but in informing the design of risk communication messages to targeted segments of high-risk populations.
Risk presentation, format and information visualisation
Previous literature on risk communication has concentrated on information framing, the interpretation of numerical information54,55 and whether presenting information numerically or in different graphical forms has greater impact. 56,57 Rothman and Kiviniemi46 group these investigations as ‘probability-based approaches’, comparing them with contextually based communication strategies. They conclude that probability-based approaches alone are unlikely to be successful, not just because people generally have difficulty understanding and using quantitative information, but because risk perceptions are ‘imbued by emotion’ and ‘always interpreted via a social and cultural lens’. 58 As an alternative, they outline contextually based approaches to risk communication, which are better at recognising that lay conceptions of risk are based on a rich mixture of cognitive and affective beliefs, and enable people to develop a mental model that delineates the personal relevance of a given risk. 46 An example of a contextually based approach would be to direct individuals to imagine themselves experiencing a symptom of a disease in order to heighten their perception of personal vulnerability.
Information visualisation is important here. It assists sense-making, which is the process of finding meaning from information. 59 For example, a study including digital photographs to contextualise and augment glucometer readings for people living with diabetes mellitus, found that the images carried deeper meaning than purely looking at the readings, and helped participants to address the social and psychological challenges of living with the condition. 60 Patients are known to use heuristics (simplified ‘rules of thumb’) to allow them to understand and make decisions. 61,62 Although heuristics may be biased by non-relevant information, such as cultural expectations and emotional responses, they are still important in allowing patients to process large amounts of complex and novel information and make decisions. 63,64 The traffic light (TL) categorisation of patients’ oral health risk is an example of an information format that provides a simple portrayal of complex sets of information, which may be useful and valuable to patients (although this has never been tested).
People’s understanding of risk is thought to be enhanced when information is presented in a vivid way, holding their attention. 65 Although all patients can benefit when pictures are used, people with low literacy skills are especially likely to benefit. 65 Very vivid and highly personalised information is increasingly available as risk communication tools, given recent advances in technologies, scans and radiographs now available that show, for example, body fat, heart function and osteoarthritis of joints. Previous studies have shown that medical imagery that gives a vivid representation of the consequences of unhealthy behaviour can enhance risk communication, although these have used general rather than personalised images, which provide less personalised information about risk status. 66–68 None of these studies investigated the extent to which patients appreciate and value this type of information.
Developments in dental photography technology allow a vivid and highly personalised way of presenting risk information to dental patients. A Quantitative Light-Induced Fluorescence (QLF™) camera (Inspektor Research Systems BV, Amsterdam, the Netherlands) can produce images of teeth showing tooth mineral loss before it is visible to the naked eye and before cavities develop. 69 Demineralised areas show up as dark spots on QLF photographs, where loss of fluorescence correlates with mineral loss in the lesions (when teeth demineralise there is a loss of fluorescence due to an increase in tooth porosity, which in turn leads to a decrease in the refractive index of the carious lesion) (Figure 1). Camera software allows changes in fluorescence of dental enamel to be quantified to estimate mineral content and, as such, can be used to evaluate changes in level of dental caries, although this requires dental plaque to be removed from teeth before the image is taken.
FIGURE 1.
Example QLF image of early tooth decay: dark patches on the image.

Quantitative light-induced fluorescence also highlights mature dental plaque in a relatively vivid way. Mature dental plaque (present for ≥ 48 hours) contains porphyrins, a by-product of the bacteria that appear as bright red/orange areas (red fluorescence)70 under QLF conditions (Figure 2). QLF images can therefore be a useful means of monitoring patients’ toothbrushing behaviour over several days rather than just behaviour related to the day of the oral examination itself. Plaque Percentage Index data gathered from QLF photographs permit plaque assessment on an interval scale and show excellent reliability when repeated measurements of the same image are analysed. 70 The tooth surface area of red autofluorescence of dental plaque can also be measured using software associated with the QLF equipment.
FIGURE 2.
Example QLF photographic image of plaque coverage: red fluorescence highlighting plaque present in the mouth for > 48 hours.

Quantitative light-induced fluorescence images can be stored in clinical records for subsequent reference and shared with the patient (digitally or as a hard copy). Images can be discussed at the dental chair-side on a computer screen or tablet, with the option of e-mailing images to patients’ mobile devices or computers as material to support the message given.
Quantitative light-induced fluorescence offers an alternative risk communication tool to TL graphics currently being used in new dental contract prototype practices. Although possibly more expensive as a higher-technology option, its potential benefits and whether or not patients value information in this form has never been properly explored. Incorporating QLF technology into the study also allows us to gather objective measures of oral health (demineralisation of teeth and plaque coverage).
Traffic light and QLF imagery have contrasting features as risk communication tools:
-
TL image –
-
simple information
-
individuals grouped by category
-
image is pictorial but not vivid
-
low technology.
-
-
Quantitative light-induced fluorescence (QLF) –
-
detailed information
-
personalised to individuals
-
vivid
-
high technology.
-
Risk work
Previous research on risk in the health context has focused mainly on either the perspective of patients or on the governance of risk by organisations. 71 By contrast, very little work has been conducted which takes a service delivery perspective. For example, dealing with how frontline health-care workers undertake activities concerned with identifying and managing risk. Against a backdrop of a ‘risk society’,6 Gale et al. 71 used the term ‘risk work’ to denote ‘working practices framed by concepts of risk’. Despite a drive from evidence-based medicine for consistent application of externally produced knowledge, dealing with uncertainty remains part and parcel of medicine, which is both an art and a science,72 so ‘risk work’ is central to everyday health care.
‘Translating’ risk information into different contexts is a common health-care activity. 71 Some of this work involves translating ‘up’, identification of individuals and creating auditable records to ensure accountability (e.g. as in the RAG categorisation of NHS dental patients in prototype practices). Translation work is also required, when clinicians take population-level data and converse with patients, translating the data into meaningful information for the individual in order to bridge the gap between scientific and lay perspectives of risk. 73
Talking to patients about risk can in itself be risky: first, balancing uncertainties in risk makes talk difficult73 (some risks may be open to medical uncertainty); second, ‘risk talk’ can be threatening for patients who may experience shame or embarrassment as a result; and, third, risk does not automatically concern an actual deviance in the patient’s body, but rather indicates a probability of something happening in the future, and hence risk talk can be anxiety inducing for patients. Risk talk can even result in a deterioration of a patient’s health: ‘once a person knows that she or he is at risk, the person often starts to feel uneasy and it is possible that she or he begins to feel sick and indeed becomes sick’. 73 While previous studies have investigated risk talk using discourse analysis,73 contextual, extraneous information in interpreting discourse data (ethnographic methods) is recommended. 74
Theoretical model of risk perception and behaviour change
Imagery and numeric risk estimates are thought to influence people’s reaction to risk messages by increasing patients’ perception of the said threat to their health and well-being, thus heightening fear regarding any negative consequences of inaction. 75 The extended parallel process model (EPPM) is therefore relevant in this context because it predicts that people engage in defensive behaviours when they perceive themselves to be at risk of a threat. 76 The EPPM model is based on the concept of ‘fight or flight’. It supposes that a person is likely to ‘flee’ if they perceive that the threat is great and that they have little hope of overcoming the obstacle, whereas they are more likely to ‘fight’ where they believe that (1) the challenge is important enough (perceived threat) and (2) they can win (perceived efficacy).
According to the EPPM, ‘perceived threat’ has two components (threat susceptibility and threat severity), as does perceived efficacy’ (response efficacy and self-efficacy). Self-efficacy refers to individuals’ subjective beliefs that they can complete behavioural changes. 77 Response efficacy relates to the person’s belief about how effective the recommended behavioural change will be to reduce the threat. The EPPM model hypothesises that when both threat and efficacy levels are high, danger control processes ensue, which lead to aversive action, whereas when threat appraisal is high and efficacy appraisal is low, this can lead people to a maladaptive action, such as rejecting the message. The EPPM, therefore, theorises that when someone is presented with information at their dental check-up appointment (e.g. about their risk of tooth decay or gum disease), they may either sense no threat and do nothing/become fearful and ignore the message or begin a danger control process, which drives them to accept the challenge and adopt the recommended course of action.
The course of action which the patient takes is therefore thought to be influenced by the extent to which the message given conveys how serious the threat is (e.g. pain, spoilt appearance from tooth decay), and how susceptible they are to such problems. The form in which information on risk is given is particularly relevant here. Imagery, in particular, has been associated with defensiveness. 78 The EPPM opens the possibility that certain risk communications can have negative as well as positive effects on individuals. 79 The EPPM will therefore be used as a framework to help understand why TL or QLF supplements to usual verbal risk communication at dental check-ups are or are not effective, and how effectiveness of risk communication may be improved.
Overview of the project
Aims and objectives
Our aim is to describe how patients value and respond to information on their oral health status and risk, and to compare the value of three different methods of presenting information on patient’s oral health and risk: verbal communication only, verbal supported by information presented as a TL graphic, or a QLF image of the patients’ own mouth.
Objectives
-
Describe what type of information patients want, need and prefer when having a dental check-up and how they use this information.
-
Describe how patients interact with the three different forms of information.
-
Investigate whether or not and how the clinician–patient relationship is influenced by patients having access to different types of information.
-
Measure individuals’ preferences, by using the economic, preference-based valuation methodology [willingness to pay (WTP)] for each of the three different methods of giving information.
-
Identify differences in preference for different types of information by differing demographic, behavioural and psychographic groups.
-
Use variables from derived established models of the behavioural change process to predict the likelihood that different forms of communication will lead to behaviour change; and to measure any actual behavioural changes and link these with differences in valuations.
-
Conduct a cost–benefit framework analysis of the three different methods and to explore financial implications for NHS dentistry.
Research plan and outline of chapters
In order to frame our research within the wider health-care context, and help address objective 1, we undertook a systematic review to identify and summarise any previous research undertaken in clinical settings concerned with how patients value and respond to health risk information given in different forms. This was focused on giving personalised feedback about health states or health risks in different forms (for example, but not limited to verbal, written, diagrammatic, photographic information), and investigated the following outcomes: patients’ preferences and economic valuations, objectively verified behavioural change, self-reported behavioural change and potential mediators of change including behavioural intentions and risk perceptions, as well as having an impact on patient-carer communication and patient satisfaction. Methods and results are given in Chapter 2.
To help address the first three objectives, we undertook an ethnographic study. This began before the experimental stage of the research [a randomised controlled trial (RCT) in NHS dental practices] and continued as a piece of qualitative research alongside the trial. The purpose of ethnography is to provide in-depth accounts of people’s views and behaviours as well as the significance of the inhabited space of the interaction. 80 As well as collecting qualitative data by interviewing patients and dental staff, we collected a wealth of ethnographic data, which included non-participant observations of dental appointments. We did this in recognition that dental staff and patients may behave differently during the dental appointment (or the ‘front stage’ according to Goffman81) than in other spaces and interactions (back stage). Cross-examining dental team and patients’ accounts with observations of everyday practices allowed us to investigate discrepancies between what patients and dental staff said and what they actually did to become apparent; this allowed us to more fully explore objectives 1–3 using the concept of ‘risk work’82 as a framework. Risk work is concerned with working practices that occur under the guise of risk, for example what do discussions of risk do in NHS dental practice, how dentists translate risk information to patients, how dentists amplify or minimise risk when giving patients information and how dentists provide care to patients when addressing risk. 71,82
The qualitative research component of the study is described and reported in Chapter 5. The qualitative component of the study was also used to identify negative outcomes from poor dental health which were important to patients, for inclusion in RCT data collection as measures to investigate potential mechanisms related to behaviour change (see Chapter 3, Secondary outcomes).
Objectives 4–7 are addressed in a RCT undertaken in four NHS dental practices, the methods and results of which can be found in Chapter 3 and 4, respectively. This research was undertaken with the active participation of four people who have a patient and public perspective in the formulation and conduct of the research, as well as in its reporting. Chapter 6 is written by this group and outlines their involvement and perspective. Chapter 7 brings together the various research components in a discussion of findings and implications for policy and practice. We also identify future research needs in this area.
Ethics and NHS Research Governance approvals
Liverpool Health Partners was the research sponsor (approval reference number UoL001042). Favourable ethics opinion for the study was confirmed by the North West – Liverpool East National Research Ethics Committee (REC) on 1 August 2014 (REC reference number 14/NW/1016). A subsequent substantial amendment in ethics approval was obtained on 18 March 2016 pertaining to the RCT [to allow a prize draw of 10 lots of £25 (amounting to £250 in total) for patients completing follow-up data collection at 6 months and, again, at 12 months]. NHS Research Governance approval was obtained from The Royal Liverpool and Broadgreen University Hospitals NHS Trust on 20 August 2014 (reference number 4819).
All participants in the study (dental staff and patients) received a written information sheet relating to their aspect of the study, written and signed consent was obtained before their involvement in the study. The information sheet provided details of the study, information on right to withdraw at any time, anonymity and confidentiality, along with contact details of the research team. Participants were given the opportunity to ask questions before consent was taken.
Records identifying participants used a system of identification (ID) numbers to preserve anonymity, with all data stored under the guidelines of the 1998 Data Protection Act. 83 No patient-identifiable information was sent via electronic means (use of coded study number, patient’s gender and age only). Details of patients participating in the RCT were recorded in a recruitment log and this was held by the NHS dental practice where they were recruited. This information was later collected in person by a member of the research team, rather than transmitted electronically, in order to conduct follow-up data collection.
Chapter 2 Systematic review
To enable us to understand the contribution of our research in the NHS dental practice context to the wider context of health care more generally, we undertook a systematic review to identify previous work that had focused on the form of risk information given to patients in a clinical setting. Our review focused on research that provided personalised feedback to patients about health states or health risks in different forms and in clinical settings (e.g. verbal, written, diagrammatic and photographic information). We also focused on research that investigated the following outcomes: patients’ preferences and economic valuations, objectively verified behavioural change, self-reported behavioural change and potential mediators of change including behavioural intentions and risk perceptions, and impact on patient–carer communication and patient satisfaction.
Review methods
Search strategy
We adopted an iterative search strategy, which involved electronic literature searching of nine databases (including grey literature and dissertation databases) and hand-searching eight specialist journals (see Appendix 1, Table 24). To strike a balance between literature search sensitivity (finding all articles in the topic area) and specificity (finding only relevant articles), we initially developed electronic search terms using TerMine ATR software (using the GENIA Tagger version 2.1 POS tagger, which is customised for texts from biomedical science) provided by The National Centre for Text Mining, University of Manchester (www.nactem.ac.uk), applying this to 35 papers previously retrieved through pilot searches undertaken in Google Scholar (Google Inc., Mountain View, CA, USA). 84 We then broadened the search strategy with general topic search terms (e.g. health education) as is customary to systematic review methods. 85 Search terms used for an example (MEDLINE) search are found in Appendix 1, Table 25. We also used forward and backward citation searches, that is, reviewing references cited in articles identified earlier in the review process and searching for publications which cited papers that met study inclusion criteria. Because we were originally only commissioned to do a scoping review, rather than a systematic review, we did not contact authors for the full article where only abstracts were available either online or via interlibrary loan. The search was last updated on 10 October 2017.
Inclusion and exclusion criteria
Literature searching was limited to publications about adults receiving risk information in clinical settings. We were aware that this was a developing field and wanted to include reports which might be likely to lead on to experimental work in the near future (we had originally been commissioned to do a scoping review). Therefore, we included all types of study design, including qualitative work and protocols, although intervention study designs were limited to those comparing delivery of tailored risk information in one form with usual care or verbal risk messages, or with a different form of risk information. We included studies involving giving tailored information about an individual’s level of health with reference to likely negative consequences, as well as those involving risk terminology and health outcome probabilities (i.e. studies involving lay concepts of risk as well as risk defined in scientific terms). We precisely defined personalised (tailored) information as that ‘given to patients which is reliant on a pre assessment of the patient’ to mirror the situation that underpins new models of NHS dental care (oral health assessments at check-ups) and the design of the RCT component of our research. Complete inclusion and exclusion criteria can be found in Appendix 1.
Data extraction and analysis
Quality assessment of included RCTs was undertaken using Cochrane risk-of-bias methodology at the study level. 86 Data extraction items consisted of type of study, intervention type, study populations, methodology, outcome measures and key results. The limited number and heterogeneity in the design and outcomes of included studies meant that meta-analysis was not undertaken. We therefore used narrative synthesis methods to summarise and synthesise findings, juxtaposing data extracted from all included studies to identify common findings. 87
Systematic review results
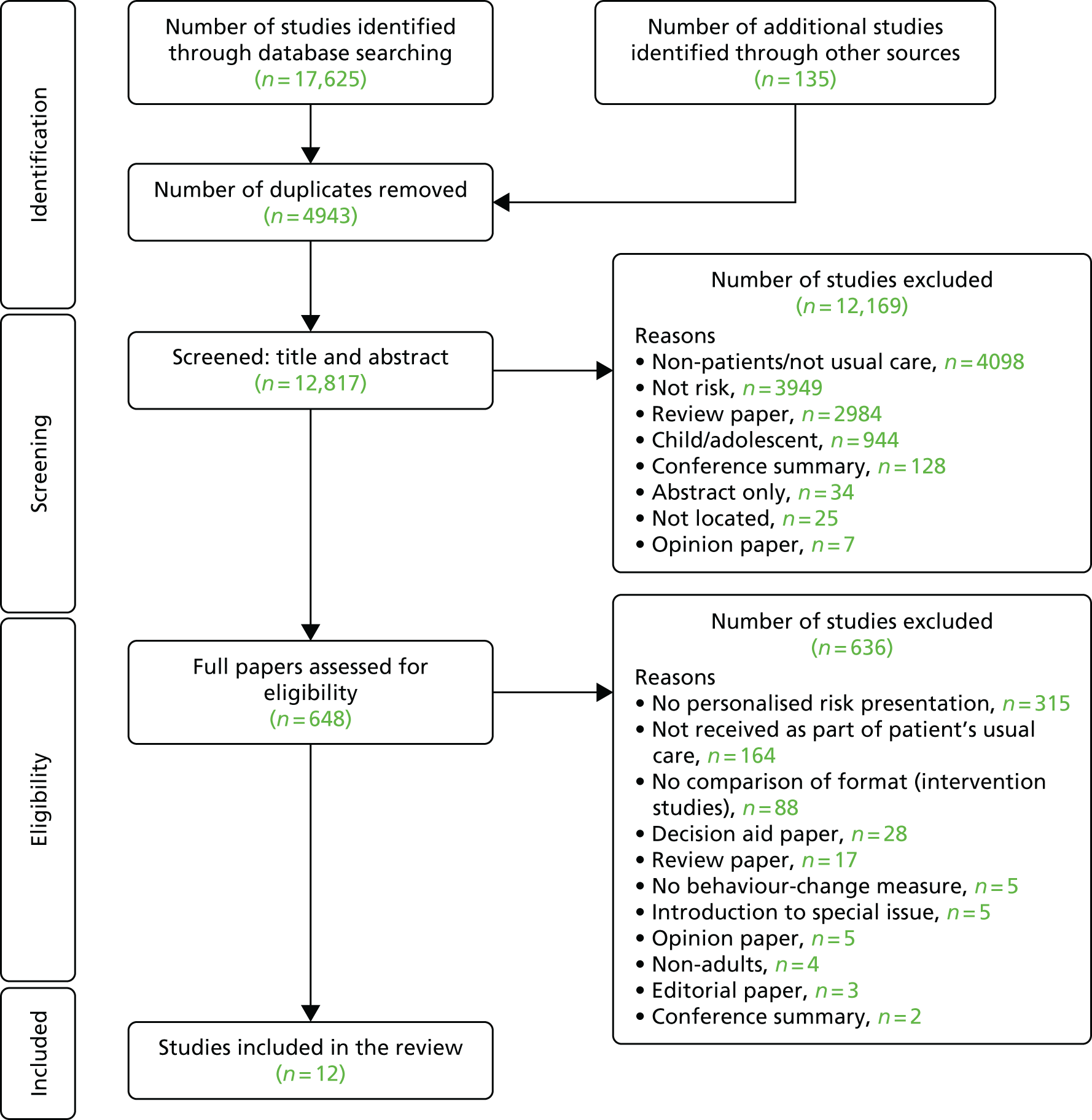
Electronic searching and hand-searching identified 17,625 papers, of which 4943 were duplicates. A further 135 papers were identified through backwards and forwards citation-chasing. Title and abstract screening was undertaken by two independent reviewers, with the full paper retrieved when at least one of the reviewers identified the study as potentially meeting inclusion criteria. This identified 648 potentially relevant papers that were then subjected to independent screening by the two reviewers, with any disagreements resolved by discussion. This identified 12 papers88–99 as being eligible for inclusion (Figure 3).
FIGURE 3.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Nine of the included studies were RCTs, although two of these were feasibility studies91,94 and two were pilot RCTs93,95 (Table 1). Of the three remaining publications, one was an intervention description,99 one was a protocol98 and the other was an iterative exploratory study that involved developing an intervention, with a qualitative analysis relating to the type of information patients preferred. 97 The quality assessment of included RCTs indicates that some of the studies were rated as having a low risk of bias in many domains (Table 2). There were no intervention studies that were not RCTs.
| Study (name, year of publication and type) | Participants (characteristics and location) | Intervention (n of participants and method of delivery) | Control (n of participants and usual care) | Follow-up (time) | Outcome measures (behaviour, communication and risk perception) | Results summary |
|---|---|---|---|---|---|---|
|
Dapp et al. (2011) 88 RCT Patients randomised by computer |
Non-disabled Aged ≤ 60 years 21 medical practices Hamburg |
n = 878 (14 practices) Written risk reports: |
n = 1702 (14 practices) Usual care: with physician training and checklists with preventative recommendations n = 746 An additional seven concurrent ‘comparison’ practices with untrained GPs |
1 year | Behaviour:
|
Adherence: ↑ in PCUB (OR 1.7, 95% CI 1.4 to 2.1) and ↑ in PHB (OR 2.0, 95% CI 1.6 to 2.6), but subgroup analyses suggest a favourable effect only with personal reinforcement NS health outcomes Preferences: Majority selected group rather than home visit reinforcement Group reinforcement is promising |
|
Harari et al. (2008) 89 RCT Patients randomised by computer |
Aged ≤ 65 years Four general practices UK 26 GPs |
n = 940 patients (18 GPs) Written risk reports: |
n = 1066 Usual care (18 GPs): Concurrent comparison group (one practice, eight GPs) |
1 year | Behaviour:
|
Adherence: ↑ in 1 PCUB (OR 1.2, 95% CI 1.01 to 1.5) and ↑ in 1 PHB (OR 1.4, 95% CI 1.0 to 2.0) NS health outcomes or patient self-efficacy Lower than expected effect attributed to lack of face-to-face reinforcement |
|
Kreuter and Strecher (1995) 90 RCT Randomisation unreported |
1317 adult patients aged 18–75 years from eight US medical practices |
n = not reported Graphical and numerical presentation of patients’ 10-year mortality risk Group 1: HRA feedback Group 2: HRA feedback plus behaviour-change information Results combined groups 1 and 2 and only given for participants recalling the intervention |
n = not reported Usual care |
6 months | Risk perception of mortality:
|
↑ in optimistic bias for risk perception of stroke mortality only (OR 1.27, 95% CI 1.02 to1.60), i.e. intervention groups were 27% more likely to have an ↑ in risk perception at follow-up ↓ in pessimistic bias for cancer risk perception only (OR 1.36, 95% CI 1.07 to 1.73), i.e. intervention groups 36% more likely to an ↓ in risk perception at follow-up |
|
Zullig et al. (2014) 91 Feasibility study Block randomisation |
US points with CVD + a modifiable risk factor Mean age 65 years |
n = 96 Web-based intervention: |
n = 49 Usual care with general health education information |
3 months | Behaviour:
|
NS Web interventions may be ineffective without guidance and accountability from clinician interactions |
|
Welschen et al. (2012) 92 RCT Patients randomised by computer |
T2D points Netherlands |
n = 131 Verbal ± pictorial: |
n = 130 Usual care |
12 weeks | Risk perception:
|
↑ in risk perception (β between-group difference 0.48, 95% CI 0.02 to 0.95) after 2 weeks, but not at 12 weeks (β between-group difference –0.03, 95% CI –0.43 to 0.37) NS risk anxiety/worry NS ICB There is no evidence that risk communication, besides an improved risk perception, will motivate patients to adopt a healthier lifestyle |
|
Hess et al. (2014) 93 Pilot RCT Cluster randomised by doctor |
Attending a single US general practice Mean age 29 years |
n = 51 (16 doctors) Computer-generated immediate feedback of risk (e.g. tobacco use, physical activity, HRQoL) before clinical appointment, to prompt initiation of discussion |
n = 48 (14 Doctors) Usual care (completing health questionnaire without feedback) |
At the end of the visit | Communication:
|
NS Patient initiation of health-related discussion but ↑ in number of doctor reports of PID on physical HRQoL only for patients with low physical HRQoL (OR 4.6, 95% CI 1.3 to 16.3) Preference: NS patient perceived discussion to be useful |
|
Neuner-Jehle et al. (2013) 94 Feasibility RCT Cluster randomised by doctor |
Swiss general practice Median age 47 years 27 GPs |
n = 114 patients Verbal ± numbers ± pictorial risk message GPs using ‘quit smoking tool’ and individualised CVD risk calculation training presented in numbers and coloured charts and training and guidelines including Motivational Interviewing (MI) |
Verbal GPs using a ‘quit smoking tool’ and training and guidelines including MI |
Not reported | Behaviour:
|
NS patients estimated motivation NS comprehensiveness, satisfaction NS counselling duration, self-confidence Feasibility and acceptability of adding a visual element is ‘equally high’ |
|
Shahab et al. (2007) 95 Pilot RCT Patients randomised by computer |
23 CVD outpatients UK |
n = 11 Print of ultrasound image of their carotid artery alongside a disease-free artery and leaflet linking smoking and CVD |
n = 12 Routine verbal feedback |
Immediately after and at 4 weeks | Behaviour:
|
All outcomes NS except ‘perceived susceptibility’ Mean difference of high perceived susceptibility = 8.04 (95% CI 5.58 to 10.50) Interviews: Only patients in the intervention group reported that the visit made them think seriously about giving up smoking High self-efficacy may be necessary to translate higher risk perception into intention to change behaviour |
|
Mauriello et al. (2016) 96 RCT Patients randomised by computer |
English/Spanish-speaking pregnant women, up to 18 weeks’ gestation |
n = 169 patients iPad-delivered tailored guidance grounded in the transtheoretical model of behaviour-change during prenatal appointments, with goal-setting, a printed report and a booklet on behaviour targeted |
n = 166 patients A March of Dimes brochure |
1 month and 4 months post partum | Behaviour:
|
Stress: NS at 1 and 4 months Fruit and vegetable consumption: at 1 month 4.31 cups in the treatment group vs. 3.32 cups in the usual care group (OR 2.74); at 4 months 4.43 cups in the treatment group vs. 3.70 cups in the usual care group (OR 2.16) |
|
Saver et al . (2014) 97 Mixed methods study |
English/Spanish-speaking adults with T2D and at least one CVD risk factor Two general practices in one US city |
n = 56 patients Verbal ± pictorial risk message First 38 patients randomised to receive bar chart/crowd chart Final 18 patients receive bar chart/crowd chart sequentially Patients were asked to explain their thinking about any changes in the ranking of risks before and after receiving the intervention |
N/A | N/A | Qualitative data on reasons for changing/not changing, motivations for change, incongruence in perceptions |
Although 80% felt that some/all of the data applied to them personally, < 40% felt it motivate changes; 75% report ‘their own body experiences’ as their motivator; 20% report a ‘warning shot’ event or a specific instance when provider urging resulted in engagement of healthy behaviours Personalised risk estimates have limited salience |
|
Ahmed et al. (2011) 98 RCT protocol Block randomisation |
18- to 69-years old Asthma patients from tertiary care pulmonary clinics, Canada |
n = 80 Web-based self-management system with asthma status presented as red (be careful), amber (needs improvement), green (keep up the good work) plus links to online educational resources tailored to patients’ gaps in knowledge and clinical information |
Usual care | 3, 6 and 9 months | Behaviour:
|
|
|
Weymann et al. (2013) 99 Outline of an intervention |
T2D patients | Tailored web-based interactive health communication application. Personalisation involves mirroring what the user says, conveying esteem and empathy, building individualised bridges, content matching and presenting users with information on themselves | N/A | N/A | N/A |
| Risk domain | Study (year of publication), level of bias | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Dapp et al. (2011)88 | Harari et al. (2008)89 | Kreuter and Strecher (1995)90 | Zullig et al. (2014)91 | Welschen et al. (2012)92 | Hess et al. (2014)93 | Neuner-Jehle et al. (2013)94 | Shahab et al. (2007)95 | Mauriello et al. (2016)96 | |
| Selection bias | |||||||||
| Random sequence generation | Low | Low | Unclear | Medium | Low | Low | Unclear | Low | Low |
| Allocation concealment | Low | Low | Unclear | Medium | Low | Low | Unclear | Low | Low |
| Performance bias | |||||||||
| Blinding of participant and personnel | High | High | High | High | High | High | High | High | High |
| Detection bias | |||||||||
| Blinding of outcome assessment | High | High | Unclear | Unclear | High | High | High | High | Low |
| Attrition bias | |||||||||
| Incomplete outcome data | Low | Low | Low | Unclear | Low | Low | Low | Low | Medium |
| Reporting bias | |||||||||
| Selective reporting | Low | Low | High | Low | Unclear | Low | Low | Low | Low |
| Other bias | |||||||||
| Bias other than those above | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
There were no studies of oral health. Most studies involved the giving of information on cardiovascular risk. 91,92,94,95,97 One study concerned asthma risk information98 and the rest covered broader ‘healthy life-check’ information. Three studies involved information for patients with type 2 diabetes mellitus. 92,97,99
Computerised information was the most common form of information studied. 88–91,93,98,99 This reflects an expanding area of technology which is starting to have an impact on clinical practice. Computers can generate customised messages on risk, including, for example, patients’ health literacy, locus of control, internet experience, attitude to self-care, decision preferences and current health knowledge. 99 After patients enter details into a database, computerised capacity (including several hundred text files, graphics and photographs) can potentially correspond with tailored options to each survey response and all possible response option combinations. 99
Two studies reported RCTs involving computerised health risk appraisals (HRAs) used in a general medical practice. 88,93 The earlier of these integrated computerised risk appraisals into practice-based information technology systems, and generated individualised feedback for both patients and general practitioners who had been trained on current care and behaviour recommendations relating to the risk domains covered. However, it was left to the discretion of doctors and patients as to how any issues identified were addressed in consultations, if at all. 89 Results showed minimal improvement in patients’ health behaviour or uptake of preventative care across the domains studied89 (see Table 1). It is interesting to note that, in the later study,88 a face-to-face reinforcement component was added (albeit outside the clinical appointment; participants were given a choice of group sessions or home visits), and a subgroup analysis showed favourable effects for HRAs delivered along with personal reinforcement, but not without. A further study of HRAs with outcomes limited to risk perception rather than clinical outcomes found that adjustments in optimistic and pessimistic bias occurred in only some disease domains studied. 90
A recent RCT96 used iPads (Apple Inc., Cupertino, CA, USA) to deliver a tailored intervention while pregnant women were waiting for their antenatal appointment. The computer activity included interactive components and incorporated feedback messages, quizzes, calculators, support messages and recipe ideas. This RCT found that this intervention increased the amount of fruit/vegetables consumed but did not increase the engagement with stress-reducing activities. However, a RCT involving a web-based intervention that gave personalised cardiovascular risk information to patients found no significant differences in health outcomes or behaviour between intervention and control groups after 3 months91 (see Table 1). In summary, although several studies conclude that computerisation makes tailoring of risk information possible100 and enables simple and visual representation of complex risk information, further reinforcement seems to be needed to interpret and discuss the information;88–91 evidence in this area is limited and more work needs to be conducted.
Studies testing other forms of presenting risk information to patients also found limited evidence for effectiveness. Studies in the clinical setting presenting risk information by way of population diagrams,92,97 coloured charts94 or photographs95 conclude that risk information presented in this way alone is insufficient to prompt patients to adopt healthier lifestyles, or even to enhance clinical communication (see Table 1). The only effect found was a short-term increase in risk perception. 92,95 Welschen92 concludes that risk communication is insufficient on its own, but should be a first stage in a more complex lifestyle intervention.
The closest previous study to the PREFER (presenting information on dental risk) study is a pilot RCT involving the use of ultrasound images to show the extent of blockage in carotid arteries (alongside contrasting photographs of a healthy artery) to cardiovascular clinic outpatients. 95 The basis for the intervention is empirical evidence, such as a study drawn from a community-based sample, showing that providing smokers with photographs of atherosclerotic lesions, together with relevant explanations, increases quit rate at 6 months compared with counselling alone (22% vs. 6%). 101 Although the pilot RCT based in outpatients showed no effect of intervention in smoking behaviour after 4 weeks, the study includes EPPM variables to investigate possible behaviour-change mechanisms. 95 The study found, first, an increase in perceived susceptibility in the intervention group and, second, that the intervention increased intentions to stop smoking only in patients with high self-efficacy (p < 0.03) and not in those with low self-efficacy (p > 0.35). This led the authors to conclude that, because their study was probably underpowered, the intervention may have the potential to alter both motivational and behavioural outcomes, and that the moderation effect may be important and could mean that such interventions may need to include procedures that increase self-efficacy in order to achieve optimal results. 95
Limitations
All systematic reviews must balance sensitivity with the precision of the literature search. In the first instance, we used text mining based on a selection of sample papers to design a precise search and then broadened this to increase sensitivity, supplementing with hand-searching. It is possible that by using text mining in the initial stages, the added precision may have limited the sensitivity of the search and some relevant papers may have been missed. To make the search manageable within the time and resources allowed, it was limited to English-language articles and the authors were not contacted for the full article where only the abstract was available online or through interlibrary loan. As a result, a few relevant papers may have been missed.
Summary
Although various studies have compared the different ways that risk messages can be framed and presented to people (e.g. comparing graphs or charts with numerical presentations), even in an era where risk profiles can be generated in the course of electronic clinical record-keeping and graphic imagery produced from scan technology with potential applications in health improvement, very few studies have been undertaken in the clinical setting. Studies that are available indicate that risk information itself may have a limited impact on health behaviour; discursive practices to define ‘who and what is normal, standard, and acceptable’ and to create meaning from the information are also needed46 (see Chapter 1, Risk presentation format and information visualisation).
Chapter 3 A randomised controlled trial in dental practice: methods
This chapter draws on the article by Harris et al. 102
Trial design, setting and population
This was a pragmatic, multicentre, three-arm, parallel-group patient RCT.
Dental practices
Patients were recruited from four NHS dental practices (practices 1–4, Table 3), located in north-west (NW) (n = 2) and north-east (NE) (n = 2) England, which were not involved in testing new models of the NHS dental contract. 103 Following pragmatic trial design principles, practices were invited to participate by sequential invitation based on random selection from a list of NHS dental practices within the two areas of England. Single-handed practices were excluded to ensure that sufficient numbers of patients could be recruited to the trial per practice. All four practices were in urban areas, with three of the four in relatively deprived areas. Practice 5 took part in qualitative work only (see Chapter 5, Observations in dental settings).
| Practice | NHS case mix (% patients) | Dental team | Location (UK) | IMD decile |
|---|---|---|---|---|
| 1 | 70% NHS, 30% private | 1 principal dentist | NE, Urban | 9 (20% least deprived) |
| 2 FT dentists; 1 PT dentist | ||||
| 1 FT hygienist; 5 dental nurses | ||||
| 1 practice manager | ||||
| 2 | 95% NHS, 5% private | 1 principal dentist | NE, Urban | 1 (10% most deprived) |
| 1 FT dentist; 1 dentist in VT | ||||
| 1 FT HT | ||||
| 6 dental nurses | ||||
| 3 | 70% NHS, 30% private | 1 principal dentist | NW, Urban | 1 (10% most deprived) |
| 3 FT dentists; 1 VT dentist | ||||
| 1 FT HT; 6 dental nurses | ||||
| 2 receptionists; 1 practice manager | ||||
| 4 | 80% NHS, 20% private | 2 PT dentists | NW, Urban | 2 (20% most deprived) |
| 1 PT HT; 1 FT dental nurse | ||||
| 1 trainee dental nurse | ||||
| 1 receptionist; 1 practice manager | ||||
| 5 | 60% NHS, 40% private | Multi-dentist practice, dental team not disclosed to preserve anonymity (involved in qualitative work only) | New contract prototype practice | 9 (20% least deprived) |
Participants
Participants were adults attending a NHS dental check-up judged to be at high/medium (red/amber) risk for poor oral health according to a nationally developed algorithm used in practices testing new models of NHS dental contract. 104,105
The algorithm, which uses a combination of social and medical history (both patient-reported) and clinical information, was applied by the recruiting dental practice. 105 Patients underwent an initial eligibility screening when making the check-up appointment (e.g. patients reporting symptoms when making the appointment could be classified as red/amber), although eligibility could be fully determined only after the dental examination by a dentist, just prior to intervention delivery. For example, categorisation of the patient as amber risk might depend on the dentist rating the patient’s dental plaque control (toothbrushing) as poor after the clinical examination.
Eligibility criteria
Inclusion:
-
aged ≥ 18 years
-
high/medium (red/amber) risk of poor oral health
-
NHS patients
-
new patients or regular attenders
-
any level of literacy.
Exclusion:
-
low (green) risk based on the absence of either clinical- or patient-related factors
-
patients attending for an emergency appointment (they do not usually receive a full check-up)
-
edentulous
-
private patients
-
patients requiring an interpreter for routine care.
Interventions
The trial had two intervention arms and a third ‘usual care’ arm.
-
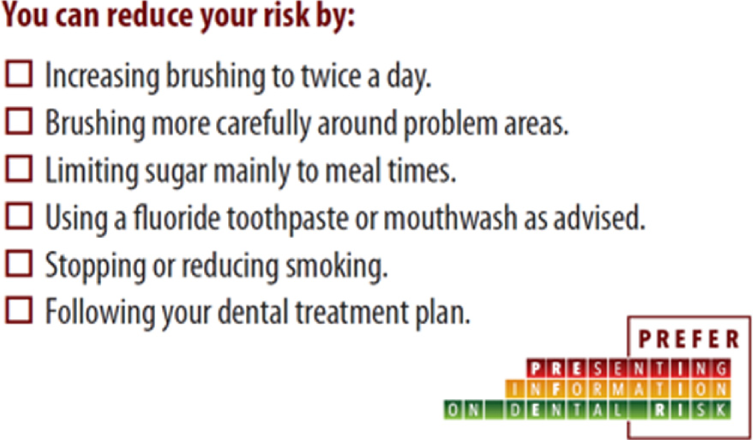
Verbal information only (usual care): dentists gave verbal information on risk in the usual way. Patients were also given a printed, credit-card-sized card with six key messages about recommended health behaviour (Figure 4). The dentist marked any messages they had covered with the patient, giving the patient the card to take away as reinforcement of advice given. When the dentist marked ‘Following your dental treatment plan’, this related to any advice about returning for further dental visits.
FIGURE 4.
Intervention card with six possible oral health behaviours (with the areas of advice covered at the check-up marked by the dentist). Reproduced with permission from Harris et al. 102 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.
-
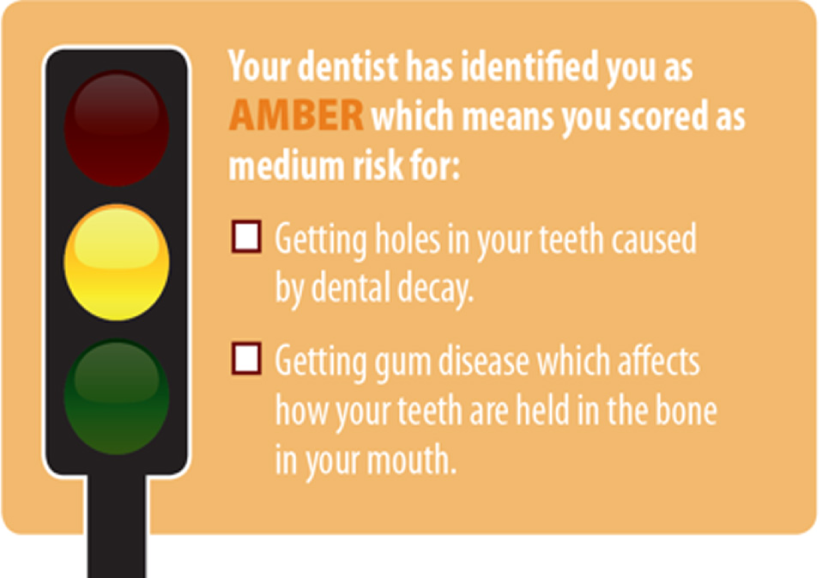
Verbal information plus TL graphic: dentists allocated the patient to one of the three RAG categories and gave them a credit card-sized card that described their risk group (Figure 5). The reverse of the card was identical to the reverse of the card given to group 1 (see Figure 4). The verbal advice covered the meaning of the RAG categorisation and oral health behaviours, as recommended by the dentist, to address any issues (which were also marked on the reverse of the card).
FIGURE 5.
Traffic light graphic cards to support verbal advice (group 2). Reproduced with permission from Harris et al. 102 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.

-
Verbal information plus QLF photograph: Dentists gave advice supported by QLF images of the patients’ anterior six (canine to canine, top and bottom) teeth. Patients received a credit-card-sized colour copy of the QLF photograph showing either demineralisation areas (see Figure 1) or plaque coverage (see Figure 2), whichever the dentist thought was most important for the patient. On the reverse of the printed photograph a sticker was placed, replicating the credit card-sized card provided to group 1, with any messages covered regarding recommended oral health behaviours marked by the dentist (see Figure 4).
Outcome measures
Primary outcome
The primary outcome measure was the mean valuation for each of the three interventions in terms of WTP. This is a common approach to the valuation of health care elicited either by observing consumer choice (the revealed preference approach) or through an expressed preference (the contingent valuation approach). 106 We used the latter method. In economics, the value of a good or service is thought of in terms of what an individual is willing to sacrifice to obtain it. A common unit of sacrifice that is well understood globally is money. If the maximum amount of money that an individual is willing to pay for a series of services or goods can be determined, then the relative values of these goods or services are revealed. In health, it is often the case that services are not paid for, or are subsidised or insured against, and so monetary payments cannot be directly observed. In these situations, values are determined by constructing a hypothetical market for the service and eliciting the maximum an individual would be willing to pay in theory, if payment was necessary.
Secondary outcomes
Secondary outcomes were collected in three ways: (1) self-reported by patients (see Report Supplementary Material 1), (2) clinical data recorded at the check-up [visit 1 (V1) – baseline] and at subsequent dental treatment visits [short-term follow-up: visit 2 (V2) and/or visit 3 (V3)], and (3) clinical outcome data extracted from QLF photographs taken at baseline and at V2 and/or V3. If clinical data were available for both V2 and V3, the V2 data were used. Secondary outcomes concerned with self-reported oral health behaviour focused on data collected 6 months post intervention (medium-term follow-up) and 12 months post intervention (long-term follow-up):
-
Clinical communication measured by the Communication Assessment Tool (CAT),107 completed by patients after receiving the risk information at V1.
-
Self-reported behaviour change between baseline and 6 and 12 months post intervention.
-
Oral hygiene –
-
Use of fluoride –
-
fluoride toothpaste prescribed by the dentist
-
fluoride mouth-rinse.
-
-
Dietary sugar intake –
-
Smoking status –
-
-
Clinical outcomes:
-
Self-rated oral health108 – change between baseline and 6 and 12 months.
-
Basic periodontal examination (BPE) score collected by dentists concentrating on conversions between codes 1 (bleeding) and 0 (healthy) between baseline V1 and V2/3.
-
Plaque Percentage Index70 [as measured on QLF images (ΔR30)] – change between baseline and V2/3.
-
Number of tooth surfaces affected by early caries – change between baseline and next dental visit measured on QLF images. 70
-
Where early carious lesions are present – change in lesion volume (ΔQ) between baseline and next dental visit measured on QLF images. 70
-
Predictor and moderator variables
-
Socioeconomic characteristics:
-
Education:
-
Patient dental visiting behaviour:
-
Oral health:
-
number of natural teeth at baseline.
-
-
Dental provider characteristics:
-
dental practice
-
clinical ID.
-
-
Behaviour-change variables (EPPM):76
-
perceived threat (severity)
-
perceived threat (susceptibility)
-
self-efficacy
-
response efficacy
-
message fear
-
affect regarding threat
-
danger control response
-
fear control response – (1) defensive avoidance, (2) perceived manipulation, (3) message derogation
-
intention to change behaviour.
-
Sample size calculation
Because valuation is the primary outcome, differences in mean and median WTP values between the three forms of information were the primary drivers of sample size. The sample size needed to be sufficiently high to detect differences between any of the three arms, either between the two intervention groups, TL and QLF photograph, or between one of these groups and the control. The sample size calculation is therefore based on a need to detect significant differences in the primary outcome (WTP) between the three arms at 80% power with an α of 0.05.
Sample size calculations for stated preference surveys, such as contingent valuation studies, are complicated by two factors. First, often no similar ‘goods’ have been valued in the past and so reliable variance estimates are impossible to determine. Second, if such data are absent, applying any effect-size estimate or minimally important difference would be arbitrary. Given these problems, and the fact that, to our knowledge, this is the first study of its kind, we calculated the samples required to show different effect sizes between any of the three groups based on numbers of standard deviations (SDs) rather than absolute numbers, as per Cohen,116 who suggests using a value of 0.5 SDs for a medium effect size where neither SD nor effect size is known. Thus, to detect a difference of 0.5 SD, 63 people were calculated to be required per arm. To detect 0.33 SD, 145 people per arm would be needed. Accepting a detectable difference of between a half and a third of a SD, and allowing for around 20% refusal to answer WTP questions (protest responses), gave a number of 133 people in each arm or a total sample size of 400 people.
We then considered the implications of this size on the detection of clinical outcome effects, particularly plaque coverage. Published data on a group of 38 college students showed a mean Plaque Percentage Index of 14.8, with a SD of 7.7. 117 As this is likely to be a more homogeneous population than that in our study, a more conservative estimate of a SD of 10 has been used to calculate a sample size of 133 people per group, which would allow us to detect a mean difference of 3.5 in the Plaque Percentage Index between groups, with 80% power at 0.05 significance level.
Trial processes
Dental practice training
Before setting up the study, whole dental teams (including the receptionist and anybody who had contact with study patients and/or procedures) at each recruiting dental practice received two sets of face-to-face training by the research team:
-
Good clinical practice training including taking informed consent, adverse event records, recruitment logs and study document and data management.
-
Study-specific training relating to the study protocol, including data collection procedures, flow of patients through the study, taking and the interpretation of QLF photographs (arm 3), the categorisation of patients to TL categories (see Report Supplementary Material 2: Study materials) and the use of intervention materials (arm 2).
The dentists or hygienists who delivered the interventions to the patients were trained in the use of the TL algorithm. Written instructions (laminated copies) on the application of the algorithm for categorising patients were provided to the dental teams. The algorithm took into account both patient and clinical factors and provided step-by-step guidance.
Specific training concerned taking QLF images to measure clinical outcomes of plaque and dental caries and included instructing staff to ask patients to clean their teeth between QLF photograph 1 (plaque) and photograph 2 (caries). If red deposits of plaque were still visible on the QLF image after brushing, the dental teams were instructed that they should ask the patients to brush their teeth again until all plaque had been removed and a further image should be taken in order to measure dental caries.
Training was supported by study materials, including a video and quick guide of how to use the QLF system, and crib sheets that included a participant procedures flow diagram (see Report Supplementary Material 2). Training on or calibration of undertaking a BPE was not provided.
Training logs were kept. Training was repeated when there was dental team staff turnover.
Randomisation, allocation concealment and blinding
Once consent was taken, dental staff took a sequentially numbered, sealed envelope containing group allocation information. The allocation sequence was prepared by the trial statistician using the ralloc procedure in Stata® version 14 (StataCorp LP, College Station, TX, USA). Allocation was stratified by practice with random block sizes of three and six. Patients were allocated with equal probability to each group.
Allocation was revealed by opening the envelope just prior to the information being given (i.e. by the dentist, witnessed by the dental nurse in the dental surgery), after the check-up had been carried out, including baseline clinical outcome data collection (BPE score).
The researcher extracting clinical outcome data from QLF photographs was blind to group allocation. Patients and dental staff were not blinded to allocation, neither was the researcher undertaking 6- and 12-month follow-up data collection nor the trial statistician (the same statistician who generated the allocation was involved in the analysis).
Piloting, trial set-up and support
The study was set up in the four practices sequentially. This meant that experience from early practices taking part was used to inform the training of later ones. Two members of practice 4 NW travelled to practice 2 NE to take part in the study training of practice 2. All dental practices received considerable support in training and during the trial (Table 4), particularly in some practices where staff turnover was high. Seven dentists per practice participated in the trial from practices 1 and 3 and three dentists in each of practices 2 and 4 (see Table 3). Study recruitment started on 17 August 2015 and ended on 5 September 2016.
| Training/support type | Practice | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Number of separate training sessions | 5 | 2 | 4 | 3 |
| Number of trial monitoring and support visits | 13 | 7 | 7, plus a period of 3 weeks with a researcher in the practice | 16 |
| Number of requests for support regarding QLF equipment failures | 5 | 0 | 2 | 3 |
Some practices particularly required support regarding issues associated with the use of the QLF camera; practice 1, for example, required the camera cable to be replaced three times. QLF software freezing was another complaint. Camera troubleshooting instructions were developed to tackle possible issues and support was provided both by telephone and by visits to practices.
Piloting included testing to see how well the use of the QLF camera to measure clinical outcomes would work in a practice setting, how well the dental teams were able to operate the camera and which members of the teams were best placed to take the QLF photographs. The pilot phase lasted 2 weeks in one practice. The pilot lasted until the dental team was happy with study processes and was deemed able to undertake them. A researcher attended the practices to provide support during this period. A total of 10 patients were involved in the pilot. As a result of the pilot, it was decided that the photographs would be taken by the dental nurses, not dentists, because of time constraints/availability issues. Patient-held dental retractors (for lips) were introduced following the pilot period. We also reduced the number of images taken per participant, related to the measurement of clinical outcomes. We had initially planned that both a central anterior and also a right and left posterior images would be taken from the buccal aspect but reduced this to taking anterior (buccal) images only.
The use of the QLF camera proved challenging for the NHS dental teams and so a simpler, less technical, version of the camera was used as a consequence of piloting. The initial version used for the pilot was the QLF-D (QLF-Digital™) Biluminator 2 system (Inspektor Research Systems BV, Amsterdam, the Netherlands) originally designed for research use (Figure 6). This customised SLR Canon 550D (Canon Ltd, Surrey, UK) camera has a polished metal tube attached to a lens with four white and 12 high-powered blue light-emitting diodes around the lens aperture.
FIGURE 6.
The QLF-D Biluminator 2 system.

Experience after a week of training in a pilot practice (practice 5) was that the dental team had found the heat and light from the camera off-putting, making them reluctant to use the device with patients. Dentists reported that it felt inappropriate to use with new patients, because the initial appointment was about developing rapport and a relationship based on mutual trust. The equipment itself was considered bulky for use in a practice setting (trailing cables, etc.) (Figure 7).
FIGURE 7.
The QLF-D system in a practice setting: camera, laptop computer, printer and cables. (a) Trailing wires from the QLF-D camera across the dental surgery; (b) photograph showing bulky equipment associated with the QLF-D camera system occupying a significant area of the dental surgery workspace.


It was decided to replace the QLF-D camera (see Figure 6) with a Q-Ray™ camera (Inspektor Research Systems, Amsterdam, the Netherlands) (Figure 8), which had been recently developed for use in the dental practice setting. The system is more like a simple camera than a sophisticated SLR camera.
FIGURE 8.
The Q-Ray camera.

Extracting clinical outcome data from quantitative light-induced fluorescence images
A single researcher, blind to allocation, first scrutinised all images for quality (focus, excessive ambient illumination, parts of teeth obscured by lips, retractors or operator’s fingers, or any other artefacts that could affect the analysis). Good-quality images were judged as photographs which were taken at a sufficiently close distance (lower and upper front teeth filling the majority of space in the middle of the frame), with the absence of excessive ambient light (lips and gums appear as dark/black), focused and not blurred due to fogging, without any object (e.g. lips, tongue, lip retractors, fingers) blocking the view of the buccal surface of any of the 12 front teeth and with tip to tip contact of opposite teeth.
Images which were out of focus, had obscured tooth surfaces and/or with excessive ambient light present were classified as unacceptable for analysis purposes and were excluded from the statistical analyses. Presence of early caries lesions and dental plaque was calculated automatically using QA2 software, version 1.26 (Inspektor Research Systems, Amsterdam, the Netherlands). If early lesions were detected, these were manually mapped by drawing a contour patch (including sound enamel) around the lesion. The software then automatically calculated the percentage of fluorescence loss (ΔF,%) within the contour patch and the area of the white spot. Multiplying both values gave the estimated volume of the lesion as Δ.
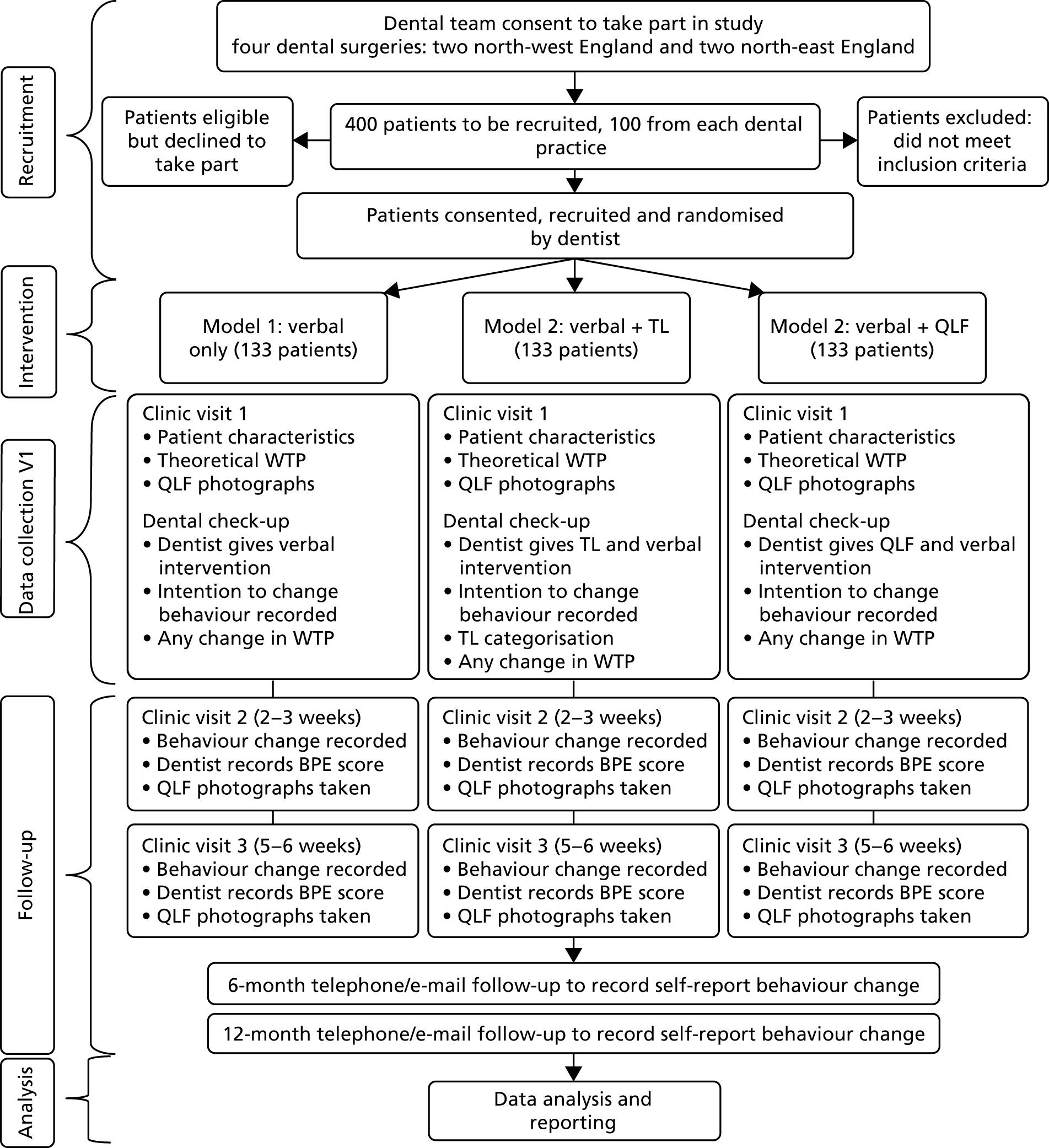
Study flow diagram
Figure 9 outlines the patient flow through the trial, with details on the study intervention arms and procedures.
FIGURE 9.
Study flow diagram.
Data collection schedule
Data were collected at baseline and at short-term (V2/V3), medium-term (6 months) and long-term (12 months) follow-up. Table 5 shows the data collection schedule and the sequence of measures collected. At each dental practice, data were entered directly onto a tablet PC computer (Samsung, Seoul, South Korea) using Qualtrics survey software [version 092017 © 2017 Qualtrics® (Provo, UT, USA)]. Trained dental nurses started by entering patients’ sociodemographic data fields and then undertook an assessment of patients’ literacy using a laminated card with REALM-R words. The tablet was then passed to the patients, who then entered data onto the tablet, including the completion of the WTP task, assisted by the dental nurse when required.
| Event | Completed by | Time point | ||||
|---|---|---|---|---|---|---|
| V1 | V2 | V3 | 6 months | 12 months | ||
| Demographics | Dental nurse | ✗ | ✗ | ✗ | ||
| REALM-R | Dental nurse | ✗ | ||||
| WTP | Patient | ✗ | ||||
| Demographics | Patient | ✗ | ||||
| Self-assessed oral health | Patient | ✗ | ✗ | ✗ | ✗ | ✗ |
| MDAS | Patient | ✗ | ✗ | ✗ | ||
| Demographics | Patient | ✗ | ||||
| QLF photo | Dental nurse | ✗ | ✗ | ✗ | ||
| BPE | Dentist | ✗ | ✗ | ✗ | ||
| WTP revision | Patient | ✗ | ||||
| EPPM and behaviour change | Patient | ✗ | ✗ | ✗ | ✗ | |
| CAT | Patient | ✗ | ✗ | |||
Quantitative light-induced fluorescence photographs were taken by the dental nurse (with the patient brushing their teeth between the two photographs taken for plaque/caries purposes). Patients then went into the surgery with the tablet, the dentist entered the BPE score and the number of natural teeth data, and after that the check-up was completed. Once group allocation was disclosed, only patients in the QLF arm received a copy of their photograph. Patients completed the remaining fields (including CAT) on the tablet after leaving the surgery.
Because participants were patients at high/medium risk of poor oral health, all would have been scheduled for return/treatment visits. Further data were collected during the initial follow-up visit (V2 at 2–3 weeks post intervention) and at a further follow-up visit (V3, 5–6-weeks post intervention) where these occurred. At V2 and V3, dentists entered data on the BPE score and further QLF photographs were taken (not shown to the patient) as a follow-up clinical outcome measure. Patients completed other fields related to behaviour at V2/V3.
Follow-up data were collected by a single member of the research team (blinded to group allocation) at both 6 and 12 months post intervention by either telephone or e-mail (preference specified by the patient). Patients who did not respond to either a telephone call or an e-mail were sent a postal questionnaire (although we did not receive any responses via this means). E-mail communication included a link to the Qualtrics survey. Telephone follow-up involved a researcher completing the Qualtrics survey while speaking to the patient. All reasonable attempts were made to contact non-respondents by telephone and by e-mail (up to five attempts for each participant).
For participants who withdrew from the study, data were retained up to the point of withdrawal. If participants withdrew, they were not replaced.
Elicitation of willingness to pay
Respondents were given descriptions and sample images of the three interventions (see Report Supplementary Material 1). They were asked to rank the three options in order of preference. Elicitation of WTP for the lowest-ranked intervention followed. Participants were asked to read a script that encouraged realistic, budget-constrained responses and emphasised that the exercise was about value rather than price. Respondents were then presented with a series of virtual cards showing different values from 50 pence to £150 and asked to drag each card to one of three boxes:
-
would pay
-
would not pay
-
not sure.
The different valued cards were presented in a random order, with a random starting card. Respondents could not see the value of subsequent cards until the current card had been placed. Once all cards had been placed, the lowest ‘would not pay’ and highest ‘would pay’ values were displayed to the respondent and they were asked for a maximum WTP value in an open-ended format. This shuffled payment card approach to WTP elicitation has been postulated to reduce starting point and range bias found with traditional WTP elicitation methods. 118
Once a WTP value for the lowest-ranked intervention had been determined, respondents were asked how much extra they would be willing to pay for their next most preferred intervention in an open-ended question and then, finally, respondents were asked how much extra they would be willing to pay on top of their value for their middle-preferred intervention. This incremental approach to eliciting WTP has been shown to give more robust valuations. 119 Where participants gave a zero value, they were asked a follow-up question to determine their reason for giving a zero value with a choice of eight predefined responses to choose from (one of these was ’other’ with the reason then recorded in free text). This particular follow-up question was taken from Ryan et al. 120 as a standard way of determining true and protest zeros, where true zeros reflect a lack of value for the intervention and protest zeros reflect an unwillingness to engage with the WTP task (but where the participant may well still value the intervention).
After their check-up (post intervention), participants returned to the task on the tablet and were reminded of the WTP value they had given for the intervention they were randomised to and then asked if they would revise their WTP given their actual experience with the intervention. If they indicated that they would revise this, the new value was determined using an open-ended question.
The initial design of the WTP task was discussed and revised by an advisory group of academic dentists, dental public health consultants, psychologists, sociologists, statisticians and patient/public representatives. It was first piloted among university staff and then with patients in a dental practice. Refinements were made to the wording of the task and the range of values was checked as plausible.
Data management
Anonymised (using patient ID) trial data were collected using Qualtrics survey software and were placed on a password-protected database. Data were monitored by the research team throughout the data collection phase as access to the data was facilitated by a cloud-based storage facility provided by Qualtrics.
Anonymised (using patient ID, gender and age) QLF photographs were stored on a password-protected laptop computer kept at each of the dental practices. A member of the research team periodically physically collected these data, transferring these to a password-protected hard drive.
Cost data
The costing element of the study was undertaken using a microcosting approach, adopting a NHS perspective (cost to the dental practice). Consumable costs were determined by assessing the consumables required for each intervention from the standard protocol and costing these from standard dental equipment suppliers. Capital items (only in the QLF arm) were costed based on the costs of procuring these for the study, split by an estimate of the number of check-ups over a period of 10 years. The number of check-ups per dentist per year was determined by dividing the total number of courses of treatment delivered in the NHS in England in 2014–15 by the total number of dentists working in the NHS in England. 121 Overhead and staff costs were determined using average times to complete each intervention multiplied by hourly rates published by Personal Social Services Research Unit (PSSRU). 122 Each practice sampled 10 consecutive patients and timed the intervention using a stopwatch.
Differential long-term costs relating to the outcomes of the different interventions (e.g. if an intervention was more effective at prevention, the costs of restorative dental work would be lower) were not considered, as this was beyond the scope of this project.
Statistical analyses
Preliminary analyses and the sensitivity analysis involving green patients
Three group logistic regression analyses were undertaken, predicting intervention group membership from variables collected before randomisation (age, gender, smoking status, diet, toothbrushing, MDAS and WTP). Preliminary analyses also described the proportion of withdrawals and attrition in each arm.
This revealed that proportionally more participants randomised to receive the TL intervention did not receive the intervention and were withdrawn from further data collection by the dental practice. It became apparent that this was because the final eligibility screen for red/amber patients, which took place after the clinical assessment, was more rigorous for green patients in the TL arm. To compensate for a potential loss of power, dental teams were encouraged to recruit beyond their target of 100 patients, leading to 412 instead of 400 patients being recruited in total.
To explore whether or not an imbalance of patients who may have had poorer oral health in the verbal and QLF arms had an impact on the results, potential green patients in the verbal and QLF arms were identified in the following way: taking patients with a healthy BPE score (all sextants < 2 except for lower anterior teeth) and then identifying any patients who were still green after all patient-reported parts of the algorithm were taken into account. Next, data on whether or not these patients had received particular post-intervention health education messages (e.g. reduce/stop smoking) were used to verify the patients’ potential RAG categorisation in the verbal/QLF arms. This mimicked the process performed by the dentists to confirm eligibility of patients in the TL arm. Analyses were re-run excluding these additional green patients in the verbal (12 potential greens identified) and QLF arms (15 potential greens identified) as a sensitivity analysis. A randomisation analysis was undertaken to assess the adequacy of identifying potential green participants in the verbal and QLF arms.
Willingness to pay
First, proportions favouring each intervention were calculated. Second, to prepare WTP data, zero WTP values were classified as true or protest zeros based on answers to follow-up questions and protest zeros were excluded from further analysis. 120 Characteristics of the group protesting were determined. There is much debate in econometrics literature123 about the reporting of either the mean or the median for WTP values elicited using bidding card formats and so both are reported here. Mean and median WTP, as well as SDs and interquartile ranges, were calculated and compared using Wilcoxon-signed rank tests (given the non-parametric nature of the data) for each intervention, as well as for the most preferred intervention (irrespective of what this was).
Factors affecting both WTP and ranking of preference were investigated econometrically, using Tobit regression models for WTP data to account for the left censoring at zero and logistic regression for preference ranks. Variable selection for the model was based on rationality of likely effect, but subsequent backwards stepwise selection was then used to check for better-fitting models using Bayesian information criterion as the principal criterion for model selection. Categorical variables were collapsed (to reduce the number of variables in the regression models) and dummied as follows (with reference levels for regression shown in italics):
-
IMD –
-
low (not deprived; IMD decile 8–10)
-
medium (reference; IMD decile 4–7)
-
high (deprived; IMD decile 1–3).
-
-
Income –
-
high income (> £31,200 per year)
-
medium (reference; £15,600 to £31,199 per year)
-
low income (< £15,600 per year).
-
-
Gender –
-
female
-
male (reference).
-
-
Education level –
-
high (undergraduate degree or higher)
-
medium [reference; General Certificate of Secondary Education (GCSE) and Advanced levels (A level)]
-
low (GCSE only or less).
-
-
Age –
-
< 35 years
-
35–64 years (reference)
-
≥ 65 years.
-
-
Number of natural teeth –
-
low (< 20 teeth)
-
functional (reference; ≥ 20 teeth).
-
-
Dental attendance frequency –
-
infrequent attender (fewer than 6 visits in the last 5 years)
-
normal attender (reference; ≥ 6 visits in the last 5 years).
-
-
Practice –
-
1
-
2
-
3
-
4 (reference).
-
Willingness-to-pay analyses were also rerun after excluding outliers (determined as those more than three interquartile ranges outside the interquartile range limits). Finally, significant changes between WTP before and after receiving the intervention were analysed using Wilcoxon signed-rank tests. We used econometric regression analyses to explore how various dental and demographic factors influence values (WTP).
Behaviour-change outcome measures
Group effects on oral health behaviour between the conditions were assessed by predicting 6- and 12-month follow-up scores from group membership. To minimise the probability of type I error, multivariate analyses were used. Overall, intervention effects on the six behavioural outcome variables at 6 and 12 months were tested using multivariate generalised linear mixed models, with baseline values of the outcomes as covariates. Logit link functions were used for the binary variables. The models were fitted using PROC GLIMMIX in SAS® software version 9.4 (SAS Institute Inc., Cary, NC, USA. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. in the USA and other countries. ® indicates USA registration). Baseline scores were used as covariates. Subsequent univariate analyses were intended to identify specific variables affected by group. The hypotheses tested were (1) TL leads to greater positive oral health behaviour change than verbal information and (2) QLF leads to greater positive behaviour change than verbal. Separate analyses examined changes from baseline to 6 months and from baseline to 12 months.
Moderation analyses involved the modelling of two-way interaction effects from the product of the predictor and moderator variables, and testing the hypothesis that the interaction term uniquely predicts behavioural change controlling main effects terms. 124 These were assessed using the multivariate generalised linear mixed models described above, with the moderator used as an additional predictor variable.
We planned that if intervention effects were found, mediation would be undertaken to assess the extent to which intermediate variables (mediators) explain variance shared between predictor and outcome variables. Potential mediators were EPPM constructs. Our mediation analysis strategy was based on recommendations by Zhao et al.,125 who specify preconditions that the predictor (group membership) be linked to the mediator (EPPM variables), and that the mediator be linked to the criterion (behavioural change) controlling the predictor. Only when these are established can path analysis be used to estimate the mediation effect. All potential mediators were to be assessed in the same analysis, reducing the likelihood of type II error that would be associated with testing mediators separately.
Clinical outcome measures
Clinical outcomes were analysed for the first follow-up visit for which data were available (V2 or V3), and where this was no more than 3 months post randomisation (i.e. short-term follow-up). All QLF images were rated as good/poor quality by the assessor. Those not judged to be of sufficient quality to accurately generate the outcome variables were excluded from the analysis. Analysis of the three QLF generated variables used generalised linear models, with value of the variable of interest at the first short-term follow-up appointment as the outcome variable and intervention group allocation as a fixed factor. Baseline value of the variable of interest was included as a covariate. All analyses followed the intention-to-treat principle, when possible.
Basic periodontal examination scores were analysed by categorising each patient into one of four outcome categories:
-
stable healthy (code 0 at baseline and at follow-up)
-
stable bleeding (code 1 or greater at baseline and at follow-up)
-
change to bleeding (code 0 at baseline, code 1 or greater at follow-up)
-
change to healthy (code 1 or greater at baseline, code 0 at follow-up).
The analysis used multinomial logistic regression to test the effect of the intervention group on outcome, with the primary hypothesis of interest between groups 2 and 4.
Multiple imputation analyses were carried out to investigate the robustness of the results to missing data. Using all the data that were available, including baseline variables, five complete-case data sets were imputed and each was analysed in the same way. The results were then combined and compared with the analysis excluding missing data to assess whether or not this would be likely to change the overall conclusions.
Chapter 4 Randomised controlled trial: results
This chapter draws on the article by Harris et al. 102
Flow of trial participants and the CONSORT flow diagram
Figure 10 describes the flow of participants through the trial. Of the 423 patients approached to take part in the study, 11 declined, most of whom cited that they were too busy to take part.
FIGURE 10.
The CONSORT (Consolidated Standards of Reporting Trials) diagram with flow of participants through the trial. Q, question. Reproduced with permission from Harris et al. 102 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.
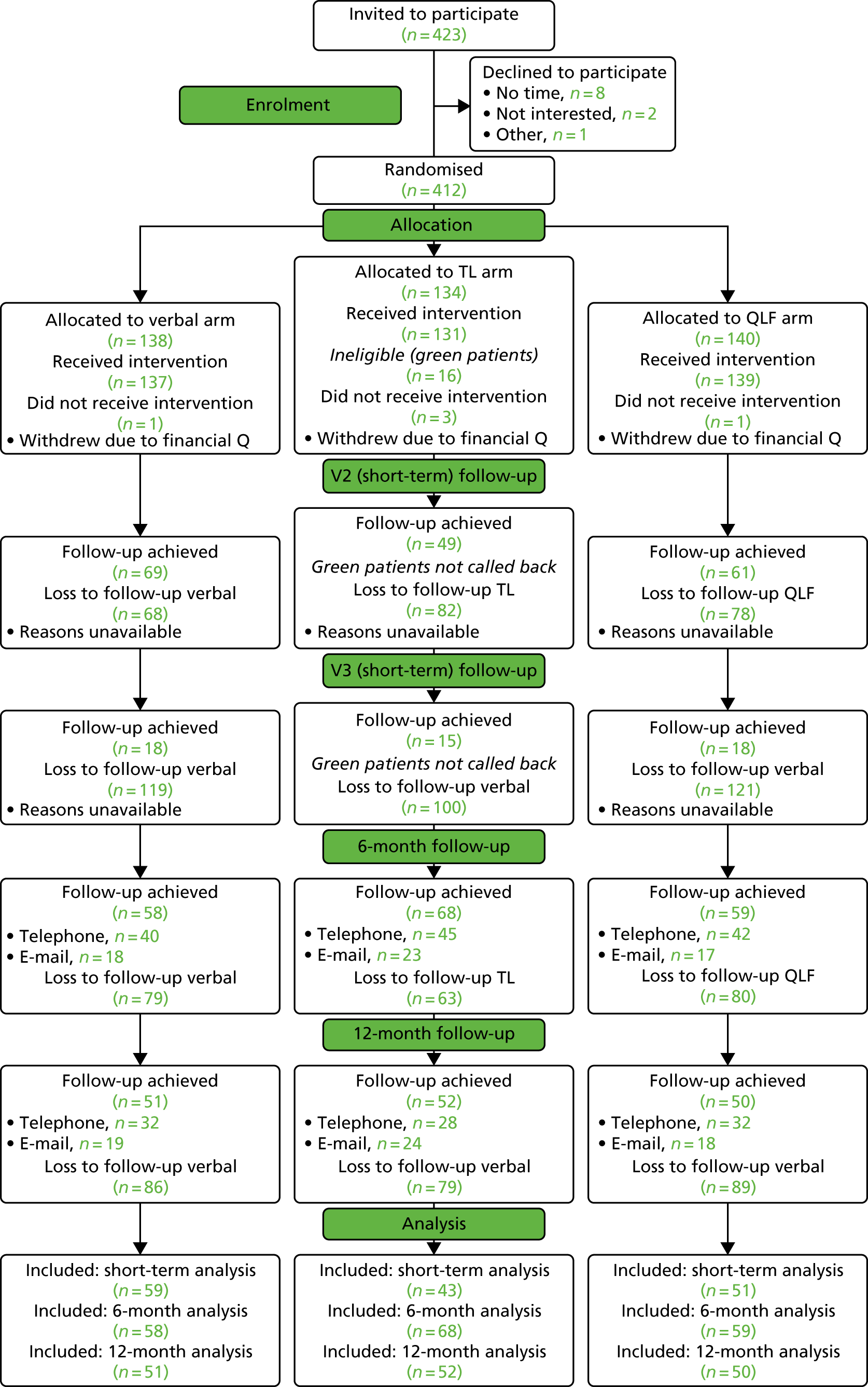
Following randomisation, five people withdrew after being asked to complete a mandatory field about personal income as part of baseline data collection. In the TL arm, after dentists had used the RAG algorithm and identified some patients as ‘green’ (n = 16), because they were technically ineligible for the trial, no further data were collected from them at that visit or V2 or V3; however, green cards were given to them at the end of the appointment. A sensitivity analysis later explored any impact of having an imbalance of proportionally more data from red/amber patients at V2/V3 in the TL arm (see Chapter 3, Preliminary analyses and the sensitivity analysis involving green patients). However, because of blinding at the 6- and 12-month follow-ups, these ‘green’ TL patients were included in long-term follow-up data analyses.
Of the 407 people receiving the intervention, 179 patients returned for V2 (43.9%) and 51 patients returned for V3 (12.5%) (excluding greens in the TL arm). For the 6-month follow-up, 185 patients responded (45.6%) and for the 12-month follow-up 153 patients responded (37.6%). However, at the point of data analysis, V2 and V3 data were collapsed into a single short-term follow-up visit and a time limit restriction of 3 months post intervention was imposed to ensure that the data collected adhered to the intended procedures in the protocol (some practices booked in their V2/3 visits outside this allotted time period and these data were excluded accordingly). Short-term follow-up data were included for 153 (37.6%) patients.
Of the 412 patients randomised, WTP (primary outcome) data were obtained for everyone. Data on the revisited WTP response for the intervention that the patients had received were obtained from 391 (95.1%) participants. Attrition in the second part of the WTP task was because of five withdrawals following the financial question and 16 green TL arm patients viewed as ineligible by dental practices.
Reasons for attrition
Not all practices kept good records of reasons for non-attendance for V2/3 follow-up. Loss to V2/3 follow-up varied by practice for organisational reasons. Follow-up in practice 2 was particularly affected by patients being required to pay in advance (at the end of the V1 consultation) for V2 dental treatment, and because the catchment area for the practice included a relatively transient (student) population. Participants did not receive any reimbursement for the time and expenses involved in taking part in the study.
Reasons for loss to follow-up at 6 months were no response (after five attempts at contact) (n = 171), incorrect contact details provided (n = 25), withdrew from the study (n = 17) or incomplete data collection (only one or two questions answered) (n = 7). A prize draw was introduced to try to address retention issues.
Sociodemographic and dental history profile of participants
Table 6 describes the 412 participants randomised to receive the intervention and from whom primary data (WTP) were obtained. There was spread in terms of gender (skewed towards female), income, age (although the ≥ 65 years group is small) and IMD (skewed towards more deprived). With regard to educational qualifications, one-third of the sample had the lowest level, although there was a reasonable number in each of the remaining groups. Most of the sample had attended 6–10 dental visits in the past 5 years and had > 20 natural teeth remaining.
| Sociodemographic and dental history variables | Time point, n (% of total) | ||||
|---|---|---|---|---|---|
| Baseline | Follow-up | ||||
| Randomised (N = 412) | Allocated (N = 407) | Short term (practice) (N = 153) | 6 months (N = 185) | 12 months (N = 153) | |
| Gender | |||||
| Male | 166 (40.3) | 164 (40.3) | 63 (41.2) | 79 (42.7) | 66 (43.1) |
| Female | 246 (59.7) | 243 (59.7) | 90 (58.8) | 106 (57.3) | 87 (56.9) |
| Age category (years) | |||||
| 18–34 | 125 (30.4) | 130 (31.9) | 39 (25.5) | 46 (24.9) | 43 (28.1) |
| 35–64 | 214 (51.9) | 205 (50.4) | 84 (54.9) | 102 (55.1) | 77 (50.3) |
| ≥ 65 | 70 (17.0) | 70 (17.2) | 28 (18.3) | 36 (19.5) | 32 (20.9) |
| Missing data | 3 (0.7) | 2 (0.05) | 2 (1.3) | 1 (0.5) | 1 (0.7) |
| Household income (£) | |||||
| 0–15,599 | 141 (34.2) | 136 (33.4) | 46 (30.1) | 51 (27.6) | 34 (22.2) |
| 15,600–31,199 | 142 (34.5) | 142 (34.9) | 51 (33.3) | 72 (38.9) | 65 (42.5) |
| ≥ 31,200 | 129 (31.3) | 129 (31.7) | 56 (36.6) | 62 (33.5) | 54 (35.3) |
| Education | |||||
| GCSE or lower | 139 (33.7) | 191 (46.9) | 69 (45.1) | 92 (49.7) | 68 (44.4) |
| A level | 145 (35.2) | 89 (21.9) | 27 (17.6) | 35 (18.9) | 33 (21.6) |
| Degree or higher | 128 (31.1) | 127 (31.2) | 57 (37.3) | 58 (31.4) | 52 (34.0) |
| IMD | |||||
| Low (1–3) | 172 (41.7) | 173 (42.5) | 56 (36.7) | 75 (40.5) | 59 (38.6) |
| Medium (4–7) | 135 (32.8) | 131 (32.2) | 54 (35.3) | 60 (32.4) | 54 (35.3) |
| High (8–10) | 100 (24.3) | 98 (24) | 40 (26.1) | 46 (24.9) | 39 (25.4) |
| Missing | 5 (1.2) | 5 (1.2) | 3 (2.0) | 4 (2.2) | 1 (0.7) |
| Natural teeth | |||||
| < 20 | 71 (17.2) | 68 (16.7) | 23 (15.0) | 28 (15.1) | 25 (16.3) |
| ≥ 20 | 341 (82.8) | 339 (83.3) | 130 (85.0) | 157 (84.9) | 128 (83.7) |
| Dental clinic attendance | |||||
| Infrequent: fewer than six appointments in 5 years | 96 (23.3) | 97 (23.8) | 31 (20.3) | 42 (22.7) | 32 (20.9) |
| Frequent: more than six appointments in 5 years | 314 (76.2) | 309 (75.9) | 122 (79.7) | 142 (76.8) | 121 (79.1) |
| Missing | 2 (0.5) | 1 (0.2) | 1 (0.5) | ||
Preference for form used to communicate information on risk
Table 7 describes participants’ preferences when asked to state the order of their preference for verbal, TL and QLF photographic information (in advance of being allocated to an arm and receiving the allocated intervention). Significantly more patients preferred verbal information delivery over other methods, such as TL and QLF photographic information (p < 0.001 binomial test).
| Form | Participants | |
|---|---|---|
| Number | % | |
| Verbal | 209 | 50.7 |
| TL | 58 | 14.1 |
| QLF photographs | 145 | 35.2 |
Factors associated with preference
To investigate whether or not demographic and dental history variables were associated with preferences, a logistic regression was performed for each intervention in turn, using variables that were collapsed and dummied as described in Chapter 3, Willingness to pay. For each intervention, the base model included all available variables with 381 participants, although a best-fit model was also determined using backwards stepwise elimination. In each case, backwards elimination-determined models did not offer any significant improvement over all variable models and did not provide different results in terms of significant variables. Therefore, only the all-variables model for each intervention is described here.
Verbal
The model had a chi-squared test likelihood ratio of 53.74 (p < 0.0001) with a pseudo-R2 of 0.102. This showed that being young (aged 18–34 years) reduced the likelihood of preferring verbal, whereas being old (aged ≥ 65 years) increased the likelihood of preferring verbal; there were also differences by practice. All other factors were non-significant (see Appendix 2, Table 27). The low pseudo-R2 suggests that the model predicts only a very small proportion of the variance in preference.
Traffic light
The all variables logistic regression model, following stepwise elimination for TL (see Appendix 2, Table 28), had a χ2 likelihood ratio of 14.42 (p = 0.49), with a pseudo-R2 of 0.046. The p-value for the Tobit regression chi-squared test suggests that the model is not significantly better than no model at all and no factors significantly affect preference for TL information.
Quantitative light-induced fluorescence
The all variables logistic regression model, following stepwise elimination for QLF preference, had a chi-squared test likelihood ratio of 41.98 (p = 0.0002), with a pseudo-R2 of 0.086 (see Appendix 2, Table 29). The model shows that the practice was a significant predictor of preferring QLF, with all other factors non-significant. The low pseudo-R2 suggests that the model predicts only a very small proportion of the variance in preference.
Trial results: willingness to pay
Willingness to pay (WTP) was elicited first for the least preferred intervention and then the additional WTP for the next preferred intervention, followed by the additional WTP for the most preferred intervention. The WTP for the most preferred intervention is, therefore, an addition of all three values.
Zero responses
When participants gave a zero valuation at any stage of the process this may mean that the participant truly does not place any valuation on the intervention (a true zero) or it may mean that participants do place some value on the intervention but do not wish to engage in the exercise (a protest zero). Protest and true zeros were differentiated as described in Chapter 3, Elicitation of willingness to pay.
In line with standard practice, protest zeros were classified as missing WTP data as their true value cannot be determined and so were excluded from analysis, but true zeros were included. The breakdown of true and protest zeros (and, therefore, the numbers excluded from analysis) for each preference level is given in Table 8. As the nature of incremental WTP is additive, if a protest zero is given at an earlier stage for a more preferred intervention then an additive WTP cannot be determined. This means that if an individual gave a protest response for their lowest-preferred intervention but then gave positive values for the additional money that they would be willing to pay for their middle-preferred intervention, then the addition of the lowest-preferred intervention plus additional funds for the middle-preferred intervention is not possible and, hence, this is also counted as missing. For this reason, the number of protests for any given intervention is higher than the number at any given preference level; the breakdown by intervention is given in Table 9. The numbers of missing and protest zeros combined in Table 9 are the numbers excluded from analysis for each of the WTP levels.
| Intervention preference | Missing | Protest zeros | True zeros | Non-zero value |
|---|---|---|---|---|
| Least preferred intervention | 1 | 97 | 57 | 257 |
| Middle preferred intervention | 2 | 123 | 58 | 229 |
| Most preferred intervention | 2 | 131 | 38 | 241 |
| Intervention preference | Missing | Protest zeros | True zeros | Non-zero value |
|---|---|---|---|---|
| Verbal | 1 | 185 | 17 | 209 |
| Verbal plus TL | 2 | 141 | 41 | 228 |
| Verbal plus QLF | 2 | 121 | 34 | 255 |
Analysis of the demographic characteristics showed that there were no differences between the protesting group and non-protesting group (χ2 test) except for age, as protestors were less likely to be older (aged ≥ 65 years). As it was not clear how to treat the protestors who gave one protest followed by at least one non-protest response, a sensitivity analysis counting all protest zeros as true zeros was also undertaken (see Chapter 4, Sensitivity analysis: removing potential ‘greens’).
Willingness-to-pay values and differences by information form
The median and mean WTP values for each intervention are shown in Table 10. There is a significant difference between verbal and TL (p < 0.0001) and QLF and TL (p < 0.0001), but not between verbal and QLF (p = 0.41). TL is valued less than either verbal or QLF. The large variances for all interventions should also be noted. It should be noted that, as expected with WTP data, the distribution is right skewed and left censored.
| WTP for intervention form | Median (£) | IQR | Mean | SD | 95% CI |
|---|---|---|---|---|---|
| WTP for verbal (n = 227) | 20 | 7–35 | 30.20 | 38.87 | 24.69 to 34.89 |
| WTP for TL (n = 271) | 10 | 2.5–27.5 | 20.93 | 29.49 | 17.46 to 24.59 |
| WTP for QLF (n = 291) | 18.8 | 5–35 | 25.52 | 30.70 | 21.76 to 28.81 |
Factors affecting willingness to pay
Factors affecting WTP were determined using Tobit regression models (Table 11). An overall model with WTP for most preferred intervention (irrespective of intervention) as the independent variable was constructed and is presented in Table 11. This model shows patients preferring TL the most, being from practice 2, having < 20 teeth and an increase in WTP (having a high IMD and a low REALM-R score decreases WTP). However, the pseudo-R2 is low, indicating that most of the variance in WTP is not explained by the model.
| Characteristics | Coefficient | Standard error | t | p > t | 95% CI |
|---|---|---|---|---|---|
| Intervention most preferred | |||||
| Verbal | Reference | ||||
| QLF | 4.87375 | 2.634868 | 1.85 | 0.066 | –0.3170022 to 10.0645 |
| Traffic light | 9.653246 | 3.808264 | 2.53 | 0.012 | 2.150874 to 17.15562 |
| Deprivation (IMD score) | |||||
| High | –7.141304 | 3.095296 | –2.31 | 0.022 | –13.23911 to –1.043497 |
| Medium | Reference | ||||
| Low | –4.167796 | 2.801527 | –1.49 | 0.138 | –9.686872 to 1.351279 |
| Income (£) | |||||
| High | –2.397248 | 2.899597 | –0.83 | 0.409 | –8.109524 to 3.315027 |
| Medium | Reference | ||||
| Low | –5.029837 | 2.885547 | –1.74 | 0.083 | –10.71443 to 0.6547596 |
| Gender | |||||
| Female | 0.2354133 | 2.459212 | 0.10 | 0.924 | –4.609294 to 5.08012 |
| Male | Reference | ||||
| Education | |||||
| High | 0.0480436 | 3.304343 | 0.01 | 0.988 | –6.461592 to 6.557679 |
| Medium | Reference | ||||
| Low | 3.249592 | 3.164322 | 1.03 | 0.305 | –2.984199 to 9.483384 |
| Age | |||||
| Young (18–35 years) | –0.7454687 | 3.038601 | –0.25 | 0.806 | –6.731585 to 5.240648 |
| Middle (36–64 years) | Reference | ||||
| Old (≥ 65 years) | –3.628658 | 3.352092 | –1.08 | 0.280 | –10.23236 to 2.975043 |
| Number of teeth | |||||
| < 20 | 6.943073 | 3.508236 | 1.98 | 0.049 | 0.0317636 to 13.85438 |
| ≥ 20 | Reference | ||||
| Dental attendance (number of visits) | |||||
| Infrequent attender | –0.4531683 | 3.021498 | –0.15 | 0.881 | –6.405592 to 5.499255 |
| Normal attender | Reference | ||||
| Literacy | |||||
| Low REALM-R | –11.02552 | 5.088937 | –2.17 | 0.031 | –21.05085 to –1.000195 |
| Normal/high REALM-R | Reference | ||||
| Practice | |||||
| 1 | 3.197624 | 3.509774 | 0.91 | 0.363 | –3.716715 to 10.11196 |
| 2 | 10.13295 | 3.409295 | 2.97 | 0.003 | 3.41656 to 16.84934 |
| 3 | 2.761299 | 3.795014 | 0.73 | 0.468 | –4.71497 to 10.23757 |
| 4 | Reference | ||||
| Constant | 8.423429 | 4.8363 | 1.74 | 0.083 | –1.104199 to 17.95106 |
In addition to this overall model, an individual model showing WTP for each intervention was developed and these are shown in Appendix 2 (see Table 30). As per the analysis plan, models of best fit were determined using backwards stepwise elimination but were not significantly better than the all variable models and did not give significantly different results in terms of significant variables. Therefore, only the all variable models for each intervention are presented and discussed here.
Verbal
The all-variables Tobit regression model for verbal information (see Appendix 2, Table 30) is based on 209 cases. The chi-squared test likelihood ratio was 29.87 (p < 0.0124) and pseudo-R2 0.0148. The model shows that living in a high-IMD area decreased WTP for verbal and being recruited from practice 2 increased WTP. The low pseudo-R2 suggests that the model only predicts a very small proportion of the variance in preference.
Traffic light
The all-variables Tobit regression model for TL information (see Appendix 2, Table 30) is based on 253 cases. The chi-squared test likelihood ratio was 26.39 (p < 0.034) and pseudo-R2 0.012. The model shows that having low educational qualification levels and being recruited from practice 2 increased WTP for TL information, although the low pseudo-R2 suggests that the model predicts only a very small proportion of the variance in preference.
Quantitative light-induced fluorescence
The all-variables Tobit regression model for QLF information shown in Appendix 2, Table 30, is based on 270 cases. The chi-squared test likelihood ratio was 26.48 (p = 0.03) and pseudo-R2 0.011. The model shows that living in a high-IMD area decreased WTP for QLF, whereas having a high income level and being recruited from practice 2 increased WTP. The low pseudo-R2 suggests that the model predicts only a very small proportion of the variance in preference.
Sensitivity analysis: willingness-to-pay values excluding outliers
Given the right-skewed nature of the data, no low outliers were identified. The number of high outliers for each intervention was 10 for the verbal intervention, eight for TL and five for QLF. The original and revised (excluding outliers) means and medians for each information form are shown in Table 12 and demonstrate that excluding outliers had no impact on results. A significant difference remained between verbal and TL (p < 0.0001) and QLF and TL (p < 0.0001), but not between verbal and QLF information (p = 0.63).
| WTP for information form | Descriptive statistic | |||
|---|---|---|---|---|
| Median | IQR | Mean | SD | |
| WTP for verbal including outliers (n = 227) | 20.0 | 7–35 | 30.20 | 38.87 |
| WTP for verbal excluding outliers (n = 217) | 18.8 | 6–30 | 23.98 | 23.66 |
| WTP for TL including outliers (n = 271) | 10.0 | 2.5–27.5 | 20.93 | 29.49 |
| WTP for TL excluding outliers (n = 263) | 10.0 | 2–25 | 17.21 | 19.80 |
| WTP for QLF including outliers (n = 291) | 18.8 | 5–35 | 25.52 | 30.70 |
| WTP for QLF excluding outliers (n = 286) | 17.5 | 5–30 | 22.89 | 23.23 |
Sensitivity analysis: removing potential ‘greens’
As described in Chapter 3, Preliminary analyses and the sensitivity analysis involving green patients, several participants were identified as having a green risk status after receiving the TL intervention and so potential greens in the other arms were also identified. A sensitivity analysis was run excluding these ‘green’ individuals. The revised descriptive statistics were median (interquartile range) WTP for verbal information £20 (£30.50), TL £11.50 (£27.00) and QLF £20.00 (£30.00). The mean (SD) WTP for verbal information was £31.40 (£39.95); for TL it was £21.98 (£30.14) and for QLF it was £26.07 (£31.32). In terms of testing for significance of differences, results were the same as with greens included, with WTP significantly different between verbal and TL and between QLF and TL but not between verbal and QLF (Wilcoxon signed-rank test at a p-value < 0.05). Rerunning the Tobit analyses produced very similar models in terms of goodness of fit and identical significant variables.
Sensitivity analysis: treating protestors as true zeros
As noted in Chapter 4, Zero responses, it is unclear how to treat cases for which one protest zero was given followed later by non-protest responses; hence a sensitivity analysis was run counting all zeros as true zeros. This is an extreme case, but there is no alternative intermediate sensitivity case that could be tested. The revised descriptive statistics were median (interquartile range) WTP for verbal £2 (£20.00), TL £2 (£20.00) and QLF £7.75 (£25.00). The mean (SD) WTP for verbal was £16.68 (£32.54), £13.84 (£25.94) for TL and £18.11 (£28.34) for QLF. In terms of testing for significance of differences, WTP between all pairs of interventions was significantly different (Wilcoxon signed-rank test at a p-value < 0.05). Rerunning the Tobit analyses produced very similar models in terms of goodness of fit and significant variables, although REALM-R scores and being from other practices (aside from practice 2, which was already significant) did become significant as predictor variables for all three interventions.
Change in willingness to pay after receiving intervention
Participants gave WTP values for all three interventions before being randomised. After being randomised and receiving one of the interventions, they were then asked if their WTP had changed for that intervention only. The before-and-after means and medians are shown in Table 13, alongside proportions that increased, decreased and kept the same WTP values. No before-and-after changes were significant (Wilcoxon signed-rank test at a p-value < 0.05). It also appears that there was a spread of people moving in different directions from their original values.
| Change in WTP | Information form | ||
|---|---|---|---|
| Verbal (n = 77) | TL (n = 84) | QLF (n = 98) | |
| Mean WTP (of those to enter that arm) before intervention (SD) | 26.35 (27.95) | 16.21 (23.11) | 27.38 (31.19) |
| Mean WTP (of those in that arm) after intervention (SD) | 19.92 (16.63) | 13.32 (18.40) | 22.39 (26.94) |
| Median WTP (of those to enter that arm) before intervention (IQR) | 20 (10–30) | 6.5 (2–20) | 20 (5–40) |
| Median WTP (of those in that arm) after intervention (IQR) | 18.8 (10–25) | 8 (2–20) | 17 (5–30) |
| Number (% of those in that arm) that increased their WTP value | 17 (22) | 22 (26) | 22 (22) |
| Number (% of those in that arm) that decreased their WTP value | 31 (40) | 34 (40) | 36 (37) |
| Number (% of those in that arm) that kept the same WTP value | 29 (38) | 28 (33) | 40 (41) |
Trial results: microcostings
Although the preferences results mean that there is no need to undertake a cost–benefit framework analysis (existing practice was preferred), costs of each intervention were quantified as part of the project. No consumable or capital items were required in the verbal or TL arms. The costs of different elements of the QLF arm are detailed in Appendix 2, Table 26. All arms received a card with information and this cost is therefore constant and excluded.
The cost of the QLF camera was calculated as £4500 with an average life of 10 years and, based on NHS Digital information reporting, an average NHS dentist provides 2000 check-ups per year;118 thus, the cost per patient was calculated at £0.24. The QLF printer was costed at £73.09 with an average life of 10 years. We included the cost of autoclavable retractors to optimise the quality of photographs, which was £61.88 per pair (or unit) with an average life of 2 years.
The QLF arm involved taking two photos and brushing teeth. The time taken was measured in one practice only and the average time for this was 213 seconds. The time taken to deliver the risk message was measured across seven patients (approximately 5%) in each arm. This was very variable, but the mean figures were 228 seconds in the verbal arm, 218 seconds in the TL arm and 245 seconds in the QLF arm. The total time for the QLF arm is, therefore, 458 seconds. The PSSRU119 published standard costs for dentist’s time (including non-consumable equipment and associated staff, e.g. nurse time) is £96 per hour or £0.27 per second. The costs for the time involved were calculated by multiplying the time by the PSSRU rate. The total cost for the QLF arm is therefore:
The costs for each information form per patient are as follows:
-
verbal – £6.15
-
TL – £5.89
-
QLF photograph – £12.62.
Trial results: self-reported oral health behaviours
Self-reported behaviour data availability
The 6-month follow-up yielded 185 cases from the initial 412 participants and the 12-month follow-up yielded 153 cases. Twenty-seven cases were included in the 12-month follow-up that did not provide data at 6 months and, therefore, 126 cases participated at all time points. Pre-intervention demographic variables, oral health status and reported dental attendance for participants responding to 6- and 12-month follow-up questionnaires are included in Table 6.
Attrition bias
Table 6 shows demographic and clinical characteristics of baseline, and 6- and 12-month samples. We used binomial logistic regression to assess attrition biases in the 6- and 12-month data set from the initial 412 participants. Pre-intervention scores on demographic variables, number of teeth, dental attendance and the six baseline variables (smoking status, not brushing twice daily, brushing duration, intake of sugar in food, sugar in drinks and sugar in hot drinks) were regressed onto a binomial variable denoting inclusion (coded as 1) or non-inclusion (coded as 0). Participants retained in the study differed slightly from the whole sample recruited to the study in some important characteristics. Although the multivariate analysis did not show a statistically significant bias at the 6-month follow-up overall [χ2 = 25.45, degrees of freedom (df) = 19, Nagelkerke R2 = 0.075; p = 0.146], Table 14 shows attrition to be more likely in the lower-income group than the middle-income group and to be associated with greater baseline sugar consumption in drinks. A significant multivariate bias was detected for the 12-month follow-up (χ2 = 35.04, Nagelkerke R2 = 0.11; p = 0.006), with attrition in low-income participants more likely than in those with middle or higher incomes and more likely for those with higher baseline sugar intake from foods.
| Characteristics | Time point, OR (95% CI) | |
|---|---|---|
| 6 months | 12 months | |
| Gender | 0.83 (0.53 to 1.31) | 0.89 (0.53 to 1.36) |
| Age (years) | ||
| 18–35 | – | – |
| 36–64 | 1.59 (0.92 to 2.76) | 1.05 (0.58 to 1.88) |
| ≥ 65 | 1.84 (0.85 to 3.98) | 1.76 (0.78 to 3.94) |
| Education | ||
| GCSE or less | – | – |
| A level | 0.84 (0.48 to 1.46) | 1.05 (0.59 to 1.89) |
| Degree and more | 1.02 (0.60 to 1.73) | 1.10 (0.64 to 1.91) |
| Household income (£) | ||
| Low (0–15,600) | – | – |
| Middle (15,601–31,200) | 1.77* (1.05 to 2.98) | 2.35* (1.35 to 4.09) |
| High (≥ 31,201) | 1.33 (0.75 to 2.35) | 2.15* (1.18 to 3.95) |
| IMD | ||
| Low (1–3) | – | – |
| Medium (4–7) | 1.04 (0.63 to 1.70) | 1.46 (0.87 to 2.47) |
| High (8–10) | 1.11 (0.65 to 1.94) | 1.21 (0.67 to 2.18) |
| Number of previous dental visits | 0.81 (0.47 to 1.37) | 1.20 (0.68 to 2.12) |
| Number of teeth | 1.47 (0.81 to 2.67) | 1.14 (0.61 to 2.12) |
| Smoking at baseline | 1.04 (0.59 to 1.84) | 0.86 (0.47 to 1.57) |
| Not brushing twice daily | 0.83 (0.44 to 1.52) | 0.92 (0.48 to 1.75) |
| Brushing duration (minutes) | 1.14 (0.85 to 1.53) | 1.32 (0.96 to 1.79) |
| Sugar intake from food | 0.92 (0.76 to 1.11) | 0.77* (0.63 to 0.95) |
| Sugar intake from drinks | 0.82* (0.68 to 0.99) | 0.91 (0.75 to 1.10) |
| Sugar from hot drinks | 1.85 (0.86 to 3.65) | 1.72 (0.77 to 3.86) |
| Intervention group | ||
| Verbal | ||
| TL | 1.50 (0.90 to 2.51) | 1.34 (0.79 to 2.28) |
| QLF | 1.30 (0.79 to 2.16) | 1.38 (0.81 to 2.33) |
Summary statistics for oral health behaviours at baseline, and at 6 and 12 months
Table 15 shows baseline, and 6- and 12-month follow-up measures for smoking status, not brushing twice daily, brushing duration, sugar intake from food and drinks and using sugar in hot drinks. Over the full sample, brushing duration increased slightly between baseline and 12 months and sugar intake in drinks decreased slightly over both the 6- and 12-month follow-up periods.
| Behaviour measure | 6-month participants | 12-month participants | ||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | Significancea | Baseline | 12 months | Significance | |
| Smoking, n (%) | 33 (17.8) | 36 (19.5) | 0.58 | 22 (14.5) | 24 (19.5) | 0.75 |
| Not brushing twice daily, n (%) | 28 (15.1) | 22 (11.9) | 0.26 | 21 (3.8) | 18 (11.8) | 0.61 |
| Brushing durationb | Mean 3.20 (SD 0.69) | Mean 3.25 (SD 0.78) | 0.43 | Mean 3.25 (SD 0.76) | Mean 3.54 (SD 0.79) | 0.000* |
| Sugar intake from foodc | Mean 3.68 (SD 1.11) | Mean 3.62 (SD 1.13) | 0.42 | Mean 3.56 (SD 1.06) | Mean 3.55 (SD 1.11) | 0.92 |
| Sugar intake from drinksc | Mean 2.71 (SD 1.30) | Mean 2.47 (SD 1.24) | 0.007* | Mean 2.70 (SD 1.31) | Mean 2.43 (SD 1.16) | 0.006* |
| Sugar in hot drinks, n (%)d | 45 (24.9) | 40 (22.1) | 0.383 | 34 (22.2) | 29 (19.2) | 0.48 |
Between-group effects on oral health behaviours
Table 16 shows 6- and 12-month frequencies or means and SDs with corresponding baseline figures, by intervention condition.
| Behaviour variable | Time point | |||
|---|---|---|---|---|
| Baseline | 6 months | Baseline | 12 months | |
| Verbal | ||||
| Smoking, n (%) | 15 (25.9) | 15 (25.9) | 10 (20.0) | 11 (21.6) |
| Not brushing twice daily, n (%) | 9 (15.5) | 7 (12.1) | 8 (16.0) | 4 (7.8) |
| Brushing durationa | Mean 3.26 (SD 0.74) | Mean 3.26 (SD 0.78) | Mean 3.27 (SD 0.75) | Mean 3.53 (SD 0.70) |
| Sugar intake from foodb | Mean 3.71 (SD 1.18) | Mean 3.64 (SD 1.22) | Mean 3.23 (SD 0.76) | Mean 3.44 (SD 0.85) |
| Sugar intake from drinksb | Mean 2.64 (SD 1.25) | Mean 2.47 (SD 1.31) | Mean 2.61 (SD 1.34) | Mean 2.27 (SD 1.04) |
| Sugar in hot drinks, n (%)c | 17 (29.3) | 17 (29.3) | 12 (23.5) | 10 (19.6) |
| TL | ||||
| Smoking, n (%) | 9 (13.4) | 11 (6.4) | 7 (13.5) | 7 (13.5) |
| Not brushing twice daily, n (%) | 9 (13.4) | 9 (13.4) | 7 (13.5) | 9 (17.6) |
| Brushing durationa | Mean 3.09 (SD 0.57) | Mean 3.18 (SD 0.76) | Mean 3.56 (SD 1.05) | Mean 3.59 (SD 1.07) |
| Sugar intake from foodb | Mean 3.66 (SD 1.21) | Mean 3.60 (SD 1.23) | Mean 3.55 (SD 1.20) | Mean 3.39 (SD 1.17) |
| Sugar intake from drinksb | Mean 2.65 (SD 1.27) | Mean 2.25 (SD 1.19) | Mean 2.78 (SD 1.24) | Mean 2.42 (SD 1.15) |
| Sugar in hot drinks, n (%)c | 11 (16.9) | 10 (15.4) | 11 (21.2) | 9 (17.6) |
| QLF | ||||
| Smoking, n (%) | 9 (15) | 10 (16.7) | 5 (10.0) | 6 (12.0) |
| Not brushing twice daily, n (%) | 10 (16.7) | 6 (10) | 6 (12.0) | 5 (10.0) |
| Brushing durationa | Mean 3.27 (SD 0.76) | Mean 3.33 (SD 0.80) | Mean 3.24 (SD 0.80) | Mean 3.66 (SD 0.80) |
| Sugar intake from foodb | Mean 3.56 (SD 0.93) | Mean 3.61 (SD 0.92) | Mean 3.59 (SD 0.93) | Mean 3.67 (SD 1.06) |
| Sugar intake from drinksb | Mean 2.83 (SD 1.40) | Mean 2.71 (SD 1.19) | Mean 2.73 (SD 1.38) | Mean 2.61 (SD 1.30) |
| Sugar in hot drinks, n (%)c | 17 (29.3) | 13 (22.4) | 11 (22.0) | 10 (20.4) |
To minimise the probability of a type I error, intervention effects were tested using multivariate generalised linear mixed models to establish the effects of the intervention on a multivariate series of follow-up outcome variables (see Table 16). All baseline values for each outcome variable were statistically controlled. The analysis did not yield a significant intervention effect for either the 6-month follow-up (F = 0.84, df = 2896; p = 0.432) or 12-month follow-up (F = 1.90, df = 2754; p = 0.150). Follow-up univariate testing did not show significant intervention group differences on any of the behavioural variables.
Moderation analyses
We investigated the possibility that findings could differ among subgroups defined by gender, age, household income, highest education level, IMD, the number of natural teeth and frequency of previous dental attendance. This is known as statistical moderation. To detect moderation, we used multivariate analyses of covariance (MANCOVAs) to test whether or not multivariate intervention effects significantly differed within categories defined by these variables. These MANCOVAs test the significance of interactions with the moderating variable. Category differences are defined by a significant interaction between the intervention group and moderator. Table 17 shows the results of the interaction terms for these analyses. No significant interactions between condition and demographic variables, oral health status and dental attendance were found in the 6- or 12-month follow-up data.
| Characteristic | Follow-up | |||||
|---|---|---|---|---|---|---|
| 6 months | 12 months | |||||
| F | df | Significance | F | df | Significance | |
| Gender | ||||||
| Male, female | 2.52 | 2896 | 0.08 | 1.59 | 12,266 | 0.09 |
| Age category (years) | ||||||
| 18–35, 36–64, ≥ 65 | 0.77 | 4891 | 0.54 | 0.89 | 2754 | 0.41 |
| Household Income (£) | ||||||
| 0–15,600, 15,601–31,200, ≥ 31,201 | 0.27 | 4896 | 0.90 | 1.04 | 2749 | 0.38 |
| Education level | ||||||
| GCSE or less, A level, degree | 0.34 | 4896 | 0.85 | 2.25 | 4754 | 0.06 |
| IMD | ||||||
| Low (1–3), medium (4–7), high (8–10) | 0.80 | 4886 | 0.53 | 0.39 | 4754 | 0.82 |
| Natural teeth | ||||||
| < 20, ≥ 20 | 0.09 | 2896 | 0.91 | 2.11 | 4749 | 0.08 |
| Previous attendance | ||||||
| Fewer than six visits in 5 years, more than six visits in 5 years | 0.42 | 2891 | 0.66 | 0.79 | 2754 | 0.46 |
| Practice | ||||||
| 1, 2, 3, 4 | 1.20 | 6896 | 0.30 | 0.78 | 6749 | 0.59 |
Mediation analysis: intervention effects on the extended parallel process model variables
The EPPM variables were proposed as mediators of intervention effects on behavioural change. We did not observe behavioural change, thus mediation was not possible. Means and SDs of EPPM variables for the full sample and intervention groups are included in Appendix 2, Table 31, for completeness.
Nonetheless, TL or QLF interventions could be seen to be of some value if they influence EPPM variables measured directly after the intervention.
In the EPPM, behavioural intention is considered the proximal determinant of behavioural change and mediates the effects of other EPPM variables. Thus, we examined the effect of intervention group on intention only. An independent groups analysis of variance failed to detect any intervention effects (F = 0.53, df = 2389; p = 0.588). An independent groups multivariate analysis of variance (MANOVA) failed to detect any intervention effects on a multivariate combination of perceived susceptibility, severity, feelings, self-efficacy, response efficacy and fear control processes (Wilks’ Lambda = 0.964, F = 1.15, df = 12,742; p = 0.318).
Trial results: clinical outcomes
Clinical outcome data availability at short-term follow-up
Table 18 shows the availability of clinical outcome data measured in the dental practices, at baseline and at short-term follow-up visits (V2/V3). This includes measurement of BPE score by dentists and data extracted from QLF images to measure plaque and early caries. QLF image quality was assessed by the researcher operating the software, with images judged to be of insufficient quality to calculate the outcomes excluded from analysis of both plaque and caries outcomes.
| Practice | Overall | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Number recruited, n | 103 | 103 | 101 | 100 | 407 |
| Plaque baseline, n (%) | |||||
| Good quality | 63 (61) | 102 (99) | 91 (90) | 97 (97) | 353 (87) |
| Unusable quality | 25 (24) | 1 (1) | 1 (1) | 3 (3) | 30 (7) |
| Not available | 15 (15) | 0 (0) | 9 (9) | 0 (0) | 24 (6) |
| Short-term follow-up plaque with good-quality baseline, n (%) | |||||
| Good quality | 11 (17) | 85 (83) | 6 (7) | 19 (20) | 121 (34) |
| Unusable quality | 3 (5) | 3 (3) | 0 (0) | 1 (1) | 7 (2) |
| No image available | 15 (24) | 3 (3) | 2 (2) | 4 (4) | 24 (7) |
| No follow-up visit | 34 (54) | 11 (11) | 83 (9) | 73 (75) | 201 (57) |
| Caries at baseline, n (%) | |||||
| Good quality | 69 (67) | 101 (98) | 92 (91) | 91 (91) | 353 (87) |
| Unusable quality | 19 (18) | 2 (2) | 0 (0) | 9 (9) | 30 (7) |
| Not available | 15 (15) | 0 (0) | 9 (9) | 0 (0) | 24 (6) |
| Short-term follow-up caries images of those with good-quality baseline, n (%) | |||||
| Good quality | 11 (16) | 2 (2) | 3 (3) | 9 (10) | 25 (7) |
| Unusable quality | 3 (4) | 0 (0) | 0 (0) | 0 (0) | 3 (1) |
| No image available | 16 (23) | 87 (86) | 5 (5) | 12 (13) | 120 (34) |
| No follow-up visit | 39 (57) | 12 (12) | 84 (91) | 70 (8) | 205 (58) |
| BPE score data at baseline, n (%) | |||||
| Available | 100 (97) | 101 (98) | 100 (99) | 100 (100) | 401 (99) |
| Unavailable | 3 (3) | 2 (2) | 1 (1) | 0 (0) | 6 (1) |
| BPE score data at short-term follow-up of those with baseline data, n (%) | |||||
| Available | 30 (30) | 89 (88) | 31 (31) | 31 (31) | 181 (45) |
| BPE not done | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) |
| No follow-up visit | 69 (69) | 12 (12) | 69 (69) | 69 (69) | 219 (55) |
At baseline, 353 (87%) out of the 407 participants had usable QLF images taken. The other images were not of sufficient quality (n = 30 images, 7%) or participants did not have a baseline image taken by the practice (n = 24 images, 6%). Of these 353, 121 (34%) had usable short-term (V2/V3) follow-up plaque images. The majority of these were from practice 2. Most of the missing data were on account of non-attendance at follow-up appointments, with 57% of patients failing to attend another appointment within 3 months of randomisation (V2/V3). Only 25 patients with post-cleaning baseline images taken to measure caries had corresponding follow-up images of a usable quality. Practice 2, which had the highest follow-up attendance rate, unfortunately failed to take almost all post-cleaning images, which meant that very limited caries clinical outcome data were available.
Relatively more BPE score data were available, with 99% of patients having baseline data and 45% of patients having follow-up data available (see Table 18). Most of the BPE score follow-up data were missing because the patient did not return for a V2/V3 visit.
Percentage plaque coverage outcome analysis
The variable used to analyse plaque coverage is the ΔR30 value produced by the QLF software. This quantity measures the percentage of visible enamel that is classified as being covered by plaque, based on the red that is fluorescence associated with the presence of porphyrins of bacterial origin.
Table 19 shows that the mean plaque coverage was similar in all three groups at baseline. Although this was available only for patients with short-term follow-up data, there is some evidence of imbalance at baseline (patients in the TL group had a lower mean ΔR30 than the verbal or QLF groups). Using a generalised linear model, adjusting for baseline plaque coverage and time to follow-up, there was no statistically significant overall effect of group allocation (p = 0.381).
| Group | N | Mean % (SD) baseline | n (non-missing short-term follow-up) | Mean % (SD) baseline for those with follow-up | Mean % (SD) time to follow-up, days | Mean % (SD) short-term follow-up | Least squares means |
|---|---|---|---|---|---|---|---|
| Verbal | 118 | 3.4 (4.2) | 42 | 4.3 (4.7) | 23 (14) | 3.7 (3.8) | 3.3 (0.3) |
| TL | 117 | 3.4 (3.6) | 38 | 2.4 (2.3) | 21 (12) | 2.5 (2.5) | 3.3 (0.3) |
| QLF | 118 | 3.6 (3.4) | 41 | 4.0 (3.6) | 19 (12) | 3.0 (2.7) | 2.7 (0.3) |
Sensitivity analysis for missing plaque coverage outcome data
As a sensitivity analysis, multiple imputation was used to create five complete data sets with imputed values for all missing plaque coverage data. Results were combined to investigate the potential effect of the missing data on the conclusions, although the overall effect of group allocation in the imputed analysis was not found to be statistically significant (p = 0.310).
Plaque coverage outcome data analysis for practice 2 only
Because 70% of available plaque data came from practice 2, we undertook an additional sensitivity analysis using data from practice 2 only (Table 20). This analysis showed a significant difference overall between the three groups (p = 0.005). Post hoc pairwise analysis using Tukey’s method shows a significant difference between the verbal and QLF groups (p = 0.004). As with the complete-case analysis, there is an apparent baseline imbalance with the TL group having a lower mean plaque coverage at baseline. However, in the other two groups where the significant difference was observed, baseline means were similar. The least squares means were adjusted for baseline plaque coverage and time to follow-up in the analysis in Table 20.
| Group | N | Mean % (SD) baseline | N (non-missing short-term follow-up) | Mean % (SD) baseline for those with follow-up | Mean % (SD) time to follow-up, days | Mean % (SD) short-term follow-up | Adjusted least squares mean plaque coverage (SD) from complete-case data set | Adjusted least squares mean plaque coverage (SD) combined from imputed data sets |
|---|---|---|---|---|---|---|---|---|
| Verbal | 35 | 3.6 (4.5) | 30 | 3.6 (3.8) | 24 (15) | 3.8 (3.9) | 3.5 (0.3) | 3.5 (0.3) |
| TL | 34 | 1.9 (2.0) | 26 | 1.6 (1.7) | 22 (12) | 1.8 (2.2) | 3.1 (0.3) | 3.1 (0.3) |
| QLF | 33 | 3.8 (3.8) | 29 | 4.2 (3.9) | 20 (13) | 2.9 (2.8) | 2.1 (0.3) | 2.3 (0.3) |
A sensitivity analysis was carried out using multiple imputation. The effect of group allocation remained significant in the imputed analysis (p = 0.035). The least squares adjusted means from the two analyses are included in Table 20.
Plaque coverage and self-reported toothbrushing behaviour
Table 16 reports the proportion of self-reported behaviour in each of the categories for toothbrushing behaviour (frequency and duration of toothbrushing) at baseline and short-term follow-up. We compared the self-reported behaviour for participants with plaque coverage clinical outcomes collected at the same visits and found little association. The mean (SD) ΔR30 for people reporting brushing more than once a day at baseline was 3.6 (SD 3.9), for those brushing twice a day was 3.4 (SD 3.7) and for those brushing once a day or less was 3.5 (SD 3.9). Moreover, at baseline, the mean (SD) ΔR30 for people reporting brushing for > 3 minutes was 3.6 (SD 4.0), for 3 minutes was 3.6 (SD 3.8), for 2 minutes was 3.4 (SD 3.8) and for ≤ 1 minute was 3.7 (SD 3.7).
We then took practice 2 data only, in which we found a difference in plaque coverage between intervention groups and categorised those with short-term follow-up into three categories of reported toothbrushing frequency, based on their questionnaire responses at the two time points (V2/V3) (Table 21). However, there were too few patients in the infrequent toothbrushing category to draw many conclusions.
| Self-reported frequency of toothbrushing | Number of patients | Time point, mean (SD) ΔR30 | |
|---|---|---|---|
| Baseline | Follow-up | ||
| Fewer than two times per day baseline, fewer than two times per day follow-up | 3 | 6.9 (6.6) | 6.0 (4.9) |
| Fewer than two times per day baseline, fewer than two times per day follow-up | 11 | 2.6 (3.5) | 2.1 (1.9) |
| Two or more times per day baseline, two or more times per day day follow-up | 71 | 3.2 (3.3) | 2.9 (3.2) |
Early caries outcome analysis
Only 25 images were usable at follow-up. Results are presented for completeness in Table 22. The available surfaces studied on the images were the buccal surfaces of anterior teeth, excluding any that were missing or obscured. If the QLF image had any patches of demineralisation on a surface it was counted as having been affected by caries.
| Group | N | Mean (SD) baseline | n, non-missing short-term follow-up | Mean (SD) baseline for those with follow-up | Mean (SD) time to follow-up, days | Mean (SD) short-term follow-up |
|---|---|---|---|---|---|---|
| Verbal | 116 | 0.07 (0.15) | 11 | 0.06 (0.12) | 18 (8) | 0.06 (0.11) |
| TL | 119 | 0.06 (0.13) | 4 | 0.04 (0.08) | 19 (18) | 0.06 (0.08) |
| QLF | 118 | 0.05 (0.12) | 10 | 0.03 (0.08) | 16 (9) | 0.03 (0.08) |
Using a generalised linear model, adjusting for baseline early caries and time to follow-up, there was no statistically significant overall effect of group allocation (p = 0.351).
We also calculated the mean values of ΔQ for each group, which were produced by QLF software that considers the area of the lesion to calculate its volume and, therefore, indicates its depth (which is of clinical importance). This is summed over all visible lesions to give a total value per patient. The units for the measurements are based on the number of pixels in the QLF image. Mean (SD) ΔQ measurements at baseline for the 25 patients with follow-up images were 6548 (SD 16,271) for verbal, 3030 (SD 6061) for TL and 6548 (SD 16,271) for QLF, with mean (SD) ΔQ at follow-up of 4501 (SD 9560) for verbal, 4512 (SD 9841) for TL and 34,606 (SD 109,434) for QLF. Using a generalised linear model, adjusting for baseline early caries and variation time to follow-up in each arm (see Table 22), we found no statistically significant overall effect of group allocation (p = 0.443).
Owing to the large number of missing data in the caries outcomes, no sensitivity analyses have been carried out using multiple imputation as these would have had to impute almost all of the data.
Basic periodontal examination outcome analysis
Patients were categorised into four categories based on their BPE score at baseline and follow-up (Table 23). We planned to analyse this outcome using a multinomial logistic regression for all four possible categories, with a focus on the difference between groups 2 and 4. However, as there were very few patients in categories 1 and 3, we have excluded these and carried out a binary logistic regression between patients in categories 2 and 4. The logistic regression analysis showed no significant effect of group allocation on BPE score category (p = 0.609).
| Category | Group, n (%) | |||
|---|---|---|---|---|
| Verbal | TL | QLF | Total | |
| 1: stable healthy (code 0 at baseline and follow-up) | 1 (2) | 0 (0) | 4 (6) | 5 (3) |
| 2: stable bleeding (code ≥ 1 at baseline and follow-up) | 46 (72) | 44 (80) | 46 (74) | 136 (75) |
| 3: change to bleeding (code 0 at baseline, code ≥ 1 at follow-up) | 2 (3) | 1 (2) | 2 (3) | 5 (3) |
| 4: change to healthy (code ≥ 1 at baseline, code 0 at follow-up) | 15 (23) | 10 (18) | 10 (16) | 35 (19) |
Sensitivity analysis at short-term follow-up for green traffic light patients
One of the exclusion criteria was that patients classed as green using the TL system were ineligible. However, during the trial, more of these patients were excluded in dental surgeries in the TL arm than in the verbal and QLF arms. To investigate possible bias, potential green patients were identified from the verbal and QLF arms using post hoc methods (see Chapter 3, Preliminary analyses and the sensitivity analysis involving green patients). However, only one patient with available short-term follow-up data in the QLF group, and no patients in the verbal group, was identified as potentially green. Therefore, this sensitivity analysis was not judged to be necessary.
Self-rated oral health
Analyses of covariance, using baseline self-perceived dental health data, were used to investigate whether or not the intervention influenced self-perceived dental health at 6 and 12 months. There were no intervention group differences at 6 months [verbal 3.84 (SD 0.81), TL 3.81 (SD 0.79), QLF 3.93 (SD 0.79); F = 0.95, df = 2177; p = 0.389] Nor were there any intervention group differences at 12 months [verbal 4.06 (SD 0.68), TL 3.96 (SD 0.68), QLF 3.92 (SD 0.70); F = 0.28, df = 2149; p = 0.758].
Chapter 5 Qualitative study
Background
Although we assume that dental practices are ‘risk contexts’ where dentists conduct ‘risk work’ (see Chapter 1, Risk work) (and that certainly appears to be the assumption in policy), there is little research to date to support this. There has been very little previous research in general, with the exception of a few studies126–129 that looked at the organisational and interactional practices in the dental field. The qualitative part of the project set out to explore the communicative approaches used and discourses drawn on when considering risk by dentists during routine dental appointments, and how patients receive and engage with these practices. We specifically focused on the following questions:
-
How do patients currently receive information on their oral health and risk in NHS dental practices?
-
How do patients respond to information given to them by dental professionals about risk in NHS dental practices?
-
How do patients feel about the information they receive in their dental appointments and how would they like to receive information in the future?
-
How do dental professionals prefer to deliver risk information to patients in dental appointments and what support is needed and necessary to improve current practice?
Qualitative methods
Design: epistemological and ontological approach
Ethnographic observations of NHS dental practices, supplemented with interviews and artefacts, were used to describe and analyse everyday routine behaviours in a naturalistic setting. 130,131 Ethnographic fieldwork took place from November 2014 to April 2016 in five NHS dental practices in the north of England. This included observations of 368 routine dental appointments and semistructured interviews with 30 patients and 16 members of staff from these practices. Artefacts including practice newsletters, posters, mission statements and photographs of the practices were also collected and compiled.
We took an interpretivist approach, which understands the social world as knowable but inseparable from subjectivity. 132 The lineage of interpretivist approaches can be linked to both symbolic interactionism, which explores how ‘through actions people create distinct social worlds’,133 and ethnomethodology, which examines ‘how social activities are done within interaction’. 134 These methods, however, have quite narrow and specific perspectives, so we used what Atkinson and Housley135 describe as sociological interactionism, which is a more inclusive approach that draws on the roots of interpretivist approaches without being as prescriptive. They define the approach of sociological interactionism as an interest in:
Social interaction and social encounters, investigations of microsocial phenomena, social construction of selves and identities, the structures of everyday knowledge, and the ordinary routines of mundane activity in social groups and institutions.
Atkinson and Housley135
Although interpretivist approaches do not automatically rely on ethnographic methods, they often go hand in hand. Indeed, as a number of authors have noted, interpretivist approaches assume that the way of knowing the world is through immersion and engagement with it. 136,137 Given that ethnography is also about treating participants as experts and paying attention to issues and processes as they emerge over time, it was an appropriate method to use to address our research questions.
Observations in dental settings
Ethnographic fieldwork took place in five NHS dental practices in areas of relative deprivation in the north of England (see Table 3 for descriptions of practices). Practices 1–4 all used the Unit of Dental Activity (UDA) system of NHS dental remuneration rather than a model involving categorisation of patients by risk, as is currently being piloted in other UK practices. 35,104 In order to include newer models of dental practice contract where risk assessment with red–amber–green categorisation of patients is being used, the ethnographic work involved a fifth NHS practice (see Table 6) that was piloting this new system. As practice 5 was not taking part in the RCT, it also piloted the study material (including the QLF camera). Several of these appointments were observed and are reported in Chapter 5, Using photographs to convey information on risk.
Each practice was studied intensively over a 4- to 12-week period, and this included extended direct observation of routine dental appointments and the practice environment, as well as formal and informal interviews of staff and patients. A single (non-dental) researcher observed and took detailed field notes of dental appointments involving 20 dentists, one dentist in vocational trainee/training (VT), three dental hygiene therapists (HTs), two prevention nurses, 19 dental nurses and three trainee dental nurses. Observations in practices 1–4 all took place before the trial involving the three different forms of information was introduced. The average number of observations in each practice was 74. Practice 1 had 53 observations, practice 2 had 59, practice 3 had 95, practice 4 had 56 and practice 5 had 105. Most of the observed appointments were NHS funded, except for 22 private appointments and a further 40 appointments that started as NHS appointments but later included some discussion, or procedures, of private treatment (such as white fillings, white crowns, whitening, private scale and polish). Although we expected that discussion on oral health risk would be positioned in dental check-up appointments, because there is no current research showing this to be the case, observations included a range of appointments in dental practices including check-ups, emergencies, treatment and review appointments.
On arrival at the dental practice, receptionists told patients that there might be an observer present at their appointment. The patient was given a leaflet with information about the study. Posters and further leaflets were also placed in the waiting rooms. When patients were called through for their appointment, the dentist introduced the observer and gave a brief explanation of the study, and the patient was given the option to consent verbally. In approximately eight appointments, the patients (who all cited anxiety) or the dentists (when they anticipated the patient would be anxious or that they would be dealing with a complaint) did not consent and the observation did not take place. In 10 further appointments, space restrictions (such as when there were several family members present) meant that the observer left the room.
Each member of the dental team was asked to consent to being observed and this was revisited during each period of observation. A few dentists later disclosed that they were initially suspicious of being ‘assessed’ by someone with a clinical background who might judge or question their clinical decisions. Once they were reassured of the observer’s non-clinical background, dental staff increasingly interpreted and explained interactions for the observer. In addition, the observer opportunistically asked staff questions for confirmation or clarification after the patient had left the room. Although the observer was treated as a ‘naive outsider’, members of staff would sometimes ask the observer questions between patients, especially when there had been a particularly difficult exchange. People’s behaviour changes when they are observed, but this change is difficult to sustain over time. The length of the observations meant that staff in the practices reported that the impact of the observer presence was minimal. The observer did not participate or talk during appointments, but sometimes patients would directly address the observer (e.g. giving feedback).
Anonymous field notes were recorded in notebooks during appointments and then typed up fully at the end of the day. Initial field notes were broad, becoming more focused over time as the observer became familiar with the structure of appointments. After a few weeks, the observer developed a structured observation-coding sheet for greater efficiency (see Appendix 3). This included recording which dental staff were present in the appointment, appointment type, patient demographics (e.g. gender, age group), length of appointment, descriptions of the appointment (e.g. verbatim when possible or through conversation and non-verbal cues) and descriptions of ‘backstage’ interaction (e.g. discussions between staff).
The types of dental appointments were noted and sorted into the following three categories, which were derived from previous research in dental settings:13 dentist-initiated check-up consultations, dentist-initiated continuing treatment consultations and patient-initiated consultations.
Dental staff were identified by consecutive numbers (dentist 1, practice 1, for example) and information on their background (e.g. years at the practice, NHS/private remuneration split, training, specialist interests) was gathered during informal conversations (between patients or in the staff room during breaks) and followed up in more detail during formal interviews (see Appendix 3). Talk during the appointment was recorded verbatim when possible, alongside descriptions of action and the non-verbal aspects of the appointment. This is important, given that dental patients often have limited scope to speak during parts of the appointments when the dentist examines or is carrying out a treatment in their mouth.
Figure 11 shows the range of types of observed appointments and Figure 12 gives an overview of the range of patient age groups observed.
FIGURE 11.
Percentage of observed appointment types.
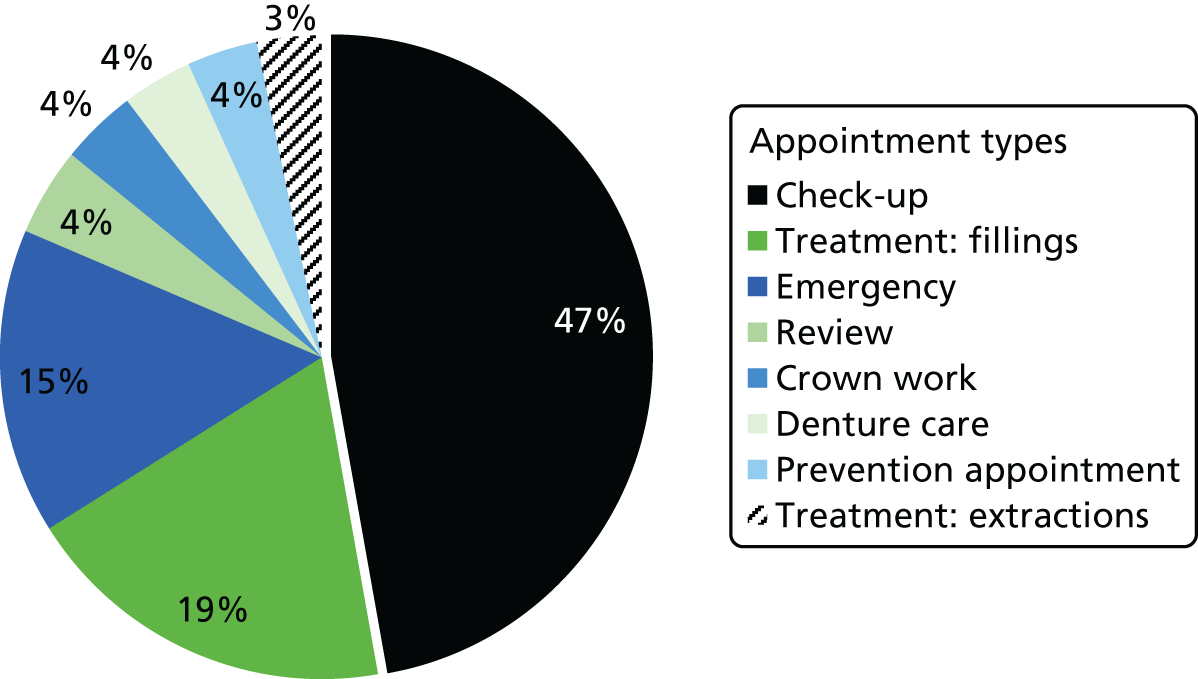
FIGURE 12.
Age groups of patients observed.
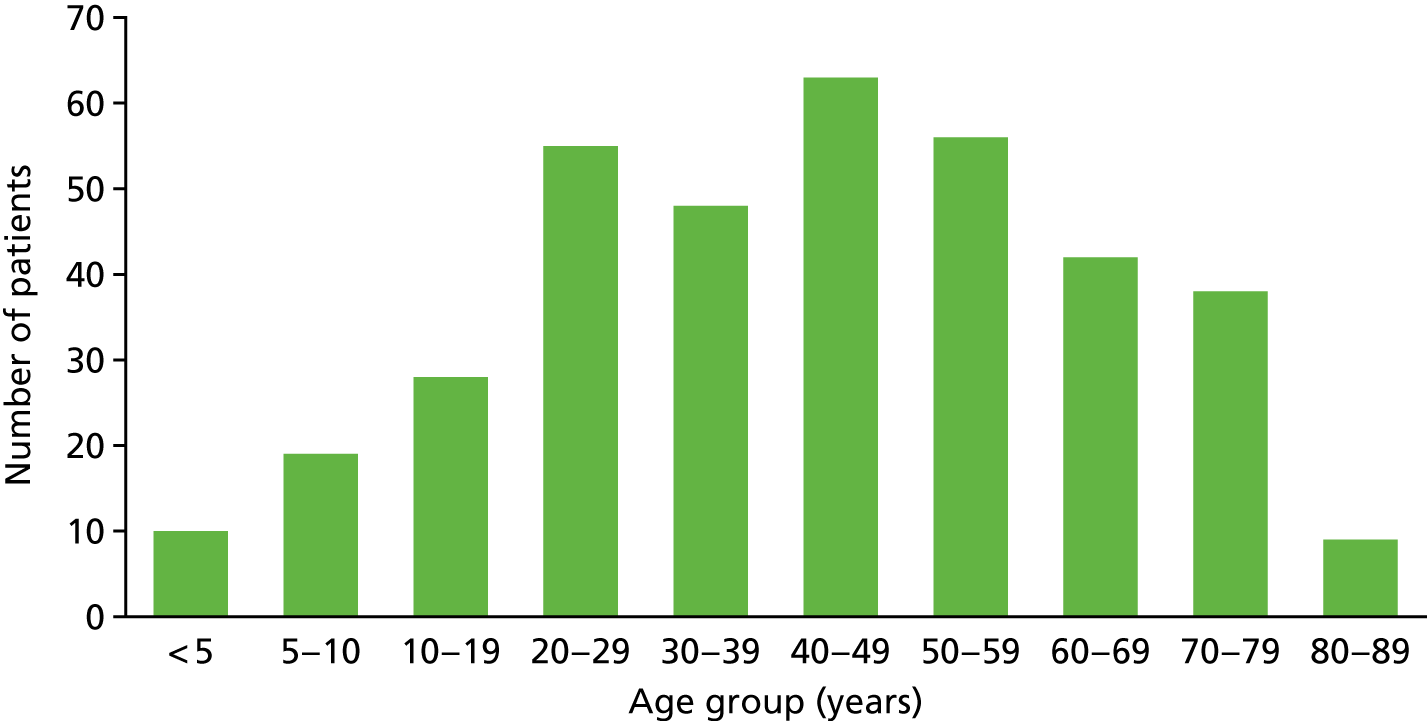
Qualitative interviews with staff and patients
Interviews with patients took place before the start of the trial during the observational period, and interviews with staff were conducted at the end of the trial to reflect on the process. The posters and leaflets given to patients on arrival gave information about interviews as well as the observations. The receptionists asked patients if they would be interested in taking part at the end of their appointment, and then called on the observer to explain the study in more detail. Some patients asked if they could take part during the observation of the appointment, and they were followed up afterwards. Although 53 patients indicated that they would be willing to be interviewed, only 30 patients participated. Patients withdrew because of time demands (especially those with caring responsibilities) or because they were feeling unwell and were unable to talk after receiving treatment during appointments. Interviews took place in a quiet section of the waiting room (n = 17), in a nearby coffee shop (n = 8) or in the patient’s home (n = 5), depending on their preference. Nineteen women and 11 men took part in the interviews, and they were aged between 18 and 70 years (median 50 years). Most participants were registered with the practice at which they were interviewed, except for five patients who were attending emergency appointments. Although most participating practices were located in disadvantaged neighbourhoods, patients often attended from outside these areas; therefore, the demographics of the participants reflect a wider mix of socioeconomic backgrounds.
All members of staff at each dental practice that were observed, or took part in the trial, were asked to take part in an interview. This comprised receptionists, dental nurses, hygienists, prevention nurses, VTs, dentists and principal dentists. Interviews often took place on the premises over lunch breaks or after the working day. Two interviews took place offsite at a local coffee shop. Demographic details of participating staff are found in Appendix 2, Table 32. The exception was practice 1, where high staff turnaround meant that all the staff who had been observed, or taken part in the trial, left during the recruitment process and were unable to be interviewed. A practice manager, two dental nurses and three dentists left practice 1 over the trial period. Only observations, patient interviews and informal conversations with staff are recorded for this practice.
A topic guide (see Appendix 3) was developed based on the current literature and insight gained through the ethnographic observations. The interviews were conducted using BNIM (Biographic-Narrative Interpretative Method), a narrative form of interview. 138 There are three sections in this interview process: first, an opening narrative-inducing invitation for participants to reflect on the place of the topic in their lives; second, the key themes and topics from the opening narrative are fed back to participants in order to obtain further detail and/or clarity; third, there is an opportunity for the researcher to ask questions that may not have been covered during the interview. This form of interview is both open and structured; participants have the opportunity to express their own ideas in their own words while also ensuring that the researcher can ask direct questions relating to the aims of the study. The opening question began by seeking a narrative of the participant’s previous experience of dental care and moved on to explore current dental care relationships in the practice. This opening question was used for both patients and staff. Patients were also asked about their views on communication in dental settings, their preferred methods of receiving information and feedback on intervention materials developed for the study. Dental staff were asked about their experiences of delivering risk information to patients, feedback on intervention materials and experience of taking part in the RCT study. Interviews were audio-taped and transcribed verbatim.
All of the qualitative work was conducted by one researcher (LL), which enabled all three strands to be pulled together and ensured that there was familiarity and immersion with the data. Analysis was conducted in collaboration with the lead author (RH), who has a dental clinical background. This supported an iterative process in which previous findings could be explored in future interviews and observations as well as aiding with recruitment.
Data analysis
The approach to analysis was predominantly inductive to ensure that themes were derived from the data. 131 A constant comparison method was used, starting with a preliminary coding framework that was refined throughout the analysis to interrogate the similarities and differences within the data. 140 As the analysis progressed, the coding framework was developed and adjusted in response to emergent themes. Analysis proceeded iteratively with data collection to allow emerging themes to be incorporated and explored in subsequent interviews.
The analysis of the observational data draws on approaches from previous research into medical encounters and talk. The analysis focused on the interpretation of meaning and action in appointments to explore the recurring themes and patterns that help explain the observations. 141 Analysis explored the form,139,142,143 structure144–146 and interaction147–151 in the appointments while paying attention to the dental setting and context (i.e. what are the explicit/implicit ethos of the practices and how do they have an impact on patients). The aim was to capture the range of activity that goes on in dental practices, from the organisation of care activities to the delivery of services. During the second round of fieldwork concerning each team, anonymised field notes were presented to participating dental staff in order to ‘member-check’ the observations and ensure that they were representative of their experience of delivering care. Through collecting and systematically comparing data from multiple sources, including direct observation, different forms of interviews and existing documents, we were able to identify inconsistencies in patterns of behaviour.
Data are presented using acronyms indicating their professional group: D for dentist, DN for dental nurse, HT for hygiene therapist, Int for interviewer and P for patient. This is followed by the appointment type (i.e. check-up or treatment), length of appointment and practice.
Key findings
Frequency and context of risk talk
Surprisingly, given the dominance of risk discourses in NHS policy (see Chapter 1, General policy context: discourse on risk and individual responsibility) and NHS dental guidance in particular,152,153 there was very little explicit ‘risk talk’ in the appointments observed. In fact, out of the 368 appointments, there were only 29 times when the term risk and its derivatives were used, occurring in just 19 appointments. The context in which the risk talk occurred and its frequency:
-
risk related to extraction – seven discussions
-
risk related to treatment – five discussions
-
risk related to orthodontic appliances (braces) – one discussion
-
risk related to radiography – one discussion
-
risk discussion between members of dental team – five discussions
-
risk to health from smoking – three discussions
-
risks of inadequate toothbrushing – one discussion
-
risk of poor oral health happening/consequences – five discussions.
Risk talk was most frequently explicit during urgent dental care appointments, and concerned potential consequences of tooth extraction or treatment. A standard set of statements was often used to give patients information about procedures and aftercare, as part of practise intended to guard against future litigation, should outcomes not be good. As such, this type of risk talk involved transferring knowledge from an expert (e.g. dental staff) to a layperson (e.g. patient) as part of procedures for obtaining informed consent. This is aligned with wider literature indicating that explicit risk discussions are more likely to occur if the topic of risk is an agenda point and the patient is in the process of being informed rather than already being under medical treatment. 154
Although we know that risk talk in medical settings varies with the type of activity involved, because previous research suggests that there would be more risk talk in check-ups rather than treatment,73 it is surprising that in the 173 check-ups observed there were only six instances of patients being given personalised oral health risk information. These occurred exclusively in practice 5 (the practice using the TL algorithm currently being piloted as a new dental contract prototype practice) (see Chapter 5, Using traffic light imagery to convey information of risk).
The form of risk talk
The following section draws on the observational data collected prior to the trial starting and interviews with members of staff at the end of the trial.
Explicit risk talk
Risk talk was occasionally found to be explicit when dentists highlighted potential harms related to smoking habits. In the observation below, for example, the dentist talked about the likelihood of mouth cancer occurring in numerical terms:
Do you smoke?
Oh, like a chimney.
I don’t want to be nagging, but I need to do my job. So smoking causes bone loss, it’s the number one cause of tooth loss. It loosens the support, so think about it like cement round a lamp post.
That happens with age anyway.
‘cause cancers, mouth cancers, six times more likely . . .
I don’t drink.
How much are you smoking?
It is varying, go down to 10 a day . . . but up to 40 again.
There is a service we can refer you to . . .
Went to the service, but it made it worse. A waste of time.
The more you go – the higher the chance of success.
Observation check-up (patient, male, 50s), practice 4
Dentists often prefaced a smoking discussion with an apology, as illustrated above and in the following example. Positioning the question just prior to operative dentistry (the dental chair being reclined) also means that there is no eye contact between dentist and patient. Risk talk undertaken in this way serves to distance the health professional from the task, turning it into a ‘neutral’ administrative task, so that it is not threatening or offensive to patients. 147,155,156 It also limits the scope for much discussion following the question:
OK going back in the chair? Here’s some glasses for you. Do you smoke?
Yes, 20.
Not here to nag you, but do need to tell you about risks of smoking. It increases your risk of mouth cancer and can cause tooth loss. Interested in giving up?
No.
Observation check-up (patient, male, 60s), practice 3
Interview data confirmed that dentists are uncomfortable when talking to patients about lifestyle issues, such as smoking, and take a cursory approach to superficially comply with professional guidance:
They do ask, but I think it’s asking because they have to ask . . . not necessarily because they want to go into detail about it. It is basically ‘Do you smoke? – well it can cause gum disease’ . . . and it doesn’t go any further than that, and I think it . . . I think, sometimes it’s just because you don’t want . . . it’s trying to tell a patient that they are not allowed to do something that they have been doing for like 30 years. They are not going to get out of that habit just because you have said that one thing and I think that’s why dentists don’t like to go into it. ‘Cause it’s like some patients say ‘Oh yeah, you say it every time, I am not stopping.’ We have to say it every time you come in, but patients don’t see that. The patients are like ‘Oh you are moaning again at me do you know about me smoking’, so I think some dentists do try and . . . they have to say it but quick enough for the patient not to realise you have said it kind of thing . . .
Interview with dental nurse, practice 4
Implicit risk talk
Recontexualisation occurs when a text or discourse is translated between different groups within a setting. Dentists were found to recontextualise risk information for patients by using metaphors or by referencing temporal dimensions (time) in relation to developing adverse outcomes. Metaphors are a means by which to translate complex information while facilitating elaboration and explanation, for example:
So . . . you’ve lost around 50–60% of bone around the teeth causing inflammation. It [plaque] nibbles around the bone.
Observation dentist 2, practice 1
Most of the implicit risk talk took place after the clinical examination (during which the dental charting and BPE scores are dictated to the dental nurse to record in the clinical notes) had occurred, and the dentist then recontextualised the clinical information by summarising it in non-medical terms. 157,158
Dentists were observed talking about the likelihood of a threat in the future, rather than making explicit reference to risk per se. This was often in the context of shared decision-making related to treatment outcomes:
So, is this tooth causing problems? I’ve seen the X-ray [radiographs].
Yeah, seen that . . . almost right across, but I’m not feeling anything. It feels good.
OK, there is a lot of decay in that tooth, just by looking. I know it is not causing issues now, but if we leave it it is going to cause problems in the future.
Observation check-up (patient, male, 50s), practice 3
Again, not using the word ‘risk’ and without reference to numerical probabilities, dentists made reference to the likelihood of adverse outcomes (risk being implicit) when communicating the need for lifestyle changes, for example in sugar consumption:
You are so young, you shouldn’t be having these problems. If you continue these habits there will be no point in doing anything – it will continue to decay.
I’ll stop! I don’t want it to happen again!
You eating sugar – it’s causing trauma to your teeth – the nerve is getting upset.
Observation check-up (patient, female, 19–25 years), practice 5
Temporal discourses were also involved in lifestyle discussions wherein dentists tried to attribute current poor oral health to previous unhealthy oral health behaviours. Reith159 proposed that risks are always perceived in relation to time, and so even though there is no explicit risk talk, by using temporal discourses dentists are carrying out implicit risk-work. Furthermore, when risk is emphasised as ‘near’, it is given more importance and presented as problematic. 160 By using negative consequences to frame these discussions, dentists highlight not only the proximity of risks in the future but also their relevance to the present. As such, there is a ‘temporal space in which future danger and present risk can be seen to co-exist simultaneously’. 160 Even though population risk cannot be easily converted to individual risk,161 leaving a degree of uncertainty, dentists tend to leave little room for doubt when framing these discussions. Dentists tell patients, under no uncertain terms, that without action there will be consequences.
Differences by dental staff type
Observations of HTs found that they also used temporal discourses, but were less likely than dentists to use negative, consequence-focused, framing-of-risk information. Rather, HTs tended to focus on the benefits of healthy behaviour. HTs also more frequently praised patients for their efforts than dentists, and consistently delivered more detailed information on patient’s oral health. Another key difference between dentists and hygienists/HTs was in their way of recontexualising clinical information. Whereas dentists recontextualised clinical information by summarising rather than trying to translate clinical information such as BPE scores to the patients, hygienists/HTs set out to translate clinical findings. Risk was still raised only implicitly, but hygienists/HTs allowed patients to interpret risk through understanding the medical terminology:
Going to do some charting today then a polish. With gum disease you need something concrete to measure. Do you know how the dentist inserts the probe? See how deep? The deeper it goes the deeper the disease is OK? How are you getting on with brushing?
Yeah, more consciously.
[Charting omitted.]
OK got a record there. So . . . 3 is 3 mm which means they are quite swollen. Anything over 3 means you have lost some support. Because there is bleeding it means that the gum disease is active. We do our cleaning here and you do yours at home. So next visit we’ll see an improvement – so we’ll have 1s and 2s. Doing great.
Observation treatment with HT (patient, male, 30s), practice 4
It’s really hard to motivate some people . . . try not to scaremonger. You’ve got to praise them for trying. It’s multifactorial, and different people react differently.
Interview with HT, practice 3
Using traffic light imagery to convey information of risk
Frequency and form of risk talk
Because observations took place before the trial was implemented in practices 1–4, the use of TL categorisation was only observed in practice 5, which was an NHS new dental prototype practice. It is notable that although the TL system was routinely used to guide the preventative care pathway in practice 5, two dentists did not communicate this information to patients during any of their observed sessions. Although all six of the personalised risk oral health discussions observed in this study took place in practice 5 (see Frequency and context of risk talk), it is striking that the TL categorisation did not prompt explicit risk talk nor facilitate expanded discussion on lifestyle risk. Even though all patients in practice 5 would have been allocated to a TL risk category using clinical software used during the check-up appointment, whenever this information was passed on to patients the implications of their TL category were usually not discussed in depth.
There is a possibility that TL categorisation may be used as a substitute for more detailed discussion on lifestyle risk (i.e. acting as a shorthand), such as in the following two observation examples:
Have a rinse out. Want to pop in and see the hygienist?
Do I need to?
It can wait. So this is your care plan, you’re green and everything. See you in a couple of years.
Observation check-up (patient, female, 20s), practice 5
Hi, I’m [name], you fit and well?
[Patient nods.]
Smoke?
No. I haven’t been to a dentist for 10 years.
Any immediate problems?
Have a bad tooth, a root canal that’s falling apart.
OK, just a check-up today – is that all right?
[Dentist lowers dental chair and hands the patient protective glasses, undertakes charting and BPE, sits patient up, then takes radiograph.]
There is some gum inflammation needs sorting out. Want to pop round?
[Dentist shows patient radiograph.]
See this tooth, it’s a difficult extraction, I could leave it, but there is decay under the filling.
OK.
Need prevention before you can have the treatment and then come back for a treatment planning session. Then come back to me. Red for decay.
How many fillings need done?
Book two appointments in with the desk.
Thanks. Bye.
Observation check-up (patient, male, 40s), practice 5
It is important to note that dentists in practice 5 often gave the patient their risk classification during the ‘farewell sequence’ of appointments. In the farewell sequence the patient is getting ready to leave, the dental nurse has started decontamination and the dentist is typing up notes and ending the appointment. In other words, important discussions happen prior to, not during, the farewell sequence, and by placing a TL category discussion in this part of the appointment the dentist signals that the information is not important. It also discourages discussion with the patient through verbal and non-verbal communication (e.g. writing notes, opening the door) that the appointment is ending.
Patients’ view of traffic light imagery
Although most of the 30 patients interviewed agreed that TL imagery was a simple way of receiving information about their oral health, patients were generally fairly indifferent about its use. In interviews, patients did not express strong feelings, commenting simply that ‘it seems self-explanatory’, ‘it wouldn’t bother me’ and ’it’s OK’. Even though some of these patients said they saw value in having the TL card as a reminder after their check-up, many admitted that they did not read material they received from the dentist:
And do you think it is something you would look at away from the dental practice?
I can’t really admit that to be fair because anything I get given at the dentist I just . . . yeah . . . I don’t look at it . . . [chuckles].
Interview with female patient in 50s, practice 2
Some patients felt particularly positive about TL information and identified two reasons for this. They felt that they wanted more information about their oral health to make better-informed decisions and that for them TL information was useful in alerting them to potential problems:
Yeah, I think it would be quite useful actually . . . to know that there is something needed flagging up or you have kind of got a clean bill of health that’s nice . . .
Interview with female patient in 30s, practice 1
I liked the traffic light card – makes you aware. Have thought about it quite a lot since and I think it really helped me to consider my oral health.
Patient telephone follow-up at 6 months
These patients were those who also said that they wanted as much information as possible about their oral health in order to help manage dental anxiety and uncertainty in particular. Good communication practices, for them, involved detailed explanations of their oral health and anticipated treatment:
. . . definitely, it’s the lack of like explaining. I like to know the ins and outs of everything, even if I don’t quite understand it, having a process of it helps me understand it.
Interview with female patient in 30s, practice 3
Patients said they liked the TL system because it provided a way to monitor their progress by providing a reference point. The value of the system is in providing a goal and a plan against which to measure progress, rather than as a one-off ‘shock factor’:
If she said ‘yeah all right you have got a red card because your teeth are going to fall out ‘cause you have not been looking after them but in six visits we can have then on a green’ . . . it can be a timescale thing.
Interview with female patient in 20s, practice 3
I thought the traffic light card was really useful and positive. It was good that I could take it home with me and then maybe compare it to the next visit, so I could maybe track my progress.
Patient telephone follow-up at 6 months
Several patients, although supportive of the simple nature of TL imagery, thought that this was unnecessary in routine dental check-ups. They explained that more information from their dentist, rather than the classification itself, was the most helpful:
I guess I don’t need a card or anything . . . as long as they explain to me what I need to do, or if there is anything that I need to buy or whatever to maintain that, I am sure they will. That’s fine for me.
Interview with female patient in 40s, practice 2
I didn’t think the traffic light was necessary – the colours I mean. I was going after just the advice personally.
Patient telephone follow-up at 6 months
Therefore, the TL imagery did not add value to their dental check-up for these patients. Several patients explained, when looking at the TL cards, that they expected dentists to provide this information to them as routine. As a result, the TL cards were meaningless to patients without additional explanation from the dentist. Moreover, some patients were unsure whether TL categories should be interpreted at an individual level (red being worse than usual, green being better than usual) or on a population basis (red is worse than expected for people like you). They were also concerned that three categories oversimplified the situation. Finally, there was some concern that the TL system might be misused, suggesting that it was open to manipulation for dentists’, rather than patients’, interests:
How might this system work for you? Would it be useful?
Well, I . . . again you are at the mercy of the person making that judgement. I mean, erm . . . if a dentist was short of patients, then there may be the temptation to classify people as amber rather than green and red rather than amber, so people come back more regularly because obviously the dentists get paid on a visitation basis.
Umm.
So erm . . . but yeah, I think something as simple as that, if the dentists were to say that, yeah I think it . . . I don’t think it is very likely that it is going to be abused but . . .
Interview with male patient in 50s, practice 4
In summary, patients overwhelmingly thought that the TL was simple to understand. What they liked most about the TL system was receiving more information from their dentist about their oral health, which, as some patients noted, did not require a TL classification in itself. There was some enthusiasm for the usefulness of a TL system to help patients manage and track their progress over time, particularly when they were arriving to the dentist with a number of problems. There were some concerns about the value of TL on top of what they expect to receive from their dentist during a check-up, and about the potential for misuse. Overall, however, there were more accounts of indifference rather than an overwhelming support or dislike of the TL.
The dental team’s view of traffic light imagery
Dental staff who took part in the RCT study had different experiences of using TL imagery that varied by practice. In practice 3, for example, situated in a high-need area, one of the dentists involved said that they did not get much of a response to TL information from patients. They described many of their patients as anxious about coming to the dentist, and when they did, they typically accepted advice without challenging or asking many questions. Because of this, when using the TL cards, the dentist was unsure about how much patients took in:
And what about the other arm with the red–amber–green group. How did you find it worked as part of the trial?
Because I don’t know the results, I wouldn’t really know. You can’t really tell with the patients . . . do they understand what that means? When I told them they were high risk (which I always do anyway whether you give them that traffic light or not), high risk or not whether that traffic light looking at it – green–red–yellow – would make an effect. So, if they keep it, obviously if they see it all the time then that’s something that may effect, well whether you give it to them and they just have a look then just throw it away it’s a different story.
Interview with dentist, practice 3
In this practice, however, there were relatively high rates of failed appointments and a high number of dentists in the practice, which meant that there were few established relationships. For this dentist, delivering a TL message during the first meeting with a patient was difficult without having the time to first develop a rapport with them.
In contrast, practice 5, which used a TL system as part of an NHS (prototype) contract, had a mix of socioeconomic groups. Their middle-class patients, for example, during observations were much more likely to challenge the dentist’s opinions or treatment choices. The practice manager at the practice explained that they had received a number of complaints about the TL system from patients who were not happy about the classification given to them:
I have had a recent complaint that I have been dealing with where the patient likened the red–amber–green pathways as being akin to Nazi Germany. Which I felt was slightly harsh but that’s how he . . . he was extreme in his feelings towards it. Hated it, absolutely hated it, thought it was an appalling system and that he was in some way being labelled as erm . . . less attractive in every sense of the word than somebody who was a green patient. He really took it to the nth degree. Didn’t like the fact that because he had some serious perio [periodontitis] and a problem with acute perio. Pretty much random caries because he was a big mint eater . . . couldn’t get that. No, no, no, no . . . it was our job was to put him back together . . . it wasn’t to give him any advice on his lifestyle and his lifestyle choices . . . that wasn’t our remit, we were just there to do what he wanted. So – no, it’s not always good.
Interview with practice manager, practice 5
During interviews, members of the dental team at practice 4, which also had a mix of socioeconomic groups, similarly reported that their patients did not respond well to the TL system and challenged the dentist on their classification. The lead research nurse for the study reported that dentists found it uncomfortable to report the TL category to patients when there was the risk that the patient would get offended. This was particularly relevant for patients who had been working on their oral health but were classed as red:
And what about the traffic light, how do you think that worked?
Erm . . . quite a lot of people have not liked the traffic light. I think quite a lot of people have said it’s a bit, I don’t know, it’s a bit erm . . . they just said it not nice to say you are a green or . . . you are either high or low, do you know, it’s a bit like not rude . . . but you know they have not found it very pleasant for someone to say, because you have maybe not brushed your gums or not flossed that you are now high risk. Not necessarily you need a filling, you are high risk because you have not done that properly and I think there is a bit of a situation with that kind of thing so you have not. So even if you need one filling you are now high risk and it’s like . . . ‘Oh this is my very first filling in 30 years, I mean how can I be high risk’ and it’s trying to explain that kind of thing to the patient that they don’t like.
Interview with research nurse, practice 4
The other dental nurse involved in the study at practice 4 reported that although some patients did not appear to like the TL system, they thought that the information on the back of the card (about recommended behaviour) might act as a bit of a reminder to patients after the appointment:
It has got things on the back of it that you need to improve, so if you have not took in all the things that the dentist has been saying it is something to take away with you to recap on . . . because obviously if you have not remembered it all it’s something you can look and say, well they did tick here that I need to improve that and need to improve that, so I think it’s better for the dentist as well to be able to give you something to say this is what you can improve on than just telling you.
Interview with dental nurse in practice 4
Practice 2 generally reported that they had a positive response to TL cards from their patients. They also found the TL cards useful as a reminder or prompt for patients. The participating dentist did acknowledge, however, that the TL algorithm was not sufficiently complex to capture a patient’s oral health in the context of their lives. As they describe, the dentist felt comfortable recontextualising TL for their patients to avoid demotivating them from engaging. This involves explaining the limits of TL to a patient and focusing on what they can do to improve. This was aided by the dentist’s experience and familiarity with patients:
How did you find the traffic light cards?
Oh, patients liked it; it was a bit new to us but not the theory behind it. Erm . . . yeah they liked it, it worked quite well and tick boxing on the back, it was quite handy to hand something to somebody that worked quite well.
And did you feel comfortable giving that to patients?
Yeah, again I think a lot of that comes with confidence, so as I have got older and more experienced I am quite happy giving, and it’s not bad news, that’s not right, but if there are areas of concern I am quite happy talking to people about that. I think maybe when I was younger in my career you maybe don’t feel as confident to do that but especially a lot of our patients who I have seen for a long time. Yeah – we are OK giving that. There are sometimes, a couple of times, where they would fall into a red traffic light, which is sometimes a little demoralising for patients who do work very hard – but obviously they do have those areas of concern and there may be some of the elderly population who technically fall into it, but you know they do their job based on their age and their ability. So, as long as you kind of explain that to them most of the time people were fine with it, therefore meant we were fine with it.
Interview with dentist, practice 2
Using photographs to convey information on risk
Visual methods used routinely in existing practice
Visual methods, such as the use of radiography, mirrors and posters, to communicate oral health risks to patients are commonplace in the observations of current practice. Some dentists used visual aids on a regular basis, but this was more of an individual professional routine rather than a general clinical practice, as reported in the interviews:
If I was to say to someone my ideal surgery that I would have . . . obviously to have more time, and then having that, you know, that intraoral camera and pictures and things like that that I could show to the patients. I used to do that in my VT [vocational training] where I would have my pictures of gum disease, what gum disease is, what it looks like, what the treatment is like, so people understand why it is important to have it and maintain it. So – I think to me pictures and videos and things like that is really, really important. Well actually, when people see the pictures and videos they understand what it is that I am talking about, just with words it is very difficult for them to kind of visualise what it is that I am saying.
Interview with dentist, practice 4
There were intraoral cameras in a few of the practices and a few dentists based in those surgeries used them with particular patients. One dentist in practice 5 used intraoral cameras with teenagers who they believed needed to see the damage being done in order to achieve behaviour change. The dentist explained that they thought that young people were more likely to remember a visual image than verbal advice. In contrast with appointments with adults when dentists were often careful to avoid lecturing or offending patients, dentists were frequently more forceful with teenagers:
Can I get intraoral camera for the molars?
[DN gets camera set up.]
Lets have a look [D charts and records BPE score].
On the whole, fine, just some areas . . .
[Turns computer screen to show P.]
See this pit, it’s like a crater. Do you think that’s normal?
No.
Know why you got it? [P shrugs] There is dotting on the teeth which is lost enamel. What do you think could have eaten that?
Don’t know.
Are you trying to work it out?
I don’t drink fizzy pop.
Drinks fresh orange juice sometimes.
[D gets out laminated picture of sugar amounts in drinks.]
See here how much sugar is in drinks you would expect. Do you drink these?
It’s mainly cordial and fruit juice.
Orange juice is healthy but still has loads of sugar and acid which damages the enamel. Drink it through a straw OK and have them at mealtimes. Don’t want to see more loss of enamel. Brushing is OK. OK?
Thanks [both leave].
Observation check-up (patient, male, 11–19 years), practice 5
Most dentists used simpler visual aids in their everyday practice, such as using radiography and mirrors. These aids helped to show patients’ areas of risk and largely eliminated the need for the dentist to tell them, making it a more comfortable exchange. Here, the examples show the dentists using mirrors, as radiographs are commonly used to show patients treatment needs rather than oral health risks. Mirrors, however, were used to give detailed oral health advice about brushing or to point out problem areas:
0, 0, 2, 3, 2, 0. That’s fine, the only area you are missing a bit is right on the inside here where there is a pocket. Concentrate here, right around the edge. Can you feel it with your tongue? Fuzzy between the tooth and gum, should be smooth.
[Hands P mirror.]
Will do my best.
Right down here, see . . .
[Uses mirror with probe to show P.]
Just do a little bit more. Everywhere else doing well.
Good, do my best.
Observation check-up (patient, female, 80s), practice 4
Dental staff who used these visual aids said that they enabled them to deliver personalised oral health advice for their patients, which could help the information resonate more:
So, I think they appreciate it because it’s not just generalised information they are getting then it’s tailored to you. You know that’s your teeth that you are seeing in the mirror and you can see the effects that it’s having on that area, you know rather than just . . . here is a model, this is where you are missing. Cause I don’t think some people can translate what they are seeing, you know like on the thingy models.
Interview with HT in practice 3
Overall, visual aids are currently being used in existing practice but tend to be used by particular dentists. Dentists had preferences for different types of visual aids for different types of patients. For dentists wanting an impact, an intraoral camera was used, especially with young people whom they were not afraid to offend. In contrast, other visual aids allowed the dentist to illustrate the problem without shocking the patient. The visual aids most commonly used were radiographs and mirrors, which do not require specialist equipment and can be easily slotted into routine appointments. Dentists doing private work tended to make the use of more complex visual aids, such as intraoral cameras or single-lens reflex cameras to show patients their teeth.
Patients’ view of the use of quantitative light-induced fluorescence photographs
As part of early piloting work, the QLF camera was also used in some observed appointments in practice 5. Two dentists agreed to allow their dental nurse to take QLF photographs over 2 days of check-ups when the observer was present. All of the patients over the 2 days agreed to have their QLF photograph taken when asked by the dentist. For some patients, the images produced appeared to shock and disgust:
Oh I’m in trouble [looking at partner], I’ve not been completely following them to be honest. I’ve been at the funeral of close family and depression so a bit hit and miss.
Still need to really work on this. Would you mind if we took a photo?
[Takes photograph and turns screen to face patient.]
Oh it shows you . . .
Can I get a copy of that – for my diet!
So, this pink is the bacteria on your teeth, so you need to be brushing this area much better, and following the advice of the prevention nurse. How did you find it?
Not too bad, interesting.
Shows you where to spend more time brushing . . .
Making me feel sick. That camera is awesome.
Observation check-up (patient, male, 40s), practice 5
How did you find having the camera?
Fine, it’s the face that looks bad . . .
[D gets up to look at the photograph on the screen.]
Need to put a hand grenade in there, flipping heck! They didn’t look too bad until the bridge broke.
Observation treatment visit (patient, male, 50s), practice 5
During the interviews, there were very strong responses to the QLF photograph in comparison with the indifference to TLs. Many patients described feeling uncomfortable with the idea of a QLF photograph. Although in the interviews patients were not referring to a QLF photograph of their own mouths (they were shown an example), their reluctance was bound up with anxieties about the look of their teeth. These patients did not want to look at their teeth, let alone a photograph displaying potential problems they did not know about. Patients discussing QLF often explained, without a prompt, their discomfort as guilt for past failings:
I think that’s awful . . . if that was me I would think ‘oh no’ . . . I would hate to see that personally, I would, I think it’s awful that. But if it aids you it’s a good thing, but just looking at that I would be thinking ‘Oh my God’ . . . cause I know I don’t clean them properly, as I say I left them for so long as a child I haven’t got the best teeth in the world erm . . . but no, I think that’s . . . not a very nice picture really, if that was mine I would be saying ‘Oh no . . .’.
Cause what we were asking is would you feel comfortable if it’s something the dentist did in your check-up?
I wouldn’t actually, I don’t think I would be personally. No, tell me what I have got to do and that would be enough for me.
Interview with female patient in 50s, practice 4
I wouldn’t like that.
No? Can you explain?
Cause I don’t like looking at my teeth, so I wouldn’t want to take a picture home with me. It would be helpful but it’s not something that I would like, does that make sense? Yeah, I wouldn’t be comfortable with [dentist] doing it erm . . . yeah, I think it’s a bit shame-y really.
Interview with female patient in 40s, practice 5
Despite patients’ dislike of QLF, it was clear that they could still see the value and utility of it. When they reflected on QLF for their own teeth, patients saw the potential of the photograph to cause shame and guilt. At the time, they recognised that the QLF photograph could give them valuable, extra information about their oral health. Some of these patients, then, said that they would be open to having QLF photographs taken once their teeth had improved as a way to show their progress. They were reluctant to have the photograph taken as a way of shocking them, as they were already keenly aware of having problems with their teeth:
How would you feel about having this photograph taken at your next check-up?
Not at the moment but once this is sorted then err . . . yeah, I guess if it is pointing out things that I have missed then that yeah . . . that’s always useful yeah.
So you would feel uncomfortable at the moment having it . . .
Yeah because of the state of my teeth yeah, I don’t want to be looking at my teeth, I don’t want anyone looking at my teeth at the moment but obviously it can’t be helped, at the end of it like when it’s all going to be hopefully clean like . . . then yeah yeah then I would find it handy. I know it sounds a bit, it’s maybe a bit backwards that when I need it the most I don’t want to look at it but do you see what I mean though yeah, it’s not a very nice thing to have.
Interview with male patient in 60s from practice 4
Yeah. I mean my initial reaction was like . . . whoooh but I mean that’s obviously a useful thing to have and there is no point in sitting there being unaware like if they can do something about it and brushing improvement it’s probably a good thing.
So if the dentist gave you a photograph of your teeth to take away with you, do you think that would be something you would look at or?
I would certainly look at it and note down but then probably get rid of it and just try and remember where to act on.
Interview with female patient in 50s, practice 4
In telephone calls at 6 and 12 months, during feedback from patients who were in the QLF arm during the RCT trial, some participants concurred that they had felt ‘embarrassed’ about the photograph but could not remember much about it, or had discarded the card, suggesting that negative emotions about the photograph may not have a long-term effect. A larger number of patients did report that they found the photograph useful for making changes to their oral health behaviours:
The photograph was useful at the time as it helped me to understand where I was failing to brush properly.
Patient telephone follow-up at 6 months
The photo was really good at demonstrating to me that I had been doing well. I liked that it was visual and that it was easy to understand and to see what I needed to do.
Patient telephone follow-up at 6 months
In summary, introduction of QLF images in dental practice for health education purposes is likely to be met with resistance. Many patients were acutely uncomfortable with the idea of the photographs being taken, even if they thought that they would be helpful. It is also clear from the observations that patients are likely to consent to the photographs when asked during appointments. Patients who received the photograph also generally reported finding it useful, even if they chose not to look at the photograph after the appointment.
The dental team’s view of the use of quantitative light-induced fluorescence photographs
Practice 5 was trained to use the QLF camera and given a few weeks to pilot it prior to the study starting. When the observer went to the practice, however, the camera was still sitting in the box from the training. Although these dentists appeared generally positive about the potential for the camera, they said that they had not had the time to use it in practice. It is also interesting to note that when visiting the trial practices after the trial had ended, none reported using the QLF camera with patients. This included the practices that had positive experiences and could see the value of its use. The current burdensome nature of the equipment (laptop computer and connecting camera shown, see Figure 7) and the need to set up and wipe down the equipment for each patient was a barrier.
Dental staff who took part in the RCT study were generally positive about the QLF photographs. Staff in practice 2 described a positive experience delivering QLF to their patients who were mostly regular attenders:
Patients love photographs. They were a big hit, they loved visual aid. Again, a lot of the demographic I had they loved something that they can see, that worked really well, taking them was really easy, they would be brilliant, it would be lovely to do that for every single check-up, that would be great. I don’t know how realistic it would be but that would be really nice.
And so, you felt the patient engaged?
Very much so, very much so with the photograph, they loved the photograph.
Interview with dentist, practice 2
The staff in the other practices also reported that they thought that QLF helped patients to understand the problem at hand and acted together with the information that was being given verbally:
There is still not a lot of information, it’s just the picture but it’s . . . I think it still does give that image to the patient thinking OK, when you show them which areas they are missing they can see it in their picture and then obviously when they are brushing their teeth that image will come to them when they are doing that. So, I think it definitely . . . will help.
Interview with dentist in practice 3
When reporting on patient responses to the QLF photographs, the dental nurses who took the photographs said that although patients were initially reluctant, the experience was not as bad as the anticipation. Despite the enthusiasm for the technology, practice 4 and other practices still reported concerns that it would not fit into their everyday practice outside the trial. Some practices suggested that they thought that it would fit in better with the work of hygienists who had more time during appointments, and similar to the patients’ view the staff thought that it was best used to show progress over time.
I wouldn’t say it would work on everybody on a day-to-day but things, but maybe things like your 3-monthly perios [periodontal examinations] or your people with gum disease that you are trying to help bring it back. I think taking pictures of them in their stages as they go along would help that patient to see where they are improving. You know if you are showing then, well this is what you started like and now look at them, they would know that they are improving, that they have done good. So I think for certain patients like that, where maybe the oral hygiene is not as good as is it should be, showing the pictures in stages would make them, you know, make them happy that we have actually done something to improve it.
Interview with dental nurse, practice 4
Summary
The qualitative work aimed to investigate at how dentists currently give patients information on their oral health risk within routine dental appointments. The key finding from the observations of dental practices is that, despite routine dental check-ups being a risk context, there is very little explicit risk talk between dentists and patients. This holds true even in the pilot/prototype contract practice, which routinely used a TL algorithm that was a mandatory part of its contractual arrangements. There was so little explicit risk talk across all appointments that this leads us to conclude that risk is not part of the normal discourse between dental staff and patients. Instead, we suggest that risk is part of a professional discourse, given its prominence in relevant policy and among staff, rather than a common concern of everyday clinical work.
In clinical encounters, dental staff used a range of ways to communicate risk implicitly, translating risk information into metaphors in order to aid understanding and using temporality to evoke risk when talking to patients. Dentists would often ask patients to offer explanations of past behaviour to explain current symptoms, as well as evoking a threatening future should action not be taken in the present. By making patients feel ‘fear’ about the future, dentists are attempting to make the risk feel real and relevant to their immediate circumstances, thus trying to avoid patients delaying treatment and requiring more extensive treatment in the future.
There are several reasons why risk work is minimal, but perhaps the most prominent one when thinking about discussing lifestyle issues is the risk of offending patients and disrupting relationships. As Linell et al. 73 note, lifestyle issues are ‘threatening to personal integrity and, therefore, interactionally sensitive’. There are several studies in a range of settings that show that health professionals often try and behave politely and civilly with patients, regardless of their personal feelings. 148 During interactions, these health professionals try and save patients’ feelings and allow patients to do face-saving work, such as excuse, repair or apologise. 162 This shows that professionals would rather deliver messages in a less confrontational way or avoid them altogether rather than risk the patient leaving after being offended. In interviews, dental staff acknowledged that talk about lifestyle could be tricky, especially around smoking. Often dentists turned to delivering rehearsed statements about smoking and sugar to patients, which enabled them to tick the box without getting into uncomfortable discussions. Dentists explained that if they gave general information about the risks to everyone, then no one would be targeted and offended. However, this tactic does not seem to work in practice and patients expressed frustration at being given general advice that was not relevant to them.
The use of traffic lights and quantitative light-induced fluorescence in dental contexts
Patients responded indifferently to the presentation of risk through TL. Most patients valued receiving more information from their dentists but did not see TL as providing additional support. On the other hand, because of the broad categories used in TL, most patients reported that they expected to be able to anticipate their risk category. Therefore, being given TL was only minimally face-threatening. This is important, given that risk is inherently a face-threatening act. In contrast, patients felt unable to anticipate the results of QLF and, as such, it was more acutely face-threatening. Anxieties about having a photograph taken, then, reflect uncertainty about the outcomes. Looking at the photograph itself can become less threatening as the dentist gives detailed information about the patient’s health. Patients reported QLF as having the potential to add value to their dental experiences. Conversely, the biggest barrier for dentists was this extra time.
Staff in dental practices also shared concerns about giving risk information to patients when it could disrupt the clinical encounter (through shame, guilt and blame). This varied, however, by practice. Some practices were comfortable delivering TL but were not met with much response by their patients, which may have led to limited discussions. Other practices met with resistance (from the patients) to being categorised. Observations made of the use of TL in practice 5 show that it does not increase discussions about risk. In some cases it reduced discussions. Staff at a number of practices reported that they also saw the value in QLF of giving personalised information to patients. Overall, staff thought that QLF would be most useful for hygienists when dealing with periodontal issues. However, even among practitioners with positive experiences, there was no adoption of QLF into routine practice.
In general, given that patients find more time and information from their dentists as most important, and that time is critical to allow for dentists to deliver risk work, it may be that adding other ways of communicating risk could be premature. Prior to introducing new methods, there first needs to be adequate time and support for dentists and patients to have these discussions. Staff and patients report discomfort from risk-related discussions during clinical practice, and, as such, risk work is not occurring. Furthermore, there is a wide variety in the communication skills of dentists and not all of it is dependent on time. Some dentists are very adept at being personable with patients in a short period of time, whereas others see communication as a low-value aspect of their job that they would like to minimise:
I think it’s totally personal. There are some dentists who are fabulous communicators, who naturally empathise with people and are just able to communicate. There are others who struggle. And I do, I don’t know if it’s something they should be taught at med [medical] school or whether it’s something that you have either got or you haven’t got. But you can see which of our dentists has the gift of the gab and those that don’t, both on a private income scale and their success rate with patient buy-in.
Interview with practice manager, practice 5
Training in communication skills needs further support so that dentists can have open discussions with their patients about oral health in a personalised, holistic way. Patients would also benefit from knowing what to expect in dental appointments, so that they can anticipate what may be talked about, reducing anxiety and improving communication.
Chapter 6 Patient and public involvement perspective
Introduction
In health research, increasing emphasis is being placed on fostering meaningful partnerships between researchers or clinicians and the patients whom the research is intended to benefit. 163 In the UK, patient and public involvement (PPI) is strongly embedded in health and social care policy: The Five Year Forward View164 emphasises the need to engage patients with a fresh perspective, involving them directly in decisions about the future of health services. In keeping with this, NHS England has committed to support PPI in its work; incorporating views from people who use health services as ‘experts by experience’ and who can make meaningful contributions ‘as a result of their lived experiences’. 165 (This paragraph contains public sector information, from an online resource provided by NHS England, which is licensed under the Open Government Licence v3.0.)
UK-based organisations that support patient engagement in research, such as National Institute for Health Reseach (NIHR) INVOLVE (funded by NIHR), have been set up to encourage research projects to be ‘coproduced’ with patients/the public, so that ‘research is being carried out ‘with’ or ‘by’ members of the public rather than ‘to’, ‘about’ or ‘for’ them’166 [Copyright of INVOLVE, National Institute for Health Research (NIHR), 2018. Materials from this site can be downloaded, printed out, copied, used and distributed free of charge for non-commercial purposes only. No alteration or adaptation of any of the materials may be made without the written permission of INVOLVE]. However, truly meaningful patient engagement and coproduction is often found to be challenging, given a landscape of inevitable constraints (ethical, practical and budgetary restrictions, among others). 167 On the other hand, possible benefits to the research community can be many, such as increased relevance of the research, more ethically sound research, diverse perspectives surrounding research questions and how to approach answering them. 168
The PREFER project sought to incorporate patient contributions at key stages throughout the study, with the main goal of ensuring that there was genuine engagement with the research processes throughout. Patient engagement was viewed by the research team as a tool to ensure that the research was relevant, applicable and communicated effectively to the patients whom the study was seeking to engage. The involvement of the PPI team members is described and reflected on in this chapter in the context of the wider literature on patient and public engagement and involvement in the research community. A range of material from discussions, meetings and documents have been collated to provide an overview of the patient contributions to the PREFER study group. Lay members also contributed by writing up their reflections (sent by e-mail) on their contribution to the PREFER study and their experience of the process of involving their views in the research.
Funding application: scoping exercise
User engagement was incorporated from the very early stages of the research, including research question development. Initial informal ‘scoping interviews’ were conducted both with an experienced PPI representative (patient 1, male) and then with eight patients of varying ages, gender and socioeconomic backgrounds attending an NHS dental practice. These discussions highlighted the relevance of the research topic to patients. Patients were interested and concerned about issues to do with communication during dental appointments. It became apparent at this stage that patients had varied reactions to different possible formats of risk information. Patients suggested ways we might engage people from a variety of different socioeconomic backgrounds in the research. A consequence of this was that we increased the time we estimated to gather research data from patients in order to better accommodate patients with low educational backgrounds.
It was during these scoping interviews in the NHS dental practice that one of these patients expressed a particular interest in the research topic and so became part of the research team as a PPI member (patient 2, female) (Figure 13).
FIGURE 13.
Timeline of PPI with sequence of patient group meetings (PG1–PG5). FMS, Faculty of Medical Sciences; rep, representative.
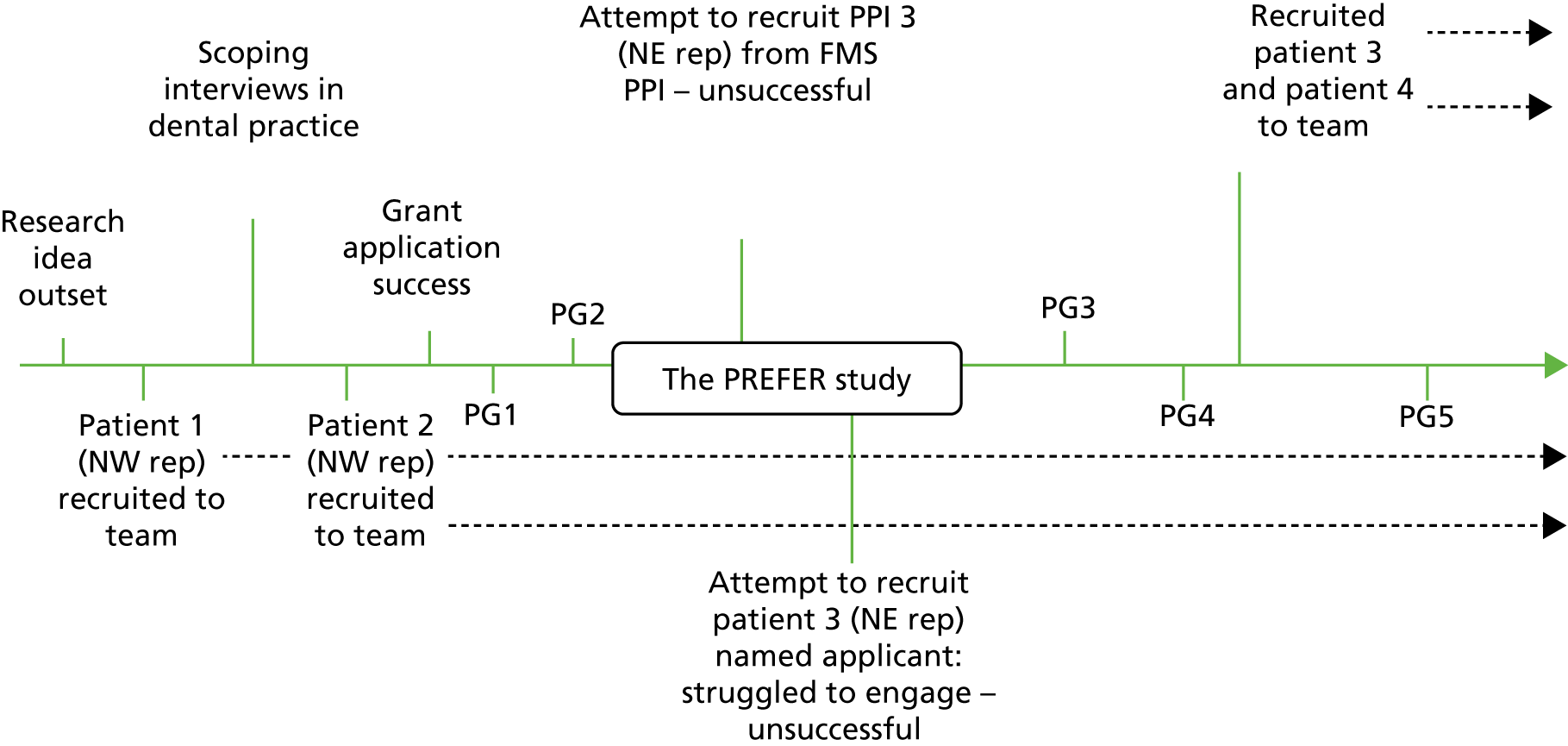
Figure 13 outlines how the first patient member [an experienced patient representative and previous chairperson of HealthWatch (Liverpool, UK) for the area] was joined by three further patient members as the research took shape.
The Patient and Public Involvement Group
The PREFER research team set up a Patient and Public Involvement Group (PG) comprising four people – two from the NW of England and two from the NE, as these were the two research activity localities chosen and we wanted to be representative of these areas. PG members were recruited through either the chief investigator or the co-applicants, following a detailed explanation of the project. In the NE, although we attempted to recruit patient and public members via the Faculty of Medical Sciences Public and Patient Engagement: VOICE North Research Support Group (www.voice-global.org/groups/), this did not come to fruition, which meant that the NE patient and public members joined the research team relatively late in the process. However, several lay people did express an interest when we tried to recruit again and we selected two candidates on the basis of written expressions of interest.
The role and scope of the PG was to review and contribute to developmental decisions surrounding the intervention, the intervention materials, recruitment processes, interpretation of results and the dissemination of findings. From the outset, the research team sought to include the patient representatives as active participants in research decisions rather than as mere observers, looking to move beyond tokenistic representation.
Patient and Public Involvement Group members consisted of three females and one male, all falling within the ‘middle-age’ age group (aged 36–64 years). All PPI members were users of dental services within their localities. Members had varied motivations for wishing to be part of the project, with all members expressing an interest in the project and dental research more broadly. They were all motivated to provide unique insights from a lay perspective:
I think it is essential to have information as clear as possible and a lay person can provide an extra insight into this.
Patient member 3: application statement
‘Bad’ dental experiences or extensive experience of dental treatment were also cited as a motivator for joining the team as a PPI member:
. . . I have had bad experiences with dentists in the past so a project like this gave me the opportunity to have a say about communication practices.
Patient member 4: informal conversation
Patient and Public Involvement Group setting
Five PG meetings were held over the life of the study, one in October 2014 at the start of the project, the second in March 2015, another in February 2016 and October 2016, and the final one in February 2017. All meetings were held at the University of Liverpool. For the most part, PG input was incorporated into the Project Advisory Group (PAG) meetings, with the exception of the final meeting, when an independent PG meeting was held (just with the four patient members) prior to the Project Advisory meeting. All four patient members then joined the PAG meeting.
Patient and public involvement members were also given a PREFER research team contact name, number and e-mail address to facilitate discussion throughout the project. Contact with patient members between meetings was on an ad hoc basis, depending on the stage of the study.
Patient members received reimbursement for their travel expenses plus £75.00 as per INVOLVE recommended rates for each session they attended. 169 During each meeting, detailed minutes were recorded and circulated to each member thereafter, including patient members. Meeting agendas and relevant papers were sent out to all members ahead of each meeting to allow time for preparation.
Patient and public involvement training
The two patient team members who were located in the NW of England attended a PPI training programme provided by Citizen Scientist (www.citizenscientist.org.uk/), a project aimed at linking lay people with research opportunities. Three training sessions took place at Salford Royal NHS Foundation Trust and involved three components:
-
Ethical implications of research – background history, governing bodies, Good Clinical Practice procedures.
-
Applied examples of Good Clinical Practice in research projects and what it means to be a PPI representative.
-
Tools and techniques that lay representatives can employ when working with research teams, including confidence building and stress management techniques.
Feedback about this training was positive, but highlighted that the different PPI members had different training needs:
I found the sessions extremely useful as a new recruit to patient and public involvement and it was also good to meet other patient and public involvement representatives and hear about their projects, so it was a good networking forum.
Patient member 2: training feedback
As an experienced patient and public involvement member I found the training sessions very useful in providing a focus. After attending I felt my approach was more structured and logical. All the sessions were very informative but 1–2 were stronger in their emphasis on involvement by participants.
Patient member 1: training feedback
In addition to general research training tailored to the role of lay people, the research team also provided study-specific training. The two NW England PPI members attended a session where the PREFER research team demonstrated study materials (including QLF camera technology), and described how the study and the technology had been implemented and co-ordinated in the dental practice setting. Following on from this, a further session was arranged with all four PPI team members during which study materials were again demonstrated and discussed with a research team member.
The timing of the two study-specific training sessions was fragmented because of difficulties with PPI recruitment in the NE. Late recruitment of the two NE patient members meant that they missed the generic research training provided by Citizen Scientist. The two NE PPI members were only involved in the second of the study-specific training sessions.
We audio-taped (with permission) discussions in the second of these study-specific training sessions in order to document their views on the study materials, technology and training materials, and to help us reflect on lay involvement in the research. Views were mixed. For example, issues about cost implications were mentioned sporadically. The four patient members expressed varying views about the different forms of information used in the study. They expressed a variety of opposing views about the QLF technology in particular, which emphasised to us the importance of including a variety of different people when incorporating lay views.
Positive opinions
I was really attracted to the photograph because it is so personal . . .
Patient member 3
It’s using technology to the perfect end for me. It sees things that you know your eyesight doesn’t . . .
Patient member 4
Negative opinions
. . . would be loath to have that done . . . I don’t want to see it, I’m one of those people in denial.
Patient member 2
. . . but how much is this all going to cost and can people afford it?
Patient member 1
Traffic light cards were viewed as a way to structure a dialogue, to supplement the information given to the patients by the dentist and as a way to prevent patients being ‘overloaded’ with written information:
The card is useful because it’s small and you’ve got more chance of having a look . . . you get sick to death of reading things on pieces of A4 paper . . .
Patient member 4: study-specific training session 2
I think the key thing for me that I’ve seen progress throughout the trial, is the forcing the dentist to have a dialogue . . .
Patient member 2: study-specific training session 2
Patient team member contributions
Patient and public involvement contributions were especially important during the study materials development phase and prior to any data collection. We were fortunate that the two patient members involved at this stage included an experienced PPI representative who had worked on projects previously in similar roles (and, therefore, understood the research process). The second representative, although new to the role as a patient team member, had a background in marketing and was able to provide advice and insight into the communication methods being tested in this study.
Specific contributions were made to editing the patient information sheets, consent forms and questionnaires in order to make the wording more patient friendly, prior to submission for ethics approval. The WTP part of the questionnaire was particularly challenging, especially trying to present the concept in an easily understandable way for patients. Patient members also advised about whether or not patients would be willing to divulge their household income, and helped the research team weigh up the benefits of including various behaviour-change questions against the downside of adding to participants’ response burden:
One of the most challenging parts . . . was making the WTP section [of the questionnaire] more understandable for the patient.
Patient member 2: reflections e-mail
As a result of my advice, patient questionnaires and data collection forms had their language amended to make them more user-friendly and accessible.
Patient member 1: reflections e-mail
Patient and public involvement contributions also helped shape the design of TL cards used in the study, resulting in a credit card-sized format rather than in an A4 sheet of paper (as is the usual case in NHS dental practices involved in testing the new dental contract model). The development of the TL cards was an iterative process between the patient members and the research team. An early prototype was shown to the patient team to garner their opinions. The feedback received had a direct impact on the design of the cards that were handed out to patients during the study.
The version below was the earliest iteration of the TL card (Figure 14). Patient feedback suggested that the card should be altered in both design and information content. It was felt that this design might stigmatise those who are categorised as red patients in this format (given a ‘red card’ – as in being sent off the pitch in a football match). Suggestions were made to dilute the red colouring. It was also proposed that the cards should carry constructive health information about what to do to change behaviours on the reverse.
FIGURE 14.
First iteration of the TL card.
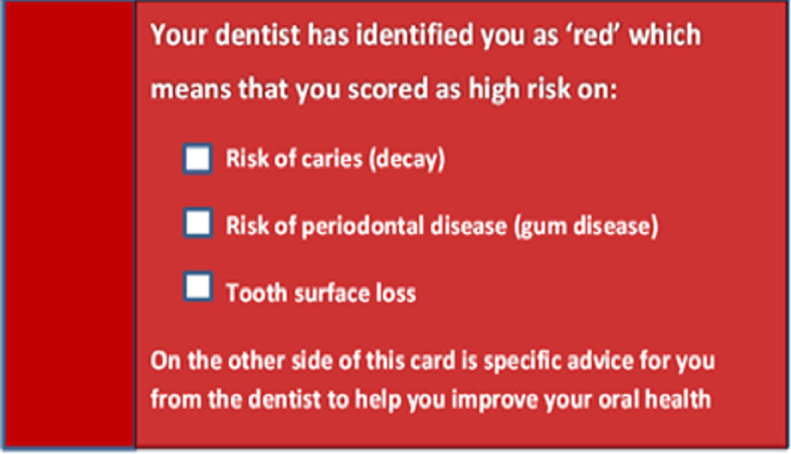
A second iteration is shown below (Figure 15), incorporating the patient comments above. The language was altered to make this more patient friendly, and specific suggestions to enact behaviour change were added to the reverse of the card. Further feedback was sought thereafter.
FIGURE 15.
Second iteration of the TL card.
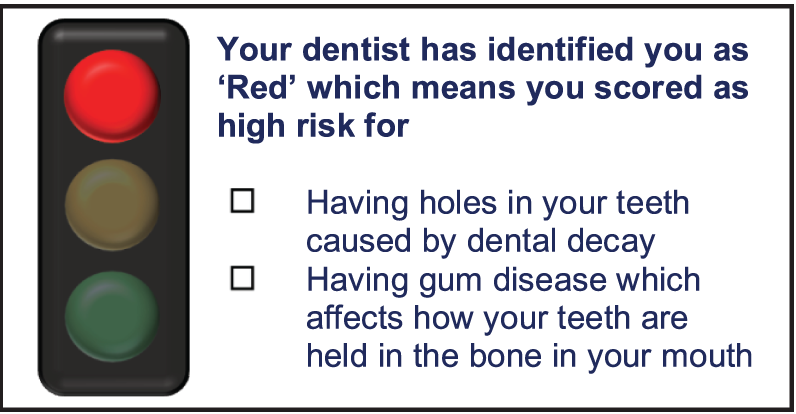
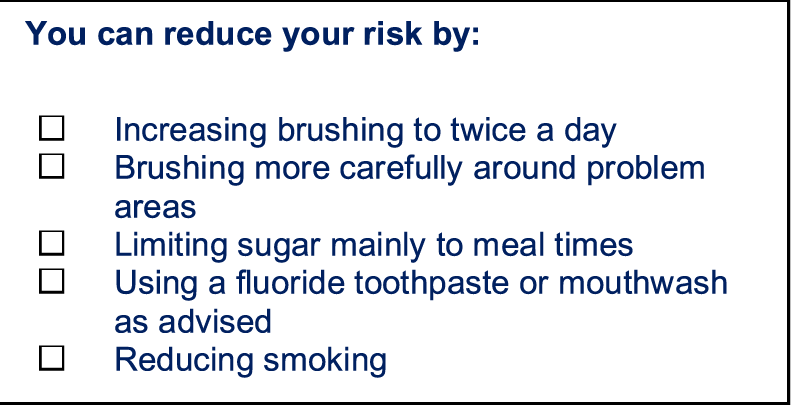
After further patient group feedback, we did some further adjustments to the format of the card, as well as to the wording of the behaviour-change information that would be presented to the patients. The red colouring was reintroduced in a lighter shade of red (see Figure 5).
Patient contributions to Project Advisory Group meetings
In addition to practical advice, throughout the course of the PREFER study development patient members voiced important considerations during PAG meetings:
What are the implications of having a ‘research ready practice’?
Patient member 1
This question prompted the research team to further explore results at the practice level:
At the dental practice, how will the addition of stress, if the patient finds the dental setting a stressful one, impact the ability of the patient to take in the information being given?
Patient member 2
This consideration resulted in a small pilot study being conducted during the development phase of the main trial:
The size of the measures pack is very large and would put me off taking part.
Patient member 2
As a result of this observation, and using input from the study team, the questionnaire pack was redrafted and shortened:
With the WTP task, this could have an impact on the patient’s suspicion of ‘upselling’ in part private practices, and we would need to explore this.
Patient member 2
It was made explicitly clear during the study task that this was a hypothetical scenario only:
People are used to paying for technology and will, therefore, expect to pay for it.
Patient member 1
How much is this additionally going to cost the NHS and the patient?
Patient member 4
Will the delivery of the traffic light card serve to reduce the amount of time the dentist spends speaking with you . . . will it just be a simple: ‘You’re red, the action you should take is written on the card’.
Patient member 2
This comment prompted us to consider this in the qualitative study.
Reflections
Patient reflections on the PREFER study
The following summarise patient members’ views on the research and their part in the process:
I can see the benefits of the three suggested methods and I was pleased to have been given the opportunity to try out the camera . . . Verbal might be ‘in one ear and out the other’ and not much communication going on. Traffic lights might encourage conversation and it’s useful to be given a card, although a ‘red card‘ might be a bit emotive! It’s much better to be made gently aware than to be terrified and not want to go back!
Patient member 3: after Project Advisory Group, by e-mail
. . . dialogue from the clinician is vital to be able to interpret the information given.
Patient member 2: after study-specific training session
I favoured the visual aspect of the photo advice as it could be used as a comparison to any follow-up photos, hopefully showing improvement if needed.
Patient member 4: after Project Advisory Group, by e-mail
For me, it was very interesting to see the work that ended up with the goals at the end – verbal feedback, traffic lights, photos. It’s a very complicated process! A bit like when you watch a film or a play which might only have a few characters that you see, there are hundreds and hundreds of people behind the scenes. It can be a surprise to hear that statisticians, analysts, psychologists are even part of the action!
Patient member 3: after Project Advisory Group, by e-mail
Patient members read the report at the draft stage. They were very engaged and provided some interesting insights:
When I had the opportunity to see (and try) the camera, I thought it was a fantastic piece of equipment but then after reading the report, I could see the pros and cons of all of the options, verbal, QLF, traffic light and understand preferences and difficulties for all of them, also the concerns that patients and dental staff may have. We might only see our face occasionally throughout the day but a photograph can be a constant and perhaps scary and uncomfortable reminder for us. I don’t think anyone likes the thought of a ‘red card’ so perhaps the dentist’s language (and the timing of it) can be very important, and the study also highlights the difference between hearing a message or seeing a message. People are all different and prefer different methods of feedback, one might have a preference of one thing over another, some might take great offence whereas others might take advice on board.
Patient member 3: comment on draft of NIHR final report
I feel that the contributions of PPI members are valued. Many of the reflective points are relevant and should inform future working methods. It would be useful to encourage the members to participate in meetings and invite interventions. I think PPI representatives could network more effectively outside meetings.
Patient member 1: reflections e-mail
From being accepted as a patient and public involvement representative on the project, I feel that I have been involved as a valued member of the team at all stages throughout the study.
Patient member 2: reflections e-mail
We were encouraged to represent the patient at all stages and excellent training (at Salford Royal) was also provided to help us better understand what our role was about and how we could best contribute . . . our contributions were also sought outside meetings as and when required. An example of this is the development of the traffic light cards and particularly on the questionnaires when we were involved in a number of iterations to ensure they were as patient friendly as possible.
Patient member 2: reflections e-mail
The main meeting, I could understand some parts fully, some parts partially and other parts were very complicated to me and I’m not sure how much sank in! Possibly a minimal amount.
Patient member 3: reflections e-mail
There was so much detail in the report, even covering the origins of the word ‘risk’, so fascinating. Even from the start, the report takes us back thousands of years . . .
I have experienced a rollercoaster of a read. Lots of surprises (perhaps) along the way. Thoughts from dental practice staff and patients were quite varied and made very interesting reading. I really enjoyed reading the interviews!
It must be impossible to gauge people’s thoughts and why they make certain decisions. Willingness to pay was an eye-opener and must be so difficult to explain, never mind write about in an understandable way . . .
Every option covered which must have been an enormous task. It makes me wonder how life has got this complicated! And . . . exciting to see my name in the report!
Patient member 3: comment on draft of NIHR final report
Patient reflections highlighted the need for PPI right from the start of the research process, as early as the idea planning stage, and certainly during the funding application stage. The PREFER study struggled to recruit the full patient team until closer to the end of the project, meaning that two of the members were not given the opportunity to contribute to the early stages of the project’s development:
The request for funding stage gave an excellent overview of the scope and aims of the project and I would recommend that this is a vital stage for PPIs [patient and public involvement representatives] to be involved in all projects.
Patient member 2: reflections e-mail
Patient and public involvement members’ reflections gave some useful suggestions as to how we might improve PPI input in future studies:
I believe that in future projects there may be opportunities to get the PPIs [representatives] more involved. One opportunity we missed in my view was to use us in the patient recruitment stage, representing the project to the patients and this would also have provided a bit more support and visibility to the dental practice.
I would also recommend that future projects consider circulating a monthly highlight report, just to keep in touch and keep the PPIs in the loop between project meetings.
I also think PPIs need to remember that they have a responsibility to represent the project to a wider patient community and I think that there is much more that I could have done to meet this responsibility.
Patient member 2: reflections e-mail
The PREFER research team reflections on patient and public involvement
Throughout the study, the research team sought to make PPI as genuine as possible and were keen that lay members took as active a role as possible. The research team had particular problems with recruiting patient members in the NE at the outset of the study. Although at the early stages of the study, a lay representative from NE England expressed an interest in being part of the team, we struggled to make contact and form an active collaboration, possibly because of the distance of their home from the main research site. This meant that patient input was not as diverse as we would have liked at the start of the project, which had implications with regard to balancing patient voice against patient representativeness.
Balancing ‘experience’ versus ‘patient representation’170 was a consideration when drawing together the PPI team. An important motivating factor when volunteering to act as a patient member is having personal experience of the topic and the empowerment that this knowledge provides (i.e. a service user, having experienced a specific disease type). 170 We recruited one patient member directly from an NHS dental practice waiting room because she expressed an interest in the research topic from an ‘experience driven’ perspective. We encountered greater difficulties recruiting patient members from existing networks of patient representatives, and so found incorporating patient representation more of a challenge. Given that our four patient members expressed diverse views regarding the three information forms tested, we were glad that we had persisted in our efforts to build a wider pool of patient members to inform the research.
Reflections from the patient members about their involvement in the research have been useful. In hindsight, we agree that the patient members may have contributed even more, especially by representing the project to a wider patient community and by raising awareness of the project among patients at the recruitment stage. On the other hand, the dissemination phase for this report is approaching and we anticipate that the patient members will be very involved in this, especially in the public-facing aspects.
In summary, the PREFER study team view its partnership with patient members as a success, particularly considering the specific contributions made to the research by the patient members, the design of the TL cards (which were used as an intervention arm), the content of the questionnaires (which were used to gather patient data) and the patient-driven discussions during project meetings, which informed the analysis, interpretation and reporting of results. We look forward to working further with the patient team in our dissemination work.
Chapter 7 Discussion and summary
Summary of key findings
Patients prefer traffic light information the least
It would appear from both direction (i.e. rankings) and strength of preference (i.e. WTP values) data that verbal information is preferred most, followed by QLF photos and TL last. This was also robust across sensitivity analyses. This is an interesting finding because the QLF and TL interventions explicitly stated that this included verbal advice (in other words, the interventions were verbal, verbal plus QLF and verbal plus TL). It is particularly surprising in this context that median WTP for verbal plus TL was half of that for verbal alone, whereas, logically, an increase in value would be expected when an additional intervention is offered. One possible explanation is that participants assumed that the addition of the TL card would diminish the quality or quantity of verbal information and that this was especially valued.
This would fit with the findings from the qualitative work: observations in a new contract prototype practice (practice 5) using TL categorisation of patients, found that the TL system did not increase discussions about risk. In some cases, it reduced discussions. Interviews with patients and dental staff regarding the TL cards indicated that patients were mostly fairly ambivalent (although in some cases patients felt TLs were an oversimplification of factors affecting their oral health, and some reacted badly against being categorised, some others appreciated being given as much information as possible, with TL information seen as a further adjunct).
On the other hand, patients and the dental team identified that the benefits of both TL and QLF as adjuncts to verbal information on risk may be in providing a basis on which to measure and reflect on progress/improvement in oral health. This is more of a longer-term prospect than the way these tools were used in this study (even though we followed patients up 6 and 12 months later). Revisiting risk status at a subsequent check-up appointment and looking back on progress (or lack of) was seen as potentially motivating for patients.
Variation by sociodemographic characteristics
The findings relating to the predictors of both the direction and strength of preference in our WTP work reflect the fact that neither are particularly predictable. Models had generally low levels of fit and few significant predictors. It also appeared that the younger patients were less likely to prefer verbal alone and the older patients were more likely to prefer verbal alone, which was an expected finding. It is interesting to reflect that the qualitative work showed that dentists appear to use visual methods more often with young people, as well as more direct language in these interactions, perhaps because they are less concerned about being confrontational or perhaps because younger people are less able to contribute to the discourse on equal terms, and the visual material acts as some sort of support when the verbal communication is a bit weak.
In terms of the influence of sociodemographic factors on WTP values, determined through regression analyses, it was surprising that income did not affect WTP more, although the amounts being elicited were relatively small, and this is not unusual for WTP studies. A recent review of WTP studies in dentistry summarised the factors affecting WTP and found that gender, education and age were only influential in a very small number of the studies, with income being the only factor found to affect WTP in a majority of studies. 106
We did, however, find that WTP was influenced by area deprivation for verbal and QLF information in particular (high IMD increased WTP for verbal but actually decreased WTP for QLF). Given that income is controlled for, what this may indicate is that the value of information may be lower in general for more deprived populations, and that there is something, such as the power relationship between patients and the dental team in deprived areas, which is not captured by other sociodemographic indicators such as income and education. The potential shame and embarrassment aspect of QLF images may explain the reduced WTP for QLF in high IMD areas. That WTP for TL was influenced by education (higher WTP with low education) is in line with our qualitative findings, which identify that TL information is perceived as being a particularly simple way of giving information.
Our study is not unusual in finding that WTP is generally unpredictable, which may be because WTP is not picking up genuine differences in valuation, or that values genuinely are very much determined by the individual. Assuming that the latter is true, the implications are that it is difficult to target different forms of information to different groups and that it actually may be better to have different options made available for all patients and to allow them to choose.
Given the fact that WTP was highest for verbal, and this was also the least costly intervention, it is obvious that this intervention would give the highest net social benefit in the immediate time frame. The intervention with the highest net social benefit over the longer term may be different, but for this to be the case there would need to be a difference in preventative effect (i.e. oral health promoting behaviour change) between the interventions, which could in turn save longer-term disease treatment costs. In the absence of any data to support this, the economic case shown here favours verbal information only.
There was little evidence of reported behaviour change
There was little evidence for behaviour change, except a reduction in consumption of sugar in drinks between baseline and 6 months, which was also seen at 12 months, and a slightly longer duration of toothbrushing among those followed up for 12 months (see Table 15). These changes did not differ by intervention group. This may either be a cohort effect, which reflects a growing awareness of the potential harms related to sugar consumption in the population in general, or the result of dietary information given by dentists at the check-up. There is virtually no evidence available on the impact of one-to-one dietary messages given in dental practice settings,171 and so this is an interesting finding irrespective of the fact that there was no intervention effect. The finding that brushing duration was also slightly increased suggests that it may be an effect of dental practice visiting.
The EPPM was used as a mediator variable because it conceptualises risk in both cognitive and emotional terms. Additionally, the EPPM proposes a specific mechanism by which people may engage defensive responses to risk-based messages that they find threatening. Although no 6- or 12-month effects were detected for behavioural change, we tested the proposal that intervention group effects may have differential effects on behavioural intentions, perceived likelihood, severity of potential negative consequences of poor oral care, and patients’ emotional responses to these. Although not directly related to a risk perception intervention, we also examined self-efficacy, confidence and response efficacy.
No effects of the intervention were found on any EPPM variable measured directly after the intervention. We did not assess effects on 6- or 12-month EPPM variables, as these are unlikely to change if the intervention does not have immediate effects. Owing to the failure of intervention group membership to influence EPPM variables, we conclude that the TL and the QLF interventions failed to change behaviour because they do not alter cognitive or emotional responses to risk.
Unlike Shahab et al. ,95 we, therefore, did not examine an interaction between the effects of intervention group membership and self-efficacy on intention or risk-related variables. This is because self-efficacy was measured after the intervention and thus cannot function as a moderating variable.
Although limited QLF clinical outcome was available, our sensitivity analysis in practice 2 (see Chapter 4, Plaque coverage outcome data analysis for practice 2 only) showed a significant reduction in plaque in the QLF arm. When compared with self-reports of toothbrushing behaviour however (see Chapter 4, Plaque coverage and self-reported toothbrushing behaviour), we did not find an expected association; indicating that either the self-reported behaviour items are subject to recall bias and are not sensitive enough to pick up true changes in behaviour or that the QLF measurement of plaque captures a different aspect of oral health (relatively mature plaque).
It is interesting to note that Han et al. 172 were only able to demonstrate a moderate correlation (r = 0.5; p < 0.01) with two conventional plaque indices (Turesky-modified Quigley–Hein and the Silness–Löe Index), collected by clinical assessment. This rather low correlation was attributed to the fact that the QLF-based planimetric method used undisclosed plaque and only detected mature plaque using red autofluorescence, as in our study.
There was some reduction in plaque coverage in the quantitative light-induced fluorescence arm in practice 2
In the complete data set, on average approximately 3.5% of patients’ anterior teeth were covered with red fluorescing dental plaque at baseline at a threshold of ΔR30, with a range of 2.4% to 4.3% for those patients at follow-up visits, with no statistically significant overall effect of group allocation (p = 0.381) for verbal, TL and QLF information. The degree of area of red fluorescent plaque coverage correlates well with previous studies involving QLF technology,172 reporting a mean plaque to area coverage of 5.4% at a lower threshold of ΔR20. Delta R (%) is the percentage increase of the ratio of the red and green component with respect to that of sound tooth tissue. It is related to the presence of porphyrins and is indirectly related to bacterial activity in and around the tooth.
Because 70% of the available data for plaque analysis came from practice 2, we did a separate analysis using data from this practice only (see Table 20). We found a significant difference for the percentage of plaque coverage at a threshold of ΔR30 between the verbal and QLF group, using a pairwise post hoc analysis. Although there was a 31% reduction (from 4.2% at baseline to 2.9%) in the QLF group at follow-up, which was based on an average of 3 weeks after the initial baseline visit, compared with the verbal only group, which had 3.8% plaque coverage at follow-up, this represents an intervention effect of about 24%. It is debatable whether or not this represents a clinically significant finding.
Patients and dentists do not generally talk about ‘risk’
Our qualitative work found that despite routine dental check-ups being a risk context, there is very little explicit risk talk between dentists and patients. This held true even in the NHS’s new dental contract practice context, in which a TL system was used. There was so little explicit risk talk across all appointments that we concluded that risk is not part of the normal discourse between dental staff and patients. Instead, we suggest that risk is part of a professional discourse, given its prominence in relevant policy and among staff, rather than a clinical one.
In clinical encounters dental staff were seen to communicate risk messages implicitly, for example by using metaphors. Although issues about the likelihood of developing adverse outcomes over time were featured in dental appointments; dentists were often observed asking patients to offer explanations of past behaviour to explain current symptoms, as well as evoking a threatening future should action not be taken in the present. Conjuring fear about the future appears to be the way dentists try to make risk feel more immediate and ‘real’ to their patients. In dentistry, patients may often present with asymptomatic problems. Therefore, there is the possibility that a patient may reject a dentist’s diagnosis or delay treatments if the risk is felt to be distant or unreal.
Face-threatening aspects of giving information on risk
A key issue about giving information on ‘risk’ is whether or not the information can be conveyed to motivate just enough, while at the same time avoiding talk which offends, shames and disrupts the relationship between the dentist and patient. This relates to what Goffman refers to as ‘face-work’. 81 He proposes that in interactions people try to avoid situations that could lead to shame or embarrassment. In other words, people use strategies to ‘save face’. As Linell et al. 73 note, lifestyle issues are ‘threatening to personal integrity and therefore interactionally sensitive’. There are several studies in a range of settings that show that health professionals often try and behave politely and civilly with patients, regardless of their personal feelings. 148 During interaction, these health professionals try and save patient’s feelings and allow patients to do face-saving work, such as excuse, repair or apologise. 162 This shows that professionals would rather deliver messages in a less confrontational way or avoid them altogether than risk the patient leaving after being offended. In interviews, dental staff acknowledged that talk about lifestyle could be tricky, especially around smoking. Often dentists turned to delivering rehearsed statements about smoking status and sugar intake to patients, which enabled them to tick the box without getting into uncomfortable discussions. Dentists explained that if they gave general information about the risks to everyone, then no one would feel targeted and offended; however, our findings show that what patients really want is detailed, personal, verbal advice, which is a difficult balance to achieve.
Because of the broad categories used in TL categorisation, many patients reported that they expected to be able to anticipate their risk category and, therefore, the information was considered only minimally face-threatening (although, at the same time, it also generally generated ambivalent feelings). By contrast, patients felt unable to anticipate the results of QLF images, were much more anxious about them and considered them potentially more acutely face-threatening. Anxieties about having a photograph taken, then, reflect uncertainty about the outcomes. Looking at the photograph itself can become less threatening when the dentist gives detailed information about the patient’s health. Patients reported QLF photographs as having the potential to add value to their dental experiences. Conversely, the biggest barrier from dentists was this extra time.
Variation between practices in preferences and trial implementation
It is noticeable that the different practices were significant influences on the direction and strength of preference, even after accounting for the other patient-level demographic variables. It is also interesting that WTP was generally higher in practice 2, despite controlling for all factors in the regression analysis (see Appendix 2, Table 30). The odds ratio for the preference of verbal information only was also especially high in this practice (see Appendix 2, Table 27). This may reflect a different ethos at the practice influencing the patients who attend it or, on the other hand, because patients who particularly value this information select that practice. It is notable, however, that practice 2 also stands out as the practice with by far the highest proportion of short-term follow-up images, with high numbers (89%) of people returning for follow-up visits (see Table 18). Practice 2 was an almost fully NHS practice working in a very deprived area (see Table 3). The dental team in practice 2 was small compared with the others but included the principal dentist, unlike practice 4, which was one of a number of practices within a group. It is possible that both the successful way the trial was implemented and the degree to which patients valued information about their oral health was down to the effective communication skills and clinical leadership demonstrated by the principal dentist in the practice.
In some practices there was a particularly high turnover of staff, such as in practice 1, where a practice manager, two dental nurses and three dentists left over the trial period. Although we undertook additional trial training sessions to address this, it is possible that the staff turnover is a barometer of staff morale in the practice, which may have had an impact on staff motivation to be involved in the study and adhere fully to study protocols. Staff turnover may have also disrupted the forming of relationships between patients and dentists, which in turn was associated with patients expressing a relatively low preference for verbal information compared with the other practices.
The trial was funded as a pragmatic trial with researchers directed to recruit practices to the trial (by invitation to participate) randomly selected from a list of NHS dental practices for the area. This meant that our participating practices, although arguably relatively representative of NHS dental practices, were mostly relatively inexperienced in participation in research (including clinical trials). This made issues such as optimising fidelity and retention challenging.
Although strategies were put in place to strengthen the fidelity of the trial, the pragmatic nature of the research added an element of difficulty in achieving this. The use of study protocols, crib sheets, step-by-step patient flow diagrams, training videos, standardised algorithms, group standardised training, regular site visits and refresher training sessions were all attempts to increase fidelity levels within the trial. The use of such measures is a recommended strategy that improves fidelity in studies;173 however, research suggests that the higher the complexity of the study being implemented, the lower the levels of fidelity maintained. 174 As this was a pragmatic trial being implemented in busy dental practices with clinical teams delivering the intervention to patients, fidelity monitoring was difficult to achieve. We did not, for example, undertake any observations as to the extent to which dentists complied with verbal advice covering the meaning of the RAG categorisation and oral health behaviours as recommended by the dentist to address any issues. Our findings indicate that practice-based effects may have been important in relation to information-giving for patients because differences between practices appeared to transcend the sociodemographics of the patient populations concerned. This is an important area in which further research is warranted.
Using quantitative light-induced fluorescence technology to measure clinical outcomes was challenging
This was the first time that QLF technology had been used to measure clinical outcomes in a trial situated in dental practices. During the initial pilot testing and training of staff in one of the dental practices selected for the study, it became apparent that the QLF-D system was too complicated and time-consuming for this setting. Consequently, the sophisticated QLF-D camera was replaced with a new, simplified clinical diagnostic system called Q-Ray, which is lighter, easier to operate and easier to clean for cross-infection control. We also introduced retractors to improve the quality of photographs. However, a proportion of images were still lost from the data set because they were of poor quality (e.g. out of focus, upper teeth covering lower arch, taken too far away from patient’s mouth, lower lip obscuring lower teeth, excessive ambient light, lip retractor obscuring lower teeth), which added to the problems with retention caused by patients’ lack of attendance at follow-up appointments.
Use of QLF images for caries analysis relied on the patient brushing their teeth after the first photograph to remove any plaque covering the teeth, and then having a second image taken. This significantly added to the complexity of implementing the trial in dental practice (patients had to go to a bathroom to brush their teeth, then return), which meant that we were only able to get relatively few second photographs, even in practice 2.
The cables linking the laptop computer and camera (see Figure 7) meant that the equipment was inconvenient to use in the confined space of a dental practice. The equipment also proved to be unreliable at times, meaning that additional support was required for practices (see Table 4) despite a troubleshooting guide being provided. This added to the logistical issues needing to be addressed when implementing the trial. It is noticeable that in practice 2, where the most complete QLF data were obtained, there were no requests for support to address camera equipment failure. Given the already complex nature of the trial, equipment failure may have caused some dental teams to become disillusioned with taking QLF photographs as part of the trial, contributing to problems with missing data. Possibly both the very high turnover of staff in practice 1 alongside five requests for support regarding camera failures contributed to a particularly low proportion (61%) of good-quality baseline QLF images being taken in this practice.
Although data from practice 2, which adopted the technology most successfully, provided some interesting findings with respect to changes in plaque coverage, further development of the technology is needed before it can have wider application measuring clinical outcomes in primary dental care research.
Strengths and limitations
Generalisability of the population
The inclusion criteria involved adults with high/medium risk of poor oral health, with most of our recruitment sites in very deprived areas. We would, therefore, expect the sociodemographics of our sample to reflect this. The highest education attainment in our population sample (see Table 6) is slightly lower than national figures for the UK, with fewer people (31%) being educated to degree level or above (national figure is 38%). 175 Table 16 summarises oral health behaviours at baseline and indicates that our participants were generally from more disadvantaged backgrounds with generally less healthy behaviours than the UK average. Baseline smoking prevalence (18%) for the sample was slightly higher in the study population than the national prevalence rate of 16%. 176 However, smoking prevalence in the regions from which the sample was drawn is 20.3%, 17.6% and 17.9% (NE and NW of England). 177 The 72% of participants reporting twice-daily toothbrushing is also slightly lower than the 75% average for Great Britain. 178
A total of 60% of our sample at baseline was made up of women, which is more than the national average population figure of 51%. 179 Therefore, this sample underrepresents men, and possibly reflects other findings, such as that women are more likely to volunteer to take part in clinical research than men. 180 Other dental studies show an even higher proportion of female participants than in our study. 181,182
Only 45% of participants who were randomised to receive the intervention completed follow-up data collection at 6 months and even fewer (37%) were retained at visit 2 or 3; the short-term follow-up during which clinical data, including QLF data, were collected can be seen in Table 6. That most of the participants were those with high/medium risk of poor oral health will have contributed to problems with retention. The trial did not include any monetary incentives for recruitment, although a prize draw was introduced in the later stages in an attempt to boost retention at 6 and 12 months. A recent non-randomised study in six NHS dental practices,103 which compared a new model involving a TL risk assessment of patients with other practices using the previous model of dental practice care, retained only 291 out of 550 (53%) participants recruited at baseline who attended follow-up appointments; this shows how challenging retention in this type of study can be.
Loss to follow-up and other factors leading to missing data have implications when reporting results in RCTs. 183 This has implications because of possible bias that can limit generalisability and the internal validity of results. 184 Therefore, we undertook an attrition bias analysis (see Chapter 4, Attrition bias). This showed that although there was no overall significant bias in sociodemographics, proportionally fewer participants from low-IMD areas and those with higher baseline sugar intake were retained at 6 and 12 months (see Table 14).
Interpretation of willingness-to-pay data
Willingness to pay is a common technique for eliciting public valuations (i.e. preferences) when valuations cannot be truly determined from consumer interactions (as might be possible in a perfect market) because the ‘good’ in question is either free at the point of consumption or subsidised in either a state-funded or private insurance-based system. The theoretical basis for contingent valuation is that preferences are measured in terms of utility; wherein the greater someone’s preference, the greater the utility gained from consuming the good. As utility cannot be measured directly, it is measured using a proxy in terms of what would be sacrificed to gain this. In contingent valuation, the sacrifice is measured in monetary terms, such that the more money someone is willing to sacrifice for something, the more utility they would gain from consuming it. Interpreting the median WTP values (see Table 10) in this light shows that the utility gained from verbal information only is double that of TL in this sample.
However, this is likely to be an oversimplification, as those who have more money available to them will, in theory, gain less utility from each additional pound (diminishing marginal returns). 185 Therefore, those with more money will, in theory, give higher WTP values for the same utility level as someone with less money. However, in this study it seems that income has little effect on WTP, as the three Tobit analyses (see Table 11) show no effect of low or high income with the exception of high income for QLF, although even for QLF the effect is weak. This may be because the income measure used here may not reflect the amount of available income (personal disposable income would be a better measure, but is very difficult for respondents to enumerate), or it may be that there are confounders hiding the effect of income that were not included in the regression analyses.
In addition to comparing the relative size of WTP across interventions, the absolute values are also useful, but are more open to bias, as they will change depending on the representativeness of the sample drawn, whereas this may be less of a problem for relative values. Typically, the absolute values are of most use in undertaking a cost–benefit analysis in which the WTP represents the benefit from which the costs can then be taken away to determine if there is a net social benefit for each intervention in turn, and also to determine which intervention has the greatest net social benefit. 186 In our study it became unnecessary to undertake a formal cost–benefit analysis, as the cheapest option of current practice was the most valued. The values obtained could be compared with the basic costs calculated in Chapter 4, Trial results: micro-costings (in which case it would appear that all interventions give a net social benefit, with verbal being highest), but this would be an oversimplification, as the time frames involved in the benefit and cost side may not be the same and they have not been standardised through a full cost–benefit analysis.
Aside from the link between the ability to pay (income) and WTP, other criticisms have been levelled at WTP in terms of its hypothetical nature and both its internal and external anchoring effects. An individual’s WTP may be influenced either by the elicitation method or external cues, such as the price of similar goods. 187 Looking at the hypothetical question, this study offered an interesting opportunity to investigate the stability of WTP values when moving from a truly hypothetical scenario to actually having experienced the intervention. The numbers were smaller for this aspect of the study, as each arm could only be investigated separately, but what is common to all three arms is that there were a significant number of patients in each of the three categories who increased valuations, decreased valuations and stayed the same. Although this experiment is not the same as the much sought after comparisons of stated and revealed preference (i.e. a WTP survey followed by an actual request for real payment), it does bear some similarities to this and the results match those of the only comparison of stated and revealed preference in dentistry;188 wherein individuals were found who increased, decreased and remained constant in terms of valuations to payments. Those who changed their valuations may have done so for at least three different reasons. First, the scenario may not have been sufficiently detailed to allow individuals to value the intervention properly; second, the actual delivery of the intervention may not have matched the intervention described (i.e. a perfect example of the intervention is described, but the reality may not be a perfect delivery of the intervention); and, third, the instrument used may not be sufficiently reliable in determining values. Without further investigation, it is difficult to know which of these is true.
Turning next to anchoring effects introduced as a result of the method, this study used a bidding method most likely to introduce the fewest problems in this respect. 118,120 The starting value and the range of values asked about are the two biggest potential internal influences on values, and the shuffled payment card method employed here means that many different starting values are used across the sample, and also that participants are unaware of the range of values until the end of the exercise. In terms of external anchoring effects, perhaps the key similar ‘good’ would be the out-of-pocket price (£X) of a NHS check-up in England at the time of the study. Although the determination of risk and communicating it is only one item that is included within the check-up fee, it is noticeable that the values do cluster around this figure and so the influence of this as an anchor for values cannot be excluded.
Finally, it is useful to explore the treatment of zero values in some more detail. Early WTP studies made the assumption that all respondents would place some value on any good. However, this was later agreed to be unlikely, as some people may not value a good at all (i.e. they would gain no utility) and so zero responses became acceptable. Once zero responses were allowed, it became apparent that some responders, although they did value the good, did not wish to engage with the WTP exercise as a way of eliciting this value and so gave it a zero value. To use this zero value in analysis would not be correct, as it is simply the case that the survey has been unable to reveal the actual value that the responder places on the goods. The accepted response to this problem has been to ask the zero responders follow-up questions to differentiate true zeros from protest zeros; follow-up questions (for those with zero valuations) with various sets of multiple choice responses have been used. 189 This is the approach adopted in this study, with the follow-up question based on that of Ryan et al. 120 However, there has been little testing of this approach to differentiating zero responses and concerns have also been raised that certain demographic sections may be more likely to protest, leading to a sample selection bias. 190 The aim of this study was not to improve the differentiation of protests or to validate the questions used for this; without the possibility of interviewing each respondent, a task not possible within the limitations of resource for this study, best practice was followed. In terms of potential sample selection bias, it appears that the protestors and non-protestors were very similar and so is not a great concern for this study.
Use of quantitative light-induced fluorescence technology to measure clinical outcomes
Dental plaque indices have been used by clinicians for decades to provide information regarding the presence of plaque surface coverage and thickness, with or without the use of disclosing agents or dyes. 191–194 There are strong correlations between plaque index scores and gingival inflammation at group, individual and tooth surface level. 195,196 These methods have a degree of subjectivity and require extensive training and examiner calibration in order to reach an acceptable level of reliability. There has also been criticism of the use of plaque indices relating, in particular, to their resolution, for example with the Quigley–Hein plaque index: it can be possible for the plaque level on the tooth to decrease by 50% but be scored at the same level. 70 Because of the limitations of the traditional indices, planimetric methods have also been developed. Planimetric analysis of plaque is a technique that uses photographic images and can utilise a plaque per cent index. 197
In recent years, particularly with the availability of digital imaging technology, planimetric methods have been developed to provide faster, more objective and more sensitive measurements of plaque accumulation. 198 The early planimetric methods that used the plaque per cent index also required the use of disclosing agents or dyes prior to photographing the tooth surfaces and analysing the images by computer. This permitted greater resolution in plaque quantification and gave more reliability,199 greater objectivity,198,200 greater sensitivity198,199 and better precision than traditional plaque indices. 200 A finding, initially reported by Amaechi and Higham201 when they were investigating optimal conditions for the use of QLF, was that heavy plaque deposits on teeth fluoresced red or orange. This has since been developed to allow the detection and quantification of mature dental plaque on teeth with the use of disclosing agents to measure total plaque presence,70 or with a non-disclosing approach wherein only mature dental plaque is detected due to red fluorescence under the lighting conditions used to illuminate the dental plaque. 172,202
It has been reported that around two-thirds of red fluorescent dental plaque is located at the gingival area in the so-called stagnation sites where plaque is initially formed. 202 Although studies show that plaque is formed fairly symmetrically, the buccal (the lip side) of upper incisor teeth is likely to accumulate the least plaque and the cheek side of lower (buccal mandibular) molars, as well as the tongue side of the lower premolar region (lingual mandibular), is likely to accumulate the most. 203 However, the lip (labial) side of lower incisors tends to accumulate almost as much plaque as the lower molars. 203 Consequently, many researchers use buccal plaque as a measure of plaque control (e.g. Needleman et al. 204).
We limited our QLF images to buccal views taken of anterior teeth and, although correlated with overall plaque levels in the mouth, this may have underestimated the extent of plaque in some areas of the mouth more prone to accumulation. It is possible to take QLF images of the lingual/palatal side of teeth and images of teeth further back in the mouth, but this would have required the use of mirrors and additional time and expertise in a trial that was already quite complex. The pilot work indicated that the dental teams would find the taking of QLF images challenging and relatively time-consuming and this led to the decision to reduce the number of QLF images taken for the purposes of measuring clinical outcomes.
Likewise, QLF technology provided an alternative to clinical epidemiological examinations to measure the prevalence of caries. With the naked eye it would be difficult to detect mineral loss in this time because decay has to be fairly well advanced (at least 15% of mineral lost) before it can be seen by eye, usually as a white spot on the tooth. QLF extends detection of tooth mineral loss from 15% down to 0%. Brochner et al.,205 using QLF, found significant regression of white spot lesions within 4 weeks in orthodontic patients after preventative care. Many other studies report similar findings.
Sensitivity, in this context, is the ability to correctly identify the presence of carious disease (true positive), whereas specificity is the ability of QLF to correctly identify those without the disease (true negative). Studies put QLF sensitivity as ranging between 0.62 and 0.74 and specificity as ranging from 0.86 to 1.0. 206–208 Thus, QLF has a higher specificity than sensitivity (i.e. it is better able to identify teeth without carious disease). Sensitivity is lower because QLF cannot differentiate between caries and other reasons for mineral loss, such as fluorosis. Other factors (e.g. extrinsic and intrinsic staining) and developmental defects (e.g. hypomineralisation) can also give a similar appearance to caries on fluorescent images. 209,210 During in vitro studies such confounding factors can be avoided by carefully selecting the teeth to be used in the study; however, in the uncontrolled world of a pragmatic trial (e.g. this study), these confounding factors may have had an impact on the sensitivity of the QLF caries diagnosis and should be recognised as a study limitation.
A further limitation in the use of QLF in a study to measure caries incidence is caused by a pragmatic decision to limit QLF photographs to anterior buccal views only. Although a more in-depth data collection could have involved taking photographs of the occlusal (biting) and lingual/palatal (the tongue/palate side of teeth) surfaces, we did not ask the dental teams to take these additional images. We were conscious that this would have been overly demanding in the busy world of an NHS dental practice. Because the teeth most susceptible to dental caries are the occlusal fissures of the first molars (along with pits on buccal surfaces),211 it is likely that limiting QLF images for caries diagnosis to anterior buccal views only would have tended to underestimate participants’ caries incidence.
Use of the basic periodontal examination score as a secondary outcome measure
A periodontal index would have been the best indicator of improved periodontal health for patients. However, our study was not intended to be a Phase III clinical trial, and the primary outcome was not a clinical measure of periodontal disease. It was difficult to justify the costs and complication of using clinical examiners to assess any improvements in clinical outcomes using conventional epidemiological approaches. Given that a BPE is familiar to dental practitioners and is a routine part of their practice (> 91% of dentists use a BPE with new patients),212 we took a pragmatic approach and used the change in BPE scores to indicate improvement in periodontal health and recognising its deficiencies as a clinical outcome measure. Because dental practitioners were required to record a periodontal score at both baseline and follow-up visits (up to 3 months post intervention), we felt that asking practitioners to undertake a full periodontal outcome measurement may have resulted in too many missing data, hence our reliance on BPE score data. However, we acknowledge that BPE scores may be insufficiently sensitive to detect changes in periodontal health over a few weeks because of BPE’s sextant scoring methods.
On the other hand, although we acknowledge that BPE scores are relatively crude in an epidemiological sense, because recording BPE score is mandatory for dental practices working under the new NHS dental contract pilot arrangements it does have its benefits as a pragmatic measurement for which there is some precedent. A BPE has been used previously as an indicator of oral health outcomes when evaluating the new NHS dental contract arrangements. 213 That and a comparison of change in BPE scores between the oral health assessment appointment and the oral health review appointment, aligned with other indicators, gave us some confidence to think that BPE score may have potential as a useful indicator of change in oral health. 213
Like the NHS Dental Contract Pilots: Learning After First Two Years of Piloting213 evaluation work, we also did not include a calibration of BPE score measurement as part of our study training. This was decided because it proved difficult for teams to set aside time for dental team research training, given that their main priority was delivering their NHS contractual targets, even though financial reimbursement for research training was available. Training sessions with dental teams were often undertaken during the lunch hour, which meant that other aspects of training needed to be prioritised. Although in the national study the number of practitioners involved may have mitigated the impact of interexaminer variability, we acknowledge that using BPE measurements as a pragmatic tool, without prior training and calibration, in just four dental practices, is a limitation. Nevertheless, the RCT design, based on individual patient randomisation, means that measurement bias would have been equally distributed between all three arms.
Qualitative work
There are very few qualitative studies that have looked at interactions in the dental setting,126,129 and none that have looked at the area of risk communication. Although our study provided a wealth of material, with over 368 observations of dental appointments, together with interviews of staff and patients, data were collected in just five dental practices. Although this provides a more ‘real-life’ portrayal of practice because those observed are more likely to forget that they are being observed, it means that it is possible that other practices, clinicians and patients elsewhere may behave differently.
We included a fifth dental practice in the qualitative work that was part of the new contract prototype practice model being tested, to ensure that when considering ‘risk communication’ environments were not significantly different in practices using the future model of dental contracting. Although data were collected in only one such practice and, therefore, may not be widely generalisable to other practices, it was important to identify that ‘risk talk’ was still very limited under the new dental contract arrangements.
It should also be noted that, in setting up the study, we encouraged dentists to deliver oral health advice and risk information to patients in the review part of the appointment, after the check-up, to ensure that there is space for discussion. In usual practice, as reflected in the ethnographic work (see Chapter 5), given fewer prompts as part of the study (even the verbal arm had a check-list card of advice topics), there may have been even fewer attempts by dentists to deliver messages on oral health risk to patients.
Implications for practice
Implications for NHS dental practice
-
Everyday practice of risk communication in NHS dental practice is very far from what is recommended in guidelines.
-
Given that NHS dental guidance documents suggest that patients should be given personalised information in order to play their part in improving and maintaining their own oral health,104 we would expect to see more discussions about oral health risk during check-ups (see Chapter 1, Risk communication). The supposition in the literature, identified at the outset of the study, that ‘risk communication should form part of every patient interaction’39 seems very far from the reality we observed in NHS dental practice. The infrequency of discussions of patients’ oral health status supports the criticism that too little preventative work goes on in existing practice under the current NHS UDA dental contract. 153
Implications for the new NHS dental contract
-
Even in NHS dental practices using a TL remuneration model built on a ‘risk’ concept, overt conversations about risk are infrequent.
-
All six discussions of patients’ oral health risk status that were observed occurred in the practice taking part in the Department of Health and Social Care pilot/prototype contracts that prioritise delivering risk information on oral health. Although this is welcomed, given that there were 105 appointments observed in this prototype practice (see Chapter 5, Observations in dental settings), it is still a disappointing outcome.
-
This may be because, as revealed in our qualitative work, dental staff and patients experience a degree of discomfort when risk-related discussions take place during clinical practice, even to the degree that it could be concluded that very little actual ‘risk work’ takes place in dental practices and that ‘risk discourse’ remains something that mainly occurs only at policy level (see Patients and dentists do not generally talk about risk). Because verbal information is so highly valued by patients from a wide range of backgrounds, our work suggests that there is a need to support staff and develop skills in dental practice teams on how best to handle these difficult conversations.
-
Therefore, in tandem with changes in the organisational structure aimed at incentivising the dental team to place a higher priority on preventative work, including conversations with patients about how to look after their own oral health, support for staff that addresses the ‘how to’ aspects of holding these potentially challenging conversations may be needed, especially because dentists deal with patients both as paying customers and as people to whom they provide health care (with associated professional responsibility).
Implications for the new NHS dental contract model: risks and benefits of a model involving traffic light information
-
In the qualitative work, we identified that oral health risk portrayed as TL categories may have more appeal to patients as a means to measure progress over time and reinforce improvements where there has been change. However, there are constraints within the TL algorithm which mean that, for example, some patients who have health problems are unlikely to move out of the amber category, which would be disheartening. As research in other health fields has found, a lack of change in risk status may be disheartening to patients who have been making a concerted effort to improve their health. 214
-
Another potential problem with giving information in the TL system is that it offers high sensitivity but low specificity. Patients are sorted into three broad categories, which means that TL could become another form of standardised information giving. As was demonstrated earlier, advice may be reduced to ‘you are red’, which does not offer personalised information in a way that patients can address. That our study has found that patients prefer this form of information less than the usual verbal communication with the dentist indicates that a potential adverse consequence of the new NHS dental contract is that the system built on a TL algorithm makes for less detailed personalised discussions of patients’ oral health and what they can do to improve their health.
-
Providing a simplified, ‘heuristic’ method to convey complex information regarding oral health risk in the form of TL symbolism was not found to appeal to patients or to be useful in prompting behaviour change, as hypothesised at the outset of the study (see Chapter 1, Risk presentation format and information visualisation). It is, however, interesting to note that whereas practice-based effects were identified as influencing patients’ preferences for verbal and QLF information, no practice-based influence on preference was seen for the TL information method (see Chapter 4, Preference for form used to communicate information on risk). It is possible, therefore, that, although TL information does not appeal to patients, it does represent a standardised message that could dilute different degrees of skills in verbal communication with patients at a practice level.
Implications for NHS dental practice: patients’ preferences for information
-
Patients’ preferences for information cannot be widely predicted based only on socioeconomic stereotypes because practice effects may supersede these.
-
An interesting finding from the trial was that the practice the patient attended influenced their preferred method of information delivery over and above a range of other factors (e.g. income, IMD, literacy). Thus, rather than categorising patients into groups that we think may prefer certain types of information, our work suggests that there is a need to focus on improving the quality of the way information is delivered to patients, especially in terms of giving personalised advice to patients verbally. There is also a particular need to consider how this could be improved at a dental practice level. Furthermore, the work does not provide any evidence to support social marketing approaches, which segment the population along the lines of various psychographic and sociodemographic characteristics (see Chapter 1, Tailoring of risk information), because our study showed that people’s preferences for information appear to transcend the stereotypical sociodemographic characteristics that might have been expected to predict their preferences.
Implications outside dentistry: alternative, innovative forms of giving information
-
Even if alternative, innovative forms of giving information are available, supporting verbal information is still important.
-
Our study found small differences in reported sugar consumption in drinks and toothbrushing duration after 12 months; these results can be seen as a consequence of dental visiting or may be a cohort effect. No such differences were seen between the three arms providing risk information in different ways, which reiterates our findings from the systematic review that, although tools to communicate risk are increasingly available, the way in which clinical communication is conducted during the appointment is still critical to whether or not there is to be any change in behaviour. The fact that patients expressed a clear preference for verbal information over either TL or QLF is indicative of the importance that patients place on the conversations that they have with the dental team about their oral health.
-
Very little previous research has been conducted on how risk is acted on and communicated in routine clinical practice,1 and in particular how newer technology, such as tailored web-based interventions, scans and radiographs, has an impact on the way in which this communication might be conducted (with possible differential impacts of newer information forms). Our study has implications for practice in health sectors beyond dentistry. We conclude that even though new technology may offer highly personalised, very visual methods of conveying information to patients, this is probably only of benefit if it is supported with an explanation of the personal meaning behind the information conveyed.
Financial implications for NHS dentistry
-
In general, given that patients find more time and information from their dentists as most important, and that time is critical to allow dentists to deliver risk work, it may be that adding alternative ways of communicating risk is premature. Prior to introducing new methods there needs to be adequate time and support for dentists and patients to have risk-related discussions. This has resource implications for the NHS. Although patients from all walks of life clearly value very highly having personalised information about their oral health, routine practice appears only to involve very brief interactions. Expanding this by using techniques, such as Brief Negotiated Interviewing, has time and, therefore, cost implications for the NHS.
-
On the other hand, in the course of our qualitative work we found a wide variety in the communication skills of dentists, indicating that, irrespective of the time available, the opportunity for risk talk during check-ups could be better used in some cases. Observing how hygiene-therapists interpreted BPE scores for patients during check-ups is a case in point. We also found that some dentists observed were particularly adept at being personable with patients in a very short period of time, whereas others appeared to view patient communication as a low-value aspect of their job that they would like to minimise:Interview with practice manager, practice 5
I think it’s totally personal. There are some dentists who are fabulous communicators who naturally empathise with people and are just able to communicate. There are others who struggle. And I do, I don’t know if it’s something they should be taught at med [medical]school or whether it’s something that you have either got or you haven’t got. But you can see which of our dentists has the gift of the gab and those that don’t, both on a private income scale and their success rate with patient buy-in.
-
Given the overall conclusion that verbal information is most preferred and cheapest, it seems that this would appear to be the best method for NHS dentistry. However, there may be some questions about the need to provide risk information at all if it has such a limited effect on behaviour change, as indicated in this study. On the other hand, there are moral and ethical arguments that the patient has a right to this information and that this service should continue to be provided. Weighing up the unpredictability of preferred methods of communication (and the subsequent argument that all forms should be offered) against the limited clinical benefit leads to a more difficult question of whether or not the extra investment to provide additional means of supporting verbal communication is necessary in order to fulfil a moral obligation.
Future research agenda
To our knowledge, this is one of the largest observational studies of the giving of information on risk to NHS dental patients, although we recognise that the sample of practices involved was relatively small. Future research is needed to look at routine practice in other dental practices, especially those piloting the new dental contract prototypes, as well as in health care more generally. For example:
-
More work is needed on how risk is acted on and communicated in other health-care settings outside dentistry – is explicit risk talk as absent in other health and care settings?
-
Given that preventative dentistry, which includes a wide range of health behaviour advice, is recommended as best practice for NHS dentistry,152 it is remarkable how little research has been undertaken to test the ways in which preventative advice can be improved within the confines of the NHS dental check-up appointment. 171,215 Thus, more research on cost-effective ways to deliver advice to patients about their oral health during check-ups is needed.
-
The ‘how to’ of delivering risk information to patients in an environment where they are both paying customers and receivers of health care is particularly challenging. Although communication skills training is routinely undertaken as part of undergraduate dental, hygiene and therapy programmes, specific training about how to handle these potentially challenging conversations within the time constraints of NHS dental practice is mostly missing. Research concerned with how best to prepare dental students to engage in risk talk with patients, how to do this confidently and effectively, and the role of other tools, such as option grids, that have been advocated as part of shared decision-making in this process, is needed.
-
Leading on from our qualitative work, dentists appear to refrain from using uncertainty in discussions. Why is this and how might their interactions with patients change if they were more able/willing to convey uncertainty?
-
This study also indicates where some further research on methodological issues is needed. Having found that the sample, on average, gave a higher WTP value for verbal than verbal plus TL prompts questions as to why a larger ‘basket of goods’ would produce less utility. This is an area of interest in terms both of understanding and risk information preferences, and how WTP methodology works, which would benefit from further exploration (probably using qualitative methods).
-
In terms of WTP methodology, a key area that emerged as needing further research is the differentiation of protest zeros, as discussed in Chapter 7, Interpretation of willingness-to-pay data. In particular, validation of published follow-up questions used when zero values are given should be undertaken.
-
The lack of association between plaque coverage measured with QLF technology and responses to behaviour-change questions raises questions about the extent to which reported behaviour measures can capture meaningful clinical outcomes for patients. In this regard, a validity trial of QLF plaque coverage measurements against clinical indices and self-reported behaviour would be useful.
Acknowledgements
The study team would like to acknowledge and express their thanks for the support in this work from staff in the five dental practices involved in the study.
We would like to acknowledge the contribution of Jimmy Steele (University of Newcastle) who helped design the study and helped with its implementation; Clare Noble (Institute of Psychology, Health and Society at the University of Liverpool) for her contribution to the selection of the health behaviour measures and involvement in the systematic review; and Gleb Komarov (Institute of Psychology, Health and Society at the University of Liverpool) who extracted clinical outcome data from QLF images and assisted with the training of dental teams in QLF technology.
We would like to acknowledge the advice and contribution of members of the PREFER Advisory Group: Gerald Humphris, Eric Rooney (Public Health England), Gail Douglas, Ben Atkins (General Dental Practitioner) and PPI members Edwin Morgan, Janet Driver, Irene Soulsby and Gwen Young.
Contributions of authors
Rebecca Harris (Professor of Dental Public Health and Honorary Consultant at Royal Liverpool and Broadgreen Hospitals Trust) was the corresponding author, designed and led the research project, managed study implementation and data analysis, and wrote the final report.
Christopher Vernazza (NIHR Clinical Scientist) and Laura Ternent (Senior Lecturer of Health Economics) designed the health economics component of the study undertook the health economic analysis and reporting. Christopher Vernazza also helped manage study implementation in north-east England sites.
Louise Laverty (Research Associate) undertook study implementation and trial monitoring, collected all the qualitative data, undertook the qualitative data analysis and reporting.
Victoria Lowers (Research Assistant) assisted study implementation and trial monitoring, assisted with the systematic review, liaised with public involvement team members, contributed to the design and analysis of the behaviour-change outcomes, collected all the 6- and 12-month follow-up data, and contributed to report writing, including the writing of the patient and public involvement chapter (see Chapter 6).
Girvan Burnside (Senior Lecturer of Biostatistics) designed the statistical aspects of the trial, analysed the clinical outcomes of the trial and contributed to the final report.
Stephen Brown (Senior Lecturer of Health Psychology) designed the psychological aspects of the trial and undertook the data analyses and reporting.
Susan Higham (Professor of Oral Biology) assisted with the dental team training relating to QLF technology, extraction of clinical outcome data from QLF images and contributed to the final report.
Publications
Harris R, Noble C, Lowers V. Does information form matter when giving tailored risk information to patients in clinical settings? A review of patients’ preferences and responses. Patient Prefer Adherence 2017;11:389–400.
Harris R, Lowers V, Laverty L, Vernazza C, Burnside G, Brown S, Ternent L. Comparing how patients value and respond to information on risk given in three different forms during dental check-ups: the PREFER randomised controlled trial. Trials 2019;21.
Data-sharing statement
Owing to the nature of this study, the type of data collected and conditions attached to ethics approval, there are no data available for wider use. All queries should be submitted to the corresponding author in the first instance. Data will be archived by the University of Liverpool.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Oxford Dictionaries . Risk n.d. https://en.oxforddictionaries.com (accessed 13 September 2017).
- Edwards A, Elwyn G. Understanding risk and lessons for clinical risk communication about treatment preferences. Qual Health Care 2001;10:i9-13. https://doi.org/10.1136/qhc.0100009.
- Althaus CE. A disciplinary perspective on the epistemological status of risk. Risk Anal 2005;25:567-88. https://doi.org/10.1111/j.1539-6924.2005.00625.x.
- Giddens A. Risk and responsibility. Mod Law Rev 1999;62:1-10. https://doi.org/10.1111/1468-2230.00188.
- Lupton D, Williams S, Gabe J, Calnan M. Health, Medicine and Society: Key Theories, Future Agendas. London: Routledge; 2000.
- Beck U. Risk Society: Towards a New Modernity. London: Sage; 1992.
- Ayo N. Understanding health promotion in a neoliberal climate and the making of health-conscious citizens. Crit Public Health 2011;22:99-105.
- Nettleton S, Bunton R, Bunton R, Nettleton S, Burrows R. The Sociology of Health Promotion: Critical Analyses of Consumption, Lifestyle, and Risk. London: Routledge; 1995.
- Petersen A, Bunton R. Foucault, Health, and Medicine. London/New York, NY: Routledge; 1997.
- Petersen A, Lupton D. The New Public Health: Health and Self in the Age of Risk. London: Sage; 1996.
- Trnka SC, Trundle C. Competing responsibilities: moving beyond neoliberal responsibilisation. Anthropol For 2014;24:136-53. https://doi.org/10.1080/00664677.2013.879051.
- Crawford R. The boundaries of the self and the unhealthy other: reflections on health, culture and AIDS. Soc Sci Med 1994;38:1347-65. https://doi.org/10.1016/0277-9536(94)90273-9.
- Crawford R, McKinlay J. Issues in the Political Economy of Health Care. New York, NY: Tavistock; 1985.
- Greco M. Psychosomatic subjects and the ‘duty to be well’ – personal agency within. Econ Soc 1993;22:357-72. https://doi.org/10.1080/03085149300000024.
- Department of Health and Social Care . The NHS Constitution for England, 2015 n.d. www.gov.uk/government/publications/the-nhs-constitution-for-england/the-nhs-constitution-for-england (accessed 14 September 2017).
- Department of Health and Social Care . Healthy Lives, Healthy People: Our Strategy for Public Health in England 2010.
- Zinn JO. Towards a better understanding of risk taking: key concepts, dimension and perspectives. Health Risk Soc 2015;17:99-114. https://doi.org/10.1080/13698575.2015.1023267.
- Lupton D. Risk and Socio-Cultural Theory: New Directions and Perspectives. Cambridge: Cambridge University Press; 1999.
- Beck U, Beck-Gernsheim E. Individualization: Institutional Individualism and its Social and Political Consequences. London: Sage; 2002.
- Gard M, Wright J. Managing uncertainty: obesity discourses and physical education in a risk society. Stud Philos Educ 2001;20:535-49. https://doi.org/10.1023/A:1012238617836.
- Douglas M, Wildavsky A. Risk and Culture: An Essay on the Selection of Technological and Environmental Dangers. Berkeley, CA: University of California Press; 1982.
- Douglas M. Risk and Blame: Essays in Cultural Theory. London/New York, NY: Routledge; 1992.
- Douglas M. Purity and Danger. London: Routledge and Kegan Paul; 1966.
- Douglas M. Risk Acceptability According to the Social Sciences. New York, NY: Russell Sage Foundation; 1985.
- NHS Digital . Statistics on Alcohol: England 2014 2014. www.hscic.gov.uk/catalogue/PUB14184/alc-eng-2014-rep.pdf (accessed 14 September 2017).
- Lash S, Adam B, Beck U, Loon JV. The Risk Society and Beyond: Critical Issues for Social Theory. London: Sage; 2000.
- Becker HS, McCall MM. Symbolic Interaction and Cultural Studies. Chicago, IL: Chicago University Press; 1990.
- Crawford R. Health as a meaningful social practice. Health 2006;10:401-20. https://doi.org/10.1177/1363459306067310.
- Prior L. Rationing through risk assessment in clinical genetics: all categories have wheels. Sociol Health Illn 2001;23:570-93. https://doi.org/10.1111/1467-9566.00266.
- Lupton D. Risk. London: Routledge; 1999.
- Hunt GP, Evans K, Kares F. Drug use and meanings of risk and pleasure. J Youth Stud 2007;10:73-96. https://doi.org/10.1080/13676260600983668.
- Vahratian A, Smith YR. Should access to fertility-related services be conditional on body mass index?. Hum Reprod 2009;24:1532-7. https://doi.org/10.1093/humrep/dep057.
- MacCormick AD, Collecutt WG, Parry BR. Prioritizing patients for elective surgery: a systematic review. ANZ J Surg 2003;73:633-42. https://doi.org/10.1046/j.1445-2197.2003.02605.x.
- Department of Health and Social Care . Dental Contract Reform: Prototypes 2015.
- Harris R, Mosedale S, Garner J, Perkins E. What factors influence the use of contracts in the context of NHS dental practice? A systematic review of theory and logic model. Soc Sci Med 2014;108:54-9. https://doi.org/10.1016/j.socscimed.2014.01.032.
- Harris R, Bridgman C. Introducing care pathway commissioning to primary dental care: the concept. Br Dent J 2010;209:233-9. https://doi.org/10.1038/sj.bdj.2010.770.
- Department of Health and Social Care . NHS Dental Contract Pilots – Early Findings: A Report by the Dental Contract Pilots Evidence and Learning Group 2012. www.ncl.ac.uk/media/wwwnclacuk/research/files/NHS-dental-contract-pilots-early-findings.pdf (accessed 18 September 2017).
- Ahmed A, Nail G, Willoughby H, Edwards AGK. Communicating risk. BMJ 2012;344:1-7. https://doi.org/10.1136/bmj.e3996.
- McCarthy C, Daly B, Asimakopoulou K. Risk communication for the dental team. Faculty Dental Journal 2016;7:144-9. https://doi.org/10.1308/rcsfdj.2016.144.
- Becker MH. The Health Belief Model and Personal Health Behaviour. San Francisco, CA: Society for Public Health Education; 1974.
- Witte K, Meyer G, Martell D. Effective Health Risk Messages: A Step-By-Step Guide. Thousand Oaks, CA: Sage; 2001.
- European Centre for Disease Prevention and Control . A Literature Review on Effective Risk Communication for the Prevention and Control of Communicable Diseases in Europe: Insights into Health Communication. Technical Report 2013. http://ecdc.europa.eu/en/healthtopics/health_communication/health-communication-topics/pages/risk-communication.aspx (accessed 14 October 2017).
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res 2008;23:454-66. https://doi.org/10.1093/her/cyn004.
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull 2007;133:673-93. https://doi.org/10.1037/0033-2909.133.4.673.
- Edwards AG, Naik G, Ahmed H, Elwyn GJ, Pickles T, Hood K, et al. Personalised risk communication for informed decision-making about taking screening tests. Cochrane Database Syst Rev 2013;2. https://doi.org/10.1002/14651858.CD001865.pub3.
- Rothman AJ, Kiviniemi MT. Treating people with information: an analysis and review of approaches to communicating health risk information. J Natl Cancer Inst Monogr 1999;25:44-51. https://doi.org/10.1093/oxfordjournals.jncimonographs.a024207.
- Abrams DB, Mills S, Bulger D. Challenges and future directions for tailored communication research. Ann Behav Med 1999;21:299-306. https://doi.org/10.1007/BF02895961.
- Lustria ML, Noar SM, Cortese J, Van Stee SK, Glueckauf RL, Lee J. A meta-analysis of web-delivered tailored health behaviour change interventions. J Health Commun 2013;18:1039-69. https://doi.org/10.1080/10810730.2013.768727.
- French J, Blair-Stevens, McVey D, Merritt R. Social Marketing and Public Health: Theory and Practice. Oxford: Oxford University Press; 2010.
- Kotler P, Zaltman G. Social marketing: an approach to planned social change. J Mark 1971;35:3-12. https://doi.org/10.1177/002224297103500302.
- Cheng H, Kotler P, Lee NR. Social Marketing for Public Health: Global Trends and Success Stories. London: Jones & Bartlett Learning; 2011.
- Maibach EW, Weber D, Massett H, Hancock GR, Price S. Understanding consumers’ health information preferences: development and validation of a brief screening instrument. J Health Commun 2006;11:717-36. https://doi.org/10.1080/10810730600934633.
- Locker D. Deprivation and oral health: a review. Community Dent Oral Epidemiol 2000;28:161-9. https://doi.org/10.1034/j.1600-0528.2000.280301.x.
- Edwards A, Elwyn G, Covey J, Matthews E, Pill R. Presenting risk information: a review of the effects of ‘framing’ and other manipulations on patient outcomes. J Health Commun 2001;6:61-82. https://doi.org/10.1080/10810730150501413.
- Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ 2002;324:827-30. https://doi.org/10.1136/bmj.324.7341.827.
- Ancker JS, Senathirajah Y, Kukafka R, Starren JB. Design features of graphs in health risk communication: a systematic review. J Am Med Inform Assoc 2006;13:608-18. https://doi.org/10.1197/jamia.M2115.
- Waldron CA, van der Weijden T, Ludt S, Gallacher J, Elwyn G. What are effective strategies to communicate cardiovascular risk information to patients? A systematic review. Patient Educ Couns 2011;82:169-81. https://doi.org/10.1016/j.pec.2010.04.014.
- Lupton D. Risk and emotion: towards an alternative theoretical perspective. Health Risk Soc 2013;15:634-47. https://doi.org/10.1080/13698575.2013.848847.
- Faisal S, Blandford A, Potts HW. Making sense of personal health information: challenges for information visualization. Health Informatics J 2013;19:198-217. https://doi.org/10.1177/1460458212465213.
- Smith BK, Frost J, Albayrak M, Sudhakar R. Integrating glucometers and digital photographs as experience capture tools to enhance patient understanding and communication of diabetes self-management practices. Pers Ubiquit Comput 2007;11:273-86. https://doi.org/10.1007/s00779-006-0087-2.
- Reyna VF. How people make decisions that involve risk: a dual-process approach. Current Directions Psychol Sci 2004;13:60-6. https://doi.org/10.1111/j.0963-7214.2004.00275.x.
- Pachur T, Hertwig R, Steinmann F. How do people judge risks: availability heuristic, affect heuristic, or both?. J Exp Psychol Appl 2012;18:314-30. https://doi.org/10.1037/a0028279.
- de Vries M, Fagerlin A, Witteman HO, Scherer LD. Combining deliberation and intuition in patient decision support. Patient Educ Couns 2013;91:154-60. https://doi.org/10.1016/j.pec.2012.11.016.
- Gigerenzer G, Gaissmaier W. Heuristic decision making. Annu Rev Psychol 2011;62:451-82. https://doi.org/10.1146/annurev-psych-120709-145346.
- Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns 2006;61:173-90. https://doi.org/10.1016/j.pec.2005.05.004.
- Lee TJ, Cameron LD, Wünsche B, Stevens C. A randomized trial of computer-based communications using imagery and text information to alter representations of heart disease risk and motivate protective behaviour. Br J Health Psychol 2011;16:72-91. https://doi.org/10.1348/135910710X511709.
- Hollands GJ, Marteau TM. The impact of using visual images of the body within a personalized health risk assessment: an experimental study. Br J Health Psychol 2013;18:263-78. https://doi.org/10.1111/bjhp.12016.
- Cameron LD, Williams B. Which images and features in graphic cigarette warnings predict their perceived effectiveness? Findings from an online survey of residents in the UK. Ann Behav Med 2015;49:639-49. https://doi.org/10.1007/s12160-015-9693-4.
- de Josselin de Jong E, Sundström F, Westerling H, Tranaeus S, ten Bosch JJ, Angmar-Månsson B. A new method for in vivo quantification of changes in initial enamel caries with laser fluorescence. Caries Res 1995;29:2-7. https://doi.org/10.1159/000262032.
- Pretty IA, Edgar WM, Smith PW, Higham SM. Quantification of dental plaque in the research environment. J Dent 2005;33:193-207. https://doi.org/10.1016/j.jdent.2004.10.017.
- Gale NK, Thomas GM, Thwaites R, Greenfield S, Brown P. Towards a sociology of risk work: a narrative review and synthesis. Sociol Comp 2016;10:1046-71. https://doi.org/10.1111/soc4.12416.
- Saunders J. The practice of clinical medicine as an art and as a science. Med Humanit 2000;26:18-22. https://doi.org/10.1136/mh.26.1.18.
- Linell P, Adelswärd V, Sachs L, Bredmar M, Lindstedt U. Expert talk in medical contexts: explicit and implicit orientation to risks. Res Lang Soc Interac 2010;35:195-218. https://doi.org/10.1207/S15327973RLSI3502_4.
- Cicourel A, Duranti A, Goodwin C. Rethinking Context: Language as an Interactive Phenomenon. Cambridge: Cambridge University Press; 1992.
- Cameron LD, Cameron LD, Leventhal H. The Self-Regulation of Health and Illness Behaviour. London: Routledge; 2003.
- Witte K. Fear control and danger control: a test of the extended parallel process model. Commun Monogr 1994;61:113-34. https://doi.org/10.1080/03637759409376328.
- Bandura A, Kazdin AE. Encyclopaedia of Psychology. New York, NY: Oxford University Press; 2000.
- Brown SL, Richardson M. The effect of distressing imagery on attention to and persuasiveness of an antialcohol message: a gaze-tracking approach. Health Educ Behav 2012;39:8-17. https://doi.org/10.1177/1090198111404411.
- Peters GJY, Ruiter RAC, Kok G. Threatening communication: a critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychol Rev 2013;7:S8-31. https://doi.org/10.1080/17437199.2012.703527.
- Nader L. Ethnography as theory. Hau J Ethnogr Theory 2011;1:211-19. https://doi.org/10.14318/hau1.1.008.
- Goffman E. The Presentation of Self in Everyday Life. London: Allen Lane; 1959.
- Horlick-Jones T. On ‘risk work’: professional discourse, accountability, and everyday action. Health Risk Soc 2005;7:293-307. https://doi.org/10.1080/13698570500229820.
- Great Britain . Data Protection Act 1998, C29 1998.
- Lefebvre C, Glanville J, Wieland LS, Coles B, Weightman AL. Methodological developments in searching for studies for systematic reviews: past, present and future?. Syst Rev 2013;2. https://doi.org/10.1186/2046-4053-2-78.
- Effective Practice and Organisation of Care . How to Develop a Search Strategy. EPOC Resources for Review Authors 2014. http://epoc.cochrane.org/epoc-specific-resources-review-authors (accessed 14 October 2016).
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011.
- Arai L, Britten N, Popay J, Roberts H, Petticrew M, Rodgers M, et al. Testing methodological developments in the conduct of narrative synthesis: a demonstration review of research on the implementation of smoke alarm interventions. Evid Policy 2007;3:361-83. https://doi.org/10.1332/174426407781738029.
- Dapp U, Anders JA, von Renteln-Kruse W, Minder CE, Meier-Baumgartner HP, Swift CG, et al. A randomized trial of effects of health risk appraisal combined with group sessions or home visits on preventive behaviors in older adults. J Gerontol A Biol Sci Med Sci 2011;66:591-8. https://doi.org/10.1093/gerona/glr021.
- Harari D, Iliffe S, Kharicha K, Egger M, Gillmann G, von Renteln-Kruse W, et al. Promotion of health in older people: a randomised controlled trial of health risk appraisal in British general practice. Age Ageing 2008;37:565-71. https://doi.org/10.1093/ageing/afn150.
- Kreuter MW, Strecher VJ. Changing inaccurate perceptions of health risk: results from a randomized trial. Health Psychol 1995;14:56-63. https://doi.org/10.1037/0278-6133.14.1.56.
- Zullig LL, Sanders LL, Shaw RJ, McCant F, Danus S, Bosworth HB. A randomised controlled trial of providing personalised cardiovascular risk information to modify health behaviour. J Telemed Telecare 2014;20:147-52. https://doi.org/10.1177/1357633X14528446.
- Welschen LM, Bot SD, Kostense PJ, Dekker JM, Timmermans DR, van der Weijden T, et al. Effects of cardiovascular disease risk communication for patients with type 2 diabetes on risk perception in a randomized controlled trial: the @RISK study. Diabetes Care 2012;35:2485-92. https://doi.org/10.2337/dc11-2130.
- Hess R, Tindle H, Conroy MB, Clark S, Yablonsky E, Hays RD. A randomized controlled pilot trial of the functional assessment screening tablet to engage patients at the point of care. J Gen Intern Med 2014;29:1641-9. https://doi.org/10.1007/s11606-014-2984-9.
- Neuner-Jehle S, Knecht MI, Stey-Steurer C, Senn O. Acceptance and practicability of a visual communication tool in smoking cessation counselling: a randomised controlled trial. Prim Care Respir J 2013;22:412-16. https://doi.org/10.4104/pcrj.2013.00086.
- Shahab L, Hall S, Marteau T. Showing smokers with vascular disease images of their arteries to motivate cessation: a pilot study. Br J Health Psychol 2007;12:275-83. https://doi.org/10.1348/135910706X109684.
- Mauriello LM, Van Marter DF, Umanzor CD, Castle PH, De Aguiar EL. Using mHealth to deliver behaviour change interventions within prenatal care at community health centres. Am J Health Promot 2016;30:554-62. https://doi.org/10.4278/ajhp.140530-QUAN-248.
- Saver BG, Mazor KM, Hargraves JL, Hayes M. Inaccurate risk perceptions and individualized risk estimates by patients with type 2 diabetes. J Am Board Fam Med 2014;27:510-19. https://doi.org/10.3122/jabfm.2014.04.140058.
- Ahmed S, Bartlett SJ, Ernst P, Paré G, Kanter M, Perreault R, et al. Effect of a web-based chronic disease management system on asthma control and health-related quality of life: study protocol for a randomized controlled trial. Trials 2011;12. https://doi.org/10.1186/1745-6215-12-260.
- Weyman N, Harter M, Petrak F, Dirmaier J. Health information, behaviour change, and decision support for patients with type 2 diabetes: development of a tailored, preference-sensitive health communication application. Patient Prefer Adherence 2013;7:1091-99. https://doi.org/10.2147/PPA.S46924.
- Campbell MK, Carr C, DeVellis B, Switzer B, Biddle A, Amanmoo MA, et al. A randomised trial of tailoring and motivational interviewing to promote fruit and vegetable consumption for cancer prevention and control. Ann Behav Med 2009;38:71-85. https://doi.org/10.1007/s12160-009-9140-5.
- Bovet P, Perret F, Cornuz J, Quilindo J, Paccaud F. Improved smoking cessation in smokers given ultrasound photographs of their own atherosclerotic plaques. Prev Med 2002;34:215-20. https://doi.org/10.1006/pmed.2001.0976.
- Harris R, Lowers V, Laverty L, Vernazza C, Burnside G, Brown S, et al. Comparing how patients value and respond to information on risk given in three different forms during dental check-ups: the PREFER randomised controlled trial. Trials 2019;21. https://doi.org/10.1186/s13063-019-3824-3.
- Pavitt SH, Baxter PD, Brunton PA, Douglas G, Edlin R, Gibson BJ, et al. The INCENTIVE protocol: an evaluation of the organisation and delivery of NHS dental healthcare to patients – innovation in the commissioning of primary dental care service delivery and organisation in the UK. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005931.
- Department of Health and Social Care . Dental Contract Reform Pilots: Notes to Support Care Pathway Approach n.d. www.networks.nhs.uk/nhs-networks/dental-pilots-network/documents/Clinical%20Pathway%20Guidance%20Final.pdf (accessed 13 July 2017).
- Department of Health and Social Care . Dental Contract Reform: Prototypes. Overview Document 2015 n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/395384/Reform_Document.pdf (accessed 13 July 2017).
- Tan SHX, Vernazza CR, Nair R. Critical review of willingness to pay for clinical oral health interventions. J Dent 2017;64:1-12. https://doi.org/10.1016/j.jdent.2017.06.010.
- Makoul G, Krupat E, Chang CH. Measuring patient views of physician communication skills: developing and testing of the Communication Assessment Tool. Patient Educ Couns 2007;67:333-42. https://doi.org/10.1016/j.pec.2007.05.005.
- NHS Digital . Adult Dental Health Survey 2009. www.hscic.gov.uk/pubs/dentalsurveyfullreport09 (accessed 14 August 2015).
- Buunk-Werkhoven YA, Dijkstra A, van der Schans CP. Determinants of oral hygiene behavior: a study based on the theory of planned behavior. Community Dent Oral Epidemiol 2011;39:250-9. https://doi.org/10.1111/j.1600-0528.2010.00589.x.
- Walker A, Gregory J, Bradnock G, Nunn J, White D. National Diet and Nutrition Survey. Volume 2: Report of the Oral Health Survey 2000.
- World Health Organization . Tobacco Questions for Surveys: A Subset of Key Questions from the Global Adult Tobacco Survey (GATS) 2011. www.who.int/tobacco/surveillance/en_tfi_tqs.pdf (accessed 14 August 2015).
- Department of Communities and Local Government . English Indices of Deprivation 2015 n.d. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 19 July 2017).
- Office for National Statistics . Primary Set of Harmonised Concepts and Questions 2015. www.ons.gov.uk/ons/guide-method/harmonisation/primary-set-of-harmonised-concepts-and-questions/index.html (accessed 14 August 2015).
- Bass PF, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med 2003;18:1036-8. https://doi.org/10.1111/j.1525-1497.2003.10651.x.
- Humphris GM, Morrison T, Lindsay SJ. The modified dental anxiety scale: validation and United Kingdom norms. Community Dent Health 1995;12:143-50.
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. New York, NY: Lawrence Erlbaum Associates; 1998.
- Aleksejūniene J, Scheie AA, Holst D. Inter-individual variation in the plaque formation rate of young individuals. Int J Dent Hyg 2006;4:35-40. https://doi.org/10.1111/j.1601-5037.2006.00167.x.
- Smith RD. It’s not just what you do, it’s the way that you do it: the effect of different payment card formats and survey administration on willingness to pay for health gain. Health Econ 2006;15:281-93. https://doi.org/10.1002/hec.1055.
- Lamiraud K, Oxoby R, Donaldson C. Incremental willingness to pay: a theoretical and empirical exposition. Theory Decis 2016;80:101-23. https://doi.org/10.1007/s11238-014-9480-x.
- Ryan M, Scott DA, Donaldson C. Valuing health care using willingness to pay: a comparison of the payment card and dichotomous choice methods. J Health Econ 2004;23:237-58. https://doi.org/10.1016/j.jhealeco.2003.09.003.
- NHS Digital . Dental Statistics England 2014 15 2015.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: PSSRU, University of Kent; 2016.
- Smith RD. Working Paper 74: Contingent Valuation – Indiscretion in the Adoption of Discrete Choice Question Formats? 1997. http://arrow4.lib.monash.edu.au:8080/vital/access/services/Download/monash:2697/DOC (accessed 2 August 2017).
- Aikin LS, West SG, Reno RR. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage Publications; 1991.
- Zhao X, Lynch, Chen Q. Reconsidering Baron and Kenny: myths and truths about mediation analysis. J Consum Res 2010;37:197-206. https://doi.org/10.1086/651257.
- Boiko OV, Robinson PG, Ward PR, Gibson BJ. Form and semantics of communication in dental encounters: oral health, probability and time. Sociol Health Illn 2011;33:16-32. https://doi.org/10.1111/j.1467-9566.2010.01268.x.
- Nettleton S. Power, Pain and Dentistry. Buckingham: Open University Press; 1992.
- Nations MK, Nuto Sde A. ‘Tooth worms’, poverty tattoos and dental care conflicts in northeast Brazil. Soc Sci Med 2002;54:229-44. https://doi.org/10.1016/S0277-9536(01)00019-3.
- Harris R, Holt R. Interacting institutional logics in general dental practice. Soc Sci Med 2013;94:63-70. https://doi.org/10.1016/j.socscimed.2013.05.038.
- Savage J. Ethnographic evidence. J Res Nurs 2006;11:383-93. https://doi.org/10.1177/1744987106068297.
- Pope C. Conducting ethnography in medical settings. Med Educ 2005;39:1180-7. https://doi.org/10.1111/j.1365-2929.2005.02330.x.
- della Porta D, Keating M. Approaches and Methodologies in the Social Sciences: A Pluralist Perspective. Cambridge: Cambridge University Press; 2008.
- Blumer H. Symbolic Interactionism: Perspective and Method. Englewood Cliffs, NJ: Prentice-Hall Inc.; 1969.
- Garfinkel H. Studies in Ethnomethodology. Malden, MA: Polity Press; 1967.
- Atkinson PA, Housley W. Interactionism. London: Sage Publications; 2003.
- Goffman E. On Fieldwork. J Contemp Ethnogr 1989;18:123-32. https://doi.org/10.1177/089124189018002001.
- Wolcott HF. Ethnography: A Way of Seeing. Oxford: AltaMira Press; 1999.
- Wengraf T. The Short Guide to BNIM. London: London East Research Institute, University of East London; 2008.
- Coleman H, Burton J. Aspects of control in the dentist–patient relationship. Int J Soc Lang 1985;51:75-104. https://doi.org/10.1515/ijsl.1985.51.75.
- Mays N, Pope C. Rigour and qualitative research. BMJ 1995;311:109-12. https://doi.org/10.1136/bmj.311.6997.109.
- Emerson RM, Fretz RI, Shaw LL. Writing Ethnographic Fieldnotes. Chicago, IL: University of Chicago Press; 2011.
- Silverman D. Going private: ceremonial forms in a private oncology clinic. Sociology 1984;18:191-204. https://doi.org/10.1177/0038038584018002003.
- Emanuel EJ, Emanuel LL. Four models of the physician–patient relationship. JAMA 1992;267:2221-6. https://doi.org/10.1001/jama.1992.03480160079038.
- Karasz A, Dowrick C, Byng R, Buszewicz M, Ferri L, Olde Hartman TC, et al. What we talk about when we talk about depression: doctor-patient conversations and treatment decision outcomes. Br J Gen Pract 2012;62:e55-63. https://doi.org/10.3399/bjgp12X616373.
- Pryce A. Frequent observation: sexualities, self-surveillance, confession and the construction of the active patient. Nurs Inq 2000;7:103-11. https://doi.org/10.1046/j.1440-1800.2000.00057.x.
- ten Have P, Boden D, Zimmerman DH. Talk and Social Structure: Studies in Ethnomethodology and Conversation Analysis. Cambridge: Polity Press; 1991.
- Goffman E. Interaction Ritual. New York, NY: Pantheon Books; 1967.
- Strong PM. The Ceremonial Order of the Clinic: Parents, Doctors and Medical Bureaucracies. London: Routledge and Kegan Paul; 1979.
- Hillyard S. Ethnography’s capacity to contribute to the cumulation of theory: a case study of Strong’s work on Goffman. J Contemp Ethnogr 2010;39:421-40. https://doi.org/10.1177/0891241610366710.
- Maynard DW. Interaction and asymmetry in clinical discourse. Am J Sociol 1991;97:448-95. https://doi.org/10.1086/229785.
- Pilnick A, Dingwall R. On the remarkable persistence of asymmetry in doctor/patient interaction: a critical review. Soc Sci Med 2011;72:1374-82. https://doi.org/10.1016/j.socscimed.2011.02.033.
- Public Health England . Delivering Better Oral Health: An Evidence-Based Toolkit for Prevention 2017. www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention (accessed 23 October 2017).
- Department of Health and Social Care . NHS Dental Services in England: An Independent Review Led by Professor Jimmy Steele 2009. www.dh.gov.uk/en/Healthcare/Primarycare/Dental/DH_094048 (accessed 23 October 2017).
- Hoffmann M, Linell P, Lindh-Astrand L, Kjellgren K. Risk talk: rhetorical strategies in consultations on hormone replacement therapy. Health Risk Soc 2003;5:139-54. https://doi.org/10.1080/1369857031000123920.
- Green J. Is it time for the sociology of health to abandon ‘risk’?. Health Risk Soc 2009;11:493-508. https://doi.org/10.1080/13698570903329474.
- Horlick-Jones T. Managing risk and contingency: interaction and accounting behaviour. Health Risk Soc 2003;5:221-8. https://doi.org/10.1080/1369857031000123975.
- Adelsward V, Sachs L. Risk discourse: recontextualization of numerical values in clinical practice. Text Interdiscip J Stud Discour 1998;18:191-210. https://doi.org/10.1515/text.1.1998.18.2.191.
- Linell P. Discourse across boundaries: on recontextualizations and the blending of voices in professional discourse. Text Talk 1998;18:143-57. https://doi.org/10.1515/text.1.1998.18.2.143.
- Reith G. Uncertain Times. Time Soc 2004;13:383-402. https://doi.org/10.1177/0961463X04045672.
- Cox SM, McKellin W. ‘There’s this thing in our family’: predictive testing and the construction of risk for Huntington Disease. Sociol Health Illn 1999;21:622-46. https://doi.org/10.1111/1467-9566.00176.
- Gifford SM, Janes CR, Stall R, Gifford SM. Anthropology and Epidemiology: Interdisciplinary Approaches to the Study of Health and Disease. Dordrecht: Springer Netherlands; 1986.
- Goffman E. Strategic Interaction. Oxford: Blackwell; 1979.
- Department of Health and Social Care . Equity and Excellence: Liberating the NHS 2010. www.gov.uk/government/publications/liberating-the-nhs-white-paper (accessed 14 August 2015).
- NHS . Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 14 August 2015).
- NHS England . Patient and Public Participation Policy 2017. www.england.nhs.uk/wp-content/uploads/2017/04/ppp-policy.pdf (accessed 14 August 2015).
- National Institute for Health Research . INVOLVE 2017. www.invo.org.uk/resource-centre/learning-and-development/whats-on-this-site/get-started/induction-materials-for-research-staff-new-to-public-involvement/ (accessed 14 August 2015).
- Szmukler G. Service users in research and a ‘well ordered science’. J Ment Health 2009;18:87-90. https://doi.org/10.1080/09638230902835028.
- Staniszewska S. Patient and public involvement in health research: a brief overview of evidence, policy and activity. J Res Nurs 2009;14:295-8. https://doi.org/10.1177/1744987109106811.
- NIHR INVOLVE n.d. www.invo.org.uk/posttypepublication/payment-for-involvement/ (accessed 31 May 2019).
- Oliver SR, Rees RW, Clarke-Jones L, Milne R, Oakley AR, Gabbay J, et al. A multidimensional conceptual framework for analysing public involvement in health services research. Health Expect 2008;11:72-84. https://doi.org/10.1111/j.1369-7625.2007.00476.x.
- Harris R, Gamboa A, Dailey Y, Ashcroft A. One-to-one dietary interventions undertaken in a dental setting to change dietary behaviour. Cochrane Database Syst Rev 2012;3. https://doi.org/10.1002/14651858.CD006540.pub2.
- Han SY, Kim BR, Ko HY, Kwon HK, Kim BI. Validity and reliability of autofluorescence-based quantification method of dental plaque. Photodiagnosis Photodyn Ther 2015;12:587-91. https://doi.org/10.1016/j.pdpdt.2015.10.003.
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004;23:443-51. https://doi.org/10.1037/0278-6133.23.5.443.
- Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. Philadelphia, PA: Wolters Kluwer Health; 2012.
- National Online Manpower Information System (NOMIS) . Regional and National Profile for United Kingdom Report, 2016 n.d. www.nomisweb.co.uk/reports/lmp/gor/2092957698/report.aspx (accessed 3 August 2017).
- Office for National Statistics . Statistical Bulletin: Adult Smoking Habits in the UK – 2016 n.d. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2016 (accessed 3 August 2017).
- Public Health England . Local Tobacco Control Profiles 2016. https://fingertips.phe.org.uk/profile/tobacco-control (accessed 14 August 2015).
- Adult Dental Health Survey . Chapter 5: Preventive Behaviour and Risks to Oral Health – a Report From the Adult Dental Health Survey 2009. https://catalogue.ic.nhs.uk/publications/primary-care/dentistry/adul-dent-heal-surv-summ-rep-them-seri-2009/adul-dent-heal-surv-summ-them-the5-2009-rep7.pdf (accessed 3 August 2017).
- Office for National Statistics . Statistical Bulletin: Overview of the UK Population – February 2016 n.d. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/february2016 (accessed 3 August 2017).
- Martin DC, Arnold JD, Zimmerman TF, Richart RH. Human subjects in clinical research: a report of three studies. N Engl J Med 1968;279:1426-31. https://doi.org/10.1056/NEJM196812262792605.
- Friesen LR, Williams KB. Attitudes and motivations regarding willingness to participate in dental clinical trials. Contemp Clin Trials Commun 2016;2:85-90. https://doi.org/10.1016/j.conctc.2015.12.011.
- Al-Amad S, Awad M, Silverman H. Attitudes of dental patients towards participation in research. East Mediterr Health J 2014;20:90-8. https://doi.org/10.26719/2014.20.2.90.
- Fewtrell MS, Kennedy K, Singhal A, Martin RM, Ness A, Hadders-Algra M, et al. How much loss to follow-up is acceptable in long-term randomised trials and prospective studies?. Arch Dis Child 2008;93:458-61. https://doi.org/10.1136/adc.2007.127316.
- Schulz KF, Grimes DA. Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet 2002;359:781-5. https://doi.org/10.1016/S0140-6736(02)07882-0.
- Donaldson C. Valuing the benefits of publicly-provided health care: does ‘ability to pay’ preclude the use of ‘willingness to pay’?. Soc Sci Med 1999;49:551-63. https://doi.org/10.1016/S0277-9536(99)00173-2.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Olsen JA, Smith RD. Theory versus practice: a review of ‘willingness-to-pay’ in health and health care. Health Econ 2001;10:39-52. https://doi.org/10.1002/1099-1050(200101)10:1<39::AID-HEC563>3.0.CO;2-E.
- Vernazza CR, Wildman JR, Steele JG, Whitworth JM, Walls AW, Perry R, et al. Factors affecting patient valuations of caries prevention: using and validating the willingness to pay method. J Dent 2015;43:981-8. https://doi.org/10.1016/j.jdent.2015.05.009.
- Jorgensen BS, Syme GJ, Bishop BJ, Nancarrow BE. Protest responses in contingent valuation. Environ Resour Econ 1999;14:131-50. https://doi.org/10.1023/A:1008372522243.
- Mekonnen A. Valuation of community forestry in Ethiopia: a contingent valuation study of rural households. Environ Dev Econ 2000;5:289-308. https://doi.org/10.1017/S1355770X00000188.
- Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc 1962;65:26-9. https://doi.org/10.14219/jada.archive.1962.0184.
- Löe H. The Gingival Index, the Plaque Index and the Retention Index systems. J Periodontol 1967;38:610-16. https://doi.org/10.1902/jop.1967.38.6.610.
- Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of vitamin C. J Periodontol 1970;41:41-3. https://doi.org/10.1902/jop.1970.41.41.41.
- Fischman SL. Current status of indices of plaque. J Clin Periodontol 1986;13:371-4. https://doi.org/10.1111/j.1600-051X.1986.tb01475.x.
- Ainamo J. Concomitant periodontal disease and dental caries in young adult males. Suom Hammaslaak Toim 1970;66:303-66.
- Axelsson P, Lindhe J. The effect of a preventive programme on dental plaque, gingivitis and caries in schoolchildren. Results after one and two years. J Clin Periodontol 1974;1:126-38. https://doi.org/10.1111/j.1600-051X.1974.tb01248.x.
- Lang NP, Ostergaard E, Löe H. A fluorescent plaque disclosing agent. J Periodont Res 1972;7:59-67. https://doi.org/10.1111/j.1600-0765.1972.tb00632.x.
- Block RP, Bouwsma OJ, Howard-Nordan KS, Miller JM, Poore CL, Sunberg RJ. Validation of computerized photo-image analysis (PIA) measurement of plaque. J Dent Res 1996;75.
- Söder B, Jin LJ, Lundquist G, Söder PO. A longitudinal investigation of the individual consistency of plaque levels in adults. Acta Odontol Scand 1995;53:72-4. https://doi.org/10.3109/00016359509005949.
- Shaloub A, Addy M. Evaluation of accuracy and variability of scoring-area-based plaque indices. A laboratory model. J Clin Periodontol 2000;27:16-21. https://doi.org/10.1034/j.1600-051x.2000.027001016.x.
- Amaechi BT, Higham SM. Quantitative light-induced fluorescence: a potential tool for general dental assessment. J Biomed Opt 2002;7:7-13. https://doi.org/10.1117/1.1427044.
- van der Veen MH, Thomas RZ, Huysmans MC, De Soet JJ. Red auto-fluorescence of dental plaque bacteria. Caries Res 2006;40:542-5. https://doi.org/10.1159/000095655.
- Söder B, Johannsen A, Lagerlöf F. Percent of plaque on individual tooth surfaces and differences in plaque area between adjacent teeth in healthy adults. Int J Dent Hyg 2003;1:23-8. https://doi.org/10.1034/j.1601-5037.2003.00003.x.
- Needleman I, Hyun-Ryu J, Brealey D, Sachdev M, Moskal-Fitzpatrick D, Bercades G, et al. The impact of hospitalization on dental plaque accumulation: an observational study. J Clin Periodontol 2012;39:1011-16. https://doi.org/10.1111/j.1600-051X.2012.01939.x.
- Brochner A, Chrisensen C, Kristensen B, Tranaeus S, Karlsson L, Sonnesen L, et al. Treatment of post-orthodontic white spot lesions with casein phosphopeptide-stabilised amorphous calcium phosphate. Clin Oral Investig 2011;15:369-73. https://doi.org/10.1007/s00784-010-0401-2.
- Shi XQ, Tranaeus S, Angmar-Månsson B. Comparison of QLF and DIAGNOdent for quantification of smooth surface caries. Caries Res 2001;35:21-6. https://doi.org/10.1159/000047426.
- Ko HY, Kang SM, Kim HE, Kwon HK, Kim BI. Validation of quantitative light-induced fluorescence-digital (QLF-D) for the detection of approximal caries in vitro. J Dent 2015;43:568-75. https://doi.org/10.1016/j.jdent.2015.02.010.
- Pontes LRA, Novaes TF, Moro BLP, Braga MM, Mendes FM. Clinical performance of fluorescence-based methods for detection of occlusal caries lesions in primary teeth. Braz Oral Res 2017;31. https://doi.org/10.1590/1807-3107bor-2017.vol31.0091.
- Alammari MR, Smith PW, de Josselin de Jong E, Higham SM. Quantitative light-induced fluorescence (QLF): a tool for early occlusal dental caries detection and supporting decision making in vivo. J Dent 2013;41:127-32. https://doi.org/10.1016/j.jdent.2012.08.013.
- Heinrich-Weltzien R, Kühnisch J, Ifland S, Tranaeus S, Angmar-Månsson B, Stösser L. Detection of initial caries lesions on smooth surfaces by quantitative light-induced fluorescence and visual examination: an in vivo comparison. Eur J Oral Sci 2005;113:494-98. https://doi.org/10.1111/j.1600-0722.2005.00255.x.
- Sheiham A, Sabbah W. Using universal patterns of caries for planning and evaluating dental care. Caries Res 2010;44:141-50. https://doi.org/10.1159/000308091.
- Tugnait A, Clerehugh V, Hirschmann PN. Use of the basic periodontal examination and radiographs in the assessment of periodontal diseases in general dental practice. J Dent 2004;32:17-25. https://doi.org/10.1016/S0300-5712(03)00126-X.
- Department of Health and Social Care . NHS Dental Contract Pilots – Learning After First Two Years of Piloting 2014. www.gov.uk/government/uploads/system/uploads/attachment_data/file/282760/Dental_contract_pilots_evidence_and_learning_report.pdf.
- Edwards A, Matthews E, Pill R, Bloor M. Communication about risk: the responses of primary care professionals to standardizing the ‘language of risk’ and communication tools. Fam Pract 1998;15:301-7. https://doi.org/10.1093/fampra/15.4.301.
- Kay EJ, Vascott D, Hocking A, Nield H. Motivational interviewing in general dental practice: a review of the evidence. Br Dent J 2016;221:785-91. https://doi.org/10.1038/sj.bdj.2016.952.
Appendix 1 Systematic review methods detail
| MEDLINE (via Ovid MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations) |
|---|
| Web of Science: Social Sciences Citation Index |
| Web of Science: Conference Proceedings Citation Index – Social Science & Humanities |
| PsycINFO |
| PsycArticle |
| Communication & Mass Media Complete |
| ProQuest Dissertations & Theses |
| The Cochrane Library – Cochrane Reviews (reviews and protocols) |
| OpenGrey |
| Health Informatics Journal |
| Patient Preference and Adherence |
| Patient Education and Counselling |
| Health Communication |
| Journal of the American Medical Informatics Association |
| Preventive Medicine |
| Journal of Health Communication |
| BMC Medical Informatics and Decision Making |
| Strategy | Example searches | Results |
|---|---|---|
| 1 | (Health care information OR Health care instruction OR Health communication OR Health information OR Health instruction OR Health message OR Health risk OR Health risk communication OR Health risk information OR Health risk message OR Health risk status OR Health status OR Health threat OR Health-related information OR Medical information OR Patient information OR Personal health information OR Personal health record OR Personalized risk feedback OR Risk communication OR Risk communication OR Risk consultation OR Risk factor information OR Risk feedback OR Risk information OR Risk presentation OR Risk Status OR Risk-relevant information).ti,ab. | 76,612 |
| 2 | (Alternative method OR Bar graph format OR Cell phone OR Coloured traffic light symbol OR Communication mode OR Communication preference OR Communication tool OR Computer presentation OR Computer tailored OR Computer-based OR Computer-based information OR Descriptive feedback OR E-health OR e-health acceptance OR e-health application OR e-health communication OR e-health technology OR Electronic communication OR Electronic medium OR e-mail communication OR Graphic datum OR Graphic format OR Graphic format preference OR Graphical display OR Graphical format OR Graphical formats OR Graphical presentation OR Graphical risk communication format OR Health information preference OR Health Information technology OR Information format OR Information leaflet OR Information presentation OR Information system OR Information technology OR Information visualisation OR Information visualization OR Information visualization tool OR Information visualisation tool OR information-seeking preference OR In-person communication OR Interactive information OR Letter OR Mobile device OR Mobile phone OR Numeric information OR Numeric risk information OR Numerical risk information OR Numerical risk presentation OR Paper-based OR Patient preference OR Pictorial display OR Preferred communication OR Presentation format OR Presentation method OR Print communication OR Printed health OR Risk communication format OR Risk communication tool OR Risk displays OR Risk graph OR Risk presentation format OR Spoken health instruction OR Spoken instruction OR Tailored message OR Telephone communication OR UV photo OR UV photography OR Verbal information OR Verbal risk communication OR Verbal risk information OR Video information format OR Visual image OR Visual message OR Visual representation OR Visual risk communication OR Visual risk feedback OR Visualization tool OR Visualisation tool OR Cellular phone OR Cellular device OR communication method OR communication methods).ti,ab. | 105,395 |
| 3 | 1 AND 2 | 5101 |
| 4 | Limit 3 to English language, humans and 1980 to current time | 3343 |
Inclusion and exclusion criteria
Inclusion
-
Personalised (tailored) information given to patients that is reliant on a pre-assessment of the patient, rather than information that is targeted according to population characteristics, such as age and gender.
-
Studies concerned with information aimed at increasing patients’ perception of health risk. These include studies involving tailored information about an individual’s level of health with reference to likely negative consequences, as well as those involving risk terminology or health outcome probabilities.
-
Studies reporting delivery of information in a certain form (e.g. written, video, online, photographic) versus no intervention/usual care controls, or comparing information in different forms. In the control group, ‘usual care’ information may or may not be tailored. Studies involving multicomponent interventions that had control group components, such as motivational interviewing, or education that was also part of the intervention group, were included.
-
Outcome measures including one or more behaviour mediators, including risk perception, health behaviour and health outcomes.
-
Adults aged ≥ 18 years.
-
Patients receiving information as part of their care.
-
Any health system.
-
English language only.
-
Dated 1980 to present time.
-
All types of study design, including qualitative studies and protocols.
Exclusion
-
Studies concerned with giving information in a verbal form compared with a control.
-
Outcomes concerned with decision-making in relation to treatment options only.
Appendix 2 Additional tables
| Item | Total costs | Cost per patient (£) | Source |
|---|---|---|---|
| Printing of photograph in QLF arm |
Cartridges, £20 each Three cartridges needed for colour printing; 300 pages of 18 stickers per cartridge |
0.01 |
Catalogue prices Assumption Details on cartridge packaging |
| Stickers for printing photograph | £10 for 1200 labels | 0.01 | Catalogue prices |
| Camera |
£4500 per camera with 10 years of life Average dentist provides 2000 check-ups per year |
0.24 |
Price to obtain a camera for the study PSSRU approach119 NHS Digital information118 |
| Printer |
£73.09 per printer with 10 years of life Average dentist provides 2000 check-ups per year |
0.01 |
Price to obtain a printer for the study PSSRU approach119 NHS Digital information118 |
| Retractors |
£61.88 per unit with 2 years of life Average dentist provides 2000 check-ups per year |
0.02 |
Price to obtain a pair of retractors for study PSSRU approach119 NHS Digital information118 |
| Characteristics | OR | SE | z | p > z | 95% CI |
|---|---|---|---|---|---|
| Deprivation (IMD) | |||||
| High | 1.14 | 0.349 | 0.44 | 0.658 | 0.63 to 2.08 |
| Medium | Reference | ||||
| Low | 1.11 | 0.303 | 0.40 | 0.691 | 0.65 to 1.90 |
| Income (£) | |||||
| High (≥ £31,201) | 0.89 | 0.249 | –0.41 | 0.682 | 0.52 to 1.54 |
| Medium (£15,601–31,200) | Reference | ||||
| Low (£0–15,600) | 0.87 | 0.247 | –0.49 | 0.625 | 0.50 to 1.52 |
| Gender | |||||
| Female | 0.86 | 0.206 | –0.61 | 0.542 | 0.54 to 1.38 |
| Male | Reference | ||||
| Education | |||||
| High (degree or more) | 0.86 | 0.275 | –0.48 | 0.631 | 0.46 to 1.61 |
| Medium (A level) | Reference | ||||
| Low (GCSE or less) | 1.48 | 0.439 | 1.33 | 0.183 | 0.83 to 2.65 |
| Age | |||||
| Young (18–35 years) | 0.53 | 0.154 | –2.18 | 0.029 | 0.30 to 0.94 |
| Middle (36–64 years) | Reference | ||||
| Old (≥ 65 years) | 1.79 | 0.593 | 1.76 | 0.079 | 0.93 to 3.43 |
| Number of teeth | |||||
| < 20 | 1.35 | 0.428 | 0.94 | 0.348 | 0.72 to 2.51 |
| ≥ 20 | Reference | ||||
| Dental attendance (by number of check-up appointments attended over the previous 5 years) | |||||
| Infrequent attender | 1.27 | 0.378 | 0.80 | 0.425 | 0.71 to 2.27 |
| Normal attender | Reference | ||||
| Literacy (REALM-R) | |||||
| Low | 0.88 | 0.412 | –0.27 | 0.789 | 0.35 to 2.20 |
| Normal/high | Reference | ||||
| Practice | |||||
| 1 | 2.45 | 0.854 | 2.57 | 0.010 | 1.24 to 4.85 |
| 2 | 4.20 | 1.439 | 4.19 | 0.000 | 2.15 to 8.22 |
| 3 | 3.13 | 1.107 | 3.23 | 0.001 | 1.57 to 6.26 |
| 4 | Reference | ||||
| Constant | 0.181 | –2.02 | 0.043 | 0.17 to 0.97 | |
| Characteristics | OR | SE | z | p > z | 95% CI |
|---|---|---|---|---|---|
| Deprivation (IMD) | |||||
| High | 1.65 | 0.700 | 1.18 | 0.239 | 0.72 to 3.79 |
| Medium | Reference | ||||
| Low | 1.23 | 0.468 | 0.55 | 0.579 | 0.59 to 2.59 |
| Income (£) | |||||
| High (≥ £31,201) | 0.63 | 0.253 | –1.15 | 0.251 | 0.29 to 1.38 |
| Medium (£15,601–31,200) | Reference | ||||
| Low (£0–15,600) | 1.21 | 0.436 | 0.53 | 0.594 | 0.60 to 2.45 |
| Gender | |||||
| Female | 1.48 | 0.500 | 1.16 | 0.246 | 0.76 to 2.87 |
| Male | Reference | ||||
| Education | |||||
| High (degree or more) | 0.83 | 0.353 | –0.44 | 0.659 | 0.36 to 1.91 |
| Medium (A level) | Reference | ||||
| Low (GCSE or less) | 0.71 | 0.283 | –0.87 | 0.384 | 0.32 to 1.55 |
| Age | |||||
| Young (18–35 years | 1.19 | 0.445 | 0.47 | 0.640 | 0.57 to 2.48 |
| Middle (36–64 years) | Reference | ||||
| Old (≥ 65 years) | 0.95 | 0.445 | –0.11 | 0.914 | 0.38 to 2.38 |
| Number of teeth | |||||
| ≤ 20 | 0.65 | 0.306 | –0.91 | 0.362 | 0.26 to 1.63 |
| ≥ 20 | Reference | ||||
| Dental attendance (by number of check-up appointments attended over the previous 5 years) | |||||
| Infrequent attender | 1.51 | 0.556 | 1.13 | 0.260 | 0.74 to 3.11 |
| Normal attender | Reference | ||||
| Literacy (REALM-R) | |||||
| Low | 1.39 | 0.846 | 0.54 | 0.586 | 0.42 to 4.58 |
| Normal/high | Reference | ||||
| Practice | |||||
| 1 | 1.12 | 0.503 | 0.25 | 0.805 | 0.46 to 2.70 |
| 2 | 0.52 | 0.253 | –1.35 | 0.179 | 0.20 to 1.35 |
| 3 | 0.94 | 0.426 | –0.14 | 0.887 | 0.38 to 2.29 |
| 4 | Reference | ||||
| Constant | 0.14 | 0.085 | –3.25 | 0.001 | 0.04 to 0.46 |
| Characteristics | OR | SE | z | P > z | 95% CI |
|---|---|---|---|---|---|
| Deprivation (IMD) | |||||
| High | 0.66 | 0.212 | –1.29 | 0.196 | 0.35 to 1.24 |
| Medium | Reference | ||||
| Low | 0.80 | 0.223 | –0.81 | 0.418 | 0.46 to 1.38 |
| Income (£) | |||||
| High (≥ £31,201) | 1.46 | 0.422 | 1.30 | 0.194 | 0.83 to 2.57 |
| Medium (£15,601–31,200) | Reference | ||||
| Low (£0–15,600) | 1.05 | 0.312 | 0.18 | 0.861 | 0.59 to 1.88 |
| Gender | |||||
| Female | 0.93 | 0.231 | –0.30 | 0.764 | 0.57 to 1.51 |
| Male | Reference | ||||
| Education | |||||
| High (degree or more) | 1.26 | 0.415 | 0.70 | 0.484 | 0.66 to 2.40 |
| Medium (A level) | Reference | ||||
| Low (GCSE or less) | 0.80 | 0.250 | –0.73 | 0.466 | 0.43 to 1.47 |
| Age | |||||
| Young (18–35 years | 1.69 | 0.493 | 1.81 | 0.071 | 0.96 to 3.00 |
| Middle (36–64 years) | Reference | ||||
| Old (≥ 65 years) | 0.50 | 0.192 | –1.80 | 0.072 | 0.24 to 1.06 |
| Number of teeth | |||||
| ≤ 20 | 0.89 | 0.310 | –0.32 | 0.746 | 0.45 to 1.76 |
| ≥ 20 | Reference | ||||
| Dental attendance (by number of check-up appointments attended over the previous 5 years) | |||||
| Infrequent attender | 0.60 | 0.187 | –1.63 | 0.102 | 0.33 to 1.11 |
| Normal attender | Reference | ||||
| Literacy (REALM-R) | |||||
| Low | 0.94 | 0.469 | –0.12 | 0.901 | 0.35 to 2.50 |
| Normal/high | Reference | ||||
| Practice | |||||
| 1 | 0.40 | 0.140 | –2.63 | 0.009 | 0.20 to 0.79 |
| 2 | 0.32 | 0.110 | –3.33 | 0.001 | 0.16 to 0.63 |
| 3 | 0.34 | 0.121 | –3.02 | 0.002 | 0.17 to 0.68 |
| 4 | Reference | ||||
| Constant | 0.611 | 0.71 | 0.475 | 0.57 to 3.28 | |
| Characteristics | Verbal information | TL information | QLF information | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | t | P > t | 95% CI | Coefficient | SE | t | P > t | 95% CI | Coefficient | SE | t | P > t | 95% CI | |
| Deprivation (IMD) | |||||||||||||||
| High | –17.26 | 7.35 | –2.35 | 0.02 | –31.76 to –2.77 | –10.14 | 5.38 | –1.88 | 0.06 | –20.74 to 0.46 | –12.52 | 5.32 | –2.36 | 0.02 | –22.99 to –2.06 |
| Medium | Reference | Reference | Reference | ||||||||||||
| Low | 1.61 | 6.65 | 0.24 | 0.81 | –11.52 to 14.73 | 0.53 | 4.91 | 0.11 | 0.91 | –9.14 to 10.20 | –1.57 | 4.89 | –0.32 | 0.75 | –11.19 to 8.06 |
| Income (£) | |||||||||||||||
| High (≥ £31,201) | –0.62 | 6.82 | –0.09 | 0.93 | –14.06 to 12.83 | –2.13 | 4.98 | –0.43 | 0.67 | –11.94 to 7.67 | 12.30 | 4.99 | 2.46 | 0.01 | 2.46 to 22.13 |
| Medium (£15,601–31,200) | Reference | Reference | Reference | ||||||||||||
| Low (£0–15,600) | –6.86 | 6.90 | –1.00 | 0.32 | –20.46 to 6.74 | –7.31 | 5.20 | –1.41 | 0.16 | –17.56 to 2.93 | 1.47 | 5.08 | 0.29 | 0.77 | –8.53 to 11.46 |
| Gender | |||||||||||||||
| Female | –0.17 | 5.74 | –0.03 | 0.98 | –11.49 to 11.16 | 0.20 | 4.30 | 0.05 | 0.96 | –8.26 to 8.67 | –1.57 | 4.25 | –0.37 | 0.71 | –9.95 to 6.81 |
| Male | Reference | Reference | Reference | ||||||||||||
| Education | |||||||||||||||
| High (degree or more) | 1.13 | 8.03 | 0.14 | 0.89 | –14.71 to 16.97 | 3.91 | 5.87 | 0.67 | 0.51 | –7.66 to 15.48 | 3.50 | 5.83 | 0.60 | 0.55 | –7.99 to 14.98 |
| Medium (A level) | Reference | Reference | Reference | ||||||||||||
| Low (GCSE or less) | 8.69 | 7.46 | 1.17 | 0.25 | –6.02 to 23.39 | 14.17 | 5.43 | 2.61 | 0.01 | 3.46 to 24.87 | 9.05 | 5.36 | 1.69 | 0.09 | –1.49 to 19.60 |
| Age | |||||||||||||||
| Young (18–35 years | –10.81 | 7.31 | –1.48 | 0.14 | –25.23 to 3.61 | –2.47 | 5.28 | –0.47 | 0.64 | –12.87 to 7.93 | 0.92 | 5.40 | 0.17 | 0.87 | –9.71 to 11.55 |
| Middle (36–64 years) | Reference | Reference | Reference | ||||||||||||
| Old (≥ 65 years) | 5.06 | 7.67 | 0.66 | 0.51 | –10.06 to 20.18 | 5.53 | 5.81 | 0.95 | 0.34 | –5.92 to 16.98 | 0.40 | 5.58 | 0.07 | 0.94 | –10.58 to 11.38 |
| Number of teeth | |||||||||||||||
| ≤ 20 | 6.94 | 8.32 | 0.83 | 0.41 | –9.48 to 23.36 | 3.96 | 6.11 | 0.65 | 0.52 | –8.08 to 16.00 | 1.15 | 5.71 | 0.20 | 0.84 | –10.10 to 12.40 |
| ≥ 20 | Reference | Reference | Reference | ||||||||||||
| Dental attendance (by number of check-up appointments attended over the previous 5 years) | |||||||||||||||
| Infrequent attender | 0.69 | 7.31 | 0.09 | 0.93 | –13.72 to 15.11 | 8.63 | 5.51 | 1.57 | 0.12 | –2.22 to 19.47 | –3.96 | 5.70 | –0.69 | 0.49 | –15.18 to 7.26 |
| Normal attender | Reference | Reference | Reference | ||||||||||||
| Literacy (REALM-R) | |||||||||||||||
| Low | –24.62 | 12.98 | –1.90 | 0.06 | –50.22 to 0.98 | –13.59 | 9.70 | –1.40 | 0.16 | –32.71 to 5.52 | –15.52 | 8.12 | –1.91 | 0.06 | –31.51 to 0.47 |
| Normal/high | Reference | Reference | Reference | ||||||||||||
| Practice | |||||||||||||||
| 1 | 17.48 | 8.97 | 1.95 | 0.05 | –0.20 to 35.17 | 13.36 | 6.80 | 1.96 | 0.05 | –0.05 to 26.76 | 8.06 | 6.98 | 1.15 | 0.25 | –5.70 to 21.81 |
| 2 | 25.37 | 8.82 | 2.88 | 0.00 | 7.97 to 42.77 | 17.70 | 6.62 | 2.67 | 0.01 | 4.66 to 30.74 | 15.70 | 6.92 | 2.27 | 0.02 | 2.07 to 29.33 |
| 3 | 10.36 | 9.51 | 1.09 | 0.28 | –8.40 to 29.11 | 10.29 | 7.06 | 1.46 | 0.15 | –3.62 to 24.21 | 2.28 | 7.19 | 0.32 | 0.75 | –11.88 to 16.43 |
| 4 | Reference | Reference | Reference | ||||||||||||
| Constant | 11.38 | 1.39 | 0.17 | –6.66 to 38.25 | 1.14 | 8.46 | 0.13 | 0.89 | –15.52 to 17.81 | 11.68 | 8.86 | 1.32 | 0.19 | –5.77 to 29.13 | |
| Sum | 37.74 | 1.93 | 33.92 to 41.55 | 30.87 | 1.52 | 27.89 to 33.86 | 31.87 | 1.48 | 28.96 to 34.79 | ||||||
| EPPM components | n | Full sample, mean (SD) | Verbal, mean (SD) | TL, mean (SD) | QLF, mean (SD) |
|---|---|---|---|---|---|
| Intention | 392 | 4.76 (0.51) | 4.76 (0.57) | 4.73 (0.50) | 4.80 (0.46) |
| Susceptibility | 392 | 4.17 (0.66) | 4.21 (0.67) | 4.17 (0.67) | 4.13 (0.65) |
| Severity | 392 | 3.91 (0.99) | 4.01 (0.97) | 3.77 (1.10) | 3.90 (0.91) |
| Feelings | 392 | 4.26 (0.68) | 4.26 (0.73) | 4.30 (0.65) | 4.17 (0.65) |
| Self-efficacy | 379 | 4.47 (0.56) | 4.49 (0.53) | 4.47 (0.51) | 4.46 (0.63) |
| Response efficacy | 385 | 4.48 (0.63) | 4.53 (0.61) | 4.46 (0.60) | 4.45 (0.68) |
| Fear control processes | 392 | 1.62 (0.83) | 1.64 (0.90) | 1.63 (0.80) | 1.61 (0.79) |
| Practice | Current position | Gender | Age (years) | Length of time since qualification (years) | Length of time in current post (years) |
|---|---|---|---|---|---|
| 3 | Dental nurse | Female | 50–59 | > 25 | 12 |
| 3 | Dentist | Male | 40–49 | 15 | 5 |
| 3 | Dentist in VT | Female | 30–39 | 1 | 1 |
| 3 | Dental HT | Female | 20–29 | 2 | 2 |
| 4 | Practice manager | Female | 30–39 | 16 | 16 |
| 4 | Receptionist | Female | 50–59 | > 25 | > 25 |
| 4 | Dental nurse | Female | 30–39 | 8 | 1 |
| 4 | Dentist | Female | 30–39 | 3 | 2 |
| 4 | Dentist | Male | 40–49 | 22 | 10 |
| 2 | Dentist | Female | 30–39 | 17 | 15 |
| 2 | Dental HT | Female | 30–39 | 17 | 10 |
| 2 | Receptionist | Female | 50–59 | > 25 | > 25 |
| 5 | Practice manager | No details given to preserve anonymity because a prototype practice might be more identifiable | |||
| 5 | Dentist | ||||
| 5 | Dentist | ||||
| 5 | Prevention nurse | ||||
Appendix 3 Interview topic guides and observation coding sheet
List of abbreviations
- A level
- Advanced level
- BPE
- basic periodontal examination
- CAT
- Communication Assessment Tool
- CONSORT
- Consolidated Standards of Reporting Trials
- df
- degrees of freedom
- EPPM
- extended parallel process model
- GCSE
- General Certificate of Secondary Education
- HRA
- health risk appraisal
- HT
- hygiene therapist
- ID
- identification
- IMD
- Index of Multiple Deprivation
- MANCOVA
- multivariate analysis of covariance
- MDAS
- Modified Dental Anxiety Scale
- NE
- north-east
- NIHR
- National Institute for Health Research
- NW
- north-west
- PAG
- Project Advisory Group
- PG
- Patient and Public Involvement Group
- PPI
- patient and public involvement
- PREFER
- presenting information on dental risk
- PSSRU
- Personal Social Services Research Unit
- QLF
- Quantitative Light-Induced Fluorescence
- QLF-D
- Quantitative Light-Induced Fluorescence-Digital
- RAG
- red–amber–green (current NHS prototype models)
- RCT
- randomised controlled trial
- REALM-R
- Rapid Estimate of Adult Literacy in Medicine, Revised
- REC
- Research Ethics Committee
- SD
- standard deviation
- TL
- traffic light
- UDA
- Unit of Dental Activity
- VT
- vocational trainee/training
- WTP
- willingness to pay
Notes
-
Questionnaires
-
Study material
Supplementary material can be found on the NIHR Journals Library report project page (www.journalslibrary.nihr.ac.uk/programmes/hsdr/133345/#/documentation).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
